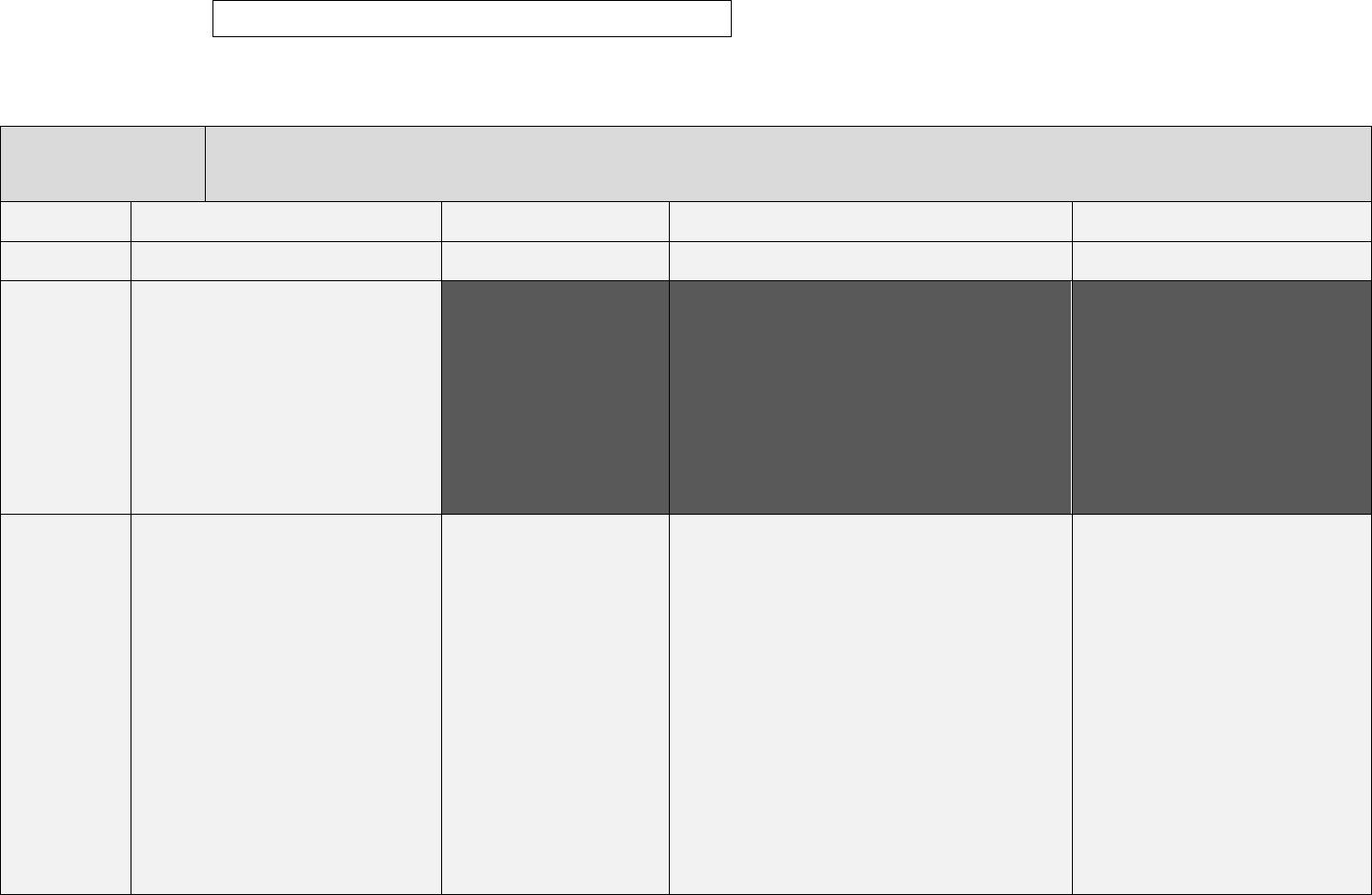
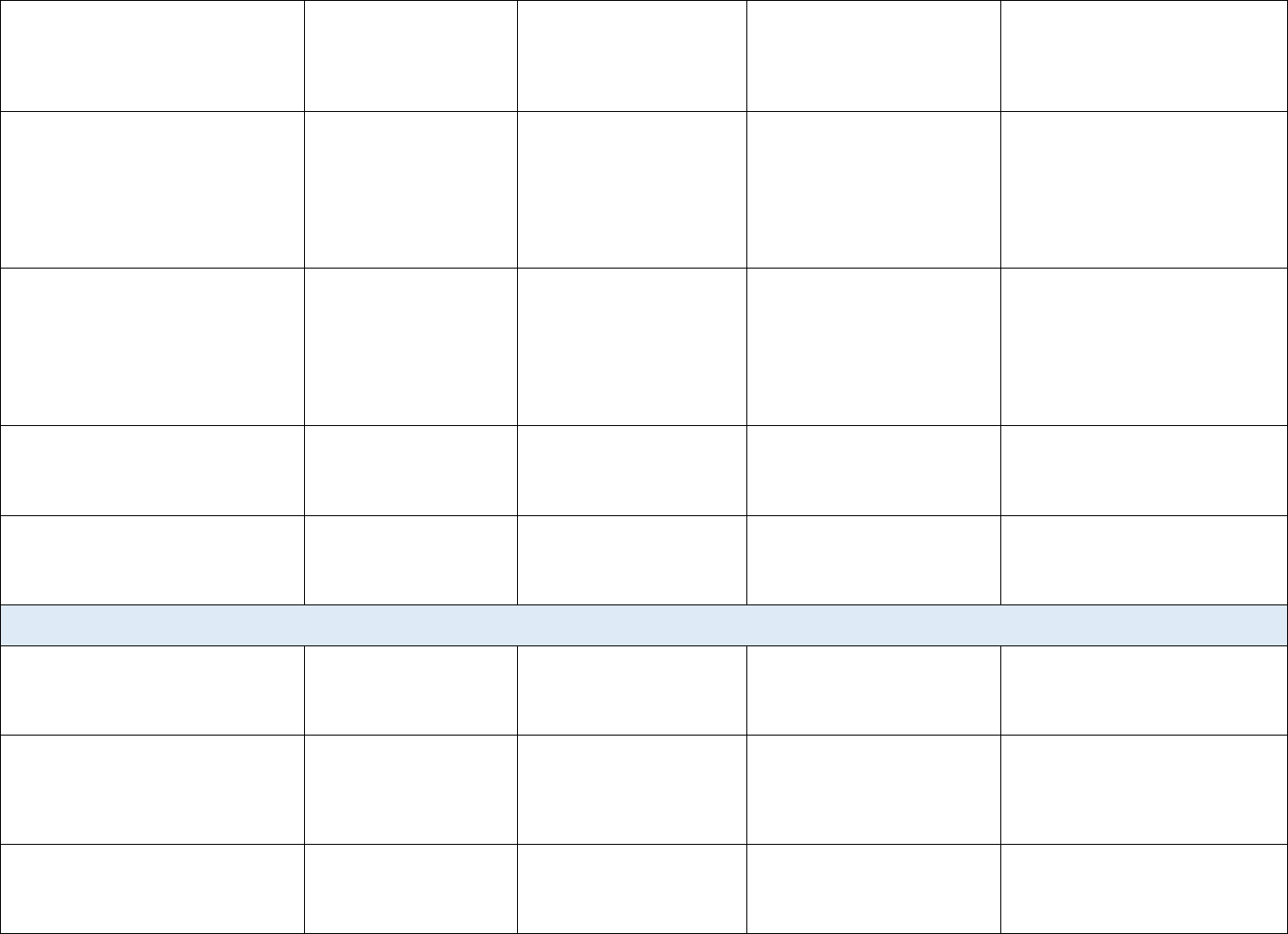
ASHP PGY1 Pharmacy
Development Plan Example
Resident Name:
The purpose of the resident development plan is to document residency program changes based upon resident strengths, opportunities for improvement, goals,
and interests. The development plan is to be shared with preceptors and the resident within 30 days from the start of the residency (initial), 90 days from the
start of the residency (Q1), and every 90 days thereafter (Q2 and Q3).
Resident’s Self-Reflection and Self Evaluation:
Self-Reflection includes Strengths, Opportunities for Improvement, Practice Interests, Career Goals, and Well-being and Resilience.
Self-Evaluation is related to the Program’s Competency Areas
Initial
Quarter 1
Quarter 2 Quarter 3
Date
6/28/2023
9/20/223
12/28/23 3/5/23
Personal
Strengths and
Weaknesses:
From Initial Self-Reflection:
Personal Strengths: enthusiastic,
detail oriented, self-motivated, and
honest.
Personal areas of Improvement:
Speaking to large group and
efficiency. I often put in long
hours/stay up all night to complete
work.
Practice
Interests/
Career Goals
From Initial Self-Reflection:
Practice Interest (in order of
preference):
• Infectious diseases
• Oncology
• Solid organ transplant
Career Goals:
• complete a PGY2 residency in a
practice area of interest
• take the BCPS exam after PGY1
residency completion
• obtain a clinical pharmacist/
specialist position at a teaching
hospital
• precept students and residents
Changes to:
Practice Interests/Career
Goals: Enjoyed ID rotation
and plan to pursue a PGY2
ID residency
Changes to:
Practice Interests/Career Goals:
PGY2: I am no longer interested in pursuing a
PGY2 residency this year. I really enjoy clinical
work but I feel tired and like I am not as good as
my preceptors.
Professional involvement:
I have enjoyed my time on the XSHP Board and
can see myself remaining involved in various
capacities throughout my career.
Changes to Practice
Interests/Career Goals:
I have accepted a position as a
clinical pharmacist generalist in a
teaching hospital near my parents
and sister. This role aligns with my
interest in practice advancement
and research and I am happy with
this decision.
Judy Jetson
• participate in research
• be actively involved in
professional organizations
Well-being
and
Resilience:
From Initial Self-Reflection
Current well-being strategies from
initial self-assessment:
• Maintain close relationships
with parents/sister’s family
• Exercise regularly
• Work on increasing hydration
and minimizing stress eating
Current well-being: I
have been able to talk to
my family on the phone or
by video at least once a
week. They are a great
support system.
I am meeting my
hydration goals but still
need to improve eating
habits. I am still stress
eating (m&ms!) and find it
hard to get to the grocery
store.
I haven’t kept up with my
sleep log since rotations
Current well-being: I am still talking with my
parents and sister’s family weekly. This time
grounds me but has also made me homesick. I’ve
stopped using the camera because they are
always saying how tired I look.
I’m not exercising regularly because I’m so busy,
am not sleeping, and feel tired all the time.
Still meeting my hydration goals and think my
eating habits have gotten worse because of
stress and lack of time…I am mostly eating from
the hospital cafeteria or gift shop.
Current well-being: Quarter two
was really hard and I had a lot of
doubts about my abilities, I wasn’t
sleeping well, and wasn’t close to
meeting my activity and nutrition
goals.
I feel like the third quarter was a
significant turning point for me.
Due to the support I received from
my family, the program, and
organization, I was able to take
some time off and recalibrate my
expectations for myself and the
remainder of the year. I have also
been able to reduce my work
hours, exercise more, eat healthier,
and get more sleep.
Strengths and
Areas of
Improvement
Related to
CAGOS
R1
From Initial Self-Evaluation
Strengths:
• Worked with a variety of
inpatient and outpatient
patient care teams during
pharmacy school
• Feel like I can easily
integrate into the team,
prioritize patients above
other responsibilities, and
form strong relationships
with patients and their
families.
• Had 2 ambulatory clinic
rotations and spent a
large portion of time
counseling patients
Opportunities for
Improvement: Worked
primarily in outpatient specialty
Progress on Previous
Opportunities for
Improvement: I feel
comfortable with my
duties in inpatient. While I
am looking forward to
transitioning to the IV
room in November, I am a
little bit nervous since I
haven’t worked in there
since the beginning of
orientation.
Strengths: Even with
limited experience prior
to residency, I believe
staffing the main
pharmacy, with the
exception of working in
the IV room, is a strength
for me now.
Progress on Previous Opportunities for
Improvement: The IV room retraining was really
helpful.
I have been able to develop alternate treatment
plans based upon changing patient parameters
or team rejection of my first plan and have
received positive feedback from my preceptor
about my progress.
Strengths: I feel that I am contributing effectively
during my staffing shifts.
New Opportunities for Improvement: I am
concerned about my progress on some R1
patient care objectives because I am having
trouble recalling the details of my patients, even
though I’ve thoroughly reviewed them. On
rounds, I start mixing up my patient’s details,
then stop making recommendations and
speaking up on rounds because I am scared that I
will say the wrong thing and hurt a patient.
Progress on Previous
Opportunities for Improvement: I
believe I’ve made a lot of positive
progress. When the preceptors
showed me through their pre-
rounding processes and challenged
me to organize my patients and
corresponding pertinent data, it
improved my confidence in my
abilities. As my confidence grew,
so did my positive contributions to
patient care decisions on rounds.
I’ve become much more efficient as
I don’t spend large portions of the
afternoon chasing down providers
and explaining my
recommendations and their
corresponding rationale.
Strengths: I feel confident to staff
all assigned areas. I also feel
confident about my abilities to
pharmacy and only have limited
experience with inpatient
pharmacy from IPPE.
New Opportunities for
Improvement: Comfort
with IV room staffing.
efficiently collect and analyze
patient data and identify a plan for
each patient.
New Opportunities for
Improvement: None identified
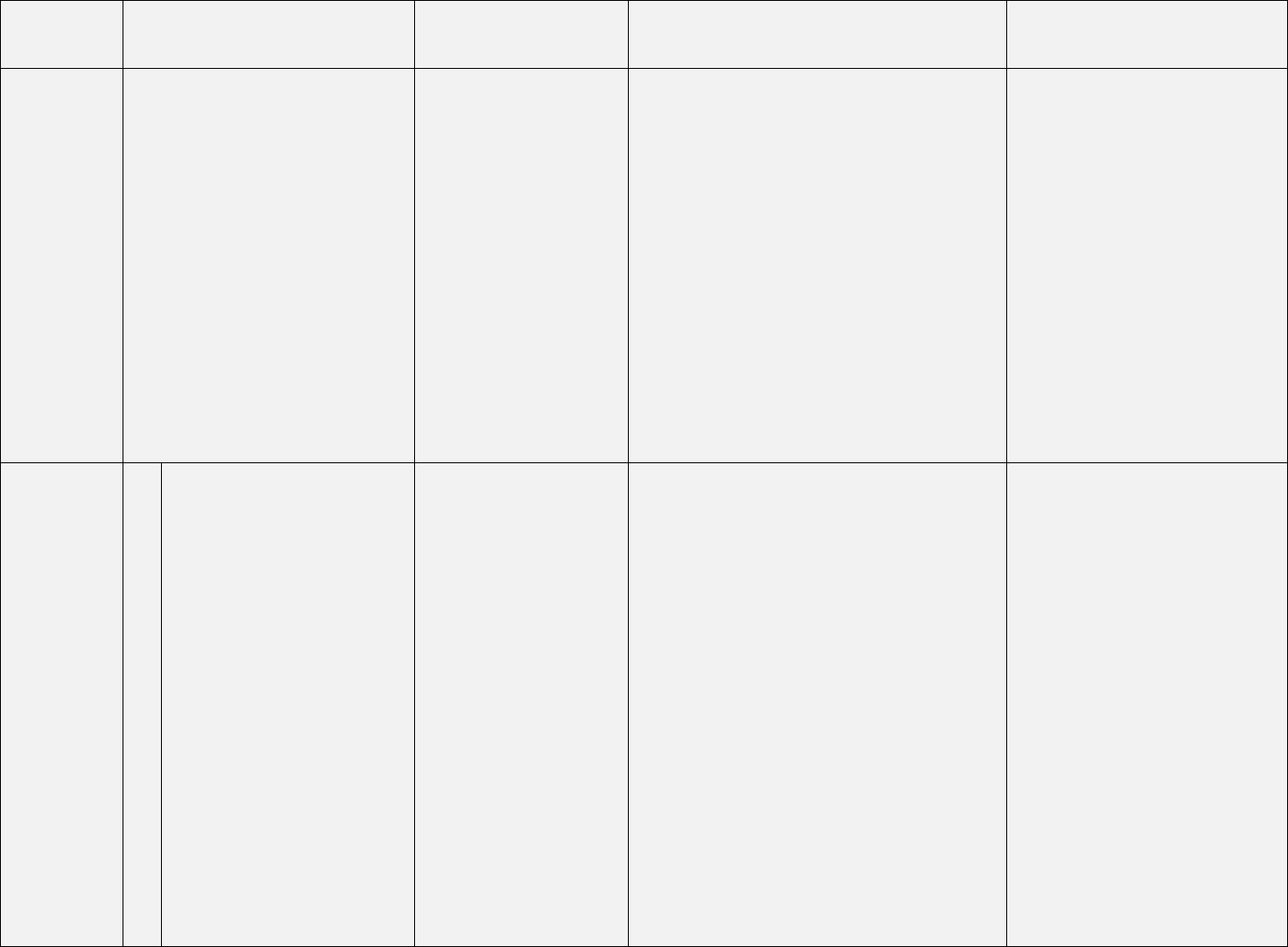
R2
From Initial Self-Evaluation:
Strengths:
• Completed a longitudinal
clinical research project in
pharmacy school that
resulted in a practice
change in the organization,
poster at ID week.
• Have submitted the
publication to a journal for
consideration
Opportunities for
Improvement:
• Have not completed a drug
monograph but did update
a treatment guideline.
• Have not independently
completed a medication
use evaluation
Progress on Previous
Opportunities for
Improvement: I have not
had the opportunity to
work on a monograph or
MUE yet
Strengths: No change
New Opportunities for
Improvement: None
Identified.
Progress on Previous Opportunities for
Improvement: I completed all of my projects in
practice management/ policy by the end of the
calendar year but not before the rotation ended.
My project is coming along as expected. I
received positive feedback from the research
committee and incorporated all of their
suggestions prior to submitting my IRB proposal.
Strengths: I am excited that the project I
completed as a student was accepted for
publication.
I was able to complete a MUE and drug
monograph this quarter.
Research project is going well.
New Opportunities for Improvement: None
identified
Progress on Previous
Opportunities for Improvement:
My project is where it should be at
this point in the year. I was able to
present my MUE and monograph at
the January P&T meeting and
received positive feedback.
Strengths: I feel like I am handling
the research project responsibilities
better than expected. My
preceptors are giving lots of praise
for my ownership.
New Opportunities for
Improvement: None identified.
R3
From Initial Self-Evaluation:
Strengths:
• Able to express opinion
and concerns in a polite
and respectful manner.
• Hold myself to a high
standard
• Experience working with a
variety of teams as head
intern, organizational
officer, and tutor.
Opportunities for
Improvement:
• Have a limited
understanding and
Progress on Previous
Opportunities for
Improvement: I am
continuing to work on my
self-evaluation skills and
recognizing what I am
doing well, not just what I
need to change/ improve.
Strengths: No change
New Opportunities for
Improvement: I am
working on my time
management and turning
things in on time. When
preparing my CE
Progress on Previous Opportunities for
Improvement: My assessment mostly aligns with
my preceptors’ assessments.
My biggest issue now is managing my time so
that I get everything done while also ensuring
rest and having non-work time. I feel that I am
failing in this area.
Strengths: Self-evaluations that align with
preceptor evaluations.
New Opportunities for Improvement: Managing
deadlines while ensuring adequate rest.
Progress on Previous
Opportunities for Improvement: I
made a lot of progress this quarter
in improving how I prioritize all of
my responsibilities. Once I reduced
obsessing about perfection,
identified when my work was ready
for preceptor review, and learned
to focus on small wins, I have
improved navigating my
responsibilities.
Strengths: No change
New Opportunities for
Improvement: None identified
experience in hospital
pharmacy management.
• Sometimes focus on “all
that I did wrong” after
receiving constructive
feedback.
presentation, I was
working past midnight to
submit the outline,
objectives, and final slides
to my preceptor.
R4
From Initial Self-Evaluation:
Strengths:
• Trained new interns
• Oversaw the scheduling of
all interns.
• Spent 2 days with IPPE
students on each of my last
2 rotations.
• Was a tutor in 2
nd
-4
th
years
of pharmacy school and
believe I am able to explain
concepts to others in
relatable terms.
Opportunities for
Improvement:
• No experience with formal
presentations to larger
audiences.
• Can fill silence with “over-
explanation”.
• Have not yet developed a
continuing education-
accredited presentation.
Progress on Previous
Opportunities for
Improvement: My Q1
rotation presentations
have gone well. All have
been in person and for
small groups (less than 15
people). I’ve received
feedback that I tend to
ramble when explaining
complicated concepts –
still a work in progress.
Strengths: No change
New Opportunities for
Improvement: None
identified
Progress on Previous Opportunities for
Improvement: The help and feedback of my
preceptor on my CE helped me work through
some of the bumpy parts. I will use what I
learned and the feedback I received when I start
preparing for my presentation at the regional
residency conference.
Strengths:
I am very happy that my CE is over and it went
well.
New Opportunities for Improvement: I think I
should also practice for my informal
presentations now that I see how much it helped
me.
Progress on Previous
Opportunities for Improvement: I
applied the tactics I used when
practicing for my CE presentation
and by I’ve been able to identify the
“rocky” places in the presentation
where I used to over-explain or
ramble. This has helped so much
and I feel much more confident in
my presentation skills
Strengths: No change
New Opportunities for
Improvement: None identified.
RPD: Assessment of Strengths and Opportunities for Improvement Related to the Program’s Competency Areas
Date 7/15/2023 10/30/2023 1/15/2024 4/1/2024
Strengths: In addition to strengths
noted on Judy’s self-assessment, also
feel the following are strengths: R1:
Judy’s inpatient APPE rotations were
completed in a teaching hospital with a
similar pharmacy practice model.
Her orientation preceptor and trainers
have shared that she has already
formed effective and positive
relationships with her trainers and all
staff, regardless of role.
Opportunities for Improvement:
R1: Medication dispensing in the
inpatient setting and sterile product
compounding due to Judy’s limited
inpatient pharmacy experience.
Also, familiarity with inpatient
regulations/ accreditation (Joint
Commission, Board of Pharmacy)
R2: Judy has limited experience with
preparing drug monographs and
completing MUE’s.
R3: So far, items that Judy has turned in
have been accurate and of a high
quality but too close to the due
date/time (11:59 PM on the day of the
deadline).
R4: During her interview last winter and
with some of the orientation sessions, it
was identified that Judy filled what
could be acceptable silence/pauses with
repeat information. Also, her pre-
residency presentations have been
limited to the following: 5 in-person and
12 virtual.
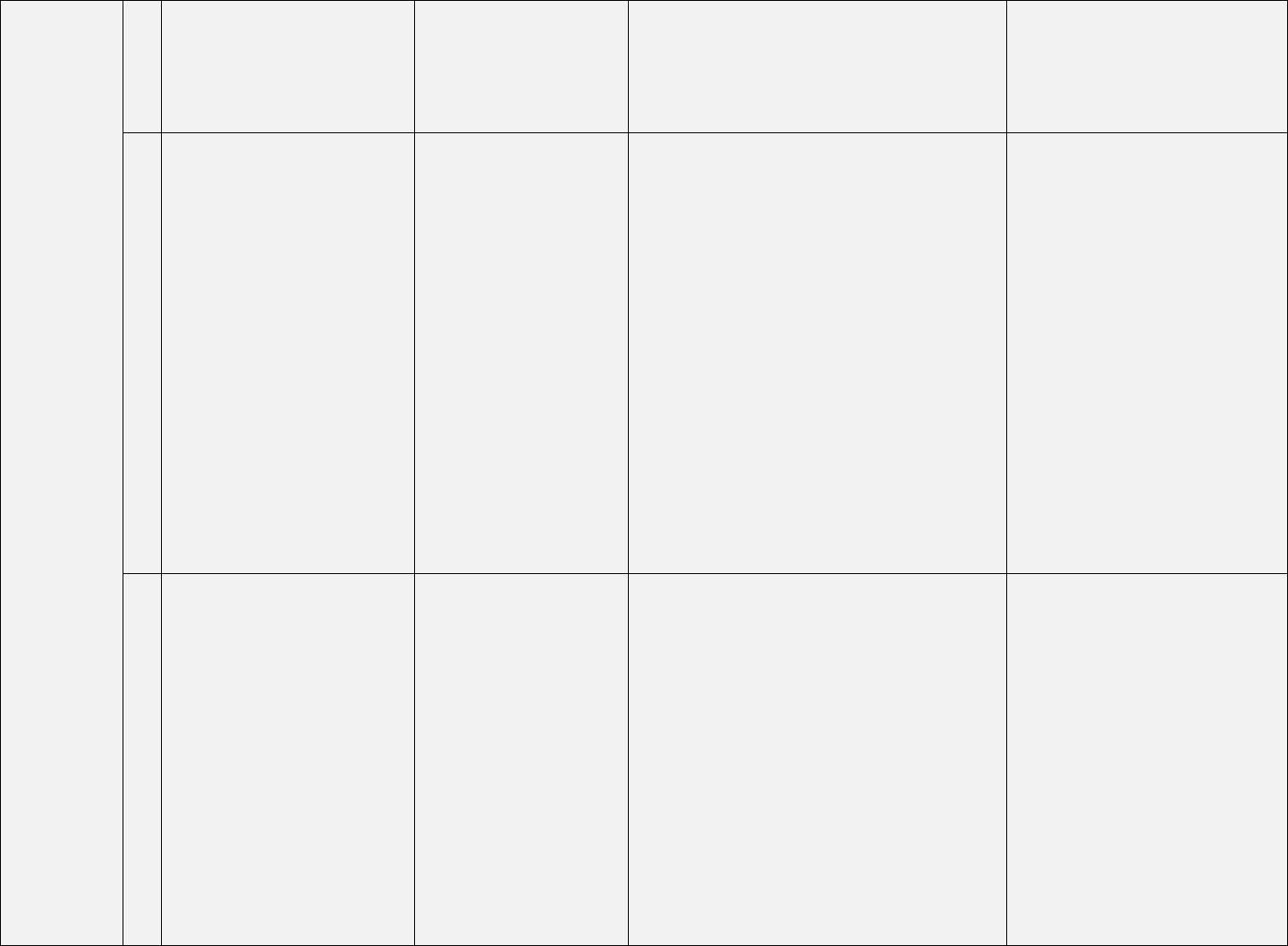
Progress on Previous Opportunities for
Improvement:
R1: Judy’s is doing well with her staffing
duties
R2: Judy has selected her research
project. Also, she will start the practice
management/ policy rotation in
October.
R3: R3.1.2 Judy’s self-evaluation skills
could be further improved. Although
Judy is able to verbalize 3 things that
went well each week (with coaching),
her focus continues to be on what she
needs to improve.
R3.2.4: For her CE requirements, she
worked long hours and into the next
day. I am concerned that as her project
and teaching certificate requirements
progress, Judy is at risk of missing
preceptor deadlines.
R4: Judy has completed several
presentations that have allowed Judy’s
preceptors to assess her presentation
skills and identify ways to help her. She
can get bogged down when explaining
the more complicated concepts and
instead of pausing/ breathing, has
become flustered, and caused confusion
of some audience members.
Strengths:
R1: Agree with Judy’s self-assessment.
Judy also has demonstrated good skills
with collection and assessment of
pertinent patient data and development
of an initial plan for patients.
R2: Judy developed a well-written
project proposal with minimal help.
R3: Judy has represented her class well
on the RPD committee. She integrates
well into any team and shows respect
for all team members.
Progress on Previous Opportunities for
Improvement:
R1: Judy has been a tremendous asset when
staffing in sterile processing. Judy has achieved
R1.3.1, R1.3.2 this quarter. Judy’s progress on
speaking up/ making recommendations on
rounds didn’t progress as expected. There were
times when she confused patient details,
became nervous, which caused her to stop
making any further recommendations.
R2: Judy’s monograph and MUE assignments
were completed in Q2 and were well-done and
required minimal preceptor input. These
objectives have been marked as ACHR. Judy’s
residency project is also progressing well. She
will begin data collection as soon as her project is
approved by IRB.
R3: R3.1.2 In most instances, Judy’s assessment
and that of her preceptors’ are aligned and Judy
is focusing on her ‘wins’. As she’s noted in her
self-reflection, time management and
prioritization are the biggest opportunities for
improvement. Judy has been compromising her
well-being to complete her work.
R4: R4.1: The effort and commitment that Judy
and her preceptors put into practice and
incorporation of feedback resulted in a
successful CE seminar and achievement of all
R4.1 objectives
Strengths:
R1: Preceptors noted Judy’s new strengths this
quarter include developing alternate treatment
plans and commitment to patient care.
R2: Judy’s research project is progressing well.
Her IRB submission was timely and with the
feedback she incorporated from her project
preceptors, has a well-designed project.
R3: Judy has excelled in representing her fellow
residents on the RPD Committee.
Progress on Previous
Opportunities for Improvement:
R1: Judy has made significant
strides since last quarter with R1.1
and is expected to fully achieve the
remaining objectives (R1.1.5-
R1.1.6) with additional exposure
and emphasis.
R2: No areas of opportunity. R2.1
objectives and most R2.2 objectives
already ACHR.
R3: The multiple adjustments made
to Judy’s plan in Q3 (routine
meetings with RPD, preceptors,
emphasis on tasks and time,
elimination of “extra projects”, and
workday/screen stop times) have
contributed positively to her
performance. Judy is meeting all
deadlines, holding herself
accountable to internal deadlines,
and effectively sharing status
updates with her RPD and
preceptors. She has made great
progress.
R4: Judy continues to improve on
her presentations.
Strengths:
R1: Agree with Judy’s self-
reflection. Judy Achieved R1.1.1-
R1.1.4 this quarter.
Judy does an excellent job
organizing her patients, the
medications, and goals
R2: Agree with Judy’s comments.
Judy is excelling in her research
longitudinal responsibilities.
This quarter her data analysis was
completed correctly and she
showed good understanding of her
data.
R4: Preceptors commented that Judy
works well with learners
New Opportunities for Improvement:
R1:Implementation of treatment plan
recommendations by sharing
recommendations on rounds and
development of alternate plans
R3: Time management
R4: Presentation skills (especially in
explaining more complicated concepts)
R4: Judy’s CE presentation was designed well
and her delivery of the presentation was
excellent. R4.1.1-4.1.4 are now ACHR.
New Opportunities for improvement:
R1: Efficiency in preparing for patient care,
organization of patient details, and making
recommendations on rounds.
R3: Time management, multi-tasking, and
prioritization.
R3: Judy continues to excel when
working with different teams and
committees.
New Opportunities for
Improvement:
R1: Identifying the most
appropriate time to share her
recommendations with the medical
team (mostly on rounds) and
ensuring the health care team
implements her recommendations.
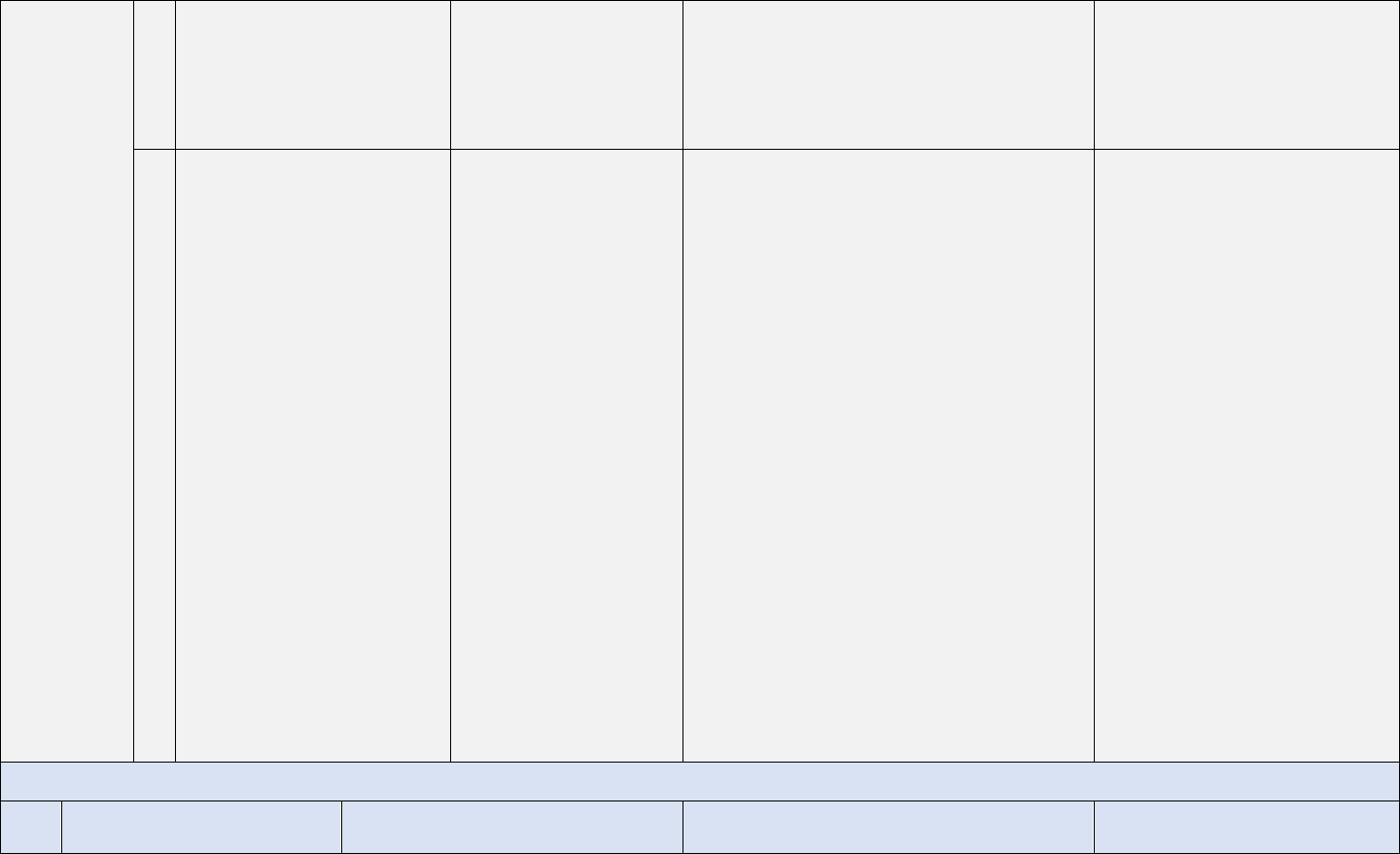
RPD: Planned Initial and Quarterly Changes to the Program*
Initial Quarter 1 Quarter 2 Quarter 2
Changes Related to CAGOS:
R1: Will assign Judy’s inpatient and IV
room orientation days with our lead
technicians in each area instead of any
staff member due to her lack of
experience with inpatient pharmacy.
Her comfort in these areas will be
assessed at the midpoint of her training
to determine if additional days are
needed.
R2: Judy will complete her practice
management/ medication policy
rotation in October to provide early
experience with both a monograph and
MUE
R3: Will appoint Judy as the RPD
Committee’s resident representative. In
this role, she will be the representative
for the entire residency class.
Judy’s 1
st
quarter preceptors will ask her
to identify 3 examples weekly of “what
went well” to help her focus on the
positives as well as areas of growth.
Changes Related to CAGOS:
R1: We will schedule an IV room
refresher for Judy prior to her transition
to IV room staffing in November. Prior
to this day, she is expected to review
the Sterile Products SOP again.
R3: Preceptors have been instructed to
“send back for edit” any evaluations
where that don’t include an example in
each of the following categories:
something to keep doing, to stop doing,
and to start doing.
Judy and her preceptors will be
establishing cut-off times after which
she should not be working unless
patient care emergencies arise.
R4: Judy’s CE presentation is in
October. Two weeks prior to scheduled
presentation, Judy will present her CE
presentation to her preceptor and me
(RPD) to help identify if additional
practices and adjustments are
necessary.
Changes Related to CAGOS:
R1: Preceptors will role model in week 1 how
they work up their patients and keep their
patient data organized to show Judy alternative
approaches to collecting and organizing patient
data. During week 2, preceptors will observe
Judy’s approach, recommend any needed
adjustments in writing to Judy, and will share this
communication with me (RPD).
To help Judy improve efficiency and
organization, Judy is to stop working up her
patients in the evening and also focus her pre-
rounding work on identifying information
pertinent to optimizing medication therapy
instead of trying to capture all patient
information.
At the start of the rotation, preceptors will
outline expectations for Judy speaking up on
rounds and sharing her recommendations. They
will also provide ongoing feedback.
R3: To address the time management, multi-
tasking, and prioritization opportunities:
Changes Related to CAGOS:
R1: In the last quarter, Judy will
bring up 100% of her
recommendations to the patient
care team on rounds every day.
R1.1.6 She will also continue to fine
tune her afternoon tasks and
responsibilities to ensure that all
time-sensitive pertinent
recommendations are
implemented.
R3: In the final quarter, Judy should
continue to implement the time
management and task prioritization
strategies that she’s optimized this
year.
The frequency of the regular
meetings between Judy and her
RPD and preceptors will be
extended from every other week to
monthly.
Changes Related to Resident’s Self
Reflection:
R4: Judy will be assigned at least one
presentation per rotation in Q1 to
increase her comfort with presentations
of varying audience sizes. Her CE
presentation will be scheduled for
October to provide early experience in
creating objectives and implementing
effective audience assessment
strategies.
Changes Related to Resident’s Self
Reflection:
The baseline program will effectively
prepare Judy for her short-term goals
(board certification and PGY2 program).
Judy will be applying to the XSHP Board
as a resident representative. This
application is due September 1 and
requires submission of her CV, letter of
intent, and a letter from me (RPD)
providing support.
Changes Related to Resident’s Self
Reflection:
No changes planned. Judy was named
the XSHP Board of Directors resident
representative.
• No “extra” projects are to be assigned by
preceptors.
• Judy, her preceptors, and I (RPD) will meet
at least every other week to review
progress.
• Judy will document and discuss a progress
report for each meeting that includes a
projected end date for each of her
longitudinal requirements as well as the
time she budgeted and the actual time
amount of time she spent on each of her
requirements.
• Judy will start implementing a stop time for
her workday.
Changes Related to Resident’s Self Reflection:
As Judy is no longer pursuing a PGY2 residency,
her learning experiences will be changed from
inpatient neurology and pulmonary clinic to
adult internal medicine and the family medicine
clinic to provide more exposure to the daily work
of clinical generalists.
Judy’s self-reflection shows some evidence of
burnout and self-doubt. Will encourage Judy to
take at least 2 days of PTO around a weekend so
she can completely unplug from work activities
and spend a long weekend with her family. Judy
is encouraged to schedule at least one
appointment with Employee Assistance.
Judy and her program director will meet weekly
to discuss her on-going well-being and make in
the moment interventions.
No further changes based on
practice interests or career goals.
Regarding well-being, Judy’s weekly
RPD formal meetings will convert to
drop-ins at least every other week.
*Changes are based on assessment of the resident’s strengths and opportunities for improvement related to the program’s Competency Areas as well as the resident’s self-
reflection of personal strengths and opportunities for improvement, practice interests, career goals, and well-being and resilience.
Completion Requirements
Tracker
Note: Completion Requirements
MUST include:
• Required deliverables for each
program type’s Competency
Areas, Goals, and Objectives
(CAGO’s)
• The threshold / percentage of
objectives that must be Achieved
for Residency (ACHR) by the end
of the program
• Appendix Requirements (if the
CAGO’s for the residency type
(e.g., PGY2) include an Appendix)
Completion Requirements MAY also
include other requirements as defined
by the program
(Standard 2.5)
End of Quarter 1
End of Quarter 2
End of Quarter 3
End of Residency - Final
Verification of Completion
Requirements
(Programs using a separate
document for the final “completion
checklist” will not need to use this
column.)
ACHR of 90% of required objectives.
2/33 (6%) objectives
marked as ACHR
14/33 (42%) objectives
marked as ACHR
22/33 (66%) objectives marked
as ACHR
30/33 (90%) objectives marked as
ACHR
No needs improvements on final
ratings.
No final rating of NI for any objective
not marked as ACHR by end of year.
None
1.1.3 was marked as NI on
Oncology (is already
assigned to 4 other learning
experiences)
1.1.3 rating was SP on Adult
Internal Medicine evaluation.
No other ratings of NI.
Completed – no final ratings of NI
for objectives not ACHR.
Completed drug class review or
monograph. (R2.1.1)
NA
Monograph completed –
11/30/2023
Monograph presented at
January P&T Committee
meeting
Completed Quarter 3
Completed medication-use
evaluation and presentation at P&T
Committee. (R2.1.2)
NA
MUE completed –
12/16/2023
MUE presented at January P&T
Committee meeting
Completed Quarter 3
Final write-up of major practice-
related project. (R2.2.5)
NA
NA NA
Completed and submitted final
write-up for major project in a
format suitable for publication to
RPD – 6/10/2024
Presentation of major practice-
related project at regional residency
conference. (R2.2.5)
NA NA NA
Delivered platform presentation of
major practice-related project at
regional residency conference –
4/23/2024
Three journal club (JC) presentations.
(R4.1.2)
NA
Completed JC #1 on DOACs
– 8/17/2023
Completed JC#2 on
antifungal prophylaxis.
10/17/2023
Completed JC #3 on Insulin in
ICU Setting - 3/5/2024
Completed JC #4 on Emerging
Infectious Diseases - 5/7/2024 (This
was in addition to required journal
club presentations – met
requirements in quarter 3)
Grand Rounds CE presentation to
pharmacy department staff (i.e.,
pharmacists/technicians).
(R4.1.2, R4.1.4)
• Include audience assessment
questions in residency portfolio
NA
Delivered Grand Rounds CE
to pharmacy staff –
11/3/2023
* Audience assessment
questions maintained in
residency portfolio
NA
Completed in 2
nd
quarter
In-services to members of the
healthcare team (at least FOUR (4)
total by the conclusion of the
program). (R4.1.2)
In-service to medical
residents on Vanc and
AMG dosing – 9/12/2023
In-service to Med/Surg
nurses on safe and proper
wasting of narcotics -
12/13/2023
In-service to newly hired
pharmacy technicians on safe
medication preparation –
1/24/2024
In-service to newly hired
pharmacists on attendance at
codes – 6/5/2024
Completed 6/5/2024
Submit ONE article for Quarterly
Departmental Newsletter (for
pharmacy staff) (R4.1.3)
NA
Completed newsletter
article on recent COVID-19
treatments – 10/18/2023
Completed 2
nd
quarter
Completed 2nd quarter
Additional Program Completion Requirements Not Required by the Standard
Teaching Certificate in conjunction
with local School of Pharmacy
NA
NA
NA
Received Certificate of Completion
for Teaching Certificate with local
School of Pharmacy – 6/21/2024
Completion and submission of FINAL
resident notebook/portfolio
Residency portfolio up-
to-date – 9/29/2023
Residency portfolio does
NOT include samples of de-
identified patient care
notes – 12/18/2023
Residency portfolio up-to-date
– 3/29/2024
FINAL residency portfolio
COMPLETE and submitted –
6/27/2024
Resident Exit Interview
NA
NA
NA
Completed Resident Exit Interview
– 6/27/2024

Office key, pager, laptop, and badge
return
NA
NA
NA
Office key, pager, laptop, and
badge ALL turned in – 6/27/2024
___________________________________ ______________________________
RPD signature Date
___________________________________ ______________________________
Resident signature Date
