
Neurogenic Bowel:
What You
Should Know
A Guide for People
with Spinal Cord Injury
CLINICAL PRACTICE CONSUMER GUIDELINE: NEUROGENIC
BOWEL
SPINAL CORD MEDICINE
Administrative and financial support provided by Paralyzed Veterans of America

Consumer Guide
Panel Members
Steven A. Stiens, MD, MS
Chair, Consumer Guide Panel and
Member, Consortium for Spinal Cord Medicine
Neurogenic Bowel Guideline Panel
U.S. Department of Veterans Affairs
VA Puget Sound Healthcare System
Seattle, Washington
University of Washington
Department of Rehabilitation Medicine
Seattle, Washington
Carol Braunschweig, PhD
Member, Consortium for Spinal Cord Medicine
Neurogenic Bowel Guideline Panel
University of Illinois of Chicago
Chicago, Illinois
John F. Cowell
Member, Consortium for Spinal Cord Medicine
Neurogenic Bowel Guideline Panel
Paralyzed Veterans of America
Washington, D.C.
C. Mary Dingus, PhD
Member, Consortium for Spinal Cord Medicine
Neurogenic Bowel Guideline Panel
U.S. Department of Veterans Affairs
VA Puget Sound Healthcare System
Seattle, Washington
Mary Montufar, MS, RN
Member, American Association of Spinal Cord Injury
Nurses Bowel Guideline Panel
U.S. Department of Veterans Affairs
VA Palo Alto Healthcare System
Palo Alto, California
Peggy Matthews Kirk, BSN, RN
Member, Consortium for Spinal Cord Medicine
Neurogenic Bowel Guideline Panel
Rehabilitation Institute of Chicago
Chicago, Illinois
Consortium Member
Organizations
American Academy of Orthopedic Surgeons
American Academy of Physical Medicine and
Rehabilitation
American Association of Neurological Surgeons
American Association of Spinal Cord Injury
Nurses
American Association of Spinal Cord Injury
Psychologists and Social Workers
American Congress of Rehabilitation Medicine
American Occupational Therapy Association
American Paraplegia Society
American Physical Therapy Association
American Psychological Association
American Spinal Injury Association
Association of Academic Physiatrists
Association of Rehabilitation Nurses
Congress of Neurological Surgeons
Eastern Paralyzed Veterans Association
Insurance Rehabilitation Study Group
Paralyzed Veterans of America
U.S. Department of Veterans Affairs

Who Should Read This Guide?
This Guide is for everyone who wants or needs to under-
stand how spinal cord injury (SCI) can affect and change
bowel* function. The clinical name for this condition is neuro-
genic bowel. It’s also for everyone who wants to learn about
ways to deal with these changes in bowel function. That
includes:
Adults with spinal cord injuries:
•People with a new SCI.
•People who’ve lived with SCI for years.
Caregivers:
•Family members.
• Friends.
•Personal care attendants.
Health-care professionals:
•Primary-care providers.
• Rehabilitation professionals.
• Other hospital staff.
This Guide is an educational tool. Feel free
to share it with your health-care professionals
when you discuss bowel management issues
with them and plans for actual changes. They
can also get a free copy of the full clini-
cal practice guideline, Neurogenic
Bowel Management in Adults with
Spinal Cord Injury, by calling
(888) 860-7244 or visiting the
Paralyzed Veterans of America
(PVA) web site at
http://www.pva.org.
A Guide for People with Spinal Cord Injury 1
*Words in italics are explained in the Glossary on page 41.
I
’m an avid sportsman and can’t get enough of the great
outdoors. Since my SCI, I’ve been experimenting with new
ways to do all the things I loved before my all-terrain vehicle
(ATV) accident. I spend all my free time camping, whitewater
rafting, kayaking, fishing, and hunting. I’ve got a T7
complete injury, so I needed some special adaptive
equipment to continue my outdoor interests.
The biggest problem I had after my injury wasn’t with
changes to my sporting equipment or other gear, but
in getting my body functions under control. I was
worried that I’d have a bowel accident while I was on
a camping or fishing trip, and that kept me from doing
the things I really enjoyed.
So I talked with my doctor, rehabilitation nurse, and
occupational therapist, and we developed a bowel program
that’s working well for me. Because I’m very physically active,
we changed the frequency of my bowel care. The occupational
therapist gave me some tips on positioning and
disposal. My doctor also linked me to a dietitian,
and we made some changes to my diet. It
worked. I’m in control of my situation and
that gives me confidence in other areas as
well.
I met a young woman I really care for.
We’ve been dating for a couple of months.
Last month she began asking some personal
questions about my injury, and I’m being really honest
with her. I gave her a copy of PVA’s Yes, You Can! book and
marked some important sections for her to read. The bowel
and bladder stuff is hard to talk about, but once she had read
the book, it was easier.
A proper
bowel program
promotes independence
and thereby improves
quality of life.
Cliff
Cliff

A Guide for People with Spinal Cord Injury 3
Contents
Why Is This Guide Important?........................................................................4
What Is the Bowel and Where Is It? ..............................................................5
How Does the Bowel Work? ..........................................................................6
How Does SCI Change the Way the Bowel Works? ........................................6
What Is a Bowel Program? ............................................................................8
What Is Bowel Care? ......................................................................................9
What Is Rectal Stimulation? ..........................................................................9
How Is Digital Rectal Stimulation Done?......................................................10
What Does My Health-Care Professional Need to Know? ............................11
How Do I Do Bowel Care?............................................................................14
Are There Other Ways to Improve a Bowel Movement? ..............................18
What Is a Bowel Care Record? ....................................................................19
Can I Be Independent in My Bowel Care? ....................................................20
Why Do I Need to Watch What I Eat and Drink?..........................................21
What Medications Are Used in Bowel Programs? ........................................26
Tips for Safe Bowel Care..............................................................................26
How Often Should My Bowel Program be Reviewed? ..................................28
What Should I Do if My Bowel Program Isn’t Working? ..............................29
Answers to Commonly Asked Questions ....................................................34
What Should I Know About Surgical Options? ............................................36
References and Resources............................................................................39
Glossary ......................................................................................................41
Food Record ................................................................................................46
Medical History............................................................................................48
Bowel Care Record ......................................................................................49
Tables and Figures
Figure 1. GI Tract ........................................................................................5
Figure 2. Colon and Anal Canal ..................................................................10
Figure 3. Digital Stimulation ....................................................................10
Figure 4. Placement of Suppository............................................................15
Figure 5. Colostomy/Ileostomy ..................................................................36
Table 1. How Much Fiber Is in Different Types of Food? ..........................23
Table 2. What You Can Do About Excessive Gas ......................................24
Table 3. Bowel Medications ......................................................................27
Table 4. Frequent Bowel Accidents: Possible Causes and Solutions..........31
Table 5. Common Bowel Problems: Solutions and Possible Causes..........32

4 NEUROGENIC BOWEL: What You Should Know
Why Is This Guide Important?
A spinal cord injury changes the way your body works and
how you will care for yourself. One important change that
may be difficult for many of us to talk about is how the bowel
functions.
Before an SCI, people don’t have to make special plans or
schedules for bowel movements. They can feel the need to use
a toilet, hold their bowels until the time is right, and then relax
and let stool pass out at the right place.
After an SCI, bowel movements require more time, thought,
and planning. People with SCI usually can’t feel when stool is
ready to come out, and they need help expelling the stool. As
people with SCI say, “The bowel rules.”
A well-designed bowel program can help you lead a healthi-
er and happier life after SCI. It can:
• Help prevent unplanned bowel movements (also called bowel
accidents, incontinence, or involuntaries).
• Help avoid physical problems such as constipation.
• Put you back in control of a bodily function that, if neglected,
can cause embarrassment.
• Improve your confidence in work and social situations.
This Guide will help you work with your family, caregivers,
and health-care professionals to create a bowel program that
fits your needs. After that, it’s up to you to stick with it.
Everyone’s body changes over time. Even if you’ve kept to a
regular bowel program for months or years, it may stop work-
ing for you as well as it once did. This Guide will tell
you what to do if that happens at any time in your life.
Talking About
Embarrassing Subjects
Most of us consider bathroom functions private and
personal. We’re not comfortable talking about them,
even with close family members or health-care pro-
fessionals. That’s one of the hardest changes
after SCI: talking about bowel functions—and
asking for help with them.
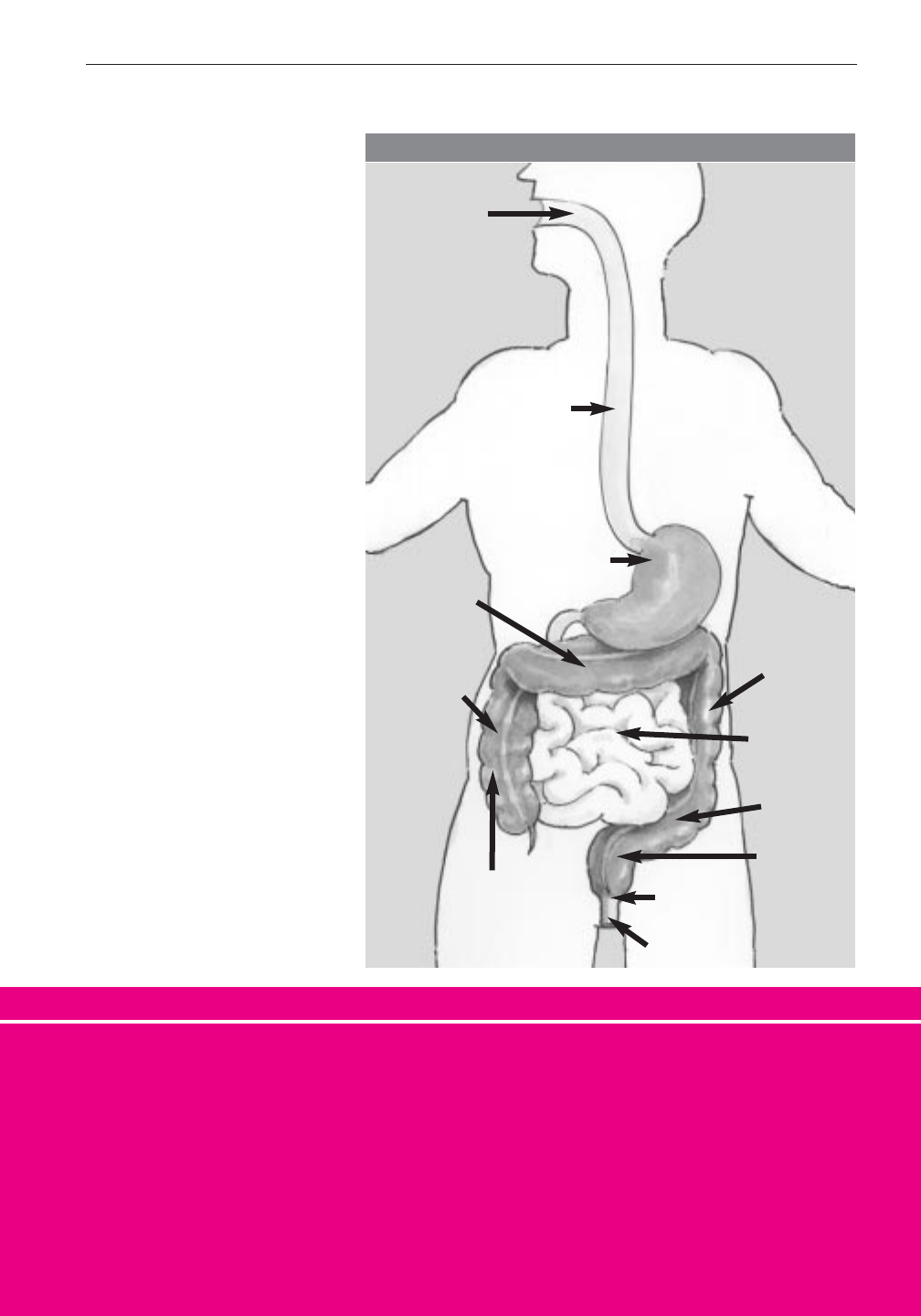
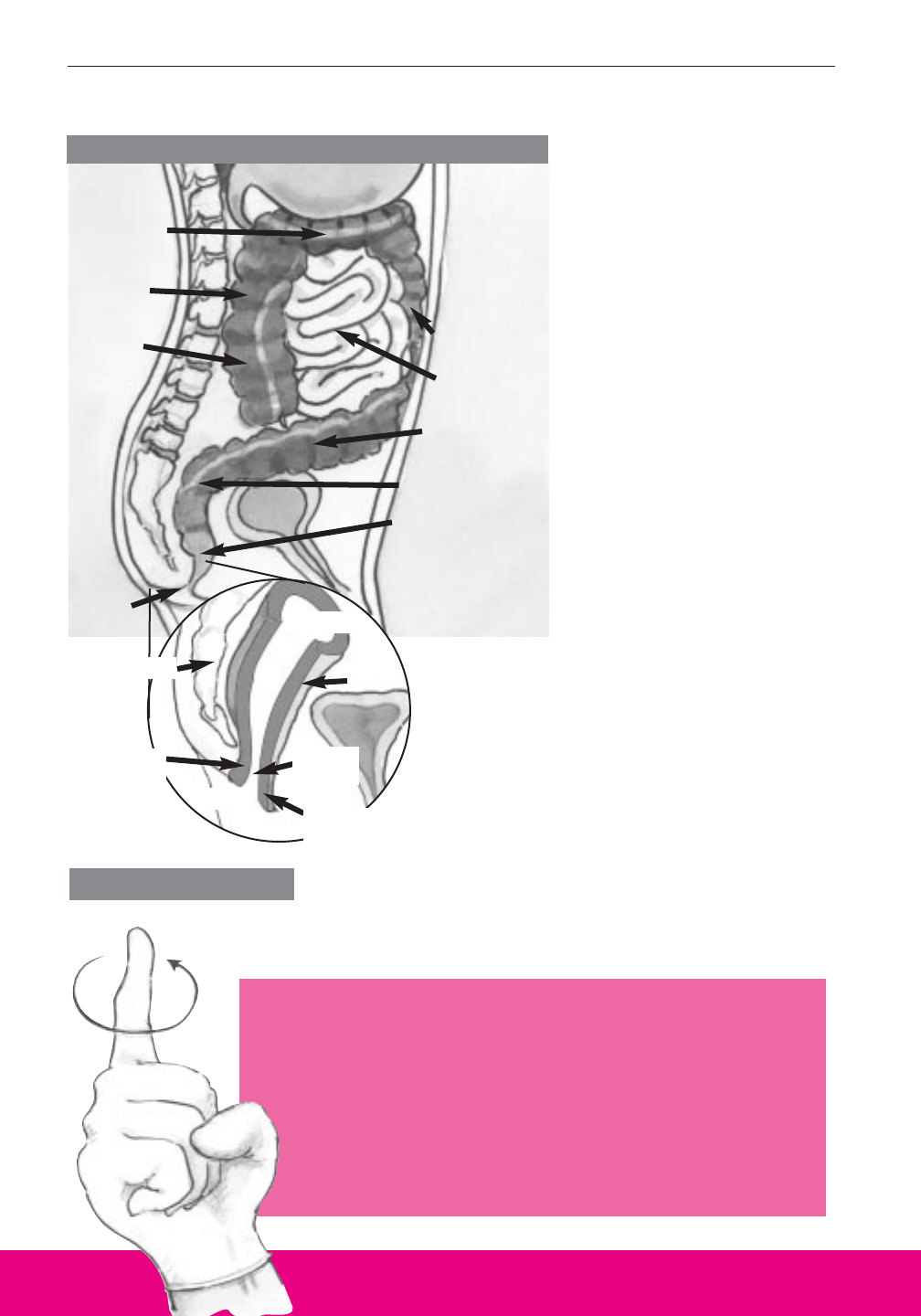
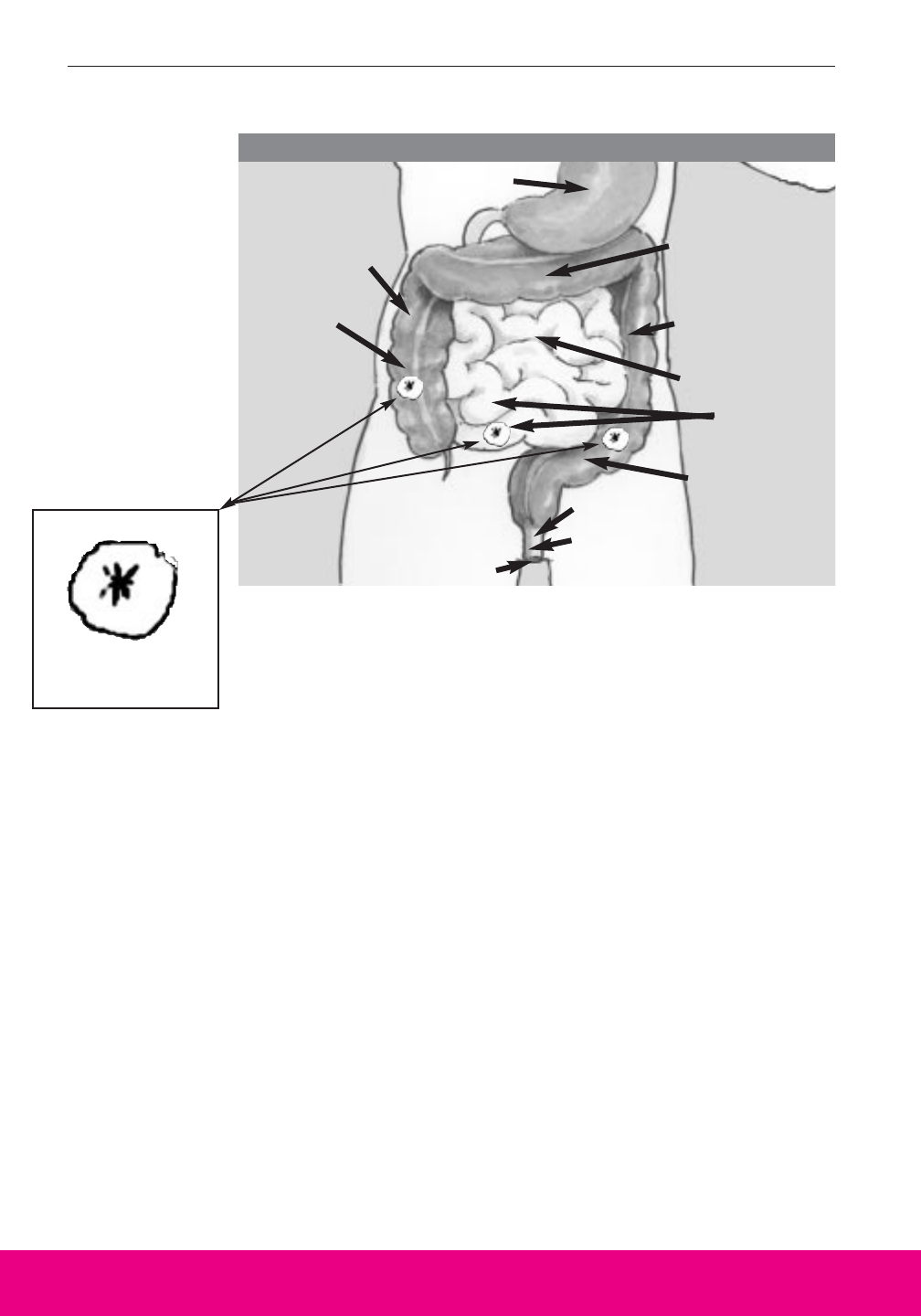
What Is the Bowel
and Where Is It?
Everything you eat
and drink travels from
your mouth through your
digestive system—also
called the gastrointesti-
nal tract or GI tract (see
Figure 1). The GI tract
includes the mouth,
esophagus, stomach,
small intestine, and
colon (also called the
large intestine) and ends
at the anus. The colon is
about 5 feet long and
forms a question mark
shape in the abdomen.
Together, the large and
small intestines are
called the bowel.
There’s no getting around it: Life is dif-
ferent now. Practice helps. The more you
talk about bowel issues, the easier it gets.
Remember that other people (except
health-care professionals) are likely to be
just as uncomfortable with bowel discus-
sions as you are at first.
Humor can be a good way to relieve
embarrassment. If you try to put other
people at ease, you’ll feel less embar-
rassed too.
A Guide for People with Spinal Cord Injury 5
Mouth
Esophagus
Stomach
FIGURE 1
Transverse
Colon
Descending
Colon
Small
Intestine
Ascending
Colon
Anus
Anal
Sphincter
Rectum
Sigmoid
Colon
Colon
(Large
Intestine)
How Does the Bowel Work?
The digestive process breaks down what you eat and drink
into nutrients your body uses and waste that you eliminate. A
wave-like action called peristalsis propels food through your GI
tract. The undigested food, waste your body doesn’t use, moves
into the colon from your small intestine. The colon takes the
moisture out of the waste and stores it. The waste follows the
question-mark shaped pathway of the colon: up the ascending
colon, across the transverse colon, down the descending colon
through the sigmoid colon, and into the rectum on its way out of
the body (see Figure 1, page 5).
People use many words to describe these wastes. Health-
care professionals call them bowel movements (BM), stool,
excrement, fecal matter, or feces. Your family and caregivers
may be more comfortable using terms like BM. (Liquid wastes
are eliminated as urine.)
How Does SCI Change the Way the Bowel Works?
Neurogenic bowel is a condition that affects the body’s
process for storing and eliminating solid wastes from food.
After SCI, the nervous system can’t control bowel functions the
way it did before.
For most people, the digestive process is controlled from
the brain by reflex and voluntary action. SCI interferes with
that process by blocking messages from parts of the digestive
system to and from the brain through the spinal cord. How it
interferes depends on where along the spinal cord the injury is.
Here’s what normally happens. The colon stores stool until
it’s propelled out as a bowel movement. When the stool is
6 NEUROGENIC BOWEL: What You Should Know
• Stick with a consistent schedule. That
means every day or every other day,
depending on your
needs.
• Find a convenient
time of day. That
means always in the
morning or always
in the evening—
whatever works for
you, but always the same time of day.
Tips for Following a Regular Bowel Care Routine
SMTWT F S
pushed into the rectum, it triggers a reflex action. This action
contracts the anal sphincter, keeping it closed so that stool
doesn’t slip out. Without SCI, people can feel stool in the rec-
tum and voluntarily contract the anal sphincter to hold in the
stool. They then find a toilet, relax the anal sphincter, and have
a bowel movement.
SCI can keep you from feeling stool in the rectum and from
controlling your anal sphincter. It can also affect peristalsis—
how stool moves through your colon.
Generally, two basic patterns of neurogenic bowel occur
after SCI, depending on which part of the spinal cord is injured.
Reflexic Bowel
This usually results from SCI at the cervical (neck) or tho-
racic (chest) level. This type of SCI interrupts messages
between the colon and the brain that are relayed by the spinal
cord. Below the injury, the spinal cord still coordinates bowel
reflexes. This means that although you don’t feel the need to
have a bowel movement, you still have reflex peristalsis. Stool
buildup in the rectum can trigger a reflex bowel movement
without warning. Between bowel movements, your anal sphinc-
ter will remain tight, and your colon will respond to digital
rectal stimulation and stimulant medications with reflex
peristalsis that pushes the stool out.
Areflexic Bowel
This results from SCI that damages the lower end of the
spinal cord (the lumbar or sacral level) or the nerve branches
that go out to the bowel. This means that you have reduced
peristalsis and reduced reflex control of your anal sphincter.
•Try to do bowel care after a meal or a
hot drink. That may help stimulate
your bowel to push stool out.
• Find a comfortable place and
positions.
•Privacy helps.
A Guide for People with Spinal Cord Injury 7

8 NEUROGENIC BOWEL: What You Should Know
Your bowel isn’t controlled by reflexes from the spinal cord. You
can’t feel the need to have a bowel movement, and your rectum
can’t easily empty stool by itself.
The location of your SCI also has a great deal to do with the
bowel program that will work best for you. (See pages 14-18 for
information about bowel care for reflexic and areflexic bowel.)
What Is a Bowel Program?
A bowel program is a total plan for regaining control of
bowel function after SCI. It deals with several aspects of your
life, including:
•Diet and fluids—what, how much, and when you eat and drink.
• Activity level—how active you are: for example, how often you
get a full range of motion of your joints, how many different
positions (sitting, standing, lying) you are in during the day and
for how long.
• Medications—what products you take for bowel care and for
other reasons. These include oral medications you take to
improve bowel function, rectal medications you use to stimulate
a bowel movement, and medications you take for other reasons
that affect bowel function.
• Bowel care—frequency and technique of scheduled, assisted
bowel movements.
A bowel program is designed to help you improve your
quality of life:
• Prevent or cut down on bowel accidents.
•Eliminate enough stool with each bowel care session at regular
and predictable times.
• Make bowel care go smoothly, allowing you to finish within a
reasonable time.
•Keep bowel-related health and other problems to a minimum.
You and your health-care professionals will work together to
design a bowel program that fits your needs.

A Guide for People with Spinal Cord Injury 9
What Is Bowel Care?
Bowel care is the term for assisted elimination of stool, and
it’s part of a bowel program. It begins with starting a bowel
movement. That’s usually done with digital rectal stimulation
and/or a stimulant medication. After the bowel movement
starts, intermittent digital rectal stimulation can also be used to
speed up defecation. (See page 18, “Are There Other Ways To
Improve a Bowel Movement?”)
What Is Rectal Stimulation?
It’s a way to turn on peristalsis in the colon, start a bowel
movement, and keep it going. Most people need to start bowel
care by stimulating the rectum to eliminate stool. There are
two main types of rectal stimulation:
• Mechanical stimulation. This method uses a finger or a
stimulant tool. It includes digital rectal stimulation and
manual evacuation.
•Stimulant medications. This method uses a suppository or
mini-enema (also called a liquid suppository).
Important:
If your SCI is at T6 or higher, stool in the rectum or any method
of rectal stimulation may cause autonomic dysreflexia. This is a
potentially life-threatening emergency medical condition! A
fast, major increase in your blood pressure is the most dangerous
sign of autonomic dysreflexia. Learn more about it and how to
prevent it. Read the guide called Autonomic Dysreflexia: What
You Should Know. For a free copy, call (888) 860-7244 or visit the
PVA web site at http://www.pva.org.
Important:
People with SCI need to stick with a regular schedule and tech-
nique of bowel care. You may have to revise your bowel pro-
gram over time, but keeping a regular schedule for doing
bowel care at a regular time is one of the best things you can
do for your health and well-being after SCI.
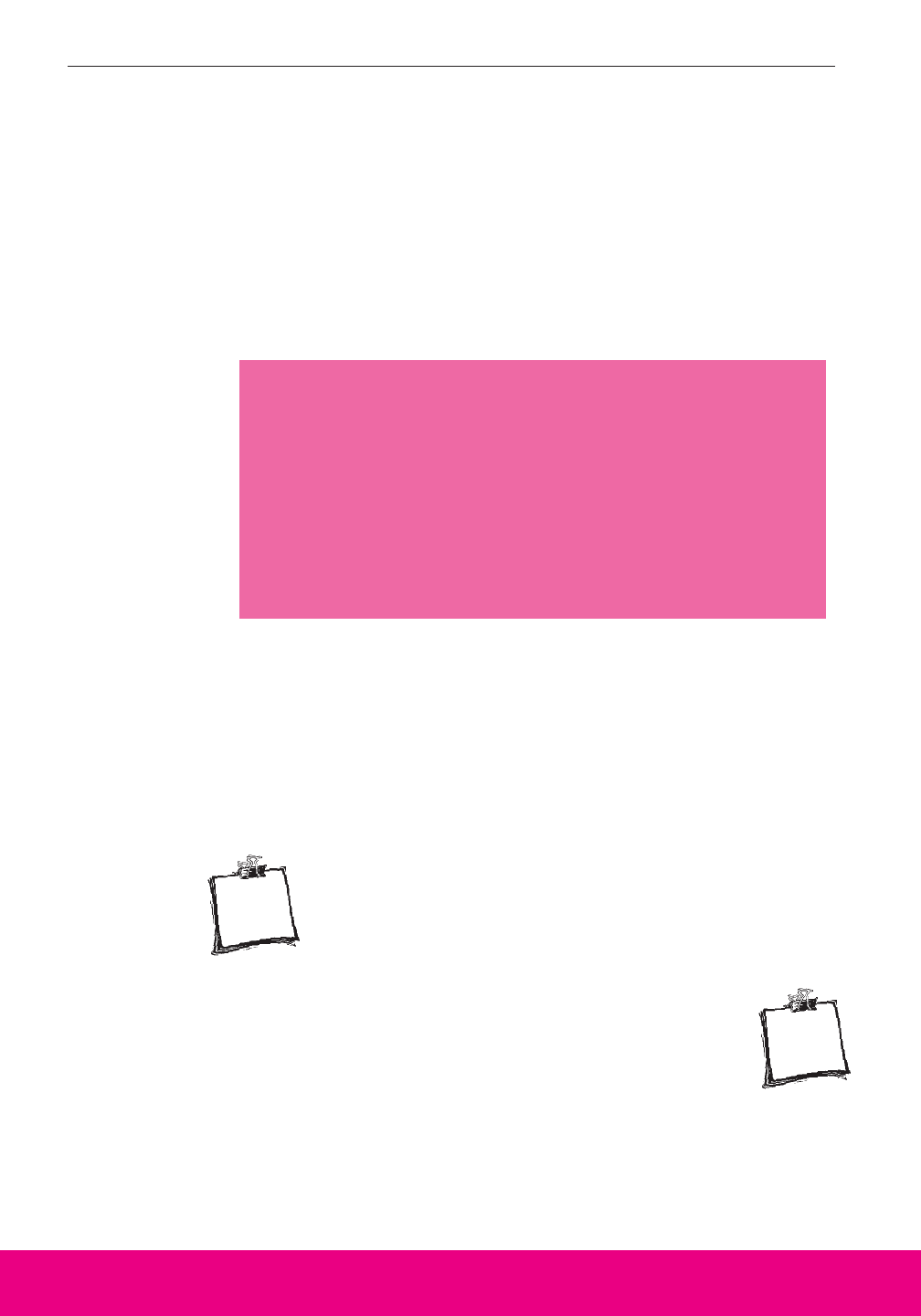
How Is Digital Rectal
Stimulation Done?
Insert a gloved, well-
lubricated finger gently
into the rectum. Direct the
stimulating finger toward
the belly button and follow
the anal canal (see Figures
2 and 3). When the finger
is inserted, digital rectal
stimulation can begin.
Move the stimulating finger
gently in a circular pattern,
keeping the finger in con-
tact with the rectal wall.
Digital rectal stimulation
usually takes 20 seconds
and should be done no
longer than 1 minute at a
time. Repeat the digital stimulation
every 5 to10 minutes until you have a
bowel movement. Sitting up or laying
on your left side may help stimulate a
bowel movement.
Digital stimulation relaxes and
opens the external anal sphincter (see
Figure 2), straightens the rectum, and
triggers peristalsis. From the time you start digital
stimulation, it should take only a few seconds to a few
minutes for stool to enter the rectum and come out.
Important:
At every stage of digital rectal stimulation, it’s important to
use plenty of lubricant and to be gentle. Pushing or rotating
the finger too roughly can irritate or tear the rectal lining
or anus and trigger autonomic dysreflexia. (For more
information about autonomic dysreflexia, see the glossary
and the guide called Autonomic Dysreflexia: What You
Should Know. For a free copy, call (888) 860-7244 or visit
the PVA web site at http://www.pva.org.)
10 NEUROGENIC BOWEL: What You Should Know
FIGURE 2
Colon
(Large
Intestine)
Sacrum
Rectal
Wall
Rectum
Anus
Internal Anal
Sphincter
Stomach
Transverse
Colon
Descending
Colon
Small
Intestine
Rectum
Sigmoid
Colon
Ascending
Colon
Anal
Sphincter
Anus
External Anal
Sphincter
FIGURE 3
Anal
Canal

A Guide for People with Spinal Cord Injury 11
What Does My Health-Care
Professional Need To Know?
No single bowel program is right for everyone. Every per-
son with SCI has a different diet, activity routine, need for med-
ication, and life schedule that regular bowel care has to fit. A
normal schedule for passing stool is whatever is usual for you.
That’s usually once a day or every other day. To find what
works best for you, tell your health-care professional about:
Any new problems with bowel function:
•Does your bowel care produce poor results, or no results?
• Do you have rectal bleeding?
• Does your bowel care routine take longer than before?
•Do you have a lot of gas or feel bloated?

Your medical history. In addition to information about
your SCI:
• Do you have, or have you had, diabetes?
• Do you have digestive problems, such as irritable bowel
syndrome, inflammatory bowel disease, or colitis?
• Have you had any bowel surgery?
Medications you’re taking:
• What prescription products are you taking and for what?
• What nonprescription products, such as laxatives, are you
taking and how often do you take them?
Alcohol and other drugs:
• Do you drink alcoholic beverages? If so, what do you drink, how
much, and how often?
• Do you use, or have you ever used, any “street” drugs? If so,
which ones, how much, and how often?
• Do you use, or have you ever used, any alternative medicines? If
so, which ones, how much, and how often?
Important:
Alcohol and drugs can affect bowel function. If you use alco-
hol or drugs, your health-care professional needs to know, to
be able to design a bowel program that will work for you.
12 NEUROGENIC BOWEL: What You Should Know
The location of your SCI affects the
amount of control you have over your
bowel and determines which methods will
work best for you. Work with your health-
care professional to create a bowel pro-
gram that fits, for example:
•Work and home situations. These
help determine the best time and place
for bowel care. They also affect meals
and food preparation.
• Supplies and equipment. They need
to be affordable, available, and acces-
sible for you.
Your Bowel Program Is as Individual as You Are

A Guide for People with Spinal Cord Injury 13
•Bowel care. You need to be able to
perform the techniques yourself or
direct an attendant or other caregiver
on when and how you need help.
Discuss whether you need an assis-
tant with your health-care professional
and if so, how to tell the assistant
what to do.
• Insurance. Find out what your
insurance covers. If some products
aren’t reimbursed, advocate for
yourself—explain why the product
is needed. Involve your health-
care professional in any decisions
about what products you use.
Your bowel habits before the SCI:
•How often did you have bowel movements?
•At what time of day did you have bowel movements?
•Did you have recurring problems with constipation or diarrhea?
Your diet:
• How much do you drink every day and what do you drink?
• What sorts of food do you usually eat, how much, and how often?
• Do any foods affect your bowel movements?
• Do you have problems with dairy products (lactose intolerance)?
• Do spicy foods give you loose stool?
Your stool:
• Is it hard, soft, or diarrhea (liquid that takes the shape of any
container it goes in)?
• How much stool usually comes out during one of your bowel
movements? For example, if your stool were formed into a ball,
would it be a golf ball, a tennis ball, a softball, or, heaven
forbid...a basketball?
If you have a bowel program now, your health-care
professional will need to know:
• When and how often do you do bowel care?
• Which bowel care techniques do you use?
• How do you start a bowel movement?
—Digital stimulation?
—Stimulant medications (suppositories, mini-enemas)?
14 NEUROGENIC BOWEL: What You Should Know
• How long does it take for the stimulants to work?
•Have you changed what you eat or drink?
• Has your activity level changed?
• Have any of your medications changed (medications you take for
bowel care or anything else)?
• Are you having problems with any part of your bowel program?
How Do I Do Bowel Care?
If I Have a Reflexic Bowel
The goal of a reflexic bowel program is soft, formed stool
that can be passed easily with minimal rectal stimulation. The
bowel care routine usually starts with a stimulant medication or
with digital stimulation.
Getting ready and washing hands. Empty your blad-
der or move your urinary drainage equipment away
from the anal area. Whoever performs bowel care—you
or an attendant—should wash their hands thoroughly.
Setting up and positioning. Prepare for a bowel
movement by getting on or ready for a transfer to a
toilet or commode. If you’re sitting up, gravity helps
empty your rectum. When sitting, keep your feet on
the floor or on a footstool or on the footrest of your commode
chair, with your hips and knees flexed. If you need help with a
transfer, position yourself before bowel care. If you don’t sit
up, lie on your left side.
Important:
Bowel care needs to be done regularly to help prevent acci-
dents! If you’re having problems sticking with your pro-
gram, tell your health-care professional. Together, you
can help identify the problem by talking about your history of
bowel care, performing a physical examination, and taking
tests to explore why you’re having problems. Then, changes
can be made—one element at a time—that will help you fol-
low a regular routine. (See page 29, “What Should I Do if My
Bowel Program Isn’t Working?”)
STEP
R1
STEP
R2

A Guide for People with Spinal Cord Injury 15
Checking for stool. Check for stool by sliding a
gloved, well-lubricated finger into the rectum. Remove
any stool that would interfere with inserting a supposi-
tory or mini-enema (manual evacuation). Use one or
two gloved and lubricated fingers to break up or hook stool and
gently remove it from your rectum.
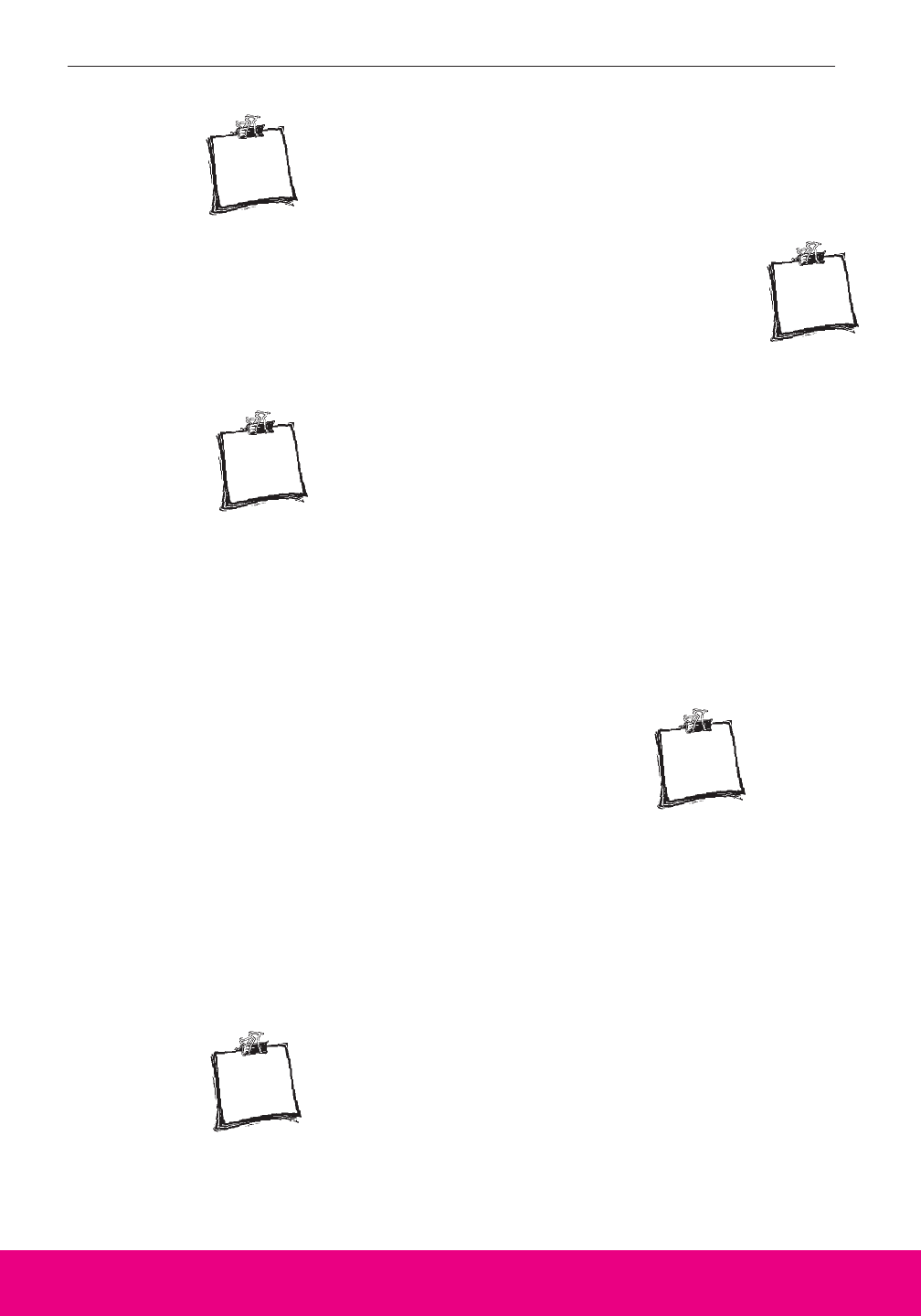
Inserting stimulant
medication. (If you
don’t use a supposito-
ry or mini-enema, go
directly to step R6.) To start a
bowel movement, insert a lubri-
cated suppository or squirt a
mini-enema high in your rec-
tum. (The suppository should
be coated with a water-soluble
lubricant.) Use a gloved and
lubricated finger or assistive
device. Place the medication
right next to the rectal wall (see
Figure 4).
STEP
R3
FIGURE 4
STEP
R4
Suppository
Sacrum
Rectal Wall
Rectum
Anus
Anal Canal
Internal Anal
Sphincter
External Anal
Sphincter
Belly Button
Waiting. Wait about 5 to 15 minutes for the stimulant to
work. If you pass gas or some stool, it’s a sign that the
stimulant is beginning to work.
Starting and repeating digital rectal stimulation.
Use digital rectal stimulation or other techniques. To
keep stool coming, repeat digital rectal stimulation every
5 to 10 minutes as needed, until all stool has passed.
(See page 10, “How Is Digital Rectal Stimulation Done?”)
Recognizing when bowel care is completed. To
make sure the rectum is empty, do a final check with a
lubricated and gloved finger or assistive device. You’ll
know that stool flow has stopped if:
— No stool has come out after two digital stimulations at
least 10 minutes apart.
— Mucus is coming out without stool.
— The rectum is completely closed around the stimulating
finger.
Cleaning up. Wash and dry the anal area.
If I Have an Areflexic Bowel
The goal of an areflexic bowel program is firm, formed stool
that: (1) can be passed manually with ease, and (2) doesn’t
pass accidentally between bowel care routines. Bowel care
doesn’t usually require chemical stimulants because the
response would be very sluggish.
Getting ready and washing hands. Empty your blad-
der or move your urinary drainage equipment away
from the anal area. Whoever performs bowel care—you
or an attendant—should wash their hands thoroughly.
16 NEUROGENIC BOWEL: What You Should Know
STEP
R8
STEP
R7
STEP
R6
STEP
R5
STEP
A1
A Guide for People with Spinal Cord Injury 17
Setting up and positioning. If possible, sit up. If
you’re sitting, gravity helps empty your rectum. When
sitting, keep your feet on the floor or on a footstool or
on the footrest of your commode chair, with your hips
and knees flexed. If you don’t sit up, lie on your left side.
Starting and repeating digital rectal simulation. Use
digital stimulation or other techniques. To keep stool
coming, repeat digital rectal stimulation every 5 to 10
minutes as needed, until all stool has passed. (See page 10,
“How Is Digital Rectal Stimulation Done?”)
Doing manual evacuation. Use one or two gloved and
well-lubricated fingers to break up stool, hook it, and
gently pull it out.
Use repeated Valsalva maneuvers. (See page 18.)
Use gentle Valsalva maneuvers to bring stool down
before and after each manual evacuation. Breathe in
and try to push air out, but block the air in your throat
to increase the pressure in your abdomen. Try to contract your
abdominal muscles as well. This technique can help you increase
pressure around the colon to push stool out. Repeat it for 30 sec-
onds at a time on and off as long as you need to expel all stool.
Bending and lifting. If you have good torso stability,
lift yourself as if doing a pressure release or do forward
and sideways bending with Valsalva maneuvers. This
helps change the position of the colon and expel stool.
Checking the rectum. To make sure the rectum is
empty, do a final check with a gloved and well-
lubricated finger. If stool is present, repeat Steps A4-7.
Cleaning up. When you are confident all stool has
passed, wash and dry the anal area.
STEP
A5
STEP
A4
STEP
A3
STEP
A2
STEP
A7
STEP
A8
STEP
A6

18 NEUROGENIC BOWEL: What You Should Know
Whether you have a reflexic or an areflexic bowel, you may be
able to rely on diet, fluids, and regular activity to give your stool a
healthy texture for bowel care. If these don’t work by themselves,
your health-care professional may suggest medications. (See
page 27, “What Medications Are Used in Bowel Programs?”)
Are There Other Ways to Improve a
Bowel Movement?
Once you have a regular bowel program that works, you and
your health-care professional may want to explore ways to sim-
plify it: doing bowel care less often, changing the stimulant you
use, or trying digital stimulation without a suppository or mini-
enema. Remember, before making any of these changes, discuss
them with your health-care professional.
Your health-care professionals may suggest a number of
assistive techniques or tips to improve your bowel care
results. The most common ones are:
•Positioning. Sitting upright in a cushioned commode chair or
padded toilet seat may help gravity to empty the lower bowel.
Placing your feet on footrests or footstools also gives you
support while you bear down (see Valsalva maneuver, below) to
push stool out.
• Abdominal massage. Rubbing or running a hand firmly over
the abdomen in a clockwise motion from the lower right across
the top and down the left helps move stool through the colon to
the rectum.
•Forward or sideways bending. For this, you need either a lap
safety belt if you’re using a commode chair or enough control of
your upper body to be able to return to a sitting position after you
bend forward or side to side at the waist. These maneuvers also
help move stool through the colon to the rectum.
• Push-ups. If you have strong upper arms, you can raise your
hips off the commode chair seat. Put yourself down in a slightly
different position to vary the pressure against your skin. Push-
ups also help move stool into the rectum.
•Valsalva maneuver. This technique works best for people with
areflexic bowel who have control over their abdominal muscles
and can help push stool out. Before doing Valsalva maneuvers,
A Guide for People with Spinal Cord Injury 19
check with your health-care professional, especially if you have a
history of heart problems. (See A5 on page 17 under “If I Have
an Areflexic Bowel.”)
• Gastrocolonic response or reflex. Eating a meal or drinking
warm liquids before bowel care may help some people with SCI
stimulate a bowel movement. Starting your bowel care within 30
minutes after you eat or drink may help it go faster and produce
more results.
What Is a Bowel Care Record?
A Bowel Care Record helps you and your health-care pro-
fessional see whether your bowel program is working. It’s
most helpful the first weeks after you leave the hospital, when-
ever you’re having problems, and a few weeks before your
annual checkup.
Use the Bowel Care Record at the back of this Guide. Every
time you do bowel care, write down:
• Date.
• Start time. The hour and minute you start stimulation or try to
start a bowel movement.
• Position. Left side lying, right side lying, sitting.
• Stimulation method. Stimulant medication, digital rectal
stimulation, or other technique you use to start a bowel movement.
• Assistive techniques. Methods used to promote bowel
emptying and the number of times used during bowel care, e.g.,
abdominal massage, bending, push-ups, Valsalva maneuver.
Important:
People with SCI need to stick with a regular schedule and
technique of bowel care. You may have to revise your bowel
program over time, but keeping a regular schedule for doing
bowel care at a regular time is one of the best things you can
do for your health and well-being after SCI.
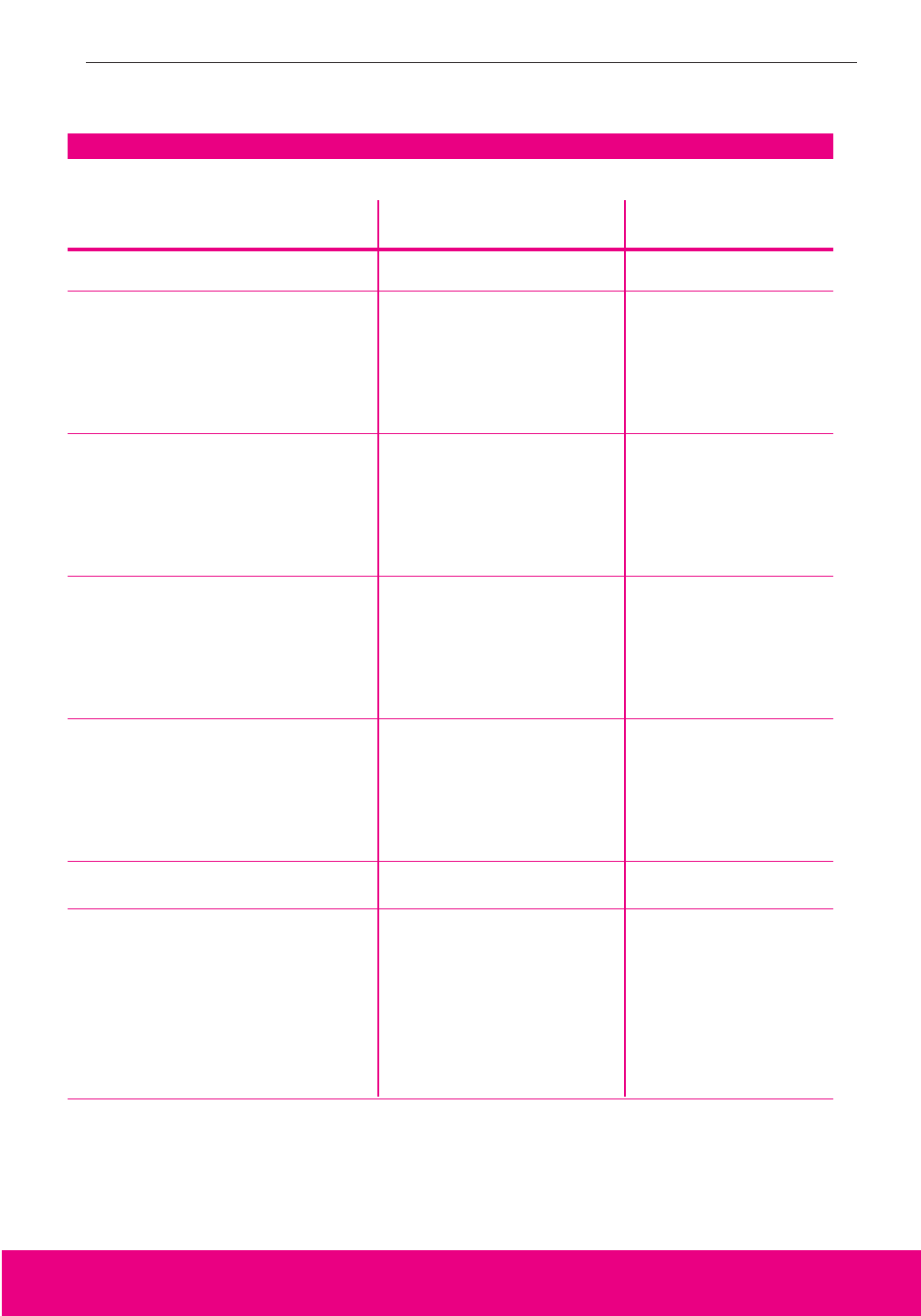
Bowel Care Record
Start Stim
ulation Assistive Tim
e of Results Stool Am
ount,
Date Tim
e Position M
ethod Techniques First/Last Consistency, Color Com
ments

20 NEUROGENIC BOWEL: What You Should Know
• Times of results. The time when the first stool begins to come
out of the anus and the time when the last stool comes out.
• Stool amount, consistency, and color. Amount: if stool were
formed into a ball—golfball, tennis ball, softball. Consistency:
hard, firm, soft, liquid. Color: especially anything unusual for
you.
• Comments. Problems such as any unplanned bowel
movements, abdominal cramps, pain, muscle spasms, pressure
ulcers, hemorrhoids, or bleeding.
If your bowel program is going well, there’s no need to keep
a Bowel Care Record.
Can I be Independent in My Bowel Care?
That depends on many factors: the level and completeness
of your SCI, your body type and general health, how strong you
are, and how much you want to be independent.
For complete independence, your arms and fingers need to
be strong enough to manage your clothes, get you into a bowel
care position, place stimulant medication, and do digital rectal
Important:
If you see any blood in your stool or any discoloration in your
stool, too dark or light, call your health-care professional right
away. It might indicate a medical problem. For example,
stool that’s dark, black, or tar-like could be a sign of bleeding
in the GI tract, like an ulcer. But be aware that iron sup-
plements will turn your stool black, and that’s not a
problem. (See page 29, “What Should I Do if My Bowel Pro-
gram Isn’t Working?”)
Alcohol and drugs can affect bowel
function and cause additional
problems for people with SCI.
• Alcohol. Alcohol, even beer,
can change your habits. It can
reduce your appetite, making it
hard to stick with the diet part
of your bowel program. It can
also cause problems in keep-
ing up with your bowel care schedule.
If you’re having trouble following your
bowel program because of alcohol
use, your health-care professional
needs to know, to be able to help.
• Drugs. Many street drugs,
as well as prescribed pills for
pain, cause constipation.
Because of that, many people
Alcohol and Drugs: What You Need To Know
R
X

stimulation. Most people with a thoracic, lumbar, or sacral SCI
are strong enough and have enough balance. Some people with
a cervical SCI at C6, C7, or C8 levels may not have enough fin-
ger strength or sitting balance to independently insert a suppos-
itory or mini-enema or do digital rectal stimulation. Special
devices like a digital stimulator and suppository inserter can
help with these activities.
Even if they can do bowel care themselves, some people
choose to have a caregiver do it. They find that it takes too
long, or it simply takes too much energy that they’d rather use
doing other things.
Whether or not you do your own bowel care, you still need
to manage your bowel program. That means watching what
you eat and drink, your activity level, your medications, and the
results of your bowel care routine. If you need assistance with
your bowel care, learn the process so that you can teach it to
caregivers and supervise your care. It’s your body and you are
the boss.
Why Do I Need to Watch What I Eat and Drink?
What you eat and drink can affect your bowel movements,
but everyone responds a bit differently to different foods. The
best way for you to learn how different foods affect you is to
keep a Food Record and Bowel Care Record. For about a
month, write down what you eat and drink each day and
describe your bowel movements. (See the Food Record and
Bowel Care Record at the back of this Guide.)
who use drugs end up overusing laxa-
tives—and that can cause more prob-
lems. If you use drugs and don’t tell
your health-care professional, there’s
a very good chance that the bowel
program you create together won’t
work. It’s also a good idea to discuss
any alternative medicines you use.
• Your bowel function is your responsi-
bility. It’s up to you to give your
health-care professionals the informa-
tion they need to help you rule your
bowel—not the other way around.
A Guide for People with Spinal Cord Injury 21

22 NEUROGENIC BOWEL: What You Should Know
Foods That Can Keep Stool Solid but Soft
Foods that have a lot of fiber can absorb liquids and help
make your stool solid but soft and easy to pass. High-fiber
foods are fresh fruits and vegetables, dried peas and beans, and
whole grain cereals and breads. It’s best to get the dietary fiber
you need from a variety of food sources. A starting goal of at
least 15 grams of fiber each day is recommended as part of a
healthy diet. An increase in fiber is recommended only if it is
necessary to produce a soft-formed stool. Table 1 gives a gen-
eral idea of how much fiber is in different types of food. It’s a
good idea to increase this amount gradually over a 6-week peri-
od to prevent a bloated feeling and too much gas.
If you can’t eat as much fiber as your health-care profession-
al suggests, you may want to try fiber supplements—natural
vegetable powders, like psyllium. You can get them at your
local drugstore and supermarket. If you take fiber supple-
ments, be sure to drink plenty of fluids. That means at
least 64 ounces a day. (Drinks with alcohol or caffeine don’t
count toward that total.) Remember, if you use fiber to vary the
consistency of your stool, you will have more total stool and
may need to do bowel care more often.
Foods That Can Cause Gas
Gas in the digestive tract may cause uncomfortable feelings
of fullness, bloating, and pain. If you’re having problems with
too much gas, you may want to cut back on or cut out foods
associated with gas. These include beans, broccoli, cabbage,
cauliflower, corn, cucumbers, onions, and turnips. (See Table
2. What You Can Do About Excessive Gas, page 24.) If your
Food Record shows that some of these foods cause problems
with gas, consider eliminating them from your diet.
Important:
Not everyone with SCI benefits from a high-fiber diet. You
need to recall how much fiber you usually had in your diet
before the SCI and how much you eat now. Talk with your
health-care professional about the amount of fiber in your diet
before and after your SCI.
A Guide for People with Spinal Cord Injury 23
TABLE 1
How Much Fiber Is in Different Types of Food?
Grams of
Food Type Quantity Fiber/Serving
LEGUMES
Baked beans 1/2 cup 8.8
Dried peas, cooked 1/2 cup 4.7
Navy beans, cooked 1/2 cup 6.0
Lima beans, cooked 1/2 cup 4.5
CEREALS
Oatmeal 3/4 cup 1.6
Bran flakes 1/3 cup 8.5
Shredded wheat 2/3 cup 2.6
Raisin-bran type 3/4 cup 4.0
FRUIT
Apple (w/ skin) 1 medium 3.5
Banana 1 medium 2.4
Orange 1 medium 2.6
Prunes 3 3.0
BREADS
Whole wheat bread 1 slice 1.4
Pumpernickel bread 1 slice 1.0
Bagels 1 bagel 0.6
Bran muffins 1 muffin 2.5
MILK ANY AMOUNT 0.0
MEAT
Beef Any amount 0.0
Pork Any amount 0.0
Poultry Any amount 0.0
Lamb Any amount 0.0
Fish Any amount 0.0
Seafood Any amount 0.0
FATS ANY AMOUNT 0.0
Certain foods may cause gas, so substitutions may be necessary.
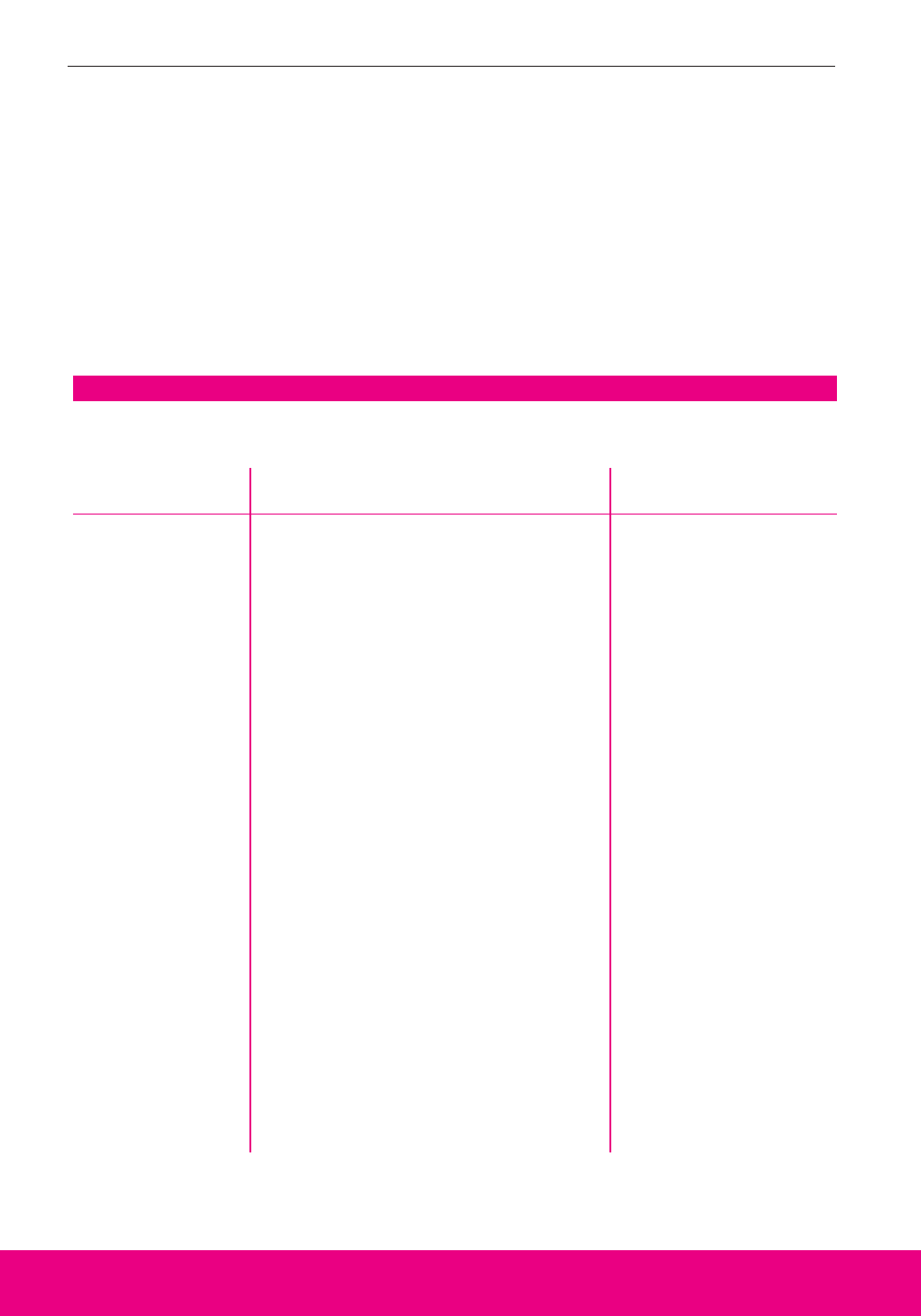
TABLE 2
What You Can Do About Excessive Gas
FOODS THAT
CAUSES SOLUTIONS CAN CAUSE GAS
Food
Constipation
Swallowing air while
you’re eating or
drinking
More bacterial
breakdown of bowel
contents than is
usual for you
Lactose
intolerance
Think about how you eat:
1. Eat your food slowly.
2. Chew with your mouth closed.
3. Try not to gulp your food.
4. Don’t talk with food in your mouth.
Experiment with foods that can cause gas:
1. Remove specific foods from your diet,
one at a time.
2. Do this for your favorite foods until
you’ve learned which, if any, cause you
to have gas.
3. Cut down on those foods.
Think about your surroundings:
1. Ceiling fans help remove odors.
2. Good ventilation, such as plenty of win-
dows or table-top fans, also helps.
3. Deodorant spray can mask the odor.
Release gas at appropriate times and
places:
1. Do digital rectal stimulation in the
morning or evening daily.
2. Do push-ups or lean to the side to
release gas when alone or before
meeting with people.
3. The bathroom is an appropriate place
to release gas.
Vegetables:
• Beans: kidney, lima,
and navy
• Broccoli
• Brussels sprouts
• Cabbage
• Cauliflower
• Corn
• Cucumbers
• Kohlrabi
• Leeks
• Lentils
• Onions
• Peas: split and
black-eyed
• Peppers
• Pimientos
• Radishes
• Rutabagas
• Sauerkraut
• Scallions
• Shallots
• Soybeans
•Turnips
Fruits:
• Apples (raw)
•Avocados
• Cantaloupe
• Melons: watermelon
and honeydew
Table 2 was adapted from Yes You Can! A Guide to Self-care for Persons with Spinal Cord Injury (Second
edition). Paralyzed Veterans of America, 1993.
24 NEUROGENIC BOWEL: What You Should Know
Foods That Can Cause Diarrhea
There are no foods that cause diarrhea in everyone. Some
people find fatty, spicy, or greasy foods seem to be related to diar-
rhea. Other people report that caffeine—found in coffee, tea,
cocoa, chocolate, many soft drinks—appears to cause diarrhea.
Diarrhea-causing bacteria can contaminate different foods as well.
If you have episodes of diarrhea, keep a Food Record of what you
eat and drink to help you identify what you’re sensitive to.
A Guide for People with Spinal Cord Injury 25
How Much Should I Drink Every Day?
You need to drink plenty of fluids every day to keep your
stool soft and to prevent constipation. Drinking enough is
especially important if you’re trying to eat more fiber. A good
guideline is 64 ounces every day (drinks with alcohol or caf-
feine don’t count). If you exercise a lot or the weather is hot,
drink more.
Some people may need to limit how much they drink because
of their bladder program. If that’s true for you, talk with your
health-care professional about a good daily fluid goal that will
work for both your bladder program and your bowel program.
Important:
If you enjoy drinks like coffee, tea, cocoa, or soft drinks, there’s
something you should know. All these drinks contain caffeine,
and caffeine is a diuretic. That means it may suck the fluid out
of your body. In fact, diuretics can cause you to lose even more
fluid than you drink. Caffeine is also a stimulant. For these
reasons, you may want to consider keeping caffeine drinks to a
minimum.

26 NEUROGENIC BOWEL: What You Should Know
What Medications Are Used in Bowel Programs?
Like the foods you eat, the medications you take can affect
your bowel activity. Some can help your body pass stool regular-
ly. Others can make regular bowel movements difficult. Table 3
lists the different types of bowel medications and examples of
each and describes what they do. For most people, the goal is to
have a successful bowel program without medications or with the
fewest medications possible.
Before taking any of the products in Table 3 regularly, dis-
cuss them with your health-care professional to learn how to
use them safely for the best results.
Tips for Safe Bowel Care
To prevent falls and pressure ulcers, follow these tips for the
safe use of equipment during bowel care. Don’t hesitate to ask
your health-care professional to show you how to use assistive
devices and stimulant medications correctly.
Toilets and Commode Chairs
•Use seats carefully to avoid skin problems. If you can,
consult an occupational therapist before you buy such
equipment.
• Make sure that seats and chairs are padded; seams shouldn’t
touch your skin.
• Don’t use a chair that has cracked or broken vinyl; it can hurt
your skin.
•Keep correct posture the whole time you’re on a toilet or
commode seat.
•Keep your weight evenly balanced over the seat.
•Do pressure releases every 15 minutes to prevent skin problems.
That means lifting yourself off the seat and shifting your position
to keep from putting pressure on the same skin area too long.
• Be careful not to forcibly separate your buttocks or squeeze
them together when you’re sitting.
• Check your skin after using your bowel care equipment. Report
any changes to your health-care professional.
A Guide for People with Spinal Cord Injury 27
TABLE 3
Bowel Medications
ORAL LAXATIVE MEDICATIONS
Stimulants
Increase the wave-like action of peristalsis to move stool through the bowel faster and
keep it soft.
• bisacodyl • castor oil
• cascara • senna
Osmotic laxatives
Increase stool bulk by pulling water into the colon. If you take these medications, you
need to drink extra fluids.
• lactulose • magnesium sulfate
•magnesium citrate • sodium biphosphate
• magnesium hydroxide • sodium phosphate
Bulk-forming laxatives
Add bulk to stool. If you take these natural vegetable fiber medications, you need to drink
extra fluids.
• hydrophilic muciloid • psyllium
• methylcellulose
Stool softeners
Help stool retain fluid, stay soft, and slide through the colon.
• docusate calcium (Doss) • docusate sodium
• docusate potassium • mineral oil
Prokinetic agents
Stimulate bowel peristalsis.
• cisapride • metoclopramide
RECTAL STIMULANTS
Suppositories
bisacodyl Increases colon activity by stimulating the nerves in the lining of the
rectum.
CO
2
Produces carbon dioxide gas in the rectum, which inflates the colon
and stimulates peristalsis.
glycerin Stimulates peristalsis in the colon and lubricates the rectum to help pass
stool.
Enemas
mineral oil Lubricates the intestine.
mini-enema Stimulates the rectal lining and softens stool.

28 NEUROGENIC BOWEL: What You Should Know
To prevent falls, be especially careful when you’re:
•Transferring to and from a toilet or commode chair.
• Doing forward or sideways bending.
• Bending to insert stimulant medication, do digital rectal
stimulation, or remove stool.
• Reaching for supplies.
Safety Straps
• Chest straps help people who have poor or no chest balance.
•Lap or waist straps help people who have spasms or tire easily.
Stimulant Medications
• Use plenty of water-based lubrication. Oil-based products, such
as petroleum jelly, can prevent stimulant medications from
working.
• Insert suppositories using lubrication, gently and correctly.
• Punch a hole in mini-enemas with a pin. Cutting them with a
knife creates a sharp edge that can slice or scrape your skin.
How Often Should My Bowel Program Be Reviewed?
Your bowel program should be reviewed at least once a year
to make sure that it’s working well for you. Your Bowel Care
Record is a key part of this review. Keep your completed Bowel
Care Records in a notebook, folder, or other handy place and
take them with you when you visit your health-care profession-
al. Ask your health-care professional how long you should
record your bowel care results.
If you use a commode chair or padded
toilet seat, avoid unpleasant surprises. It’s
a good idea to record the date you get
your equipment; cushions and pads tend
to wear out in about 18 months. Inspect all
your bathroom equipment every month:
• Check screws and other hardware for
loose or missing pieces.
• Lubricate axles to prevent rust.
• Check for cracks or splits in vinyl cov-
ering. If cracks develop, ask a mem-
ber of your rehabilitation team to
inspect the equipment to consider
replacement or repair.
Maintaining Bowel Care Equipment

A Guide for People with Spinal Cord Injury 29
What Should I Do if My Bowel Program
Isn’t Working?
If there is a problem, you have to get to the bottom of it
immediately. If you’re having bad reactions with your bowel
program, call and work with your health-care professional right
away. Bad reactions include:
•Fainting or loss of consciousness.
• Symptoms of autonomic dysreflexia, like a pounding headache
during bowel care. (For more information about autonomic
dysreflexia, see the glossary and the guide called Autonomic
Dysreflexia: What You Should Know. For a free copy, call
(888) 860-7244 or visit the PVA web site at http://www.pva.org.)
•Blood in your stool, on your rectum, or on your clothes.
• Any sudden change in the color of your stool—if it becomes
lighter, red, or black.
You may be able to take care of other problems yourself.
The most common bowel problems after SCI are:
• Repeated bowel accidents.
• Delayed results from bowel care.
Important:
If you’re having constipation or other bowel problems (see Table
4 on page 31, Frequent Bowel Accidents: Possible Causes and
Solutions), don’t wait for your annual bowel program review.
Call your health-care professional to discuss the problem and
what you can do about it.
• Check for water-logged or soggy cush-
ions or padded seats. Pushing on the
cushion or seat can squeeze out extra
water.
•Watch for worn-out cushions and
padded seats. If they stay flattened
after you get off, they’re probably
worn out.
• Replace worn, frayed safety straps and
broken buckles.

30 NEUROGENIC BOWEL: What You Should Know
• Prolonged bowel care (lasts more than 1 hour).
• Constipation.
• Inadequate or no stool results after two bowel care sessions.
• Diarrhea.
• Hemorrhoids.
•Too much gas or a bloated feeling.
Table 4 lists possible causes of and solutions to frequent
bowel accidents (more than once a week). Table 5 on pages
32-33 describes other problems, their possible causes, and
solutions. For many people with SCI, gas is a cause of embar-
rassment in public and private situations. Table 2 on page 24
provides information about excessive gas.
If you visit your health-care professional to discuss changing
your bowel program, bring your Bowel Care Record with you.
Be ready to discuss anything that might have changed in your
bowel program. Even one change in what you usually eat or
drink, for example, can affect how your program works for you.
Figuring out what’s changed and switching back to your previ-
ous habits may correct the problem.
If that doesn’t work, or if there’s a good reason for you not
to return to your previous routines, your health-care profession-
al will help you modify your bowel program. It’s important
for you to change only one of the following components
of your bowel program at a time:
• Diet.
• Fluids.
• Activity.
• Bowel care schedule.
•Position during bowel care.
• Rectal stimulant medications.
• Mechanical stimulation.
• Assistive techniques for bowel care.
• Oral medications.
With this approach, you can see which changes improve
your results.
A Guide for People with Spinal Cord Injury 31
Stools are too soft and If you are taking stool softeners, cut down on quantity
are oozing out. and/or frequency or stop taking them altogether.
Look at your diet to: (1) make sure you’re eating
enough high fiber foods, and (2) check for too many
foods that can soften stools (such as spicy or greasy
food).
You are eating more food Try doing your bowel care routine more often. For
than you did before. example, if your bowel care schedule is every other
day, you may need to do it every day.
Overuse of laxative medications If you are more active than you used to be or if you
to help food move through your are eating more fiber, you may not need bowel
stomach and bowel (peristalsis). medications anymore. Cut down on the number of
laxatives you take each day until you have:
(1) stopped having accidents, or (2) stopped taking
the laxatives.
Bowel care sessions are not Consider: (1) taking an oral laxative medication to
emptying your bowel well enough. help move food through your digestive system,
(2) using a stronger rectal stimulant and more fre-
quent digital stimulation, and (3) discussing the prob-
lem with your health-care professional.
Information in table 4 was adapted in part from Educational Guide for Individuals and Families Following
SCI. Rehabilitation Institute of Chicago, 1995.
TABLE 4
Frequent Bowel Accidents: Possible Causes and Solutions
NOTE: When changing your bowel program, change only ONE COMPONENT at a time, such as fre-
quency of bowel care, time of bowel care, or diet, so that each change can be fully evaluated.
POSSIBLE CAUSE SOLUTIONS
SCI may make it more difficult to spot
symptoms of colorectal cancer. That’s why
your health-care professional may want to
do tests for this condition, especially if
you’re 50 or older and have (1) a positive
test for unseen blood in the stool (fecal
occult blood test) or (2) a change in the
way your bowel works that doesn’t
improve after treatment.
Ask your doctor to help you follow cur-
rent recommendations about checking for
colorectal cancer. If you’re 40 or older, it’s
recommended that you have a rectal exam
and fecal occult blood test every year.
Other tests may include using a special
flexible scope to view the inside of the
colon.
Checking for Colorectal Cancer
32 NEUROGENIC BOWEL: What You Should Know
Delayed Results
Bowel movements start 1-6 hours after you begin
your bowel care.
Constipation or hard stools
Less than normal amounts of stool for at least 3 days
(and it’s usually hard); small or no bowel movements
for 24 hours or 2 or more bowel care routines. May
cause rectal bleeding that you can see as bright red
blood on your stool, toilet paper, or glove.
If you get constipated every few weeks, you may
need to change your bowel program.
IMPORTANT: If you are constipated and you have
(1) abdominal pain, (2) autonomic dysreflexia* that
doesn’t go away after stool is removed from your rec-
tum, or (3) sudden swelling in your abdomen, call
your health-care professional right away!
If you are not already doing digital stimulation, start; if
you are already doing it, try to do it more often.
If you can, sit up on the toilet or commode for bowel care
techniques.
Consider taking an oral laxative 6-8 hours before starting
bowel care (talk with your health-care professional first).
Try eating more fiber and drinking more liquids.
Consider using a strong rectal stimulant medication: (a) if
you are using a glycerin suppository, try a bisacodyl sup-
pository or enema, and (b) if you are using a bisacodyl
suppository, try a stimulant mini-enema, or a polyethyene
glycol-based bisacodyl suppository.
Do a rectal check.
—If you feel stool: (a) remove it gently with a gloved and well-
lubricated finger, using an anesthetic cream or jelly, and
(b) do your regular bowel care (suppository or mini-
enema).
—If you do not feel stool: (a) take a laxative or take more of
the one you’ve already taken, and (b) wait 6-8 hours and
do your regular bowel care (suppository or mini-enema).
Increase the frequency of your bowel care to daily until
normal volumes of stool results return.
If the above steps do not produce a bowel movement,
call your health-care professional. Suggestions may
include taking a product to add bulk to your stool or a
laxative at least 8 hours before you do your bowel care
routine.
Stool is too dry.
Stimulant is too weak or you’re not using enough.
Medications such as narcotics, iron, aluminum
hydroxide.
Not enough fiber in diet.
Inadequate rectal stimulation.
Performing bowel care in a lying position.
Digested food moving too slowly through the GI
tract.
Not following a regular bowel program.
Incomplete passing of stool.
Not enough fiber in diet.
Bed-rest or not much physical activity.
Medications such as narcotics, iron, aluminum
hydroxide.
TABLE 5
Common Bowel Problems: Solutions and Possible Causes
Note: When changing your bowel program, change only ONE COMPONENT at a time so that each change can be fully evaluated.
PROBLEMS SOLUTIONS POSSIBLE CAUSES
*Autonomic dysreflexia is a life-threatening condition. For more information, please refer to the consumer guide Autonomic Dysreflexia: What You Should Know, August 1997,
Consortium for Spinal Cord Medicine. To order your free copy, call toll-free (888) 860-7244 or visit the PVA web site at http://www.pva.org.

A Guide for People with Spinal Cord Injury 33
POSSIBLE CAUSES
Not following a regular bowel program.
Incomplete passing of stool.
Not enough fiber in diet.
Bed-rest or not much physical activity.
Medications such as narcotics, iron, aluminum
hydroxide.
Spicy or greasy foods.
Drinks with caffeine (coffee, tea, cocoa, many
soft drinks).
Overuse of laxatives and bowel softeners.
Severe constipation or impaction.
Viral infection, flu, or intestinal infection.
Stress.
Antibiotics.
Persistence of hard stools.
Rectal straining.
Too vigorous digital stimulation or manual evacu-
ation. Suppositories, enemas, and digital stimu-
lation can irritate and worsen hemorrhoids.
Information in table 5 was adapted in part from Educational Guide for Individuals and Families Following SCI. Rehabilitation Institute of Chicago, 1995.
PROBLEMS
Fecal Impaction
See Constipation, but usually happens over a longer
period of time. You also may have small amounts of
liquid or watery stools.
Diarrhea
Loose watery stools, usually 3 or more times a day.
IMPORTANT: Call your health-care professional
right away if you have any of the following:
(1) abdominal pain, (2) dehydration (dry or chapped
mouth or lips, a lot less urine than usual, or dark urine
with a strong smell), or (3) diarrhea that lasts 3 or
more days.
Hemorrhoids
The first signs may be bright red blood on your
clothes, glove, or toilet paper after a bowel movement.
You may also see or feel bulging areas outside your
rectum.
IMPORTANT: Hemorrhoids are the most common
problem in bowel programs. You can help prevent
them by preventing constipation. Keep your stools
soft but formed.
SOLUTIONS
Start with the first step, and try others ONLY if previous steps
do not help:
Do a rectal check; if you feel stool, remove it gently with
a gloved and lubricated finger. Use an anesthetic cream
or jelly.
Drink 1 ounce of mineral oil to make the stool easier to
eliminate.
Take 1 or 2 tablets of senna or bisacodyl (bisacodyl is
stronger) to help move the stool down into your rectum.
Wait 6-8 hours and do your bowel care routine.
If the above steps do not produce a bowel movement, call
your health-care professional.
Stop taking any bowel medications. After the diarrhea
stops, you may start taking them again slowly.
Stay away from foods that can irritate your bowel (such
as spicy, fried, and greasy foods).
Eat foods that help make your stools hard (such as
yogurt with fruit, whole grain breads and cereals, rice,
and bananas).
Drink plenty of water, estimating what you are losing with
the loose stools and replacing it.
Make sure it is not a fecal impaction. If you do have an
impaction, your diarrhea may be very watery. If you are
taking antibiotics, try eating yogurt every day. If you have
diarrhea anyway, don’t stop taking the antibiotics but do
call your health-care professional.
After each bowel movement, use a cream or suppository
made for hemorrhoids as recommended by your health-
care professional.
If you have active hemorrhoids (bleeding, swelling, pain):
(a) try to avoid or minimize digital stimulation and manual
removal until the tissue heals, or (b) increase the amount
of stool softener or take them more often.
Use more lubricant.

Answers to Commonly Asked Questions
Q: What should I do if I have a bowel accident at school,
work, or a movie?
If you have an accident, don’t just sit there! If you can,
leave wherever you are and find a bathroom. Here are three
good reasons for you to deal promptly with the situation:
•Blocking stool flow can cause autonomic dysreflexia.
• Allowing your skin to be in contact with stool too long can cause
skin problems.
• Putting others at ease and calmly doing what you have to do can
help everyone get past the awkwardness. Accidents can be
touchy situations, not just for you but for other people.
A regular bowel program can help you take charge of your
bowel function and cut down on accidents. But accidents do
happen; be prepared. Many people keep a change of clothes
with them in a gym bag or overnight bag, just in case. The bag
might contain some toilet paper, moist wipes, exam gloves, a
diaper, clean underwear, loose-fitting pants, a water proof pad,
and a plastic bag for storage of soiled clothes. Some people use
disposable undergarments when they know they might be away
from a bathroom for a long time.
When you have to talk about bowel management, it may
help you and others if you are calm and matter of fact. As you
learn to live with SCI, it’ll become easier to discuss uncomfort-
able subjects like bowel functions and habits with your family
and friends, attendants, and health-care professionals.
34 NEUROGENIC BOWEL: What You Should Know
The best things you can do to prevent
bowel problems are to:
•Stick with your bowel program. If
you’re having trouble following any part
of your program, call your health-care
professional. Together, you should be
able to adapt your program to your life
demands, privacy needs, and
tolerance for various treatments.
• Pay attention to your body, your stool,
and your bowel care routine. You
know yourself best; you’ll be the first to
notice changes that may be important.
• If you need to change any aspect of
your bowel program, change only one
component at a time. And give
yourself plenty of time to decide if the
change has helped. A good rule is to
Preventing Bowel Problems

A Guide for People with Spinal Cord Injury 35
Q: What should I do if I pass a lot of gas? Passing gas in
public is embarrassing, especially if it smells.
Have a frank talk with your health-care professional. You
might be referred to a dietitian in case the gas and odor are
related to foods you’re eating. Think back to what you’d have
done before the SCI. Whatever you do, don’t try too hard to
hold in the gas. That can give you a stomachache or headache.
And remember: Passing gas means your digestive system is
working right. It was OK to pass gas before your SCI; it’s
still OK to pass gas now.
Passing gas and odor are just as embarrassing now as they
were before the SCI. With or without SCI, most people aren’t
comfortable with their bodily functions.
Some gas smells bad, and some gas doesn’t. Your gas will
probably smell bad after you eat food that’s high in protein,
such as meat, fish, or eggs. If you eat a vegetarian diet, your
gas probably won’t smell so bad, but you’ll have a lot of it.
Increasing the frequency of bowel care may reduce the amount
of stool you store in your colon to produce gas.
What did you do about gas odor before the SCI? Ventilation
is a good idea; fans and open windows help. Some people keep
room deodorizers or air fresheners in their office, home, and
bathroom.
allow 1 week or 3 to 5 bowel care
cycles before you make more
changes.
• If you’re having problems keeping a
healthy weight (you’re gaining or losing
too much), talk to your health-care
professional. Information about diet
and exercise and an evaluation may
be helpful.
• Get a checkup at least once a year.
Bring a completed copy of the Bowel
Care Record at the back of this Guide,
and review it with your health-care
professional.
These steps can’t prevent all bowel
problems related to SCI. If the tips in
Tables 2, 4, and 5 don’t help, talk with your
health-care professional.
36 NEUROGENIC BOWEL: What You Should Know
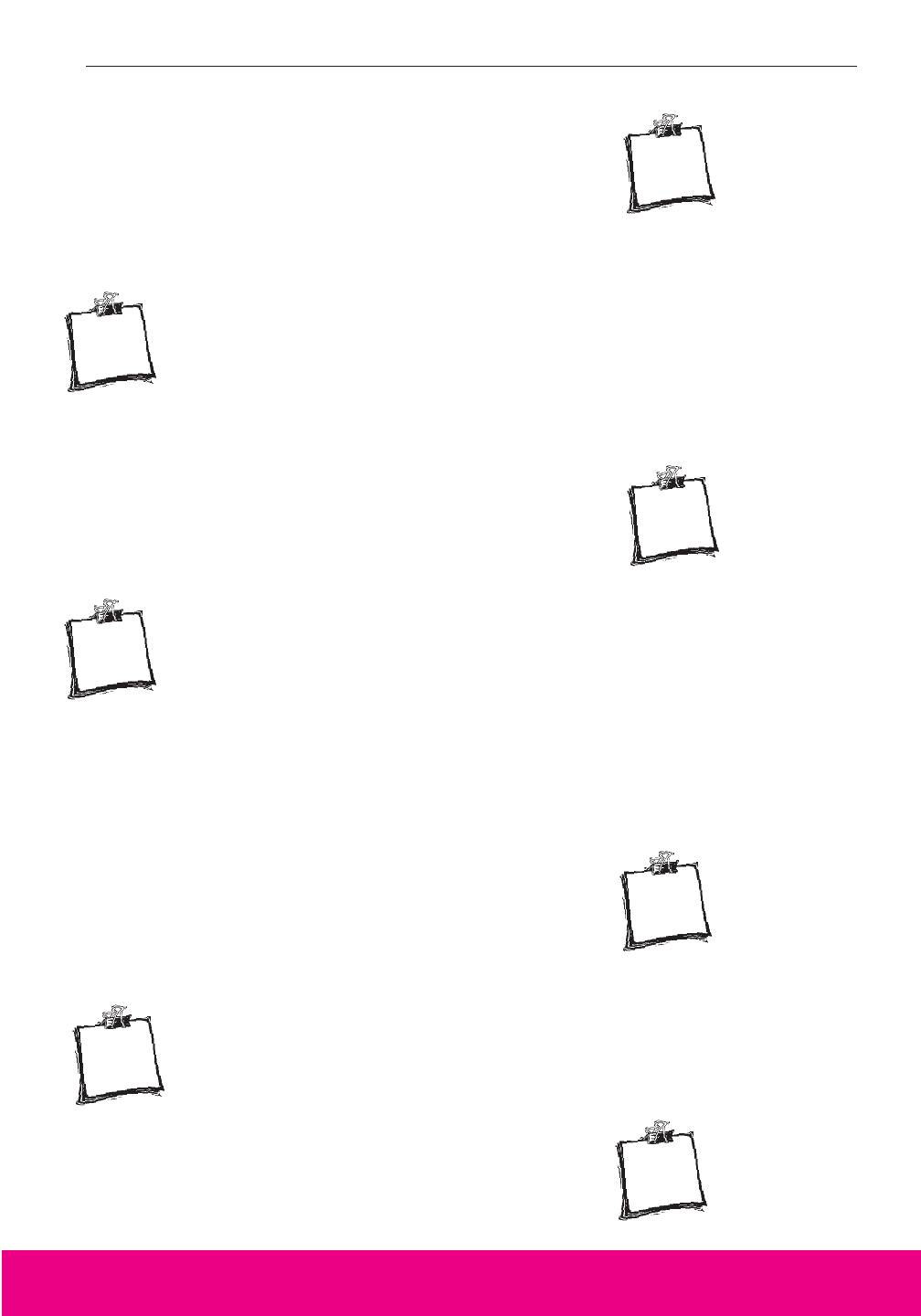
What Should I Know About
Surgical Options?
One common surgical procedure creates a new opening
(called a stoma) on the abdomen where stool can be pushed
into an attached, disposable bag. This surgery is called colosto-
my or ileostomy, depending on where the opening is made.
The choice between a colostomy or an ileostomy should depend
upon the results of studies examining how your stool moves
through your colon and consultations with your health-care pro-
fessionals. The site on your abdomen for the stoma placement
should maximize both your functional independence and your
body image (see Figure 5).
An important goal of this type of surgery is to improve your
quality of life by:
• Making you more independent in bowel care.
• Reducing the time and effort bowel care requires.
• Preventing bowel accidents.
People consider surgery for many reasons, including some
or all of the following:
• BM accidents or leaking of stool.
• Recurring pressure ulcers.
FIGURE 5
Stomach
Transverse
Colon
Colon
(Large
Intestine)
Descending
Colon
Small
Intestine
Ascending
Colon
Sigmoid
Colon
Rectum
Anal
Sphincter
Anus
Ileum
(~12” length)
Stoma—always
moist and red

A Guide for People with Spinal Cord Injury 37
•Persistent pelvic or rectal infections.
• Safety issues (transferring accidents).
• Skin problems from a toilet or commode seat.
• Bleeding hemorrhoids.
• Sweating.
• Nausea.
• Anorexia.
•Fatigue.
• Effects of aging.
• Abdominal pains.
•Too much time spent on bowel care.
Surgery is a serious matter. Before deciding if it’s the
right choice for you, you need to consider all other med-
ical therapies thoroughly. If they don’t work, discuss surgical
options with members of your rehabilitation team: your primary
care practitioner, psychologist, occupational therapist, rehabili-
tation nurse, family members, and other people who are impor-
tant in your life. Different team members can give you the
information you need to make your decision carefully. They can:
• Make sure you understand what the
surgery can—and can’t—do to make
you more independent.
• Discuss specific screening studies that
provide information for decision making.
• Predict how well the procedure will
work for you.
• Explain the risks you’ll face during
and after surgery.

38 NEUROGENIC BOWEL: What You Should Know
If you’re considering surgery, team members may suggest a
conference to discuss important issues. These include how to
take care of the opening, use of bags and other equipment, and
where on your abdomen the opening should be. Things you
need to consider in choosing a stoma site:
•Your preference (where you want it to be, and why).
•Your body image (how your clothes will fit and how you’ll feel
about the way you look).
• Independence in bowel care (how easy it is to reach and
care for).
This type of surgery is intended to produce permanent
changes in how the colon empties. It can be reversed, but only
in some circumstances. If you aren’t happy with the results,
you may be able to go back to your previous bowel care rou-
tine. Even though you can change your mind, reversing
the procedure requires more surgery. That’s why you
should ask as many questions as you need, to feel comfortable
with your choice before anything is done.
Even though surgery is seldom required, the decision should
include careful consideration of all alternatives. There are a
variety of surgical options available to improve management of
the neurogenic bowel. Evaluation of options should include
contact with a spinal cord center and, if possible, discussion of
the outcome with someone who has had the procedure.

References
Consortium for Spinal Cord Medicine. Neurogenic Bowel Management in
Adults with Spinal Cord Injury. Washington, DC: Paralyzed Veterans of
America, 1998.
Rehabilitation Institute of Chicago. “Educational Guide for Individuals and
Families Following SCI.” Chicago: Rehabilitation Institute of Chicago, 1995.
Stiens, S.A., S. Biener-Bergman, and L.L. Goetz. Neurogenic bowel dysfunction
after spinal cord injury: Clinical evaluation and rehabilitation management. Arch
Phys Med Rehabil 78 (1997): S86–S102.
Resources
Autonomic Dysreflexia: What You Should Know. Consortium for Spinal Cord
Medicine. Washington, DC: Paralyzed Veterans of America, 1997. (Available by
calling (888) 860-7244 or visiting the PVA web site at http://www.pva.org.
“Bowel Management: A Fantastic Voyage!” In Take Control: A Multimedia
Guide to Spinal Cord Injury, Vol 3. University of Arkansas for Medical
Sciences, 1998. (CD ROM available by calling (800) 543-2119.)
“Bowel Management Program.” In Yes, You Can! A Guide to Self-Care for
Persons With Spinal Cord Injury, Second Edition, edited by Margaret C.
Hammond, Robert Umlauf, Brenda Matteson, and Sonya Perduta-Fulginiti.
Washington, DC: Paralyzed Veterans of America, 1993. (Available by calling
(888) 860-7244.)
Bowel Management Programs: A Manual of Ideas and Techniques, edited
by Raymond C. Cheever and Charle D. Elmer. RPT: Accent Press, 1975.
Constipation and Spinal Cord Injury: A Guide to Symptoms and Treatment.
D. Harari, J. Quinlan, and S.A. Stiens, Paralyzed Veterans of America: Washington
DC, 1996. (Available by calling (888) 860-7244.)
A Guide for People with Spinal Cord Injury 39

I
’m 24. Three years ago I had a spinal
cord injury at C6. They sent me home
from the hospital too fast. I didn’t have
time to learn much about bowel care and
neither did Mom, who had to do all
my attendant care. I wouldn’t do
pressure releases in public because I
was afraid of having an accident or
passing gas. It got so I was afraid to leave the house. My
bowel program was a mess, and I was embarrassed and
worried all the time.
Fortunately, I started working with a home health nurse who
really cared and understood my fears and my dreams. She
helped my mom and me train an attendant to help me with
bowel care. Having that taken care of gave me enough
confidence to move out of my parents’ house. Now I live in
a dormitory at school and “have a life!”
Regular bowel care really cut down on all the
gas I was passing, I have more confidence in
myself, and feel comfortable doing pressure
releases in public.
At first I was afraid to tell my boyfriend the
details of my bowel care needs and what
could happen. As it turns out, he finds how
I overcome problems very interesting. Our
relationship has grown, and we’ve been
physically close often. It helps that we talk
about it.
A successful bowel program has made a big difference in my
quality of life. It’s not foolproof, but I have the assurance that
others will understand if there are problems.
Having the
right information
and sharing it
with family and
significant others
can improve
understanding
about embarrassing
matters.
Bridget
Bridget

A Guide for People with Spinal Cord Injury 41
anal sphincter—A circular band of
muscle that keeps the colon closed,
like a drawstring on a purse.
areflexic bowel—A pattern of bowel
dysfunction caused by injury to the
nerves that travel from the spinal cord
to the bowel. No reflex bowel
processes are possible. Also called
flaccid bowel or lower motor-neuron
(LMN) bowel. A person with this
condition can’t feel the need to have a
bowel movement, the rectum doesn’t
empty by an automatic reflex action,
and the anal sphincter doesn’t close as
tightly as it did to keep stool in.
assistive device—Any device that
increases the independence of a
person with a disability. An example is
a digital stimulator, which helps a
person with limited hand function to
be more independent with bowel care.
Also called adaptive device.
assistive technique—Any movement
that increases the speed of bowel care
or the amount of stool produced.
Includes digital rectal stimulation,
abdominal massage, manual
evacuation, forward and sideways
bending, and push-ups.
attendant—See personal care
attendant.
autonomic dysreflexia—An
abnormal response to a problem in the
body below a spinal cord injury that
causes high blood pressure. It’s most
likely to happen if the SCI is at or
above the 6th thoracic vertebra (T6).
See Autonomic Dysreflexia: What
You Should Know, a free guide you
can get by calling (888) 860-7244 or
visiting the PVA web site at
http://www.pva.org.
bowel—The intestines, tube-like
structures that propel and store food
(small intestine) and waste (large
intestine).
bowel care—The process of triggering
and assisting a bowel movement. Bowel
care is part of a bowel program.
Bowel care can include any or all of
the following steps: getting ready,
positioning, checking for stool,
inserting stimulant medications,
performing digital rectal stimulation
or manual evacuation, recognizing
when done, and cleaning up.
bowel program—A total treatment
plan designed to prevent or cut down
on bowel accidents (unplanned bowel
movements), to eliminate stool at a
regular and predictable time through
bowel care, and to keep bowel-related
health and other problems to a
minimum. The components of a bowel
program are diet and fluid, activity
level, medications, and a consistent
routine schedule for bowel care
(including rectal stimulation).
Glossary

colitis—Inflammation of the colon.
colostomy—A surgical opening from
the intestine through the abdominal
wall that allows stool to be pushed out
into an attached, disposable bag. This
opening is built by disconnecting the
colon from the rectum and connecting
it to the abdominal wall.
constipation—A condition in which
stool does not pass as often, as fast, or
as completely, and it’s hard and dry.
defecation—Elimination of fecal
matter from the bowel through the
anus; bowel movement.
digestive system—The mouth,
esophagus, stomach, small intestine,
colon (or large intestine), rectum, and
anus. Also called the gastrointestinal
tract, GI tract, or gut (see bowel).
digital rectal stimulation—The
process of inserting a gloved, well-
lubricated finger into the rectum and
moving the finger in a circular funnel-
shaped pattern, keeping contact with
the rectal wall. This technique helps
trigger peristalsis in people with
reflexic bowel and helps remove stool
from people with areflexic bowel.
gastrointestinal tract—See digestive
system.
ileostomy—A surgical opening from
the ileum (the end of the small
intestine) through the abdominal wall
that allows liquid stool to be pushed
into an attached, disposable bag. This
opening is built by disconnecting the
ileum from the colon and connecting it
to the abdominal wall.
impaction—A collection of hard stool
located within a segment of the colon
that is obstructing peristalic stool
movement.
incontinence—Involuntary passage of
stool or urine. Also called an accident.
inflammatory bowel disease—A
chronic condition associated with
abdominal cramping, frequent stools,
and diarrhea.
irritable bowel syndrome—A
condition associated with colon
cramping and alternating constipation
and diarrhea.
lactose intolerance—Sensitivity to
lactose, a sugar in dairy products.
People with this condition can’t digest
lactose properly and may experience
abdominal discomfort ranging from
gas and bloated feelings to pain and
diarrhea.
laxatives—Medications and
substances found in certain foods or
herbs that stimulate bowel
movements.
lower motor-neuron bowel—See
areflexic bowel.
42 NEUROGENIC BOWEL: What You Should Know

A Guide for People with Spinal Cord Injury 43
manual evacuation—Use of one or
two gloved and lubricated fingers to
break up or hook stool and remove it
from the rectum. This is the standard
way to empty the rectum for people
with areflexic bowel. People with
reflexic bowel also use it sometimes
to remove stool before they insert a
rectal stimulant medication.
mechanical stimulation—Use of the
fingers or other mechanical device
(such as a digital stimulator) to
remove stool from the rectum.
Manual evacuation and digital
rectal stimulation are two methods
used by people with SCI to empty the
rectum.
mini-enema—Medication in a small
amount of liquid (usually 1 ounce or
less) that’s injected into the rectum to
stimulate a bowel movement. Also
called a liquid suppository.
neurogenic bowel—A medical
condition caused by an injury to the
spinal cord that damages the nervous
system’s control of the colon and
interferes with the body’s natural
process for storing and eliminating
solid wastes. There are two patterns
of neurogenic bowel: reflexic and
areflexic.
peristalsis—A wave-like action of the
muscular gut wall that moves food
through the gastrointestinal tract.
personal care attendant—A
person—such as a family member,
friend, or hired helper—who assists
with personal care or household tasks
on a routine basis.
positioning—Putting a person with
SCI into a posture for skin protection,
comfort, and efficiency of bowel care.
A cushioned commode chair or
padded toilet seat helps empty the
lower bowel by taking advantage of
the effects of gravity. Lying on the left
side (for people who can’t sit up) takes
advantage of gravity in moving waste
through the transverse colon.
range of motion—An arc of
movement of a joint of your body.
rectal stimulation—Treatment of the
rectum to encourage elimination of
stool. There are two types of rectal
stimulation: digital rectal
stimulation is a manual or mechanical
technique, and use of rectal stimulant
medications in a suppository or
mini-enema form is a chemical
technique.
rectum—the last segment of the colon
that ends just inside the anus.
reflex—An automatic (requiring no
conscious thought) response
coordinated by connections between
nerves. An example is an increase in
peristalsis in the colon caused by
digital rectal stimulation.
T
his spinal cord injury is old news for
me. I was on patrol near Da Nang,
Vietnam, when I was wounded
in action. It’s hard to believe I’ve
been living with a T5 SCI for more than
30 years now. Those first couple of years were
rough, but little by little, I was able to get my life back
on track.
The VA’s SCI system has been great to me and my
family. I don’t know what I’d have done over the
years if these services weren’t available.
During rehab at the VA hospital in
Sunnydale, California, I adopted a bowel
care routine that worked well for 27 years.
There was one phase in my life when I did
have a lot of accidents. I was drinking my
share of beer and had a lot of fun. Even
though I had bowel accidents on a regular
basis after I drank, it took me a long time to
make the connection between the accidents and
the beer. I’m not saying that beer is responsible for all
accidents, but if you’re having a similar problem, you may
want to consider that drinking beer and other alcohol may be
a cause.
My biggest problem came about 3 years ago when my body
seemed to be going through some changes. Bowel care was
like mission impossible every time. So I called the VA SCI
center near my home and scheduled an appointment. VA’s
SCI staff are really professional and know their stuff. In a
short time we worked out some new procedures for my rou-
tine, and I’ve been on the go ever since.
Aging can
bring on changes
in an individual’s
bowel care program
that must
be identified
and thoughtfully
resolved.
Douglas
Douglas

A Guide for People with Spinal Cord Injury 45
reflexic bowel—A pattern of
neurogenic bowel dysfunction that
affects storage and elimination of stool
that results from an injury to the spinal
cord in the cervical (neck) or thoracic
(chest) area. Also called spastic bowel
and upper motor-neuron (UMN) bowel.
A person with this condition may or
may not be able to feel the need to
have a bowel movement. In either
case, the rectum will still empty by an
automatic reflex action, the same as it
did before the SCI.
spastic bowel—see reflexic bowel.
stimulant medications—Substances
given rectally as a suppository or
mini-enema.
stoma—An opening on the abdomen
created by surgery for removal of
stool.
suppository—A solid form of
medication (usually small and bullet-
shaped) that’s inserted in the rectum
to stimulate a bowel movement.
upper motor-neuron bowel—see
reflexic bowel.
Valsalva maneuver—Breathing in
and trying to push air out while at the
same time blocking the air in your
throat to increase the pressure in your
abdomen. For people with areflexic
bowel, gentle Valsalva maneuvers can
help push stool out.
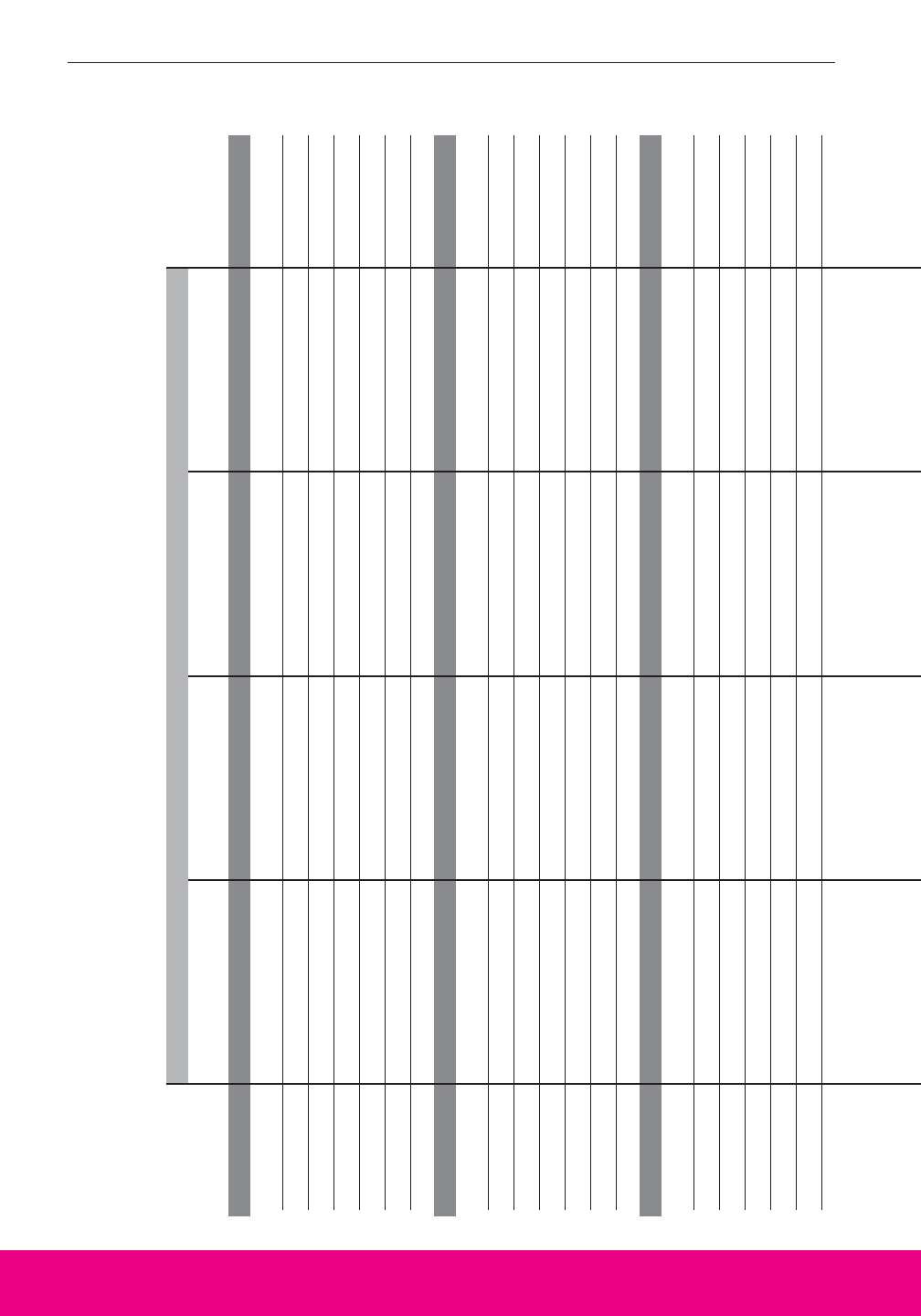
46 NEUROGENIC BOWEL: What You Should Know
Food Record
For about a month, write down what you eat and drink each day and describe your bowel movements.
Food DESCRIPTION AND QUANTITY FOR EACH MEAL CATEGORY Successful
Category Breakfast Lunch Dinner Snacks Bowel Care?
MONDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
TUESDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
WEDNESDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
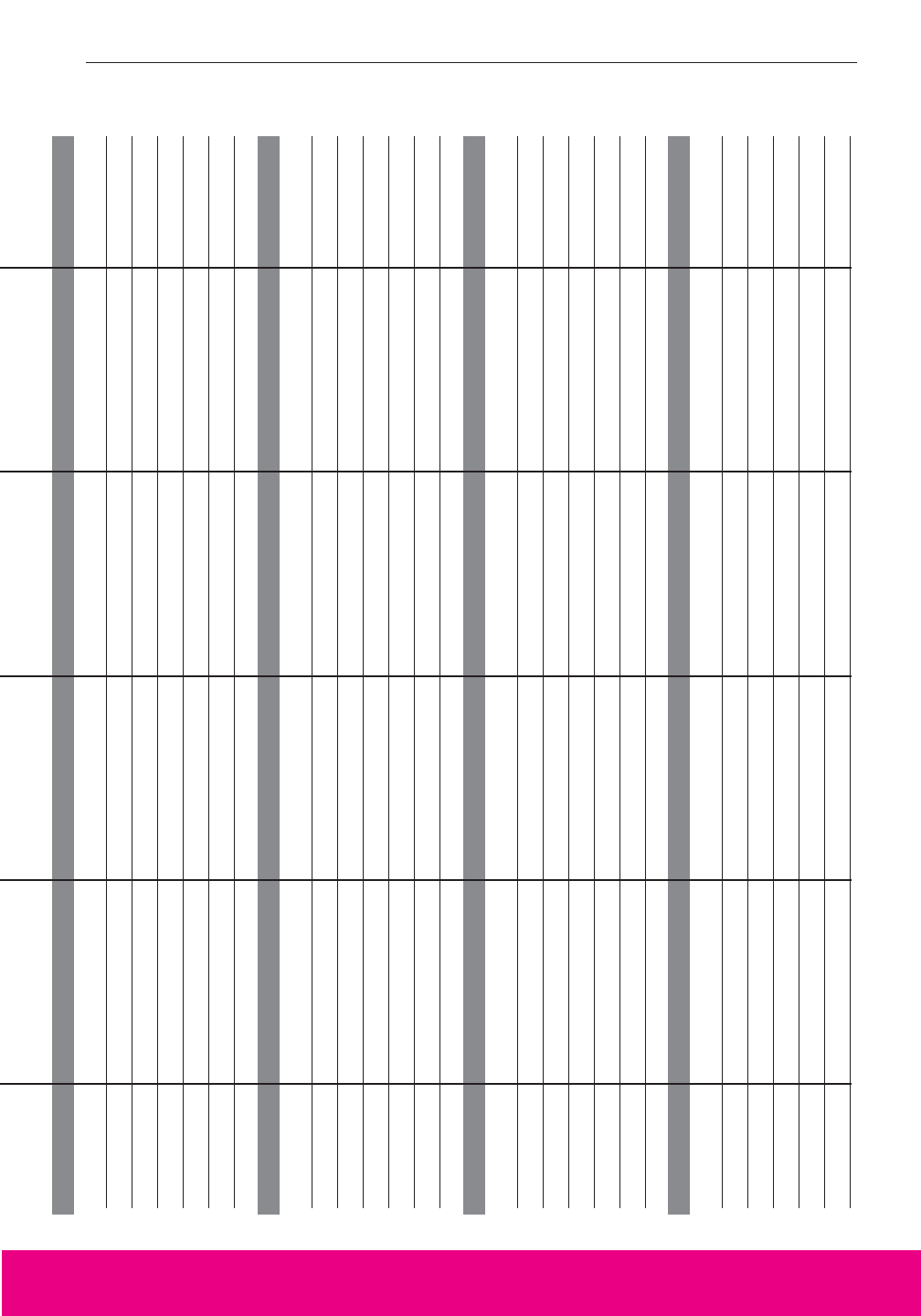
A Guide for People with Spinal Cord Injury 47
THURSDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
FRIDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
SATURDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
SUNDAY
Starch
Vegetables
Fruits
Milk
Meat
Fat
Medical History
Complete the following. Share this information with your health-care professionals.
Name: ________________________________________________________________________________
Date of Birth: __________________________________________ Sex: M or F
Date of Spinal Cord Injury: ______________________________________________________________
Neurologic location of injury: Complete_________________ Incomplete_______________
Description of bowel function before spinal cord injury (include usual frequency, time of day, prob-
lems such as constipation, hemorrhoids, etc.):______________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
Sensation around the anus? Yes No
Sensation of stool in the rectum? Yes No
Ability to contract the anal sphincter? Yes No
Reflexic or areflexic bowel? ______________________________________________________________
Allergies?______________________________________________________________________________
Poorly tolerated foods? __________________________________________________________________
Oral medications? Yes No
If yes, please complete the following section.
List medications taken regularly: ________________________________________________________
List medications taken as needed: ________________________________________________________
Rectal stimulants? ______________________________________________________________________
EMERGENCY INFORMATION
In case of emergency, call: ______________________________________________________________
Relationship: ____________________________ Phone number: ( ) ______________________
INSURANCE INFORMATION
Name of insurance company: ____________________________________________________________
Identification number: __________________________________________________________________
Group number: __________________________ Phone number: ( ) ______________________
48 NEUROGENIC BOWEL: What You Should Know
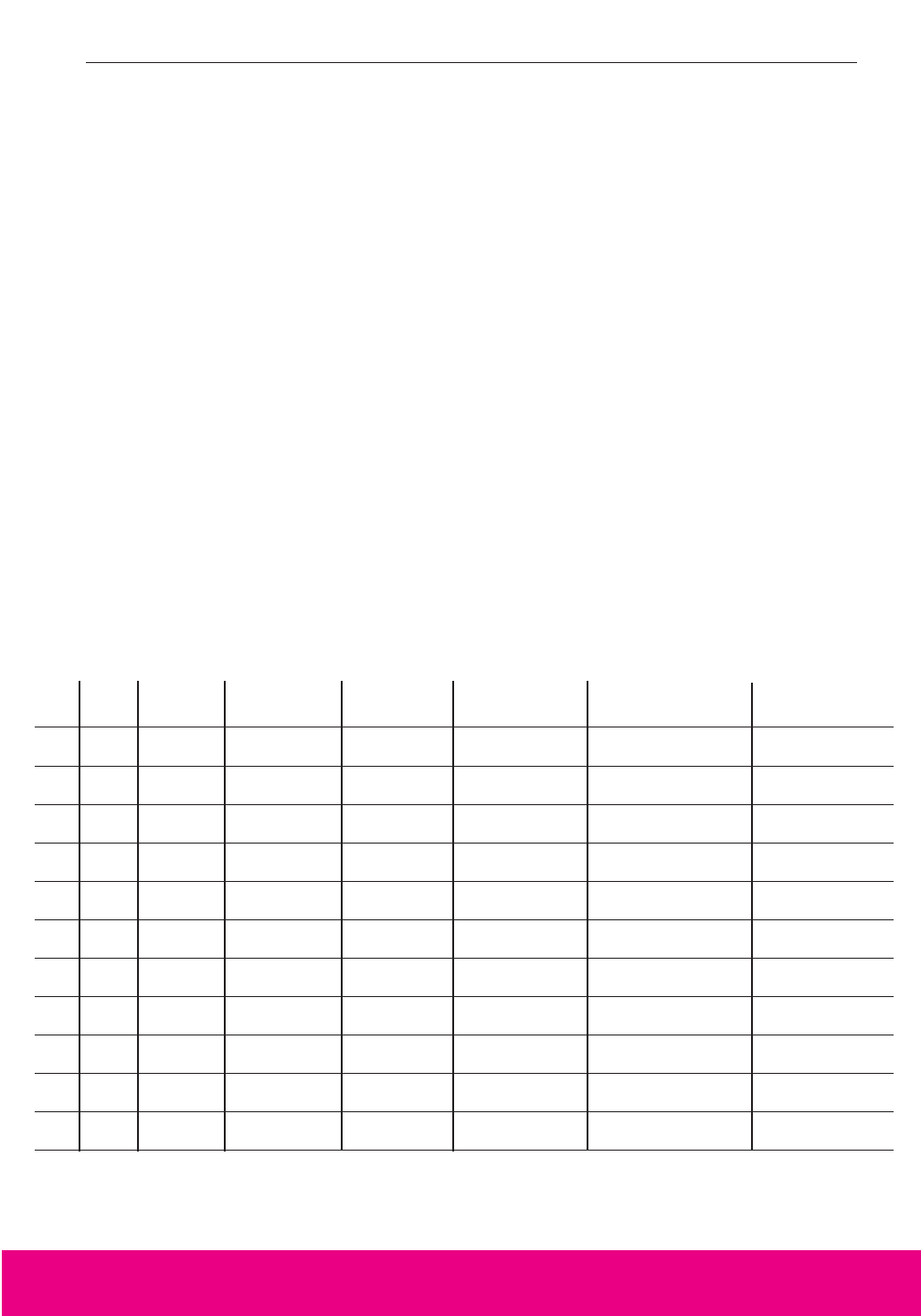
A Guide for People with Spinal Cord Injury 49
Bowel Care Record
Every time you do bowel care, write down:
• Date.
• Start time. The hour and minute you start stimulation or try to start a bowel movement.
• Position. Left side lying, right side lying, sitting.
• Stimulation method. Stimulant medication, digital rectal stimulation, or other technique you use
to start a bowel movement.
• Assistive techniques. Methods used to promote bowel emptying and the number of times
used during bowel care, e.g., abdominal massage, bending, push-ups, Valsalva maneuver.
• Times of results. The time when the first stool begins to come out of the anus and the time
when the last stool comes out.
• Stool amount, consistency, and color. Amount: if stool were formed into a ball—golfball,
tennis ball, softball. Consistency: hard, firm, soft, liquid. Color: especially anything unusual
for you.
• Comments. Problems such as any unplanned bowel movements, abdominal cramps, pain,
muscle spasms, pressure ulcers, hemorrhoids, or bleeding.
Start Stimulation Assistive Time of Results Stool Amount,
Date Time Position Method Techniques First/Last Consistency, Color Comments
continued on back
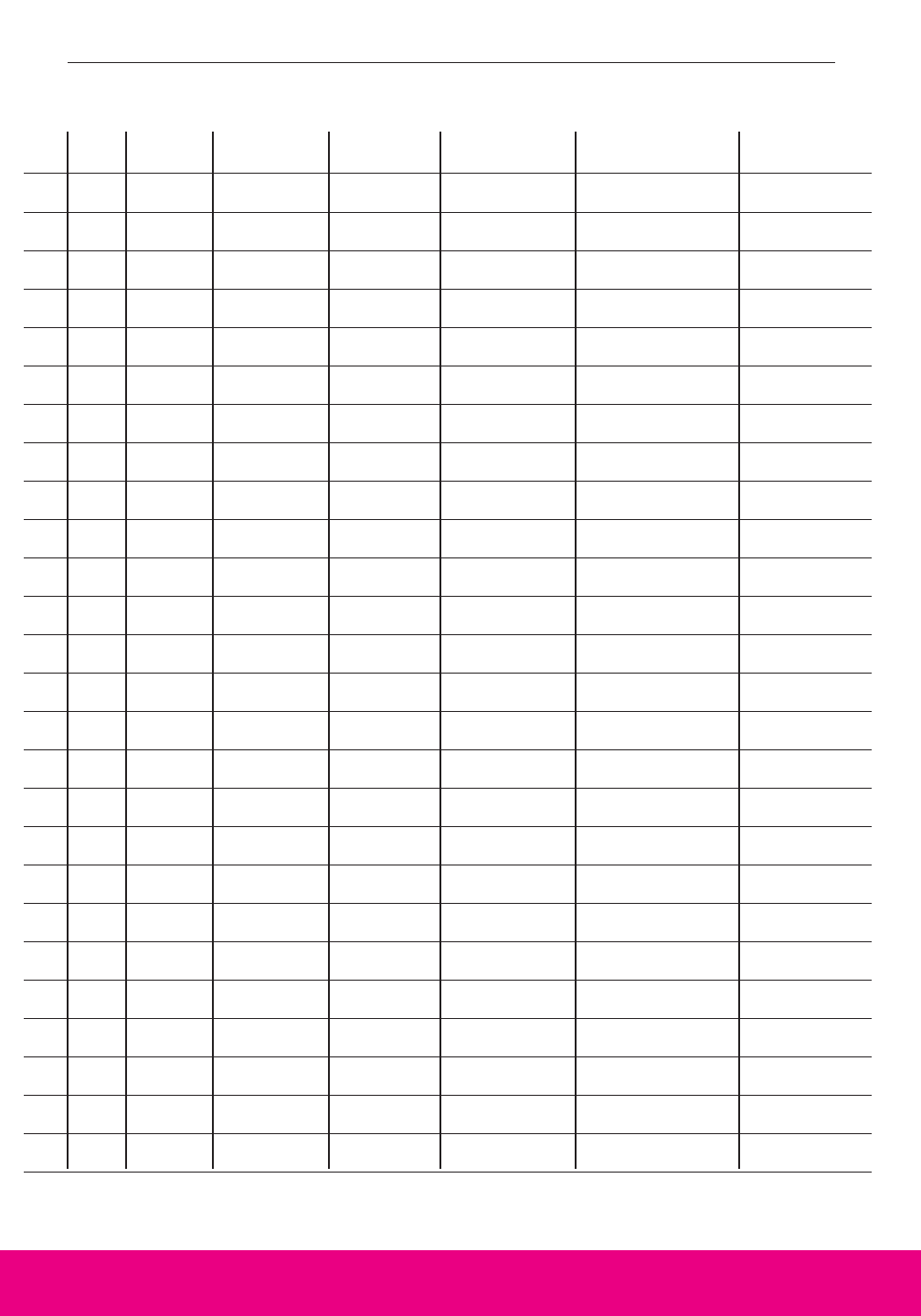
Start Stimulation Assistive Time of Results Stool Amount,
Date Time Position Method Techniques First/Last Consistency, Color Comments
50 NEUROGENIC BOWEL: What You Should Know
I
t’s been over a year since the parachute
accident that left me a paraplegic at the T6
chest level. One of the biggest challenges
I’ve had is bowel management. I wanted
to be as independent as possible, so I
worked closely with my rehab team to
learn how to take care of bowel care myself. I follow my bowel
program like a flight plan.
As a young, single, career guy, the last thing I want
to worry about is an unplanned bowel
movement. If accidents happen, I handle
them myself because I live alone and really
feel this is something I need to take care of.
Now for the challenge. I work for a major
airline, and my job has me traveling all over
the country. Staying in hotels makes my
bowel program a little different from how I
manage at home. While I try to keep the same
schedule, access to a toilet and bathroom
conditions often change. At home, things are pretty
routine. But on the road, I never know what facilities I’ll find
at different hotels. Sometimes the bathroom accommodations
just don’t work for me and I’m forced to do my bowel care in
bed using the side-lying technique. When I fly, I do my bowel
care at least 6 hours before I need to be at the airport. I think
it’s important for people with SCI to know it’s OK to use
whatever method works best for them.
Things are going OK for me. I watch what I eat and drink and
have a regular schedule for my bowel care. I carry a backup
bag with a change of clothes, just in case. It’s like my
parachute; I hope I don’t have to use it, but it’s there when I
need it. My life is on course.
Knowing
your own body
and being prepared
can allow you to
have an
active full life
with lots of
independence.
Orville
Orville

The Consortium for Spinal Cord
Medicine Clinical Practice Guidelines is
composed of 18 organizations interest-
ed in spinal cord injury (SCI) care and
treatment. The Consortium Steering
Committee established a guideline
development panel to make recommen-
dations on the management and reha-
bilitation of neurogenic bowel
dysfunction in individuals with SCI.
The recommendations within this con-
sumer guide are based on scientific
research compiled from 1966 to 1997
and used in the Consortium’s clinical
practice guideline (CPG) Neurogenic
Bowel Management in Adults with
Spinal Cord Injury. The CPG devel-
opment panel was assisted by an expert
team from the University of North Car-
olina at Chapel Hill who reviewed the
literature and determined the quality of
the research. The Paralyzed Veterans
of America (PVA) provided financial
support and administrative resources
for all aspects of guideline and con-
sumer guide development.
The consumer panel was chaired by
Steven A. Stiens, MD, MS, and consist-
ed of five members with experience in
the management and treatment of the
neurogenic bowel in individuals with
SCI. For many with SCI, bowel dys-
function is a major life-limiting prob-
lem. Creation of a consumer guide that
addresses the problems of, and the
solutions for, living with a neurogenic
bowel required a diverse, experienced,
and sensitive panel. The Consortium
thanks all members of the consumer
guide panel for providing the essential
ingredients of knowledge, experience,
empathy, and practicality.
The Consortium is also appreciative
of the outstanding work of the entire
PVA publications support team. In par-
ticular, the Consortium would like to
recognize the professional writer Bar-
bara Shapiro, the PVA senior editor
Patricia E. Scully, DesignS by Sarah for
the graphic design, and the illustrators
who made our concepts of characters
come alive as figures.
In the end, it is those with SCI who
are living with and learning about neu-
rogenic bowel who are the best evalua-
tors of a teaching tool such as this
consumer guide. The Consortium
thanks the consumer focus group for
their critical review and comments on
the manuscript, including Frank W.
Anderson, Victoria Christensen,
Edward R. Jasper, Joseph A. Kiren,
Patrick J. Marron, Delatorro L.
McNeal, and Charles J. Sabatier, Jr.
Their varied life experiences with SCI
provided wise perspectives that refined
and improved the consumer guide.
Finally, it is essential to recognize
all investigators studying the effects of
SCI on the digestive system. Research
is the source of solutions; there is still
much to be done in the future. Bowel
dysfunction continues to be a fertile
area for research!
The Consortium will continue to
develop clinical practice guidelines
and consumer guides on topics in
spinal cord injury care. Look for con-
sumer guides on other topics in spinal
cord injury.
Acknowledgments
Administrative and financial
support provided by
PARALYZED VETERANS OF AMERICA
801 Eighteenth Street, NW
Washington, DC 20006-3517
(800) 424-8200 • (800) 795-3427 tty • www.pva.org
(888) 860-7244 (toll-free distribution center)
March 1999
