
Corresponding Author: Rebecca L Stearns, Rebecc[email protected]
Original Publication Date: June 2, 2020 1
Return to Sports and Exercise during the COVID-
19 Pandemic: Guidance for High School and
Collegiate Athletic Programs
Contributing Authors
Rebecca L. Stearns, PhD, ATC, Korey Stringer Institute, University of Connecticut, Storrs, CT
Samantha E. Scarneo-Miller, PhD, ATC, Korey Stringer Institute, University of Connecticut, Storrs, CT
Robert A. Huggins, PhD, ATC, Korey Stringer Institute, University of Connecticut, Storrs, CT
Lindsay B. Baker, PhD, Gatorade Sports Science Institute, PepsiCo R&D, Barrington, IL
Tony Caterisano, PhD, CSCS*D, Collegiate Strength and Conditioning Coaches Association, Furman University,
Greenville, SC
George Chiampas, DO, Chief Medical Officer United States Soccer Federation, Northwestern University Feinberg School
of Medicine, Chicago, IL
Don Decker, MS, CSCS, SCCC, Collegiate Strength and Conditioning Coaches Association, New Mexico State University,
Las Cruces, NM
Jonathan A. Drezner, MD, University of Washington, Seattle, WA
John F. Jardine, MD, Korey Stringer Institute, University of Connecticut, Storrs, CT
Michael C. Koester, MD, National Federation of State High School Associations, Slocum Center for Orthopedics and Sports
Medicine, Eugene, OR
Kristen L. Kucera, PhD, MSPH, ATC, National Center for Catastrophic Sport Injury Research, University of North
Carolina, Chapel Hill, NC
Eric McMahon, M.Ed, CSCS, RSCC*D, National Strength and Conditioning Association, Colorado Springs, CO
Neha P. Raukar, MD, Mayo Clinic, Rochester, MN
Jennifer D. Rheeling, MS, ATC, National Athletic Trainers’ Association, Washington DC Public Schools, Washington DC
Chuck Stiggins, Ed.D, SCCC, Collegiate Strength and Conditioning Coaches Association, Provo, UT
Brady L. Tripp, PhD, ATC, National Athletic Trainers’ Association, University of Florida, Gainesville, FL
The following organizations endorsed this document: American College of Sports Medicine (ACSM), Collegiate
Strength and Conditioning Coaches Association (CSCCa), Gatorade Sports Science Institute (GSSI), Korey Stringer
Institute (KSI), National Athletic Trainers’ Association (NATA), National Center for Catastrophic Sport Injury Research
(NCCSIR), National Federation of State High School Associations (NFHS), National Strength and Conditioning
Association (NSCA).
he COVID-19 pandemic has sparked dramatic
changes across all aspects of our daily lives. The
combination of lifestyle modifications and potential
comorbidities associated with COVID-19 also presents
important, athlete specific, health and safety risks as return
to sport plans emerge. While it is clear that transition periods
have a higher risk for catastrophic sport injury,1–6 some of the
factors that place athletes at higher risk during these periods
may be amplified as a result of social distancing measures.
These risk factors may also be amplified at various levels –
so even athletes within the same team may have a spectrum
of risk profiles. As plans for a return to organized sport begin,
and over 10 million high school and college athletes emerge
from this unprecedented period,7,8 healthcare providers and
administrators must give greater consideration for how to
reduce risk while re-introducing sport.
The purpose of this document is to create an overarching
consensus statement across high school and collegiate
athletics to address return to physical activity considerations
during or immediately following physical distancing. This
document is meant to serve as a resource, providing a
streamlined approach that sport organizations and those
involved in high school and college sport programs (i.e.
athletes, coaches, strength and conditioning coaches, athletic
trainers, athletic directors, and physicians) may use. It is
important to remember that organizations must always refer
to federal and state authorities, departments of public health,
and sport specific organizational governing bodies when
considering health and safety policies and procedures. The
recommendations provided in this document are based on
published best practices and hold value for prioritizing
athlete health and safety. However, in the absence of this
evidence, expert opinion is utilized. It is acknowledged that
resources across and between high school and collegiate
programs differ, therefore the application of these
recommendations must be considered within the context of
T
2
the sport setting, compliance and individual school
resources. It should also be noted that some of these
recommendations may be accomplished over a timeline and
not at the immediate resumption of sport activity. Similarly,
these recommendations are written to apply across all sport
seasons and are not limited to only fall athletes.
The specific objectives of this document are as follows:
1. Discuss how and why physical distancing presents
added and unique risk to athletes.
2. Identify various risk profiles.
3. Identify how to mitigate risk with tools and resources
already available.
4. Discuss considerations for interruptions to normal
seasons, and when this document may be
implemented.
5. Specifically address the following topics:
• Pre-participations evaluations
• Return to physical activity/conditioning
• Heat acclimatization
• Injury prevention (preventative training programs)
• Education for related items
This document is not intended to:
1. Provide a recovery plan specific for COVID-19
patients.
2. Discuss administrative considerations and practices.
3. Discuss cleaning procedures or personal protection
practices.
4. Provide detailed discussion of screening, testing,
isolating and contact tracing for sport programs.
Preparticipation Physical Evaluation
Physical Evaluations
The preparticipation physical evaluation (PPEval) is
considered best practice for identifying potentially serious
medical conditions which may lead to injury or illness during
athletic competition. The National Federation of State High
School Associations (NFHS) and National Collegiate
Athletic Association (NCAA) recommend a history and
physical evaluation prior to athletic participation. All state
high school athletic associations require a PPEval, but the
scope, medical providers approved to conduct the exam, and
required time interval between exams vary.
During the COVID-19 pandemic, many healthcare offices
have significantly scaled back or canceled routine well care
visits, including PPEval appointments. As healthcare offices
slowly re-open in the coming months, there is a concern that
the demand for regular routine care and maintenance of
chronic medical conditions may overburden healthcare
offices, making it difficult, or impossible, for athletes to
obtain a PPEval in a timely manner. Given the unprecedented
loss of employment nationwide, many young athletes may
also lose health insurance benefits and see delays in primary
care provider assignment when or if they enroll in a state
Medicaid program.
While the recommendations below are in agreement with
the NFHS Statement on PPE’s and Athletics Participation
(released in April 2020),9 the recommendations are also
generalizable to the college setting across all levels (Junior
College, NCAA DIII, DII, DI, and NAIA).
As such, we recommend the following minimum
recommendations for both high school and collegiate
athletes:
1) Be familiar with state and local laws as well as
organizational policy requirements for PPEvals.
2) Discuss with local health departments and state medical
associations prior to making a final decision on how best
to approach this issue.
3) If needed, and absent indications to the contrary, a one-
year extension should be considered for any student who
has a PPEval that “expires” before or during the 2020-21
academic year.
4) Access to the PPEval should be assessed at a local level
as much as is organizationally possible. When the
opportunity for an in-office encounter is unavailable, an
interim history update and a review of any chronic
medical conditions with an athletic trainer or a
telemedicine visit with a primary care provider should be
strongly encouraged.
5) Athletes who have not had a PPEval, such as incoming
freshmen and students who are first time participants in
athletics, or athletes who did not have a PPEval during
the 2019-2020 academic year, should still be required to
have a PPEval prior to athletic participation. Therefore,
athletes, parents and guardians should be informed of the
need to obtain a PPEval prior to the start of the 2020-21
academic year and should schedule the appointment with
their primary care provider as soon as possible.
Past Medical History
Severe acute respiratory syndrome coronavirus 2 (SARS-
CoV-2), the novel coronavirus that causes COVID-19,
presents unique health issues that should be considered prior
to a return to sports and exercise. While the vast majority of
young persons afflicted with the coronavirus have mild
symptoms or remain asymptomatic, rarely the infection can
cause direct injury or inflammation to the heart or kidneys.
Concerns for cardiac complications from COVID-19 arise
from data in the sickest of hospitalized patients, and evidence
on the prevalence and risks of myocardial injury during more
mild illness remains limited. Likewise, acute kidney injury
has been seen in critically ill patients, affecting nearly one-
third of patients requiring intensive care. Nonetheless, the
sports medicine community believes that patients with prior
COVID-19 should undergo a medical assessment before
returning to exercise.

3
1) We recommend that every student-athlete with a prior
diagnosis of COVID-19, symptoms suggestive of
COVID-19, or a “close exposure” to someone with
COVID-19 should contact their medical provider to
determine if further evaluation is warranted prior to
returning to sports. A close exposure is defined as having
a household member with COVID-19, prolonged
exposure (>10 minutes) within 6 feet of an individual
with confirmed COVID-19, direct exposure to infectious
secretions (e.g., being coughed on) or direct physical
contact during sports from an individual with COVID-
19.
2) A medical evaluation is strongly recommended for
student-athletes with a confirmed diagnosis of COVID-
19.
3) Those at greater risk for developing severe COVID-19
disease or complications should undergo an informed
decision-making process with their medical provider
before a return to sports as exposure to teammates and
opponents may increase their risk of becoming infected.
Individuals at higher risk of severe COVID-19 include
those with a serious heart condition, uncontrolled or
moderate to severe asthma, chronic lung disease,
diabetes, obesity, pre-existing kidney disease, or a
weakened immune system.
a) Although the Centers for Disease Control and
Prevention states that patients with these conditions
may be at greater risk for more severe disease, there
are limited published data in young athletes to
support this determination at this time.
4) All athletes with prior COVID-19 should be screened for
ongoing symptoms of chest pain/pressure with exercise,
difficulty breathing or dizziness with exercise, or
decreased exercise tolerance.
5) Additional cardiac testing, such as an electrocardiogram
(ECG), cardiac biomarkers (i.e. hs-troponin), and an
echocardiogram may be indicated depending on the
severity of past COVID-19 illness, ongoing symptoms,
or clinical suspicion. Specific medical guidance can be
found from a publication by Baggish et al.10
6) Tests to evaluate kidney function (i.e. urinalysis, serum
creatinine) should be considered to evaluate kidney
function after recovery from COVID-19.
7) Athletes with ongoing respiratory symptoms associated
with COVID-19 should undergo cardiac and pulmonary
testing as guided by a physician.
8) Secondary schools and collegiate athletic programs
should consider a supplemental questionnaire addressing
COVID-19 specific medical issues (see Appendix A).
Positive responses from this questionnaire should trigger
an evaluation by a medical provider prior to participation
in sports.
PPEval Resources:
1. NFHS Statement on PPE and Athletic Participation:
Ramifications of the COVID-19 Pandemic
2. American Academy of Pediatrics Preparticipation
Physical Evaluation (PPE)
3. National Athletic Trainers’ Association Position
Statement: Preparticipation Physical Examinations and
Disqualifying Conditions
4. AMSSM Position Statement on Cardiovascular
Preparticipation Screening in Athletes: Current
evidence, knowledge gaps, recommendations and future
directions
5. The resurgence of sport in the wake of COVID-19:
cardiac considerations in competitive athletes
Return to Physical Activity
Exercise Adaptations
The COVID-19 crisis and physical distancing policies have
resulted in high school and college athletes being separated
from their normal training facilities and workout routines for
several months. Because of this crisis, athletes will be
returning with a variety of conditioning levels, creating the
potential for “a perfect storm” of detrained athletes returning
to shorter training preparation time.
In June 2019, a joint position paper was published in the
Strength and Conditioning Journal entitled “CSCCa and
NSCA Joint Consensus Guidelines for Transition Periods:
Safe Return to Training Following Inactivity.”11 These
guidelines apply to those athletes with any period of
inactivity of two weeks or greater. If a two-week break or
longer occurs after the resumption of training, the
recommendation is to re-start the guidelines in the 2019
consensus document, which may even need to be done
multiple times. While these recommendations were written
specifically for the collegiate athlete, many of these
recommendations should be considered for the high school
athlete when possible. It is recommended that coordination
occurs between the coach, strength and conditioning staff
and athletic trainer to be sure that training is developmentally
appropriate and not superfluous or excessive.
As such, we recommend the following:
1) Register your written training programs with athletics
administrators.
a) Prior to restarting training workouts, coaches should
record a written strength and conditioning program.
This record should adhere to established
recommendations of training protocols within the
field of strength and conditioning by organizations
such as the Collegiate Strength and Conditioning
Coaches Association (CSCCa), the National
Strength and Conditioning Association (NSCA), the
NFHS, the individual state high school athletic
association, and the NCAA, and a copy of the
conditioning program should be held on file by an
appropriate member of the athletics administration.
b) This program should reflect the upper limit for
exercise intensity and volume. The “upper limit”
4
workout would be the highest level of intensity and
volume an athlete would be able to tolerate when in
peak condition. This workout will be utilized to
determine the maximum allowable limits using the
50/30/20/10 and F.I.T. (Frequency, Intensity, Time
of Weight Training) rules.
2) Follow the 50/30/20/10 Rule11
a) The 50/30/20/10 Rule for athletes is a testing
protocol, and a daily and weekly conditioning
protocol.
b) College Student-Athletes
i) It is recommended that weekly conditioning
volume be reduced by 50% from the uppermost
volume on file in week 1 with a 1:4 or greater
Work to Rest Ratio (W:R) and 30% in week 2
with a 1:3 or greater W:R. Based on the protocol,
the returning athletes can then return to normal
training volumes and intensities based upon the
professional judgment of the coach. For athletes
who are new to the program, it is recommended
that a minimum of a 20%, and 10% reduction
takes place in weeks 3 and 4, respectively.
ii) If conditioning testing is completed for returning
athletes, then the workload (whether through
intensity, volume, rest time, or a combination)
should be reduced by 20% in the first week and
10% in the second week. Because of the
reduction in workload, there is no mandate to
change the W:R for these testing sessions.
iii) For new athletes, conditioning testing must be
completed on the first day of return to training
and should be performed at 50% of the standard
volume of the test on file with the administrator,
using 1:4 or greater W:R. Although not
mandatory, testing may be repeated, but should
follow the rule for conditioning activities, with a
30/20/10% weekly reduction in volume at
standard intensities and rest times.
c) High School Student-Athletes
i) High school programs might use training
regimens that are different from collegiate
programs, but the recommendation is being
made that a reduction be applied to exercise
programs in order to create a phased re-
introduction of physical activity. Because a
consensus statement on transition periods for
high school athletes has not been published, the
50/30/20/10 rule provides the best
recommendations available to guide exercise
modifications within the high school setting.
These recommendations would allow the re-
introduction of exercise over the first 4 weeks
based on reductions from the normal exercise
load/plan: Week 1 a 50% reduction, Week 2 a
30% reduction, Week 3 a 20% reduction and
Week 4 a 10% reduction in conditioning
volume.
ii) For that reason, the recommendation is that in
week one of training, if a conditioning test is
done, a reduction of 50% should be applied to
the chosen measuring tool with a W:R of 1:4 or
greater. This should remain consistent , and the
same is true for all daily and weekly
conditioning programs. This is a recommended
“ceiling”. If at any time prior to achieving the
50% volume prescribed athletes begin to
struggle, they should be removed from the drill.
In Week 2 the volume, whether for testing or
general conditioning, is reduced by 30% with a
1:3 W:R or greater; Week 3 by 20% with no
added accommodation for work rest; and week
4 by 10% with no added accommodations for
work rest.
iii) Athletes involved in multiple sports should
consider not participating in multiple sport
practices or conditioning sessions during the
pre-season or should reduce the workload in
each of the sports practices or conditioning
sessions by at least 50%.
3) Follow The F.I.T. Rule (Frequency, Intensity, Time of
Weight Training)11
a) The F.I.T. Rule provides guidance for phasing in
weight training and should be used following a
period of active rest or periods of minimal training
(See Appendix B).
b) The F.I.T. Rule has been described in the Joint
Consensus Document for collegiate athletics.
Because a consensus statement on transition periods
for high school athletes has not been published, the
F.I.T. Rule provides the best recommendations
available to guide weight training modifications
within the high school setting.
c) The F.I.T. rule is designed to ensure that frequency,
intensity relative volume (IRV), and time of rest
interval are appropriately administered to minimize
the chance of severe muscle damage during weight
training.
d) Frequency is defined as the number of training
sessions completed per week for a specific muscle
group or movement type. For example, the student-
athlete might train a total of 5 days in the week, but
only train the lower body for 3 days, so the frequency
for lower-body movements equals 3. Following a
period of inactivity, it is recommended that
frequency not exceed 3 days in the first week and no
more than 4 days in the second week. IRV is a
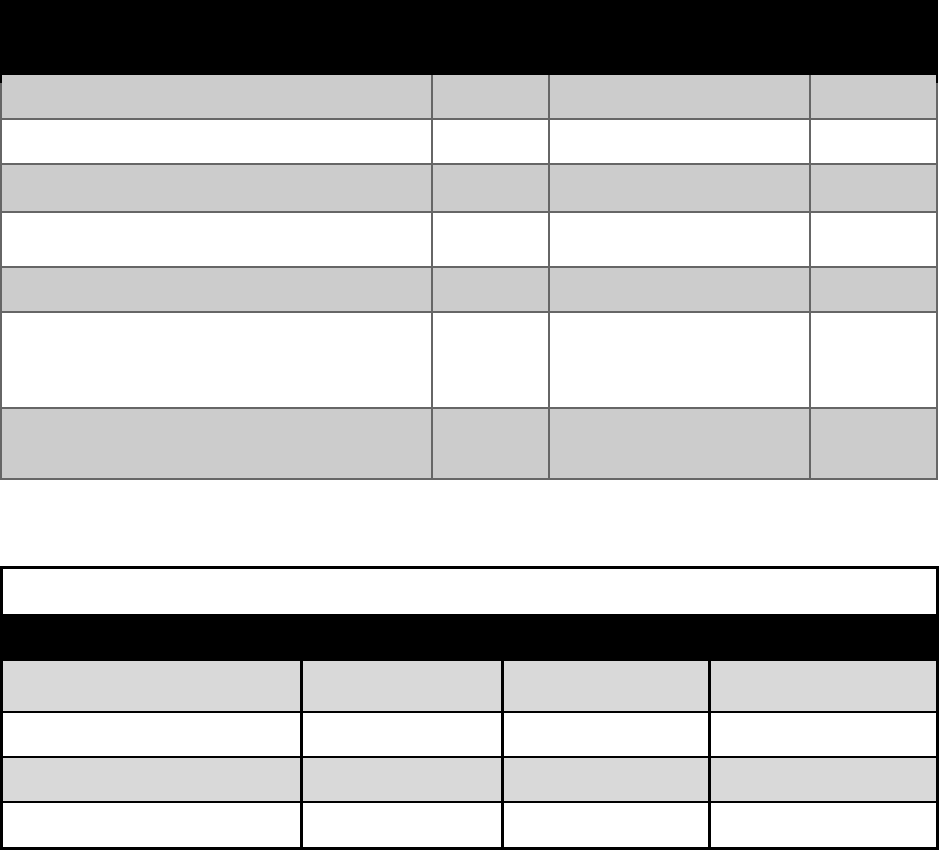
derivation of volume load that includes the %1RM
(one repetition maximum) and is calculated with the
following equation: Sets x Reps x % of 1RM (as a
decimal) = IRV
5
i) Example: 3 sets x 10 reps x 0.50 (which would
be 50% 1RM) = 15 IRV
e) The recommendation is to keep IRV between 11 –
30 with a W:R of 1:4 or greater the first week and
1:3 or greater the second week. IRVs of greater than
30 are contraindicated in the first 2 weeks following
a period of inactivity in addition to coaches’ own
professional judgment regarding limitations on the
return to training program.
f) Examples and specific usage of the F.I.T. principle
can be found within the 2019 CSCCa and NSCA
Joint Consensus Guidelines for Transition Periods:
Safe Return to Training Following Inactivity.11
Exercise Adaptations Resources:
1. CSCCa and NSCA Joint Consensus Guidelines for
Transition Periods: Safe Return to Training Following
Inactivity
2. National Athletic Trainers’ Association – Key Facts
about Detraining
Heat Acclimatization
Exercising in the heat imposes significant strain on the
cardiovascular system to simultaneously support
thermoregulatory and metabolic demands, thus presenting a
serious challenge to body core temperature regulation.
Routine exposure to exercise in the heat elicits physiological
adaptations that gradually improve exercise heat tolerance.
As such, a proper heat acclimatization program is essential
to reduce the risk of exertional heat illness, death from
exertional heatstroke, and death from other causes such as
sudden cardiac and exertional sickling that are exacerbated
by heat intolerance. Established heat acclimatization
guidelines are clearly outlined and take into account summer
and pre-season scheduling, however the timing of a return to
activity during or following social distancing may alter the
feasibility of these guidelines.
Thus, consider the following to properly heat acclimatize
athletes:
1) Time course of adaptations
a) An important consideration is that fitness
acclimatization may overlap and even
enhance/jumpstart the heat acclimatization process.
b) Once physical fitness is established (see exercise
adaptations section), gradually increase the duration
and intensity of exercise in the heat over a minimum
of 7 days, with full adaptations occurring at 10-14
days (see Appendix C). Repeated maximal physical
efforts over a prolonged period and competitive play
should be avoided until both fitness and heat
acclimatization are achieved.
c) While some adaptations can be obtained from
exposure to hot environments without exercise as
well as from exercise without heat exposure, these
approaches do not maximize the adaptations.
d) Organizations should consider modifying regular
season start dates and/or shortening the length of the
regular season to allow sufficient time for heat
acclimatization to occur.
e) If training is paused for more than 5-7 days due to
“stay at home orders” or due to individual/team
quarantines, schools should consider restarting or
extending the heat acclimatization process prior to
the resumption of activity.
2) Hydration considerations
a) Hydration plays an important role in maintenance of
thermoregulatory function and can influence the risk
of exertional heat illness. Therefore, it is critical to
allow for frequent and open access to cool, palatable
fluids to promote proper hydration in hot weather.12–
14
b) Hydration status should be monitored daily via pre-
practice body mass, urine concentration, and thirst.
See GSSI Sport Science Exchange: Hydration
Assessment of Athletes or NATA Position
Statement: Fluid Replacement15 for the Physically
Active for more information.
c) To reduce the risk of viral transmission, the sharing
of bottles and water sources should be avoided. All
efforts should be made to have individualized and
labeled bottles for each athlete. Good hygiene
practices (e.g., hand washing) and personal
protective equipment (i.e. gloves, masks) should be
used when filling bottles for athletes. Heightened
awareness should be taken to support access to
individualized fluids containers.
d) Other means of fluid delivery besides individual
bottles/containers (like hoses, PVC pipes, mass
drinking stations etc.) should not be utilized as
individual drinking stations.
e) If proper access to fluids during exercise in the heat
is not possible due to COVID-19 transmission
concerns, sessions should be modified or cancelled.
3) Modifying exercise based on environmental conditions
a) During and after the heat acclimatization period,
modification or cancellation of physical activity
(consistent with organizational, state, and regional
policies) based on routine measurements of
environmental conditions (ideally via wet-bulb
globe temperature per best practices) is strongly
recommended.4,16
b) As environmental heat stress increases,
modifications, such as the removal of unnecessary
equipment or clothing, increased frequency of rest
breaks, and access to hydration, or rescheduling the
session to an earlier/later (i.e., cooler) time of the day
should be implemented.4,16–18
6
Heat Acclimatization Resources:
1. 2013-2014 NCAA Sports Medicine Handbook
2. Korey Stringer Institute Heat and Hydration
3. National Athletic Trainers’ Association: Preseason
Heat Acclimatization Guidelines for Secondary
School Athletics
4. National Athletic Trainers’ Association – Heat
Acclimatization
5. National Federation of State High School
Associations – Heat Acclimatization and Heat
Illness Prevention Position Statement
6. GSSI Sport Science Exchange: Hydration
Assessment of Athletes
7. NATA Position Statement: Fluid Replacement for
the Physically Active
Injury Prevention
There is an increased risk of musculoskeletal injury
following a prolonged period of physical inactivity. Given
lower extremity injuries make up approximately 66% of all
sports injuries, preventative training programs (also known
as injury prevention programs, multicomponent training
programs) may reduce the likelihood of these injuries during
sport.19 Preventative training programs that require more
than 1 type of exercise (e.g., strength, balance, agility,
flexibility, plyometrics) are more effective at reducing
injuries.
The following guidelines are recommended to reduce lower
extremity injuries:
1) Preventative training programs:
a) Should include exercises in at least 3 of the
following categories: strength, balance, plyometrics,
agility, and flexibility.19
b) Should be performed at least 2-3 times per week
throughout the pre-season and in-season.19
c) Are easily implemented to replace, or in conjunction
with, a team’s warm-up program or strength and
conditioning program. The programs are typically
10-15 minutes and dynamic in nature.19
2) It is important to note that the pre-participation physical
evaluation may also assist with injury prevention (See
Preparticipation Physical Evaluation section).
Injury Prevention Resources:
1. National Athletic Trainers’ Association Position
Statement: Prevention of Anterior Cruciate
Ligament Injury
2. Stanford Orthopedics Sports Medicine
Education
It is important to remember that it is the responsibility of
sport organizations to interpret these recommendations and
apply what is relevant and feasible to their setting.
Additionally, an educational plan should be in place to
ensure a timely, streamlined communication of the policies
and procedures that should be in place.
The following considerations are recommended to achieve
this:
1) Education of all entities involved. This may include (but
not limited to): coaches, athletes, administrators,
parents/guardians, healthcare team, maintenance staff,
etc.
2) Designate a point person to disseminate information
pertaining to policies/procedures that should be
disseminated/implemented.
3) Define targets/audience for the dissemination of this
information.
4) Determine mode of information dissemination (email,
conference call, video conference, etc.).
5) Determine timing of this information and future updates.
6) Recommendations and guidelines may be subject to
change in response to an increased viral burden or other
evolving situations.
7) Re-education and policy re-evaluation given developing
circumstances.
Disclaimer
This document is intended to provide relevant practice
parameters for high school and collegiate sport programs to
use when performing their responsibilities in providing
services to athletes or other participants. The
recommendations presented here are based on published
scientific studies, position statements, inter-association task
force documents, personal communications, and a
consensus of expert views available based on the time of
publication. However, this information is not a substitute
for individualized judgment or independent professional
advice.
Neither the Korey Stringer Institute/The University of
Connecticut, nor the contributors to this project assume any
duty owed to third parties by those reading, interpreting, or
implementing this information. When rendering services to
third parties, these recommendations cannot be adopted for
use with all participants without exercising independent
judgment and decision making.
Sport programs using this information are encouraged to
seek and obtain advice from licensed healthcare
professionals responsible for the health and safety of their
programs (e.g. athletic trainer, team physician, school nurse
etc).
References:
1. Casa DJ, Anderson SA, Baker L, et al. The Inter-
Association Task Force for Preventing Sudden Death
in Collegiate Conditioning Sessions. Strength and
Conditioning Journal. 2015;37(6):113–116.
2. Yau RK, Kucera KL, Thomas LC, Price H, Cantu RC.
Catastrophic Sports Injury Research Thirty-Fifth
7
Annual Report: Fall 1982 – Spring 2017. National
Center for Catastrophic Sport Injury Reearch at the
University of North Carolina at Chapel Hill; 2018.
3. Kay MC, Register-Mihalik JK, Gray AD, Djoko A,
Dompier TP, Kerr ZY. The Epidemiology of Severe
Injuries Sustained by National Collegiate Athletic
Association Student-Athletes, 2009–2010 Through
2014–2015. Journal of Athletic Training.
2017;52(2):117-128. doi:10.4085/1062-6050-52.1.01
4. Casa DJ, Guskiewicz KM, Anderson SA, et al.
National athletic trainers’ association position
statement: preventing sudden death in sports. Journal
of Athletic Training. 2012;47(1):96–118.
5. Parsons JT, Anderson SA, Casa DJ, Hainline B.
Preventing catastrophic injury and death in collegiate
athletes: interassociation recommendations endorsed
by 13 medical and sports medicine organisations. Br J
Sports Med. 2020;54(4):208-215.
doi:10.1136/bjsports-2019-101090
6. Casa DJ, Almquist J, Anderson SA, et al. The inter-
association task force for preventing sudden death in
secondary school athletics programs: best-practices
recommendations. Journal of Athletic Training.
2013;48(4):546–553.
7. National Federation of State High School
Associations. 2018-2019 High School Athletics
Participation Survey Results. Published online 2019.
8. Irick E. NCAA Sports Sponsorship and Participation
Rates Report: 1981-82 - 2018-19. National Collegiate
Athletic Association; 2019.
9. Statement on PPE and Athletic Participation:
Ramifications of the COVID-19 Pandemic. Published
online April 2020.
10. Baggish A, Drezner JA, Kim JH, Martinez M, Prutkin
JM. The resurgence of sport in the wake of COVID-
19: cardiac considerations in competitive athletes.
Blog British Journal of Sports Medicine. Published
April 24, 2020. Accessed May 27, 2020.
https://blogs.bmj.com/bjsm/2020/04/24/the-
resurgence-of-sport-in-the-wake-of-covid-19-cardiac-
considerations-in-competitive-athletes/
11. Caterisano A, Decker D, Snyder B, et al. CSCCa and
NSCA Joint Consensus Guidelines for Transition
Periods: Safe Return to Training Following Inactivity.
Strength and Conditioning Journal. 2019;41(3):23.
12. Armstrong LE, Maresh CM. The induction and decay
of heat acclimatisation in trained athletes.
1991;12(5):302–312.
13. Sawka MN, Leon LR, Montain SJ, Sonna LA.
Integrated physiological mechanisms of exercise
performance, adaptation, and maladaptation to heat
stress. Compr Physiol. 2011;1(4):1883-1928.
doi:10.1002/cphy.c100082
14. Pandolf KB. Time course of heat acclimation and its
decay. Int J Sports Med. 1998;19 Suppl 2:S157-160.
doi:10.1055/s-2007-971985
15. McDermott BP, Anderson SA, Armstrong LE, et al.
National Athletic Trainers’ Association Position
Statement: Fluid Replacement for the Physically
Active. J Athl Train. 2017;52(9):877-895.
doi:10.4085/1062-6050-52.9.02
16. Casa DJ, DeMartini JK, Bergeron MF, et al. National
Athletic Trainers’ Association Position Statement:
Exertional Heat Illnesses. Journal of Athletic
Training. 2015;50(9):986–1000.
17. Cooper ER, Ferrara MS, Broglio SP. Exertional heat
illness and environmental conditions during a single
football season in the southeast. Journal of Athletic
Training. 2006;41(3):332–336.
18. Cooper ER, Ferrara MS, Casa DJ, et al. Exertional
Heat Illness in American Football Players: When Is
the Risk Greatest? Journal of Athletic Training.
2016;51(8):593–600.
19. Padua DA, DiStefano LJ, Hewett TE, et al. National
Athletic Trainers’ Association Position Statement:
Prevention of Anterior Cruciate Ligament Injury.
Journal of Athletic Training. 2018;53(1):5-19.
doi:10.4085/1062-6050-99-16
8
Summary Points
• While it is clear that transition periods have a higher risk for catastrophic sport injury,1–3 some of the
factors that place athletes at higher risk during these periods may be amplified as a result of social
distancing measures.
• PPEs may be difficult to coordinate or obtain, and flexibility may be called for, such as a one-year
extension for any student who has a PPEval that "expires" before or during the 2020-21 academic
year.
o Every student-athlete with a prior diagnosis of COVID-19, symptoms suggestive of COVID-19, or a
“close exposure” to someone with COVID-19 should contact their medical provider to determine if
further evaluation is warranted prior to returning to sports.
• Exercise programs will need to be modified upon returning from any period of inactivity of two weeks
or greater. The 50/30/20/10 rule and F.I.T. rule are the best guidelines for achieving this.
• Once physical fitness is established, gradually increase the duration and intensity of exercise in the
heat over a minimum of 7 days to establish heat acclimatization.
• Preventative Training Programs should include three of the following: strength, balance, plyometrics,
agility, and flexibility,19 and be performed at least 2-3 times per week19 and last ~ 10-15 minutes.
9
Additional Resources
1) Pre-Participation Exam:
i) NFHS Statement on PPE and Athletic Participation: Ramifications of the COVID-19 Pandemic
ii) American Academy of Pediatrics Preparticipation Physical Evaluation (PPE)
iii) National Athletic Trainers’ Association Position Statement: Preparticipation Physical
Examinations and Disqualifying Conditions
iv) AMSSM Position Statement on Cardiovascular Preparticipation Screening in Athletes: Current
evidence, knowledge gaps, recommendations and future directions
v) The resurgence of sport in the wake of COVID-19: cardiac considerations in competitive
athletes
2) Exercise Adaptations:
i) CSCCa and NSCA Joint Consensus Guidelines for Transition Periods: Safe Return to Training
Following Inactivity
ii) NSCA Strength and Conditioning Professional Standards and Guidelines
iii) National Athletic Trainers’ Association – Key Facts about Detraining
3) Heat Acclimatization:
i) National Athletic Trainers’ Association: Preseason Heat Acclimatization Guidelines for
Secondary School Athletics
ii) National Athletic Trainers’ Association – Heat Acclimatization
iii) 2013-2014 NCAA Sports Medicine Handbook
iv) KSI: Heat and Hydration
v) National Federation of State High School Associations – Heat Acclimatization and Heat Illness
Prevention Position Statement
vi) GSSI Sport Science Exchange: Hydration Assessment of Athletes
vii) National Athletic Trainers’ Association Position Statement: Fluid Replacement for Athletes
4) Injury Prevention Resources:
i) National Athletic Trainers’ Association Position Statement: Prevention of Anterior Cruciate
Ligament Injury
ii) Stanford Orthopedics Sports Medicine
5) Additional Resources:
i) NFHS Guidance for Opening Up High School Athletics and Activities
ii) USOPC Youth Sport Return to Play Report (Aspen Project Play.org)
iii) Preventing catastrophic injury and death in collegiate athletes: interassociation recommendations
endorsed by 13 medical and sports medicine organizations
iv) The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics
Programs: Best-Practices Recommendations
v) The Inter-Association Task Force for Preventing Sudden Death in Collegiate Conditioning
Sessions: Best Practices Recommendations
vi) Association of Chief Executives for Sport (ACES): Return to Play
vii) NSCA COVID-19 Return to Training – Guidance on Safe Return to Training for Athletes
viii) National Center for Catastrophic Sport Injury Research (NCCSIR)
ix) U.S. Soccer “PLAY ON”
x) World Health Organization. Considerations for sports federations/sports event organizers when
planning recommendations for Mass Gatherings in the
context of COVID-19: interim guidance.
xi) World Health Organization. Guidance for the use of the WHO Mass Gatherings Sports:
addendum: risk assessment tools in the context of COVID-19.
10
Appendix A
COVID-19 Supplemental Questionnaire
1. Have you had any of the following symptoms in the past 2 weeks?
a. Fever
b. Cough
c. Shortness of breath or difficulty breathing
d. Shaking chills
e. Chest pain, pressure, or tightness
f. Fatigue or difficulty with exercise
g. Loss of taste or smell
h. Persistent muscle aches or pains
i. Sore throat
j. Nausea, vomiting, or diarrhea
2. Do you have a family or household member with current or past COVID-19?
3. Do you have moderate to severe asthma, a heart condition, diabetes, pre-existing kidney
disease, or a weakened immune system?
4. Have you been diagnosed or tested positive for COVID-19 infection?
5. If you had COVID-19:
a. During the infection did you suffer from chest pain, pressure, tightness or
heaviness, or experience difficulty breathing or unusual shortness of breath?
b. Since the infection, have you had new chest pain or pressure with exercise, new
shortness of breath with exercise, or decreased exercise tolerance?
11
Appendix B
Examples of Frequently Used High School Football Conditioning Drills (a),
Example Application of 50/30/20/10 Rule (b) and F.I.T. Rule (c)
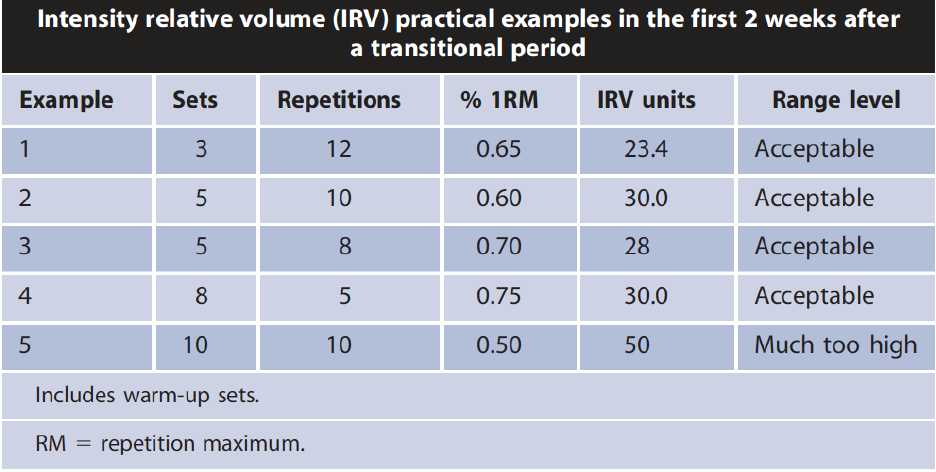
Table 1a. Sampling of High School Football Conditioning Drills
(Collected from personal communication with various high school football strength & conditioning
coaches within Arkansas, Kansas, Louisiana, Mississippi, Oklahoma, Texas)
Drill
Reps
Time in Seconds
(Skill/Power/Linemen)
Rest
110's Drill
16
16/18/21
45
Staggered 110/100/90 Drill
16
16
45
Half Gasser Drill (Over & Back)
14
17/18/21
45
300 yd. Shuttles (25 yds.)
3
65/70/75
2:30
300 yd. Shuttles (50 yds.)
3
59/66/70
2:30
300 yd. Shuttles
(50&Back/40&Back/30&Back/20&Back
/10&Back
3
62/68/73
2:30
50 (25&Back)/40 (20&Back)/30
(15&Back) Drill
20
8/7/6
35/30/25
Table 1b. Example of the Application of 50/30/20/10 to the 110 Drill
New Athletes - 110 Drill
Reduction
Reps
Time
Rest
Week 1 - 50%
50% = 8
16/18/20
64/72/80
Week 2 - 30%
30% = 11
16/18/20
48/54/60
Week 3 - 20%
20% = 13
16/18/20
45
Week 4 - 10%
10% = 14
16/18/20
45
12
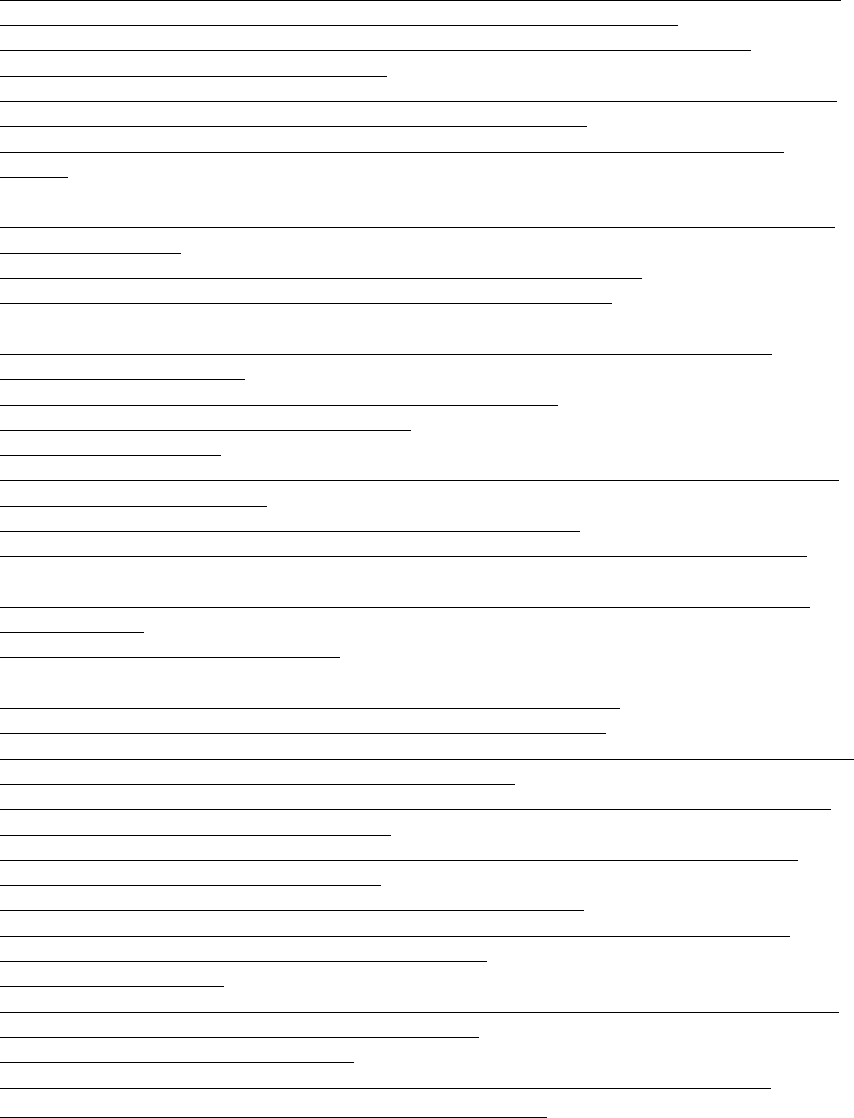
Table 1c. Example Application of the F.I.T. Rule
Reprinted with permission from: Caterisano A, Decker D, Snyder B, et al. CSCCa and NSCA Joint
Consensus Guidelines for Transition Periods: Safe Return to Training Following Inactivity. Strength and
Conditioning Journal. 2019;41(3):23.
13
Appendix C
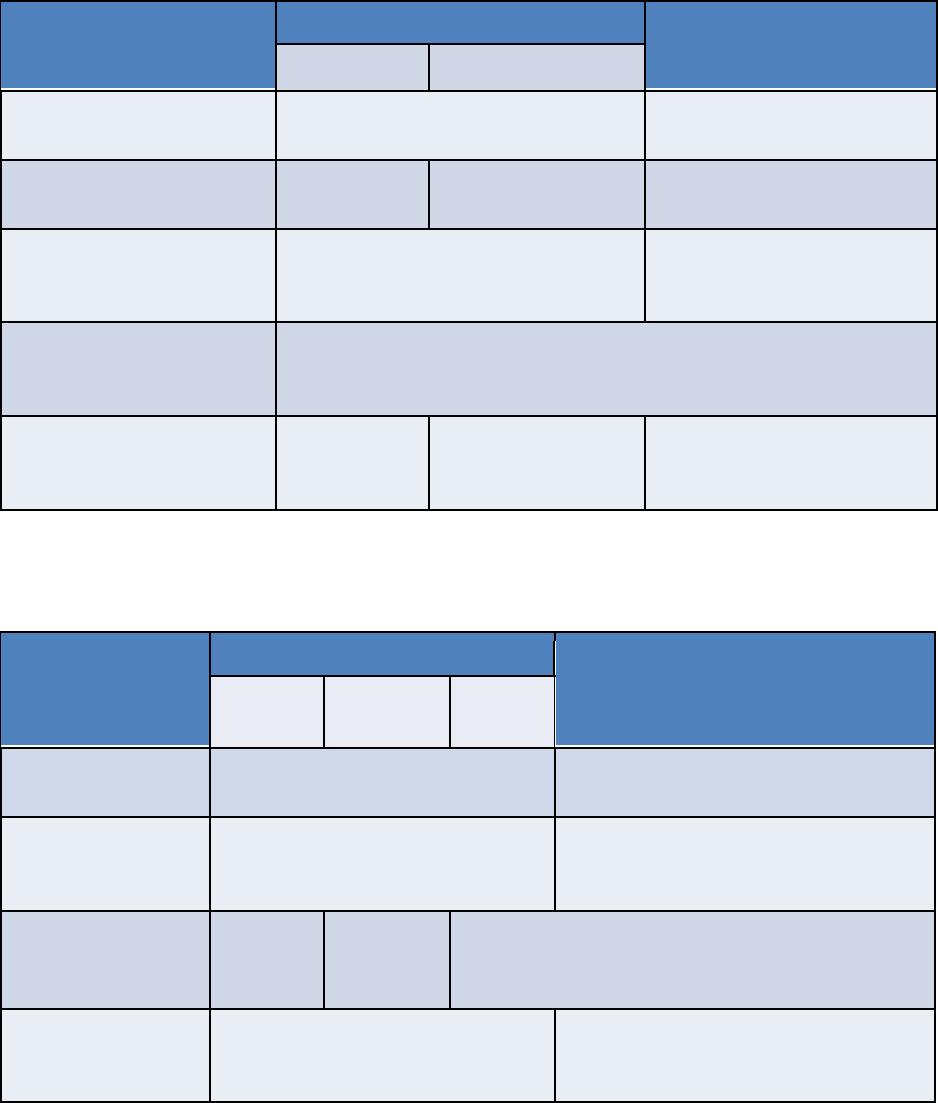
High School (a) and NCAA (b) Preseason Heat Acclimatization Guidelines
Table 2a. High School Preseason Heat Acclimatization Guidelines
Area of Practice
Modification
Practices 1-5
Practices 6-14
Practices 1-2
Practices 3-5
# of Practices Permitted Per
Day
1
2, only every other day
Equipment
Helmets only
Helmets & Shoulder
Pads
Full Equipment
Maximum Duration of
Single Practice Session
3 hours
3 hours (a total maximum of
5 hours on double session
days)
Permitted Walk Through
Time (not included as
practice time)
1 hour (but must be separated from practice for 3 continuous hours)
Contact
No Contact
Contact only with
blocking
sleds/dummies
Full, 100% live contact drills
NOTE: warm-up, stretching, cool-down, conditioning, and weight-room activities are Included as part of
practice time
Table 2b. NCAA Football Preseason Heat Acclimatization Guidelines
Area of Practice
Modification
Practices 1-5
Practices 6+
Practices
1-2
Practices
3-4
Practice
5
# of Practices
Permitted Per Day
1
>1, if not consecutive days with
multiple practices
Maximum Duration
of Single Practice
Session
3 hours
3 hours on days with 1 practice
Equipment*
Helmets
only
Helmets &
Shoulder
Pads
Full Pads
Full Equipment
Double Practice
Days
None
No more than 5 total hours of on-field
practice permitted - with at least 3
continuous hours between practices
