
Services and Supports for
Longer-Term Impacts of
COVID-19
August 2022
2
Preparation Notice
Services and Supports for Longer-Term Impacts of COVID-19
This Services and Supports for Longer-Term Impacts of COVID-19 Report was prepared by the
Department of Health and Human Services.
Electronic Access
This publication may be downloaded from COVID.gov - Find COVID-19 guidance
for your
community
Disclaimer Notice
This publication lists non-federal resources to provide additional information. The views and
content in those resources have not been formally approved by the Department of Health and
Human Services (HHS). Listing of the resources is not an endorsement by HHS or its
components.
Public Domain Notice
All material appearing in this publication is in the public domain and may be reproduced or
copied without permission from Department of Health and Human Services. Citation of the
source is appreciated.
Suggested Citation
Department of Health and Human Services, Office of the Assistant Secretary for Health. 2022.
Services and Supports for Longer-Term Impacts of COVID-19, 200 Independence Ave SW,
Washington, DC 20201.

3
Services and Supports for Longer-Term Impacts of COVID-19
Contents
Executive Summary................................................................................................ 5
Letter from the Secretary of Health and Human Services ...................................... 8
Chapter 1: Introduction ....................................................................................... 10
Disparities and COVID-19 .......................................................................................................... 11
Bereavement ............................................................................................................................. 12
Mental Health and Substance Use ............................................................................................ 13
Long COVID ............................................................................................................................... 14
Individuals Who Experience Disabilities from Long COVID ...................................................... 17
Purpose of the Report ............................................................................................................... 18
Methodology for Assembling this Report ................................................................................. 19
References ................................................................................................................................ 20
Chapter 2: Federal Supports and Services for Americans Experiencing Long COVID
............................................................................................................................. 27
Know Your Rights ...................................................................................................................... 28
Health Care Coverage and Access............................................................................................. 31
Community Services and Supports ........................................................................................... 41
Income and Financial Assistance .............................................................................................. 48
Job Assistance ........................................................................................................................... 53
Housing ..................................................................................................................................... 58
Food and Nutrition Support ...................................................................................................... 62
Child Care and Early Childhood Development and Education .................................................. 65
Education Supports ................................................................................................................... 67
Caregiving and Family Support ................................................................................................. 71
Chapter 3: Enabling Health Care Personnel to Improve Treatment of People
Experiencing Long COVID ..................................................................................... 76
Resources for Health Care Personnel Caring for Individuals with Long COVID ........................ 77
Support for Health Care Personnel Experiencing Stress and Trauma Related to COVID-19 .... 88

4
Services and Supports for Longer-Term Impacts of COVID-19
Chapter 4: Services for Individuals Dealing with Mental Health, Substance Use, or
Bereavement Challenges in the Wake of the Pandemic ....................................... 91
Mental Health Supports and Services ....................................................................................... 92
Substance Use Supports and Services .................................................................................... 101
Bereavement Supports ........................................................................................................... 107
References .............................................................................................................................. 111
Chapter 5: Future Directions .............................................................................. 112
Engagement of Public and Private Stakeholders in the Development of the Report ............ 113
Challenges with Addressing the Longer-Term Impacts of COVID-19 ..................................... 116
The National Research Action Plan on Long COVID................................................................ 118
Conclusion ............................................................................................................................... 118
Appendix A: Report Abbreviations ..................................................................... 119
Appendix B: Contributing U.S. Government Departments ................................. 124

5
Services and Supports for Longer-Term Impacts of COVID-19
Executive Summary
On April 5, 2022, President Biden issued the Memorandum on Addressing the Long-Term
Effects of COVID-19 outlining actions needed to support the American people in addressing the
longer-term effects of COVID-19. The President charged the Secretary of Health and Human
Services with coordinating a U.S. government-wide response to Long COVID. An element of that
response was for the Department of Health and Human Services, in collaboration with federal
partners, to develop two reports: the Services and Supports for Longer-Term Impacts of COVID-
19 Report (Services Report and the National Research Action Plan on Long COVID (Research
Plan. The Services Report outlines current federal services and mechanisms of support
available to the American public in addressing the longer-term effects of COVID-19, including
Long COVID and related conditions, medical health and substance use challenges, and
bereavement. The Research Plan provides the first U.S. government-wide national research
agenda focused on advancing prevention, diagnosis, treatment, and provision of services and
supports for individuals and families experiencing Long COVID.
Longer-term effects of COVID-19 including Long COVID
COVID-19 has affected all aspects of health, including mental health, and disrupted daily life. It
created additional obstacles for those experiencing mental health and substance use
challenges. Further, many people have been forced to cope with the death of loved ones,
especially children, and face the aftermath of those losses. Millions of Amercians continue to
experience lingering symptoms after an initial infection with SARS-CoV-2, the virus that causes
COVID-19. This report outlines federally funded supports and services for individuals
experiencing the effects of COVID-19 in the areas of mental health, substance use, and
bereavement. In addition, the Services Report lists federally funded supports and services for
individuals experiencing disabilities due to Long COVID and associated conditions.
Long COVID
In April 2020, shortly after the beginning of the pandemic, anecdotal reports from patients
started to emerge that previously healthy individuals were experiencing lingering symptoms
and were not fully recovering from infection with SARS-CoV-2, the virus that causes COVID-19.
Recovery from infection can vary from person to person, most individuals seem to recover
quickly and completely; however, some individuals report symptoms that persist or emerge
weeks or even months after the acute phase of the infection has passed, even when the
infection was asymptomatic. These sets of conditions are often referred to as “Long COVID.”
Long COVID is a term created and promulgated by patients, and recognizes the importance of
two technical terms, Post-COVID-19 conditions, or PCC, broadly equivalent to Long COVID, and
Post-acute Sequalae of SARS-CoV-2 infection, focused on the direct effects of the virus.

6
Services and Supports for Longer-Term Impacts of COVID-19
• Individuals experiencing Long COVID and associated conditions
• Health care personnel who work with and treat individuals experiencing Long COVID
• Individuals experiencing longer-term impacts of COVID-19, including mental health and
substance use challenges
• Individuals dealing with the loss of family members or loved ones to COVID-19.
The report serves as an initial resource guide to help individuals, their families, and caregivers
find needed supports, services, and reasonable modifications
to receive health care and
treatment, work, go to school, and stably live in the community. It is also useful for community
organizations,
health care enterprises, and public health agencies who work with individuals
experiencing longer-term effects of COVID-19. It will inform the development of additional
resources and tools created by the federal government for individuals, families, and
communities to naviagate the federal supports and services available to them.
The COVID-19 pandemic has placed significant stresses on health systems, hospitals, primary
care practices, and health care personnel. H
ealth care personnel have faced a novel clinical
entity threatening the life and well-being of u
nprecedented numbers of people. They worked
with limited available knowledge or consensus on basic treatment protocols. Th
ese health care
personnel continue to face challenges at work and home due to the pandemic’s sustained
impact. To
better support these personnel and their continued efforts to care for individuals
with COVID-19 and Long COVID, this report provides resources along with supports to deal with
the stresses and traumas experienced from being on the front lines of the COVID-19 response.
There are critical barriers to equitable access to and utilization of health care and other services
and supports for both COVID-19 and Long COVID as well as associated conditions, mental
health and subsutance use challenges, and bereavement, all exasperated by the pandemic. To
achieve our vision, this report is guided by health equity principles, building upon prioritized
recommendations made by the Presidential COVID-19 Health Equity Task Force. These critical
barriers include, but are not limited to, understanding how racism, ableism, and discrimination
are associated with health care access, symptom recog
nition, disease progression, and severity
of Long COVID in communities of color, people with disabilities, and other underserved
populations; and the resultant limitations on access to appropriate services and supports.
Future Direction
The U.S. government will continue to invest in supports, further refine the scope of services,
and address gaps as we learn more through experience and research about Long COVID and the
About this Report
This report provides webpage information and telephone numbers that are relevant for

7
Services and Supports for Longer-Term Impacts of COVID-19
other longer-term impacts of COVID-19. Engagement with public and private partners has
informed both reports and will continue to be integral to our process as we ensure resources
are accessible to those who need them.

8
Letter from the Secretary of Health and
Human Services
Thank you, President Biden, for the opportunity to coordinate a U.S. government effort that
outlines federally-funded resources available to the American public in the face of COVID-19,
titled the Report on Services and Supports for Longer-Term Impacts of COVID-19.
On January 20, 2020, health officials identified the first case of COVID-19 on U.S. soil. Eleven
days later, the Department of Health and Human Services declared a public health emergency.
On March 11, 2020, the World Health Organization declared the COVID-19 outbreak a
pandemic in light of the alarming spread and severity of the disease across the world. Now, two
years later, not only has the United States experienced over 86 million confirmed COVID-19
cases and a staggering one million deaths from COVID-19, but also these numbers continue to
rise. The pandemic has disproportionately impacted communities of color and other
underserved groups, especially those with disabilities and older adults, exacerbating the
existing health inequities in our country and highlighting social and racial injustices that impede
equitable health outcomes.
We have lost neighbors, parents, spouses, children, friends, and colleagues because of the
pandemic, and millions continue to grieve the loss of loved ones.
Beyond the human toll, COVID-19 changed the way we live. It contributed to job losses,
business closures, children staying home from school, food insecurity, and housing instability.
Efforts to reduce the spread of the disease have contributed to social isolation, loneliness, and
detriments to mental and emotional health.
Today, we continue to make advancements in addressing this pandemic by improving vaccine
availability, increasing access to testing, expanding treatment for COVID-19, and enhancing
research to advance our understanding of the epidemiology and impact of the disease. The
American Rescue Plan has led to a remarkable and historically equitable economic recovery.
Although much work remains, we are thankfully moving towards a future in which we have
additional tools to prevent, treat, and mitigate the risks associated with COVID-19.
Despite these gains, emerging evidence suggests that, for many people, COVID-19 can have
long-lasting health implications, commonly known as “Long COVID.” Long COVID refers to the
constellation of symptoms that can linger or arise anew long after the acute phase of SARS-
CoV-2 infection. For persons affected by Long COVID, symptoms like fatigue,
shortness of
breath, heart palpitations, and joint pain can persist long after the acute infection. Individuals
with Long COVID can have symptoms that persist or emerge four weeks or longer after
contracting COVID-19, and our understanding of the longer-term persistent symptoms remains
uncertain. Long COVID can hinder an individual’s ability to work, attend school, participate in
community life, and engage in normal everyday activities. Further, the pandemic has increased
Services and Supports for Longer-Term Impacts of COVID-19

9
Services and Supports for Longer-Term Impacts of COVID-19
the burden of mental health and substance use challenges, both directly and indirectly related
to COVID-19. Although our nation continues to make advancements in addressing this
pandemic, a new emphasis is necessary to address the impact of Long COVID and associated
conditions.
Further, we recognize the extensive leadership and work of state and local governments in
delivering supports and services. It is only through continued collaboration that we can hope to
mitigate the longer-term effects of COVID-19 and plan for future pandemics. In response to the
President’s directive to coordinate a federal response and provide individuals with the
resources they need, this report outlines the services and mechanisms of support across
agencies that can assist people in America with addressing the longer-term impacts of COVID-
19. Principles guiding this report include a commitment to health equity, patient and
stakeholder engagement, and public-private collaboration.
I want to thank the staff in the 14 Departments and agencies who worked diligently to prepare
this report. I also want to thank the Assistant Secretary for Health and the Assistant Secretary
for Mental Health and Substance Abuse for their leadership in conceptualizing and driving the
production of this report. Finally, I want to express my sincere gratitude to numerous
organizations and individuals who contributed their time, resources, contacts, and invaluable
conversations with us. This collaboration remains critically important in advancing the science
and paving the way for progress. Those with lived experiences are central to these efforts.
Sincerely,
Xavier Becerra
Secretary of Health and Human Services
10
COVID-19 has affected every U.S. community and so
many aspects of our lives.
Services and Supports for Longer-Term Impacts of COVID-19
• There have been 86.6 million confirmed cases
of the illness, 4.8 milli
on hospitalizations, and
over one million deaths from COVID-19
3
• Over 200,000 children have lost a parent to
COVID-19.
4
• Almost 50 million people either did not work
or worked fewer hours due to COVID-19
5
• In the first year of the pandemic ninety-three percent of children switched from
classroom education to distance learning
6
• In July 2020 thirty million people reported their household did not have enough to eat
7
• In July 2020 fifteen million people reported being behind in paying rent
7
• In August 2020 sixty-six percent of adults and 75percent of young adults reported
feeling socially isolated.
8
Chapter 1: Introduction
COVID-19 is a viral disease caused by SARS-CoV-2, a coronavirus that emerged in 2019. The
virus spreads mainly from person to person through aerosolized respiratory droplets produced
when an infected person coughs, sneezes, or talks. Some people who are infected may not have
symptoms. For others, symptoms may appear 2 to 14 days after exposure and can include
fever, chills, and cough. Symptomatic and asymptomatic infected persons can be contagious.
Adults 65 years and older and people of any age with underlying medical conditions are at
higher risk for severe illness, but anyone can have severe illness from COVID-19. Not only has
the pandemic affected individuals, but it has also had major economic and social impacts on
communities and reduced the availability of resources for individuals who live and work in
those communities. COVID-19 has caused major economic disruptions, disconnected many
from community resources and support systems, and created widespread uncertainty and fear.
This in turn placed considerable stress on individuals and communities and may contribute to or
exacerbate interpersonal or community violence. The COVID-19 pandemic has placed
significant stresses on health systems, hospitals, primary care, practices and health care
personnel. It is only through extensive coordination and collaboration with state, tribal, and
local governments that we can together achieve our aims.
2
1
COVID-19 was the third
leading cause of death in
2020 and 2021 and second
leading cause of death in
January 2022.
11
109

11
Services and Supports for Longer-Term Impacts of COVID-19
In 2020, the unemployment rate reached its highest peak since data collection began in 1948,
a
nd almost 50 million pe
o
p
le
eit
h
e
r
d
id
n
ot wo
rk or w
o
rked fewer hours due to COVID-19.
Although the unemployment rate has since returned to roughly its pre-pandemic level, the
labor force participation rate is lower than it was before the pandemic.
13
5
1
2
At
o
ne time, early in the pandemic, , 77 percent of public schools and 73 percent of private
schools reported moving classes to online distance-learning formats. Though most children
have since returned to the classroom, more than 80 percent of public schools reported that the
COVID-19 pandemic has negatively impacted student behavior and socio-emotional
development. Children receiving virtual instruction are less active, less social, and have worse
mental and emotional health. As children struggle with the challenges of maturing in a new
and uncertain virtual world, parents struggle to balance their financial security with the safety
of their families.
16
15
1
4
E
s
t
imates from the Department of Agriculture show the number of people in food-insecure
households increased from 35.2 million in 2019 to 38.3 million in 2020, and the number of
children in households where at least one child was food insecure rose from 5.3 million in 2019
to 6.1 million in 2020. In addition, analysis of the Census Household Pulse Survey showed that
food insecurity doubled overall, and tripled in households with children at the start of the
pandemic, and that 30 million people reported their household did not have enough to eat in
January 2021.
7
18
1
7
T
ho
ugh only limited data on homelessness has been collected since the start of the pandemic,
we know that housing insecurity is still an issue for many Americans: 15 million people reported
that their household was behind on rent in January 2021.
7
St
udies
show that social isolation can have a significant negative impact on health, including
increased risk of dementia, heart disease, and stroke. COVID-19’s death toll, which has left
millions grieving, and its health, social, and financial effects have also brought mental health to
the forefront of public concern.
8
D
i
sparities and COVID-19
Though everybody is at risk of COVID-19 and its effects, research shows that some racial and
ethnic minority groups, older adults, people with disabilities, and people with lower incomes
are disproportionately affected by COVID-19 and its impacts. COVID-19 data show that Black,
African American, Hispanic, Latino, American Indian
and Alaska Native persons in the U
nited
States experience higher rates of COVID-19-related hospitalization and death compared with
non-Hispanic White populations, and that these disparities persist even when accounting for
other demographic and socioeconomic factors.
30
Age-adjusted case, hospitalization, and death
rates were highest in American Indian, Alaska Native individuals.
31, 32
Non-Hispanic Black or
African American people and Hispanic people are both more than twice as likely to be
hospitalized due to COVID-19 than non-Hispanic White people. In 2020, residents of long-
term care facilities made up less than 1percent of the U.S. population but accounted for more
33
12
Services and Supports for Longer-Term Impacts of COVID-19
than 35percent of all COVID-19
deaths, with even more
disproportionate impacts in nursing
homes with higher percentages of
residents from racial and ethnic
minority groups. Compared with
ages 18 to 29 years, the rate of
death is 330 times higher in those
who are ages 85 years and older.
In addition, people ages 18 years
and older with certain underlying
medical conditions and certain
disabilities are at increased risk for
severe illness from COVID-19. In
addition, immunocompromised
individuals may experience weaker
immune responses to COVID-19
vaccines.
36
26
35
34
Disparities and COVID-19
Racial and Ethnic Minority Populations
Older Adults
•
Age is the strongest risk factor for severe COVID-
19 outcomes
26
•
•
U.S. adults ages 65 years and older accounted for
81% of COVID-19 related deaths in 2020
26
• Had higher rates of positive test results,
hospitalizations, severe illness, and death from
COVID-19, even after adjusting for age
19-22
• Experienced greater unemployment and were
more likely to be behind on rent
7
12
• Had higher rates of anxiety symptoms,
depressive symptoms and suicidal ideation
2423
• Were twice as likely to report having lost a
relative or close friend to COVID-19
25
People with disabilities, including attention-
deficit/hyperactivity disorder, cerebral palsy,
intellectual and developmental disabilities, spinal
cord injuries, Down syndrome, and other chronic
health conditions such as HIV/AIDS may be more
likely to get very sick from COVID-19 because of
underlying medical conditions, living in
congregate settings, or systemic health and
social inequities.
27-29
•
•
Social determinants of health
(SDOH) are conditions in the
environment that affect a wide
range of health outcomes and
risks. These SDOH include
neighborhood and the physical
environment, health and health
care, occupation and job conditions,
income and wealth, and education.
Discrimination, including racism,
ableism, and associated chronic
stress, influences each of these
important topic areas. Together,
disparities in each of these areas
have contributed to
disproportionately worse COVID-19
related outcomes for people from
racial and ethnic minority groups, people with disabilities, and for older people.
37
, , 3
8 3729
People with Disabilities
Bereavement
Over 1 million people have lost their lives to COVID-19. They were beloved parents,
grandparents, children, siblings, spouses, neighbors, and friends. Each soul is irreplaceable, and
the families and communities left behind are still reeling from profound loss. Many families and
communities have already received support from federal programs that help with the loss they
Services and Supports for Longer-Term Impacts of COVID-19
13
COVID-19 Impacts on
Mental Health and
Substance Use
• Thirteen percent of
Americans started or
increased substance use as
a way to cope with the
stress of COVID-19
43
• Individuals infected with
COVID-19 were 60% more
likely to have a mental
health condition or mental
health-related
prescription
45
• Drug overdose deaths
increased throughout the
pandemic reaching a
record of 107,000.
44
• More than half of parents
expressed concern about
their children’s mental
well-being
46
have experienced. As we move forward, we commit to ensuring that families and communities
can access these support programs and connect to resources they may need to help with their
healing, health, and well-being.
Every COVID-19 death leaves behind approximately nine bereaved kin. One-fifth of Americans
had lost a relative or close friend in early 2021, when there were roughly half as many deaths
from COVID-19 as today.
39
Over 200,000 children have lost a parent to COVID-19.
Compared
with the group at lowest risk, White children, we found American Indian and Alaska Native
children, Black children, Hispanic children, and Asian
children were 4.5, 2.4, 1.8, and 1.1 times more likely,
respectively, to lose a parent or caregiver. Providing
support and resources to individuals who have lost
loved ones during the pandemic remains an important
priority in the process of grief and bereavement.
41
440
Mental Health and Substance
Use
Fear, anxiety, anger, and depression have been common
emotions as individuals cope with the stressors
associated with the COVID-19 pandemic. Over 41percent
of Americans, more than four times the amount in 2019,
reported feelings of anxiety and depression during the
peak of the pandemic. Thoughts of suicide increased
and over a quarter of Americans experienced stress-
related symptoms. In a nationally representative survey
conducted by CDC in June 2020, it was determined that
thirteen percent of Americans started or increased
alcohol or substance use as a way to cope with the stress
of COVID-19. Substance use in the study was defined as
use of alcohol, legal or illegal drugs, or prescriptions
drugs that are taken in a way not recommended by your
doctor.
43
43
42
Drug overdose deaths, already on the rise before 2020,
increased rapidly during the COVID-19 pandemic,
reaching a record 107,000 in 2021.
44
Social, emotional, and economic stressors, as well as disruptions in health and emergency
services, may have contributed to increases in interpersonal violence. Studies have
documented increases in domestic violence and gender-based violence during the COVID-19
pandemic.
47, 48
A CDC analysis also found that the firearm homicide rate grew nearly 35percent
from 2019 to 2020, a historic increase that resulted in the highest firearm homicide rate in
more than 25 years. Multiple studies found that suicide risk increased during the COVID-19
49
14
Long COVID
“I went to the emergency room because
I was exhausted all the time. It was a
horrible experience! They admitted me
to an inpatient psychiatric ward. Much
later, after many scary medical
problems, I was diagnosed with Long
COVID.”
—Person with Long COVID
Services and Supports for Longer-Term Impacts of COVID-19
Long COVID is broadly defined as signs,
symptoms, and conditions that continue or
develop after initial COVID-19 or SARS-CoV-
2 infection. The signs, symptoms, and
conditions
• are present four weeks or more after
the acute phase of infection;
• may be multisystemic;
• and may present with a relapsing–
remitting pattern and progression or
worsening over time, with the
possibility of severe and life-threatening
events even months or years after
infection.
Long COVID is not one condition. It
represents many potentially overlapping
entities, likely with different biological
causes and different sets of risk factors and
outcomes.
pandemic across a range of population
groups. For example, 25% of young adults
age 18 to 24 years, 15percent of non-
Hispanic Black adults, and 19percent of
Hispanic respondents in one survey reported
experiencing suicide ideation in the past 30
days. Emergency department visits for
suspected suicide attempts among young
females aged 12 to 17 years increased
51percent in 2021 compared to the same
period in 2019.
50
43
The COVID-19 pandemic has contributed to
substantial economic and social impacts that
have reduced the availability of resources
and supports for individuals, and these
impacts have in turn exacerbated the effects
on individuals. Although this report focuses
on services for individuals, it is important to
note that, because COVID-19 impacted family
members, caregivers, organizations, and
communities, the federal response includes
community-level programs and services.
These community-level programs and
services, however, remain outside the scope
of this report.
Long COVID
Amidst the many challenges of the pandemic are the persistent health effects some individuals
face well after their acute COVID-19 infection. Recovery from infection with SARS-CoV-2, the
virus that causes COVID-19, can vary from person to person. Most people seem to recover
quickly and completely. However, some report
symptoms that persist or emerge weeks or even
months after the acute phase of illness has
passed, sometimes even in asymptomatic cases.
This condition is often referred to as “Long
COVID.”
At this time, no laboratory test can definitively
distinguish post-COVID conditions from other
causes. A positive SARS-CoV-2 viral or antibody
test result may help determine if there is a
15
Common Symptoms of
“Long COVID”
51
Services and Supports for Longer-Term Impacts of COVID-19
current or previous infection; however, these laboratory
tests are not required to establish a diagnosis of post-
COVID conditions.
The medical, scientific, and public health communities
have developed precise terms with agreed-upon, interim
definitions of Long COVID, such as Post-COVID-19
conditions (PCC) and Post-acute Sequelae of SARS-CoV-2
infection (PASC), to use for communicating about clinical,
research, and public health activities (see Appendix C in
the Research Report). The first, Post-COVID-19 Conditions,
is equivalent to Long COVID and includes both direct and
indirect effects of the virus. It is useful in various clinical
setting, assessing the burden to the health care system,
and surveillance. The second, is Post-acute Sequalae of
SARS-CoV-2 infection, which aims to capture the direct
effects of the virus. It is used often in clinical contexts and
critical to the medical research community aiming to
understand the root causes of Long COVID. Additional
research is needed to sufficiently separate the various
forms and conditions of Long COVID, including from pre-
existing ones. The differences and nuances among the
definitions reflect the central challenge of defining,
studying, and addressing the impact of Long COVID. In
addition, some scientists and patient advocate
communities point to the importance of conditions
associated with Long COVID, drawing parallels in
symptoms and underlying biology to other diseases, such
as post-infectious conditions. The terminology of Long
COVID and associated conditions leverages existing
experience and knowledge to recognize commonalities to
better treat and care for the many affected individuals,
including the domains of disability and insurance
coverage. Although the definitions will likely change as we
learn more, using terms with commonly understood
definitions helps research and public health communities
compare findings across studies and facilitates turning
surveillance and research findings into action to improve
patient care.
Throughout this report, it will be noted if and where
specific research uses a more specific term (i.e., PCC,
PASC). Also, it is emphasized that “Long COVID” is not just
General symptoms
• Tiredness or fatigue that interferes
with daily life
• Symptoms that get worse after
physical or mental effort (also
known as “post-exertional malaise”)
• Fever
Respiratory and heart symptoms
• Difficulty breathing or shortness of
breath
• Cough
• Chest pain
• Fast-beating or pounding heart
(also known as heart palpitations)
Neurological symptoms
• Difficulty thinking or concentrating
(sometimes referred to as “brain
fog”)
• Headache
• Sleep problems
• Dizziness when you stand up
(lightheadedness)
• Pins-and-needles feelings
• Change in smell or taste
• Depression or anxiety
Digestive symptoms
• Diarrhea
• Stomach pain
Other symptoms
• Joint or muscle pain
• Rash
• Changes in menstrual cycles

16
Services and Supports for Longer-Term Impacts of COVID-19
one condition, and the use of the term Long COVID in this report should not be construed as
such.
Long COVID can affect nearly every organ system and hinder an individual’s ability to work,
attend school, participate in community life, and engage in normal everyday activities. Long
COVID can affect people regardless of race, age, gender, or baseline health status. It is more
common in people with severe COVID-19 who require hospitalization or intensive care,
individuals with underlying health conditions, unvaccinated individuals, and people affected by
health disparities.
51
A new CDC study reports that at least 30 days after having COVID-19, one in five COVID-19
survivors aged 18–64 years and one in four survivors aged 65 years or older have a health
condition that might be related to their previous COVID-19 illness. People who had previous
COVID illness had twice the risk for developing pulmonary embolism or respiratory conditions.
52
The study looked at rates of 26 conditions known to occur after COVID-19 (post-COVID
conditions). The report found that people that had past COVID-19, had twice the risk of
developing a new condition compared with people without evidence of COVID-19. The highest
risks were for conditions involving the lungs, including blood clots in the lungs, and respiratory
symptoms, although the conditions examined affected multiple body systems. The most
common new conditions were respiratory symptoms and musculoskeletal pain.
52
Estimates from the CDC study may not be generalizable to the broader U.S. population, but the
breadth of symptoms and conditions that are manifestations of Long COVID, and the potential
scale, are consistent throughout the scientific literature. Despite more precise estimates of risk,
it is evident that Long COVID already impacts a substantial number of people. This number may
continue to grow, although vaccinations and prevention measures can help. The response to
Long COVID will have to be at a scale and scope necessary to respond to the short-term and
longer-term health care needs of persons with this lived experience.
Human-centered design and human-centered research, such as the HHS Health+ (“health plus”)
cycle for Long COVID, will be necessary to understand common experiences of individuals living
with Long COVID. Health+ involves over 1,000 hours of interviews, workshops, listening
sessions, and human-centered research to co-create solutions with—not for—those impacted
by Long COVID. Through human-centered research Health+ will identify opportunity areas that
matter most to patients and help to guide federal action.
53
Beyond the health complications it causes, Long COVID has resulted in decreased employment
and billions of dollars in lost income. As individuals experiencing Long COVID
disproportionately work in the service sector, this has led to a labor shortage in this industry,
which may contribute to inflation. Health care cost burdens are also expected to increase for
new chronic conditions, such as heart disease, diabetes, and kidney disease, that may be
attributable to COVID-19.
55
54
54
17
Services and Supports for Longer-Term Impacts of COVID-19
Individuals Who Experience
Disabilities from Long COVID
For some, whose Long COVID substantially limits their
major life activities, their illness may qualify as a
disability under disability rights laws. Whether Long
COVID is a disability depends on how Long COVID
affects the individual. Other laws define disability
differently, and individuals will need to meet those
definitions to qualify for those programs. The following
examples highlight cases where Long COVID may be a
disability according to the Americans for Disabilities Act
(ADA) and other disability rights laws.
56
• A person with Long COVID who has lung damage
that causes shortness of breath, fatigue, and
related effects is substantially limited in
respiratory function, among other major life
activities
• A person with Long COVID who has symptoms
of intestinal pain, vomiting, and nausea that
have lingered for months is substantially limited
in gastrointestinal function, among other major
life activities
• A person with Long COVID who experiences
memory lapses and cognitive impairment (or
“brain fog”) is substantially limited in brain
function, concentrating, and thinking.
When Long COVID qualifies as a disability under federal
disability rights laws, individuals are eligible for
reasonable accommodations, such as
, 5756
• Modifying a policy to allow a person who
experience dizziness when standing to be
accompanied by their service animal that is
trained to stabilize them
• Providing an employee who has fatigue issues a
modified work schedule
Long COVID and Disability
56
• According to official guidance
from the Office for Civil Rights of
the Department of Health and
Human Services, the Civil Rights
Division of the Department of
Justice, and the Equal
Employment Opportunity
Commission, Long COVID can be a
disability under the ADA, Sections
501 and 504 of the Rehabilitation
Act, and Section 1557 of the
Affordable Care Act if it
substantially limits one or more
major life activities
• These federal laws provide
protection from discrimination for
people with disabilities
• Major life activities include, but
are not limited to, caring for
oneself, performing manual tasks,
seeing, hearing, eating, sleeping,
walking, standing, sitting,
reaching, lifting, bending,
speaking, breathing, learning,
reading, concentrating, thinking,
writing, communicating,
interacting with others, and
working. The term also includes
the operation of a major bodily
function, such as the functions of
the immune system,
cardiovascular system,
neurological system, circulatory
system, or the operation of an
organ
• The limitations do not need to be
severe, permanent, or long-term
18
Services and Supports for Longer-Term Impacts of COVID-19
• Modifying procedures so a customer who finds it too tiring to stand in line can
announce their presence and sit down without losing their place in line
• Allowing an employee who has joint or muscle pain caused by walking to the meeting
place the ability to participate in staff meetings by video
• Providing an employee who is having respiratory problems with a portable air purifier in
their office.
Long COVID may be less prevalent in children, but it can still occur. Children especially may have
trouble describing their experiences with Long COVID. Extra accommodations, such as extra
time on tests, scheduled rest periods throughout the day, or a modified class schedule may be
necessary for children experiencing Long COVID. This guidance also applies to colleges and
universities, although they are not required to identify students with disabilities. Rather, college
and university students may request accommodations.
59
58
A student may also qualify for special education based on the Individuals with Disability
Education Act (IDEA) if the student has limited strength, vitality, or alertness due to a chronic or
acute health problem that adversely affects the child’s educational performance, as determined
by a comprehensive evaluation. For example, children with developmental delays due to severe
cases of Long COVID may qualify. IDEA requires states to have a system in place to identify and
evaluate children with a disability and provide early intervention services as soon as possible.
Purpose of the Report
On April 5, 2022, President Biden issued the
Memorandum on Addressing the Long-Term
Effects of COVID-19, charging the Secretary of
Health and Human Services (Secretary) with
coordinating the federal response, in
engagement with public- and private-sector
partners, to the longer-term effects of COVID-19.
As part of the federal response, President Biden
directed the Secretary, with input from federal
agencies, to produce two reports within 120
days. This first report, the Report on Services and
Supports for Longer-Term Impacts of COVID-19,
outlines the services and mechanisms of support across agencies that assist the American
public in addressing the longer-term effects of COVID-19, including mental health, substance
use, bereavement, Long COVID and related conditions. The second report, titled the National
Research Action Plan, provides the first government-wide national research agenda focused on
understanding and treating Long COVID.
“Honestly, I don’t know where to refer
people who have Long COVID
symptoms. There are so many people
suffering. Even when there is a Long
COVID expert in the area, there is a
wait time of at least 4 months for an
appointment.”
—Community health worker

Services and Supports for Longer-Term Impacts of COVID-19
The purpose of this report is to outline the current services and supports across federal
agencies to address the far-reaching and longer-term effects of COVID-19, including Long
COVID and associated conditions, mental health and substance use challenges, and
bereavement. This report highlights over 200 services and supports that are currently
supported by the U.S. government. This report, as well as the National Research Action Plan on
Long COVID, are intended to serve as two tools in the larger ecosystem of the needed
response to the longer-term impacts of COVID-19. The federal government will continue to
invest in services and supports, and strive to improve how these programs can address the
specific needs of the population as we continue to learn more. In development of this report
and through engagement with a broad group of partners it is recognized that more will be
needed. In addition, it is recognized that some individuals may need supports across multiple
domans such as services for Long COVID and supports for bereavement. Finally, many of the
resources listed are accessible to broader populations with disabilities. In addition, many
federal agencies have resources that are specific to individuals with pre-existing medical
conditions, such as individuals with HIV and AIDS. Those resources are beyond the scope of
the report.
This report provides practical information and describes the federally funded services and
supports available for
• Individuals experiencing Long COVID and associated conditions
• Health care personnel who work with and treat individuals experiencing Long COVID
• Individuals experiencing longer-term impacts of COVID-19, including mental health and
substance use challenges
• Individuals dealing with losing a family member or loved one to COVID-19.
Methodology for Assembling this Report
This report is published by the Secretary of Health and Human Services, supported within the
Department of Health and Human Services by the Assistant Secretary for Health and the
Assistant Secretary for Mental Health and Substance Use. The content of the report was guided
by the recommendations issued last year by the Presidential COVID-19 Health Equity Task
Force. The Department of Health and Human Services’ Office of Intergovernmental and
External Affairs hosted a series of interactive listening sessions from April through June 2022 to
help develop this report. The sessions included a broad range of individual stakeholders
including persons affected by the longer-term impacts of COVID-19, researchers, health
professionals and their specialty organizations, and advocacy organizations. The messages that
U.S. government leadership and workgroup members heard across sessions are reflected in the
development of this report. Contributors included relevant nongovernmental experts,
organizations and stakeholders, including individuals affected directly by the longer-term
effects of COVID-19. For a full list of the U.S. federal departments and agencies that contributed
to this report, please see the Acknowledgements in Appendix B.
19
20
Services and Supports for Longer-Term Impacts of COVID-19
The Biden Administration has made a commitment to combat and respond to the COVID-19
pandemic with the full capacity of the federal government. Federal agencies, working in
partnership with health care professionals, clinical workforce, and community support
organizations will continue to work with and for individuals experiencing longer-term effects of
COVID-19.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19).
cdc.org. Updated December 21, 2021. Accessed May 24, 2022.
https://www.cdc.gov/dotw/covid-
19/index.html#:~:text=COVID%2D19%20is%20a%20respiratory,infected%20may%20not
%20have%20symptoms
2. Substance Abuse and Mental Health Services Administration. Intimate Partner Violence
and Child Abuse Considerations during COVID-19. samhsa.gov. Accessed June 14, 2022.
https://www.samhsa.gov/sites/default/files/social-distancing-domestic-violence.pdf
3. Centers for Disease Control and Prevention. COVID Data Tracker. cdc.gov. Updated June
2, 2022. Accessed June 2, 2022. https://covid.cdc.gov/covid-data-tracker
4. Imperial College London. COVID-19 Orphanhood. imperialcollegelondon.github.io.
Updated May 24, 2022. Accessed May 24,
2022. https://imperialcollegelondon.github.io/orphanhood_calculator/#/country/Unite
d%20States%20of%20America
5. Bureau of Labor Statistics. Table 3. Persons unable to work at some point in the last 4
weeks because their employer closed or lost business due to the coronavirus pandemic
by receipt of pay from their employer for hours not worked and selected characteristics,
Tables for 2020, May. bls.gov. Updated May 12, 2022. Accessed May 24,
2022. https://www.bls.gov/cps/effects-of-the-coronavirus-covid-19-
pandemic.htm#table3
6. McElrath K. Nearly 93% of Households With School-Age Children Report Some Form of
Distance Learning During COVID-19. census.gov. Published August 26, 2020. Updated
December 21, 2021. Accessed May 24, 2022.
https://www.census.gov/library/stories/2020/08/schooling-during-the-covid-19-
pandemic.html
7. Center on Budget and Policy Priorities. The COVID-19 Economy’s Effects on Food,
Housing, and Employment Hardships. cbpp.org. Updated February 10, 2022. Accessed
June 20, 2022. https://www.cbpp.org/research/poverty-and-inequality/tracking-the-
covid-19-economys-effects-on-food-housing-and
21
Services and Supports for Longer-Term Impacts of COVID-19
8. Murthy VH. COVID-19 pandemic underscores the need to address social isolation and
loneliness. Public Health Reports. 2021;136(6):653-655.
https://doi.org/10.1177/00333549211045425
9. Ahmad FB, Cisewski JA, Miniño A, Anderson RN. Provisional Mortality Data — United
States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(14);519-522.
http://dx.doi.org/10.15585/mmwr.mm7014e1
10. Ahmad FB, Cisewski JA, Anderson RN. Provisional Mortality Data — United States, 2021.
MMWR Morb Mortal Wkly Rep. 2022;71:597-600.
http://dx.doi.org/10.15585/mmwr.mm7117e1
11. Ortaliza J, Amin K, Cox C. COVID-19 leading cause of death ranking. Kaiser Family
Foundation. Published March 24, 2022. Accessed June 27, 2022.
https://www.healthsystemtracker.org/brief/covid-19-leading-cause-of-death-ranking/
12. Falk G, Romero PD, Nicchitta IA, Nyhof EC. Unemployment Rates during the COVID-19
Pandemic. Congressional Research Service. Updated August 20, 2021. Accessed May 24,
2022. https://sgp.fas.org/crs/misc/R46554.pdf
13. U.S. Bureau of Labor Statistics. Employment Situation Summary. bls.gov. Published June
3, 2022. Accessed June 3, 2022. https://www.bls.gov/news.release/empsit.nr0.htm
14. Berger M, Kuang M, Jerry L, Freund D. Impact of the Coronavirus (COVID-19) Pandemic
on Public and Private Elementary and Secondary Education in the United States
(Preliminary Data): Results from the 2020–21 National Teacher and Principal Survey
(NTPS). U.S. Department of Education. Published February 2022. Accessed July 19, 2022.
https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2022019
15. National Center for Education Statistics. More than 80 Percent of U.S. Public Schools
Report Pandemic Has Negatively Impacted Student Behavior and Socio-Emotional
Development. nces.ed.gov. Published July 6, 2022. Accessed July 19, 2022.
https://nces.ed.gov/whatsnew/press_releases/07_06_2022.asp
16. Verlenden JV, Pampati S, Rasberry CN, et al. Association of children’s mode of school
instruction with child and parent experiences and well-being during the COVID-19
pandemic—COVID Experiences Survey, United States, October 8–November 13, 2020.
MMWR Morb Mortal Wkly Rep. 2021;70:369–376.
http://dx.doi.org/10.15585/mmwr.mm7011a1
17. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the
United States in 2020. U.S. Department of Agriculture, Economic Research Service.
Published September 2021. Accessed May 24,
2022. https://www.ers.usda.gov/webdocs/publications/102076/err-298.pdf?v=6253.5
22
Services and Supports for Longer-Term Impacts of COVID-19
18. Schanzenbach DW, Pitts A. How much has food insecurity risen? Evidence from the
Census Household Pulse Survey. Northwestern Institute for Policy Research. Published
June 10, 2020. Accessed May 24,
2022. https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-
researchreports-pulse-hh-data-10-june-2020.pdf
19. Centers for Disease Control and Prevention. Disparities in COVID-19 Illness. cdc.gov.
Updated December 10, 2020. Accessed May 24, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-
disparities/increased-risk-illness.html
20. Centers for Disease Control and Prevention. Disparities in COVID-19-Associated
Hospitalizations. cdc.gov. Updated May 23, 2022. Accessed May 24,
2022. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-
ethnic-disparities/disparities-hospitalization.html
21. Centers for Disease Control and Prevention. Disparities in Deaths from COVID-19.
cdc.gov. Updated December 10, 2020. Accessed May 24, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-
disparities/disparities-deaths.html
22. Centers for Disease Control and Prevention. Risk of Severe Illness or Death from COVID-
19. cdc.gov. Updated December 10, 2020. Accessed May 24,
2022. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-
ethnic-disparities/disparities-illness.html
23. Panchal N, Kamal R, Cox C, Garfield R. The Implications of COVID-19 for Mental Health
and Substance Use. Kaiser Family Foundation. Published February 10, 2021. Accessed
May 24, 2022. https://www.kff.org/report-section/the-implications-of-covid-19-for-
mental-health-and-substance-use-issue-brief/
24. Czeisler MÉ , Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal
ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR
Morb Mortal Wkly Rep. 2020;69:1049–1057.
http://dx.doi.org/10.15585/mmwr.mm6932a1
25. Neergaard L, Fingerhut H, Renault M. AP-NORC poll: 1 in 5 in US lost someone close in
pandemic. The Associated Press. Published March 11, 2021. Accessed May 24, 2022.
https://apnorc.org/ap-norc-poll-1-in-5-in-us-lost-someone-close-in-pandemic/
26. Centers for Disease Control and Prevention. Underlying Medical Conditions Associated
with Higher Risk for Severe COVID-19: Information for Health care Professionals.
cdc.gov. Updated February 15, 2022. Accessed June 14, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-
23
Services and Supports for Longer-Term Impacts of COVID-19
care/underlyingconditions.html#:~:text=Age%20is%20the%20strongest%20risk,U.S.%20
COVID%2D19%20related%20deaths
27. Centers for Disease Control and Prevention. People with Certain Medical Conditions.
cdc.gov. Updated May 2, 2022. Accessed June 14, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-
medical-conditions.html
28. Weech-Maldonado R, Lord J, Davlyatov G, Ghiasi A, Orewa G. High-minority nursing
homes disproportionately affected by COVID-19 deaths. Front Public Health.
2021;9:606364. doi:10.3389/fpubh.2021.606364
29. U.S. Department of Health and Human Services Office for Civil Rights. Civil Rights and
COVID-19. hhs.gov. Updated May 20, 2022. Accessed June 14, 2022.
https://www.hhs.gov/civil-rights/for-providers/civil-rights-
covid19/index.html#:~:text=STANDARDS%20OF%20CARE-
,At%20the%20beginning%20of%20the%20COVID%2D19%20public%20health%20emerg
ency,including%20COVID%2D19%20%2D%20PDF
30. Centers for Disease Control and Prevention. Health Equity Considerations and Racial and
Ethnic Minority Groups. cdc.gov. Updated January 25, 2022. Accessed June 14, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-
ethnicity.html
31. Ward LA, Black KP, Britton CL, Tompkins ML, Provost EM. COVID-19 cases,
hospitalizations, and deaths among American Indian or Alaska Native persons—Alaska,
2020–2021. MMWR Morb Mortal Wkly Rep. 2022;71:730–733.
http://dx.doi.org/10.15585/mmwr.mm7122a2
32. Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization,
and Death By Race/Ethnicity. cdc.gov. Updated June 2, 2022. Accessed June 14 2022.
https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-
discovery/hospitalization-death-by-race-ethnicity.html
33. Centers for Disease Control and Prevention. Disparities in COVID-19-Associated
Hospitalizations. cdc.gov. Updated May 23, 2022. Accessed June 14, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-
disparities/disparities-hospitalization.html
34. Weech-Maldonado R, Lord J, Davlyatov G, Ghiasi A, Orewa G. High-minority nursing
homes disproportionately affected by COVID-19 deaths. Front Public Health.
2021;9:606364. doi:10.3389/fpubh.2021.606364
35. Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization,
and Death by Age Group. cdc.gov. Updated June 2, 2022. Accessed June 14, 2022.
24
Services and Supports for Longer-Term Impacts of COVID-19
https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-
discovery/hospitalization-death-by-age.html
36. Centers for Disease Control and Prevention. COVID-19 Vaccines for People who are
Moderately or Severely Immunocompromised. cdc.gov. Updated June 24, 2022.
Accessed June 27, 2022. https://www.cdc.gov/coronavirus/2019-
ncov/vaccines/recommendations/immuno.html
37. U.S. Department of Health and Human Services Office of Disease Prevention and Health
Promotion. Social Determinants of Health. health.gov. Accessed June 14, 2022.
https://health.gov/healthypeople/priority-areas/social-determinants-health
38. U.S. Department of Health and Human Services Office for Civil Rights. HHS Issues New
Guidance for Health Care Providers on Civil Rights Protections for People with
Disabilities. hhs.gov. Published February 4, 2022. Accessed June 7, 2022.
https://www.hhs.gov/about/news/2022/02/04/hhs-issues-new-guidance-health-care-
providers-civil-rights-protections-people-disabilities.html
39. Verdery AM, Smith-Greenaway E, Margolis R, Daw J. Tracking the reach of COVID-19 kin
loss with a bereavement multiplier applied to the United States. Proceedings of the
National Academy of Sciences. 2020;117(30):17695-17701.
https://doi.org/10.1073/pnas.2007476117
40. Neergaard L, Fingerhut H, Renault M. AP-NORC poll: 1 in 5 in US lost someone close in
pandemic. The Associated Press. Published March 11, 2021. Accessed May 24,
2022. https://apnorc.org/ap-norc-poll-1-in-5-in-us-lost-someone-close-in-pandemic/
41. Hillis SD, Blenkinsop A, Villaveces A, et al. COVID-19–Associated Orphanhood and
Caregiver Death in the United States. Pediatrics. 2021;148(6).
https://doi.org/10.1542/peds.2021-053760
42. Panchal N, Kamal R, Cox C, Garfield R. The Implications of COVID-19 for Mental Health
and Substance Use. Kaiser Family Foundation. Published February 10, 2021. Accessed
May 24, 2022. https://www.kff.org/report-section/the-implications-of-covid-19-for-
mental-health-and-substance-use-issue-brief/
43. Czeisler MÉ , Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal
ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR
Morb Mortal Wkly Rep. 2020;69:1049–1057.
http://dx.doi.org/10.15585/mmwr.mm6932a1
44. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National
Center for Health Statistics. Published 2021. Accessed May 24,
2022. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
25
Services and Supports for Longer-Term Impacts of COVID-19
45. Nordenberg T. VA research spells out COVID's down-the-road risks for cardiovascular
and mental health. U.S. Department of Veterans Affairs. Published February 16, 2022.
Accessed May 24, 2022. https://www.research.va.gov/currents/0222-VA-research-
spells-out-COVIDs-down-the-road-risks-for-cardiovascular-and-mental-health.cfm
46. American Psychiatric Association (2021). New APA Poll Shows Sustained Anxiety among
Americans; More than Half of Parents are Concerned about the Mental Well-being of
their Children. psychiatry.org. Published May 2, 2021. Accessed May 24,
2022. https://www.psychiatry.org/newsroom/news-releases/new-apa-poll-shows-
sustained-anxiety-among-americans-more-than-half-of-parents-are-concerned-about-
the-mental-well-being-of-their-children
47. Piquero AR, Jennings WG, Jemison E, Kaukinen C, Knaul FM. Domestic violence during
the COVID-19 pandemic - Evidence from a systematic review and meta-analysis. Journal
of Criminal Justice. 2021;74(101806). https://doi.org/10.1016/j.jcrimjus.2021.101806
48. Flor LS, Friedman J, Spencer CN, et al. Quantifying the effects of the COVID-19 pandemic
on gender equality on health, social, and economic indicators: a comprehensive review
of data from March, 2020, to September, 2021. The Lancet. 2022;399(10344):2381-
2397. https://doi.org/10.1016/S0140-6736(22)00008-3
49. Kegler SR, Simon TR, Zwald ML, et al. Vital Signs: Changes in Firearm Homicide and
Suicide Rates — United States, 2019–2020. Morb Mortal Wkly Rep. 2022;71(19):656-
663. http://dx.doi.org/10.15585/mmwr.mm7119e1
50. Yard E, Radhakrishnan L, Ballasteros M, et al. Emergency Department Visits for
Suspected Suicide Attempts Among Persons Aged 12–25 Years Before and During the
COVID-19 Pandemic — United States, January 2019–May 2021. Morb Mortal Wkly Rep.
2021;70(24): 888-894. http://dx.doi.org/10.15585/mmwr.mm7024e1
51. Centers for Disease Control and Prevention. Long COVID or Post-COVID Conditions.
cdc.org. Updated May 5, 2022. Accessed May 24,
2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-
effects/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F
2019-ncov%2Flong-term-effects.html
52. Bull-Otterson L, Baca S, Saydah S, et al. Post–COVID Conditions Among Adult COVID-19
Survivors Aged 18–64 and ≥65 Years — United States, March 2020–November 2021.
Morb Mortal Wkly Rep. 2022;71(21):713-717.
http://dx.doi.org/10.15585/mmwr.mm7121e1
53. Office of the Assistant Secretary for Health. Health+ Human-Centered Design.
Department of Health and Human Services. Updated May 19, 2022. Accessed June 28,
2022. https://www.hhs.gov/ash/osm/innovationx/human-centered-design/index.html
Services and Supports for Longer-Term Impacts of COVID-19
54. Cutler DM. The Costs of Long COVID. JAMA Health Forum. 2022;3(5):e221809.
doi:10.1001/jamahealthforum.2022.1809
55. Centers for Disease Control and Prevention. Health and Economic Costs of Chronic
Diseases. cdc.gov. Updated June 6, 2022. Accessed July 19, 2022.
https://www.cdc.gov/chronicdisease/about/costs/index.htm
56. Office for Civil Rights. Guidance on “Long COVID” as a Disability Under the ADA, Section
504, and Section 1557. Department of Health and Human Services. Updated July 26,
2021. Accessed May 24, 2022. https://www.hhs.gov/civil-rights/for-providers/civil-
rights-covid19/guidance-long-covid-disability/index.html#footnote4_i76jbi5
57. Equal Employment Opportunity Commission. Section N of What You Should Know About
COVID-19 and the ADA, the Rehabilitation Act, and Other Laws. eeoc.gov. Updated
December 14, 2021. Accessed July 14, 2022. https://www.eeoc.gov/wysk/what-you-
should-know-about-covid-19-and-ada-rehabilitation-act-and-other-eeo-laws
58. Centers for Disease Control and Prevention. Caring for People with Post-COVID
Conditions. cdc.gov. Updated Mar 21, 2022. Accessed May 24, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/care-post-covid.html
59. Department of Education Office for Civil Rights and Office of Special Education and
Rehabilitative Services. Long COVID under Section 504 and the IDEA: A Resource to
Support Children, Students, Educators, Schools, Service Providers, and Families.
Published July 26, 2021. Accessed May 24, 2022. https://sites.ed.gov/idea/files/ocr-
factsheet-504-20210726.pdf
26

27
Services and Supports for Longer-Term Impacts of COVID-19
Chapter 2: Federal Supports and Services
for Americans Experiencing Long COVID
Some people with Long COVID, as well as their families or caregivers, may need a variety of
services, supports or reasonable modifications to access health care and treatment, work, go to
school, and stably live in the community. They may not know where to start
.
This chapter is intended to be a resource guide to help people navigate needed supports,
services, and modifications. It provides a list of federal programs, supports and services that can
help individuals with Long COVID and their families and caregivers. In addition, some of the
resources may also support individuals, their families and caregivers are experiencing the
longer-term impacts of the COVID-19 pandemic, such as mental health and substance use
challenges, and bereavement.
The chapter is divided into ten sections that cover common areas of need
1. Know Your Rights
2. Health care Coverage and Access
3. Community Services and Supports
4. Income and Financial Assistance
5. Job Assistance
6. Housing
7. Food and Nutrition Support
8. Child Care and Early Childhood Development and Education
9. Education Supports
10. Caregiver and Family Support
Each section begins with a “Not Sure Where to Start?” section that provides navigation
resources for the topic, like a website or phone number. The sections include a list of relevant
programs, supports and services for each topic, with a short description and a telephone
number or hyperlink to a website to get more information. You do not need to have Long
COVID to access these resources. Most of the resources are relevant to anyone with a disability
or who meets the program criteria.
28
Services and Supports for Longer-Term Impacts of COVID-19
Know Your Rights
If you have Long COVID, you may be considered an
“individual with a disability” under civil rights laws,
including the Americans with Disabilities Act (ADA),
Section 501 of the Rehabilitation Act of 1973 (Section
501), Section 504 of the Rehabilitation Act of 1973
(Section 504) and Section 1557 of the Patient Protection
and Affordable Care Act (Section 1557). Under these
laws, someone with Long COVID has a disability if the
individual’s condition or any of its symptoms is a physical
or mental impairment that substantially limits one or
more major life activities. There are additional rights
discussed throughout this chapter.
Each of these federal laws protects individuals with
disabilities from discrimination by “covered entities,”
which are the employers and providers who must
comply. Each law is slightly different in terms of rights
and obligations, but there is information about how
these laws can help meet the needs of people with Long
COVID in different topic areas, such as in workplaces,
schools, housing, or in accessing community services. In
some topic areas, such as education, there are additional
federal laws that require services for someone with a
disability.
The Department of Health and Human
Services (HHS) Office for Civil Rights (OCR)
and the Department of Justice (DOJ) Civil
Rights Division have issued Guidance on
“Long COVID” as a Disability Under the ADA,
Section 504, and Section 1557
The Equal Employment Opportunity Commission
(EEOC) addresses Long COVID as a disability and
the employment rights of individuals with Long COVID. See section N within their
guidance document What You Should Know About COVID-19 and the ADA, the
Rehabilitation Act, and Other EEO Laws | U.S. Equal Employment Opportunity
Commission (eeoc.gov)
DOJ and HHS OCR also provide education to the public on the rights and responsibilities
of individuals and entities under the ADA and Section 504 during the COVID-19
pandemic. For more information, visit Emergency Preparedness and Response | U.S.
Not Sure Where to Start?
Q. Do you believe that you
have been discriminated
against because of your race,
color, national origin,
disability, age, gender, or
religion?
A. Visit Office for Civil Rights |
U.S. Department of Health and
Human Services (hhs.gov) or
Contact the Civil Rights Division
| Department of Justice or
Home | U.S. Equal Employment
Opportunity Commission
(eeoc.gov)
-------------------------------------------
Q. Do you have a complaint
about housing, law
enforcement, labor, education
or employment discrimination?
A. Find other Federal civil rights
agencies that can help you
Visit Contact the Civil Rights
Division | Department of Justice
29
Services and Supports for Longer-Term Impacts of COVID-19
Department of Justice (ada.gov) and Civil Rights and COVID-19 | U.S. Department of
Health and Human Services (hhs.gov)
DOJ also has a team of ADA Specialists available by phone, Monday through Friday, to
provide technical assistance on the requirements of the ADA. These Specialists can be
reached at 1 (800) 514-0301 (Voice) and 1 (800) 514-0383 (TTY)
The federal government recognizes that equity requires non-discrimination in the availability of,
and access to, care, treatment, supports and services, and employment opportunities for people
with Long COVID. Federal civil rights laws not only protect individuals with Long COVID from
discrimination on the basis of disability, but also on the basis of race, color, national origin
(including limited English proficiency), age, religion, pregnancy, sexual orientation, and gender
identity.
For additional resources on addressing civil rights issues related to the COVID-19
pandemic, more can be found in the Department of Justice (DOJ) Civil Rights Division’s
Statement on a Coordinated Civil Rights Response to Coronavirus: Statement by the
Principal Deputy Assistant Attorney General for Civil Rights Leading a Coordinated Civil
Rights Response to Coronavirus (COVID-19) | OPA | Department of Justice.
The U.S. Equal Employment Opportunity Commission has issued What You Should Know
About COVID-19 and the ADA, the Rehabilitation Act, and Other EEO Laws, a series of
technical assistance questions and answers on COVID-19 issues, such as return to work,
hiring, vaccinations, caregivers, the definition of disability that includes Long COVID,
reasonable accommodation, and retaliation.
The Department of Health and Human Services Office for Civil Rights has issued a
bulletin: Bulletin: Ensuring the Rights of Persons with Limited English Proficiency in
Health Care During COVID-19 | Guidance Portal (hhs.gov).
Legal Assistance and Information
Sometimes people with Long COVID may have questions about their eligibility for some of the
programs discussed in this chapter. They or their family member may have been told they are
not eligible, or that services are not covered, and they want to know their legal rights. They may
be subject to a legal proceeding, such as an eviction or a collection on a bill they could not pay
because they lost their job. They may be eligible for free legal help for some or all of these
questions.
Legal Assistance for People with Disabilities through Protection and Advocacy
Systems
Protection and Advocacy Systems (P&As) are congressionally mandated agencies that provide a
range of legal advocacy services to people with disabilities. P&As can assist if a person has been
denied access to a service or an opportunity to take part in an activity, such as employment or
30
Services and Supports for Longer-Term Impacts of COVID-19
education, and can address allegations of neglect or abuse and conduct monitoring and
investigations of facilities. For people with Long COVID, their local P&A may help assess their
status and needs, provide case management, ensure access to services, and address
accessibility barriers. There are 57 P&As—one in each state and territory, as well as one which
serves the Navajo and Hopi Nations in Colorado, New Mexico, Arizona, and Utah.
Find a local P&A, visit Member Agencies | National Disability Rights Network (ndrn.org)
Legal Assistance for Older Americans
The Older Americans Act (OAA) provides funding for legal assistance to older adults ages 60 and
older provided through Area Agencies on Aging (AAAs). There are approximately 1,000 OAA-
funded legal services providers nationwide. The legal services network can provide important
assistance for older persons in accessing long-term care options and other community-based
services. Legal services also protect older persons against direct challenges to their
independence, choices, and financial security. These legal services are specifically targeted to
“older individuals with economic or social needs.” OAA-funded legal services providers may
address issues such as health care coverage, income security, housing, utilities, protective
services, abuse, neglect, and age discrimination.
Find local services, visit Eldercare Locator | Administration for Community Living
(eldercare.acl.gov) or call 1 (800) 677-1116
Americans with Disabilities Act National Network
The Americans with Disabilities Act (ADA) National Network provides information, training, and
technical assistance to individuals, including students with Long COVID, educators, businesses,
and agencies with rights and responsibilities under the ADA. There are 10 Regional ADA Centers
located throughout the United States and an ADA Knowledge Translation Center (ADAKTC),
providing technical assistance about the ADA, Sections 501 and 504 of the Rehabilitation Act,
and the Individuals with Disabilities Education Act (IDEA).
Learn more about the ADA National Network, visit ADA National Network | Information,
Guidance and Training on the Americans with Disabilities Act (adata.org)
Reach a representative, call the ADA National Network hotline 1 (800) 949-4232 or visit
Email Us | ADA National Network (adata.org)
31
Services and Supports for Longer-Term Impacts of COVID-19
Health Care Coverage and
Access
The COVID-19 pandemic has highlighted the critical
importance of having health care coverage for yourself
and your family. The pandemic has worsened the
inequities that underlie our health care system, and the
federal government is continually working on both
federal and state levels to improve access to and quality
of care for everyone. Symptoms of Long COVID, which
may present differently in each person and often appear
similar to other conditions, can pose significant
challenges to our health care system and to patients,
especially those with other underlying disabilities. Some
of the resources in this section may also support
individuals, their families and caregivers who are
experiencing the longer-term impacts of the COVID-19
pandemic, such as mental health and substance use
challenges, and bereavement. Indivuidals who many
have lost a loved one whose health care coverage you
depended or who lost health coverage due to job loss
may also benefit from the supports and services in this
chapter. This section covers eight topics.
• Health Insurance Coverage
• Health Insurance Support after Job Loss
• Community Health Centers and Health Care for
Underserved Communities
• Veterans, Military Service Members, and Military
Families
• Tribal Communities
• Home Medical Equipment
• Telehealth and Long COVID
• Long COVID Study Enrollment.
Not Sure Where to Start?
Q. Need health insurance
coverage?
A. Contact a Health Insurance
Navigator and Assister. Search -
Local Assistance for Health
Insurance Application |
(HealthCare.gov)
-------------------------------------------
Q. Need help paying for your
health care costs?
A. Find out if you might save on
Marketplace premiums, or
qualify for Medicaid or
Children's Health Insurance
Program (CHIP), based on your
income at Saving Money on
Healthcare Costs |
(HealthCare.gov)
-------------------------------------------
Q. Need assistance with
Medicare coverage,
enrollment, or costs?
A. Contact Medicare at
1 (800) MEDICARE or
1 (800) 633-4227 and 1 (877)
486-2048 (TTY). Welcome to
Medicare | Medicare
(medicare.gov)
-------------------------------------------
Q. In need of health insurance
coverage after job loss?
A. Contact a Benefits Advisor.
Ask EBSA | U.S. Department of
Labor (dol.gov)
32
Services and Supports for Longer-Term Impacts of COVID-19
If you have problems getting health insurance coverage or getting services you need, you may
want to review the Legal Assistance portion of the Know Your Rights section.
Health Insurance Coverage
HealthCare.gov
If you have private insurance through the individual market, the Affordable Care Act’s (ACA)
“Essential Health Benefits” generally provide coverage for the diagnosis and treatment of
COVID-19, including Long COVID. Coverage and cost-sharing details can vary by plan. Generally,
individuals can enroll in coverage during the annual open enrollment period or if they qualify
for a special enrollment period. You may be eligible for a special enrollment period if you loose
your health insurance because you lost your job. Uninsured people under age 65 who are
eligible to enroll in coverage through the ACA Marketplaces and consumers who are currently
enrolled in Marketplace coverage can get help with plan enrollment and consult with health
insurance Navigators and Assisters.
Find assistance near you, visit Search - Local Assistance for Health Insurance Application
(HealthCare.gov)
Find out if you can lower your Marketplace premium costs, visit Saving Money on
Healthcare Costs | (HealthCare.gov)
For translated resources, visit Other Language Resources | HealthCare.gov
Medicaid and the Children’s Health Insurance Program
Medicaid and the Children’s Health Insurance Program (CHIP) are joint federal-state programs.
Medicaid provides health coverage to eligible adults with lower incomes, children, pregnant
individuals, older individuals, and people with disabilities. CHIP provides health coverage to
uninsured children in families with incomes too high to quality for Medicaid, but too low to
afford private coverage. COVID-19-related treatment is available with no cost-sharing for most
Medicaid and CHIP beneficiaries. These coverage requirements and cost-sharing prohibitions
generally end in the year following the end of the COVID-19 public health emergency. This
coverage includes treatments and therapies for Post-COVID-19 conditions, including Long
COVID. Additionally, states must cover the treatment of a condition, which is usually covered
under Medicaid and CHIP, and that may otherwise seriously complicate the treatment of
COVID-19. Medicaid and CHIP also cover a wide range of other health care benefits, services,
and treatments that are relevant for individual's with Long COVID.
Medicaid and CHIP also cover a wide range of health care benefits and treatments.
Learn whether you are eligible for Medicaid or CHIP, visit Get Coverage. Health
Insurance Marketplace® | HealthCare.gov
33
Services and Supports for Longer-Term Impacts of COVID-19
Medicare
Medicare provides health insurance coverage for people who are 65 and older and for some
people with disabilities. This includes coverage of diagnosis and treatment for Long COVID as
well as a wide range of health care benefits and treatments.
Learn about Medicare coverage of Long COVID by calling 1 (800) MEDICARE or 1 (800)
633-4227 and 1 (877) 486-2048 (TTY)
Explore how Medicare can best fit your needs, visit Welcome to Medicare | Medicare
For translated resources, visit Information in Other Languages | Medicare
(medicare.gov)
If you need help paying for your Medicare costs, see Medicare Savings Program and
Extra Help for Medicare Part D topics below
If you are enrolled in a Medicare Advantage Plan, you should check your plan details for
COVID-19 related benefits
Medicare Savings Programs
If you are eligible for Medicare, you can get help from your state for paying your Medicare
premiums. In some cases, Medicare Savings Programs may also pay Medicare Part A (Hospital
Insurance) and Medicare Part B (Medical Insurance) deductibles, coinsurance, and copayments
if you meet certain conditions.
Contact your state Medicaid agency, visit Talk to someone | Medicare, select your state
and then choose "Other insurance programs" from the menu on the left
Extra Help for Medicare Part D Participants
If you are eligible for Medicare and meet certain income and resource limits, you may qualify
for Extra Help with your prescriptions. This program helps pay for your Medicare drug coverage,
such as plan premiums, deductibles, and costs when you fill your prescriptions, called copays or
coinsurance.
Some people automatically qualify for Extra Help. You'll get the Extra Help program if you have
Medicare and get any of the following: full Medicaid coverage; help from your state Medicaid
program paying your Part B premiums (from a Medicare Savings Program); or Supplemental
Security Income (SSI) benefits. If you do not automatically qualify, you can apply for Extra Help
at any time.
Apply for Extra Help online, visit Welcome!, Extra Help With Medicare Prescription Drug
Plan Costs, Social Security (ssa.gov) or call Social Security toll-free at 1 (800) 772-1213
and 1 (800) 325-0778 (TTY)
34
Services and Supports for Longer-Term Impacts of COVID-19
State Health Insurance Assistance Program
State Health Insurance Assistance Program (SHIP) is a national program that offers one-on-one
assistance, counseling, and education to Medicare beneficiaries, their families, and caregivers
to help them make informed decisions about their care and benefits.
Find your local SHIP, visit Home | State Health Insurance Assistance Programs
(shiphelp.org)
Talk to a counselor by calling (877) 839-2675
Federal Employees Health Benefits Program
There are approximately 250 Federal Employees Health Benefits (FEHB) Program plan options
available to the more than 8.2 million federal employees, retirees, and family members. The
plans offer comprehensive benefits that include inpatient, outpatient, office-based care,
pharmacy services, and telehealth. The diagnosis of Long COVID and related conditions is
covered by FEHB plans, and there are no general exclusions based on this condition or cluster of
conditions. Federal employees and retirees can join the program during the annual Open
Season (November to December) or when they join federal service.
Learn more about FEHB, visit Eligibility (opm.gov)
Health Insurance Support after Job Loss
Consolidated Omnibus Budget Reconciliation Act Continuation Coverage
If you’ve lost your job or had your hours reduced, there are options available to workers and
their families to maintain health coverage, including the Consolidated Omnibus Budget
Reconciliation Act (COBRA). COBRA provides a way for workers and their families to temporarily
maintain their employer-provided health insurance during situations such as job loss or a
reduction in hours worked.
Find out if you qualify for COBRA, call 1 (866) 444-3272; dial 7-1-1 to access
telecommunications relay services
Request assistance from a Benefits Advisor, visit Ask EBSA | U.S. Department of Labor
(dol.gov)
Employer-Sponsored Insurance
The Employee Benefits Security Administration (EBSA) provides answers to your questions and
assists you if you believe you have been inappropriately denied employee benefits, including
health benefits. They can help answer questions on issues such as denied health or disability
benefits, COBRA, or plan administration and compliance.
35
Services and Supports for Longer-Term Impacts of COVID-19
Reach a Benefits Advisor, visit Ask EBSA | U.S. Department of Labor (dol.gov)
Speak to a Benefits Advisor, call (866) 444-3272; dial 7-1-1 to access
telecommunications relay services
Community Health Centers and Health Care for Underserved
Communities
Federally Qualified Health Centers
Federally Qualified Health Centers (FQHCs) are community-based health care organizations that
provide comprehensive, culturally competent, high-quality primary health care services for
people who have lower incomes, who are uninsured, or face other obstacles to getting health
care. FQHCs provide services regardless of patients’ ability to pay and charge for services on a
sliding fee scale.
Find a health center near you, visit Find a Health Center (hrsa.gov)
While not part of the FQHCs, many state and local health (and public health)
departments provide health care. To find find a public health department near you, visit
Directory of Local Health Departments - NACCHO
Rural Health Clinics
Rural Health Clinics (RHCs) make up a critical part of the rural health care infrastructure and
help address health equity gaps in medically underserved rural communities to improve health
outcomes for rural residents. There are nearly 5,000 RHCs in 45 states located in rural,
underserved areas.
Find additional information about RHCs, visit Expanding COVID-19 Response in Rural
Communities through Rural Health Clinics | Official web site of the U.S. Health
Resources and Services Administration (hrsa.gov)
Rural Hospitals
More than half of all hospitals in the United States are in rural areas. Rural hospitals serve
individuals living in rural areas.
Find additional information about rural hospitals, visit Rural Hospital Programs | HRSA
Veterans, Military Service Members, and Military Families
Veterans Affairs Health Care
Veterans enrolled in the Veterans Affairs (VA) Health Care System can access primary and
specialty care appointments, including those to cardiologists, gynecologists, and mental health
36
Services and Supports for Longer-Term Impacts of COVID-19
providers). In addition, veterans enrolled in VA health care can also access VA health care
services like home health care, and you can get medical equipment, prosthetics, and
prescriptions. Veterans with Long COVID and those with health needs related to the longer-
term impact of the pandemic may access health services through the VA Health Care System.
Find out more about eligibility for VA health care and learn how to apply for these
benefits by calling Health benefits hotline at (877) 222-VETS or (877) 222-8387
Find more information about VA health care services, visit VA Health Care | Veterans
Affairs (va.gov)
Find a VA service provider near you, visit Find VA Locations | Veterans Affairs (va.gov)
Military Health System and TRICARE
The Department of Defense provides treatment and care to Military Health System
beneficiaries through TRICARE. TRICARE is the health care program for eligible uniformed
service members, retirees, and their families around the world. TRICARE provides
comprehensive coverage to all beneficiaries, and most TRICARE health plans meet the
requirements for minimum essential coverage under the Affordable Care Act. Depending on
their plan type, TRICARE beneficiaries, including those with persistent Long COVID symptoms
may be able to access care through military medical treatment facilities (MTFs) or through the
community network.
Patients concerned about prolonged symptoms or symptoms associated with Long
COVID, any non-COVID-19 symptoms, or other health questions may call the Military
Health System Nurse Advice Line at 1 (800) TRICARE or 1 (800) 874-2273 and select
option 1
Find military treatment facilities and TRICARE providers close to you, visit Find a Military
Hospital or Clinic | TRICARE (www.tricare.mil)
Find a network or non-network provider, visit Find a Doctor | TRICARE (www.tricare.mil)
Tribal Communities
Indian Health Service
If you are an American Indian or Alaska Native (AI/AN) person affected by any longer-term
consequences of COVID-19, the Indian Health Service (IHS) supports a comprehensive health
service delivery system through a series of Federal, Tribal, and Urban Indian Organization
programs. The IHS offers primary care, mental health, substance use treatment, emergency
services, and hospital care, although the range of services may vary by location. AI/AN persons
with Long COVID and those with health needs related to the longer-term impact of the
pandemic may seek primary health services at IHS.
37
Services and Supports for Longer-Term Impacts of COVID-19
Find a health center near you, visit Find Health Care | Indian Health Service (IHS.gov)
Indian Health Service Community Health Representative Program
The Community Health Representative (CHR) Program is a culturally oriented and tailored
concept for providing health care, health promotion, and disease prevention services. CHRs are
frontline public health workers who are trusted members of the community with a close
understanding of the community, language, and traditions. They assist by increasing health
knowledge of patients and communities through a broad range of activities, such as
transportation to health visits, outreach, community education, informal counseling, social
support, and advocacy.
Learn more about the CHR program, visit Community Health Representative | Indian
Health Service (IHS)
Indian Health Service Pharmacy Program
The Indian Health Service Pharmacy Program serves as an integral part of a comprehensive,
community-based, health care delivery system. Pharmacy services are patient-centered and are
directed toward optimal patient care outcomes, health promotion, and disease prevention.
Learn more about the Pharmacy Program, visit Pharmacy Program | Division of Clinical
and Community Services (ihs.gov)
For information on Pharmacy Expanding Vaccine Access, visit Pharmacy Expanding
Vaccine Access (PEVA) | Commissioned Corps of the U.S. Public Service
(dcp.psc.gov/OSG/pharmacy)
Indian Health Service Division of Behavioral Health
The Indian Health Service Division of Behavioral Health (DBH) serves as the primary source of
national advocacy, policy development, management, administration of mental health, alcohol
and substance use challenges, and family violence prevention programs for AI/AN people.
Working in partnership with Tribes, Tribal organizations, and Urban Indian health organizations,
DBH coordinates national efforts to share knowledge and build capacity through the
development and implementation of evidence-based, practice-based and culturally-based
activities in Indian Country. DBH also established Long-Term COVID resources to develop a DBH
IHS planning document of long-term recovery and resilience from mental and behavioral
impacts of COVID-19.
Learn more about DBH, visit Division of Behavioral Health | Indian Health Service (IHS)
38
Services and Supports for Longer-Term Impacts of COVID-19
Indian Health Service Telehealth Resources
Indian Health Service offers telehealth services to help achieve the mission of raising the
physical, mental, social, and spiritual health of AI/AN people to the highest level. IHS telehealth
services support and promote long-distance clinical health care, patient and professional
health-related education, and public health and health administration. Using telehealth brings
specialty care locally to the AI/AN population including patients affected by any longer-term
consequences of COVID-19.
Learn more about the IHS Telehealth resources, visit Telehealth | IHS (ihs.gov)
The Indian Health Service Teleophthalmology Program
Established in 2000, this program uses telemedicine technology to provide high-quality, cost-
effective, annual diabetic eye exams to AI/AN people.
Learn more about the Teleophthalmology Program, visit Joslin Vision Network
Teleophthalmology Program | IHS (ihs.gov)
Find a list of sites, visit List of Facilities (ihs.gov)
The Indian Health Service Telebehavioral Health Program
Provides direct, ongoing care via televideo to patients of all ages at IHS, Tribal, and Urban
Indian operated facilities across the country. Current clinical services include: Adult Psychiatry;
Addictions Psychiatry; Geriatric Psychiatry; Child and Adolescent Psychiatry; Adult Therapy;
Family, Couples, and Group Therapy; Child and Adolescent Therapy; and Trauma and PTSD
Therapy.
Learn more about the Telebehavioral Health Program, visit IHS Telebehavioral Health
Center of Excellence (TBHCE)
Find a list of TBHCE sites, visit Current TBHCE Sites | Telebehavioral Health (ihs.gov)
Tribal Employer Health Insurance via the Federal Employees Health Benefits
Program
Health insurance coverage through the Federal Employees Health Benefits Program (FEHB) can
be purchased by Tribes or tribal organizations carrying out programs under the Indian Self-
Determination and Education Assistance Act (ISDEAA) or the Tribally Controlled Schools Act of
1988 (TCSA) (25 U.S.C. 2501 et seq.), and urban Indian organizations carrying out programs
under Title V of the Indian Health Care Improvement Act (IHCIA). It can be offered to eligible
employees and their family members. The plans offer comprehensive benefits that include
inpatient, outpatient, office-based care, pharmacy services, and telehealth. Similar to FEHB
coverage for federal employees, retirees, and their families, there are not health plan
restrictions in coverage for Long COVID.
39
Services and Supports for Longer-Term Impacts of COVID-19
Learn more about Tribal Employee Health Insurance by visiting Tribal Employers
(opm.gov).
Find a Quick Guide to FEHB for Tribal Employees, visit Quick Guide to FEHB for Tribal
Employees (opm.gov)
Home Medical Equipment
Home Medical Equipment
Health insurance may cover a range of home medical equipment (sometimes known as durable
medical equipment). Home medical equipment includes, but is not limited to oxygen
equipment, crutches, home infusion pumps and supplies, nebulizers, wheelchairs, and walkers.
Check with your health insurance to see if it covers home medical equipment if needed.
See the Health Care Coverage and Access section for more information.
Telehealth and Long COVID
Health and Human Services Telehealth Guidance for Patients
Telehealth has been extended across many health programs. It is safe, convenient, and more
cost-effective for patients who may have mobility and transportation concerns that make
getting to the office difficult. However, for people experiencing Long COVID, including older
adults, people with limited English proficiency, and people with low digital literacy, there may
be accessibility issues.
For more information on HHS Telehealth Guidance, visit For Patients | Telehealth
(telehealth.hhs.gov)
For information about accessibility, visit Improving Access to Telehealth |
(Telehealth.hhs.gov)
See telehealth resources for specific populations such as tribal communities within the
Health Care Coverage and Access section
Long COVID Study Enrollment
Innovative Support for Patients with SARS-CoV-2 Infections
A Centers for Disease Control and Prevention funded study called the Innovative Support for
Patients with SARS-CoV-2 Infections (INSPIRE) will describe and increase our understanding of
the longer-term effects of COVID-19 infection. Participants will be asked to describe how they
are feeling by completing online surveys and sharing their medical information through a
secure, confidential, cloud-based personal health platform.
40
Services and Supports for Longer-Term Impacts of COVID-19
Learn more about how you can be involved in INSPIRE, visit Covid Inspire
Researching COVID to Enhance Recovery Initiative
The Researching COVID to Enhance Recovery (RECOVER) Initiative at the National Institutes of
Health (NIH) is a major study to improve the understanding of and ability to predict, treat, and
prevent Long COVID. RECOVER is a patient-centered study of national scale with inclusive
diverse participation and community and patient engagement. It includes longitudinal
observational studies across the lifespan, ancillary clinical studies leveraging cohort data and
specimens, clinical trials, a patient registry, pathobiology studies, a mobile health platform, and
electronic health record studies. Studies include children, adults, and pregnant people.
Learn more about how you can be involved in RECOVER, visit About the Initiative |
RECOVER COVID (RecoverCOVID.org)
41
Services and Supports for Longer-Term Impacts of COVID-19
Community Services and Supports
If you have Long COVID, you may need assistance to do
things you did by yourself in the past. You also may need
to make changes in your life or to your home to adapt to
the changes in your abilities. Below are networks and
programs that offer a wide range of services and
supports to meet your needs. Some of the resources in this
section may also support individuals, their families
and caregivers who are experiencing the longer-term
impacts of the COVID-19 pandemic, such as mental
health and substance use challenges and bereavement.
This section includes six topics
• Community Based Services to Assist with
Activities of Daily Living
• Navigation Support
• Transportation
• Assistive Technology
• Consumer Supports
• Community Economic Development.
If you need legal assistance with accessing community
services, including the right to receive services in the
most integrated setting under disability rights laws, you
may want to review the Legal Assistance section of the
Know Your Rights section.
Community Based Services to Assist with Activities of Daily Living
Access to Services in the Community
One form of discrimination prohibited by non-discrimination laws that is specific to community
services is the unnecessary segregation of people with disabilities. States and local
governments must provide the services and supports they offer in the most integrated setting
appropriate, meaning a setting that enables people with and without disabilities to interact to
the fullest extent possible. When states and local governments provide services and supports to
people with Long COVID, they must offer those services in community settings, such as a
Not Sure Where to Start?
Q. Looking for information
about community-based
supports and services that you
are eligible to receive?
A. Contact the Disability
Information and Access Line
(DIAL). To use DIAL, call (888)
677-1199 Monday through
Friday, 9:00 a.m. to 8:00 p.m. ET
or email
DIAL@usaginganddisability.org.
Learn more at acl.gov/DIAL.
-------------------------------------------
Q. Are you an older adult or a
caregiver for an older adult
looking for local support
resources?
A. Call the Eldercare Locator at
1 (800) 677-1116 or visit
eldercare.acl.gov to chat live or
browse resources.
Services and Supports for Longer-Term Impacts of COVID-19
42
person’s own home, as opposed to only in nursing facilities or other institutional settings, when
doing so would not fundamentally change their program of services and supports.
Learn more about the guidance for public entities to provide services and supports to
qualified individuals with disabilities in integrated settings, visit Statement of the
Department of Justice on Enforcement of the Integration Mandate of Title II of the
Americans with Disabilities Act and Olmstead v. L.C. (ada.gov)
Navigation Support
Aging and Disability Resource Centers
Aging and Disability Resource Centers (ADRC) provide objective information, advice, counseling
and assistance, and help people access public and private programs that assist with community
living. For people with Long COVID, ADRCs can help navigate state systems of services, including
determining eligibility and connecting individuals to the organizations, critical resources, and
services that can help meet their needs.
Find an ADRC near you, visit Eldercare Locator | Administration for Community Living
(eldercare.acl.gov)
Disability Information and Access Line
Disability Information and Access Line (DIAL) provides information about community-based
supports and services that people with Long COVID may be eligible for to live independently, go
to school and work, and fully participate in all of life's activities.
Learn more about DIAL, visit Disability Information and Access Line | ACL Administration
for Community Living
Reach DIAL at (888) 677-1199, Monday through Friday, 9:00 a.m. to 8:00 p.m. ET or
email DIAL@usaginganddisability.org
Eldercare Locator
The Eldercare Locator is a nationwide service that connects older adults and their caregivers
with trustworthy local support resources. The Eldercare Locator can provide information to
help older adults and caregivers find transportation to medical appointments, make repairs or
modifications to their homes, receive in-home assistance, get meals delivered to the home, and
more.
Reach out to Eldercare Locator, call 1 (800) 677-1116 or visit Eldercare Locator (acl.gov)
to chat live
43
Services and Supports for Longer-Term Impacts of COVID-19
Family-to-Family Health Information Centers
Family-to-Family Health Information Centers (F2F) are family-staffed centers that
provide critical support to families caring for children and youth with special health care
needs, particularly families of children with complex needs and those from diverse
communities. F2Fs help people find effective care and services, apply for Medicaid, Children’s
Health Insurance Program, or private insurance, get referrals to providers, address insurance
denials, identify and access community support programs, advocate to ensure effective and
cost-efficient care and connect with parent mentors.
Find F2Fs near you, visit Affiliate Archive - Family Voices | (familyvoices.org)
State Health Insurance Assistance Program
State Health Insurance Assistance Program (SHIP) is a national program that offers one-on-one
assistance, counseling, and education to Medicare beneficiaries, their families, and caregivers
to help them make informed decisions about their care and benefits. If you have Long COVID,
you may want to find out if you can reconsider your Medicare options to make sure you have
the best Medicare coverage for you.
Review your options and learn about enrollment periods, contact your local SHIP by
visiting Home | State Health Insurance Assistance Programs (shiphelp.org)
Talk to a counselor, call (877) 839-2675
Area Agencies on Aging
Area Agencies on Aging (AAA) serve older adults (age 60 years and greater) and family
caregivers. Most also serve people with disabilities. AAAs contract with 20,000+ local providers
nationwide to provide services and programs that may include congregate and home-delivered
meals, information and assistance, evidence-based chronic disease prevention programs,
caregiver respite, case management, transportation, homemaker and chore support, and
personal care.
Find your local AAA, visit Eldercare Locator | Administration for Community Living
(eldercare.acl.gov) or call 1 (800) 677-1116
Centers for Independent Living
Centers for Independent Living (CIL) support people of all ages with all types of disabilities and
are in communities in every state and most territories. They offer, at a minimum, the following
services: information and referral, independent living skills training, peer counseling, individual
and systems advocacy, transition and diversion from nursing homes and other institutional
settings back into the community, and transition of youth to postsecondary life.
Find a CIL near you, visit CIL Center and Association Directory | ILRU (ilru.org)
Services and Supports for Longer-Term Impacts of COVID-19
44
Home and Community-Based Services
Home and Community-Based Services (HCBS) provide opportunities for Medicaid beneficiaries
to receive services in their own home or community rather than institutions or other isolated
settings. These programs serve a variety of targeted populations groups, such as people with
intellectual or developmental disabilities, physical disabilities, or mental health disabilities.
Eligibility for HCBS varies by state.
Learn more about HCBS, visit State Resources Map | CMS
Learn about your eligibility for Medicaid, how to apply, and other frequently asked
questions, visit Medicaid & You: Frequently Asked Questions | Medicaid (medicaid.gov)
Tribal and Native American Grantees
Native American Elderly Service Centers provide supportive services, nutrition services, and
caregiver support to native elders and their families. Age for eligibility is determined by each
tribe; there are 282 grantees serving over 400 tribes. For tribal and Native American elders with
Long COVID, these programs may provide case management and assistance organizing
transportation. They may also help educate individuals and communities on Long COVID and
the resources available to assist people with Long COVID and caregivers.
Find services in your area, visit Service Locator | National Resource Center on Native
American Aging (nrcnaa.org)
Transportation
Area Agencies on Aging
Area Agencies on Aging (AAA) serve older adults (age 60 and older) and family caregivers. Most
also serve people with disabilities. AAAs contract with more than 20,000 local providers
nationwide to provide services and programs including transportation.
Find your local AAA, visit Eldercare Locator | Administration for Community Living
(eldercare.acl.gov) or call 1 (800) 677-1116
Centers for Independent Living
Centers for Independent Living (CIL) support people of all ages with all types of disabilities and
are in communities in every state and most territories. They offer a range of services, including
assistance with transportation.
Find a local CIL, visit CIL Center and Association Directory | ILRU (ilru.org)
45
Services and Supports for Longer-Term Impacts of COVID-19
Disability Information and Access Line
Disability Information and Access Line (DIAL) provides information about community-based
supports and services that people experiencing Long COVID may be eligible for, including
transportation.
Learn more, visit Disability Information and Access Line | ACL Administration for
Community Living
Reach a representative, call (888) 677-1199, Monday through Friday from 9:00 a.m. to
8:00 p.m. ET or email DIAL@usaginganddisability.org
Eldercare Locator
The Eldercare Locator is a nationwide service that connects older adults and their caregivers
with trustworthy local support resources, including transportation.
Reach Eldercare, call the Eldercare Locator at 1 (800) 677-1116 or visit
to chat live or browse resources
eldercare.acl.gov
Half or Reduced Fare, Urbanized Area Formula Grants
This program makes federal resources available to urbanized areas (population over 50,000) for
public transportation, buses, commuter trains, ferries, etc. Public transportation law requires
grantees receiving funding under this program to offer half fare or reduced fare to people with
disabilities and older adults during off-peak hours for fixed-route services. Local transit agencies
may also have a reduced fare policy for additional groups of riders such as children, students,
active-duty military members, or military Veterans.
Learn more, visit Understanding Half Fare/Reduced Fare Requirements | The National
Aging and Disability Transportation Center (NADTC.org)
National Aging and Disability Transportation Center
National Aging and Disability Transportation Center (NADTC) serves professionals in the fields
of transportation, aging, disability, human services, and caregiving. It supports the availability
and accessibility of transportation options for older adults, people with disabilities, and their
families to find the best transportation options in their local communities.
Explore NADTC resources, trainings, and information, visit National Aging and Disability
Transportation Center (nadtc.org)
For technical assistance, email at contact@nadtc.org or call at (866) 983-3222, Monday
through Friday, 9:00 a.m. to 5:00 p.m. ET
46
Services and Supports for Longer-Term Impacts of COVID-19
Assistive Technology
State Assistive Technology Programs
State Assistive Technology (AT) programs help make AT devices and equipment and services
available. Their efforts range from “low tech” (e.g., built-up handle on spoon to improve ability
to grasp) to “high tech” (e.g., computers controlled with eye movement). Other examples of
supports are home automation solutions and services to obtain and use devices. AT support can
also include assessment, customization, repair, and training. For people with Long COVID, their
state program may be able to provide them with AT, subject matter expertise, and technical
assistance related to accessibility and AT.
Find a local AT program, visit Find a local AT program | Assistive Technology Act
Technical Assistance and Training Center (at3center.net)
Consumer Supports
Centers for Independent Living
Centers for Independent Living (CIL), discussed in more detail above, support people of all ages
with all types of disabilities and are in communities in every state and most territories.
Find a local CIL, visit CIL Center and Association Directory | ILRU (ilru.org)
Area Agencies on Aging
Area Agencies on Aging (AAA), discussed in more detail above, serve older adults (age 60 and
older) and family caregivers. Most also serve people with disabilities. AAAs contract with more
than 20,000 local providers nationwide to provide services and programs including
transportation.
Find your local AAA, visit Eldercare Locator | Administration for Community Living
(eldercare.acl.gov) or call 1 (800) 677-1116
State Long-Term Care Ombudsman Programs
State Long-Term Care Ombudsman Programs (LTCOP) advocate for people living in nursing
homes, board-and-care homes, assisted living facilities, and similar facilities to resolve
individual problems and to bring about changes that improve their care, quality of life, and
rights. For people with Long COVID living in long-term care facilities, their ombudsman may
serve as a resource to provide information on Long COVID and help if any issues arise in
meeting new needs as a result of Long COVID.
Reach a representative, call 1 (800) 677-1116
Find an ombudsman program near you, visit Program Locator | ConsumerVoice.org
47
Services and Supports for Longer-Term Impacts of COVID-19
Community Economic Development
Community Action Agencies
A network of Community Action Agencies (CAA) throughout the United States connects people
to greater opportunities and could be a good resource for people with Long COVID. CAAs are
the frontline resource for people living in poverty, providing education, employment and family
support services for families with low incomes. Community Action Agencies also promote
community economic development through community partnerships and collaborations that
enhance business development and create jobs.
Learn more about Community Action Partnership, visit National CAP | Community
Action (communityactionpartnership.com)
Find a CAA near you, visit Find A CAP | National CAP (communityactionpartnership.com)
or call (202) 265-7546
48
Not Sure Where to Start?
Q. Lost your job and want to
know whether you are eligible
for unemployment benefits?
A. Find out about the programs
in your state by visiting
Unemployment Benefits Finder
| CareerOneStop.org
-------------------------------------------
Q. Does your family need some
financial assistance since you
were diagnosed with Long
COVID?
A. Find out if your family is
eligible to participate in the
Temporary Assistance for
Needy Families (TANF) by
contacting a program in your
area by visiting Help for Families
| The Administration for
Children and Families (hhs.gov)
Services and Supports for Longer-Term Impacts of COVID-19
Income and Financial Assistance
People experiencing Long COVID may need financial
assistance due to lost wages or unemployment. There
are federal programs to help you address financial
difficulties that are the result of Long COVID. In addition,
some of the resources may also support individuals, their
families and caregivers are experiencing the longer-term
impacts of the COVID-19 pandemic, such as mental
health and substance use challenges and bereavement.
Individuals who lost income due to the loss of a loved
one my also find assistance from these federal supports.
This section covers five topics
• Disability and Survivor Benefits
• Unemployment Benefits
• Tax Credits
• Retirement Benefits
• Assistance Programs for Families with Children.
If you need help applying for financial assistance, or have
applied for financial assistance and been denied, you
may want to review the Legal Assistance section in the
Know Your Rights section.
Disability and Survivor Benefits
Social Security Disability Insurance
The Social Security Disability Insurance (SSDI) program provides assistance to people who are
disabled under the Social Security Act. The SSDI program may pay benefits to you and certain
family members if you are “insured.” This means that you worked long enough—and recently
enough—and paid Social Security taxes on your earnings. To be eligible for SSDI you also have
to meet the program requirements to be found disabled, which may be different from the
requirements to be considered disabled under the ADA. If you meet the requirements, monthly
benefits are paid if you have a medical condition that prevents you from working and is
expected to last at least one year or result in death.
Learn about the SSDI program and apply online, visit Disability Benefits | (ssa.gov)
49
Services and Supports for Longer-Term Impacts of COVID-19
Make an appointment to file your application, call 1 (800) 772-1213 and 1 (800) 325-
0778 (TTY)
Find a Social Security Office near you, visit Social Security/SSA Office Locator I (ssa.gov)
Supplemental Security Income
The Supplemental Security Income (SSI) program pays benefits to adults and children with
disabilities who have limited income and resources. Like the SSDI program, the SSI program can
provide assistance to people who qualify as disabled due to a medical condition like COVID-19,
if it results in functional limitations that prevent a person from working. The SSI program
provides assistance to some people who are disabled under the Social Security Act, which may
be different from the requirements to be considered disabled under the ADA. Unlike SSDI, for a
person to receive SSI, they also must have limited limited income and resources. SSI payments
are also made to people age 65 and older without disabilities who meet the financial
qualifications. You may be eligible to receive monthly SSI payments even if you are receive SSDI
or retirement benefits.
Learn more about the SSI program or apply online, visit Supplemental Security Income |
(ssa.gov)
Make an appointment to complete your application and call 1 (800) 772-1213 and 1
(800) 325-0778 (TTY)
Find a Social Security Office near you, visit Social Security/SSA Office Locator | (ssa.gov)
Survivors Benefits
If someone in your family dies from for any reason, including from a medical impairment such
as COVID-19, you may be entitled to Survivors Benefits. If the deceased individual was
employed and paid into Social Security, then their spouse, children, and parents could be
eligible for benefits based on their earnings.
Learn more about Survivors Benefits, visit Survivors Benefits | SSA (ssa.gov)
Make an appointment to complete your application, call 1 (800) 772-1213 and 1 (800)
325-0778 (TTY)
Find a Social Security Office near you, visit Social Security/SSA Office Locator | SSA
(ssa.gov)
50
Services and Supports for Longer-Term Impacts of COVID-19
Unemployment Benefits
Unemployment Insurance Programs
Unemployment Insurance provides unemployment benefits, usually in the form of
weekly payments, to eligible workers who become unemployed through no fault of their
own and meet certain other eligibility requirements. Unemployment Insurance is
administered by the states. Each state develops their own system for delivering
benefits. Find more information and check your eligibility, visit Unemployment
Insurance I U.S. Department of Labor (dol.gov)
Find information about your state’s Unemployment Insurance opportunities, visit
Unemployment Benefits Finder | CareerOneStop.org
Extended Unemployment Benefits
Extended Benefits are available during periods of elevated unemployment to workers who have
exhausted regular unemployment insurance benefits. The basic Extended Benefits program
provides up to 13 additional weeks of benefits. Some states have also enacted a voluntary
program to pay up to seven additional weeks (20 weeks maximum) of Extended Benefits during
periods of extremely high unemployment. Contact your state’s Unemployment Insurance
Agency to ask whether your state supports an Extended Unemployment Benefits program.
To find Extended Unemployment Benefits program contact information for your state,
visit Unemployment Benefits Finder | CareerOneStop.org
Unemployment Compensation for Ex-Service Members Program
The Unemployment Compensation for Ex-Service members (UCX) Program provides
unemployment compensation benefits to individuals transitioning from military service to the
civilian labor market.
Contact your state’s Unemployment Insurance Agency to ask about UCX program in
your state, visit Unemployment Benefits Finder | CareerOneStop.org
Unemployment Compensation for Federal Employees Program
The Unemployment Compensation for Federal Employees (UCFE) program provides
unemployment compensation for federal employees who lost their employment through no
fault of their own. In general, the unemployment insurance law of the state in which the former
federal employee had his or her last official duty station in federal civilian service will be used
to determine eligibility for UCFE benefits.
Contact your state’s Unemployment Insurance Agency to ask about UCFE program in
your state, visit Unemployment Benefits Finder | CareerOneStop.org
51
Services and Supports for Longer-Term Impacts of COVID-19
Workers’ Compensation for Federal Employees
The Federal Employees' Compensation Act (FECA) covers injury in the performance of duty;
injury includes COVID-19 proximately caused by federal employment. The FECA provides
medical benefits and compensation for disability or death of an employee who is diagnosed
with COVID-19 while in the performance of duty. Coverage is extended for Long COVID if it
develops as the result of the initial, work-related COVID-19 infection. Further, the American
Rescue Plan Act of 2021 (ARPA) has made it much easier for federal workers diagnosed with
COVID-19 to establish coverage under the FECA.
Learn more about filing a claim, visit Claims under the Federal Employees'
Compensation Act due to COVID-19 | U.S. Department of Labor (dol.gov)
Employer-Sponsored Insurance
The Employee Benefits Security Administration (EBSA) provides answers to your questions and
assists you if you believe you have been inappropriately denied employee benefits, including a
retirement, disability, or other employee benefit. They can help answer questions on issues
such as denied health or disability benefits, COBRA, or plan administration and compliance.
Reach a Benefits Advisor, visit Ask EBSA | U.S. Department of Labor (dol.gov)
Speak to a Benefits Advisor, call (866) 444-3272; Dial 7-1-1 to access
telecommunications relay services
Tax Credits
Earned Income Tax Credit
The Earned Income Tax Credit, sometimes called EITC, is a tax credit for workers with low to
moderate income. Eligibility for the tax credit is based on various factors including family size,
IRS filing status, and income.
For more information on EITC, visit EITC | IRS (irs.gov)
To check your eligibility, visit Use the EITC Assistant | (irs.gov)
Retirement Benefits
Social Security Retirement for Workers and Some Dependents
When you reach age 62 years, you may be eligible to start receiving monthly Social Security
benefits. The age you begin receiving your retirement benefit affects how much your monthly
benefits will be for as long as you receive benefits. The longer you wait to begin receiving
benefits, the higher your monthly benefit amount will be.
52
Services and Supports for Longer-Term Impacts of COVID-19
Learn more and apply online, visit Retirement Benefits | SSA (ssa.gov)
To talk with a Social Security Administration (SSA) representative about your eligibility
or to apply by phone, call 1 (800) 772-1213 and 1 (800) 325-0778 (TTY), Monday through
Friday, 8:00 a.m. to 7:00 p.m. local time
Find a local Social Security office, visit Social Security/SSA Office Locator | (ssa.gov)
Assistance Programs for Families with Children
Temporary Assistance for Needy Families
The Temporary Assistance for Needy Families (TANF) program provides states, territories, and
tribes with funds to operate programs designed to help families with lower incomes and
children achieve economic self-sufficiency. The program provides monthly cash assistance
payments to families with lower incomes and children, as well as a wide range of services.
Find more information regarding the TANF program, visit TANF | The Administration for
Children and Families (acf.hhs.gov)
Find information about your state’s TANF program, visit Help for Families | The
Administration for Children and Families (acf.hhs.gov)
53
Not Sure Where to Start?
Q. Need accommodations to
perform your job since being
diagnosed with Long COVID?
A. Contact the Job
Accommodations Network
(JAN). JAN is a free service that
provides confidential guidance
to individuals regarding job
accommodations and disability
employment issues.
For more information contact
JAN at 1 (800) 526-7234 (VOICE)
and 1 (877) 781-9403 (TTY)
You can also reach JAN via
online chat, email or JAN on
Demand by visiting Information
By Role (askjan.org)
-------------------------------------------
Q. Recently unemployed and
unsure of what benefits you
may be entitled to?
A. Find unemployment
programs and benefits in your
state by visiting Unemployment
Benefits Finder |
CareerOneStop
Services and Supports for Longer-Term Impacts of COVID-19
Job Assistance
People experiencing Long COVID may need
accommodations in the workplace or assistance with
finding a new job. There are federal programs to help
you address job-related needs—whether in your search
for a new job or issues dealing with your current
job/employer—that are the result of Long COVID. In
addition, some of the resources may also support
individuals, their families and caregivers are experiencing
the longer-term impacts of the COVID-19 pandemic, such
as mental health and substance use challenges, and
bereavement. Individuals who are newly seeking
employment due to the loss of a loved one my find
assistance through these federal supports and services.
Topics covered in this section include
• Workplace Accommodations
• Job Training and Reemployment Assistance
• Support for Employers.
If you need legal assistance in getting workplace
accommodations due to Long COVID or because you
have faced discrimination in the workplace, you may
want to review the Legal Assistance section of the Know
Your Rights section, in addition to the information
below.
Workplace Accommodations
Workplace Accommodations under the
Americans with Disabilities Act
Long COVID can be a disability under the Americans with
Disabilities Act (ADA) and Sections 501 and 504 of the
Rehabilitation Act of 1973, if it substantially limits one or more major life activities. The ADA
prohibits employers from discriminating on the basis of disability. It also requires employers to
make reasonable accommodations, unless doing so would cause significant difficulty or expense
for the employer. A reasonable accommodation is any change in the work environment (or in
the way things are usually done) to help a person with a disability apply for a job, perform the
duties of a job, or enjoy the benefits and privileges of employment. For example, reasonable
accommodations may include
54
job restructuring, part-time or modified work schedules, telework, exceptions to workplace
policies, or reassignment to a vacant position.
Learn more about your rights and the types of accommodations available to individuals
with Long COVID, visit What You Should Know About COVID-19 and the ADA, the
Rehabilitation Act, and Other EEO Laws | U.S. Equal Employment Opportunity
Commission (eeoc.gov)
For more information on COVID-19 and the ADA, visit: COVID-19 and the Americans
with Disabilities Act | Beta.ADA.gov
Learn about your rights, visit Home | U.S. Equal Employment Opportunity Commission
(eeoc.gov), or call 1 (800) 669-4000 (voice) and 1 (800) 669-6820 (TTY), or (844) 234-
5122 (ASL Video Phone)
Find more information, call JAN at 1 (800) 526-7234 (voice) and 1 (877) 781-9403 (TTY)
Reach a representative by phone, live chat, or email, visit Information By Role
(askjan.org)
Services and Supports for Longer-Term Impacts of COVID-19
Job Accommodation Network
Job Accommodation Network (JAN) is the leading source of free, expert, and confidential
guidance on job accommodations and disability employment issues. Serving customers for
more than 35 years, JAN provides individualized consultation to assist
• Employers and their representatives seeking guidance on practical ways to engage in
the interactive process, provide job accommodation solutions, and comply with Title I of
the ADA
• Individuals with medical conditions and disabilities seeking information about job
accommodation solutions, employment rights under the ADA, and self-employment and
entrepreneurship opportunities
• Family members and rehabilitation, medical, educational, and other professionals in
their effort to support successful employment outcomes for individuals with medical
conditions and disabilities.
Ticket to Work
Social Security's Ticket to Work (Ticket) Program supports career development for people ages
18 through 64 who receive SSDI or SSI and want to work. The Ticket Program is free. It helps
people with disabilities move toward financial independence and connects them with the
services and support they need to succeed in the workforce.
55
Learn more about achieving your work goals, ident
ifying providers, service
s, and
job
re
sources, visit Find
Help - Ticke
t to
Wor
k - Social
Security (ssa.gov)
Speak to a representative, call the Ticket to Work Help Line at 1 (866) 968-7842 and 1
(866) 833-2967 (TTY), Monday through Friday, 8:00 a.m. to 8:00 p.m. ET
Reach the helpline and email [email protected]
To learn more about the State Vocational Rehabilitation Services Program in your state,
visit RSA State Vocational Rehabilitation Service Agencies (rsa.ed.gov/about/states)
To learn more about other vocational rehabilitation programs, visit Rehabilitation
Services Administration (rsa.ed.gov)
If you get disability benefits, call the Ticket to Work Help Line for PABSS contact
information at 1 (866) 968-7842 and 1 (866) 833-2967 (TTY), Monday through Friday,
8:00 a.m.to 8:00 p.m. ET
Services and Supports for Longer-Term Impacts of COVID-19
Vocational Rehabilitation
The State Vocational Rehabilitation (VR) Services Program, funded by the Rehabilitation
Services Administration in the Department of Education, provides employment-related services
for individuals with disabilities so that they may prepare for and engage in competitive,
integrated, and gainful employment that is consistent with their strengths, resources, priorities,
concerns, abilities, capabilities, interests, and informed choice. To be eligible for the VR
program, individuals must have a physical or mental impairment, which can include Long
COVID, that results in a substantial impediment to employment and who require and can
benefit from VR services to achieve employment and maximize career goals.
Protection and Advocacy for Beneficiaries of Social Security
The Protection and Advocacy for Beneficiaries of Social Security (PABSS) program serves people
with disabilities who receive SSDI or SSI who want to work by helping to remove barriers to
employment. PABSS staff help recipients understand and secure employment protections. They
provide legal representation when needed.
Job Training and Employment Assistance
Comprehensive American Job Centers
There are nearly 2,400 American Job Centers located throughout the United States that provide
free help and training to job seekers for a variety of career and employment-related needs.
Many have special programs to accommodate the needs of individuals experiencing Long
COVID.
56
Find a Comprehensive American Job Center near you, visit American Job Center Finder |
CareerOneStop.org
Self-Employment Assistance Program
Some states offer the Self-Employment Assistance (SEA) program. SEA programs provide
qualifying disloca
ted workers the opportunity for early re-employment through self-
employment. The program is designed to encourage and enable unemployed workers to create
their own jobs by starting their own small businesses. S
tates operating an SEA program can pay
participants a weekly allowance while they are getting their businesses off the ground.
Find SEA program contact information for your state, visit Unemployment Benefits
Finder | CareerOneStop.org
Work Incentives Planning and Assistance
Social Security's Ticket to Work (Ticket) Work Incentives Planning and Assistance (WIPA)
projects provide free bene
fits counseling to help people receiving disability benefits make
informed choices about work. Trained Community Work Incentive Coordinators provide
personalized counseling about services and supports and explain how working may affect
benefits. More than 70 organizations provide these services.
Learn more about WIPA, call the Ticket to Work Help Line at 1 (866) 968-7842 and 1
(866) 833-2967 (TTY), Monday through Friday, 8:00 a.m.to 8:00 p.m. ET
Reemployment Services and Eligibility Assessment Program
This program is for unemployment compensation claimants determined to be most likely to
exh
aust b
enefits and former U.S. military service members receiving unemployment
c
ompensation for the Ex-Service Members Program. In some states, this service is also open to
other unemployment claimants. The program is administered by the states, and not all states
support this program. The foundational element of the Reemployment Services and Eligibility
Assessment (RESEA) Program is an in-person meeting between the claimant and a trained
employment specialist.
Find RESEA program contact information for your state, visit Unemployment Benefits
Finder | CareerOneStop.org
Support
for Employers
The Employer Assistance and Resource Network on Disability Inclusion
The Employer Assistance and Resource Network on Disability Inclusion (EARN) offers
information
and resources to help employers recruit, hire, retain and advance people with
disabilities. It helps employers build inclusive workplace cultures and meet diversity, equity,
inclusion and accessibility goals.
Services and Supports for Longer-Term Impacts of COVID-19
57
Find more information about EARN and additional resources, visit Employer Assistance
and Resource Network on Disability Inclusion | (AskEARN.org)
Community Economic Development
Community Economic Development (CED) is a federal grant program funding Community
Development Corporations that address the economic needs of low-income individuals and
families through the creation of sustainable business development and employment
opportunities. CED awards funds to private, non-profit organizations Community Development
Corporations, including faith-based organizations and Tribal and Alaskan Native organizations.
CED-funded projects create or expand businesse
s, create new jobs for individuals with low
incomes, and leverage funding investments in communities.
Find more information about CED, visit Community Economic Development (CED) |
Administration for Children and Families (acf.hhs.gov) or call the Office of Community
Services at (202) 401-9333
Services and Supports for Longer-Term Impacts of COVID-19
58
Do you have a question? Contact the Department
of Housing and Urban Development Office of Fair
Housing and Equal Opportunity (FHEO) intake
specialist by calling 1 (800) 669-9777 or 1 (800)
877-8339.
Would you like more information about filing a
complaint? Visit How to File a Complaint | U.S.
Department of Housing and Urban Development
FHEO (hud.gov)
Not Sure Where to Start?
Q. Worried about falling
behind on rent for your home?
A. Find emergency rental
assistance programs in your
area by visiting Find Help with
Rent and Utilities | Consumer
Financial Protection Bureau
(ConsumerFinance.gov).
Visit the HUD Housing
Counseling Office at Office of
Housing Counseling | HUD.gov /
U.S. Department of Housing and
Urban Development (HUD)
You can also visit the Office of
Fair Housing and Equal
Opportunity to File a Complaint
– Main Page | HUD.gov / U.S.
Department of Housing and
Urban Development (HUD)
-------------------------------------------
Q. Are you homeless or have
you recently lost your home?
A. Reach out to the Housing
Authority in your state at PHA
Contact Information - HUD |
HUD.gov / U.S. Department of
Housing and Urban
Development (HUD).
Find Homeless Assistance
programs in your area by
visiting Need Homeless
Assistance? - HUD Exchange.
Services and Supports for Longer-Term Impacts of COVID-19
Housing
Individuals experiencing Long COVID may need financial
assistance to maintain their home or housing assistance
to find affordable housing. If you are experiencing
housing insecurity due to the loss of a loved one from
COVID, then you may have options through federal
supports. Several federal programs are available that can
help. This section covers five topics
• Fair Housing Act
• Assistance for Renters
• Assistance for Homeowners
• Affordable Housing Programs
• Utilities Assistance.
If you are facing eviction because you could not pay your
rent or need other legal assistance related to housing
benefits, you may want to review the Legal Assistance
section in the Know Your Rights section.
Fair Housing Act
The Fair Housing Act protects people, including people
with disabilities such as Long COVID, from discrimination
when they are renting or buying a home, getting a
mortgage, seeking housing assistance, or engaging in
other housing-related activities. Additional
protections apply to federally-assisted housing.
59
Emergency Rental Assistance Program
State and local organizations can help landlo
rds and renters struggling to keep up with rent and
other bills. Many programs take applications from both landlords and renters.
Find rental assistance program in your area, visit Find Help with Rent and Utilities |
Consumer Financial Protection Bureau (ConsumerFinance.gov)
If you are facing eviction because you could not pay your rent, you may want to review the
Legal Assistance section in the Know Your Rights section.
Assistance for Homeowners
Homeowner Assistance Fund
The purpose of the Homeowner Assistance Fund (HAF) is to prevent homeowners from losing
their homes d
ue to mortgage delinquencies, foreclosures, loss of utilities or home energy
services, and displacement of homeowners experiencing financial hardship after January 21,
2020. Funds from the HAF may be used for assistance with mortgage payments, homeowner’s
insurance, utility payments, and other specified purposes.
Find out if you are eligible for HAF, visit Help for Homeowners | Consumer Financial
Protection Bureau ConsumerFinance.gov
Find a HAF program in your state or tribal community, visit Homeowner Assistance Fund
| National Council of State Housing Agencies (ncsha.org)
Rural Housing Repair Loans and Grants
The Rural Housing Repair Loans and Grants program provides loans and grants to very low-
income ho
meowners to repair, improve, modernize, or to remove health and safety hazards in
their rural dwellings. Grants may be arranged for recipients who are 62 years and older and can
be used only to pay for repairs and improvements to remove health and safety hazards.
Find information about the Rural Housing Repair Loans program, visit Single Family
Housing Repair Loans Grants | U.S. Department of Agriculture Rural Development
(rd.usda.gov) or call the USDA Information Hotline (202) 720-2791
Apply for a loan or grant, visit USDA Service Center Agencies eForms
(forms.sc.egov.usda.gov)
Contact your state's Rural Development field office, visit USDA Service Centers Locator
(offices.sc.egov.usda.gov/locator/app)
Assistance for Renters
Services and Supports for Longer-Term Impacts of COVID-19
60
Affordable Housing Programs
Housing Voucher Programs
HUD has several voucher programs, which provide ongoing rental assistance to eligible
households, including ones targeted to people with disabilities, older adults, and Veterans, to
help them access affordable housing.
Find information on housing choice voucher programs, visit HCV Programs and
Initiatives | HUD.gov / U.S. Department of Housing and Urban Development (HUD)
Learn more about voucher options from public housing agencies in your state, territory
or tribal community, visit PHA Contact Information | U.S. Department of Housing and
Urban Development (HUD.gov)
Homelessness As
sistance Programs
Homelessness assistance programs provide funding to states and local governments and
nonprofit providers to serve individuals and families who are affected by homelessness.
Learn more about homelessness assistance programs in your area, visit Need
Homeless
Assistance? - HUD Exchange
Find resources about homelessness assistance programs, visit Homelessness Resources
and Programs | HHS.gov
Public Housing
Public housing was established to provide decent and safe rental housing for eligible low-
income families, the elderly, and persons with disabilities. Local housing authorities operate
public housing in all sizes and types, from scattered single-family houses to high rise
apartments for elderly families.
Learn more about public housing, visit HUD's Public Housing Program | U.S. Department
of Housing and Urban Development (HUD.gov)
Learn more about public housing in your state, territory or tribal community, visit PHA
Contact Information | U.S. Department of Housing and Urban Development (HUD.gov)
Find contact information for the Housing and Urban Development field offices, visit
Local Offices | HUD.gov / U.S. Department of Housing and Urban Development
(HUD)Local Offices | U.S. Department of Housing and Urban Development (HUD.gov)
Services and Supports for Longer-Term Impacts of COVID-19
61
Learn more about private assisted multifamily housing: Rental Assistance | U.S.
Department of Housing and Urban Development (hud.gov)
Search for an assisted multifamily apartment: Resource Locator | U.S. Department of
Housing and Urban Development (resources.hud.gov)
Utilities Assistance
Low Income Home Energy Assistance Program
The Low In
come Home Energy Assistance Program (LIHEAP) assist families with energy costs.
The program provides federally funded assistance in managing costs associated with home
energy bills, energy crises, weatherization, and energy-related minor home repairs.
Find information about LIHEAP programs in your state or territory, visit LIHEAP Map
State and Territory Contact Listing | The Administration for Children and Families
(hhs.gov)
Find information about LIHEAP programs in your tribal community, visit LIHEAP Map
Tribal Contact Listing | The Administration for Children and Families (hhs.gov)
Reach a representative, call the National Energy Assistance Referral (NEAR) hotline at 1
(866) 674-6327
Low Income Household Water Assistance Program
Low Income Household Water Assistance Program (LIHWAP) provides funds to assist
households that are behind in paying their water or wastewater bills. States, territories and
tribes administer the program.
Learn more about the LIHWAP program, visit LIHWAP | The Administration for Children
and Families (hhs.gov)
Find information about LIHWAP programs in your state or territory, visit LIHWAP Map
State and Territory Contact Listing | The Administration for Children and Families
(hhs.gov)
Find information about LIHWAP programs in your tribal community, visit LIHWAP Tribal
Contact Listing | The Administration for Children and Families (hhs.gov)
Services and Supports for Longer-Term Impacts of COVID-19
Assisted Multifamily Housing
Private owners of multifamily developments offer housing at assisted rents under contract with
HUD. Some types of developments are designed to serve older people or individuals with
disabilities and offer service coordinators.
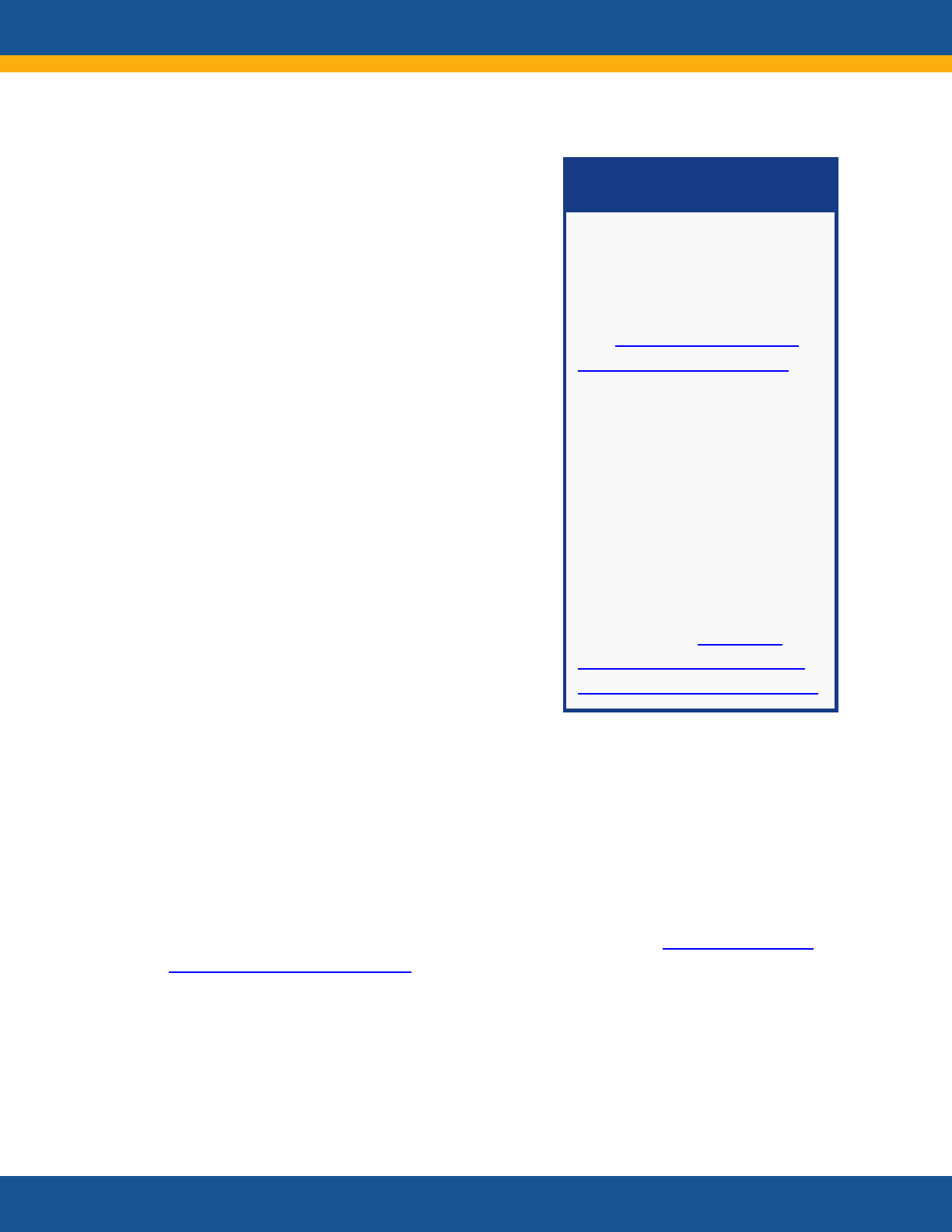
62
Not Sure Where to Start?
Q. Concerned about being able
to feed your family?
A. Find emergency food
distribution programs in your
area Contact Map | Food and
Nutrition Service (usda.gov).
-------------------------------------------
Q. Wondering if you are
eligible for the Supplemental
Nutrition Assistance Program
(SNAP) which can help you
purchase healthy foods for your
family?
A. Find your local SNAP office
and talk to them about whether
you are eligible SNAP State
Directory of Resources | Food
and Nutrition Service (usda.gov)
Find information about the nutrition programs in your state, visit Contact Map | Food
and
Nutrition Service (usda.gov)
Special Supplemental Nutrition
Program for Women, Infants, and Children
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides
federal
grants to states for supplemental foods, health care referrals, and nutrition education
for women with lower incomes, pregnant, breastfeeding, and non-breastfeeding postpartum
Services and Supports for Longer-Term Impacts of COVID-19
Food and Nutrition Support
People with Long COVID may be unable to continue to
work and earn money, putting them at risk of being
unable to afford food or getting enough nutrition for
themselves and their families. If you or your immediate
family members need help purchasing food, there are
several federal programs that can help you put nutritious
food on your family’s table. Some of the resources in this
section may also support individuals, their families and
caregivers who are experiencing the longer-term impacts
of the COVID-19 pandemic, such as mental health and
substance use challenges and bereavement. Individuals
who may be experiencing food insecurity due to the loss
of loved one may also find assistance through these
federal supports and services. This section covers three
topics
• Child and Family Nutrition Programs
• Food Distribution Programs
• Nutrition Program for Seniors.
If you are found ineligible for food assistance programs
like SNAP, or if your SNAP benefits are being reduced or
discontinued, you may want to review the Legal
Assistance section of the Know Your Rights section.
Child and Family Nutrition Programs
National School Lunch Program
The National School Lunch Program (NSLP) is a federally assisted meal program operating in
public and nonprofit private schools and residential child care institutions. It provides
nutritionally balanced, low-cost or free lunches to children each school day.
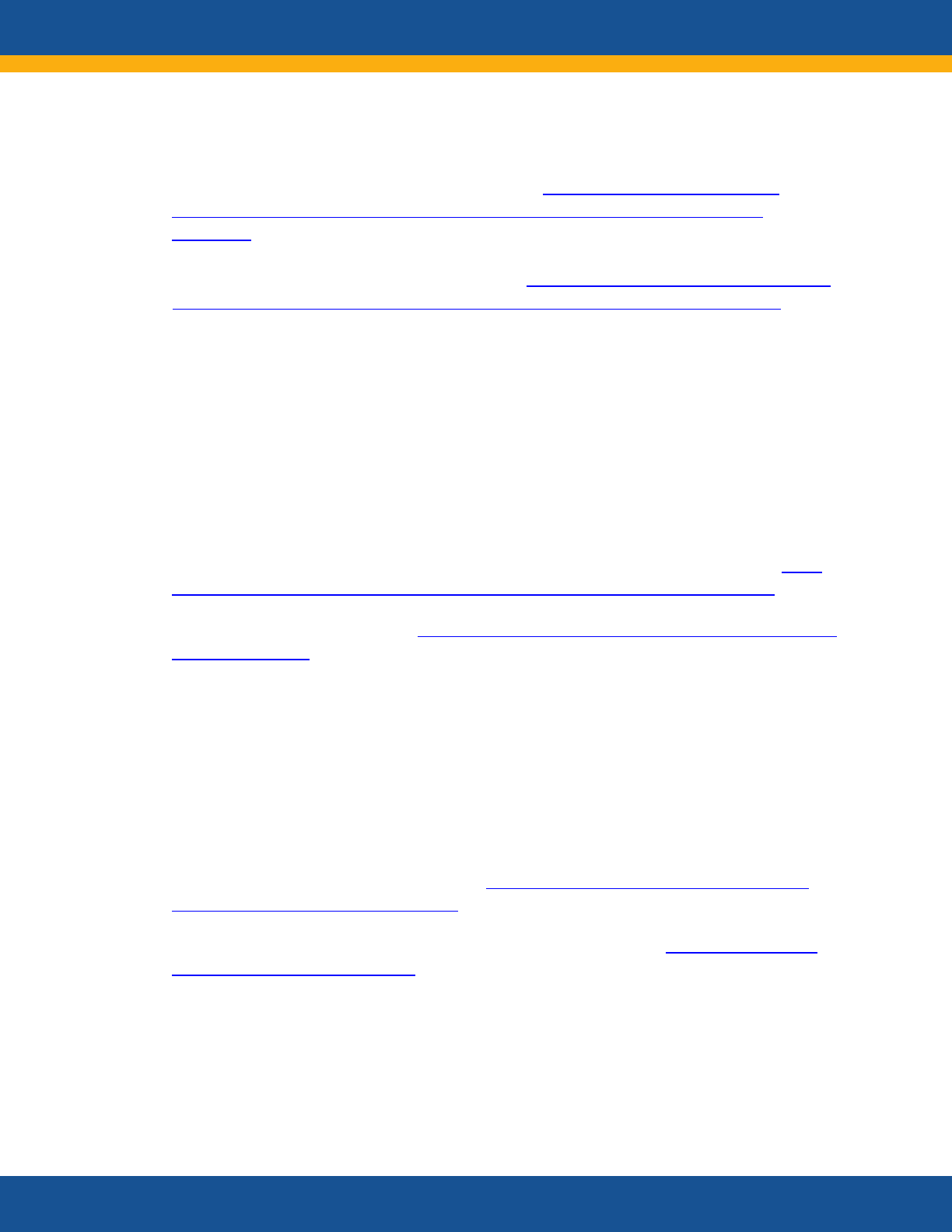
63
Find information and to learn how to apply, visit Special Supplemental Nutrition
Program for Women, Infants, and Children (WIC) | Food and Nutrition Service
(usda.gov)
Learn more about programs in your state, visit Special Supplemental Nutrition Program
for Women, Infants, a
nd Childre
n (WIC)
|
Food and Nutritio
n Service (usda
.gov)
Supplemental
Nutrition Assistance Program
Supplemental Nutrition Assistance Program (SNAP) provides nutrition benefits to supplement
the food budget of families with low incomes so they can purchase healthy food and move
towards self-sufficiency. Most SNAP eligibility rules apply to all households, but there are
some special rules for households with members who are older or have a disability, including
those that experience disability due to Long COVID. For people with disabilities or older
adults, allowable medical costs that are more than $35 a month may be deducted unless an
insurance company or someone who is not a household member pays for them.
Learn about the SNAP rules for individuals with disabilities and older adults, visit SNAP
Special Rules for the Elderly or Disabled | Food and Nutrition Service (usda.gov)
Find your local SNAP office, visit SNAP State Directory of Resources | Food and Nutrition
Service (usda.gov)
Food Distribution Programs
Emergency Food Assistance Program
The Emergency Food Assistance Program (TEFAP) is a federal program that helps supplement
the diets of Americans with low incomes by providing them with emergency food assistance at
no cost.
Find more information about TEFAP, visit The Emergency Food Assistance Program |
Food and Nutrition Service (usda.gov)
Find information about the nutrition programs in your state, visit Contact Map | Food
and Nutrition Service (usda.gov)
Emergency Food and Shelter Program
Food Distribution Program on Indian Reservations
The Food Distribution Program
on Indian Reservations (FDPIR) provides USDA Foods to income-
eligible households living on Indian reservations and to Native American households residing in
Services and Supports for Longer-Term Impacts of COVID-19
individuals, and to infants and children up to age five years who are found to be at nutritional
risk.
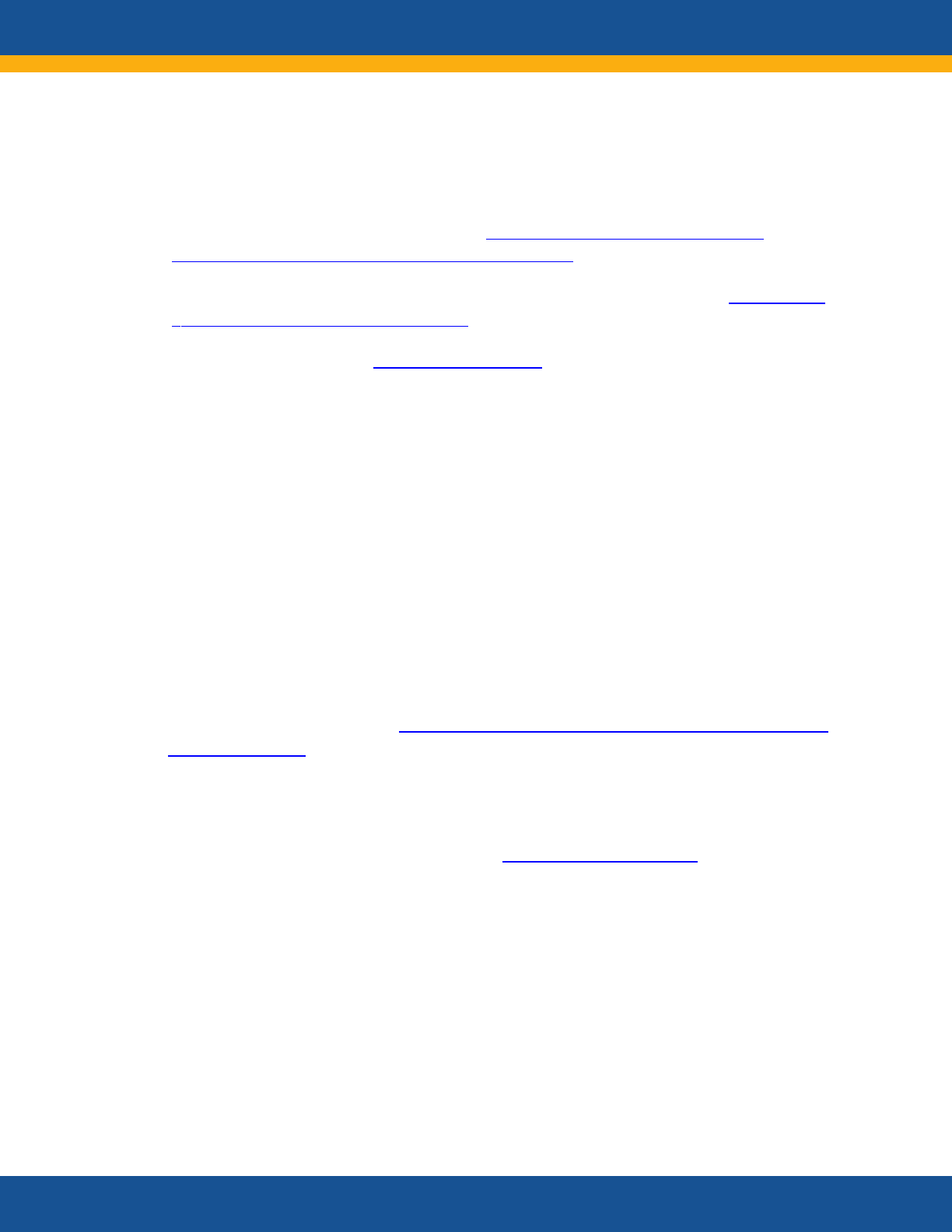
64
Find more information about FDPIR, visit Food Distribution Program on Indian
Reservations | Food and Nutrition Service (usda.gov)
Learn more about eligibility contact
your state or tribal organization, visit Contact Map
|Food and Nutrition Service (usda.gov)
Contact USDA by emailing [email protected]
Nutrition
Program for
Older Adults
Learn about elder care programs in your area and
to participate in an online chat with
an information specialist, visit Eldercare Locator | Administration for
Community Living
(eldercare.acl.gov)
Talk with a specialist, call 1 (800) 677-1116, Monday through Friday, 9:00 a.m. to 8:00
p.m. ET
Learn more about the program by emailing [email protected]
Services and Supports for Longer-Term Impacts of COVID-19
designated areas near reservations or in Oklahoma. The program supplements and expands the
ongoing work of local nonprofit and governmental social service organizations to provide
shelter, food, and supportive services to individuals and families who are experiencing, or at
risk of experiencing hunger and homelessness.
Senior Nutrition Program
Older adults (age 60 and older) and in some cases, their caregivers, spouses and persons with
disabilities may be eligible for certain nutrition programs. The services include both home-
delivered meals and healthy meals served in group settings, such as senior centers and faith-
based locations. In addition, the programs provide a range of services including nutrition
screening, assessment, education, and counseling. Nutrition services also provide an important
link to other supportive in-home and community-based supports, such as homemaker, chore
and home-health aide services, transportation, physical activity and chronic disease self-
management programs, home repair and modification, and falls prevention programs.
65
Child Care and Early Childhood Development and
Education
Not Sure Where to Start?
Q. Worried about paying for
child care?
A. To find out more about child
care financial assistance
resources in your state, visit See
Your State's Resources |
Childcare.gov
-------------------------------------------
Q. Worried about finding
affordable learning
opportunities for your
preschool age children?
A. Reach out to the Head Start
Programs and check your
eligibility
Call 1 (866) 763-6481, Monday
through Friday, 8:00 a.m. to
6:00 p.m. ET.
Visit How to Apply | ECLKC
(hhs.gov)
Find
out more a
bout CCDF
resources
in
your
state, visit See
Your
State
's
Resources |
Childcare.gov
Services and Supports for Longer-Term Impacts of COVID-19
Individuals experiencing Long COVID may need
assistance with childcare or preschool. In addition, young
children with Long COVID might need services, supports
or accommodations. Several federal programs are
available that may be able to help you. Some of the
resources in this section may also support individuals,
their families and caregivers who are experiencing the
longer-term impacts of the COVID-19 pandemic, such as
mental health and substance use challenges, and
bereavement. Individuals who may need additional
assistance due to the loss of a caregiver may also find
assistance
through these supports and services.
This section covers three topics
• Child Care
• Early Childhood Development and Education
• Tax Credits.
If you need legal assistance with c
hild care or early
childhood benefits, you may want to review the Legal
Assistance section of the Know Your Rights section.
Child Care
Child Care Financial Assistance Options
Several federal funding sources are available to help pa
y for child care. These programs are
intended to help eligible working families with low incomes access child care and improve the
quality of child care for all children. Subsidized child care services are available to eligible
families through certificates (vouchers) or grants and contracts with providers. The Child Care
and Development Fund (CCDF) also improves the quality of care to promote children’s healthy
development and learning by supporting child care licensing, quality improvement systems to
help programs meet higher standards, and training and education for child care workers.
66
Early Childhood Development and Education
Head Start and Early Head Start Programs
Head Start and Early Head Start programs provide families with free learning and
development services for their children ages birth to five years. Head Start programs must
ensure that at least 10 percent of children enrolled are Individuals with Disabilities Education
Act eligible children with disabilities, which may include children with Long COVID. Some
Early Head Start programs also provide prenatal services for pregnant people. Families
qualify for the Head Start program if their household income is at or below the poverty level.
Families who receive public assistance (TANF, SSI, or SNAP), those with children in foster
care, or children who are homeless also qualify regardless of income.
Find more information about Head Start and Early Head Start Programs, visit Frequently
Asked Questions About
Head Start | ECLKC (hhs.gov)
Check to see if your family qualifies, visit Poverty Guidelines | ASPE (hhs.gov)
Find a Head Start program near your home, call 1 (866) 763-6481, Monday through
Friday, 8:00 a.m. to 6:00 p.m. ET or visit How to Apply | ECLKC (hhs.gov)
Tax Credits
The Child and Dependent
Care Credit
The Child and Dependent Care Credit is a tax credit that may help families pay for the care of
eligible children and other dependents, referred to as “qualifying persons.” The credit is
calculated based on income and a percentage of expenses that you incur for the care of
qualifying persons (e.g., childcare, day treatment, in home care), to enable you to go to work,
look for work, or attend school.
For more information visit Child and Dependent Care Credit FAQs | Internal Revenue
Service (irs.gov)
The
Child
Tax Credit
The Child Tax Credit provides money to support American families—helping them make ends
meet, more easily afford the costs of raising children, or save for their children’s future. On
March 11, 2021, President Biden signed into law the American Rescue Plan Act, expanding the
Child Tax Credit for 2021 and providing additional tax relief to the vast majority of families.
For more information and to check your eligibility visit C
hild Tax Credit | Internal
Revenue Service (irs.gov)
Services and Supports for Longer-Term Impacts of COVID-19
For 2021 visit The 2021 Child Tax Credit | Information About Payments & Eligibility
67
Education Supports
Students with Long COVID may need supports, services
and accommodations to succeed in school. They also are
protected against discrimination by federal law. Some of
the resources in this section may also support
individuals, their families and caregivers who are
experiencing the longer-term impacts of the COVID-19
pandemic, such as mental health and substance use
challenges, and bereavement.This section covers four
topics
• The Americans with Disabilities Act
• Section 504 of the Rehabilitation Act
• Special Education under the Individuals with
Disabilities Education
• Higher Education.
Laws Related to Students with
Disabilities, including Long COVID
Not Sure Where to Start?
Q. Do you need more
information about education
supports for someone, age
birth to 26 years, with Long
COVID?
A. Find your Parent Center by
visiting Find Your Center |
(ParentCenterHub.org)
Q
. Do yo
u n
eed an
adv
o
cate or
attorney to assist with
accessing services,
su
pports o
r
a
ccommodations?
A. Co
n
n
ect with a Protection
&
Ad
v
o
cacy System by visiting
Member Agencies | NDRN
In addition to the resources in that section, there are other resources that specifically help
students with disabilities, including Long COVID.
Services and Supports for Longer-Term Impacts of COVID-19
Department of Education’s Office for Civil Rights and Office of Special Education and
Rehabilitative Services “Long COVID under Section 504 and the IDEA: A Resource to
Support Children, Students, Educators, Schools, Service Providers, and Families”
The Department of Education’s Office for Civil Rights enforces civil rights laws on behalf
of students, including students with disabilities.
If you believe your student has faced discrimination at school, including on the basis of
disability, you can file a complaint with the Department of Education’s OCR How to File
a Discrimination Complaint with the Office for Civil Rights (ed.gov), or the Department
of Justice’s Civil Rights
Division and Contact the Civil Rights Division | Department of
Justice.
Long COVID can be a disability under the Americans with
Disabilities Act, Section 504 of the Rehabilitation Act of 1973, and Individuals with Disabilities
Education Act (IDEA). These laws collectively require covered entities to provide services,
supports and accommodations to students with disabilities. You may want to review the Know
Your Rights section for more information.
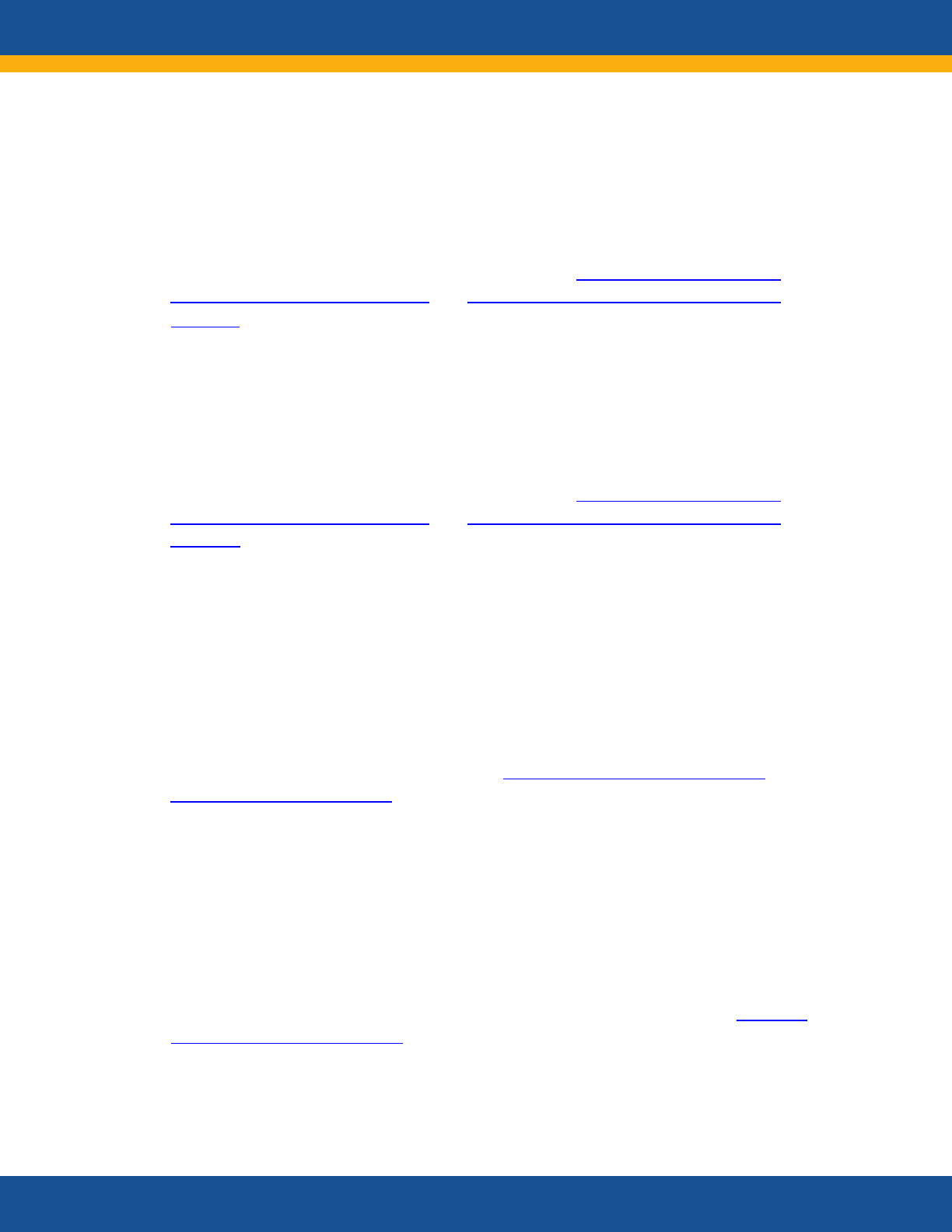
68
Section 504 of the Rehabilitation Act of 1973
Section 504 prohibits discrimination based on disability in any program or activity operated by
recipients of federal funds. Section 504 requires programs to provide students with disabilities
ages 3 to 22 years equal access to the program, including by making reasonable
accommodations and modifications.
Find out more and learn how to file a complaint, visit Office for Civil Rights | U.S.
Department of Education (ed.gov) and Civil Division | U.S. Department of Justice
(ada.gov)
The Americans with Disabilities Act
The Americans with Disabilities Act (ADA) is a federal civil rights law that prohibits
discrimination against people with disabilities in everyday activities. The ADA applies to public
schools and certain private schools.
Find out more and learn how to file a complaint, visit Office for Civil Rights | U.S.
Department of Education (ed.gov) and Civil Division | U.S. Department of Justice
(ada.gov)
Sp
ecial Education
Services
under
the
Individuals
with Disabilities Education Act
The Individuals with Disabilities Education Act (IDEA) is a federal civil rights law that makes
available a free appropriate public education (FAPE) to eligible children with disabilities
from ages birth to 21 years throughout the nation and ensures special education and related
services to those children. Parents and caregivers who suspect their child may need special
education services should contact their local public school and request an evaluation to
determine eligibility.
Find more information about IDEA, visit the IDEA website | U.S. Department of
Education (sites.ed.gov/idea)
Parent Training and Information Centers
Parent Training and Information Centers (PTI) work with families of infa
nts, toddlers,
children,
and
yout
h wit
h disa
bilities, including
those
e
xperiencing
Long
COVID,
from
ages
birt
h to
26
years.
PTIs
help
parents
participate
effectively in their children’s education and
development and partner with professionals and policy makers to improve outcomes for all
children with disabilities.
Services and Supports for Longer-Term Impacts of COVID-19
Find your Parent Center listed alphabetically by sta
te or
U.S.
Territory,
visit
Find
Your
Center
|
Pare
ntCenterHub.org
69
Branch—Military Families Technical Assistance Center
The Branch—Military Families Technical Assistance Center provides resources for military
families of children and youth with disabilities, as well as young adults between ages 18 to 26
years who have a disability and who grew up in a military family.
Learn more about the Branch program, visit Home - Military Parent Technical Assistance
Center (branchta.org)
Charting the Lifecourse™ & Charting the LifeCourse Nexus
Charting the Lifecourse™ helps students with disabilities, including those experiencing Long
COVID, families, c
aregivers, and those who support them organize their ideas, vision, and goals,
as well as problem-solve, navigate, and advocate for supports, including primary medical care,
behavioral health care (mental health and substance use challenges), health education, case
management, and nutrition education. The LifeCourse Nexus provides workshops and technical
assistance to shape and support innovation in policy, practice, procedure, and culture, including
around school-based supports for children with Long COVID.
Learn more about LifeCourse, visit LifeCourse Nexus – Exchange Knowledge | Build
Capacity | Engage Collaboratively (lifecoursetools.com)
4-H
Funded by the Department of Agriculture, 4‑H is delivered by Cooperative Extension—a
community of more than 100 publ
ic universities across the nation that provides experiences
where young people learn by doing. Individuals with Long COVID may benefit from these
programs. 4‑H programs and resources are available at home or through local in-person and
virtual 4‑H clubs, 4‑H camps, in-school and after-school programs. With the support of adult
mentors, youth select from a menu of hands-on project ideas to complete. 4‑H programs are
available for kids and teens ages 8 to 18 years. 4‑H Cloverbud programs are available for
children ages five to seven years.
Find your local 4-H program, visit Find Your Local 4-H | 4-H
Higher Education
Services and Supports for Longer-Term Impacts of COVID-19
Colleges and universities are required by Section 504 and the ADA to provide students with
disabilities with appropriate academic adjustments and auxiliary aids and services that are
necessary to afford an individual with a disability an equal opportunity to participate in the
school’s program. An example of an academic adjustment is extra time to take a test. Examples
of auxiliary aids include note takers, interpreters, readers, and specialized computer
equipment.
70
The National Center for College Students with Disabilities
The National Center for College Students with Disabilities (NCCSD) is the only federally-funded
national center in the United States for college and graduate students with any type of
disability, chronic health condition, or mental or emotional disabilities. College students
experiencing Long COVID can access a variety of resources using the NCCSD Clearinghouse.
Learn more about NCCSD, visit National Center for College Students with Disabilities
Clearinghouse (nccsdclearinghouse.org)
Services and Supports for Longer-Term Impacts of COVID-19
71
Caregiving and Family Support
Not Sure Where to Start?
Q. Wondering what support
services are available for
caregivers in your area?
A. Call the Eldercare Locator at
1 (800) 677-1116 or visit
Eldercare Locator (acl.gov) to
chat live or browse resources
Q. Are you caring for a veteran
or are you a veteran caring for
a non-veteran family member?
A. Call the Caregiver Support
Line at 1 (855) 260-3274 or visit
Caregivers Support Line (CSL) -
VA Caregiver Support Program
Services and Supports for Longer-Term Impacts of COVID-19
Caregivers who are experiencing Long COVID, are caring
for someone who has Long COVID, or both, may find they
now need additional support. That support may come in
the form of respite care, which gives caregivers
temporary r
elief from their caregiving responsibilities,
which can range from a few hours to a few days or
weeks. It may also include paid leave from work to care
for themselves or their loved ones, training to adapt to
changes in their abilities or the abilities of their loved
ones, or counseling and support groups. Some of the
resources in this section may also support individuals,
their families and caregivers who are experiencing the
longer-term impacts of the COVID-19 pandemic, such as
mental health and substance use challenges and
bereavement. Individuals who may need additional
assistance with family acare due to the loss of a lovd one
my a
lso find assistance through these federal supports
and s
ervices.
This section covers five topics
• Navigation Support
• Family and Medical Leave and Sick Leave
• Respite Care
• Individual Counseling and Support Groups
• Child Welfare.
If you need legal assistance with caregiving and family supports, you may want to review the
Legal Assistance section of the Know Your Rights section.
Navigation Support
Kinship Navigator
The Kinship Navigator assists grandparents and other kin caring for children, including families
involved in the child welfare system. Kinship Navigator programs assist kinship caregivers in
learning about, finding, and using programs and services to meet the needs of the children they
are raising and their own needs.
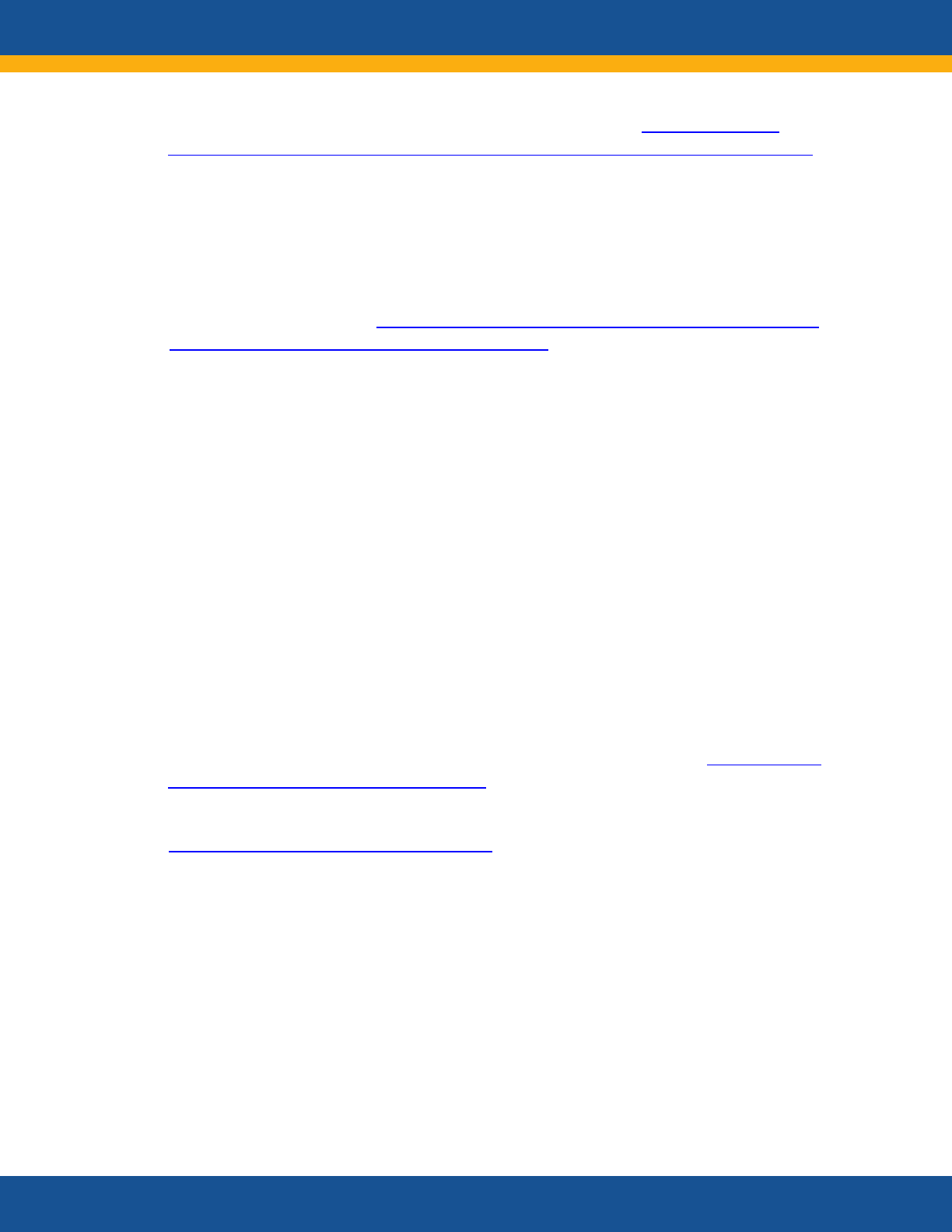
People with Long COVID may need time away from work—whether a few occasional sick days
or longer periods of leave—to seek treatment or for recovery. Workers may also need to take
time off to care for family members experiencing Long COVID.
For more information, visit COVID-19 and the Family and Medical Leave Act Questions
and Answers | U.S. Department of Labor (dol.gov)
Family and Medical Leave Act
Employees impacted by Long COVID may be able to take leave from work under the Family
and Medical Leave Act (FMLA). The FMLA entitles eligible employees of covered employers to
take up to 12 weeks each year of unpaid, job-protected leave for certain qualifying reasons,
including for a serious mental or physical health condition that makes the employee unable to
work or care for the employee’s spouse, child, or parent who has a serious health condition.
FMLA leave may be taken intermittently in short increments of time or in longer blocks of up
to 12 weeks in leave a year for FMLA serious health conditions. FMLA does not require
employers to provide paid leave, but employees may elect, or employers may require
concurrent use of paid leave, such as accrued vacation or sick leave. The FMLA also requires
employers to continue group health insurance coverage under the same terms and conditions
as if the employee had not taken leave. The Department of Labor's Wage and Hour Division
(WHD) is responsible for administering and enforcing the FMLA. Your state may offer stronger
protections for family and medical leave than those under the FMLA, including paid family and
medical leave benefits.
For more information about your FMLA eligibility and use of leave, visit
Fact Sheet #28:
The Family and Medical Leave Act of 1993
If you have questions or concerns, you can contact WHD at 1 (866) 487-9243 or visit
WHD | U.S. Department of Labor (dol.gov)
State Paid Family and
Medical Leave Programs
Some states operate
programs that entitle eligible workers to receive wage replacement when
t
hey c
annot work du
e to
c
o
v
er
e
d
f
amily
c
are
g
iv
i
n
g
or
m
e
d
ic
al r
e
a
sons. Eligibility rules and wage
replacement rates vary by state and are based on prior earnings and work history. Eligible
workers are entitled to paid leave benefits for qualifying reasons including a serious health
condition that makes them unable to work and caregiving leave for family members with a
serious health condition. As of 2022, paid family and medical leave benefits can be accessed
through state programs in California, New Jersey, Rhode Island, New York, the District of
Columbia, Washington, Massachusetts, and Connecticut.
Family and Medical Leave and Sick Leave
Services and Supports for Longer-Term Impacts of COVID-19
Find a program or contact in your state, territory or tribe, visit State Kinship Care
Contacts and Programs | Administration for Children and Families (ChildWelfare.gov)
72
73
• California: State Disability Insurance (ca.gov)
• New Jersey: Division of Temporary Disability and Family Leave Insurance | Family
Leave Insurance (nj.gov)
• Rhode Island: Temporary Disability / Caregiver Insurance | RI Department of Labor &
Training
• N
ew York: Ne
w York State Paid Family Leave (ny.gov) or Introduction to the Disa
bility
Benefits Law (ny.gov)
• District of Columbia: DC Paid Family Leave | does
• Washington: Washington State's Paid Family and Medical Leave – Washington
workers will have up to 12 weeks
of paid family or medical leave starting in 2020.
Employers begin payroll withholding in 2019
• Massachusetts: Paid Family and Medical Leave (PFML)
overview and benefits |
Mass.gov
• Connecticut:
CT Paid Leave Authority
(PFMLA)| Home | Official Site
Paid Leave for Federal Employees
Leave options available to federal employees who are experiencing Long COVID symptoms
include sick leave, annual leave, advance sick and annual leave, and donated leave under the
Voluntary Leave Transfer or Leave Bank programs. Federal employees on an alternative work
schedule may request to adjust their hours of duty to accommodate medical appointments or
accrue and use credit hours. Federal employees may also use any accumulated and accrued
compensatory time.
Learn more about federal policies, visit Pay & Leave | OPM (opm.gov), Work Schedules |
OPM (opm.gov), Fact Sheets | OPM (opm.gov)
Services and Supports for Longer-Term Impacts of COVID-19
For more information about state paid family and medical leave programs, visit
74
Respite Care
Respite care provides short-term relief
for caregivers. It is an important component of family
support and home and community-based lon
g-term services and supports. Respite services
strengthen family systems while protecting the health and well-being of both caregivers and
care recipients.
National Caregiver Family Support Program
National Caregiver Family Support Program (NFCSP) provides a range of services that assist
family and other caregivers to care for their family members at home for as long as possible.
Services to family caregivers include information about caregiver services and supports,
connecting caregivers with services, caregiver education and training, respite care provided by
trained caregivers, and other supplemental services.
Find services available near you, call the Eldercare Locator at 1 (800) 677-1116 or visit
Eldercare Locator (acl.gov) to chat live or browse resources
Learn more about the program, visit National Family Caregiver Support Program | ACL
Administration for Community Living (acl.gov)
Individual Counseling and Support Groups
Veterans Affairs Caregiver Support Program
The VA Caregiver Support Program (CSP) offe
rs an array of supports and services to family
members and friends who care for Veterans, including online courses, face-to-face classes,
telephone support, and peer support. These services are offered in addition to the support
provided to families and caregivers across VA by clinicians as part of a Veteran’s care. Every VA
Services and Supports for Longer-Term Impacts of COVID-19
Paid Sick Leave for Employees of Federal Contractors
Employees of certain federal contractors may be entitled to paid sick leave to care for
themselves or a family member experiencing Long COVID. Executive Order 13706, Establishing
Paid Sick Leave for Federal Contractors, requires certain employers that contract with the
federal government to provide employees working on or in connection with those contracts
with one hour of paid sick leave for every 30 hours they work—up to 56 hours of paid sick leave
each year. The Wage and Hour Division (WHD) is responsible for making sure covered
employers comply with this requirement.
For information on whether you are entitled to accrue and use paid sick leave, visit How
do I know if I am working on a federal contract under which I am entitled to accrue and
use paid sick leave?
If you have questions or concerns, you can contact WHD at 1 (866) 487-9243 or visit
www.dol.gov/agencies/whd.
75
Find more information, call the Caregivers Support Line (CSL) - VA Caregiver Support
Program toll-free at 1 (855) 260-3274, Monday through Friday, 8:00 a.m. to 10:00 p.m.
ET, and Saturday, 8:00 a.m. to 5:00 p.m. ET
Visit the CSP Teams/Caregiver Support Coordinators Locator at Caregiver Support
Program (CSP) Teams/Caregiver Support Coordinators - VA Caregiver Support Program
Learn more about the program, visit VA Caregiver Support Program Home | VA
(caregiver.va.gov)
Child Welfare
Child Welfare programs focus on improving the lives of children and families by reducing
child abuse and neglect, increasing the number of adoptions, and strengthening foster care.
They may provide some assistance to individuals who are caring for children who lost their
parents due to COVID-19 and Long COVID.
• The Title IV-E Foster Care Program provides board and care payments for eligible
children under the supervision of the state and placed in foster family homes or child
care institutions that are safe and licensed
• The Title IV-E Prevention Program provides time-limited prevention services for mental
health conditions, substance use concerns, and in-home parent skill-based programs
for children or youth who are candidates for foster care, pregnant or parenting youth
in foster care, and the parents or kin caregivers of those children and youth
• The Title IV-E Guardianship Assistance Program to support relatives who become legal
guardians of children for whom they previously cared for as foster parents
Access more information about child welfare programs, visit Children's Bureau (CB) |
The Administration for Children and Families (hhs.gov) or call (202) 205-8618
Services and Supports for Longer-Term Impacts of COVID-19
medical center has dedicated Caregiver Support Program staff who assist with information and
referrals to these programs.

76
Chapter 3: Enabling Health Care
Personnel to Improve
Treatment
o
f
People Experiencing Long COVID
The longer-term effects of COVID-19 encompass not just the ongoing challenge of providing
care for people with Long COVID, but also the physical and psychological stresses on health
care personnel, their patients, and their families due to the pandemic’s disruptions.
At the pandemic’s onset, health care personnel faced a novel clinical entity threatening
morbidity and mortality to unprecedented numbers of people. Health care personnel worked
with limited available knowledge or consensus on basic treatment protocols. We have since
gained more clinical knowledge about the prevention, diagnosis and management of acute
COVID-19 infection, while evidence for Long COVID is just emerging. However, health care
personnel are now coping with the still novel entity of Long COVID, and once again confronting
uncertainty and rapidly evolving evidence.
COVID-19 initially presented as acute pulmonary disease with high rates of mortality but
rapidly was recognized as a multisystem disease. The virus demonstrated its ability to attack a
wide range of organ systems, creating serious neurologic, cardiac, hematologic, renal,
pulmonary, rheumatologic and other consequences that make support and treatment of
individuals with COVID-19 exceptionally complex. Long COVID presents with an unusually
broad set of symptoms and affects multiple organ systems, creating additional challenges in
identifying and treating patients.
The COVID-19 pandemic has placed significant stresses on health systems, hospitals and
individual health care personnel. While hospitals are less crowded with people with COVID-19,
many challenges remain in the ongoing function of health systems. These include increased
demand due to delayed preventive and chronic care during the pandemic, supply chain delays
for some medical equipment, and national shortages of staff, especially nurses. The resulting
pressure to get by with fewer staff members leaves remaining health care personnel under
great stress, potentially resulting in further shortage and increasing the risk of providers
themselves contracting COVID-19.
In addition to stress at work, many health care personnel face challenges at home due to the
impact of COVID-19 on their family members, including both children and older people. The
majority of health care personnel are women, many of whom shoulder considerable caregiving
responsibilities.1 The psychological stress of providing health care during the pandemic is
powerful, with greater impact on those who are younger, people from racial and ethnic
minority groups, and those with minor children or an ill family member.2 In addition, health
care personnel are now confronting the consequences of delayed preventive care and chronic
Services and Supports for Longer-Term Impacts of COVID-19
77
• Resources for healthcare personnel caring for individuals with Long COVID
• Supports for healthcare personnel who are dealing with the stressors and traumas of
serving on the front lines in the COVID-19 response and the continued challenges of
working in a system under stress.
Resources for Health Care Personnel Caring for
Individuals with Long COVID
Resources for
Healthcare Personnel
This section includes
• Federal Clinical Care
Guidance for Long COVID
• Sample of Clinical Care
Guidance from Professional
Associations
• Federally Sponsored
Educational Programs for
Healthcare Personnel
• Healthcare Delivery Systems
Equipped for Long COVID
Care
• Development of Best
Practices for Long COVID
Clinical Care.
Services and Supports for Longer-Term Impacts of COVID-19
This chapter presents U.S. government resources
available to guide health care personnel in treating
individuals with Long COVID. A sample of non-federal
sources is also included.
Clinical practice guidelines for treating individuals with
Long COVID are emerging. As the state of evidence is
still evolving, there is a need for living evidence reviews,
guidelines, and clinical decision support to bring the
best evidence to the point of care. This report and
referenced resources help mitigate provider
misconceptions and biases, where they exist, in making
the diagnosis of Long COVID.
The resources linked in this section use what is known
so far. Enhanced coordination will be required to ensure
optimal consistency in best practices. Health care
personnel referring to these websites should check back
re
gularly for updates.
Federal Clinical Care Guidance for Long
COVID
Agency for Healthcare Research and Quality
Evidence-Based Practice Centers Program
Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Centers (EPCs)
produce evidence reports on medications, devices, and other health care services with the goal
of helping consumers, health care professionals, and policymakers make informed and
disease management resulting from the pandemic along with higher rates of mental health and
substance use.
This chapter covers two main components
78
Centers for Disease Control and Prevention
Interim Guidance on Evaluating and Caring for Patients with Post-COVID Conditions
Centers for Disease Control and Prevention (CDC) has many resources for health care
personnel addressing the needs of Long COVID patients. The interim guidance documents
provide practical guidance for providers caring for people with Post-COVID-19 conditions.
See the full list of topics, visit Interim Guidance on Evaluating and Caring for Patients
with Post-COVID Conditions | CDC
View the CDC overview for healthcare personnel working with patients with post-COVID
conditions, visit Post-COVID Conditions: Information for Healthcare Providers (cdc.gov)
CDC-INFO offers live agents by phone and email to help the public find the latest,
reliable, and science-based health information on more than 750 health topics. For
example, help your patient find a vaccine provider or learn more about other CDC
resources, visit CDC INFO | CDC
Department of Defense
Military Health System COVID-19 Toolbox
The Department of Defense (DOD) provides resources to health care personnel to facilitate the
treatment and care of Military Health System (MHS) beneficiaries infected with COVID-19,
including those that have persistent Long COVID symptoms.
Resources in the COVID-19 Toolbox help DOD clinical staff address the needs of their COVID-19
patients. The Toolbox includes the Practice Management Guide which provides information to
assist in decision-making, general information on symptoms persisting for four or more weeks
after infection, presentation of potential symptoms by patients, recommendations for patient
evaluation and diagnosis, treatment and clinical management for patients with sustained
symptoms, and summary of the prospective prognosis of Long COVID. The Toolbox website
includes additional patient care clinical skills augmentation that may be necessary and
provides just-in-time training videos with critical care training for health care personnel.
Learn more about the Toolbox, visit COVID-19 Toolbox | Health.mil
Services and Supports for Longer-Term Impacts of COVID-19
evidence-based health care decisions. The EPC Program has created several COVID-19
resources that may be helpful to health care personnel.
Learn more about EPC’s COVID-19 resources, visit COVID-19 Resources Developed by
AHRQ's Evidence-based Practice Centers | Effective Health Care (EHC) Program
79
Health Center Resource Clearinghouse
HRSA and the National Association of Community Health Centers, a HRSA-funded National
Training and Technical Assistance Partners (NTTAP), developed the Health Center Resource
Clearinghouse, which provides an up-to-date selection of high-quality technical assistance
resources relevant to health centers, including COVID-19.
Learn more about COVID-19 Resources, visit COVID-19 | Health Center Resource
Clearinghouse (healthcenterinfo.org)
AIDS Education and Training Center
The AIDS Education and Training Center Program, National Coordinating Resource Center
supports national HIV priorities by building clinician and care team capacity and expertise
along the HIV care continuum.
Find COVID-19 Resources for HIV Providers, visit COVID-19 Resources for HIV Providers |
AIDS Education and Training Centers National Coordinating Resource Center (AETC
NCRC) (aidsetc.org)
Substance Abuse and Mental Health Services Administration
Center for Mental Health Services Expert Summit on Behavioral Effects of Long COVID
SAMHSA convened an expert panel of researchers, clinical care professionals, and individuals
experiencing firsthand the cognitive and other behavioral health effects of Long COVID to
create guidance on the identification and management of the mental health conditions that
some with Long COVID experience. A report and materials to guide health care personnel and
individuals with Long COVID address the neurological and mental health symptoms of Long
COVID will be available on the SAMHSA.gov website.
Sample of Clinical Care Guidance from Professional Associations
Below are some consensus statements and guidance documents developed by various
professional groups. It is outside the scope of this report to vet the methodological rigor and
quality of current professional association guidance related to Long COVID. As such, none of
the resources below are endorsed by the U.S. government.
Services and Supports for Longer-Term Impacts of COVID-19
Health Resources and Services Administration
Tens of millions of Americans receive quality, affordable health care and other services through
Health Resources and Services Administration’s (HRSA) 90-plus programs and more than 3,000
grantees. HRSA programs have been leveraged to enable the nation’s health care safety net to
address COVID-19 and emerging priorities and issues, such as Long COVID.
80
American Academy of Physical Medicine and Rehabilitation
Consensus Guidance Statements Related to Long COVID
Services and Supports for Longer-Term Impacts of COVID-19
Lea
rn more about the methodology used by American Academy of Physical Medicine
a
nd Rehabilitation, visit Consensus methodology for the development of postacute
sequelae of SARS-CoV-2 guidance
state
ments -Maley -2021 - PM&R - Wi
le
y Online
Libra
ry
Read about the consensus guidance regarding fat
igue among SARS-COV-2 infection
patients, visit
Multidisciplinary collaborative
consensus
guidance state
ment
on the
assessment and treatment of fatigue in postacute sequelae of SARS-CoV-2 infection
(PASC) patients - Herrera - 2021 - PM&R - Wiley Online Library
Read
about
the
consensus guidance regarding breathing discomfort among Long COVID
patients, visit
Multi
-disciplinary
collaborative
consensus
guidance statement on the
assessment and treatment of breathing discomfort and respiratory sequelae in patients
with post-acute sequelae of SARS-CoV-2 infection (PASC) - Maley - 2022 - PM&R -
Wiley Online Library
Read
about
the
consensus
guidance regarding
cogniti
ve symptoms among Long COVID
patients, visit Multi-disciplinary collaborative consensus guidance statement on the
assessment and treatment of cognitive symptoms in patients with post-acute sequelae
of SARS-CoV-2 infection (PASC) - Fine - 2022 - PM&R - Wiley Online Library
Read
about
the
consensus guidance regarding Long COVID Cardiovascular
Complications, visit AAPM&R Long COVID
Cardiovascular
Complications
Guidance
State
ment Released (aapmr.org)
American College of Cardiology
Expert Consensus Decision Pathway
Read about the consensus decision pathway regarding cardiovascular sequelae among
COVID-19 patients, visit 2022 ACC Expert Consensus Decision Pathway on Cardiovascular
Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, Post-
Acute Sequelae of SARS-CoV-2 Infection, and Return to Play: A Report of the American
College of Cardiology Solution Set Oversight Committee | Journal of the American
College of Cardiology (jacc.org)
The body of evidence on Long COVID is rapidly evolving, so clinical practice guidance will need
to be kept up-to-date through living reviews, regular updates to practice guidelines, and
strategies to effectively make the latest evidence available at the point of care. This guidance
can let clinicians know what works and what is not effective, and may also help clinicians
address misinformation among the people and communities they serve.
81
Services and Supports for Longer-Term Impacts of COVID-19
American Nurses Association
American Nurses Association’s Well-Being Initiative
Resource includes free tools and apps to support the mental health and resilience of all nurses.
Learn more about the American Nurses Association’s Well-Being Initiative, visit
Coronavirus | Well-Being Initiative | Mental Health | ANA (nursingworld.org)
European Respiratory Society
Read the European Respiratory Society statement on Long COVID
Follow-Up, visit
European Respiratory Society Statement on Long COVID-19 Follow-Up | European
Respiratory Society (ersjournals.com)
Other Extern
al Resources for Long COVID Information Relevant to Clinicians
R
ead the
N
ational Instit
ute
for
He
alth Care Excellence
guideline on managing the longer-
term effects of COVID-19, visit Overview | COVID-19 rapid guideline: managing the long-
term effects of COVID-19 | Guidance | NICE
Read the National Health Service guidance on when you need to seek help, visit When
Do I Need To Seek Help? | Your COVID Recovery
Read about the neurological effects of Long COVID, visit Long-COVID: neurological
manifestations and management - PMC (nih.gov)
Read about proposed clinical guidelines for Long COVID diagnosis and disease
management, visit IJERPH | Free Full-Text | Long Covid-19: Proposed Primary Care
Clinical Guidelines for Diagnosis and Disease Management (mdpi.com)
Read the Chartered Society of Physiotherapy’s Long COVID clinical guidance, visit Long
COVID clinical guidance | The Chartered Society of Physiotherapy (csp.org.uk)
Read the Indiana Department of Health’s Long COVID clinical guidance, visit COVID-19-
LTC-Clinical-Guidance-2.8.22.pdf
Federally Sponsored
Educational
Programs
for
Healthcare Personnel
Clinicians have struggled throughout the pandemic to access reliable and up-to-date
information to identify COVID-19-related symptoms and treatments. This task is exacerbated
by the large amount of inaccurate advice that is not e
vidence-based and can be harmful to
patients. This section provides links to trusted channels of dissemination to help clinicians
access the most current and accurate information and training related to treating Long COVID.
82
Centers for Disease Control and Prevention
Clinician Outreach and Communication Activity
Clinician Outreach and Communication Activity (COCA) helps prepare clinicians to respond to
emerging health threats and public health emergencies by communicating relevant, timely
information related to disease outbreaks, disasters, terrorism events, and other health alerts.
Read about Clinician Outreach and Communication Activity, visit Home | Clinician
Outreach and Communication Activity (COCA) (cdc.gov)
View a webinar on evaluating and supporting COVID-19 patients with cognitive
symptoms, visit Webinar Thursday, May 5, 2022 - Evaluating and Supporting Patients
Presenting with Cognitive Symptoms Following COVID (cdc.gov)
View a webinar on evaluating and supporting COVID-19 patients with fatigue, visit
Webinar September 30, 2021 - Evaluating and Supporting Patients Presenting With
Fatigue Following COVID-19 (cdc.gov)
View a webinar on evaluating and caring for patients with Long COVID, visit Webinar
June 17, 2021 - Evaluating and Caring for Patients with Post-COVID Conditions (cdc.gov)
View a webinar on what clinicians, pharmacists, and public health partners need to
know about antibiotic prescribing for COVID-19, visit Webinar Thursday, November 18,
2021 -What Clinicians, Pharmacists, and Public Health Partners Need to Know about
Antibiotic Prescribing and COVID-19 (cdc.gov)
TeleECHO Program
Project ECHO, “Extension for Community Healthcare Outcomes,” is an innovative knowledge-
on-demand model for providing treatment to patients with chronic, common, and complex
diseases who do not have direct access to specialty health care providers. There are several
examples of ECHO or ECHO-like programs that have been adopted by federal agencies.
One example is CDC’s Long COVID and Fatiguing Illness Recovery Program, which aims to
improve the health of people who are medically underserved who have Long COVID and other
complex chronic conditions with similar symptoms, such as myalgic encephalomye
litis and
chronic fatigue syndrome (ME/CFS) and other post-infectious fatiguing illnesses. This low-cost,
scalable model has potential to reduce health inequities by increasing the capacity of health
care providers in underserved communities to deliver effective care informed by the latest
clinical advances. The program implements a randomized trial at the Family Health Centers of
San Diego, a large, Federally Qualified Health Center and a cohort comparison with patients at
the University of Washington Long COVID Rehabilitation and Recovery Clinic. The program is
evaluating telementoring involving multi-specialty case consultation and peer-to-peer sharing
of emerging promising clinical practices for managing Long COVID and improving provider- and
patient-level outcomes. The program also disseminates educational content in monthly topic-
Services and Supports for Longer-Term Impacts of COVID-19
83
focused webinars and quarterly short courses open to providers nationwide. Although the
main focus is Long COVID, the similarities to ME/CFS and other post-infectious fatiguing
illnesses is recognized and included in the curriculum, with the idea that the clinics could serve
patients with Long COVID-like symptoms, whether or not they had a positive COVID test result.
Multi-speciality faculty/mentors include national experts in the care of Long COVID, ME/CFS,
and other post-infectious chronic illnesses, as well as lived experience experts (patients,
patient advocates, and caregivers). The program has attracted 40 nationally recognized
faculty/mentors representing multiple medical specialties who have started a social media
discussion group for sharing evolving knowledge and emerging clinical practice. Investigators
have documented increasing webinar attendance of up to 650 participants and have received
inquiries indicating interest in participation from health care providers nationally and
internationally
Register to start receiving invitations to monthly Long COVID and Fatiguing Illness
Recovery Program
webinars: Webinar Registration - Zoom
Read more about the Long COVID and Fatiguing Illness Recovery Program, visit Does a
Technology Enabled Multi-disciplinary Team-based Care Model for the Management of
Long COVID and Other Fatiguing Illnesses Improve Clinical Care of Patients and
Represent a Sustainable Approach Within a Federally Qualified Health Center? - Full Text
View - ClinicalTrials.gov
Read about the Family Health Centers of San Diego, visit Family Health Centers of San
Diego: Low Cost Clinic - No Insurance (fhcsd.org)
Read about Project ECHO, visit Project ECHO | Agency for Healthcare Research and
Quality (ahrq.gov)
Read about the University of Washington’s guidance on Long COVID rehabilitation and
recovery, visit Post-COVID Rehabilitation | UW Medicine
Read about Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, visit What is
ME/CFS? | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | CDC
Services and Supports for Longer-Term Impacts of COVID-19
Centers for Medicare & Medicaid Services
Centers for Medicare & Medicaid Services Medicare Learning Network
Centers for Medicare & Medicaid Services (CMS) works with providers to advance recognition
and understanding of Long COVID and associated conditions, including by sharing culturally
competent information and resources through platforms like the CMS Medicare Learning
Network (MLN) and engaging stakeholders across the health sector to share best practice and
new findings from research occurring across HHS.
The MLN offers a weekly email newsletter for health care personnel. It compiles news from
across CMS into a single source for program and policy details; news and announcements;
press
84
releases; upcoming educational event registration and reminders; claim, price, and code
information; and updates new and revised MLN Matters Articles® and publications.
As more clinical information on the diagnosis for Long COVID and its treatment become available
from ongoing research at the Department’s research agencies, CMS can use its established
channels and ability to convene stakeholders to get this information directly to providers.
Accurate and Effective Use of Long COVID Diagnostic Code
This year, the Administration is set to develop and launch targeted clinician and medical coder
education on the ICD-10-CM code U09.9, which became effective last year to support
diagnosis, billing, and tracking of Long COVID.
Read about the Long COVID diagnostic code, visit page 30
of FY2022 April1 update ICD-
10-CM Guidelines (cms.gov)
Veterans Affairs
COVID-19 ECHO
The Veterans Health Administration provides live, interactive, hour-long educational sessions
which cover evidence-based care recommendations, discussion of models of care, optimizing
virtual care delivery during the pandemic, and best practices. All sessions offer continuing
education. Sessions vary from weekly, bi-weekly, or monthly. Learners include clinical
providers and allied health; management, administration, and leadership; non-clinical team
members; and health care trainees. Non-VA clinicians are also welcome at most sessions at no
cost.
Register and start receiving invites to the COVID-19 VA-ECHO sessions, visit VA-ECHO
(iths.org)
Health Resources and Ser
vices Administration
Telehealth
Technology
-Enabled
Learning
Program
The purpose of Telehealth Technology-Enabled Learning Programs (TTELP) is to connect
specialists at academic medical centers with primary care providers who work with people from
rural areas and those who are medicall
y underserved, providing evidence-based training and
support to help them treat patients with complex conditions in their communities. TTELP
recipients develop learning community models that emphasize collaborative partnerships
between such providers (i.e., telementoring models such as Project ECHO, distance learning,
clinical decision support, and other emerging models in the field), to provide training and
facilitate the dissemination of best practice specialty care to PCPs and care teams in rural areas,
frontier, and underserved populations. The $4.28 million in funding, which began in FY2021,
funds nine grantee recipients. The grants assist specialists at academic medical centers to
provide training and support to primary care providers in rural, frontier, and other underserved
Services and Supports for Longer-Term Impacts of COVID-19
85
areas to help treat patients with complex conditions ranging from Long COVID to substance
use challenges in their communities. TTELP is in its first year of the five-year program. Five
out of the nine TTELP grantees are working on Long COVID issues with the potential of two
additional grantees adding it to their work plans over the course of the program’s five years.
View grantee recipients, visit FY 2021 Telehealth Awards | HRSA
Learn about the Telehealth Technology-Enabled Learning Program, visit Telehealth
Technology-Enabled Learning Program | Official web site of the U.S. Health
Resources &
Services Administration (hrsa.gov)
Indian Health Service
National Pharmacy
and Therapeutics Committee
The National Pharmacy and Therapeutics Committee (NPTC) provides COVID-19 Emergent
Treatment Updates to IHS clinical providers. Updates include new and changing
recommendations and guidelines, authorizations for relevant medications related to COVID-19,
and vaccinations.
View all Emergent Treatment Updates, visit COVID-19 | National Pharmacy &
Therapeutics Committee (ihs.gov)
COVID-19 ECHO
This COVID-19 ECHO Program is designed to connect Federal, Tribal, and Urban IHS clinicians,
administrators, and staff with up-to-date information on clinical care and emerging health
topics. ECHO sessions are open to those interested in staying current on the rapidly evolving
pandemic to inform their COVID-19 response efforts. This program is focused on Federal, Tribal,
and Urban IHS clinical providers, administrators, and staff, and it is free to register.
Learn more about this ECHO program, visit COVID-19 ECHO Programs - Indian Country
ECHO
Register for a myECHO account, visit Login - Indian Country ECHO
Pharmacy Program
The IHS Pharmacy Program is the primary
source of national advocacy, management, and policy
development for IHS pharmacies across the United States. IHS pharmacists are intimately
involved in improving patient care through active involvement with Pharmacy and Therapeutics
Committees, formulary management, policy and procedure development and education across
the healthcare spectrum. The IHS Pharmacy Program provides vaccine training and certification
for Federal, Tribal, and Urban Pharmacists and Ph
armacy Technicians to expand the number of
people eligible to administer vaccines available during COVID-19. Some IHS facilities lead the
Pharmacy Expanding Vaccine Access (PEVA) workgroup, an initiative to decrease the prevalence
of vaccine-preventable diseases. The primary focus of PEVA is to increase access to and demand
Services and Supports for Longer-Term Impacts of COVID-19
86
for immunization services by using subject matter experts to advise, educate and implement
improved immunization practices to the public health service field.
Rea
d more
a
bout the
Pharmacy
Program, visit
Pharmacy
Program
| Division
of
Clinical
and Community Services (ihs.gov)
Read more about Pharmacy Expanding Vaccine Access, visit Pharmacist Professional
Advisory Committee (psc.gov)
Healthcare Delivery Systems Equipped for Long COVID Care
Clinical expertise on Long COVID is not equally available across the United States. This section
aims to give examples of existing programs that can be leveraged to address Long COVID and to
provide information for clinicians who wish to refer patients who need resources beyond what
is locally available.
Health Resources and Services Administration
Federally Qualified Health Centers
Health centers funded by the Health Resources and Services Administration (HRSA) operate
more than 14,000 service delivery sites across all U.S. states and territories. Nearly 29 million
people, or 1 in 11 nationwide, rely on a HRSA-funded health center for affordable, accessible
health care. These centers provide care to people who are medically underserved, including
people with HIV, people who are pregnant, mothers and their families, those with low
incomes, residents of rural areas, AI/AN persons, and those otherwise unable to access high-
quality health care. Health centers are located in medically underserved communities,
providing access to affordable, comprehensive, and high-quality primary health care services
for people who have low incomes, who are uninsured, or face other obstacles to getting
health care.
Read more about Health Centers, visit What is a Health Center? | Bureau of Primary
Health Care (hrsa.gov)
Find a Health Center, visit Find a Health Center (hrsa.gov)
National Maternal Mental Health Hotline
The National Maternal Mental Health Hotline provides 24/7, free, confidential support before,
during, and after pregnancy. Any expecting or new mom experiencing mental health challenges,
and their support networks and providers can call the hotline. The Hotline offers callers phone
or text access to trained, professional counselors who are culturally and trauma-informed; real-
time support and information; response within a few minutes, 24 hours a day, 7 days a week;
resources; referrals to local and telehealth providers and support groups; culturally sensitive
support; counselors who speak English and Spanish; and interpreter services in 60 languages.
Services and Supports for Longer-Term Impacts of COVID-19
87
Read more about the Hotline, visit 1-833-9-HELP4MOMS – National Maternal Mental
Health Hotline | MCHB (hrsa.gov)
Access the Hotline, call or text 1 (833) 9-HELP4MOMS or 1 (833) 943-5746. TTY users can
use a preferred relay service or dial 711 and then 1 (833) 943-5746.
Indian Health Service
Federal, Tribal, and Urban Health Centers
COVID-19 has amplified health inequities in AI/AN communities because of underfunded and
under-resourced health systems, limited access to health services, poor infrastructure, and
underlying health disparities. For example, according to the latest rates reported by CDC, AI/AN
individuals are three times more likely to be hospitalized with COVID-19.3
IHS offers comprehensive health services to AI/AN individuals through a series of Federal,
Tribal, and Urban health centers. Availability of services (e.g., primary care, emergency
services, hospital care, behavioral health, substance use treatment) is dependent on each
clinic. Eligible AI/AN individuals affected by longer-term effects of COVID-19—whether
physical, mental, social, or spiritual—are encouraged to use the provided website to locate
those IHS services nearest to them. Identify the nearest IHS, Tribal or Urban (I/T/U) Indian
Health Program facility using the provided website and call to schedule an appointment. Each
center will communicate what is needed to register as a patient.
Find a Federal, Tribal, or Urban health center, visit Find Health Care | Indian Health
Service (IHS)
Department of Veterans Affairs
Programs and Services Offered
VA clinics are offering a combination of in-person and telehealth services for Long COVID care
to maximize patient access to these services. As of early 2022, an environmental scan
identified that 22 VA facilities offer coordinated Long COVID care and many other facilities are
working to stand up similar clinics. A second environmental scan of these rapidly evolving
clinics is currently underway and will be completed in mid-2022. Services offered vary based
on location and may include physical therapy, occupational therapy, speech therapy, mental
health assessment and intervention, pulmonary rehabilitation, cardiac rehabilitation,
psychology groups, neuropsychological testing, and medical specialties including geriatrics,
primary care, physiatry, psychiatry, neurology, pulmonology, and cardiology.
Services and Supports for Longer-Term Impacts of COVID-19
88
Development of Best Practices for Long COVID Clinical Care
Veterans Affairs
VA standards of care for Long COVID are being developed nationally through a Community
of Practice (CoP) concurrent with the development of a Long COVID Integrated Practice
Team driven by VHA leadership. These groups are actively working to establish
• Best practices and guidelines for clinical interventions
• Standardized referral processes, tools, and templates
• Data and metric consensus
• Resources and model of care planning
• Training and education for VA employees, Veterans, and external audiences.
Resources are being developed to guide services for both primary care and specialty care
providers across a broad range of VA facilities, including development of note templates and
best practice management recommendations.
Providers interested in contacting or coordinating with the VA Long COVID CoP can send
inquiries to the email address VHALongCOVID@va.gov
Support for Health Care Personnel Experiencing Stress
and Trauma Related to COVID-19
The realities of our health care system are driving many health care personnel to burnout. They
are at an increased risk for mental health challenges and are choosing to leave the health
workforce early.4 They work in distressing environments that strain their physical, emotional,
and psychological well-being, making it harder for patients to get care when they need it.
COVID-19 has created enormous stresses on both health care systems and their personnel. The
vast increase in seriously ill patients, the resulting lack of sufficient medical resources during
surges, and the lack of established effective treatments, especially early in the pandemic,
affected health care personnel who also had ill family members and children forced out of their
ordinary school routine. Current shortages of medications, other medical supplies, and staffing
contribute to high ongoing stress levels in medical workplaces. These multiple factors created a
devastating impact on health care personnel. We describe several federal employee assistance
programs provided by health systems to support their clinical workers at an individual level.
Services and Supports for Longer-Term Impacts of COVID-19
89
Services and Supports for Longer-Term Impacts of COVID-19
Health Resources and Services Administration
To address stress on health care personnel, Department of Health and Human Services (HHS),
through the Health Resources and Services Administration (HRSA) provided $103 million in
awards to improve the retention of health care personnel and help respond to the nation’s
critical staffing needs by reducing burnout and promoting mental health and wellness among
the health care workforce. These awards will fund evidence-informed programs, practices and
training, with a specific focus on providers in areas where people are medically underserved
and in rural communities.
Learn more about the federal grants to reduce burnout and promote mental health and
wellness among health care personnel, visit HRSA Workforce Program Initiatives Fact
Sheet
Learn more about health care personnel burnout, visit Health Worker Burnout —
Current Priorities of the U.S. Surgeon General (hhs.gov)
Department of Veterans Affairs
Staff Support Programs
The Employee Whole Health program offers VA staff a holistic approach to self-care, with
numerous virtual tools for employees related to stress management, trauma-informed peer
support, well-being, professional fulfillment, and personal or family emergencies.
Read more about Employee Whole Health, visit Employee Whole Health - Whole Health
(va.gov)
Read the Whole Health Blog, visit #LiveWholeHealth Archives - VAntage Point
In addition, the Reduce Employee Burnout and Optimize Organizational Thriving (REBOOT) task
force is working to help alleviate burnout and promote VA employee well-being. The task force
engages with employees to identify major contributors to burnout and recommend existing
efforts that might be complemented or amplified to address those contributors.
Access resources on mental health, women Veterans, cultural competency, and
common clinician concerns when working with members of the National Guard,
Reserve, and Veterans transitioning to civilian work environments, visit Employee
Assistance Program (EAP) Providers - Veterans Employment Toolkit (va.gov)
Learn more about the REBOOT task force, visit Reducing Employee Burnout (va.gov)
90
Services and Supports for Longer-Term Impacts of COVID-19
Indian Health Service
Employee Assistance Program
The Employee Assistance Program (EAP) is a resource for IHS health care personnel and
employees. The voluntary, work-based program offers free and confidential assessments, short-
term counseling, referrals, and follow-up services to employees who have personal and work-
related problems. EAPs address a broad and complex body of issues affecting mental and
emotional well-being, such as alcohol and other substance use challenges, stress, grief, family
problems, and psychological conditions. EAP counselors also work in a consultative role with
managers and supervisors to address employee and organizational challenges and needs.
Read more about the Employee Assistance Program, visit Employee Assistance Program
| Working at IHS
Read more about Federal Occupational Health where suicide information and
prevention resources can be found, visit FOH4YOU
Mental Health Training
Some of the IHS areas are providing Mental Health First Aid training and train-the-trainer
education. This provides supervisors with the tools to evaluate staff for possible mental health
intervention needs. Also, agency-wide training for QPR (Question, Persuade and Refer) was
provided by the Department of Behavioral Health. This provides an effective tool to screen for
suicidal ideation and provide immediate intervention and referral.
References
1. Day J, Christnacht C. Women Hold 76% of all Health Care Jobs, Gaining in Higher-Paying
Occupations. United States Census Bureau. Updated August 14, 2019. Accessed July 19,
2022. https://www.census.gov/library/stories/2019/08/your-health-care-in-womens-
hands.html
2. Kisely S, Warren N, McMahon L, Dalais, C, Henry I, Siskind D. Occurrence, prevention, and
management of the psychological effects of emerging virus outbreaks on health care
workers: rapid review and meta-analysis.” BMJ. 2020;369:m1642.
3. Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization, and
Death By Race/Ethnicity. Updated June 24, 2022. Accessed July 19, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-
discovery/hospitalization-death-by-race-ethnicity.html
4. National Academy of Medicine. Action Collaborative on Clinician Well-being and Resilience.
National Plan for Health Workforce Well-Being. Updated May 5, 2022. Accessed July 19,
2022. https://nam.edu/initiatives/clinician-resilience-and-well-being/national-plan-for-
health-workforce-well-being/
91
Services and Supports for Longer-Term Impacts of COVID-19
Chapter 4: Services for Individuals
Dealing with Mental Health, Substance
Use, or Bereavement Challenges in the
Wake of the Pandemic
The COVID-19 pandemic impacted our lives in numerous ways, and as a result, many of us have
faced a variety of stressful challenges that can be overwhelming. The COVID-19 pandemic has
affected people’s mental health and created additional obstacles for those in need of
behavioral health care to include mental health and substance use care. A growing number of
adults in the United States reported mental health concerns since the start of the pandemic,
2
and many children and adolescents have experienced challenges to their emotional health and
well-being.
,
While already increasing before COVID-19, substance use and drug overdoses
increased in the United States after the COVID-19 pandemic began, and we have learned that
people with substance use challenges and some mental illnesses are at increased risk for poor
COVID-19 outcomes. In addition, as the full impact of COVID-19 unfolds, many Americans have
been forced to cope with the death of loved ones and face the aftermath of those losses.
5
43
1,
Resources are available to help. In this chapter, you will find three sections that feature
federally funded supports and services for individuals experiencing the effects of COVID-19 in
the areas of
1. Mental Health
2. Substance Use
3. Bereavement.
Although we have separated these sections, the social and medical factors underlying them are
strongly inter-related and relevant as are the resources to assist those in need. Therefore, there
is some repetition in each section. For each support or service, a telephone number or a
hyperlink to appropriate websites are provided. You do not need to have Long COVID to access
these resources. Most of the resources are relevant to anyone with a disability or who meets
the program criteria.
For information about mental health and substance use, please visit SAMHSA -
Substance Abuse and Mental Health Services Administration
92
Not Sure Where to Start?
Q. Are you thinking about taking
your life, or are you worried about a
friend or
loved one who is talking
about suicide?
Find support, visit Lifeline
You may also contact the National
Suicide Prevention Lifeline at 1 (800)
273-8255; TTY Users can use your
preferred relay service or dial 711
then 1 (800) 273-8255.
-------------------------------------------------
Q. Do you need to find treatment to
help you cope with depression,
anxiety or your emotions generally?
A. Call the National Helpline at
1 (800) 662-HELP (4357) and 1 (800)
487-4889 (TTY)
Find treatment through the
Behavioral Health Treatment
Services Locator at Home - SAMHSA
Behavioral Health Treatment
Services Locator, through the
Department of Veterans Affairs at
Find VA Locations | Veterans Affairs
or the Department of Defense
Treatment Locator at Find a Military
Hospital or Clinic | TRICARE
A. Call, t
ext, or chat the N
ational
Suicide prevention Lifeline by
pressing 988 to connect to
counselors who will listen, provide
support, and connect you to
treatment and other resources.
Services and Supports for Longer-Term Impacts of COVID-19
For information about the protection and
advocacy of individuals with mental illness,
please visit Protection & Advocacy for
Individuals with Mental Illness (PAIMI)
Program | SAMHSA
For information about non-discrimination
protections for individuals with mental
health or substance use conditions, please
visit File a Complaint | Beta.ADA.gov
For more information about the rights of
students, please visit Supporting and
Protecting the Rights of Students at Risk of
Self-Harm in the Era of COVID-19 (PDF)
(ada.gov).
Mental Health Supports and
Services
The COVID-19 pandemic brought about
unprecedented changes to our lives that had
implications for not only our physical health, but
also our mental health and well-being. People
experienced a variety of stressors, including
uncertainty about the future, changes in daily
routines, financial concerns, employment instability,
and social isolation. Challenges from the pandemic
often prompted mental health challenges to
develop and worsened existing mental health
concerns. Studies show increases in the number of
U.S. adults who report symptoms of stress, anxiety,
and depression during the pandemic, compared to
reports before the pandemic. A variety of federal
mental health resources and supports are available
to help. This section covers five topics
6-7
• Treatment Locators
• Helplines
• Self-Help Resources

93
Early Serious Mental Illness Treatment Locator
The Early
Serious Mental Illness Treatment Locator provides a confidential and anonymous
source of information for people and their family members
who are seeking treatment for a
recent onset of serious mental illnesses such as psychosis, schizophrenia, bipolar disorder and
other conditions. These evidence-based programs provide medication, therapy, family and peer
support, assistance with education and employment and other services.
Find early serious mental illness treatment, visit Early Serious Mental Illness Treatment
Locator | SAMHSA
Helplines
The Lifeline and 988
988 is the new
three-digit dialing code that will route callers to the National Suicide Prevention
Lifeline. When people call, text, or chat 988 on their phone, they will be connected to
trained
counselors that are part of the existing National Suicide Prevention Lifeline network. These
trained counselors will listen, understand how their problems are affecting them, provide
support, and connect them to resources if necessary.
Connect with a trained counselor, call,
text, or chat 988
Find support, call 1 (800) 273-8255; (TTY) Dial 711 then 1 (800) 273-8255
Learn more about The Lifeline and 988 : Lifeline (suicidepreventionlifeline.org)
Disaster Distress Helpline
The Disa
ster Distress Helpline provides 24 hours-a-day, 365-day-a-year crisis counseling and
support to people experiencing emotional distress related to natural or human-caused
Services and Supports for Longer-Term Impacts of COVID-19
• Resources for Military Veterans, Service Members, and their Families
• Indian Health Service Resources.
Treatment Locators
Behavioral Health Treatment Services Locator
This Behavioral Health Treatment Services Locator provides confidential and anonymous
information for anyone seeking treatment facilities in the United States or U.S. Territories for
substance use challenges and mental health problems.
Find treatment, call 1 (800) 622 HELP or 1 (800) 622-4357 or visit Home - SAMHSA
Behavioral Health Treatment Services Locator
94
Health Resources and Services Administration, Maternal & Child Health Bureau,
Nationa
l Maternal Mental Health Hotline
The National Maternal
Mental Health Hotline provides 24-hours-a-day, free, confidential
support before, during, and after pregnancy. Any expecting or new mom experiencing mental
health challenges, and their support networks and providers, can call the hotline. The Hotline
offers callers voice or text access to professional counselors, real-time support and information,
referrals to local and telehealth providers and support groups,
and counselors who speak
English and Spanish. Interpreter services are available in 60 languages.
Find support, call or text 1 (833) 9-HELP4MOMS or 1 (833) 943-5746; (TTY) Dial 711 and
1 (833) 943-5746
For support and resources, visit 1-833-9-HELP4MOMS – National Maternal Mental
Health Hotline | MCHB (hrsa.gov)
Self-Help Resources
COVID-19 Parental Resources Kit
COVID-19 can affec
t children and young people
directly and indirectly. Beyond getting sick,
many young p
eople’s social, emotional, and mental well-being are impacted by the pandemic.
The COVID-19 Parental Resource Kit provides information about ensuring children and young
people’s social, emotional, and mental well-being.
Find parenting resources, visit COVID-19 Parental Resources Kit (cdc.gov)
Disaster Behavioral Health Information Series Resource Center
The SAMHSA Disaster Technical Assistance Center (DTAC) provides resources and useful
information for those in the disaster behavioral health field and those who have experienced
disasters.
Services and Supports for Longer-Term Impacts of COVID-19
disasters, including the COVID-19 pandemic. Callers to the hotline can also connect with
counselors in over 100 other languages via 3rd-party interpretation services.
Connect with a trained crisis counselor, call or text 1 (800) 985-5990
Connect directly to an agent in American Sign Language, call 1 (800) 985-5990 from your
videophone
Learn more about the Disaster Distress Helpline | SAMHSA
Access Disaster Distress Helpline informational on-page documents in multiple
languages, visit disasterdistresshelpline Publisher Publications - Issuu
95
Access resources about coping with stress at Home | MentalHealth.gov
Stress and Coping with COVID-19
Centers for Disease Control and Prevention (CDC) provides resources for adults experiencing
stress from COVID-19.
Find resources for stress and COVID-19, visit Stress and Coping (cdc.gov)
Support for Teens and Young Adults
Stress and coping resources are available to help support teens and young adults struggling
during the COVID-19 pandemic.
Find resources for young people and visit Support For Teens and Young Adults (cdc.gov)
Tools for Supporting Emotional Wellbeing in
Children and Youth
Easy-to-use and interactive web tools are available to help children and teens cope with stress
and worries and deal with thoughts and feelings in a healthy way.
Learn more about supporting children and teens, visit | The National Academies Press |
Tools for Supporting Emotional Wellbeing in Children and Youth
Mental Health and Wellbeing Resources for Youth
The Youth.gov website includes a list of resources to help youth learn about topics related to
mental health, find places where they can get help if they need it, hear from other youth about
their struggles with mental health challenges, and help others get through tough times.
Services and Supports for Longer-Term Impacts of COVID-19
Find resources for youth and visit Mental Health and WellBeing (engage.youth.gov)
Learn more about the Resource Center | SAMHSA
How Right Now
How Right Now is a communications campaign designed to promote and strengthen the
emotional well-being and resiliency of populations adversely affected by COVID-19-related
stress, grief, and loss. The website includes tools and information to help individuals cope and
be resilient.
Access How Right Now resource, visit How Right Now | Finding What Helps (cdc.gov)
MentalHealth.gov
This resource provides one-stop access to mental health and mental health-related problems,
including coping with stress related to the COVID-19 pandemic.
96
Resources for Military Veterans, Service Members, and their Families
Department of Veterans Affairs Treatment Locator
The Department of Veterans Affairs (VA) provides a resource to identify VA treatment locations
or in-network community care providers. Just enter a location (street, city, state, or postal
code), the type of facility, and the type of service for a list of providers.
Department of Veterans Affairs COVID Coach
The COVID Coach app
was created for everyone, including Veterans and Service members, to
support self-care and overall mental health during the COVID-19 pandemic. The app is available
on Apple and Android devices.
Learn more about COVID Coach, visit
COVID Coach | VA Mobile
Department of Veterans Affairs Mindfulness Coach 2 App
Mindfulness Coach 2 was developed to help Veterans, Service Members, and others learn
how to practice mindfulness. The app provides a gradual, self-guided training program
designed to help individuals understand and adopt a simple mindfulness practice.
Mindfulness Coach 2 also offers a library of information about mindfulness, 12 audio-guided
mindfulness exercises, a growing catalog of additional exercises available for free download,
goal-setting and tracking, a mindfulness mastery assessment to help you track your progress
over time, customizable reminders, and access to other support and crisis resources.
Department of
Veterans Affairs National Center for Posttraumatic Stress Disorder
The National Center for Posttraumatic Stress Disorder (PTSD) has strategies that can help with
the stress, grief, and anxiety related to COVID-19. Information is available to support self-care,
the work of providers, and community efforts.
Services and Supports for Longer-Term Impacts of COVID-19
Access information about VA treatment , visit Find VA Locations | Veterans Affairs
National Child Traumatic Stress Network
The National Child Traumatic Stress Network (NCTSN) is federally funded and was created to
raise the standard of care and increase access to services for children and families who
experience or witness traumatic events.
Find resources on supporting children and families impacted by COVID-19, visit Search |
The National Child Traumatic Stress Network (nctsn.org)
Access the Mindfulness Coach 2 app, visit Mindfulness Coach | VA Mobile
97
Services and Supports for Longer-Term Impacts of COVID-19
Learn more about the COVID-19 resources, visit COVID-19: Resources for Managing
Stress - PTSD: National Center for PTSD (va.gov)
Department of Veterans Affairs Veterans Crisis Line
Veterans Crisis Line, text-messaging service, and online chat provides free confidential support
for all Service members, including members of the National Guard and Reserve, and all
Veterans, even if they are not registered with the VA or enrolled in VA health care.
Find support, dial 988, then select 1
Text 838255 from your mobile device
Access the online chat, visit Chat (veteranscrisisline.net)
Department of Veterans Affairs Whole Health Resources
The self-help VA Whole Health app is a free, easy-to-use tool created for Veterans and others
who are ready to take the next step in their Whole Health journey. Available on Apple and
Android devices, Whole Health is the VA’s holistic approach to care that supports your health
and well-being. With this app, you can fill out your personal health inventory, set goals, and
learn more about Whole Health.
Access the Whole Health Mobile app and other on-line resources, visit Mobile Apps and
Online Tools - Whole Health (va.gov)
Department of Defense Treatment Locator
Military hospitals and clinics are found at military bases and posts around the world. They are
also referred to as "military treatment facilities" or "MTFs." Use this resource to find a military
hospital or clinic near you.
Access military treatment facilities, visit Find a Military Hospital or Clinic | TRICARE
Department of Defense Military OneSource
Military OneSource is a free helpline service provided 24-hours-a-day, 7-days-a-week by the
Department of Defense to service members and their families to help with a broad range of
concerns, including possible mental health problems.
Find support, call 1 (800) 342-9647 or visit Support for Military Personnel & Families •
Military OneSource
98
Services and Supports for Longer-Term Impacts of COVID-19
Department of Defense Psychological Health Center of Excellence
The Psychological Health Center of Excellence (PHCoE) provides psychological health research
self-help consultation and expertise to leaders, providers, service members, and their families,
with a helpline available 24 hours-a-day.
Learn more about this service, visit Psychological Health Center of Excellence |
Health.mil or call 1 (866) 966-1020
You may also Live Chat or email the Center at dha.ncr.j-9.mbx.intransition@mail.mil
Department of Defense Psychological Health Resource Center
A free, trusted Department of Defense source of psychological health information and
resources related to how to get into treatment, types of treatment for mental health
conditions, and many other topics. Individuals have access to professional health resource
consultants, all of whom are master's-level mental health clinicians that understand military
culture. This is not a treatment or counseling center, but helps service members, Veterans,
family members, clinicians and commanders to access mental health care.
To find a psychological health resource center, call 1 (866) 966-1020, 24 hours-a-day, 7
days-a-week
Learn more about the Psychological Health Resource Center, visit Crisis Hotlines |
TRICARE
Department of Defense inTransition Program
This is a free confidential program that provides a helpline with specialized coaching and
assistance for service members, National Guard members, reservists, Veterans, and retirees.
Resources are available to those who need access to mental health care when relocating to
another assignment, returning from deployment, transitioning between active duty and reserve
component, preparing to leave military service, or any other time they need a new mental
health provider, or need a provider for the first time.
Talk with an inTransition Program specialist, call 1 (800) 424-7877
Learn more about inTransition, visit inTransition | Health.mil
Indian Health Service Resources
Indian Health Service Mental Health Program
Many tribes run their own mental health programs. The Indian Health Service’s Mental Health
Program is a community-based clinical and preventive service program that provides access to
vital outpatient mental health counseling, dual diagnosis services, mental health crisis response
Services and Supports for Longer-Term Impacts of COVID-19
and triage teams, case management services, community-based prevention programming,
outreach, and health education activities.
Access local treatment, visit IHS Mental Health Programs | Mental Health and check
"Behavioral Health" under "Choose facility types"
Learn more about mental health resources, visit Mental Health | Indian Health Service
(IHS)
Resource for the Healing Process
In Tribal communities, schools, health care services, and tribal programs play an important role
in providing the necessary services to aid in the healing of mental and behavioral health issues
including suicide, substance use, depression, and trauma. These resources are available to
those seeking assistance.
Find behavioral health resources, visit Resources for the Healing Process | Mental
Health (ihs.gov)
Stronghearts Native Helpline
This helpline provides access to a confidential and anonymous domestic, dating, and sexual
violence hotline for American Indian or Alaska Native (AI/AN) individuals, offering support,
referrals, and advocacy. The trained professionals can assist family members or friends of abuse
victims with information to give to loved ones.
Access the Stronghearts Native Helpline, call 1 (844) 762-8483 or 1 (844) 7NATIVE
Learn more about this resource, visit StrongHearts Native Helpline
Suicide Prevention Resources
Depression and suicide affect people of all ages and populations. AI/AN populations experience
a higher rate of suicide than any other group in the United States. If you are experiencing a
crisis, there are options available to help.
Access support resources through Suicide Prevention | Health Topics (ihs.gov)
Treatment Locator for Indian Health Service, Tribal or Urban Indian Health
Program
This online locator and map can be used to find Indian Health Service, Tribal or Urban Indian
Health Program facilities, including behavioral health facilities.
Find local services, visit Find Health Care | Indian Health Service (IHS)
99
100
Two-Spirits and the LGBTQ+ Community
Two-Spirits provides resources for Two-Spirit and LGBTQ+ individuals and loved ones (third
party) within the American Indian and Alaska Native community. Includes information on
finding a provider, community support, mental health care, and legal rights.
Find more information, visit Two-Spirit | Health Resources (ihs.gov)
WERNATIVE
WERNATIVE provides comprehensive health resources and information for Native youth, by
Native youth. It includes information about culture, environment, mental health, physical
health, relationships, life tips, spirituality, wellness, and activism.
Find resources, visit Home - We R Native
Services and Supports for Longer-Term Impacts of COVID-19
Indian Health Service Telebehavioral Health Program
Provides direct, ongoing care via televideo to patients of all ages at IHS, Tribal, and Urban
Indian operated facilities across the country. Current clinical services include: Adult Psychiatry;
Addictions Psychiatry; Geriatric Psychiatry; Child and Adolescent Psychiatry; Adult Therapy;
Family, Couples, and Group Therapy; Child and Adolescent Therapy; and Trauma and PTSD
Therapy.
Learn more about the Telebehavioral Health Program, visit IHS Telebehavioral Health
Center of Excellence (TBHCE)
Find a list of TBHCE sites, visit Current TBHCE Sites | Telebehavioral Health (ihs.gov)
101
Substance Use Supports and Services
The ongoing stress and uncertainty prompted by the
pandemic continues to have an impact on people’s
health and well-being. Increases in substance use and
drug overdoses have emerged in the United States
since the COVID-19 pandemic was declared a national
emergency in March 2020. Research shows that 13%
of Americans started or increased substance use as a
way of dealing with stress or e
motions related to
COVID-19, and people with substance use conditions
are at increased risks for poor COVID-19 outcomes.
The federal government has resources available to
help address substance use issues. This section covers
four topics
8
• Treatment Locators
• Self-Help Resources
• Resources for Military Veteran, Service
Members, and their Families
• Indian Health Service Resources.
Treatment Locators
Behavioral Health Services Treatment Locator
The Locator provides confidential
and anonymous
information for anyone seeking treatment facilities for
substance use challenges and mental health problems.
Not Sure Where to Start?
Q. Are you looking for substance
use treatment?
A. Visit the Behavioral Health
Treatment Services Locator
through Home - SAMHSA
Behavioral Health Treatment
Services Locator
-----------------------------------------------
Q. Do you feel like you need to
talk with someone to figure out
your treatment options?
A. Call the National Helpline at 1
(800) 662-HELP (4357); For TYY
Users Dial 1 (800) 487-4889
This helpline provides free,
confidential information, 24 hours-
a-day, 365 days-a-year, in English
and Spanish, for individuals and
family members facing mental
health conditions and substance
use challenges.
Finding treatment, call 1 (800) 622 HELP (4357) or visit Home | FindTreatment.gov
Buprenorphine Practitioner Locator
This easy-to-use resource helps you to use an interactive map to find practitioners
authorized to treat opioid dependency with buprenorphine by state
.
Find local opioid dependency treatment, visit Buprenorphine Treatment Practitioner
Locator | SAMHSA
Services and Supports for Longer-Term Impacts of COVID-19
102
Opioid Treatment Program Directory
This resource allows you to find opioid treatment programs in your state.
Find opioid treatment programs in your state, visit OTP Directory (samhsa.gov)
Self-Help Resources
Alcohol and COVID-19
Alcohol misuse is a public health c
oncern in the United States.
Access resources about alcohol treatment at Alcohol and COVID-19 | National Institute
on Alcohol Abuse and Alcoholism (NIAAA) (nih.gov)
COVID-19 Information, Support, and Resources
Substance use concerns can make people more likely to become severely ill from COVID-19,
and as such additional precautions are needed for protection against COVID-19.
Find information, support, and resources, visit COVID-19 Information, Support, and
Resources | Drug Overdose | CDC Injury Center
Find additional resources, visit COVID-19 & Substance Use | National Institute on Drug
Abuse (NIDA) (nih.gov)
Resources for Families Coping with Mental
Health Conditions and Substance Use
Challenges
Every family is different, but families may share a bond that can be used to support one
another during trying times including this pandemic. Family support can play a major role in
helping a loved one with mental health conditions and substance use challenges.
Find resources for families, visit Resources for Families Coping with Mental and
Substance Use Disorders | SAMHSA
Services and Supports for Longer-Term Impacts of COVID-19
Alcohol Screening Tool
CDC has launched a new tool for adults to anonymously check their drinking, identify barriers
and motivators for drinking less, and print or save a personalized change plan. This evidence-
based tool is a free resource.
Access the Alcohol Screening Tool, visit Check Your Drinking | Alcohol | CDC
103
Services and Supports for Longer-Term Impacts of COVID-19
Resources on Harm Reduction
Harm reduction practices aim to reduce the harms associated with substance use by providing
non-judgmental services and supports to people who use drugs.
Find resources on harm reduction strategies at Harm Reduction | SAMHSA
Learn about CDC’s National Harm Reduction Technical Assistance Center, visit Home
(cdc.gov)
Find resources on novel harm reduction and treatment strategies to support individuals
with opioid use concerns, visit Harm Reduction - National Council for Mental Wellbeing
(thenationalcouncil.org)
Resources for Military Veterans, Service Members, and their Families
Department of Veterans Affairs Substance Use Treatment for Veterans
If you are struggling with substance use concerns, you are not alone. Many Veterans have
problems with the use of alcohol, tobacco, street drugs, and prescription medicines.
Find out how to get support for substance use concerns, visit Substance Use Treatment
For Veterans | Veterans Affairs (va.gov)
Department of Veterans Affairs Substance Use Resources
The VA has substance use resources, information, treatment options, and more—all accessible to
Veterans, Veterans’ supporters, and the general public. Explore these pages to learn more about a
substance use topic or to find information specifically tailored to your needs.
Find more information on substance use resources, visit Mental Health Home (va.gov)
Department of Veterans Affairs Veterans Crisis Line
Veterans Crisis Line, text-messaging service, and online chat provide free confidential VA
support for all Service members, including members of the National Guard and Reserve, and all
Veterans, even if they are not registered with VA or enrolled in VA health care.
Dial 988, then press 1
Text 838255 from your mobile device
Chat with a representative by visiting Chat (veteranscrisisline.net)
104
Department of Defense Military OneSource
Military OneSource is a free service provided by the Departme
nt of Defense to service
members and their families to help with a broa
d ra
nge of
co
n
ce
r
ns, including possible mental
health problems.
Call and talk anytime, 24 hours-a-day, 7 days-a-week, at 1 (800)-342-9647. For more
information, visit Support for Military Personnel & Families • Military OneSource
Department of Defense Psychological Health Center of Excellence
The Psychological Health Center of Excellence (PHCoE) provides psychological health research
consultation and expertise to leaders, providers, service members, and their families, with a
help line available 24 hours-a-day.
To talk with someone at PHCoE call 1 (866) 966
-1020
You may also Live Chat or email the Center at dha.ncr.j-9[email protected]
For more information about this service, visit Psychological Health Center of Excellence
| Health.mil
Department of Defense Psychological
Health Resource Center
A free
, trusted Department
o
f Defense
source
o
f psychological
health
information
and
res
o
u
rc
e
s
related to how to get into treatment, types of treatment for mental health conditions
and substance use challenges. Provides access to professional health resource consultants, all
of whom are master's-level mental health clinicians that understand military culture. This is not
a treatment or counseling center, but we can help service members, veterans, family members,
clinicians and commanders to access mental health care.
To find a resource center, call 1 (866) 966-1020, 24 hours-a-day, 7 days-a-week
For more information, visit Crisis Hotlines | TRICARE
Services and Supports for Longer-Term Impacts of COVID-19
Department of Veterans Affairs Whole Health Resources
The VA Whole Health app is a free, easy to use tool created for Veterans and others who are
ready to take the next step in their Whole Health journey. Available on Apple and Android
devices, Whole Health is VA’s holistic approach to care that supports health and well-being.
With this app, you can fill out your personal health inventory, set goals, and learn more about
Whole Health.
Learn more about Whole Health, visit Employee Whole Health - Whole Health (va.gov)
105
Learn more about ASAP, visit Alcohol and Substance Abuse Program | Indian Health
Service (IHS)
Indian Health Service’s Mental Health
Program
Find mental health programs in your area, search the IHS Mental Health Programs |
Mental Health
by checking "Behavioral Health" under "Choose facility types"
Learn more, visit Mental Health | Indian Health Service (IHS)
Resources for Substance Use Challenges
Understanding the warning signs, risk factors, and protective factors associated with substance
use challenges are critical to providing effective prevention, intervention, and treatment. This
Indian Health Service page includes information and resources.
Find resources and more information, visit Substance Abuse | Health Topics (ihs.gov)
Resource for the Healing Process
In Tribal communities, schools, healthcare services, and tribal programs play an important role
in providing the necessary services to aid in the healing of mental and behavioral health issues
including suicide, substance use, depression, and trauma.
Find supportive resources, visit Resources for the Healing Process | Mental Health
(ihs.gov)
Services and Supports for Longer-Term Impacts of COVID-19
Indian Health Service Resources
Alcohol and Substance Abuse Program
The Alcohol and Substance Abuse Program (ASAP) is designed to reduce the incidence and
prevalence of alcohol and substance use challenges among AI/AN persons to a level at or below
the general U.S. population. ASAP strives to meet this goal through the implementation of
alcohol and substance use programs within Tribal communities, including emergency
treatment, inpatient and outpatient treatment, and rehabilitation services, in rural and urban
settings.
The Indian Health Service Mental Health Program is a community-based clinical and preventive
service program that provides access to vital outpatient mental health counseling, dual
diagnosis services, mental health crisis response and triage teams, case management services,
community-based prevention programming, outreach, and health education activities.
Services and Supports for Longer-Term Impacts of COVID-19
106
Treatment Locator for Indian Health Service, Tribal or Urban Indian Health
Program
This resource includes a map that can be used to find Indian Health Service, Tribal or Urban
Indian Health Program facilities, including behavioral health facilities.
Identify local treatment, visit Find Health Care | Indian Health Service (IHS)
107
Not Sure Where to Start?
Q. Need help paying COVID-19-
related funeral expenses?
A. Call the Federal Emergency
Management Agency (FEMA) to
see if you are eligible for financial
assistance to cover COVID-19-
related funeral expenses. Toll free
number: (844) 684-6333, Monday-
Friday, 9:00 a.m. to 9:00 p.m. ET. If
you use a relay service, please
provide FEMA with the specific
number assigned to you for the
service so FEMA can follow up with
you about your application.
Multilingual services are also
available.
For more information you may also
want to visit COVID-19 Funeral
Assistance | FEMA.gov
Q. Having problems coping with
your loss?
A. Call the National Helpline at 1
(800) 662-HELP (4357); 1 (800)
487-4889 (TTY)
Access local services through the
Behavioral Health Treatment
Services Locator and visit Home -
SAMHSA Behavioral Health
Treatment Services Locator
Services and Supports for Longer-Term Impacts of COVID-19
• Treatment Locators
• Self-Help Resources
• Caring for Children Who Lost Caregvers
• Survivor Benefits
• Funeral Assistance.
Treatment Locators
Behavioral Health Services Treatment Locator
The Locator provides confidential and anonymous
information for anyone seeking treatment facilities for
substance use challenges and mental health
problems.
Finding treatment, call 1 (800) 622 HELP
(4357) or visit Home | FindTreatment.gov
Bereavement Supports
Millions are coping with the death of loved ones since
the COVID-19 pandemic. One-fifth of Americans had
lost a relative or close friend in early 2021, when
there were roughly half as many deaths from COVID-
19 as today. Providing support and resources to
individuals who have lost loved ones during the
pandemic remains an important priority in the
process of grief and bereavement. People cope with
losses in different ways. If you need bereavement
support or help dealing with your loss, federal
resources are available to help. This section includes
federal supports and services. There are additional
community and state supported services that may be
available to individuals who have lost a loved one.
27
This section covers five topics
108
Self-Help Resources
Resources on Grief and Loss
CDC has resources available that can help you cope with the loss of loved one during the
COVID-19 pandemic.
Learn more information and access resources, visit Grief and Loss (cdc.gov)
Helping Children Cope
CDC provides information for adults on how to help children cope with loss, and help support
their mental health in l
ight of the COVID-19 pandemic.
Learn more information about children and coping, visit Helping Children Cope (cdc.gov)
Bereavement Resources
MedlinePlus links to health information from the National Institutes of Health and other federal
government agencies and provides resources on bereavement, grief, and loss.
Find bereavement resources, visit Bereavement: MedlinePlus
Services and Supports for Longer-Term Impacts of COVID-19
Department of Defense Resources on Understanding Grief
Grief is a natural response with the loss of a loved one. This resources provides tools and
services to help you cope, make informed decisions, grieve in healthy ways, and begin to
envision a life with new opportunities.
How Children Grieve and How Parents and Other Adults Can Support Them
SAMHSA provides a resource for parents and other adults to help children who have suffered
the loss of a parent or loved one.
Learn more on supporting children with grief, visit After a loved one dies - how children
grieve: And how parents and other adults can support them | SAMHSA
Department of Veterans Affairs Bereavement Counseling
If you are the surviving spouse, child, or parent of a service member who died while serving
their country, you may qualify for bereavement counseling through the VA. Bereavement
counseling (also sometimes called “grief counseling”) provides assistance and support for
people going through emotional and psychological stress after the death of a loved one.
Access information about VA Bereavement Counseling, visit Bereavement Counseling |
Veterans Affairs (va.gov)
109
Survivors Benefits
Social Security Survivors Benefits
The Social Security Administration provides information on the basics of survivor benefits, how
to apply, what documents you need, and other related information.
Apply for benefits, call 1 (800) 772-1213 and 1 (800) 325
-0778 (TTY), Monday through
Friday, 8:00 a.m. to 7:00 p.m. ET.
Find the phone number for your local office by using the SSA Social Security Office
Locator here: Social Security Office Locator, SSA Office Locator Social Security Office
Locator, Social Security
Services and Supports for Longer-Term Impacts of COVID-19
Find more bereavement resources, visit Grief and Loss • Bereavement • Military
OneSource
Coping with Grief: Life after Loss
This resource from the National Institute of Mental Health provides information on adapting to
loss, types of grief, and discusses life beyond the loss of a loved one.
Learn more about coping with grief, visit Coping With Grief | NIH News in Health
Caring for Children Who Lost Caregivers
Children Who Have Lost a Parent or Caregiver to COVID-19
Thousands of children in the United States have lost a parent or caregiver during the COVID-19
pandemic. These children have experienced the deaths of one or both parents, and
grandparent caregivers. CDC and the Administration for Children and Families, Children’s
Bureau has resources about family-based care support services and protecting children who
experienced the loss of a parent or caregiver.
9
Find additional information: Children: The Hidden Pandemic 2021. A joint report of
COVID-19 associated orphanhood and a strategy for action (cdc.gov)
Learn more about global orphanhood: Global Orphanhood Associated with COVID-19 |
CDC
Child Welfare Information Gateway provides information and resources on a wide range
of child welfare topics, covering the continuum from preventing child abuse and neglect
through adoption. To support professionals working with children and families involved
with child welfare, we offer current information, research, statistics, best practices, and
other materials. Access information and resources on child welfare topics, visit Topics -
Child Welfare Information Gateway

Services and Supports for Longer-Term Impacts of COVID-19
110
Learn more about the basics of survivor benefits, visit Survivors Benefits | SSA
Funeral Assistance
COVID-19 Funeral Assistance
If you are responsible for COVID-19-related funeral expenses, the Federal Emergency
Management Agency (FEMA) may be able to help.
Call FEMA’s toll-free helpline to learn more and apply for assistance: (844) 684-6333,
Monday through Friday, 9:00 a.m. to 9:00 p.m. ET
If you use a relay service, please provide FEMA with the specific number assigned to you
for the service so FEMA can follow up with you about your application
Multilingual services are also available
Find additional information and visit COVID-19 Funeral Assistance | FEMA.gov
111
References
1. Panchal N, Kamal R, Fox C, Garfield R. The implications of COVID-19 for mental health
and substance use, Kaiser Family Foundation Web site. Published Feb 10, 2021.
Accessed June 1, 2022. https://www.kff.org/report- section/the-implications-of-
covid-19-for-mental-health-and-substance-use-issue-brief.
2. Czeisler MÉ , Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal
ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR
Morb Mortal Wkly Rep. 2020;69:1049–1057.
https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm?s_cid=mm6932a1_w.
3. American Psychiatric Association. New APA poll shows sustained anxiety among
Americans; more than half of parents are concerned about the mental well-being of
their children. American Psychiatric Association Web site. Published May 2, 2021.
Accessed June 1, 2022.https://www.psychiatry.org/newsroom/news-releases/new-
apa- poll-shows-sustained-anxiety-among-americans-more-than-half-of-parents-are-
concerned-about-the-mental-well-being-of-their-children
.
4. U.S. Surgeon General Advisory. Protecting Youth Mental Health. The U.S.
Surgeon General’s Advisory Web site. Published 2021. Accessed June 1, 2022.
https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-
advisory.pdf.
5. National Institute of Drug Abuse (NIDA). COVID-19 & Substance Use. National
Institute of Drug Abuse Web site. Published February 25, 2022. Accessed June
1, 2022.
https://nida.nih.gov/drug-topics/comorbidity/covid-19-substance-use.
8. Czeisl
er MÉ, Lane RI, Petrosky E, et al. Mental
health, substance use, and suicidal ideation
during the COVID-19 pandemic — United St
ates,
June 24–30, 2020. MMWR Morb Mortal
Wkly Rep. 2020;69:1049–
1057. http://dx.doi.org/10.15585/mmwr.mm6932a1
9. Hills S, Blenkinsop A, Villaveces A. COVID-19 Associated orphanhood and caregiver death
in the United States. Ped. 2021;148(6):e2021053760. https://doi.org/10.1542/
peds.2021-053760
Services and Supports for Longer-Term Impacts of COVID-19
6.
7.
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of
depression symptoms in U.S. adults before and during the COVID-19 pandemic. JAM A
Netw Open. 2020;3(9):e2019686.
Panchal N, Kamal R, Cox C. The implications of COVID-19 for mental health and substance
use. Kaiser Family Fund website. Published February 10, 2021. Accessed June 20, 2022.
https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-
mental-health-and-substance-use/
112
Chapter 5: Future Directions
On April 5, 2022, President Biden pledged to harness the full potential of the federal
government in coordination with public and private sector partners to respond to the longer-
term effects of COVID-19 fully and effectively. The President emphasized a strong
commitment to ensuring that individuals, families, and communities affected by COVID-19
and Long COVID have access to programs and resources to help support healing, health, and
well-being.
The Services and Supports for Longer-Term Impacts of COVID-19 Report is an important
component of the overall federal response. It provides resources that are relevant to
individuals with Long COVID, health care personnel addressing the needs of those with Long
COVID, and individuals and their families who are experiencing the longer-term effects of
COVID-19. To address the longer-term effects of COVID-19, the report includes supports and
services that can help address mental health and substance use challenges that have
escalated during the pandemic. The report also includes a section on resources for those
mourning the loss of their loved ones.
This report compiles federal services and
supports into one document. It includes a
description of the resources as well as
information on how to access them. For each
of the resources, a website or phone number is
provided.
“People experiencing Long COVID
symptoms don’t know where to go.
Even when there is a COVID-19
specialist nearby, the wait is 6-12
months for an initial visit.”
—Person with Long COVID
Services and Supports for Longer-Term Impacts of COVID-19
The Department of Health and Human Services
hosted a series of interactive listening sessions
to inform the development of this Report and its companion report, the National Research
Action Plan on Long COVID. The sessions included a broad range of participants, including
persons affected by Long COVID, researchers, health care personnel, organizations representing
health care professionals, public health partners, and advocacy organizations. In parallel, the
Department of Health and Human Services’ Office of the Assistant Secretary for Health ran its
Health+™, pronounced “health plus,” research model for human-centered design. This Health+
Long COVID cycle involves over 1,000 hours of patient interviews, workshops, listening sessions,
and human-centered research to co-create solutions with—not for—those impacted by Long
COVID. The Health+ model positions people as active participants—experts in their own life
challenges—listening and learning from their lived experiences, to uncover their needs and
understand their challenges.
Across listening sessions and Health+ engagements, stakeholders repeatedly emphasized the
need for accessible supports and services. They indicated that a compilation of these resources
could help lessen the burden of COVID-19 on individuals and their families.
113
It is worth repeating that this report is only the first step. In the coming months, the
information within this report will be posted on federal websites. Navigable web pages will
help individuals and others affected by COVID-19 and Long COVID quickly and efficiently find
services and supports. Printable fact sheets will help health care personnel connect the people
they serve to the resources they need. At the same time, the implementation of the National
Research Action Plan will inform the development and deployment of additional resources. The
work of the federal government will continue to support individuals and communities
experiencing the longer-term effects of the ongoing COVID-19 pandemic.
Engagement of Public and Private Stakeholders in the
Development of the Report
Listening Session with Stakeholders
Informed both Reports
Listening sessions included:
A few of the most common messages heard
during the listening sessions are
summarized below.
Increase Awareness of Long
COVID, Behavioral Health
Challenges, and Bereavement
During the listening session, a recurring
theme was that more information needs to
be available and accessible about the longer-
term effects of COVID-19. Many
acknowledged that a part of the population
remains skeptical about COVID-19 generally.
With the combination of lack of information
and skepticism, many people do not know
what is happening to them when they
experience symptoms. They can feel alone,
frightened, and sometimes ashamed.
Several suggested that establishing a central
location for information, such as a national
website, would be a step in the right
direction. It would allow individuals
experiencing Long COVID and other
problems related to the pandemic and
others to have confidence in the source of
information.
Services and Supports for Longer-Term Impacts of COVID-19
• Long COVID advocates
• Disability and chronic illness advocates
• Provider groups and organizations
(health care organizations
and
systems, community health centers,
mental health, hospitals)
• Researchers, including patient
researchers
• Public health partners
• Professional organizations
• Mental health advocates
• Children’s advocates.

114
Make Information, Services, and Supports Available to People with
Affected by the Pandemic
—Parent of a child with Long
COVID
Many individuals affected by the pandemic, including Long COVID, are not getting the services
they require and are at risk of losing their jobs, their homes, and their families. For example,
participants in the listening session voiced their experiences with community service providers
and their health care providers being reluctant to label their Long COVID symptoms as being a
disability. They noted that many of the people who administer public support programs are not
aware that Long COVID can cause disabilities.
They mistakenly assume they cannot help people
with Long COVID by providing financial assistance and other supports. Further, several
individuals reported that their employers were unwilling to make workplace accommodations,
such as allowing them to telework from home, they had no recourse, and they lost their jobs.
Clarify that Long COVID can be a Post-Infectious Condition
Many reported that health care providers were too quick to dismiss or ignore some of the
features of Long COVID. Features of Long COVID overlap with many mental health conditions,
and health care providers need to be able to identify Long COVID to help people manage their
symptoms. One person noted that current depression and anxiety disorder screening questions
Services and Supports for Longer-Term Impacts of COVID-19
Increase Attention on the Impact of the
Pandemic on Children
Participants in the listening sessions identified the lack of information, research, and education
about children with Long COVID as a high priority area to address. Many parents of children
with Long COVID and other consequences of the pandemic talked about their frustration with
having their pediatricians and school administrators tell them that anxiety disorder, depression,
or puberty were to blame for their children’s Long COVID symptoms. Many parents re
ported
feeling helpless when their children’s doctors wrongly indicated that Long COVID does not occur
in children.
Additional Services and Supports for
those Experiencing Longer-term
Impact of the Pandemic Including
Bereavement
Participants in the listening sessions acknowledged the
profound impact of the death of a loved one and the
reality that some of us experienced numerous losses
without time to process and grieve. The loss of a loved one
can impact a sense of financial security, cause depression
and loneliness, and underscores the need to take
intentional action. Participants suggested expanded
mental health services, particulary school based services, creation of a registry of providers who can support those
in need of grief counseling, to focus particularly on the communities hardest hit by the pandemic including the black
and American Indican/Alaskan Native communities.
“Parents seeking Long COVID care for
their children do not have relevant
information to challenge pediatricians
or teachers who dismiss children’s
symptoms as puberty, growing pains,
or moodiness.”
115
may falsely classify individuals with Long COVID as having a mental illness (or vice versa) and
may miss the association with having had COVID-19. Another person related that emergency
department staff informed her that rapid heartbeat, anxiety about her health, and
hopelessness were indications of an anxiety disorder rather than recognizing these as common
features of Long COVID.
Ensure that Services are Accessible, Culturally Informed and
Linguistically Effective
Many of the individuals in the listening sessions emphasized that communications should be
accessible, clear, and provided in the language of the population served. People from racial and
ethnic minority groups and the LGBTQI+ community discussed the barriers to receiving services
in their communities. They described the stigma
, racism, ableism, and provider bias within
their communities regarding COVID-19. They noted the lack of COVID-19 research with diverse
populations and the lack of providers who work close by and are able and willing to work with
non-English speakers. People with disabil
ities are experiencing barriers in receiving services,
including long wait times, and problems with access and safety.
Reduce Long Waits
for Services
A critical workforce shortage exists within the health care system. Not enough providers are
available to serve the needs of the anticipated number of individuals experiencing Long COVID
symptoms. People with Long COVID reported
waiting 4 to 12 months for an initial
appointment with a medical specialist, such as a
neuropsychologist, cardiologists, or
pulmonologist. An individual shared that very
few medical care providers have
multidisciplinary practices, so they were forced
to visit four to five different provider’s offices
when they were so tired they could hardly walk.
Listening session participants highly
recommended telemedicine and clear guidance
about how to access immediate care. Several
people urged that states eliminate barriers to cross-state telehealth and expand cell phone
coverage in rural areas.
Services and Supports for Longer-Term Impacts of COVID-19
“I got COVID-19 and I was embarrassed
that I continued to have symptoms
after the 14 day quarantine. I am 70
years old. I doubted my own symptoms
for so long. I was afraid to even go to
my doctor because I thought they
wouldn’t believe me.”
—Person with Long COVID
Provide Clinical Guidance and Support
for Healthcare Personnel
Health care personnel who participated in the l
istening sessions reported the need for guidance
on how to address the multiple needs of patients with pandemic consequences. They reported
treating individual symptoms without having a clear understanding of how to address the
overall condition. Very few said that they worked within a Long COVID medical center, and so
they felt overwhelmed by the number of people coming to see them since the pandemic
116
Services and Supports for Longer-Term Impacts of COVID-19
started. They voiced the need for clinical
guidance on care coordination and referrals
for Long COVID patients. They identified
needs for continuing education on topics
such as common post-infectious conditions
and common Long COVID symptoms, and
treatment.
COVID-19 has exacerbated existing shortages
in health care personnel, and a critical
imperative remains to grow, support, retain,
and efficiently deploy the health care
workforce. In particular, it is important to
identify which factors (e.g., wages,
opportunity for career advancement,
schedule flexibility, engagement) and which
system-level strategies (e.g., education,
staffing and safety policies, coaching) can
improve the job satisfaction, engagement,
and well-being of the health care workforce.
Challenges with
Addressing the Longer-
Term Impacts of COVID-
19
Influenced by the public listening sessions, 14
U.S. government departments and agencies
coordinated to draft this report.
Departments identified current supports and
services available for those experiencing Long COVID and the longer-term effects of COVID-19.
Many of the resources existed before the pandemic and offer services and supports to
individuals and their family members who have disabilities. Depending on their level of
disability and need, many individuals experiencing the longer-term effects of COVID-19 can
access these programs to meet their needs.
As part of their work in compiling this report, federal departments also identified challenges to
ensuring accessible resources to those in need. The five challenges most commonly reported by
federal departments were lack of awareness; difficulties reaching individuals and families due
to COVID-19 precautions; statutory limitations; limited resources; and insufficient data. The U.S.
government will work to address each of these challenges. These challenges provide an
opportunity for federal departments and agencies to improve services and supports.
Federal Government Efforts That
Will Improve Identification of Long
COVID and Connect Patients to Care
• Convene public and private partners to
better align the definitions of Long
COVID and develop agreed upon
terminology for clinical care,
surveillance, and research
• Develop comprehensive and equitable
Long COVID diagnosis, care, and
treatment guidance
• Make available tools to help individuals
recognize symptoms of Long COVID and
to discuss their symptoms with their
health care providers
• Advance research that helps separate
the broader effects of the pandemic on
an individual’s physical and mental
health from those of the initial SARS-
CoV-2 infection and re-infections
• Use findings from Health+ Long COVID
patient-centered research to improve
the way individuals access and receive
health care and services.

117
Services and Supports for Longer-Term Impacts of COVID-19
Lack of Awareness
Public awareness of the full range of government services and supports for individuals
experiencing longer-term effects of the ongoing pandemic remains limited. Individuals
experiencing the impacts of COVID-19, their family members, health care providers, schools,
employers, and state agencies that administer federally-funded programs may be unaware of
the resources and services available through U.S. government programs. Many were also
unaware of changes to eligibility criteria for these programs that now allow for individuals with
Long COVID to participate. Other times, individuals may know about a resource but not know
how to access it. Expanding awareness will require enhanced coordination and outreach to
ensure consistency in various activities and programs.
Difficulties Reaching Individuals and Families
Some federal programs leverage technology to create flexible ways of connecting with
individuals. Other programs have difficulty maintaining sufficient engagement with patients
through remote settings. The problem has persisted and created a gap in services and supports,
especially among those focused on recovery support services for substance use concerns.
The COVID-19 pandemic expanded how federal agencies use technology to engage with clients,
and efforts are underway to determine how technology can be further and effectively
leveraged.
Insufficient Data
We are only beginning to understand the exact nature of Long COVID. Insufficient data about
the longer-term impacts of COVID-19 make it difficult to accurately inform federal programs
serving target populations. For example, some people have well-recognized longer-term
illnesses related to COVID-19, such as myocarditis, lung fibrosis, or diabetes. Management of
these illnesses can follow established medical approaches. Others with Long COVID may
experience non-specific symptoms, such as periodic fatigue, “brain fog,” or anxiety, which can
be more challenging to recognize and manage. Enhancing the capacity to capture and analyze
data may accelerate learning about how to prevent, diagnose, and manage the longer-term
effects of COVID-19. As the evidence accumulates, living evidence reviews, guidelines, and
clinical decision supports will need to be developed so that individuals and their families receive
the full array of services and supports that they need. With more knowledge from persons
affected by Long COVID, based on their experiences of living with it, programs can offer
relevant and needed services.
Limited Resources
Limited resources, such as staffing or funding, limit the impact of programs. The most common
gap identified was created due to stagnant funding levels. Understanding and articulating the
impact of these limited resources will support future requets to Congress for funding to address

118
Services and Supports for Longer-Term Impacts of COVID-19
the longer-term impact of COVID-19, including Long COVID and associated conditions, mental
health and substance use challenges, and bereavement.
The National Research Action Plan on Long COVID
The companion document to this report, the National Research Action Plan on Long COVID, will
be essential in advancing progress in the provision of services and supports for individuals and
families experiencing Long COVID.
Understanding the need for and access to services and supports, including disability services
and caregiver supports, is part of the National Research Action Plan. Research must identify
strategies to address the pandemic’s disproportionate impact on certain communities and
populations. We must identify ways to translate research into equitable service delivery.
Qualitative and quantitative research methods are complementary for a more complete
understanding of the health and socioeconomic burdens on individuals affected by COVID-19,
and among different races, ethnicity groups, pregnant people, and those with underlying
disabilities.
Conclusion
Although we are still learning about Long COVID and the longer-term impacts of COVID-19, a lot
has been done, and there are substantial services and supports through many U.S. government
programs to support those affected. This report is the first iteration of a compendium of
supports for use by individuals, communities, and health enterprises. In upcoming months and
years, the U.S. government will continue to invest in supports and further refine the scope of
services as we learn more through lived experiences and research about Long COVID and the
other longer-term impacts of COVID-19.
Moving forward, federal departments will continue to engage with partners, including state and
local governments. Engagement of nongovernmental experts, organizations, and stakeholders,
including individuals affected directly by the longer-term effects of COVID-19, has played an
essential role in shaping the government’s response to COVID-19 and Long COVID, including the
development of this Report and the National Research Action Plan.

119
Appendix A: Report Abbreviations
AAA
ACA
ADA
ADAKTC
ADRC
AHRQ
AI/AN
ASAP
AT
CAA
CCDF
CDC
CDS
CED
CHIP
CHR
CIL
CMS
COBRA
COCA
CoP
COVID-19
CSL
Area Agency on Aging
Affordable Care Act
Americans with Disabilities Act
ADA Knowledge Translation Center
Aging and Disability Resource Center
Agency for Healthcare Research and Quality, HHS
American Indian, Alaska Native
Alcohol and Substance Abuse Program
Assistive Technology
Community Action Agencies
Child Care and Development Fund
Centers for Disease Control and Prevention, HHS
Clinical Decision Support
Community Economic Development
Children’s Health Insurance Program
Community Health Representative
Center for Independent Living
Centers for Medicare & Medicaid Services, HHS
Consolidated Omnibus Budget Reconciliation Act
Clinician Outreach and Community Activity
Community of Practice
Coronavirus disease 2019
Caregivers Support Line
Caregiver Support Program
CSP
Services and Supports for Longer-Term Impacts of COVID-19

120
DBH
DHS
DIAL
DOD
DOJ
DSM
DTAC
EAP
EARN
EBSA
ECHO
EEOC
EHV
EIC
EITC
EPC
F2F
FAPE
FDA
FDPIR
FEHB
FEMA
FHCSD
FHIR
FQHC
Division of Behavioral Health, IHS, HHS
Department of Homeland Security
Disability Information and Access Line
Department of Defense
Department of Justice
Diagnostic and Statistical Manual of Mental Disorders
Disaster Technical Assistance Center
Employee Assistance Program
Employer Assistance and Resource Network on Disability
Inclusion
Employee Benefits Security Administration
Extension for Community Healthcare Outcomes
Equal Employment Opportunity Commission Emergency
Housing Voucher
Earned Income Credit
Earned Income Tax Credit
Evidence-based Practice Center
Family-to-Family
Free Appropriate Public Education
Food and Drug Administration, HHS
Food Distribution Program on Indian Reservations
Federal Employees Health Benefits
Federal Emergency Management Agency, DHS
Family Health Centers of San Diego
Fast Healthcare Interoperability Resources
Federally Qualified Health Center
Fiscal Year
FY
Services and Supports for Longer-Term Impacts of COVID-19

121
HAF
HCBS
HHS
HIV/AIDS
HRS&D
HRSA
HUD
IDEA
IHS
IPT
IT
JAN
LC&FIRP
LIHEAP
LIHWAP
LTCOP
MCC
ME/CFS
MHS
MLN
M
TF
NADTC
NCCSD
NEAR
Homeowner Assistance Fund
Home and Community-Based Services
Department of Health and Human Services
Human Immunodeficiency Virus / Acquired
Immunodeficiency Syndrome
Health Services Research and Development
Health Resources and Services Administration, HHS
Department of Housing and Urban Development
Individuals with Disability Education Act
Indian Health Service, HHS
Integrated Practice Team
Information Technology
Job Accommodations Network
Long COVID and Fatiguing Illness Recovery Program
Low Income Home Energy Assistance Program
Low Income Household Water Assistance Program
Long-Term Care Ombudsman Program
Multiple Chronic Conditions
Myalgic Encephalomyelitis, Chronic Fatigue Syndrome
Military Health System
Medicare Learning Network
Medical Treatment Facility
National Aging and Disability Transportation Center
National Center for College Students with Disabilities
National Energy Assistance Referral
National Family Caregiver Support Program
National Institutes of Health, HHS
NFCSP
Services and Supports for Longer-Term Impacts of COVID-19
NIH

122
NPTC
NSLP
OAA
OCR
P&A
PABSS
PASC
PCC
PCOR
PCP
PHCoE
PMG
PMHCA
PTI
PTSD
QPR
RECOVER
RESEA
RHC
SAMHSA
SARS-CoV-2
SDOH
SEA
SHIP
National Pharmacy and Therapeutics Committee N
ational
School Lunch Program
Older Americans Act
Office for Civil Rights
Protection and Advocacy System
Protection and Advocacy for Beneficiaries of Social
Security Post-Acute Sequelae of COVID-19
Post-COVID Conditions
Patient-Centered Outcomes Research
Primary Care Provider
Psychological Health Center of Excellence
Practice Management Guide
Pediatric Mental Health Care Access
Parent Training and Information Centers
Post-Traumatic Stress Disorder
Question, Persuade, and Refer
Researching COVID to Enhance Recovery
Reemployment Services and Eligibility Assessment
Rural Health Clinic
Substance Abuse and Mental Health Services
Administration, HHS
Severe Acute Respiratory Syndrome Coronavirus 2
Social Determinants of Health
Self-Employment Assistance
State Health Insurance Assistance Program Supplemental
Supplemental Nutrition Assistance Program
Social Security Administration
Social Security Disability Insurance
SNAP
Services and Supports for Longer-Term Impacts of COVID-19
SSA
SSDI

123
SSI
TANF
T
E
FAP
TTELP
TTY
UCFE
UCX
USDA
VA
VR
WIC
WIPA
Supplemental Security Income
Temporary
Assistance for Needy Families
The Emergency Food Assistance Program Telehealth
Technology-Enabled Learning Program Teletypewriter
Teletypewriter
Unemployment Compensation for Federal Employees
Unemployment Compensation for Ex-Service members
Department of Agriculture
Department of Veterans Affairs
Vocational Rehabilitation
Women, Infants, and Childre
n
Work Incentives Planning and Assistance
Services and Supports for Longer-Term Impacts of COVID-19
124
Appendix B: Contributing U.S.
Government Departments
Departments
Department of Defense (DOD) Department of Labor (DOL)
Department of Education (ED)
Department of the Treasury
(DOT)
Department of Energy (DOE)
Department of Veterans Affairs
(VA)
Department of Health and
Human Services (HHS)*
National Council on Disability
(NCD)
Department of Homeland
Security (DHS)
Federal Emergency
Management Agency (FEMA)
Office of Personnel
Management (OPM)
Department of Housing and
Urban Development (HUD)
Social Security Administration
(SSA)
Department of Justice (DOJ)
HHS Divisions
Administration for Children and Families (ACF)
Administration for Community Living (ACL)
Agency for Healthcare Research and Quality (AHRQ)
Centers for Disease Control and Prevention (CDC)
Centers for Medicare & Medicaid Services (CMS)
Food and Drug Administration (FDA)
Health Resources and Services Administration (HRSA)
Indian Health Service (IHS)
National Institutes of Health (NIH)
Office for Civil Rights (OCR)
Office of Global Affairs (OGA)
Office of Intergovernmental and External Affairs (IEA)
*
Office of
the Assistant Secretary for Administration (ASA)
Office of the Assistant Secretary for Health (OASH)
Office of the Assistant Secretary for Planning and
Evaluation (ASPE)
Office of the Assistant Secretary for Preparedness and
Response (ASPR)
Office of the Secretary (IOS)
Office of the Surgeon General (OSG)
Substance Abuse and Mental Health Services
Administration (SAMHSA)
Services and Supports for Longer-Term Impacts of COVID-19
Equal Employment Opportunity
Commission (EEOC)
