
PHYSICIANS
SERVICES
PROVIDER
MANUAL
SEPTEMBER 1, 2024
South Carolina
Department of Health and Human Services

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
2
CONTENTS
1. Program Overview ...................................................................................................................... 5
2. Eligible Providers ........................................................................................................................ 6
• Provider Qualifications .......................................................................................................... 6
• Provider Enrollment and Licensing ...................................................................................... 13
3. Covered Services and Definitions ............................................................................................. 16
• Primary Care Services ........................................................................................................ 16
• Physician Services .............................................................................................................. 16
• Office/Outpatient Exams Definitions .................................................................................... 17
• Ambulatory Care Visit Guidelines ........................................................................................ 17
• Evaluation and Management Services ................................................................................ 18
• Non-Covered Services ...................................................................................................... 144
4. Utilization Management ........................................................................................................... 152
• Prior Authorization ............................................................................................................. 152
• Other Service Limitations .................................................................................................. 164
5. Reporting/Documentation ....................................................................................................... 175
• Co-Signatures ................................................................................................................... 175
• Evaluation and Management Services Records and Documentation Requirements .......... 175
• Documentation of the Teaching Physician ......................................................................... 176
• Convenient Care Clinics .................................................................................................... 176
• Telehealth ......................................................................................................................... 176
• Obstetrics and Gynecology ............................................................................................... 176

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
3
• Psychiatric and Counseling Services ................................................................................. 179
• Tuberculosis (TB) Policy ................................................................................................... 181
• Breast Cancer Susceptibility Gene 1 and 2 (BRCA) .......................................................... 181
• Chiropractic Services ........................................................................................................ 182
• Pain Management Services ............................................................................................... 184
6. Billing Guidance ...................................................................................................................... 185
• Services Outside of the Country ........................................................................................ 185
• Direct Physician Supervision ............................................................................................. 185
• Physician’s Office within an Institution ............................................................................... 185
• Physician Administered Drugs ........................................................................................... 185
• Teaching Physician Policy Billing Requirements ............................................................... 186
• Fee-For-Time Compensation arrangements ...................................................................... 187
• Evaluation and Management Services .............................................................................. 188
• Immunizations ................................................................................................................... 197
• Pediatrics and Neonatology ............................................................................................... 197
• Tobacco Cessation ........................................................................................................... 207
• Obstetrics and Gynecology ............................................................................................... 207
• Psychiatric and Counseling Services ................................................................................. 213
• Nephrology and End Stage Renal Disease Services ......................................................... 213
• Part II — Diagnostic Ophthalmology Services ................................................................... 215
• Hyperbaric Oxygen Therapy .............................................................................................. 219
• General Surgery Guidelines .............................................................................................. 220
• Surgical Guidelines for Specific Systems .......................................................................... 226

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
4
• Anesthesia Services .......................................................................................................... 227
• Pain Management Services ............................................................................................... 230
• Pathology and Laboratory Services ................................................................................... 231
• Radiology and Nuclear Medicine ....................................................................................... 235
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
5
1
PROGRAM OVERVIEW
The State of South Carolina (South Carolina or State) Medicaid program recognizes professional
medical services that are medically necessary unless limitations are noted within the Other Service
Limitations section of this manual. Information in this manual includes South Carolina Medicaid
policies for general medical care, such as office exams.
These services are predominantly billed to Medicaid by Primary Care Physicians (PCPs), such as
family physicians, internists, general practitioners, obstetricians/gynecologists (OB/GYN),
pediatricians, Nurse Practitioners (NPs) and Certified Nurse Midwives (CNMs). However, the
guidelines are written for all providers rendering services to South Carolina citizens who are
Medicaid beneficiaries.
Note: References to supporting documents and information are included throughout the manual.
This information is found at the following locations:
• Provider Administrative and Billing Guide
• Forms
• Procedure Codes

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
6
2
ELIGIBLE PROVIDERS
PROVIDER QUALIFICATIONS
Physician
For Medicaid billing purposes, the term “physician” includes Doctor of Medicine and Doctor of
Osteopathy currently licensed in the state in which they are rendering services by that state’s Board
of Medical Examiners.
Hospital-Based Physician
A hospital-based physician is defined as a physician licensed to practice medicine or osteopathy
who is employed by a hospital, and whose payment for services is claimed by the hospital as an
allowable cost under the Medicaid program and billed by the contracted hospital.
Physician’s Assistant
A physician assistant (PA) may provide medically necessary covered services if the services
provided are allowed by State Law and consistent with the agreement between the PA and the PA’s
supervising physician. PAs providing services to Healthy Connections beneficiaries must be
enrolled as South Carolina Medicaid providers.
Services rendered and billed under the PA’s individual National Provider Identifier (NPI) number are
reimbursed at 80% of the current Medicaid Family and General Practitioners physician’s fee
schedule for professional services.
Nurse Practitioner
A Nurse Practitioner (NP) is defined as a registered nurse who has completed an advanced formal
education program at the master's level or doctoral level acceptable to the board, and who
demonstrates advanced knowledge and skill in assessment and management of physical and
psychosocial health, and illness status of persons, families, and groups. Nurse practitioners who
perform medical acts must do so pursuant to a practice agreement in compliance with Section 40-
33-34 of the Nurse Practice Act. Reimbursement is 80% of the physician rate.
Certified Nurse Midwife
A Certified Nurse Midwife (CNM) is defined as an advanced practice registered nurse who holds a
master's degree in the specialty area, maintains an American Midwifery Certification Board
certificate, and is trained to provide management of women's health care from adolescence beyond
menopause, focusing on gynecologic and family planning services, preconception care, pregnancy,
childbirth, postpartum, care of the normal newborn during the first twenty-eight days of life, and the
notification and treatment of partners for sexually transmitted infections. A CNM performing medical

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
7
acts must do so pursuant to a practice act agreement in compliance with Section 40-33-34 of the
Nurse Practice Act. Reimbursement is 100% of the physician rate.
Licensed Midwife
A Licensed Midwife is defined as a person who is not a medical or nursing professional licensed by
the South Carolina Department of Public Health (SCDPH), for the purpose of providing specifically
defined prenatal, delivery and postpartum services to low-risk women. Reimbursement is 65% of the
physician rate. Regulations can be found on the SCDPH website at R.61-24.pdf (sc.gov)
Certified Registered Nurse Anesthetist (CRNA)
A CRNA must be licensed to practice as a registered nurse in the state in which he or she is
rendering services and currently certified by the Council on Certification of Nurse Anesthetists or the
Council on Recertification of Nurse Anesthetists. A recent graduate is a new graduate of an
advanced formal education program for nurse anesthetist accredited by the national accrediting
organization who must achieve certification within one year of graduation. Upon obtaining
certification, recent graduates must notify Provider Enrollment to continue practicing as a Medicaid
provider. CRNAs may work under the medical direction of a surgeon or under the supervision of an
anesthesiologist. CRNAs working under the medical direction of a surgeon or under the supervision
of an anesthesiologist will be reimbursed at 50% of the physician rate. CRNAs not working under
the direction of an anesthesiologist or supervised by a physician will be reimbursed 90% of the
physician rate.
Anesthesiologist Assistant (AA)
An AA must be licensed to practice as an AA in the state he or she is rendering services. AAs may
only work under the supervision of an anesthesiologist.
Licensed Pharmacist
A licensed pharmacist is defined as an individual health care provider licensed by the South
Carolina Board of Pharmacy to engage in the practice of pharmacy. A pharmacist is a learned
professional authorized to provide patient care services within the scope of their knowledge and
skills. A pharmacist providing services to Healthy Connections beneficiaries must be enrolled as a
South Carolina Medicaid provider and have an individual National Provider Identifier (NPI) and shall
be affiliated with the pharmacy that the services will be paid to. The service a pharmacist renders is
limited to those that are allowed under State Law.
Dietitian
A dietitian is defined as any individual meeting the licensure and educational requirements in South
Carolina and/or the border states of Georgia and North Carolina. All services must be rendered
within the South Carolina Medicaid Service Area (SCMSA). The SCMSA is defined as South
Carolina and adjacent areas within 25 miles of its borders.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
8
Paramedical Professionals
The following medical professionals may render services to Medicaid patients under the direct
supervision of a licensed physician:
• Audiologists
• Speech pathologists
• Physical therapists
• Occupational therapists
• Licensed master social workers (LMSWs)
• Psychiatric nurse practitioners (NPs)
• X-ray or lab technicians
• Licensed respiratory therapists
• Nurse midwives
• NPs
Reimbursement will be made to the supervising physician or hospital where the professional is
employed, and where the service is rendered, under the restrictions set forth in this manual. If any of
these medical professional services are included in a hospital cost report, they cannot also be billed
separately as professional services.
Certified Nurse Practitioner (CNP) and Clinical Nurse Specialist (CNS)
The CNP/CNS may enroll with South Carolina Medicaid and be assigned a Medicaid ID number if
he or she meets all of the following criteria:
• Licensed to practice as a registered nurse,
• Licensed as a CNS/CNP in the state in which he or she is rendering services, and
• Practicing under a physician preceptor according to a mutually agreed-upon protocol.
CNP/CNSs may bill for services under their physician preceptor’s NPI number or under their
individual NPI number (NP + 4 digits).
The services they render are limited to those that are allowed under State Law and are documented
in the approved written protocol.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
9
Delegated acts and protocols that outline the scope of practice guidelines for NPs, CNMs, CNS or
PAs must be current and available in the personnel file of the supervised practitioner. Upon
submission of a claim, the rendering physician is attesting that the services have been accurately
and fully documented in the medical record and that he or she assumes responsibility for the NP,
CNM, CNS or PA. The claim also confirms that the provider has certified the medical necessity and
reasonableness for the service(s) submitted to Medicaid for payment. This policy does not
supersede State Law, as it relates to requirements, for off-site practice protocols that outline co-
signature guidelines for PAs. These requirements can be found in Article 7, Section 40-47-955, of
the South Carolina Physician Assistants Practice Act.
Services rendered and billed under the NP individual NPI number are reimbursed at 80% of the
physician’s fee schedule for Evaluation and Management (E&M) codes and all professional codes,
and 100% for supplies and pathology services. Fee schedules are located on the South Carolina
Department of Health and Human Services (SCDHHS) website at https://www.scdhhs.gov
.
Any CNP/CNS employed by a hospital will be ineligible to submit claims for his or her services, as
these services are included in the hospital cost report.
To request a CNP/CNS Enrollment Form, contact Provider Enrollment at +1 888 289 0709.
Optician
An optician fits and dispenses corrective lenses for the correction of a person’s vision.
Self-Employed Optometrist
A self-employed licensed provider who examines the eyes to evaluate health and visual abilities,
diagnoses eye diseases and conditions of the eye and visual system and provides necessary
treatment such as eyeglasses and contact lenses.
Chiropractors
To qualify as a Medicaid provider for chiropractic services, an individual must be licensed by the
South Carolina Board of Chiropractic Examiners as a Doctor of Chiropractic. In order to participate
in the Medicaid Program, a chiropractor must enroll with Medicaid and receive a Medicaid ID
number. Both individual chiropractors and chiropractic groups are eligible to enroll. For questions
regarding enrollment, please contact Medicaid Provider Enrollment at +1 888 289 0709.
Psychiatric and Counseling Services
Psychiatric and psychotherapy services must be prescribed by an individual listed below:
• Physician/Psychiatrist
• Psychiatric NP

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
10
SCDHHS will reimburse an eligible provider for covered psychiatric and psychotherapy services
personally provided by the physician or NP or by an allied professional under the direct supervision
of the physician/NP. Allied professionals rendering the service cannot be directly reimbursed under
the Medicaid Physician Services program. All allied professionals must be under the direct
supervision of the physician/NP to whom reimbursement is made. Covered services differ based on
the provider providing the service.
Medicaid reimburses for medically necessary services delivered by the following allied professional
under the supervision and direction of a physician or NP:
• LMSW — A master’s or doctoral degree from a social work program accredited by the Council
on Social Work Education and one year of experience working with the population to be served.
All allied professionals are responsible for providing services within their scope of practice as
prescribed by South Carolina State Law. Interns are not eligible to provide services to Medicaid
beneficiaries and their services are non-billable.
Subsection I: Accessibility of the Teaching Physician
Accessibility of the teaching physician while the resident is providing a service is defined as follows
for particular service types.
Ambulatory Services
Accessibility of the teaching physician for supervision of ambulatory services requires the teaching
physician to be present in the clinic or office setting while the resident is treating patients. The
physician is thus immediately available to review the patient’s history, personally examine the
patient, if necessary, review the records of the encounter and laboratory tests, confirm or revise the
diagnoses, and determine the course of treatment.
Inpatient Services
Accessibility of the teaching physician for supervision of non-procedural inpatient services requires
that the teaching physician evaluate the patient within 24 hours of admission and on each day
thereafter for which services are billed. The teaching physician must review the patient’s history,
personally examine the patient as needed; review the records of the encounter and laboratory tests,
confirm or revise the diagnoses; and determine the course of treatment.
Procedures
Minor Procedures
For supervision of procedures that take only a few minutes to complete or involve relatively little
decision-making once the need for the procedure is determined, accessibility requires that the
teaching physician be on the premises and immediately available to provide services during the
entire procedure.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
11
All Other Procedures
For supervision of all other procedures, accessibility requires that the teaching physician be
physically present during all critical and key portions of the procedure and be immediately available
to provide services during the entire procedure.
Special Coverage Groups
Pediatric Anesthesia Services
Board-eligible and/or board-certified Pediatric Intensivists are allowed to be reimbursed for a limited
number of anesthesia Current Procedural Terminology (CPT) codes. Board-eligible and/or board-
certified pediatric emergency medicine physicians may also be reimbursed for this service if they
practice in a facility where a board-eligible and/or board-certified pediatric anesthesiologist and/or a
board-eligible and/or board-certified pediatric intensivist is on staff. In addition, the pediatric
intensivist or pediatric emergency medicine physician must have a current Pediatric Advanced Life
Support (PALS) certification. Anesthesia services performed by Pediatric Intensivist or Pediatric
Emergency Medicine Physician must be filed with modifier G9 listed as the first modifier on the
claim form.
The Pediatric Sub-Specialist Program
SCDHHS will reimburse an enhanced rate to certain pediatric sub-specialists that meet the
enrollment requirements. Fee schedules are located on the SCDHHS website at
http://www.scdhhs.gov
.
Pediatric Sub-Specialist Program Participation Requirements
To be eligible for participation in this program, a physician must meet the following criteria:
• Practice within the SCMSA. The South Carolina service area is defined as within 25 miles of the
State line.
• At least 85% of total practice, including after-hours patients, is dedicated to children age
18 years or younger.
• Practice in at least one of the following sub-specialties recognized by the American Board of
Pediatrics available at https://www.abp.org/
:
– Adolescent Medicine
– Allergy
– Cardiology
– Cardiothoracic Surgery
– Child Abuse Pediatrics

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
12
– Critical Care
– Developmental — Behavioral
– Emergency Medicine
– Endocrinology
– Gastroenterology/Nutrition
– Genetics
– Hematology/Oncology
– Infectious Disease
– Neonatology
– Nephrology
– Neurology
– Neurological Surgery
– Ophthalmology
– Orthopedic Surgery
– Otolaryngology
– Psychiatry
– Pulmonology
– Radiology
– Rheumatology
– Surgery
– Urology
– Other pediatric subspecialty areas as may be determined by SCDHHS
• Complete and return a copy of the attestation statement found in the forms section of the
Physician Services Provider Manual.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
13
PROVIDER ENROLLMENT AND LICENSING
Clinics and Ancillary Services
Under the Omnibus Budget Reconciliation Act of 1989 (OBRA ’89), several specific types of health
professionals and facilities are eligible for enrollment in the South Carolina Medicaid program. Their
services are compensable only for beneficiaries with special needs, age 21 and under, and are
related to an Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) exam.
These providers include physical therapists, occupational therapists, speech therapists and
audiologists. Facilities and private therapists providing rehabilitative services have to meet certain
qualifications. Guidelines for these services are outlined in the Rehabilitative Therapy and
Audiological Services Provider Manual available online at www.scdhhs.gov
.
EPSDT Provider
Professional practitioners and other providers must be licensed and/or certified by the appropriate
standard setting agency to provide services covered by South Carolina Healthy Connections
Medicaid program.
• Registered nurses working in county health department offices must meet the standards for
performing EPSDT screenings established by SCDPH.
• Registered nurses who perform screenings in schools must have successfully completed the
SCDHHS-approved Child Health Maintenance Course. A physician must be available for
consultation, if necessary.
• Registered nurses in physicians’ offices or clinics who assist in the performance of EPSDT
screenings must do so under the direct supervision of a physician/NP who assumes
responsibility for quality of care. They are encouraged to successfully complete the SCDPH
course.
• Registered nurses in physicians’ offices or clinics who assist in the performance of EPSDT
screenings must do so under the direct supervision of a physician/NP who assumes
responsibility for quality of care. They are encouraged to successfully complete the SCDPH
course.
Maternal Fetal Medicine Physician Ultrasound Override
Providers must register as a Maternal Fetal Medicine (MFM) specialist in order to receive an
authorization number to bypass the limitation on antenatal ultrasounds. The provider’s medical
license must have the MFM specialty designation to be accepted.
To register as an MFM specialist, providers must send a written request by mail or fax to:
Medicaid Provider Enrollment
PO Box 8809

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
14
Columbia, SC 29202-8809
Fax: +1 803 870 9022
Questions may be directed to the PSC at +1 800 289 0709 or providers may submit an online
inquiry at Contact a Provider Representative | SCDHHS
Hyperbaric Oxygen (HBO) Therapy Units
Hyperbaric units must be contracted with a hospital even if certified as a freestanding clinic by the
Centers for Medicare and Medicaid Services (CMS). This contractual agreement with the hospital
involves reimbursement for the technical portion of the therapy only.
Independent Laboratories
Medicaid requires that all enrolled independent laboratories meet Clinical Laboratory Improvement
Amendments (CLIA) regulations. CLIA is a regulatory program administered by CMS.
Information concerning CLIA regulations and participation may be obtained through South Carolina
Department of Environmental Services (SCDES) Division of Certification at +1 803 545 4205. For
Medicaid enrollment information, call or write to:
Medicaid Provider Enrollment
PO Box 8809
Columbia, SC 29202-8809
+ 1 888 289 0709
All independent laboratories must be certified by CMS to perform laboratory tests. CLIA certification
must be on file with Medicaid Provider Enrollment. Procedures performed and/or charged when the
lab is not certified to perform a particular test will be rejected. Medicaid will not reimburse for
services performed prior to certification or prior to enrollment. Independent laboratories that have
not enrolled in CLIA also cannot bill Medicaid beneficiaries directly for any services rendered.
Clinical Laboratory Improvement Amendments (CLIA)
Just as Medicaid requires all enrolled independent laboratories meet CLIA regulations, in
accordance with federal regulations (42CFR 493.1809), SCDHHS requires that in order to perform
laboratory tests, all laboratory testing sites must have one of the following CLIA certifications:
• Certificate of Registration
• Certificate of Accreditation or Partial Accreditation
• Certificate of Compliance
• Certificate of Waiver
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
15
• Physician Performed Microscopy Procedures (PPMP) Certificate
In addition, each site must have an assigned unique 10-digit certification number. Information
concerning CLIA regulations and participation guidelines may be obtained from SCDES at
+1 803 545 4203 or by writing to:
SCDES
Division of Certification
2600 Bull Street
Columbia, SC 29201-1708
Independent Imaging Centers and Mobile Imaging Units
Freestanding imaging centers and mobile imaging units must be enrolled with SCDHHS in order to
be reimbursed for services provided. Mobile imaging units must meet SCDES certification.
Freestanding imaging centers and mobile ultrasound units must be certified by Medicare.
For enrollment information, contact provider enrollment at + 1 888 289 0709 or visit the website at
Contact a Provider Representative | SCDHHS

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
16
3
COVERED SERVICES AND DEFINITIONS
PRIMARY CARE SERVICES
These services are predominantly billed to Medicaid by Primary Care Providers (PCPs) such as
family physicians, internists, general practitioners, OB/GYNs, pediatricians, certified nurse midwives
and nurse practitioners. However, guidelines are written for all physicians rendering services to
South Carolina citizens who are Medicaid beneficiaries.
SCDHHS will implement 42 CFR Part 438, 441, and 447 for services provided January 1, 2013,
through December 31, 2014. This action implements the Affordable Care Act (ACA) requirement
that increases payments to physicians with a specialty designation of family medicine, general
internal medicine, pediatric medicine, and related subspecialists for specified primary care services
and charges for vaccine administration under the Vaccines for Children (VFC) Program.
To qualify for the enhanced rate, a physician must self-attest to one of the following criteria:
• Board certification in one of the specialty designations by the American Board of Medical
Specialties (ABMS), the American Board of Physician Specialties (ABPS) or the American
Osteopathic Association (AOA).
• Newly enrolled, non-board-certified physicians in one of the designated specialties are eligible if
they attest to meeting the 60% threshold in the billing of E&M codes in the prior month.
For additional information, providers may contact the PSC at +1 888 289 0709 or submit an online
inquiry at Contact a Provider Representative | SCDHHS
for more information.
PHYSICIAN SERVICES
Physician services rendered either in the patient’s home, a hospital, a skilled nursing facility (SNF),
a physician’s office, a clinic, or elsewhere are defined as those services provided by, or under the
personal supervision of, an individual licensed under State Law to practice medicine or osteopathy
in the state in which he or she is rendering services. When billing for services, the provider of
service must be the same as the provider of service noted in the patient’s medical record, unless
working in an exceptional situation such as supervision, or Fee-For-Time Compensation
Arrangements. Additionally, Medicaid providers must bill actual charges for their services rather
than the anticipated reimbursement. Please refer to the Billing Guidance section of this manual for
more detailed Medicaid billing instructions.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
17
OFFICE/OUTPATIENT EXAMS DEFINITIONS
Some phrases commonly used to describe a patient’s relationship to a physician or practice group
are defined as follows:
• New Patient — Medicaid defines a new patient as one visiting the office for the first time. A new
patient is one who has not received any professional services from the physician or another
physician of the same specialty who belongs to the same group practice within the past three
years. An exception can be justified if all records are lost or destroyed.
• Established Patient — An established patient is one who has received professional services
from the physician or another physician of the same specialty who belongs to the same group
practice within the past three years.
The designation of a new or established patient does not preclude the use of a specific level of
services. Medicaid will reimburse no more than one visit per day unless medically justified. If a
second visit is medically necessary, the second visit must be clearly documented in the patient's
chart.
In the instance where a physician is on-call for or covering for another physician, the patient’s
encounter is classified as it would have been by the physician who is not available. For example, if
the patient is an established patient of the physician who is not available, then the covering
physician would also report his or her services as an established patient visit.
COVID-19 TREATMENT
COVID-19 treatment is covered as required by the American Rescue Plan act. COVID-19
treatment, including specialized equipment and therapies, will be covered for full-benefit Medicaid
members without amount, duration or scope limitations that would otherwise apply when covered for
purposes outside of the treatment or prevention of COVID-19.
AMBULATORY CARE VISIT GUIDELINES
Ambulatory care is defined as all outpatient (OP) examinations, to include paid claims for the
following types of examinations:
• Encounters
• Psychiatric Diagnostic Exam
• Physician Examinations
• Consultations
• Healthy Adult Physicals

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
18
• Maternal care, including antepartum and postpartum care
• Family Planning visits (service provided as part of Family Planning Program) or family planning
• EPSDT screenings
• Minimal exams performed without a physician's direct involvement for ongoing therapies, blood
pressure checks, injections, etc., if billed using the appropriate CPT code
• Emergency department services
When services are rendered, providers must always request the beneficiary's Medicaid card and
verify coverage. Possession of a Medicaid card does not guarantee Medicaid eligibility.
Beneficiaries may become ineligible for Medicaid for a given month, only to regain eligibility later. It
is possible a beneficiary will present a card during a period of ineligibility. It is very important to
verify Medicaid eligibility, coverage and type prior to providing services.
Medicaid eligibility can be verified through the South Carolina Medicaid Web-Based Claims
Submission Tool (Web Tool). Please contact the SCDHHS Medicaid PSC at +1 888 289 0709 for
further information.
EVALUATION AND MANAGEMENT SERVICES
Please refer to the CPT when multiple E&M services are provided on the same date of service
(DOS).
Convenient Care Clinics
Effective with dates of services on or after August 1, 2012, the SCDHHS will now allow Convenient
Care Clinics (CCC) to enroll as a provider group for billing purposes. CCCs are in retail stores,
supermarkets and pharmacies and may treat uncomplicated minor illnesses and provide
preventative healthcare services. They are often referred to as retail clinics, retail-based clinics or
walk-in medical clinics.
Episodic Care for adults and children is defined as a pattern of medical and nursing care in which
services are provided to a person for a particular problem, without an ongoing established
relationship between the patient and health care professionals. Examples of Episodic Care include,
but are not limited to allergies, bronchitis, ear infections, flu-like symptoms, mononucleosis, motion
sickness, blisters, minor burns, minor cuts, sprains and strains. Episodic Care (i.e., sick visits) is
covered for all ages and subject to the CCCs internal policies governing initial age for treatment.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
19
Covered Services
EPSDT for this provider type is limited to children five years and older. For additional program,
billing, and reimbursement policy information, please refer to EPSDT Standards in this section.
Immunizations
Vaccinations are covered as indicated under Immunization in this section.
Diabetes Patient Education
Diabetes Management services are medically necessary, comprehensive self-management and
counseling services provided by programs enrolled by SCDHHS. Enrolled programs must adhere to
the National Standards for Diabetes Self-Management Education and be recognized by the
American Diabetes Association, American Association of Diabetes Educators, Indian Health
Services or be managed by a Certified Diabetes Educator. An eligible beneficiary must have a
diabetes diagnosis and be referred by their PCP. For details on this service, please refer to the
Enhanced Services Manual. Contact the PSC for a list of recognized programs in your area or
information on how to become a provider of diabetes education.
Preventive Services
Preventive services are defined as any routine service exam for adults or children when the
procedures are performed in the absence of an illness or complaint(s). A well visit and a sick visit
may be billed on the same DOS. Generally, the South Carolina Medicaid program requires that a
complaint or illness be recorded before a service is compensable.
Preventive Screening
Providers must follow the United States Preventive Services Task Force (USPSTF) grade A and B
recommendations available on the USPSTF's website at
A and B Recommendations | United States
Preventive Services Taskforce (uspreventiveservicestaskforce.org) when providing preventive
screenings to full benefit Healthy Connections Medicaid members.
For preventive screenings for Family Planning Limited benefit members, please refer to the Family
Planning section of this manual.
Immunizations
Providers must follow the Advisory Committee on Immunization Practices (ACIP) recommendations
on vaccines for both children and adults available at ACIP Vaccine Recommendations | CDC
, when
administering vaccines to full benefit Healthy Connections Medicaid Members.
For immunizations for Family Planning Limited benefit members, please refer to the Family Planning
section of this manual.
All vaccines and vaccine administration are covered without cost-sharing.
https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-a-and-b-
recommendations

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
20
Family Planning Services
Family planning services are defined as preconception services that prevent or delay pregnancies
and do not include abortion or abortion-related services.
Family Planning is a limited benefit program available to men and women who meet the appropriate
federal poverty level percentage in order to be eligible. This program provides coverage for physical
examinations, Family Planning services, Family Planning-related services, and some preventive
health screenings. Family Planning promotes the increased use of primary medical care; however,
beneficiaries enrolled in this program only receive coverage for a limited set of services. Services
provided to men and women enrolled in Family Planning that are not specifically outlined below are
the sole responsibility of the beneficiary.
Family Planning services do not require a referral or prior authorization for beneficiaries in
Medicaid’s managed care programs. All services rendered to dually eligible (Medicare and
Medicaid) patients must be filed to Medicare first. Family Planning services that are non-covered
services by Medicare are reimbursed by Medicaid. Providers may contact the PSC at +1 888 289
0709 or submit an online inquiry at Contact a Provider Representative | SCDHHS
for billing
procedures.
Covered Services
Family Planning services may be prescribed and rendered by physicians, hospitals, clinics,
pharmacies, or other Medicaid providers recognized by state and federal laws and enrolled as a
Medicaid provider. Services include family planning examinations, counseling services related to
pregnancy prevention, contraceptives, laboratory services related to family planning, etc., and
sterilizations (including vasectomies) accompanied by a completed Sterilization Consent Form
(DHHS Form 687, located in the forms section of the provider portal).
Long-Acting Reversible Contraceptives (LARC) are covered under both the pharmacy benefit and
under the medical benefit using the traditional “buy and bill” method. Any LARC billed to Medicaid
through the pharmacy benefit will be shipped directly to the provider’s office for insertion. Providers
must only bill Medicaid for the insertion of the device when it is purchased through the pharmacy.
All Family Planning services must be billed using the appropriate CPT or Healthcare Common
Procedure Coding System (HCPCS) code with an FP modifier and/or an appropriate diagnosis
code.
Note: Pregnancy testing (when the test result is negative) is a reimbursable family-planning-related
service in two situations:
1. The test is provided at the time family planning services are initiated for an individual.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
21
2. The test is provided after the initiation of family planning services, when the patient may not
have used the method properly, or when the patient is having an unusual response to the family
planning method.
Examinations/Visits
Four types of visits are covered for beneficiaries enrolled in the Family Planning Program. These
visits include biennial (once every two years) physical examinations, annual family planning E&M
visits, periodic family planning visits and contraceptive counseling visits.
Initial Family Planning Visit
New patients are not required to have a physical examination during an initial Family Planning visit
in order to receive hormonal contraceptives or other family planning procedures as prescribed. A
new patient is one who has not received any professional services from the physician or another
physician of the same specialty who belongs to the same group practice within the past three years.
This visit must be billed using the appropriate level of CPT E&M codes with an FP modifier.
The initial visit is the first visit and requires the establishment of the medical record, an
establishment of baseline laboratory data, contraceptive and sexually transmitted disease
prevention counseling, medically necessary lab tests, and an issuance of supplies or prescriptions.
The initial Family Planning Physical Assessment is an integral part of the initial Family Planning
visit.
The following services, at a minimum, must be provided during the initial visit:
• Medical history.
• Reproductive life plan.
• Sexual health assessment.
• Height, blood pressure and weight check.
• Documentation of any treatment and/or counseling including administration and/or issuance of
contraceptive supplies.
• Counseling and education, as necessary, regarding pregnancy prevention and/or sexually
transmitted diseases.
The following services, at a minimum, must be provided during the initial visit:
• Breast exam, >20 years of age for females
• Cervical Cytology, ≥21 years of age for females

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
22
Genital exam, to include inspection of skin, hair and perianal region, as well as palpation of inguinal
nodes, scrotum and penis for males.
Biennial Physical Examination
The Family Planning Program sponsors adult physical examinations under the following guidelines:
• Examinations are allowed once every two years per beneficiary.
• The examinations are preventive visits.
• There are separate codes for initial patient visits and established patient visits.
• A FP modifier must be used when billing these codes for Family Planning beneficiaries.
• Diagnosis code Z00.00 or Z00.01 must be used when billing these codes for Family Planning
beneficiaries.
• The examinations can be performed by a NP, PA or physician.
The adult physical examination for Family Planning beneficiaries is a preventive, comprehensive
visit and must contain the following components, at a minimum:
– A past family, social, and surgical history for a new patient or an interval history for an
established patient
– Height, weight and body mass index (BMI)
– Blood pressure
– A generalized physical overview of the following organ systems:
› Abdomen
› Heart
› Back
› Lungs
› Breasts (female)
› Pelvic (female)
› Brief muscular
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
23
› Peripheral vascular
› Brief neurological
› Prostate (male)
› Brief skeletal
› Rectal
› Head, Eye, Ear, Nose and Throat (HEENT)
› Skin
› External genitalia
– Age, gender and risk appropriate preventive health screenings, according to the United
States Preventive Services Task Force (USPSTF) Recommendations (Grade A and B with
the addition of Grade C prostate cancer screening recommendation).
For more information on these recommendations, please visit
https://www.uspreventiveservicestaskforce.org/
Screenings
Family Planning covers a limited amount of prevention screening. Please refer to the USPSTF
recommendations listed in the chart below.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
24
DESCRIPTION
APPROPRIATE
FOR THE
FOLLOWING
FAMILY
PLANNING
BENEFICIARIES
ALLOWABLE
CODES
REQUIRED
MODIFIER
PROVIDER TYPE
REQUIREMENTS
NOTES
Age and Risk-
Appropriate
Screenings for the
Following:
Alcohol Misuse
BRCA Screening
Questions
Depression
Intimate Partner
Violence
Obesity
Tobacco Use
Low-Intensity
Counseling for the
Following:
Healthy Diet
Skin Cancer
Prevention
All adults 96150
96151
96152
FP
NP, PA or Physician
Must occur during physical
exam
Cholesterol
Abnormalities
Screening
Men aged 35+
Men aged 20-35 if at
increased risk for
coronary heart disease
Women ages 20+ if at
increased risk for
coronary heart disease
80061
82465
83718
FP
NP, PA or Physician
Must occur during physical
exam
Diabetes Screening
Asymptomatic adults
with sustained blood
pressure (either treated
or untreated) greater
than 135/80 mm Hg
82947
82950
82951
83036
FP
NP, PA or Physician
Must occur during physical
exam
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
25
DESCRIPTION
APPROPRIATE
FOR THE
FOLLOWING
FAMILY
PLANNING
BENEFICIARIES
ALLOWABLE
CODES
REQUIRED
MODIFIER
PROVIDER TYPE
REQUIREMENTS
NOTES
Hepatitis C Virus
Infection Screening
All adults at high risk for
virus infection
One-time screening for
all adults born between
1945-1965
86803
86804
FP
NP, PA or Physician
Must occur during physical
exam
Breast Cancer
Screening
(Mammography)
Women aged 40-74 77067
77066
FP
Physician
/Provider/Qualified
Practitioner
Can occur outside physical
exam
Abdominal Aortic
Aneurysm Screening
Men aged 65-75 who
have ever smoked
76706 FP Physician Only
Can occur outside physical
exam
Colorectal Cancer
Screening
Men and Women ages
50-75
45331 45378
82270 82274
88305 G0105
FP
Physician Only
Can occur outside physical
exam
Colorectal Cancer
screening using
Multi-targeted stool
DNA (MT-sDNA) test
Cologuard
Men and Women ages
45-75
81528 FP Physician Order Only
Can occur outside physical
exam.
Allowed every three years
for asymptomatic, low-
average risk members,
Lung Cancer
Screening for
Smokers
Adults ages 55 - 80 who
have a 30-pack-year
smoking history and
currently smoke or have
quit within the past 15
years
71250 FP
Physician Only
Can occur outside physical
exam
Prostate Cancer
Screening
Men aged 55-69
G0102 G0103
84153
FP Physician Only
Can occur outside physical
exam

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
26
The following screenings have age, sex, and/or patient history limitations:
• Breast Cancer Screens (mammography) are covered for women ages 40 to 74 years with a
recommended frequency of one screening every 2 years.
• Abdominal Aortic Aneurysm (AAA) screens are limited to men who have had a smoking history
and are between the ages of 65 and 75 years.
• Colorectal Cancer screens are covered for both men and women who are between the ages of
50 and 75 years.
– The mt-sDNA test (Cologuard) is recommended every three years for asymptomatic, low-
average risk members, aged 45 to 75 years who:
› Have not had any colorectal screening in the past, or
› Have had a negative colonoscopy at least seven years prior.
– The mt-sDNA test is not recommended for high-risk individuals who:
› Have a personal history of colorectal cancer and adenomas.
› Have had a positive result from another colorectal cancer screening at any time.
› Have been diagnosed with a condition associated with high risk for colorectal cancer
such as IBD, chronic ulcerative colitis, or Crohn’s disease; or have a family history of
colorectal cancer, or certain hereditary syndromes.
• Lung Cancer screens cover both men and women between the ages of 55 and 80 years and
meet one or more of the following criteria:
– Beneficiary is a current smoker
– Beneficiary has a 30-pack per year history
– Beneficiary quit smoking within 15 years
• Prostate Cancer screens are covered for men between the ages of 55 and 69 years.
Family Planning Counseling must be offered to Family Planning beneficiaries during the physical
examination.
Portions of the physical may be omitted if not medically applicable to the beneficiary’s condition or if
the beneficiary is not cooperative and resists specific system examinations (despite encouragement

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
27
by the physician, NP or office staff). A note must be written in the record explaining why part of the
exam was omitted.
Note: If a medical condition and/or problem is identified during the physical examination and the
provider is unable to offer free or affordable care based on the individual’s income, the provider
must refer the beneficiary to a provider who can offer services to uninsured individuals (examples
include FQHCs, RHCs, free clinics, etc.). Please refer to “Referral Instructions for Family Planning”
in this section for important information about billing for beneficiary referrals.
The following lab procedures are included in the reimbursement for the physical examination:
• Hemoccult
• Urinalysis
• Blood Sugar
• Hemoglobin
Note: College physicals, direct observed therapy (DOT) physicals, and administrative physicals are
not covered.
Annual Family Planning Evaluation/Management Visits
The Family Planning Program sponsors annual Family Planning Evaluation/Management visits. The
annual visit is the re-evaluation of an established patient requiring an update to the medical record,
interim history, physical examination, appropriate diagnostic laboratory tests and/or procedures,
Family Planning Counseling, and adjustment of contraceptive management as indicated. This visit
must be billed using the appropriate level of CPT E&M with an FP modifier.
The following services, at a minimum, must be provided during the annual visit:
• Medical history
• Sexual health assessment
• Weight
• Blood pressure check
• Symptom appraisal, as needed
• Documentation of any treatment and/or counseling including administration and/or issuance of
contraceptive supplies

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
28
• Counseling and education, as necessary, regarding pregnancy prevention and/or sexually
transmitted diseases
• Breast exam, annually if >19 years of age; then every three years if 20–39 years of age
• Cervical Cytology:
– Every three years if ≥21 years of age
– Every five years if ≥30 years of age
• Genital exam, to include inspection of skin, hair and perianal region, as well as palpation of
inguinal nodes, scrotum and penis
• Laboratory tests
• Issuance of birth control supplies or prescription
Periodic Revisit
The Family Planning Program sponsors periodic revisits for beneficiaries, as needed. The periodic
revisit is a follow-up of an established patient with a new or an existing family planning condition.
These visits are available for multiple reasons such as change in contraceptive method due to
problems with that method (e.g., breakthrough bleeding or the need for additional guidance) or
issuance of birth control supplies. This visit must be billed using the appropriate level of E&M with
an FP modifier.
For E&M, the following services, at a minimum, must be provided during the revisit:
• Weight and blood pressure check
• Interim history
• Documentation of any treatment and/or counseling including administration and/or issuance of
contraceptive supplies
The following services, at a minimum, must be provided during the periodic visit:
• Symptom appraisal, as needed
• Laboratory tests
• Issuance of birth control supplies or prescription

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
29
Family Planning Counseling Visits
The Family Planning Program sponsors Family Planning Counseling Visits for beneficiaries. The
Family Planning Counseling/Education visit is a separate and distinct service (Preventative
Medicine Counseling and/or Risk Factor Reduction Intervention) with an FP modifier. Family
Planning Counseling/Education is a face-to-face interaction to enhance a beneficiary’s
comprehension of, or compliance with, his or her family planning method of choice. These services
are for the expressed purpose of providing education/counseling above and beyond the routine
contraceptive counseling that are included in the clinic/office visits.
Note: This service may not be billed on the same day as another visit.
Covered Contraceptive Supplies and Services
The Family Planning Program provides coverage for contraceptive supplies (for example, birth
control pills or male condoms) and contraceptive services such as an injection, intrauterine device
(IUD), Essure®, or sterilization. When billing for contraceptive services and supplies, all claims must
bill using a relevant Family Planning diagnosis code.
Long-Acting Reversible Contraceptives (LARCs)
LARCs are covered under both the pharmacy benefit and under the medical benefit using the
traditional “buy and bill” method. Any LARC billed to Medicaid through the pharmacy benefit will be
shipped directly to the provider’s office for insertion. Providers must only bill Medicaid for the
insertion of the device when it is purchased through the pharmacy.
Note: Pregnancy testing (when the test result is negative) is a reimbursable Family Planning service
in two situations:
1. The test is provided at the time family planning services are initiated for an individual.
2. The test is provided after the initiation of family planning services, when the patient may not
have used the method properly, or when the patient is having an unusual response to the family
planning method.
Covered Screenings and Testing
The Family Planning Program provides coverage for sexually transmitted infections (STI)
screenings including syphilis, chlamydia, gonorrhea, herpes, candidiasis, trichomoniasis and HIV,
when performed at the time of the physical examination, initial or annual family planning visits. All
diagnostic tests will require the FP modifier to be appended to the CPT/HCPCS codes. All claims
must contain a relevant Family Planning diagnosis code.
Immunization
The Family Planning Program provides coverage for the Human Papillomavirus (HPV) 9-valent
vaccine for members between the ages of 19- 45 years in alignment with the Centers for Disease
Control and Prevention (CDC) adult immunization schedule and the Advisory Committee on

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
30
Immunization Practices (ACIP) vaccine recommendations and guidelines, ACIP Vaccine
Recommendations and Schedules | CDC as follows:
– Routine HPV vaccination is recommended for everyone through age 26 years if not
adequately vaccinated when younger. HPV vaccination is given as a series of either two or
three doses, depending on age at initial vaccination.
– HPV vaccination for adults aged 27-45 is based on recommendations for shared clinical
decision-making, which is individually based and informed by a decision process between
the health care provider and the patient. Clinicians may consider discussing HPV
vaccination with members aged 27-45 who are most likely to benefit from it.
Covered Medication
If, during a physical examination or annual family planning E&M visit, any of six specific STIs are
identified, antibiotic treatment will be allowed under the Family Planning Program. The six STIs are
syphilis, chlamydia, gonorrhea, herpes, candidiasis and trichomoniasis. STI testing and treatment
are only covered during the beneficiaries’ physical examination or annual family planning visit.
Breast and Cervical Cancer Early Detection Program (Best Chance Network)
The South Carolina Breast and Cervical Cancer Early Detection Program (Best Chance Network)
provides coverage for women under the age of 65 who have been diagnosed and found to be in
need of treatment for either breast or cervical cancer or pre-cancerous lesions (CIN 2/3 or atypical
hyperplasia). For further information, providers or beneficiaries may call toll-free +1 888 549 0820.
Department of Public Health
SCDPH provides outreach and direct FP services as part of the waiver and will assist women in
finding a PCP or clinic to provide Family Planning services. Participants in the FP program can call
toll-free +1 855 472 3432 for more information about covered services and health department
locations. Also, SCDPH contracts with private physicians who will offer FP services to participants.
Tobacco Cessation
Tobacco use is the leading cause of preventable disease and premature death in South Carolina.
SCDHHS provides comprehensive coverage for tobacco cessation treatment through
pharmacotherapy and counseling for all full-benefit Medicaid beneficiaries. SCDHHS also partners
with SCDPH to communicate about programs available to assist Medicaid beneficiaries with quitting
tobacco use.
Providers are encouraged to screen beneficiaries for tobacco use during medical encounters and
document nicotine dependence using the appropriate diagnosis codes.
Medication
SCDHHS covers prescriptions for the following tobacco cessation and nicotine replacement therapy
(NRT) products:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
31
• Bupropion sustained release (SR) products for tobacco use (Zyban)
• Varenicline (Chantix) tablets
• Nicotine gum
• Nicotine lozenge
• Nicotine nasal spray
• Nicotine inhaler
• Nicotine patch
Tobacco cessation products are exempt from prior authorization requirements. There is no limit to
the number of quit attempts in a calendar year. The following medically appropriate combination
therapies are also covered:
• Long-term nicotine patch + other NRT product (gum or spray)
• Nicotine patch + nicotine inhaler
• Nicotine patch + Bupropion SR
General edits on day supply are based on product dosing in manufacturer package inserts.
Prescribers are encouraged to reference the AAFP Pharmacologic Product Guide for Food and
Drug Administration (FDA)-approved medications for smoking cessation for more information on
product guidelines.
As with all other pharmaceuticals, SCDHHS reimburses only rebated products (brand or generic) for
fee-for-service (FFS) beneficiaries. A beneficiary must provide a prescription to receive any
medication, including over-the-counter (OTC) products. A dual-eligible member can receive OTC
products through Medicaid coverage, but the individual’s Medicare Part D prescription drug plan
must cover prescriptions for legend (non-OTC) tobacco cessation products.
For further questions about this benefit, prescribers may contact the pharmacy benefit administrator.
For contact information refer to the Provider Administrative and Billing Manual.
Counseling
Tobacco cessation counseling in individual and group settings are covered when billed with the
appropriate code. Reimbursement for counseling is limited to four sessions per quit attempt for up to
two quit attempts annually. Tobacco cessation counseling may be billed on the same day as an
office visit using an appropriate modifier.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
32
SCDHHS policy requires that all tobacco cessation treatment must be ordered by a qualified
practitioner defined as a physician, NP, CNM or PA. Medical documentation including time spent
counseling the patient, treatment plan, and pharmacotherapy records must be maintained in the
patient record.
South Carolina Tobacco Quitline
One-on-one telephone counseling with web-based support are available to all South Carolinians
without charge through the South Carolina Tobacco Quitline. Participants in the Quitline program
are connected with a personal Quit Coach, who helps the participant develop a quit plan and uses
cognitive behavioral coaching and motivational interviewing techniques to support the quit process.
This evidence-based program has been clinically proven to help participants quit tobacco use, and
tailored programs are available for Hispanic, Native American, pregnant and youth callers, and
smokeless tobacco users, as well as participants who have chronic medical and mental health
conditions.
SCDHHS strongly encourages prescribers and pharmacists to refer patients to the South Carolina
Tobacco Quitline at +1 800 QUIT NOW. Services are available 24 hours a day, seven days a week.
Additional information is available at
https://www.dph.sc.gov/health-wellness/tobacco-prevention-control/tobacco-cessationTelehealth
Telehealth is defined as the provision of healthcare via electronic communications technology
between a provider in one location and a patient in another location without loss of quality of care.
Electronic communication means the use of interactive telecommunication equipment that typically
includes audio and video equipment permitting two-way, real-time interactive communication
between the patient and the provider at the referring site.
Children and adult beneficiaries are eligible to receive services via telehealth modality under the
State Plan benefit (authority).
Though there are differences in the definitions of telehealth and telemedicine, the two terms are
generally used interchangeably, and SCDHHS will reference telehealth in this and other provider
manuals addressing the provision of services via electronic communications.
Telehealth includes consultation, diagnostic and treatment services. Telehealth as a service delivery
option, in some cases, can provide beneficiaries with increased access to specialists, better
continuity of care, and eliminate the hardship of traveling extended distances.
Telehealth services are not an expansion of Medicaid-covered services but an option for the
delivery of certain covered services. Quality of health care must be maintained regardless of the
mode of delivery.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
33
Consultant Sites
A consultant site (also called the distant site) is the site at which the provider is located at the time
the telehealth service. The provider performing the medical care must be currently and appropriately
licensed in South Carolina.
Referring Sites
A referring site (also called the patient site) is the location of an eligible Medicaid beneficiary at the
time the telehealth service is being furnished. Medicaid beneficiaries are eligible for telehealth
services only if they are presented from a referring site located in the SCMSA. Referring site
presenters may be required to facilitate the delivery of this service. Referring site presenters must
be a knowledgeable person on how the equipment works and able to provide clinical support if
needed during a session.
Covered referring sites are:
• The office of a qualified practitioner defined as a physician, NP, CNM, PA, or LIP
• Hospital (inpatient and OP)
• RHCs
• FQHCs
• Community Mental Health Centers
• Public Schools
• Act 301 Behavioral Health Centers
• Patient home
Telehealth Providers
Providers who meet the Medicaid credentialing requirements and are currently enrolled with the
South Carolina Medicaid program are eligible to bill for telehealth and telepsychiatry when the
service is within the scope of their practice.
If a referral is needed for a beneficiary’s plan of care, providers utilizing telehealth as the mode of
delivery will be described below. The referring provider is the provider who has evaluated the
beneficiary, determined the need for a consultation, and has arranged the services of the consulting
provider for the purpose of consultation, diagnosis and/or treatment.
The consulting provider is the provider who evaluates the beneficiary via telehealth upon the
recommendation of the referring provider.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
34
In situations where a referral is not needed, the provider will not need to be confined to the
definitions above.
Practitioners at the distant site who may furnish and receive payment for covered telehealth
services are:
• Physicians
• NPs
• PAs
• Licensed Independent Practitioners (and associates)
• Physical, occupational, and speech therapists
Covered Services
Services that are eligible for reimbursement include consultation, office visits, individual
psychotherapy, pharmacologic management, and psychiatric diagnostic interview examinations and
testing, delivered via a telecommunication system. Audio-only (telephonic) care is available for
established patients only. A licensed physician, NP, PA, licensed psychologist, licensed professional
counselor, licensed independent social worker, and licensed marriage and family counselor may
provide telepsychiatry services.
As a condition of reimbursement, an audio and video telecommunication system that is Health
Insurance Portability and Accountability Act of 1996 (HIPAA) compliant must be used. This
telecommunication system must permit interactive communication between the provider at the
consultant site and the beneficiary at the referring site.
Office and OP visits that are conducted via telehealth are counted towards the applicable benefit
limits for these services.
Medicaid covers telehealth when the service is medically necessary and under the following
circumstance:
• The medical care is individualized, specific, and consistent with symptoms or confirmed
diagnosis of the illness or injury under treatment, and not in excess of the beneficiary’s need.
• The medical care can be safely furnished.
• No equally effective, more conservative or less costly treatment is available Statewide.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
35
A list of Medicaid telehealth services can be found in the Procedure Codes section of this manual.
Coverage Guidelines
The following conditions apply to all services rendered via telehealth.
• The beneficiary must be present and participating in the telehealth visit. Any exemptions to this
condition (such as interprofessional consultation services) will be otherwise listed under the
exempted service section of this manual respectively.
• The referring provider must provide pertinent medical information and/or records to the
consulting provider via a secure transmission.
• Interactive audio and video telecommunication must be used, permitting encrypted
communication between the distant site physician or practitioner and the Medicaid beneficiary.
The telecommunication service must be secure and adequate to protect the confidentiality and
integrity of the telehealth information transmitted.
• The telehealth equipment and transmission speed and image resolution must be technically
sufficient to support the service billed. Any staff involved in the telehealth visit must be trained in
the use of the telehealth equipment and competent in its operation.
• A trained healthcare professional at the referring site (patient site presenter) is required to
present the beneficiary to the provider at the consulting site and remain available as clinically
appropriate (this condition is waived when the referring site is the patient home).
• If the beneficiary is a minor (under 18 years old), a parent and/or guardian must present the
minor for telehealth service unless otherwise exempted by State or Federal law. The parent
and/or guardian need not attend the telehealth session unless attendance is therapeutically
appropriate.
• The beneficiary retains the right to withdraw from the telehealth visit at any time.
• All telehealth activities must comply with the requirements of HIPAA: Standards for Privacy of
individually identifiable health information and all other applicable State and Federal Laws and
regulations.
• The beneficiary has access to all transmitted medical information, except for live interactive
video, as there is often no stored data in such encounters.
• The provider at the distant site must obtain prior approval for service when services require prior
approval, based on service type or diagnosis.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
36
Unusual Travel
This service is compensable only when a patient must be transported to a medical facility and is
accompanied by a physician because there is no other recourse available based on the necessary
medical skills and expertise required for the patient's condition. Documentation must be submitted
with the claim. Coverage and reimbursement will be determined on a claim-by-claim basis.
Unlisted Services or Procedures
A service or procedure may be provided that is not listed in the CPT. When reporting such a service,
the appropriate "unlisted” procedure code may be used to indicate the service, identifying it by
special report.
Appropriate records to justify the use of the unlisted code, the complexity of the service, and the
charge must accompany the unlisted procedures. The reimbursement will be directly related to the
support documentation submitted with the claim. To ensure proper interpretation and payment, a
complete description of the performed service is required.
Procedures that are considered an integral part of an examination shall not be charged separately
(i.e., simple vision test, blood pressure check, ophthalmoscopy, otoscopy). Charges for these
services in addition to an E&M visit will be denied.
Preventive/Rehabilitative Services for Primary Care Enhancement (P/RSPCE)
P/RSPCE are provided to support primary medical care in patients who exhibit risk factors that
directly impact their medical status. These services are designed to help the physician maximize the
patient’s treatment benefits and outcomes by supplementing routine medical care.
These services can be provided by public health nurses, social workers, dietitians, health educators,
home economists, and public health assistants who have special training and experience in working
in the home or other community setting to assist the client in meeting mutually developed health
care objectives.
Following are examples of P/RSPCE:
• Comprehensive assessments/evaluations of a client's medical, nutritional or psychosocial needs
by health professionals.
• Home or community follow-up as requested by a PCP to monitor the medical plan of care,
reinforce the treatment regime, counsel, provide anticipatory guidance, and support the client’s
medical needs. Nurses can apply the nursing process with the overall aim of optimizing the
health outcomes of the client.
• Social work assessment, counseling or anticipatory guidance relative to the medical plan of care

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
37
• Medical nutrition therapy for clients with chronic disease, growth problems, medically diagnosed
anemias, elevated blood lead or other nutritional disorders.
• Coordination of medical services for clients with multiple providers and/or complex needs.
Counseling interventions address the client’s attitude, knowledge base, beliefs, behaviors and
values relative to the medical condition. Individual and group interventions are tailored to meet the
patient’s needs and include specific targeted actions that are more than simple didactic
presentations of information. These actions are intended to be collaborations between the
P/RSPCE, the PCP and the patient.
Contact the PSC for more details on P/RSPCE services.
Missed Appointments
Medicaid beneficiaries cannot be charged for missed appointments. A missed appointment is not a
distinct reimbursable Medicaid service, but a part of provider’s overall costs of doing business. The
Medicaid rate covers the cost of doing business, and providers may not impose separate charges
on beneficiaries.
Home Health Services — Physician Requirements
Home health services are provided only by home health agencies that are certified by SCDES and
have contracted with SCDHHS. Coverage is dependent upon a physician's orders and payable only
to a contracted home health agency.
Plan of Care
Covered home health services must be ordered by the beneficiary’s attending physician as part of a
written plan of care, consistent with the functions the practitioner is legally authorized to perform.
The plan of care must specify the treatment, services, items or personnel needed by the patient and
the expected outcome. The care must be appropriate to the home setting and to the patient's needs.
For additional information, providers may contact the PSC at +1 888 289 0709 or submit an online
inquiry at Contact a Provider Representative | SCDHHS
.
Long-Term Living Program
The Community Long-Term Care (CLTC) Program is designed to serve Medicaid-eligible aged and
disabled adults who require long-term care. Careful assessment, service planning, and counseling
allow each client to receive care in his or her own home, thus avoiding premature and costly nursing
home admission.
For additional information, providers may contact the PSC or submit an online inquiry.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
38
Nursing Home/Rest Home Facility Services
Services provided by a physician for a patient residing in a nursing home or long-term care facility
must be medically necessary, requested by the patient or responsible party, or performed to meet
the requirements of continued long-term care.
Services such as physical therapy (PT), occupational therapy (OT), recreational therapy, dietary
consultation, social services, and nursing care are reimbursable only through the nursing home
facility charges, according to the per diem rate.
If nursing home placement is not available, please refer to “Administrative Days” under “Inpatient
and Outpatient Hospital Services” in this section.
The attending physician must submit signed and dated certification by the 60
th
day of the patient’s
stay at the SNF in order for the patient to remain certified.
Injections
Coverage Guidelines
Injectable drugs are covered if the following criteria are met:
• They are of the type that cannot be self-administered. The usual method of administration and
the form of the drug given to the patient are two factors in determining whether a drug should be
considered self-administered. If a form of the drug given to the patient is usually self-injected
(e.g., insulin), the drug is excluded from coverage unless administered to the patient in an
emergency (e.g., diabetic coma).
• The medical record must substantiate medical necessity. When acceptable oral and parenteral
preparations exist for necessary treatment, the oral preparation must be the route of
administration. If parenteral administration is necessary, the record must document the reason
for choosing this route.
• Use of a drug or biological must be safe and effective, and otherwise reasonable and necessary.
Drugs or biologicals approved for marketing by the FDA are considered safe and effective for
purposes of this requirement when used for indications specified on the labeling. Occasionally,
FDA-approved drugs are used for indications other than those specified on the labeling.
Provided the FDA has not specified such use as non-approved, coverage is determined
considering the generally accepted medical practice in the community.
• Drugs and biologicals that have not received final marketing approval by the FDA are not
covered unless CMS advises otherwise.
• The injection must be furnished and administered by a physician, or by auxiliary personnel
employed by the physician and under his or her personal supervision.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
39
• When billing for a drug administered in the office, the physician must bill an injection code. A
prescription cannot be filled by a pharmacist and then returned to a physician's office for
administration.
Orphan Drugs
An orphan drug is a drug or biological product used for the treatment or prevention of a rare disease
or condition. Prior approval is required for orphan drugs that are not listed on the injection code list.
Unlisted Injections
If an injection is not listed, the appropriate J code must be used. A description of the drug, the
National Drug Code (NDC) number, and the dosage, along with the office record, flow record (if
possible), and an invoice indicating the cost of the drug, must all be attached to the claim to be
considered for payment. Claims containing this code without the required documentation will be
rejected. Additional documentation may be required if the unlisted injection is being submitted for
reimbursement for the first time. When a claim is rejected, providers must submit a new claim and
attach the required documentation for medical review.
When billing multiple unlisted injection codes on the same claim, the documentation must identify
the specific unlisted code that is to be considered for reimbursement.
The appropriate procedure code is billed per injection for administration.
Botox®, Dysport®, Myobloc®, and Xeomin®
Botox®, Injection, OnabotulinumtoxinA
Botox® is FDA-approved for strabismus, blepharospasm, severe primary axillary hyperhidrosis,
upper limb spasticity in adults, cervical dystonia in adults, and for the prophylaxis of headaches in
adult patients with chronic headache and chronic migraine prophylaxis (≥15 days per month with
headache lasting four hours a day or longer). In addition, Botox® is FDA-approved to treat urinary
incontinence due to detrusor overactivity associated with a neurologic condition [e.g., spinal cord
injury, multiple sclerosis (MS)] in adults who have an inadequate response to or are intolerant of an
anticholinergic medication.
• Dysport®
• Dysport® is FDA-approved for cervical dystonia in adults
• Myobloc® injection, rimabotulinumtoxinb
• Myobloc® is FDA-approved for cervical dystonia in adults
• Xeomin® injection, incobotulinumtoxina

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
40
• Xeomin® is FDA-approved for cervical dystonia in adults and for blepharospasm in adults
previously treated with onabotulinumtoxinA (Botox®)
The botulinum toxin products listed on the left share certain properties and some FDA-approved
indications. However, these agents are not identical. They have differing therapeutic and adverse
even profiles. Botulinum toxin products are not directly interchangeable with one another.
SCDHHS requires support documentation to be submitted with claims filed for Botox®, Dysport®,
Xeomin® or Myobloc®. Medicaid will pay claims for Botox®, Dysport®, Xeomin® or Myobloc® only
when administered for FDA-approved indications. Therefore, medical records submitted with the
claim must:
• Include the beneficiary’s age
• Clearly delineate the symptom or circumstance that necessitates the administration of Botox®,
Dysport®, Xeomin® or Myobloc®
Claims will reject if information is omitted or if it cannot be determined that the product was given for
an FDA-approved indication.
All Botulinum toxin products must be preauthorized by Magellan Rx Management except for those
being administered to patients who are dually eligible for Medicare and Medicaid (please refer to
Utilization Review Services in this section for more information) Magellan Rx Management will pre-
authorize all Botulinum Toxin — Type A for Botox® and Type B (Myobloc®) when administered for
FDA-approved indications.
Xolair® (Omalizumab)
Xolair® is FDA-approved for patients 12 years of age or older under some circumstances (see
below for more detail). Physician CMS-1500 claims must be billed using the appropriate HCPCS J
code and must include the prior authorization number. Claims submitted without prior authorization
number will be rejected. Providers must submit prior authorization requests to Magellan Rx
Management at http://ih.magellanrx.com
or by calling +1 800 424 8219.
SCDHHS requires prior approval for Xolair® (Omalizumab), 150 mg powder/vial. Prior authorization
requests must be telephoned or faxed, toll-free, to the pharmacy benefit administrator. For contact
information, refer to the Provider Administrative and Billing Manual.
Authorizations will be based on the following criteria:
FDA-Labeled Indications:
• Approved for treatment of patients 12 years of age or older with moderate persistent or
severe persistent asthma for at least one year, who have had positive skin test or in vitro
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
41
reactivity to a perennial aeroallergen and whose symptoms are inadequately controlled with
inhaled corticosteroids.
• Symptoms not adequately controlled with the following three treatments:
– Patient must have tried or have a contraindication to inhaled corticosteroids.
– Patient must have tried or have a contraindication to long-acting Beta 2 agonists
(Reference: National Heart, Lung, and Blood Institute (NHLBI) guidelines).
– Patient must have tried or have a contraindication to a leukotriene receptor antagonist.
Length of Prior Authorization:
• Six months
• Provider must verify clinical improvement at each subsequent renewal, if approved.
The Physician Requesting the Prior Approval Must be one of the Following:
• Allergist/Immunologist
• Pulmonologist
Required Labs:
• History of positive skin test or radioallergosorbent (RAST) test to a perennial aeroallergen.
• Pretreatment serum lgE level must be 30 to 700 IU/ml.
• Weight and height
Preventive Care Services
Preventive measures are defined as any routine service exam for adults or children when the
procedures are performed in the absence of an illness or complaint(s). Generally, the South
Carolina Medicaid program requires that a complaint or illness be recorded before a service is
compensable. The exceptions to this policy are listed below:
Cancer Screening Services
Please refer to the current edition of the ICD-10 for the most appropriate diagnosis code. If a more
appropriate code is not available, use diagnosis code Z00.8.
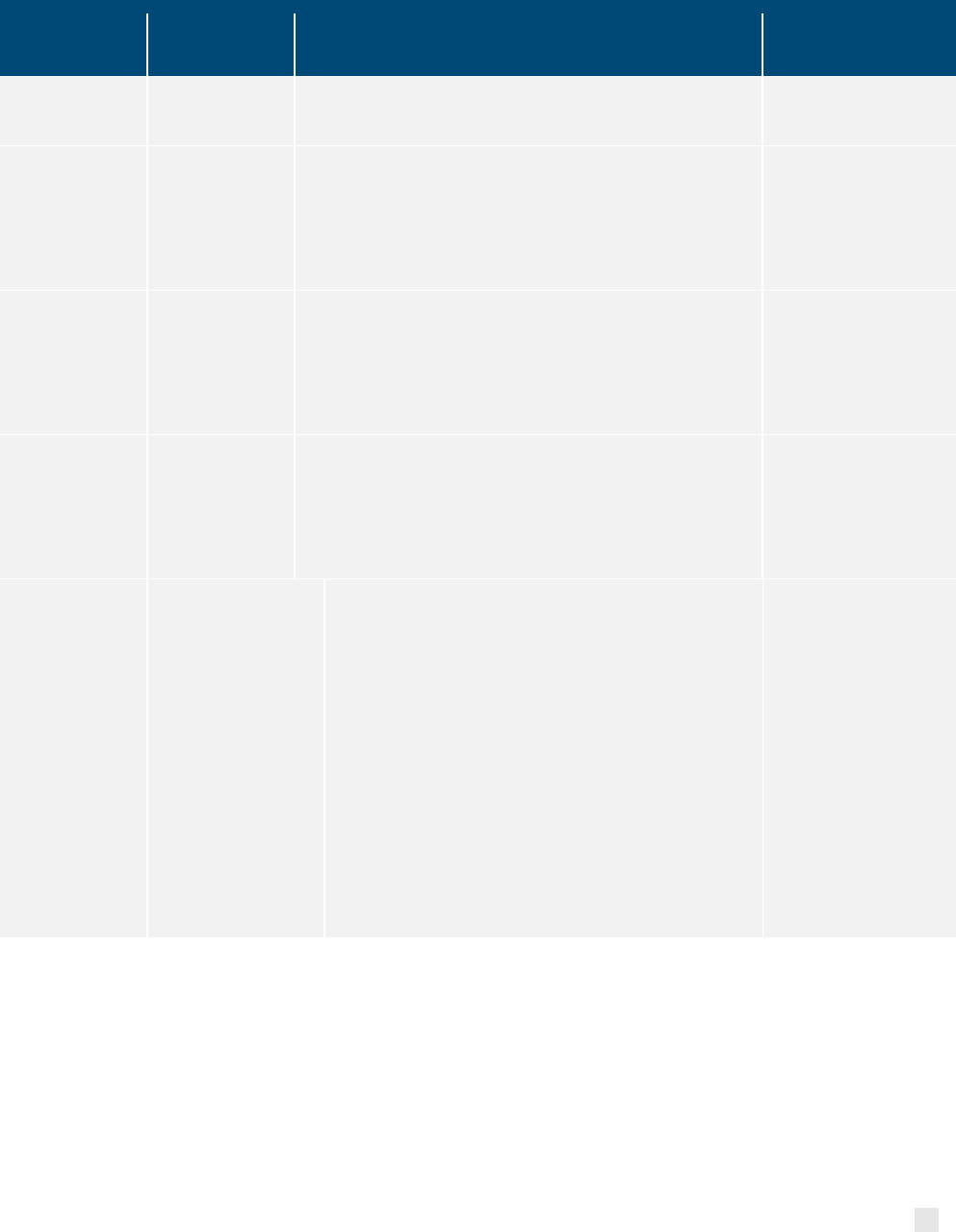
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
42
SERVICE
PROCEDURE
CODE
FREQUENCY LIMITATIONS COMMENTS
Mammography 77067 Baseline (ages 35-39*).
1 per 2 years (ages 40-74).
Must be referred by a
qualified licensed provider
Hemoccult Test
One of the
following:
82270, 82271
or 82272
• 1 per year age 50 and up for low-risk individuals (no risk
factors known).
• Age 40 and up for high-risk individuals with personal history
of polyps, ulcerative colitis, or colorectal cancer; family
history of breast or gynecological cancer
The hemoccult code
includes both the
collection of the stool and
interpretation of the test.
Sigmoidoscopy G0104
• 1 per 5 years age 50 and up for low-risk individuals (no risk
factors known).
• Age 40 and up for high-risk individuals with personal history
of polyps, ulcerative colitis, or colorectal cancer; family
history of breast or gynecological cancer
Must be referred/order by
a qualified licensed
provider
Screening
Colonoscopy
G0121
G0105
• 1 per 10 years age 50 and up for low-risk individuals (no risk
factors known).
• Age 40 and up for high-risk individuals with personal history
of polyps, ulcerative colitis, or colorectal cancer; family
history of breast or gynecological cancer
Must be referred/order by
a qualified licensed
provider
Multi-targeted stool
DNA (mt-sDNA)
test (Cologuard)
81528
• The mt-sDNA test is allowed every three years for
asymptomatic, low-average risk individuals, aged 45 to
75 years who:
o Have not had any colorectal screening in the
past, or
o Have had a negative colonoscopy at least
seven years prior.
• The mt-sDNA test is not allowed for high-risk
individuals who:
o Have a personal history of colorectal cancer or
adenomas
o Have had a positive result from another
colorectal screening at any time
o Have been diagnosed with Irritable Bowel
Disease (IBD), chronic ulcerative colitis, or
Crohn’s disease; or have a family history of
colorectal cancer, or certain hereditary
syndromes.
Must be referred/order by
a qualified licensed
provider
* The age limits on the cancer screening services are the recommended ages to begin screening
services. If medically indicated, screening services are reimbursable to younger beneficiaries
provided the medical documentation supports the screening service.
Obesity Management/Intervention Program
This policy currently targets those obese individuals who do not meet the criteria for gastric bypass
surgery or related services. Beneficiaries eligible for the Obesity Management Program are:
• Adults, age of 21 or older with a body mass index (BMI) of 30 or greater.
• Children, age 12 to 21 years with BMI greater than or equal to 95
th
percentile for age
and sex.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
43
Currently, this program will exclude the following categories of beneficiaries:
• Pregnant women
• Beneficiaries who have had or are scheduled to have bariatric surgery/gastric
banding/gastric sleeve.
• Beneficiaries actively being treated with gastric bypass surgery/vertical-banded
gastroplasty/ sleeve gastrectomy.
Obesity Management Program consists of:
• Screening for obesity in adults using measurement of BMI. The BMI is calculated by
dividing the patient’s weight in kilograms by square height in meters.
• Dietary (nutritional) assessment and intensive behavioral counseling and behavioral
therapy to promote sustained weight loss through high intensity interventions related
to diet and exercise.
• Therapeutic treatment to support weight loss in conjunction with intensive lifestyle
therapy. Providers must follow the SCDHHS Preferred Drug List (PDL) when
prescribing therapeutic treatment.
Provider Services
A provider is defined as a physician, PA or NP meeting the licensure and educational requirements
within the State of South Carolina.
During the patient’s routine physical exam or office visit, the provider will assess the patient’s need
for an obesity intervention program.
All obesity visits must include the following components listed below:
• Assess: Ask about and assess behavioral health risks and factors affecting
behavioral change goals/methods.
• Advise: Give clear, specific and personalized behavioral advice, including information
about personal health, harms and benefits.
• Agree: Collaborate with the patient to select appropriate treatment goals and
methods based on the patient’s interest and willingness to change behavioral
patterns and habits.
• Assist: Use behavioral change techniques (self-help and/or counseling) to aid the
patient in achieving agreed-upon goals by acquiring the skills, confidence, and social,
environmental supports for behavioral change, supplemented with adjunctive medical
treatments when appropriate.
• Arrange: Schedule follow-up contacts to provide ongoing assistance and/or support
and to adjust the treatment plan as needed, including referral to more intensive or
specialized treatment.
The provider must also emphasize the importance of exercise, developing a realistic exercise plan
with goals. The obesity intervention plan must be documented in the patient’s medical health
record.
The provider will arrange for an individual nutritional assessment to be provided by a licensed and
Medicaid-enrolled dietitian.
A follow-up exam must be completed by the provider to evaluate the progress the patient has made,
reviewing compliance with the exercise and nutritional plan of the patient. Documentation of each
service must include the patient’s BMI, progress toward weight management goals, activities and
compliance with the treatment plan. The provider must record the patient’s BMI in the chart.
Providers may bill for all medically necessary diagnostic testing.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
44
Dietitian Services
The dietitian is responsible for reviewing the patient’s habits, providing dietary education, reinforcing
the importance of exercise, developing a nutritional plan and establishing goals. The dietitian must
document the patient’s progress, activities, and compliance with the nutritional and exercise plan. A
written progress report must be submitted within 48 hours of the nutritional counseling visit to the
ordering provider each time the patient is seen individually or in a group/class setting. The dietitian
must maintain complete medical records of the patient’s nutritional and exercise plan, and his or her
compliance with the obesity treatment regimen.
Additional Resources
For additional resources, providers may visit the SCDPH’s Nutrition, Physical Activity & Obesity
Prevention webpage at
Nutrition, Physical Activity, & Obesity Prevention | South Carolina
Department of Public Health (sc.gov)
Nutritional Counseling Services
Eligible members: Nutritional counseling will be allowed for full benefit Medicaid beneficiaries
with a diagnosis of one of the conditions listed in the criteria below.
Eligible Providers: Physicians, Physician Assistant, Nurse Practitioners, Dietitians, FQHC,
RHC.
Place of Service: Dietary evaluation and counseling is allowed in hospital outpatient clinics;
public agencies such as health departments, federally qualified health centers, and rural health
clinics; private agencies; physician offices, residential facilities (billed by healthcare
professionals).
Clinical Criteria: Nutritional counseling is allowed when there is a chronic, episodic, or acute
condition for which nutrition therapy is a critical component of medical management, including
any one of the following:
• Inappropriate growth or weight gain such as inadequate weight gain, inappropriate weight
loss, underweight, obesity, inadequate linear growth, or short stature
• Nutritional anemia
• Eating or feeding disorders that result in a medical condition such as failure to thrive,
anorexia nervosa, or bulimia nervosa
• Physical conditions that have an impact on growth and feeding, such as very low birth
weight, necrotizing enterocolitis, cleft palate, cerebral palsy, and neural tube defects
• Chronic or prolonged infections that have a nutritional treatment component, such as HIV or
hepatitis
• Genetic conditions that affect growth and feeding, such as Cystic Fibrosis, Prader-Willi
Syndrome, or Down Syndrome
• Chronic medical conditions, such as cancer, chronic or congenital cardiac disease,
hypertension, hyperlipidemia, gastrointestinal diseases, liver disease, pulmonary disease,
malabsorption syndromes, renal disease, significant food allergies, and diseases of the
immune system
• Metabolic disorders such as inborn errors of metabolism (phenylketonuria (PKU),
galactosemia) and endocrine disorders such as diabetes
• Non-healing wounds due to chronic conditions

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
45
• Acute burns over significant body surface area
• Metabolic Syndrome
• Documented history of a relative of the first degree with cardiovascular disease or
possessing factors that significantly increase the risk of cardiovascular disease, such as a
sedentary lifestyle, elevated cholesterol, smoking, high blood pressure, and higher than ideal
body weight
• Pregnant women when the pregnancy is threatened by chronic, episodic, or acute conditions
for which nutrition therapy is a critical component of medical management and postpartum
women who need follow-up for these conditions or who develop such conditions early in the
postpartum period, including any one of the following:
o Conditions that affect the length of gestation or the birth weight, where nutrition is an
underlying cause, such as:
Severe anemia [Hemoglobin (Hgb) less than 10m/dl or Hematocrit (HCT) less
than 30]
Preconceptionally underweight (less than 90% standard weight for height)
Inadequate weight gain during pregnancy.
Intrauterine growth retardation.
Very young maternal age (under the age of 16).
Multiple gestation; or
Substance use or abuse
o Metabolic disorders, such as diabetes, thyroid dysfunction, maternal PKU, or other
inborn errors of metabolism.
o Chronic medical conditions, such as cancer, heart disease, hypertension,
hyperlipidemia, inflammatory bowel disease, malabsorption syndromes, or renal
disease.
o Auto-immune diseases of nutritional significance, such as systemic lupus
erythematosus.
o Eating disorders, such as severe pica, anorexia nervosa, or bulimia nervosa.
o Obesity when the following criteria are met:
Body Mass Index (BMI) greater than 30 in same woman pre-pregnancy and
postpartum.
BMI greater than 35 at 6 weeks of pregnancy; or
BMI greater than 30 at 12 weeks of pregnancy. or
o Documented history of a relative of the first degree with cardiovascular disease or
possessing factors that significantly increase the risk of cardiovascular disease, such
as a sedentary lifestyle, elevated cholesterol, smoking, high blood pressure, and
higher than ideal body weight.
Utilization Management: Nutritional counseling services do not require prior authorization;
however, a referral is necessary when services are performed by dietitians.
Additional Services:
If the total 12 hours per fiscal year have been utilized and additional units
of nutritional counseling are needed, the provider must submit documentation of medical
necessity justifying the need for additional units to:
SCDHHS
Attention: Medical Director
PO Box 8206
Columbia, SC 29202

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
46
Documentation to be maintained in the Patient Record:
At minimum a patient’s record must include:
1. Referral (when applicable)
2. Review of medical management, an evaluation of medical and psychosocial history,
and treatment plan as they impact nutrition interventions
3. Assessment of living conditions related to nutrition evaluation such as possession of
a working stove, refrigerator, and access to city water or tested well water
4. Diagnostic nutritional assessment, consisting of:
a. Review and interpretation of pertinent laboratory and anthropometric data.
b. Analysis of dietary and nutrient intake.
c. Determination of nutrient–drug interactions, and
d. Assessment of feeding skills and methods.
5. Development of an individualized nutrition care plan, consisting of:
a. Recommendations for nutrient and calorie modification.
b. Calculation of a therapeutic diet for disease states such as diabetes, renal
disease, galactosemia, and
c. Referral to other health care providers.
6. Counseling on nutritional or dietary management of nutrition-related medical
conditions
7. Consultation with the beneficiary’s primary care provider
8. Education on reading food labels.
Pharmacist Services
Licensed pharmacists are allowed to provide evaluation and management services for new and
established patients when delivering contraceptives or performing urine pregnancy tests to
members of childbearing age enrolled in the Healthy Connections full benefit program or the Family
Planning Limited benefit.
Adult Physical Exams
This exam may also be offered to patients with Medicare and Medicaid. The physical exam is
expected to include the following:
• A past history for a new patient or an interval history on an established patient.
• A generalized physical overview of the following organ systems:
– Abdomen
– Back
– Breasts (female)
– Brief Muscular
– Brief Neurological

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
47
– Brief Skeletal
– External genitalia
– Heart
– HEENT
– Lungs
– Pelvic (Female)*
– Peripheral Vascular
– Prostate (Male)
– Rectal
– Skin
• Family Planning Counseling must be offered. An additional Family Planning code may be billed
for this service when provided. Please refer to Obstetrics and Gynecology in this section of the
manual for the description of codes.
• The following lab procedures are included in the reimbursement for the physical:
– Blood Sugar
– Hemoccult
– Hemoglobin
– Urinalysis
Any other lab procedures, x-rays, etc., may be billed separately. Portions of the physical may be
omitted if not medically applicable to the patient's condition or if the patient is not cooperative and
resists specific system examinations (despite encouragement by the physician and office staff). A
note must be written in the record explaining why that part of the exam was omitted.
Diabetes Patient Education
Diabetes Management services are medically necessary, comprehensive self-management and
counseling services provided by programs enrolled by SCDHHS. Enrolled programs must adhere to
the National Standards for Diabetes Self-Management Education and be recognized by the
American Diabetes Association, American Association of Diabetes Educators, Indian Health
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
48
Services, or be managed by a Certified Diabetes Educator. An eligible beneficiary must have a
diabetes diagnosis and be referred by their PCP.
For details on this service, please refer to the Enhanced Services Provider Manual. Contact the
PSC for a list of recognized programs in your area or information on how to become a provider of
diabetes education.
Immunizations
Immunizations for Children
The VFC Program is a federally funded program created by the Omnibus Budget Reconciliation Act
of 1993 that provides vaccines at no cost to children who qualify. Children who are eligible for VFC
are entitled to receive pediatric vaccines that are recommended by the Advisory Committee on
Immunization Practices (ACIP). In South Carolina, the VFC Program is managed by the SCDPH.
Medicaid providers may obtain free vaccines from the SCDPH through the VFC Program. Vaccines
are delivered free of charge to providers enrolled in the program. For additional information on the
VFC Program or to enroll as a provider in the program, you may contact SCDPH at +1 803 898
0460 (local) or +1 800 27 SHOTS (outside the Columbia area). You may also visit the SCDPH
website at Vaccinations | South Carolina Department of Public Health (sc.gov)
Note: The Rabies vaccine is non-covered through the VFC for children as it is not considered
routine. However, the Rabies vaccine is covered by Medicaid for children. Providers may bill the
appropriate administration and vaccine code to receive reimbursement from Medicaid.
Immunizations for Adults
Providers must follow the Advisory Committee on Immunization Practices (ACIP) recommendations
on vaccines for adults with full Medicaid benefits available here
.
https://www.cdc.gov/vaccines/hcp/acip-recs/index.html
Pediatrics and Neonatology
All procedures, with the following exceptions, must be submitted under the child's own Medicaid
number regardless of the child's age.
Newborn Care for the Sick Newborn
A sick child is defined as a newborn not considered a well-baby, but not sick enough to be
considered a neonate or critically ill.
High Risk Channeling Project (HRCP) Neonatal Risk Screening
Please refer to Best Practice Guidelines for Perinatal Care (Replaces High Risk Channeling
Project — HRCP) under “Obstetrics and Gynecology” in this section.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
49
Postpartum Infant Home Visit
The postpartum infant home visit is designed to assess the environmental, social, and medical
needs of the infant and mother. All Medicaid-sponsored postpartum mothers and newborns are
eligible for this visit, within six weeks of delivery. Providers must be enrolled as a Postpartum Infant
Home visit provider to perform this service. The Division of Care Management may be contacted for
enrollment at +1 803 898 4614. For further details on this service, providers may refer to the
Enhanced Services Provider Manual.
Sudden Infant Death Syndrome (SIDS)
SIDS is defined as the unexpected and sudden death of an apparently normal and healthy infant
that occurs during sleep and with no physical or autopsy evidence of disease.
Sick Child Care
Physicians are reimbursed for all services provided to Medicaid-eligible children if services are
medically necessary and a diagnostic reason for the service is documented in the physician's
records. Children (age birth through the end of the month of 21
st
birthday) are eligible for unlimited
office visits if previously mentioned criteria are met.
Neonatology
Pre-Discharge Home Visit
The pre-discharge home visit is designed to assess the condition of the home of an infant who is, or
has been a patient, in a neonatal intensive care unit (NICU), or who has had a significant medical
problem. The goal is to ensure a safe environment, conducive to maintaining the health status of the
infant, after discharge from the hospital.
The visit must be made in response to a referral by a physician directly involved in the care of the
infant while hospitalized (unless the infant is a member of a Managed Care Organization [MCO]).
This also applies to infants who have been transported from the Level III hospital back to their
county of residence.
Routine Newborn Circumcision
Routine newborn circumcisions are covered services for beneficiaries 28 days old and younger
without prior approval.
Forensic Medical Evaluations
Medicaid covers forensic medical evaluations for beneficiaries up to age 21. The purpose of the
forensic evaluation is to:
• Determine if a child has been abused, and to identify possible perpetrators.
• Gather forensically sound facts necessary to assist law enforcement officials and protect the
child.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
50
• Allow the child to disclose information in a non-threatening environment and assess the extent
and nature of the alleged abuse.
• Evaluate the child’s social and behavioral functioning in order to make treatment
recommendations, and to establish a foundation for effective treatment if needed.
This service will be covered when billed in association with a South Carolina State Office of Victim
Assistance (SOVA) service that meets the threshold of State Law Section 16-3-1350 that governs
criminal sexual conduct or child sexual abuse. Coverage will also include those events that meet the
reporting requirements of the South Carolina Department of Social Services (DSS) Child Protective
Services State Law Section 63-7-310 identifying and reporting child abuse and neglect. An event is
defined as each original occurrence that meets the forensic evaluations requirements of SOVA and
DSS.
Early and Periodic Screening, Diagnosis, and Treatment (EPSDT)
The South Carolina Healthy Connections Medicaid Program, in accordance with federal
requirements, Section 1905(r) of the Social Security Act, has developed an EPSDT benefit for
Medicaid-eligible children from birth to age 21.
EPSDT Standards
• To provide early health assessments for the child who is Medicaid eligible so that potential
diseases can be prevented.
• To periodically assess the child’s health for normal growth and development.
• To screen the child through simple tests and procedures for conditions needing closer medical
attention.
• To diagnose the nature and cause of conditions requiring attention, by synthesizing findings of
the health history and physical examination.
• To treat abnormalities detected in their preliminary stages or make the appropriate referral
whenever necessary.
Services Covered under EPSDT
The EPSDT benefit in South Carolina provides comprehensive and preventive health services
needed to diagnose and treat a child’s health and developmental conditions as early as possible.
Periodic Screening Services
EPSDT covers regular screening services (check-ups) for infants, children and adolescents. At a
minimum, children will receive services which constitute evaluations of their physical and mental
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
51
health; their growth and development; vision, hearing and dental health; and their nutritional and
immunization status.
The SCDHHS has adopted the Bright Futures/AAP Recommendations for Pediatric Preventive
Health Services that is comprised of a set of periodic screenings and procedures applicable at each
stage of the child’s life, also called the “Periodicity Schedule” available at
Periodicity Schedule |
EPSDT (scdhhs.gov).
The age-appropriate required periodic screenings and procedures during an EPSDT visit are as
follows:
• Comprehensive Health and Physical Examination:
– Includes history, measurements, unclothed age-appropriate physical examination.
• Sensory Screening:
– includes vision and hearing.
• Developmental/Behavioral Health Screenings:
– Includes a general screening as part of the EPSDT screening component.
• Procedures:
– Includes laboratory tests and procedures.
• Appropriate Immunization:
– If at the time of screening, it is determined that immunization is needed and appropriate to
provide, then immunization treatment must be provided at that time. For an age-
appropriate immunization schedule, the provider must reference the CDC at
https://www.cdc.gov/vaccines/vpd/vaccines-age.html
.
• Oral Health:
– Includes oral screening at each visit and when applicable, fluoride varnish and fluoride
supplementation.
• Health Education and Anticipatory Guidance:
– Includes age-appropriate health education (including anticipatory guidance) at each
screening.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
52
For details of pediatric preventive health care screening services and their frequency, please refer to
the Bright Futures/AAP Periodicity Schedule at https://msp.scdhhs.gov/epsdt/site-page/ periodicity-
schedule.
Note: Additionally, the SCDHHS policy exceeds the frequency and coverage recommended by the
AAP and providers are required to follow the South Carolina-specific information for the following
areas:
• Immunization:
– For an age-appropriate immunization schedule, the provider must reference the CDC at
https://www.cdc.gov/vaccines/schedules/hcp/index.html
.
– Every visit should be an opportunity to update and complete a child’s immunizations. If a
child is unable to be immunized at the recommended time, the reason must be
documented in the child’s record.
• Developmental/Behavioral Health Assessments:
– Follow-up developmental and behavioral health assessments are allowed as indicated by
the general screening during a periodic or inter-periodic visit.
• Lead Screening:
– Children enrolled in Medicaid must receive blood lead screening at ages 12 months and
24 months. Additionally, any child between ages 24 and 72 months with no record of a
previous blood lead screening test must receive one. The completion of a risk assessment
does not meet SCDHHS requirements.
– In collecting blood samples for lead testing, providers are required to follow the specimen
and collection guidelines developed by the SCDPH. These guidelines are available on the
SCDPH Bureau of Laboratories webpage at
Public Health Laboratory (PHL) | South
Carolina Department of Public Health (sc.gov)
– The South Carolina Code of Laws, Section 44-53-1380, mandates that any physician,
hospital, public health nurse or other diagnosing person or agency must report known or
suspected cases of lead poisoning to the SCDPH within seven days. If you would like
more information about the South Carolina Childhood Lead Poisoning Prevention
Program, please call: +1 866 466 5323.
• Oral Health:
– Oral screenings are performed during each EPSDT visit through the month of the
beneficiary’s 21
st
birthday. For details on physicians’ oral health services, please refer to
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
53
the SCDHHS Oral Health Section of the Periodicity Schedule at
https://www.scdhhs.gov/resources/programs-and-initiatives/epsdt/providers/periodicity-
schedule.
Inter-periodic Screening Services
EPSDT also covers medically necessary “inter-periodic” screenings outside of the periodicity
schedule when there is an indication of a medical need to diagnose an illness or condition that was
not present at the regularly scheduled screening or to determine if there has been a change in a
previously diagnosed illness or condition that requires additional services.
Note: All health-related problems that are identified during an EPSDT visit must include referral
(when indicated) to the proper entity for further evaluation and treatment. Referrals may include
such services and evaluations to determine the need for assistive technology if it is determined that
these services are medically necessary, and that the child may benefit from them. These services
must be medical in nature and not for educational purposes.
Diagnostic Services
EPSDT covers diagnostic services when a screening indicates the need for further evaluation.
Treatment Services
• State Plan Covered Services:
– EPSDT covers necessary health care services for treatment of all physical and mental
illnesses or conditions discovered by any screening and diagnostic procedure.
• Non-State Plan Covered Services — Medically Necessary Services:
– Additional health care services are available under the federal Medicaid program if they
are medically necessary to treat, correct or ameliorate illnesses and conditions discovered
regardless of whether the service is covered by the South Carolina Medicaid State Plan.
Medical necessity is determined by South Carolina Medicaid on a case-by-case basis.
Arbitrary limitations on services are not allowed within the EPSDT benefit (e.g., one pair of
eyeglasses or 10 PT visits per year). South Carolina Healthy Connections Medicaid will
make the final determination as to which treatment it will cover among equally effective,
available alternative treatments. All in-state resources must be exhausted prior to
treatment outside of the State.
Additional Tests/Procedures
• Sickle Cell Test — A screening test is administered when indicated by family, medical history or
in the presence of anemia.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
54
• Parasites Test — A test for parasites is administered when indicated by medical history,
physical assessment or a positive result of a previous test.
• Tuberculin Skin Test — Mantoux test (with five tuberculin units [TUs] of purified protein
derivative [PPD] administered intradermally) must be considered for all children at increased risk
of exposure to individuals with tuberculosis (TB). Providers may want to check with local, State
or regional TB control officials (public health department) for more specific information relating to
the epidemiology of TB in their area.
• Topical Fluoride Varnish — South Carolina Healthy Connections children can receive topical
fluoride varnish during sick or well-child visits from the eruption of their first tooth through the
month of their 21
st
birthday. Children ages zero through six may receive a maximum of four
applications per year, while children ages seven through 20 may receive one application per
year.
• Developmental/Behavioral Health Assessments — Follow-up developmental and behavioral
health assessments are allowed as indicated by the general screening during a periodic or
interperiodic visit.
Transportation Services
Transportation services, including Non-Emergency Medical Transportation (NEMT), are available for
EPSDT-eligible beneficiaries. To schedule NEMT trips to a medical appointment for beneficiaries
not residing in a nursing facility, contact the Transportation Broker at
https://memberinfo.logisticare.com/scmember/
. To schedule NEMT trips to a medical appointment
for beneficiaries residing in a nursing facility, contact the nursing facility directly.
Beneficiary Eligibility for EPSDT Services by Provider Location
Based on the qualified healthcare practitioner’s location, EPSDT services can be rendered to the
beneficiaries as follows:
• In the physician’s office:
– EPSDT services can be rendered for beneficiaries ages 0–20 (through the month of the
21
st
birthday).
• In CCCs:
– EPSDT services can be rendered only for children ages 5–20 (through the month of the
21
st
birthday).

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
55
Pharmacy Services
Please see the Pharmacy Services Provider Manual for specific information regarding Pharmacy
Services.
Durable Medical Equipment/Supply
Please see the Durable Medical Equipment (DME) Services Provider Manual for specific information
regarding DME and Supply Services.
Continuous Glucose Monitoring (CGM)
Continuous glucose monitoring devices are covered for full benefit Healthy Connections Medicaid
beneficiaries.
CGM is covered under the Pharmacy or DME State Plan benefits with prior authorization that meets
the following criteria:
1. CGM must be prescribed by one of the following qualified healthcare providers:
a. Primary care provider (a physician, physician assistant or advance practice
registered nurse)
b. Obstetrician
c. Endocrinologist
2. Eligible beneficiary must have one of the following clinical criteria:
a. Type 1 diabetes mellitus
b. Gestational diabetes
c. Type 2 diabetes with one of the following:
i.Any type of insulin dependency
ii.Non-insulin-treated diabetes with recurrent moderate (Level 2) or at
least one severe (Level 3) hypoglycemic event.
Services for AIDS Patients
In an effort to find a medical home for AIDS patients covered under the Medicaid program and to
properly reimburse physicians for the complications involved with treating these patients,
supplemental codes have been developed for physicians treating Medicaid beneficiaries diagnosed
with AIDS or AIDS Related Complex (ARC).
Additional Long-Term Living Services
Aside from traditional Medicaid services (physician, hospital, drugs, etc.), SCDHHS offers additional
services through a home and community-based services (HCBS) waiver program. In addition to
being HIV positive, the individual must meet an established medical level of care prior to receiving
these services. Services available are listed below:
• Case management services
• Private duty nursing services
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
56
• Personal care aide services
• Modified and therapeutic-diet home-delivered meals
• Limited nutritional supplements
• Environmental modifications
• Attendant care
• Companion services
• Pest control services
Incontinence Products
For incontinence products policy and procedures, please refer to the Home Health Services
Provider Manual located on the SCDHHS website at Provider Manual List | SCDHHS
.
CLTC Offices
There are 11 areas and three satellite CLTC offices Statewide. Each office is staffed by service
managers who are professional social workers and Registered Nurses. These service managers
work with the person and/or the family to plan and coordinate the services the beneficiary may
need.
If you have clients, who you feel may benefit from any of these services, or if you have questions
about the CLTC program, please call your area CLTC office as listed in the table below.
For additional information, please contact the PSC at +1 888 289 0709, submit an online inquiry at
Contact a Provider Representative | SCDHHS
or write to:
SCDHHS
Community Long-Term Care Department
PO Box 8206
Columbia, SC 29202
AREAS COUNTIES SERVED PHONE NUMBERS
Area 1 — Greenville Greenville, Pickens +1 864 660 4131
+1 888 535 8523
Area 2 — Spartanburg Cherokee, Spartanburg, Union +1 864 594 4964
+1 888 551 3864
Area 3 — Greenwood, IMS
Abbeville, Edgefield, Greenwood,
Laurens, McCormick, Saluda
+1 864 223 8622
+1 800 628 3838
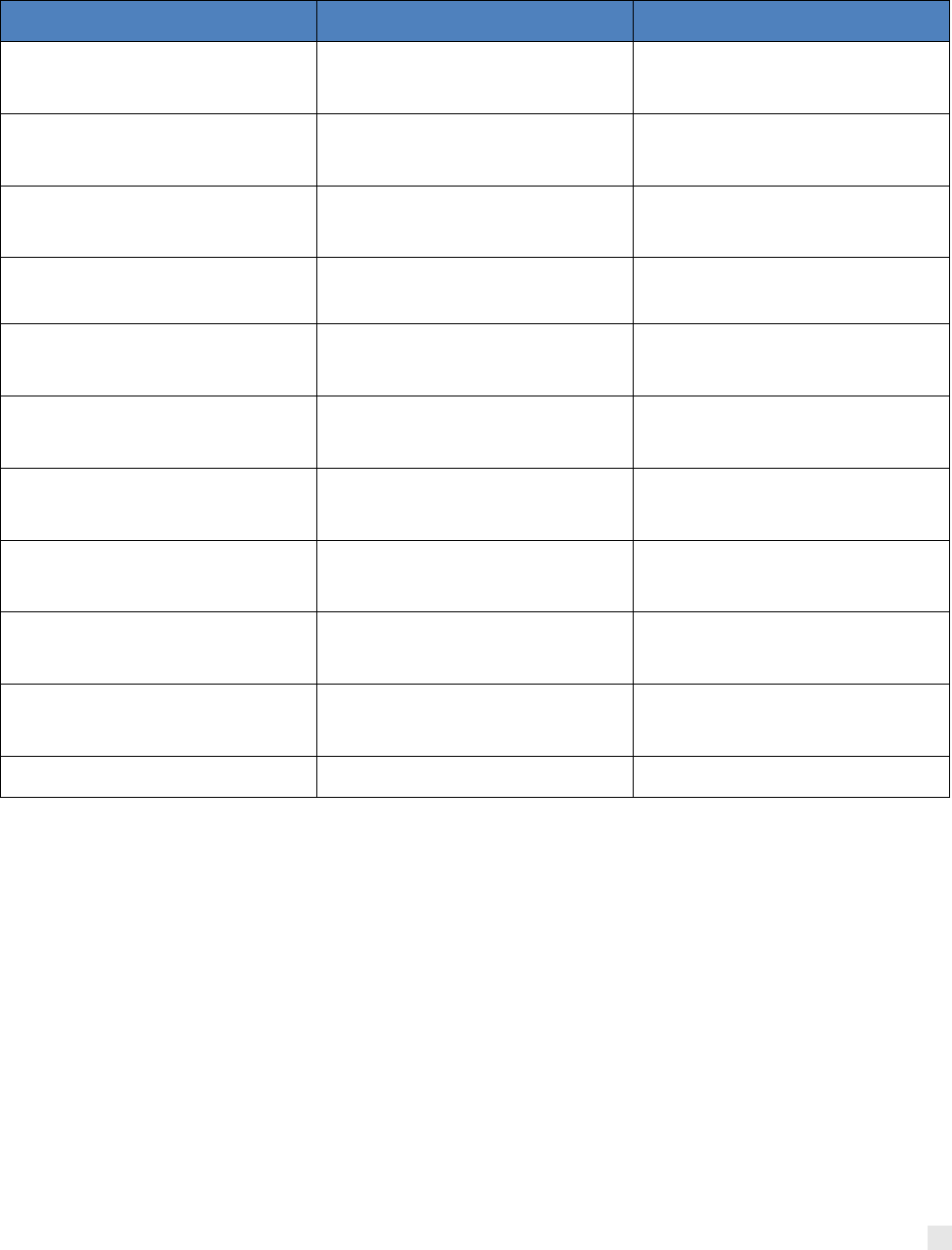
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
57
AREAS COUNTIES SERVED PHONE NUMBERS
Area 4 — Rock Hill Chester, Lancaster, York +1 803 560 6457
+1 888 286 2078
Area 5 — Columbia
Fairfield, Lexington, Newberry,
Richland
+1 803 764 8319
+1 888 847 0908
Area 6 — Orangeburg
Allendale, Bamberg, Calhoun,
Orangeburg
+1 803 536 0122
+1 888 218 4915
Area 7 — Sumter
Clarendon, Kershaw, Lee,
Sumter
+1 803 567 3110
Area 8 — Florence
Chesterfield, Darlington, Dillon,
Florence, Marlboro
+1 843 667 8718
+1 888 798 8995
Area 9 — Conway
Georgetown, Horry, Marion,
Williamsburg
+1 843 279 2011
+1 888 539 8796
Area 10 — Charleston Berkeley, Charleston, Dorchester +1 843 529 0142
+1 888 805 4397
Area 11 — Anderson, IMS Anderson, Oconee +1 864 660 4100
+1 800 713 8003
Area 13 — Ridgeland
Beaufort, Colleton, Hampton,
Jasper
+1 843 726-5353
+1 800 262 3329
Area 14 — Aiken Aiken, Barnwell +1 803 641 7680
+1 888 364 3310
Area 17 — Centralized Intake Statewide +1 888 971 1637
Outpatient Pediatric Aids Clinics
Outpatient Pediatric AIDS Clinics (OPACs) are designed to provide specialty care, consultation, and
counseling services for HIV-infected and exposed, Medicaid-eligible children and their families.
These clinics are contracted providers with SCDHHS. The mission of OPAC is to follow children
who have been exposed to HIV perinatally. Additional information on these clinics can be found in
the Clinic Services manual.
Alcohol and Drug Abuse Rehabilitation Services
The medical benefits package for Medicaid beneficiaries includes OP alcohol and drug (A&D)
rehabilitative services. Crisis Management is also available for patients who are experiencing
emotional, physical and/or psychological trauma.
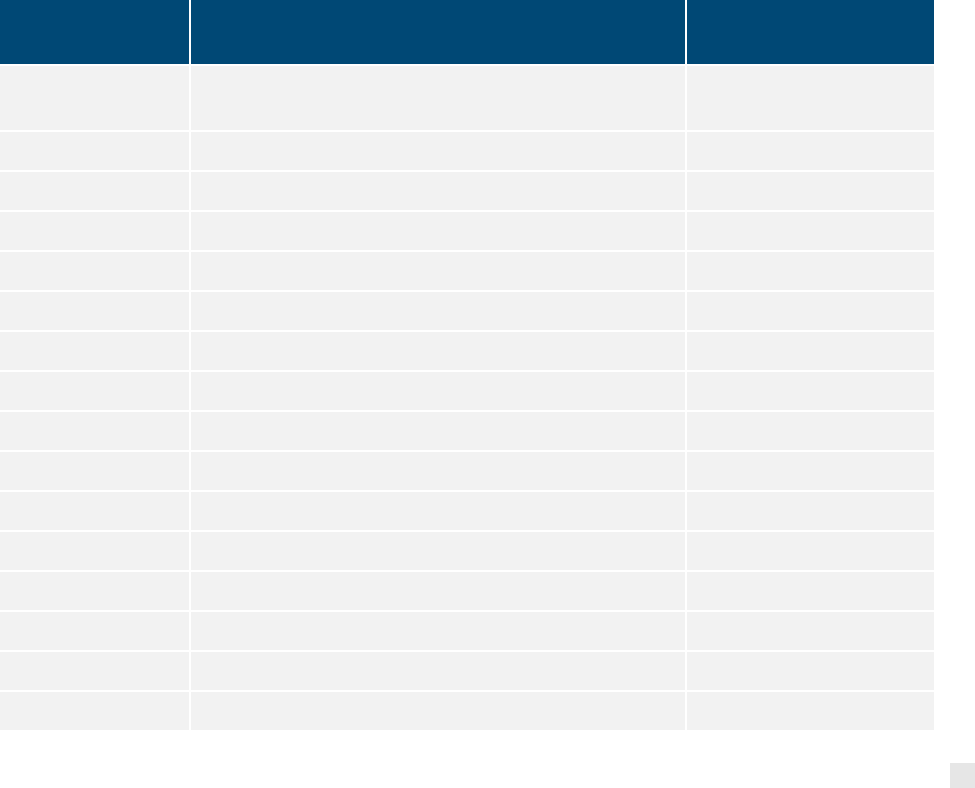
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
58
The effectiveness of this program relies on the referrals by physicians. There are several
alternatives a physician can use to refer a Medicaid beneficiary for A&D services. Likewise, there
are several ways to bill for referral services.
Initial Medical Assessment and Referral
Face-to-face contact between physician and client to assess the patient status, provide diagnostic
evaluation screening, and provide physician’s referral for A&D rehabilitative services must be billed
using the appropriate code. This includes the completion of the A&D Medical Assessment signed
and dated by the physician. A sample copy of the form can be found in the Forms section of the
provider portal. Additional forms are available upon request from your county A&D abuse program.
This form will be placed in the client’s file at the local A&D abuse authority site. A copy must be
retained in the patient’s file. The assessment form completion is included in the reimbursement fee.
Local Alcohol and Drug Authorities Currently Enrolled in Medicaid
The chart beginning on the following page includes an address and telephone number for all of the
local A&D authorities currently enrolled in Medicaid:
COUNTY PROGRAM NAME AND ADDRESS
TELEPHONE
NUMBER
South Carolina Department of Alcohol and Drug
Abuse (DAODAS)
101 Executive Center Drive, Suite 215 +1 803 896 5555
Columbia, South Carolina 29210
Cornerstone
Abbeville 112 Whitehall Street +1 864 366 9661
Abbeville, South Carolina 29620
Aiken Center
Aiken 1105 Gregg Highway +1 803 649 1900
Aiken, South Carolina 29801
New Life Center
Allendale 570 Memorial Avenue +1 803 584 4238
Allendale, South Carolina 29810
Anderson/Oconee Behavioral Health Services
Anderson 226 McGee Road +1 864 260 4168
Anderson, South Carolina 29625
Dawn Center (Tri-County Commission of A&D Abuse)
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
59
COUNTY PROGRAM NAME AND ADDRESS
TELEPHONE
NUMBER
Bamberg 608 North Main Street +1 803 245 4360
Bamberg, South Carolina 29003
Axis I Center of Barnwell
Barnwell 644 Jackson Street +1 803 541 1245
Barnwell, South Carolina 29812
Beaufort County Department of Alcohol and
Other Drug Services
Beaufort 1905 Duke Street +1 843 470 4545
Beaufort, South Carolina 29901
Ernest E. Kennedy Center
Berkeley 306 Airport Drive +1 843 761 8272
Monks Corner, South Carolina 29461
Dawn Center (Tri-County Commission of A&D Abuse)
Calhoun Herlong Extension Industrial Park +1 803 655 7963
St. Matthews, South Carolina 29135
Charleston Center
Charleston 5 Charleston Center Drive +1 843 958 3300
Charleston, South Carolina 29401
Cherokee County Commission of Alcohol and Other
Drug Services
Cherokee 201 West Montgomery Street +1 864 487 2721
Gaffney, South Carolina 29341
Hazel Pittman Center
Chester 130 Hudson Street +1 803 377 8111
Chester, South Carolina 29706
Alpha Center
Chesterfield 1218 East Boulevard +1 843 623 7062
Chesterfield, South Carolina 29709
Clarendon County Commission on ADA
Clarendon 14 North Church Street +1 803 435 2121
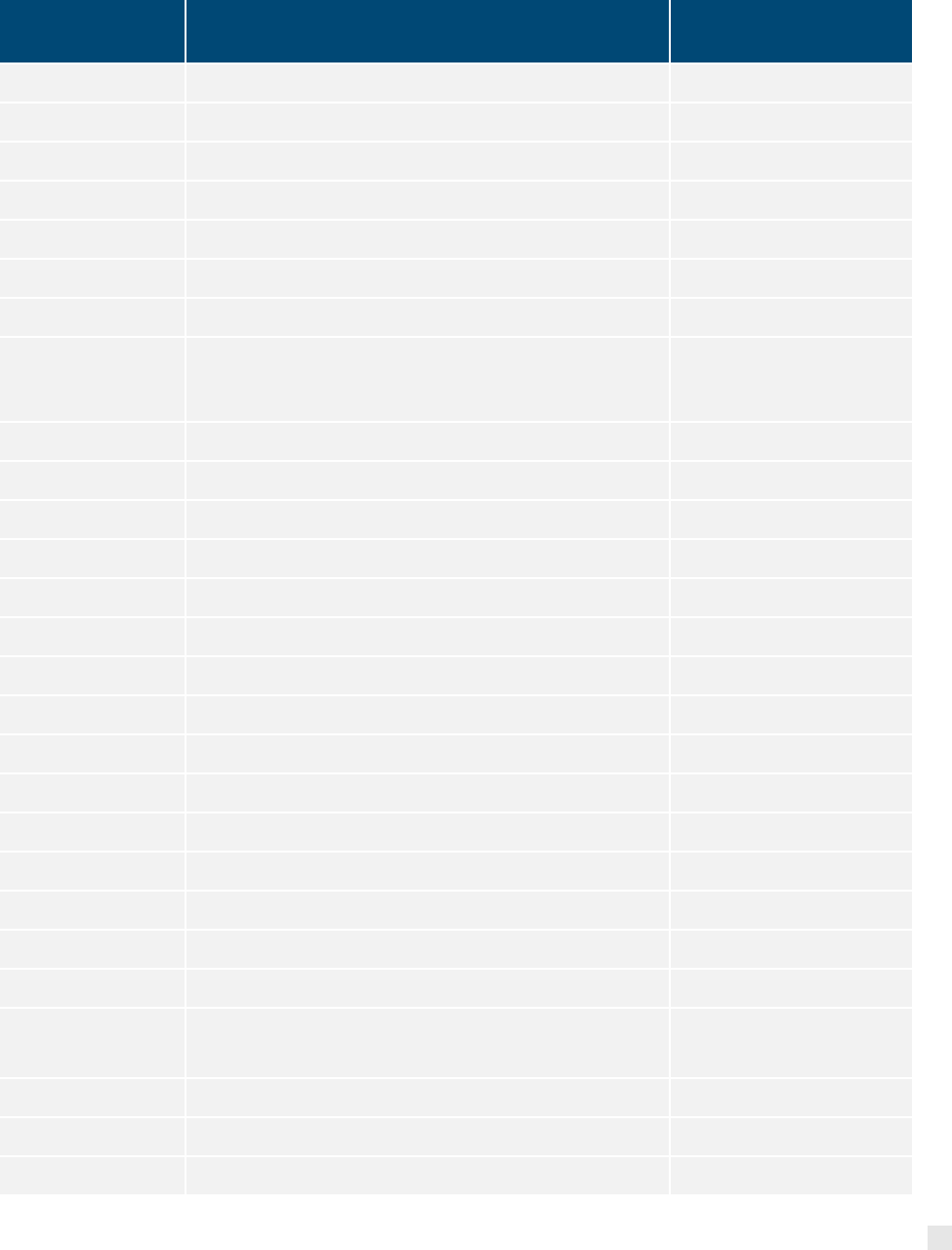
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
60
COUNTY PROGRAM NAME AND ADDRESS
TELEPHONE
NUMBER
Manning, South Carolina 29102
Colleton County Commission on ADA
Colleton 1439 Thunderbolt Drive +1 843 538 4343
Walterboro, South Carolina 29488
Rubicon Inc.
Darlington 510 East Carolina Avenue +1 843 332 4156
Hartsville, South Carolina 29550
Trinity Behavioral Care
Dillon 204 Martin Luther King Jr. Blvd. +1 843 774 6591
Dillon, South Carolina
Dorchester Alcohol & Drug Commission
Dorchester 500 North Main Street, Suite 4 +1 843 871 4790
Summerville, South Carolina 29483
Cornerstone
Edgefield 400 Church Street, Room 112 +1 803 637 4050
Edgefield, South Carolina 29824
Fairfield County Substance Abuse Commission
Fairfield 200 Calhoun Street +1 803 635 2335
Winnsboro, South Carolina
Circle Park Behavioral Health Services
Florence 601 Gregg Avenue +1 843 665 9349
Florence, South Carolina 29501
Georgetown County ADA Commission
Georgetown 1423 Winyah Street
Georgetown, South Carolina 29440
+1 843 546 6081
The Phoenix Center
Greenville 1400 Cleveland Street +1 864 467 3739
Greenville, South Carolina 29607
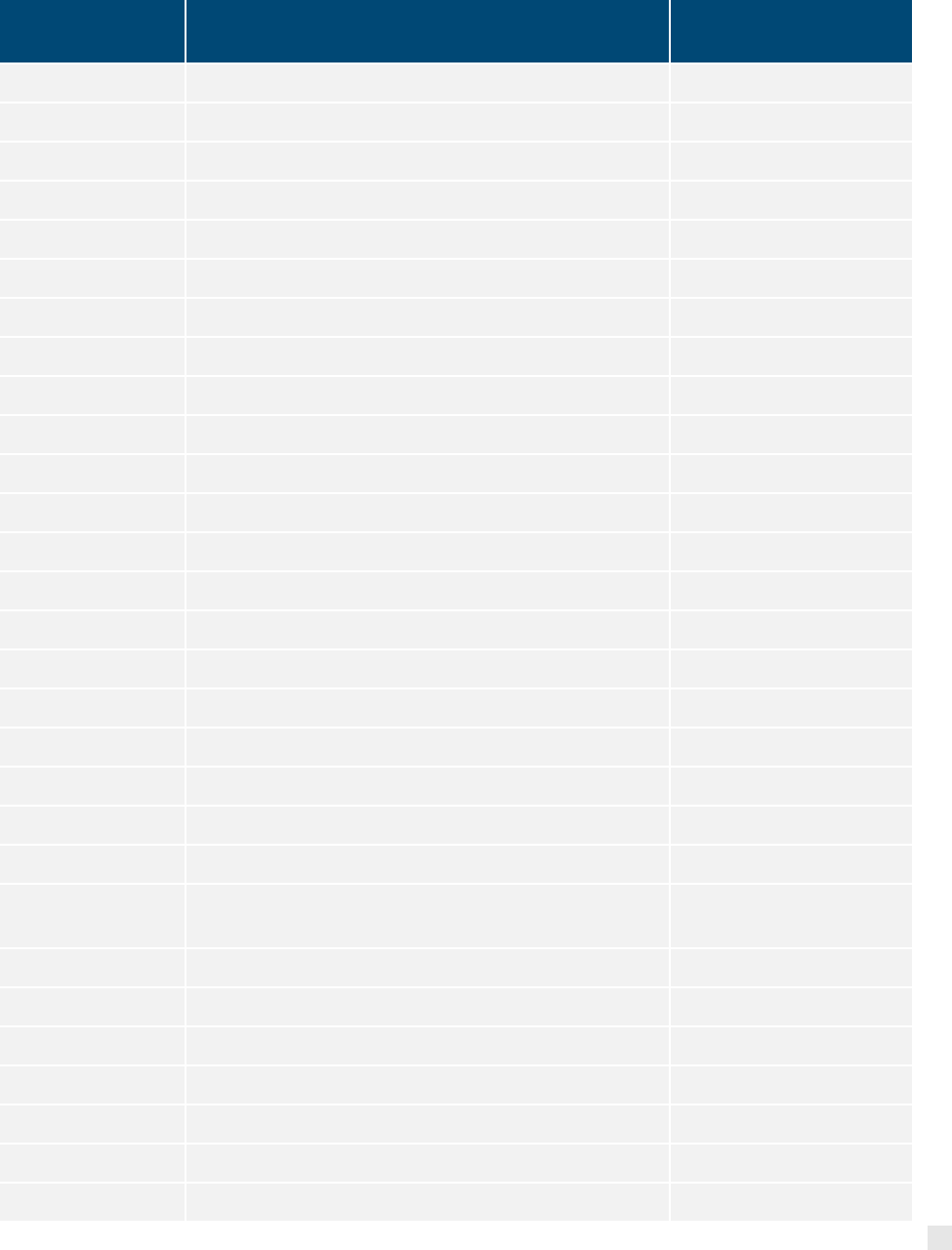
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
61
COUNTY PROGRAM NAME AND ADDRESS
TELEPHONE
NUMBER
Cornerstone
Greenwood 1510 Spring Street +1 864 227 1001
Greenwood, South Carolina 29646
New Life Center
Hampton 102 Ginn Altman Avenue, Suite C +1 803) 943-2800
Hampton, South Carolina 29924
Shoreline BHS
Horry 2404 Wise Road +1 843 365 8884
Conway, South Carolina 29526
New Life Center
Jasper 113 East Wilson Street +1 843 726 5996
Ridgeland, South Carolina 29936
Alpha Center
Kershaw 709 Mill Street +1 803 432 6902
Camden, South Carolina 29020
Counseling Services of Lancaster
Lancaster 114 South Main Street +1 803 285 6911
Lancaster, South Carolina 29720
Gateway Counseling Center
Laurens 219 Human Services Road +1 864 833 6500
Clinton, South Carolina 29325
The Lee Center Family Counseling and Addiction
Services
Lee 108 East Church Street +1 803 484 6025
Bishopville, South Carolina 29010
Lexington/Richland Alcohol and Drug Abuse Council
Lexington 130 North Hospital Drive +1 803 733 1390
West Columbia, South Carolina 29169
Trinity Behavioral Care
Marion 103 Court Street +1 843 423 8292
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
62
COUNTY PROGRAM NAME AND ADDRESS
TELEPHONE
NUMBER
Marion, South Carolina 29571
Trinity Behavioral Care
Marlboro 211 North Marlboro Street, 2nd Floor +1 843 479 5683
Bennettsville, South Carolina 29512
Cornerstone
McCormick 504 North Mine Street +1 864 465 2631
McCormick, South Carolina 29835
Westview Behavioral Health Services
Newberry 800 Main Street or 909 College Street +1 803 276 5690
Newberry, South Carolina 29108
Anderson/Oconee Behavioral Health Services
Oconee 691 South Oak Street +1 864 882 7563
Seneca, South Carolina 29678
Dawn Center (Tri-County Commission of Alcohol and
Drug Abuse)
Orangeburg 910 Cook Road +1 803 536 4900
Orangeburg, South Carolina 29118
Behavioral Health Services of Pickens County
Pickens 309 East Main Street +1 864 898 5800
Pickens, South Carolina 29671
Lexington/Richland Alcohol and Drug Abuse Council
Richland 2711 Colonial Drive +1 803 726 9300
Columbia, South Carolina 29203
Saluda Behavioral Health System
Saluda 204 Ramage Street +1 864 445 2968
Saluda, South Carolina 29138
Spartanburg County Alcohol and Drug Abuse
Commission
Spartanburg 187 West Broad Street, Suite 200 +1 864 582 7588
Spartanburg, South Carolina 29306
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
63
COUNTY PROGRAM NAME AND ADDRESS
TELEPHONE
NUMBER
Sumter County Commission on ADA
Sumter 115 North Harvin Street, 3rd Floor +1 803 775 6815
Sumter, South Carolina 29150
Union county Commission on ADA
Union 201 South Herdon Street +1 864 429 1656
Union, South Carolina 29379
Williamsburg Commission on ADA
Williamsburg 115 Short Street +1 843 354 9113
Kingstree, South Carolina 29556
Keystone Substance Abuse Services
York 199 South Herlong Avenue +1 803 324 1800
Rock Hill, South Carolina 29732
Alcohol and Drug Testing Policy
Effective for dates of service beginning January 1, 2016, the SCDHHS will cover the following
presumptive and definitive drug testing classifications. SCDHHS will reimburse for a maximum of
one screening per procedure code, per DOS, not to exceed 18 screenings per 12-month period.
Providers must bill the most appropriate Healthcare Common Procedure Coding System (HCPCS)
code for the service rendered.
Drug test(s), presumptive, any number of drug classes; any number of devices or procedures, (e.g.,
immunoassay) capable of being read by direct optical observation only (e.g., dipsticks, cups, cards,
cartridges), includes sample validation when performed, per DOS.
Drug test(s), presumptive, any number of drug classes; any number of devices or procedures by
instrumented chemistry analyzers utilizing immunoassay, enzyme assay, TOF, MALDI, LDTD,
DESI, DART, GHPC, GC mass spectrometry), includes sample validation when performed, per
DOS.
Drug test(s), definitive, utilizing drug identification methods able to identify individual drugs and
distinguish between structural isomers (but not necessarily stereoisomers), including, but not limited
to GC/MS (any type, single or tandem) and LC/MS (any type, single or tandem and excluding
immunoassays (e.g., IA, EIA, ELISA, EMIT, FPIA) and enzymatic methods [e.g., alcohol
dehydrogenase]); qualitative or quantitative, all sources(s), includes specimen validity testing, per
day, 1–7 drug class(es), including metabolite(s) if performed.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
64
SCDHHS policy has been and continues to be A&D screenings, as with all lab tests, must be
ordered by a qualified practitioner operating within their scope of practice and as allowed by State
Law. Qualified practitioners may authorize certain laboratory tests to be performed at defined
intervals over a period of 60 days with one “standing order” only when used in connection with an
extended course of treatment for substance abuse disorders. The ordering practitioner must
document in the beneficiary’s clinical record the medical necessity for the testing and the results of
each test. Qualified practitioners ordering unnecessary tests for which Medicaid is billed may be
subject to civil penalties.
A qualified practitioner is defined as a physician, NP or a PA. The qualified practitioner may write an
individualized standing order for the beneficiary but must be updated every 60 days.
Laboratory standing orders must be in a written form, patient-specific, and include a duration that
cannot exceed 60 days. In all instances, standing orders are rendered invalid after 60 days from the
date the initial test was ordered. Existing standing orders must be reviewed regularly to ensure their
continuing validity.
Standing orders must include the following information:
• The treating physician, NP or PA name, address, telephone number, license number and NPI
number.
• The name, date of birth, sex, Medicaid ID number, diagnosis and statement of clinical symptoms
that justify medical necessity of the beneficiary for whom the tests are ordered.
• The date the test was ordered.
• The name of all tests performed, listed individually.
• Specific intervals, at which each individual test may be performed, based on the individual
treatment needs.
• Signature, title and date of qualified practitioner that evaluated the beneficiary and confirmed the
medical necessity.
A&D screens for employment purposes or for a court-ordered A&D screen are not covered under
the Medicaid program.
Tobacco Cessation
Tobacco use is the leading cause of preventable disease and premature death in South Carolina.
SCDHHS provides comprehensive coverage for tobacco cessation treatment through
pharmacotherapy and counseling for all full-benefit Medicaid beneficiaries. SCDHHS also partners

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
65
with SCDPH to communicate about programs available to assist Medicaid beneficiaries with quitting
tobacco use.
Providers are encouraged to screen beneficiaries for tobacco use during medical encounters and
document nicotine dependence using the appropriate diagnosis codes.
Medication
SCDHHS covers prescriptions for the following tobacco cessation and NRT products:
• Bupropion SR products for tobacco use (Zyban)
• Varenicline (Chantix) tablets
• Nicotine gum
• Nicotine lozenge
• Nicotine nasal spray
• Nicotine inhaler
• Nicotine patch
Tobacco cessation products are exempt from prior authorization, requirements. There is no limit to
the number of quit attempts in a calendar year. The following medically appropriate combination
therapies are also covered:
• Long-term nicotine patch + other NRT product (gum or spray)
• Nicotine patch + nicotine inhaler
• Nicotine patch + Bupropion SR
General edits on day supply are based on product dosing in manufacturer package inserts.
Prescribers are encouraged to reference the AAFP Pharmacologic Product Guide for FDA-approved
medications for smoking cessation for more information on product guidelines.
As with all other pharmaceuticals, SCDHHS reimburses only rebated products (brand or generic) for
FFS beneficiaries. A beneficiary must provide a prescription to receive any medication, including
OTC products. A dual-eligible member can receive OTC products through Medicaid coverage, but
the individual’s Medicare Part D prescription drug plan must cover prescriptions for legend (non-
OTC) tobacco cessation products.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
66
For further questions about this benefit, prescribers may contact the Magellan Medicaid
Administration’s Clinical Call Center at +1 866 247 1181.
Counseling
SCDHHS policy requires that all tobacco cessation treatment must be ordered by a qualified
practitioner defined as a physician, NP, CNM or PA. Medical documentation including time spent
counseling the patient, treatment plan, and pharmacotherapy records must be maintained in the
patient record.
South Carolina Tobacco Quitline
One-on-one telephone counseling with web-based support are available to all South Carolinians
without charge through the South Carolina Tobacco Quitline. Participants in the Quitline program
are connected with a personal Quit Coach, who helps the participant develop a quit plan and uses
cognitive behavioral coaching and motivational interviewing techniques to support the quit process.
This evidence-based program has been clinically proven to help participants quit tobacco use, and
tailored programs are available for Hispanic, Native American, pregnant and youth callers, and
smokeless tobacco users, as well as participants who have chronic medical and mental health
conditions.
SCDHHS strongly encourages prescribers and pharmacists to refer patients to the South Carolina
Tobacco Quitline at +1 800 QUIT NOW. Services are available 24 hours a day, seven days a week.
Additional information is available at
Quitline Information for Healthcare Providers | South Carolina Department of Public Health (sc.gov)
Hospice
Please see the Hospice Services Provider Manual for specific information regarding Hospice
Services.
Inpatient and Outpatient Hospital Services
General Policy Guidelines
Services performed by the physician in a hospital are compensable if medically necessary. Special
procedures are compensable if deemed a separate and reimbursable service. Services or supplies
administered by the hospital or hospital employee are considered a part of the overall hospital
service and are reimbursable only under the hospital allowable costs.
A physician who is either salaried or contracted by the hospital (a hospital-based physician), and
who performs services under said contract or employment, may not bill for those services separately
under his or her individual Medicaid provider number. The contracting hospital may claim these
services under the professional fees allowable for the hospital under its hospital-based physician
Medicaid number.
Inpatient Only Procedures
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
67
The Centers for Medicare and Medicaid Services (CMS) publishes a list of designated procedures
that Medicare will pay for only when care takes place in a hospital setting. Any procedures not
included on the list must be performed on an outpatient basis.
SCDHHS follows the CMS Inpatient Only List for designation of inpatient only procedures. A link to
the Outpatient Prospective Payment System (OPPS), Addendum E, can be found below:
Hospital Outpatient PPS | CMS
Hospital Outpatient PPS | CMS
Levels of Service
The terminology for levels of service as defined in the American Medical Association (AMA) CPT
guidelines will be recognized. The medical record must reflect the level of service billed.
Records and Documentation Requirements
Both the physician and hospital are expected to comply with South Carolina Medicaid policy in
providing the agency with medical records if requested.
Hospital Visits
Initial Hospital Care
Please refer to the current CPT when multiple E&M services are prescribed on the same date as
initial hospital care.
Only one physician for each hospital admission is reimbursed. If two physicians of different
specialties perform a comprehensive exam on admission day, one may use a consultation code
(with the exception of a transfer), as long as the service meets the criteria of a consultation.
A comprehensive level of service is not allowed for readmission for the same illness or problem. A
reduced level of service must be used if the patient is discharged and readmitted.
If a patient is transferred from one hospital to another, the receiving physician may bill for a
comprehensive level of service (even if the transfer occurs on the day of admission).
Initial hospital care codes are exempt from the surgical package. For instructions on surgical
package billing, please refer to General Surgery Guidelines within this section of the manual.
Subsequent Hospital Care
Subsequent hospital care is generally allowable one visit per day, per physician.
Post-operative visits by the surgeon are not allowed as a separate reimbursement since the visits
are included in the surgical package unless the surgical procedure is not part of a surgical package.
Subsequent hospital care codes will "multiply" and must be reported as one line item, with the
number of visits indicated in the “units” column.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
68
Hospital Discharge
Hospital discharge is a covered service. This charge is acceptable only if billed in lieu of a
hospital visit code. It may not be charged if a surgical procedure was performed, and the surgery
is considered a surgical package. Reimbursement is made for only one physician for each hospital
discharge.
Concurrent Care Guidelines
When two or more physicians render subsequent hospital care, consultations (office or inpatient),
critical care, emergency room (ER), nursing home, rest home or office medical care to the same
patient at the same time, this is referred to as "medical concurrent care".
Concurrent Care Criteria
If physicians of the same specialty or similar specialty render care for the same condition at the
same time, benefits are provided only for the attending physician.
When two physicians render care for unrelated conditions at the same time, benefits are provided to
each physician if both of the following apply:
• The physicians are not of the same or similar specialty.
• Each physician is treating the patient for a condition unique to his specialty.
Medical/Surgical
Benefits are provided for in-hospital medical services performed by a physician other than the
admitting surgeon in addition to benefits for in-hospital surgical services under the following
circumstances:
• The medical care rendered was not related to the condition causing surgery and was not part of
routine pre and post-operative care.
• The medical care required supplemental skills not possessed by the attending surgeon.
• A physician other than a surgeon admits a patient for medical treatment, and the need for
surgery arises later during the hospitalization.
• A cardiovascular surgeon performs cardiac surgery, and a cardiologist follows the patient during
hospitalization even though the diagnosis is the same.
Critical Care Services
Follow current CPT guidelines indicating services are considered a part of critical care and not
reimbursed separately. Up to four hours of critical care per day are allowed. Critical care must be
billed per DOS. Critical care services are not included in the surgical package and may be billed
separately.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
69
EKG interpretations would not be covered separately when performed as part of, or in conjunction
with, critical care.
Critical Care first hour is used to report the services of a physician providing constant attention to an
unstable, critically ill patient for a total of 30 minutes to 74 minutes on a given day. Reimbursement
is limited to one per day. If the total duration of critical care on a given day is less than 30 minutes,
the appropriate E&M code must be used. In the hospital setting, the higher-level code would most
often apply. Time must be clearly documented in the medical record.
Critical Care, each additional 30 minutes is used to report the services of a physician providing
constant attention to an unstable, critically ill patient for up to 30 minutes beyond the first 74 minutes
of care on a given day.
Reimbursement is limited to six per day for a total of three hours per day. Time must be clearly
documented in the medical record.
Prolonged Services
Medicaid will reimburse for prolonged physician services with direct (face-to-face) patient contact.
Documentation for CPT codes must clearly indicate that the service provided was direct
(face-to-face) contact between the physician and the patient for more than one hour beyond the
usual service for the level of E&M code billed. These codes are billed in addition to the appropriate
E&M code. Please refer to the CPT guidelines for coding these services. Prolonged Services each
additional 30 minutes are non-covered.
Prolonged Physician Services without Direct (face-to-face) Patient Contact will remain non-covered.
ER Services
Outside Attending Physician
A private physician called to the hospital in an emergency situation may bill for ER services in the
following instances:
• When a hospital-based ER physician is not available.
• The physician is called in by the ER physician.
• If a life-threatening situation develops.
Hospital-Salaried or Hospital-Based ER Physicians
Medicaid has established policies and procedures for OP hospital services to distinguish between
OP clinic services and ER services. Since some hospitals do not have separate and distinct OP
clinics, the ER physician must designate in the patient's records if the patient's visit to the ER was
an emergency.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
70
Professional services rendered in an OP hospital environment must be charged on a CMS-1500
form. If a hospital-based or salaried physician renders a professional service in an ER, all services
must be charged separately by submitting a CMS-1500 or by using a PAID or billing through the
PAID Spin Off Program.
The physician's service must be charged using an appropriate CPT code. Procedures identifiable as
a unique and separate service may be reported separately.
Levels of Service
Each level of service includes examinations, evaluations, and treatments that are medically
necessary, and that are presented as an emergency in a hospital ER setting. These levels of
service exclude the interpretation of diagnostic tests. Medicaid will only reimburse for one ER visit
per day for the same or related diagnosis.
Emergency Life Support
Physician direction of an emergency medical system (EMS) or ambulance transport service for
advanced life support is covered when medically indicated. The service is compensable, in addition
to other medically necessary services performed by a physician. Emergency services performed by
other hospital professionals are considered part of a technical charge by the hospital and may not
be billed or charged as a separate professional service.
Pediatric Inpatient Rehabilitation Services
Professional services of a physician or a qualified healthcare professional delivered in a pediatric
inpatient rehabilitation unit are covered when medically necessary and are reimbursed separately
from the facility services. For details on medical necessity and clinical criteria for pediatric inpatient
rehabilitation services, please refer to the Hospital Services Provider Manual.
Transportation of Self-Administered Oxygen Dependent Beneficiaries
This policy applies to beneficiaries who are admitted, as an inpatient of a hospital or hospital ER,
are oxygen dependent and currently do not have their portable oxygen system in their possession,
and do not require transportation via ambulance for their return trip to their residence for any other
reason. The hospital is responsible for arranging and acquiring a portable oxygen system complete
with all medically necessary accessories, upon discharge. Hospitals and ambulance providers will
no longer receive reimbursement for non-essential, non-medically necessary ambulance
transportation for self-administered oxygen-dependent beneficiaries. All provider types and services
are subject to post-payment review by the Division of PI.
It is the responsibility of both the hospital and DME provider to coordinate and dispense oxygen to
the Medicaid beneficiary who is currently admitted to the hospital or hospital ER in order for the
appropriate mode of non-emergent transportation to be arranged with the transportation broker
upon discharge. The dispensing DME provider will be responsible for arranging the return of the

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
71
portable oxygen system dispensed by their company at the time of discharge from the admitting
hospital facility.
SCDHHS will reimburse for a portable oxygen system billed with a U1 modifier, and the dispensing
DME provider will be reimbursed per occurrence. SCDHHS will limit the number of occurrences per
patient to no more than three occurrences per calendar month. Services that exceed three
occurrences per calendar month will not be reimbursed.
It is the responsibility of EMS providers whenever possible to transport oxygen dependent
beneficiaries with the beneficiary’s personal portable oxygen system in anticipation of the
beneficiary’s medical/health needs.
Observation Unit
Medicaid will sponsor the professional reimbursement for E&M services provided to patients
requiring observation in a hospital. Please refer to the current CPT for coding guidelines.
Observation codes must be billed with place of service 22.
Administrative Days
Medicaid sponsors Administrative Days in any South Carolina-enrolled acute care hospital and
acute care hospitals enrolled within the South Carolina service area for Medicaid-eligible patients
who no longer require acute hospital care but need nursing home placement that is not available at
the time.
Physicians who are treating these patients can bill for their services rendered to these patients using
the same procedure codes that they use for their patients in nursing homes and rest home facilities.
The specific code you use would depend on whether it is a new or established patient and on the
level of care given. Use place of service 21 when billing.
One limited examination per 30 days is required for all Administrative Day patients. Additional visits
may be allowed if medical justification is submitted.
Obstetrics and Gynecology
Healthy Mothers/Healthy Futures Obstetrical Program
Obstetrical care provided under the Healthy Mothers/Healthy Futures program (HM/HF) must be
billed as separate charges (fragmented), not as global OB care. The program includes health
education, referral to the Women, Infants, and Children (WIC) program at the local county health
department, and follow-up on missed appointments.
HM/HF Checklist
One way of documenting the additional services is the HM/HF checklist. A sample copy of the
checklist can be found in the Forms section of provider portal. The checklist is only an option for
documenting services and is by no means a requirement. The only requirement is that services be

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
72
documented. If a practice chooses to use the HM/HF checklist, the physicians must sign and date
the back of the checklist at the time of the initial visit so that it is not forgotten at a later date.
It is not necessary to cover all the educational components on the checklist with each patient, but
only the ones that pertain to each individual patient’s health. If one component is discussed with the
patient on more than one occasion, it may be checked and dated for each time. It is very important
that at least one educational component on the checklist be checked and dated for each HM/HF
enhanced visit that is billed to Medicaid.
Best Practice Guidelines for Perinatal Care (Replaces HRCP)
South Carolina Medicaid remains committed to the concept(s) of risk-appropriate care and
enhancing maternal and child health outcomes. Therefore, the following Medicaid Best Practice
guidelines are recommended:
• Early and continuous risk screening must be provided for all pregnant women.
– SCDHHS has adopted the American College of Obstetricians and Gynecologists (ACOG)
recommendations for screening serologically for syphilis during each pregnancy with the
following frequency:
› At the first prenatal care visit,
› Once during the third trimester,
› On the delivery date, at birth
• Early entry into prenatal care must be encouraged.
– Care for all prenatal women must be delivered by the provider level and specialty best
suited to the risk of the patient. (AAP, American College of Obstetricians and
Gynecologists. Guidelines for Perinatal Care. 8th ed. Elk Grove Village (IL): AAP;
Washington, DC: American College of Obstetricians and Gynecologists, 2017.)
– All infants must receive risk-appropriate care in a setting that is best suited to the level of
risk presented at delivery. (AAP, American College of Obstetricians and Gynecologists.
Guidelines for Perinatal Care. 8th ed. Elk Grove Village (IL): AAP; Washington, DC:
American College of Obstetricians and Gynecologists, 2017.)
– Risk assessment of the infant must be performed prior to discharge from the hospital.
– Every Medicaid-eligible mother and infant must receive a Postpartum/Infant Home Visit.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
73
– Effective communication/coordination regarding the perinatal plan of care between each
provider is essential (i.e., the specialist physician must communicate pertinent information
back to the community-level physician).
– A medical home must be established for the mother-infant unit after delivery to handle the
long-term health care needs.
– P/RSPCE referrals must be made when medically indicated.
For additional recommendations and guidelines for risk-appropriate ambulatory prenatal care for
pregnant women, the “Guidelines for Perinatal Care,” which are endorsed by the AAP and the
American College of Obstetrics and Gynecology (ACOG) may be referenced.
Ultrasounds
SCDHHS policy allows three obstetrical ultrasounds per pregnancy for OB/GYN providers.
Ultrasounds in the first trimester are performed to establish viability, gestational age or to detect
malformations. Two additional ultrasounds, performed during the second or third trimester,
establishes more detailed anatomy and/or interval growth.
Additional Services
Fetal Biophysical Profile
Fetal biophysical profiles must also be medically justified. The medical record must reflect medical
necessity.
Non-Invasive Prenatal Screening
SCDHHS covers Non-Invasive Prenatal Screening (NIPS) of pregnant women for the detection of:
• Fetal chromosomal aneuploidy genomic sequence analysis panel, circulating cell-free DNA in
maternal blood, must include analysis of chromosomes 13, 18 and 21.
• Fetal chromosomal microdeletion(s) genomic sequence analysis, circulating cell-free fetal DNA
in maternal blood.
• Fetal aneuploidy (trisomy 21, 18 and 13) DNA sequence analysis of selected regions using
maternal plasma, algorithm reported as a risk score for each trisomy.
NIPS is considered medically necessary for pregnant women meeting all of the following criteria:
• Underwent pretest counseling.
• A cell-free fetal DNA test has not been performed yet in this pregnancy.
• Current pregnancy is not a multiple gestation.
• Current pregnancy greater than or equal to ten weeks and less than 23 weeks at the time the
blood will be drawn.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
74
Amniocentesis
Amniocentesis is a covered service when medically necessary. Justification must be documented in
the medical record. Please refer to Genetic Studies within this manual for coverage criteria.
Reimbursement is the same in the office or hospital (do not use the 26 modifier for place of service
21 or 22).
Ultrasound for Amniocentesis Guidance
When performed in the hospital, do not use the 26 modifier since the code is for supervision and
interpretation only.
Non-Stress Test
Non-stress tests (NSTs) are reimbursed when medically necessary. Reimbursement is not allowed
when performed in the hospital-by-hospital personnel. If the physician provides the interpretation in
place of service 21 or 22, he or she must bill with the 26 modifier. The physician’s interpretation of
the NST must be clearly documented in the patient’s record.
Tocolytic
Tocolysis is non-compensable as a separate reimbursement under the Physician Services program.
If a patient is admitted for tocolysis, the physician may bill for the appropriate hospital visits,
prolonged services, or critical care services when applicable. The medical record must reflect the
level of service billed. Tocolysis agents and monitoring are considered an integral part of the
hospital allowable charged.
Lab Procedures
If the physician sends a specimen to an independent lab, the lab will bill for their services.
• The collection of a urine specimen is included in the office visit.
• Finger/heel/ear stick for collection of specimen(s) is included in office visit reimbursement or lab
test reimbursement and may not be billed as collection of venous blood by venipuncture. Lab
tests performed in the office may be billed as a separate charge by billing the appropriate code
allowed by the laboratory’s CLIA certification category. Medicaid does not reimburse the
maternal care provider for tests performed at an independent lab.
Venipuncture
When performing a venipuncture, bill the service as collection of venous blood by venipuncture. No
documentation is required to be sent with the claim. If more than one venipuncture is performed on
the same DOS, the claim must be billed hard copy with documentation of the number of
venipunctures attached.
Non-Self-Injectable Drugs
The physician must provide any drugs that are not self-injectable and bill Medicaid the appropriate
procedure code for the cost of the drug in addition to the procedure code for the administration of

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
75
the drug. A physician may not write the patient a prescription for the medication to be filled at a
pharmacy with the expectation that the beneficiary return to the physician’s office for administration.
The pharmacy will not be reimbursed for the prescription.
Enhanced Services for Pregnant Women Offered by SCDPH
In addition to traditional medical care, pregnant women often have nutritional, environmental,
psychosocial, and educational needs that may influence pregnancy outcomes.
To address these needs, all Medicaid pregnant women are eligible for the following Family Support
Services through SCDPH:
• Psychosocial Intervention — Patients may be referred to SCDPH for services by an
appropriately credentialed social worker for an assessment followed by services based on an
individualized plan of care (IPOC).
• Nutritional Services — Patients may be referred to SCDPH for services by an appropriately
credentialed nutritionist or dietitian for an assessment followed by treatment that responds to
individual patient needs and problems.
• Health Education — Information and process-oriented activities may be provided on an
individual or group basis to predispose, enable, or reinforce patient adaptation or behavior
conducive to health at the local health department.
For information on referrals to authorized providers of these services, call the PSC at
+1 888 289 0709 or submit an online inquiry at Contact a Provider Representative | SCDHHS
.
17 Alpha Hydroxyprogesterone Caproate (Makena
®
and 17P)
Makena
®
and compounded hydroxyprogesterone caproate are covered without a prior authorization.
SCDHHS currently covers the use of 17 alpha hydroxyprogesterone caproate (17-P) intramuscular
injections to support the prevention of preterm births. The therapy is considered effective in reducing
negative outcomes and improving the quality of care in pregnant women. Makena
®
and
compounded 17-P will be covered on a weekly basis beginning at 16 weeks’ gestation through 36
weeks’ gestation when the patient presents with a history of spontaneous preterm delivery in a
single pregnancy, before 37 weeks' gestation. All other risk factors for preterm delivery and for the
use of hydroxyprogesterone caproate are considered investigational and not medically necessary.
Perinatal Care
Emergency Room Visit
When the physician meets the maternal patient in the ER or labor and delivery unit for immediate
medical attention, the appropriate level emergency department code must be billed.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
76
Observation Admission
When the physician meets the maternal patient at the ER or labor and delivery unit and admits the
patient to the hospital for observation (less than 24 hours), the physician must bill the appropriate
level hospital observation code with place of service 22.
External Version
External version is reimbursable as a separate procedure. The physician may bill this procedure in
addition to the delivery charge. If applicable, prolonged services may also be billed. The medical
record must document the service billed. This procedure is compensable at 100% of the established
rate when performed on the same day of delivery.
Note: No assistant is allowed for this procedure.
Uncomplicated (Routine) Deliveries
Both vaginal and Caesarean section (C-section) deliveries are considered surgical packages. The
following are inclusive in the surgical packages:
• Pitocin induction
• Surgical or mechanical induction
• Fetal monitoring (internal or external)
• Amnioinfusion
• Episiotomy
• Laceration repair
• Suture removal
• Standby for delivery
• Subsequent routine hospital care
• Hospital discharge
• Any related E&M visits within 30 days following the delivery
• Routine follow-up care (one postpartum visit may be billed separately using the appropriate
code. Please refer to Postpartum Care under Obstetrics and Gynecology in this section of the
manual).

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
77
• Insertion of cervical dilator (e.g., laminaria, prostaglandin) is considered included in the surgical
package and may not be billed in addition to the CPT code for the delivery. This applies whether
being placed the day of delivery, or several days prior to delivery, if placed by the delivering
physician or physician within the same practicing group.
Providers are required to append the following modifiers, and in some cases complete the ACOG
Patient Safety Checklist or a comparable patient safety justification form, when scheduling an
induction of labor or a planned C-section for deliveries less than 39 weeks’ gestation. The provider
is responsible for maintaining a copy of this documentation in their files and in the hospital record,
which are subject to SCDHHS PI review.
Providers may append the following modifiers to all CPT codes when billing for vaginal deliveries
and C-sections:
• GB — 39 weeks’ gestation and or more:
– For all deliveries at 39 weeks' gestation or more regardless of method (induction, C-section
or spontaneous labor).
• CG — Less than 39 weeks' gestation:
– For deliveries resulting from patients presenting in labor, or at risk of labor, and
subsequently delivering before 39 weeks, or
– For inductions or C-sections that meet the ACOG or BOI-approved medically necessary
guidelines, the appropriate ACOG Patient Safety Checklist must be completed and
maintained for documentation in the patient’s file, or
– For inductions or C-sections that do not meet the ACOG or BOI-approved medically
necessary guidelines, the appropriate ACOG Patient Safety Checklist must be completed.
In addition, the provider must obtain approval from the regional perinatal center’s MFM
physician and maintain this documentation in the patient’s file.
No Modifier — Elective Non-Medically Necessary Deliveries Less Than 39 Weeks Gestation
For deliveries less than 39 weeks gestation that do not meet ACOG or approved BOI guidelines or
are not approved by the designated regional perinatal center’s MFM physician.
Delivery in Cases of Prolonged Labor
Effective with dates of service on or after January 1, 2012, SCDHHS modified the delivery policy in
cases of prolonged labor when a vaginal delivery with failure to progress converts to a C-section.
For beneficiaries that have been admitted to the hospital and have been in active labor for at least
six hours, the procedure code and modifier UA must be used when billing for the C-section delivery.
The patient records must indicate the time the beneficiary was admitted to the hospital with active

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
78
labor and the start time of the C-section. All claims and reimbursements are subject to an audit by
the Division of Program Integrity.
Hospital Admission for Delivery
The hospital admission codes are not allowed if the delivering physician or group has provided
prenatal care to the beneficiary. The appropriate level admission code may be billed with drop-in
vaginal and C-section deliveries only.
Emergency Deliveries
If the patient gives birth outside the hospital setting and the patient’s private physician did not
perform the delivery, but later meets the maternal patient at the hospital for post-delivery services,
the following procedures apply:
• The private physician may bill for delivery of the placenta, if applicable.
• The private physician may also bill for subsequent hospital care and the hospital discharge, if
applicable.
If a hospital-based physician performs the delivery and the private physician arrives in time to assist
the hospital-based physician or arrives shortly after the delivery, the following apply:
• The hospital-based physician would bill for the delivery.
• The private physician would bill for the post-delivery services if the private physician performed
the services.
• The private physician may also bill for subsequent hospital care and the hospital discharge, if
applicable.
If the private physician is not involved in the delivery or post-delivery services, then the following
applies:
• The physician may bill for the admission (if appropriate), subsequent hospital care, and the
discharge, if applicable, during the hospitalization for the delivery.
If a physician or CNM is preparing to deliver a baby and it is decided that the baby must be
delivered by an emergency C-section and an OB must be called in, then the following applies:
• The physician or certified midwife may receive payment from Medicaid for his or her involvement
in the case by billing the C-section code with an 80 modifier, assistant surgeon. Technically, the
physician or CNM would be billing as an assistant surgeon on the C-section. Reimbursement for
this procedure is 20% of the C-section rate.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
79
Multiple Births
Please refer to Multiple Births within the Billing Guidance section of this manual for the policy on
billing for multiple babies.
Pre-Term Deliveries
Please refer to the “Abortion Guidelines” below for the policy on coding for a vaginal delivery or non-
elective abortion.
Postpartum Care
Routine Postpartum Visit
The postpartum visit includes an uncomplicated routine GYN examination of the mother following a
vaginal or C-section delivery. Only one postpartum exam per delivery is allowed. Reimbursement for
all other routine postpartum visits is included in payment for the delivery.
Family Planning Counseling or instruction may not be billed in addition to the postpartum code when
Family Planning services are rendered and documented. Please refer to Family Planning in this
section of the manual for the code description and more details.
Complication/Other Medical Attention During 30-Days Post Delivery
If E&M services unrelated to routine postpartum care are necessary during the 30 days’ post-
delivery, bill these services using modifier 24. Documentation in the patient’s chart must
substantiate that the visit was unrelated to the delivery.
Note: Wound infection is not considered routine postpartum care.
Abortion Guidelines
Non-Elective Abortions
All non-elective abortions, including spontaneous, missed, incomplete, septic, hydatidiform mole,
etc., require only that the medical record verify such a diagnosis. Medical procedures necessary to
care for a patient with an ectopic pregnancy are not modified by this section and are compensable
services.
Therapeutic Abortions
In compliance with federal regulations (42 CFR 441.203 and 441.206), SCDHHS requires
documentation for all charges associated with instances of therapeutic abortion. This includes the
attending physician, the anesthesiologist, and the hospital.
Therapeutic abortions are sponsored only in cases that a physician has found, and certified in
writing to the Medicaid agency, that on the basis of his or her professional judgment, the pregnancy
is the result of an act of rape or incest; or the woman suffers from a physical disorder, physical
injury, or physical illness, including a life-endangering physical condition caused by or arising from
the pregnancy itself, that would place the woman in danger of death unless an abortion is
performed.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
80
The abortion statement must contain the name and address of the patient, the reason for the
abortion, and the physician’s signature and date. The patient’s certification statement is only
required in cases of rape or incest. The medical record must document that continued pregnancy
would endanger the life of the mother or that the pregnancy is the result of an act of rape or incest.
This may be reflected in the office admission history notes and physical, discharge summary,
consultation reports, operative records and/or pathology reports. Both the abortion statement and
the appropriate medical records must be submitted with the claim. A sample copy of the Abortion
Statement Form can be found in the Forms section of the provider portal. If documentation is
insufficient or the abortion statement is improperly completed, the claim will be rejected.
Questions may be directed to the PSC at +1 888 289 0709 or providers may submit an online
inquiry at Contact a Provider Representative | SCDHHS
Licensed Midwives
Medicaid sponsors the enrollment of licensed midwives. The scope of practice is limited to that
defined in the South Carolina State Register, Volume 17, Issue 7, Chapter 61.
As Medicaid providers, licensed and certified midwives are required to maintain and disclose their
records consistent with the Provider Administrative and Billing Manual. As allied health
professionals, licensed midwives are required by State Law (SC Code Section 20-7-510) to report
any signs of abuse or neglect to children that they may encounter in the office or home setting.
Additional enrollment and documentation requirements are specified below. For more information on
Medicaid-sponsored midwifery services, please contact the PSC at +1 888 289 0709 or submit an
online inquiry at Contact a Provider Representative | SCDHHS
.
Requirements for Physician Back-up
The same physician or group must agree to provide the following services:
• Two assessment visits as required by regulations.
• Appropriate prescriptions for any medications that the midwife may administer at the time of the
delivery according to the regulations (e.g., Pitocin, RhoGAM, eye prophylaxis, etc.).
• Medical evaluation and treatment in the event of a complication during pregnancy.
• Delivery services in the event of an emergency.
Birthing Centers
Medicaid will contract with birthing centers for obstetrical and newborn services. The birthing center
must be licensed by SCDPH prior to enrolling in the Medicaid program. For enrollment information,
please contact our enrollment department at +1 888 289 0709.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
81
OB/Newborn Care with Technical Component (TC) Modifier
Medicaid will reimburse for an all-inclusive facility fee. The facility fee will include all technical
services provided by the birthing center including, but not limited to, administration, nursing, drugs,
surgical dressings, supplies and materials for anesthesia.
Observation for Maternity/Labor
This service is billable for observation of maternity/labor. This code is billable only if the patient is at
the birthing center laboring, but the labor does not progress, and the patient is sent home to return
later or discharged to the hospital.
Pulse Oximetry Policy
SCDHHS accepts the SCDPH Pulse Oximetry Screening test on newborns to detect congenital
heart defects. Pulse oximetry is a non-invasive test that estimates the percentage of hemoglobin in
blood that is saturated with oxygen.
The “Emerson Rose Act” (Act) became effective September 11, 2013, mandating that SCDPH
require each birthing facility it licenses to perform a pulse oximetry screening test, or other SCDPH
approved screening to detect critical congenital heart defects, on every newborn in its care. A
newborn may be exempt from the required screening if the parent of the newborn objects, in writing,
for reasons pertaining to religious beliefs only.
In accordance with the Act, birthing facilities shall perform a pulse oximetry screening test, or other
SCDPH-approved screening to detect critical congenital heart defects, on every newborn when the
baby is 24 to 48 hours of age, or as late as possible if the baby is discharged from the hospital
before reaching 24 hours of age. Pulse oximetry screening for newborns shall be performed in the
manner designated by SCDPH guidelines located at
Homepage | South Carolina Department of
Public Health (sc.gov)The hospital reimbursement for newborns is an all-inclusive payment for
services rendered during that hospital stay and thus includes the pulse oximetry screen.
In compliance with SCDPH policy, licensed midwives and certified nurse midwives that deliver a
newborn in a birthing center must also perform this test. In addition, SCDHHS requires the test to be
performed when a newborn is delivered in place of service home. When billing SCDHHS for the
screening:
• Licensed midwives delivering in a birthing center or home must bill the appropriate code
appended with the SB modifier.
• Certified nurse midwives or other clinician delivering in place of service birthing center or home
must bill the appropriate code appended with a UD modifier, Medicaid level of care 13, as
defined by each state.
The birthing center is responsible for following the policy as outlined by SCDPH. Medicaid
reimbursement for this procedure will be paid at the line level.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
82
Levonorgestrel-Releasing Intrauterine System (Mirena®) Coverage
Medicaid will sponsor reimbursement for the Levonorgestrel-Releasing Intrauterine System
(Mirena®). To bill for Mirena®, the provider may use the appropriate HCPCS J code. Please include
the FP modifier on the claim form. Providers must continue to use the appropriate Family Planning
diagnosis codes and CPT codes for the insertion and removal of the device.
Etonogestrel Implant (Implanon®) Coverage
Medicaid will sponsor reimbursement for the Etonogestrel Implant (Implanon®/Nexplanon®), a
single-rod implantable contraceptive that is effective for up to three years. To bill for
Implanon®/Nexplanon®, the provider may use the appropriate HCPCS J code. Please include the
FP modifier on the claim form. Providers must continue to use the appropriate Family Planning
diagnosis codes and CPT codes for the insertion and removal of the device.
Zithromax (Oral Suspension)
Medicaid will sponsor reimbursement for Zithromax (Azithromycin) for oral suspension in one-gram
dose packets by prescription or when provided in the physician’s office. An appropriate code may be
used when this oral drug is provided in the physician’s office.
Lupron Depot® (Leuprolide Acetate)
Medicaid will sponsor reimbursement for Lupron Depot® injections. The provider must supply the
drug.
Pessary
Medicaid will sponsor reimbursement for pessaries; the physician must provide the pessary.
Salpingectomy and/or Oophorectomy
The operative report must be submitted with the claim. The medical record must reflect medical
necessity for the procedure performed. Reimbursement using these codes is not allowed if
performed as a sterilization procedure, unless a copy of the Sterilization Consent Form is attached.
A sample copy of the form can be found in the Forms section of the provider portal.
Depo-Provera for Other than Contraceptive Purposes
An appropriate code is used to report Depo-Provera for other than contraceptive purposes. Dosage
is 50 mg. Frequency is limited to 500 mg and must be billed in units of 50 mg.
Family Planning Program
See Family Planning within this section of the manual for more information.
Elective Sterilization
SCDHHS is required to have a completed Sterilization Consent Form that meets the federal
regulations for all charges associated with elective sterilization. Photocopies are accepted if legible.
The physician must submit a properly completed consent form with his or her claim so that other
providers involved with the sterilization procedure may also be reimbursed.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
83
Definitions (as stated in the Code of Federal Regulations 42 CFR 441.251)
Sterilization — Any medical procedure, treatment, or operation for the purpose of rendering an
individual permanently incapable of reproducing.
Institutionalized Individual — An individual who is:
• Involuntarily confined or detained under a civil or criminal statute, in a correctional or
rehabilitative facility, including a mental hospital or other facility for the care and treatment of
mental illness, or
• Confined, under a voluntary commitment, in a mental hospital or other facility for the care and
treatment of mental illness.
Mentally Incompetent Individual — Means an individual who has been declared mentally
incompetent by a federal, state, or local court of competent jurisdiction for any purpose, unless the
individual has been declared competent for purposes which include the ability to consent to
sterilization.
All sections of the Sterilization Consent Form (DHHS Form 687) must be completed when submitted
with the claim for payment. Each Sterilization Claim and Consent Form are reviewed for compliance
with federal regulations (42 CFR 441.250–441.259 subpart F).
****The sterilization consent form is codified in federal regulations as an Appendix to 42 CFR
441 Subpart F. Because the form is codified in federal regulation it never expires and must be
used regardless of whether there is a current OMB date. For Medicaid purposes the form does
not require an expiration date to be valid. This is the only form that can be used, and it may
not be altered in any way. The lack of a current form is not a valid reason to deny a claim
providing the form has not been altered and is compliant with regulations. ****
Requirements
For Medicaid financial coverage of an elective sterilization for a male or female, the following
requirements must be met:
• The Sterilization Consent Form must be signed at least 30 days prior to, but no more than
180 days prior to, the scheduled date of sterilization.
• The individual must be 21 years old at the time the consent form is signed.
• The individual cannot be institutionalized or mentally incompetent. If the physician questions the
mental competency of the individual, he or she may contact the PSC at +1 888 289 0709 or
submit an online inquiry at Contact a Provider Representative | SCDHHS
.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
84
• The individual must voluntarily give consent. All questions must be answered and all topics in
the consent form discussed. (A witness of the patient’s choice may be present during the
consent interview.) The Family Planning Counseling or family planning education/instruction
procedure code may be billed when this service is rendered and documented.
• A copy of the consent form must be given to the patient after Parts I, II, and III are completed.
• At least 30 days, but not more than 180 days, must have passed between the signing of the
consent form and the date of the sterilization procedure. The date of the beneficiary’s signature
is not included in the 30 days (e.g., day one begins the day after the signature). No one can sign
the form for the individual.
Exceptions to the 30-day waiting period are:
• Premature Delivery — The informed consent must have been signed at least 30 days prior to
the expected date of delivery. In cases involving a C-section, the scheduled date of the
C-section is considered the expected date of delivery. At least 72 hours must have elapsed
since the informed consent was given.
• Emergency Abdominal Surgery — The emergency does not include the operation to sterilize the
patient. At least 72 hours must have elapsed since the informed consent was given. An
explanation must accompany the consent form.
Note: If the beneficiary is pregnant, premature delivery is the only exception to the 30-day waiting
period.
Informed consent may not be obtained while the patient to be sterilized is:
• In labor or childbirth.
• Seeking or obtaining an abortion.
• Under the influence of alcohol or other substances which may affect the patient’s judgment.
Specialty Care Services
This section of the manual contains policies and guidelines for services that are primarily performed
and billed by specialty physicians who treat specific body systems. However, all physicians are
subject to all guidelines in this manual.
Consultations
A consultation is a request for an opinion and/or advice only. A consultation may involve a complete
or a single organ system examination, followed by a written report in the patient's medical record.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
85
The attending physician makes the request and continues in the role of primary physician unless he
releases the patient to the consultant. The request for a consultation must be documented in the
patient's record. The date the attending physician turns the patient's care over to the consultant
must be documented, and the initial physician ceases billing.
When the consultant assumes responsibility or management of a portion or all of the patient's
condition, services are considered subsequent hospital visits, office visits or concurrent care.
A follow-up consultation involves the consultant's re-evaluation of a patient on whom he or she has
previously rendered an opinion or advice. As in initial consultations, the consultant provides no
patient management or treatment.
Coverage — Consultation may be covered when the following conditions are met:
• A consultation or follow-up consultation is requested from a physician whose specialty or
sub-specialty is different from the attending physician, for the opinion and/or advice in the further
evaluation or management of the patient.
• Multiple consultations for the same patient must be determined to be medically necessary. Each
consultation must relate to a different diagnosis or document that unusual circumstances exist,
such as severity of condition or complexity of care.
Initial Inpatient Consultation — Using the CPT guidelines for terminology and levels of service, one
initial consultation is allowed per patient per admission.
Documentation must reflect the request for the follow-up consultation and indicate that the
consulting physician has not assumed responsibility for any portion of the patient's care. The third
follow-up visit and all subsequent visits during that hospitalization must be billed with subsequent
hospital visit codes.
Office or Other OP Consultations — Use the CPT guidelines for terminology and levels of service.
Interprofessional Consultation
Interprofessional consultation is defined as a situation in which the patient’s treating physician or
other qualified health care practitioner (hereafter referred to as the treating practitioner) requests the
opinion and/or treatment advice of a physician or other qualified health care practitioner with specific
specialty expertise (hereafter referred to as the consulting practitioner) to assist the treating
practitioner with the patient’s care.
Interprofessional consultation is intended to expand access to specialty care and foster
interdisciplinary input on patient care. It is not intended to be a replacement for direct specialty care
when such care is clinically indicated.
Reimbursement of interprofessional consultation is permissible, even when the beneficiary is not
present, as long as the consultation is for the direct benefit of the beneficiary. The consulting

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
86
provider must be an enrolled Medicaid provider. Interprofessional consultation services may be
provided via telehealth and reimbursed with the use of the appropriate modifier.
Referral
A referral is the transfer of the total or specific care of a patient from one physician to another and
does not constitute a consultation. Use proper codes for initiation of treatment (i.e., office or hospital
visit codes).
Psychiatric and Counseling Services
Psychiatric services include E&M, psychotherapy, and other services to an individual, family, or
group and are compensable when medically indicated and in compliance with Medicaid policies. In
order to be covered under the Medicaid program, a service must be medically necessary. Medical
necessity means the need for treatment services is necessary to diagnose or treat, an illness.
Medicaid-eligible beneficiaries may receive psychiatric and psychotherapy services when there is a
confirmed psychiatric diagnosis from the current edition of the American Psychiatric Association’s
Diagnostic and Statistical Manual of Mental Disorders (DSM) or the ICD. Any psychiatric services
provided to a child less than three years of age must be carefully documented to show medical
necessity.
Covered psychiatric and psychotherapy services include the following:
• Psychiatric diagnostic evaluation
• Environmental intervention for medical management
• Psychological testing
• Psychotherapy
• Family Psychotherapy with patient present
• Family Psychotherapy without patient present
• Group psychotherapy
• Psychotherapy for crisis
• Medical E&M
These services are provided to, or directed exclusively toward, the treatment of the Medicaid-eligible
beneficiary for the purpose of ameliorating disabilities, improving the beneficiary’s ability to function
independently and restoring maximum functioning.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
87
Please refer to Covered Services in this manual for appropriate codes for each covered service
listed above and who is eligible to bill for these services.
Referral to Allied Professionals
The psychiatric diagnostic evaluation completed by the physician/NP (also referred to as the
supervising clinician) shall result in a determination of the beneficiary’s need for psychiatric services
and/or psychotherapy services. The physician/NP must document all treatment services authorized
to be provided to the beneficiary. If appropriate, the physician/NP may authorize services to be
rendered by an allied professional. The physician/NP must:
• See each beneficiary initially unless the beneficiary was accepted as a referral from another
physician.
• Authorize the treatment services to be provided by the allied professional.
• Participate in patient staffing with the allied professional to document progress summaries.
If the beneficiary is referred by a non-physician (e.g., DSS, school counselor, etc.), the referral
source must be documented in the chart.
When scheduling is a problem or the beneficiary’s condition requires immediate treatment, a
maximum of two psychotherapy visits in 14 days will be allowed by an allied professional under
supervision prior to an initial psychiatric diagnostic evaluation by the supervising clinician. The
supervising clinician must then perform the initial psychiatric diagnostic evaluation before any further
psychotherapy services can be provided.
In all cases, the supervising clinician must assume all professional liability for services rendered by
staff under his or her supervision. In the event of a post-payment review, the supervising clinician
who is reimbursed by Medicaid is responsible for all records. Credentials of allied professionals who
provided services must be on file and will be part of the post-payment review. If the allied
professional’s credentials are not on file or do not meet the qualifications, the supervising clinician’s
payments will be subject to recoupment.
Supervision
Direct supervision in the physician’s office, group practice or clinic setting means that the
supervising clinician must be responsible for all services rendered and be accessible at all times
during the diagnosis and treatment of the beneficiary.
Services provided under direct supervision are covered only if the following conditions are met:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
88
• The allied professional must be a part-time, full-time, or contracted employee of the supervising
clinician, physician group practice, or of the legal entity that employs the supervising clinician; or
the allied professional must be an independent contractor engaged by the physician/NP through
a written agreement.
• The supervising clinician cannot be employed by the allied professional.
• The supervising clinician must be accessible to the allied professional while services are being
delivered and must meet with the allied professional at a minimum of every 90 days to review
beneficiary progress.
• The service must be furnished in connection with a covered physician/NP service that was billed
to SCDHHS; therefore, the beneficiary must be one who has been seen by the physician/NP.
• A psychiatric diagnostic evaluation must be performed by the supervising clinician.
The allied professional providing psychotherapy personally works with the beneficiary to develop the
IPOC and the supervising clinician meets with the beneficiary periodically during treatment to
monitor the service being delivered and to review the need for continued services. There must be
subsequent services by the supervising clinician of a frequency that reflects his/her continued
participation in the management of the course of treatment. The supervising clinician assumes
professional responsibility and liability for all services provided by allied professionals.
The supervising clinician must spend as much time as necessary directly supervising the services to
ensure that patients are receiving services in a safe and efficient manner in accordance with
accepted standards of practice. The supervising clinician must meet with the allied professional and
document the monitoring of performance, consultation, guidance and education at a minimum of
every 90 days to ensure the delivery of medically necessary services.
A supervising clinician is limited to supervising no more than three allied professionals who meet the
qualifications to render psychotherapy services. Prior to services being rendered by allied
professionals, the names and credentials of the three allied professionals being supervised must be
submitted to:
SCDHHS
Division of Behavioral Health
Post Office Box 8206
Columbia, SC 29202-8206
Fax: +1 803 255 8204
This information must be updated as necessary or at least every 12 months. To satisfy this
requirement, complete and return a copy of the Allied Professional Supervision Form found in the

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
89
Forms section of the provider portal. Additionally, the credentials of the allied professionals must be
maintained on file at the office where services are being provided.
Individualized Plan of Care (IPOC)
If it is determined through the psychiatric diagnostic evaluation that a beneficiary needs
psychotherapy services and a referral is made to an allied professional OR psychotherapy services
will be provided by the physician/NP, an IPOC is required within 45 days of the date of the initial
psychiatric diagnostic evaluation. The IPOC is an individualized, comprehensive treatment plan,
which is based on the assessment and is created in partnership with the beneficiary and/or legally
responsible person, except in the case of an emergency. The IPOC is designed to improve and/or
stabilize the beneficiary’s condition and must encompass all treatment goals and objectives.
The following services are not required to be listed on the IPOC:
• Psychiatric diagnostic evaluation
• Psychotherapy for crisis
• Environmental intervention
• E&M
• Psychological testing
Services not outlined in the treatment plan, other than those listed above, are non-billable and
subject to recoupment. The allied professional providing psychotherapy services under the
supervision of a physician/NP may develop the IPOC, but the IPOC must be signed by both the
allied professional and the supervising clinician when psychotherapy is being provided by an allied
professional.
The IPOC provides the overall direction for the treatment of the beneficiary and must include the
following elements:
• Individualized treatment goals developed in conjunction with the beneficiary and/or family.
• Specific interventions and strategies that will be used to meet goals.
• Outcomes that are anticipated to be achieved by provision of the service and projected date of
achievement.
• A projected schedule for service delivery, including the expected frequency and duration of each
treatment method.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
90
• The beneficiary and/or legally responsible person must sign the IPOC indicating that they were
involved in the planning process and were offered a copy of the IPOC. If the beneficiary does
not sign the IPOC, the reason must be documented in the clinical record.
• The physician/NP’s signature is required on the IPOC to confirm the diagnosis, medical
necessity of the treatment, and the appropriateness of care.
The original IPOC supervising clinician’s signature date stands as the date to be used for all
subsequent progress summaries, reviews and reformulations. Each page of the IPOC must be
signed, titled and signature dated by the supervising clinician. Services added or frequencies of
services changed in an existing IPOC must be signed and dated by the supervising clinician. An
updated copy must be provided to the beneficiary. The IPOC must be filed in the beneficiary’s
clinical record with any supporting clinical documentation.
Progress Summary
A progress summary is a periodic evaluation and review of the beneficiary’s progress toward the
treatment goals, the appropriateness of the services being provided, and the need for the
beneficiary’s continued participation in treatment. If psychotherapy services are being provided by
an allied professional, the supervising clinician and allied professional must meet to review the
beneficiary’s participation in all services every 90 days with completion during the calendar month in
which it is due. Reviews may be conducted more frequently if the nature of needed services
changes or if there is a change in the beneficiary’s condition or status as determined by the
physician/NP.
Progress summaries shall be documented in detail in the beneficiary’s record and include:
• The beneficiary’s progress towards treatment goals.
• The appropriateness of the services provided and their frequency.
• The need for continued treatment.
• Recommendations for continued services.
• The signature and title of the supervising clinician and allied professional.
If it is determined during the progress summary that the IPOC needs to be modified, then an
updated IPOC also must be developed.
IPOC Reformulation
The maximum duration of an IPOC is 12 months (365 days) from the date of the signature of the
supervising clinician. The allied professional must evaluate with the beneficiary his/her progress in
reference to each of the treatment goals and desired outcomes. Based on the progress of the

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
91
beneficiary, the IPOC must be reformulated annually to include updated treatment goals and
outcomes. The signature of the supervising clinician is required on the reformulated IPOC.
Transition/Discharge
The supervising clinician is responsible for determining the duration of treatment based on the
individual needs of the beneficiary. The allied professional involved in the delivery of services to the
beneficiary may gather and/or give information to assist with this process. Beneficiaries may be
discharged from treatment when they meet one of the following criteria:
• Level of functioning has significantly improved with respect to goals outlined in treatment plan.
• All treatment goals have been achieved.
• Beneficiary has developed skills and resources needed to transition to a lower level of care.
• Beneficiary requests discharge (and is not imminently dangerous to self or others).
• Beneficiary requires a higher level of care (e.g., inpatient hospitalization or Psychiatric
Residential Treatment Facility [PRTF]).
Psychiatric Diagnostic Evaluation
Psychiatric diagnostic evaluation is an integrated biopsychosocial assessment, including history,
mental status and recommendations. The evaluation may include communication with family or
other sources and review and ordering of diagnostic studies.
Psychiatric diagnostic evaluation with medical services is an integrated biopsychosocial and medical
assessment, including history, mental status, other physical examination elements as indicated, and
recommendations. The evaluation may include communication with family or other sources,
prescription of medications, and review and ordering of laboratory or other diagnostic studies.
• Psychiatric diagnostic evaluation
• Psychiatric diagnostic evaluation with medical services
These procedures may be reported once every six months and not on the same day as an E&M
service performed by the same individual for the same beneficiary.
Eligible to bill: Physician/Psychiatrist or Psychiatric NP
Psychological Testing
Psychological testing includes psycho-diagnostic assessment of emotionality, intellectual abilities,
personality and psychopathology (e.g., MMPI, Rorschach, WAIS) per hour of the physician’s time,
both face-to-face time administering tests to the beneficiary and time interpreting these test results
and preparing the report.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
92
• Psychological testing.
• Psychological testing evaluation services by physician or other qualified health care
professional, including integration of patient data, interpretation of standardized test results and
clinical data, clinical decision making, treatment planning and report and interactive feedback to
the patient, family member(s) or caregiver(s), when performed; first hour.
• Each additional hour is listed separately in addition to code for primary procedure.
These procedures are reimbursed per hour, not per test. Report time as face-to-face time with
patient and the time spent interpreting and preparing the report. Only three hours are allowable per
day with a maximum limit of 12 hours in one year.
Eligible to bill: Physician/Psychiatrist or Psychiatric NP
Environmental Intervention for Medical Management
Environmental intervention for medical management purposes on a psychiatric patient's behalf,
including coordination of services. This code can be billed when the supervising clinician meets with
an allied professional to coordinate services, discusses treatment issues, and review the treatment
plan for a beneficiary and must be clearly documented in the progress summary and signed by the
supervising clinician. This code cannot be billed each time the clinician signs the chart only. One
progress summary is required every 90 days. Medicaid will reimburse only the supervising clinician
for this service.
• Environmental intervention for medical management purposes on a psychiatric patient's behalf
with agencies, employers or institutions.
This procedure is reimbursed in 30-minute increments (units), not to exceed an hour and a half per
day. The supervising clinician, when coordinating services with allied professionals, may bill one unit
of this code.
Eligible to bill: Physician/Psychiatrist or Psychiatric NP
Psychotherapy
Psychotherapy is the treatment of mental illness and behavioral disturbances in which the physician
or other qualified healthcare professional, through definitive therapeutic communication, addresses
the emotional disturbance, reverses or changes maladaptive patterns of behavior, and encourages
personality growth and development. Psychotherapy times are for face-to-face services with
beneficiary and/or family member. The beneficiary must be present for all or some of the service.
• Psychotherapy, 30 minutes
• Psychotherapy, 45 minutes

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
93
• Psychotherapy, 60 minutes
One session, regardless of time, is allowed per day within this range of procedures. If this service is
being billed, an IPOC must have been completed for the beneficiary.
Eligible to bill: Physician/Psychiatrist, Psychiatric NP or LMSW — with HO Modifier
Psychotherapy with Medical Evaluation and Management Services
Some psychiatric patients receive a medical E&M service on the same day as a psychotherapy
service by the same physician/NP. To report both E&M and psychotherapy, the two services must
be significant and separately identifiable. Please refer to the current CPT for further instruction.
These services are reported by using the following codes specific for psychotherapy when
performed with E&M services as add-on codes to the E&M service:
• Psychotherapy, 30 minutes
• Psychotherapy, 45 minutes
• Psychotherapy, 60 minutes
One session, regardless of time, is allowed per day within this range of codes. If this service is being
billed, an IPOC must have been completed for the beneficiary.
Eligible to bill: Physician/Psychiatrist or Psychiatric NP
Family Psychotherapy
Family psychotherapy is a face-to-face intervention with family members of the beneficiary with the
purpose of treating the beneficiary’s condition and improving the interaction between the beneficiary
and family member(s) so that the beneficiary may be restored to their best possible functional level.
Family Psychotherapy may be rendered with or without the beneficiary to family members of the
identified beneficiary if the identified beneficiary is the focus of the sessions. The identified
beneficiary is the family member with the symptom that has brought the family into treatment. Only
issues pertinent to the identified beneficiary may be addressed under this service.
• Family Psychotherapy including patient, 50 minutes
• Family Psychotherapy, 50 minutes
One session, regardless of time, is allowed per day within this range of codes. If this service is being
billed, an IPOC must have been completed for the beneficiary.
Eligible to bill: Physician/Psychiatrist, Psychiatric NP or LMSW — with HO Modifier

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
94
Group Psychotherapy
Group psychotherapy is a face-to-face intervention with a group of beneficiaries who are addressing
similar issues with the purpose of restoring the beneficiary to his/her best possible functional level.
Therapy is conducted in small groups. The group must be a part of an active treatment plan and the
goals of group therapy must match the overall treatment plan for the individual beneficiary. The
focus of the therapy sessions must not be exclusively educational or supportive in nature. Groups
must consist of one professional and no more than eight beneficiaries.
• Group Psychotherapy — other than of a multiple-family group.
This code is covered for eligible beneficiaries in a group, even when the whole group is not
Medicaid eligible. Medicaid will reimburse a clinician for one group session per day per
Medicaid-eligible beneficiary. If this service is being billed, an IPOC must have been completed for
the beneficiary.
Eligible to bill: Physician/Psychiatrist, Psychiatric NP or LMSW — with HO Modifier
Psychotherapy for Crisis
Psychotherapy for Crisis is an urgent assessment and history of a crisis state, a mental status exam
and a disposition. The treatment includes psychotherapy, mobilization of resources to defuse the
crisis and restore safety, and implementation of psychotherapeutic interventions to minimize the
potential for psychological trauma. The presenting problem is typically life-threatening or complex
and requires immediate attention to a beneficiary in high distress.
• Psychotherapy for Crisis — This procedure is used to report the first 30–74 minutes of
psychotherapy for crisis on a given date. It must be used only once per date even if the time
spent by the physician or other qualified health care professional is not continuous on that date.
The beneficiary must be present for all or some of the service.
• A separate code is used in conjunction with Psychotherapy for Crisis to report each additional
30 minutes of crisis for psychotherapy.
Eligible to bill: Physician/Psychiatrist, Psychiatric NP or LMSW — with HO Modifier
Medical Evaluation and Management Services
Some psychiatry services may be reported with Medical E&M services or other services when
performed. E&M services may be reported for treatment of psychiatric conditions, rather than using
Psychiatry Services codes, when appropriate. Please refer to the current CPT as E&M codes are
classified by type of service, place of service and the patient’s status.
Eligible to bill: Physician/Psychiatrist or Psychiatric NP

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
95
Interactive Complexity
Interactive complexity refers to specific communication factors that complicate the delivery of a
psychiatric procedure. Please refer to the current CPT for complete definition. For billing purposes,
this is an add-on code for interactive complexity to be reported in conjunction with codes for
diagnostic psychiatric evaluation, psychotherapy, psychotherapy when performed with an E&M
service and group psychotherapy.
Eligible to bill: Physician/Psychiatrist or Psychiatric NP
Ophthalmology and Optometry Services
SCDHHS recognizes parity between ophthalmologists and optometrists as defined by State Law
with respect to reimbursement. Services rendered by optometrists must comply with SC Optometry
Practice Act.
Routine vision services are covered for beneficiaries from birth up to the last day of the month of
their 21
st
birthday. Routine vision services for adult beneficiaries 21 years and older are non-
covered services. Routine vision services are defined as services related to refractive care: routine
eye exams, refractions, corrective lenses and glasses. Services related to disease of the eye are
covered, for an example glaucoma, conjunctivitis and cataracts.
Providers are responsible for accurately billing a valid and appropriate procedure code the level of
which reflects services rendered to Medicaid beneficiaries. Providers must use the appropriate
place of services (POS) code as defined by the Centers for Medicare and Medicaid Services (CMS).
For services rendered via a mobile optometry unit on-site of a Title I public school, providers must
enter the POS=03 on the claim form. For a complete listing of POS codes please visit the CMS
website: Place of Service Code Set | CMS
. Reimbursement for vision services delivered in Title I
schools via mobile units is the same as services delivered in an office setting.
When reporting services provided in an office, home, SC Title I public schools, hospital, or an
institutional facility that are not specific ophthalmology codes providers must utilize E&M codes
listed in the AMA CPT manual. Providers are responsible for all National Correct Coding Initiative
(NCCI) rules and regulations.
If an E&M code is used for treatment of a disease, it cannot be used in conjunction with a
comprehensive exam code for treatment on the same DOS (as defined by NCCI). The provider
must bill either the E&M code or the comprehensive exam code. Providers must refer to the CPT
manual to determine which E&M code is the most appropriate. The patients’ record must reflect the
level of service performed and must be well documented in the patients’ chart. All services billed are
subject to a PI review. During post-payment reviews (audits), auditors will monitor these codes
closely to ensure that the code reflects the service billed and best meets the description reflected in
the documentation. The use of E&M codes will count toward the 12 maximum visits allowed for all
patients over the age of 21, for the fiscal year. The fiscal year begins July 1
st
of every year and ends
June 30
th
of every year.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
96
Part I — Vision Care Services
Vision care services are defined as those that are medically necessary for the diagnosis and
treatment of conditions of the eye. Refractive care is defined as the exam and treatment of visual
states such as, but not limited to, the correction of amblyopia, presbyopia and for all services that
can be corrected by the provision of corrective lenses. Referrals from local DSS offices or staff,
schools, and patient's actual complaints of visual acuity constitute justification to provide eye exams
and other refractive services for children under the age of 21. Providers must note these referrals
and complaints in the patient’s medical records.
Exam and Glasses for Birth to Age 21
For the treatment of children under the age of 21, one complete comprehensive eye exam is
covered within a 365-day period (12 consecutive months).
A complete set of glasses is provided every 365 days when medically necessary.
Repair and Replacement
Eyeglasses must be repaired without additional reimbursement when the repair or replacement of
eyeglass parts is required due to defects in quality of materials or workmanship. Reimbursement is
available for repair or replacement of eyeglass parts in situations where the damage is the result of
causes other than defective materials or workmanship. Replacement parts must replicate the
original prescription and frame style. Repairs to frames may be rendered as necessary.
Providers must use the appropriate procedure code for the repair or replacement of component
parts of eyeglasses. When a component part of eyeglasses is replaced, the U8 modifier may be
affixed to the appropriate procedure code for the component part that is being replaced. The reason
for the repair or replacement of parts must be documented in the recipient’s records.
Replacement of a Complete Pair of Eyeglasses
Reimbursement is available for one complete pair of replacement eyeglasses that has been lost or
destroyed within twelve consecutive months. The replacement for a complete pair of eyeglasses
must replicate the original prescription and frames. The U9 modifier is affixed to the appropriate
procedure codes identifying fitting of eyeglasses and materials when claiming replacement of a
complete pair of eyeglasses that has been lost or destroyed. An explanation of the circumstances
surrounding replacement of the complete pair of eyeglasses must be maintained in the enrollee's
record.
If a beneficiary has surgery or prescriptive change with a minimum of one-half diopter (0.50) during
12 consecutive months, only replacement lenses (not frames) will be covered. Providers must
document medical necessity in the patient’s medical record.
Contact lenses are allowed when prescriptive glasses are medically unsuitable. Documentation
must indicate the medical necessity for contact lenses over glasses.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
97
Guidelines for Lenses and Frames
Fabrication of eyeglasses shall conform to the current American National Standards Institute
prescription requirements, and all lenses, frames and frame parts must be guaranteed against
defects in manufacture and assembly. The provider who receives reimbursement for dispensing the
eyeglasses has the final responsibility for this guarantee.
When adjustments to eyeglasses are required, the adjustment must be made without additional
reimbursement whenever the enrollee returns to the original dispenser.
If the enrollee selects frames or lenses that are not Medicaid reimbursable, the enrollee must be
informed prior to the fabrication of the eyeglasses that he/she will be financially responsible. In such
cases, Medicaid may not be billed for all or part of the cost of said frames or lenses.
Lenses
All lenses for children under the age of 21 are to be first quality impact resistant lenses meeting FDA
regulations, free of surface imperfections such as pits, scratches or grayness. The lenses shall not
contain bubbles, striations or other surface abrasions.
Special Types of Lenses
Polycarbonate Lenses
All lenses provided to beneficiaries up to the age of 21, must be polycarbonate lenses and billed
with the appropriate HCPCS vision code; non-polycarbonate lenses are not covered by SCDHHS.
High-I
ndex Lenses
A 10 diopters (10DS) or greater lens is reimbursable at acquisition cost that is documented by an
itemized invoice when such cost is greater than the fee listed for the lens code in the fee schedule.
The fee schedule can be found on the SCDHHS website:
http://www.scdhhs.gov/.
Frames
Frames supplied are to be first quality frames. All frames must have eye size, bridge size, temple
length and manufacturer's name or trademark imprinted on them.
If the enrollee returns to the original dispenser to obtain the service, future fittings must be made by
that dispenser without additional reimbursement:
• Frame Complete
• Deluxe Frame
Guidelines for Contact Lenses
Daily wear contact lenses will be covered for beneficiaries under the age of 21, if medical necessity
has been established and prescription glasses are not suitable for the beneficiary. Daily wear
contact lenses will be supplied in monthly increments. Contact lens procedure codes are per lens

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
98
and the correct number of units must be indicated in the “units” column of the claim form/electronic
record.
Providers must file for payment using the examination date as the DOS. Use CPT procedure codes
for the fitting and dispensing of contact lens. These codes include the contact lens fitting, all follow-
up visits, solutions and supplies. This reimbursement does not include the initial eye examination.
Special Requests
If the covered contacts do not meet the needs of the patient, providers can contact the PSC at
+1 888 289 0709 or submit an online inquiry at Contact a Provider Representative | SCDHHS
before dispensing the contacts. Special requests will require medical justification prior to dispensing.
The PSC will forward all requests to the Division of Health and Medical Services, which will review
the requests and contact the provider with a decision. Health and Medical Services are responsible
for all reviews and exceptions.
Covered Contact Lens Products
The following covered contact lens products includes:
• Contact lens, PMMA, spherical, per lens
• Contact lens, PMMA, toric or prism ballast, per lens
• Contact lens, gas permeable, spherical, per lens
• Contact lens, gas permeable, toric, and prism ballast per lens, or a high plus or minus gas
permeable post cataract, per lens
• Contact lens, hydrophilic, spherical, per lens
• Contact lens, hydrophilic, toric or prism ballast, per lens
• UV lens, per lens
• Contact lens, other type. (Providers must contact and send documentation via the PSC. The
PSC will forward the documentation to the Division of Health and Medical Services.)
Dispensing Codes for Contact Lenses and Glasses
The following dispensing codes and fees for contacts and glasses may be used when applicable for
the services to be rendered.
92310 — Prescription of optical and physical characteristics of the fitting of contact lenses, with
medical supervision of adaptation; corneal lenses. The dispensing procedure is bilateral, and the fee
listed is for both eyes.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
99
92311 — Prescription of a corneal lens for aphakia. The dispensing procedure is unilateral, and the
fee listed is for one eye.
92312 — Prescription of corneal lenses for aphakia. The dispensing procedure is bilateral, and the
fee listed is for both eyes.
92313 — Prescription of a corneoscleral (large lens). The dispensing procedure is unilateral, and
the fee listed is for one eye.
92340 — Fitting of spectacles, except for aphakia. This code must only be filed when the glasses
are physically received at the physician’s office for the dispensing of glasses. The DOS when filing
this procedure must always be the date the eye exam was performed.
92370 — Repair and refitting of spectacles; except for aphakia.
Optician
Providers must show eligible recipients the complete selection of Medicaid-reimbursable frames and
explain that Medicaid pays only for frames that falls within the reimbursement limit.
Providers must have a selection of nickel-free frames for beneficiaries that have allergies to nickel.
Providers must have a selection of oversized frames or special needs frames for children readily
available as an option in the frame selection. See guidance above under Guidelines for Lenses and
Frames.
Providers must file for payment using the examination date as the DOS. Reimbursement for
eyewear does not include the initial eye examination. All records and medical justification must be
documented and located in the patient’s charts for auditing purposes.
Prescription requests must be written in language common to all health care practitioners providing
vision care in the United States. Criteria for the prescription requests include, but are not limited to,
the following:
• Unaided visual acuity at distance and near must be 20/30 or less. Aided and unaided visual
acuities must be stated in the patient's records.
• Corrective lenses must be at least plus or minus 0.50 sphere or more, or plus or minus 0.50
cylinder or more in each eye; or 0.75 in one eye.
• Vertical and horizontal prisms will be authorized if medically necessary. The prescription must
be remedial and not training — by nature.
• Replacement of lenses requires medical justification. Self-Employed Optometrist
Reimbursement is provided for the following materials and services in accordance with the fee
schedule:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
100
• Complete optometric eye examination.
• Office-based E&M services, consultations, diagnostic examinations, and non-invasive
procedures for the diagnosis and treatment of diseases of the eye and the prescribing of
pharmaceutical agents authorized under State Law.
• Eyeglass lenses.
• Contact lenses.
• Repairs and refitting of eyeglasses.
• Fitting of eyeglasses.
Retail Optical Establishments and Ophthalmic Dispensers
Reimbursement is provided for the following materials and services in accordance with the fee
schedule:
• Complete optometric eye examination (limited to retail optical establishments and ophthalmic
dispensers who employ an optometrist).
• Office-based E&M services, consultations, diagnostic examinations and non-invasive
procedures for the diagnosis and treatment of diseases of the eye and the prescribing of
pharmaceutical agents authorized under State Law (limited to retail optical establishments and
ophthalmic dispensers who employ and optometrist).
• Eyeglass lenses.
• Contact lenses.
• Repairs and refitting of eyeglasses.
• Fitting of eyeglasses.
The fee schedule for vision services is located on the SCDHHS website at http://www.scdhhs.gov/
.
Part II — Diagnostic Ophthalmology Services
Diagnostic services included in the CPT coding range 92018–92287 are compensable as separate
procedures if performed as a distinct and individual service and not included in the ophthalmological
or E&M exam, with the following restrictions:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
101
Covered Services
Refractions
The determination of the refractive state is allowed as a separate procedure in addition to the
ophthalmology exam.
Ophthalmoscopy
Routine ophthalmoscopy (direct or indirect) is a part of general and specific ophthalmologic
services, whenever indicated. It is not reported separately. Ophthalmoscopy, extended, with retinal
drawing, as for retinal detachment, melanoma, with interpretation and report, may be billed in
addition to an ophthalmological exam or an E&M services procedure code. If medically necessary,
this code may be billed one time per eye per DOS.
Visual Field Examination
This exam is compensable when medically indicated as separate from the ophthalmological or E&M
exam.
Vision Therapy
The following procedures are allowed for vision therapy services only:
• Unlisted neurological or neuromuscular diagnostic procedure (Support documentation of therapy
service must be attached to the claim.)
• Developmental testing; limited (e.g., Developmental Screening Test II, Early Language
Milestone Screen) with interpretation and report.
• Developmental testing: extended (includes assessment of motor, language, social, adaptive,
and/or cognitive functioning by standardized developmental instruments) with interpretation and
report.
• Neurobehavioral status exam (clinical assessment of thinking, reasoning and judgment, e.g.,
acquired knowledge, attention, language, memory, planning, problem solving, and visual-spatial
abilities), per hour of the psychologist’s or physician’s time, both face-to-face time with the
patient and time interpreting test results and preparing the report.
Note: If an eye examination indicates a need for corrective lenses, the examining provider
performing the comprehensive exam must complete the course of treatment. This includes the
eye examination and written prescription (Rx) for ordering the glasses for the Medicaid
beneficiary.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
102
Part III — Ocular Surgery
Post-Operative Management of Cataract Surgery
South Carolina Medicaid allows optometrists to bill for post-operative management only for
appropriate CPT procedure codes. These are global codes and cover both the surgical care and
post-operative management.
For an optometrist to bill and be reimbursed for post-operative management, optometrists must bill
the above-referenced codes using modifier 55 only. Ophthalmologists must bill the above-
referenced codes with modifier 54, surgical care only. If the ophthalmologist does not bill using a
modifier, the provider will be reimbursed for the entire global fee, which includes both surgical care
and post-operative management.
Ocular Prosthesis: The prescription and fitting of ocular prostheses are covered for all eligible
beneficiaries. The molding and manufacturing of the actual prosthesis is through our Agent, MUSC
Maxillofacial Prosthodontic Clinic. Providers must contact MUSC Maxillofacial Prosthodontic Clinic
at:
Phone Number: +1 843 876 1001
Fax Number: +1 843 876 1098
Providers are responsible for forwarding all medically necessary documentation to our Agent in
order for services to be rendered.
Intraocular Lenses: Physicians who supply these lenses may bill using the codes listed below. The
codes are for the supply of lenses and must be billed in addition to the surgical procedure.
• Anterior chamber angle fixation lens.
• Posterior chamber lens.
Ptosis: Lid correction procedures are covered only when there is documented medical necessity for
the improvement of visual disabilities. Services must be preauthorized by the Quality Improvement
Organization (QIO) contractor, for utilization review.
Note: Simple blepharoplasty is considered a cosmetic procedure and therefore non-compensable.
Keratoplasty: Corneal transplants are compensable. Physician reimbursement includes only the
surgery. Reimbursement to the hospital includes all technical services including donor preparation.
Special Ophthalmological Services
The following medical ophthalmology codes may be billed separately from an ophthalmology exam
or an E&M services code. These codes may be billed one time per eye per DOS when medically
necessary.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
103
• Ophthalmoscopy, extended, with retinal drawing, as for retinal detachment, melanoma with
interpretation and report; initial.
• Ophthalmoscopy extended; subsequent.
• Fluorescein angioscopy with interpretation and report.
• Fluorescein angiography (includes multiframe imaging) with interpretation and report, unilateral
or bilateral.
• Indocyanine-green angiography (includes multiframe imaging) with interpretation and report,
unilateral or bilateral.
• Ophthalmodynamometry.
• Electrooculography with interpretation and report.
• Electroretinography with interpretation and report.
• External ocular photography with interpretation and report for documentation of medical
progress.
• Special anterior segment photography with interpretation and report; with specular endothelial
microscopy and cell count.
• Special anterior photography with fluorescein angiography.
Use of Modifiers with Procedure Codes
If it is medically necessary to repeat an ophthalmology procedure on the same DOS and the
procedure is bilateral (i.e., the procedure is for both eyes), then the total charge amount for both
eyes must be listed on the first line and again on the line recording the repeated procedure.
For the claim to process, the modifier on the first line must be “00” (two zeros), and the modifier on
the line recording the repeated procedure must be (76). This is the only time these two modifiers
must be used. It is imperative that the medical record of this patient indicates and justifies the
medical necessity of repeating this service on the same day. The use of two modifiers indicates that
the procedure was done bilaterally on the first occurrence and again bilaterally on the second
occurrence. Indicate a “1” in the “units" column for the number of units on each line.
When medically necessary to repeat the same procedure on the same DOS and the procedure is
unilateral, then the total charge amount for one eye must be listed on the first line utilizing an RT,
right side (used to identify procedures performed on the right side of the body) or LT modifier, left
side (used to identify procedures performed on the left side of the body). The second line for the

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
104
repeated procedure must be billed utilizing a 76 modifier. The medical record of the patient must
indicate and justify the medical necessity for the repeat procedure.
Reminder: In all cases, the fee listed for all ophthalmological procedures is for both eyes, unless
otherwise indicated.
The use of modifiers AP (determination of refractive state was not performed in the course of
diagnostic ophthalmological examination) is not reimbursed by SCDHHS and will result in rejected
claims.
The following modifiers must be used for replacement of parts:
U8 = Replacement of a part of frames
U9 = Replacement of a part
Otorhinolaryngology (ENT)
General ENT Services
Diagnostic or treatment procedures usually included in an ENT exam are reported as an integrated
medical service and must not be reported separately.
Microsurgical Techniques are procedures that describe “microsurgical techniques requiring use of
operating microscope.” It can be billed in addition to the primary surgical procedure if it is not an
inclusive part of the surgical procedure and if the documentation supports the use of microsurgical
techniques. It is not for visualization of the operative field alone but is intended to be employed
when the surgical services are performed using the techniques of microsurgery.
If the use of the operating microscope is an inclusive component of a procedure, the use of the
operating microscope cannot be unbundled.
Endoscopic Procedures: Please refer to guidelines for endoscopic procedures under General
Surgery Guidelines in this section of the manual.
Uvulopalatopharyngoplasty: Documentation (admission history and physical and operative report)
is required with claims submitted for this procedure. The record must substantiate medical necessity
as well as clarify the procedures performed.
Septoplasty, Turbinectomy: These and any other nasal reconstructive surgeries are covered only
when there is a loss or serious impairment of bodily function, usually as a result of trauma, and the
surgery restores the disabled function. The office record must document the functional deficit or the
need for prompt correction.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
105
Speech Therapy (ST) and Hearing Therapy Services
Services rendered by ENT specialists or therapists supervised by a physician are compensable
using the appropriate code in the CPT with the following restrictions:
• ST and Hearing Therapy: Non-compensable. Please refer to Specialized Speech and Hearing
Services for Children Under 21 below regarding services for children.
• Vestibular Function Test without Recording: Non-compensable (included in visit code).
• Ear Protector Attenuation Measurements (ear plugs): non-compensable.
• Hearing Aids and Hearing Aid Accessories: Must be pre-authorized and obtained through the
SCDPH. Services are limited to children under age 21. For prior approval, send request to:
Division of Children’s Rehabilitative Services
Box 101106, Mills Complex
Columbia, SC 29211
+1 803 898 0784
• Ear Molds: To report, physicians must use the following supplemental codes:
– Ear mold, not disposable, any type.
– Ear mold, disposable, any type.
– Use modifiers RT (right side) and LT (left side) to indicate which ear.
– These codes are allowed four times every 12 months per ear for children under age 21.
• Cochlear Implants and related services:
– Beneficiaries under the age of 21 years with unilateral or bilateral hearing loss may receive
medically necessary placement, replacement and maintenance of cochlear implants that
delivered in accordance with clinical standards of medical and audiological practice.
– Beneficiaries aged 21 years and older with unilateral or bilateral severe to profound
sensorineural hearing loss may receive medically necessary placement, replacement and
maintenance of cochlear implants that delivered in accordance with clinical standards of
medical and audiological practice. Hearing aid trial is not required to qualify for the
cochlear implantation.
– Replacement of cochlear implants are allowed once in 5 years. Maintenance services are
allowed as necessary.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
106
– Cochlear Device Implantation: Requires prior approval from QIO one of the following
methods:
QIO Customer Service: +1 855 326 5219
QIO Fax: +1 855 300 0082
• Specialized Speech and Hearing Services for Children Under 21: Services are available through
clinics certified by SCDPH and through individual speech-language pathologists/audiologists
who are licensed by the South Carolina State Board of Examiners in Speech-Language
Pathology and Audiology and enrolled with the South Carolina Medicaid program.
Speech/language and audiology services rendered by these providers must be pre-authorized
by SCDPH, South Carolina Department of Disabilities and Special Needs, or a school district.
• ENT specialists who provide these specialized services in their office or clinic may apply for
certification. If certified by SCDPH, the physician must enroll as a speech and hearing clinic with
South Carolina Medicaid in order to obtain payment for these services (for children
under 21). For information on SCDPH certification requirements, you may write to:
Department of Public Health
Clinic Certification
2600 Bull Street
Columbia, SC 29201
Cardiology
Physicians performing these services in their office may bill for the complete procedure code, which
includes the tracing, interpretation and report. Those providers interpreting the recording only must
use the code that stipulates interpretation and report only. The modifier 26 is not necessary when
the code clearly defines the professional component only (interpretation and/or report).
For more detail regarding EKG interpretations, please refer to Radiology Reimbursement Limitations
under Radiology and Nuclear Medicine in this section of the manual.
Pulmonary Medicine
Oxygen therapy given in the office is compensable when medically indicated and clearly identifiable
as a separate procedure. Documentation must be submitted with the claim.
Questions regarding oxygen therapy equipment for home use may be directed to the PSC at
+1 888 289 0709. Providers may also submit on online inquiry at
Contact a Provider Representative
| SCDHHS for additional information.
A separate code is used to report tracheostomy tube change in the office setting. This may be used
in addition to the appropriate level office E&M visit codes.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
107
Overnight sleep apnea study services must be billed using the appropriate code.
Tuberculosis (TB) Policy
TB services cover treatment directly related to the care of TB which falls under the following
categories:
• Prescribed medications
• Physician services
• OP hospital services
• Public health clinics
• Laboratory
• Radiology
• Case management
Note: This policy does not cover hospital stays, room and board or observation stays.
Treatment of a beneficiary with TB is most successful within a comprehensive framework that
addresses both clinical and social issues of relevance to the beneficiary. It is essential that
treatment be tailored and supervised based on each beneficiary’s individual clinical and social
needs (patient-centered care). SCDPH is ultimately responsible for ensuring that adequate,
appropriate diagnostic and treatment services are available, and for monitoring the results of
therapy.
Initial TB Screening
The initial TB screening will be covered when performed by a NP, PA or Registered Nurse
employed by the SCDPH clinic. The initial screening includes, but is not limited to the following:
• Brief mental and physical assessment
• Exposure history
• Referral for laboratory testing and or radiology services
• Referral for social services
• Referral for other medical services
• Consultation with TB medical clinician

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
108
SCDPH will bill SCDHHS for an E&M code.
For beneficiaries that are not in the limited benefits category (Family Planning and/or TB only),
SCDPH will provide a referral for the beneficiary to be seen by a physician if medically necessary
and maintained in the beneficiary’s medical health record. The physician must bill SCDHHS utilizing
a new patient examination 99203 CPT code. The physician will be reimbursed for the initial
consultation as long as the consultation is done within a 30-day period from the date of the initial TB
screening service provided by SCDPH, or all initial and subsequent treatment will be denied. If
SCDPH determines that it is medically necessary for the beneficiary to see a physician for
subsequent visits, they are responsible for providing authorization, which must be maintained in the
beneficiary’s medical health records. All services are subject to audit by SCDHHS Division of
Program Integrity.
Subsequent Nursing Services
Subsequent nursing services are covered services when performed by an NP, Registered Nurse,
and Licensed Practical Nurse, in the SCDPH clinic or home setting. SCDPH must bill all medically
necessary exams to SCDHHS utilizing the appropriate E&M code. The maximum number of visits
allowed for a treatment cycle is 360 for a beneficiary with latent TB infection and 360 for a
beneficiary with TB disease. Medical necessity must be maintained within the beneficiary’s medical
health records.
Case Management
All Case Management services will be patient-centered and will include an adherence plan that
emphasizes DOT, in which a beneficiary is observed to ingest each dose of anti-TB medications, to
maximize the likelihood of completion of therapy. Each beneficiary’s management plan must be
individualized to incorporate strategies that facilitate adherence to the treatment regimen. Such
measures may include, for example, social service support, treatment incentives and enablers,
housing assistance, referral for treatment of substance abuse, and coordination of the TB services
with those of other providers.
SCDPH is responsible for providing all Case Management services. Case Management services
include, but are not limited to:
• Medication monitoring
• Providing services in the patient’s home
• Referring all medically necessary laboratory tests
• Referring all medically necessary radiology tests
• Referring patient to a physician for consultation when medically necessary

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
109
Case Management services are limited to 360 visits per year, one visit per day. Case Management
services will be covered when performed by a NP, PA, Registered Nurse or Social Worker
employed by the SCDPH clinic.
Multidrug-Resistant Tuberculosis (MDR-TB) Treatment Protocol
MDR-TB is a form of TB that is resistant to two or more of the primary drugs (isoniazid and rifampin)
used for the treatment of TB. The MDR-TB patient treatment model may involve a step approach.
First high-dose oral medications are used that may include drugs such as isoniazid, pyrazinamide
and ethambutol. Then treatment can move to injectable drugs, such as capreomycin, kanamycin
and amikacin. Treatment length may be extended to manage the disease.
The use of this very intense treatment regimen also requires that the MDR-TB patient receive
additional services. For these patients the below additional procedures codes are covered. For all
services providers must follow NCCI correct coding.
• Vision screens up to six times per year
• Labs
• Peripherally inserted central catheter (PICC) line insertion
Pharmacotherapy
All treatment medications will be provided by SCDPH for SCDPH patients who have been
diagnosed with TB disease and/or latent TB infection regardless of enrollment status (FFS or
TB -only eligible). All medications will be reimbursed via 340B pricing. SCDPH must submit the
acquisition cost plus dispensing fee to SCDHHS. SCDHHS will then reimburse SCDPH for the TB
medications submitted.
Laboratory Tests
All laboratory tests are subject to medical necessity guidelines and documentation must be
maintained in the beneficiary’s chart.
Laboratory tests must be billed with a “00” (two zeros) modifier. If the laboratory tests are referred to
an outside laboratory, then SCDPH will provide authorization which will be maintained in the
beneficiary’s medical health records.
Radiology Tests
Radiology tests including interpretation of exams are covered if performed by a NP, PA or
Physician:
All radiology procedures must be billed with the appropriate modifiers. See below for a list of
modifiers and descriptions:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
110
• Modifier 00 must be appended to the CPT code when the provider has rendered both the TC
(the physical taking of an x-ray) and the professional component (interpretation of results).
• Modifier TC must be appended to the CPT code when the provider has only rendered the taking
of the x-ray.
• Modifier 26 must be appended to the CPT code when the provider has rendered the
interpretation only. Providers are required to write a report and sign, and date.
Obstructive Sleep Apnea
Treatment of mild obstructive sleep apnea (OSA) is covered via use of eXciteOSA, a Food and Drug
Administration (FDA) approved prescription medical device, under the Durable Medical Equipment
benefit. The device will be allowed without prior authorization for full-benefit Healthy Connections
Medicaid members ages 18 years or older. Eligible members must have a diagnosis of mild OSA,
indicated by a sleep study, with a score of apnea-hypopnea index of more than 5 and less than 15.
Medical providers must follow the FDA guidelines for use, indications and contraindications when
prescribing the device.
The device has the following two units:
• Power Source and Control Unit
One prescription per lifetime is allowed for the power source and control unit. During the first
two years, repairs or replacement covered under the product manufacturer’s warranty are
not billable to SCDHHS. If the power source unit is damaged or lost after two years of usage
or ownership, SCDHHS may allow a replacement power source unit with prior authorization.
Providers must file the prior authorization request to the SCDHHS Quality Improvement
Organization (QIO).
• Oral Appliance Unit
The prescription for the oral appliance unit must be renewed annually. During the first two
years, repairs or replacement covered under the product manufacturer’s warranty are not
billable to SCDHHS. If additional units of oral appliance are needed during a 12-month
period, the provider must file a prior authorization request to the SCDHHS QIO justifying the
need for the additional unit. Only one additional unit may be allowed.
To be eligible for reimbursement for eXciteOSA, Healthy Connections Medicaid-enrolled DME
providers must maintain a copy of the Medicaid Certificate of Medical Necessity (MCMN) in the
patient’s record.
DME Providers must utilize the following procedure codes, criteria, and limitations when billing for
the prescription of eXciteOSA:
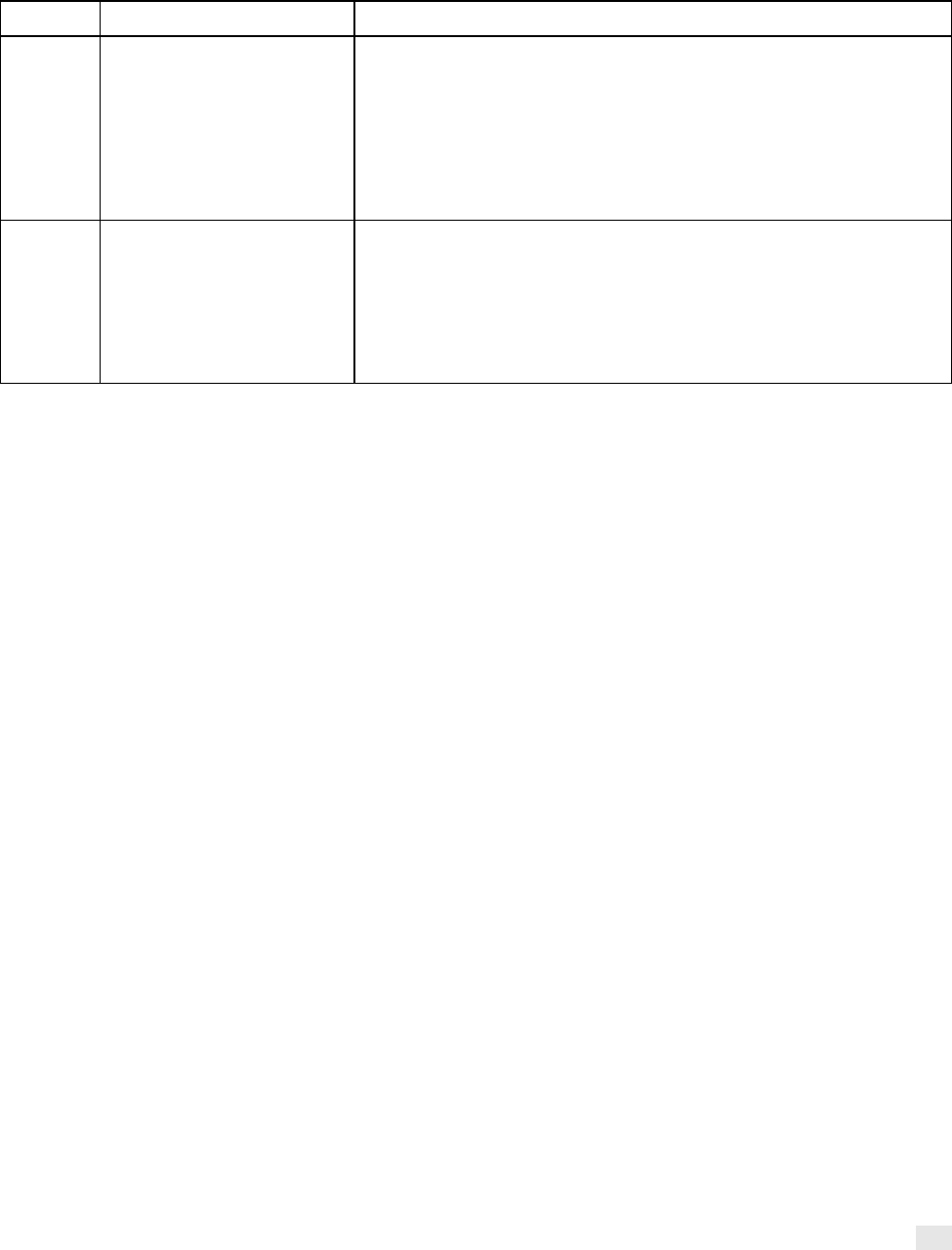
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
111
Code
Descriptor
Limitations and Billing
E0490
Power source and control
electronics unit for oral
device/appliance for
neuromuscular electrical
stimulation of the tongue
muscle, controlled by
hardware remote
Allowed one (1) power source & control unit per patient per lifetime. This
is a capped rental device. Procedure code may be billed monthly for up
to13 months
KH-
DMEPOS item, initial claim, purchase of first month rental.
KI – DMEPOS item, the second or third month of the capped rental
period. KJ- DMEPOS item, month four to thirteen of
the capped rental period.
E0491
Oral device/appliance for
neuromuscular electrical
stimulation of the tongue
muscle, used in conjunction
with the power source and
control electronics unit,
controlled by hardware
remote, 90-day supply
Supply Purchase. Oral device allowed one (1) per day per patient and up
to four (4) per 12 months.
No modifier is required.
Allergy and Immunotherapy
Allergy Testing
Scratch testing is the gold standard for Allergy Testing and is a covered service. Allergy testing
under anesthesia and RAST testing is not a covered service. Allergy testing for food allergies is not
normally considered medically necessary. Therefore, if the provider is testing for food allergies, they
must clearly state the medical necessity and supporting documentation in the beneficiary’s medical
record. All services are subject to audit through the SCDHHS Division of Program Integrity.
Allergen Immunotherapy
Allergen Immunotherapy is performed by providing injections of pertinent allergens to the patient on
a regular basis with the goal of reducing the signs and symptoms of an allergic reaction or
prevention of future anaphylaxis. This is usually done with allergen dosages that gradually increase
over a period of months.
Providers may bill for professional services for allergen immunotherapy not including provision of
allergenic extracts. These codes are for professional services only and do not cover reimbursement
for antigen extract or venom.
Antigen and Preparation
Refer to code information on the provider portal for information on covered services.
Allergy Testing and Immunotherapy
Allergy Testing
The MPFSDB fee amounts for allergy testing services are established for single tests. Therefore,
the number of tests must be shown on the claim.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
112
Example: If a physician performs 25 percutaneous tests (scratch, puncture or prick) with allergenic
extract, the physician must bill the appropriate code and specify 25 in the “units” field of form
CMS-1500 (paper claims or electronic format). To compute payment, the Medicare carrier multiplies
the payment for one test (i.e., the payment listed in the fee schedule) by the quantity listed in the
“units” field.
Allergy Immunotherapy
For services rendered on or after January 1, 1995, all antigen/allergy immunotherapy services are
paid for under the Medicare physician fee schedule. Prior to that date, only the antigen injection
services, were paid for under the fee schedule. Codes representing antigens and their preparation
and single codes representing both the antigens and their injection were paid for under the
Medicare reasonable charge system. A legislative change brought all of these services under the
fee schedule at the beginning of 1995 and the following policies are effective as of January 1, 1995:
• Separate coding for injection-only codes and/or the codes representing antigens and their
preparation must be used.
– If both services are provided, both codes are billed.
– This includes allergists who provide both services using treatment boards.
• Single-dose vials of antigen may be billed only if the physician providing the antigen is providing
it to be injected by some other entity. Single-dose vials, which may be used only as a means of
insuring proper dosage amounts for injections, are costlier than multiple-dose vials and therefore
their payment rate is higher. Allergists who prepare antigens are assumed to be able to
administer proper doses from the less costly multiple-dose vials. Thus, regardless of whether
they use or bill for single or multiple-dose vials while they are billing for an injection service, they
are paid at the multiple-dose vial rate.
• The fee schedule amounts for the antigen codes are for a single dose. When billing those
codes, physicians are to specify the number of doses provided. When making payment, carriers
multiply the fee schedule amount by the number of doses specified in the “units” field.
• If a patient's doses are adjusted, e.g., because of patient reaction, and the antigen provided is
more or fewer doses than originally anticipated, the physician is to make no change in the
number of doses for which he or she bills. The number of doses anticipated at the time of the
antigen preparation is the number of doses to be billed. This is consistent with the notes on
page 30 of the Spring 1994 issue of the AMA's CPT Assistant. Those notes indicate that the
antigen codes mean that the physician is to identify the number of doses “prospectively planned
to be provided”. The physician is to "identify the number of doses scheduled when the vial is
provided". This means that in cases where the patient gets more doses than originally
anticipated (because dose amounts were decreased during treatment) and in cases where the
patient gets fewer doses (because dose amounts were increased), no change is to be made in

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
113
the billing. In the first case, carriers are not to pay more because the number of doses provided
in the original vial(s) increased. In the second case, carriers are not to seek recoupment (if
carriers have already made payment) because the number of doses is less than originally
planned. This is the case for both venom and non-venom antigen codes.
• Venom doses and catch-up billing — Venom doses are prepared in separate vials and not
mixed — except in the case of the three-vespid mix (white and yellow hornets and yellow
jackets). Separate codes must be used for venom combinations of 2, 3, 4 or 5 venoms. Some
amount of each of the venoms must be provided. Questions arise when the administration of
these venoms does not remain synchronized because of dosage adjustments due to patient
reaction. For example, a physician prepares ten doses utilizing the four-venom code in two vials
— one containing 10 doses of three vespid mix and another containing 10 doses of wasp
venom. Because of dose adjustment, the three vespid mix doses last longer, i.e., they last for 15
doses. Consequently, questions arise regarding the amount of "replacement" wasp venom
antigen that is prepared and how it is billed. Medicare pricing amounts have savings built into
the use of the higher venom codes. Therefore, if a patient is in two-venom, three-venom, four-
venom or five-venom therapy, the carrier objective is to pay at the highest venom level possible.
This means that, to the greatest extent possible, the two-venom code is to be billed for a patient
in two-venom therapy, the three-venom code is to be billed for a patient in three-venom therapy,
the four-venom code is to be billed for a patient in four venom therapy, and five venom code is
to be billed for a patient in five venom therapy. Thus, physicians are to be instructed that the
venom antigen preparation, after dose adjustment, must be done in a manner that, as soon as
possible, synchronizes the preparation back to the highest venom code possible. In the above
example, the physician must prepare and bill for only five doses of "replacement" wasp venom
— billing five doses of the single venom code. This will permit the physician to get back to
preparing the four venoms at one time and therefore billing the doses of the "cheaper" four
venom code. Use of a code below the venom treatment number for the patient must occur only
for the purpose of “catching up”.
• Preparation of vials of non-venom antigens. As in the case of venoms, some non-venom
antigens cannot be mixed, i.e., they must be prepared in separate vials. An example of this is
mold and pollen. Therefore, some patients will be injected at one time from one vial —
containing in one mixture all of the appropriate antigens — while other patients will be injected at
one time from more than one vial. In establishing the practice expense component for mixing a
multi-dose vial of antigens, we observed that the most common practice was to prepare a 10-cc
vial; we also observed that the most common use was to remove aliquots with a volume of 1 cc.
Our PE computations were based on those facts. Therefore, a physician's removing 10 1-cc
aliquot doses captures the entire PE component for the service.
This does not mean that the physician must remove 1 cc aliquot doses from a multi-dose vial. It
means that the practice expenses payable for the preparation of a 10-cc vial remain the same
irrespective of the size or number of aliquots removed from the vial. Therefore, a physician may

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
114
not bill this vial preparation code for more than 10 doses per vial; paying more than 10 doses
per multi-dose vial would significantly overpay the practice expense component attributable to
this service.
Note: This code does not include the injection of antigen(s); injection of antigen(s) is separately
billable.
When a multi-dose vial contains less than 10-cc, physicians may bill Medicare for the number of
1-cc aliquots that may be removed from the vial. That is, a physician may bill Medicare up to a
maximum of 10 doses per multi-dose vial but may bill Medicare for fewer than 10 doses per vial
when there is less than 10-cc in the vial.
If it is medically necessary, physicians may bill Medicare for preparation of more than one
multi-dose vial.
Examples:
– If a 10-cc multi-dose vial is filled to 6-cc with antigen, the physician may bill Medicare for
six doses since six 1-cc aliquots may be removed from the vial.
– If a 5-cc multi-dose vial is filled completely, the physician may bill Medicare for five doses
for this vial.
– If a physician removes ½ cc aliquots from a 10-cc multi-dose vial for a total of 20 doses
from one vial, he/she may only bill Medicare for 10 doses. Billing for more than 10 doses
would mean that Medicare is overpaying for the practice expense of making the vial.
– If a physician prepares two 10-cc multi-dose vials, he/she may bill Medicare for 20 doses.
However, he/she may remove aliquots of any amount from those vials. For example, the
physician may remove ½ aliquots from one vial, and 1-cc aliquots from the other vial, but
may bill no more than a total of 20 doses.
– If a physician prepares a 20-cc multi-dose vial, he/she may bill Medicare for 20 doses,
since the practice expense is calculated based on the physician's removing 1-cc aliquots
from a vial. If a physician removes 2-cc aliquots from this vial, thus getting only 10 doses,
he/she may nonetheless bill Medicare for 20 doses because the PE for 20 doses reflects
the actual practice expense of preparing the vial.
– If a physician prepares a 5-cc multi-dose vial, he may bill Medicare for five doses, based
on the way that the practice expense component is calculated. However, if the physician
removes ten ½ cc aliquots from the vial, he/she may still bill only five doses because the
practice expense of preparing the vial is the same, without regard to the number of
additional doses that are removed from the vial.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
115
• Allergy Shots and Visit Services on the Same Day:
– Visits must not be billed with allergy injection services unless the visit represents another
separately identifiable service.
» For a physician to receive payment for a visit service provided on the same day that
the physician also provides a service in the allergen immunotherapy series, the
physician is to bill a modifier 25 with the visit code, indicating that the patient's
condition required a significant, separately identifiable visit service above and beyond
the allergen immunotherapy service provided.
• Reasonable Supply of Antigens:
– See CMS Manual System, Internet Only Manual, Medicare Benefits Policy Manual, CMS
Pub. 100-02 Chapter 15, section 50.4.4, regarding the coverage of antigens, including
what constitutes a reasonable supply of antigens.
– Providers must only bill Medicaid for a 90-day (three-month) supply of Antigens and/or
Venoms for each Medicaid beneficiary. When the provider notices that the beneficiary is
running low on antigens, he or she may arrange for more antigens to be made and
delivered. Please note that these services cannot be overlapped and reimbursed.
Dermatology
The acne diagnosis codes (L70.0 - L70.9, L73.0) are covered only when the patient is 18 years of
age or younger (non-covered beginning on the 19
th
birthday), and the acne condition is infected,
cystic or pustular.
The keloid scar diagnosis L91.0 is covered only in severe cases with pain, intractable itching, or
interference with range of movement.
Oncology and Hematology
If a physician or physician group leases space in a clinic or hospital, they may bill for the
chemotherapy administration and drugs provided all the following criteria are met:
• They are using their own employees, equipment, supplies and drugs.
• The services are provided in the leased area of the hospital designated as an office.
• The patient is not a registered inpatient or OP of the hospital.
A physician’s office within an institution must be confined to a separately identified part of the facility
that is used solely as the physician’s office and cannot be construed to extend throughout the entire
institution. Services performed outside the “office” area will be subject to coverage rules applicable
to services furnished outside the office setting.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
116
A distinction must be made between the physician’s office practice and the institution. For services
to be covered, auxiliary medical staff must be office staff rather than institution staff, and the cost of
supplies must represent an expense to the physician’s office practice. The physician must directly
supervise services performed by his or her employees outside the office area; the physician’s
presence in the facility would not be sufficient.
If services are provided in an inpatient, OP, or infusion center setting, the physician can only bill for
the E&M service and/or prolonged care, critical care services when appropriate. Reimbursement for
chemotherapy administration, drugs, supplies, equipment and nursing are included in the hospital or
infusion center’s reimbursement.
Oncotype DX Breast Cancer Assay
The Oncotype DX Breast Cancer Assay is a genetic test used for gene expression profiling by real-
time RT-PCR of 21 genes, utilizing formalin-fixed paraffin embedded tissue.
Benefit Criteria and Limitations:
Allowed one test per lifetime for adult beneficiaries with full benefit. This includes members enrolled
in the Breast and Cervical Cancer Program (BCCP). No prior authorization is required. Medicaid
members must have the following findings and diagnosis:
• recently diagnosed with stage I, stage II, or stage III invasive breast cancer; and
• cancer is estrogen receptor-positive; and
• cancer is HER2-negative; and
• cancer is lymph node-positive or lymph node-negative;
Billing Guidance
• Providers with CLIA certification are eligible to bill for this service.
• Providers must file claims with primary diagnosis of the conditions listed above.
Breast Cancer Susceptibility Gene 1 and 2 (BRCA)
Definition
BRCA1 and BRCA2 genes encode for tumor suppressor proteins that function to preserve
chromosome structure, repair damaged DNA, manage the cell cycle and transcription of DNA, and
maintain the stability of genetic material.
Background
Individuals who inherit a mutated copy of the BRCA1 or BRCA2 gene are predisposed to developing
breast, ovarian, tubal, peritoneal, pancreatic and prostate cancers. In rare cases, duplications or
deletions of one or more exons, or coding regions, can occur and are classified as BRCA large cell
rearrangements. Familial inheritance, of a mutated BRCA1 or BRCA2 gene, encompasses 5%–10%
of all breast cancer cases. Screening and genetic testing is essential to identify individuals who
have a family history of breast cancer and determine if they carry inherited mutations in BRCA1 or
BRCA2 genes.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
117
Coverage Guidelines
Criteria
The SCDHHS may cover BRCA genetic testing for eligible men and women who meet medical
necessity criteria. Medical necessity criteria are based on the current National Comprehensive
Cancer Network (NCCN) Clinical Practice Guidelines in Oncology — Genetic/Familial High-Risk
Assessment: Breast and Ovarian SCDHHS policy guidelines. To review the current NCCN
guidelines you may visit:
https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf
Meeting one or more of the breast and ovarian cancer criteria warrants further personalized risk
assessment, genetic counseling and oftentimes, genetic testing and management. Testing of an
individual without a cancer diagnosis must only be considered when an appropriate affected family
member is unavailable for testing.
Age Requirements
Recipients of BRCA genetic testing must be 18 years of age or older. SCDHHS will not cover BRCA
testing or associated genetic counseling for minors.
Genetic Counseling
Genetic counseling must be received before and after genetic testing for BRCA1, BRCA2 and
BRCA large cell rearrangement. Pre- and post-genetic counseling are considered medically
necessary and is a covered service in addition to genetic testing. Genetic counseling is required to
inform beneficiaries about the risks and benefits of genetic testing. Genetic counseling must be
performed by an appropriately trained genetic counselor.
Genetic Testing
A blood test is performed on an individual to identify mutations in either of the two breast cancer
susceptibility genes. The test will determine if an individual carries a mutated BRCA1 or BRCA2
gene.
Generally, genetic testing for a particular disease is limited to once in a lifetime; however, there may
be exceptional instances that permit genetic testing more than once in a lifetime. SCDHHS will
cover cases for additional BRCA testing for beneficiaries who:
• Have previously been tested for BRCA1 and BRCA2 comprehensive sequencing gene mutation
analysis testing and received negative results. Documentation of negative results for BRCA1
and BRCA2 comprehensive sequencing gene mutation analysis is required for medically
necessary BRCA large cell rearrangement gene mutation testing.
• Results are not available, and every reasonable attempt has been made to obtain the results.
Documentation of reasonable attempts to obtain results from the genetic testing physician or the
testing laboratory must be submitted to QIO when requesting prior authorization.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
118
Cancer Risk-Reducing Interventions
The USPSTF recommends that primary care providers screen women who have family members
with breast, ovarian, tubal or peritoneal cancer or have an ethnicity or ancestry associated with
BRCA1 or BRCA2 gene mutations with one of the several screening tools designed to identify a
family history that may be associated with an increased risk for potentially harmful mutations in
breast cancer susceptibility genes (BRCA1 or BRCA2). Women with positive screening results must
receive genetic counseling, and if indicated after counseling, BRCA genetic testing.
Based on the results of the BRCA test, beneficiaries may select a treatment that may reduce their
chances of developing cancer. Medical necessity must be established for the selected risk reducing
treatment option in accordance with the NCCN Guidelines for Genetic/Familial High-Risk
Assessment: Breast and Ovarian. The specific guidelines may be accessed through this link:
https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf
Note: Beneficiaries may also elect not to pursue treatment options.
Treatments include:
• Increased cancer screenings:
– Cancer screenings may be received if a beneficiary does or does not desire risk-reducing
therapy. Screening and follow-up options must be discussed between the beneficiary and
their provider.
• Risk-reducing agent:
– Risk-reducing agents may be covered for a beneficiary with a BRCA genetic mutation or
compelling family history conferring a high risk for breast, ovarian, tubal, peritoneal,
pancreatic or prostate cancers.
• Risk-reducing surgery:
– Risk-reducing prophylactic mastectomy or oophorectomy may be covered for a beneficiary
with a BRCA genetic mutation or a compelling family history conferring a high risk for
breast or ovarian cancer.
Gastroenterology
Diagnostic procedures listed are covered as separate procedures if medically necessary and
justified.
Obesity is now recognized as a disease state. Policy is currently being written and will be published
later.
The following services are non-covered by Medicaid:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
119
• Supplemental fasting
• Intestinal bypass surgery
• Gastric balloon for treatment of obesity
The following procedures to treat obesity are covered based on InterQual criteria. QIO must
preauthorize all claims for these services. Approval will be based on medical records that document
established InterQual criteria.
Panniculectomy
Panniculectomy is the surgical excision of the abdominal apron containing superficial fat in obese
individuals. The Lipectomy and Abdominoplasty procedure codes can be covered by Medicaid if:
• It is medically appropriate and necessary for the individual to have such surgery.
• The surgery is performed to correct an illness caused by or aggravated by the pannus.
Gastrostomy Button Device Feeding Tube Kit
This service will be covered for beneficiaries under the age of 21 when performed in the physician’s
office setting to cover the cost associated with purchasing the device.
Physical Medicine and Therapy
PT, OT and/or ST may be rendered in an office, or OP setting. The licensed therapist performing
these services must meet the state licensure regulations specified by the South Carolina
Department of Labor, Licensing, and Regulation (SCLLR). Licensed therapists may bill directly and
be reimbursed for services rendered following billing and benefit limitations as described in the
Rehabilitative Therapy and Audiological Services Provider Manual.
At a minimum, PT services must improve or restore physical functioning as well as prevent injury,
impairments, functional limitations and disability following disease, injury or loss of limb or body part.
OT must prevent, improve, or restore physical and/or cognitive impairment following disease or
injury.
Speech-language pathology must improve or restore cognitive functioning, communication skills
and/or swallowing skills following congenital or acquired disease or injury.
Physicians/NPs are required to submit the applicable CPT codes as defined in the CPT reference
manual for the specified therapy. Therapy procedures are defined in 15-minute sessions, SCDHHS
will define 15 minutes as one unit.
For children under the age of 21, PT/OT/ST services are available through rehabilitation centers
certified by SCDES, and through individual licensed practitioners. Policy guidelines are located in

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
120
the Rehabilitative Therapy and Audiological Services Provider Manual on our website located at
www.scdhhs.gov
.
Osteopathic Manipulative Treatment
Osteopathic Manipulative Treatment (OMT) is allowed as a separate procedure when medically
necessary, justified, and performed by a physician, or licensed physical therapist employed by the
physician. These procedures must be reported using procedure codes 98925–98929.
Chiropractic Services
SCDHHS provides Medicaid reimbursement for a limited array of chiropractic services provided to
Medicaid beneficiaries. Coverage is limited to treatment by means of manual manipulation of the
spine for the purpose of correcting a subluxation demonstrated on x-ray. For the purposes of this
program, “subluxation” means an incomplete dislocation, off centering, misalignment, fixation, or
abnormal spacing of the vertebrae anatomically that is demonstrable on a radiographic film (x-ray).
It is the provider’s responsibility to ensure that services provided are due to medical necessity and
are documented in the patient’s medical charts, and that the beneficiary’s Medicaid eligibility is
current before chiropractic services are provided.
The provider must check the beneficiary’s Medicaid card before rendering services. Providers must
call the toll-free number (+1 888 549 0820) listed on the back of the Medicaid insurance card to
verify eligibility every time the Medicaid beneficiary is seen for chiropractic services. Eligibility
changes on the first of each month. If services are provided, and are later denied because eligibility
was not checked, Medicaid will not pay for the services and providers must not bill the patient for
these services.
Eligible Medicaid beneficiaries, regardless of age, are allowed six chiropractic visits per year,
commencing on July 1 of each year.
Neurology
Neurological testing procedure codes include the TC, interpretation, and the physician's
professional services. Physicians doing only the interpretation must use the 26 modifier with the
appropriate procedure code. All procedures must be medically justified.
Nerve Conduction Studies are covered as medically necessary when performed with needle
electromyography (EMG) studies to confirm the diagnosis. It is recommended by the American
Association of Neuromuscular and Electrodiagnostic Medicine (AANEM) that the nerve conduction
study and a needle EMG be performed together to ensure an accurate diagnosis. Neurological
testing includes the TC, the interpretation, and the physician's professional services. Physicians
performing only the interpretation must use the 26 modifier with the appropriate procedure code.
Nerve conduction studies must be billed using CPT guidelines indicating each nerve and all site(s)
along the nerve, not each site. Codes that indicate "each nerve" will multiply for payment and must

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
121
be submitted on one line with the number of tests (or hours) indicated in the “units” column on the
claim form. Claims submitted with more than the allowed number of units will reject with Edit
Code 713. Providers may submit a new claim with documentation for medical review. If justified,
reimbursement may be made to the provider.
Hyperbaric Oxygen Therapy
For purposes of coverage, HBO therapy is a modality in which the entire body is exposed to oxygen
under increased atmospheric pressure.
Covered Conditions
Program reimbursement for HBO therapy will be limited to that which is administered in a chamber
(including the one-man unit) for the following conditions:
• Acute carbon monoxide intoxication.
• Decompression illness.
• Gas embolism.
• Gas gangrene.
• Acute traumatic peripheral ischemia. (HBO therapy is a valuable adjunctive treatment to be used
in combination with accepted standard therapeutic measures, when loss of function, limb or life
is threatened.)
• Crush injuries and suturing of severed limbs. (As in the previous conditions, HBO therapy would
be an adjunctive treatment employed when loss of function, limb or life is threatened.)
• Meleney ulcers. (The use of HBO in any other types of cutaneous ulcer is not covered.)
• Acute peripheral arterial insufficiency.
• Preparation and preservation of compromised skin grafts.
• Chronic refractory osteomyelitis that is unresponsive to conventional medical and surgical
management.
• Osteoradionecrosis as an adjunct to conventional treatment.
• Cyanide poisoning.
• Actinomycosis, but only as an adjunct to conventional therapy when the disease process is
refractory to antibiotics and surgical treatment.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
122
• Soft tissue radionecrosis.
General Surgery Guidelines
Criteria outlined in this section are contingent upon demonstrated medical necessity. The medical
record must substantiate the need for surgical services including information to support the medical
justification. Compensable services include correcting conditions that meet any of the following
criteria:
• Conditions that directly threaten the life of the beneficiary.
• Conditions that have the potential for causing irreparable physical damage.
• Conditions that can result in the loss or serious impairment of a bodily function.
• Conditions that can result in the impairment of normal physical growth and development.
• Conditions that result from trauma and must be promptly corrected (i.e., as soon as medically
feasible).
When care is furnished outside of these conditions, documentation must be included in the medical
record, or when designated, justification must be attached to the CMS-1500 claim form for payment.
This includes the history and physical, operative report, discharge summary and pathology report.
If a claim is submitted that requires support documentation, and the required documentation is not
attached to the claim form, the claim will be rejected. In this case, the documentation must be
attached to a new claim for review.
Note: All unlisted procedure codes must have documentation attached to the claim form to ensure
equitable pricing of the procedure.
To avoid delay in the processing of your claim, do not use an unlisted code when a descriptive code
is available. All unlisted codes suspend for review and pricing.
If the reviewer finds a code comparable for the procedure, the unlisted code will be priced at the
same rate as the descriptive code. The reviewer may also choose to notify the provider of the
proper code to use for future reference.
Surgical Supplies
Please refer to Supplies under Additional Ambulatory Services in this section of the manual for more
detail.
Ambulatory Surgical Services
Many surgical procedures ordinarily performed on an inpatient or OP basis consistent with sound
medical practice can be performed in an Ambulatory Surgical Center (ASC) for less cost. South

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
123
Carolina Medicaid recognizes these procedures as compensable if performed in an ASC and
included on the ASC list of covered procedures.
Surgeons must utilize only those ASC facilities contracted with South Carolina Medicaid for their
Medicaid patients. South Carolina Medicaid reimburses the ASC for the facility charges under strict
guidelines. Each ASC contracted is provided with a list of covered procedures (which is subject to
change from time to time).
Note: The surgeon must verify with the ASC that the elective procedure is covered under ASC
guidelines.
Assistant Surgeon
All guidelines that apply to the primary surgeon also apply to the assistant surgeon. The CPT
surgical procedure codes that allow an assistant surgeon's fee are listed on the provider portal.
Note: These allowances are subject to change and may be used as a reference only.
Surgical Guidelines for Specific Systems
Integumentary System
Lesion Removal
Excision/treatment of non-malignant dermal lesions and other dermal anomalies are not covered
routinely. However, Medicaid will provide coverage of these anomalies if the therapy conforms with
accepted treatment standards of the problem and meets one of the following conditions:
• The lesion is pre-cancerous or suspected to be cancerous by physical findings, appearance or
changes in characteristics.
• The anomaly causes pain, irritation, or numbness that result in the functional impairment of
bodily functions or normal growth and development.
• At least two alternative methods of treatment (i.e., steroid injection, compression, silicone gel
treatment, etc.) have been attempted and found ineffective.
• The anomaly is responsible for the loss of a bodily function and the treatment restores the
disabled function.
Keloid/Scar Conditions
Medicaid will provide coverage of excision and/or treatment of a Keloid scar and scar conditions and
fibrosis of the skin if the therapy conforms to accepted standards of the problem and meets one of
the following conditions:
• The scar causes functional impairment which interferes with daily living.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
124
• The scar is symptomatic with a history of ulceration or inflammation that causes repeat office
visits. At least two methods of treatment such as radiation (silicone gel treatment), compression,
steroids and laser surgery have been tried and failed.
• There is a history of repeated infections with the scar.
Destruction Codes
Treatment must be medically indicated according to the criteria set forth in the guidelines previously
stated. Certain procedures are considered cosmetic and therefore non-compensable.
Chemosurgery (Mohs Technique)
Procedures are compensable if medically justified and not performed for cosmetic purposes.
Mohs micrographic surgery is defined by the AMA’s CPT as a technique for the removal of complex
or ill-defined skin cancer with the histologic examination of 100% of the surgical margins. It requires
a single physician to act in two integrated but separate and distinct capacities: surgeon and
pathologist.
Musculoskeletal System
Facial Reconstructive Codes
Certain facial reconstructive procedures are covered. The criteria are contingent upon medical
necessity as outlined in the General Surgery guidelines. Justification includes result of severe
trauma and/or congenital malformations; each claim must have support documentation attached. If
there is no documentation, the claim will be rejected.
If the reconstructive process must be performed in stages, each claim must have documentation
that includes all prior stages. A consultant for the specialty will review each claim and make a
determination.
Under no circumstances is payment allowed for reconstructive surgery performed for cosmetic
reasons alone.
Fracture Repair (For Acute Care of an Injured Part)
All codes listed in the musculoskeletal section of the CPT are considered surgical packages with the
exceptions of those listed in this manual.
The original application of a cast, splint, strapping, or traction device is included in the treatment of a
fracture or dislocation and may not be billed separately.
Grafts
Most bone, cartilage and fascia graft procedures include the obtaining of the graft by the operating
surgeon. When the assistant surgeon obtains the graft for the operating surgeon, the additional
service may be identified and reported separately.
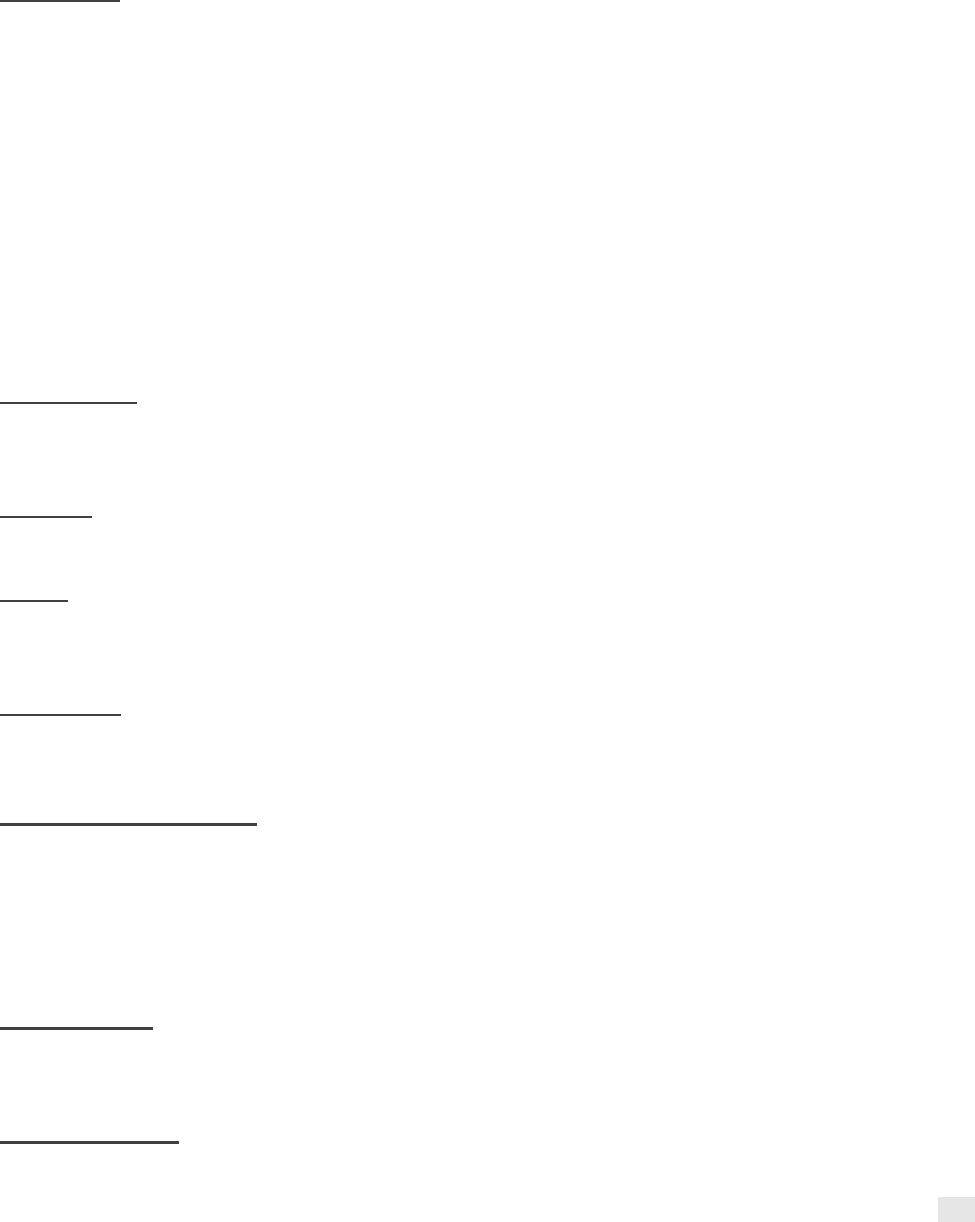
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
125
Casts
Application
The original application of a cast, splint, strapping or traction device is included in the treatment of a
fracture or dislocation and may not be billed separately except for the application of a halo-type
body cast, Risser jacket, turnbuckle jacket, body cast, or hip spica cast. Plaster or fiberglass can be
billed additionally for cast supplies.
Plaster casts for rehabilitation are compensable using the appropriate CPT codes for the upper or
lower extremity. Reimbursement includes the actual application of the cast. Supply codes may be
billed in addition to the application.
Synthetic casts (fiberglass) are covered but may only be billed one time during the patient's course
of treatment. A delayed or non-union replacement or the replacement of a patellar-tendon-bearing
(PTB) cast is covered.
Replacement
The application of a cast, splint, strapping or traction device is reimbursable if it is a replacement, or
subsequent replacement to the original cast, splint, strapping or traction device.
Removal
Codes for cast removals are reimbursable only if another physician applied the cast.
Repair
To report any repairs made to a cast, use the supplemental codes plaster cast supplies, or
fiberglass cast supplies.
Cast Codes
Cast codes will reimburse in an OP setting when the physician applies the cast. If these codes are
applied by a hospital technician, then no reimbursement to the physician will be allowed.
Application or Strapping
If cast application or strapping is provided as an initial service (e.g., casting of a sprained ankle or
knee) in which no other procedure or treatment (e.g., surgical repair, reduction of a fracture or joint
dislocation) is performed, or is expected to be performed by a physician rendering the initial care
only, use the casting, strapping, and/or supply code in addition to an E&M code, as appropriate.
Splints
Plaster Splints
Plaster splints are compensable using the appropriate CPT codes for the upper or lower extremity.
The reimbursement includes the materials used as well as the actual application of the splint.
Synthetic Splints

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
126
Synthetic splints (fiberglass) are covered but may only be billed one time during the patient's course
of treatment. Any replacement is non-covered and cannot be billed except a PTB, delayed, or non-
union cast.
Custom Splints
Custom-made splints are recognized as a viable part in the patient's rehabilitative period of
treatment. Reimbursement is allowed for these splints only when made by a licensed orthotist or
occupational therapist. To report any repairs or adjustments made to a splint, use and appropriate
supply code.
Prefab Splints
Prefabricated splints (Velcro closure) are non-compensable under the Physician Services program.
Orthotic Supplies
Please refer to the heading “Durable Medical Equipment/Supply” in this section of the manual.
Cardiovascular System
Vascular Injection Procedures
Listed services for injection procedures include necessary local anesthesia, introduction of needles
or catheters, injection of contrast medium with or without automatic power injection, and/or
necessary pre- and post-injection care specifically related to the injection procedure. For injection
procedures in conjunction with cardiac catheterization, please refer to Cardiology under Specialty
Care Services in this section of the manual.
Radiological vascular injections performed by a single physician are compensable separate from the
radiology service. Catheters, drugs and contrast media are not included in the listed service for
these injection procedures.
For insertion of a Swan-Ganz catheter not associated with cardiac catheterization, use an
appropriate assistant surgeon code in lieu of a heart catheter code.
Implantable Vascular Access Portal/Catheter
For port-a-cath maintenance, use the appropriate J codes, supply codes and office visit code when
applicable. Do not use an unlisted CPT code for catheter maintenance.
Digestive System (et al.)
Contralateral Inguinal Exploration
Medicaid will reimburse for a contralateral inguinal exploration when a unilateral herniorrhaphy has
been performed on an infant (under five years of age). To report this service, use an appropriate
assistant surgeon code along with the procedure code for herniorrhaphy and attach support
documentation for medical review.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
127
Gastric Bypass
Please refer to Gastroenterology under Specialty Care Services in this section of the manual
regarding treatment of obesity and bariatric surgical procedures.
Urinary System
Services listed in this section are covered when medically necessary, with the following restrictions:
• Endoscopic Procedures: Follow guidelines for endoscopic procedures under General Surgery
Guidelines within this manual.
• Urodynamics: These procedures may be billed in addition to the appropriate surgical code
(Cystourethroscopy); reimbursement includes equipment and supplies.
• When performed (and billed) on the same DOS as the surgery, these services are not
considered surgical and will be reimbursed at 100% of the established rate. Documentation
must include the urine measurement.
• Urinary Supplies: Please refer to the Durable Medical Equipment/Supply section of this manual.
• Lithotripsy: Percutaneous, extracorporeal shock wave, and cystourethroscope lithotripsy are
covered services when medically necessary. The physician is reimbursed only for the
professional service. If the procedure is performed bilaterally, bill on two lines adding no modifier
to the first procedure, and a 50 modifier to the second (bilateral) procedure.
Nervous System
No special restrictions apply other than those defined in the general surgery and pain therapy
guidelines.
Spinal Procedures for Injection of Anesthetic Substance
These procedures are reimbursed for the initial placement of an indwelling catheter for anesthesia
purposes. Subsequent injections of the anesthetic agent are not allowed under the injection code.
For maintenance of an epidural, please refer to Anesthesia Services and Pain Management
Services in this section of the manual for additional information.
Implantable Infusion Pumps
An implantable infusion pump is covered when used to administer anti-spasmodic drugs
intrathecally (e.g., Baclofen) to treat chronic intractable spasticity in patients who have proven
unresponsive to less invasive medical therapy as determined by the following criteria:
• As indicated by at least a six-week trial, the patient cannot be maintained on non-invasive
methods of spasm control.
• Prior to pump implantation, the patient must have responded favorably to a trial intrathecal dose
of the anti-spasmodic drug.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
128
Each claim will be reviewed for these criteria; claims submitted without documentation will be
rejected.
Implantable infusion pumps are also covered for treatment of pain. Please refer to Pain
Management Services in this section of the manual for additional information.
Organ Transplantation
SCDHHS covers medically necessary and non-investigational/experimental organ and tissue
transplant and transplant-related services. SCDHHS will only support the referral of patients for an
evaluation to CMS-certified transplant centers. This will include certified facilities that are contracted
with SCDHHS as well as certified facilities that are located outside of the SCMSA (more than 25
miles of the South Carolina borders). For a complete list of CMS-approved centers, visit the CMS
website at
https://www.cms.gov/Medicare/Provider-Enrollment-and-
Certification/CertificationandComplianc/Transplant.html
Covered transplant services fall into two groups:
• Group I: includes corneal and kidney transplants for which coverage is applicable in all
medically necessary instances without restriction and without prior approval.
• Group II: includes pancreas, bone marrow, heart, liver, liver with small bowels, and lung
transplants when medically necessary and clinically acceptable. Coverage of these
transplants is limited to facilities within the geographic boundaries of South Carolina and
require prior approval. All authorization requests for pancreas, bone marrow, heart, liver,
liver with small bowel and lung transplants will be evaluated utilizing uniform professional
and administrative guidelines as to medical necessity.
See the Utilization Management, Prior Approval section of this manual for more information
regarding organ transplants.
Anesthesia Services
Anesthesia services consist of services rendered by a physician, a CRNA, or anesthetist assistant
(AA) other than the attending surgeon or his or her assistant and shall include the administration of
spinal or rectal anesthesia, or a drug, or other anesthetic agent. The agent may be administered by
injection or inhalation, except by local infiltration, the purpose and effect of which administration is
the obtaining of muscular relaxation, loss of sensation or loss of consciousness. The reporting of
anesthesia services is appropriate by or under the responsible supervision of a physician.
Use of the surgical procedure code for billing anesthesia services will result in a rejection. When
multiple surgical procedures are performed during the same period of anesthesia, only the
anesthesia procedure code for the major procedure may be billed and the total time must reflect

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
129
coverage for all procedures. Base time associated with the procedure code will be automatically
assigned from the procedure code billed.
There is no additional payment for anesthesia services rendered by the attending surgeon or
assistant surgeon when performed on an inpatient or OP basis.
Time Reporting
Anesthesia time involves the continuous, actual presence of the anesthesiologist or the medically
directed CRNA/AA. It starts when the anesthesiologist begins to prepare the patient for anesthesia
care in the operating room and ends when the anesthesiologist is no longer in continuous, actual
attendance. See the Billing Guidance section of this manual for billing information.
Pain Management Services
The complaint of pain remains the single greatest reason for seeking medical attention. Pain is
defined as an unpleasant sensory and emotional experience associated with actual or potential
tissue damage. The condition is considered chronic pain when it has been present continuously or
intermittently for six months or more, or it has extended two to three months beyond the expected
recovery time. It is of utmost importance that medical providers seek the source of the pain in
addition to working to relieve and resolve the pain. Patient history must be reviewed to ensure all
areas of treatment have been explored. Appropriate referrals for concurrent medical or
psychological treatment must be made. This requires all physicians, not just pain specialists, to
understand the pain symptoms and their underlying cause.
The primary objectives of pain management must be to accomplish the following:
• Eliminate the use of optional health care services for primary pain complaints.
• Increase physical activities and return the patient to productive activity.
• Increase the patient's ability to manage pain and related problems.
• Reduce the use and misuse of medication.
• Decrease the intensity of subjective or illusory pain.
The policies outlined in the remainder of the Pain Management Services section of this manual
apply to physicians of all specialties.
Evaluation and Management Visits
SCDHHS will cover one office or inpatient consultation necessary for screening a beneficiary
focusing on identifying the cause of the pain and developing a pain management plan. When the
consultant assumes responsibility for a portion or all of the patient's condition, appropriate office visit
or subsequent hospital care codes must be used after the initial consultation. Consultative services

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
130
related to any direct or indirect patient care are included in the basic value of an anesthesia
payment and cannot be billed separately.
E&M guidelines apply to office, inpatient and OP hospital care for pain management.
External Infusion Pumps
The condition of external infusion pumps is covered for the following:
• Opioid drugs for intractable cancer pain.
• Treatment for acute iron poisoning or iron overload.
• Chemotherapy for liver cancer.
• Treatment for thromboembolic disease and/or pulmonary embolism.
Other uses of the external infusion pump may be reimbursable if the provider can document the
medical necessity and appropriateness of this type of therapy and pump for the individual patient.
Prior approval must be requested in writing for a condition other than those listed above.
Implantable Infusion Pumps
The use of implantable infusion pumps is covered for the following conditions:
• Chemotherapy treatment of liver cancer.
• Delivery of anti-spasmodic drugs for severe spasticity.
• Treatment of chronic intractable pain.
Chemotherapy for Liver Cancer
The implantable pump is covered for the treatment of liver cancer in patients in whom the
metastases are limited to the liver, and where one of the following applies:
• The disease is unresponsive.
• The patient refuses surgical excision of the tumor.
Anti-Spasmodic Drugs for Severe Spasticity
An implantable infusion pump is covered when used to administer antispasmodic drugs intrathecally
(e.g., Baclofen) to treat chronic intractable spasticity in patients who have proven unresponsive to
less invasive therapy when both of the following criteria are met:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
131
• As indicated by at least a six-week trial, the patient cannot be maintained on non-invasive
methods of spasm control such as oral anti-spasmodic drugs, because these methods either fail
to adequately control the spasticity, or they produce intolerable side effects.
• Prior to pump implantation, the patient must have responded favorably to a trial intrathecal dose
of anti-spasmodic drug.
Treatment of Chronic Intractable Pain
An implantable pump is covered when used to administer opioid drugs (e.g., morphine) intrathecally
or epidurally for the treatment of severe or chronic intractable pain in patients who have a life
expectancy of at least three months, and who have proven unresponsive to less invasive medical
therapy when ALL of the following criteria have been met:
• Coordination must be made with other attending physicians in order to identify and treat the
cause of the pain, rather than symptoms, if possible.
• The patient's history must indicate that he or she would not respond adequately to non-invasive
methods of pain control.
• A preliminary trial of intraspinal opioid drug administration must be undertaken with a temporary
catheter to monitor acceptable pain relief, degree of side effects and patient acceptance.
Refilling and maintenance of the implantable pump will be allowed when administered by a
physician.
Determinations may be made on coverage of other uses for implantable infusion pumps if the
provider can verify ALL the following:
• The drug is reasonable and necessary for treatment of the individual patient.
• It is medically necessary that the drug be administered via an implantable infusion pump.
• The FDA-approved labeling for the pump specifies that the drug being administered and the
purpose for its administration is an indicated use for the pump.
Pathology and Laboratory Services
In accordance with federal regulations (42 CFR 493.1809), all laboratory testing sites (except for
physician’s offices) are required to have an appropriate CLIA certificate. CLIA is a regulatory
program administered by the CMS. For more detail, please refer to Clinical Laboratory Improvement
Amendments within this section of the manual.
Pathology includes services rendered by attending physicians and pathologists. Hospital
laboratories must reference the Hospital Services Provider Manual. Independent laboratories will be
covered in this section.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
132
Laboratory services/tests must be ordered by the attending physician, appropriate to the study of
the patient (i.e., consistent with the diagnosis and treatment of the patient's condition and medically
necessary for the appropriate care of the patient). Medicaid reimbursement will generally include
obtaining the specimen, the performance of the test, supplies used in the performance of the test,
and recording of the test(s). In addition, the reimbursement includes reporting of the test results.
The DOS for all billing must be the date the specimen was collected. For specimen collections that
span more than a 24-month period, the DOS must be reported as the date the collection began. For
laboratory tests that require a specimen from stored collections, the DOS must be defined as the
date the specimen was obtained from archives. Procedures reimbursed in components will be
identified later and separate allowable handling fees will be defined in this section.
Attending Physician Services
The attending physician is responsible for the study of the patient, medical necessity, and
appropriateness of procedures ordered. Physicians may not bill for lab tests performed outside their
offices. Physicians may not bill a patient for lab services performed in the office that are normally
covered by Medicaid when the service would have been paid if a Medicaid claim was submitted,
provided the physician has accepted the patient's Medicaid benefits for the office visit or other
procedure on the same date.
The performance of a test(s) prior to seeing the patient is a screening procedure and is not
compensable. The only exceptions are pregnancy tests and prenatal lab work.
All laboratory tests must be ordered for the appropriate diagnosis and treatment of the patient's
illness. Laboratory services requested or performed as general screening services are
non-compensable, except for services rendered under the healthy adult physical as outlined in the
Preventive Care Services section of this manual. General health panels are
non-compensable; fertility tests are non-compensable. Routine paternity tests are non-covered, but
medically necessary exceptions will be considered. Claims must be submitted with documentation
justifying the service.
The chlamydia rapid test procedure code is used to report the chlamydia rapid test.
Venipuncture
A separate handling charge for blood products drawn through venipuncture is allowed and
compensable. To report a routine venipuncture, use the collection of venous blood by venipuncture
procedure code. Finger/heel/ear stick for collection of specimen(s) will be included in the office visit
or lab test reimbursement and may not be billed separately. Filing for only the collection of
specimen(s) is permissible, but an office visit or lab test reimbursement charge cannot be filed for
the same DOS. The physician or clinic provider may charge a separate venipuncture code if he or
she provided the entire diagnostic lab service or only extracted the blood for referral to an outside
lab.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
133
Catheterization
Urine specimens collected by all methods are not considered a separate compensable charge. The
patient is also not liable for the charge since the collection fee is considered part of the lab test or
office examination. The provider may charge for a separate catheterization regardless of whether
the specimen was collected for a test in the office or for referral to an outside laboratory.
Automated Chemistry Tests and Panels
Clinical laboratory tests are covered under Medicaid if they are reasonable and necessary for the
diagnosis or treatment of an illness or injury. A physician who orders a series of clinical lab tests
must specify the actual tests to be performed. If a panel is requested, the professional judgment of
the physician must dictate the medical necessity of the complete panel instead of an individual test.
Likewise, individual tests ordered by a physician must indicate a medical reason for the individual
test in lieu of a panel that is less expensive.
Automated Multi-Channel Chemistry Tests
Refer the codes information on the provider portal for acceptable services. If three or more of the
tests are performed on the same DOS, they will be grouped together and paid according to the
number of tests performed. Duplicate payments and payments that are not consistent with Medicaid
policy will be recouped at post-payment review.
Pathology Panels
Please refer to the current CPT for guidelines on acceptable criteria for billing organ or
disease-oriented panels.
Clinical Pathology Services
South Carolina Medicaid will recognize both a professional and TC for all pathology codes. Refer to
the code information on the provider portal for pathology codes requiring a 26 modifier in a hospital
setting.
Professional Pathology Services
Anatomical
Medicaid recognizes the expertise of professional pathology services when charged separately for
the interpretation of all anatomical and surgical tissues. Postmortem examinations are non-covered
by Medicaid.
Blood Smears, Bone Marrows and Blood Bank Services
The 26 modifier is not required when performed in a hospital setting.
Bone marrows, including smears, aspiration, staining, biopsy and interpretation, are compensable
as separate professional services. Care must be taken when coding bone marrow interpretation
procedures; the 26 modifier is not required.
Blood bank services are covered; no modifier is required when performed in a hospital setting.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
134
Cytopathology and Surgical Pathology
These procedures include accession, handling and reporting. The handling and interpretation of
surgical tissues must be charged separately if rendered by a pathologist in a hospital or office when
only the professional interpretation is necessary, using a distinct physician provider number and a
26 modifier. Only an independent laboratory may charge for the total lab procedure when the
laboratory has performed the total service (i.e., both technical and professional component related
to the surgical tissue).
Some surgical pathology codes will multiply by units for payment. When filing a claim, list the
appropriate CPT code for the DOS one time and the number of units in the “days/units” column and
the total charges for the number of units billed.
Pap Smears
Medicaid reimburses a pathologist for a professional interpretation of a Pap smear. An attending
physician must specifically order the appropriate cytopathology code with definite hormonal
evaluation.
Medicaid covers Pap smears for dually eligible Medicare/Medicaid beneficiaries who have exceeded
the Medicare frequency limit. When the Medicare denial is received, the charges must be billed
using the CMS-1500 claim form. Please refer to Cancer Screening Services within this section of
the manual for frequency limitations.
Specimen Referrals
The pathologist must use the appropriate procedure codes to designate review and report of
referred material only. A separate procedure code is used for comprehensive consultation with
review of medical records and specimens, with report, on referred material.
Referral Out-of-State (OOS)
Specimens must be referred to a South Carolina Medicaid-enrolled independent laboratory,
pathologist or hospital. OOS referrals to non-enrolled providers are not compensable through the
Medicaid program. Providers cannot bill Medicaid beneficiaries when Medicaid would have paid the
lab service if appropriate billing and referral procedures had been followed.
Genetic Studies
Medicaid will reimburse for genetic studies if ordered by an attending physician and requested as a
direct diagnosis and treatment tool. The genetic study may be ordered as a preventive measure;
however, the prevention must have a direct correlation with the treatment of the patient and the
patient's family or serve as an inhibitor to institutionalization. Medicaid will not reimburse for genetic
research.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
135
Chromosome Analysis
Genetic centers are permitted to fragment chromosome charges into the “tissue culture for
chromosome analysis” charge and the analysis charge. Chromosome studies must be medically
necessary.
In addition, reimbursement may be allowed for the following expanded services: extended
chromosome analysis, R-Bands, and Fragile X DNA analysis.
The following conditions may be used as indications of analysis:
• Intellectual disabilities
• Dysmorphic fractures
• Multiple congenital abnormalities
• Abnormal sexual development
• Abnormalities of growth
• Certain types of malignancies
Genetic Studies Also Covered by Medicaid
Lysosomal Enzyme Analysis for Developmental Regression (e.g., Tay-Sachs Disease)
The following indications must be present:
• Growth failure
• Development regression
• Clouding of corneas
• Hepatosplenomegaly
• Coarsening of facial features
• Abnormalities of skeletal system
Amino Acid Analysis for Infants and Children
The following indications must be present:
• Feeding abnormalities
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
136
• Growth failure
• Development failure
• Seizures
• Uncommon acidosis
Organic Acid Analysis for Infants
The following indications must be present:
• Feeding abnormalities
• Unexplained acidosis
• Growth failure
• Seizures
Carbohydrate Analysis for Infants and Children
One of the following indications must be present:
• Cataracts
• Hepatosplenomegaly
• Jaundice
• Growth failure
• Acidosis
• Seizures
Other Tests for Infants and Children
These tests include the following:
• Metabolic screen
• Alpha-fetoprotein
• Sialic acid
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
137
• Sulfate incorporation
Amniocentesis for Prenatal Diagnosis
Allowable for the following categories of patient:
• Women over 35 years of age
• Previous child with chromosomal disorder
• Multiple spontaneous abortions
• Patients with neural tube defects
• Patients at risk for having children with X-linked disorder (i.e., hemophilia or Duchenne muscular
dystrophy, or metabolic disorders such as Tay-Sachs disease)
Tests for the Detection of Other Genetic Diseases
These tests include the following:
• Skeletal Dysplasias
• Huntington's disease
• Sickle Cell
• Hemoglobinopathies
Neuropharmagen Genomic Testing
Neuropharmagen is a pharmacogenomic test (PGx) that allows providers to see how patients would
interact with different medications for mental health diagnoses without going through a trial and error
process to determine optimal medication and dosage. Adult beneficiaries with full benefit are eligible
to receive this test.
Prior authorization must be obtained for this genomic test and must meet the following criteria:
1. Test must be ordered by a board-certified psychiatrist or by a psychiatrist extender
(psychiatric physician assistant, psychiatric nurse practitioner) under the supervision of a
board-certified psychiatrist. AND
2. Patient must have one of the following mental health conditions: general anxiety disorder,
major depressive disorder, obsessive compulsive disorder, bipolar or schizophrenia; AND
3. The Medicaid member must meet at least one of the following:
o Has experienced a trial and failure of two previous psychoactive drugs for the mental
health condition being treated. OR

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
138
o Is currently taking more than two medications to treat the mental health condition.
Prior authorization form for this test can be found in the Forms section of this manual.
Radiology and Nuclear Medicine
Radiology services are those services performed by a radiologist/physician in conjunction with an
x-ray, ultrasound, Positron Emission Tomography (PET scan), computerized axial tomogram
(CAT scan), or magnetic resonance imaging (MRI). Radiological services are covered only when
such services are consistent with the diagnosis and treatment of an illness or injury. Screening
procedures are not reimbursable unless outlined as covered items in this manual.
Effective March 1, 2014, SCDHHS will no longer prior authorize high-tech radiology services. All
radiology services will be based on medical necessity and held to the American College of
Radiology (ACR) standards. ACR standards can be found at http://www.acr.org
.
This policy pertains to all FFS recipients and SCDHHS will no longer exclude anyone based on
category or whether they have third-party liability primary coverage. Providers must continue to refer
members in an MCO to the appropriate MCO provider in order to determine if prior authorization
applies to radiology services.
Positron Emission Tomography (PET) Scans
PET scan reimbursement will be limited to two scans in a 12-consecutive month period. PET scans
will only be covered for the staging and restaging of cancer malignancies.
Staging
• The stage of the cancer remains in doubt after completion of a standard diagnostic work-up,
including conventional imaging such as CAT scan, MRI or ultrasound, or
• The use of a PET scan could potentially replace one or more conventional imaging studies when
it is expected that conventional study information is insufficient for the clinical management of
the patient, and
• Clinical management of the patient would differ depending on the stage of the cancer identified.
Restaging
• Detecting residual disease.
• Detecting suspected recurrence or metastasis.
• Determining the extent of recurrence.
• Potentially replacing one or more conventional imaging studies when it is expected that
conventional study information is insufficient for the clinical management of the patient.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
139
PET scans will not be utilized for screening purposes and the use of PET scans to monitor tumor
response during a planned course of treatment will not be covered. Restaging only occurs after a
course of treatment is completed and 90 days has lapsed prior to the restaging PET scan. PET
scans will be subject to retrospective review to include paid inpatient/OP hospital and physician
claims. Documentation must be maintained in the beneficiary’s medical records and must support
medical necessity. SCDHHS will not cover any additional PET scans over the frequency limitation of
two in a 12-consecutive month period.
Diagnostic Radiology
Medicaid requires that all facilities providing screening and diagnostic mammography services meet
FDA regulations. Medicaid claims for mammography services will be reviewed to ensure FDA
criteria are met. Medicaid will not reimburse for mammography services performed by providers who
are not certified, and providers cannot bill the Medicaid beneficiaries for the denied Medicaid
services. An FDA certificate for screening mammography services must be in the provider
enrollment file. Questions regarding enrollment may be directed at:
Medicaid Provider Enrollment
Post Office Box 8809
Columbia, SC 29202-8809
Phone: +1 888 289 0709
Diagnostic Ultrasound
Ultrasound procedures are recorded as complete, limited or repeat procedures. Full documentation
must justify the use of the complete procedure code. A complete procedure is one that the provider
furnished both the professional and TCs. Please refer to Obstetrics and Gynecology in this section
of the manual for pregnancy-related guidelines.
Radiology Oncology
A preliminary evaluation/consultation of the patient is allowed prior to the decision to treat and must
be identified by the appropriate E&M code. Once the therapist assumes responsibility for the
treatment and care of the patient, a separate consultation or E&M code will not be covered.
Please refer to CPT reference manual for appropriate codes for the treatment planning, radiation
physics, treatment delivery and treatment management of radiation oncology.
Clinical Treatment Planning
Please refer to the CPT reference manual for appropriate codes for the treatment and planning
process. These services include test interpretation, tumor localization, treatment volume
determination, time/dosage determination, treatment modality, number and size of ports and
selection of treatment devices.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
140
Medical Radiation Physics
Please refer to the CPT reference manual for appropriate codes for services by the physician and
physicist involved in radiation physics, dosimetry calculation, construction of treatment devices and
other special services.
Radiation Treatment Delivery
Radiation treatment codes reflect the technical portion of radiation therapy services. The codes will
be found in your CPT reference manual and represent individual sessions of service delivery or
daily services. Multiple treatment sessions on the same DOS are allowed as long as there is a
distinct break in therapy services/individual session.
Clinical Treatment Management
Please refer to the CPT reference manual for appropriate codes. Clinical treatment management
codes reflect the professional component of treatment on a weekly basis. These codes are used to
describe the physician’s weekly radiotherapy management services at all energy levels. A weekly
unit is equal to five fractions or treatment sessions, regardless of whether the fraction or treatment
sessions are furnished on consecutive days or without regard to the actual time period in which the
services are provided.
Hyperthermia
Treatments include external and internal procedures. Hyperthermia is used only as an adjunct to
radiation/chemotherapy. It may be initiated by microwave, ultrasound, low-energy radio-frequency
conduction or by probes.
Clinical Brachytherapy
Please refer to your CPT reference manual for all codes. Services bundled within the procedure
codes include hospital admission, daily visits, follow-up care, dilation, insertion and removal of
applicators. They do not include preparation of the element calculation of dosage or loading of the
element.
Nuclear Medicine
Please refer to the CPT reference manual for appropriate codes for services related to diagnostic
and therapeutic nuclear medicine. The procedures may be performed and charged separately, or as
part of a course of treatment. Radioimmunoassay tests are found in the Clinical Pathology section of
the CPT reference manual.
Contrasts and Radiopharmaceuticals
For appropriate codes for billing contrasts and radiopharmaceuticals providers must refer to the
HCPCS reference manual. Physicians must not bill for radiopharmaceuticals and/or contrasts that
are provided by the hospital.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
141
Independent Imaging Centers and Mobile Imaging Units
Independent Imaging Centers and Mobile Imaging Units: Medicaid will reimburse for services
provided by a freestanding imaging centers, mobile ultrasound units, and mobile imaging units when
the services are consistent with diagnosis, treatment, injury or covered preventative services as
found in Family Planning.
Independent imaging centers, mobile ultrasound units and mobile imagining units can only be
reimbursed for the technical portion of an x-ray or other imaging service. Separate reimbursement
will be made to the physician for the professional interpretation of the radiology procedure. The
physician’s name must be on the radiology report as the reading/interpreting physician.
Reimbursement will be sent to the reading/interpreting physician or reading/interpreting physician
group practice. The reading/interpreting physician must be enrolled with SCDHHS as an in-state
provider. All OOS providers must go through the OOS approval process. OOS physicians must
attach a copy of the approval letter to each CMS-1500 form submitted for reimbursement.
Podiatry Services
Podiatry services are those services that are responsible and necessary for the diagnosis and
treatment of foot conditions. These services are limited to the specialized care of the foot as outlined
under the laws of the State of South Carolina.
Office Examinations
Level of service guidelines must be followed as described in the current CPT. Podiatric exams may
be charged at all levels of services as medically necessary for new or established office E&M visits.
Treatment of Subluxation of the Foot
Subluxation of the foot is defined as partial dislocation to displacement of joint surfaces, tendons,
ligaments or muscles of the foot.
Reasonable and necessary diagnosis and treatment (except using orthopedic shoes or other
supportive devices for the foot) of symptomatic conditions such as osteoarthritis, bursitis, tendonitis,
etc., that result from or are associated with partial displacement of foot structures are covered
services. Surgical correction of a subluxed foot structure that is either an integral part of the
treatment of a foot injury, or that is undertaken to improve the function of the foot, or that is
undertaken to alleviate an induced or associated symptomatic condition, is a covered service. The
presentation of symptoms is clearly the paramount factor in coverage. Surgical and non-surgical
treatments undertaken for the sole purpose of correcting the subluxed structure of the foot as an
isolated entity are not covered.
Treatment of Flat Foot
The term “flat foot” is defined as a condition in which one or more of the arches of the foot have
flattened out. Services directed toward the care or correction of such a condition is not covered.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
142
However, the services or procedures required to make the initial diagnosis may be considered
reasonable and necessary and are covered.
Supportive Devices for the Feet
Orthopedic shoes and other supportive devices for the feet are not covered unless the shoe is an
integral part of a leg brace.
Prosthetic Shoe
A prosthetic shoe (a device used when all or a substantial portion of the front part of the foot is
missing) can be covered as a terminal device (i.e., a structural supplement replacing a totally or
substantially absent foot). The beneficiary must be referred to a DME supplier for such devices.
Excision of Nail
When a procedure indicates a partial or total permanent nail removal, separate billing is not to be
used for the medial and lateral borders of the same toe. The number of toes must be indicated if
multiple toes are corrected at the same time.
Plantar Warts
Treatment for Verruca vulgaris and intractable plantar keratoma are covered services.
Mycotic Nail
Mycotic nail and other infections of the feet and toenails require professional services that are
outside the scope of routine foot care and are covered services if the subsequent criteria are met.
Treatment of a fungal (mycotic) infection of the toenail can be covered under the following
circumstances:
• Clinical evidence of mycosis of the toenail.
• Medical documentation that the patient has either a limitation of ambulation requiring active
treatment of the foot, or in the case of a non-ambulatory patient, a condition that is likely to result
in significant medical complications in the absence of such treatment.
Routine Foot Care
Routine foot care includes the cutting or removal of corns or calluses, the trimming of nails, and
other hygienic and preventative maintenance care.
Reimbursement for routine foot care is allowed under the medical conditions listed below when the
patient is under the active care of a physician, licensed practitioner. It is essential that the patient
has seen a physician for treatment and/or evaluation of the complicating disease process during the
six months prior to the DOS. The allowable conditions are as follows:
• Diabetes mellitus

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
143
• Chronic thrombophlebitis
• Peripheral neuropathies involving the feet associated with:
– Malnutrition and vitamin deficiency
– Malnutrition (general, pellagra)
– Alcoholism
– Malabsorption (celiac disease, tropical sprue)
– Pernicious anemia
– Carcinoma
– Diabetes mellitus
– Drugs and toxins
– MS
– Uremia (chronic renal disease)
In evaluating whether the routine services can be reimbursed, a presumption of coverage is made
where the evidence available discloses certain physical and/or clinical findings consistent with the
diagnosis, and indicative of surface peripheral involvement.
The presumption of coverage is applied when a physician rendering the routine foot care has
identified one Class A finding as noted below, two Class B findings, or one Class B and two Class C
findings as follows:
Class A Findings:
• Non-traumatic amputation of the foot or an integral skeletal portion thereof
Class B Findings:
• Absent posterior tibial pulse
• Absent dorsalis pedis pulse
• A minimum of three trophic changes as follows:
– Hair growth (decrease or absence)

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
144
– Nail changes (thickening)
– Pigmentary changes (discoloration)
– Skin texture (thin, shiny)
– Skin color (rubor or redness)
Class C Findings:
• Claudication
• Temperature changes (e.g., cold feet)
• Edema
• Paresthesia (abnormal spontaneous sensations in the feet)
• Burning
Additional services ordinarily considered routine may also be covered if they are performed as a
necessary and integral part of otherwise covered services, such as diagnosis and treatment of
diabetic ulcers, wounds and infections.
Nursing Home Visits
Podiatry care may be rendered to patients in nursing or rest home facilities, provided the service is
medically necessary and meets the policies defined in this manual. Podiatry care must be requested
by one of the following:
• The attending physician
• The patient
• The patient’s family when the patient is incompetent
• Nursing service*
• Nursing service requests must be documented in the patient’s chart. The podiatrist’s records
must indicate who made the request for services in this situation.
NON- COVERED SERVICES
Evaluation and Management Services
Telehealth
The following interactions do not constitute reimbursable telehealth or telepsychiatry services and
will not be reimbursed:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
145
• Telephone conversations
• Email messages
• Video cell phone interactions
• Facsimile transmissions
• Services provided by allied health professionals
Unusual Travel
CPT procedure codes indicating medical testimony, special reports for insurance, educational
services for groups, and data analysis are non-compensable by Medicaid.
EPSDT
The following services are not covered under EPSDT:
• Experimental or investigational treatments (except qualifying clinical trials- for details refer to the
Provider Administrative and Billing Manual).
• Services or items not generally accepted as effective and/or not within the normal course and
duration of treatment.
• Services for caregiver or provider convenience.
• HCBS Waiver
• Services for which South Carolina Healthy Connections Medicaid has a waiver program are not
considered to be State Plan benefits, and therefore, are not a benefit under EPSDT. For
example, items such as respite, vehicle modifications and home modifications are not covered.
• Sports, camp or college physical examination.
Obstetrics and Gynecology
Infertility Procedures
Any medications, tests, services, or procedures performed for the diagnosis or treatment of
infertility are non-covered.
Gender Transition
Services and procedures related to gender transition are not covered.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
146
Family Planning
Family Planning services required to manage or to treat medical conditions and/or diseases,
whether such procedures are also related to preventing or delaying pregnancy, are not covered.
Services to address side effects or complications (e.g., blood clots, strokes, abnormal Pap smears,
etc.) associated with various family planning methods requiring medical interventions (e.g., blood
clots, strokes, abnormal Pap smears, etc.) other than changing the birth control method, should not
be billed using an FP modifier or Family Planning diagnosis code.
Many procedures that are performed for “medical” reasons also have family planning implications.
When services other than Family Planning are provided during a family planning visit, these
services must be billed separately using the appropriate CPT/HCPCS codes and modifiers if
applicable. Examples of these services include:
• Sterilization by hysterectomy.
• Abortions.
• Hospital charges incurred when a beneficiary enters an OP hospital/facility for sterilization
purposes, but then opts out of the procedure.
• Inpatient hospital services.
• Removal of an IUD due to a uterine or pelvic infection.
• Colposcopy and biopsy of cervix/vagina performed to identify and treat medical conditions.
• Diagnostic or screening mammograms.
• Treatment of medical complications (e.g., perforated bowel or bladder tear) caused by, or
following a Family Planning procedure.
• Any procedure or service provided to a woman who is known to be pregnant.
• Removal of contraceptive implants due to medical complications.
• Routine gynecological exams (diagnosis code Z01.411 or Z01.419) in which contraceptive
management is not provided.
Note: Beneficiaries are allowed one permanent sterilization procedure per lifetime.
Specialty Care Services
Consultations Exclusions
Situations in which consultations generally are excluded from coverage are as follows:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
147
• Physicians within the same specialty who are partners cannot be paid consultation fees for visits
to the same patient unless one partner's sub-specialty is unique to a particular situation.
• Consultations required by hospital rules and regulations, or consultations between colleagues
who exchange medical opinions as a matter of courtesy and normally without charge, are not
covered.
• Anesthesia consultations are not covered on the same date as surgery or the day prior to
surgery, if part of the pre-operative assessment.
• Follow-up consultations are not covered when the total or specific care of a patient is transferred
from the attending physician to the consultant.
Psychiatric and Counseling Services
The following services are non-compensable:
• Psychoanalysis
• Multiple-family group psychotherapy
• Narcosynthesis for psychiatric diagnostic and therapeutic purposes (e.g., sodium amobarbital
[amytal] interview)
• Individual psycho-physiological therapy incorporating biofeedback training (20–30 minutes)
• Individual psycho-physiological therapy incorporating biofeedback training (45–50 minutes)
• Hypnotherapy
Psychotherapy services are non-covered in an inpatient setting when reimbursement of this service
is included in the hospital reimbursement.
Ophthalmology and Optometry Services
Part I — Vision Care Services
The following services are non-covered under the Vision Care program:
• Routine eye exams for beneficiaries beginning on their 21
st
birthday and older.
• Refractions for beneficiaries beginning on their 21
st
birthday.
• Lenses and frames for beneficiaries beginning on their 21
st
birthday.
• Optometric hypnosis.
• Broken appointments.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
148
• Special reports.
• Extended wear contact lenses, cosmetic lenses, tinted and/or colored contacts.
• Transitional and progressive lenses.
Part II — Diagnostic Ophthalmology Services
Glare Testing
This is considered non-standardized and has not been proven effective in the diagnosis of visual
disabilities. Therefore, no separate reimbursement is allowed for this procedure.
Schirmer Test
This is considered an integral part of the ophthalmological or E&M exam; separate reimbursement
for this test is not allowed.
Orthotic or Pleoptic Training: Non-covered
Color Vision Examination: Non-covered
Dark Adaptation Examination: Non-covered
Radial Keratotomy: Non-covered
Vision Screenings: Non-covered for those individuals aged 21 or over
Cardiology
Vascular Studies
Thermography is non-covered.
Dermatology
Services provided for cosmetic reasons are non-covered.
Physical Medicine and Therapy
Biofeedback therapy may be utilized as a modality of treatment, but it is not reimbursable
separately.
Hyperbaric Oxygen Therapy
No program payment may be made for HBO in the treatment of the following conditions:
• Cutaneous, decubitus and stasis ulcers
• Chronic peripheral vascular insufficiency
• Anaerobic septicemia and infection other than clostridial

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
149
• Skin burns (thermal)
• Senility
• Myocardial infarction
• Cardiogenic shock
• Sickle cell crisis
• Acute thermal and chemical pulmonary damage (i.e., smoke inhalation with pulmonary
insufficiency)
• Acute or chronic cerebral vascular insufficiency
• Hepatic necrosis
• Aerobic septicemia
• Non-vascular causes of chronic brain syndrome (Pick’s disease, Alzheimer’s disease,
Korsakoff’s disease)
• Tetanus
• Systemic aerobic infection
• Organ transplantation
• Organ storage
• Pulmonary emphysema
• Exceptional blood loss anemia
• MS
• Arthritic disease
• Acute cerebral edema
Topical Application of Oxygen
This method of administering oxygen does not meet the definition of HBO therapy as stated above.
Also, its clinical efficacy has not been established. Therefore, no reimbursement is allowed for the
topical application of oxygen.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
150
General Surgery Guidelines
Certain surgical procedures are routinely not covered. These non-covered procedures typically fall
into one of the following categories:
• Do not restore a bodily function.
• Are performed for cosmetic reasons.
• Have an alternative non-operative treatment.
• Frequently are performed for less than adequate diagnostic indications.
• Are not proven effective.
• Are experimental/investigational in nature.
• Are for the convenience of the patient.
No reimbursement will be made for subsequent procedures that do not add significantly to the
complexity of the major surgery or are rendered incidentally and performed at the same time as the
major surgery (e.g., incidental appendectomies, incidental scar excisions, puncture of ovarian cysts,
simple lysis of adhesions, simple repair of hiatal hernias).
Surgical Guidelines for Specific Systems
Integumentary System
Lesion Removal
Medicaid will not provide coverage for excision/treatment of non-malignant dermal lesions and
dermal anomalies under the following circumstances:
• The treatment is performed for cosmetic or emotional purposes.
• The therapy is experimental or investigational.
Cosmetic Procedures
Cosmetic surgery or expenses incurred in connection with such services are non-covered. Cosmetic
surgery includes any surgical procedure directed at improving appearance, except when required
for the prompt repair of accidental injury (i.e., as soon as medically feasible), or for the improvement
of the functioning of a malformed body member. This exclusion does not apply to surgery for
therapeutic purposes which coincidentally also serves some cosmetic purposes.
Cosmetic otoplasty is not covered under normal circumstances. Payment will be considered for
otoplasty procedures for children under 21, but only if there is documented evidence of
psychological trauma because of their appearance. A psychiatric evaluation performed by a
psychiatrist recommending treatment, plus pertinent medical documentation, must be attached to

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
151
the claim. Lack of, or insufficient documentation will result in a rejected claim. All otoplastic
procedures must be preauthorized by the QIO contractor.
Repair of the following birth defects is not considered cosmetic surgery: cleft lip, cleft palate,
clubfoot, webbed fingers and toes, congenital ptosis, and other birth defects which impair bodily
functions.
Male Genital System
Routine newborn circumcisions are covered services for beneficiaries 28 days and younger without
the necessity for prior approval.
Anesthesia Services
The following CPT modifiers are non-covered:
P1 — A normal healthy patient
P2 — A patient with mild systemic disease
P3 — A patient with severe systemic disease
P4 — A patient with severe systemic disease that is a constant threat to life
P5 — A moribund patient who is not expected to survive without the operation
P6 — A declared brain-dead patient whose organs are being removed for donor purposes
These risk factor codes are non-covered.
Pain Management Services
There is no reimbursement to physicians or CRNAs for the set-up or subsequent daily management
of patient-controlled analgesia pumps. Behavioral modification, PT, psychiatric services, and related
services are also non-compensable as pain management or pain therapy services.
Pathology and Laboratory Services
Clinical Laboratory Improvement Amendments (CLIA)
The following codes are non-covered:
• Ovulation tests by visual color comparison methods for human luteinizing hormone.
• Fern test.
• Post-coital direct, qualitative examinations of vaginal or cervical mucous.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
152
4
UTILIZATION MANAGEMENT
PRIOR AUTHORIZATION
Pre- and Post-Payment Review
All Medicaid claims, including claims for surgery, are paid through an automated claims processing
system. These claims are subject to pre-payment edits and may require documentation. If a
pre-payment edit is received, providers must file a new claim and submit documentation to support
medical necessity.
Post-payment reviews are conducted regarding utilization, appropriateness, medical necessity and
other factors.
All claims and reimbursements are subject to post-payment monitoring and recoupment if review
indicates a claim was paid inappropriately or incorrectly. Providers are required to maintain and
disclose their records consistent with the Provider Administrative and Billing Manual.
SCDHHS reserves the right to request medical records at any time for purposes of medical
justification and/or review of billing practices.
Utilization Review Services
SCDHHS contracts for utilization review services with the current QIO contractor.
The QIO review consists of:
• Pre-surgical justification for all hysterectomies.
• Select preauthorization review.
• Support documentation review.
• A retrospective review of a sample of paid inpatient/OP hospital claims.
• Select project studies as determined by SCDHHS.
Screening criteria may be obtained upon request from QIO. Any questions or concerns should be
directed to QIO customer service at +1 855 326 5219 or emailed to: [email protected]om.
Please be advised that a beneficiary may not contact QIO directly.
Telephone or written approval from the QIO is not a guarantee of Medicaid payment. All cases will
be subject to retrospective review to validate the medical record documentation.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
153
SCDHHS reserves the right to review retrospectively any case that has received prior approval to
assure accuracy and compliance with South Carolina Medicaid guidelines and federal requirements.
Instructions for Obtaining Prior Approval
The responsibility for obtaining pre-admission/pre-procedure review rests with the attending
physician. The physician must submit all necessary documents, including the Request for Prior
Approval Review Form, to QIO.
Requests for prior authorizations from QIO may be submitted using one of the following methods:
QIO Customer Service: +1 855 326 5219
QIO Fax: +1 855 300 0082
Provider Issues Email: atrez[email protected]
Unless otherwise stated within SCDHHS policy or procedure, if the beneficiary has a primary
coverage through Medicare or any other private health insurance, prior authorization by QIO is not
required. The QIO reviewer will screen the medical information provided, using appropriate QIO or
InterQual criteria for non-physician review.
If criteria are met, the procedure will be approved, and an authorization number assigned.
Notification of the approval and authorization number will be given by written confirmation to the
physician. Write this number in block 23 of the CMS-1500 claim form.
If criteria are not met, or a case is otherwise questioned, the QIO reviewer will refer the procedure
request to a physician reviewer. If the physician reviewer cannot approve the admission/procedure
based on the initial information provided, he or she will make a reasonable effort to contact the
attending physician for additional supporting documentation of the need for the procedure.
The physician reviewer will document any additional information provided, as well as his/her
decision regarding the medical necessity and appropriateness of the procedure.
Review personnel will assign an authorization number (if the procedure is approved), and a written
copy of the authorization number will be sent to the physician.
If the physician reviewer cannot approve the procedure based on the additional information, he or
she will document the reasons for the decision. QIO review personnel will attempt to notify the
attending physician’s office of the denial.
QIO will verify all initial procedure denial decisions by issuing written notices to the attending
physician.
The attending physician may request a reconsideration of the initial denial decision by submitting a
written request outlining the rationale for recommending the procedure. Reconsideration may be

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
154
requested whether the case was pre-procedure or post-procedure reviewed. The request must be in
writing to QIO. If a case is denied upon reconsideration, the determination is final and binding upon
all parties (CFA 473.38).
Points of Emphasis for Prior Authorization
QIO will accept medical review documentation via facsimile, telephone or via their website.
Providers are responsible for verifying beneficiary eligibility prior to the prior authorization request
being submitted and again prior to performing a service. Eligibility and managed care enrollment
status may change during the time a request is submitted and approved and the actual date the
procedure is performed.
A prior authorization request for beneficiaries enrolled in a MCO must be handled by the MCO. If
you have any additional questions regarding the MCO you may contact the MCO’s Provider
Services department, or the Managed Care area at +1 803 898 4614. Contact information for the
MCOs is in the Managed Care Supplement.
Physician providers are responsible for providing the prior authorization number to any facility or
medical provider who will submit a Medicaid claim.
The hysterectomy policy has changed.
Quality Improvement Organization (QIO) Authorization
SCDHHS will allow for the review and prior authorization of additional mental health visits
(psychotherapy, family psychotherapy and group psychotherapy). The beneficiary’s physician must
request, in writing, prior authorization through SCDHHS to override the 12 allowable mental health
visits. The prior authorization request must be submitted to the SCDHHS designated QIO by faxing
the DHHS Mental Health Form (in the Forms section of the provider portal). The signature of the
physician making the request must be on the form. The prior authorization request must include
sufficient clinical information to determine the need for additional mental health visits. The physician
will be notified via QIO approval letter if the authorization request is approved, and prior
authorizations will only be indicated for a six-month period.
All requests must be sent to the current QIO using one of the following methods:
Fax: +1 855 300 0082
Web portal: http://scdhhs.kepro.com

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
155
Other QIO contact information:
Customer Service: +1 855 326 5219
Provider Issues Email: [email protected]
When an emergency arises and there is insufficient time to obtain prior approval, the treating
physician must prepare the required documentation and submit it for retrospective review. Claims
requiring retrospective review are still subject to timely filing guidelines.
Breast Cancer Susceptibility Gene 1 and 2 (BRCA)
Effective August 1, 2019, prior authorization must be obtained from QIO prior to initial or subsequent
BRCA testing. One or more of the NCCN Clinical Practice Guidelines in
Oncology — Genetic/Familial High-Risk Assessment: Breast and Ovarian criteria must be met.
A completed Hereditary Breast and Ovarian Cancer (HBOC) Genetic Testing Prior Authorization
Request Form must be submitted to QIO. The form must be completed in its entirety, signed and
dated by the referring provider. The provider’s signature submitted on the HBOC is their attestation,
to the best of their knowledge, that the information provided in the document is true, accurate and
complete.
The physician must indicate one of the following on the HBOC form:
• The request is for initial BRCA1 and BRCA2 testing.
• The request is for repeat BRCA1 and BRCA2 comprehensive sequencing testing for the
beneficiary because initial results are negative, or are not available, and large cell
rearrangement testing is necessary.
Hysterectomies
All hysterectomies must be preauthorized by QIO except for those being performed on patients that
are dually eligible for Medicare and Medicaid. (Please refer to Utilization Review Services within this
section of the manual for more information.) All prior approval requests for hysterectomies must be
in writing. The South Carolina Medicaid Surgical Justification Form and the Consent for Sterilization
(DHHS 687) must be completed and submitted to QIO. The forms are available on the provider
portal; both forms must be submitted at least 30 days prior to the scheduled surgery to QIO via
facsimile at +1 855 300 0082.
InterQual criteria will be used to for screening prior authorization request. In addition to meeting
InterQual criteria a hysterectomy must be medically necessary and meet the following requirements:
• The individual or her representative, if any, must be informed orally and in writing that the
hysterectomy will render the individual permanently incapable of reproducing.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
156
• The individual or her representative, if any, must sign and date the acknowledgement of receipt
of hysterectomy information (DHHS Form 1729) prior to the hysterectomy.
Requests for prior authorizations must be submitted before the service is rendered. Exceptions to
this policy include emergency, urgent case or retroactive eligibility. Emergency or urgent cases must
also be submitted for approval before the claim is sent for processing.
Prior authorization, support documentation, quality assurance and quality care inquires must be
submitted to QIO using one of the following methods:
QIO Customer Service: +1 855 326 5219
QIO Fax: +1 855 300 0082
Provider Issues Email: atrez[email protected]
QIO urgent and emergent hysterectomy cases will be reviewed retrospectively. Please refer to
Special Coverage Issues in this manual for additional Medicaid policies for hysterectomies. Cases
that do not meet the QIO criteria will be referred for physician review. The physician will use clinical
judgment to determine whether the proposed treatment was appropriate to the individual
circumstances of the referred case. Pre-approved cases will not be subject to retrospective review
by the QIO. However, SCDHHS reserves the right to review any paid claim and recoup payment
when medical necessity requirements are not met. The patient and physician shall make the final
decision as to whether to undergo surgery. Medicaid will not sponsor the hospital -related expenses
associated with the surgery if the QIO physician consultant determines that the proposed surgery is
not appropriate.
The Consent for Sterilization Form is not required if the individual was already sterile before the
surgery, or if the individual required a hysterectomy because of a life-threatening emergency in
which the physician determined that prior acknowledgement was not possible. In these
circumstances, a physician statement is required. The statement must indicate the cause of the
sterility or the diagnosis and description of the nature of the emergency.
Specialty Care Services
All services provided and billed are contingent upon medical necessity. SCDHHS reserves the right
to request documentation to substantiate medical necessity at any time.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
157
Certain procedures are always subject to medical review on a pre-payment basis. These
procedures are listed in their respective specialty areas in this manual. If a claim is denied for
reasons of "Not Medically Necessary”, the provider may request a reconsideration. The request
must be in writing and sent to the Division of Hospital Services at the following address:
SCDHHS
Division of Hospital Services
PO Box 8206
Columbia, SC 29202-8206
If the claim is denied a second time, the provider has the right to request an appeal within 30 days
of the notice of denial. The request for an appeal must be in writing and sent to the Division of
Appeals and Hearings at the following address:
SCDHHS
Division of Appeals and Hearings
PO Box 8206
Columbia, SC 29202-8206
If a hearing is necessary, a date will be arranged by the Division of Appeals and Hearings for the
appellant and SCDHHS to formally review the claim(s).
Medicaid contracts with our QIO contractor, for utilization review services and pre-payment
authorization of hysterectomies. Certain other procedures are subject to prior authorization through
the Division of Hospital Services. For specific details, please refer to the Provider Administrative and
Billing Manual.
Psychiatric and Counseling Services
Inpatient Admissions
SCDHHS will require prior authorization for all acute (general hospital) inpatient admissions. The
Medicaid QIO, will perform the review and will accept prior authorization review requests via:
Fax: +1 855 300 0082
Web Portal: http://scdhhs.kepro.com
QIO nurse reviewers will screen the medical information provided using InterQual criteria. It is the
responsibility of the attending physician to submit the Request for Prior Approval Review Form and
all current medical documents that support the medical necessity of the admission to QIO. If criteria
are met, the admission will be approved, and an authorization number assigned and faxed to the
requesting provider.
For emergent or urgent admissions, providers must contact QIO for authorization within
24 hours of the date of the admission.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
158
For admission to PRTF’s or inpatient psychiatric hospitals for beneficiaries under age 21, please
refer to the Psychiatric Hospital Services Provider Manual.
Gastroenterology
Panniculectomy
Prior authorization is needed and must be obtained by submitting documentation to QIO via fax,
email or website; InterQual criteria apply.
Physical and Medicine Therapy
Recipients aged 21 years and older who receive treatment services in one of the settings listed in
the covered services section under Physical and Medicine Therapy within this manual must be pre-
authorized by the QIO.
Medical documentation must be submitted to the QIO to justify the medical necessity for
rehabilitative therapy services. Documentation includes, but not limited to, patient medical history,
radiology, pharmacology records and letter of medical necessity which clearly indicates the medical
justification for the service being requested. Any requests sent without medical documentation will
be administratively denied. InterQual criteria will be used to make all determinations.
Patients with Medicare or any other payer are only required to obtain a prior authorization if
Medicare or the primary carrier denied the service, or the service is considered not covered.
SCDHHS will require prior authorization for rehabilitative therapy treatment for children when the
combined allowed 420 units have been met. The accumulative units will apply to any rehabilitative
therapy treatment delivered to a patient either in a practice setting or in an OP hospital clinic.
Requests for therapy services for children that exceed the combined 420 units of rehabilitative
therapy treatment services, must be submitted to QIO for authorization. The QIO will use InterQual’s
OP Rehabilitation criteria for medical necessity determinations. Requests for therapy services may
be submitted by the PCP, NP, PA, physical, occupational or speech therapist. but must follow the
guidelines outlined in the Rehabilitative Therapy and Audiological Services Provider Manual.
Surgical Guidelines for Specific Systems
Prior Authorization for Mammaplasty and Mastectomy and Reconstructive Procedures
Reduction mammaplasty and gynecomastia, mastectomy procedures must be preauthorized by QIO
using InterQual criteria. A Request for Prior Approval Form must be used when submitting a request
for these services. A sample copy of the Request for Prior Approval Form can be found in the Forms
section of the provider portal. The attending physician shall obtain prior authorization and submit all
necessary documentation to QIO.
The following policies must be followed for reduction mammaplasty and gynecomastia:
• Prior authorization is required for all ages.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
159
• Photographs must be submitted with all requests.
• Pathology/operative reports are no longer needed.
• QIO will conduct all reviews.
• Physicians are responsible for verifying beneficiary eligibility prior to the prior authorization
request being submitted.
• Physicians are responsible for providing the prior authorization number to any facility or medical
provider who will submit a Medicaid claim.
Reduction Mammaplasty
Reduction mammaplasty for large, pendulous breasts on a female may be considered medically
necessary when InterQual screening criteria are met. Prior authorization is required for all ages. A
claim is reviewed for medical necessity and must be submitted with the preoperative assessment
from the patient’s record.
Reconstructive Breast Surgery
Reimbursement is allowed for reconstructive breast surgery following a mastectomy performed for
the removal of cancer or for prompt repair of accidental injury. Prior authorization and/or support
documentation must be obtained. QIO is responsible for prior authorization and support
documentation requests; InterQual screening criteria applies.
Breast reconstruction done for cosmetic reasons is non-covered. Augmentation is non-covered
under all circumstances. Payment is made for special bras through the DME program for women
who have undergone any type of mastectomy.
Gynecomastia
Although unilateral or bilateral mastectomy in a male is rarely indicated, this procedure may be
allowed when medically necessary. Prior authorization must be obtained by the attending physician.
South Carolina Medicaid Request for Prior Approval Form and all necessary documentation must be
sent to QIO; InterQual screening criteria applies.
Male Gynecomastia
Repeat Male Gynecomastia may be considered when supporting documentation meets InterQual
screening criteria.
Male Genital System
Circumcisions to be performed for beneficiaries older than 28 days due to medical justification
require prior approval, which must be granted utilizing the Request for Prior Approval Review Form
found in the “Forms” section of the appendices section within the Provider Administrative and Billing
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
160
Manual. Support documentation must accompany the form and be faxed “Attention Circumcision
Review” to +1 803 255 8255. Cosmetic reconstruction of the penis is non-compensable without
medical justification. Prior approval must be granted by Medical Services Review before services
are considered for payment.
Penile implants are non-covered unless prior approval is obtained. Reimbursement will not be
allowed for penile prosthesis if the only reason is sexual dysfunction. The criteria for approval are
based on medical necessity. Examples would be chronic depression as a result of sexual
dysfunction or a paraplegic with decubitus problems who would benefit from better condom urine
drainage.
The following support documentation is required:
• Summary of psychiatric care.
• The medical condition that surgery is expected to improve.
• History and physical.
As with cosmetic reconstruction, prior approval must be granted by the QIO contractor. A complete
list of procedures requiring prior authorization is located on the provider portal.
Sterilization requirements are the same as for females. (Please refer to Elective Sterilization under
Obstetrics and Gynecology within this section of the manual.)
Organ Transplants and Transplant-Related Services
South Carolina Medicaid covers medically necessary and non-investigational/experimental organ
and tissue transplant and transplant-related services. SCDHHS will only support the referral of
patients for an evaluation to CMS-certified transplant centers. This will include certified facilities that
are contracted with SCDHHS as well as certified facilities that are located outside of the SCMSA
(more than 25 miles of the South Carolina borders). For a complete list of CMS-approved centers,
visit the CMS website at
https://www.cms.gov/Medicare/Provider-Enrollment-and-
Certification/CertificationandComplianc/Transplant.html
– Covered transplant services fall into two groups:
– Group I: includes corneal and kidney transplants for which coverage is applicable in all
medically necessary instances without restriction and without prior approval.
–
– Group II: includes pancreas, bone marrow, heart, liver, liver with small bowels, and lung
transplants when medically necessary and clinically acceptable. Coverage of these
transplants is limited to facilities within the geographic boundaries of South Carolina and
require prior approval. All authorization requests for pancreas, bone marrow, heart, liver,
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
161
liver with small bowel and lung transplants will be evaluated utilizing uniform professional
and administrative guidelines as to medical necessity.
The contracted Quality Improvement Organization (QIO) will be responsible for in-state or out of
state evaluations and transplant requests, the determination of medical necessity for the services for
members in the FFS program. The QIO will issue an authorization determination letter. The letter
will also contain an authorization number that must be entered in the prior authorization field of all
the UB-04 claim forms submitted for reimbursement.
Referral requests for organ transplants to both in-state and OOS centers must be submitted to QIO
before services are rendered.
Requests for prior authorizations from QIO may be submitted using one of the following methods:
QIO Customer Service: +1 855 326 5219
QIO Fax: +1 855 300 0082
Provider Issues Email: [email protected]
In addition to completing the Transplant Prior Authorization Request Form, the request must also
include a letter from the attending physician with the following patient information:
• The description of the type of transplant needed.
• The patient’s current medical status.
• The patient’s course of treatment.
• The name of the center to which the patient is being referred.
Upon approval, QIO will issue an authorization number to the requesting physician with instructions
for its use. The approval letter will serve as authorization for the following services:
– pre-transplant services (medically necessary services rendered in preparation for the
transplant within 72 hours prior to the transplant event/surgery),
– the transplant event (surgery and services rendered through discharge),
– post-transplant services (medically necessary services from discharge up to 90 days post
discharge).
The transplant authorization number must be included on all claims submitted for reimbursement.
The Transplant Prior Authorization Request Form can be found in the Forms section of the
Physicians Services Provider Manual webpage
.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
162
QIO reserves the right to make recommendations to the provider for services at a certified center
that has provided transplant services to Medicaid beneficiaries in the past. Please note that the
approval of a transplant evaluation does not guarantee the approval of the actual transplant.
Once the authorization letter is received, the provider must notify the beneficiary that if
transportation is needed, the beneficiary must contact the SCDHHS transportation broker in his or
her region.
Kidney Transplantation
Medicaid will reimburse for kidney transplants. Professional services, including the nephrectomy
and transplantation of the new organ, performed by a physician team, are reimbursed separately.
Inclusive charges are compensable for the services rendered on behalf of the Medicaid-eligible
beneficiary. Medicare coverage is primary, and Medicaid will only pay if Medicare benefits are either
not available or have been denied.
A Medicare denial of benefits must accompany the claim, and the patient must be End Stage Renal
Disease (ESRD) enrolled with Medicaid. (Please refer to “Nephrology and End Stage Renal Disease
Services” under “Specialty Care Services” in this section of the manual.)
Corneal Transplantation (Keratoplasty)
Corneal transplants are compensable. The reimbursement to the hospital includes all technical
services, including donor testing and preparation.
Professional services are compensable using the appropriate CPT codes 65710-65755. All general
surgery guidelines apply when billing for keratoplasty.
SCDHHS will cover the cost of the corneal tissue when a corneal transplant is performed in an ASC.
The ASC will be reimbursed for the transplant surgical procedure and the corneal tissue must be
submitted with the HCPCS procedure code V2785 (processing, preserving and transporting covered
tissue). ASC providers must attach a copy of the invoice reflecting the cost of the tissue along with
the claim to avoid delays in payment.
Transportation for Medicaid Beneficiaries Requiring Transplants
Transportation arrangement for transplants is coordinated through the transportation broker. Once
the authorization letter is received, the provider must notify the beneficiary that if transportation is
needed, the beneficiary must contact the SCDHHS transportation broker in his or her region.
For information on the transportation program, you may call the PSC at
+1 888 289 0709, or submit an online inquiry at Contact a Provider Representative | SCDHHS
Spinal Cord Neurostimulators
Neurostimulator now require prior authorization by the QIO. Please refer to the provider portal for a
complete list of procedures that require prior authorization. The implantation of spinal cord

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
163
neurostimulators will be covered for the treatment of severe and chronic pain. Implantation of this
device, related services and supplies, may be covered if InterQual criteria are met.
The implantation of the neurostimulator may be performed on an inpatient or OP basis according to
medical necessity.
Procedure codes 63650, 63655, or 63685 may be used to bill for the implantation.
Post-Payment Review
Post-payment review of pain management services will be conducted regularly, at which time
documentation of treatment and methods of resolving the source of the pain will be requested from
the provider.
Radiology and Nuclear Medicine
SCDHHS will include in post-payment reviews an assessment of providers’ compliance with the
following policies and payment rules. Post-payment reviews indicating unnecessary radiological
procedures and interpretations, or non-covered or unallowable services will result in recoupment of
any Medicaid payments.
• When both the ER physician and radiologist or cardiologist interpret an x-ray or EKG done in the
ER, payment will be made for the interpretation and report that directly contributes to the
diagnosis and treatment of the patient. The specialty of the physician rendering the service will
not be the primary factor considered. The interpretation billed by the cardiologist or radiologist is
payable if the interpretation is performed at the time of the diagnosis and treatment of the
patient. Separate payment to the hospital medical staff is not made for interpretations performed
solely for quality control and liability purposes under hospital policy.
• Reinterpretations, unordered images and second opinions are not reimbursable. Medical
necessity must be documented for additional or repeat procedures for the same DOS (i.e.,
additional images were needed, patient in congestive heart failure, catheter placement, etc.).
• CPT procedures are compensable if ordered by an attending/ordering physician and deemed
medically necessary for the diagnosis and treatment of the patient's condition.
• Routine chest x-rays without a diagnostic reason are not reimbursable.
• Radiological procedures performed as a screening mechanism, without a diagnostic reason for
justification, are non-covered.
• Separate consultative procedures are non-covered. SCDHHS will also use post-payment review
to determine adherence to correct coding to include:
– Correct use of modifiers.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
164
– Correct use of supervision and consultation codes when used in conjunction with a
radiological procedure.
– Use of unlisted procedure code.
– All other service and coverage requirements listed in this section.
The incorrect use of modifiers or coding which results in an over-payment or improper payment to
the provider will result in recovery of the over-payment and will result in a recovery action and/or
sanction.
OTHER SERVICE LIMITATIONS
Medical Necessity
Chiropractic Services
Medicaid will only pay for services that are medically necessary. The patient must have a significant
health problem in the form of a neuromusculoskeletal condition necessitating treatment.
Additionally, the manipulative services rendered must have a direct therapeutic relationship to the
patient’s condition. Spinal axis aches, strains, sprains, nerve pains and functional mechanical
disabilities of the spine are considered to provide therapeutic grounds for chiropractic manipulative
treatment (CMT). Most other non-spinal diseases and pathological disorders (e.g., rheumatoid
arthritis, muscular dystrophy, MS, pneumonia and emphysema) are not considered therapeutic
grounds for CMT.
Dermatology
Visits and treatments for dermatological services must be medically necessary. The patient’s record
must clearly document the condition and medical necessity.
EPSDT Services
Providers must obtain a prior authorization for all medically necessary non-State Plan EPSDT
services prior to service provision. Providers must submit documentation of medical necessity and
any additional information that will assist in the determination of service coverage.
Gastroenterology
Bariatric Surgery
Bariatric surgery is a covered service for members who meet InterQual guidelines for medical
necessity. Prior authorization is required for these procedures and must be requested from QIO.
Radiology and Nuclear Medicine
All radiology and diagnostic services must be medically necessary and directed to the diagnosis,
maintenance, improvement, and treatment of illness and/or disability. All providers must use ACR
best practice guidelines when determining the need for radiology services. The purpose of the
guidelines is to improve the quality of services to patients and to promote the safe and effective use
of diagnostic and therapeutic radiology. Therefore, the justification for any radiological treatment or

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
165
service will align with best practice guidelines and must be documented in the patient medical
record.
Medicaid requires that the attending/ordering physician must order all radiology services. The NPI of
the attending ordering physician must be present on the claim in order for Medicaid to reimburse for
services. The attending/ordering physician will be responsible for maintaining and/or providing
access to the required documentation, regardless of whether the radiology procedures were
provided in a hospital, OP facility, office, freestanding imaging center or mobile unit. As noted in the
Documentation Standards below, this information may be recorded in the patient medical chart,
nursing reports, radiology records, inpatient or OP medical information storage areas, or in the
electronic health record. Services rendered in a hospital setting must be adequately documented,
including the above-cited records by the physician, with corresponding records retained by the
hospital.
High-Tech Radiology
SCDHHS will review Medicaid reimbursements for high-cost diagnostic radiology procedures to
determine medical necessity. Claims received with duplicated diagnosis and services ordered by
multiple providers are not reimbursable and are not considered medically necessary. Physicians,
when referring patients to specialists for consultations, must send their patients with copies of films
and/or a portable device (thumb drive, CD).
Standards for Documenting Medical Necessity and Provision of Services
Failure to maintain documentation that follows the above referenced (ACR/Society of Interventional
Radiology [SIR]) guidelines, as well as failure to comply with other payment rules established by the
policies in this section, may result in a recovery action by SCDHHS and may result in provider
sanctions.
The following standards are taken from the ACR and SIR practice guidelines (http://www.sirweb.org
)
for the Reporting and Archiving of Interventional Radiology Procedures revised in 2009. The
guidelines must be followed when documenting medical necessity in the patient records. A medical
record consists of a patient’s medical information recorded in either written or electronic format. This
information may be recorded in the patient medical chart, nursing reports, radiology records,
inpatient or OP medical information storage areas. The medical record must include, as appropriate,
the following information:
• Documentation of pre-procedural inpatient and/or office consultation.
• Immediate pre-procedure note.
• Immediate post-procedure note.
• Final report.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
166
• Documentation of post-procedure inpatient and/or office contact.
Pre-Procedure Documentation
The pre-procedural documentation provides a baseline record of patient status and documents the
indication/justification for the procedure; it must be written in the chart before the procedure.
Pre-procedural documentation , as appropriate, depending on the complexity and/or clinical urgency
of the procedure, must include the following information:
• The plan for each procedure to be performed.
• Indication/justification for procedure and brief history.
• Findings of targeted physical examination.
• Relevant laboratory and other diagnostic findings.
• Risk stratification, such as the American Society of Anesthesiologists Physical Status
Classification.
• Documentation of informed consent (consistent with state and federal laws) or, in the case of an
emergency, that this was an emergency medical procedure.
Immediate Post-Procedure Note
Before a patient is transferred to the next level of care, an immediate post-procedure note, or a final
report must be completed and available. The immediate post-procedure note must include, as
appropriate:
• Diagnosis
• Procedure
• Physician
• Assistant
• Sedation
• Medications
• Findings
• Blood loss
• Specimen

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
167
It is not necessary for the listed items to be recorded in the order given above.
Final Report
A final report is required:
• To transmit procedural information to all members of the health care community who may
participate in subsequent care of the patient.
• For legal purposes.
• For reimbursement.
Specific information to be included in this report depends on the procedure. The following elements
are recommended, although all of them may not be applicable:
• Procedure
• Date
• Operator(s)
• Indication
• Method of anesthesia or sedation
• Procedure/technique: a technical description of the procedure. This information must include, as
appropriate, access site (and attempted access sites), guidance modalities,
catheters/guidewires/needles used, vessels or organs accessed technique, and hemostasis.
Each major vessel catheterized for imaging or intervention mustnnoted specifically.
• For inserted medical devices, appropriate identifying information such as the product name,
vendor and lot numbers.
• Medications, dosages, and route of administration, including any pre-medications and contrast
agents.
• Estimated radiation dose (fluoroscopy time if no other measurement is available)
• Findings and results
• Complications
• Conclusion

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
168
• Post-procedure disposition
Out-of-State (OOS) Services
South Carolina Medicaid Service Area
All services must be rendered within the SCMSA. The SCMSA is defined as South Carolina and
adjacent areas within 25 miles of its borders.
Treatment Rendered Outside the South Carolina Medical Service Area
The term SCMSA refers to South Carolina and areas in North Carolina and Georgia within 25 miles
of the South Carolina State border. Charlotte, Augusta and Savannah are considered within the
service area. Medicare/Medicaid beneficiaries do not require prior approval from Medicaid for
covered services from providers located within the SCMSA.
The South Carolina Medicaid Program will compensate medical providers outside the SCMSA in the
following situations:
• Emergency medical services for beneficiaries traveling outside the SCMSA whose health would
be endangered if care was postponed until their return to South Carolina. This includes all
pregnancy-related services and delivery.
• When a SCMSA physician certifies that needed services are not available within the SCMSA
and properly refers the beneficiary to an OOS provider.
Prior Approval
In all but emergency situations, the referring physician must request approval prior to the OOS
service. Referrals must be made to an OOS provider only when the procedure or service is not
available within the SCMSA. All available resources must have been considered and indicated in
the request to SCDHHS for the OOS referral. The referring physician is the one most aware of the
client’s medical history and needs and will best be able to justify the necessity for the OOS referral.
Prior to contacting SCDHHS, the referring physician must first contact any OOS provider who will
render a service to the client and inform them of the client’s medical status. The OOS provider must
confirm, in writing, that he or she will enroll in the South Carolina Medicaid program and will accept
Medicaid reimbursement as payment in full. The written confirmation must be submitted to SCDHHS
along with the completed Referral Request Form for OOS services.
The referring physician must complete the Referral Request for OOS Services Form. A sample copy
of the form can be found in the Forms section of the Provider Administrative and Billing Manual. The
written requests for OOS referral must include the following information:
• Beneficiary’s name and Medicaid number.
• DOS (state as “tentative” if unscheduled at the time of request).

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
169
• An explanation as to why you feel these services must be rendered OOS versus within the
SCMSA.
• Name, address, telephone and fax number of the OOS providers(s) who will render the medical
services. (For example, hospital and physicians(s) involved in that patient’s medical treatment.)
• A copy of the beneficiary’s medical records for the past year relating to the treatment of the
condition.
• Any experimental and/or investigational services identified by the referring physicians that are
sponsored under a research program or performed in only a few medical centers across the
United States.
SCDHHS reserves the right to determine, based on medical advisement, that the needed medical
services, or necessary supplementary resources, are more readily available in the other state.
SCDHHS will reject referrals for the following reasons:
• All information required on the referral form is not provided with the requested attached
documentation.
• The provider rendering the service(s) is not willing to enroll in South Carolina Medicaid and
adhere to the enrollment criteria.
• The provider rendering the service(s) will not accept the South Carolina Medicaid
reimbursement as payment in full.
To obtain approval for OOS referrals, the OOS coordinator can be reached by fax at
+1 803 255 8255, or by mail at:
Medicaid Claims Receipt
PO Box 1412
Columbia, SC 29202-1412
The referring physician is responsible for communicating with the OOS provider coordinating
services for the patient. Patients being referred OOS, as well as their escorts, can be provided
transportation when necessary. Transportation and any other assistance are only provided when
there are no other means available to the patient to meet the needs connected with OOS travel.
Adequate advance notice, as well as prior approval, is mandatory in order to make the necessary
travel arrangements. Providers may contact the PSC at +1 888 289 0709 or submit an online inquiry
at Contact a Provider Representative | SCDHHS
: for additional information.
When a beneficiary is in one of the Medicaid MCOs, the requests for OOS services must be
completed through the MCO. For assistance with authorizations for MCO-enrolled members,
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
170
providers must contact the MCO’s Provider Services department, or the Managed Care area at +1
803 898 4614. Contact information for the MCOs is in the Managed Care Supplement.
Exceptions to Prior Approval
Medicaid will accept and review for medical necessity OOS claims from medical providers who did
not seek any type of approval before filing their claim. However, experience has proven that these
providers put themselves at an otherwise avoidable risk of non-payment or delayed payment due to
the lack of knowledge of the South Carolina Medicaid claim filing policies and procedures.
Foster Children Residing Out of the SCMSA
The DSS will be responsible for all Medicaid-eligible foster children when they reside OOS. The
county case manager assigned to the case must assist with medical services. Prior approval is not
required for services rendered to foster children who live OOS; however, medical necessity remains
a requirement. The OOS coordinator must be contacted for two reasons:
1. The coordinator must determine whether the medical services can be reimbursed through the
Medicaid program or whether DSS will reimburse the medical provider.
2. If Medicaid can reimburse for the services, proper enrollment and billing information needs to be
sent to the medical providers involved.
Providers must contact the PSC at +1 888 289 0709 or submit an online inquiry at
Contact a
Provider Representative | SCDHHS for additional information.
Retroactive Eligibility
When retroactive eligibility for Medicaid is granted, the beneficiary is responsible for notifying the
medical provider that retroactive eligibility has been granted.
For additional information regarding retroactive eligibility, please refer to the Provider Administrative
and Billing Manual.
Dually Eligible Beneficiaries
When a beneficiary has both Medicare and Medicaid coverage, Medicare is considered the primary
payer. However, if the beneficiary does not have Part A benefits, medically necessary inpatient
hospital services will require approval.
In order to verify eligibility on Medicare/Medicaid patients, contact the PSC at +1 888 289 0709 or
submit an online inquiry at Contact a Provider Representative | SCDHHS
.
Ancillary and Other OOS Services
Other health care services are compensable under the South Carolina Medicaid OOS program. For
OOS referral questions, please contact the PSC, submit an online inquiry, or write to SCDHHS for
more information. For professional claims, providers must write to:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
171
Medicaid Claims Receipt
PO Box 1412
Columbia, SC 29202-1412
For institutional claims, providers must write to:
Medicaid Claims Receipt
PO Box 1458
Columbia, SC 29202-1458
Office/Outpatient Exams
Laboratory Services
If the provider only extracts the specimen to send to an outside independent laboratory or hospital
laboratory, then the physician cannot charge for the lab test. When the specimen is sent to the
independent lab or hospital lab, report the patient's Medicaid number and the lab will bill for their
service. The physician must send the specimen(s) to Medicaid-enrolled labs, or the beneficiary will
be responsible for the lab charges and must be informed prior to having the specimen taken.
A handling service is compensable to the physician if the specimen is collected by venipuncture or
catheterization. In addition, collection of Pap smears may be charged. Please refer to Initial OB
Exam within this section of the manual for handling service codes for Pap smears. Medicaid will not
reimburse for special handling of specimens using either procedure code 99000 or 99001.
X-Ray and EKG Services
Medicaid will reimburse only one provider for the interpretation of diagnostic x-rays and EKGs.
Reinterpretations, after a physician has interpreted and reported the test, are not allowed. Please
refer to Radiology within this section of the manual for guidelines and further details.
If an outside source performed the technical part of an x-ray or EKG, then the physician may bill
only the professional component.
Convenient Care Clinics
Preventative Services
The Medicaid program sponsors adult physical exams under the following guidelines:
• The exams are allowed once every two years per patient.
• The patient must be 21 years of age or older.
This exam may also be offered to patients with Medicare and Medicaid (dually eligible or qualified
Medicare beneficiary).
• A past history for a new patient or an interval history on an established patient.
• A generalized physical overview of the following organ systems:
o HEENT
o Lungs

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
172
o Abdomen
o Skin
o Breasts (female)
o External genitalia
o Heart
o Back
o Pelvic (female)
o Prostate (male)
o Rectal
o Brief neurological
o Brief muscular
o Brief skeletal
o Peripheral vascular
Family Planning Counseling must be offered if the patient is female within childbearing years or for
men. (An additional Family Planning code may be billed for this service when provided. Please refer
to Obstetrics and Gynecology within this section of the manual for the description of codes.)
The following lab procedures are included in the reimbursement for a physical:
• Hemoccult
• Urinalysis
• Blood Sugar
• Hemoglobin
Any other lab procedures, x-rays, etc., may be billed separately. Portions of the physical may be
omitted if not medically applicable to the patient’s condition or if the patient is not cooperative and
resists specific system examinations (despite encouragement by the physician, NP or office staff). A
note must be written in the record explaining why that part of the exam was omitted.
Note: College physicals, DOT physicals and administrative physicals are not covered services.
Family Planning Services
Not all Family Planning Services can be performed in all CCCs therefore, please review your
licensure and requirements from the SCLLR authority and SCDES.
Synagis® (Palivizumab) 90378
Medicaid covers the administration of Synagis® in accordance with the current ACIP
recommendations and current clinical guidelines published by the American Academy of Pediatrics
(AAP). The AAP guidelines are available at http://www.aap.org
.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
173
Prior approval is not required for up to six doses when given at least 30 days apart and meet the
most current guidelines of the AAP for Synagis® administration. Any dose over the limit of six or
administered outside the RSV season (as defined by the AAP) requires prior approval. If prior
approval is needed, please submit requests to:
South Carolina Department of Health and Human Services
Attention: Medical Review/Synagis® Program
PO Box 8206
Columbia, SC 29202-8206
Providers must use discretion in the administration of Synagis® to infants born between 32 and 35
weeks of gestation who do not have chronic lung disease (CLD). SCDHHS will not reimburse
providers for Synagis® administration to children in this age group that do not have two or more risk
factors listed in the AAP guidelines.
Ultrasounds
Additional ultrasounds may be approved if supporting documentation is attached to the claim clearly
indicating that the service provided is medically necessary. Examples of appropriate documentation
include ultrasound reports and patient clinical records and history. If the documentation is
insufficient or illegible, reimbursement for additional ultrasounds will be rejected. Claims for
obstetrical ultrasounds that exceed the defined limits will be reviewed by QIO for medical necessity.
For MFM specialists, there is no limit on the number of ultrasounds that can be submitted for
reimbursement. However, all ultrasounds provided by MFM specialists must have documentation to
support medical necessity in the patient’s medical record.
All ultrasound services that appear to fall outside of best practice guidelines are subject to
post-payment review by the Division of Program Integrity. Multiple gestations billed with CPT add-on
codes will be counted as one ultrasound if billed on the same claim with primary CPT codes.
Ultrasounds requested by the patient to determine the sex of the fetus or for other reasons are the
responsibility of the patient.
When ultrasounds are performed at the hospital, a 26 modifier is required if the physician provides
the interpretation. When the ultrasounds are performed in the office, no modifier is required if the
physician owns the equipment. The physician’s interpretation of the ultrasound must be documented
in the patient’s record.
No prior authorization is necessary for ultrasounds when performed within the guidelines as stated
in the CPT book. Repeat ultrasounds are allowed when medically necessary. The medical record
must substantiate the reason for the follow-up ultrasounds.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
174
Hyperbaric Oxygen Therapy
Reasonable Utilization Parameters
Reimbursement is allowed for HBO therapy when it is considered medically necessary. HBO
therapy must not be a replacement for other standard, successful therapeutic measures. Depending
on the response of the individual patient and the severity of the original problem, treatment may
range from less than one week to several months’ duration, with the average being two to four
weeks. The medical necessity for use of HBO for more than two months, regardless of the condition
of the patient, must be reviewed and documented before further reimbursement is requested.
Preventive Services
Preventive measures are defined as any routine service exam for adults or children when the
procedures are performed in the absence of an illness or complaint(s). Generally, the South
Carolina Medicaid program requires that a complaint or illness be recorded before a service is
compensable. The exceptions to this policy are the EPSDT program and the Healthy Adult Physical
Exam.
The EPSDT program provides preventive health services to Medicaid-eligible children from birth to
age 21 through periodic medical screenings. This includes the application of topical fluoride varnish
in a primary care setting. An EPSDT screening is considered an encounter. A screening and an
encounter code may not be billed on the same DOS. All EPSDT screenings must be billed using the
appropriate CPT codes (99381–99385 and 99391–99395). EPSDT screening must be billed at the
FQHC contract rate. For additional program policy information, please refer to the EPSDT heading
within this section of the manual.
The Medicaid program sponsors adult physical exams under the following guidelines:
• The exams are allowed once every two years per patient.
• The patient must be 21 years of age or older.
This encounter code may also be offered to dually eligible Medicare and Medicaid clients until
Medicare covers physicals. If a patient has both Medicare and Medicaid coverage, bill Medicaid
directly.
For additional program policy guidelines, please refer to Adult Physical Exams under Preventive
Care Services in this section.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
175
5
REPORTING/DOCUMENTATION
CO- S IGNATURES
Effective with dates of service on or after January 1, 2010, SCDHHS will discontinue the
requirement of the physician’s co-signature in a medical record when services are performed by the
following professionals:
• NP
• Certified Nurse-Midwife (CNM)
• Certified Nurse Specialist (CNS)
• PA
Delegated acts and protocols that outline the scope of practice guidelines for NP, CNM, CNS or PA
must be current and available in the personnel file of the supervised practitioner. Upon submission
of a claim, the rendering physician is attesting that the services were accurately and fully
documented in the medical record and that he or she assumes responsibility for the NP, CNM, CNS
or PA. The claim also confirms the provider has certified the medical necessity and reasonableness
for the service(s) submitted to Medicaid for payment.
This policy update does not supersede State Law as it relates to requirements for off-site practice
protocols that outlines when co-signatures are required for PAs. These requirements can be found
in Article 7 of the South Carolina Physician Assistants Practice Act section 40-47-955.
EVALUATION AND MANAGEMENT SERVICES RECORDS AND
DOCUMENTATION REQUIREMENTS
The appropriate medical documentation must appear in the patient's medical record to justify
medical necessity for the level of service reimbursed, including the illness, history, physical findings,
diagnosis and prescribed treatment. The record must reflect the level of service billed and must be
legible.
Nursing Home/Rest Home Facility Services
Progress notes are required in the patient’s record for all visits, including those performed to meet
the requirements of continued long-term care. The medical record must justify and reflect the level
of service billed. Nursing home visits are subject to post-payment review under the same Medicaid
guidelines as any other medical services.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
176
DOCUMENTATION OF THE TEACHING PHYSICIAN
Documentation for services must include a description of the presence and participation of the
teaching physician. The resident may document the encounter, to include a note that describes the
involvement of the teaching physician. The teaching physician’s signature is then adequate to
confirm agreement.
Documentation of an encounter by the teaching physician may reference portions of a medical
student’s notes. The combined entries of the medical student, resident, and teaching physician must
be adequate to substantiate the level of service required and billed. Documentation must include the
teaching physician’s signature for each encounter.
CONVENIENT CARE CLINICS
CCCs are required to send information regarding a service to the PCP by facsimile within 24 hours
of the visit and maintain confirmation of receipt of the facsimile in the patient’s file.
TELEHEALTH
Documentation in the medical records must be maintained at the referring and consulting locations
to substantiate the service provided. A request for a telehealth service from a referring provider and
the medical necessity for the telehealth service must be documented in the beneficiary’s medical
record. Documentation must indicate the services were rendered via telehealth. All applicable
documentation requirements for services delivered face-to-face also apply to services rendered via
telehealth. Examples may include but are not limited to the following based on provider specialty:
• The diagnosis and treatment plan resulting from the telehealth service and progress note by the
health care provider.
• The location of the referring site and consulting site.
• Documentation supporting the medical necessity of the telehealth service.
• Start and stop times.
OBSTETRICS AND GYNECOLOGY
Licensed Midwife
The following documentation must be maintained for all services provided by a Licensed Midwife:
• The midwife’s initial claim for prenatal services for each beneficiary must be accompanied by
signed documentation from a physician credentialed in obstetrics who agrees to provide medical
backup in the event of a complication or emergency.
• Documentation of the physician’s hospital privileges must be provided to SCDHHS.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
177
• Any changes in the physician back-up must be reported in writing to the Division of Physician
Services.
• The physician who agrees to provide back-up must be enrolled as a Medicaid provider.
The following additional documentation regarding the Licensed Midwife must be kept in the patient’s
medical record:
• A signed consent form that documents the beneficiary’s awareness that her choice of provider
can be made or changed at any point in the pregnancy.
• A certification statement provided to the physician by the midwife that the home is an acceptable
environment for a birth.
• A copy of the plan for accessing emergency care with a confirmed source of transportation to
the hospital provided to the beneficiary.
• Documentation that the beneficiary has been advised of Family Support Services available
through the SCDES.
Sterilization Consent Form
If the consent form is correctly completed and meets the federal regulations, the claim can be
approved for payment. If the consent form does not meet the federal regulations, the claim will be
rejected, and a letter sent to the physician explaining the rejection. If the consent form is not
submitted with the claim, the claim will be rejected. If the line is rejected, a new claim must be
submitted with the consent form. A sample copy of the consent form and instructions can be found
in the Forms section of the Administrative and Billing Manual.
Listed below is an explanation of each field that must be completed on the consent form and
whether it is a correctable error.
Consent to Sterilization
• Name of the physician or group scheduled to do the sterilization procedure. (If the physician or
group is unknown, put the phrase “OB on Call”): Correctable Error.
• Name of the sterilization procedure (e.g., bilateral tubal ligation): Correctable Error.
• Birth date of the beneficiary (The beneficiary must be 21 years old when he or she gives
consent by signing the consent form 30 days prior to the procedure being performed.):
Correctable Error.
• Beneficiary’s name (Name must match name on CMS-1500 form.): Correctable Error.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
178
• Name of the physician or group scheduled to perform the sterilization or the phrase “OB on call”:
Correctable Error.
• Name of the sterilization procedure: Correctable Error.
• Beneficiary’s signature. (If the beneficiary signs with an “X,” an explanation must accompany the
consent form.): non-correctable error.
• Date of signature: non-correctable error without detailed medical record documentation.
• Beneficiary’s Medicaid ID number (10 digits): Correctable Error.
Interpreter’s Statement
If the beneficiary had an interpreter translate the consent form information into a foreign language
(e.g., Spanish, French, etc.), the interpreter must complete this section. If an interpreter was not
necessary, put “N/A” in these fields: Correctable Error.
Statement of Person Obtaining Consent
• Beneficiary’s name: Correctable Error.
• Name of the sterilization procedure: Correctable Error.
• Signature and date of the person who counseled the beneficiary on the sterilization procedure:
This date must be the same date of the beneficiary’s signature date.
– Signature is not a correctable error.
– Date is not a correctable error without detailed medical record documentation.
– If the beneficiary signs with an “X”, an explanation must accompany the consent form: Not
a correctable error without detailed medical record documentation.
• A complete facility address: An address stamp is acceptable if legible.
Physicians Statement
• Beneficiary’s name: Correctable Error.
• Date of the sterilization procedure (This date must match the DOS that you are billing for on the
CMS-1500.): Correctable Error.
• Name of the sterilization procedure: Correctable Error.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
179
• Estimated Date of Confinement is required if sterilization is performed within the 30-day waiting
period and the beneficiary was pregnant. At least 72 hours are required to pass before the
sterilization procedure may be done: Correctable Error.
• An explanation must be attached if emergency abdominal surgery was performed within the
30-day waiting period. At least 72 hours are required to pass before the sterilization, and the
sterilization procedure may not be the reason for the emergency surgery.
• Physician signature and date: a physician’s stamp is acceptable. The rendering or attending
physician must sign the consent form and bill for the service. The physician’s date must be
dated the same as the sterilization date or after.
The date is not a correctable error if the date is prior to the sterilization without detailed medical
record documentation. In the license number field, put the rendering physician’s Medicaid Provider
ID or NPI number (the same number that is in block 33 on the CMS-1500 claim form). Either the
group or individual Medicaid Provider ID or NPI is acceptable.
PSYCHIATRIC AND COUNSELING SERVICES
Clinical Records
Providers must maintain a clinical record for each Medicaid eligible beneficiary receiving services
that fully describes the extent of the treatment services provided. The clinical record must contain
sufficient medical documentation to justify medical necessity for the level of service reimbursed and
clearly specify the course of treatment. The absence of appropriate and complete records may
result in recoupment of previous payments by SCDHHS. Each beneficiary’s clinical record must
contain the following documentation:
• Full demographic information, including beneficiary’s full name, contact information, date of
birth, race, gender and admission date.
• Consent forms, pertinent medical history, assessments and instructions to the beneficiary.
• All physician’s orders, reports of treatments and medications, and other pertinent information
necessary to monitor the beneficiary’s progress.
• Reports of physical examinations, diagnostic and laboratory results and consultative findings.
• Documentation of communication regarding coordination of care activities.
• The beneficiary’s name on each page generated by the provider.
• The beneficiary’s Medicaid number on all clinical documentation and billing records.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
180
Clinical Service Notes
All psychiatric and psychotherapy services must be documented in a clinical service note (CSN)
upon the delivery of services. The purpose of the CSN is to record the nature of the beneficiary’s
treatment, any changes in treatment, discharge, crisis interventions and any changes in medical,
behavioral or psychiatric status. The CSN must include:
• DOS
• Name of the service provided
• Place of service
• Purpose of the contact (for psychotherapy notes, this must be tied back to the IPOC treatment
goals)
• Description of treatment or interventions performed
• Effectiveness of the intervention(s) and the beneficiary’s response or progress
• Duration of the service (start and end time for each service delivered)
• Signature, title, and signature date of the person responsible for the provision of services and
supervising clinician, if appropriate
CSN’s must be completed and placed in the clinical record within 10 business days from the date of
rendering the service.
Error Correction
Medical records are legal documents. Providers must be extremely cautious in making alterations to
records. If errors are made, adhere to the following guidelines:
• Draw one line through the error and write “error”, “ER”, “Mistaken Entry”, or “ME” to the side of
the error in parenthesis. Enter the correction, sign or initial and date it.
• Errors cannot be totally marked through, the information in error must remain legible.
• No correction fluid may be used.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
181
Late Entries
Late entries may be necessary at times to handle omissions in the documentation. Late entries must
be rarely used and then only used to correct a genuine error of omission or to add new information
that was not discovered until a later date. Whenever late entries are made, adhere to the following
guidelines:
• Identify the new entry as “late entry”.
• Enter the current date and time.
• Identify or refer to the date and incident for which the late entry is written.
• If the late entry is used to document an omission, validate the source of additional information as
much as possible.
• When using late entries, document as soon as possible.
TUBERCULOSIS (TB) POLICY
Documentation Requirements
All providers must keep documentation in the beneficiary’s medical record to justify medical
necessity for the level of service reimbursed, including history, illness, physical findings, diagnosis,
laboratory results, radiology results, and records on medications prescribed and delivered.
Providers must follow NCCI and coding rules and practices. All services are subject to retrospective
review by our Division of Program Integrity.
BREAST CANCER SUSCEPTIBILITY GENE 1 AND 2 (BRCA)
The following documentation must be maintained in the beneficiary’s medical record:
• The HBOC Genetic Testing Prior Authorization Form.
• Pre-testing genetic counseling clinical notes, to include but not limited to the following:
– Pre-test counseling date with the name and qualifications of the counseling professional.
– The risks, benefits and limitations discussed with the beneficiary.
– The beneficiary’s consent to proceed with specific gene mutation testing to be performed
as attested by the beneficiary’s signature on the consent form.
• The beneficiary’s BRCA test results.
• Post-testing genetic counseling clinical notes, to include, but not limited to, the following:
– Post-test counseling date with the name and qualifications of the counseling professional.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
182
– The beneficiary’s acknowledgment of the test results.
CHIROPRACTIC SERVICES
As a condition of participation in the South Carolina Medicaid program, providers are required to
maintain and allow appropriate access to clinical records that fully disclose the extent of services
provided to the Medicaid patient. The maintenance of adequate records is regarded as essential for
the delivery of appropriate services and quality medical care.
Providers must be aware that these records are key documents for post-payment review. In the
absence of appropriately completed clinical records, previous payments may be recovered by
SCDHHS. It is essential for the provider to conduct internal record reviews to ensure that services
are medically necessary, and that service delivery, documentation, and billing comply with Medicaid
policies and procedures.
Clinical Records
Providers are required to maintain a clinical record on each Medicaid patient that includes
documentation of all Medicaid-reimbursable services. This documentation must be sufficient to
justify Medicaid participation. Clinical records must be current and consistently organized, meet
documentation requirements, and provide a clear description of services rendered and progress
toward treatment goals. Clinical records must be arranged logically, so that information may be
easily reviewed, copied and audited.
Each Medicaid patient’s clinical record must include, at a minimum, the following:
• A Release of Information Form signed by the patient authorizing the release of any medical
information necessary to process Medicaid claims and requesting payment of government
benefits on behalf of the patient.
• The initial written physician prescription (original or fax) and documentation of subsequent
prescriptions required after every third visit.
• Patient history to include the following:
– A general patient history, including review of systems.
– Chief complaint/systems causing patient to seek chiropractic treatment.
– Onset and duration of symptomatic problem, which may include quality and character of
problem, intensity, frequency, location and radiation, onset, duration, aggravating or
relieving factors, prior interventions and treatments, including medications and secondary
complaints.
– Family history (if indicated).

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
183
– Past health history to include general health statement, prior illnesses, surgical history,
prior injuries or traumas, past hospitalizations, medications, allergies, and pregnancies and
outcomes.
• A physical examination report to include:
– Evaluation of the musculoskeletal and nervous system.
– Evaluation of the cardiovascular and gastrointestinal systems, and of the eye, ear, nose,
and throat (both vascular and endocrine), if appropriate to symptoms causing patient to
seek chiropractic treatment.
– Analytical procedures used to determine vertebral subluxation (level and severity) and
contraindications to treatment (e.g., inspection, palpation).
• Radiographic film (x-ray) and interpretation.
• A written report/assessment of the patient’s condition, including the precise area of subluxation.
• A treatment plan.
• CSNs.
Treatment Plan
If an evaluation indicates that treatment is warranted, the chiropractor must develop and maintain a
treatment plan that outlines short- and long-term goals, as well as the recommended scope,
frequency and duration of treatment. The treatment plan must serve as a comprehensive plan of
care by outlining the service delivery that will address the specific needs of the patient. The
treatment plan must be individualized and must specify the problems to be addressed, goals and
objectives of treatment, types of interventions to be utilized, planned frequency of service delivery,
criteria for achievement, and estimated duration of treatment. The treatment plan must contain the
signature and title of the chiropractor and the date signed.
The individualized treatment plan must be reviewed and updated according to the level of progress.
If a determination is made during treatment that additional services are required, these services
must be added to the treatment plan. When long-term treatment is required, a new treatment plan
must be developed each year. If services are discontinued, the chiropractor must ensure that the
reason for discontinuing treatment is indicated in the treatment plan.
Clinical Service Notes
Chiropractic services must be documented by CSNs. A CSN is a written summary of each treatment
session. The purpose of these notes is to record the nature of the patient’s treatment by recording
the service provided and summarizing the patient’s participation in treatment.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
184
CSNs must do the following:
• Furnish a pertinent clinical description of the activities that took place during the session,
including an indication of the patient’s response to treatment as related to stated goals and
objectives.
• Reflect delivery of a specific billable service as identified in the patient’s treatment plan.
• Document that the services rendered correspond to billing as to DOS, type of service rendered,
and length of time-of-service delivery.
Error Correction Procedures
The patient’s clinical record is a legal document; therefore, extreme caution must be used when
altering any part of this record. Appropriate error correction procedures must be followed when
correcting an error in the patient’s clinical record.
Errors in documentation must never be totally eradicated, and correction fluid must never be used.
Draw one line through the error, enter the correction, and add signature (or initials) and date next to
the correction. If warranted, an explanation of the correction may be appropriate. In extreme
circumstances, having the corrected notation witnessed may be appropriate.
X-Rays
The documenting radiographic film (x-ray) must have been taken at a time reasonably proximate to
the initiation of the course of treatment. Unless the chiropractor concludes that more specific X-ray
evidence is warranted, an X-ray is considered reasonably proximate if it was taken no more than six
months prior to the initiation of a course of chiropractic treatment. Neither an MRI nor CAT scan
may be used instead of an X-ray to document subluxation.
The x-ray is required Medicaid documentation and must be maintained in the patient’s medical
record. X-ray films must have permanent identification of the patient’s name, the date the film was
taken, and the name of the facility where taken. Films must be marked right or left side. If the x-ray
was taken elsewhere (e.g., doctor’s office or other medical facility), the written report must be
present in the patient’s medical record.
P AIN M ANAGEMENT S ERVICES
Patient records must indicate medical necessity and are subject to post-payment review.
Documentation in the record must indicate the treatment process, which includes the service(s) to
be provided, diagnostic procedures and treatment goals. Goals must be specific according to patient
needs and the services to be rendered.
Progress summaries must be documented at a minimum of every three months. The summaries
must address the patient's progress toward treatment goals, appropriateness of services rendered
and recommendations for the continued need for services.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
185
6
BILLING GUIDANCE
SERVICES OUTSIDE OF THE COUNTRY
Medicaid will not provide any payments for items or services provided under the State Plan or under
a waiver to any financial institution or entity located outside of the United States.
DIRECT PHYSICIAN SUPERVISION
For Medicaid billing purposes, direct supervision means that the supervising physician is accessible
when the services being billed are provided, and the supervising physician is responsible for all
services rendered, fees charged, and reimbursements received.
PHYSICIAN’S OFFICE W ITHIN AN INSTITUTION
When a physician establishes an office within a nursing home, hospital or other institution, coverage
of services and supplies furnished in the office must be determined in accordance with the “incident
to a physician’s professional services” criteria as determined by federal regulations. A physician’s
office within an institution must be confined to a separately identified part of the facility that is used
solely as the physician’s office and cannot be construed to extend throughout the entire institution.
Thus, services performed outside the “office” area will be subject to coverage rules applicable to
services furnished outside the office setting (i.e., a TC that is included in the institutional
reimbursement).
Consideration must be given to the physical proximity of the institution and the physician’s office.
When his or her office is located within a facility, a physician may not be reimbursed for services,
supplies, or use of equipment that falls outside the scope of services “commonly furnished” in
physician’s offices. Additionally, a distinction must be made between the physician’s office practice
and the institution, especially when the physician is the administrator or owner of the facility. Thus,
for their services to be covered, the auxiliary medical personnel must be members of the office staff
rather than of the institution’s staff, and the cost of supplies must represent an expense of the
physician’s office practice. Finally, the physician must directly supervise services performed by the
employees of the physician outside the “office” area; his or her presence in the facility as a whole is
not sufficient.
PHYSICIAN ADMINISTERED DRUGS
National Drug Code (NDC) Billing Requirements for Drug-Related HCPCS Codes
Medicaid requires providers billing for physician-administered drugs in an office, a clinic, or other OP
setting to report the NDC when using a drug-related HCPCS code. The HCPCS code must include
the correct NDC 5-4-2 format (11 digits total) to receive reimbursement from Medicaid. The NDC
must be used on all claim submissions (e.g., electronic, Web Tool and CMS-1500).
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
186
Additionally, providers must implement a process to record and maintain the NDC(s) of the drug(s)
administered to the beneficiary as well as the quantity of the drug(s) given.
Billing Unlisted/Not Otherwise Specified HCPCS Codes
In addition to documentation detailing the drug that was administered and the medical necessity,
providers must also include the product’s 11-digit NDC. The claim will suspend for review. Please
note that the drug-related procedure code is not payable if the 11-digit NDC is omitted.
NDC Not Found on the NDC to HCPCS Crosswalk
For a drug-related HCPCS code to be reimbursable by SCDHHS, the manufacturer of the drug must
participate in the Federal Drug Rebate program. To determine whether the pharmaceutical
manufacturer participates in the rebate program, please visit the following website for the
NDC/HCPCS crosswalk at
https://www.cms.gov/medicare/medicare-part-b-drug-average-sales-
price/2020-asp-drug-pricing-files.
The first five digits of the NDC identify the manufacturer of the product. Prescribers must use the
crosswalk and the criteria below to determine if the drug is reimbursable by SCDHHS:
• If the first five digits of the 11-digit NDC are listed on the crosswalk, the manufacturer
participates in the rebate program and the claim must be submitted to Medicaid. The claim will
suspend for review.
• If the first five digits of the 11-digit NDC are not on the crosswalk, the manufacturer does not
participate in the rebate program. South Carolina Medicaid does not provide coverage of
non-rebated drugs.
Please refer to the Provider Administrative and Billing Manual for information and instructions for
claims submission.
TEACHING PHYSICIAN POLICY BILLING REQUIREMENTS
Services provided by residents under the direct supervision of a teaching physician are billable to
Medicaid. For Medicaid billing purposes, direct supervision means that the teaching physician is
accessible, as defined in Subsection I, when the resident provides the services being billed. The
teaching physician is responsible for all services rendered, fees charged, and reimbursements
received. The services must be documented, as defined in Subsection II, in the patient’s medical
record. The supervising physician must sign the patient’s medical record, indicating that he or she
accepts responsibility for the services rendered.
For the purpose of the policy, the following definitions apply:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
187
• Resident: A resident is an individual who participates in an approved graduate medical
education (GME) program, or a physician who is not in an approved GME program but who is
authorized to practice only in a hospital setting. The term includes interns and fellows in GME
programs recognized as approved for purposes of direct GME payments made by the fiscal
intermediary.
• Medical Student: A medical student is an individual who is enrolled in a program culminating in
a degree in medicine. Any contribution of a medical student to the performance of a billable
service or procedure must be performed in the physical presence of a teaching physician or
jointly with a resident while providing a service meeting the requirements set forth for teaching
physician billing.
• Teaching Physician: A teaching physician is an individual who, while functioning under the
authority and responsibility of a resident program director, involves resident and/or medical
students in the care of his or her patients or supervises residents in the care of patients.
FEE- FOR- TIME COMPENSATION ARRANGEMENTS
Physicians may retain a substitute physician to take over their professional practice for reasons
such as pregnancy, illness, or continuing medical education. Physicians are able to bill and receive
payment for services provided by the substitute physician and then pay the substitute physician
under a fee-for-time compensation arrangement. The substitute physician serves as an independent
contractor rather than an employee.
The following requirements must be met:
• The regular physician is unavailable to provide services.
• The substitute physician must meet the same licensing requirements as required by Medicaid;
however, Medicaid enrollment is not required.
• The beneficiary has arranged or seeks to receive services from the regular physician.
• The regular physician pays the substitute physician for services provided.
• The substitute physician shall not provide services to beneficiaries over a continuous period of
longer than 60 days subject to the following exception:
o The regular physician is called to active duty in the Armed Forces.
• The regular physician indicates services were provided by a substitute physician under a fee-for
time compensation arrangement by entering HCPCS code modifier Q6 (service furnished under a
fee-for-time compensation arrangement) after the procedure code.
If the only services a physician performs in connection with an operation are post-operative services
furnished during the period covered by the global fee, these services do not need to be identified on
the claim as services furnished by a substitute physician.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
188
The regular physician must keep on file a record of each service provided by the substitute
physician and make this record available to Medicaid upon request. Covered visit services include
those services ordinarily characterized as a covered physician visit, as well as any other covered
items and services furnished by the substitute physician or by others as incident to the physician
services.
EVALUATION AND MANAGEMENT SERVICES
Convenient Care Clinics
CCCs must bill Medicaid using Place of Service Code 17 as defined by the AMA’s CPT for a
walk-in, retail health clinic. Covered services for this place of service are limited to Episodic Care
and wellness/preventative services. Wellness/preventative services are covered for recipients five
years and older.
Family Planning Services Referral and Billing
Family Planning beneficiaries have Medicaid coverage for a limited set of medical services.
Beneficiaries enrolled in Family Planning are covered for preventive physical examinations and
preventive health screenings, but do not have full Medicaid coverage for follow-up visits, treatment
or medication (apart from those specifically outlined in the benefit structure).
If a health condition or problem is identified during the physical examination or after the provider
receives lab results from a preventive screening that was performed, the provider must refer the
patient to a source of free or subsidized care. SCDHHS strongly encourages providers to connect
uninsured Family Planning beneficiaries to sources of care such as FQHCs, RHCs, free clinics,
subsidized hospital clinics, etc. Providers will be compensated for the administrative costs
associated with making referrals for Family Planning beneficiaries.
For more information about where to refer Family Planning patients for follow-up care, please visit
the South Carolina Primary Health Care Association website, https://www.scphca.org/
or contact the
SCDHHS PSC at +1 888 289 0709.
Instructions
Providers that refer uninsured Family Planning beneficiaries for follow-up care or treatment for a
problem or condition identified during the physical examination or annual family planning visit can
bill for this referral activity. Providers must use the procedural coding and modifiers listed below.
These referral codes may only be used in instances when the follow-up care is not covered as a
component of the Family Planning Program.
Note: At least one of the modifiers listed below is required when billing for referral codes.
Note: Providers must NOT use the FP modifier when billing for referral codes.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
189
Providers that refer uninsured Family Planning patients for follow-up care or treatment for any health
issue identified during or after (lab results) the physical examination or annual family planning visit
may bill for this referral activity using one of the following referral codes:
• Same Day Referral or Telephone Referral: Utilized when a patient is referred to follow-up care
immediately after the physical exam or family planning visit OR if lab results are received after
the physical exam or family planning visit, and a) results can be explained to the patient by
phone and b) referral to follow-up care can occur by phone.
• Different Day Referral (In-Person): Utilized when a patient is required to receive lab results
in-person, on a different day than the physical exam or family planning visit occurs.
Billing Instructions
• Providers may include Same Day Referral or Telephone Referral on the same claim form as the
physical examination or annual family planning visit.
• Providers may bill for the Same Day Referral or Telephone Referral on a separate claim form. If
submitting a separate claim form, diagnosis code Z00.00 or Z00.01 must be used.
• Providers must bill for the in-person, Face-to-Face Referral on a separate claim form. Diagnosis
code Z00.00 or Z00.01 must be used.
• Providers must include at least one modifier and up to four modifiers from the list below when
billing for both referral codes.
Modifier Instructions
Providers must use the appropriate modifier from the list below. Up to four modifiers can be used for
each referral code (e.g., if a patient is referred to follow-up care for more than one positive
screening, include modifiers for all positive screenings):
• If referring a patient for a positive diabetes screen, use modifier P1.
• If referring a patient for a positive cardiovascular screen, use modifier P2.
• If referring a patient for any positive cancer screen, use modifier P3.
• If referring a patient for any mental or behavioral health screens, use modifier P4.
• If referring a patient for any other condition or problem, use modifier P5.
Referral Instructions for Family Planning Providers who do offer free or subsidized care to
uninsured individuals (e.g., FQHCs, hybrid clinics, RHCs, subsidized hospital clinics, etc.).

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
190
Providers that offer free or subsidized care to uninsured individuals must schedule follow-up visits
with Family Planning beneficiaries when a problem or condition is identified during or after the
physical examination or family planning visit. This “self-referral” activity is captured in the encounter
rate for the physical examination or family planning visit. However, for data collection and monitoring
purposes, providers who fall into this category must include the referral code and appropriate
modifiers listed above as a separate line on the Encounter Claim Form (these codes will bill to
$0.00). The referral codes and accompanying modifiers will provide important data to SCDHHS
regarding the utilization of follow-up care among the Family Planning population.
Note: Uninsured Family Planning patients will be responsible for any fees associated with follow-up
visits. As Family Planning beneficiaries are considered uninsured for purposes of follow-up care, all
visits must follow the provider’s established policies and procedures for treating uninsured patients.
Referral Instructions for Family Planning Providers who refer patients for additional, preventive
screenings
• If you are a provider that performs a physical examination for a Family Planning beneficiary and
are unable to perform certain preventive health screenings (e.g., include mammography,
colonoscopy, AAA screening, and lung cancer screening using computerized tomography), you
must refer the patient to a provider who is able to perform these screenings.
• Providers are not allowed to submit a referral claim for this type of referral.
Office/Outpatient Exams
After Hour Services
Primary Care Providers (Pediatrician’s, Family Practice, General Practice, Internal Medicine and
OB/GYN) may bill the E&M code that best describes the level of service being rendered.
• Services provided in the office at times other than regularly scheduled office hours or days when
the office is normally closed (i.e., holidays, Saturday or Sunday), in addition to basic service.
• Service provided in the office during regularly scheduled evening, weekend, or holiday office
hours, in addition to basic service.
The purpose of this coverage is to encourage expanded office hours. SCDHHS defines CPT code
99050 to mean all patients scheduled outside published business hours; this would not include a
visit that was scheduled at 4:00 pm and the patient was not seen by the physician until 6:30 pm. For
CPT code, SCDHHS defines evening hours to be any time after 6:00 pm and before 8:00 am.
Weekends are defined as Saturday 8:00 am to Monday 8:00 am. Providers may only bill for the
following holidays, the day of New Year’s, Independence, Labor, Thanksgiving and Christmas.
Holidays are defined as 8:00 am the morning of the holiday, until 8:00 am the following morning.
After-hours procedure codes are not covered when the service is provided in a hospital emergency
department, an inpatient setting, OP setting or an urgent care facility (place of service codes 20, 21,

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
191
22 and 23). All claims submission could be subject to review by the Department of Program
Integrity.
Additional Ambulatory Services
Services commonly rendered in addition to an office exam are compensable if medically necessary.
Diagnostic procedures such as lab and x-ray are compensable as separate charges.
Laboratory Services
Diagnostic lab services are compensable as separate charges when the provider renders the
service and CMS’s CLIA certification standards are met. The appropriate lab service must be used.
Special Services/Visits
Post-Operative Follow-up Visit
This service is non-compensable. Please refer to surgical package guidelines under General
Surgery Guidelines within this section of the manual.
Emergency Office Services
Services may be billed in addition to the appropriate level office E&M code when office services are
provided on an emergency basis (after posted office hours).
Supplies
Supplies are reimbursable when provided in the physician's office using the following list of
procedure codes only. All other supplies are reimbursable through DME providers only.
Major Surgical Tray — Reimbursement may be allowed for a surgical tray when minor surgery is
performed in a physician’s office that necessitates local anesthesia and other supplies (i.e., gauze,
sterile equipment, suturing material, etc.). If the procedure code description includes anesthesia,
only the minor surgical tray can be billed. When a major surgical tray is used, local anesthesia
cannot be billed separately. Reimbursement will not be provided when a hospital OP department or
SNF supplies the tray.
To report, use the appropriate supplemental procedure code for a major surgical tray. A major
surgical tray may not be charged for a suture removal tray.
Minor Surgical Tray — A minor surgical tray includes those trays necessary for suture removal,
minor debridement, superficial foreign body removal, or incision and drainage of superficial abscess.
Small Supplies and Materials — Used to bill for supplies provided by the physician (except
spectacles), which are over and above those usually included with the office visit or other services
rendered. This can be used when a starter dose of a one-to-three-day supply purchased by the
physician is given to assist in the diagnostic or treatment process. Surgical dressings are

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
192
compensable if the supplies are medically necessary. Documentation must indicate what supply
was used or provided. Charges billed must indicate the actual cost to the physician.
Splints and Casts –- These items are reimbursable only under certain circumstances. For details,
refer to the musculoskeletal system under the heading Surgical Guidelines for Specific Systems in
this section of the manual.
The following additional supplies are listed below:
•
Lacrimal Puncture
Plugs
•
Indwelling Catheter
•
Urinary Drainage Bag
•
Urinary Leg Bag
•
Major Surgical Tray
(including anesthetic
injection)
•
Splint
•
Cast Supplies (e.g.,
plaster)
•
Special Casting
Material
(e.g., fiberglass)
•
Spacer, bag or
reservoir with/without
mask
•
Sestamibi
•
Supply of
Radiopharmaceutical
(Technetium)
•
Technetium
Medronate (up to 30
mCi)
•
Thallous Chloride
•
Strontium
•
Crutches, wooden,
pair
•
Paragard® IUD, cost
•
Cervical Collar,
flexible, foam
•
Philadelphia Cervical
Collar, semi-rigid
•
Pavlik Harness
•
Knee Immobilizer,
canvas longitudinal
•
Shoulder Immobilizer
•
Figure 8 Mobilizer
•
Acromioclavicular
Brace
•
Family Planning
Condoms
•
Contraceptive Supply,
Spermicide (e.g.,
vaginal foam/cream,
suppositories,
contraceptive
gel/sponge)
•
Minor Surgical Tray
•
Peak Flow Meter
•
Ear Mold, not
disposable, any type
(use LT or RT
modifier)
•
Ear Mold, disposable,
any type (use LT or RT
modifier)
•
Zithromax, oral, 1-
gram, single dose
•
Contact Lens,
spherical, per lens
•
Contact Lens,
toric/prism ballast, per
lens
•
Contacts, gas
permeable, spherical,
per lens
•
Contacts, gas
permeable, toric/prism,
per lens
•
Contacts, hydrophilic,
spherical, per lens
•
Contacts, hydrophilic,
toric/ballast, per lens
•
Anterior Chamber
Intraocular Lens
•
Posterior Chamber
Intraocular Lens
•
Application of Long
Arm Splint
•
Application of Short
Arm Splint, static
•
Application of Short
Arm Splint, dynamic
•
Application of Finger
Splint, static
•
Application of Finger
Splint, dynamic
•
Application of Rigid
Total Contact Cast
•
Application of Long
Leg Splint
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
193
• Application of Short
Leg Splint
•
Supplies and Materials
•
Educational Supplies
This supply list is not all-inclusive. Some supplies specific to certain specialties may be listed in
those sections.
Telehealth Reimbursement
Professional Services
Reimbursement to the health professional delivering the medical service is the same as the current
fee schedule amount for the service provided. Consulting site physicians and practitioners submit
claims for telehealth or telepsychiatry services using the appropriate CPT code for the professional
service along with the telehealth modifier GT, “via interactive audio and video telecommunications
system”. By coding and billing the “GT” modifier with a covered telehealth procedure code, the
consulting site physician and/or practitioner certifies that the beneficiary was present at the referring
site when the telehealth service was furnished. Fee schedules are located on the SCDHHS website
at http://www.scdhhs.gov
.
Originating Site Facility Fee
The referring site, also known as the originating site, is only eligible to receive a facility fee for
telehealth services. Claims must be submitted with an appropriate HCPCS code (telehealth
originating site facility fee). If a provider from the referring site performs a separately identifiable
service for the beneficiary on the same day as telehealth, documentation for both services must be
clearly and separately identified in the beneficiary’s medical record, and both services are eligible
for full reimbursement.
Hospital Providers
Hospital providers are eligible to receive reimbursement for a facility fee for telehealth when
operating as the referring site. Claims must be submitted with the appropriate telehealth revenue
code. There is no separate reimbursement for telehealth services when performed during an
inpatient stay, OP clinic or ER visit, or OP surgery, as these are all-inclusive payments.
Injections
A list of injection codes is provided on the provider portal. Injection codes include the cost of the
drug only, not the administration.
The unit of measure for reimbursement for injectable drugs corresponds to the unit of measure
noted in the code description. Indicate the same unit of measure in the “days/units” field (24G) on
the claim form. For example, if the injection code lists one unit as 50 mg, be sure to indicate 50 mg
as one unit. If 100 mg was administered, two units would be indicated on the claim.
Office E&M visits and additional office services are allowed as separate reimbursement from
injection codes. If the administration of the drug is the only reason for the visit, then only a minimal
established office E&M visit is allowed in addition to the administration code and the drug code.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
194
Therapeutic, prophylactic or diagnostic injection (specify substance or drug); subcutaneous or
intramuscular includes the syringe and administration of the drug. Minimal office visits include the
observation time if indicated.
On rare occasions, parenteral medications are provided by someone other than the physician
(pharmaceutical company research, patient, etc.). In these cases, the physician may bill South
Carolina Medicaid for a minimal office visit if this is the only reason for the visit and providing the
service is normally covered.
Note: Beneficiaries are not allowed to use their Medicaid card to obtain non-self-injectable drugs.
The reason this practice is not allowed is to prevent a possible duplicate payment from being made
by Medicaid (i.e., payment for drug to both the pharmacy provider and to the physician).
Guidelines on allergen immunotherapy can be found under the heading “Allergen and Clinical
Immunology” and those for chemotherapy under the heading “Oncology and Hematology” in this
section of the manual. Immunization guidelines can be located under the heading “Preventive Care
Services”.
Synagis® (Palivizumab)
If a 50 mg vial of Synagis® is administered to an infant up to 2 years old, the appropriate revenue
code must be billed in combination with the appropriate service.
SCDHHS has established a 50 mg rate and a 100 mg rate. For multiples of 50 mg dosages
(150 mg) or 3 units, SCDHHS will pay the 100 mg price plus the 50 mg price not to exceed 4 units.
Therapeutic, prophylactic or diagnostic injections may also be billed for the administration of the
drug. Providers must use the dosage that is appropriate for each child according to his or her
weight.
In order to ensure consistency, reimbursement for Synagis® is limited to physicians, hospitals and
infusion centers. To avoid possible duplicate reimbursement, SCDHHS will not reimburse pharmacy
providers for Synagis®. Payment for Synagis® administration will be limited to six doses per RSV
season.
Physician-Administered Injectable Drug Reimbursement Methodology
The reimbursement for drugs within each tier is set as follows:
• Tier 1 contains certain generic and injectable drugs in classes with therapeutic alternatives and
is priced at Maximum Allowable Cost/Least Cost Alternative.
• Tier 2 contains newer agents and higher-cost drugs and is priced at Average Sales Price (ASP)
plus 6%.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
195
• Tier 3 contains moderately priced agents and older drugs where there are often significant
Average Wholesale Price (AWP)/ASP differences and is priced at ASP plus 10%.
• Tier 4 contains drugs where ASP pricing is not available and is priced at AWP minus 18%.
The SCDHHS will adjust the provider-administered injectable drug fee schedule quarterly so that
reimbursement levels reflect changes in market prices for acquiring and administering drugs. Fee
schedules are located on the SCDHHS website at http://www.scdhhs.gov
.
Cancer Screening Services
South Carolina will sponsor reimbursement for mammography for dually eligible Medicare/Medicaid
beneficiaries according to the frequency limitations listed. Claims rejected by Medicare for having
exceeded their frequency limitations must be filed with Medicaid on a CMS-1500 claim form with no
Medicare information provided.
All services must be physician-generated, and the physician must be currently enrolled in the
Medicaid program.
Nutritional Counseling Services
The following billing instructions apply to FFS only. Providers who submit claims to a MCOs must
refer to the provider contract with the appropriate MCO for billing instructions.
All providers and dietitians are required to bill the appropriate CPT codes with a primary diagnosis
code.
All qualified providers and dietitians must follow the criteria and limitations described below:
• Total of twelve (12) hours of combined initial, re-assessment and group medical nutrition
therapy per fiscal year per patient is allowed. Services must be provided as in-person or via
telehealth, face-to-face encounter with the beneficiary and the beneficiary’s parent or
guardian (when applicable).
• Nutritional counseling services are allowed to be performed via telehealth. A telehealth
encounter must be billed with GT modifier, and it counts towards the twelve (12) hours of
combined medical nutrition therapy services provided to a patient per fiscal year.
Procedure
Code
Description Benefit Criteria and Limitations
97802
Medical nutrition therapy; initial
assessment and intervention,
individual, face-to-face with the
patient, each 15 minutes.
Allowed up to four (4) units of 97802 per same provider, provider
location or billing entity. Allowed to be performed via telehealth with GT
modifier. These units count towards the 12 hours of combined medical
nutrition therapy services per patient per fiscal year. Not allowed on the
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
196
same date of service as 97803 or 97804 by the same provider,
provider location or billing entity.
97803
Medical nutrition therapy; re-
assessment and intervention,
individual, face-to-face with the
patient, each 15 minutes
Allowed up to twelve (12) units of 97803 per month, per patient, up to
four (4) units per date of service/visit, with at least 7 calendar days
between visits. Allowed to be performed via telehealth with GT modifier.
These units count towards the 12 hours of combined medical nutrition
therapy services per patient per fiscal year. Not allowed on the same
date of service as 97802
or 97804 by the same provider, provider
location or billing entity.
97804
Medical nutrition therapy; group (2
or more individual(s), each 30
minutes
Allowed one (1) 97804 per date of service. Up to 4 units per month per
patient, with at least 7 calendar days between visits. Group size
allowed is 2-8 patients. Allowed to be performed via telehealth with GT
modifier. These units count towards the 12 hours of combined medical
nutrition therapy services per patient per fiscal year. Not allowed on the
same date of service as 97802 or 97803 by the same provider,
provider location or billing entity.
Total of 12 hours of combined initial, re-assessment and group nutritional counseling therapy
per state fiscal year per patient is allowed. Services must be provided as in person, face-to-
face encounter with the beneficiary and the beneficiary’s parent or guardian (when
applicable). A minimum of 6 hours of intensive nutritional counseling must occur prior to the
member being eligible for the obesity management therapy.
All providers and dietitians are responsible for clearly documenting the patient’s chart with all
information referenced in this policy. All services provided by both providers and dietitians are
subject to review by the Division of Program Integrity. Services not meeting the requirements
reflected in this policy may be subject to recoupment by SCDHHS.
The provider can either schedule the patient for an independent visit or may bill the initial medical
nutrition therapy visit on the same day as a routine physical exam or E&M service. If the provider
chooses to bill for both services on the same day, the provider will need to append the 25 modifier
to the billed claim for the second E&M service.
Pharmacist Services
Licensed pharmacists are allowed to bill new and established patient E&M codes, contraceptive
injection administration, and urine pregnancy tests to members of childbearing age, enrolled in the
Healthy Connections full benefit program or Family Planning Limited benefit program. Services
rendered by a pharmacist must be billed on a CMS 1500 claim form with FP modifier. The claim
must indicate the pharmacist individual NPI as the rendering provider and the affiliated pharmacy
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
197
NPI as the billing provider. There is no prior authorization required for these services.
Reimbursement of pharmacist services is 80% of the Medicaid physician base rate.
Adult Physical Exams
Adult physical exams are covered under the following guidelines:
• The exams are allowed once every two years, per patient.
• The patient must be 21 years of age or older.
The following appropriate age and diagnosis code Z00.8 must be used when billing:
• Preventive visit, new, age 18–39
• Preventive visit, new, age 40–64
• Preventive visit, new, age 65+
• Preventive visit, established, 18–39
• Preventive visit, established, 40–64
• Preventive visit, established, 65+
IMMUNIZATIONS
Immunizations for Children
Providers may bill for the administration of vaccines that are obtained through the VFC Program and
administered in the doctor’s office. When billing for immunization services for children under the age
of 19, both the administration code and the vaccine code for the administered vaccine must be listed
on the claim to receive reimbursement for the vaccine administration only. For this code
combination, only the administration code will be reimbursable.
Immunizations for Adults
When billing for vaccines for beneficiaries 19 years of age and older, the provider must bill for both
the vaccine and the immunization administration code. For vaccines billed under the pharmacy
benefit, only the administration fee can be billed on the medical side. Claims submitted for dually
eligible patients must first be submitted to Medicare. Covered codes may be found on the
Physicians Injectable Drug Fee Schedule located at https://www.scdhhs.gov
.
PEDIATRICS AND NEONATOLOGY
Routine Newborn Care Exam
This procedure is an all-inclusive code for any visits made during the first day of the newborn's birth.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
198
Routine Newborn Follow-up Care
Follow-up nursery visits made to a healthy newborn on subsequent days are reimbursable. Only
one follow-up nursery visit is reimbursed per day regardless of the number of visits made to the
nursery.
Newborn Discharged Early
This procedure must be used only to report the history and examination of a normal newborn who is
assessed and discharged from the hospital on the day of delivery.
Physicians following a newborn who is discharged before a routine follow-up exam can be
performed may bill for the office follow-up exam. This procedure code has a frequency limit of one
every 10 months.
Healthy Mothers/Healthy Futures Newborn Health Initiatives
If a physician performs the services listed below in addition to the newborn care exam, Medicaid will
provide enhanced reimbursement.
• Mother and infant referral to the WIC program at the county health department (for supplemental
food and nutritional counseling).
• Referral to the county health department to set up an infant home visit.
Referral to the county DSS for infant eligibility and an appointment for the first EPSDT well-baby
examination.
Newborn Care
The following procedures may also be billed under the newborn’s mother’s Medicaid number:
• Routine newborn care exam in hospital or birthing center.
• Normal newborn care not in hospital or birthing room setting.
• Follow-up care in nursery for a healthy newborn.
• History and examination.
• Newborn resuscitation.
• Mother/newborn WIC referral.
• Standby for newborn care, limited to two units (e.g., C-section/high-risk delivery).
• E&M Initial comprehensive preventative medicine.
• E&M Periodic Comprehensive Preventative Medicine.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
199
Note: Any other pediatric charges not noted in the above exceptions must be billed under the
Child’s Medicaid number.
Newborn Care for the Sick Newborn
Used to report the newborn care exam for a sick newborn. If the newborn becomes critically ill,
please refer to Neonatology in this section of the manual for coding instructions.
Follow-up Care for the Sick Newborn
Follow-up visits made to a sick newborn may be billed using the appropriate level subsequent
hospital care code or critical care code depending on the severity of illness.
Sick Newborn Care Billing Notes
Sick childcare may not be billed under the newborn's mother's Medicaid number. Sick childcare
must be billed under the newborn's Medicaid number.
Sudden Infant Death Syndrome (SIDS)
Appropriate procedure codes must be used to bill for infants being tested for SIDS. They are
allowed once and are all-inclusive.
Neonatology
Hospital Care for Sick Newborns
Hospital care for newborns who do not meet the criteria for NICU codes must be billed using
hospital care codes or critical care codes, if appropriate.
When the neonate no longer requires the intensity or level of care described in the NICU codes and
remains under the care of the same group or physician, subsequent hospital care or critical care
codes, if appropriate, may be used. When a neonate is transferred from one hospital to another
hospital and remains under the same group or same physician's care, the appropriate level critical
care or subsequent hospital care codes may be billed. NICU codes may not be billed if the neonate
does not meet the severity of illness or intensity of treatment as defined in the CPT manual.
Newborns Stabilized for Transport
If a physician treats a critically ill newborn in a hospital and stabilizes the newborn for transport to a
higher-level hospital appropriate critical care codes may be used for those services. Arterial
puncture, withdrawal of blood for diagnosis may not be billed in addition to the critical care.
However, arterial catheterization or cannulation for sampling, monitoring or transfusion;
percutaneous and catheterization, umbilical artery, newborn, for diagnosis or therapy are allowed in
addition to critical care.
Neonatal Intensive Unit Care Codes
Neonatology codes are used to report services provided by a physician directing the inpatient care
of a critically ill neonate/infant. Use of these codes must reflect the severity of the neonate's illness,
the intensity of treatment, and the level of care as defined in the CPT.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
200
Critical care codes may be used in place of NICU codes when direct physician care is given for an
extended period of time exclusively to one neonate. Time must be clearly documented for critical
care services.
Additionally, physician standby service and newborn resuscitation are to be used when the
physician is standing by for the C-section and newborn resuscitation is required.
Once the neonate is no longer considered to be critically ill, the codes for subsequent hospital care
and, when appropriate, subsequent normal newborn hospital care must be used. Initial and
subsequent neonatal care includes monitoring and treatment of the patient including nutritional,
metabolic, and hematologic maintenance; parent counseling; and personal direct supervision of the
health care team in the performance of cognitive and procedural activities.
Initial pediatric critical care, per day — This code reflects initial E&M of a critically ill infant or young
child, 29 days up through 24 months of age. This code is allowed only once per day and includes
24 hours of care provided by the attending physician.
If a physician treats a critically ill infant/young child in a hospital and stabilizes the infant/young child
for transport to a higher-level hospital, critical care codes would be appropriate for those services.
Arterial puncture, withdrawal of blood for diagnosis may not be billed in addition to the critical care.
However, arterial catheterization or cannulation for sampling, monitoring or transfusion;
percutaneous and catheterization, umbilical artery, newborn, for diagnosis or therapy are allowed in
addition to critical care.
The initial NICU code is also allowed for an infant/young child who has been treated for more than
one day in one facility and is then transported to another facility for specialized treatment under
another group or physician's care. The admitting physician at each facility may report the admission
using this code. If the infant/young child is transferred back to the original facility, the appropriate
subsequent level of care must be billed since this is considered a continuation of the same
hospitalization.
If the neonate is released home and subsequently readmitted to the hospital, NICU codes cannot be
billed. You must bill hospital care codes or critical care codes.
Subsequent pediatric critical care, per day — This code reflects subsequent E&M of a critically ill
infant or young child, 29 days up through 24 months of age. This code is allowed only once per day
and includes 24 hours of care provided by the attending physician.
Initial NICU care, once per physician or group — This code reflects the admission of a critically ill
neonate when the intensity of care meets the definition set forth in the CPT. This code is allowed
only one time and includes 24 hours of care provided by the attending physician.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
201
Subsequent NICU care, per day — This code reflects subsequent E&M of a critically ill neonate,
28 days of age or less. This code is allowed only once per day and includes 24 hours of care
provided by the attending physician.
Subsequent NICU care, per day — This code reflects subsequent E&M of the recovering very low
birth weight infant (present body weight less than 1,500 grams). This code is allowed only once per
day and includes 24 hours of care provided by the attending physician.
Subsequent NICU care, per day — This code reflects subsequent E&M of the recovering low birth
weight infant (present body weight 1,500-2,500 grams). This code is allowed only once per day and
includes 24 hours of care provided by the attending physician.
Additional Services
The following services may be billed in addition to the NICU codes. Documentation that the billing
physician rendered the services or directly supervised the rendering of the services must be
recorded in the medical record. The following list is not a complete list of additional services
allowed, but the most frequently billed services only:
• Tracheal Lavage*
• 99255 — SIDS evaluation
• Venipuncture, under age 3 years, femoral, jugular or sagittal sinus*
• Scalp vein*
• Other vein*
• Push transfusion, blood, 2 years or under*
• Exchange transfusion, blood; newborn
• Cut down arterial catheterization*
• Arterial catheterization for prolonged infusion therapy, (chemotherapy), cut down
• Catheterization, umbilical artery, newborn, for diagnosis or therapy*
• Physician Standby Service, requiring prolonged physician attendance, each 30 minutes (limited
to two units)**
• Newborn Resuscitation
* These codes are included in the description of the NICU codes in the CPT, however, Medicaid
policy has made an exception, and these codes may be billed in addition to the NICU codes.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
202
** This code is used only for prolonged physician attendance prior to delivery.
Primary or assistant surgeon charges may be billed in addition to the neonatal or critical care codes.
Extracorporeal Membrane Oxygenation Support (ECMO)
ECMO services are reimbursed by the following CPT codes:
• Insertion of cannula(s) for prolonged extracorporeal circulation for cardiopulmonary insufficiency.
• Prolonged extracorporeal circulation for cardiopulmonary insufficiency, each additional 24 hours.
Prolonged extracorporeal circulation for cardiopulmonary insufficiency will be paid for each
additional 24 hours up to four days. However, starting with day five, progress notes must be sent
attached to the claim for appropriate reimbursement.
The initial and subsequent NICU care codes may be billed in addition to the ECMO codes.
All other specific CPT surgical procedures that are not included in the 24-hour neonatal codes may
be billed separately.
Step Down Neonatal Services
When a neonate is transferred from a Level III hospital to a Level II hospital and remains under the
same group or same physician's care, the appropriate level of subsequent, critical care or hospital
care codes may be billed depending on the service(s) provided. This coding is also applicable for
neonates transferred from the NICU in a hospital to a lower-level nursery or unit in the same
hospital while remaining under the care of the same group or physician.
Back Transfer of Neonatal Intensive Care Unit Infants
Care must be transferred to another group or another physician's care in order to establish a
permanent medical home for these high-risk infants. This coding is also applicable for neonates
transferred from the NICU in a level III hospital to a lower-level nursery or unit in the same hospital
when their care is transferred to another group or physician.
• NICU discharge home visit.
The following six codes can be billed as appropriate, depending on level of care:
• Initial pediatric critical care, per day
• Subsequent pediatric critical care, per day
• Initial NICU care, once per physician or group
• Subsequent NICU care, per day

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
203
• Subsequent NICU care, per day, recovering very low birth weight (body weight less than
1,500 grams)
• Subsequent NICU care, per day, recovering low birth weight (body weight 1,500–2,500 grams)
Forensic Medical Evaluations
All forensic evaluations must be medically necessary. Use the following HCPCS codes to bill for
these services:
• Prolonged E&M service before and/or after direct (face-to-face) patient care (e.g., review of
extensive records and test, communication with other professionals and/or the patient/family);
first 30 minutes (list additional minutes separately) for other physician service(s) and/or inpatient
or OP E&M service.
Note: this service is used to report the accumulated duration of the time spent by a health care
professional providing prolonged care, even if the time spent spans over more than one DOS.
(The last DOS must be billed.)
– Each additional 15 minutes (list separately); must be used in conjunction with this service.
• Medical team conference with interdisciplinary team of healthcare professionals, face-to-face
with patient and/or family; 15 minutes or more participation by non-physician qualified healthcare
professional.
Note: A non-physician qualified health care professional includes, but is not limited to, NPs and
PAs.
• Medical team conference with interdisciplinary team of healthcare professionals, without patient
and/or family; 15 minutes or more participation by physician.
• Participation by non-physician qualified healthcare professional; 15 minutes or more.
All forensic evaluations must be medically necessary. Only physicians and NPs may bill SCDHHS
directly, using their NPI, for services rendered. Registered Nurses (P-SANE) and PAs must bill
using the supervising Physicians NPI number in order to be reimbursed by SCDHHS. Modifiers will
indicate which medical professional rendered services. All provider information must be maintained
in the patient’s records.
Early and Periodic Screening, Diagnosis, and Treatment (EPSDT)
Providers can bill for EPSDT services and immunizations on the CMS-1500 claim form using the
appropriate CPT codes. Providers who are set up for electronic billing may bill using the electronic
billing system when using these CPT codes. Providers using the CMS-1500 claim form must bill
under the Medicaid provider numbers they currently use for billing on the claim form such as:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
204
• Physicians must bill under their group or individual provider numbers.
• Clinics must bill under their clinic numbers.
Providers using the CMS-1500 will be responsible for handling their own EPSDT scheduling for
patients in their practice.
Periodic and Inter-periodic Screening Services
• All EPSDT screenings must be billed using the appropriate CPT codes regardless of provider
type or location.
• Prior authorizations are NOT required for Periodic or Inter-periodic screening services.
• Medicaid providers enrolled with SCDPH in the VAFAC program may bill an immunization
administration fee.
The following indicators must be used in field 24H of the CMS-1500 claim form when billing a
screening:
Indicator 1 — Well child care with treatment of an identified problem treated by the physician
Indicator 2 — Well child-care with a referral made for an identified problem to another provider
Indicator N — No problems found during visit
Medically Necessary Services
Providers must bill using the appropriate diagnosis and treatment code for each procedure.
Providers must obtain a prior authorization for all medically necessary non-State Plan EPSDT
services; submitting documentation of medical necessity and any additional information will assist in
this determination.
Reimbursement for EPSDT Services
Note: This policy applies only to the Physician’s office and CCCs.
Well-care visits conducted via telehealth must be billed with the appropriate EPSDT code and a GT
modifier.
EPSDT Periodic Screening
EPSDT periodic screenings will be reimbursed at a uniform rate. Although screening services vary
according to age and schedule, the reimbursement is intended to be an equitable average fee. Any
other test or treatment service performed may be billed separately. The following guidelines must be
used when billing for periodic screening:
• Screening components can be fragmented and billed separately.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
205
• The screening provider can bill an office visit on the same day a screening is billed.
• South Carolina Medicaid policy allows providers to bill an EPSDT well-child screening on the
same day as a sick visit.
• If individual components of a screening are not performed, the reason must be appropriately
documented. Reimbursement for the screening fee may be subject to recoupment if each
age-appropriate component is not performed and not documented.
EPSDT Inter-periodic Screening
Reimbursement for an inter-periodic screening is the same as a periodic screening. The following
guidelines must be used when billing for inter-periodic screenings:
• The provider must indicate the diagnosis code of the condition to justify the medical necessity
for performing an inter-periodic screening.
• The inter-periodic screening must include all the required screening components appropriate to
the child’s age.
• Individual screening components or follow-up treatment cannot be billed as an inter-periodic
screening.
Additional Services
Additional services performed during an EPSDT visit may be covered separately from the EPSDT
visit utilizing the appropriate CPT code and billed at a frequency according to the periodicity
schedule available at
https://www.scdhhs.gov/resources/programs-and-
initiatives/epsdt/providers/periodicity-schedule. The additional services include:
• Immunization Administration:
– When billing for an immunization administration and an EPSDT examination code on the
same day, the provider must use modifier XU when billing the immunization administrative
code in order to receive additional reimbursement.
– Providers may bill for the administration of vaccines that are obtained through the VFC
Program and administered in the physician’s office.
– When billing for immunization services for children under the age of 19, both the
administration code and the vaccine code for the administered vaccine must be listed on
the claim to receive reimbursement for the vaccine administration only. For this code
combination, only the administration code will be reimbursable.
• Topical Fluoride Varnish

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
206
• Laboratory Tests and Analysis:
– Reimbursement for the lab analysis is not part of the EPSDT service rate.
– Blood level assessments:
› If the provider office sends the blood lead samples to an outside laboratory for analysis,
the laboratory will bill Medicaid directly for the blood lead analysis.
› If the provider office is using the ESA LeadCare Blood Lead Testing System to analyze
the blood lead samples internally, then the office may bill Medicaid directly using.
– Age Limited Screenings
– Elective Tests
– Developmental and Behavioral Assessments
EPSDT providers are allowed to bill for standardized developmental, mental, emotional, behavioral
and psychosocial assessments utilizing standardized screening tools that are culturally sensitive
and have a moderate to high sensitivity, specificity and validity level. A general screening is
recommended with follow-up screening, as indicated. Documentation must include a copy of the
completed screening tool and the score per instrument screening tool. Billing for screenings follow
coding guidelines and NCCI edits.
• Childhood and Adolescent Developmental Levels:
– This code is limited to a frequency of two times per day for beneficiaries up to 18 years of
age. Examples of standardized screening instruments include, but are not limited to:
› Ages and Stages Questionnaire, 3rd Edition (ASQ)
› Parents Evaluation of Developmental Status (PEDS)
› Modified Checklist of Autism in Toddlers (MCHAT)
• Emotional and/or Behavioral Health Assessment:
– This code is limited to a frequency of two times per day for beneficiaries up to 18 years of
age. Examples of standardized screening instruments include, but are not limited to:
› Ages and Stages Questionnaire: Social-Emotional (ASQ: SE)
› Pediatric Symptom Checklist (PSC) or Pediatric Symptom Checklist — Youth Report
(PSC-Y)

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
207
› Modified Patient Health Questionnaire (PHQ-9)
› Screen for Child Anxiety Related Emotional Disorders (SCARED)
› Vanderbilt Diagnostic Rating Scale (Vanderbilt)
• Patient Focused Health Risk Assessment (e.g., health hazard appraisal). This code is limited to
a frequency of two times per day for beneficiaries through 18 years of age. Examples of
standardized screening instruments include, but are not limited to:
– Acute Concussion Evaluation (ACE)
– CRAFFT Screening Interview
– Guidelines for Adolescent Preventative Services (GAPS)
• Caregiver-Focused Health Risk Assessment (e.g., depression inventory) for the benefit of the
patient. This code is limited to a frequency of two times per DOS. Examples of standardized
screening instruments include, but are not limited to:
– Edinburgh Maternal Depression Screen
– Safe Environment for Every Kid (SEEK)
TOBACCO CESSATION
Counseling
Tobacco cessation counseling in individual and group settings are covered when billed with
appropriate CPT codes. Reimbursement for counseling is limited to four sessions per quit attempt
for up to two quit attempts annually. Tobacco cessation counseling may be billed on the same day
as an office visit using a 25 modifier.
OBSTETRICS AND GYNECOLOGY
Screening Brief Intervention and Referral to Treatment Initiative
The following billing procedures must be utilized in order to receive payment for SBIRT services.
SCDHHS began coverage for SBIRT in 2011 to improve birth outcomes and the overall health of
moms and babies. SCDHHS has partnered with stakeholders across the state to help identify and
treat pregnant beneficiaries who may experience alcohol or other substance abuse issues,
depression, tobacco use or domestic violence. SBIRT services (screening and, when applicable, a
brief intervention) are reimbursable in addition to an E&M code for pregnant women and/or those
who are in the 12-month postpartum period.
SCDHHS will continue to use the screening and intervention HCPCS codes. The HD modifier is
required when the services rendered indicate a positive result and/or when a referral is completed.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
208
Providers must use the appropriate HCPCS code and the HD modifier when an SBIRT screening
result is positive. Additionally, providers must use the appropriate HCPCS code with the HD modifier
when a referral to treatment is made in conjunction with the brief intervention. These changes in
billing procedures apply for Healthy Connections Medicaid members enrolled in both the Medicaid
FFS and Medicaid Managed Care program.
• Screening — once per fiscal year
• Brief Intervention — twice per fiscal year
The Institute for Health and Recovery’s Integrated Screening Tool, which is a validated and
objective resource, must be used to receive reimbursement for screening and intervention. A copy
of this screening tool is located in the Forms section of the Provider Administrative and Billing
Manual.
When billing for SBIRT services using appropriate HCPCS codes, providers must bill using both
their individual and group NPI numbers on the CMS-1500 form or an electronic claim.
Pregnancy Visits
Providers have two options when choosing how to bill for an initial pregnancy visit:
• Providers may bill an initial visit for each pregnancy using the Current Procedural
Terminology (CPT) evaluation and management (E/M) code. Under this option, a provider
would bill for a new patient E/M code even if the Medicaid member is a patient of record at
that practice. The claim must contain a pregnancy diagnosis code.
OR
• Providers may bill the appropriate E/M code that meets the CPT description for level of
complexity when billing for initial or antepartum visits. The level of complexity must be
documented in the patient’s medical record. The claim must contain a pregnancy diagnosis
code.
Please refer to the information regarding ICD-10-CM pregnancy diagnosis codes on the provider
portal.
17 Alpha Hydroxyprogesterone Caproate (Makena
®
and 17P)
Providers must bill the HCPCS code for Injection, hydroxyprogesterone caproate, (Makena
®
), 10 mg
and/or Injection, hydroxyprogesterone caproate, not otherwise specified, 10 mg and bill for the
appropriate number of units administered. Providers billing for compounded 17 alpha
hydroxyprogesterone caproate will continue to bill the appropriate HCPCS code using the TH
modifier (obstetrical treatment/services, prenatal or postpartum) in order to be reimbursed. When
billing for Makena
®
or Compounded 17-P, the appropriate CPT code can be billed for administration

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
209
of the drug, which must be given in the physician’s office or clinic. The reimbursement for Makena
®
(injection, hydroxyprogesterone caproate (Makena
®
), 10 mg) and/or injection, hydroxyprogesterone
caproate, not otherwise specified, 10 mg is listed on our Other Physician’s Fee Schedule at
www.scdhhs.gov
. When billing Medicaid, providers must include the NDC in field 24A of the
CMS-1500 claim form and the number of units in field 24G.
All providers must keep documentation showing the medical necessity for either Makena
®
or 17-P in
the patient’s chart. All claims are subject to potential PI audits and therefore, it is the provider’s
responsibility to maintain the patient’s records.
Multiple Births
For multiple births of more than two, the claim must be sent a hardcopy with operative notes
attached.
If the patient delivers multiple babies, all either vaginally or by C-section, the first birth must be billed
with modifier GB (39 weeks or more) or CG (less than 39 weeks), and each consecutive birth must
be billed using modifier 51.
Example: Delivery of triplets, all vaginally at 39 weeks:
(GB) Vaginal Delivery
(51) Vaginal Delivery
(51) Vaginal Delivery
If the patient delivers multiple babies, the first vaginally and one (or more) via C-section, the first
birth must be billed with modifier GB (39 weeks or more) or CG (less than 39 weeks), and the
following birth, via C-section, must be billed using modifier 79.
Example: Delivery of triplets, 1
st
birth vaginally, 2
nd
and 3
rd
via C-Section at 38 weeks:
(CG) Vaginal Delivery
(79) C-section Delivery
(51) C-section Delivery
For further questions regarding multiple births, please contact PSC at
+1 888 289 0709 or submit an online inquiry at Contact a Provider Representative | SCDHHS
Abortion
When billing for any type of abortion, the procedures must be billed using the abortion procedure
codes. There are separate codes for spontaneous, missed, and septic abortions, and hydatidiform

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
210
mole, and for therapeutic abortion. The vaginal delivery code must not be used to report an abortion
procedure.
The only exception to this rule is if the physician performs the delivery of the fetus and only when
the gestation is questionable and there is a probability of survival. The medical record must contain
documented evidence that the fetus was delivered by the physician. If the physician did not perform
the delivery, but problems necessitated his or her presence, then the appropriate E&M codes must
be used to report these services.
Diagnosis codes to be used only to report therapeutic abortions and diagnosis codes to be used to
report spontaneous, inevitable and missed abortions. Please refer to the provider portal for
ICD-10-CM diagnosis codes for these services. Abortions, which are reported with diagnosis and
procedure codes for therapeutic abortion, must be accompanied by complete medical records which
substantiate life endangerment to the mother or that the pregnancy is a result of rape or incest, and
the signed abortion statement.
Please refer to the provider portal for diagnosis codes do not require documentation.
Licensed Midwife
Required Modifier for Licensed Midwives
When filing claims for services rendered by licensed midwives, all procedure codes must be filed
with an SB modifier.
Initial OB Exam by the Licensed Midwife
Pregnancy Visits
Providers have two options when choosing how to bill for an initial pregnancy visit:
• Providers may bill an initial visit for each pregnancy using the Current Procedural
Terminology (CPT) evaluation and management (E/M) code. Under this option, a provider
would bill for a new patient E/M code even if the Medicaid member is a patient of record at
that practice. The claim must contain a pregnancy diagnosis code.
OR
• Providers may bill the appropriate E/M code that meets the CPT description for level of
complexity when billing for initial or antepartum visits. The level of complexity must be
documented in the patient’s medical record. The claim must contain a pregnancy diagnosis
code.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
211
Physician Back-up Coding
Each of the two obstetrical examinations by the backup physician must be billed using the
appropriate level of complexity E&M CPT procedure code.
Delivery Supply Code
An additional code has been developed to reimburse for supplies used for delivery in the home
setting. This procedure code may be billed by the Licensed Midwife in addition to the vaginal
delivery code.
Newborn Care
The newborn examination must be billed with this CPT code using the SB modifier.
Newborn Metabolic Screening+
In compliance with SCDPH Newborn Screening regulations, if there is no attending physician, then
the Licensed Midwife is responsible for the collection of specimens. Providers who collect
specimens for the newborn metabolic screening in a birthing center or home birth setting must
follow the guidance established in Section V of the Department of Public Health (DPH) Public Health
Laboratory Complete Services Guide for specimen submission and invoicing
Hysterectomies
Reimbursement for a hysterectomy is not allowed if the hysterectomy is performed solely for the
purpose of rendering an individual permanently incapable of reproducing. A hysterectomy may not
be covered if there was more than one purpose for performing the hysterectomy, but the primary
purpose was to render the individual permanently incapable of reproducing.
A hysterectomy can be reimbursed by Medicaid in cases of retroactive eligibility only if the physician
certifies in writing ONE of the following:
• The individual was already sterile before the hysterectomy and the physician who performs the
hysterectomy certified in writing that the individual was sterile at the time of the hysterectomy.
The certification must state the cause of the sterility.
• The individual requires a hysterectomy because of a life-threatening emergency, and the
physician who performs the hysterectomy certified in writing that the hysterectomy was
performed under a life-threatening situation in which the physician determined prior
acknowledgement was not possible. The certification must include a diagnosis and description
of the nature of the emergency. If timing permits, prior approval may be requested, but
appropriate and timely medical care must not be delayed obtaining approval.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
212
Ectopic Pregnancy
For surgical treatment of an ectopic pregnancy, bill the appropriate code. No documentation is
required with the claim when using these codes.
Pelvic Exam
A pelvic exam under anesthesia may only be billed if performed separately and if medically
indicated. Pelvic exams at the time of surgery involving the vagina or through a vaginal incision are
included in the surgical procedure and must not be billed in addition to the surgical procedure (e.g.,
vaginal hysterectomy, laparoscopic elective sterilization, conization of the cervix, etc.).
Sterilization and Other Related Procedures
Under the following circumstances, bill the corresponding sterilization procedure codes:
Essure® Sterilization Procedure
Effective with dates of service prior to May 31, 2010, SCDHHS will reimburse for the Essure®
Sterilization procedure only when certain criteria are met. This procedure is available to women who
have risk factors that prevent a physician from performing a safe and effective laparoscopic tubal
ligation. Reimbursement will be provided for any of the following criteria:
• Morbid obesity (BMI of 35 or greater).
• Abdominal mesh that mechanically interferes with the laparoscopic tubal ligation.
• Permanent colostomy.
• Multiple abdominal/pelvic surgeries with documented severe adhesions.
• Artificial heart valve requiring continuous anticoagulation.
• Any severe medical problems that would contraindicate laparoscopy because of anesthesia
considerations. (This must be attested in the request for prior approval that general anesthesia
would pose a substantial threat to the beneficiary’s life.)
The procedure will be covered when performed in an inpatient or OP hospital setting or in a
physician’s office. SCDHHS will reimburse the implantable device by utilizing the HCPCS code with
the FP modifier, and the professional service will be reimbursed utilizing the CPT code with the FP
modifier.
Hysterosalpingogram and Radiological Supervision and Interpretation may be billed as follow-up
procedures 90 days after the sterilization. A Sterilization Consent form must be completed and
submitted with the claim.
Federal guidelines for sterilization procedures will remain a requirement which includes completing
and submitting a Sterilization Consent Form.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
213
• Tubal ligation following a vaginal delivery by a method except laparoscope.
• Tubal ligation following C-section or other intra-abdominal (tubal ligation as the minor procedure)
surgery.
• Ligation, transection of fallopian tubes; abdominal or vaginal approach.
• Occlusion of fallopian tubes by device.
• Laparoscopic sterilization by fulguration or cauterization.
• Laparoscopic sterilization by occlusion by device.
• Vasectomy.
When billing for a vaginal delivery as well as a tubal ligation performed on the same DOS, the tubal
ligation must be billed using modifier 79 (unrelated procedure or service by the same physician or
other qualified health care professional during the postoperative period) to ensure proper
reimbursement.
Claims for sterilization services must always be billed hardcopy with a copy of the Sterilization
Consent Form attached.
Salpingectomy and/or Oophorectomy — The operative report must be submitted with the claim. The
medical record must reflect medical necessity for the procedure performed. Reimbursement using
these codes is not allowed if performed as a sterilization procedure, unless a copy of the
Sterilization Consent Form is attached.
Dilation and Curettage — When a D&C is performed at the same time as sterilization, medical
necessity for the D&C must be clearly documented in the patient’s operative report.
PSYCHIATRIC AND COUNSELING SERVICES
Additional Billable Codes
Additional codes may be billed by a physician specializing in psychiatric care.
Pediatric Sub-Specialist Program
SCDHHS will reimburse an enhanced rate to certain pediatric sub-specialists that meet the
enrollment requirements. Please refer to The Pediatric Sub-Specialist Program under Special
Coverage Groups in this section of the manual for full eligibility criteria to participate in this program.
NEPHROLOGY AND END STAGE RENAL DISEASE SERVICES
Physician-related Dialysis Procedures
In-Center Dialysis — Medicaid reimburses the nephrologist or other supervising internist an
all-inclusive monthly fee for the supervision of ESRD services. These services are defined as

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
214
monthly supervision of medical care, dietetic services, social services and procedures directly
related to the physician's role in the treatment of ESRD.
If billing for a complete month of treatment supervision, the monthly code must be used. The DOS
must be the last date in the month and the “days” unit block must be a “one”, indicating one full
month of supervision.
The monthly ESRD code includes all services rendered to the patient for all days of the month.
Office visits must not be billed in addition to the monthly supervision. Special procedures may be
billed separately (e.g., shunt revision, cannula declotting).
If the patient is hospitalized, or for some reason did not have a full month of in-center treatments,
the partial month procedure code must be used with the appropriate number of days of supervision
in the days/unit column on the CMS-1500 claim form and the appropriate “to” and “from” dates of
service.
Inpatient Dialysis — If an ESRD patient is hospitalized, the hospitalization may or may not be due to
a renal-related condition. In either case, the patient must continue dialysis.
Inpatient dialysis usually requires more intense physician involvement for a prolonged period and/or
multiple visits. Physicians will be reimbursed for inpatient dialysis services to either acute renal
failure (ARF) or ESRD patients on a FFS basis. Guidelines are the same for inpatient dialysis
whether the patient is ARF or ESRD.
Complications or hospitalization for reasons not related to dialysis or the treatment of dialysis may
be charged separately. However, when dialysis codes are charged, hospital visits may not be
charged for the same DOS.
Visits may be charged on alternate dialysis days when applicable. Special procedures (e.g., an
EKG) may be charged when clearly justified as a service outside of the normal dialysis
management.
For inpatient dialysis, services Medicaid will apply the same rules as it does for all reasonable
charge determinations. The services must meet the following criteria:
• They must be covered physician services.
• They must be medically necessary.
• They must be personally furnished by the physician.
• They must be within the requirements under Part B Medicare.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
215
Home Dialysis — Medicare is the primary sponsor for patients receiving home dialysis services and
Medicaid, if available, is the secondary sponsor of coinsurance and deductibles. The Social Security
Administration does not require a delayed period for home services, and Medicare will reimburse
from the initial course of treatment.
In this case, Medicaid will not reimburse for home treatments during the first ninety days of services
as primary sponsor but will pay coinsurance and deductibles.
In certain instances, where Medicaid is the primary sponsor, the physician supervising the home
dialysis patient must adhere to policies for in-center supervision. Reimbursement will be per full
month of supervision, or per day for partial months. The monthly supervision fee includes all the
services outlined for the alternate method of reimbursement. A home training supervision fee is
allowed for the first month of home dialysis in addition to the regular monthly fee for treatment
supervision.
Dialysis Training — Dialysis training is a covered service for ESRD patients. The initial completed
course and per training session may be billed for training services for any mode (self, peritoneal or
hemodialysis). The initial course is allowed only once in a lifetime. Training services for
self-dialysis performed after the initial course is completed (retraining) are compensable on a per
day basis, and under the following Medicare guidelines:
• The patient changes from one mode of dialysis to another.
• The patient's home dialysis equipment changes.
• The patient's dialysis setting changes.
• The patient's dialysis partner changes.
• The patient's medical condition changes (the patient must continue to be an appropriate patient
for self-dialysis).
Home support services (e.g., reviewing the patient's technique and instructing him or her in any
corrections) are not compensable as training services. Support services are included in the monthly
or partial month ESRD supervision fees.
PART II — DIAGNOSTIC OPHTHALMOLOGY SERVICES
Diagnostic services included in the CPT coding range 92018-92287 are compensable as separate
procedures if performed as a distinct and individual service and not included in the ophthalmological
or E&M exam, with the following restrictions:

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
216
Cardiology
Cardiac Catheterization
The cardiologist must bill for the catheterization that describes the procedure and technique utilized;
fragmenting the codes is not allowed.
If medically indicated, intracardiac electrophysiological procedures may be billed in addition to the
catheterization angiogram procedure.
Cardiac MRI of the heart procedure codes are used to report the physician’s attendance and
participation in the MRI of the heart. When filing for this procedure, bill appropriate MRI code
depending on level of service. Use modifier 26 when billing the professional component only. The
technical portion will be reimbursed to the hospital under the revenue code for MRI. Medical
necessity for both the MRI and heart catheter (if needed) must be documented in the beneficiary’s
chart. The procedure may be performed in lieu of heart catheterization, when possible. The code will
be allowed reimbursement only once per DOS, regardless of how many sessions or images are
performed.
Vascular Studies
Reimbursement to a provider for services purchased from an outside supplier or lab is not allowed.
Reimbursement is only allowed to the provider who performed the service and is enrolled with South
Carolina Medicaid.
Independent physiology labs performing monitoring services must be enrolled for participation. The
physician requesting the service may only bill for the interpretation of the study if performed.
Oncology and Hematology
Infusion start and stop time must be clearly documented. Start time does not include the E&M
service or delivery of adjunctive therapy by a nurse or physician.
Chemotherapy administrations, push technique, are only for pushing a chemotherapy agent and are
not to be billed when pushing pre-medications or providing other incidental services. Only one push
technique code will be allowed per day. These codes cannot be billed when given in a hospital
setting.
If routine maintenance (flushing with heparin and saline) of an access device is the only service
rendered, and is rendered by the nurse, the office visit code is appropriate.
Therapeutic or diagnostic infusions codes may only be billed when a therapeutic or diagnostic agent
other than chemotherapy must be infused over an extended period. Payment of these codes is
considered bundled into the payment for chemotherapy infusion when administered simultaneously.
Separate payment is allowed when these services are administered sequentially or as a separate
procedure. These codes cannot be billed in a hospital setting or in addition to prolonged service
codes.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
217
Blood transfusions may be billed only when the physician or an employee of the physician performs
the transfusion. It must be billed per unit of blood. If the transfusion requires prolonged physician
attendance, then it is appropriate to charge for this service. The medical record must substantiate
this service. If hospital personnel administer the blood transfusion, it is reimbursable only under the
hospital allowable costs.
A listing of chemotherapy drug codes can be found on the provider portal. The codes include the
cost of the drug only, not the administration. Chemotherapy agents provided by a hospital are
considered a technical cost and may not be charged by a physician. The hospital is reimbursed for
all technical costs.
When a patient receives the entire regimen of chemotherapy in an office setting, including lab work,
hydration, pre-medication and all chemotherapy agents, these procedures indicate an infusion or
injection by the physician or an employee of the physician. The following are appropriate codes to
bill:
• If the patient received chemotherapy over four hours in the office via IV infusion:
– Chemotherapy administration, intravenous infusion technique; up to an hour, single or
initial substance/drug
– Each additional hour, 1 to 8 hours
– J Codes — Appropriate medication charges
• E&M services are allowed when a separate and identifiable medical necessity exists and is
clearly documented in the patient’s chart. The physician must not routinely bill an E&M service
for every patient prior to chemotherapy administration. Only one E&M service is billable per
patient per day.
• Prolonged services may be billed in addition to the E&M code when there is more than an hour
of actual face-to-face physician time required beyond the usual service for the level of the E&M
code billed. This code must only be used when the physician’s expertise is medically necessary
in evaluating and managing the patient over a prolonged period and specific documentation
describes the content and duration of the service.
• Critical care services may only be used in situations requiring constant physician attendance of
an unstable or critically ill patient. These codes may only be used in situations significantly more
complex than other chemotherapy situations.
Inpatient and Outpatient Hospital Services
Services or supplies administered by the hospital or hospital employees are considered a part of the
overall hospital service and are reimbursable only under the hospital allowable costs. A physician

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
218
who is either salaried or contracted by the hospital, and who performs services under contract or
employment, may not bill for those services separately under his or her individual Medicaid provider
number. The contracting hospital may claim these services under the professional fees allowable for
the hospital under their hospital-based physician Medicaid number.
Gastroenterology
Gastrostomy Button Device Feeding Tube Kit
Claims must be processed on a CMS-1500 claim form and include a copy of the invoice and
appropriate documentation supporting the medical necessity of the device.
Physical Medicine and Therapy
Osteopathic Manipulative Treatment
An E&M office code may be billed in addition to an OMT code if the E&M service performed is
documented as a significant, separately identifiable service.
Breast Cancer Susceptibility Gene 1 and 2 (BRCA)
The following services are covered for BRCA genetic testing and genetic counseling:
• BRCA1, BRCA2 gene analysis; full sequence analysis and full duplication/deletion analysis (i.e.,
detection of large gene rearrangements)
• BRCA1, BRCA2 gene analysis; full sequence analysis
• BRCA1, BRCA2 gene analysis; full duplication/deletion analysis (i.e., detection of large gene
rearrangements)
• BRCA1, gene analysis; full sequence analysis
• BRCA1 gene analysis; full duplication/deletion analysis (i.e., detection of large gene
rearrangements)
• BRCA2 gene analysis; full duplication/deletion analysis (i.e., detection of large gene
rearrangements)
• BRCA1, BRCA2 gene analysis; 185delAG, 5385insC, 6174delT variants
• BRCA1 gene analysis; known familial variant
• BRCA2 gene analysis; full sequence analysis
• BRCA2 gene analysis; known familial variant
• Medical genetics and genetic counseling services, each 30 minutes face-to-face with
patient/family

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
219
• Genetic counseling, under physician supervision, each 15 minutes
Chiropractic Services
Billing for CMT is limited to one procedure per visit and one visit per day, with a maximum of six
visits during a state fiscal year (July 1–June 30), with no exceptions. Eligible Medicaid beneficiaries,
regardless of age, will be allowed six chiropractic visits per state fiscal year providers must call the
toll-free telephone number on the back of the Medicaid insurance card to verify a patient’s current
eligibility and number of visits used to date during the current state fiscal year. Visits not used in one
year do not carry over to the next year.
Note: For dually eligible Medicaid and Medicare beneficiaries, Medicare is the primary payer. Bill all
chiropractic services to Medicare first. Once a dually eligible beneficiary has exhausted his or her
Medicare-allowed chiropractic services, Medicaid reimbursement for chiropractic services is no
longer available.
Medicaid-reimbursable CMT services are limited to the following three services only:
• CMT; Spinal, 1 to 2 Regions
• CMT; Spinal, 3 to 4 Regions
• CMT; Spinal, 5 Regions
Radiologic Examination (X-Ray)
Billing for radiologic examination is limited to two x-rays per beneficiary per state fiscal year
(July 1–June 30). Medicaid-reimbursable radiology services are limited to the following:
• Radiologic Examination; Spine, Entire, Survey Study; Anteroposterior and Lateral
• Radiologic Examination; Spine, Cervical; Anteroposterior and Lateral
• Radiologic Examination; Spine, Thoracic; Anteroposterior and Lateral
• Radiologic Examination; Spine, Thoracolumbar; Anteroposterior and Lateral
• Radiologic Examination; Spine, Lumbosacral; Anteroposterior and Lateral
HYPERBARIC OXYGEN THERAPY
Technical Component
All technical services must be billed on the UB-04 hospital claim form. Payment for OP hyperbaric
therapy is allowed. Inpatient therapy cannot be billed separately as the fee is included in the hospital
DRG or per diem rate.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
220
Professional Component
If a physician directly supervises the HBO therapy, procedure codes for HBO may be billed on the
CMS-1500 claim form; no modifier is necessary. The professional component must be coded as one
of the following:
• Initial Treatment — An initial treatment is compensable only once per course of treatment for a
specific diagnosis. HBO initial treatment is not billed in units of time, but rather the first day of
the initial therapy.
• Subsequent Care — All subsequent HBO therapy treatments must be coded as such.
Subsequent therapy is defined as any length of therapy following the initial treatment on any
given day. If two subsequent treatments are performed on the same DOS (at different times of
the day), a second charge may be used with a 76 modifier. HBO therapy is not billed in units of
time, but rather in episodes of treatment.
GENERAL SURGERY GUIDELINES
Hospital Acquired Conditions (HACs)
SCDHHS will make zero payments to providers for other provider preventable conditions which
includes Never Events. The reporting requirements for Never Events include ASCs and
practitioners. These providers will be required to report Never Events on the CMS-1500 claim form
or the 837-P claim transaction. Avoidable errors that fall under this policy include:
• Wrong surgical or other invasive procedure performed on a patient.
• Surgery or other invasive procedure on the wrong body part.
• Surgical or other invasive procedure performed on the wrong patient.
Providers are required to follow the following procedures for reporting avoidable errors (Never
Events):
Claims submitted using the CMS-1500 claim form or 837-P claim transaction, must include the
appropriate modifier appended to all lines that relate to the erroneous surgery(s) or procedure(s)
using one of the following applicable National Coverage Determination modifiers:
• PA — Surgery wrong body part
• PB — Surgery wrong patient
• PC — Wrong surgery on patient
The non-covered claim must also include one of the following ICD-10-CM diagnosis codes reported:
• Y65.51 — Performance of wrong procedure (operation) on correct patient

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
221
• Y65.52 — Performance of procedure (operation) on patient not scheduled for surgery
• Y65.53 — Performance of correct procedure (operation) on wrong side or body part
Related Claims
Within 30 days of receiving a claim for a surgical error, SCDHHS shall begin to review beneficiary
history for related claims as appropriate (both claims already received and processed and those
received after the notification of the surgical error). Also, the PI Division or its designee will audit all
claims for the recipient to determine if they relate to or have the potential to be related to the original
Never Event claim. When the PI or designee identifies such claims, it will take appropriate action to
deny such claims and to recover any overpayments on claims already processed.
Every 30 days for an 18-month period from the date of the surgical error, PI or its designee will
continue to review recipient history for related claims and take appropriate action as necessary.
Related services do not include performance of the correct procedure.
General Provisions
Medicaid will not pay any claims for “provider-preventable conditions” for any member who is
Medicare/Medicaid eligible.
No reduction in payment will be imposed on a provider for a provider preventable condition, when
the condition defined as a PPC for the member existed prior to the initiation of the treatment for that
member by that provider.
Reductions in provider payments may be limited to the extent that the following apply:
• The identified PPC would otherwise result in an increase in payment.
• The SCDHHS can reasonably isolate for non-payment the portion of the payment directly
related to treatment for and related to the PPC.
To review the complete Health Acquired Conditions policy, please visit:
http://www.cms.gov/HospitalAcqCond
.
Exploratory Procedures
If a procedure is carried out through the laparotomy incision, the physician may choose to bill for
either the laparotomy or the actual procedure performed during the surgery; most likely, it will be the
code that reimburses the higher rate. In any case, South Carolina Medicaid will sponsor payment for
either the procedure or the laparotomy, not both.
Under the same principle, when a surgical procedure is performed through an endoscope, the
diagnostic endoscopy is inclusive in the reimbursement. The physician may be reimbursed for either
the endoscopic procedure or the diagnostic endoscopy, not both.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
222
When endoscopy procedures are performed in the office, small supplies and materials provided by
the physician over and above those usually included with the office visit may be billed. A minor
surgical tray may also be billed.
Multiple Surgery Guidelines
Multiple surgeries include separate procedures performed through a single incision, or separate
procedures performed through second and subsequent incisions or approaches. All surgical
procedures for the same DOS must be filed on one claim form when possible.
Payment Guidelines
When multiple surgeries are performed at the same operative session, the procedure that
reimburses the highest established rate will be considered the primary procedure and will be
reimbursed at 100% of the established rate. All second and subsequent surgeries performed at the
same operative setting will be reimbursed at 50% of the established rate. Procedure codes that are
exempt from multiple procedure reduction as outlined by the AMA in the CPT Standard Edition are
reimbursed at 100%.
A vaginal delivery and tubal ligation performed on the same DOS will not be affected by this policy.
Both procedures are reimbursed at 100%, even when performed on the same day. Use the
79 modifier on the tubal ligation to ensure correct reimbursement.
Modifiers
Listed services and procedures may be modified under certain circumstances. When applicable, the
modifying circumstance must be identified by the addition of the appropriate modifier code, which
must be reported by adding a two-digit number (modifier) placed after the procedure number.
Modifiers commonly used in surgery are listed in the surgery section of the CPT and on the provider
portal. Only the first modifier indicated will be used to process the claim — Medicaid will key only the
first modifier indicated for each procedure.
Billing
Claims for surgery must be filed using the CPT code that most closely describes the surgical
procedure that was performed. When this is not applicable, an unlisted procedure code may be
used, and the appropriate documentation must be attached to the claim form for adequate
reimbursement.
Claims for more than one surgical procedure performed at the same time by the same physician
must be billed as follows:
• On a single claim form, unless more than six procedures are performed.
Note: If more than one surgical procedure is billed for the same DOS on different claims, the
second claim that processes may reject. To avoid this delay, file all surgical procedures for the
same DOS on one claim form.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
223
• Only for subsequent procedures which add significantly to the major surgery or are not
incidental to the major surgery.
• Using the appropriate modifier (Medicaid will key the first modifier indicated for each procedure
only).
• With charges listed separately for each procedure.
When identical procedures (not bilateral) are billed for the same day, the first must be billed without
a modifier, and the second with modifier 51. If the same procedure is billed a third time, the claim
must be filed hardcopy with supporting documentation.
Modifier 62 is used to indicate that the skills of two surgeons were required. Modifier 66 is used to
indicate circumstances requiring a surgical team. These modifiers will ensure proper reimbursement
for each provider involved.
Modifier 52 is used to describe reduced services. Modifier 53 is used to describe a discontinued
procedure. Both modifiers will be reimbursed at 50% when billed with a surgical procedure.
Separate Procedures Performed on the Same DOS
When two separate surgical procedures are performed on the same DOS at different operative
sessions, both procedures will be allowed 100% of the established rate.
To report, submit the second procedure with the 78 or 79 modifier. This will ensure that both
procedures will be paid at 100%. If not reported in this manner, the lower priced of the two
procedures will be reimbursed at 50%. All surgical procedures performed on the same DOS must be
filed on the same claim form whenever possible.
Procedure Codes That Multiply
Occasionally the CPT defines certain procedure codes as "each", indicating the possibility of
multiple procedures. When filing these types of codes, list the code one time for the DOS and bill
the appropriate number of units in the “units” column of the claim form and the total charge for the
number of units billed. If there is only one surgical procedure for the DOS and multiple units are
billed, payment for codes that multiply will be 100% of the established rate for the first unit and 50%
for each additional unit(s) filed. If a surgical procedure with a higher established rate is performed on
the same DOS, the higher established rate will be allowed and the code(s) to multiply will pay 50%
of the established rate per unit filed.
Automatic Adjustments to Paid Surgical Procedures
All surgical procedure codes for the same patient and same DOS must be filed on the same claim
form. This ensures that the correct procedure will reimburse at 100% of the established rate. At
times, however, surgical codes are filed on separate claim forms, causing incorrect payments and
the need for adjustments.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
224
Automatic adjustments work in the following manner: When a claim for a surgical procedure code is
submitted, the system will review the paid claims history for that patient, DOS and provider. If there
is no previously paid surgical code(s) on file for that DOS, the surgery will pay at 100% of the
established rate. If, however, there is a previously paid surgery on file for that patient, DOS, and
provider, the system will compare the previously paid surgery and the newly submitted surgical
code. It will then determine which of the codes would correctly reimburse the provider at 100%. If
the newly submitted surgical code would pay at 100%, the system will make an automatic
adjustment against the previously paid surgical code by subtracting 50% of the previously paid
procedure from the amount to be reimbursed for the newly submitted surgical code. Therefore, the
newly submitted surgical code will be allowed at 100% although the payment may not reflect the full
amount due because of the recoupment of 50% of the previously paid procedure.
When the system reviews paid claims history for a patient, DOS and provider, and finds that the
previous surgical claim paid correctly at 100% and the second surgical claim would pay at 50% of
the established rate, there will be no adjustment as the claim will pay correctly.
Bilateral Surgery
To report a bilateral procedure, bill the first procedure with no modifier, and the second procedure
with a 50 modifier. Report on two lines instead of one. A bilateral procedure billed with only one line
will result in underpayment. Codes with bilateral descriptions may not be billed with a 50 modifier.
Claims filed for an assistant surgeon performing a bilateral procedure must be filed hardcopy with
documentation using the 80, 81 or 82 modifier on both lines of the procedure code that is bilaterally
performed.
Bilateral procedures will be reimbursed at 100% for the first procedure, and 50% for the second
procedure (same as multiple procedures). If the bilateral procedure is billed in conjunction with
another procedure that is normally reimbursed at a higher rate than the bilateral procedure, then
each of the bilateral procedures will be reimbursed at 50%.
Billing Procedures
Surgical endoscopic procedures always include the diagnostic endoscopy. Therefore, the
diagnostic endoscopy code is not allowed in addition to the surgical endoscopy for the same
anatomical site.
Under the same principle, when a surgical procedure is performed through an endoscope, the
diagnostic endoscopy is inclusive in the reimbursement. The physician may be reimbursed for either
the endoscopic procedure, or the diagnostic endoscopy, not both.
Endoscopic procedures do not require a 26 modifier when performed in the inpatient or OP hospital
setting.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
225
When two endoscopic procedures are performed on the same DOS, the first procedure must be
reported without a modifier, and the second procedure must be reported with modifier 51.
Ambulatory Surgical Services
To bill for the professional service, the surgeon must submit claims following the usual surgical
guidelines, using place of service “24”.
Surgical Package
The surgical package includes post-operative care for 30 days following surgery. Post-operative
services rendered and billed during this 30-day period will be rejected for an 854-edit code. Normal
post-operative care is considered part of the surgical package and includes office examinations and
all hospital follow-up visits, including discharge management. Hospital and office E&M visits are
allowed up to and including the day of surgery.
ER services and critical care are not considered part of the surgical package. They may be billed in
addition to the surgery performed. For guidelines on delivery admissions, please refer to Perinatal
Care under Obstetrics and Gynecology within this section of the guide.
Surgical procedures that are billed within 30 days prior to a paid office or hospital visit will suspend
for review. If applicable, the office or hospital visit(s) will be recouped, and the surgery claim will
process for payment. The surgical procedure may be rejected with edit 855. In that case, providers
must submit a new claim and indicate that the surgery to be paid, and the visits to be recouped.
Ambulatory Surgical Services
Complications or services rendered for a diagnostic reason unrelated to the surgery may be billed
with a separate examination code if the primary diagnosis reflects a different reason for the service.
To report post-operative visits unrelated to surgery, submit the visit code(s) with modifier 24 or 25.
The medical record must substantiate that a visit(s) was justified outside of the surgical package
limitation.
Follow-up care in the office and/or hospital may be billed if the surgery is an exception to the
surgical package.
Assistant Surgeon
When billing for the assistant surgeon's fee, the modifier 80, 81, or 82 must accompany all
procedure codes filed. Assistant surgeons must be physicians. Medicaid will not reimburse
non-physician surgery assistants.
If, due to unforeseen circumstances, the surgery did require an assistant, and an assistant surgeon
is not allowed for the surgical procedure, Medicaid will review the claim for reimbursement.
Providers may submit a new claim with documentation for medical review. The medical record must
justify the special need for an assistant surgeon.
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
226
An assistant surgeon will be reimbursed at 20% of the total allowable fee per procedure.
An assistant surgeon must use the same CPT procedure codes as the primary operating surgeon.
The assistant surgeon modifier is the only modifier required for each procedure billed. Medicaid will
only key the first modifier indicated.
The claim for the assistant surgeon must be submitted with a different individual provider number
(rendering physician) from the primary surgeon. The assistant surgeon must be enrolled with South
Carolina Medicaid in order to receive reimbursement.
Claims filed for an assistant surgeon performing a bilateral procedure must be filed using the 80, 81
or 82 modifiers.
SURGICAL GUIDELINES FOR SPECIFIC SYSTEMS
Organ Transplant and Transplant related services
Billing and Reimbursement Policy
Providers must enter the prior authorization number issued by QIO in the appropriate authorization
field of all CMS-1500 claim forms submitted for reimbursement. All general surgery guidelines apply
when billing for organ transplants including keratoplasty. Reimbursement for transplants include
technical services and professional services, which are billed separately from each other. For kidney
transplants, if Medicare coverage is primary, Medicaid will only pay if Medicare benefits are either
not available or have been denied. A Medicare denial of benefits must accompany the claim, and
the patient must be End Stage Renal Disease (ESRD) enrolled with Medicaid.
Providers must follow the guidance below when billing for transplant and transplant-related services
for a Medicaid member in the FFS program:
FFS Members
• Corneal transplants and related services
Medically necessary corneal transplants delivered to a FFS member will be reimbursed by
SCDHHS. The reimbursement to the hospital includes all technical services, including donor
testing and preparation. Professional services are compensable separately using the
appropriate Code of Procedural Terminology (CPT) codes for Keratoplasty. The Ambulatory
Surgery Centers (ASC) will be reimbursed for the transplant surgical procedure and the
corneal tissue must be submitted with the appropriate HCPCS procedure code for
processing, preserving and transporting covered tissue. ASC providers must attach a copy
of the invoice reflecting the cost of the tissue along with the claim to avoid delays in
payment.
• All other transplants and transplant-related services

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
227
Only QIO-approved authorizations will be considered for reimbursement. Provider must file
claims for a FFS member to the South Carolina Healthy Connections Medicaid for all the
approved transplants and transplant-related services which include:
pre-transplant services (medically necessary services rendered in preparation for
the transplant within 72 hours prior to the transplant event/surgery),
the transplant event (surgery and services rendered through discharge),
Medically necessary post-transplant services (from discharge up to 90 days post
discharge).
MCO Members
• All transplants and transplant-related services
Medically necessary transplants delivered to a MCO member will be covered by the MCO
plan. Providers must file the claims to the MCO following the MCO’s billing guidance.
Integumentary System
Lesion Removal
Supporting documentation is required for a claim submitted for a lesion and a dermal anomaly
removal or revision with diagnosis codes L91.0 and L90.5. Medicaid will not cover treatment that is
considered to be experimental, investigational (i.e., chemical peels, cryosurgery, dermabrasion,
punch grafts, bleomycin, interferon and verapamil injections), or done for cosmetic or emotional
purposes.
Keloid/Scar Conditions
Claims for these treatments must be accompanied by documentation that supports the criteria as
outlined above. Medicaid will not provide coverage for excision and/or treatment of non-malignant
dermal lesions, dermal anomalies and Keloid/scar conditions under the following circumstances:
• The treatment is performed for cosmetic or emotional purposes.
• The therapy is experimental or investigational.
Examples include chemical peels, cryosurgery, dermabrasion and punch grafts.
Skin Grafts
Providers must follow CPT guidelines when billing for skin grafts. Procedures are identified by size
and location of the defect (beneficiary area) and the type of graft. Skin graft codes that pertain to
subsequent (each additional square centimeter) areas must be billed in units.
ANESTHESIA SERVICES
Time Reporting
South Carolina Medicaid only accepts actual time when billing for anesthesia services. Report time
in minutes, in the “units” field (Item 24G) of the CMS-1500 claim form.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
228
Example:
Anesthesia Start Time — 1:15 pm
Anesthesia Stop Time – 2:45 pm
Total Anesthesia Time Billed in Minutes — 90 minutes
Modifiers of Anesthesia Services
The following modifiers are acceptable when billing In conjunction with the appropriate anesthesia
CPT procedure code based on medical direction involved in the procedure:
• AA – Anesthesia services performed personally by an anesthesiologist. The anesthesiologist
must remain in constant attendance of the patient.
• QY — Medical direction of one CRNA by an anesthesiologist.
• QK — Medical direction of two, three or four concurrent anesthesia procedures involving
qualified individuals.
• AD — Medical direction of more than four concurrent anesthesia procedures involving
qualified individuals.
• QX – Anesthesia services performed by CRNA with medical direction by a physician
(anesthesiologist).
• QZ- Anesthesia services performed by CRNA without medical direction by a physician
(anesthesiologist).
If the complexity of a surgery or complications that develop during surgery require both the CRNA
and the anesthesiologist to be involved completely and fully in a single anesthesia case, both
providers may bill for their services. The complexity of service or complications must be clearly
documented in the patient's records and submitted with the claim. The anesthesiologist must bill
using the AA modifier, anesthesia services performed personally by anesthesiologist. The CRNA
must bill using the QZ modifier. These claims must be filed hardcopy with documentation supporting
the need for both professionals.
Routine scheduling of a CRNA/AA, resident or intern to assist an anesthesiologist in the care of a
single patient does not justify medical necessity.
The monitored anesthesia care modifiers QS, G8 and G9 do not describe medical direction involved
in the anesthesia procedure. The monitored anesthesia care modifiers describe the type of
anesthesia care. These are secondary modifiers. It is important to use a modifier that describes the
medical direction involved as the first modifier when using more than one; Medicaid only accepts
one modifier.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
229
Procedures
Intubation
Payment is allowed for intubation (31500) performed in the intensive care unit or ER by an
anesthesiologist or CRNA. Intubation is considered a regular part of anesthesia services and may
not be a fragmented charge when performed in conjunction with anesthesia services.
Catheter Placement
Anesthesiologists are reimbursed for placement of central venous, subclavian, arterial or
Swan-Ganz catheters in addition to anesthesia services. CRNA/AAs will not be reimbursed for these
codes. Refer to the provider portal for a list of codes.
Spine and Spinal Cord Puncture for Injection
Medicaid reimburses personally performing anesthesiologists and CRNAs for the following spine
and spinal cord puncture codes. Either the anesthesiologist or CRNA may bill for the codes listed
below without a modifier, but not both.
For placement of the continuous epidural catheter, an anesthesiologist or CRNA, personally
performing or supervised, bills the appropriate code with the appropriate modifier. Please refer to
the provider portal for a list of appropriate codes.
Laboring Epidural
The continuous epidural codes for the vaginal delivery and a vaginal delivery becoming a C-section
reimburses a flat rate regardless of the time involved. The anesthesiologist and CRNA must bill with
the appropriate modifier indicating personally performed or as part of an anesthesia team.
When a vaginal delivery becomes a C-section and the catheter remains in place for the C-section,
you must bill for the vaginal delivery and then use the add-on code. This is an add-on code and
therefore must be billed in conjunction with the procedure code.
If the C-section is performed under general anesthesia, you may bill the time for the C-section only,
in addition to the labor and delivery epidural.
For a scheduled C-section, an anesthesiologist or CRNA bills with payment based on time.
When a tubal is performed at a later surgical session and the same catheter remains in place and is
re-dosed, it is not appropriate to bill general anesthesia based on time.
Anesthesia Consultations
Consultative services rendered on behalf of any direct or indirect patient care are included in the
basic value of the anesthesia payment and may not be charged separately. However, if an
anesthesiologist is requested to consult with another physician or hospital anesthetist or examines a
patient to determine the appropriate anesthetic agent and does not furnish direct anesthesia

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
230
services or assume direct supervision of the anesthesia service, then the anesthesiologist may bill a
separate consultation code based on the appropriate level of service.
The anesthesiologist may bill a consultative code if the surgery is canceled. An anesthesiologist
may not charge a consultative service in addition to any anesthesia service (either for supervision or
direct care).
Fragmented Charges
Services considered an integral part of anesthesia services, such as blood gases, venipuncture,
oxygen capacity, blood transfusions, administration of medications, intubation in the operating room,
etc., are non-compensable when billed separately.
PAIN MANAGEMENT SERVICES
Post-Operative Pain Management
Physicians billing for post-operative pain management must bill the single or continuous procedure
code when the insertion of the epidural catheter is for purposes other than surgical anesthesia.
These codes include an allowance for insertion of the needle or catheter into the epidural space,
and an allowance for injecting the drug or medication through the portal. If a continuous epidural is
used for surgical anesthesia and remains in for post-operative pain, an additional insertion cannot
be billed for management of the post-operative pain. These procedures must be billed without a
modifier for the initial insertion.
Daily management of the epidural analgesia must be billed on days after the day of insertion of the
epidural catheter. Up to five days of post-operative pain management may be allowed without
additional documentation to justify the extended service. Unless a separately identifiable service has
been rendered on the same day, do not bill any other service, including an E&M code.
Modifier QZ or AA (anesthesia services performed personally by anesthesiologist) must be used
with the appropriate service. Please refer to Anesthesia Services within this section of the manual
for a description of these modifiers.
Nerve Blocks
Physicians are reimbursed for injection of anesthetic agents for nerve blocks. Anesthesiologists bill
for these services without a modifier. Use separate procedure codes for trigger point injections that
may also be billed by the anesthesiologist with no modifier.
Injecting any substance through the needles, including small amounts of contrast to confirm the
position of the needle, is considered an integral part of the procedure and is not reimbursed
separately.
When destruction of the facet joint nerve is performed following the block, only the codes for the
nerve destruction must be billed, since their allowance includes the nerve block procedure.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
231
PATHOLOGY AND LABORATORY SERVICES
In accordance with Title XIX of the Social Security Act, Medicaid reimbursement for laboratory fees
cannot be higher than the Medicare fee schedule established for laboratory services. Fee schedules
are located on the SCDHHS website at http://www.scdhhs.gov
.
It is further mandated that only the actual provider of the service or the provider performing the test
may charge and receive Medicaid reimbursement. Providers cannot bill Medicaid patients when
Medicaid would have paid for the lab service if the appropriate billing procedures and referral
procedures had been followed.
Services or supplies administered by the hospital or hospital employees are considered a part of the
overall hospital service and are reimbursable only under the hospital allowable costs. A physician
who is either salaried or contracted by the hospital, and who performs services under contract or
employment, may not bill for those services separately under his or her individual Medicaid provider
number. The contracting hospital may file for these services under the professional fees allowable
for the hospital under their hospital-based physician’s Medicaid number.
Professional component services constitute the professional interpretation and report and must be
charged using the 26 modifier. Claims for professional pathology services indicating a hospital as
the place of service will be rejected if submitted without the 26 modifier. Only anatomical, surgical,
and the clinical pathology procedures listed earlier in this section are reimbursable with a
26 modifier.
TC services are those services usually performed by a hospital in the administration of a hospital
lab. These services include payment for a lab technician, equipment and supplies. Only a hospital
may bill for separate technical lab services.
Total lab procedures are a combination of both the professional and TCs. Usually, an independent
laboratory or a private practicing physician performing his or her own lab services is the only
provider eligible for a total lab reimbursement rate. Pathologists and laboratories may bill for
beneficiaries that are in the Family Planning Eligibility category only, but a valid family planning
diagnosis code must be present on the claim, along with the FP modifier.
Automated Chemistry Tests and Panels
Providers billing for automated multi-channel chemistry tests may bill these tests individually as
described in the CPT coding manual. The system will bundle specific tests and reimburse one rate
based on the number of tests performed. Claims with less than three of these tests will pay each
individual test based on the fee schedule. The list above identifies those codes, when billing three or
more, that are bundled to pay one rate based on the number of tests. A provider may also bill for
individual tests that are assigned to a panel. If the individual tests are included on the list, these
tests will also bundle when three or more are filed on the same claim form and pay one rate based
on the number of tests.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
232
Fee schedules are located on the SCDHHS website at http://www.scdhhs.gov.
Blood
Medicaid requires that the securing supplier of blood products bill those products or packed cells. If
a hospital laboratory secures the packed cells and washes, then the hospital must charge for the
blood. A physician, clinic or other non-securing provider may not bill for the blood. In addition to the
products, the securing provider may only bill for additional type and cross matching, if appropriate,
and the transfusion.
Professional Pathology Services
A pathologist may charge for a clinical lab interpretation if requested by the attending physician and
reported as a contribution to direct patient care. This diagnostic procedure must be charged for
limited and comprehensive services, respectively.
Interpretation of clinical lab tests will not be reimbursed. Only charges for consultations on clinical
lab tests may be recognized. A professional component modifier is not required (26). General
consultation procedures are not compensable for professional clinical lab services.
Independent Laboratories
Whenever an independent laboratory charges Medicaid with an unlisted procedure, support
documentation is required. Since SCDHHS and most independent laboratories recognize the mutual
benefits of automated claims processing, steps must be taken to insure timely and efficient claims
submission.
When a laboratory initiates a new lab test(s) or a new combination, notification must be sent to the
Pathology program manager. This preliminary process will quicken the assignment of a code and
approval for Medicaid payment.
Independent laboratories must submit charges on a CMS-1500 claim form with the appropriate CPT
or supplemental code. The place of service must be an "81" and the DOS when the test was
performed must be indicated.
Independent labs may bill for beneficiaries who are in the Family Planning Eligibility category only. A
valid family planning diagnosis and modifier must be present on the claim.
Clinical Laboratory Improvement Amendments (CLIA)
Claims Editing
Claims will be denied for lab services delivered by any lab site meeting one or more of the following
descriptions:
• A lab that does not have CLIA certification.
• A lab that submits claims for services not covered by CLIA certificate.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
233
• A lab that submits claims for services rendered outside the effective dates of the CLIA
certificate.
Individual physicians who are members of a group must bill under the group number. The CLIA
editing is based on the provider number in field 33 of the CMS-1500. For more detailed information,
please refer to the Provider Administrative and Billing Manual.
Lab Procedures
The following sections indicate the lab procedures allowed for each type of certification. Current
CLIA information can be found on the Internet at http://www.cms.hhs.gov/clia/
.
Labs issued a Certificate of Registration, Certificate of Accreditation or Partial Accreditation, or
Certificate of Compliance are allowed to perform and bill for the following procedures:
• All pathology and lab procedures
• Plasma volume, radiopharmaceutical volume-dilution technique (separate procedure); single
sampling
• Plasma volume, radiopharmaceutical volume-dilution technique (separate procedure); multiple
areas
• Red cell volume determination (separate procedure); single sampling
• Red cell volume determination (separate procedure); multiple samplings
• Whole blood volume determination, including separate measurement of plasma volume and red
cell volume (radiopharmaceutical volume-dilution technique)
• Red cell survival study
• Platelet survival study
• Vitamin B-12 absorption study (e.g., Schilling test); without intrinsic factor
• Vitamin B-12 absorption study (e.g., Schilling test); with intrinsic factor
• Vitamin B-12 absorption studies combined, with and without intrinsic factor
• Culture and sensitivity urine only
Labs issue a Certificate of Waiver limited to performing only the following procedures:
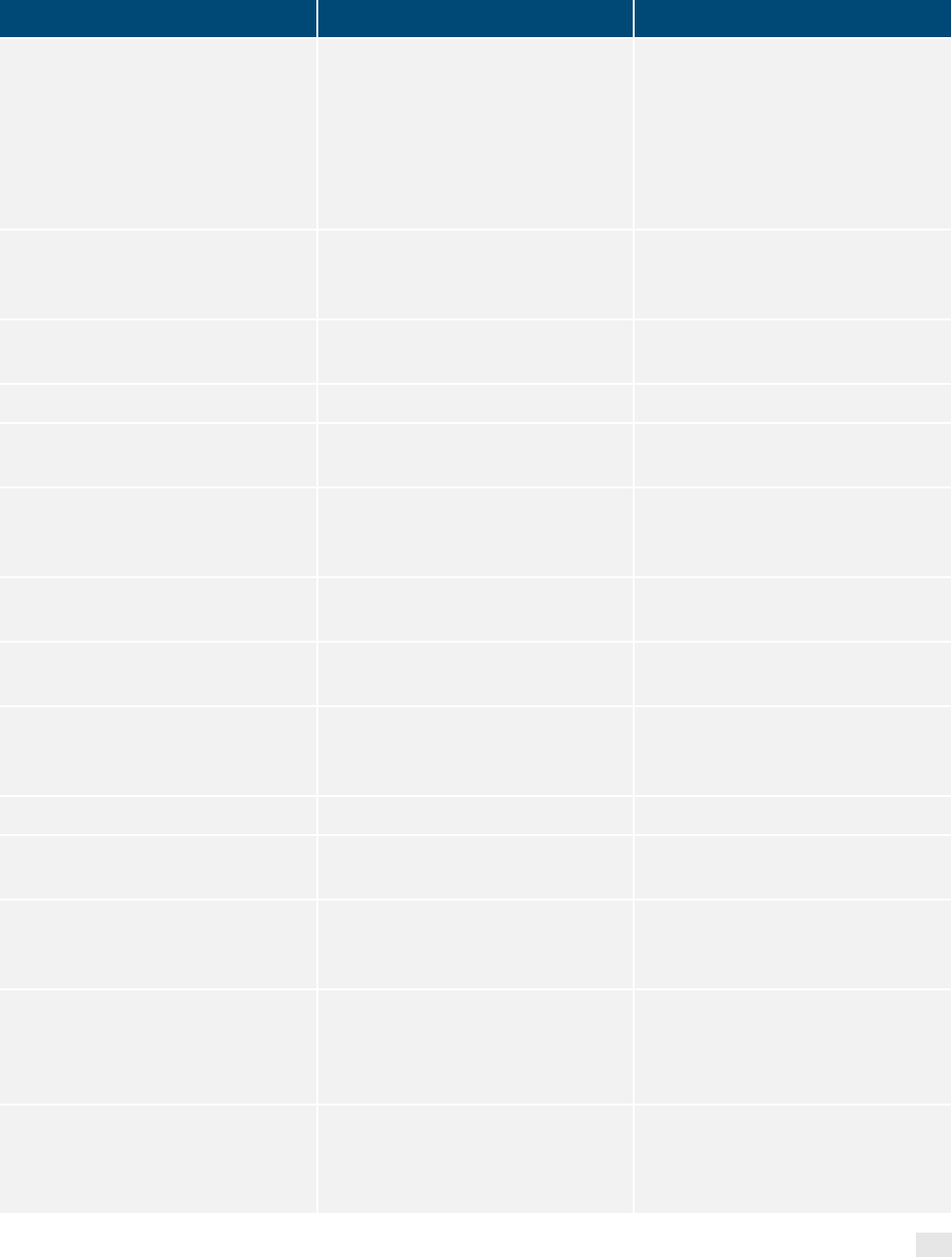
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
234
PROCEDURE
Lipid panel
Urinalysis, by dipstick or tablet
reagent for bilirubin, glucose,
hemoglobin, ketone, leukocytes,
nitrite, pH, protein specific gravity,
urobilinogen, any number of
constituents; non-automated,
without microscopy
Urinalysis, by dipstick or tablet
reagent for bilirubin, glucose,
hemoglobin, ketone, leukocytes,
nitrite, pH, protein specific gravity,
urobilinogen, any number of
constituents; automated, without
microscopy
Bacteriuria screen, exp
culture/dips
Urine pregnancy test, by visual
color comparison methods
Albumin, urine, microalbumin,
semiquantitative (e.g., reagent
strip assay)
Amines, vaginal fluid, qualitative
Blood, occult; feces, one to three
simultaneous determinations
Cholesterol, serum, total
Collagen cross links; any links Creatinine; other source Glucose; quantitative
Glucose: post glucose dose
(includes glucose)
Glucose: tolerance test, three
specimens (includes glucose)
Glucose; tolerance test, each
additional beyond three specimens
Glucose, blood, by glucose
monitoring device(s) cleared by
the FDA specifically for home use
Glutathione Reductase RBC Glycated protein
Gonadotropin; follicle stimulating
hormone
Gonadotropin; luteinizing hormone
Hemoglobin; by copper sulfate
method, non-automated
Hemoglobin; glycated
Immunoassay analyte not
antibody, single step method
Lactate (Acetic acid)
Lipoprotein, direct measurement;
high-density cholesterol
(HDL cholesterol)
pH, body fluid, except blood Transferase; alanine amino
Triglycerides Gonadotropin chorionic qualitative Unlisted chemistry procedure
Blood count; spun microhematocrit
Blood count; other than spun
hematocrit
Blood count; hemoglobin
Prothrombin time
Sedimentation rate, erythrocyte;
non-automated
Immunoassay for tumor antigen,
qualitative or semiquantitative;
(EG, bladder tumor antigen)
Heterophile antibodies; screening
Immunoassay for infectious agent
antibody, qualitative or
semiquantitative, single step
method (e.g., reagent strip)
Antibody; borrelia burgdorferi
(Lyme Disease)
Culture, bacterial; aerobic isolate,
additional methods for definitive
identification, each isolate
Infectious agent antigen detection
by enzyme immunoassay
technique qualitative or
semiquantitative; multiple step
Infectious agent antigen detection
by immunoassay with direct optical
observation; influenza
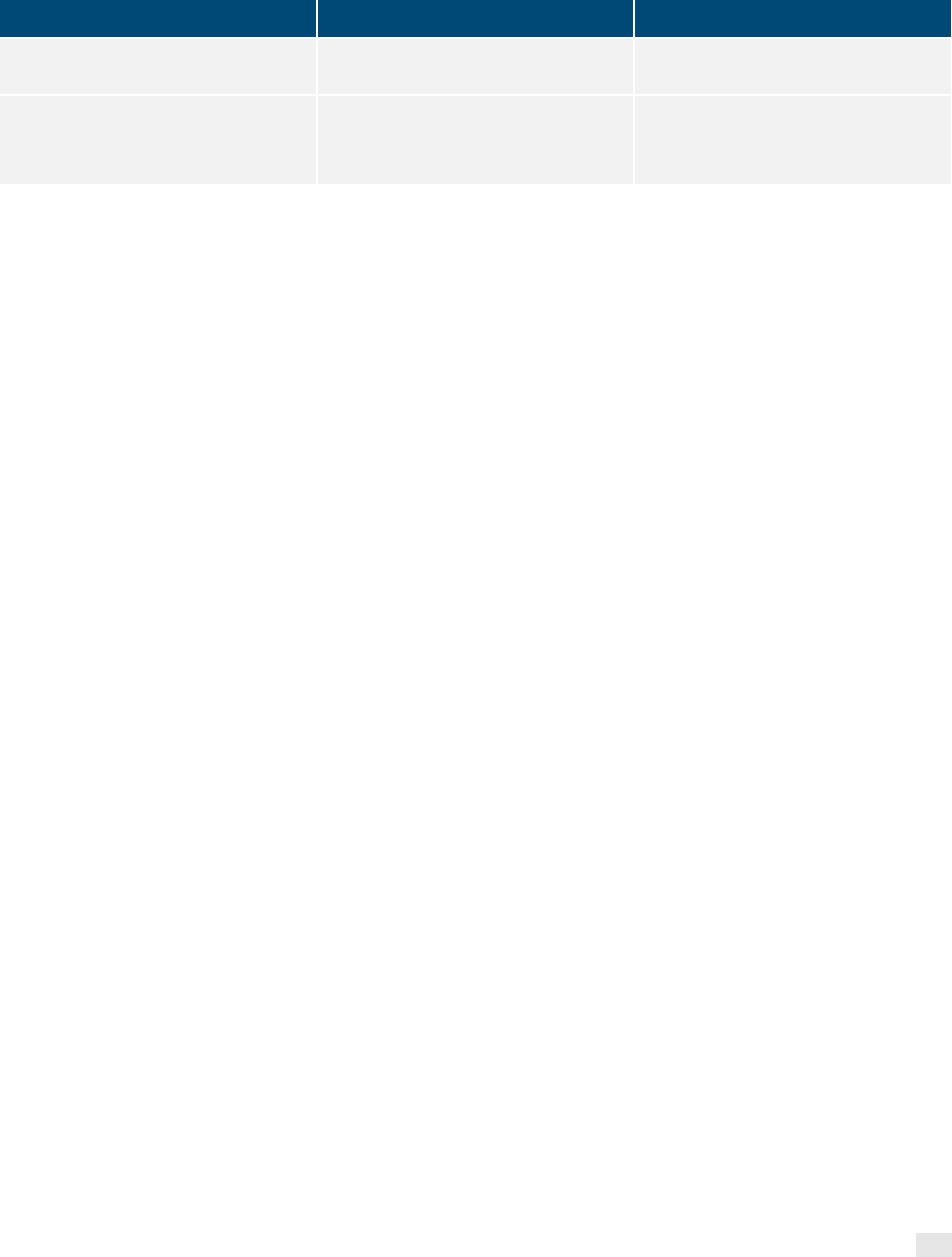
PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
235
PROCEDURE
method, not otherwise specified,
each organism
Streptococcus, screen, direct
Anaerobic isolate, additional
methods required for definitive
identification, each isolate
Aerobic isolate, additional methods
required for definitive identification,
each isolate
Labs issued PPMP Certificates are allowed to perform the above listed procedures for Certificate of
Waiver and the following procedures:
• Fecal Leukocyte examination
• Semen analysis
• Wet mount, including preparations of vaginal, cervical, or skin specimens
• All potassium hydroxide preparations
• Pinworm examinations
• Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes,
nitrite, pH, protein, specific gravity, urobilinogen, any number of these constituents,
non-automated, with microscopy
• Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes,
nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; automated,
with microscopy
• Urinalysis; microscopic only
• Urinalysis; two or three glass test
• Nasal smear for eosinophil
RADIOLOGY AND NUCLEAR MEDICINE
Positron Emission Tomography (PET) Scans
Providers billing for radiopharmaceutical diagnostic imaging agents utilizing a CMS-1500 claim form
must select the appropriate HCPCS code. When billing for an unlisted radiopharmaceutical agent
the provider must include a copy of the invoice with the CMS-1500 claim form for review.
Clinical Treatment Management
If at the final billing of the treatment course, there are three or four fractions beyond a multiple of
five, those three or four fractions are considered a week. If there are only one or two fractions

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
236
beyond a multiple of five, reimbursement for the sessions will be considered as having been
covered through prior payment.
When the patient receives a mixture of simple, intermediate, and/or complex services, bill the code
that represents the majority of the fractions furnished during the five-fraction week.
Independent Imaging Centers and Mobile Imaging Units
Mobile units may bill the following codes for set-up and transportation in addition to the x-ray or EKG
when the patient would require special transportation. These codes must be billed without a
modifier:
• Set up of portable x-ray equipment in a nursing facility, per radiological procedure (other than
re-takes of the same procedure). Medicaid will not reimburse for re-takes.
• Round trip transportation of portable x-ray equipment and personnel to nursing home, per trip to
facility or location; one patient seen.
• Round trip transportation of portable x-ray equipment and personnel to nursing home, per trip to
facility or location; more than one patient seen, per patient.
• Round trip transportation of portable EKG to facility or location; per patient.
Charges must be submitted on a CMS-1500 claim form with the following restrictions:
• All CPT procedure codes must be submitted with a TC modifier.
• Separate charges for injection of contrast mediums, radiopharmaceuticals or catheterizations
are not covered.
Modifiers and Components
Radiology services are divided into the following defined components:
• TC — Includes equipment, supplies and technician time and effort. Provider must bill using the
TC modifier.
• Professional Component — Includes the physician’s supervision, interpretation, and report, and
when appropriate, the physician’s administration of an injection or catheterization. Payment will
be made to the physician or radiologist who performed the interpretation and written report at
the time of the diagnosis and treatment. Provider must bill using the 26 modifier.
• Complete Procedure — Is the combination of both the technical and professional services.
Provider must bill 00 modifier.

PHYSICIANS SERVICES PROVIDER MANUAL
SOUTH CAROLINA DEPARTMENT OF
HEALTH AND HUMAN SERVICES
237
• 76 modifier — The use of the 76 modifier can only be used on medically necessary repeat
radiology procedures performed on the same DOS and must include both the technical and
professional components.
Providers must bill using the appropriate modifiers which are determined by the parameters of
services rendered. Therefore, if a rendering provider is only submitting the TC of the procedure, use
the TC modifier along with the procedure code performed. If the claim is submitted utilizing the UB
format, the modifier TC will be assumed. No further payment will be made to any additional provider
for the TC for this procedure.
If the rendering provider is submitting the professional component/interpretation of the radiological
procedure, use the 26 modifier along with the procedure code performed. No further payment will be
made to any additional providers for the professional component of the procedure.
