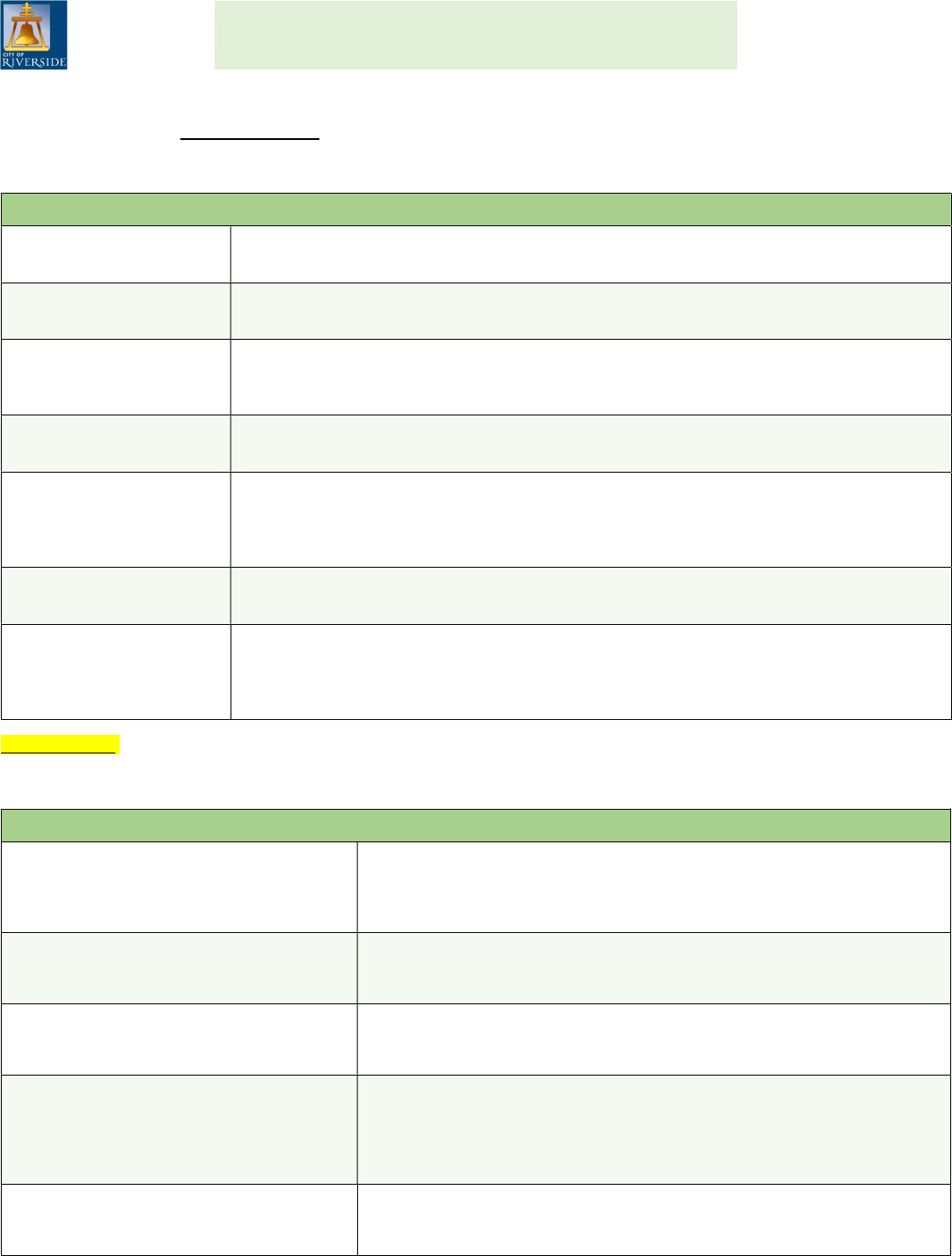
WHAT IS A QUALIFYING EVENT?
The City of Riverside allows employees to add or drop dependents from their medical, vision, dental and/or make changes
to their flexible spending account plans (FSAs) when a “Qualifying Event” is experienced. All employees experiencing a
qualifying event have 30 calendar days from the qualifying event date to make a benefit election change (add/drop
dependents or enroll/cancel coverage). If the 30 day deadline is missed, employees can make these changes, in addition
to plan changes during Open Enrollment in November of each year for coverage effective January 1 of the following year.
The following are the types of qualifying events and their descriptions:
Marital Status Change
Marriage, registered domestic partnership, death of spouse, dissolution of registered
domestic partnership, divorce or legal separation.
Eligible Dependent
Change
Birth or death of child, legal guardianship, adoption, disabled child or placement for foster
care. Note: Foster children are ONLY eligible to be covered under the City’s dental plans.
Gain or Loss of
Dependent’s Eligibility
An event that causes an employee’s eligible dependent to satisfy or cease to satisfy
coverage requirements under the City’s plan due to: attainment of the maximum plan age
or change in employment status.
Employee’s Benefit Status
Change
A change in employment status that affects the individual’s eligibility under the City’s plan;
such as a promotion from a non-benefitted to a benefitted position.
Court Order
If a Court judgment, decree, or order from a divorce, legal separation, change in legal
guardianship, or order of child support requires that you provide health and/or dental
insurance coverage for your dependent, you may change your election to provide
insurance coverage for a dependent child/former spouse consistent with terms of the order.
Open Enrollment Under a
Spouse’s Employer Plan
You can make a benefit election change when your spouse makes an Open Enrollment
change such as selecting or declining coverage under their Employer’s Plan.
Other
An example of a qualifying event not defined above includes an employee’s loss of
coverage through their spouse’s plan. For further assistance in defining acceptable
qualifying event criteria, please contact the Human Resources, Benefits Division at
951-826-5639 or email us directly at CityBenefits@Riversideca.gov.
Important note: All qualifying event changes require supporting documentation (e.g., marriage certificate, birth certificate,
etc.) to be submitted to Human Resources, Benefits Division by the 30 calendar day deadline. Please refer to Human
Resources policy V-9 for more information on medical/vision and dental enrollment rules.
Frequently Asked Questions:
Can I drop my eligible dependent (s) any
time during the year?
No, you may not drop eligible dependents from your medical, vision or
dental plan unless you experience a qualifying event (i.e. divorce, max
age). If you don’t experience a qualifying event you will need to wait until
the next open enrollment period to remove them from your plan(s).
If I drop or add a dependent due to a
qualifying event, when does the coverage
end or become effective?
If you drop or add an eligible dependent to a medical, vision or dental plan,
the coverage will end/begin the FIRST of the month following the qualifying
event date.
If I add or drop an eligible dependent, can I
also switch my medical and/or dental
plan?
No, if you add or drop an eligible dependent, you CANNOT switch your
medical and/or dental plan. Switching to a new plan may only be done
during the open enrollment period.
If I waived the medical, vision, or dental
coverage and I lost other group coverage,
can I enroll in a City insurance plan mid-
year?
Yes, you can enroll in the medical, vision, and dental plan if you have lost
other group insurance coverage
*
. The health opt-out stipend will be
forfeited upon enrolling in health insurance. Supporting documentation of
the loss of coverage is required and must be submitted to the HR Benefits
Division within 30 days of the loss of coverage date.
What if I DO NOT add an eligible dependent
to a medical, vision or dental plan within 30
days of the qualifying event?
If you do not add an eligible dependent within 30 days of the qualifying
event date, you must wait until the next open enrollment period to add your
eligible dependent.
*If you previously elected to waive City medical, vision or dental insurance, please contact HR before submitting a request to enroll in City
benefits.
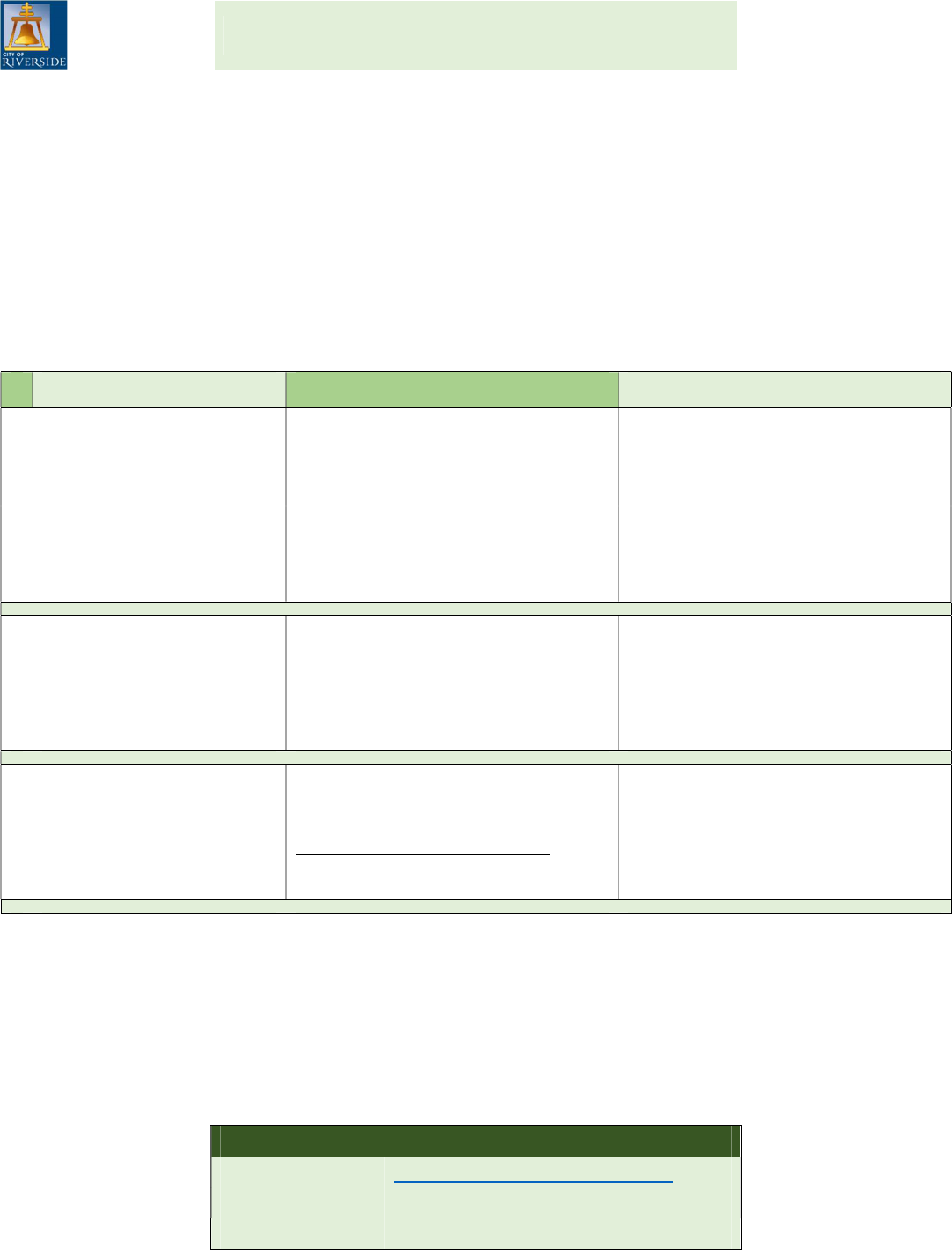
QUALIFYING EVENT CHECKLIST
Employees may add or drop coverage for new or existing dependents to their Health/Vision, Dental,
and Flexible Spending Account (FSA) plans when experiencing a qualifying event. Examples of
qualifying events include marriage, registered domestic partnership, new births, adoptions, or divorce.
Enrollments/change requests to a health/vision, dental or FSA plan MUST be submitted within 30 days
of the qualifying event date via Employee Online. Proof of dependent eligibility (i.e. marriage
certificate, birth certificate, divorce decree) must also be submitted by the 30-day deadline.
Employee Online may be accessed at www.RiversideCA.gov under Online Services or via the City’s
Intranet site.
The following checklist will assist you in the process of making benefit enrollment changes. Visit our
benefit website at www.RiversideCA.gov/benefits to find detailed information regarding each benefit.
Benefit Plan Where to find information: How to enroll or make changes:
Health/Vision Insurance
City Benefits website; click on the
Health Plans, Vision Plan, or
Dental Plans links (Vision
coverage is provided with all
health plans)
Submit request via EO system to
add or drop an eligible
dependent.
Dental Insurance
Flexible Spending
Accounts (FSA)
Benefits website; click on Flexible
Spending Account (FSA) link
Submit request via EO system to
add or modify the FSA annual
amount.
Additional Life Insurance
The Standard’s Website;
www.standard.com/enroll/
Apply and complete medical
history statement online and
submit electronically.
Important Note: In addition to adding/dropping coverage for dependents, it is important to update
your beneficiary designation if you experience a qualifying event.
All supporting documentation must be submitted to Human Resources within 30 days of the qualifying
event. Documents may be emailed, faxed, sent via interoffice mail, or brought in person to Human
Resources.
Contact Information:
Human Resources, Benefits Division (5
th
Floor, City Hall)
E-Mail:
CityBenefits@RiversideCA.gov
Phone:
951-826-5639
Fax:
951-826-2421
