Walden University
ScholarWorks
Walden Dissertations and Doctoral Studies
Walden Dissertations and Doctoral Studies
Collection
2019
Accounts Receivable Management Strategies to
Ensure Timely Payments in Rural Clinics
Anthony N. Medel
Walden University
Follow this and additional works at: h)ps://scholarworks.waldenu.edu/dissertations
Part of the Finance Commons
(is Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies Collection at ScholarWorks. It has been
accepted for inclusion in Walden Dissertations and Doctoral Studies by an authorized administrator of ScholarWorks. For more information, please
contact ScholarW[email protected].

Walden University
College of Management and Technology
This is to certify that the doctoral study by
Anthony Natividad Medel
has been found to be complete and satisfactory in all respects,
and that any and all revisions required by
the review committee have been made.
Review Committee
Dr. Roger Mayer, Committee Chairperson, Doctor of Business Administration Faculty
Dr. Warren Lesser, Committee Member, Doctor of Business Administration Faculty
Dr. Judith Blando, University Reviewer, Doctor of Business Administration Faculty
Chief Academic Officer
Eric Riedel, Ph.D.
Walden University
2019
Abstract
Accounts Receivable Management Strategies to Ensure Timely Payments in Rural
Clinics
by
Anthony Natividad Medel
MBA, University of Phoenix, 2005
BSHS, University of Phoenix, 2003
Doctoral Study Submitted in Partial Fulfillment
of the Requirements for the Degree of
Doctor of Business Administration
Walden University
April 2019
Abstract
Healthcare business leaders in a rural clinic setting can enhance profitability by
implementing strategies to ensure timely payments. The purpose of this multiple case
study was to examine strategies applied by healthcare leaders in rural clinics to improve
profitability. The population included 10 rural clinic managers and billing staff from 5
rural clinics in the southwestern region of the United States. The conceptual framework
for this study was Wernerfelt’s resource-based value theory. Implementing Yin’s
multiple-step data analysis process, data from semistructured interviews were transcribed,
coded, and analyzed to identify strategies used by rural clinic managers and billing staff
to enhance profitability. Four primary themes emerged regarding revenue cycle
management that could increase profitability, including developing effective
communication between medical providers and billing staff, implementing payment plan
strategies, ensuring accuracy of billing claims, and consistently reviewing open
receivable accounts. The implications of this study for positive social change include
insights for clinic managers in the development of strategies to increase cash from
accounts receivables, which may contribute to the financial stability of the clinic and
improve the provision of healthcare for citizens of the southwestern region of the United
States.

Accounts Receivable Management Strategies to Ensure Timely Payments in Rural
Clinics
by
Anthony Natividad Medel
MBA, University of Phoenix, 2005
BSHS, University of Phoenix, 2003
Doctoral Study Submitted in Partial Fulfillment
of the Requirements for the Degree of
Doctor of Business Administration
Walden University
April 2019
Dedication
I dedicate my study to my wife, Karen. You have been with me through every
step of this process, and I could never thank you enough for standing by side in this
process. I love you very much, and I look forward to sharing the rest of my life with you.
To my children, Cheryl, Andrew, Kaitlan, and Alexander, for all of the times that I
missed your activities. To my brothers and sister Steve, Manuel, Rene, and Christina, as
the family is everything. Also, I dedicate this doctoral study to the memory of my parents
Manuel Young and Clementina Natividad Medel for instilling in me a strong work ethic
and a faith in God that can never be broken.
Acknowledgments
First, I thank God the Father Almighty for his guidance, and granting me the
strength, patience, and perseverance to complete this educational journey. With God, all
things are possible and I would not have made it without the strength and faith that His
presence in my life.
I thank my family, friends, and coworkers for their support, encouragement, and
listening to me throughout this process and providing uplifting words during the most
difficult times in this process. Thank you to my maternal Aunts and Uncles as we have
had some pass away during this time, but I have kept them all in my heart and blessed
that they were a part of my life. Thank you to Dr. David E. Bealer (1955-2016), for a
meeting we had back in 2016 and providing words of wisdom, encouragement, and
support, your memory will not be forgotten.
Finally, I thank my Chair, Dr. Roger Mayer. You have worked with and assisted
many doctoral graduates by providing your time, encouragement, and most of all support.
Thank you for everything that you have done to help students reach their educational
goals, and you came into my life at a time when I needed direction and you far exceeded
this task. Also, thank you to my committee members Dr. Warren Lesser, Dr. Robert
Hockin (1950-2019), Dr. Jill Murray, and Dr. Judith Blando for your feedback and
dedication to help students place an emphasis on the quality of work produced. This has
been an unforgettable journey, and I will be eternally grateful for all those who have been
there for me along the way.
i
Table of Contents
Section 1: Foundation of the Study ......................................................................................1
Background of the Problem ...........................................................................................1
Problem Statement .........................................................................................................2
Purpose Statement ..........................................................................................................2
Nature of the Study ........................................................................................................3
Research Question .........................................................................................................4
Interview Questions .......................................................................................................4
Conceptual Framework ..................................................................................................5
Operational Definitions ..................................................................................................6
Assumptions, Limitations, and Delimitations ................................................................7
Assumptions ............................................................................................................ 7
Limitations .............................................................................................................. 8
Delimitations ........................................................................................................... 8
Significance of the Study ...............................................................................................8
Contribution to Business Practice ........................................................................... 9
Implications for Social Change ............................................................................... 9
A Review of the Professional and Academic Literature ..............................................10
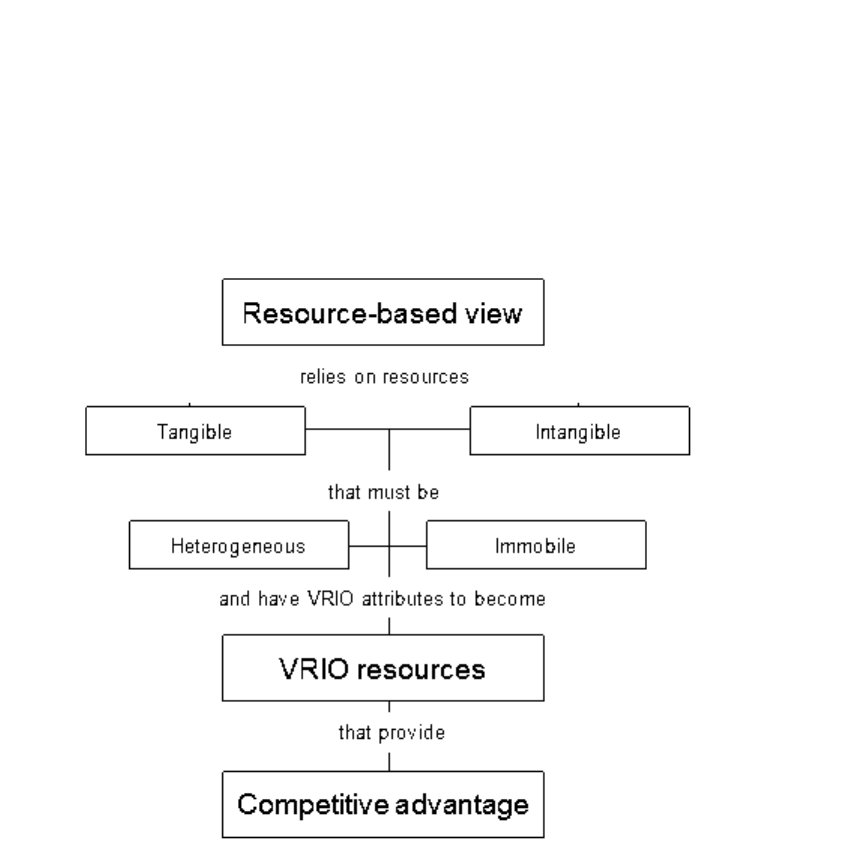
Resource-Based Value Theory ............................................................................. 12
Alternative Theories.............................................................................................. 19
Historical Involvement by Government in the Health Care System..................... 22
Health Care Financial Options and Medical Care ................................................ 26
ii
Fee-For-Service (FFS) vs. Value-Based Purchasing (VBP) ................................. 31
Accounts Receivable Management and Health Care ............................................ 38
Transition .....................................................................................................................41
Section 2: The Project ........................................................................................................42
Purpose Statement ........................................................................................................42
Role of the Researcher .................................................................................................42
Participants ...................................................................................................................45
Research Method and Design ......................................................................................47
Research Method .................................................................................................. 47
Research Design.................................................................................................... 48
Population and Sampling .............................................................................................50
Ethical Research...........................................................................................................52
Data Collection Instruments ........................................................................................54
Data Collection Technique ..........................................................................................57
Data Organization Technique ......................................................................................59
Data Analysis ...............................................................................................................61
Reliability and Validity ................................................................................................63
Reliability .............................................................................................................. 64
Validity ................................................................................................................. 65
Transition and Summary ..............................................................................................67
Section 3: Application to Professional Practice and Implications for Change ..................68
Introduction ..................................................................................................................68
iii
Presentation of the Findings.........................................................................................68
Theme 1: Communication Between Medical Providers and Billing Staff ........... 70
Theme 2: Payment Plan Setup .............................................................................. 73
Theme 3: Accuracy of Billing Claims .................................................................. 77
Theme 4: Consistent Accounts Receivable Reviews ............................................ 79
Overall Findings Applied to the Conceptual Framework ..................................... 83
Applications to Professional Practice ..........................................................................84
Implications for Social Change ....................................................................................85
Recommendations for Action ......................................................................................86
Recommendations for Further Research ......................................................................87
Reflections ...................................................................................................................88
Conclusion ...................................................................................................................88
References ..........................................................................................................................90
Appendix A: Interview Protocol ......................................................................................136
Appendix B: Interview Questions ....................................................................................137
iv
List of Figures
Figure 1. The resource-based view ....................................................................................16
1
Section 1: Foundation of the Study
Effective revenue cycle management in rural clinics is essential to their economic
sustainability (Lubberink, Blok, van Ophem, & Omta, 2017). In the initial phase of a
revenue cycle strategy, a healthcare organization summarizes potential revenue outlets
based on the volume of patients and mix of insurance payers (Johnson & Garvin, 2017).
Revenue, in the form of accounts receivable collection processes, of healthcare
organizations are unlike most with other industries (Mindel & Mathiassen, 2015).
Healthcare providers must deal with multiple payers and unique rules such as bundled
payments, case-based payments, copayers, and contractual allowances (Hernandez,
2017). Healthcare managers must deal with payment delays, challenges by payers for
services provided and unreimbursed services (Cascardo, 2015). Thus, healthcare clinic
managers must develop strategies to address these revenue cycle challenges in order to
obtain timely payments from patients and their insurance payers.
Background of the Problem
Developing an effective means to collect payment for health services rendered
during a routine visit is a challenging task in the health care industry. Rural clinics that
serve a high number of indigent patients would close without adequate reimbursement.
The goal of the Medicaid program enacted in 1965 was to provide medical services to
lower income individuals and families (Leemon, 2014). The passage of the Affordable
Care Act (ACA) in 2010 became another form of health coverage introduced to the
public. It provides health insurance to the uninsured, which constitutes approximately
27.3 million individuals or 8.6% of the population (United States Census Bureau, 2016).
2
Other forms of coverage or payment can include private pay insurance plans, direct
payment, and a sliding fee scale based on one’s ability to pay (Barbaresco,
Courtemanche, & Qi, 2015). Clinic managers and financial support staff will benefit from
successful strategies to obtain timely payment for medical services from patients, which
relate to strategies for collecting accounts receivables.
Problem Statement
Rural clinic managers struggle to generate cash flow from unpaid patient accounts
(Lail, Laird, McCall, Naretto, & York, 2016). Healthcare organizations spend roughly
$26 billion on revenue cycle management addressing reimbursement and collection
processes (Hayes, Subhan, & Lakatos, 2015). The general business problem was that
healthcare leaders do not develop effective revenue cycle strategies and cash flow
shortfalls may threaten the survival of the organization. The specific business problem
was that some rural clinic managers lack strategies to obtain timely payments from
patients and insurance payers.
Purpose Statement
The purpose of this qualitative multiple case study was to explore strategies rural
clinic managers use to obtain timely payment from patients and insurance payers. Study
subjects included clinic managers from five rural clinics in southwestern region of the
United States who have incorporated strategies to obtain timely payment from patients
and insurance payers. The implication for positive social change could come from
insights for clinic managers when they develop strategies to increase cash from accounts
3
receivables, which may improve the financial stability of the clinic and increase the
wellbeing of individuals in southwestern region of the United States.
Nature of the Study
The three research methods are qualitative, quantitative, and mixed methods
(Denzin & Lincoln, 2011). Qualitative researchers gather in-depth data, discover the
meaning of the unknown, and reconstruct stories of participants on a conceptual level
(Guba & Lincoln, 1994). I have selected the qualitative methodology to recognize
multifaceted comprehensive medical services performed in rural clinics. A quantitative
researcher focuses on empirical evidence by using statistical processes (Petrescu &
Lauer, 2017). A quantitative methodology was not an appropriate method, because I was
not examining numeric data with statistical processes. The mixed methods methodology
incorporates both quantitative and qualitative components (Polit & Beck, 2010). This was
not a suitable choice, as I do not intend to incorporate statistical methods to explore my
research question.
I considered four qualitative research designs, including (a) phenomenology, (b)
ethnography, (c) narrative design, and (d) case study. Phenomenology researchers
emphasize the meaning of participants’ lived experiences (Moustakas, 1994). The
phenomenology design was not appropriate for this study because my goal was not to
explain the meaning of the participants’ lived experiences. Ethnography researchers
emphasize the meaning of the participants’ expression of culture (Symons & Maggio,
2014). I do not propose to explore a participant’s individual customs or culture and an
ethnography design was not appropriate for this study. A narrative design provides the
4
researcher the opportunity to focus on the lives of individuals as told through their own
stories (Denzin & Lincoln, 2011). I did not intend to focus on the lives of the participants
through their own stories and rejected a narrative design for this study. I used a case
study design to explore the research question as the case study approach allows the
researcher to view the issue in a natural setting.
Research Question
What strategies do rural clinic managers use to obtain timely payments from
patients and insurance payers?
Interview Questions
1. What strategies do you use to obtain timely payments from your patients and
insurance payers?
2. What strategies do you use to collect from uninsured and underinsured
patients?
3. What strategies do you use to manage doubtful accounts and bad debt?
4. What strategies does your organization use to ensure staff complete billing
forms correctly with no errors that delay payments?
5. What techniques does your office staff use to collect copayment either before
or after the patient visit?
6. How does the organization provide training to the billing staff to ensure they
are able to meet the organization’s standard for timely collections?
7. How does the organization ensure that the billing staff has the current training
or professional development regarding health information technology?
5
8. What billing techniques does the organization use that would be a
competitive advantage over other similar organizations?
9. What are the necessary attributes and abilities of a biller to ensure continued
profitability and sustainability for the organization?
10. What additional information can you make available that accounts receivable
strategies ensure timely payment from patients and insurance payers?
Conceptual Framework
The resource-based value theory (RBV) served as the foundation for this
qualitative multiple case study. Wernerfelt (1984) provided an approach in finding a
balance between manipulation of existing resources and the expansion of resources to an
organization’s firm strategic management design to yield increased profits. The RBV
indicates a correlation between profitability and resources as well as managing
organizations’ resources for the long term (Wernerfelt, 1984). RBV theorists and
strategists are contributors in the RBV development.
The healthcare industry exemplifies the RBV within the internal organizational
resources to include attributes, abilities, organizational procedures, and expertise
formulated at the administrative level of an organization (Patidar, Gupta, Azbik, &
Weech-Maldonado, 2016). RBV theorists Warnerfelt (1984) and Barney (1991),
proposed to improve an organization’s efficiency and effectiveness with an increase in
profitability and sustainability. The prevalence of internal resources to maintain a
competitive advantage over rival competitors can be found using RBV. A turbulent
period for the healthcare industry is transpiring due to competition, an adjustment in
6
reimbursement for services rendered, and struggles in keeping current with health
information technology and electronic medical records (Angeli & Norwood, 2017). The
RBV combines superior resources and competencies to achieve increased financial
earnings. The RBV perspective emphasizes the development of dynamic capabilities and
useful resources as possible foundations for a definite competitive advantage (Kash,
Spaulding, Gamm, & Johnson, 2014).
Operational Definitions
Arizona Health Care Cost Containment System (AHCCCS): A version of the
Medicaid system in the state of Arizona that provides medical benefits to those with
lower to moderate incomes (Langellier, de Zapien, Rosales, Ingram, & Carvajal, 2014).
Contractual adjustments: The difference between healthcare organizations’ fully
charged amounts for services and payments received (Chen et al., 2015).
Contractual allowances: The financial difference between what the healthcare
organization bills and the agreement entered into financial conditions with a third party
payer (Rosolio, 2016).
Customary allowable rate: The rate of reimbursement intended to mirror the
value of the services provided by the provider (Panning, 2014).
Government-funded health plans: A provision as part of social wellbeing to
provide healthcare services to lower income individuals (i.e., disabled, children, and the
elderly; Bradbury, 2015).
7
Multifaceted health care organization: Healthcare organization with many
different elements or combinations of services or roles provided to customers/patients
(Prowle & Harradine, 2014).
Reimbursement rate (normal/customary): The fee or charge associated based on
the volume of services provided to a customer or patient during an encounter with a
medical provider (Jones & Ku, 2015).
Timely payments: A reimbursement for services rendered by the health care
provider within a payment timeframe defined by the payor (Fitzpatrick, Butler,
Pitsikoulis, Smith, & Walden, 2014).
Assumptions, Limitations, and Delimitations
Assumptions, limitations, and delimitations can limit the methods and
examination of the research within the study. Assumptions and limitations are outside the
scope of the researcher’s control. Delimitations are essential within the context of the
research managed by the researcher. Furthermore, these concepts are integral in outlining
methodology within the context of the research detailed as part of the study.
Assumptions
The rural clinic acknowledged a responsibility to provide the patient with quality
healthcare services regardless of the volume of ailments during an encounter with the
assumption the clinic would be paid. Another assumption was the accounts receivable
management strategies in collecting co-payments or deductibles imposed by
organizational leadership was determinate in the collection of timely payments from the
patient. Second, an essential assumption was specific strategies and methods pertaining to
8
the collection process were abided by according to company financial policy (Grant,
2014). The last assumption was that implemented revenue management strategies
developed by clinic managers would positively affect payments from patients and
insurance payers.
Limitations
Marshall and Rossman (2016) defined limitations as elements of the study outside
the control of the researcher. A significant limitation of this study was that payment
information could not be gathered from patients or insurance providers. One of the
limitations of this study was that participants potentially could withdraw at any time in
the study thereby skewing the data due to the small sample size. The participants’
interview responses are subject to their personal presumptions (Yin, 2017).
Delimitations
Delimitations define the scope of the research study determined by the researcher
(Yazan, 2015). This study included 10 clinic managers from southwestern region of the
United States to include South County and East County. This study included clinic
managers who reside in Arizona and live in southwestern region of the United States and
who confirmed insurance payers for treated patients.
Significance of the Study
Rural clinic managers and individuals residing in southwestern region of the
United States could benefit from the outcomes of this study. The healthcare industry
prevails as a change agent for reducing costs and improving patient outcomes. Reducing
costs, lowering or bundling healthcare services, and establishing strategic processes in
9
obtaining payments from insurance payers may result in a higher volume of patients. An
examination of the accounts receivable management processes may provide awareness to
rural clinic managers regarding attaining payment from patients and insurance payers.
Contribution to Business Practice
Rural clinic managers could benefit from this study by understanding their role as
it relates to reimbursement practices. Healthcare leaders must demonstrate strategic
business practices interpreting the development of volume and scale of insurance payors
in conjunction with the business model (Kemperman et al., 2016). The healthcare
business model requires transparency in the reimbursement process of services rendered.
. Ideally, a healthcare organization must provide patients with a high quality of care at
affordable prices to form an organizational culture of accountability (Mkanta, Katta,
Basireddy, English, & de Grubb, 2016). Rural clinic business leaders may gain awareness
of strategies to increase cash flow, which could increase resources necessary to provide
quality services.
Implications for Social Change
Organizational leadership, hospitals, and physician-based groups considering
collaboration could benefit from the results of this study on rural clinics while
influencing the quality of care. The healthcare business model of requiring payment in
advance of services has demonstrated ineffective in the inability to provide adequate
healthcare to underserved communities (LeFevre, Shillcutt, Broomhead, Labrique, &
Jones, 2017). Patients decide their healthcare needs based on the qualities and expertise
of the medical provider (Reddy & Mythri, 2016). Effective cash collection strategies that
10
allow for payments of co-pays, deductibles and uninsured payments may increase the
likelihood of health care services to residents in underserved communities, which will
impact the patients’ well-being.
A Review of the Professional and Academic Literature
Reviewing prior published research is a strategy researchers use to gain a more in-
depth understanding of a research topic. Lubberink et al. (2017) stated that the literature
review is an essential component of the research because it provides systemic, activities-
based approach to reported context. The purpose of this qualitative multiple case study
coincides with research related to evolving changes in reimbursement. Included in this
section is a review of the academic and professional literature on the RBV theory as used
by other researchers to investigate related research topics. I examined literature from
other scholars who deliberated regarding rural clinic managers’ strategies to obtain timely
payments from patients and insurance payers and my findings aim to help managers
reduce the interruption or delay in receiving payment from patients and insurance payers
for medical services rendered.
The information gathered from this study came from a multitude of sources
including ABI/INFORM Global, ProQuest, SAGE Publications, Google scholar, Wiley
Online, Academic Search Complete, Emerald Insight, MEDLINE, Proquest Central,
Proquest Health and Medical Collection, Proquest Nursing & Allied Health Source, and
EBSCOHost. The keyword search terms for this research included: health care, health
care industry, business model, government involvement, financial options, medical care,
11
Medicaid, ACA, fee-for-service, value-based purchasing, Resource Base Value, and total
quality management. .
The financial health care models in the literature illustrate how healthcare services
can be efficient and which methods are cost-effective. The reimbursement models
indicate the delivery of healthcare services, efficiency of effective billing procedures, and
exhibit cost-effective methods to develop the success of a healthcare operation. I
presented the value-based purchasing model, which was the defining standard for
healthcare operations’ performance. The core business values of this model consist of
cost control, financial stability, and sustainability of healthcare operations. Consistency
of adequate reimbursement of healthcare organizations maintains sustainability. With this
intention, healthcare organizations determine adequate reimbursement fee schedules
concerning payment for the businesses to remain flexible for future success.
The U.S. healthcare sector has changed as health insurance plans provide an array
of healthcare services. The clinic manager is responsible for reimbursement and assessing
strategic business models for obtaining timely payment within the clinic. The continuity
of care diminishes when patients are required to choose their provider solely based on
insurance coverage. The delivery of healthcare is a focal point for patients who can be
loyal to a medical provider or turn to a competitor for the same services based on
insurance (Hegwer, 2014). The value-based purchasing model holds medical providers
accountable for the cost and quality of care. Healthcare organizations using a value-based
purchasing model focused on cost containment accompanied by quality care, presuming
patients will choose quality. The literature review consists of 299 references from peer-
12
reviewed journals, government reports, and books with at least 94% of the sources
published between 2013 and 2018, or within 5 years of my expected graduation.
Resource-Based Value Theory
The RBV is a relevant framework for service-based industries where there is a
requirement of trust. The organization’s ability to gain the patient’s trust will increase its
competitive advantage and improve its financial performance (Lin, Chang, & Dang,
2015). The central tenet of RBV theory is that healthcare leaders should focus on
efficient and strategic uses of resources to remain viable (Ozuru & Igwe, 2016). The
profitability of an organization stems from the implementation of strategies based on
resources identified by organizational leaders (Liu, Zhu, & Seuring, 2017). The RBV
model concentrates on the service-concept methodology and is dependent on the
performance of individuals executing roles within the organization. It becomes necessary
to apply resources to provide medical services that benefit the patient. An organization
must consider the implementation of services and equipment, specialty amenities, and
quality improvement for their patients as assets and strengths.
Only recently have researchers and business leaders applied RBV to the
healthcare field. It is a relevant framework because it claims product-based endeavors are
part of a grand business strategy. RBV indicates resources are scarce and unique in
stature; these strategic resources are necessary to maintain a competitive advantage in a
healthcare market (Gerber & Hess, 2017). The financial and operational well-being of the
organization hinges on internal resources within the business (Neghina, Bloemer, van
Birgelen, & Caniëls, 2017). Managers can use RBV to develop a strategic plan for using

13
internal resources to enhance financial success and sustainability.
Managers in the healthcare industry face difficulties in implementing
RBV strategies when the business is at an early stage of development (Voss, Perks,
Sousa, Witell, & Wünderlich, 2016). Healthcare leaders can base organizational policies
on the RBV theory to specify assets that support the delivery of medical care to patients
(Wilden & Gudergan, 2017). In the healthcare industry, the roles of patients, healthcare
organizations, and medical providers are still evolving. The RBV framework includes a
service delivery model emphasizing employee skills and knowledge expertise which is a
foundational piece of financial success (Ozuru & Igwe, 2016). As healthcare systems
develop towards financial prosperity, the connection with RBV amplifies.
The RBV framework includes strategies to remain competitive. RBV when
applied as a business strategy exposes possible disadvantages involving profitability and
reputation to the organization (Jain & Singal, 2014). The RBV as a strategic business
model proposes using internal resources to outperform competitors. The healthcare
organization used resources to strategically coordinate with the medical practice to secure
a competitive advantage (Abidemi, Halim, & Alshuaibi, 2017), and key resources are
employees, who all need to be included in the strategy (Pinto, 2017). Rural clinics leaders
also consider the revenue cycle process to guarantee payment, a resource that
organizational leaders need to manage. Business leaders manage internal resources in
order to keep revenue consistent with the long-term financial growth of the organization.
In rural clinics, the focal point is services provided to patients (check-up, follow-
up care, or consultation). The healthcare industry is a service-model based exchange, and
14
with the flow of internal resources and potential employees’ capabilities, a creation of
value will develop over time indicating innovation as the focal theme (Schneider &
Sachs, 2017). RBV within a healthcare organization improves patient outcomes through
the use of internal resources within the healthcare organization towards continuity of care
(Szymaniec-Mlicka, 2016) and guides business strategies towards competitiveness in the
marketplace (Li, Jiang, Pei, & Jiang, 2017). The healthcare industry has integrated RBV
into its business models to drive potential success, economic prosperity, and strategic
preparation.
RBV in the management environment. The methodology of RBV strategy in a
management setting focuses on internal business resources. The healthcare industry is
service-based and must ensure approaches are successful and services provided exceed
those of competitors (Jali, Abas, & Ariffin, 2016). The indicators regarding internal
resources needs rethinking with the managerial emphasis placed on varying differences
and unique characteristics of health care services (Neghina et al., 2017). Successes stem
from creating new and innovative ways to deliver services by reducing costs and passing
on the value to the patients.
Rural health clinics need to develop new and innovative ways to build their
patient base and management’s ability to expound, implement, and reintroduce strategic
resources. The healthcare industry must adapt to healthcare reform and seek innovative
processes regarding internal resources to attain a competitive advantage (Lillis,
Szwejczewski, & Goffin, 2015). The control over strategic resources gives businesses a
unique competitive advantage that creates barriers to entry (Ferlie et al., 2015). Managers

15
following RBV concentrate on their most valuable assets to achieve continued
sustainability. The progression of the RBV is achievable, but a path towards
organizational development follows a period of increased growth to meet an
organization’s financial goals (Maurer & Ryan, 2016). The objective of rural clinics is to
enable access to medical providers, establish growth, become more productive, and
maintain a consistent and sustainable profit margin.
RBV within rural clinics emphasizes using internal resources to improve the
quality of care for patients, stressing improvements toward operational goals and
objectives. The operational and performance goals of a healthcare organization include
balancing healthcare services, reducing costs, and improving patient outcomes
(Adebanjo, Laosirihongthong, & Samaranayake, 2016). Thus, essential characteristics
surrounding RBV within the healthcare environment include producing positive results
while managing revenue collections to provide long-term fiscal sustainability. Healthcare
leaders must continue to focus on the improvement of patient care while ensuring the
financial growth of the medical practice.
RBV methods can contribute to a medical practice’s success by building its
strategic resources and hence improving its competitive advantage (Maurer & Ryan,
2016). Corporate social responsibility also builds organizational goodwill by improving
reputation (Sheikh, 2017). Some medical practices focus on collecting payments from
insurance payers without any impediment or delay in payment (Lai & Gelb, 2015).
Increasing the timeliness of payments is a strategy that increases the competitive
advantage of a clinic.
16
An organization’s resources align with RBV based upon the value to the
organization (Lin et al., 2015). The service-based model is grounded on an ecosystem of
multiple variables as internal resources become tangible for the strategic betterment of
the organization (Voss et al., 2016). The service-based model goes through a shift where
the focus is on tangible resources creating capabilities for future strategic planning
(Wilden & Gudergan, 2017).
Figure 1. The resource-based view.
RBV in the healthcare setting. RBV principles emphasize the importance of the
delivery of services and resources for rural clinics to set themselves apart from
competitors. Healthcare organizations allocate resources efficiently to give legitimacy to
management and leadership in the decision-making process of RBV (Angelis, Kanavos,

17
& Montibeller, 2017). Business leaders consider the healthcare organization’s resources
to be valuable assets. The healthcare organization is poised to use all available internal
resources to provide consistency and continuity of care to patients. The internal resources
available to the healthcare organization are well thought-out, have identifiable
characteristics, and designated as VRIO (valuable, rare, inimitable, and organized; Lin et
al., 2015). The VIRO characteristics selected are the foundation for RBV.
The connection between products and services are intertwined and generate
combinations of resources (Benedettini, Neely, & Swink, 2015). The resulting resources
are significant to the rural clinic advantage over competitors, but are not sustainable and
will not benefit the healthcare organization over the course of time (Mweru & dan Muya,
2015). Rural clinic managers use RBV strategies to recognize and implement approaches
to make improvements in efficiency and effectiveness (Teece, 2017). Rural clinics
incorporate resources into their strategic planning for the purposes of financial
achievement (Patidar et al., 2016). Healthcare organizations value internal resources,
which are components of their competitive advantage (Helmig, Hinz, & Ingerfurth,
2014). Their competitive positions regarding administration efficiency influence potential
operational development of competitive strategies (Krzakiewicz & Cyfert, 2017). The
rural clinics’ used for this doctoral study have strategic approaches in line with RBV, as
cost and organizational performance are devices providing the business with
sustainability and competitive advantage for years to come (Abidemi et al., 2017).
Through strategic planning, an organization can establish a competitive
dominance over its rivals (Kash et al., 2014). RBV is becoming a strategic management
18
model trending towards organizational management, and developing applicability of
external resources within the healthcare industry (Hitt, Xu, & Carnes, 2016). The RBV
framework in the healthcare industry is an innovative approach within the confines of the
management structure and all internal resources within the organization has not been
sufficient to establish RBV within healthcare strategic planning. However, healthcare
organizations are willing to be a part of this rapidly growing model. The U.S. healthcare
sector follows and identifies common strategic initiatives put into practice by hospitals,
community health centers, and urgent care facilities. Accordingly, a broader view of
RBV includes internal viable resources, adding to increased capabilities, employees and
staff, and financial assets (Wilden & Gudergan, 2017).
The healthcare industry consists of operational and clinical professionals and their
collaboration within the health care environment is essential. Business leaders consider
VIRO attributes to be valuable, inimitable, rare, and organized difficult to replace that
lead towards a competitive advantage for the health care organization. The health care
organization’s administration explores competitive advantages coming from within the
firm’s specific resources and limitations, depending on the location (Yang, 2014). The
healthcare profession has organizations that can strategically manage resources to
improve their performance (Evans, Brown, & Baker 2015). RBV’s place within rural
clinics in combination with strategic resource planning remains driven by healthcare
professionals whose objective is quality care.
RBV methods put into place the needed resources to provide patients with the
continuum of care and offer a strategy to sustain competitive advantage (Popli, Ladkani,
19
& Gaur, 2017). The strategic business model is a representation of the view of a health
care organization reflecting potential sustainability and viability (Goyal, Sergi, &
Kapoor, 2014). The RBV approach, a health care business implementation, is the
building block of competitiveness not only in the present but in the future and reinforces
sustainable benefits for the long-term (Teece, 2017). Rural clinic managers can use RBV
as a reliable business model to properly use internal resources to facilitate sustainment.
The financial results were referencing accounts receivable segments of the business focus
on the strategies implemented by leaders within the establishment. A rural clinic manager
uses RBV in conjunction with its business model to develop financially and clinically to
build the community’s trust.
Alternative Theories
RBV addresses the roles or control of one’s resources as a primary method to
create a strategic advantage over competitors (Popli et al., 2017). Critics indicate the
RBV approach is limited because it focuses on the user of the resource (Gerber & Hess,
2017). The utilization of internal organizational resources becomes part of the landscape,
and the user of the resource takes on a far lesser role in the overall encounter. The
potential for the business to sustain its resources over an extended period will prolong a
fierce competitive advantage during specific phases of time (Lee, 2017). Resource
dependence theory (RDT) has similarities to RBV with the role of the RDT taking on
external environmental linkages within the organization (Shaukat, Qiu, & Trojanowski,
2016). I used both RDT and TQM as analytical frameworks to explore health care
20
organization management strategies. Wernerfelt (1984) details RBV as a means to use
internal resources and includes components to separate businesses from its competitors.
Resource dependence theory. In 1978, Pfeffer and Salancik addressed resource
dependencies and indicated the effect external resources had on the role of an
organization. Pfeffer and Salancik (2003) detailed that health care organizations are
providers of significant resources, and like other organizations, they need to make
changes to fulfill positive outcomes. RDT indicates organizations require resources from
competing organizations within a similar market to innovate, resulting in distinctive
qualities within competing organizations (Van den Broek, Boselie, & Paauwe, 2017).
Pfeffer and Salancik (2003) stated that organizations have more power drawing from the
interdependence of others and the need for their positions in the marketplace. RDT
describes dependent players in the organization as having a weaker position within the
competitive market to offset structures to collaborate (Christensen, 2016). From the
organizational aspect, minimal information in the form of external constraints affecting
management decisions ought yet to be determined (Pfeffer & Salancik, 2003). RDT has
three specific factors: the significance of the resource to the organization, scarceness of
the resource, and the level of internal organization competition (Selviaridis, Matopoulos,
Thomas-Szamosi, & Psychogios, 2016). Business leaders manage potential constraints
and uncertainties potentially resulting in the acquisition of external resources (Pfeffer &
Salancik, 2003).
The viability of the health care organization is contingent on RDT in which a
strategy may alter a power-dependent relational dynamic (Doyle, Kelly, & O’Donohoe,
21
2016). Management sets the strategy, and these individuals play a crucial role in the
process and scheming of resource dependencies. Any organization can build resources
both internally and externally to assemble competencies to enter and leave the market and
to take a competitive advantage (Pfeffer & Salancik, 2003). RDT researchers focus on the
use and outcomes of resources utilization (Coupet & McWilliams, 2017). An
organization’s management may devise a scheme to ensure resources remain supported
and seek a clear competitive advantage over market rivals (Pfeffer & Salancik, 2003).
Total quality management. In 1985, Deming addressed the Western style of
management called total quality management (TQM), which introduces organizational
attempts to deliver quality products and services. TQM emphasizes planning and
introducing methods to improve an organization’s products and services to decrease costs
(Deming, 1985). The focus of enhancing quality concentrates on the customer (Deming,
2000), which is supervised by management. Health care managers introduced TQM into
the field in the late 1980s, intending to increase patient satisfaction, reduce costs, and
increase productivity at all levels within the organization (Chiarini & Vagnoni, 2017).
Management is fully responsible for creating processes, ensuring stability, and
establishing strategies for the success of the organization (Deming, 2000).
Deming’s approach centered on process improvement (Matthews & Marzec,
2017). Deming (2000) provides a thorough concept showing that any considerable
improvement must come from actions introduced by operations management. TQM
methodology has in the past focused on the supply side of operations, but now has a
presence in an organization’s services sector (Iqbal et al., 2017). The service-based
22
industries such as health care apply various TQM improvement practices by enhancing
services and reducing costs for patients during a routine encounter (Deming, 2000). The
implementation of TQM within a health care organization has led to improved processes
in the quality of patient care, patient satisfaction, and increased financial prosperity
(Mosadeghrad, 2015). RBV is the best choice for this study, as the theoretical lens
focuses on quality improvement organizational concepts.
Historical Involvement by Government in the Health Care System
Governmental involvement in the health care system has gone through an
evolutionary process since the initial phase in the early 1900s. The U.S. government
implemented health care services emphasizing the health and welfare of its citizens. The
first model of health care reform began with the Sheppard-Towner Act of 1921, one of
the catalysts in the health care reform movement (Haeder & Weimer, 2015). In
subsequent years following the Sheppard-Towner Act, President Harry S. Truman
tendered a plan for universal health care, a measure unable to pass through the
government (Manchikanti, Helm, Benyamin, & Hirsch, 2017). Haeder and Weimer
(2015) stated that federal health care programs aimed to expand health care services to
influence care reimbursement and financial outcomes, with an overarching goal of
universal health care.
As the movement towards universal health care continued, the health concern
continued into the Great Depression. The Social Security Act of 1935 provided stability
in the health care system and identified residents who were either elderly or disabled to
receive health care through Medicare and Medicaid (Haeder & Weimer, 2015). Federal
23
and state governments were delivering health services and sharing the cost provided
stability for U.S. citizens and medical providers taking care of the sick and infirm.
Welfare state policies became part of society with the combination of health care
insurance and retirement funding for the public (Mayhew, 2015).
The enactment of Medicare and Medicaid as health care programs did not appeal
to both the federal and state governments and not all states participated initially (Haeder
& Weimer, 2015; Leemon, 2014). The health care recipients in those states receiving
government-funded health care plans have to use either of these health care plans based
on income and age requirements. Individuals who are apathetic regarding health care
dwell on the ineffectiveness of programs established by government leaders. The
individuals receiving health care assistance viewed government intervention in a negative
context by the lack of transparency of the government regarding cost, quality of care, and
treatment outcomes (Maurer et al., 2017).
The principles of health care were to ensure services of value and quality is
accessible to individuals with moderate to lower incomes. The design of health care
reform existed as a social and societal norm, and economic instability has occurred in the
form of a conservative fiscal approach or terms of limited government intervention for
health care services (Schimmel, 2013). Reforming the health care system based on an
economic point of view will provide health care to all citizens as a cheaper and more
efficient alternative (Pineda & Hermes, 2015). In addition, the scope of health care
expansion is to ensure all citizens have access to health care services (i.e., hospitals,
public clinics, and health centers). The health care claim is that individuals pay from their
24
income if they do not need health care services. However, people should receive health
care services based on need, not income (Nardin, Zallman, Sayah, & McCormick 2016).
Government’s role in health care is not the solution and may hinder positive
advancements in health care reform (Manchikanti et al., 2017). Approximately 45 million
Americans are without health care coverage and millions more deal with lapses in their
health care insurance and are considered to be underinsured (Schimmel, 2013). The
concern with health care reform continues to come from the involvement of the
government, and the government has only marginally controlled health care costs
(Howrigon, 2016). There is market demand for health care services for the millions of
individuals without health care insurance. The health care industry is in a phase of
fluctuation, and the challenge ahead for rural clinics is to identify proactively potential
changes in health care reform.
The reform of health care insurance does not follow in the footsteps of socialized
medicine, as services remain vulnerable now and in the upcoming future. The idea
concerning health care as an inalienable right would regulate and conflict with other’s
rights and freedoms, as coordinating health care services is not the primary focus
(Roberts, 2012). The marketplace is a determinant regarding financial control in health
care with the emphasis placed on profitability and not necessarily on treating the illness
(Darrow, 2015). The concern of state or federal government officials is not to engage in
the agreement of social, economic, or even cultural rights between citizens but to play a
role in the scope of health care reform. Early health care reform had a lasting effect on
legislation in the United States (Durenberger, 2015). There is controversy about
25
government involvement in health care today, and without consensus, reform cannot take
place. The debate over universal health care is prevalent and divisive, but the right to
have health care remains unsettled with the advent of the ACA.
During the past 50 years, much of the health care system remains pieced together
ensuring individuals have access to hospitals, clinics, doctors, and medical supplies
(Farnsworth, 2015). Business leaders seeking for-profit benefits focus financially on
volume while spending less time providing adequate care (Joynt, Orav, & Jha, 2014). The
extension of health care benefits aimed to ensure those who were uninsured received
sufficient health care assistance, though a segment of the population is still without health
care insurance or is underinsured because of cost control means put in place by the
government (Schimmel, 2013).
The progression of health care services within the American health care system
results from the efforts of the public, private, government, businesses, and other
industries to create a universal health system. The evolutionary process of the American
health care system from a historical perspective exists in addressing enhanced
accessibility to services, upgrading the quality of care, and cost-effectiveness, or control
(Farnsworth, 2015). The U.S. health care system remains segmented into three groups:
government-assisted insurance, private insurance, and no insurance (Marshall et al.,
2016). There are differences between public and private health care, and evidence shows
that private health care according to US standards remains the best option (Nardin et al.,
2016). The idea persists that each citizen is responsible for his or her health care services
26
and may need to seek health care by any means possible through state-funded, federally
based, or private options.
The American legislature has different methodologies regarding health care
reform, and hence nothing has emerged as a clear means for all citizens to have adequate
health care. The past 50 years of government involvement has led from
Medicare/Medicaid to the ACA with no affordable options to all citizens (Durenberger,
2015). The selection of health care reform models comes from a form of compensation
for health care organizations who can deliver skilled and superior care (Barinaga et al.,
2017). The decision for health care reform comes from the government, which can
fluctuate between liberal and conservative perspectives, but operational or business
functions must address the financial stability of the organizations (Noh, 2016). The
selection of different reimbursement methods, such as fee-for-service (FFS) or value-
based purchasing (VBP) determines the economic outcome of a health care organization
and will be the catalyst for creating a cost-effective health care system (Schneider & Hall,
2017).
Health Care Financial Options and Medical Care
Health insurance representatives base their coverage decisions on factors such as
cost, effectiveness, and outcomes of care. A misunderstanding is to base a model of
health insurance with the resulting cost of delivering care. The government related
options available to U.S. citizens are minimal regarding health care, as they are referred
to as “safety nets.” The fail-safe system set up by the federal government to ensure
necessary care exists for individuals with lower to moderate income (Chokshi, Chang, &
27
Wilson, 2016). Thirty-one million Americans are without health care coverage, and
health care organizations need possible financial outcomes to provide coverage and care
(Hall & Lord, 2014). The rural clinic manager’s goal is viability in providing a public
health commodity and service (Reddy & Mythri, 2016). Medicaid and the ACA provide
stability of health care services, but individuals at or below the poverty level will use one
model or another irrelevant of the cost (Durenberger, 2015). The number of Americans
without health care coverage is a determining factor regarding reimbursement progress
affecting health care organizations (Kessell et al., 2015).
The quality of health care is a crucial financial consideration in addressing
adequate health care. The viability of health care concerning Medicaid and the ACA was
due to the expansion of Medicaid support to the states ensuring health insurance would be
accessible to low-income adults (Nguyen & Sommers, 2016). The premise towards the
expansion of Medicaid services was not only to meet the growing need for new patients,
but a determinant of the ACA to deliver quality care (Franz, Skinner, & Murphy, 2016).
Patients choose their health care services based on their health insurance and the
necessity of medical treatment or service. Uninsured individuals may experience lower
quality health care in comparison to those with private health care insurance (Nardin et
al., 2016). A rural clinic should implement services and treatment models following
private health care insurance.
The fiscal model for private insurance may not be adequate for all health care
organizations, as there are regional differences in access to appropriate health care. Thus,
if the area does not have a medical specialist, Medicaid and ACA patients, who depend
28
on the safety-net providers such as community-based health care services, will visit
primary care providers (Nguyen & Sommers, 2016). The advantage of health care
organizations is in facilitating and examining costs to the health care facility, while in
turn ensuring the quality of health care services promoting positive patient outcomes
(Shortell et al., 2015). Rural clinics build a kinship with patients in their regions with an
undertaking that medical services are available in each community. Ultimately, the care
and treatment is available for individuals who are in federal or state health care plans
regardless of the ailment or sickness, and the medical practice will build an assortment of
various payer sources.
The financial barriers associated with the ACA originated from the Massachusetts
Health Reform of 2006. The proposal is to expand Medicaid in a provision to decrease
the number of uninsured individuals. The financial obligation has been the ability of
health care organizations to provide affordable health care insurance to individuals with
moderate to low incomes (Nardin et al., 2016). The quality of health care in the United
States has languished over the past several years; however, costs have soared caused by
the reimbursement process (Choi, Lai, &Lai, 2016). Since the introduction of the ACA in
2010, the number of insured persons has increased by around 20 million, which has
reduced the number of persons not insured (Oberlander, 2017). The rural clinic benefits
with growth in the number of insured but the provision of quality health care is also
essential.
Limitations of both Medicaid and the ACA are a focus of legislators (Nardin et
al., 2016). The changes to the delivery of health care to Medicaid or ACA should not
29
affect the utilization of health care services or deny needed care (Nardin et al., 2016).
Health care organizations benefit from ACA because providers can generate high net
revenues from the increase in expanded coverage (Glied & Jackson, 2017). The quality of
care given a patient does not affect the amount of reimbursement (Glied & Jackson,
2017).
There is a movement towards personalized health care to hold patients
accountable for their lifestyles and tailored treatments. The principle of customized health
care has a dual purpose of enhancing the quality of health care services while lowering
costs (Teng, 2015). The rural clinic must ensure accountability for the total costs and
move away from past FFS beliefs towards risk-sharing measures (Blumenthal, 2016).
Similarly, the idea of personalized health care and price do not associate with each other,
but there are segments of the health care system to indicate care and treatment are
universal (Teng, 2015). The evidence-based information shows personalized health care
is a cost-effective approach to health care in the United States (Kuramoto, 2014). Overall,
implementing personalized care will bring focus on patient-centered care, but other
aspects are involved such as cost-effectiveness and containment.
The cost savings to the rural clinic does not appear to be evidence indicating
improved patient satisfaction. Personalized health care can educate, teach, and encourage
patient care, leading to financially supportive reimbursement arrangements (Teng, 2015).
Health economics plays an essential role in the identification of a payment system, but
the assurance of quality care will come at a significant cost (Chen & Goldman, 2016).
Preventative care is a necessary part of the quality goals of health care reform. Such an
30
incentive-based health care policy will enable cost-effective health care for all citizens:
the right care at the right time for the appropriate individuals (Kuramoto, 2014).
Health care reform potentially harms insurance profitability over time due to
shifts in reimbursement payments (Teng, 2015). Health care insurance existed before the
ACA in the form of private insurance, government funded, subsidized, regulated health
care, as Medicaid and Medicare coverage was primarily for the poor and elderly. The
objective was to have health care reform much like Canada, a single-payer system
emulating universal health care (Hall & Lord, 2014). The concept of a universal health
care system exceeds the financial accountability of Medicaid, and expanding Medicaid
would ease the financial burden on the states (Langellier et al., 2014). The concept of a
temporary health care system is universal and far exceeds financial accountability based
on poverty. Expanding Medicaid to ease the financial burden on the states to cover
medical services for individuals who remain uninsured is a temporary solution
(Langellier et al., 2014).
The correlation between financial preferences and health care is a crucial way to
solve the problems that overwhelm state and federal governments. The payment
structures for receiving medical care historically centered on FFS (fee-for-service) and
the capitation rate structure (predetermined rate to reimburse medical providers or
capitated rate or managed care) (Leemon, 2014). Health care organizations are
developing an infrastructure to move from previous ways of thinking about payment
modalities and creating revenue (Conrad, Vaughn, Grembowski, & Marcus-Smith, 2016).
Consequently, risk/reward plays a factor in financial preferences and the delivery of
31
services to the patient. The customary allowable rates are a risky proposition for rural
clinics due to the flat rate becoming a point of contention for the rural clinic depending
on the negotiation of the signed contract. Health care reform in Medicaid and ACA has
benefits for most Americans, regardless of the patient’s ability to pay. The objective of
health care reform is to provide adequate health care to the patient at a reasonable cost.
The challenges are facing health care financing options and medical care rest on
the patient’s ability to pay. Rural health care facilities face increased challenges in
comparison to urban areas due to differences in levels of income of patients (Allen,
Davis, Hu, & Owusu-Amankwah, 2015). The U.S. government offers rural health clinic
services through Medicare and Medicaid to the needy (Ortiz, Meemon, Zhou, & Wan,
2013). The rural health hospitals in smaller communities are financially unstable, but they
become viable substitutes for the patient in search of health care (Allen et al., 2015). The
mission of rural health clinics is to provide medical services to an underserved population
due to financial and operational issues. The rural clinic managers must contend with the
increased patient flow while managing costs and quality.
Fee-For-Service (FFS) vs. Value-Based Purchasing (VBP)
The duality of rural clinics is to serve the patients who walk through their doors
and manage the financial well-being of the operation. Reimbursements to health care
organizations are important considerations within the health care reform framework
(Oberlander, 2017). Business leaders will need to address reimbursement approaches in
preparing a profitable business model for the future (Gurganious, 2016). With health care
costs rising, reducing costs will lead to a decline in accessibility or value of the American
32
health care industry (Rudnicki et al., 2016). Thus, changes in coverage for patients to
visit hospitals, health care facilities, and providers will have a profound impact on the
operational bottom line.
Rural clinics link prospective payment for medical services to either FFS or VBP,
which encompasses payment through improved performance and reduced cost. This form
of payment holds health care providers responsible for the costs and quality of their care
and attempts to reduce and identify and reward inappropriate care (Kessell et al., 2015).
In order to establish continuity, rural clinics need a strategy for collecting reimbursement
and payment. FFS or VBP are important financial choices to a health care organization
and for the provider of medical services (Feldman, 2015). The future of health care
reform centers on price and value, and less on status, with the emphasis on conventional
health care economics (Gerben, 2016). Operations management makes decisions
regarding the volume or value of these payment options. Overall, rural clinics select the
most common and reliable payment types to establish consistency in the changing
landscape of health care reform.
The modes of payment for health care services have reached critical levels as
proponents of both sides view each system with flaws. The FFS model places
accountability for costs on medical providers (Feldman, 2015). The majority of health
care leadership analyzes payment reform as an approach to motivate medical providers to
incorporate the delivery of services (Murphy, Ko, Kizer, & Bindman, 2015). However,
the objective is to maximize profits, and the number of services and potential outcomes is
difficult for rural clinics to predict. The rural clinic distinguishes the best possible
33
payment opportunity for the business to create increased volume. Many contend having
one payment source and a financial plan to address lengthy payment delays is better for
the health care organization (Cascardo, 2015).
Health care reform interests should bring about restrictions on the way rural
clinics decide to accept or deny revenue streams. Health care providers recognize the FFS
model, but in some areas, the bundled payment is part of VBP and is standard for medical
generalists (Kuramoto, 2014). Business leaders determine the soundest payment structure
to ensure medical providers and the business receive compensation while still
emphasizing quality and efficiency (Ojeifo & Berkowitz, 2015). A mode of collection is
not to isolate specialists from accepting one form of payment for services (Palinkas et al.,
2015). Rural clinics comprise of a mixture of general practitioners and specialists.
Health care organizations must anticipate changes in health care reform as cost
conflicts could take place among medical providers regarding lower reimbursement rates.
The perception of clinical equity is something an organization must confront due to cost-
effectiveness or the anticipation of high-quality care and treatment (Kuramoto, 2014).
The health care system has gone through changes in the language of policy and
inconsistency with the delivery of medical services, leading to gaps in coverage,
conflicting outcomes, and inexcusable costs (Larkin, Swanson, Fuller, & Cortese, 2016).
The perspective of the business is to follow any advantage obtained or accept one payer
source over another, focusing on the overall value of the provided services. Rural clinics
address possible changes in the reimbursement fee schedule while identifying potential
opportunities to expand business and cost-effectiveness (Abidemi et al., 2017). Finally,
34
business leaders establish strategies to separate themselves from competitors and limit the
need for unnecessary risk-taking.
The U.S. health care system has migrated away from an FFS option regarding
reimbursement and is trending towards VBP as a financial alternative. Health care
clinicians are progressing towards VBP for services rendered (Joynt et al., 2017). The
transformation of the reimbursement revenue cycle has caused business leaders to assess
operational infrastructure with the limited resources available in the selection of a
payment model (Granata & Hamilton, 2015). Additionally, enrollment of individuals in
the ACA or Medicaid remains scripted as these plans continue for persons with lower to
moderate incomes (Durenberger, 2015). Business leaders will initiate a plan for accepting
either reimbursement arrangement (FFS or VBP), and the economic impact of the
decision-making process may result in financial implications for days, weeks, months,
and years.
The financial impact of health care reform on health care organizations is not
entirely clear. The FFS model remains monetarily centered on one particular service-
taking place for the patient (Leemon, 2014). Conversely, the VBP payment modality
provides a consistent financial revenue flow for the health care organization, along with
the element of increased quality of care and higher health outcomes for patients (Joynt et
al., 2017). Health care organizations seek revenue streams that provide an incentive base
for the business and do not discourage utilizing capitation rates (Doran, Maurer, & Ryan,
2017). Overall, payment modalities have a financial impact on the organization, and
sustainability is the groundwork for success.
35
Rural clinics need to focus on the delivery of services to address prospective
payment reimbursement concerns to ensure a consistent source of revenue. This analysis
should emphasize the elements of risk and reward to incentivize to include expectations
on treatment expenses, value, and results (Halfon et al., 2014). Higher expectations fuel
increasing health care costs, as health care organizations plan to improve patient
satisfaction and reduce costs (Moraros, Lemstra, & Nwankwo, 2016). While the U.S.
health care system is meant to provide affordable services, they are often ineffective and
high priced. The business strategies implied by an association with an FFS model serves
as a volume-driven entity, while the modality of VBP promotes costs and quality of care
(Noether & May, 2017). Rural clinics identify a recurring payer source as suitable for
financial growth while providing patients viable health care solutions.
The reimbursement process considers aspects such as improvement in the quality
of care, managed spending, and a patient’s access to health care services. The
involvement of federal and state governments regarding health care is a primary source,
and the Centers for Medicare and Medicaid Services (CMS) is presently in the middle
(Haeder & Weimer, 2015). The directive is to initiate replacing the reimbursement model
of FFS with the model of VBP (Schneider & Hall, 2017). CMS established an enhanced
version of paying for the quality of care (Cassel, Kerr, Kalman, & Smith, 2015). The
justification for change stems from the quality and quantity of the medical services
provided to the patient by the medical provider. Overall, the financial risk implied with
this VBP process emphasizes the value of health care services provided to patients.
36
The concern about health care exchanges with Medicaid and the ACA focuses on
inducements that reduce health care costs and provide improved service quality. The
research regarding FFS and VBP or bundling of services has lasting fiscal effects on
federal and state governments (Noh, 2016). The budgetary durability of our health care
system rests with federal and state governments determining a balance between cost
containment and quality care (Landers et al., 2016). Accordingly, federal and state
governments have addressed changes regarding health care reform and considered
reducing funds due to sustained debt at federal and state levels (Maurer et al., 2017). The
financial implications of health care reform with the implementation of the ACA remain
a temporary solution with the revamping of health care, as it currently exists.
Medicaid and ACA address cost, utilization of services, and trends in the health
care system. The forecasting of federal and state budgets regarding health care services is
a complex task; roughly, 20% of a state’s budget consists of health care funds, second
only to education (Gerstorff & Gibson, 2016). Health care spending is a national issue
and reforms can result in increased health care expenses (Duijmelinck & van de Ven,
2016). Data collection is important because the resulting reports illustrate the cost
efficiency of programs relative to the type of reimbursement model used (Eggbeer &
Bowers, 2014). Financial and operational strategies that result from data collection
prioritize cost containment, and health care outcomes are essential for the operation to be
successful.
Many individuals affected by health care reform and who are covered by
Medicaid (AHCCHS-Arizona) or the ACA reside in rural communities. Most of these

37
areas are underserved locations or populations that have other forms of payment for
medical services, including deductibles or co-pays or, for patients with lower to moderate
income, a sliding fee scale payment (Gao, Nocon, Sharma, & Huang, 2017). The
reduction in health care costs may become pivotal to enhance our current health care
system (Nocon et al., 2016). Consequently, smaller community clinics associated with an
entirely different patient base may limit the number of health care providers. The health
care coverage will fall into Medicaid and ACA categories, as they may be a split between
either of these payer sources (Noether & May 2017). Conversely, demand for rural health
care clinics to serve patients with low to moderate incomes remains essential within the
community.
The economic impact of FFS and VBP revolves around increased patient volume
for the rural clinic. Engagement with payer sources remains crucial for the organization,
but a fixed amount of revenue from the FFS or the provision of high-quality care implied
by VBP needs to be taken into account (Noether & May, 2017). Providing better care for
patients, lowering costs, expanding health care coverage for individuals, and reinforcing
infrastructure are the prime objectives (Kessell et al., 2015). Rural clinics thrive on
increased volume, and the distribution of a higher quality of care will equate to lower
costs. The organization’s selection of a particular payment revenue cycle will translate
into future financial success (Lubberink et al., 2017). Overall, the health care industry
faces pressures for reform and to ensure health care services are cost-effective and
delivered with quality.
38
Accounts Receivable Management and Health Care
An accounts receivable management strategy is a factor in the success of rural
clinics (Aidoo-Buameh, 2014). Members of the management team with expertise in
accounts management and those within the financial department who consult regarding
payment collection are responsible for strategic planning (Lai & Gelb, 2015). Health care
organizations manage their revenue cycles from billing and reimbursement from
insurance companies (Boden, 2014). This highlights the importance of accounts
receivable management, which is vital for the financial well-being of the medical
practice.
The operational working capital is critical to profitability (Talonpoika, Kärri,
Pirttilä, & Monto, 2016), which relies on accounts receivable management (Foerster,
Tsagarelis, & Wang, 2017). A revenue cycle manager aims to ensure the collection of
revenue for the organization (Mindel & Mathiassen, 2015). Payment delays are typical in
the health care profession, unlike shopping at the grocery store or having a vehicle
serviced.
Accounts receivable management involves collecting payment from patients and
insurance payers. The accounts receivable component of any health care organization is
paramount to the level of profitability (Shorr, 2015). Health services are available before
payment, and the provider relies on the patient’s intention to pay. The business model for
reimbursement for services provided by health care organizations is the intention to pay
for the medical provider’s service (Gurganious, 2016). Accounts receivable management
apply strategies to ensure payments made by patients and insurance payers for services
39
rendered are effective and efficient (Aidoo-Buameh, 2014). Rural clinic managers’ ability
to collect compensation from patients and insurance payers is essential for sustainability
and financial independence.
The collection process enlisted by health care organizations attempts to maximize
the revenue cycle management for the medical practice. The collection of payment for
medical services rendered is not a direct process, but it is essential for the practice to
thrive (Weinstock, 2015). Barriers to the collection process can include billing mistakes,
insurance payers underpaying, or an inability to collect from the right patient due to
misinformation (Shi, Zurada, Guan, & Goyal, 2015). Consequently, the incorporation of
strategic planning within the rural clinic and implementing processes to prevent the lack
of payment from patient and insurance payers becomes significant in the collection
process. The monitoring of accounts receivables ensures payment is timely and that the
dollar amounts owed to the organization decrease over time (Lail et al., 2016). The
traditional form of compensation is the FFS model, as insurance companies pay for each
service provided to the patient (Mabotuwana, Hall, Thomas, & Wald, 2017), and
collecting payment on time is a formula for sustainability.
The accounts receivable management role influences the financial future of the
rural clinic. The knowledge of where the revenue is coming from and the cost associated
with services are vital components. The strategic planning implemented by the financial
manager creates a primary construct for good fiscal control within the health care
organization (Sheet, 2017). Health care organizations receive payment from patients and
insurance payers through a mix of insurance types and payment methods (Loy et al.,
40
2016). Ultimately, the financial stability of the organization supports the accounts
receivable management strategies, and financial management staff incorporates plans to
maximize profits.
Analyzing accounts receivable revolves around the number of days it takes to
receive reimbursement from the payer including patients, insurances payers, and
government entities (Dong, 2015). The accounts receivable cycle breaks down into time
increments by days, weeks, or months; an improvement in accounts receivable
management will increase efficiency and profits (Aidoo-Buameh, 2014). Additionally,
the incorporation of accounts receivable management strategies into the operations
management will improve the consistency of payment from patients and insurance
payers. Financial managers analyze the mix of patients and insurer plans (Johnson &
Garvin, 2017). The accounts receivable manager strategizes with operations to identify
ways to improve profitability and sustainability through the selection of patients and
insurance types.
The financial and operational benefit of accounts receivable management is
narrowing the margin between profitability and the cost incurred by the health care entity.
The health care industry is going through extreme changes in which reimbursements are
steadily decreasing (Yaduvanshi & Sharma, 2017). Operations management strategies
must direct health care professional towards dealing with financial survival concerns
(Krzakiewicz & Cyfert, 2017). Managing earnings within the context of a health care
organization include reducing costs and increasing cash flow (Dong, 2016). Accounts
receivable management must integrate strategic procedures in collecting payment from
41
patients and insurance payers to avoid cutting costs or provide ineffective care.
Transition
Section 1 consisted of the foundation of the study; I provided the background of
the problem and purpose statements, nature of the study, research question, interview
questions, and conceptual framework. As part of Section I, I also presented operational
definitions, assumptions, and delimitations. In Section 1, I discussed the importance of
the study and the review of the professional and academic literature on accounts
receivable management strategies used by rural health care clinics to obtain timely
payment.
As part of Section 2, I presented data collection techniques and data analysis. I
finish Section 2 with the reliability and validity of the study. In Section 3, I introduced
the findings and implications of my research. The information consists of the data
collected, applications to professional practice, implications for social change,
recommendations for action, further study, and my reflections as the researcher.
42
Section 2: The Project
In Section 2, I focus on the factors employed by rural healthcare clinic managers
to implement accounts receivable management strategies to ensure timely payments from
patients and insurance payers. The section included the restatement of the purpose
statement, the role of the researcher, study participants, and the research method and
design. Also in this section, I covered population and sampling, ethical standards, data
collection instruments, and techniques. Furthermore, I concluded Section 2 with data
analysis, reliability, and validity of the study.
Purpose Statement
The purpose of this qualitative multiple case study was to explore strategies rural
clinic managers use to obtain timely payment from patients and insurance payers. Study
subjects included clinic managers from five rural clinics located in southwestern region
of the United States who have incorporated strategies to obtain timely payment from
patients and insurance payers. The implication for positive social change could come
from insights for clinic managers when they develop strategies to increase cash from
accounts receivables, which may improve the financial stability of the clinic and increase
the wellbeing of individuals in southwestern region of the United States.
Role of the Researcher
The role of the researcher is to ensure the quality and value of the study results
(Isaacs, 2014). The qualitative researcher plays a significant role in the methodology and
interpretation of the collected data (Swafford, 2014). In my role as a qualitative case
study researcher, I identified participants and maintained a working relationship with
43
these participants during the study. I involved myself in every facet of this study
including the selection of participants, selection of an appropriate research method,
collection of data, transcribing interviews, data analysis, and writing an account on the
outcomes.
Researchers incorporate their unique perspective to the research study (Brett et
al., 2014). I have 12 years of healthcare management experience, in which I
independently and objectively collected and analyzed relevant data. This experience
provided me with knowledge that assisted in this doctoral study. In addition, I understand
how my experience could predispose me to bias and this knowledge will help me
minimize my personal bias.
Researchers must possess knowledge of ethical issues and challenges involving
the study with the goal to attain accurate results (Sanjari, Bahramnezhad, Fomani,
Shoghi, & Cheraghi, 2014). The Belmont Report issued in 1979 identified ethical
standards and procedures for researchers to implement while researching human subjects
(U.S. Department of Health and Human Services [USDHHS], 1979). The Belmont
Report includes principles of respect for individuals, beneficence, and justice (USDHHS,
1979). The application of the Belmont Report provides research participants protection
from undue harm or exploitation and ensures confidentiality for participants.
During the study, researchers recognize the potential harmful effects of defined
beliefs or opinions regarding the phenomenon under study (Bradbury-Jones, Taylor, &
Herber, 2014). Researchers implementing a case study methodology should have an
awareness of the issues studied, as this awareness may become influential with the
44
understanding of the data collected (Yin, 2017). Some researchers may use other
resources and place an emphasis on reviewing the data, as opposed to doing additional
research to determine whether the data is acceptable or unacceptable (D’Andrea &
O’Dwyer, 2017). Researchers need to be neutral during interpretation of the data and
adopting neutrality will assist with potential future studies (Morgado, Meireles, Neves,
Amaral, & Ferreira, 2017). In my role as the researcher, I reduced bias by maintaining
high moral and ethical standards through integrity, professional competence, and
extensively reading prior research related to the study. Researchers must be wary of bias,
and at the same time, avoid having a negative mindset, which could affect objectivity
(Simons, Bester, & Moll, 2017). Hence, to mitigate bias, I maintained an understanding
of the topic and expectations of a researcher.
Researchers can increase the consistency of data collection using an interview
protocol, which enhances the validity of the study (Yin, 2017). With the use of the
protocol, a case study researcher can increase continuity and efficiency with the
collection of data (Yin, 2017). The interview protocol is a vital aspect of the data
collection process, as research design will have an influence on the data obtained and
define the kind of analysis used in exploring the data (Manning & Kunkel, 2015). During
the collection phase of gathering information, it is vital to review the information
immediately as there could be a need to obtain further evidence (Yin, 2017). The setting
up of the interview protocol for a case study is the basis for the audit path leading to the
trustworthiness of data and eventually the quality of the research (Ang, Embi, & Yunus,
2016). Consequently, I used an interview protocol (see Appendix A) to determine a level
45
of trustworthiness during this study. A researcher must prevent misinterpretations or
decrease bias (Thomas, 2017). The use of the interview protocol will assist me in
reducing bias by treating each of the participants in the same manner.
Participants
A crucial element in choosing participants is that researchers identify participants
with reliable knowledge of the research question (McCalman et al., 2017). The
participants in a study focused on a balance between operational issues surrounding a
patient-centered approach or using the older fee-for-service model for the collection of
payment for services rendered (Pittmam, Masselink, Bade, Frogner, & Ku, 2016).
Research participants should include only those who are readily available and willing to
participate (Yin, 2017). The eligibility criteria for the participants in this study was
individuals who work at a management level, (southwestern region of the United States,
and who confirmed insurance payers for treated patients. Participants included clinic
managers, accounts receivable managers, and the director of revenue cycle. These
individuals remain involved in the direction of payment cycles and putting strategies into
action to ensure payments occur promptly with no disruption to the organization.
The researcher must use strategies for gaining access to each of the preferred
participants from each of the sites. Researchers may use specific resources and
community support to acquire ideal study participants (Katigbak, Foley, Robert, &
Hutchinson, 2016). A gatekeeper is an individual who has power and control over
specific access within an organization, and negotiate terms and conditions to ensure the
best interest of all parties was met (Caretta & Riaño, 2016). The ability to have access to
46
the gatekeeper is a challenge and building a relationship is a critical aspect of the
foundation of the study (Brooks & Jean-Marie, 2015). Gatekeepers exist within the
organization as responsible representation of the organization and protect the
organizations’ best interests (Rattani & Johns, 2017). As part of the study, I asked the
gatekeeper, Director of Revenue Cycle Management to sign a letter of cooperation (see
Appendix B) in conjunction with IRB approval process from Walden University to work
with the gatekeeper identifying appropriate participants. I used the gatekeeper to identify
appropriate documentation for triangulation of data in this study. Subsequently, after the
gatekeeper signed the letter of cooperation and identified appropriate participants, I
included an introductory letter (see Appendix C) to the participants inviting them to
participate in the study. As part of the introductory letter, I incorporated the informed
consent form which provides confidentiality and protects their privacy. Before
conducting an interview, I asked participants to read, review, and sign the informed
consent form.
Participants have a significant impact on the researcher. The roles of the
researcher and participant deemed to be essential in all aspects of the study (Råheim et
al., 2016). The formation of a working relationship existed early in the study with
participants, as I provided a detailed explanation of the study, events, disadvantages and
advantages of participating in the study, and adherence to confidentiality for participants.
I also went over the study with the potential participants to make sure they fully
understood the purpose of this study before agreeing to participate.
47
Research Method and Design
The purpose of this qualitative multiple case study was to explore strategies rural
clinic managers use to obtain timely payment from patients and insurance payers. The
researcher can choose between qualitative, quantitative, or mixed research methodologies
to delineate an occurrence (Wilson, 2016). Researchers use a qualitative multiple case
study design to explore and enlighten human experience (Yin, 2017).
Research Method
Rebs, Brandenburg, Seuring, and Stohler (2017) argued that quantitative research
methods like analysis of empirical data produce stronger results than illustrated durable
numerical examples. A quantitative researcher uses systemic numerical indicators, along
with empirical inquiry to comprehend the existence of a phenomenon (Chang, 2017). A
researcher’s selection of quantitative methodology exists as an expertly constructed
process in obtaining clear, concise results either validating or disapproving a hypothesis
(Saxena, 2017). A quantitative research method was not appropriate for this proposed
study due to no testing of relationships among variables. Also, did not use the
quantitative research method for the reason no hypotheses exist for this study.
The researcher bringing a mixed method approach incorporates strategies from
both the qualitative and quantitative methods, and to integrate these practices to reflect
inquire of importance (Mertens et al., 2016). The carrying out of a mixed methods
research is difficult, as opposed to implementing a single research method (Yin, 2017).
The mixed method researchers implement this method of research primarily based on the
phenomenon under inquiry, which needs to be understood (Annansingh & Howell, 2016).
48
I eliminated the use of the mixed method research model, as I did not incorporate
numerical data in this study. I implemented the qualitative method approach to
investigate and interpret occurrences encountered by the participants.
To remain alert when a research question occurs, it is vital in fulfilling an
outcome in the research methodology (Isaacs, 2014). The exploration of strategies used
by rural health care clinic managers to ensure timely payment from patients and
insurance payers dictate that I selected a qualitative research method. Qualitative
researchers focus on what and how components of events revolve around individual
experiences (Bazzano, Martin, Hicks, Faughnan, & Murphy, 2017). With the use of a
qualitative research method, I improved my understanding of how clinic managers
promptly collect payments amid difficult circumstances. The implementation of a
qualitative research method entails the use of interviewing skills and observation and a
systematic form of deduction to confirm or contradict findings (Arino, LeBaron, &
Milliken, 2016). Researchers use a qualitative methodology to gain more in-depth
information to provide further meaning.
Research Design
I used a multiple case study design to explore the research question as the case
study approach allows the researcher to view the issue in a natural setting. The primary
reason for the research design of a study is to lead the researcher through the collection of
the data, analyze the information, and provide a deduction to the findings (Yin, 2017).
The researcher’s research design focuses on the research question and remains suitable to
conduct the study (Santiago-Delefosse, Gavin, Bruchez, Roux, & Stephen, 2016). The
49
qualitative researcher can seek to use different design methods including case study,
ethnography, and phenomenological (Colorafi & Evans, 2016).
Researchers use a qualitative multiple case study to reinforce study findings
through replicating research at multiple sites (Solomon & Casey, 2017). Researchers use
the case study design to explore phenomena using numerous data collection methods
(Wang, Sadler, & Shee, 2017). Researchers use a qualitative case study design to focus
on the how and why questions within a study (Fitzsimmons, 2017). I used a qualitative
multiple case study to look at strategies rural clinic managers use to obtain timely
payments from patients and insurance payers.
Ethnographers construct the possibility of exploration of insight and examination
of shared patterns within individuals and cultures (Jaimangal-Jones, 2014). The
researcher using ethnography design engages and learns more about a particular group of
participants based on the interest (Desmond, 2014). Ethnographers engage extensive
periods in the field investigating and connecting with a specific culture group (Rouleau,
de Rond & Musca, 2014).
The examination of the culture within the rural clinic staff potentially could have
provided valuable information. However, the purpose of the study did not include
observation of the rural clinic staff, but reporting strategies applied by rural clinic
managers to ensure timely payments from patients and insurance payers. For this study,
an ethnographic design was not appropriate. Researchers utilizing a phenomenological
design concentrated on the line of inquiry that focuses on the participant lived occurrence
(Ziakas & Boukas, 2014). A phenomenological researcher’s interest is to illustrate what
50
and how all participants’ respond to the phenomenon encounter (Bourne, 2015). Using a
phenomenological research design, a researcher firmly situates to describe and analyze
possible interpretations from all participants during this investigative process (DeFelice
& Janesick, 2015). The phenomenological research design was not an appropriate design
for this study, as my objective was to delve into strategies used by clinic managers to
obtain timely payment and not to look at participants lived experiences.
The data saturation approach used by the researcher exists on concepts identified
as part of the study, along with the research method and design (Saunders et al., 2017).
Boddy (2016) indicates that data saturation occurs at the point where no new information
or themes detected in the data. A researcher conducting a qualitative research
methodology uses exact data collection methods towards receiving an answer to the
research question (Fusch & Ness, 2015). An occurrence may take place during a study in
which a novice researcher due to their level of data saturation inexperience maybe at risk
and unachievable (Wilkinson & Hayward, 2017). I interviewed rural clinic managers and
financial personnel until I reached a point of data saturation, as indicated by no further
substantial information or new themes emerged.
Population and Sampling
The purpose of this qualitative multiple case study was to explore strategies used
by rural health care clinic managers to ensure timely payment from patients and
insurance payers. The sample population for this study consisted of clinic managers and
financial personnel from rural health care clinics in southwestern region of the United
States. Researchers will select participants based on the role they play within the
51
organization concerning the research question (Palinkas et al., 2015). A researcher should
be able to justify the inclusion of participants in a study (Cleary, Horsfall, & Hayter,
2014). The participants must meet parameters within the purpose of the study to reduce
the potential risk for inauthentic or improper settings and processes (Khan, 2014). The
selection of participants exists on the premise that the information generated is plentiful
and insightful to the research topic (Mountford & Kessie, 2017). Consequently, the
sampled population supported the research question: What strategies do rural clinic
managers use to obtain timely payments from patients and insurance payers?
I used purposive sampling as the sampling method for this research study.
Researchers use the purposive sampling method to obtain participants based on their
extensive knowledge or verbal expression within a group or subculture of their belonging
(Gentles, Charles, Ploeg, & McKibbon, 2015). The sampling of a study must represent an
accurate alignment of the purpose and ideas throughout the study (Solomon & Casey,
2017). Researchers use sampling to enhance the effectiveness used through the collection
of data to validate the study (Sharafizad & Coetzer, 2017). For this study, I purposively
selected rural clinic managers and financial staff because they are in the position to
provide detailed information and insight into their experience and familiarity with timely
payments.
Data saturation and gathering takes place after which data collected is repetitious,
and no additional data can be acquired (Pourghane, Ahmadi, & Salimi, 2017). Data
saturation is confirmation of high-quality information tested to solidify the validity and
reliability of the study (Wang, Gellynck, & Verbeke, 2016). A qualitative researcher will

52
cease the interviewing of additional participants recognizing no further information will
emerge complementing the phenomenon studied (Gligor, Esmark, & Gölgeci, 2016).
Data saturation happens through the beginning analysis of data collected when rural
clinic managers and financial staff provide no new information on strategies to obtain
payments from patients and insurance payers. The sample size of this study was 10 rural
clinic managers and financial staff within the rural clinic setting.
A researcher can use interview surroundings to put the participants in a state of
increased comfort or feelings of ease by conducting interviews in a place of neutrality
and privacy (McGhie-Anderson, 2017). I conducted face-to-face in-depth interviews at
the location of the clinic managers or financial staff members to ensure the wellbeing of
all participants in the study. The participants in the study chose their work setting as a
place of comfort and security to conduct the interviews. The participants feel comfortable
in a face-to-face interview and are placed in a setting to discuss feedback results relevant
to the event studied (Strasser, 2017). The participants provided commentary with
confidence in an environment free from disruption with an ability to share their
observations (Wardale & Lord, 2017).
Ethical Research
The participant informed consent process is critical to control ethics regarding the
research of the study (Graham, Powell, & Truscott, 2016). The method of informed
consent keeps the lines of communication open with the participant and provides
comprehension and education within the context of the study (Gordon, Mullee, Skaro, &
Baker, 2016). By presenting and reviewing the consent form (see Appendix D) with

53
participants, I ensured the explanation of the study, their rights as participants, and my
contact information as the researcher. Before interviewing the participants, I ensured that
I attained a signed informed consent from each participant. Also, each participant
received a copy of the document for his or her records.
A researcher must allow a participant the opportunity to withdraw from the
research study at any time and without reason (Hinnekens, Vanhee, De Schryver, Ickes,
& Verhofstadt, 2016). The participants received a copy of the informed consent in the
initial phase of the study; provisions within the context of the informed consent allow the
participants to withdrawal at any time (Nilsson et al., 2016). I explicitly stated that the
participants may request to withdrawal or opt out of the study at any time, without
repercussions.
I reiterated to participants that participation was strictly voluntary and no financial
incentives were part of this study. McNaughton, Adams, and Shucksmith (2016) asserted
that offering financial incentives may be ineffective and counterproductive. The
provision to provide monetary incentives or stipends reduced the level of participation
(Begley, McCarron, Huntley-Moore, Condell, & Higgins, 2014). Some financial
incentives offered by researchers encourage participants to provide valuable information
(Smaglik, 2016). I restated that participation in this study was strictly voluntary and there
are no incentives for participation in the study.
I protected the confidentiality of the names of the participants by not including
identifiers that may allow others to determine the names of the participants in the study.
The concealing of participant identities is a primary goal of researchers to ensure

54
discretion (Raman & Pramod, 2017). To protect the anonymity of participants, I used
pseudonyms to ensure privacy. I ensured that only I have access to the interview
information.
After I collected and analyzed study data, I stored all confidential study
information in a secured file cabinet at my home. After 5 years of securely storing the
data, I intend to shred all interview notes, paper files, consent forms, and delete any
electronic files or data stored in my possession. Finally, I remained compliant with the
requirements outlined by Walden University Institutional Review Board to ensure the
welfare of the participants.
Data Collection Instruments
In qualitative studies, a researcher is the principal data collection instrument (Yin,
2017). As a primary data collection instrument, a qualitative researcher engages directly
with participants, and the engagement will have an impact on the study (Forsythe et al.,
2016). Hasle, Limborg, Grøn, and Refslund (2017) stated that qualitative researchers
collect data through interviews, a review of written organizational and archival
documents, email correspondence, and observations. As a qualitative researcher, I was
the primary data collector for this research study, and I ensured the implementation of the
semistructured interviews as part of this research study.
A qualitative researcher can use semistructured interviews to seek information
and clarification on vital points in the study (Shalhoub, Marshall, & Ippolito, 2017). I
conducted face-to-face semistructured interviews utilizing open-ended formatted
questions to collect data for this study. Researchers who use semistructured interviews
55
connect with participants and elicit responses about experiences in the study (Fowler,
Coffey, & Dixon-Fowler, 2017). A researcher using semistructured interviews has a
predetermined list of questions going into the study (Van den Berg & Struwig, 2017).
The semistructured interviews for this study comprised 10 prearranged open-ended
questions that primarily focus on the pivotal phenomenon of the study. Each
semistructured interviews lasted 30-45 minutes. During the semistructured interview
process, I asked participants constructive interview questions, stayed accommodative,
and avoided biases.
A qualitative researcher will use triangulation of multiple data sources to develop
a comprehension of the phenomena within the study (Carter, Bryant-Lukosius, DiCenso,
Blythe, & Neville, 2014). A qualitative researcher applies triangulation less as a strategy
for the validation of results than an option to validate the consistency, intensity, and range
of a study (Wilson, 2014). A researcher needs to be exact about the collection and
analyzing of the data to support rigor within the study (Tibben, 2015). I implemented
methodological triangulation to promote the authenticity, consistency, and accuracy of
the study. As a researcher, I employed methodological triangulation by including referred
organizational documental evidence to include IRS Form 990 form, specific health center
data from Health Resources and Service Administration (HRSA), and casual observations
of the environment to enhance my data collected from face-to-face interviews. Arfaoui,
Damak-ayadi, Ghram, and Bouchekoua (2016) stated the selection of methodological
triangulation allows for control over possible bias and the empirical justification for the
study. The data collection methods I used included informal observation, semistructured
56
interviews utilizing open-ended questions, and an examination of the documental support
within the study. Documental support that I collected consists of policies, internal
organizational data, and other relevant in-house documentation.
Member checking is a proven technique used by qualitative researchers to ensure
the validity and accuracy of the study (Schaik, O'Brien, Almeida, & Adler, 2014). A
researcher will use member checking to ensure the findings become available to the
participants before the completion of the study (McNulty, 2015). To make sure accuracy
and authenticity exist as part of the data collection process, a qualitative researcher can
make use of member checking (West, 2015). I applied member checking by asking
participants to validate my conclusions and emergent themes from the interviews.
A qualitative researcher is the prime data collection instrument and must prevent
any or all misinterpretations from decreasing bias (Thomas, 2017). Researchers use
interview protocols steadily as a gradual progression to direct them through the interview
process (Karen, Kennedy, Hunter, & Maksabedian, 2016). Yin (2017) stated a researcher
could use interview protocols to obtain access to significant participants and coordinate
schedules to complete the collection of data at any time during the study. A researcher
will use interview protocols to focus and concentrate on structural boundaries of the
study to reduce the risk of bias (Venkat, Shank, Rickard-Aasen, Pringle, & Johnjulio,
2017). I consistently applied the same questions, in the same order, to help minimize
investigator bias. Using an interview protocol (see Appendix A), I was able to adapt each
interview consistently reducing researcher bias.
57
Data Collection Technique
Data collection included open-ended semistructured face-to-face interviews and a
review of documental resources. The data collection techniques of researchers include
detail processes aimed at assembling relevant information connected to the phenomenon
of interest (Eisenhardt, Graebner, & Sonenshein, 2016). A researcher will use multiple
data sources within the same study to ensure validity (Aslinda & Ibrahim, 2016). Data
collection techniques for this doctoral study involved 10 face-to-face semistructured
interviews utilizing open-ended questions (see Appendix E), documental evidence, and
informal observations. All interviews were conducted at the business site and conducted
during regular business hours. Researchers use semistructured interviews to probe
beyond the participant’s responses to gain further insights, perceptions, and experiences
related to the research phenomenon (Peters & Halcomb, 2015). A qualitative researcher
uses semistructured interviews to allow participants to offer their experiences as a
contributor to the study (Campbell, Manns, Hemmelgarn, Sanmartin, & King-Shier,
2016). As a qualitative researcher, I implemented documental support, and informal
observations to explore the strategies required by rural health care clinic managers to
obtain timely payments from patients and insurance payers.
Participants who were willing to participate in the study received the consent form
in advance through an in-person visit. Before conducting interviews, I visited each
prospective participant during an in-person onsite visit to provide and review the
informed consent form (see Appendix D). After the meetings, participants signed the
informed consent documents and provided a copy to me of each signed form. The
58
following week I called or emailed each of the 10 participants to schedule a date, time,
and place for the interview. Before conducting each interview, I informed participants
that I would be recording the interview using a portable electronic audio recording device
to ensure accurate data transcription.
Researchers use semistructured interviews to explore further insight from the
participant’s perspective to expand on added knowledge of the phenomenon studied
(Yagasaki, Komatsu, & Takahashi, 2015). I used audio recorded semistructured face-to-
face interviews and documental analysis to explore strategies implemented by health care
leaders to increase profitability. A researcher will use semistructured interviews to collect
data identified by participants as experiences during the study (Spinks, Chaboyer,
Bucknall, Tobiano, & Whitty, 2015). The rationale for using this protocol was to make
the process easier and more manageable for the participants. Researchers utilizing
semistructured interviews will have a comprised set of listed open-ended questions with
no preconceived designed response options (Alhaddad, Smith, Robertson, Watman, &
Taylor, 2015).
I followed my prescribed interview protocol (Appendix A) questions to engage in
an extensive exchange with the participants. A prepared researcher will effectively
employ interview questions to evoke hidden or imperceptibly improper data (Mlinar,
Petek, Cotic, Metka, & Zaletel, 2016). A researcher will use informal observations to
access pertinent information as depicted by the participants in the study (Joe, Young,
Moses, Knoki-Wilson, & Dennison, 2016). A researcher will interject realistic actions or
events of participants while observing (Yin, 2017). I carefully assured all these elements
59
during the interview process by reviewing all journal entries and documented notes at the
conclusion of each interview.
The qualitative researcher uses member checking to allow the participants to
review the interview transcript or data interpreted in the study (Birt, Scott, Cavers,
Campbell, & Walter, 2016). Member checking is the method a qualitative researcher uses
concerning the acquisition of participant feedback and confirming the authenticity of the
findings (Charmaz, 2006; Harvey, 2015). A researcher implements member checking as
part of the interpretative portion of the data collection for increasing confidence and
validity (Dorsey, Conover, & Revillion-Cox, 2014). To ensure reliability within this
study, I presented my findings to the participants with my interpretations of the
interviews and provided them with the opportunity to corroborate the accuracy of my
interpretation of the collected data as part of this study. I emailed my summary to the
participants within 7 days of the interview and asked for a response within 14 days of
receiving the summary. There were no significant changes during the review process, and
all information was confirmed through an email sent to participants verifying all
interview responses. As part of the member checking process, participants confirmed the
accuracy of my interpretations during the interview.
Data Organization Technique
A researcher organizes data based on the relevance of the data to the study
framework (Nielsen & Nielsen, 2015). Yin (2017) detailed that a qualitative case study
researcher should organize data based on the relevance of the research question. A
researcher will organize data in a form that safeguards the integrity and confidentiality of
60
the information (Van Zyl, Mathafena, & Ras, 2017). My objective was to develop a
proficient data technique; I created a research log utilizing an Excel spreadsheet to keep a
structured record of the dates of the interviews, names of the interviewees, and other data
acquired from participants and online searches. A researcher uses reflective journaling to
document personal accounts with participants along with a provisional for opportunities
for questions, feedback, and critiquing (Baillie, 2015). Also, I maintained a reflective
journal that includes notes from interviews, observations, and analysis of organizational
documents. A qualitative researcher applies coding to aid in the process of data
organization (Chowdhury, 2015). Thus, I used the coding process to assist in the
organizing and retrieval of data in my research log.
Researchers ensure sensitive information remains encrypted and compliant with
ethical guidelines. Researchers initiate protective measures stay in place by using a
password-protected filing system secured in a locked cabinet (Fairfield & Shtein, 2014).
A researcher must ensure data remains secure to prevent unauthorized discovery or use
(Peng & Gala, 2014). To ensure the confidentiality of participants, I stored all data
collected in a password-protected personal computer, and hard copies of information
accumulated will remain secure in a locked file cabinet. Researchers need to
predetermine a retention policy (Cullington et al., 2016). After 5 years of securely storing
the participant data, I intend to destroy all written documents and electronic data from all
electronic devices used to gather information.
61
Data Analysis
Qualitative data analysis coincides with the exploration, categorizing, and coding
of data into themes (Iancu, Zweekhorst, Veltman, & van Balkom, 2015). Data analysis
entails multifaceted and contextually rooted data generated with the intent to prepare,
manage, and report from the perspective of multiple sources (Patterson, Smith, &
Bellamy, 2015). Data analysis is one of the most challenging aspects of research,
especially for a beginning researcher (Yin, 2017). The data analysis process suitable for
this case study research was methodological triangulation. Wilson (2014) provided a
practical approach regarding the four aspects of triangulation including data, investigator,
methodological, and theory. In methodological triangulation, a researcher implements a
series of data collection techniques and analysis in the exploration of a phenomenon
(Oleinik, 2015). Thus, I employed three collection methods including face-to-face
semistructured interviews utilizing open-ended questions (see Appendix E), review of
organization documents, and informal observations to enhance the validity of the findings
of this study.
Using a logical and sequential process addressing multiple facets of the study is a
crucial component of the researcher’s data analysis process (Pradabwong, Braziotis,
Pawar, & Tannock, 2015). The data analysis process for a researcher begins immediately
after conducting the initial interview and throughout the research process (Fletcher,
2017). A case study researcher will have strategies in place to ensure a prominent role in
linking the collected data to the research question is at the forefront (Yin, 2017). Rose
and Lennerholt (2017) defined the data analysis process consisting of (a) acquiring data
62
and related sources, (b) extracting, coding, and formatting information in an orderly
manner, (c) grouping data into subject matter, (d) analyzing and assessing text, and (e)
interpreting results and formulation a conclusion. After collecting the data from the
participants through semistructured face-to-face interviews, document reviews, and
informal observations, I immediately transcribed each interview and field notes.
Subsequently, I organized the data into thematic relevance as recommended (Percy,
Kostere, & Kostere, 2015). The coding process ensures themes remain grouped into
categories (Percy et al., 2015). Once coding the data into segmented themes, I presented
my preliminary findings to the participants to confirm the emerging themes through
member checking and follow-up emails to the participants. A qualitative researcher
interprets the data to ensure consistency and significance (Chavira, Bustos, Garcia, Ng, &
Camacho, 2017). I complied, disassembled, and reassembled data to develop a final list
of emergent themes.
The use of computer-based software in the process of data analysis assists
researchers reflect on the data in the thematic development process (Zamawe, 2015). The
options of qualitative data analysis vendors include NVivo, ATLAS.ti, RQDA, and
MaxQDA (Chandra & Shang, 2017). NVivo is an efficient system used by researchers to
assist in interpretation and time management while developing qualitative themes
(Heisler, Firmin, Firmin, & Hundley, 2015). A researcher can use NVivo to influence
data by deriving codes and rules connected to the data to affect bias (Sotiriadou,
Brouwers, & Le, 2014). I applied NVivo 12 Plus software in the data analysis portion to
assist in the retrieval of information and to salvage time.
63
A researcher will implement a thematic analysis to uncover a collection of
patterns associated with the themes (Braun & Clarke, 2006; Fugard & Potts, 2015).
Researchers use thematic analysis as a means to capture and organize data in a way to
derive meanings and create a detailed understanding (Crowe, Inder, & Porter, 2015). A
researcher should ensure thematic interpretations are a direct reflection concerning the
research question (Henning et al., 2015). Researchers use a thematic analytic process to
ensure appropriate analysis of data (Gallagher, Phillips, Lee, & Carroll, 2015). I used
NVivo 12 Plus for my thematic analysis to create and organize essential themes. Through
the triangulation process, I developed themes with supporting documentation from
financial information reported in the IRS Form 990, specific health center data from the
HRSA form, and my journal notes. Included in my journal notes were comments I made
related to my observations of the environment. The RBV theory was the framework I
used to explore the themes related to improving receivable collections of accounts.
Reliability and Validity
Reliability and validity of a qualitative research study are essential components of
research dependability (Bengtsson, 2016). Reliability and validity are critical standards to
the construct of a qualitative researcher emphasizing objectivity as the primary purpose
of research (Power & Gendron, 2015). In evaluating reliability and validity of a
qualitative study, a researcher can use the criterion of dependability, credibility,
transferability, confirmability, and data saturation (Dubois & Gadde, 2014; Yin, 2017).
The reliability and validity of a study substantiate rigor and integrity of the research
64
findings (Cypress, 2017). I incorporated reliability and validity strategies during my
study to improve trustworthiness.
Reliability
A researcher should consider reliability within the context of a research study
(Fida et al., 2016). Dependability contains the essentials of stability of data over time
under different conditions (Holm & Severinsson, 2014). A researcher will establish
reliability to ensure details of the qualitative study transpire in a detailed manner
(Eriksson, 2015). To assess dependability, a researcher addresses internal and external
auditing to ensure the reviewing process occurs in a research study (Smith & Smyer,
2015). As a researcher, I preserved an auditing path to augment the assessment of
dependability of this study. The relationship between dependability and quality ensures
the processes and rigor in the study (Lin, Han, & Pan, 2015). In alignment with (Lin et
al., 2015), I employed member checking with participant follow up. Participants
reviewed my preliminary themes and validated my interpretation of the collected data.
Makola (2015) provided a detailed approach that a qualitative researcher uses member
checking to concentrate on emerging themes, confirm findings, and elicit precise results.
A qualitative researcher uses intrinsic and extrinsic motivation in member checking, thus
ensuring themes are precise, thorough, and interpretations are practical (Bassous, 2015).
To enhance the reliability and validity of findings in this study, I established several
sources of data collection including face-to-face semistructured interview using open-
ended questions, a review of organizational documents, and observations. Organizational

65
documents will include policy and procedures, collection templates, and other significant
internal documents.
Validity
According to Leung (2015), reliability and validity are primary principles for a
study. Validity entails the degree of accuracy of data (Chahal & Dutta, 2015). A
researcher can confirm the validity of a research discovery by upholding the formulation
of internal consistencies in the research process (Slife, Wright, & Yanchar, 2016). To
confirm the validity of the study, a researcher can use to support the fundamentals of
credibility, transferability, confirmability, and data saturation (Bennett & McWhorter,
2016; Yin, 2017).
Credibility. Qualitative researchers can augment the credibility of the findings in
a study by determining dependability from the perspective of the participants (Munn,
Porritt, Lockwood, Aromataris, & Pearson, 2014). Schipper et al. (2014) purposed the use
of reflective journaling and member checking as methods researchers can implement to
confirm findings in the study. A qualitative researcher can establish credibility when a
participant confirms the findings brought about by the researcher (Rosenthal, 2016).
Researchers use member checking to gain further insight into the phenomenon of the
study (Welch, 2017). To address credibility, I established member checking and
reflective journaling. Both techniques allowed me to maintain a comprehensive, detailed
account of the participant interviews and subsequent interpretation of the data.
Transferability. Researchers meet the criteria of transferability if the findings
add meaning to studies in different settings (Rapport, Clement, Doel, & Hutchings,
66
2015). Researchers can ensure transferability when the results of the research involve a
degree of importance to other groups (Pompeii, 2015). The intensity of transferability
increases as researchers present a detailed description of data (Vermeulen, Niemann, &
Kotzé, 2016). In demonstrating transferability future researchers crossing multiple
disciplines and readers of a study could find the data resourceful and valuable (Smith et
al., 2015). To enhance transferability, I ensured to provide adequate information
regarding the details of my study.
Conformability. The conformability criteria arise from the data accuracy of
information and data provided by participants (McInnes, Peters, Bonney, & Halcomb,
2017; Polit & Beck, 2010). Rich, Viney, Needleman, Griffin, and Woolf (2016) assert
that conformability as the neutrality of the researcher in the research process. A
qualitative researcher can apply conformability by establishing an audit trail by ensuring
the research method is engaged in the study (Ang et al., 2016). I used methodological
triangulation to assure conformability. In methodological triangulation, researchers
employ multiple data collection methods to investigate a phenomenon (Fusch & Ness,
2015). I used different data collection methods including face-to-face semistructured
interview using open-ended questions, a review of organizational documents, and
observations.
Researchers reach data saturation at the point when collecting additional data does
not produce new ideas relating to the phenomenon of the study (Saunders et al., 2017).
Researchers use data saturation to increase the level of reliability and validity of the
findings of a study (Fusch & Ness, 2015). At the point of sufficient data saturation, a
67
qualitative researcher will cease with interviews (Boddy, 2016). To ensure data
saturation, I continued to conduct interviews until no new or sufficient data to replicate
the themes identified in the study.
Transition and Summary
Section 2 consisted of a comprehensive description of this study. I started Section
2 by restating my purpose statement. Next, I expanded on my role as the researcher with
provisions including in-depth accounts about the participants selected for the study. As
part of Section 2, I described the research method and design along with the population
and sampling. Next, I included ethical research and established data collection
instruments, techniques, and organization. Furthermore, I concluded Section 2 with data
analysis, and methodology addressing reliability and validity.
In Section 3, I presented the research findings and the application of professional
practice and implications for change. In the introduction, I reiterated the purpose
statement and research question. I also presented study findings and applications to
professional practice. Finally, I inquired into the applications for social change,
recommendations for action, further research, reflect on the research process, and
concluded the study.
68
Section 3: Application to Professional Practice and Implications for Change
Introduction
The objective of this qualitative multiple case study was to explore strategies rural
clinic managers use to obtain timely payment from patients and insurance payers. The
processes and strategies used by rural clinic billing staff establish and maintain
profitability and sustainability for the entire organization. As a result, multiple revenues
generating strategies exist that financial billing staff uses to increase economic prosperity.
After interviewing participants and reviewing other document sources, I identified four
major accounts receivable management strategy themes: (a) communication between
medical providers and billing staff, (b) payment plan set up, (c) accuracy of billing claims
and (d) consistent accounts receivable reviews. These themes represented strategic
approaches to assist financial leaders in collecting payments from patient and insurance
payers in a timely and efficient manner.
Presentation of the Findings
The overarching research question for this study was: What strategies do rural
clinic managers use to obtain timely payments from patients and insurance payers? To
answer the overarching research question, I conducted semistructured face-to-face
interviews with a combination of 10 clinic managers and billing staff from rural clinics in
southwestern region of the United States. During the interview process, I followed an
interview protocol (see Appendix A). I called and spoke with both the Director of
Revenue Management and Accounts Receivable Supervisor to obtain permission to meet
with each participant individually and asked each participant the same set of questions in
69
the same order. I informed each participant that each interview would be audio recorded
and I would be integrating their responses into the documented results. The
semistructured face-to-face interviews occurred at the request of the Director of Revenue
Cycle, and dates and times were allotted to meet the needs of the research participants. At
the instruction of the Director of Revenue Cycle, who was also the gatekeeper, I received
a list of participants and used the list to organize each individual interview. The
interviews took place over a 2-day time span; however, I returned on a third day to meet
individually with the Director of Revenue Cycle for a followup interview.
The data collection configuration appropriate for this study was methodological
triangulation. Triangulation is collecting and examining multiple data sources (Wilson,
2014). To gain a dynamic understanding of strategies implemented by rural clinic billing
staff and clinic managers to maintain profitability and sustainability for the organization,
I chose this method.
I coded the participants CL1 through CL10. I confirmed my interview data
through methodological triangulation. Additional data sources confirming my interviews
included data from reviewing HRSA documentation and the IRS-990 form along with
casual observations. I also met with both the Accounts Receivables Supervisor and
Director of Revenue Cycle to process accounts receivables strategies for capturing
payment from patients and insurance payers to ensure sustainability and profitability.
Yin (2017) provided researchers with a multiple step data analysis process: (a)
collection, (b) dismantling, (c) aggregation, and (d) interpretation. I used each of these
steps for data collection and analysis. I collected information by taking notes during the
70
interview process. After each interview prior to ending the recording, I verified the
identity of the participant, their specific job title, and the date and time of the interview. I
also emailed a transcription copy to each participant to allow them to corroborate the
data. I transcribed the taped results with Microsoft Word. The aggregation of the
information occurred as I transferred transcribed audio interview results into NVivo 12. I
used queries, narratives, accounting of the results, and coding to identify significant
themes during the interpretation process.
I wrote up my conclusions following the data interpretation. Throughout the data
analysis process, four main themes emerged: (a) communication between medical
providers and billing staff, (b) payment plan setup, (c) accuracy of billing claims, and (d)
consistent accounts receivable reviews. The rural clinic managers and billing staff were
all consistent in terms of their standards regarding these four major themes for accounts
receivables strategies that improve sustainability and profitability.
Theme 1: Communication Between Medical Providers and Billing Staff
All but one of the 10 study participants articulated how consistent communication
between medical providers and billing staff provides stability, which increases
profitability. CL1 explained that specific departments, for example obstetrics and
gynecology, will incorporate billing requirement changes from specific payers regarding
billing for obstetrics and referrals. These changes are communicated to the billing office.
CL1 mentioned that medical assistants (MAs) provide required information regarding
encounters with patients, and all billing codes are used and sent to the insurance company
71
for reimbursement. CL1 stated, “Without the front desk, without the MAs, and without
the doctors, we wouldn’t be able to bill the claim.”
CL2 explained that it was essential to ensure that billing staff update patient
demographics with correct information. Obtaining correct and timely information
requires a high level of communication between the medical provider and billing staff.
CL2 stated, “We make sure that we [billing staff] go from time to time to the front office
to make sure that they are doing everything correctly and entering everything correctly.”
CL2 explained the importance of ensuring charges match medical diagnoses and
procedures performed by the medical provider. In order to increase communication with
medical providers, billing staff monitors patient accounts to determine if the accounts are
current or inactive. CL4 described effective communication as the process of updating
patient information. CL5 also confirmed the importance of consistent communication
with other departments:
It [billing] affects our doctors, our medical records staff; it is a team effort.
Whatever the front desk person does, what the medical doctor does in the notes,
whatever he is going to charge and a bill to when we get it, as it is truly a team
effort. There is no way to get around it.
CL7 added that they review patients’ financial charts to ensure that payments
occur and verify previous payments. CL8 identified that the primary indicator of prompt
billing was the timely documentation of the services received from the provider to submit
for billing purposes. CL8 in addition stated “the encounter [patient visit] is complete and
72
submitted for billing within 72 hours.” The timeliness of the billing will ensure that
claims submitted to the insurance payer are received and payment occurs.
CL9 further added that communication with other departments improves billing
accuracy. CL10 focused on how accurate information reduces the possibility of insurance
payers denying or rejecting a claim. CL10 described the importance of closing the
encounter and promptly submitting the claim. CL10 alluded to the open lines of
communication between medical providers and billing staff was important to ensure
correct billing information resulting in increased revenue. During the interview process at
the central billing location, I observed interaction between billing staff, coding staff,
accounts receivable supervisor, and the Director of Revenue Cycle Management. I noted
collaboration within the various departments, which ensured the accuracy and timeliness
of claims.
Gurganious (2016) said that the reimbursement model for services provided by
healthcare organizations is intended to pay for the services the patient received from the
healthcare provider. The profitability of healthcare organizations depends on effective
communication between medical providers and billing staff, who oversee the
reimbursement process for the services provided. The RBV is a relevant framework for a
service-based industry such as healthcare. The concept of providing continuity of care for
the patient and the ability of the organization to win the confidence of the patient
increases its competitive advantage and improves its financial performance (Lin et al.,
2015). Al Achkar et al. (2018) indicated apart from ensuring clinical services remain
adequately compensated, accurate coding and billing reflect the appropriate assessment
73
of the complexity of medical conditions. CL2 stated ensuring demographic information is
correct, in order to assure correct billing information and avoid declined claims, and
communication between the medical providers and the billing staff are crucial for timely
reimbursement.
CL1, CL3, CL5, CL9, and CL10 shared that consistent communication
departmentally between providers and billing staff are vital and without one another the
claim could not be submitted for payment. These comments align with Mkanta et al.
(2016) who stated that the U.S. health care officials must focus on the cost and quality of
health care and evaluate operational aspects, including scheduling of providers, clinical
methods, payment methods, and management structures. All, but one of the 10
participants confirmed that communication between medical providers and the billing
staff are imperative towards the consistency of billing which affects increased
profitability.
Theme 2: Payment Plan Setup
The second identified theme from this study was the payment plan setup to ensure
that payment occurs at the time of the medical encounter. All 10 participants mentioned
the flexibility of setting up a payment plan that meets the needs of the patients and their
monthly budgetary constraints was important. During the interview process, the study
participants each expressed collectively the ease in which payment plans are setup
specifically to address the patient’s financial needs. CL1 shared that discounts and sliding
fee scale payment are arranged for those patients who are uninsured or under-insured.
CL1 stated:
74
We can offer a small payment plan for those patients before sending them to
collections even if we do send them to collections, $5.00 or $10.00 a month,
something that can work for them. We work on a payment plan, even if it is a
small dollar amount. Whatever the patient’s financial needs are, that’s what we
work with.
CL2 further added that the sliding fee scale payment option was available and if a
patient comes in with no health care insurance, they are offered a 30-day discount. The
objective of the biller is to collect a form of payment or instead of no payment, a partial
payment is an acceptable means of collection. A sliding fee scale intends to assist the
patient to make a form of payment and helping the patients is a form of excellent
customer service. CL3 stated, “Usually it depends on what the patient can give, and some
patients give $20, and some give $50, it depends on what the patient can do at that time.”
CL4 indicated that if a patient was already in collections, an alternative to making a
payment to the collection company would be that the organization accepts payment in the
billing office. CL4 stated, “We do take a lot of payments from people who are already in
collections. They always say they would much rather talk to us than the people in the
collections.”
CL5 added that a discounted payment plan applies to single individuals, as well as
families and children. CL5 also mentioned that before the patient visits the front desk,
personnel inform the patient of the co-pay or deductible. If the patient cannot afford to
make the entire co-payment or deductible, arrangements occur at the time of the
appointment for payment options. CL6 stated, “We always try to work around and help
75
them [patients] out if they have little income.” The implementation of the payment plan
ensures revenue for the organization and the ease in which the patient can make a
payment promotes community engagement.
CL7 indicated the flexibility of the payment plan and the expectation is not that
the patient makes the full amount at one time. CL8 added that discounts are offered
depending on a patient’s level of income. CL8 stated, “Payments can pay as little as $15,
$20, $38, and up to $43. Again, based on their income, how many in the household, we
can reduce down their office visits.” CL9 shared the uniqueness of the organization is
their ability to engage the patients in a payment plan that serves both the uninsured and
under-insured population. During the interview process, I had the opportunity to observe
clinic staff engage patients, address their co-pays, and address methods of payment for
their medical encounters. CL10 added that for some of the patients the sliding fee scale is
a primary option. As CL10 stated, “Using a sliding fee scale is a requirement of being a
federally-funded community health center. We offer a type of discounts to low income
patients. We also offer payment arrangements up to 12-month for balances over $150.”
CL10 further added that the health center accepts credit and debit cards and can set up the
payment arrangement through the credit or debit card. Having a payment plan setup
increases flexibility and improves financial options.
Theme 2 findings, payment plan setup, are also relevant to RBV conceptual
theory and an ability of billing staff to win the confidence of patients, which improves
accounts receivable collections. According to Lai and Gelb (2015), the goal of billing
department managers is collecting payments from insurance payers with limited obstacles

76
or delays. Business leaders manage internal resources to keep revenue consistent with the
organization’s long-term financial growth. The profitability of an organization relies on
the implementation of strategies based on organizational resources (Liu et al., 2017). One
of these corporate organizational procedures is a payment plan. Once the payment plan
setup is confirmed, commitment to consistency in the collections process is essential.
Study participants were specific that operational approaches, such as payment plan setup,
produced positive results by improving customer satisfaction and improving the medical
care experience.
Farnsworth (2015) further confirmed in the literature the evolutionary process of
improving accessibility to services, improving quality of care, and reducing costs affects
the generated revenue. Health care leaders are developing an infrastructure to move away
from previous approaches to payment methods and revenue generation (Conrad et al.,
2016). The evolutionary process of billing from paper to electronic has quickened the
timeframe in which providers receive revenue. In recent literature since this study,
payment collection methodology focusing on factors involving a patient’s insurance plan
as reimbursement potentially may become modified with minimal notice (Tamblyn,
Winslade, Qian, Moraga, & Huang, 2018).
Evidential to the second theme, all 10 participants discussed the importance of
offering a payment plan setup for uninsured and under-insured patients. As a result, the
participants identified that making a payment plan setup available to patients established
a consistent flow of revenue for the organization. The payment plan set up option gives
patients financial flexibility which, in turn, builds community rapport. Chen and

77
Goldman (2016) alluded to health economics playing a pivotal role in identifying a
payment system that benefits the providers and the patient. By introducing a payment
plan, patients are able to receive care and rural clinic mangers are able to receive timely
payments
Theme 3: Accuracy of Billing Claims
I observed how the billing staff focused on gathering accurate information for
billing claims. All 10 participants mentioned that accuracy in billing was one of the
primary results of prompt revenue collection. Themes 2 and 3 relate to revenue and
profitability, which are connected. Study participants mentioned effective billing ideas
and processes 53 times, which reinforced foundational components for organizational
leaders, clinic managers, and billing.
CL1 stated, “Make sure the ‘I’s are dotted, that everything is completed the first
go around because the more you submit the greater chance you have of the claim not
being paid in a timely manner. The more you work on it, the more it costs the company to
get paid on that claim.” CL2 indicated that the biller who is placing the information on
the claim must ensure that the information is correct with no mistakes. This strategy of
focusing on accuracy reduces the number of claim resubmission due to errors. CL5
further stated, “Each insurance has their time in which we can bill before it is either
processed to pay or it can be denied and they we have some additional time that we have
for denials.” CL5 stressed the importance of gathering the information correctly to
process the claim promptly with an emphasis on receiving the reimbursement quickly
without delay.

78
CL6 stated, “If there are any errors in the claim, we want to make sure we get that
fixed as soon as possible.” CL6 added that billing on time was the key component; but if
charges remain denied, working on the claim quicker will increase the process of
receiving payment in a shorter period. CL8 added, “As a biller, keeping up with the
changes in the organization with regard to claims billing and processing is important. It is
important to read, research, and keep informed of what is coming up that may affect your
organization, so you can help the organization.” CL10 explained that with the
information technology (IT) and software any errors or missing information that does not
relate to the medical encounter could be detected. The comment from CL10 supported
this conclusion:
A lot of our staff members review the denials and will sparse it out depending on
who is responsible for what aging. Then the charge entry sends them back to the
staff for reviews so not only are they correcting the staff but learning for future
claims the help reduce the same mistakes.
Further, health care leaders must deal with payment delays and unreimbursed
services (Cascardo, 2015). Theme 3 substantiated the overarching research question:
What strategies do rural clinic managers use to obtain timely payments from patients and
insurance payers? In health care, organizations emphasized improved patient satisfaction,
reduced costs and increased productivity at all levels of the organization (Chiarini &
Vagnoni, 2017). Cascardo (2018) concluded that staff training increases the productivity
of billing staff. Revenue cycle leadership must be involved in all aspects of the billing
staff from training, continuing education, coder application, and audit resources to be
79
successful in the billing of claims (Cascardo, 2018). The goal of leaders is to develop a
fully engaged billing department, which is a critical element of the reimbursement
process.
Other forms of payment include private payment insurance, direct payment, and a
sliding rate based on the ability of the patient to pay (Barbaresco et al., 2015). Angeli and
Norwood (2017) concluded the health care industry is experiencing a turbulent period
due to competition, contractual adjustments in reimbursement for services rendered and a
struggle to keep up with health information technology (electronic medical records). The
transformation of the reimbursement revenue cycle leads to the evaluation of the
operational infrastructure with the limited resources available to select a payment model
(Granata & Hamilton, 2015). Revenue cycle managers, clinic managers and billing staff
must collaborate to ensure that consistent accounts receivable reviews are occurring
steadily.
Theme 4: Consistent Accounts Receivable Reviews
All but two of the 10 participants expressed the importance of consistent accounts
receivable reviews, as a critical component in determining patient accounts and method
of payment. Consistent accounts receivable reviews coincide with theme two, payment
plan setup and theme three, accuracies of billing claims. CL1 shared the importance of
completing a more extensive review of patient accounts. CL1 stated “Make sure that
everything charged is correct; if something is incorrect, we correct it immediately. This
has more to do with doubtful accounts for the collection of payment and consistent
review of patient accounts.” CL2 described the billing activity of the patient accounts and
80
the importance of determining if the patient has made a payment towards the statement or
if there has been no activity in that patient’s claim. CL2 added:
Once the billing process is done, there is a report that shows a claim rejected, if
something is incorrect, if the claim wasn’t put in right, if the policy number was
wrong, it rejects them. Doing the charge entry daily and then the billing is done
daily, also once that is done and if they are rejected we correct them at the
moment and they get billed again.
CL3 explained that charge entries are corrected based on the accounts receivable
reports that are run on a daily basis. CL3 reiterated that the report flags claims prior to
submission for reimbursement. CL6 emphasized that they run reports daily to ensure that
accounts remain reviewed and that claims to insurance payers are not getting behind due
to lack of payment from the insurance companies. The timeliness of the review of
accounts receivables is dependent on the week, but these reports are worked on
consistently by revenue cycle management leaders, clinic manager, and billing staff. CL7
commented that data analyst staff review the report to determine if the patent is self-pay
or has insurance. Billers review the reports to confirm that third-payer collectors have not
received payment and to follow up on accounts that have not completed payment as this
list could be used for double or triple checking of lost revenue.
CL8 revealed that they continually monitor the patient aged-trial balance to
identify accounts with old outstanding balances. The objective is to review and identify
accounts that require assistance from other departments. CL8 stated, “We send these
reports daily, if these accounts are sitting there for 120 days with no payments, they are
81
sent back to us, and we then flag them and send them to a third-party collector.” If no
payments transpire on the patient accounts sent by the third-party collector, these
accounts are taken off the books as non-collectible accounts. CL8 added that these reports
are easily located to find out exactly what is going on with these accounts, and those
billing staff who look at the accounts take ownership and ensure that there is not going to
be revenue lost due to irresponsibility or losing focus due to lack of follow-up.
CL9 noted that when accounts receivable staff review reports, they could detect
where the errors occur in the billing process, and the information in the reports are
available to the staff to prevent future mistakes. CL9 added that revenue cycle managers
and billing staff use ageing reports to identify old claims that require additional work. I
observed substantive conversation among billing staff members who discussed collecting
accounts receivable in accordance with organizational standards. CL10 stated, “I think
accounts receivables within the name itself is just making sure all parties are accountable
for their ownership within the process.”
Supporting theme 4, leadership within the accounts receivable component of any
health care organization is of the utmost importance concerning profitability (Shorr,
2015). The consistency of accounts receivable reviews is to decrease barriers to the
collection process may include billing errors, underpayment of insurance payers, or
failure to collect information from the correct patient (Shi et al., 2015). The leaders of
rural clinics also consider the revenue cycle process to guarantee payment as a resource
to be managed by organizational leaders. Accounts receivables claims are reviewed
promptly to ensure the dollar amounts due to the organization decrease over time. (Lail et
82
al., 2016). The utilization of the consistent accounts receivable reviews is the revenue
cycle manager's strategic plan to create a primary structure for good fiscal control in the
health care organization (Sheet, 2017). The key concept is to ensure the follow through of
the accounts receivable review on a consistent basis leading towards organizational
sustainability.
An example of research contribution for consistent accounts receivable reviews
since the initial proposal approval of this study included Zenilman and Freischlag (2018).
Zenilman and Freischlag addressed the element of a detailed review process examining
every facet of the patient encounter. The pillar of system integration at the organization
includes administrative infrastructure to support the essentials of the review process for
the collection of each patient encounter (Zenilman & Freischlag, 2018). The objective of
the organization is to achieve financial transparency, and this occurs by scheduling a
regular meeting, one-to-one meetings with staff, and ensuring that follow-up happens to
address any concerns brought up by staff members (Zenilman & Freischlag, 2018).
I reviewed available IRS Form 990 and HRSA documentation to support data
collected from interviews. Abzug, Olbrecht, Sabrin, and DeLeon (2016) noted IRS Form
990 information is publically available and includes financial information reported to the
IRS. I calculated two critical metrics of accounts receivable management including
turnover and days sales outstanding (DSO). Turnover (credit sales divided by average
accounts receivable) and DSO (turnover divided by 365) represent key ratios in accounts
receivable management. Turnover at the research site increased from 3.1 to 4.6 between
2015 and 2016, and DSO decreased to from 119 days to 80 days for the same period.
83
Both ratios represent improvements in accounts receivable management. In the same two
year period the organization saw an increase in total patients (9.4%), uninsured patients
(0.26%), and dual eligible patients with both Medicare and Medicaid (1.27%; HRSA,
2018). The documentation I reviewed supported the importance the organization placed
on account receivable management. CL10 added the following comment:
It has been tedious for the billing department to run all those reports, but in the
long run we benefit. Because now they don’t have to write off because of
eligibility. So it decreases the aging. Because before we would just check the
patient in and we were done. Even as coordinator, we did not know that we were
writing off thousands of dollars just because this wasn’t being done. We were so
separate from them (billers), and we didn’t know the long-term effect it would
have or how much was being written off.
Overall Findings Applied to the Conceptual Framework
The findings revealed strategies rural clinic managers used to obtain timely
payments from patients and insurance payers. These findings supported the conceptual
framework, and Wernerfelt’s RBV as the basis for this study. Wernerfelt’s theory
included a detailed approach to an organizational resource as a strategic management
design to yield higher profits (Wernerfelt, 1984). The RBV indicated a connection
between profitability and resources and the long-term management of the organization’s
resources (Wernerfelt, 1984). Barbaresco et al. (2015) identified forms of payment
including private insurance, direct payments, and a sliding rate based on one’s ability to
pay. The tenets of RBV can be relevant for health care leaders regarding organizational
84
resources, including administratively formulated attributes, skills, organizational
procedures, and expertise. (Patidar et al., 2016). The concepts established by Wernerfelt
enhanced the theory of resource-based value by Barney (1991) with the concepts of
organizational resources, competitive advantage, and the utilization of sustained
competitive advantage.
Managers play a crucial role in ensuring that billing staff assess the patient’s
insurance coverage and potential form of payment (Barbaresco et al., 2015). Rural clinic
managers must deal with reimbursement delays, insurance payers’ denials for services
provided, and unreimbursed services (Casardo, 2015). Organizational leaders examine
the competitive advantages of the specific resources and limitations of each location
(Yang, 2014). Strategic findings from this study are pertinent to the professional practice
for revenue cycle manager and medical billers.
Applications to Professional Practice
Health care leaders could benefit from this study’s findings by identifying
strategies to increase the collection of payment from patients and insurance payers.
According to Gerstorff and Gibson (2016), roughly 20% of a state’s budget consists of
health care funds. The findings of this study indicate the professional practice procedure
steps followed by rural clinic managers maintaining profitability and sustainability are:
(a) communication between medical providers and billing staff, (b) payment plan setup,
(c) accuracy of billing claims, and (d) consistent accounts receivable reviews.
The findings corroborate findings of other researchers, showing that
communication between clinical and billing departments, setting up payment plans,
85
accuracy in the filing of billing claims and reviewing accounts consistently provide a path
to long-term profitability. The results of this study could be relevant across other
industries and may enhance further understanding of those with minimal management
experience as well as qualified managers. Furthermore, health care policies formulated at
the administrative level incorporate organizational resources including attributes,
abilities, organizational procedures, and expertise (Patidar et al., 2016). Each of the
themes identified supportive strategies to ensure timely payments from patients and
insurance payers to sustain profitability. Organizations increase awareness of ensuring
payments from patients and insurance payers by developing dynamic capabilities and
increasing resources (Kash et al., 2014). Emergent themes in the study represent
strategies that apply to professional practice.
Implications for Social Change
Society could benefit from the results of this study. Approximately 45 million
Americans are without health care coverage insurance and are underinsured (Schimmel,
2013). The findings from this study could lead to tangible improvements to individuals,
communities, and organizations. The findings include strategies to improve the
sustainability of health care organizations. In this study, I focused on rural clinics.
Financial stability of rural clinics directly benefits the health of individuals and the public
health of communities. I found that strategies including communication, attention to
detail, and consistent patient account reviews impact cash flow. Engagement with payer
sources is also crucial to the collection cycle (Noether & May 2017). The staff of rural
86
clinics provides support to underserved populations. Increased collection rates can result
in the support that rural clinics provide to the wellbeing of underserved communities.
Recommendations for Action
The objective of this qualitative multiple case study was to explore strategies rural
clinic managers use to obtain timely payment from patients and insurance payers. Study
findings identified four major accounts receivable management strategy themes to
increase sustainability and profitability are: (a) communication between medical
providers and billing staff, (b) payment plan setup, (c) accuracy of billing claims, and (d)
consistent accounts receivable reviews. I noted some recommendations to financial
leaders in collecting payments from patients and insurance payers in a timely and
efficient manner to increase overall profitability.
Health care leaders may consider attempting to establish an atmosphere
encouraging a strategic approach for collecting payments from patients and insurance
payers. The leadership develops accounts receivable management strategies and ensures
that the organization’s staff abides by company financial practices, policies, and
procedures (Grant, 2014). The five rural clinics I chose for this multiple case study were
successful clinics committed to helping build a healthy community. Each participant I
interviewed appeared committed to using effective strategies into their daily, weekly, and
monthly schedule to increase collections from patients and insurance payers.
How a company’s managers and staff use their resources is a critical strategic
factor in many industries, and many other fields could benefit from this study. Multi-
faceted health care organizations must adapt to identify new and innovative processes
87
regarding the use of internal resources to achieve a competitive advantage (Lillis et al.,
2015). The participants from the research organization I selected were reliable and
concise in their approaches to ensure timely collection of payments from patients and
insurance payers. These strategies could assist leaders in other industries.
Recommendations for Further Research
The purpose of this qualitative multiple case study was to explore strategies rural
clinic managers use to obtain timely payment from patients and insurance payers. The
targeted population included 10 rural clinic managers and billing staff from five rural
clinics located in southwestern region of the United States, who have incorporated
strategies to obtain timely payment from patients and insurance payers to maintain
sustainability and profitability. The study findings concerned further research for
numerous reasons. First, the results of the study may extend to other industries in a way
that improves cash collection and payment management.
Second, there are numerous facets of research that other investigators can explore.
For example, there were less significant themes that emerged, such as ways to elicit
information from patients and insurance payers instead of going directly to rural clinic
mangers and billing staff. Finally, researchers could also consider accounts receivable
management strategies, insurance payer-mix types, location, and short and long-term
financial goals of the organization. To promote further discussion of the results, I will
share a summary of the findings with the research participants. Additionally, I will
publish this study through the ProQuest/UMI dissertation database for future researchers
88
to use and work with my Doctoral Chair to present the results of this study at professional
health care conferences or seminars and to publish my findings in peer-reviewed journals.
Reflections
Completing a DBA has been one of the most demanding, yet, rewarding
opportunities of my life. I knew going into the program would be challenging; however, I
accepted the challenge. Also, I had prior experience in the health care field, but I did not
have any outside experience with the participants before collecting the data. As a
researcher, I understood the importance of maintaining high scholarly and research
standards when conducting interviews. Also, I gained new knowledge about how rural
clinic managers and billing staff are regarding the accounts receivable process to increase
profitability.
My goal as a qualitative researcher was to collect data without personal bias or
preconceived views. I made sure that I consistently addressed the guidelines I wrote in
the initial proposal to ensure the process demonstrated legitimacy. The research
participants provided detailed responses. I was appreciative for that part of the process.
Participants provided precisely and detail orientated responses and conveyed how each
person defined their task and how it related to the team. I learned from participants about
accounts receivable management strategies used to ensure payment for patients and
insurance payers to improve profitability.
Conclusion
Accounts receivable management strategies are essential to organizational
strategic success. The overarching research question of this multiple qualitative case
89
study was: What strategies do rural clinic managers use to obtain timely payments from
patients and insurance payers? I conducted face-to-face semistructured interviews to
obtain data. I also reviewed HRSA documentation and IRS Form 990s to complement the
data collection. I applied information from the methodological triangulation data
collection process to validate data source themes
Study findings revealed four significant themes regarding accounts receivable
strategies applied by rural clinic billing staff to increase profitability: (a) communication
between medical providers and billing staff, (b) payment plan setup, (c) accuracy of
billing claims, and (d) consistent accounts receivable reviews. The social change
enrichment exists when the rural clinic is successful: operations are effective and
efficient, profits increase, job opportunities proliferate, and cohesion develops within the
community.

90
References
Abidemi, B. T., Halim, F. B., & Alshuaibi, A. I. (2017). Marketing capabilities and
organizational performance: A proposed model on the moderating effect of
technological turbulence. International Journal of Management Research and
Reviews, 7(6), 626-636. Retrieved from http://ijmrr.com
Abzug, R., Olbrecht, A., Sabrin, M., & DeLeon, E. (2016). Nonprofit financing to the
rescue? The slightly twisted case of local educational foundations and public
education in New Jersey. Nonprofit and Voluntary Sector Quarterly, 45,133-149.
doi:10.1177/0899764014564577
Adebanjo, D., Laosirihongthong, T., & Samaranayake, P. (2016). Prioritizing lean supply
chain management initiatives in health care service operations: A fuzzy AHP
approach. Production Planning & Control, 27, 953-966.
doi:10.1080/09537287.2016.1164909
Aidoo-Buameh, J. (2014). The effect of NHIA debt on accounts payables management in
public hospitals. Asian Economic and Financial Review, 4(8), 1001-1015.
Retrieved from http://www.aessweb.com
Al Achkar, M., Kengeri-Srikantiah, S., Yamane, B. M., Villasmil, J., Busha, M. E., &
Gebke, K. B. (2018). Billing by residents and attending physicians in family
medicine: the effects of the provider, patient, and visit factors. BMC medical
education, 18(1), 1-7. doi:10.1186/s12909-018-1246-7
Alhaddad, B., Smith, F. J., Robertson, T., Watman, G., & Taylor, K. M. G. (2015).
Patients' practices and experiences of using nebuliser therapy in the management

91
of COPD at home. British Medical Journal Open Respiratory Research, 2(1), 1-9.
doi:10.1136/bmjresp-2014-000076
Allen, J., Davis, A., Hu, W., & Owusu-Amankwah, E. (2015). Residents' willingness-to-
pay for attributes of rural health care facilities. Journal of Rural Health, 31, 7-18.
doi:10.1111/jrh.12080
Angeli, E. L., & Norwood, C. D. (2017). Responding to public health crises: Bridging
collective mindfulness and user experience to create communication
interventions. Communication Design Quarterly Review, 5, 29-39. doi:10.11
45/3131201.3131204
Angelis, A., Kanavos, P., & Montibeller, G. (2017). Resource allocation and priority
setting in health care: A multi‐ criteria decision analysis problem of value. Global
Policy, 8, 76-83. doi:10.1111/1758-5899.12387
Annansingh, F., & Howell, K. (2016). Using phenomenological constructivism (PC) to
discuss a mixed method approach in information systems research. Electronic
Journal of Business Research Methods, 14(1), 39-49. Retrieved from
http://www.ejbrm.com/main.html
Ang, C. K., Embi, M. A., & Yunus, M. M. (2016). Enhancing the quality of the findings
of a longitudinal case study: Reviewing trustworthiness via ATLAS.ti. The
Qualitative Report, 21(10), 1855-1867. Retrieved from
http://nsuworks.nova.edu/tqr
Arfaoui, F., Damak-ayadi, S., Ghram, R., & Bouchekoua, A. (2016). Ethics education
and accounting students' level of moral development: Experimental design in

92
Tunisian audit context. Journal of Business Ethics, 138, 161-173.
doi:10.1007/s10551-015-2643-z
Arino, A., LeBaron, C., & Milliken, F. J. (2016). Publishing qualitative research in
academy of management discoveries. Academy of Management Discoveries, 2,
109-113. doi:10.5465/amd.2016.0034
Aslinda, A., & Ibrahim, M. A. (2016). The state-centric model of transportation policy in
Mamminasata areas, South Sulawesi. Bisnis & Birokrasi, 23(1), 55-62. Retrieved
from http://journal.ui.ac.id/jbb
Baillie, L. (2015). Promoting and evaluating scientific rigour in qualitative research.
Nursing Standard, 29, 36-42. doi:10.7748/ns.29.46.36.e8830
Barbaresco, S., Courtemanche, C. J., & Qi, Y. (2015). Impacts of the affordable care act
dependent coverage provision on health-related outcomes of young adults.
Journal of Health Economics, 40, 54-68. doi:10.1016/j.jhealeco.2014.12.004
Barinaga, G., Sayeed, Z., Anoushiravani, A., Scaife, S., El-Othmani, M., & Saleh, K. J.
(2017). Using a comanagement model to develop a hip fracture integrated care
pathway. Journal of Health care Management, 62, 107-117. doi:10.1097/JHM-D-
17-00011
Barney, J. (1991). Firm resources and sustained competitive advantage. Journal of
Management, 17, 99-120. doi:10.1177/014920639101700108
Bassok, O. (2015). Interpretative theories as roadmaps to constitutional identity: The case
of the United States. Global Constitutionalism, 4, 289-327. doi:10.1017/S204538
1715000167

93
Bassous, M. (2015). What are the factors that affect worker motivation in faith-based
nonprofit organizations? Voluntas, 26, 355-381. doi:10.1007/s11266-013-9420-3
Bazzano, A. N., Martin, J., Hicks, E., Faughnan, M., & Murphy, L. (2017). Human-
centred design in global health: A scoping review of applications and
contexts. PLoS One, 12(11), 1-24. doi:10.1371/journal.pone.0186744
Begley, C., McCarron, M., Huntley-Moore, S., Condell, S., & Higgins, A. (2014).
Successful research capacity building in academic nursing and midwifery in
Ireland: An exemplar. Nurse Education Today, 34, 754-760.
doi:10.1016/j.nedt.2013.09.016
Benedettini, O., Neely, A., & Swink, M. (2015). Why do servitized firms fail? A risk-
based explanation. International Journal of Operations & Production
Management, 35(6), 1-37. doi:10.1108/IJOPM-02-2014-0052
Bengtsson, M. (2016). How to plan and perform a qualitative study using content
analysis. NursingPlus Open, 2, 8-14. doi:10.1016/j.npls.2016.01.001
Bennett, E. E., & McWhorter, R. R. (2016). Opening the black box and searching for
smoking guns. European Journal of Training and Development, 40(8/9), 691-718.
doi:10.1108/EJTD-07-2015-0049
Birt, L., Scott, S., Cavers, D., Campbell, C., & Walter, F. (2016). Member checking: A
tool to enhance trustworthiness or merely a nod to validation? Qualitative Health
Research, 26, 1802-1811. doi:10.1177/1049732316654870
Blumenthal, D. (2016). Better health care: A way forward. Journal of American Medical
Association, 315, 1333-1334. doi:10.1001/jama.2016.0590

94
Boddy, C. R. (2016). Sample size for qualitative research. Qualitative Market
Research, 19, 426-432. doi:10.1108/QMR-06-2016-0053
Boden, T. W. (2014). Fighting the "golden rule". The Journal of Medical Practice
Management: MPM, 30(3), 201-202. Retrieved from https://greenbranch.com
Bourne, B. (2015). Phenomenological study of generational response to organizational
change. Journal of Managerial Issues, 27(1-4), 141-159. Retrieved from
https://www.questia.com
Bradbury, C. J. (2015). Determinants of physicians’ acceptance of new Medicaid
patients. Atlantic Economic Journal, 43, 247-260. doi:10.1007/s11293-015-9454-
6
Bradbury-Jones, C., Taylor, J., & Herber, O. (2014). How theory is used and articulated
in qualitative research: Development of a new typology. Social Science &
Medicine, 120, 135-141. doi:10.1016/j.socscimed.2014.09.014
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative
Research in Psychology, 3, 77-101. doi:10.1191/1478088706qp063oa
Brett, J., Staniszewska, S., Mockford, C., Herron-Marx, S., Hughes, J., Tysall, C., &
Suleman, R. (2014). Mapping the impact of patient and public involvement on
health and social care research: A systematic review. Health Expectations, 17,
637-650. doi:10.1111/j.1369-7625.2012.00795.x
Brooks, M. C., & Jean-Marie, G. (2015). The challenges to and the need for international
research in educational leadership. International Journal of Educational
Management, 29, 874-887. doi:10.1108/IJEM-05-2015-0069

95
Campbell, D. T., Manns, B. J., Hemmelgarn, B. R., Sanmartin, C., & King-Shier, K. M.
(2016). Development of a conceptual framework for understanding financial
barriers to care among patients with cardiovascular-related chronic disease: A
protocol for a qualitative (grounded theory) study. Canadian Medical Association
Journal Open, 4, 304-308. doi:10.9778/cmajo.20160030
Caretta, M. A., & Riaño, Y. (2016). Feminist participatory methodologies in geography:
Creating spaces of inclusion. Qualitative Research, 16, 258-266. doi:10.1177/
1468794116629575
Carter, N., Bryant-Lukosius, D., DiCenso, A., Blythe, J., & Neville, A. J. (2014). The use
of triangulation in qualitative research. Oncology Nursing Forum, 41, 545-547.
doi:10.1188/14.ONF.545-547. Retrieved from
Cascardo, D. (2018). The importance of a revenue cycle game plan is that your revenue
team manages it. The Journal of Medical Practice Management : MPM, 33, 231-
233. Retrieved from https:// greenbranch.com
Cascardo, D. (2015). Physician challenges in 2015. The Journal of Medical Practice
Management: MPM, 30, 395-398. Retrieved from https:// greenbranch.com
Cassel, J. B., Kerr, K. M., Kalman, N. S., & Smith, T. J. (2015). The business case for
palliative care: Translating research into program development in the US. Journal
of Pain and Symptom Management, 50, 741-749.
doi:10.1016/j.jpainsymman.2015.06.013
Chahal, H., & Dutta, K. (2015). Measurement and impact of customer experience in
banking sector. Decision, 42(1), 57-70. doi:10.1007/s40622-014-0069-6

96
Chandra, Y., & Shang, L. (2017). An RQDA-based constructivist methodology for
qualitative research. Qualitative Market Research, 20, 90-112. doi:10.1108/QMR-
02-2016-0014
Chang, C. (2017). Methodological issues in advertising research: Current status, shifts,
and trends. Journal of Advertising, 46(1), 2-20. doi:10.1080/00 913367.2016.127
4924
Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative
research. London, England: Sage.
Chavira, D. A., Bustos, C. E., Garcia, M. S., Ng, B., & Camacho, A. (2017). Delivering
CBT to rural Latino children with anxiety disorders: A qualitative study.
Community Mental Health Journal, 53, 53-61. doi:10.1007/s10597-015-9903-3
Chen, A., & Goldman, D. (2016). Health care spending: Historical trends and new
directions. Annual Review of Economics, 8, 291-319. doi:10.1146/annurev-
economics-080315-015317
Chen, J., O’Brien, M. J., Mennis, J., Alos, V. A., Grande, D. T., Roby, D. H., & Ortega,
A. N. (2015). Latino population growth and hospital uncompensated care in
California. American Journal of Public Health, 105, 1710-1717.
doi:10.2105/AJPH.2015.302583
Chiarini, A., & Vagnoni, E. (2017). TQM implementation for the health care sector. the
relevance of leadership and possible causes of lack of leadership. Leadership in
Health Services, 30, 210-216. doi:10.1108/LHS-02-2017-0004

97
Choi, A., Lai, D., Lai, T. (2016). Health analytics, economics and medicine toward a
21st Century health care system. Health, 8, 428-443.
doi:10.4236/health.2016.85046
Chokshi, D. A., Chang, J. E., & Wilson, R. M. (2016). Health reform and the changing
safety net in the United States. The New England Journal of Medicine, 375, 1790-
1796. doi:10.1056/NEJMhpr1608578
Chowdhury, M. F. (2015). Coding, sorting and sifting of qualitative data analysis:
Debates and discussion. Quality and Quantity, 49, 1135-1143.
doi:10.1007/s11135-014-0039-2
Christensen, J. K. B. (2016). Does telecare improve interorganisational collaboration?
International Journal of Integrated Care, 16(4). 1-10. doi:10.5334/ijic.2462
Christoun, L. (2015). Prioritizing key academic support systems for Latino English
language learners in Northern Illinois public school districts. Academy of
Educational Leadership Journal, 19(3), 63-83. Retrieved from
https://www.abacademies.org/journals/academy-of-educational-leadership-
journal-home.html
Cleary, M., Horsfall, J., & Hayter, M. (2014). Data collection and sampling in qualitative
research: Does size matter? Journal of Advanced Nursing, 70, 473-475.
doi:10.1111/jan.12163
Colorafi, K. J., & Evans, B. (2016). Qualitative descriptive methods in health science
research. HERD: Health Environments Research & Design Journal, 9(4), 16-25.
doi:10.1177/1937586715614171

98
Connelly, L. M. (2013). Limited section. MEDSURG Nursing, 22(5), 325-336. Retrieved
from http://www.medsurgnursing.net
Conrad, D. A., Vaughn, M., Grembowski, D., & Marcus-Smith, M. (2016). Implementing
value-based payment reform: A conceptual framework and case examples.
Medical Care Research and Review, 73, 437-457. doi:10.1177/10775587156157
74
Coupet, J., & McWilliams, A. (2017). Integrating organizational economics and resource
dependence theory to explain the persistence of quasi markets. Administrative
Sciences, 7(3), 1-13. doi:10.3390/admsci7030029
Crowe, M., Inder, M., & Porter, R. (2015). Conducting qualitative research in mental
health: Thematic and content analyses. Australian & New Zealand Journal of
Psychiatry, 49, 616-623. doi:10.1177/0004867415582053
Cullington, H., Kitterick, P., DeBold, L., Weal, M., Clarke, N., Newberry, E., & Aubert,
L. (2016). Personalised long-term follow-up of cochlear implant patients using
remote care, compared with those on the standard care pathway: Study protocol
for a feasibility randomized controlled trial. British Medical Journal Open, 6(5),
1-9. doi:10.1136/bmj open-2016-011342
Cylus, J., Papanicolas, I., & Smith, P. C. (2016). A framework for thinking about health
system efficiency. Health System Efficiency, 46(1), 1-20. Retrieved from
https://www.ncbi.nlm.nih.gov

99
Cypress, B. S. (2017). Rigor or reliability and validity in qualitative research:
Perspectives, strategies, reconceptualization, and recommendations. Dimensions
of Critical Care Nursing, 36, 253-263. doi:10.1097/DCC.0000000000000253
D’Andrea, R., & O’Dwyer, J. P. (2017). Can editors save peer review from peer
reviewers? Public Library of Science One, 12(10), 1-14.
doi:10.1371/journal.pone.0186111
Darrow, W. W. (2015). The decline and disorganization of public health in the United
States: Social implications. The International Journal of Social Quality, 5, 29-45.
doi:10.3167/IJSQ.2015.050203
DeFelice, D., & Janesick, V. J. (2015). Understanding the marriage of technology and
phenomenological research: From design to analysis. The Qualitative
Report, 20(10), 1576-1593. Retrieved fromhttp://nsuworks.nova.edu/tqr
Deming, W. E. (2000). Out of the crisis. Cambridge, MA. MIT press.
Deming, W. E. (1985). Transformation of western style of management. Interfaces,
15(3), 6-11. doi:10.1287/inte.15.3.6
Denzin, N. K., & Lincoln, Y. S. (Eds.). (2011). The Sage handbook of qualitative
research (4th ed.). Thousand Oaks, CA: Sage.
Desmond, J. (2014). Ethnography as ethics and epistemology: Why American studies
should embrace fieldwork, and why it hasn't. American Studies, 53(1), 27-56.
Retrieved from https://journals.ku.edu/amerstud/
Dong, G. N. (2016). Earnings management in U.S. hospitals. Journal of Health and
Human Services Administration, 39(1), 41-71. https://jhhsa.spaef.org

100
Dong, G. N. (2015). Performing well in financial management and quality of care:
Evidence from hospital process measures for treatment of cardiovascular
disease. BMC Health Services Research, 15(1), 1-15. doi:10.1186/s12913-015-
0690-x
Doran, T., Maurer, K. A., & Ryan, A. M. (2017). Impact of provider incentives on quality
and value of health care. Annual Review of Public Health, 38, 449-465.
doi:10.1146/annurev-publhealth-032315-021457
Dorsey, S., Conover, K. L., & Revillion-Cox, J. (2014). Improving foster parent
engagement: Using qualitative methods to guide tailoring of evidence-based
engagement strategies. Journal of Clinical Child and Adolescent Psychology,
53, 877-889. doi:10.1080/15374416.2013.876643
Doyle, G., Kelly, R., & O’Donohoe, S. (2016). Resource dependence as a mechanism for
survival: The case of the mater Misericordiae university hospital. Voluntas:
International Journal of Voluntary and Nonprofit Organizations, 27, 1871-1893.
doi:10.1007/s11266-016-9735-y
Dubois, A., & Gadde, L. E. (2014). “Systematic combining”-A decade later. Journal of
Business Research, 67, 1277-1284. doi:10.1016/j.jbusres.2013.03.036
Duijmelinck, D., & van de Ven, W. (2016). What can Europe learn from the managed
care backlash in the United States? Health Policy, 120, 509-518.
doi:10.1016/j.healthpol.2016.03.010
Durenberger, S. D. (2015). Health care reform and the American congress. The Milbank
Quarterly, 93, 663-666. doi:10.1111/1468-0009.12155

101
Eggbeer, B., & Bowers, K. (2014). Health care's new game changer. Thinking like a
health plan. Health care Financial Management: Journal of The Health Care
Financial Management Association, 68(10), 52-59. Retrieved from
https://www.hfma.org
Eisenhardt, K. M., Graebner, M. E., & Sonenshein, S. (2016). Grand challenges and
inductive methods: Rigor without rigor mortis. Academy Of Management
Journal, 59, 1113-1123. doi:10.5465/amj.2016.4004
Eriksson, D. (2015). Lessons on knowledge creation in supply chain management.
European Business Review, 27(4), 346-368. Retrieved from
http://www.europeanbusinessreview.com/
Evans, J. M., Brown, A., & Baker G. R. (2015). Intellectual capital in the health care
sector: A systematic review and critique of the literature. BMC Health Services
Research, 15(1), 1-14. doi:10.1186/s12913-015-1234-0
Fairfield, J., & Shtein, H. (2014). Big data, big problems: Emerging issues in the ethics of
data science and journalism. Journal of Mass Media Ethics, 29, 38-51.
doi:10.1080 08900523.2014.863126
Farnsworth, S. S. (2015). Enduring conflicts in the American health care system. The
Journal of Health Administration Education, 32(2), 159-164. Retrieved from
http://www.aupha.org
Feldman, R. (2015). The economics of provider payment reform: Are accountable care
organizations the answer? Journal of Health Politics, Policy & Law, 40, 745-760.
doi:10.1215/03616878-3150038

102
Ferlie, E., Crilly, T., Jashapara, A., Trenholm, S., Peckham, A., & Currie, G. (2015).
Knowledge mobilization in health care organizations: A view from the resource-
based view of the firm. International Journal of Health Policy and Management,
4, 127-130. doi:10.15171/ijhpm.2015.35
Fida, R., Tramontano, C., Paciello, M., Kangasniemi, M., Sili, A., Bobbio, A., &
Barbaranelli, C. (2016). Nurse moral disengagement. Nursing Ethics, 23, 547-
564. doi:10.1177/0969733015574924
Fitzpatrick, P. G., Butler, M., Pitsikoulis, C., Smith, K., & Walden, L. (2014). The case
for integrating health care management courses into the curricula of selected
health care providers. Journal of Management Policy & Practice, 15(4), 92-102.
Retrieved from http://www.na-businesspress.com/jmppopen.html
Fitzsimmons, A. P. (2017). Soldier readiness: Past to present, initial entry training.
Journal of Leadership, Accountability and Ethics, 14(2), 117-122. Retrieved from
http://www.na-businesspress.com/JLAE/jlaescholar.html
Fletcher, A. J. (2017). Applying critical realism in qualitative research: Methodology
meets method. International Journal of Social Research Methodology, 20, 181-
194. doi:10.1080/13645579.2016.1144401
Foerster, S., Tsagarelis, J., & Wang, G. (2017). Are cash flows better stock return
predictors than profits? Financial Analysts Journal, 73(1), 73-99.
doi:10.2469/faj.v73.n1.2
Forsythe, L. P., Ellis, L. E., Edmundson, L., Sabharwal, R., Rein, A., Konopka, K., &
Frank, L. (2016). Patient and stakeholder engagement in the PCORI pilot projects:

103
Description and lessons learned. Journal of General Internal Medicine, 31(1), 13-
21. doi:10.1007/s11606-015-3450-z
Foundation Center. (2018). 990 form. Retrieved from http://foundationcenter.org/find-
funding/990-finder
Fowler, E. A. R., Coffey, B. S., & Dixon-Fowler, H. (2017). Transforming good
intentions into social impact: A case on the creation and evolution of a social
enterprise. Journal of Business Ethics 146, 1-14. doi:10.1007/s10551-017-3754-5
Franz, B. A., Skinner, D., & Murphy, J. W. (2016). Changing medical relationships after
the ACA: Transforming perspectives for population health. SSM-Population
Health, 2, 834-840. doi:10.1016/j.ssmph.2016.10.015
Fugard, A. J., & Potts, H. W. (2015). Supporting thinking on sample sizes for thematic
analyses: A quantitative tool. International Journal of Social Research
Methodology, 18, 669-684. doi:10.1080/13645579.2015.1005453
Fusch, P. I., & Ness, L. R. (2015). Are we there yet? Data saturation in qualitative
research. The Qualitative Report, 20(9), 1408-1416. Retrieved from
http://nsuworks.nova.edu/tqr/
Gallagher, S., Phillips, A. C., Lee, H., & Carroll, D. (2015). The association between
spirituality and depression in parents caring for children with developmental
disabilities: Social support and/or last resort. Journal of Religion and Health, 54,
358-370. doi:10.1007/s10943-014-9839-x

104
Gao, Y. N., Nocon, R. S., Sharma, R., & Huang, E. S. (2017). What factors are associated
with Medicaid patients’ use of health centers? Journal of Primary Care &
Community Health, 8, 141-146. doi:10.1177/2150131916687919
Gentles, S. J., Charles, C., Ploeg, J., & McKibbon, K. A. (2015). Sampling in qualitative
research: Insights from an overview of the methods literature. The Qualitative
Report, 20(11), 1772-1789. Retrieved from http://nsuworks.nova.edu/tqr/
Gerben, D. (2016). Coming to terms with the IMPACT Act of 2014. The American
Journal of Occupational Therapy, 70(3), 1-6. doi:10.5014 /ajot .2016.703003
Gerber, J. D., & Hess, G. (2017). From landscape resources to landscape commons:
Focusing on the non-utility values of landscape. International Journal of the
Commons, 11. 708-732. doi:10.18352/ijc.745
Gerstorff, J. L., & Gibson, S. (2016). Medicaid encounter data: The next national data set.
Milliman, 6-14. Retrieved from http://us.milliman.com/
Gligor, D. M., Esmark, C. L., & Gölgeci, I. (2016). Building international business
theory: A grounded theory approach. Journal of International Business Studies,
47, 93-111. doi:10.1057/jibs.2015.35
Glied, S., & Jackson, A. (2017). The future of the Affordable Care Act and insurance
coverage. American Journal of Public Health, 107, 538-540.
doi:10.2105/AJPH.2017.303665
Gordon, E. J., Mullee, J., Skaro, A., & Baker, T. (2016). Live liver donors’ information
needs: A qualitative study of practical implications for informed consent.
Surgery, 160, 671-682. doi:10.1016/j.surg.2016.04.022

105
Goyal, S., Sergi, B. S., & Kapoor, A. (2014). Understanding the key characteristics of an
embedded business model for the base of the pyramid markets. Economics &
Sociology, 7(4), 26-40. doi:10.14254/2071-789X.2014/7-4/2
Graham, A., Powell, M. A., & Truscott, J. (2016). Exploring the nexus between
participatory methods and ethics in early childhood research. Australasian
Journal of Early Childhood, 41(1), 82-89. Retrieved from
http://earlychildhoodaustralia.org.au
Granata, R. L., & Hamilton, K. (2015). Exploring the effect of at-risk case management
compensation on hospital pay-for-performance outcomes: Tools for change.
Professional Case Management, 20(1), 14-27.
doi:10.1097/NCM.0000000000000067
Grant, A. (2014). Troubling 'lived experience': A post-structural critique of mental health
nursing qualitative research assumptions. Journal of Psychiatric and Mental
Health Nursing, 21, 544-549. doi:10.1111/jpm.12113
Guba, E. G., & Lincoln, Y. S. (1994). Competing paradigms in qualitative
research. Handbook of qualitative research. Thousand Oaks, CA: Sage
Gurganious, V. S. (2016). Four simple steps to conduct an assessment of your practice.
The Journal of Medical Practice Management: MPM, 31(6), 329-331. Retrieved
from Retrieved from https:// greenbranch.com
Haeder, S. F., & Weimer, D. L. (2015). Inching toward universal coverage: State-federal
health-care programs in historical perspective. Journal of Policy History, 27, 746-
770. doi:10.1017/S0898030615000330

106
Halcomb, E., & Peters, K. (2016). Research would not be possible without participants.
Nurse Researcher, 24(1), 6-7. doi:10.7748/nr.24.1.6.s2
Halfon, N., Long, P., Chang, D., Hester, J., Inkelas, M., & Rodgers, A. (2014). Applying
a 3.0 transformation framework to guide large-scale health system reform. Health
Affairs, 33, 2003-2011. doi:10.1377/hlthaff.2014.0485
Hall, M. A., & Lord, R. (2014). Obamacare: What the Affordable Care Act means for
patients and physicians. British Medical Journal, 349, 1-10.
doi:10.1136/bmj.g5376
Harvey, G., & Kitson, A. (2015). Necessary but not sufficient: Comment on "knowledge
mobilization in health care organizations: A view from the resource-based view of
the firm". International Journal of Health Policy and Management, 4, 865-868.
doi:10.15171/ijhpm.2015.159
Harvey, L. (2015). Beyond member-checking: A dialogic approach to the research
interview. International Journal of Research & Method in Education, 38(1), 23-
38. doi:10.1080/1743727X.2014.914487
Hasle, P., Limborg, H. J., Grøn, S., & Refslund, B. (2017). Orchestration in work
environment policy programs. Nordic Journal of Working Life Studies, 7(3), 43-
62. doi:10.18291/njwls.v7i3.97092
Hay-Smith, E. J. C., Brown, M., Anderson, L., & Treharne, G. J. (2016). Once a
clinician, always a clinician: A systematic review to develop a typology of
clinician-researcher dual-role experiences in health research with patient-

107
participants. BMC medical research methodology, 16(1), 1-17. doi:10.1186/s1287
4-016-0203-6
Hayes, D., Subhan, Z., & Lakatos, J. (2015). Encompass software: Getting started, The
first months and fueling growth. Journal of the International Academy for Case
Studies, 21(5), 83-91. Retrieved from http://www.abacademies.org
Health Resources and Service Administration (2018) Health data center. Retrieved from
https://bphc.hrsa.gov/datareporting/index.html
Hegwer, L. R. (2014). 5 strategies for combating market uncertainty to deliver value:
Innovative health systems are taking aggressive approaches as they prepare for
value-based business models and other changes ahead. Health Care Financial
Management, 68(10), 74-82. Retrieved from https://www.ncbi.nlm.nih.gov
Heisler, E., Firmin, M. W., Firmin, R. L., & Hundley, A. E. (2015). Intrinsic values that
affect men's motivation to participate in female abuse prevention. North American
Journal of Psychology, 17(2), 267-285. Retrieved from http://najp.us/
Helmig, B., Hinz, V., & Ingerfurth, S. (2015). Valuing organizational values: Assessing
the uniqueness of nonprofit values. Voluntas: International Journal of Voluntary
& Nonprofit Organizations, 26, 2554-2580. doi:10.1007/s11266-014-9530-6
Hernandez, N. (2017). Essential financial metrics. Journal of Medical Practice
Management, 32(6), 387-389. Retrieved from https://www.ncbi.nlm.nih.gov
Hinnekens, C., Vanhee, G., De Schryver, M., Ickes, W., & Verhofstadt, L. L. (2016).
Empathic accuracy and observed demand behavior in couples. Frontiers in
Psychology, 7, 1-5. doi:10.3389/fpsyg.2016.01370

108
Hitt, M. A., Xu, K., & Carnes, C. M. (2016). Resource based theory in operations
management research. Journal of Operations Management, 41, 77-94.
doi:10.1016 /j.jom.2015.11.002
Holm, A. L., & Severinsson, E. (2014). Surviving depressive ill‐ health: A qualitative
systematic review of older persons' narratives. Nursing & Health Sciences, 16,
131-140. doi:10.1111/nhs.12071
Howrigon, R. (2016). Payer negotiations in the new health care environment: How to
prepare for and succeed in a value-based world. The Journal of Medical Practice
Management: MPM, 31(6), 354-356. Retrieved from https://greenbranch.com
Iancu, S. C., Zweekhorst, M. B., M., Veltman, D. J., & van Balkom, A. J. (2015).
Outsourcing mental health care services? The practice and potential of
community-based farms in psychiatric rehabilitation. Community Mental Health
Journal, 51, 175-184. doi:10.1007/s10597-014-9742-7
Iqbal, J., Shabbir, M. S., Zameer, H., Tufail, M. S., Sandhu, M. A., & Ali, W. (2017).
TQM practices and firm performance of Pakistani service sector firms.
Paradigms, 11(1), 87-96. Retrieved from http://paradigms.ucp.edu.pk/
Isaacs, A. N. (2014). An overview of qualitative research methodology for public health
researchers. International Journal of Medicine & Public Health, 4, 318-323.
doi:10.4103/2230-8598.144055
Jain, A. K., & Singal, A. K. (2014). Mapping vulnerability: How emerging markets
respond to multinationals. Journal of Business Strategy, 35, 41-48.
doi:10.1108/JBS-11-2013-0112

109
Jaimangal-Jones, D. (2014). Utilizing ethnography and participant observation in festival
and event research. International Journal of Event and Festival Management,
5(1), 39-55. Retrieved from http://www.ijemr.org
Jali, M. N., Abas, Z., & Ariffin, A. S. (2016). Social innovation: A new paradigm of
innovation outcome strategy in the context of strategic knowledge management
processes. Sains Humanika, 8, 47-50. doi:10.1108/JBS-11-2013-0112
Joe, J. R, Young, R. S., Moses, J. Knoki-Wilson, U., & Dennison, J. (2016). A
collaborative case study: The office of native medicine. American Indian and
Alaska Native Mental Health Research (Online), 23(2), 50-63. Retrieved from
http://www.ucdenver.edu/academic s/colleges
Johnson, J. E., & Garvin, W. S. (2017). Advanced practice nurses: Developing a business
plan for an independent ambulatory clinical practice. Nursing Economics, 35(3),
126-141. Retrieved from http://www.nursingeconomics.net
Jones, E. B., & Ku, L. (2015). Sharing a playbook: Integrated care in community health
centers in the United States. American Journal of Public Health, 105, 2028-2034.
doi:10.2105/AJPH.2015.302710
Joynt, K. E., De Lew, N., Sheingold, S. H., Conway, P. H., Goodrich, K., & Epstein, A.
M. (2017). Should medicare value-based purchasing take social risk into account?
New England Journal of Medicine, 376, 510-513. doi:10.105 6/N EJM p1616278
Joynt, K. E., Orav, E. J., & Jha, A. K. (2014). Association between hospital conversions
to for-profit status and clinical and economic outcomes. Journal of American
Medical Association, 312, 1644-1652. doi:10.1001/jama.2014.13336.

110
Jung-Sik, W., & Han-Sung, K. (2016). Study of in-patient cost analysis using hospital
database in Korea. International Journal of Database Theory and
Application, 9(11), 107-118. Retrieved from http://www.sersc.org
Karen, C. O., Kennedy, D. P., Hunter, S. B., & Maksabedian, E. (2016). Feasibility of a
computer-assisted social network motivational interviewing intervention for
substance use and HIV risk behaviors for housing first residents. Addiction
Science & Clinical Practice, 11(1), 1-11. doi:10.1186/s13722-016-0061-x
Kash, B. A., Spaulding, A., Gamm, L. D., & Johnson, C. E. (2014). Health care strategic
management and the resource based view. Journal of Strategy & Management, 7,
251-264. doi:10.1108/JSMA-06-2013-0040
Katigbak, C., Foley, M., Robert, L., & Hutchinson, M. K. (2016). Experiences and
lessons learned in using community‐ based participatory research to recruit Asian
American immigrant research participants. Journal of Nursing Scholarship, 48,
210-218. doi:10.1111/jnu.12194
Kemperman, J., Geelhoed, J., & In Hoog, J. (2017). Brilliant business models in health
care: Get inspired to cure health care. Switzerland: Springer.
Kessell, E., Pegany, V., Keolanui, B., Fulton, B., Scheffler, R., & Shortell, S. (2015).
Review of Medicare, Medicaid, and commercial quality of care measures:
Considerations for assessing accountable care organizations. Journal of Health
Politics Policy and Law, 40, 761-796. doi:10.1215/03616878-3150050.
Khan, S. N. (2014). Qualitative research method: Grounded theory. International Journal
of Business and Management, 9, 224-233. doi:10.5539/ijbm.v9n11p224

111
Krzakiewicz, K., & Cyfert, S. (2017). Dynamic capabilities in strategic choice processes
within organizations. Management, 21(1), 7-19. doi:10.1515/manment-2015-0077
Kuramoto, R. (2014). Specialties: Missing in our health care reform strategies? Journal
of Health care Management, 59(2), 89-94. Retrieved from https://www.ache.org
Lai, C. J., & Gelb, B. D. (2015). Key account teams: Success factors for implementing
strategy. Journal of Business Strategy, 36, 48-55. doi:10.1108/JBS-07-2014-0079
Lail, P. J., Laird, S. S., McCall, K., Naretto, J., & York, A. (2016). Facility closure: How
to get in, get out, and get what is important. Perspectives in Health Information
Management, 13(1). 1-11. Retrieved from http://perspectives.ahima.org/
Landers, S., Madian, E., Leff, B., Rosati, R. J., McCann, B. A., Hornbake, R., & Breese,
E. (2016). The future of home health care: A strategic framework for optimizing
value. Home Health Care Management & Practice, 28, 262-278.
doi:10.1177/1084822316666368.
Langellier, B. A., de Zapien, J. G., Rosales, C., Ingram, M., & Carvajal, S. C. (2014).
State medicaid expansion, community interventions, and health care disparities in
a United States–Mexico border community. American Journal of Public
Health, 104, 94-100. doi:10.2105/AJPH.2014.302013
Larkin, D. J., Swanson, R. C., Fuller, S., & Cortese, D. A. (2016). The Affordable Care
Act: A case study for understanding and applying complexity concepts to health
care reform. Journal of Evaluation in Clinical Practice, 22, 133-140.
doi:10.1111/jep.12271

112
Lee, J. (2017). A review of competitive repertoire-action-based competitive advantage.
International Journal of Business and Management, 12, 120-129.
doi:10.5539/ijbm.v12n11p120
Lee, N. S. (2015). Framing choice: The origins and impact of consumer rhetoric in US
health care debates. Social Science & Medicine, 138, 136-143.
doi:10.1016/j.socscimed.2015.06.007
Leemon, J. (2014). Medicaid under the affordable care act: Fixing the gaps before the
revolution. Public Contract Law Journal, 43(2), 333-351. Retrieved from
http://pclj.org
LeFevre, A. E., Shillcutt, S. D., Broomhead, S., Labrique, A. B., & Jones, T. (2017).
Defining a staged-based process for economic and financial evaluations of
mHealth programs. Cost Effectiveness and Resource Allocation, 15(1), 1-16.
doi:10.1186/s12962-017-0067-6
Leung, L. (2015). Validity, reliability, and generalizability in qualitative research.
Journal of Family Medicine & Primary Care, 4, 324-327. doi:10.4103 /2249-
4863.161306
Lidén, E., & Yaghmaiy, K. S. (2017). The meaning of encounters with health
professionals in primary health care as reported by patients with medically
unexplained symptoms. Nordic Journal of Nursing Research, 37, 70-77.
doi:10.1177/2057158516671449

113
Li, L., Jiang, F., Pei, Y., & Jiang, N. (2017). Entrepreneurial orientation and strategic
alliance success: The contingency role of relational factors. Journal of Business
Research, 72, 46-56. doi:10.1016/j.jbusres.2016.11.011
Lillis, B., Szwejczewski, M., & Goffin, K. (2015). The development of innovation
capability in services: Research propositions and management implications.
Operations Management Research, 8, 48-68. doi:10.1007/s12063-015-0099-z
Lin, C. S., Chang, R. Y., & Dang, V. T. (2015). An integrated model to explain how
corporate social responsibility affects corporate financial performance.
Sustainability, 7, 8292-8311. doi:10.3390/su7078292.
Lin, C., Han, C., & Pan, I. (2015). A qualitative approach of psychosocial adaptation
process in patients undergoing long-term hemodialysis. Asian Nursing Research,
9(1), 35-41. doi:10.1016/j.anr.2014.10.007
Liu, Y., Zhu, Q., & Seuring, S. (2017). Linking capabilities to green operations strategies:
The moderating role of corporate environmental proactivity. International
Journal of Production Economics, 187, 182-195. doi:10.1016/j.ijpe.2017.03.007
Loy, A, Shkedy C. I., Powell A. C., Happe, L. E., Royalty, J. A., & Miao, M. T. (2016).
Do case rates affect physicians' clinical practice in radiation oncology? An
observational study. Public Library of Science ONE, 11(2), 1-9.
doi:10.1371/journal.pone.0149449
Lubberink, R., Blok, V., van Ophem, J., & Omta, O. (2017). Lessons for responsible
innovation in the business context: A systematic literature review of responsible,
114
social and sustainable innovation practices. Sustainability, 9(5), 1-31.
doi:10.3390/su9050721
Mabotuwana, T., Hall, C. S., Thomas, S., & Wald, C. (2017). A model to determine
payments associated with radiology procedures. International Journal of Medical
Informatics, 108, 71-77. doi:10.1016/j.ijmedinf.2017.09.012
Makola, S. (2015). The effectiveness of a meaning-centered intervention in protecting the
well-being HIV/AIDS health educators. Systemic Practice and Action Research,
28(1), 37-49. doi:10.1007/s11213-014-9321-4
Manchikanti, L., Helm, I. S., Benyamin, R. M., & Hirsch, J. A. (2017). Evolution of US
health care reform. Pain Physician, 20(3), 107-110. Retrieved from
http://www.painphysicianjournal.com/
Manning, J., & Kunkel, A. (2015). Qualitative approaches to dyadic data analyses in
family communication research: An invited essay. Journal of Family
Communication, 15, 185-192. doi:10.1080/15267431.2015.1043434
Marshall, C., & Rossman, G. B. (2016). Designing qualitative research (6th ed.).
Thousand Oaks, CA: Sage.
Marshall, A., Nazroo, J., Feeney, K., Lee, J., Vanhoutte, B., & Pendleton, N. (2016).
Comparison of hypertension health care outcomes among older people in the
USA and England. Journal of Epidemiology and Community Health, 70, 264-270.
doi:10.1136/jech-2014-205336
Mason, D. J. (2017). Professionalism in health care organizations. Journal of the
American Medical Association, 317, 1203-1204. doi:10.1001/jama.2017.1753

115
Matthews, R. L., & Marzec, P. E. (2017). Continuous, quality and process improvement:
Disintegrating and reintegrating operational improvement? Total Quality
Management & Business Excellence, 28, 296-317.
doi:10.1080/14783363.2015.1081812
Maurer, M., Mangrum, R., Carman, K. L., Ginsburg, M., Gold, M. R., Sofaer, S., &
Siegel, J. (2017). Setting boundaries: Public views on limiting patient and
physician autonomy in health care decisions. Journal of Health Politics, 42, 579-
605. doi:10.1215/03616878-3856079
Maurer, K. A., & Ryan, A. M. (2016). No hospital left behind? Education policy lessons
for value‐ based payment in health care. Journal of Hospital Medicine, 11, 62-64.
doi:10.1002/jhm.2483
Mayhew, D. R. (2015). Congress as a handler of challenges: The historical record.
Studies in American Political Development, 29, 185-212. doi:10.1017/S0898588
X15000061
McCalman, J., Heyeres, M., Campbell, S., Bainbridge, R., Chamberlain, C., Strobel, N.,
& Ruben, A. (2017). Family-centered interventions by primary health care
services for indigenous early childhood wellbeing in Australia, Canada, New
Zealand and the United States: A systematic scoping review. BMC Pregnancy and
Childbirth, 17(1), 1-21. doi:10.1186/s12884-017-1247-2
McGhie-Anderson, R. (2017). Advanced nursing education: Critical factors that influence
diploma and associate degree nurses to advance. Nursing Education
Perspectives, 38(6), 1-6. doi:10.1097/01.NEP.000000000000022

116
McInnes, S., Peters, K., Bonney, A., & Halcomb, E. (2017). An exemplar of naturalistic
inquiry in general practice research. Nurse Researcher 24(3), 1-10.
doi:10.7748/nr.2017 .e1509
McNaughton, R. J., Adams, J., & Shucksmith, J. (2016). Acceptability of financial
incentives or quasi-mandatory schemes to increase uptake of immunizations in
preschool children in the United Kingdom: Qualitative study with parents and
service delivery staff. Vaccine, 34, 2259-2266. doi:10.1016/j.vaccine.2016.03.009
McNulty, Y. (2015). Till stress do us part: The causes and consequences of expatriate
divorce. Journal of Global Mobility, 3, 106-136. doi:10.1108/JGM-06-2014-0023
Mertens, D. M., Bazeley, P., Bowleg, L., Fielding, N., Maxwell, J., Molina-Azorin, J. F.,
& Niglas, K. (2016). Expanding thinking through a kaleidoscopic look into the
future: Implications of the mixed methods international research association’s
task force report on the future of mixed methods. Journal of Mixed Methods
Research, 10, 221-227. doi:10.1177/1558689816649719
Mindel, V., & Mathiassen, L. (2015). Contextualist inquiry into IT-enabled hospital
revenue cycle management: Bridging research and practice. Journal of the
Association for Information Systems, 16(12), 1016-1057. Retrieved from
https://aisel.aisnet.org
Mkanta, W. N., Katta, M., Basireddy, K., English, G., & de Grubb, M. M. (2016).
Theoretical and methodological issues in research related to value-based
approaches in health care. Journal of Health care Management, 61(6), 402-418.
Retrieved from http://journals.lww.com/jhmonline

117
Mlinar, S., Petek, D., Cotic, Z., Metka, M. C., & Zaletel, M. (2016). Persons with
epilepsy: Between social inclusion and marginalisation. Behavioural Neurology
2016, 1-10. doi:10.1155/2016/2018509
Moraros, J., Lemstra, M., & Nwankwo, C. (2016). Lean interventions in health care: Do
they actually work? A systematic literature review. International Journal for
Quality in Health Care, 28, 150-165. doi:10.1093/intqhc/mzv123
Mosadeghrad, A. M. (2015). Developing and validating a total quality management
model for health care organizations. Total Quality Management Journal, 27,
544-564. doi:10.1108/TQM-04-2013-0051
Morgado, F. F., Meireles, J. F., Neves, C. M., Amaral, A. C., & Ferreira, M. E. (2017).
Scale development: Ten main limitations and recommendations to improve future
research practices. Psicologia: Reflexão e Crítica, 30(1), 1-20.
doi:10.1186/s41155-016-0057-1
Mountford, N., & Kessie, T. (2017). Towards a more holistic understanding of whole
organizational networks: Anthropological approaches in evolving markets.
Electronic Journal of Business Research Methods, 15(2), 74-84. Retrieved from
http://www.ejbrm.com
Moustakas, C. (1994). Phenomenological research methods. Thousand Oaks, CA: Sage.
Munn, Z., Porritt, K., Lockwood, C., Aromataris, E., & Pearson, A. (2014). Establishing
confidence in the output of qualitative research synthesis: The ConQual
approach. BMC Medical Research Methodology, 14, 108-114. doi:10.1186/1471-
2288-14-108

118
Murphy, J., Ko, M., Kizer, K., & Bindman, A. (2015). Safety net integration: A shared
strategy for becoming providers of choice. Journal of Health Politics Policy and
Law, 40, 403-419. doi:10.1215/03616878-2882267
Mweru, M. C., & dan Muya, M. T. (2015). Features of resource based view theory: An
effective strategy in outsourcing. International Journal of Management and
Commerce Innovation, 3(2), 215-218.Retrieved from
http://www.researchpublish.com/journalss/IJMCI
Nardin, R., Zallman, L., Sayah, A., & McCormick, D. (2016). Experiences applying for
and understanding health insurance under Massachusetts health care reform.
International Journal for Equity in Health, 15(1), 1-8. doi:10.1186/s12939-016-
0397-6
Neghina, C., Bloemer, J., van Birgelen, M., & Caniëls, M. J. (2017). Consumer motives
and willingness to co-create in professional and generic services. Journal of
Service Management, 28, 157-181. doi:10.1108/JOSM-12-2015-0404
Nguyen, K. H., & Sommers, B. D. (2016). Access and quality of care by insurance type
for low-income adults before the affordable care act. American Journal of Public
Health, 106, 1409-1415. doi:10.2105/AJPH.2016.303156
Nielsen, S., & Nielsen, E. H. (2015). The balanced scorecard and the strategic learning
process: A system dynamics modeling approach. Advances in Decision Sciences
2015, 1-20. doi:10.1155/2015/213758
Nilsson, U., Jaensson, M., Dahlberg, K., Odencrants, S., Grönlund, Å., Hagberg, L., &
Eriksson, M. (2016). RAPP, A systematic e-assessment of postoperative recovery

119
in patients undergoing day surgery: Study protocol for a mixed-methods study
design including a multicentre, two-group, parallel, single-blind randomized
controlled trial and qualitative interview studies. British Medical Journal
Open, 6(1), 1-7. doi:10.1136/bmjopen-2015-009901
Nocon, R. S., Lee, S. M., Sharma, R., Ngo-Metzger, Q., Mukamel, D. B., Gao, Y., &
Huang, E. S. (2016). Health care use and spending for Medicaid enrollees in
federally qualified health centers versus other primary care settings. American
Journal of Public Health, 106, 1981-1989. doi:10.2105/AJPH.2016.303341
Noether, M., & May, S. (2017). Hospital merger benefits: Views from hospital leaders
and econometric analysis. 2017, 1-24. Retrieved from http://www.crai.com
Noh, S. (2016). Federal strategies to induce resistant states to participate in the ACA
health exchanges. State and Local Government Review, 48, 227-235.
doi:10.1177/0160323X16685371
Oberlander, J. (2017). The end of obamacare. New England Journal of Medicine, 376(1),
1-3. doi:10.1056/NEJMp1614438
Ojeifo, O., & Berkowitz, S. A. (2015). Cardiology and accountable care. Circulation:
Cardiovascular Quality and Outcomes, 8, 213-217. doi:10.1161./114.001482
Oleinik, A. (2015). On content analysis of images of mass protests: A case of data
triangulation. Quality and Quantity, 49, 2203-2220. doi:10.1007/s11135-014-
0104-x

120
Ortiz, J., Meemon, N., Zhou, Y., & Wan, T. H. (2013). Trends in rural health clinics and
needs during U.S. health care reform. Primary Health Care Research &
Development, 14, 360-366. doi:10.1017/S1463423612000503
Ozuru, H. N., & Igwe, P. (2016). Service expertise and marketing success of government
owned hospitals in Rivers state. Journal of Marketing Development, 1, 66-84.
Retrieved from https://jmdcopen.html
Palinkas, L. A., Horwitz, S. M., Green, C. A., Wisdom, J. P., Duan, N., & Hoagwood, K.
(2015). Purposeful sampling for qualitative data collection and analysis in mixed
method implementation research. Administration and Policy in Mental Health and
Mental Health Services Research, 42, 533-544. doi:10.1007/s10488-013-0528-y
Panning, R. (2014). Current status of clinical laboratory reimbursement. Clinical
Laboratory Science: Journal of the American Society for Medical
Technology, 27(2), 119-126. Retrieved from http://www.ascls.org/
Patidar, N., Gupta, S., Azbik, G., & Weech-Maldonado, R. (2016). Succession planning
and financial performance: Does competition matter? Journal of Health care
Management, 61(3), 215-227. Retrieved from http://journals.lww.com/jhmonline/
Patterson, J. J., Smith, C., & Bellamy, J. (2015). Enabling and enacting 'practical action'
in catchments: Responding to the 'wicked problem' of nonpoint source pollution
in coastal subtropical Australia. Environmental Management, 55, 479-495.
doi:10.100 7/s00267-014-0409-5

121
Peng, G. C. A., & Gala, C. (2014). Cloud ERP: A new dilemma to modern organizations?
The Journal of Computer Information Systems, 54(4), 22-30.
doi:10.1080/08874417.2014.11645719
Percy, W. H., Kostere, K., & Kostere, S. (2015). Generic qualitative research in
psychology. The Qualitative Report, 20(2), 76-85. Retrieved from
http://nsuworks.nova.edu/tqr/
Peters, K., & Halcomb, E. (2015). Interviews in qualitative research. Nurse Researcher
22(4), 6-7. doi:10.7748/nr.22.4.6.s2
Petrescu, M., & Lauer, B. (2017). Qualitative marketing research: The state of journal
publications. The Qualitative Report, 22(9), 1-42. Retrieved from
http://nsuworks.nova.edu/tqr/
Pineda, G., & Hermes, F. (2015). Incorporation of the health care system in the
west. Colombia Médica, 46(3), 144-149. Retrieved from
http://colombiamedica.univalle.edu
Pinto, J. (2017). A multifocal framework for developing intentionally sustainable
organizations. Current Opinion in Environmental Sustainability, 28, 17-23.
doi:10.1016/j.cosust.2017.07.002
Pittmam, P., Masselink, L., Bade, L., Frogner, B., & Ku, L. (2016). Factors determining
medical staff configurations in community health centers: CEO perspectives.
Journal of Health care Management, 61(5), 364-378. Retrieved from
http://journals.lww.com/jhmonline

122
Polit, D. F., & Beck, C. T. (2010). Generalization in quantitative and qualitative research:
Myths and strategies. International Journal of Nursing Studies, 47, 1451-1458.
doi:10.1016/j.ijnurstu.2010.06.004
Pompeii, B. (2015). The use of public radio as a tool in qualitative geographic research.
GeoJournal, 80, 791-802. doi:10.1007/s10708-015-9647-1
Popli, M., Ladkani, R. M., & Gaur, A. S. (2017). Business group affiliation and post-
acquisition performance: An extended resource-based view. Journal of Business
Research, 81, 21-30. doi:10.1016/j.jbusres.2017.08.003
Pourghane, P., Ahmadi, F., & Salimi, S. (2017). An exploration in women’s perception of
the use of over-the-counter drugs: A content analysis. Iranian Red Crescent
Medical Journal, 19(1), 1-10. doi:10.5812/ircmj.43364
Power, M. K., & Gendron, Y. (2015). Qualitative research in auditing: A methodological
roadmap. Auditing: A Journal of Practice & Theory, 34, 147-165.
doi:10.2308/ajpt-10423
Pradabwong, J., Braziotis, C., Pawar, K. S., & Tannock, J. (2015). Business process
management and supply chain collaboration: A critical comparison. Logistics
Research, 8(1), 1-20. doi:10.1007/s12159-015-0123-6
Pfeffer, J., & Salancik, G. R. (2003). The external control of organizations: A resource
dependence perspective. Stanford, CA: Stanford University Press.
Prowle, M., & Harradine, D. (2014). Austerity and financial governance: A UK case
study of the National Health Service. International Journal of Public Sector
Management, 27, 212-224. doi:10.1108/IJPSM-02-2013-002

123
Råheim, M., Magnussen, L. H., Sekse, R. J. T., Lunde, Å., Jacobsen, T., & Blystad, A.
(2016). Researcher–researched relationship in qualitative research: Shifts in
positions and researcher vulnerability. International Journal of Qualitative
Studies on Health and Well-Being, 11(1), 1-12. doi:10.3402/qhw.v11.30996
Raman, R., & Pramod, D. (2017). A strategic approach using governance, risk and
compliance model to deal with online counterfeit market. Journal of Theoretical
and Applied Electronic Commerce Research, 12(3), 13-26. doi:10.4067/S0718-
18762017000300003
Rapport, F., Clement, C., Doel, M. A., & Hutchings, H. A. (2015). Qualitative research
and its methods in epilepsy: Contributing to an understanding of patients' lived
experiences of the disease. Epilepsy & Behavior, 45, 94-100.
doi:10.1016/j.yebeh.2015.01.040
Rattani, A., & Johns, A. (2017). Collaborative partnerships and gatekeepers in online
research recruitment. The American Journal of Bioethics, 17(3), 27-29.
doi:10.108/15265161.2016.1274800
Rebs, T., Brandenburg, M., Seuring, S., & Stohler, M. (2017). Stakeholder influences and
risks in sustainable supply chain management: A comparison of qualitative and
quantitative studies. Business Research, 1-41. doi:10.1007/s40685-017-0056-9
Reddy, M. S., & Mythri, S. V. (2016). Health-care ethics and the free market value
system. Indian Journal of Psychological Medicine, 38, 371-375. doi:10.4103/0
253-7176.191387

124
Rich, A., Viney, R., Needleman, S., Griffin, A., & Woolf, K. (2016). 'You can't be a
person and a doctor': The work-life balance of doctors in training-a qualitative
study. British Medical Journal Open, 6(12), 1-9. doi:10.1136/bmjopen-2016-
013897
Roberts, C. J. (2012). Dynamics of health care reform: Bitter pills old and
new. Vanderbilt Journal of Transnational Law, 45(5), 1341-1380. Retrieved from
https://www.vanderbilt.edu/jotl/
Rosado-Serrano, A., Dikova, D., & Paul, J. (2018). International franchising: A literature
review and research agenda. Journal of Business Research, 85, 238-257.
doi:10.1016/j.jbusres.2017.12.04 9
Rose, J., & Lennerholt, C. (2017). Low cost text mining as a strategy for qualitative
researchers. Electronic Journal of Business Research Methods, 15(1), 2-16.
Retrieved from http://www.ejbrm.com/
Rosenthal, M. (2016). Qualitative research methods: Why, when, and how to conduct
interviews and focus groups in pharmacy research. Currents in Pharmacy
Teaching and Learning, 8, 509-516. doi:10.1016/j.cptl.2016.03.021
Rosolio, C. E. (2016). Hospital contracts: Important issues for medical groups. The
Journal of Medical Practice Management: MPM, 31(4), 219-222. Retrieved from
https://greenbranch.com
Rouleau, L., de Rond, M., & Musca, G. (2014). From the ethnographic turn to new forms
of organizational ethnography. Journal of Organizational Ethnography, 39(1), 2-
9. doi:10.1108/JOE-02-2014-0006

125
Rudnicki, M., Armstrong, J. H., Clark, C., Marcus, S. G., Sacks, L., Moser, A. J., &
Reid-Lombardo, K. M. (2016). Expected and unexpected consequences of the
affordable care act: The impact on patients and surgeons-pro and con
arguments. Journal of Gastrointestinal Surgery: Official Journal of the Society
for Surgery of the Alimentary Tract, 20, 351-360. doi:10.1007/s11605-015-3032-8
Sage, W. M. (2014). Putting insurance reform in the ACA’s rear-view mirror. Houston
Law Review, 51, 1-33. Retrieved from http://www.houstonlawreview.org/
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., & Jinks, C.
(2017). Saturation in qualitative research: Exploring its conceptualization and
operationalization. Quality & Quantity 52(4), 1-15. doi:10.1007/s11135-017-
0574-8
Sanjari, M., Bahramnezhad, F., Fomani, F. K., Shoghi, M., & Cheraghi, M. A. (2014).
Ethical challenges of researchers in qualitative studies: The necessity to develop a
specific guideline. Journal of Medical Ethics and History of Medicine, 7(14), 1-6.
Retrieved from http://jmehm.tums.ac.ir
Santiago-Delefosse, M., Gavin, A., Bruchez, C., Roux, P., & Stephen, S. L. (2016).
Quality of qualitative research in the health sciences: Analysis of the common
criteria present in 58 assessment guidelines by expert users. Social Science &
Medicine, 148, 142-151. doi:10.1016/j.socscimed.2015.11.007
Saxena, R. (2017). Muddling through the passage of qualitative research: Experiences of
a novice researcher. Vision, 21, 314-322. doi:10.1177/0972262917721423

126
Schaik, S. M., O'Brien, B. C., Almeida, S. A., & Adler, S. R. (2014). Perceptions of
interprofessional teamwork in low-acuity settings: A qualitative analysis. Medical
Education, 48, 583-592. doi:10.1111/medu.12424
Schimmel, N. (2013). The place of human rights in American efforts to expand and
universalize health care. Human Rights Review, 14(1), 1-29. doi:10.1007/s12142-
012-0247-x
Schipper, K., Abma, T. A., Koops, C., Bakker, I., Sanderman, R., & Schroevers, M. J.
(2014). Sweet and sour after renal transplantation: A qualitative study about the
positive and negative consequences of renal transplantation. British Journal of
Health Psychology, 19, 580-591. doi:10.1111/bjhp.12057
Schneider, E. C., & Hall, C. J. (2017). Improve quality, control spending, maintain
access—can the merit-based incentive payment system deliver? New England
Journal of Medicine, 376, 708-710. doi:10.1056/NEJMp1613876
Schneider, T., & Sachs, S. (2017). The impact of stakeholder identities on value creation
in issue-based stakeholder networks. Journal of Business Ethics, 144, 41-57.
doi:10.1007/s10551-015-2845-4
Selviaridis, K., Matopoulos, A., Thomas Szamosi, L., & Psychogios, A. (2016). Reverse
resource exchanges in service supply chains: The case of returnable transport
packaging. Supply Chain Management, 21, 381-397. doi:10.1108/SCM-07-2015-
0265
Shalhoub, J., Marshall, D. C., & Ippolito, K. (2017). Perspectives on procedure-based
assessments: A thematic analysis of semistructured interviews with 10 UK

127
surgical trainees. British Medical Journal Open, 7(3), 1-8. doi:10.1136/bmjopen-
2016-013 417
Sharafizad, J., & Coetzer, A. (2017). Women business owners' start-up motivations and
network structure. Journal of Management and Organization, 23, 206-223.
doi:10.1017/jmo.2016.51
Shaukat, A., Qiu, Y., & Trojanowski, G. (2016). Board attributes, corporate social
responsibility strategy, and corporate environmental and social performance
Journal of Business Ethics, 135, 569-585. doi:10.1007/s10551-014-2460-9
Sheet, B. (2017). Understanding the finances of oncology practice, part 1. Journal of
Oncology, 4, 146-149. doi:10.1200/JOP.0836501
Sheikh, S. (2017). Is corporate social responsibility a value-increasing investment?
Evidence from antitakeover provisions. Global Finance Journal, 1-12
doi:10.1016/j.gfj.2017.08.002
Shi, D., Zurada, J., Jian, G., & Goyal, S. (2015). An adaptive neuro-fuzzy system with
semi-supervised learning as an approach to improving data classification: An
illustration of bad debt recovery in health care. Journal of International
Technology & Information Management, 24(4), 1-24.
doi:10.1109/HICSS.2015.376
Shorr, J. (2015). Ten most commonly asked questions about collections in the medical
practice. The Journal of Medical Practice Management: MPM, 30(4), 281-283.
Retrieved from https://greenbranch.com

128
Shortell, S. M., Colla, C. H., Lewis, V. A., Fisher, E., Kessell, E., & Ramsay, P. (2015).
Accountable care organizations: The national landscape. Journal of Health
Politics, Policy and Law, 40, 647-668. doi:10.1215/03616878-3149976
Simons, R. C., Bester, A., & Moll, M. (2017). Exploring variability among quality
management system auditors when rating the severity of audit findings at a
nuclear power plant. South African Journal of Industrial Engineering, 28, 145-
163. doi:10.7166/28-1-1512
Slife, B. D., Wright, C. D., & Yanchar, S. C. (2016). Using operational definitions in
research: A best-practices approach. The Journal of Mind and Behavior, 37(2),
119-139. Retrieved from https://umaine.edu/jmb/
Smaglik, P. (2016). Activism: Frustrated postdocs rise up. Nature, 530, 505-506.
doi:10.1038/nj7591-505a
Smith, A., & Smyer, T. (2015). Black African nurses educated in the United States.
Journal of Nursing Education, 54, 72-79. doi:10.3928/01484834-20150120-05
Smith, L. M., Wade, C. M., Case, J. L., Harwell, L. C., Straub, K. R., & Summers, J. K.
(2015). Evaluating the transferability of a U.S. human well-being index (HWBI)
framework to Native American populations. Social Indicators Research, 124,
157-182. doi:10.1007/s11205-014-0775-7
Solomon, J., & Casey, A. (2017). A hierarchical model of organizational identification.
Journal of Organizational Psychology, 17(3), 93-111. Retrieved from
http://www.na-businesspress.com

129
Sommers, B. D. (2015). Health care reform's unfinished work--remaining barriers to
coverage and access. The New England Journal of Medicine, 373, 2395-2397.
doi:10.1056/NEJMp1509462
Sotiriadou, P., Brouwers, J., & Le, T. A. (2014). Choosing a qualitative data analysis
tool: A comparison of NVivo and Leximancer. Annals of Leisure Research, 17,
218-234. doi:10.1080/11745398.2014.902292
Spinks, J., Chaboyer, W., Bucknall, T., Tobiano, G., & Whitty, J. A. (2015). Patient and
nurse preferences for nurse handover-using preferences to inform policy: A
discrete choice experiment protocol. British Medical Journal Open, 5(11), 1-8.
doi:10.1136/bmjopen-20 15-008941
Strasser, A. (2017). Delphi method variants in information systems research: Taxonomy
development and application. Electronic Journal of Business Research
Methods, 15(2), 120-133. Retrieved from http://www.ejbrm.com
Swafford, L. G. (2014). Elements and evaluation of qualitative research. Radiation
Therapist, 23(1), 90-91. Retrieved from https://www.asrt.org
Symons, J., & Maggio, R. (2014). 'Based on a true story': Ethnography's impact as a
narrative form. Journal of Comparative Research in Anthropology & Sociology,
5(2), 1-6. Retrieved from http://compaso.eu/
Szymaniec-Mlicka, K. (2016). Impact of strategic orientation adopted by an organization
on its performance, as shown on the example of public health care entities.
Management, 20, 278-290. doi:10.1515/manment-2015-0065.
130
Talonpoika, A.M., Kärri, T., Pirttilä, M., Monto, S. (2016). Defined strategies for
financial work capital management, International Journal of Managerial
Finance, 12, 277-294. doi:10.1108/IJMF-11-2014-0178
Tamblyn, R., Winslade, N., Qian, C. J., Moraga, T., & Huang, A. (2018). What is in your
wallet? A cluster randomized trial of the effects of showing comparative patient
out-of-pocket costs on primary care prescribing for uncomplicated
hypertension. Implementation Science, 13(1),1-14. doi:10.1186/s13012-017-0701-
x
Teece, D. J. (2017). Towards a capability theory of (innovating) firms: Implications for
management and policy. Cambridge Journal of Economics, 41, 693-720.
doi:10.1093/cje/bew063
Teng, K. (2015). A shift toward personalized health care: Does the Affordable Care Act
provide enough incentive for change? Personalized Medicine, 12, 231-235.
doi:10.2217/pme.14.78
Thomas, D. R. (2017). Feedback from research participants: Are member checks useful
in qualitative research? Qualitative Research in Psychology, 14(1), 23-41.
doi:10.1080/14780887.2016.1219435
Tibben, W. J. (2015). Theory building for ICT4D: Systemizing case study research using
theory triangulation. Information Technology for Development, 21, 628-652.
doi:10.1080/02681102.2014.910635
United States Census Bureau (2016) Arizona population estimates. Retrieved from
https://www.census.gov

131
U.S. Department of Health and Human Services. (1979). The Belmont report. Retrieved
from http://www.hhs.gov/ohrp/humansubjects/guidance/belmont.html.
Van den Berg, A., & Struwig, M. (2017). Guidelines for researchers using an adapted
consensual qualitative research approach in management research. Electronic
Journal of Business Research Methods, 15(2), 109-119. Retrieved from
http://www.ej brm.com
Van den Broek, J., Boselie, P., & Paauwe, J. (2017). Cooperative innovation through a
talent management pool: A qualitative study on coopetition in health care.
European Management Journal. 36(1), 1-10. doi:10.1016/j.emj.2017.03.012
Van Zyl, E. S., Mathafena, R. B., & Ras, J. (2017). The development of a talent
management framework for the private sector. SA Journal of Human Resource
Management, 15(1), 1-19. doi:10.4102/sajhrm.v15i0.820
Venkat, A., Shank, G., Rickard-Aasen, S., Pringle, J. L., & Johnjulio, W. (2017).
Screening, brief intervention and referral to treatment implementation in the
emergency department. The Qualitative Report, 22(3), 745-756. Retrieved from
http://nsuworks.nova.edu/tqr
Vermeulen, Y., Niemann, W., & Kotzé, T. (2016). Supply chain integration: A
qualitative exploration of perspectives from plastic manufacturers in Gauteng.
Journal of Transport and Supply Chain Management, 10(1), 1-13.
doi:10.4102/jtscm.v10i1.223

132
Voss, C., Perks, H., Sousa, R., Witell, L., & Wünderlich, N. V. (2016). Reflections on
context in service research. Journal of Service Management, 27(1), 30-36.
doi:10.1108/JOSM-04-2015-0115
Wang, J. J., Sadler, I., & Shee, H. (2017). Managing logistics outsourcing to China:
Business problems and solutions for Australian firms. The Journal of Business
Diversity, 17(2), 10-29. Retrieved from http://www.na-business press.com
Wang, O., Gellynck, X., & Verbeke, W. (2016). Perceptions of Chinese traditional food
and European food among Chinese consumers. British Food Journal, 118, 2855-
2872. doi:10.1108/BFJ-05-2016-0180
Wardale, D., & Lord, L. (2017). Psychogeography – providing a lens on corporate culture
and its potential impact on career success: A novel and efficient approach.
Electronic Journal of Business Research Methods, 15, 99-108. Retrieved from
http://www.ejbrm.com
Weil, A. R. (2015). Medicaid moving forward. Health Affairs, 34, 1092-1095.
doi:10.1377/hlthaff.2015.0526
Weinstock, D. (2015). Does your front desk staff maximize collections? The Journal of
Medical Practice Management: MPM, 31(1), 6-8. Retrieved from
https://greenbranch.com
Welch, S. (2017). Virtual mentoring program within an online doctoral nursing education
program: A phenomenological study. International Journal of Nursing Education
Scholarship, 14, 128-130. doi:10.1515/ijnes-2016-0049

133
Wernerfelt, B. (1984). A resource‐ based view of the firm. Strategic Management
Journal, 5, 171-180. doi:10.1002/smj.4250050207
West, J. L. (2015). A mixed method analysis of the better business bureau's third-party
seal and the extent to which it inculcates trust among consumers. Journal of
Research in Interactive Marketing, 9, 214-238. doi:10.1108/JRIM-09-2014-0055
Wilden, R., & Gudergan, S. (2017). Service-dominant orientation, dynamic capabilities
and firm performance. Journal of Service Theory and Practice, 27, 808-832.
doi:10.1108/JSTP-04-2016-0077
Wilkinson, S., & Hayward, R. (2017). Band 5 nurses' perceptions and experiences of
professional development. Nursing Management, 24, 30-37.
doi:10.7748/nm.2017.e1537
Wilson, V. (2011). Research ethods: Design, methods, case study…oh my!. Evidence
Based Library and Information Practice, 6, 90-91. doi:10.18438/B87W5S
Wilson, V. (2014). Research methods: Triangulation. Evidence Based Library and
Information Practice, 9, 74-75. doi:10.18438/B8WW3X
Wisker, G. (2015). Developing doctoral authors: Engaging with theoretical perspectives
through the literature review. Innovations in Education and Teaching
International, 52, 64-74. doi:10.1080/14703297.2014.981841
Yaduvanshi, D., & Sharma, A. (2017). Lean six sigma in health operations: Challenges
and opportunities—‘nirvana for operational efficiency in hospitals in a resource
limited settings’. Journal of Health Management, 19, 203-213.
doi:10.1177/0972063417699665

134
Yagasaki, K., Komatsu, H., & Takahashi, T. (2015). Inner conflict in patients receiving
oral anticancer agents: A qualitative study. British Medical Journal Open, 5(4), 1-
8. doi:10.1136/bmjo pen 2014-006699
Yang, H. Y. (2014). A cause-effect study on the relationship between human capital
investment practice and human capital for health care management
strategy. Journal of Accounting, Finance & Management Strategy, 9(1), 33-50.
Retrieved from http://performancesforum.org/
Yazan, B. (2015). Three approaches to case study methods in education: Yin, Merriam,
and Stake. The Qualitative Report, 20(2), 134-152. Retrieved from
http://nsuworks.nova.edu/tqr/
Yin, R. K. (2017). Case study research: Design and methods (6th ed.). Thousand Oaks,
CA: SAGE Publications.
Zamawe, F. C. (2015). The implication of using NVivo software in qualitative data
analysis: Evidence-based reflections. Malawi Medical Journal, 27(1), 13-15.
doi:10.4314/mmj.v27i1.4
Zenilman, M. E., & Freischlag, J. A. (2018). The changing paradigm in surgery is system
integration: How do we respond? The American Journal of Surgery, 216(1), 2-6.
doi:10.1016/j.amjsurg.2017.11.031
Ziakas, V., & Boukas, N. (2014). Contextualizing phenomenology in event management
research. International Journal of Event and Festival Management, 5(1), 56-73.
Retrieved from https://www.emeraldinsight.com/journal/ijefm
136
Appendix A: Interview Protocol
Interview Title: Finding out about competitive strategies rural clinic managers need to
obtain timely payments from patients and health insurance payers.
1. I will begin the interviews with greetings and thank them for their participation in
the interview process. Next, I will make sure I introduce the research topic and
myself to the participants.
2. I will explain the voluntary nature to participate in the study and the opportunity
to withdrawal from the study at any time.
3. I will ensure that participants read and ask any questions related to the study
before agreeing to sign the informed consent form.
4. I will ensure that the participants have a copy of the signed consent form for their
records.
5. I will inform participants that the interview will last between 30 to 45 minutes,
and the interview procedures and that the interview will be audio recorded.
6. I will begin the interview process.
7. I will explain to all participants that as part of member checking procedure, I will
present my interpretations of the interviews to them for corroboration.
8. At the end of the interview process, I will stop audio recording, and thank the
participants again for taking part in the research study.
137
Appendix B: Interview Questions
1. What strategies do you use to obtain timely payments from your patients and
insurance payers?
2. What strategies do you use to collect from uninsured and under-insured
patients?
3. What strategies do you use to manage doubtful accounts and bad debt?
4. What strategies does your organization use to ensure staff complete billing
forms correctly with no errors that delay payments?
5. What techniques does your office staff use to collect copayment either before
or after the patient visit?
6. How does the organization provide training to the billing staff to ensure they
are able to meet the organization’s standard for timely collections?
7. How does the organization ensure that the billing staff has the current training
or professional development regarding health information technology?
8. What billing techniques does the organization use that would be a
competitive advantage over other similar organizations?
9. What are the necessary attributes and abilities of a biller to ensure continued
profitability and sustainability for the organization?
10. What additional information can you make available that accounts receivable
strategies ensure timely payment from patients and insurance payers?

