Form 405-D (rev. 9/1/2022)
Notice of Intent to Arbitrate Form
Please complete this form and send it to: BBVA@scc.virginia.gov
Attach copies of both the notice of payment and payment, if both are available.
This request must be submitted to both the SCC and the non-initiating
party within 40
days of the earlier of the provider’s receipt of the payment or payment notification;
otherwise, the request will be rejected. For bundled claims, attach a separate sheet
listing all requested information. All claims within the bundle must meet the timeframes set below, the dates of service
must be within two months of each other, the claims must relate to similar CPT codes and involve the same carrier and
health care professional or facility.
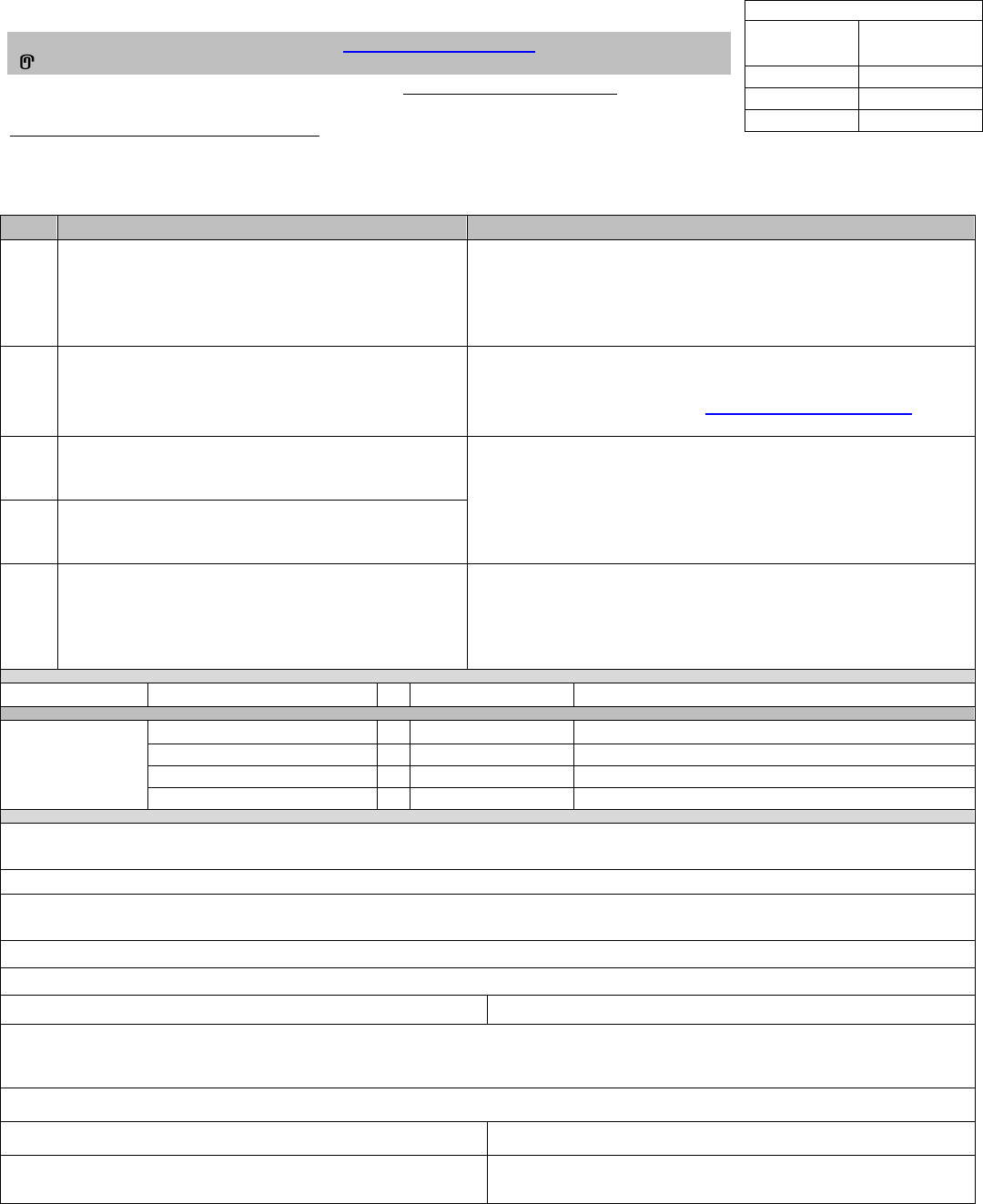
To be completed by SCC
SCC Tracking
No.:
Received Date
Date Closed
Closed reason
Step
Claim Payment Negotiation History
Screening Information
1.
Date the provider received the payment(s) or
payment notification related to the claim(s),
whichever is earlier. Attach all copies of notice
of payment(s) and payments received by
provider related to the claim(s):
Are all claims submitted related to a plan regulated by the
SCC Bureau of Insurance, the state employee health plan, or
an elective group health plan?
(See Information and Instructions
below)
Yes □ No □ If “no,” do not submit this request.
2.
Date notice was provided to non-initiating party
putting claim payment into dispute (must be
within 30 days of Step 1):
Do all claims relate to services rendered in Virginia?
Yes □ No □
If “no,” STOP and contact BBVA@scc.virginia.gov
prior to submitting this request.
3.
Date of completion of 30-day period of good faith
negotiation (add 30 days to Step 1 date):
Name of the health care professional initiating arbitration, and
name, phone number and email address of the submitter:
4.
Date of request to SCC to initiate arbitration
(must be within 10 days after Step 3 date – do
not submit prior to Step 3 date):
5.
Date notice of intent to initiate arbitration was
provided to non-initiating party
(must be within 10
days after Step 3 date):
If the party initiating arbitration is a provider, indicate the
provider’s employer or business entity in which the provider
has an ownership interest and address:
Services are:
Emergency
□
Non-emergency
□
The party
requesting
arbitration is a:
Health care facility:
□
License type:
Health care professional:
□
Specialty type:
Other health care provider:
□
Type:
Carrier or administrator:
□
Indicate which:
Provide the name and address of the facility:
Is the facility In-Network for the service? Yes □ No □
Description of health care services provided (including any applicable CPT codes):
Is this request for multiple claims? Yes □ No □ (If so, all claims must meet the above stated requirements)
Date(s) of service: (for bundled claims, must be within two months of each other)
Group/plan number:
Claim number:
Complete name of non-initiating party (carrier), and name, phone number and email address of its contact person to
which notice was sent/is being sent:
(For bundled claims, report the sum of all charges to be arbitrated for each offer below)
Initial billed amount of covered services:
Carrier/TPA allowed amount (use latest EOB):
Provider final offer provided with this request:
Most recent carrier/TPA payment offer (if different from
latest EOB allowed amount):
Form 405-D (rev. 9/1/2022)
Information and Instructions
• Only claim payments made in connection with managed care plans regulated by SCC, the
state employee health plan and eligible group health plans defined in 14 VAC 5-405-20 can
use the arbitration process. Examples of health benefit plans that are not included are:
Medicar
e and Medicaid
Federal Employee Health Benefit Plans
• Please check the list of elective group health plans at: Search Elective Group Health Plans |
Balance Billing (virginia.gov) to determine whether a plan has elected to participate in balance
billing protections for their members.
• An out-of-net
work provider or facility subject to Virginia law and providing emergency services
at a hospital or non-emergency services if those services involve surgical or ancillary services
at an in-network facility may submit this arbitration request to both the SCC and the non-
initiating party if it is believed that the payment offered for the covered services was not a
commercially reasonable amount. A carrier or an elective group plan may also submit a
request for arbitration.
• Upon SCC review and acceptance of a request for arbitration, both the initiating and non-
initiating parties must choose an arbitrator from a list of arbitrators approved by the SCC. If
the parties cannot agree on an arbitrator, the SCC will choose one and notify the parties,
using the process outlined in § 38.2-3445.02 of the Code of Virginia and 14 VAC 5-405-40
.
• Within 10 business days of the initiating party notifying the SCC and the non-initiating party
of intent to initiate arbitration, both parties must agree to and execute a nondisclosure
agreement.
• Once the arbitrator has been chosen, the SCC will send the arbitrator a copy of the Notice of
Intent to Arbitrate Form. Both parties have 30 days from the date of notice of intent to arbitrate
to make written submissions to the arbitrator. The non-initiating party must provide the
initiating party their final offer at this time. The arbitrator’s fee is payable within 10 calendar
days of the assignment of the arbitrator, with the health carrier and the provider to divide the
fee equally. A party that fails to make timely written submissions without good cause shown
will be in default and agrees to pay the final offer amount submitted by the party not in default.
The arbitrator also can require the party in default to pay expenses incurred to date in the
course of arbitration, including the arbitrator's fee.
• N
o
l
at
er than 15 calendar days after the receipt of the parties' written submissions, the
arbitrator will:
o Issue a written decision to the parties and the SCC requiring payment of the final offer
amount of either the initiating party or the non-initiating party;
o Provide each party with the other’s written submissions, and
o Provide the additional information described in § 38.2-3445.02 E of the Code of
Virginia and 14 VAC 5-405-40 G to the SCC.
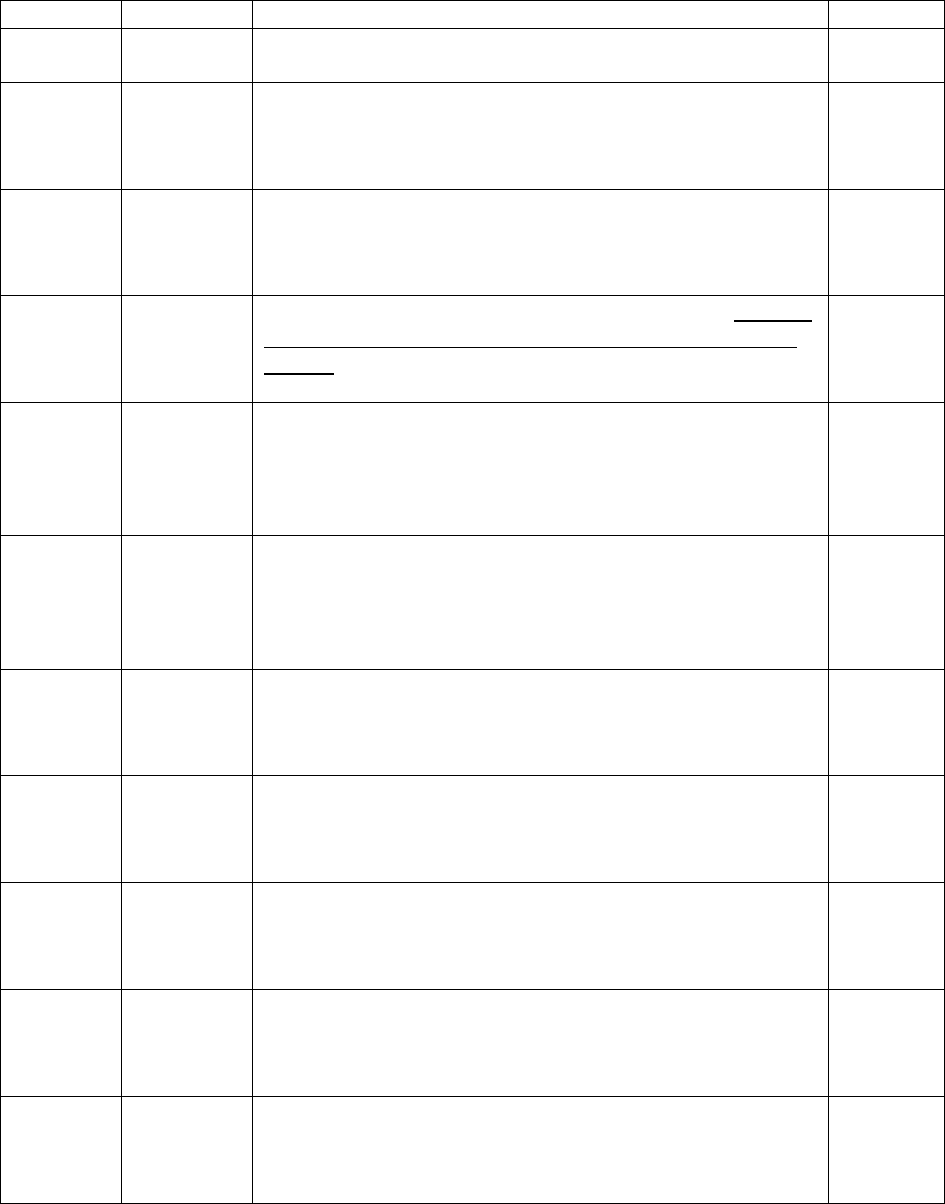
Form 405-D (rev. 9/1/2022)
Arbitration Timeline
Example
Step 1
Out-of-network provider submits clean claim to
carrier/payer.
2/15/21
Step 2
Within 30
days of
Step 1
date
Carrier/payer pays or offers to pay out-of-network
provider.
3/1/21
Step 3
Within 30
days of
Step 2
date
Provider may dispute payment or payment offer by
notifying carrier/payer.
3/15/21
Step 3
continued
Ends 30
days after
Step 2
date
Parties are engaged in good faith negotiation. Parties
must complete the full 30-day good faith negotiation
period.
3/31/21
Step 4
Within 10
days of
the end of
Step 3
continued
Carrier/payer or provider can request arbitration by
sending this form to the SCC and to the non-initiating
party. Initiating party must include their final offer with
request.
4/9/21
Step 5
Within 10
business
days of
Step 4
date
Nondisclosure agreement signed by the initiating and
non-initiating parties. The parties decide on the
agreement to sign.
4/23/21
Step 6
Within 20
days of
Step 4
date
Arbitrator is chosen. Commission notifies initiating and
non-initiating parties of chosen arbitrator and copies
chosen arbitrator.
4/29/21
Step 7
Within 30
days of
Step 4
date
Both parties must make written submissions in
support of final offer.
5/9/21
Step 8
Within 10
days of
Step 6
date
Parties each pay arbitrator their half of the applicable
fee.
5/9/21
Step 9
Within 15
days of
Step 7
date
Arbitrator issues decision.
5/24/21
Step 10
Within 10
days of
Step 9
date
Claim payment is made.
6/3/21
Parties can come to an agreement at any time during this process; however, once an
arbitrator is chosen, the arbitrator must receive payment. Claim must be paid within 10 days
of agreement.
