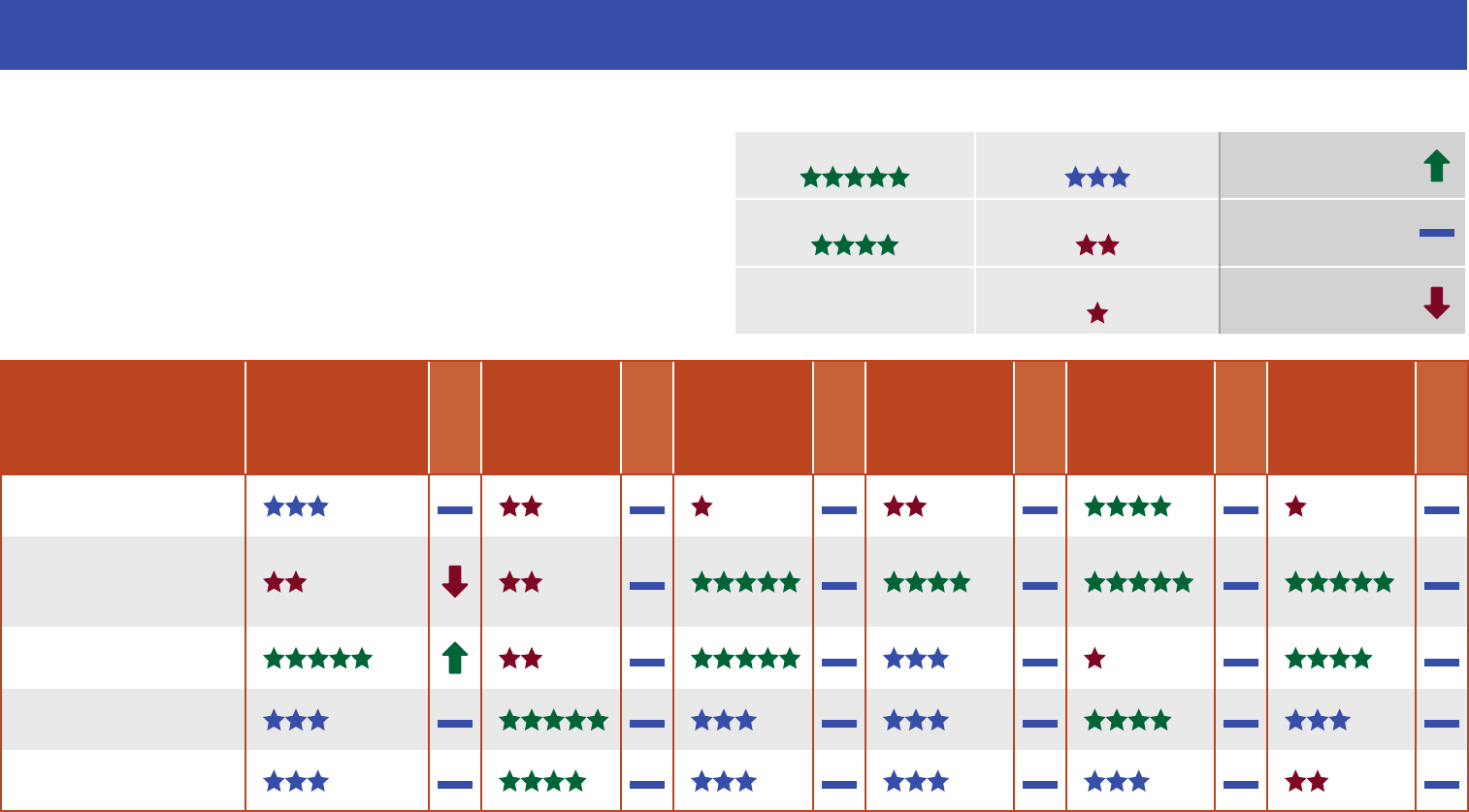
HealthChoice Illinois: 2022 HealthChoice Illinois Plan Report Card
Comparing HealthChoice Illinois Plans
This report card is for individuals in the HealthChoice Illinois Managed
Care Program in Cook County. The report shows how the managed
care plans compare to one another in key performance areas. The
ratings for each plan are to help pick a plan that is best for you. The
change for each performance area shows if the plan’s rating got
better, worse, or stayed the same from last year’s report card.
Performance Rating Performance Change
Highest Performance
Average Performance Rating
Got Better
High Performance
Low Performance Rating Stayed
the Same
Lowest Performance Rating
Got Worse
Plan
Doctors’
Communication
Change
Access
to Care
Change
Women’s
Health
Change
Living With
Illness
Change
Behavioral
Health
Change
Keeping
Kids Healthy
Change
Aetna Better Health
Blue Cross
Community
Health Plans
CountyCare
Health Plan
MeridianHealth
Molina Healthcare
What is Rated in Each Performance Area?
Doctors’ Communication
• Doctors explain things well to members
• How happy members are with their doctor
Access to Care
• Members get the care they need when they need it
Women’s Health
• Women get screenings and tests for female cancers and diseases
• Women receive care before and after their babies are born
Living With Illness
• Members living with conditions, like diabetes and high blood
pressure, get the care they need by getting tests, checkups, and the
right medicines
Behavioral Health
• Members with behavioral health conditions get the follow-up care
they need
• Members who use drugs and alcohol get the help they need
Keeping Kids Healthy
• Children get regular checkups and important shots that help them
stay healthy
Choosing a HealthChoice Illinois Plan
Choosing the plan that best meets your health care needs is important. Here are some questions to ask before you pick a plan:
• Have you read all of the materials that were included in this enrollment packet?
• Which plans have the extra services you want? (See Your Health Plan Choices that came with this packet.)
• How did the plans rate in each area on the front of this report card? Do the doctors in the plan I like communicate with
their members?
— Do the members in the plan I like get care when they need it?
— Do women get the care they need?
— Do members with behavioral health conditions get the care they need?
— Do kids get the care they need to stay healthy?
• Which plans have the doctors, clinics, hospitals, specialists, long term care waiver service providers, and other
providers you use? Call your providers to nd out which HealthChoice Illinois plans they accept.
• Do you need providers that speak a certain language?
• How far do you want to travel to see your providers?
• Which plans have co-pays?
• Did the plan receive any sanctions from the state?
— For more information, visit the website here.
Need More Information on Your HealthChoice Illinois Plan Options?
Visit the Illinois Department of Healthcare and Family Services online at:
hfs.illinois.gov. You can contact Illinois Client Enrollment Services by phone at
1-877-912-8880 (TTY 1-866-565-8576) or visit the website at: enrollhfs.illinois.gov.
You can also contact the plans directly. All plan contact information is found on the
Your Health Plan Choices that came with this Report Card.
About This Report Card
The information in this report card included measures collected for calendar
year 2022 as required by the health plan contract. The information was reviewed
for accuracy by independent organizations. The 2023 (calendar year 2022 results)
National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data
and Information Set (HEDIS®) and Consumer Assessment of Healthcare Providers
and Systems (CAHPS®) data were used in this report card to rate the plans. HEDIS®
is a registered trademark of NCQA and CAHPS® is a registered trademark of the
Agency for Healthcare Research and Quality (AHRQ).
Published 8/2023
You can get this information in other languages or formats, such as large print or audio.
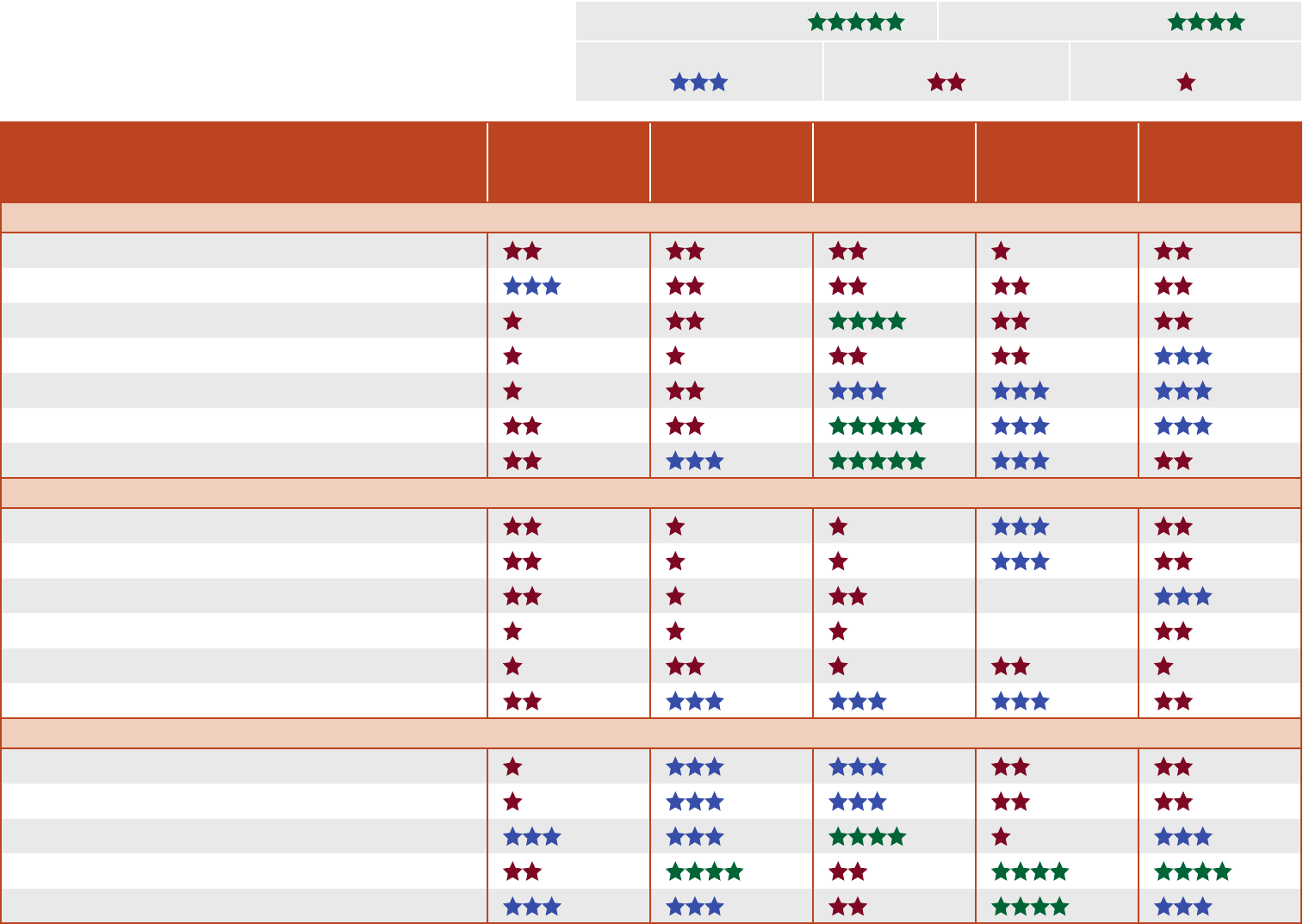
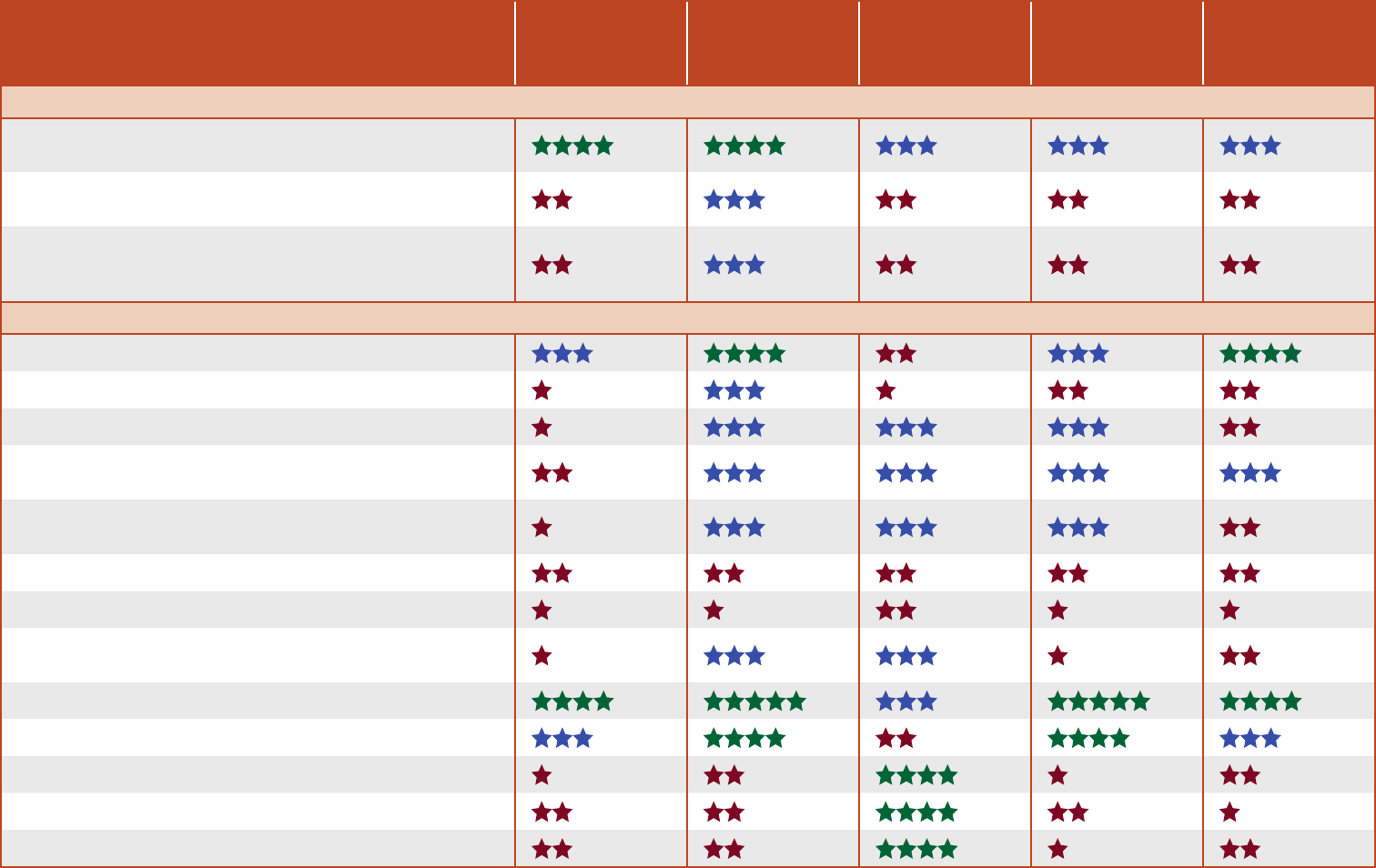
HealthChoice Illinois Plans’ National Ratings
The star ratings below show how the managed care plans in
Cook County compare to national Medicaid ratings for each
measure within key performance areas.
Key
Highest Performance High Performance
Average Performance Low Performance Lowest Performance
Plan
Aetna
Better Health
Blue Cross
Community
Health Plans
CountyCare
Health Plan
MeridianHealth
Molina
Healthcare
Doctors’ Communication
Adult—How Well Doctors Communicate
Child—How Well Doctors Communicate
Adult—Rating of Personal Doctor
Child—Rating of Personal Doctor
Talking to Tobacco Users About How to Quit
Talking About Medicines to Stop Tobacco Use
Talking About Plans to Stop Tobacco Use
Access to Care
Adult—Getting Needed Care
Child—Getting Needed Care
Adult—Getting Care Quickly NA
Child—Getting Care Quickly NA
Outpatient or Preventive Care Visits
Annual Dental Visits
Women’s Health
Breast Cancer Screening
Cervical Cancer Screening
Chlamydia Screening in Women
Moms Got Care Before Babies Were Born
Moms Got Care After Babies Were Born
NA = not enough data.
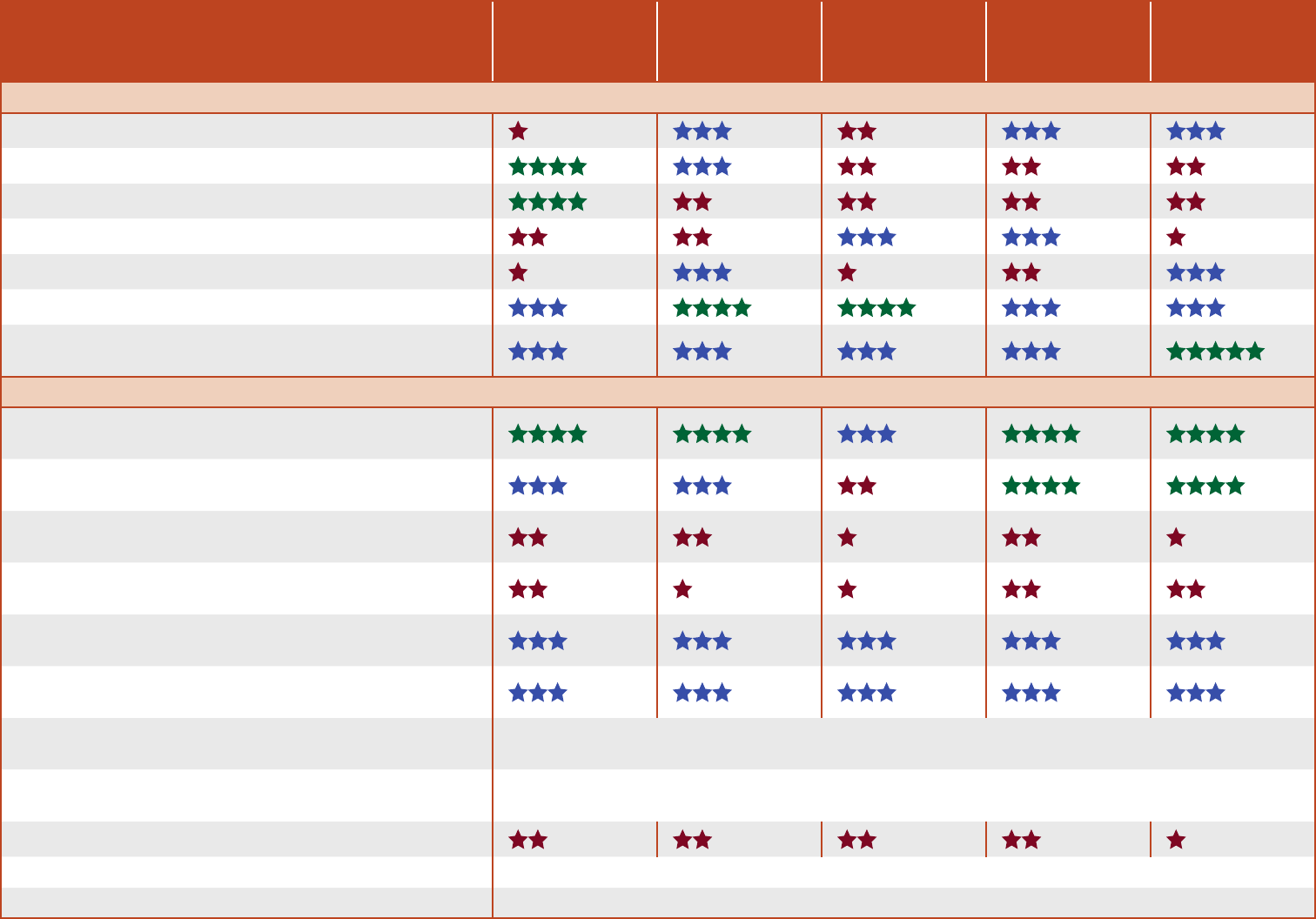
Plan
Aetna
Better Health
Blue Cross
Community
Health Plans
CountyCare
Health Plan
MeridianHealth
Molina
Healthcare
Living With Illness
Diabetics Have Controlled High Blood Pressure
Diabetics Have Controlled HbA1c
Diabetics With Poorly Controlled HbA1c
Diabetics Had an Eye Exam
Adults Have Controlled High Blood Pressure
Diabetics Received Statin Drugs
Diabetics Received Statin Drugs and Stayed
on Them
Behavioral Health
Follow-Up Care Within 7 Days After an Emergency
Room Visit Due to Mental Illness
Follow-Up Care Within 30 Days After an Emergency
Room Visit Due to Mental Illness
Follow-Up Care Within 7 Days After a Hospital Visit
Due to Mental Illness
Follow-Up Care Within 30 Days After a Hospital Visit
Due to Mental Illness
Follow-Up Care Within 7 Days After Care for
Addiction Treatment
Follow-Up Care Within 30 Days After Care for
Addiction Treatment
Follow-Up Care Within 7 Days After an Emergency
Room Visit for Addiction
National rules on how to collect and report these data changed.
Follow-Up Care Within 30 Days After an Emergency
Room Visit for Addiction
National rules on how to collect and report these data changed.
Received Medications to Help With Opioid Use
Start of Addiction Treatment National rules on how to collect and report these data changed.
Start and Continue Addiction Treatment National rules on how to collect and report these data changed.
Plan
Aetna
Better Health
Blue Cross
Community
Health Plans
CountyCare
Health Plan
MeridianHealth
Molina
Healthcare
Behavioral Health
Checkups for Kids/Teenagers on Mental Health
Medications—Antispychotics (Blood Sugar Testing)
Checkups for Kids/Teenagers on Mental Health
Medications—Antispychotics (Cholesterol Testing)
Checkups for Kids/Teenagers on Mental Health
Medications—Antispychotics (Blood Sugar and
Cholesterol Testing)
Keeping Kids Healthy
Doctor Visits for Kids Younger Than 15 Months
Doctor Visits for Kids 15 to 30 Months
Doctor Visits for Kids Ages 3 to 11 Years
Doctor Visits for Kids/Teenagers Ages 12 to
17 Years
Doctor Visits for Teenagers/Adults Ages 18 to
21 Years
Kids Received Immunizations, Combo 3
Kids Received Immunizations, Combo 10
Human Papillomavirus (HPV) Immunization for
Teenagers
Meningitis Immunization for Teenagers
Tdap Immunization for Teenagers
BMI Percentile for Kids/Teenagers
Counseling for Nutrition for Kids/Teenagers
Counseling for Physical Activity for Kids/Teenagers
