
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 1
DEFINITIONS FOR BILLED, ALLOWED AND PAID AMOUNTS
AND OTHER PAYMENT TERMS
A. INTRODUCTION
Under RCW 43.371.010(3), the mandated Washington All Payer Claims Database (APCD) data
suppliers include the state Medicaid program, Public Employees Benefits Board (PEBB) programs,
all health carriers operating in this state, all third-party administrators paying claims on behalf of
health plans in this state and the state Labor and Industries program. The data suppliers must submit
claims data, including billed amounts, allowed amounts and paid amounts, and such additional
information as defined by the Office of Financial Management (OFM) director in rule. Paper 3
provides background information for the three required definitions — billed, allowed and paid
amounts. As for ‘“such additional information,” OFM identifies and provides background
information on other health care claim payment terms that may be defined in the rule. OFM
acknowledges there may be additional claim data that should be defined in rule, and that these terms
will be identified in the rule-making process.
For this paper, OFM reviewed health care claim payment definitions from federal and state rules and
the definitions provided by Washington state health insurers. OFM also reviewed the descriptions of
payment data elements found in the other state APCD data submission guides. The information
sources for this paper are:
The Uniform Glossary
The rules for the Patient Protection and Affordable Care Act
1
(ACA)
require health insurers
and group health plans to provide a summary of benefits and coverage (SBC) and a Uniform
Glossary to their enrollees and beneficiaries. The SBC is intended to provide an easy-to-
understand summary of the benefits and coverage available under their plans. The Uniform
Glossary provides definitions of common insurance-related and medical terms to help
consumers understand the terms of coverage. The Uniform Glossary definitions do not pre-
empt definitions in state law or definitions in a health plan or health insurance policy. Health
insurers are required to make the Uniform Glossary available, upon request, to their
subscribers. In Washington, the health care insurers, the Office of the Insurance
Commissioner, Health Care Authority, Health Benefits Exchange and Department of Health
post the Uniform Glossary on their websites.
Title 182 WAC
Title 182 WAC contains the definitions and rules for the Washington state Medicaid program, a
mandated data supplier to the Washington APCD
2
. See Appendix A: Title 182 WAC
definitions.
Commercial health insurers in Washington
OFM asked Premera Blue Cross, Regence BlueShield and Group Health Cooperative to
provide the definitions they use for billed, allowed and paid amounts and other payment terms.
1
For the Uniform Glossary, see https://www.cms.gov/CCIIO/Resources/Files/Downloads/uniform-glossary-
final.pdf. The U.S. departments of Health and Human Services, Treasury and Labor worked with the National
Association of Insurance Commissioners to draft the rules for the SBC and Uniform Glossary.
2
See definitions Chapter 182-500 WAC and Chapter 182-550 WAC http://apps.leg.wa.gov/wac/default.aspx?cite=182.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 2
OFM chose these health insurers because they are the three largest data suppliers to the WA-
APCD. OFM also reviewed their online samples of explanation of benefits
3
(EOB).
Medicare Glossary
To receive Medicare data, RCW 43.371.020(2)(b) requires the APCD lead organization to apply
to become a Centers for Medicare and Medicaid Services (CMS) qualified entity. CMS has a
Medicare glossary that includes analogous definitions for billed and paid amounts and other
payment terms
4
. See Appendix B: CMS Medicare glossary terms related to claim payments.
Other state APCD rules
Maine, New Hampshire, Oregon and Vermont define payment terms in their APCD rules. A
review of these rules shows that:
› None of these states define billed amount.
› Oregon and Vermont define charge which is an analogous definition to billed amount.
› Oregon is the only state that defines allowed amount and paid amount.
› These states also define other payment terms in their rules, including capitated services, co-
payment, coinsurance, deductible and prepaid amount.
APCD data submission guides
The other states describe payment data elements in their data submission guides (DSGs). The
data element descriptions provide insight into the claim payment data that are actually collected.
APCD Council core data elements
National health insurers express concern with the complexity and cost of submitting health care
claims data to multiple state APCDs that have differing rules and data element specifications.
To address this concern, the APCD Council, the U.S. Department of Health and Human
Services Agency for Healthcare Research and Quality (AHRQ) and other stakeholders
developed a list of APCD core data elements for medical claims file submission, medical
eligibility file submission and pharmacy claims file submission. Each data element is named and
assigned a data element ID. States provide the definitions for the data elements. To review the
APCD Council core set of data elements, see https://ushik.ahrq.gov/mdr/portals/apcd.
The following paper presents OFM’s findings for the definitions for billed, allowed and paid
amounts and other health care claim payment terms. The paper also lists the questions and issues for
consideration in developing payment definitions for the WA-APCD.
3
Health care insurers send EOBs to covered individuals to explain the medical treatments and/or services paid on their
behalf. For sample EOBs, see the links below.
Premera Blue Cross https://www.premera.com/wa/member/manage-my-account/explanation-of-benefits
Regence Uniform Medical Plan
https://www.regence.com/documents/10192/286192/UMP+Explanation+of+Benefits/2fca7dd3-576c-4fb3-
9ccd-a169e9cf25fe
Group Health https://provider.ghc.org/open/workingWithGroupHealth/forms/payment.pdf
4
For the full Medicare glossary of terms, see https://www.medicare.gov/glossary/e.html.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 3
Paper 3 is divided into the following sections:
A. Introduction
B. Billed amount
C. Allowed amount
D. Paid amount
E. Other payment terms
F. Considerations for developing definitions
Appendices and References
Appendix A: Title 182 WAC Definitions
Appendix B: CMS Medicare glossary terms related to claim payments
References
B. BILLED AMOUNT
After reviewing the definitions in rules or provided by the health insurers, OFM found that:
Billed amount is not defined in rule by any of the states with an APCD.
Billed amount can be either the total amount billed (Premera, Group Health) or the dollar
amount charged on the service line for a service (Regence).
The Medicaid definition is not definite on whether the billed charge is the total dollar amount
or a line item charge.
Billed amount is generated by the provider billing the health plan for services.
Billed/submitted amount can also be generated by Group Health members when submitting
charges for reimbursement.
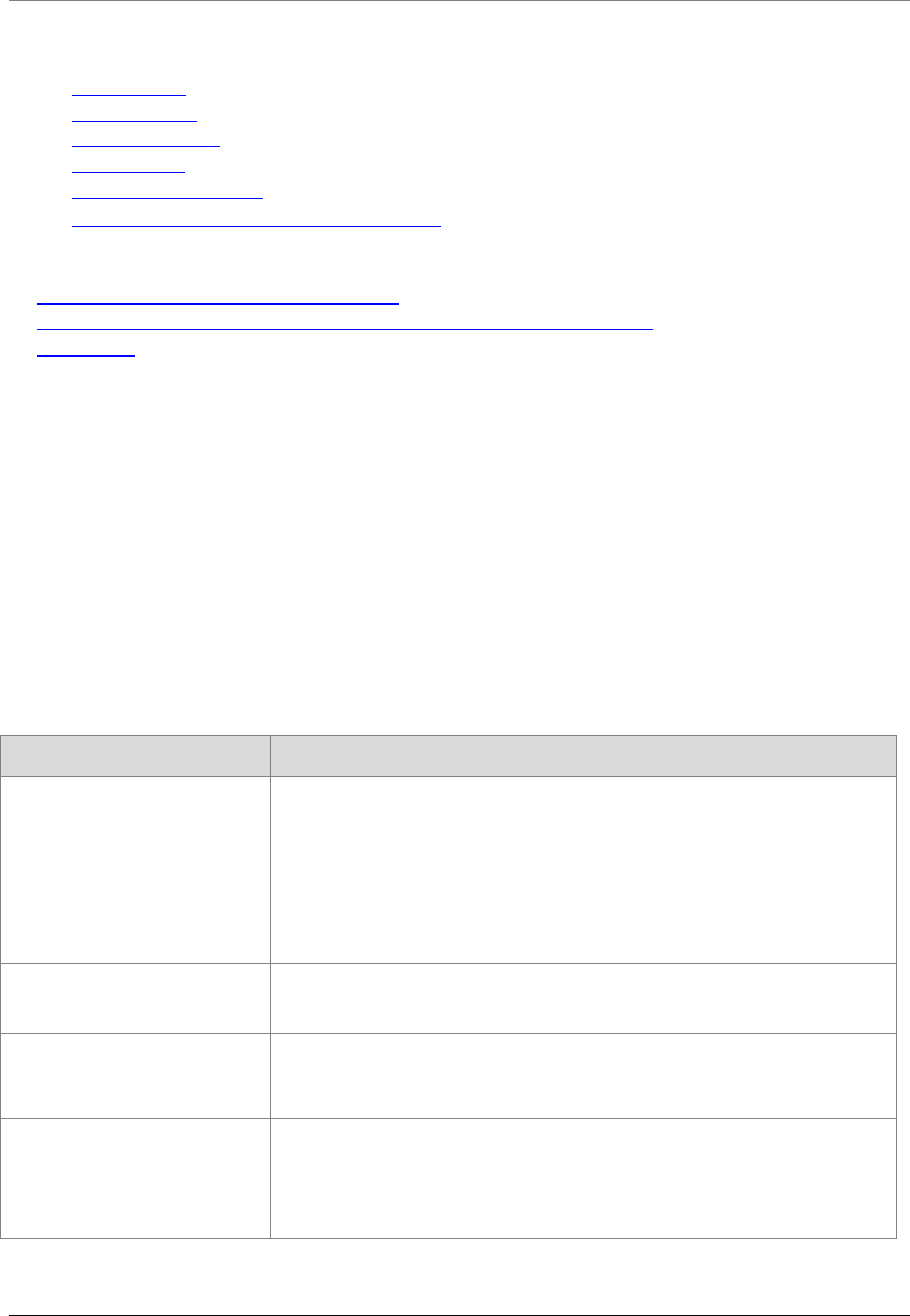
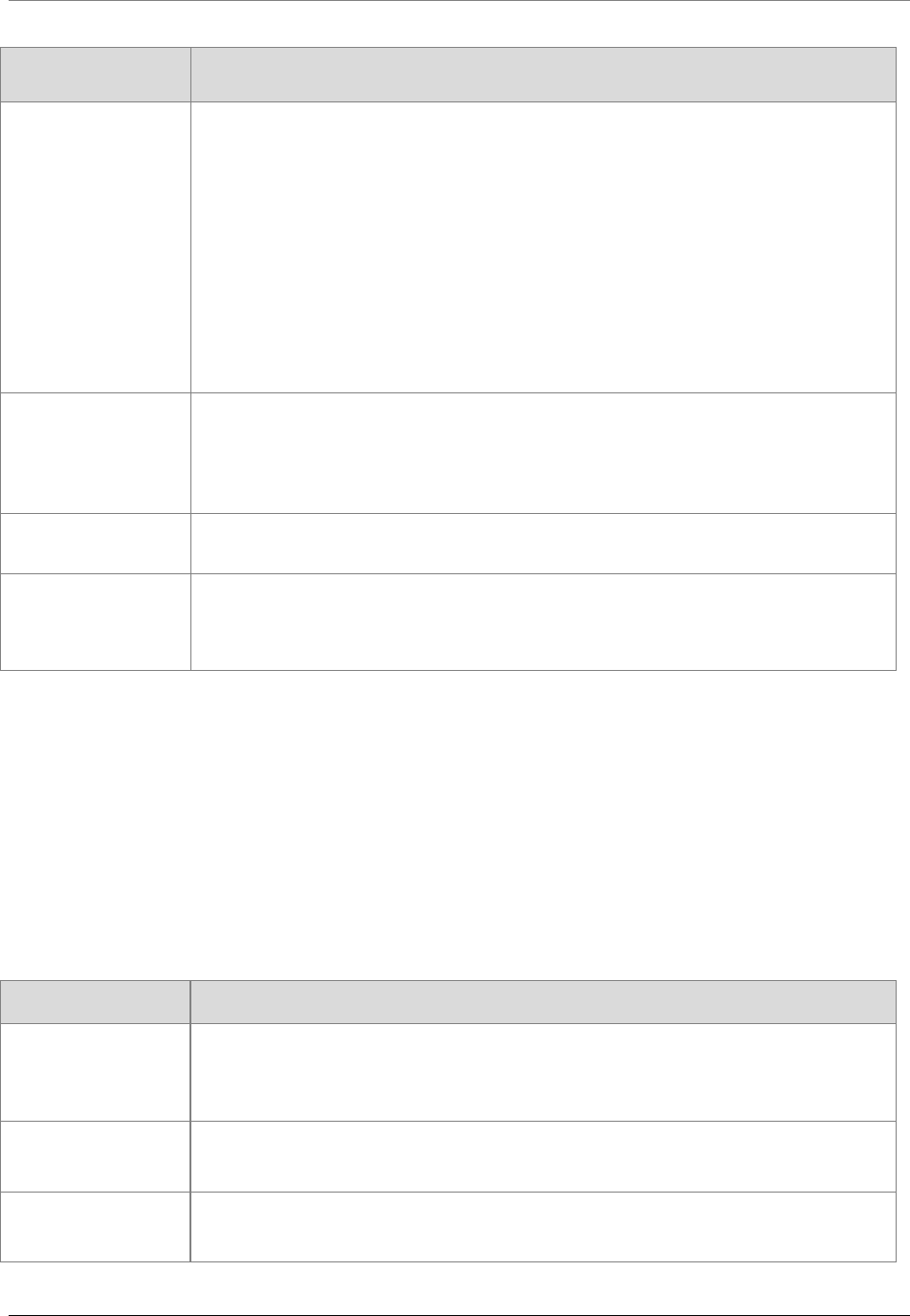
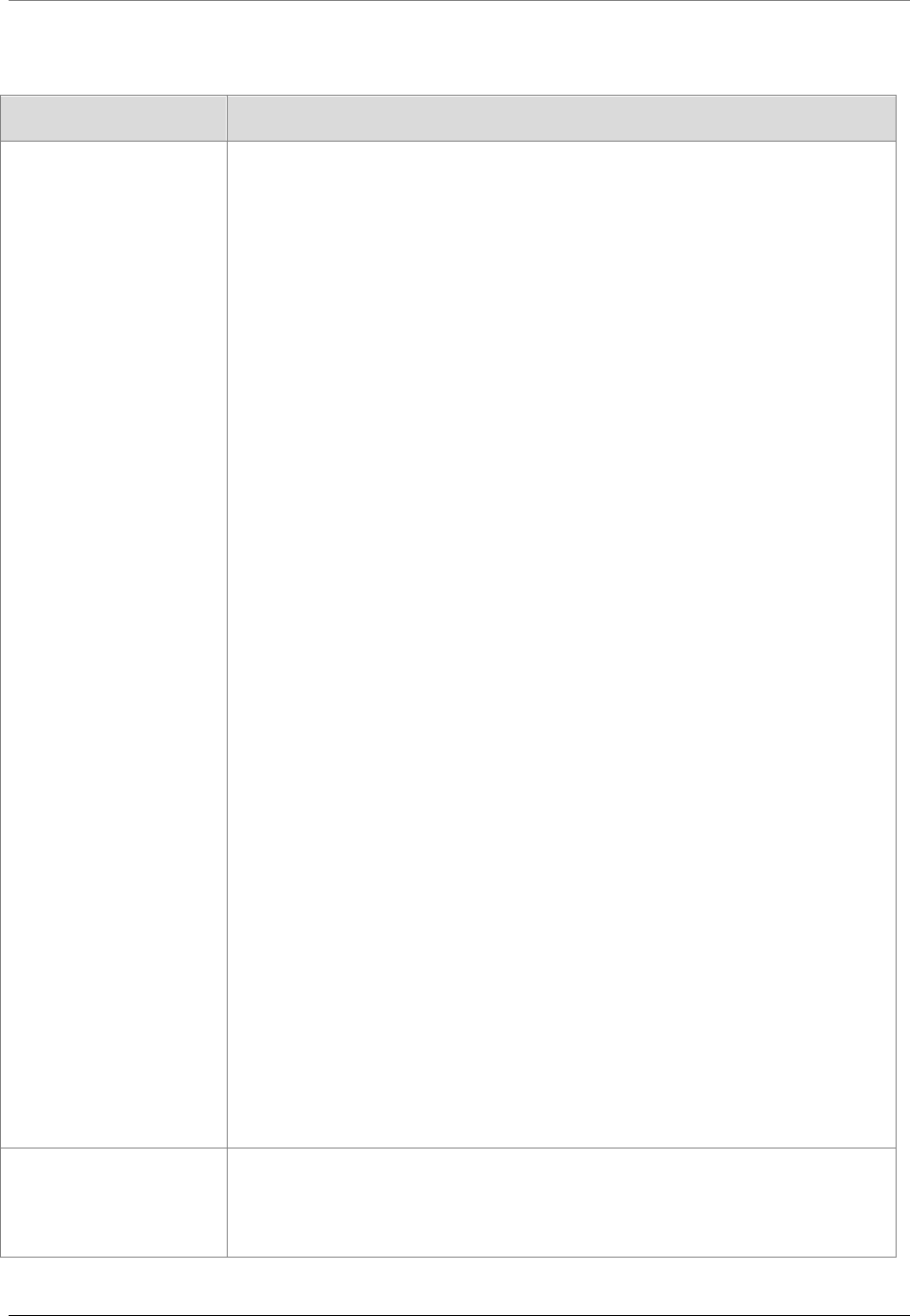
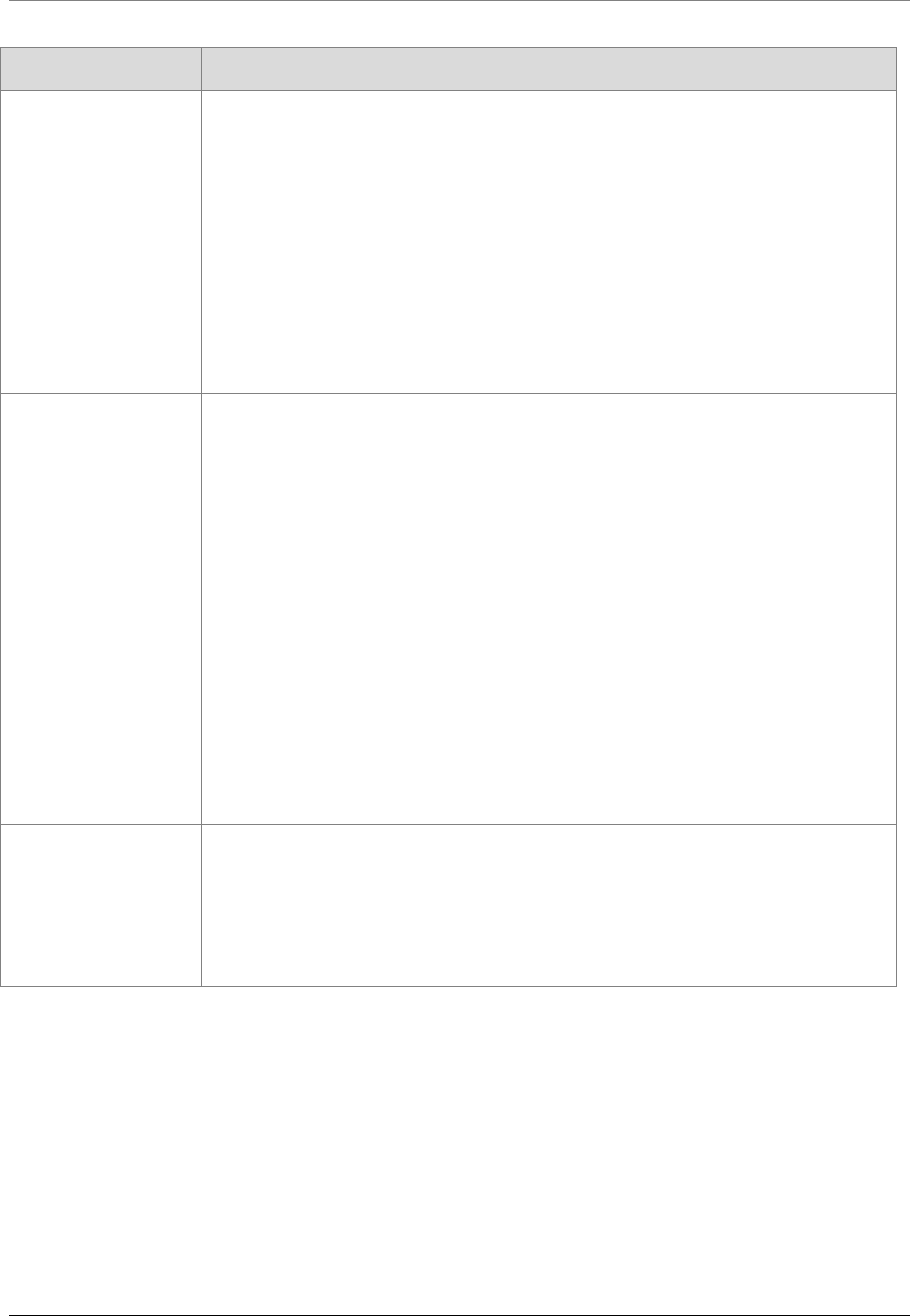
Table 1: Definitions for billed amount in rules and from health insurers
SOURCE TERM AND DEFINITION
WAC 182-550-1050 Hospital
Services Definitions
Billed charge – The charge submitted to the agency by the provider.
Allowed charges – The total billed charges for allowable services.
Allowed covered charges – The total billed charges for services minus the
billed charges for noncovered and/or denied services.
Premera Blue Cross Amount billed – The full amount billed by your provider to your health plan.
Regence BlueShield Billed – The dollar amount the provider charged on the service line for the
service rendered.
Group Health Cooperative Billed/submitted charges – The charges submitted by the provider or
member for reimbursement.
Total charges – The total amount billed to Group Health by a provider.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 4
SOURCE TERM AND DEFINITION
Oregon APCD Rule Charge – The actual dollar amount charged on the claim.
Vermont APCD Rule Charge – The actual dollar amount charged on the claim.
After reviewing the descriptions of payment data elements in the other state APCD data submission
guides (DSGs), OFM found:
Minnesota and Maryland require submittal of total charges for the service billed.
Maryland has a separate data element for billed charge for pharmacy that requires the submittal
of the retail amount of the drug, including dispensing fees and administrative cost.
Connecticut and Massachusetts require submittal of the amount of the provider charges for the
claim line.
Table 2 lists the data elements and descriptions for billed amount in other state DSGs.
Table 2: Data elements and descriptions for billed amount in other state APCDs
SOURCE APCD DATA ELEMENT AND DESCRIPTION
APCD Council
core data element
Charge amount – States add their own descriptions.
Connecticut DSG Charge amount – Amount of provider charges for the claim line.
Maryland DSG Billed charge – Practitioner billed charges.
Billed charge – Retail amount for drug, including dispensing fees and administrative
cost.
Massachusetts DSG Charge amount – Amount of provider charges for the claim line.
Minnesota DSG Charge amount – Total charges for the service as reported by the provider.
C. ALLOWED AMOUNT
After reviewing the definitions in rules or provided by the health insurers, OFM found that:
Allowed amount is the maximum amount that a payer will pay a provider for a service.
Allowed amount applies to services that are included or allowed in the health care plan or the
government program.
Allowed amount applies to services provided by providers who are contracted with the health
care plan (in-network).
Allowed amount varies for providers who are not contracted with the subscriber’s health care
plan (out-of-network).
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 5
Allowed amount may not cover all the provider’s charges. In some cases, subscribers may have
to pay the difference.
Allowed amount may be determined by a fee schedule such as Medicare’s.
Usual customary and reasonable (UCR) amount is sometimes used to determine the allowed
amount.
Oregon is the only state that defines allowed amount (see Table 3).
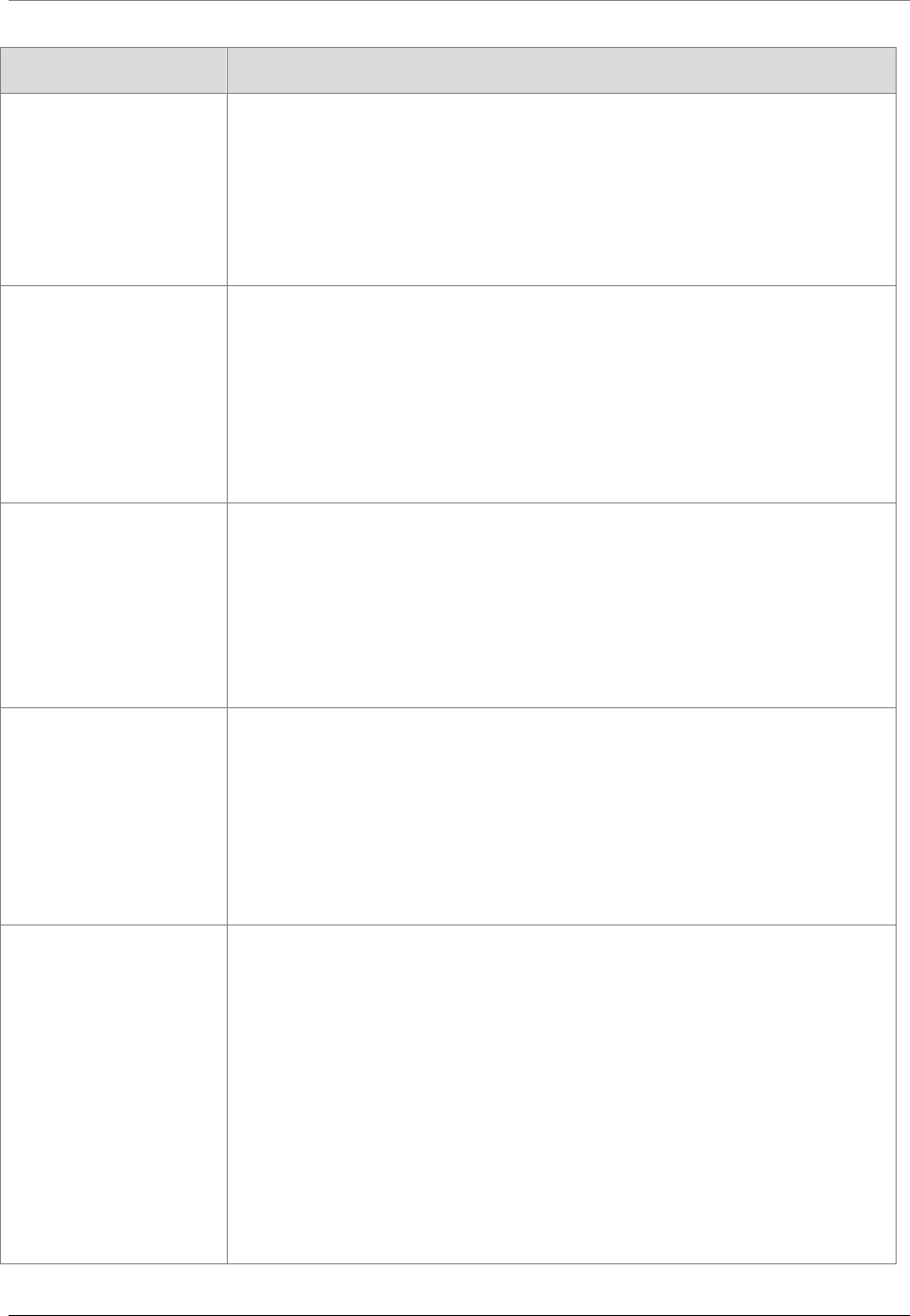
Table 3 lists the sources and definitions in rules and from health insurers for allowed amount.
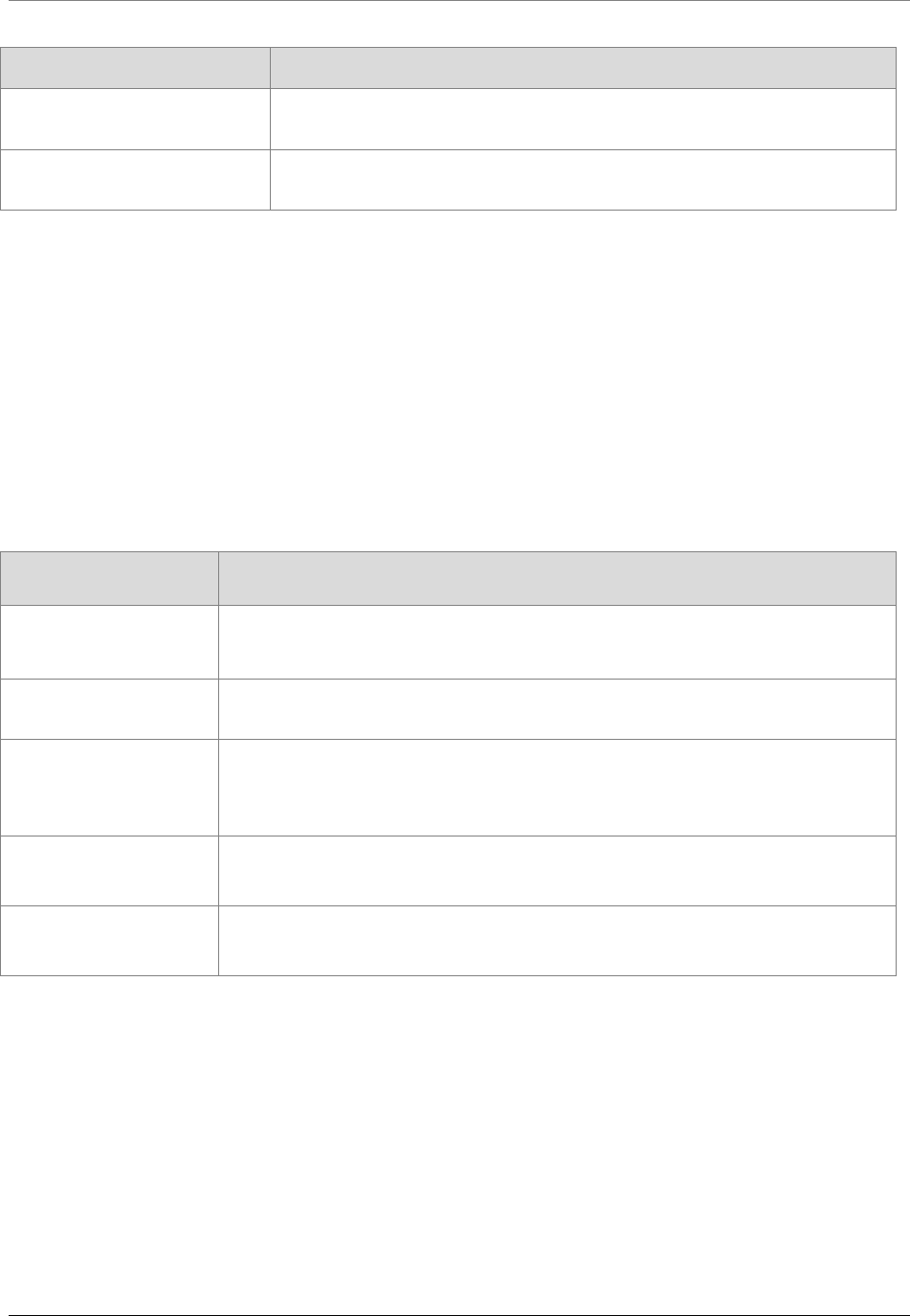
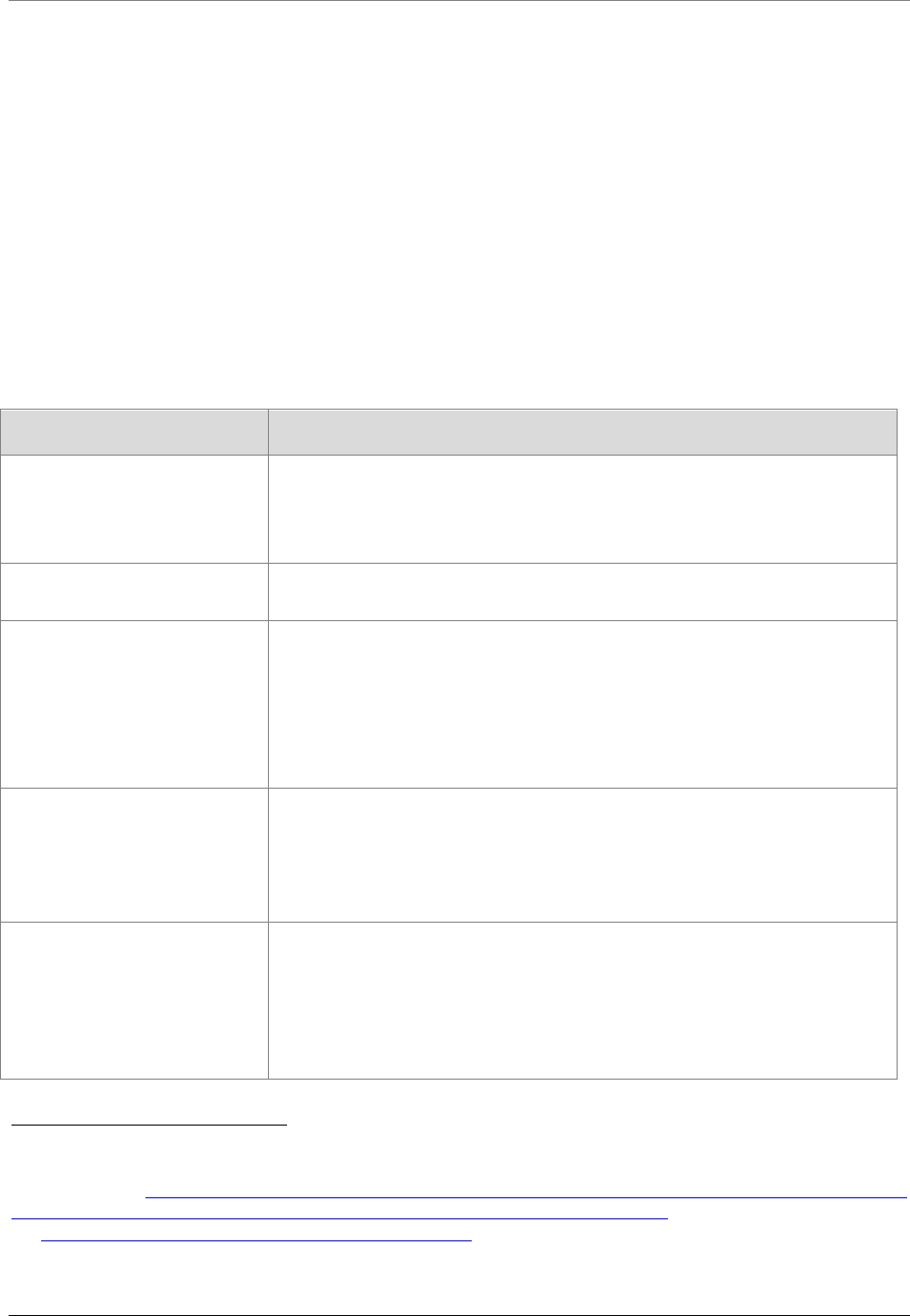
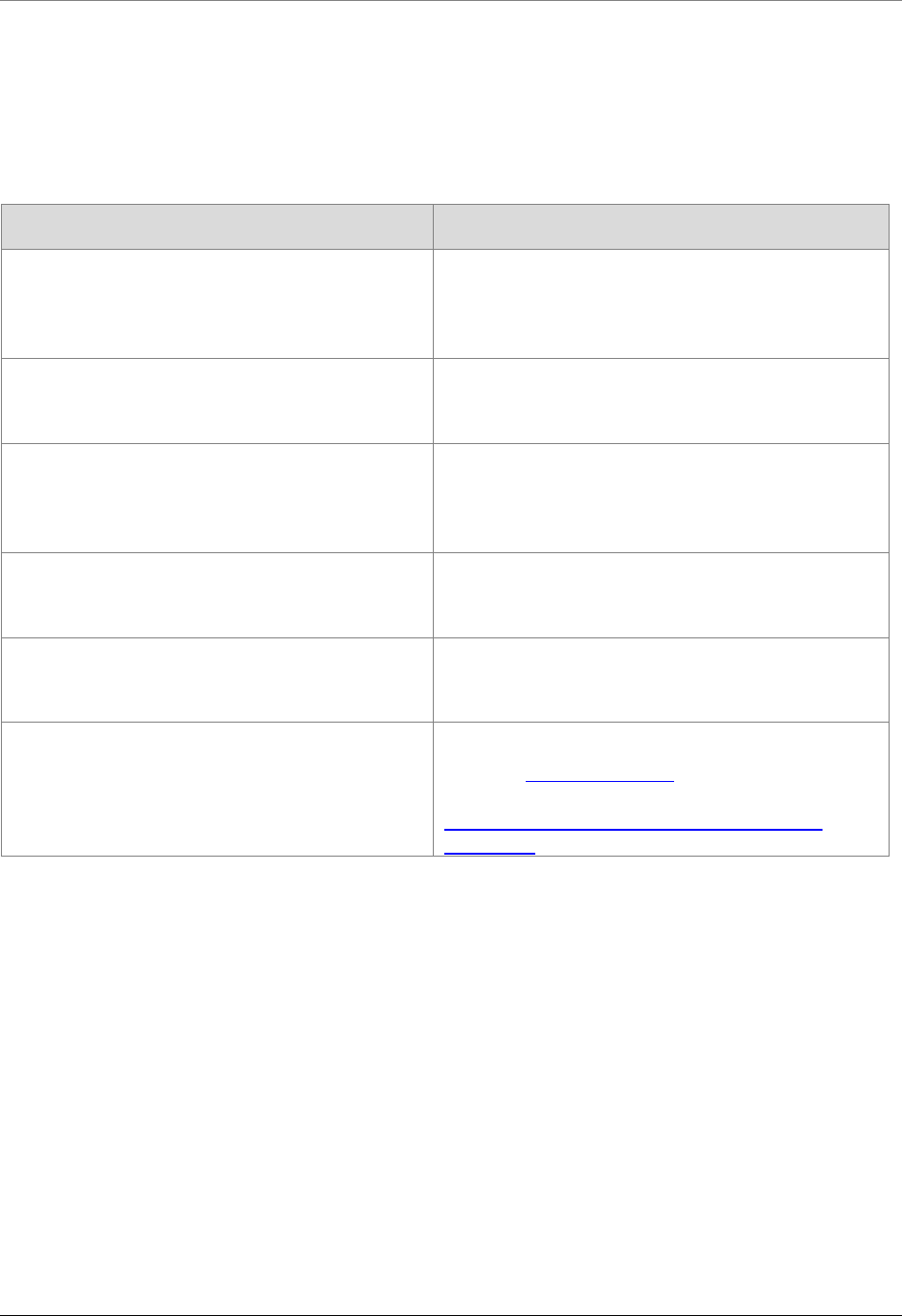
Table 3: Definitions for allowed amount in rule and from health insurers
SOURCE TERM AND DEFINITION
Uniform Glossary Allowed amount – Maximum amount on which payment is based for covered health care
services. This may be called eligible expense, payment allowance or negotiated rate. If
your provider charges more than the allowed amount, you may have to pay the
difference.
UCR (usual, customary and reasonable) – The amount paid for a medical service in a
geographic area based on what providers in the area usually charge for the same or
similar medical service. The UCR amount sometimes is used to determine the allowed
amount.
Medicare Glossary
of Terms
Medicare approved amount – In Original Medicare, this is the amount a doctor or
supplier who accepts assignment can be paid. It may be less than the actual amount a
doctor or supplier charges. Medicare pays part of this amount and you’re responsible for
the difference.
WAC 182-550-1050
Hospital services
definitions
Allowed amount – The initial calculated amount for any procedure or service, after
exclusion of any nonallowed service or charge, that the agency allows as the basis for
payment computation before final adjustments, deductions and add-ons.
Premera Blue Cross
Allowable charge – This plan provides benefits based on the allowable charge for
covered services. We reserve the right to determine the amount allowed for any given
service or supply. The allowable charge is described below.
Providers in Washington and Alaska who agreements with us – For any given
service or supply, the amount these providers have agreed to accept as payment in full
pursuant to the applicable agreement between us and the provider. These providers
agree to seek payment from us when they furnish covered services to you. You'll be
responsible only for any applicable calendar year deductibles, co-pays, coinsurance,
charges in excess of the stated benefit maximums and charges for services and supplies
not covered under this plan. Your liability for any applicable calendar year deductibles,
coinsurance, co-pays and amounts applied toward benefit maximums will be calculated
on the basis of the allowable charge.
Providers outside Washington and Alaska who have agreements with other Blue
Cross Blue Shield licensees – For covered services and supplies received outside
Washington and Alaska, or in Clark County, Washington, allowable charges are
determined as stated in the What Do I Do If I'm Outside Washington And Alaska? Section
(BlueCard® Program And Other Inter-Plan Arrangements) in this booklet.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 6
SOURCE TERM AND DEFINITION
Providers who don't have agreements with us or another Blue Cross Blue Shield
licensee – The allowable charge for Washington or Alaska providers that don't have a
contract with us is the least of the three amounts shown below. The allowable charge for
providers outside Washington or Alaska who don't have a contract with us or the local
Blue Cross and/or Blue Shield Licensee is also the least of the three amounts shown
below.
An amount that is no less than the lowest amount we pay for the same or similar
service from a comparable provider who has a contracting agreement with us.
125 percent of the fee schedule determined by the Centers for Medicare and
Medicaid Services (Medicare), if available.
The provider’s billed charges, if applicable law requires a different allowable charge
than the least of the three amounts above; this plan will comply with that law.
Regence BlueShield
Allowed – The dollar amount that is allowed for services rendered by providers based on
their contractual agreements with Regence. For those providers who serve Regence
members, but don't have a contract with Regence (participating or nonparticipating), this
field represents the amount upon which the members' benefits are based.
Group Health
Cooperative
The maximum amount that Group Health will pay for a specific type of service.
Oregon rule Allowed amount – The actual amount of charges for health care services, equipment or
supplies that are covered expenses under the terms of an insurance policy or health
benefits plan.
After reviewing descriptions of payment data elements in other state DSGs, OFM found that:
In Connecticut and Massachusetts, allowed amount is the maximum amount that is
contractually allowed and that a carrier will pay to a provider for a particular procedure or
service.
In Maryland, allowed amount includes total patient and payer liability. It is the retail amount for
the specified procedure code.
Table 4 lists the APCD data elements and descriptions for allowed amount in other state DSGs.
Table 4: Data elements for allowed amount in other state APCDs
SOURCE APCD DATA ELEMENT AND DESCRIPTION
Connecticut DSG
Allowed amount – The maximum amount contractually allowed and that a carrier will
pay to a provider for a particular procedure or service.
Maryland DSG
Allowed amount – Total patient and payer liability. Retail amount for the specified
procedure code.
Massachusetts DSG
Allowed amount – The maximum amount contractually allowed and that a carrier will
pay to a provider for a particular procedure or service.

WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 7
D. PAID AMOUNT
After reviewing the definitions in rules or provided by the health insurers, OFM found that paid
amount:
Can have several meanings:
› Actual dollar amount paid for whole claim by health care insurer.
› Actual dollar amount paid for a claim line by health care insurer.
› Portion of the charges the health insurer is liable for.
› Amount paid for a medical service in a geographic area based on what providers in the area
usually charge for the same or similar medical service, also known as UCR.
Can be paid by the health plan and by other source.
Does not include co-pay, deductibles, coinsurance or network discount.
On pharmacy claims, paid amount may mean amount billable to the customer/group; the client
total amount due.
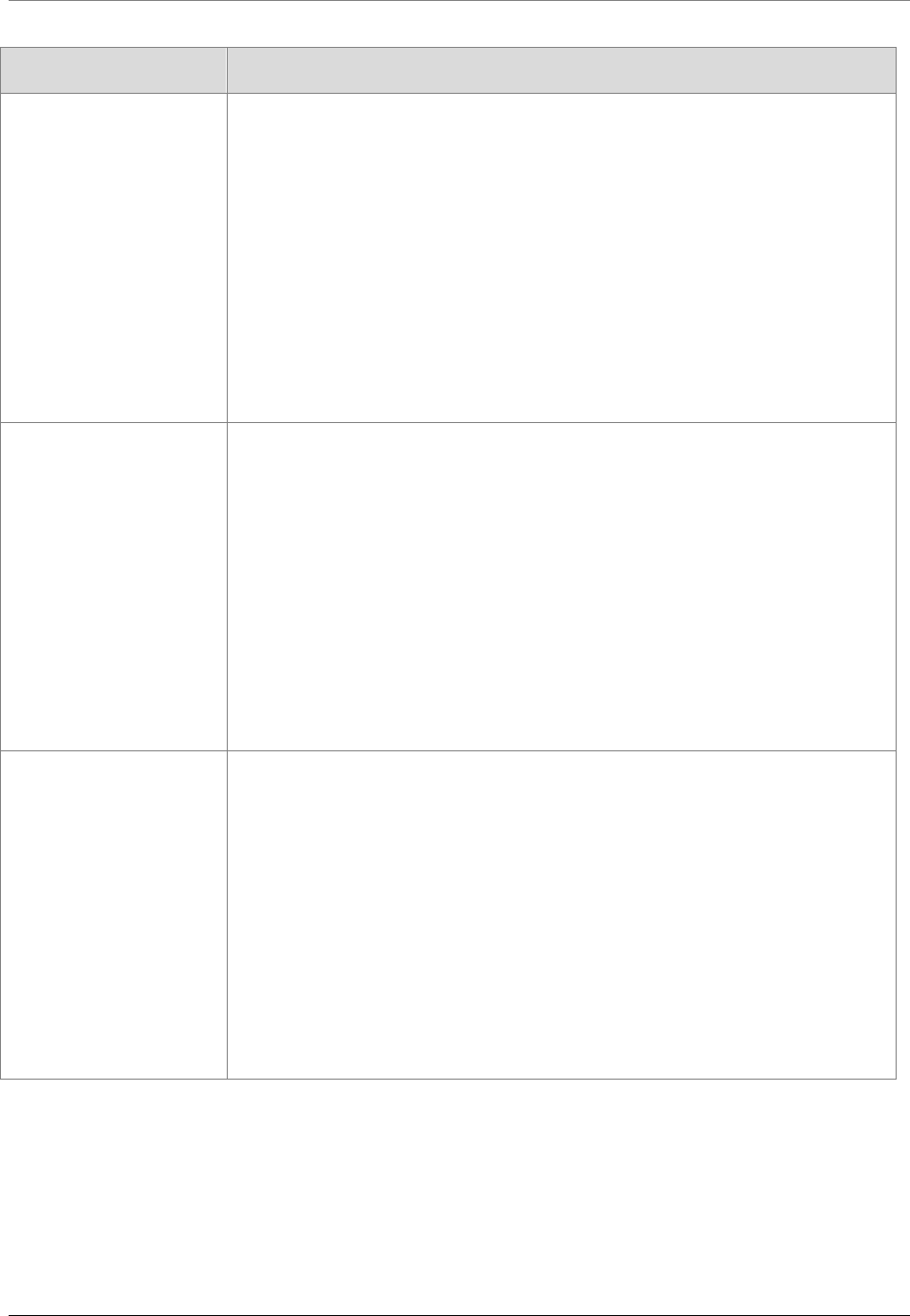
Table 5 lists the source and definition in rules and from health insurers for paid amount.
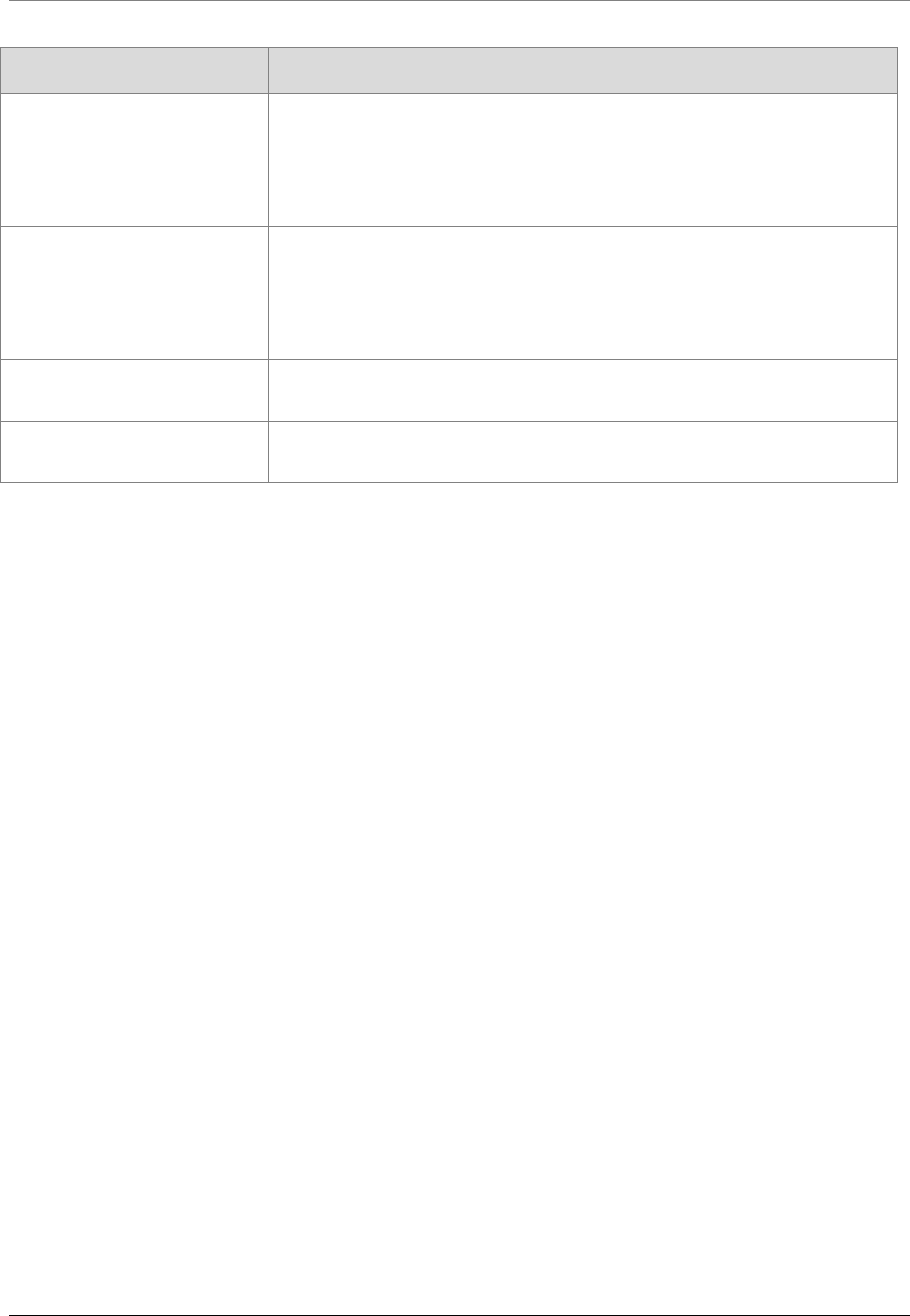
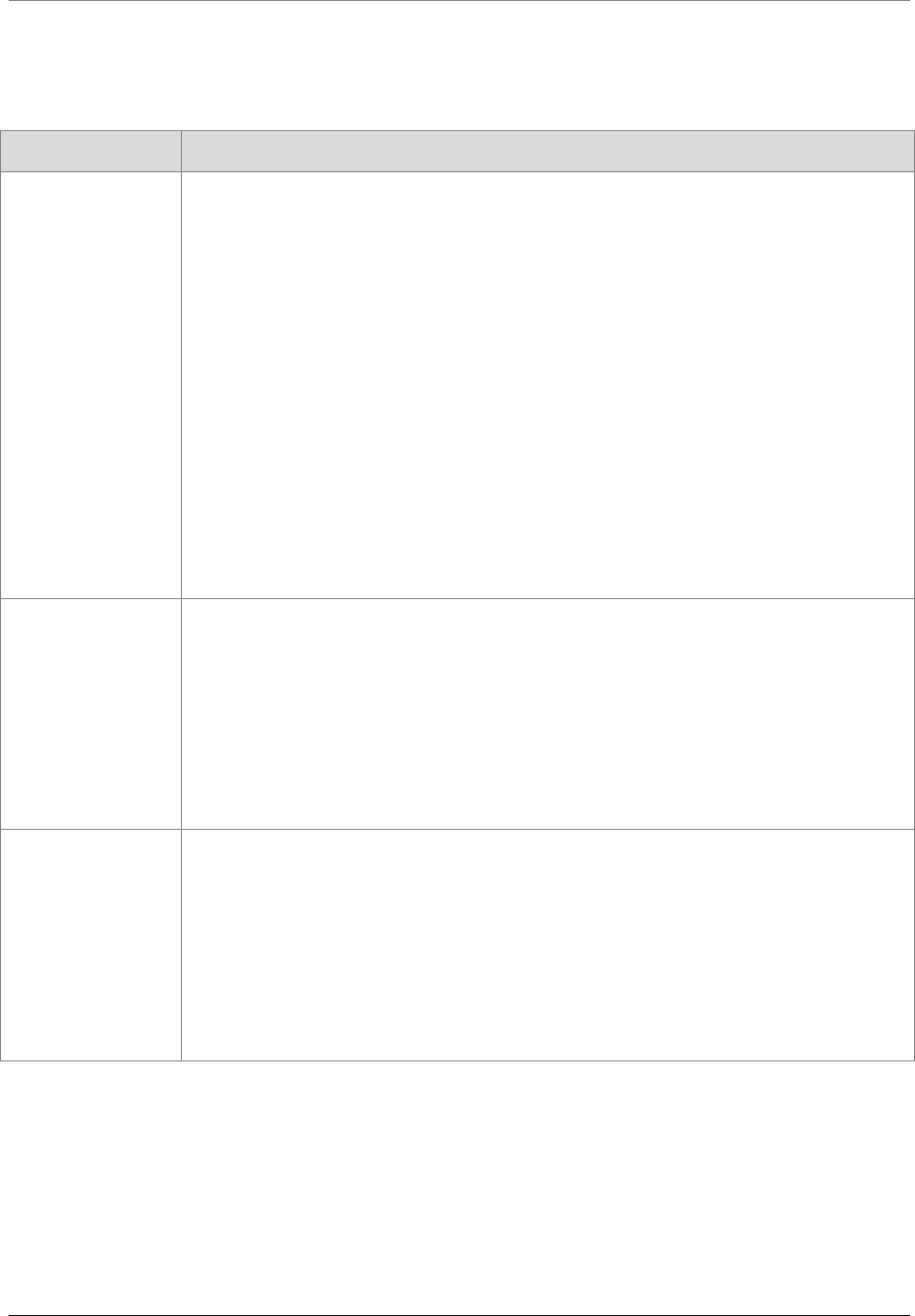
Table 5: Definitions for paid amount from rules and health insurers
SOURCE TERM AND DEFINITION
Uniform Glossary UCR (usual, customary and reasonable) – The amount paid for a medical
service in a geographic area based on what providers in the area usually
charge for the same or similar medical service. The UCR amount sometimes is
used to determine the allowed amount.
Premera Blue Cross Amount paid by your health plan – The portion of the charges eligible for
benefits minus your co-pay, deductible, coinsurance, network discount and
amount paid by another source, up to the billed amount.
Amount paid by another source – Examples of other sources: a health
funding account, other health insurance, automobile insurance, homeowners’
insurance, disability insurance, etc.
Regence BlueShield Paid – The dollar amount of the insurer, corporation or health plan's liability for
the services. On pharmacy claims, amount billable to customer/group; the client
total amount due.
Group Health Cooperative Allowance – The maximum amount payable by the health plan for certain
covered services under the coverage agreement.
Oregon Rule Paid amount – The actual dollar amount paid for claims.
Vermont Rule Payment – The actual dollar amount paid for a claim by a health insurer.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 8
After reviewing descriptions of payment data elements in other state DSGs, OFM found that:
Paid amount means the total amount paid to the provider.
Some states include withhold amounts in the paid amount
5
.
Exclusions from paid amount include withhold amounts, sales tax and members’ payments.
Some state APCDs have data elements for the difference sources of the payment such as:
› Other insurance paid amount – Amount already paid by primary carrier.
› Medicare paid amount – Any amount Medicare paid toward the claim line.
› Member self-pay amount – Amount member/patient paid out of pocket on the claims line
for pharmacy.
Table 6 lists the APCD data elements and descriptions for paid amount in other state DSGs.
Table 6: Data elements for paid amount in other state APCDs
SOURCE APCD DATA ELEMENT AND DESCRIPTION
APCD Council core data
elements
Paid amount – State determines description.
Other amount paid – State determines description.
Other payer amount recognized – State determines description.
Colorado DSG Paid amount – Includes any withhold amounts.
Connecticut DSG Paid amount – Amount paid by the carrier for the claim line.
Other insurance paid amount – Amount already paid by primary carrier.
Medicare paid amount – Any amount Medicare paid toward the claim line.
Member self-pay amount – Amount member/patient paid out of pocket on the
claims line (for pharmacy claims data).
Maine DSG For medical claim file specifications, paid amount includes any withhold
amounts.
For pharmacy claims file specifications, paid amount includes all health plan
payments and excludes all member payments.
Maryland DSG Amount paid to the pharmacy by payer. Do not include patient co-payment or
sales tax.
Reimbursement amount – Amount paid to a practitioner, other health
professional, office facility or institution.
5
Withhold – Means a percentage of payment or set dollar amounts that are deducted from the payment to the physician
group/physician that may or may not be returned, depending on specific predetermined factors. For more information
on withholds, see
http://www.ama-assn.org/ama/pub/advocacy/state-advocacy-arc/state-advocacy-campaigns/private-
payer-reform/state-based-payment-reform/evaluating-payment-options/withholds.page.
See http://www.geom.uiuc.edu/usenate/payreport/how.html for more information on how health care plans pay
physicians.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 9
SOURCE APCD DATA ELEMENT AND DESCRIPTION
Massachusetts DSG Paid amount – Amount paid by the carrier for the claim line.
Medicare paid amount – Amount Medicare paid on claim.
Other insurance paid amount – Amount paid by a primary carrier.
Minnesota DSG Total amount paid – This field includes all health plan payments and excludes
all member payments.
Paid amount – This field includes all health plan payments and excludes all
member payments and withholds from providers.
New Hampshire DSG Paid amount – Includes any withholds.
Utah DSG Paid Amount – Includes all health plan payments and excludes all member
payments.
E. OTHER PAYMENT TERMS
After reviewing other health care claim payment terms, OFM found five terms that are used by two
or more of the sources for this paper: coinsurance, coordination of benefits/third party liability, co-
payment, deductible and prepaid. These terms have very similar meanings regardless of the source.
OFM found that:
Coinsurance – Means the subscriber’s share of the costs.
› Usually calculated as a percentage of the cost of the medical service.
› Coinsurance for an out-of-network provider is usually a higher percentage than coinsurance
for an in-network provider.
› Medicare has per-day coinsurance for Part A and percentage coinsurance for Part B.
› Coinsurance is a payment in addition to any deductibles the subscriber pays.
Coordination of benefits/third party liability (TPL) amount – Means the amount due from a
secondary carrier, when known.
Co-payment – Means a payment by the subscriber to the health care provider.
› Is a fixed dollar amount.
› Usually paid at the time of service.
› Applies to covered services.
› May be higher for covered services from an out-of-network provider.
› May also be the full cost of the service if the full cost is less than the fixed dollar amount.
Deductible – Means the amount a subscriber pays for health care services before the health
plan begins to pay.
› There is a timeframe for deductibles, usually a year.
› Applies only to services covered in the health plan.
› May not apply to all services.
Prepaid – Has two meanings.
› In the state APCD rules, prepaid means the fee for the service equivalent that would have
been paid for a specific service if the service had not been capitated.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 10
› In several of the DSGs, prepaid means the amount the carrier has prepaid toward the claim
line.
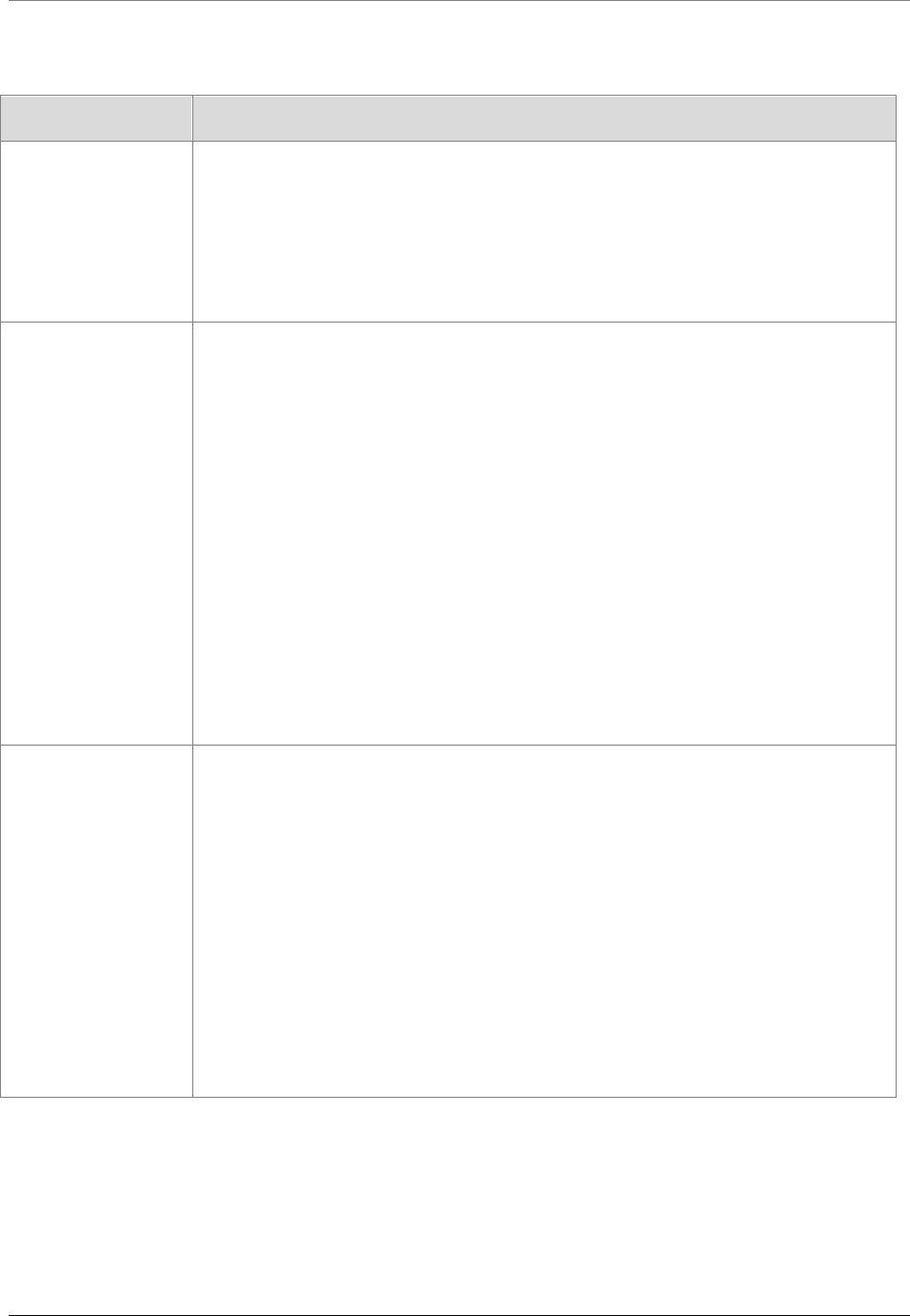
Table 7 lists the other payment terms by source. Table 8 lists the definitions for other payment
terms in rules and provided by the health insurers. Table 9 lists the descriptions for the other
payment data elements in other state APCDs.
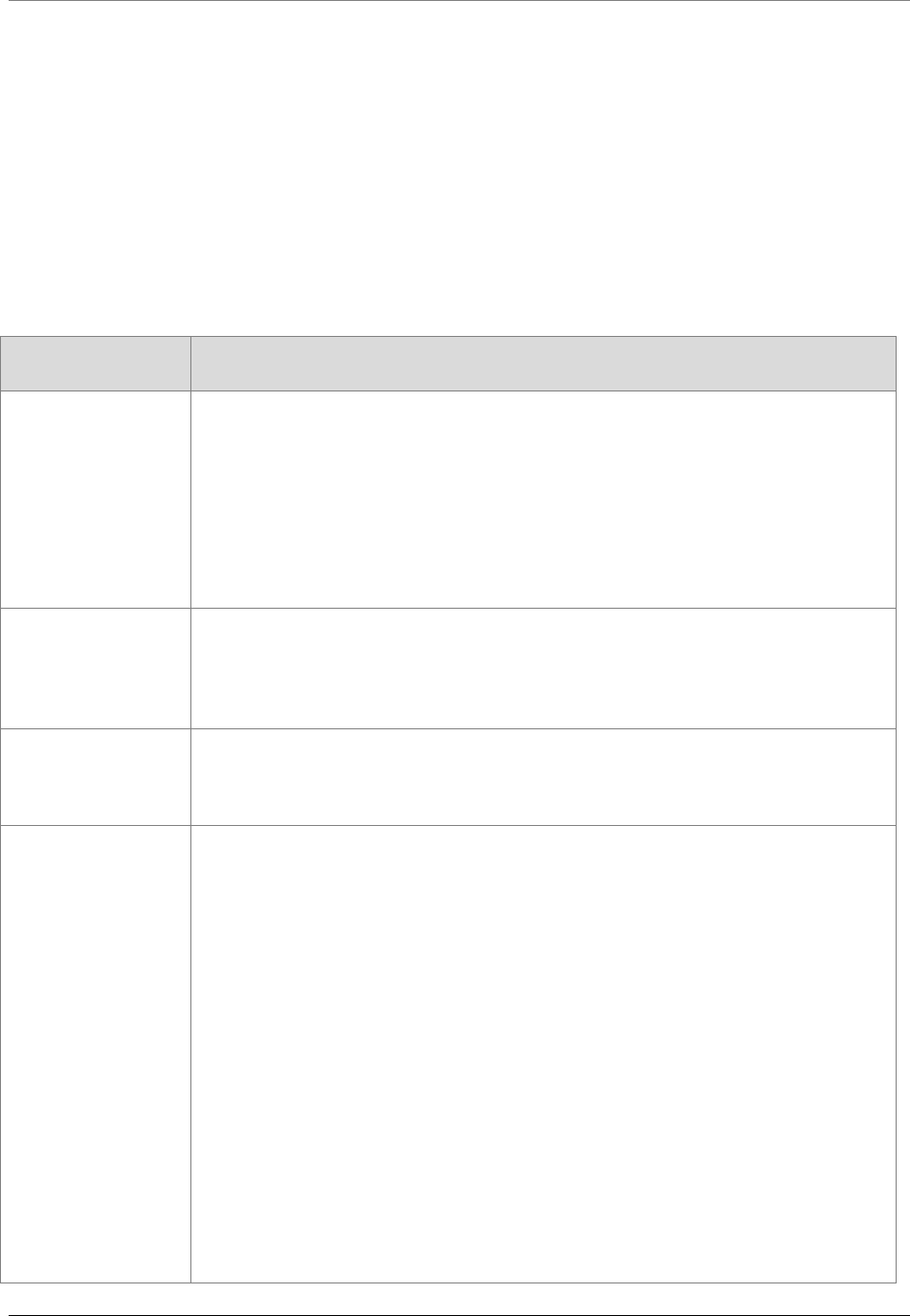
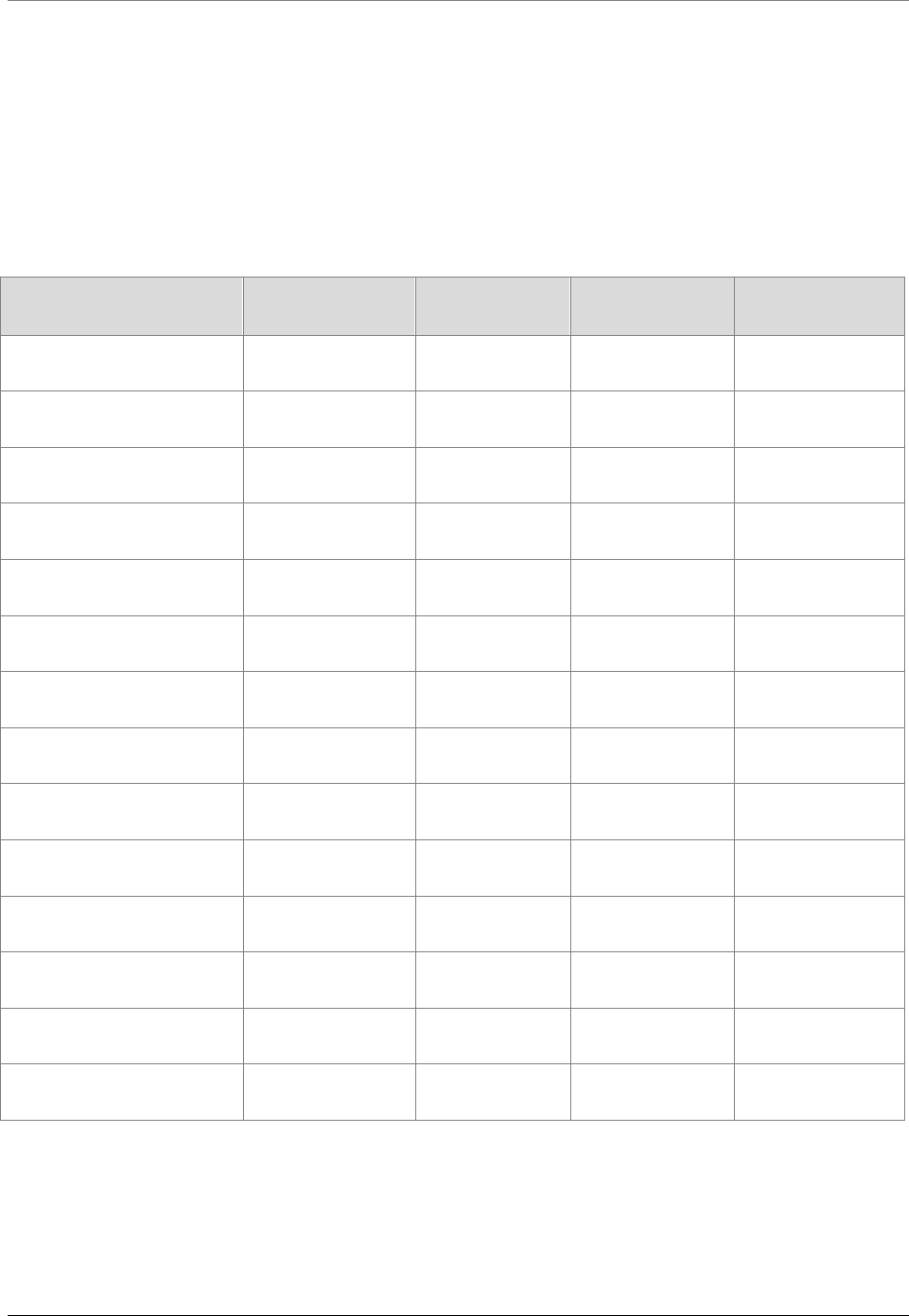
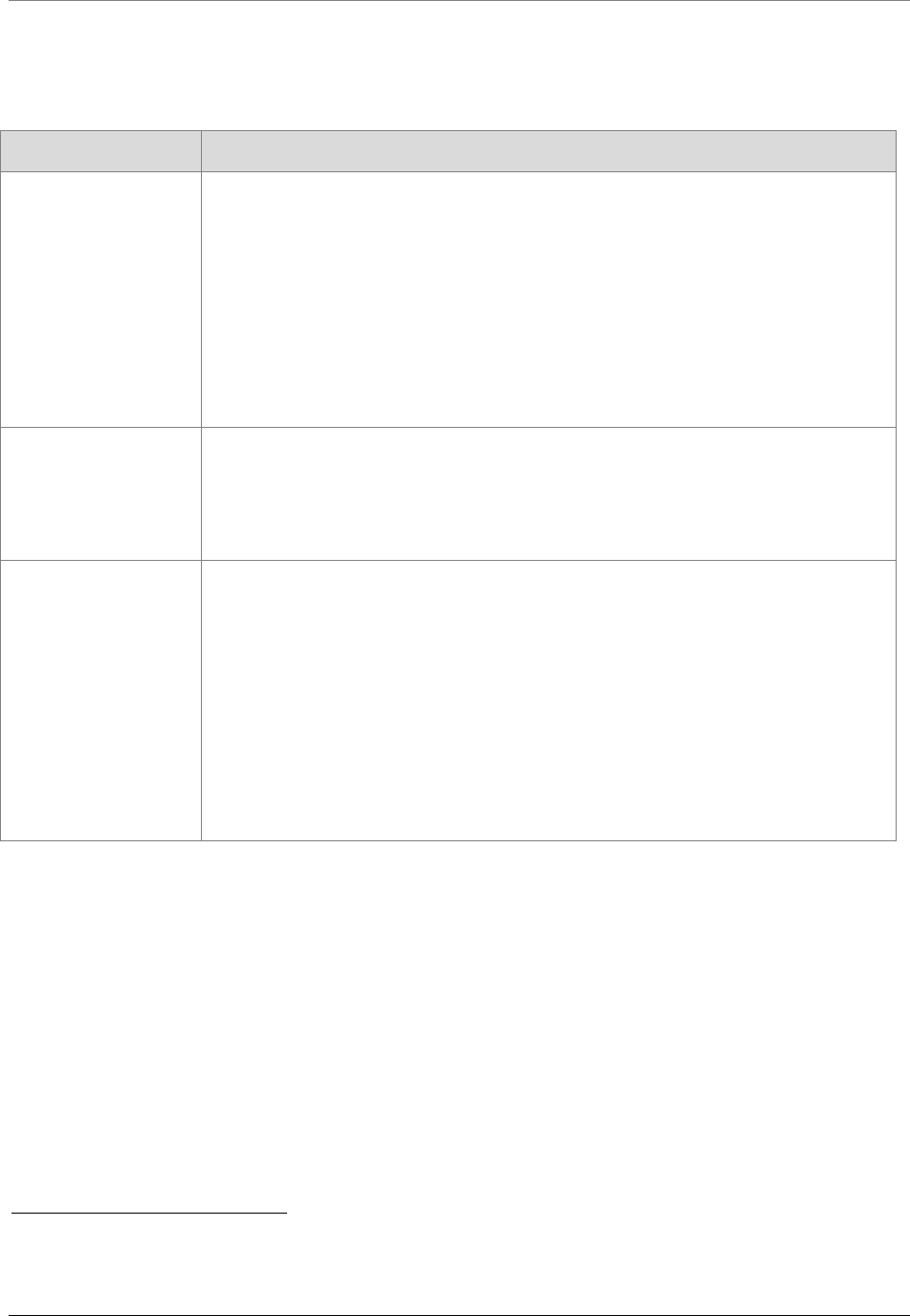
Table 7: Other payment terms by source
OTHER PAYMENT TERMS
RULES &
GLOSSARIES
HEALTH
INSURERS
OTHER STATE
APCD DSGs
APCD CORE DATA
ELEMENTS
Balance billing
Balance due
Capitated services
Coinsurance
Coordination of benefits/
TPL amount
Co-payment
Deductible
In-network coinsurance
In-network co-payment
Other patient obligations
Out-of-network coinsurance
Out-of-network co-payment
Noncovered amount
Prepaid amount
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 11
Table 8: Other payment terms in rule or used by health plans
SOURCE OTHER PAYMENT TERMS AND DEFINITIONS
Uniform Glossary Balance billing – When a provider bills you for the difference between the provider’s
charge and the allowed amount. For example, if the provider’s charge is $100 and
the allowed amount is $70, the provider may bill you for the remaining $30. A
preferred provider may not balance bill you for covered services.
Coinsurance – Your share of the costs of a covered health care service, calculated
as a percentage (for example, 20 percent) of the allowed amount for the service.
You pay coinsurance plus any deductibles you owe. For example, if the health
insurance or plan’s allowed amount for an office visit is $100 and you’ve met your
deductible, your coinsurance payment of 20 percent would be $20. The health
insurance or plan pays the rest of the allowed amount.
Co-payment – A fixed amount (for example, $15) you pay for a covered health care
service, usually when you get the service. The amount can vary by the type of
covered health care service.
Deductible – The amount you owe for covered health care services before your
health insurance or plan begins to pay. For example, if your deductible is $1,000,
your plan won’t pay anything until you’ve met your $1,000 deductible for covered
health care services subject to the deductible. The deductible may not apply to all
services.
In-network coinsurance – The percentage (for example, 20 percent) you pay of the
allowed amount for covered health care services to providers who contract with your
health insurance or plan. In-network coinsurance usually costs you less than out-of-
network coinsurance
In-network co-payment – A fixed amount (for example, $15) you pay for covered
health care services to providers who contract with your health insurance or plan. In-
network co-payments usually are less than out-of-network co-payments.
Out-of-network coinsurance – The percentage (for example, 40 percent) you pay
of the allowed amount for covered health care services to providers who do not
contract with your health insurance or plan. Out-of-network coinsurance usually
costs you more than in-network coinsurance.
Out-of-network co-payment – A fixed amount (for example, $30) you pay for
covered health care services from providers who do not contract with your health
insurance or plan. Out-of-network co-payments usually are more than in-network co-
payments.
Medicare Glossary of
Terms
Coinsurance – An amount you may be required to pay as your share of the cost for
services after you pay any deductibles. Coinsurance is usually a percentage (for
example, 20 percent).
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 12
SOURCE OTHER PAYMENT TERMS AND DEFINITIONS
Co-payment – An amount you may be required to pay as your share of the cost for
a medical service or supply, like a doctor’s visit, hospital outpatient visit or
prescription. A co-payment is usually a set amount rather than a percentage. For
example, you might pay $10 or $20 for a doctor’s visit or prescription.
Deductible – The amount you must pay for health care or prescriptions before
Original Medicare, your prescription drug plan or your other insurance begins to pay.
WAC 182-500 and
WAC 182-550
Cost-sharing – Any expenditure required by or on behalf of an enrollee with respect
to essential health benefits; such term includes deductibles, coinsurance, co-
payments or similar charges, but excludes premiums, balance billing amounts for
nonnetwork providers and spending for noncovered services. (WAC 182-500-0020).
Deductible – The dollar amount a client is responsible for before an insurer, such as
Medicare, starts paying, or the initial specific dollar amount for which the client is
responsible. (WAC 182-550-1050 Hospital services definitions).
Premera Blue Cross Co-pay – A set amount you pay for certain covered services such as office visits or
prescriptions. Co-pays are usually paid at the time of service.
Deductible – Your deductible is the amount you need to pay each year for covered
services before your plan starts paying benefits.
Coinsurance – A percentage of covered expenses that you pay after you meet your
deductible.
Group Health
Cooperative
Coinsurance – The percentage amount that a member (or possibly a member's
secondary health plan) is required to pay for covered services. For example, the
health plan may pay 80 percent of the cost of care or services and the member may
pay 20 percent.
Co-payment/co-pay – The dollar amount a member is required to pay at the time of
service for certain covered services. For example, an office visit may have a set co-
pay of $10 or $20 per visit.
Maine
Coinsurance – The dollar amount a member pays as a predetermined percentage
of the cost of a covered service after the deductible has been paid.
Co-payment – The fixed dollar amount a member pays to a health care provider at
the time a covered service is provided or the full cost of a service when that is less
than the fixed dollar amount.
Deductible – The total dollar amount a member pays toward the cost of covered
services over an established period of time before any payments are made by the
contracted third-party payer.
Prepaid amount – The fee for service equivalent that would have been paid by the
health care claims processor for a specific service if the service had not been
capitated.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 13
SOURCE OTHER PAYMENT TERMS AND DEFINITIONS
Oregon Coinsurance – The percentage an enrolled member pays toward the cost of a
covered service.
Co-payment – The fixed dollar amount an enrolled member pays to a health care
provider at the time a covered service is provided or the full cost of a service when
that is less than the fixed dollar amount.
Deductible – The total dollar amount an enrolled member pays toward the cost of
covered services over an established period of time before the carrier or third-party
administrator makes any payments under an insurance policy or health benefit plan.
Prepaid amount – The fee for the service equivalent that would have been paid for
a specific service if the service had not been capitated.
New Hampshire
Capitated services – Services rendered by a provider through a contract in which
payments are based upon a fixed dollar amount for each member on a monthly
basis.
Coinsurance – The percentage a member pays toward the cost of a covered
service.
Co-payment – The fixed dollar amount a member pays to a health care provider at
the time a covered service is provided or the full cost of a service when that is less.
Prepaid amount – The fee for the service equivalent what would have been paid by
the health care claims processor for a specific service if the service has not been
capitated.
Vermont Coinsurance – The percentage a member pays toward the cost of a covered
service.
Co-payment – The fixed dollar amount a member pays to a health care provider at
the time a covered service is provided or the full cost of a service when that is less
than the fixed dollar amount.
Deductible – The total dollar amount a member pays toward the cost of covered
services over an established period of time before the contracted third-party payer
makes any payments.
Prepaid amount – The fee for the service equivalent that would have been paid for
a specific service if the service had not been capitated.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 14
Table 9: Data elements for other payment terms in state APCDs
SOURCE APCD TERMS AND DESCRIPTIONS
Colorado
DSG
Co-pay amount – The pre-set fixed dollar amount for which the individual is responsible.
Coinsurance amount – The dollar figure for which the individual is responsible; not a
percentage amount.
Deductible amount – Collect this data but no description of data element.
Prepaid amount – For capitated services, the fee for service equivalent amount.
Connecticut
DSG
Deductible amount – Amount of deductible member/patient is responsible to pay on the
claim line.
Member deductible – Annual maximum out-of-pocket member deductible across all
benefit types.
Dental deductible – Maximum out-of-pocket amount of member's deductible applied to
dental benefits.
Vision deductible – Maximum out-of-pocket amount of member's deductible applied to
vision benefits.
Co-pay amount – Amount co-pay member/patient is responsible to pay.
Coinsurance amount – Amount of coinsurance member/patient is responsible to pay.
Noncovered amount – Amount of claim line charge not covered due to eligibility
limitations or unmet provider requirements.
Prepaid amount – Amount carrier has prepaid toward the claim line.
Maryland
DSG
Patient deductible – Fixed amount that the patient must pay for covered services before
benefits are payable.
Patient coinsurance/co-payment – The specified amount or percentage the patient is
required to contribute toward covered medical services after any applicable deductible.
Co-pay amount – Amount of co-pay member/patient is responsible to pay.
Coinsurance amount – Amount of coinsurance member/patient is responsible to pay.
Deductible amount – Amount of deductible member/patient is responsible to pay on the
claim line.
Other patient obligations – Any patient liability other than deductible or coinsurance/co-
payment. Includes obligations for out-of-network care (balance billing), non-covered
services or penalties.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 15
SOURCE APCD TERMS AND DESCRIPTIONS
Massachusetts
DSG
Co-pay amount – Amount of co-pay member/patient is responsible to pay.
Coinsurance amount – Amount of coinsurance member/patient is responsible to pay.
Deductible amount – Amount of deductible member/patient is responsible to pay on
the claim line.
Coordination of benefits/TPL amount – Amount due from a secondary carrier when
known.
Noncovered amount – Report the amount that was charged on a claim that is not
reimbursable due to eligibility limitations or provider requirements.
Prepaid amount – Amount carrier has prepaid toward the claim line.
Minnesota DSG
Co-pay amount – Amount of co-pay member/patient is responsible to pay.
Coinsurance amount – Amount of coinsurance member/patient is responsible to pay.
Deductible amount – Amount of deductible member/patient is responsible to pay on
the claim line.
Coordination of benefits/TPL amount – Amount due from a secondary carrier when
known.
Noncovered amount – Report the amount that was charged on a claim that is not
reimbursable due to eligibility limitations or provider requirements.
Prepaid amount – Amount carrier has prepaid toward the claim line.
New Hampshire DSG Co-pay amount – The preset fixed dollar amount for which the individual is responsible.
Coinsurance amount – The dollar amount an individual is responsible for.
Prepaid amount – For capitated services, the fee for service equivalent amount.
Utah DSG Co-pay amount – The pre-set fixed dollar amount for which the individual is
responsible.
Coinsurance amount – The dollar amount an individual is responsible for, not the
percentage.
Prepaid amount – For capitated services, the fee for service equivalent amount.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 16
F. CONSIDERATIONS FOR DEVELOPING CLAIM DATA DEFINITIONS
Table 10 identifies the other considerations and related questions and issues that will be discussed in
the rule-making process. This list is not exhaustive; OFM welcomes input from stakeholders.
Table 10: Considerations for developing claim data definitions
CONSIDERATIONS QUESTIONS / ISSUES
1. Are there other payment terms that should be
defined in rule besides billed, allowed and paid
amounts?
There are some common health care claims processing
terms: co-payment, coinsurance, deductible, prepaid,
coordination of benefits.
2. Do we need to consider definitions to capture
alternative payments?
There are other payment methods besides fee for
service.
3. WA-APCD data suppliers may have IT,
accounting and possibly other organizational
systems tied to their definitions.
What are the impacts that the WA-APCD definitions
have, if any, on current programs and organizational
systems?
4. Are there other claims data terms that should be
defined in rule rather than the WA-APCD data
submission guide?
It takes longer to change a term in a rule than it does in
a data submission guide.
5. Over time the definitions in the Universal Glossary
will shape the public’s understanding of these
terms.
Does this need to be taken into consideration when
developing definitions?
6. Other considerations? Please add your questions, issues, comments and send
to OFM at [email protected]ov
.
Please reference WA-APCD Rules Paper 3 in the
subject line.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 17
APPENDIX A
Title 182 WAC definitions
TERMS DEFINITIONS
Billed amount Allowed charges – The total billed charges for allowable services. (WAC 182-550-1050
Hospital services definitions)
Allowed covered charges – The total billed charges for services minus the billed charges
for non-covered and/or denied services. (WAC 182-550-1050 Hospital services definitions)
Billed charge – The charge submitted to the agency by the provider (WAC 182-550-1050
Hospital services definitions)
Noncovered charges – Billed charges a provider submits to the agency on a claim and
indicates them on the claim as noncovered. (WAC 182-550-1050 Hospital services
definitions)
Usual and Customary Charge – The amount a provider typically charges to 50 percent or
more of patients who are not medical assistance clients. (WAC 182-500-0110 Medical
assistance definitions)
Allowed amount Allowed – The initial calculated amount for any procedure or service, after exclusion of any
nonallowed service or charge that the agency allows as the basis for payment computation
before final adjustments, deductions and add-ons. (WAC 182-550-1050 Hospital services
definitions)
Allowable – The calculated amount for payment, after exclusion of any nonallowed service
or charge, based on the applicable payment method before final adjustments, deductions
and add-ons. (WAC 182-550-1050 Hospital services definitions)
Other such terms Cost-sharing – Any expenditure required by or on behalf of an enrollee with respect to
essential health benefits; such term includes deductibles, coinsurance, co-payments or
similar charges, but excludes premiums, balance billing amounts for nonnetwork providers
and spending for noncovered services. (WAC-182-500-0020 Washington apple health
definitions)
Deductible – The dollar amount a client is responsible for before an insurer, such as
Medicare, starts paying or the initial specific dollar amount for which the client is responsible.
(WAC 182-550-1050 Hospital services definitions)
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 18
APPENDIX B
CMS Medicare glossary terms related to claim payments
TERMS DEFINITIONS
Billed amount
Limiting charge – In Original Medicare
6
, the highest amount of money you can be
charged for a covered service by doctors and other health care suppliers who don’t
accept assignment. The limiting charge is 15 percent over Medicare’s approved amount.
The limiting charge applies only to certain services and doesn’t apply to supplies or
equipment.
Excess charge – If you have Original Medicare, and the amount a doctor or other
health care provider is legally permitted to charge is higher than the Medicare-approved
amount, the difference is called the excess charge.
Allowed amount Medicare approved amount – In Original Medicare, this is the amount a doctor or
supplier that accepts assignment can be paid. It may be less than the actual amount a
doctor or supplier charges. Medicare pays part of this amount and you’re responsible for
the difference.
Other such terms Coinsurance – An amount you may be required to pay as your share of the cost for
services after you pay any deductibles. Coinsurance is usually a percentage (for
example, 20 percent).
Co-payment – An amount you may be required to pay as your share of the cost for a
medical service or supply, like a doctor’s visit, hospital outpatient visit or prescription. A
co-payment is usually a set amount, rather than a percentage. For example, you might
pay $10 or $20 for a doctor’s visit or prescription.
Deductible – The amount you must pay for health care or prescriptions before Original
Medicare, your prescription drug plan or your other insurance begins to pay.
6
Original Medicare is fee-for-service coverage under which the government pays your health care providers directly for
your Part A and/or Part B benefits.
WA-APCD Rules Background Paper #3 September 2015
OFM Forecasting and Research Division 19
REFERENCES
1. Colorado:
Statute:
http://www.leg.state.co.us/CLICS/CLICS2010A/csl.nsf/fsbillcont3/7772EFE1E998E6278725
76B700617FA4?Open&file=1330_enr.pdf
Rules: http://www.civhc.org/getmedia/2a315773-cbcd-4f75-805a-759d3cf96888/Rules-
Governing-Data-Submissions-to-APCD-2011-08-24.pdf.aspx/
2. Connecticut
Statute: http://www.cga.ct.gov/2012/ACT/Pa/pdf/2012PA-00166-R00HB-05038-PA.pdf
3. Maine
Statute: http://www.mainelegislature.org/legis/statutes/22/title22sec8703.html
Rules: https://mhdo.maine.gov/claims.htm
4. Maryland
Statute: http://www.dsd.state.md.us/comar/SubtitleSearch.aspx?search=10.25.06
Rules: http://www.dsd.state.md.us/comar/SubtitleSearch.aspx?search=10.25.06
5. Massachusetts
Statute: http://chiamass.gov/relevant-regulations-5
Rules: http://chiamass.gov/assets/docs/g/chia-regs/957-8.pdf
6. Minnesota
Statute: https://www.revisor.mn.gov/rules/?id=4653
Rules: https://www.revisor.mn.gov/rules/?id=4653.0300
7. New Hampshire
Statute: http://www.gencourt.state.nh.us/rsa/html/XXXVII/420-G/420-G-11-a.htm
Rules: http://www.gencourt.state.nh.us/rules/state_agencies/ins4000.html
8. Oregon
Statute: http://www.oregon.gov/oha/ohpr/Pages/Statutes-
Health%20Care%20Data%20Reporting.aspx
Rules: http://www.oregon.gov/oha/OHPR/rulemaking/notices/409-
025_PermComplete_2.1.13.pdf
9. Tennessee
Statute: http://state.tn.us/sos/acts/106/pub/pc0611.pdf
Rules: http://www.state.tn.us/sos/rules/0780/0780-01/0780-01-79.20100908.pdf
10. Utah
Statute: http://le.utah.gov/~2007/bills/hbillenr/hb0009.pdf
Rules: http://www.rules.utah.gov/publicat/code/r428/r428-015.htm
11. Vermont
Statute:
http://www.leg.state.vt.us/statutes/fullsection.cfm?Title=18&Chapter=221&Section=09410
Rules: http://gmcboard.vermont.gov/sites/gmcboard/files/REG_H-2008-01.pdf
