
The Dental Council hosted the annual conference of FEDCAR, the Federation of European Dental Competent Authorities and Regulators on the 20 April
BITESIZE
BITESIZE
Ocial Newsletter of the Dental Council of Ireland
VOLUME 2, ISSUE 1 | JUNE 2018
VOLUME 2, ISSUE 1 | JUNE 2018
President’s Address
Welcome to our Summer 2018 newsletter. I am
delighted to say that the Dental Council hosted
the annual conference of FEDCAR, the
Federation of European Dental Competent
Authorities and Regulators on the 20 April. We
hold the FEDCAR presidency this year and we
held the conference in Dublin Castle. A
combination of the fine facilities and the first
gloriously sunny days of the New Year showed Dublin and
Ireland off positively to our European colleagues.
The main focus of the meeting was to discuss ways of ensuring
that there is quality assurance of dental training across all
European dental schools. The European Union project allows
dental health professionals to move relatively freely across
Europe. It is important for patients that they can be assured that
there is an appropriate system in place to ensure that someone
graduating with a dental qualification has the required skills to
treat patients. This is presently not the case and it is a significant
weakness in the European systems. We had a positive
engagement with the other stakeholders representing dental
educators, the professional organisations and the dental
students. We look forward to progressing this important work
over the coming months.
THE REGISTRAR’S
Frequently Asked Questions
As Registrar, David O’Flynn receives many phone calls and
emails from both registrants and members of the public and
there are some themes that come forward regularly.
Do you get many calls about
communication issues?
In 2017, the main issue for approximately 30%
of the patients who contacted the council
concerned communications. These patients
reported problems ranging from sharp or
brusque responses to questions, to anger, to
the patient feeling that the treatment plan was
not properly explained to them.
The number of calls and emails we receive is
small in the context of the total number of
patient/dentist interactions that take place
every day in Ireland. However, sometimes the
patient’s heightened general anxiety about
going to the dentist and the draws on the
dental team’s attention that can occur in a busy
dental surgery collide and leave the patient
worried or annoyed about something that
happened in the surgery.
It is important for all members of the dental
team to continually remind themselves of the
paramount importance of fully engaging with
your patients.
Is complex treatment at the heart of many
complaints to the Dental Council?
Surprisingly, no. Most of the complaints we
receive about treatment are routine general
practise dentistry, such as fillings falling out, ill-
fitting dentures, fabricating and affixing crowns
and bridgework. In many cases, the patient has
already discussed the issue with the dentist and
is still dissatisfied. While we generally ask the
patient to discuss their treatment with the
dentist, the fact that they have contacted us
generally means they are losing confidence in
their dentist’s willingness to deal with their
problem.
We do also receive complaints about more
complex treatment and an increasing number
of these concern implant retained bridges.
A recurring problem is the failure of the dentist
to realise when specialist assistance may be
required. We accept that problems will arise
during even the most routine treatment, and it
is important for dentists to reflect on the point
when the patient should be referred on.
IN THIS
ISSUE
How the Council Works
Minimata
General Data Protection
Regulations (GDPR)
Practitioner Health Matters
Programme
Renewal Fee’s
Communicating with the
Registration Department
Civil Liability (Amendment) Act
BT Young Scientist
Dental Council Updates
FAQ’s
Dr Gerry McCarthy,
President
57 Merrion Square, Dublin 2, D02 EH90, Ireland
Telephone: (01) 676 2226. Email: [email protected]
www.dentalcouncil.ie
Update from David O’Flynn, Registrar
F
itness to Practise
In this edition of the Newsletter I would like to set out some information about the
Dental Council’s Fitness to Practise procedures. This is an area that is of interest to
many dentists and the general public alike.
Most allegations we receive are of professional misconduct which is defined as
being a serious falling short in the standards expected of a dentist, and in this
context the word ‘serious’ is important. Professional misconduct is intended to sit
above negligence in terms of a hierarchy of seriousness. The process is intended to
deal with matters where the allegation gives rise to a serious concern about the dentist’s practise.
We receive over 150 calls or emails from patients every year. Most patients contact us because they
are unhappy with their experience with a dentist and they are looking for advice. In most cases, we
recommend that the patient discuss the matter with the dentist directly. Often, when the patient
contacts the council, they are close to escalating the matter further, and resolving the matter
promptly is usually the best option for everyone.
Each year about 8-10 calls and emails result in a formal allegation of professional misconduct being
m
ade. The dentist is always given an opportunity to provide their comments and observations on an
allegation prior to the matter being considered by the Fitness to Practise Committee.
In order for the matter to proceed to Inquiry, the committee must be satisfied that there is prima facie
evidence of professional misconduct. The prima facie test is met if the committee is satisfied that the
allegation, if proven, would amount to professional misconduct, and that there is a likely prospect of
the allegation being proven beyond reasonable doubt. Beyond reasonable doubt is the burden of
p
roof required at an inquiry. As you can see from the table, only 1-2 of the applications received
annually will result in an inquiry.
The Dental Council may apply any of 6 sanctions if an allegation of professional misconduct is proven.
These sanctions are: erasure, suspension for a period of time, conditions attached to practise, censure,
admonishment, and advisement. Shortly, all sanctions will need to be confirmed by the High Court.
How the council works
F
itness to Practise Committee
Nine members of the Dental Council sit on the Fitness to Practise Committee. Under the Dentists Act,
1985, the majority of the committee must have been elected by the profession and at least one must
be appointed by the Department of Health and must not be a dentist. The full committee considers
allegations up to the prima facie decision, and usually three members of the committee are delegated
to hear each inquiry. The present membership is:
F
itness to Practise Journey
Initial Contact
R
eferred back to practice or to Dental Complaints Resolution Service
Allegation
No prima facie (case closed)
Inquiry
No finding of professional misconduct
Council
Sanctions imposed after proven finding of professional misconduct
Year Total
Ave per
contact
(
min)
W
rite
to DC
A
llegations
received
I
nquiry
Decision
Subject of Complaint
F
ees
B
ehaviour
T
reatment
O
thers
2017 153 23 15 5 1 17% 30% 53% 0%
2016 150 24 12 9 2 19% 19% 59% 3%
2015 171 19 13 2 1 12% 20% 60% 8%
2014 163 18 16 13 1 16% 19% 60% 6%
2013 228 24 N/A 9 2 25% 25% 45% 4%
Fitness to Practise Activity 2013-2017
F
F
F
i
i
t
t
t
n
n
n
e
e
e
s
s
s
s
s
t
t
t
o
o
o
P
P
P
P
r
r
r
a
a
c
c
t
t
t
i
i
s
s
e
e
C
C
C
O
O
O
M
M
M
M
M
M
I
I
I
T
T
T
T
T
E
E
E
E
D
r Bernard
Murphy
Chair and elected
dentist
Dr Danielle
Colbert
Elected
member
Mr James
Doorley
Nominated by
D
ept of Health
(lay member)
Dr Rory
F
leming
Elected member
Prof Martin
Kinirons
Nominated
by UCC
Dr Liam
Lynch
Elected member
Dr Ray
McCarthy
Elected member
Dr Eleanor
O’Higgins
Nominated by
Dept of Health
(lay member)
Vacant
Nominated by
D
ept of Health
(lay member)
The Dental Council expects all dentists to have a formal complaints procedure in place (Section
5.4 of the Code of Practice regarding Professional Behaviour and Ethical Conduct).

The Dental Council hosted the annual conference of FEDCAR, the Federation of European Dental Competent Authorities and Regulators on the 20 April
BITESIZE
BITESIZE
Ocial Newsletter of the Dental Council of Ireland
VOLUME 2, ISSUE 1 | JUNE 2018
VOLUME 2, ISSUE 1 | JUNE 2018
President’s Address
Welcome to our Summer 2018 newsletter. I am
delighted to say that the Dental Council hosted
the annual conference of FEDCAR, the
Federation of European Dental Competent
Authorities and Regulators on the 20 April. We
hold the FEDCAR presidency this year and we
held the conference in Dublin Castle. A
combination of the fine facilities and the first
gloriously sunny days of the New Year showed Dublin and
Ireland off positively to our European colleagues.
The main focus of the meeting was to discuss ways of ensuring
that there is quality assurance of dental training across all
European dental schools. The European Union project allows
dental health professionals to move relatively freely across
Europe. It is important for patients that they can be assured that
there is an appropriate system in place to ensure that someone
graduating with a dental qualification has the required skills to
treat patients. This is presently not the case and it is a significant
weakness in the European systems. We had a positive
engagement with the other stakeholders representing dental
educators, the professional organisations and the dental
students. We look forward to progressing this important work
over the coming months.
THE REGISTRAR’S
Frequently Asked Questions
As Registrar, David O’Flynn receives many phone calls and
emails from both registrants and members of the public and
there are some themes that come forward regularly.
Do you get many calls about
communication issues?
In 2017, the main issue for approximately 30%
of the patients who contacted the council
concerned communications. These patients
reported problems ranging from sharp or
brusque responses to questions, to anger, to
the patient feeling that the treatment plan was
not properly explained to them.
The number of calls and emails we receive is
small in the context of the total number of
patient/dentist interactions that take place
every day in Ireland. However, sometimes the
patient’s heightened general anxiety about
going to the dentist and the draws on the
dental team’s attention that can occur in a busy
dental surgery collide and leave the patient
worried or annoyed about something that
happened in the surgery.
It is important for all members of the dental
team to continually remind themselves of the
paramount importance of fully engaging with
your patients.
Is complex treatment at the heart of many
complaints to the Dental Council?
Surprisingly, no. Most of the complaints we
receive about treatment are routine general
practise dentistry, such as fillings falling out, ill-
fitting dentures, fabricating and affixing crowns
and bridgework. In many cases, the patient has
already discussed the issue with the dentist and
is still dissatisfied. While we generally ask the
patient to discuss their treatment with the
dentist, the fact that they have contacted us
generally means they are losing confidence in
their dentist’s willingness to deal with their
problem.
We do also receive complaints about more
complex treatment and an increasing number
of these concern implant retained bridges.
A recurring problem is the failure of the dentist
to realise when specialist assistance may be
required. We accept that problems will arise
during even the most routine treatment, and it
is important for dentists to reflect on the point
when the patient should be referred on.
IN THIS
ISSUE
How the Council Works
Minimata
General Data Protection
Regulations (GDPR)
Practitioner Health Matters
Programme
Renewal Fee’s
Communicating with the
Registration Department
Civil Liability (Amendment) Act
BT Young Scientist
Dental Council Updates
FAQ’s
Dr Gerry McCarthy,
President
57 Merrion Square, Dublin 2, D02 EH90, Ireland
Telephone: (01) 676 2226. Email: [email protected]
www.dentalcouncil.ie
Update from David O’Flynn, Registrar
F
itness to Practise
In this edition of the Newsletter I would like to set out some information about the
Dental Council’s Fitness to Practise procedures. This is an area that is of interest to
many dentists and the general public alike.
Most allegations we receive are of professional misconduct which is defined as
being a serious falling short in the standards expected of a dentist, and in this
context the word ‘serious’ is important. Professional misconduct is intended to sit
above negligence in terms of a hierarchy of seriousness. The process is intended to
deal with matters where the allegation gives rise to a serious concern about the dentist’s practise.
We receive over 150 calls or emails from patients every year. Most patients contact us because they
are unhappy with their experience with a dentist and they are looking for advice. In most cases, we
recommend that the patient discuss the matter with the dentist directly. Often, when the patient
contacts the council, they are close to escalating the matter further, and resolving the matter
promptly is usually the best option for everyone.
Each year about 8-10 calls and emails result in a formal allegation of professional misconduct being
m
ade. The dentist is always given an opportunity to provide their comments and observations on an
allegation prior to the matter being considered by the Fitness to Practise Committee.
In order for the matter to proceed to Inquiry, the committee must be satisfied that there is prima facie
evidence of professional misconduct. The prima facie test is met if the committee is satisfied that the
allegation, if proven, would amount to professional misconduct, and that there is a likely prospect of
the allegation being proven beyond reasonable doubt. Beyond reasonable doubt is the burden of
p
roof required at an inquiry. As you can see from the table, only 1-2 of the applications received
annually will result in an inquiry.
The Dental Council may apply any of 6 sanctions if an allegation of professional misconduct is proven.
These sanctions are: erasure, suspension for a period of time, conditions attached to practise, censure,
admonishment, and advisement. Shortly, all sanctions will need to be confirmed by the High Court.
How the council works
F
itness to Practise Committee
Nine members of the Dental Council sit on the Fitness to Practise Committee. Under the Dentists Act,
1985, the majority of the committee must have been elected by the profession and at least one must
be appointed by the Department of Health and must not be a dentist. The full committee considers
allegations up to the prima facie decision, and usually three members of the committee are delegated
to hear each inquiry. The present membership is:
F
itness to Practise Journey
Initial Contact
R
eferred back to practice or to Dental Complaints Resolution Service
Allegation
No prima facie (case closed)
Inquiry
No finding of professional misconduct
Council
Sanctions imposed after proven finding of professional misconduct
Year Total
Ave per
contact
(
min)
W
rite
to DC
A
llegations
received
I
nquiry
Decision
Subject of Complaint
F
ees
B
ehaviour
T
reatment
O
thers
2017 153 23 15 5 1 17% 30% 53% 0%
2016 150 24 12 9 2 19% 19% 59% 3%
2015 171 19 13 2 1 12% 20% 60% 8%
2014 163 18 16 13 1 16% 19% 60% 6%
2013 228 24 N/A 9 2 25% 25% 45% 4%
Fitness to Practise Activity 2013-2017
F
F
F
i
i
t
t
t
n
n
n
e
e
e
s
s
s
s
s
t
t
t
o
o
o
P
P
P
P
r
r
r
a
a
c
c
t
t
t
i
i
s
s
e
e
C
C
C
O
O
O
M
M
M
M
M
M
I
I
I
T
T
T
T
T
E
E
E
E
D
r Bernard
Murphy
Chair and elected
dentist
Dr Danielle
Colbert
Elected
member
Mr James
Doorley
Nominated by
D
ept of Health
(lay member)
Dr Rory
F
leming
Elected member
Prof Martin
Kinirons
Nominated
by UCC
Dr Liam
Lynch
Elected member
Dr Ray
McCarthy
Elected member
Dr Eleanor
O’Higgins
Nominated by
Dept of Health
(lay member)
Vacant
Nominated by
D
ept of Health
(lay member)
The Dental Council expects all dentists to have a formal complaints procedure in place (Section
5.4 of the Code of Practice regarding Professional Behaviour and Ethical Conduct).

The Dental Council hosted the annual conference of FEDCAR, the Federation of European Dental Competent Authorities and Regulators on the 20 April
BITESIZE
BITESIZE
Ocial Newsletter of the Dental Council of Ireland
VOLUME 2, ISSUE 1 | JUNE 2018
VOLUME 2, ISSUE 1 | JUNE 2018
President’s Address
Welcome to our Summer 2018 newsletter. I am
delighted to say that the Dental Council hosted
the annual conference of FEDCAR, the
Federation of European Dental Competent
Authorities and Regulators on the 20 April. We
hold the FEDCAR presidency this year and we
held the conference in Dublin Castle. A
combination of the fine facilities and the first
gloriously sunny days of the New Year showed Dublin and
Ireland off positively to our European colleagues.
The main focus of the meeting was to discuss ways of ensuring
that there is quality assurance of dental training across all
European dental schools. The European Union project allows
dental health professionals to move relatively freely across
Europe. It is important for patients that they can be assured that
there is an appropriate system in place to ensure that someone
graduating with a dental qualification has the required skills to
treat patients. This is presently not the case and it is a significant
weakness in the European systems. We had a positive
engagement with the other stakeholders representing dental
educators, the professional organisations and the dental
students. We look forward to progressing this important work
over the coming months.
THE REGISTRAR’S
Frequently Asked Questions
As Registrar, David O’Flynn receives many phone calls and
emails from both registrants and members of the public and
there are some themes that come forward regularly.
Do you get many calls about
communication issues?
In 2017, the main issue for approximately 30%
of the patients who contacted the council
concerned communications. These patients
reported problems ranging from sharp or
brusque responses to questions, to anger, to
the patient feeling that the treatment plan was
not properly explained to them.
The number of calls and emails we receive is
small in the context of the total number of
patient/dentist interactions that take place
every day in Ireland. However, sometimes the
patient’s heightened general anxiety about
going to the dentist and the draws on the
dental team’s attention that can occur in a busy
dental surgery collide and leave the patient
worried or annoyed about something that
happened in the surgery.
It is important for all members of the dental
team to continually remind themselves of the
paramount importance of fully engaging with
your patients.
Is complex treatment at the heart of many
complaints to the Dental Council?
Surprisingly, no. Most of the complaints we
receive about treatment are routine general
practise dentistry, such as fillings falling out, ill-
fitting dentures, fabricating and affixing crowns
and bridgework. In many cases, the patient has
already discussed the issue with the dentist and
is still dissatisfied. While we generally ask the
patient to discuss their treatment with the
dentist, the fact that they have contacted us
generally means they are losing confidence in
their dentist’s willingness to deal with their
problem.
We do also receive complaints about more
complex treatment and an increasing number
of these concern implant retained bridges.
A recurring problem is the failure of the dentist
to realise when specialist assistance may be
required. We accept that problems will arise
during even the most routine treatment, and it
is important for dentists to reflect on the point
when the patient should be referred on.
IN THIS
ISSUE
How the Council Works
Minimata
General Data Protection
Regulations (GDPR)
Practitioner Health Matters
Programme
Renewal Fee’s
Communicating with the
Registration Department
Civil Liability (Amendment) Act
BT Young Scientist
Dental Council Updates
FAQ’s
Dr Gerry McCarthy,
President
57 Merrion Square, Dublin 2, D02 EH90, Ireland
Telephone: (01) 676 2226. Email: [email protected]
www.dentalcouncil.ie
Update from David O’Flynn, Registrar
F
itness to Practise
In this edition of the Newsletter I would like to set out some information about the
Dental Council’s Fitness to Practise procedures. This is an area that is of interest to
many dentists and the general public alike.
Most allegations we receive are of professional misconduct which is defined as
being a serious falling short in the standards expected of a dentist, and in this
context the word ‘serious’ is important. Professional misconduct is intended to sit
above negligence in terms of a hierarchy of seriousness. The process is intended to
deal with matters where the allegation gives rise to a serious concern about the dentist’s practise.
We receive over 150 calls or emails from patients every year. Most patients contact us because they
are unhappy with their experience with a dentist and they are looking for advice. In most cases, we
recommend that the patient discuss the matter with the dentist directly. Often, when the patient
contacts the council, they are close to escalating the matter further, and resolving the matter
promptly is usually the best option for everyone.
Each year about 8-10 calls and emails result in a formal allegation of professional misconduct being
m
ade. The dentist is always given an opportunity to provide their comments and observations on an
allegation prior to the matter being considered by the Fitness to Practise Committee.
In order for the matter to proceed to Inquiry, the committee must be satisfied that there is prima facie
evidence of professional misconduct. The prima facie test is met if the committee is satisfied that the
allegation, if proven, would amount to professional misconduct, and that there is a likely prospect of
the allegation being proven beyond reasonable doubt. Beyond reasonable doubt is the burden of
p
roof required at an inquiry. As you can see from the table, only 1-2 of the applications received
annually will result in an inquiry.
The Dental Council may apply any of 6 sanctions if an allegation of professional misconduct is proven.
These sanctions are: erasure, suspension for a period of time, conditions attached to practise, censure,
admonishment, and advisement. Shortly, all sanctions will need to be confirmed by the High Court.
How the council works
F
itness to Practise Committee
Nine members of the Dental Council sit on the Fitness to Practise Committee. Under the Dentists Act,
1985, the majority of the committee must have been elected by the profession and at least one must
be appointed by the Department of Health and must not be a dentist. The full committee considers
allegations up to the prima facie decision, and usually three members of the committee are delegated
to hear each inquiry. The present membership is:
F
itness to Practise Journey
Initial Contact
R
eferred back to practice or to Dental Complaints Resolution Service
Allegation
No prima facie (case closed)
Inquiry
No finding of professional misconduct
Council
Sanctions imposed after proven finding of professional misconduct
Year Total
Ave per
contact
(
min)
W
rite
to DC
A
llegations
received
I
nquiry
Decision
Subject of Complaint
F
ees
B
ehaviour
T
reatment
O
thers
2017 153 23 15 5 1 17% 30% 53% 0%
2016 150 24 12 9 2 19% 19% 59% 3%
2015 171 19 13 2 1 12% 20% 60% 8%
2014 163 18 16 13 1 16% 19% 60% 6%
2013 228 24 N/A 9 2 25% 25% 45% 4%
Fitness to Practise Activity 2013-2017
F
F
F
i
i
t
t
t
n
n
n
e
e
e
s
s
s
s
s
t
t
t
o
o
o
P
P
P
P
r
r
r
a
a
c
c
t
t
t
i
i
s
s
e
e
C
C
C
O
O
O
M
M
M
M
M
M
I
I
I
T
T
T
T
T
E
E
E
E
D
r Bernard
Murphy
Chair and elected
dentist
Dr Danielle
Colbert
Elected
member
Mr James
Doorley
Nominated by
D
ept of Health
(lay member)
Dr Rory
F
leming
Elected member
Prof Martin
Kinirons
Nominated
by UCC
Dr Liam
Lynch
Elected member
Dr Ray
McCarthy
Elected member
Dr Eleanor
O’Higgins
Nominated by
Dept of Health
(lay member)
Vacant
Nominated by
D
ept of Health
(lay member)
The Dental Council expects all dentists to have a formal complaints procedure in place (Section
5.4 of the Code of Practice regarding Professional Behaviour and Ethical Conduct).
BITESIZE
O
cial Newsletter of the Dental Council of Ireland
NEWS
IN BRIEF
P
ractitioner Health
Matters Programme
We feel it’s important to bring
this service to the attention of
the dental profession once again.
This programme was launched in
2
015 and since then has
expanded with a steady increase
in the number of practitioners
availing of the service. It gives
support to those going through
mental health difficulties, stress,
or alcohol or drug misuse
problems and we would like to
r
emind all dental professionals
that this service is available to
help in a completely confidential
manner. Ph; 012970356 or
p
ractitionerhealth.ie
D
ental Renewal Fees
We would like to thank the
p
rofession for their co-operation
in using our online payments
system this year. We
acknowledge that a small
number of practitioners had
some difficulty but overall the
online payment system worked
very well. The Dental Council will
continue to use this online
payment system and would
encourage dentists and auxiliary
workers to retain their sign in
details somewhere safe to allow
easy access next year.
Auxiliary Renewal Fees
All auxiliary renewal fees are due
on August 31st 2018. Dental
nurses who have joined
additional registers such as
Dental Hygienist or Orthodontic
Therapists and who no longer
wish to be included on the
Dental Nurse register need to
inform us of this via e-mail. The
fee can only be paid online
through the Dental Council
website. We are unable to accept
cheques, cash or any other form
of payment. Your payment will
be returned if you pay this way.
You should also inform us if you
have changed your address or
are no longer practising.
Please e-mail us at
Communicating with
the Registration
Department
While you will all have dealt with
the registration department
upon registering to practice for
the first time, it is important to
know your responsibilities going
forward. It is easy to keep your
information up-to-date on the
Register. Drop us an email to
[email protected] with any
changes to your details and we
will let you know if you are
required to send in any
additional information in order
for us to make these changes
happen.
Minimata:
The European Union has introduced
regulation 2017/852 to implement
the Minimata Convention on
Mercury. This is an environmental
regulation rather than a health
regulation and its purpose is to
r
educe the amount of mercury used in
many industries and professional sectors, including
dentistry. This EU Regulation is binding in its entirety and
directly applicable in all member states.
K
ey dates for dentists;
1 January 2018;
• Amalgam separators put into service from this date must provide retention level of at least 95% of
amalgam particles and be maintained in accordance with manufacturer's instructions.
1 July 2018;
•
Dental amalgam shall not be used for dental treatment of deciduous teeth, of children under 15
years and of pregnant or breastfeeding women, except when deemed strictly necessary by the
dental practitioner based on the specific medical needs of the patient.
1 January 2019;
• Operators of dental facilities in which dental amalgam is used, or dental amalgam fillings or teeth
containing such fillings are removed, shall ensure that their facilities are equipped with amalgam
separators for the retention and collection of amalgam particles, including those contained in used
water.
• Dental amalgam shall only be used in pre-dosed encapsulated form. The use of mercury in bulk by
dental practitioners shall be prohibited.
• All separators must provide a retention level of at least 95%.
Dental practitioners should note that failure to comply with the waste management regulations may
separately result in proceedings under the Waste Management Regulations, S.I. No. 126/2011 –
European Communities (Waste Directive) Regulations 2011.
The Dental Council intends issuing guidance for the profession on complying with the new regulations
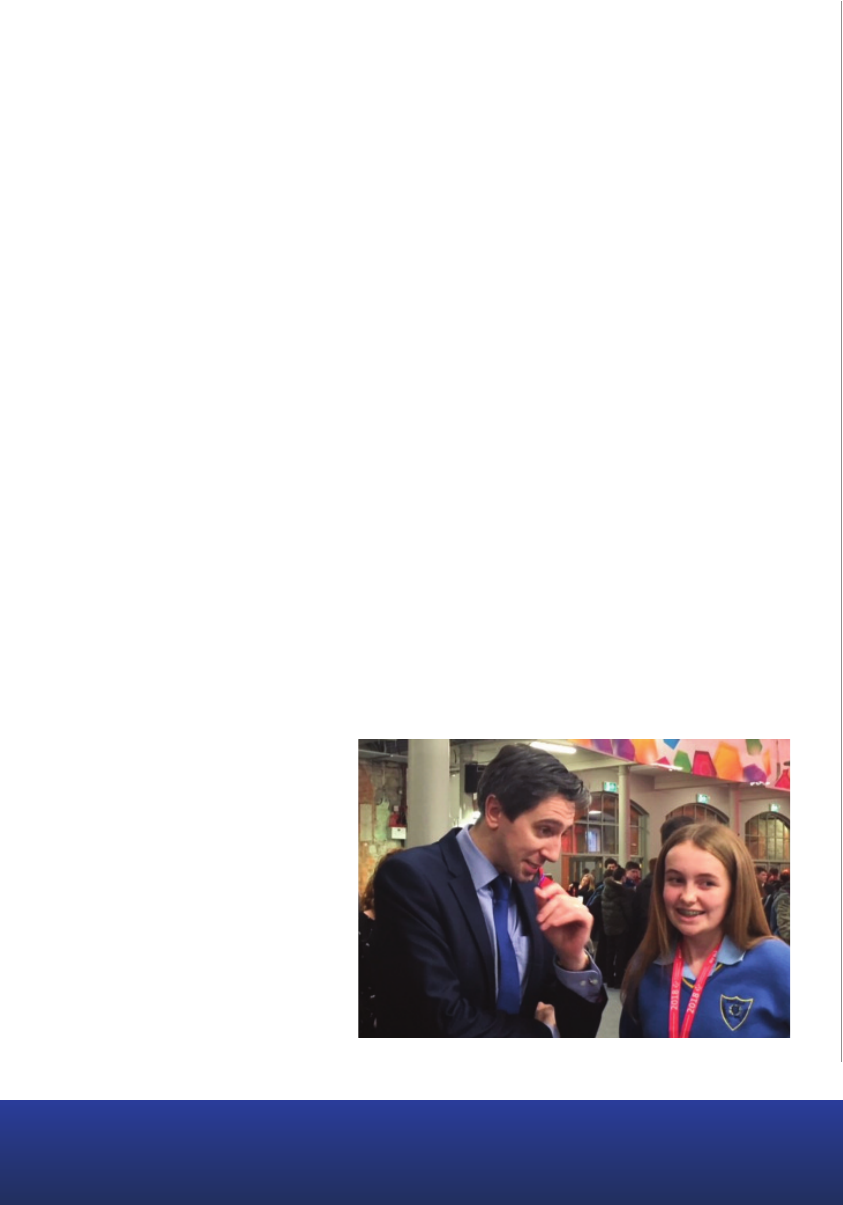
BT Young Scientist
We would like to congratulate Lily Fitzgerald for her prize winning project on dental phobia
and anxiety.
Lily is a second year student at Kinsale Community School and her project was well received. She was
interested in researching the prevalence of dental phobia and dental anxiety and who this affected
attending a dentist, and some other matters. Her main objectives were to:
• Establish how prevalent dental anxiety and dental phobia is.
• Assess its causes.
• Try to measure anxiety and identify factors that enhance or lessen their perceived anxiety.
• Establish the extent to which people avoid the dentist due to anxiety and phobia.
• Establish what is most common: attending the dentist for a check-up or attending for an
emergency.
• Establish whether people are aware of the age a child should rst visit a dentist.
• Find people’s preferences for their dentists and whether the participants own gender and age
aected their preferences.
Lily undertook a survey of 1074 participants and the respondents were predominantly female (79%)
aged 35-54, mainly educated up to third level and higher and predominantly Irish. She found that the
most common reason for having a fear of the dentist was “bad memories of a dentist visit”. She further
found that 59.9% of respondents avoided the dentist because of dental anxiety, and 43.3% of
respondents avoided attending a dentist because of dental phobia. Delays in being called into the
surgery would make 39.3% of the survey respondents feel more anxious.
Almost 40% of those who only attend at least every 4 years said that this was because of dental
phobia. Interestingly, Lily found that male patients are not as anxious as female patients.
Of the people who stated that they were “a little to very much afraid” to visit a dentist, 26% said it was
due to having bad memories of a
previous dental visit and 25% said it
was because they were afraid of
experiencing pain.
The survey is indicative of how
important it is for all the dental team
to ensure that their patients are put
at ease. In our experience of patients
contacting the council, the
heightened anxiety that can
sometimes stem from comment or a
slight complication in treatment
which can result in complaints to the
council that could have been readily
dealt with in the practice.
General Data
Protection
Regulations (GDPR)
You are probably
already aware that the
new EU General Data
Protection Regulations
came into force on 25
May 2018. These
regulations further
strengthen an
individual’s right to
have their information held and processed
appropriately and securely. Failing to comply may
result in significant fines.
The concept of confidentiality of patient information
has been a bedrock of dentistry over the years, and
there should be little difficulty for the dental
profession in meeting these enhanced requirements.
However there are other areas that dentists should
reflect on to ensure that they have appropriate
policies and procedures in place.
Dentists should only retain records for as long as they
are reasonably required and it would be advisable to
prepare a data retention policy. Under the Dental
Council’s Code of Practise regarding Professional
Behaviour and Ethical Conduct, dentists should retain
records for at least 8 years (9 years, in certain cases).
Dentists should consult with their indemnity provider
regarding an appropriate duration for them to hold
records. This is likely to vary from practice to practice,
depending on the nature of the treatments provided.
We also regularly hear from patients stating that
dentists are failing to release records or are being slow
to do so. This is frustrating for your patients and is
contrary to the regulations. We would suggest putting
a notice in your practice informing patients how they
can go about obtaining a copy of their records and the
costs involved.
Further information on GDPR can be found on the
Data Protection Commissioner’s website:
https://www.dataprotection.ie/docs/GDPR/1623.htm
Civil Liability
(Amendment)
Act
2 0 1 8 A U X I L I A R Y R E N E W A L F E E D E A D L I N E - 3 1 s t A U G U S T 2 0 1 8
In November 2017, an amendment to the Civil
Liability Act, 1961 was signed into law. The
a
mendment Act allows healthcare professionals
to make an open disclosure of patient safety
r
elated incidents in the interests of the
common good. The amendment Act provides
certain restrictions to prohibit information
provided by way of an open disclosure being
u
sed in civil and regulatory processes.
The Act is prescriptive as to how an open disclosure
should be made and by whom. New regulations will,
in due course, set out the exact format of disclosures
made under the Act. All healthcare providers are
encouraged to prepare procedures for making an
open disclosure to patients when:
• Unintended or unanticipated injury or harm has
occurred in the course of treatment
• Where a patient was put at risk of unanticipated
injury and harm (even if harm or injury was not
actually caused)
•
Unintended or anticipated injury or harm was
prevented through a timely intervention or by
chance
The Civil Liability (amendment) Act, 2017 (Number
30 of 2017) can be viewed in full on
www.irishstatutebook.ie.
The Minister for Health Simon Harris TD visiting Lily’s stand
BITESIZE
O
cial Newsletter of the Dental Council of Ireland
NEWS
IN BRIEF
P
ractitioner Health
Matters Programme
We feel it’s important to bring
this service to the attention of
the dental profession once again.
This programme was launched in
2
015 and since then has
expanded with a steady increase
in the number of practitioners
availing of the service. It gives
support to those going through
mental health difficulties, stress,
or alcohol or drug misuse
problems and we would like to
r
emind all dental professionals
that this service is available to
help in a completely confidential
manner. Ph; 012970356 or
p
ractitionerhealth.ie
D
ental Renewal Fees
We would like to thank the
p
rofession for their co-operation
in using our online payments
system this year. We
acknowledge that a small
number of practitioners had
some difficulty but overall the
online payment system worked
very well. The Dental Council will
continue to use this online
payment system and would
encourage dentists and auxiliary
workers to retain their sign in
details somewhere safe to allow
easy access next year.
Auxiliary Renewal Fees
All auxiliary renewal fees are due
on August 31st 2018. Dental
nurses who have joined
additional registers such as
Dental Hygienist or Orthodontic
Therapists and who no longer
wish to be included on the
Dental Nurse register need to
inform us of this via e-mail. The
fee can only be paid online
through the Dental Council
website. We are unable to accept
cheques, cash or any other form
of payment. Your payment will
be returned if you pay this way.
You should also inform us if you
have changed your address or
are no longer practising.
Please e-mail us at
Communicating with
the Registration
Department
While you will all have dealt with
the registration department
upon registering to practice for
the first time, it is important to
know your responsibilities going
forward. It is easy to keep your
information up-to-date on the
Register. Drop us an email to
[email protected] with any
changes to your details and we
will let you know if you are
required to send in any
additional information in order
for us to make these changes
happen.
Minimata:
The European Union has introduced
regulation 2017/852 to implement
the Minimata Convention on
Mercury. This is an environmental
regulation rather than a health
regulation and its purpose is to
r
educe the amount of mercury used in
many industries and professional sectors, including
dentistry. This EU Regulation is binding in its entirety and
directly applicable in all member states.
K
ey dates for dentists;
1 January 2018;
• Amalgam separators put into service from this date must provide retention level of at least 95% of
amalgam particles and be maintained in accordance with manufacturer's instructions.
1 July 2018;
•
Dental amalgam shall not be used for dental treatment of deciduous teeth, of children under 15
years and of pregnant or breastfeeding women, except when deemed strictly necessary by the
dental practitioner based on the specific medical needs of the patient.
1 January 2019;
• Operators of dental facilities in which dental amalgam is used, or dental amalgam fillings or teeth
containing such fillings are removed, shall ensure that their facilities are equipped with amalgam
separators for the retention and collection of amalgam particles, including those contained in used
water.
• Dental amalgam shall only be used in pre-dosed encapsulated form. The use of mercury in bulk by
dental practitioners shall be prohibited.
• All separators must provide a retention level of at least 95%.
Dental practitioners should note that failure to comply with the waste management regulations may
separately result in proceedings under the Waste Management Regulations, S.I. No. 126/2011 –
European Communities (Waste Directive) Regulations 2011.
The Dental Council intends issuing guidance for the profession on complying with the new regulations
BT Young Scientist
We would like to congratulate Lily Fitzgerald for her prize winning project on dental phobia
and anxiety.
Lily is a second year student at Kinsale Community School and her project was well received. She was
interested in researching the prevalence of dental phobia and dental anxiety and who this affected
attending a dentist, and some other matters. Her main objectives were to:
• Establish how prevalent dental anxiety and dental phobia is.
• Assess its causes.
• Try to measure anxiety and identify factors that enhance or lessen their perceived anxiety.
• Establish the extent to which people avoid the dentist due to anxiety and phobia.
• Establish what is most common: attending the dentist for a check-up or attending for an
emergency.
• Establish whether people are aware of the age a child should rst visit a dentist.
• Find people’s preferences for their dentists and whether the participants own gender and age
aected their preferences.
Lily undertook a survey of 1074 participants and the respondents were predominantly female (79%)
aged 35-54, mainly educated up to third level and higher and predominantly Irish. She found that the
most common reason for having a fear of the dentist was “bad memories of a dentist visit”. She further
found that 59.9% of respondents avoided the dentist because of dental anxiety, and 43.3% of
respondents avoided attending a dentist because of dental phobia. Delays in being called into the
surgery would make 39.3% of the survey respondents feel more anxious.
Almost 40% of those who only attend at least every 4 years said that this was because of dental
phobia. Interestingly, Lily found that male patients are not as anxious as female patients.
Of the people who stated that they were “a little to very much afraid” to visit a dentist, 26% said it was
due to having bad memories of a
previous dental visit and 25% said it
was because they were afraid of
experiencing pain.
The survey is indicative of how
important it is for all the dental team
to ensure that their patients are put
at ease. In our experience of patients
contacting the council, the
heightened anxiety that can
sometimes stem from comment or a
slight complication in treatment
which can result in complaints to the
council that could have been readily
dealt with in the practice.
General Data
Protection
Regulations (GDPR)
You are probably
already aware that the
new EU General Data
Protection Regulations
came into force on 25
May 2018. These
regulations further
strengthen an
individual’s right to
have their information held and processed
appropriately and securely. Failing to comply may
result in significant fines.
The concept of confidentiality of patient information
has been a bedrock of dentistry over the years, and
there should be little difficulty for the dental
profession in meeting these enhanced requirements.
However there are other areas that dentists should
reflect on to ensure that they have appropriate
policies and procedures in place.
Dentists should only retain records for as long as they
are reasonably required and it would be advisable to
prepare a data retention policy. Under the Dental
Council’s Code of Practise regarding Professional
Behaviour and Ethical Conduct, dentists should retain
records for at least 8 years (9 years, in certain cases).
Dentists should consult with their indemnity provider
regarding an appropriate duration for them to hold
records. This is likely to vary from practice to practice,
depending on the nature of the treatments provided.
We also regularly hear from patients stating that
dentists are failing to release records or are being slow
to do so. This is frustrating for your patients and is
contrary to the regulations. We would suggest putting
a notice in your practice informing patients how they
can go about obtaining a copy of their records and the
costs involved.
Further information on GDPR can be found on the
Data Protection Commissioner’s website:
https://www.dataprotection.ie/docs/GDPR/1623.htm
Civil Liability
(Amendment)
Act
2 0 1 8 A U X I L I A R Y R E N E W A L F E E D E A D L I N E - 3 1 s t A U G U S T 2 0 1 8
In November 2017, an amendment to the Civil
Liability Act, 1961 was signed into law. The
a
mendment Act allows healthcare professionals
to make an open disclosure of patient safety
r
elated incidents in the interests of the
common good. The amendment Act provides
certain restrictions to prohibit information
provided by way of an open disclosure being
u
sed in civil and regulatory processes.
The Act is prescriptive as to how an open disclosure
should be made and by whom. New regulations will,
in due course, set out the exact format of disclosures
made under the Act. All healthcare providers are
encouraged to prepare procedures for making an
open disclosure to patients when:
• Unintended or unanticipated injury or harm has
occurred in the course of treatment
• Where a patient was put at risk of unanticipated
injury and harm (even if harm or injury was not
actually caused)
•
Unintended or anticipated injury or harm was
prevented through a timely intervention or by
chance
The Civil Liability (amendment) Act, 2017 (Number
30 of 2017) can be viewed in full on
www.irishstatutebook.ie.
The Minister for Health Simon Harris TD visiting Lily’s stand
BITESIZE
O
cial Newsletter of the Dental Council of Ireland
NEWS
IN BRIEF
P
ractitioner Health
Matters Programme
We feel it’s important to bring
this service to the attention of
the dental profession once again.
This programme was launched in
2
015 and since then has
expanded with a steady increase
in the number of practitioners
availing of the service. It gives
support to those going through
mental health difficulties, stress,
or alcohol or drug misuse
problems and we would like to
r
emind all dental professionals
that this service is available to
help in a completely confidential
manner. Ph; 012970356 or
p
ractitionerhealth.ie
D
ental Renewal Fees
We would like to thank the
p
rofession for their co-operation
in using our online payments
system this year. We
acknowledge that a small
number of practitioners had
some difficulty but overall the
online payment system worked
very well. The Dental Council will
continue to use this online
payment system and would
encourage dentists and auxiliary
workers to retain their sign in
details somewhere safe to allow
easy access next year.
Auxiliary Renewal Fees
All auxiliary renewal fees are due
on August 31st 2018. Dental
nurses who have joined
additional registers such as
Dental Hygienist or Orthodontic
Therapists and who no longer
wish to be included on the
Dental Nurse register need to
inform us of this via e-mail. The
fee can only be paid online
through the Dental Council
website. We are unable to accept
cheques, cash or any other form
of payment. Your payment will
be returned if you pay this way.
You should also inform us if you
have changed your address or
are no longer practising.
Please e-mail us at
Communicating with
the Registration
Department
While you will all have dealt with
the registration department
upon registering to practice for
the first time, it is important to
know your responsibilities going
forward. It is easy to keep your
information up-to-date on the
Register. Drop us an email to
[email protected] with any
changes to your details and we
will let you know if you are
required to send in any
additional information in order
for us to make these changes
happen.
Minimata:
The European Union has introduced
regulation 2017/852 to implement
the Minimata Convention on
Mercury. This is an environmental
regulation rather than a health
regulation and its purpose is to
r
educe the amount of mercury used in
many industries and professional sectors, including
dentistry. This EU Regulation is binding in its entirety and
directly applicable in all member states.
K
ey dates for dentists;
1 January 2018;
• Amalgam separators put into service from this date must provide retention level of at least 95% of
amalgam particles and be maintained in accordance with manufacturer's instructions.
1 July 2018;
•
Dental amalgam shall not be used for dental treatment of deciduous teeth, of children under 15
years and of pregnant or breastfeeding women, except when deemed strictly necessary by the
dental practitioner based on the specific medical needs of the patient.
1 January 2019;
• Operators of dental facilities in which dental amalgam is used, or dental amalgam fillings or teeth
containing such fillings are removed, shall ensure that their facilities are equipped with amalgam
separators for the retention and collection of amalgam particles, including those contained in used
water.
• Dental amalgam shall only be used in pre-dosed encapsulated form. The use of mercury in bulk by
dental practitioners shall be prohibited.
• All separators must provide a retention level of at least 95%.
Dental practitioners should note that failure to comply with the waste management regulations may
separately result in proceedings under the Waste Management Regulations, S.I. No. 126/2011 –
European Communities (Waste Directive) Regulations 2011.
The Dental Council intends issuing guidance for the profession on complying with the new regulations
BT Young Scientist
We would like to congratulate Lily Fitzgerald for her prize winning project on dental phobia
and anxiety.
Lily is a second year student at Kinsale Community School and her project was well received. She was
interested in researching the prevalence of dental phobia and dental anxiety and who this affected
attending a dentist, and some other matters. Her main objectives were to:
• Establish how prevalent dental anxiety and dental phobia is.
• Assess its causes.
• Try to measure anxiety and identify factors that enhance or lessen their perceived anxiety.
• Establish the extent to which people avoid the dentist due to anxiety and phobia.
• Establish what is most common: attending the dentist for a check-up or attending for an
emergency.
• Establish whether people are aware of the age a child should rst visit a dentist.
• Find people’s preferences for their dentists and whether the participants own gender and age
aected their preferences.
Lily undertook a survey of 1074 participants and the respondents were predominantly female (79%)
aged 35-54, mainly educated up to third level and higher and predominantly Irish. She found that the
most common reason for having a fear of the dentist was “bad memories of a dentist visit”. She further
found that 59.9% of respondents avoided the dentist because of dental anxiety, and 43.3% of
respondents avoided attending a dentist because of dental phobia. Delays in being called into the
surgery would make 39.3% of the survey respondents feel more anxious.
Almost 40% of those who only attend at least every 4 years said that this was because of dental
phobia. Interestingly, Lily found that male patients are not as anxious as female patients.
Of the people who stated that they were “a little to very much afraid” to visit a dentist, 26% said it was
due to having bad memories of a
previous dental visit and 25% said it
was because they were afraid of
experiencing pain.
The survey is indicative of how
important it is for all the dental team
to ensure that their patients are put
at ease. In our experience of patients
contacting the council, the
heightened anxiety that can
sometimes stem from comment or a
slight complication in treatment
which can result in complaints to the
council that could have been readily
dealt with in the practice.
General Data
Protection
Regulations (GDPR)
You are probably
already aware that the
new EU General Data
Protection Regulations
came into force on 25
May 2018. These
regulations further
strengthen an
individual’s right to
have their information held and processed
appropriately and securely. Failing to comply may
result in significant fines.
The concept of confidentiality of patient information
has been a bedrock of dentistry over the years, and
there should be little difficulty for the dental
profession in meeting these enhanced requirements.
However there are other areas that dentists should
reflect on to ensure that they have appropriate
policies and procedures in place.
Dentists should only retain records for as long as they
are reasonably required and it would be advisable to
prepare a data retention policy. Under the Dental
Council’s Code of Practise regarding Professional
Behaviour and Ethical Conduct, dentists should retain
records for at least 8 years (9 years, in certain cases).
Dentists should consult with their indemnity provider
regarding an appropriate duration for them to hold
records. This is likely to vary from practice to practice,
depending on the nature of the treatments provided.
We also regularly hear from patients stating that
dentists are failing to release records or are being slow
to do so. This is frustrating for your patients and is
contrary to the regulations. We would suggest putting
a notice in your practice informing patients how they
can go about obtaining a copy of their records and the
costs involved.
Further information on GDPR can be found on the
Data Protection Commissioner’s website:
https://www.dataprotection.ie/docs/GDPR/1623.htm
Civil Liability
(Amendment)
Act
2 0 1 8 A U X I L I A R Y R E N E W A L F E E D E A D L I N E - 3 1 s t A U G U S T 2 0 1 8
In November 2017, an amendment to the Civil
Liability Act, 1961 was signed into law. The
a
mendment Act allows healthcare professionals
to make an open disclosure of patient safety
r
elated incidents in the interests of the
common good. The amendment Act provides
certain restrictions to prohibit information
provided by way of an open disclosure being
u
sed in civil and regulatory processes.
The Act is prescriptive as to how an open disclosure
should be made and by whom. New regulations will,
in due course, set out the exact format of disclosures
made under the Act. All healthcare providers are
encouraged to prepare procedures for making an
open disclosure to patients when:
• Unintended or unanticipated injury or harm has
occurred in the course of treatment
• Where a patient was put at risk of unanticipated
injury and harm (even if harm or injury was not
actually caused)
•
Unintended or anticipated injury or harm was
prevented through a timely intervention or by
chance
The Civil Liability (amendment) Act, 2017 (Number
30 of 2017) can be viewed in full on
www.irishstatutebook.ie.
The Minister for Health Simon Harris TD visiting Lily’s stand

BITESIZE
O
cial Newsletter of the Dental Council of Ireland
NEWS
IN BRIEF
P
ractitioner Health
Matters Programme
We feel it’s important to bring
this service to the attention of
the dental profession once again.
This programme was launched in
2
015 and since then has
expanded with a steady increase
in the number of practitioners
availing of the service. It gives
support to those going through
mental health difficulties, stress,
or alcohol or drug misuse
problems and we would like to
r
emind all dental professionals
that this service is available to
help in a completely confidential
manner. Ph; 012970356 or
p
ractitionerhealth.ie
D
ental Renewal Fees
We would like to thank the
p
rofession for their co-operation
in using our online payments
system this year. We
acknowledge that a small
number of practitioners had
some difficulty but overall the
online payment system worked
very well. The Dental Council will
continue to use this online
payment system and would
encourage dentists and auxiliary
workers to retain their sign in
details somewhere safe to allow
easy access next year.
Auxiliary Renewal Fees
All auxiliary renewal fees are due
on August 31st 2018. Dental
nurses who have joined
additional registers such as
Dental Hygienist or Orthodontic
Therapists and who no longer
wish to be included on the
Dental Nurse register need to
inform us of this via e-mail. The
fee can only be paid online
through the Dental Council
website. We are unable to accept
cheques, cash or any other form
of payment. Your payment will
be returned if you pay this way.
You should also inform us if you
have changed your address or
are no longer practising.
Please e-mail us at
Communicating with
the Registration
Department
While you will all have dealt with
the registration department
upon registering to practice for
the first time, it is important to
know your responsibilities going
forward. It is easy to keep your
information up-to-date on the
Register. Drop us an email to
[email protected] with any
changes to your details and we
will let you know if you are
required to send in any
additional information in order
for us to make these changes
happen.
Minimata:
The European Union has introduced
regulation 2017/852 to implement
the Minimata Convention on
Mercury. This is an environmental
regulation rather than a health
regulation and its purpose is to
r
educe the amount of mercury used in
many industries and professional sectors, including
dentistry. This EU Regulation is binding in its entirety and
directly applicable in all member states.
K
ey dates for dentists;
1 January 2018;
• Amalgam separators put into service from this date must provide retention level of at least 95% of
amalgam particles and be maintained in accordance with manufacturer's instructions.
1 July 2018;
•
Dental amalgam shall not be used for dental treatment of deciduous teeth, of children under 15
years and of pregnant or breastfeeding women, except when deemed strictly necessary by the
dental practitioner based on the specific medical needs of the patient.
1 January 2019;
• Operators of dental facilities in which dental amalgam is used, or dental amalgam fillings or teeth
containing such fillings are removed, shall ensure that their facilities are equipped with amalgam
separators for the retention and collection of amalgam particles, including those contained in used
water.
• Dental amalgam shall only be used in pre-dosed encapsulated form. The use of mercury in bulk by
dental practitioners shall be prohibited.
• All separators must provide a retention level of at least 95%.
Dental practitioners should note that failure to comply with the waste management regulations may
separately result in proceedings under the Waste Management Regulations, S.I. No. 126/2011 –
European Communities (Waste Directive) Regulations 2011.
The Dental Council intends issuing guidance for the profession on complying with the new regulations
BT Young Scientist
We would like to congratulate Lily Fitzgerald for her prize winning project on dental phobia
and anxiety.
Lily is a second year student at Kinsale Community School and her project was well received. She was
interested in researching the prevalence of dental phobia and dental anxiety and who this affected
attending a dentist, and some other matters. Her main objectives were to:
• Establish how prevalent dental anxiety and dental phobia is.
• Assess its causes.
• Try to measure anxiety and identify factors that enhance or lessen their perceived anxiety.
• Establish the extent to which people avoid the dentist due to anxiety and phobia.
• Establish what is most common: attending the dentist for a check-up or attending for an
emergency.
• Establish whether people are aware of the age a child should rst visit a dentist.
• Find people’s preferences for their dentists and whether the participants own gender and age
aected their preferences.
Lily undertook a survey of 1074 participants and the respondents were predominantly female (79%)
aged 35-54, mainly educated up to third level and higher and predominantly Irish. She found that the
most common reason for having a fear of the dentist was “bad memories of a dentist visit”. She further
found that 59.9% of respondents avoided the dentist because of dental anxiety, and 43.3% of
respondents avoided attending a dentist because of dental phobia. Delays in being called into the
surgery would make 39.3% of the survey respondents feel more anxious.
Almost 40% of those who only attend at least every 4 years said that this was because of dental
phobia. Interestingly, Lily found that male patients are not as anxious as female patients.
Of the people who stated that they were “a little to very much afraid” to visit a dentist, 26% said it was
due to having bad memories of a
previous dental visit and 25% said it
was because they were afraid of
experiencing pain.
The survey is indicative of how
important it is for all the dental team
to ensure that their patients are put
at ease. In our experience of patients
contacting the council, the
heightened anxiety that can
sometimes stem from comment or a
slight complication in treatment
which can result in complaints to the
council that could have been readily
dealt with in the practice.
General Data
Protection
Regulations (GDPR)
You are probably
already aware that the
new EU General Data
Protection Regulations
came into force on 25
May 2018. These
regulations further
strengthen an
individual’s right to
have their information held and processed
appropriately and securely. Failing to comply may
result in significant fines.
The concept of confidentiality of patient information
has been a bedrock of dentistry over the years, and
there should be little difficulty for the dental
profession in meeting these enhanced requirements.
However there are other areas that dentists should
reflect on to ensure that they have appropriate
policies and procedures in place.
Dentists should only retain records for as long as they
are reasonably required and it would be advisable to
prepare a data retention policy. Under the Dental
Council’s Code of Practise regarding Professional
Behaviour and Ethical Conduct, dentists should retain
records for at least 8 years (9 years, in certain cases).
Dentists should consult with their indemnity provider
regarding an appropriate duration for them to hold
records. This is likely to vary from practice to practice,
depending on the nature of the treatments provided.
We also regularly hear from patients stating that
dentists are failing to release records or are being slow
to do so. This is frustrating for your patients and is
contrary to the regulations. We would suggest putting
a notice in your practice informing patients how they
can go about obtaining a copy of their records and the
costs involved.
Further information on GDPR can be found on the
Data Protection Commissioner’s website:
https://www.dataprotection.ie/docs/GDPR/1623.htm
Civil Liability
(Amendment)
Act
2 0 1 8 A U X I L I A R Y R E N E W A L F E E D E A D L I N E 3 1 s t A U G U S T 2 0 1 8
In November 2017, an amendment to the Civil
Liability Act, 1961 was signed into law. The
a
mendment Act allows healthcare professionals
to make an open disclosure of patient safety
r
elated incidents in the interests of the
common good. The amendment Act provides
certain restrictions to prohibit information
provided by way of an open disclosure being
u
sed in civil and regulatory processes.
The Act is prescriptive as to how an open disclosure
should be made and by whom. New regulations will,
in due course, set out the exact format of disclosures
made under the Act. All healthcare providers are
encouraged to prepare procedures for making an
open disclosure to patients when:
• Unintended or unanticipated injury or harm has
occurred in the course of treatment
• Where a patient was put at risk of unanticipated
injury and harm (even if harm or injury was not
actually caused)
•
Unintended or anticipated injury or harm was
prevented through a timely intervention or by
chance
The Civil Liability (amendment) Act, 2017 (Number
30 of 2017) can be viewed in full on
www.irishstatutebook.ie.
The Minister for Health Simon Harris TD visiting Lily’s stand

The Dental Council hosted the annual conference of FEDCAR, the Federation of European Dental Competent Authorities and Regulators on the 20 April
BITESIZE
BITESIZE
Ocial Newsletter of the Dental Council of Ireland
VOLUME 2, ISSUE 1 | JUNE 2018
VOLUME 2, ISSUE 1 | JUNE 2018
President’s Address
Welcome to our Summer 2018 newsletter. I am
delighted to say that the Dental Council hosted
the annual conference of FEDCAR, the
Federation of European Dental Competent
Authorities and Regulators on the 20 April. We
hold the FEDCAR presidency this year and we
held the conference in Dublin Castle. A
combination of the fine facilities and the first
gloriously sunny days of the New Year showed Dublin and
Ireland off positively to our European colleagues.
The main focus of the meeting was to discuss ways of ensuring
that there is quality assurance of dental training across all
European dental schools. The European Union project allows
dental health professionals to move relatively freely across
Europe. It is important for patients that they can be assured that
there is an appropriate system in place to ensure that someone
graduating with a dental qualification has the required skills to
treat patients. This is presently not the case and it is a significant
weakness in the European systems. We had a positive
engagement with the other stakeholders representing dental
educators, the professional organisations and the dental
students. We look forward to progressing this important work
over the coming months.
THE REGISTRAR’S
Frequently Asked Questions
As Registrar, David O’Flynn receives many phone calls and
emails from both registrants and members of the public and
there are some themes that come forward regularly.
Do you get many calls about
communication issues?
In 2017, the main issue for approximately 30%
of the patients who contacted the council
concerned communications. These patients
reported problems ranging from sharp or
brusque responses to questions, to anger, to
the patient feeling that the treatment plan was
not properly explained to them.
The number of calls and emails we receive is
small in the context of the total number of
patient/dentist interactions that take place
every day in Ireland. However, sometimes the
patient’s heightened general anxiety about
going to the dentist and the draws on the
dental team’s attention that can occur in a busy
dental surgery collide and leave the patient
worried or annoyed about something that
happened in the surgery.
It is important for all members of the dental
team to continually remind themselves of the
paramount importance of fully engaging with
your patients.
Is complex treatment at the heart of many
complaints to the Dental Council?
Surprisingly, no. Most of the complaints we
receive about treatment are routine general
practise dentistry, such as fillings falling out, ill-
fitting dentures, fabricating and affixing crowns
and bridgework. In many cases, the patient has
already discussed the issue with the dentist and
is still dissatisfied. While we generally ask the
patient to discuss their treatment with the
dentist, the fact that they have contacted us
generally means they are losing confidence in
their dentist’s willingness to deal with their
problem.
We do also receive complaints about more
complex treatment and an increasing number
of these concern implant retained bridges.
A recurring problem is the failure of the dentist
to realise when specialist assistance may be
required. We accept that problems will arise
during even the most routine treatment, and it
is important for dentists to reflect on the point
when the patient should be referred on.
IN THIS
ISSUE
How the Council Works
Minimata
General Data Protection
Regulations (GDPR)
Practitioner Health Matters
Programme
Renewal Fee’s
Communicating with the
Registration Department
Civil Liability (Amendment) Act
BT Young Scientist
Dental Council Updates
FAQ’s
Dr Gerry McCarthy,
President
57 Merrion Square, Dublin 2, D02 EH90, Ireland
Telephone: (01) 676 2226. Email: [email protected]
www.dentalcouncil.ie
Update from David O’Flynn, Registrar
F
itness to Practise
In this edition of the Newsletter I would like to set out some information about the
Dental Council’s Fitness to Practise procedures. This is an area that is of interest to
many dentists and the general public alike.
Most allegations we receive are of professional misconduct which is defined as
being a serious falling short in the standards expected of a dentist, and in this
context the word ‘serious’ is important. Professional misconduct is intended to sit
above negligence in terms of a hierarchy of seriousness. The process is intended to
deal with matters where the allegation gives rise to a serious concern about the dentist’s practise.
We receive over 150 calls or emails from patients every year. Most patients contact us because they
are unhappy with their experience with a dentist and they are looking for advice. In most cases, we
recommend that the patient discuss the matter with the dentist directly. Often, when the patient
contacts the council, they are close to escalating the matter further, and resolving the matter
promptly is usually the best option for everyone.
Each year about 8-10 calls and emails result in a formal allegation of professional misconduct being
m
ade. The dentist is always given an opportunity to provide their comments and observations on an
allegation prior to the matter being considered by the Fitness to Practise Committee.
In order for the matter to proceed to Inquiry, the committee must be satisfied that there is prima facie
evidence of professional misconduct. The prima facie test is met if the committee is satisfied that the
allegation, if proven, would amount to professional misconduct, and that there is a likely prospect of
the allegation being proven beyond reasonable doubt. Beyond reasonable doubt is the burden of
p
roof required at an inquiry. As you can see from the table, only 1-2 of the applications received
annually will result in an inquiry.
The Dental Council may apply any of 6 sanctions if an allegation of professional misconduct is proven.
These sanctions are: erasure, suspension for a period of time, conditions attached to practise, censure,
admonishment, and advisement. Shortly, all sanctions will need to be confirmed by the High Court.
How the council works
F
itness to Practise Committee
Nine members of the Dental Council sit on the Fitness to Practise Committee. Under the Dentists Act,
1985, the majority of the committee must have been elected by the profession and at least one must
be appointed by the Department of Health and must not be a dentist. The full committee considers
allegations up to the prima facie decision, and usually three members of the committee are delegated
to hear each inquiry. The present membership is:
F
itness to Practise Journey
Initial Contact
R
eferred back to practice or to Dental Complaints Resolution Service
Allegation
No prima facie (case closed)
Inquiry
No finding of professional misconduct
Council
Sanctions imposed after proven finding of professional misconduct
Year Total
Ave per
contact
(
min)
W
rite
to DC
A
llegations
received
I
nquiry
Decision
Subject of Complaint
F
ees
B
ehaviour
T
reatment
O
thers
2017 153 23 15 5 1 17% 30% 53% 0%
2016 150 24 12 9 2 19% 19% 59% 3%
2015 171 19 13 2 1 12% 20% 60% 8%
2014 163 18 16 13 1 16% 19% 60% 6%
2013 228 24 N/A 9 2 25% 25% 45% 4%
Fitness to Practise Activity 2013-2017
F
F
F
i
i
t
t
t
n
n
n
e
e
e
s
s
s
s
s
t
t
t
o
o
o
P
P
PP
r
r
r
aa
c
c
t
t
t
ii
s
s
ee
C
C
C
O
O
O
M
M
M
M
M
M
I
I
I
T
T
T
T
T
E
E
E
E
D
r Bernard
Murphy
Chair and elected
dentist
Dr Danielle
Colbert
Elected
member
Mr James
Doorley
Nominated by
D
ept of Health
(lay member)
Dr Rory
F
leming
Elected member
Prof Martin
Kinirons
Nominated
by UCC
Dr Liam
Lynch
Elected member
Dr Ray
McCarthy
Elected member
Dr Eleanor
O’Higgins
Nominated by
Dept of Health
(lay member)
Vacant
Nominated by
D
ept of Health
(lay member)
The Dental Council expects all dentists to have a formal complaints procedure in place (Section
5.4 of the Code of Practice regarding Professional Behaviour and Ethical Conduct).
