
MILLIMAN CLIENT REPORT
Average annual beneficiary
health care costs for various
Medicare coverage options 2023
Commissioned by UnitedHealth Group (UHG)
September 2023
David Mike, FSA, MAAA
Philip Nelson, FSA, CERA, MAAA
Brad Schliesmann, ASA, MAAA, JD
MILLIMAN CLIENT REPORT
Table of contents
1. EXECUTIVE SUMMARY ........................................................................................................................................ 1
2. BACKGROUND ..................................................................................................................................................... 4
3. NATIONWIDE COMPARISON OF THE COVERAGE VALUE TO MEDICARE BENEFICIARIES ....................... 7
Nationwide comparison of annual health care costs for an average aged Medicare enrollee ......................... 8
Average lifetime cost differential for 65-year-old Medicare beneficiary ............................................................ 9
Annual health care costs for specific age groupings ...................................................................................... 10
Considerations for beneficiaries who incur high health care costs ................................................................. 12
Additional considerations not measured by annual health care costs ............................................................ 12
Demographic information ............................................................................................................................... 15
4. STATE-LEVEL RESULTS ................................................................................................................................... 16
5. METHODOLOGY ................................................................................................................................................. 20
6. CAVEATS AND LIMITATIONS ............................................................................................................................ 21

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 1 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
1. EXECUTIVE SUMMARY
UnitedHealth Group (UHG) commissioned Milliman to compare the beneficiary costs of the Medicare Advantage (MA)
program relative to other public and private health insurance options available to Medicare-eligible seniors. This
report is an update to our 2020 analysis
1
comparing average annual health care costs
2
paid by seniors across various
popular coverage options. We compared an integrated Medicare Advantage and Prescription Drug (MA-PD) plan, the
most popular type of MA plan,
3
to Traditional Medicare Fee-for-Service (FFS) and Medigap Plan G, which are
supplemented by standalone Medicare Prescription Drug Plans (PDPs), the most popular drug coverage option for
seniors choosing FFS and Medigap.
As of 2023, approximately 59.8 million people were enrolled in Medicare Parts A and B, of which over 86% are
seniors eligible for Medicare due to age.
4
Approximately 31 million seniors chose an individual MA plan for coverage,
while over 14 million chose Medigap plans.
5
,
6
Approximately two-thirds of people who purchased a Medigap plan
between 2019 and 2021 purchased Plan G.
7
Additionally, many Medicare beneficiaries receive supplemental
coverage through Medicaid or their employers (employer coverage may be provided through MA plans, Medigap
plans, or other employer-sponsored health plans). The most recent published information shows that of the 51.6
million non-institutionalized Medicare beneficiaries, approximately 4.6 million, or 8.9%, have no supplemental
coverage.
8
Most Medicare beneficiaries are on fixed incomes, with half having annual incomes below $29,650 as of
2019,
9
,
10
rendering average annual health care costs a significant portion of income for many Medicare beneficiaries
and a key determinant in the choice of health care coverage for Medicare beneficiaries.
This analysis considers average annual health care costs borne by seniors of average age and health status, not
eligible to receive income-based assistance with medical costs, and eligible for the Medicare program due to age
rather than disability.
RESULTS
For 2023, we estimate that such a beneficiary (one not eligible to receive income-based assistance with medical
costs and eligible for the Medicare program due to age) will incur approximately $3,396 in health care costs annually
under MA-PD, about $5,597 annually under FFS and PDP, and about $6,200 under the most popular Medigap plan
option currently available to new enrollees, Plan G. Please note that these cost estimates represent averages.
Individual beneficiaries will experience actual out-of-pocket (OOP) costs that vary from averages. We highlight
considerations for beneficiaries with annual OOP costs that differ significantly from averages in a special section of
this report dedicated to high-cost beneficiaries.
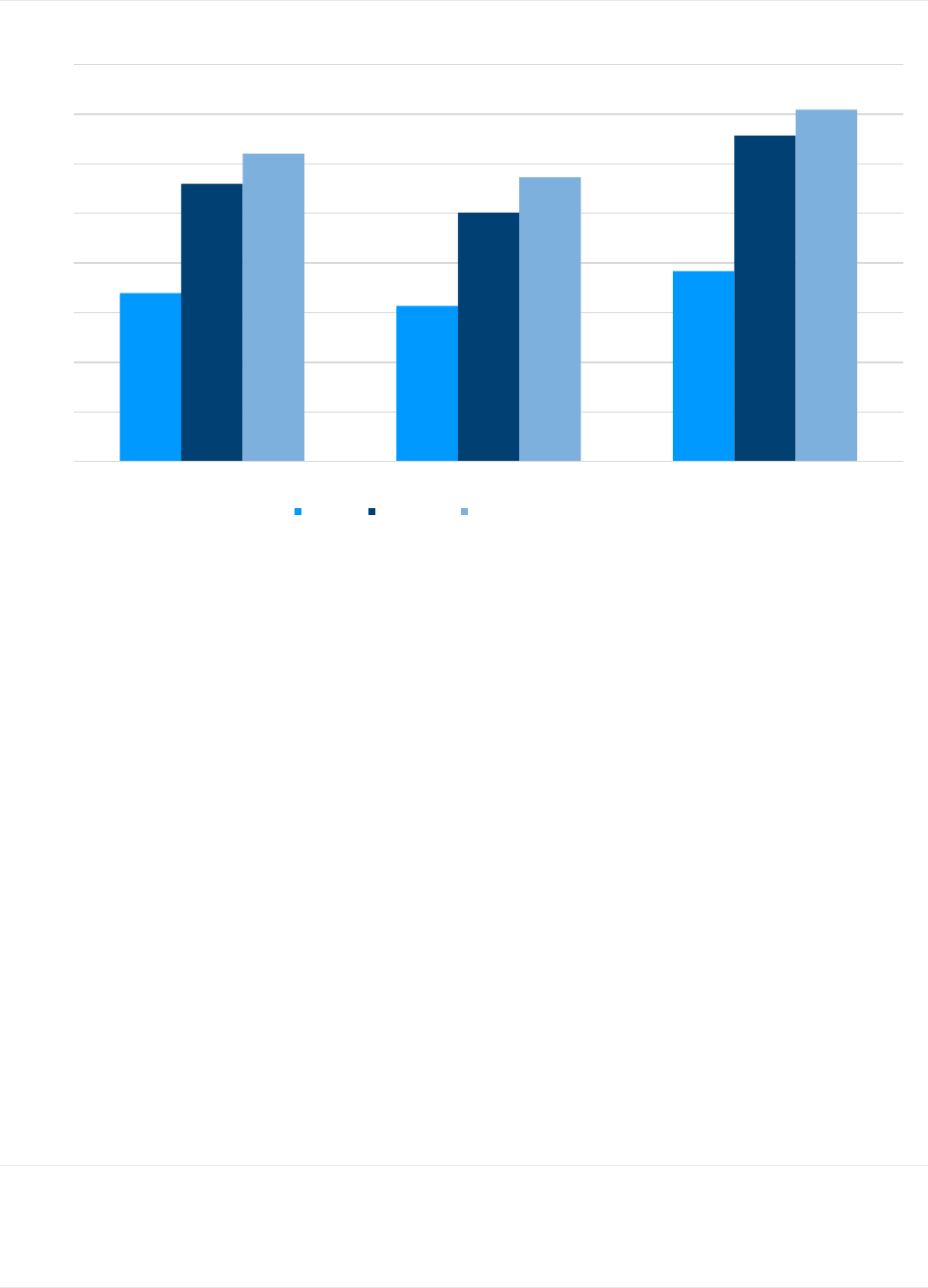
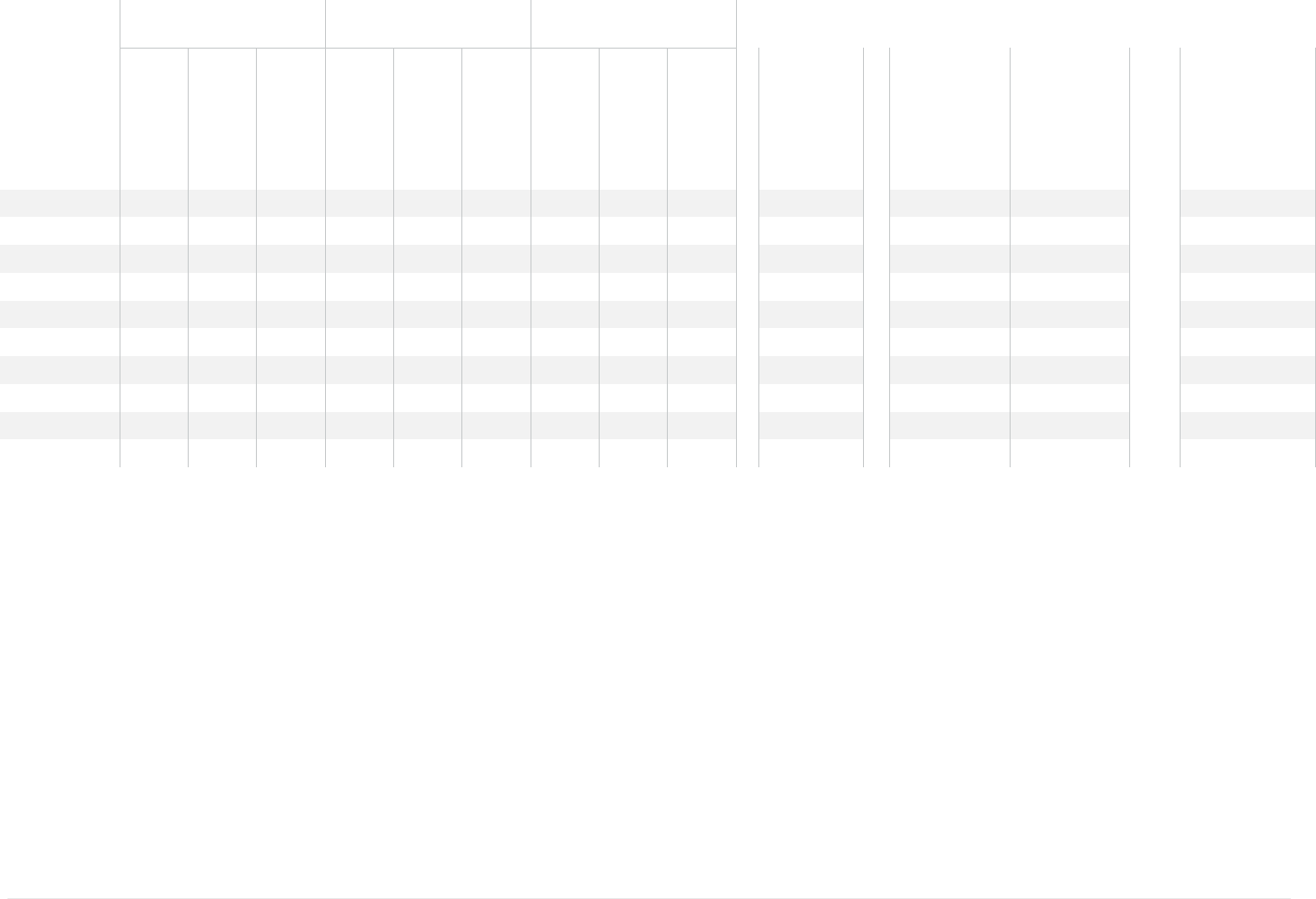
We performed this analysis for hypothetical average 65-year-old and 85-year-old Medicare beneficiaries under the
same coverage options—these results are adjusted for differences in the underlying health status. Results are
summarized in Figure 1.
1
Mike, D. & Yilmaz, G. (April 2021). Average annual beneficiary health care costs for various Medicare coverage options 2021. Retrieved February 1,
2023 from https://us.milliman.com/en/insight/average-annual-beneficiary-health-care-costs-for-various-medicare-coverage-options-2021 .
2
Annual health care costs represent total health care-related spending by an individual beneficiary, including premiums and out-of-pocket (OOP) costs
on deductibles, coinsurances, and copays for medical, drug, and ancillary services.
3
Not all MA plans cover prescription drug costs. Those that do are known as MA-PD plans. The majority of MA plans do cover prescription drug costs,
but some plans, which are less common, are known as MA-only plans and do not cover Part D. MA-PD plans are the focus of this report.
4
MedPAC July 2023 Data Book: Health Care Spending and the Medicare Program, Section 2: Medicare beneficiary demographics. Retrieved August
18, 2023, from https://www.medpac.gov/wp-content/uploads/2023/07/July2023_MedPAC_DataBook_SEC.pdf.
5
Freed M. et al., Kaiser Family Foundation (August 2023) Medicare Advantage in 2023: Enrollment Update and Key Trends. Retrieved August 18,
2023, from https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2023-enrollment-update-and-key-trends/.
6
American Association of Medicare Supplement Insurance, Medicare Insurance Statistics 2022 – Medicare Advantage – Medigap – Data – Costs –
Facts & More. Retrieved February 1, 2023, from https://medicaresupp.org/medicare-insurance-statistics-2022/#enrollment-2022.
7
Mark Farrah Associates 2021 Med Supp Database. Retrieved April 1, 2023.
8
MedPAC July 2023 Data Book: Health Care Spending and the Medicare Program, Section 3: Medicare beneficiary and other payer financial liability.
Retrieved August 18, 2023, from https://www.medpac.gov/wp-content/uploads/2023/07/July2023_MedPAC_DataBook_SEC.pdf.
9
Kaiser Family Foundation (April 2020). Medicare Beneficiaries’ Financial Security Before the Coronavirus Pandemic. Retrieved February 1, 2023,
from https://www.kff.org/medicare/issue-brief/medicare-beneficiaries-financial-security-before-the-coronavirus-pandemic/.
10
All dollar amounts in this report reflect the nominal dollar amount. Reported amounts are not adjusted for inflation.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 2 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
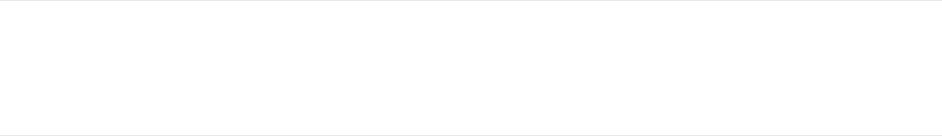
FIGURE 1: ESTIMATED ANNUAL BENEFICIARY HEALTH CARE COSTS BY COVERAGE OPTION AND AGE
These beneficiary health care cost estimates include premiums (total member premium, that is, including the Part B
premium, as well as the member premium for the MA-PD, PDP, and/or Medigap plan) and cost sharing for medical
services, pharmacy services, and ancillary services, such as dental, vision, and hearing. While premium is the most
visible cost to prospective beneficiaries when deciding what coverage to purchase, total health care costs, which are
generally less understood by beneficiaries shopping for coverage, ultimately determine whether a coverage option is
the best option financially. Results are outlined in greater detail in the Nationwide Comparison of the Coverage Value
to Medicare Beneficiaries section below.
A key design feature required to be included in all MA plans is an annual maximum out-of-pocket (MOOP) limit; the
average in-network MOOP is approximately $4,680 in 2023.
11
Fee-for-Service Medicare has no cap on total annual
OOP costs. Most Medigap plan designs do not offer an explicit cap on total OOP costs, but significantly limit
beneficiary cost sharing. Care management programs and provider networks included in MA plans are designed, in
part, to generate savings, though they may be viewed by beneficiaries as limiting choice or creating administrative
barriers.
12
Medigap plans, while relatively more expensive, do offer an option to Medicare beneficiaries for maximizing provider
choice and minimizing variability in OOP costs. These plans tend to offer premiums in excess of the reduction in
expected OOP costs they provide, but with a hard cap on beneficiary costs for Medicare-covered services. In the
case of Plan G, this cap is $226 in 2023, which is the Part B deductible. Medigap plans, however, do not offer
protection for services not traditionally covered by Medicare FFS, such as drugs, vision, and dental.
KEY FINDINGS RELATIVE TO 2020 REPORT
Relative to our prior report, which outlined beneficiary estimated annual health care costs for 2020, we expect that a
beneficiary’s total annual health care costs for those enrolled in MA-PD plans will decrease by about $160 in 2023
relative to 2020, despite the Part B premium increasing in that timeframe. We expect beneficiaries in FFS and with a
PDP, whether they purchase a Medigap plan to supplement coverage under Part A and Part B or not, will face higher
11
By regulation, an MA plan’s in-network maximum out-of-pocket limit (MOOP) may not exceed $8,300 in 2023.
12
O'Connor, J.T. & Spector, J.M. (July 2, 2014). High-Value Healthcare Provider Networks. Milliman Report. Retrieved September 12, 2019, from
https://www.ahip.org/wp-content/uploads/2016/02/High-Value-Provider-Networks-Issue-Paper-2014_07_01.final-pdf.pdf.
$3,396
$3,138
$3,837
$5,597
$5,021
$6,573
$6,200
$5,726
$7,092
$0
$1,000
$2,000
$3,000
$4,000
$5,000
$6,000
$7,000
$8,000
Average Medicare Beneficiary 65-Year Old Medicare Beneficiary 85-Year Old Medicare Beneficiary
MA-PD FFS, PDP FFS, PDP, Medigap Plan G

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 3 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
annual health care costs in 2023 relative to 2020. Note that the 2020 costs from our prior report did not include the
impact of the COVID-19 pandemic.
Medical OOP costs for Medicare-covered services remain flat for the average MA-PD beneficiary relative to 2020,
offsetting medical cost trends, which generally exceed overall inflation. Out-of-pocket costs for these same core
services will be higher, relative to 2020, for beneficiaries choosing FFS, and Medigap premiums increase
correspondingly, mirroring the increase in OOP costs for FFS beneficiaries. On the pharmacy side, Part D OOP costs
for MA-PD beneficiaries decreased approximately $80 relative to 2020, while corresponding Part D OOP costs for
PDP, for FFS and Medigap beneficiaries, decreased approximately $40 in the same period.
A portion of total annual health care costs is attributable to premiums. All beneficiaries pay the Part B premium,
unless eligible for income-related subsidies. Beneficiaries who enroll in MA and Medigap plans pay additional
premiums for these coverage options, though some MA plans are offered with no additional premium. The average
member premium for MA-PD plans decreased relative to 2020 from $300 per member per year to $189 in 2023. This
is due to a large increase in the number of plans offering $0 premiums and beneficiaries choosing to enroll in those
plans. Nearly three-quarters of all members enrolled in MA-PD plans in 2023 will be in a $0 premium plan, up from
60% of members in 2020. Annual Part B premiums increased $244 between 2020 and 2023; however, some MA-PD
plans offer a Part B premium “buydown,” offsetting Part B premiums. The value of the Part B buydown benefit for MA-
PD beneficiaries has increased by $40 since 2020, resulting in a lower effective Part B premium increase for MA-PD
beneficiaries relative to FFS and Medigap beneficiaries.
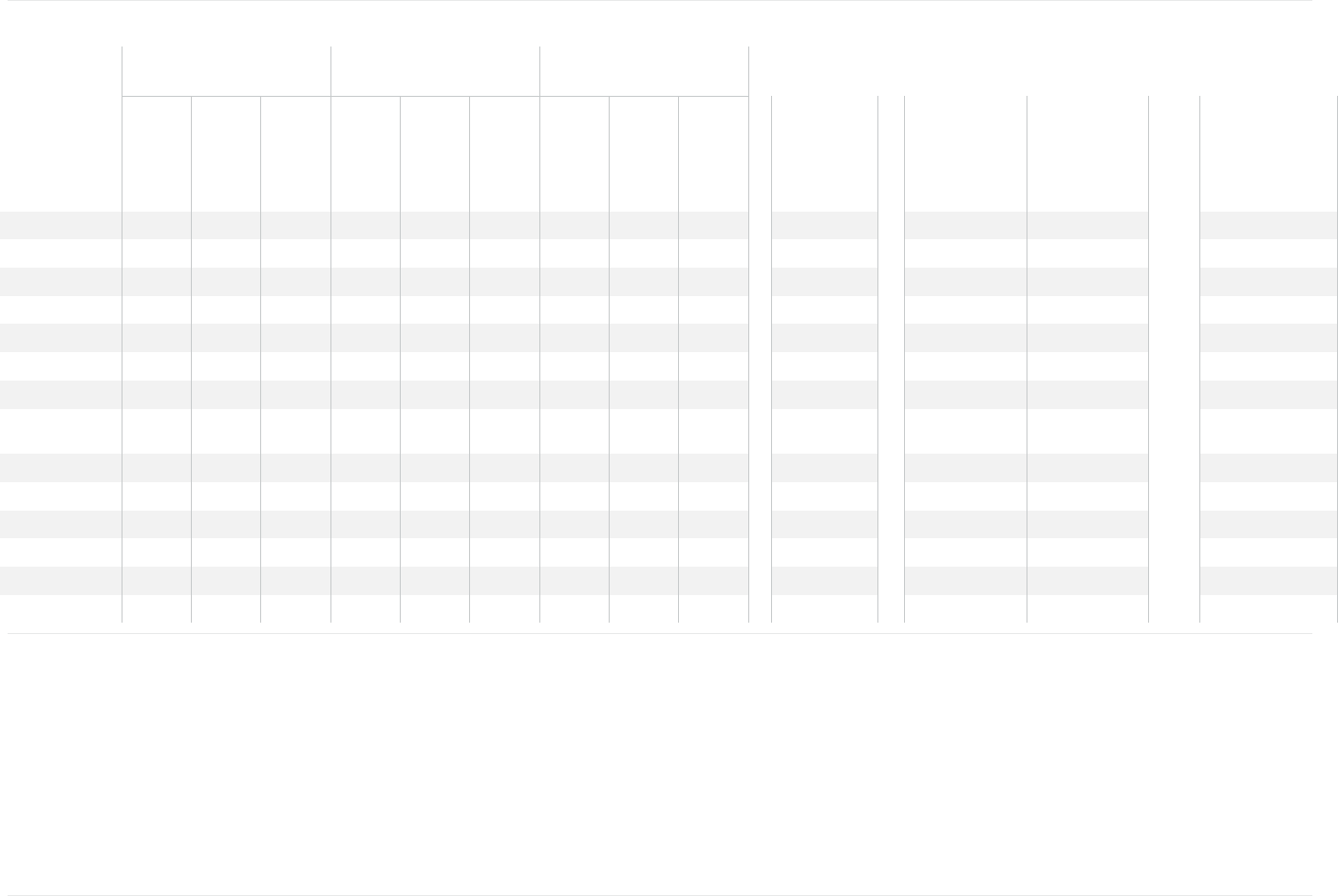
FIGURE 2: CHANGES IN ANNUAL BENEFICIARY COSTS BETWEEN 2020 AND 2023 FOR A SENIOR OF AVERAGE AGE
Category
2020
2023
Change
Annual Premiums
MA-PD beneficiaries
$2,013
$2,106
$93
FFS and PDP beneficiaries
$2,186
$2,470
$284
FFS, PDP, and Medigap beneficiaries
$4,393
$4,901
$509
Medical OOP costs for Medicare-covered services
MA-PD beneficiaries
$857
$854
($3)
FFS and PDP beneficiaries
$1,773
$2,053
$280
FFS, PDP, and Medigap beneficiaries
$198
$226
$28
Drug OOP costs
MA-PD beneficiaries
$471
$388
($83)
FFS and PDP beneficiaries
$659
$622
($38)
FFS, PDP, and Medigap beneficiaries
$659
$622
($38)
Dental, Vision, & Hearing OOP costs
MA-PD beneficiaries
$217
$48
($169)
FFS and PDP beneficiaries
$742
$452
($291)
FFS, PDP, and Medigap beneficiaries
$742
$452
($291)
Total annual health care costs
MA-PD beneficiaries
$3,558
$3,396
($162)
FFS and PDP beneficiaries
$5,361
$5,597
$236
FFS, PDP, and Medigap beneficiaries
$5,992
$6,200
$208
Note: The sum of individual components in this figure may not equal totals due to rounding.
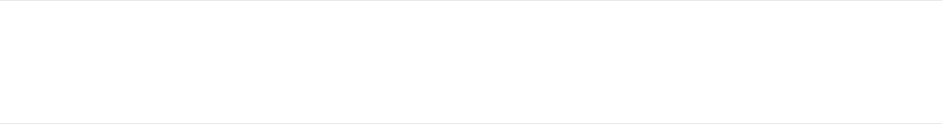
For the remainder of this report, we will refer to the dental, vision, and hearing non-Medicare covered services as
“supplemental benefits.” These costs have decreased about $170 annually for MA-PD members, partly driven by a
substantial increase in the number of MA-PD beneficiaries enrolled in plans newly offering these services relative to
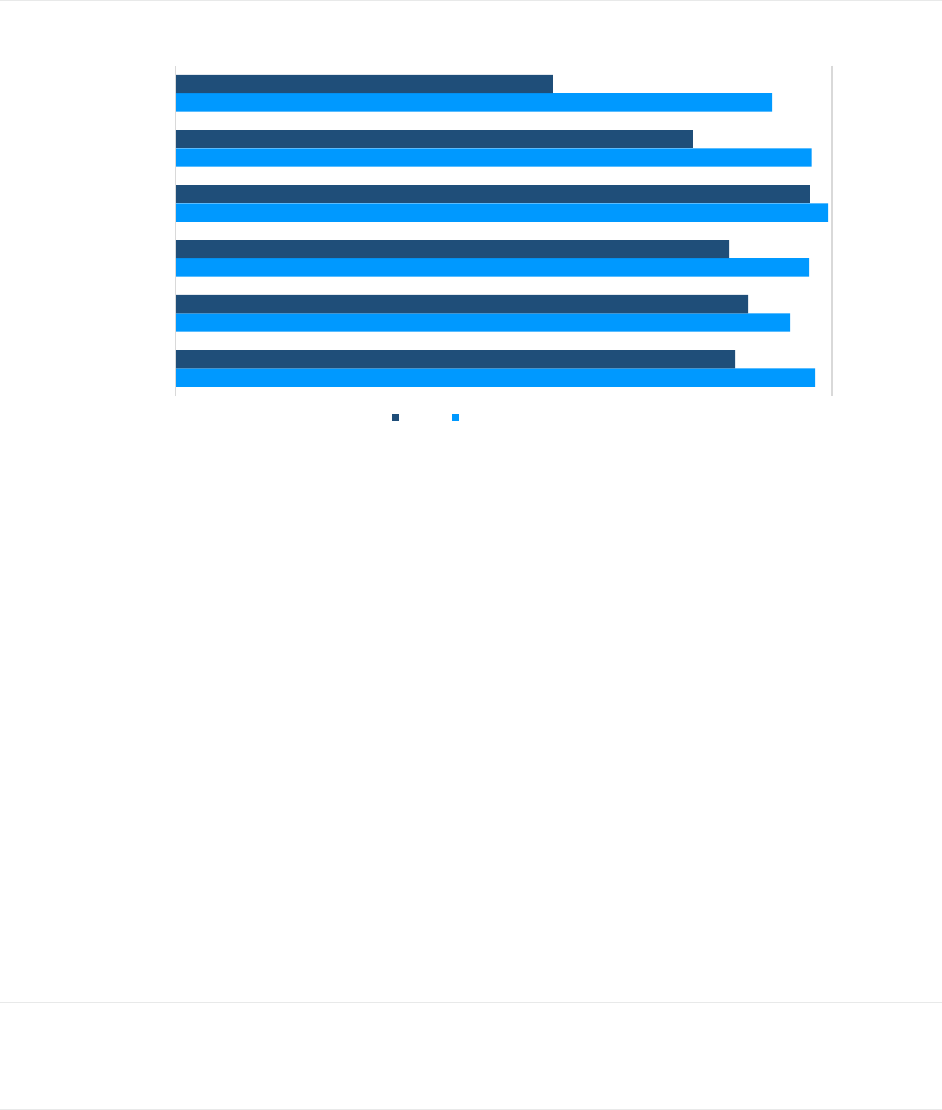
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 4 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
2020. In the absence of these benefits, we estimate that Medicare beneficiaries will pay $452 OOP annually in 2023
for these services. The decrease in the supplemental benefit cost estimate relative to our 2020 report is primarily
driven by a refinement in our dental modeling. As substantially more MA plans have offered dental benefits since
2020, we made refinements to more accurately reflect expected Medicare beneficiary dental costs. The percentage of
non-SNP MA beneficiaries receiving these supplemental benefits in 2020 and 2023 is shown in Figure 3.
13
FIGURE 3: PERCENT OF BENEFICIARIES ENROLLED IN PLANS OFFERING SELECT SUPPLEMENTAL BENEFITS
2. BACKGROUND
UnitedHealth Group (UHG) commissioned Milliman to compare the beneficiary costs of the Medicare Advantage (MA)
program relative to other public and private health insurance options available to seniors. In this report, we highlight
differences in average annual beneficiary health care costs (i.e., premiums and cost sharing) among Medicare
coverage options. We also describe several qualitative differences among the options.
The options analyzed, described in detail below, include Medicare Advantage (MA), Traditional Medicare Fee-For-
Service (FFS), Prescription Drug Plans (PDPs), and Medicare Supplement policies (Medigap). We do not analyze
options subsidized by employers for active or retired employees, nor do we analyze options for Medicare
beneficiaries receiving financial assistance from Medicaid or other programs due to income.
▪ Medicare Advantage: Medicare Advantage Organizations (MAOs) contract with the Centers for Medicare and
Medicaid Services (CMS) to offer privately managed insurance plans covering Part A, Part B, and frequently
Part D (prescription drug) services—they are known as Medicare Advantage and Prescription Drug (MA-PD)
plans. The MA program is an alternative to FFS, and beneficiary premiums for MA-PD coverage vary from $0
to over $3,600 per year in 2023, with an average of $189 in addition to the standard Medicare Part B premium
($1,979 per year in 2023). In many cases, additional health care services not covered by FFS are offered by
MAOs, known as ancillary or supplemental benefits. These types of services vary widely by MA plan and
include benefits such as hearing, vision, dental, over-the-counter (OTC) drug cards, and non-emergency
medical transportation (NEMT). MAOs, through capitated payments from CMS, are incentivized to manage and
coordinate the care of the beneficiaries enrolling in their plans.
13
Laktas J., Yeh, M., & Friedman, J. (March 2023) Prevalence of Supplemental Benefits in the general enrollment Medicare Advantage marketplace:
2019 to 2023. Retrieved March 21, 2023, from https://www.milliman.com/en/insight/prevalence-supplemental-benefits-general-enrollment-ma-
marketplace-2023.
97%
94%
96%
99%
97%
91%
85%
87%
84%
97%
79%
57%
0% 100%
Hearing Hardware
Hearing Exams
Vision Hardware
Vision Exams
Preventive Dental
Comprehensive Dental
2020 2023

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 5 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
▪ Traditional Medicare FFS (FFS): Only Part A (facility services) and Part B (ambulatory services) services are
covered by FFS, so beneficiaries opting for FFS must select a PDP plan or have some alternative drug
coverage, such as Veterans Administration coverage or employer-provided insurance, if they would like
coverage for pharmacy costs. All FFS beneficiaries pay a premium for Part B services, which is $1,979 per
year in 2023. Higher-income beneficiaries may pay higher Part B premiums than the standard amount. Those
who are enrolled in FFS can go to any doctor or hospital that accepts Medicare.
▪ Prescription Drug Plans (PDP): While Part D benefits are typically bundled with MA-PD coverage, PDP
organizations contract with CMS to provide Part D plans that cover only prescription drug benefits—mainly for
FFS beneficiaries (including those who enroll in Medigap plans). Premiums for PDP plans in 2023 range from
just under $24 to over $2,400 per year, with an average of about $491 per year. If a beneficiary is not enrolled
in an MA-PD plan that provides both medical and drug coverage, they must enroll in a PDP plan to avoid facing
penalties from CMS.
14
▪ Medigap: Those in FFS can purchase private supplemental “wraparound” insurance known as Medigap
15
,
16
for
a premium, in addition to the standard Part B premium paid by Medicare beneficiaries. Medigap plans, such as
Plan G,
17
are purchased from private insurance companies. Plan G is currently the most comprehensive and
most popular Medigap plan actively sold on the market and, therefore, commands high premiums. The
premiums are exchanged for certainty in OOP costs; Plan G covers all OOP costs for Medicare covered
services but the Part B deductible. The high premiums are driven by the need for an administrative cost and
profit load, as well as what some argue to be induced utilization due to lack of beneficiary cost sharing,
18
and
the lack of tools to control underlying cost and utilization of medical services.
19
Less generous Medigap plans
are available, with lower premiums to reflect leaner benefits. Medigap plans do not offer coverage for services
not otherwise covered by FFS, including prescription drug coverage, so any coverage for services not covered
by FFS must be obtained separately. Beneficiaries who choose MA are not eligible to purchase Medigap plans.
Most Medicare beneficiaries are on a fixed income, with half having annual incomes below $29,650 as of 2019.
20
In
order to mitigate the unexpected OOP costs associated with FFS coverage, and because FFS does not have a
maximum limit on a beneficiary’s annual OOP costs, many beneficiaries choose MA-PD plans or Medigap plans to
replace or supplement their FFS coverage, respectively. Additionally, MA plans offer supplemental benefits beyond
those offered by FFS or Medigap plans, such as integrated prescription drug coverage, hearing, dental, and vision.
Approximately 22% of non-institutionalized Medicare beneficiaries choose Medigap, while 45% choose Medicare
Advantage, and 9% choose Medicare FFS only
21
,
22
. The remainder obtain supplemental coverage via their employer,
Medicaid, or other public sector programs, such as the VA. In this report, we provide estimates of beneficiary health
care costs associated with each of these programs for an average aged beneficiary (that is, the average of all
Medicare beneficiaries ages 65 and older), as well as a new entrant into Medicare (age 65) and an older Medicare
enrollee (age 85). We also review plan features that beneficiaries may consider when selecting a type of coverage.
14
Note, members who enroll in MA-only plans are not the focus of this paper because they typically have their pharmacy needs covered under
something other than Part D, like creditable coverage from an employer or the Veterans Administration. Beneficiaries in MA-only plans are restricted
from buying PDP coverage except in very limited circumstances.
15
Medigap is also known as Medicare Supplement.
16
Medigap is not technically health insurance. It is insurance against the potential of very high cost sharing under FFS—that is, it provides financial
indemnification for cost sharing associated with health events where the primary insurance is FFS.
17
There are 10 standardized Medigap plan designs, designated by letters A through N. Three states, Massachusetts, Minnesota, and Wisconsin, have
different standardized plans through federal waivers.
18
Induced utilization is the expected increased use of a benefit or service when a person is protected from its financial consequences, e.g., by
insurance.
19
Medigap plans lack the traditional tools used by health insurers to contain costs, such as care management and negotiation with providers.
20
Kaiser Family Foundation, Medicare Beneficiaries’ Financial Security Before the Coronavirus Pandemic, 2019, op cit.
21
MedPAC July 2023 Data Book: Health Care Spending and the Medicare Program, Section 3: Medicare beneficiary and other payer financial liability.
Retrieved August 18, 2023, from https://www.medpac.gov/wp-content/uploads/2023/07/July2023_MedPAC_DataBook_SEC.pdf.
22
The July 2023 MedPAC Data Book uses 51.6 million non-institutionalized Medicare beneficiaries and the Medicare Current Beneficiary Survey
(MCBS) from 2020 as the basis for their supplemental coverage analysis. In other parts of this report, we use all 59.8 million Medicare beneficiaries
enrolled in Medicare Part A and Part B, subject to limitations outlined, as the basis of our analyses.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 6 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
The demographic makeup of seniors choosing various coverage options differs; however, we adjust for this in our
analysis using publicly available cost data and Milliman proprietary benchmark claim data. Over half of Medicare
beneficiaries are female, with the mix differing between MA (56%), FFS (50%), and Medigap (57%). Beneficiaries
over the age of 75 are more prevalent in both MA (39%) and Medigap (45%) than in FFS (31%). Around half of
beneficiaries in MA (48%) and in FFS (48%) have incomes less than twice the federal poverty level, while about one-
quarter of the Medigap members have an income less than twice the federal poverty level. This report focuses on
beneficiaries not eligible for government subsidies due to income, as discussed above.
23
This report provides results specific to average annual health care costs (premium and cost sharing) borne by
beneficiaries in the above age groups. Results exclude beneficiaries receiving additional assistance from Medicaid,
beneficiaries obtaining active employee or retiree coverage through an employer, beneficiaries in MA Special Needs
Plans (SNPs), and institutionalized beneficiaries (i.e., beneficiaries residing in nursing homes or other long-term care
facilities). We assume that the sample beneficiaries analyzed in the report obtain coverage for pharmacy costs
through either an MA-PD plan or a PDP plan.
23
MedPAC July 2023 Data Book: Health Care Spending and the Medicare Program, Section 3: Medicare beneficiary and other payer financial liability.
Retrieved August 18, 2023, from https://www.medpac.gov/wp-content/uploads/2023/07/July2023_MedPAC_DataBook_SEC.pdf.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 7 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
3. NATIONWIDE COMPARISON OF THE COVERAGE VALUE TO
MEDICARE BENEFICIARIES
We estimated average annual health care costs for Medicare beneficiaries under three different coverage options, using
publicly available premium, enrollment, and benefit data, as well as proprietary Milliman MA-PD pricing models. We
analyzed these coverage options for three groupings of Medicare beneficiaries intended to represent beneficiaries of
average health status at various ages: average age non-dual beneficiaries eligible for Medicare due to age,
24
average 65-
year-old newly eligible Medicare beneficiaries, and average older Medicare beneficiaries, with an average age of 85. For
each coverage option and average beneficiary age grouping, we examine average annual OOP costs for cost sharing (i.e.,
copays, deductibles, and coinsurance), insurance premiums, and other OOP costs for health-related products and services
on a calendar year (CY) 2023 basis.
The three coverage options are as follows:
Medicare Advantage coverage: This scenario reviews the medical, pharmacy, and ancillary benefit OOP
costs, as well as total premiums paid by the member—MA-PD premium and Part B premium—under the MA
program. This coverage option assumes that all members choose to obtain Part D coverage under an MA-
PD plan, and that supplemental benefits (like dental, vision, and hearing) are partly covered by the MA-PD
plan.
Traditional Medicare FFS and PDP coverage: This scenario reviews the medical OOP costs for Medicare-
covered services under FFS and pharmacy OOP costs under a PDP plan and the premiums for Part B and
PDP coverage, as well as the expected costs of additional supplemental benefits that are not covered under
FFS.
Traditional Medicare FFS, PDP, and Plan G Medigap coverage: This scenario assumes that, in addition
to FFS and PDP coverage, all members purchase the richest available Medigap plan on the market—Plan
G. Average PDP and Part B premiums are included in this scenario as well. Results would be different for
enrollees that choose leaner Medigap plans, which have lower premiums but cover fewer OOP costs for
beneficiaries. Also, we consider the expected OOP costs for the Part B deductible (not covered by Plan G);
for additional core supplemental benefits, defined in our analysis as dental, vision, and hearing, that are not
covered under FFS; and for drugs under the PDP plan, which are not covered by Medigap plans.
24
The average Medicare beneficiary in our analysis is approximately 73 years old and of average health for a beneficiary eligible for Medicare due to
age. We exclude beneficiaries dually-eligible for Medicare and Medicaid, as well as those eligible for Medicare due to disability and/or end-stage
renal disease (ESRD). Both groups are known to have extremely different cost profiles and they are also limited in their coverage options,
particularly under Medigap.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 8 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
Nationwide comparison of annual health care costs for an average aged Medicare enrollee
Figure 4 illustrates our estimates of average annual health care costs for an average aged Medicare beneficiary, split
by type of cost to the beneficiary.
FIGURE 4: ESTIMATED ANNUAL HEALTH CARE COSTS FOR AVERAGE AGED BENEFICIARY, BY TYPE OF COST
Note: The sum of individual components in this figure may not equal totals due to rounding.
MA-PD plan coverage has the lowest overall average total annual health care costs for beneficiaries, followed by FFS
with PDP coverage. The Medigap coverage option analyzed has a higher average total annual cost than either the
MA-PD or FFS with PDP options, though Medigap enrollees generally exchange higher premiums for limited
variability in annual OOP costs and expanded provider availability.
The average annual costs for a beneficiary who chooses Medigap Plan G are $604 higher annually than an average
beneficiary who forgoes Medigap coverage and only has Medicare FFS and PDP coverage, and they are about
$2,805 higher than for an average beneficiary who chooses to purchase an MA-PD plan. These costs are intended to
represent the average, and an individual beneficiary will experience different costs based on that person's own
circumstances.
These differences in OOP costs also indicate that the estimated actuarial value for the MA-PD coverage is 91.3%,
while the actuarial value for the FFS coverage options is 83.9%.
25
Said another way, for every dollar of health care
cost, MA-PD plans pay 91.3 cents and the member cost sharing is 8.7 cents. Similarly, under each of the two FFS
coverage options, FFS pays 83.9 cents of every dollar of health care costs, while the member pays the remaining
16.1 cents through cost sharing.
25
We define actuarial value as the percentage of total Medicare-covered claim costs that are covered by each coverage option, i.e., (Payer Liability /
[Payer Liability + Member Cost Sharing]). Claim costs are for core Medicare-covered benefits plus pharmacy claims, and exclude ancillary benefits,
such as dental, vision, and hearing. Pharmacy claims exclude the impact of federal subsidies and rebates.
$1,917
$1,979 $1,979
$189
$491 $491
$2,431
$48
$452
$452
$388
$622
$622
$854
$2,053
$226
$3,396
$5,597
$6,200
$0
$1,000
$2,000
$3,000
$4,000
$5,000
$6,000
$7,000
MA-PD FFS, PDP FFS, PDP, Medigap Plan G
Medicare Covered Medical OOP
Part D OOP
Supplemental OOP
Medigap Premium
PDP Premium
MA-PD Premium
Part B Premium

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 9 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
Some drivers of the differences in annual health care costs across coverage options are as follows:
MA-PD plans: MAOs attract and retain members by offering lower cost sharing, which is required to be at
least equivalent to, but is generally better than, FFS cost sharing, at a competitive premium. Based on our
analysis, shown in Figure 4, the average annual health care costs for an MA-PD member are lower than
those of FFS and Medigap members for reasons that include the following:
− MA plans provide care management and coordination for their members, including directing members to
specific services and providers to manage their health care, as well as disease management programs
aimed at improving health outcomes. Utilization management typically generates cost savings but can
be viewed as a limitation by some beneficiaries, as they may be required to obtain prior authorization,
use specific providers, or try alternative treatments during the course of care.
− Furthermore, MA plans typically provide a selection of supplemental benefits for no additional premium,
often with no or low cost sharing, to attract membership, as well as to assist in care management. In our
estimates listed above, we included only dental, vision and hearing cost sharing under each coverage
option. We estimate the average MA-PD member pays approximately $48 annually OOP for dental,
vision and hearing supplemental benefits in 2023, compared to $452 for beneficiaries choosing FFS
with or without Medigap, a $404 difference in OOP costs. MA plans also usually offer additional
supplemental benefits that members may choose to forgo without coverage, such as cards to subsidize
OTC drugs, NEMT, or fitness benefits. On average, MA-PD plans offer additional supplemental benefits
worth $190 in 2023. These benefits vary significantly by plan.
− MA plans may also implement provider networks, some of which limit coverage to a specific subset of
providers. Medicare Health Maintenance Organization (HMO) plans offer lower cost sharing to
beneficiaries by limiting the network to a defined set of preferred providers. Preferred Provider
Organization (PPO) and point-of-service (POS) plans may offer lower cost sharing to members if they
choose providers specified by the MA plan, but still allow the member the option of going outside the
network.
− MA plans implement an in-network maximum out-of-pocket (MOOP) cost limit for beneficiaries. While
the regulatory in-network annual maximum is $8,300 in 2023,
26
many MA-PD plans offer lower MOOP
limits—in 2023, the average MOOP in MA-PD plans is just under $4,680. FFS has no such limit on a
beneficiary’s OOP medical costs, making the MOOP particularly important for those members who are
likely to incur high medical costs.
PDP plans: PDP plans generally offer leaner Part D benefits, in the form of higher cost sharing and a more
restrictive formulary, than MA-PD plans, which results in higher drug-related health care costs for FFS and
Medigap members relative to MA-PD members.
Medigap plans: While the magnitude of OOP costs for FFS members may not be known in advance, it is
generally assumed that beneficiaries choosing Plan G knowingly do so to “lock-in” OOP costs for Medicare-
covered services. As a result, the premiums for Plan G significantly exceed average Medicare-covered health
care costs under FFS (approximately $2,400 vs. $2,000) in order to cover administrative costs, profit, and risk
loads inherent in Medigap premiums, as well as what some argue to be induced utilization caused by the lack
of beneficiary cost sharing—that is, beneficiaries are able to obtain covered care without limits or any utilization
management controls.
27
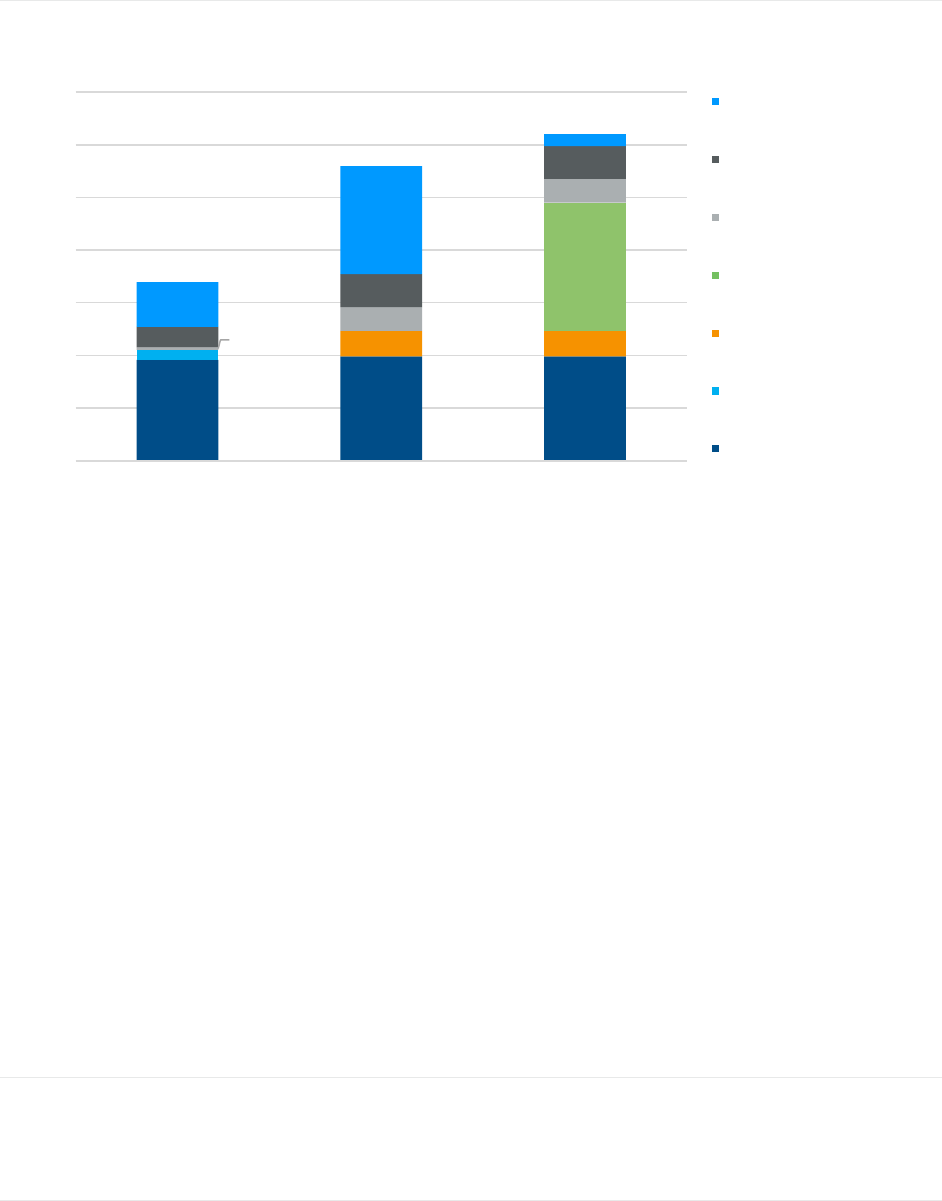
Average lifetime cost differential for 65-year-old Medicare beneficiary
A typical 65-year-old will live for an average of about 21 more years, or through age 85.
28
,
29
We projected the annual
health care costs of each Medicare coverage option for the average 65-year-old using assumptions for medical cost
inflation and cost increases due to age, and then summed these costs over the average expected lifetime to
26
The regulatory in-network maximum was raised to $8,300 in 2023 by CMS.
27
Induced utilization is a term used by actuaries to describe increased use in health care services due to moral hazard.
Moral Hazard in Health Insurance: What We Know and How We Know it. Retrieved December 1 2020, from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6128379.
28
https://www.ssa.gov/planners/lifeexpectancy.html
29
The Social Security Administration website calculates different life expectancies for male and female, which are both slightly different than 21 years.
However, we used 21 years for this lifetime calculation because the male and female life expectancies average to approximately 21 years.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 10 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
demonstrate the total expected financial outlay over that same timeframe. FFS, PDP and Plan G represent
approximately $111,889 more in health care costs compared to MA-PD, while FFS and PDP represent $77,582 more
than MA-PD over the same 21-year time horizon.
FIGURE 5: ESTIMATED FUTURE LIFETIME HEALTH CARE COSTS FOR AVERAGE 65-YEAR-OLD BENEFICIARY, BY COVERAGE OPTION
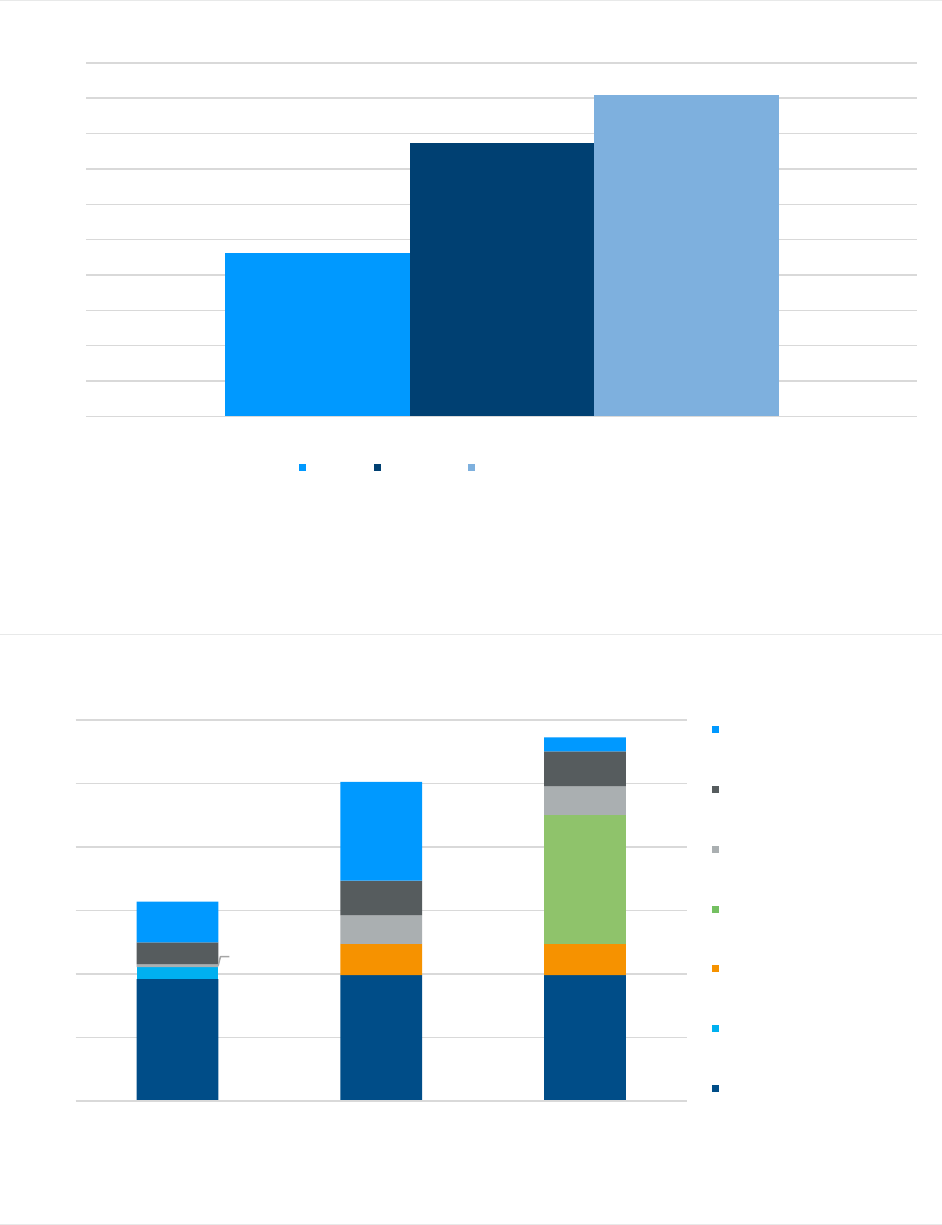
Annual health care costs for specific age groupings
The differences in costs between coverage options for the average beneficiary, shown in Figure 4, holds for an
average 65-year-old newly eligible Medicare beneficiary, as well as for older Medicare beneficiaries. Figure 6
illustrates our estimates of average annual health care costs for an average 65-year-old Medicare beneficiary, split by
type of cost to the beneficiary.
FIGURE 6: ESTIMATED ANNUAL HEALTH CARE COSTS FOR AVERAGE 65-YEAR-OLD BENEFICIARY, BY TYPE OF COST
Note: The sum of individual components in this figure may not equal totals due to rounding.
$115,451
$193,033
$227,340
$0
$25,000
$50,000
$75,000
$100,000
$125,000
$150,000
$175,000
$200,000
$225,000
$250,000
Total Lifetime Expenditures
MA-PD FFS, PDP FFS, PDP, Medigap Plan G
$1,917
$1,979 $1,979
$189
$491 $491
$2,033
$48
$452
$452
$345
$546
$546
$639
$1,554
$226
$3,138
$5,021
$5,726
$0
$1,000
$2,000
$3,000
$4,000
$5,000
$6,000
MA-PD FFS, PDP FFS, PDP, Medigap Plan G
Medicare Covered Medical OOP
Part D OOP
Supplemental OOP
Medigap Premium
PDP Premium
MA-PD Premium
Part B Premium
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 11 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
Similar to the average beneficiary results, an average 65-year-old new entrant to Medicare can expect to incur lower
annual health care costs under an MA-PD plan than under the combinations of FFS and PDP, with or without
Medigap coverage ($1,884 to $2,588 lower). This differential is smaller than for the average beneficiary ($2,201 to
$2,805 lower). The primary driver of the difference in annual health care costs between options at age 65 relative to
the average Medicare beneficiary is the Medigap premium, which varies by age in most states. The 65-year-old
Medigap member will have lower premiums than the average Medigap member. MA-PD plans, in contrast, are
community-rated i.e., the rates do not vary by age, gender, or health status. As such, the MA-PD premium is the
same for a 65-year-old as it is for a beneficiary at any other age. These costs are intended to represent the average
for a 65-year-old. Individual beneficiaries will experience different costs based on that person’s own circumstances.
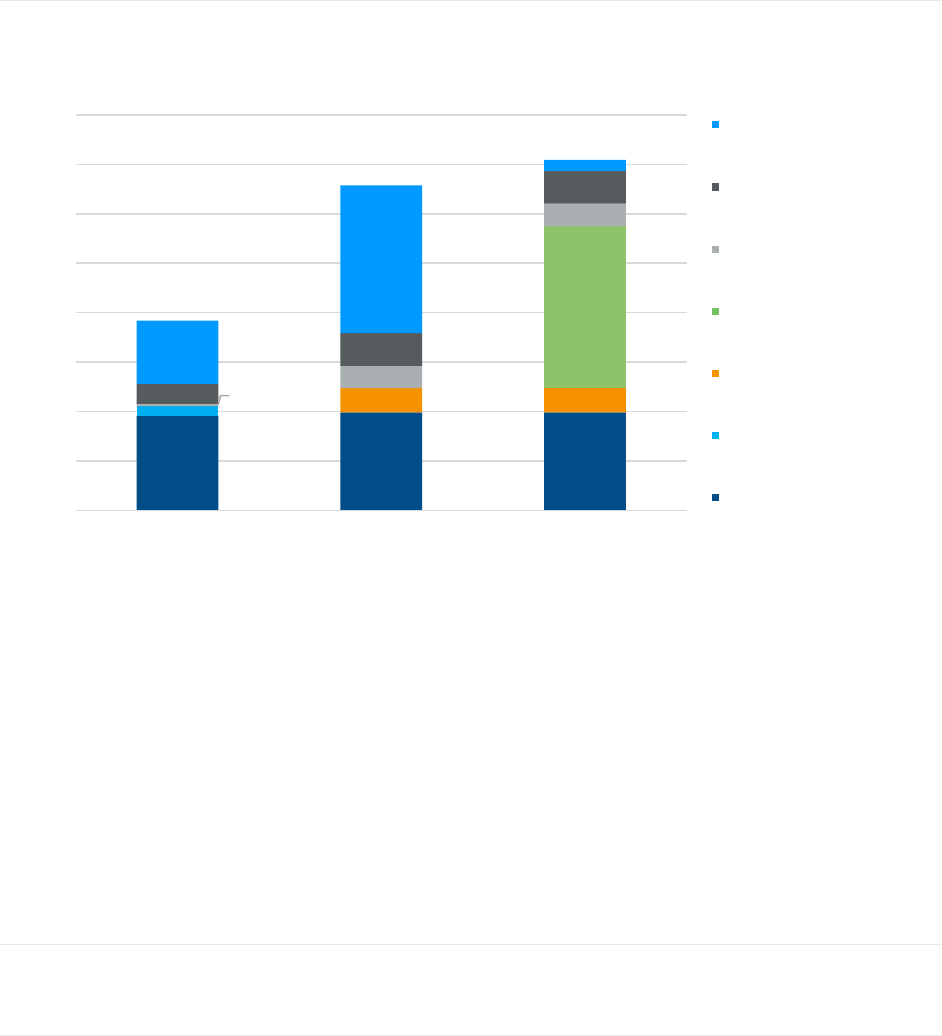
Figure 7 illustrates our estimates of average annual health care costs for an average 85-year-old Medicare
beneficiary, split by type of cost to the beneficiary.
FIGURE 7: ESTIMATED ANNUAL HEALTH CARE COSTS FOR AVERAGE 85-YEAR-OLD BENEFICIARY, BY TYPE OF COST
Note: The sum of individual components in this figure may not equal totals due to rounding.
Similar to the previous two examples, an average 85-year-old Medicare beneficiary can expect to incur lower annual
health care costs under an MA-PD plan than under the combinations of FFS and PDP, with or without Medigap
coverage (about $2,737 to $3,256 lower), though the differential between FFS and PDP with and without Medigap
narrows at this age, as Medigap premiums align more closely to FFS costs at higher ages.
30
The estimated annual
Medigap premiums in this scenario are much higher than in the previous average age beneficiary and average age
65-year-old scenarios. We also expect that medical and drug OOP costs will be higher in this scenario given the
morbidity of this population. These costs are intended to represent the average for an 85-year-old, and an individual
beneficiary will experience different costs based on that person’s own circumstances.
30
The narrower differential between FFS and PDP-only and FFS and PDP with Medigap Plan G at age 85 relative to the differential for the age 65 and
for the average age cohorts may, in part, be due to higher up-front administrative costs and commissions associated with Medigap plans.
$1,917
$1,979 $1,979
$189
$491 $491
$3,283
$48
$452
$452
$402
$662
$662
$1,280
$2,990
$226
$3,837
$6,573
$7,092
$0
$1,000
$2,000
$3,000
$4,000
$5,000
$6,000
$7,000
$8,000
MA-PD FFS, PDP FFS, PDP, Medigap Plan G
Medicare Covered Medical OOP
Part D OOP
Supplemental OOP
Medigap Premium
PDP Premium
MA-PD Premium
Part B Premium

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 12 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
Considerations for beneficiaries who incur high health care costs
While our report focuses on averages within groupings of beneficiaries, for a beneficiary expecting to incur
significantly greater than average health care costs (for example, for Part B infusion medications), both Medigap
policies and MA plans (including MA-PD plans) offer financial protections in the form of a hard cap on OOP costs not
offered by FFS on its own. While all MA plans have an in-network MOOP of $8,300 or less as of 2023, most Medigap
plans limit total annual health care costs to significantly less than $8,300. To better understand which enrollees would
benefit from theses financial protections, we studied FFS claim data for enrollees with more than $8,300 in annual
OOP costs (i.e., cost sharing expenses) for Medicare-covered services.
Figure 8 demonstrates that only about 2.5% of FFS enrollees exceed $8,300 in annual OOP costs, with average
OOP costs of approximately $15,000 for those exceeding this amount. These beneficiaries incur approximately
$100,000 in annual claims and may incur lower OOP costs by choosing an MA-PD plan or a Medigap plan than FFS
coverage alone.
Further, beneficiaries who expect to have over $2,700 annually in OOP costs (the approximate average annual Plan
G premium plus the annual Part B deductible in 2023) for copays, coinsurance, and deductibles for Part A and Part B
services over a multiyear time horizon may incur lower OOP costs with a Medigap plan than with an MA-PD plan, as
beneficiaries in MA-PD plans may continue to accrue cost sharing up to $8,300, while a Plan G enrollee will not
accrue Medicare-covered costs beyond the Medigap premium and the Part B premium and deductible. However,
depending on MA plans available in a beneficiary’s geography, they may be able to purchase a Medicare Advantage
plan with a low MOOP to protect themselves against high OOP costs. In some instances, a beneficiary could enroll in
an MA-PD plan with a lower combined premium plus MOOP than the available Medigap Plan G premium plus the
annual Part B deducible. By purchasing an MA-PD plan, most of these beneficiaries are also able to access the
additional supplemental benefits offered by MA-PD plans but not covered by FFS or Medigap plans.
Average premiums for Plan G by year are included below for comparison with OOP costs for this high-cost
population.
Our analysis is based on 2023 benefits and premiums. Note that the COVID-19 pandemic affected 2020 medical
costs. Nonetheless, we include 2020 results from the CMS 5% Sample, as the values align with 2017 through 2019
amounts.
FIGURE 8: FFS ENROLLEES EXCEEDING $8,300 IN ANNUAL MEDICAL (PART A AND PART B) OUT-OF-POCKET COSTS
YEAR
SHARE OF FFS
ENROLLEES
AVERAGE ANNUAL
TOTAL CLAIMS
AVERAGE ANNUAL
MEMBER OOP COSTS
AVERAGE PLAN G
PREMIUM
2017
2.4%
$96,851
$14,191
$1,557
2018
2.6%
$98,022
$14,439
$1,530
2019
2.7%
$99,989
$14,671
$1,860
2020
2.5%
$101,424
$15,111
$2,206
Note: Results are based on 2017 to 2020 data from the CMS 5% Sample, and are limited to non-Dual, non-ESRD, and non-Hospice members from these
data sets, including those enrolled in FFS regardless of PDP or Medigap enrollment.
Additional considerations not measured by annual health care costs
The previous sections outlined the estimated annual health care costs for a Medicare beneficiary under various
coverage options. In addition to beneficiary costs, there are many additional considerations when a prospective
beneficiary is deciding what type of coverage is best for them. These additional considerations include, in no
particular order:
▪ Care management: Most MA plans provide care management and coordination. Many plan sponsors
incorporate programs to direct members to the specific services and sites of service in order to improve
access to preventive care and to coordinate the total care spectrum for members with numerous and
complex conditions. As such, members with complex health profiles may benefit from the coordinated and
holistic approach to their health care needs. In recent years, CMS has implemented a series of value-based
care programs (such as the Medicare Shared Savings Program), which encourage providers to coordinate

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 13 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
care delivery to benefit high acuity and complex members. However, these programs, if implemented
improperly, may burden the member due to administrative hurdles.
▪ Availability of supplemental benefits in Medicare Advantage: Many MA-PD plans offer ancillary
benefits, including but not limited to routine dental, vision, hearing, meals, NEMT, nutritional therapy, OTC
drugs, and gym memberships. In recent years, CMS has allowed greater flexibility for MA plans to offer
supplemental benefits, including provision of benefits that address social determinants of health. Relative to
our prior report, more MA-PD plans are offering benefits that address social determinants of health and
more beneficiaries are enrolled in plans offering such benefits.
Relative to our prior report, combo benefits (which allow plans to group together multiple supplemental
benefits under a single benefit limit) and reduction in cost sharing (RICS)
31
offerings are available to more
beneficiaries under recent benefit flexibilities available to MA plans. In 2023, approximately one-fourth of
beneficiaries enrolled in a non-SNP plan will be enrolled in a plan that offers a combined benefit with a
single limit covering multiple supplemental service categories.
32
Also, based on research from the 2023
Milliman MACVAT
®
, approximately one in 10 MA beneficiaries enrolled in a non-SNP plan will be enrolled in
a plan that offers a RICS benefit.
In contrast, FFS and Medigap policies do not include any supplemental benefits, and a member would have
to buy standalone plans or pay full OOP costs to receive these benefits or services. According to the 2017
Medicare Current Beneficiary Survey, the most frequently self-identified chronic condition is related to vision
(99.6% of respondents self-reporting as having vision issues).
33
Additionally, many Medicare beneficiaries
use OTC drugs. Many MA-PD plans offer an OTC drug benefit, which is valued at approximately $65 in
2023. Therefore, supplemental benefits are likely a significant source of OOP savings for MA-PD members
who need and utilize these supplemental services and benefits that are not covered under FFS.
▪ Existence of Special Needs Plans in Medicare Advantage: There are several types of SNPs in the MA
program, listed below. These plans may offer targeted ancillary benefits, which are not available in FFS, for
members who qualify based on their health conditions or income-based characteristics to address their
specific conditions or characteristics, such as maintenance drugs for members with diabetes and meals
benefits for low-income members in a dual eligible SNP.
− Chronic SNP (C-SNP): Plans for members with specified chronic conditions (e.g., diabetes, chronic heart
failure)
− Institutionalized SNP (I-SNP): Plans for members who are institutionalized in a nursing home, or
functionally impaired seniors living in the community
− Dual eligible SNP (D-SNP): Plans for members who are eligible for both Medicare and Medicaid
− ESRD SNP: Plans for members with ESRD
Special supplemental benefits for the chronically ill, uniformity flexibility, and value-based insurance
design benefits in Medicare Advantage: CMS encourages MAOs to offer coordinated care through these
various options to personalize the experience and to reduce health care costs for specific individuals who
need more intensive therapies. As of CY 2020 for special supplemental benefits for the chronically ill
(SSCBI), CY 2019 for uniformity flexibility (UF), and CY 2017 for value-based insurance design (VBID),
MAOs are allowed to design benefits that target a specific population, and these benefits may be offered
non-uniformly to members in plans with these offerings.
31
RICS benefits allow an MA-PD plan to reimburse any beneficiary in that plan for OOP costs up to a specific dollar amount for a defined set of
services. For example, a plan could offer a $500 RICS allowance on dental, vision, and hearing benefits. A particular member could incur OOP costs
for glasses, hearing aid, etc. and then be reimbursed by the plan for those OOP costs up to $500.
32
Friedman, J., Yeh, M. & Yen, I. (January 2023). 2023 Combined Benefits in Medicare Advantage: Tracking Benefit Strategy and Options. Retrieved
February 1, 2023 from https://us.milliman.com/en/insight/2023-combined-benefits-in-medicare-advantage-tracking-benefit-strategy
33
Milliman analysis of CMS-provided Medicare Current Beneficiary Survey Chartbook 2017, accessed November 19, 2020 from
https://www.cms.gov/research-statistics-data-and-systemsresearchmcbsdata-tables/2017-medicare-current-beneficiary-survey-annual-chartbook-
and-slides.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 14 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
Part D financial penalties: A beneficiary who goes without Part D or other creditable drug coverage after
their initial Medicare enrollment period will generally be liable for a late enrollment penalty on future PDPs, if
and when the beneficiary eventually enrolls.
34
Therefore, beneficiaries who actively choose to not enroll in
Part D for their lifetime may see potential premium savings; but if those same beneficiaries choose to enroll
in Part D later in life, they could face steep financial costs depending on the length of time they have gone
without Part D or other creditable drug coverage.
Guaranteed issue and premium protections in Medicare Advantage: General enrollment MA plans
(i.e., non-SNP) are guaranteed issue, with no underwriting. The only restriction to guaranteed issue in MA is
that potential SNP beneficiaries need to prove they are eligible for those MA-PD plan types. The same
premium is charged to each member, regardless of health status. Premiums may vary due to subsidies
available to low-income beneficiaries, but not due to age or health conditions. While MA plans can increase
their member premiums each year, there are strict filing restrictions around allowable premium increases. In
contrast, while Medigap policies are guaranteed issue at age 65, many Medigap policies allow underwriting
by age, health status, geography, and tobacco use, though some states only allow community rating.
Therefore, premiums typically vary widely for an individual depending on their demographic, geographic,
and/or health characteristics. In addition, many Medigap policies’ premiums increase as the member ages. It
is worth noting that Medigap premiums frequently increase with age, and future premiums are generally not
known by beneficiaries with certainty at the time they first enroll in their Medigap plans.
Beneficiary access to providers (e.g., network access): MA plans rely on provider networks to
coordinate care, implement programs, and reduce plan cost through preferred network rates. In an HMO, a
member going outside the network would not receive any insurance benefit and would be obligated to pay
all billed charges OOP. In a PPO, a member would pay the predetermined out-of-network benefit cost
sharing, which is typically less generous than in-network benefit cost sharing. As a trade-off for including
out-of-network access, many PPOs charge higher premiums. In contrast, FFS and Medigap policies typically
do not offer any restrictions on provider access and members would not need to verify that their physicians
and providers are in-network before receiving care or worry about unexpected bills for out-of-network labs or
procedures. Medigap “select” plans are an exception because they do have a preferred provider network for
Part A services, and, frequently, lower premiums as a trade-off for the network restriction.
Medigap plan offerings: Plan G is currently the most popular Medigap option because it covers all OOP
costs for Part A and Part B services except the Part B deductible for FFS beneficiaries, making it easy for
beneficiaries to plan their annual expected health care costs for that year. In 2023, the annual Part B
deductible is $226, the Part B Premium is $1,979, and the Plan G premium is approximately $2,430.
Because the Part B deductible is the only beneficiary cost sharing for Medicare-covered services under Plan
G, beneficiaries purchasing this plan will have a comprehensive Medigap option ensuring predictable annual
health care costs for Medicare-covered services in 2023.
Predictable medical costs in the future: Many seniors are on a fixed income each year. By enrolling in a
comprehensive Medigap plan like Plan G, they have more predictable medical OOP spending each year,
without dealing with the uncertainty of high cost sharing due to a long hospitalization or coverage of Part B
infusion medications under FFS and a PDP. The peace of mind for a beneficiary of having predictable OOP
costs each year without network restrictions is in some cases worth more to them than the actual higher
lifetime health care costs under Medigap. Additionally, as most Medigap policies allow underwriting, it is
advantageous to the beneficiary to purchase the coverage prior to a health event that may preclude them
from obtaining Medigap coverage.
34
This penalty is calculated as a percentage of the nationwide base beneficiary premium each year, which is $32.74 in 2023. The percentage
increases with the length of time between when a beneficiary first gains Medicare eligibility or their last period of creditable drug coverage, whichever
is later.

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 15 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
Demographic information
The demographic makeup of beneficiaries selecting various coverage options differs across several measures,
including gender, age, income, and geography. Figure 9 outlines several demographic measures across coverage
options for 2020. These metrics are calculated based on Medicare enrollment distributions from the MedPAC July
2023 Databook.
35
FIGURE 9: DEMOGRAPHIC INFORMATION FOR 2020
CATEGORY
MEDICARE ADVANTAGE
FFS EXCLUDING
MEDIGAP
MEDIGAP
ALL MEDICARE
BENEFICIARIES
GENDER
Male
44%
50%
43%
45%
Female
56%
50%
57%
55%
AGE GROUP
Younger than 65 Years
13%
21%
2%
13%
65 to 69 Years
23%
22%
26%
22%
70 to 75 Years
26%
25%
28%
25%
75 to 79 Years
17%
14%
21%
18%
80 to 84 Years
11%
9%
12%
11%
85 Years and Older
11%
8%
11%
11%
GEOGRAPHIC LOCATION
Urban
87%
75%
77%
82%
Rural
13%
25%
23%
18%
INCOME-TO-POVERTY RATIO
<1.0
17%
11%
4%
15%
1.0 to 1.2
9%
9%
4%
7%
1.2 to 1.35
9%
11%
5%
7%
1.35 to 2.0
14%
17%
11%
12%
>2.0
52%
52%
76%
59%
Note: The percentages in this table may not sum to 100 percent due to rounding.
35
MedPAC July 2023 Data Book: Health Care Spending and the Medicare Program, Section 3: Medicare beneficiary and other payer financial liability.
Retrieved August 18, 2023, from https://www.medpac.gov/wp-content/uploads/2023/07/July2023_MedPAC_DataBook_SEC.pdf.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 16 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
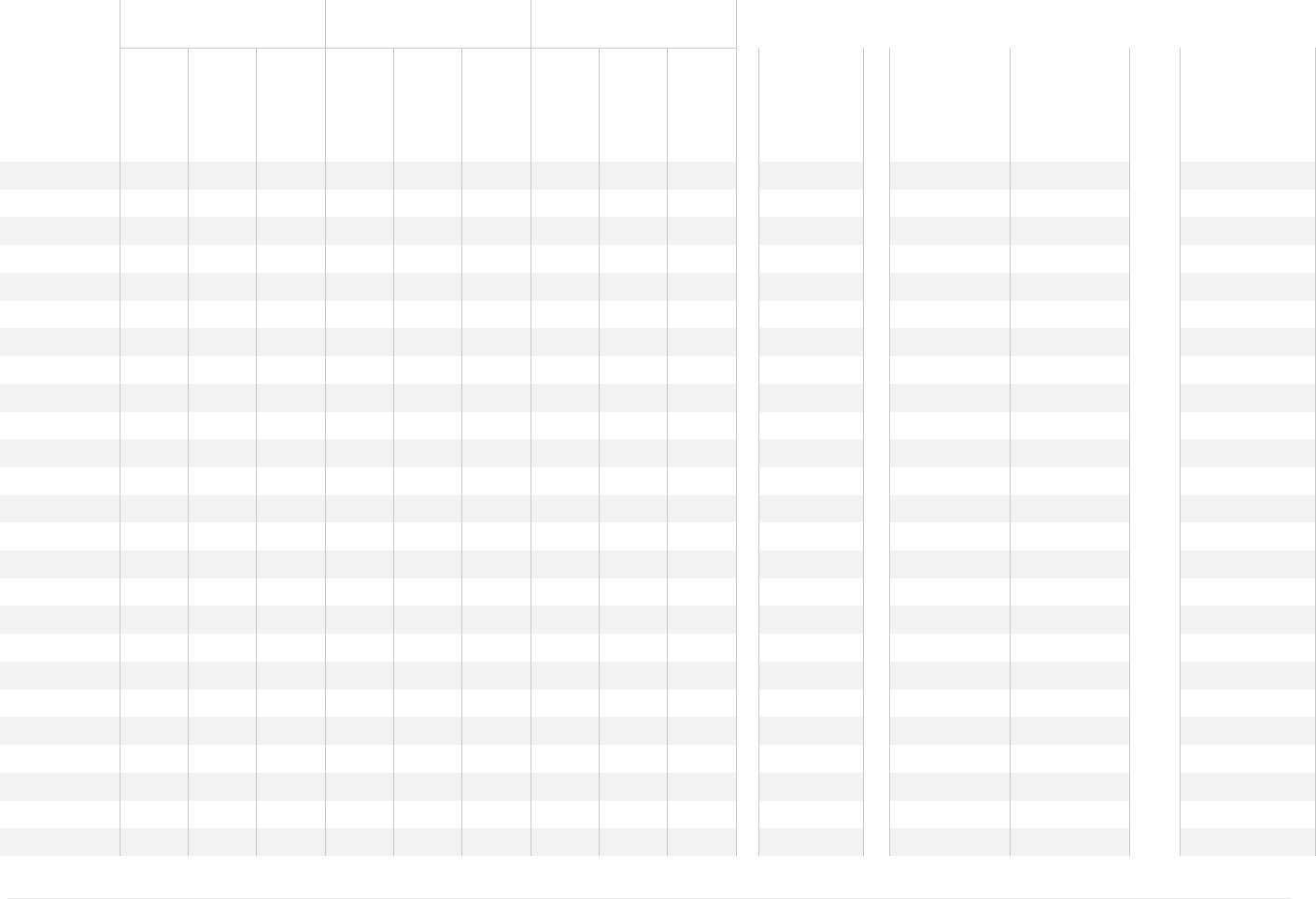
4. STATE-LEVEL RESULTS
Figure 10 details our analysis by state for each of the enrollment options discussed above, for an average Medicare
beneficiary. There is expected variation across each state and coverage option due to differences in cost and
utilization patterns, differences in MA-PD and PDP plan offerings, and Medigap premiums.
We excluded Alaska from the state level summary due to a lack of MA-PD plan offerings. We excluded all U.S.
territories due to the unique nature of the Medicare program in US territories.
Since Medigap is a product largely regulated at a state level, there are some differences in the structure of the rates
for beneficiaries of different ages. For example, states like Arkansas, Connecticut, Massachusetts, Maine, Minnesota,
New York, Vermont, and Washington do not allow age-issue underwriting, which means that rates are the same,
regardless of the age of a beneficiary when they choose to enroll. Three states—Massachusetts, Wisconsin and
Minnesota—do not offer standardized benefits. For these three states, we included rates for each set of state-level
Medigap products that correspond most closely to Plan G.
36
There is significant variation in MA-PD premiums across states. While the Part B premium is the same for all
beneficiaries, the MA-PD premium offered by health plans varies significantly by product type, geography, and plan
offerings. Notably, in Florida the premium is much lower due to the prevalence of $0 MA-PD premium plans and
plans offering Part B premium reductions. Conversely, in states such as North Dakota, South Dakota and Wyoming,
the MA-PD premiums are higher due to the low number of MA-PD plans, or plans are designed to mimic high-
premium Medicare Cost or Medigap plans, which are currently more prevalent in these less densely populated states.
36
The equivalent plans in these three states were determined to be: MA1 Supplement 1 for Massachusetts; Minnesota Basic Coverage with the Usual
and Customary Rider for Minnesota; Wisconsin Basic Coverage with the following riders: Part A Deductible Rider, Additional Home Health Rider,
Part B Excess Charges Rider, and Foreign Travel Rider.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 17 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
FIGURE 10 2023 OUT-OF-POCKET AND PREMIUM COSTS BY STATE (CONTINUED ON PAGES 19 AND 20)
MA-PD
FFS and PDP
FFS, PDP and
Medigap Plan G
State
Total
OOP
Cost
37
Total
Premium
38
Total
Cost
Total
OOP
Cost
39
Total
Premium
40
Total
Cost
Total
OOP
Cost
41
Total
Premium
42
Total
Cost
MA-PD Value
of
Supplemental
Benefits
43
FFS
and PDP
compared
to MA-PD
FFS, PDP, and
Medigap Plan G
Compared
to MA-PD
FFS, PDP, and
Medigap Plan G
Compared to FFS
and PDP Only
Alabama
44
$1,368
$2,028
$3,396
$3,176
$2,494
$5,669
$1,353
$4,587
$5,940
$154
167%
175%
105%
Arizona
$1,119
$1,997
$3,115
$3,037
$2,462
$5,499
$1,229
$4,744
$5,973
$209
177%
192%
109%
Arkansas
$1,439
$2,028
$3,467
$3,174
$2,424
$5,598
$1,361
$4,381
$5,741
$194
161%
166%
103%
California
$740
$2,081
$2,821
$3,058
$2,478
$5,536
$1,268
$5,114
$6,381
$192
196%
226%
115%
Colorado
$1,051
$2,090
$3,141
$2,932
$2,443
$5,376
$1,248
$4,651
$5,899
$205
171%
188%
110%
Connecticut
$1,906
$2,113
$4,019
$3,242
$2,490
$5,732
$1,275
$5,399
$6,673
$173
143%
166%
116%
Delaware
$1,325
$2,077
$3,401
$3,216
$2,500
$5,716
$1,292
$4,796
$6,088
$190
168%
179%
107%
District of
Columbia
$1,330
$2,271
$3,602
$2,856
$2,500
$5,356
$1,292
$4,914
$6,206
$172
149%
172%
116%
Florida
$1,048
$1,694
$2,742
$3,539
$2,528
$6,067
$1,310
$5,869
$7,180
$204
221%
262%
118%
Georgia
$1,473
$1,986
$3,459
$3,080
$2,479
$5,559
$1,328
$4,501
$5,828
$187
161%
169%
105%
Hawaii
$1,294
$2,574
$3,868
$2,384
$2,434
$4,818
$1,210
$4,526
$5,736
$128
125%
148%
119%
Idaho
$1,311
$2,211
$3,522
$2,856
$2,421
$5,277
$1,290
$4,743
$6,033
$185
150%
171%
114%
Illinois
$1,193
$2,105
$3,298
$3,212
$2,436
$5,647
$1,300
$4,707
$6,007
$205
171%
182%
106%
Indiana
$1,405
$2,042
$3,446
$3,116
$2,401
$5,517
$1,333
$4,426
$5,760
$201
160%
167%
104%
37
Milliman analysis of medical OOP costs, drug OOP costs, estimated OOP for dental, vision, and hearing supplemental benefits, based on plan design and described in the Methodology section.
38
Includes average Part C plan premium by state, in addition to Part B premium, reduced by the average state Part B Buydown.
39
Milliman analysis of Medicare FFS medical OOP costs, drug OOP costs for the average PDP, estimated OOP costs for dental, vision, and hearing supplemental benefits, assuming other or no coverage.
40
Includes Part B premium, as well as the average PDP premium.
41
Milliman analysis of medical OOP costs, accounting for Plan G plan design, drug OOP costs for the average PDP, estimated OOP for dental, vision, and hearing supplemental benefits, assuming other or no coverage.
42
This premium reflects average Medigap premium for Plan G in each state, in addition to Part B premium, and average PDP premium.
43
Dental, vision, and hearing OOP costs are excluded from this column because they are included in the Total OOP Cost.
44
The Alabama Medigap market has historically had a higher share of Medicare Select Medigap plans, offered by Blue Cross and Blue Shield of Alabama. We excluded Medicare Select products nationwide due to low
overall prevalence and the network requirement as a trade-off for lower premiums.
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 18 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
MA-PD
FFS and PDP
FFS, PDP and
Medigap Plan G
State
Total
OOP
Cost
37
Total
Premium
38
Total
Cost
Total
OOP
Cost
39
Total
Premium
40
Total
Cost
Total
OOP
Cost
41
Total
Premium
42
Total
Cost
MA-PD Value
of
Supplemental
Benefits
43
FFS
and PDP
compared
to MA-PD
FFS, PDP, and
Medigap Plan G
Compared
to MA-PD
FFS, PDP, and
Medigap Plan G
Compared to FFS
and PDP Only
Iowa
$1,327
$2,021
$3,348
$3,059
$2,386
$5,445
$1,324
$4,558
$5,882
$171
163%
176%
108%
Kansas
$1,330
$2,024
$3,354
$3,181
$2,363
$5,544
$1,344
$4,662
$6,006
$177
165%
179%
108%
Kentucky
$1,531
$2,014
$3,545
$3,134
$2,401
$5,535
$1,333
$4,581
$5,914
$224
156%
167%
107%
Louisiana
$1,293
$1,967
$3,260
$3,165
$2,470
$5,635
$1,365
$4,549
$5,915
$168
173%
181%
105%
Maine
$1,441
$2,078
$3,519
$2,933
$2,485
$5,419
$1,229
$5,297
$6,526
$169
154%
185%
120%
Maryland
$1,641
$2,424
$4,064
$3,384
$2,500
$5,884
$1,292
$5,122
$6,414
$172
145%
158%
109%
Massachusetts
$1,449
$2,556
$4,005
$3,139
$2,490
$5,629
$1,275
$5,372
$6,646
$170
141%
166%
118%
Michigan
$1,416
$2,229
$3,645
$3,045
$2,445
$5,489
$1,248
$4,729
$5,977
$221
151%
164%
109%
Minnesota
$1,231
$2,959
$4,190
$3,080
$2,386
$5,466
$1,324
$4,958
$6,282
$163
130%
150%
115%
Mississippi
$1,481
$2,095
$3,576
$3,219
$2,425
$5,644
$1,369
$4,237
$5,606
$170
158%
157%
99%
Missouri
$1,262
$2,011
$3,273
$3,196
$2,442
$5,638
$1,351
$5,154
$6,506
$191
172%
199%
115%
Montana
$1,530
$2,296
$3,826
$2,953
$2,386
$5,339
$1,324
$4,418
$5,741
$164
140%
150%
108%
Nebraska
$1,350
$2,063
$3,413
$3,147
$2,386
$5,532
$1,324
$4,485
$5,809
$175
162%
170%
105%
Nevada
$795
$1,960
$2,756
$3,074
$2,468
$5,542
$1,263
$4,759
$6,022
$229
201%
219%
109%
New Hampshire
$1,695
$2,148
$3,843
$3,005
$2,485
$5,491
$1,229
$5,177
$6,406
$158
143%
167%
117%
New Jersey
$1,583
$2,087
$3,671
$3,445
$2,516
$5,961
$1,325
$4,936
$6,262
$155
162%
171%
105%
New Mexico
$1,237
$2,049
$3,286
$2,574
$2,458
$5,032
$1,227
$4,438
$5,665
$193
153%
172%
113%
New York
$1,704
$2,190
$3,894
$3,144
$2,581
$5,725
$1,294
$6,215
$7,509
$163
147%
193%
131%
North Carolina
$1,331
$2,017
$3,348
$3,072
$2,515
$5,587
$1,316
$4,481
$5,797
$192
167%
173%
104%
North Dakota
$1,475
$2,462
$3,937
$3,065
$2,386
$5,451
$1,324
$4,532
$5,856
$177
138%
149%
107%
Ohio
$1,433
$2,104
$3,538
$3,074
$2,434
$5,508
$1,286
$4,488
$5,774
$220
156%
163%
105%
Oklahoma
$1,359
$2,098
$3,456
$3,288
$2,447
$5,735
$1,423
$4,439
$5,862
$181
166%
170%
102%
Oregon
$1,289
$2,402
$3,691
$2,701
$2,452
$5,153
$1,214
$5,107
$6,321
$161
140%
171%
123%
Pennsylvania
$1,412
$2,307
$3,719
$3,039
$2,482
$5,521
$1,290
$4,596
$5,886
$202
148%
158%
107%
Rhode Island
$1,257
$2,306
$3,563
$3,040
$2,490
$5,530
$1,275
$4,944
$6,219
$276
155%
175%
112%
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 19 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
MA-PD
FFS and PDP
FFS, PDP and
Medigap Plan G
State
Total
OOP
Cost
37
Total
Premium
38
Total
Cost
Total
OOP
Cost
39
Total
Premium
40
Total
Cost
Total
OOP
Cost
41
Total
Premium
42
Total
Cost
MA-PD Value
of
Supplemental
Benefits
43
FFS
and PDP
compared
to MA-PD
FFS, PDP, and
Medigap Plan G
Compared
to MA-PD
FFS, PDP, and
Medigap Plan G
Compared to FFS
and PDP Only
South Carolina
$1,410
$1,954
$3,364
$3,036
$2,495
$5,531
$1,316
$4,714
$6,030
$181
164%
179%
109%
South Dakota
$1,443
$2,213
$3,656
$3,078
$2,386
$5,464
$1,324
$5,129
$6,453
$173
149%
176%
118%
Tennessee
$1,284
$2,136
$3,420
$3,103
$2,494
$5,597
$1,353
$4,435
$5,788
$192
164%
169%
103%
Texas
$1,256
$1,987
$3,243
$3,202
$2,431
$5,633
$1,321
$4,442
$5,762
$190
174%
178%
102%
Utah
$1,228
$2,102
$3,330
$2,991
$2,421
$5,412
$1,290
$4,554
$5,844
$194
163%
176%
108%
Vermont
$1,692
$2,179
$3,871
$2,881
$2,490
$5,370
$1,275
$5,723
$6,997
$149
139%
181%
130%
Virginia
$1,330
$2,067
$3,398
$3,024
$2,460
$5,485
$1,295
$4,371
$5,666
$201
161%
167%
103%
Washington
$1,333
$2,331
$3,664
$2,803
$2,452
$5,256
$1,214
$5,053
$6,266
$172
143%
171%
119%
West Virginia
$1,550
$2,156
$3,706
$3,029
$2,482
$5,511
$1,290
$4,631
$5,921
$197
149%
160%
107%
Wisconsin
$1,343
$2,305
$3,648
$2,954
$2,425
$5,379
$1,344
$5,007
$6,351
$184
147%
174%
118%
Wyoming
$1,347
$2,373
$3,721
$2,954
$2,386
$5,340
$1,324
$4,609
$5,932
$150
144%
159%
111%
MILLIMAN CLIENT REPORT
UnitedHealth Group Page 20 August 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
5. METHODOLOGY
We used detailed publicly available benefit design, premium, and plan information, and county-level enrollment
information, for all 2023 MA plans provided by CMS. We used this information, along with proprietary Milliman MA-PD
pricing models, to calculate the value of the medical cost sharing in the MA-PD program for all calendar year 2023
non-SNP MA-PD plans under the current MA payment methodology in each county. We also calculated the value of
medical cost sharing under the FFS program at the county level. We summarized the premium paid for MA-PD plans
and any Part B premium reductions in the MA-PD program. We applied a similar exercise to calculate the value of
cost sharing under the Part D portion of an MA-PD plan and of PDP plans for FFS members, and also captured the
PDP premium paid.
Medical costs are calculated for a non-disabled average age Medicare beneficiary not receiving income-based
assistance with medical costs. Part D costs are calibrated to published CMS values, for a non-low income (NLI)
population. We adjusted for the cost impact of geography and average CMS HCC (Part A and Part B) and RxHCC
(Part D) payment risk scores when developing medical cost estimates and other assumptions. In calculating expected
lifetime costs for an average 65-year-old, we assumed an annual inflation rate of 4.3% and an average remaining life
span of approximately 21 years. We also included the impact of aging in our medical and pharmacy cost trends,
which is in addition to the 4.3% annual trend. We include the impact of aging in the lifetime cost projections because
we expect OOP costs to increase as beneficiaries age. We projected the costs based on these assumptions for each
of those 21 years and summed them to demonstrate the lifetime costs for an average 65-year-old.
45
,
46
The annual
inflation rate of 4.3% is commensurate with the long-term trend rate as measured in the 2022 Medicare Trustees
Report and includes all components of trend that are applicable to costs outlined in this report. We did not consider
the impact of the Inflation Reduction Act (IRA) on OOP costs when calculating lifetime costs. The provisions in the
IRA that pertain to the Medicare market will substantially change Part D OOP costs for both the PDP and MA-PD
markets; however, as of the time of this analysis, there are too many unknowns regarding the changes instituted by
this new law to accurately project OOP costs two decades into the future.
To calculate the imputed costs for a 65-year-old and an 85-year-old, we applied relativities based on calculated member
spending for medical costs and drugs, separately. This analysis was performed using the CMS Medicare 2018 5%
Sample and Milliman’s 2019 Part D Consolidated Database (PDCD). The CMS 5% Sample was used as a proxy for
medical costs to determine the average Part A and Part B cost sharing for the non-dual-eligible beneficiaries by age
band relative to the overall average, while the PDCD was used to determine the average Part D cost sharing for NLI
beneficiaries by age band relative to the average. Adjustment factors were then calculated from this information, relative
to a 1.00 factor representing the average cost of the entire over-65 population. We exclude disabled Medicare
beneficiaries from the medical adjustment factors, as these disabled beneficiaries are likely not reflective of a NLI
population, as most beneficiaries eligible for Medicare due to disability receive income-related subsidies. The adjustment
factors are then applied to the average OOP costs for MA-PD, FFS, and PDP to calculate OOP costs by age.
We only analyzed general enrollment MA-PD plans and did not analyze employer group waiver plans (EGWPs),
SNPs, Program of All-inclusive Care for the Elderly (PACE) organizations, Medical Savings Account (MSA) plans,
Medicare cost plans (1876 and 1833), and Medicare-Medicaid Plans (MMPs). We also focused exclusively on MA-PD
plans under the MA program; that is, we excluded MA-only plans in this analysis. We focused our discussion around
a non-SNP and NLI population.
Our nationwide analysis excludes the state of Alaska, as there are currently no MA-PD offerings in that state other
than two MSA plans. We also exclude the U.S. territories in this analysis. The Medigap nationwide premium averages
also exclude the states of Massachusetts, Minnesota, and Wisconsin, as Medigap is offered though a different set of
standardized plans under a federal waiver in those states. Medigap premiums are sourced from Weiss Ratings,
provided by Weiss Ratings at a state, age, and gender level. We sourced the Medigap membership from Mark Farrah
Associates. We excluded Medigap rates for Medicare Select products due to the low prevalence of these types of
plans as of 2022. We weighted these 2022 rates using enrollment by carrier, and female and male membership splits
summarized from the 2022 Quarter 1 CMS Master Beneficiary Summary File Limited Data Set.
45
CMS (June 2, 2022). 2022 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical
Insurance Trust Funds. Retrieved February 1, 2023, from https://www.cms.gov/files/document/2022-medicare-trustees-report.pdf.
46
SSA. Social Security: Benefits Planner/Life Expectancy. Retrieved February 1, 2023, from https://www.ssa.gov/planners/lifeexpectancy.html.

MILLIMAN CLIENT REPORT
UnitedHealth Group Page 21 September 2023
Average annual beneficiary health care
costs for various Medicare coverage options 2023
6. CAVEATS AND LIMITATIONS
The authors of this report are consulting actuaries for Milliman, Inc. They are members of the American Academy of
Actuaries, and meet the qualification standards of the American Academy of Actuaries to render the actuarial opinion
contained herein.
The material in this report represents the opinion of the authors and is not representative of the views of Milliman. As
such, Milliman is not advocating for, or endorsing, any specific policy changes to the Medicare FFS or Medicare
Advantage programs in this report.
The figures presented in this report are illustrative estimates for hypothetical average Medicare beneficiaries and
based on publicly available information and Milliman proprietary data and models. This report is intended to illustrate
average beneficiary cost differences among various Medicare coverage options and should not be used for any other
purpose. Actual beneficiary health costs will vary from the estimates in this report, and will depend on the
beneficiary’s age, gender, geography, health status, available health plans, and other factors.
In completing this analysis, we relied on information from CMS, Mark Farrah Associates, and Weiss Ratings, which
we accepted without audit. However, we did review this information for general reasonableness. If this information is
inaccurate or incomplete, conclusions drawn from this information may change.
Milliman is among the world’s largest providers of actuarial, risk
management, and technology solutions. Our consulting and
advanced analytics capabilities encompass healthcare, property &
casualty insurance, life insurance and financial services, and
employee benefits. Founded in 1947, Milliman is an independent firm
with offices in major cities around the globe.
milliman.com
CONTACT
David Mike
david.mike@milliman.com
Philip Nelson
philip.nelson@milliman.com
Brad Schliesmann
brad.schliesmann@milliman.com
© 2023 Milliman, Inc. All Rights Reserved. The materials in this document represent the opinion of the authors and are not representative of the views of Milliman, Inc.
Milliman does not certify the information, nor does it guarantee the accuracy and completeness of such information. Use of such information is voluntary and should not be
relied upon unless an independent review of its accuracy and completeness has been performed. Materials may not be reproduced without the express consent of Milliman.
