
January 2022
Guidelines: Bowel Management for Patients with
Neurogenic Bowel Dysfunction
Neurogenic Bowel Dysfunction
‘Neurogenic bowel’ is the term used to describe dysfunction of the colon due to loss of
normal sensory and/or motor control or both, as a result of central neurological disease or
damage (trauma). Damage to the spinal cord and brain interrupts the neural pathways and
the outcome will vary depending on the location and severity of the damage.
Neurogenic bowel dysfunction (NBD) is a temporary or permanent disruption of bowel
function. NBD can be life altering, affecting all aspects of a patient’s social, physical and
emotional wellbeing. Patients likely to present with NBD are patients with Spinal Cord Injury
(SCI), Cauda Equina Syndrome, Multiple Sclerosis, Guillain Barre Syndrome, and some
patients with Stroke. NBD can present in any situation where there is interruption of the
normal innervation of the bowel.
Purpose of Guidelines:
The purpose of this document is to provide front line health care providers and physicians with
guidance to assist and support (empower) patients and their care providers to develop and /
maintain a bowel management routine. The goal of the bowel routine is to minimize or eliminate
the occurrence of unplanned or difficult evacuations; to evacuate stool at a regular, predictable
time within 60 minutes of bowel care; and to minimize gastrointestinal (GI) complications.
Key Messages:
1. Bowel movements are usually a personal and private function. Loss of independence
and control of something so private may cause the patient to feel vulnerable. It can be
very stressful and elicit a range of emotions including anxiety and grief.
2. The goal of a bowel routine is to minimize or eliminate the occurrence of unplanned or
difficult evacuations.
3. It is important to plan a consistent, regularly scheduled bowel routine in collaboration
with the patient, as well as their possible caregivers.
4. If a patient with an SCI at T6 (or occasionally T7-8) or above begins to experience signs
and symptoms of Autonomic Dysreflexia (AD) during the bowel routine, bowel care
should be stopped, and AD resolved before resuming.
5. Bowel routine should be initiated as early as possible in the acute phase of injury to help
establish the bowel routine and to prevent complications.
6. An effective bowel routine will need trial and evaluation, close monitoring, and careful
adjustments that can take up to months to establish.
7. Bowel management and education is important in supporting the patient in rehabilitation
and empowering their independence over time.
Types of NBD: Reflexic (spastic) vs Areflexic (flaccid)
Nearly everyone who experiences a spinal cord injury (SCI) will have some level of NBD.
NBD can be classified into two types: reflexic (spastic) neurogenic bowel and areflexic
(flaccid) neurogenic bowel.
Reflexic (spastic) NBD is seen with injuries above approximately vertebral level T12. It
results in a hypertonic and spastic bowel because the defecation reflex centre, which causes

Bowel Management for Patients with Neurogenic Bowel Dysfunction | 2
January, 2022
the involuntary contraction of muscles of the rectum and anus, remains intact. However, the
nerve damage results in disruption to the nerve signals and therefore there is an inability to
relax the anal sphincters and defecate, often leading to constipation.
Areflexic (flaccid) NBD is typically seen with injuries below approximately vertebral level
T12. There is damage to the defecation reflex. There is a significant risk of incontinence due
to the atonic or flaccid external anal sphincter and lack of control over the muscle that
causes the lumen of the rectum to open. The patient cannot feel the need to have a bowel
movement, and the rectum can’t easily empty by itself. There is a significant risk of
incontinence due to the atonic or flaccid external anal sphincter and lack of control over the
muscle that causes the lumen of the rectum to open.
Note: The commonly used terminology upper motor neuron versus lower motor neuron has
generally been abandoned for NBD. (PVA 2020 guidelines)
After an acute SCI, a patient may initially have an areflexic bowel. Once reflexes return, the
bowel may become reflexic. Management of NBD may be required for a short time in
reversible syndromes, or may be a permanent part of life going forward for patients with SCI
and other irreversible neurological disorders. Bowel symptoms are more severe in patients
with complete SCI than in those with incomplete SCI.
Principle of Care
A comprehensive evaluation of bowel function, impairment, and possible problems should
be completed by the most responsible health practitioner (MRHP), often a Physiatrist, at the
onset of NBD and at least annually throughout the continuum of care.
Starting early bowel management and education is important in supporting the patient in
rehabilitation and regaining their independence. A basic bowel management routine should be
used in individuals with both reflexic and areflexic NBD during the acute phase of care. It is a
treatment plan designed to eventually minimize or eliminate the occurrence of unplanned or
difficult bowel evacuations.
Each cycle of bowel care should be scheduled at the same time of day to facilitate habituation.
This is important to support the patient in resuming activities such as school, work, leisure and
recreation on discharge and transition back to community. Build the plan with the patient. An
effective bowel routine will need trial and evaluation, close monitoring, and careful adjustments
that can take up to months to establish.
For most individuals with a reflexic (spastic) NBD, a minimum of 3 adequate bowel movements
per week is recommended to avoid constipation. For persons with areflexic (flaccid) NBD, a
minimum of daily bowel care is typically needed in order to minimize the risk of unplanned bowel
evacuations. The ideal frequency of bowel movements per week should factor in an individual’s
lifestyle and bowel history prior to their SCI.
Patient and Family Education and Engagement
Education for patients with NBD and/or caregivers should be provided and tailored to their level
of understanding. It is important to understand what education the patient / family has, and what
additional information they need to become confident with managing their bowel routine.
It is important to plan the bowel routine with the patient with NBD, as well as their possible
caregivers.
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 3
January, 2022
If a patient with an SCI at T6 or above begins to experience signs and symptoms of Autonomic
Dysreflexia (AD), the bowel routine should be stopped and AD resolved before resuming.
Persons who live with chronic neurological disorders (including SCI), and have managed their
neurogenic bowel are usually the experts in their own bowel care. It is important to consider this
expertise when changes are required to their bowel plan. Situations like admission to hospital,
health changes, illness, or even normal aging may affect the bowel function or patterns of a
person with a neurological disorder (including SCI). Collaborative problem solving between care
providers and patients is recommended to find bowel management solutions that work for the
patient and their family.
As the patient and care providers learn more about the patient’s bowel habits and patient-
centered needs and concerns, the bowel routine is expected to be adjusted and adapted over
time.
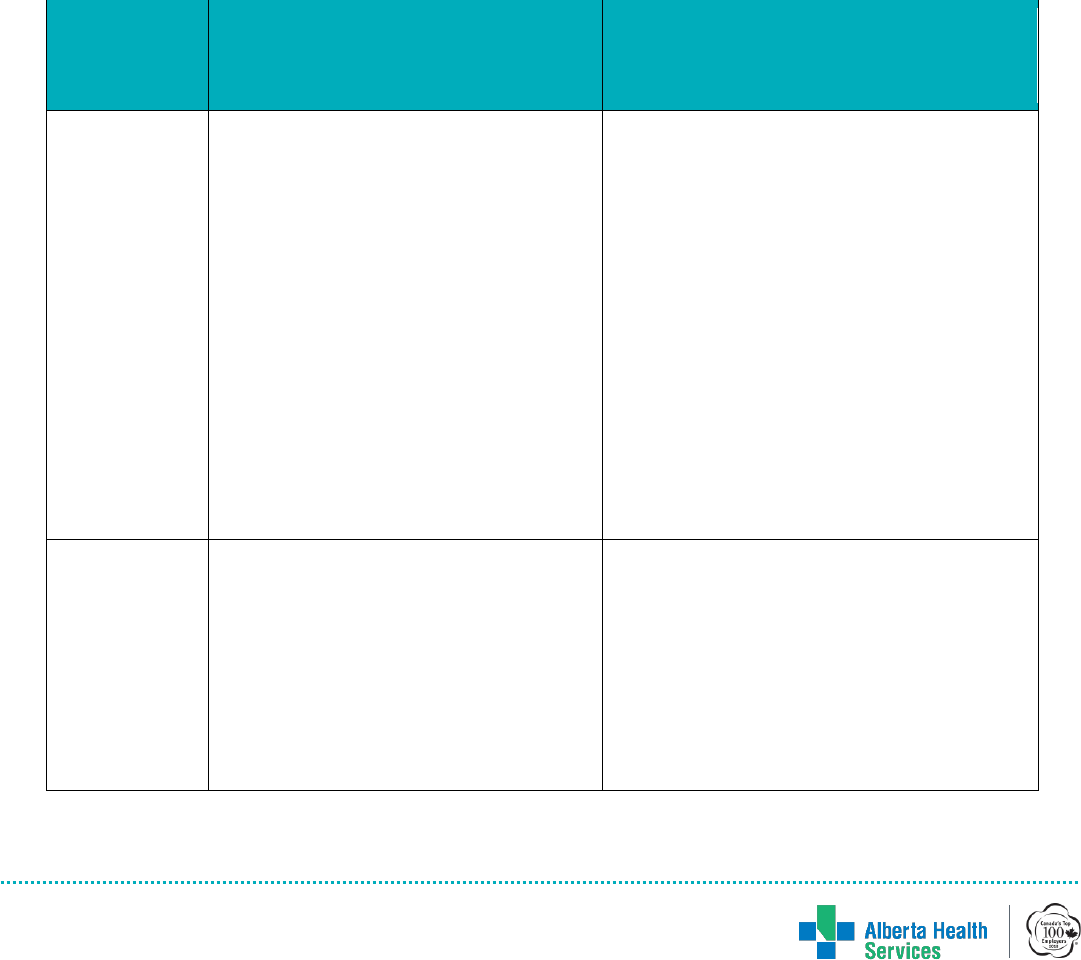
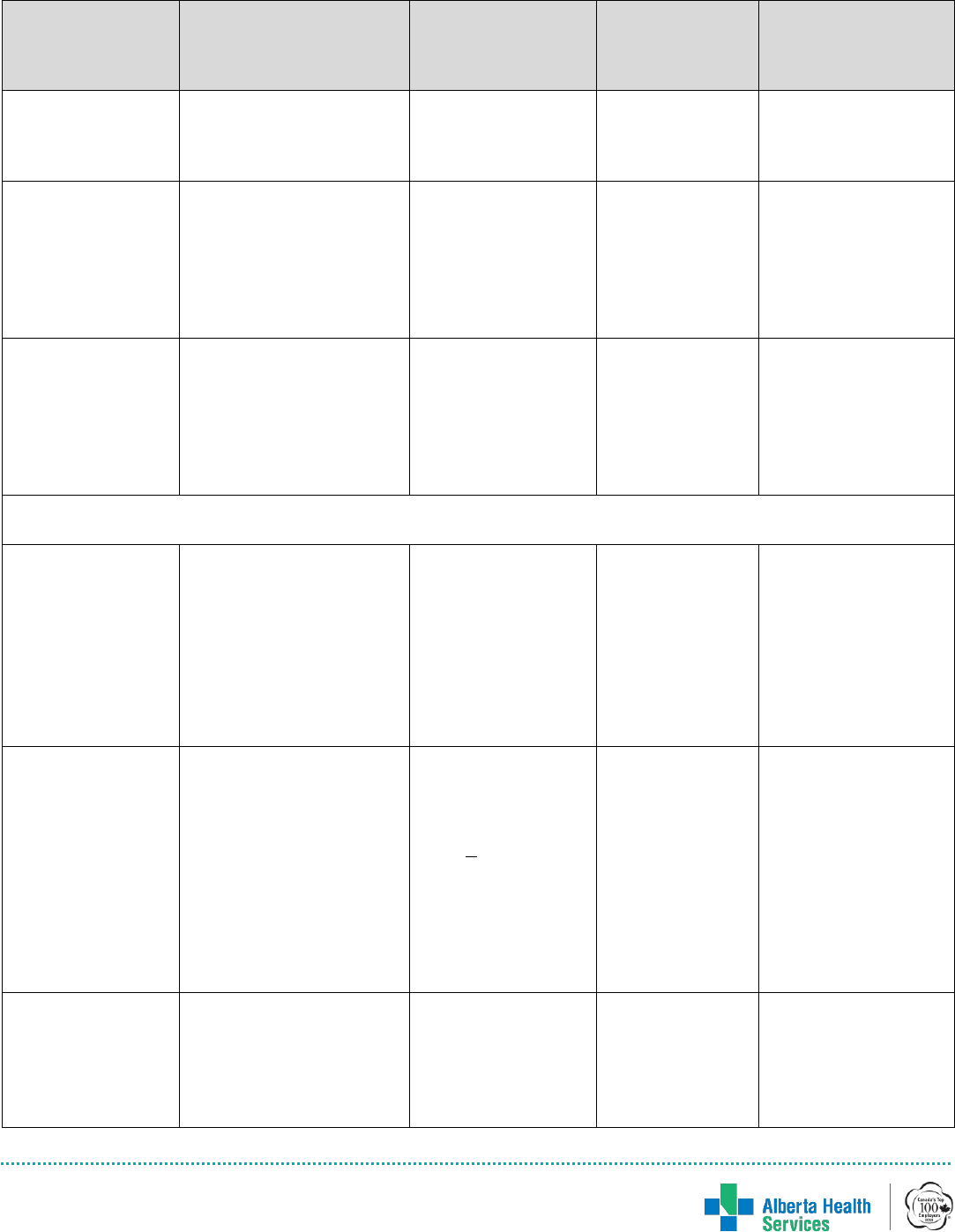
Table 1: Summary of Care: Reflexic (Spastic) vs. Arreflexic (Flaccid) Bowel
Reflexic (Spastic) Bowel
(previously referred to as
upper motor neuron lesion)
Areflexic (Flaccid) Bowel
(previously referred to as
lower motor neuron lesion)
Patho-
physiology
• More common in spinal cord injuries
or lesions above T12
• Lesion allows for impulses to get to
and from the spinal cord, resulting in
the presence of bowel reflexes
• Patients with reflexic NBD benefit
from mechanical and chemical rectal
stimulation because the defecation
reflex is intact.
• More common in spinal cord injuries or
lesions below T12 (cauda equina
syndrome)
• Lesions in the peripheral nerves block
impulses from getting to and from the
spinal cord, resulting in the absence of
reflexes
• Patients with areflexic NBD require
manual evacuation of stool because of
the absence of the defecation reflex.
• May occur in some lesions above T12
during the first days to months after
injury, resolving to reflexic bowel with the
return of reflex activity.
Characteristics
• Patient does not feel the need to
have a bowel movement, but the
reflex to have a movement is still
intact.
• The rectum may evacuate more
stool after a bowel movement when
the anus is stimulated (ie with
cleaning/peri-care)
• The rectum empties at irregular times,
especially when the patient is upright
(due to gravity) or on movement
transitioning from bed to chair, and
laying to sitting
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 4
January, 2022
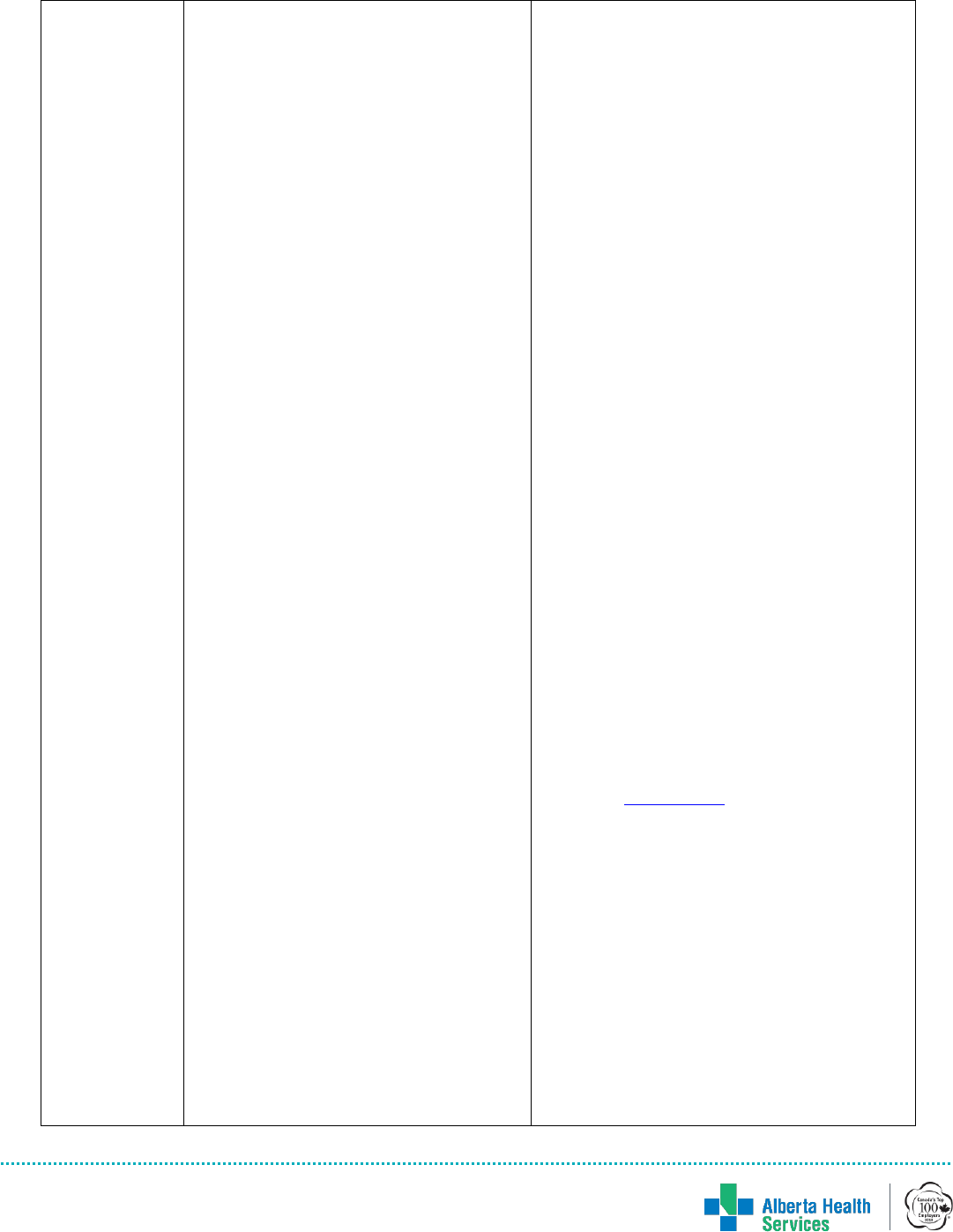
Management
start as early as
possible
Including in
acute care
• This type of bowel can be “trained”
to respond to stimulus, although the
training can take a long time to
develop.
• It is recommended that the bowel
care occur daily in the acute phase
of injury and during the
establishment of a bowel routine. As
the bowel routine becomes more
established and efficient, individuals
may choose to decrease their bowel
care to a minimum of 3 times a
week because of different life
considerations. (This usually does
not occur until several weeks or
months after injury.)
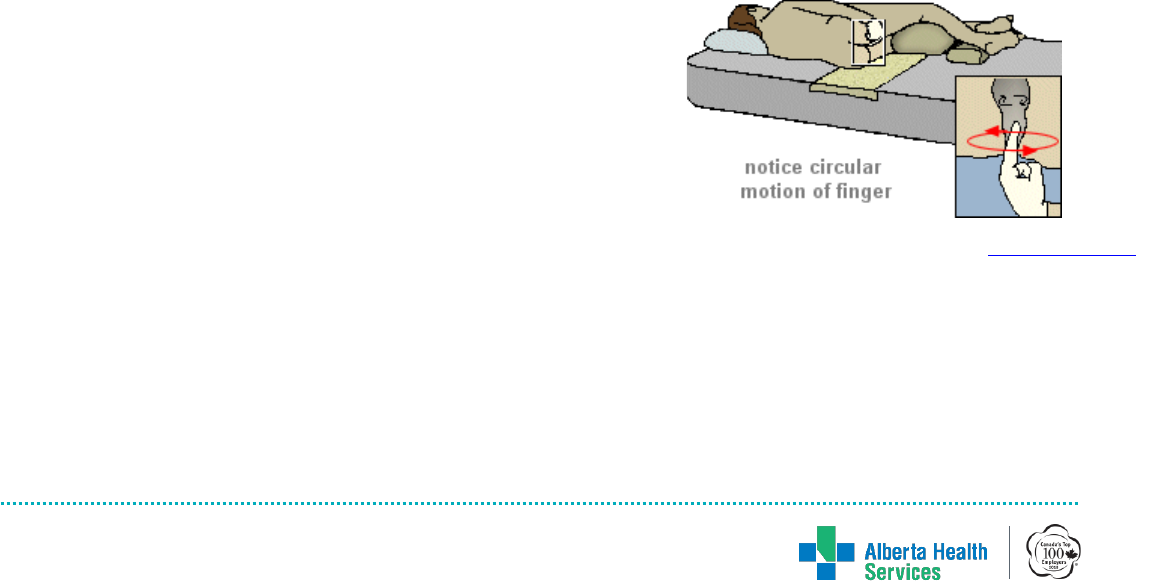
• Mechanical rectal stimulation is
used to trigger anorectal reflexes to
increase motility and relax
sphincters. (This stimulation can be
done with a finger or with an
adaptive device.)
• Digital rectal stimulation is a form
of mechanical rectal stimulation that
is most commonly used. This
procedure may be performed side
lying or over a commode.
• Digital rectal stimulation is
performed by the affected individual
or caregiver by placing a gloved,
lubricated finger into the rectum and
performing slow rotation in a circular
movement for no longer than 10 to
20 seconds at a time. Repeat the
rectal stimulation sequence every 5
to 10 minutes until evacuation of the
stool is achieved. Using additional
fingers or excessive dilation has
shown no benefit and can contribute
to complications.
• Having the patient consume food or
a beverage 30 minutes prior to
bowel care, can stimulate the
• This type of bowel requires more
frequent manual evacuation of stool and
may not be successful in bowel training.
Digital inspection and evacuation of
bowels will likely be required two or
more times per day, especially in the
initial stages.
• Manual evacuation of stool is indicated
as treatment and is performed with the
affected individual side-lying in bed or
positioned on a padded commode if
prescribed to be performed in an upright
position. The individual with SCI or
caregiver inserts a single, gloved,
lubricated finger into the rectum to
disimpact and remove stool that is
present in the rectal vault.
• Manual rectal disimpaction /removal of
stool – minimum daily, up to TID after
meals
• Care note: If there is stool in the rectum
when a patient with an areflexic bowel
sits upright, gravity may cause that stool
to be expelled. If this happens at an
unplanned time, it is likely to impact the
patient’s schedule and rehab, requiring
care and cleanup. The rectum should be
inspected for stool before the patient is
moved to an upright position.
• Goal is for stool to be firm (Bristol Type
3). See Appendix C
• Once a routine has been established
manual evacuation may only need to be
performed daily (but may be more often
depending on the patient’s individual
needs)
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 5
January, 2022
gastrocolic reflex, and help facilitate
a bowel movement.
• Goal is for stool to be soft and
formed (Bristol Type 4). See
Appendix C.
Typical routine
see Appendix A
Complications
• Complications associated with
mechanical rectal stimulation
include potential for AD (for those at
risk), hemorrhoids, abdominal
distension, and anal fissures.
• If during mechanical rectal
stimulation an individual has signs
and symptoms of AD, such as
bradycardia, cardiac arrhythmia,
pounding headache, anxiety,
sweating above the level of their
SCI, flushing, blurry vision, nasal
congestion, and/or piloerection,
rectal stimulation should be
discontinued immediately.
(Lidocaine gel for lubrication is
commonly used to reduce the risk of
AD episodes caused by mechanical
rectal stimulation.)
• Complications associated with manual
evacuation of the bowel include: AD (for
those at risk), hemorrhoids, and anal
fissures.
Changes over
time
• Bowel routines will require customization for each patient. The initial plan
described above will likely change over the months and years following acquired
spinal cord injury according to patient response.
Medication
management
Medications
commonly
prescribed to
facilitate bowel
routine (as per
SCI order set)
Bowel will respond to peristaltic
stimulants.
Bowel training:
1. Daily polyethylene glycol (PEG)
3350 17g packet* daily or QHS
2. Sennosides (Senna)* 1-2 tablets PO
daily or QHS
Bowel Routine:
1. PEG based Bisacodyl* suppository
10mg 10-15 minutes before planned
evacuation (some stool may
Bowel will not respond to peristaltic
stimulants. Osmotics or lubricant
medications to make stool pass more
easily through the intestine may be
prescribed.
1. Psyllium mucilloid powder 1 packet daily
up to TID (Each packet to provide 3.4 g
psyllium)
Caution: patients will need appropriate
fluid intake to prevent constipation while
taking psyllium
2. Lidocaine 2% gel 5 to 10 mL rectally
PRN prior to disimpaction
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 6
January, 2022
evacuate when suppository is
inserted.)
2. Lidocaine gel 2% prn for lubrication
is commonly used to reduce the risk
of AD episodes caused by
mechanical rectal stimulation.
3. If bleeding or uncomfortable
hemorrhoids with digital stimulation,
add Anusol-HC 2.5% cream after
bowel movement for 14 days
3. If bleeding or uncomfortable
hemorrhoids with manual dis-impaction,
add Anusol-HC 2.5% cream after bowel
movement for 14 days
Dietary
Consideratio
ns
• Water and other healthy fluids: Fluids are crucial to maintaining a healthy
bowel routine. Many other factors will not be effective without taking in enough
fluids. Healthy fluids should not include caffeine or alcohol beverages, as these
will cause dehydration (unless there are intake restrictions). Patients should be
encouraged to avoid dehydration to reduce the tendency to experience
constipation.
• Diet: Fibre plays a key role in establishing a successful bowel routine. A person
with a SCI must learn how fibre impacts their bowel routine as well as which
foods affect their bowel routine.
• Consult a registered dietitian if the patient has poor appetite, poor oral intake, or
significant weight changes, or if guidance is required for fluid and fibre intake.
• Patients with SCI should not be routinely placed on high-fibre diets. Increases in
fibre intake should be done gradually to assess tolerance.
* medications require an order from an authorized prescriber.
** patients with spinal cord injury and/or at risk of pressure ulcers should never be seated on a
commode without appropriate padding or pressure redistribution material between the patient
and the seat.
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 7
January, 2022
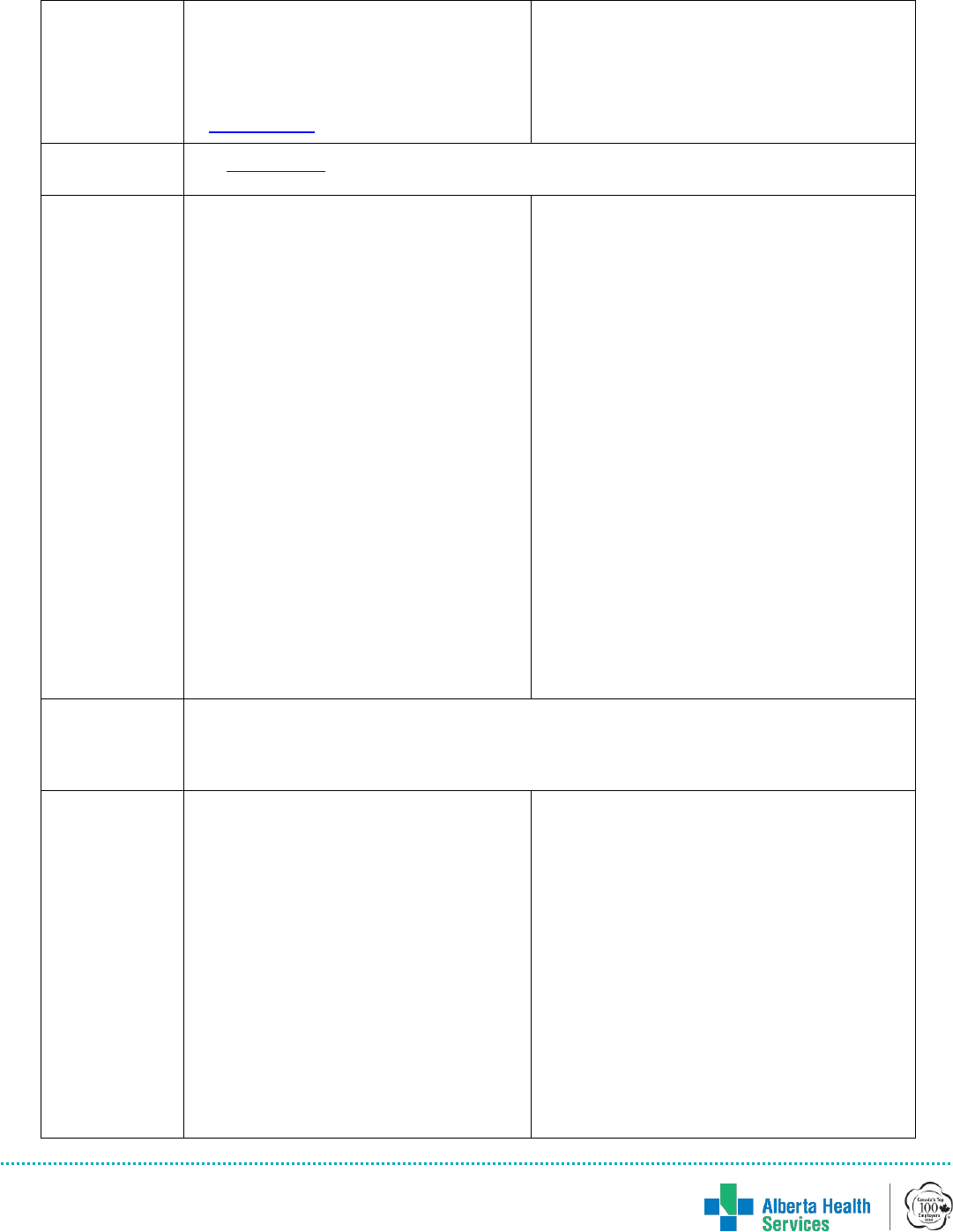
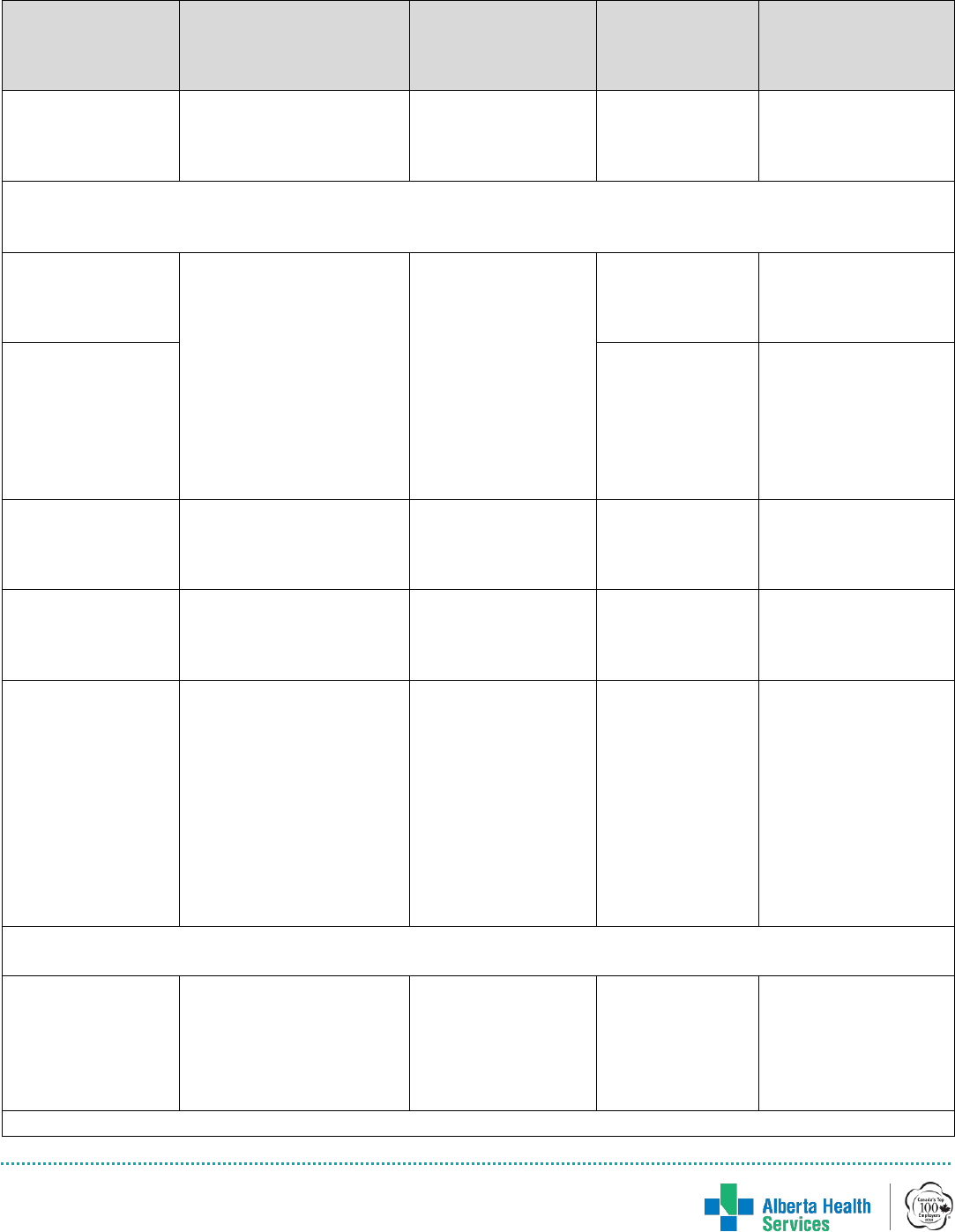
Appendix A: Typical Routine for Management of NBD
Reflexic (Spastic) Bowel
Areflexic (Flaccid) Bowel
• Bowel care is best performed approximately 30
minutes after eating
• Bisacodyl suppository (if ordered) 10-15
minutes before planned evacuation
• Bowel care is best performed approximately 30-
60 minutes after eating
• Psyllium mucilloid powder 1 packet daily up to
TID (Each packet to provide 3.4 g psyllium)
• Caution, patients will need appropriate fluid
intake to prevent constipation while taking
psyllium
• If occurrence of pain or history of autonomic
dysreflexia (AD) with bowel evacuation, follow
AHS AD protocol or obtain an order for
application of topical lidocaine 2%* to anus.
• Explain procedure and get permission to
proceed
• Daily AM or PM routine (depending on
patient’s’ schedule):
1. Have patient sitting on padded
commode**, in sling of mechanical lift, or
lying on left side
2. Digital rectal stimulation (for no longer than
10 to 20 seconds at a time); allow stool to
evacuate unassisted; repeat every 5-10
minutes X 2 until evacuation of the stool is
achieved.
3. Digital disimpaction may be required for any
stool that does not evacuate with
stimulation alone.
4. Perform this routine even if the bowels have
emptied spontaneously earlier in the day
• NOTE: simply inserting a suppository and
waiting for results without stimulation and
manual disimpaction will not likely be effective,
and can cause impaction of stool in the rectum
• If patients displays signs and symptoms of
AD, stop bowel care. AD is a medical
emergency. Manage AD (See AD protocol)
Caution: vagal response (syncope) may
occur with bowel routine
• Explain procedure and get permission to
proceed
• Routine should be performed twice per day and
prn (eg. prior to getting the patient up in their
wheelchair).
• If patient having more incontinence—may need
to increase frequency of routine.
1. Have patient sitting on padded commode, in
sling of mechanical lift, or lying on left side
2. Digitally inspect the rectum for stool
3. If stool is present, remove it by performing
digital disimpaction
4. If stool is too hard to remove, consider
administering a glycerin suppository* (as per
prescriber’s orders) into the bulk of stool,
then trying to remove stool after 30 minutes.
NOTE: Incontinence may be more frequent due to
areflexic bowel, therefore nursing may need to
assess more frequently for incontinence, and
provide assistance as required.
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 8
January, 2022
Appendix B: Glossary
Autonomic Dysreflexia: Autonomic Dysreflexia (AD) is a potentially life-threatening
condition that most commonly occurs in patients with a SCI at or above the T6 neurological
level; and sometimes in patients with a SCI at level T7-8. AD is a medical emergency that
causes a sudden rise in the patient’s blood pressure. AD is a usually the result of a noxious
stimuli below the level of the spinal cord injury, that the patient with SCI may not be able to
feel or is unaware of. Early management includes recognition and removal of the cause of
the noxious stimuli. If conservative management is unsuccessful, medical management with
anti-hypertensive medication may be required to prevent serious complications. If left
untreated, AD may result in serious complications (e.g., stroke, seizure, cardiac arrest, and
death).
Bowel Care: is the process of assisted defecation, typically at a scheduled interval, which
can include rectal stimulation (chemical, mechanical, or both), manual evacuation of stool,
positioning, and adaptive equipment. Mechanical rectal stimulation should be used for
individuals with reflexic NBD. Manual evacuation of stool should be used for individuals with
areflexic NBD.
Manual Evacuation or Digital Disimpaction: is indicated as treatment for areflexic bowel
management and fecal impaction. Performed with the affected individual side-lying in bed or
positioned on a padded commode if prescribed to be performed in an upright position. Insert
a single, gloved, lubricated finger into the rectum to disimpact and remove stool that is
present in the rectal vault.
Mechanical Rectal Stimulation: manual procedures to stimulate bowel evacuation in the
setting of reflexic neurogenic bowel dysfunction.
Digital Rectal Stimulation: is a form of mechanical
rectal stimulation that is most commonly used for
those with reflexic NBD. Insert a gloved, lubricated
finger into the rectum and perform slow rotation in a
circular movement for no longer than 10 to 20
seconds at a time. Repeat the rectal stimulation
sequence every 5 to 10 minutes until evacuation of
the stool is achieved. Using additional fingers or
excessive dilation has shown no benefit and can contribute to complications.
Assistive Device (adaptive digital stimulator): Any device that increases the
independence of a person with a disability. An example is a digital stimulator, which
helps a person with limited hand function to be more independent with bowel care.
Also called adaptive device.
My Shepherd Connection
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 9
January, 2022
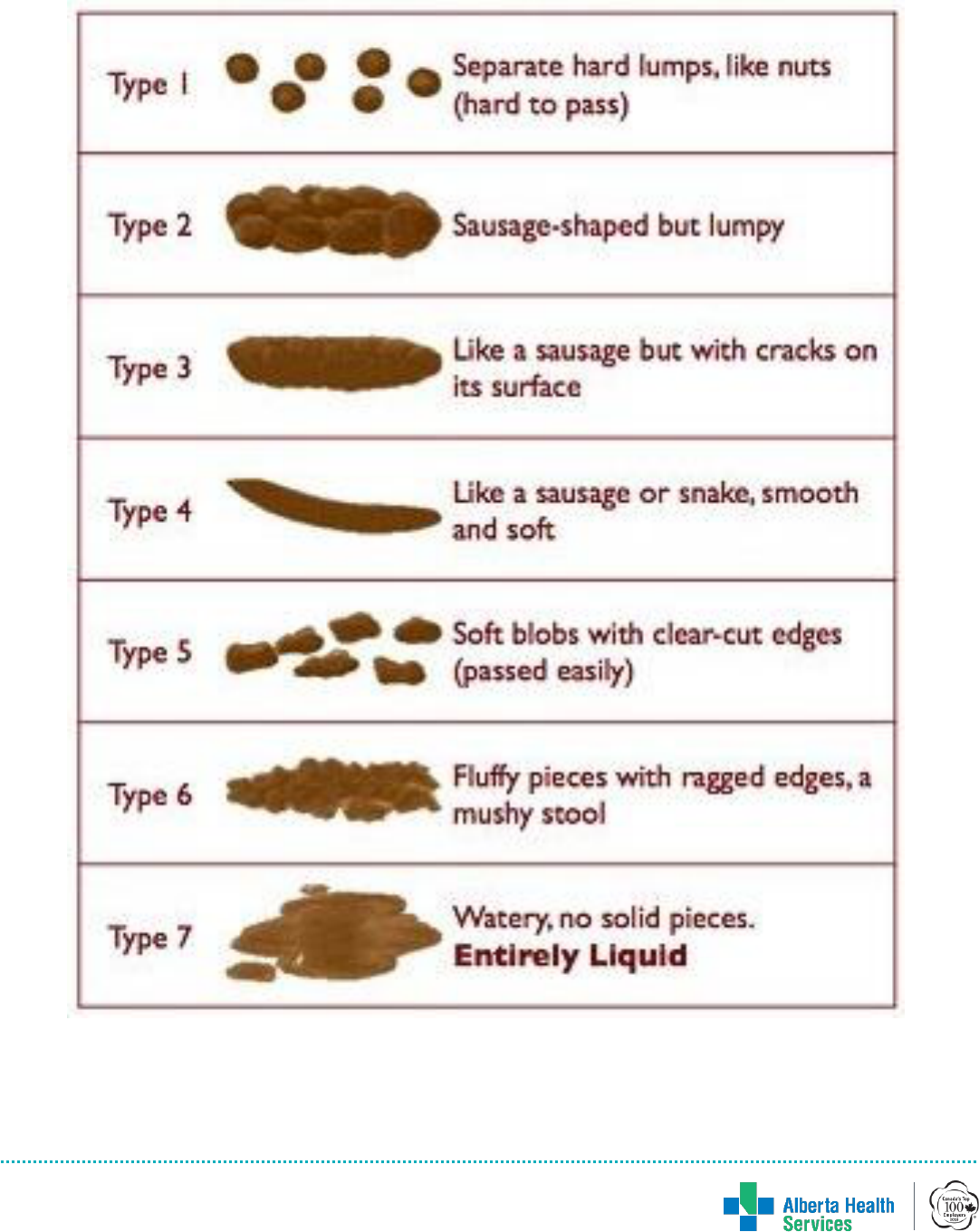
Appendix C: Bristol Stool Chart
The Bristol Stool Scale (Heaton et al 1992)
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 10
January, 2022
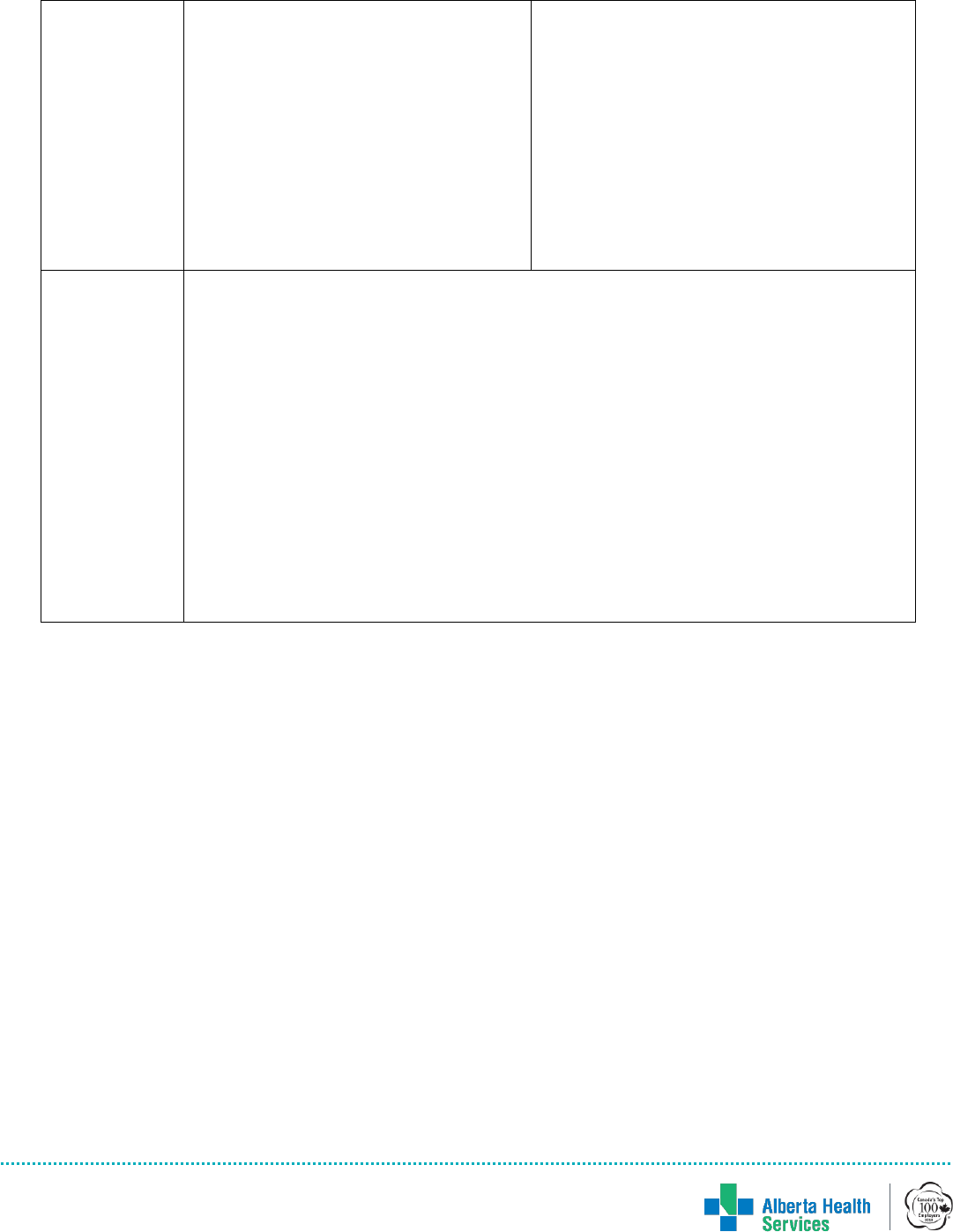
Appendix D: Bowel Management Medications: Tips and Tricks
Medication
Mechanism
of Action
Ideal for
Purpose
(Prevention,
Rescue or
Management)
Tips
Bulk Forming Agents
Psyllium
(Metamucil®)
Increases physical bulk
of feces, which
stimulates peristalsis in
normal bowel; promotes
growth of health gut
flora. Acts within 12- 72
hours.
Patients with loose
or liquid stools, or
fibre deficit in diet;
may be helpful in
preventing
accidents in
patients with
flaccid bowel;
patients whose
stools are difficult
to pass
Prevention;
Chronic
Management
Not appropriate
for acute bowel
impaction
Can cause
distention and gas.
Can be taken up to
TID. Take with a full
glass of water; avoid
with enteral
administration –
likely to clog tubing.
Fruit Lax
(contains soluble
and insoluble fruit
fibre)
Osmotic and bulking
agent
Patients with fibre
poor diets
Prevention;
Chronic
Management
Take with meals
and lots of water,
consult a dietitian
for frequency. Too
much fibre too
quickly can cause
bloating and
cramping
Osmotics and Hyperosmotics
Polyethylene
Glycol (PEG)
3350 (Colyte®)
with electrolytes
Draws water into the
lumen of the gut,
distending the colon
with promotes
peristalsis; causes
abdominal distention
and subsequent
evacuation of the bowel.
Acts within 48 hours.
Patients preparing
for bowel
procedures
Bowel prep
Reconstitute with
water. Makes 4
liters of solution.
Lactulose
Oral
Draws water into the
lumen of the gut,
distending the colon
with promotes
peristalsis; causes
abdominal distention
and subsequent
evacuation of the bowel.
Acts within 24-48 hours.
Chronic or
subacute
constipation
Prevention or
Chronic
Management
Max 60 mL per day
May cause gas,
distension, belching
and discomfort in
the first week. May
take up to 48 hours
for results.
Glycerin
Suppository
Rectal
Osmotic and softens,
lubricates. May also
stimulate. Acts within
15-60 minutes.
Acute constipation
with rectal
impaction of stool
that is too hard and
Treatment of
Constipation
Usually works 15-60
minutes. Patient to
stay in side-lying
position while
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 11
January, 2022
Medication
Mechanism
of Action
Ideal for
Purpose
(Prevention,
Rescue or
Management)
Tips
bulky to pass.
suppository is in
place. Try to insert
suppository directly
into stool.
Tap water enema
Rectal
Adds water to stool;
causes bowel
distention, stimulating
peristalsis and
expulsion of stool
Only to be used as
last resort as bowel
prep prior to
endoscopy or
rectal procedures/
diagnostics.
Not
recommended
except in bowel
prep
Can cause fluid and
electrolyte
imbalance with
repeated
administration.
Uses 500-1000 mL
warm water.
Sorbitol 70%
Oral
Adds water to stool;
causes bowel
distention, stimulating
peristalsis and
expulsion of stool.
Onset of action: 24-48
hours.
Less sweet than
lactulose, may
cause less nausea.
Saline Laxatives (Osmotics and Hyper-Osmotics containing magnesium or phosphates)
Sodium
phosphate enema
(Fleet®)
Rectal only
Draws water into the
lumen of the gut,
creating softer stools,
potentially affecting
systemic fluid and
electrolyte balance. Acts
quickly with results
usually within 3 to 5
minutes.
Acute constipation
Rescue (Use
with caution)
Rectal
administration will
increase serum
phosphorus levels.
Don’t give more
than once in 24 h
period. May result
in acute kidney
injury.
Magnesium
hydroxide
(Milk of
Magnesia®)
Oral
Draws water into the
lumen of the gut,
distending the colon
which promotes
peristalsis; causes
abdominal distention
and subsequent
evacuation of the bowel
Acts in 30 minutes to 3
hours.
Chronic or
subacute
constipation; only
for patients with
GFR > 30 mL/min
Management
Max dose 60 mL in
24 h; one 30 mL
dose contains 2400
mg of elemental
magnesium;
magnesium toxicity
can occur with
excessive oral
doses. Also helps
with symptoms of
indigestion/reflux
Magnesium
Citrate
(Citromag®)
Draws water into the
lumen of the gut,
distending the colon
which promotes
peristalsis; causes
abdominal distention
Acute Constipation
Rescue
Results within 3
hours. May cause
electrolyte
imbalance,
especially in young
children or patients
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 12
January, 2022
Medication
Mechanism
of Action
Ideal for
Purpose
(Prevention,
Rescue or
Management)
Tips
and subsequent
evacuation of the bowel.
Acts within 30 minutes
to 3 hours.
with renal
insufficiency.
Peristaltic Stimulants
(Give for spastic or non-neurogenic bowel. Will not be effective for flaccid bowel.)
Bisacodyl
(Dulcolax®) oral
Directly stimulates the
colonic mucosa to
produce peristalsis.
Tablets act in 6 to 12
hours.
Suppositories act in 15
minutes to 1 hour.
Give for spastic or
non-neurogenic
bowel. Will not be
effective for flaccid
bowel.
Prevention and
treatment
Given in the evening
to produce a bowel
movement in the
morning.
Bisacodyl
suppository
Routine
Maintenance of
neurogenic
bowel;
Rescue for non-
neurogenic
bowel
Give in the evening
to avoid lengthy AM
bowel management.
Ensure suppository
is placed in contact
with the rectal wall.
Cascara oral
Irritates the intestinal
mucosa; increases
motility and alters fluid/
electrolyte secretion.
Management
May cause
cramping
Senna oral
(Senokot®)
Stimulates neuro-
peristaltic response.
Acts in 6 to 10 hours.
Prevention and
Management
Take with a large
glass of water, or
large enteral flush.
Soap and water
enema
Distends the bowel,
increasing peristalsis;
irritates/stimulates the
mucous membranes of
the bowel.
Only to be used as
a last resort as
bowel prep prior to
endoscopy or
rectal procedures /
diagnostics.
Not
recommended
except in bowel
prep as may
cause colonic
mucosa irritation
Use the pre-
prepared kit/
package or, if no kit
available, mix 5 mL
mild liquid soap in
1000 mL warm
water. Can causes
fluid and electrolyte
imbalance with
repeated
administration.
Lubricants
Mineral Oil
Enema
Lubricates stool for
easier passing. Acts
within 2-15 minutes.
When straining
may be painful or
dangerous; difficult
to pass or very
hard stools
Management,
Rescue
Usually works within
2-15 minutes.
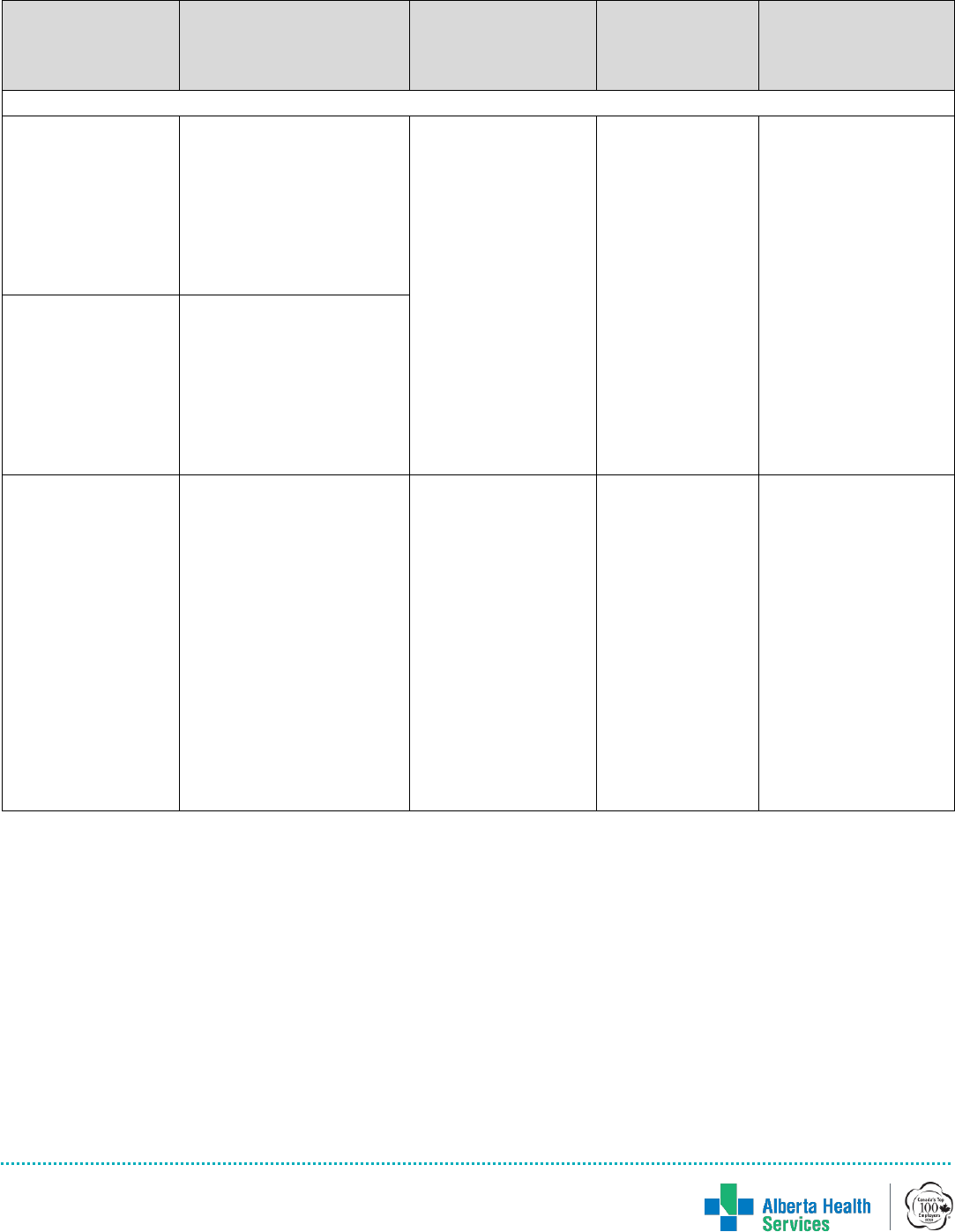
Bowel Management for Patients with Neurogenic Bowel Dysfunction | 13
January, 2022
Medication
Mechanism
of Action
Ideal for
Purpose
(Prevention,
Rescue or
Management)
Tips
Medications with a unique mechanism of action to treat constipation
Methylnaltrexone
(Relistor®)
injectable
Opioid receptor
antagonist that acts
upon GI tract to prevent
opioid induced
decreased GI motility
and delay in GI transit
time. Acts within 30-60
minutes.
Opioid induced
constipation
Rescue (only in
those with
opioid induced
constipation)
Should not be used
with other laxatives;
Monitor for opioid
withdrawal.
Naloxegol
(Movantik®) oral
Opioid receptor
antagonist that acts
upon GI tract to prevent
opioid induced
decreased GI motility
and delay in GI transit
time. Acts within 6 to 12
hours.
Prucalopride
(Resotran®)
Serotonin agonist
whose action at the
receptor site promotes
stimulation of peristaltic
reflex, intestinal
secretions and GI
motility. Acts within 2-3
hours
Chronic idiopathic
constipation
Management of
chronic
idiopathic
constipation
refractory to a 4-
week trial of
osmotic
laxatives;
Management of
chronic
intestinal
pseudo-
obstruction
refractory to
other laxatives.
Only indicated for
females in Canada

Bowel Management for Patients with Neurogenic Bowel Dysfunction | 14
January, 2022
References
Basson, M.D. (2014, October 1). Constipation Medication. Medscape. Retrieved from
http://emedicine.medscape.com
Canadian Pharmacists Association. (n.d.) Retrieved April 1, 2015, from http://www.e-cps.ca.
Ottawa, ON.
Consortium for Spinal Cord Medicine. (2020). Management of Neurogenic Bowel
Dysfunction in Adults after Spinal Cord Injury: Clinical Practice Guideline for Health Care
Providers. Retrieved from www.pva.org on November 5, 2020.
Cotterill, Nikki; Madersbacher, Helmut; Wyndaele, Jean J.; Apostolidis, Apostolos; Drake,
Marcus J.; Gajewski, Jerzy; Heesakkers, John; Panicker, Jalesh; Radziszewski, Piotr (2017-
06-22). "Neurogenic bowel dysfunction: Clinical management recommendations of the
Neurologic Incontinence Committee of the Fifth International Consultation on Incontinence
2013". Neurourol Urodyn. 37 (1): 46–53. doi:10.1002/nau.23289. PMID 28640977.
den Braber-Ymker, Marjanne; Lammens, Martin; van Putten, Michel J.A.M.; Nagtegaal, Iris D.
(2017-01-06). "The enteric nervous system and the musculature of the colon are altered in
patients with spina bifida and spinal cord injury". Virchows Archiv. 470 (2): 175–184.
doi:10.1007/s00428-016-2060-4. PMC 5306076. PMID 28062917.
Hallin, P.A., Herndon, C.M., Jackson, K.C. (2002). Management of opioid-induced
gastrointestinal effects in patients receiving palliative care. Pharmacotherapy, 22(2).
Retrieved from http://www.medscape.com/
Hunter, R. (2014). Nursing management of constipation in the medical-surgical setting. Med-
Surg Matters, 23(2), 4-9.
Jamshed, N., Lee, Z., Olden, K.W. (2011). Diagnostic approach to chronic constipation in
adults. American Family Physician, 84(3), 299-306.
Krogh, K; Christensen, P; Laurberg, S (June 2001). "Colorectal symptoms in patients with
neurological diseases". Acta Neurol Scand. 103 (6): 335–343. doi:10.1034/j.1600-
0404.2001.103006335.x. PMID 11421845.
Micromedex® Drugdex. (n.d.). Retrieved October 30, 2014, from
www.micromedexsolutions.com/micromedex2/librarian. Greenwood Village, CO: Truven
Health Analytics.
Rauck RL. (2013). Treatment of opioid-induced constipation: focus on the peripheral mu-
opioid receptor antagonist methylnaltrexone. Drugs, 73, 1297-306.
Timby, B.K. (2009). Fundamental nursing skills and concepts. Philadelphia, PA: Lippincott
Williams & Wilkins.
