January 2020 Advising Congress on Medicaid and CHIP Policy
Medicaid Payment Policy for Out-of-State
Hospital Services
Although most Medicaid enrollees obtain medical services within their state of residence, some enrollees
seek care out-of-state under certain circumstances. Current Medicaid regulations describe four situations
in which states must provide out-of-state coverage:
• a medical emergency;
• the beneficiary’s health would be endangered if required to travel to the state of residence;
• services or resources are more readily available in another state; or,
• it is general practice for recipients in a particular locality to use medical resources in another state (42
CFR § 431.52).
States have broad flexibility to determine payment rates for services provided out of state and the
processes that providers must follow to enroll as an out-of-state Medicaid provider. Specifically, many
states pay out-of-state providers at lower rates than in-state providers and require out-of-state providers to
undergo provider screening and enrollment even if the provider is already enrolled in Medicare or Medicaid
in another state. Some providers have raised concerns that these policies may reduce providers’
willingness to serve out-of-state Medicaid beneficiaries and may result in delays in care while provider
enrollment is processed (Manetto et al. 2018).
Hospital services comprise the largest category of Medicaid spending and the only one for which we have
reliable data about out-of-state service use. This brief reviews the use of out-of-state hospital services in
Medicaid and the various ways that states pay out-of-state hospitals. Overall, we find that children who are
eligible for Medicaid on the basis of a disability are more likely to have out-of-state hospital stays than
other types of Medicaid enrollees and that children’s hospitals serve a higher share of patients from out-of-
state than other types of hospitals.
The use of out-of-state care may increase in the future as a result of the Advancing Care for Exceptional
Kids Act (ACE Kids Act, P.L. 116-16), which includes provisions intended to facilitate out-of-state care for
children with disabilities. The ACE Kids Act also requires the Centers for Medicare & Medicaid Services
(CMS) to issue guidance by October 2020 on best practices for ensuring that children with complex
medical conditions receive prompt care out of state when medically necessary.
More information about state payment policies for hospital services is available in MACPAC’s compendia
of state payment policies for inpatient and outpatient services (MACPAC 2018, 2016).
2
Use of Out-of-State Hospital Services
In fiscal year (FY) 2013, about 2 percent of Medicaid hospital stays occurred out of the patient’s state of
residence (Table 1). About half of these stays occurred at hospitals in neighboring states that were located
in the same hospital-referral region (HRR) where the patient lived. An HRR is a geographical designation
that describes regional health care markets tertiary medical care.
1
In 2017, about one-third of HRRs
overlapped multiple states.
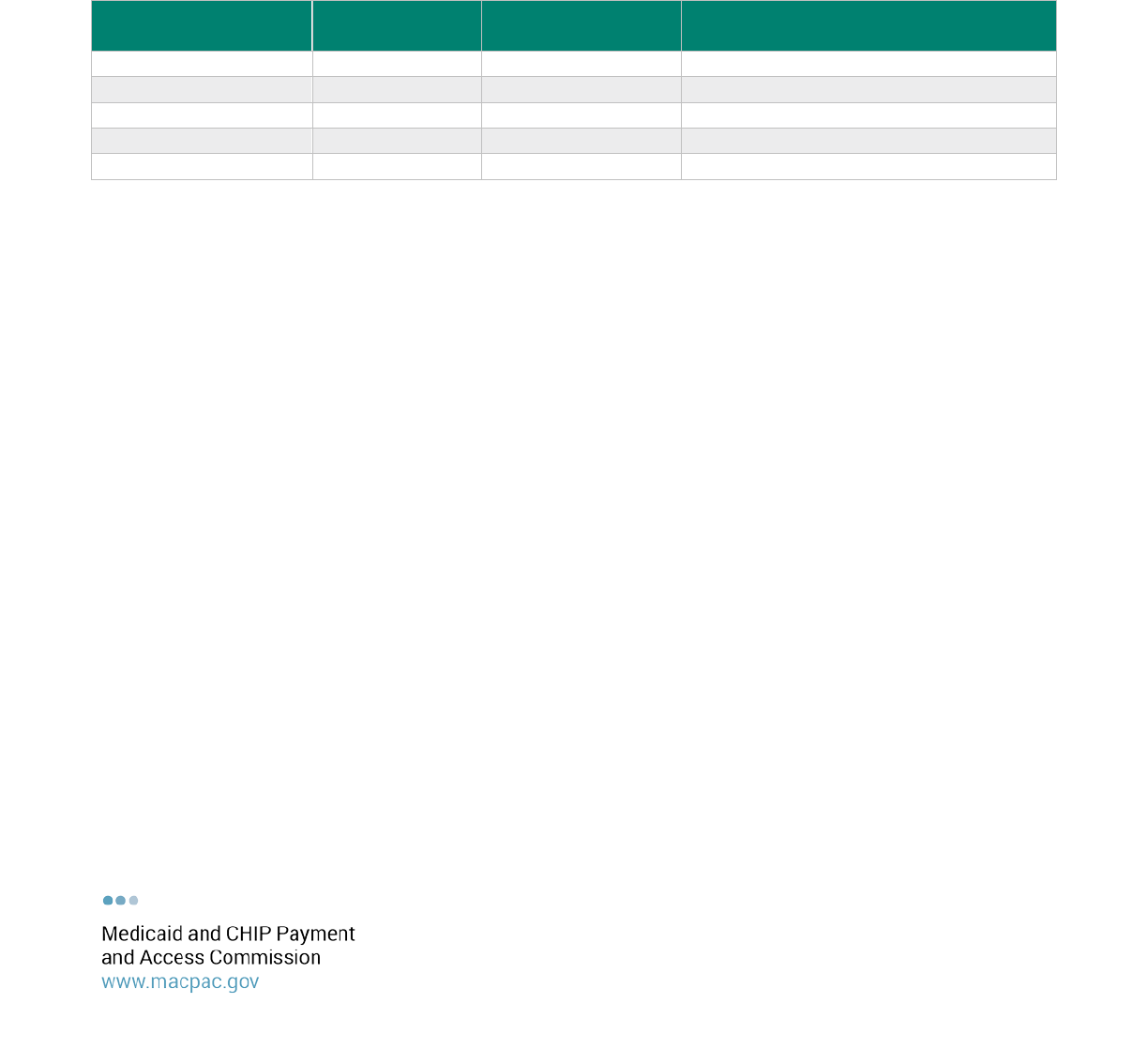
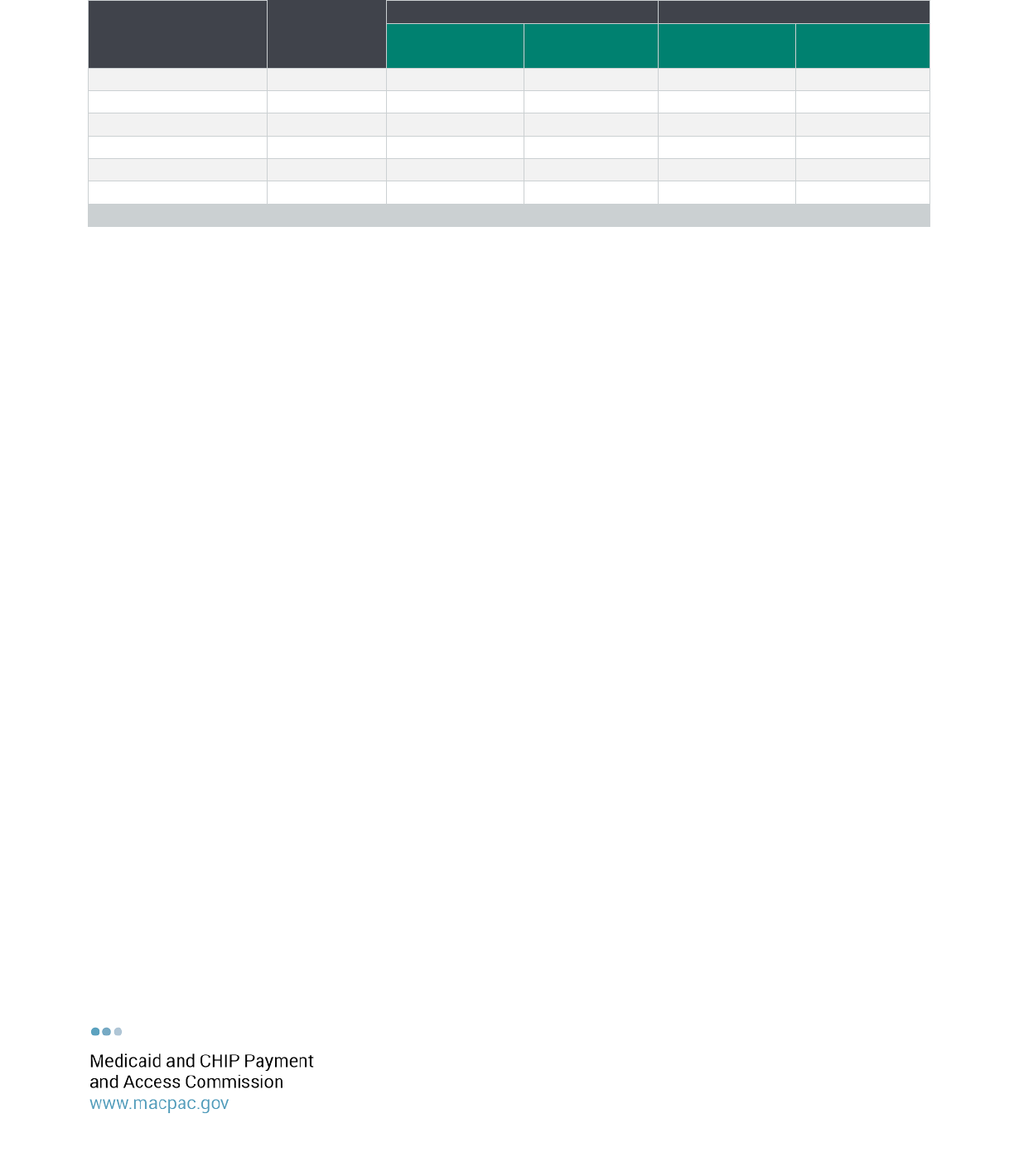
TABLE 1. Out-of-State Medicaid Inpatient Hospital Stays by Eligibility Group, FY 2013
Eligibility group
Total number of
stays (millions)
Share of stays out of
state
Share of out-of-state stays in a different
HRR than enrollee
Total
6.5
1.9%
1.0%
Non-disabled children
2.2
2.2
1.1
Non-disabled adults
2.7
1.5
0.7
Disabled children
0.2
4.1
2.7
Disabled adults
1.5
2.0
1.0
Notes: FY is fiscal year. HRR is hospital-referral region. Analysis excludes individuals enrolled in both Medicare and Medicaid and
those age 65 and older. Ten states are excluded because of lack of complete managed care encounter data (Alaska, Kansas,
Maryland, Missouri, Nebraska, Nevada, Oregon, Rhode Island, Washington, and West Virginia). For more information on our method
for classifying out-of-state hospital stays, see Appendix B.
Source: MACPAC, 2020, analysis of FY 2013 Medicaid Statistical Information System data.
Children who qualify for Medicaid on the basis of a disability have a higher share of out-of-state inpatient
hospital stays than other eligibility groups. These children are also more likely to access care outside of
the HRR where they reside.
Use of out-of-state hospitals varies widely by state, based in part on the extent to which residents live near
other states. For example, Hawaii, which does not border any states, had the lowest share of Medicaid
hospital stays out of state (0.1 percent), while Vermont had the highest (19.0 percent). As discussed
further below, Vermont reduces barriers to out-of-state care by designating certain border hospitals as
Vermont Medicaid providers and paying these hospitals the same rates as in-state hospitals. Complete
information on the distribution of out-of-state hospital stays by state is provided in Appendix A.
Hospital characteristics
In FY 2013, less than half of hospitals (44.9 percent) provided care to Medicaid enrollees who resided
outside the state where the hospital was located (Table 2). However, 86.4 percent of children’s hospitals
served out-of-state patients, a higher share than other types of hospitals. Psychiatric, long-term care, and
children’s hospitals were more likely to serve out-of-state patients from outside their HRR than from within
their HRR, while the majority of out-of-state stays for other hospital types came from within the same HRR
as the hospital.
3
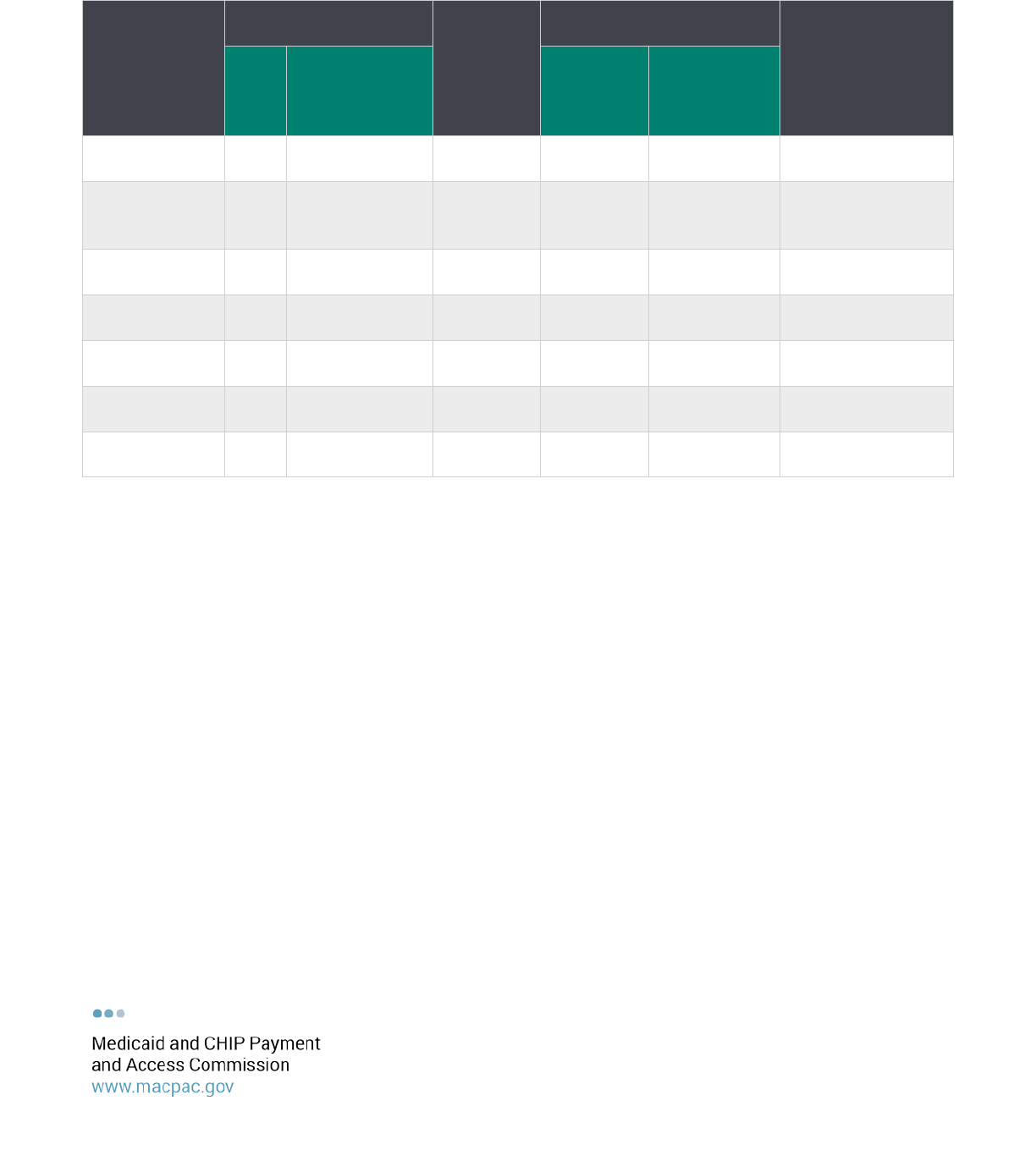
TABLE 2. Medicaid Stays by Hospital Type and Out-of-State Status, FY 2013
Hospital type
Number of hospitals in
analysis
Total
Medicaid
stays
Out-of-state stays as a
share of total Medicaid stays
Average number of
states represented
by out-of-state
Medicaid stays
Total
Share of
hospitals with
out-of-state
Medicaid stays
Share from
out-of-
state
patients
Share from
out-of-state
patients in a
different HRR
Total 4,616 44.9% 6,024,307 1.4% 0.6% 3.1
Short-term
acute care
hospital
2,966
59.4
5,600,348
1.3
0.5
3.2
Critical access
hospital
998
16.2
91,488
1.5
0.4
1.2
Psychiatric
hospital
172
18.6
50,049
1.0
0.8
1.2
Long-term care
hospitals
238
11.3
7,483
2.2
1.6
1.3
Rehabilitation
hospital
161
11.8
6,654
2.2
0.7
1.4
Children's
hospitals
81
86.4
268,285
3.8
2.9
6.6
Notes: FY is fiscal year. HRR is hospital-referral region. Average number of states out-of-state Medicaid patients are from excludes
hospitals without out-of-state visits and does not include the state the hospital is located in. Analysis excludes individuals enrolled
in both Medicare and Medicaid and those age 65 and older. Ten states are excluded because of lack of complete managed care
encounter data (Alaska, Kansas, Maryland, Missouri, Nebraska, Nevada, Oregon, Rhode Island, Washington, and West Virginia).
Analysis also excludes stays that could not be linked to Medicare cost report data (n=512,407). For more information on our method
for classifying out-of-state hospital stays, see Appendix B.
Source: MACPAC, 2020, analysis of FY 2013 Medicaid Statistical Information System data and Medicare cost report data.
States also vary in the extent to which hospitals receive Medicaid payments from multiple states. On
average, hospitals with out-of-state Medicaid patients received Medicaid payments from about three
different states in FY 2013, but children’s hospitals received Medicaid payments from more than six states,
on average. Some children’s hospitals received Medicaid payments from more than 25 states in FY 2013.
Provider Enrollment Requirements
In order to receive payment for Medicaid services, providers must enroll with the program in the patient’s
state of residence and meet federal screening requirements. These requirements are similar to those under
Medicare, and states are not required to conduct additional screening for limited risk providers, such as
hospitals, that have been previously screened by Medicare or another state (CMS 2018). However, states
are not required to use screening data from Medicare or other states and they are allowed to conduct
additional screening beyond the minimum federal requirements. As of June 2019, 24 states and the

4
District of Columbia relied on screenings conducted by Medicare to facilitate their Medicaid provider
enrollment (GAO 2019).
Current state requirements for screening and enrolling out-of-state providers vary widely (GAO 2019 and
HMSA 2018). Some states, such as California, do not require separate screening for out-of-state providers
and have established an express enrollment process for out-of-state providers (DHCS 2020). Other states
require out-of-state providers to follow the same process as in-state providers regardless of whether they
are enrolled in Medicaid in another state. In addition, state requirements for screening and enrolling
providers sometimes differ for services provided under fee-for-service (FFS) and managed care delivery
systems.
Payment Methods for Out-of-State Hospital Services
States have considerable flexibility in how they set hospital rates, including those for hospitals in other
states. States that establish different rates generally pay out-of-state hospitals less than in-state
providers.
As of November 2018, 18 states and the District of Columbia paid out-of-state hospitals using the in-state
rate for inpatient hospital services in their fee-for-service (FFS) Medicaid programs, and the remaining 32
states paid a different out-of-state rate (MACPAC 2018). As of July 2016, 14 states paid out-of-state
hospitals the in-state rate for outpatient services provided under FFS, and the remaining 36 states and the
District of Columbia paid a different out-of-state rate (MACPAC 2016). We do not have information on how
managed care plans pay hospitals.
Most states pay for inpatient hospital services using diagnosis-related groups (DRGs) and many of these
use the same underlying methodology for in-state and out-of-state providers even if the payment rate is
different. For example, Colorado pays out-of-state hospitals a DRG base rate that is 10 percent lower than
the rate paid to in-state hospitals, and Michigan does not apply the same DRG wage adjustment to out-of-
state hospitals that it applies to in-state hospitals (MACPAC 2018).
Some states base payments to out-of-state hospitals using the payment rates for the state in which the
hospital is located. For example, New Jersey pays out-of-state hospitals the lower of the New Jersey state
rate or the Medicaid payment rate for the state in which the hospital is located for both inpatient and
outpatient hospital services (MACPAC 2018 and 2016).
States can establish different payment rates for out-of-state hospitals located in particular geographic
areas. For example, Vermont’s Medicaid state plan designates eight hospitals in neighboring states as
border hospitals that are paid the same rate as in-state hospitals due to their close proximity and the
general practice of Vermont residents to access care at these hospitals (DVHA 2017). However, Vermont
makes lower payments to other out-of-state hospitals that are not designated as border hospitals.
Some states also make supplemental payments to out-of-state hospitals, including disproportionate share
hospital (DSH) payments.
2
However, the vast majority of supplemental payments are made to in-state

5
hospitals. In state plan rate year (SPRY) 2015, 10 states made $44.3 million in DSH payments to out-of-
state hospitals (0.2 percent of total DSH payments in that year). Most of these hospitals also received DSH
payments from the state in which they were physically located.
Endnotes
1
The Dartmouth Atlas defines HRRs based on where patients are referred for major cardiovascular surgical procedures and
for neurosurgery (Dartmouth 1999).
2
The two broad categories of Medicaid payments to hospitals are (1) base payments for services and (2) supplemental
payments, which are typically made in a lump sum for a fixed period of time. For more information, see MACPAC’s issue brief
on
Medicaid Base and Supplemental Payments to Hospitals
.
References
California Department of Health Care Services (DHCS). 2020. Provider enrollment. Sacramento, CA: DHCS. http://files.medi-
cal.ca.gov/pubsdoco/prov_enroll.asp.
Centers for Medicare and Medicaid Services (CMS), U.S. Department of Health and Human Services. 2018.
Medicaid provider
enrollment compendium.
Baltimore, MD: CMS. https://www.medicaid.gov/affordable-care-act/downloads/program-
integrity/mpec-7242018.pdf.
The Dartmouth Atlas of Health Care (Dartmouth). 1999.
Appendix on the geography of health care in the United States.
http://archive.dartmouthatlas.org/downloads/methods/geogappdx.pdf.
Department of Vermont Health Access (DVHA). 2017.
Elective out-of-state inpatient medical care admission
. Waterbury, VT:
DVHA. https://dvha.vermont.gov/for-providers/out-of-state-admissions-010317.pdf.
Hawaii Medical Services Association Provider Resource Center (HMSA). 2018.
QUEST integration—Medicaid provider
enrollment requirements by state as of March 1, 2016.
Honolulu, HI: HMSA.
https://hmsa.com/portal/provider/zav_QI.03.MED.50.htm.
Manetto, N., J. Greenberg, and M. Gaulin. 2018. Medicaid’s unnecessary barriers delay care for children with complex needs.
Stat News
. May 1. https://www.statnews.com/2018/05/01/medicaid-barriers-delay-care-children-complex-needs/.
Medicaid and CHIP Payment and Access Commission (MACPAC). 2018.
State Medicaid payment policies for inpatient
hospital services.
December 2018. Washington, DC: MACPAC. https://www.macpac.gov/publication/macpac-inpatient-
hospital-payment-landscapes/.
Medicaid and CHIP Payment and Access Commission (MACPAC). 2016.
State Medicaid payment policies for outpatient
hospital services.
July 2016. Washington, DC: MACPAC. https://www.macpac.gov/publication/macpac-outpatient-hospital-
payment-landscapes/.
U.S. Government Accountability Office (GAO). 2019.
CMS oversight should ensure state implementation of screening and
enrollment requirements.
Report no. GAO-20-8. Washington, DC: GAO. https://www.gao.gov/products/GAO-20-8.
6
Appendix A: State-Level Data
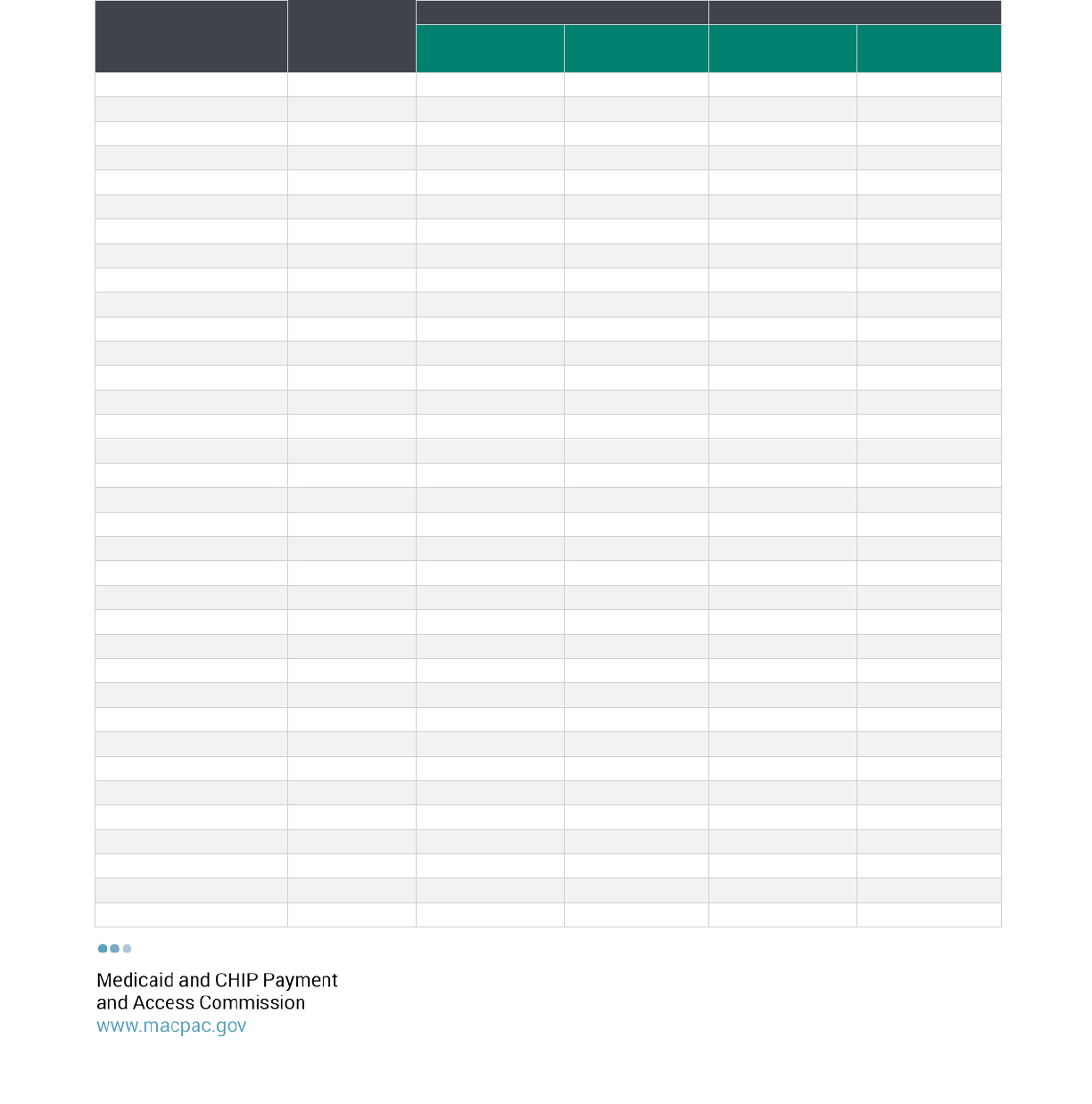
TABLE A-1. Out-of-State Medicaid Hospital Stays by State, FY 2013
State
Total number
of stays
Total out of state
Different HRR
Number of
stays
Share of total
Number of
stays
Share of total
Alabama
111,217
2,407
2.2%
776
0.7%
Arizona
177,524
1,824
1.0%
754
0.4%
Arkansas
76,531
5,660
7.4%
1,190
1.6%
California
554,236
3,137
0.6%
2,371
0.4%
Colorado
62,445
330
0.5%
255
0.4%
Connecticut
93,911
1,046
1.1%
853
0.9%
Delaware
23,016
1,177
5.1%
789
3.4%
District of Columbia
23,619
1,275
5.4%
974
4.1%
Florida
426,310
1,425
0.3%
922
0.2%
Georgia
242,698
4,333
1.8%
1,753
0.7%
Hawaii
23,522
34
0.1%
32
0.1%
Idaho
29,805
1,987
6.7%
647
2.2%
Illinois
247,043
10,867
4.4%
3,404
1.4%
Indiana
135,191
2,749
2.0%
996
0.7%
Iowa
54,517
4,566
8.4%
2,533
4.6%
Kentucky
81,068
4,138
5.1%
2,606
3.2%
Louisiana
136,446
1,328
1.0%
1,019
0.7%
Maine
25,738
581
2.3%
366
1.4%
Massachusetts
168,977
2,235
1.3%
1,813
1.1%
Michigan
228,034
2,125
0.9%
958
0.4%
Minnesota
101,837
4,166
4.1%
939
0.9%
Mississippi
103,636
4,813
4.6%
2,100
2.0%
Montana
17,443
518
3.0%
482
2.8%
New Hampshire
13,477
924
6.9%
623
4.6%
New Jersey
120,451
4,460
3.7%
3,570
3.0%
New Mexico
58,687
4,165
7.1%
713
1.2%
New York
1,103,320
5,498
0.5%
3,380
0.3%
North Carolina
226,278
2,145
0.9%
953
0.4%
North Dakota
10,115
388
3.8%
242
2.4%
Ohio
288,754
7,001
2.4%
2,573
0.9%
Oklahoma
118,329
3,907
3.3%
1,220
1.0%
Pennsylvania
239,792
2,185
0.9%
1,447
0.6%
South Carolina
137,559
17,080
12.4%
12,322
9.0%
South Dakota
19,027
981
5.2%
481
2.5%
Tennessee
132,831
1,301
1.0%
575
0.4%
7
State
Total number
of stays
Total out of state
Different HRR
Number of
stays
Share of total
Number of
stays
Share of total
Texas
642,368
959
0.15%
689
0.1%
Utah
50,855
348
0.7%
249
0.5%
Vermont
12,359
2,350
19.0%
607
4.9%
Virginia
111,570
4,522
4.1%
2,171
1.9%
Wisconsin
95,537
3,239
3.4%
1,059
1.1%
Wyoming
10,641
1,449
13.6%
978
9.2%
Total
6,536,714
125,623
1.9%
62,384
1.0%
Notes: FY is fiscal year. HRR is hospital-referral region. Analysis excludes individuals enrolled in both Medicare and Medicaid and
those age 65 and older. Ten states are excluded because of lack of complete managed care encounter data (Alaska, Kansas,
Maryland, Missouri, Nebraska, Nevada, Oregon, Rhode Island, Washington, and West Virginia). For more information on our method
for classifying out-of-state hospital stays, see Appendix B.
Source: MACPAC, 2020, analysis of FY 2013 Medicaid Statistical Information System data.

8
Appendix B: Methodology and Data Limitations
Out-of-state hospital stays were examined using fiscal year (FY) 2013 claims and encounter data from the
Medicaid Statistical Information System (MSIS). Below we describe the data included in our analysis and
our method for classifying out-of-state stays.
Data Included in Analysis
Using MSIS, we examined Medicaid fee-for-service claims and managed care encounter data for inpatient
hospital stays that began during FY 2013. Claims that occured on the same, consecutive, or overlapping
days were merged into a single stay for this analysis.
Because hospital care for patients dually eligible for Medicare and Medicaid is primarily covered by
Medicare, this analysis excluded stays for dually eligible patients and patients over age 65. We also
excluded stays without complete data on Medicaid enrollee’s age and basis of eligibility.
We excluded data from ten states without complete claims or encounter data for FY 2013:
• three states (Alaska, Kansas, and Rhode Island) had no data for at least one quarter in in FY 2013;
• two states (Nevada and West Virginia) did not have managed care encounter data; and,
• five states (Oregon, Washington, Nebraska, Missouri and Maryland) did not have valid national provider
identifiers (NPIs) for at least 80 percent of inpatient hospital stays.
Classifying Hospital Stays
For inpatient hospital stays included in our analysis, we collected information about the hospital’s NPI, the
enrollee’s zip code, and the enrollee’s basis of Medicaid eligibility. A total of 6,770,107 stays were identified
at this stage of the analysis.
The National Plan and Provider Enumeration System was used to validate each NPI and get information
about the zip code associated with the provider’s practice location. Zip codes for providers and enrollees
were then used to determine the state and hospital referral regions (HRR) for the enrollee and provider and
classify out-of-state visits. A total of 233,393 stays (3.4 percent) were excluded because they did not have
valid zip code information that could be linked to a HRR.
To provide descriptive information about the types of hospitals that serve out-of-state patients, each
hospital’s NPI was linked to the CMS certification number (CCN), which was used to identify hospitals in
Medicare cost reports. CCN data were not available for 512,407 stays (7.8 percent of the stays in our
analysis with valid zip codes).
