This report summarizes the ndings and recommendations of the
Texas CASA Mental Health Task Force. With the support of the Hogg Foundation
for Mental Health, child welfare experts, stakeholders, advocates and consumers came together to
address the variety of mental health issues facing children and youth in the child welfare system. Membership
was comprised of physical and mental health care practitioners, judges, social workers, psychologists and state agency
personnel.
Texas CASA wanted to ensure that the urgent mental health needs of the children remained a constant focus of the Task Force’s work. Therefore, a
vision was developed to guide their work and advocacy:
We envision a system of care that:
• respects the needs of traumatized children and youth in substitute care;
•places the utmost importance on ensuring they have access to the best mental health services and systems of support; and
• provides them with a real opportunity to heal from their traumatic experiences and grow into successful adults.
Task Force members were charged with:
• identifying problems facing children and youth in state custody in regards to their mental health;
• developing actionable solutions (recommendations) that will improve the well-being of children and youth in foster care; and
• advocating for those solutions.
This report represents the Task Force’s recommendations around three major issue areas identied by Task Force members as the most impactful issues affecting mental health outcomes of children and youth in foster care in Texas:
Diagn o s is an d tre atm e n t o f m e n tal h e alth is s ue s in ch ild re n an d yo u th in s u bs titute ca re
:
an accurate and appropriate m ental health diagnoses for children and y outh in substitute care. Furtherm ore, w hen diagnoses are assigned, accurate or
unclear w hether therapeutic or non-pharm acological strategies or m odels are av ailable and/ or used appropriately .
in norm alcy activities. These obstacles can prev en t y oung people in care from engaging in norm al adolescent experiences and building social and life
skills. This struggle can be made more difcult depending on how restrictive a child’s placement is and depending on their cultural and spiritual identity and/or what special needs they may have.
supported to successfully care for children and youth struggling w ith sy m ptom s of traum a. This challenge is one of m any existing obstacles in attem pts
The Texas CASA Mental Health Task Force also recognized a number of barriers to achieving needed system and care improvements. Predictably, the most prominent barriers recognized by the Task Force are the same as those recognized by many mental health
stakeholders and advocacy groups:
Medicaid reimbursements are too low and discourage well-trained and specialty practitioners from choosing to become Medicaid providers.
There is a lack of providers overall, especially those who are well-trained in treating trauma and specically trained to treat trauma experienced by children.
To research and create recommendations around these challenges, Task Force members were divided into sub-committees around the three major issue areas. These sub-committees met many times over the course of one and a half years and worked with the larger
Task Force to produce the recommendations found in this report.
RESPECTING THE NEEDS OF CHILDREN AND
YOUTH IN TEXAS FOSTER CARE:
ACKNOWLEDGING TRAUMA AND PROMOTING POSITIVE MENTAL
HEALTH THROUGHOUT THE SYSTEM
RECOMMENDATIONS OF THE
TEXAS CASA MENTAL HEALTH TASK FORCE
Acknowledgements
This report was prepared by Stephanie LeBleu and Sarah Crockett, with
generous support from Cristina Masters, Andy Homer, Elizabeth Krog and
Jemila Lea. It would not have been possible without the input of the experts
who served on the Texas CASA Mental Health Task Force and volunteered
their time to think critically about how to improve the lives and experiences
of children and youth in foster care in Texas. This endeavor was facilitated
by Texas CASA under the leadership of its CEO, Vicki Spriggs.
This project was made possible through a generous grant from the
Hogg Foundation for Mental Health at the University of Texas.
Texas CASA Mental Health
Task Force Members
Tymothy Belseth
Texas Department of Family
and Protective Services
Gail Biro
DePelchin Children’s Center
Duncan Cormie
Texas Network of Youth
Services
Sheila Craig
Center for Elimination of
Disproportionality and
Disparities
Texas Health and Human
Services Commission
Cheryl Fisher
Cenpatico
Michael Greenwood, MSSW
Giocosa Foundation
William Holmes, MD
Cenpatico
Andy Homer
Texas CASA
Richard Lavallo, JD
Disability Rights Texas
Jemila Lea, JD
Hogg Foundation for Mental
Health
Molly Lopez, PhD
Texas Institute for Excellence in
Mental Health
Jon Olson, MSSW
Center for Elimination of
Disproportionality and
Disparities
Texas Health and Human
Services Commission
Anu Partap, MD
Foster Care Clinic
Children’s Medical Center
Dallas
Courtney McElhaney Peebles
Center for Elimination of
Disproportionality and
Disparities
Texas Health and Human
Services Commission
Karyn Purvis, PhD
Institute of Child Development
Texas Christian University
Cindy Rains
CASA of the Permian Basin
Area, Inc.
Debbie Sapp
CASA of Walker County, Texas
Kristopher Sharp
Texas Foster Care Alumni
Andrea Sparks
Texas Regional Ofce
National Center for Missing
and Exploited Children
Yolanda Valenzuela
Child Advocates of San Antonio
Dianna Velasquez
Governor’s Ofce of Budget,
Planning and Policy
Ofce of Texas Governor Rick
Perry
Sara Wood, RN, PMHNP,
APRN-BC,
Ex Ofcio Members
Debra Emerson
Child Protective Services
Texas Department of Family
and Protective Services
Judge John Hathaway
Travis County, Texas
Monica Thyssen
Medicaid and Chip Division
Texas Department of Health
and Human Services
Jennifer Sims
Department of Family and
Protective Services
Kristi Taylor, JD
Texas Children’s Commission
Technical Assistance
Dan Capouch
Texas Department of Family
and Protective Services
Shannon Ramsey
Texas Department of Family
and Protective Services
Kathy Teutsch
Texas Department of Family
and Protective Services
RESPECTING THE NEEDS OF CHILDREN AND
YOUTH IN TEXAS FOSTER CARE:
ACKNOWLEDGING TRAUMA AND PROMOTING POSITIVE
MENTAL HEALTH THROUGHOUT THE SYSTEM
RECOMMENDATIONS OF THE
TEXAS CASA MENTAL HEALTH TASK FORCE
December 2014
TABLE OF CONTENTS
Introduction..................................................................................................6
Executive Summary.......................................................................................8
Section 1: Diagnosis and treatment of mental health issues
in children and youth in substitute care.......................................14
Integrated care is the standard, not the reality........................................................................18
The term “non-pharmacological interventions” is not well-dened or
understood..............................................................................................................................21
Medical and mental health providers serving this population are not
beholden to American Academy of Pediatrics standards and the current
Medicaid reimbursement rates in Texas deter providers...........................................................22
Limited information is available regarding the array of mental health
services available under STAR Health and understanding of how to
utilize the Medicaid appeals process and other legal options is limited....................................23
Texas youth who aged out of care are not auto-enrolled in Medicaid and
youth who aged out in other states are not extended coverage in Texas...................................24
Section 2: Empowerment and normalization of youth in
substitute care............................................................................26
The current system inhibits caregivers’ ability to make decisions about
a child’s participation in normalcy activities and experiences...................................................28
Service plans can be too prescriptive and unwittingly block a young
person from participating in an activity or experience and caregivers can
be discouraged from allowing for participation in normalcy activities.......................................30
Youth are not empowered to address concerns within their placements
or to report abuse and are not aware of their individual rights or what
recourse is available to them when rights are violated.............................................................32
Section 3: Appropriate caregiving environments for children
and youth in substitute care.......................................................35
Caregivers are not adequately trauma-informed and efforts to establish
a trauma-informed care system are slow, disconnected, and vary in how
they are dened......................................................................................................................36
Current practice does not include an assessment for adult attachment
for alternate caregivers...........................................................................................................40

MENTAL HEALTH TASK FORCE REPORT | PAGE 6
INTRODUCTION
This report summarizes the ndings and recommendations of the Texas CASA Mental Health Task
Force. Child welfare experts, stakeholders, advocates and former foster youth came together to address
the variety of mental health issues facing children and youth in the child welfare system. Membership
was comprised of physical and mental health care practitioners, judges, social workers, psychologists,
attorneys and state agency personnel.
Texas CASA wanted to ensure that the urgent mental health needs of the children remained a constant
focus of the Task Force’s work. Therefore, the following vision was developed to guide their work and
advocacy:
We envision a system of care that:
• Respects the needs of traumatized children and youth in substitute care;
• Places the utmost importance on ensuring they have access to the best mental health
services and systems of support; and
• Provides them with a real opportunity to heal from their traumatic experiences and grow
into successful adults.
Task Force members were charged with:
• Identifying problems facing children and youth in state custody in regards to their mental
health;
• Developing actionable solutions (recommendations) that will improve the well-being of children
and youth in foster care; and
• Advocating for those solutions.
This report represents the Task Force’s recommendations around three major issue areas identied by
Task Force members as the most impactful issues affecting mental health outcomes of children and
youth in foster care in Texas:
1. Diagnosis and treatment of mental health issues in children and youth in substitute care:
There is currently a lack of emphasis on achieving an accurate and appropriate
mental health diagnoses for children and youth in substitute care. Furthermore,
when diagnoses are assigned, accurate or not, it is unclear whether therapeutic
or non-pharmacological strategies or models are available and/or used
appropriately.
2. Empowerment and normalization of youth in substitute care:
Systemic obstacles exist for young people in care who wish to participate in
normalcy activities. These obstacles can prevent young people in care from
engaging in normal adolescent experiences and building social and life skills.
This struggle can be made more difcult depending on how restrictive a child’s
placement is and depending on the child’s cultural and spiritual identity and/or
what special needs he or she may have.

MENTAL HEALTH TASK FORCE REPORT | PAGE 7
3. Appropriate caregiving environments for children and youth in substitute care:
Currently, caregivers in Texas are not effectively recruited,
screened, prepared or supported to successfully care for children
and youth struggling with symptoms of trauma. This challenge
is one of many existing obstacles in attempts to achieve a truly
trauma-informed system of child welfare.
The Texas CASA Mental Health Task Force also recognized a number of barriers to
achieving needed system and care improvements. Predictably, the most prominent barriers
recognized by the Task Force are the same as those recognized by many mental health
stakeholders and advocacy groups:
• Medicaid reimbursements are too low and discourage well-trained and specialty
practitioners from choosing to become Medicaid providers.
• There is a lack of providers overall, especially those who are well-trained in treating
trauma and specically trained to treat trauma experienced by children.
To research and create recommendations around these challenges, Task Force members
were divided into sub-committees around the three major issue areas. These sub-
committees met individually numerous times over the course of one-and-a-half years and
worked as a part of the larger Task Force to produce the recommendations found in this
report.

MENTAL HEALTH TASK FORCE REPORT | PAGE 8
EXECUTIVE SUMMARY
Mental health has found its way to center stage over the last few years in our country. Tragic incidents
have occurred across the nation that have forced states and communities to look at issues of mental
health and gure out more effective ways to care for people who need help and support.
Texas engaged in this effort as well. Last legislative session Texas appropriated $2.6 billion toward
providing mental and behavioral health services for its residents (approximately a 15% increase from
the 2012-2013 budget).
1
The Texas CASA Mental Health Task Force believes that the same emphasis
and imperative placed on addressing general mental health should be placed on addressing the
unique mental health needs of children and youth in the child welfare system. While it remains to be
seen how or if this infusion of funding will impact the children and youth in the Texas child welfare
system, research has shown that their need for mental health care and services is great and based
on a unique set of needs and complex circumstances.
Children in foster care experience mental illness at a rate almost 30% greater than the average
population of children.
2
Children and youth in care are also less likely to receive adequate treatment
and services for their mental health needs.
3
Given these facts, it is no surprise that children in care
experience negative outcomes at a much higher rate as well.
Child welfare advocates have learned that unresolved trauma plays an enormous role in driving
these negative outcomes. Trauma can cause both long and short-term problems for children.
“Consequences of trauma include difculties with learning, ongoing behavior problems, impaired
relationships and poor social and emotional competence. Children and youth exposed to trauma,
especially violence, experience more learning and academic difculties and behavioral and mood-
related problems.”
4
This means that children who experience trauma may still struggle to attach
to caregivers or regulate their emotions and behaviors, even if they are placed in an ideal home,
where loving and consistent care is available to them.
The Texas CASA Mental Health Task Force believes that these complex physical and behavioral
health needs have been poorly addressed or not addressed at all for children and youth in Texas.
There are a number of reasons why children in foster care may not get the care or support they need.
These include:
• Frequently changing providers due to placement moves
• Lack of physical and mental health providers who accept Medicaid
• Lack of providers well-trained in trauma, grief and loss
1 Ligon, Katharine. Sizing Up the 2014-15 Texas Budget: Mental Health. Rep. Center for Public Policy Priorities, Sept. 2013. Web. 15 Dec.
2014. <http://forabettertexas.org/images/2013_10__PP_Budget_MentalHealth.pdf>.
2 Texas Medicaid Managed Care and Children’s Health Insurance Program: EQRO Summary of Activities and Trends in Healthcare Quality.
Rep. Institute for Child Health Policy at the University of Florida Texas External Quality Review Organization, 28 Mar. 2014. Web. 15 Dec. 2014. <http://
www.hhsc.state.tx.us/reports/2014/EQRO-Summary.pdf>.
3 Carrillo, Sarah, and Elisa Ashton. Improving Care Coordination for Foster Children: An Update on California’s Audacious Goal. Rep.
California Ofce for Health Information Integrity, 20 Jan. 2013. Web. 15 Dec. 2014.
4 Cooper, Janice L. “Facts about Trauma for Policymakers: Children’s Mental Health.” National Center for Children in Poverty. Columbia
University Mailman School of Public Health Department of Health Policy & Management, July 2007. Web. 4 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 9
• Lack of providers who are specically trained to treat children
• Lack of understanding of the root cause of a child’s behavior
• Overburdened caseworkers and other parties in the case
• Systemic resistance to using non-pharmacological interventions other than therapy
• Systemic inability to make decisions about a child’s outcomes based on their emotional and
mental health needs
• Lack of access to normal life experiences that contribute to positive mental health outcomes
The Texas CASA Mental Health Task Force decided to focus its efforts on three major areas of
concern and make recommendations about issues within those three areas. A summary of the issues
and recommendations are as follows:
I. DIAGNOSIS AND TREATMENT OF MENTAL HEALTH ISSUES IN CHILDREN AND
YOUTH IN SUBSTITUTE CARE
Issue 1: Integrated care is the standard, not the reality
Recommendations:
1. The Health and Human Services Commission should activate and publicize Medicaid
billing codes that will allow providers to bill for collaborative consultation, which
allows practitioners to bill for “peer consults” between primary care physicians
(PCPs) and other PCPs; PCPs and Psychiatrists; and PCPs and other mental health
practitioners.
2. Ensure the Health Passport is being utilized and includes updated information on the
child’s medical history, mental health, developmental and psychosocial functioning—
any information pertinent to any course of care for the child.
Issue 2: The term “non-pharmacological interventions” is not well dened or
understood
Recommendation:
1. Adoption of the following denition of “non-pharmacological interventions” by the
judicial system, medical care providers, insurers, CASA, CPS and others:
• “Non-pharmacological interventions” is terminology meant to represent an
array of strategies, supports and interventions intended to help children recover
and heal from trauma, build resilience and meet developmental milestones.
Non-pharmacological interventions must be used in lieu of or concurrently with
psychotropic medications and should be informed by accurate and continuous
assessment and/or diagnosis. Non-pharmacological interventions include both
evidence-based interventions, promising practices and those interventions
proven effective by peer-reviewed research.

MENTAL HEALTH TASK FORCE REPORT | PAGE 10
Issue 3: Medical and mental health providers serving this population are
not beholden to American Academy of Pediatrics standards and the current
Medicaid reimbursement rates in Texas deter providers
Recommendations:
1. Implement, require and train on American Academy of Pediatrics standards for
physicians treating children in substitute care on health screenings in foster care.
2. Provide equivalent reimbursement rates for all licensed professionals who provide
Medicaid mental health services to children in foster care.
Issue 4: Limited information is available regarding the array of mental
health services available under STAR Health and understanding of how to
utilize the Medicaid appeals process and other legal options is limited
Recommendations:
1. Revise STAR Health Member Handbook to include:
• Information on trauma and trauma-informed care
• Information on behavioral health services, including a list of covered services,
denition of services, and information on how to access services and who can
provide services
• A simpler explanation of the Medicaid appeals process
2. Train consumers, attorneys, judges, CASA volunteers, medical consenters and
youth (especially those 16 and older) on:
• What behavioral health services are available through STAR Health, including
denitions of services, how to access services and who can provide services
• The Medicaid appeals process, including how to appeal when a requested
medically necessary service is denied
3. Train attorneys, CASA volunteers, judges, medical consenters and youth on how to
petition the court for an order related to the medical care for a foster child. This is not
a formal Medicaid appeal but the use of the exclusive jurisdiction of the court could
help to ensure that foster children receive appropriate medical care, including mental
health and behavioral health services.

MENTAL HEALTH TASK FORCE REPORT | PAGE 11
Issue 5: Texas youth who aged out of care are not auto-enrolled in Medicaid
and youth who aged out in other states are not extended coverage in Texas
Recommendations:
1. Create automatic enrollment transfers from STAR Health to STAR when a child turns
21, assuring that former foster children will have Medicaid coverage until age 26
regardless of reapplication.
2. Extend Medicaid eligibility to former foster youth from any state until age 26.
II. EMPOWERMENT AND NORMALIZATION OF YOUTH IN SUBSTITUTE CARE
Issue 1: The current system inhibits caregivers’ ability to make decisions
about a child’s participation in normalcy activities and experiences
Recommendations:
1. Dene the Reasonable and Prudent Parenting Standard and include what to consider
when caregivers are making decisions.
2. Require DFPS to verify that private contracted agencies promote and protect
the ability of a child to participate in normalcy activities by requiring that private
agencies have the same provisions of “reasonable and prudent parenting standards”
as foster caregivers.
Issue 2: Service plans can be too prescriptive and unwittingly block a young
person from participating in an activity or experience and caregivers can be
discouraged from allowing for participation in normalcy activities
Recommendations:
1. Address service plan limitations by listing normalcy activities and/or experiences the
child has/is participating in rather than listing activities as a limited list of activities in
which a child can participate.
2. Mandate that the foster parent and/or the associated child placing agency shall not be
held responsible for potentially negative outcomes beyond their reasonable control as
a result of the child’s participation in an age-appropriate normalcy activity, provided
the activity is approved by the foster parent using the reasonable and prudent parent
standard.
3. Require training for residential staff, child placing agency staff, foster parents, kinship
providers and residential child care licensing staff. This training should include
instruction on decision-making as a “reasonable and prudent parent”, appropriate
and trauma-informed ways to deal with a child or youth’s misbehavior, the importance
of a child’s participation in normal adolescent activities and experiences, and the

MENTAL HEALTH TASK FORCE REPORT | PAGE 12
benets of such participation to a child’s social, emotional and developmental growth,
well-being and mental health.
Issue 3: Youth are not empowered to address concerns within their
placements or to report abuse and are not aware of their individual rights or
what recourse is available to them when rights are violated
Recommendations:
1. Establish an independent Ombudsman ofce or establish autonomy within the OCA,
ensuring that the Department of Family and Protective Services shall have no authority
to:
• Create or change the policy and practice of the Ofce of Consumer Affairs;
• Determine the budget of the Ofce of Consumer Affairs; or
• Make decisions regarding personnel of the Ofce of Consumer Affairs
2. Caseworkers and CPA personnel should provide foster children and youth with better
access to the Children’s Bill of Rights by making copies available at court hearings
and at site visits and provide ongoing education around these rights in order to fully
empower them.
3. Require Child Placing Agencies and foster care placements to provide access to the
OCA or independent Ombudsman’s ofce contact information in private spaces, such
as bathrooms or on the back of bedroom doors.
4. Require the OCA or independent Ombudsman’s ofce to establish a written policy on
foster youth’s provisions and protections from retaliation by a caregiver, including a
procedure of investigation of such retaliation and consequences for caregivers who are
found to have engaged in retaliation against a child or youth in foster care.
5. Require the OCA to establish a secure form of communication with the child or youth
in order to ensure that he or she is made aware of the investigation including the
substantiation of any complaints that are brought to the attention of or determined by
the OCA.
6. Require the OCA to establish specic procedures for working with youth in foster care
who call to make an inquiry or complaint.

MENTAL HEALTH TASK FORCE REPORT | PAGE 13
III. APPROPRIATE CAREGIVING ENVIRONMENTS FOR CHILDREN AND YOUTH
IN SUBSTITUTE CARE
Issue 1: Caregivers are not adequately trauma-informed and efforts to establish
a trauma-informed care system are slow, disconnected, and vary in how they
are dened
Recommendations:
1. Dene trauma-informed care for caregivers within Minimum Standards.
2. Require all residential child care administrators and staff to complete trauma-informed
care training, as dened by the Department of Family and Protective Services.
3. Incentivize Child Placing Agencies (CPAs) to incorporate trauma-informed care into
their assessments, training and support of caregivers of children with increased
reimbursement rates.
4. Evaluate the utilization and effectiveness of implementing trauma-informed care models,
as dened by the Department of Family and Protective Services, within the eligible CPAs.
Issue 2: Current practice does not include an assessment for adult attachment
for alternate caregivers
Recommendations:
1. Require all agencies that screen potential caregivers to include an attachment screening
as a component of the overall assessment to better understand that caregiver’s
ability to form meaningful and trust-promoting relationships with children who have
experienced trauma. There are several free attachment screening options and the Task
Force recommends that the Department of Family and Protective Services create a
standardized list of tools for agencies to utilize for these screenings.
2. Train Child Placing Agency staff to screen potential caregivers using attachment
screening and ensure they have the proper assessment tools, as dened by the
Department of Family and Protective Services.
3. Require a set of standardized assessments of prospective caregivers, dened by the
Department of Family and Protective Services, across child placing agencies.

MENTAL HEALTH TASK FORCE REPORT | PAGE 14
I. DIAGNOSIS AND TREATMENT OF
MENTAL HEALTH ISSUES IN CHILDREN AND YOUTH
IN SUBSTITUTE CARE
Background
Children in care more likely to experience poor mental and physical health
Children and youth in the child welfare system have a higher prevalence of physical, developmental,
dental and behavioral health conditions than any other group of children.
1
Physical trauma, such as
a blow to the head or body or violent shaking, can result in negative effects on physical development.
Neglect, such as inadequate nutrition, lack of adequate stimulation or withholding of medical treatment,
can also negatively impact physical development. Additionally, maltreatment in the rst few years of
life can negatively affect brain development and have repercussions into adolescence and adulthood.
2
There is also a great body of research, especially the Adverse Childhood Experiences (ACE) Study,
that documents the conversion of traumatic experiences in childhood into organic disease later in life,
including all of the major causes of adult mortality in the United States.
3
The Task Force on Health Care
for Children explains the issue this way:
“Children and adolescents in foster care are a group with special health care needs. They
are a uniquely disadvantaged group. Prior to foster care, the vast majority lived with families
devastated by substance abuse, mental health disorders, poor education, unemployment,
violence, lack of parenting skills, and involvement with the criminal justice system. High
rates of premature birth, prenatal drug and alcohol exposure, and postnatal abuse and
neglect contribute to the extremely poor health status of children and adolescents entering
foster care. In addition, health care prior to foster care placement often is inadequate,
meaning that children and adolescents entering foster care have multiple unmet health
care needs, far exceeding even those of other children who are poor.”
4
These challenges are reected in the statistics on this issue, especially when one compares the
differences between the three major health insurance programs that serve low-income children: STAR
(typical Medicaid), CHIP (the Children’s Health Insurance Program, which is for families with incomes
slightly higher than what Medicaid allows), and STAR Health (the Medicaid program exclusively for
children in the child welfare system). According to the FY 2012 STAR Health Caregiver Survey, it
served a considerably higher percentage of child MSHCN (members with special health care needs)
than other programs (48 percent). This was more than double the rates observed in STAR (18
percent) or CHIP (20 percent). In STAR Health, more than one-third of recipients were prescribed
1 “Fostering Health: Health Care for Children and Adolescents in Foster Care.” Task Force on Health Care for Children 2 (2005): n. pag. Http://
www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-foster-care-america/Documents/FosteringHealthBook.pdf. 2005. Web. 9 Dec. 2014.
2 Health and Mental Health. Child Welfare Information Gateway, n.d. Web. 9 Dec. 2014. <https://www.childwelfare.gov/can/impact/longterm/
health.cfm>.
3 Felitti, Vincent J. “The Relationship of Adverse Childhood Experiences to Adult Health: Turning Gold into Lead.”Z Psychsom Med Psychother 48.4
(2002): 359-69. Web. 9 Dec. 2014. <http://www.acestudy.org/les/Gold_into_Lead-_Germany1-02_c_Graphs.pdf>.
4 “Fostering Health: Health Care for Children and Adolescents in Foster Care.” Task Force on Health Care for Children 2 (2005): n. pag. Http://
www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-foster-care-america/Documents/FosteringHealthBook.pdf. 2005. Web. 9 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 15
medications for mental illness (35 percent) or had problems that required mental health treatment
or counseling (36 percent). More than a quarter of STAR Health recipients also need more medical
care, mental health or educational services than is typical for children (29 percent). The percentage of
STAR Health recipients who had functional/ability limitations or needed special therapies in 2012 was
16 percent and 14 percent, respectively.
5
Children in Substitute Care Exist Within Complex Systems
Children in state custody are served simultaneously by many systems, including the child welfare system,
the judicial system, the education system, the medical system and mental health systems. All of these
systems are structured and function differently. It is difcult to imagine how a child could experience
positive outcomes within all of these systems when few people, including those who work with and
advocate for these children, understand the intricacies of each of them. This labyrinth of systems,
processes and services and the general lack of knowledge about how to navigate them can create
signicant barriers to children receiving the services they need.
Task Force members found this complexity difcult as they set out to identify specic issues regarding
how children in state custody receive mental health diagnoses and how they receive treatment for those
issues. The Task Force sought to ensure that each child in the system is receiving an accurate and
appropriate mental health diagnosis based on that child’s individual needs. However, what Task Force
members found was that because of the extremely complex nature of the systems that touch the lives
of these children, they would rst have to gain a better understanding of how these systems interact.
Due to limited time and resources, Task Force members decided to focus solely on the system of mental
health care established to treat children in substitute care, its interaction with the child welfare system
and how the functioning of these two systems can discourage appropriate and accurate diagnosis and
treatment for individual children in care. Current functioning and interaction between these systems
limits the possibility for every child to be accurately and appropriately diagnosed based on their
individualized needs.
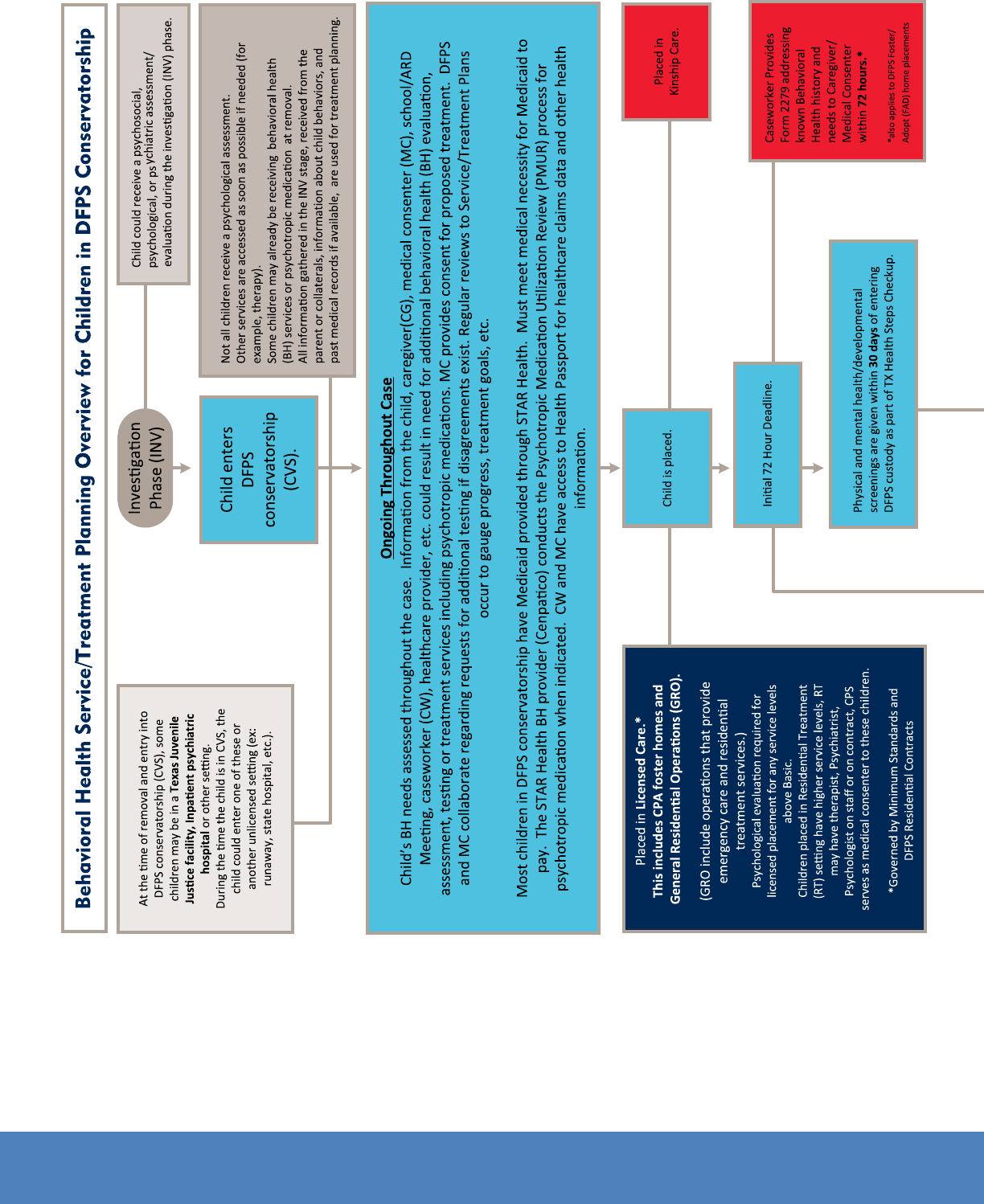
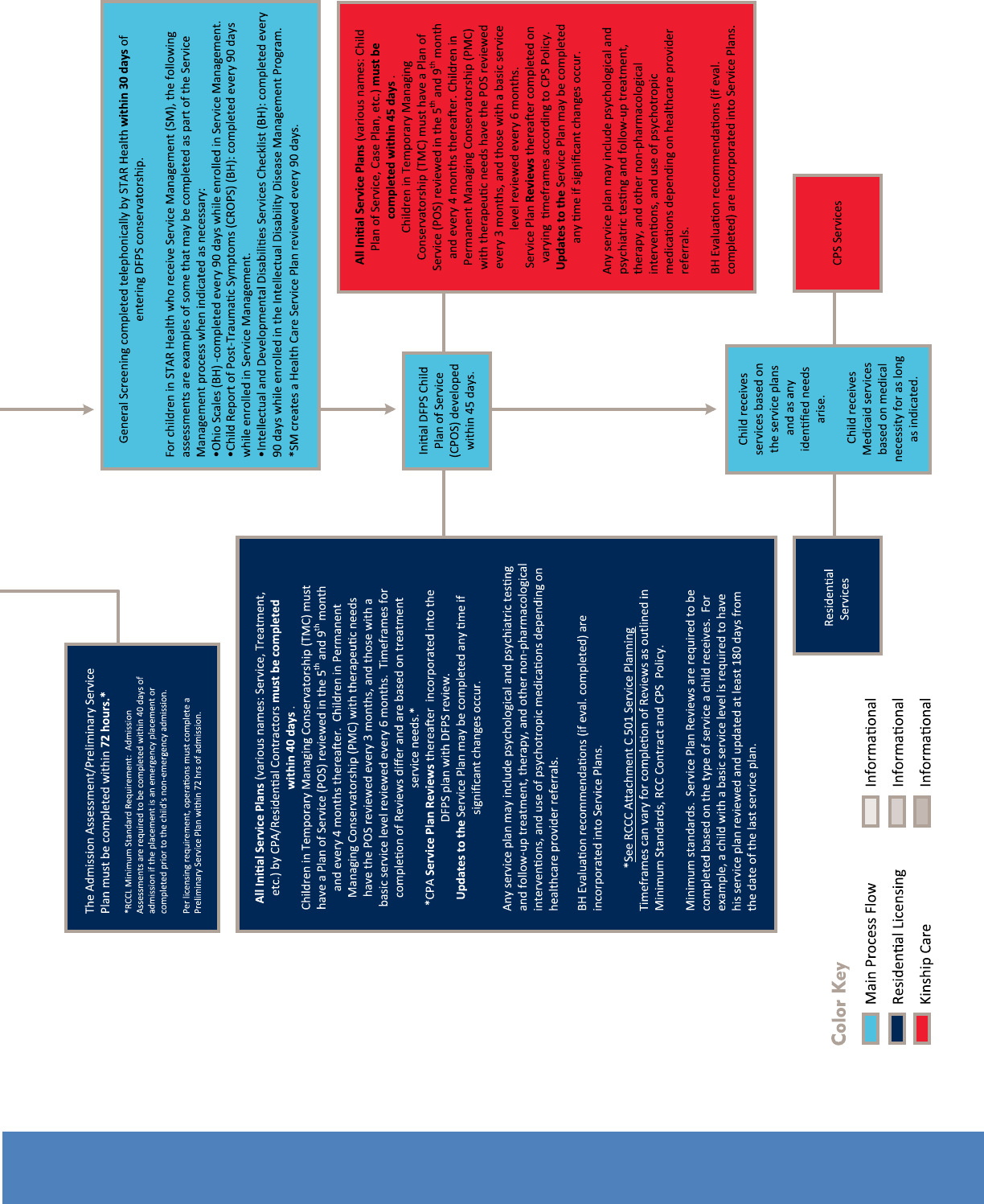
In order to gain a better understanding of how the mental health care system and child welfare system
interact, Task Force members worked with Pamela Baker, Well-Being Specialist, and other Department
of Family and Protective Services staff to create a guide to demonstrate the systems’ interactions and
to identify keys points in the systems where a child receives mental health-related services. Figure 1a
demonstrates the process of how a child in CPS custody is assessed, diagnosed and treated through the
mental health system.
5 Texas Medicaid Managed Care and Children’s Health Insurance Program: EQRO Summary of Activities and Trends in Healthcare Quality. Rep.
Institute for Child Health Policy at the University of Florida Texas External Quality Review Organization, 28 Mar. 2014. Web. 15 Dec. 2014. <http://www.hhsc.
state.tx.us/reports/2014/EQRO-Summary.pdf>.
MENTAL HEALTH TASK FORCE REPORT | PAGE 16
MENTAL HEALTH TASK FORCE REPORT | PAGE 17

MENTAL HEALTH TASK FORCE REPORT | PAGE 18
As is demonstrated by Figure 1a, navigating the interwoven systems of mental health care and child
welfare can be difcult. The complexity raises the question: How do we know that the best mental
health decisions are being made for our state’s most vulnerable children?
The Texas child welfare system houses our state’s most vulnerable children. Members of the Task Force
believe these children face great challenges and deserve the best care. They deserve to heal from
the pain and trauma of being abused or neglected. They deserve to grow up feeling normal and safe.
They deserve to nish high school and get a college degree. They deserve to grow into healthy adults.
Therefore, they deserve the best system and services that exist in order to help them achieve these
things.
The Texas CASA Mental Health Task Force believes that the current system that provides medical and
mental health care for the children in state custody can greatly improve its services and delivery.
KEY ISSUES
Issue 1: Integrated Care is the standard, not the reality
A major concern that Task Force members identied is that children in state custody often do not
receive accurate or appropriate diagnoses. This has been an ongoing concern for Texas and a number
of efforts have been employed to address this issue. While those efforts have mostly been benecial,
Texas must not stop short of realizing a system that works effectively for children in care. If Texas
wishes to ensure accurate and appropriate diagnoses for children and youth in foster care then it
needs to create a truly integrated, collaborative system that is staffed with well-trained, trauma-
informed medical and mental health professionals.
The mental health care, medical care and child welfare systems may be independently helping children,
however, the situations of children in state custody are extremely complex and thus require a smarter,
more exible, and collaborative integrated system of care.
Current System
STAR Health is the Medicaid program that covers medical and behavioral health care for children
in substitute care. Superior Health is the managed care organization for STAR Health. Cenpatico
manages the behavioral health benets for STAR Health. According to STAR Health, their coverage
offers each child in their network an “integrated medical home where each foster care child has access
to primary care physicians, behavioral health clinicians, specialists, dentists, vision services and more”.
6
Integrated care is dened as:
“The care a patient experiences as a result of a team of primary care and behavioral health
clinicians, working together with patients and families, using a systematic and cost-effec-
tive approach to provide patient-centered care for a dened population. This care may
address mental health and substance abuse conditions, health behaviors (including their
contribution to chronic medical illnesses), life stressors and crises, stress-related physical
symptoms, and ineffective patterns of health care utilization.”
7
6 Welcome to STAR Health. Superior Health Plan, 2014. Web. 18 Dec. 2014. <http://www.fostercaretx.com/welcome-to-star-health/>.
7 “What Is Integrated Behavioral Health Care?” Agency for Healthcare Research and Quality. U.S. Department of Health and Human Services,
2014. Web. 18 Dec. 2014. <http://integrationacademy.ahrq.gov/atlas/What%20Is%20Integrated%20Behavioral%20Health%20Care>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 19
The Texas Department of State Health Services (DSHS) denes a medical home as:
“A partnership between a child, the child’s family, and the place where the child gets
primary health care. At a medical home, the child’s family and health care experts are a
team. They work together to nd and get all the services the child and family need, even
if they are not medical services.”
8
DSHS continues its denition, suggesting a medical home offers “health care that is accessible, family-
centered, continuous, comprehensive, coordinated, compassionate, [and] culturally competent”.
9
While these are lofty and strong denitions about the current system, the Task Force believes that this
is not how the system actually functions. CASA volunteers and staff around the state, as well as other
child welfare advocates and professionals on the Task Force, have expressed concern over the ability of
the current medical and mental health care system to provide truly integrated, quality care to children
based on the child’s specic needs and with the goal of healing as the focus. Concerns raised regarding
the integration of mental and physical health care of children include:
• Moving between placements and changing providers interrupts continuity of care. Additionally,
new providers may add new diagnoses on top of an already inappropriate diagnosis or they may
not appropriately treat or even be made aware of chronic issues.
• Children’s medical histories are often non-existent, unknown or not properly acquired by either
caseworkers or the medical and mental health professionals treating the child. Therefore, their
histories may not be used to inform the process of continued treatment for the child.
• Children’s medical care information, while shared with caseworkers and courts, is not required
to be shared with medical or mental health providers treating the child.
• The Health Passport, while benecial in some ways, has not historically contained the most
important health information, nor does it organize information in a way that is efcient for
providers to access and use. It is often under-utilized and not updated, so it can lack in-depth
information about the child’s medical history, mental health, developmental and psychosocial
functioning—information pertinent to any course of care for the child.
If health conditions, medications and medical events are not recorded, maintained, and delivered to the
child’s provider as the child moves between different providers and living situations, the consequences
may include missed diagnoses, inappropriate treatment, duplications in therapy and more. “Such com-
plications can lead to signicant adverse health outcomes and poor quality of life for the child, as well
as increased healthcare costs for the state.”
10
The statistics about this issue reect the concerns that
the Texas CASA Mental Health Task Force laid out above. In fact, on average, children in care experi-
ence eleven placements in a three-year period.
11
8 Every Child Deserves a Medical Home. Texas Department of Family and Protective Services, 14 May 2014. Web. 18 Dec. 2014. <http://www.dshs.
state.tx.us/layouts/contentpage.aspx?pageid=29472&id=2019&terms=%22medical+home%22+and+%22denition%22>.
9 Every Child Deserves a Medical Home. Texas Department of Family and Protective Services, 14 May 2014. Web. 18 Dec. 2014. <http://www.dshs.
state.tx.us/layouts/contentpage.aspx?pageid=29472&id=2019&terms=%22medical+home%22+and+%22denition%22>.
10 Carrillo, Sarah, and Elisa Ashton. Improving Care Coordination for Foster Children: An Update on California’s Audacious Goal. Rep. California
Ofce for Health Information Integerity, 20 Jan. 2013. Web. 18 Dec. 2014.
11
Ramshaw, Emily. “Lawsuit Can’t Cover All Kids in Long-Term Foster Care.” The Texas Tribune. N.p., 23 Mar. 2012. Web. 07 Aug. 2014. <https://
www.texastribune.org/2012/03/23/lawsuit-texas-failing-foster-children/>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 20
Given the amount of upheaval and the rapid nature in which transitions to new placements must be
made, it is often difcult to transfer medical and mental health records or to ensure that providers
are communicating the needs of each child to new care providers, especially when those placements
are in different cities, counties or states.
Another indication that Texas’ integrated system of health care is not functioning as is intended can be
seen in the high number of potentially preventable readmissions (PPRs) of children enrolled in STAR
Health. These types of readmissions result from “poor coordination of services at time of discharge…
or deciencies in the process of care and treatment, including actions taken or omitted during the
initial hospital stay”.
1
Children enrolled in STAR Health had PPRs at a rate over ten percentage points
higher (15.5%) than children enrolled in CHIP (5.1%).
2
A truly integrated, coordinated system of care
should not experience this high a rate of PPRs, nor should the children in state care be subjected to
repeat hospital visits when proper care coordination could have prevented them.
One of the most challenging components of achieving positive outcomes for children in state custody
is the ability of the state to create stability and establish continuity across systems as children shufe
through homes, courts, medical and mental health providers and caseworkers. So much is lost for
these children along the way, including the rapport and trust they have potentially built with a provider,
as well as information regarding their needs, what treatments
may have been employed and the success of those treatment options.
The Collaborative Care Model
It is the responsibility of the Department of Family and Protective Services, STAR Health and its
managed care organizations to provide care that is thoughtful, continuous, well-coordinated,
collaborative, trauma informed and sensitive to the child’s experiences and unique needs. Given the
problems that were outlined above, this kind of care is not consistently available in the current system
in Texas.
While STAR Health is supposed to be an integrated system, there is a lack of consideration for the
role that the Department should play in integration efforts. To be a truly integrated care model
serving this population, integration must include not only physical and mental health care but also
care within the child welfare system. This means doctors and mental health professionals need to
collaborate better with each other and they must collaborate with key care partners within the child
welfare system such as the CPS caseworker, the judge and the CASA.
The Task Force recommends that Texas consider adopting the Collaborative Care model. Collaborative
Care is dened as:
“Ongoing working relationships between clinicians, rather than a specic product of
service. Providers combine perspectives and skills to understand and identify problems
1 Texas Medicaid Managed Care and Children’s Health Insurance Program: EQRO Summary of Activities and Trends in Healthcare Quality. Rep.
Institute for Child Health Policy at the University of Florida Texas External Quality Review Organization, 28 Mar. 2014. Web. 15 Dec. 2014. <http://www.
hhsc.state.tx.us/reports/2014/EQRO-Summary.pdf>.
2 Texas Medicaid Managed Care and Children’s Health Insurance Program: EQRO Summary of Activities and Trends in Healthcare Quality. Rep.
Institute for Child Health Policy at the University of Florida Texas External Quality Review Organization, 28 Mar. 2014. Web. 15 Dec. 2014. <http://www.
hhsc.state.tx.us/reports/2014/EQRO-Summary.pdf>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 21
and treatments, continually revising as needed to hit goals.”
3
Establishing a truly integrated, well-coordinated, collaborative system with a medical home could lead
to more positive and healthy outcomes for children. Research suggests that “collaborative care has
consistently demonstrated higher effectiveness than usual care”.
4
“Studies have shown that integrated
health care approaches, such as the Collaborative Care model are more effective than usual care for
depression, anxiety disorders and more serious conditions such as bipolar disorder and
schizophrenia.”
5
Because of the often mobile nature of a child’s life in state care, an integrated method of health care
should include a collaborative element. As a child moves from one provider to the next, past providers
should speak with new providers and share all pertinent information about his or her care. Caseworkers,
CASA volunteers and court systems should also contribute to this collaborative approach by assisting
in the timely transfer of medical and insurance information so that the child’s care is seamless as they
transition.
By establishing an integrated, collaborative system, Texas can be sure that a child’s social, behavioral,
psychological and medical histories can travel along with them. When practitioners have a fuller
understanding of what is going on for a child, they are more likely to make an accurate diagnosis
and suggest more useful treatment options. Integrated, collaborative and holistic systems of health
care mean all practitioners (medical care providers, mental health professionals, psychiatrists, etc.)
are communicating, frequently assessing the progress of the child’s care, regularly re-evaluating the
treatment plan and referring to outside, community-based services that may also be useful to the child.
Recommendations:
1. The Health and Human Services Commission should activate and publicize Medicaid billing codes
that will allow providers to bill for collaborative consultation, which allows practitioners to bill for
“peer consults” between primary care physicians (PCPs) and other PCPs; PCPs and Psychiatrists, and
PCPs to other mental health practitioners.
2. Ensure the Health Passport is being utilized and includes updated information on the child’s medical
history, mental health, developmental and psychosocial functioning—any information pertinent to any
course of care for the child.
Issue 2: The term “non-pharmacological interventions” is not well dened or
understood
The 83
rd
Texas Legislature passed House Bill 915, establishing added protections from the overuse of
psychotropic medications for children and youth in state custody. The new law states that the Depart-
ment of Family and Protective Services (DFPS) and judges are now responsible for ensuring non-phar-
3 Peek, C.J. Lexicon for Behavioral Health and Primary Care Integration: Concepts and Denitions Developed by Expert Consensus. Rep. Agency for
Healthcare Research and Quality, Apr. 2013. Web. 18 Dec. 2014.
4 Unutzer, J., Harbin, H., Schoenbaum, M., and Druss, B., The Collaborative Care Model: An Approach for Integrating Physical and Mental Health
Care in Medicaid Health Homes. 2013. http://www.medicaid.gov/State-Resource-Center/Medicaid-State-Technical-Assistance/Health-Homes-Technical-
Assistance/Downloads/HH-IRC-Collaborative-5-13.pdf.
5 Ybarra, Rick. “Our Journey Through Integrated Health Care and What We Have Learned.” Web log post. Hogg Blog. Hogg Foundation for Mental
Health, 5 Aug. 2014. Web. 18 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 22
macological interventions are considered in lieu of or along with psychotropic medications. Shortly after
this bill became law, questions arose regarding the denition of “non-pharmacological interventions”.
The purpose of this law was to ensure that children and youth in state custody are only treated with
psychotropic medications when absolutely necessary and that other methods of mental health inter-
vention be employed to assist a child in coping with symptoms of mental health conditions and trauma.
Yet, there is no broad understanding between DFPS, the courts, caregivers, stakeholders, practitioners
or advocates about what “non-pharmacological interventions” means.
The Texas CASA Mental Health Task Force set out to establish a denition for “non-pharmacological
interventions” to provide clarity to those working within the child welfare system and to ensure that
children and youth in substitute care have access to a wide array of services that have proven benets
for their mental health outcomes. In developing a denition, the Task Force demanded that space be
made for both what professional mental health providers refer to as “evidence-based practices” and for
other interventions that have been proven through research to have a positive effect on mental health
outcomes.
Recommendation:
1. Adoption of the following denition of “non-pharmacological interventions” by the judicial system,
medical care providers, insurers, CASA, CPS and others:
• “Non-pharmacological interventions” is terminology meant to represent an array of strategies,
supports and interventions intended to help children recover and heal from trauma, build
resilience and meet developmental milestones. Non-pharmacological interventions must be used
in lieu of or concurrently with psychotropic medications and should be informed by accurate
and continuous assessment and/or diagnosis. Non-pharmacological interventions include both
evidence-based interventions, promising practices and those interventions proven effective by
peer-reviewed research.
Issue 3: Medical and mental health providers serving this population are
not beholden to American Academy of Pediatrics standards and the current
Medicaid reimbursement rates in Texas deter providers
Not only does the current functioning and interplay between the child welfare, mental health care and
medical care systems raise questions regarding coordination of services for children, there are also
challenges around the quality of and access to services.
Like many other states, Texas struggles to host quality medical and mental health providers and that
struggle is further complicated as fewer providers choose to serve Medicaid clients. In fact, in 2011,
less than 33 percent of Texas’ practicing doctors accepted Medicaid patients.
6
There are a number
of reasons why providers choose not to become a Medicaid provider, including the huge amount of
paperwork involved and inadequate reimbursement rates for services. In Texas, licensed clinical social
workers and licensed professional counselors are reimbursed at only 70 percent of the rate paid to
licensed psychologists and psychiatrists, even though they are providing the majority of the Medicaid
mental health services to children and youth in foster care.
7
Since Texas is already struggling to recruit
6 Crisis Point: Mental Health Workforce Shortages in Texas. Rep. Hogg Foundation for Mental Health and Methodist Healthcare Ministries, Mar.
2011. Web. 19 Dec. 2014. <http://www.hogg.utexas.edu/uploads/documents/Mental_Health_Crisis_nal_032111.pdf>.
7 “Texas Medicaid Fee-For-Service Reimbursement.” Texas Medicaid Provider Procedures Manual 1 (2014): 2-1--11. American Medical Association,
Dec. 2014. Web. 19 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 23
and maintain quality Medicaid mental health providers, it should not create additional challenges for
providers by not reimbursing all licensed professionals at the same rates for the same services.
The Task Force members also believe that mental health and medical providers who care for children
in the child welfare system should be expected to adhere to the American Academy of Pediatrics (AAP)
standards and recommendations on Health Screenings in Foster Care. The AAP requirements for health
screenings in foster care detail information about how to conduct a comprehensive evaluation, how
to create a medical home, the importance of preventative health care for this population and how
to properly maintain medical records for children and youth in foster care.
8
In order to meet these
standards, physicians need to spend more time with each patient. Allowing more time with the children
is imperative because they will be better able to develop a trusting relationship with the child and should
(if they adhere to AAP standards) be eliciting important medical and mental health related information
from the child throughout their time in state care.
9
Training on national standards, including the
American Academy of Pediatrics standards, is not widely available or required for physicians in Texas,
even if they are providing care for the vulnerable children and youth in the foster care system.
Recommendations:
1. Implement, require and train on American Academy of Pediatrics standards for
physicians treating children in substitute care on health screenings in foster care.
2. Provide equivalent reimbursement rates for all licensed professionals who provide
Medicaid mental health services to children in foster care.
Issue 4: Limited information is available regarding the array of mental health
services available under STAR Health and understanding of how to utilize the
Medicaid appeals process and other legal options is limited
Task Force members experienced difculty in attempting to nd a comprehensive list of services covered
by STAR Health and had further challenges dening the services that are covered. Despite their best
efforts, Task Force members were unsuccessful at compiling a list of covered services, and it was even
unclear to members what the services entail as there are no easily available denitions of services.
Given the difculty seasoned advocates experienced nding a comprehensive list of mental health
services and their denitions, how can caregivers, consenting youth or other medical consenters be
expected to understand the variety of options available to the children they care for?
Additionally, Task Force members found that the complexity of the Medicaid appeals process and other
legal avenues to challenge denial of services present signicant, unnecessary challenges for stakeholders
and caregivers in Texas. The basic appeals process overseen by Superior Health Plan is available to
all enrollees in STAR Health but it can be difcult to access and to navigate for consumers without
experience in the process. The appeals process is important for caregivers to understand because it
allows them to seek coverage for services not explicitly covered by STAR Health, as long as the services
are deemed medically necessary by the child’s physician. Additionally, currently provided services must
continue to be provided during an appeal if the appeal is requested in a timely manner. STAR Health
8 “Requirements for Health Screenings in Foster Care.” Healthy Children. The American Academy of Pediatrics, 03 Oct. 2013. Web. 19 Dec. 2014.
<http://www.healthychildren.org/English/family-life/family-dynamics/adoption-and-foster-care/Pages/Requirements-for-Health-Screenings-in-Foster-Care.
aspx>.
9 “Requirements for Health Screenings in Foster Care.” Healthy Children. The American Academy of Pediatrics, 03 Oct. 2013. Web. 19 Dec. 2014.
<http://www.healthychildren.org/English/family-life/family-dynamics/adoption-and-foster-care/Pages/Requirements-for-Health-Screenings-in-Foster-Care.
aspx>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 24
members also have the right to initiate a fair hearing appeal process that is separate from the fair
hearing appeals process and adjudicated by the Health and Human Services Commission, rather than
Superior Health Plan.
Gaining a better understanding of what services are available under STAR Health and knowledge about
how to navigate the Medicaid fair hearing appeals process would allow those making medical decisions
for children in care to advocate appropriately for the individual needs of the children they are caring for
and promote better health outcomes.
Recommendations:
1. Revise STAR Health Member Handbook to include:
• Information on trauma and trauma-informed care
• Information on behavioral health services, including a list of covered services, denition of
services, and information on how to access services and who can provide services
• A simpler explanation of the Medicaid appeals process
2. Train consumers, attorneys, judges, CASA volunteers, medical consenters and youth (especially
those 16 and older) on:
• What behavioral health services are available through STAR Health, including denitions of ser-
vices, how to access services and who can provide services
• The Medicaid appeals process, including how to appeal when a requested medically necessary
service is denied
3. Train attorneys, CASA volunteers, judges, medical consenters and youth on how to petition the
court for an order related to the medical care for a foster child. This is not a formal Medicaid appeal
but the use of the exclusive jurisdiction of the court could help to ensure that foster children receive
appropriate medical care, including mental health and behavioral health services.
Issue 5: Texas youth who aged out of care not auto-enrolled in Medicaid and
youth who aged out in other states are not extended coverage in Texas
With the passage of The Patient Protection and Affordable Care Act (ACA), states are now required
to provide Medicaid coverage to individuals under the age of 26 who were in foster care and receiving
Medicaid at the time of aging out of care.
10
According to the Texas Department of Family and Protec-
tive Services (DFPS), the changes set forth by the ACA have expanded the Former Foster Care Children
Program. So, depending a child’s age, the child will have Medicaid coverage until the age of 26 in
Texas. DFPS has altered the structure of the program and has laid out how this Medicaid expansion
will be accessible to foster youth.
11
While the expansion is well-needed, concern exists regarding the
implementation of these changes. The Texas CASA Mental Health Task Force identied two potential
barriers that youth might experience when they try to access this program.
10 Deckinga, Audrey. “Former Foster Care Children Program-Medicaid Healthcare Coverage for Former Foster Youth Ages 18 through 25.”
Memorandum to CPS Regional Directors. 18 Nov. 2013. Texas Department of Family and Protective Services. 1-6. Print.
11
Deckinga, Audrey. “Former Foster Care Children Program-Medicaid Healthcare Coverage for Former Foster Youth Ages 18 through 25.”
Memorandum to CPS Regional Directors. 18 Nov. 2013. Texas Department of Family and Protective Services. 1-6. Print.

MENTAL HEALTH TASK FORCE REPORT | PAGE 25
Foster youth face immense challenges when they age out of foster care, including lack of family and/
or social support, poverty, potential unemployment, inadequate living arrangements and little or no
coordination of their physical and mental health services. In spite of the fact that they are supposed
to be enrolled in Medicaid services, foster youth are likely to face untreated medical and mental health
problems.
12
According to the American Academy of Pediatrics, children who have aged out of state care
lack access to health and mental health services, which are critically important and have a signicant
impact on the child’s transition into adulthood.
13
Under current Texas statute, former foster youth in the initial Medicaid coverage plan, STAR health,
are covered until age 21. At that time, the former foster youth must request and apply to be enrolled
into the second coverage plan, STAR, extending coverage to age 26. This is Texas’ approach to com-
pliance with the Affordable Care Act requirements. The Task Force views the fact that foster youth
must reapply for Medicaid benets at age 21 as a signicant barrier that prevents many foster youth
from obtaining critical physical and mental medical care. The Task Force recommends changing this
practice to include seamless and automatic enrollment transfers from STAR Health to STAR when the
child turns 21, assuring that former foster children will have Medicaid coverage until age 26 regardless
of reapplication.
Another barrier for foster youth that the Task Force identied is the lack of Medicaid coverage for for-
mer foster youth who relocate to Texas after they age out of care. DFPS’s recent statutory changes
include a provision that alters the eligibility of the Medicaid Transitioning Foster Care Youth (MTFCY)
program from including former foster care children from any state to only those who aged out in Texas.
14
This leaves a gap of coverage for former foster youth from other states who newly reside in Texas. For
example, if a former foster care youth moves to Texas (to reunite with family, seek employment or pur-
sue educational opportunities), the eligibility change will roll back coverage for the youth. This means
that youths in this situation were covered until age 21 in the original program and now they are only
covered until age 18.
This change prevents former foster youth from accessing the resources necessary to lead healthy lives
and could potentially impact their overall life outcomes.
Recommendations:
1. Create automatic enrollment transfers from STAR Health to STAR when a child turns 21, assuring
that former foster children will have Medicaid coverage until age 26 regardless of reapplication.
2. Extend Medicaid eligibility to former foster youth from any state until age 26.
12 “Health Care of Youth Aging Out of Foster Care.” Pediatrics 130.6 (2012): 1170-173. Council on Foster Care, Adoption, and Kinship Care and
Committee on Early Childhood. American Academy of Pediatrics, 26 Nov. 2012. Web. 19 Dec. 2014.
13
“Health Care of Youth Aging Out of Foster Care.” Pediatrics 130.6 (2012): 1170-173. Council on Foster Care, Adoption, and Kinship Care and
Committee on Early Childhood. American Academy of Pediatrics, 26 Nov. 2012. Web. 19 Dec. 2014.
14 Deckinga, Audrey. “Former Foster Care Children Program-Medicaid Healthcare Coverage for Former Foster Youth Ages 18 through 25.”
Memorandum to CPS Regional Directors. 18 Nov. 2013. Texas Department of Family and Protective Services. 1-6. Print.

MENTAL HEALTH TASK FORCE REPORT | PAGE 26
II. EMPOWERMENT AND NORMALIZATION OF
YOUTH IN SUBSTITUTE CARE
Background
Normalcy shapes children and youth in the state’s care
As children develop into adolescence and then adulthood, their growth is marked by experiences that
contribute to their autonomy and their social functioning, shaping who they will become as adults and
how successful they may be in life and relationships. These experiences can include things from spending
the night at a friend’s house, volunteering in the community, having an after school job, playing sports,
running for student government, to going on a rst date or attending senior prom. The list of activities a
young person may experience during their adolescence is extensive. All of these experiences help shape
the person this youth will ultimately become.
These types of activities are referred to as “normalcy” activities and are dened as “the opportunity
for children and youth to participate in and experience age and culturally appropriate activities,
responsibilities, and life skills that promote normal growth and development”.
1
The Texas Department
of Family and Protective Services has made efforts to ensure that all children/youth in its care have
access to normalcy activities. These guidelines are laid out in communication from the agency, within
their minimum standards and residential contracts.
Empowerment and normalcy activities are key to mental health and healthy
development
Access to normalcy activities and opportunities for empowering young people in substitute care can
improve mental health outcomes. Simple experiences such as having friends and spending time with them
can vastly improve a young person’s disposition. Friendship and socialization are essential in maintaining
health and psychological well-being.
2
Positive relationships are correlated with happiness, quality of
life, resilience and cognitive capacity.
3
Friendships are essential for foster youths and friendships with
peers outside of the foster care program are especially important. Research has shown these friendships
may act as a deterrent against victimization, promote social skills and increase emotional health.
4
The types of experiences offered through friendships are sometimes taken for granted, but it is important
to understand that establishing, maintaining and enjoying friendships is not something easily achieved
by our young people in foster care. Youth in substitute care move often, change schools frequently and
are sometimes housed in isolated facilities. Even in stable placements, youth face prohibitions on simple
1 “Normalcy Recommendations: Improving Well-Being by Addressing Normalcy for Foster Youth.” The National Foster Care Youth & Alumni Policy
Council. N.p., 16 Apr. 2013. Web. 16 Dec. 2014.
2 Blieszner, R. The Worth of Friendship: Can Friends Keep Us Happy and Healthy? Journal of the American Society on Aging. Spring 2014 Vol. 38.
No. 1
3 Fowler, J.H., Christakis, N.A., Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart
Study. Dec. 2008.
4 Skrzypiec, G., Slee P., Askel-Williams, H. and Lawson, M. Associations between types of involvement in bullying, friendships and mental health
status. Emotional and Behavioral Difculties
Vol. 17, Nos. 3–4, September–December 2012, 259–272.

MENTAL HEALTH TASK FORCE REPORT | PAGE 27
things like staying the night with friends or having friends stay the night at their home.
In addition to building relationships with friends, young people’s mental health is greatly beneted
by participating in recreational activities. Age-appropriate recreational activities can promote positive
emotions, increase relationship skills and advance mental and physical health. Part of the positive
benet of physical activity on mental health occurs through the socialization that happens when young
people engage in physical activities with their peers.
5
Other social activities such as band, religious
involvement, drama club and others contribute to a young person’s self-esteem, moral and cognitive
development.
6
These social activities help foster youth create and maintain relationships and help
them develop important life skills and coping strategies. Recreational activities that involve play and
playfulness have also been shown to reduce defensiveness, enhance well-being and foster maturation
in children.
7
While normalcy and access to age-appropriate activities are important for foster children in general,
they are even more critical for foster youth with poor mental health. Due to the stigma associated with
mental health issues, many foster youth create coping strategies outside of professional mental health
interventions, including many of the normalcy activities described above. Mental health professionals
have drastically underestimated the importance of therapeutic lifestyle interventions, including self-help
and coping mechanisms. Unlike what occurs in sometimes rigid and highly structured mental health
therapies, these activities are free of stigma and have profound effects on self-esteem and quality of
life.
8
Normalcy activities are essential for the mental health of foster youth. In fact, these activities may
lessen the need for professional intervention in the mental health of children in state care, providing
nancial incentive for DFPS and foster care providers to help children and youth access normalcy
activities.
The current status of foster youth decision-making and normalcy activities in Texas Department of
Family and Protective Services is troubling. In depth-interviews conducted with former Texas foster youth
conrm the need of normalcy activities in foster youth lives. This report, entitled Voices of Experiences,
identied many alarming facts regarding the mental health of children in substitute care in Texas.
More than one third of the youth who aged out of care in Texas reported they had no input on their
mental health diagnoses or mental health services. Many of the youth also reported they had negative
experiences with mental health services while in state custody. Youth in Texas also indicated a desire
to have a gradual increase of responsibilities and liberties as their age and maturity increased.
They
reported that they believe the child welfare system kept them “isolated from the real world”.
9
Similar
information was revealed in the youth surveys conducted by Texas Department of Family and Protective
Services. Some youth felt they were not given chances to make decisions about their lives as they
prepared for adulthood.
10
5 VanKim N., Nelson T. Vigorous Physical Activity, Mental Health, Perceived Stress, and Socializing Among College Students. American Journal of
Health Promotion. September/October 2013, Vol. 28, No. 1
6 Alexander, C.N. & Langer, E. (1990). Higher stages of human development: Perspectives on adult growth. New York, NY: Oxford University Press
7 Walsh, Roger. “Lifestyle and Mental Health.” American Psychologist 66.7 (2011): 579-92. Web. 16 Dec. 2014.
8 Walsh, Roger. “Lifestyle and Mental Health.” American Psychologist 66.7 (2011): 579-92. Web. 16 Dec. 2014.
9 Gendron, Christine. Voices of Experience: Improving Mental Health Supports for Homeless & Transitioning Youth. Rep. Texas Network of Youth
Services, 2011. Web. 16 Dec. 2014.
10 Improving the Quality of Services to Youth in Substitute Care: A Report on Surveyed Youth in Foster Care FY 2007. Rep. Texas Department of
Family and Protective Services, Sept. 2008. Web. 16 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 28
A recurring challenge in helping children in foster care achieve a sense of normalcy is the lack of
consistency in their lives. Numerous personal narratives and testimonies of children shine light on
the traumatizing feelings associated with moving from placement to placement. In 2007, focus group
studies were conducted in order to examine the mental health of foster youth dealing with the ongoing
stresses of substitute care. According to the study, youth interviewed noted the importance of routine
and control over life situations:
“[They have a] need for normalcy related to feelings of lack of control and confusion as
a result of constant life changes. These feelings affected the informants’ self-esteem,
security, and identity. The foster children described the desire for foster care professionals
to allow them to participate in decisions about home placements”.
11
Foster children have desire for autonomy and involvement in decisions inuencing their lives and well-
being. They have repeatedly emphasized their wish to be involved in their own mental health decisions.
12
Foster children also expressed a desire to have autonomy over other important decisions, such as
placement options and the type of preparation they need for aging out of state custody.
Examining testimonies of former foster children led the Task Force to the conclusion that foster youth
may be reluctant to participate in mental health resources or therapy.
13
Youth in state custody often have
resentment about being forced to receive therapy before they feel they are ready for such services.
14
Due to negative experiences in the child welfare and mental health systems, foster youth may distrust
mental health professionals, which further elevates the importance of normalcy activities and decision-
making for children in care. Children in state custody should be allowed to be actively involved in
normalcy activities and have more autonomy to make decisions regarding their care, leading to better
mental and physical health outcomes.
The challenge is that access to these activities is difcult to achieve for many young people who are
cared for by a system. The system wants youth to be able to participate in normalcy activities but it is
set up to discourage such participation.
KEY ISSUES
Issue 1: The current system inhibits caregivers’ ability to make decisions
about a child’s participation in normalcy activities and experiences
In the Department of Family and Protective Services (DFPS) literature, normalcy activities are guaranteed
to foster youth through a Bill of Rights. This Bill of Rights states “I have the right to attend my choice
of community, school, and religious services and activities (including extracurricular activities) to the
extent that is right for me, as planned for and discussed by my caregiver and caseworker, and based on
11 Ellermann, Caroline. “Inuences on the Mental Health of Children Placed in Foster Care.” Family & Community Health 2nd ser. 30.25 (2007):
S23-32. Web. 16 Dec. 2014.
12 Ellermann, Caroline. “Inuences on the Mental Health of Children Placed in Foster Care.” Family & Community Health 2nd ser. 30.25 (2007):
S23-32. Web. 16 Dec. 2014.
13 Gendron, Christine. Voices of Experience: Improving Mental Health Supports for Homeless & Transitioning Youth. Rep. Texas Network of Youth
Services, 2011. Web. 16 Dec. 2014.
14 Ellermann, Caroline. “Inuences on the Mental Health of Children Placed in Foster Care.” Family & Community Health 2nd ser. 30.25 (2007):
S23-32. Web. 16 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 29
my caregiver’s ability”.
15
DFPS published the Guidelines of Normalcy Activities, setting expectations
and providing examples of normalcy activities for residential contract caseworkers and foster caregivers.
The same activities parents can arrange for biological children should be considered and arranged for
every child, youth and young adult in foster care.
16
Some of the activities mentioned and outlined in this
document are: boy scouts, dating, cheerleading, etc. According to the Guidelines, in order to deem an
activity age-appropriate and allow a foster youth to participate, caseworkers and caregivers must apply
the “reasonable and prudent parent standard”, asking, “What information would I require before I gave
my biological child permission to engage in an activity?”
17
A signicant issue identied as a roadblock to normalcy is concern for foster youth in Residential
Treatment Centers (RTCs) and other restrictive settings. Many of these children and youth attend unique
settings of education, such as a charter school or home-schooling. In these instances, these settings
may not offer sports or social recreation, the placement is more restrictive and the opportunities to
participate in activities with other youth are lacking, ultimately depriving foster youth of the opportunity
to be social and meet children not in state care.
Although DFPS has provided guidelines for normalcy activities, the reality and implementation of these
activities into foster youth’s lives is inconsistent and, in many cases, is not creating opportunities for
foster youth to participate in these activities. With the importance of normalcy activities becoming
more evident in scholarly research, the implementation of normalcy activities in foster care is crucial to
improve children’s lives.
Many child welfare agencies throughout the United States have already increased discussion of the
importance of normalcy activities for foster youth. This issue has been researched and evaluated in
the child welfare sector throughout the country and legislative momentum has increased dramatically.
Not only has the federal government examined the lack of normalcy in foster youth’s lives, many state
legislatures have examined the issue and a few states have passed legislation to try to reduce the barriers
to normalcy in this population. These states (Florida, Utah and Washington) all passed legislation with
similar language.
In 2014, Congress enacted Federal H.R. 4980, which requires the Secretary of Health and Human
Services to provide assistance to states on best practices for devising strategies, in order to assist foster
parents in applying a reasonable and prudent parent standard in a manner that promotes child safety
and normalcy activities. According to the bill, state child welfare agencies will be required to establish
standards of reasonable and prudent parenting for the child’s participation in age or developmentally
appropriate extracurricular, enrichment, cultural and social activities.
18
These standards will extend to
foster family homes and child care institutions and will be required to include policies related to the
liability of foster parents/institutions using a reasonable and prudent parenting standard.
The Task Force recognizes the need for state-level legislation to address the lack of normalcy activities
in foster youth’s lives. With federal legislation being implemented around this issue, Texas legislators
should prepare for the need to update the Department’s policies in order to stay in compliance with
15 Rights of Children and Youth in Foster Care. Texas Department of Family and Protective Services, n.d. Web. 16 Dec. 2014. <https://www.dfps.
state.tx.us/Adoption_and_Foster_Care/About_Foster_Care/rights.asp>.
16 Deckinga, Audrey. “Normalcy Activities for Children.” Letter to Residential Contractors. 8 Aug. 2013. Texas Department of Family and Protective
Services, 8 Aug. 2013. Web. 16 Dec. 2014. <http://www.tffa.org/wp-content/uploads/2013/08/Normalcy-Activities-for-Children-Final_8-8-2013.pdf>.
17 Deckinga, Audrey. “Normalcy Activities for Children.” Letter to Residential Contractors. 8 Aug. 2013. Texas Department of Family and Protective
Services, 8 Aug. 2013. Web. 16 Dec. 2014. <http://www.tffa.org/wp-content/uploads/2013/08/Normalcy-Activities-for-Children-Final_8-8-2013.pdf>.
18 H.R. 4980, 113th Cong. (2014) (enacted). Print.

MENTAL HEALTH TASK FORCE REPORT | PAGE 30
federal standards. Legislation should also specify what things to consider when deciding if an activity
is appropriate for a foster child. The normalcy legislation passed in Florida, HB215 or “The Quality
Parenting for Children in Foster Care Act”, provides helpful language on requirements for decision-
making:
“When using the reasonable and prudent parent standard, the caregiver shall consider:
• The child’s age, maturity, and developmental level to maintain the overall health and
safety of the child.
• The potential risk factors and the appropriateness of the extracurricular, enrichment,
and social activity.
• The best interest of the child based on information known by the caregiver.
• The importance of encouraging the child’s emotional and developmental growth.
• The importance of providing the child with the most family-like living experience
possible.
• The behavioral history of the child and the child’s ability to safely participate in the
proposed activities, as well as with any other child.”
19
If Texas were to pass legislation with similar language, it would provide caregivers with a guideline to
help them assess if activities are appropriate for foster children in their care. Due to the complexity of
Texas’ foster care system, it is important for any legislation on this issue to require that these normalcy
standards are implemented in private contracted agencies throughout the state, including child placing
agencies and residential treatment centers.
Recommendations:
1. Dene the Reasonable and Prudent Parenting Standard and include what to consider when caregivers
are making decisions.
2. Require DFPS to verify that private contracted agencies promote and protect the ability of a child
to participate in normalcy activities by requiring that private agencies have the same provisions of
“reasonable and prudent parenting standards”.
Issue 2: Service plans can be too prescriptive and unwittingly block a young
person from participating in an activity or experience and caregivers can be
discouraged from allowing for participation in normalcy activities
Secondly, the Task Force believes that the prescriptiveness of service plans is limiting foster children’s
access to normalcy. For foster youth living in foster care placements, a service plan is designed by the
foster parent and caseworker to “meet the child’s needs for safety, permanency and well-being while
the child is in substitute care”.
20
Service plans include exploring what is in the best interest of the child
19 Florida House of Representatives. Quality Parenting for Children in Foster Care Act. 2013. Web. http://www.senate.gov/Session/Bill/2013/0215/
BillText/er/PDF
20 Texas Department of Family and Protective Services Program Handbook: The Child’s Service Plan, § 6251 (2014). Web. http://www.dfps.state.
tx.us/handbooks/cps/les/CPS_pg_6240.asp

MENTAL HEALTH TASK FORCE REPORT | PAGE 31
based on development level, discussing the foster youth’s input and determining the necessary level of
supervision. According to the guidelines set forth by DFPS, foster parents and caseworkers should have
a discussion about the expectations for allowing the child to participate in age-appropriate activities
and should ensure these activities are referenced in the service plan at a level that allows for exibility
yet provides guidance as to which activities a child is ready to participate.
21
Although DFPS has established these guidelines of exibility in the service plan, the implementation of
this practice has not been consistent. Service plans are meant to set standards for activities that are
appropriate, but the Task Force found that many caseworkers or contracted agencies have practices
that establish and maintain very prescriptive service plans. The challenge stems from the words of the
service plan itself. The child’s service plan currently lists the activities a child is allowed to participate in.
In the event a child participates in an activity other than one outlined on their service plan, the caregiver
faces the potential for a licensing violation.
Additionally, when foster care children are allowed to participate in normal, age-appropriate activities,
Child Care Licensing may reprimand agencies, contractors or foster parents if the child is injured during
these normalcy activities, even if the parent used a “reasonable and prudent standard” in deciding the
appropriateness activity.
For example, if a foster youth’s plan states that he/she may participate in
football but then gets hurts playing basketball, a foster parent could be punished for not following the
service plan, even though the activities are very similar in nature and appropriateness. It is important
for caregivers to have some leniency when using a “reasonable and prudent standard” to assess the
appropriateness of activities for foster children and youth. Without this leniency, caregivers may fear
child care licensing punishments or the increased liability. In order to fully empower caregivers to use a
reasonable and prudent parent standard, which is essential for ultimately increasing normalcy activities
in foster youth’s lives, they must be granted protection from liability of injury sustained during normalcy
activities. Moreover, in order for everyone to understand these sometimes complex issues, residential
staff, child placing agency staff, foster parents kinship providers and residential child care licensing
staff should be trained on them.
Recommendations:
1. Address service plan limitations by listing normalcy activities and/or experiences the child has/is
participating in rather than listing activities as a limited list of activities in which a child can participate.
2. Mandate that the foster parent and/or the associated child placing agency shall not be held
responsible for potentially negative outcomes beyond their reasonable control as a result of the child’s
participation in an age-appropriate normalcy activity, provided the activity is approved by the foster
parent using the reasonable and prudent parent standard.
3. Require training for residential staff, child placing agency staff, foster parents, kinship providers
and residential child care licensing staff. This training should include instruction on decision-making
as a “reasonable and prudent parent”, appropriate and trauma-informed ways to deal with a child
or youth’s misbehavior, the importance of a child’s participation in normal adolescent activities and
experiences, and the benets of such participation to a child’s social, emotional and developmental
growth, well-being and mental health.
21 Texas Department of Family and Protective Services Program Handbook: The Child’s Service Plan, § 6250 (2014). Web. http://www.dfps.state.
tx.us/handbooks/cps/les/CPS_pg_6240.asp

MENTAL HEALTH TASK FORCE REPORT | PAGE 32
Issue 3: Youth are not empowered to address concerns within their
placements or to report abuse and are not aware of their individual rights or
what recourse is available to them when rights are violated
It is important for the health, safety and well-being of foster youth to feel empowered and to have their
voices heard. However, due to the nature of Child Protective Services and the foster care system, many
foster youth feel they have little to no control over their lives and have no safe place to voice concerns
about their care. With this in mind, it is extremely important for the Department of Family and Protective
Services (DFPS) to equip youth in foster care with the tools and resources to voice their concerns about
the treatment they receive while they are in state custody.
In order for youth to be fully empowered, they must be educated about their rights and have control and
decision-making power in matters that impact their care. Empowerment of foster children refers to the
level of choice, inuence and control that youth can exercise over events in their lives. In order for youth
to access necessary resources and gain a sense of empowerment over their lives and outcomes, formal
and informal structures may need to be dismantled. According to research published by the Child Welfare
Consensus Conference, ensuring youth empowerment is considered best practice for positive mental
health outcomes for children in the child welfare system.
22
Best practice guidelines state that “child
welfare agencies and their partners [should] strive to help children and youth understand, at their level
of functioning, their rights, entitlements, and opportunities, by providing a range of communications,
engagements, and supports”.
23
Research also suggests that child welfare agencies should be held
accountable through measurable outcomes related to youth empowerment.
Some resources currently exist for youth in the Texas foster care system to express concerns about
their care while in state custody and to ask questions regarding their case. One of these resources is
the Ofce of Consumer Affairs (OCA), the purpose of which is to serve as an independent ofce that
answers inquiries and takes complaints regarding Adult Protective Services, Child Care Licensing and
Child Protective Services. The OCA is considered an independent ofce although its policies, personnel
choices and budget are under the purview of DFPS. The Ofce is mentioned in the Foster Youth Bill of
Rights, created by the Department of Family and Protective Services:
“I have the right to complain to the DFPS Consumer Affairs Ofce at 1/800/252/5400
to report abuse, neglect, exploitation, or violation of personal rights without fear of
punishment, interference, coercion, or retaliation.”
24
While the OCA is currently in the process of creating pamphlets aimed at educating youth in foster care,
the Task Force believes it is necessary to increase these efforts so youth understand the purpose of the
OCA and how to access it. The Task Force found that there are many roadblocks that deter youth in
foster care from making reports to the OCA. Some of the deterrents identied were a lack of knowledge
about the OCA, lack of access to OCA information, lack of trust in reporting to a system that oversees
their care and the fear of retaliation if they le complaints and/or report concerns.
22 Romanelli, L.H., Hoagwood, K.E., Kaplan, S.J., Kemp, S. P., Hartman, R.L., Trupin, C., et al. (2009). Best Practices for Mental Health in Child
Welfare: Parent Support and Youth Empowerment Guidelines. Child Welfare 88(1), 189-218.
23 Romanelli, L.H., Hoagwood, K.E., Kaplan, S.J., Kemp, S. P., Hartman, R.L., Trupin, C., et al. (2009). Best Practices for Mental Health in Child
Welfare: Parent Support and Youth Empowerment Guidelines. Child Welfare 88(1), 189-218.
24 Rights of Children and Youth in Foster Care. Texas Department of Family and Protective Services, n.d. Web. 16 Dec. 2014. <https://www.dfps.
state.tx.us/Adoption_and_Foster_Care/About_Foster_Care/rights.asp>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 33
In order to ensure that quality care and effective accountability are being provided to children
within the child welfare system, an independent or autonomous agency should be established to
review all complaints about placement and care. According to the World Health Organization,
in order to fulll user empowerment in mental health, an agency must ensure that independent
review bodies are in place to review the lawfulness of treatment and services.
25
The Ofce
of Consumer Affairs is currently housed at the Department of Family and Protective Services
and does not have autonomy from the Department, including the lack of a separate budget.
Establishing an independent or autonomous ombudsman’s ofce would give youth in foster care a secure
outlet to voice their concerns and grievances, which would ultimately result in greater empowerment
for the youth as well as assurance that the state is appropriately protecting youth in its care. Children
and youth in foster care also need private access to information about their rights and about how to
make a complaint to the OCA or ombudsman’s ofce in order for them to feel safe enough to seek
help or information. When they do call the OCA, their inquiries or complaints should be handled with
special care given that these children are under the state’s authority. Along with private access to
OCA information and strengthening foster youth protections, this Task Force identied the need for the
complaint process to be transparent. In order for youth to be empowered, they must be informed about
the actions taken to investigate and resolve their complaints. This transparency should be incorporated
into all of the OCA’s processes and every complaint report should have an element of transparency,
including investigation movements and actions taken or not taken. This information should not only be
reported to the Health and Human Services Commission and DFPS, but also to the legislature in a yearly
report that details ndings, underlying causes and systemic remedies.
This Task Force also noted concern over the lack of child protections against caretaker retaliation after
a foster youth reports his/her concerns to the OCA. The Texas Department of Family and Protective
Services Rights of Children and Youth in Foster Care currently states that foster children have the right
to complain to DFPS Consumer Affairs Ofce or Disability Rights of Texas if the youth feels that his/her
rights have been violated or ignored.
26
It also states that the youth cannot be punished or threatened
with punishment for making such complaints. Other than this statement, there are no specic policies
that guarantee youth are protected from retaliation. There are also are no consequences in place to
address retaliation by staff or caregivers.
Recommendations:
1. Establish an independent Ombudsman ofce or establish autonomy within the OCA, ensuring that
the Department of Family and Protective Services shall have no authority to:
• Create or change the policy and practice of the Ofce of Consumer Affairs;
• Determine the budget of the Ofce of Consumer Affairs; or
• Make decisions regarding personnel of the Ofce of Consumer Affairs.
2. Caseworkers and Child Placing Agency personnel should provide foster children and youth with
better access to the Children’s Bill of Rights by making copies available at court hearings and at site
visits and provide ongoing education around these rights in order to fully empower them.
25 User Empowerment in Mental Health: A Statement by the WHO Regional Ofce for Europe. Rep. World Health Organization Europe, 2010. Web.
16 Dec. 2014. <http://www.euro.who.int/__data/assets/pdf_le/0020/113834/E93430.pdf?ua=1>.
26 Rights of Children and Youth in Foster Care. Texas Department of Family and Protective Services, n.d. Web. 16 Dec. 2014. <https://www.dfps.
state.tx.us/Adoption_and_Foster_Care/About_Foster_Care/rights.asp>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 34
3. Require Child Placing Agencies and foster care placements to provide access to the OCA or
independent Ombudsman’s ofce contact information in private spaces, such as bathrooms or on the
back of bedroom doors.
4. Require the OCA or independent Ombudsman’s ofce to establish a written policy on foster youth’s
provisions and protections from retaliation by a caregiver, including a procedure of investigation of such
retaliation and consequences for caregivers who are found to have engaged in retaliation against a
child or youth in foster care.
5. Require the OCA to establish a secure form of communication with the child or youth in order to
ensure that he/she is made aware of the investigation including the substantiation of any complaints
that are brought to the attention of or determined by the OCA.
6. Require the OCA to establish specic procedures for working with youth in foster care who call to
make an inquiry or complaint.

MENTAL HEALTH TASK FORCE REPORT | PAGE 35
III. APPROPRIATE CAREGIVING ENVIRONMENTS
FOR CHILDREN AND YOUTH IN SUBSTITUTE CARE
Background
Children in substitute care have experienced trauma
All children that enter the child welfare system have experienced trauma. They experience trauma
when they are abused or neglected, when they are removed from their home and in countless other
ways as they negotiate the child welfare system in Texas. Perhaps most damaging to children in
the child welfare system is the relational trauma that they experience—the trauma of being hurt or
neglected by the person or people they trust the most. This type of trauma often occurs in families
across generations and can be especially difcult to overcome.
1
Numerous research articles and
studies detail the impact of trauma on developing children and youth. Trauma can cause both long
and short-term problems for children. “Consequences of trauma include difculties with learning,
ongoing behavior problems, impaired relationships and poor social and emotional competence.
Children and youth exposed to trauma, especially violence, experience more learning and academic
difculties and behavioral and mood-related problems.”
2
Part of the reason that trauma has such a detrimental and potentially long-lasting effect is that
chronic, prolonged and sustained trauma actually alters brain development, especially in young
children. When children grow up in chaotic environments where they are in physical danger or
they are not getting what they need to survive on a consistent basis, the “child’s brain may be
hyper-alert for danger…if this environment persists and the child’s brain is focused on developing
and strengthening its strategies for survival, other strategies may not develop as fully. The result
may be a child who has difculty functioning when presented with a world of kindness, nurturing
and stimulation.”
3
This means that children who experience trauma may still struggle to attach to
caregivers or regulate their emotions and behaviors, even if they are placed in an ideal home where
loving and consistent care is available to them.
Trauma can have profound and life-long detrimental impacts on individuals
The widely renowned Adverse Childhood Experiences (ACE) Study, clearly demonstrates the long-
term, costly impact of trauma and maltreatment in childhood. The study was a collaboration between
the Centers for Disease Control and Prevention and the Kaiser Permanente’s Health Appraisal
Clinic in San Diego, California and is the largest examination of the correlation between childhood
maltreatment and adult health and well-being outcomes. Findings from the study indicated that some
negative experiences in childhood are risk factors or causes for various illnesses and poor health.
Indeed, the study found that the more adverse experiences that individuals had in childhood, including
abuse and neglect by their caregivers, the more likely they were to experience a wide variety of health
and social problems as adults. These range from liver and heart disease to increased risk for intimate
1 Children and Relational Trauma. Ackerman Institute for the Family, 2014. Web. 12 Dec. 2014. <https://www.ackerman.org/centers/children-and-
relational-trauma/>.
2 Cooper, Janice L. “Facts about Trauma for Policymakers: Children’s Mental Health.” National Center for Children in Poverty. Columbia University
Mailman School of Public Health Department of Health Policy & Management, July 2007. Web. 4 Dec. 2014.
3 “Understanding the Effects of Maltreatment on Brain Development.” Child Welfare Information Gateway. U.S. Department of Health and Human
Services Administration on Children and Families, Nov. 2009. Web. 4 Dec. 2014.
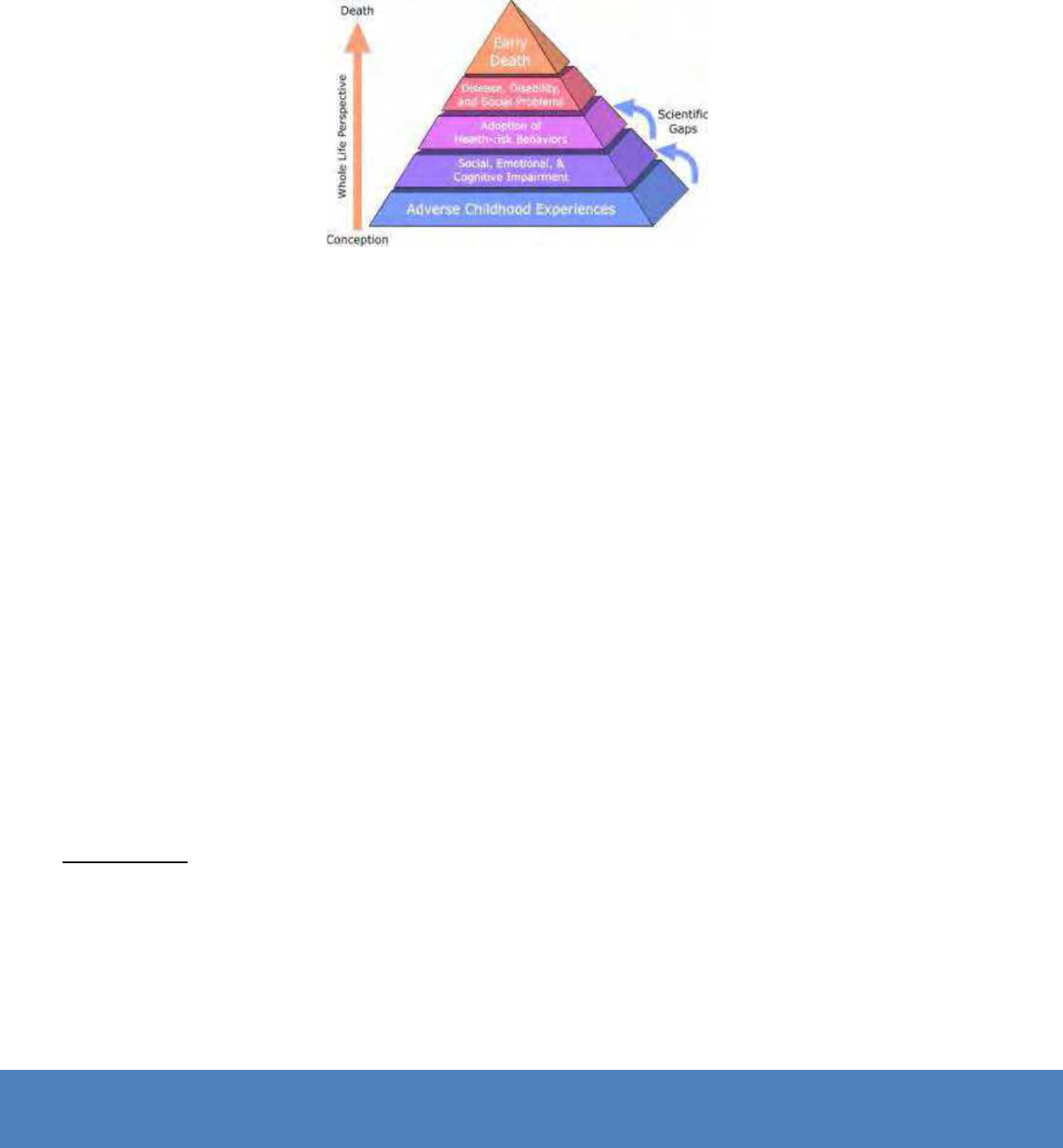
MENTAL HEALTH TASK FORCE REPORT | PAGE 36
partner violence, adolescent pregnancy and illicit drug use
4
.
The study found that the more adverse childhood experiences that a child faced, the greater their
likelihood of experiencing health and social problems as an adult.
The chart below demonstrates the impact of these types of experiences over a lifetime
5
:
In spite of these daunting facts, there are many factors that help to bolster resiliency in children and
youth and could help to combat the long-term impact of trauma. Research has shown that if children
are surrounded by protective factors, or developmental assets, they are more likely to develop a
sense of resiliency that might alter the impact that trauma has on their development and long-term
outcomes.
6
These factors occur across different aspects of the child’s daily life and occur at the community,
relationship and individual levels. At the community level, factors like a positive school environment,
positive community environment and economic opportunities are all considered protective factors
that help to promote resiliency in children. At the relationship level, parenting competencies, positive
peers and caring adults are all important. And, nally, at the individual level, self-regulation skills,
problem solving skills, relational skills and involvement in positive activities all contribute to protecting
children and youth from the effects of trauma in their lives.
7
All of these protective factors are interrelated and impact each other, which adds to the challenges
of those trying to understand the impact of trauma and how to help children who have experienced
trauma in their lives.
4 ACE Study: Major Findings.” Injury Prevention & Control: Division of Violence Prevention. Centers for Disease Control and Prevention, 13 May
2014. Web. 4 Dec. 2014.
5 ACE Study.” Injury Prevention & Control: Division of Violence Prevention. Centers for Disease Control and Prevention, 13 May 2014. Web. 4 Dec.
2014.
6 “40 Developmental Assets for Adolescents.” Discovering What Kids Need to Succeed. Search Institute, 2007. Web. 4 Dec. 2014.
7 “Promoting Protective Factors for In-Risk Families and Youth: A Brief for Researchers.” The Administration on Children, Youth and Families, 2014.
Web. 4 Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 37
KEY ISSUES
Issue 1: Caregivers are not adequately trauma-informed and efforts to
establish a trauma-informed care system are slow, disconnected, and vary in
how they are dened
As more and more research comes out about trauma and its impact on the brain development of
young children, professionals have increased their efforts to address trauma in their practices. The
Texas CASA Mental Health Task Force found that the term “trauma-informed care” has become a
buzzword that is beginning to be overused and misunderstood among professionals and policy
makers. In order to effectively address the impact of trauma in homes, communities and systems,
it is essential to establish a common denition for trauma-informed care. The Substance Abuse and
Mental Health Services Administration National Center for Trauma-Informed Care denes trauma-
informed care as “an approach to engaging people with histories of trauma that recognizes the
presence of trauma symptoms and acknowledges the role that trauma has played in their lives”.
8
Trauma-informed care focuses on the provision of developmentally appropriate, gender-
specic care through the lens of research and evidence of effective practice for children
and youth who have experienced events that are psychologically overwhelming.
9
The Department of Family and Protective Services (DFPS) does not require any annual training on
trauma or trauma-informed care, but does list the following as a best practice suggestion for annual
training: “Special needs of children in care, which may include areas such as sexualized behavior,
trauma, medical needs, and/or developmental disorders”.
10
Since the State of Texas does not require training on the impact of trauma, it is safe to assume that
many foster parents have not received any training on it. Additionally, those who have been trained on
trauma may be trained to understand its impact, but not necessarily on how to interact and help children
who have experienced trauma heal. Given the list of challenges that children who have experienced
trauma face, it is essential for those who interact with children and youth in the foster care system
to understand trauma and its impact so that they can understand the meaning behind challenging
behaviors and relationship decits that children and youth in the child protection system struggle with.
Once foster parents have this foundational knowledge, they should then be given tools and strategies
to utilize in their interactions and relationships with the children in their care in order to help them heal
and improve long-term outcomes.
To date, there have been numerous efforts to train different types of professionals, advocates,
service providers and parents about trauma and how to be trauma-informed. Some notable examples
identied by the Mental Health Task Force are: The Texas Children Recovering from Trauma Initiative, a
Department of State Health Services grant project; the Travis County Collaborative for Children, a Texas
Christian University Institute of Child Development pilot project; the Trauma-Informed Care Consortium
of Central Texas, led by the Austin Child Guidance Center; the Trauma and Grief Clinic for Youth, a
University of Texas Health Science Center at Houston initiative; and others. Even domestic violence
8 “About NCTIC.” National Center for Trauma-Informed Care & Alternatives to Seclusion and Restraint. Substance Abuse and Mental Health
Services Administration, 17 Oct. 2014. Web. 17 Dec. 2014. <http://www.samhsa.gov/nctic/about>.
9 “About NCTIC.” National Center for Trauma-Informed Care & Alternatives to Seclusion and Restraint. Substance Abuse and Mental Health
Services Administration, 17 Oct. 2014. Web. 17 Dec. 2014. <http://www.samhsa.gov/nctic/about>.
10 Texas Department of Family and Protective Services. Licensing Division. Minimum Standards for Child-Placing Agencies. N.p., Sept. 2014. Web. 5
Dec. 2014.

MENTAL HEALTH TASK FORCE REPORT | PAGE 38
and juvenile justice providers are thinking critically about how to utilize the research on trauma with the
populations that they serve. The challenge is that none of the initiatives have the scope or funding to
create a consistent, coordinated and evidence-based trauma-informed system for children and youth
in foster care in Texas. These efforts have been largely disjointed, slow and focused on narrow groups,
who often only see children and youth in foster care for short periods of time and not daily.
An Ideal Trauma-Informed Care System
The Task Force asserts that Texas will not have a truly trauma-informed system until professionals and
policy makers begin to think of “caregivers” as anyone involved in the life of a child who has experienced
trauma. This would include anyone who is with the child in the home, school, community, medical or
mental health system, child protection system and the legal system. A successful trauma-informed
system of care would share a common culture of supportive, consistent interactions with the child
by all individuals and systems that touch that child. The majority of the training efforts to date have
focused on providing training to mental health providers and direct service staff. These professionals
are important to a child’s healing, but they often only interact with the child for two or fewer hours
each week. While it is the case that some aspects of trauma-informed care practices are more easily
accessible if an individual has formal training in counseling or social work, “there are a few consistent
propositions that much of the healing from trauma can take place in non-clinical settings…[and] there
is some evidence to suggest that trauma-informed living environments in which healing and growth
can take place are a necessary precursor to any formal therapy that might be offered to a traumatized
child.”
11
Some researchers believe that without trauma-informed living environments, the child cannot truly heal
or fully engage in the therapeutic process. Dr. Howard Bath argues that children need three primary
things in order to begin to heal from trauma, none of which require an intensive training in mental
health interventions: the development of safety, the promotion of healing relationships and the teaching
of self-management and coping skills.
12
These three “pillars” of trauma-informed care have been widely adopted by researchers and trauma
experts around the world. Feelings of safety and self-regulation skills are both highly dependent on the
connections that children and youth are able to form with the adults in their lives. The individuals who
most impact the child are those that the child spends the most time with, including adults who live with
the child and teachers at school. The Task Force believes that the approach to trauma-informed care
must shift to training and working with those individuals who are in the home and school environment,
while continuing to train mental and physical health providers, legal professionals and advocates, and
child protection system staff. Individuals in the community where the child plays and interacts must also
be considered, including coaches, religious leaders, child care providers, mentors and others. If Texas
could begin to think of everyone that interacts with a child in the foster care system as a “caregiver” for
the child, an approach to a truly trauma-informed system could begin. The Task Force developed the
diagram below to illustrate the type of trauma-informed care system that the members envision for the
children and youth in foster care in Texas:
11 Bath, Howard. “The Three Pillars of Trauma-Informed Care.” Reclaiming Children and Youth 17.3 (2008): 17-21. 2008. Web. 5 Dec. 2014.
<https://reclaimingjournal.com/sites/default/les/journal-article-pdfs/17_3_Bath.pdf>.
12 Bath, Howard. “The Three Pillars of Trauma-Informed Care.” Reclaiming Children and Youth 17.3 (2008): 17-21. 2008. Web. 5 Dec. 2014.
<https://reclaimingjournal.com/sites/default/les/journal-article-pdfs/17_3_Bath.pdf>.

MENTAL HEALTH TASK FORCE REPORT | PAGE 39
While Task Force members would like to see the term “caregiver” expanded as mentioned above, they
recognize the importance of starting with tangible rst steps in an effort to create an ideal trauma-
informed system. For the purposes of the Task Forces’ recommendations, the term “caregiver” will be
used to refer to anyone serving in a parenting role for the child, including biological parents, kinship
caregivers, adoptive caregivers, foster parents and residential staff.
With this in mind, the Task Force developed a list of principles that it would like to apply to every caregiver
of a child in foster care in an ideal trauma-informed care system. The Task Force recommends that
eventually all caregivers serving children in the Texas child welfare system will be recruited, selected,
trained, supported and expected to:
• Understand the complex needs of the children with histories of trauma and understand
the comprehensive damage to brain, body, biology and beliefs that drive behaviors.
• Understand specic challenges of children who’ve suffered trauma, such as fear,
ashbacks, aggression and other symptoms of PTSD.
• Employ effective methods of response to behavioral problems helping them recognize
trauma-driven behaviors (fear, sadness, loss, pain) and to respond appropriately without
reactivating the original trauma.
• Create comprehensive environments that disarm fear and help children heal, including the
children’s need of a “safe base” relationship with caregivers.
Home: Biological family, kinship caregivers, foster family,
adoptive family, residential staff, siblings
School: Teachers, administrators, foster care liaisons,
pre-k
Community: Coaches, religious leaders, mentors, child
care providers
Emotional Well-Being: Psychiatrists, psychologists,
therapists, social workers, mental health professionals
Physical Well-Being: Pediatricians, nurses, medical
doctors
Child Protection: CPS investigators, caseworkers, case
supervisors, child placing agency staff
Legal System:
Judges, attorneys, guardian ad litems, law
enforcement ofcers, juvenile justice system staff

MENTAL HEALTH TASK FORCE REPORT | PAGE 40
• Recognize parenting strategies that are effective vs. those that drive further aberrations
in behavior.
• Prevent secondary trauma that is often induced by behavioral intervention approaches
that exacerbate fear.
• Spend quality one-on-one time with each child in the home.
• Create a meaningful connection and nurturing, trusting relationship with each child in the
home.
• Collaborate effectively with the various systems that impact the child, such as medical,
mental health, education, judicial, etc.
While many efforts have already begun and there is much focus by policy makers and stakeholders
around this issue, the Task Force had a few additional recommendations to offer as rst steps to a new
kind of approach to a trauma-informed care system in Texas.
Recommendations:
1. Dene trauma-informed care for caregivers within Minimum Standards.
2. Require all residential child care administrators and staff to complete trauma informed care training,
as dened by the Department of Family and Protective Services.
3. Incentivize Child Placing Agencies (CPAs) to incorporate trauma-informed care into their assessments,
training and support of caregivers of children with increased reimbursement rates.
4. Evaluate the utilization and effectiveness of implementing trauma-informed care models, as dened
by the Department of Family and Protective Services, within the eligible CPAs.
Issue 2: Current practice does not include an assessment for adult attachment
for alternate caregivers
Frequent placement changes have historically been a challenge for the Department of Family and
Protective Services. In 2013, Texas children in permanent foster care for more than three years would,
on average, experience eleven placement changes.
13
Obstacles in placement stability have led the
Department and child welfare professionals to study better methods to evaluate if a child is a good t
for his/her caregiver. Currently, the system fails to observe a caregiver’s ability to attach to individual
children.
The attachment style of a foster parent or caregiver has signicant implications on the care of children
and these implications follow children and youth into adulthood. According to research conducted
in coordination with The Attachment Style Interview (an assessment used to determine caregiver’s
attachment style), a child’s caregiver’s attachment style has been linked to the child’s attachment
style, choice of partner and ability to access emotional support. Research shows that there is a clear
correlation between the adult attachment styles of those parenting a child and their capacity to promote
13 Ramshaw, Emily. “Lawsuit Can’t Cover All Kids in Long-Term Foster Care.” The Texas Tribune. N.p., 23 Mar. 2012. Web. 07 Aug. 2014. <https://
www.texastribune.org/2012/03/23/lawsuit-texas-failing-foster-children/>

MENTAL HEALTH TASK FORCE REPORT | PAGE 41
well-being and safety for children who have been traumatized.
14
Given this research, understanding
a caregiver’s attachment style can help the system predict if a child will be successful in a particular
placement and whether the caregiver can, with proper support, employ trauma-informed interventions
to assist the child in his/her healing. Ideally, policies and procedures should exist to properly screen
caregivers and to match children to caregivers who are best equipped to provide such involved care. In
referencing the necessity for caregiver assessments and training, all adults qualifying as a “caregiver”
are subject to recommendations.
Recommendations:
1. Require all agencies that screen potential caregivers to include an attachment screening as a
component of the overall assessment to better understand that caregiver’s ability to form meaningful
and trust-promoting relationships with children who have experienced trauma. There are several free
attachment screening options and the Task Force recommends that the Department of Family and
Protective Services create a standardized list of tools for agencies to utilize for these screenings.
2. Train child placing agency staff to screen potential caregivers using attachment screening and
ensure they have the proper assessment tools, as dened by the Department of Family and Protective
Services.
3. Require a set of standardized assessments of prospective caregivers, dened by the Department of
Family and Protective Services, across child placing agencies.
14 Bufulco, Antonia, Catherine Jacobs, Amanda Bunn, Geraldine Thomas, and Karen Irving. “The Attachment Style Interview: A Support-based
Adult Assessment Tool for Adoption and Fostering Practice.” Adoption & Fostering 32.3 (2008): 33-45. Print.

1501 W Anderson Lane Suite B2 | Austin, Texas 78757 | www.texascasa.org
