BY ORDER OF THE
SECRETARY OF THE AIR FORCE
AIR FORCE MANUAL 41-210
10 SEPTEMBER 2019
Incorporating Change 1, 22 June 2021
Health Services
TRICARE OPERATIONS AND PATIENT
ADMINISTRATION
COMPLIANCE WITH THIS PUBLICATION IS MANDATORY
ACCESSIBILITY: Publications and forms are available on the e-Publishing website at
www.e-Publishing.af.mil for downloading or ordering.
RELEASABILITY: There are no releasability restrictions on this publication.
OPR: AF/SG3/4S
Supersedes: AFI 41-210, 06 June 2012
Certified by: AF/SG3/4
(Maj Gen Robert I. Miller)
Pages: 233
This publication implements Air Force Policy Directive (AFPD) 41-2, Medical Support. It
identifies and defines the requirements, policies, procedures, activities, and minimum expectations
necessary to ensure a successful Air Force Medical Treatment Facility (MTF) TRICARE
Operations and Patient Administration mission. This publication describes how to manage
TRICARE Operations and Patient Administration including determining eligibility for care,
protecting medical information, managing health records, the preparation and disposition of
medical documentation and managing other administrative activities to support patients.
Organizational alignment of these functions may vary among MTFs. This publication applies to
all civilian employees and uniformed members of the Regular Air Force, Air Force Reserve and
Air National Guard who perform TRICARE Operations and Patient Administration. Ensure all
records created as a result of processes prescribed in this publication are maintained in accordance
with Air Force Manual 33-363, Management of Records, and disposed of in accordance with the
Air Force Records Disposition Schedule located in the Air Force Records Information
Management System Records Disposition Schedule. Refer recommended changes and questions
about this publication to Air Force Medical Readiness Agency (AFMRA)/SG3S using the Air
Force Form (AF Form) 847, Recommendation for Change of Publication; route AF Forms 847
from the field through the appropriate functional chain of command. All field publications that
either implement or supplement this publication must be submitted to AFMRA/SG3S for
coordination prior to approval. (T-2). The authorities to waive wing/unit level requirements in
this publication are identified with a Tier (“T-0, T-1, T-2, T-3”) number following the compliance
statement. See AFI 33-360, Publications and Forms Management, for a description of the
authorities associated with the Tier numbers. Submit requests for waivers through the chain of

2 AFMAN41-210 10 SEPTEMBER 2019
command to the appropriate Tier waiver approval authority, or alternately, to the requestor’s
commander for non-tiered compliance items. The use of the name or mark of any specific
manufacturer, commercial product, commodity, or service in this publication does not imply
endorsement by the Air Force. This manual requires the collection and/or maintenance of
information protected by Title 5 United States Code Section 552a, Privacy Act of 1974, authorized
by 10 U.S.C. Chapter 55, Medical and Dental Care, and E.O. 9397 (SSN). The applicable SORN
F044 AF SG D, Automated Medical/Dental Record System (August 29, 2003, 68 FR 51998) is
available at http://dpclo.defense.gov/Privacy/SORNs.aspx.
SUMMARY OF CHANGES
This interim change revises AFMAN 41-210 by (1) adding guidance that ensures proper care hand-
off for Reserve Component members who transition from active duty orders to inactive status and
(2) deleting Section 4K in its entirety. A margin bar (|) indicates newly revised material.
Chapter 1—OVERVIEW, ROLES AND RESPONSIBILITIES 10
Section 1A—TRICARE 10
1.1. TRICARE Overview. .............................................................................................. 10
1.2. TRICARE Operations Overview. ............................................................................ 10
Section 1B—Patient Administration 10
1.3. Patient Administration Overview. ........................................................................... 10
1.4. Patient Administration Officer, Director and Noncommissioned Officer (NCO). ... 10
1.5. HIPAA Privacy Officer. .......................................................................................... 11
1.6. Registered Health Information Administrator (RHIA), Registered Health
Information Technician (RHIT), or Air Force member with equivalent education
and experience. ....................................................................................................... 11
Section 1C—Medical Coding 11
1.7. Medical Coders. ...................................................................................................... 11
1.8. Air Force Medical Operations Agency (AFMOA) Coding Program Office. ........... 11
Section 1D—Unit Commanders 12
1.9. Unit Commanders. .................................................................................................. 12
Section 1E—Administrative Assistant to the Secretary of the Air Force (SAF/AA) 12
1.10. SAF/AA. ................................................................................................................. 12
AFMAN41-210 10 SEPTEMBER 2019 3
Chapter 2—HEALTHCARE BENEFITS AND REQUIREMENTS 13
Section 2A—Healthcare Entitlements for Current and Former Uniformed Services Personnel and
Foreign Forces Members 13
2.1. General Administration of Healthcare Benefits. ...................................................... 13
2.2. RC Members. .......................................................................................................... 14
2.3. Foreign Forces and Their Dependents. .................................................................... 15
2.4. Cadets and Midshipmen. ......................................................................................... 16
2.5. Senior College or University Reserve Officer Training Corps (ROTC) Cadets;
ROTC Membership Applicants; Uniformed Service Applicants; and Service
Academy Applicants. .............................................................................................. 16
2.6. Medal of Honor Recipients. .................................................................................... 16
Section 2B—Healthcare for Current and Former Uniformed Service Family Members 16
2.7. Un-remarried Former Spouses. ............................................................................... 16
2.8. Abused Family Members and Dependents. ............................................................. 16
Section 2C—Healthcare for Eligible Civilians and Special Categories of Beneficiaries and Their
Family Members 17
2.9. Federal Civilian Employees. ................................................................................... 17
2.10. Family Members (Dependents) of Federal Civilian Employees. ............................. 20
2.11. Secretarial Designees. ............................................................................................. 20
2.12. Members of Uniformed Services Auxiliaries. ......................................................... 20
2.13. Emergency Care. ..................................................................................................... 20
2.14. Contractors. ............................................................................................................. 20
2.15. Family Members (Dependents) of Contractors. ...................................................... 20
2.16. Expanded Medical Care for Caregivers. .................................................................. 20
2.17. Volunteers. .............................................................................................................. 20
Section 2D—Other Services and Authorizations 21
2.18. Additional MTF Requirements ............................................................................... 21
2.19. Primary Care Manager Assignments. ...................................................................... 24
2.20. Sexual Dysfunctions, Inadequacies, or Paraphilic Disorders Treatment.................. 26
Chapter 3—TRICARE OPERATIONS 28
Section 3A—Access to Care Guidance 28
3.1. Access to Care Standards. ....................................................................................... 28
4 AFMAN41-210 10 SEPTEMBER 2019
Section 3B—Beneficiary Counseling and Assistance Coordinator 28
3.2. Beneficiary Counseling and Assistance Coordinator Position and Procedural
Information. ............................................................................................................ 28
Section 3C—Debt Collection Assistance Officer 28
3.3. Debt Collection Assistance Officer Position and Procedural Information. .............. 28
Section 3D—Service Change Requests 29
3.4. Changes in Clinical Services. .................................................................................. 29
Section 3E—Referral Management Program 33
3.5. Referral Management Program. .............................................................................. 33
Section 3F—Medical In/Out-Processing Program 33
3.6. Medical In/Out-Processing Program Overview. ...................................................... 33
3.7. In-processing Requirements. ................................................................................... 34
3.8. Out-processing Requirements. ................................................................................ 35
3.9. Limited Capability Out-processing. ........................................................................ 35
3.10. Retirement/Separation Out-processing. ................................................................... 35
Section 3G—External Resource Sharing Agreements 36
3.11. External Resource Sharing Agreement. ................................................................... 36
Chapter 4—PATIENT ADMINISTRATION FUNCTIONS 37
Section 4A—Legal Aspects of Protected Health Information (PHI), Release of Information and
Patient Self-Determination 37
4.1. Laws and Provisions Affecting Disclosure of Medical Information. ....................... 37
4.2. Health Record Custody and Control. ....................................................................... 38
4.3. General Guidelines on Releasing Medical Information. .......................................... 41
4.4. Patient Requests for Copies of Medical Records and Restrictions. ......................... 43
4.5. Patient Rights (Reference DoDI 6000. .................................................................... 46
Section 4B—Patient Registration & Multiple Healthcare Eligibility 47
4.6. Patient Registration. ................................................................................................ 47
4.7. Patients with Multiple-Eligibility. ........................................................................... 48
Section 4C—Patient Travel 49
4.8. Patient Accountability for Service Members Traveling to Attend Medical ............. 49
4.9. Patient Travel Benefit. ............................................................................................ 50
4.10. Transferring Patients Through the Aeromedical Evacuation System. ..................... 53
AFMAN41-210 10 SEPTEMBER 2019 5
Section 4D—Quarters Administration 53
4.11. Quarters Status. ....................................................................................................... 53
Section 4E—Line of Duty Program Administration 54
4.12. Line of Duty Determinations. .................................................................................. 54
Section 4F—Air Force Secretarial Designee Program Administration 57
4.13. Authority. ................................................................................................................ 57
4.14. U.S. Air Force Secretarial Designee Criteria. .......................................................... 59
4.15. Applying for Air Force Designee Status. ................................................................ 62
4.16. Certain Senior Officials of the United States Government. ..................................... 64
4.17. Operating the Air Force Secretarial Designee Program Overseas. .......................... 64
4.18. Designee Status Used in Claims Against the United States. .................................... 64
Section 4G—Exceptional Family Member Program 65
4.19. Exceptional Family Member Program (EFMP). ...................................................... 65
4.20. Family Member Relocation Clearance Coordinator (FMRCC). .............................. 65
Section 4H—Admissions and Dispositions Program Administration 65
4.21. Responsibility for Admission Processing. ............................................................... 65
4.22. Administrative Admission and Disposition Requirements. ..................................... 65
4.23. Assuming Administrative Responsibility for Military Members Hospitalized in
Non-Military Medical Facilities also known as Absent Sick Status. ....................... 65
4.24. Assuming Administrative Responsibility for AD U. S. Air Force Members
Hospitalized in DoD Facilities. ............................................................................... 68
4.25. Admitting Infants Born Outside the MTF. .............................................................. 68
4.26. Admitting Generals/Admirals (Flag Officers), Colonels, and Prominent Persons. .. 68
4.27. Reporting Aircraft Accident Admissions. ............................................................... 70
4.28. Managing Military Patients Expected To Be Hospitalized Over 90 Days. .............. 71
4.29. Deployed Military Members who are Aeromedically Evacuated from
Contingency Operations to CONUS MTF. ............................................................. 71
4.30. Readmission of Patients. ......................................................................................... 71
4.31. Canceling Admissions. ............................................................................................ 71
4.32. Inpatient Disposition Procedures. ............................................................................ 72
4.33. Convalescent Leave. ............................................................................................... 75
Table 4.1. (Added) Recommendations: Convalescent Leave after Perinatal Loss ................... 75
6 AFMAN41-210 10 SEPTEMBER 2019
4.34. Reporting AD Soldiers, Sailors, and Marines Hospitalized in Civilian or Non-
Military Medical Facilities. ..................................................................................... 77
Section 4I—Casualty Reporting Program Administration 78
4.35. Reporting Patients in Casualty Status. ..................................................................... 78
4.36. Assigning Responsibility......................................................................................... 78
4.37. Requesting and Arranging Travel for Legally Authorized Representative under
the Emergency Family Member Travel Program. ................................................... 79
4.38. Preparing the AF Form 1403, Roster of Seriously Ill/Very Seriously Ill. ................ 80
4.39. Responsibility for Preparing Death Cases. .............................................................. 81
4.40. Policies Regarding Deaths. ..................................................................................... 81
4.41. Performing Postmortem (Autopsy) - Non-Forensic Cases. ..................................... 83
4.42. Disposition of Outpatient Records on Deceased AD Personnel. ............................. 85
4.43. Deceased Patient Kit. .............................................................................................. 85
Section 4J—Birth Registration Program Administration 86
4.44. Birth Registration in the CONUS. ........................................................................... 86
4.45. Registering Births Overseas. ................................................................................... 86
Section 4K—Medical Evaluation of Service Members for Continued Military Service 86
4.46. DELETED .............................................................................................................. 86
4.47. DELETED .............................................................................................................. 86
4.48. DELETED .............................................................................................................. 86
4.49. DELETED .............................................................................................................. 87
4.50. DELETED .............................................................................................................. 87
4.51. DELETED .............................................................................................................. 88
4.52. DELETED .............................................................................................................. 89
4.53. DELETED .............................................................................................................. 89
4.54. DELETED .............................................................................................................. 89
4.55. DELETED .............................................................................................................. 89
4.56. DELETED .............................................................................................................. 89
4.57. DELETED .............................................................................................................. 89
4.58. DELETED .............................................................................................................. 89
4.59. DELETED .............................................................................................................. 89
4.60. DELETED .............................................................................................................. 90
4.61. DELETED .............................................................................................................. 90
AFMAN41-210 10 SEPTEMBER 2019 7
4.62. DELETED .............................................................................................................. 90
4.63. DELETED .............................................................................................................. 91
4.64. DELETED .............................................................................................................. 91
4.65. DELETED .............................................................................................................. 91
4.66. DELETED .............................................................................................................. 91
4.67. DELETED .............................................................................................................. 92
4.68. DELETED .............................................................................................................. 92
4.69. DELETED .............................................................................................................. 94
4.70. DELETED .............................................................................................................. 94
4.71. DELETED .............................................................................................................. 94
4.72. DELETED .............................................................................................................. 94
4.73. DELETED .............................................................................................................. 95
Section 4L—Tumor Registry Program Administration 97
4.74. The Tumor Registry Program.................................................................................. 97
Chapter 5—HEALTH RECORDS MANAGEMENT 98
Section 5A—General Program Administration 98
5.1. Managing Health Records. ...................................................................................... 98
5.2. Documenting Health Records. ................................................................................ 99
5.3. Correcting Health Records. ..................................................................................... 99
5.4. The Electronic Health Record. ................................................................................ 101
5.5. Electronically-Generated Forms. ............................................................................. 110
5.6. Overprinting of Forms............................................................................................. 111
5.7. Service Treatment Record Disposition Instructions for Airman Retiring,
Separating and Transitioning to the RC. ................................................................. 112
5.8. Base Closures and Medical Records Management. ................................................. 135
5.9. Health Record Review Committee/Functions. ........................................................ 136
Section 5B—Outpatient Records Administration 137
5.10. Creation of Outpatient Record Folders. ................................................................... 137
Table 5.1. Preparing Outpatient Record Folders Table. ........................................................... 137
5.11. Labeling File Folders. ............................................................................................. 140
Table 5.2. Terminal Digit Health Record Filing System. ......................................................... 140
5.12. Contents of the Outpatient Record. ......................................................................... 142
5.13. Filing Outpatient Records. ...................................................................................... 146
8 AFMAN41-210 10 SEPTEMBER 2019
5.14. Managing ARC Outpatient Records. ....................................................................... 148
5.15. Active Association and Geographically Separated Unit Outpatient Records
Management. ........................................................................................................... 149
Figure 5.1. Sample GSU Label.................................................................................................. 152
Figure 5.2. Sample GSU Record Copy ...................................................................................... 152
5.16. Custody and Control of Health Records. ................................................................. 152
5.17. Filing Outpatient Computer Generated Clinical Diagnostic Results. ...................... 154
5.18. Researching Appropriate Host MTF Record Locations. ......................................... 155
5.19. Loose Leaf, Orphaned, or Miscellaneous Medical Documents. .............................. 156
5.20. Missing and Lost Health Records............................................................................ 159
5.21. Health Records Availability, Accountability, and “Tracking” Standards. ............... 160
5.22. Medical Documentation Requirements for Partial Hospitalization. ........................ 167
5.23. Supplemental Documentation Guidance. ................................................................ 168
5.24. Mental Health Records Documentation Requirements. ........................................... 168
5.25. Prenatal Records Documentation Requirements. .................................................... 168
5.26. Family Advocacy Program (FAP) Documentation Requirements. .......................... 169
5.27. Documentation Requirements to Support Graduate Medical Education Programs. 169
5.28. Managing Service Treatment Records for Service Members Assigned to the
Personnel Reliability Assurance Program and Presidential Support Program ......... 169
5.29. Transferring Health Records Between MTFs or Medical Units. ............................. 170
5.30. Providing Health Records to AD Members During Temporary Duty Periods. ........ 176
Section 5C—Inpatient Records Administration 177
5.31. Creating Inpatient Records. ..................................................................................... 177
5.32. Creation of the Master Patient Index. ...................................................................... 178
5.33. Preparing Inpatient Record Folders. ........................................................................ 178
Table 5.3. Preparing Inpatient Record Folders. ........................................................................ 178
5.34. Contents of the Inpatient Record. ............................................................................ 179
5.35. Inpatient Record Documents, Forms, and Patient Identification. ............................ 180
5.36. Filing Inpatient Records. ......................................................................................... 180
5.37. Coding and Documenting Inpatient Records. .......................................................... 181
5.38. Prenatal Records. .................................................................................................... 187
5.39. The Extended Ambulatory Record. ......................................................................... 187
5.40. Creating, Coding, and Documenting, Ambulatory Procedure Visit Records. .......... 187
AFMAN41-210 10 SEPTEMBER 2019 9
5.41. Creating, Coding, and Documenting Observation Records. .................................... 189
5.42. Patients Discharged Without Definitive Diagnosis. ................................................ 190
5.43. Disposition of Inpatient Records. ............................................................................ 190
5.44. Medical Transcription. ............................................................................................ 191
Section 5D—Deployed Assignment Medical Record Management 192
5.45. Minimum Deployed Medical Documentation and Record Management
Requirements. ......................................................................................................... 192
5.46. Expeditionary Electronic Health Record Management Platforms and Systems. ..... 195
5.47. Emergency Medical Service and AF Form 552, Air Force Patient Care Report. .... 195
Attachment 1—GLOSSARY OF REFERENCES AND SUPPORTING INFORMATION 196
Attachment 2—SECRETARY OF THE AIR FORCE DESIGNEE EXAMPLE REQUEST 212
Attachment 3—CONSULT NOTES AND SPECIALTY STUDIES GUIDE 214
Attachment 4—INITIAL RILO COVER SHEET/ CHECKLIST 216
Attachment 5—PERSONNEL RELIABILITY ASSURANCE PROGRAM ADMIN CERT
HAIMS SCAN GUIDE 218
Attachment 6—ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES,
HEALTH RECORD OUTPATIENT SECTION 1 220
Attachment 7—ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES,
HEALTH RECORD OUTPATIENT SECTION 2 224
Attachment 8—ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES,
HEALTH RECORD OUTPATIENT SECTION 3 225
Attachment 9—ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES,
HEALTH RECORD OUTPATIENT SECTION 4 227
Attachment 10—ARRANGEMENT OF FORMS IN THE INPATIENT RECORD 229
Attachment 11—SERVICE TREATMENT RECORDS MAILING ADDRESSES FOR
OTHER SERVICES 233

10 AFMAN41-210 10 SEPTEMBER 2019
Chapter 1
OVERVIEW, ROLES AND RESPONSIBILITIES
Section 1A—TRICARE
1.1. TRICARE Overview. TRICARE is the Department of Defense’s (DoD) managed
healthcare program for active duty (AD) military and their families, Reserve Component (RC)
members and their families, retirees and their families, and other beneficiaries. The TRICARE
Program offers options for healthcare coverage including: TRICARE Prime, TRICARE Select,
TRICARE Prime Remote, TRICARE for Life, TRICARE Plus, TRICARE Young Adult, and
several other programs. For detailed information on the various TRICARE health plans and to
access the TRICARE manuals go to the TRICARE website at https://manuals.health.mil/.
Throughout this AFMAN, the TRICARE Operations and Patient Administration staff are
responsible for the execution of the programs and processes outlined, unless explicitly stated.
1.2. TRICARE Operations Overview. The following activities are functions of TRICARE
Operations: managed care support, beneficiary counseling and assistance, debt collection
assistance, medical in/out-processing briefings, TRICARE plan marketing and education, health
plan analysis, enrollment management, external resource sharing agreements, clinical support
agreements, and the referral management center.
Section 1B—Patient Administration
1.3. Patient Administration Overview.
1.3.1. Patient Administration provides healthcare support services as part of the delivery of
basic and comprehensive medical treatment to eligible beneficiaries and manages or provides
appropriate guidance and oversight of all aspects of medical records functions within the
Military Treatment Facility (MTF).
1.3.2. The following activities are functions of Patient Administration: admissions and
dispositions, birth registration, death processing, casualty reporting, inpatient records
management, HIPAA privacy compliance, non-clinical aeromedical evacuation duties, line of
duty (LOD) determinations/coordination, outpatient records management, medical evaluation
boards administration, physical evaluation board liaison officer, organ donor program, patient
registration, release of information, Secretary of the Air Force designee program, sensitive
duties program records management, and the tumor registry program administration.
1.4. Patient Administration Officer, Director and Noncommissioned Officer (NCO).
1.4.1. The MTF commander or director will appoint a Patient Administration Officer,
Director, Senior NCO (SNCO) or NCO, depending on the size of the MTF, to manage and
provide oversight of all patient administration functions performed throughout the MTF. (T-
3). The individual appointed by the MTF commander or director has primary authority to
facilitate and/or enforce the policies, on behalf of the commander, identified in this manual.
1.4.2. Responsibilities: The Patient Administration Officer, Director, SNCO or NCO will
manage functions listed in paragraph 1.3.2. (T-1).
AFMAN41-210 10 SEPTEMBER 2019 11
1.5. HIPAA Privacy Officer. The duties and responsibilities of the MTF HIPAA privacy officer
are discussed in AFI 41-200, Health Insurance Portability and Accountability Act (HIPAA).
1.6. Registered Health Information Administrator (RHIA), Registered Health Information
Technician (RHIT), or Air Force member with equivalent education and experience.
1.6.1. The RHIA or RHIT must be credentialed by the American Health Information
Management Association, and if a civilian, must be rated eligible by the Office of Personnel
Management (OPM) Qualification Standard for the GS 669 or GS 675 series. (T-1).
1.6.2. The RHIA or RHIT will manage the inpatient records department, inpatient records
coding, and inpatient professional service encounters (rounds), ambulatory procedure visits,
medical transcription, outpatient record documentation, and coding oversight.
1.6.3. The RHIA or RHIT will work closely with the Information System Security Office and
HIPAA privacy officer to ensure security of, and controlled access to, both the paper-based
and automated medical records, and ensure release of information procedures conform to all
legal requirements.
Section 1C—Medical Coding
1.7. Medical Coders. For recording diagnoses and procedures, MTFs will include in their
position descriptions (PD) that coding staff will be required to complete the appropriate training
and certification exam from the American Academy of Professional Coders or American Health
Information Management Association within 18 months of placement under the PD indicated for
their position in accordance with Defense Health Agency Interim Procedures Memorandum
(DHA-IPM) 18-016, Medical Coding of the DoD Health Records.
1.7.1. Professional Services Coding: certified professional coder, American Academy of
Professional Coders; or certified coding specialist-physician, American Health Information
Management Association.
1.7.2. Institutional (Facility) Coding: certified outpatient coder (outpatient facility only),
certified inpatient coder (inpatient facility only), American Academy of Professional Coders;
or certified coding specialist, American Health Information Management Association.
1.7.3. An American Health Information Management Association RHIT or RHIA credential
may be counted in lieu of the certified coding specialist or certified coding specialist –
physician credential.
1.8. Air Force Medical Operations Agency (AFMOA) Coding Program Office. The AFMOA
Coding Program Office will be the office of primary responsibility for all Air Force Medical
Service (AFMS) coding related issues, composed of the Coding Manager and the AFMOA Coding
Consultants.
1.8.1. Responsibilities:
1.8.1.1. Represent the AFMS in tri-Service meetings and discussions involving coding
policy and guidance.
1.8.1.2. Provide program management oversight, expertise, and technical support to
AFMS coding operations.
12 AFMAN41-210 10 SEPTEMBER 2019
1.8.1.3. Define coder qualifications and provide AFMS coder manning and funding
recommendations.
Section 1D—Unit Commanders
1.9. Unit Commanders. The responsibilities of the unit commander are discussed throughout
this AFMAN. In particular commander authorizations, notifications and coordination with MTF
staff may occur. See paragraphs 2.9, 2.18.4, 2.20.2, 4.11.2, 4.23.10, 4.24, 4.50.4, 4.65.8, 4.68.5,
5.4.5, 5.7.2.4, 5.15.6, 5.21.5.7.
Section 1E—Administrative Assistant to the Secretary of the Air Force (SAF/AA)
1.10. SAF/AA. The responsibilities of SAF/AA include delegated authority of the Air Force
Secretarial Designee Program. See paragraphs 4.13, 4.14, 4.15.
AFMAN41-210 10 SEPTEMBER 2019 13
Chapter 2
HEALTHCARE BENEFITS AND REQUIREMENTS
Section 2A—Healthcare Entitlements for Current and Former Uniformed Services Personnel
and Foreign Forces Members
2.1. General Administration of Healthcare Benefits. MTFs will administer healthcare benefits
to uniformed service members, family members, retirees, and other eligible persons in accordance
with Department of Defense Directive (DoDD) 6010.04, Healthcare for Uniformed Services
Members and Beneficiaries, and Health Affairs Policy 11-005, TRICARE Policy for Access to
Care. (T-0).
2.1.1. MTFs will provide care without regard to the sponsor’s Service affiliation, rank or
grade. (T-0).
2.1.2. Active Duty (AD) service members must be enrolled to TRICARE Prime. (T-0).
Reference Health Affairs Policy 05-014, Policy Guidance for Active Duty Service Member
Enrollment to TRICARE Prime and 32 CFR Part 199.17, TRICARE program.
2.1.3. Eligibility Verification. MTFs will require that all persons, including members in
uniform, show satisfactory evidence of their beneficiary status before receiving MTF care. (T-
0). MTFs will not provide routine care to patients whose eligibility cannot be verified unless a
competent medical authority determines a delay in care would create an unreasonable risk to
the patient’s health. (T-0). In such cases, the MTF will require the patient to sign a statement
of eligibility that indicates the patient’s requirement to provide proof of eligibility within 30
days or be held responsible for the costs associated with the care provided. (T-0). After the
30th day, if the individual has not produced evidence that satisfactorily verifies eligibility, the
TRICARE Operations and Patient Administration Flight will forward the patient’s information
to the Resource Management Flight to initiate the billing process. (T-1). This process applies
to outpatient care, inpatient care, and ancillary care; however, for emergency cases, MTFs will
always provide care first and verify eligibility after treatment. (T-0). The Military Personnel
Section (MPS) establishes eligibility, whereas the MTFs verify eligibility. Reference: 10 USC
Chapter 55, “Medical and Dental Care;” DoDI 1341.02, Defense Enrollment Eligibility
Reporting System (DEERS) Program and Procedures and AFI 36-3026_IPV1, Identification
Cards for Members of the Uniformed Services, Their Eligible Family Members, and Other
Eligible Personnel.
2.1.3.1. MTFs will require that all patients requesting care present a valid government
identification card that satisfactorily establishes the identity of the patient except when the
patient is aged 10 or under. (T-0). Beneficiaries aged 10 and under may receive MTF care
without providing a valid government identification when the child passes a Defense
Enrollment Eligibility Reporting System (DEERS) check and a legally authorized
representative with a military identification validates the child’s identity. Legally
authorized representatives who lack a military identification may not validate the child’s
identity. In cases where the legally authorized representative lacks military identification,
the child must show government identification that satisfactorily confirms the child’s
identity. (T-0).
14 AFMAN41-210 10 SEPTEMBER 2019
2.1.3.2. MTFs will perform DEERS checks for eligibility on all patients requesting care.
(T-0). Eligible beneficiaries enrolled in a Uniformed Services Family Health Plan are not
eligible for routine care at MTFs; however, all other patients reflecting eligibility in
DEERS are authorized care within MTFs. RC service members and their family members
who present a government, state or country photo identification card and pass a DEERS
check should not be asked for a copy of AD orders.
2.1.3.2.1. If a patient fails a DEERS check, MTFs may still provide routine care within
the direct care system in the following circumstances and as otherwise authorized in
this manual, or by statute:
2.1.3.2.1.1. The patient is a member of the RC on active or inactive duty for less
than 30 days and presents a copy of their orders or other administrative
documentation.
2.1.3.2.1.2. The patient is a member of the RC on active or inactive duty status,
and is seeking healthcare related to an in line of duty (LOD) medical or dental
condition or a condition which is currently under LOD investigation in accordance
with AFI 36-2910, Line of Duty (LOD) Determination, Medical Continuation
(MEDCON) and Incapacitation (INCAP) Pay.
2.1.3.2.1.3. If a RC service member is issued delayed-effective-date AD orders for
more than 30 days in support of a contingency operation, the member and the
member’s family are eligible for early TRICARE medical and dental benefits
beginning on the latter of either: (a) the date their orders were issued or (b) 90 days
before the service member reports for duty or is activated to AD.
2.1.3.2.1.4. The patient has a Secretarial Designee letter that authorizes the care.
Ensure the patient only receives care limited to the specific dates and diagnosis
annotated in the approval letter. (T-0).
2.2. RC Members. MTFs will administer health benefits to RC service members on AD tours,
on AD orders, and under circumstances directed in Department of Defense Instruction (DoDI)
1241.01, Reserve Component (RC) Line of Duty Determination for Medical and Dental Treatments
and Incapacitation Pay Entitlements and AFI 36-2910. (T-0).
2.2.1. When not in an Extended Active Duty military status (orders for greater than 30 days),
TRICARE Early Mobilization or Transitional Assistance Management Program status; RC
member military healthcare is limited. Refer to DoDI 1241.01 for entitlements.
2.2.2. RC service members placed on orders for more than 30 days for non-contingency
related operations are authorized TRICARE benefits equal to the AD component.
Additionally, TRICARE benefits are extended to the RC service member’s authorized family
members during the same period.
2.2.2.1. Officer direct accessions: Members commissioned as reserve officers in the
uniformed services may be entitled to full medical and dental benefits prior to commencing
AD service on Extended AD orders when: Extended AD orders will be issued but have
not been issued yet, or the orders have been issued but the member has not yet entered AD;
and the member does not have healthcare insurance and is not covered by any other health
plan. Reference 10 USC § 1074.

AFMAN41-210 10 SEPTEMBER 2019 15
2.2.2.2. (Added) MTFs will ensure RC service members undergoing an LOD in
accordance with paragraph 4.12 receive thorough hand-off between facility providers and
supporting reserve medical unit or civilian providers.
2.2.3. RC service members ordered to Federal AD for more than 30 days in support of
contingency operations are also authorized full TRICARE benefits. Healthcare coverage is
also extended to each of the RC service member’s authorized family members. Additionally,
if the RC service member is issued delayed-effective-date AD orders for more than 30 days in
support of a contingency operation, the member and sponsored family members are eligible
for early TRICARE medical and dental benefits beginning on the latter of either: (a) the date
orders were issued or (b) 180 days before the member reports for duty or is activated to AD.
2.2.4. Air Reserve Component (ARC) members do not have to be in a duty status to make an
appointment. However, the member must show they are on duty status (active, inactive or
points only) at the time of any treatment/care (i.e. any annual military requirement exam,
immunization, or deployment-related exam). (T-1). MTFs verify ARC members are in a duty
status (active, inactive, or points only) for annual military requirements such as Periodic Health
Assessment, flight physicals and immunizations with the AF Form 40A, Record of Individual
Inactive Duty Training, or a copy of the member’s orders.
2.3. Foreign Forces and Their Dependents. MTFs will provide healthcare to foreign forces,
and their eligible dependents when applicable, in accordance with DoDI 6025.23, Health Care
Eligibility Under the Secretarial Designee (SECDES) Program and Related Special Authorities,
DoDI 6015.23, Foreign Military Personnel Care and Uniform Business Offices in Military
Treatment Facilities (MTFs); DoDI 1000.13, Identification (ID) Cards for Members of the
Uniformed Services, their Dependents, and other Eligible Individuals. (T-0).
2.3.1. MTFs will provide authorized care for the categories of foreign nationals listed below,
and seek reimbursements that are consistent with international agreements (i.e. Status of Forces
Agreement or Reciprocal Health Care Agreement). (T-0). If a Reciprocal Health Care
Agreement exists that establishes different benefits or charges from those associated with a
training program, then the Reciprocal Health Care Agreement takes precedence. Foreign
nationals and their family members must present approved identification and/or Invitational
Travel Orders as appropriate when requesting care. (T-0). Treatment of foreign nationals and
their family members is subject to the provisions of approved international agreements.
2.3.1.1. North Atlantic Treaty Organization (NATO) and Partnership for Peace Status of
Forces Agreement personnel and their authorized family members eligibility is determined
by DoDI 6015.23.
2.3.1.2. Foreign diplomatic or other senior foreign officials and the dependents of such
officials may be provided inpatient or outpatient services in MTFs only in compelling
circumstances, including both medical circumstances and mission interests, and through
case-by-case approval. Refer to DoDI 6025.23.
2.3.1.3. Foreign military personnel assigned or attached to United States military units for
duty and their family members eligibility is determined by DoDI 6015.23.
2.3.1.4. International students assigned or attached to United States military units for
training and their authorized family members eligibility is determined by DoDI 6015.23.

16 AFMAN41-210 10 SEPTEMBER 2019
2.3.1.5. Detainees, Enemy Prisoners of War, refugees, and other displaced personnel will
be provided medical care equal to that of United States Service Members. See for example,
Article 91 of Geneva Convention Relative to the Protection of Civilian Persons in Time of
War of August 12, 1949: 75 U.N.T.S. 287 (1950) which can be located at
https://ogc.osd.mil/LoW_Treaties.html. Consult with Staff Judge Advocate regarding
Law of War compliance.”
2.4. Cadets and Midshipmen. MTFs will administer health benefits to cadets enrolled at the
United States Air Force Academy, the United States Military Academy at West Point, the United
States Coast Guard Academy, and midshipmen enrolled at the United States Naval Academy. (T-
0). Enrollment into TRICARE is authorized. Reference 10 USC § 1074b.
2.5. Senior College or University Reserve Officer Training Corps (ROTC) Cadets; ROTC
Membership Applicants; Uniformed Service Applicants; and Service Academy
Applicants. MTFs will provide limited healthcare to ROTC Cadets and applicants to the Service
Academies, ROTC and the Uniformed Services. (T-0). Reference 10 USC § 1074b.
2.5.1. MTFs will provide cadets medical and dental care for any injury or illness incurred
while traveling to and from, and participating in, any summer field training or other practical
military training. (T-0)
2.5.2. If a ROTC cadet’s college, university, or institution does not have the ability to perform
a physical exam, the cadet will be provided an examination(s) at a MTF, per Health Affairs
Policy 99-003, Physical Examination for ROTC Applicants, including admission if required to
satisfy clinical diagnostic requirements. (T-0). Uniformed Service or Service Academy
applicants may receive initial service eligibility examination(s) at a MTF. For remedial ROTC
commissioning, Uniformed Service, or Service Academy entrance examinations that require
additional diagnostic care beyond a MTFs capabilities, refer the cadet or applicant to the closest
MTF (with the required capabilities) for required medical testing.
2.5.3. Cadets requiring additional follow-up medical care after hospitalization and/or after
completing summer training, military exercise training, practical military training, etc., are
authorized Department of Defense (DoD) MTF care only, regardless of the cadet’s distance
from a MTF.
2.6. Medal of Honor Recipients. MTFs will administer medical and dental benefits to otherwise
non-eligible Medal of Honor recipients and their immediate dependents as if the Medal of Honor
recipient is a retiree entitled to retired pay. (T-0). Reference 10 USC § 1074h.
Section 2B—Healthcare for Current and Former Uniformed Service Family Members
2.7. Un-remarried Former Spouses. MTFs will administer healthcare benefits to certain un-
remarried former spouses of Uniformed Service Members. (T-0). Reference 10 USC § 1072 and
1086a.
2.8. Abused Family Members and Dependents. MTFs will administer health benefits to abused
family members and dependents in accordance with 32 CFR Part 199.3, DoDI 1342.24,
Transitional Compensation for Abused Dependents, and in accordance with 10 USC § 1076,
1408(h), 1059. (T-0).
AFMAN41-210 10 SEPTEMBER 2019 17
Section 2C—Healthcare for Eligible Civilians and Special Categories of Beneficiaries and
Their Family Members
2.9. Federal Civilian Employees. MTFs will provide limited health care to Federal civilian
employees in accordance with DoDI 1400.32, DoD Civilian Work Force Contingency and
Emergency Planning Guidelines and Procedures; DoDI 6490.03, Deployment Health; and Health
Affairs Policy 08-002, Policy for Billing Care Furnished by Military Treatment Facilities to
Federal Employees for On-the-Job Injuries and for Occupational Health to support DoD civilian
personnel deployment and occupation health. (T-0).
2.9.1. Conditional Employment/Annual Occupational Exam Requirements. MTFs will
provide occupational exams when they have the capability. (T-3). Reference 5 Code of Federal
Regulations 339.301, Authority to Require an Examination.
2.9.1.1. When the local MTF does not have the capability to provide a medical
examination (or a portion of the exam) required for Air Force civilian employment, then
the MTF may arrange to have the examination (lab tests, etc.) completed in the civilian
sector (non-DoD) healthcare community after receiving payment authorization from the
employee’s unit commander.
2.9.1.2. The employee’s unit commander must authorize payment for all civilian sector
(non-DoD) examinations in advance of the MTF making the arrangements. (T-1). Payment
is made from the same appropriation that funds the employee’s salary. The Defense Health
Program appropriation will not be used for the examinations, unless the employee’s salary
is Defense Health Program-funded (e.g., a MTF employee). (T-0).
2.9.1.3. The Installation Occupational and Environmental Medicine Consultant will
provide clinical oversight of referrals/consults to ensure they are appropriate and justified.
(T-3).
2.9.1.4. The MTF provider’s support staff will notify the MTF Resource Management
Office (RMO) that a private sector exam is needed for a civil service employee (the clinic
must include the estimated cost of the exam or test). (T-3).
2.9.1.5. The RMO will send a request for unit commander’s Authorization of Payment for
Civilian Medical Exam packet to the employee’s unit commander. (T-3). The packet
contains two attachments: (1) Commander’s Authorization of Payment for Civilian
Medical Exam, and (2) Instructions for the unit resource advisor.
2.9.1.6. Commander’s Authorization of Payment for Civilian Medical Exam: This letter
serves as the MTF’s authorization to process the employee’s referral. It also expresses the
unit commander’s acknowledgement that unit funds will be used for payment of the exam.
(T-3).
2.9.1.7. Instructions to unit resource advisor: This information sheet explains to the
employee’s unit resource advisor the steps the advisor must take in order for payment to
be made to the civilian healthcare provider. (T-3). Payment will not be made until exam
results are received by the MTF. (T-3).
2.9.1.8. Once the RMO receives the unit commander’s Authorization of Payment for a
Civilian Medical Exam from the employee’s unit, a copy is provided to the MTF clinic.
The clinic will then schedule the employee’s exam. (T-3).
18 AFMAN41-210 10 SEPTEMBER 2019
2.9.1.9. The MTF clinic that schedules the employee’s exam should emphasize to the
civilian sector provider’s office that results of the exam and the associated invoice for full
and final payment must be sent to the MTF’s Referral Management Center. (T-3). Note:
MTF must provide the address, fax, and point of contact information. (T-3).
2.9.1.10. The Referral Management Center will: (1) Forward the exam results to the MTF
provider that requested the exam, and (2) Forward the invoice for the exam to RMO. (T-
3).
2.9.1.11. The RMO will: (1) Verify that the invoice contains “Full” or “Final” payment
on the invoice. If the invoice does not state that it is for full/final payment, then RMO
should contact the civilian provider’s billing office in order to receive a revised bill; (2)
Process payment according to the option indicated by the employee’s unit commander on
the bottom of the Commander’s Authorization of Payment for Civilian Medical Exam, and
per the Instructions to the unit resource advisor. The RMO should not proceed with
payment until exam results are received by the MTF. (T-3).
2.9.2. Workers’ Compensation Eligibility for Medical Services. Under the Federal
Employee’s Compensation Act, an employee injured while in the performance of duty is
entitled to compensation. This compensation may include services, appliances, and supplies
prescribed or recommended by a qualified physician. The Secretary of Labor must consider
the compensation likely to cure, give relief, and reduce the degree or period of disability or aid
in lessening the amount of monthly compensation. Reference 5 USC § 8103. Said services,
appliances, and/or supplies may be furnished by MTFs, Veterans Affairs (VA), or, United
States Public Health facilities; however, this instruction does not guarantee that the required
service(s) or supplies will be available at any one particular MTF, VA, or, United States Public
Health facility. When the local MTF has the capacity and supplies to provide this care, the
employee may choose to seek care through either the MTF or the civilian sector.
2.9.2.1. Direct MTF medical care, also known as in-house care, for job related injuries or
illnesses require: (1) Presentation of a completed Department of Labor Form LS-1,
Request for Examination and/or Treatment, LS-201, Notice of Employee’s Injury or Death,
or LS-202, Employer’s First Report of Injury or Occupational Illness along with Form
Compensation Act (CA)-16, Authorization for Examination and/or Treatment. A separate
Form CA-16 is not required for each episode of follow-up care if a Form CA-16 was
provided on the initial visit. If follow-up care is required beyond 60 days of the initial
issuance of the Form CA-16, the supervisor contacts the United States Department of Labor
(DOL) for authorization to issue another Form CA-16; (2) the care being provided is for
the same illness or injury as on the initial visit; and (3) the MTF has the capability to
provide the care.
2.9.2.1.1. A Form CA-16 authorizes an injured employee to obtain a medical
examination and/or treatment for up to 60 days. The Form CA-16 is used to authorize
payment for medical care of injuries only and cannot be used for illnesses. The Form
CA-16 is required for MTF care and prior to referring the patient outside of the MTF
for a consult or special study.
2.9.2.2. If the patient is referred/transferred to a specialist, the worker’s supervisor will
complete the Form CA-16 to authorize payment to the specialist (again, only for the first
60 days following injury). (T-1). The form is prepared by the individual’s supervisor and
AFMAN41-210 10 SEPTEMBER 2019 19
must be presented prior to treatment outside the MTF unless it is a medical emergency. (T-
1). In an emergency, the supervisor prepares the form within 48 hours after treatment is
rendered. If a Form CA-16 is created, a copy is scanned/uploaded into the individual’s Air
Force electronic health record. The MTF Patient Administration function does not provide
advice to employees or supervisors regarding form completion. Refer to the United States
Department of Labor, Office of Worker’s Compensation Programs.
2.9.3. Non-Deployment, non-work related illness/injury MTF Healthcare. Federal civilian
employees may be provided limited MTF medical treatment at the discretion of the MTF
commander or director for non-work related conditions on an outpatient basis for the purpose
of preventing excessive loss of duty time, or when immediate occupational requirements
dictate. Outpatient MTF medical care provided to federal civilian employees must be limited
to urgent relief of minor illnesses (e.g., sunburn, insect bite/stings, etc.) during the duty period
when care from a private medical provider would require a disproportionate amount of time
lost from the job. (T-1). The MTF commander or director must limit treatment to what is
needed to complete the work shift. (T-3). Surgical procedures, intravenous fluids and
prolonged course of care should not be provided. Controlled substances must not be
administered. (T-1). If simple outpatient medical care is approved by the MTF commander or
director and care is provided, the MTF should not assume responsibility for continued
treatment for any condition that could not be reasonably resolved during the initial episode of
treatment.
2.9.4. Federal Civilian employees employed outside the United States. Federal civilian
employees employed outside the United States who require treatment for conditions not
covered by the Office of Workers’ Compensation Program, who are not beneficiaries of any
other federal agency listed in this chapter, and dependents of such employees may receive
space available care in MTFs outside the United States. Charges will be collected locally in
accordance with DoD 6010.15-M, MTF Uniformed Business Office Manual, from the
individual at the interagency rate, except that no charge will be made for immunizations
authorized by AR 40-562/BUMEDINST 6230.15B /AFI 48-110/CG COMDTINST
M6230.4G, Immunizations and Chemoprophylaxis for the Prevention of Infectious Diseases,,
or for occupational health services as authorized elsewhere in this chapter. (T-0).
2.9.5. Non-Appropriated Fund employees. Non-Appropriated Fund employees are generally
not considered to be United States Government employees for most benefits, but may receive
occupational health services such as pre-employment, pre-deployment, and annual physicals
at MTFs in accordance with Health Affairs Policy 08-002. Such services are billed to the Non-
Appropriated Fund instrumentality.
2.9.6. Armed Forces Retirement Home. Title 24 United States Code Section 411 establishes
the Armed Forces Retirement Home as an independent federal organization. The purpose of
the Armed Forces Retirement Home is to provide residences and related services to certain
retired and former members of the Armed Forces in two locations—the Washington, D.C. area
and the Gulfport, MS area. Title 24 United States Code Section 413 authorizes the DoD to
provide secondary and tertiary hospital care, to the extent available, for both retiree and non-
retiree residents that is not available at the Armed Forces Retirement Home itself. As such,
Armed Forces Retirement Home residents do not require Secretarial Designation and are
eligible for secondary and tertiary hospital care at those MTFs that have been identified by the
DoD to provide these services (currently the Walter Reed National Military Medical Center
20 AFMAN41-210 10 SEPTEMBER 2019
and Keesler Air Force Base). Armed Forces Retirement Home leadership is responsible for
transportation to and from these MTFs.
2.10. Family Members (Dependents) of Federal Civilian Employees. When available, MTFs
will provide limited care to dependents who reside overseas under applicable laws and directives.
(T-0). Reference AFI 36-3026_IPV1; 24 USC § 34; DoDI 6000.11, Patient Movement; DoDI
6025.23. When their civil service sponsor is stationed overseas, family members are eligible to
receive space available healthcare and space available routine dental at MTFs at the Interagency
Outpatient Rate or Interagency Rate. Family members of civilians stationed in the United States
are not eligible for any routine healthcare or dental at MTFs.
2.11. Secretarial Designees. MTFs will administer medical and dental care to secretarial
designees, when applicable, in accordance with DoDI 6025.23. (T-0).
2.12. Members of Uniformed Services Auxiliaries. MTFs will provide limited healthcare to
senior adult and cadet members of the Uniformed Services Auxiliaries, who are injured while on
official government business. (T-0).
2.13. Emergency Care. Medical and dental care is authorized to the extent necessary to save life
or limb and prevent undue suffering. Patients are transferred to a civilian medical facility as soon
as they are stabilized. Collect the full-reimbursement rate from the individual or the individual’s
insurance company.
2.14. Contractors.
2.14.1. MTFs will provide care in accordance with contract terms and applicable laws and
policies to support contractor deployments and occupational health requirements. (T-0).
Elective care is not authorized, and in most instances, routine care is not authorized. Always
check the contract for specific terms. Reference DoDI 3020.41, Operational Contract Support.
2.14.2. MTF Contractor Occupational Health. Exams, evaluations, and immunizations
necessary to comply with MTF occupational health requirements are authorized at MTFs,
except when the provision of these occupational health services are designated as a contractor
responsibility under the terms of the contract.
2.15. Family Members (Dependents) of Contractors. Contractors may request approval from
the overseas Major Command (MAJCOM) Commander for medical care for their family members
beyond emergency care when specified requirements are met. Agreements reached under this
paragraph are annotated in the annual report for Secretarial Designees. Elective care is not
authorized. (T-1).
2.16. Expanded Medical Care for Caregivers. MTFs will inform individuals designated as
caregivers for seriously ill/very seriously ill service members of their authorization for space-
available inpatient/outpatient medical care at MTFs. (T-0). Reference 38 USC 1720G, Assistance
and support for caregivers.
2.17. Volunteers. MTFs will treat DoD volunteers, who are not TRICARE eligible, as federal
employees for volunteer-related injury or stabilization for illness. (T-0). Reference 10 USC §
1588, 5 USC § 8103, 5 USC § 8141 and DoDI 1100.21, American Red Cross (ARC)-DoD MOU.
If a DoD volunteer, regardless of volunteer organization affiliation, e.g., Red Cross, military retiree
activities office, etc., is normally entitled to MTF Direct Care or TRICARE benefits, then provide
the necessary healthcare coverage without delay. Otherwise, volunteers may be authorized
AFMAN41-210 10 SEPTEMBER 2019 21
outpatient and inpatient direct MTF healthcare for volunteer-related injury or illness for
stabilization.
Section 2D—Other Services and Authorizations
2.18. Additional MTF Requirements
2.18.1. Healthcare at Department of VA and Other Government Agencies. MTF commanders
or directors may authorize active duty and other DoD beneficiaries to receive space available
care at other federal agencies through resource sharing agreements. MTF commanders or
directors may also authorize beneficiaries from other federal agencies to purchase care from
MTFs when an appropriate agency official requests the services in writing from the MTF, and
the request will not interfere with medical care for persons entitled to MTF care. Reference
AFI 41-126, Department of Defense/Veterans Affairs Health Care Resource Sharing Program.
2.18.2. Dependency Determinations for Incapacitated Children. MTFs will process
dependency determinations for incapacitated children to assist in applying for continued
benefits for a child who becomes incapacitated before losing eligibility. (T-1). MTFs will
provide a medical sufficiency statement and follow process and eligibility guidance in AFI 36-
3026_IPV1. (T-1). Children enrolled in TRICARE Young Adult do not fall under the
provisions of this paragraph.
2.18.2.1. The Defense Finance and Accounting Service-Indianapolis Center is the final
approving authority for dependency determinations. The Military Personnel Section and
Base Finance Office will review the DD Form 137-5, Dependency Statement, and other
documentation to determine if the initial eligibility criteria warrant further processing and
forwarding to Defense Finance and Accounting Service-Indianapolis Center.
2.18.2.2. A medical statement in narrative format from the attending physician, or primary
care manager, including a medical sufficiency statement must be included in the
dependency determination application package provided from the MTF. (T-1). The MTF
commander or director is responsible for completing the Medical Sufficiency Statement;
however, the MTF commander or director may delegate the responsibility to the Chief of
the Medical Staff.
2.18.2.3. The patient and/or sponsor is responsible for obtaining and providing any
supporting medical documentation required for the application package. The TRICARE
Operations and Patient Administration Office will coordinate all requests for dependency
determinations with the Chief of Medical Staff. (T-3). Final medical sufficiency review
rests with the MTF commander or director, or Chief of Medical Staff if delegated. If the
MTF commander or director has delegated endorsement authority to the MTF/Chief of
Medical Staff, the application package does not need the MTF commander’s or director’s
signature before it is forwarded to officials at the installation personnel/finance office.
2.18.2.4. If the patient’s care is rendered outside of the MTF, and it would be a burden on
the patient or sponsor to travel to a MTF, a civilian provider may complete the medical
sufficiency statement and submit it to the nearest Air Force MTF for endorsement.
2.18.2.5. In order to establish medical incapacity, the patient’s illness must be substantial
and truly disabling. (T-1). In addition, the medical incapacity must occur before the
individual’s 21st birthday (or 23rd birthday if enrolled as a full-time student when
22 AFMAN41-210 10 SEPTEMBER 2019
incapacitation occurred). (T-1). The Air Force does not consider a diagnosis of alcoholism
or drug abuse as an incapacitating illness for the purposes of dependency determinations.
The likelihood of future medical expenditures and/or the existence of a medical condition
that will worsen over time, do not justify a determination of medical incapacity if no
incapacitation currently exists.
2.18.2.6. The civilian or MTF provider will include the following information in the
medical sufficiency statement (T-2):
2.18.2.6.1. Diagnosis (use medical and layperson’s terms).
2.18.2.6.2. Summary of the individual’s incapacitation, including the nature and extent
of the illness or disease. Non-medical personnel should be able to understand this
summary.
2.18.2.6.3. Explain how the incapacity affects the individual’s ability to perform
routine life activities, such as self-care.
2.18.2.6.4. Age when the incapacitation began (might not be the same as when medical
personnel diagnosed the illness or disease).
2.18.2.6.5. Probable duration of the incapacitation. Indicate if the incapacity predated
the individual’s 21st or 23rd birthday and has been continuous since diagnosis.
2.18.2.6.6. Based on the healthcare provider’s professional opinion, indicate if the
incapacity makes the individual incapable of self-support.
2.18.2.6.7. Depending on the circumstances involved in the sufficiency review, the
MTF commander or director/designee selects one of the four statements as described
in attachment 15 of AFI 36-3026_IPV1.
2.18.2.7. The MTF completing the Medical Sufficiency Statement shall provide the
sponsor with the completed request package; however, only an approved Medical
Sufficiency Statement must be submitted to Defense Finance and Accounting Service. (T-
1). The sponsor is responsible for coordinating with the appropriate finance and Military
Personnel Section officials.
2.18.2.8. A copy of the Medical Sufficiency Statement and any other supporting medical
documentation should be scanned/uploaded in the appropriate section of the patient’s
electronic health record.
2.18.2.9. The applicant may submit a request for reconsideration to the MTF commander
or director if there is new or compelling information. The MTF can review, and if the
commander determines a change from original recommendation to the Military Finance
Office is warranted, will notify that office. (T-2). Defense Finance and Accounting
Service-Indianapolis Center remains the ultimate decision authority for granting
dependency status based on the Medical Sufficiency Statement and financial support (over
50%) from the sponsor.
2.18.3. TRICARE Extended Care Health Option. MTFs will administer the TRICARE
Extended Care Health Option program in accordance with Title 32, Code of Federal
Regulations, Part 199.5(g), TRICARE Extended Health Care Options (ECHO), current edition
AFMAN41-210 10 SEPTEMBER 2019 23
and Title 32, Code of Federal Regulations, Part 199.7, Claims Submission, Review, and
Payment, current edition (T-0).
2.18.3.1. Extended Care Health Option Home Healthcare. Custodial care services, as
defined in Title 32, Code of Federal Regulations, Part 199.2, Definitions, current edition
may be provided to the extent such services are provided in conjunction with authorized
TRICARE Extended Care Health Option home healthcare services, including the Extended
Care Health Option Home Healthcare respite care benefit specified in this section.
Authorized beneficiaries will receive all home healthcare services and no portion will be
provided under the TRICARE Basic Program. (T-0). Reference 32 CFR Part 199.4(e).
2.18.4. Elective Medical Care from Civilian Sources for AD Members. Elective medical and
dental care provided at civilian medical facilities or from other civilian sources is not
authorized at the government’s expense. Service Members who seek medical/dental care
outside the Military Health System without prior approval or coordination with the MTF
responsible for their primary care, do so at their own risk. Any unfavorable outcome resulting
from elective care provided by civilian sources could result in a not-in-line-of duty finding and
potentially impact disability benefits. All members assigned or attached to a sensitive duty
program, e.g., the Personnel Reliability Program (PRP), Presidential Support Program (PSP),
or other national security dependent program, must obtain written permission from their unit
Commander and local MTF Commander prior to treatment. If approved, personnel in these
uniquely critical programs must have their treatment reviewed by the MTF PRP consultant or
designated competent medical authority. (T-1). In addition, any service member seeking
elective surgery must comply with AFI 44-102, Medical Care Management. (T-1).
2.18.4.1. Service members must arrange for the civilian medical facility to send a
summary of treatment to the servicing MTF. (T-1). For additional information regarding
elective civilian medical care for AD service members, refer to AFI 44-102 and AFI 36-
3003, Military Leave Program.
2.18.5. Requirements for Organ Donation Requests. All AD members must follow the
requirements in AFI 44-102 in order to serve as organ donors. (T-1).
2.18.6. Authorization for Physical Examinations Other than Flying.
2.18.6.1. Operational Health Assessments (Periodic Health Assessment, Mental Health
Assessment, Deployment-Related Health Assessment). Operational Health Assessments
are authorized in accordance with DoDI 6200.06, Periodic Health Assessment (PHA)
Program; DoDI 6490.03; and DoDI 6490.12, Mental Health Assessments for Service
Members Deployed in Connection with a Contingency Operation, and 10 US Code §1074.
Scheduling is managed by the Operational Medicine Clinic or Force Health Management
as determined by the MTF.
2.18.6.2. Civilian occupational health examinations are performed in accordance with 29
CFR §1910.
2.18.6.3. The MTF commander or director may authorize medical evaluations in the
context of a public health emergency in accordance with DoDI 6200.03, Public Health
Emergency Management within DoD; exposure to bloodborne pathogen in accordance with
29 CFR §1910.1030; and food safety in accordance with AFMAN 48-147, Tri-Service
Food Code.
24 AFMAN41-210 10 SEPTEMBER 2019
2.19. Primary Care Manager Assignments. MTFs shall provide enrollees with the opportunity
to register personal preferences for Primary Care Managers from a list of choices as required by
DoDI 6000.14, DoD Patient Bill of Rights and Responsibilities in the Military Health System
(MHS). (T-0). The MTF commander or director will also make a provider directory easily
accessible to beneficiaries, which is inclusive of all MTF Primary Care Managers alongside the
provider information required by DoDI 6000.14. (T-0).
2.19.1. MTFs shall not deny Primary Care Manager empanelment/enrollment to beneficiaries
based on the sponsor’s Service affiliation. (T-0). MTFs shall not deny patients the opportunity
to initiate Primary Care Manager changes by phone or by web through the Beneficiary Web
Enrollment application, or otherwise limit Primary Care Manager change requests to face-to-
face transactions. (T-1).
2.19.2. MTFs shall only make credentialed and privileged Primary Care Managers available
for empanelment. (T-1). Primary care managers loaded into DEERS and/or the Composite
Health Care System (CHCS) shall be entered using the credentialed provider's name as listed
in the MTFs provider directory, not team names or other names that are non-specific to a
particular credentialed and privileged provider. (T-1). MTFs shall not enter primary care
managers into DEERS or CHCS for short-term administrative purposes such as managing
disenrollment, over-enrollment, or provider panel acuity/complexity. (T-1). MTFs may allow
a recently departed primary care manager to remain in DEERS and/or CHCS temporarily until
the departed primary care manager’s panel can be transferred; however, one or more
credentialed and privileged providers must be accountable for the panel until it is transferred.
(T-1).
2.19.3. MTFs shall honor enrollee primary care manager preference requests subject to the
primary care manager’s availability, matching patient medical needs with the appropriate level
of healthcare provider, and other operational requirements established by the MTF commander
or director. (T-3). MTFs shall minimize primary care manager changes not requested by
enrollees, and shall not disrupt established patient-provider relationships for the sole purpose
of rebalancing provider panels; instead, provider panels should be balanced through new
patient enrollments and patient attrition. (T-3).
2.19.4. MTFs shall not initiate a primary care manager change that transfers an enrollee from
a MTF primary care manager to a network primary care manager unless the enrollee’s medical
needs exceed the MTFs capabilities. (T-1). MTFs planning any forced disempanelment of
beneficiaries require pre-approval from the Air Force Medical Support Agency and must
coordinate with the Defense Health Agency. (T-1). Poor patient behavior and/or non-
compliance with medical care are insufficient grounds to involuntarily disengage an enrollee
from a MTF primary care manager to a network primary care manager, except in rare
circumstances where the patient’s behavior is so abusive or belligerent that it significantly
interferes with execution of the MTF’s mission and threatens the safety and wellbeing of the
other patients and/or MTF staff. In these cases, the MTF should seek advice from the local
Staff Judge Advocate and regional Medical Legal Consultant. If legal authorities advise the
patient’s abusiveness or belligerency warrants disengagement of the patient from the MTF,
and that the individual’s entitlement to care doesn’t prevent transferring their care to the
network, the MTF shall coordinate a transfer of care to a network healthcare team to ensure
continuity of care. (T-3). If there is an immediate danger to staff or patients, the healthcare
team should contact security forces.
AFMAN41-210 10 SEPTEMBER 2019 25
2.19.4.1. In written documentation, the MTF commander or director will describe the
disruptive behavior, its effect, the investigative and determination process, and the
probable consequences of disruptive behavior. MTF leadership will consult their servicing
legal office early in all cases of disruptive beneficiary behavior.
2.19.4.2. When an active duty service member displays abusive or seriously disruptive
behavior in the MTF, the following actions are recommended:
2.19.4.2.1. Obtain objective assessment and documentation of the abusive behavior by
witnesses. Documentation should clearly demonstrate how the behavior threatens
patient or staff safety.
2.19.4.2.2. Advise the active duty service member of paragraph 2.19.4.5, referencing
the patient’s responsibility to show respect and consideration to others, and the MTF’s
authority to respond to the abusive or disruptive behavior.
2.19.4.2.3. If the active duty service member’s misconduct continues, ask the
member’s command authority to arrange security police escort when the member is
seeking medical or dental care. Definitive administrative or punitive action is a military
command issue.
2.19.4.3. When an active duty family member enrollee engages in disruptive behavior, the
MTF commander or director may:
2.19.4.3.1. Arrange a discussion between a senior hospital leader and the beneficiary,
with the sponsor present, to dissuade future disruptive behavior and describe potential
consequences.
2.19.4.3.2. With the active duty family member’s consent, empanel the family member
to a network provider, ensuring that the TRICARE contractor is informed of the
disruptive issue. Note: When an active duty family member is empaneled to the
network, if network empanelment is unable to accommodate, the MTF must empanel
the beneficiary to a MTF primary care manager unless the family member enrollee
elects TRICARE Select.
2.19.4.3.3. Issue a warning letter, in accordance with written MTF policy, conveying
the beneficiary's responsibility to uphold appropriate behavior including respect and
consideration to other patients and staff in accordance with DoDI 6000.14.
2.19.4.3.4. Ask the installation commander, or designee, to bar the active duty family
member from base under 18 USC § 1382. In some instances, an installation bar letter
may permit an active duty family member limited access to base for medical care; in
such cases, a military police escort may be required.
2.19.4.3.5. When the active duty family member’s disruptive behavior amounts to
criminal activity, in consultation with the base Staff Judge Advocate, seek to have the
family member prosecuted.
2.19.4.4. When confronted with disruptive behavior by a retiree, a retiree’s family
member, or a TRICARE Plus enrollee, the MTF commander or director has the same
options as with an active duty family member enrollee with a notable addition: the MTF
commander or director may involuntarily transfer the individual’s routine direct care and
access to ancillary services to a site outside the MTF. In this case the MTF commander or

26 AFMAN41-210 10 SEPTEMBER 2019
director will make efforts, in coordination with the TRICARE contractor, to find an
accepting network primary care manager. The TRICARE contractor and network primary
care manager must be made aware of past disruptive behavior. A coordinated handoff of
care to the network healthcare team is necessary to avoid any appearance of patient
abandonment. Should obtaining a network primary care manager prove impossible, self-
managed health care using TRICARE Select is likely the beneficiary's only TRICARE
option. For those TRICARE Plan and Medicare ineligible (a small minority of TRICARE
Plus enrollees) with no other health insurance, finding an accepting primary care manager
may be improbable; nonetheless if warranted, the MTF commander or director may transfer
empanelment of a TRICARE Plus beneficiary without other insurance to a network
provider for routine care and ancillary services.
2.19.4.5. Care providers must document patients’ abusive behavior. Commanders must
document actions taken to mitigate poor behavior. Transferring care to the network for
routine care and ancillary services is not to be used in an arbitrary or capricious manner,
such as for an argumentative patient or for patients not compliant with the treatment team
recommendations. It must be a compelling situation where the welfare and safety of the
patients or staff is seriously threatened. Additionally, if the patient has a history of, or is
exhibiting actions that may be due to mental illness or neurological impairment, the MTF
must manage these circumstances as a medical matter. MTF commanders and directors
should also notify leadership at other multi-service markets for the potential of a seriously
threatening patient who may seek care in their facilities.
2.19.5. MTFs with current capacity to provide primary care services to additional patients may
reassign TRICARE Prime beneficiaries from network primary care managers to MTF primary
care managers when beneficiaries live within a 30-minute drive time of the MTF.
2.19.5.1. When recapturing network Prime enrollees, MTF commanders or directors shall
recapture AD family members first and retiree beneficiaries second. (T-1). An exception
to this requirement are beneficiaries who require a primary care manager with a skillset
unavailable at the MTF, or there are strong continuity of care reasons against changing the
primary care manager.
2.19.5.2. Involuntary recapture campaigns must include communication with the
beneficiaries, multi-service market, if applicable, local elected officials, public affairs
officials, the TRICARE regional office, and the managed care support contracts. (T-1).
See “Enrollments” on Air Force Medical Operations Agency (AFMOA) Health Benefits
Knowledge Exchange (Kx) for best practices on conducting involuntary recapture
campaigns. https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
2.20. Sexual Dysfunctions, Inadequacies, or Paraphilic Disorders Treatment. For benefit
guidelines and instructions reference TRICARE Policy Manual 6010.60-M, Chapter 4, Section
16.1, Intersex Surgery.
2.20.1. Surgical procedures related to gender dysphoria may be provided within a MTF if there
is a provider appropriately credentialed, trained, current and privileged to perform the
procedure. Requests for surgery related to gender dysphoria for active duty must utilize the
Supplemental Health Care Program waiver process, in accordance with current Defense Health
Agency policy. (T-1). Patient travel may be authorized for patients who are referred to the Air
AFMAN41-210 10 SEPTEMBER 2019 27
Force Medical Multi-Disciplinary Team at the Wilford Hall Ambulatory Surgical Center in
San Antonio, TX for evaluation.
2.20.2. The patient must have appropriate endorsement from the Air Force Medical Multi-
Disciplinary Team and their unit commander. (T-1). Appropriate rules for billing and duty
status apply depending on the type of surgery being provided. Refer to AFI 44-102, for rules
on elective care and cosmetic care.

28 AFMAN41-210 10 SEPTEMBER 2019
Chapter 3
TRICARE OPERATIONS
Section 3A—Access to Care Guidance
3.1. Access to Care Standards.
3.1.1. Access to care for beneficiaries is a top priority for the MHS. All enrolled beneficiaries
regardless of their location, must be afforded access to care according to the standards
published in Health Affairs Policy 11-005. (T-0). See AFI 44-176, for additional information
and DHA IPM 18-001, Standard Appointing Processes, Procedures, Hours of Operation,
Productivity, Performance Measures and Appointment Types in Primary, Specialty, and
Behavioral Health Care in Medical Treatment Facilities (MTFs).
Section 3B—Beneficiary Counseling and Assistance Coordinator
3.2. Beneficiary Counseling and Assistance Coordinator Position and Procedural
Information.
3.2.1. Beneficiary Counseling and Assistance Coordinators are mandated at each MTF and
TRICARE regional office. Beneficiary Counseling and Assistance Coordinators will execute
roles and responsibilities in performance of their duties as stated in DoDI 6015.23. (T-0).
Duties include:
3.2.1.1. Inputting beneficiary associated casework into the Assistance Reporting Tool.
3.2.1.2. Tracking, managing, referring categorizing, and documenting case workload in
the Assistance Reporting Tool. Any cases that need referral to a DHA Program Office (to
DHA or a TRICARE regional office) must be sent via the Assistance Reporting Tool.
Assistance Reporting Tool credentials are requested by e-mailing
dha.ncr.comm.mbx.bcacdca[email protected] .
3.2.2. In the event of system connectivity issues, MTF personnel are encouraged to create and
utilize a temporary internal tracking mechanism. MTFs shall move information from their
internal tracking tool to the Assistance Reporting Tool when the tool is once again operational.
(T-2). For training, visit https://mhs.health.mil/customerservicecommunity/.
Section 3C—Debt Collection Assistance Officer
3.3. Debt Collection Assistance Officer Position and Procedural Information.
3.3.1. Debt Collection Assistance Officers are mandated at each MTF and TRICARE regional
office. Debt Collection Assistance Officers will execute roles and responsibilities in
performance of duties as stated in DoDI 6015.23. (T-0).
3.3.2. TRICARE Prime Remote members may contact DHA Great Lakes Debt Collection
Assistance Officer Representative at 1-(888)-647-6676 for assistance with debt collection
issues related to line-of-duty determinations; otherwise, members should work with the
appropriate regional managed care support contractor first.

AFMAN41-210 10 SEPTEMBER 2019 29
3.3.3. Beneficiary Counseling and Assistance Coordinator - Debt Collection Assistance
Officer Directory. Debt Collection Assistance Officers should ensure that contact information
is accurately reflected in the online public Beneficiary Counseling and Assistance Coordinator
- Debt Collection Assistance Officer directory found on the TRICARE website at
(http://www.tricare.mil/bcacdcao/). Changes and updates should be forwarded to the
TRICARE regional office.
Section 3D—Service Change Requests
3.4. Changes in Clinical Services. DoDI 6015.23 provides that the Secretaries of the Military
Departments and the Director, DHA, act on requests for changes in clinical services at MTFs as
recommended by respective military command authorities. Headquarters Air Force (HAF)
Mission Directive 1-48, The Air Force Surgeon General (AF/SG), states that the Secretary of the
Air Force further delegated authority to AF/SG to implement policy, assign responsibilities, and
prescribe procedures on provisions of care in the delivery of health care at MTFs pursuant to DoDI
6015.23. Per HAF Mission Directive 1-24, Assistant Secretary of the Air Force Manpower and
Reserve Affairs (SAF/MR) retains Secretarial oversight responsibility for all aspects of the Air
Force Active Duty, Reserve, and Auxiliary Component Affairs concerning health program benefits
and entitlements, to include those authorities delegated directly to the AF/SG. Thus, all service
change requests are coordinated with AF/SG, SAF/MR, and DHA before they are approved. (T-
1). Congressional reporting is required in accordance with NDAA 2019, Section 711, in the
interest of maintaining a positive relationship with members of the community and Congress, the
Congressional and Public Affairs office (AF/SGL) should be included in the process to provide
guidance.
3.4.1. MTFs will submit written request packages, already coordinated with their TRICARE
regional offices and MAJCOM command surgeon to Air Force Medical Readiness Agency
(AFMRA). AFMRA will then prepare requests and coordinate the package for AF/SG,
SAF/MR, and DHA approval. (T-0).
3.4.1.1. Permanent changes in services that significantly affect the current annual volume
of care provided to one or more categories of beneficiaries at a MTF for one or multiple
specialty or ancillary service(s).
3.4.1.2. Changes that impact users in a way that may stimulate local public or
congressional objections.
3.4.1.3. Temporary closures of services that are projected to last 90 days or more, or for
an indefinite period.
3.4.1.4. Changes in enrollment that result in the recapture or disengagement of 400 or more
beneficiaries in a single disengagement or recapture campaign or over a 1 year period.
3.4.2. MAJCOM command surgeons, AFMOA/SGAT, and MTF operational and resource
planners should include projected changes in services in their strategic planning documents
such as strategic plans, business plans, and/or strategic resourcing portfolios. Notify
AFMOA/SGAT as soon as possible of any projected changes in service, keeping in mind the
various planning cycles involved in accommodating changes. The planning cycle is at least
three fiscal years to facility modifications that involve major construction projects, at least two
years for manpower and financial resources, and at least twelve months for personnel
30 AFMAN41-210 10 SEPTEMBER 2019
assignments. The content and submission requirements for change in service requests may
vary depending on impact and cause of the proposed change.
3.4.2.1. Change in service requests shall include information as outlined below and must
arrive at AF/SG at least six months prior to the proposed effective date when the change
involves significant downgrading or upgrading in level of services. (T-2). This includes
downgrading from hospital to clinic, permanent closure of services, and adding a service
which has been previously unavailable at the facility. MTFs should not assume their
request will be approved.
3.4.2.2. Abbreviated requests or notifications may be submitted for any changes in service
which result in minor changes in type of services (such as discontinuing a subspecialty
service) or for any changes resulting from circumstances beyond the control of the
MAJCOM command surgeon, AFMOA/SGAT, or the MTF. This includes actions due to
resource management decisions, economic analyses for Military Construction Projects, and
for situations described below. Abbreviated requests or notifications should be coordinated
through respective MAJCOM command surgeons and AFMOA/SGAT, with information
copies sent to TRICARE regional offices, and should arrive at AF/SG not later than 90
days prior to the effective date of the change.
3.4.2.3. If a temporary change in services occurs as a result of sudden staffing changes or
reassignments, equipment breakdowns, supply shortages, or other unexpected
circumstance, immediately notify the TRICARE regional office, command surgeon,
AFMOA/SGAT, and prepare an abbreviated package as soon as possible but arriving at
AF/SG no later than 30 days following the change. If the change eventually results in a
permanent closure of services, a more detailed package is required within 90 days of the
original closure.
3.4.2.4. Changes in services which are made under the following circumstances do not
require prior notification to AF/SG and SAF/MR approval, but the MTF commander or
director shall report the change in services to the chain of command (T-1):
3.4.2.4.1. A facility rendered structurally unsound by a natural disaster.
3.4.2.4.2. A change in a Status of Forces Agreement.
3.4.2.4.3. An initial response to an emergency deployment of healthcare personnel.
3.4.2.4.4. A change in local Force Protection Condition.
3.4.3. The service change request will include or address the following information:
3.4.3.1. Name and location of the facility.
3.4.3.2. Type of change in service and, if applicable, the Medical Expense and
Performance Reporting System specialty area.
3.4.3.3. Proposed effective date of the change and/or the estimated duration of the change.
3.4.3.4. Reason or Justification for the change.
3.4.3.5. Summary of the impact on beneficiaries, including access and quality of
alternatives and difference in cost, if any (e.g., estimated increase or decrease in out-of-
pocket expenses).
AFMAN41-210 10 SEPTEMBER 2019 31
3.4.3.6. Evidence of briefing and feedback to wing commanders and/or line commanders
and beneficiary groups supported by MTF (such as retiree and veterans associations and
staff of congressional field offices), and concerns resolved or addressed by MTF; may
include beneficiary marketing and education plan in package.
3.4.3.7. Impact on readiness capability, including how training needs will be affected
and/or addressed to maintain technical and clinical skills and currency, knowledge, tasks
required for wartime, enhancement of a fit force, and improvements in force protection.
3.4.3.8. Description of how the change(s) is/are consistent with the overall health services
mission and strategy for the medical facility, MAJCOM command surgeon, and AFMOA,
Department of Defense (DoD) Health Services Region, Air Force, MHS, etc., including
implementation of new and innovative ways for promoting better health among
beneficiaries and the military community.
3.4.3.9. Estimated workload changes, by Medical Expense and Performance Reporting
System specialty area and beneficiary category, including number of non-availability
statements, beneficiary visits, admissions, bed days, and/or ancillary service work units.
Beneficiary categories should include Active Duty (AD), non-TRICARE eligible, and
TRICARE-eligible, with the latter broken down into AD dependents, and non-AD
dependents.
3.4.3.10. Projected savings (or cost) to the government, by fiscal year, resulting from the
change, including operations and maintenance funds (including civilian staffing), military
personnel, impact from estimated bid price adjustment, and military construction project
costs, if applicable. Submit all calculations used in determining final estimates, including
methodology for both full and marginal cost estimates.
3.4.3.11. Net manpower, equipment, and facilities resources resulting from the proposed
change, and projected methodology for redistributing resources, if applicable; include how
surplus resources will be used in other functions or eliminated.
3.4.3.12. Analysis of alternative ways to provide care to the beneficiaries affected,
including projected increases in cost of each alternative, as well as, the financial
implications to the beneficiary. The analysis should include the following:
3.4.3.12.1. Quality and Utilization of Services: Provider qualifications, accreditation,
preventive measures, health outcomes, beneficiary satisfaction, and projected volume
and level of care based on beneficiary needs and/or referrals.
3.4.3.12.2. Cost: Government as well as beneficiary savings or costs.
3.4.3.12.3. Access: Availability of civilian or other federal healthcare providers in the
community, including options such as DoD/VA sharing, contracting, TRICARE
resource sharing or resource support agreements.
3.4.3.12.4. Other: Local market factors which may influence the use of alternatives
such as quality, cost, access and other unique factors specific to the MTF, local
community, or region that could potentially generate future benefits or problems
resulting from the requested service change.
32 AFMAN41-210 10 SEPTEMBER 2019
3.4.3.12.5. Projected impact in terms of increased reliance on TRICARE managed care
support contractor and/or Medicare providers in the service area in which the MTF is
located.
3.4.3.12.6. Long-term costs and savings in infrastructure such as information systems
requirements, contracts, and facilities (including minor construction, major repair or
military construction projects) currently underway, recently completed, and/or
planned.
3.4.3.12.7. Explanation of how the change is/is not consistent with the MTF strategic
resourcing portfolio, business plan, goals and objectives, etc.
3.4.3.13. TRICARE regional office input may include, but is not limited to:
3.4.3.13.1. How the change is/is not consistent with the TRICARE regional office
business plan/strategic plan/regional health plan, including comparison with any
regional alternatives or initiatives, particularly those involving the TRICARE managed
care support contractor.
3.4.3.13.2. Impact on the managed care support contractor, and if available, the net
negative or positive cost impact to the region and/or another DoD MTF, particularly in
overlapping prime service areas, also known as the areas in which the contractor offers
enrollment in TRICARE Prime.
3.4.3.13.3. Coordination/feedback from other Services, MAJCOM command
surgeons, and/or AFMOA/SGAT, particularly if impacting graduate medical education
programs.
3.4.3.13.4. Recommendations, including estimated timeline.
3.4.3.14. MAJCOM command surgeons must submit evidence of coordination with
MAJCOM commanders (through MAJCOM Plans and Programs offices) and shall include
in their evaluation (T-1):
3.4.3.14.1. Impact on readiness baseline and how MAJCOM command surgeon or
AFMOA/SGAT proposes to make any necessary changes to operational mission within
the command to accommodate change.
3.4.3.14.2. Validation of military personnel disposition (e.g., if Military Personnel
savings are expected and, if applicable, how MAJCOM command surgeon or Air Force
Medical Operations Agency, Manpower Division (AFMOA/SGAP) proposes to
redistribute resources in accordance with projected limits to downsizing force in
accordance with Air Force Medical Service (AFMS) rightsizing efforts, Base
Realignment and Closure plans, and other factors).
3.4.3.14.3. Explanation of how the change is/is not consistent with the MAJCOM
command surgeon’s business plan, strategic plan, or strategic resourcing portfolio.

AFMAN41-210 10 SEPTEMBER 2019 33
Section 3E—Referral Management Program
3.5. Referral Management Program.
3.5.1. Guidance, Policy, and information regarding referral management business rules can be
found in AFI 44-176. Best practices regarding referral management can be found on the Air
Force Medical Service (AFMS) Kx Referral Management website at
https://kx.health.mil/kj/kx8/AccesstoCare/Pages/referral_management.aspx.
3.5.2. Support to Geographically Separated Units (GSU)/TRICARE Prime Remote enrollees.
3.5.2.1. GSU members are usually enrolled to a civilian Primary Care Manager through
the TRICARE Prime Remote program. When a TRICARE Prime Remote member’s
medical condition warrants referral to a MTF for either administrative reasons (e.g., Line
of Duty, Medical Evaluation Board, etc.) or specialty care, the MTF becomes clinically
responsible for that patient. If the MTF subsequently refers the patient to the local network,
while maintaining clinical oversight of the patient’s care, the approval and authorization
process rests with the referring MTF. Under no circumstance will the Specified
Authorization Staff at the DHA-Great Lakes be asked to place an authorization into the
system for a TRICARE Prime Remote enrolled patient when a MTF initiated the referral.
If the patient’s clinical needs exceed the MTF’s oversight capability, care management is
returned to the civilian Primary Care Manager through the Specified Authorization Staff.
These same guidelines apply to RC personnel referred to MTFs for medical and
administrative support.
Section 3F—Medical In/Out-Processing Program
3.6. Medical In/Out-Processing Program Overview.
3.6.1. Air Force medical units will apprise all beneficiaries, in particular military service
members, of their healthcare benefits as they move from one assignment to another.
Specifically, members must be informed of the scope of their benefits; how to access healthcare
in their local community; how to access healthcare while away from home or enroute to a new
duty station; and how to resolve problems related to medical care and access during this
transitional period, should they arise. (T-0). Reference DoDI 6000.14.
3.6.2. Medical In/Out-Processing Program Roles and Responsibilities.
3.6.2.1. MTF Commanders or Directors. MTF commanders or directors will establish
medical in/out-processing programs designed to ensure enrolled beneficiaries have a basic
understanding of their individual health benefits, the MTF’s capabilities, and a basic
overview of preventative health programs available to patients. (T-0). Reference DoDI
6000.14.
3.6.2.2. MTF commanders or directors will ensure MTF staff members are familiar with
the typical subject issues and topics discussed at in/out-processing briefings. (T-0).
Reference DoDI 6000.14.
3.6.2.3. MTF staff members should have a basic understanding of TRICARE benefit
options and be able to clearly communicate these options to beneficiaries when required –
or at least know to refer patients who have TRICARE enrollment or general health benefits
34 AFMAN41-210 10 SEPTEMBER 2019
questions to the appropriate office to obtain further information. Health benefits briefings
may be combined with other installation information briefings normally provided to
arriving and departing service members. Although not specifically limited as an exclusive
TRICARE Operations and Patient Administration obligation, generally, MTF staff
members assigned to this office are responsible for providing the healthcare benefits
portion of each in/out-processing function.
3.7. In-processing Requirements. At a minimum, the following information or procedures must
be accomplished with, or briefed to, each sponsor during the in-processing briefing(s) by
TRICARE Operations and Patient Administration staff (T-3):
3.7.1. TRICARE enrollment options.
3.7.2. Choosing a new primary care manager and how to contact their provider or clinical
support team.
3.7.3. How to change their primary care manager at the new location.
3.7.4. Benefits of enrolling in TRICARE Prime, including Point of Service option for Non AD
Beneficiaries.
3.7.5. Local polices on TRICARE Prime enrollment and CHCS registration data collection.
3.7.6. How to enroll family members in the dental plan.
3.7.7. MTF/TRICARE regional office/managed care support contractor/TRICARE service
points of contact.
3.7.8. Exceptional Family Member Program with a brief description of each of the MTF
partner programs that support Exceptional Family Member Program, Exceptional Family
Member Program-Medical and the Family Member Relocation Clearance processes.
3.7.9. Family Advocacy Program.
3.7.10. How to schedule/cancel appointments.
3.7.11. Out of area care procedures.
3.7.12. Services available at local MTF (s).
3.7.13. How to access services not available at the local MTF and after hours.
3.7.14. Services available in the network.
3.7.15. AFMS health record custody policy.
3.7.16. Mental Health.
3.7.17. Local prescription services.
3.7.18. Personnel Reliability Assurance Program, Presidential Support Program, and other
sensitive duties program overview.
3.7.19. How to file a civilian medical or dental claim.
3.7.20. Contact information for the Beneficiary Counseling and Assistance Coordinator/Debt
Collection Assistance Officer.
3.7.21. Co-payments and cost-share/deductible fees for care outside the direct care system.
AFMAN41-210 10 SEPTEMBER 2019 35
3.7.22. How to enroll or update TRICARE Online member profiles to gaining MTF.
3.7.23. Collect any medical or dental records that the member may be carrying and return to
the MTF records room or primary care management team for which the beneficiary is or will
be assigned.
3.7.24. Procedures for participation in Secure Messaging, if available at the MTF.
3.8. Out-processing Requirements. At a minimum, the following information or procedures
must be accomplished with, or be briefed to, each sponsor during the out-processing
appointment(s) by TRICARE Operations and Patient Administration staff (T-3):
3.8.1. Ensure all laboratory and radiology results are scanned/uploaded into in the individual’s
electronic health record within 0-5 business days prior to final out-processing appointment for
Permanent Change of Station (PCS), separation or retirement.
3.8.1.1. For individuals enrolled in Exceptional Family Member Program, or navigating
the Family Member Relocation Program/Process, scan/upload medical documents into
their electronic health record prior to the screening as required in accordance with AFI 40-
701, Medical Support to Family Member Relocation and Exceptional Family Member
Program (EFMP).
3.8.2. The DoD and AFMS health records custody and control policies.
3.8.3. The process required to file medical claims for care while in transit.
3.8.4. The process required to schedule appointments in transit.
3.8.5. The process required to locate a MTF at the next assignment.
3.8.6. The process required to obtain prescription services while in transit.
3.8.7. The process required to transfer/change the Primary Care Manager to a new MTF.
3.8.8. The process required to avoid point of service charges while in transit.
3.8.9. How to obtain emergency care and the patient responsibilities for contacting her/his
Primary Care Manager.
3.9. Limited Capability Out-processing. If a member is going to a medical facility without
access to Composite Healthcare System (CHCS)/Health Artifact and Image Management Solution
(HAIMS)/Armed Forces Health Longitudinal Technology Application (AHLTA) or MHS
GENESIS (such as geographically separated or remote locations, recruiters not near an installation,
or Navy members going to a ship, etc.), all electronic health records will be printed and filed in
the hard copy record. (T-0). If the member is moving to a traditional location/MTF, only medical
records created prior to the implementation of AHLTA (2006) need to be filed in the hard copy
record and forwarded to the gaining MTF.
3.10. Retirement/Separation Out-processing. For AD Service Treatment Record disposition
(member is separating or retiring), the Air Force Service Treatment Record Processing Center
needs all hardcopy encounters/records not captured in AHLTA. AHLTA Web Print will capture
all electronic medical records documented. For Non-Service Treatment Record disposition, all
records are required to be printed in hard copy format, as the records are legally required to be
complete upon arrival at the National Processing Records Center. (T-0). Reference DoDI 6040.45,
DoD Health Record Life Cycle Management.
36 AFMAN41-210 10 SEPTEMBER 2019
Section 3G—External Resource Sharing Agreements
3.11. External Resource Sharing Agreement.
3.11.1. MTF Responsibilities. MTFs seeking External Resource Sharing Agreements must
coordinate approval with AFMOA/SGAT prior to signing. (T-1).
3.11.2. MTFs will request a child Defense Medical Information System Identifier through the
Air Force Defense Medical Information System ID coordinator (AF/SGY) for new External
Resource Sharing Agreements within 30 days of being signed by the TRICARE regional office
director. (T-1).
3.11.2.1. MTFs will capture all workload performed under an External Resource Sharing
Agreement in the Defense Medical Information System ID set up for the External Resource
Sharing Agreement. (T-1).
3.11.2.2. Workload performed under a Training Affiliation Agreement shall not be
captured under an External Resource Sharing Agreement Defense Medical Information
System ID. (T-1).
3.11.3. MTFs will forward a copy of new External Resource Sharing Agreements to
AFMOA/SGAT within 30 days of being signed by the TRICARE regional office director. (T-
2).
3.11.4. MTFs will internally review all External Resource Sharing Agreements annually, and
document the review locally. (T-1). External Resource Sharing Agreements that are no longer
active and not anticipated to become active before the next annual review should be terminated
in accordance with the External Resource Sharing Agreement’s terms.
3.11.5. MTF commanders or directors may only authorize Medicare dual eligible beneficiaries
to be seen under an External Resource Sharing Agreements for care that is a non-covered
benefit under Medicare. (T-1).
AFMAN41-210 10 SEPTEMBER 2019 37
Chapter 4
PATIENT ADMINISTRATION FUNCTIONS
Section 4A—Legal Aspects of Protected Health Information (PHI), Release of Information
and Patient Self-Determination
4.1. Laws and Provisions Affecting Disclosure of Medical Information.
4.1.1. Privacy Act of 1974.
4.1.1.1. Medical records are maintained within a system of records protected by the
Privacy Act. Disclosure to third parties is prohibited, except pursuant to the written
authorization of the individual to whom the record pertains or in specified limited
circumstances as outlined in the Privacy Act (as implemented by Air Force Instruction
(AFI) 33-332, Air Force Privacy and Civil Liberties Program), and the HIPAA Privacy
Rule (as implemented by AFPD 41-2, Medical Support and AFI 41-200).
4.1.1.2. Refer to AFI 41-200 for guidance on the collection, safeguarding, use,
maintenance, access, amendment and disclosure of information. AFI 41-200 explains
policy on access, disclosure, time periods, denial authority, judicial sanctions, and
accounting of disclosures.
4.1.1.3. DD Form 2005, Privacy Act Statement - Healthcare Records, eliminates the need
for a separate Privacy Act statement for each medical, dental or related document requiring
individual identifying information. The DD Form 2005 is not a consent form. It serves as
evidence that, as prescribed by the Privacy Act, the individual was informed of the purpose
and uses of the information collected and was advised of rights and obligations with respect
to supplying the data. The patient’s signature is not mandatory. When the Privacy Act
statement is printed on the reverse of AF Form 560, Authorization and Treatment
Statement, or on the record folder, the DD Form 2005 is not required.
4.1.2. Alcohol and Drug Abuse Prevention and Treatment (ADAPT) Records. Alcohol and
Drug Abuse Prevention Program information collected and maintained as part of Alcohol and
Drug Abuse Prevention treatment or aftercare services are maintained in accordance with AFI
44-121, Alcohol and Drug Abuse Prevention and Treatment (ADAPT) Program and AFI 44-
172, Mental Health. These records are protected from public disclosure and afforded special
protections.
4.1.3. Freedom of Information Act (FOIA). See DoDM 5400.07, AFMAN 33-302, Freedom
of Information Act Program, for specific guidance and procedures related to the release of
information from health records.
4.1.4. HIPAA. Reference AFI 41-200.
4.1.5. Provisions Regarding the Release of Mental Health Information. Mental health
information will be protected in accordance with AFI 33-332, AFI 41-200, and AFI 44-172.
4.1.6. State Laws, Reporting Guidance for Medical Personnel, and Medical Documentation of
Restricted Reports.
38 AFMAN41-210 10 SEPTEMBER 2019
4.1.6.1. Providers must consult the supporting medical law consultant or Staff Judge
Advocate’s office when child abuse, domestic abuse, or sexual assault is evident or
suspected. (T-3).
4.1.6.2. Some states require medical providers to report to civilian authorities in situations
addressed by DoD policies, to include those DoD polices that provide for restricted
reporting. Mandatory reporting laws are typically based on the law of the state where care
is currently being provided and not to the state of licensure. However, while working in a
MTF, follow DoD and AF policy. If federal law, DoD policy or AF policy require
reporting, follow the provisions in such policy. However, any state law or regulation that
would require a healthcare professional to disclose the PII or PHI of an adult victim or
alleged perpetrator of sexual assault to law enforcement shall not apply, except when
reporting is necessary to prevent or mitigate a serious and imminent threat to health and
safety.
4.1.6.3. Medical record documentation under restricted reporting must contain sufficient
information to allow for continuity of care and coding. (T-0). The following wording in
bold type should be placed at the top of each notation in the approved electronic health
record or paper record: "Restricted from disclosure unless and until determined to be
releasable by the MTF commander, director or designee. Do not release without
specific patient authorization or as specifically authorized by federal law or DoD or
Air Force policy." Electronic records in AHLTA may also be secured via a "break the
glass," (means for a person who does not have access privileges to certain information to
gain access when necessary) or disclosure function with the above notation in place. This
function highlights those entries as restricted and prompts additional review prior to release
or electronic review.
4.2. Health Record Custody and Control.
4.2.1. Each MTF will develop policies and procedures for defining levels of access to health
information by individuals or groups of individuals (work centers) based on requirements in
fulfillment of assigned duties. (T-1). At a minimum, guidance should address:
4.2.1.1. Standardized matrix for evaluating specific roles against access requirements.
4.2.1.2. Review and approval process, to include approval authority.
4.2.1.3. Procedures for periodically validating access requirements.
4.2.1.4. Termination of access procedures.
4.2.2. Maintaining custody and control of original medical, dental, and inpatient records.
4.2.2.1. Take necessary precautions to avoid compromise of medical information during
the movement of the record inside and outside the MTF.
4.2.2.2. Original health records are not to be released to anyone outside the MTF without
specific and verifiable operational mission related, legal or medical necessity requirements.
4.2.2.3. MTF commander or director approval and authorization is required for unescorted
access to medical records areas. Written authorization memorandum must be posted near
each entrance for ready reference. (T-2). If commander’s written authorization is required
prior to electronic access identification card swipe activation, individuals with
AFMAN41-210 10 SEPTEMBER 2019 39
identification card swipe access do not need to be identified on the posted listing. This
does not apply to keypad access due to the potential for security compromise.
4.2.3. Establish written procedures to ensure highly sensitive records and sensitive medical
information are safeguarded. This includes safeguarding x-rays and fetal monitoring strips.
Examples of highly sensitive records include mental health records, substance abuse treatment
records, records related to sexual assault, records related to child or adult abuse, and records
relevant to a claim or suit against the United States. To protect the sensitive nature of the
information, medical records staff will only release Mental Health notes that are marked
sensitive with approval from the treating mental health provider. Consults marked sensitive
will be released only after review and approval by the primary care provider (or mental health
provider, if the patient is being treated in mental health).
4.2.4. Sequestering Health Records. Sequestering a health record is the storage and securing
of a health record separate from other health records for added security or for legal purposes.
The MTF may sequester the original medical record or a certified copy when the situation
warrants. A notice should be placed on the original record to ensure personnel do not allow
the patient to hand-carry the record while there is an active claim or litigation. If a certified
copy is made for sequestering, return the original record to the file room and suspense and
label it for periodic updates. Records will be sequestered under the following conditions (T-
2):
4.2.4.1. When an administrative claim or lawsuit against the government has been filed.
4.2.4.2. When a patient has tried to tamper, alter or illegally remove a record from the
facility.
4.2.4.3. When a request is received from an attorney under circumstances indicating claim
or law suit is being considered.
4.2.4.4. When an Inspector General (IG), congressional inquiry or investigation has been
initiated and when the medical record is relevant to an IG or congressional inquiry/
investigation.
4.2.4.5. When the record becomes relevant to an Air Force Office of Special Investigation
(AFOSI) or Security Forces investigation. Annotate sequestered record form with the
AFOSI/Security Forces agent’s name and case number for annual review process. Contact
the medical law consultant, Staff Judge Advocate or HIPAA privacy officer for questions.
4.2.4.5.1. Investigative agencies, such as AFSOI have the authority to request a delay
in disclosure reporting. The individual’s right to receive an accounting of disclosures
to the law enforcement may be temporarily suspended if the agency or official indicates
that such an accounting would impede the agency‘s activities. Verbal requests for
suspension shall not exceed 30 days; suspensions beyond 30 days require a written
request. (T-2). Account for the disclosure per AFI 41-200 if no request for temporary
suspension is made or upon the expiration of a temporary suspension.
4.2.4.5.2. Address military Service Member agents of the AFOSI as “Special Agent,”
followed by their last name. Refrain from addressing a military Service Member agent
using the member’s military rank.
40 AFMAN41-210 10 SEPTEMBER 2019
4.2.4.6. For purposes of safety or mishap investigations, the MTF Release of Information
Office will facilitate the appropriate collection of medical and/or dental records for
disclosure to a Safety Investigation Board and/or Accident Investigation Board.
4.2.4.6.1. Original hard copy paper medical and dental records of persons of interest
in a safety investigation must be immediately sealed in envelopes and sequestered in a
secure location. (T-3). Provide a copy of the original records to the Interim Safety
Board Medical Officer as soon as one is appointed.
4.2.4.6.2. Records that are only maintained in electronic format will need to be printed
or downloaded as encrypted electronic files (CD-ROM, USB drive, etc.), if the
investigating medical officer(s) will not have access to the electronic record systems
(AHLTA, CHCS, HAIMS, or other approved electronic health record). (T-2). Seal
these in a separate envelope and also provide to the Safety Investigation Board.
4.2.4.6.3. During the investigation, the Safety Investigation Board or Accident
Investigation Board may periodically request an update of any medical
records/documents related to the investigation and continuing care.
4.2.4.6.4. At the conclusion of the Safety Investigation Board and/or Accident
Investigation Board, all medical and dental records, including any electronic copies,
will be returned to the MTF Release of Information Office and handled in accordance
with Air Force document retention and destruction requirements.
4.2.4.7. It is the MTF commander’s or director’s responsibility (with advice from the
Quality Services Manager, medical law consultant, or Staff Judge Advocate) to establish
local operating instructions regarding sequestered medical records safekeeping policy and
procedure. At a minimum, the records will be kept in a separate, locked location, with
limited staff and patient access. If the patient is actively being treated at the MTF, copy
the original record for the outpatient records room and annotate on the jacket “Clinic
Copy.” Create the clinic copy in CHCS as a unique record type for tracking purposes in
the Medical Records Tracking module.
4.2.4.8. Place a cover sheet on the original medical record stating the record has been
sequestered. Maintain a separate file on why the record has been sequestered and the date
(or occurrence of an event) when the record should be reviewed to determine the need for
continued sequestering. Place a charge out, which details where the record is located, in
appropriate records room with statement that the record has been sequestered. If a clinic
copy is made, ensure that original documentation is forwarded to the sequestered file and
a copy is placed in the clinic copy.
4.2.4.9. Coordinate an annual review of sequestered records with the base legal office to
determine whether the records should continue to be sequestered. In addition, ensure that
records are reviewed prior to patient relocation to see if sequestering is still applicable. If
sequestering is still required, mail the outpatient records to the gaining MTF. Include a
cover letter stating the records are to be sequestered and an explanation of the
circumstances. The losing MTF will make a certified true copy of the record before
mailing. Maintain the copy until the claim or litigation is resolved and the base legal office
or Air Force Legal Operations Agency, Claims and Tort Litigation Division
(AFLOA/JACC) concurs.
AFMAN41-210 10 SEPTEMBER 2019 41
4.3. General Guidelines on Releasing Medical Information.
4.3.1. Original medical documents or records are not released to any non-federal government
agency, except in compliance with a valid court order or as otherwise required by law. Always
consult the medical law consultant or Staff Judge Advocate prior to releasing medical
information under these circumstances.
4.3.1.1. Documentation received via fax can be scanned into Health Artifact and Image
Management Solution (HAIMS) or other approved patient electronic health record.
4.3.1.2. The use of a fax machine to transmit provider’s orders is permissible. To verify
their authenticity, the provider should sign the orders prior to transmission. Reference AFI
44-102, for additional information. If the orders were not signed, do not carry them out
until the ordering provider verifies them. (T-1). Unless otherwise required by applicable
law or regulation, the faxed copy does not require countersignature.
4.3.1.3. Documentation transmitted on thermal paper will fade over time. If a fax machine
uses thermal paper, make a photocopy of the document and scan/upload into HAIMS or
approved electronic health record. Destroy the thermal paper document and photocopy
after scanning/uploading.
4.3.2. Health records may contain information from non-military sources. A patient can be
referred to a non-military source for ancillary, diagnostic care, and/or treatment.
Documentation from the non-military source that supports the diagnosis and treatment will be
scanned/uploaded into HAIMS or approved electronic health record. This documentation will
then become a part of the patient’s medical record and subsequent releases of information from
the patient’s record will include this information from non-military sources.
4.3.3. Special Handling of Medical Records.
4.3.3.1. Records of Newborns Released for Adoption. Take special care releasing
information from the records of newborns who have been released for adoption. Delete all
references to the child’s natural parents. Stamp or identify the newborn inpatient record
with the following statement, “Release of Information Restricted according to AFMAN
41-210, Chapter 4.” Do not forward AF Form 560, AF Form 565, Record of Inpatient
Treatment, SF 502, Medical Record - Narrative Summary (Clinical Resume), or SF 535,
Medical Record - Newborn in the outpatient record.
4.3.3.2. Radiographs, Radiographic Images or Film (also known as X-Ray). Generally,
only the provider’s paper document radiographic interpretation or analysis report is
provided to the requestor. The cost of producing this paper report is usually free, unless
repeated requests for the same document are submitted. Copies of actual radiographs,
sometimes referred to as, radiographic film, x-ray film or x-ray images, may be provided
upon specific request via hard copy or CD/DVD.
4.3.3.3. All provider social security numbers must be redacted from the health record
before issuing a copy. (T-0). This mandate applies to all forms of health records (including,
but not limited to, the outpatient medical, dental treatment, inpatient, and extended
ambulatory record). This policy applies to copies provided for any purpose or request,
including an individual’s request for copies of the member’s own health records. Original
medical records shall remain intact and unaltered. The original provider’s social security
42 AFMAN41-210 10 SEPTEMBER 2019
number must never be deleted from the original health record. (T-0). Other social security
numbers should be redacted when warranted.
4.3.3.4. All sponsor social security numbers must be redacted from the health record
before issuing a copy, unless the copy request is made by the actual sponsor for their own
record. (T-0). This mandate applies to all forms of health records (including, but not
limited to, the outpatient medical, dental treatment, inpatient, and extended ambulatory
record). This policy applies to copies provided for any purpose or request. Original
medical records shall remain intact and unaltered. The original sponsor social security
number must never be deleted from the original health record. (T-0). Other Social security
numbers should be redacted when warranted.
4.3.3.5. Prior to the release of information, the health record should be reviewed to ensure
that information pertaining to other individuals is not contained in the record.
4.3.3.5.1. Erroneously filed documents should be removed in accordance with
paragraph 5.3.
4.3.3.5.2. Information pertaining to other individuals (e.g., other family members,
Edinburgh Postnatal Depression Scale in infant record) should be considered for
redaction. Consult the servicing legal office.
4.3.3.6. If a MTF provides health records electronically (e.g., scanned copy in lieu of
paper), the MTF must use standardized nomenclature when naming the file. (T-3). This
will allow outside agencies and others, as applicable, to easily identify a beneficiary’s
treatment record. At a minimum, the file name should contain the following: the term
“Outpatient Record,” “Dental Record,” or “Inpatient Record” as applicable, last name of
the beneficiary, and date the copy was made, e.g., OUTPATIENT RECORD_ [SMITH]
_15MAR2010] .pdf.
4.3.3.7. Scan all correspondence, e.g., requests for PHI from the patient’s health insurance
company, state worker’s compensation agency, or federal and state disability agencies,
with an attached information release statement regarding the release of information into
HAIMS, Section III of the electronic health record repository or approved electronic health
record for permanent safekeeping.
4.3.3.8. Fees for copying. The MTF is permitted to charge a reasonable, cost-based fee
for responding to requests for copies of health records, as outlined in AFI 41-200.
4.3.3.8.1. If the patient requests a copy of the medical record and the copy request is
complete, provide the patient with copies at no charge.
4.3.3.8.2. Upon local approval of the MTF commander or director, the Release of
Information Office may charge beneficiaries or their agents/representatives, for
excessive and repeated personal requests for the same document or repeated requests
for partial or complete volume copies that have already been provided to the patient or
his representative, within the same 12-month period.
4.3.3.8.2.1. If the individual requests a copy of the PHI or agrees to a summary or
explanation of such information, the covered entity may impose a reasonable, cost-
based fee, provided that the fee includes only the cost of:
4.3.3.8.2.1.1. Labor for the PHI requested by the individual, whether in paper
AFMAN41-210 10 SEPTEMBER 2019 43
or electronic form;
4.3.3.8.2.1.2. Supplies for creating the paper copy or electronic media if the
individual requests that the electronic copy be provided on portable media; and
4.3.3.8.2.1.3. Preparing an explanation or summary of the PHI, if agreed to by
the individual.
4.3.3.8.3. Advance payments for information requests from insurance companies and
other agencies may be accepted. If the request is for a large volume or requires
extensive research, notify the requester of any additional charges.
4.3.3.8.3.1. If the payment is incorrect, inform the requesting agency that the
information is being provided even though the required fee (specify amount) has
not been paid, to avoid possible adverse effect to the patient. Advise the requester
to send payment promptly to the Medical Service Account office by check or
money order payable to the Treasurer of the United States.
4.3.3.8.4. Send payment to the Medical Service Account office with the completed
copy of the transmittal letter if correct payment is received with the request. If the
requested information cannot be obtained on the day the request is received, complete
only the required items and send the form and payment to the Medical Service Account
office before the ordinary close of business each day.
4.3.3.8.5. If prepayment is not made, use a locally developed form to identify and
request the fees. Prepare the form in three copies; send the original to the requester,
file the second copy in part 3 of the health record with the patient's signed authorization
for release of information, and forward the third copy to the RMO. When answering
requests for information on injury cases that appear to involve medical affirmative
claims action, create a fourth copy of the form and send it to the medical law consultant
or Staff Judge Advocate.
4.4. Patient Requests for Copies of Medical Records and Restrictions. This section outlines
the patient’s right to request copies of their PHI, including copies produced from paper-based and
electronic-based medical records, and their right to request restrictions on uses or disclosures of
their PHI IAW AFI 41-200. Note that a patient may also be a member of the MTF workforce, as
Active Duty (AD), Reservist, civilian, or contractor. MTF workforce members should not be
accessing health records systems to obtain copies of their own medical records. MTF workforce
members should request copies of medical records in the same manner as any other patient as
outlined in paragraph 4.4.5.
4.4.1. Patient or Authorized Representative: Information may be released directly to the
patient or to a representative they designate in writing. An abstract of a patient's relevant
medical history (or copies of pertinent pages of the record) may be furnished to the patient, or
authorized representative, when the patient departs on a temporary absence from home and
requires medical care while away. While AFI 41-200 provides conditions upon which a
covered entity may deny an individual access to their PHI, since medical records are contained
in Privacy Act systems of records, access is generally required. Consult with the medical law
consultant or Staff Judge Advocate prior to denying an individual access to their own medical
records.
44 AFMAN41-210 10 SEPTEMBER 2019
4.4.1.1. If a provider determines that direct disclosure to the patient could have an adverse
effect on either the physical or mental health, safety, or welfare of the individual, or other
persons with whom the patient may have contact, the disclosure will be made to a
healthcare provider named by the individual, or to a person qualified to make psychiatric
or mental health determinations.
4.4.2. Provide patients or their designated representatives’ access to their health records upon
written request. The original record is always retained at the MTF, but copies will be provided
if requested. Per HIPAA and AFI 41-200, process copy requests within 30 days of receipt of
the DD Form 2870, Authorization for Disclosure of Medical or Dental Information, or other
written request. If, however, the requested medical record copies cannot be provided within
30 days, contact the requestor in writing and inform them of the delay and when the records
will be available. Copy requests not completed by the 30th calendar day will be elevated to
the squadron commander for immediate explanation and resolution. (T-3).
4.4.2.1. Military healthcare providers are encouraged to discuss, with their patients, the
contents of their patients’ health records at least once a year. Providers should encourage
their patients to review the healthcare information stored in their medical record to ensure
all necessary documents are included in the record, including referral results from civilian
network providers.
4.4.2.2. Healthcare providers may recommend ways of disclosing health records other
than by direct patient access. On occasion, a healthcare provider may elect to disclose
information on specific diagnoses of terminal illness or psychiatric conditions to a patient’s
designated representative, and not directly to the patient, with the patient’s concurrence.
4.4.3. Urgent copy requests for referral appointments. If a patient requests to remove the
medical record from the medical facility, MTF personnel are required to inform the patient of
the DoD policy prohibiting patients from hand-carrying their record(s). Primary Care
Managers and/or referring MTF providers are responsible for ensuring that a patient has copies
of any necessary paperwork from the outpatient, inpatient, dental records, other paper or
electronic health record required to ensure adequate medical reference and continuity of care
between the MTF and the external provider or civilian medical facility. These copies are
provided free of charge. If a patient has not obtained the necessary documents for the referral
visit for an external MTF patient appointment, copy the pertinent section/document(s) and
provide the copy to the patient. Requests of this type must be expedited so the patient can
provide this information to the referral provider at the time of the appointment. (T-3). Unless
specifically requested by either the referring or accepting physician, do not copy the entire
medical or dental record. Copies of pertinent medical documents may also be faxed or mailed
from the MTF to the receiving provider or civilian medical facility provided the necessary
coordination with the external provider has been accomplished.
4.4.4. Urgent copy requests to meet short-notice or no-notice service member separations or
discharges resulting from accelerated Force Management related personnel action. When
informed or notified by an appropriate service separation or discharge authority of a service
member’s request to obtain a complete copy of the member’s Service Treatment Record to
meet expedited Force Management related separation or discharge installation out-processing
requirements, the MTF Release of Information office will immediately prioritize the request
above all other non-urgent, routine requests. The service member is required to complete the

AFMAN41-210 10 SEPTEMBER 2019 45
necessary record copy request, DD Form 2870, for submission to the MTF Release of
Information office.
4.4.5. Non-Urgent, Routine Copy Requests. Refer the patient to the appropriate Release of
Information office. Release of Information personnel will inform the patient of the average
MTF wait-time for non-urgent requests and should use DD Form 2870.
4.4.5.1. The timeline for such request are established in paragraph 4.4.2. The time
duration may be based upon a variety of factors, including, but not limited to the staffing,
the size of the individual record(s) or record portion(s) to be copied, the number of non-
urgent daily and weekly requests, the number of emergent and/or urgent daily and weekly
requests and the time it takes to redact Social Security Numbers. The staff assigned to the
Release of Information Office should keep their supervisors appraised on any current or
impending delays. Unforeseen delays can be documented by the leadership and affected
beneficiaries should be notified.
4.4.5.2. The patient can elect to receive their records by unencrypted/unsecured e-mail or
to another individual designated by the patient. Documentation of patient permission to
send and receive medical information via electronic communication should be maintained
in the medical records or tracked internally in a Release of Information tracking
binder/spreadsheet for future requests. Reference AFI 41-200, paragraph 7.6, for a
description of requirements.
4.4.6. General rules and individual state laws specify when a power of attorney is required.
Refer any questions about power of attorney to the medical law consultant or Staff Judge
Advocate.
4.4.7. Amendments to Erroneous Information. A patient has a right to request an amendment
to their medical record. The amendment must be granted if it is determined that the information
contained in the record created by the MHS is inaccurate or incomplete. (T-0). Refer to the
MTF’s HIPAA Privacy Officer or the Air Force Medical Operations Agency (AFMOA) Health
Information Compliance Team Kx website for information on this process
(https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx).
4.4.7.1. The MTF commander or director will appoint in writing the MTF HIPAA privacy
officer as the primary point of contact for all matters related to erroneously entered
information in AHLTA. (T-3).
4.4.7.1.1. The appointment letter can include language that the MTF HIPAA privacy
officer is the commander’s designee for purposes of signing the “Request for AHLTA
Legal Correction of Erroneous Data or Erroneous Personal Health Information”
memorandum (MTF Commander’s or Director’s Memorandum). This letter is required
for each AHLTA amendment submission.
4.4.7.2. The MTF HIPAA privacy officer will ensure that policies and procedures are
developed at the local level (e.g., Medical Group Instruction) to address patient requests
for amendment of PHI. (T-1).
4.4.7.3. In the event that erroneous information in an AHLTA record is discovered by
someone other than the patient (e.g., provider, Release of Information personnel), the same
process for correction as referenced in paragraph 4.4.7 should be followed.
46 AFMAN41-210 10 SEPTEMBER 2019
4.4.7.3.1. The MTF HIPAA privacy officer will act on any correction/amendment to
the record as soon as practicable, but no later than 30 business days after receiving it in
accordance with AFI 33-332. (T-1). If the MTF is unable to act on the amendment
within 30 days, the time may be extended for no more than an additional 30 days. This
may occur if the Medical Group (MDG) provides the patient with a written statement
of the reason for delay, and the date by which the amendment request will be completed
in accordance with AFI 41-200. (T-1).
4.5. Patient Rights (Reference DoDI 6000. 14). MTF staff must inform patients of their rights,
according to state law, to make decisions regarding their medical care. (T-0). This includes the
right to accept or refuse treatment and the right to prepare advance directives. An advance
directive is defined as a written instruction by the patient, in the form of what is commonly known
as a living will or a durable power of attorney for healthcare, recognized under state law (some
states require both) and related to the provision for such care when the patient is incapacitated.
Signed advance directives shall become a part of the patient’s medical record. (T-1).
4.5.1. Each MTF will establish and maintain written policies and procedures to implement
patients’ rights to make decisions concerning their medical care. (T-0). Ensure compliance
with state law (whether statutory or as recognized by the courts of the state) respecting advance
directives.
4.5.2. Each MTF will provide to all adult patients written information on their rights under the
host state’s law to make decisions concerning their medical care, including the right to execute
an advance directive. (T-0).
4.5.3. Document whether or not each patient has an advance directive. This information will
be documented on the AF Form 560 for inpatient care or the DD Form 2766, Adult Preventive
and Chronic Care Flowsheet for outpatient care, and on the automated cover sheet for
ambulatory procedure visit cases. (T-1). Note: Utilize the DD Form 2766 and/or DD Form
2882, Pediatric and Adolescent Preventive and Chronic Flowsheet or Tri-Service Workflow
Pediatric Alternate Input Method forms for all new records. See Chapter 5, Health Records
Management, paragraph 5.12.5 for more information regarding this DD form 2766. Provider
teams are encouraged to ensure comprehensive notes are placed within AHLTA or Essentris
(system for inpatient medical care) to document whether or not each patient has an advance
directive, however, the hard copy documentation shall remain available. (T-1).
4.5.4. Each MTF will provide for education of the staff and community on issues concerning
advance directives. (T-1).
4.5.5. Check with the servicing medical law consultant or installation Staff Judge Advocate
for further guidelines.
4.5.6. Military advance medical directives are exempt from any requirements of form,
substance, formality or recording required by state law. For example, if an Air Force member
has a military living will prepared in Florida, but then becomes severely injured in California,
the military living will is honored in California even though the document may not conform to
California Law.
AFMAN41-210 10 SEPTEMBER 2019 47
Section 4B—Patient Registration & Multiple Healthcare Eligibility
Note: Section 4B applies to the Legacy System, CHCS only. As MHS GENESIS implementation
efforts continue, additional information will be provided.
4.6. Patient Registration.
4.6.1. The Patient Administration function has direct oversight of MTF patient registration.
MTF clinical work centers such as the pharmacy, laboratory, and the emergency department,
require the ability to register patients in CHCS or approved electronic health record. To ensure
a balanced and responsible registration process throughout the MTF, Patient Administration
personnel, in partnership with CHCS Administrators and Information Management officials,
will provide user training and are the only MTF approval authorities authorized to grant
registration access and/or similar capabilities. (T-3). Requests for registration training should
be coordinated and approved by the flight superintendent or flight commander before
submitting requests to the MTF TRICARE OPERATIONS AND PATIENT
ADMINISTRATION Flight Commander, Patient Administration Officer, Systems or
Information Management Flight Commander.
4.6.2. Patient Administration officials will conduct periodic reviews of all MTF personnel
with registration capabilities to verify training requirements have been met and registration
capabilities remain valid. (T-3). Reference MHS, Patient Identity Management and
Registration Guidance.
4.6.3. When registering a patient for the first time, MTF personnel should obtain as much
information as possible without degrading medical care. At a minimum, the following patient
information must be captured (T-3):
4.6.3.1. Patient’s name (first, last & middle initial).
4.6.3.2. Sponsor’s name.
4.6.3.3. Sponsor’s Social security number.
4.6.3.4. Patient’s relationship code/family member prefix e.g., 20-Sponsor, 30-Spouse,
01-Child, etc.
4.6.3.5. Patient Category (e.g., F11/Active United States Air Force, A11/Active United
States Army, F31/Retired United States Air Force Service Member, M12/Marine Corps
RC Member, N41/AD Navy Family Member, etc.).
4.6.3.6. Patient’s date of birth.
4.6.3.7. Patient’s gender.
4.6.3.8. Patient’s Service (sponsor only).
4.6.3.9. Patient’s station/unit (sponsor only).
4.6.3.10. Patient’s rank (sponsor only).
4.6.3.11. Patient’s address & telephone contact information.
4.6.3.12. Organ donor declaration (yes, no, or unknown).
4.6.3.13. Third party health insurance information.

48 AFMAN41-210 10 SEPTEMBER 2019
4.6.3.14. MTF where medical record(s) are normally maintained.
4.6.3.15. Marital status (if full registration is used).
4.6.3.16. Race (if full registration is used).
4.6.3.17. Ethnicity (if full registration is used).
4.6.3.18. Individual Patient Social Security Number or available/authorized unique
“Person or Personal Identifier” (DoD Identification Number, Foreign Identification
Number, Temporary Identification Number, Individual Taxpayer Identification Number,
etc.).
4.6.3.18.1. Person or Personal Identifiers. Most patients treated in the AFMS possess
a Social Security Number. Individual identification using a person’s unique Social
Security Number provides a solid framework from which to build a personal eligibility
profile in Defense Enrollment Eligibility Reporting System (DEERS) and within the
MTF.
4.6.3.18.2. Social Security Numbers are considered Person or Personal Identifiers and
are used as the default numeric account number for which CHCS partly bases
individual identification. Some patients, however, may not possess a Social Security
Number for various reasons. Frequently, alternative Person or Personal Identifiers are
used to reduce the use of Social Security Numbers or identify patients as individuals
who may not possess a Social Security Number. There are multiple alternative Person
Identifiers issued, used, and/or created depending on the patient’s particular situation.
For more technical information on the use of personal identifiers refer to AFMOA Kx
Patient Registration Training located at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
4.6.3.19. Command Security if applicable, e.g., Personnel Reliability Assurance
Program/Presidential Support Program.
4.6.3.20. Active Flight Status (if patient is assigned to an active flight position). This is a
full registration demographic question and minimal full registration data must be available
to properly complete the registration for this category of patient. (T-2).
4.6.3.21. Length of Service (years).
4.6.4. The MHS, when feasible, will limit the use and display of Social Security Numbers
while migrating systems and business processes to use the DoD Identification Number. (T-0).
Reference DoDI 1000.30, Reduction of Social Security Number (SSN) Use Within DoD.
4.6.5. Registration Options. Please refer to the MHS, Patient Identity Management and
Registration Guidance for current, accurate and complete information on all registration
options. For best practices on registration see AFMOA Kx Patient Registration Training
located at https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
4.7. Patients with Multiple-Eligibility. Beneficiaries will only be registered one time on each
CHCS host according to their highest level of eligibility. (T-0) See MHS, Patient Identity
Management and Registration Guidance, for technical information.
AFMAN41-210 10 SEPTEMBER 2019 49
4.7.1. The TRICARE Operations and Patient Administration and systems offices must ensure
that all MTF staff members who possess registration capabilities are aware of the problems
associated with multi-eligible patients and other current patient identity problems. (T-1).
4.7.1.1. Providers and MTF staff must be aware of the potential problems associated with
dual or multiple-eligibility patients and how to implement corrective measures and
alternative processes to ensure the patient’s healthcare is properly documented. (T-1).
4.7.1.2. MTF TRICARE Operations and Patient Administration staff or system managers
are authorized to merge erroneous duplicate records by merging the alias record with the
surviving record using the Former Patient Name functionality within CHCS. An alias
record indicates that a record is also known or more familiar under another specified record.
A surviving record is the complete record remaining after the merge of duplicate records.
AHLTA changes must be processed in accordance with current MHS merge/unmerge
guidelines. (T-1). Reference Assistant Secretary of Defense for Health Affairs
Memorandum, Guidance for Requesting Correction of Erroneously Entered Information
in the Armed Services Longitudinal Health Technology Application.
4.7.1.3. Potential Duplicate Patient Report. Collectively, CHCS Administrators, Patient
Administration, and Information Assurance officials will produce a monthly report
identifying duplicate records to aggressively find, fix and prevent unnecessary duplicate
patient registrations. (T-1).
4.7.1.3.1. When duplicate patient records are detected in either CHCS or AHLTA,
duplications shall be reported in the Patient Safety Reporting tool. Once the duplicate
record is reported, it will be routed through the Patient Safety Reporting tool to the
TRICARE Operations and Patient Administration flight for resolution by either
merging the records or submitting a MHS Helpdesk Ticket. (T-1).
4.7.1.3.2. There are instances when patients may have multiple eligibilities or are
eligible for care under more than one patient category. Refer to websites in paragraph
4.5.5 for a complete listing of the most common patient categories, the multiple
eligibility that it presents and clear guidance on how to avoid duplicating patients. The
patient category is not static and can be changed; however, it is not automatically
updated when the beneficiary’s status changes in DEERS. The patient category can
and must be changed within CHCS by MTF personnel, when required. (T-1).
Section 4C—Patient Travel
4.8. Patient Accountability for Service Members Traveling to Attend
Medical Appointments and/or Specialty Care.
4.8.1. All service members traveling to any MTF for outpatient medical follow-up or referred
specialty medical care must have the following messages annotated on their travel orders. (T-
1).
4.8.1.1. Section 11 shall indicate, “MTF – TRICARE Operations and Patient
Administration Function and/or AMTU.” (T-1).
4.8.1.2. Section 16 will indicate, “Service members must report to the MTF TRICARE
Operations and Patient Administration Function to have their travel orders validated within
50 AFMAN41-210 10 SEPTEMBER 2019
24-hours of arrival, or the next duty day if arriving on a weekend or holiday. (T-1). All
service members traveling to attend official medical-related appointments or treatment are
required to contact the MTF TRICARE Operations and Patient Administration function
every two weeks to revalidate their orders.” (T-3).
4.9. Patient Travel Benefit.
4.9.1. Travel Reimbursement/Funding. For patients enrolled to a direct care MTF, the travel
benefit is administered by the MTF. For patients enrolled to a network Primary Care Manager,
the TRICARE regional office administers the travel benefit. Exceptions: Travel orders and
funding for AD service members must be the responsibility of the sponsor’s respective Service
branch. (T-1).
4.9.1.1. MTF commander or director will ensure processes are in place for the
accountability of patients entered into the Patient Movement system, see paragraph 4.9.1.2.
This includes using the designated Patient Movement Automated Information Systems
when transport is in excess of 100 miles for ground transportation and for all air
transportation provided under the Defense Travel System. Reference DoDI 6000.11.
4.9.1.2. All staff members utilizing Transportation Command (TRANSCOM) Regulating
and Command & Control Evacuation System (TRAC
2
ES) will complete a basics user
course and submit a certificate of completion to obtain a TRANSCOM TRAC
2
ES account.
Training can be requested at transcom.scott.tcsg.mbx.gpmic-global-training@mail.mil.
(T-1). Reference DoDI 6000.11.
4.9.1.2.1. TRANSCOM Regulating and Command & Control Evacuation System
(TRAC
2
ES) BASICS training can be accomplished three ways:
4.9.1.2.1.1. In residence classroom training at USTRANSCOM Command
Surgeon’s Office; 4.9.1.2.1.2. Online through Joint Knowledge Online (JKO) web
based training; or
4.9.1.2.1.2.1. In-house with a TRAC
2
ES Trainer that has completed the in-
residence course at the USTRANSCOM Command Surgeon’s Office.
4.9.1.2.2. In-residence class schedules are available by contacting the TRAC
2
ES
training coordinator via email at transcom.scott.tcsg.mbx.gpmic-global-
training@mail.mil.
4.9.1.2.3. Funding is the responsibility of the member’s unit. Reference DoDI
6000.11.
4.9.2. TRICARE Prime Travel Benefit. When MTF TRICARE Prime enrollees (family
members or military retirees) are referred by their Primary Care Manager for medically
necessary, non-emergency specialty care to a location greater than 100 miles from the referring
primary care manager’s office, the patient must be reimbursed for reasonable travel expenses
in accordance with the Joint Travel Regulations available at available at
https://www.dfas.mil/militarymembers/travelpay/regulations.html. (T-0). Travel
expenses are charged to the MTF.
4.9.2.1. Military Retirees with a Combat-Related Disability Who are Not Enrolled in
TRICARE Prime. When a retired service member with a combat-related disability, who is
not a TRICARE Prime enrollee, is referred by a Primary Care Manager for follow-on
AFMAN41-210 10 SEPTEMBER 2019 51
specialty care, services and supplies, for that particular disability, to a location greater than
100 miles from the primary care provider’s office, the patient must be reimbursed for
reasonable travel expenses in accordance with the Joint Travel Regulation. (T-0). Note:
This also applies to subsequent specialty referrals authorized by a primary care provider.
This benefit is not available overseas.
4.9.2.2. GSU Members. The supporting MTF commander or director has direct control of
patient travel funding for GSU members. When it is unclear who the supporting MTF
commander or director is, the responsibility will default to the nearest Air Force MTF
commander or director to the member’s permanent duty station, unless MAJCOM policy
designates an alternative MTF to provide patient travel support. (T-2).
4.9.3. Non-Medical Attendant Travel. Non-medical attendants are appointed by medical
authority. Local area travel/transportation expense coverage is authorized when serving as a
non-medical attendant for a service member traveling on official business. Non-medical
attendants assisting patients who are referred to medical facilities located beyond the local
permanent duty station area will be reimbursed travel/transportation expenses in accordance
with the Joint Travel Regulation. (T-0).
4.9.3.1. Non-Concurrent Non-Medical Attendant Travel. Non-concurrent non-medical
attendant travel may be authorized or approved when the need for an attendant arises during
treatment or when there is need for an attendant only during a portion of the patient's travel.
4.9.4. Civil Service Family Member of a Seriously Ill or Injured Uniformed Service Member.
A civilian employee, who is authorized travel under a competent travel authorization/order as
a family member of an AD service member who is seriously ill, seriously injured, or when
death is imminent, is treated as an employee in a Temporary Duty (TDY) status.
4.9.5. Travel for Families of Inpatient Service Members who are Very Seriously Ill/Seriously
Ill, or Hostile Not Seriously Injured. Travel for family members of inpatient service members
who are Very Seriously Ill/Seriously Ill or Hostile Not Seriously Injured is governed by the
Emergency Family Member Travel Program (AFI 36-3002, Casualty Services, paragraph
2.25). Emergency Family Member Travel Program is not funded by the MTF. Emergency
Family Member Travel Program is centrally funded by the Air Force, and managed by Air
Force Personnel Center, Casualty Affairs Division (AFPC/DPFC).
4.9.6. Medical Referrals within the Local Permanent Duty Station Area. Travel by personally
owned conveyance to obtain medical care within the local permanent duty station area is
reimbursable only when a service member is ordered (see note below) to a medical facility
within the local area to take a required physical or to obtain a medical diagnosis or treatment.
When ordered, service members are considered to be on official business and must be
reimbursed for the transportation, unless government transportation is available (see Joint
Travel Regulation). (T-0). Note: “Ordered” in this context is defined as an order/command
that could result in disciplinary action if not obeyed (e.g., commander-directed or required by
regulation).
4.9.6.1. Medical Referral Travel at the Member’s Expense. Travel to medical
appointments within the permanent duty station other than as described in the above
paragraph is generally not reimbursable.
52 AFMAN41-210 10 SEPTEMBER 2019
4.9.6.2. Service members traveling on official travel orders outside the permanent duty
station may be authorized travel and transportation allowances in accordance with the Joint
Travel Regulation. Travel must be authorized by the proper medical authority. (T-0).
4.9.7. Medical Referral Travel for Government Employees Overseas and Their Family
Members. When local medical facilities (military or civilian) at a foreign Outside Continental
United States (CONUS) area are not able to accommodate an employee’s dependent’s needs,
transportation to another location may be authorized for appropriate medical or dental care.
Healthcare related travel expenses for an employee or eligible dependent are funded by the
employee’s unit. Travel and transportation expenses and/or reimbursement are authorized in
accordance with the Joint Travel Regulation.
4.9.8. Convalescent Leave Transportation for Illness/Injury. A service member is authorized
transportation allowances (without per diem) for one trip when traveling for convalescent leave
for illness/injury incurred while eligible for hostile fire pay under 37 USC § 310. The
convalescent travel will be funded by the fund cite on the member's deployment travel orders.
(T-1). TDY orders are prepared by the member’s unit. Additional trips, if deemed necessary
by the attending physician, may be authorized through the Secretarial Process. The Secretarial
Process is an action by the Per Diem Travel and Transportation Allowance Committee
(PDTATAC) Principal member or a subordinate level specified by the Principal. The
Secretarial Process is in administrative and procedural issuances issued under the JTR
Introduction (Service or DoD Agency Regulation Review Process).
4.9.9. Travel and Per Diem Allowance. Service members traveling to a medical facility to
obtain an examination or when traveling to Lackland Air Force Base, TX to attend a formal
Physical Evaluation Board, receive travel and per diem (including meals and lodging)
allowance (10 USC § 1210 and Joint Travel Regulation). The service member is authorized
an escort to the place of examination when the member is not physically or mentally able to
travel without assistance.
4.9.9.1. Approximately 20-30 days prior to the reporting date, Air Force Personnel Center,
Disability Division (AFPC/DPFD) will send travel orders to the service member. The
orders will indicate the exact date, time and place to report and includes the authority for
payment of travel costs. (T-1).
4.9.9.2. The destination or examining medical facility will endorse the order with the date
and time the service member reported as verification that the service member was
examined as an inpatient or outpatient. (T-3). The endorsement also serves to verify the
service member was released following the examination.
4.9.9.3. If the service member received an examination as an outpatient, the destination
MTF must indicate whether the service member occupied government quarters during the
stay. (T-3). The examining or destination facility must ensure the service member has an
endorsed order to submit the claim for reimbursement. (T-3). Upon return to the departure
location, the service member is required to submit a travel voucher to their local accounting
and finance office to obtain reimbursement for travel-related expenses. (T-3). Refer to the
Joint Travel Regulation for further travel entitlement information.

AFMAN41-210 10 SEPTEMBER 2019 53
4.10. Transferring Patients Through the Aeromedical Evacuation System. See AFI 48-
307V1, En Route Care and Aeromedical Evacuation Medical Operations, AFPD 10-29,
Worldwide Aeromedical Evacuation Operations.
Section 4D—Quarters Administration
4.11. Quarters Status.
4.11.1. Quarters is a full duty excuse provided to AD uniformed service members receiving
medical or dental treatment for a disease or injury that, based on sound professional judgment,
does not require inpatient care. A quarters patient is treated on an outpatient basis, and is to
remain in their home during the quarters period. Quarters periods generally last 24-72 hours
depending on the providers prescribed rest/recovery period.
4.11.2. The provider or support staff will notify the member’s unit commander or
commander’s designee regarding the patient’s quarters status. The Aerospace Services
Information Management System (ASIMS) Quarters-Airman Medical Notification Module is
the required mechanism for quarters notifications. (T-1). Refer to AFI 41-200, paragraph
3.7.1, 4.3.11.1.1, and 5.1.1.1.2.1 for additional guidance.
4.11.2.1. Disclose only the minimum information necessary.
4.11.2.2. ASIMS automatically accounts for the disclosures at the time it is accessed by
the commander or designee.
4.11.2.3. In the event that ASIMS is not available or the member is from another Service:
4.11.2.3.1. Command authority notification must be documented on DD Form 689,
Individual Sick Slip, or a locally created form. (T-3). See examples located in patient
administration misc. document folder on the AFMOA Health Benefits Kx page at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
4.11.2.3.2. Forward a copy of the quarters notification or DD Form 689 to the
member’s unit commander or designee to receive quarters information. Provide a
second copy of the DD Form 689 to the member to provide to the member’s supervisor.
4.11.2.3.3. If it is necessary to accomplish quarters notification outside of the ASIMS
mechanism, disclosures must be accounted for in the PHI Management Tool or AFMS
approved centralized disclosure accounting tool. (T-2). Reference AFI 41-200.
4.11.3. Develop local procedures for program management, including, but not limited to (T-
3):
4.11.3.1. Notifying Public Health for communicable disease tracking, in the event that
ASIMS is not available or the member is from another Service.
4.11.3.2. Extending quarters past the initial rest period.
4.11.3.2.1. Establishing time limits on 24, 48, & 72-hour quarters. For example, when
an individual is placed on 24-hour quarters, the period expires the next day at the start
of patient’s regular work shift not 24-hours from the time the patient was placed on
quarters.
54 AFMAN41-210 10 SEPTEMBER 2019
4.11.3.2.2. Equally, for 48 hours, the period extends to the start of work on the second
day and for 72 hours, it extends to the start of work on the third day, not to exceed 24,
48, or 72 hours respectively. Unless instructed otherwise, clinic personnel will inform
the patient to report for duty in accordance with the guidelines above.
4.11.4. Unit commanders and supervisors have the authority to grant up to 24 hours sick status
at their discretion if a member’s illness/injury does not require MTF intervention. If the
illness/injury persists beyond 24 hours, then the commander or supervisor must refer the
member to the MTF for treatment and subsequent clinical examination. (T-3).
Section 4E—Line of Duty Program Administration
4.12. Line of Duty Determinations.
4.12.1. Authority: AFI 36-2910. AFI 36-3212, Physical Evaluation for Retention, Retirement,
and Separation.
4.12.2. According to AFI 36-2910, a Line of Duty determination, “Is a finding made after an
investigation into the circumstances of a member’s illness, injury, disease or death.” A service
member who dies or sustains an illness, injury or disease prior to service, while absent without
authority, or due to the member’s own misconduct is not eligible for certain government
benefits.
4.12.3. Following the start of a Line of Duty determination, initial direct care and/or
TRICARE network healthcare may not be denied to any AD service member or RC service
member.
4.12.4. Following the completion of a Line of Duty determination:
4.12.4.1. Direct care and/or TRICARE network healthcare may not be denied to any AD
service member for a Line of Duty determination of Not in Line of Duty is found or
identified.
4.12.4.2. Continued direct care and/or TRICARE network healthcare entitlements of RC
service member may be impacted by Line of Duty determinations.
4.12.5. The Line of Duty determination process is an AF/A1, Manpower, Personnel and
Services, program. The AFMS is not the office of primary responsibility. However, the Line
of Duty determination process is initiated with a medical officer’s review of the member’s
illness, injury, disease, or death. The Line of Duty determination process must be
accomplished in accordance with AFI 36-2910. (T-1). Refer to AFI 36-2910 for information
regarding when to initiate a Line of Duty determination.
4.12.6. The service member’s personnel status and branch of Service usually dictates what
type of Line of Duty form should be used when initiating a Line of Duty determination case.
4.12.6.1. For AD service members and members of the ARC, MTF providers must use the
AF Form 348, Line of Duty Determination or AF Form 348-R, Line of Duty Determination
for Restricted Report of Sexual Assault, for restricted reports. (T-1).
4.12.6.2. For service members assigned to other Service branches (i.e., United States
Army, Navy, Marines), Air Force MTF providers should use the specific Service Line of
AFMAN41-210 10 SEPTEMBER 2019 55
Duty form or the DD Form 261, Report of Investigation Line of Duty and Misconduct
Status when initiating a Line of Duty determination case.
4.12.6.3. An illness, injury, disease or death sustained by member in a duty status is
presumed to be In the Line of Duty. The presumption can be rebutted when evidence
shows the member was not in the Line of Duty. A Line of Duty determination case must
be initiated, whether a member is hospitalized or not, for certain illnesses and injuries. (T-
2). Refer to AFI 36-2910, paragraph 1.6 for definitive information regarding when to
initiate a Line of Duty determination for AD service members and RC service members.
4.12.7. For AD service members, the inability to perform one’s job for 24 hours or more, and
the subsequent placement upon simple quarters for minor injuries and illnesses (including
obstetrical quarters) will likely not require the submission of an AF Form 348 provided:
4.12.7.1. None of the mandatory circumstantial factors or Line of Duty determination/case
initiation triggers identified by AFI 36-2910 are present.
4.12.7.2. The injury or illness is minor and meets the criteria provided under the
Administrative Line of Duty Determination allowances of AFI 36-2910.
4.12.8. If an injured RC service member is taken to a non-MTF for care, the medical officers
assigned to the MTF, Reserve Medical Unit (RMU) or Guard Medical Unit (GMU) who
provided the initial treatment or had first contact with the RC service member should initiate
the Line of Duty determination process.
4.12.9. The medical officer initiating the AF Form 348 will complete blocks 1-11 of the AF
Form 348, sign, stamp or type printed name and title, and date the form. (T-3). The provider
will then contact the appropriate MTF or RC Line of Duty patient administration representative
to initiate the administrative coordination process. (T-3). The Line of Duty patient
administration representative shall ensure that all applicable supporting medical documents
and/or any other medical-related incident or information reports are attached to the AF Form
348 before forwarding the package to the appropriate officials designated in AFI 36-2910. (T-
2). The Line of Duty administrative representative will fill in the “TO, THRU, and FROM”
blocks at the top of the form. (T-3).
4.12.10. In cases where the healthcare provider has determined a Line of Duty determination
review is required for an inpatient admission, the admitting clerk must obtain the time, place
and manner of occurrence of the incident from the patient, other witnesses and/or available
sources and records the information on the reverse of the AF Form 560. (T-3). Again, the
initiating provider completes the appropriate blocks on the AF Form 348, signs the form and
coordinates with the appropriate MTF or RC Line of Duty representative. The Line of Duty
representative will forward the package to the service member’s Military Personnel Section.
(T-1).
4.12.11. The MTF or RC Line of Duty Medical Focal Point representative shall be appointed
in writing by the MTF or RC commander. (T-3). The Line of Duty Medical Focal Point
representative is responsible for (T-3):
4.12.11.1. Educating MTF or RC staff on medical responsibilities for the Line of Duty
process.
4.12.11.2. Processing of all LOD paperwork within the MTF quickly and accurately.
56 AFMAN41-210 10 SEPTEMBER 2019
4.12.11.3. Routing Line of Duties to the appropriate Military Personnel Section special
actions unit or RC personnel processing office in accordance with AFI 36-2910.
4.12.11.4. Ensuring Line of Duties are initiated for local unit attached Individual
Mobilization Augmentee and Participating Individual Ready Reserves reservists.
4.12.11.5. Identifying cases requiring Line of Duty and determinations for AD and RC
service members.
4.12.11.6. Ensuring the appropriate medical officer signs the AF Form 348 before
distributing the AF Form 348 as follows:
4.12.11.6.1. Original: Forward the original and all supporting medical summaries and
supporting documentation to the member’s servicing Military Personnel Section
Special Actions Office.
4.12.11.6.2. Copy: Scan/upload one copy into the member’s approved electronic
health record.
4.12.11.6.3. Copy: File one copy in the Line of Duty - Medical Focal Point Office.
4.12.12. Line of Duty Requirements for Members of the Reserve Component. Reference
DoDI 1241.01, AFI 36-2910 and AFI 36-3212.
4.12.12.1. Government sponsored (Direct Care or TRICARE) healthcare is not authorized
at government expense beyond the period of Inactive Duty Training or drill status orders
for any medical condition that is determined to be not in line of duty. Attempts to complete
Line of Duty determinations should occur prior to the end of the AD orders.
4.12.12.2. The LOD process should be initiated as soon as possible. If the LOD
determination process cannot be initiated by the point of first contact, the process will be
initiated by the RC service member’s servicing MTF, RMU or GMU. (T-1). The LOD
determination process must be accomplished in accordance with AFI 36-2910. (T-1).
4.12.12.3. Any RC service member seeking government sponsored healthcare must
produce at least a partially completed AF Form 348 (1st side completed and signed by the
provider initiating the Line of Duty determination process). (T-1). The partially completed
Line of Duty determination form may be used as healthcare eligibility verification source
when the service member seeks government sponsored healthcare without possessing
current AD status orders or when a DEERS healthcare eligibility check indicates no current
coverage.
4.12.12.4. If a Line of Duty determination cannot be made before the tour of duty ends,
and the individual requires further hospitalization or treatment, continue with any
necessary healthcare related to the potentially service-connected injury or illness.
4.12.12.5. If the final determination is “Not in Line of Duty,” medical care at government
expense ends. Document the notification of the Line of Duty determination in the patient's
medical record(s). If the service member is still hospitalized, advise the patient that as of
the day of notification, care will be provided at the full reimbursement rate until transfer to
a civilian medical facility.
4.12.12.6. If the final Line of Duty determination is “In Line of Duty,” document the
notification and advise the patient that care continues at government expense until service
AFMAN41-210 10 SEPTEMBER 2019 57
member is found fit and returned to duty or separated by the Disability Evaluation System
for the documented medical condition.
4.12.12.7. “Interim” Line of Duty Determination for Healthcare: An informal or formal
Line of Duty investigation, still ongoing, and where a final Line of Duty determination has
not yet been determined. An Interim Line of Duty determination for healthcare is
comprised of the completed medical portion (front part) of the AF Form 348 (with a
provider signature). The form should contain a description of the service member’s illness,
injury or disease, and date of occurrence. In accordance with AFI 36-2910, the military
officer’s signature does not constitute a completed Line of Duty determination. The
Interim Line of Duty determination for healthcare is used to provide eligibility for direct
or TRICARE network healthcare when DEERS indicates a RC service member may not
be eligible for medical or dental benefits. In other words, the completed first side of the
AF Form 348 (including a provider signature) may be used to verify a RC service member’s
entitlement to medical care at government expense when not on AD orders.
4.12.12.8. If the MTF initiates the AF Form 348, the form must be submitted to the
reservist’s Air Force Reserve (AFR) unit or to the RC responsible for uploading the
information into the Electronic Case Tracking. (T-1). The RC will initiate the AF Form
348 through the RC Electronic Case Tracking. (T-1).
4.12.12.9. For Individual Mobilization Augmentee and Participating Individual Ready
Reserves Service Members: The MTF should initiate an AF Form 348 (1st side with
provider signature) and routed in accordance with AFI 36-2910. Notification of ARC
Surgeon General’s Office of initiated Line of Duties for Individual Mobilization
Augmentee and Participating Individual Ready Reserves Service Members is not
necessary.
4.12.12.10. Air National Guard (ANG) Service Members: The medical officers who first
provide treatment or the medical officers stationed nearest to the non-Air Force medical
facility that first provides treatment, in cooperation with the MTF or GMU patient
administration or Line of Duty representative, should initiate the AF Form 348.
4.12.12.11. If the MTF initiates the AF Form 348, the form must be submitted to the ANG
service member’s unit or to the GMU responsible for completing Part I. (T-1).
Section 4F—Air Force Secretarial Designee Program Administration
4.13. Authority. Reference DoDI 6025.23. The use of regulatory authority to establish DoD
healthcare eligibility for individuals without a specific statutory entitlement or eligibility shall be
used very sparingly, and only when it serves a compelling DoD mission interest. (T-0). The
Secretary of Defense and/or the Secretaries of the Army, Navy, and Air Force may designate
individuals not otherwise entitled, for DoD healthcare (medical and dental) in MTFs. The
Secretarial Designee Program only authorizes care within MTFs. Under HQ Air Force Mission
Directive 1-6, Administrative Assistant to the Secretary of The Air Force, the Secretary of the Air
Force has delegated authority to approve medical designee status to the Administrative Assistant
to the Secretary of the Air Force (SAF/AA). Healthcare authorized under this section shall be
provided on a reimbursable basis, unless non-reimbursable care is authorized by this AFMAN or
waived by the Office of the Under Secretary of Defense for Personnel and Readiness or the
58 AFMAN41-210 10 SEPTEMBER 2019
Secretaries of the Military Departments as the approving authorities. (T-0). The level of benefit
and reimbursement rate is determined by the Military Services, using Military Services-specific
criteria.
4.13.1. Reciprocity Among Military Departments and the Defense Health Agency (DHA). Air
Force MTFs will provide treatment to Secretarial Designees from other Military services and
the DHA, subject to the capabilities of the MTF professional staff, availability of space and
facilities, and any other limitations imposed by the approving authority. (T-0). Each
Secretarial Designee agreement must identify the specific MTF in which medical care is
requested, requiring close coordination among service program managers. (T-0).
4.13.2. Each approved Secretary of the Air Force Designee must obtain a signed letter from
the SAF/AA establishing eligibility for care. (T-0). Exception: When a MTF commander or
director authorizes care for newborns of dependent daughters. The letter will include an
effective date, coverage period, aeromedical evacuation/transport determination, the specific
treatment or care authorized in relation to the specific medical condition/incident, and the rate
(charges) for care. (T-2).
4.13.3. Authorization does not entitle a Designee to utilize TRICARE benefits/entitlements.
Approved Designees receive space-available care at the MTF commander’s or director’s
determination, in accordance with Health Affairs Policy 11-005. Unless the authorization
letter specifies otherwise, individual Designees may not use the aeromedical evacuation
system. If aeromedical evacuation becomes a requirement after the SAF/AA has approved the
initial request, a supplemental Designee request must be submitted. (T-2). Designated MTF
personnel may contact AFMOA/SGAT for assistance.
4.13.4. The SAF/AA normally authorizes care for no more than two years. However,
extensions for continuity of care are limited as detailed in paragraph 4.14.4., below. This
program is not intended to provide life-long medical care. Individuals may request renewal of
Designee status and reapply for Designation as outlined in this chapter; however, continued
approval is not guaranteed. Secretarial Designee requests will not be approved for financial or
humanitarian purposes. (T-1). It will not be the process in which to offer an individual debt
relief.
4.13.5. Individuals being considered for Secretarial Designee status (not currently eligible for
care) shall not receive treatment at Air Force MTFs until Secretarial Designee status has been
approved. (T-2). An exception to this requirement is Extracorporeal Membrane Oxygenation,
or partial heart-lung bypass. In this situation, the MTF is required to initiate a verbal request
via telephone communication through the Air Force Surgeon General’s Medical Operations
Center. (T-2).
4.13.6. MTF Secretarial Designee Program Managers should educate MTF professionals,
medical support (outpatient and inpatient) and ancillary staff members of the purpose of the
Secretarial Designee Program and its basic requirements. Clinical professionals and
immediate medical support staff are best positioned to identify patients who may benefit from
potential Secretarial Designee status.
4.13.6.1. If Secretarial Designee status is identified as a potential option, clinicians and
medical support staff should proactively submit a timely application. The staff may
identify a potential designee through the normal course of treatment for a MHS beneficiary
AFMAN41-210 10 SEPTEMBER 2019 59
for whom healthcare benefits are soon to expire; in such case, staff should determine
eligibility loss date and begin the application process. Staff may also identify a potential
designee when that person is treated as an emergency patient.
4.13.6.2. MTF requests must be received by AFMOA/SGAT no later than 30 days prior
to expiration of medical benefits. (T-2). Individuals who have lost their military medical
benefits and are being considered for Secretarial Designee status will no longer receive
treatment at Air Force MTFs until Designee status has been approved.
4.13.6.3. Situations where patient healthcare eligibility has expired and Secretarial
Designee approval has not been granted could potentially leave the patient without
healthcare coverage; further, these situations could force the applicant to incur a financial
burden, especially if the designee request is disapproved.
4.13.6.4. Application denials for healthcare already provided will automatically generate
charges at the full reimbursement rate. Retroactive requests should be limited to absolutely
unavoidable situations such as short-notice separations. The MTF must notify
AFMOA/SGAT immediately of urgent cases. (T-2).
4.13.7. Each application shall include a DEERS and identification check to verify the status
of the patient and sponsor. (T-2). The MTF law consultant or base Legal Office will review
applications and include the review as part of the Secretarial Designee request. (T-3).
4.13.8. Typically, in emergency (life, limb, eyesight, or relief of undue suffering) cases that
present at a MTF, healthcare personnel can provide necessary treatment to stabilize the
individual without the need to pursue a Secretarial Designation. However, for longer-term
care, there could be a need to pursue approval to treat via this Secretarial Designee process
identified in this AFMAN.
4.14. U.S. Air Force Secretarial Designee Criteria. Individuals who meet one or more of the
following criteria may apply for Secretarial Designee status through the requesting MTF using the
sample format in Attachment 2. When submitting applications, choose the most appropriate
category for the request.
4.14.1. Teaching Case. When the case presents a unique teaching opportunity for the MTF
staff or residency programs, an individual may request Designee status. If this option is
selected, the MTF attending physician or primary physician advocate must include a thorough,
written, signed statement that identifies the specific benefits to the Air Force. (T-2). The
application must then be endorsed by the attending physician’s department chairperson, the
Director of Graduate Medical Education, and the Chief of the Medical Staff. Each signature
is required to validate the teaching significance of the case. For example, the case is critical
for continued accreditation of a training program; is an extremely rare case; the case is a
necessary part of a training program protocol and the patient case mix is not available in the
beneficiary population. MTF healthcare will, under most circumstances, be provided at the
family member rate. Use this paragraph for teaching cases that fall outside paragraph 4.14.2.2
for Extracorporeal Membrane Oxygenation Program cases.
4.14.2. SAF/AA Delegated Approval Authority Programs.
4.14.2.1. Civilian Trauma Program. In certain instances and at certain locations, SAF/AA
designates authority to the MTF commander or director to identify civilian trauma patients
60 AFMAN41-210 10 SEPTEMBER 2019
as Secretarial Designees under the parameters SAF/AA determines appropriate. Upon
expiration of eligibility initially established through this delegated authority, additional or
continued care requires a full Secretarial Designee application and approval by the
SAF/AA. (T-2). If the additional or continued care is approved, the Designee will pay the
Full Reimbursement Rate for healthcare provided under the Secretarial Designee program.
4.14.2.2. Extracorporeal Membrane Oxygenation Program (partial heart-lung bypass). If
a patient requires Extracorporeal Membrane Oxygenation or partial heart-lung by-pass, the
MTF will initiate the application with a verbal request through the Air Force Surgeon
General’s Medical Operations Center to the SAF/AA. (T-2). All verbal requests to grant
Secretarial Designee status for Extracorporeal Membrane Oxygenation treatment must
include: patient demographics, citizenship of patient, pick up location, type of military
transport (air/ground), diagnosis, justification for the mission, requested length of
Secretarial Designee status, if follow-on inpatient care at a MTF is required and if patient
has health insurance. (T-2). Transportation on civilian air or ground ambulances or
treatment at a civilian medical facility is not authorized under the Secretarial Designee
Program. To gain approval of all requests the Medical Operations Center will notify the
appropriate point of contacts. The Medical Operations Center will coordinate with the
AF/SG and the Air Force Deputy Surgeon General (AF/DSG) prior to engagement with
SAF/AA. The Medical Operations Center will simultaneously notify Secretary of the Air
Force International Affairs (SAF/IA) if the request involves a non-United States citizen or
a foreign country. The MTF will submit the full and complete electronic application within
24 hours to AFMOA/SGAT. AFMOA will email the formal package directly to SAF/AA
with a courtesy copy to the Medical Operations Center. (T-2).
4.14.2.3. Human Immunodeficiency Virus (HIV) Research Program.
4.14.3. Best Interest of the Air Force. This category of Designees includes those for whom it
is in the best interest of the Air Force to provide continued care. For cases when the
justification is in the best interest of the government, include a letter from the MTF, addressing
the effects of denying Designee status (e.g., litigation risk, cost, negative press coverage). Care
will under most circumstances be provided at the family member rate. (T-0).
4.14.4. Continuity of Care. If continuity of care is a significant clinical issue in the individual's
course of treatment and civilian medical care is not available or appropriate, this individual
may request Designee status. Care is limited to a period of six months, or in the case of
pregnancy, until the completion of the pregnancy. For cases when the justification is continuity
of care, the case must be medically supportable. (T-0). Include a statement on the medical
impact if the Air Force were to deny the individual Designee status.
4.14.4.1. Obstetrics, Maternal, and Pediatric Care Sub-Category: The MTF commander
or director or designated representative may approve Designee status for applicants
identified below at the family member rate unless the Designee has other health insurance.
4.14.4.1.1. Newborns of eligible family member daughters.
4.14.4.1.2. Pregnant former AD members and their newborns.
4.14.4.1.3. Spouses of former AD and their newborns.
AFMAN41-210 10 SEPTEMBER 2019 61
4.14.4.1.4. Family member dependent daughters who became pregnant prior to losing
eligibility and their newborns.
4.14.4.1.5. Newborns of widows losing transitional survivor benefits.
4.14.4.2. In the case the Designee has other health insurance, the rate will be the Full
Reimbursement Rate. MTF healthcare is generally limited to pre-partum obstetrical care,
MTF newborn delivery, one post-partum check-up (for the mother), well baby outpatient
visits for the infant and any necessary immunizations for the infant, all to be provided no
later than six weeks following delivery.
4.14.5. Abused Family Members and Dependents. This section is only applicable if all or
some transitional benefits are denied by the Air Force Personnel or Finance Authorities, and/or
the Defense Finance and Accounting Service. If all or some transitional benefits, discussed in
AFI 36-3024, Transitional Compensation for Abused Dependents, are denied, a discharged or
separated service member’s family member/dependents may apply for consideration of limited
(MTF direct care only) medical benefits under the Secretarial Designee program. Approval is
not guaranteed. If approved, healthcare is specifically limited to medical services necessary to
treat injuries or illnesses suffered as a direct result of the sponsor’s abuse.
4.14.5.1. Notification or receipt of denial of transitional compensation benefits (from the
installation Military Personnel Section or Finance Office) does not necessitate MTF
obligation to automatically submit a Secretarial Designee application on behalf of the
abused family member(s). The MTF is only required to submit an Air Force Secretarial
Designee application to the SAF/AA (via AFMOA/SGAT intermediary), if requested in
writing by one or more family members of the discharged service member. (T-2).
4.14.5.2. Confirmation of this action must be coordinated with the abused family member
dependent(s) or legally authorized representative(s). (T-0). The MTF location responsible
for assembling the Secretarial Designee package should include the standard application
package documentation identified at Attachment 2 and, to include the application letter and
medical summary or statement that clearly identifies the medical illness, injury or condition
(related to, or as a consequence of abuse) for which military healthcare is requested. See
example at Attachment 2.
4.14.6. Foreign Military Sales Case. If the country has an open Foreign Military Sales case,
the Air Force may bill the costs for the additional study to that case number. In other situations,
the requesting country may have the Air Force bill sent to another United States controlled
fund or may have the bill sent to their Embassy. The applicant must provide billing information
before the Air Force decides on the availability of the requested service.
4.14.7. Special Foreign Nationals. The Secretary of the Air Force may authorize Air Force
healthcare benefits to foreign nationals considered to be critically important to the interests of
the United States The Secretary of the Air Force may use this authority for individual
designations, on a case-by-case basis. Such a designation does not create a new category of
beneficiaries.
4.14.7.1. Criteria for selection as a Secretary of the Air Force Designee for foreign
nationals:
62 AFMAN41-210 10 SEPTEMBER 2019
4.14.7.1.1. Foreign nationals nominated for Designee status must be Heads of State,
Cabinet members (Minister), Chiefs of Staff of the Armed Forces, or hold equivalent
positions. (T-0).
4.14.7.1.2. Appropriate healthcare must not be available in the nominee's country or
in a civilian healthcare facility in the United States. (T-0).
4.14.7.1.3. The nominee or his government must agree to assume responsibility for
payment of DoD healthcare services (at the Full Reimbursement Rate) if the individual
requested and the Air Force approved the cost of aeromedical evacuation. (T-0).
4.14.7.2. Designation procedures:
4.14.7.2.1. Foreign governments seeking Designee status will submit requests to the
State Department through the mission chief of the country involved. The request must
contain the full name and title of the individual, an explanation of why the individual
is critical to United States’ interests, the pertinent medical information, the billing
address, individual or office, and a certification that the nominee meets the necessary
criteria. (T-0).
4.14.7.2.2. Refer inquiries from foreign embassies in Washington, or other sources to
the United States Chief of Mission in the country concerned.
4.14.7.2.3. The State Department reviews the request and refers it to the appropriate
agency Secretary with a recommendation for approval.
4.14.7.2.4. The Request is submitted to the Secretary of the Air Force for review. If
approved, the Secretary's office forwards it to the Office of the AF/SG for appropriate
action. AFMOA/SGAT prepares the request and assigns responsibility for moving the
Designee through the Patient Movement Requirements Center to the specific overseas
or CONUS MTF.
4.15. Applying for Air Force Designee Status. When evaluating a Designee application, MTF
commanders or directors should consider the availability of MTF capabilities and resources. If
adequate capabilities exist, and the applicant does not meet or qualify for any initial or continued
sponsor service affiliation for DEERS enrollment, eligibility, and/or medical entitlement identified
in AFI 36-3026_IPV1, then the MTF commander or director should review and sign the
application package recommending whether or not Designee status is warranted. The package is
then forwarded to AFMOA/SGAT for processing. The MTF shall electronically submit (via e-
mail encryption) a Secretarial Designee application to AFMOA/SGAT no later than 30 days prior
to expiration of medical benefits or requested Designee start date. (T-2). The 30 day window
allows enough coordination time to submit the Secretarial Designee application to the SAF/AA
for review and approval consideration. See example of Designee application at Attachment 2.
4.15.1. Forward all United States Air Force Secretarial Designee requests electronically to
AFMOA/SGAT. Because designee applications may contain PHI or sensitive medical
information, e-mail messages must only be forwarded to higher HQ using government
Common Access Card digital signature and encryption protocols. (T-0). If unable to send an
encrypted message, the package may be sent using Encryption Wizard/AMRDEC SAFE
requirements in accordance with AFI 41-200, paragraph 7.8, or mailed using a commercial
AFMAN41-210 10 SEPTEMBER 2019 63
overnight express mail shipping company or First Class United States Postal Service overnight
or express mail with return receipt or other package tracking option.
4.15.2. Each request is required to be coordinated with an AFMOA/SGAT representative. (T-
2). AFMOA/SGAT will review and coordinate the request package for a legal review prior to
submitting to the SAF/AA. AFMOA will submit all “retroactive” requests to the AF/SG for
coordination and approval consideration prior to further submission to the SAF/AA. All
request packages must contain the AFMOA electronic Staff Summary Sheet, the MTF
application, and a legal review. (T-0).
4.15.3. If the request pertains to a sponsor or member who is due to separate and/or be
discharged from the Air Force, the request package must include a copy of the sponsor’s or
member’s separation orders and DD Form 214, Certificate of Release or Discharge from Active
Duty, and the line of duty determination for RC service members, when applicable (T-3).
4.15.4. AFMOA/SGAT officials, with concurrence of respective MAJCOM command
surgeons, are authorized to reject applications that do not meet the requirements identified in
this chapter. Applications that are denied or rejected by AFMOA officials and the MAJCOM
command surgeon do not need to be routed through or submitted to the SAF/AA. Ensure
request packages are accurate, current and contain all necessary supporting documentation.
4.15.5. AFMOA will forward United States Air Force Secretarial Designee requests via e-
mail to the SAF/AA.
4.15.6. The electronic Staff Summary Sheet must contain (at a minimum) purpose,
background, discussion, options and recommendation. (T-1). The discussion must include a
justification that specifies which of the criteria in paragraph 4.14 the request is based upon,
and an explanation of how the request relates to those criteria. (T-1). The discussion must also
include the eligibility duration being requested. (T-1).
4.15.7. The Secretarial Designee approval letter must contain the designee’s name, eligibility
duration, designation criteria being met, aeromedical evacuation determination,
reimbursement rate, statement limiting care to MTF authorized care only for the specified
illness or injury and any applicable third party insurance. (T-1).
4.15.8. The determinations of all designee cases and respective application packages
submitted to and returned from the SAF/AA will be returned to AFMOA/SGAT who will then
notify the applicable MTF and/or MAJCOM so the individual can be notified. MTF will file
a copy of the letter in the individual’s outpatient medical record. (T-3).
4.15.9. Reporting. The annual Secretarial Designee Log will be forwarded annually (FY) to
AFMOA/SGAT no later than 15 October. (T-1). Following report collection and quality
review, officials at AFMOA/SGAT will then forward the reports to the SAF/AA no later than
30 October.
4.15.9.1. Overseas MAJCOM commander surgeons, MTF commanders and directors will
report data on the individuals approved under SAF/AA delegated authority (locally
approved). (T-3).
4.15.9.2. All reporting data is PHI and will be transmitted in accordance with appropriate
safeguards. (T-0).
64 AFMAN41-210 10 SEPTEMBER 2019
4.16. Certain Senior Officials of the United States Government. Certain senior officials
within the Government, including the DoD and the Military Departments, have Secretary of
Defense Designee status for medical care and dental care in military medical or dental treatment
facilities.
4.16.1. The Secretary of the Air Force recognizes Secretary of Defense Designees in
accordance with DoDI 6025.23, Enclosure 2. Family members are not included unless
otherwise stated. See DoD 6025.23 for instructions on Health Care Eligibility Under the
Secretarial Designee (SECDES) Program.
4.16.2. Applicable charges for Secretary of the Air Force Designees. The Secretary of the Air
Force has authorized the individuals listed in DoDI 6025.23 Enclosure 2 to receive space-
available inpatient and outpatient health care services from United States Air Force MTFs on
a reimbursable basis.
4.16.3. See AFI 48-307V1 for instructions on Aeromedical Evacuation operations.
4.17. Operating the Air Force Secretarial Designee Program Overseas. In accordance with
HAF Mission Directive 1-6, Administrative Assistant to the Secretary of the Air Force, HAF
Mission Directive 1-48, The Air Force Surgeon General, and DoDI 6065.23 Health Care
Eligibility Under the Secretarial Designee (SECDES) Program and Related Special Authorities,
the Command surgeons at HQ United States Air Force Europe Air Forces Africa (HQ USAFE-
AFAFRICA) and HQ Pacific Air Forces (HQ PACAF) for their respective theater have the
authority to designate individuals for care in overseas MTFs. This authority does not extend to
authorizing transportation to the CONUS.
4.17.1. United States Citizens. The Air Force tries to keep the number of United States
citizens who commanders can designate to an absolute minimum. Most United States citizens
who fall under this paragraph are returning hostages and individuals involved in prisoner
exchanges. There may be other occasions when designating United States citizens would be
appropriate.
4.17.2. Foreign Nationals. Commanders who use the authority under this paragraph must
issue guidelines on medical care for nationals of foreign nations. (T-2). These guidelines must
identify the categories of persons, both military and civilian, who have authorization for
medical care within the provisions of this paragraph. (T-0). Individuals, whom the commander
designated under this paragraph, must contribute to the advancement of United States public
interests. (T-0). Generally, only officials of high national prominence are made Designees.
Sometimes, a commander grants designee status when there are special, unusual or
extraordinary circumstances. The Air Force may not provide care for foreign nationals with
incurable diseases or who require excessive nursing care. Commanders should seek
recommendations from the chief of the diplomatic mission or embassy to the country involved
before authorizing care to any foreign national. The Air Force collects charges for the
Designee’s care locally.
4.18. Designee Status Used in Claims Against the United States. Designee status is not used
in the claims process.
AFMAN41-210 10 SEPTEMBER 2019 65
Section 4G—Exceptional Family Member Program
4.19. Exceptional Family Member Program (EFMP). MTFs will standardize the location of
Exceptional Family Member Program enrollment and relocation clearance functions within
Medical Management offices. (T-1). Refer to AFI 40-701, for additional information.
4.20. Family Member Relocation Clearance Coordinator (FMRCC). The individual
responsible for ensuring administrative process requirements are met is the Family Member
Relocation Clearance Coordinator. Refer to AFI 40-701, for additional information.
Section 4H—Admissions and Dispositions Program Administration
4.21. Responsibility for Admission Processing. Unless otherwise specified, Patient
Administration is responsible for administrative needs required for the admission and disposition
of patients.
4.22. Administrative Admission and Disposition Requirements. The Admissions and
Dispositions Office will verify authorized eligibility for healthcare for 100% of inpatient
admissions.
4.22.1. For all admissions, enter the patient’s demographic and personal data via the FULL
patient registration menu.
4.22.2. Notify the military patient’s commander, first sergeant or other appropriately
appointed commander’s designee, of member’s admission. All disclosures of PHI to
commanders will be tracked in accordance with AFI 41-200. (T-0)
4.22.3. Determine at the time of admission if the patient will opt in or opt out of the Facility
Directory and make appropriate documentation. See AFI 41-200, paragraph 4.2.1, for
additional information.
4.22.4. If communication with the member’s commander, first sergeant, or other appropriately
appointed commander’s designee is not possible, then contact the service member’s
installation command post or installation operations/control center. Release only Sanitized
Healthcare Information to the member’s installation command post or control center staff.
4.23. Assuming Administrative Responsibility for Military Members Hospitalized in Non-
Military Medical Facilities also known as Absent Sick Status.
4.23.1. The MTF commander or director at the nearest Air Force MTF shall assume the
primary administrative support responsibility (including appropriate service member
identification, monitoring, “tracking,” clinical secondary support, advice, analysis, and/or
consultation) for any AD service member referred to, hospitalized, or admitted to a non-
military medical facility. (T-1). AD service members admitted to non-military civilian medical
facilities are referred to as being in an “Absent Sick” or ABS status (menu path in CHCS).
4.23.2. If necessary, the nearest Air Force MTF shall serve as an information conduit between
the civilian or non-military medical facility, the service member’s family, and the service
member’s chain of command. (T-1).
4.23.3. Each MTF TRICARE Operations and Patient Administration function or Admissions
and Dispositions Office is responsible for identifying and tracking each known Air Force AD
66 AFMAN41-210 10 SEPTEMBER 2019
service member hospitalized or admitted to a civilian or non-military medical facility.
Established or perceived geographic boundaries, TRICARE Prime Service Areas, or other
distance or mileage restrictions or arguments, shall not relieve a MTF from its obligation to
identify, monitor, track, or support a hospitalized Airman unless another Air Force MTF, has,
or will assume primary administrative support responsibility. (T-1). Support obligations may
extend hundreds of miles if no other Air Force MTF exists in a particular region or if no other
Air Force MTF has been identified as having primary administrative support responsibility.
4.23.4. Notwithstanding the provisions identified immediately above this paragraph, the
nearest MTF will assume primary administrative support responsibility for all known Air Force
AD service members, regardless of type of injury or illness, whether hospitalization was
planned, scheduled, resulted from emergent, urgent, non-emergency, non-urgent, battle or non-
battle related circumstances.
4.23.5. All known Air Force Wounded Warriors will be identified, tracked, and supported by
the nearest Air Force MTF. (T-3).
4.23.6. Any seriously ill or injured Air Force AD service members will be identified, tracked,
and supported by the nearest Air Force MTF. (T-3).
4.23.7. All Air Force AD service members referred from the MTF, to a civilian or non-military
medical facility will be monitored and tracked. (T-3).
4.23.8. Minimum Processes Required to Identify, Monitor, and Track Absent Sick Patients.
4.23.8.1. Tracking Requirements for Inpatient or Bedded MTFs:
4.23.8.1.1. At a minimum, the Admissions and Dispositions Office will use the CHCS
automated computer system to support their identification, monitoring, and tracking,
efforts of each known Absent Sick patient. (T-3).
4.23.8.1.2. Record the admission in the CHCS Patient Administration module using
the Admissions, Discharges, and Transfer secondary menu and Admissions sub-menu.
4.23.8.1.3. If a decision to transfer the service member-patient from the civilian or
non-military medical facility to the MTF is authorized, then the MTF Chief of the
Medical Staff is responsible for identifying the admitting MTF physician. The
Admissions and Dispositions Office leaves the admission category type as ABI (menu
path in CHCS) and enters the transfer date and time into CHCS. Maintain the same
register number.
4.23.8.1.4. If the service member-patient remains in the civilian or non-military
facility for the duration of inpatient treatment, the MTF Admissions and Dispositions
Office will change the admission category type from ABI to ABS (Absent Sick). After
confirming the service member-patient has been discharged from the civilian or non-
military medical facility, then discharge the service member-patient in CHCS.
4.23.8.1.5. Request a complete summary of the patient’s treatment from the civilian or
non-military medical facility before the patient is transferred to the MTF or after the
patient has been discharged from the civilian medical facility.
4.23.8.2. Tracking Requirements for Outpatient or Non-Bedded MTFs: Place any medical
documents received from the civilian or non-military medical facility into a secure, locked
AFMAN41-210 10 SEPTEMBER 2019 67
transitory file within the office responsible for providing or facilitating the majority of the
administrative support responsibility. Upon discharge from the civilian medical facility,
the office responsible for administrative support will scan/upload the documents into the
patient’s electronic health record.
4.23.9. The nearest MTF should recommend to the hospitalized AD service member that an
information release authorization should be signed to allow the civilian or non-military medical
facility to disclose treatment information to the supporting MTF.
4.23.10. Obtain full patient identification from the civilian or non-military medical facility and
promptly notify the patient’s unit commander by telephone with the patient’s name and
location.
4.23.11. When possible, obtain comprehensive medical information regarding the AD service
member’s condition. The civilian or non-military medical facility is financially reimbursed
for the patient’s care based on the Diagnosis Related Group, known as a patient classification
system that standardizes prospective payment to hospitals. A complete summary of the
patient’s treatment while under the care of the civilian healthcare provider is required after the
patient has been discharged.
4.23.12. When no MTF has assumed administrative support responsibility, Air Force points
of contact at DHA-Great Lakes should contact the MTF located nearest to the AD service
member’s location if DHA-Great Lakes received information from:
4.23.12.1. The admitting civilian or non-military medical facility
4.23.12.2. The TRICARE managed care support contractor or regional office
4.23.12.3. An AD service member’s family member.
4.23.12.4. Other sources of information.
4.23.13. When hospitalized at a uniformed services treatment facility or VA hospital, the
nearest MTF assumes administrative support responsibility. The responsible MTF will arrange
for a transfer to a MTF when it is safe to transport the service member. (T-2).
4.23.14. If the service member is referred to a Uniformed Services Treatment Facility or VA
hospital, the referral MTF maintains administrative support responsibility.
4.23.15. Unit commanders must notify the nearest Air Force MTF and the DHA-Great Lakes
(1-888-647-6676) as soon as possible if one of the commander’s unit members in the following
categories is hospitalized in a civilian or non-military medical facility:
4.23.15.1. ARC service members (related to an In-Line-of-Duty occurrence or incident),
4.23.15.2. AD service members assigned to GSU,
4.23.15.3. TRICARE Prime Remote AD Service Member.
4.23.16. Admissions and Dispositions Office will notify the base occupational safety office
and resource management office in accident cases using AF Form 1488, Daily Log of Patients
Treated for Injuries. (T-1). Account for disclosure in accordance with AFI 41-200, paragraph
3.7.
68 AFMAN41-210 10 SEPTEMBER 2019
4.24. Assuming Administrative Responsibility for AD U. S. Air Force Members Hospitalized
in DoD Facilities.
4.24.1. The nearest Air Force MTF commander or director assumes administrative
responsibility and Patient Administration staff ensures that the following procedures are
carried out for Air Force personnel hospitalized in Army or Navy MTFs:
4.24.1.1. Facilitates necessary communication between members’ unit commander, and
officials at the Army or Navy MTF. All disclosures of PHI to commanders will be tracked
in accordance with AFI 41-200. (T-0).
4.24.1.2. Keeps rosters and pertinent data on hospitalized Air Force patients and notifies
the members’ unit commander immediately upon notification.
4.24.1.3. Prepares AF Form 348, when applicable, in accordance with AFI 36-2910.
4.24.1.4. Notifies the base occupational safety officer in accident cases.
4.24.2. Within the CONUS, patients may be administratively assigned or attached to the
closest Air Force MTF Airman Medical Transition Unit nearest to the Army or Navy MTF
providing medical care. See paragraph 4.68 for Airman Medical Transition Unit assignments.
4.24.2.1. Prepares AF Form 1488 when applicable and forwards it to the base occupational
safety office and Resource Management Flight.
4.24.2.2. Serves as the admitted member’s local representative for all patient
administration related matters.
4.24.3. See Section 4I, Casualty Reporting Program Administration, for Seriously Ill and/or
death cases.
4.25. Admitting Infants Born Outside the MTF.
4.25.1. Infants born outside the MTF (e.g., at home or enroute to the hospital) are admitted to
the MTF as “Liveborn” or “Newborn” when the mother is also admitted for post-partum care
within 24 hours following delivery. If the infant is admitted outside the 24 hour window or if
the mother is not admitted at the same time as the infant, then the infant is admitted as a direct
admission.
4.25.2. If the infant’s birth and subsequent admission first occurred in a civilian hospital and
the mother and baby are later transferred to a MTF, admit the infant in CHCS using the CIV-
INITIAL ADM TO NON-U.S. MILITARY HOSP, MOVED TO MIL MTF (NON AD)
admission/transfer code (Source of Admission Code 5) instead of a Direct, Newborn, or
Liveborn admission.
4.25.3. When a newborn infant is transferred from one MTF to another MTF, the receiving
MTF generally admits the infant using the TAF-TRANSFER FROM AF HOSPITAL; TAR-
TRANSFER FROM ARMY HOSPITAL; or TNF-TRANSFER FROM NAVY HOSPITAL
admission/transfer code instead of a Direct, Newborn, or Liveborn admission.
4.26. Admitting Generals/Admirals (Flag Officers), Colonels, and Prominent Persons. All
disclosures of PHI to Commanders will be tracked in accordance with AFI 41-200. (T-0).
4.26.1. Terms:
AFMAN41-210 10 SEPTEMBER 2019 69
4.26.1.1. General/Admiral Officer (GO): Includes all AD, RC (of any Uniformed Service
branch) and foreign general flag officers (0-7 and above).
4.26.1.2. Colonel: Applies only to AD Air Force colonels that are Seriously Ill /Very
Seriously Ill, expected to be hospitalized for a non-scheduled emergency hospital stay
greater than 10 days, or any Air Force colonel provided a profile change for any serious
medical or surgical condition affecting the member’s assignment availability or command
obligation. This reporting rule also includes any AFMS colonel (Medical Corps (MC),
Dental Corps (DC), Nurse Corps (NC), Medical Service Corps (MSC), and Biomedical
Sciences Corps (BSC)) who has been admitted as an inpatient under emergent
circumstances.
4.26.1.3. Prominent Persons:
4.26.1.3.1. Senior Executive Service (SES) federal civilian officials, political officials
or officers, high-ranking public officials, federal judges who are expected to be
hospitalized for a non-scheduled, emergency hospital stay greater than 10 days.
Notifications for persons in this category require the patient’s authorization.
4.26.1.3.2. Current Chief Master Sergeant of the Air Force and any AD AFMS Chief
Master Sergeant.
4.26.1.4. Admission and Extended Ambulatory Care: Admission to a MTF, non-federal
hospital, or any facility for which the nearest MTF assumes administrative responsibility.
This includes inpatient units and other extended care services (e.g., ambulatory patient
visits, observation and partial hospitalization).
4.26.1.5. Information Conduits: Command Posts, Operations Centers at the installation or
MAJCOM level. AF/SGXO, Air Force Medical Operations Center can be reached at
Defense Switched Network (DSN) 227-9075 or commercial (703) 697-9075.
4.26.2. Local and MAJCOM Notification Procedures when a General/Flag Officer, Colonel,
or Prominent Person (fitting the description listed in the above paragraphs), is Admitted.
4.26.2.1. The Admissions and Dispositions Office (or similar Patient Administration
location or office) will contact the MTF commander or director and provide sanitized
information regarding the admission. (T-1).
4.26.2.2. The Admissions and Dispositions Office (or similar Patient Administration
location or office) will contact the local base or wing command post and the command post
or operations center of the admitted military official. Provide only sanitized information.
(T-2).
4.26.2.3. The Admissions and Dispositions Office (or similar Patient Administration
location or office) will contact their MAJCOM command surgeon or AFMOA Health
Benefits Regional Branch. (T-2).
4.26.2.4. The MTF commander or director will notify the installation commander (via
appropriate information conduits) and release only minimum necessary information. (T-
2).
4.26.2.5. Notifications will be made as soon as possible, no later than 12 hours after
admission or initial treatment. (T-2).
70 AFMAN41-210 10 SEPTEMBER 2019
4.26.3. HQ USAF Notification Procedure when a General/Flag Officer, Colonel or Prominent
Person is admitted or remains in the MTF.
4.26.3.1. Inpatient/bedded MTFs will contact the Pentagon AF/SG Military Operations
Center by 0600 Eastern Time every duty day to include negative replies. (T-1).
4.26.3.2. Provide only sanitized information to the Medical Operations Center. Include
telephone call back phone numbers so Medical Operations Center officials can obtain
comprehensive medical information as needed.
4.26.3.2.1. In unusual circumstances, if the MTF commander or director determines
the AF/SG should be notified during non-duty hours, call the Air Force Service Watch
Cell, DSN 227-6103, commercial (703) 697-6103.
4.26.4. HQ USAF/Medical Operations Center Responsibilities:
4.26.4.1. Medical Operations Center officials will create two word-processing (letter)
documents from the information. (T-1).
4.26.4.1.1. The first document includes sanitized information only.
4.26.4.1.1.1. The sanitized information document is transmitted, in password
protected or encrypted mode only, to the Chief, United States Air Force General
Officer Matters Office (AFGOMO) via the Pentagon e-mail address.
4.26.4.1.1.2. AF/SG, AF/DSG or a representative will receive the information via
live brief or in password protected or encrypted electronic format. AF/SG,
AF/DSG or a representative will provide the information to Chief of Staff, United
States Air Force (CSAF). (T-1).
4.26.4.1.1.3. If the document contains information regarding any colonel that has
been admitted or treated and meets the criteria indicated in paragraph 4.25.1.2., the
password protected or encrypted electronic transmission will be provided to the
United States Air Force Colonel Matters Office Support Division. (T-1).
4.26.4.1.2. The second document will include comprehensive medical information and
be provided only to AF/SG, AF/DSG or a representative. (T-1).
4.27. Reporting Aircraft Accident Admissions.
4.27.1. For specific instructions, see AFI 91-204, Safety Investigation and Hazard Reporting.
The Medical Group, Chief Aerospace Medicine (MDG/SGP) makes initial notification to the
command surgeon of the MAJCOM. The command surgeon of the MAJCOM that the aircraft
is assigned notifies Air Force Medical Support Agency (AFMSA)/SG3P, DSN 761-7242 or
DSN 761-7616, commercial 703-681-7616) of any admission resulting from an aircraft
accident (regular Air Force, AFR, or ANG).
4.27.2. Provide the diagnosis, estimated period of hospitalization, and probable disposition of
personnel.
4.27.3. During regular duty hours, notify AFMSA/SG3P (Aerospace Medicine) by telephone.
After duty hours, notify AF/SG Duty Officer through the AFMOA, DSN 227-9075 or
commercial (703) 697-9075. The MAJCOM command surgeon is required to provide the date
of the victim’s initial clinic visit, diagnosis, estimated period of treatment, and the probable
AFMAN41-210 10 SEPTEMBER 2019 71
disposition of all personnel who are examined or received treatment for injuries incurred as a
result of an aircraft accident.
4.28. Managing Military Patients Expected To Be Hospitalized Over 90 Days.
4.28.1. MTF staff must notify the patient’s servicing MTF and Military Personnel Section
when a patient will be reassigned or hospitalized over 90 days. (T-2).
4.28.2. For patients hospitalized while traveling to a CONUS port for permanent change of
station overseas, the staff at the admitting MTF must advise the local Traffic Management
Office and Military Personnel Section of the patient’s hospitalization and the expected
duration. (T-2).
4.28.3. The patient may be assigned or attached to the Airman Medical Transition Unit. See
paragraph 4.67 in this AFMAN.
4.28.4. Under this section, all disclosures of PHI to commanders will be tracked in accordance
with AFI 41-200. (T-0).
4.29. Deployed Military Members who are Aeromedically Evacuated from Contingency
Operations to CONUS MTF.
4.29.1. Deployed Air Force service members (who are on Contingency, Exercise, Deployment
(CED) orders) and are aeromedically evacuated to a CONUS MTF from a Contingency Area
of Responsibility (for example, from Landstuhl Regional Army Medical Center to National
Naval Medical Center) will remain on CED orders until returned to their home station
(permanent duty station). (T-1). Medical TDY orders will not be prepared. (T-1). The
member’s per diem is covered by their CED orders.
4.29.2. CED orders will be extended, if necessary, until the member returns to their home
station. (T-2).
4.29.3. Ambulance Transport for members on CED orders is funded by Defense Health
Program Overseas Contingency Operations (OCO) Supplemental Funds.
4.29.4. Travel per diem expenses of Air Force members transported from a MTF to a
Comprehensive Care Facility are covered by member’s (CED) orders.
4.29.5. Travel and per diem expenses of Air Force members transported from a MTF to home
station is covered by member’s CED orders.
4.29.6. Travel and per diem expenses of Air Force members from home station MTF to a
referral facility, refer to Section 4C, Patient Travel in this AFMAN.
4.30. Readmission of Patients.
4.30.1. Re-activate an inpatient record of hospitalization if a patient is re-admitted before
midnight (2400 hours) on the same day as previously discharged only if the re-admission is for
the same diagnosis or reason documented during the initial admission process. The attending
provider annotates the reason for re-admission and the hospitalization is considered as one
continuous period.
4.31. Canceling Admissions. Annotate the admission work sheet with the reason for cancellation
and gather all paperwork generated by the admission (e.g., History and Physical, progress notes,
laboratory and x-ray reports, etc.) as one package. Scan/upload into the patient’s electronic health
72 AFMAN41-210 10 SEPTEMBER 2019
record or mail the package to the MTF where the patient’s outpatient medical record is normally
maintained.
4.32. Inpatient Disposition Procedures.
4.32.1. Discharge to Duty (Military Patient) or Discharge (Non-military Patient).
4.32.1.1. Review the AF Form 577, Patient’s Clearance Record, to ensure the patient has
cleared all necessary sections. Annotate the form with the date and time of discharge and
enter the information into the current automated system. The patient is then released from
the MTF.
4.32.1.2. Maintain the AF Form 577 in the Admissions and Dispositions Office for a
period of three months and then destroy.
4.32.1.3. Remove any pertinent information from the suspense file and scan/upload in the
patient’s electronic health record.
4.32.2. Discharging Non-AD Patients Requiring Domiciliary or Custodial Care.
4.32.2.1. Discharge retirees eligible for care in VA facilities as follows:
4.32.2.1.1. Arrange for admission and transportation to a VA medical facility, if
acceptable to the patient or legally authorized representative.
4.32.2.1.2. Release retirees declining assistance in getting into a VA facility to the
legally authorized representative.
4.32.2.1.3. If the legally authorized representative declines acceptance, contact civil
authorities in the patient’s state of residence for permission to transfer the patient to
their custody. If the original request for permission is disapproved, contact the
servicing legal office for assistance.
4.32.2.1.4. Provide complete information from the attending healthcare provider (in
narrative form) on the diagnosis, date the condition started, history of previous
hospitalization(s) for the condition, patient’s legal residence, place and date of birth,
length of patient’s military service, and name and address of patient’s legally
authorized representative.
4.32.2.1.5. Coordinate the patient’s move, with proper escort, to the legally authorized
representative or to the civilian authority accepting custody. Advise the accepting party
of the expected time of patient’s arrival.
4.32.2.2. Discharge other non-AD patients requiring domiciliary or custodial care
following procedures similar to those in paragraph 4.31.1 and 4.31.2.1.
4.32.2.2.1. Discharge alternatives must be acceptable to the patient or the legally
authorized representative. (T-3).
4.32.2.2.2. Release the patient to the legally authorized representative if the arranged
or recommended alternatives are declined.
4.32.2.2.3. Request permission to transfer patient custody to civil authorities if the
legally authorized representative declines acceptance. Contact the Staff Judge
Advocate if the request is denied.
AFMAN41-210 10 SEPTEMBER 2019 73
4.32.3. Discharging Patients Not Eligible for Care at VA Expense.
4.32.3.1. Discharge a military patient who, upon expiration of term of service, has physical
or mental disabilities and requires custodial care or is not competent to care for themselves
as follows:
4.32.3.1.1. Contact the legally authorized representative to determine whether they are
assuming custody of the patient and responsibility for care.
4.32.3.1.2. The legally authorized representative must produce affidavits certifying
their willingness to make suitable arrangements for the patient and the financial means
to do so.
4.32.3.1.3. See 4.32.2.1.3 – 4.32.2.1.4 for procedures to follow when the legally
authorized representative declines acceptance.
4.32.3.1.4. Coordinate the patient’s move, with proper escort, to the legally authorized
representative or to the civilian authority accepting custody. Advise the accepting party
of the expected time of the patient’s arrival.
4.32.3.2. When the patient is stable enough, transfer a federal civilian employee patient
with a physical or mental disability requiring hospital care that exceeds the MTF’s
capabilities or if the civilian employee is not a beneficiary under the Federal Employee’s
Compensation Act. Coordinate proposals to move a civilian employee hospitalized in a
medical facility outside the United States, or when it is necessary to separate the employee
from Federal service for medical or other reasons, with the appropriate Civilian Personnel
Office.
4.32.4. Discharging Patients with Chronic Physical or Mental Conditions. The following
instructions apply to a civilian or military member who is separated or retired because of a
chronic physical or mental condition.
4.32.4.1. A patient who does not exhibit suicidal or homicidal tendencies may request
release to the legally authorized representative. See 4.32.3.1.2.
4.32.4.2. Discharge a patient who exhibits suicidal or homicidal tendencies as follows:
4.32.4.2.1. Transfer a member or former member of the Uniformed Services entitled
to treatment by the VA to a location designated by the VA. This requires the request
of the legally authorized representative and authorization for admission from the
hospital concerned. A patient with a mental health condition requiring inpatient
hospitalization may be eligible for involuntary inpatient admission pursuant to
applicable state law.
4.32.4.2.2. Discharge a military or civilian patient not entitled to treatment by the VA
to civil authorities who are legally authorized to assume care in such case; or to an
acceptable private hospital at the written request of the legally authorized
representative. This will also require authorization from the destination hospital. (T-
1).
4.32.4.3. A non-military psychotic (mental disorder) patient admitted to an Air Force MTF
overseas is handled by the liaison, through the American Embassy and civil authorities, to
resolve problems associated with hospitalization and transfer to CONUS.
74 AFMAN41-210 10 SEPTEMBER 2019
4.32.4.3.1. By law, the Department of Health and Human Services may receive and
provide care for non-military mental health patients returned to CONUS.
4.32.4.3.2. If the patient is not releasable to the legally authorized representative, and
is not authorized further Air Force hospitalization, the overseas commander should ask
local United States diplomatic representatives to arrange, through the Department of
State, for the Department of Health and Human Services to receive the patient upon
arrival in CONUS.
4.32.5. Disposition of Prisoner Patient. When discharging prisoner patients, Federal Bureau
of Prisons exercises administrative control over prisoners confined in a DoD regional or long-
term corrections facility. This agency’s responsibility extends to all matters except clemency,
parole, restoration to duty and enlistment. When a prisoner is under the administrative control
of the Air Force, the Air Force is responsible as follows:
4.32.5.1. If a prisoner, whose sentence includes an executed punitive discharge, has a
disabling condition (including psychosis requiring closed unit treatment), hospitalize the
prisoner at the nearest DoD hospital which can provide the required care. Move the patient
in accordance with AFI 31-105, Air Force Corrections System.
4.32.6. Discharging Patients with Communicable Diseases. Notify Force Health Management
if a patient has a communicable disease when the term of service ends and if the patient elects
to separate and be discharged from the hospital.
4.32.7. Discharging Non-AD Patients Refusing to Comply with Rules. Contact the Staff
Judge Advocate for assistance when a non-AD patient fails or refuses to comply with
established patient behavior rules in paragraph 2.19.4.
4.32.8. Discharging Patients with Terminal Illness.
4.32.8.1. Transfer non-Air Force members according to the latest joint service
medical/patient regulating guidance.
4.32.8.2. Final decision on the discharge of the patient depends on MTF capability,
demand for services and humanitarian considerations.
4.32.8.3. If the AD terminal patient is referred to the Physical Evaluation Board, follow
the procedures in Section 4K and AFI 36-3212.
4.32.9. Discharging Patients Absent Without Leave (AWOL). Report a military patient who
is AWOL from a medical facility to the individual’s servicing Military Personnel Section. Do
not carry AWOL patients on the Admissions and Dispositions Office list or the census reports
more than 10 days. Close out the medical records after 10 days. Under this section, all
disclosures of PHI to commanders will be tracked in accordance with AFI 41-200. (T-0).
4.32.10. Discharging Patients through action by Medical Evaluation Board and Physical
Evaluation Board. See Section 4K and AFI 36-3212.
4.32.11. Retention of Enlisted or Officer Patients Beyond the Discharge Date. See AFI 36-
3208, Administrative Separation of Airmen.
4.32.12. Discharging Persons Refusing Professional Care. See Section 4K. Notations are
placed in the health record documenting the refusal and explaining the risks of refusal that
were provided to the patient. Beneficiaries are encouraged to sign the notation.
AFMAN41-210 10 SEPTEMBER 2019 75
4.33. Convalescent Leave. Initiate convalescent leave for military patients in accordance with
AFI 36-3003. Convalescent leave is not to be used as an alternative for placing a member in an
excused from duty status or when an individual could instead be returned to limited duty without
adversely affecting full recovery. (T-1).
4.33.1. MTF commanders or directors may recommend convalescent leave up to a total of 90
days for a single period of hospitalization. Convalescent leave over 30 days requires additional
medical review and consent with the exception of obstetrical leave. The MTF’s MAJCOM
command surgeon’s office must approve convalescent leave in excess of 90 days. (T-2).
4.33.2. (Added) Per AFI 36-3003, Military Leave Program, Maternity Convalescent Leave
is limited to a covered Service member birthparent after a qualifying birth event. It is limited
to 42 days of non-chargeable leave, unless additional Maternity Convalescent Leave is
specifically recommended, and must be taken prior to any caregiver leave (for a maximum of
84 days in conjunction with Primary Caregiver Leave). (T-1).
4.33.2.1. In cases where a baby is stillborn, the member suffers a miscarriage/termination,
or where the baby is given up for adoption immediately following birth, unit commanders
will grant convalescent leave, other than Maternity Convalescent Leave, up to 42 days,
based on the patient-specific time of gestational age of the fetus, as noted in Table 4.1,
RECOMMENDATIONS: Convalescent Leave after Perinatal Loss. (T-1).
4.33.2.2. (Added) Table 4.1 provides a guide regarding convalescent leave.
4.33.2.2.1. Provider convalescent leave recommendations shall also be guided by best
clinical judgment, however, they are recommended to be no less than the time periods
as listed in Table 4.1. (T-1).
Table 4.1. (Added) Recommendations: Convalescent Leave after Perinatal Loss
GESTATION
(WEEKS +
DAYS)
CONVALESCENT LEAVE
RECOMMENDATION
PROFILE
RECOMMENDATION
COMMENTS
First Trimester
Less than or
equal to twelve
weeks and zero
days (≤ 12+0)
7 days
60 days no Physical Fitness
Testing (PFT)
With or without
surgical intervention
Second
Trimester
Twelve weeks,
one day to
sixteen weeks,
zero days (12+1
– 16+0)
14 days
180 days no PFT testing
With or without
surgical intervention
76 AFMAN41-210 10 SEPTEMBER 2019
Second
Trimester
Sixteen weeks,
one day to
nineteen weeks,
six days (16+1 –
19+6)
21 days
180 days no PFT testing
In accordance with
DAFI 34-501 and the
commonly used
definition for ‘fetal
death’, if neonate is
>20+0 weeks
gestation OR has a
fetal weight of 350
grams or more,
mother should receive
42 days of
convalescent leave.
In cases of multiple
pregnancies (such as
twins or triplets), if
one fetus meets the
fetal weight of 350
grams or more,
mother should receive
42 days convalescent
leave).
Second
Trimester
Twenty weeks,
zero days to
twenty seven
weeks, six days
(20+0 – 27+6)
42 days
365 days no PFT testing
Intentionally left
blank
Third Trimester
Twenty eight
weeks, zero days
to term (28+0 –
term)
42 days
365 days no PFT testing
Intentionally left
blank
Baby born alive
at any gestation
42 days
Intentionally left blank
Qualifying birth event
– mother would

AFMAN41-210 10 SEPTEMBER 2019 77
receive Maternity
Convalescent Leave
4.33.3. Recommendations for convalescence are also used for outpatients (without related
inpatient episode) when the medical condition warrants it.
4.34. Reporting AD Soldiers, Sailors, and Marines Hospitalized in Civilian or Non-Military
Medical Facilities.
4.34.1. Upon notification of an AD Soldier, Sailor, or Marine hospitalized in a nearby or
regional civilian or non-military medical facility, the TRICARE Operations and Patient
Administration or Patient Administration Function at the nearest Air Force MTF shall obtain
the patient’s name, rank, unit name and location, and additional identifying data and notify the
nearest Army or Navy MTF, as appropriate, and notify the individual’s unit commander. (T-
3).
4.34.2. Contact the DHA-Great Lakes at 1-888-647-6676 when notified of an AD Soldier,
Sailor, or Marine hospitalized at a local or regional civilian or non-military medical facility.
The Air Force MTF will make every effort to contact the AD service member’s unit
commander. On occasion, the Air Force MTF nearest to the hospitalized Soldier, Sailor, or
Marine may be asked to assume temporary administrative support responsibility. In this event,
TRICARE Operations and Patient Administration personnel at the nearest Air Force MTF shall
initiate the necessary action to keep the designated parent service representative and member’s
unit commander informed of the patient’s status. (T-3).
4.34.3. Coast Guard, United States Public Health Service or foreign military personnel
admitted to civilian or non-military medical facilities are not admitted and/or tracked as
“Absent Sick” definition listed in paragraph 4.22 and are not entered into the current automated
inpatient admission system. Additionally, there is no need to contact the MAJCOM command
surgeon’s office, AFMOA/SGAT, or the Air Force Medical Operations Center at the Pentagon
unless the admitted Coast Guard, United States Public Service or foreign military member
meets the “prominent persons” definition listed in paragraph 4.25.
4.34.4. In any situation where the MTF receives information about any Uniformed Service
Member admitted to a local or regional civilian or non-military medical facility, it is imperative
that the MTF commander, director or designee notify the nearest appropriate sister service
MTF and/or member’s unit commander, first sergeant, or other appropriately appointed
commander’s designee, of the hospitalization.
4.34.5. Admissions and Dispositions Office will notify the base ground occupational office in
accident cases using AF Form 1488. (T-1).
4.34.6. All disclosures of PHI to commanders will be tracked in accordance with AFI 41-200.
(T-0).
78 AFMAN41-210 10 SEPTEMBER 2019
Section 4I—Casualty Reporting Program Administration
4.35. Reporting Patients in Casualty Status.
4.35.1. This section describes patients and MTF reporting procedures for patients placed in a
casualty status in accordance with AFI 36-3002. Categories of patients requiring special
casualty reports are as follows:
4.35.1.1. Very Seriously Ill Patients. A Very Seriously Ill patient requires medical
attention and medical authority declares it more likely than not that death will occur within
72 hours.
4.35.1.2. Seriously Ill Patients. A Seriously Ill patient requires medical attention, medical
authority declares that death is possible, but not likely within 72 hours, and/or the severity
is such that it is permanent and life-altering.
4.35.1.3. Under this section, all disclosures of PHI to commanders will be documented in
accordance with AFI 41-200. Disclosure of PHI associated with the Seriously Ill-Very
Seriously Ill status of Non-AD patients to external MTF agencies (including, but not
limited to, the installation command post or Casualty Affairs office) is authorized only after
obtaining the patient's authorization or as required by law. In situations where the patient
is incapacitated or otherwise unable to agree or object to the disclosure, the MTF may, in
the exercise of professional judgment, make such notification in accordance with AFI 41-
200. All disclosures of PHI must be properly documented in the PHI Management Tool
or AFMS approved disclosure accounting tool. (T-0).
4.36. Assigning Responsibility.
4.36.1. The patient’s attending healthcare provider classifies a patient as Very Seriously Ill or
Seriously Ill and records an entry on the AF Form 3066, Doctor’s Orders, 3066-1, Doctor’s
Orders, or in Essentris. The provider is also responsible for completing the clinical
condition/status portions of the AF Form 570, Notification of Patient’s Medical Status, and
signing and applying signature stamp where required. Additionally, MTF Patient
Administration staff or designated Casualty Affairs Liaison may be required (depending on
local installation Casualty Affairs Office reporting rules) to complete an additional local form
to secure emergency government sponsored travel for an AD patient's immediate family
member(s). The MTF Casualty Affairs Liaison is responsible for submitting all MTF Casualty
reporting forms/documents/information to the installation Casualty Affairs or Casualty
Assistance Representative. At inpatient MTFs, the Casualty Affairs Liaison may be the
Admissions and Dispositions Office supervisor, one or more members of the Admissions and
Dispositions Office staff, and/or the on-call administrative NCO or Officer of the Day. At
outpatient MTFs, the Casualty Affairs Liaison may be the NCOIC, Patient Administration.
4.36.1.1. Preparation of AF Form 570.
4.36.1.1.1. Complete sections I, II, and, III when the report is prepared. Complete
section IV when reporting Seriously Ill and Very Seriously Ill patients. If the patient
is an organ donor, check the appropriate block and indicate organ to be donated. The
Casualty Affairs Liaison will complete section V. Section VI may be used to continue
entries from other sections, provide additional information, or request administrative
action.
AFMAN41-210 10 SEPTEMBER 2019 79
4.36.1.1.2. Upon receiving the AF Form 570, the Casualty Affairs Liaison completes
section V and immediately notifies the installation commander via the command post
and/or Casualty Assistance Representative in accordance with AFI 36-3002. The
Casualty Affairs Liaison provides enough information to make the first notification and
required progress reports on the patient’s status. If the patient has not authorized the
release of their information, ensure only the minimum necessary amount of information
is released and properly documented in the PHI Management Tool or AFMSA
approved disclosure accounting tool.
4.36.2. For AD personnel in a Seriously Ill, Very Seriously Ill, or Not Seriously Ill/Injured
casualty status, the attending physician, MTF commander or director, member’s commander,
or designated representative or AFPC/DPFC notifies the legally authorized representative in
accordance with AFI 36-3002.
4.36.3. If the status of a patient previously reported as Seriously Ill or Very Seriously Ill
changes the attending physician or dentist prepares an AF Form 570.
4.36.4. Regardless of the patient category, document all notifications for Seriously Ill and
Very Seriously Ill status in the appropriate casualty status remarks module/section in the CHCS
or other automated inpatient monitoring and documentation system. The patient must be
admitted and an active inpatient register number must exist before casualty status changes can
be made. (T-1). Document the release of information (for all patient categories) in the PHI
Management Tool or AFMS approved disclosure accounting tool. (T-2).
4.36.5. Absent Sick Patients: The Chief of Medical Staff, designee, or other appropriate
medical authority at the MTF assigned to monitor the civilian medical facility admission,
should contact the member’s attending physician and obtain enough medical information to
determine appropriate Seriously Ill or Very Seriously Ill status (if warranted). If such a
condition exists, an AF Form 570 must be completed by the physician and forwarded to the
office responsible for coordinating with the Casualty Assistance Representative and member’s
unit commander or installation command post. (T-3). If the patient has not authorized the
release of their information, ensure only the minimum necessary amount of information is
released and properly documented in the PHI Management Tool or AFMS approved disclosure
accounting tool. (T-2).
4.37. Requesting and Arranging Travel for Legally Authorized Representative under the
Emergency Family Member Travel Program.
4.37.1. In situations where an AD or RC service member patient in a on duty and/or in-line of
duty status has been placed on the inpatient Seriously Ill or Very Seriously Ill roster, the
attending physician must provide written recommendation to the MTF commander or director
that indicates the presence of the designated travelers is considered beneficial to the patient’s
recovery or when the member’s designated travelers' presence is warranted given the patient’s
critical or terminal prognosis. (T-3). If the MTF commander or director approves the request
(in writing), the Casualty Affairs Liaison or the administrative officer or noncommissioned
officer of the day must immediately contact the installation Casualty Assistance
Representative. (T-3). The Casualty Assistance Representative is then responsible for
coordinating the MTF commander’s or director’s recommendation/approval for Emergency
Family Member Travel Program with Air Force Personnel Center Casualty Affairs officials.
Air Force Personnel Center Casualty Affairs Program management officials are responsible
80 AFMAN41-210 10 SEPTEMBER 2019
for arranging military or commercial transportation arrangements (including commercial
airline travel) for no more than three designated travelers provided all the required legally
authorized representative information is obtainable. A comprehensive explanation of the entire
Emergency Family Member Travel Program is available in AFI 36-3002.
4.37.2. The MTF commander or director or designee must concur and approve the attending
physician’s request on Emergency Family Member Travel Program Request Memorandum
prior to Air Force Personnel Center Casualty Affairs Program securing emergency designated
traveler travel arrangements. (T-3). Prior to approving the Emergency Family Member Travel
Program Request Memorandum, the MTF commander or director or designee must ensure
there are no more than a total of three designated travelers between the Emergency Family
Member Travel Program and Non-Medical Attendant Program. (T-2).
4.37.3. Final emergency designated traveler travel approval is not to be authorized at the MTF.
4.37.4. The Emergency Family Member Travel Program benefit does not apply to Service
academy cadets, high school, college, or university ROTC participants.
4.38. Preparing the AF Form 1403, Roster of Seriously Ill/Very Seriously Ill.
4.38.1. The Casualty Affairs Liaison prepares the AF Form 1403, just after midnight each day
to document the preceding 24-hour casualty status activity period. Negative activity rosters
are not required. Typically, this report is generated automatically or user requested from the
CHCS automated system. Distribute the report internally within the MTF in accordance with
local guidance. External MTF reporting should be limited to the installation Casualty Affairs
office and/or the installation Command Post (in case of Very Important Person reporting).
Report initial Seriously Ill/Very Seriously Ill placement status and again if the status changes
or is removed.
4.38.1.1. Reporting Seriously Ill and Very Seriously Ill status PHI to external MTF
agencies (including, but not limited to, the installation command post or casualty affairs
office) regarding non- AD service member, is generally authorized only after obtaining the
patient’s authorization or exercising professional judgment in the disclosure of relevant
information in emergency situations.
4.38.2. Providing Follow-up Information. The Casualty Affairs Liaison provides the
installation commander and Casualty Assistance Representative with information received
from the patient’s healthcare provider for follow-up action in accordance with AFI 36-3002.
4.38.3. Removing Patients from the Roster.
4.38.3.1. When the attending healthcare provider determines that the patient can be
removed from AF Form 1403, prepare AF Form 570 and send it to the Casualty Affairs
Liaison.
4.38.3.2. The Casualty Affairs Liaison will notify the installation commander and
Casualty Assistance Representative once the patient is removed from the roster so that
action can be taken in accordance with AFI 36-3002, Casualty Services. Notify interested
persons or agencies, as defined by local guidance, quickly and complete Section V of AF
Form 570. File AF Form 570 in the patient’s suspense file. Annotate the remarks section
of the work copy of the AF Form 1403 to indicate the time of removal.
AFMAN41-210 10 SEPTEMBER 2019 81
4.39. Responsibility for Preparing Death Cases. As described in the following paragraphs, the
individual who is responsible for preparing death cases varies depending on the status of the
patient.
4.39.1. Death of a person while being attended outside the MTF: The attending Air Force
medical officer.
4.39.2. Death of a person in an Air Force-owned or leased aircraft: The MTF serving the base
that investigated the accident.
4.39.3. Death of other Air Force personnel who are not patients in a MTF at time of death:
The MTF serving the base that investigated the circumstances of death.
4.39.4. Death of a non-military person on an Air Force base: The MTF serving the base.
4.39.5. Death of a person being staged through an Enroute Patient Staging flight: The MTF
supporting the Enroute Patient Staging Flight.
4.39.6. Death of a person while in transit and in inpatient status: The MTF receiving the
remains. Note: Treat as transfer-in patients those who die while in transit (either while in flight
or in an ambulance between facilities) or while being staged through an Enroute Patient
Staging Flight.
4.39.7. Notwithstanding any other international, federal, state, or county law, or any other
DoD or Air Force Issuance, MTF providers, usually the member’s Primary Care Manager or
specialist, may be asked to sign the death certificates for retired military members or family
members who have died in their off-base homes of natural causes. Check with the wing or
base mortuary affairs office, local county sheriff’s office, or county coroner before preparing
the death certificate or authorizing or obtaining a MTF provider’s signature. Providers should
not document or certify a cause of death unless, based on their knowledge of the patient and
the circumstances of death, they are able to determine the cause of death to a reasonable degree
of medical certainty. Consult with the servicing legal office with any questions or concerns.
4.40. Policies Regarding Deaths.
4.40.1. See AFI 34-501, Mortuary Affairs Program, for instructions on preparing, inspecting
and shipping remains and completing related forms and reports.
4.40.2. A healthcare provider verifies all deaths occurring at an Air Force MTF and on an Air
Force installation.
4.40.3. If a member of the Uniformed Services on AD dies outside the limits of an Air Force
installation, do not remove the body without permission of civil authorities or local coroner.
4.40.3.1. The installation commander consults with the Armed Forces Medical Examiner
System when uniformed services personnel die within installation limits under exclusive
federal jurisdiction. When uniformed services personnel die beyond installation limits the
commander consults local civil authorities to identify procedures to follow.
4.40.3.2. Obtain a transient or burial permit from the proper civil authority before
removing a body from an Air Force base for shipment or burial.
4.40.3.3. Release remains to mortuary personnel within 24 hours after death unless
extenuating circumstances exist. Ensure that the death certificate is completed and signed
82 AFMAN41-210 10 SEPTEMBER 2019
by the responsible medical officer before releasing the remains. The mortuary
representative (military or civilian) taking custody of the remains signs a receipt for the
remains. Scan/upload the receipt in the deceased’s electronic health record.
4.40.4. Initial movement of remains is accomplished as follows:
4.40.4.1. Typically, a provider pronounces death at the site or at the MTF; prepares a death
certificate; and obtains a decision regarding an autopsy. If no autopsy is required, officials
from Mortuary Affairs are responsible for arranging transportation to move the body from
the site or from the MTF to the interment location.
4.40.4.1.1. If an autopsy is required, it must be authorized by the base commander or
by the Armed Forces Medical Examiner System. (T-2). If the local coroner has right
of first refusal (in accordance with applicable state law) to conduct the autopsy and the
local coroner defers to the Armed Forces, the following guidance takes effect (T-2):
4.40.4.1.1.1. For deaths occurring on a military installation, or under federal
jurisdiction, if the MTF on that installation has the capability and capacity to
perform the autopsy, then the MTF is responsible for performing the autopsy. If
the installation MTF does not have the capability or capacity to perform the autopsy
then the installation Mortuary Affairs office is responsible for either arranging
transportation of the body to another MTF where autopsy capabilities exist or
arranging a postmortem examination with a contracted civilian pathologist.
4.40.4.1.1.2. If the death of an Air Force AD service member occurs outside a
military installation, the nearest Air Force installation Mortuary Affairs office is
responsible for arranging transportation of the body from the death site or local
coroner’s office back to the closest MTF with histopathology-autopsy capabilities
or to a contracted civilian pathologist in accordance with local and Air Force
Mortuary Affairs policy. In accordance with AFMAN 65-605V1_AFGM2018-01,
Budget Guidance and Technical Procedures autopsies performed by civilian
pathologists, not employed by the Air Force, are funded using “O&M funds of the
organization to which the deceased was assigned.”
4.40.4.1.2. If an autopsy is required and the local coroner is authorized right of first
refusal to conduct the autopsy and the coroner decides to conduct the autopsy
themselves, officials from Mortuary Affairs are responsible for arranging
transportation to move the body to the coroner and then to interment location. Refer to
AFI 34-501 for more information regarding available postmortem Mortuary Affairs
responsibilities and services.
4.40.4.2. Local civil authorities, namely the local coroner, exercise control over the
movement of remains in the event of an off-installation death. Once the remains of an AD
member are released from the civil authorities, determine if an autopsy will be performed.
If yes, medical personnel provide or arrange transport of the remains to the MTF. If an
autopsy is not required, mortuary services transports the remains to the contract funeral
home or government mortuary. Note: In the event of a military aircraft accident, an
autopsy is usually required and will be funded with Defense Health Program money
regardless of who performs the examination.
AFMAN41-210 10 SEPTEMBER 2019 83
4.40.4.2.1. In the case of a death in a foreign country, refer to any applicable treaty,
Status of Forces Agreement or other international agreement to determine authorization
for autopsy. Reference DoDI 5154.30, Armed Forces Medical Examiner System
(AFMES) Operations.
4.40.4.2.2. In a disaster or multiple death situation, the mortuary officer calls the motor
pool for transportation to move the remains during search and recovery operations.
Remains are placed in body bags for movement.
4.40.5. When a patient dies, notify the Casualty Affairs Liaison or their representative
immediately.
4.40.6. Collect and inventory all personal property of the deceased in the presence of a witness
as soon as possible following the death of any patient. Send personal effects of a military
patient to the summary court officer. Send personal effects of civilians to an executor or
administrator, or (if none appointed) to the nearest legally authorized representative. The
executor, administrator or nearest legally authorized representative, as appropriate, signs the
inventory as a receipt for effects. Scan/upload the receipt in the patient’s electronic health
record.
4.40.7. Certificate of Death. Usually the provider pronouncing death, or other authorized
personnel, prepares a death certificate and sends it to the proper authorities according to state
requirements. However, the death certificate must be signed by a physician with knowledge
of the primary and contributory cause(s) of death. (T-1). This may be the pronouncing
physician, the deceased’s primary physician, or another member of the medical staff with that
knowledge. Scan or upload one copy of the certificate in the deceased patient’s electronic
health record or extended ambulatory record. In overseas locations, prepare DD Form 2064,
Certificate of Death (Overseas), per AFI 34-501.
4.40.8. Reporting Deaths. The MTF commander or director reports deaths as required by AFI
36-3002 when a person dies at an Air Force MTF or enroute to the MTF.
4.40.9. Reporting Stillbirths. Prepare a death certificate and file it as required by state and
civil law. File one copy of the fetal death certificate with the mother’s inpatient record. In the
case of an abortion, send the surgical specimen to the laboratory the same as for other surgical
specimens. Note: Even when not required by state law, a fetal death certificate may be issued
if the legally authorized representative requests the coroner or medical examiner to do so.
4.40.10. Comply with AFI 34-501 when deceased, uniformed services personnel cannot be
identified by local means. Utilize the resources of the Armed Forces Medical Examiner
System to the maximum extent possible to support the identification of remains.
4.41. Performing Postmortem (Autopsy) - Non-Forensic Cases.
4.41.1. Perform a hospital or non-forensic postmortem only with the consent of the legally
authorized representative, person(s) having a right of burial, or at the request of the local
coroner or medical examiner (except in the circumstances described in paragraph 4.40.4). Scan
or upload the authorization to perform a postmortem examination in the deceased’s electronic
health record.
4.41.2. Under normal circumstances, complete the postmortem within 24 hours after the
remains are received, appropriate records are available and authorization has been granted.
84 AFMAN41-210 10 SEPTEMBER 2019
4.41.3. Record the postmortem on SF 503, Medical Record-Autopsy Protocol, except those
performed under AFI 91-204. Scan and upload the original copy in the electronic health record
of the deceased. Maintain a completed copy of the certificate in the clinical laboratory.
4.41.4. A death, military or civilian, is a medical examiner case subject to forensic autopsy
when it meets the criteria listed under DoDI 5154.30. These cases do not require consent from
the legally authorized representative. If the death meets any one of the criteria listed in DoDI
5154.30, it must be referred to the Armed Forces Medical Examiner System. (T-0). The Armed
Forces Medical Examiner System may be contacted 24 hours a day, seven days a week at
commercial 302-346-8648. Reference DoDI 5154.30.
4.41.5. Authorization for Postmortem on United States Uniformed Services Personnel. The
installation commander or Armed Forces Medical Examiner is the approving authority for the
postmortem examinations in areas exclusive to Federal jurisdiction and in other areas when the
civil authority has released jurisdiction to the Uniformed Services. In areas outside the United
States and its Territories, existing Status of Forces Agreements apply. When the host
government relinquishes its authority, the Armed Forces Medical Examiner or installation
commander authorizes the postmortem. This approving authority may be delegated to the
MTF commander or director, but must be written and always current. (T-2).
4.41.6. Performing a Postmortem Examination on a Civilian.
4.41.6.1. Obtain the written, signed permission of the nearest legally authorized
representative, or an order by an appropriate civil or military authority if the death occurred
in unusual or suspicious circumstances. Develop procedures incorporating the
requirements of this instruction, relevant laws, existing legal agreements and other
requirements of local authorities.
4.41.6.2. For postmortem purposes, treat the remains of members of the National Guard,
Reserve Officers Training Corps and other RCs not on AD for training, as civilians.
4.41.6.3. When consent of the legally authorized representative is required, check to verify
notification and obtain the required consent on SF 523, Medical Record-Authorization for
Autopsy.
4.41.6.4. After deliverance of casualty notice to the family or legally authorized
representative and confirmation of its receipt, the MTF commander or director sends a
condolence letter to the family or legally authorized representative and requests permission
for a postmortem. The consent is scanned/uploaded in the patient’s electronic health
record.
4.41.6.5. At overseas installations, request the family or legally authorized representative
send the reply to the request for postmortem consent to AFMOA/Chief of Medical Staff.
Upon receipt of reply, AFMOA/Chief of Medical Staff will send a priority wire through
military message channels advising of the decision and then send the original message by
mail to the MTF for scanning/uploading into the patient’s electronic health record. (T-2).
4.41.7. Performing a Postmortem Examination on Foreign Military Personnel. When
performing a postmortem examination on foreign military personnel, obtain permission from
the military attaché of the foreign embassy. Include this request for permission in the casualty
report required by AFI 36-3002.
AFMAN41-210 10 SEPTEMBER 2019 85
4.41.8. Organ Disposal Following Postmortem. Return all organs and tissues removed during
postmortem to the body, except those organs, tissues and tissue fluids essential to diagnose the
cause of death or intended for studies authorized by the family or legally authorized
representative or required by law (see DoDI 6465.03, Anatomic Gifts and Tissue Donation).
4.42. Disposition of Outpatient Records on Deceased AD Personnel. See AFI 36-2608,
Military Personnel Records System and AFI 36-3002 for guidance on the disposition of the
outpatient record when an AD member of the United States Armed Services expires.
4.43. Deceased Patient Kit.
4.43.1. Local or state law may require the local medical examiner or coroner to respond for
each fatality that occurs on a military installation.
4.43.2. The response may include managing, reviewing or pronouncing death in these cases.
Sometimes these responsibilities are deferred to the installation MTF. Such deferrals are more
likely when no suspicious circumstances exist that require an investigation by the local medical
examiner or coroner. These deferrals are also more likely when the MTF has histopathology
or postmortem examination capability.
4.43.3. When practical and only when approved by the appropriate installation Plans,
Programs, and Operations officials, the MTF may enter into a support agreement with the local
medical examiner or coroner and the installation Mortuary Affairs office. Any agreement
should identify specific forms and instructions necessary to process a deceased body.
4.43.4. To adequately prepare for any contingency, each non-bedded Air Force MTF is
required to compile and maintain at least five pre-positioned death processing packages. Each
package will contain all of the forms and documents (described below).
4.43.5. When the MTF is required or authorized to officially respond and process a human
being’s death occurring on a military installation, each package will be used to document the
fatality whether the death occurred in the MTF or elsewhere on the military installation.
4.43.6. Inpatient MTFs will maintain a minimum of ten packages. The packages should be
kept in a central location such as the TRICARE Operations and Patient Administration Flight,
Admissions and Dispositions Office, or the emergency department. Each package shall
contain, at a minimum, the following forms. (T-1).
4.43.6.1. SF Form 523.
4.43.6.2. AF Form 146, Death Tag.
4.43.6.3. AF Form 570.
4.43.6.4. Release of Remains.
4.43.6.5. Request for Postmortem Examination.
4.43.6.6. AF Form 1122, Personal Property and Personal Effects Inventory.
4.43.6.7. Fax Notification.
4.43.6.8. Death Certificate Worksheet.
4.43.6.9. Death Certificate (Issued by state. If overseas use, DD Form 2064).
86 AFMAN41-210 10 SEPTEMBER 2019
Section 4J—Birth Registration Program Administration
4.44. Birth Registration in the CONUS.
4.44.1. A birth certificate will be prepared for each infant born in an Air Force MTF. Follow
State laws with regard to the forms used, format, and number of copies required.
4.44.2. Updating Personnel Records. Advise parents to report to the Military Personnel
Section to update personnel records and register the child in DEERS as part of birth
registration. This must be accomplished within 120 days or the member will receive a bill for
care. (T-3). When both the parents are AD, recommend that the same sponsor be identified in
CHCS and DEERS in order to eliminate confusion with the records.
4.44.3. Refer parents to the TRICARE customer service phone number for TRICARE options,
including TRICARE Prime enrollment.
4.45. Registering Births Overseas.
4.45.1. Overseas Air Force MTFs must cooperate with consular officers in registering births
of infants born to United States citizens in areas overseas. (T-0). Exceptions: Register births
in American Samoa, Guam, Puerto Rico, the Trust Territories, and the United States Virgin
Islands through the special offices of the Vital Statistics Division, Public Health Services,
United States Department of Department of Health and Human Services, or specified local
United States Government offices.
4.45.2. Completing Department of State Form DS-2029, Application for Consular Report of
Birth Abroad of a Citizen of the United States of America, available at
https://eforms.state.gov/Forms/ds2029.pdf. The form DS-2029 will be completed in four
copies. The (U.S. citizen) parent will sign each copy of the forms under oath before a military
officer qualified to administer oaths. (T-0).
4.45.3. If the mother is not a U.S. citizen, the U.S. citizen father must sign form DS-2029 if
he is available. (T-0). If the father is not available (or if there is any question about his
citizenship status), ask the parent(s) to get in touch with the U.S. Consular Office. (T-0).
4.45.4. Registration of Birth. Advise the parents that a fee for registering the child’s birth will
be charged. The U.S. Consular Officer issues them a copy of the Department of State Foreign
Form FS-240, Consular Report of Birth Abroad when the birth is reported, available at
https://travel.state.gov/content/travel/en/international-travel/while-abroad/birth-
abroad.html.
Section 4K—Medical Evaluation of Service Members for Continued Military Service
4.46. DELETED
4.46.1. DELETED
4.47. DELETED
4.48. DELETED
4.48.1. DELETED
4.48.1.1. DELETED
AFMAN41-210 10 SEPTEMBER 2019 87
4.48.1.2. DELETED
4.48.1.2.1. DELETED
4.48.1.2.2. DELETED
4.48.1.3. DELETED
4.48.1.4. DELETED
4.49. DELETED
4.49.1. DELETED
4.49.1.1. DELETED
4.49.1.2. DELETED
4.49.1.3. DELETED
4.49.1.4. DELETED
4.49.1.5. DELETED
4.49.2. DELETED
4.49.2.1. DELETED
4.49.2.2. DELETED
4.49.3. DELETED
4.49.3.1. DELETED
4.49.4. DELETED
4.49.4.1. DELETED
4.49.4.2. DELETED
4.49.4.3. DELETED
4.49.4.4. DELETED
4.49.4.5. DELETED
4.49.5. DELETED
4.49.5.1. DELETED
4.49.5.2. DELETED
4.49.5.3. DELETED
4.49.6. DELETED
4.50. DELETED
4.50.1. DELETED
4.50.1.1. DELETED
4.50.1.2. DELETED

88 AFMAN41-210 10 SEPTEMBER 2019
4.50.1.2.1. DELETED
4.50.1.2.2. DELETED
4.50.1.2.3. DELETED
4.50.1.2.4. DELETED
4.50.1.2.5. DELETED
4.50.1.3. DELETED
4.50.1.4. DELETED
4.50.1.5. DELETED
4.50.1.6. DELETED
4.50.1.6.1. DELETED
4.50.1.6.1.1. DELETED
4.50.1.6.1.2. DELETED
4.50.1.6.1.3. DELETED
4.50.1.6.1.4. DELETED
4.50.1.6.1.5. DELETED
4.50.1.6.1.6. DELETED
4.50.1.6.1.7. DELETED
4.50.1.6.2. DELETED
4.50.1.6.3. DELETED
4.50.2. DELETED
4.50.2.1. DELETED
4.50.2.2. DELETED
4.50.3. DELETED
4.50.4. DELETED
4.51. DELETED
4.51.1. DELETED
4.51.2. DELETED
4.51.3. DELETED
4.51.3.1. DELETED
4.51.3.2. DELETED

AFMAN41-210 10 SEPTEMBER 2019 89
4.52. DELETED
4.53. DELETED
4.54. DELETED
4.54.1. DELETED
4.54.2. DELETED
4.54.3. DELETED
4.54.4. DELETED
4.54.5. DELETED
4.55. DELETED
4.55.1. DELETED
4.55.2. DELETED
4.56. DELETED
4.56.1. DELETED
4.56.2. DELETED
4.56.3. DELETED
4.57. DELETED
4.57.1. DELETED
4.57.1.1. DELETED
4.57.1.2. DELETED
4.57.1.3. DELETED
4.57.1.4. DELETED
4.57.2. DELETED
4.57.3. DELETED
4.58. DELETED
4.58.1. DELETED
4.58.2. DELETED
4.58.3. DELETED
4.59. DELETED
4.59.1. DELETED
4.59.2. DELETED
4.59.3. DELETED
4.59.4. DELETED
90 AFMAN41-210 10 SEPTEMBER 2019
4.59.5. DELETED
4.60. DELETED
4.60.1. DELETED
4.60.2. DELETED
4.60.3. DELETED
4.60.4. DELETED
4.60.5. DELETED
4.60.6. DELETED
4.60.6.1. DELETED
4.60.6.2. DELETED
4.60.6.3. DELETED
4.60.7. DELETED
4.60.7.1. DELETED
4.60.8. DELETED
4.60.8.1. DELETED
4.60.8.1.1. DELETED
4.60.8.1.2. DELETED
4.60.8.1.3. DELETED
4.60.8.1.3.1. DELETED
4.60.8.1.3.2. DELETED
4.61. DELETED
4.61.1. DELETED
4.61.2. DELETED
4.61.3. DELETED
4.61.4. DELETED
4.61.5. DELETED
4.61.6. DELETED
4.62. DELETED
4.62.1. DELETED
4.62.2. DELETED
4.62.2.1. DELETED
AFMAN41-210 10 SEPTEMBER 2019 91
4.63. DELETED
4.63.1. DELETED
4.63.1.1. DELETED
4.64. DELETED
4.64.1. DELETED
4.64.2. DELETED
4.64.3. DELETED
4.64.4. DELETED
4.64.5. DELETED
4.64.5.1. DELETED
4.64.6. DELETED
4.65. DELETED
4.65.1. DELETED
4.65.2. DELETED
4.65.3. DELETED
4.65.4. DELETED
4.65.5. DELETED
4.65.6. DELETED
4.65.7. DELETED
4.65.7.1. DELETED
4.65.7.2. DELETED
4.65.8. DELETED
4.65.8.1. DELETED
4.65.8.2. DELETED
4.66. DELETED
4.66.1. DELETED
4.66.2. DELETED
4.66.2.1. DELETED
4.66.2.2. DELETED
4.66.2.3. DELETED
4.66.3. DELETED
4.66.4. DELETED

92 AFMAN41-210 10 SEPTEMBER 2019
4.66.5. DELETED
4.66.5.1. DELETED
4.66.5.2. DELETED
4.66.5.2.1. DELETED
4.66.5.2.1.1. DELETED
4.66.5.2.1.2. DELETED
4.66.5.2.1.3. DELETED
4.66.5.2.1.4. DELETED
4.66.5.2.1.5. DELETED
4.67. DELETED
4.67.1. DELETED
4.67.1.1. DELETED
4.67.1.1.1. DELETED
4.67.1.1.2. DELETED
4.67.1.1.3. DELETED
4.67.1.2. DELETED
4.67.2. DELETED
4.67.3. DELETED
4.68. DELETED
4.68.1. DELETED
4.68.1.1. DELETED
4.68.1.2. DELETED
4.68.1.2.1. DELETED
4.68.1.2.2. DELETED
4.68.2. DELETED
4.68.2.1. DELETED
4.68.2.2. DELETED
4.68.3. DELETED
4.68.3.1. DELETED
4.68.3.2. DELETED
4.68.3.3. DELETED
4.68.3.4. DELETED
AFMAN41-210 10 SEPTEMBER 2019 93
4.68.3.5. DELETED
4.68.4. DELETED
4.68.5. DELETED
4.68.6. DELETED
4.68.6.1. DELETED
4.68.6.2. DELETED
4.68.6.2.1. DELETED
4.68.6.3. DELETED
4.68.6.4. DELETED
4.68.7. DELETED
4.68.8. DELETED
4.68.9. DELETED
4.68.10. DELETED
4.68.11. DELETED
4.68.11.1. DELETED
4.68.11.2. DELETED
4.68.11.3. DELETED
4.68.11.4. DELETED
4.68.11.5. DELETED
4.68.11.6. DELETED
4.68.11.7. DELETED
4.68.11.8. DELETED
4.68.11.9. DELETED
4.68.11.10. DELETED
4.68.11.11. DELETED
4.68.11.12. DELETED
4.68.11.13. DELETED
4.68.11.14. DELETED
4.68.11.14.1. DELETED
4.68.11.14.2. DELETED
4.68.11.14.3. DELETED
4.68.11.14.4. DELETED

94 AFMAN41-210 10 SEPTEMBER 2019
4.68.11.14.5. DELETED
4.68.12. DELETED
4.69. DELETED
4.69.1. DELETED
4.69.2. DELETED
4.70. DELETED
4.70.1. DELETED
4.70.1.1. DELETED
4.70.1.2. DELETED
4.70.1.3. DELETED
4.70.2. DELETED
4.70.2.1. DELETED
4.70.2.2. DELETED
4.70.2.3. DELETED
4.70.2.4. DELETED
4.70.2.5. DELETED
4.71. DELETED
4.71.1. DELETED
4.71.2. DELETED
4.71.3. DELETED
4.71.3.1. DELETED
4.71.3.2. DELETED
4.71.3.3. DELETED
4.71.3.4. DELETED
4.71.4. DELETED
4.71.5. DELETED
4.71.5.1. DELETED
4.71.5.2. DELETED
4.71.5.3. DELETED
4.71.5.4. DELETED
4.72. DELETED
4.72.1. DELETED

AFMAN41-210 10 SEPTEMBER 2019 95
4.72.1.1. DELETED
4.72.1.2. DELETED
4.72.1.3. DELETED
4.72.1.4. DELETED
4.72.1.5. DELETED
4.72.1.6. DELETED
4.72.1.7. DELETED
4.72.1.8. DELETED
4.72.1.8.1. DELETED
4.72.1.8.2. DELETED
4.72.1.8.3. DELETED
4.72.1.8.4. DELETED
4.72.1.8.5. DELETED
4.72.1.8.5.1. DELETED
4.72.1.8.5.2. DELETED
4.72.1.8.6. DELETED
4.72.1.8.7. DELETED
4.72.1.8.8. DELETED
4.72.1.8.9. DELETED
4.73. DELETED
4.73.1. DELETED
4.73.2. DELETED
4.73.2.1. DELETED
4.73.2.1.1. DELETED
4.73.2.1.2. DELETED
4.73.2.1.3. DELETED
4.73.2.2. DELETED
4.73.2.3. DELETED
4.73.3. DELETED
4.73.3.1. DELETED
4.73.3.1.1. DELETED
4.73.3.1.2. DELETED

96 AFMAN41-210 10 SEPTEMBER 2019
4.73.3.1.3. DELETED
4.73.3.1.4. DELETED
4.73.3.2. DELETED
4.73.3.2.1. DELETED
4.73.3.3. DELETED
4.73.3.3.1. DELETED
4.73.3.3.2. DELETED
4.73.3.3.3. DELETED
4.73.3.3.4. DELETED
4.73.3.4. DELETED
4.73.3.4.1. DELETED
4.73.3.4.2. DELETED
4.73.3.4.3. DELETED
4.73.3.5. DELETED
4.73.3.5.1. DELETED
4.73.3.5.2. DELETED
4.73.3.5.2.1. DELETED
4.73.3.5.2.2. DELETED
4.73.4. DELETED
4.73.4.1. DELETED
4.73.4.1.1. DELETED
4.73.4.1.2. DELETED
4.73.4.1.3. DELETED
4.73.4.2. DELETED
4.73.4.2.1. DELETED
4.73.4.2.2. DELETED
4.73.4.2.3. DELETED
4.73.4.3. DELETED
4.73.4.3.1. DELETED
4.73.4.3.2. DELETED
4.73.4.3.3. DELETED
4.73.4.3.4. DELETED

AFMAN41-210 10 SEPTEMBER 2019 97
4.73.5. DELETED
Section 4L—Tumor Registry Program Administration
4.74. The Tumor Registry Program.
4.74.1. All Air Force MTFs will maintain a tumor registry of reportable diagnoses (a condition
of malignancy, precancerous lesion, benign central nervous system, brain tumor, or certain
hematopoietic conditions). (T-1). All Air Force MTFs that diagnose and/or treat patients with
reportable diagnoses must have a cancer program or cancer reporting process (for Reporting
MTFs) and will comply with the requirements of the American College of Surgeons’
Committee on Cancer (ACoS CoC). (T-1). The Cancer Program, in accordance with AFI 44-
110, The Cancer Surveillance Program, is based on the size and services of the facility. The
guidance in this chapter applies to Patient Administration only if the MTF is not authorized its
own histopathology department and is thus referred to as a Reporting MTF.
4.74.2. The Reporting MTF will perform a case finding function and report all new cancer
cases to its lead Regional Cancer Registry monthly. (T-1).
4.74.2.1. MTFs in multi-service markets may establish a memorandum of understanding
with Army or Navy MTFs and will be coordinated with the Air Force Cancer Registry
Consultant. (T-1).
4.74.2.2. Case finding may be performed by working a query of reportable diagnosis codes
as well as review/obtain available pathology, radiology, procedure/operative, and other
appropriate reports.
4.74.2.3. Ensures all new cancer cases, including TRICARE beneficiaries who are
diagnosed and/or treated in civilian facilities, are reported.
4.74.2.4. Cancer case information will be transmitted from the Reporting MTF to the
Regional Cancer Registry via encrypted e-mail reports or other HIPAA compliant methods.
(T-1).
4.74.3. The Tumor Registry is the principal database for evaluating the care of cancer patients
in the MTF. Patient Administration actions will include:
4.74.3.1. Use of Automated Central Tumor Registry to create and track cases. Requests
for Automated Central Tumor Registry access (limited to cancer registry personnel) are
made through the Air Force Cancer Registry Consultant.
4.74.3.2. Reporting MTFs retain the responsibility for maintaining follow-up information
for the lifetime of each cancer patient according to American College of Surgeons’
guidelines.
4.74.4. Data requests for research using Automated Central Tumor Registry reports are routed
through the Air Force Cancer Registry Consultant.
4.74.5. Release of Information to Non-Air Force Tumor Registries. Refer to Section 4A on
health information release procedures and requirements.
98 AFMAN41-210 10 SEPTEMBER 2019
Chapter 5
HEALTH RECORDS MANAGEMENT
Section 5A—General Program Administration
5.1. Managing Health Records.
5.1.1. Health records are the property of the United States Government, not the individual
beneficiary. This designated record set consists of electronic health records, outpatient records,
inpatient records, extended ambulatory records, fetal monitor strips, mental health records,
dental records, obstetrical and gynecological (pre and post-partum records), radiographic
images and film, and any other official record or media format (physical, analog, digital, video)
that provides a permanent record of a patient’s medical or dental care. Maintenance of records
at the MTF is required in accordance with this AFI. Refer to Army Regulation (AR) 40-66,
Medical Record Administration and Healthcare Documentation for additional information on
United States Army health records maintenance. Refer to Manual of the Medical Department
(MANMED), NAVMED P-117, Chapter 16, Health Records for additional information on
health records maintenance of Navy personnel. Inform beneficiaries of this requirement
through appropriate media. Initiate action to retrieve records maintained outside the MTF.
Regardless of the status of the individual, if the beneficiary is enrolled to the MTF, it is
mandatory that their health records are maintained in the MTF of enrollment. (T-0). Reference
DoDI 6040.45 and DHA Interim Procedures Memorandum 18-018, Physical Custody and
Control of the DoD Health Record.
5.1.2. Management of medical records includes quality and security assurance which is the
responsibility of administrative, clinical, and information technology staff.
5.1.3. MTF Commander or Director. The MTF commander or director will serve as Custodian
of Records and ensure that all health records are prepared, maintained, used, protected, and
controlled as required in accordance with this manual. (T-2).
5.1.3.1. Ensures that records and loose documents are retired or disposed of according to
the Air Force Records Information Management System (AFRIMS), Records Disposition
Schedule.
5.1.3.2. Must be knowledgeable concerning the control of health records and protected
health information (PHI), release of information from the records, and provider of care
documentation requirements. Commanders ensure that these important functions are
properly supported.
5.1.3.3. Manages custody and control, and security assurance of paper-based and
automated or electronic medical records.
5.1.4. Chief of Dental Services. The Chief of Dental Services serves as the custodian of the
dental records and is responsible to the MTF commander or director for dental record
management functions including custody, control and security assurance of paper-based and
automated or electronic dental records.
5.1.5. Healthcare Providers. Healthcare providers (physicians, dentists, and other authorized
healthcare providers) will include in appropriate health records, an accurate, legible, and

AFMAN41-210 10 SEPTEMBER 2019 99
complete description of all services rendered to patients. (T-2). This description must
adequately address current medical, administrative, and legal requirements. (T-1). Ensure that
proper identification information is entered on various forms and that records are returned to
the appropriate file as quickly as practical, but no later than 72 hours after treatment is rendered.
Note: Dental encounters should follow guidance as outlined in AFMAN 47-101, Managing
Dental Services.
5.1.6. Records created and maintained at a joint DoD/VA facility are shared by the two
organizations. Develop local policies to ensure that the needs of both organizations are met.
Records disposition instructions can be found at the AFRIMS System Records Disposition
Schedule website: https://www.my.af.mil/afrims/afrims/afrims/rims.cfm, the Medical
Record Tracking, Retirement and Retrieval User Guide is located at the AFMS Knowledge
Exchange.
5.2. Documenting Health Records. Health records are completed to meet the highest possible
standards of completeness, promptness, clinical pertinence, and standards of the Joint
Commission. The Joint Commission accredits and certifies nearly 21,000 health care
organizations and programs in the United States. Only authorized individuals make entries in the
original hard copy medical record using black or blue-black ink. No other annotations are
authorized. For care received outside of the Direct Care System ensure that the memorandum of
understanding and TRICARE contracts include a mechanism for obtaining documentation (i.e.,
summaries, operative reports, etc.) to be incorporated into the individual’s health record.
5.3. Correcting Health Records.
5.3.1. Patients have the right, under HIPAA and the Privacy Act, to access their health records
and request amendment if they think the documentation is in error. However, there is no
requirement for the MTF to agree to the proposed amendment. Furthermore, at no time should
any documentation be removed from the record (including automated record documentation
systems) unless it is determined that the documentation does not pertain to the patient in
question or any one of the following applies:
5.3.1.1. Records or Primary Care Manager support staff may remove an outdated DD
Form 2766C as long as the most current version of this form documents the latest
immunization history for the patient.
5.3.1.2. Outdated or expired DD Form 2992, Medical Recommendation for Flying or
Special Operational Duty and AF Form 1418, Recommendation for Flying or Special
Operational Duty – Dental with recommendations for special operations and/or flying
status in accordance with Attachment 8.
5.3.2. The request to amend any part of the health record (electronic or paper) must be made
in writing and be signed by the patient or authorized representative and filed in section 3 of AF
Form 2100A, Health Record - Outpatient or left side of AF Form 2100B, Health Record -
Dental. (T-1).
5.3.3. Refer to AFI 33-332 and AFI 41-200 for response timeline.
5.3.4. Denial of requests is allowed if any of the following conditions are met:
5.3.4.1. The PHI is not part of a designated record set available for inspection under
HIPAA or a system of records under the Privacy Act.
100 AFMAN41-210 10 SEPTEMBER 2019
5.3.4.2. The information requested to be amended is accurate and complete.
5.3.4.3. The MTF did not originally create the PHI requested for amendment (e.g., copies
of records from treatment at another MTF or civilian facility provider). However, if the
requestor can prove that the MTF that originally created the information no longer exists,
the MTF will handle the request as if it had created the information.
5.3.5. Upon receipt of a request for record amendment, forward it immediately to the
applicable provider for research.
5.3.6. If an error is identified and the responsible practitioner is available and recalls the
circumstances, for paper records:
5.3.6.1. Line through the incorrect data with one straight line. Do not erase, scratch out or
otherwise destroy the original data. Amendment of erroneous data should be done by the
initial provider or practitioner. If that is impractical, enter a brief explanation of why the
originating provider did not make the correction. Enter the correct data next to the lined
through data if space permits. Only privileged providers, authorized to document patient
care, will make corrections. Each supplemental or corrected entry must be dated, signed
and stamped. (T-1).
5.3.6.2. If there is not enough space on the record next to the incorrect data to enter the
correction, draw one straight line through the entry, initial, date and make a referral note
to where in the record the correction is documented. Then enter the correction
chronologically as indicated on the referral note. If the correction is not self-explanatory,
also enter the reason for the correction. Provider will sign, date, and stamp the new entry.
(T-1). If other practitioners are associated with the patient’s care and have a need-to-know
concerning the change, inform them of the correction. Major changes may require
documentation on a separate form (i.e., a new, blank form). Follow the same procedures
stated above and file the corrected information as near as possible to the document
containing the lined through information.
5.3.7. If an error is identified after a claim or lawsuit has been filed or after a substantial lapse,
then the provider with personal knowledge of the erroneous data must consult Air Force legal
counsel prior to correcting an erroneous entry in accordance with paragraphs 5.3.6.1 and
5.3.6.2 (T-0). The provider with personal knowledge of the erroneous data should immediately
notify all practitioners involved with the patient’s care.
5.3.8. Patients who believe their medical records contain erroneous entries or information
have several options to remedy perceived errors. Several instructions, such as AFI 33-332 and
AFI 36-2603, Air Force Board for Correction of Military Records (AFBCMR), allow patients
to seek relief when they believe their medical records should be amended and the MTF has
denied their requests. If a patient files such a request to the Air Force Board of Correction of
Military Records, SAF/MRBR, 550 C Street West, Suite 40, Randolph Air Force Base TX
78150-4742, the MTF will take no action until contacted by the board representatives. See
AFI 36-2603 Chapter 3 for application procedures and who may apply. If there are questions
regarding an amendment, contact the Staff Judge Advocate or area medical law consultant.
5.3.9. MTF should ensure careful adherence to the process of legal corrections of erroneous
data or information in a patient’s electronic health record. Legal corrections of erroneous data
may require Tier III Help Desk Support. Tier III Help Desk Support is a resource external to

AFMAN41-210 10 SEPTEMBER 2019 101
the MTF that handles advanced technical issues. Defense Health Agency (DHA) has
developed a specific process to request the legal correction of erroneous PHI in situations
where the incorrect information identifies another individual and the MTF is not able to make
the correction at the local level. This direction is located in the "Policy for Legal Correction
of AHLTA Erroneous Data or Information” and the process is contained in updated guidance
found on AFMOA Health Benefits Kx at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.3.10. All provider Social security numbers must be redacted and made unreadable prior to
issuing a copy of any health record (including, but not limited to, the outpatient medical, dental
treatment, inpatient, ambulatory procedure visit, and extended ambulatory record). (T-2).
Specifically, the MTF will make an initial copy of the record(s), then within the copy, sanitize
the entire Social security number, and then recopy the health record(s) before releasing a copy
to the requestor. This policy applies to copies for any purpose, to include individual’s
requesting copies of the individual’s own records for any reason. Original medical records
should remain intact. The original provider’s social security number must never be deleted
from the original health record. (T-0).
5.4. The Electronic Health Record.
5.4.1. Since 2006, the AFMS has used AHLTA; the Department of Defense’s (DoD) approved
electronic health record for the day-to-day outpatient care documentation processes. Until
completely transitioned to an electronic health record, the AFMS will use a hybrid record
consisting primarily of the electronic health record and include traditional paper-based records
and forms to meet unique operational mission requirements.
5.4.2. The following applications are the only approved electronic health record applications
authorized for use within the AFMS:
5.4.2.1. AHLTA and CHCS – outpatient medical and dental care which is stored in the
Central Data Repositories.
5.4.2.2. Essentris – inpatient medical care which is stored in the MTF Global Data
Repositories.
5.4.2.3. Composite Health Care System (CHCS) II-Theater (Armed Forces Health
Longitudinal Technology Application-Theater (AHLTA-T)).
5.4.2.4. Health Artifact and Image Management Solution (HAIMS) – enterprise-wide data
sharing capability for all types of artifacts and images.
5.4.2.5. Military Health System (MHS) GENESIS – new electronic health record for MHS
providing a single health and dental record for beneficiaries.
5.4.3. Medical Systems and Applications Not Considered Part of the Official Air Force
Medical System electronic health record:
5.4.3.1. Unless approved by competent authority, MTFs may not acquire, deploy or use
electronic health record systems other than those described in paragraph 5.4.2. This
prohibition applies to applications, systems or components of electronic health records
intended to temporarily or permanently document patient healthcare. Competent authority
resides with the Assistant Surgeon General, Health Care Operations; the Air Force Surgeon
102 AFMAN41-210 10 SEPTEMBER 2019
General (or deputy); or officials of the Office of the Assistant Secretary of Defense, Health
Affairs (ASD/HA).
5.4.3.2. Any non-AFMS or non-MHS standardized electronic system, application, or
clinical management tool is not considered part of the official Air Force electronic health
record. The documents contained within these tools are not considered part of the
electronic health record. To be approved for use, these tools must provide for the
permanent transferability of electronically generated or documented health information
into the following:
5.4.3.2.1. MHS Central Data Repositories,
5.4.3.2.2. Individual or regional MTF inpatient Global Data Repositories,
5.4.3.2.3. MHS or Air Force standardized and approved data repository or database,
5.4.3.2.4. Official VA single medical data repository. (T-1).
5.4.3.3. If the clinical information and/or PHI contained therein is meant to be permanently
stored or may possibly be relied upon in the future to support the delivery of healthcare,
then all PHI must be immediately transferred to an approved electronic health record or
standardized and AF/SG approved data repository or printed and scanned into HAIMS. (T-
1).
5.4.4. MTF commanders or directors may require that all or some of the medical records
maintained within the MTF be filed in hard copy format, regardless of electronic health record
capabilities, to fulfill mission requirements and to ensure comprehensive continuity of care.
MTF commanders or directors must be knowledgeable of health record management practices
as they apply to members assigned to the Sensitive Duties Programs. (T-2).
5.4.5. Service Members assigned to Sensitive Duties may be temporarily or permanently
decertified, suspended, or removed from their duty position(s). This determination may be
based on their medical, dental, mental health status, or the type of medications prescribed.
Sensitive duties programs include the Personnel Reliability Assurance Program, Presidential
Support Program, or other sensitive duty national security program(s). The current DoD
electronic health record cannot automatically provide for the mandatory notification and
receipt confirmation documentation. Notification must occur between the MTF competent
medical authority and individual unit commanders or installation operational assurance
officials. (T-1). This notification must include the service member’s health status, operational
capabilities/limitations, or fitness for duty following each patient encounter. (T-1). Following
proper notification and documentation (either electronic or written), all documents will be
uploaded into the service member’s outpatient medical electronic health record via HAIMS or
filed in the dental treatment record. (T-1).
5.4.6. The combination of the electronic health record and the paper record constitutes a
complete health record for a beneficiary and both record types need to be available for
inspection, review, and copying when required. Failure to maintain the paper medical record
as outlined in this instruction will result in a program deficiency and may violate HIPAA
safeguard requirements, Air Force Inspection Agency and Joint Commission standards.
5.4.7. Prior to a beneficiary’s Permanent Change of Station (PCS) reassignment, personal
geographic location move, MTF reassignment, or change to TRICARE enrollment location,
AFMAN41-210 10 SEPTEMBER 2019 103
all laboratory and radiology CHCS results, must be printed and filed into the patient’s health
record. (T-2). Since AHLTA is operational at all Active Duty (AD) MTFs, MTF health records
personnel are not required to print AHLTA patient encounter notes. However, if a beneficiary
is moving or has a PCS to a remote location without access to AHLTA, then all historical
AHLTA patient encounter notes must be printed and filed into the patient’s health record. (T-
1).
5.4.8. MTF personnel must establish procedures to provide beneficiaries copies of their
medical documentation from their electronic record when requested. (T-0). The format of the
documentation can be either paper or electronic; whichever is acceptable by the beneficiary.
If the documentation is provided in electronic format, MTF personnel must ensure their facility
is in compliance with the HIPAA, and any revisions to DoDM 6025.18 regarding modes of
transmission to the beneficiary. (T-0). Refer to AFI 41-200, paragraph 7.6 for additional
information.
5.4.9. Documenting MTF Healthcare in AHLTA (Minimum Operational Rules).
5.4.9.1. It is a prohibited activity to enter, upload, or transfer information, documents, files,
or images to the electronic health record that would not normally be available to patients.
Examples of these inappropriate entries are documents created or governed by quality
assurance, business rules, including peer review results or any Quality Assurance related
information; root cause analysis or other information not normally considered part of a
medical record. Information of this type will not be entered or uploaded into the Central
Data Repositories. (T2)
5.4.9.2. The operational processes listed herein were current at the time of this publication.
Advances in technology often outpace policy development; therefore this policy attempts
to outline rules of the current technology and to clarify operating parameters when
advances occur. This manual also includes actions for moving to an electronic
environment (1) the paper record is only retrieved by exception, (2) the filing of all paper
documents is eliminated, and, (3) when to “retire” or disposition paper records. These
actions include firm policy guidance. When certain milestones are reached, a specific set
of actions must occur.
5.4.9.3. The development of alternative plans independent of AF/SG and/or DoD
guidelines is not authorized without permission from AF/SG3. Alternative data capture
and documentation methods not originally identified or engineered for permanent storage
into the Central Data Repositories, are not authorized without approval from AF/SG3. Any
other use of technology contrary to guidance provided in this manual must be discontinued
until permission is granted for process continuation. (T-2). Forward all requests for
permission to depart from these operational rules to AFMSA/SG3S. Exceptions must
clearly state why the facility cannot change to an approved methodology. (T-1). Waiver
requests will be considered with a global or Service-wide standardization impact
perspective. (T-1).
5.4.9.4. Every Air Force MTF will use AHLTA or approved electronic health record to
document outpatient care. (T-1). All outpatient MTF entries (except emergency
department entries and dental treatment entries) must be entered into AHLTA. (T-1). Use
of structured text within approved electronic health records is highly encouraged. As other
automated methods of entry become available, these processes will likely be authorized
104 AFMAN41-210 10 SEPTEMBER 2019
following analysis by AF/SG3. Clinical data collection and document template use is
encouraged, using AHLTA capabilities to leverage documentation technique.
5.4.9.5. Printing AHLTA Information and Encounters. Printing and filing of patient
encounters stored in AHLTA is not required. Exception: Until further notice, all
information in AHLTA for non-service treatment records must be printed and filed prior
to disposition of the medical and dental record before physically mailing the record(s). (T-
1). Any automated clinical encounters, results, or notes that a provider feels a patient would
need or benefit from are authorized to be printed during a patient visit and handed to the
patient.
5.4.9.6. Electronic/Digital File Types and Files Size. Use only the following electronic
file types when capturing documents, files, or images into an AHLTA patient encounter
note: TXT, RTF, HTML, TIF, JPG, BMP, and DOC. Note: PDF files cannot be directly
uploaded into AHLTA; however, the information contained within a PDF file may be
copied and pasted into the “Add Note” using the Adobe Reader Snapshot tool. Imported
documents, files, or images will not exceed 500kb.
5.4.9.7. Placement of Scanned/Uploaded/Imported Documents, Files, and Images into
AHLTA.
5.4.9.7.1. Within a patient encounter note: A scanned document, file, or image may
be uploaded or imbedded into an AHLTA patient encounter note, provided the
document or image a) is directly related to the current patient encounter, b) will not
delay the coding of the patient encounter note, and c) can be uploaded into the patient
encounter note before the provider electronically signs the encounter. By signing the
encounter, the provider is acknowledging that the scanned/uploaded image or
document was acceptable for its intended purpose.
5.4.9.7.1.1. Appending a patient encounter note after the note is Closed/Signed. If
the document cannot be imbedded into the note before the provider electronically
signs, or if an image is captured, or scanned and uploaded in support of a previous
episode of care, the document or image should be appended to the desired note.
This action will generate an automatic notification to the provider or user who
created the original encounter note. The notification mechanism lets the original
creator know that someone has appended the member’s original patient encounter
note.
5.4.9.7.1.2. Appending a previously closed encounter with an uploaded image will
not change the original encounter information. The user adding the additional
image or document must also electronically sign the appended patient encounter
notes. (T-2). Appending a note is a permanent action and cannot be reversed.
Appended documentation is not searchable. Without prior knowledge that a
specific encounter note has been appended with an image, subsequent users may
have significant difficulty finding the appended image or they may not even know
of its existence.
5.4.9.7.2. Within clinical notes or as a stand-alone document. The practice of creating,
importing, or uploading scanned documents and images into AHLTA (not directly
imbedded within a patient encounter note), is not authorized without approval from

AFMAN41-210 10 SEPTEMBER 2019 105
AFMSA/SG3S. Managing the capability to create, import, or upload, stand-alone
scanned documents should be accomplished through HAIMS application.
5.4.9.7.3. Alternative methods to capture consults and referral results. AHLTA is not
to be used for volume storage of TRICARE network consultation report or referral
results storage without approval from AFMSA/SG3S. Identified below is an optional
method that allows temporary data collection, storage, authorized user viewing, and
data sharing of electronic copies of consultation reports and referral results received
from civilian medical providers, is.
5.4.9.7.3.1. MTFs are authorized to use a local, secure, shared computer server or
data storage device, to temporarily store consultation reports and referral results
received from civilian medical providers and specialists.
5.4.9.7.3.2. No later than 30 days following the date they create the electronic file,
staff must destroy the contents the file. Those contents include reports or referral
results received, scanned and imported into HAIMS from external MTF providers.
This rule assumes AFMSA/SG3S did not authorize an exception that allows
importing and/or uploading reports or results into HAIMS. (T-3).
5.4.9.7.3.3. There is no limitation (unless prescribed locally) to specific file size or
type (in the MTF shared computer server).
5.4.9.7.3.4. The MTF will create specific processes and business rules to a) ensure
the referring provider has access to the temporary electronically stored consultation
report or referral results and is aware that those electronic document(s), file(s), or
image(s), will only be available for viewing 30 days following the creation of the
electronic copy, and b) processes are in place to ensure the original consultation
report or referral result(s) is scanned into HAIMS. (T-3).
5.4.9.7.3.5. The official government e-mail transfer of consultation reports and
referral results is authorized as long as the message(s) is digitally signed and
encrypted. Access to shared MTF computer folders and files, containing PHI, must
be limited to users who can demonstrate a verifiable need for access. (T-0). Shared
computer folders and files must offer limited user access and password protection.
(T-0). Once a data-at-rest solution is deployed, PHI on shared drives must be
encrypted in accordance with security standards. (T-0).
5.4.9.8. Filing, Scanning and Uploading New Documents into HAIMS. All specialty care
and urgent primary care results, Emergency Room (ER) notes, discharge summary reports,
laboratory results, and radiology reports generated by providers and health care
organizations external to the MTF shall be scanned and imported into HAIMS within three
working days from receipt of results. (T-0). Referring providers/Primary Care Managers
will be notified of the new results/report via telephone consult or locally established
protocol. (T-0). Providers will have three business days from the date of receipt to review
the results. (T-0). Tips on importing/scanning and standard naming conventions can be
found in "The Management of Artifacts Scanned into HAIMS” located in Medical
Records/HAIMS folder on the AFMOA Health Benefits Kx page at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx. If a particular
type of paper document was regularly reviewed and signed (by hand) by a provider and
106 AFMAN41-210 10 SEPTEMBER 2019
filed into the paper record, the same document must still be signed (by hand) before
scanning into HAIMS. (T-2). See 5.4.7 and 5.7.1 for additional instructions on printing.
5.4.9.9. Scanning Entire Paper Health Records for Importing or Uploading into HAIMS
or other Secure Database.
5.4.9.9.1. The practice of scanning entire original paper health records for permanent
storage, importing, or uploading into HAIMS or similar DoD approved document
management system is unauthorized.
5.4.9.9.2. The only exception to bulk scanning is when the MTF is processing records
for service members on active Presidential Support Program or Personnel Reliability
Assurance Program status and the mission needs require rapid electronic access to the
service treatment record. The MTF is then authorized to bulk scan the record into
HAIMS and mail the hard copy in accordance with standard procedures.
5.4.9.9.3. In support of the Personnel Reliability Assurance Program Administrative
Qualification Central Cell process, all paper health treatment records will be requested
from the losing MTF. (T-3). Paper medical and dental records must be scanned into
HAIMS within seven calendar days. (T-3).
5.4.9.9.4. Refer to Attachment 5: PERSONNEL RELIABILITY ASSURANCE
PROGRAM ADMIN CERT HAIMS SCAN GUIDE, also located at:
https://kx2.afms.mil/kj/kx2/AFMOAHealthBenefits/Documents/Forms/ShowFol
ders.aspx?RootFolder=%2Fkj%2Fkx2%2FAFMOAHealthBenefits%2FDocume
nts%2FMedical%20Records%2FHAIMS&FolderCTID=0x0120000459EFB11C
132E479D3C03001C859239&View=%7BDB7164E0%2DEF02%2D4CE4%2DA
D97%2DF6B6ED3D1D7B%7D.
5.4.9.10. Scanning in Lieu of Paper Copies. The practice of scanning original health
records in lieu of copying (for MTFs that offer this option) is authorized, as long as:
5.4.9.10.1. Digital or electronic memory, compact or read-writable discs or storage
media are marked with the following statement, “This electronic storage media may
contain information covered under the Privacy Act, and/or HIPAA and its various
implementing regulations and must be protected in accordance with those provisions.”
(T-0).
5.4.9.10.2. Scanned documents, files, and images are not stored on any local computer
or MTF computer hard drive permanently. Scanned images and documents must be
deleted from all computer, copier, and scanner hard drives, or the computer drives or
memory devices within these machines. (T-0).
5.4.9.10.3. Digital or electronic memory, compact or read-writable discs or storage
media are not included with paper health records when forwarded to the National
Personnel Records Center or to the VA Records Management Center via approved Air
Force health records disposition intermediary.
5.4.9.11. Electronic signatures on forms and documents. Handwritten (“wet”) signatures
and initials are not required on printouts of electronic forms and documents created by the
following systems: CHCS, AHLTA, Armed Forces Health Longitudinal Technology
AFMAN41-210 10 SEPTEMBER 2019 107
Application –Theater (AHLTA-T), Essentris, and TRICARE Online. Electronic signatures
and initials in these systems are equivalent to full handwritten signatures and initials.
5.4.9.12. Retrieving Outpatient Medical Records by Exception. The MTF commander or
director, with the recommendations from the Executive Committee of the Medical Staff
and Health Records Committee may stop or suspend the practice of routinely retrieving
paper outpatient medical or dental treatment records for provider use. It should be done
only after careful consideration and on the recommendations of the Executive Committee
of the Medical Staff and Health Records Committee. Only after addressing the following
minimum questions should a requesting work center, clinic, specialty group, or Family
Health Element team submit a request for retrieval and delivery of paper records to the
Executive Committee of the Medical Staff function.
5.4.9.12.1. Have procedures been developed to validate the beneficiary’s
acknowledgement of the MHS Notice of Privacy Practices? See AFI 41-200 paragraph
3.2 for additional information and requirements.
5.4.9.12.2. If a provider needs a paper record on a specific patient during treatment,
how will the clinic ensure the patient’s health record can be quickly obtained and
delivered to the requesting provider?
5.4.9.12.3. How will the transition from the traditional health record pull all to pull by
exception MTF business rule affect the requesting work center’s record availability
rate?
5.4.9.12.4. With recommendation from the Health Records Management Committee,
medical record retrieval variations may exist within a MTF that require specific clinics
to retrieve/receive the paper outpatient or dental treatment record in addition to
accessing AHLTA. This requirement should be reviewed annually (at a minimum) in
order to ensure that resources required to manage records are used to the best advantage
of overall operations.
5.4.9.13. Historic scanning by exception. If a provider identifies any document from the
patient's paper medical or dental record the document must be uploaded into the electronic
health record. (T-3). Following scanning, the original source document, file, or image must
be re-filed into the paper health record. (T-3). Once an item is uploaded into HAIMS, the
provider should determine whether the data is specific to an episode of care. If it is, the
item should be uploaded to the current patient encounter note without delaying the coding
process. The provider should also determine if the item should be uploaded as an
independent, stand-alone document.
5.4.10. HAIMS. HAIMS is a MHS strategic project that enhances medical informatics through
seamless integration of medical digital images into the electronic health record. The objective
of HAIMS is to give healthcare providers global awareness and access to essential health
artifacts and images throughout the continuum of care from Theater to the Sustaining Base to
the VA. HAIMS provides a single enterprise-wide image sharing capability for all types of
artifacts and images, including radiographs, photographs, wave forms, audio files, video files
and scanned documents.
5.4.10.1. Using HAIMS in the MTF. HAIMS is required to be used at all MTFs.

108 AFMAN41-210 10 SEPTEMBER 2019
5.4.10.2. HAIMS Administration. The MTF (outpatient records, referral management
centers, clinical departments, etc.), must use HAIMS exclusively to scan loose paperwork.
(T-3).
5.4.10.2.1. MTF Staff will cease filing loose paperwork in the hard-copy medical
record and instead scan/upload them into HAIMS. (T-3).
5.4.10.2.2. Once a loose document has been scanned, validated and uploaded into
HAIMS, the document shall be destroyed. (T-3).
5.4.10.2.3. Lackland Air Force Base, Maxwell Air Force Base, and United States Air
Force Academy will bulk scan entry paperwork. New paper records will not be created.
Members will not hand-carry medical records. (T-3).
5.4.10.2.4. New paper records will not be created for new dependents. (T-3).
5.4.10.3. HAIMS Training. MTF clinical systems trainers and super users are responsible
for training any users.
5.4.10.4. HAIMS Guidance. Tips on how to use HAIMS can be located on the Kx at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.4.10.4.1. HAIMS provides functionality that can be used to support the clinical
practice of medicine by making artifacts and images that are not already part of the
electronic health record accessible to providers.
5.4.10.4.2. Business Process Standardization. The requirement of appending artifacts
and images, by copying and pasting Clear and Legible Reports into AHLTA clinical
notes, is no longer in effect at MTFs due to the full implementation of HAIMS. The
standardized business process will now include placing these items into HAIMS. In
multi-service market areas, there must be close coordination between the Services
regarding this policy so that all the providers in those market areas will be able to access
the Clear and Legible Reports for individual patients. (T-3).
5.4.10.4.3. Artifacts and Images scanned into HAIMS are called assets. These assets
are identified by a process known as metadata tagging. Metadata must be entered
before an asset is saved in HAIMS. (T-3). In The HAIMS Clinical User Guide Table
1, there is a brief explanation of nearly 20 data entry fields. (T-2).
5.4.10.4.3.1. Patient Name: Auto-populates when the patient is selected in the
search function. Provides Patient Name, Social security number, Date of Birth,
Gender, and family member prefix/sponsor social security number. Search
function is similar to that currently employed with AHLTA.
5.4.10.4.3.2. Author Name: Free text. The author is considered the person
responsible for the original artifact (e.g. ordering provider or network provider).
Enter the full name of the author of the asset in “last name, first name” format.
5.4.10.4.3.3. Document Type: (Dropdown Menu). Click on the down arrow,
scroll down to and highlight the appropriate document type (e.g. Encounter Note,
Consultation) and enter.
5.4.10.4.4. In addition to the above three required metadata tags, HAIMS users will
utilize the following fields as much as possible within the constraints of local resources:

AFMAN41-210 10 SEPTEMBER 2019 109
5.4.10.4.4.1. Mark as Sensitive: Click on Box. Mark the document as “Sensitive”
to restrict access to it. When an asset is restricted, unauthorized users will not have
access to the document. All authorized users have access after acknowledging they
will be viewing sensitive data and will be subject to auditing. If in doubt whether
a document would be marked sensitive, HAIMS users will consult with the provider
or the mental health clinic to determine sensitive information.
5.4.10.4.4.2. MHS Form Number: Auto-Populate Field. Type a few characters
contained in the form number (e.g. 600). Highlight the proper form number (e.g.
SF 600, Chronological Record of Medical Care) and enter. Use this field when
there is a known form number.
5.4.10.4.4.3. Procedure or Service: Auto-Populate Field. Type a few characters
contained in the procedure or service code number. Highlight the proper service
(e.g. Ultrasound) or code number (e.g. 335.20) and enter.
5.4.10.4.4.4. Installation/Facility: Auto-Populate Field. Enter the first letter(s) of
the installation/facility. A dropdown list will appear. Select the appropriate
installation/facility and enter.
5.4.10.4.4.5. Facility Name: Free Text Field. If the asset was received from a
place not listed in the “Installation/Facility” field, enter the name of the
organization where the asset originated.
5.4.10.4.4.6. Clinic: Dropdown Menu. Click on the down arrow, scroll down to
and highlight the proper clinic type (e.g. Cardiology) and enter.
5.4.10.4.4.7. Specialty: Auto-complete field. Type a few characters contained in
the specialty name (e.g. obstet). Highlight the proper service (e.g. Obstetrics) and
enter.
5.4.10.4.5. Enclosures. There are 8 enclosures found within the clinical use of HAIMS
Guidance. Each enclosure provides guidance for acquiring assets and using assets in
the HAIMS embedded mode within AHLTA. The enclosures are listed below and
examples can be found on the Kx at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.4.10.4.5.1. ACQUIRING ASSETS
5.4.10.4.5.2. SCANNING ARTIFACTS
5.4.10.4.5.3. ENTERING HAIMS METADATA
5.4.10.4.5.4. ACCESSING HAIMS VIA “EMBEDDED MODE”
5.4.10.4.5.5. ASSOCIATING ASSET TO AHLTA CURRENT ENCOUNTER
5.4.10.4.5.6. ASSOCIATING ASSET TO AHLTA PREVIOUS ENCOUNTER
5.4.10.4.5.7. ASSOCIATING ASSET TO AHLTA PROBLEM
5.4.10.4.5.8. ASSOCIATION REMOVAL
5.4.10.4.6. Guidance for Making the Service Treatment Record Available for Access
by the VA
110 AFMAN41-210 10 SEPTEMBER 2019
5.4.10.4.6.1. Air Force Service Treatment Record Processing Center: The AFMS
has opted to centralize the Service Treatment Record digitization, for
retiring/separating members, into HAIMS for access by the VA. The Service
Treatment Record disposition process can be found in this manual in paragraph 5.7.
5.4.10.4.6.2. The home MTF/Dental Treatment Facility is responsible for securing
the service member’s paper Service Treatment Record, collecting all unfiled, loose
and late flowing documents and artifacts at the MTF and filing them properly in the
Service Treatment Record. This does not include electronic encounter information
maintained in AHLTA. Any loose and late flowing documents will be scanned and
uploaded into HAIMS by the MTF.
5.5. Electronically-Generated Forms.
5.5.1. Use only the Air Force-approved forms package. Word processing packages are
directly forbidden because there is no method of locking the form so that it cannot be changed
by the user. See AFI 33-360. Most Air Force, Standard Forms (SF) and Optional Forms (OFs)
can be obtained from the Air Force e-Publishing website at: http://www.e-publishing.af.mil.
5.5.2. The only exception to the rule in 5.5.1 is permission to use the forms for which
AFMOA/SGAT has identified standard data elements. For these forms, the standard elements
are required but mirror imaging of the paper form is no longer required. (T-1). Additional data
elements that would change the meaning of the form cannot be added. Standard patient
information is required on these forms.
5.5.3. Include the following patient information blocks on both inpatient and outpatient forms:
Name (last, first, middle), patient family member prefix/last four digits of the sponsor’s social
security number, DoD Identification Number, Sex, Date of Birth, Rank/Grade,
Department/Service Where Records Maintained, and Relationship to Sponsor. Under Sponsor
Information, include Name (last, first, middle) and last four digits of the Sponsors Social
security number and/or DoD Identification Number. Under Facility Information, include
Name of MTF. Additionally, add blocks for Register Number and Ward Number on inpatient
forms.
5.5.4. To date, the forms for which standard data elements have been identified for the body
of the form are: SF 93, Report of Medical History, SF 505, Medical Record – History Parts 2
and 3, SF 506, Medical Record – Physical Examination, SF 509, Medical Record – Progress
Report, SF 526, Medical Record – Interstitial/Intercavitary Therapy, SF 551, Medical Record
– Serology, SF 558, Medical Record – Emergency Care and Treatment, SF 559, Medical
Record – Allergen Extract Prescription – New and Refill, SF 600, and OF 523B. Contact
AFMOA/SGAT for a list of the identified standard data elements for these and any subsequent
forms for which standard data elements have been identified.
5.5.5. OF 275, Medical Record Report, may be used in lieu of SFs, Air Force forms and DoD
forms, available at https://www.gsa.gov/forms-library/medical-record-report. OF 275, if
used, must indicate the form number and title of the form being replaced. (T-3). Information
entered on the form must include all of the same information as the form it represents. (T-2).
Scan and upload the OF 275 into the patient’s electronic health record. This form is not to be
used for the creation of local forms.
AFMAN41-210 10 SEPTEMBER 2019 111
5.5.6. If a MTF desires to create a local form in lieu of a form that already exists, a waiver
must be requested from AFMOA/SGAT. (T-1).
5.5.7. In an effort to reduce the unnecessary use of Social security numbers, DoD has begun
the use of alternative Personal Identifiers in place of the Social security number. The
alternative Personal Identifiers include the DoD Identification Number which uniquely
identifies individuals and the DoD Benefits Number that identifies individuals eligible to
receive DoD benefits such as commissary, exchange, and TRICARE benefits. The MHS, when
feasible, should limit the use and display of Social security numbers while migrating systems
and business processes to use the DoD Identification Number.
5.5.7.1. Local MTF forms must be reviewed for the necessity of Social security number
use. (T-3). MTFs are encouraged to use DoD Identification Numbers in place of Social
security numbers on local forms. To locate Social security numbers, MTFs may obtain the
Social security number from General Inquiry of Defense Enrollment Eligibility Reporting
System (DEERS) Web Application by cross matching the DoD Identification Number on
the Identification card or form with the DoD Identification Number in the system.
5.5.7.2. If the MTF determines the continued use of the Social security number on a local
form is necessary, the MTF must comply with the justification procedures set forth in AFI
33-332. (T-2).
5.6. Overprinting of Forms. An overprint is a form displaying identical entries in an
appropriately captioned area or fillable field existing on a form. Overprints do not change the
information collected on a form and are authorized in accordance with AFI 33-360. The specific
overprint must be a) approved by the local body responsible for the medical record review function,
b) recorded in the minutes of that body, and c) approved by the MTF commander or director. (T-
3). Follow instructions in AFI 33-360 concerning inclusion of the name of the organization
followed by “overprint” in the lower right margin of the form; for example, 579 Medical Group
(MDG) Overprint. The list of Air Force forms authorized for overprint follows:
5.6.1. AF Form 230, Request for Patient Transfer.
5.6.2. AF Form 250, Health Record Charge Out Request.
5.6.3. AF Form 560, Authorization and Treatment Statement.
5.6.4. AF Form 565, Record of Inpatient Treatment.
5.6.5. AF Form 570, Notification of Patient’s Medical Status.
5.6.6. AF Form 577, Patient’s Clearance Record.
5.6.7. AF Form 2700L, Health Record Year Grid.
5.6.8. AF Form 745, Sensitive Duties Program Record Identifier.
5.6.9. AF Form 1403, Roster of Seriously Ill/Very Seriously Ill.
5.6.10. AF Form 1942, Clinic Index.
5.6.11. AF Form 3066, Doctor’s Orders (multiple copy format).
5.6.12. AF Form 3066-1, Doctor’s Orders (cut sheet format).
112 AFMAN41-210 10 SEPTEMBER 2019
5.7. Service Treatment Record Disposition Instructions for Airman Retiring, Separating
and Transitioning to the RC. There are two categories of Health Records: The first category is
the Service Treatment Record - the outpatient medical record and dental treatment record for a
member of the United States Military. It is made up of the patient’s medical and dental encounters
incurred throughout the course of their military career. The Service Treatment Record begins upon
entry to AD (Military Entrance Processing Station/intake physical or commissioning physical) and
ends upon discharge, retirement, separation or death (if death occurred while on AD). The second
category is the Non-Service Treatment Record - outpatient medical records for patients in all other
categories (dependents, civilians, foreign military, retirees, etc.). The following sections contain
guidance regarding the proper procedures to transfer, disposition, and retire all types of heath
records to the appropriate location. Dependent, Non-NATO Foreign military, and Retiree Non-
Service Treatment Records are retired to the National Personnel Records Center using the Medical
Record Tracking application in CHCS. Federal Civilian Employee Non-Service Treatment
Records are provided to the local Civilian Personnel Office or retired to National Personnel
Records Center.
5.7.1. The Service Treatment Record on-time submission goals to meet the Under Secretary
of Defense Personnel and Readiness expectations are 95% on-time submission of Active
Component Service Treatment Records and 75% on-time submission of RC Service Treatment
Records.
5.7.1.1. The Service Treatment Record process mandated that all AD Air Force MTFs and
ARCs begin mailing Service Treatment Records for retiring and separating Airmen (with
a separation or retirement date effective 1 January 2009 and thereafter) to the Air Force
Service Treatment Record Processing Center instead of forwarding records to the Air Force
Personnel Center.
5.7.1.2. Service Treatment Records shall be sent to the Air Force Service Treatment
Record Processing Center at 3370 Nacogdoches Rd, Suite 116, San Antonio, TX 78217.
(T-1). The cell will continue to receive bulk shipments of paper Service Treatment Records
for retiring and separating Air Force Service Members. Upon receipt, the cell will digitize
the paper records into HAIMS. (T-1). The original paper Service Treatment Record will
then be dispositioned according to DoD and National Archives and Records Administration
guidance.
5.7.1.3. Total Force Applicability: This Service Treatment Record disposition policy
applies equally to the AD MTFs and the RCs. Although the language that follows in this
paragraph specifically mentions MTF responsibilities and expectations, the guidance also
applies to Air Force Reserve (AFR), Air National Guard (ANG) medical units, and
organizations responsible for the day-to-day maintenance and storage of ARC Service
Treatment Records. Air Force Service Treatment Record Processing Center is the only Air
Force agency authorized to forward AD and RC Service Treatment Records to the VA.
MTFs and RCs are not authorized to mail records directly to the VA. (T-0). Reference
DoDI 6040.45.
5.7.1.4. All MTF and Dental Treatment Facility records management personnel will apply
the following directions to their Service Treatment Record disposition plan. (T-0). MTF
records managers and supervisors must work closely with their Dental Treatment Facility
counterparts and local Military Personnel Section, Military Personnel Element, Military
AFMAN41-210 10 SEPTEMBER 2019 113
Personnel Squadron or Force Support Squadron officials to make this transition as smooth
as possible. (T-0). Reference DoDI 6040.45.
5.7.1.5. Incorporate the Service Treatment Record disposition instructions into all
standard MTF, Dental Treatment Facility, and RC Service Treatment Record disposition
instructions for retiring, separating, discharging, and transitioning members. Reference
DoDI 6040.45.
5.7.2. AFPC Retirement/Separation Notification Roster (also known as LOSS Roster).
5.7.2.1. In order to streamline the process and standardize LOSS Rosters acquisition
procedures, a Medical Records Management SharePoint website was created so MTF,
Dental Treatment Facility, and ARC records managers could easily obtain this time
sensitive information.
5.7.2.2. Personnel LOSS rosters include a listing of all projected retiring, separating,
transitioning, and discharging Air Force service members (AD and ARC), to include those
assigned to GSU. The rosters also identify Airmen who retired or separated in previous
months which the Air Force Service Treatment Record Processing Center has not received
a complete Service Treatment Record. The column with a header of “Record Required”
on each roster indicates the original component(s) which have still not been received by
the Air Force Service Treatment Record Processing Center. Note: These records will
continue to remain on the roster until the Air Force Service Treatment Record Processing
Center receives the records or a Non-Availability Letter.
5.7.2.3. Identified MTF, Dental Treatment Facility, and ARC personnel must obtain the
LOSS roster from the Medical Records Management SharePoint each month. (T-1). The
local Military Personnel Section will continue to provide support in the case of short-notice
changes and any other questions which might arise. As the LOSS rosters contain
Personally Identifiable Information, and the SharePoint site contains all rosters for all
facilities, access to the page is restricted to only those individuals who require access to
perform Service Treatment Record disposition duties.
5.7.2.4. Each MTF or ARC is authorized one primary and four alternate points of contact,
for a total of five (5). ARCs are authorized an additional two members in order to identify
the Senior Air Reserve Technician and the Medical Administrative Officer. It is
recommended that the primary point of contact should be the individual with direct
oversight of the records process (NCOIC, in most cases). (T-1). Alternates should be a
dental representative, flight commander or superintendent. Each member must be
designated in writing by the unit commander. (T-1). An example of an appointment letter
is available on the Medical Records Management SharePoint and the AFMOA Health
Benefits Kx page. As the rosters are in Excel format, they can be downloaded, saved and
distributed locally as the facility deems necessary. However, given the information on the
spreadsheet, access must be limited to only those with a need to know. (T-0). E-mail
messages containing Personally Identifiable Information must be digitally signed and
encrypted. (T-0).
5.7.2.4.1. The appointment letter must include the reason for request and must be
signed by the squadron commander. (T-1). Appointment letters can be
updated/resubmitted at any time; letters will be updated at least annually. (T-1).
114 AFMAN41-210 10 SEPTEMBER 2019
5.7.2.4.2. Address appointment letters to AFMOA/SGAT and scan/e-mail the
document to usaf.jbsa.afmoa.mbx.str-processing-center@mail.mil.
5.7.2.4.3. Once the appointment letter has been submitted and approved, the Air Force
Service Treatment Record Processing Center Managers will grant access to the Medical
Records Management SharePoint. (T-1).
5.7.2.5. At MTFs with decentralized medical record filing rooms, the TRICARE
Operations and Patient Administration office is responsible for distributing the LOSS
rosters to each record room.
5.7.2.6. Once the appointment letter has been submitted and approved, the Air Force
Service Treatment Record Processing Center Managers will grant access to the Medical
Records Management SharePoint. (T-1).
5.7.2.7. The LOSS rosters are located in the main folder "Medical Record Rosters”, and
then in the sub-folder “Medical Record Departure Rosters” for the applicable month. The
folders correspond with the month the roster was run.
5.7.2.8. Each roster on the SharePoint is listed separately by Personnel Accounting
Symbol (PAS) Code. A number of installations have RCs assigned/co-located with the
AD MTF; therefore, these bases will appear to be listed more than once. The first 2 digits
of the PAS Codes determine the applicability of the roster. Generally, AD PAS Codes are
two ALPHA characters, whereas RC PAS Codes are identified by an ALPHA Numeric
code. For instance, McConnell Air Force Base could appear three times: McConnell
(MK); McConnell (D6); and McConnell (R2). The AD MTF roster is identified by (MK),
the Guard roster is identified by (D6) and the Reserve unit is identified by (R2).
5.7.2.9. Some larger MTFs have more than one Military Personnel Section providing
services at their installation; therefore, MTFs and RCs also need to know the two-digit PAS
Code for each of those Military Personnel Section/GSU for which they provide
care/maintain records. A memorandum of understanding/memorandum of agreement is
required for each MTF or RC if co-located with another MTF/RC (regardless of Service
affiliation) to ensure correct Records Management procedures/policies are followed and
addressed.
5.7.2.10. PAS codes can be obtained from the AFPC secure web site at:
https://mypers.af.mil/app/login/redirect/home. After accessing the site, click “OK,”
then “PAS CODES.” The PAS codes are also located on the Medical Records Management
SharePoint in the Departure Rosters folder.
5.7.2.11. For questions regarding which roster to obtain, contact the local Force Support
Squadron, or the Reserve, Guard, or AFMOA Health Benefits regional representative for
assistance.
5.7.2.12. Facilities have a window of opportunity when records should be mailed to arrive
at the Air Force Service Treatment Record Processing Center. The LOSS roster contains
two columns for shipment dates for the Service Treatment Record to arrive at the Air Force
Service Treatment Record Processing Center, “no earlier than” and is due “no later than.”
The no earlier than date is the member’s date of retirement/separation; the no later than
date is 30 days after the member’s date of retirement/separation. Medical records
AFMAN41-210 10 SEPTEMBER 2019 115
personnel at all Air Force MTFs and ARCs must mail a retiring/separating member’s
Service Treatment Record to arrive at the Air Force Service Treatment Record Processing
Center no earlier than the Date of Retirement/Date of Separation and no later than 30 days
past the Date of Retirement/Date of Separation. (T-0). Reference DoDI 6040.45.
5.7.2.13. GSU: Service Treatment Records for retiring and separating Air Force service
members assigned to remote units or GSU must be maintained at the MTF serviced by the
Military Personnel Section to which the member is assigned. (T-3). If the Airman is
enrolled to a TRICARE network Primary Care Manager, civilian medical documents are
maintained at the network Primary Care Manager Office. If the individual appears on the
MTFs/Reserve Medical Units roster, that specific MTF/RC is responsible and will be held
accountable for its disposition. (T-1).
5.7.2.14. Outside Continental United States (OCONUS) Based Member
Retiring/Separating: Based on AFPC guidance, retiring/separating members assigned
OCONUS are directly retired/separated by the OCONUS Military Personnel Section;
members are no longer allowed to receive a PCS to CONUS for retirement/separation
processing. However, even if a retiring/separating member based at an OCONUS MTF
returns stateside just for the purpose of retiring/separating, the OCONUS MTF Service
Treatment Record LOSS roster normally reflects the member as retiring/separating. It is
the OCONUS MTF’s responsibility to ensure the Service Treatment Record is
appropriately dispositioned to the Air Force Service Treatment Record Processing Center.
5.7.2.15. ARC LOSS Rosters will be assessed and downloaded from the AFPC Medical
Records Management SharePoint. (T-1).
5.7.3. Retirement/Separation/Transition Orders.
5.7.3.1. AD Personnel Responsibilities:
5.7.3.1.1. Retiring/Separating Airmen are required to report to the central MTF health
records customer service location and the installation Dental Treatment Facility with
their retirement orders no later than five days prior to the member’s final out-processing
appointment. The member is required to provide four copies of their retirement orders
(or, in the case of separations, the AF Form 100, Request and Authorization for
Separation); two for the MTF and two for the Dental Treatment Facility records
departments.
5.7.3.1.2. Airmen transitioning from the AD to the RC are required to report to the
central MTF health records customer service location with their service transition
order, PCS order, or AD separation order no later than five days prior to the member’s
final out-processing appointment. The member is required to provide two copies of the
service transition order, PCS order, or AD separation order. (Specific rules regarding
the disposition or the transfer of Service Treatment Records for Airmen transitioning
from the Active to the RC are identified in paragraph 5.7.5.11.)
5.7.3.2. MTF/Dental Treatment Facility Responsibilities:
5.7.3.2.1. The MTF and Dental Treatment Facility will each place one copy of the
orders in the member’s outpatient medical and dental treatment records. (T-1). In the
outpatient medical record, the member’s orders will be placed in Section II. (T-1). In
116 AFMAN41-210 10 SEPTEMBER 2019
the dental treatment record, the member’s orders will be placed on the inside right-side
folder section. (T-1).
5.7.3.2.2. The second copy of the orders will be placed into a plastic AF Form 885-
887 series, Medical Record Charge-Out Guide and filed in place of the record. (T-0).
It is also recommended to include a reference to where the record is located (transitory
file) until the record is mailed. Reference DoDI 6040.45.
5.7.3.2.3. Missing Orders. MTFs and RCs should not delay processing Service
Treatment Records for transfer to the Air Force Service Treatment Record Processing
Center due to missing service member orders. If, after contacting the Military
Personnel Section or accessing the Virtual Military Personnel Section, a copy of the
orders cannot be obtained, the Service Treatment Record may be sent without the
orders. MTFs and RCs must verify or check with the military personnel section prior
to shipment to ensure the Airman did not re-enlist or extend the enlistment. (T-1).
5.7.3.2.4. AD Virtual Military Personnel Section Checklist Confirmation. Outpatient
medical and dental records managers and Force Health Management officials will work
together to ensure each outbound Airmen has fulfilled all of the MTF out-processing
responsibilities. (T-0). Reference DoDI 6040.45.
5.7.3.2.5. Checklist Operation. Multiple (at least two) staff members assigned to MTF
and Dental Treatment Facility records departments will be granted Virtual Military
Personnel Section Checklist access to ensure each departing service member is
informed of the requirement to provide the MTF and Dental Treatment Facility with
copies of the member’s orders at the time of MTF/Dental Treatment Facility out-
processing. (T-1). Access will also allow MTF records managers to obtain and print
individual retirement/separation orders when necessary. Once added to the process or
granted access to the Virtual Military Personnel Section system, records managers can
forecast the timeframe when separating and/or retiring Airmen will visit the MTF and
Dental Treatment Facility to out-process. (T-1). MTF and Dental Treatment Facility
records managers may also be able to add special notes to the Virtual out-processing
checklists to inform out-processing Airmen to obtain a copy of their Service Treatment
Record no earlier than 179 calendar days and no later than 30 days prior to the date of
their final separation or retirement date.
5.7.3.3. AFR Personnel. Each month, the servicing Reserve Military Personnel Section
will provide the servicing RMU a copy of the retirement/discharge/transition orders. (T-
1). Alternatively, the AF Form 1288, Application for Ready Reserve Assignment may be
provided. Orders are provided to the RMU for assigned Airmen serviced by the Military
Personnel Section, including GSU personnel, with a 60-day projected retirement,
discharge, or transition to inactive status date.
5.7.3.4. ANG Personnel. Guard members receive their retirement/discharge orders from
the Retirements/Separations department of the Military Personnel Section located at their
ANG Wing. These retirement/separation orders should be received at the monthly Unit
Training Assembly immediately preceding the final service obligation date.
5.7.4. Making Copies of Outpatient Medical and Dental Records.
5.7.4.1. For the AD Service Member:
AFMAN41-210 10 SEPTEMBER 2019 117
5.7.4.1.1. Separating and retiring Airmen may request one complete copy of their
Service Treatment Record no earlier than 179 calendar days and no later than 30
calendar days prior to the date of their final out-processing appointment. Only one
copy free of charge is authorized. The goal is to have one complete Service Treatment
Record copy ready for the separating or retiring Airman by the time of his final
MTF/Dental Treatment Facility out-processing appointment. The copy can be
provided as a hard-copy record or in electronic or digital media format, whichever the
member requests. Note: This copy is for the member’s personal use, not for the VA
as the VA requires the record in electronic format. Do not scan the medical or dental
record into HAIMS, as the Air Force Service Treatment Record Processing Center is
the only entity that has the authority to place complete records into HAIMS. Ensure
patient understands they are only authorized one complete copy free of charge. They
will not receive another copy (free of charge) if they give their copy to the VA.
5.7.4.1.2. Copy requests should be fulfilled no later than 30 calendar days from the
date of copy request receipt. Records managers must use all available resources within
their means to ensure separating and retiring Airmen understand the importance of
submitting their Service Treatment Record copy requests as early as possible. (T-3).
The volume of electronic patient encounter documents generated from MTF or Dental
Treatment Facility visits that fall within the 30-day cut-off copy request date through
the Airman’s MTF/Dental Treatment Facility out-processing date are usually not that
significant. These few documents should be reasonably easy to identify and print from
AHLTA or CHCS, on the spot, or copy from the paper outpatient medical or dental
records and added to the copy package or provided to the member at the time of out-
processing.
5.7.4.1.3. MTF records managers are expected to notify the Transition Assistance
Program (TAP) of the member’s right to one free copy of their record upon separation
or retirement. MTF records personnel will ensure local installation Transition
Assistance Program officials are aware that each AD Airman enrolled in Transition
Assistance Program class may receive a copy of their Service Treatment Record no
earlier than 179 calendar days, but not later than 30 calendar days prior to their final
retirement or separation date.
5.7.4.2. For the ARC Service Member:
5.7.4.2.1. Separating and discharging ARC service members may request one
complete copy of their Service Treatment Record no earlier than 179 calendar days and
no later than 90 calendar days prior to the date of their final out-processing
appointment. Only one free copy is authorized. The goal is to have one complete
Service Treatment Record copy ready for the retiring or discharging Airman by the
completion of the final medical unit out-processing appointment.
5.7.4.2.2. Copy requests from MTFs should be fulfilled no later than 30 days from the
date of copy request receipt. Requests for copies from ARCs will be fulfilled. (T-1).
ARCs are not regularly staffed as well as full-time AD MTFs. Opportunities to make
copies for retiring or discharging members may be diminished, sometimes limited to
only drill weekends. Ninety calendar days is a reasonable period of time to complete
the copy request. Records managers must use all available resources within their means
118 AFMAN41-210 10 SEPTEMBER 2019
to ensure ARC retiring and discharging Airmen understand to submit their Service
Treatment Record copy requests as early as possible. (T-3). The volume of electronic
patient encounter documents generated from MTF, Dental Treatment Facility or RC
visits that fall within the period from the 90-day cut-off copy request date through the
Airman’s MTF, Dental Treatment Facility or ARC out-processing date should not be
that significant. These few documents should be reasonably easy to identify and print
from AHLTA or CHCS on the spot, or copy from the paper outpatient medical or dental
records and added to the copy package or provided to the member at the time of out-
processing.
5.7.4.2.3. For those ARCs without AHLTA, CHCS, or HAIMS access, records
managers are required to contact the AD MTF to obtain copies of all AHLTA/CHCS
encounters, ancillary laboratory and radiology results. (T-1). Provide a copy of the
service member’s pharmacy prescription medication history only upon specific request.
5.7.4.2.4. Although the Transition Assistance Program may not be available for many
ARC Airmen, ARC unit commanders, first sergeants, personnel staff, and medics are
encouraged to inform retiring or discharging ARC Airmen of the necessity to obtain a
complete copy of their Service Treatment Record as soon as possible.
5.7.4.3. Service Treatment Record Composition.
5.7.4.3.1. The Service Treatment Record includes traditional paper outpatient medical
and dental documents stored in the outpatient medical and dental records as well as
ancillary laboratory and radiology reports stored and printed from CHCS, outpatient
patient encounter notes and any other PHI reports, data, or information stored and
printed from AHLTA. Copies of clinical narrative summaries and operation reports
from previous inpatient, ambulatory procedure visit, and/or Medical Evaluation Board
actions should already be filed in Part I or III of the member’s outpatient record.
However, MTF records managers or Release of Information staff will verify that any
narrative summaries and/or operation reports generated from past inpatient, ambulatory
procedure visit or Medical Evaluation Board actions completed at the same MTF
responsible for the Service Treatment Record disposition, are included in the paper
outpatient medical record. (T-1).
5.7.4.3.1.1. AHLTA Web Print. AHLTA Web Print is a feature in AHLTA that
allows a user to print or generate a PDF file of a patient’s entire electronic health
record, or specific sections thereof, with one command. The AHLTA Web Print
menu will appear as a link in the AHLTA folder tree. The user interface screen
permits configuration and setting of desired report options. These options allow
the user to customize the printed report by limiting the report to a specified date
range or clinical domains to be included in the report, and to even generate a mailing
page.
5.7.4.3.1.2. Given that AHLTA Web Print file comes complete with a Table of
Contents which specifies page numbers for each item, it is no longer logical to file
individual items in each applicable section of the record (i.e. SF600's in Section 2,
labs/rads in Section 4, etc.). As such, the entire printed copy of the electronic health
record should be kept together as one file, to reduce confusion on where an
encounter identified in the Table of Contents is located. In the event a patient’s
AFMAN41-210 10 SEPTEMBER 2019 119
entire electronic health record must be printed/filed, MTFs/RCs (utilizing AHLTA
Web Print) should file the AHLTA Web Print PDF as a complete packet in one of
the following ways (T-3):
5.7.4.3.1.2.1. If the patient's original paper record is small enough, the entire
packet can be filed as the top documents in Section 2.
5.7.4.3.1.2.2. If the patient's original paper record is too large, the AHLTA
Web Print packet should be placed in its own jacket (another volume), filed in
Section 2.
5.7.4.3.2. AHLTA Web Print and Service Treatment Record Disposition. The
availability of AHLTA Web Print in the AFMS has provided significant benefits to
reducing the workload associated with printing electronic health record documentation.
As such, patient encounter notes, printable clinical notes, radiology procedures, and
laboratory test results electronically stored in AHLTA are no longer required to be
printed and filed in the outpatient medical record prior to forwarding to the Air Force
Service Treatment Record Processing Center. The Service Treatment Record
Processing Center will utilize AHLTA Web Print to generate all AHLTA electronic
health record documents into the AHLTA Web Print PDF and upload it into HAIMS
during Service Treatment Record digitization, thereby making the complete Service
Treatment Record available to the VA in one process. (T-1).
5.7.4.3.3. AHLTA Web Print and Non-Service Treatment Record Retirement. Non-
Service Treatment Record, outpatient medical records for patients in all other
categories (dependents, civilians, foreign military, retirees, etc.), are retired to National
Personnel Records Center using e7m,8Treatment Record Retirement, is outlined in
detail in paragraph 5.7.12. Until necessary data communication links are permanently
established between both the MHS and National Personnel Records Center electronic
health record systems. MTF records personnel must continue to print and file (into the
patient’s paper record) all available ancillary, diagnostic or clinical information
electronically stored electronic health record prior to final records retirement
processing and shipment. (T-0). If MTF records personnel do not have access to
necessary AHLTA or CHCS systems to identify and print patient encounters, radiology
reports, and laboratory reports, then the patient’s Primary Care Manager support staff
is expected to complete this requirement and forward the documents to the MTF
outpatient medical and/or dental departments for inclusion into the Non-Service
Treatment Record.
5.7.4.4. To ensure reasonable continuity of care and or VA disability
evaluation/consideration, documents generated from civilian healthcare providers, stored
in any MTF health record, are included in the Service Treatment Record. Examples
include:
5.7.4.4.1. Reports and documents received from civilian referral healthcare providers.
5.7.4.4.2. Reports and documents from TRICARE Prime and TRICARE Prime
Remote civilian network providers. When a service member assigned to a remote unit
or GSU is enrolled to a TRICARE network Primary Care Manager, civilian documents
are owned and maintained at the network civilian Primary Care Manager office. At the
120 AFMAN41-210 10 SEPTEMBER 2019
time of the separating or retiring Airman’s MTF, Dental Treatment Facility or ARC
records department out-processing appointment, each Airman enrolled to a TRICARE
civilian Primary Care Manager should complete an authorization to obtain healthcare
information from the civilian Primary Care Manager and/or any civilian healthcare
provider. These documents should be forwarded to the MTF where the Service
Treatment Record is maintained so that Release of Information staff can make the
patient a copy, then include these civilian documents into the Service Treatment
Record. MTF records managers are expected to communicate this process to separating
and retiring Airmen attending Transition Assistance Program class so last minute
civilian Primary Care Manager requests do not delay Service Treatment Record
disposition.
5.7.4.5. Providing Copies for the Benefits Delivery at Discharge Program.
5.7.4.5.1. The Benefits Delivery at Discharge Program is a joint initiative between the
VA and the DoD. This program enables VA representatives to help transitioning
Airmen assemble and prepare their disability claim packages for VA disability
compensation and benefits review prior to their service separation or retirement. The
original Service Treatment Record is not provided to the Benefits Delivery at Discharge
office. Instead, the MTF will provide the member with a paper copy or electronic copy
(CD/DVD) of the Service Treatment Record at the member’s request. (T-1). Note:
this copy is counted as the member’s one complete copy free of charge.
5.7.4.5.2. Regardless of who maintains the records, if the individual appears on the
MTF/Reserve Medical Units roster, that specific MTF/ARC is responsible for
searching and sending the record or an acceptable Non-Availability Letter to the Air
Force Service Treatment Record Processing Center and will be held accountable for its
disposition.
5.7.4.5.3. Service Treatment Record records managers, as stewards of the Medical
Corps and appointed maintainers of the medical/dental records, have an obligation to
Veterans – to ensure their complete Service Treatment Record is ready and available
to the VA when the member chooses to file a claim. While a claim can be initiated
with a copy of the medical record, it is not official or complete without the original
records. Without the original record, the member’s claim will be left incomplete and
unfiled and the member will not receive their due compensation.
5.7.5. Collecting and Preparing Service Treatment Records for Shipment.
5.7.5.1. Once the LOSS rosters are obtained, retrieve the applicable outpatient medical
records and place them in a staging area separate from the main file located within a secure,
limited access room. File the Service Treatment Records in chronological order according
to the LOSS Roster shipment date. This will help ensure the Service Treatment Records
are mailed to arrive at the Air Force Service Treatment Record Processing Center by the
deadline. Service Treatment Records must be mailed no earlier than Date of
Separation/Date of Retirement and no later than 30 days after the member’s final date of
separation/retirement. (T-1).
5.7.5.2. No later than one business day after the Airman’s date of separation/retirement,
MTF and Dental Treatment Facility records personnel will ensure the dental treatment

AFMAN41-210 10 SEPTEMBER 2019 121
records for each separating and retiring Airman are forwarded to a central MTF location
where they will be bundled with the outpatient medical record and staged until ready for
mailing to the Air Force Service Treatment Record Processing Center. (T-1). Note: The
outpatient medical and dental records for each Airman must be bundled together before
shipping to the Air Force Service Treatment Record Processing Center. (T-0). Reference
DoDI 6040.45. Do not mail the outpatient and dental records separately. (T-0). Reference
DoDI 6040.45. Exception: Separate shipment may be necessary, for those medical or
dental records or other record volume that may be at another installation. Do not hold
medical or dental records after the member’s Date of Separation to include documentation
or encounters generated for any care they may receive after Date of Separation.
5.7.5.3. Missing Records: With the DoD-wide implementation of AHLTA, almost all
Service Members have patient medical encounters documented electronically. MTFs/RCs
must have and implement thorough in and out-processing procedures to ensure all records
for a patient are available as soon as possible. (T-0). Reference DoDI 6040.45.
5.7.5.3.1. Each Service has developed its own process to provide Service Treatment
Records to the VA. The VA provides metrics for each Service (similar to the Service
Treatment Record metrics) to Office of the Secretary of Defense (OSD), the White
House and Congress.
5.7.5.3.2. Each Service is held 100% accountable for missing records/record
components. Regardless of who maintains the records, if the individual appears on the
MTF/Reserve Medical Units roster, that specific MTF/ARC is responsible for
searching and sending the record or an acceptable Non-Availability Letter to the Air
Force Service Treatment Record Processing Center and will be held accountable for its
disposition. (T-1).
5.7.5.4. Non-Availability Letter, Verification Checklist, for Lost Original Paper Records:
5.7.5.4.1. If the original hardcopy dental or outpatient medical records cannot be
located send a Non-Availability Letter and completed Verification Checklist indicating
which original record is lost. If both hardcopy records cannot be located, include a
Non-Availability Letter and two completed verification checklists. An example is
available on the Medical Records Management SharePoint and the AFMOA Health
Benefits Kx page at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx. Note: If
both the original paper dental and original paper outpatient medical record(s) are lost,
include a Non-Availability Letter and two completed Verification Checklists.
5.7.5.4.1.1. If a Service Treatment Record cannot be located upon notification of a
member separating or retiring, the Verification Checklist and signed Non-
Availability Letter to declare unavailability must be completed. (T-0). These items
must arrive to the Air Force Service Treatment Record Processing Center no later
than the member’s Date of Separation/Date of Retirement plus 30 calendar days
(Date of Separation/Date of Retirement + 30). (T-0). Also, bundle these items with
all available parts of the Service Treatment Records. (T-2). Note: If the MTF
cannot find a full or partial Service Treatment Record but sends a compliant
package, the Air Force Service Treatment Record Processing Center will complete
due diligence for 10-12 days. If Service Treatment Record components are not

122 AFMAN41-210 10 SEPTEMBER 2019
located the Air Force Service Treatment Record Processing Center will certify all
available documents to the VA with AHLTA Web Print, prior to the Date of
Separation +45 deadline. Despite this certification by the Air Force Service
Treatment Record Processing Center, the MTF is still required to process a Non-
Availability Letter and complete due diligence, to include initiating a HIPAA
breach report.
5.7.5.4.1.2. MTFs will mail complete Service Treatment Records or any loose
documentation to the Air Force Service Treatment Record Processing Center no
later than date of Separation/Date of Retirement +30 days in order to allow the Air
Force Service Treatment Record Processing Center enough time to certify the
Service Treatment Record by Date of Separation/Date of Retirement +45 days.
5.7.5.4.1.2.1. The Air Force Service Treatment Record Processing Center will
provide the unit a list of records that were certified, after due diligence, without
MTF input. MTFs will complete HIPAA breaches, defined as the acquisition,
access, use, or disclosure of PHI in a manner not permitted under the HIPAA
Privacy Rule which compromises the privacy or security of the PHI for
incomplete Service Treatment Records. Refer to AFI 41-200.
5.7.5.4.1.2.2. MTFs will support the Air Force Service Treatment Record
Processing Center (respond to queries) as the Air Force Service Treatment
Record Processing Center completes due diligence during its research of
incomplete Service Treatment Records. (T-1).
5.7.5.4.1.2.3. MTFs will mail any Service Treatment Records that are found to
the Air Force Service Treatment Record Processing Center, even after the
Service Treatment Record has been certified. (T-1).
5.7.5.4.2. The commander of the MTF, group, or clinic responsible for the day-to-day
maintenance and storage of the lost record identified in the letter must wet or digitally
CAC sign the Non-Availability Letter. (T-1). Exception: The Medical Administrative
Officer is allowed to sign ANG letters and the Senior Air Reserve Technician is
allowed to sign AFR letters. The signature block must reflect the job title of the person
signing. (T-1). Signature delegation is not authorized. (T-1).
5.7.5.4.3. Air Force Members Empaneled to Sister-Service MTFs: Service Treatment
Records for AD service members are normally maintained at the MTF where the
member receives primary care, regardless of service affiliation. The health record
management officials at the Air Force MTF located nearest to the member’s Sister-
Service Primary Care Manager/MTF location must establish a local Service Treatment
Record Support Agreement (memorandum of understanding/memorandum of
agreement) (For an example of the memorandum, see AFMOA Health Benefits Kx
page at (https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx)
with the Sister-Service MTF. (T-1). Memorandum of understanding verbiage should
include both service processes. The agreement should identify how the Service
Treatment Records will be transferred from the Sister-Service MTF. How this is
accomplished is jointly decided by the MTFs, but acceptable methods include:
5.7.5.4.3.1. The Sister-Service MTF may mail the Service Treatment Record to the
AFMAN41-210 10 SEPTEMBER 2019 123
nearest Air Force MTF for subsequent mailing to the Air Force Service Treatment
Record Processing Center.
5.7.5.4.3.2. The Sister-Service MTF may forward the Service Treatment Record
directly to the Air Force Service Treatment Record Processing Center if they use
the instructions outlined in this document. Include a copy of the Service Treatment
Record disposition instructions with the agreement if this method is chosen.
5.7.5.4.4. There may be instances when the member is assigned to a GSU and the
responsible Air Force MTF is not the nearest MTF to the member’s Sister-Service
Primary Care Manager/MTF location. In these cases, see rules for managing GSU
records in the instructions that follow.
5.7.5.5. Non-Air Force Service Members Empaneled to Air Force MTFs:
5.7.5.5.1. Service Treatment Records for non-Air Force service members are normally
maintained at the Air Force MTF when the member is empaneled to the Air Force MTF.
Unless there is a local Service Treatment Record Support Agreement stating otherwise,
Service Treatment Records for Sister-Service members should be mailed to the
applicable address included in Attachment 11 of this AFMAN, with the appropriate
documentation (i.e. orders, Non-Availability Letter, etc.).
5.7.5.5.2. If a local Service Treatment Record Support Agreement is established with
another Service, the agreement must identify how the Service Treatment Record will
be transferred to the applicable Service. (T-1).
5.7.5.6. Personnel Assigned to GSU.
5.7.5.6.1. If the MTF identified on the LOSS Roster is not the MTF that maintains the
retiring/separating member’s Service Treatment Record, the LOSS-Roster-named
MTF must coordinate with the MTF where the record is regularly maintained in order
to ensure the Service Treatment Records are mailed to the Air Force Service Treatment
Record Processing Center. (T-1). (Note: Names and numbers of the points of contact
at each Air Force MTF and RC are located on the Medical Records Management
SharePoint).
5.7.5.6.2. Once contacted, the MTF maintaining the Service Treatment Record must
mail the Service Treatment Record to the Air Force Service Treatment Record
Processing Center in accordance with this guidance. (T-1).
5.7.5.7. Packaging and Shipping Service Treatment Records
5.7.5.7.1. Items included in Service Treatment Record Bundles:
5.7.5.7.1.1. Outpatient medical record or Non-Availability Letter, Verification
Checklist.
5.7.5.7.1.2. Dental record or Non-Availability Letter, Verification Checklist.
5.7.5.7.1.3. Include a copy of the retirement/separation or discharge order in each
record. In the outpatient medical record, the member’s orders will be placed in
Section II. (T-1). In the dental treatment record, the member’s orders will be placed
on the inside right-side folder section, on top of all other pages. (T-1).
124 AFMAN41-210 10 SEPTEMBER 2019
5.7.5.7.2. Include the following items in the shipment box; the LOSS roster as an
inventory sheet stapled to an AF Form 330, Records Transmittal/Request and the
records bundles. (T-1).
5.7.5.7.2.1. Print the LOSS roster inventory sheet with only the following columns
showing: Social security number, Name, Date of Separation, Medical Records
(Yes/No)/In Health Artifact and Image Management Solution, Dental Records
(Yes/No)/Never Created, Date Record Mailed, Remarks, and NCOIC Signature.
5.7.5.7.2.2. Place the records bundles in order of the listed records on the LOSS
roster. 5.7.5.7.2.3. Write "SEE ATTACHED ROSTER" in the “Name” block on
the AF Form 330 type and staple together with the roster (inventory sheet). (T-1).
5.7.5.7.2.3.1. The NCOIC or records department supervisor must sign the
roster stating they have quality checked the shipment. (T-1). Annotate the
mailing date and annotate any remarks relevant to shipping. (T-1).
5.7.5.7.2.4. Note: MTF records management personnel must keep a copy of the
AF Form 330 and LOSS roster permanently or until the Office of the Under
Secretary of Defense for Personnel and Readiness and the Services establish a
disposition rule for AD records. (T-0). Reference DoDI 6040.45. Place together
with the postage tracking/arrival confirmation notice in a central location within the
Outpatient Records department.
5.7.5.8. Shipment Containers.
5.7.5.8.1. Boxes - Records personnel are required to use standard white record
retirement boxes or other same-sized box, purchased specifically for shipping. (T-1).
The maximum weight per shipping box is 50 pounds. Do not bundle standard shipping
boxes within larger containers for shipment as the Air Force Service Treatment Record
Processing Center mailroom will not accept large or heavy packages or containers.
MTF records personnel are responsible for ensuring boxes are thoroughly and securely
packed, labeled, and taped for shipping so as to prevent inadvertent opening during
shipment and subsequent loss of Service Treatment Records or delays in arriving at
destination.
5.7.5.8.2. Envelopes – If the Service Treatment Record bundle will easily fit into an
envelope, one may be used. Envelopes must be tear resistant (i.e. fiber/cloth-like
construction, such as TYVEK), securely packed, labeled, and taped for shipping so as
to prevent inadvertent opening during shipment and subsequent loss of Service
Treatment Records or delays in arriving at destination. (T-1).
5.7.5.9. Shipping Service Treatment Records.
5.7.5.9.1. Service Treatment Records will be mailed to arrive at the Air Force Service
Treatment Record Processing Center no earlier than the member’s Date of
Retirement/Date of Separation and should arrive no later than 30 calendar days after
the member’s date of retirement/separation/discharge or transition to inactive status.
(T-0). Reference DoDI 6040.45. All OCONUS MTFs will use commercially available
global delivery services to mail the Service Treatment Record to arrive at the Air Force
Service Treatment Record Processing Center on the no-earlier-than date to prevent the
AFMAN41-210 10 SEPTEMBER 2019 125
Service Treatment Record from arriving late at Air Force Service Treatment Record
Processing Center.
5.7.5.9.2. Do not mail a member’s outpatient and dental records separately; they must
be mailed together as a bundle. (T-0). Reference DoDI 6040.45.
5.7.5.9.3. Service Treatment Record bundles of outpatient and dental records for more
than one individual may be combined into one shipment box provided the destination
is to the same location.
5.7.5.10. Preferred Mailing Method.
5.7.5.10.1. Forward Service Treatment Record boxes/envelopes to the Air Force
Service Treatment Record Processing Center using standard First Class United States
mail with immediate delivery confirmation/acknowledgment, certified mail, or other
commercially available option, e.g., FedEx, that offers package tracking and
delivery/arrival confirmation.
5.7.5.10.2. If standard first class United States Postal Service is used, package tracking
and delivery/arrival confirmation or shipment via Certified Mail is required. These
services are typically available via the Base Information Transfer System or the Base
Information Transfer Center (BITC) at each major installation.
5.7.5.10.3. Commercial priority mailing services are usually offered through the MTF
mailroom.
5.7.5.10.4. Records personnel must keep postage tracking/arrival confirmation notice
permanently or until the Office of the Under Secretary of Defense for Personnel and
Readiness and the Services establish a disposition rule for AD records. (T-0). Place
together with the Air Force Form 330 and LOSS roster in a central location within the
Outpatient Records department.
5.7.5.10.5. Use of standard First Class United States Postal Service mailing method
alone, without package tracking and immediate delivery
confirmation/acknowledgment or certified mail receipt, is prohibited. (T-1). Return
receipt confirmation must not be dependent upon the timeliness or willingness of the
destination MTF to complete a DD Form 2825, Internal Receipt, or other manual
delivery confirmation receipt option. (T-1).
5.7.5.11. For Airmen transitioning from AD to the RC, records personnel will forward the
AD component to the Air Force Service Treatment Record Processing Center. The AD
service period will be available electronically for the RCs.
5.7.5.12. Medical Record Tracking Transition in CHCS. Update the CHCS Medical
Record Tracking Function to annotate the record has been mailed to the Air Force Service
Treatment Record Processing Center. Health records personnel will TRANSFER the
record in the CHCS Medical Record Tracking menu to the appropriate location. (T-1).
5.7.5.13. Handling Clarification Queries from the Air Force Service Treatment Record
Processing Center. Queries for clarification on Service Treatment Records (e.g., requests
for missing documents/records) must receive immediate MTF/ARC record management
action. (T-2). The Air Force Service Treatment Record Processing Center only has a 15-

126 AFMAN41-210 10 SEPTEMBER 2019
day window from time of Service Treatment Record receipt to ensure it is digitized
appropriately in HAIMS.
5.7.5.13.1. Track Air Force Service Treatment Record Processing Center queries and
their outcome in a local database. The method is left up to the MTF/ARC and could
include an electronic spreadsheet, simple ledger, or other method.
5.7.5.13.2. MTF/Dental Treatment Facility/ARC records managers have only two (2)
duty days from receipt of the inquiry to investigate and provide a response. Delayed
responses will require immediate explanation to AFMOA/SGAT. (T-1).
5.7.5.13.3. The MTF/Dental Treatment Facility/ARC may be contacted by phone or e-
mail. MTF/Dental Treatment Facility/ARC records managers may contact officials at
the Air Force Service Treatment Record Processing Center via telephone or return e-
mail with the results of the inquiry, whether or not the record or missing item was found
and when it will be sent to the Air Force Service Treatment Record Processing Center.
Annotate the results in the computer spreadsheet.
5.7.6. Managing Loose and/or Late-Flowing Medical Documents Following Service
Treatment Record Shipment. Loose and/or late-flowing medical documents are those medical
or dental documents discovered in the MTF or Dental Treatment Facility after the Service
Treatment Record has already been mailed to the Air Force Service Treatment Record
Processing Center or the departing member’s gaining RC.
5.7.6.1. Loose and/or Late-Flowing Medical Documents must be digitized into HAIMS in
accordance with the HAIMS scanning policy. (T-0).
5.7.6.2. Loose paperwork may be digitized at any facility with HAIMS access.
5.7.7. Large Shipments of Pre 1 Jan 14 Medical and Dental Records/Loose Documents
Processing:
5.7.7.1. The following guidance applies only to records collected for Airmen who
separated/retired before 1 January 2014. Due to limited space and storage capabilities at
the Air Force Service Treatment Records Processing Center, shipments of Pre-January
2014 Service Treatment Records must be coordinated and approved prior to sending. (T-
1).
5.7.7.2. MTF records personnel are required to temporarily stage the outpatient and dental
records together in a central records storage location, separate from the main MTF file or
records room. (T-1). Ensure the following steps are taken:
5.7.7.2.1. If the information on hand is only loose documentation or less than 10 pages,
digitize it in HAIMS. Exception: If the service member is an Entry Level Separation,
the record may be less than 10 pages and should be mailed to the Air Force Service
Treatment Records Processing Center.
5.7.7.2.2. Complete an AF Form 330 along with an inventory list containing the
required data elements listed below. See examples located in patient administration
misc. document folder on the AFMOA Health Benefits Kx page at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.7.7.2.2.1. NAME (Last, First).

AFMAN41-210 10 SEPTEMBER 2019 127
5.7.7.2.2.2. SOCIAL SECURITY NUMBER.
5.7.7.2.2.3. MEDICAL RECORD (YES/NO).
5.7.7.2.2.4. DENTAL RECORD (YES/NO).
5.7.7.2.2.5. COMMENTS.
5.7.7.2.2.6. SIGNATURE BLOCK (Flight Commander, NCOIC, or Records
Department Supervisor).
5.7.7.3. Maintain the records in the central records storage location until directed by
AFMOA/SGAT to mail them to the Air Force Service Treatment Record Processing
Center. Do not mail these records until directed to do so by AFMOA. Large pre-
coordinated shipments of Service Treatment Records will be mailed to the Air Force
Service Treatment Record Processing Center at the following address: (T-1).
AF STR Processing Center
3370 Nacogdoches Road, Suite 116
San Antonio, TX 78217
5.7.8. AD and ARC records disposition rules are subject to frequent changes. For the latest
information, contact the Records Management Support Team, AFMOA/SGAT via e-mail at
usaf.jbsa.afmoa.mbx.str-processing-center@mail.mil.
5.7.9. Sequestered/Deceased Member’s Records. In the event a Service Treatment Record is
sequestered for legal reasons or has already been provided to the installation Casualty or
Mortuary Affairs office in the event of an AD or ARC service member’s death, MTF records
managers must notify the Air Force Service Treatment Record Processing Center via email at
usaf.jbsa.afmoa.mbx.str-processing-center@mail.mil that the Service Treatment Record is
sequestered. (T-1). If unable to forward original record, the Service Treatment Record Center
will accept a certified copy of the original record along with a notarized affidavit.
5.7.9.1. Service Treatment Records for Service Members Killed in Action. Immediately
following an AD service member’s death at an overseas battle zone or theater of operations,
the on-site Casualty or Mortuary Affairs office is authorized to take possession of the
remains and prepare the body for transport to the Dover Air Force Base Port Mortuary
Facility as soon as medical actions are complete. Available paper health treatment
documents and records must be surrendered to the Mortuary Affairs/Casualty Affairs
representative(s) upon request. (T-1). Document the records transfer using the appropriate
electronic records tracking mechanism.
5.7.9.1.1. If outpatient medical or dental treatment records are discovered (at a location
not specifically identified as the AD service member’s home-of-station support MTF),
after the remains have been transported to the Dover Air Force Base Port Mortuary
Facility, contact the nearest Casualty or Mortuary Affairs unit responsible for arranging
transportation of the remains. If medical and/or dental records cannot be transferred to
the nearest Casualty or Mortuary Affairs office, forward the medical record(s) to the
MTF responsible for the regular maintenance and storage of the deceased member’s
record. Contact the deceased service member’s deployed unit chain of command or
Personnel Support for Contingency Operations unit to ascertain from which installation
the Airman deployed. In the records package, include a completed AF Form 330, DD
128 AFMAN41-210 10 SEPTEMBER 2019
Form 2138 Request for Transfer of Outpatient Records or other appropriate form or
letter that informs the receiving MTF that, a) the AD service member has died, and b)
informs the receiving MTF the health records they received were intentionally
forwarded.
5.7.9.1.2. Home Station MTF Service Treatment Records Disposition Responsibility:
If notified by an official agency or unit (e.g., unit commander or chain of command
representative, installation Command Post, Mortuary or Casualty Affairs) that an AD
service member was killed in action while deployed, remove the deceased service
member’s outpatient medical and dental records from the main file and contact the
installation Casualty or Mortuary Affairs office. Forward the Service Treatment
Record to the Air Force Service Treatment Record Processing Center according to
processes identified earlier within this section, no later than 30 days following
notification of the service member’s death. The Air Force Service Treatment Record
Processing Center will digitize the Service Treatment Record in HAIMS, thus making
it available to the VA. (T-1). Surviving family members may be eligible for Service
or VA death benefits or compensation. The deceased Airman’s Service Treatment
Record may be required as part of the VA death benefits or compensation evaluation.
If, at any time, while preparing to ship the Service Treatment Record to the Air Force
Service Treatment Record Processing Center, the installation Mortuary or Casualty
Affairs unit, or Air Force Institute of Pathology specifically requests the outpatient
medical or dental records for official purposes, provide a certified copy of the Service
Treatment Record.
5.7.9.2. Service Members Placed in Appellate Review Leave Status or When a Prisoner is
transported to a Correctional Detention Facility Immediately Following a Trial.
5.7.9.2.1. Appellate Review Leave. Under the Uniform Code of Military Justice, a
punitive service discharge or dismissal may not be executed until the appellate review
is completed. During this appellate process, service members are still entitled to AD
healthcare benefits and are required to remain enrolled in TRICARE Prime. The
appellate process can sometimes be quite lengthy and requires the service member to
be placed on an involuntary excess leave status called “Appellate Review Leave.” The
following guidance provides instruction on how to manage the enrollment and medical
records of members on appellate review leave.
5.7.9.2.2. Service members subject to appellate review may relocate and reside
anywhere within the CONUS, to meet unique administrative and personnel
accountability requirements. Service members placed on appellate review leave are
assigned to the Air Force Security Forces Center (AFSFC), Joint Base San Antonio
(JBSA) Lackland, TX.
5.7.9.2.3. While on appellate review leave, the service member must remain enrolled
in TRICARE Prime and be enrolled to a MTF. (T-0). If the service member relocates
to another area, prior to departure the servicing MTF must brief the member on the
processes required for obtaining health care for themselves and any dependents. (T-0).
Service members on appellate leave cannot enroll into TRICARE Prime Remote or
choose a civilian Primary Care Manager. Reference 32 CFR Part 199.17. Also, see
Section 2A for additional information on enrollment.
AFMAN41-210 10 SEPTEMBER 2019 129
5.7.9.2.4. When a member is placed on appellate leave, the service member’s Service
Treatment Record will be forwarded (in a sealed envelope) to the Wilford Hall
Ambulatory Surgical Center at Lackland Air Force Base, TX where it will be
maintained until the appellate review period has completed. (T-1).
5.7.9.2.5. If the service member is available to complete MTF out-processing actions,
obtain or reproduce two copies of the individual’s discharge orders and follow the steps
identified below.
5.7.9.2.5.1. Place one copy in a charge-out guide.
5.7.9.2.5.2. Locate and retrieve the service member’s outpatient medical record.
5.7.9.2.5.3. Place the second copy of the discharge orders inside the record and file
the document in Section II on top of all other medical documents.
5.7.9.2.5.4. Locate and retrieve the dental treatment record – bundle together with
the Outpatient Medical Record.
5.7.9.2.5.5. Properly TRANSFER/INACTIVATE the medical records in the
CHCS Medical Records Tracking menu. Select “APPELATE LEAVE” or create
another easily identifiable records location destination that clearly distinguishes
these types of medical records from medical records transferred to the 59th Medical
Wing under routine PCS transfer rules. See the Medical Record Tracking,
Retirement and Retrieval User Guide on the AFMOA Health Benefits Kx to learn
how to create or set-up new records borrower/destination locations.
5.7.9.2.5.6. Place the complete Service Treatment Record in shipping package.
5.7.9.2.5.7. Prepare, complete, and sign an AF Form 330 and insert the form into
the package. Keep a copy of the AF Form 330.
5.7.9.2.5.8. No later than three days following the start of the appellate review
period, mail the complete Service Treatment Record and AF Form 330 to the
address identified below: following the steps outlined in paragraph 5.29.5.5.
Wilford Hall Ambulatory Surgical Center
ATTENTION: Lackland STR Manager
1100 Wilford Hall Loop
JBSA-Lackland Air Force Base, TX 78236-9908
5.7.9.3. Upon completion of the appellate review, if the service member is officially and
permanently discharged from the Service, the member’s name will appear on the
installation personnel LOSS roster for Lackland Air Force Base. The records department
at Wilford Hall Ambulatory Surgical Center is responsible for forwarding the original
Service Treatment Record to the Air Force Service Treatment Record Processing Center.
If the service member is removed from appellate leave and returned to duty, Wilford Hall
will transfer the original Service Treatment Record to the service member’s previous
assignment support MTF or to another MTF based upon written direction or orders. (T-1).
Medical records personnel will not release or forward the Service Treatment Record to
anyone, any place, or any agency without obtaining written direction or orders. (T-1).

130 AFMAN41-210 10 SEPTEMBER 2019
5.7.9.4. Prisoners Transported to a Correctional Detention Facility Immediately Following
Court-Martial Trial. Following the court’s Ruling and/or Sentencing, a service member
may be immediately escorted to a correctional detention facility.
5.7.9.4.1. During the appellate review period, even if a service member is immediately
transported to a correctional facility, the MTF where the service member’s Service
Treatment Record is normally maintained is responsible for forwarding the original
Service Treatment Record to Wilford Hall Ambulatory Surgical Center in accordance
with the instructions (associated with appellate review record disposition) previously
identified in this section. (T-1).
5.7.9.4.2. Records personnel at the service member’s support MTF and/or the Wilford
Hall Ambulatory Surgical Center are prohibited from providing or forwarding the
original Service Treatment Record to any prisoner escort detail or correctional facility.
(T-1). Instead, provide the escort detail or confinement facility with a complete Service
Treatment Record copy. If a copy cannot be immediately provided, a copy will be
mailed to the destination military correctional facility within five duty days. (T-1).
Copies of Service Treatment Records may be mailed to state and federal prisons upon
proper request. If available, obtain a copy of the service member’s orders or court
confinement order from the prisoner escort detail.
5.7.9.4.3. Address questions concerning this program to the Records Management
Support Team, AFMOA/SGAT at usaf.jbsa.afmoa.mbx.str-processing-
5.7.9.5. United States Air Force Academy Cadets and Airmen with Less than 180 days of
Continued Service. This applies to members of the United States Air Force Academy and
all other Air Force recruits separated or discharged prior to accruing 179 days or less days
of military service. Forward Service Treatment Records for these two beneficiary
categories to the Air Force Service Treatment Record Processing Center. Follow the same
Service Treatment Record disposition instructions as identified for AD and ARC service
members identified earlier in this manual. Place a copy of the separation or retirement
order or personnel document ordering the separation, discharge, or retirement inside the
Service Treatment Record.
5.7.10. NATO Military Personnel and NATO Family Member Non-Service Treatment
Records. Deliver outpatient records of NATO military personnel and their family members in
a sealed envelope to the individual concerned upon transfer to another United States military
base. Upon return of personnel to the NATO country, transfer records to the specific national
military medical authority. Address questions concerning this program to the Records
Management Support Team, AFMOA/SGAT at [email protected]il.
5.7.11. Non-NATO Foreign Military Personnel Non-Service Treatment Records. Retire
outpatient records for non-NATO foreign military personnel to National Personnel Records
Center two years after the end of the calendar year of the last date of treatment, in accordance
with AFRIMS Records Disposition Schedule, Series 41 Internet website, accessible via the Air
Force Portal website, and the Medical Record Tracking, Retirement and Retrieval User Guide,
available for download on the AFMOA Health Benefits Kx.

AFMAN41-210 10 SEPTEMBER 2019 131
5.7.12. Non-military (including family members and retired personnel) Non-Service
Treatment Records. Air Force MTFs are required to at least annually (no later than the end of
the same month from the previous year’s record retirement), retire or purge outpatient medical
records for family members and retired personnel to the National Personnel Records Center
Annex, 1411 Boulder Boulevard, Valmeyer, IL 62295. If records were last retired in April
2010, the next records retirement process should be completed by 30 April 2011. Retire
records two years after the end of the calendar year of the last date of treatment. Note: Do not
use the most current treatment date identified inside the paper health record. Review the
patient’s appointment history in the electronic health record. Retire or purge records in
accordance with AFRIMS Records Disposition Schedule, Series 41, accessible via the Air
Force Portal website and the Medical Record Tracking, Retirement and Retrieval User Guide,
available for download on the AFMOA Health Benefits Kx.
5.7.13. Non-Service Treatment Records for Family Members of Service Members Assigned
to GSU. Outpatient medical records are usually maintained at the MTF for two years after the
calendar year in which the last treatment occurred. However, this rule does not apply to Non-
Service Treatment Records for family members of service members assigned to a GSU, and/or
enrolled to TRICARE Prime Remote. As such, a family member’s Non-Service Treatment
Record may be kept on file at the MTF closest to the service member’s GSU TRICARE
enrollment. If this is the case, there may be no evidence in either the military electronic health
record or paper health record to indicate the family member has received MTF care within the
last two years. If records personnel suspect a family member, for whom the MTF maintains
an outpatient medical record, may be receiving care at a civilian network healthcare provider,
the record technician researching the record must verify the sponsor and family member
TRICARE enrollment status via DEERS. (T-1). If the enrollment information indicates the
family member is enrolled into TRICARE Prime Remote, then flag the outpatient medical
record according to the instructions in paragraph 5.15. If the DEERS information indicates no
TRICARE Prime or Prime Remote enrollment, then retire the record(s).
5.7.14. Federal Civilian Employee Non-Service Treatment Records. Federal Civilian
Employee Non-Service Treatment Records are maintained in SF 66D, Employee Medical
Folder and is a chronological, cumulative record of occupational and non-occupational
information pertaining to the health of a civilian employee during the course of employment.
A SF 66D can be obtained at https://www.gsa.gov.
5.7.14.1. This record consists of personal and occupational health histories, exposure
records, medical surveillance records, Office of Worker’s Compensation Programs
records, and the documented notes, evaluations and tests results generated by healthcare
providers in the course of examination, treatment and counseling.
5.7.14.2. Maintain Non-Service Treatment Records of civilian Air Force employees until
the employee is transferred to another activity within the Federal government or is
separated from the Federal Service. Upon employee transfer or separation, forward the SF
66D to the Military Personnel Section, Civilian Personnel Section within 10 days of
transfer or separation.
5.7.14.3. It is the responsibility of the Military Personnel Section to forward the Non-
Service Treatment Record to the appropriate custodian. However, federal civilian
132 AFMAN41-210 10 SEPTEMBER 2019
employees must complete installation and unit and/or installation out-processing checklists
similar to their AD counterparts (as applied to MTF out-processing requirements). (T-1).
5.7.14.4. Typically, AD members are required to visit the installation Outpatient Record
department to make sure their record(s) and the record(s) of their family members will be
forwarded to the next base, regardless of any pre-arranged Military Personnel Section -
MTF transfer process.
5.7.14.5. Federal civilian employees are also required to visit the local servicing MTF
Outpatient Record department where their Non-Service Treatment Record is maintained.
This process will ensure that the MTF receives notice from the civilian employee of an
upcoming transfer or retirement, regardless of any Military Personnel Section records
relocation/retirement notification.
5.7.14.6. Information regarding creation and maintenance of these Non-Service Treatment
Records is available for download on the AFMOA Health Benefits Kx.
5.7.14.7. If civilian employee records are found years after the employee has relocated or
retired, then:
5.7.14.7.1. Ensure records are in a SF 66D. Each employee will have his own folder.
5.7.14.7.2. Annotate the SF 66D with the employee’s last name, first name, middle
initial and Social security number on the upper right hand corner - preferably typed on
a white folder tab.
5.7.14.7.3. Box the records in a container which will safely make it through the United
States Postal Service mailing process.
5.7.14.7.4. Create a shipping list for each container. Detail the contents by name and
Social security number of each employee’s record. A SF 135, Records Transmittal and
Receipt is not needed.
5.7.14.7.5. Mail the container(s) to:
National Personnel Records Center Annex
1411 Boulder Boulevard
Valmeyer, IL 62295
5.7.14.7.6. Mail the record containers using standard first class mail, certified mail, or
other available option. If standard first class United States Postal Service is used, return
receipt confirmation is required.
5.7.15. Retirement of Inpatient Records, Extended Ambulatory Records, and Fetal Monitor
Strips to National Personnel Records Center. Additional information regarding creation and
maintenance of these records is available for download on the AFMOA Health Benefits Kx.
5.7.15.1. Inpatient Records. Retire inpatient records of all service members and their
family member dependents to National Personnel Records Center, in accordance with
AFRIMS Records Disposition Schedule, Series 41 Internet website, accessible via the Air
Force Portal website and the Medical Record Tracking, Retirement and Retrieval User
Guide available for download on the AFMOA Health Benefits Kx.
AFMAN41-210 10 SEPTEMBER 2019 133
5.7.15.1.1. Dispose or retire inpatient records according to the year of hospitalization
discharge, not date of admission.
5.7.15.1.2. Teaching facilities will retire records 5 years after the end of the calendar
year of the last date of treatment unless a waiver to retire earlier has been approved by
the Air Force Records Officer and National Personnel Records Center. Contact
AFMOA/SGAT for assistance when requesting a waiver. Non-teaching MTFs will
retire inpatient records one year following the end of the calendar year of the last date
of treatment.
5.7.15.2. NATO Military Personnel Inpatient Records: in accordance with NATO
Standardization Agreement for Basic Military Hospital (Clinical) Records, Inpatient and/or
Clinical records will accompany the patient upon transfer between hospitals, and will be
forwarded to the patient’s specific national military medical authority. See NATO
STANAG, Basic Military Medical Record, AMedP-8.2 Edition B, 15 January 2018.
5.7.15.3. Non-NATO Military Personnel Inpatient Records: Retire inpatient records in
accordance with AFRIMS, Records Disposition Schedule, Series 41 and the Medical
Record Tracking, Retirement and Retrieval User Guide, available for download on the
AFMOA Health Benefits Kx.
5.7.15.4. Extended Ambulatory Records. The retirement rules for extended ambulatory
records are the same as those for inpatient records. For teaching MTFs, the extended
ambulatory record should be retired five years following the end of the calendar year of the
last documented episode of care unless a waiver to retire earlier has been approved by the
Air Force Records Officer and National Personnel Records Center. Contact
AFMOA/SGAT for assistance when requesting a waiver. For non-teaching facilities, the
extended ambulatory record will be retired one year after the end of the calendar year of
the last documented episode of care.
5.7.15.4.1. Retire the extended ambulatory record folder to National Personnel
Records Center along with the inpatient records and any applicable fetal monitor strips
(i.e., in the same box.)
5.7.15.4.2. Place the extended ambulatory record folder behind any fetal monitor strips
for that patient, or behind the applicable inpatient record folder if there are no fetal
monitor strips.
5.7.15.4.3. If the patient does not have an inpatient record but does have an extended
ambulatory record, the extended ambulatory record is still included in the shipment of
inpatient records.
5.7.15.5. Fetal Monitor Strip. Retire the fetal monitor strips to National Personnel Records
Center in accordance with AFRMS Records Disposition Schedule, Series 41 Internet
website, accessible via the Air Force Portal website and the Medical Record Tracking,
Retirement and Retrieval User Guide, available for download on the AFMOA Health
Benefits Kx. (Note: Digitized, or other format, fetal monitor strips that can be printed out
on an 8 ½” X 11” sheet of paper are filed in the infant’s inpatient record or the mother’s if
the infant is stillborn and are retired as a part of the inpatient record).
134 AFMAN41-210 10 SEPTEMBER 2019
5.7.15.5.1. Retire the fetal monitor strips to National Personnel Records Center using
the same disposition schedule as that for inpatient records.
5.7.15.5.2. Attach the envelopes containing the fetal monitor strips to the inside of an
appropriately labeled folder (only two envelopes per patient per folder).
5.7.15.5.3. Annotate the outside of the folder with the name and register number of the
infant, sponsor’s name and Social security number, name of the MTF and date of
infant’s birth.
5.7.15.5.4. File these folders in the same box as the applicable inpatient record (baby’s
or mother’s) directly after that record.
5.7.16. General Inpatient Records Disposition Procedures:
5.7.16.1. Prepare National Personnel Records Center required index of records shipment
file. Outpatient and Inpatient medical records require separate indexes (fetal monitor strips
and extended ambulatory records must be included on the Inpatient records index). (T-3).
5.7.16.2. Follow the applicable tables and rules in accordance with AFRIMS, Records
Disposition Schedule, Series 41, to determine record retirement eligibility.
5.7.16.3. Utilize the step-by-step instructions provided in the Medical Record Tracking,
Retirement and Retrieval User Guide to create/run the retirement index. The Medical
Record Tracking, Retirement and Retrieval User Guide is available for download on the
AFMOA Health Benefits Kx. Address questions concerning this program to the Records
Management Support Team, AFMOA/SGAT at [email protected]il.
5.7.16.4. The CHCS will maintain shipment indices until all records listed have been
destroyed or transferred to the National Archives, or when no longer needed, whichever is
later. For future use, print and maintain a copy of each index. This information is
invaluable when determining whether or not a record has been retired to National Personnel
Records Center.
5.7.16.5. Forward a copy of each shipment index to the Base Records Management Office
for their files.
5.7.16.6. Requests for Medical Records from the National Personnel Records Center.
5.7.16.6.1. When requesting medical records retired to National Personnel Records
Center prior to CY 2003, use the DD Form 877-1, Request for Medical/Dental Records
from the National Personnel Records Center (NPRC) (St Louis, Missouri) or other
specific form identified by National Personnel Records Center records managers.
National Personnel Records Center request forms contain space for the minimal
information required for their agency to institute a search for the requested record.
5.7.16.6.2. To obtain medical records retired to the National Personnel Records Center
from CY 2003 and beyond, use the National Personnel Records Center Medical
Registry System to request the record(s). This computer application can be accessed
through a web interface. To register, requesting MTF personnel must complete the VA
Form 9957, ACRS Time Sharing Request Form. (T-2). An electronic version of the
form along with instructions for completion can be obtained at the Medical Registry
System website at https://www.archives.gov/st-louis/military-

AFMAN41-210 10 SEPTEMBER 2019 135
personnel/agencies/medical-registry-system.html. Additionally, MTF personnel
may use the step-by-step records retrieval instructions provided in the Medical Record
Tracking, Retirement and Retrieval User Guide available for download on the AFMOA
Health Benefits Kx.
5.7.16.6.3. Use the DD Form 2138 or 877, Request for medical/Dental Records or
Information when requesting records from another MTF.
5.8. Base Closures and Medical Records Management.
5.8.1. Inpatient Records are retired to the National Personnel Records Center upon
inactivation of the hospital (or upon downsizing to a clinic) in accordance with AFRIMS
Records Disposition Schedule at https://www.my.af.mil/afrims/afrims/afrims/rims.cfm and
the Medical Record Tracking, Retirement and Retrieval User Guide available for download on
the AFMOA Health Benefits Kx website and the AF/SG’s Contingency Operations Plan.
Reference AFI 41-106, Medical Readiness Program Management.
5.8.2. If early retirement is desired (i.e., out of cycle), the MTF commander or director must
request early retirement from Secretary of the Air, Chief Information Officer, Compliance
Division (SAF/CIO A6XA). (T-1). Coordinate the request with the local Information
Management Office before submission.
5.8.3. Submit requests for early retirement as soon as possible because of the time required
for approval. The request is coordinated with National Personnel Records Center who will
notify the MTF commander or director of the decision. The request must include the following
(T-3):
5.8.3.1. Reason for request.
5.8.3.2. Closure date (or date realigning to a clinic).
5.8.3.3. Type(s) of records to be retired.
5.8.3.4. Number of records (volume) involved.
5.8.3.5. All information normally included on the shipment index when requesting an
accession number from National Personnel Records Center.
5.8.4. Health records of AD members and their family members are transferred to the
member’s gaining base.
5.8.5. Health records of retirees and others are transferred as follows:
5.8.5.1. If another MTF is identified by the patient as the new facility of treatment, forward
the health records to that facility with a cover letter explaining why the records were
forwarded.
5.8.5.2. If a civilian medical facility is identified as the new treatment facility, copy
pertinent portions of the record for the patient to take to that facility. Retire the original
record to National Personnel Records Center in accordance with AFRIMS Records
Disposition Schedule and the Medical Record Tracking, Retirement and Retrieval User
Guide. Maintain an AF Form 1942 for six months or until the base closes, whichever
comes first, then destroy.
136 AFMAN41-210 10 SEPTEMBER 2019
5.8.6. For sequestered records, each MAJCOM will designate repository bases within the
command to administer medical records involved in projected or active litigation.
5.8.7. If a medical malpractice claim was filed for AD family members, forward the original
inpatient or outpatient record (as applicable) to the Risk Manager or Hospital Administrator at
the gaining MTF. Do not allow the patient to hand-carry the record. In addition, send a letter
explaining why the records are being forwarded.
5.8.8. Use the following guidance if a medical malpractice claim was filed for a retiree or
other patient.
5.8.8.1. If the continued care will be provided at an Air Force MTF, forward the original
record with the appropriate letter of explanation.
5.8.8.2. If the care will be provided by a civilian or non-Air Force MTF, provide the patient
with a copy of the record and forward the original with the appropriate letter to the Risk
Manager or Medical Facility Administrator at the designated repository.
5.8.9. Use the following guidance for potential claims.
5.8.9.1. If there is a potential claim in reference to inpatient records, forward the original
inpatient record with the accompanying letter of explanation to the Risk Manager or
Quality Services Manager at the gaining Air Force MTF or designated repository base.
5.8.9.2. If there is a potential claim in reference to outpatient records, as a general rule,
follow procedures outlined in this section. Coordinate special concerns and circumstances
with the local base Staff Judge Advocate. Maintain the record in a sequestered location.
5.8.10. Closure bases must establish a “Chain of Custody” document that lists each patient’s
name, Social security number, DoD Identification Number and location to which the medical
record was forwarded. (T-3). Forward a copy of the Chain of Custody document to the
MAJCOM command surgeon and the Records Management Support Team, AFMOA/SGAT.
5.8.11. Upon inactivation of the MTF, the old retained SF 135s, (these were produced prior to
CY 03) and copies of the CHCS shipment indices (produced CY 03 and later) will be forwarded
to the next higher records management office at the MAJCOM command surgeon’s office and
the Records Management Support Team, AFMOA/SGAT.
5.9. Health Record Review Committee/Functions.
5.9.1. Record review functions will be performed at each MTF by either an established
Medical Record Review Committee or incorporated into other committees that review records.
(T-1). Record review function examines and evaluates the following: record quality and
clinical pertinence; information assurance practices; and, inpatient and outpatient records
completion times. Also examined are whether the records are prepared and maintained
according to directives and Joint Commission standards. Finally the records review function
is the approval authority for locally created forms. (T-0). Cross-service representation will be
included in the performance of these committees, i.e., representatives of the various clinic
services, dental services, nursing services, medical record departments, management and
administrative services, and other departments, as appropriate. These review functions are part
of the Air Force Quality Assurance program. Reference under DoDI 6025.13, Medical Quality
Assurance (MQA) and Clinical Quality Management in the Military Health System (MHS).
Responsibilities of this committee will include but not be limited to the following items (T-0):
AFMAN41-210 10 SEPTEMBER 2019 137
5.9.1.1. Cross-Functional Sampling of Clinical Documentation: The review function
should include an adequate number of both inpatient and outpatient records (sampling ratio
should represent clinical facility workload levels). For example: Provider monthly
workload < 30, review 100% of cases; Workload = 30-100, review 30 cases; Workload =
101-500, review 50 cases; Workload > 500, review 70 cases. Records will be reviewed to
ensure the highest possible standards of quality control, record completion periods,
legibility, promptness in documentation, and clinical pertinence are met. Records of recent
deaths, hospital infections, complications and unusual problem cases are reviewed. A
representative sample of records from every provider will be reviewed throughout the year.
5.9.1.2. Review the monthly medical record availability and accountability rates and
report to the Executive Committee of the Medical Staff or as directed by the MTF
commander or director.
5.9.1.3. Review the Service Treatment Record disposition process and progress on
meeting the standards of completeness and timeliness and report to the Executive
Committee of the Medical Staff or as directed by the MTF commander or director.
5.9.1.4. Written reports of the review function contain conclusions, recommendations,
actions taken and after-action results. These data reports are quality assurance records.
These data reports are then forwarded to the Executive Committee of the Medical Staff for
review or as directed by the MTF commander or director.
5.9.2. Committees tasked with records review must approve locally overprinted SFs filed in
health records. (T-2). Overprints are authorized only when the material added does not conflict
with the purpose for which the form was intended. See AFI 33-360 and DoD 7750.07-M for
further instructions on the authorized use of overprinted forms.
Section 5B—Outpatient Records Administration
5.10. Creation of Outpatient Record Folders. The AFMS no longer creates hard copy
outpatient record folders. Outpatient records will be created and maintained in the approved
electronic health record. (T-0). Arrangement of content, record filing methodology and use of
electronic health records are consistent throughout Air Force MTFs. For those existing hard copy
original paper medical records in the MTF that may need a replacement folder see Table 5.1 for
preparing outpatient records folders and Attachments 6, 7, 8 and 9.
Table 5.1. Preparing Outpatient Record Folders Table.
If the patient is:
Use Social security number of:
AD/ARC
Member
Family Member
Sponsor
Family Member and RC Service Member
Sponsor
Civilian Employee
Employee
Retired Military
Retired Military (Note paragraph
5.10.4.)
Civilian Emergency
Patient
5.10.1. Dual eligibility presents a concern for both medical records personnel and clinicians.
Medical records personnel must ensure that the correct Social security number is used when
138 AFMAN41-210 10 SEPTEMBER 2019
creating the Service Treatment Record/Non-Service Treatment Record for a dual eligible
member who presents for care at the MTF. (T-0). In accordance with DoDI 1000.13 and AFI
36-3026_IPV1, medical records personnel will create a record based upon the highest level of
eligibility. (T-0). Refer to paragraph 4.7 for additional information regarding multiple same-
patient dual eligibility situations. However, for this section, the two most notable dual eligible
scenarios that usually apply to medical records are covered:
5.10.1.1. A dependent who is also a member of the RC. Usually, in this instance, the
dependent is a spouse of another AD or retired military member. However, another
possibility may indicate that the dependent is a child (son or daughter); under 21 years of
age or under 23 years of age if enrolled in a full-time college program.
5.10.1.2. The second likely scenario may be a dependent spouse who is also a retired
military member.
5.10.2. Generally, medical records personnel should create a record based upon the highest
level of eligibility. If a cross-reference situation exists, specifically for family members who
are also RC service members, locate the block labeled, “Specify Service & Grade for Military
& Retired Military Member,” near the middle of the front of the outpatient medical record
jacket. Of the three categories, select the NONMILITARY category. This is the selection that
should correspond to the patient’s primary MTF dependent empanelment status. Then blot the
corresponding square/block. Next, print the member’s dependent status and Social security
number here and status as a member of the AFR or ANG, or other multi-service RC as
appropriate. Additionally, print in black felt-tip marker or stamp the words, “CROSS-
REFERENCE” in 2-inch block letters on the upper left side of the front of the jacket.
5.10.3. Outpatient medical and dental records for (Category A) RC service members are
usually maintained with the member’s reserve unit. Already existing paper based records will
be maintained as listed below. Only create one electronic health record per dual eligible
patient. If the RC service member is also a family member-dependent, another outpatient
medical record should be created at the servicing MTF to document all medical care the patient
received under the dependent patient category. The following provides guidance for
establishing two record volumes – using 000-00-0000 as the patient’s Social security number
and 999-99-9999 as the sponsor’s Social security number:
5.10.3.1. Volume 1 will be the primary record used for the dependent information (30/999-
99-9999). Dependent documentation will be filed in this record jacket (99-RED). The
label should be the printed label from CHCS (30/999-99-9999). Write “CROSS-
REFERENCE” on the cover and annotate RC/AD family member prefix/social security
number 20/000-00-0000.
5.10.3.1.1. File the record in the main central file with a Charge-out Guide. Inside the
guide place a word document referring to the separate RC record, e.g., “STOP! This
member is also a Reservist/Individual Mobilization Augmentee/ANG Member.
Separate RC record maintained on xxxxxx shelf.”
5.10.3.1.2. In the small pocket where the AF Form 250 would go, print/place an extra
label from CHCS that states where to re-file the guide on the shelf.
5.10.3.2. Volume 2 will be the record used for the RC/AD paperwork (20/000-00-0000).
Activated RC service member documentation will be filed in this jacket (00-ORANGE).
AFMAN41-210 10 SEPTEMBER 2019 139
The label can be handwritten OR, if printed label from CHCS is used, cover the 30/999-
99-9999 family member prefix/social security number with a label or white tape and
annotate the correct family member prefix/social security number for this record (20/000-
00-0000).
5.10.3.2.1. Write “CROSS-REFERENCE” on the cover and annotate “RC/AD family
member prefix/social security number 20/000-00-0000.”
5.10.3.2.2. File the record in a separate location from the main central file.
5.10.3.3. When records are retrieved for appointments by exception, pull both volumes,
the dependent record and the RC/AD record, and wrap a rubber-band around both record
volumes. Ensure the clinic staff knows in which record to annotate the encounter.
5.10.4. Military retired patients who are also eligible for care as a dependent spouse may
produce a unique situation when selecting appropriate CHCS automated system registration
formats and when creating the corresponding outpatient medical record. Generally, medical
records for dual or multiple healthcare eligibility patients should be created using the family
member prefix and social security number that corresponds to highest level of eligibility or
according to the patient category that is most advantageous to the patient.
5.10.5. If a beneficiary has received medical care under a previous social security number as
a result of remarriage to another military sponsor, record forms filed under the former Social
security number should be consolidated under the current sponsor Social security number.
Once the patient has been registered in CHCS under the current sponsor’s Social security
number, merge the old and new patient file. For future inquiries, a cross-reference from the
old number to the new number should be indicated in the outpatient files as well as in the
current automated system.
5.10.6. A temporary or pseudo Social security number may be created for beneficiaries
without a Social security number. This process occurs in DEERS when the personnel
technician issues an identification card or enters the beneficiary into DEERS. Either a Foreign
Identification Number or a Temporary Identification Number is generated.
5.10.7. Civilian Emergencies. No paper based records will be created for civilian
emergencies. Already existing records will be filed by Social security number in a manila
folder and maintained separately from the main file if desired. However, they must be
interfiled by Social security number with the rest of the records when retired to National
Personnel Records Center. (T-1).
5.10.8. Civilian employees [including Air Reserve Technicians] who are also members of a
RC will have one medical record maintained as indicated in paragraph 5.14. The only
exception will be if the individual is not employed as a civilian at the same base where the
individual’s RC unit is assigned. In these cases, a civilian medical record will be maintained
as described in the beginning of this paragraph. Civilian employees who are also assigned to
a Personnel Reliability Assurance Program/Presidential Support Program or Sensitive Duties
Program position or job will have one medical record maintained as indicated in paragraph
5.12.5.7 until such time as they are removed from the program or are transferred to another
federal agency or separated from federal service.
140 AFMAN41-210 10 SEPTEMBER 2019
5.10.9. When individuals who are not attached to the base are receiving medical care on base
(for example, Air Force Institute of Technology (AFIT) students), identify their records by
entering their status on the record folder, in pencil. Do not forward these records except at the
patient’s specific request.
5.11. Labeling File Folders.
5.11.1. AF Forms 2100A Series, Forms 2100A, 2110A, 2120A, 2130A, 2140A, 2150A,
2160A, 2170A, 2180A and 2190A, Health Record – Outpatient.
5.11.2. Select an Air Force form in the 2100A series according to the last two digits of the
applicable Social security number:
Table 5.2. Terminal Digit Health Record Filing System.
Last two digits of Social
security number:
Use AF Form:
00-09
2100
10-19
2110
20-29
2120
30-39
2130
40-49
2140
50-59
2150
60-69
2160
70-79
2170
80-89
2180
90-99
2190
5.11.3. Print the first name, middle initial, and last name of the patient in the space provided
with a black pen or black felt-tip marker. Address labels prepared by the Personnel Data
System may be used to provide names of military personnel. Do not use pencil for any entry
except rank. Always place information in the upper right-hand corner of the cover in the
patient Identification area.
5.11.4. Print the sponsor’s Social security number in the preprinted blocks in the upper right-
hand corner of the record.
5.11.4.1. Print the family member prefix in the two circles next to the Social security
number. Check the TRICARE DEERS website for the DEERS Dependent Suffix for the
patient or if not available, number in birth date order for family member children.
5.11.4.2. The family member prefix will not change as long as the patient is still associated
with the same sponsor and social security number.
5.11.4.3. When a military member marries a person with children, assign family member
prefix numbers in sequence following the last family member prefix already assigned to
children of the sponsor (if any). Assign the oldest child the next number in numerical
sequence, etc.
5.11.4.4. Spouse Prefix Assignment: Assign the family member prefix “30” to the first
spouse authorized care. If the member remarries due to spousal death, divorce, etc., assign
AFMAN41-210 10 SEPTEMBER 2019 141
the number “31” to the next authorized current spouse. Increase prefix numbers by 1 (e.g.,
32, 33) for any additional dependent spouse authorized care. Only one current dependent
spouse is authorized medical care.
5.11.4.5. Un-remarried Former Spouses: All un-remarried former spouses are now self-
sponsored. Un-remarried former spouses who have met the requirements in accordance
with AFI 36-3026_IPV1 are treated in the MTF as their own sponsor. Create medical
records for these patients using a “20” family member prefix and the un-remarried spouse’s
own social security number. If the patient’s previous record, filed under the deceased
sponsor’s Social security number, is still in the file, remove the documents and place in
this new record. Annotate previous folder with cross reference to new folder. If the patient
is still in CHCS under the deceased sponsor’s Social security number, work with the
Systems Office to correct. See paragraph 2.7 for more definitive information regarding
authorized care for former spouses of military members.
5.11.5. Standard Folder Markings: Blot out the ½ inch square block, along the right edge of
the rear leaf of the folder that corresponds to the sponsor’s last Social security number digit.
Use a black pen, black felt-tip marker or ½ inch-wide black tape. If a pen or marker is used,
be sure to darken the digit block on the reverse side of the record jacket. For tape, cover the
appropriate digit on the front side of the folder, then fold an equal amount of ½ inch-wide tape
to the rear side of the folder and cover the digit on the reverse. Keep tape cuts neat and even.
5.11.5.1. Do not make any entries in the small preprinted, numbered blocks, the “R” and
“S” blocks at the top of the folder, or the “R” and “S” blocks on the side of the folder (these
are for Army use only).
5.11.5.2. On the front leaf cover, on the right side of the record jacket, blot out the year
that corresponds to the patient’s most recent documented visit with a black pen or black
felt-tip marker. Note: Do not prepare another folder if the available year selections on the
original record jacket fill-up. Attach AF Form 2700L, Health Record Year Grid, to AF
Form 2100A series over the old year markings.
5.11.5.3. Located near the center of the outside of the record jacket, in the block labeled,
Specify Service, Grade for Military and Retired Military Member, select the appropriate
category, blot the corresponding block, and document the patient’s status. Enter the
Service and rank for AD and retired military personnel. Enter the country for non-United
States military personnel. (A copy of the non-United States military member’s orders
should be placed in the health record). Use pencil for rank only. See paragraph 5.10.5 for
family members who are also members of the AFR or ANG.
5.11.6. Personnel Reliability Assurance Program/Presidential Support Program, or Sensitive
Duties Program Folder Markings: Use red pen, red permanent marker or red tape instead of
black to identify a Personnel Reliability Assurance Program/Presidential Support Program
member’s folder. Cover the appropriate last Social security number digit (both sides of the
record jacket) located along the folder’s right edge.
5.11.6.1. Stamp or label the outside of the record jacket with the abbreviation “PRP” or
“PSP” in approximately 2-inch red block letters. The stamp marking should be placed on
the left hand side of the front of the record jacket to identify persons who participate in the
142 AFMAN41-210 10 SEPTEMBER 2019
Personnel Reliability Assurance Program. Cover the red marking with a black marking or
black tape when a member is removed from the program. All other colors are unauthorized.
5.11.6.2. An AF Form 745 will be affixed to Section 2 of the active Volume of the
outpatient medical record. Note: In existing records, the use of the AF Form 745 in
closed/inactive volumes is authorized, but not required.
5.11.7. Aerospace or Flight Medicine Record Markings: To help identify patients in the
categories listed in paragraph 5.13.5., blot out with black pen, black felt-tip marker or place a
½ inch-wide strip of black tape along the right side of the folder beginning at the bottom of the
“9” block and end at the bottom of the folder. Cover the “R” and “S” blocks. One inch-wide
black tape may also be used. If using 1 inch-wide tape, place the tape on the folder so that half
of the strip folds to the rear side of the folder. If a marker is used, mark out the same distance
on the rear of the folder jacket. If the record is filed in a filing cabinet instead of on a shelf,
apply another narrow strip of black tape to the top edge of the rear folder leaf. Ensure the tape
strip covers both the “R” and “S.” Start tape strip over the left side edge of the first numerical
digit block of the sponsor’s last 4 digits of the Social security number and continue to the right
edge of the numerical digit block “9” at the top of the folder. Place the tape on the folder so
that half of the strip folds to the rear side of the folder. Never cover the family member prefix
or social security number.
5.11.7.1. Stamp or label the outside of the record jacket with the word “FLY” (ALL IN
CAPS) in approximately 2-inch black block letters. The stamp marking should be placed
on the left hand side of the front of the record jacket to identify persons who participate in
an aerospace/flying program or dependents of persons who participate in an
aerospace/flying program.
5.11.8. Stamping or labeling the front cover of the medical record with any large-letter
identifiers other than a) FLY, b) PRP or PSP, c) CROSS-REFERENCE, d) with infant-
adoption related notifications (see paragraph 4.3.3.1.) or, e) MEDICATION ALLERGIES is
discouraged.
5.11.9. If the patient is a food handler, the Force Health Management office enters the date of
the current food handler examination in pencil on the appropriate line of the preprinted format.
5.11.10. If the patient is allergic to medication, display this information prominently under the
patient identification data on the right hand side of the folder.
5.11.11. Attach the CHCS Medical Record Tracking bar code label to the health record folder
in the upper right hand corner. See the Medical Record Tracking, Retirement and Retrieval
User Guide for instructions on label requirements.
5.11.12. Acknowledgement of Notice of Privacy Practices. Each patient will receive a copy
of the MHS Notice of Privacy Practices. (T-0). See AFI 41-200, paragraph 3.2 for additional
information on providing the notice and documenting receipt. Reference DoDM 6025.18.
5.12. Contents of the Outpatient Record.
5.12.1. Outpatient records must contain enough information to identify the patient, support the
diagnosis/condition, justify the care, treatment, and service, accurately document the results of
care, treatment and service rendered, and promote continuity of care. (T-1). Documents will
contain the name and location of the MTF maintaining the record to ensure the document is
AFMAN41-210 10 SEPTEMBER 2019 143
sent to the proper MTF. (T-1). The documents will also contain the name of the outpatient
record location. (T-1).
5.12.2. Embossed plastic cards may be used to record patient identification information on
forms. Each document in the record contains, as a minimum, patient’s name, family member
prefix, full Social security number under which the record is to be filed, name of the MTF
maintaining the patient’s record, and name of the outpatient record location. The only
exception is the display sheet on which laboratory and x-ray slips are filed. Since the individual
slips contain the necessary data, it is not necessary to repeat identification information on the
same sheet. However, if the information is not there, it needs to be added.
5.12.3. Paperwork Filing Order for the AF Form 2100A Series, Health Record-Outpatient
(four-part folder). Refer to the tables located at attachment(s) 6-9 in this AFMAN.
5.12.4. Electronically generated forms.
5.12.4.1. Tri-Service Workflow is the standard documentation method for Patient
Centered Medical Home in Family Medicine, Internal Medicine, and Pediatrics for the
entire MHS.
5.12.4.2. No matter the form automation mechanism, when electronically generated forms
are used in place of SF, DD, or Air Force forms, each automated form must contain the
statement “SF, DD or AF Form XXXX (EF) [name and producer/vendor (if any) of the
software used].” (T-1). See Section 5A for guidance on overprinted and electronically
generated forms. Reference DoDI 7750.07-M.
5.12.5. Documenting the DD Form 2766 for AD Service Members/ RC Service Members –
Continuity of Care Documentation.
5.12.5.1. The DD Form 2766 is the primary folder used to document medical and dental
treatment for AD, AFR, ANG, and deployable federal civilian employees while in a
deployed environment. The original outpatient medical and dental records for each
deployed AD, RC service member and deployed federal employee remain at the host base.
During a deployment, the cardstock DD Form 2766 is the only authorized folder used to
document a service member or federal employee’s adult preventative and chronic care
history, unless exempted by COCOM/Component reporting instructions. During non-
deployment periods the DD Form 2766 is filed inside the service member’s outpatient
medical record. Federal civilian employees who have not deployed in support of a
contingency operation should not have a DD Form 2766. Reference DoDI 6490.03.
5.12.5.2. The Tri-Service Workflow Core Alternate Input Method form (“Tri-Service
Workflow Core”) in AHLTA will serve as the initial intake form for all primary care visits
(both AD and non-AD) and serves as the primary mechanism for communicating
continuum of care information between healthcare team members and MTFs.
5.12.5.3. MTF providers and clinical support staff are required to update the Tri-Service
Workflow Core continuum of care elements at each visit, but are not required to review or
update the cardstock DD Form 2766. If information is handwritten on the card stock DD
Form 2766, it should be validated and transferred to the Aerospace Services Information
Management System (ASIMS) DD Form 2766 for AD and ARC service members. The
form should then be marked (with a stamp or hand-printed in bold letters) “Data
144 AFMAN41-210 10 SEPTEMBER 2019
Transferred to electronic ASIMS Form 2766 on (insert date of transfer)” at the top of
each card stock page.
5.12.5.3.1. No medical information is to be hand-written on an ASIMS DD Form 2766
generated document. Information collected on the card stock DD 2766 during a
deployment will be merged with the electronic ASIMS DD Form 2766 within 30 days
following a service member’s return from deployment in accordance with DoDI
6490.03.
5.12.5.3.2. The electronic ASIMS DD Form 2766 will be updated during the annual
Periodic Health Assessment and/or from information obtained from pre and post-
deployment questionnaires, patient interviews, patient-provider encounters, clinical
reviews, and updated prior to any service member PCS. Unless, exempted by
COCOM/Component reporting instructions, the most current version of the ASIMS
DD Form 2766 and DD Form 2766C will be printed and placed into the cardstock DD
Form 2766 (secured with the metal prongs) for all AD and ARC service members
during pre-deployment screening, and prior to completing PCS out-processing for PCS
locations that do not utilize AHLTA. Insert a copy of the most current DD Form 2766
and DD Form 2766C into the cardstock DD Form 2766 for any Federal civilian
employee during the pre-deployment screening process.
5.12.5.4. Absent an automated DoD solution that captures and transfers the same
preventive and chronic care medical information from non-combat host MTFs to a
deployed theater location, the card stock DD Form 2766 will remain a permanent part of
the paper-based outpatient medical record. (T-3).
5.12.5.5. Immediately following the pre-deployment clinical review/screening, photocopy
all sections of the cardstock DD Form 2766 and file the copy in the original outpatient
medical record.
5.12.5.6. For service members assigned to Sensitive Duties Programs (e.g., Personnel
Reliability Assurance Program and Presidential Support Program), MTF records personnel
will attach an AF Form 745, inside the DD Form 2766 cardstock record at the time of
deployment. (T-3). Additionally, stamp “Personnel Reliability Assurance Program” or
“Presidential Support Program” in approximately 2-inch letters on the cover of the DD
Form 2766 prior to a service member’s deployment. Note: This only applies to existing
records.
5.12.6. Documenting Preventative and Chronic Care for Non-AD Adult Beneficiaries.
5.12.6.1. The Tri-Service Workflow Core template in AHLTA will serve as the initial
intake form for all primary care visits (for both AD and non-active-duty adult patients) and
serves as the primary mechanism for communicating.
5.12.6.2. Tri-Service Workflow Core will replace the need for completing the card-stock
DD Form 2766 for non-AD adult beneficiaries. (T-3). All discontinued DD 2766 forms,
already filed in the medical record, must remain in the outpatient medical record. (T-3).
Do not destroy old or seemingly irrelevant medical documents.
5.12.7. Documenting and Filing the DD Form 2882.

AFMAN41-210 10 SEPTEMBER 2019 145
5.12.7.1. This form will be used for all DoD TRICARE Prime pediatric and adolescent
beneficiaries to provide continuity of care in the TRICARE system. (T-3). The form may
also be used for non-TRICARE Prime pediatric and adolescent beneficiaries at the
discretion of the MTF or provider. The DD Form replaces the AF Form 4320. All AF
Forms 4320 and AF Forms 3923 already in the medical records must remain in the
outpatient medical record. (T-3). Do not destroy old or seemingly irrelevant medical
documents.
5.12.7.2. Pages one and two are mandatory for all newborns and all current Service
specific forms used for the summary of care that are worn, torn or which otherwise need to
be replaced. (T-3).
5.12.7.3. Pages 3 and 4 are used to track immunizations and are available for use if there
is not a Service specific form currently in use.
5.12.7.4. Pages 5, 6, and 7 are designed to track clinical preventive services, as identified
by the current edition of the United States Preventive Services Task Force Guide to Clinical
Preventive Services (https://www.uspreventiveservicestaskforce.org) and the
TRICARE Prime benefit package. This form is not intended to be used as current age-
specific recommendations for care of newborns through adolescence ages (0 - 18 years).
5.12.7.5. The DD Form 2882 is available in hard copy only. To obtain copies of the
current form, contact the MTF Forms Management Office.
5.12.7.6. Tri-Service Workflow Pediatric Alternate Input Method forms have replaced DD
Form 2882 for documentation of pediatric and adolescent preventive and chronic medical
information. Although DD Form 2882 has been replaced, it may still be present in original
paper medical records and utilized at locations that do not have access to AHLTA.
5.12.8. Documenting and Transcribing Information from Historical Patient Preventative and
Chronic Care Flow Sheets.
5.12.8.1. Health records support personnel are not authorized to transcribe pertinent
information from the old form to the new form. Only the patient’s Primary Care Manager
medical staff are authorized to transcribe pertinent medical information from this document
to the electronic health record or to another DD Form 2766.
5.12.8.2. Do not remove or destroy the old AF Form 1480, Summary of Care, 1480A,
Adult Preventive and Chronic Care Flowsheet (aka Summary of Care); DD Form 2766; or
DD Form 2882 from the paper outpatient medical record. Keep these documents in
outpatient medical record. Instead, for an outdated DD Form 2766 (from the current filing
position in part I of the AF Form 2100A Series Outpatient Medical record), close the form
and then double hole punch the bottom of the form/folder and replace the form back into
Section I with page 1 of 4 face-up.
5.12.8.3. For service members, place the new DD Form 2766 on top of the old form so
that the form can be opened inside the medical record. Non-AD adult beneficiaries do not
need a replacement DD Form 2766.
5.12.9. Unauthorized Storage of Second, Back-up, or Shadow Files. There will be only one
storage area for medical records. (T-0). Medical information which documents, illustrates,
depicts, or describes clinical data will not be stored in more than one MTF location. (T-0).
146 AFMAN41-210 10 SEPTEMBER 2019
This data includes but not limited to outpatient encounters, dental encounters, inpatient
healthcare, same day surgeries, ambulatory surgery, or diagnostic care. (T-0).
5.12.9.1. Official medical records and medical documents created to permanently
document the healthcare provided to a patient are maintained in either the electronic health
record or officially recognized rigid, cardstock record (for which an approved Air Force or
DoD record/form number exists). Copies of original medical or dental treatment records,
sometimes referred to a “back-up” or “shadow files” kept in any work center for the
purpose of convenience, quick reference availability, or to maintain a clinic mini-file
system, are unauthorized.
5.12.9.2. The minimum official record sets used by the AFMS include: outpatient
medical, dental treatment, inpatient, ambulatory procedure, extended ambulatory, and
mental health record folders. Any officially recognized paper/cardstock record(s) are
stored with like records in a central or decentralized, secure, limited access records file
room(s). Following each individual treatment or patient encounter, and only after all
necessary administrative and/or coding or quality review processes are complete, original
medical or dental treatment forms or records documenting provider-patient interaction, will
be placed or filed into the patient’s electronic health record or applicable cardstock medical
record. Copies will not be maintained anywhere. (T-0).
5.13. Filing Outpatient Records.
5.13.1. “Terminal Digit” Filing System: File records by Social security number, according to
a terminal digit, color-coded and blocked filing system. Divide the central files into 100 equal
sections. Establish a minimum of 100 files guides identifying primary Terminal Digit
numbers, “00” through “99.”
5.13.2. File record folders in numerical sequence according to their secondary numbers within
each section. The secondary number is the pair of digits immediately to the left of the primary
number.
5.13.3. All outpatient records and forms will be maintained in a single numerical file in a
central location except when the MTF commander or director authorizes decentralization of
the numerical file to the patient’s major primary or family care team location or to the Flight
and Operational Medicine Clinic, if applicable, see paragraph 5.13.5. (T-3). The numerical
files of personnel assigned to the Personnel Reliability Assurance Program, Presidential
Support Program or any other sensitive duty program are also maintained in a separate secured
location. See paragraph 5.13.6. In MTFs with authorized decentralized records rooms, the
CHCS Medical Record Tracking function will identify where the numerical file is regularly
stored and will document inter-facility borrower history. Use of AF Form 614, Charge Out
Record will not be required unless the CHCS Medical Record Tracking function is not used or
the MTF Records Custodian deems non-use appropriate.
5.13.4. Annual AD Inventory. MTFs will establish local procedures to perform an annual
inventory of all AD Air Force records by 31 March. (T-1). AFMOA will contact the local
Military Personnel Section and obtain a roster of all assigned and/or attached AD personnel
and provide a copy to medical records personnel. (T-1). Medical records personnel should sort
the roster by terminal digit order. If missing record(s) and/or volumes(s) are discovered during
AFMAN41-210 10 SEPTEMBER 2019 147
the initial audit, records personnel will perform monthly follow-up audits until the missing
record(s) and/or volumes(s) are retrieved or located. (T-1).
5.13.5. Flight and Operational Medicine Records: If authorized by the MTF commander or
director, outpatient records for Airmen and family members empaneled to the Flight and
Operational Medicine Clinic may be maintained in the Flight and Operational Medicine Clinic.
Flight and Operational Medicine records are usually maintained on individuals assigned to: air
crew duty, missile launch duty, air traffic control duty, physiological training duty, parachute
duty, and weapons control duty, and on the family members of Airmen on flight status who
are empaneled to the Flight Clinic.
5.13.6. Outpatient medical and dental treatment records for personnel assigned to the
Personnel Reliability Assurance Program, Presidential Support Program, or any other sensitive
duty program will be maintained in a separate, secured location. (T-3). Again, as mentioned
in paragraph 5.13.3., proper use and management of the CHCS Medical Record Tracking
module will provide MTF personnel with the mechanism to determine where a paper medical
record is located.
5.13.7. Outpatient and dental health records for authorized family members and sponsors who
reside at locations outside of approved MTF TRICARE PRIME enrollment prime service areas
or who are assigned to a) United States Air Force Recruiting Service posts, b) Reserve Officer
Training Corps (ROTC) units, c) GSU, d) authorized TRICARE Prime Remote locales, e)
health records for TRICARE Prime family members enrolled to civilian Primary Care
Managers and f) overseas United States embassy support will be maintained at the nearest
MTF to the member/sponsor’s remote assignment location or home address, whichever is more
advantageous to the sponsor and family member(s). There may be instances when the
responsible Air Force MTF is not the nearest MTF to where the member is assigned or the
family member is enrolled. In these instances, the responsible Air Force MTF must coordinate
with the nearest MTF maintaining the records to ensure the records are correctly processed
when the member retires, separates, receives a PCS to another location or enrolls to another
MTF. (T-2). Family members and sponsors will not hand-carry their Service Treatment
Records/Non-Service Treatment Records to these locations. (T-0). See paragraphs 5.15 and
5.29 for additional instructions.
5.13.8. Splitting Records aka Closing Record Volumes: In order to optimize file space for
current and future outpatient records, it is permissible to split or separate outpatient records
that consist of more than one volume.
5.13.8.1. If an additional record volume is needed or to separate the current volume from
older volumes, records personnel will mark on the front cover of the new outpatient record
volume jacket cover, in the upper left corner or in another area where other identifying
record information is not obscured, in 2” capital letters, with bold, black marker, the
appropriate volume number, e.g., “Volume 2, 3, or 4” or “Volume II, III, or IV,” etc. (T-
3).
5.13.8.2. Login to CHCS and from the Medical Record Tracking module, verify that the
multi-volume record is properly referenced, and if not, create a new electronic volume
reference, print a new bar-scan Identification label and affix to the new record volume
jacket in the upper right corner.
148 AFMAN41-210 10 SEPTEMBER 2019
5.13.8.3. Place the new record volume back into main file and relocate older volume(s) to
a designated location within the secure records department. Label older volume(s) with
the same type of bold, black marker, clearly indicating the volume number and be sure the
bar-scan Identification label reflects the older volume number(s).
5.13.9. Deceased Patients: Place outpatient records of deceased patients in a separate, secured
file location within the records department. Retire the non-AD medical record to the National
Personnel Records Center in accordance with established record retirement procedures. For
records of deceased AD and RC service members, refer to the Sequestered/Deceased
Member’s Records. See paragraph 5.7.2.
5.13.10. Use of AF Form 1942, to manage records is optional. However, if a MTF Records
Custodian chooses to continue using the form, prepare and maintain an AF Form 1942 for each
record permanently forwarded to another facility. Keep the form in an alphabetical file for 180
days, and then destroy. See paragraph 5.29 for further information regarding permanently
transferring medical records to other MTFs.
5.13.11. Record custodians will comply with Air Force records management and maintenance
instructions when maintaining Army and Navy records. (T-1).
5.13.12. When personnel from the United States Army and United States Navy are:
5.13.12.1. Attached to an Air Force facility for medical care, the Air Force assumes
custody of their health records. When patients from other Services are treated in Air Force
facilities and require certain Service specific forms be completed and filed in the records,
the documents will be filed in their record. The documents will be placed in the appropriate
section of their outpatient record based on the type of form.
5.13.12.2. Treated in a MTF but their records are not available, send documents, routinely
included in Air Force outpatient records, to the custodian of their records. If unknown,
forward these documents using guidelines provided in appropriate subsections of
paragraph 5.19.
5.13.13. When Air Force personnel are treated at a United States Army or United States Navy
facility; send the documentation to the MTF where the record is maintained.
5.13.14. Interfile Army and Navy records with Air Force records. Replace folders with the
AF Form 2100A series only if the color and blocking do not permit interfiling.
5.13.15. Do not use the AF Form 2100A series to document or maintain Mental Health or
Family Advocacy notes, documents, or records. These files are separated from the outpatient
record and are secured in either the Mental Health Clinic or Family Advocacy Office.
5.14. Managing ARC Outpatient Records.
5.14.1. Health records for members of the AFR (Category A) and ANG or members of the
ARC who are on tours of active duty for less than 30 days are normally maintained with their
respective medical units, unless a local agreement or memorandum of understanding exists
between the MTF and the ARC unit(s) requires the MTF to maintain them.
5.14.1.1. The MTF may maintain health records for members of the AFR (Category A)
and ANG who have or are, a) placed on AD orders for more than 30 days; b) are currently
empaneled to a MTF Primary Care Manager; or c) the service member or unit has provided
AFMAN41-210 10 SEPTEMBER 2019 149
the MTF records department with the original health record and a copy of the member’s
activation orders. In these instances, the member is required to notify the MTF records
department upon completion or removal from AD and/or removal from active MTF
enrollment.
5.14.1.2. If the service member’s ARC unit does not provide the outpatient medical
records to the MTF during the ARC service member’s period of AD activation and/or
empanelment, the missing outpatient record will not negatively count against the MTF’s
paper records availability and accountability percentages.
5.14.2. Maintain separate paper-based health records for dual or multiple healthcare eligibility
patients, (e.g., a patient who is a family member husband and a RC service member) that have
already been created. Only maintain one electronic health record per dual eligible patient. See
Section 4B for additional guidance regarding dual or multiple eligibility patient record
maintenance. Medical and dental records for Category B (Individual Mobilization
Augmentee) and E (Participating Individual Ready Reserves) are maintained at the Individual
Mobilization Augmentee service member’s servicing MTF usually co-located at or near the
service member’s unit of attachment. Individual Mobilization Augmentee medical and dental
records will be maintained in accordance with the paragraph below. (T-3).
5.14.3. Maintain health records for Individual Mobilization Augmentees (Category B)
according to the following instructions:
5.14.3.1. Maintain records for centrally managed Individual Mobilization Augmentees
(HC, JA, and SG) with the AD MTF unit of attachment.
5.14.3.2. Maintain records of non-centrally managed Individual Mobilization Augmentees
with the AD MTF unit of assignment.
5.14.3.3. Complete an annual inventory of all ARC health records on file as of 31 March.
5.14.3.3.1. Readiness Management Group/Individual Reservist Medical Section
maintains a registry of Individual Mobilization Augmentee/Participating Individual
Ready Reserves records/locations, and can furnish a list of the records identified in
paragraph 5.14.3.1. Notify AFRC/Chief of Aerospace Medicine if records are not
located or if a records transfer (due to reassignment, retirement) is required.
5.14.3.3.2. The inventory will include:
5.14.3.3.2.1. Identify and remove Service Treatment Records of personnel no
longer assigned, or those who have retired or separated.
5.14.3.3.2.2. Identify records which are unaccounted, find or replace the records,
and take actions as required in AFI 41-200, paragraph 6.3.
5.14.3.3.2.3. Report summarized results of the inventory to the Executive
Management Committee.
5.15. Active Association and Geographically Separated Unit Outpatient Records
Management.
5.15.1. An Active Association is a construct which an AFR or ANG Sponsor Organization
shares a mission with one or more Regular Air Force Associate Organizations. The majority
of service members assigned to an Active Association and their family members will be

150 AFMAN41-210 10 SEPTEMBER 2019
enrolled in TRICARE Prime Remote. Similar to GSU, the nearest MTF will maintain the
official health records of Active Association members.
5.15.1.1. The nearest Air Force MTF commander or director and service member’s GSU
commander will ensure mechanisms are in place to access medical documentation
generated from civilian medical facilities and update the service member and family
member’s official health record.
5.15.1.2. For additional details on Active Association refer to AFI 90-1001, Planning
Total Force Association (TFAS) and for best practices AFMOA Health Benefits Kx page
at: https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.15.1.3. Personnel who are assigned to Active Associations will follow the same
guidelines as those assigned to Geographically Separated Units as outlined below this
section.
5.15.2. GSU personnel are AD service members, and their family members, assigned to a unit
with no on-site military medical support, and/or those who reside more than 50 miles or
approximately one hour of driving time from the nearest MTF.
5.15.3. In accordance with DoDI 6040.42, Medical Standards for Medical Coding of DoD
Health Records, all beneficiary medical records are the property of the DoD. Their
maintenance and availability are key to appropriate medical care and legal and administrative
proceedings. As such, the original health records of GSA service members and their family
members (if family members accompany the sponsor) will not be hand-carried or maintained
by the sponsor, the family members, or provided to the sponsor or family members’ civilian
Primary Care Manager Office. Alignment of Geographically Separated Unit s with MTFs for
medical records support will be based on proximity, past history, and Major Command
(MAJCOM) prerogatives. For tips and best practices see AFMOA Health Benefits Kx page at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.15.4. Affix the following statement to the outside of each original health record(s) using an
address label: “Assigned to an Active Association/GSA at or near (Enter City, State, Territory,
or Province name here). In accordance with AFMAN 41-210, Section 5B, DO NOT RETIRE
THIS OUTPATIENT RECORD.” See Figure 5.1 GSA Label.
5.15.5. Place a copy of the sponsor’s PCS orders in Section I of the health record on top of
most current DD Form 2766. Place a copy of the sponsor’s PCS orders in Section I of all
health records of family members identified on the PCS order to depart with the sponsor to the
Active Association/GSU. Forward these records to the appropriate MTF and inform the
sponsor which MTF will maintain their and their family members’ records. AD personnel and
their family members preparing to PCS to an Active Association/GSU may obtain, and hand-
carry, a complete copy of their records to these locations (to be obtained from the losing MTF
prior to departure). Members must request copies of their records no later than 30 days prior
to departure, to allow the MTF sufficient time to fill the request. (T-3). Place the copies in a
new AF Form 2100 Series record jacket. The record jacket of the copy should indicate the
record is a copy and identify the MTF where the official record is being maintained. See Figure
5.2 GSU Record Copy. When the members relocate to a non-remote location, upon in-
processing, they should notify the gaining MTF to request the records from the original losing
MTF.
AFMAN41-210 10 SEPTEMBER 2019 151
5.15.6. Exception for Sensitive Duties Program Participants: The original Service Treatment
Record of service members assigned to a GSU may be required to be maintained or stored at
the unit to maintain sensitive duties program participation. If the original Service Treatment
Record is required to be kept at the unit, the outpatient medical and dental records will be
maintained by the unit commander, and secured in a locked container behind at least one locked
door during non-duty hours. Access is restricted to the commander and the commander’s
designee for the Personnel Reliability Assurance Program, Presidential Support, and FLY
programs. A good example of this type of scenario would apply to service members assigned
to remote Munitions Sites (MUNS) GSU in USAFE-AFAFRICA. The nearest Air Force MTF
commander or director and service member’s GSU commander will ensure mechanisms are in
place to ensure all medical documentation generated from civilian medical facilities are added
into the service member’s Service Treatment Record and that all health records are maintained
in accordance with this manual. (T-3).
5.15.7. The MTF will educate the service members and family members on the process for
receiving medical and dental care at the new assignment. If the service members and family
members will be enrolled into TRICARE Prime Remote, educate beneficiaries on the
TRICARE Prime Remote program and assist with enrollment into the program.
5.15.8. When health record copies are provided, Air Force MTF records personnel will place
a “Property of the U.S. Air Force” label containing the appropriate MTF address on the record
jacket. (T-3). See Figure 5.2 GSU Record Copy.
5.15.9. Miscellaneous or loose medical documents generated by an MTF for Active
Association/GSU members and/or their family members will be scanned into Health Artifact
and Image Management Solution (HAIMS).
5.15.10. Upon reassignment from the Active Association/GSU to a military installation and
subsequent MTF Primary Care Manager assignment, the gaining MTF will send a DD Form
877 or DD Form 2138, so that the member’s original outpatient medical record(s) are
forwarded to the new location. Upon receipt of the original health record, cover the GSU label
with a blank label, create a new facility location label, and remove the PCS order to the
previous GSU location. The gaining MTF/Primary Care Manager shall complete a release of
information authorization for the patient to request copies of medical record documentation
from their civilian provider to be added into the official medical record. (T-3).
5.15.11. The MTF will educate the service members and family members on the process for
receiving medical and dental care at the new assignment. If the service members and family
members will be enrolled into TRICARE Prime Remote, educate beneficiaries on the
TRICARE Prime Remote program and assist with enrollment into the program.
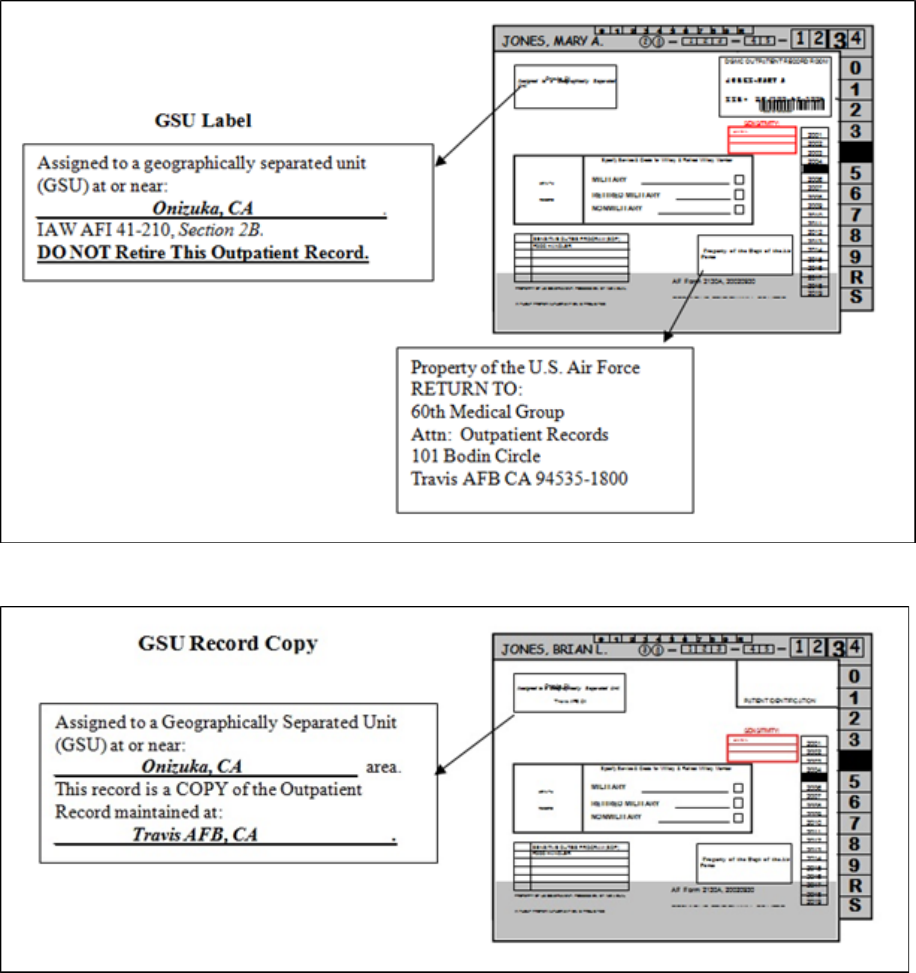
152 AFMAN41-210 10 SEPTEMBER 2019
Figure 5.1. Sample GSU Label
Figure 5.2. Sample GSU Record Copy
5.16. Custody and Control of Health Records.
5.16.1. Beneficiary health records are the property of the United States Government. The
information contained in the record belongs to the patient. In accordance with the Privacy Act
of 1974 and HIPAA of 1996, the patient has the right to the information in the record.
However, the maintenance of the record at the MTF is a legal requirement. Refer to DoDI
6040.42. Agency obligations mandate the health records be available for continuity of care
purposes and to support national accreditation and DHA clinical coding auditing actions. The
lack of medical records and documentation may adversely impact individual patient medical
continuity of care as well as Joint Commission accreditation. Generally, beneficiaries are not
AFMAN41-210 10 SEPTEMBER 2019 153
authorized to hand-carry their health records in accordance with DHA policy and Air Force
policy identified in this manual. Local MTF records management policy must include
measures to (T-1):
5.16.1.1. Establish a methodology to obtain beneficiary medical record(s) upon arrival on-
station if hand-carried.
5.16.1.2. Establish custody of the health record upon the patient’s initial visit.
5.16.1.3. Ensure health records are available so that patients may obtain a copy of their
complete medical record. Refer to paragraph 4.4 for instructions on responding to patient
requests for copies of health records.
5.16.2. MTF personnel will not return an original medical or dental record to the patient’s
control after an outpatient visit unless authorized to do so by the MTF commander or director.
(Only on a case by case basis.) (T-3).
5.16.3. All miscellaneous, loose or late-flowing documents must contain sufficient patient
identification information to allow for proper scanning into HAIMS and or filing into paper
record when authorized in accordance with paragraph 5.12. (T-3). Additionally, these
documents must identify the outpatient records location and the MTF where the record is
maintained. (T-3).
5.16.4. Generally, borrowed records will be returned to the MTF record section by the end of
the day. However, records may be charged out or borrowed by an internal MTF requester for
up to five days if the record is needed to accomplish an official task, audit, review, etc. The
borrower must provide the rank (if applicable), first and last name, office symbol, name of
duty or work location, and telephone contact number. (T-3). The record must be returned to
the records library as soon as possible. (T-3). The records department supervisor may grant
extensions to the 5-day rule on a case-by-case basis. While in the borrower’s possession, the
record(s) must be secured and immediately produced upon request if required for patient care.
(T-3). When an extension is granted, “RE-CHARGE” the record to the borrower.
5.16.5. Service Treatment Record and Non-Service Treatment Record In-processing. Upon
receipt of each new Service Treatment Record not already maintained in the MTF records file
system, outpatient records personnel will perform a quality assurance inspection of the medical
record. (T-3). Inspection checks shall include the following, but are not limited to: a) ensure
the health record jacket is in satisfactory condition and labeled/documented properly, b) ensure
that medical documents are filed in their appropriate place, c) remove any misfiled wrong-
patient documents and forward the documents to the appropriate patient record or MTF, and
d) ensure Service Treatment Records contain the patients’ complete history of documented
healthcare (including all record volumes). (T-3). In the event a record is missing (i.e. received
Vol. 2 without Vol.1) the gaining MTF will contact the losing MTF to retrieve the missing
record. The losing MTF will mail the missing record as soon as possible but no later than five
days after request. (T-3).
5.16.6. As often as necessary, and whenever medical documents are filed into a health record,
records personnel will correct any obvious misfiles or other noticeable errors in each health
record. (T-3). MTFs should establish local guidance to best facilitate this process.
154 AFMAN41-210 10 SEPTEMBER 2019
5.16.7. Using Charge-Out Guides. Use AF Forms 885, 886, and 887 and AF Form 250, to
indicate the location of an outpatient record removed from the file. Use of the Medical Record
Tracking module in CHCS is required as a tool to track movement of outpatient records. (T-
3). It also enhances the management of records accountability and availability.
5.16.8. Authorized Exceptions that Allow Service Members to Hand-Carry Their Health
Records.
5.16.8.1. Every effort should be made to ensure patients do not leave the MTF with their
records unless authorized to do so. However, paragraph 5.30.1 and the two reasons below
indicate when MTF records managers are allowed to provide health records to
beneficiaries.
5.16.8.1.1. Exception #1. Applies to service members assigned to: Personnel
Reliability Assurance Program, Presidential Support Program, and overseas United
States embassy support. These members may also hand-carry their dental records. See
paragraph 5.28 for additional Personnel Reliability Assurance Program records transfer
instructions.
5.16.8.1.2. Exception #2. The MTF commander or director (Custodian of Records)
or delegate is authorized to grant exceptions (in writing) to this policy on a case-by-
case basis to satisfy unique individual situations where providing the original medical
and/or dental records to the requesting beneficiary is in the patient’s and/or the
government’s best interest. MTF commanders or directors may not issue general
blanket orders or MTF policy that allows any beneficiary to hand-carry medical or
dental records without careful analysis of all of the circumstances surrounding the
individual request. Additional exceptions may include circumstances in which a
significant inconvenience to the patient may occur or where continuity of care may be
negatively impacted if records were to be mailed. No sponsor is authorized to possess
or hand-carry the original health records or copies of health records for any member of
his family aged 18 years or older without written authorization from the family
member.
5.17. Filing Outpatient Computer Generated Clinical Diagnostic Results.
5.17.1. Daily filing of outpatient clinical diagnostic and/or test results is generally no longer
required. Diagnostic results and tests are easily obtained using available automated computer
system clinical diagnostic and test results retrieval mechanisms.
5.17.1.1. If there is a particular standard in the local community that requires the
maintenance of hard copy diagnostic test results or specifically prohibits the storage of
these results in electronic media, then the MTF must also comply. (T-0). Otherwise, there
is no requirement to print and file (into the paper outpatient medical record) a hardcopy
diagnostic or clinical test result.
5.17.1.2. Prior to any PCS reassignment, personal geographic location move, MTF
reassignment, or change to TRICARE enrollment location, MTF records personnel will
identify and print any CHCS laboratory, radiology, and/or clinical diagnostic results that
have accumulated from the departure or losing MTF for each departing beneficiary that are
not available in AHLTA due to age (i.e. prior to 2004/2005 depending on the
implementation date of AHLTA at the specific MTF). (T-2). This rule applies to Services
AFMAN41-210 10 SEPTEMBER 2019 155
Members, retirees, and family members alike. The losing MTF must still transfer the paper
record to the gaining MTF. (T-3). The gaining MTF will usually not be able to access or
view older clinical diagnostic reports and information completed and stored at another
MTF or on a CHCS host computer server other than their own. These procedures are
required to ensure the gaining MTF has access to the beneficiary’s complete health record.
5.18. Researching Appropriate Host MTF Record Locations.
5.18.1. Scan health record documents in the appropriate electronic health record as soon as
possible. The practice of blindly mailing medical documents or records to the MTF closest to
where the beneficiary lives or works is prohibited. (T-1). Confirmation of the exact MTF
responsible for maintaining the beneficiary’s health record(s) is required. If confirmation
cannot be obtained, then contact the specific Uniformed Service personnel office according to
the instructions in the following sections.
5.18.2. AD Service Members: AD service members may incur several PCS assignments;
same station - Permanent Change of Assignment (PCA) relocations; TDY, deployments, and
personal Leave absences that may include travel to various locations throughout the United
States and abroad. Along the way, MTF medical records personnel may receive medical
documents from internal facility clinics for AD patients who have received transient medical
care during these periods. Whatever the reason, the process of tracking down and locating
current duty assignment stations is sometimes challenging. Several options for locating the
primary record custody locations are listed below.
5.18.2.1. Primary AD Research Methods: Locate a patient’s primary record location by
accessing the CHCS-DEERS eligibility menu option or by referencing the General Inquiry
of DEERS Internet website at https://www.dmdc.osd.mil/opsconnect/. Defense Medical
Information System Identification location, military installation name, and current patient
address are listed. Sponsor Social security number is required to complete search. User
Identification and personal password are required to access this website application.
Contact the Site Security Manager (SSM) to obtain necessary access. Contact
AFMOA/SGAT if the Site Security manager is not known.
5.18.2.2. Alternate Methods:
5.18.2.2.1. When researching Air Force service member, access the Air Force Portal
website’s “White Pages” locator at https://www.my.af.mil/. User Identification and
personal password are required. Additionally, the Air Force Global e-mail directory
may be used as another alternative reference method.
5.18.2.2.2. Although not a medical records or MTF locator, the DefenseLink Internet
website at http://www.defenselink.mil/faq/pis/PC04MLTR.html may be of some
limited use when researching an individual service member’s duty address or duty
contact information.
5.18.3. Family Members, Retired Military Members, and Other Non-Military Personnel:
Health records of Air Force AD family members are usually maintained at the MTF where the
sponsor is assigned unless the sponsor is stationed at a remote or unaccompanied tour
assignment. File medical documents for family members of AD or retired military in the
medical record at the MTF where the majority of care is provided or where the dependents are

156 AFMAN41-210 10 SEPTEMBER 2019
empaneled or enrolled in TRICARE. If the medical document(s) do not belong at the MTF
where the research is accomplished, follow the instructions below.
5.18.3.1. Research Methods for Family Members, Retired Military Members, and Other
Non-Military Personnel: Locate a patient’s primary record location by accessing the
CHCS-DEERS eligibility menu option or by referencing the General Inquiry of DEERS
Internet website at https://www.dmdc.osd.mil/opsconnect/. Defense Medical
Information System Identification location, military installation name, and current patient
address are listed. Sponsor Social security number is required to complete search. User
Identification and personal password are required to access this website application.
Contact the SSM to obtain necessary access. Contact AFMOA/SGAT if the Site Security
Manager is not known.
5.18.3.2. In all other cases where the record cannot be located use the patient’s
identification to scan the documents into the approved electronic health record.
5.18.4. If patient cannot be properly identified, return document(s) to the originating clinic for
required identification data completion.
5.18.5. Develop local procedures between clinic and ancillary services personnel to correct
errors and avoid omissions. Do not ask the patient to return an improperly completed form to
the originator.
5.18.6. If the referring clinic cannot sufficiently identify the documents for filing/scanning,
contact the Medical Record Review Committee chairperson or the Chief of Medical Staff. If
after an extensive review the documents in questions cannot be identified by name, Social
security number, date of birth, or by any other available means, the Record Review Committee,
with approval from the Chief of Medical Staff, may destroy unidentifiable health documents.
5.19. Loose Leaf, Orphaned, or Miscellaneous Medical Documents.
5.19.1. Health record documents, separated from the primary health record will follow the
HAIMS guidance referenced in paragraph 5.4.10.2.1.
5.19.1.1. AD Air Force Personnel. Locate a patient’s primary record location by accessing
the CHCS-DEERS eligibility menu option or by referencing the General Inquiry of DEERS
Internet website at https://www.dmdc.osd.mil/opsconnect/. Follow the same instructions
as listed in paragraph 5.18.2.1. If there is not enough patient data listed on the form(s) to
properly identify the patient, then submit the documents to the MTF Health Records
Committee. The committee is authorized to order the destruction of unidentifiable medical
documents. Do not send loose or unidentifiable medical documents to the AFPC Service
Treatment Record disposition center or to the AFPC world-wide personnel locator office.
5.19.1.2. AFR Personnel. Although the CHCS-DEERS eligibility menu option or the
General Inquiry of DEERS Internet website may not identify the service member’s AFR
location, it may identify the individual’s home address, unit Personnel Accounting Symbol
Code, and/or last known AD Defense Medical Information System Identification location
(if the service member was activated at some point in the recent past). Follow the same
instructions as listed in paragraph 5.18.2.1. If unable to locate member’s primary records
custody location, or if there isn’t enough patient data listed on the form(s) to properly
identify the patient, and/or the service member’s unit, contact the AFRC Command

AFMAN41-210 10 SEPTEMBER 2019 157
Surgeon’s Office, Robbins Air Force Base, Georgia (GA) for additional guidance. Do not
forward medical documents to AFRC without prior approval from an AFRC official.
Furthermore, do not forward dependent or retiree health records or loose/orphaned
documents to AFRC, nor to any AFR unit as they do not maintain records for retirees or
dependents.
5.19.1.3. ANG Personnel. Although the CHCS-DEERS eligibility menu option or the
General Inquiry of DEERS Internet website may not identify the service member’s Guard
Medical Unit location, it may identify the individual’s home address, unit Personnel
Accounting Symbol Code, and/or last known AD Defense Medical Information System
Identification location (if the service member was activated at some point in the recent
past). Follow the same instructions as listed in paragraph 5.18.2.1. If unable to locate
member’s primary records custody location, or if there isn’t enough patient data listed on
the form(s) to properly identify the patient and/or member’s unit, contact Office of the Air
Surgeon (NGB/Chief of Aerospace Medicine), NGB, Joint Base Andrews, Maryland, for
additional guidance. Do not forward medical documents to NGB without prior approval
from a NGB official. Furthermore, do not forward dependent or retiree health records or
loose/orphaned documents to this HQ command, nor to any ANG Unit as they do not
maintain records for retirees or dependents.
5.19.1.4. United States Air Force Individual Mobilization Augmentee Personnel. Locate
a patient’s primary record location by accessing the CHCS-DEERS eligibility menu option
or by referencing the General Inquiry of DEERS Internet website at
https://www.dmdc.osd.mil/opsconnect/. Follow the same instructions as listed in
paragraph 5.18.2.1. If unable to locate member’s primary records custody location, or if
there isn’t enough patient data listed on the form(s) to properly identify the patient, and/or
Individual Mobilization Augmentee’s unit of attachment, contact Readiness Management
Group/Individual Reservist Medical Section, Warner Robins Air Force Base, Georgia, for
additional guidance. Do not forward medical documents to AFRC without prior approval
from an AFRC official. Do not forward dependent family member or retiree service
member health records to this command.
5.19.1.5. United States Army Personnel. Forward United States Army health records or
document(s) according to the instructions listed below:
5.19.1.5.1. Locate a patient’s Primary Care Manager and primary record location by
referencing the General Inquiry of DEERS Internet website at
https://www.dmdc.osd.mil/opsconnect/. Defense Medical Information System
Identification location, military installation name, and current patient address are listed.
Follow the same instructions as listed in paragraph 5.18.2.1. If unable to locate
member’s primary records custody location, forward AD officer, warrant officer, and
enlisted health records to:
AMEDD Record Processing Center
3370 Nacogdoches Road, Suite 116
San Antonio, TX 78217
5.19.1.6. United States Navy Personnel. Forward United States Navy health records or
document(s) according to the instructions listed below.
158 AFMAN41-210 10 SEPTEMBER 2019
5.19.1.6.1. Locate a patient’s primary record location by accessing the CHCS-DEERS
eligibility menu option or by referencing the General Inquiry of DEERS System
Internet website at https://www.dmdc.osd.mil/opsconnect/. Defense Medical
Information System Identification location, military installation name, and current
patient address are listed. Follow the same instructions as listed in paragraph 5.18.2.1.
If unable to locate member’s primary records custody location, then draft and forward
a generic letter with the name and Social security number of the AD, Reserve, or retiree
to the Department of the Navy, Navy Personnel Command (NPC), PERS-312, 5720
Integrity Drive, Millington, TN 38055-3120, commercial voice contact at (901) 874-
3388, DSN Voice at 882-3388, or FAX to DSN 882-2766. The NPC should provide
advice as to whether the document(s) and/or record(s) should be retired to National
Personnel Records Center or to the VA Records Management Center. For more
information, visit the United States Navy Personnel Command website at
http://www.npc.navy.mil/.
5.19.1.7. United States Marine Corps Personnel. Forward United States Marine Corps
health records or document(s) according to the instructions listed below.
5.19.1.7.1. Locate a patient’s primary record location by accessing the CHCS-DEERS
eligibility menu option or by referencing the General Inquiry of DEERS Internet
website at https://www.dmdc.osd.mil/opsconnect/. Defense Medical Information
System Identification location, military installation name, and current patient address
are listed. Follow the same instructions as listed in paragraph 5.18.2.1. If unable to
locate the member’s primary records custody location, forward the medical record(s)
or form(s) to the United States Marine Corps (USMS) Worldwide Locator Service,
Commandant of the Marine Corps, Headquarters USMC, Code MMSB-10, Quantico,
VA 22134-5030.
5.19.1.8. United States Coast Guard. Locate a patient’s primary record location by
accessing the CHCS-DEERS eligibility menu option or by referencing the General Inquiry
of DEERS) Internet website at https://www.dmdc.osd.mil/opsconnect/. Defense Medical
Information System Identification location, military installation name, and current patient
address are listed.
5.19.1.9. United States Public Health Service Commissioned Corps records or documents
with a complete name and social security number should be forwarded to the Office of
Commissioned Corps Support Services, Medical Branch, 5600 Fishers Lane, Parklawn
Building, Room 4C-04, Rockville, MD 20857-0435.
5.19.1.10. National Oceanic and Atmospheric Administration records or documents with
a complete name and social security number, should be forwarded to:
U.S. Public Health Service
Commissioned Personnel Center
Attn: CDR Hobson-Powell
National Oceanic and Atmospheric Administration
8403 Colesville Road, Suite 500
Silver Spring, Maryland 20910.

AFMAN41-210 10 SEPTEMBER 2019 159
5.19.1.11. Retired Military and Family Members. Locate a patient’s primary record
location by accessing the CHCS-DEERS eligibility menu option or by referencing the
General Inquiry of DEERS Internet Website at https://www.dmdc.osd.mil/opsconnect/.
Defense Medical Information System Identification location, military installation name,
and current sponsor/patient address are listed. Sponsor’s social security number is
required. If unable to locate the family member’s Primary Care Manager and/or primary
records custody location, place the loose documents in a charge-out guide and follow
instructions listed in paragraph 5.18.3.1.
5.19.2. Remember to identify the primary health records custody location Identification for all
patient categories, in all services. First try the CHCS-DEERS System eligibility menu option,
then reference the General Inquiry of m Internet Website at:
https://www.dmdc.osd.mil/opsconnect/. Finally, be sure to follow the individual Uniformed
Services forwarding instructions or contact the agency in question before mailing the
documents via the United States Postal System.
5.19.3. If the gaining/servicing MTF cannot be clearly identified, do not mail the medical
documents or record. Mailing medical documents or records to the MTF closest to where the
beneficiary lives or works is prohibited. Confirmation of the exact MTF responsible for
maintaining the beneficiary’s health record(s) is required. The losing MTF must maintain the
record until it is requested or eligible for retirement to National Personnel Records Center. (T-
3).
5.19.3.1. National Personnel Records Center. For loose documents belonging in records
stored at National Personnel Records Center and those recalled from National Personnel
Records Center.
5.19.3.2. When loose documents are identified but the original medical record has already
been transferred to the National Personnel Records Center, then:
5.19.3.2.1. Place documents in a folder (manila folder is acceptable).
5.19.3.2.2. Label the folder with the patient identifiers using a standard CHCS label to
include at a minimum; last name and first name, sponsor social security number, patient
date of birth, and record volume number (e.g., volume 2). Note: the label can be
handwritten vs. CHCS output.
5.19.3.3. Add the record to the retirement index (via CHCS) for transfer to National
Personnel Records Center in accordance with the disposition rules in AFRIMS.
5.19.3.4. Do not mail or return recalled records to National Personnel Records Center
directly. Recalled records must be created within CHCS as a new volume and retired when
eligible in the MTF’s next scheduled retirement. (T-3).
5.20. Missing and Lost Health Records.
5.20.1. Health records, both in electronic and paper form are considered PHI and Personally
Identifiable Information subject to HIPAA and the provisions of the Privacy Act. Once a health
record is deemed “lost,” specific steps must be taken in order to report the information and
notify the affected beneficiary or party. (T-3).
5.20.2. There are several instances when a health record may be considered “missing.” Some
of the most common examples are:
160 AFMAN41-210 10 SEPTEMBER 2019
5.20.2.1. A health record may be considered “missing” immediately following a record
room supervisor’s investigation of the circumstances surrounding the record’s
disappearance.
5.20.2.2. When a health record is discovered missing from the main Record File with no
documented borrower location or date.
5.20.2.3. When a record is discovered missing from the main Record File with a
documented borrower location and date, but the physical record has not returned to the
Main File following a period of 30 calendar days or more - without a documented
explanation.
5.20.3. MTFs must exhaust all reasonable means to locate a missing health record. (T-1).
When records are discovered to be missing, each MTF staff member is responsible for
searching their immediate work area(s). MTF personnel will mobilize and help search for a
missing record.
5.20.3.1. The following procedures are required after discovering a record is missing:
Check to identify possible borrower charge-out locations in the automated Medical Record
Tracking module; check for record misfiles in each record storage room; search provider
offices and exam rooms; ensure the record has not been forwarded to a peer review or
clinical review committee, meeting, or function; verify the record has not been sequestered
from main file; verify the record has not been temporarily separated from the main file for
any other official review function; if known, contact the previous MTF responsible for
maintaining the beneficiary’s health records; contact the service member/beneficiary to see
if the member/beneficiary is in possession of the record. (T-1). If the record still has not
been located following the preceding minimum search requirements, begin processing the
Non-Availability Letter for Service Treatment Records and breach notifications. In
addition, the MTF Verification Checklist must be completed in accordance with paragraph
5.7.5.4. (T-0).
5.20.3.2. After all efforts to find the lost health record(s) are exhausted the MTF
commander or director may deem the missing health record as “lost.” Once the MTF
commander or director has deemed a record “lost,” MTF HIPAA privacy officer must
follow the guidelines and procedures identified in AFI 41-200, paragraph 6.5., in
consultation with the installation public affairs officer, as applicable and available
installation legal staff and/or the medical law consultant. (T-0).
5.21. Health Records Availability, Accountability, and “Tracking” Standards.
5.21.1. All MTFs and/or medical units with CHCS computer capabilities must utilize the
CHCS Medical Record Tracking function to properly manage, track, and locate health records.
(T-1). Efficient use of associated Medical Record Tracking system tools like the records bar
code scanner and electronic AF Form 250 will save time and reduce misplaced paper health
records. Any non-MTF organization authorized to maintain AD service member or RC health
records without using the CHCS computer Medical Record Tracking module to identify and
manage their record inventory, shall establish a manual tracking system. (T-1).
5.21.2. The CHCS computer Medical Record Tracking function will be used to charge in and
charge out records between the medical records department and every authorized requesting
borrower location in the MTF or within the medical unit. (T-1). Records managers should
AFMAN41-210 10 SEPTEMBER 2019 161
create or build borrowing locations within the Medical Record Tracking module for all
locations/borrowers that regularly request health records. Contact the site CHCS systems
office for assistance.
5.21.3. Monthly Outpatient Medical Record Accountability Review: Every 30 days, records
managers in each MTF record room will review all of the medical records that have been
loaned or charged out to borrowers for more than 5 days. (T-1). Records personnel are required
to identify each overdue record and contact the last known borrower to inquire about the status
of the record. (T-1). Establish a local process to retrieve records that have been loaned to
borrowers for more than 5 days. Overdue records will be identified by viewing the CHCS
Overdue Records List Report or similar CHCS records management reporting mechanism. (T-
1). Maintain monthly overdue/missing record statistics by documenting the overall records
assigned to the individual record room (denominator) and comparing this number to the
number of overall missing and/or overdue medical records (numerator). To obtain the
percentage of missing and/or overdue records, divide the numerator by the denominator.
Report findings monthly to the Health Record Review Committee (or similar records review
function), and to the TRICARE Operations and Patient Administration Flight Commander or
Patient Administration Officer. The TRICARE Operations and Patient Administration
function is responsible for creating an aggregate MTF total of overdue or missing records. The
TRICARE Operations and Patient Administration Flight Commander or Patient
Administration Officer will use the submitted information to identify duty locations and/or
individuals who routinely borrow records without returning them to the main file. (T-1). Refer
to paragraph 5.14 for potential medical records availability exceptions for RC service members
on AD orders. Refer to paragraph 5.20., lost medical records, for additional information
regarding obligations required when reporting missing or lost medical records.
5.21.4. Health Record Availability Standards: With the implementation of the DoD electronic
health record, immediate reliance upon outpatient paper medical records should diminish, not
cease. Eventually, the AFMS will completely transition from a paper-based to a
comprehensive, all-inclusive, electronic health record system. However, to satisfy DoD, Joint
Commission, and functional and provider point-of-service outpatient medical record
availability, and various auditing requirements, paper outpatient paper medical records must
still be maintained and accounted for at each MTF. (T-1). The two basic medical records
availability metrics standards outlined below measure a MTF’s compliance.
5.21.4.1. Service Provider Point of Service Record Availability Standard. Unless a MTF
has implemented a local policy to retrieve or pull outpatient paper medical records by
exception, MTFs will continue to implement a system to meet the minimum 95% (goal is
100 percent) AFMS provider point-of-service availability standard. (T-1). AFMS Provider
Point of Service availability is defined as the physical presence of the paper record for use
at the point-of-service or when needed for specific review or audit. This standard applies
to MTF records rooms (whether centralized or decentralized).
5.21.4.1.1. Methodology. Outpatient records availability percentages are generated by
tracking and maintaining the numbers of records that were retrieved and delivered to
the point-of-service, then dividing by the number of record requests (manual entry AF
Form 250 and electronic record requests) received. The overall monthly MTF records
availability percentage is generated by combining the monthly number of records
delivered to the point-of-service (for each individual records room) then dividing this
162 AFMAN41-210 10 SEPTEMBER 2019
total number by the total number of all MTF outpatient record room requests (manual
and electronic). Report this data to the MTF Health Record Review Committee or
function and to the AFMOA/SGAT office by the 10th duty day following the close of
the previous reporting month.
5.21.4.1.2. For patients with multiple appointments on the same day, count the record
as being available for all of the appointments as long as the record(s) was delivered to
the first scheduled appointment. However, records personnel should attach a note or
locally created notice or flag to the record, before distribution to the first appointment
location. The note should inform the record(s) borrower that the patient has multiple
same-day appointments. The note or flag will alert clinic staff to forward the patient’s
record to the next clinic. Clinic personnel are required to forward the record to the next
location.
5.21.4.2. DoD Minimum Functional Control Record Availability Standard. MTF records
managers must ensure their outpatient records control process include procedures to ensure
95% percent availability of all outpatient medical records. (T-1). Availability is defined
as any outpatient medical record located within the MTF having functional responsibility
for maintaining the record. DoD availability is not to be confused with provider or point
of service availability as described in the previous paragraph.
5.21.4.2.1. Methodology. DoDI 6040.40, Military Health System Data Quality
Management Control Procedures, Enclosure 1, paragraph C.6., identifies a minimum
on hand records availability audit formula. From a random sample of CHCS outpatient
appointments from the reporting month, medical record personnel will determine the
percentage of available or on hand outpatient paper medical records that can be
physically located in a record room file system. If an outpatient record is not
immediately physically available in the record room file, but a properly documented
AF Form 250 and plastic record charge-out guide are filed in place of the paper record,
then count the record as available.
5.21.4.2.2. If a MTF can prove record availability, according to this standard, by
pinpointing the specific location of the record within a MTF medical records
department(s) or MTF borrower location, using the CHCS computer Medical Record
Tracking module or from a properly documented AF Form 250, then count the record
as available. Records loaned to a borrower with a check-out date older than 30 days,
must be physically located and verified with the borrower. (T-1).
5.21.4.3. Report monthly AFMS availability and Office of the ASD for Health Affairs
availability percentages to the MTF Health Record Review Committee. The committee
chairperson will report this information monthly to the Executive Committee of the
Medical Staff unless otherwise directed by the MTF commander or director. (T-1).
5.21.4.4. Refer to paragraph 5.14 for potential records availability exceptions for RC
service members placed on AD.
5.21.5. Converting to a Paper Medical Records Retrieval or by Exception Process: The Health
Record Review Committee and the Executive Committee must support any decision to suspend
or discontinue retrieving or pulling outpatient medical records for daily outpatient
appointments. (T-3).
AFMAN41-210 10 SEPTEMBER 2019 163
5.21.5.1. The MTF Chief of Medical Staff, in coordination with the unit commander(s) are
responsible for health records maintenance and management, must determine, based on
program management analysis and input from the entire clinical staff that all providers who
use AHLTA, are using the system the way it was designed to be used. (T-2).
5.21.5.2. If the Chief of Medical Staff and respective unit commander(s) support the
decision to suspend daily paper outpatient medical records retrieval and distribution, the
MTF commander or director may approve the decision or determine another course of
action. Approval may be for defined specialty groups, Family Health Elements, clinics
and/or entire facilities. Documentation of approval must include any sub-groups that will
continue to require paper records on a regular basis. (T-3).
5.21.5.3. Prior to approving any retrieve or pull records by exception policy, the MTF
commander or director must ensure that the requesting clinical work center(s) have created
a process to verify patients have signed the MHS Notice of Privacy Practices for each
empaneled patient. (T-0). Refer to AFI 41-200, paragraph 3.2 for specific information and
expectations regarding HIPAA (MHS Notice of Privacy Practices requirements.
5.21.5.4. If the MTF commander or director decides to suspend traditional daily paper
outpatient medical records retrieval and distribution processes, an immediate six-month
trial phase will begin starting from the date of the decision or other designated
implementation date.
5.21.5.5. During this period, the AFMS Provider or Point of Service records availability
percentage, for patients with a) an established electronic medical record history, b) new
patients with no previous outpatient paper medical record, and c) patient encounters for
which the provider does not need to reference the traditional paper outpatient medical
record, will be deemed to be 100%. Records room managers will meet with the CHCS site
manager and/or information systems managers to suspend the automated function that
produces the pre-printed AF Form 250, prior to each patient’s appointment. Records
personnel will inform clinic staff that individual records requests are still possible using
CHCS.
5.21.5.6. During this period, if a provider(s) requests the traditional paper outpatient
medical record prior to a patient encounter, and assuming there is an established traditional
paper record on file, records room personnel will retrieve and distribute the requested
record(s). For all requested traditional outpatient paper medical records requested
separately from the AHLTA system, records room supervisors will apply the same record
availability methodology previously referenced in paragraph 5.21.5.1., and report this
records availability statistic monthly to the Health Record Review Committee and to
AFMOA/SGAT. (T-1).
5.21.5.7. After the six-month trial phase, the chief of medical stall will coordinate options
with the unit commander responsible for health records. Also, the chief of medical staff
will receive input from the Health Record Review Committee, the Executive Committee
of the Medical Staff and the provider staff. After these coordination efforts, the chief of
medical staff will recommend one of the following option to the MTF commander or
director:
164 AFMAN41-210 10 SEPTEMBER 2019
5.21.5.7.1. Permanently or temporarily cease MTF daily outpatient paper medical
records retrieval and distribution processes,
5.21.5.7.2. Implement a limited cessation or selective cessation (based on MTF-unique
circumstances) of paper medical records retrieval and distribution,
5.21.5.7.3. Institute another trial period, or
5.21.5.7.4. Determine some other appropriate action. Additionally, whatever process
is chosen, paper documents from internal and external sources will be scanned and
uploaded into Health Artifact and Image Management Solution (HAIMS) or the
approved electronic health record. (T-1).
5.21.5.7.5. Exception: For official auditing purposes, the MTF must either supply the
auditor with a paper copy of the applicable patient encounters, or provided access to
AHLTA to review the outpatient encounter documentation. (T-3).
5.21.6. Using Charge-Out Guides. Use AF Forms 885, 886, and 887 and AF Form 250, to
indicate the location of an outpatient record removed from the file. Use of the Medical Record
Tracking module in CHCS is required as a tool to track movement of outpatient records. It
also enhances the management of records accountability and availability.
5.21.7. Loaning Records to Clinics/Units. MTFs must establish strict, but sensible,
procedures to manage the loaning of records. (T-3). The following instructions must be
adhered to ensure sound health records management operations (T-3):
5.21.7.1. Limit access to all outpatient medical records areas to only authorized personnel.
MTF personnel should not be granted access based solely on the proximity of their clinic
or work center to the secure records area.
5.21.7.2. When a paper medical record is requested or removed from file by an authorized
borrower, records room personnel will ensure the borrower uses a charge-out guide and
completes the AF Form 250 with accurate, adequate, and legible, information or requests
the record through the CHCS Medical Record Tracking module. Whenever possible,
automated CHCS AF Form 250s should be used to place inside the charge-out guide.
5.21.7.3. The outpatient records department and clinic personnel will ensure the outpatient
record is available prior to the patient’s appointment.
5.21.7.4. Medical records staff must notify the requesting clinic or clinical work center
when the medical record is not available. If the record is not available at the clinic or
borrower’s location before the patient arrives the clinic staff should access the Medical
Record Tracking module to locate the health record(s) or contact the medical records
department if an explanation has not been provided. If the record is not available, the
provider should make an entry on the form used to document care that the record was not
available for review.
5.21.7.5. Generally, health records are only to be loaned to internal work centers.
However, there may be very unique instances when the original health record(s) may be
released to an outside agency, MTF, civilian medical facility, or even the patient. The MTF
commander or director is the only official authorized to release original health record(s) to
external MTF requestors. Note: If a health record(s) is involved in a potential Medical
Affirmative (MAC) Claim, or other potential claim either for or against the United States
AFMAN41-210 10 SEPTEMBER 2019 165
Government, or for potential litigation, or for use as evidence in a court of law, do not give
the original record to the patient. All parties with legitimate and legal authorization to
receive either the health record(s) or copies will be provided the information once all
security validation and/or authorization requirements have been met. Refer to AFI 41-200,
paragraphs 4.1.-4.3., Use and Disclosure of PHI, for further guidance.
5.21.7.5.1. The Medical Cost Reimbursement Program (MCRP) replaced the Hospital
Recovery (HR) claims program administered by base legal offices and is now
administered through 8 regional offices. Medical Cost Reimbursement Program
recoveries are made pursuant to the Federal Medical Care Recovery Act and the
Coordination of Benefits statute, as well as any applicable state laws allowing for
recovery.
5.21.7.5.2. All money recovered will be returned to the MTFs or DHA. Medical Cost
Reimbursement Program legal personnel may require access to health records and
MTFs should coordinate the appropriate access to needed health information. For more
information on Medical Cost Reimbursement Program, contact the Air Force Legal
Operations Agency, Claims and Tort Litigation Division (AFLOA/JACC).
5.21.7.6. Health records for military retired service members and the records of a retired
service member’s family members must be maintained at a MTF. (T-1).
5.21.8. Medical Records Custody Responsibility and Records Borrower Training.
5.21.8.1. TRICARE Operations and/or Patient Administration officials will brief newly
assigned staff members during initial in-processing or MTF newcomer’s orientation and
again annually thereafter, about their responsibilities regarding expected health records
custody management. (T-1). Training should provide, but not be limited to, how to request
a paper medical record, information regarding appropriate records control, release,
availability, accountability of health records, and the transition from paper-based to
electronic health records. Training may be informal, formal, or computer-based. This
records awareness training is separate from initial and annual HIPAA training requirements
outlined in AFI 41-200.
5.21.8.2. Training will be documented in the Career Field Education and Training Plan or
other official record of personnel training accomplishments. (T-1).
5.21.8.3. Just as important as the availability of health records so is the completeness of
the documentation for the same. MTFs will establish procedures to ensure that records
contain accurate and complete documentation of outpatient visits. (T-1).
5.21.8.4. MTFs should inform beneficiaries of DoD and AFMS health records custody
rules whenever and wherever possible (e.g., at town hall meetings, via patient newsletters,
time of MTF registration, etc.).
5.21.9. Obtaining Government Owned Medical Record(s) from Patients: When it is known
that a patient has custody of their record(s), initiate the following procedures to retrieve the
record from the patient:
5.21.9.1. Contact the patient and/or the sponsor and inform the party(s) the record(s) is the
property of the United States Government and must be returned immediately. (T-3).
166 AFMAN41-210 10 SEPTEMBER 2019
Inform the patient they may receive a free copy of the record but the original must be
maintained at the MTF. (T-3).
5.21.9.2. If the patient does not return the record after contact, take the following actions:
5.21.9.2.1. AD and their Family Members: Contact the sponsor’s first sergeant or unit
commander for assistance in retrieving the health record(s). Inform the sponsor’s unit
commander or first sergeant of the previous attempts to collect the record(s) in
accordance with this manual. If, after contacting the sponsor’s chain of command, the
patient still has not returned the record(s), send a certified letter to the sponsor’s and/or
patient’s home address notifying the sponsor and/or patient that the record(s) are the
property of the United States Government. Inform the sponsor or patient that a
complete copy may be provided at no charge, but that a signed authorization is required
to obtain the record of any dependent authorized to consent for their own care.
Reference any known previous attempts or actions to collect the record(s) and instances
(if any) of refusals to cooperate. Request the record(s) be returned to the MTF within
10 calendar days from receipt of the letter. Inform the sponsor that failure to comply
will result in an additional notification to the first sergeant or unit commander which
may result in potential administrative or corrective personnel action.
5.21.9.2.2. For all other beneficiaries enrolled to the MTF: If, after requesting the
record(s) in accordance with the directions found in this manual, the patient(s) still has
not returned the record(s), send a certified letter to the sponsor’s and/or patient’s home
address notifying that the record(s) are the property of the United States Government.
Inform the sponsor or patient, that a complete copy may be provided (at no charge) to
the sponsor and/or patient. Reference any known previous attempts or actions to collect
the record(s) and instances (if any) of refusals to cooperate. Request the record(s) be
returned to the MTF within 10 calendar days from receipt of the letter. Inform the
patient and/or sponsor that failure to comply will result in notification to local law
enforcement or installation Security Forces which may result in a criminal investigation
for theft of United States Government property.
5.21.10. Clinic Personnel Record Accountability and Tracking Responsibilities:
5.21.10.1. Clinic personnel must keep outpatient record entries up-to-date and use the
following disposition rules (T-3):
5.21.10.1.1. As a general rule, records are to be returned to the Outpatient Records
location at the end of the duty day associated with each episode of care. Any provider
requiring extended use of a record to complete necessary healthcare documentation
requirements should re-charge the health record to their clinic every three-days using
the CHCS Medical Records Tracking module.
5.21.10.1.2. Admission to Hospital. Send the outpatient record to the designated
inpatient nursing unit. Clinic personnel will update the CHCS Medical Record
Tracking module to document that the record has been transferred to the appropriate
inpatient nursing unit
5.21.10.1.3. Transfer of Patient to Another Military Facility for Treatment. Outpatient
medical records may be transferred to another MTF without obtaining a patient’s
AFMAN41-210 10 SEPTEMBER 2019 167
permission. MTF personnel are required to document the record transfer using the
CHCS Medical Record Tracking module.
5.22. Medical Documentation Requirements for Partial Hospitalization.
5.22.1. Partial hospitalization is defined as a facility or unit that provides a planned therapeutic
program for patients who do not require full time hospitalization, but who need broader
programs than are possible from outpatient visits in a hospital-based or hospital-affiliated
facility. Patients would spend a portion or majority of a day (less than 24-hour daily care) in
a hospital setting and then return to their homes or places of residence in the evening. They
would then return to the facility on the following day.
5.22.1.1. Partial hospitalizations are characterized by structured, daily supervised,
outpatient activities over a prolonged period (usually 2-6 weeks) tailored to treat or
rehabilitate individuals with generic-like illnesses, dependencies or psychological profiles.
Partial hospitalization may be used for crisis stabilization, treatment of partially stabilized
mental health disorders for adults and adolescents, chemical dependency treatment
programs, or as a transition from an inpatient program when medically necessary.
5.22.1.2. All documentation for partial hospitalization must comply with the current Joint
Commission documentation standards. (T-1). SFs, or other forms, as noted, are
recommended for use in the partial hospitalization records. At a minimum, the
documentation in the medical record will include (T-1):
5.22.1.2.1. SF 504, Clinical Record-History Parts I and II.
5.22.1.2.2. SF 505, Clinical Record-History Parts II and III.
5.22.1.2.3. SF 506, Clinical Record-Physical Examination.
5.22.1.2.4. Nursing assessments and interventions.
5.22.1.2.5. SF 509, Medical Record – Progress Notes written daily, which reflects a
brief summary of the therapeutic activity, observation of the patient’s status and
responses in the course of the therapeutic contact and the therapist’s plans for any
subsequent therapeutic contact.
5.22.1.2.6. AF Form 3066 or 3066-1.
5.22.1.2.7. AF Form 3069, Medication Administration Record as applicable.
5.22.1.2.8. Supporting documentation such as case management notes, treatment team
notes, weekly progress summaries, and physician summaries including physician
supervision, evaluation, and certification.
5.22.1.2.9. Patient education, release instructions, and plans for follow-up care.
5.22.1.3. All documentation related to a partial hospitalization stay will be filed as a
package in the mental health record in accordance with AFI 44-172, in Section III of the
outpatient medical record, or scanned and uploaded into HAIMS as applicable. (T-1).
Illnesses related to mental health will be filed in the mental health record. (T-1).
168 AFMAN41-210 10 SEPTEMBER 2019
5.23. Supplemental Documentation Guidance.
5.23.1. Inpatients Seen in Outpatient Clinics. Occasionally, inpatients may have appointments
in an outpatient clinic during their admission. After the appointment, the outpatient clinic staff
will forward the outpatient appointment document(s) to the inpatient’s nursing unit or place
into the inpatient medical record.
5.23.2. Withdrawing Documents. When documents in an outpatient record are relevant to
further treatment as an inpatient, the documents may be withdrawn and inserted in the inpatient
record. Note the withdrawal on SF 600. Other than this exception, original medical
document(s) will not be removed from a medical record after filing.
5.23.3. Dead on Arrival and Emergency Room (ER) Death. All MTF Dead on Arrival and
ER Death encounters will be reported in the automated ambulatory data collection system or
other ambulatory data collection and coding system. Appropriate clinical coding and Medical
Expense and Performance Reporting System code assignment is required. Any documents
created for these patients will be filed in an extended ambulatory record and maintained in a
secure, limited access area, separate from inpatient/outpatient health records. (T-3).
5.23.4. Variations in the disposition and maintenance of records in clinics are not authorized.
The MTF commander or director ensures that the health records are maintained as required by
current Air Force directives.
5.23.5. Request for Ancillary Services. Clinic personnel will ensure the appropriate ancillary
request form is properly completed and lists all patient identification and other data required
by directives. (T-3). Develop local procedures between clinic and ancillary services to correct
errors and avoid omissions.
5.23.6. When health record documents are received without adequate identification, records
personnel may return the documents to the point of origin. The originating clinical work center
must add the missing information for each incomplete entry and then return the document(s)
to the appropriate health record section. (T-3).
5.24. Mental Health Records Documentation Requirements. Mental health records are a
separate category of records that contain detailed psychiatric notations of evaluations,
consultations, tests, and treatment provided on an outpatient or inpatient status. Do not use AF
Form 2100 or 2100A series for records kept in the mental health clinic. These records must be
kept in properly secured files in the mental health clinic. (T-1). See AFI 44-172, Chapter 5, for
details on mental health records and records management.
5.25. Prenatal Records Documentation Requirements. Prenatal records may be maintained
separately by the prenatal clinic and then must be incorporated, as a package, into the inpatient
record at the time of delivery, see Attachment 10 for filing instructions. (T-1). For exceptions, see
the following:
5.25.1. If a patient is transferred or relocates before delivery, give the patient a copy of the
prenatal record to hand-carry to the next MTF. If the patient does not expect to deliver in a
MTF, copies of the prenatal record should be given to the patient and the original documents
scanned into HAIMS.
5.25.2. Prenatal records shall be screened quarterly. (T-1). When the expected date of delivery
has passed or there is no indication that the patient is being followed, the prenatal record should

AFMAN41-210 10 SEPTEMBER 2019 169
be withdrawn from the prenatal file and forwarded to the outpatient records department for
inclusion in the patient’s electronic health record.
5.26. Family Advocacy Program (FAP) Documentation Requirements.
5.26.1. The Family Advocacy clinic or office maintains the original Family Advocacy
Program patient record. The Family Advocacy Program record contains detailed, confidential
information regarding alleged or verified family maltreatment. For every patient visit to the
Family Advocacy clinic, an abbreviated continuity of care entry must be documented in
AHLTA. (T-1). Treatment entries, documenting only minimal information, are inserted into
AHLTA by Family Advocacy Program providers. The continuity of care AHLTA entry most
commonly used indicates: “Patient was seen in Family Advocacy for assessment due to
allegations of family maltreatment.” Other abbreviated or minimally documented statements
or references to one’s suicidal/homicidal assessment and/or a maltreatment risk assessment
will also be included in an AHLTA entry. (T-1). The initial Family Advocacy Program
Clinical Case Staffing (CCS) recommendations will be placed in AHLTA, as well as the
transfer/closure summary for each patient treated in Family Advocacy Program.
5.26.2. When patients are seen in Family Advocacy Program for prevention services, there is
only a requirement for an AHLTA note when there is a clinically significant finding, requiring
documentation for continuity of care or a referral to a medical provider.
5.27. Documentation Requirements to Support Graduate Medical Education
Programs. Documentation requirements will be as outlined by the Accreditation Council for
Graduate Medical Education (https://www.acgme.org) in their common and specific program
requirements. (T-1).
5.28. Managing Service Treatment Records for Service Members Assigned to the Personnel
Reliability Assurance Program and Presidential Support Program
5.28.1. Transferring Service Treatment Records for service members Assigned to a Personnel
Reliability Assurance Program position. Medical records personnel will take all steps
necessary to ensure the gaining MTF has access to the service member’s complete service
treatment record. For service members being assigned to a duty location that does not have
access to the electronic health record [AHLTA/Health Artifact and Image Management
Solution (HAIMS)], a complete copy of their medical record in paper or digital format will be
provided to the service member. (T-0). Reference DoDM 5210.42, Nuclear Weapons
Personnel Reliability Program.
5.28.2. The only exception for hand-carry of outpatient medical records are those service
members in or going into an active Personnel Reliability Assurance Program status whose
record will not be reviewed by the Administrative Qualification Central Cell. Note: These
members must also hand-carry their dental records.
5.28.3. Physical Separation from the Main File for Service Treatment Records of service
members assigned to Personnel Reliability Assurance Program. Outpatient medical and dental
treatment records for Airmen assigned to Personnel Reliability Assurance Program, shall be
maintained in a separate, secured location. (T-1). Access to these physical Service Treatment
Records must be restricted to only those medical personnel with an official need for access.
(T-1).

170 AFMAN41-210 10 SEPTEMBER 2019
5.28.4. Airmen meeting the personnel status conditions identified in Section 5.28.2 are
required to hand-carry their health treatment records (in a sealed envelope) from the losing
MTF or RC to the gaining MTF or to the medical unit responsible for maintaining health
records. Upon arrival to the gaining MTF or to the medical unit, the health records must be
surrendered to the MTF clinic or office responsible for the daily maintenance of these special
records. (T-1).
5.28.5. Before health records are provided to the service member, outpatient and/or dental
records medical and dental record personnel will seal the record(s) in an appropriately sized
envelope, then write or place a pre-worded ink stamp that indicates, “During Transport, Open
Only for Medical Emergencies,” across the envelope sealed flap seam. Then place one strip
of clear or transparent ½ inch adhesive tape down the entire length of the envelope along the
sealed flap seam. Finally, the records management official that seals the envelope must write
official’s initials along the sealed flap seam and legibly write or place a pre-worded ink stamp
that identifies the losing MTF or installation Dental Treatment Facility unit name, office
symbol, address, installation name, zip code, point of contact name and contact telephone
number. (T-3).
5.29. Transferring Health Records Between MTFs or Medical Units.
5.29.1. Transferring Service Treatment Records During PCS, PCA or Permanent Duty
Location Reassignment for Airmen Not Assigned to Sensitive Duties or Active Flight Status.
5.29.1.1. Custody and Control of Outpatient Medical and Dental Records: Hand-carry of
outpatient medical and dental records in a sealed envelope during a PCS or PCA
reassignment is now prohibited for all Airmen, with the exception of Airmen assigned, or
who will likely be assigned, to Personnel Reliability Assurance Program, Presidential
Support Program, and overseas United States embassy support.
5.29.1.2. MTF and RC records managers at the departure or losing MTF or RC are
required to forward the Service Treatment Records for departing service members, to the
gaining MTF or RC responsible for maintaining the service member’s health records. (T-
1). Service Treatment Records will be mailed no later than five duty days following the
service member’s PCS/PCA departure or date of separation/transition to the gaining MTF
or RC. (T-1). Records managers will not mail the records in conjunction with the monthly
purge. (T-3). Records will be mailed on a daily basis as needed. (T-3). Mail the records
via standard First Class United States mail with immediate delivery
confirmation/acknowledgment, certified mail, or other commercially available option, e.g.,
FedEx, that offers package tracking and delivery/arrival confirmation. Use of standard First
Class United States Postal Service mailing method alone
usaf.jbsa.afmoa.mbx.sgat@mail.mil, without package tracking and immediate delivery
confirmation/acknowledgment or certified mail receipt, is prohibited. Return receipt
confirmation must not be dependent upon the timeliness or willingness of the destination
MTF to complete a DD Form 2825 or other manual delivery confirmation receipt option.
(T-3).
5.29.1.2.1. MTF and RC records managers at the departure or losing MTF or RC are
required to expedite the mailing of original outpatient medical and dental treatment
records for departing service members and accompanied family members on PCS
orders to all overseas locations utilizing a commercial carrier (i.e. FedEx or DHL). (T-

AFMAN41-210 10 SEPTEMBER 2019 171
3). The expedited mailing ensures scheduled/guaranteed and tracked delivery of no
more than seven calendar days from the mailing date. United States Postal Service first
class and certified mail do not currently meet this standard – generally taking four to
six weeks for delivery to any OCONUS location. All MTF and RC Outpatient Records
sections have been provided updated and tested mailing addresses for commercial
carriers such as FedEx that only utilize local/physical addresses. The current list of
addresses can be located on the AFMOA Health Benefits Kx page at
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
5.29.1.2.2. In addition to the requirements of paragraph 5.29.1.2, MTR and RC records
managers will coordinate mail-outs with the Dental clinic to ensure the complete
medical and dental records are mailed together to the gaining MTF/RC. Records will
be mailed with a copy of the member's orders and contain "ATTN: OUTPATIENT
RECORDS" in the address. (T-3).
5.29.1.3. The service member is required to present military PCS orders or duty location
reassignment orders to the departure or losing MTF or to the RC prior to final departure
from the installation or organization. (T-3). Records managers at the losing MTF or RC
will include a copy of the service member’s PCS orders in the same mailing shipment
package bound for the gaining MTF or destination medical unit. (T-3). In the event a copy
of the service member’s PCS orders are not available, the MTF or RC will include a
completed AF Form 330 in place of the orders. (T-3).
5.29.1.4. MTF and Dental Treatment Facility In/Out-Processing PCS Customer Service
Locations: Ideally, each MTF and Dental Treatment Facility should provide one central
in-processing and out-processing customer service location for health records respective to
each facility. For the installation Dental Treatment Facility, this location is usually the
front clinic reception desk. However, some MTFs have decentralized outpatient medical
record rooms. Although one central MTF outpatient medical records customer service
and/or reception area is recommended, MTF commanders or directors may choose instead
to align multiple outpatient medical customer service locations alongside or co-located
with Primary Care Manager or Patient Centered Medical Home clinic operations.
5.29.1.5. Airmen PCS Departure Out-Processing Procedures: All service members
empaneled to the MTF and scheduled for reassignment to another station are required to
out-process through the MTF and Dental Treatment Facility before final installation
departure. The purpose of the out-processing visit is to ensure MTF and Dental Treatment
Facility records managers know to remove the service member’s outpatient medical and
dental records from the main file and prepare the record(s) for shipment to the gaining
MTF.
5.29.1.6. Airmen projected for installation departure related to a PCS reassignment are
required to clear the Dental Treatment Facility and MTF no earlier than the fifth duty day
before their final installation out-processing Military Personnel Section appointment. (T-
3). This time period restriction ensures outpatient medical and dental records will be
readily available to medical and dental providers up until the time the member leaves the
base.
5.29.1.7. During each respective out-processing appointment, Airmen are required to
provide four copies of their orders (two copies for the Dental Treatment Facility, two copies
172 AFMAN41-210 10 SEPTEMBER 2019
for the MTF). (T-3). Depending on local operating policy, service members may be
required to visit a centrally located MTF records customer service office or out-process
through their Primary Care Manager records room location. MTF & Dental Treatment
Facility records personnel will ensure local installation out-processing checklists include
MTF & Dental Treatment Facility records out-processing requirements. (T-3).
5.29.1.8. Dental Treatment Facility Record Processing: No later than the close of business
each duty day, Dental Treatment Facility records managers will ensure two copies of each
departing Airman’s PCS reassignment orders are filed properly. (T-3). One copy will be
placed on top of all other documents in Section II of the AF Form 2100B series. The
second copy will be placed in a plastic AF Form 885-887 series.
5.29.1.8.1. Complete an AF Form 250 and insert into the upper right identification slot
on the charge-out-guide. File the charge-out guide into the main file according to
terminal-digit order - just like the original dental record. The charge-out guide will
remain for 90 calendar days. At the end of this period, if any loose, late-flowing dental
documents are discovered, place the documents and the copy of the PCS reassignment
order in an envelope and mail directly from the Dental Treatment Facility to the
member’s gaining Dental Treatment Facility. Do not forward these late, loose flowing
documents to the MTF outpatient records office.
5.29.1.8.2. No later than the close of business on the duty day following the member’s
out-processing visit, Dental Treatment Facility records managers will forward the
dental treatment record(s) to either a central MTF records room or to the Primary Care
Manager records room where the service member is empaneled. (T-3). After receiving
the dental treatment record(s), MTF records managers may temporarily stage the
records in a separate location, away from the main outpatient medical file. Local MTF
policy must be established to identify the best method for transferring the dental
treatment records from the dental clinic to the MTF. (T-3).
5.29.1.8.3. Dental record managers will document the date and forwarding location of
each dental treatment record removed from the dental records main file using the
current local or standard dental records tracking mechanism. (T-3)
5.29.1.9. MTF Record Processing: No later than the close of business each duty day, MTF
records managers will ensure two copies of each departing Airman’s PCS reassignment
orders are filed properly. (T-3). One copy will be placed on top of all other documents in
Section II of the AF Form 2100A series. The second copy will be placed in a plastic AF
Form 885-887 series.
5.29.1.9.1. Complete an AF Form 250 and insert into the upper right identification slot
on the charge-out-guide. File the charge-out guide into the main file according to
terminal-digit order - just like the original outpatient medical record. The charge-out
guide will remain for 90 calendar days. (T-3).
5.29.1.9.2. MTF records managers must mail the medical and dental records bundled
together and follow the procedures outlined in paragraph 5.29.1.2. (T-3).
5.29.1.9.3. Select and enter the appropriate transfer code in the CHCS Medical Record
Tracking module and enter the name of gaining MTF in the “MTF Location Remarks
Section.”
AFMAN41-210 10 SEPTEMBER 2019 173
5.29.1.9.4. After 90 days, retrieve the charge-out guide from the main file and scan
any loose or late flowing documents that may have collected in the charge-out guide
into the HAIMS repository or into another approved electronic health record.
5.29.2. Transferring Service Member Service Treatment Records During PCS, PCA or Duty
Location Reassignment to Forward or Foreign Combat/Combat Support Theater of Operations
Locations, or Other Overseas Deployment Locations for Airmen Not Assigned to Sensitive
Duties or Active Flight Status.
5.29.2.1. For 365-day PCS and/or extended deployments the service member’s original
service treatment record will remain at the MTF where the service member is enrolled. (T-
3). Upon return records staff will forward the original service treatment record to the
gaining assignment once written direction or orders are received. (T-3). Obtain two copies
of the PCS orders and place one copy of each inside the original outpatient medical and
dental treatment records in Section I or attach to the left side folder flap on top of most
current DD Form 2766, dental treatment encounter form, service transition order, or AF
Form 1288.
5.29.2.2. Unless exempted by the COCOM/Component Reporting Instructions, following
the AD or RC service member’s deployment medical clearance, established during the
MTF pre-deployment screening, and before the service member finishes departure PCS
out-processing, print the most current version of the ASIMS DD 2766 and place them into
the cardstock DD Form 2766 (secured with the metal prongs). Include paper copies of any
medical information that documents chronic medical conditions or any documents ordered
to be copied and placed into the service member’s DD Form 2766. The service member
(or deployment team leader) is responsible for transporting the original DD Form 2766
along with the documents listed above, leaving the original Service Treatment Record and
a copy of the DD Form 2766 behind at the service member’s home MTF.
5.29.2.3. When the service member returns to home installation, the DD Form 2766 and
any documents generated in theater are removed from the DD Form 2766 and scanned into
patient’s electronic health record. If the service member has received an order to proceed
to a follow-on PCS re-assignment installation, the gaining MTF will request the service
member’s original Service Treatment Record from the departure or losing home
installation MTF. (T-3).
5.29.2.4. Exception: When a service member receives a 365-day PCS order to a deployed
location where the site is adequately resourced to manage medical records, exercise 24/7
operations and have an approved waiver authorizing the maintenance of medical records,
the member may hand-carry a copy of their service treatment record. The losing MTF will
forward the original service treatment record to the gaining deployed location (in a sealed
package secured by the departure MTF). (T-2). Upon arrival, the service member is
required to relinquish their Service Treatment Record to the Expeditionary Medical
Support facility or to the installation MTF. (T-3). These facilities will be identified and
added to the exception list maintained by the AFMOA/SGAT.
5.29.3. Transferring service member Service Treatment Records During PCS, PCA or Duty
Location Reassignment for Air Force Members Empaneled to Sister-Service MTFs. The fact
that some Airmen are enrolled to non-Air Force MTFs does not prohibit the accurate and timely
health records transfer process. Health records for service members are normally maintained
174 AFMAN41-210 10 SEPTEMBER 2019
at the MTF where the member obtains primary care, regardless of service affiliation. To
facilitate appropriate health records transfer procedures for Air Force service members the
following actions must occur. (T-3). Health records staff at Air Force MTFs nearest to the
service member’s sister-service Primary Care Manager/MTF location must establish a local
memorandum of agreement or memorandum support agreement. (T-3). The agreement with
the sister-service MTF and the service member’s servicing Military Personnel Section will
ensure all final out-processing documents, checklist requirements, Military Personnel Section-
generated PCS notices, and PCS orders are completed and/or forwarded. (T-3). The agreement
must identify how the health records of Air Force personnel will transfer to the MTF at the
next duty location. (T-3). Transfer options may include, but are not limited to instructions that
specify health records, a) be mailed to the requesting Air Force MTF by the sister-service MTF
or, b) forwarded to the MTF at the Airman’s next duty location.
5.29.3.1. Note: Local procedures may be required if an agreement on how to forward
medical records cannot be reached between the sister-service primary care manager or
MTF, the local installation military personnel section and the MTF nearest the service
member’s GSU. If such an impasse occurs, the local military personnel section and the
nearest MTF to the GSU may have to initiate local procedures to ensure the Airman’s
health records are properly forwarded and delivered to the Airman’s next duty station.
5.29.4. AD Virtual Military Personnel Section Checklist Confirmation. Although the Force
Health Management staff may have additional medical out-processing checklist approval
authority or obligations, they should not sign or approve any outpatient medical or dental
treatment record out-processing tasks on a service member’s Virtual Military Personnel
Section out-processing checklist. Outpatient medical and dental records managers and Force
Health Management officials will work together to ensure each outbound Airmen has fulfilled
all the MTF out-processing responsibilities.
5.29.4.1. Checklist Operation: Multiple (at least two) staff members assigned to MTF and
Dental Treatment Facility records departments should be granted Virtual Military
Personnel Section Checklist access to ensure each departing service member is informed
of the requirement to provide the MTF and Dental Treatment Facility with copies of orders
at the time of MTF/Dental Treatment Facility out-processing.
5.29.4.2. Access will also allow MTF records managers to obtain and print individual
retirement/separation orders when necessary.
5.29.5. Transferring Outpatient Medical and Dental Records between MTFs for Family
Members, Retired Military Service Members, or Any Other Category of Beneficiary Not
Specifically Captured in this Section.
5.29.5.1. MHS beneficiaries are prohibited from hand-carrying their medical records. The
standard procedure throughout the AFMS is to mail family member hard-copy outpatient
medical records from one MTF to another during reassignments. Only the MTF
commander or director can make a case-by-case exception to deviate from this process.
5.29.5.2. Upon notification from the sponsor of being re-assigned to another installation
several actions must take place. MTF records personnel will check the typed PCS/PCA
orders to determine if the reassignment is to be “ACCOMPANIED” (with family members)
or “UNACCOMPANIED” (without family members). (T-3). If the service member’s
AFMAN41-210 10 SEPTEMBER 2019 175
orders indicate an ACCOMPANIED assignment, records personnel will ask the service
member if all of the family members are to accompany. (T-3). If all family members are
accompanying the service member, then records personnel will verify the departure date
with the sponsor. (T-3). Records personnel will obtain any available dental treatment
records, and then combine all of the family member health records into one package. (T-
3). MTF records personnel may also add the sponsor’s Service Treatment Record into the
same package. If the package is too big or it becomes impractical to combine all of the
family’s records together, then separate the service member’s record from the package and
mail separately. Enclose a copy of the sponsor’s typed PCS/PCA reassignment orders in
each package. Mail the health records package(s) to the destination MTF no later than five
calendar days following the sponsor’s departure date.
5.29.5.3. If the sponsor’s orders indicate UNACCOMPANIED or the sponsor indicates
one or more family members are not accompanying, records personnel must validate family
member enrollment. Records personnel must verify with the sponsor if the remaining
family members will stay enrolled at the current MTF. (T-3). If not the remaining health
records should be forwarded to another facility where TRICARE enrollment is expected.
(T-3). The following actions must take place when family members are expected to receive
direct healthcare at another MTF, apart from where the sponsor. (T-3). Upon re-enrollment
at the new MTF, the sponsor, spouse, or legally-aged (per state law) family member must
contact the records department to complete the necessary records request paperwork. (T-
3). After receiving a completed DD Form 2138, or DD Form 877 from the requesting
MTF, the current MTF will release and forward the requested records. (T-3).
5.29.5.4. For Retired Service Members, and/or Their Family Members, and AD Family
Members Who Wish to Change Their MTF TRICARE Enrollment Location Without
Associated Sponsor PCS/PCA. This process is required whether the move be across the
country or within a multi-market service location (e.g., changing MTF/Primary Care
Manager location within the San Antonio, TX; Washington, DC; or Hampton
Roads/Norfolk/Portsmouth, VA - Tidewater area). Inform the sponsor that upon arrival
and/or TRICARE re-enrollment at the new MTF, the sponsor, spouse, or legally-aged
family member must contact the outpatient medical records department to complete the
necessary records request paperwork. (T-3). Only after receiving a properly completed
DD Form 2138 or a DD Form 877 or another suitable request form (from the requesting
MTF) will the MTF (where health records are currently maintained) release and forward
the requested records. If the sponsor contacts the departure or losing MTF before the
anticipated MTF change, provide the sponsor with a DD Form 2138. Instruct the sponsor
to complete Sections I and II of the form and deliver the form to the MTF records
department at the gaining MTF where TRICARE re-enrollment is expected.
5.29.5.5. Under all circumstances, CONUS based MTFs/RCs mailing health records or
loose, late flowing medical documents to other stateside CONUS MTFs/RCs will follow
the mailing procedures outlined in paragraph 5.29.1.2. (T-3).
5.29.5.5.1. Under all circumstances, OCONUS based MTFs/RCs mailing health
records or loose, late flowing medical documents to other OCONUS and CONUS
MTFs/RCs will use a commercial carrier (i.e. FedEx or DHL). (T-3).
176 AFMAN41-210 10 SEPTEMBER 2019
5.29.5.5.2. Use of United States Postal Service first class and certified mail are not
authorized.
5.29.5.6. MTF commanders or directors (Custodians of Record or their delegates) may
make exceptions to the hand-carrying policy on a case-by-case basis if extenuating
circumstances warrant it. No sponsor is authorized to possess or hand-carry the original
health records or copies of health records for any member of the family aged 18 years or
older without written authorization from the family member.
5.29.5.7. Forward health records critical to potential, pending, or active litigation using
only shipping options with an immediate delivery confirmation/acknowledgment feature.
(T-3). Shipping options may include certified mail via official military mail, United States
Postal System or other commercially available option, e.g., FedEx, that offers package
tracking and arrival confirmation. Use of standard First Class United States Postal Service
mailing method alone, without immediate delivery confirmation/acknowledgment, is
prohibited. (T-3).
5.29.6. Disposition of Family Member Outpatient Medical and Dental Records When the
Sponsor has a 365-day PCS to an Overseas Location in Support of Contingency Operations.
5.29.6.1. If the service member’s PCS is identified as ACCOMPANIED on the sponsor’s
orders, the outpatient medical and dental records for all family members will remain at the
losing or “home base” facility until the service member either returns from deployment or
receives a follow-on PCS assignment to another location. (T-3). Only upon request,
provide copies of family member medical records (including AHLTA patient encounters)
to the sponsor and/or any legally-aged family member.
5.29.6.2. Upon return from a 365-day PCS overseas location, if the sponsor receives a
follow-on assignment to a different installation the member will contact the gaining MTF
upon arrival (at the new installation) and initiate a formal request to obtain family-member
dependent medical records from the losing MTF. (T-3).
5.29.6.3. If the service member’s PCS is identified as UNACCOMPANIED on the orders,
determine where the family member’s MTF TRICARE enrollment is expected and follow
protocol outlined in Section 5.29.5.3.
5.29.6.4. Insert a charge out guide with a copy of PCS orders, DD Form 877, or DD Form
2138. Scan all loose medical documents in the approved electronic health record.
5.29.7. Transferring Mental Health Records. See AFI 44-172 for procedures detailing the
transfer of Mental Health Records.
5.30. Providing Health Records to AD Members During Temporary Duty Periods.
5.30.1. With the enterprise-wide use of the electronic health record, there are very few
situations where an Airman would be required to bring paper outpatient and/or dental records
to a TDY location. Most Professional Military Education (PME) and technical training schools
no longer require students to bring a copy of their medical record or copies of recent
encounters. As a general rule, MTF outpatient records departments should only provide a
complete copy of outpatient medical record to the member if, a) specifically required per
formal training requirements (TDY orders must include this requirement in writing on the
orders), b) if the member has a chronic medical condition where reference of the medical record

AFMAN41-210 10 SEPTEMBER 2019 177
could be useful during treatment at the TDY location, or c) in any situation that a provider
deems medically necessary for the member to hand-carry the record while TDY. Ensure all
pertinent electronic health record documents are printed and filed into the record prior to the
service member’s departure. If a copy of the health record is to be provided, the record(s) must
be enclosed in a strong envelope or package and sealed. (T-3).
5.30.2. MTF Staff who care for Personnel Reliability Assurance Program members while
member is in TDY status will help to ensure that appropriate documentation and notifications
are made to member’s home unit. (T-3). Following the completion of all official TDY
assignments, the TDY assignment location MTF staff will ensure that the member receives a
copy of all medical documentation that occurred during the member’s TDY assignment. (T-
3).
5.30.3. All TDY Airmen normally assigned to a Personnel Reliability Assurance Program
position who are not expected to perform or fill an active operational Personnel Reliability
Assurance Program position or job at the TDY location, are not required to hand-carry their
Service Treatment Record to the TDY. Following each episode of care at the TDY location,
personnel assigned to the Personnel Reliability Assurance Program, flight medicine clinic or
any official(s) responsible for managing the integrity of the MTF portion of the Personnel
Reliability Assurance Program notification system, will print out a copy of the electronic health
record note and mail a copy (via Certified military or United States Mail with immediate
delivery confirmation/package tracking) to the MTF at the Airman’s home station. (T-3). MTF
personnel at the TDY location will also provide a copy of the printed electronic health record
note to the service member. (T-3). The service member is required to bring the printed
electronic health record note to the provider at home station. The returning Airman’s provider
is required to review the electronic health record document (either the mailed copy or the copy
provided by the service member) to identify any potential medical issues that could jeopardize
overall program integrity or reliability based upon the patient’s capabilities/limitations (if any)
documented or identified at the TDY location. (T-3)
5.30.4. Before copies of health records are provided to the member, outpatient and/or dental
records personnel will follow the procedures for sealing the records that are set out in paragraph
5.28.5. (T-3).
Section 5C—Inpatient Records Administration
5.31. Creating Inpatient Records.
5.31.1. MTFs that create and maintain inpatient records will use guidelines from this chapter
and from Joint Commission standards. (T-0). Records must to be completed within 30 days
after the patient’s discharge in accordance with Joint Commission standards. (T-0) Reference
The Joint Commission Standards at
https://www.jointcommission.org/facts_about_joint_commission_accreditation_standar
ds/.
5.31.2. MTFs will create an inpatient record for the following episodes (T-0):
5.31.2.1. Patients admitted to an inpatient unit of an Air Force MTF including patients
admitted and discharged before midnight on the day of admission regardless of the type of
discharge.
178 AFMAN41-210 10 SEPTEMBER 2019
5.31.2.1.1. Reactivate the record of hospitalization if the patient is readmitted before
midnight on the same day as discharged for the same reason as the first admission. The
attending provider annotates the reason for readmission and the hospitalization is
considered as one continuous period.
5.31.2.1.2. If the patient is readmitted after midnight, or the reason for readmission is
different from that of the previous admission, create a new record.
5.31.2.2. Live births occurring in an Air Force MTF. Note: Do not create a separate
record for stillbirth infants. All paperwork, including the autopsy (if performed), will be
filed in the mother’s inpatient record. (T-3).
5.31.2.3. Patients who die in transit. The MTF receiving the remains processes the records
and completes the AF Form 565 as if the patient had transferred in.
5.31.2.4. All patients admitted to an Expeditionary Medical Support facility or fixed
contingency hospital during deployment. See Section 5D, Deployed Assignment Medical
Record Management for further instructions.
5.31.3. A canceled admission may be appropriate in some instances. Annotate the admission
worksheet with the reason for cancellation and place all paperwork generated by the admission
(e.g., history and physical, progress notes, laboratory and x-ray reports, etc.) in the patient’s
electronic health record. Record and code the episode as an outpatient encounter.
5.32. Creation of the Master Patient Index.
5.32.1. The Master Patient Index serves as an alphabetical index of all hospital patients and
patients for whom administrative responsibility is assumed (e.g., AD military in non-federal
hospital). Note: Do not destroy - maintain for 50 years.
5.32.2. The Master Patient Index is created by and stored in the current automated system.
5.32.3. MTFs without automated Admissions & Dispositions Office functions will maintain
hard-copy paper index cards.
5.33. Preparing Inpatient Record Folders.
5.33.1. Create records at time of disposition and completion of each patient hospitalization for
future retirement. Ensure discharge summary is scanned/uploaded into approved electronic
health record. Number folders according to the sponsor’s social security number. Place an
automated bar code patient identification label in the upper right corner of the record jacket
cover in the Patient Identification block. Document the record jacket cover according to the
following table:
Table 5.3. Preparing Inpatient Record Folders.
If the patient is:
Use social security number of:
AD/RC
Service Member
Family Member
Sponsor
Civilian Employee
Employee
Retired military
Member
Civilian Emergency
Patient

AFMAN41-210 10 SEPTEMBER 2019 179
Foreign national, allied or other military member
without social security number
Construct a social security number
5.33.2. See paragraph 5.10.6 for guidance regarding the creation of a pseudo social security
number when a patient’s own social security number is not known or does not exist.
5.33.3. MTFs that create and maintain inpatient records will use AF Form(s) 788A-788J
series, as appropriate, according to the last two digits of the applicable social security number.
To increase the likelihood that the paper inpatient record will be filed and retrieved easily,
enter information on the front of the folder as indicated by the following paragraphs. See
paragraph 5.36 for filing instructions.
5.33.3.1. Print the first name, middle initial, and last name of the patient in the space
provided with a black pen, felt-tip marker, or embossed card. Address labels prepared by
the Personnel Data System may be used to provide names of military personnel. DO NOT
use pencil for any entry. Always place information in the upper right-hand corner of the
jacket cover in the patient Identification area.
5.33.3.2. Enter the sponsor’s social security number in the preprinted blocks in the upper
right-hand corner of the record.
5.33.3.3. Enter the family member prefix in the two circles next to the social security
number.
5.33.3.4. Fill in the ½-inch square block, along the right edge of the back leaf of the folder,
containing the same digit as the last digit of the social security number, with a black ink
pen, felt-tip marker, or black tape.
5.33.3.5. On the outside, front cover of the inpatient record jacket, in the pre-printed or
labeled treatment year grid section, fill-in the current treatment year that corresponds to the
patient’s most recent inpatient treatment. Use a black felt-tip marker or black pen.
5.33.3.6. Indicate the patient’s status in the appropriate block on the front.
5.33.3.7. Attach the CHCS Medical Record Tracking bar code label to the inpatient record
folder. See the Medical Record Tracking, Retirement and Retrieval User Guide for
instructions on label requirements.
5.33.3.8. Stamping or labeling the front cover of the inpatient record with any large-letter
identifiers other than “CROSS-REFERENCE,” or with infant-adoption related
notifications is discouraged. See paragraph 4.3.3.1 for detailed information regarding
infant-adoption medical information release instructions.
5.33.4. Documents placed in the folder may be held together with a 3-inch fastener or fastened
into the folder. When records are retired to the National Personnel Records Center, documents
are permanently affixed to the folder.
5.34. Contents of the Inpatient Record.
5.34.1. Upon the patient’s disposition, MTFs will arrange paper copies of forms in the order
listed below as applicable to the case. (T-1). Note: As MTFs increase their use of Essentris
or other automated systems to create a computer-based patient record, the style and
arrangement of data in the electronic record may vary from the guidance provided here.
Records printed from automated systems should be assembled as closely as possible to the
180 AFMAN41-210 10 SEPTEMBER 2019
traditional inpatient record until more detailed instructions are published. An asterisk “*”
denotes that the form may not be filed in the order listed. See special instruction column in
Attachment 10 for proper filing location. Command and locally developed medical forms
should be filed in the appropriate order as according to purpose. See Attachment 10 for
arrangement of forms in the inpatient record.
5.34.2. Problem Oriented Medical Record. If a MTF elects to use the Problem Oriented
Medical Record format, then the MTF will develop local directives to prescribe which cases
will use this format, the method by which the forms are used and the manner in which the
forms will be filed. (T-3).
5.34.3. Self-Determination Act (Advance Directive) Documents. When provided by the
patient (at each admission), the documents (which may include the living will, durable power
of attorney, and/organ donation paperwork) will be filed with the other administrative
documents in the record. (T-3). After discharge, the patient may take the original documents
home with them and bring them back if admitted again at some future date. At the time of
discharge, the MTF inpatient nursing ward clerk will make a copy of the Advance Directive
document(s) and replace into the electronic health record for reference. (T-3).
5.35. Inpatient Record Documents, Forms, and Patient Identification.
5.35.1. Inpatient records consist of the original copy of the forms listed in Attachment 10 as
applicable to the case. Each form filed in the inpatient record must contain, at a minimum:
Patient name (last, first, middle name or initial), Register Number, patient’s DoD Identification
Number, patient’s family member prefix, patient’s and sponsor’s social security number, and
MTF organization and/or treatment name. (T-1).
5.35.2. SFs Available on Internet. Many SFs are now available at the GSA Forms Library
website. Most forms are in “PDF” format and should be downloaded with the Adobe Reader,
available on the website. Forms not available on the website must be ordered from: (T-1).
GSA-FSS
General Products Commodities Center
ATTN: 7FSM
819 Taylor Street
Fort Worth, TX 76102
5.35.3. See Section 5A for guidance on overprinted and electronically generated forms.
5.35.4. Dictated and Transcribed Medical Forms. Providers, at the time of dictation, will
indicate the date and time of the dictation, their clinical occupational specialty, and their Air
Force Specialty Code (AFSC), if applicable. Transcriptionists will include the aforementioned
data, the transcribed clinical content, and the date of transcription on all transcribed reports,
such as SFs 502, 504-506, 516, Operation Report, etc. (T-1).
5.36. Filing Inpatient Records.
5.36.1. Preparation of folders, arrangement of content, and record filing methodology is
consistent throughout Air Force MTFs.
5.36.2. File records in terminal digit format by social security number.
AFMAN41-210 10 SEPTEMBER 2019 181
5.36.3. For discharges in Calendar Year 2003 and earlier, records of previous admissions may
be brought forward and filed, as a separate entity, in the folder of the current admission record.
5.36.4. Beginning with discharges as of 1 January 2004, file each admission in a separate
folder. There is no requirement to re-file admissions in a separate folder for discharges
occurring prior to 1 January 2004.
5.36.5. Only authorized personnel at the MTF may access inpatient records. Substitute an AF
Form 614 for the inpatient record when removed from the file and charge out the record in the
Medical Record Tracking module of CHCS.
5.36.6. Fetal Monitor Strip Filing Procedures. Maintain the fetal monitor strips on the
obstetrical unit with the prenatal record until delivery.
5.36.6.1. After discharge of the infant, send the fetal monitor strips to the inpatient records
department for maintenance until retirement to the National Personnel Records Center.
Annotate the envelope with the name and register number of the infant, sponsor’s name
and social security number, name of the MTF, and date of infant’s birth.
5.36.6.2. Place strips in envelopes that will be filed in record folders when retired to
National Personnel Records Center. Note: Digitized, or other format, fetal monitor strips
which can be printed out on an 8 1/2” X 11” document are filed in the infant’s inpatient
record or the mother’s if the infant is stillborn. Attach the CHCS Medical Record Tracking
bar code label to the folder.
5.36.6.3. When an undelivered patient is transferred, send all fetal monitor strips prepared
with the copy of inpatient records to the receiving MTF.
5.36.6.4. Send the fetal monitor strips with the patient, when a newborn is transferred to
another MTF during initial hospitalization.
5.36.6.5. File fetal monitor strips for stillborn infants, as defined by the Center for Disease
Control and Prevention (CDC) and/or State guidelines as appropriate, under the register
number of the mother.
5.36.6.6. In instances where the case outcome is unclear, send the outpatient fetal monitor
strips to the inpatient record department. File the fetal monitor strips in a record created
under the mother’s name, family member prefix and sponsor’s social security number.
5.36.6.7. All fetal monitor strips will be retired to National Personnel Records Center in
the same shipment as the inpatient records and the extended ambulatory record. (T-3).
5.37. Coding and Documenting Inpatient Records.
5.37.1. Coding of Inpatient Records.
5.37.1.1. All diagnoses and procedures are to be written in full, without symbols or
abbreviations, in acceptable provider terminology.
5.37.1.2. Sequence and code the diagnoses and procedures according to the current version
of the International Classification of Diseases (ICD) or other government approved coding
classification system.
5.37.1.3. Signatures are required on all documentation before the record is coded. (T-2)
182 AFMAN41-210 10 SEPTEMBER 2019
5.37.1.4. After coding the record, prepare and print the final cover sheet (AF Form 565 or
automated equivalent).
5.37.1.5. At the end of each month, create the Standard Inpatient Data Record and transmit
it by the 5th working day.
5.37.2. The provider’s social security number must not appear anywhere in the patient’s
inpatient record. (T-1).
5.37.3. AF Form 560 - Use this form as a worksheet for admitting the patient and for recording
final diagnoses and procedures.
5.37.3.1. Demographic information can be entered directly into the current automated
system, without duplicate entry of the same information on AF Form 560. It is not
necessary that the AF Form 560 be an exact copy of the final automated coversheet.
5.37.3.2. The appropriate healthcare provider completes AF Form 560 at discharge and
authenticates the entry and identifies himself or herself by signature, initials and use of a
signature block/name stamp.
5.37.3.3. Upon receipt of the inpatient record, inpatient records personnel review the entire
record to ensure completeness and accuracy of diagnostic and procedure information on
the AF Form 560. If a question arises, consult the provider for clarification. The provider
completing the form makes the final decision regarding additions and deletions of
diagnoses and procedures.
5.37.3.4. Sequence and code the diagnoses and procedures using the current version of the
International Classification of Diseases. Prepare the final cover sheet (AF Form 565 or
automated equivalent) after all information has been checked and completed.
5.37.3.5. Disposition of the AF Form 560.
5.37.3.5.1. The original worksheet is filed in the inpatient record.
5.37.3.5.2. A copy of the AF Form 560 is scanned and uploaded when used in lieu of
an AF Form 565.
5.37.4. AF Form 565. Use this form or automated equivalent as the final cover sheet of each
record to provide an administrative and clinical summary of each admission.
5.37.4.1. The cover sheet is used to summarize the inpatient episode of care with the
identification of the principal diagnosis and procedure, any co-morbidities (presence of one
or more conditions simultaneously with a primary condition), or complications, and the
sequencing of the diagnoses and procedures. Provider terminology will be used for
diagnoses and procedures. (T-3). No provider signature is required on the cover.
5.37.4.2. At local MTF option, a stamp indicating that the record was created for
administrative purposes only may also be used.
5.37.4.3. Use AF Form 565 in death cases for persons who are inpatients at the time of
death.
5.37.4.4. Disposition of AF Forms 565.
5.37.4.4.1. Insert the original AF Form 565 in the inpatient record.

AFMAN41-210 10 SEPTEMBER 2019 183
5.37.4.4.2. Scan and upload a copy of the AF Form 565 in the outpatient record after
final disposition of the case.
5.37.4.4.3. Scan and upload a copy of the AF Form 565 in the outpatient record of
patients being transferred to another facility.
5.37.5. The Joint Commission (https://www.jointcommission.org) mandates that “a concise
discharge summary providing information to other caregivers facilitating continuity of care
includes the following: the reason for hospitalization; significant findings; procedures
performed and care, treatment, and services provided; patient’s condition at discharge; and
instructions to the patient and family as appropriate.” Consideration should be given to
instructions relating to physical activity, medication, diet and follow-up activity. The condition
of the patient on discharge should be stated in terms that permit a specific measurable
comparison with the condition on admission, avoiding the use of vague relative terminology,
such as “improved.” When preprinted instructions are given to the patient or family, the record
should so indicate and a sample of the instruction sheet in use at the time should be on file in
the medical record department.
5.37.5.1. The healthcare provider dictates a concise clinical resume (narrative summary)
which is transcribed on the SF 502 for:
5.37.5.1.1. Patients hospitalized eight days or longer.
5.37.5.1.2. Patients received by transfer from another MTF for further medical
treatment regardless of the length of stay.
5.37.5.1.3. Patients who die after admission.
5.37.5.2. The narrative summary may be handwritten on the SF 502 if the patient has been
hospitalized less than eight days.
5.37.5.3. When a patient is transferred to another medical facility for further care, a
handwritten summary will be completed. If, for expediency’s sake, a quick transfer note
is written, a written or dictated summary will follow. (T-3).
5.37.5.4. Final progress notes on SF 509 may be substituted for narrative summaries on
patients with minor problems requiring less than a 48-hour stay, normal newborn infants
or uncomplicated obstetrical deliveries. Include any instructions given to the patient or
family in the final progress note. Scan and upload a copy in the patient’s outpatient record.
5.37.5.5. Disposition of SF 502:
5.37.5.5.1. File the original in the patient’s inpatient record.
5.37.5.5.2. Scan and upload a copy in the patient’s outpatient record.
5.37.5.5.3. Send one copy to the Commandant (G-KMA), United States Coast Guard,
Washington DC 20590, when United States Coast Guard members on AD are
discharged.
5.37.5.5.4. Upon disposition of a uniformed services member who is already on the
Temporary Disability Retired List when admitted, send a copy of the AF Form 565 and
SF 502 to the parent service as indicated below:
Air Force:
184 AFMAN41-210 10 SEPTEMBER 2019
HQ AFPC/DPSD
550 C Street West
Randolph AFB TX 78150
Navy:
Department of the Navy
Bureau of Medicine and Surgery (MED-25)
2300 E St., NW
Washington DC 20372-5300
Public Health Service and National Oceanic Atmospheric Administration
Medical Affairs Branch
ATTN: Dr. David Hooper
Department of Health and Human Services
5600 Fishers Lane, Rm 4C-06
Rockville, MD 20857
5.37.6. For an AD patient pending final disposition of PCS to home or transfer to a VA
hospital, place all additional copies of the AF Form 565 (or AF Form 560 when used in lieu
of) and SF 502 in a suspense file. Keep the patient in a change-of-status category until final
disposition of the case. Upon disposition, patient administration personnel complete the
administrative data on the final cover sheet (i.e., regarding type of disposition, etc...) and file
the following forms as specified in Attachment 10.
5.37.7. SF 504, SF 505, and SF 506.
5.37.7.1. Healthcare providers complete the history and physical examination records
within 24 hours after admission.
5.37.7.1.1. Completion of any part of the history or physical examination by a medical
student/physician’s assistant student does not relieve the attending healthcare provider
of the responsibility to ensure that an adequate history and physical examination is
performed and documented. See AFI 44-119, Medical Quality Operations for
procedures concerning histories and physicals conducted by medical/physician’s
assistant students.
5.37.7.1.2. The certified nurse mid-wife completes the history and physical
examination on obstetrical patients for whom the mid-wife is responsible.
5.37.7.1.3. A properly credentialed oral surgeon completes the physical examination
for patients admitted for dental services.
5.37.7.1.4. Podiatrists complete the history and physical as applicable to the podiatry
problem.
5.37.7.2. If an adequate history and physical examination is sent with transfer-in patients,
the provider may document an interval note on SF 509 stating no changes. The provider
will document any important changes.
AFMAN41-210 10 SEPTEMBER 2019 185
5.37.7.3. Enter a note in the SF 509 referring to the previous history and physical
examination for patients readmitted within one month to the same MTF for the same
condition. Document any changes. If desired, place a copy of the previous history and
physical in the current record.
5.37.7.4. If a history and physical examination was performed within 30 days before
admission, such as in the physician’s office, place a durable, legible copy in the inpatient
record and document any changes in the SF 509.
5.37.8. DD Form 2770, Abbreviated Medical Record may be used for the following:
5.37.8.1. Hospitalizations of five days or less for minor medical conditions normally
treated on an ambulatory basis when care in the patient’s residence is inadequate.
5.37.8.2. Hospitalizations of two days or less for minor surgical procedures performed
under local or peripheral nerve block anesthesia. This includes stable anesthesia Class III
or IV with minor procedure under local or regional anesthesia with or without IV sedation.
5.37.8.3. Hospitalizations of five days or less for delivering obstetric patients whose intra-
partum and postpartum course is uncomplicated, provided that a complete prenatal record
is included in the inpatient record.
5.37.8.4. Hospitalizations of 48 hours or less for surgeries when the patient is clearly
anesthesia Class I or II, regardless of type of anesthesia used.
5.37.9. Prepare SF 535 in duplicate for all newborn infants. Include the original in the
newborn’s inpatient record. Scan and upload information into the patient’s electronic health
record.
5.37.10. Record the patient’s diagnosis, treatment and care on the SF 509 to chronologically
describe the clinical course of the patient.
5.37.10.1. Determine the frequency of the notes based on the patient’s condition. Make
daily notations for the following: the first five days after a patient has undergone a major
operation; if the patient is seriously ill.
5.37.10.2. Record the postoperative note on the SF 509. The form may be overprinted
locally to provide a format.
5.37.10.3. Document the informed consent on the SF 509. See AFI 44-102 for
instructions.
5.37.11. Report surgical operations, including those performed in the ambulatory surgery unit,
on SF 516.
5.37.11.1. According to Joint Commission requirements, providers/surgeons will dictate
the report immediately following surgery. (T-0).
5.37.11.1.1. If immediate dictation is not feasible, dictate the report no later than 24
hours following the end of the surgical procedure.
5.37.11.1.2. If the operative report is not placed in the medical record immediately
after surgery, then prior to the patient’s release from the Recovery Room, the provider
will draft and enter an operative note into the inpatient or ambulatory procedure record
indicating pertinent clinical information to ensure continuity of care.
186 AFMAN41-210 10 SEPTEMBER 2019
5.37.11.2. Providers, at the time of dictation, must include the date and time of the
dictation, their clinical occupational specialty, and their AFSC, if applicable. (T-2).
Transcriptionists will include the aforementioned data, the transcribed clinical content, and
the date of transcription on all transcribed reports, including operative reports, SFs: 502,
504-506, 516, etc. (T-3).
5.37.11.3. Include in the report a description of the findings, the technique used, the tissue
removed or altered, estimated blood loss, as indicated, the postoperative diagnosis, the
condition of the patient at the end of the operation, and the name of the primary surgeon
and assistants.
5.37.12. Laboratory and Radiology Reports. When a computerized or automated summary of
all laboratory and radiology report results compiled during the patient’s hospitalization is
provided, file only the cumulative final report with the exception of preadmission labs and x-
rays. Destroy all previous duplicated computerized/automated report results. For inpatient
records unlike outpatient, all laboratory and radiology results must be filed in the record upon
discharge from the hospital. (T-3).
5.37.13. AF Form 3066 or 3066-1. A provider signs and dates orders on the AF Form 3066
or 3066-1, or enters the information into the current automated system.
5.37.13.1. When a hardcopy AF Form 3066 or 3066-1 is utilized, maintain the original
with the patient’s inpatient record.
5.37.13.2. When medications are ordered, send a copy to the Pharmacy. The provider’s
Drug Enforcement Agency (DEA) number is required in the provider’s signature
block/name stamp for any hand written prescriptions for controlled substances. Non-
United States physicians and dentists assigned to overseas facilities use their medical or
dental license number instead of a Drug Enforcement Agency number. (See AFI 44-102).
5.37.13.3. A verbal or telephone order may be given to a registered nurse. Each verbal
order is dated by the individual taking the order and identifies the names of the individuals
who gave and received it. In such cases, the provider confirms the order, signs, dates, and
stamps it within 48 hours.
5.37.14. Reverse of AF Forms 3068, PRN Medication Administration Record and 3069,
Medication Administration Record.
5.37.14.1. The reverse of these forms contain a section for the initials and signatures of
nursing staff administering the medications. Instead of signing the reverse of these forms,
utilize a separate sheet that contains the names, signatures and initials of the nursing staff.
5.37.14.2. When there is a separate sheet with the names, signatures and initials, the
nursing staff is only required to initial the reverse of the AF Form 3068 and 3069 when
administering medications.
5.37.14.3. File the sheet after the AF Form 3068 or 3069.
5.37.15. Maintain inpatient records received with a transfer-in patient as a component part of,
and attach to, the current inpatient record. Do not break up the transfer record and interfile its
forms among the forms of the current record. Note: If the original record was sent, copy and
maintain the pertinent portions, returning the original record to the transferring MTF.
AFMAN41-210 10 SEPTEMBER 2019 187
5.38. Prenatal Records. Prenatal documentation is maintained in the OB/GYN clinic until the
mother delivers.
5.38.1. If delivery is in the mother’s home MTF, maintain the documents, as a package, with
the inpatient documentation and file in the mother’s inpatient record.
5.38.2. If the delivery was not performed in the MTF, scan and upload the prenatal package
(as a whole package with prenatal treatment documents filed chronologically between the SF
533, Prenatal and Pregnancy Medical Record and AF Form 3915, Labor and Delivery
Flowsheet) in the mother’s electronic health record.
5.39. The Extended Ambulatory Record.
5.39.1. The extended ambulatory record is a folder that contains information on treatment
received during an ambulatory procedure visit, an observation stay, ER Death, Dead on
Arrival, or other similar status.
5.39.1.1. Create records at time of disposition and completion of each episode of care for
future retirement. Ensure discharge summary is scanned/uploaded into approved
electronic health record. Create a separate folder for each episode.
5.39.1.2. Maintain the extended ambulatory record folder in a method similar to the
inpatient record, using the inpatient record folder (AF Form 788A-J, Inpatient Record).
Annotate the folder with the patient’s name, family member prefix, and sponsor’s social
security number. Attach the CHCS Medical Record Tracking bar code label to the folder.
The extended ambulatory record will be filed by the sponsor’s social security number
(same as the outpatient and inpatient records). (T-3).
5.39.1.3. The extended ambulatory record will be maintained in a limited access area.
5.39.1.4. Although the paperwork for these cases is filed in the extended ambulatory
record folder, these episodes are coded as an outpatient episode in the appropriate
ambulatory data collection system.
5.40. Creating, Coding, and Documenting, Ambulatory Procedure Visit Records.
5.40.1. File original documentation on a patient seen during an ambulatory procedure visit
episode in the extended ambulatory record folder.
5.40.2. Create an ambulatory procedure visit record for those cases when a patient is seen in
the ER or specialty procedure room, an ambulatory procedure visit procedure is performed,
and the patient is discharged within 23 hours and 59 minutes of the time the patient was
checked in by the nurse for preliminary work-up for the procedure.
5.40.3. Maintain the record in a limited access area (preferably in the inpatient records
department). The ambulatory procedure visit record will be filed by the sponsor’s social
security number, (same as the outpatient and inpatient records). (T-3).
5.40.4. Clinical Application of Ambulatory Procedure Visit Records.
5.40.4.1. The medical record documentation for the ambulatory procedure visit must meet
the standards of documentation similar to the short-term stay (abbreviated medical record).
(T-1). The record documentation must comply with Joint Commission standards. (T-0).
At a minimum, the record must include an abbreviated history and physical, progress notes,
188 AFMAN41-210 10 SEPTEMBER 2019
doctor’s orders, patient’s informed consent, operative report, tissue report (if any),
anesthesia record, summary of care, to include discharge instructions and any Advance
Directive. (T-2). Copies of the summary, operative report, and any tissue reports are
forwarded to the outpatient record.
5.40.4.2. Physicians will sign and stamp an automated cover sheet or ambulatory
encounter summary form for the ambulatory procedure visit records. All diagnoses and
procedures will be written in full, without symbols or abbreviations, and in acceptable
provider terminology. (T-3).
5.40.4.3. The following forms are recommended for use in ambulatory procedure visit
records:
5.40.4.3.1. AF Form 560 or automated coversheet.
5.40.4.3.2. DD Form 2770.
5.40.4.3.3. SF 509.
5.40.4.3.4. SF 516.
5.40.4.3.5. OF 522, Anesthesia Medical Record or locally produced form.
5.40.4.3.6. OF 517, Request for Administration of Anesthesia and for Performance of
Operations and Other Procedures.
5.40.4.3.7. AF Form 3066 or 3066-1.
5.40.4.3.8. AF Form 3069.
5.40.4.3.9. AF Form 3068.
5.40.4.3.10. AF Form 3067, Intravenous Record.
5.40.4.4. Until Standard, Air Force or DD Forms (for ambulatory procedure visit records)
are developed, each MTF may elect to develop local forms, as an alternative to the
established forms listed in paragraph 5.40.4.3 to integrate documentation requirements into
the comprehensive records. The MTF Medical Records Function approves all requests for
locally developed forms before use in the health record. The MTF may utilize an
ambulatory encounter summary form.
5.40.5. Coding of Ambulatory Procedure Visits.
5.40.5.1. Code diagnoses according to current version of the International Classification
of Diseases (ICD) or current government approved coding classification system.
5.40.5.2. Code procedures/operations according to Current Procedure Terminology
coding references or current government approved coding classification system.
5.40.5.3. Utilize the Ambulatory Data Module in CHCS to capture the coded information
on each ambulatory procedure visit.
5.40.5.4. Utilize the Ambulatory Data Module Patient Encounter Forms or the automated
ambulatory procedure visit form used for coding in the ambulatory procedure visit record
for auditing and quality assurance purposes.
5.40.6. Admission of Ambulatory Procedure Visit Patients.
AFMAN41-210 10 SEPTEMBER 2019 189
5.40.6.1. Admit as an inpatient an ambulatory procedure visit patient that stays beyond the
time limit of 23 hours and 59 minutes. Time commences when the patient is checked in
for preliminary work-up for the procedure.
5.40.6.2. Do not backdate or change the time of the admission date and time to the point
when the patient’s ambulatory procedure visit episode began. Use the date and time when
the admission to the hospital occurs. Enter the following statement in the administrative
section of the cover sheet “Patient admitted from APU. Information on the ambulatory
procedure visit procedure is maintained in the ambulatory procedure visit record.”
5.40.6.3. Do not combine the original ambulatory procedure visit documentation with the
inpatient record but maintain it separately in the extended ambulatory record folder.
5.40.6.4. Include copies of the Ambulatory Data Module Patient Encounter Form or
automated cover sheet, the abbreviated history and physical, operative report, and any other
pertinent documentation in the inpatient record, as applicable.
5.40.6.5. Code the inpatient record with the reason that caused the admission.
5.41. Creating, Coding, and Documenting Observation Records.
5.41.1. Observation patients are outpatients with acute or chronic medical problems who
require assessment monitoring or diagnostic evaluation in order to determine final disposition.
The decision to place a patient in observation status is based upon the complexity, intensity,
and duration of care required as determined by the provider.
5.41.2. Outpatient observation stays generally should not exceed 23 hours and 59 minutes.
However, up to 48 hours may be authorized when medical necessity has been clearly
demonstrated.
5.41.3. Observation patients may be cared for in either dedicated observation units or in any
designated bed space. Appropriate Joint Commission standards will apply. (T-3).
5.41.4. Documentation of Observation Records.
5.41.4.1. Documentation for an observation patient must meet the standards for a short-
term stay (abbreviated medical record) and must comply with the current Joint Commission
documentation standards. (T-3).
5.41.4.2. SFs, or other forms as noted, are recommended for use in observation records.
At a minimum, the documentation in the medical record will include:
5.41.4.2.1. Summary of pertinent diagnostic findings.
5.41.4.2.2. A plan of care to include reasons for observation, diagnoses, and risks of
complication, patient education, release instructions, medication orders, and plans for
follow-up care.
5.41.4.2.3. SF 558.
5.41.4.2.4. SF 509.
5.41.4.2.5. All diagnostic reports (e.g., laboratory, radiology, or electrocardiogram) as
applicable.
5.41.4.2.6. AF Form 3066 or 3066-1.
190 AFMAN41-210 10 SEPTEMBER 2019
5.41.4.2.7. AF Form 3069 as applicable.
5.41.4.2.8. AF Form 3068 as applicable.
5.41.4.2.9. AF Form 3067 as applicable.
5.41.4.2.10. Advance Directive (if previously accomplished by the patient).
5.41.4.3. File all documentation related to an observation stay in the extended ambulatory
record folder.
5.41.4.4. Forward the following documents to the outpatient treatment record: release note
with summary of pertinent diagnostic findings, status of patient upon release, and release
instructions with plans for follow-up care.
5.41.5. Coding of Observation Records.
5.41.5.1. Code diagnoses according to the current version of the ICD coding references or
current government approved coding classification system.
5.41.5.2. Code procedures/operations according to the Current Procedural Terminology
coding references or current government approved coding classification system.
5.41.5.3. Utilize the Ambulatory Data Module in CHCS to capture the coded information
on each observation episode, except when an observation patient is admitted.
5.41.6. Admission of Observation Patients. When a patient is admitted from an observation
status, file the observation documentation in the extended ambulatory record folder. Place
copies of pertinent documentation in the inpatient record.
5.42. Patients Discharged Without Definitive Diagnosis. The inpatient records department
maintains in a suspense file, records that the provider has indicated should be held pending
pathology reports, laboratory test results, or other confirmations. Never maintain the records in
suspense longer than one month after the month of disposition. (T-1). Process the record with
whatever information is available. The record may be corrected at a later date if information,
which alters the final diagnosis, is received.
5.43. Disposition of Inpatient Records.
5.43.1. When transferring patients to another MTF, send a complete and legible copy of the
current inpatient record, original outpatient record, and copies of any previous admissions
pertinent to the patient’s current condition. If complete and legible copies cannot be made in
time for the patient’s transfer, send the original current inpatient record. Note: The receiving
MTF returns original records to the transferring MTF when they have served their purpose.
Also, send any x-ray films and duplicate slides or surgical specimens when the findings have
a direct bearing on the diagnosis and treatment.
5.43.2. The admitting facility notifies the originating MTF of patients admitted while on
directed convalescence, PCS home, or Absent Without Leave (AWOL) from another medical
facility while in patient status. If the patient will remain at the new MTF, the initial facility
transfers the individual to the new MTF and forwards the patient’s records.
5.43.3. When transferring patients to non-military MTFs, a transcript or copy of pertinent
pages may accompany the patient. Never release the original records; however, pertinent x-
ray films are furnished to the receiving non-military MTF as required.
AFMAN41-210 10 SEPTEMBER 2019 191
5.43.4. Send a copy of the current inpatient record and any x-ray films when an AD patient is
transferred to a VA hospital pending separation or retirement from the uniformed services.
5.43.5. Forward original records of NATO military personnel and their family members
(including x-ray film and medical examination reports) in a sealed envelope with the individual
concerned upon transfer to another MTF. When the individual is discharged, return the record
to the parent country. Retain copies of pertinent records necessary for quality assurance
review.
5.43.6. Handle inpatient records of non-NATO military personnel and their family members
the same as any other inpatient record.
5.43.7. When mailing records pertinent to litigation cases, mail medical records and claims
files via certified mail/return receipt.
5.44. Medical Transcription.
5.44.1. Responsibilities of Medical Transcription: Medical transcription services provide
timely and accurate transcription of provider dictation dealing with inpatient and ambulatory
patient care. It is a patient administration responsibility and is usually managed by the inpatient
medical records department supervisor in cooperation with the transcription quality assurance
evaluator and/or contracting officer’s technical representative.
5.44.2. Production Goals: Each medical transcription center should produce an acceptable
quantity and quality of medical transcription in a timely manner. Normally, these services are
employed to generate transcription services for inpatient episodes of care. If transcription
staffing and inpatient workload allow, transcription services can be expanded to ambulatory
and outpatient clinic services. Inpatient and ambulatory procedure visits dictated operative
reports must be transcribed and filed in the medical record immediately following surgery. (T-
3). In accordance with The Joint Commission, MTFs must generate clear policy/guidance to
all providers in their facility regarding the scope of medical transcription services they intend
to offer. (T-3).
5.44.2.1. Quantity: Suggested production goals for medical transcriptionist are 800 lines
per day per transcriptionist. The senior transcriptionist or supervisor, in a smaller medical
transcription center, contributes to the work center output; however, their goals are lower
than those established for other medical transcriptionists and decrease as the size of the
medical transcription center and supervisory responsibilities increase. Personnel in
training should be able to achieve the production goals within a reasonable period of time,
not to exceed 1 year.
5.44.2.2. Counting and Reporting: Medical transcriptionists count and record their output
according to the following suggested instructions. (Output is reported daily to the senior
transcriber or supervisor)
5.44.2.2.1. Margins should be adjusted to ensure full lines that average 80 strokes.
Narrative lines of 80 strokes should average 13 words. Count each typed line with six
words or more as a line; any narrative line with five words or less is not counted.
5.44.2.2.2. Form-style typing:
5.44.2.2.2.1. Count each line with two or more names, dates or words as one line.
192 AFMAN41-210 10 SEPTEMBER 2019
5.44.2.2.2.2. Physician signature elements are counted as two lines when a two-
line signature element is used, and counted as one line when a one-line signature
element is used.
5.44.2.2.2.3. Patient identification data is counted as two lines.
5.44.2.2.3. The senior transcriptionist or supervisor reports individual production to
the supervisor or Quality Assurance Evaluator/Contracting Officer’s Technical
Representative of inpatient records.
5.44.2.3. The supervisor or Quality Assurance Evaluator/Contracting Officer’s Technical
Representative of inpatient records, through the senior transcriptionist or supervisor,
monitors the quality of all medical transcription. When medical transcriptionists are
required to retype work which does not meet quality standards, do not include lines retyped
in production counts.
5.44.2.4. Work should normally be completed within 24 hours of receipt of dictation.
Transcribed narrative summaries and operative reports should be filed in the medical
record prior to inpatient/ambulatory procedure visit coding to provide complete
documentation and ensure accurate coding.
Section 5D—Deployed Assignment Medical Record Management
5.45. Minimum Deployed Medical Documentation and Record Management Requirements.
5.45.1. Unless exempted by COCOM/Component reporting instructions, the DD Form 2766is
the principle folder used to document primary medical and dental care for AD, AFR, ANG,
and deployed federal civilian employees. Inpatient documents generated from a theater MTF
will likely be maintained and documented separately from the medical information stored in
the DD Form 2766.
5.45.2. Health records located at deployed combat theater locations are maintained by unit
medical personnel. Deployed medical commanders will ensure effective re-deployment
medical out-processing procedures are in place, and will work with deployed unit commanders
to ensure required actions are completed for all re-deploying personnel, to include all DoD
uniformed members, civilians, and contractors in accordance with DoDI 6490.03, AFI 10-403,
Deployment Planning and Execution, and AFI 48-122, Deployment Health. (T-0).
5.45.3. Unless exempted by the COCOM/Component reporting instructions, deployed
medical unit records managers will use the cardstock DD Form 2766 to document primary
medical and dental care. (T-0). Reference DoDI 6490.03. Deployed records personnel are
required to file all primary local, Service-specific, SFs, and OFs generated from primary care
provider-patient encounters, into the cardstock DD Form 2766. (T-0). Reference DoDI
6490.03. File documents inside the cardstock DD Form 2766 in chronological order, with the
most recent encounter filed on top of older documents.
5.45.4. Theater Electronic Health Records and/or Applications: Although advances in
electronic medical record technology support comprehensive regional healthcare operations in
the deployment environment, unless the medical information maintained in these systems can
provide reliable, secure, and timely medical record data transfer from the deployed medical
unit to the DoD’s Central Data Repository, or otherwise exempted by COCOM/Component
AFMAN41-210 10 SEPTEMBER 2019 193
reporting instructions, deployed medical records personnel are required to print each primary
care patient encounter and file the printed form into the cardstock DD Form 2766.
5.45.5. Documenting Patient Care: Proper documentation of medical/surgical care is
accomplished on all patients treated at the Expeditionary Medical Support/Air Force Theater
Hospital. Utilization of the SF 600, is the primary form used to document most ambulatory
care. AF Form 3910, Critical Care Flow Sheet (Small MTF) is used to record critical care
patients’ treatment/progress. All ambulatory care healthcare forms and documents must be
filed into the DD Form 2766. (T-0). Reference DoDI 6490.03. The outpatient healthcare
information collected on these forms must return to the member’s host MTF. (T-0). Reference
DoDI 6490.03.
5.45.5.1. For patients entering the aeromedical evacuation system, the AF Form 3830,
Patient Manifest (5 copies minimum) should be completed for each Aeromedical
Evacuation mission. If not available, substitute this form with the DD Form 601, Patient
Evacuation Manifest. The AF Form 3899, Aeromedical Evacuation Patient Record,
accompanies the patient to ensure appropriate care during transport. This document is
primarily used to direct and record en route care. If AF Form 3899 is not available, use
DD Form 602, Patient Evacuation Tag. Medical orders should be clearly written on either
the AF Form 3899 or the DD Form 1380, Tactical Combat Casualty Care (TCCC) Card.
The DD Form 1380 normally is used by the originating facility during contingencies. The
information on the DD Form 1380 is transcribed to the AF Form 3899/DD Form 602 upon
entry into the Aeromedical Evacuation System. Information should include both primary
and secondary diagnoses, correct patient classification, and orders for all enroute
medications, care, and special diets. A concise, pertinent nursing note from the referral
MTF should be written on the form as a transfer note. At a minimum, the note should
include the dates and times of last medications, vital signs, and treatment rendered.
5.45.5.2. Required deployed healthcare minimum documentation forms include (T-1): SF
Form 600; DD Form 1380; DD Form 2992; AF Form 422; AF Form 579, Controlled
Substances Register; SF 516, OF 517; and DD Form 599, Patient’s Effects Storage Tag.
5.45.6. Deployed MTF medical staff will:
5.45.6.1. Conduct redeployment processing in accordance with DoDI 6490.03, AFI 10-
403 and AFI 48-122. Work with the deployed Military Personnel Section and unit
commanders to ensure all returning or re-deploying personnel are identified in a timely
manner and have completed medical re-deployment screening and/or out-processing no
earlier than 30 days prior to scheduled/projected departure.
5.45.6.2. If required, conduct DD Form 2796, Post-Deployment Health Assessment, in
accordance with Air Force Instruction 48-122.
5.45.6.3. Complete DD Form 2796 electronically via ASIMS. Hard copy forms will not
be accepted.
5.45.6.4. A legible copy of the DD Form 2796 must be documented in the deployer’s
electronic health record, if the capability exists. (T-0). Otherwise, MTF medical personnel
are required to print a hard copy of the electronic DD Form 2796 and place it in the
member’s deployment medical record (DD Form 2766). (T-2). For more specific
instructions for ASIMS/AHLTA documentation, see AFI 48-122.
194 AFMAN41-210 10 SEPTEMBER 2019
5.45.6.5. If the deployer is unable to complete the form electronically due to computer
failure, network interruption, or the unavailability of an automated process, deployed
medical staff must prominently place the following notice in the DD Form 2766; “Member
unable to Electronically Complete DD Form 2796 in Theater. (T-3). Member must report
to Public Health within 5 duty days of returning to home unit to complete the electronic
DD Form 2796.” (T-2).
5.45.7. Deployed MTF support (records) staff will (T-1):
5.45.7.1. File the signed/stamped hard copy DD Form 2796 into the DD Form 2766 for
later transcription into ASIMS and documentation in AHLTA by a host station MTF
provider, when the location does not have electronic health record capability.
5.45.7.2. Package and seal the medical records for each returning service member.
Individual records may be bundled together (but not inter-filed) and sealed together in a
bulk courier package. Identify the troop commander for each returning or re-deploying
group and transfer the sealed medical records to the troop commander. If no troop
commander exists, identify the senior ranking member in the group and transfer the records
to the ranking member, or authorized delegate. Obtain a chain of custody receipt before
completing the transfer. If records are to be packaged and sealed for a single returning or
re-deploying service member, first check with a mental health provider to ensure the
service member should not be physically or mentally harmed if the member were to open
the sealed package and read the documents inside. If the mental health provider decides
the sealed medical documents for a returning or re-deploying service member could
potentially cause harm if the member were to read the documents, contact the service
member’s host MTF and arrange for the records to be mailed back to the medical unit. If
the mailing option is used, ensure the package is mailed with a package-tracking or return-
receipt confirmation service (if available).
5.45.7.3. Each DD Form 2766 should contain all primary care medical documents
generated during the length of the deployment. The minimum number and name of
documents to be filed into each DD Form 2766 include:
5.45.7.3.1. Smallpox vaccination screening forms (SF 600 Overprint).
5.45.7.3.2. All primary care patient documents (if no automated data transfer
mechanism exists that guarantees reliable, secure, and timely medical record data
transfer from the deployed location to DoD’s Central Data Repository, print each
primary care patient encounter and file the printed form into the cardstock DD Form
2766).
5.45.7.3.3. Environmental/Occupational Health Exposure Data (SF 600 Overprint).
5.45.7.3.4. Physical therapy and dental visit records.
5.45.7.3.5. Mental health provider documentation: (Note: If a mental health provider
decides that sealed medical documents for a returning or re-deploying service member
could potentially cause harm if the member were to read the documents, contact the
service member’s host MTF and arrange for the records to be mailed back to the
medical unit).
5.45.7.3.6. Provider signed, dated, and Identification stamped DD Form 2796.
AFMAN41-210 10 SEPTEMBER 2019 195
5.45.7.3.7. Insert a shipping roster of names and ranks for each corresponding DD
Form 2766 placed inside each bulk courier package. Label individual sealed envelopes
with the returning or re-deploying member’s name, rank, home unit, and assignment
installation. For bulk courier and individual medical record packages, address the
outside envelope or package with the following pre-printed or stamped message, “PHI
ENCLOSED. THIS ENVELOPE MUST BE DELIVERED TO THE FORCE
HEALTH MANAGEMENT OFFICE AT YOUR HOME DUTY STATION.”
5.46. Expeditionary Electronic Health Record Management Platforms and Systems. A
complete list of expeditionary electronic health record management platforms and systems can be
found at the Defense Health Clinical Systems website: https://www.health.mil/.
5.47. Emergency Medical Service and AF Form 552, Air Force Patient Care Report.
5.47.1. Patients transported to a MTF for care/treatment/admission. If the patient is
transported to the MTF, the information on the AF Form 552 is relevant to their care. The
healthcare provider should include the AF Form 552 as part of the patient's health record.
5.47.1.1. A copy should be sent to the Medical Director for peer review and a copy to
TRICARE Operations and Patient Administration for billing considerations.
5.47.1.2. Copies should be retained in accordance with normal retention standards.
5.47.2. Patients transported to a non-DoD facility with existing record. If the patient is
empaneled to the MTF or otherwise has an existing record (e.g., occupational health record)
the AF Form 552 is relevant to their care and should be included as part of the patient’s health
record.
5.47.2.1. A copy should be sent to the Medical Director for peer review and a copy to
TRICARE Operations and Patient Administration for billing considerations.
5.47.2.2. Copies should be retained in accordance with normal retention standard.
5.47.3. Patients transported to DoD facility (non-beneficiary). Due to legal and liability
considerations, maintain a copy of the AF Form 552 for a minimum of two years. If the patient
is not a beneficiary, the form can be kept in an alphabetical file and maintained similar to
AFRIMS rule T41-08 R 09.00 https://afrims.cce.af.mil/afrims/rims.cfm.
5.47.4. Any copies of the AF Form 552 provided to or used by other areas of the MTF, as
deemed appropriate by the Medical Director, should be maintained in accordance with existing
retention standards.
DOROTHY A. HOGG
Lieutenant General, USAF, NC
Surgeon General
196 AFMAN41-210 10 SEPTEMBER 2019
Attachment 1
GLOSSARY OF REFERENCES AND SUPPORTING INFORMATION
References
5 CFR Part 339.301, Authority to Require an Examination, 18 January 2017
32 CFR Part 199, Civilian health and Medical Program of the Uniformed Services (CHAMPUS),
1 July 1986
42 CFR Part 493, Laboratory Requirements, 14 March 1990
45 CFR Part 164, Security and Privacy, 28 December 2000
5 USC § 552a, User Training for TRANSCOM Reporting and Command & Control Evacuation
System (TRAC2ES), 16 March 2018
5 USC § 8103, Medical Services and Initial Medical and Other Benefits, 19 May 2019
5 USC § 8141, Civil Air Patrol Volunteers, 15 August 1994
5 USC § 8142, Peace Corps Volunteers, 9 October 2018
5 USC § 8143, Job Corps Enrollees, Volunteers in Service to America, 21 September 1993
10 USC § 1072, Definitions, 12 December 2017
10 USC § 1074, Medical and Dental Care for Members and Certain Former Members, 12
December 2017
10 USC § 1074b, Medical and Dental Care: Academy Cadets and Midshipmen; Members of,
and Designated Applicants for Membership in, Senior ROTC, 28 October 2004
10 USC § 1074h, Medical and Dental Care: Medal of Honor Recipients; Dependents, 13
August 2018
10 USC § 1076, Medical and Dental for Dependents: General Rule, 28 December 2001
10 USC § 1095, Healthcare Services Incurred on Behalf of Covered Beneficiaries: Collection
From Third Party Payers, 30 November 1993
10 USC § 1210, Members on Temporary Disability Retired List: Periodic Physical
Examination; Final Determination of Status, 23 December 2016
10 USC § 1588, Authority to Accept Certain Voluntary Services, 19 December 2014
24 USC § 34, Hospitalization of Persons Outside Continental Limits of United States; Persons
Entitled; Availability of Other Facilities; Rate of Charges; Disposition of Payments, 26 October
2015
37 USC § 310, Special Pay: Duty Subject to Hostile Fire or Imminent Danger, 2 January 2013
38 USC § 1720G, Assistance and support for caregivers, 29 September, 2018
National Defense Authorization Act for Fiscal Year 2019, Section 711, Transition of
Administration by Defense Health Agency of Military Medical Treatment Facilities, 15 May,
2018
AFMAN41-210 10 SEPTEMBER 2019 197
DFAS DEM 177-373, Department of Defense (DoD) Financial Management Regulation,
February 1999
DHA IPM 18-001, Standard Appointing Processes, Procedures, Hours of Operation,
Productivity, Performance Measures and Appointment Types in Primary, Specialty, and
Behavioral Health Care in Medical Treatment Facilities (MTFs), 3 July 2018
DHA IPM 18-016, Medical Coding of the DoD Health Records, 19 October, 2018
DHA IPM 18-018, Physical Custody and Control of the DoD Health Record, 8 November 2018
DoDI 1000.13, Identification (ID) Cards for Members of the Uniformed Services, Their
Dependents, and Other Eligible Individuals, 23 January 2014
DoDI 1000.30, Reduction of Social Security Number (SSN) Use Within DoD, 1 August 2012
DoDI 1241.01, Reserve Component (RC) Line of Duty Determination for Medical and Dental
Treatments and Incapacitation Pay Entitlements, 19 April 2016
DoDI 1332.18, Disability Evaluation System, 5 August 2014
DoDI 1341.02, Defense Enrollment Eligibility Reporting System (DEERS) Program and
Procedures, 8 August 2016
DoDI 1342.24, Transitional Compensation for Abused Dependents, 23 May 1995
DoDI 1400.32, DoD Civilian Work Force Contingency and Emergency Planning Guidelines and
Procedures, 24 April 1995
DoDI 3020.41, Operational Contract Support (OCS), 20 December 2011
DoDI 5154.30, Armed Forces Medical Examiner System (AFMES) Operations, 29 December
2015
DoDI 6000.11, Patient Movement, 22 June 2018
DoDI 6000.14, DoD Patient Bill of Rights and Responsibilities in the Military Health System
(MHS), 26 September 2011
DoDI 6015.23, Foreign Military Personnel Care and Uniform Business Offices in Military
Treatment Facilities (MTFs), 23 February 2015
DoDI 6025.13, Medical Quality Assurance (MQA) and Clinical Quality Management in the
Military Health System (MHS), 17 February 2011
DoDI 6025.23, Health Care Eligibility Under the Secretarial Designee (SECDES) Program and
Related Special Authorities, 16 September 2011
DoDI 6040.40, Military Health System Data Quality Management Control Procedures, 26
November 2002
DoDI 6040.42, Management Standards for Medical Coding of DoD Health Records, 8 June 2016
DoDI 6040.45, DoD Health Record Life Cycle Management, 16 November 2015
DoDI 6200.06, Periodic Health Assessment (PHA) Program, 8 September 2016
DoDI 6465.03, Anatomic Gifts and Tissue Donation, 8 June 2016

198 AFMAN41-210 10 SEPTEMBER 2019
DoDI 6490.03, Deployment Health, 11 August 2006
DoDI 6490.12, Mental Health Assessments for Service Members Deployed in Connection with a
Contingency Operation, 26 February 2013
DoD 7750.07-M, DoD Forms Management Program Procedures Manual, 7 May 2008
DoD 5400.11-R, Department of Defense Privacy Program, 14 May 2007
DoDM 6025.18, Implementation of the Health Insurance Portability and Accountability Act
(HIPAA) Privacy Rule in DoD Health Care Programs, 13 March 2019
DoDM 5210.42, Nuclear Weapons Personnel Reliability Program, 13 January 2015
AFI 10-203, Duty Limiting Conditions, 20 November 2014 AFI 10-403, Deployment Planning
and Execution, 20 September 2012
AFI 16-108, Managing the Aviation Leadership Program, 17 August 2015
AFI 31-105, The Air Force Corrections System, 15 June 2015
AFI 33-332, Air Force Privacy and Civil Liberties Program, 12 January 2015
AFI 33-360, Publications and Forms Management, 1 December 2015
AFI 34-1101, Warrior and Survivor Care, 6 May 2015
AFI 34-501, Mortuary Affairs Program, 16 April 2019
AFI 36-2110, Total Force Assignments, 5 October 2018
AFI 36-2603, Air Force Board for Correction of Military Records (AFBCMR), 18 September
2017
AFI 36-2608, Military Personnel Records Systems, 26 October 2015
AFI 36-2910, Line of Duty Misconduct Determination, 8 October 2015
AFI 36-3002, Casualty Services, 26 April 2019
AFI 36-3003, Military Leave Program, 11 May 2016
AFI 36-3024, Transitional Compensation for Abused Dependents, 24 January 2018
AFI 36-3026V1_IP, Identification Cards for Members of the Uniformed Services, Their Eligible
Family Members, and Other Eligible Personnel, 4 Aug 2017
AFI 36-3208, Administrative Separation of Airman, 9 July 2004
AFI 36-3212, Physical Evaluation for Retention, Retirement, and Separation, 2 February 2006
AFI 40-301, Family Advocacy Program, 16 November 2015
AFI 40-701, Medical Support to Family Member Relocation and Exceptional Family Member
Program (EFMP), 19 November 2014
AFI 41-106, Medical Readiness Program Management, 9 June 2017
AFI 41-126, DoD/Veterans Affairs Health Care Resource Sharing Program, 4 September 2018
AFI 41-200, Health Insurance Portability and Accountability Act (HIPAA), 25 July 2017
AFMAN41-210 10 SEPTEMBER 2019 199
AFI 44-102, Medical Care Management, 17 March 2015
AFI 44-110, The Cancer Program, 18 September 2014
AFI 44-119, Medical Quality Operations, 16 August 2011
AFI 44-121, Alcohol and Drug Abuse Prevention and Treatment (ADAPT) Program, 18 July
2018
AFI 44-172, Mental Health, 13 November 2015
AFI 44-176, Access to the Care Continuum, 8 September 2017
AFI 48-122, Deployment Health, 18 August 2014
AFI 48-123, Medical Examinations and Standards, 5 November 2013
AFI 48-307V1, En Route Care and Aeromedical Evacuation Medical Operations, 9 January
2017
AFI 90-1001, Planning Total Force Association (TFAS), 9 January 2017
AFI 90-6001, Sexual Assault Prevention and Response (SAPR) Program, 21 May 2015
AFI 91-204, Safety Investigation and Reports, 27 April 2018
AFMAN 33-363, Management of Records, 1 March 2008
AFMAN 65-605V1_AFGM2018-01, Budget Guidance and Technical Procedures, 24 October
2018
AFMAN 65-116V1, Defense Joint Military Pay System Active Component (DJMS-AC) FSO
Procedures, 1 April 2007
AFPD 10-29, Worldwide Aeromedical Evacuation Operations, 13 February 2019
AFPD 41-2, Medical Support, 17 May 2018
AR 40-562/BUMEDINST 6230.15B /AFI 48-110/CG COMDTINST M6230.4G, Immunizations
and Chemoprophylaxis for the Prevention of Infectious Diseases, 7 October 2013
Headquarters Air Force Mission Directive 1-6, Administrative Assistant to the Secretary of the
Air Force, 22 December, 2014
Headquarters Air Force Mission Directive 1-48, The Air Force Surgeon General, 7 May 2015
Headquarters Air Force Mission Directive 1-24, Special Management, 28 January, 2019
Health Affairs Policy 05-014, Policy Guidance for Enrollment of AD Service Members into
TRICARE Prime, 19 August 2005, https://www.health.mil/Reference-Center/Policies
Health Affairs Policy 08-002, Policy for Billing Care Furnished by MTFs to Federal Employees
for On-the-Job Injuries and for Occupational Health, 26 March 2008,
https://www.health.mil/Reference-Center/Policies
Health Affairs Policy 11-005, TRICARE Policy for Access to Care, 23 February 2011,
https://www.health.mil/Reference-Center/Policies
200 AFMAN41-210 10 SEPTEMBER 2019
Health Affairs Policy Memorandum 99-003, Physical Examinations for Reserve Officer Training
Corps (ROTC) Applicants, 18 December 1999, https://www.health.mil/Reference-
Center/Policies
Joint Travel Regulations, https://www.dfas.mil/militarymembers/travelpay/regulations.html
Medical Department (MANMED), NAVMED P-117, Chapter 16, Health Records, 23 December
1994, https://www.med.navy.mil/directives/Pages/BUMEDInstructions.aspx
Medical Record Tracking, Retirement and Retrieval User Guide,
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx
MHS, Patient Identity Management and Registration Guidance, 28 October 2013,
https://www.health.mil/
MHS, Notice of Privacy Practices, 1 October 2013 https://www.health.mil/
The Joint Commission,
https://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx
TRICARE Policy Manual 6010.60-M, Chapter 4, Section 16.1, Intersex Surgery, 1 April 2015
https://www.health.mil/
Prescribed Forms
AF Form 146, Death Tag
AF Form 230, Request for Patient Transfer
AF Form 250, Health Record Charge Out Request
AF Form 552, Air Force Patient Care Report
AF Form 560, Authorization and Treatment Statement
AF Form 565, Record of Inpatient Treatment
AF Form 570, Notification of Patient’s Medical Status
AF Form 577, Patient’s Clearance Record
AF Form 614, Charge Out Record
AF Form 788A-J, Inpatient Record
AF Form 1403, Roster of Seriously Ill/Very Seriously Ill
AF Form 1480, Summary of Care (Canceled)
AF Form 1480A, Adult Preventive and Chronic Care Flowsheet
AF Form 1480B, Adult Preventive and Chronic Care Flowsheet Continuation Sheet
AF Form 2100A, Health Record - Outpatient
AF Form 2100B, Health Record - Dental
AF Form 2110A, Health Record - Outpatient
AF Form 2120A, Health Record - Outpatient
AFMAN41-210 10 SEPTEMBER 2019 201
AF Form 2130A, Health Record - Outpatient
AF Form 2140A, Health Record - Outpatient
AF Form 2150A, Health Record - Outpatient
AF Form 2160A, Health Record - Outpatient
AF Form 2170A, Health Record - Outpatient
AF Form 2180A, Health Record - Outpatient
AF Form 2190A, Health Record - Outpatient
AF Form 3066, Doctor’s Orders
AF Form 3066-1, Doctor’s Orders
AF Form 3068, PRN Medication Administration Record
Adopted Forms
AF Form 40A, Record of Individual Inactive Duty Training
AF Form 100, Request and Authorization for Separation
AF Form 330, Records Transmittal/Request
AF Form 348, Line of Duty Determination
AF Form 348-R, Line of Duty Determination for Restricted Report of Sexual Assault
AF Form 422, Notification of Air Force Member’s Qualification Status
AF Form 469, Duty Limiting Condition Report
AF Form 579, Controlled Substances Register
AF Form 745, Sensitive Duties Program Record Identifier
AF Form 797, Job Qualification Standard Continuation/Command JQS
AF Form 885, Medical Record Charge Out Guide (Red) (For use by USAF Medical Treatment
Facilities ONLY)
AF Form 886, Medical Record Charge Out Guide (Yellow) (For use by USAF Medical
Treatment Facilities ONLY)
AF Form 887, Medical Record Charge Out Guide (Blue) (For use by USAF Medical Treatment
Facilities ONLY)
AF Form 847, Recommendation for Change of Publication
AF Form 1122, Personal Property and Personal Effects Inventory
AF Form 1185, AF Form 1185, Commander’s Impact Statement for Medical Evaluation Board
AF Form 1288, Application for Ready Reserve Assignment
AF Form 1418, Recommendation for Flying or Special Operation Duty - Dental
AF Form 1488, Daily Log of Patients Treated for Injuries
202 AFMAN41-210 10 SEPTEMBER 2019
AF Form 1942, Clinic Index
AF Form 2005, Issue/Turn-In-Request
AF Form 2700L, Health Record Year Grid
AF Form 3067, Intravenous Record Medical/Dental Records or Information
AF Form 3069, Medication Administration Record
AF Form 3830, Patient Manifest
AF Form 3899, Aeromedical Evacuation Patient Record
AF Form 3910, Critical Care Flow Sheet (Small MTF)
AF Form 3915, Labor and Delivery Flowsheet
DD Form 137-5, Dependency Statement
DD Form 214, Certificate of Release or Discharge from Active Duty
DD Form 261, Report of Investigation Line of Duty and Misconduct Status
DD Form 599, Patient’s Effects Storage Tag
DD Form 601, Patient Evacuation Manifest
DD Form 602, Patient Evacuation Tag
DD Form 689, Individual Sick Slip
DD Form 877-1, Request for Medical/Dental Records from the National Personnel Records
Center (NPRC) (St. Louis, Missouri)
DD Form 1380, Tactical Combat Casualty Care (TCCC) Card
DD Form 2005, Privacy Act Statement - Healthcare Records
DD Form 2064, Certificate of Death (Overseas)
DD Form 2138, Request for Transfer of Outpatient Records
DD Form 2499, Health Care Practitioner Action Report
DD Form 2766, Adult Preventive and Chronic Care Flowsheet
DD Form 2766C, Adult Preventive and Chronic Care Flowsheet (Continuation Sheet)
DD Form 2770, Abbreviated Medical Record
DD Form 2796, Post-Deployment Health Assessment
DD Form 2825, Internal Receipt
DD Form 2870, Authorization for Disclosure of Medical or Dental Information
DD Form 2882, Pediatric and Adolescent Preventive and Chronic Care Flowsheet
DD Form 2992, Medical Recommendation for Flying or Special Operational Duty
DoL Form LS-1, Request for Examination and/or Treatment
DoL Form LS-201, Notice of Employee’s Injury or Death
AFMAN41-210 10 SEPTEMBER 2019 203
DoL Form LS-202, Employer’s First Report of Injury or Occupational Illness
DS-2029, Application for Consular Report of Birth Abroad of a Citizen of the United States of
America
Form Compensation Act (CA)-16, Authorization for Examination and/or Treatment
FS-240, Consular Report of Birth
OF 275, Medical Record Report
OF 517, Request for Administration of Anesthesia and for Performance of Operations and Other
Procedures
OF 522, Anesthesia Medical Record
OF 523B, Medical Record – Authorization for Tissue Donation
SF 66D, Employee Medical Folder
SF 93, Report of Medical History
SF 135, Records Transmittal and Receipt
SF 502, Medical Record – Narrative Summary (Clinical Resume)
SF 503, Medical Record-Autopsy Protocol
SF Form 504, Clinical Record-History Parts I and II
SF 505, Medical Record – History Parts 2 and 3
SF 506, Medical Record – Physical Examination
SF 509, Medical Record – Progress Report
SF 516, Operation Report
SF 523, Medical Record-Authorization for Autopsy
SF 526, Medical Record – Interstitial/Intercavitary Therapy
SF 535, Medical Record - Newborn
SF 551, Medical Record – Serology
SF 558, Medical Record – Emergency Care and Treatment
SF 559, Medical Record – Allergen Extract Prescription – New and Refill
SF 600, Chronological Record of Medical Care
VA Form 21-0819, DoD Referral to Integrated Disability Evaluation System (IDES)
VA Form 9957, ACRS Time Sharing Request Form
Abbreviations and Acronyms
AAC—Assignment Availability Code
AD—Active Duty
ADAPT—Alcohol and Drug Abuse Prevention and Treatment
204 AFMAN41-210 10 SEPTEMBER 2019
AFI—Air Force Instruction
AFMOA—Air Force Medical Operations Agency
AFMS—Air Force Medical Service
AFMSA—Air Force Medical Support Agency
AFOSI—Air Force Office of Special Investigation
AFR—Air Force Reserve
AFRC—Air Force Reserve Command
AFRIMS—Air Force Records Information Management System
AFSC—Air Force Specialty Code
AHLTA—Armed Forces Health Longitudinal Technology Application
AMTU—Airman Medical Transition Unit
ANG—Air National Guard
ARC—Air Reserve Component
ASD—Assistant, Secretary of Defense
ASIMS—Aerospace Services Information Management System
AWOL—Absent Without Leave
CED—Contingency, Exercise, Deployment
CHCS—-Composite Healthcare System
CLIA—Clinical Laboratory Improvements Amendments
COCOM—Combatant Command
CONUS—Continental United States
DC—Dental Corps
DEERS—Defense Enrollment Eligibility Reporting System
DHA—Defense Health Agency
DoD—Department of Defense
DoDD—Department of Defense Directive
DoDI—Department of Defense Instruction
DoDM—Department of Defense Manual
DSN—Defense Switched Network
EFMP—Exceptional Family Member Program
ER—Emergency Room
FOIA—Freedom of Information Act
AFMAN41-210 10 SEPTEMBER 2019 205
GSU—Geographically Separated Unit
HAIMS—Health Artifact and Image Management System
HIPAA—Health Insurance Portability and Accountability Act
HIV—Human Immunodeficiency Virus
IG—Inspector General
Kx—Knowledge Exchange
MAJCOM—Major Command
MC—Medical Corps
MDG—Medical Group
MDSS—Medical Support Squadron
MHS—Military Health System
MTF—Military Treatment Facility
NATO—North Atlantic Treaty Organization
NC—Nurse Corps
NCO—-Non-Commissioned Officer
OCO—Overseas Contingency Operations
OCONUS—Outside Continental United States
OSD—Office of the Secretary of Defense
PAS—Personnel Accounting Symbol
PCA—Permanent Change of Assignment
PCS—Permanent Change of Station
PHI—Protected Health Information
PME—Professional Military Education
RC—Reserve Component
RMO—Resource Management Office
ROTC—Reserve Officer Training Corps
SAF—Secretary of the Air Force
SAF/MR—Assistant Secretary of the Air Force for Manpower and Reserve Affairs
SAPR—Sexual Assault Prevention and Response
SECAF—Secretary of the Air Force
SES—Senior Executive Service
SF—Standard Form
206 AFMAN41-210 10 SEPTEMBER 2019
SM—Service Member
SNCO—Senior Non-commissioned Officer
TOL—Tricare Online
TRAC2ES—TRANSCOM Regulating and Command & Control Evacuation System
USC—United States Code
VA—Veterans Affairs
Terms
Active Duty (AD)—Applies to members serving full-time duty in the active military service of
the United States. It includes members of the RC serving on AD or full-time training duty, but
does not include full-time National Guard duty. The term Inactive Duty for Training does not apply
to this definition when considering healthcare eligibility.
AD Training or AD for Training—A tour of AD which is used for training members of the
Reserve components to provide trained units and qualified persons to fill the needs of the Armed
Forces in war or national emergency and such other times as the national security requires. The
member is under orders that provide for return to non-active status when the period of AD training
is completed. It includes annual training, special tours of AD for training, school tours, and the
initial duty for training performed by non-prior service enlistees.
Active Guard and Reserve—National Guard and Reserve members who are on voluntary active
duty providing full-time support to National Guard, Reserve, and Active Component organizations
for the purpose of organizing, administering, recruiting, instructing, or training the Reserve
Components. Also called AGR.
AHLTA—The Department of Defense legacy electronic health record, is a clinical information
system that generates, maintains, stores and provides secure electronic access to comprehensive
patient records.
Air Reserve Component (ARC)—Units, organizations, and members of the ANG and the AFR.
Attending Physician—The physician who has the primary responsibility for the medical
diagnosis and treatment of the patient.
Beneficiary—Persons entitled to benefits under the Uniformed Services Health Benefits Program
and this manual.
Business Associate—A person or entity that performs certain functions or activities that involve
the use or disclosure of protected health information on behalf of, or provides services to, a covered
entity defined in terms.
Child—The natural or adopted child of a sponsor, or in some cases for purposes of determining
eligibility for military health benefits, the unadopted step-child of a sponsor, or the legal ward of
a sponsor. To determine whether a minor child may consent to certain classes of healthcare, refer
to applicable state law, or for overseas locations local Medical Group (MDG) Operating
Instructions.
Chronic Medical Condition—A medical condition that active medical treatment cannot cure or
control. Chronic conditions may involve periodic acute episodes and may require intermittent
AFMAN41-210 10 SEPTEMBER 2019 207
inpatient care. Sometimes medical treatment may control a chronic medical condition sufficiently
to permit continuation of daily living activities such as work, or school.
Commander—The principle commissioned officer responsible for all activities, operations, and
resources under the officer’s control. Synonymous with commanding officer and commanding
officer in charge.
Comprehensive Medical Information—Patient’s name, rank, age, status (e.g., AD, RC) unit of
assignment or government occupational position, date of admission and/or date of treatment,
diagnosis, current medical status, whether the admission was routine or happened under emergent
circumstances, and the projected length of stay.
Convalescent Leave—An authorized leave status granted to AD uniformed service members
while under medical or dental care that is a part of the care and treatment prescribed for a member’s
recuperation or convalescence.
Continental United States (CONUS)—United States territory, including the adjacent territorial
waters, located within North America between Canada and Mexico (Alaska and Hawaii are not
part of CONUS).
Covered Entity—In the HIPAA rules as (1) health plans, (2) health care clearinghouses, and (3)
health care providers who electronically transmit any health information in connection with
transactions for which HHS has adopted standards. Generally, these transactions concern billing
and payment for services or insurance coverage.
Custodial Care—Healthcare for a patient who:
- Is mentally or physically disabled and expected to continue as such for prolonged period.
- Requires a protected, monitored, or controlled environment in an institution or home.
- Requires assistance to support the essentials of daily living.
- Is not under active and special medical, surgical, or psychiatric treatment that reduces the
disability to the extent necessary to enable the patient to function outside a protected, monitored,
or controlled environment.
Deceased Member—A person who was, at the time of death, a uniformed service AD member or
retired; or a retired member of a RC who elected to participate in the Survivor Benefit Plan (for
information on this plan, contact the Personal Affairs department at the local Military Personnel
Section), but died before reaching age 60.
Definitive Diagnosis—For purposes of an Medical Evaluation Board evaluation, any condition
that significantly interferes with performance of duties appropriate to a service member’s office,
grade, rank, or rating.
Dependency Determination—A determination by the Air Force Accounting and Finance Center,
that individuals may retain their status as dependents of an AD or retired member of the uniformed
services. A favorable dependency determination does not in itself establish an entitlement to
medical care. The dependency determination must also provide specifically for medical care.
Dependent—A term that has generally been replaced with “family member.” An immediate
family member of an AD or retired Uniformed Services member. See AFI 36-3002 for a detailed
explanation.
Direct Care System—The system of military hospitals and clinics around the world.
208 AFMAN41-210 10 SEPTEMBER 2019
Disability Evaluation System—A process maintained by the military Services to ensure a fit and
vital force by determining a service member’s fitness for continued military service. The Disability
Evaluation System should include a medical evaluation board, a physical evaluation board, an
appellate review process, and a final disposition.
Disposition—The removal of a patient from a MTF because of a return to duty or to home, transfer
to another MTF, death, or other termination of medical care. The term may also refer to change
from inpatient to outpatient status (for example, inpatient to subsisting elsewhere or convalescent
leave).
Emergency Care—The immediate medical or dental care necessary to save a person’s life, limb,
or sight, or to prevent undue suffering or loss of body tissue.
Extended AD—A tour of AD, normally for more than 90 days, that members of the RC perform.
Strength accountability changes from the RC to the AD force. AD for training is not creditable as
Extended AD.
Foreign Military Sales—That portion of United States security assistance authorized by the
Foreign Assistance Act of 1961, as amended, and the Arms Export Control Act of 1976, as
amended. This assistance differs from the Military Assistance Program and the International
Military Education and Training Program in that the recipient provides reimbursement for defense
articles and services transferred.
Former Spouse—As the status relates to this manual, an individual who is no longer married to
an AD member, but was in the past for a sufficient length of time to become eligible for healthcare.
Health Artifact and Image Management Solution (HAIMS)—Provides an enterprise-wide data
sharing and content management capabilities for all types of artifacts and images, including
radiographs, clinical photographs, electrocardiographs, waveforms, audio files, video files and
scanned documents.
Health Insurance and Portability Accountability Act (HIPAA) Breach—The acquisition,
access, use, or disclosure of protected health information (PHI) in a manner not permitted under
the HIPAA Privacy Rule which compromises the privacy or security of the PHI.
Highly Sensitive Records—Health records, correspondence (including working papers), and
laboratory results, which may have an adverse effect on the morale or character of the patient or
other person(s). Highly sensitive records include but are not limited to alleged or confirmed
information relating to the treatment of patients for sexual assault, criminal actions (including child
or spouse abuse), psychiatric or social conditions, or venereal disease. Claims against the
government (including malpractice) are also considered highly sensitive.
Inactive Duty Training—Authorized training performed by a member of a RC not on published
active orders and consisting of regularly scheduled unit training assemblies, additional training
assemblies, periods of appropriate duty of equivalent training, and any special additional duties
for RC personnel that an authority designated by the Secretary concerned, and performed by them
in connection with the prescribed activities of the organization in which they are assigned with or
without pay. Does not include work or study associated with correspondence courses.
Integrated Disability Evaluation System—The Integrated Disability Evaluation System
integrates the Disability Evaluation System with the Veterans Affairs (VA), and delivers the
AFMAN41-210 10 SEPTEMBER 2019 209
advantage of single-sourced disability ratings that are accepted by both the DoD and the VA, so
the member will receive a VA benefits decision shortly after separation or retirement.
International Military Education and Training—Formal or informal instruction provided to
foreign military students, and forces on a non-reimbursable (grant) basis by offices or employees
of the United States, contract technicians, and contractors. Instruction may include
correspondence courses; technical, educational or informational publications; and media of all
kinds.
Legally Aged Family Member—The age of 18 years and older, however, can vary by state law
with respect to the matter at issue.
Medical Care—Inpatient, outpatient, dental care, and related professional services.
MHS GENESIS—The new electronic health record for the
MHS, provides enhanced, secure technology to manage health information. MHS GENESIS
integrates inpatient and outpatient solutions that will connect medical and dental information
across the continuum of care, from point of injury to the military treatment facility.
Military Patient—A patient who is a member of the Uniformed Services of the United States on
AD, or RC status eligible for military care, or an AD member of a foreign government eligible for
military care.
Military Treatment Facility—A military treatment facility is every fixed facility established for
the purpose of furnishing medical and/or dental care to eligible individuals, including all
operations of each such facility and all health care delivery associated with each such facility.
Military Treatment Facility Commander or Director—The person appointed on orders as the
commanding officer of the MTF.
North Atlantic Treaty Organization—Security alliance of 28 countries with the fundamental
goal to safeguard the Allies’ freedom and security by political and military means. North Atlantic
Treaty Organization nations are: Albania, Belgium, Bulgaria, Canada, Croatia, Czech Republic,
Denmark, Estonia, France, Germany, Greece, Hungary, Iceland, Italy, Latvia, Lithuania,
Luxembourg, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain,
Turkey, the United Kingdom, and the United States.
Non-appropriated Fund Employee—A Government employee whose pay comes from other
than appropriated funds (for example, bowling alley and Base Exchange employees).
Power of Attorney—A legal document authorizing an individual to act as the attorney or agent
of the grantor. General rules and individual state laws specify when a power of attorney is
required. Refer any questions pertaining to powers of attorney to the legal office.
Prime Service Areas (PSAs)—Are areas in which the contractor offers enrollment in TRICARE
Prime in compliance with the travel time access standard. PSAs encompass the entire area of all
the ZIP codes lying within or intersected by the 40 mile radius around enrolling MTFs/enhanced
Multi-Service Markets (eMSMs) (both hospitals and clinics) and Base Realignment and Closure
(BRAC) sites. Zip codes enclosed entirely within a PSA’s boundary shall also be included. For
BRAC sites, the 40 mile radius shall be determined based on the physical address of the former
MTF location. If the former MTF address is no longer valid, the 40 mile radius shall be determined
from the geographic center of the BRAC site zip code as of the date of contract award.

210 AFMAN41-210 10 SEPTEMBER 2019
Reserve Components—Reserve components of the Armed Forces of the United States are: the
ANG of the United States, the AFR, the Army National Guard of the United States, the Army
Reserve, the Naval Reserve, the Marine Corps Reserve, and the Coast Guard Reserve. For the
purpose of this manual, the term also includes the reserve members of the commissioned corps of
the United States Public Health Service and National Oceanic and Atmospheric Administration.
Retiree—A former member of a uniformed service who is entitled to retired, retainer, or
equivalent pay, based on duty in a uniformed service.
Sanitized Healthcare Information—A patient’s name, rank, age, military status (AD, RC), unit
of assignment or government occupational position, date of admission and/or treatment date, and
whether the admission was routine or happened under emergent circumstances, as this information
applies to reporting an AD service member’s status to the authorized AD service member’s
commander or the commander’s properly appointed designee.
Sensitive Medical Information—Information that may affect the patient’s morale, character,
medical progress, or mental health. This includes the specific location or description of illness or
injury, which may prove embarrassing to the patient or reflect poor taste. If the patient consents,
information relating to the description of disease or injury and general factual circumstances may
be released. Note: To protect the sensitive nature of the information, records or documents will
be sent directly through medical channels when considered advisable by the healthcare provider
or MTF commander or director.
Transitional Assistance Management Program—Offers transitional healthcare coverage under
TRICARE Prime where offered, TRICARE Extra, and TRICARE Standard to certain separating
AD members and their eligible family members. Care is available for a limited time. Sponsors
may verify eligibility for themselves and their family members by visiting or contacting the nearest
uniformed services Identification card facility or contacting the Defense Manpower Data Center
Support Office toll free at (800) 538-9552. To locate the nearest Identification card facility, visit
www.dmdc.osd.mil/rsl/. Refer to paragraph 2.21 for additional information. Effective 1 January
2018, TRICARE Standard and Extra are replaced by TRICARE Select.
Treatment—A procedure or medical service that medical persons expect to lead to or assist in the
patient’s recovery.
TRICARE—The military’s managed healthcare program, overseen by the DoD in cooperation
with regional civilian contractors. TRICARE uses the MHS as the main delivery system
augmented by a civilian network of providers and facilities serving AD (including
Reservists/National Guard), their families and retired military/families and survivors world-wide.
TRICARE Prime Remote—TRICARE Prime Remote provides healthcare coverage through
civilian providers for those United States Uniformed Service Members and their families who are
on remote assignment. It applies to members of the Army, Navy, Marine Corps, Air Force, Coast
Guard, United States Public Health Service, and National Oceanic and Atmospheric
Administration. Eligible beneficiaries must live and work more than 50 miles or approximately
one hour's drive time from the nearest MTF. TRICARE Prime Remote is offered in the 50 United
States only.
Uniformed Services—The Army, Navy, Air Force, Marine Corps, Coast Guard, National Oceanic
and Atmospheric Administration, and United States Public Health Service.
AFMAN41-210 10 SEPTEMBER 2019 211
Uniformed Services Family Health Plan—US Family Health Plan is a TRICARE Prime option
There is a TRICARE Prime option available to eligible persons - including those who are age 65
and over - who live near selected civilian medical facilities around the country. These facilities
are called “designated providers” (DPs) - formerly known as Uniformed Services Treatment
Facilities.
United States—The 50 states and the District of Columbia, Puerto Rico, the US Virgin Islands,
and Guam.
Veteran—A person who served in the active military, Army, Navy, Coast Guard or Air Force. A
person who originally enlisted in a regular component of the Armed Forces after 7 September
1980, or who entered AD after 16 October 1981, is not eligible for benefits from the Department
of Veterans Affairs unless the member completes the lesser of 24 continuous months of AD or the
full period for which the person was called or ordered to duty. This provision does not apply to
veterans who have a compensable service-connected disability or who were discharged close to
the end of an enlistment term because of hardship, or a disability incurred or aggravated in line of
duty.
Wounded Warrior—Any service member who has sustained a combat or hostile-related injury
or illness requiring long-term care that will require a Medical Evaluation Board or Physical
Evaluation Board to determine fitness for duty.
Written Authorization—Written consent from the patient or authorized representative allowing
release or disclosure of information.
212 AFMAN41-210 10 SEPTEMBER 2019
Attachment 2
SECRETARY OF THE AIR FORCE DESIGNEE EXAMPLE REQUEST
Date
MEMORANDUM FOR (MAJOR COMMAND NAME AND ADDRESS)
FROM: (MILITARY TREATMENT FACILITY NAME AND ADDRESS)
SUBJECT: Secretary of the Air Force Designee Program Application
1. Request the following individual be granted Secretarial Designee status. The following
information is provided in accordance with AFMAN 41-210, Chapter 4.
a. The patient's full name.
b. The patient’s date of birth.
c. The patient’s relationship to sponsor.
d. Sponsor’s full name.
e. Sponsor’s rank.
f. Sponsor’s branch of service.
g. Last four numbers of the Sponsor’s social security number.
h. Sponsor’s military status (active duty retired, deceased) and reason for discharge or
separation.
i. The exact date Designee status should begin.
j. The recommended length of Designation.
k. Transportation aboard an aeromedical evacuation aircraft is/is not requested. Identify
whether the patient requesting Designee status might require transportation on aeromedical
evacuation. If so, include patient's home address and estimated cost of military transport.
l. Reason for Designation: for example, age (specify date of birth), marriage status, sponsor
leaving the service.
m. Justification: Identify both the primary program category/criteria best suited for the situation
and a supporting narrative.
n. Diagnosis: The application should include diagnosis in both clinical and layman's terms.
o. Brief Case History: The application needs a brief (one or two paragraph) case history. For
complex cases, attach a separate letter with additional details. Include a long-term prognosis, the
patient's age when medical providers first diagnosed the problem, and when and where DoD
sponsored care began. Histories must be understandable to non-medical personnel.
p. Name of attending physician.
q. Medical specialty required: Application should specify the type of medical specialist
(orthopedics, pediatrics, etc.) who would provide care for the patient.
r. Name, rank, and duty phone (Defense Switched Network and commercial) of the Secretarial
Designee caseworker.
s. Third Party Insurance Carrier: Identify if the sponsor, and or, applicant has Third Party
Insurance.
t. Third Party Insurance Carrier Policy Number.
u. Space Availability: Indicate if the military treatment facility (MTF) has the capacity to treat
the applicant.
AFMAN41-210 10 SEPTEMBER 2019 213
v. Like-care TRICARE Prime patients are/are not being deferred to the network. Indicate if
other TRICARE Prime beneficiaries with the same diagnosis are being deferred to the network.
w. Right of First Refusal status: Indicate if the MTF accepts/does not accept Right of First
Refusals.
2. For additional information please call the caseworker at the above phone number.
//SIGNATURE BLOCK//
214 AFMAN41-210 10 SEPTEMBER 2019
Attachment 3
CONSULT NOTES AND SPECIALTY STUDIES GUIDE
Table A3.1. Consult Notes and Specialty Studies Guide.
Diagnosis
Required Consults
Required Studies/Info
Asthma
Pulmonology (ONLY if
Complicated)
Spirometry (MCT or HC if diagnosis in
doubt)
Burns
% BSA, ROM, Photographs of
affected areas
Collagen Vascular Disease
Rheumatology
Arthritis
Rheumatology
Fibromyalgia
Rheumatology
Trigger point summary
Coronary Artery Disease
Cardiology
ETT, Echo or Cath, NYHA class
Diabetes
Endocrinology if Insulin
Dependent
FBS, A1C, Optometry or
Ophthalmology
Hearing
ENT
Audiogram
Eyes
Ophthalmology
Visual Acuity and Visual Field exam
Neuromuscular
Orthopedics (PT if available)
ROM (percent), Strength, Function,
EMG if appropriate
Musculoskeletal
Orthopedics (PT if available)
ROM (percent), Strength, Function
Cancer (Brain)
Oncology, neurosurgery, & psych
5 year prognosis
Cancer (Skin)
Dermatology
5 year prognosis
Cancer (Head and Neck)
ENT
5 year prognosis
Cancer (renal or GU)
Urology
5 year prognosis
Cancer (other)
Oncology
5 year prognosis
Multiple Sclerosis
Neurology
MRI, spinal tap
Headache
Neurology
MRI, Log with # prostrating HA’s last
12 months
Seizure
Neurology
EEG, MRI, Log of seizure frequency
Renal
Neurology
Lab progression over time
Crohn’s/Ulcerative Colitis
GI
Scope/Biopsy, Log of flare freq &
severity
Psych
MD/DO Psych review and cosign
Military & Social-Industrial
Impairment
TBI
Neuropsychiatry
MRI, Military & Social-Industrial

AFMAN41-210 10 SEPTEMBER 2019 215
Impairment
216 AFMAN41-210 10 SEPTEMBER 2019
Attachment 4
INITIAL RILO COVER SHEET/ CHECKLIST
Figure A4.1. Initial RILO Cover Sheet/Checklist.
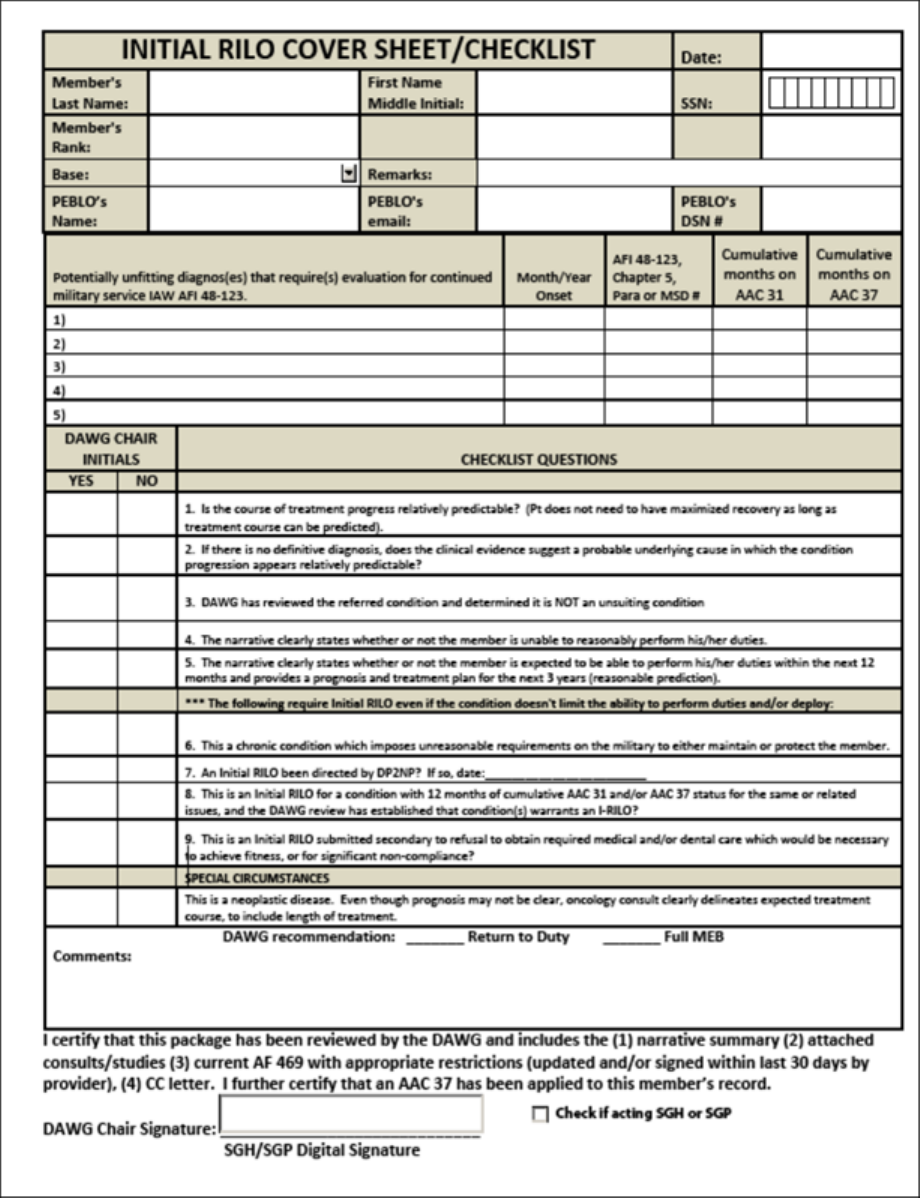
AFMAN41-210 10 SEPTEMBER 2019 217
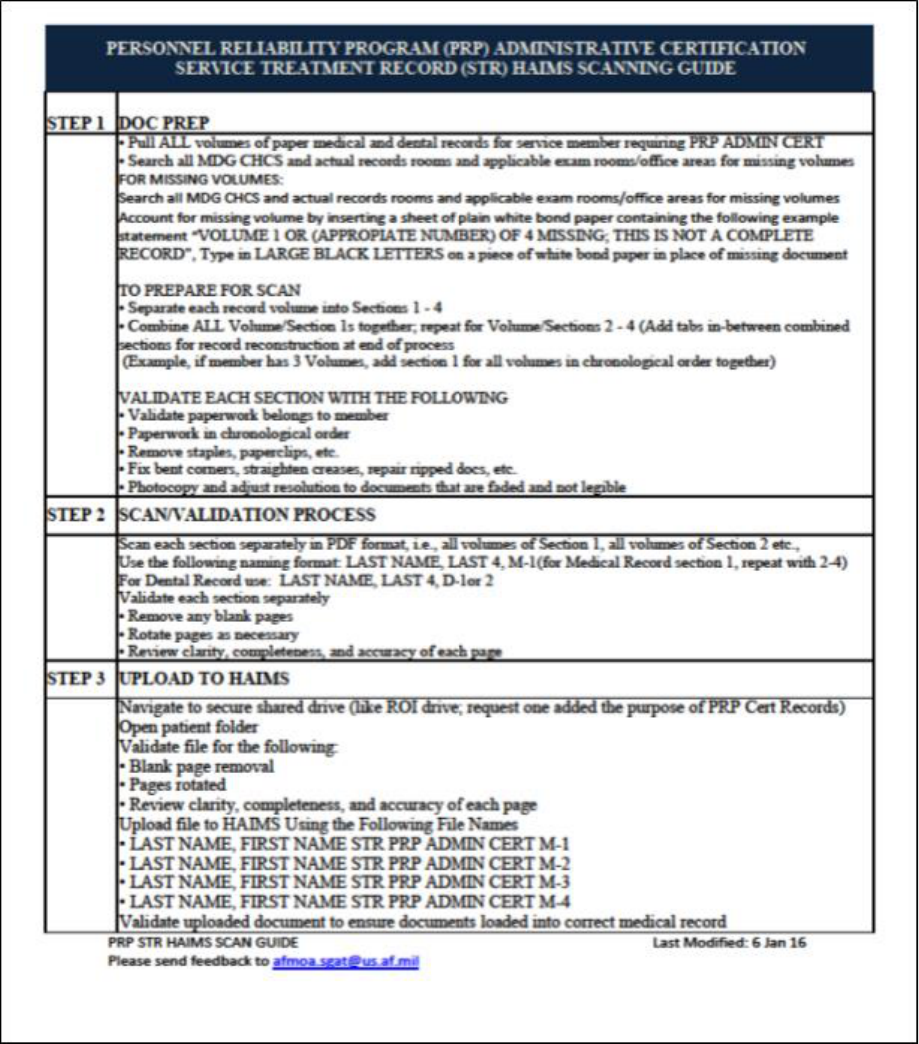
218 AFMAN41-210 10 SEPTEMBER 2019
Attachment 5
PERSONNEL RELIABILITY ASSURANCE PROGRAM ADMIN CERT HAIMS SCAN
GUIDE
Figure A5.1. Personnel Reliability Assurance Program Admin Cert HAIMS Scan Guide.
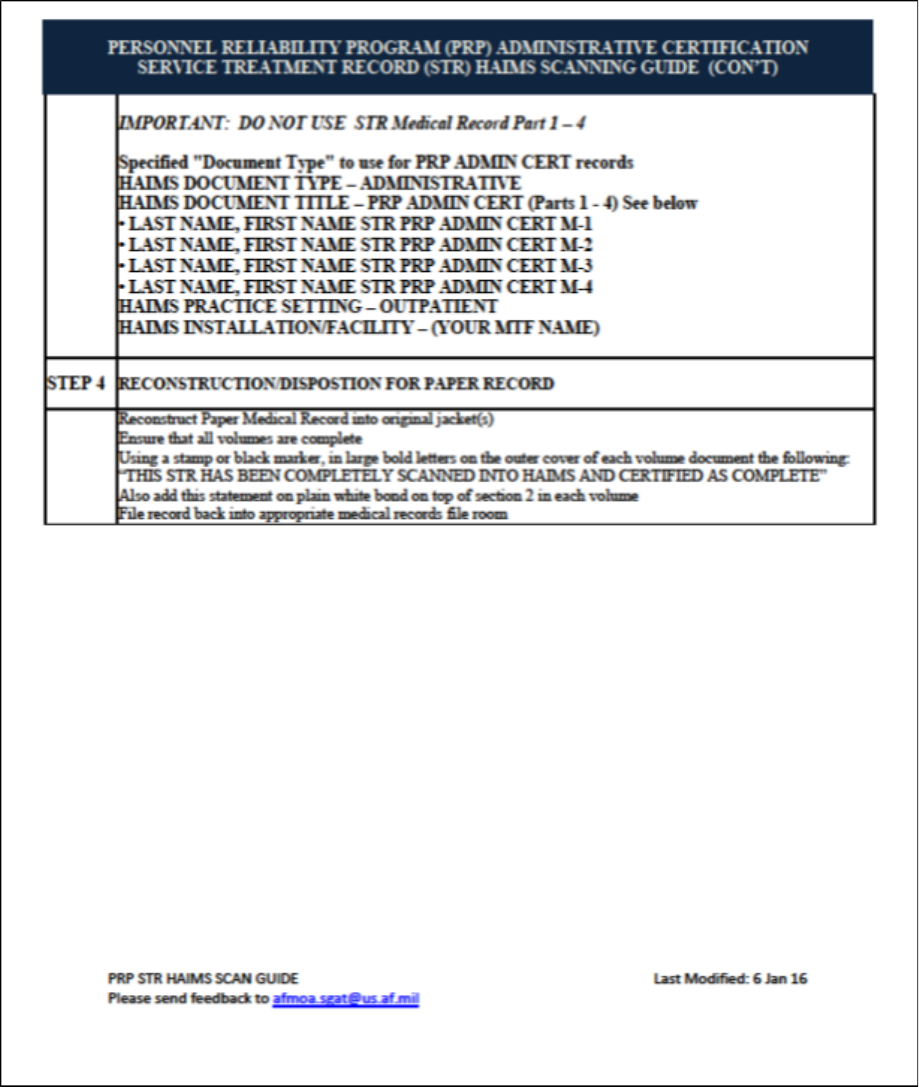
AFMAN41-210 10 SEPTEMBER 2019 219
220 AFMAN41-210 10 SEPTEMBER 2019
Attachment 6
ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES, HEALTH RECORD
OUTPATIENT SECTION 1
Table A6.1. Arrangement of Forms in the AF Form 2100A Series, Health Record
Outpatient Section 1.
Form Number and Title
Special Instructions
DD Form 2766, Adult Preventive and Chronic
Care Flowsheet , and/or, AF Form 1480a, Adult
Preventive and Chronic Care Flowsheet
Note: AF Form 1480A, and the AF Form
4320 have been replaced by DD forms,
same title. Whichever form is used, (DD
Form 2766, AF Form 1480, or AF Form
4320), this form is always the top form
filed in section I. Transcribe pertinent
information from older forms to each
subsequent new form(s) and file the old
form(s) underneath the newer form in
section I. DO NOT remove/discard the
old forms. File old forms underneath the
current version.
DD Form 2882, Pediatric & Adolescent
Preventive and Chronic Care Flowsheet, and/or,
AF Form 4320, Pediatric & Adolescent
Preventive and Chronic Care Flowsheet
DD Form 2766C or AF Form 1480B, Adult
Preventive and Chronic Care Flowsheet –
Continuation Sheet
File after/behind the DD Form 2766, AF
Form 1480A, or AF Form 4320. This
form is used as a continuation form for
documenting information that cannot fit on
DD Form 2766 or AF Form 1480A, or for
local requirements. The Aerospace
Services Information Management System
(ASIMS) also utilizes an automated
version of the form. Each time a member
receives an updated immunization, ASIMS
may generate an updated paper form. If an
updated form is generated, discard the
previous form ONLY after ensuring the
latest form contains BOTH historical and
current immunization data, then file the
new form in its place.
DD Form 2795, Pre-Deployment Health
Assessment Questionnaire
File the DD Form 2796, DD Form 2844,
and DD Form 2900 (post deployment
assessment forms) after the corresponding
DD Form 2795 that each form is
associated with.
DD Form 2796, Post-Deployment Health
Assessment
DD Form 2844, Medical Assessment Post-
Deployment
DD Form 2900, Post-Deployment Health RE-
Assessment
Form Number and Title
Special Instructions
AFMAN41-210 10 SEPTEMBER 2019 221
AF Form 1480, Summary of Care
Information will be transcribed from the
AF Form 1480 onto the DD Form 2766 or
AF Form 1480A. Do not discard old
forms. File under the oldest DD Form
2766.
AF Form 3922, Adult Preventive Care –
Flowsheet
Transcribe the AF Form 3922 information
in the same way as the AF Form 1480 and
file it after the AF Form 1480.
AF Form 3923, Child Preventive Care –
Flowsheet
Transcribe the AF Form 3923 information
onto the AF Form 4320.
DD Form 2569, Third Party Collection Program
(TPCP) – Record of Other Health Insurance
1. File here unless military treatment
facility (MTF) policy is to maintain the
form in the resource management
(business) office or in an authorized
electronic format and stored in an
enterprise-wide electronic clinical
documentation database. File the most
current form. Remove older, outdated
forms. This form must be updated
annually or upon change of patient
information. The form must be validated
at every encounter as being current and
correct. This form contains Personally
Identifiable Information and must be
safeguarded if maintained apart from the
outpatient medical record.
2. Filing Options:
a. Continue with current process of
maintaining a hardcopy of this form filed
in the outpatient medical record.
b. Capture and store the form
electronically. The stored e-file must be
saved with the following naming
convention: Last Name (or first 8
characters), First Initial, family member
prefix, Last 4 of Sponsor’s social security
number, Month/Year of patient or adult
family member signature with dashes
separating each data entry, e.g., (Jones, D-
20-4567-0910). Stored electronic forms
will not be available to anyone without
authorized, need to know, TPCP or clinic
staff member access. MTF Data Quality
auditors and TPCP contract support
personnel must have access to the
Form Number and Title
Special Instructions
222 AFMAN41-210 10 SEPTEMBER 2019
electronic forms database. Obsolete or
outdated electronic forms may be
deleted/destroyed in accordance with
applicable records management rules.
c. Maintain the original hardcopy form in
the MTF RMO, business office, or TPCP
office. The form should be filed by
signature date/month and alphabetically
thereafter. During non-business hours,
store in a secure location, which offers at
least one locked door between the filed
documents and the outside hallway or
office entrance. Destroy form/file one year
after date of signature of the form, or when
replaced by an updated signed form.
d. File this form for non-enrolled/non-
empaneled patients who otherwise do not
receive regular direct care from the MTF
and/or there is no paper medical record
already on file, in either the MTF
outpatient records department or in the
RMO/business office, TPCP office. File
forms by signature date/month and
alphabetically thereafter. During non-
business hours, store in a secure location,
which offers at least one locked door
between the filed documents and the
outside hallway or office entrance.
Destroy form/file one year after date of
signature of the form, or when replaced by
an updated signed form.
3. Each MTF will choose one option for
filing the form. If not already
accomplished, the MTF must communicate
the option of choice to their TPCP contract
partner. Regardless of the filing option
choice, the TPCP contractor must receive
the original or copy of all DD Forms 2569
before final filing.
AF Form 565, Record of Inpatient Treatment
(or approved Composite Health Care System
(CHCS) computer generated form)
Copy of original, or similar document used
by the United States Army, United States
Navy, or Department of Veterans Affairs
medical facilities.
Form Number and Title
Special Instructions
AFMAN41-210 10 SEPTEMBER 2019 223
AF Form 560, Authorization and Treatment
Statement
Original – Only necessary if admission
was cancelled. Previously filed AF Forms
560 will not be removed.
SF 502, Medical Record - Narrative Summary
Copy of original.
SF 509, Medical Record – Progress Notes
File a copy of original, when used as a
final discharge note or discharge
instruction.
SF 515, Medical Record – Tissue Examination
File a copy of original report if the
procedure relates to inpatient care; file the
original report if the procedure relates to
outpatient care if not already filed in an
EAR.
SF 516, Medical Record – Operation Report
File a copy of original report if the
procedure relates to inpatient care; file the
original report if the procedure relates to
outpatient care if not already filed in the
EAR.
OF 517, Clinical Record – Anesthesia
File a copy of the original document if
episode of care relates to inpatient report
(if there was an anesthetic incident); file
the original document if the care relates to
an outpatient episode.
OF 522, Medical Record – Request for
Administration of Anesthesia and for
Performance of Operations and Other
Procedures
Copy of all documentation relating to
ambulatory surgery.
224 AFMAN41-210 10 SEPTEMBER 2019
Attachment 7
ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES, HEALTH RECORD
OUTPATIENT SECTION 2
Table A7.1. Arrangement of Forms in the AF Form 2100A Series, Health Record
Outpatient Section 2.
Form Number and Title
Special Instructions
AF Form 745, Sensitive Duties Program Record
Identifier
Always the top form in this section when
used.
AF Form 966, Registry Record
Filed after AF Form 745, if used.
SF 600, Health Record – Chronological Record
of Medical Care
SF 600s from single-visit encounters (e.g.
Health Assessment Overprints), with no
other associated supporting paperwork,
should be filed in chronological order,
most current form filed on top of the other
single-visit SF 600s.
OF 558, Medical Record – Emergency Care and
Treatment
Interfile OF 588 with applicable SF 600s
in date order. Forward original to the
inpatient unit and file with the inpatient
record if the patient is admitted.
DD Form 2161, Referral for Civilian Medical
Care
File these forms on top of the SF 600 to
which it belongs.
SF 513, Consultation Report
AF Form 1535, Physical Therapy Consult
AF Form 1352, Hyperbaric Patient Information
and Therapy Record
Original if treatment was on an outpatient
basis. File the most recent form on top of
all others.
AF Form 1446, Medical Examination – Flying
Personnel
Signed original.
DD Form 2697, Report of Medical Assessment
OF 178, Certificate of Medical Examination
Applies to civilian employees only.
SF 88, Report of Medical Examination or DD
Form 2808, Report of Medical Examination
Signed copy of each report. When DD
Form 2161 or any other form is prepared
in conjunction with the SF 88/DD Form
2808, it is filed with the SF 88/DD Form
2808.
SF 93, Report of Medical History, DD Form
2807-1, Report of Medical History or DD Form
2807-2, Medical Prescreen of Report of Medical
History
Signed copy of each report. File civilian
employee’s SF 93/DD Form 2807-1/DD
Form 2807-2 in the health record.
Note:
Ensure inter-related documents for the same episode of care or subsequent referral care
documents are filed on top of the initial encounter document.
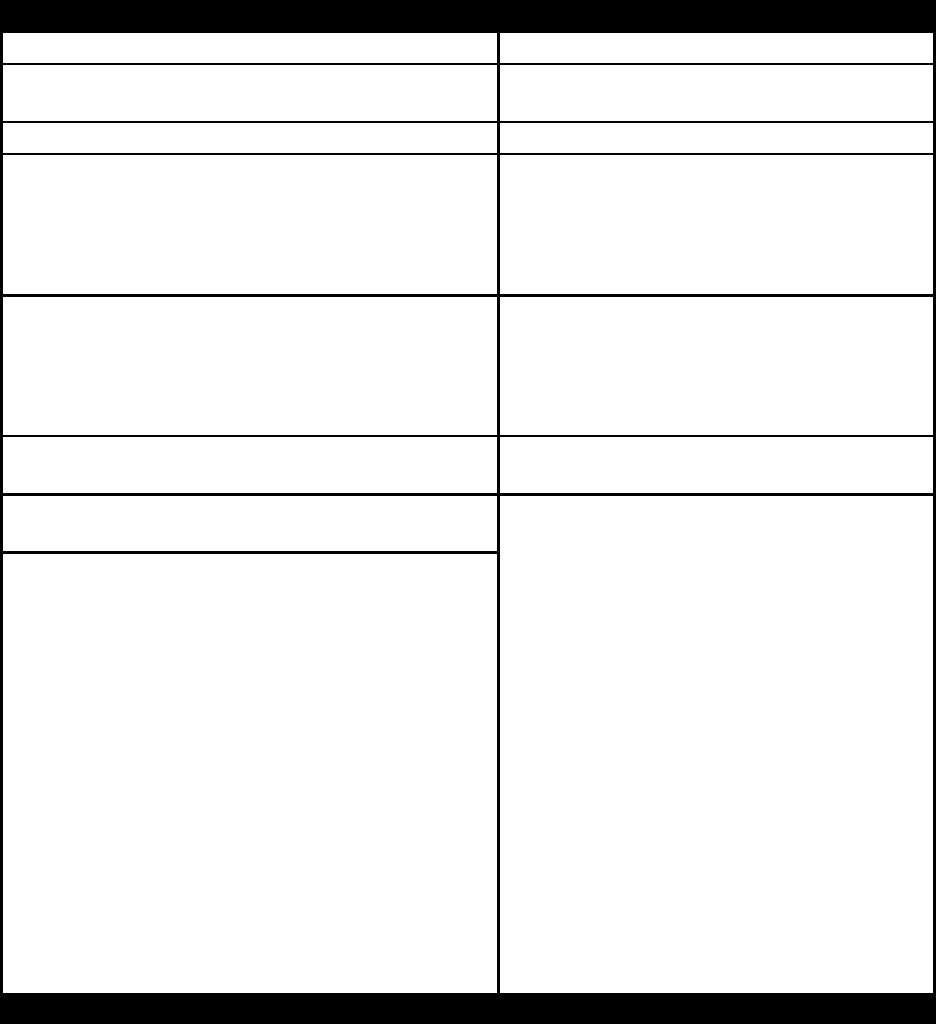
AFMAN41-210 10 SEPTEMBER 2019 225
Attachment 8
ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES, HEALTH RECORD
OUTPATIENT SECTION 3
Table A8.1. Arrangement of Forms in the AF Form 2100A Series, Health Record
Outpatient Section 3.
Form Number and Title
Special Instructions
AF Form 348, Line of Duty Determination
AF Form 422, Physical Profile Serial Report
Filed chronologically with most recent
report on top.
AF Form 469, Duty Limiting Condition Report
Most recent
Prenatal Forms
Prenatal forms will be maintained in the
OB-GYN clinic until the mother delivers.
If the mother delivers in a civilian facility
the forms will be filed in the outpatient
record.
SF 533, Medical Record – Prenatal and
Pregnancy
If the mother did not deliver in the
hospital, the prenatal record is filed as a
whole package with all forms pertaining to
prenatal treatment filed chronologically
between the SF 533 and AF Form 3915.
AF Form 618, Medical Board Report
Signed copy of original and associated
documents.
DD Form 2992, Medical Recommendation for
Flying or Special Operational Duty
File a copy of the most current
recommendation for or against (either
temporary or permanent suspension) flying
status or special operational duty. File the
AF Form 1418 with the DD Form 2992,
the SF 88, or any other form prepared in
conjunction with DD Form 2992. Keep all
supporting documents even though the DD
Form 2992 may be destroyed. Remove the
DD Form 2992, specifically prepared for
annual or incoming clearance, from the
record and destroy when it expires.
Remove and destroy any DD Form 2992
excusing, grounding, or disqualifying an
individual for flying or special operational
duty after the new DD Form 2992
returning the individual to medically
approved/cleared status is filed.
AF Form 1418, Recommendation for Flying
or Special Operational Duty – Dental
Form Number and Title
Special Instructions
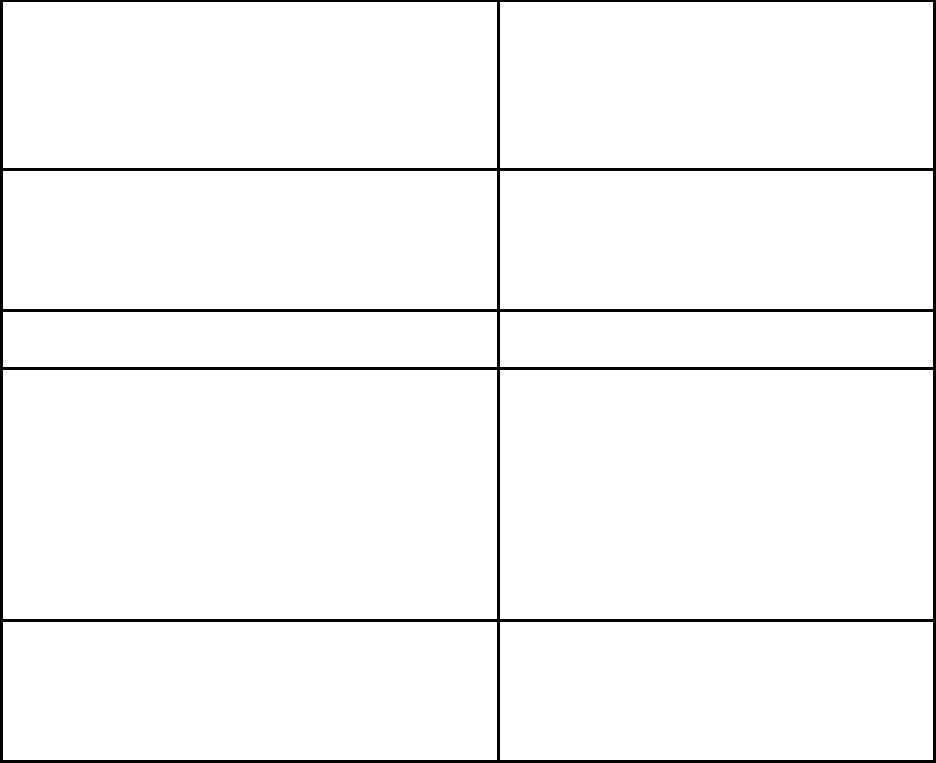
226 AFMAN41-210 10 SEPTEMBER 2019
AF Form 137, Footprint Record
AF Form 137 is filed on top of DD Form
2005. Note: The September 1988 edition
of AF Form 2100A series has the Privacy
Act Statement printed on the folder. It is
not required to place DD Form 2005 in
these folders.
All other forms not listed in Section 1, 2, and 4
File all other forms in chronological order
by date, including letters and copies of
reports of care from civilian sources
(reviewed by the military healthcare
provider) and locally generated forms.
DD Form 2005
For records that do not have a Privacy Act
statement preprinted on the record folder.
Disclosure Accounting Record
The purpose of the document is to
maintain a record of patient information
released. This document will contain the
following information: individual’s name
(e.g., patient); requestor’s name and
address; nature of disclosure; individual’s
consent with a block for annotating “Yes”
or “No, not required;” and date of
disclosure.
Disclosure Accounting Record (continued)
Until such time as this form is printed on
the AF Form 2100A series folder, each
MTF will develop a local form containing
space for the requested information with
space for entry of multiple requests.
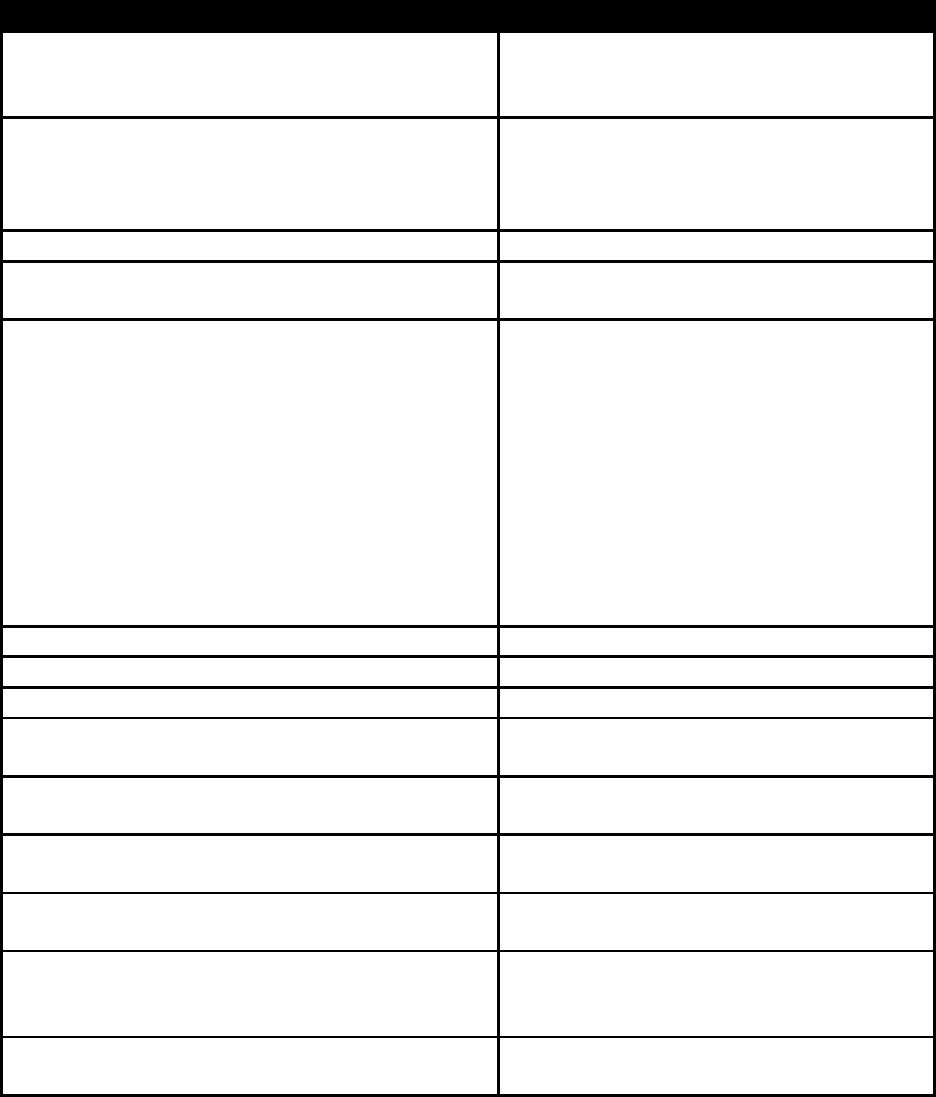
AFMAN41-210 10 SEPTEMBER 2019 227
Attachment 9
ARRANGEMENT OF FORMS IN THE AF FORM 2100A SERIES, HEALTH RECORD
OUTPATIENT SECTION 4
Table A9.1. Arrangement of Forms in the AF Form 2100A Series, Health Record
Outpatient Section 4.
Form Number and Title
Special Instructions
Laboratory Forms
File in chronological order with most
current laboratory results/report filed on
top.
SF 601, Health Record – Immunization Record
Used by United States Army, United
States Navy, Air National Guard (ANG),
and United States Air Force Reserve
(AFR).
SF 602, Health Record – Serology Record
SF 519B, Medical Record – Radiological
Consultation Request Report
Filed in chronological order by date with
the most recent on top.
OF 520, Medical Record-Electrocardiographic
Record, (or automated EKG report)
Filed together in chronological order by
date (the most recent on top), except when
OFs 520 attached as documentation to
reports, are filed with other reports. Filing
a copy of the inpatient electrocardiograms
(EKGs) in the outpatient record is
optional. Facilities with computer
generated EKG reports may destroy OF
520 after the test has been ordered and if
all patient identification is on the
automated report.
AF Form 1721, Spectacle Prescription
DD Form 2215, Reference Audiogram
DD Form 2216, Hearing Conservation Data
AF Form 1671, Detailed Hearing Conservation
Data Follow-up
AF Form 190, Occupational Illness/Injury
Report
AF Form 1527, History of Occupational
Exposure to Ionizing Radiation
USAFSAM Form 1527-1, Annual Report of
Individual Exposure to Ionizing Radiation
USAFSAM Form 1527-2, Cumulative
Occupational Exposure History to Ionizing
Radiation
AF From 1753, Hearing Conservation
Examination
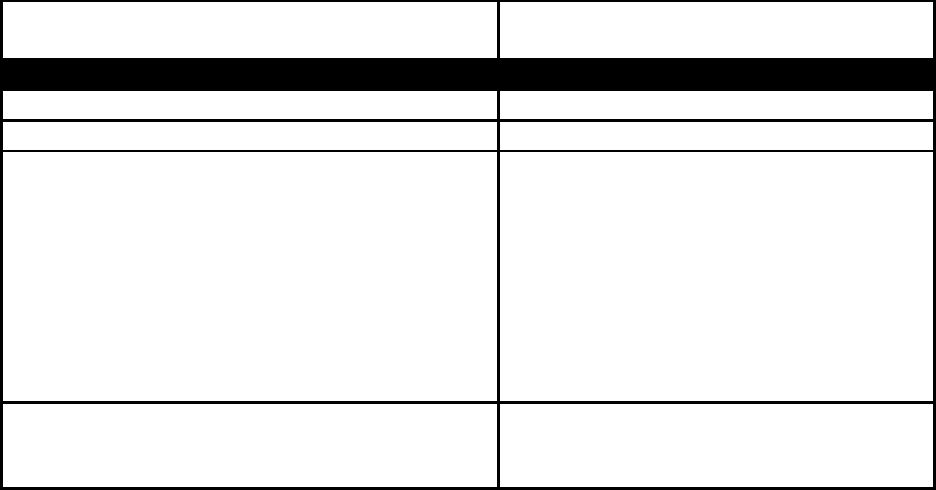
228 AFMAN41-210 10 SEPTEMBER 2019
AF Form 2755, Master Workplace Exposure
Data Summary
Form Number and Title
Special Instructions
AF Form 2769, Supplemental Data Sheet
AF Form 895, Annual Medical Certificate
OTHER DIAGNOSTIC TEST RESULTS and/or
flat disc digital MEDIA not already stored in the
patient’s electronic health record or specifically
mentioned in this attachment.
Note: Some MTFs may receive referral
results from civilian providers in the form
of CD-ROM digital media. If no
capability exists to transfer/convert this
information into Armed Forces Health
Longitudinal Technology Application
(AHLTA), print the information from the
CD-ROM and file in the appropriate
outpatient records department.
Advance Directives (Self Determination Act
forms), durable Power of Attorney forms, organ
donor forms
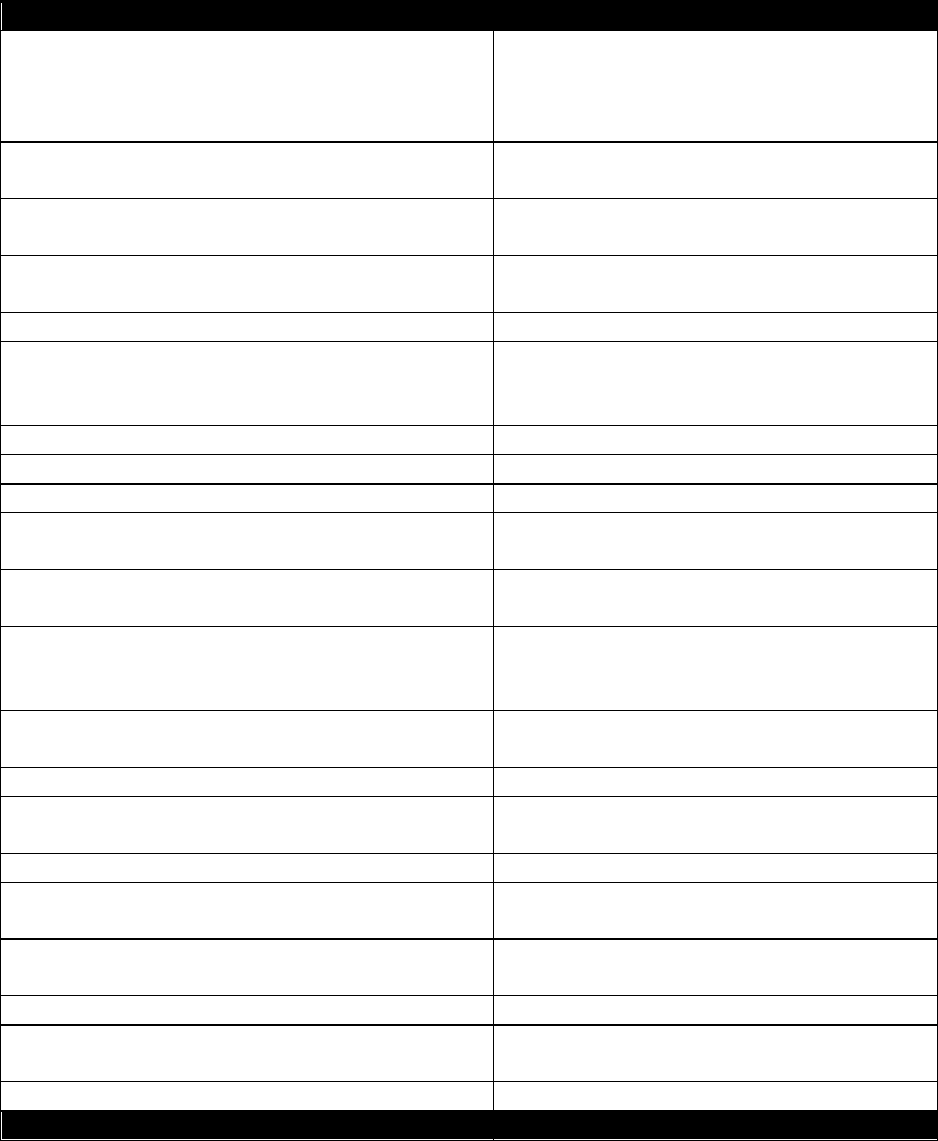
AFMAN41-210 10 SEPTEMBER 2019 229
Attachment 10
ARRANGEMENT OF FORMS IN THE INPATIENT RECORD
Table A10.1. Arrangement of Forms in the Inpatient Record.
Form Number and Title
Special Instructions
AF Form 565, Record of Inpatient Treatment
Original, typed, or electronic. Filed on top
of all other applicable forms. File all other
forms (listed below) for the same episode
of care beneath this form in listed order.
AF Form 560, Authorization and Treatment
Statement
Original with physician’s signature, or
initials, and signature stamp at bottom.
*AF Form 618, Medical Board Report
With attachments as a complete package
when prepared.
SF 502, Medical Record-Narrative Summary
(Clinical Resume)
Unless included in Medical Board package.
SF 503, Medical Record-Autopsy Protocol
DD Form 1322, Aircraft Accident Autopsy
Report
When used instead of SF 503 for reporting
autopsies performed on aircraft accident
fatalities.
SF 504, Clinical Record-History Parts I and II
SF 505, Clinical Record-History Parts II&III
SF 506, Clinical Record-Physical Examination
SF 539 (or DD Form 2770), Medical Record-
Abbreviated Medical Record
When used instead of, or in addition to SF
504-506.
SF 558, Medical Record-Emergency Care and
Treatment
When patient is admitted through the ER;
Original.
*SF 507, Clinical Record Report On ____ or
Continuation of SF Report_______
Always file as an attachment to the form to
which it pertains. Do not separate from
that form.
*OF 275, Medical Record Report
When used in lieu of a SF, AF or DD form,
file in place of that form.
SF 535, Clinical Record-Newborn
SF 509, Medical Record-Progress Notes
When appropriate place preadmission SF
600s in front of SF 509
SF 513, Consultation Report
DD Form 2161, Referral for Civilian Medical
Care
SF 515, Medical Record-Tissues Examination
If an AFIP report is prepared, file it beneath
the SF 515 to which it pertains
SF 516, Clinical Record-Operation Report
OF 517, Medical Record-Anesthesia Recovery
Room Record
AF Form 1864, Preoperative Nursing Record
Form Number and Title
Special Instructions
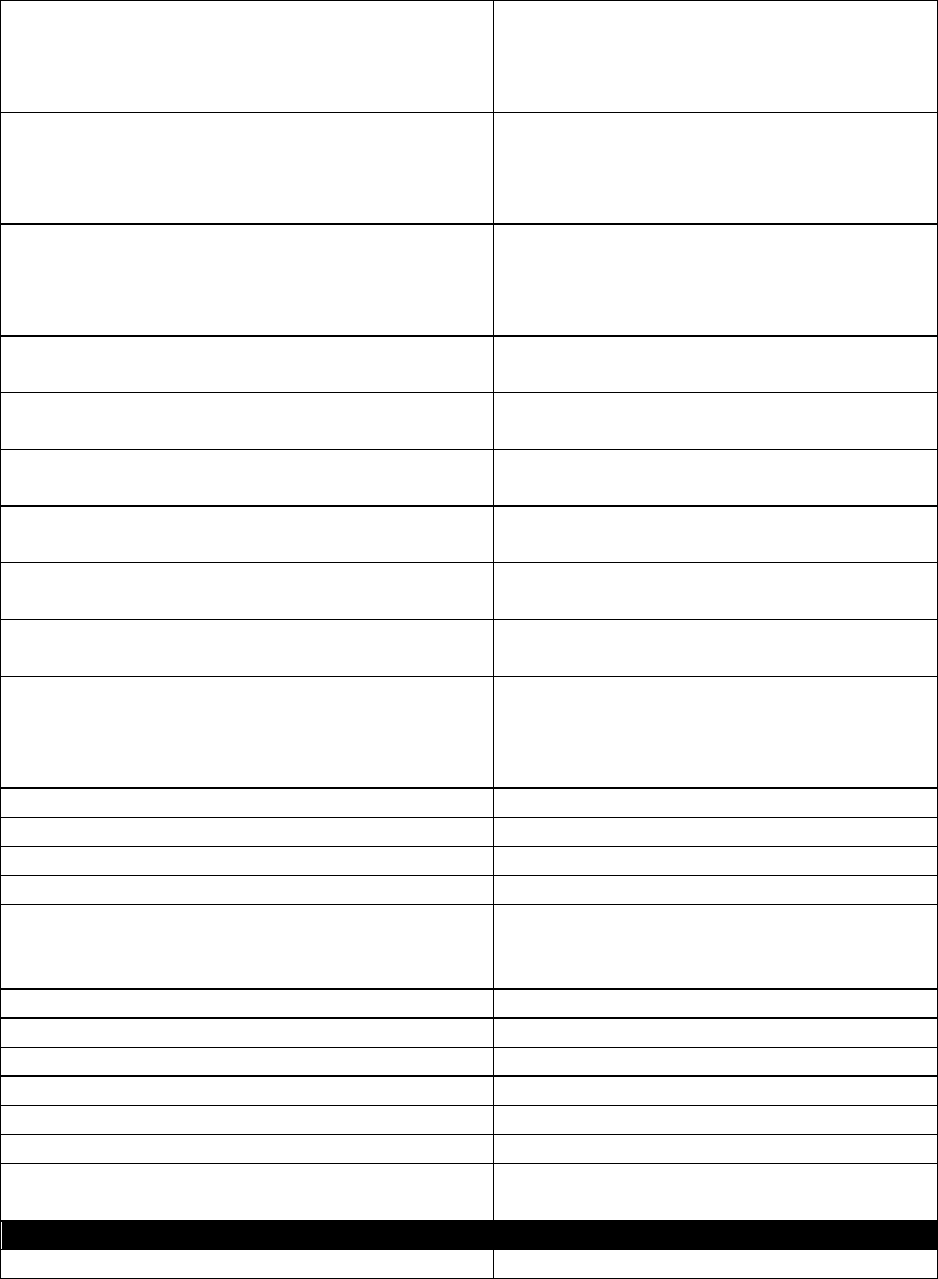
230 AFMAN41-210 10 SEPTEMBER 2019
OF 522, Medical Record-Request for
Administration of Anesthesia and for
Performance of Operations and Other
Procedures
Or locally approved form (check with State
Requirements).
SF 533, Medical Record – Prenatal and
Pregnancy
Prenatal record is filed as a whole package
with all forms pertaining to prenatal
treatment filed chronologically between the
SF 533 and AF Form 3915.
AF Form 3915, Labor and Delivery Flow Sheet
Prenatal record is filed as a whole package
with all forms pertaining to prenatal
treatment filed chronologically between the
SF 533 and AF Form 3915.
AF Form 1302, Request and Consent for
Sterilization
AF Form 1225, Informed Consent for Blood
Transfusion
SF 523, Medical Record-Authorization for
Autopsy
OF 523B, Medical Record-Authorization for
Tissue Donation
SF 518, Medical Record-Blood or Blood
Component
SF 519B, Medical Record – Radiological
Consultation Request Report
OF 520, Medical Record-Electrocardiographic
Record or automated electrocardiograph (EKG)
report
Facilities with computer generated EKG
reports may destroy the OF 520 after the
test is ordered and all patient identification
is on the automated report.
SF 546, Chemistry I
SF 541, Medical Record-Gynecologic Cytology
SF 547, Chemistry II
SF 548, Chemistry III (urine)
SF 549, Hematology
Facilities having Coulter Counter Model S,
Use AF Form 1976-Hematology instead of
SF 549.
SF 550, Urinalysis
SF 551, Serology
SF 552, Parasitology
SF 553, Microbiology I
SF 554, Microbiology II
SF 555, Spinal Fluid
SF 557, Miscellaneous (Note: Laboratory
Reports may be computerized)
Form Number and Title
Special Instructions
DD Form 741, Eye Consultation
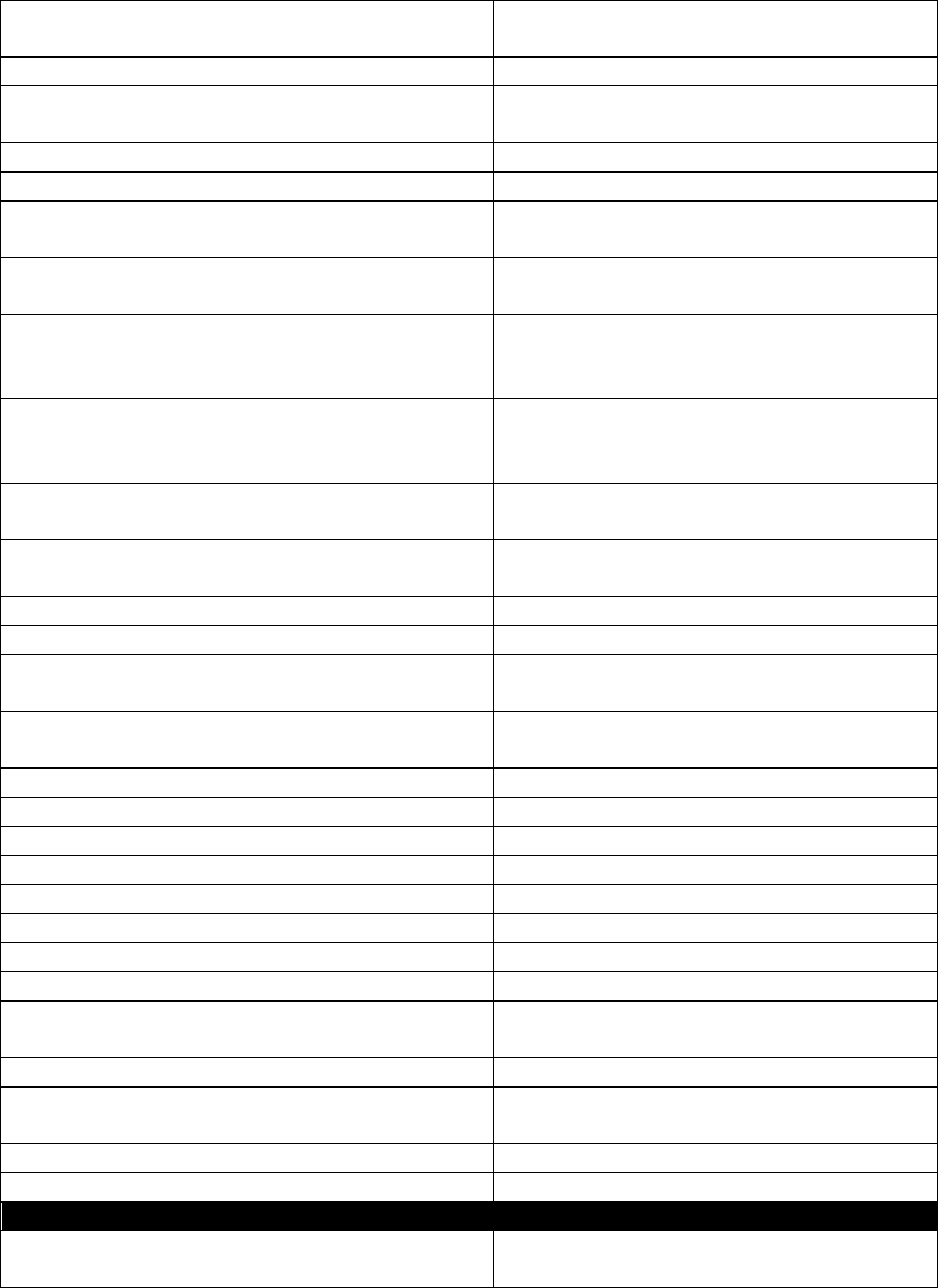
AFMAN41-210 10 SEPTEMBER 2019 231
AF Form 1412, Occupational Therapy
Treatment Record
AF Form 1535, Physical Therapy Consultation
AF Form 1536, Physical Therapy Consultation
Continuation Sheet Record
SF 521, Medical Record-Dental
SF 524, Medical Record-Radiation Therapy
SF 525, Medical Record-Radiation Therapy
Summary
SF 526, Medical Record-
Interstitial/Intercavitary Therapy
SF 527, Medical Record-Group Muscle
Strength, Joint R.O.M., Girth and Length
Measurements
SF 528, Medical Record-Muscle Function by
Nerve Distribution: Face, Neck and Upper
Extremity
SF 529, Medical Record-Muscle Function by
Nerve Distribution: Trunk and Lower Extremity
SF 530, Medical Record-Neurological
Examination
SF 531, Medical Record-Anatomical Figure
AF Form 3066 (or 3066-1), Doctor’s Orders
AF Form 3069, Medication Administration
Record
AF 3068, PRN Medication Administration
Record
AF 3067, Intravenous Record
AF Form 3241, Adult Admission Note
AF Form 3242, Adult Patient Care Plan
AF Form 3244, Pediatric Admission Note
AF Form 3245, Pediatric Patient Care Plan
AF Form 3247, Neonatal Admission Note
AF Form 3248, Neonatal Patient Care Plan
AF Form 3250, Obstetric Patient Care Plan
AF Form 3252A, Mental Health Patient Care
Plan
AF Form 3254, Patient Care Plan
AF Form 3256, Patient/Family Teaching Flow
Sheet
SF 511, Medical Record-Vital Signs Record
SF 512, Medical Record-Plotting Chart
Form Number and Title
Special Instructions
SF 512A, Medical Record-Plotting Chart-Blood
Pressures
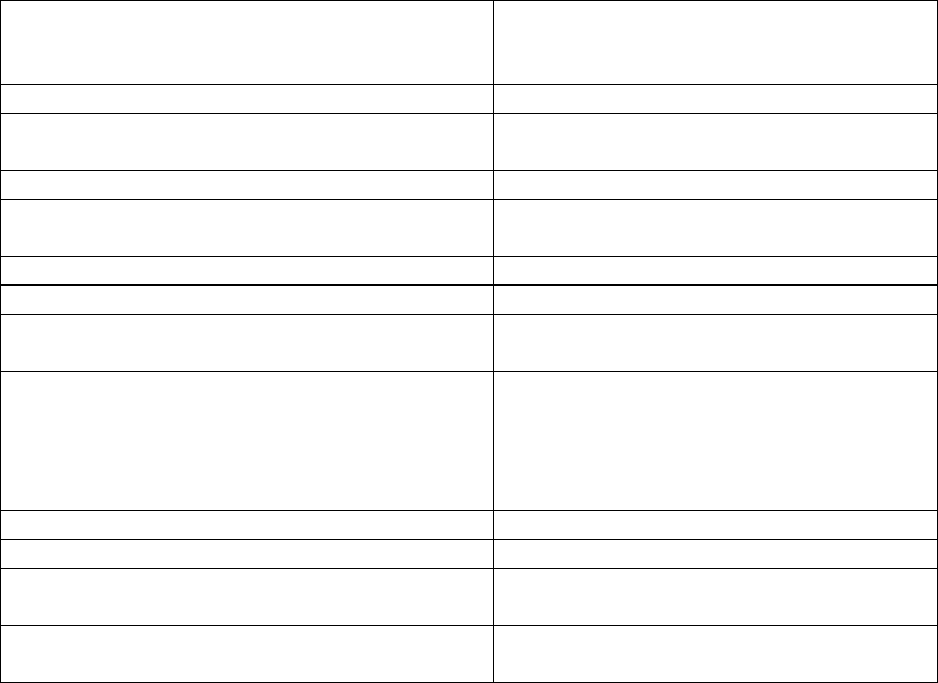
232 AFMAN41-210 10 SEPTEMBER 2019
DD Form 792, Twenty-Four Hour Patient Intake
and Output Worksheet (if local requirements to
file)
Other prescribed nursing forms
AF Form 570, Notification of Patient’s Medical
Status
AF Form 1122, Personal Property Inventory
AF Form 1122A, Personal Property Inventory
(Continuation Sheet)
Birth Certificate and Worksheet
Death Certificate
AF Form 438, Medical Care - Third Party
Liability Notification
DD Form 2569, Third Party Collection Program
– Other Health Information
File the most up-to-date form signed by the
patient or legally authorized representative.
Admitted patients or legally authorized
representative will sign this form prior to or
at the time of admission.
Other command and local administrative forms
Other release of information forms
Correspondence Records received with
transferred patients
*DD Form 602, Patient Evacuation Tag
File beneath the SF 502 from the
transferring MTF.

AFMAN41-210 10 SEPTEMBER 2019 233
Attachment 11
SERVICE TREATMENT RECORDS MAILING ADDRESSES FOR OTHER SERVICES
U.S. Army:
AMEDD Record Processing Center
3370 Nacogdoches Road, Suite 116
San Antonio, TX 78217
U.S. Navy:
Navy Medicine Records Activity (NMRA)
BUMED Detachment St. Louis
4300 Goodfellow Blvd, Bldg. 103
St. Louis, MO 63120
U.S. Marine Corps:
Marine STR Processing Center (MRA)
Attn: STRRCC
3280 Russell Road
Quantico, VA 22134
U.S. Coast Guard:
Commanding Officer
USCG Health, Safety, and Work-Life Service Center (MA)
300 E. Main Street, Suite 1000
Norfolk, VA 23510-9109
USPHS – U.S. Public Health Service
Office of Commissioned Corps Support Services
Medical Affairs Branch
5600 Fishers Lane, Parklawn Building, Room 4C-04
Rockville, MD 20857-0001
NOAA – National Oceanic and Atmospheric Administration
U.S. Public Health Service
Commissioned Personnel Center
Attn: CDR Hobson-Powell
National Oceanic and Atmospheric Administration
8403 Colesville Road, Suite 500
Silver Spring, MD 20910
See AFMOA Kx/Health Benefits/STR/STR Guidance for address updates at:
https://kx.health.mil/kj/kx2/AFMOAHealthBenefits/Pages/home.aspx.
