Dental Services Among Medicare Beneficiaries
Dental Services Among Medicare Beneficiaries:
Source of Payment and Out-of-Pocket Spending
Introduction
Oral health is an important aspect of general health and
wellbeing. Poor oral health is linked with respiratory
disease, cardiovascular disease, and diabetes.
(1)
The
relationship between poor dental health and disease is
especially relevant for vulnerable populations, such as
individuals with disabilities or the elderly.
(2, 3, 4)
Although Medicare does cover dental services that are
an essential part of a medical procedure such as jaw
surgery, routine dental services, including exams, check-
ups, and cleanings, are not covered by Medicare.
Beneficiaries must pay for these routine services
directly out-of-pocket (OOP), or rely on dental coverage
through private plans or Medicaid. This lack of dental
coverage can be a barrier to seeking dental care for
beneficiaries. More than half of all beneficiaries do not
use any dental services in a given year.
(5)
This data highlight examines sources of payment and
OOP spending for dental services among Medicare
beneficiaries for two time periods, 2002 and 2012, and
by select beneficiary characteristics. The analysis uses
the Medicare Current Beneficiary Survey (MCBS) which
has been widely used to study total Medicare costs and
health care utilization, but comparatively little research
has been done on the dental information collected in
the survey. The MCBS collects detailed self-reported
information on different sources of payment for a
dental event.
Source of Payment for Dental Services and Average
Dental Costs over Time
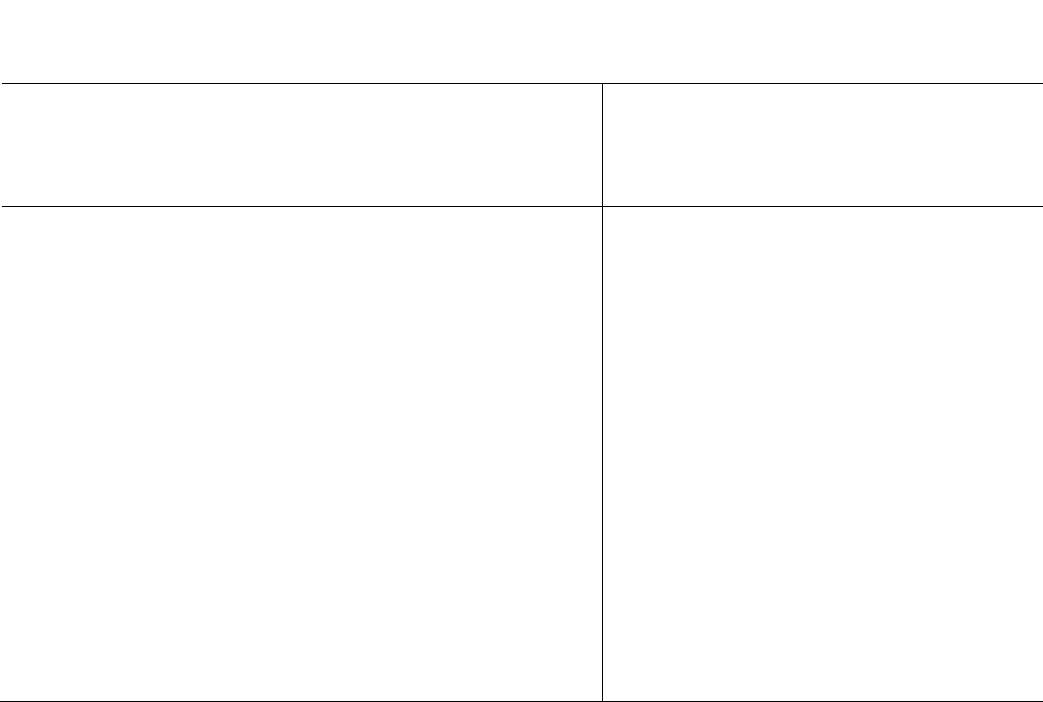
Figure 1 illustrates sources of payment for dental
services in 2002 and 2012 among Medicare
beneficiaries with at least one reported dental service.
The majority of dental costs were covered directly by
beneficiary OOP spending, at about 75%. Employer
sponsored insurance was the next largest payer, at 12%.
Other payers
1
combined paid about 10% of dental
costs.
1
The other payer category was determined by combining some of the
smallest sources of payment, which included Medicare Fee-for-
Service. A complete description of other payers can be found in the
technical notes.
KEY FINDINGS
Medicare beneficiaries paid out-of-pocket nearly
three-fourths of the costs of dental services.
The percentage of out-of-pocket spending on
dental services by all Medicare beneficiaries did
not change in 2012 compared to 2002.
Beneficiaires without supplemental insurance paid
a higher proportion of dental costs in 2012
compared to 2002.
Data Highlight March 2016
Data Highlight March 2016
Dental Services Among Medicare Beneficiaries
Medicare Advantage covered less than 5% of dental
costs, and Medicaid paid less than 1%.
Across sources of payment, the percentage of costs
covered by payers did not change between 2002 and
2012. Average dental costs per beneficiary increased
significantly from $798 in 2002 to $929 in 2012
2
.
Total Dental Costs and Medicare Beneficiary Out-of-
Pocket Spending
Although the percentage of beneficiary OOP spending
for dental services did not significantly vary over time
(~75%) in the Medicare population, we also examined
total dental costs and OOP spending by key beneficiary
characteristics for 2002 and 2012. From 2002 to 2012
there were no trends in the percentage of OOP
2
For more detailed numbers, including standard errors, please
reference Tables 1 and 2 in the Appendix.
spending on dental services over time for any of the
examined age groups, by gender, or by education
status. However, OOP spending on dental services did
differ between 2002 and 2012 by supplemental
insurance categories (Table 1).
Beneficiaries with no supplemental insurance (Fee-for-
Service (FFS) only) directly paid a significantly higher
portion of dental costs in 2012 (96.3%) than in 2002
(80.8%). Similarly, beneficiaries with only Medicaid
supplemental insurance (that is, FFS and Medicaid) paid
55.3% OOP in 2002, which increased to 75.0% in 2012.
Beneficiaries with only private health insurance and FFS
saw no change over the selected years, while those with
Medicare Advantage or another managed care plan
paid 70.3% OOP in 2002, increasing to 81.3% in 2012.
However, beneficiaries with multiple supplemental
insurance experienced no change in the percentage of
OOP spending.
Data Highlight March 2016
Dental Services Among Medicare Beneficiaries
Conclusion
On average, Medicare beneficiaries cover nearly three-
fourths of the costs of dental services. While inflation-
adjusted dental costs increased from 2002 to 2012, the
percentage of OOP spending on dental services by
Medicare beneficiaries remained the same and this
persisted when examining key socio-demographic
characteristics, such as age, gender, and education.
However, beneficiaries without supplemental insurance
paid a higher portion of dental costs in 2012, compared
to 2002. Similar trends were found for beneficiaries
with Medicaid or managed care supplemental
insurance. Beneficiaries with private health insurance
coverage or multiple supplemental insurance plans saw
no increase in their percentage of OOP spending.
Furthermore, beneficiaries with multiple supplemental
insurance paid the smallest percent of total costs OOP.
These findings highlight an important issue for Medicare
beneficiaries, particularly that beneficiaries pay the
majority of routine dental costs OOP, and most
beneficiaries do not have private or public plans to help
offset this cost. This has been consistent over time,
and may serve as a deterrent to dental care. Future
research should further examine the effects of
supplemental insurance, the burden of OOP spending in
relation to income, the association between insurance
coverage and service utilization, and the relationship
between oral health and quality of life. The MCBS is
uniquely suited to examine many of these issues.
Table 1. Mean Total Dental Costs and Out-of-Pocket Spending with Standard Errors for Medicare Beneficiaries With
At Least One Dental Service by Year and Beneficiary Characteristics, in 2012 Dollars
2002
2012
n
Mean Total
Dental Costs
(SE)
Mean OOP
Dental
Spending (SE)
Percent of OOP
Spending (SE) n
Mean Total
Dental Costs
(SE)
Mean OOP
Dental Spending
(SE)
Percent of OOP
Spending (SE)
Age
64 years old or younger
661
$717 (62)
$409 (46)
57.1% (3.86)
662
$821 (82)
$535 (68)
65.1% (4.06)
65 to 84 years old
3,757
$816 (25)
$613 (21)
75.1% (1.09)
3,614
$940 (32)
$707 (30)
75.2% (1.09)
85 years old or older
538
$730 (58)
$583 (49)
79.8% (2.29)
666
$980 (110)
$782 (106)
79.8% (2.62)
Sex
Male
2,227
$812 (32)
$588 (28)
72.4% (1.71)
2,197
$987 (42)
$744 (43)
75.3% (1.62)
Female
2,729
$787 (33)
$587 (27)
74.6% (1.26)
2,745
$883 (34)
$652 (38)
73.9% (1.35)
Education
Less than HS
930
$714 (50)
$509 (40)
71.4% (2.57)
586
$873 (92)
$675 (94)
77.4% (3.53)
High School
1,466
$734 (41)
$556 (32)
75.8% (1.86)
1,298
$727 (43)
$554 (40)
76.2% (2.06)
Any College
2,545
$863 (35)
$631 (29)
73.2% (1.49)
3,039
$1,016 (40)
$749 (37)
73.8% (1.29)
Supplemental Insurance
No Supplemental
278
$697 (83)
$563 (73)
80.8% (3.73)
208
$1,219 (199)
$1,174 (195)
96.3% (2.40)
Medicaid Only
383
$496 (59)
$275 (32)
55.3% (5.79)
344
$579 (70)
$434 (69)
75.0% (4.57)
Private Insurance only
2,984
$813 (29)
$635 (26)
78.1% (1.12)
1,937
$995 (40)
$754 (37)
75.8% (1.35)
HMO only
657
$809 (59)
$569 (47)
70.3% (2.58)
1,156
$814 (57)
$661 (55)
81.3% (1.95)
Multiple Supplemental
654
$897 (57)
$543 (40)
60.6% (2.59)
1,297
$957 (73)
$600 (62)
62.7% (2.50)
Data Highlight March 2016
Dental Services Among Medicare Beneficiaries
References
(1) Institute of Medicine and National Research Council. Improving access to oral health care for vulnerable and
underserved populations. Washington, DC: National Academies Press, 2011.
(2) Griffin SO, Jones JA, Brunson D, Griffin PM, and Bailey WD. “Burden of oral disease among older adults and
implications for public health priorities.” American Journal of Public Health. 2012; 102(3), 411-418.
(3) U.S. Department of Health and Human Services. Oral health in America: a report of the Surgeon General. Rockville,
MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research,
National Institutes of Health; 2000.
(4) Dolan TA and Atchison KA. “Implications of access, utilization and need for oral health care by the non-
institutionalized and institutionalized elderly on the dental delivery system.” Journal of Dental Education. 1993;
57(12), 876-887.
(5) Huang J, Saulsberry L, Damico A, Licata R, Neuman T. Oral Health and Medicare Beneficiaries: Coverage, Out-of-
Pocket Spending, and Unmet Need. Washington, DC: Kaiser Family Foundation. June 2012. Available at
<https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8325.pdf>.
______________
This data brief was written by Jessie Parker at CMS, in partnership with Matthew DiFiore, Sukanya Kadam, Robert Kosarowich, and
Ida Chiang at Carnegie Mellon University (CMU), under the direction of CMU’s Dr. Martin Gaynor. Lisa Mirel and Kim Lochner at CMS
provided invaluable editorial feedback. For more information about the MCBS, visit www.cms.gov
. To purchase MCBS files, contact
the Research Data Assistance Center (ResDAC) at www.resdac.org or (888) 973-7322.
Data Highlight March 2016
Dental Services Among Medicare Beneficiaries
Technical Notes
The Medicare Current Beneficiary Survey (MCBS)
collects data from the total Medicare population,
whether aged or disabled, living in the community or a
facility, or served by managed care or traditional Fee-
for-Service (FFS). The MCBS is an in-person,
longitudinal panel survey. Respondents are interviewed
three times a year over a period of four years to form a
continuous profile of their health care experience. Two
types of interviews are conducted in the MCBS: a
community interview done in the home, and an
interview of knowledgeable staff on behalf of
beneficiaries in a facility setting.
This data highlight is based upon the 2002 and 2012
MCBS Cost and Use (CAU) research files, which
represent a full year of data captured in the Winter, Fall
and Summer interviews. The CAU research files include
demographic and health insurance data as well as
information on health care utilization and costs,
regardless of payer. In addition, the CAU files are
enhanced with available CMS administrative data and
Medicare claims data for survey participants who
received services through traditional FFS Medicare.
Special steps are taken to expand sample coverage in
the CAU files to include all beneficiaries who were
enrolled during the calendar year. This mix of
continuing enrollees, accretions (i.e., new enrollees),
and terminations is referred to as the “ever-enrolled”
population. The ever-enrolled population includes
everyone who was enrolled in Medicare for any period
during the year. These steps are necessary because
official Medicare program statistics cover all persons
entitled to Medicare during the year, and omitting part-
year enrollees and persons who died during the year
could substantially bias the results of these analyses. In
2002, 12,697 sampled beneficiaries represented an
ever-enrolled population of 41,808,000. In 2012,
11,299 sampled beneficiaries represented an ever-
enrolled population of 52,079,000.
Beneficiaries who reported that they received dental
care (or service) from a dentist, dental surgeon,
endodontist, periodontist, or dental hygienist were
subsequently asked about costs for that care and the
sources of payments to cover the costs. Any beneficiary
from the 2002 and 2012 MCBS CAU file that reported a
dental service and the associated cost was included in
this analysis. For this analysis source of payments
include Medicare Advantage, Medicaid, OOP, employer-
sponsored insurance, other payer. To create the ‘other’
category for source of payment in this analysis, the
existing ‘other’ category was combined with Medicare
FFS ( “Original Medicare”), Veteran’s Administration,
individually-purchased insurance, unknown private
insurance, private HMO, and uncollected liability.
In this data highlight, cost and source of payment
information is from the service summary dataset (RIC
SS). This dataset summarizes cost and utilization by
event type for all beneficiaries (e.g. there is a one
record per beneficiary for all the dental utilization for
the year).
Subgroup analyses included age, sex, education and
supplemental insurance. Age categories were defined
using the sampling age strata variable (D_STRAT) from
the Record Identification Code (RIC) 1 and were
grouped as: (1) disabled beneficiaries, who were under
age 65 and were entitled to Medicare benefits by either
receiving two years of Social Security or Railroad
Retirement Board benefits, or who had a qualifying
disability; (2) beneficiaries ages 65 to 84, who were
enrolled in Medicare, regardless of their original reason
for Medicare enrollment; and (3) beneficiaries ages 85
and older, who were enrolled in Medicare, regardless of
their original reason for Medicare enrollment. Sex was
determined using data from the administrative records
in the data file RIC A (variable name H_SEX). Education
was categorized based on the self-reported education
level found in RIC 1 (variable name SPDEGRCV).
Supplemental insurance categories were defined using
both self-reported and administrative data on insurance
status based on the annual summary variables for
Medicaid (D_CAID), Private Health Insurance (D_PHI),
Private Managed Care (D_PMC) and Medicare
Advantage (D_MA) found in RIC 4. For 2002, the annual
summary variable for Health Maintenance Organization
(D_HMO) was used to instead of D_PMC and D_MA
Data Highlight March 2016
Dental Services Among Medicare Beneficiaries
since earlier years of data on Medicare Advantage and
Private Managed Care were not available. Beneficiaries
with Medicare Advantage (MA) without other
supplemental insurance were categorized as “HMO
only” for all years. Beneficiaries with FFS without other
supplemental insurance were categorized as “No
Supplemental.” Beneficiaries with FFS and
supplemental private health insurance (PHI) were
categorized as “PHI only” but beneficiaries with MA and
PHI were categorized as “Multiple Supplemental.”
All costs are presented in 2012 dollars and are adjusted
for inflation using the Consumer Price Index available at
http://www.bls.gov/cpi/home.htm
The CAU files contain cross-sectional weights that
represent the “ever-enrolled” Medicare population. The
survey weights incorporate the selection probability of
each sample person, are post-stratified to control totals
based on when beneficiaries became eligible for
Medicare, age, sex, race, region, and metropolitan area
status and are adjusted to account for non-response.
Unweighted sample sizes (n’s) are displayed, but all
estimates presented in this data highlight were
calculated using the cross-sectional weights, and all
variance estimates were calculated using the balanced
repeated replicate weights with the Fay adjustment. A
two-sided p-value of less than 0.05 was used to assess
statistically significant differences between estimates.
No adjustments were made for multiple comparisons.
Appendix Tables
Appendix Table 1. (Figure 1) Distribution of Sources of
Payment for Dental Services Among Medicare
Beneficiaries, with Standard Errors
2002
2012
Estimate
SE
Estimate
SE
Sources of Payment
Out of Pocket
73.59%
1.11
74.57%
1.08
Employer Sponsored
11.98%
0.66
11.57%
0.75
Other
9.96%
0.73
8.98%
0.58
Medicare Advantage
3.17%
0.49
4.07%
0.47
Medicaid
1.16%
0.23
0.72%
0.15
Appendix Table 2. Average Total
Cost for Dental Services Among
Medicare Beneficiaries, with
Standard Errors
Estimate
SE
Year
2002
$798.14
22.39
2012
$928.76
31.14
Data Highlight March 2016
