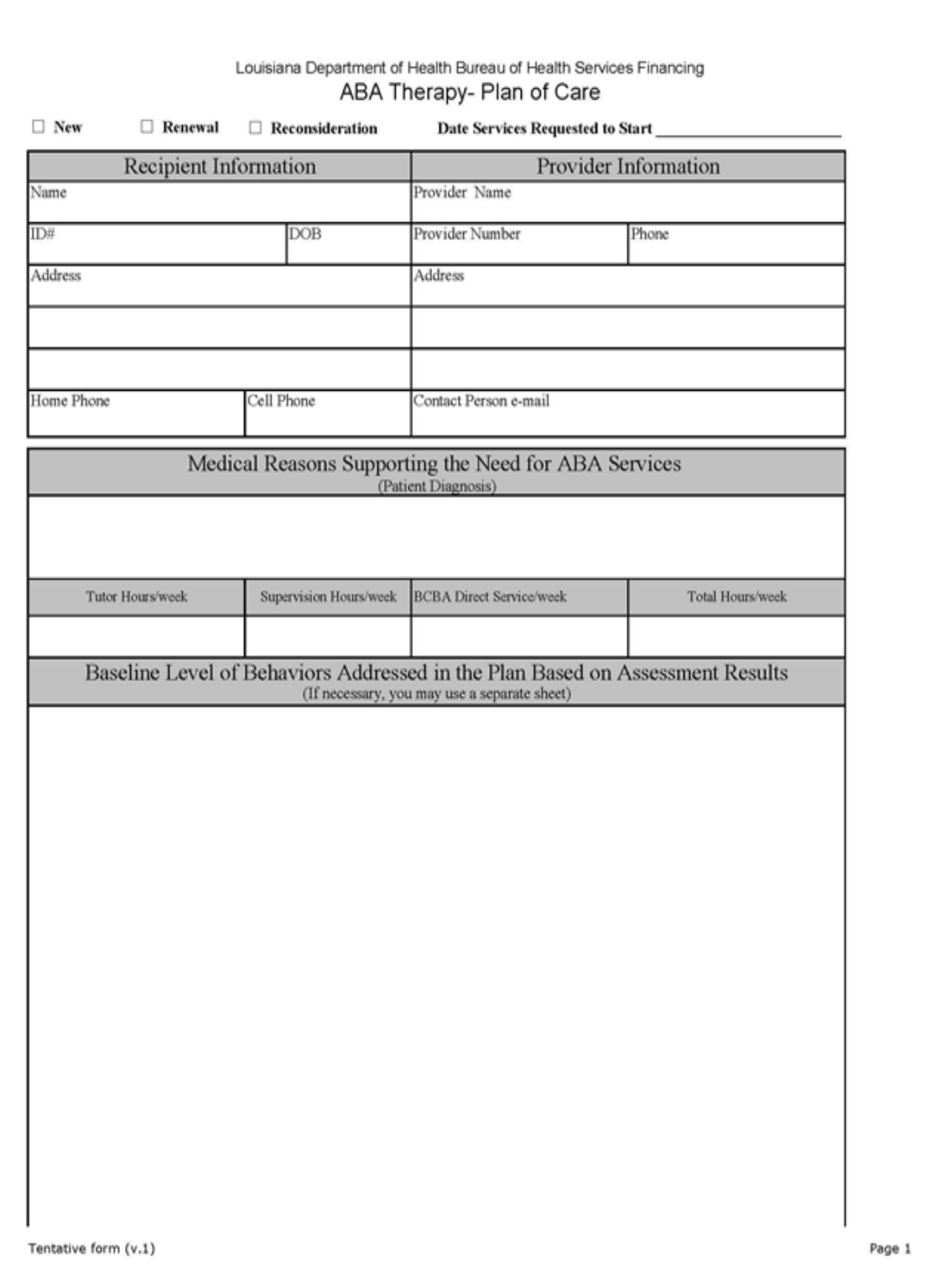
Page 1 of 4
BEHAVIOR TREATMENT PLAN
Instructions for Completion of the Behavioral Treatment Plan of Care
The provider is not required to use this plan of care form. However, if not using this form, the plan
of care must address all the information specified in the Medicaid State Plan for Applied Behavior
Analysis (ABA) and the most recent version of the ABA Provider Manual.
Recipient Information
Type or print the patient’s full name, Medicaid ID number, date of birth, address and home and
cell phone number in the space provided.
Provider Information
Type or print the name of the provider, the provider’s Medicaid ID number, phone number, address
and contact person’s email address.
Medical Reason Supporting the Need for ABA Services
Type or print the recipient’s diagnosis.
Requested Hours of Services
• Type or print the number of tutor/RBT hours requested per week.
• Type or print the number of supervision hour conducted by the (BCBA/-D) per
week.
• Type or print the number of direct services hour provided by a BCBA/-D per week
(this may include caregiver training as well).
• Type or print the total number of requested hours for all services per week.
Baseline Level of Behaviors Addressed in the Plan Based on Assessment Results
•
Type or write a narrative description of the baseline level of all behaviors assessed
for which a goal is developed. This section must be completed.
Examples:
• “Daniel did not use words to communicate during the assessment.”;
• “James used ten mand forms inconsistently during assessment.”;
• “Sharlee could tact ten animals and four colors during assessment.”; and
• “Silvia made eye-contact two of 12 times after given the direction, look at
me.”

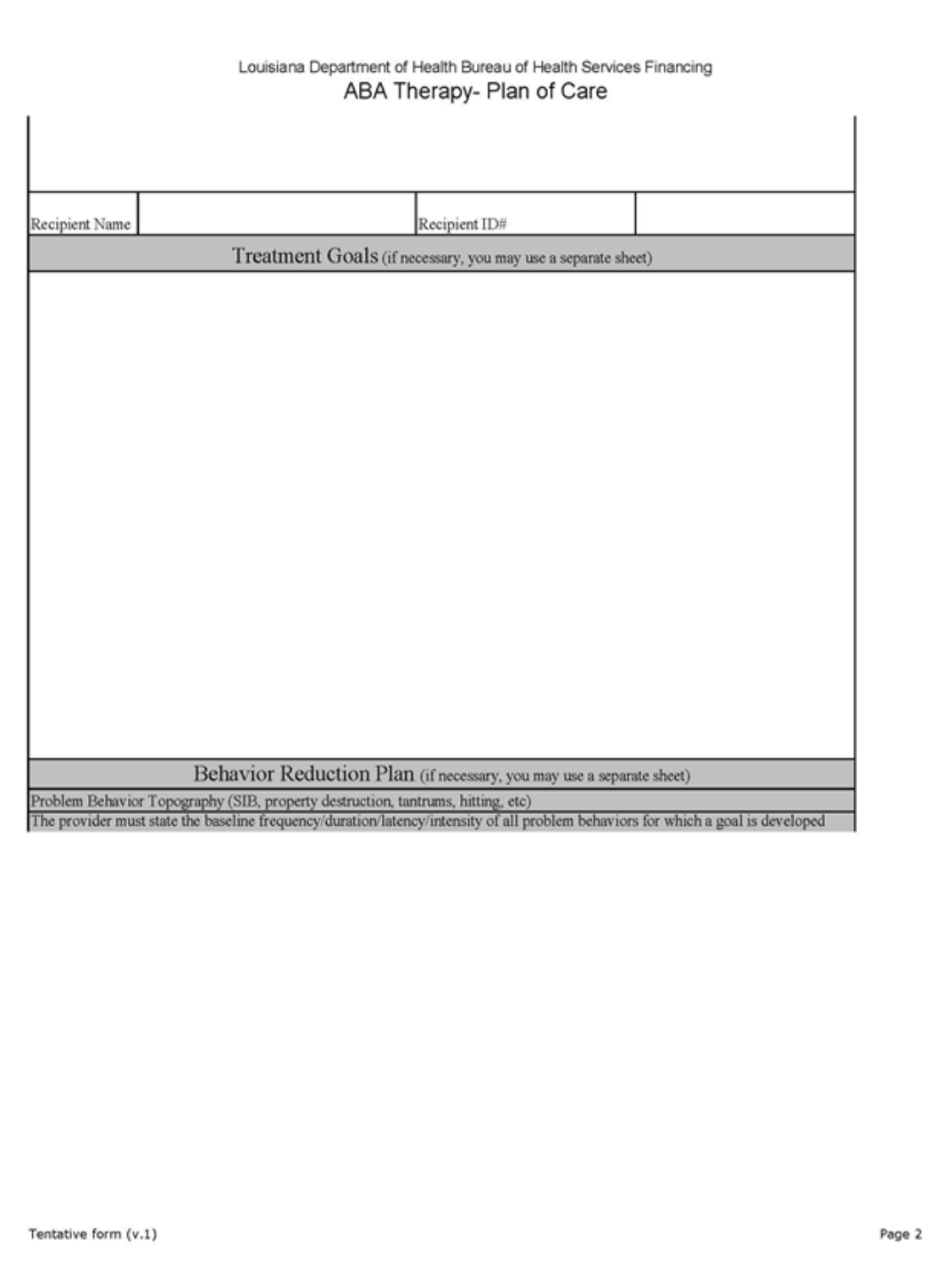
Page 2 of 4
• If the document is a treatment plan renewal, list the present level of performance
for skills under treatment and any goals mastered during the previous authorization
period.
• Do not refer to idiosyncratic, proprietary assessment instrument results to describe
baseline performance.
Examples:
• “Harry could perform skills 4L to 5G on ABEL4 assessment”; and
• “Wilma performed at a level 2 across all language skills on VBMZT
assessment.”
NOTE: May use another sheet for this section and attach it to this form, but the section must be
labeled.
Treatment Goals
• Type or write a goal for each behavior/skill identified for treatment not including
behavior reduction goals. Each goal should have a performance standard and
criterion for mastery.
Examples
• “Jon will tact 26 upper case letters independently across two consecutive
treatment sessions;
• “Susan will use quantifying autoclitics while manding for chips, (e.g., Can
I have two chips please) for ten mand forms.”; and
• “Marvin will make eye contact when his name is called on 90% of the
instructional trials across three tutors.”
• The provider may NOT use idiosyncratic, proprietary nomenclature to specify
treatment goals.
Examples:
• “Seth will complete goals A-K, M-R, and Q-T on the MASP.”;
• “Roger will master ADL skills 1-2 to 4-6 on the ACQMOT program.”
NOTE: A separate sheet may be used for this section and attach it to this form, but the
section must be labeled.
Behavior Reduction Plan
According to state guidelines, if the provider is going to intervene on problem behaviors, the
provider MUST conduct a functional assessment or a functional analysis (preferred method) and
develop a function based treatment plan.

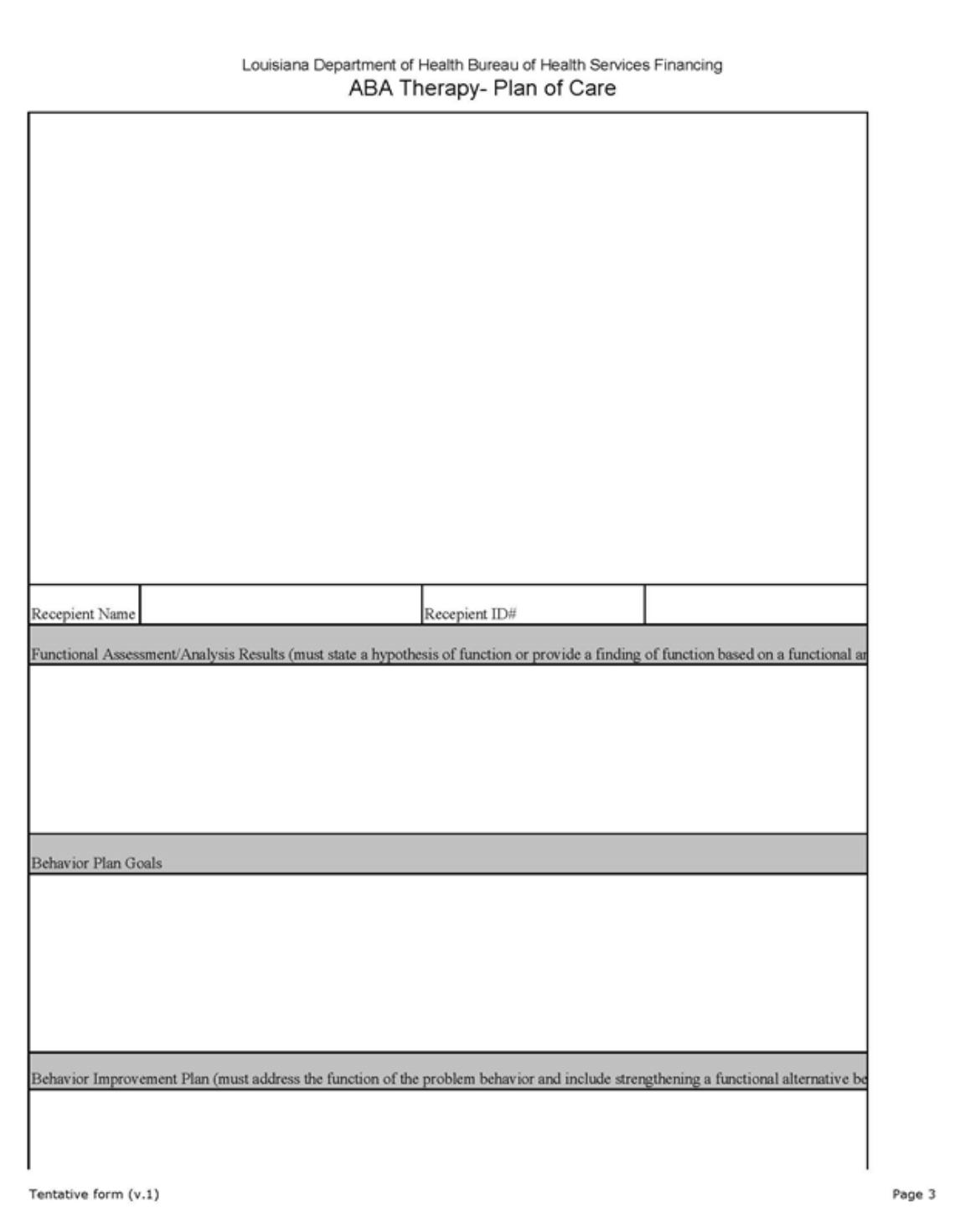
Page 3 of 4
• The provider may NOT make a grid sheet with intervention tactics that is not tied
to a narrative description/date analysis of the results of a functional
assessment/analysis.
• Type or write the behavior topography of the problem behavior and state the
frequency/duration/latency/intensity of all the problem behaviors for which a goal
is developed.
• Type or write the results of the functional assessment and type or write a hypothesis
statement or describe the results of a functional analysis.
• Type or write a behavior improvement goals with a performance standard and
criteria for mastery.
Examples:
• “Terrance will decrease hitting others by 50 percent week for four
consecutive weeks. Terrance will ask mand for attention by saying “help”
when prompted on 100 percent of the opportunities.”; and
• “William ask mand for an independently break at least five times/session.”
• Type or write the behavior intervention plan that addresses the function of the
problem behavior that includes strengthening a functional replacement behavior.
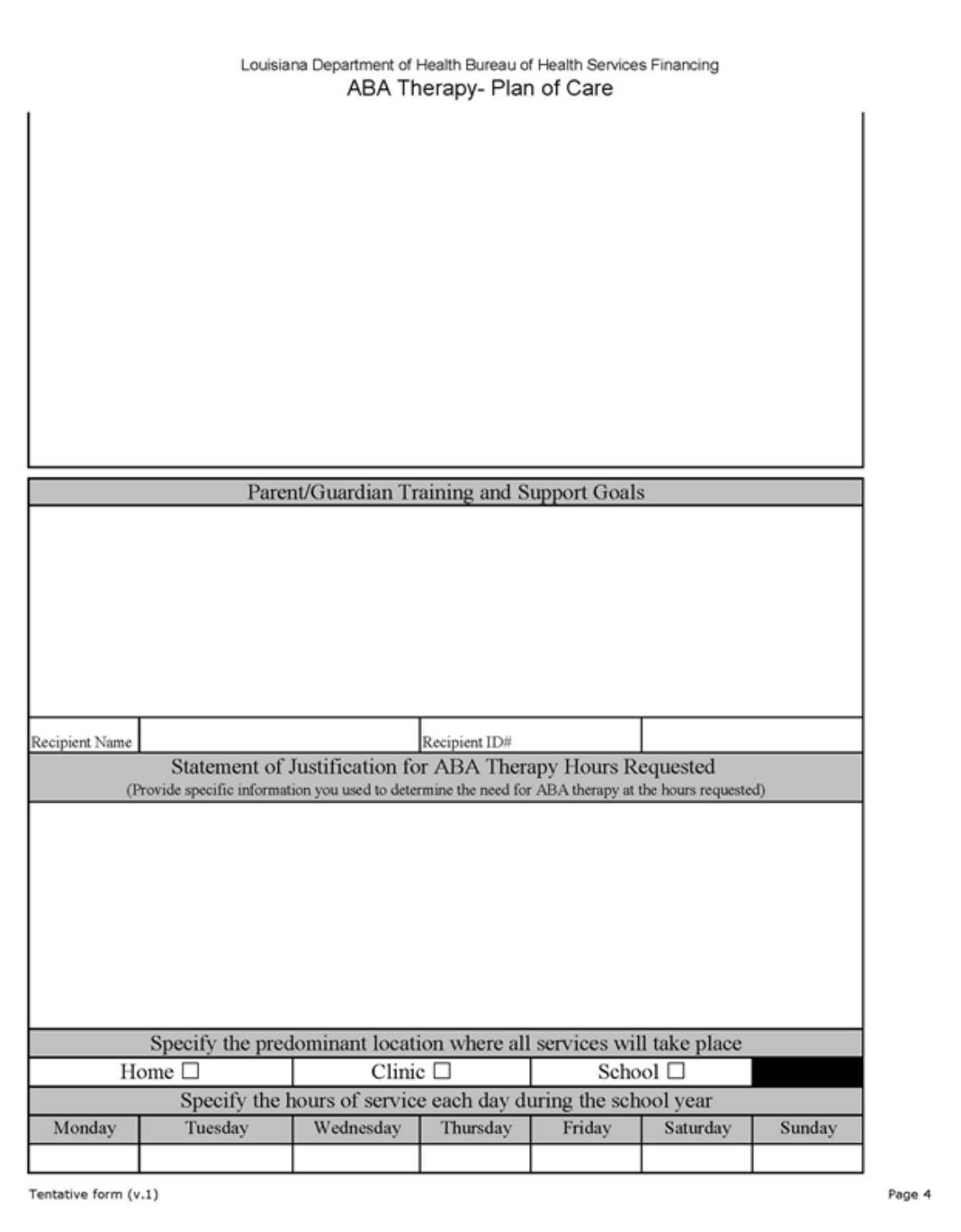
Parent/Guardian Training and Support Goals
Type or write caregiver training with a performance standard and criteria for mastery.
Example:
• After role-play training, Mrs. Jones will implement Terrance’s behavior
reduction plan with 100 percent fidelity across three sessions
Statement of Justification for ABA Therapy Hours Requested
Type or write the specific criteria used to determine the need for ABA therapy at the hours
requested.
Example:
• Terrance presents with clinically significant deficits in listener behavior
(receptive identification, direction following) and currently does not use
vocal verbal, sign language or augmentative communication to
communicate. He engages in high frequency and high intensity aggressive
and self-injurious behavior that presents a substantial risk to himself, others,
and property.

Page 4 of 4
Predominant Location
Specify the predominant location where all services will take place.
Check off the environment where services will occur. If services will occur in more than one
setting, you may check more than one box.
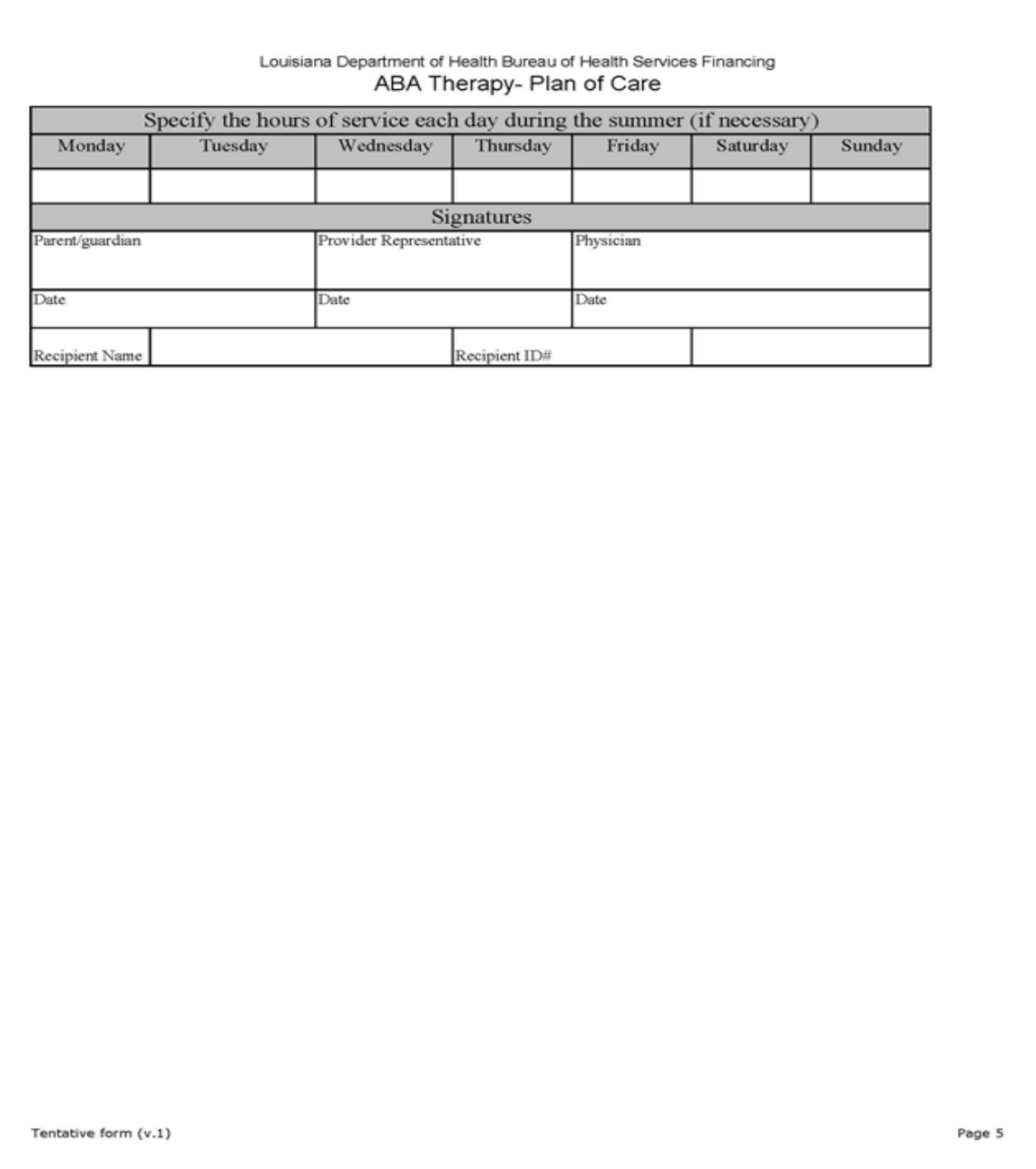
Hours of Service
Specify the hours of service each day during the school year and summer (if necessary).
Type or write the anticipated total hours (therapy + supervision) for each day.
Signatures
Provide signatures as necessary. Must sign and date the plan.