
COVID-19 OPERATIONS MANUAL
H1.V56.L1.20210729
3
TABLE OF CONTENTS
OPERATIONAL GUIDANCE
INTRODUCTION ...................................................................................................................................................... 6
1.1. CHANGE LOG (ABRIDGED) .............................................................................................................. 6
2. SAFETY .............................................................................................................................................................. 8
2.1. DUTY OF CARE ..................................................................................................................................... 8
2.2. FULLY-VACCINATED GREYSHIRT POLICY ................................................................................. 8
2.3. RECEIVING AN ON-SITE VACCINE POLICY ............................................................................... 9
2.4. MAINTENANCE OF HYGIENE ...................................................................................................... 10
2.5. POST-OPERATION DECONTAMINATION ............................................................................... 10
2.6. TR COVID-19 EXPOSURE POLICY .............................................................................................. 10
2.7. TR MINIMUM PPE REQUIREMENTS .......................................................................................... 16
3. OUTFITTING ................................................................................................................................................. 17
3.1. BILLETING ............................................................................................................................................ 17
TRANSPORTATION .................................................................................................................................... 27
3.3. AIR TRAVEL ......................................................................................................................................... 29
3.4. PERSONNEL ........................................................................................................................................ 23
3.5. INFORMATION .................................................................................................................................. 25
4. ADMINISTRATION ..................................................................................................................................... 25
4.1. DOCUMENTATION .......................................................................................................................... 25
5. ORGANIZATIONAL SUPPORT................................................................................................................ 25
5.1. MOBILIZATION .................................................................................................................................. 26
APPENDIX A: GLOSSARY................................................................................................................................... 28
APPENDIX B: COVID-19 STRATEGIC TOOLKIT ........................................................................................ 32
APPENDIX C: HYGIENE GUIDE ....................................................................................................................... 35
APPENDIX D: TRAVEL GUIDE .......................................................................................................................... 40
APPENDIX E: CORE OPS COVID-19 SAFETY PROTOCOLS .................................................................. 43
APPENDIX F: JOB AIDS ...................................................................................................................................... 46
APPENDIX G: FORMS AND LETTERS ............................................................................................................ 73
APPENDIX H: ACTIVITY RISK AWARENESS ............................................................................................... 80
APPENDIX I: RISK CATEGORIES ..................................................................................................................... 81
APPENDIX J: EVALUATION PLAN .................................................................................................................. 85
APPENDIX K: BACKGROUND AND DESIGN ELEMENTS ...................................................................... 86
4
DEMAND ............................................................................................................................................................. 86
IMPACT ................................................................................................................................................................ 86
COMMANDER’S INTENT............................................................................................................................... 86
ASSUMPTIONS.................................................................................................................................................. 87
SCOPE .................................................................................................................................................................. 87
APPENDICES
APPENDIX A: GLOSSARY................................................................................................................................... 28
APPENDIX B: COVID-19 STRATEGIC TOOLKIT ........................................................................................ 32
APPENDIX C: HYGIENE GUIDE ....................................................................................................................... 35
APPENDIX D: TRAVEL GUIDE .......................................................................................................................... 40
APPENDIX E: CORE OPS COVID-19 SAFETY PROTOCOLS .................................................................. 43
APPENDIX F: JOB AIDS ...................................................................................................................................... 46
APPENDIX G: FORMS AND LETTERS ............................................................................................................ 73
APPENDIX H: ACTIVITY RISK AWARENESS ............................................................................................... 80
APPENDIX I: RISK CATEGORIES ..................................................................................................................... 81
APPENDIX J: EVALUATION PLAN .................................................................................................................. 85
APPENDIX K: BACKGROUND AND DESIGN ELEMENTS ...................................................................... 86
DEMAND ............................................................................................................................................................. 86
IMPACT ................................................................................................................................................................ 86
COMMANDER’S INTENT............................................................................................................................... 86
ASSUMPTIONS.................................................................................................................................................. 87
SCOPE .................................................................................................................................................................. 87
FIGURES
FIGURE 1. EXPOSURE PROTOCOL PROCESS ............................................................................................ 12
FIGURE 2. DAILY HYGIENE SAFETY BRIEFING ......................................................................................... 47
FIGURE 3. SYMPTOMS OF COVID-19 .......................................................................................................... 48
FIGURE 4. STOP THE SPREAD OF GERMS .................................................................................................. 49
FIGURE 5. VEHICLE AND EQUIPMENT DECONTAMINATION GUIDE ............................................ 52
FIGURE 6. DISINFECTING HIGH-TOUCH SURFACES ............................................................................. 53
FIGURE 7. MIX AND USE OF DISINFECTING DILUTED BLEACH SOLUTION ................................ 54
FIGURE 8. ALTERNATIVE PPE TABLE ........................................................................................................... 56
FIGURE 9. SEQUENCE FOR PUTTING ON PPE.......................................................................................... 57
FIGURE 10. HOW TO SAFELY REMOVE PPE ............................................................................................. 58
5
FIGURE 11. PPE TRAINED OBSERVER CHECKLIST ................................................................................. 61
FIGURE 12. USE AND REUSE OF N95 RESPIRATOR MASKS AND FACE SHIELDS ...................... 62
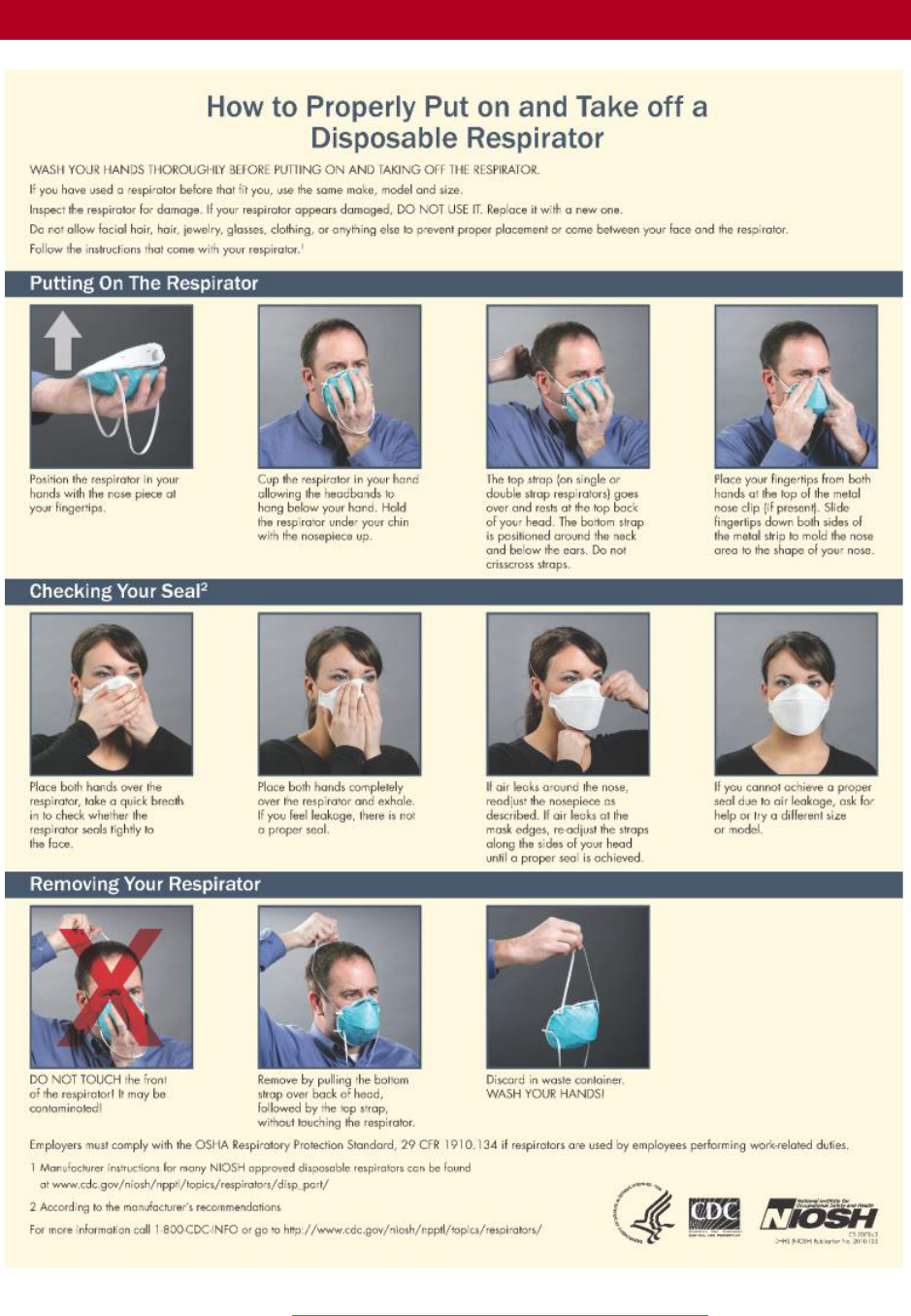
FIGURE 13. HOW TO PUT ON AND TAKE OFF A DISPOSABLE RESPIRATOR ............................. 63
FIGURE 14. N95 RESPIRATORS WITH VALVES/WITHOUT VALVES ................................................ 64
FIGURE 15. TEMPERATURE CHECK OPTIONS ......................................................................................... 68
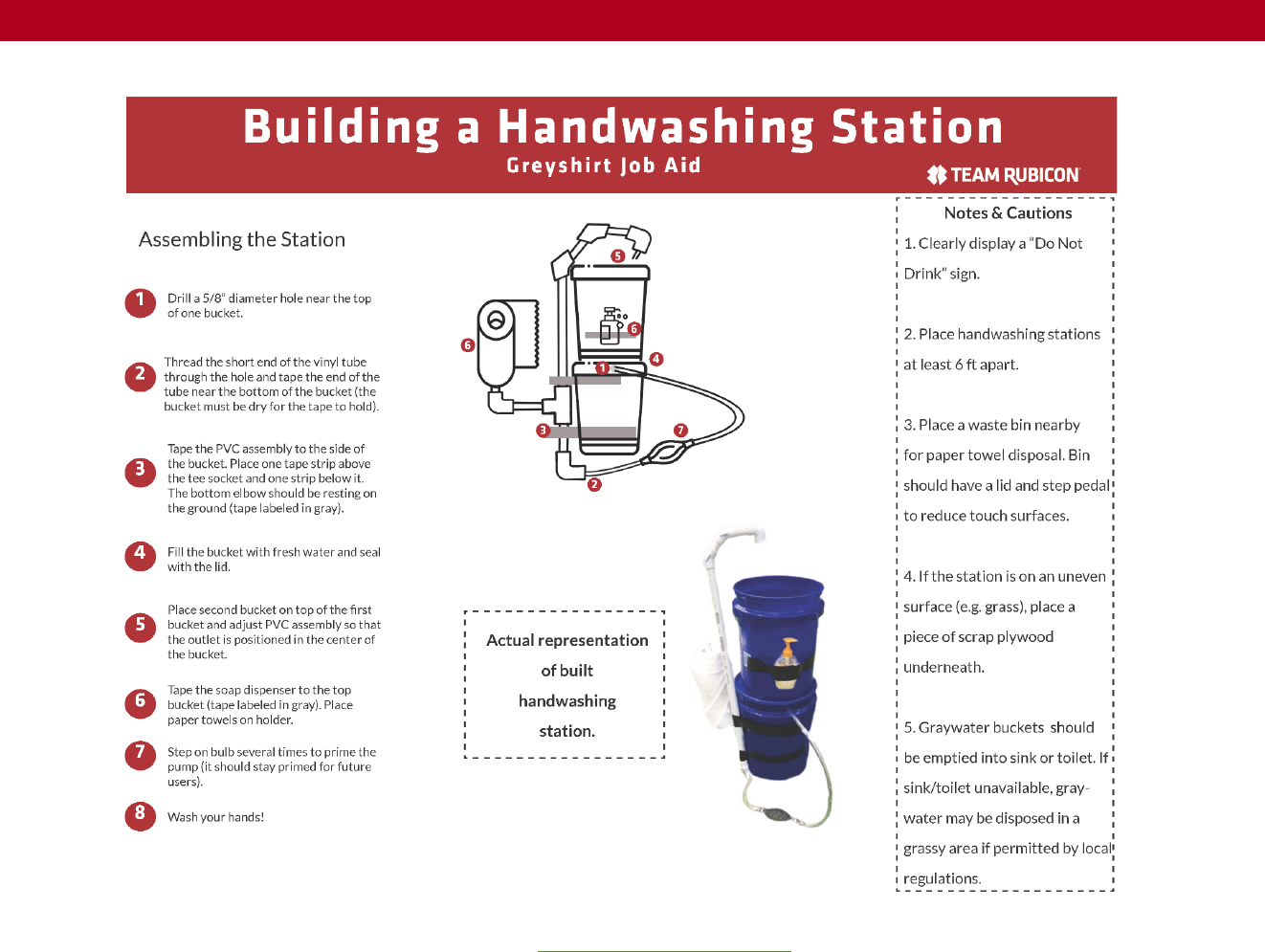
FIGURE 16. BUILDING A HANDWASHING STATION ............................................................................. 70
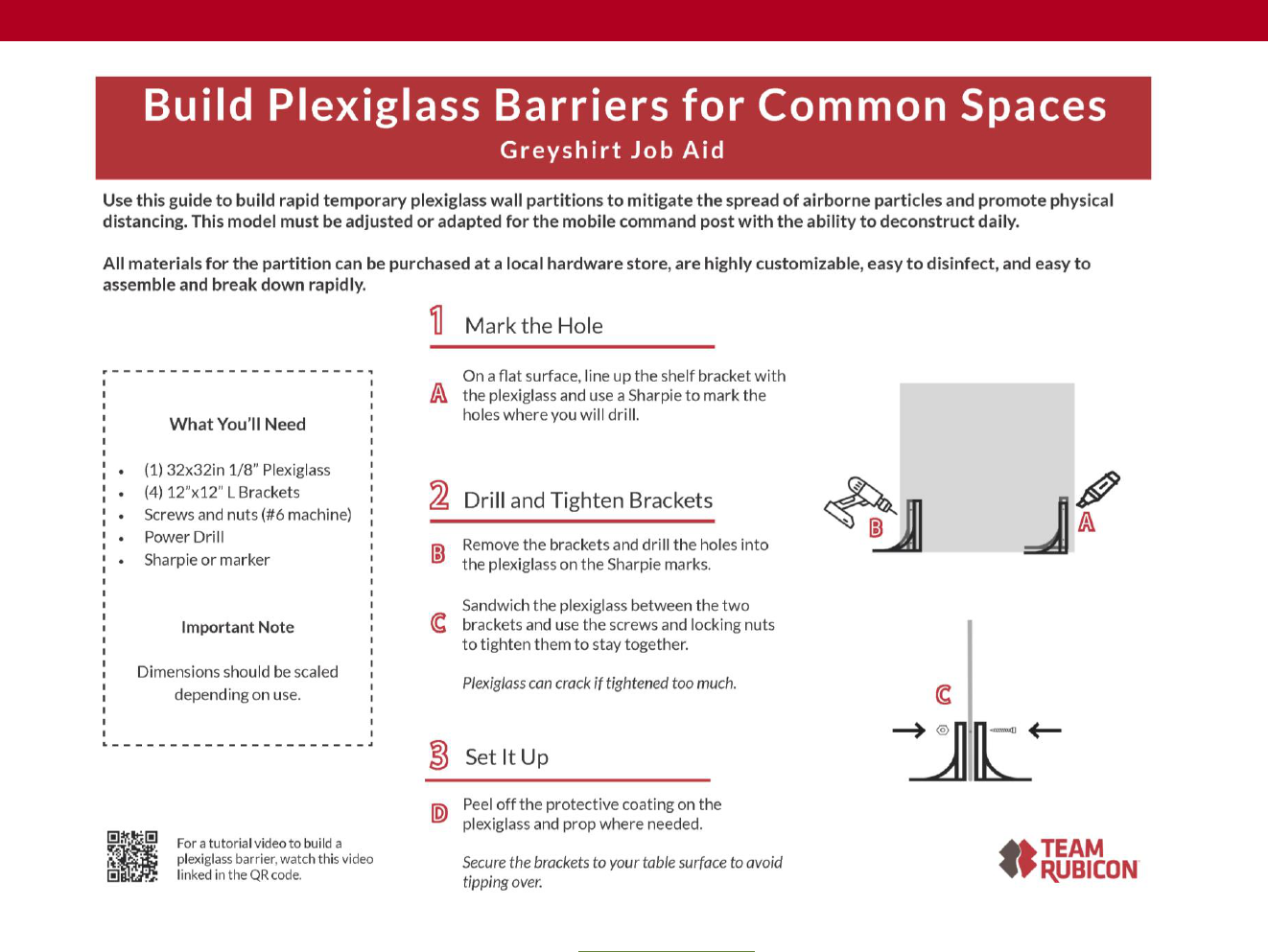
FIGURE 17. BUILD PHYSICAL BARRIERS ..................................................................................................... 72
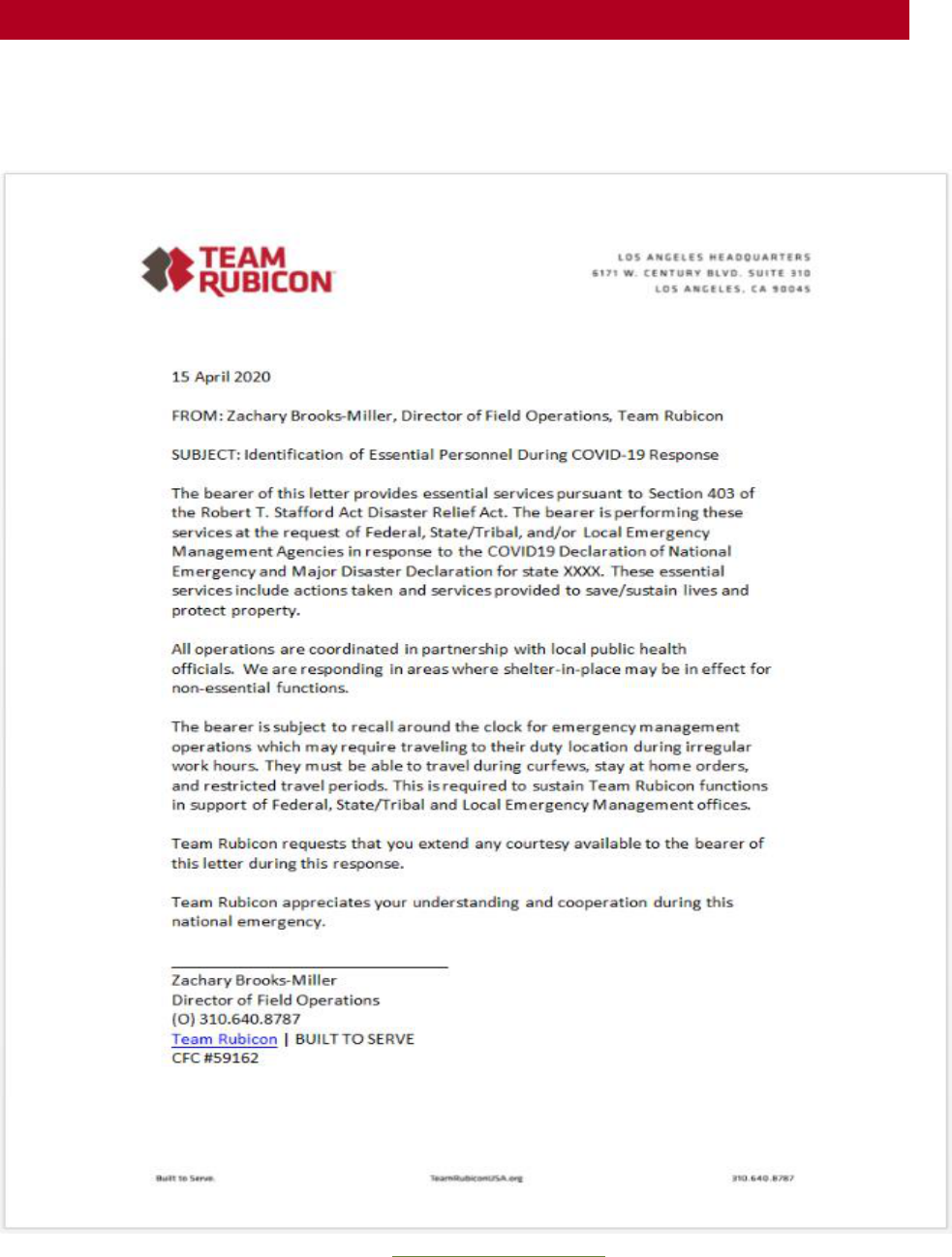
FIGURE 18. JURISDICTIONAL TRAVEL LETTER ........................................................................................ 73
FIGURE 19. ACKNOWLEDGEMENT OF POLICY FORM......................................................................... 74
FIGURE 20. SPONTANEOUS VOLUNTEER COVID-19 MOU ................................................................ 75
FIGURE 21. PII SECURITY AND CONFIDENTIALITY POLICY FORM ................................................. 79
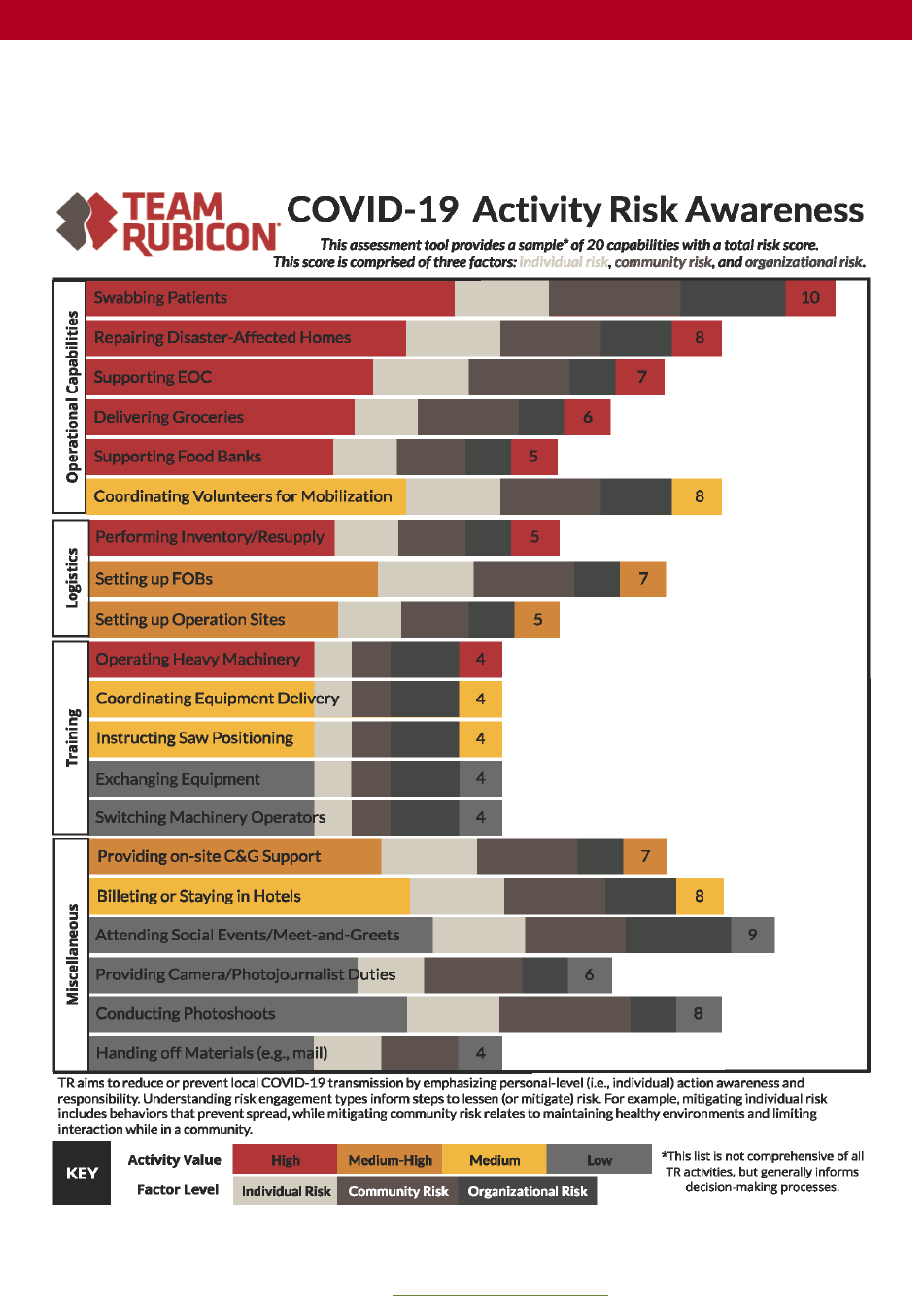
FIGURE 22. COVID-19 RISK AWARENESS .................................................................................................. 80
FIGURE 22. OPERATIONS EVALUATION PLAN ........................................................................................ 85
6
INTRODUCTION
This document serves as the overarching guidance for all activities, tools, training, and
communications to be followed by TR staff and Greyshirts during all in-person operations and
events.
This document includes a comprehensive collection of best practices for operational activities
and specific guidelines for effective coordination with government agencies and partner
organizations. The appendices include supplemental information, checklists, and one-page flyers.
Greyshirts should also complete the applicable COVID FLASH LEARNINGS. These can be found
where an online learning icon is shown:
Job aids are available in printable size and resolution by clicking on the green link in the caption
(See green link example below):
Figure 1. Symptoms of COVID-19
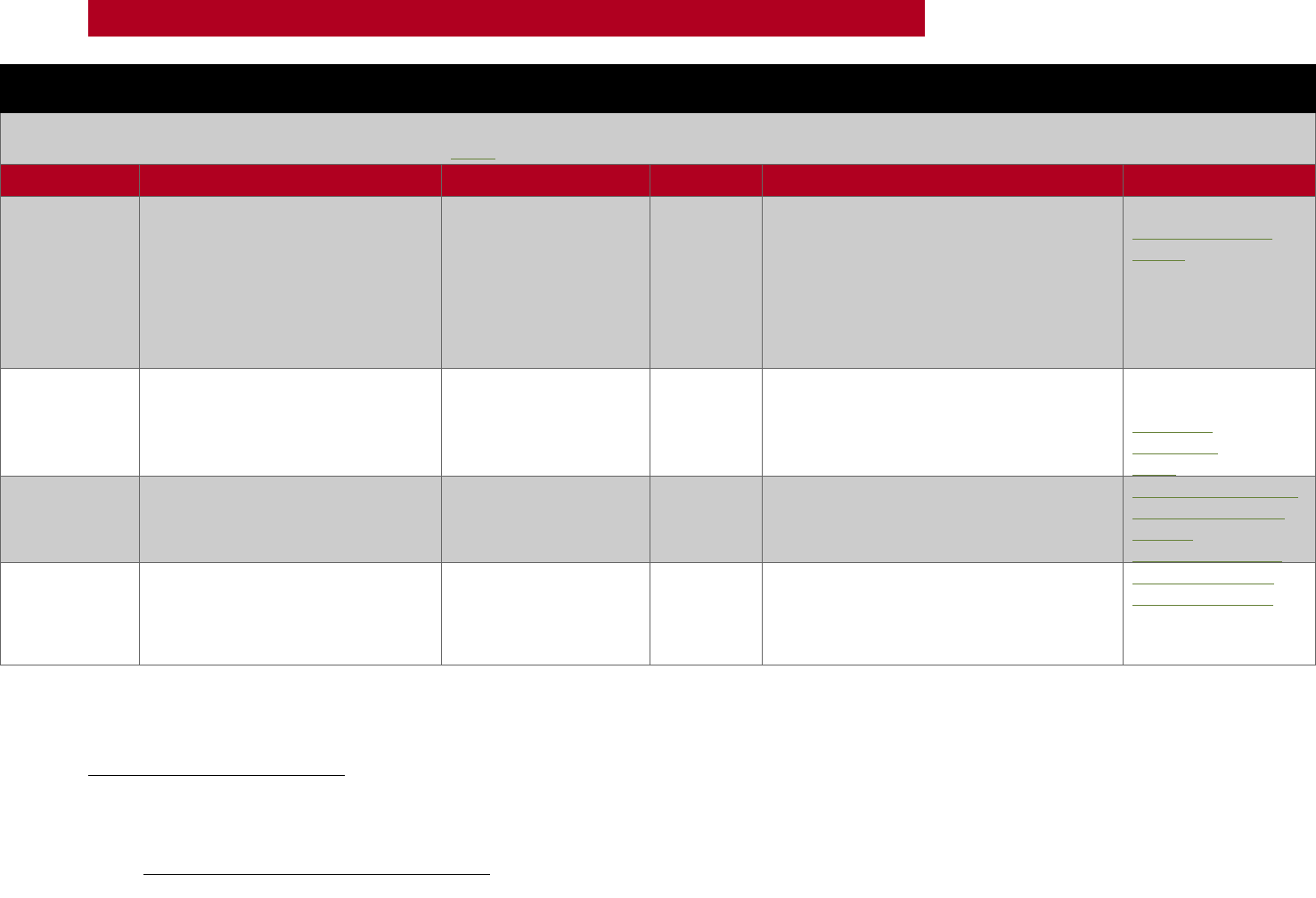
1.1. CHANGE LOG (ABRIDGED)
This log contains entries from past iterations of this document.
Section
Page
Description
Reviser
Revision Date
2.6.2
12
Add deployment
restriction for GSs
exhibiting symptoms to
Pre-Op Monitoring
Melissa Stone
07/27/21
2.7
17
Update to minimum PPE
requirements (masking
indoors/outdoors)
Melissa Stone
07/27/21
3.1.1
18
Update to billeting policy
(spacing between cots,
maximize
outdoor/virtual
interactions, disinfect
cots after use, limit
sharing)
Melissa Stone
07/27/21
3.1.1
19
Update to CPAP policy
(can deploy if op
supports a single-use
room)
Melissa Stone
07/27/21
3.1.1
20
Update to hotel stay
policy (single-occupancy
rooms when necessary;
removed extraneous
information)
Melissa Stone
7/27/21
Appendix G
74
Replaced PII form with
updated version
Kathleen Anaza
07/27/21

7
COVID-19
OPERATIONS MANUAL
OPERATIONAL GUIDANCE

8
OPERATIONAL GUIDANCE
2. SAFETY
2.1. DUTY OF CARE
Team Rubicon assesses risk throughout the Mission Planning process and during all operational
periods to ensure the health, wellbeing, and security of all Greyshirts, personnel, and community
members are prioritized. Greyshirts in the field represent Team Rubicon and are held to a high
standard for protecting vulnerable communities served. Therefore, all interactions within
communities will continue to adhere to mitigation strategies for COVID-19-related risks.
2.2. FULLY-VACCINATED GREYSHIRT POLICY
Team Rubicon aims to increase response capacity in the field and reduce the risk presented to
families in vulnerable communities served. As such, all Greyshirts and external/corporate
volunteers are required to be fully-vaccinated to participate in any in-person activities and will
adhere to all related guidance herein.
An individual is considered fully-vaccinated, when the following conditions are met:
• Two weeks have passed after completing the second dose of a two-dose COVID-19
vaccine (e.g., Pfizer or Moderna), OR two weeks have passed after receiving a single dose
of a one-dose vaccine (e.g., Johnson & Johnson/Janssen), AND
• Greyshirt acknowledges vaccination status at the time of activity registration and attests
to their vaccination status on their Roll Call profile.
Fully-vaccinated Greyshirts (18 years and older):
• Are required to be fully-vaccinated in order to participate in any in-person activities
hosted by Team Rubicon.
• May attend in-person activities that were previously closed, including but not limited to:
training events, leadership meetings, service projects, operational and partnership
meetings, and socials.
Registering for In-Person Activities:
All Greyshirts will be prompted to verify vaccination status during activity registration as well as
attest to their vaccination status on their personal profile in Roll Call.
Unvaccinated Greyshirts or Greyshirts with unverified vaccination status:
Greyshirts who are unable to verify vaccination status may still participate in many virtual events
and activities listed in Roll Call and can continue to make a difference in communities in virtual
and remote capacities.
De-Conflicting Policies:
In cases where local, state, or territory regulations conflict with any rules or regulations stated in
this COVID-19 Operations Manual, Team Rubicon staff and Greyshirts will always abide by

9
OPERATIONAL GUIDANCE
regulations led by local, state, or territory initiatives when they are more conservative than our
own.
2.3. RECEIVING AN ON-SITE VACCINE POLICY
2.3.1. Policy Principles:
• Mission First: Our clients and communities come first, and no action should be taken that
jeopardizes or could be perceived to jeopardize those individuals.
• Greyshirts Always: We believe that Greyshirts volunteering themselves to be on the
frontlines of the COVID-19 pandemic should qualify as a high-priority group for
vaccination to maximize impact in communities across the country.
• Your Mother’s A Donor: This principle extends to our organizational partners as well as
Team Rubicon. Waste and inefficiency should be minimized. In this case, the challenging
logistics of vaccine delivery may result in daily surpluses. If there are vaccines that will
expire and Greyshirts in need of the vaccine, Team Rubicon can acquire the vaccine if the
supporting organization deems Greyshirts eligible and in accordance with all tracking,
reporting and follow up requirements.
Team Rubicon has positioned Greyshirts across the country to provide critically needed frontline
support to local jurisdictions’ COVID-19 vaccination efforts. If the type of work Greyshirts are
providing qualifies Greyshirts for COVID-19 vaccination within the jurisdiction's qualification
criteria, Greyshirts are encouraged to be vaccinated. Wherever possible, Team Rubicon mission
planning teams will inquire about jurisdictions’ vaccination qualification criteria to determine if
Greyshirts qualify as prioritized frontline workers.
Greyshirts should not sign up for vaccination operations with an expectation that they will be
vaccinated.
If the opportunity arises and volunteers can receive a vaccination for the reasons listed above,
Greyshirts should use discretion when publicizing their vaccination. Misperceptions or
misrepresented images about how the vaccinations were obtained could challenge the validity of
vaccine distribution, putting future operations in jeopardy and questioning TR’s integrity in the
process.
Note that Greyshirts who have been vaccinated may be approached to share their experience when
the vaccination is available to the general population.
Team Rubicon supports the recommendations from the CDC’s Advisory Committee on
Immunization Practices regarding the prioritization of access to the COVID-19 vaccine. Team
Rubicon also recognizes that the decision of prioritization is determined at the local level.
2.3.2. Post-Vaccination Deployments
If a Greyshirt has been vaccinated on site, (s)he may not deploy to another operation within 72
hours of receiving a vaccine as they could exhibit signs and symptoms that mimic COVID
infection like fever, body aches, or fatigue that may interfere with site operation. If a Greyshirt is
10
OPERATIONAL GUIDANCE
vaccinated on site and exhibits symptoms, (s)he will be asked to forego participation and begin
isolation, with a few exceptions:
• If an operation site has a more stringent policy, site policy will take precedence and TR
policy will be suspended.
• If symptoms do not align to those expected post vaccinations, Greyshirts will be treated
accordingly to the rest of the COVID symptom policy within this manual.
• TR will not be expected to enforce or monitor quality control of on site vaccination
policy.
2.4. MAINTENANCE OF HYGIENE
To mitigate infection and spread and continue hygienic standards, Greyshirts are expected to
practice proper hygiene during and while in transit to an operation. See APPENDIX C: HYGIENE
GUIDE for expectations.
2.5. POST-OPERATION DECONTAMINATION
At the end of operations and/or operational periods, Greyshirts will decontaminate personal and
operational gear in accordance with TR protocol. Instructions for this are provided in APPENDIX
F: JOB AIDS. Additionally, TR may suggest Greyshirts take
measures after deployment to prevent community spread, such as
physical isolation or self-quarantine. Greyshirts returning to homes
shared with other unvaccinated members should follow guidance
from the CDC’s Information for Healthcare Professionals about
Coronavirus (COVID-19)4F
1
, immediately disrobe outside (backyard,
garage, etc.), and wash clothes in hot water on high heat to
minimize the chance of spreading COVID-19.
2.6. TR COVID-19 EXPOSURE POLICY
Any member of the TR team experiencing signs and symptoms associated with COVID-19
should immediately contact a healthcare provider and reduce
contact with others. While on, or immediately following an
operation or event, Greyshirts and staff must also inform their
designated supervisor. All Greyshirts should be prepared to self-
quarantine for 14 days following any TR event. TR may recommend
this self-quarantine be enacted pursuant to the conditions outlined
in this Exposure Policy. Greyshirts deployed on an operation will
strictly adhere to the protocols outlined in the Exposure Policy.
1
Centers for Disease Control and Prevention (2020, August 25). Information for Healthcare Professionals about
Coronavirus (COVID-19). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html
MAINTENANCE
OF HYGIENE
POST-OPERATION
DECONTAMINATION
PROTOCOL
11
OPERATIONAL GUIDANCE
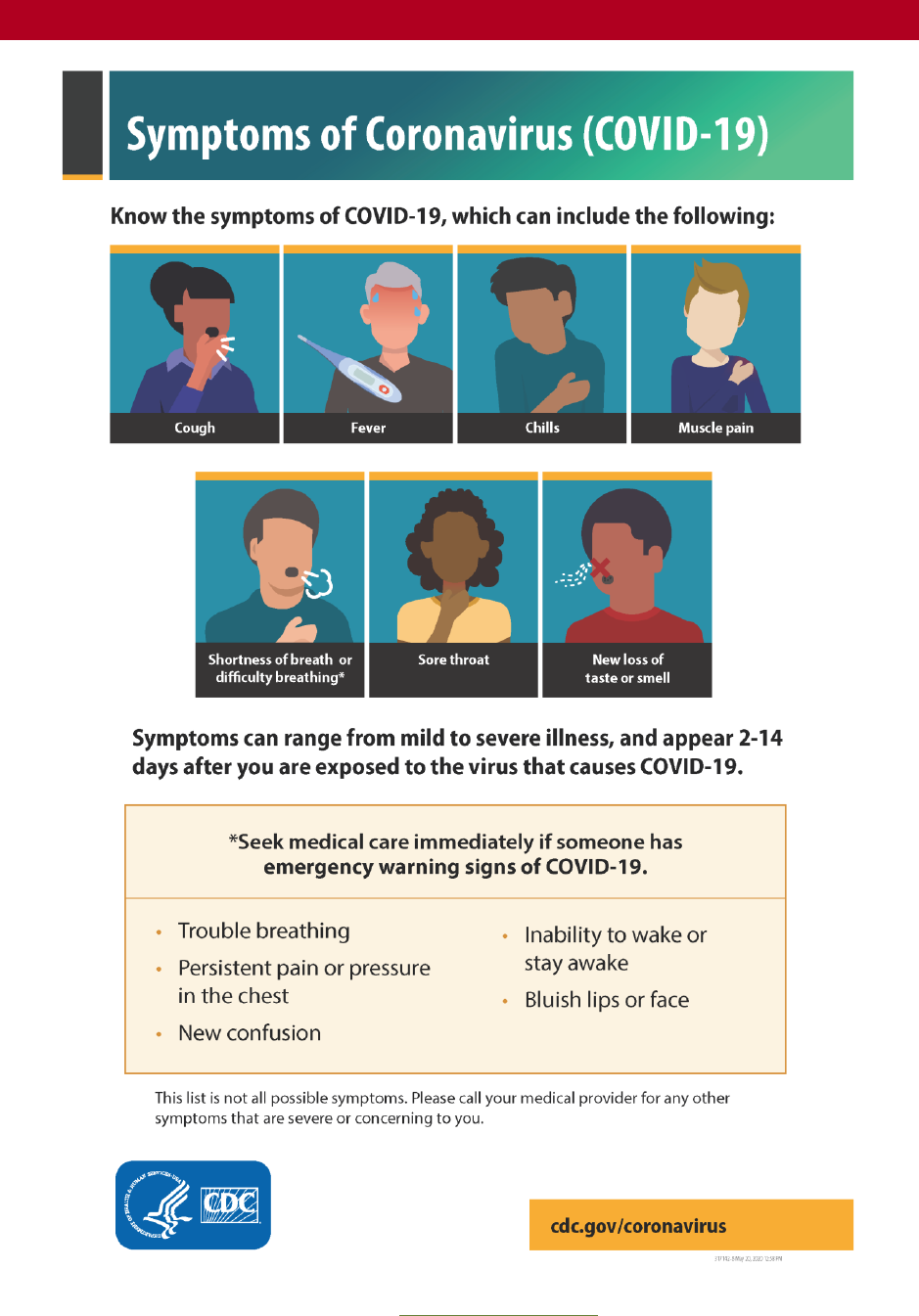
2.6.1. Signs and Symptoms
COVID-19 symptoms include
2
, but are not limited to cough,
shortness of breath, or difficulty breathing. Symptoms may also
include at least two of the following:
• Fever
• Chills
• Muscle or body aches
• Fatigue
• Headache
• Sore throat
• New loss of taste or smell
• Congestion or runny nose
• Nausea or vomiting
• Diarrhea
Symptoms appear 2–14 days after exposure to the virus. Refer to the CDC for further guidance
2
. See Appendix B: Job Aids for CDC Symptoms of COVID-19.
2.6.2. Pre-Operation Check-In and Monitoring During Operations
When a Greyshirt receives their dispatch instructions, they will acknowledge risk through
informed consent (waiver through the availability and mobilization process) to self and possible
post-event exposure to household members. Greyshirts will not deploy, but will isolate and get
tested, if exhibiting any symptoms of COVID-19 (see Section 2.6.1 Signs & Symptoms).
All traveling GSs will refer to local channels as well as TR’s COVID-19 High-Output Decision
Indicators Dashboard to confirm they are not traveling from a county with high disease burden.
Indicators of low disease burden include:
• Weekly decline in daily deaths
• Rolling 7-day average daily cases staying below 50,000
2
Centers for Disease Control and Prevention (2020, May 13). Symptoms of Coronavirus. Retrieved from
https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
SIGNS AND SYMPTOMS
EXPOSURE PROTOCOLS
12
OPERATIONAL GUIDANCE
• Daily average deaths below 1000
• ICU Hospitalizations remains below 10,000 daily.
Strike Team Leaders will assess the needs of all team members throughout the day and monitor
intermittently for signs of COVID-19 symptoms. Command and General (C&G) Staff will pair up
to monitor and check in with teams as needed.
If symptoms are exhibited by any Greyshirt or personnel on site, Team Leaders will document
the date and details related to the case, as well as any details related to time of potential onset.
Greyshirts exhibiting symptoms of COVID-19 will not be permitted to take commercial
transportation (including commercial air travel) until cleared through local health department
policy.
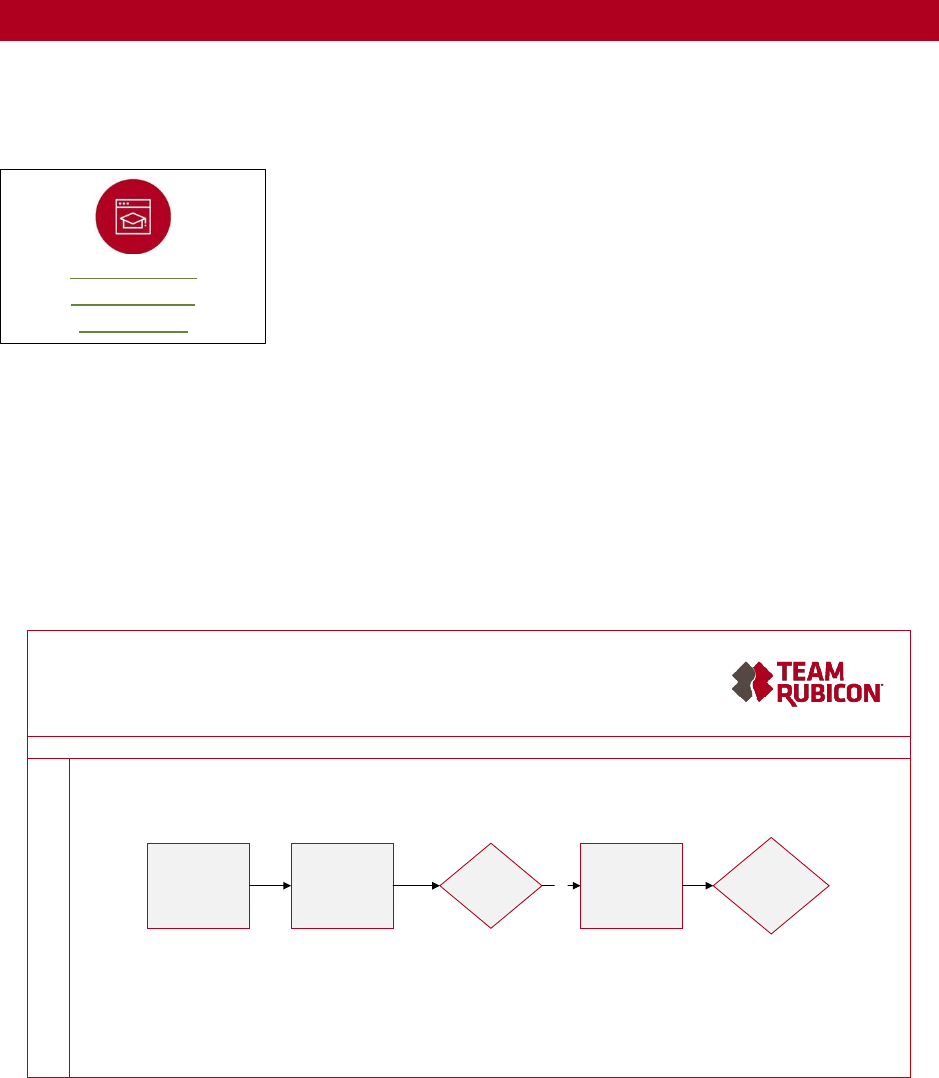
Figure 1. Exposure Protocol Process
2.6.3. (X-1) Protocol for Signs of Illness
If a Greyshirt develops COVID-19 symptoms during an operation, their designated field leader
will immediately give the individual a surgical mask and direct them to perform hand hygiene.
The individual will isolate and maintain physical distancing protocols. The workspace of the
affected person will be decontaminated.
Exposure ProtocolExposure Protocol
Last Update: 20200420 Last Update: 20200420
X-1
Protocol for signs of
illness
X-2
Medical assessment
& demobilization
X-3
GS tests positive
Yes
X-4
Exposure notification
X-5
Site decon & Demob
decision
DAILY HEALTH
MONITORING
PROTOCOLS

13
OPERATIONAL GUIDANCE
The designated field leader will notify the Safety Officer about the symptomatic individual. The
Safety Officer will notify and provide details to the IC.
The designated field leader will also notify Greyshirts who worked alongside the symptomatic
Greyshirt of possible risk. Should other Greyshirts wish to demobilize as a precaution, designated
field leaders will accommodate their requests. Meanwhile, designated field leaders will continue
to enforce strict symptom checks and hygiene measures at the work site.
The IC will submit the Incident Report, prompting the IMT and the Greyshirt Support Team to
complete the COVID-19 Incident Form and follow standard Incident Report procedure.
2.6.4. (X-2) Medical Assessment & Demobilization
The Greyshirt Support Team will contact the Safety Officer, who will consult the 206 to identify
local testing facilities and phone numbers. The Safety Officer will direct the Greyshirt Support
Team and the individual showing symptoms to the appropriate local resources for COVID-19
screening and/or testing.
Greyshirt Tests Negative:
The IMT, in consultation with the Greyshirt Support Team, will direct the IC to send the
Greyshirt home. While waiting to depart, the Greyshirt will remain isolated and standard
syndrome precautions will be implemented (e.g., physical distancing, hand hygiene, surgical
mask). If the Greyshirt drove to the operation, they will return to their Home of Record (HOR)
and notify a primary care provider. If the Greyshirt took commercial transportation or carpooled,
the IC will consult with the National Operations Center (NOC) and IMT who will coordinate and
seek guidance from public health officials as necessary. The IMT will keep the Greyshirt Support
Team informed.
Healthcare assessment determined additional in-person testing requested/required for Greyshirt:
The Greyshirt will remain isolated and standard syndrome precautions will be implemented (e.g.,
physical distancing, hand hygiene, surgical mask). The Greyshirt Support Team will notify NOC,
TR Med, IMT, and IC. Greyshirt will be transported to the testing site.
• If Greyshirt is able to drive and has a vehicle, the Greyshirt showing symptoms will drive
his/her own vehicle to the hospital while being followed by a Greyshirt in a separate car
to ensure safe arrival at the testing site.
• If Greyshirt is unable to drive due to symptoms, 911 will be called. The 911 operator
should be notified the individual is showing symptoms of COVID-19.
• Greyshirt will receive treatment per hospital/protocol.
2.6.5. (X-3) Greyshirt Tests Positive
Testing facility confirms positive COVID-19 in Greyshirt:
The Greyshirt will conform to all medical advice and notify Greyshirt Support Team of a positive
test result. The Greyshirt will remain hospitalized or under treatment per public health protocol
or will be sent home to self-isolate and monitor symptoms. The IMT, in consultation with the
Greyshirt Support Team, will instruct the Greyshirt to demobilize and isolate, and the Greyshirt

14
OPERATIONAL GUIDANCE
will comply. TR will coordinate transportation home as appropriate via commercial or personal
transport at hospital release.
If a Greyshirt is told to return home and isolate but refuses to comply due to concern of infecting
family, the Greyshirt Support Team, IMT, and NOC, in consultation with public health officials,
will determine a safe and secure place for Greyshirt to isolate, as well as the duration and
conditions upon which the Greyshirt can safely exit isolation. In cases where a local
care/isolation site is not available, the Greyshirt Support Team, IMT, and NOC will coordinate to
secure a hotel for the Greyshirt for the duration of their isolation.
2.6.6. (X-4) Exposure Notification
TR actions if COVID-19 confirmed positive and the operation is still ongoing:
The Greyshirt Support Team will contact IMT and Mobilization. The IMT will notify deployed
Greyshirts of potential COVID-19 exposure. Mobilization will notify Greyshirts dispatched to the
operation. Local authorities will be responsible for contact tracing and TR will provide any
requested information to this end. If the Greyshirt is tested outside of the county of operation,
the Greyshirt Support Team will notify public health authorities in the county of operation. If any
other Greyshirts develop symptoms, the above protocol should be followed for everyone
showing signs of illness.
TR actions if COVID-19 confirmed positive and the operation is already demobilized:
If a Greyshirt is confirmed positive after an operation has been demobilized, but had symptoms
during the operation, s/he will notify the Greyshirt Support Team at
greyshirts[email protected]. Greyshirts will also receive an e-mail from Mobilization
confirming safe arrival home and notifying that Greyshirts can report a positive COVID-19 test
by responding to the message. The Greyshirt Support Team will notify impacted locations’ public
health authorities and Mobilization, who will notify Greyshirts who were deployed on the
operation of potential exposure.
Direct exposure to COVID-19:
The following procedures apply if a Greyshirt comes into direct contact with an individual either
suspected or confirmed to have COVID-19, who was not wearing a cloth face covering or
facemask and were exposed to respiratory droplets or airborne particles without the proper use
of PPE.
Upon identification of direct exposure, the following notification actions will occur
immediately:
• Greyshirts involved in or who witnessed the exposure will notify the designated field
leader.
• The designated field leader will report the exposure event to the Safety Officer.
• The Safety Officer:
• Will investigate the exposure and determine if other Greyshirts were affected.
• Will notify the IC, who submits the Incident Report.
15
OPERATIONAL GUIDANCE
• The IMT will coordinate with the Greyshirt Support Team and the TR Medical Team to
recommend immediate quarantine of the affected Greyshirt and determine the course of
demobilization.
As soon as possible, TR will coordinate plans for transporting the exposed Greyshirt home. The
Greyshirt will immediately report any COVID-19 symptoms or change in health status.
Transportation Modality
Primary Method:
If within an 8-hour drive of HOR, Greyshirt is immediately demobilized via
Privately Owned Vehicle (POV).
Alternate Method:
If within an 8-hour drive of HOR, Greyshirt is immediately demobilized via
TR-provided rental vehicle.
Contingency Method:
Greyshirt is demobilized via commercial air.
Demobilization by commercial air requires the Greyshirt to:
• Target departure within 24 hours of exposure and reach HOR before 48
hours after exposure
• Be asymptomatic
• Undergo a temperature check by the TR Medical Team immediately prior
to departing the operation and produce a temperature of less than 100.0
orally
• Practice Universal Source Control in accordance with CDC guidance6F
3
• Wear a surgical mask (NOT a cloth mask or N95) for the duration of the
travel
• Follow hand hygiene guidance
Emergency Method:
Greyshirt is quarantined on site.
The Greyshirt Support Team will reach out to the exposed Greyshirt daily for 14 days to inquire
about symptoms and support fulfilling daily needs (e.g., groceries). If a Greyshirt refuses
to quarantine at home due to concern of infecting family, the Greyshirt Support Team, IMT, and
NOC (in consultation with public health officials) will determine a safe and secure place for the
Greyshirt to quarantine, the duration, and conditions upon which the Greyshirt can safely exit
quarantine. In cases where a local care/quarantine site is not available, the Greyshirt Support
Team, IMT, and NOC will coordinate to secure a hotel for the Greyshirt for the duration of their
quarantine. The TR Medical Team will work with the IMT and NOC to track exposures and assist
with Greyshirt medical needs as able.
Upon returning home, the Greyshirt is requested to quarantine for 14 days and monitor
symptoms. Greyshirts wishing to return to their place of employment need to follow the
3
Centers for Disease Control and Prevention (2020, July 15). Interim Infection Prevention and Control
Recommendations for Healthcare Personnel During the Coronavirus Disease 19 (COVID-19). Retrieved from
https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
16
OPERATIONAL GUIDANCE
guidelines set forth by their employer. The decision to allow the Greyshirt to sign up for future
TR operations will be based on the CDC Discontinuation of Isolation Guidance7F
4
.
If a Greyshirt becomes symptomatic, they will immediately contact their healthcare provider and
follow local jurisdictional guidelines for COVID-19 evaluation. During routine check-in, the
Greyshirt will immediately notify the Greyshirt Support Team or the IMT if they become
symptomatic or test positive.
2.6.7. (X-5) Site Decontamination and Demobilize Decision
The site will be decontaminated following. Cleaning and Disinfecting CDC Guidance8F
5
. IMT will
decide whether to demobilize the site or reopen and continue operations.
Second-Degree Contact
Second-degree contact is defined in this manual as contact with a healthy (or presumably
healthy) individual who had direct contact with another individual who tested positive for
COVID-19. In cases where a Greyshirt experienced second-degree contact, the operation will
proceed as planned and no action will be required. If the situation evolves (e.g., Greyshirt
develops COVID-19 symptoms or a COVID-19 case is confirmed at the operation site), TR and
the Greyshirt will adhere to the protocols outlined above.
2.7. TR MINIMUM PPE REQUIREMENTS
Due to an increase in COVID-19 infections across the country and at the recommendation of the
CDC, (effective 7/27/2021), Team Rubicon will require masking indoors at all in-person events,
operations and in Team Rubicon offices even if all Greyshirts are vaccinated.
• Community Settings: In all interactions with the community, we will continue to wear
masks and practice social distancing to reduce the risk of and prevent potential spread of
COVID-19, even if all Greyshirts are vaccinated.
• Outdoor Settings: We will resume the practice of social distancing for outdoor activities.
Where social distancing is not feasible, masking is required. For isolated, independent
activities like sawyer or HEO work, masking is not required.
Non-Medical Face Covering Policy
4
Centers for Disease Control and Prevention (2020, July 20). Discontinuation of Isolation for Persons with COVID-19
Not in Healthcare Settings. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-
patients.html
5
Centers for Disease Control and Prevention (2020, September 10). Cleaning and Disinfection for Community
Facilities. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/cleaning-
disinfection.html

17
OPERATIONAL GUIDANCE
Based on the CDC’s recommendation, when masks are required as stated in PPE policy,
Greyshirts are required to wear a non-medical face covering11F
6
(e.g., homemade cloth mask,
bandana, scarf, old t-shirt) to cover their mouth and nose while participating on all TR operations.
• This does not replace the need for additional PPE per TR's Minimum PPE guidelines.
• Greyshirts are expected to provide their own non-medical face covering. Non-medical
face coverings do not sufficiently prevent illness. All other COVID protocols to this end
(e.g., hand hygiene, physical distance, disinfecting) must be followed.
3. OUTFITTING
The following are operational guidelines for all TR facilities, equipment, FOBs, and billeting
locations for fully-vaccinated Greyshirts participating in in-person activities:
3.1. BILLETING
3.1.1. Billeting Capacity and Access Restrictions
Billeting and FOB locations will be separate. Limited time should be spent in shared spaces (e.g.,
spend time outside except during nighttime hours). Social interaction between different working
groups should be avoided as much as possible. Staff should not enter billeting spaces unless
necessary and will use virtual communications and check-ins (e.g., phone, video chat) as
available.
Non-TR members, visitors, and non-essential volunteers are not allowed access to the FOB and
billeting areas including bathrooms, eating areas, and shared spaces. Billeting will not be shared
with other organizations.
Buildings with open floor plan billeting will be chosen with consideration on air flow, ceiling
height, and ventilation. Areas that promote physical spacing, support large occupancy, and
accommodate Heating, Ventilation, and Air Conditioning (HVAC) systems will be considered to
reduce potential airborne spread of the virus. Spaces with operable windows will be preferred if
potential ventilation issues exist.
The following ventilation options will also be used to increase ventilation:
• Open windows or screened doors as much as possible. Do not open windows and doors
if this will pose a safety or health risk (e.g., falling, triggering asthma symptoms).
• Turn on fans to increase air ventilation with minimal air recirculation.
• Operate a window air conditioner with an outdoor air intake or vent, with the vent open.
Some window air conditioners do not have outside air intakes.
• Open the outside air intake of the HVAC system, if there is one. (This is not common.)
6
Centers for Disease Control and Prevention (2020, June 28). Use Masks to Help Slow Spread of COVID-19.
Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html
18
OPERATIONAL GUIDANCE
• Create cross-ventilation by opening windows (or doors) at opposite sides of a building,
and keeping internal doors open. Preferably not directly opposite of each other.
• Open the highest and lowest windows, especially on different floors.
• Use air filtration/purification/HEPA air scrubbers when possible and position to pull air
out of buildings.
Billeting Setup and Sleeping Arrangements
• Cots will be spaced at least six feet apart. Additionally:
• Use the entire floor plan to arrange cots as far as possible to maximize distancing (room
occupancy is recommended at about 113 sq. Ft/person)
• Stagger the direction of cots (i.e., not in direct line with one another)
• Use painter’s tape on the floor to maintain positions
• Make sure personal belongings remain stowed under each bunk and aren’t left out in
common areas
• Once a cot is occupied, try not to share or switch cots until demobilization by that
Greyshirt until the Greyshirt demobilizes. Greyshirts will not switch cots
• Disinfect cots using appropriate cleaners before the cot will be occupied by another
Greyshirt.
Billeting for CPAP Users
Greyshirts who wear a CPAP to sleep may billet in individual rooms separated by a door from
other rooms or shared spaces. The room must be:
• Closed off by four walls from the main billeting area or any common areas like the
kitchen
• Equipped to accommodate the power source for the CPAP, if required
• If the facility does not have an appropriate space available for a separate sleeping area, an
alternate lodging option may be arranged
Conduct As-Needed Screenings
Designated field leaders assigned to billeting sites will be equipped to conduct temperature
checks as needed during operations and at events. See APPENDIX F: JOB AIDS for
recommendations for temperature screening but note that there is no requirement to screen
Greyshirts at regular intervals each day. Greyshirts with temperatures of 100.4°F or above (i.e.,
fever) will be screened and subject to the provisions of TR COVID-19 EXPOSURE POLICY. The
Medical & Technical Advisory Team will review each escalation case to ensure correct actions
are taken.
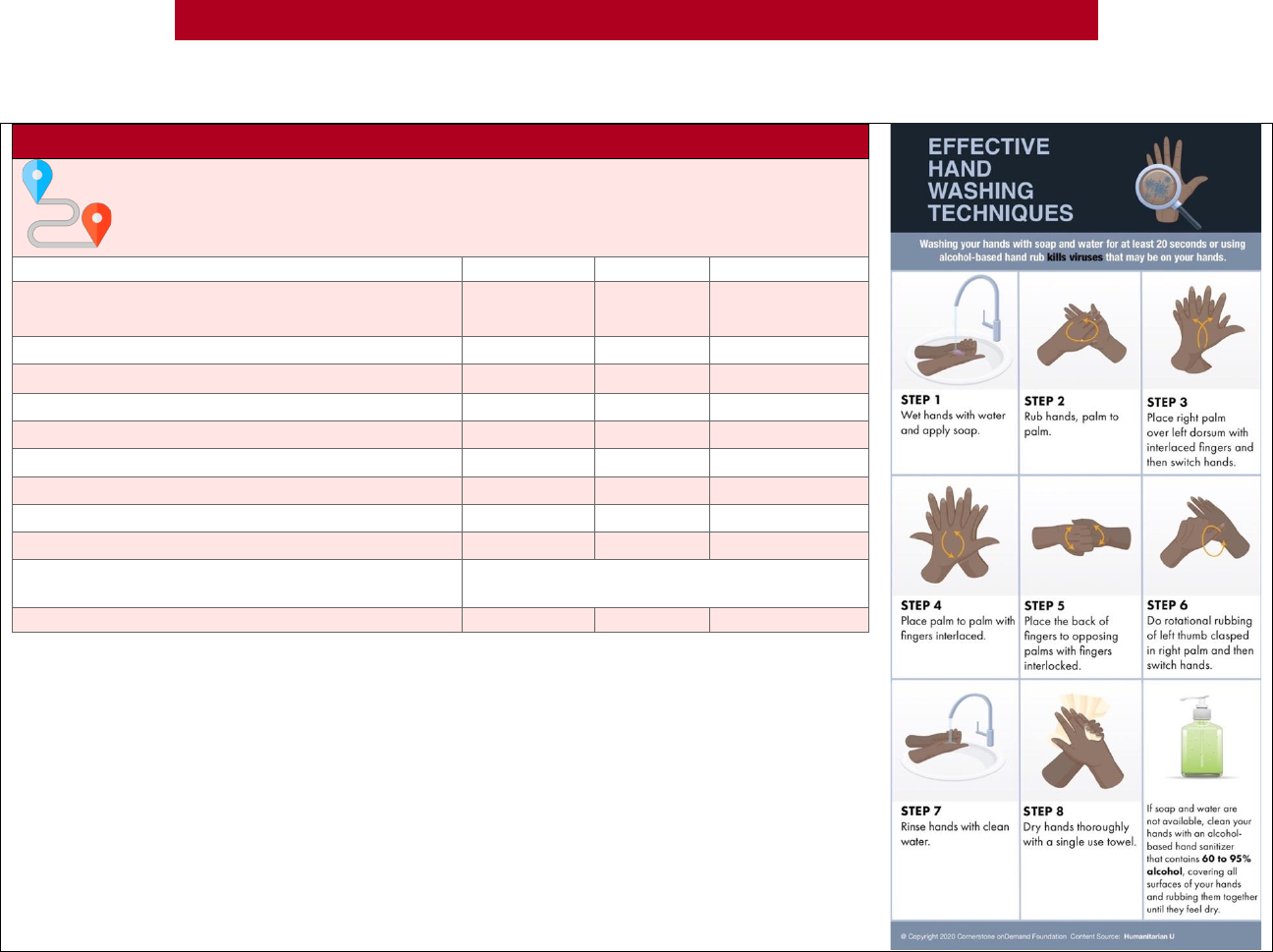
Posting Information
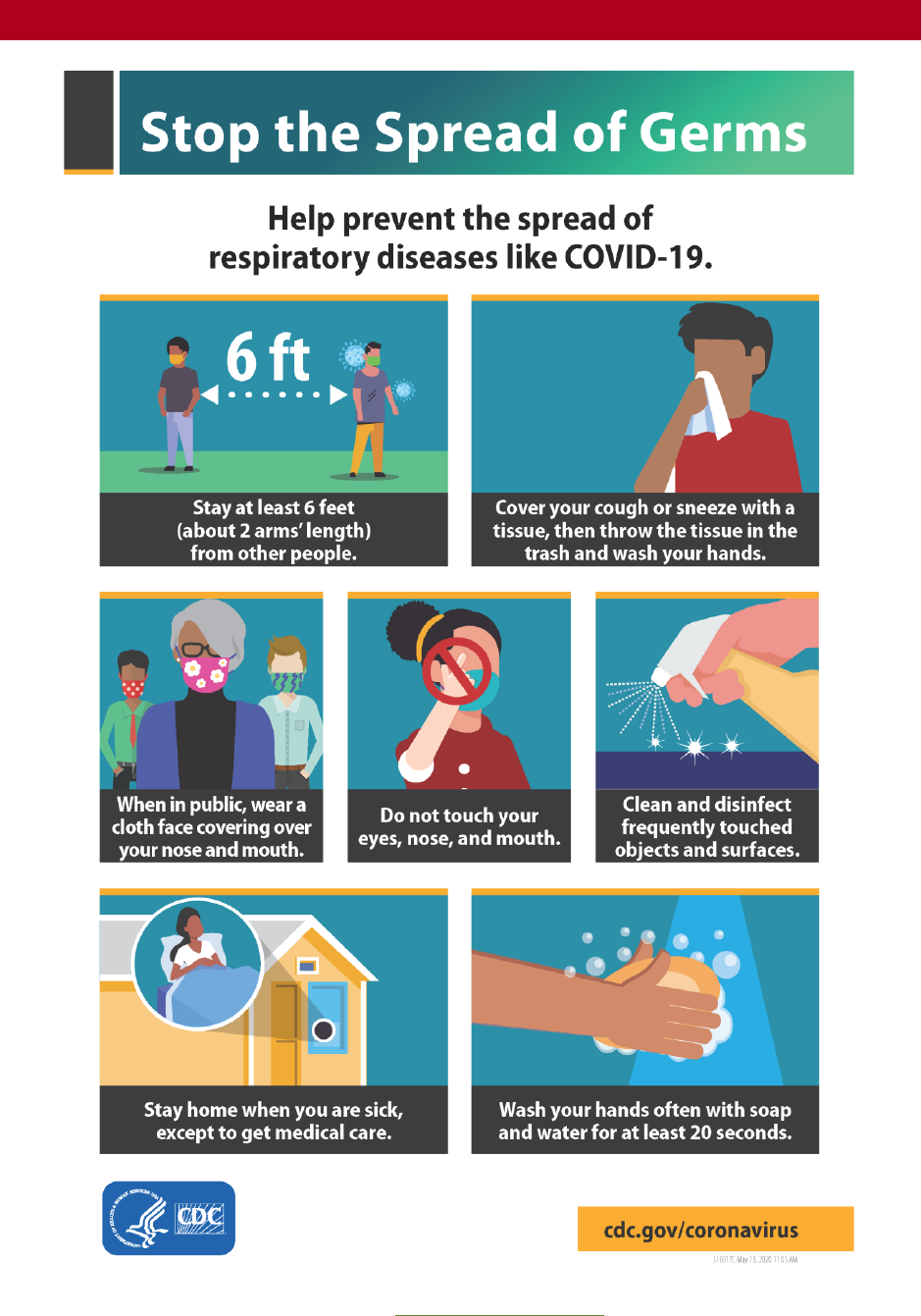
Health and safety CDC fact sheets, including at a minimum Stop the Spread of Germs and
Effective Handwashing Techniques, will be posted at entrances and in strategic places providing
instructions on hand hygiene, respiratory hygiene, and cough etiquette. Additionally, signs will be
posted at exterior doors reading, “Wash hands upon entering.” If hand sanitizer is available, the
sign may read, “Wash hands or use hand sanitizer upon entering.” All new Greyshirts will be
given a one-time hygiene orientation when first working at the FOB or entering a billeting
19
OPERATIONAL GUIDANCE
location. This orientation will include distribution of the hygiene guidelines in APPENDIX C:
HYGIENE GUIDE.
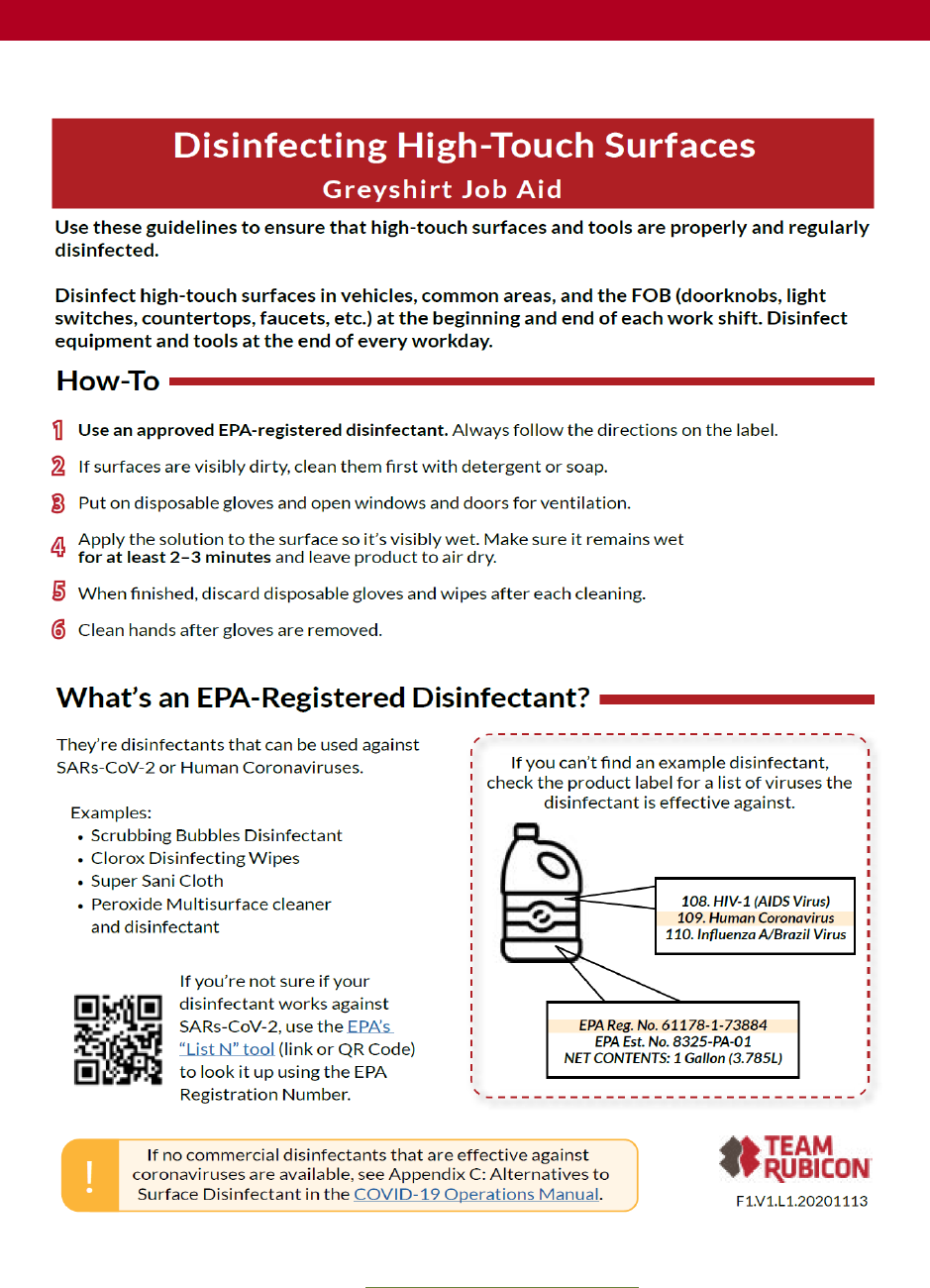
General Sanitation
High-touch surfaces, such as doorknobs and handles, will be cleaned throughout the FOB.
Billeting facilities, including restrooms, will be cleaned at least twice daily following the CDC
guidance, Cleaning and Disinfection for Community Facilities
5
. If possible, disinfecting wipes will
be available in high-touch areas such as break rooms or workstations. Individuals will wipe off
the area when they depart. Adequate disinfecting supplies will be made available.
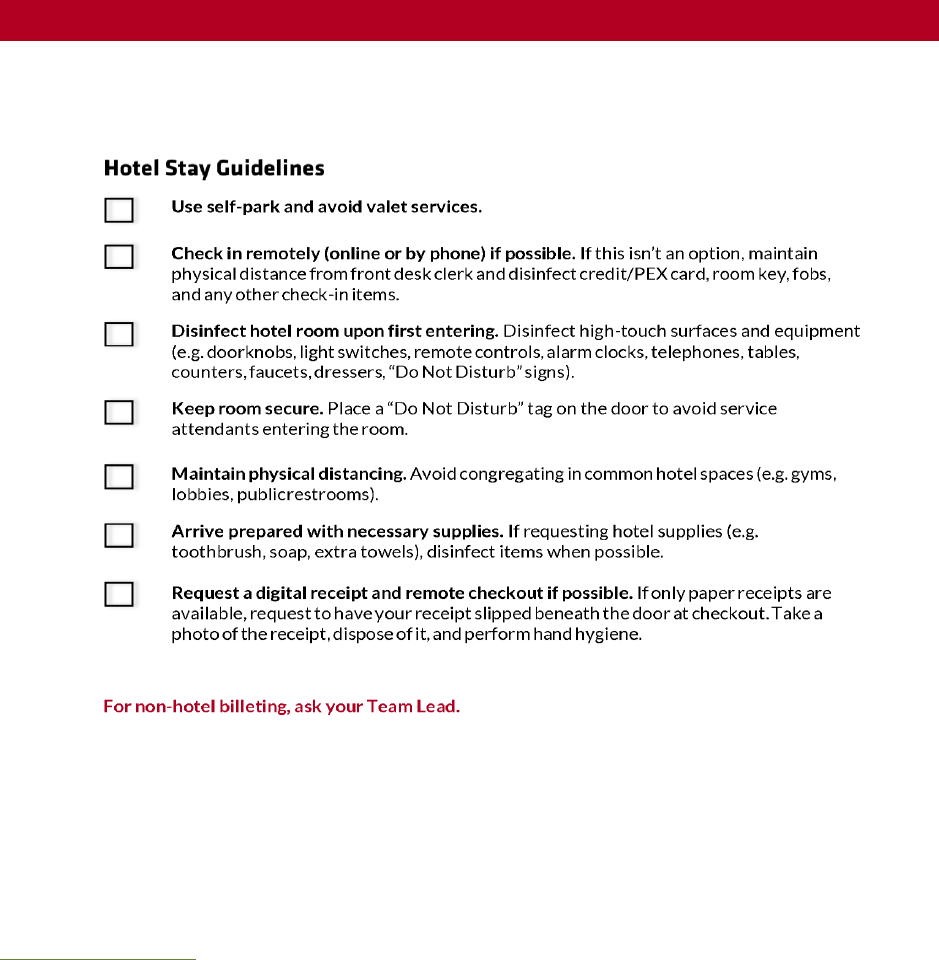
Hotel Stays
When it is necessary, Greyshirts will stay in single-occupancy hotel rooms, unless operationally
unavidable. When staying in hotels, Greyshirts will adhere to all provisions in APPENDIX C:
HYGIENE GUIDE.
Disinfecting Billeting/FOB After Confirmed Exposure
If a Greyshirt or staff member has confirmed COVID-19 status, regardless of vaccination status,
on any billeting, FOB, or office location, Team Rubicon staff will shut down the operation as
outlined in TR COVID-19 EXPOSURE POLICY. A certified cleaning service will be hired
immediately to clean and disinfect the facilities in line with the CDC guidelines below. If such
service is inaccessible, Greyshirts will be assigned to clean according to these guidelines:
• Close areas visited by the ill person(s). Open outside doors and windows. Use ventilating
fans to increase air circulation in the area.
• Wait 24 hours, or as long as practical, before beginning cleaning and disinfection.
• Clean and disinfect all areas such as offices, bathrooms, common areas and shared
electronic equipment like tablets, touch screens, keyboards, and remote controls used by
the ill person(s), focusing on high-touch surfaces.
Adhere to CDC-prescribed guidance for hygiene as outlined in APPENDIX C: HYGIENE GUIDE.
Food Preparation and Distribution
The Food Unit Lead (FUL) should be the only person in contact with food or related supplies and
equipment for food distribution during the operation, but other duties can be delegated. The
FUL will not be responsible for cleaning the kitchen or food service areas. The FUL will maintain
the standards of hygiene outlined in the Food Unit Leader Handbook, including sanitizing all food
prep surfaces and utensils after every use.
The FUL should have access to effective surface disinfectant products (such as bleach, hydrogen
peroxide, quaternary ammonium) to use against SARS-CoV-2 (the novel coronavirus that causes
COVID-19).
During COVID-19, the FUL and Greyshirts involved in food handling should increase hand
hygiene. All Greyshirts involved with food handling and related equipment will wash their hands
often.
The FUL will ensure barriers such as tongs, gloves, or other utensils are being used effectively
when handling ready to eat food or packaged food.

20
OPERATIONAL GUIDANCE
The FUL will remind food handlers to avoid touching their eyes, nose, and mouth to help slow
the spread of germs. Hand sanitizers with at least 60% ethyl alcohol will be readily available. The
FUL will also remind food handlers of the guidelines of ‘minimal touch’ food distribution as listed
in the Food Unit Leader Handbook to minimize touch points.
Coronavirus is a respiratory virus spread through respiratory droplets. The Centers for Disease
Control and Prevention (CDC) does not consider COVID-19 to be a foodborne illness, but similar
actions to prevent foodborne illness can be taken to mitigate the spread of COVID-19. The most
important actions to take include proper handwashing using soap and water and scrubbing for at
least 20 seconds, frequent cleaning and sanitation of touch points. Whenever possible, the FUL
should maintain 6 feet of distance from others. The FUL and Greyshirts feeling sick should avoid
food service areas.
During Covid-19, the FUL should avoid buffet style service distribution. Food is encouraged to
either be purchased separately packaged when possible. When bulk food is purchased (e.g.
catering trays) it should be separated into individual packages by the FUL and distributed ‘grab
and go’ style.
Food Delivery
When possible, acquiring food via delivery services is preferred because it can reduce potential
exposure.
Food delivered from external organizations (e.g., churches, food kitchens, outside organizations)
will be subject to tougher rules for drivers delivering to the FOB or billet.
Delivery drivers should remain in their vehicle and the FUL/LSC will meet them in appropriate
PPE to receive the food.
If there are multiple deliveries. The FUL should coordinate to stagger deliveries for crowd
control.
3.2. TRANSPORTATION
rtFFully-vaccinated Greyshirts who are carpooling are required to wear well-fitting masks
throughout the duration of their ride. However, these do not need to be N95 masks. If
necessary, fully-vaccinated groups may fill the car to their maximum capacity (e.g., as many GSs
as there are seatbelts).
Rental or TR vehicles will be used for all activities requiring
transportation during an operation. Greyshirts are not permitted to
use personal vehicles or partner organization’s vehicles while
executing activities during an operation or working with partner
organizations.
In the event a Greyshirt will be driving a vehicle rented or owned by TR, the designated
supervisor will ensure the Greyshirt possesses a current non-expired driver’s license. During
operations, any Greyshirt tasked with driving a motor vehicle to perform specific duties is
required to have their driver’s license in their possession and present it to the designated
supervisor prior to assuming their role.
SAFE FOOD
HANDLING
21
OPERATIONAL GUIDANCE
The designated supervisor will visually confirm the Greyshirt assigned to drive has a non-expired
motor vehicle driver’s license in their possession. If the Greyshirt cannot provide a non-expired
driver’s license, the designated supervisor is responsible for assigning the Greyshirt to a non-
driver role.
The vehicle rideshare process below will be followed when Greyshirts travel in a vehicle during
an operation (see Appendix B: Job Aids, Vehicle Rideshare Checklist):
3.2.1. Vehicle Ridesharing
Wear PPE/Face Coverings
Anytime there is more than one person in a TR vehicle, precautions will be taken to decrease
potential viral transmission. Vaccinated Greyshirts will wear personal and well-fitting masks for
the duration of the shared ride.
Maintain Ventilation
• Primary: Roll down all windows to increase air ventilation throughout the duration of the
trip. Maximize in/out air flow and avoid using the recirculated air option for car
ventilation.
• Contingency (when weather is limiting): Roll down windows intermittently (as weather
permits) to increase air ventilation throughout the entire
duration of the trip.
• At all Times: Avoid using the recirculated air option for car
ventilation.
Ensure Passenger and Vehicle Sanitization
Apply the universal risk mitigation strategies outlined in the
following table:
Universal Risk Mitigation Strategies
Mitigation Strategy
More Information
Ensure the car has been disinfected prior to and
following use.
Pay close attention to frequently touched surfaces
like door handles, steering wheels, ignition,
operating buttons, seat buckles, keys, etc. Wear
disposable gloves when cleaning and only use
them once. Disinfectants should be EPA-
registered antimicrobial, diluted household bleach
according to manufacturer instructions, or alcohol
solutions with at least 70% alcohol.
Carry hand sanitizer and tissues.
Consider having appropriate disinfectant tools on
hand including cleaning and disinfectant spray, or
disposable wipes and a small trash bag for each
vehicle.
Wash your hands before and after entering the
vehicle with soap and water for at least 30
seconds.
Use an alcohol-based hand sanitizer that contains
at least 60% alcohol if soap and water are not
available.
Avoid touching your face with unwashed hands.
Specifically avoid touching your eyes, nose, or
mouth.
TRANSPORTATION
REQUIREMENTS AND
RESTRICTIONS
22
OPERATIONAL GUIDANCE
Cover your mouth and nose with a tissue when
you cough or sneeze.
Throw the tissue in the trash and wash your
hands.
Refer to TR COVID-19 EXPOSURE POLICY if you experience signs and symptoms associated
with COVID-19, isolating immediately. Inform your designated supervisor if you participated in
any carpooling activities during an operation and are experiencing signs and symptoms.
3.2.2. Air Travel
In cases pre-authorized by the Director of Field Operations, Greyshirts may fly to and from an
operation. In these cases, Greyshirts will adhere to CDC-endorsed best practices20F
7
for flying
including wearing face coverings, the airline’s rules and regulations, and TR’s hygiene guidelines
detailed in APPENDIX C: HYGIENE GUIDE.
Priority will be given to booking flights on airlines following strict COVID-19 precautions. When
flying to and from a site through commercial air travel, the following mitigation strategies MUST
be taken:
Prior to Your Flight, Conduct Self-Health Screening
If you answer “yes” to any of the questions in the box to
the right, do not travel and contact mobilization.
Wear Face Coverings
Wear face coverings for the entirety of travel (e.g., in
the airport, aircraft, throughout subsequent travel - see
new guidance related to vehicle travel). Abide by air
travel guidance for the type of mask used.
Perform Hand Hygiene
Before entering the aircraft, wash your hands with soap
and water for at least 30 seconds. If soap is not
available, use an alcohol-based hand sanitizer containing
at least 60 percent alcohol throughout the flight as
needed. Avoid touching your eyes, nose, or mouth with
unwashed hands. Cover your mouth and nose with a
tissue when you cough or sneeze; throw the tissue in
the trash and wash your hands.
Greyshirts deployed on an operation will strictly adhere to the protocols outlined in the TR
Exposure Policy. All Greyshirts should be prepared to self-quarantine for 14 days following any
7
Centers for Disease Control and Prevention (2020, October 21). Travel During the COVID-19 Pandemic. Retrieved
from https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-
covid19.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-
ncov%2Ftravelers%2Ftravel-in-the-us.html
HEALTH SCREENING QUESTIONS
In the last two weeks, have you
experienced:
• Fever or feeling feverish?
• Chills?
• A new cough?
• Shortness of breath?
• A new sore throat?
• New muscle aches?
• New headache?
• New loss of smell or taste?
• Have you been exposed to
someone with a confirmed
case of COVID-19?

23
OPERATIONAL GUIDANCE
TR event. TR may recommend this self-quarantine be enacted pursuant to the conditions
outlined in the Exposure Policy. Symptomatic Greyshirts are not permitted to take commercial
flights until cleared through local health department policy.
3.3. PERSONNEL
3.3.1. Personnel Eligibility
While delivery of service will always involve certain amount of risk, TR is committed to mitigating
such risks whenever possible. Individuals with increased vulnerability to COVID-19, or who
could pose a danger through infection to team and community members, will not be deployed to
COVID-19 related activities. In the interest of keeping Greyshirts and community members safe,
TR will adhere to the following personnel guidelines:
As part of our continued commitment to the service of others and fight the spread of COVID-19,
Team Rubicon requires the acknowledgement and attestation of COVID-19 vaccination status
from all Greyshirts participating in in-person events and operations. Greyshirts will be required
to provide accurate information about their vaccination status during the registration process, or
alternatively may decline to provide vaccination status. If a Greyshirt declines to provide
information about vaccination status, TR will be required to assume the Greyshirt is
unvaccinated for purposes of policies that are different for vaccinated or unvaccinated
volunteers.
FULLY-VACCINATED GREYSHIRT POLICY will outline which individuals are considered “fully-
vaccinated”
Finally, TR asks that Greyshirts experiencing common symptoms of COVID-19 avoid
engagement in any TR activity or event. CDC guidelines advise screeners to watch for the
following symptoms:
• Cough
• Shortness of breath
• Difficulty breathing
• Fever
• Chills
• Muscle or body aches
• Headache
• Sore throat
• A new loss of taste or smell
• Fatigue
• Congestion or runny nose
• Nausea or vomiting
• Diarrhea
Greyshirts exhibiting the following symptoms should seek immediate medical attention:
• Trouble breathing
• Persistent pain or pressure in the chest
24
OPERATIONAL GUIDANCE
• New confusion or inability to arouse
• Bluish lips or face
Note this list identifies the most common symptoms of COVID-19. It is not a complete list of
COVID-19 symptoms and will not be used to diagnose COVID-19.
These criteria are based on the most accurate and up-to-date
information provided by the Centers for Disease Control and
Prevention (CDC) and the World Health Organization (WHO).
These organizations also suggest that people with underlying
conditions including chronic kidney disease, cancer, chronic
obstructive pulmonary disease (COPD), immunocompromised
(weakened immune system), obesity, serious heart conditions,
sickle cell disease, and diabetes type 2 are at an increased risk of developing severe COVID-19
illness.21F
8
If a Greyshirt is ineligible to deploy due to symptoms or a confirmed case of COVID-19, the
decision to allow a return to work will be based on the CDC Discontinuation of Isolation
Guidance
4
. TR is not responsible for verifying Greyshirt COVID-19 status and all Greyshirts are
expected to honestly report their status.
3.3.2. Deployability Requirements
Greyshirts must be prepared to quarantine for 14 days following deployment, if necessary.
Spontaneous volunteers working under TR COVID-19 response activities will adhere to the
policies and protocols laid out in this manual. Spontaneous volunteers will only assist with low
exposure risk operations. TR will not provide billeting for spontaneous volunteers. Spontaneous
volunteers will sign the Memorandum of Understanding located in Figure 20. Spontaneous
Volunteer COVID-19 MOU.
“Close Contact” Deployment Constraint
Greyshirts who have come into close contact with COVID-19 positive individuals without the
use of respiratory protection (e.g., N95, PAPR) in the past 14 days should not sign up for TR
events. Close Contact is defined as one of the following:
• Living in the same household as a sick person with COVID-19
• Caring for a sick person with COVID-19
• Being within six feet of a sick person with COVID-19 for about 10 minutes
• Being in direct contact with secretions from a sick person with COVID-19 (e.g., being
coughed on, kissing, sharing utensils, etc.)
8
Centers for Disease Control and Prevention (2020, October 16). People with Certain Medical Conditions. Retrieved
from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
SIGNS AND SYMPTOMS
25
OPERATIONAL GUIDANCE
3.3.3. Travel Restrictions
When regional policies restrict travel to and from an operation, Greyshirts may present the
“Jurisdictional Travel Restrictions” letter to checkpoint authorities. Jurisdictional restrictions may
include COVID-19 checkpoints, established curfews, and any other travel restriction issued by
local, state, or tribal authorities. This official letter is a template sent with dispatch instructions,
which will need to be edited for personal use. An example of the Jurisdictional Travel letter is
located in Figure 18. Jurisdictional Travel Letter.
Prior to deployment, Greyshirts should anticipate travel restrictions along the way to, or on the
way back from, an operation. Read local and government websites, as well as other sources for
information. Full adherence to local polices, including travel restrictions (e.g., mandatory
quarantine, testing, screening) is extremely important.
If a Greyshirt is denied entry into a jurisdiction, they will follow the recommendations of the local
authority, contact their designated supervisor, and wait for further instruction.
3.4. INFORMATION
Whenever possible, TR will request to be plugged in to the Requesting Organization’s current
information gathering operations. Key data points will be compiled with the support of
Marcomms and Development. For further information, to the Information Management section,
of the Domestic Emergency Operations Plan.
4. ADMINISTRATION
4.1. DOCUMENTATION
TR and Requesting Organizations will sign the Acknowledgement of Policy Form, in Figure 19.
Acknowledgement of Policy Form to confirm they have shared all relevant policy, guidelines, and
protocol related to COVID-19 and general execution of operations with each other. This form
also ensures that, regardless of Greyshirt participation in different activities with the Requesting
Organization, Greyshirts will adhere to minimum standards as dictated in TR doctrine and this
COVID-19 Operations Manual.
The Acknowledgement of Policy Form must be signed by the TR POC and Requesting
Organization POC for MPT to move the mission planning process from Warning Order
(WARNO) to Operations Order (OPORD). The signed and completed Acknowledgement of
Policy form will be stored in the operations folder by MPT. If a Requesting Organization refuses
to sign, or there are other difficulties involving capturing signatures on the Acknowledgement of
Policy Form, the MPT can consult with either the Director of Territory Operations or The Deputy
Director of Operations Support on how to work towards a “yes” with the Requesting
Organization.
5. ORGANIZATIONAL SUPPORT

26
OPERATIONAL GUIDANCE
5.1. MOBILIZATION
Greyshirts will follow standard operating procedures as detailed in the Mobilization-
Demobilization Manual. Greyshirts will be deployed for no longer than 14 days. Greyshirts will be
deployed within a 50-mile radius whenever possible and will not work more than 12 hours per
day, including travel time. Additional guidance specific to this capability is below.
The following deployment guidelines will apply:
• Incident Command Support, Non-Medical Testing Operations, and Shelter General
Support are preferred to deploy within a 450-mile radius by driving only when billeting is
confirmed.
• Medical Operations will deploy within a 450-mile radius by driving only, however airline
travel for Greyshirts providing medical services will be authorized with DFO approval.
• TR Core Operations are preferred to deploy within a 450-mile radius by driving when
there is confirmed billeting and DFO approval.
• Training instructors will be authorized to travel when their respective training is identified
as capacity-building and approved at the Deputy Director level. Instructors will be
prioritized by their proximity to an operations site. Instructors (registered as leased
employees) are preferred to drive to the training site.
• In all cases of deployment, Greyshirts are expected to adhere to the safety and hygiene
guidelines as outlined in this COVID-19 Operations Manual.
27
SUPPLEMENTAL INFORMATION/APPENDICES
COVID-19
OPERATIONS MANUAL
SUPPLEMENTAL INFORMATION
28
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX A: GLOSSARY
Definitions
Capability – TR service provided to individuals and/or communities affected by disaster.
Clients –End-recipient (e.g., individual, family, household, and/or community) of TR’s services.
Close Contact – Immediate contact without PPE with a person who is COVID-19 positive.
Community Spread – Indicates people are infected with the virus in an area, including those who
are not sure how or where they became infected. Typically measured at the county, parish, or
metropolitan area level.
COVID-19 – Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a newly
discovered coronavirus, first detected in Wuhan, China, in 2019.
Direct Exposure – An epidemiological mode of disease transmission involving either direct
contact with an infectious agent (e.g., skin-to-skin, kissing, sexual intercourse) or droplet spread
(e.g., sneezing, coughing, talking). See CDC Intro to Epidemiology.
Extended Use – Wearing the same N95 respirator or face shield for repeated close-contact
encounters with several patients.
Hastysling Capability – An ad hoc new service created amid a response to an urgent demand
prompted by a sudden onset disaster.
High Exposure Risk – Both immediate contact with COVID-19-infected individuals and with the
surfaces and spaces they may have come into contact with.
High-Touch Surfaces – Surfaces handled frequently throughout the day by multiple people (e.g.,
doorknobs, light switches, phones).
Indirect Exposure – An epidemiological mode of disease transmission involving contact with
suspended air particles (e.g., dust), inanimate objects/vehicles (e.g., food, water, biologic
products), or vectors (e.g., mosquitoes, fleas, ticks). See CDC Intro to Epidemiology.
Isolation – Separating sick people with a contagious disease from people who are not sick.
Limited Reuse – Using the same N95 respirator or face shield for multiple encounters with
patients, doffing the respirator or face shield, storing, and donning again for further encounters
with patients.
Low Exposure Risk – No contact with COVID-19 infected individuals, or with the surfaces and
spaces they may have encountered.
Medium Exposure Risk – No contact with COVID-19 infected individuals; however, contact may
have been made with the surfaces and spaces they encountered.

29
SUPPLEMENTAL INFORMATION/APPENDICES
N95 Respirator/Mask – Type of PPE worn over one’s mouth and nose to prevent the
transmission of airborne particles, including droplets containing COVID-19.
Non-Operational Travel – Routine travel performed during TR operations not directly ordered
by the OSC. This includes travel, billeting to FOB, off-duty runs, etc.
Operation – A temporary organizational TR structure that delivers capabilities to individuals and
communities.
Operational Travel – Routine travel during TR operations directly ordered by the OSC and is
mission critical.
Physical Distancing [previously referred to as “Social Distancing”] – Increasing the space
between individuals, and decreasing the frequency of contact, to reduce the risk of spreading a
disease (ideally, maintain at least 6-feet between all individuals, even those who are
asymptomatic). See CDC guidance.
Plug-n-Play Service – TR providing Greyshirts to support another organization’s response
activities.
Quarantine – Separating and restricting the movement of people exposed to a contagious
disease to see if they become sick.
Requesting Organization – An external entity who has submitted a Request for Assistance to TR.
Request for Assistance (RFA) – A direct ask from a Requesting Organization to TR for support
and/or a plug-n-play service.

30
SUPPLEMENTAL INFORMATION/APPENDICES
Acronyms
C&G – Command and General
CDC – Centers for Disease Control and Prevention
CDL – Commercial Driver’s License
CONOPS – Concept of Operations
COPD – Chronic Obstructive Pulmonary Disease
COVID-19 – Novel Coronavirus of 2019
CPAP – Continuous Positive Airway Pressure
CSSE – Center for Systems Science and Engineering
DDRO – Deputy Director of Regional Operations
EMAC – Emergency Management Assistance Compact
EMS – Emergency Medical Service
EMS – Enterprise Management System
EMT – Emergency Medical Technician
EOC – Emergency Operations Center
EPA – Environmental Protection Agency
ER – Emergency Room
FEMA – Federal Emergency Management Agency
FOB – Forward Operating Base
FRAGO – Fragmentary Order
FSMB – Federation of State Medical Boards
FUL – Food Unit Leader
HOR – Home of Record
IAP – Incident Action Plan
IC – Incident Commander
ICS – Incident Command System
ICU – Intensive Care Unit
IMT – Incident Management Team
JD – Job Description

31
SUPPLEMENTAL INFORMATION/APPENDICES
LSC – Logistics Section Chief
MPT – Mission Planning Team
N95 – N95 Respirator Mask
NIOSH – National Institute for Occupational Safety and Health
NGO – Non-Governmental Organization
NOC – National Operations Center
NREMT – National Registry of Emergency Medical Technician
NRP – Nationally Registered Paramedic
NUAF – New User Access Form
OPORD – Operations Order
OSC – Operations Section Chief
OSHA - Occupational Safety and Health Administration
PAPR – Powered Air Purifying Respirator
PII – Personal Identifiable Information
POC – Point of Contact
POV – Privately Owned Vehicle
PPE – Personal Protective Equipment
PSC – Planning Section Chief
TR – Team Rubicon
RESL – Resource Unit Leader
RFA – Request for Assistance
SitRep – Situation Report
SS – Superior Staffing
UEVHPA – Uniform Emergency Volunteer Health Practitioner Act
VOAD – Voluntary Organizations Active in Disaster
WARNO – Warning Order
WHO – World Health Organization
32
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX B: COVID-19 STRATEGIC TOOLKIT
COVID-19 Strategic Toolkit for In-Person Activities
The indicators and triggers toolkit assists stakeholders in establishing boundaries for the health
and safety of all TR volunteers and personnel, preventing the spread of virus in communities.
Together, indicators and triggers guide decision making in providing training and logistics
readiness activities as we navigate a rapidly changing environment.
As a standard of care, Team Rubicon will closely monitor the indicators (measures or predictors)
below in conjunction with domestic in-person activities. This toolkit does not apply to any TR
operations. If at least one trigger (decision point) is present in a location of interest, a
contingency strategy will be implemented based on an appropriate situational response.
Indicators and Triggers Toolkit
Regional
Indicator
Regional Trigger(s)
Restriction Details
Information Review
Travel
Restrictions
If interstate restrictions
have been enacted in a
state where a high-output
non-operational in-person
activity is scheduled to
take place, restrict
attendance to only
internal state attendees.
To mitigate the spread
of COVID-19, certain
states have enacted
restrictions on
interstate travel. Local
policy could enforce a
14-day quarantine,
either mandatory or
advised. Some
restrictions are only
applicable if
individuals traveling
from states are
deemed high risk.
Frequently updated state-by-
state responses and
restrictions.
Currently (updated August
18, 2020) interstate travel
restrictions exist in Alaska,
Connecticut, District of
Columbia, Hawaii, Illinois,
Kansas, Kentucky, Maine,
Maryland, Massachusetts,
Montana, Nebraska, Nevada,
New Hampshire, New Jersey,
New Mexico, New York,
Ohio, Oklahoma,
Pennsylvania, Rhode Island,
South Carolina, Utah,
Vermont, Virginia, and
Wisconsin.
Stay at Home or
Shelter-in-Place
Mandates
If a stay-at-home
mandate, shelter-in-place,
or any other request from
a Public Health Agency
has been enacted in an
area where a high-output
non-operational in-person
activity is scheduled to
take place, implement a
contingency strategy.
Nearly every state is
enacting daily changes
to their responses to
COVID-19.
State-by-state policy.
Recent history of legislative
changes by state.
Risk in Positive
COVID-19 Cases
If an upturn in infections
is reported in a state
where a high-output non-
operational in-person
Multiple sources are
providing clear and
consistent information
on COVID-19 risk
TR Situational Awareness
Dashboard, provides COVID-
19 cases 14-day difference
33
SUPPLEMENTAL INFORMATION/APPENDICES
Regional
Indicator
Regional Trigger(s)
Restriction Details
Information Review
activity will take place,
implement a contingency
strategy measured in one
of the following two
ways:
1) 10 infections per
100,000 residents on
a 7-day rolling
average.
2) 10 percent or higher
of the state’s total
positive test rate on a
7-day rolling average.
levels in different
jurisdictions to assist
decisions for policy
makers.
per 100,000 layer to identify
the state percentage.
Johns Hopkins Daily State-
by-State Testing Trends may
help determine the positive
test rates.
Harvard Global Health
Institute dashboard provides
a 7-day rolling average.

34
SUPPLEMENTAL INFORMATION/APPENDICES
Contingency Strategy
This strategy discusses what to do once a trigger has been identified and when the risk of
conducting an in-person event or activity outweighs the positive outcome of the activity itself.
If a concern for the safety and health of attendees exists, and a trigger has been identified, the
information will be immediately directed to Territory Directors, or assigned leaders in the
associated territory. From here, two different contingency strategies can be followed:
1) Future Scheduled Event—Implement this strategy if an in-person activity has been
scheduled in the future. The Event Lead will immediately coordinate with Territory staff
to determine the course of demobilization leading to shutdown (and potential
rescheduling). All communication will be sent directly via email and phone to any
volunteer, personnel, or other attendee expecting to deploy to the scheduled activity.
The Event Lead, in concert with the Territory Team, will ensure either verbal or written
confirmation of the cancellation has been attained for every attendee on the roster.
Updates will be posted on Roll Call, TR’s website, or social media platforms (e.g., TR
Facebook groups) when needed.
2) Event in Progress—Implement this strategy if a high-output non-operational in-person
activity is currently in progress when the trigger has been identified. The Event Lead will
coordinate with Territory staff to determine the immediate course of demobilization.
35
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX C: HYGIENE GUIDE
When Should You Wash Your Hands?
“Destination to destination:” wash your hands any time you arrive or depart from a
location, including immediately after you arrive at an operation, and before you
leave. When you return to your place of residence, wash your hands again.
Wash Your Hands
Before
During
After
Animals, Animal Feed, and Animal Waste
(handling)
X
Bathroom Use
X
Coughing, Sneezing, or Nose-Blowing
X
Cuts and wounds (treating)
X
X
Diaper Changes or Potty Assistance
X
Eating
X
Food Preparation
X
X
X
Garbage
X
Pet Food (handling)
X
Visible Dirt
Wash hands properly with soap and water for
at least twenty seconds.
Vomiting and/or diarrhea (caring for the sick)
X
X
Other Hygiene Requirements
• Cover your mouth and nose with a tissue when you cough or sneeze. Put your used tissue
in a waste basket. If you don’t have a tissue, cough or sneeze into your upper sleeve, not
your hands.
• Don’t touch your face.
• Practice “physical distancing”– stand at least 6-feet away from others.
• Don’t shake hands or have other personal contact. When you meet people, wave or greet,
but do not touch.
• Minimize hand contact with high touch surfaces as much as possible.
• Frequently disinfect surfaces that people routinely touch.
• Wipe down any general areas with a disinfectant wipe.
36
SUPPLEMENTAL INFORMATION/APPENDICES
Alternatives to Surface Disinfectant32F
9
NOTE: Many commercial disinfection products may be used against COVID-19. If products are commercially available, they're probably most
convenient to use. Check the N list. The table below provides options if no commercial solution is available.
Product
How to Use
What to Use On
PPE
Details
Product Links
Bleach (0.1%
or 1,000 ppm
concentration
Apply with a sponge or cloth. Leave
solution on the surface for at least
1 minute.
Hard surfaces, goggles
and face shields
Typical household bleach is ~6%. Make
sure bleach isn't expired and read label to
make sure it's suitable for disinfection. To
make a bleach solution, mix:
5 tablespoons (1/3rd cup) bleach per gallon
of water
OR
4 teaspoons bleach per quart of water
For Example:
Clorox Germicidal
Bleach
Chlorine
Concentrate
Apply with a sponge or cloth. Leave
solution on the surface for at least
1 minute.
Hard surfaces, goggles
and face shields
Electro chlorinators are devices that use
electrolysis to turn table salt and water into
a chlorine solution. Dilute as needed for
disinfection.
Manufactures
include:
MSR Gear
WaterStep
H2go
Shockwave
Apply with a sponge, thoroughly
wet and allow to sit 10 minutes
before wiping or air drying
Hard surfaces, porous,
semi porous
TBD (see
comments)
Use in accordance with manufacturer’s
specifications. Can be irritating to skin.
Fiberlock Shockwave
RTU Disinfectant &
Cleaner
Product Fact Sheet
Rubbing
Alcohol (70%
or greater)
Spray or wipe on surface. Dry
surface thoroughly to avoid pooling
of liquids.
Hard surfaces,
electronics
It can irritate skin, so wear cleaning gloves
if possible. Note: This is not alcohol for
drinking, it can easily poison you!
Isopropyl Rubbing
Alcohol, 70% USP
9
Note: NEVER mix ammonia and bleach-based cleaners! The combination of ammonia and bleach produces dangerous chlorine gas, which in small doses can
cause irritation to the eyes, skin and respiratory tract. In large doses, it can kill.
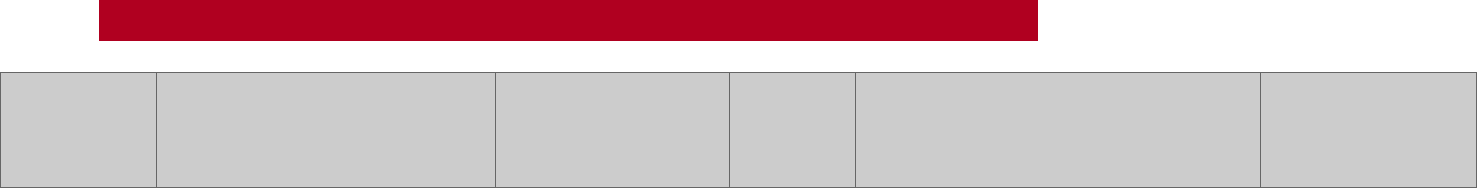
37
SUPPLEMENTAL INFORMATION/APPENDICES
Grain alcohol
(60% or
greater)
Spray or wipe on surface. Dry
surface thoroughly to avoid pooling
of liquids.
Hard surfaces,
electronics
You can use grain alcohol (liquor) to
disinfect. Make sure you have at least 120
proof (60%) and don't drink too much of it
during your disinfection process.
Try your local liquor
store (suggest
something like
Everclear)
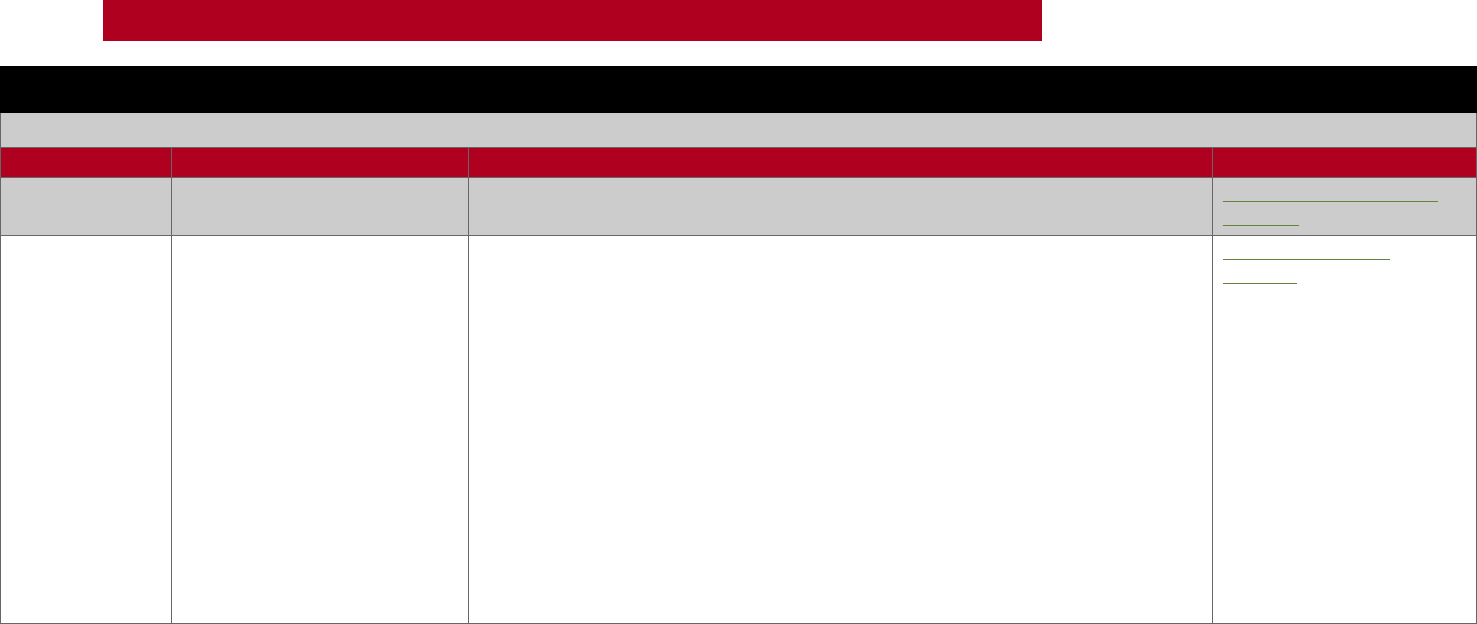
38
SUPPLEMENTAL INFORMATION/APPENDICES
Alternatives to Hand Sanitizer
Note: First alternative and preferred option is washing your hands with soap and water.
Product
How to Use
Comments
Product Links
Hand Sanitizer
from Distilleries
Liquid/gel applied to hands
In the product link are distilleries by state. Many are making hand sanitizer.
Distilleries Making Hand
Sanitizer
DIY Hand
Sanitizer
Liquid/gel applied to hands
Note:
Use DIY hand sanitizers when no other option is available. Avoid use on children
below the age of 12.
Hand sanitizer recipe:
• 3/4 cup of isopropyl or rubbing alcohol (99 percent)
• 1/4 cup of aloe vera gel
10 drops of essential oil (ex. lavender oil, or even lemon juice)
Directions:
Pour all ingredients into a bowl, ideally one with a pouring spout like a glass
measuring container. Mix with a spoon and then beat with a whisk to turn the
sanitizer into a gel. Pour the ingredients into an empty bottle for easy use, and
label it “hand sanitizer.”
NOTE: Only use homemade hand sanitizers in extreme situations when
handwashing isn’t available for the foreseeable future.
Don’t use homemade hand sanitizers on children’s skin as they may be more
prone to use them improperly, leading to a greater risk of injury.
How to make hand
sanitizer
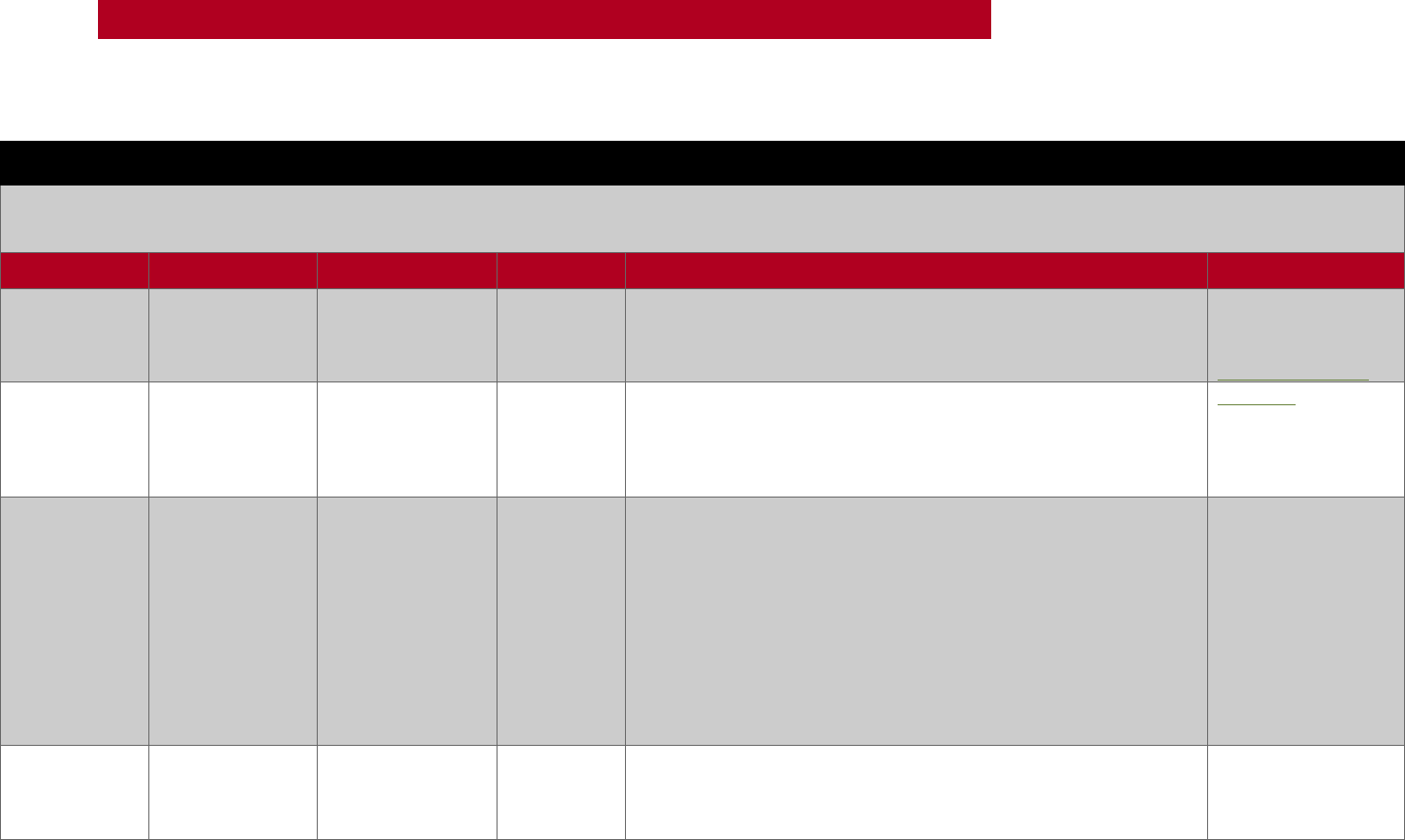
39
SUPPLEMENTAL INFORMATION/APPENDICES
Alternatives for Disinfecting PPE
Note: First alternative is to use and dispose of used PPE as recommended by manufacturer. Options are provided if we must reuse PPE (and/or it
was designed for reuse and standard disinfecting products are unavailable).
Product
How to Use
What to Use On
PPE
Comments
Product Links
Moist heat
Microwave
steam bag
Filtering Face
Respirators (e.g.,
N95)
Filtering
Face
Respirators
(e.g., N95)
Approximately 99.9% reduction in virus. For low risk applications
this is a good option. Note: if there are any metal parts to a filtering
face respirator, it may spark in the microwave and could be a fire
hazard.
There are multiple
options on the
market, for example:
Micro Steam Bags
Protex90
Various forms as
a POST
disinfection
treatment.
Cloth masks
Laundry
product may
be used for
cloth mask
treatment
Note: NOT for disinfection. This is a good alternative for low risk
environments where people are wearing cloth masks.
Protex90
Neutral
detergent/
cleaner wipe/
hospital
disinfectant
See comments
Eye protection/
face shields
Eye
protection/
face shields
Per CDC: While wearing gloves, carefully wipe the inside, followed
by the outside of the face shield or goggles using a clean cloth
saturated with neutral detergent solution or cleaner wipe.
Carefully wipe the outside of the face shield or goggles using a
wipe or clean cloth saturated with EPA-registered hospital
disinfectant solution (see list N).
Wipe the outside of face shield or goggles with clean water or
alcohol to remove residue.
Fully dry (air dry or use clean absorbent towels).
NA
Bleach
solution
See comments
Eye protection/
face shields
Eye
protection/
face shields
• Dip 3 times in 0.5% chlorine
• Soak in 0.05% chlorine for 30 minutes
• Rinse with clean water
• Hang to dry
NA
40
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX D: TRAVEL GUIDE
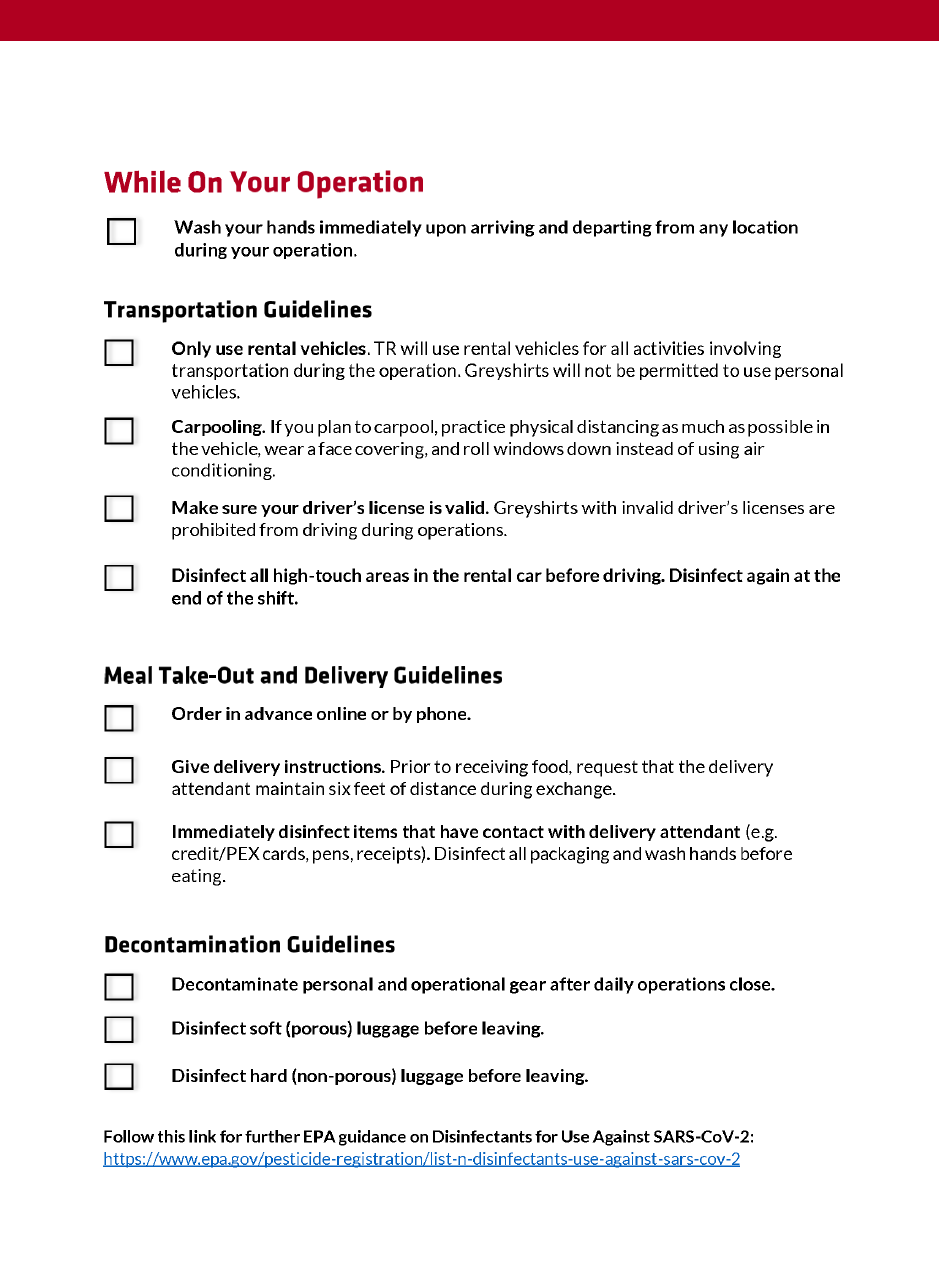
41
SUPPLEMENTAL INFORMATION/APPENDICES

43
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX E: CORE OPS COVID-19 SAFETY
PROTOCOLS
OVERVIEW
Pre-Work Disinfecting Guidelines
In addition to the standard worksite preparation and decontamination protocols in the Core Ops
Manual, Greyshirts will take the following steps to prevent the spread of COVID-19 at worksites:
• Disinfect at the beginning of each work shift
• Disinfect all high-touch surfaces (see examples below)
o Doorknobs, light switches, countertops, faucets, etc.
o Use 10 to 15 percent bleach solution, or other approved disinfectant cleaner,
before starting work
Post-Work Disinfecting Guidelines
Greyshirts will disinfect the following items at the end of each work shift:
• High-touch surfaces (e.g., doorknobs, light switches, countertops, faucets)
• Equipment, materials, and tools
Use bleach solution or other approved and appropriate disinfecting cleaner, for surfaces. See TR
MINIMUM PPE REQUIREMENTS for further guidance.
Tools and Equipment
Greyshirts will take turns accessing tools and materials to maintain physical distancing.
Greyshirts should avoid exchanging tools, if possible, and passing equipment or materials.
Disinfect each tool before it will be used by someone else or placed back in the trailer. Refer to
the Vehicle and Equipment Decontamination Guide in Figure 5. Vehicle and Equipment
Decontamination Guide.
Performing Work
While some situations may require additional hands and/or greater proximity, Greyshirts will
adhere to the following guidelines to the extent practicable:
• Physical distancing (6 feet of space) will be maintained while performing work tasks,
including working in different rooms
• Work tasks should be performed individually
• Avoid more than two people in a room at a time, except when necessary to complete a
joint work task
Port-O-Johns and Handwashing Facilities

44
SUPPLEMENTAL INFORMATION/APPENDICES
When using Port-O-Johns, Greyshirts will adhere to TR’s Hygiene Guidelines (See APPENDIX C:
HYGIENE GUIDE) and wash hands thoroughly after each use. Greyshirts should also limit
touching surfaces and door handles. If handwashing facilities are not available, see the
instructions on how Building a Handwashing Station in Figure 16. Building a Handwashing
Station.
The Team Leader or assigned Greyshirt will disinfect exterior handles of Port-O-Johns in the
morning when unlocking. They will disinfect high-touch surfaces on the Port-O-John (e.g., door
handles, toilet paper holster, toilet seats) and handwashing facilities at a minimum twice a day—
once before lunch and once at the end of shift. The Team Leader or assigned Greyshirt will check
daily to ensure Port-O-Johns are adequately stocked and will procure new materials as
necessary. The Port-O-John vendor will clean and re-stock these facilities weekly.
The Team Leader, or assigned Greyshirt, will secure Port-O-Johns each night. If surgical masks
are unavailable, follow the instructions below for a no-sew cloth face covering37F
10
. Materials
needed:
• Bandana (or square cotton cloth approximately 20”x20”)
• Coffee filter
• Rubber bands (or hair ties)
• Scissors (if cutting your own cloth)
10
Centers for Disease Control and Prevention (2020, June 28). Use of Cloth Face Coverings to Help Slow the Spread
of COVID-19. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-
coverings.html
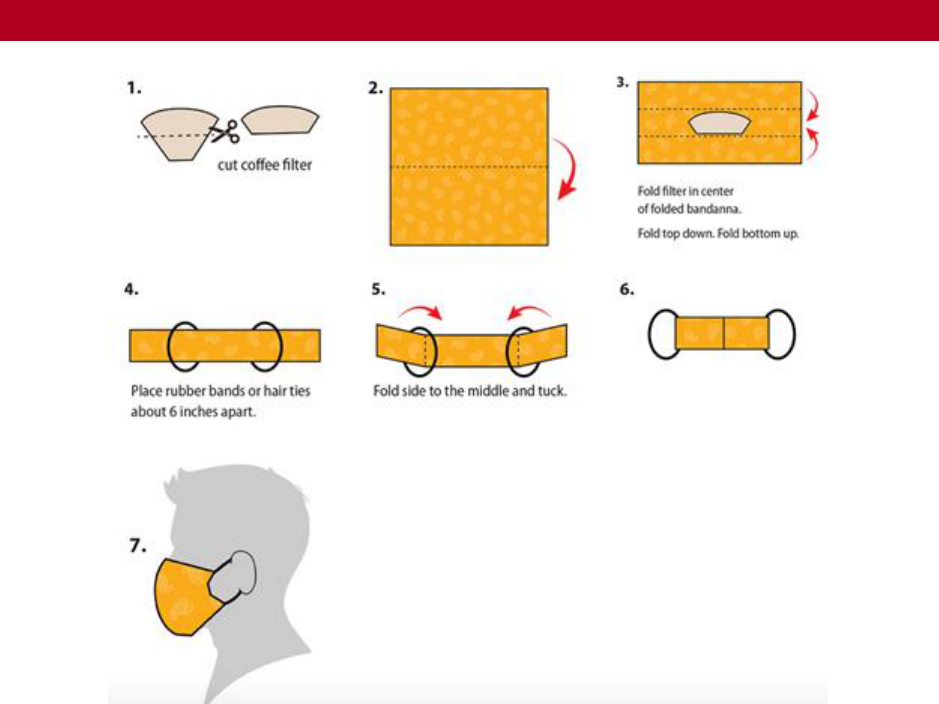
45
SUPPLEMENTAL INFORMATION/APPENDICES
No-Sew Cloth Face Covering
• Mask users should take care not to touch their eyes, nose, and mouth when removing
their face covering and wash hands immediately after removing.
• Replace the coffee filter daily at minimum or as needed (e.g., if coffee filter becomes wet
or soiled).
• Cloth face coverings should be washed routinely after use in a washing machine with hot
water and detergent.
46
SUPPLEMENTAL INFORMATION/APPENDICES
CORE OPS DAILY COVID-19 CHECKLIST
Date:
Location:
Person completing checklist:
ITEM
TIME
OPS MANUAL
SECTION
Y / N
DAILY SAFETY BRIEF/COVID-
19 UPDATE
START OF DAY
APPENDIX B
REQUIRED PPE/NON-
MEDICAL FACE COVERINGS
PRESENT
START OF DAY
1. SAFETY
DISINFECT WORK AREA
BEFORE WORK BEGINS
START OF DAY
APPENDIX I
DISINFECT PORT-A-JOHN &
HANDWASH STATION
BEFORE LUNCH &
END OF DAY
APPENDIX I
DISINFECTANT AND
HYGIENE SUPPLIES PRESENT
START OF DAY
APPENDIX C
GREYSHIRTS FOLLOWING
TOOL HANDLING &
DISINFECTANT GUIDELINES
THROUGHOUT
APPENDIX I
GREYSHIRTS FOLLOWING
TECHNOLOGY AND VEHICLE
DISINFECTANT GUIDELINES
THROUGHOUT
APPENDIX B
GREYSHIRTS FOLLOWING
HYGIENE GUIDELINES
THROUGHOUT
APPENDIX C
CLEAN/DISINFECT WORK
AREAS
END OF DAY & END
OF OP
APPENDIX I
CLEAN/DISINFECT
OPERATIONAL GEAR &
TOOLS
END OF DAY
3.1.1 TR FACILITIES
AND EQUIPMENT
SECURE PORT-A-JOHN &
HANDWASH STATION
END OF DAY
APPENDIX I
DESCRIBE ANY COVID-19-RELATED RISKS OR CONCERNS DURING THIS SHIFT:
APPENDIX F: JOB AIDS
47
SUPPLEMENTAL INFORMATION/APPENDICES
For Printing and Display: Job aids are available in printable size and resolution by clicking on the
blue link in the caption.
This COVID-19 job aid should be included in daily safety briefings.
Daily Hygiene Safety Briefing
1. FACILITIES
Tell team members the locations of the following:
Bathrooms and hand washing stations
Emergency exits
Posted Health and Safety information (ex. hand hygiene poster)
Food (including mealtimes if applicable)
2. HYGIENE & SANITATION
Tell team members the following:
Wash your hands with soap and water for at least 20 seconds after eating or drinking,
touching one’s face, using the bathroom, or any other activity that may contaminate one’s
hands.
Non-medical face covering is required at all times.
Team members should stay 6 feet apart at all times.
If using equipment or vehicles, be sure to sanitize them per protocol.
Assign one team member to clean high-touch surfaces (e.g., doorknobs, light switches) with
disinfecting wipes throughout the shift.
3. COVID-19 INFORMATION
Tell team members the following:
COVID-19 symptoms include, but are not limited to: cough, shortness of breath, or difficulty
breathing. Symptoms may also include at least two of the following:
• Fever
• Chills
• Fatigue
• Muscle or body aches
• Nausea or vomiting
• Headache
• Sore throat
• A New loss of taste or smell
• Congestion or runny nose
• Diarrhea
If you experience any of these symptoms, or any other signs of illness at any time during
your deployment, immediately report to your supervisor.
Figure 2. Daily Hygiene Safety Briefing

50
FIELD GUIDES
Vehicle Rideshare Checklist
Vehicle Rideshare Checklist
In vehicles with more than one occupant, the front row passenger will serve as the vehicle safety
officer. This Greyshirt will have responsibility for ensuring that COVID-19 mitigation practices are
adhered to include proper supply of PPE and sanitization materials, prescreening of passengers,
cleaning of the vehicle, physical distancing, and proper environmental practices.
The following checklist serves to ensure every Greyshirt does their part to support the safety of our
Greyshirts and survivors we serve.
Wear PPE/face coverings.
Maintain proper ventilation in the vehicle.
Ensure proper vehicle sanitization and passenger preparations.
Universal Risk Mitigation Strategies
Mitigation Strategy
More Information
Ensure the car has been disinfected prior to
and following use.
Pay close attention to frequently touched surfaces like
door handles, steering wheels, ignition, operating buttons,
seat buckles, keys, etc. Wear disposable gloves when
cleaning and only use them once. Disinfectants should be
EPA-registered antimicrobial, diluted household bleach
according to manufacturer instructions, or alcohol
solutions with at least 70% alcohol.
Carry hand sanitizer and tissues.
Consider having appropriate disinfectant tools on hand
including cleaning and disinfectant spray, or disposable
wipes and a small trash bag for each vehicle.
Wash your hands before and after entering
the vehicle with soap and water for at least
30 seconds.
Use an alcohol-based hand sanitizer that contains at least
60% alcohol if soap and water are not available.
Avoid touching your face with unwashed
hands.
Specifically avoid touching your eyes, nose, or mouth.
Cover your mouth and nose with a tissue
when you cough or sneeze.
Throw the tissue in the trash and wash your hands.
Vehicle and Equipment Decontamination Guide
Gloves should be worn when cleaning and decontaminating surfaces and equipment. If gloves
are not available, hand hygiene (preferably hand washing but hand sanitizer is also acceptable)
must be performed after cleaning is completed.
51
FIELD GUIDES
What are you
disinfecting?
Equipment
Actions
Hardware, PCs,
Monitors or
Display Screens,
Docking
Stations,
Keyboards, and
Mice
• Disinfecting
wipe, or
• Microfiber cloth,
or
• Paper towel
moistened with
a mixture of
70% isopropyl
alcohol / 30%
water.
***The cloth should
be damp, but not
dripping wet.
Remove excess
moisture if the cloth
is wet before wiping
the product.***
1. Turn off the device you plan to clean and
disconnect AC power. Also, to the extent
practicable, remove batteries from items
like wireless keyboards. Never clean a
product while it is powered on or plugged
in.
2. Disconnect external devices.
3. Never spray liquids directly on the product.
4. Gently wipe the moistened cloth on the
surfaces to be cleaned. Do not allow
moisture to drip into areas like keyboards,
display panels, etc. Moisture entering the
inside of an electronic product can cause
damage. Excessive wiping could potentially
damage some surfaces.
5. When cleaning a display screen, carefully
wipe in one direction moving from the top
of the display to the bottom.
6. Surfaces must be completely air dried
before turning the device on after cleaning.
No moisture should be visible on the
surfaces of the product before it is
powered on or plugged in.
7. After cleaning or disinfecting a glass
surface, it may be cleaned again using a
glass cleaner designed for display surfaces
and following directions for that specific
cleaner. Avoid glass cleaning products
containing ammonia.
8. Discard disposable gloves used after each
cleaning. Clean hands immediately after
gloves are removed and disposed.
52
FIELD GUIDES
What are you
disinfecting?
Equipment
Actions
Vehicles and
Equipment
after Contact
with or
Transporting a
Confirmed
COVID-19
Patient
• Disposable gown
and gloves
• Face shield or
facemask and
goggles will also
be worn if
splashes or
sprays during
cleaning are
anticipated
• Disinfectants for
Use Against
SARS-CoV-2 on
the EPA website
1. After transporting the patient, leave the
doors of the transport vehicle open to
allow for sufficient air changes to remove
potentially infectious particles. The time to
admit the patient to the receiving facility
should provide sufficient air changes.
2. Ensure environmental cleaning and
disinfection procedures are followed
consistently and correctly, to include the
provision of adequate ventilation when
chemicals are in use. Keep doors open
when cleaning the vehicle.
3. Clean and disinfect the vehicle in
accordance with standard operating
guidance procedures. All surfaces that may
have come in contact with the patient, or
materials contaminated during patient
assessment, will be thoroughly cleaned and
disinfected using an EPA-registered
hospital-grade disinfectant in accordance
with the product label.
4. Clean and disinfect reusable patient-care
equipment before using on another patient
and according to manufacturer’s
instructions.
5. Follow standard operating guidance for the
containment and disposal of used PPE and
regulated medical waste.
Figure 5. Vehicle and Equipment Decontamination Guide
54
FIELD GUIDES
Mix and Use of Disinfecting Diluted Bleach Solution
Mix
• 5 tablespoons of bleach per gallon of water
• 4 teaspoons of bleach per quart of water24F
11
Use
1. Open windows and doors.
2. If surfaces are visibly dirty, clean them first with detergent or soap.
3. Apply the solution to the surface to be disinfected, leave for 1 minute.
4. Let the surface air dry.
5. When finished, follow hand-washing protocol immediately.
Do:
Use on hard non-porous surfaces (e.g., glass, plastic, varnished wood).
Mix solution outside or in a well-ventilated area.
Wear PPE (e.g., eye protection, gloves, face shield) when handling bleach.
Add bleach to measured water to prevent splashes.
Check the bleach’s expiration date.
Store in a cool location out of direct sunlight and away from metal.
Don’t:
Use on porous surfaces (e.g., untreated wood, cardboard, fabric).
Mix with ammonia or other cleaning product.
Eat, drink, or smoke during or after handling bleach.
Figure 7. Mix and Use of Disinfecting Diluted Bleach Solution
11
Centers for Disease Control and Prevention (2020, July 10). Cleaning and Disinfection for Households. Retrieved
from https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cleaning-disinfection.html
55
FIELD GUIDES
Alternative PPE
Required PPE
PPE Descriptions/
Specifications
Acceptable Alternative(s)25F
12
NOTE: Ensure all reused PPE is disinfected between uses per CDC guidelines.
LOW RISK
There are currently no alternatives to low risk PPE.
MEDIUM RISK
Gloves
Use for handling potentially
contaminated supplies. Ideally use
waterproof disposable gloves (e.g.,
medical gloves) and dispose of
them after each incidence of
touching potentially contaminated
material.
Reusable waterproof gloves (e.g.,
cleaning gloves) are acceptable;
however, those gloves must be
dedicated for cleaning and disinfection
of potential COVID-19 exposed
surfaces and not used for other
purposes.
Isolation Gown
Use fluid-resistant and
impermeable protective clothing
options (isolation gowns and
surgical gowns).
• Hospital grade
reusable/washable isolation
gown
• Coveralls (such as Tyvek)
HIGH RISK
Gloves
Medical gloves
• NA
Isolation Gown
Use fluid-resistant and
impermeable protective clothing
options (isolation gowns and
surgical gowns).
• Hospital grade
reusable/washable isolation
gown
• Coveralls (such as Tyvek)
• Gowns or coveralls conforming
to international standards
(Note: Situations with
moderate-to-high amounts of
body fluids)
Bouffant Cap
A loose disposable cap, so called
because of its puffy shape, typically
secured around the head with an
elastic. Required for patient
contact.
For non-patient contact, a cloth
bouffant cap is acceptable. Also, fabric
covering (such as a bandana or
headscarf, as long as it covers all hair)
Face shield
(including eye
protection)
A face shield is a mask, typically
made of clear plastic, that protects
the mucous membranes of the
eyes, nose, and mouth during
patient-care procedures and
activities that carry the risk of
Reusable face shields or extended use
of a disposable face shield that can be
properly disinfected
12
Centers for Disease Control and Prevention. (2020, July 16). Optimizing Supply of PPE and Other Equipment
during Shortages. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html
56
FIELD GUIDES
Required PPE
PPE Descriptions/
Specifications
Acceptable Alternative(s)25F
12
generating splashes of blood, body
fluids, excretions, or secretions.
N95 Mask
Disposable N95 filtering facepiece
respirators
• Powered Air Purifying
Respirators (PAPRs) or full-face
elastomeric respirators which
have built-in eye protection
(and for which proper fit
test/training have occurred)
• Substitution of other NIOSH-
certified respirators (e.g., R95,
P100), including elastomeric
half facepiece respirators (if
initial fit test has been
conducted)
• Use of certain (identified by
CDC by make/model) N95
masks beyond their stated
shelf life
• Use of respirators approved
under international standards
similar to NIOSH-approved
respirators
Figure 8. Alternative PPE Table
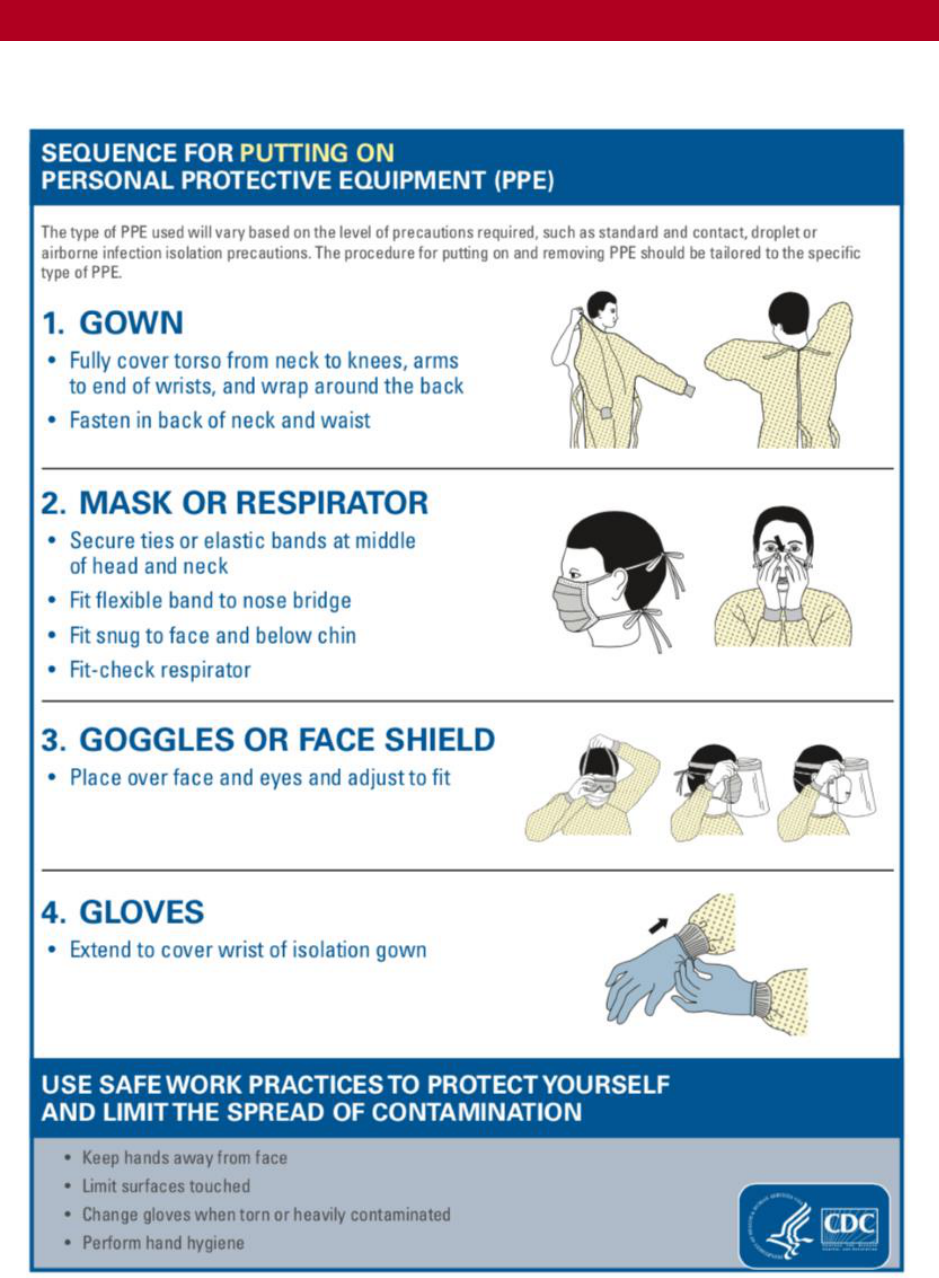
57
FIELD GUIDES
PPE Donning and Doffing Guide
Follow the instructions below when donning PPE:
Figure 9. Sequence for Putting On PPE

58
FIELD GUIDES
Follow the instructions below when doffing PPE:
Figure 10. How to Safely Remove PPE
59
FIELD GUIDES
PPE Trained Observer
A PPE Trained Observer is an individual whose sole responsibility is to guide responders as they
don and doff PPE. The role of the Trained Observer will be fulfilled at TR high COVID-19
exposure risk operations.
The Trained Observer will verbally assist the responders with donning and doffing PPE piece-by-
piece, according to the donning and doffing checklists, to ensure proper protection and minimize
contamination in the process.
Prior to serving in this role, Greyshirts should complete the PPE TRAINED OBSERVER FLASH
LEARNING.
PPE Trained Observer Checklist
As a PPE Trained Observer, it is your responsibility to lead and protect your team members
through the following PPE donning and doffing procedures. The following checklists are
appropriate for operations with high exposure risk requiring the use of full PPE (bouffant cap,
face shield, respirator, isolation gown, and two pairs of gloves). If there are any variations in the
PPE utilized at a job site, the checklist should be modified to reflect such changes to best guide
the Trained Observer and the responders.
Preparation
Prior to assisting with PPE donning and doffing, conduct the following:
Confirm enough of each PPE item is available
Confirm appropriate decontamination area set up including biohazard trash bins
Confirm your own safety by donning PPE (e.g., gloves) to allow you to safely
observe and assist as needed
Undergo a pre-brief with each team member
• Together identify the equipment the individual requires; ensure they are
aware of its location and it is both present and of good quality
• Confirm team member has been respirator fit-tested and knows their mask
size and suitable mask type
Donning
Verbally direct and observe each team member undergoing the following procedures. As
team members don equipment, ensure appropriate seals and fit of all gear and call out any
rips or damages. Encourage slow and purposeful movement throughout the donning process
to prevent contamination.
Wash hands with soap and water for a minimum of 20 seconds and dry thoroughly
(if hand washing station not available, hand sanitizer is appropriate)
Don first pair of gloves
Don isolation gown (observer may help with tying into gown as needed)
Tape gown sleeve onto base layer glove to form a seal (suggested)
Or
Optional Alternative: (If gown can withstand thumb poke) Make a thumb hole in
each gown sleeve and secure gloved hand in place
60
FIELD GUIDES
Use hand sanitizer to clean gloved hands
Put on respirator mask top strap first, taking care to not touch the inside of the
respirator (and outside of the respirator if mask is being reused)
Place bottom strap of the respirator in place and ensure proper seal (visualize seal
of respirator onto face and nosepiece. Point out to team members any apparent
loose spaces around their respirator that would prevent effective filtration or
damages that warrant grabbing a new respirator)
Clean gloved hands with hand sanitizer
Put on bouffant cap or surgical cap
Clean gloved hands with hand sanitizer
Put on face shield
Clean gloved hands with hand sanitizer
Don second pair of gloves
Turn in a circle with the observer reviewing and communicating any gaps or PPE
damage
Final check: Each participant confirms all equipment is appropriately placed and
fitted
Doffing
As team members remove equipment, ensure they do not accidentally touch exposed skin. Be
vigilant and remind team members they are not decontaminated and need to continue to not
touch exposed skin. Be careful about placement of contaminated gear into biohazard trash or
designated storage for reuse to prevent transfer of particles on equipment.
If any breaches occur, that step will be completed followed with conducting disinfection of
the exposed area and an additional check for any other exposures.
Upon team member communicating they are ready to exit the hot zone, advise
team member to wait for your confirmation to exit
When you are ready, communicate to the team member to enter warm zone
Remove and dispose of outer pair of gloves into biohazard trash bin
Cut ties to back of isolation gown
Remove tape used for base layer gloves if applied previously (assist if necessary and
ensure even if tape is removed that base layer gloves remain on)
Remove gown slowly with minimal disruption and turn it inside out with
removal
Dispose of isolation gown in biohazard trash bin
Clean gloved hands with hand sanitizer
Remove face shield and drop it into the decon bucket (i.e diluted bleach solution if
being reused or into the biohazard trash bin if not being reused
Clean gloved hands with hand sanitizer
If face shield is being reused, Trained Observer will retrieve it from the decon
bucket and take it over to the designated clean face shield storage area

61
FIELD GUIDES
Remove bouffant cap and dispose in biohazard trash (if using surgical cap, remove
and place in receptacle until it can be laundered)
Clean gloved hands with hand sanitizer
Remove the bottom strap of the respirator mask and then the top strap, taking care
not to touch the inside of the respirator
If respirators are being reused, carefully place them into a brown paper bag labeled
with responder name (if not being reused, drop respirator into biohazard trash bin)
Remove base layer of gloves
Wash hands and all areas below the elbows with soap and water for a minimum of
20 seconds and dry thoroughly
Figure 11. PPE Trained Observer Checklist
Storage and Reuse of N95 Respirator Masks and Face Shields
Keep used respirators in a clean, breathable paper bag between uses by following the steps
below:
1. Perform hand hygiene and don a clean pair of gloves.
2. Obtain clean paper bag and write name and date on the outside of the bag.
3. Open the paper bag.
4. Remove the N95 mask by only touching the straps or the outermost rim of the N95
mask.
5. Place N95 mask in the labeled paper bag, handling only the straps or the outermost rim
of the N95 mask.
6. Remove gloves.
7. Perform hand hygiene.
8. Close bag by folding over itself two times. Take care to not fold, bend or crush the N95
mask inside the bag. Place one N95 respirator per paper bag.
9. Store bags in the designated area in the designated warm zone. Ensure bag is 3 feet or
more from a sink or potential splash zone.
10. Perform hand hygiene prior to leaving warm zone/doffing area.
When it is time to reuse the stored N95 respirator, follow the steps below:
1. Perform hand hygiene and don a clean pair of gloves.
2. Remove your previously used N95 mask from the labeled paper bag by only touching
the straps or the outermost rim of the N95 mask. If contact with the front or inside
surface of the mask occurs, place N95 mask on top of bag, remove gloves, perform
hand hygiene and put on new pair of gloves.
3. Place N95 mask on face by only touching the straps and the outermost rim of the N95
mask.
4. Perform seal check by only by touching outermost rim of N95 mask
a. To perform a negative/positive seal check26F
13
:
13
Nebraska Medicine (2020, April 20). Nebraska Medicine COVID-19 PPE Guidance: Extended Use and Reuse of
Facemasks, Respirators and Protective Eyewear for Healthcare Personnel. Retrieved from
https://www.nebraskamed.com/sites/default/files/documents/covid-19/COVID-Extended-Use-Reuse-of-PPE-and-
N95.pdf
62
FIELD GUIDES
i. No air should be felt around the perimeter while blowing out. If you feel
air coming out it is not a tight seal.
ii. When taking a small breath in, the mask should pucker in slightly. If it
does not, it is not a tight seal.
iii. When breathing out you should feel the respirator expand slightly. If it
does not, it is not a tight seal.
iv. If you cannot achieve a tight seal, the respirator must be discarded.
5. Throw the paper bag away. Do not reuse paper bag.
6. Remove gloves and perform hand hygiene.
Steps for reprocessing face shields and goggles:
1. While wearing gloves, carefully wipe the inside followed by the outside of the face
shield or goggles using a clean cloth saturated with neutral detergent solution of
cleaner wipe.
2. Carefully wipe the outside of the face shield or goggles using a wipe or clean cloth
saturated with EPA-registered hospital disinfectant solution.
3. Wipe the outside of the face shield or goggles with clean water or alcohol to remove
residue.
4. Fully dry (air dry or use clean absorbent towels).
5. Remove gloves and perform hand hygiene.
Figure 12. Use and Reuse of N95 Respirator Masks and Face Shields
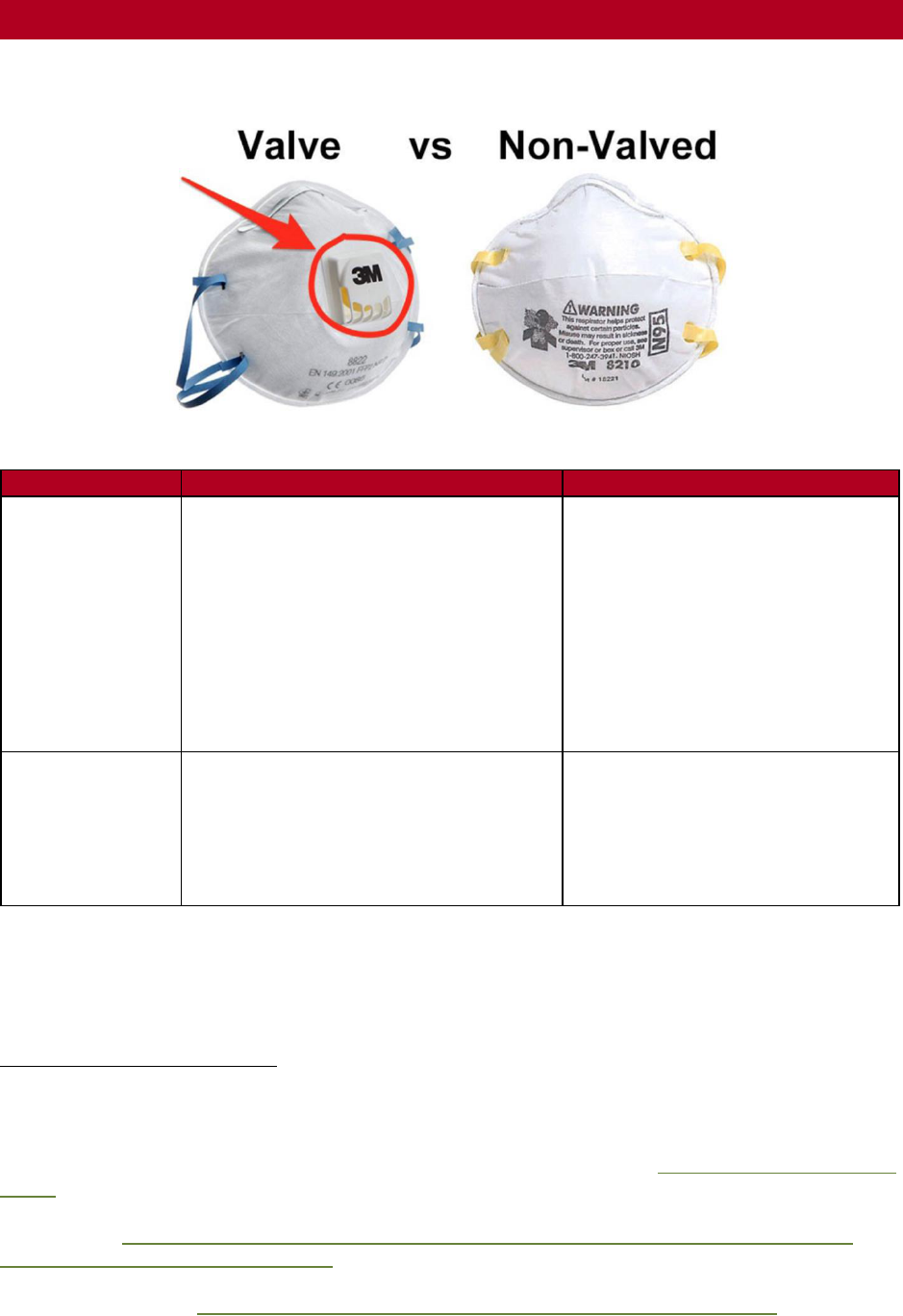
64
FIELD GUIDES
Protection Differences Between Valved and Non-Valved N95 Respirators
Figure 14. N95 Respirators with Valves/Without Valves
14
N95 Valve Respirator
N95 Respirator without Valve
Purpose
Respirators with exhalation valves were
developed for ease of breathing and less
moisture build-up for construction site
workers.
Valve respirators provide one-way
protection by filtering the air inhaled by
the wearer. However, this respirator
does not filter the air exhaled by the
wearer as it leaves the mask through the
valve.
Worn primarily in healthcare
settings to reduce the wearer’s
exposure to airborne particles, from
small particle aerosols to large
droplets28F
15
.
Appropriate for
COVID-19?
The use of a valve respirator does not
effectively mitigate COVID-19 exposure
risk to the individuals around the wearer
who are not wearing respiratory
protection.
Respirators without valves filter
breath as it leaves the mask. Both
the wearer and those around them
are effectively protected from
microorganisms, body fluids, and
particulate material29F
16
.
14
Fast Life Hacks (2020, July 12). N95 vs FFP3 & FFP2 Masks - what's the difference? https://fastlifehacks.com/n95-
vs-ffp/
15
U.S. Food and Drug Administration. (2020, August 20). N95 Respirators, Surgical Masks, and Face Masks.
Retrieved from https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-
respirators-and-surgical-masks-face-masks
16
Centers for Disease Control and Prevention (2020, August 8). Personal Protective Equipment: Questions and
Answers. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirator-use-faq.html
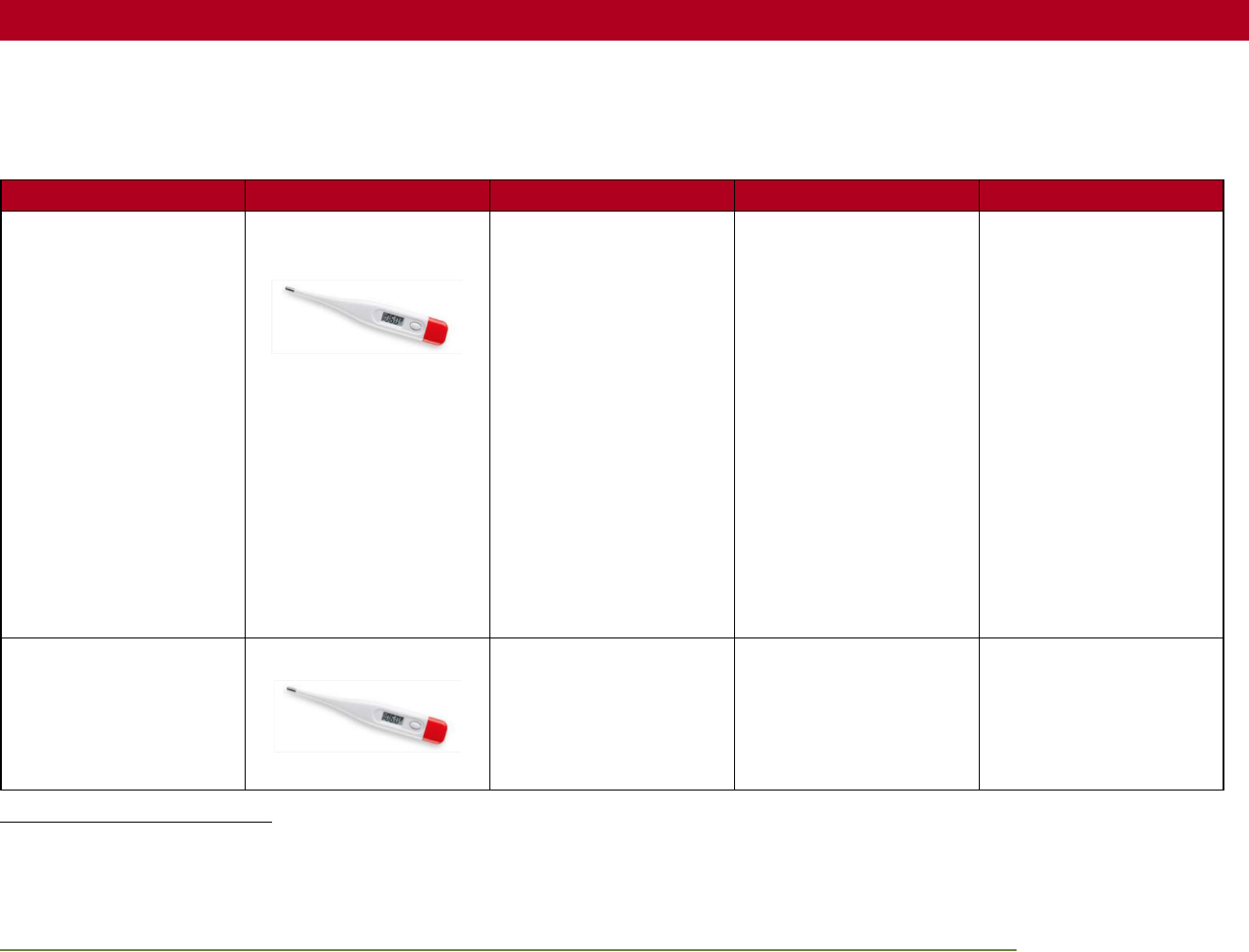
65
SUPPLEMENTAL INFORMATION/APPENDICES
Recommended Temperature Check Options
Temperature takers will keep as much distance from the Greyshirt as possible, wash their hands with soap and water or use alcohol-
based hand sanitizer (at least 60% alcohol) regularly, and use gloves if available30F
17
.
Option
Tool
Method
Cleaning
Notes
Oral temperature
Digital thermometer with
probe cover
1. Thoroughly clean
thermometer
2. Place new probe
cover
3. Place tip of
thermometer under
the tongue
4. Close mouth
5. Keep in place for 1
minute, or until
thermometer signals
6. Remove thermometer
and check
temperature reading
7. Remove probe cover
8. Thoroughly clean
thermometer
Use alcohol wipes or
isopropyl alcohol to
thoroughly wipe down the
entire thermometer after
each use.
Note: If probe covers are
not available, oral
temperature option is not
recommended.
Eating or drinking liquids
and solids within 30
minutes can cause
inaccurate readings.
Axillary (armpit)
temperature
Digital thermometer
1. Thoroughly clean
thermometer
2. Place thermometer tip
at the center of the
armpit
Use alcohol wipes or
isopropyl alcohol to
thoroughly wipe down the
entire thermometer after
each use.
17
Centers for Disease Control and Prevention. (2020, August 3). Screening Clients for COVID-19 at Homeless Shelters or Encampments. Retrieved from
https://www.cdc.gov/coronavirus/2019-ncov/community/homeless-shelters/screening-clients-respiratory-infection-symptoms.html
66
SUPPLEMENTAL INFORMATION/APPENDICES
Option
Tool
Method
Cleaning
Notes
3. Tuck arm against body
to keep thermometer
in place
4. Keep in place for 1
minute, or until
thermometer signals
5. Remove thermometer
and check
temperature reading
6. Thoroughly clean
thermometer
Temporal (forehead)
temperature
Digital temporal
thermometer
1. Thoroughly clean
thermometer
2. Gently sweep the
thermometer across
the forehead to the
temple
3. Remove the
thermometer and
check temperature
reading
4. Thoroughly clean
thermometer
Clean the thermometer
with an alcohol wipe (or
isopropyl alcohol on a
cotton swab) between
each use. You can reuse
the same wipe as long as
it remains wet.
17
Note: Ambient
temperature, sunlight, and
wind can cause inaccurate
readings with a forehead
(temporal) thermometer
when used outdoors31F
18
.
Temporal (forehead)
temperature
Infrared non-contact
thermometer
1. Thoroughly clean
thermometer
2. Power on the
thermometer gun and
If you did not touch the
person being screened,
you do not need to wipe
Note: Ambient
temperature, sunlight, and
wind can cause inaccurate
18
San Francisco Department of Public Health. (2020, May 26). Interim Guidance: Measuring Temperatures when Screening for COVID-19 Symptoms. Retrieved
from https://www.sfcdcp.org/wp-content/uploads/2020/05/COVID19-Temperature-Measurement-UPDATE-05.26.2020.pdf
67
SUPPLEMENTAL INFORMATION/APPENDICES
Option
Tool
Method
Cleaning
Notes
hold the trigger until
the laser appears
3. Once the laser is
emitted from the
thermometer, hold the
sensing area
perpendicular to the
forehead and instruct
the person to remain
still during
measurement
4. Continue holding
down the
thermometer’s trigger
while it reads the
temperature
5. Once the temperature
has been read, the
thermometer will
display reading on the
screen
6. Thoroughly clean
thermometer
down the thermometer or
change gloves between
each check.
Use alcohol wipes or
isopropyl alcohol to
thoroughly wipe down the
thermometer at the
beginning and end of the
temperature check.
readings with an infrared
thermometer when used
outdoors
18
.
Tympanic (ear)
temperature
Tympanic thermometer
1. Thoroughly clean
thermometer
2. Gently tug ear up and
back to straighten the
ear canal
3. Insert tympanic
thermometer tip
4. Keep in place for 1
minute, or until
thermometer signals
Use alcohol wipes or
isopropyl alcohol to
thoroughly wipe down the
thermometer after each
use.
Note: Temperature
reading may not be
accurate if thermometer is
not correctly placed in the
ear.

68
SUPPLEMENTAL INFORMATION/APPENDICES
Option
Tool
Method
Cleaning
Notes
5. Remove thermometer
and check
temperature reading
6. Thoroughly clean
thermometer
If performing a temperature check on multiple individuals, ensure a clean pair of gloves is worn and the thermometer has been
thoroughly cleaned between each check. If non-contact thermometers are used, and you did not have physical contact with an
individual, you do not need to change gloves before the next check. Clean and disinfect thermometers according to manufacturer’s
instructions.
Figure 15. Temperature Check Options
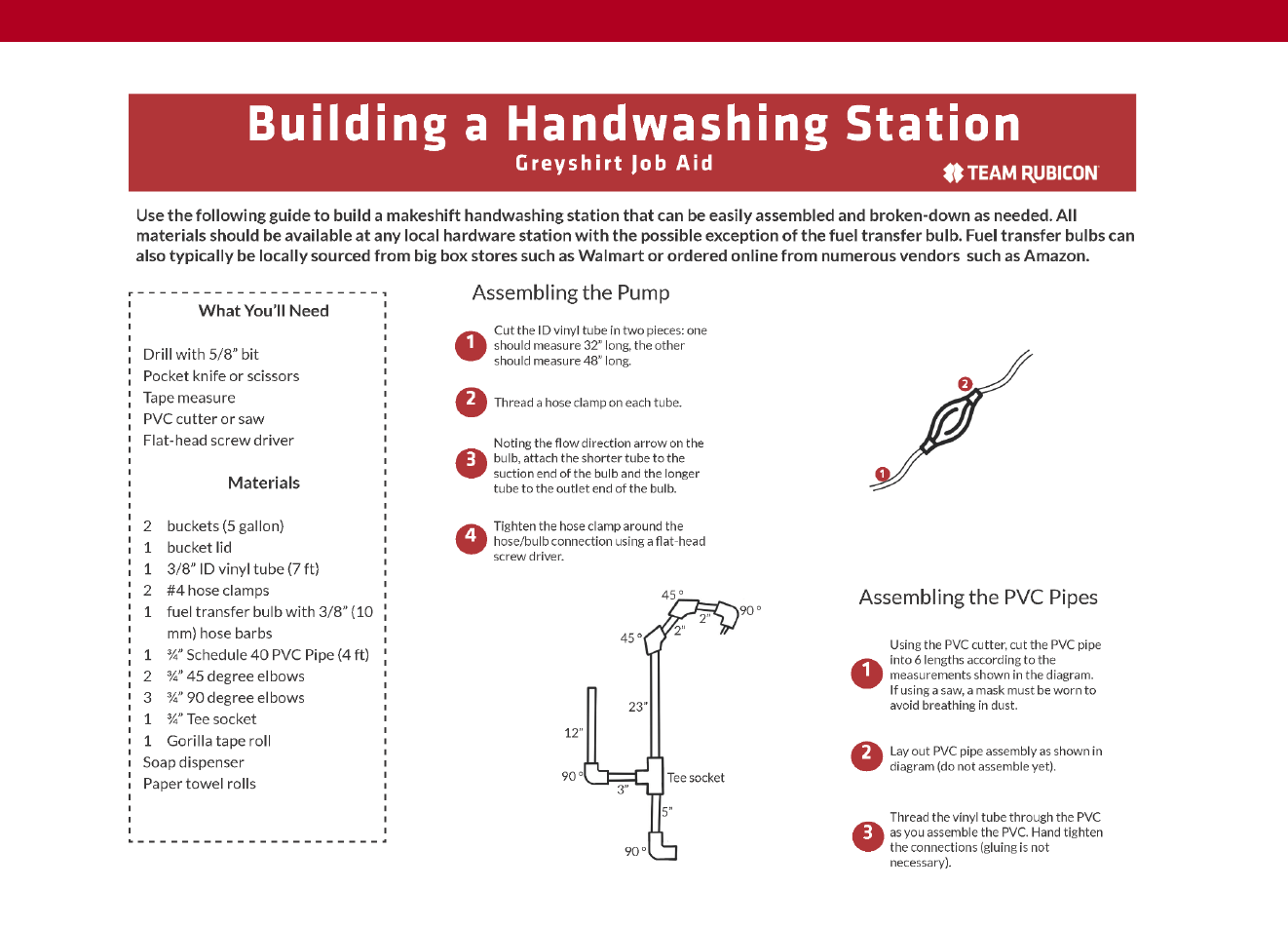
69
SUPPLEMENTAL INFORMATION/APPENDICES
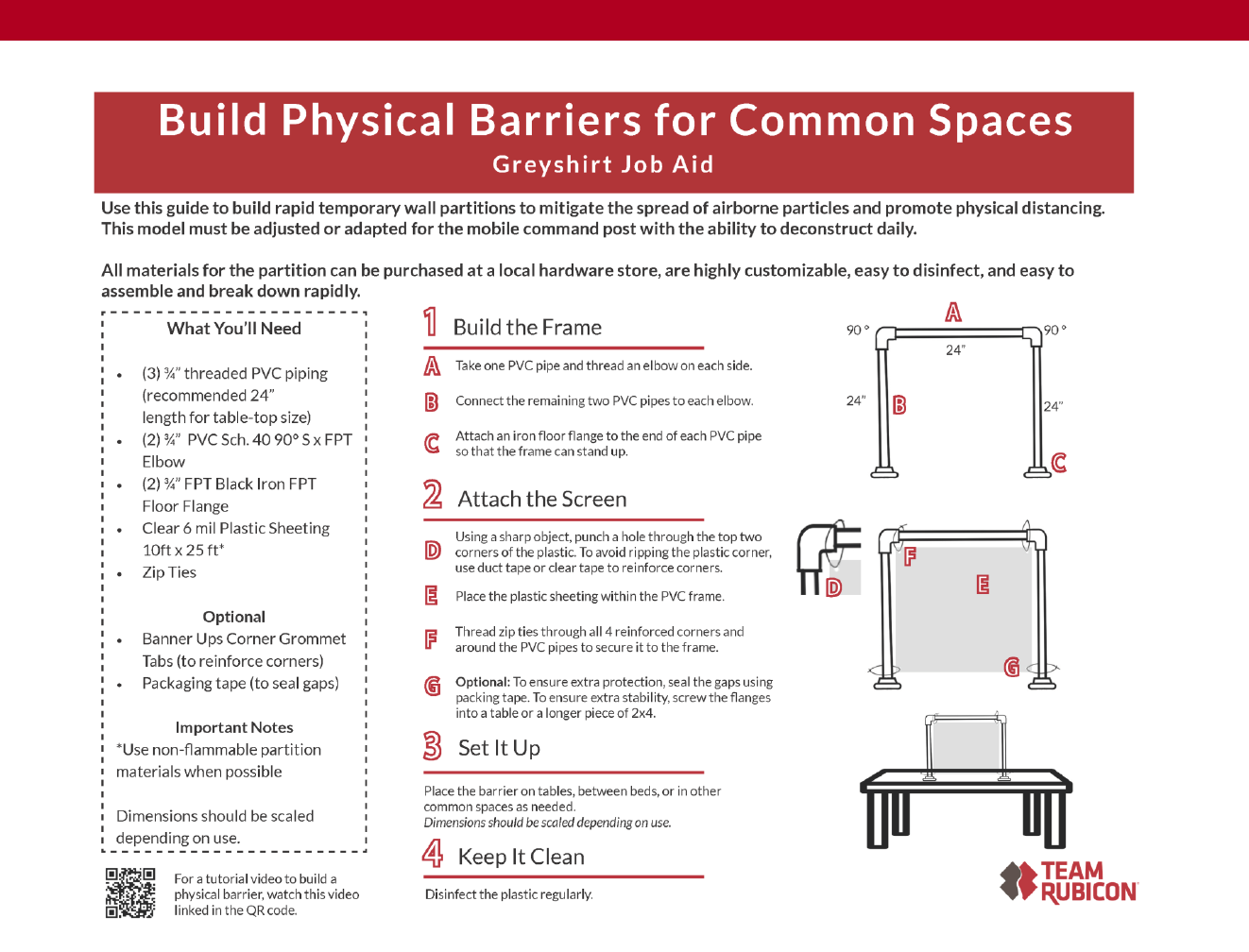
71
SUPPLEMENTAL INFORMATION/APPENDICES
74
SUPPLEMENTAL INFORMATION/APPENDICES
Figure 19. Acknowledgement of Policy Form
Acknowledgement of Policy
Team Rubicon is committed to maintaining the health and safety of Team Rubicon volunteers and
the communities we serve. To meet this commitment, Team Rubicon reviews each request for
assistance for alignment with our organizational guidelines and relevant local, state, and federal
guidance; and asks that requesting organizations share materials related to the scope of requested
activities and the health and safety standards of its operations, including:
• Manuals
• Protocols
• Policies
• Standard operation guidelines or
procedures
• Job aids
• Training curricula
• Certifications
By signing below, [REQUESTING ORGANIZATION] acknowledges that they have shared the
requested materials with Team Rubicon and commit to upholding health and safety standards that
meet or exceed Team Rubicon’s organizational guidelines.
_______________________________________________
[Requesting Organization]
_______________________________________________
[Representative Name – Print]
_______________________________________________
[Representative Name – Sign]
Materials shared (please list below):
_______________________________________________
_______________________________________________
_______________________________________________
_______________________________________________
_______________________________________________
_______________________________________________
_______________________________________________
75
SUPPLEMENTAL INFORMATION/APPENDICES
Spontaneous Volunteer COVID-19 Memorandum of Understanding
Team Rubicon is committed to the health and safety of all volunteers supporting its operations.
In pursuit of that goal, TR has implemented policies, protocols, and personnel eligibility
requirements for all volunteers, including spontaneous volunteers. By signing this document, I
certify I meet TR’s Personnel Eligibility and Deployability Requirements and will adhere to TR’s
COVID-19 policies and protocols.
Personnel Eligibility and Deployability Requirements Self-Certification
✓
I am fully-vaccinated. I have completed my first and second dose of COVID-19
vaccination (in needed) and it has been at least 14 days past my vaccination completion
date.
I am not currently experiencing COVID-19 symptoms as described by the CDC and have
not experienced COVID-19 symptoms in the past 14 days.
I agree to adhere to all policy and guidance provided to me by my assigned field leader.
Signature of Acknowledgement
Printed Name
Date
Email Address/Phone Number
Figure 20. Spontaneous Volunteer COVID-19 MOU
76
SUPPLEMENTAL INFORMATION/APPENDICES
77
SUPPLEMENTAL INFORMATION/APPENDICES
78
SUPPLEMENTAL INFORMATION/APPENDICES
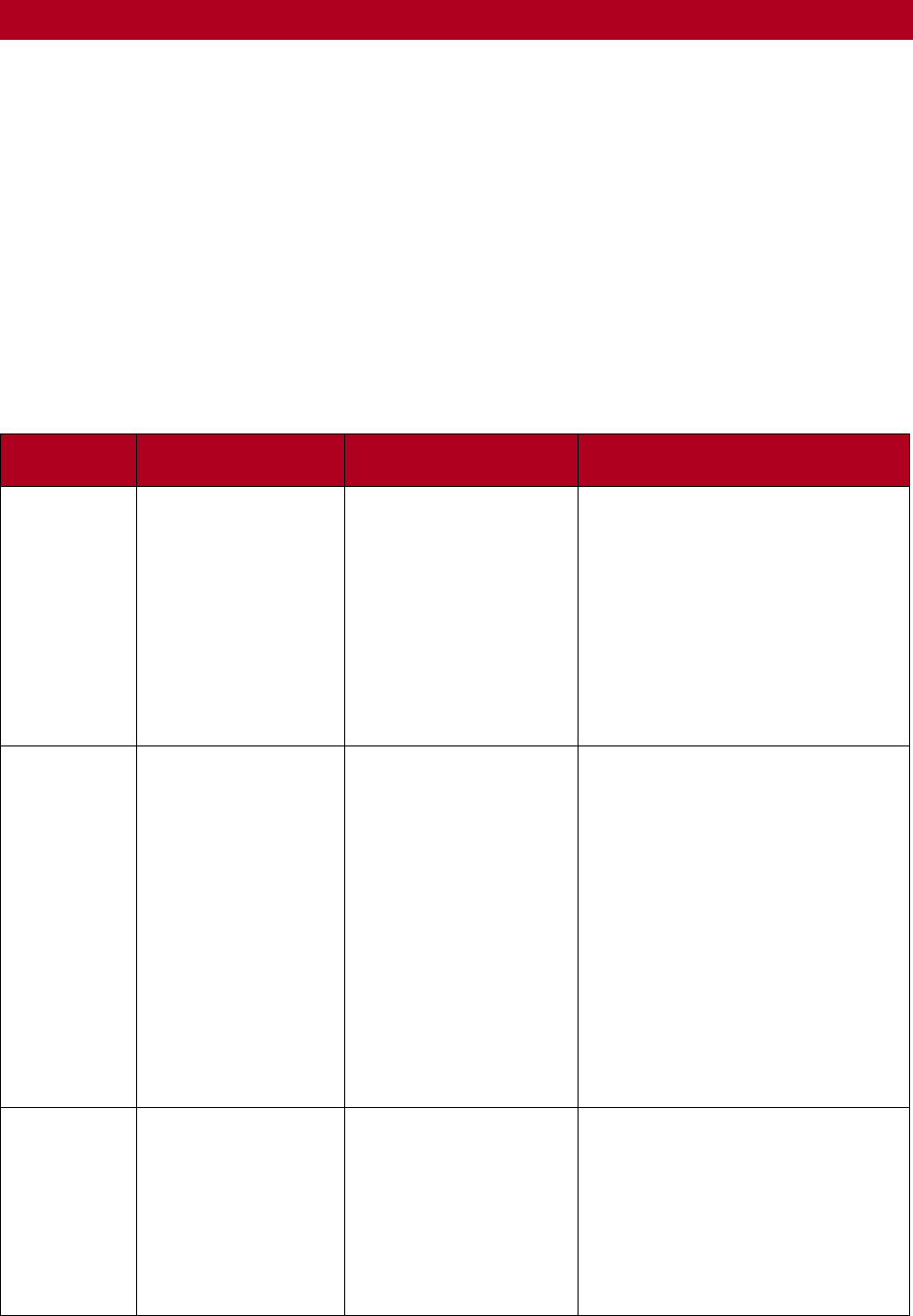
81
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX I: RISK CATEGORIES
The following categories and definitions of risk are outlined and defined based on potential for
direct contact with COVID-19. Fully vaccinated Greyshirts should continue to take precautions
especially when working in communities and inside of facilities interacting directly with patients
being treated for COVID-19. Greyshirts assigned to service sites equipped with less than
minimum standard PPE are authorized to opt out of operations. Greyshirts are discouraged from
using PPE unless required or recommended due to the international shortages and to reserve
equipment for those with the most critical needs. PPE should only be used in situations that have
potential for exposing Greyshirts to COVID-19.
PPE Requirements for Exposure Risk Levels
Exposure
Risk Level
Description
Example Activities
Recommended PPE
Low Risk
No contact with
COVID-19-infected
individuals or
surfaces and spaces
they may have
come into contact.
Warehouse and
packaging support,
remote support
Standard precautions including:
• Contained, GS-Only: No
mask or social distancing
• In Community: Well-
fitting mask and
continued social
distancing
• Hand hygiene
• Clean and disinfect
surfaces
Medium
Risk
No contact with
COVID-19 infected
individuals;
however, there
may be contact
with the surfaces
and spaces they
may have come
into contact.
Handling potentially
contaminated supplies
or equipment,
occupying spaces that
previously contained
COVID-19+
individuals
Standard precautions plus:
• Nitrile gloves (when
contacting or cleaning
contaminated surfaces or
items)
• Isolation gown (when
contacting or cleaning
contaminated surfaces or
items)
• N95 mask if working in
spaces occupied by
COVID-19+ individuals;
otherwise, wear a non-
medical face covering
High Risk
Both immediate
contact with
COVID-19 infected
individuals and with
the surfaces and
spaces they may
have come into
contact.
Direct interaction
with clients suspected
or confirmed to be
COVID-19+, working
inside of a facility
treating COVID-19+
patients
Standard precautions plus:
• Nitrile gloves
• Face shield/goggles
• Isolation gown
• N95 mask
• Bouffant cap (available,
but optional, for outdoor
mobile testing sites)
82
SUPPLEMENTAL INFORMATION/APPENDICES
All “high exposure risk” operations will provide a method for
Greyshirts to be properly fit tested for use of N95 respirator masks
(or other respirator masks of similar droplet protective quality). For
further information about donning and doffing PPE see Figure 9.
Sequence for Putting On PPE.
All “high exposure risk” operations will provide a method for Greyshirts to be properly fit tested
for use of N95 respirator masks (or other respirator masks of similar droplet protective quality).
For further information see Figure 12. Use and Reuse of N95 Respirator Masks and Face Shields
.
Minimum PPE required per risk level and example activities to use proper PPE are provided in a
one-page job aid found in Figure 8. Alternative PPE Table. Alternative PPE options are noted.
See for a graphic on how to properly put on and remove a disposable respirator.
PPE Extended Use and Reuse Policy
TR responders will follow the protocols outlined below for the extended use and reuse of PPE on
medium-to-high exposure risk operations. This policy has been developed specifically
in response to a critical shortage of PPE due to a pandemic or other disaster and when all other
options of obtaining these items have been exhausted.
Note particulate respirators, including N95 respirators, are not to be mistaken for surgical masks.
Use N95 respirators without breathing valves as much as possible. Breathing valves do not filter
contaminated breath as it leaves the respirator, which may leave others vulnerable to
contaminated air. If available, use respirators without breathing valves or take precautions as
referenced in Figure 12.
Extended Use of Particulate and N95 Respirators
In these instances, the respirator will continue to be worn between patient encounters9F.
Extended use may be implemented when multiple patients are infected with the same
respiratory pathogen and patients are placed together in dedicated waiting rooms or hospital
wards.
Discard N95 respirators under the following conditions:
• After aerosol-generating procedures (unless covered with a
disposable mask during the aerosol-generating procedure).
• Visible contamination with blood or other bodily fluids from
patients.
• Obvious damage or becomes hard to breathe through.
• A tight seal cannot be achieved.
Limited Reuse of N95 Respirators
N95 Extended Use
“Extended use” refers to the
practice of wearing the same
N95 respirator for repeated
close contact encounters
with several patients.
PPE TRAINED OBSERVER

83
SUPPLEMENTAL INFORMATION/APPENDICES
Refer to for instructions on storing and reusing N95 respirators. Discard masks after five uses.10F
CDC guidelines recommend use of face shields that can be thoroughly cleaned over N95
respirators. Follow the protocol below:
• Clean hands with soap and water or an alcohol-based hand sanitizer (at least 60 percent
ethanol or 70 percent isopropanol) before and after touching the respirator.
• Immediately after donning a used N95 respirator and performing a user seal, check to
ensure a good seal using the following
steps:
o Ensure no air comes through the
perimeter of the mask when the
user blows out. If air comes out,
it is not a tight seal.
o A light intake of breath should
cause a slight inward puckering
of the mask. If it does not, then
it is not a tight seal.
o A light exhale should cause a
slight expansion of the mask. If
it does not, then it is not a tight seal.
• Observe hand hygiene and change gloves regularly.
Face Shield Reuse and Decontamination
A face shield is a device used to protect the user’s eyes and face from bodily fluids, liquid
splashes, and potentially infectious materials. The following guidelines allow for the reuse of face
shields:
• Full face shields are dedicated to individual healthcare workers as foam pieces and elastic
headbands cannot be fully disinfected.
• The user will don gloves and disinfect inside and then outside surfaces.
• Do not use germicidal wipes on foam and elastic bands.
• Store reused full face shield alongside labeled paper bag containing reused N95 mask.
Face shields will be discarded under the following conditions:
• Face shield can no longer fasten securely.
• Visibility is obscured and reprocessing does not restore visibility.
• Physical damage (e.g., breakage, bending, degradation of materials).
For more information about reprocessing face shields for reuse refer to Appendix C: Job Aids
N95 Reuse
“Reuse”
refers to the practice of using
the same N95 respirator for multiple
encounters with patients and doffing
(removing) the respirator after multiple
patient encounters
Error! Bookmark not defined.
. T
he respirator will be stored between
encounters to be donned prior to the
next encounter with a patient.

84
SUPPLEMENTAL INFORMATION/APPENDICES
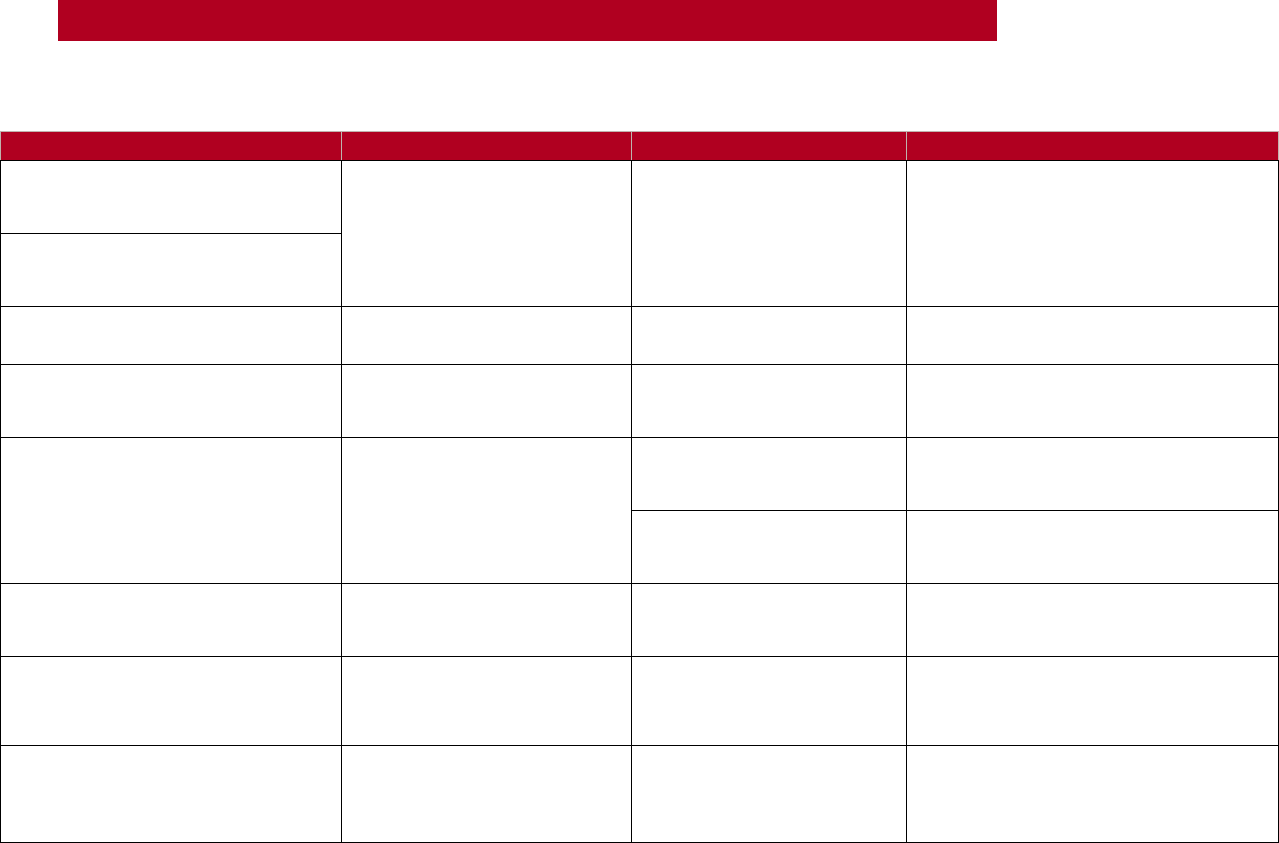
85
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX J: EVALUATION PLAN
Assumptions
Indicators
Outputs
Definition
1) Government and NGO response
at the local, state, and federal level
will be overwhelmed.
# of RFAs received by TR (as a
measure of need of
Government, NGO, local
community need)
# of RFAs received
# of total RFAs received regardless of
TRs ability to respond, disaggregated by
Requesting Organization (Government
level, NGO, other).
2) The needs of the community
throughout the US and globally, are
beyond the local capacity.
3) Requests for assistance
communication is effective.
TR can respond to requests
for assistance
# of RFAs
# of RFAs that go to OPORD
disaggregated by capability type.
4) Appropriate PPE and other
safety equipment will be available
to TR.
Appropriate health and safety
measures and equipment
were provided to Greyshirts
% Greyshirts provided with
PPE, when needed
PPE provided is defined as appropriate
PPE for a task is assigned every time.
5) The number of quarantined
communities will increase in the
coming weeks.
# of quarantined communities
over time
% of Greyshirts given health
and safety training and/or
protocols
Greyshirts given a briefing or required
to read protocols for health and safety.
# of total communities
quarantined mapped over
time
# of total communities (by county) with
any community spread order tracked as
total per week.
6) The number of confirmed
positive cases will increase in the
coming weeks.
# of confirmed cases over
time
# of total cases mapped over
time
# of total confirmed cases tracked as
total per week.
7) Specific community needs will
vary by geographic location.
# and type of capabilities
launched over the course of
the operation
# of RFAs disaggregated by
geographic location and
activity type
# of RFAs disaggregated by geographic
location and activity type.
8) Some portion of TR staff
and Greyshirts will become
infected with COVID-19, related, or
not related, to TR activities
# of confirmed or suspected
cases during or after
deployment
% of Greyshirts that contract
COVID-19 (confirmed or
suspected cases) during or
after deployment
# of confirmed or suspected cases
during or after deployment/# of total
Greyshirts deployed.
Figure 23. Operations Evaluation Plan
86
SUPPLEMENTAL INFORMATION/APPENDICES
APPENDIX K: BACKGROUND AND DESIGN
ELEMENTS
DEMAND
In December of 2019, China notified the World Health Organization (WHO) of an outbreak in
Wuhan Province that would be identified as Coronavirus disease 2019 (COVID-19)33F
19
. By March
11, 2020, WHO characterized the virus as a pandemic and on March 13, the President of the
United States declared a National Emergency. While the situation is extremely fluid, as of the
current iteration of this document, over 3,926,000 cases of COVID-19 have been confirmed
worldwide resulting in more than 374,000 deaths34F
20
and those numbers continue to rise.
It quickly became clear that government agencies at all levels, as well Non-Governmental
Organizations (NGOs) and Voluntary Organizations Active in Disasters (VOADs), would struggle
to fulfill the needs of impacted communities. Because COVID-19 is most deadly to those 65
years of age and older,35F
21
or people with compromised immune systems, personnel able to safely
work within infected communities has become limited.
There is an overwhelming need for human resources to support unique needs arising as well as
to augment existing life-sustaining services in the context of COVID-19. There is need for TR’s
support in delivering a wide range of services through affiliations with government agencies and
other partner organizations, and we are fielding various requests for aid. To successfully stretch
our capabilities into this new realm, it is imperative that a process for working within this space is
developed.
IMPACT
The intended impact of this capability is to swiftly mobilize human resources to support
communities in meeting unique life safety needs secondary to the COVID-19 pandemic. TR will
provide swift and timely services to communities as aligned with the organization’s mission. The
provided services will improve the sense of well-being, safety, and connectedness among the
communities we serve, and our activities will ensure that people in affected communities have
access to food and other life-sustaining resources.
COMMANDER’S INTENT
19
World Health Organization. COVID-19: Operational Planning Guidelines and COVID-19 Partners Platform to
support country preparedness and response. (2020, March 4). Retrieved from https://openwho.org/courses/UNCT-
COVID19-preparedness-and-response-EN/items/6tSiNrZnrCUJsYthaH6449
20
Johns Hopkins University & Medicine. (2020, October 27) COVID-19 Dashboard by Center for Systems Science
and Engineering (CSSE) at Johns Hopkins University (JHU). Retrieved from https://coronavirus.jhu.edu/map.html
21
Centers for Disease Control and Prevention (2020, September 11). Older Adults. Retrieved from
https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications/older-adults.html

87
SUPPLEMENTAL INFORMATION/APPENDICES
Aggressively and responsibly deploy our resources (current and developing) to effectively and
safely assist a Whole of America response to, and recovery from, COVID-19 and all other
hazards that occur in this backdrop.
ASSUMPTIONS
General Assumptions:
• Government and non-governmental organization response at the local, state, and federal
level will be overwhelmed
• Travel to locations with service needs will be possible
• Specific community needs will vary by geographic location
• Resources will become limited for citizens, either due to physical access or financial
strain
• Appropriate Personal Protective Equipment (PPE) and other safety equipment will be
available to TR
• The number of confirmed positive cases will increase in the coming weeks
• The number of quarantined communities will increase in the coming weeks
• The needs of communities throughout the US and globally are beyond the local capacity
• Greyshirts and TR staff can safely provide services without increasing the spread of
COVID-19
• Some portion of TR staff and Greyshirts will become infected with COVID-19, related, or
not related, to TR activities
• Some portion of TR staff and Greyshirts will be personally impacted by COVID-19
• Virus risk factors and pathologies will remain consistent
• The situation will remain fluid, meaning guidance on self-isolation, quarantine, and other
public health actions may change
SCOPE
Throughout the COVID-19 pandemic, TR expects to receive multiple requests for a variety of
services. To provide timely response to these requests, TR will maintain the concept of
operations described in the Domestic Emergency Operations Plan. TR will adhere to standard
Incident Command System (ICS) structure, unless explicitly stated elsewhere within this
document, and in accordance with best practices during a pandemic. This will enable TR to
provide support in multiple capacities with the flexibility and speed necessary to contribute to
the national COVID-19 response. TR will engage in two categories of response operations:
Requesting Organization Activities and TR-Led Activities. Actions specific to the COVID-19
response not otherwise covered in other doctrine are outlined in this manual.