
INTERNATIONAL COUNCIL FOR HARMONISATION OF TECHNICAL
REQUIREMENTS FOR PHARMACEUTICALS FOR HUMAN USE
ICH HARMONISED GUIDELINE
GOOD CLINICAL PRACTICE (GCP)
E6(R3)
Draft version
Endorsed on 19 May 2023
Currently under public consultation
At Step 2 of the ICH Process, a consensus draft text or guideline, agreed by the appropriate
ICH Expert Working Group, is transmitted by the ICH Assembly to the regulatory authorities
of the ICH regions for internal and external consultation, according to national or regional
procedures.
ii
E6(R3)
Document History
Code
History
Date
E6
Approval by the Steering Committee under Step 2
and release for public consultation.
27 April 1995
E6
Approval by the Steering Committee under Step 4
and recommended for adoption to the three ICH
regulatory bodies.
1 May 1996
E6(R1)
Approval by the Steering Committee of Post-Step 4
editorial corrections.
10 June 1996
E6(R2)
Adoption by the Regulatory Members of the ICH
Assembly under Step 4. Integrated Addendum to
ICH E6(R1) document. Changes are integrated
directly into the following sections of the parental
Guideline: Introduction, 1.63, 1.64, 1.65, 2.10, 2.13,
4.2.5, 4.2.6, 4.9.0, 5.0, 5.0.1, 5.0.2, 5.0.3, 5.0.4,
5.0.5, 5.0.6, 5.0.7, 5.2.2, 5.5.3 (a), 5.5.3 (b), 5.5.3 (h),
5.18.3, 5.18.6 (e), 5.18.7, 5.20.1, 8.1
9 November 2016
E6(R3)
Endorsement by the Members of the ICH Assembly
under Step 2 and release for public consultation.
19 May 2023
Legal notice: This document is protected by copyright and may, with the exception of the ICH logo, be
used, reproduced, incorporated into other works, adapted, modified, translated or distributed under a
public license provided that ICH's copyright in the document is acknowledged at all times. In case of
any adaption, modification or translation of the document, reasonable steps must be taken to clearly
label, demarcate or otherwise identify that changes were made to or based on the original document.
Any impression that the adaption, modification or translation of the original document is endorsed or
sponsored by the ICH must be avoided.
The document is provided "as is" without warranty of any kind. In no event shall the ICH or the authors
of the original document be liable for any claim, damages or other liability arising from the use of the
document.
The above-mentioned permissions do not apply to content supplied by third parties. Therefore, for
documents where the copyright vests in a third party, permission for reproduction must be obtained
from this copyright holder.
ICH E6(R3) Guideline
i
ICH HARMONISED GUIDELINE
GOOD CLINICAL PRACTICE (GCP)
E6(R3)
ICH Consensus Guideline
TABLE OF CONTENTS
I. INTRODUCTION........................................................................................................ 1
Guideline Scope ........................................................................................................................ 1
Guideline Structure ................................................................................................................. 1
II. PRINCIPLES OF ICH GCP ....................................................................................... 2
III. ANNEX 1 ...................................................................................................................... 7
1. INSTITUTIONAL REVIEW BOARD/INDEPENDENT ETHICS COMMITTEE
(IRB/IEC)...................................................................................................................... 7
1.1 Responsibilities ............................................................................................................. 7
1.2 Composition, Functions and Operations ................................................................... 9
1.3 Procedures .................................................................................................................... 9
1.4 Records........................................................................................................................ 10
1.5 Submission and Communication .............................................................................. 11
2. INVESTIGATOR ...................................................................................................... 11
2.1 Qualifications and Training ...................................................................................... 11
2.2 Resources .................................................................................................................... 11
2.3 Responsibilities ........................................................................................................... 11
2.4 Communication with IRB/IEC ................................................................................. 12
2.5 Compliance with Protocol ......................................................................................... 12
2.6 Premature Termination or Suspension of a Trial ................................................... 13
2.7 Participant Medical Care and Safety Reporting..................................................... 13
2.7.1 Medical Care of Trial Participants ........................................................... 13
2.7.2 Safety Reporting ........................................................................................ 14
2.8 Informed Consent of Trial Participants .................................................................. 14
2.9 End of Participation in a Clinical Trial ................................................................... 18
2.10 Investigational Product Management ...................................................................... 19
2.11 Randomisation Procedures and Unblinding ........................................................... 19
ICH E6(R3) Guideline
ii
2.12 Records........................................................................................................................ 20
2.13 Clinical Trial/Study Reports ..................................................................................... 21
3. SPONSOR ................................................................................................................... 22
3.1 Trial Design ................................................................................................................ 22
3.2 Resources .................................................................................................................... 22
3.3 Allocation of Activities ............................................................................................... 22
3.4 Qualification and Training........................................................................................ 22
3.4.1 Medical Expertise ...................................................................................... 22
3.5 Financing .................................................................................................................... 23
3.6 Agreements ................................................................................................................. 23
3.7 Investigator Selection................................................................................................. 24
3.8 Communication with IRB/IEC and Regulatory Authority(ies) ............................ 24
3.8.1 Notification/Submission to Regulatory Authority(ies) .............................. 24
3.8.2 Confirmation of Review by IRB/IEC ......................................................... 25
3.9 Sponsor Oversight ...................................................................................................... 25
3.10 Quality Management ................................................................................................. 26
3.10.1 Risk Management ...................................................................................... 26
3.11 Quality Assurance and Quality Control .................................................................. 27
3.11.1 Quality Assurance ..................................................................................... 27
3.11.2 Audit .......................................................................................................... 27
3.11.3 Quality Control .......................................................................................... 28
3.11.4 Monitoring ................................................................................................. 28
3.12 Noncompliance ........................................................................................................... 33
3.13 Safety Assessment and Reporting............................................................................. 33
3.13.1 Sponsor Review of Safety Information ...................................................... 34
3.13.2 Safety Reporting ....................................................................................... 34
3.13.3 Managingan Immediate Hazard ................................................................ 35
3.14 Insurance/Indemnification/Compensation to Participants and Investigators ..... 35
3.15 Investigational Product(s) ......................................................................................... 35
3.15.1 Information on Investigational Product(s) ................................................ 35
3.15.2 Manufacturing, Packaging, Labelling and Coding Investigational
Product(s) ............................................................................................................. 35
ICH E6(R3) Guideline
iii
3.15.3 Supplying and Handling Investigational Product(s) ................................. 36
3.16 Data and Records ....................................................................................................... 37
3.16.1 Data Handling ........................................................................................... 37
3.16.2 Statistical Programming and Data Analysis ............................................. 41
3.16.3 Record Keeping and Retention .................................................................. 41
3.16.4 Record Access ............................................................................................ 42
3.17 Reports ........................................................................................................................ 42
3.17.1 Premature Termination or Suspension of a Trial ..................................... 42
3.17.2 Clinical Trial/Study Reports ...................................................................... 42
4. DATA GOVERNANCE – INVESTIGATOR AND SPONSOR ............................ 43
4.1 Safeguard Blinding in Data Governance ................................................................. 43
4.2 Data Life Cycle Elements .......................................................................................... 44
4.2.1 Data Capture ............................................................................................. 44
4.2.2 Relevant Metadata, Including Audit Trails ............................................... 44
4.2.3 Review of Data and Metadata ................................................................... 45
4.2.4 Data Corrections ....................................................................................... 45
4.2.5 Data Transfer, Exchange and Migration .................................................. 45
4.2.6 Finalisation of Data Sets Prior to Analysis ............................................... 45
4.3 Computerised Systems............................................................................................... 45
4.3.1 Procedures for the Use of Computerised Systems ..................................... 46
4.3.2 Training ..................................................................................................... 46
4.4 Security of Computerised Systems ........................................................................... 46
4.5 Validation of Computerised Systems ....................................................................... 46
4.6 System Failure ............................................................................................................ 47
4.7 Technical Support ...................................................................................................... 47
4.8 User Management ...................................................................................................... 48
GLOSSARY............................................................................................................................ 49
APPENDICES ........................................................................................................................ 58
Appendix A. INVESTIGATOR’S BROCHURE ................................................................ 58
A.1 Introduction ................................................................................................................ 58
A.2 General Considerations ............................................................................................. 59
A.2.1 Title Page .................................................................................................. 59
ICH E6(R3) Guideline
iv
A.2.2 Confidentiality Statement .......................................................................... 59
A.3 Contents of the Investigator’s Brochure .................................................................. 59
A.3.1 Table of Contents ....................................................................................... 59
A.3.2 Summary .................................................................................................... 59
A.3.3 Introduction ............................................................................................... 59
A.3.4 Physical, Chemical and Pharmaceutical Properties and Formulation .... 59
A.3.5 Nonclinical Studies .................................................................................... 60
A.3.6 Effects in Humans ...................................................................................... 61
A.3.7 Summary of Data and Guidance for the Investigator ............................... 62
Appendix B. CLINICAL TRIAL PROTOCOL AND PROTOCOL AMENDMENT(S)
...................................................................................................................................... 64
B.1 General Information .................................................................................................. 64
B.2 Background Information .......................................................................................... 64
B.3 Trial Objectives and Purpose ................................................................................... 64
B.4 Trial Design ................................................................................................................ 65
B.5 Selection of Participants ............................................................................................ 65
B.6 Withdrawal of Consent or Discontinuation of Participation ................................. 65
B.7 Treatment and Interventions for Participants ........................................................ 66
B.8 Assessment of Efficacy ............................................................................................... 66
B.9 Assessment of Safety .................................................................................................. 66
B.10 Statistical Considerations .......................................................................................... 66
B.11 Direct Access to Source Records .............................................................................. 67
B.12 Quality Control and Quality Assurance .................................................................. 67
B.13 Ethics ........................................................................................................................... 67
B.14 Data Handling and Record Keeping ........................................................................ 67
B.15 Financing and Insurance ........................................................................................... 67
B.16 Publication Policy....................................................................................................... 67
Appendix C. ESSENTIAL RECORDS FOR THE CONDUCT OF A CLINICAL TRIAL
...................................................................................................................................... 68
C.1 Introduction ................................................................................................................ 68
C.2 Management of Essential Records ........................................................................... 68
C.3 Essentiality of Trial Records ..................................................................................... 69
1

ICH E6(R3) Guideline
1
I. INTRODUCTION
1
Good Clinical Practice (GCP) is an international, ethical, scientific and quality standard for the
2
conduct of trials that involve human participants. Clinical trials conducted in accordance with
3
this standard will help to assure that the rights, safety and well-being of trial participants are
4
protected; that the conduct is consistent with the principles that have their origin in the
5
Declaration of Helsinki; and that the clinical trial results are reliable. The term “trial conduct”
6
in this document includes processes from planning to reporting, including planning, initiating,
7
performing, recording, oversight, evaluation, analysis and reporting activities as appropriate.
8
The objective of this ICH GCP Guideline is to provide a unified standard to facilitate the mutual
9
acceptance of clinical trial data for ICH member countries and regions by applicable regulatory
10
authorities.
11
This guideline builds on key concepts outlined in ICH E8(R1) General Considerations for
12
Clinical Studies. This includes fostering a quality culture and proactively designing quality into
13
clinical trials and drug development planning, identifying factors critical to trial quality, and
14
engaging stakeholders, as appropriate, using a proportionate risk-based approach.
15
Clinical trials vary widely in scale, complexity and cost. Careful evaluation of the priorities
16
involved in each trial and the risks associated with the priorities will help ensure efficiency by
17
focusing on activities critical to achieving the trial objectives.
18
Guideline Scope
19
This guideline applies to interventional clinical trials of investigational products
1
that are
20
intended to be submitted to regulatory authorities. This guideline may also be applicable to
21
other interventional clinical trials of investigational products that are not intended to support
22
marketing authorisation applications in accordance with local requirements.
23
Guideline Structure
24
This ICH GCP Guideline is composed of principles and annexes that expand on the principles,
25
with specific details for different types of clinical trials. The principles are intended to apply
26
across clinical trial types and settings and to remain relevant as technological and
27
methodological advances occur. The principles outlined in this guideline may be satisfied using
28
differing approaches and should be applied to fit the intended purpose of the clinical trial.
29
Annex-1 is intended to provide information on how the principles can be appropriately applied
30
to clinical trials. Additional annexes may be developed to respond to stakeholder needs and to
31
address emerging innovations in trial design and conduct. This guideline should be read in
32
conjunction with other ICH guidelines relevant to the design and conduct of clinical trials,
33
including multiregional trials.
34
1
For the purpose of this guideline, the term “investigational products” should be considered synonymous with
drugs, medicines, medicinal products, vaccines and biological products.
ICH E6(R3) Guideline
2
II. PRINCIPLES OF ICH GCP
35
Clinical trials are a fundamental part of clinical research that support the development of new
36
medicines or uses of existing medicines. Well-designed and conducted clinical trials help
37
answer key questions in healthcare and drug development. Their results are essential for
38
evidence-based healthcare decisions. Trials with inadequate design and/or poorly conducted
39
trials may place participant safety at risk and yield inadequate or unreliable evidence and are
40
unethical. They waste resources and the efforts and time of investigators and participants.
41
The principles of GCP are designed to be flexible and applicable to a broad range of clinical
42
trials. This guideline, along with ICH E8(R1), encourages thoughtful consideration and
43
planning to address specific and potentially unique aspects of an individual clinical trial. This
44
includes evaluation of trial characteristics, such as the design elements, the investigational
45
product being evaluated, the medical condition being addressed, the characteristics of the
46
participants, the setting in which the clinical trial is being conducted, and the type of data being
47
collected. Careful consideration of factors relevant to ensuring trial quality is needed for each
48
clinical trial.
49
The principles are intended to support efficient approaches to trial design and conduct. For
50
example, innovative digital health technologies, such as wearables and sensors, may expand
51
the possible approaches to trial conduct. Such technologies can be incorporated into existing
52
healthcare infrastructures and enable the use of a variety of relevant data sources in clinical
53
trials. This will aid in keeping clinical trial conduct in line with advancing science and
54
technological developments. The use of technology in the conduct of clinical trials should be
55
adapted to fit the participant characteristics and the particular trial design. This guideline is
56
intended to be media neutral to enable the use of different technologies for the purposes of
57
documentation.
58
The use of innovative clinical trial designs and technologies may help include diverse patient
59
populations, as appropriate, and enable wider participation. The design of the trial, to ensure
60
appropriate quality and meaningful trial outcomes, may be supported by the perspectives of
61
stakeholders; for example, patients and/or healthcare providers. Their input can increase the
62
likelihood of meaningful trial outcomes, which are relevant to both trial participants and future
63
patients. This input will also guide decisions on the feasibility of data collection and assure that
64
participation in the trial does not become unduly burdensome for those involved.
65
Clinical trials should be designed to protect the rights, safety and well-being of participants and
66
assure the reliability of results. Quality by design should be implemented to identify the factors
67
(i.e., data and processes) that are critical to ensuring trial quality and the risks that threaten the
68
integrity of those factors and ultimately the reliability of the trial results. Clinical trial processes
69
and risk mitigation strategies implemented to support the conduct of the trial should be
70
proportionate to the importance of the data being collected and the risks to trial participant
71
safety and data reliability. Trial designs should be operationally feasible and avoid unnecessary
72
complexities.
73
The overarching principles provide a flexible framework for clinical trial conduct. They are
74
structured to provide guidance throughout the life cycle of the clinical trial. These principles
75
are applicable to trials involving human participants. The principles are interdependent and
76
should be considered in their totality to assure ethical trial conduct and reliable results.
77
ICH E6(R3) Guideline
3
1. Clinical trials should be conducted in accordance with the ethical principles that
78
have their origin in the Declaration of Helsinki and that are consistent with GCP
79
and applicable regulatory requirement(s). Clinical trials should be designed and
80
conducted in ways that ensure the rights, safety and well-being of participants.
81
82
1.1 The rights, safety and well-being of the participants are the most important
83
considerations and should prevail over interests of science and society.
84
1.2 The safety of the participants should be reviewed periodically as new safety
85
information becomes available, which could have an impact on the participant
86
or the conduct of the trial.
87
1.3 Foreseeable risks and inconveniences should be weighed against the anticipated
88
benefits for the individual participants and society. A trial should be initiated
89
and continued only if the anticipated benefits justify the known and anticipated
90
risks.
91
1.4 When designing a clinical trial, the scientific goal and purpose should be
92
carefully considered so as not to unnecessarily exclude particular participant
93
populations. The participant selection process should be representative of the
94
anticipated population who is likely to use the medicinal product in future
95
clinical practice to allow for generalising the results across the broader
96
population. Certain trials (e.g., early phase, proof of concept trials,
97
bioequivalence studies) may not require a heterogeneous population.
98
1.5 A qualified physician or, when appropriate, a qualified dentist (or other
99
qualified healthcare professionals in accordance with local regulatory
100
requirements) should have the overall responsibility for the trial-related medical
101
care given to, and medical decisions made on behalf of, participants; however,
102
the practical interactions and the delivery of medical care and decisions can be
103
carried out by appropriately qualified healthcare professionals in accordance
104
with applicable regulatory requirements.
105
1.6 The confidentiality of information that could identify participants should be
106
protected in accordance with applicable privacy and data protection
107
requirements.
108
109
2. Informed consent is an integral feature of the ethical conduct of a trial. Clinical
110
trial participation should be voluntary and based on a consent process that
111
ensures participants (or their legally acceptable representatives, where
112
applicable) are well-informed.
113
114
2.1 Freely given informed consent should be obtained and documented from every
115
participant prior to clinical trial participation. For potential participants unable
116
to provide informed consent, their legally acceptable representative should
117
provide consent prior to clinical trial participation.
118
2.2 The process and information provided should be designed to achieve the
119
primary objective of enabling potential trial participants to evaluate the benefits
120
and risks of participating in the trial and to make an informed decision on
121
whether or not to participate in the trial. The information provided during the
122
ICH E6(R3) Guideline
4
informed consent process should be clear and concise so as to be understandable
123
by potential participants or legally acceptable representatives.
124
2.3 The informed consent process should take into consideration relevant aspects
125
of the trial, such as the characteristics of the participants, the trial design, the
126
anticipated benefit and risk of medical intervention(s), the setting and context
127
in which the trial will be conducted (e.g., trials in emergency situations), and
128
the potential use of technology to inform participants (or their legally
129
acceptable representatives) and obtain informed consent.
130
131
3. Clinical trials should be subject to an independent review by an institutional
132
review board/independent ethics committee (IRB/IEC).
133
134
3.1 A trial should always be conducted in compliance with the protocol that
135
receives prior IRB/IEC approval/favourable opinion.
136
3.2 Periodic review of the trial by the IRB/IEC should also be conducted in
137
accordance with applicable regulatory requirements.
138
139
4. Clinical trials should be scientifically sound for their intended purpose and based
140
on robust and current scientific knowledge and approaches.
141
142
4.1 The available nonclinical and clinical information on an investigational
143
product(s) should be adequate to support the proposed clinical trial.
144
4.2 Clinical trials should be scientifically sound and reflect the state of knowledge
145
and experience with the investigational product(s), including, if applicable, the
146
condition to be treated, diagnosed or prevented; the current understanding of
147
the underlying biological mechanism (of both the condition and the treatment);
148
and the population for which the investigational product is intended.
149
4.3 There should be periodic review of current scientific knowledge and approaches
150
to determine whether modifications to the trial are needed, since new or
151
unanticipated information may arise once the trial has begun.
152
153
5. Clinical trials should be designed and conducted by qualified individuals.
154
155
5.1 Individuals with different expertise and training may be needed across all
156
phases of a clinical trial, such as physicians, scientists, ethicists, technology
157
experts, trial coordinators, monitors, auditors and statisticians. Individuals
158
involved in a trial should be qualified by education, training and experience to
159
perform their respective task(s).
160
161
6. Quality should be built into the scientific and operational design and conduct of
162
clinical trials.
163
164
6.1 Quality of a clinical trial is considered in this guideline as fit for purpose. The
165
quality and amount of the information generated during a clinical trial should
166
support good decision making.
167
ICH E6(R3) Guideline
5
6.2 Factors critical to the quality of the trial should be identified. These factors are
168
attributes of a trial that are fundamental to the protection of participants, the
169
reliability and interpretability of the trial results and the decisions made based
170
on those trial results. Quality by design involves focusing on the design of all
171
components of the trial in order to maximise the likelihood of trial success (i.e.,
172
that the trial will answer the research question).
173
6.3 Strategies should be implemented to avoid, detect and address serious non-
174
compliance with GCP, the trial protocol and applicable regulatory requirements
175
to prevent recurrence.
176
177
7. Clinical trial processes, measures and approaches should be implemented in a
178
way that is proportionate to the risks to participants and to the importance of
179
the data collected.
180
181
7.1 Trial processes should be proportionate to the risks inherent in the trial and the
182
importance of the information collected. Risks in this context include risks to
183
the rights, safety and well-being of trial participants as well as risks to the
184
reliability of the trial results.
185
7.2 The focus should be on the risks to participants beyond those associated with
186
standard medical care. The risks relating to investigational products that have a
187
marketing authorisation when used in the clinical trial context may differ from
188
the routine care of patients and should be taken into consideration.
189
7.3 Risks to critical to quality factors should be managed prospectively and
190
adjusted when new or unanticipated issues arise once the trial has begun.
191
192
8. Clinical trials should be described in a clear, concise and operationally feasible
193
protocol.
194
195
8.1 A well-designed trial protocol is fundamental to the protection of participants
196
and for the generation of reliable results.
197
8.2 The scientific objectives of any trial should be clear and explicitly stated in the
198
protocol.
199
8.3 The clinical trial protocol as well as the plans or documents for the protocol
200
execution (e.g., statistical analysis plan, data management plan, monitoring
201
plan) should be clear, concise and operationally feasible.
202
203
9. Clinical trials should generate reliable results.
204
205
9.1 The quality and amount of the information generated in a clinical trial should
206
be sufficient to provide confidence in the trial’s results and support good
207
decision making.
208
9.2 Systems and processes that aid in data capture, management and analyses, as
209
well as those that help ensure the quality of the information generated from the
210
trial, should be fit for purpose, should capture the data required by the protocol
211
and should be implemented in a way that is proportionate to the risks to
212
participants and the importance of acquired data.
213
ICH E6(R3) Guideline
6
9.3 Trial processes should be operationally feasible and avoid unnecessary
214
complexity, procedures and data collection. Trial processes should support the
215
key trial objectives.
216
9.4 Computerised systems used in clinical trials should be fit for purpose, and
217
factors critical to their quality should be addressed in their design or adaptation
218
for clinical trial purposes.
219
9.5 Clinical trials should incorporate efficient and well-controlled processes for
220
managing records through appropriate management of data integrity,
221
traceability and protection of personal information, thereby allowing the
222
accurate reporting, interpretation and verification of the clinical trial-related
223
information.
224
9.6 Clinical trial-related records should be retained securely by sponsors and
225
investigators for the required period of time and should be available to
226
regulatory authorities upon request to enable reconstruction of the trial conduct
227
and results in order to ensure the reliability of trial results.
228
9.7 The transparency of clinical trials in drug development includes registration on
229
publicly accessible and recognised databases and the public posting of clinical
230
trial results.
231
232
10. Roles and responsibilities in clinical trials should be clear and documented
233
appropriately.
234
235
10.1 The sponsor may transfer or the investigator may delegate some or all their
236
tasks, duties or functions (hereafter referred to as activities), but they retain
237
overall responsibility for their respective activities.
238
10.2 Agreements should clearly define the roles, activities and responsibilities for
239
the clinical trial and be documented appropriately. Where activities have been
240
transferred or delegated to service providers, the responsibility for the conduct
241
of the trial, including quality and integrity of the trial data, resides with the
242
sponsor or investigator, respectively.
243
10.3 The sponsor or investigator should maintain appropriate oversight or
244
supervision of the aforementioned activities, respectively.
245
246
11. Investigational products used in a clinical trial should be manufactured in
247
accordance with applicable Good Manufacturing Practice (GMP) standards and
248
be stored, shipped, handled and disposed of in accordance with the product
249
specifications and the trial protocol.
250
251
11.1 Investigational products used in a clinical trial should be manufactured in
252
accordance with applicable GMP standards.
253
11.2 Measures should be in place to ensure that the investigational product provided
254
to trial participants retains its quality.
255
11.3 Investigational products should be used in accordance with the protocol and
256
relevant trial documents.
257
ICH E6(R3) Guideline
7
11.4 Manufacturing, handling and labelling of investigational products should be
258
undertaken in a manner that aligns with treatment assignment and maintains
259
blinding, where applicable.
260
11.5 Investigational product labelling should follow applicable regulatory
261
requirements.
262
11.6 Adequate measures to ensure that the investigational product is handled and
263
shipped appropriately should be implemented.
264
265
III. ANNEX 1
266
1. INSTITUTIONAL REVIEW BOARD/INDEPENDENT ETHICS COMMITTEE
267
(IRB/IEC)
268
The IRB/IEC is responsible for the ethical review of the trial. The requirements for
269
the IRB/IEC in this guideline should be read in conjunction with local regulatory
270
requirements.
271
1.1 Responsibilities
272
1.1.1 The purpose of an IRB/IEC is to safeguard the rights, safety and well-being of all trial
273
participants.
274
275
1.1.2 The IRB/IEC should review the following information, where applicable:
276
277
(a) protocol and any amendments;
278
279
(b) informed consent material(s), assent form(s), where applicable, and any
280
updates, including the description of the process for how informed consent is
281
to be obtained;
282
283
(c) Investigator’s Brochure or current scientific information, such as a basic
284
product information brochure (e.g., Summary of Product Characteristics
285
(SmPC), package leaflet or labelling), as appropriate, including their updates;
286
287
(d) any other information to be provided to the trial participant(s), including a
288
description of the media through which such information will be provided;
289
290
(e) advertisement for participant recruitment (if used) and information on the
291
recruitment process;
292
293
(f) plans to compensate participants (if any);
294
295
(g) ongoing updates to safety information (dependent on requirements of the
296
IRB/IEC);
297
298
(h) investigator’s current curriculum vitae and/or other documentation evidencing
299
qualifications;
300
301
ICH E6(R3) Guideline
8
(i) any other documents that the IRB/IEC may need to fulfil its responsibilities.
302
303
1.1.3 The IRB/IEC should review a proposed clinical trial within a reasonable time and
304
document its reviews clearly identifying the trial, the documents reviewed and the
305
dates for the following:
306
307
(a) approval/favourable opinion;
308
309
(b) modifications required prior to its approval/favourable opinion;
310
311
(c) disapproval/negative opinion;
312
313
(d) termination/suspension of any prior approval/favourable opinion.
314
315
1.1.4 The IRB/IEC should conduct continuing review of each ongoing trial at intervals
316
appropriate to the degree of risk to participants.
317
318
1.1.5 The IRB/IEC may request more information than is outlined in section 2.8.11 be given
319
to participants when, in the judgement of the IRB/IEC, the additional information
320
would add meaningfully to the protection of the rights, safety and/or well-being of the
321
participants.
322
323
1.1.6 Where the protocol indicates that prior consent of the trial participant or the
324
participant’s legally acceptable representative is not possible (see section 2.8.9), the
325
IRB/IEC should determine that the proposed protocol and/or other document(s)
326
adequately address relevant ethical concerns and meet applicable regulatory
327
requirements for such trials (e.g., in emergency situations).
328
329
1.1.7 If minors are to be included in a trial, the IRB/IEC should review the assent
330
information considering the age, maturity and psychological state of the minor, as
331
well as applicable regulatory requirements.
332
333
1.1.8 If the trial participants are compensated for their participation in the trial, the IRB/IEC
334
should review both the amount and method of payment to participants to assure that
335
neither presents problems of coercion or undue influence on the trial participants.
336
Payments to a participant should be prorated and not wholly contingent on completion
337
of the trial by the participant. Reasonable reimbursement of participants for travel and
338
lodging is not typically coercive.
339
340
1.1.9 The IRB/IEC should ensure that information regarding payment to participants,
341
including the methods, amounts and schedule of payment to trial participants, is set
342
forth in the informed consent material and any other information to be provided to
343
participants.
344
ICH E6(R3) Guideline
9
1.2 Composition, Functions and Operations
345
1.2.1 The IRB/IEC should consist of a reasonable number of members who collectively
346
have the qualifications and experience to review and evaluate the science, medical
347
aspects and ethics of the proposed trial. It is recommended that the IRB/IEC should
348
include:
349
350
(a) at least five members;
351
352
(b) at least one member whose primary area of interest is not in medical sciences;
353
354
(c) at least one member who is independent of the institution/investigator site.
355
356
Only those IRB/IEC members who are independent of the investigator and the sponsor
357
of the trial should vote/provide an opinion. A list of IRB/IEC members and their
358
qualifications should be maintained.
359
360
1.2.2 The IRB/IEC should perform its functions according to documented operating
361
procedures, should maintain records of its activities and minutes of its meetings, and
362
should comply with GCP and with the applicable regulatory requirement(s).
363
364
1.2.3 An IRB/IEC should make its decisions at announced meetings at which at least a
365
quorum, as stipulated in its documented operating procedures, is present.
366
367
1.2.4 Only members who participate in the IRB/IEC review and discussion should
368
vote/provide their opinion and/or advise.
369
370
1.2.5 The investigator, investigator site staff and/or sponsor, where appropriate, may
371
provide information on any aspect of the trial but should not participate in the decision
372
making of the IRB/IEC or in the vote/opinion of the IRB/IEC.
373
374
1.2.6 An IRB/IEC may invite non-members with expertise in special areas for assistance.
375
1.3 Procedures
376
The IRB/IEC should establish, document in writing or electronically, and follow its procedures,
377
which should include:
378
1.3.1 Determining its composition (names and qualifications of the members) and the
379
authority under which it is established;
380
381
1.3.2 Scheduling, notifying its members of and conducting its meetings;
382
383
1.3.3 Conducting initial and continuing review of trials;
384
385
1.3.4 Determining the frequency of continuing review, as appropriate;
386
387
ICH E6(R3) Guideline
10
1.3.5 Providing, according to the applicable regulatory requirements, expedited review and
388
approval/favourable opinion of minor change(s) in ongoing trials that have the
389
approval/favourable opinion of the IRB/IEC;
390
391
1.3.6 Specifying that no participant should be admitted to a trial before the IRB/IEC issues
392
its documented approval/favourable opinion of the trial;
393
394
1.3.7 Specifying that no deviations from the protocol should be initiated without prior
395
documented IRB/IEC approval/favourable opinion, except when necessary to
396
eliminate immediate hazards to the participants;
397
398
1.3.8 Specifying that the investigator/institution should promptly report to the IRB/IEC (see
399
section 1.5):
400
401
(a) deviations from the protocol to eliminate immediate hazards to the trial
402
participants (see sections 1.3.7, 2.5.3 and 2.5.4);
403
404
(b) changes increasing the risk to participants and/or significantly affecting the
405
conduct of the trial (see section 2.4.6);
406
407
(c) all suspected unexpected serious adverse reactions (SUSARs) in line with
408
applicable regulatory requirements;
409
410
(d) new information that may affect adversely the safety of the participants or the
411
conduct of the trial.
412
413
1.3.9 Ensuring that the IRB/IEC (see section 1.5) promptly notifies in writing or
414
electronically the investigator/institution or sponsor concerning:
415
416
(a) its trial-related decisions/opinions;
417
418
(b) the reasons for its decisions/opinions;
419
420
(c) procedures for appeal of its decisions/opinions.
421
1.4 Records
422
1.4.1 The IRB/IEC should retain all relevant records (e.g., documented procedures,
423
membership lists, lists of occupations/affiliations of members, submitted documents,
424
minutes of meetings and correspondence) in accordance with applicable regulatory
425
requirements and make them available upon request from the regulatory
426
authority(ies).
427
428
1.4.2 The IRB/IEC may be asked by investigators, sponsors or regulatory authorities to
429
provide its documented procedures and membership lists.
430
ICH E6(R3) Guideline
11
1.5 Submission and Communication
431
For the submission to or communication with the IRB/IEC, it is recognised that in most regions,
432
there is also a requirement to make a submission to the relevant regulatory authority, and these
433
may be combined, in line with applicable regulatory requirements, in a single submission in
434
some regions. In addition, applicable regulatory requirements may require that submissions to
435
the IRB/IEC are made in some regions by the investigator/institution and in others by the
436
sponsor.
437
438
2. INVESTIGATOR
439
2.1 Qualifications and Training
440
2.1.1 The investigator(s) should be qualified by education, training and experience to
441
assume responsibility for the proper conduct of the trial and should provide evidence
442
of such qualifications.
443
444
2.1.2 The investigator should be familiar with the appropriate use of the investigational
445
product(s) as described in the protocol, in the current Investigator’s Brochure, in the
446
product information and/or in other information sources provided by the sponsor.
447
2.2 Resources
448
2.2.1 The investigator should be able to demonstrate (e.g., based on retrospective or
449
currently available data) a potential for recruiting the proposed number of eligible
450
participants within the recruitment period as agreed with the sponsor.
451
452
2.2.2 The investigator should have sufficient time, an adequate number of available and
453
qualified staff, and adequate facilities for the foreseen duration of the trial to conduct
454
the trial properly and safely.
455
2.3 Responsibilities
456
2.3.1 The investigator may delegate trial-specific activities to other persons or parties.
457
The investigator may be supported by the sponsor to identify a suitable service
458
provider(s); however, the investigator retains the final decision on whether the service
459
provider intended to support the investigator is appropriate based on information
460
provided by the sponsor (see section 3.6.6).
461
The investigator retains the ultimate responsibility and maintains appropriate
462
supervision of the persons or parties undertaking the activities delegated to ensure the
463
rights, safety and well-being of the trial participants and data reliability.
464
465
2.3.2 The investigator should ensure that persons or parties to whom the investigator has
466
delegated trial-specific activities are appropriately qualified and supervised and are
467
adequately informed about the protocol, the investigational product(s) and their
468
assigned trial activities (including activities conducted by staff provided by other
469
parties, for example, home nurses arranged by the sponsor). Trial-related training to
470
ICH E6(R3) Guideline
12
persons assisting in the trial should correspond to what is necessary to enable them to
471
fulfil their delegated trial activities that go beyond their usual training and experience.
472
473
2.3.3 The investigator should ensure a record is maintained of the persons and parties to
474
whom the investigator has delegated significant trial-related activities. In situations
475
where the clinical trial activities are performed in accordance with routine clinical
476
care, delegation documentation may not be required.
477
478
2.3.4 Agreements made by the investigator/institution with service providers for trial-
479
related activities should be documented.
480
481
2.3.5 The investigator/institution should permit monitoring and auditing by the sponsor and
482
inspection by the appropriate regulatory authority(ies).
483
2.4 Communication with IRB/IEC
484
2.4.1 Submission to the IRB/IEC may be made by the investigator/institution or sponsor in
485
accordance with applicable regulatory requirements (see section 1.5).
486
487
2.4.2 Before initiating a trial, the investigator/institution should have a documented and
488
dated approval/favourable opinion from the IRB/IEC for the trial protocol, informed
489
consent material, participant recruitment procedures (e.g., advertisements) and any
490
other information to be provided to participants.
491
492
2.4.3 As part of the investigator’s/institution’s or sponsor’s (in accordance with applicable
493
regulatory requirements) submission to the IRB/IEC, a current copy of the
494
Investigator’s Brochure or basic product information brochure should be provided
495
(see section A.1.1 of Appendix A. Investigator’s Brochure). If the Investigator’s
496
Brochure is updated during the trial, the IRB/IEC should receive the current version
497
in accordance with applicable regulatory requirements.
498
499
2.4.4 As the trial progresses, the investigator/institution or sponsor should provide any
500
updates to the participant information according to applicable regulatory
501
requirements.
502
503
2.4.5 The investigator or the sponsor should submit documented summaries of the trial
504
status to the IRB/IEC in accordance with local regulatory requirements or upon
505
request.
506
507
2.4.6 The investigator or the sponsor should promptly communicate to the IRB/IEC (see
508
section 1.3.8) and, where applicable, the institution about any changes significantly
509
affecting the conduct of the trial and/or increasing the risk to participants.
510
2.5 Compliance with Protocol
511
2.5.1 The investigator should comply with the protocol and GCP and applicable regulatory
512
requirements. The investigator/institution should sign the protocol or an alternative
513
contract to confirm agreement with the sponsor.
514
ICH E6(R3) Guideline
13
2.5.2 The investigator should document all protocol deviations and review deviations
515
communicated to them by the sponsor. For important deviations, the investigator
516
should explain the deviation and implement appropriate measures to prevent a
517
recurrence, where applicable, see section 3.9.3.
518
519
2.5.3 The investigator should follow the protocol and deviate only where necessary to
520
eliminate an immediate hazard(s) to trial participants. In case of deviations undertaken
521
to eliminate immediate hazard to trial participants, the investigator should inform the
522
sponsor, IRB/IEC and/or regulatory authorities promptly.
523
524
2.5.4 The investigator should report information on the immediate hazard, the implemented
525
change and the subsequent proposed protocol amendment to the IRB/IEC and/or
526
regulatory authorities.
527
2.6 Premature Termination or Suspension of a Trial
528
2.6.1 If the trial is prematurely terminated or suspended for any reason, the
529
investigator/institution should promptly inform the trial participants and should assure
530
appropriate therapy and follow-up for the participants.
531
532
2.6.2 Where the investigator terminates or suspends their involvement in a trial without
533
prior agreement by the sponsor, the investigator should promptly inform the sponsor,
534
the IRB/IEC and the regulatory authorities in accordance with applicable regulatory
535
requirements and should provide a detailed explanation of the reasons.
536
537
2.6.3 If the sponsor terminates or suspends a trial, the investigator/institution, or the
538
sponsor, in accordance with applicable regulatory requirement(s), should promptly
539
inform the IRB/IEC and the regulatory authorities. See section 3.17.1.
540
541
2.6.4 If the IRB/IEC terminates or suspends its approval/favourable opinion of a trial (see
542
sections 1.1.3 and 1.3.9), the investigator should inform the institution, where
543
applicable, and the investigator/institution should promptly notify the sponsor.
544
2.7 Participant Medical Care and Safety Reporting
545
2.7.1 Medical Care of Trial Participants
546
(a) A qualified physician or, where appropriate, a qualified dentist (or other
547
qualified healthcare professionals in accordance with local regulatory
548
requirements) who is an investigator or a sub-investigator for the trial should
549
have the overall responsibility for trial-related medical care and decisions.
550
551
(b) Other appropriately qualified healthcare professionals may be involved in the
552
medical care of trial participants, in line with their normal activities and in
553
accordance with local regulatory requirements.
554
555
(c) During and following participation in a trial, the investigator/institution should
556
ensure that adequate medical care is provided to a participant for any adverse
557
events, including clinically significant laboratory values, related to the trial.
558
ICH E6(R3) Guideline
14
The investigator/institution should inform a participant when medical care is
559
needed for intercurrent illness(es) of which the investigator becomes aware.
560
561
(d) The investigator should inform the participant’s primary physician about the
562
participant’s involvement in the trial if the participant has a primary physician
563
and agrees to the primary physician being informed.
564
2.7.2 Safety Reporting
565
(a) Adverse events and/or laboratory abnormalities required for safety evaluations
566
(as outlined in the protocol) should be reported to the sponsor according to the
567
reporting requirements and within the time periods specified in the protocol.
568
569
(b) All serious adverse events (SAEs) should be reported immediately (after the
570
investigator reasonably becomes aware of the event) to the sponsor. In
571
accordance with applicable regulatory requirements, the protocol may identify
572
SAEs not requiring immediate reporting, for example, deaths or other events
573
that are endpoints. Subsequent information should be submitted as a follow-
574
up report, as necessary.
575
576
(c) For reported deaths, the investigator should supply the sponsor, the IRB/IEC
577
and, where applicable, the regulatory authority with any additional requested
578
information (e.g., autopsy reports and terminal medical reports) when they
579
become available.
580
581
(d) The investigator may delegate activities for safety reporting to qualified
582
investigator site staff but retains the overall responsibility for safety of
583
participants under their responsibility and compliance with the reporting
584
requirements.
585
2.8 Informed Consent of Trial Participants
586
2.8.1 In obtaining and documenting informed consent (paper or electronic format), the
587
investigator should comply with the applicable regulatory requirement(s) and should
588
adhere to GCP and to the ethical principles that have their origin in the Declaration of
589
Helsinki. See the glossary term “informed consent.” The informed consent process
590
should include the following:
591
592
(a) Prior to consenting and enrolling participants, the investigator should have the
593
IRB/IEC’s documented approval/favourable opinion of the informed consent
594
materials and process;
595
596
(b) The information should be as clear and concise as possible, use simple
597
language and avoid unnecessary volume and complexity. This is to ensure that
598
the trial participants or their legally acceptable representatives have an
599
adequate understanding of the objectives of the trial, alternative treatments,
600
the potential benefits and risks, burdens and their rights and obligations to be
601
able to make an informed decision as to their participation in the trial;
602
ICH E6(R3) Guideline
15
(c) Varied approaches (e.g., text, images, videos and other interactive methods)
603
may be used in the informed consent process including for providing
604
information to the participant. Obtaining consent remotely may be considered
605
where appropriate.
606
607
2.8.2 The participant or the participant’s legally acceptable representative should be
608
informed in a timely manner if new information becomes available that may be
609
relevant to the participant’s willingness to continue trial participation. The
610
communication of this information and confirmation of the willingness to continue
611
trial participation should be documented.
612
613
New information that could impact a participant’s willingness to continue
614
participation should be assessed to determine if re-consent is needed (e.g., depending
615
on the stage of the trial, consideration should be given to whether the new information
616
is relevant only to new participants or to existing participants). If re-consent is needed
617
(e.g., information on emerging safety concerns), new information should be clearly
618
identified in the revised informed consent materials. Revised informed consent
619
materials should receive the IRB/IEC’s approval/favourable opinion in advance of
620
use.
621
622
2.8.3 Neither the investigator nor the investigator site staff should coerce or unduly
623
influence a participant to participate or to continue their participation in the trial.
624
625
2.8.4 None of the information provided to the participant during the informed consent
626
process should contain any language that causes the participant or the participant’s
627
legally acceptable representative to waive or to appear to waive any legal rights, or
628
that releases or appears to release the investigator, the institution, the sponsor or their
629
service providers from liability for negligence.
630
631
2.8.5 The informed consent process should be conducted by the investigator or other
632
investigator site staff delegated by the investigator, in accordance with applicable
633
regulatory requirements. If the participant is unable to provide consent themselves,
634
the participant’s legally acceptable representative should provide their consent on
635
behalf of the participant.
636
637
2.8.6 The information provided during the informed consent process and translations should
638
be relevant, clear, simple, concise and understandable to the participant or the
639
participant’s legally acceptable representative and the impartial witness, where
640
applicable.
641
642
2.8.7 Before informed consent may be obtained, the investigator or investigator site staff
643
delegated by the investigator, in accordance with the protocol and conditions of
644
IRB/IEC favourable opinions/approvals, should provide the participant or the
645
participant’s legally acceptable representative ample time unless justified (e.g., in an
646
emergency situation) and opportunity to enquire about trial details and to decide
647
whether or not to participate in the trial. Questions about the trial should be answered
648
ICH E6(R3) Guideline
16
to the satisfaction of the participant or the participant’s legally acceptable
649
representative.
650
651
2.8.8 Prior to trial participation, the informed consent form should be signed and dated by
652
the participant or by the participant’s legally acceptable representative and, where
653
appropriate, impartial witness and by the investigator or delegated investigator site
654
staff who conducted the informed consent discussion. The informed consent process
655
may involve a physical signature or an electronic signature.
656
657
2.8.9 In emergency situations, when prior consent of the participant is not possible, the
658
consent of the participant’s legally acceptable representative, if present, should be
659
requested. When prior consent of the participant is not possible and the participant’s
660
legally acceptable representative is not available, enrolment of the participant should
661
require measures described in the protocol and/or elsewhere, with documented
662
approval/favourable opinion by the IRB/IEC, to protect the participant’s rights, safety
663
and well-being and to ensure compliance with applicable regulatory requirements.
664
The participant or the participant’s legally acceptable representative should be
665
informed about the trial as soon as possible, and consent as appropriate (see section
666
2.8.10) should be requested.
667
668
2.8.10 If a participant or the legally acceptable representative is unable to read, an impartial
669
witness should be present (remotely or in-person) during the entire informed consent
670
discussion. After the informed consent form and any other information is read and
671
explained to the participant or the participant’s legally acceptable representative and
672
they have orally consented to the participant’s trial participation and, if capable of
673
doing so, have signed and personally dated the informed consent form, the witness
674
should contemporaneously sign and personally date the consent form. By signing the
675
consent form, the witness attests that the consent information was accurately
676
explained to and apparently understood by the participant or the participant’s legally
677
acceptable representative and that informed consent was freely given by the
678
participant or the participant’s legally acceptable representative.
679
680
2.8.11 The informed consent discussion and the informed consent materials to be provided
681
to participants should explain the following as applicable:
682
683
(a) the purpose of the trial;
684
685
(b) that the trial involves research and summary of the experimental aspects of the
686
trial;
687
688
(c) the trial’s investigational product(s) and the probability for random
689
assignment to the investigational product, if applicable;
690
691
(d) the trial procedures to be followed including all invasive procedures;
692
693
(e) the participant’s obligations;
694
ICH E6(R3) Guideline
17
(f) the reasonably foreseeable risks or inconveniences to the participant and, when
695
applicable, the participant’s partner, to an embryo, foetus or nursing infant;
696
697
(g) the reasonably expected benefits. When there is no intended clinical benefit to
698
the participant, the participant should be made aware of this;
699
700
(h) the alternative procedure(s) or course(s) of treatment that may be available to
701
the participant and their important potential benefits and risks;
702
703
(i) the compensation and/or treatment available to the participant in the event of
704
trial-related injury;
705
706
(j) any anticipated prorated compensation to the participant for trial participation;
707
708
(k) any anticipated expenses to the participant for trial participation;
709
710
(l) that the participant’s trial participation is voluntary, and the participant may
711
refuse to participate or may withdraw, at any time, without penalty or loss of
712
benefits to which the participant is otherwise entitled;
713
714
(m) the process by which the participant’s data will be handled, including in the
715
event of the withdrawal of participation in accordance with regulatory
716
requirements;
717
718
(n) that by agreeing to participate in the trial, the participant or their legally
719
acceptable representative allows direct access to original medical records, per
720
applicable regulatory requirements, while safeguarding the confidentiality of
721
the participant. This access is limited for the purpose of reviewing trial
722
activities and/or reviewing or verifying data and records by the IRB/IEC(s),
723
regulatory authority(ies) and the sponsor’s representatives, for example,
724
monitor(s) or auditor(s);
725
726
(o) that records identifying the participant will be kept confidential and, to the
727
extent permitted by the applicable regulatory requirements, will not be made
728
publicly available. If the trial results are published, the participant’s identity
729
will remain confidential. The trial may be registered on publicly accessible
730
and recognised databases, per applicable regulatory requirements;
731
732
(p) that the participant or the participant’s legally acceptable representative will
733
be informed in a timely manner if information becomes available that may be
734
relevant to the participant’s willingness to continue trial participation;
735
736
(q) the person(s) to contact for further trial information and the trial participant’s
737
rights, and whom to contact in the event of suspected trial-related injury;
738
739
ICH E6(R3) Guideline
18
(r) the foreseeable circumstances and/or reasons under which the participant’s
740
trial participation may be terminated;
741
742
(s) the expected duration of the participant’s trial participation;
743
744
(t) the approximate number of participants involved in the trial;
745
746
(u) that trial results and information on the participant’s actual treatment, if
747
appropriate, will be made available to them should they desire it.
748
749
2.8.12 Prior to participation, the participant or the participant’s legally acceptable
750
representative should receive a copy (paper or electronic) of the signed informed
751
consent form and any other informed consent materials provided to the participants,
752
or in accordance with applicable regulatory requirements. During trial participation,
753
the participant or the participant’s legally acceptable representative should receive a
754
copy of the consent form updates and any other updated informed consent materials
755
provided to participants.
756
757
2.8.13 Where a minor is to be included as a participant, age-appropriate assent information
758
should be provided and discussed with the minor as part of the consent process, and
759
assent from the minor to enrol in the trial should be obtained as appropriate. A process
760
for re-consent should be considered if, during the course of the trial, the minor reaches
761
the age of legal consent, in accordance with applicable regulatory requirements.
762
763
2.8.14 When a clinical trial includes participants who may only be enrolled in the trial with
764
the consent of the participant’s legally acceptable representative (e.g., minors, patients
765
with severe impaired decision-making capacity), the participant should be informed
766
about the trial to the extent compatible with the participant’s understanding and, if
767
capable, the participant should sign and personally date the informed consent form or
768
assent form as appropriate.
769
770
2.8.15 In exceptional circumstances (e.g., public health emergencies), when the usual
771
methods to obtain and document informed consent are not possible, the use of
772
alternative measures and technologies in accordance with local IRBs/IECs and
773
applicable regulatory requirements should be considered.
774
2.9 End of Participation in a Clinical Trial
775
2.9.1 When a participant decides to stop treatment with the investigational product, stop
776
trial visits or completely withdraw from a trial; is discontinued from the trial; or
777
reaches routine end of trial, the investigator should follow the protocol and other
778
sponsor instructions to determine appropriate follow-up measures. This may include
779
instructions to avoid unnecessary loss of already collected critical data in accordance
780
with applicable regulatory requirements.
781
782
2.9.2 Although a participant is not obliged to provide a reason(s) for withdrawing
783
prematurely from a trial, the investigator should make a reasonable effort to ascertain
784
ICH E6(R3) Guideline
19
the reason(s), while fully respecting the participant’s rights. The investigator should
785
consider discussing with the participant or the participant’s legally acceptable
786
representative the reasons for withdrawal to determine if there are ways to address the
787
concerns. The investigator site staff should make an effort to explain to the participant
788
the value and importance of continuing their participation to minimise trial
789
participants withdrawal.
790
791
2.9.3 Where relevant, the investigator should inform the participant about the trial results
792
and treatment received when this information is available from the sponsor after
793
unblinding, with due respect to the participant’s preference to be informed.
794
2.10 Investigational Product Management
795
2.10.1 Responsibility for investigational product(s) accountability rests with the
796
investigator/institution. The sponsor may facilitate this process.
797
798
2.10.2 When the investigator/institution assigns some or all of their activities for
799
investigational product(s) accountability to a pharmacist or another individual, they
800
should be under the supervision of the investigator/institution.
801
802
2.10.3 The investigator/institution and/or a pharmacist or other appropriate individual should
803
maintain records of the product’s delivery, the inventory, the use by each participant
804
(including documenting that the participants were provided the doses specified by the
805
protocol) and the return to the sponsor and destruction or alternative disposition of
806
unused product(s). These records should include dates, quantities, batch/serial
807
numbers, expiration dates (if applicable) and the unique code numbers assigned to the
808
investigational product(s) and trial participants. For authorised medicinal products,
809
alternative approaches to the aforementioned may be considered, in accordance with
810
local regulatory requirements.
811
812
2.10.4 The investigational product(s) should be stored as specified by the sponsor and in
813
accordance with applicable regulatory requirement(s).
814
815
2.10.5 The investigator should ensure that the investigational product(s) are used only in
816
accordance with the approved protocol.
817
818
2.10.6 Where applicable, the investigator or a person designated by the
819
investigator/institution should explain the correct use of the investigational product(s)
820
to each participant and should check, at intervals appropriate for the trial, that each
821
participant is following the instructions properly.
822
2.11 Randomisation Procedures and Unblinding
823
The investigator should follow the trial’s randomisation procedures, if any, and, in the case of
824
an investigator-blinded trial, should ensure that the identification code is broken only in
825
accordance with the protocol. In the case of an emergency, to protect patient safety, the
826
investigator should be prepared and capable from the start of the trial to perform unblinding
827
without undue delay and hinderance. The investigator should promptly document and explain
828
ICH E6(R3) Guideline
20
to the sponsor any premature unblinding (e.g., accidental unblinding, emergency unblinding to
829
protect trial participant, unblinding due to an SAE) of the investigational product(s).
830
2.12 Records
831
2.12.1 In generating, recording and reporting trial data, the investigator should ensure the
832
integrity of data under their responsibility, irrespective of the media used.
833
834
2.12.2 The investigator/institution should maintain adequate source records that include
835
pertinent observations on each of the trial participants under their responsibility.
836
Source records should be attributable, legible, contemporaneous, original, accurate
837
and complete. Changes to source records should be traceable, should not obscure the
838
original entry and should be explained if necessary (via an audit trail). The
839
investigator should define what is considered to be a source record(s), the methods of
840
data capture and their location prior to starting the trial and should update this
841
definition when needed. Unnecessary transcription steps in between the source record
842
and the data acquisition tool should be avoided.
843
844
2.12.3 The investigator should have timely access to and be responsible for the timely review
845
of data, including relevant data from external sources (e.g., central laboratory data,
846
centrally read imaging data, other institution’s records and, if appropriate, electronic
847
patient-reported outcome (ePRO) data) which can have an impact on, for example,
848
participant eligibility, treatment or safety. The protocol may provide exceptions for
849
access, for instance, to protect blinding.
850
851
2.12.4 The investigator should ensure that data acquisition tools and other systems deployed
852
by the sponsor for clinical trial purposes are used as specified in the protocol or trial-
853
related instructions.
854
855
2.12.5 The investigator should ensure the accuracy, completeness, legibility and timeliness
856
of the data reported to the sponsor in the data acquisition tools completed by the
857
investigator site (e.g., case report form (CRF)) and in all required reports. The
858
investigator should review and endorse the reported data at milestones agreed upon
859
with the sponsor (e.g., interim analysis).
860
861
2.12.6 Data reported to the sponsor should be consistent with the source records or the
862
discrepancies explained. Changes or corrections in the reported data should be
863
traceable, should be explained (if necessary) and should not obscure the original entry.
864
865
2.12.7 The investigator/institution should implement appropriate measures to protect the
866
privacy and confidentiality of personal information of trial participants in accordance
867
with applicable regulatory requirements on personal data protection. Data reported to
868
the sponsor should be identified by an unambiguous participant code that can be traced
869
back to the identity of the participant by the investigator/institution.
870
871
2.12.8 For systems deployed by the investigator/institution that maintain and retain trial
872
data/information, the investigator/institution should ensure that such data are
873
ICH E6(R3) Guideline
21
protected from unauthorised access, disclosure, dissemination or alteration and from
874
inappropriate destruction or accidental loss.
875
876
2.12.9 When using computerised systems in a clinical trial, the investigator/institution should
877
do the following:
878
879
(a) for systems deployed by the investigator/institution, ensure that appropriate
880
individuals have secure and attributable access;
881
882
(b) for systems deployed by the investigator/institution specifically for the
883
purposes of clinical trials, ensure that the requirements for computerised
884
systems in section 4 are addressed;
885
886
(c) where equipment for data acquisition is provided to trial participants by the
887
investigator, ensure that traceability is maintained and participants are
888
provided with appropriate training;
889
890
(d) ensure that incidents in the use and operation of computerised systems, which
891
in their judgement may have a significant and/or persistent impact on the trial
892
data, are reported to the sponsor and, where applicable, to the IRB/IEC.
893
894
2.12.10 The investigator/institution should maintain the trial records as specified in Appendix
895
C. Essential Records for the Conduct of a Clinical Trial and as required by the
896
applicable regulatory requirement(s). The investigator/institution should have control
897
of all essential records generated by the investigator/institution before, during and
898
after the trial. The investigator/institution should take measures to prevent accidental
899
or premature destruction of these records. If the investigator closes a site or leaves a
900
site during or after the end of the clinical trial, the sponsor should be notified of the
901
appropriate individual responsible for retention of the site’s essential records.
902
903
2.12.11 The investigator/institution should retain the essential records for the required
904
retention period in accordance with applicable regulatory requirements or until the
905
sponsor informs the investigator/institution that these records are no longer needed,
906
whichever is the longer (see Appendix C).
907
908
2.12.12 Upon request of the monitor, auditor, IRB/IEC or regulatory authority, the
909
investigator/institution should make available for direct access all requested trial-
910
related records.
911
2.13 Clinical Trial/Study Reports
912
2.13.1 Upon completion of the trial, the investigator, where applicable, should inform the
913
institution. The investigator/institution should provide the IRB/IEC with a summary
914
of the trial’s outcome and, if applicable, the regulatory authority(ies) with any
915
required reports.
916
917
ICH E6(R3) Guideline
22
2.13.2 Where a coordinating investigator is involved in a trial, consideration should be given
918
to them being a signatory on the clinical trial report; see ICH E3 Structure and Content
919
of Clinical Study Reports.
920
921
3. SPONSOR
922
The responsibility of the sponsor entails the implementation of risk-proportionate processes to
923
ensure the safety of the trial participants and the reliability of the trial results throughout the
924
clinical trial life cycle.
925
3.1 Trial Design
926
3.1.1 When planning trials, the sponsor should ensure that sufficient safety and efficacy
927
data from nonclinical studies and/or clinical trials and/or real-world data are available
928
to support human exposure by the route, at the dosages, for the duration and in the
929
trial population to be studied.
930
931
3.1.2 Sponsors should incorporate quality into the design of the clinical trial by identifying
932
factors that are critical to the quality of the trial and by managing risks to those factors.
933
934
3.1.3 Sponsors should consider inputs from a wide variety of stakeholders, for example,
935
healthcare professionals and patients, to support the development plan and clinical
936
trial protocols as described in ICH E8(R1) and when developing the informed consent
937
material and any other participant-facing information.
938
939
3.1.4 The sponsor should ensure that all aspects of the trial are operationally feasible and
940
should avoid unnecessary complexity, procedures and data collection. Protocols, data
941
acquisition tools and other operational documents should be fit for purpose, clear,
942
concise and consistent, when applicable.
943
3.2 Resources
944
The sponsor should ensure that sufficient resources are available to appropriately conduct the
945
trial.
946
3.3 Allocation of Activities
947
Prior to initiating clinical trial activities, the sponsor should determine the roles and allocate
948
trial-related activities accordingly.
949
3.4 Qualification and Training
950
The sponsor should utilise appropriately qualified individuals for the activities to which they
951
are assigned (e.g., biostatisticians, clinical pharmacologists, physicians, data scientists/data
952
managers, auditors and monitors) throughout the trial process.
953
3.4.1 Medical Expertise
954
The sponsor should have medical personnel readily available who will be able to
955
advise on specific trial-related medical questions or problems.
956
ICH E6(R3) Guideline
23
3.5 Financing
957
The financial aspects of the trial should be documented in an agreement between the sponsor
958
and the investigator/institution.
959
3.6 Agreements
960
3.6.1 Agreements made by the sponsor with the investigator/institution, service providers
961
and any other parties (e.g., independent data monitoring committee (IDMC),
962
adjudication committee) involved with the clinical trial should be documented prior
963
to initiating the activities.
964
965
3.6.2 Agreements should be updated when necessary to reflect significant changes in the
966
activities delegated.
967
968
3.6.3 The sponsor should obtain the investigator’s/institution’s and, where applicable,
969
service provider’s agreement:
970
971
(a) to conduct the trial in accordance with the approved protocol and in
972
compliance with GCP and applicable regulatory requirement(s);
973
974
(b) to comply with procedures for data recording/reporting;
975
976
(c) to retain the trial-related essential records for the required retention period in
977
accordance with applicable regulatory requirements or until the sponsor
978
informs the investigator/institution or, where applicable, the service provider,
979
that these documents are no longer needed, whichever is longer;
980
981
(d) to permit monitoring, auditing and inspections by sponsors, IRB/IECs and
982
regulatory authorities (domestic and foreign) including providing direct access
983
to source records and facilities, including to those of service providers.
984
985
3.6.4 The responsibilities of coordinating investigator(s) and the other participating
986
investigators should be documented prior to the start of the trial.
987
988
3.6.5 Any of the sponsor’s trial-related activities that are transferred to and assumed by a
989
service provider should be documented in an agreement. The sponsor’s trial-related
990
activities that are not specifically transferred to and assumed by a service provider are
991
retained by the sponsor.
992
993
3.6.6 The sponsor should provide information to the investigator on any service provider
994
identified by the sponsor to undertake any activities under the responsibility of the
995
investigator. The responsibility for such activities remains with the investigator.
996
997
3.6.7 A sponsor may transfer any or all of the sponsor’s trial-related activities to a service
998
provider; however, the ultimate responsibility for the sponsor’s trial-related activities,
999
including protection of participants’ rights, safety and well-being and reliability of the
1000
trial data, resides with the sponsor. Any service provider used for clinical trial
1001
ICH E6(R3) Guideline
24
activities should implement appropriate quality management and report to the sponsor
1002
any incidents that might have an impact on the safety of trial participants or/and trial
1003
results.
1004
1005
3.6.8 The sponsor is responsible for assessing the suitability of and selecting the service
1006
provider to ensure that they can adequately undertake the activities transferred to
1007
them. The sponsor should provide the service providers with the protocol where
1008
necessary as well as any other documents required for them to perform their activities.
1009
1010
3.6.9 The sponsor should have access to relevant information (e.g., SOPs and performance
1011
metrics) for selection and oversight of service providers.
1012
1013
3.6.10 The sponsor should ensure appropriate oversight of important trial-related activities
1014
that are transferred to service providers and further subcontracted.
1015
1016
3.6.11 Trial-related activities performed by service providers should be conducted in
1017
accordance with relevant GCP requirements, which may be fulfilled by a service
1018
provider’s existing processes.
1019
1020
3.6.12 A clinical trial may have one or several sponsors where permitted under applicable
1021
regulatory requirements. In trials with more than one sponsor, the sponsors should
1022
have a documented agreement that sets out their respective responsibilities, in
1023
accordance with local regulatory requirements and/or practice. Where the documented
1024
agreement does not specify to which sponsor a given responsibility is attributed, that
1025
responsibility lies with all sponsors.
1026
3.7 Investigator Selection
1027
3.7.1 The sponsor is responsible for selecting the investigator(s)/institution(s). Each
1028
investigator should be qualified by education, training and experience and should
1029
demonstrate they have adequate resources and facilities to properly conduct the trial.
1030
If organisation of a coordinating committee and/or selection of coordinating
1031
investigator(s) are to be utilised in multicentre trials, their organisation and/or
1032
selection are the sponsor’s responsibility, and their roles should be documented prior
1033
to their involvement in the trial.
1034
1035
3.7.2 The sponsor should provide the investigator(s)/institution(s) with the protocol and an
1036
up-to-date Investigator’s Brochure as well as sufficient time for the review of the
1037
protocol and the information provided.
1038
3.8 Communication with IRB/IEC and Regulatory Authority(ies)
1039
3.8.1 Notification/Submission to Regulatory Authority(ies)
1040
In accordance with applicable regulatory requirement(s), before initiating the clinical
1041
trial(s), the sponsor (or the sponsor and the investigator) should submit any required
1042
application(s) to the appropriate regulatory authority(ies) for review, acceptance
1043
and/or permission to begin the trial(s). Any notification/submission should be dated
1044
and contain sufficient information to identify the protocol.
1045
ICH E6(R3) Guideline
25
3.8.2 Confirmation of Review by IRB/IEC
1046
(a) Where reference is made to a submission to the IRB/IEC, this can be made by
1047
the investigator/institution or sponsor in accordance with applicable regulatory
1048
requirements (see section 1.5).
1049
1050
(b) The sponsor should ensure that the following is obtained:
1051
1052
(i) The name and address of the relevant IRB/IEC along with:
1053
1054
(aa) a statement that it is organised and operates according to GCP
1055
and the applicable regulatory requirements;
1056
1057
(bb) documented initial and subsequent IRB/IEC
1058
approval/favourable opinion as well as any termination of the
1059
trial or the suspension of approval/favourable opinion.
1060
3.9 Sponsor Oversight
1061
3.9.1 The sponsor should ensure that the trial design and trial conduct, the processes
1062
undertaken, and the information and data generated are of sufficient quality to ensure
1063
reliable trial results, trial participant’s safety and appropriate decision making.
1064
1065
3.9.2 The sponsor should ensure that trial processes are conducted in compliance with the
1066
trial protocol and related documents as well as with applicable regulatory
1067
requirements and ethical standards.
1068
1069
3.9.3 The sponsor should determine necessary trial-specific criteria for classifying protocol
1070
deviations as important (i.e., those that impact the rights, safety and well-being of trial
1071
participants and the reliability of results).
1072
1073
3.9.4 Decisions related to the trial should be appropriately assessed for their impact on
1074
participant’s rights, safety and well-being and the reliability of trial results. Risks
1075
related to such decisions should be suitably managed throughout the planning,
1076
conduct and reporting of the trial.
1077
1078
3.9.5 The range and extent of oversight measures should be fit for purpose and tailored to
1079
the complexity of and risks associated with the trial. The selection and oversight of
1080
investigators and service providers are fundamental features of the oversight process.
1081
Oversight by the sponsor includes quality assurance and quality control processes
1082
relating to the trial-related activities of investigators and service providers.
1083
1084
3.9.6 The sponsor should ensure appropriate and timely escalation and follow-up of issues
1085
to allow the implementation of appropriate actions in a timely manner.
1086
1087
3.9.7 The sponsor may consider establishing an IDMC to assess the progress of a clinical
1088
trial including the safety data and the efficacy endpoints at intervals and to recommend
1089
to the sponsor whether to continue, modify or stop a trial.
1090
ICH E6(R3) Guideline
26
3.9.8 Where appropriate, sponsors may also establish an endpoint assessment/adjudication
1091
committee in certain trials to review important endpoints reported by investigators to
1092
determine whether the endpoints meet protocol-specified criteria. Such committees
1093
should typically be blinded to the assigned treatments when performing their
1094
assessments, regardless of whether the trial itself is conducted in a blinded manner, to
1095
ensure that the data reviewed by committee are as free of bias as possible.
1096
1097
3.9.9 Committees established for purposes that could impact participant safety or the
1098
reliability of trial results should include members with relevant expertise and with
1099
managed conflicts of interest, have written operating procedures (e.g., charters) and
1100
document their decisions.
1101
3.10 Quality Management
1102
The sponsor should implement an appropriate system to manage quality throughout all stages
1103
of the trial process. Quality management includes the design and implementation of efficient
1104
clinical trial protocols including tools and procedures for trial conduct (including for data
1105
collection and management) in order to support participant’s rights, safety and well-being and
1106
the reliability of trial results. The sponsor should adopt a proportionate and risk-based approach
1107
to quality management, which involves incorporating quality into the design of the clinical trial
1108
(i.e., quality by design) and identifying those factors that are likely to have a meaningful impact
1109
on participant’s rights, safety and well-being and the reliability of the results (i.e., critical to
1110
quality factors as described in ICH E8(R1)). The sponsor should describe the quality
1111
management approach implemented in the trial in the clinical trial report (see ICH E3).
1112
3.10.1 Risk Management
1113
A proportionate approach to the identification and management of risk is described below:
1114
3.10.1.1 Risk Identification
1115
The sponsor should identify risks that may have a meaningful impact on critical to
1116
quality factors. Risks should be considered across the processes used in the clinical
1117
trial (e.g., patient selection, informed consent process, randomisation and
1118
investigational product administration, data handling, and service provider activities).
1119
3.10.1.2 Risk Evaluation
1120
The sponsor should evaluate potential risks by considering:
1121
(a) the likelihood of harm/hazard occurring;
1122
1123
(b) the extent to which such harm/hazard would be detectable;
1124
1125
(c) the impact of such harm/hazard on trial participant protection and the
1126
reliability of trial results.
1127
3.10.1.3 Risk Control
1128
(a) Risk control should be proportionate to the importance of the risk to
1129
participants’ rights, safety and well-being and the reliability of trial results.
1130
ICH E6(R3) Guideline
27
Risk mitigation activities may be incorporated in protocol design and
1131
implementation, monitoring plans, agreements between parties defining roles
1132
and responsibilities, systematic safeguards to ensure adherence to SOPs, and
1133
training in processes and procedures.
1134
1135
(b) The sponsor should set acceptable ranges to support this process within which
1136
variation can be accepted. Where deviation beyond these ranges is detected,
1137
an evaluation should be performed to determine if there is a possible systemic
1138
issue and if action is needed.
1139
3.10.1.4 Risk Communication
1140
The sponsor should communicate the identified risks and mitigating activities, if
1141
applicable, to those who are involved in taking action or are affected by such activities.
1142
Communication also facilitates risk review and continual improvement during clinical
1143
trial conduct.
1144
3.10.1.5 Risk Review
1145
The sponsor should periodically review risk control measures to ascertain whether the
1146
implemented quality management activities remain effective and relevant, taking into
1147
account emerging knowledge and experience.
1148
3.10.1.6 Risk Reporting
1149
The sponsor should summarise and report the risks and the remedial actions taken in
1150
relation to important deviations from the acceptable ranges as detailed in section
1151
3.10.1.3(b) and document them in the clinical trial report (ICH E3).
1152
3.11 Quality Assurance and Quality Control
1153
The sponsor is responsible for establishing, implementing and maintaining
1154
appropriate quality assurance and quality control processes and documented
1155
procedures to ensure that trials are conducted and data are generated, recorded and
1156
reported in compliance with the protocol, GCP and the applicable regulatory
1157
requirement(s).
1158
3.11.1 Quality Assurance
1159
Quality assurance should be applied throughout the clinical trial and includes
1160
implementing strategies to identify potential or actual causes of serious non-
1161
compliance with the protocol, GCP and/or applicable regulatory requirements to
1162
enable their corrective and/or preventive actions.
1163
3.11.2 Audit
1164
When performed, audits should be conducted in a manner that is proportionate to the
1165
risks associated with the conduct of the trial.
1166
The purpose of a sponsor’s audit, which is independent of and separate from routine
1167
monitoring or quality control functions, is to evaluate whether the processes put in
1168
place to manage and conduct the trial are effective and compliant.
1169
ICH E6(R3) Guideline
28
3.11.2.1 Selection and Qualification of Auditors
1170
(a) The sponsor should appoint individuals who are independent of the clinical
1171
trial being audited.
1172
1173
(b) The sponsor should ensure that the auditors are qualified by training and
1174
experience to conduct audits properly.
1175
3.11.2.2 Auditing Procedures
1176
(a) The sponsor should ensure that the auditing of clinical trials/processes is
1177
conducted in accordance with the sponsor’s documented procedures on what
1178
to audit, how to audit (i.e., on-site or remote), the frequency of audits and the
1179
form and content of audit reports.
1180
1181
(b) The sponsor’s audit plan, program and procedures for a trial audit should be
1182
guided by the importance of the trial to submissions to regulatory authorities,
1183
the number of participants in the trial, the type and complexity of the trial, the
1184
level of risks to the trial participants and any identified problem(s).
1185
1186
(c) The observations and findings of the auditor(s) should be documented.
1187
1188
(d) To preserve the independence and value of the audit function, the regulatory
1189
authority(ies) should not routinely request the audit reports. Regulatory
1190
authority(ies) may seek access to an audit report on a case-by-case basis when
1191
evidence of serious GCP non-compliance exists or in the course of legal
1192
proceedings.
1193
1194
(e) When required by applicable regulatory requirements, the sponsor should
1195
provide an audit certificate.
1196
3.11.3 Quality Control
1197
Quality control should be applied to each stage of the data handling to ensure that data
1198
are reliable and have been processed correctly. Within clinical trials, monitoring and
1199
data management processes are the main quality control activities.
1200
1201
The quality control of sites (other than investigator sites, such as centralised imaging
1202
reading facilities), including on site and/or centralised activities, may be undertaken
1203
and reported using a risk-based approach.
1204
3.11.4 Monitoring
1205
The aim of monitoring is to ensure the participants’ rights, safety and well-being and
1206
the reliability of trial results as the trial progresses. Monitoring is one of the principal
1207
quality control activities.
1208
Monitoring involves a broad range of activities including, but not limited to,
1209
communication with investigator sites, verification of the investigator and investigator
1210
site staff qualifications and site resources, training and review of trial documents and
1211
ICH E6(R3) Guideline
29
information using a range of approaches including source data review, source data
1212
verification, data analytics and visits to institutional facilities undertaking trial-related
1213
activities. Some of these monitoring activities may be conducted by different methods
1214
and persons with different roles. However, monitoring should be performed by
1215
persons not involved in the clinical conduct of the trial being monitored. The
1216
monitoring approach should consider the activities and services involved, including
1217
decentralised settings, and be included in the monitoring plan. Monitors and other trial
1218
staff should adhere to data protection and confidentiality requirements in accordance
1219
with applicable regulatory requirements, institution policy and established data
1220
security standards.
1221
Monitoring activities may include site monitoring (performed on-site or remotely) and
1222
centralised monitoring, depending on the monitoring strategy and the design of the
1223
clinical trial.
1224
The sponsor should determine the appropriate extent and nature of monitoring, based
1225
on identified risks. Factors such as the objective, purpose, design, complexity,
1226
blinding, number of trial participants, investigational product, current knowledge of
1227
the safety profile and endpoints of the trial should be considered.
1228
3.11.4.1 Investigator Site Monitoring
1229
(a) Monitoring may be performed in relation to the clinical trial activities at the
1230
investigator sites (e.g., including their pharmacies and local laboratories, as
1231
appropriate). The frequency of monitoring activities should also be determined
1232
based on identified risks. Monitoring activities and their frequency should be
1233
modified as appropriate using knowledge gained.
1234
1235
(b) This monitoring activity may be performed on-site or remotely depending on
1236
the nature of the activity and its objectives.
1237
1238
(c) Monitoring may include secure, remote, direct read-only access to source
1239
records, other data acquisition tools and essential record retention systems.
1240
3.11.4.2 Centralised Monitoring
1241
(a) Centralised monitoring is an evaluation of accumulated data, performed in a
1242
timely manner, by the sponsor’s qualified and trained persons (e.g., medical
1243
monitor, data scientist/data manager, biostatistician).
1244
1245
(b) Centralised monitoring processes provide additional monitoring capabilities
1246
that can complement and reduce the extent and/or frequency of site monitoring
1247
or be used on its own. Use of centralised data analytics can help identify
1248
systemic or site-specific issues, including protocol non-compliance and
1249
potentially unreliable data.
1250
1251
(c) Centralised monitoring may support the selection of sites and/or processes for
1252
targeted site monitoring.
1253
ICH E6(R3) Guideline
30
3.11.4.3 Monitoring Plan
1254
The sponsor should develop a monitoring plan that is tailored to the identified
1255
potential safety risks, the risks to data quality and/or other risks to the reliability of
1256
the trial results. Particular attention should be given to procedures relevant to
1257
participant safety and to trial endpoints. The plan should describe the monitoring
1258
strategy, the monitoring activities of all the parties involved, the various monitoring
1259
methods and tools to be used, and the rationale for their use. The monitoring strategy
1260
should ensure appropriate oversight of trial conduct and consider site capabilities and
1261
the potential burden. The plan should focus on aspects that are critical to quality. The
1262
monitoring plan should reference the sponsor’s applicable policies and procedures.
1263
Monitoring of key data and processes (e.g., those related to primary endpoints and key
1264
secondary endpoints and processes intended to assure patient safety) performed
1265
outside the investigator site (e.g., central reading facilities, central laboratories) should
1266
be addressed in the monitoring plan.
1267
3.11.4.4 Monitoring Procedures
1268
Persons performing monitoring should follow the sponsor’s monitoring plan and
1269
applicable monitoring procedures.
1270
3.11.4.5 Monitoring Activities
1271
Monitoring in accordance with the sponsor’s requirements and monitoring plan
1272
should generally include the following activities across the clinical trial life cycle, as
1273
applicable.
1274
3.11.4.5.1 Communication with Parties Conducting the Trial
1275
(a) Establishing and maintaining a line of communication between the
1276
sponsor and the investigator and other parties and individuals involved
1277
in the trial conduct (e.g., centrally performed activities). In general, each
1278
site should have an assigned monitor as their contact point.
1279
1280
(b) Informing the investigator or other parties and individuals involved in
1281
the trial conduct of identified deviations from the protocol, GCP and the
1282
applicable regulatory requirements and taking appropriate action
1283
designed to prevent recurrence of the detected deviations. Important
1284
deviations should be highlighted and should be the focus of remediation
1285
efforts as appropriate.
1286
1287
(c) Informing the investigator or other parties and individuals involved in
1288
the trial conduct of source record(s) or entry errors or omissions in data
1289
acquisition tools and ensuring that corrections, additions or deletions are
1290
made as appropriate, dated, explained (if necessary) and that approval
1291
of the change is properly documented.
1292
1293
(d) Actions taken in relation to the deviations, errors or omissions should be
1294
proportionate to their importance.
1295
ICH E6(R3) Guideline
31
3.11.4.5.2 Investigator Site Selection, Initiation, Management and Close-out
1296
(a) Selecting the site and confirming that the investigator and individuals or
1297
parties involved in the trial conduct have adequate qualifications,
1298
resources (see sections 3.1, 3.2, and 4.7) and facilities, including
1299
laboratories, equipment and investigator site staff, to safely and properly
1300
conduct the trial.
1301
1302
(b) Confirming that the investigator, investigator site staff and other parties,
1303
and individuals involved in the trial conduct are adequately informed
1304
about the trial and follow the current approved protocol and other
1305
protocol-related documents, such as the current Investigator’s Brochure
1306
and relevant information related to the investigational product and
1307
instructions related to their delegated activities.
1308
1309
(c) Confirming that the investigator is maintaining the essential records (see
1310
Appendix C).
1311
1312
(d) Confirming that informed consent was obtained before participation in
1313
the trial (see section 2.8) for all enrolled participants at the site.
1314
1315
(e) Determining whether adverse events are appropriately reported within
1316
the time periods required by the protocol, GCP and the applicable
1317
regulatory requirement(s).
1318
1319
(f) Clarifying the sponsor’s protocol requirements for source records and
1320
the site’s location of such data.
1321
1322
(g) Verifying that the blinding is maintained, where applicable.
1323
1324
(h) Reviewing and reporting the participant recruitment and retention rates.
1325
1326
(i) Confirming that the investigator provides the required reports,
1327
notifications or other information in accordance with the protocol and
1328
trial procedures.
1329
1330
(j) Confirming the arrangement for the retention of the essential records and
1331
the final accountability of the investigational product (e.g., return and
1332
destruction or alternative disposition, if appropriate) during site close-
1333
out activity.
1334
3.11.4.5.3 Monitoring of Investigational Product Management
1335
(a) Confirming, for the investigational product(s):
1336
1337
(i) that storage conditions are acceptable and in accordance with the
1338
storage requirement specified in the protocol;
1339
1340
ICH E6(R3) Guideline
32
(ii) that supplies are sufficient throughout the trial and are used
1341
within their shelf-life;
1342
1343
(iii) that the correct investigational product(s) are supplied only to
1344
participants who are eligible to receive it at the protocol-
1345
specified dose(s) and, where appropriate, in accordance with the
1346
randomisation procedures;
1347
1348
(iv) that the participants, investigator, investigator site staff and other
1349
relevant parties and individuals involved in the trial conduct are
1350
provided with necessary instruction on properly using, handling,
1351
storing, returning and destroying, or alternative disposition of the
1352
investigational product(s);
1353
1354
(v) that the receipt, use, return and destruction, or alternative
1355
disposition of the investigational product(s) are controlled and
1356
documented adequately;
1357
1358
(vi) that the disposition of unused investigational product(s)
1359
complies with applicable regulatory requirement(s) and is in
1360
accordance with the sponsor requirements;
1361
1362
(vii) where product available on the market is dispensed and used in
1363
accordance with applicable regulatory requirements, some of the
1364
previously outlined considerations may not be applicable.
1365
3.11.4.5.4 Monitoring of Clinical Trial Data
1366
(a) Verifying that the investigator is enrolling only eligible trial participants.
1367
1368
(b) Checking the accuracy, completeness and consistency of the reported
1369
trial data against the source records and other trial-related records and
1370
whether these were reported in a timely manner. This can be done on the
1371
basis of using samples and supported by data analytics, as appropriate.
1372
The sample size may need adjustment based on previous monitoring
1373
results or other indications of insufficient data quality. Monitoring
1374
should:
1375
1376
(i) verify that the data required by the protocol and identified as
1377
critical in the monitoring plan are consistent with the source;
1378
1379
(ii) identify missing data, inconsistent data, data outliers,
1380
unexpected lack of variability and protocol deviations;
1381
1382
(iii) examine data trends, such as the range, consistency and
1383
variability of data within and across sites;
1384
1385
ICH E6(R3) Guideline
33
(c) Identifying significant errors in data collection and reporting at a site or
1386
across sites, potential data manipulation and data integrity problems.
1387
3.11.4.6 Monitoring Report
1388
(a) Reports of monitoring activities should include a summary of what was
1389
reviewed, a description of significant findings, conclusions and actions
1390
required to resolve them and follow-up on their resolution including those not
1391
resolved in previous reports. The requirements of monitoring reports
1392
(including their content and frequency) should be described in the sponsor’s
1393
procedures.
1394
1395
(b) Reports of investigator site and/or centralised monitoring should be provided
1396
to the appropriate sponsor staff as described in the sponsor’s procedures in a
1397
timely manner for review and follow-up.
1398
1399
(c) When needed, the report should describe findings requiring escalation for
1400
action and resolution. The sponsor should decide on the appropriate action to
1401
be taken, and these decisions and the resolution of the actions involved, where
1402
needed, should be recorded.
1403
3.12 Noncompliance
1404
3.12.1 Noncompliance with the protocol, SOPs, GCP and/or applicable regulatory
1405
requirement(s) by an investigator/institution or by member(s) of the sponsor’s staff
1406
should lead to appropriate and proportionate action by the sponsor to secure
1407
compliance.
1408
1409
3.12.2 If noncompliance that significantly affects or has the potential to significantly affect
1410
trial participant’s rights, safety or well-being or the reliability of trial results is
1411
discovered, the sponsor should perform a root cause analysis, implement appropriate
1412
corrective and preventive actions and confirm their adequacy unless otherwise
1413
justified. Where the sponsor identifies issues that could significantly impact
1414
participant’s rights, safety and well-being or the reliability of trial results, the sponsor
1415
should notify the regulatory authority and/or IRB/IEC in line with applicable
1416
regulatory requirements.
1417
1418
3.12.3 If the monitoring and/or auditing identifies serious noncompliance on the part of an
1419
investigator/institution that persists despite efforts at remediation, the sponsor should
1420
terminate the investigator’s/institution’s participation in the trial. When an
1421
investigator’s/institution’s participation is terminated because of noncompliance, the
1422
sponsor should promptly notify the regulatory authority(ies) and IRB/IEC as
1423
appropriate.
1424
3.13 Safety Assessment and Reporting
1425
The sponsor is responsible for the ongoing safety evaluation of the investigational product(s).
1426
ICH E6(R3) Guideline
34
The Investigator’s Brochure or, where applicable, the current scientific information such as a
1427
basic product information brochure, forms the basis of safety assessment and reporting for the
1428
clinical trial. For further information, see Appendix A.
1429
3.13.1 Sponsor Review of Safety Information
1430
The sponsor should aggregate, as appropriate, and periodically review relevant safety
1431
information. This may result in the update of the protocol, Investigator’s Brochure,
1432
informed consent materials and related documents.
1433
The sponsor should review the available emerging safety information to assess
1434
whether there is any new data that may affect the participant’s willingness to continue
1435
in the trial, impact the conduct of the trial, or alter the approval/favourable opinion of
1436
the IRB/IEC and/or regulatory authority(ies), as applicable. Any information of this
1437
nature should be communicated to the participants, investigator, IRB/IEC and
1438
regulatory authorities, as applicable, in a timely manner.
1439
3.13.2 Safety Reporting
1440
(a) The sponsor should submit to the regulatory authority(ies) safety updates and
1441
periodic reports, including changes to the Investigator’s Brochure, as required
1442
by applicable regulatory requirements.
1443
1444
(b) The sponsor should, in accordance with the applicable regulatory
1445
requirement(s) and with ICH E2A Clinical Safety Data Management:
1446
Definitions and Standards for Expedited Reporting, expedite the reporting to
1447
the regulatory authority(ies) of all adverse drug reactions (ADRs) that meet
1448
three criteria: suspected, unexpected and serious (i.e., SUSARs).
1449
1450
(c) Safety reporting to regulatory authorities should be undertaken by assessing
1451
the expectedness of the reaction in relation to the applicable product
1452
information (e.g., the reference safety information (RSI) contained within the
1453
Investigator’s Brochure or alternative documents) in accordance with
1454
applicable regulatory requirements. Refer to ICH E2F Development Safety
1455
Update Report for more information about RSI.
1456
1457
(d) The reporting of SUSARs to investigator(s)/institutions(s) and to the
1458
IRB(s)/IEC(s) should be undertaken in a manner that reflects the urgency of
1459
action required and should take into consideration the evolving knowledge of
1460
the safety profile of the product. Reporting of SUSARs to the
1461
investigators/institutions should be made in accordance with regulatory
1462
requirements. In some regions, periodic reporting of line listings with an
1463
overall safety assessment may be appropriate.
1464
1465
(e) Urgent safety issues requiring immediate attention or action should be
1466
reported to the IRB/IEC and/or regulatory authority(ies) and investigators
1467
without undue delay and as specified in regulatory requirements.
1468
1469
ICH E6(R3) Guideline
35
(f) Alternative arrangements for safety reporting to regulatory authorities,
1470
IRBs/IECs, and investigators and for reporting by investigators to the sponsor
1471
should be prospectively agreed upon with the regulatory authority(ies) and the
1472
IRB/IEC if applicable, and described in the clinical trial protocol, (e.g., SAEs
1473
considered efficacy or safety endpoints, which would not be subject to
1474
unblinding and expedited reporting; see ICH E2A). See ICH E19.
1475
3.13.3 Managing an Immediate Hazard
1476
The sponsor should take prompt action to address immediate hazards to participants.
1477
The sponsor should determine the causes of the hazard and based on this, take
1478
appropriate remedial actions.
1479
The sponsor should consider whether the protocol requires amendment in response to
1480
an immediate hazard. The information on the immediate hazard, if required, and any
1481
subsequent protocol amendment should be submitted to the IRB/IEC and/or
1482
regulatory authorities by the investigator/institution or sponsor (in accordance with
1483
applicable regulatory requirements).
1484
3.14 Insurance/Indemnification/Compensation to Participants and Investigators
1485
3.14.1 If required by the applicable regulatory requirement(s), the sponsor should provide
1486
insurance or should indemnify (legal and financial coverage) the investigator/the
1487
institution against claims arising from the trial except for claims that arise from
1488
malpractice and/or negligence.
1489
1490
3.14.2 The sponsor’s policies and procedures should address the costs of treatment of trial
1491
participants in the event of trial-related injuries in accordance with the applicable
1492
regulatory requirement(s).
1493
1494
3.14.3 The approach to compensating trial participants should comply with applicable
1495
regulatory requirement(s).
1496
3.15 Investigational Product(s)
1497
3.15.1 Information on Investigational Product(s)
1498
1499
The sponsor should ensure that an Investigator’s Brochure is developed and updated
1500
as significant new information on the investigational product becomes available.
1501
Alternatively, for authorised medicinal products, the sponsor should identify the basic
1502
product information to be used in the trial (see Appendix A).
1503
3.15.2 Manufacturing, Packaging, Labelling and Coding Investigational Product(s)
1504
(a) The sponsor should ensure that the investigational product(s) (including active
1505
control(s) and placebo, if applicable) is characterised as appropriate to the
1506
stage of development of the product(s), is manufactured in accordance with
1507
any applicable GMP and is coded and labelled in a manner that protects the
1508
blinding, if applicable. In addition, the labelling should comply with
1509
applicable regulatory requirement(s).
1510
1511
ICH E6(R3) Guideline
36
(b) The sponsor should determine acceptable storage temperatures and other
1512
storage conditions (e.g., protection from light) for the investigational
1513
product(s), appropriate reconstitution fluids and procedures, and devices for
1514
product infusion, if any. The sponsor should inform all involved parties (e.g.,
1515
monitors, investigators, pharmacists, storage managers) of these
1516
determinations.
1517
1518
(c) The investigational product(s) should be packaged to prevent contamination
1519
and unacceptable deterioration during transport and storage.
1520
1521
(d) In blinded trials, the sponsor should implement:
1522
1523
(i) a process to blind the sponsor staff, trial participant and/or investigator
1524
as appropriate to the investigational product identity and assignment to
1525
prevent and detect inappropriate unblinding;
1526
1527
(ii) a procedure and mechanism that permits the investigator to rapidly
1528
identify the product(s) in case of a medical emergency where
1529
unblinding is considered necessary, while protecting the identity of the
1530
treatment assignment of the other trial participants;
1531
1532
(iii) a mechanism that protects the blinding of the trial where a participant’s
1533
treatment assignment is unblinded for the purpose of safety reporting
1534
to regulatory authorities and/or IRB/IEC, where appropriate.
1535
1536
(e) If significant formulation changes are made in the investigational product(s)
1537
(including active control(s) and placebo, if applicable) during the course of
1538
clinical development, the results of any additional studies of the formulated
1539
product(s) (e.g., stability, dissolution rate, bioavailability) needed to assess
1540
whether these changes would significantly alter the pharmacokinetic profile
1541
of the product should be available prior to the use of the new formulation in
1542
clinical trials.
1543
3.15.3 Supplying and Handling Investigational Product(s)
1544
(a) The sponsor is responsible for supplying the investigator(s)/institution(s) with
1545
the investigational product(s) or, where appropriate, supplying trial
1546
participants in accordance with applicable regulatory requirements and after
1547
obtaining the required approval/favourable opinion from the IRB/IEC and the
1548
regulatory authority(ies) for the trial.
1549
1550
(b) The sponsor should ensure that instructions are available for the
1551
investigator/institution or trial participants on the handling and storage of
1552
investigational product(s). The procedures should consider adequate and safe
1553
receipt, handling, storage, dispensing, retrieval of unused product from
1554
participants and return of unused investigational product(s) to the sponsor (or
1555
ICH E6(R3) Guideline
37
alternative disposition if authorised by the sponsor and in compliance with the
1556
applicable regulatory requirement(s)).
1557
1558
(c) The sponsor should:
1559
1560
(i) ensure timely delivery of investigational product(s) to the
1561
investigator(s) or, where appropriate, to trial participants in accordance
1562
with applicable regulatory requirements to avoid any interruption to
1563
the trial as well as for the continuation of treatment for participants.
1564
1565
(ii) maintain records that document the identity, shipment, receipt, return
1566
and destruction, or alternative disposition of the investigational
1567
product(s) (see Appendix C);
1568
1569
(iii) maintain a system for retrieving investigational products and
1570
documenting this retrieval (e.g., for deficient product recall, return and
1571
destruction, or alternative disposition after trial completion, or expired
1572
product reclaim);
1573
1574
(iv) maintain a system for the disposition of unused investigational
1575
product(s) and for the documentation of this disposition;
1576
1577
(v) take steps to ensure that the investigational product(s) are stable over
1578
the period of use and only used within the current shelf-life;
1579
1580
(vi) maintain sufficient quantities of the investigational product(s) used in
1581
the trials to reconfirm specifications should this become necessary and
1582
maintain records of batch sample analyses and characteristics. The
1583
samples should be retained either until the analyses of the trial data are
1584
complete or as required by the applicable regulatory requirement(s),
1585
whichever represents the longer retention period. The samples do not
1586
need to be kept by the sponsor in trials where an authorised medicinal
1587
product is used as an investigational product unmodified from its
1588
authorised state, since samples are kept by the manufacturer.
1589
3.16 Data and Records
1590
3.16.1 Data Handling
1591
(a) The sponsor should ensure the integrity and confidentiality of data generated
1592
and managed.
1593
1594
(b) The sponsor should apply quality control to the relevant stages of data
1595
handling to ensure that the data are of sufficient quality to generate reliable
1596
results. The sponsor should focus their quality assurance and quality control
1597
activities and data review on critical data, including its relevant metadata.
1598
1599
ICH E6(R3) Guideline
38
(c) The sponsor should pre-specify data to be collected and the method of its
1600
collection in the protocol (see Appendix B. Clinical Trial Protocol and
1601
Protocol Amendment(s)). Where necessary, additional details, including a
1602
data flow diagram, should be contained in a protocol-related document (e.g.,
1603
a data management plan).
1604
1605
(d) The sponsor should ensure that data acquisition tools are fit for purpose and
1606
designed to capture the information required by the protocol. They should be
1607
validated and ready for use prior to their required use in the trial.
1608
1609
(e) The sponsor should ensure that documented processes are implemented to
1610
ensure the data integrity for the full data life cycle.
1611
1612
(f) The sponsor should implement measures to ensure the safeguarding of the
1613
blinding, if any (e.g., maintain the blinding during data entry and processing).
1614
1615
(g) The sponsor should provide guidance to investigators/institutions, service
1616
providers and trial participants, where relevant, on the expectations for data
1617
capture, data changes, data retention and data disposal.
1618
1619
(h) The sponsor should not make changes to data entered by the investigator or
1620
trial participants unless justified and documented by the sponsor and agreed
1621
upon by the investigator.
1622
1623
(i) The sponsor should allow correction of errors to data, including data entered
1624
by participants, where requested by the investigators/participants. Such data
1625
corrections should be justified and supported by source records around the
1626
time of original entry.
1627
1628
(j) The sponsor should ensure that the investigator has access to data collected in
1629
accordance with the protocol during the course of the trial including relevant
1630
data from external sources, for example, central laboratory data, centrally read
1631
imaging data and, if appropriate, ePRO data that are necessary to enable the
1632
investigators to make decisions (e.g., on eligibility, treatment, continuing
1633
participation in the trial and care for the safety of the individual trial
1634
participants). The sponsor should pay special attention to data that may
1635
unblind the investigator and include the appropriate provisions in the protocol.
1636
1637
(k) The sponsor should not have exclusive control of data captured in data
1638
acquisition tools.
1639
1640
(l) The sponsor should ensure that the investigator has access to the required data
1641
for retention purposes.
1642
1643
ICH E6(R3) Guideline
39
(m) The sponsor should ensure that the investigator receives instructions on how
1644
to navigate systems, data and relevant metadata for the trial participants under
1645
their responsibility.
1646
1647
(n) The sponsor should seek investigator endorsement of their data at
1648
predetermined milestones.
1649
1650
(o) The sponsor should document the data management steps to be undertaken
1651
prior to data analysis. These steps may vary depending on the purpose of the
1652
analysis to be conducted (e.g., data for IDMC, for interim analysis or the final
1653
analysis).
1654
1655
(p) Prior to provision of the data for analysis, edit access to the data acquisition
1656
tools should be restricted as appropriate to the purpose of the analysis; for
1657
example, for interim analysis, the restriction may only be temporary or
1658
managed differently compared to the final analysis.
1659
1660
(q) Deviations from the planned statistical analysis or changes made to the data
1661
analysis set after the trial has been unblinded (where applicable) should be
1662
clearly documented and justified and should only occur in exceptional
1663
circumstances (e.g., data discrepancies that must be resolved for the reliability
1664
of the trial results). Data changes should be authorised by the investigator and
1665
reflected in an audit trail. Post-unblinding data changes and deviations from
1666
the planned statistical analyses should be reported in the clinical trial report.
1667
1668
(r) The sponsor should use an unambiguous trial participant identification code
1669
(see glossary term) that allows identification of all the data reported for each
1670
participant.
1671
1672
(s) The sponsor should implement appropriate measures to protect the privacy and
1673
confidentiality of personal information of trial participants, in accordance with
1674
applicable regulatory requirements on personal data protection.
1675
1676
(t) In accordance with applicable regulatory requirements, the sponsor should
1677
document what happens to data when a participant withdraws or discontinues
1678
from the trial.
1679
1680
(u) The sponsor should ensure that trial data are protected from unauthorised
1681
access, disclosure, dissemination or alteration and from inappropriate
1682
destruction or accidental loss.
1683
1684
(v) The sponsor should have processes and procedures in place for reporting
1685
incidents (including security breaches) that have a significant impact on the
1686
trial data to relevant parties, including regulatory authorities, where relevant.
1687
1688
1689
ICH E6(R3) Guideline
40
(w) When using computerised systems in a clinical trial, the sponsor should:
1690
1691
(i) have a record of the computerised systems used in a clinical trial. This
1692
should include the use, functionality, interfaces and validation status
1693
of each computerised system, and who is responsible for its
1694
management should be described. The record should also include a
1695
description of implemented access controls and internal and external
1696
security measures;
1697
1698
(ii) ensure that the requirements for computerised systems deployed by the
1699
sponsor (e.g., requirements for validation, audit trails, user
1700
management, backup, disaster recovery and IT security) are addressed
1701
and implemented and that documented procedures and adequate
1702
training are in place to ensure the correct development, maintenance
1703
and use of computerised systems in clinical trials (see section 4). These
1704
requirements should be proportionate to the importance of the
1705
computerised system and the data or activities they are expected to
1706
process;
1707
1708
(iii) maintain a record of the individual users who are authorised to access
1709
the system, their roles and their access privileges:
1710
1711
(iv) ensure that access rights granted to investigator site staff are in
1712
accordance with delegations by the investigator and visible to the
1713
investigator;
1714
1715
(v) for systems deployed by the investigator/institution, assess whether
1716
such systems, if identified as containing source records in the trial,
1717
(e.g., electronic health records and other record keeping systems for
1718
source data collection and investigator site files) are fit for purpose or
1719
whether the known issue(s) can be appropriately mitigated. This
1720
assessment should occur during the process of selecting clinical trial
1721
sites and should be documented;
1722
1723
(vi) ensure that there is a process in place for service providers and
1724
investigators to inform the sponsor of system defects identified or
1725
incidents that could potentially constitute a serious non-compliance
1726
with the clinical trial protocol, trial procedures or GCP in accordance
1727
with section 3.13.
1728
ICH E6(R3) Guideline
41
3.16.2 Statistical Programming and Data Analysis
1729
This section concerning documentation of operational aspects of clinical trial
1730
statistical activities should be read in conjunction with ICH E9 Statistical Principles
1731
for Clinical Trials, which provides detailed guidance on statistical principles for
1732
clinical development, trial design, conduct, analysis and reporting.
1733
(a) The sponsor should ensure that appropriate and documented quality control of
1734
statistical programming and data analysis is implemented (e.g., for sample size
1735
calculations, results for IDMC, outputs for clinical trial report, statistical or
1736
centralised monitoring).
1737
1738
(b) The sponsor should ensure the traceability of data transformations and
1739
derivations during data processing and analysis.
1740
1741
(c) The sponsor should ensure that the allocation to or exclusion of each trial
1742
participant from any analysis set is predefined (e.g., in the protocol or the
1743
statistical analysis plan). The rationale for inclusion or exclusion for any
1744
participant (or particular data point) should be clearly described and
1745
documented.
1746
1747
(d) Procedures should be in place to describe unblinding; these descriptions
1748
should include:
1749
1750
(i) who was unblinded, at what timepoint and for what purpose they were
1751
unblinded;
1752
1753
(ii) who should remain blinded;
1754
1755
(iii) the safeguards in place to preserve the blinding.
1756
1757
(e) The sponsor should retain the statistical programming records that relate to the
1758
output contained or used in reports of the trial results, including quality
1759
control/validation activities performed. Outputs should be traceable to the
1760
statistical software programs, and they should be dated and time stamped and
1761
protected against any changes.
1762
3.16.3 Record Keeping and Retention
1763
(a) The sponsor (or subsequent owners of the data) should retain all of the
1764
sponsor-specific essential records pertaining to the trial in conformance with
1765
the applicable regulatory requirement(s).
1766
1767
(b) The sponsor should inform the investigator(s)/institution(s) and service
1768
providers, when appropriate, in writing of the need for essential records
1769
retention and should notify the investigator(s)/institution(s) and service
1770
providers, when appropriate, in writing when the trial-related records are no
1771
longer needed.
1772
ICH E6(R3) Guideline
42
(c) The sponsor should report any transfer of ownership of the essential records
1773
to the appropriate authority(ies) as required by the applicable regulatory
1774
requirement(s).
1775
3.16.4 Record Access
1776
(a) The sponsor should ensure that it is specified in the protocol or other
1777
documented agreement that the investigator(s)/institution(s) provide direct
1778
access to source records for trial-related monitoring, audits, IRB/IEC review
1779
and regulatory inspection.
1780
1781
(b) The sponsor should ensure that trial participants have consented to direct
1782
access to their original medical records and other participant-related trial
1783
documents for trial-related monitoring, audit, IRB/IEC review and regulatory
1784
inspection as part of the informed consent.
1785
3.17 Reports
1786
3.17.1 Premature Termination or Suspension of a Trial
1787
If a trial is prematurely terminated or suspended, the sponsor should promptly inform
1788
the investigators/institutions and the regulatory authority(ies) of the termination or
1789
suspension and the reason(s) for the termination or suspension. The IRB/IEC should
1790
also be informed promptly and provided with the reason(s) for the termination or
1791
suspension by the sponsor or by the investigator/institution, in accordance with
1792
applicable regulatory requirement(s).
1793
3.17.2 Clinical Trial/Study Reports
1794
(a) Whether the trial is completed or prematurely terminated or an interim analysis
1795
is undertaken for regulatory submission, the sponsor should ensure that the
1796
clinical trial reports, including interim reports, are prepared and provided to
1797
the regulatory agency(ies) as required by the applicable regulatory
1798
requirement(s). The sponsor should also ensure that the clinical trial reports in
1799
marketing applications meet the standards of ICH E3 or are otherwise in
1800
accordance with applicable regulatory requirements. (Note: ICH E3 specifies
1801
that abbreviated study reports may be acceptable in certain cases.)
1802
1803
(b) Investigators should be provided with a summary of the trial results.
1804
1805
(c) Consideration should be given to providing the investigator with information
1806
about the final treatment taken by their participants for blinded trials and a
1807
brief summary of the overall outcome of the trial. Where this information is
1808
provided to participants, the language should be non-technical, understandable
1809
to a layperson and non-promotional. The sponsor should only supply this
1810
information after the trial has been unblinded and all relevant
1811
analyses/conclusions have been completed and finalised.
1812
ICH E6(R3) Guideline
43
4. DATA GOVERNANCE – INVESTIGATOR AND SPONSOR
1813
This section provides guidance to investigators and sponsors (i.e., the responsible parties) on
1814
appropriate management of data integrity, traceability and security, thereby allowing the
1815
accurate reporting, verification and interpretation of the clinical trial-related information. This
1816
section should be read in conjunction with corresponding responsibilities for the investigator
1817
and the sponsor as defined in sections 2 and 3, along with ICH E8(R1) and ICH E9.
1818
The quality and amount of the information generated in a clinical trial should be sufficient to
1819
address trial objectives, provide confidence in the trial’s results and support good decision
1820
making.
1821
The systems and processes that help ensure this quality should be designed and implemented
1822
in a way that is proportionate to the risks to participants and the reliability of trial results.
1823
The following key processes should address the full data life cycle with a focus on the criticality
1824
of the data and should be implemented proportionately and documented appropriately:
1825
(a) processes to ensure data protection of trial participants’ confidential data;
1826
1827
(b) processes for managing computerised systems to ensure that they are fit for
1828
purpose and used appropriately;
1829
1830
(c) processes to safeguard essential elements of the clinical trial, such as
1831
randomisation, dose escalation and blinding;
1832
1833
(d) processes to support key decision making, such as data finalisation prior to
1834
analysis, unblinding, allocation to analysis data sets, changes in clinical trial
1835
design and, where applicable, the activities of, for example, an IDMC.
1836
4.1 Safeguard Blinding in Data Governance
1837
4.1.1 Maintaining the integrity of the blinding is important in particular in the design of
1838
systems, management of users’ account, delegation of responsibilities with respect to
1839
data handling and provision of data access at sites, data transfers, database review
1840
prior to planned unblinding and statistical analysis across all appropriate stages of the
1841
trial.
1842
1843
4.1.2 Roles, responsibilities and procedures for access to unblinded information should be
1844
defined and documented by all relevant parties according to the protocol; this
1845
information may also be included in the data management plans and statistical
1846
analysis plans. For example, in blinded trials, sponsor staff or designated third parties
1847
who are involved in operation of the trial and directly or indirectly interact with site
1848
investigator staff should not have access to unblinding information.
1849
1850
4.1.3 The potential for unblinding should be part of the risk assessment of a blinded trial.
1851
Any planned or unplanned unblinding, including accidental or emergency unblinding,
1852
should be documented and assessed for impact to trial results.
1853
ICH E6(R3) Guideline
44
4.2 Data Life Cycle Elements
1854
Procedures should be in place to cover the full data life cycle.
1855
4.2.1 Data Capture
1856
(a) The requirements for and extent of data verification, when data captured on
1857
paper or in an electronic health record are manually transcribed into a
1858
computerised system, should take the criticality of the data into account. Refer
1859
to section 4.2.3 for data entered directly in data acquisition tools.
1860
(b) Acquired data from any source should be accompanied by relevant metadata.
1861
At the point of data capture, automated data validation checks should be
1862
considered as required based upon risk, and their implementation should be
1863
controlled and documented.
1864
1865
4.2.2 Relevant Metadata, Including Audit Trails
1866
The approach used by the responsible party for implementing, evaluating, accessing,
1867
managing and reviewing relevant metadata associated with critical data should entail:
1868
1869
(a) Evaluating the system for the types and content of metadata available to ensure
1870
that:
1871
(i) computerised systems maintain logs of user account creation, changes
1872
to user roles and permissions and user access;
1873
1874
(ii) systems are designed to permit data changes in such a way that the
1875
initial data entry and any subsequent changes or deletions are
1876
documented, including, where appropriate, using a risk-based
1877
evaluation, the reason for the change if it is not implicit;
1878
1879
(iii) systems record and maintain workflow actions in addition to direct
1880
data entry/changes into the system.
1881
(b) Ensuring that audit trails, reports and logs are not disabled or modified except
1882
in rare circumstances and only if a log of such action and justification is
1883
maintained;
1884
1885
(c) Ensuring that audit trails and logs are decipherable and can facilitate analysis;
1886
1887
(d) Ensuring that the automatic capture of date and time of data entries or transfer
1888
using data acquisition tools are unambiguous (e.g., coordinated universal time
1889
(UTC));
1890
1891
(e) Determining which of the identified metadata require review and retention.
1892
ICH E6(R3) Guideline
45
4.2.3 Review of Data and Metadata
1893
Procedures for review of trial-specific data, audit trails and other relevant metadata
1894
should be in place. It should be a planned activity, and the extent and nature should
1895
be adapted to the individual trial and adjusted based on experience during the trial.
1896
4.2.4 Data Corrections
1897
There should be processes to correct data errors that could impact the reliability of the
1898
trial results. Corrections should be attributed to the entity making the correction,
1899
justified and supported by source records around the time of original entry, and
1900
performed in a timely manner.
1901
4.2.5 Data Transfer, Exchange and Migration
1902
Validated processes or other appropriate processes such as reconciliation should be in
1903
place to ensure that electronic data transferred between computerised systems retains
1904
its integrity and preserves its confidentiality. The transfer process should be
1905
documented to ensure traceability, and data reconciliation should be implemented as
1906
appropriate.
1907
4.2.6 Finalisation of Data Sets Prior to Analysis
1908
(a) Data of sufficient quality for interim and final analysis are achieved by
1909
implementing timely and reliable processes for data capture, verification,
1910
validation, review and rectification of errors and omissions that have a
1911
meaningful impact on the safety of trial participants and/or the reliability of
1912
the trial results.
1913
1914
(b) Activities undertaken to finalise the data sets prior to analysis should be
1915
confirmed and documented in accordance with pre-specified procedures.
1916
These activities may include reconciliation of entered data and data sets or
1917
reconciliation of relevant databases, correction of data errors and omissions,
1918
medical coding, compilation and addressing the impact of non-compliance
1919
including protocol deviations.
1920
1921
(c) Data extraction and determination of data analysis sets should take place in
1922
accordance with the planned statistical analysis and should be documented.
1923
4.3 Computerised Systems
1924
As described in sections 2 and 3, the responsibilities of the sponsor, investigator and
1925
the activities of other parties with respect to a computerised system used in clinical
1926
trials should be clear and documented. In summary, the sponsor is responsible for
1927
ensuring that for computerised systems which they put in place, the expectations for
1928
computerised systems as described in this section are addressed in a risk proportionate
1929
manner. The sponsor should review whether the systems used by the
1930
investigator/institution (e.g., electronic health records and other record keeping
1931
systems for source data collection) are fit for purpose in the context of the trial. In the
1932
event that the investigator/institution deploys systems specifically for the purposes of
1933
ICH E6(R3) Guideline
46
conducting clinical trials, the investigator/institution should ensure that the
1934
expectations are proportionately addressed and implemented.
1935
The responsible party should ensure that those developing computerised systems for
1936
clinical trials are aware of the intended purpose and the regulatory requirements that
1937
apply to them.
1938
It is recommended that representatives of intended participant populations and
1939
healthcare professionals are involved in the design of the system, where relevant, to
1940
ensure that computerised systems are suitable for use by the intended user population.
1941
4.3.1 Procedures for the Use of Computerised Systems
1942
Documented procedures should be in place to ensure the appropriate use of
1943
computerised systems in clinical trials for essential activities related to data collection,
1944
handling and management.
1945
4.3.2 Training
1946
The responsible party should ensure that those using computerised systems are
1947
appropriately trained in their use.
1948
4.4 Security of Computerised Systems
1949
4.4.1 The security of the trial data and records should be managed throughout the data life
1950
cycle.
1951
1952
4.4.2 The responsible party should ensure that security controls are maintained for
1953
computerised systems. These controls should include user management and ongoing
1954
measures to prevent, detect and/or mitigate security breaches. Aspects such as user
1955
authentication requirements and password management, firewall settings, antivirus
1956
software, security patching, system monitoring and penetration testing should be
1957
considered.
1958
1959
4.4.3 The responsible party should maintain adequate backup of the data.
1960
1961
4.4.4 Procedures should cover the following: system security measures, data backup and
1962
disaster recovery.
1963
4.5 Validation of Computerised Systems
1964
4.5.1 The responsible party is responsible for the validation status of the system throughout
1965
its life cycle. The approach to validation of computerised systems should be based on
1966
a risk assessment that considers the intended use of the system; the purpose and
1967
importance of the data/record that is collected/generated, maintained and retained in
1968
the system; and the potential of the system to affect the well-being, rights and safety
1969
of trial participants and the reliability of trial results.
1970
1971
4.5.2 Validation should demonstrate that the system conforms to the established
1972
requirements for completeness, accuracy, and reliability and is consistent with
1973
intended performance.
1974
ICH E6(R3) Guideline
47
4.5.3 Systems should be appropriately validated prior to use with adequate change control
1975
procedures implemented.
1976
1977
4.5.4 Validation of changes should be based on risk and consider both previously collected
1978
and new data.
1979
1980
4.5.5 Both basic system functionality and protocol specific configurations and
1981
customisations, including automated data entry checks and calculations, should be
1982
validated. Interfaces between systems should also be defined and validated. Different
1983
degrees of qualification/validation may be needed for bespoke systems, systems
1984
designed to be configured or systems where no alterations are needed.
1985
1986
4.5.6 Where relevant, procedures should cover the following: system design, validation,
1987
and functionality testing; release; setup; installation and change control until
1988
decommissioning.
1989
1990
4.5.7 The responsible party should ensure that the computerised systems used in clinical
1991
trial processes are qualified and validated, including those developed by other parties.
1992
They should ensure that qualification and validation documentation is maintained and
1993
retained.
1994
1995
4.5.8 Validation should generally include defining the requirements and specifications for
1996
the system and their testing, along with the associated documentation, to ensure the
1997
system is fit for purpose, especially for critical functionality, such as randomisation,
1998
dosing and dose titrations and reductions, and collection of endpoint data.
1999
2000
4.5.9 Unresolved issues, if any, should be justified and, where relevant, addressed by
2001
mitigations prior to and/or during the continued use of the system.
2002
2003
4.5.10 The trial-specific systems (including updates resulting from protocol amendments)
2004
should only be implemented to enable the conduct of the trial by the investigator after
2005
all necessary approvals for the clinical trial have been received.
2006
4.6 System Failure
2007
Contingency procedures should be in place to prevent loss or lack of accessibility to data
2008
essential to participant safety, trial decisions or trial outcomes.
2009
4.7 Technical Support
2010
4.7.1 Where appropriate, there should be mechanisms (e.g., help desk support) in place to
2011
document, evaluate and manage issues with the computerised systems (e.g., raised by
2012
users), and there should be periodic review of these cumulative issues to identify those
2013
that are repeated and/or systemic.
2014
2015
4.7.2 Defects and issues should be resolved according to their criticality. Issues with high
2016
criticality should be resolved in a timely manner.
2017
ICH E6(R3) Guideline
48
4.8 User Management
2018
4.8.1 Access controls are integral to computerised systems used in clinical trials to limit
2019
system access to authorised users and to ensure attributability to an individual. The
2020
security measures should be selected in such a way that they achieve the intended
2021
security and do not unduly impact user-friendliness.
2022
4.8.2 Procedures should be in place to ensure that user access rights are appropriately
2023
assigned based on a user’s duties and functions, blinding arrangements and the
2024
organisation to which users belong. Access rights should be revoked when they are
2025
no longer needed.
2026
4.8.3 Authorised users and access privileges should be clearly documented, maintained and
2027
retained. These records should include any updates to a user’s roles, access rights and
2028
permissions, and time of access privileges given (e.g., time stamp).
2029
ICH E6(R3) Guideline
49
GLOSSARY
2030
Adverse Events and Adverse Reaction-related definitions:
2031
Adverse Event (AE): Any unfavourable medical occurrence in a trial participant. The
2032
adverse event does not necessarily have a causal relationship with the treatment.
2033
Adverse Drug Reaction (ADR):
2034
• in the pre-approval clinical experience with a new investigational product or its new
2035
usages (particularly as the therapeutic dose(s) may not be established):
2036
unfavourable and unintended responses, such as a sign (e.g., laboratory results),
2037
symptoms or disease related to any dose of a medicinal product where a causal
2038
relationship between a medicinal product and an adverse event is a reasonable
2039
possibility. The level of certainty about the relatedness of the adverse drug reaction
2040
to an investigational product will vary. If the ADR is suspected to be medicinal
2041
product-related with a high level of certainty, it should be included in the reference
2042
safety information (RSI) and/or the Investigator’s Brochure (IB).
2043
2044
• for marketed medicinal products: a response to a drug that is noxious and
2045
unintended and that occurs at doses normally used in humans for prophylaxis,
2046
diagnosis or therapy of diseases or for modification of physiological function.
2047
(See ICH E2A Clinical Safety Data Management: Definitions and Standards for
2048
Expedited Reporting).
2049
Serious Adverse Event (SAE): Any unfavourable medical occurrence that is considered
2050
serious at any dose if it:
2051
• results in death
2052
• is life-threatening
2053
• requires inpatient hospitalisation or prolongation of existing hospitalisation
2054
• results in persistent or significant disability/incapacity
2055
• is a congenital anomaly/birth defect (see ICH E2A)
2056
Suspected Unexpected Serious Adverse Reaction (SUSAR): an adverse reaction that
2057
meets three criteria: suspected, unexpected and serious.
2058
• Suspected: There is a reasonable possibility that the drug caused the adverse drug
2059
reaction.
2060
2061
• Unexpected: An adverse reaction, the nature or severity of which is not consistent
2062
with the applicable product information (e.g., the RSI, see glossary term contained
2063
within the Investigator’s Brochure or alternative documents according to applicable
2064
regulatory requirements. Refer to ICH E2F Development Safety Update Report for
2065
more information about RSI.
2066
2067
• Serious: See above for SAE.
2068
2069
ICH E6(R3) Guideline
50
Agreement
2070
A document or set of documents describing the details of any arrangements on delegation or
2071
transfer, distribution and/or sharing of activities and, if appropriate, on financial matters
2072
between two or more parties. This could be in the form of a contract. The protocol may serve
2073
as the basis of an agreement.
2074
Applicable Regulatory Requirement(s)
2075
Any law(s) and regulation(s) addressing the conduct of clinical trials of investigational
2076
products.
2077
Assent
2078
Affirmative agreement of a minor to participate in clinical trial. The absence of expression of
2079
agreement or disagreement should not be interpreted as assent.
2080
Audit
2081
A systematic and independent examination of trial-related activities and records performed by
2082
the sponsor, service provider (including contract research organisation (CRO)) or institution to
2083
determine whether the evaluated trial-related activities were conducted and the data were
2084
recorded, analysed and accurately reported according to the protocol, applicable standard
2085
operating procedures (SOPs), Good Clinical Practice (GCP) and the applicable regulatory
2086
requirement(s).
2087
Audit Certificate
2088
A declaration of confirmation by the auditor that an audit has taken place.
2089
Audit Report
2090
A record describing the conduct and outcome of the audit.
2091
Audit Trail
2092
Metadata records that allow reconstruction of the course of events by capturing details on
2093
actions (manual or automated) performed relating to information and data collection and, where
2094
applicable, to activities in computerised systems. The audit trail should show activities, initial
2095
entry, and changes to data fields or records, by whom, when and, where applicable, why. In
2096
computerised systems, the audit trail should be secure, computer generated and timestamped.
2097
Blinding/Masking
2098
A procedure in which one or more parties to the trial are kept unaware of the treatment
2099
assignment(s). Single-blinding usually refers to the participant(s) being unaware, and double-
2100
blinding usually refers to the participant(s), investigator(s) or other trial staff, as appropriate,
2101
being unaware of the treatment assignment(s).
2102
Case Report Form (CRF)
2103
A tool designed to record protocol-required information to be reported by the investigator to
2104
the sponsor on each trial participant (see Data Acquisition Tool).
2105
2106
ICH E6(R3) Guideline
51
Certified Copy
2107
A copy (irrespective of the type of media used) of the original record that has been verified
2108
(i.e., by a dated signature or by generation through a validated process) to have the same
2109
information as the original, including relevant metadata, where applicable.
2110
Clinical Trial
2111
Any interventional investigation in human participants intended to discover or verify the
2112
clinical, pharmacological and/or other pharmacodynamic effects of an investigational
2113
product(s); and/or to identify any adverse reactions to an investigational product(s); and/or to
2114
study absorption, distribution, metabolism and excretion of an investigational product(s) with
2115
the object of ascertaining its safety and/or efficacy.
2116
Clinical Trial/Study Report (CSR)
2117
A documented description of a trial of any investigational product conducted in human
2118
participants, in which the clinical and statistical description, presentations and analyses are
2119
fully integrated into a single report (see ICH E3 Structure and Content of Clinical Study
2120
Reports).
2121
Comparator
2122
An investigational or authorised medicinal product (i.e., active control), placebo or standard of
2123
care used as a reference in a clinical trial.
2124
Compliance (in relation to trials)
2125
Adherence to the trial-related requirements, GCP requirements and the applicable regulatory
2126
requirements.
2127
Confidentiality
2128
Prevention of disclosure to other than authorised individuals of a sponsor’s proprietary
2129
information or of a participant’s identity or their confidential information.
2130
Coordinating Investigator
2131
An investigator assigned the responsibility for the coordination of investigators at different
2132
investigator sites participating in a multicentre trial (if appropriate).
2133
Computerised Systems Validation
2134
A process of establishing and documenting that the specified requirements of a computerised
2135
system can be consistently fulfilled from design until decommissioning of the system or
2136
transition to a new system. The approach to validation should be based on a risk assessment
2137
that takes into consideration the intended use of the system and the potential of the system to
2138
affect trial participant protection and the reliability of trial results.
2139
Contract Research Organisation (CRO)
2140
See Service Provider.
2141
2142
ICH E6(R3) Guideline
52
Data Acquisition Tool (DAT)
2143
A paper or electronic tool designed to collect data and associated metadata from a data
2144
originator in a clinical trial according to the protocol and to report the data to the sponsor.
2145
The data originator may be a human (e.g., the participant or trial staff), a machine (e.g.,
2146
wearables and sensors) or an electronic transfer of data from one system to another (e.g.,
2147
extraction of data from an electronic health record or laboratory system).
2148
Examples of DATs include but are not limited to CRFs, interactive response technologies
2149
(IRTs), patient-reported outcomes (PROs), clinical outcome assessments (COAs) and wearable
2150
devices, irrespective of the media used.
2151
Direct Access
2152
Permission to examine, analyse and verify records that are important to the evaluation of a
2153
clinical trial and may be performed in person or remotely. Any party (e.g., domestic and foreign
2154
regulatory authorities, sponsor’s monitors and auditors) with direct access should take
2155
reasonable precautions within the constraints of the applicable regulatory requirement(s) to
2156
maintain the confidentiality of participants’ identities and their data and sponsor’s proprietary
2157
information.
2158
Essential Records
2159
Essential records are the documents and data (and relevant metadata), in any format, associated
2160
with a clinical trial that facilitate the ongoing management of the trial and collectively allow
2161
the evaluation of the methods used, the factors affecting a trial and the actions taken during the
2162
trial conduct to determine the reliability of the trial results produced and the verification that
2163
the trial was conducted in accordance with GCP and applicable regulatory requirements (see
2164
Appendix C. Essential Records for the Conduct of a Clinical Trial).
2165
Good Clinical Practice (GCP)
2166
A standard for the planning, initiating, performing, recording, oversight, evaluation, analysis
2167
and reporting of clinical trials that provides assurance that the data and reported results are
2168
reliable and that the rights, safety and well-being of trial participants are protected.
2169
Impartial Witness
2170
A person who is independent of the trial who cannot be unfairly influenced by people involved
2171
with the trial, who attends the informed consent process if the participant or the participant’s
2172
legally acceptable representative cannot read, and who reads the informed consent form and
2173
any other documented information supplied or read to the participant and/or their legally
2174
acceptable representative.
2175
Independent Data Monitoring Committee (IDMC)
2176
An independent data monitoring committee (e.g., data safety monitoring board) that may be
2177
established by the sponsor to assess at intervals the progress of a clinical trial, the safety data
2178
and the critical efficacy endpoints, and to recommend to the sponsor whether to continue,
2179
modify or stop a trial.
2180
2181
ICH E6(R3) Guideline
53
Informed Consent
2182
A process by which a participant or their legally accepted representative voluntarily confirms
2183
their willingness to participate in a trial after having been informed and been provided with the
2184
opportunity to discuss all aspects of the trial that are relevant to the participant’s decision to
2185
participate. Varied approaches to the provision of information and the discussion about the trial
2186
can be used. This can include, for example, providing text in different formats, images and
2187
videos and using telephone or video conferencing with investigator site staff. Informed consent
2188
is documented by means of a written or electronic, signed and dated informed consent form.
2189
Obtaining consent remotely may be considered when appropriate.
2190
Inspection
2191
The act by a regulatory authority(ies) of conducting an official review of documents, facilities,
2192
records and any other resources that are deemed by the authority(ies) to be related to the clinical
2193
trial and that may be accessed at the investigator site, at the sponsor’s and/or service provider’s
2194
(including CRO’s) facilities, or at other establishments deemed appropriate by the regulatory
2195
authority(ies). Some aspects of the inspection may be conducted remotely.
2196
Institution
2197
Any public or private entity or agency or medical or dental organisation in whose remit clinical
2198
trials are conducted.
2199
Institutional Review Board (IRB)/Independent Ethics Committee (IEC)
2200
An independent body (a review board or a committee, institutional, regional, national or
2201
supranational) constituted of medical professionals and non-medical members whose
2202
responsibility it is to ensure the protection of the rights, safety and well-being of human
2203
participants involved in a trial and to provide public assurance of that protection by, among
2204
other things, reviewing and approving/providing favourable opinion on the trial protocol, the
2205
suitability of the investigator(s), the facilities, and the methods and material to be used in
2206
obtaining and documenting informed consent of the trial participants. The legal status,
2207
composition, function, operations and regulatory requirements pertaining to IRBs/IECs may
2208
differ among countries but should allow the IRB/IEC to act in agreement with GCP as
2209
described in this guideline.
2210
Interim Clinical Trial/Study Report
2211
A report of intermediate results and their evaluation based on analyses performed during the
2212
course of a trial.
2213
Investigational Product
2214
A pharmaceutical form of an active ingredient or placebo being tested or used as a reference in
2215
a clinical trial, including a product with a marketing authorisation when used or assembled
2216
(formulated or packaged) in a way different from the approved form, or when used for an
2217
unapproved indication, or when used to gain further information about an approved use.
2218
2219
2220
ICH E6(R3) Guideline
54
Investigator
2221
A person responsible for the conduct of the clinical trial, including the trial participants for
2222
whom that person has responsibility during the conduct of the trial. If a trial is conducted by a
2223
team of individuals, the investigator is the responsible leader of the team and may be called the
2224
principal investigator. Where an investigator/institution is referenced in this guideline, it
2225
describes expectations that may be applicable to the investigator and/or the institution in some
2226
regions. Where required by the applicable regulatory requirements, the “investigator” should
2227
be read as “investigator and/or the institution.”
2228
Investigator’s Brochure (IB)
2229
A compilation of the clinical and nonclinical data on the investigational product(s) that is
2230
relevant to the study of the investigational product(s) in human participants (see Appendix A.
2231
Investigator’s Brochure).
2232
Investigator Site
2233
The location(s) at or from where trial-related activities are conducted under the
2234
investigator’s/institution’s supervision.
2235
Legally Acceptable Representative
2236
An individual or juridical or other body authorised under applicable law to consent, on behalf
2237
of a prospective participant, to the participant’s participation in the clinical trial.
2238
Metadata
2239
The contextual information required to understand a given data element. Metadata is structured
2240
information that describes, explains or otherwise makes it easier to retrieve, use or manage
2241
data. For the purpose of this guideline, relevant metadata are those needed to reconstruct the
2242
trial conduct.
2243
Monitoring
2244
The act of overseeing the progress of a clinical trial and of ensuring that the clinical trial is
2245
conducted, recorded and reported in accordance with the protocol, SOPs, GCP and the
2246
applicable regulatory requirement(s).
2247
Monitoring Plan
2248
A document that describes the strategy, methods, responsibilities and requirements for
2249
monitoring the trial.
2250
Monitoring Report
2251
A documented report following site and/or centralised monitoring activities.
2252
Multicentre Trial
2253
A clinical trial conducted according to a single protocol but at more than one investigator site.
2254
Nonclinical Study
2255
Biomedical studies not performed on human participants.
2256
ICH E6(R3) Guideline
55
Original Medical Record
2257
See Source Records.
2258
Protocol
2259
A document that describes the objective(s), design, methodology, statistical considerations and
2260
organisation of a trial. The protocol usually also gives the background and rationale for the
2261
trial, but these could be provided in other protocol referenced documents. Throughout the ICH
2262
GCP Guideline, the term protocol refers to protocol and protocol amendments.
2263
Protocol Amendment
2264
A documented description of a change(s) to a protocol.
2265
Quality Assurance (QA)
2266
All those planned and systematic actions that are established to ensure that the trial is performed
2267
and the data are generated, documented (recorded) and reported in compliance with GCP and
2268
the applicable regulatory requirement(s).
2269
Quality Control (QC)
2270
The operational techniques and activities undertaken to verify that the requirements for quality
2271
of the trial-related activities have been fulfilled.
2272
Randomisation
2273
The process of deliberately including an element of chance when assigning participants to
2274
groups that receive different treatments in order to reduce bias.
2275
Reference Safety Information (RSI)
2276
Contains a cumulative list of ADRs that are expected for the investigational product being
2277
administered to participants in a clinical trial. The RSI is included in the Investigator’s
2278
Brochure.
2279
Regulatory Authorities
2280
Bodies having the power to regulate, including those that review submitted protocols and
2281
clinical data and those that conduct inspections. These bodies are sometimes referred to as
2282
competent authorities.
2283
Service Provider
2284
A person or organisation (commercial, academic or other) providing a service used during the
2285
conduct of a clinical trial to either the sponsor or the investigator to fulfil one or more of their
2286
trial-related activities.
2287
Signature
2288
A unique mark, symbol or entry in line with applicable regulatory requirements and/or practice
2289
to show expression of will and allow authentication of the signatory.
2290
2291
ICH E6(R3) Guideline
56
Source Records
2292
Original documents or data (which includes relevant metadata) or certified copies of the
2293
original documents or data, irrespective of the media used. This may include trial participants’
2294
medical/health records/notes/charts; data provided/entered by trial participants (e.g., electronic
2295
patient-reported outcome (ePROs)); healthcare providers’ records from pharmacies,
2296
laboratories and other facilities involved in the clinical trial; and data from automated
2297
instruments, such as wearables and sensors.
2298
Sponsor
2299
An individual, company, institution, or organisation that takes responsibility for the initiation,
2300
management and arrangement of the financing of a clinical trial. A clinical trial may have one
2301
or several sponsors where permitted under regulatory requirements. All sponsors have the
2302
responsibilities of a sponsor set out in this guideline. In accordance with regulatory
2303
requirements, sponsors may decide in a documented agreement setting out their respective
2304
responsibilities. Where the agreement does not specify to which sponsor a given responsibility
2305
is attributed, that responsibility lies with all sponsors.
2306
Sponsor-Investigator
2307
An individual who both initiates and conducts, alone or with others, a clinical trial, and under
2308
whose immediate direction the investigational product is administered to, dispensed to or used
2309
by a participant. The term does not include any person other than an individual (e.g., the term
2310
does not include a corporation or an agency). The obligations of a sponsor-investigator include
2311
both those of a sponsor and those of an investigator.
2312
Standard Operating Procedures (SOPs)
2313
Detailed, documented instructions to achieve uniformity of the performance of a specific
2314
activity.
2315
Sub-investigator
2316
Any individual member of the clinical trial team designated and supervised by the investigator
2317
to perform critical trial-related procedures and/or to make important trial-related decisions
2318
(e.g., associates, residents, research fellows).
2319
Trial Participant
2320
An individual who participates in a clinical trial, either as a recipient of the investigational
2321
product(s) or as a control.
2322
Trial Participant Identification Code
2323
A unique identifier assigned to each trial participant to protect the participant’s identity and
2324
used in lieu of the participant’s name when the investigator reports adverse events and/or other
2325
trial-related data.
2326
Vulnerable Participants
2327
Individuals whose willingness to volunteer in a clinical trial may be unduly influenced by the
2328
expectation, whether justified or not, of benefits associated with participation or of a retaliatory
2329
ICH E6(R3) Guideline
57
response from senior members of a hierarchy in case of refusal to participate. Examples are
2330
members of a group with a hierarchical structure, such as medical, pharmacy, dental and
2331
nursing students; subordinate hospital and laboratory personnel; employees of the
2332
pharmaceutical industry; members of the armed forces and persons kept in detention. Other
2333
vulnerable participants may include persons in nursing homes, unemployed or impoverished
2334
persons, patients in emergency situations, ethnic minority groups, homeless persons, nomads,
2335
refugees, minors and those incapable of giving consent.
2336

ICH E6(R3) Guideline
58
APPENDICES
2337
Appendix A. INVESTIGATOR’S BROCHURE
2338
A.1 Introduction
2339
The Investigator’s Brochure (IB) is a compilation of the clinical and nonclinical data on the
2340
investigational product(s)
1
that are relevant to the study of the product(s) in human participants.
2341
Its purpose is to provide the investigators and others involved in the trial with the information
2342
to facilitate their understanding of the rationale for and their compliance with many key
2343
features of the protocol, such as the dose, dose frequency/interval, methods of administration
2344
and safety monitoring procedures.
2345
2346
A.1.1 Development of the Investigator’s Brochure
2347
Generally, the sponsor is responsible for ensuring that an up-to-date IB is developed.
2348
In the case of an investigator-initiated trial, the sponsor-investigator should determine
2349
whether a brochure is available from the product license/marketing authorisation
2350
holder. If the investigational product is provided by the sponsor-investigator, then they
2351
should provide the necessary information to the investigator site staff. Where
2352
permitted by regulatory authorities, the current scientific information such as a basic
2353
product information brochure (e.g., summary of product characteristics package
2354
leaflet, or labelling) may be an appropriate alternative, provided that it includes
2355
current, comprehensive and detailed information on all aspects of the investigational
2356
product that might be of importance to the investigator. If an authorised medicinal
2357
product is being studied for a new use (i.e., a new indication), an IB specific to that
2358
new use should be prepared unless there is a rationale for only one IB. The IB should
2359
be reviewed at least annually and revised as necessary in compliance with a sponsor’s
2360
documented procedures. More frequent revision may be appropriate depending on the
2361
stage of development and the generation of relevant new information. Relevant new
2362
information may be so important that it needs to be communicated to the investigators
2363
and possibly to the IRBs/IECs and/or regulatory authorities before it is included in a
2364
revised IB.
2365
2366
A.1.2 Reference Safety Information and Risk-Benefit Assessment
2367
The reference safety information (RSI) contained in the IB provides an important
2368
reference point for expedited reporting of suspected unexpected serious adverse
2369
reactions (SUSARs) in the clinical trial. The IB also provides insight to support the
2370
clinical management of the participants during the course of the clinical trial. The
2371
information should be presented in a concise, simple, objective, balanced and non-
2372
promotional form that enables a clinician or potential investigator to understand it and
2373
make their own unbiased risk-benefit assessment of the appropriateness of the
2374
proposed trial. For this reason, a medically qualified person should be involved in the
2375
generation of an IB, but the contents of the IB should be approved by the disciplines
2376
that generated the described data.
2377
1
For the purpose of this guideline, the term “investigational products” should be considered synonymous with
drugs, medicines, medicinal products, vaccines and biological products.
ICH E6(R3) Guideline
59
A.2 General Considerations
2378
These considerations delineate the minimum information that should be included in an IB. It is
2379
expected that the type and extent of information available will vary with the stage of
2380
development of the investigational product.
2381
The IB should include;
2382
A.2.1 Title Page
2383
This should provide the sponsor’s name, the identity of each investigational product
2384
(i.e., research number, chemical or approved generic name and trade name(s) where
2385
legally permissible and desired by the sponsor) and the release date. It is also
2386
suggested that an edition number and a reference to the number and date of the edition
2387
it supersedes be provided along with the cut-off date for data inclusion in the version.
2388
Where appropriate, a signature page may be included.
2389
A.2.2 Confidentiality Statement
2390
The sponsor may wish to include a statement instructing the investigator and other
2391
recipients to treat the IB as a confidential document for the sole information and use
2392
of the investigator/institution, investigator site staff, regulatory authorities and the
2393
institutional review board/independent ethics committee (IRB/IEC).
2394
A.3 Contents of the Investigator’s Brochure
2395
The IB should contain the following sections, each with literature references (publications or
2396
reports) included at the end of each chapter, where appropriate;
2397
A.3.1 Table of Contents
2398
A.3.2 Summary
2399
A brief summary (preferably not exceeding two pages) should be given, highlighting
2400
the significant physical, chemical, pharmaceutical, pharmacological, toxicological,
2401
pharmacokinetic, metabolic and clinical information available that is relevant to the
2402
stage of clinical development of the investigational product.
2403
A.3.3 Introduction
2404
A brief introductory statement should be provided that contains the chemical name
2405
(and generic and trade name(s) when approved) of the investigational product(s); all
2406
active ingredients; the pharmacological class of the investigational product(s) and its
2407
expected position within this class (e.g., advantages); the rationale for performing
2408
research with the investigational product(s); and the anticipated prophylactic,
2409
therapeutic or diagnostic indication(s). Finally, the introductory statement should
2410
provide the general approach to be followed in evaluating the investigational product.
2411
A.3.4 Physical, Chemical and Pharmaceutical Properties and Formulation
2412
A description should be provided of the investigational product substance(s)
2413
(including the chemical and/or structural formula(e)), and a brief summary should be
2414
given of the relevant physical, chemical and pharmaceutical properties.
2415
ICH E6(R3) Guideline
60
To permit appropriate safety measures to be taken in the course of the trial, a
2416
description of the formulation(s) to be used, including excipients, should be provided
2417
and justified if clinically relevant. Instructions for the storage and handling of the
2418
dosage form(s) should also be given.
2419
Any structural similarities to other known compounds should be mentioned.
2420
A.3.5 Nonclinical Studies
2421
Introduction
2422
The results of all relevant nonclinical pharmacology, toxicology, pharmacokinetic and
2423
investigational product metabolism studies should be provided in summary form. This
2424
summary should address the methodology used, the results and a discussion of the
2425
relevance of the findings to the investigated therapeutic and the possible unfavourable
2426
and unintended effects in humans.
2427
The information provided may include the following, as appropriate, if
2428
known/available:
2429
• species tested
2430
• number and sex of animals in each group
2431
• unit dose (e.g., milligram/kilogram (mg/kg))
2432
• dose interval
2433
• route of administration
2434
• duration of dosing
2435
• information on systemic distribution
2436
• duration of post-exposure follow-up
2437
• results, including the following aspects:
2438
- nature and frequency of pharmacological or toxic effects
2439
- severity or intensity of pharmacological or toxic effects
2440
- time to onset of effects
2441
- reversibility of effects
2442
- duration of effects
2443
- dose response
2444
Tabular format/listings should be used whenever possible to enhance the clarity of the
2445
presentation.
2446
The following sections should discuss the most important findings from the studies,
2447
including the dose response of observed effects, the relevance to humans and any
2448
aspects to be studied in humans. If applicable, the effective and nontoxic dose findings
2449
in the same animal species should be compared (i.e., the therapeutic index should be
2450
discussed). The relevance of this information to the proposed human dosing should
2451
be addressed. Whenever possible, comparisons should be made in terms of
2452
blood/tissue levels rather than on a mg/kg basis.
2453
(a) Nonclinical Pharmacology
2454
A summary of the pharmacological aspects of the investigational product and, where
2455
appropriate, its significant metabolites studied in animals should be included. Such a
2456
ICH E6(R3) Guideline
61
summary should incorporate studies that assess potential therapeutic activity (e.g.,
2457
efficacy models, receptor binding and specificity) as well as those that assess safety
2458
(e.g., special studies to assess pharmacological actions other than the intended
2459
therapeutic effect(s)).
2460
(b) Pharmacokinetics and Product Metabolism in Animals
2461
A summary of the pharmacokinetics and biological transformation and disposition of
2462
the investigational product in all species studied should be given. The discussion of
2463
the findings should address the absorption and the local and systemic bioavailability
2464
of the investigational product and its metabolites and their relationship to the
2465
pharmacological and toxicological findings in animal species.
2466
(c) Toxicology
2467
A summary of the toxicological effects found in relevant studies conducted in
2468
different animal species should be described under the following headings where
2469
appropriate:
2470
• single dose
2471
• repeated dose
2472
• carcinogenicity
2473
• special studies (e.g., irritancy and sensitisation)
2474
• reproductive toxicity
2475
• genotoxicity (mutagenicity)
2476
A.3.6 Effects in Humans
2477
Introduction
2478
A thorough discussion of the known effects of the investigational product(s) in
2479
humans should be provided, including information on pharmacokinetics, metabolism,
2480
pharmacodynamics, dose response, safety, efficacy and other pharmacological
2481
activities. Where possible, a summary of each completed clinical trial and ongoing
2482
trials where interim results are available that may inform the safety evaluation should
2483
be provided. Information should also be provided regarding results of any use of the
2484
investigational product(s) other than from in clinical trials, such as from experience
2485
during marketing.
2486
(a) Pharmacokinetics and Product Metabolism in Humans
2487
A summary of information on the pharmacokinetics of the investigational product(s)
2488
should be presented, including the following, if available:
2489
• pharmacokinetics (including metabolism, as appropriate, and absorption,
2490
plasma protein binding, distribution and elimination)
2491
• bioavailability of the investigational product (absolute, where possible, and/or
2492
relative) using a reference dosage form
2493
• population subgroups (e.g., sex, age and impaired organ function)
2494
• interactions (e.g., product-product interactions and effects of food)
2495
ICH E6(R3) Guideline
62
• other pharmacokinetic data (e.g., results of population studies performed within
2496
clinical trial(s))
2497
2498
(b) Safety and Efficacy
2499
A summary of information should be provided about the investigational
2500
product’s/products’ (including metabolites, where appropriate) safety,
2501
pharmacodynamics, efficacy and dose response that was obtained from preceding
2502
trials in humans (healthy volunteers and/or patients). The implications of this
2503
information should be discussed. In cases where a number of clinical trials have been
2504
completed, the use of summaries of safety and efficacy across multiple trials by
2505
indications in subgroups may provide a clear presentation of the data. Tabular
2506
summaries of adverse drug reactions for all the clinical trials (including those for all
2507
the studied indications) would be useful. Important differences in adverse drug
2508
reaction patterns/incidences across indications or subgroups should be discussed.
2509
The IB should provide a description of the possible risks and adverse drug reactions
2510
to be anticipated on the basis of prior experiences with the product under investigation
2511
and with related products. There should be a list of adverse reactions, clearly identified
2512
as the reference safety information section, including information on their frequency
2513
and nature. This list should be used for determining the expectedness of a suspected
2514
serious adverse reaction and subsequently whether it needs to be expedited in
2515
accordance with regulatory requirements. A description should also be provided of
2516
the precautions or special monitoring to be done as part of the investigational use of
2517
the product(s).
2518
(c) Marketing Experience
2519
The IB should identify countries where the investigational product has been marketed
2520
or approved. Any significant information arising from the marketed use should be
2521
summarised (e.g., formulations, dosages, routes of administration, adverse drug
2522
reactions). The IB should also identify all the countries where the investigational
2523
product did not receive approval/registration for marketing or was withdrawn from
2524
marketing/registration.
2525
A.3.7 Summary of Data and Guidance for the Investigator
2526
This section should provide an overall discussion of the nonclinical and clinical data
2527
and should summarise the information from various sources on different aspects of
2528
the investigational product(s), wherever possible. In this way, the investigator can be
2529
provided with the most informative interpretation of the available data and with an
2530
assessment of the implications of the information for future clinical trials.
2531
Where appropriate, the published reports on related products should be discussed.
2532
This could help the investigator to anticipate adverse drug reactions or other problems
2533
in clinical trials.
2534
The overall aim of this section is to provide the investigator with a clear understanding of the
2535
possible risks and adverse reactions and of the specific tests, observations and precautions that
2536
may be needed for a clinical trial. This understanding should be based on the available physical,
2537
ICH E6(R3) Guideline
63
chemical, pharmaceutical, pharmacological, toxicological and clinical information on the
2538
investigational product(s). Guidance should also be provided to the clinical investigator on the
2539
recognition and treatment of possible overdose and adverse drug reactions that is based on
2540
previous human experience and on the pharmacology of the investigational product.
2541
ICH E6(R3) Guideline
64
Appendix B. CLINICAL TRIAL PROTOCOL AND PROTOCOL AMENDMENT(S)
2542
Clinical trials should be described in a clear, concise and operationally feasible protocol. The
2543
protocol should be designed in such a way as to minimise unnecessary complexity and to
2544
mitigate or eliminate important risks to the rights, safety, and wellbeing of trial participants
2545
and the reliability of data. Protocol development processes should incorporate input from
2546
relevant stakeholders, where appropriate. Building adaptability into the protocol, for example,
2547
by including acceptable ranges for specific protocol provisions, can reduce the number of
2548
deviations or in some instances the requirement for a protocol amendment. Such adaptability
2549
should not adversely affect participant safety or the scientific validity of the trial. For additional
2550
information, refer to ICH E8(R1) General Considerations for Clinical Studies and ICH E9
2551
Statistical Principles for Clinical Trials.
2552
The contents of a trial protocol should generally include the following topics, which may vary
2553
depending on the trial design. Investigator site-specific information may be provided on
2554
separate protocol page(s) or addressed in a separate agreement, and some of the information
2555
listed below may be contained in other protocol referenced documents, such as an
2556
Investigator’s Brochure.
2557
B.1 General Information
2558
B.1.1 Protocol title, unique protocol identifying number, and date. Any amendment(s)
2559
should also bear the amendment number(s) and date(s).
2560
B.1.2 Name and address of the sponsor.
2561
B.1.3 Name and title of the person(s) authorised to sign the protocol and the protocol
2562
amendment(s) for the sponsor.
2563
B.2 Background Information
2564
B.2.1 Name and description of the investigational product(s).
2565
B.2.2 A summary of findings from nonclinical studies that potentially have clinical
2566
significance and from clinical trials that are relevant to the trial.
2567
B.2.3 Summary of the known and potential risks and benefits, if any, to human participants.
2568
B.2.4 Description of and justification for the route of administration, dosage, dosage
2569
regimen and treatment period(s).
2570
B.2.5 A statement that the trial will be conducted in compliance with the protocol, Good
2571
Clinical Practice (GCP) and the applicable regulatory requirement(s).
2572
B.2.6 Description of the population to be studied.
2573
B.2.7 References to literature and data that are relevant to the trial and that provide
2574
background for the trial.
2575
B.3 Trial Objectives and Purpose
2576
A clear description of the scientific objectives and the purpose of the trial. Information on
2577
estimands, where appropriate, if not included in any other trial-related document, see ICH
2578
ICH E6(R3) Guideline
65
E9(R1) Addendum on Estimands and Sensitivity Analysis in Clinical Trials to the Guideline
2579
on Statistical Principles for Clinical Trials.
2580
B.4 Trial Design
2581
The scientific integrity of the trial and the reliability of the results from the trial depend
2582
substantially on the trial design. A description of the trial design should include:
2583
B.4.1 A specific statement of the primary endpoints and the secondary endpoints, if any, to
2584
be measured during the trial.
2585
B.4.2 A description of the type and design of trial to be conducted (e.g., double-blind,
2586
placebo-controlled, parallel design, adaptive design, platform/umbrella/basket, trials
2587
with decentralised elements) and a schematic diagram of trial design, procedures and
2588
stages.
2589
B.4.3 A description of the measures taken to minimise/avoid bias, including:
2590
(a) Randomisation
2591
(b) Blinding
2592
B.4.4 A description of the trial treatment(s) and the dosage and dosage regimen of the
2593
investigational product(s), including a description of the dosage form, packaging and
2594
labelling.
2595
B.4.5 The expected duration of the participant’s involvement in the trial and a description
2596
of the sequence and duration of all trial periods, including follow-up, if any.
2597
B.4.6 A description of the “stopping rules” or “discontinuation criteria” and “dose
2598
adjustment” or “dose interruption” for individual participants, parts of trial and entire
2599
trial.
2600
B.4.7 Accountability procedures for the investigational product(s), including the placebo(s)
2601
and other comparator(s), if any.
2602
B.4.8 Maintenance of treatment randomisation codes and procedures for breaking codes.
2603
B.5 Selection of Participants
2604
B.5.1 Participant inclusion criteria.
2605
B.5.2 Participant exclusion criteria.
2606
B.5.3 Mechanism for pre-screening, where appropriate, and screening of participants.
2607
B.6 Withdrawal of Consent or Discontinuation of Participation
2608
The investigator may choose to discontinue the participant, or the participant may
2609
withdraw their consent. The protocol should specify:
2610
(a) when and how to discontinue participants from the trial/investigational product
2611
treatment;
2612
ICH E6(R3) Guideline
66
(b) the type and timing of the data to be collected for withdrawn/discontinued
2613
participants, including the process by which the data are handled, in accordance
2614
with applicable regulatory requirements;
2615
(c) whether and how participants are to be replaced;
2616
(d) the follow-up for participants who have discontinued the use of the
2617
investigational product.
2618
B.7 Treatment and Interventions for Participants
2619
B.7.1 The treatment(s) to be administered, including the name(s) of all the product(s), the
2620
dose(s), the dosing schedule(s), the criteria for dose adjustment(s), the route/mode(s)
2621
of administration and the treatment period(s), including the follow-up period(s) for
2622
participants for each investigational product treatment/trial treatment group/arm of the
2623
trial.
2624
B.7.2 Medication(s)/treatment(s) permitted (including concomitant and rescue medication)
2625
and not permitted before and/or during the trial.
2626
B.7.3 Strategies to monitor the participant’s adherence to treatment.
2627
B.8 Assessment of Efficacy
2628
B.8.1 Specification of the efficacy parameters, where applicable.
2629
B.8.2 Methods and timing for assessing, recording and analysing of efficacy parameters.
2630
Where any trial-related committees (e.g., independent data monitoring committee
2631
(IDMC)/adjudication committees) are utilised for the purpose of assessing efficacy
2632
data, procedures, timing and activities should be described in the protocol or a separate
2633
document.
2634
B.9 Assessment of Safety
2635
B.9.1 Specification of safety parameters.
2636
B.9.2 The methods, extent and timing for recording and assessing safety parameters. Where
2637
any trial-related committees (e.g., IDMC) are utilised for the purpose of assessing
2638
safety data, procedures, timing and activities should be described in the protocol or a
2639
separate document.
2640
B.9.3 Procedures for obtaining reports of and for recording and reporting adverse event and
2641
intercurrent events; see ICH E9(R1).
2642
B.9.4 The type and duration of the follow-up of participants after adverse events.
2643
B.10 Statistical Considerations
2644
B.10.1 A description of the statistical methods to be employed, including timing and purpose
2645
of any planned interim analysis(ses) and the criteria for the stopping of the trial.
2646
B.10.2 The number of participants planned to be enrolled and the reason for the choice of
2647
sample size, including reflections on or calculations of the power of the trial and
2648
clinical justification.
2649
ICH E6(R3) Guideline
67
B.10.3 The level of significance to be used or the threshold for success on the posterior
2650
probability in a Bayesian design.
2651
B.10.4 The criteria for the termination of the trial and the criteria for the stopping of the trial.
2652
B.10.5 The selection of participants to be included in the planned analyses (e.g., all
2653
randomised participants, all dosed participants, all eligible participants, all evaluable
2654
participants).
2655
B.10.6 Procedures for accounting for missing, unused and spurious data.
2656
B.10.7 Statement that any deviation(s) from the statistical analysis plan will be described and
2657
justified in the clinical study report.
2658
B.11 Direct Access to Source Records
2659
The sponsor should ensure that it is specified in the protocol or other documented agreement
2660
that the investigator(s)/institution(s)/service provider(s) will permit trial-related monitoring,
2661
audits, institutional review board/independent ethics committee (IRB/IEC) review and
2662
regulatory inspection(s), providing direct access to source records.
2663
B.12 Quality Control and Quality Assurance
2664
B.12.1 Description of identified quality factors and associated risks in the trial unless
2665
documented elsewhere.
2666
B.12.2 Description of the monitoring approaches that are part of the quality control process
2667
for the clinical trial.
2668
B.12.3 Description of the process for the handling of non-compliance with the protocol or
2669
GCP.
2670
B.13 Ethics
2671
Description of ethical considerations relating to the trial.
2672
B.14 Data Handling and Record Keeping
2673
B.14.1 Specification of data to be collected and the method of its collection. Where necessary,
2674
additional details should be contained in a clinical trial-related document.
2675
B.14.2 The identification of records to be recorded directly into the data acquisition tools
2676
(i.e., no prior written or electronic record of data) and considered to be source data.
2677
B.14.3 A statement that records should be retained in accordance with applicable regulatory
2678
requirements.
2679
B.15 Financing and Insurance
2680
Financing and insurance, if not addressed in a separate agreement.
2681
B.16 Publication Policy
2682
Publication policy, if not addressed in a separate agreement.
2683
ICH E6(R3) Guideline
68
Appendix C. ESSENTIAL RECORDS FOR THE CONDUCT OF A CLINICAL TRIAL
2684
C.1 Introduction
2685
C.1.1 Many records are generated before and during the conduct of a clinical trial. The
2686
nature and extent of those records generated and maintained are dependent upon the
2687
trial design, its conduct, application of proportional approaches and the importance
2688
and relevance of that record to the trial.
2689
2690
C.1.2 Determining which records are essential will be based upon consideration of the
2691
guidance in this appendix.
2692
2693
C.1.3 The essential records permit and contribute to the evaluation of the conduct of a trial
2694
and the reliability of the results produced. They serve to demonstrate the compliance
2695
of the investigator and sponsor with the standards of Good Clinical Practice (GCP)
2696
and applicable regulatory requirements. The essential records are used as part of the
2697
sponsor oversight or investigator supervision of the trial. These records are used by
2698
the sponsor’s independent audit function and during inspections by regulatory
2699
authority(ies) to assess the trial conduct and the reliability of the trial results. The
2700
investigator/institution should have access to and the ability to maintain and retain the
2701
essential records generated by the investigator/institution before, during and after the
2702
trial.
2703
C.2 Management of Essential Records
2704
C.2.1 Records should be identifiable and version controlled, and should include authors,
2705
reviewers and approvers as appropriate, along with date and signature (electronic or
2706
wet ink), where necessary.
2707
2708
C.2.2 For activities that are transferred or delegated to service providers by the sponsor or
2709
investigator/institution respectively, arrangements should be made for the access and
2710
management of the essential records throughout the trial and for their retention
2711
following completion of the trial.
2712
2713
C.2.3 These essential records should be maintained in or referred to from repositories,
2714
including, for example, the trial master file (TMF) or investigator site file (ISF). The
2715
TMF is held by the sponsor or by the investigator; in the latter case, it is often called
2716
the ISF.
2717
2718
C.2.4 The sponsor and investigator/institution should maintain a record of where essential
2719
records are located, including source records. The storage system(s) used during the
2720
trial and for archiving (irrespective of the type of media used) should provide for
2721
appropriate identification, version history, search and retrieval of trial records.
2722
2723
C.2.5 The sponsor and investigator/institution should ensure that the essential records are
2724
collected and filed in a timely manner, including those required to be in place prior to
2725
the trial start, which can greatly assist in the successful management of a trial.
2726
ICH E6(R3) Guideline
69
C.2.6 The sponsor and investigator/institution should retain the essential records in a way
2727
that ensures that they remain complete, readable and readily available and are directly
2728
accessible upon request by regulatory authorities. Alteration to the essential records
2729
should be traceable.
2730
2731
C.2.7 The original version of the essential record should be retained by the responsible party
2732
(sponsor or investigator). When a copy is used to permanently replace the original
2733
essential record, the copy should fulfil the requirements for certified copies.
2734
2735
C.2.8 In order to fulfil their responsibilities in the conduct of the trial, the sponsor and
2736
investigator/institution may need access to or copies of one another’s relevant
2737
essential records before, during and after the trial is completed. This will determine
2738
whether the record resides in the repositories of the sponsor, the
2739
investigator/institution, or both. There should be careful consideration of sharing of
2740
records subject to data protection legislation and blinding considerations in line with
2741
applicable regulatory requirements. For the sharing of essential records with service
2742
providers, see section C.2.2.
2743
2744
C.2.9 Certain essential records may not be specific to a trial but may be related to the
2745
systems and processes involved in running multiple trials and retained outside the
2746
trial-specific repositories (e.g., standard operating procedures validation records,
2747
master services agreements).
2748
C.3 Essentiality of Trial Records
2749
C.3.1 Whether a specific clinical trial record generated before, during and after the trial is
2750
essential and needs to be retained should be based on the following criteria:
2751
(a) Is a document that is submitted to or issued by the regulatory authority or
2752
IRB/IEC, including related correspondence and those documenting regulatory
2753
decisions or approvals/favourable opinions;
2754
(b) Is a trial-specific procedure or plan;
2755
(c) Is relevant correspondence or documentation of meetings related to important
2756
discussions and/or trial-related decisions that have been made related to the
2757
conduct of the trial and the processes being used;
2758
(d) Documents the conduct of relevant trial procedures;
2759
(e) Documents the arrangements between parties and insurance/indemnity
2760
arrangements;
2761
(f) Documents the compliance with the requirements and any conditions of
2762
approval from the regulatory authority or the favourable opinion of the
2763
institutional review board/independent ethics committee (IRB/IEC);
2764
(g) Documents the composition and, where appropriate, the functions,
2765
correspondence and decisions of any committees involved in the trial approval
2766
or its conduct.
2767
ICH E6(R3) Guideline
70
(h) Demonstrates that a trial-specific computerised system is validated and that
2768
non-trial-specific systems have been assessed as fit for purpose for their
2769
intended use in the trial;
2770
(i) Is a document that has been authorised/signed by the sponsor and/or
2771
investigator to confirm review or approval;
2772
(j) Is, where necessary, documentation that demonstrates signatures/initials of staff
2773
undertaking trial-specific activities; for example, completing data acquisition
2774
tools;
2775
(k) Documents what information was provided to potential trial participants and
2776
that participants’ informed consent was appropriately obtained and maintained;
2777
(l) Documents that sponsor personnel involved in the trial conduct and individuals
2778
performing trial-specific activities on their behalf are qualified by education,
2779
training and experience to undertake their activities;
2780
(m) Documents that the investigator and those individuals delegated trial-specific
2781
activities by the investigator are qualified by education, training and experience
2782
to undertake their activities, particularly where the activities are not part of their
2783
normal role;
2784
(n) Contains the data as well as relevant metadata that would be needed to be able
2785
to reconstruct the trial;
2786
(o) Are documents related to the sponsor and investigator oversight of safety of
2787
trial participants during the trial, including compliance with safety reporting
2788
requirements between sponsors and investigators, regulatory authorities and
2789
IRBs/IECs and informing trial participants of safety information as necessary;
2790
(p) Documents that service providers are suitably qualified for conducting their
2791
delegated or transferred activities;
2792
(q) Documents that laboratory activities and other tests used in the trial are fit for
2793
purpose;
2794
(r) Documents sponsor oversight of investigator site selection and monitoring and
2795
audit of the trial, where appropriate, and provides information on arising
2796
issues/non-compliance and deviations detected and implementation of
2797
corrective and preventative actions;
2798
(s) Documents the compliance with the protocol and/or procedures for
2799
management and statistical analysis of the data and production of any interim
2800
report and the final report;
2801
(t) Documents the collection, chain of custody, analysis and retention or
2802
destruction of biological samples;
2803
(u) Provides relevant information on the investigational product and its labelling;
2804
(v) Provides information about the shipment, storage, packaging, dispensing,
2805
randomisation and blinding of the investigational product;
2806
(w) Provides, where appropriate, traceability and accountability information about
2807
the investigational product from release from the manufacturer to dispensation,
2808
ICH E6(R3) Guideline
71
administration to trial participants, and return and destruction, or alternative
2809
disposition;
2810
(x) Provides information on the identity and quality of the investigational product
2811
used in the trial;
2812
(y) Documents processes and activities relating to unblinding;
2813
(z) Documents the recruitment, pre-trial screening and consenting process of trial
2814
participants and their identity and chronological enrolment as appropriate;
2815
(aa) Documents the existence of the trial participants and substantiates the integrity
2816
of trial data collected. Includes source records related to the trial and medical
2817
treatments and history of the trial participants;
2818
(bb) Defines processes/practices in place in the event of a security breach in order to
2819
protect participants’ rights, safety and well-being and the integrity of the data.
2820
C.3.2 Applying the criteria in section C.3.1, the trial records for every trial that are
2821
considered essential, except in justifiable and documented exceptional circumstances,
2822
are set out in Table 1, and these should be retained.
2823
2824
C.3.3 For other trial records, their presence and nature are dependent upon the trial design,
2825
its conduct and risk proportional management. Table 2 lists potential trial records that
2826
when generated, would be considered essential by applying the criteria in section
2827
C.3.1 and should be retained. This is not an exhaustive list, and other trial records may
2828
also be considered essential by the sponsor or the investigator.
2829
2830
Table 1 – Essential Records for All Trials
1.1
Investigator’s Brochure or basic product information brochure (e.g., summary of
product characteristic, package leaflet or labelling) and relevant updates
1.2
signed protocol and amendments during the trial
1.3
dated, documented approval/favourable opinion of IRB/IEC of information provided
to them before and during the trial
1.4
IRB/IEC composition
1.5
regulatory authority(ies) authorisation, approval and/or notification of the protocol
and subsequent protocol amendments during the trial (where required)
1.6
completed signed and dated informed consent forms
1.7
completed participant identification code list and enrolment log
1.8
- notification by originating investigator to sponsor of serious adverse events (SAEs)
and related reports, where required
- notification by sponsor and/or investigator, where required, to regulatory
authority(ies) and IRB(s)/IEC(s) of suspected unexpected serious adverse reactions
(SUSARs) and of other safety information
- notification by sponsor to investigators of safety information, where required
1.9
interim or annual reports to IRB/IEC and regulatory authority(ies)
1.10
source records
ICH E6(R3) Guideline
72
Table 1 – Essential Records for All Trials
1.11
data and relevant metadata (including documentation of data corrections) in the data
acquisition tools
1.12
final report by investigator to IRB/IEC and regulatory authority(ies), where required
1.13
interim (where applicable) and final clinical trial reports
2831
Table 2 – Potential Essential Records
2.1
sample of data acquisition tools (e.g., case report forms (CRFs), diaries, clinical
outcome assessments, patient-reported outcomes) that are provided to the investigator
and/or IRB/IEC
2.2
sample of information given to trial participants and revisions during the trial
- informed consent materials (including all applicable translations)
- any other documented information, e.g., instructions for use of an investigational
product or a device
- advertisement for participant recruitment
2.3
financial aspects of the trial
2.4
insurance statement
2.5
signed agreement between involved parties, e.g.,
- investigator/institution and sponsor
- investigator/institution and service providers
- sponsor and service providers
- sponsor and independent data monitoring committee (IDMC) members
2.6
curriculum vitae and/or other relevant documents evidencing qualifications of
investigator(s) and sub-investigator(s) involved in conducting the trial
2.7
trial-specific training records
2.8
documentation of delegation of activities by the investigator to investigator site staff
2.9
signature sheet documenting signatures and initials of delegated investigator site staff
2.10
normal value(s)/range(s) for medical/laboratory/technical procedure(s) and/or test(s)
included in the protocol and updates during the trial conduct
2.11
certification or accreditation or established quality control and/or external quality
assessment or other validation (where required) of medical/laboratory/technical
procedures/tests used during the trial conduct and any updates
2.12
documentation of collection, processing and shipment of body fluids/tissue samples
2.13
documentation of body fluids/tissue samples storage conditions
2.14
record of retained body fluids/tissue samples at the end of the trial
2.15
sample of label(s) attached to investigational product container(s)
2.16
instructions for handling of investigational product(s) and trial-related materials (if
not included in protocol or Investigator’s Brochure), for example, pharmacy manual
2.17
shipping records for investigational product(s) and trial-related materials
2.18
certificate(s) of analysis of investigational product(s) shipped
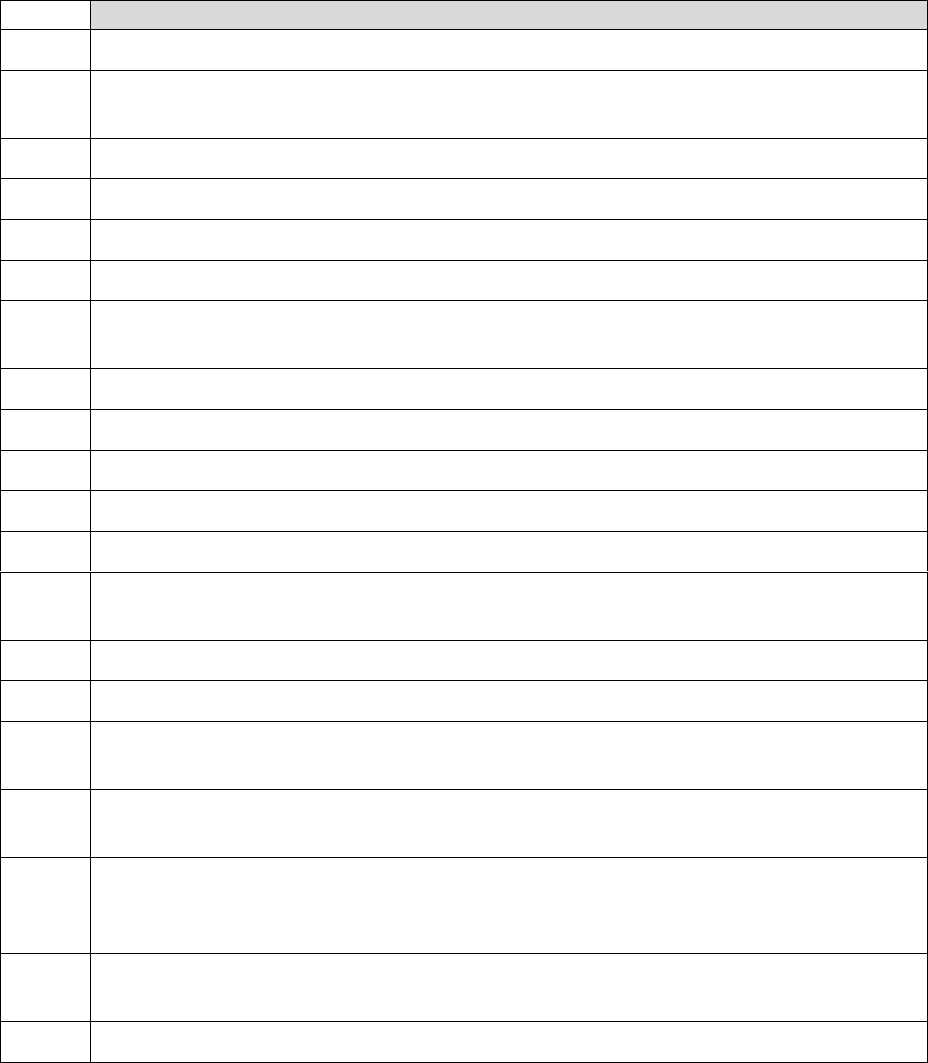
ICH E6(R3) Guideline
73
Table 2 – Potential Essential Records
2.19
investigational product(s) accountability at investigator site
2.20
documentation of investigational product storage conditions during shipment and at
the trial site
2.21
records of relabelling of investigational product at trial site
2.22
documentation of investigational product destruction
2.23
emergency decoding procedures for blinded trials
2.24
master randomisation list
2.25
instructions for use for critical trial-specific systems (e.g., interactive response
technologies (IRT) user manual, electronic CRF (eCRF) manual)
2.26
maintenance and calibration records for critical trial-specific equipment
2.27
treatment allocation and decoding documentation
2.28
completed participants screening log
2.29
site monitoring reports (including site selection, initiation, routine and close-out)
2.30
centralised monitoring reports
2.31
records and reports of protocol and GCP non-compliance/deviations and corrective
and preventative actions
2.32
documentation of relevant communications and meetings
2.33
audit certificate
2.34
documentation relating to data finalisation for analysis (e.g., query resolutions, SAE
reconciliation, quality control reports, coding completion, output data sets)
2.35
documentation of trial-specific computerised system validation (e.g., specifications,
testing, validation report, change control)
2.36
documentation relating to the statistical considerations and analysis (e.g., sample size
calculations, analysis sets decisions, analysis datasets, analysis programs, quality
control records and output)
2.37
trial-specific plans (e.g., risk management, monitoring, safety, data management, data
validation and statistical analysis) and procedures
2.38
procedures, meeting minutes and submissions to the IDMC
2832
