
The Maine Death with Dignity Act
Annual Report
Pursuant to 22 MRS §2140
Data from Calendar Year 2023
Submitted April 2024 to the Joint Standing Committee
on Health and Human Services
Maine State Legislature
Produced by Data, Research, and Vital Statistics
Maine Center for Disease Control and Prevention
Department of Health and Human Services

Death with Dignity Act CY 2023 Annual Report
Executive Summary
In accordance with 22 MRS § 2140(17), the Department of Health and Human Services
(Department) shall generate and make available to the public an annual statistical report of
information collected under the Maine Death with Dignity Act (Act). The Department is
mandated to submit a copy of the report to the Joint Standing Committee of the Legislature
having jurisdiction over health matters, annually by March 1. This report is for patients who
completed a written request for medication to hasten their death in calendar year 2023. Patients
who completed the oral request but not a written request within the calendar year will be
included in the subsequent year’s report.
This report provides statistics concerning the utilization of Patient-directed Care, 22 MRS
chapter 418. Specifically, this report provides information about patients who have reportedly
met the requirements of the Act, the underlying causes of qualified patient deaths, and the
number of prescriptions for life-ending medication written or dispensed to qualified patients.
In 2023, there were 80 patients who started the process (19 more than in 2022). Four
individuals died before they could make their written requests. There were nine patients still
alive at the time of this report, although three of these completed their requirements at the end
of 2023 and six months has not passed. Patients resided in 14 counties. The two counties
where patients did not reside were Piscataquis and Washington. Patients were more likely to
be older. There was no significant difference in the split of male or female and cancer was the
condition reported most often.
Introduction
The 129
th
Maine Legislature passed Public Law 2019 Chapter 271 known and cited as the
Death with Dignity Act (Appendix A). The Act enables physicians to prescribe medication to a
Maine resident diagnosed with a terminal condition with the intent that the medication be self-
administered for the purpose of hastening the patient’s death. The Act set forth conditions for
the patient and the physician for this action to be taken lawfully. Those conditions include, but
are not limited, to an oral and written request by the patient to the physician, a reminder that all
steps in the process must be voluntary and that the patient be capable of making such a
decision, confirmation of the diagnosis and prognosis by a second physician, and an attestation
by a qualified witness to these steps.
Once the prescribing physician fulfills all the statutory requirements, the physician is required
to attest to compliance with the Act and submit required report forms to the Department. The
fact that a health care provider participates in activities under this Act may not be the sole basis
for a complaint or report by another health care provider to the appropriate licensing board
under Title 32, including, but not limited to, the Board of Licensure in Medicine, the Board of
Osteopathic Licensure and the Maine Board of Pharmacy.
Within six months of the effective date of the Act, the Department was directed to adopt major
substantive rules to facilitate the collection of information regarding compliance with the Act.
The information collected is confidential, is not a public record, and may not be made available
for inspection by the public.
On June 12, 2019, Governor Janet Mills issued executive order number 9 FY19/20, directing the

Death with Dignity Act CY 2023 Annual Report
Department to conduct rulemaking on an emergency basis following the enactment of Public
Law 2019 c. 271. Emergency rulemaking was conducted in accordance with 5 MRS §8054, and
the Death with Dignity Act Reporting Rule, 10-146 CMR chapter 15, was in place when the law
became effective on September 19, 2019 (Appendix B). The emergency rule provided guidance
on reporting requirements for physicians to demonstrate that the individual made an informed
decision about their end-of-life care and to ensure compliance with the law. Reporting forms
were developed to collect the information required both in law and in the Governor’s executive
order.
To coincide with expiration of the emergency rule as means to ensuring continuity, the
Department submitted for provisional adoption, a major substantive rule in January 2020. In
accordance with the Maine Administrative Procedures Act, this major substantive rule was
submitted to the Legislature for review and approval for final adoption.
In March 2020, the Legislature voted to enact LD 2068, Resolve, Regarding Legislative Review
of Portions of Chapter 15: Death with Dignity Act Reporting Rule, a Major Substantive Rule of
the Department of Health and Human Services, Maine Center for Disease Control and
Prevention.
Currently in effect, the Death with Dignity Act Reporting Rule requires up to five documents for
reporting and compliance purposes. The content of reporting forms required by the Department is
consistent with the statute. Forms are found on the Data, Research, and Vital Statistics (DRVS)
website
1
or by request to the State Registrar and these forms include:
• Request for Medication to End My Life in a Humane and Dignified Manner Form
that is to be completed and signed by the patient and two witnesses;
• Interpreter Attachment Form, if applicable;
• Consulting Physician Form that is to be signed by a physician who has reviewed and
confirmed the medical opinion of the attending physician;
• Attending Physician End-of Life Reporting Form which certifies all the requirements
of the Act have been met, including adherence to the waiting periods set forth by the
Act; and
• End-of-Life Closure Form to be completed by the attending physician within 30 days
of the death of the qualified patient
General Statistics
•
There were 80 patients who started the process; however, four patients died before
completing the request process. The remaining 76 patients met all the requirements of the
Act. At the time of this report, there are nine individuals for whom a death certificate
could not be found. It was confirmed with the attending physician that these patients are
still alive. Three of these nine, completed the requests near the end of the year and are
still less than six months into the process from when the first request was made.
1
Maine CDC Office of Data, Research and Vital Statistics; https://www.maine.gov/dhhs/mecdc/public-health-
systems/data-research/vital-records/forms/index.shtml
Death with Dignity Act CY 2023 Annual Report
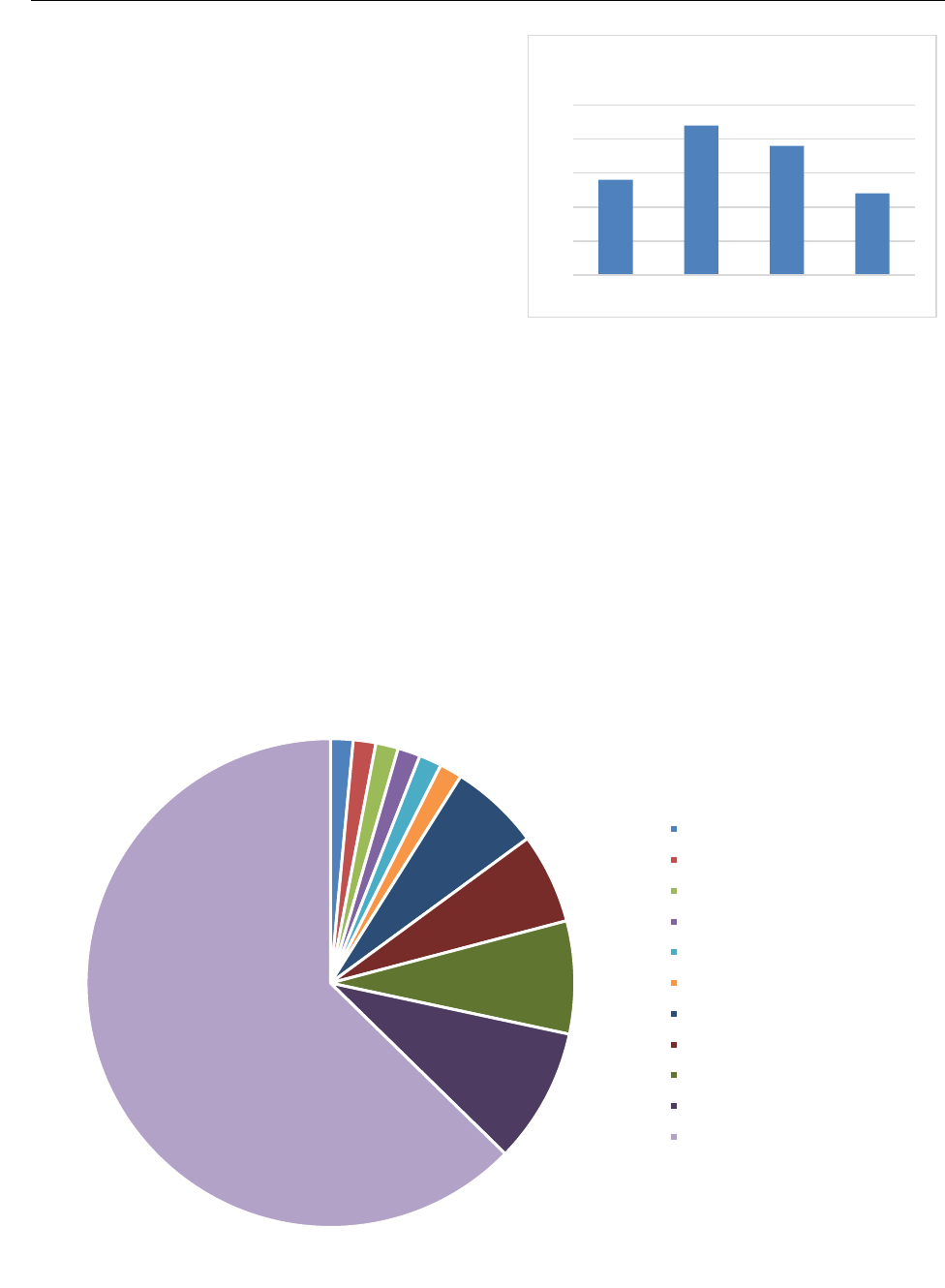
• Ages ranged from the youngest of 31 to the
oldest of 98. Distribution across age groups
were similar with nearly half being 75 and
older.
• Over 35% of those who died had attained a
high school education, while 18% had
attended college but did not have a degree
and 47% had college degrees.
• Of the 67 patients who died, 53 died by
patient choice, 12 from the underlying illness and two unknowns. The average number of
days between the time the prescription was written and the date of death for those patients
who died from administering the prescription was 20 days.
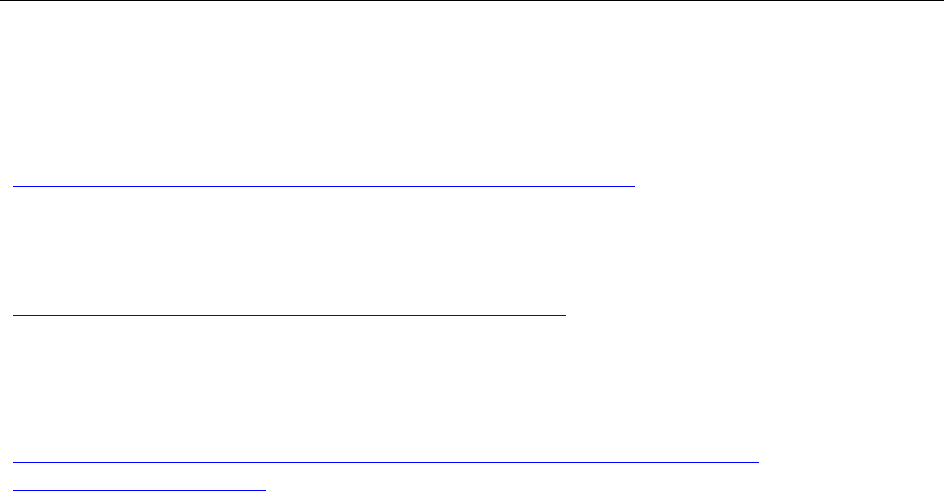
• Cancer was the terminal condition in 42 of the cases of death of patients under the Act.
This represented 63% of the total. Amyotrophic lateral sclerosis (ALS) was indicated in six
deaths, heart disease in five deaths, chronic obstructive pulmonary disease (COPD) and
end stage renal disease in four deaths each. The six other conditions were Parkinson’s
Disease, Muscular Dystrophy, Crohn’s disease, cerebral amyloid angiopathy, multiple
system atrophy, and inclusive body myositis with one case each.
1
1
1
1
1
1
4
4
5
6
42
Terminal Condition in Cases of Patient Death
Cerebral Amyloid Angiopathy (1)
Crohn's Disease (1)
Inclusive Body Myositis (1)
Multiple System Atrophy (1)
Muscular Dystrophy (1)
Parkinson's Disease (1)
COPD (4)
End Stage Renal Disease (4)
Heart Disease/Cardiac (5)
ALS (6)
All Cancers (42)
0
5
10
15
20
25
<65 65-74 75-84 >84
Number of Patients by Age
Death with Dignity Act CY 2023 Annual Report
Attachments
Appendix A
22 MRS chapter 418, available for download at:
http://legislature.maine.gov/legis/statutes/22/title22sec2140.html
Appendix B
10-146 CMR chapter 15, available for download at:
http://www.maine.gov/sos/cec/rules/10/chaps10.htm#146
Reporting Forms (Attending Physician End-of-Life Reporting Form, Consulting Physician
Form, Interpreter Attachment Form, Request for Medication to End My Life in a Humane
and Dignified Manner Form, End of Life Closure Form) are available for download at:
http://www.maine.gov/dhhs/mecdc/public-health-systems/data-research/vital-
records/forms/index.shtml

Death with Dignity Act CY 2023 Annual Report
APPENDIX A
MRS Title 22, §2140. PATIENT-DIRECTED CARE AT THE END OF LIFE
§2140. Patient-directed care at the end of life
1. Short title. This chapter may be known and cited as "the Maine Death with Dignity Act."
[PL 2019, c. 271, §4 (NEW).]
2. Definitions. As used in this chapter, unless the context otherwise indicates, the following
terms have the following meanings.
A. "Adult" means a person who is 18 years of age or older. [PL 2019, c. 271, §4 (NEW).]
B. "Attending physician" means the physician who has primary responsibility for the care of a
patient and the treatment of that patient's terminal disease. [PL 2019, c. 271, §4 (NEW).]
C. "Competent" means that, in the opinion of a court or in the opinion of the patient's attending
physician or consulting physician, psychiatrist or psychologist, a patient has the ability to make
and communicate an informed decision to health care providers, including communication
through persons familiar with the patient's manner of communicating if those persons are
available. [PL 2019, c. 271, §4 (NEW).]
D. "Consulting physician" means a physician who is qualified by specialty or experience to make
a professional diagnosis and prognosis regarding a patient's disease. [PL 2019, c. 271, §4
(NEW).]
E. "Counseling" means one or more consultations between a state-licensed psychiatrist, state-
licensed psychologist, state-licensed clinical social worker or state-licensed clinical professional
counselor and a patient for the purpose of determining that the patient is competent and not
suffering from a psychiatric or psychological disorder or depression causing impaired judgment.
[PL 2019, c. 271, §4 (NEW).]
F. "Health care provider" means:
(1) A person licensed, certified or otherwise authorized or permitted by law to administer
health care services or dispense medication in the ordinary course of business or practice of a
profession; or
(2) A health care facility. [PL 2019, c. 271, §4 (NEW).]
G. "Informed decision" means a decision by a qualified patient to request and obtain a
prescription for medication that the qualified patient may self-administer to end the qualified
patient's life in a humane and dignified manner that is based on an appreciation of the relevant
facts and that is made after being fully informed by the attending physician of:
(1) The qualified patient's medical diagnosis;
(2) The qualified patient's prognosis;
(3) The potential risks associated with taking the medication to be prescribed;
(4) The probable result of taking the medication to be prescribed; and
(5) The feasible alternatives to taking the medication to be prescribed, including palliative
care and comfort care, hospice care, pain control and disease-directed treatment options. [PL
2019, c. 271, §4 (NEW).]
H. "Medically confirmed" means the medical opinion of an attending physician has been
confirmed by a consulting physician who has examined the patient and the patient's relevant
medical records. [PL 2019, c. 271, §4 (NEW).]
I. "Patient" means an adult who is under the care of a physician. [PL 2019, c. 271, §4 (NEW).]
J. "Physician" means a doctor of medicine or osteopathy licensed to practice medicine in this
State. [PL 2019, c. 271, §4 (NEW).]
Death with Dignity Act CY 2023 Annual Report
APPENDIX B
STATE OF MAINE
DEATH WITH DIGNITY ACT
REPORTING RULE
10-146 CODE OF MAINE RULES
CHAPTER 15
Department of Health and Human Services
Maine Center for Disease Control and Prevention
11 State House Station
Augusta, Maine 04333-0011
Effective Date: August 30, 2020 (Major Substantive Rule)
Death with Dignity Act Reporting Rule
(Major Substantive Rule)
10-144 CMR, Ch. 15
TABLE OF CONTENTS
SECTION 1. PURPOSE AND DEFINITIONS ................................................................................... 1
A. Purpose ............................................................................................................................. 1
B. Definitions ........................................................................................................................ 1
SECTION 2. SCOPE ............................................................................................................................. 1
SECTION 3. RESPONSIBILITIES OF HEALTHCARE PROVIDERS ........................................ 2
A. Compliance ....................................................................................................................... 2
B. Request for Medication to End My Life in a Humane and Dignified Manner ................. 2
C. Interpreter Attachment ...................................................................................................... 2
D. Consulting Physician End-of-Life Care Form .................................................................. 2
E. Attending Physician End-of-Life- Reporting Form .......................................................... 3
F. End-of-Life Closure Form ................................................................................................ 3
SECTION 4. REPORTING AND RECORD RETENTION ............................................................. 3
A. Reporting .......................................................................................................................... 3
B. Record Retention .............................................................................................................. 4
C. Confidentiality .................................................................................................................. 4
STATUTORY AUTHORITY AND HISTORY ..................................................................................... 5
SECTION 1. PURPOSE AND DEFINITIONS
A. Purpose. This major substantive rule implements 22 MRS chapter 418, the Maine Death with
Dignity Act (Act), and specifies the Department’s authority to collect and use information related
to patient-directed care at the end of life.
B. Definitions. As used in this rule, unless the context indicates otherwise, the following terms have
the following meanings:
1. Act means the Maine Death with Dignity Act, 22 MRS Chapter 418.
2. Attending physician means the physician who has primary responsibility for the care of
a patient and the treatment of that patient’s terminal disease.
3. Competent means that, in the opinion of a court or in the opinion of the patient’s
attending physician or consulting physician, psychiatrist or psychologist, a patient has the
ability to make and communicate an informed decision to health care providers, including
communication through persons familiar with the patient’s manner of communicating, if
those persons are available.
4. Consulting physician means a physician who is qualified by specialty or experience to
make a professional diagnosis and prognosis regarding a patient’s disease.
5. Department means the Department of Health and Human Services, Maine Center for
Disease Control and Prevention (Maine CDC).
6. Form means a form prescribed by the Department that the Department requires to be
completed for purposes of compliance with this rule. Forms that are missing required
signatures, dates or information will not be considered valid or acceptable.
7. Life-ending medication means the medication prescribed or dispensed by a licensed
healthcare provider in accordance with the Act to be self-administered by the qualified
patient suffering from a terminal disease to end the qualified patient’s life in a humane
and dignified manner.
8. Physician means a doctor of medicine or osteopathy licensed pursuant to 32 MRS
chapter 48 or 36.
9. Qualified patient means a competent adult who is a resident of this State and who has
satisfied the requirements of the Act in order to obtain a prescription for medication that
the qualified patient may self-administer to end the qualified patient’s life in a humane
and dignified manner.
SECTION 2. SCOPE
This rule applies to healthcare providers involved in the decisions pursuant to the Act. This rule
establishes reporting requirements related to patient-directed care at the end of life and
responsibilities of healthcare providers participating in specific conduct under the Act. This rule
does not require a healthcare provider to provide life-ending medication to a qualified patient.

SECTION 3. RESPONSIBILITIES OF HEALTHCARE PROVIDERS
A. Compliance. The attending physician must verify that all requirements of the Act have been met
before prescribing or dispensing life-ending medication. The attending physician is responsible
for ensuring that copies of all required forms are received by the Department. The attending
physician must ensure that each original, completed form is retained in the qualified patient’s
medical record. Copies of required forms must be filed within 30 days after the date the
prescription for life-ending medication is written, unless otherwise specified.
B. Request for Medication to End My Life in a Humane and Dignified Manner. The Request
for Medication to End My Life in a Humane and Dignified Manner Form must be used for all
written requests for life-ending medication. This form must be completed by the competent
patient and two witnesses no sooner than 15 days following the patient’s first oral request for life-
ending medication, in accordance with 22 MRS §§ 2140(5) and 2140(24). A copy of the
completed form must be provided to the qualified patient.
1. Witnesses. The qualified patient’s signature on this form must be witnessed by at least
two individuals who, in the presence of the qualified patient, attest that to the best of their
knowledge and belief, the patient is competent, is acting voluntarily, and is not being
coerced to sign the request.
a. One witness must be a person who is not:
i. A relative of the patient by blood, marriage, or adoption;
ii. A person who at the time the form is signed would be entitled to any
portion of the estate of the patient upon death, under any will or by
operation of any law; or
iii. An owner, operator or employee of a health care facility where the
patient is receiving medical treatment or is a resident.
b. Attending Physician. The patient’s attending physician at the time the written
request is signed may not be a witness.
c. Patient in a Long-Term Care Facility. If the patient resides in a long-term care
facility at the time of the patient’s written request, one witness must be a licensed
healthcare provider designated by the facility. The facility’s designee may be an
owner, operator or employee of the healthcare facility where the patient resides.
C. Interpreter Attachment. The Interpreter Attachment Form is only required if an interpreter is
used pursuant to 22 MRS §2140(5)(B), to interpret conversations or consultations between the
patient and the patient’s attending or consulting physician in a language other than English,
regarding the written request for life-ending medication. If an interpreter is used, this form,
containing the elements required by 22 MRS §2140 (25), must accompany the Request for
Medication to End My Life in a Humane and Dignified Manner Form.
D. Consulting Physician End-of-Life Care Form. The Consulting Physician End-of-Life Care
Form, containing the reporting requirements of 22 MRS §§ 2140 (7) and 2140 (14)(D), must be
completed by the consulting physician who has examined the patient, has reviewed the patient’s
medical record, and who has confirmed the medical opinion of the attending physician that the

patient is suffering from a terminal disease and has verified that the patient is competent, is acting
voluntarily, and has made an informed decision.
E. Attending Physician End-of-Life Reporting Form. The Attending Physician End-of-Life-
Reporting Form must be completed by the attending physician to certify that all requirements of
the Act have been met, including the attending physician’s responsibilities at 22 MRS §2140(6),
the documentation requirements at 22 MRS §2140(14), and the waiting periods set forth at
22 MRS §2140(13). A copy of the written prescription record must accompany this form.
F. End-of-Life Closure Form. The End-of-Life Closure Form must be completed by the attending
physician within 30 days after the qualified patient’s death, in accordance with 22 MRS
§2140(17)(B)(1). The Department, in receipt of a death certificate registration for a patient who
has been prescribed life-ending medication, may contact the attending physician to complete
reporting under this rule, including the End-of-Life Closure Form, and submit to the State
Registrar within 30 days following notification of the patient’s death.
SECTION 4. REPORTING AND RECORD RETENTION
A. Reporting
1. Reporting must be in the manner prescribed by the Department, using the forms specified
in this rule. Copies of the forms may be accessed at the Department’s Data Research and
Vital Statistics website at http://www.maine.gov/dhhs/mecdc/public-health-systems/data-
research/vital-records/forms/index.shtml, or by request to the State Registrar.
2. Copies of completed forms must be sent via postal mail to the following address or
submitted to the State Registrar electronically by encrypted email. Fax filing of reports is
not accepted under this rule.
DHHS - Office of Data, Research, and Vital Statistics
Attn: State Registrar
11 State House Station
220 Capitol Street
Augusta, Maine 04333-0011
3. All forms must be completed in accordance with the Act and this rule. Unless otherwise
specified, all forms must be submitted to the State Registrar no later than 30 days after
the date the prescription for life-ending medication is written. The Department will
contact the qualified patient’s attending physician when it appears that any required form
has not been filed.
4. The Department will collect information from attending physicians who have prescribed
or dispensed life-ending medication to ensure compliance with the Act and this rule, and
for use in assembling an annual statistical report as required by the Act. Required
information will include any information requested on the forms prescribed by the
Department and specified in this rule. Additionally, the Department may request from an
attending physician any other information reasonably necessary to determine compliance
with the Act and this rule.

B. Record Retention.
1. The attending physician prescribing or dispensing life-ending medication to a qualified
patient must retain the original of each required form in the patient’s medical record.
2. Paper forms submitted to the State Registrar will be retained by the Department to inform
the annual report and may be destroyed only after the Department publishes the yearly
report required by the Act.
C. Confidentiality. Except as otherwise provided by law, information collected by the Department
pursuant to this rule is confidential, is not a public record, and may not be made available for
inspection by the public.
STATUTORY AUTHORITY AND HISTORY
STATUTORY AUTHORITY:
22 MRS §42; 22 MRS §2140
EFFECTIVE DATE:
September 19, 2019 – filing 2019-170 (Emergency adoption, major substantive)
January 13, 2020 – filing LR-2020-7 (Provisional adoption, major substantive)
August 30, 2020 - filing 2020 -173 (Final adoption, major substantive)
