Behaviour Research and Therapy 142 (2021) 103874
Available online 5 May 2021
0005-7967/© 2021 Published by Elsevier Ltd.
Relationship to CBT outcome and dropout of decision support tools of the
written case formulation, list of treatment goals and plot of symptom scores
Vael Gates
a
, Megan Hsiao
b
, Garret G. Zieve
a
, Rebecca Courry
b
, Jacqueline B. Persons
b
,
a
,
*
a
University of California, Berkeley, USA
b
Oakland Cognitive Behavior Therapy Center, USA
ARTICLE INFO
Keywords:
Outcome
Dropout
Case formulation
Decision support
Measurement-based care
Private practice
ABSTRACT
Many patients who receive cognitive behavior therapy (CBT) for mood and anxiety disorders fail to respond or
drop out of treatment. We tested the hypotheses that therapist use of each of three decision support tools, a
written case formulation, a list of treatment goals, and a plot of symptom scores, was associated with improved
outcome and reduced dropout in naturalistic CBT provided to 845 patients in a private practice setting. We
conducted regression analyses to test the hypotheses that the presence of each tool in the clinical record was
associated with lower end-of-treatment scores on the Beck Depression Inventory (BDI) and the Burns Anxiety
Inventory (BurnsAI), and lower rates of premature and uncollaborative dropout. We found that the presence of a
written case formulation in the clinical record was associated with lower rates of both types of dropout. A list of
treatment goals was associated with lower end-of-treatment scores on the BDI and the BurnsAI, and a lower rate of
uncollaborative but a higher rate of premature dropout. A plot of symptom scores was associated with lower end-
of-treatment scores on the BDI, and lower rates of both types of dropout. Results suggest that therapist use of a
written case formulation, list of treatment goals, and a plot of symptom scores can contribute to improved
outcome and reduced dropout in CBT.
Despite its strong evidence base, many patients who receive cogni-
tive behavior therapy (CBT) for mood and anxiety and related disorders
fail to respond to it. For example, Cuipers et al. (2014) reported that
response rates of empirically-supported treatments for major depressive
disorder ranged from 44% to 53%. In addition, many patients terminate
treatment prematurely and thus fail to receive a full dose of treatment.
Fernandez et al. (2015), in a meta-analysis, reported that more than 25%
of patients dropped out of cognitive behavioral therapy (CBT).
Clinicians who use the methods of evidence-based practice rely on a
range of strategies and decision support tools to guide decision-making
and solve problems that can otherwise lead to nonresponse and dropout
(American Psychological Association, 2006). First, clinicians of all
theoretical orientations view the case formulation as a key tool (Eells,
2007). The case formulation describes the factors that appear to cause
and maintain a particular patient’s particular symptoms and problems,
and it thus identies the treatment targets and guides the therapist’s
efforts to overcome problems that can arise in treatment. Despite its
importance to practitioners, the case formulation is under-studied, and
we have little information about the relationship of the case formulation
to outcome and dropout (Persons & Hong, 2016). Second, cognitive
behavioral therapists develop with their patients an agreed-upon list of
treatment goals. The list of treatment goals individualizes the treatment
and focuses it on concrete, specic, achievable objectives. A shared list
of goals is considered to be part of the therapeutic alliance (Bordin,
1994), and we know that the alliance is related to both outcome (Hor-
vath et al., 2011) and dropout (Roos, J. & Werbart, A., 2013), but we
don’t know whether the strategy of writing down a list of the patient’s
concrete, specic treatment goals and using them to guide treatment
affects outcome and dropout.
Third, evidence-based practitioners rely on a plot of symptom scores.
The patient completes a symptom scale before the session, and the
therapist and patient together review the plot showing the trajectory of
scores and use it to guide decision-making. A recent review showed that
measurement-based care, dened as “the systematic evaluation of pa-
tient symptoms before or during each clinical encounter to inform
behavioral health treatment” leads to improved psychotherapy outcome
(Lewis et al., 2018). But only one of the samples that Lewis et al.
reviewed were American samples of outpatients with mood and anxiety
disorders (Hawkins et al., 2004). All three of these tools (the case
formulation, the list of treatment goals, and progress monitoring data)
* Corresponding author. Oakland Cognitive Behavior Therapy Center, 5625 College Avenue, Suite 215, Oakland, CA, 94618, USA.
E-mail address: [email protected] (J.B. Persons).
Contents lists available at ScienceDirect
Behaviour Research and Therapy
journal homepage: www.elsevier.com/locate/brat
https://doi.org/10.1016/j.brat.2021.103874
Received 26 April 2020; Received in revised form 30 December 2020; Accepted 19 April 2021

Behaviour Research and Therapy 142 (2021) 103874
2
represent elements of evidence-based practice as dened by the Amer-
ican Psychological Association (2006), and appear in widely-used clin-
ical manuals (J. S. Beck, 1995; Eells, 2007; Persons, 2008), but little is
known about their contribution to outcome and dropout in routine
clinical practice. More empirical support is needed for these tools that
are widely viewed as core elements of evidence-based practice.
To address this gap in the literature, we tested the hypotheses that
therapist use of each of the decision support tools of the written case
formulation, list of treatment goals, and plot of symptom scores were asso-
ciated with improved outcome and reduced dropout in a large sample of
patients who received naturalistic cognitive behavior therapy (CBT) for
symptoms of depression and anxiety in a private practice setting. We
studied outcome as dened by scores on two symptom measures at the
end of treatment: the Beck Depression Inventory and the Burns Anxiety
Inventory. We studied dropout as dened in two ways. We studied
premature dropout, dened as ending treatment before, in the therapist’s
judgment, the treatment has been tried for long enough to help the
patient accomplish their treatment goals, and uncollaborative dropout,
dened as ending treatment against the therapist’s advice or without
discussing the termination with the therapist. We predicted that the
presence in the clinical record of a written case formulation, a list of
treatment goals, and a plot of scores on a measure of depression or anxiety
would be associated with improved outcome and reduced premature
and uncollaborative dropout.
1. Method
1.1. Participants
Participants were 845 adults who received individual naturalistic
cognitive behavior therapy during the years 1981–2009 from the second
author or one of 20 therapists at the group private practice she estab-
lished in 1995. All participants gave written consent for data from their
clinical record to be used for research purposes. The procedures used to
establish and maintain the Persons Archival Database we studied in this
investigation were reviewed and approved by the Behavioral Health
Research Collective Institutional Review Board. The Persons Archival
Database is a completely de-identied database, and no master code list
links the data in the database to the names of the patients in the
database.
Patients in the sample had an average age of 36.2 years (SD = 12.3)
and had completed an average of 16.6 years (SD = 2.6) of education.
Patients identied as 58.6% female and 41.2% male; 0.2% were of un-
specied gender. 80.9% patients were Caucasian, 2.5% were African
American, 2.6% were Hispanic, 6.3% were Asian, 1.9% were of other
ethnicity, and 5.8% were of unspecied ethnicity. 20.0% of patients
received adjunctive psychosocial treatment (e.g., group therapy or
couple therapy), 63.2% did not, and 16.8% were unspecied. 50.7% of
patients received adjunctive pharmacotherapy, while 38.1% did not,
and 11.1% were unspecied. 86.4% of patients had an anxiety or
depressive disorder or both. Diagnoses were assigned by the treating
therapist based on the most current version of the Diagnostic and Sta-
tistical Manual of Mental Disorders at the time the patient was treated.
Patients were treated by one of twenty therapists.
1
The 845 patients studied here were drawn from a database of 1469
adult patients. Patients were excluded from the larger sample if they had
incorrect or missing data describing how many total sessions they
completed (n = 14) or sought consultation only, not treatment (n = 24).
Most importantly, patients were excluded if they had fewer than three
sessions in the database (n = 586). We excluded these cases so that the
computations required to carry out the multiple imputation strategy we
used to interpolate missing data could be carried out in a reasonable
length of time, and so we could use the same patient sample for all data
analyses we conducted. If patients completed more than one course of
treatment, only the rst course was analyzed to simplify analysis.
1.2. Treatment
Treatment consisted of individual cognitive behavior therapy (CBT),
typically provided weekly and based on a case formulation-driven mode
of treatment (Persons, 1989, 2008). The case formulation-driven mode
of treatment called for the therapist to develop, with the patient, an
individualized formulation of the case and a written list of treatment
goals, to make a plot in each session of scores on symptoms relevant to
the patient’s treatment goals, and to use these three tools to guide
decision-making in therapy. However, therapists worked in a group
private practice, not a clinic, and there was no policy or requirement in
the practice that clinicians use these decision support tools, and thus
therapists made their own decisions about use of the tools. The most
common symptom measures used by the therapists in the practice were
the Beck Depression Inventory and the Burns Anxiety Inventory, and
therefore we selected those two scales as our outcome measures for this
study. Treatment was naturalistic because it did not depend on a pro-
tocol that described a pre-determined number and frequency of sessions,
and it allowed the therapist to make adjustments in the treatment (e.g.,
increasing session frequency or adding adjunctive psychosocial treat-
ment, such as couple therapy, or adjunctive pharmacotherapy) based on
the results of the progress monitoring data and other factors (e.g., the
patient’s preference). Treatment was open-ended in duration and ended
ideally when patient and therapist agreed that the patient had reached
the patient’s goals but sometimes ended for other reasons (e.g., the
patient moved, the therapist left the practice, the patient felt they had
accomplished all that could be done in the therapy, or the patient ended
treatment against the therapist’s advice). Most therapists were Ph.D.
psychologists; one was an L.C. S.W. The mean (and standard deviation)
of the length of treatment in days was 286.0 (SD = 573.9), and the
number of sessions was 24.0 (SD = 32.7).
1.3. Measures
Symptoms of depression. We assessed symptoms of depression
with the original version of the Beck Depression Inventory (A. T. Beck
et al., 1961). The BDI is a widely-used, 21-item self-report measure of
the severity of depressive symptoms that has been shown to have good
internal consistency (
α
= 0.86 for psychiatric patients) and good
convergence with other measures of depressive symptoms (A. T. Beck
et al., 1988). Total score could range from 0 to 63.
Symptoms of anxiety. We assessed symptoms of anxiety with the
Burns Anxiety Inventory (BurnsAI), a 33-item self-report inventory
measuring 6 anxious feelings (e.g., anxiety, nervousness, worry or fear),
11 anxious thoughts (e.g., feeling that you’re on the verge of losing
control) and 16 physical symptoms (e.g., a lump in the throat). Each
symptom was rated on a 0 to 3 scale ranging from 0 (not at all) to 3 (a
lot). Total score could range from 0 to 99. Burns and Eidelson (1998)
reported, in a sample of 483 outpatients, that the BurnsAI had a Cron-
bach’s alpha of 0.94, indicating high internal consistency, and it was
correlated 0.86 (p < 0.001) with the Anxiety subscale of the Symptom
Check List-90 (Derogatis et al., 1976). We used the BurnsAI because it
covered the full range of anxious symptoms we observed in our patients,
its classication of anxiety symptoms as feelings, thoughts, or physical
symptoms was clinically helpful, and it was sensitive to change.
Premature dropout. Premature dropout was coded as present (a
score of 1) when, after treatment ended and the database was being
1
Of the 845 patients, 2 were seen by Therapist 1; 107 by Therapist 2; 23 by
Therapist 3; 20 by Therapist 4; 3 by Therapist 5; 25 by Therapist 6; 2 by
Therapist 7; 1 by Therapist 8; 70 by Therapist 9; 54 by Therapist 10; 16 by
Therapist 11; 16 by Therapist 12; 3 by Therapist 13; 315 by Therapist 14 (last
author); 28 by Therapist 15; 66 by Therapist 16; 3 by Therapist 17; 42 by
Therapist 18; 12 by Therapist 19; 36 by Therapist 20; and 1 by an unspecied
therapist.
V. Gates et al.
Behaviour Research and Therapy 142 (2021) 103874
3
assembled, the patient’s therapist answered “no” to the question: “Has
the therapy been given a fair shake/tried for long enough to help patient
accomplish their treatment goals?” Reasons for the therapist’s judgment
that termination was premature varied widely from case to case
depending on the patient’s treatment goals.
Uncollaborative dropout. Uncollaborative dropout was coded as
present (a score of 1), when, after treatment ended and the database was
being assembled, the patient’s therapist answered “no” to the question:
“Did the patient and therapist work well together on the termination,
agree on it and discuss it fully?” The termination was coded as uncol-
laborative, for example, if the patient ended treatment by simply
cancelling a session and never rescheduling it.
Premature and uncollaborative dropout were not mutually exclusive,
and each patient received a score of 1 (yes) or 0 (no) for each type of
dropout.
Therapist use of decision support tools: written case formula-
tion, list of treatment goals, and plot. To assess therapist use of the
decision support tools of case formulation-driven CBT, the therapist
reviewed each patient’s clinical record after treatment had ended, and
coded each tool (written case formulation, list of treatment goals, or plot
of behavior or symptoms) 1 if it was present, and 0 if it was not present.
Therapists used a coding manual to make these coding decisions. The
coding manual called for a code of 1 on the case formulation item “if there
was a written case formulation of any quality in the chart, and 0 other-
wise. This should be a written formulation of the case, not just a brief
mini-formulation, e.g., a Thought Record or diagram of a panic cycle.”
The coding manual called for a code of 1 on the list of treatment goals if
“the goals or objectives of treatment are stated in the clinical chart prior
to the termination note. . . . This is not the goals/objectives for what the
patient wants to accomplish between one session and another but must
be the Goals or Objectives of treatment. The word ‘Goals’ or ‘Objectives’
must appear, and there should be a list, except in rare cases where there
is a single goal. It is not sufcient to state, ‘The patient seeks treatment to
work on OCD symptoms,’ or similar.” Plot was coded 1 if a plot of scores
on the Beck Depression Inventory or Burns Anxiety Inventory appeared
in the chart with at least one score entered on the plot, and 0 otherwise.
1.4. Data analysis
We tested the hypotheses that the presence in the clinical record of
the three decision support tools (case formulation, treatment goals, and
plot), was associated with lower end-of-treatment scores on the Beck
Depression Inventory and Burns Anxiety Inventory, and reduced likeli-
hood of premature and uncollaborative dropout. We conducted a linear
regression to predict each outcome variable (end-of-treatment symptom
scores on the Beck Depression Inventory (BDI) and the Burns Anxiety
Inventory (BurnsAI)), and we conducted a logistic regression to predict
each dropout variable (premature and uncollaborative dropout). In each
analysis, the independent variables were the three decision support tools
(coded 0/1 to indicate whether the tool was present in the clinical re-
cord), the number of sessions the patient spent in therapy, and the
identity of the patient’s therapist. In the analyses of end-of-treatment
BDI and BurnsAI scores, we also controlled for the patient’s score on
the measure in the rst session. We included all the decision support
tools in the regressions in order to examine the effect of each tool on
outcome and dropout while controlling for the contributions of the other
tools.
To control for therapist identity, we included therapist as a variable
in the regression analyses. Thus, our analyses examined the relationship
between the decision tools and outcome/dropout within each therapist’s
caseload. To enter therapist identity into the regressions, we created one
dummy-coded categorical variable (coded 0–1) for each of the 20
therapists. Rather than report effects for each individual therapist, we
reported a cumulative result of the effect of therapist identity on the
dependent variable. To do that, for each regression analysis, we
compared two nested models, one including the therapist variable and
one without the therapist variable. We computed the p-value using the F
distribution for each regression to determine whether the larger model
that included the therapist variable was statistically signicantly
different from the smaller model that did not include the therapist
variable.
We handled the therapist variable as a xed effect rather than a
random effect. Our rationale for this decision was two-fold. Random-
effects and xed-effects models usually give similar results, and random-
effects models require making an assumption (Gardiner et al., 2009) that
we did not believe was justied, the assumption that therapist effects are
uncorrelated with therapist propensity to use the decision support tools
we are studying.
As an additional aid to understanding the relationship between the
decision support tools and the dropout variables, we computed a mea-
sure of correlation between each independent variable and each dropout
variable, the Jaccard similarity coefcient (Jaccard index). The Jaccard
index ranges from 0 to 1, with 1 indicating maximal similarity.
Effect size. Because our sample size was so large, very small effects
could be statistically signicant. Therefore, we calculated effect sizes. In
the linear regressions examining the relationship between the tools and
outcome, we used the change in adjusted R
2
(designated as ΔR
2
) as an
effect size. Adjusted R
2
, the coefcient of determination adjusted for the
number of variables, is a statistical measure of how much variance a
regression model explains. We calculated the ΔR
2
by subtracting the
adjusted R
2
of a regression model that omitted the variable of interest
(case formulation, treatment goals, or plot) from the adjusted R
2
of the
model that included the variable of interest.
In the logistic regressions examining the relationship between the
tools and dropout, we used the odds ratio (e
Est.
) as an effect size. The
odds ratio describes the relative odds of the dependent variable (pre-
mature or uncollaborative dropout) occurring given the inclusion of the
specied independent variable. We are most interested in the odds ratio
(e
Est.
) for each decision support tool parameter of the regressions, which
indicates the estimated odds of a premature/uncollaborative dropout by
a patient whose clinical record has the decision support tool (case
formulation, list of treatment goals, or plot) as compared to the odds of
dropout by a patient whose chart does not have the decision support
tool. To increase the interpretability of the odds ratio, we converted the
odds ratio to a relative risk ratio for a baseline risk level, using as the
baseline risk level the percentage of patients in our sample who dropped
out prematurely or uncollaboratively.
We carried out the analyses using R Core Team (2018) and Python
(Python Software Foundation, n.d.), using Jupyter Notebooks (Project
Jupyter, n.d.), and used the packages Amelia II (Honaker et al., 2012)
and Zelig (R Core Team, 2007) to conduct the multiple imputations
analyses.
2. Results
2.1. Preliminary analyses
Missing data. Our dataset contained 845 patients with 15987 ses-
sions of data. 104 patients (12.3%) were missing data about case
formulation, 100 patients (11.8%) were missing data about treatment
goals, and 88 patients (10.4%) were missing data about plot. 70 patients
(8.3%) did not have any BDI scores, and 8427 sessions (52.7%) did not
have a BDI score. 177 patients (20.9%) did not have any BurnsAI scores,
and 10,357 sessions (64.8%) did not have a BurnsAI score. 91 patients
(10.8%) were missing data about premature dropout, and 83 patients
(9.8%) were missing data about uncollaborative dropout. Data about the
decision support tools and dropout were missing when we were unable
to interview the treating therapist to obtain this information. BDI and
Burns AI scores were missing when we could not locate the medical
record or when the therapist did not monitor outcome with a symptom
scale or selected another measure (e.g., the YBOCS or a daily log of skin-
picking behavior) to monitor outcome.
V. Gates et al.
Behaviour Research and Therapy 142 (2021) 103874
4
Multiple imputation. To handle missing data, we used the statisti-
cal technique of multiple imputation (Enders, 2017). In this approach,
missing data were estimated from existing data multiple times (multiple
“imputations”) with some degree of randomness, and these multiple
estimates were pooled for a nal result. By averaging multiple ran-
domized imputations, we can incorporate the variance of estimated
values, so that estimates that the system has low condence in will have
high variance, and estimates that are highly supported by the existing
data will have low variance. This strategy reduces bias in the estimated
values. We used the package Amelia II (Honaker et al., 2012) to carry out
the imputations. We computed ve imputations. To improve our
imputed values, we incorporated our data’s structure into the imputa-
tion model. Specically, we modeled our data as time series within
patient cross-sections, meaning we assumed that patients’ values would
vary over time, and that each patient could have a different starting
point and rate of change. Amelia II modeled patients’ patterns by
computing rst-order polynomial regressions for each patient, using
session number to represent time. We included the following as vari-
ables for each patient: number of sessions in treatment, number of days
in treatment, age, number of years of education, gender, ethnicity,
whether adjunctive pharmacotherapy was provided, whether adjunctive
psychosocial treatment was provided, whether they had a
depression-related diagnosis, whether they had an anxiety-related
diagnosis, the identity of their therapist (numerically coded), whether
they had a written case formulation in their chart, whether they had a
list of treatment goals in their chart, whether they had a plot of symptom
scores in their chart, whether they were coded as a premature dropout,
whether they were coded as an uncollaborative dropout, and their BDI
and BurnsAI scores for each session. Imputed BDI and BurnsAI scores
were lower-bounded at 0 and upper-bounded at the maximum score for
each measure, and the number of sessions, days in treatment, age, and
years of education were lower-bounded at 0, 0, 18 and 0 respectively. All
missing data for these variables were imputed. Final BDI and BurnsAI
scores were determined after this multiple imputation analysis. To speed
up computation, we used a ridge prior that was set to 10% of the total
number of sessions (for details on Amelia II’s statistical options,
including ridge priors, see Honaker et al. (2012)).
Reliability of coding for therapist decision support tools: writ-
ten case formulation, list of treatment goals, and plot. To evaluate
the inter-rater reliability of coding of the clinical record for presence of a
written case formulation, a list of treatment goals, and a plot of symptom
data, we conducted a small study of clinical records of 20 patients
treated by the last author during the years 2008–2020. These records
were randomly selected from a larger database the last author has
collected. Patients gave consent for use of their records for research
purposes, and this study was reviewed by the IRB of the Behavioral
Health Research Collective. We were unable to conduct this study using
the data from the Persons Archival Database used in the present study
because no master code list exists to link the patient clinical record to the
data in the Persons Archival Database. Two authors (R.C. and J.B.P.)
rated each of the 20 clinical records using the same coding manual
(described on page 9) that therapists used to rate these variables in the
Persons Archival Database. The two therapists showed nearly perfect
agreement on ratings of the presence in the clinical record of all three
decision support tools: a written case formulation, a list of treatment
goals, and a plot of symptom data. The clinicians agreed on 19 of 20
ratings of a written case formulation, 19 of 20 ratings of a list of treat-
ment goals, and 20 of 20 ratings of a plot of progress monitoring data,
indicating that the presence in the clinical record of the decision support
tools in the clinical record can be reliably rated.
Therapist use of the decision support tools. We had data about the
presence of a written case formulation (present or absent) for 741 par-
ticipants; of those 741 cases, 581 (78%) had a written case formulation
in the chart. We had data for 745 participants about the presence of a list
of treatment goals; of those 745 cases, 505 (68%) had a list of treatment
goals in the chart. We had data for 757 participants about the presence
of a plot of BDI or BurnsAI data; of those 757 cases, 424 (56%) had a plot
in the chart.
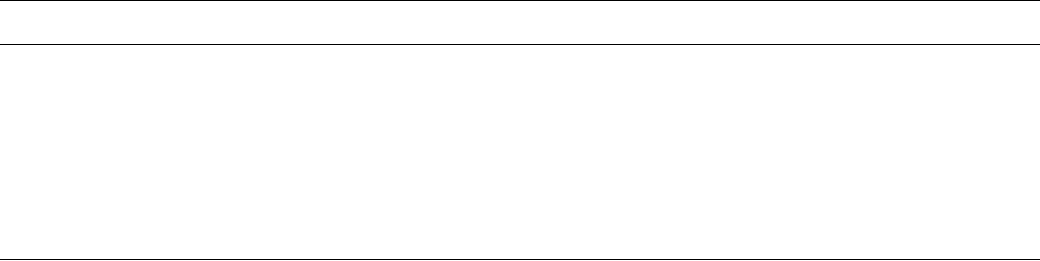
Patient outcome. Table 1 presents imputed scores on the Beck
Depression Inventory and Burns Anxiety Inventory for all patients, and
for patients whose charts did and did not include a case formulation, list
of treatment goals, and plot. (The equivalent information for the original
data, before the multiple imputation procedure, is presented in Sup-
plementary Table 1.)
Patient dropout. We had data on premature dropout for 754 pa-
tients; of those, 394 (52%) were premature dropouts. We had data on
uncollaborative dropout for 762 patients; of those, 231 (30%) were
uncollaborative dropouts. These percentages were used as “baseline
risk” estimates for the relative risk ratio calculations for each type of
dropout.
2.2. The effect of decision support tools on outcome and dropout
We hypothesized that the presence in the clinical record of decision
support tools of case formulation, treatment goals, and plot would be
associated with reduced end-of-treatment BDI and BurnsAI scores, and
reduced premature and uncollaborative dropout. To test our hypotheses
about end-of-treatment BDI and BurnsAI scores, we conducted a linear
regression for each symptom score, where the dependent variable was
the end-of-treatment score on the symptom measure, and the indepen-
dent variables were the three decision support tools (coded as present or
absent), the initial score on the symptom measure, the identity of the
therapist, and the total number of sessions of treatment. To test our
hypotheses about dropout, we conducted a logistic regression for each
type of dropout, where the dependent variable was premature or
uncollaborative dropout, and the independent variables were the deci-
sion support tools (coded as present or absent), the identity of the
therapist, and the total number of sessions of treatment. We multiplied
all p values by four to Bonferroni-correct for the number of regression
analyses. Table 2 reports the results of these regressions. We examine
results for outcome and dropout in turn.
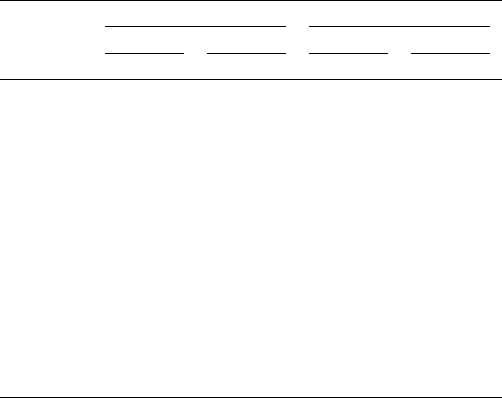
Outcome. First we examine the degree to which the presence of the
decision support tools in the clinical record was related to improved
patient outcome on the Beck Depression Inventory (Table 2). We found
that Treatment Goals (β = − 1.4, p = 0.007) and Plot (β = − 1.6, p = 0.04)
but not Case Formulation (β = − 0.6, p = 0.6) were statistically signi-
cant predictors of end-of-treatment Beck Depression Inventory (all p
Table 1
Estimated means and standard deviations (S.D.) of initial and nal outcome
scores of subcategories of patients, after multiple imputation replaced missing
data. Lower scores indicate fewer symptoms.
n = 845 Beck Depression Inventory Burns Anxiety Inventory
Initial Score Final Score Initial Score Final Score
Mean ± S.D. Mean ± S.D. Mean ± S.D. Mean ± S.D.
All Patients 17.45 ± 8.89 12.03 ± 9.02 28.79 ±
15.61
19.98 ±
14.62
Sorted by Tool
Case Formulation
Present 17.16 ± 8.41 11.66 ± 8.68 28.55 ±
15.58
19.73 ±
14.52
Absent 18.53 ±
10.41
13.35 ±
10.08
29.65 ±
15.73
20.89 ±
14.98
Treatment Goals
Present 17.22 ± 8.64 11.48 ± 8.72 28.36 ±
15.84
18.62 ±
14.42
Absent 17.93 ± 9.37 13.16 ± 9.54 29.65 ±
15.12
22.77 ±
14.64
Plot
Present 18.21 ± 8.87 12.01 ± 9.00 29.96 ±
15.52
19.64 ±
14.48
Absent 16.48 ± 8.83 12.04 ± 9.07 27.29 ±
15.62
20.41 ±
14.80
V. Gates et al.
Behaviour Research and Therapy 142 (2021) 103874
5
values are Bonferroni-corrected). These beta coefcients indicate that
we would expect that patients whose clinical record included a list of
treatment goals would have an end-of-treatment BDI score that was 1.4
points lower on average compared to patients whose clinical record did
not include a list of treatment goals, and that patients whose clinical
record included a plot of symptoms would have an end-of-treatment BDI
score that was 1.6 points lower. So although statistically signicant, the
effects of the Treatment Goals and Plot variables on end-of-treatment
BDI score were small, about 1.5 points on the Beck Depression In-
ventory. The measure of effect size, ΔR
2
, reported in Table 2 also shows
that the effects of Treatment Goals and Plot on end-of-treatment BDI
scores were small.
For the Burns Anxiety Inventory, our linear regression analysis
showed that Treatment Goals was a statistically signicant predictor of
end-of-treatment score on the Burns Anxiety Inventory (β = − 4.2, p =
0.04), but not Plot (β = − 3.4, p = 0.09) or Case Formulation (β = 0.09, p
= 3.8) (all p values were multiplied by 4 to Bonferroni-correct for the
total number of regression analyses). These beta coefcients indicate
that we would expect that patients whose clinical record included a list
of treatment goals would have an end-of-treatment BurnsAI score that
was 4.2 points lower on average (fewer symptoms) than patients whose
clinical record did not include a list of treatment goals. As the size of the
beta coefcient indicates, the effect of the Treatment Goals variable on
end-of-treatment Burns Anxiety Inventory score was small (the score on
the measure ranges from 0 to 99). The measure of effect size, ΔR
2
, re-
ported in Table 2 also shows that the effect of Treatment Goals on end-
of-treatment BurnsAI score was small.
In both the BDI and BurnsAI analyses, the initial score on the mea-
sure and therapist identity were statistically signicant predictors of the
end-of-treatment score on the measure (p < 0.0001), but total number of
therapy sessions and the intercept parameters were not.
In sum, two decision support tools, Treatment Goals and Plot, were
statistically signicantly related to end-of-treatment scores on one or
two of the outcome measures. Treatment Goals was a statistically sig-
nicant predictor of both end-of-treatment BDI and Burns AI scores, and
Plot was a statistically signicant predictor of end-of-treatment BDI
score. All effects were small in size.
Dropout. First we examine the degree to which the presence of the
decision support tools in the clinical record was related to Premature
dropout. As predicted and shown in Table 2, Case Formulation (β =
− 0.5, p < 0.0001) and Plot (β = − 0.4, p < 0.0001) were statistically
signicantly related to reduced Premature dropout compared to when
these tools were not present in the clinical record. However, contrary to
prediction, Treatment Goals was positively related to Premature dropout
(β = 0.3, p < 0.0001), indicating that a list of Treatment Goals was in the
chart was statistically signicantly related to increased premature
dropout.
The effect sizes (estimated odds ratios) of the decision support tools
on Premature dropout were 0.6 for Case Formulation, 1.3 for Treatment
Goals, and 0.7 for Plot. The fact that the odds ratio for Case Formulation
was less than one indicates that if patients had a case formulation in
their clinical record, they were less likely to drop out prematurely than if
they did not have a case formulation in their clinical record; the same is
true for Plot. The fact that the odds ratio for Treatment Goals was greater
than one indicates that if patients had a list of treatment goals in their
clinical record, they were more likely to drop out prematurely than if
they did not have a list of treatment goals in the clinical record. Another
way to consider the odds ratio is to convert it to a risk ratio for a given
baseline risk level. Using a baseline risk level of premature dropout of
52% and the odds ratios generated from our model t, we calculated
that a patient whose chart had a case formulation was 0.74 times as
likely to drop out prematurely as a patient without a case formulation, a
patient whose chart had a list of treatment goals was 1.13 times as likely
to drop out prematurely as a patient without a list of treatment goals,
and a patient whose chart had a plot was 0.80 times as likely to drop out
prematurely as a patient without a plot.
Next we examine the degree to which the presence of the decision
support tools in the clinical record was related to Uncollaborative
dropout. As Table 2 shows, Case Formulation (β = − 0.3, p = 0.0004),
Treatment Goals (β = − 0.4, p < 0.0001), and Plot (β = − 0.6, p < 0.0001)
were each statistically signicantly related to Uncollaborative dropout
in the predicted direction, indicating that the presence of a case
formulation, a list of treatment goals, or a plot in the clinical record each
predicted reduced uncollaborative dropout compared to when these
tools were not present in the clinical record.
As reported in Table 2, the estimated odds ratios for Case Formula-
tion, Treatment Goals, and Plot were 0.8, 0.7, and 0.5, respectively. The
fact that all odds ratios were less than one indicates that patients with
each of these tools in their clinical record were less likely to drop out
uncollaboratively than patients without each of these tools. Using a
baseline risk level of uncollaborative dropout of 30%, and the model-
derived odds ratios, we calculated that patients who had a case formu-
lation were 0.82 times as likely to drop out uncollaboratively as patients
without a case formulation, 0.77 times as likely to drop out
Table 2
Parameter estimates for linear and logistic regression models predicting outcome and dropout from the decision support tools of a written case formulation, list of treatment goals,
and plot of symptom scores.
n = 845 Beck Depression
Inventory Est. ± S.E.
ΔR
2
p Burns Anxiety
Inventory Est. ± S.E.
ΔR
2
p Premature Est.
± S.E.
e
Est.
p Uncollaborative Est.
± S.E.
e
Est.
p
Intercept − 2.5 ± 2.7 1.4 5.3 ± 7.3 1.9 2.8 ± 0.6 0 1.3 ± 0.3 4e-
4
Case
Formulation
− 0.6 ± 0.4 4e-4 0.6 0.09 ± 1.8 9e-4 3.8 − 0.5 ± 0.08 0.6 0 − 0.3 ± 0.07 0.8 4e-
4
Treatment
Goals
− 1.4 ± 0.4 0.005 7e-3 − 4.2 ± 1.6 0.02 0.04 0.3 ± 0.05 1.3 0 − 0.4 ± 0.05 0.7 0
Plot − 1.6 ± 0.6 0.007 0.04 − 3.4 ± 1.5 0.01 0.09 − 0.4 ± 0.05 0.7 0 − 0.6 ± 0.05 0.5 0
Total # Sessions 4e-4 ± 0.007 3.8 − 0.001 ± 0.01 3.8 − 0.01 ± 6e-4 0 − 0.002 ± 3e-4 0
Initial Score 0.3 ± 0.04 0 0.3 ± 0.02 0
Therapist F(19,76.3) = 8.3 0 F(19,76.1) = 3.9 0 F(19,10901.4) = 85.8 0 F(19,463.4) = 20.5 0
Note. All p-values were Bonferroni-corrected for the number of regression analyses. A p-value of 0 represents signicance at <0.0001. ΔR
2
signies the difference
between adjusted R
2
for the full regression model, and adjusted R
2
for the regression model without the decision support tool. e
Est.
is the odds ratio. Both ΔR
2
and e
Est.
are effect size measures. Reported ΔR
2
are means over the ve imputations; means ± standard errors across imputations are as follows: Case formulation/BDI: 4e-4 ±
1e-4; Treatment Goals/BDI: 0.0047 ± 0.0013; Plot/BDI: 0.0068 ± 0.0019; Case formulation/BurnsAI: 9e-4 ± 5e-4; Treatment Goals/BurnsAI: 0.017 ± 0.0053; Plot/
BurnsAI: 0.0113 ± 0.0038. Condence intervals around odds ratios are as follows: Case formulation/Premature Dropout: 0.58, CI = [0.50,0.67]; Treatment Goals/
Premature Dropout: 1.31, CI = [1.19,1.44]; Plot/Premature Dropout: 0.66, CI = [0.60,0.72]; Case formulation/Uncollaborative Dropout: 0.76, CI = [0.67,0.87];
Treatment Goals/Uncollaborative Dropout: 0.70, CI = [0.63,0.77]; Plot/Uncollaborative Dropout: 0.53, CI = [0.48,0.59].
V. Gates et al.
Behaviour Research and Therapy 142 (2021) 103874
6
uncollaboratively as patients without a list of treatment goals, and 0.62
times as likely to drop out uncollaboratively as patients without a plot.
The total number of sessions a patient completed (p < 0.0001), the
therapist identity (p < 0.0001), and the intercept parameter (p
premature
< 0.0001, p
uncollaborative
= 0.0004) were all statistically signicant pre-
dictors of both types of dropout.
The mean Jaccard index across imputations for the relationship be-
tween the decision support tools and Premature dropout was 0.31, 0.36,
and 0.27, for Case Formulation, Treatment Goals, and Plot, respectively.
The mean Jaccard index across imputations for the relationship between
the decision support tools and Uncollaborative dropout was 0.22, 0.17,
and 0.18, respectively, for Case Formulation, Treatment Goals, and Plot,
respectively. These indices describe the relationship between each de-
cision support tool and type of dropout, separate from the presence of
the other tools, therapist, or number of sessions.
In sum, Case Formulation, Treatment Goals, and Plot each predicted
statistically signicant reductions in both Premature and Uncollabor-
ative dropout, with the exception that, contrary to our prediction,
Treatment Goals predicted an increased rate of Premature dropout.
3. Discussion
We found that all three of the decision support tools we studied, a
written case formulation, a list of treatment goals, and a plot of symptom
scores, were associated with improved outcome and/or reduced dropout
in our sample of outpatients treated with naturalistic CBT in a private
practice setting. Tools had differing effects on dropout and outcome. We
found that two of the three decision support tools we studied, a list of
treatment goals, and a plot of symptom scores, were associated with
improved outcome. Patients whose medical record included a written
list of treatment goals had lower end-of-treatment scores on the Beck
Depression Inventory and Burns Anxiety Inventory than patients whose
medical record did not include a list of treatment goals. Patients whose
medical record included a plot of symptom scores had lower end-of-
treatment scores on the Beck Depression Inventory than patients
whose medical record did not include a plot. Effects of the decision
support tools on outcome were statistically signicant but small. The
tools with statistically signicant effects were associated with expected
average reductions in the end-of-treatment BDI score of 1.4 points (a
written list of treatment goals) and 1.6 points (a plot of symptom scores),
and an expected average reduction in the end-of-treatment BurnsAI
score of 4.2 points (a written list of treatment goals). These small effects
are similar to the small effects of decision support tools seen in some
other studies (e. g., Delgadillo et al., 2018; Kendrick et al., 2016), and
several of the studies reviewed by Lewis et al. (2018). We might have
obtained larger effects if we had been able to measure the degree to
which therapists actually used each tool; instead, we had only an indi-
rect measure of the therapist’s use of the tool, namely whether the tool
was present in the clinical record. Therapists may have had a written
formulation in the chart, for example, but not relied on it in their work,
or they may have relied on a case formulation without writing it down.
We might have also obtained larger effects if we had assessed the quality
of the case formulation; Abel et al. (2016) showed that therapist
competence in case conceptualization was related to sudden gains in
patients with treatment-resistant depression. And the list of treatment
goals might have been more convincingly related to outcome if we had
assessed outcome by assessing progress toward the goals on the list.
Unfortunately, our eld has not yet developed a strong measure for
assessing progress toward idiographic goals. Also, there is some evi-
dence that decision support tools contribute more to outcome when the
patient begins treatment with a poor outcome than when early progress
is good (cf. Lambert et al., 2005; Vittengl et al., 2019) and that the
currently-available tools are most effective at predicting deterioration
than outcome (e.g., Delgadillo et al., 2018; Lambert & Shimokawa,
2011).
The decision support tools we studied were more predictive of
dropout than of outcome in our sample. All three tools were statistically
signicantly related to a lower rate of both types of outcome we studied,
with the exception that a list of treatment goals was a statistically sig-
nicant predictor of a higher rate of premature termination. Based on our
model-derived odds ratios and estimated baseline sample rates, we
calculated that patients were 0.74 or 0.80 times as likely to drop out
prematurely when the clinical record had a written case formulation or a
plot of symptom scores, respectively. We calculated that patients were
0.82, 0.77, or 0.62 times as likely to drop out uncollaboratively when the
clinical record had a written case formulation, list of treatment goals, or
plot of symptom scores, respectively.
Contrary to our prediction, we calculated that patients whose chart
included a list of treatment goals were more likely (1.13 times more
likely) to drop out prematurely than patients whose chart did not
include a list of treatment goals. Perhaps this nding resulted from the
fact that the rating of whether the dropout was premature was made by
the therapist, and perhaps the therapist who had a written list of the
patient’s treatment goals in the chart was more likely to be aware of the
patient’s unmet goals and to rate the patient who wanted to end treat-
ment before accomplishing all of their goals as ending treatment pre-
maturely. Relatedly, therapists seem often to have more goals for
patients than do the patients themselves. This is reected by the fact that
in our sample (in which patients were only included if they had had at
least three therapy sessions), a very large proportion of patients were
judged by the therapist to have terminated prematurely (52% of the
patients for whom we had premature dropout data) yet had completed a
substantial number of therapy sessions (mean ± std.err of 16.3 ± 0.9) at
the time they terminated treatment. (For all patients in the sample, the
mean ± std.err was 24.0 ± 1.1 sessions.)
We speculate that the effects of the tools on outcome and dropout
was mediated at least in part by the benecial effects of the use of the
tools on the therapeutic alliance. Notice that all of the decision support
tools we studied entailed a written document that therapist and patient
could review together and use to guide treatment. Thus, the sharing of
the case formulation (Kuyken et al., 2009) and the list of treatment
goals, and the collaborative discussion of progress and decision-making,
may all contribute to the development of a strong therapeutic alliance.
(For example, one of the last author’s patients, a business executive,
volunteered that the author’s practice of collecting and reviewing
outcome data conveyed a willingness to be held accountable that
increased his respect for her.) This notion is consistent with the facts that
agreement on the tasks and goals of therapy is widely viewed as an
element of the therapeutic alliance (Bordin, 1994), and uncollaborative
dropout would seem to be the quintessential example of an alliance
rupture (Safran et al., 2011). A strong alliance has been shown to be
related to both improved outcome (Horvath et al., 2011) and reduced
dropout (Roos & Werbart, 2013).
Of the three tools we studied in our sample, the one that most aligned
with our predictions was the plot of symptom scores, which predicted
reduced end-of-treatment Beck Depression Inventory score, marginally
predicted reduced end-of-treatment Burns Anxiety Inventory score (p =
0.09), and predicted lower rates of both types of dropout. This obser-
vation is consistent with a growing body of studies showing that
measurement-based care and routine outcome monitoring are associ-
ated with improved outcome (see reviews by Carlier et al., 2012;
Goodman et al., 2013; Lewis et al., 2018) and reduced dropout (Janse
et al., 2020; meta-analysis by; de Jong et al., 2012).
The data analyzed in the present study were collected over a long
time period that ended more than 10 years ago (1981–2009). Many
changes occurred in our eld over this time period, including changes in
therapists’ training, the development of new interventions and new
diagnostic systems, and the advent of online tools for the medical record
and progress monitoring. The question of whether these developments
have implications for our results is worth considering. However, our
hypotheses and data analyses were constructed in such a way that in-
sulates our ndings from these changes. We tested the hypothesis that
V. Gates et al.
Behaviour Research and Therapy 142 (2021) 103874
7
therapist use of decision support tools of a written case formulation, a
list of treatment goals, and a plot of symptom scores affected outcome
and dropout. These questions remain of interest today. In fact, our study
provides some empirical support for the treatment utility of online tools
that make it easier for clinicians to maintain a useful clinical record that
includes a written case formulation and a list of treatment goals, and to
collect and plot progress monitoring data.
Our study has several limitations. Use of the decision support tools
was not randomly assigned, and as a result we cannot conclude that the
therapist’s use of a formulation, plot, and treatment goals caused the
effects on outcome and dropout that we observed. However, because we
controlled for the main effect of therapist in our analyses, we can rule
out the competing account that the decision support tools were related
to outcome and dropout because the use of the tools reects the
conscientiousness or skill level of the therapist rather than the use of the
tools.
Several limitations affect our independent variables, the decision
support tools. We do not have any information about the content or
adequacy of the case formulations or lists of treatment goals; we have
only a rating of whether the tool was present in the clinical record.
Therapists may have used a case formulation to guide the treatment
even if a written formulation was not present in the clinical record. And
the fact that the clinical record included a plot does not indicate that the
therapist reviewed the plot with the patient. We also have no informa-
tion about when in the course of treatment the tools were developed and
the degree to which the therapist used the tool to guide the treatment.
Another limitation is that results cannot be assumed to generalize to
therapists other than the ones studied here, who are not typical of
therapists in the community. All of these therapists collected and plotted
symptom data for at least some of their patients; in contrast, less than
20% of providers use measurement-based care (Lewis et al., 2018). This
fact limits the generalizability of our ndings, as does the fact that pa-
tients were a homogeneous group of highly educated predominantly
White adults who paid high fees for their treatment.
Strengths of our investigation include our study of a sample of pa-
tients with multiple comorbidities who received treatment in a clinical
rather than a research setting, and the fact that most of the data we
studied here were collected in the course of routine clinical practice,
both of which are research strategies that increase the external validity
of our ndings (Weisz et al., 2014). Additional strengths of our study
include our focus on key elements of evidence-based practice (American
Psychological Association, 2006), and our examination of a large sample
of private practice patients that are infrequently represented in the
research literature. A nal strength of our study is that the decision
support tools we studied (the written case formulation, the list of
treatment goals, and the plot of symptom scores) can be used by any
psychotherapist of any discipline or psychotherapy orientation to treat
patients who seek treatment for any disorder or presenting problem.
Author declaration template
There are no nancial conicts of interest.
CRediT authorship contribution statement
Vael Gates: devised and conducted the data analysis and wrote most
of the Results section and some of the Discussion. Megan Hsiao: made
major contributions to organizing and cleaning the database. Garret G.
Zieve: assisted with the database organization, cleaning, and coding.
Rebecca Courry: assisted with coding for the inter-rater reliability
study. Jacqueline B. Persons: collected the data and drafted the
manuscript.
Acknowledgments
The rst author received funding from Defense Advanced Research
Projects Agency grant D17AC0004. We thank Thomas L. Grifths for his
support as the rst author’s thesis advisor, M. D. Edge for statistical
consultation, Cannon Thomas for helpful comments, and Connie Fee for
help cleaning and organizing the database. An earlier version of this
paper was presented at the Association for Behavioral and Cognitive
Therapies in Atlanta on November 22, 2019.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.
org/10.1016/j.brat.2021.103874.
References
Abel, A., Hayes, A. M., Henley, W., & Kuyken, W. (2016). Sudden gains in
cognitive–behavior therapy for treatment-resistant depression: Processes of change.
Journal of Consulting and Clinical Psychology, 84(8), 726–737. https://doi.org/
10.1037/ccp0000101. PsycINFO.
American Psychological Association. (2006). Evidence-based practice in psychology.
American Psychologist, 61(4), 271–285.
Beck, J. S. (1995). Cognitive therapy: Basics and beyond. Guilford press.
Beck, A. T., Steer, R. A., & Garbin, M. G. (1988). Psychometric properties of the Beck
depression inventory: Twenty-ve years of evaluation. Clinical Psychology Review, 8,
77–100. https://doi.org/10.1016/0272-7358(88)90050-5.
Beck, A. T., Ward, C. H., Mendelsohn, M., Mock, J., & Erbaugh, J. (1961). An inventory
for measuring depression. Archives of General Psychiatry, 4, 561–571. https://doi.
org/10.1001/archpsyc.1961.01710120031004.
Bordin, E. S. (1994). Theory and research on the therapeutic working alliance: New
directions. In A. O. Horvath, & L. S. Greenberg (Eds.), The working alliance: Theory
research and practice. Wiley.
Burns, D. D., & Eidelson, R. J. (1998). Why are depression and anxiety correlated? A test
of the tripartite model. Journal of Consulting and Clinical Psychology, 66(3), 461.
Carlier, I. V. E., Meuldijk, D., Van Vliet, I. M., Van Fenema, E., Van der Wee, N. J. A., &
Zitman, F. G. (2012). Routine outcome monitoring and feedback on physical or
mental health status: Evidence and theory. Journal of Evaluation in Clinical Practice,
18(1), 104–110. https://doi.org/10.1111/j.1365-2753.2010.01543.x.
Cuijpers, P., Karyotaki, E., Weitz, E., Andersson, G., Hollon, S. D., & van Straten, A.
(2014). The effects of psychotherapies for major depression in adults on remission,
recovery and improvement: A meta-analysis. Journal of Affective Disorders, 159,
118–126. https://doi.org/10.1016/j.jad.2014.02.026.
Delgadillo, J., de Jong, K., Lucock, M., Lutz, W., Rubel, J., Gilbody, S., Ali, S., Aguirre, E.,
Appleton, M., Nevin, J., O’Hayon, H., Patel, U., Sainty, A., Spencer, P., &
McMillan, D. (2018). Feedback-informed treatment versus usual psychological
treatment for depression and anxiety: A multisite, open-label, cluster randomised
controlled trial. The Lancet Psychiatry, 5, 564–572. https://doi.org/10.1016/S2215-
0366(18)30162-7.
Derogatis, L. R., Rickels, K., & Rock, A. F. (1976). The SCL-90 and the MMPI: A step in the
validation of a new self-report scale. The British Journal of Psychiatry, 128(3),
280–289.
Eells, T. D. (Ed.). (2007). Handbook of psychotherapy case formulation (2nd ed.). Guilford.
Enders, C. K. (2017). Multiple imputation as a exible tool for missing data handling in
clinical research. Behaviour Research and Therapy, 98, 4–18. https://doi.org/
10.1016/j.brat.2016.11.008.
Fernandez, E., Salem, D., Swift, J. K., & Ramtahal, N. (2015). Meta-analysis of dropout
from cognitive behavioral therapy: Magnitude, timing, and moderators. Journal of
Consulting and Clinical Psychology, 83(6), 1108–1122. https://doi.org/10.1037/
ccp0000044.
Gardiner, J. C., Luo, Z., & Roman, L. A. (2009). Fixed effects, random effects and GEE:
What are the differences? Statistics in Medicine, 28(2), 221–239. https://doi.org/
10.1002/sim.3478.
Goodman, J. D., McKay, J. R., & DePhilippis, D. (2013). Progress monitoring in mental
health and addiction treatment: A means of improving care. Professional Psychology:
Research and Practice, 44(4), 231–246. https://doi.org/10.1037/a0032605.
Hawkins, E. J., Lambert, M. J., Vermeersch, D. A., Slade, K. L., & Tuttle, K. C. (2004). The
therapeutic effects of providing patient progress information to therapists and
patients. Psychotherapy Research, 14(3), 308–327. https://doi.org/10.1093/ptr/
kph027.
Honaker, J., King, G., & Blackwell, M. (2012). Amelia II: A Program for Missing Data
(1.6.2) [Computer Software]. https://gking.harvard.edu/amelia.
Horvath, A. O., Del Re, A. C., Flückiger, C., & Symonds, D. (2011). Alliance in individual
psychotherapy. Psychotherapy, 48(1), 9.
Janse, P. D., de Jong, K., Veerkamp, C., van Dijk, M. K., Hutschemaekers, G. J. M., &
Verbraak, M. J. P. M. (2020). The effect of feedback-informed cognitive behavioral
therapy on treatment outcome: A randomized controlled trial. Journal of Consulting
and Clinical Psychology, 88(9), 818–828. https://doi.org/10.1037/ccp0000549.
de Jong, K., van Sluis, P., Nugter, M. A., Heiser, W. J., & Spinhoven, P. (2012).
Understanding the differential impact of outcome monitoring: Therapist variables
that moderate feedback effects in a randomized clinical trial. Psychotherapy Research,
22(4), 464–474. https://doi.org/10.1080/10503307.2012.673023. PsycINFO.
Kuyken, W., Padesky, C. A., & Dudley, R. (2009). Collaborative case conceptualization.
Guilford.
V. Gates et al.
Behaviour Research and Therapy 142 (2021) 103874
8
Lambert, M. J., Harmon, C., Slade, K., Whipple, J. L., & Hawkins, E. J. (2005). Providing
feedback to psychotherapists on their patients’ progress: Clinical results and practice
suggestions. Journal of Clinical Psychology, 61(2), 165–174. https://doi.org/10.1002/
jclp.20113.
Lambert, M. J., & Shimokawa, K. (2011). Collecting client feedback. Psychotherapy, 48
(1), 72–79. https://doi.org/10.1037/a0022238.
Lewis, C. C., Boyd, M., Puspitasari, A., Navarro, E., Howard, J., Kassab, H., … Douglas, S.
(2018). Implementing measurement-based care in behavioral health: A review.
JAMA Psychiatry, 76(3), 324–335. https://doi.org/10.1001/jamapsychiatry.2018.
3329.
Persons, J. B. (1989). Cognitive therapy in practice: A case formulation approach. Norton &
company.
Persons, J. B. (2008). The case formulation approach to cognitive-behavior therapy. Guilford.
Persons, J. B., & Hong, J. J. (2016). Case formulation and the outcome of cognitive
behavior therapy. In N. Tarrier, & J. Johnson (Eds.), Case formulation in cognitive
behaviour therapy (2nd ed., pp. 14–37) Routledge.
Project Jupyter. (n.d.). Jupyter Notebook. https://jupyter.org.
Python Software Foundation. (n.d.).Python Language Reference (3.6.5) [Computer
software]. http://python.org.
R Core Team. (2007). ls: Least squares regression for continuous dependent variables.
http://zeligproject.org.
R Core Team. (2018). R: A language and environment for statistical computing. R
foundation for statistical computing. https://www.r-project.org/.
Roos, J., & Werbart, A. (2013). Therapist and relationship factors inuencing dropout
from individual psychotherapy: A literature review. Psychotherapy Research, 23,
394–418. https://doi.org/10.1080/10503307.2013.776628.
Safran, J. D., Muran, J. C., & Eubanks-Carter, C. (2011). Repairing alliance ruptures.
Psychotherapy, 48(1), 80–87. https://doi.org/10.1037/a0022140. PsycINFO.
Vittengl, J. R., Clark, L. A., Thase, M. E., & Jarrett, R. B. (2019). Estimating outcome
probabilities from early symptom changes in cognitive therapy for recurrent
depression. Journal of Consulting and Clinical Psychology, 87(6), 510.
Weisz, J. R., Ng, M. Y., & Bearman, S. K. (2014). Odd couple? Re-envisioning the relation
between science and practice in the dissemination-implementation era. Clinical
Psychological Science, 2(1), 58–74. https://doi.org/10.1177/2167702613501307.
V. Gates et al.
