
2 Bowel Management (Part 1)
Introduction
If you have a spinal cord injury (SCI) then a regular bowel management
routine is vitally important, both physically and socially. Establishing an
effective routine will bring the confidence and freedom needed to live a full
and active life.
There is no single, infallible method to suit everyone – you will need to
experiment to find the method which best suits your own needs and
lifestyle, but if you do have a problem it is wise to discuss the matter with
your GP, District Nurse, Spinal Unit Community Liaison Nurse or Spinal
Consultant, as there may be a medical reason why you are having
problems.
A SCI changes the way your body works and how you will have to care for
yourself and probably the most significant change is how the bowel works.
After SCI your bowel movements require more time, thought, and
planning. Usually a SCI person cannot feel when the bowel is ready to
empty and help is required to expel the stool: this requires a well-designed
bowel management programme/bowel care routine.
A proper bowel management programme will help prevent unplanned
bowel movements, and avoid complications like constipation. A
personalised bowel management programme, ideally put in place before
discharge from hospital, will improve your confidence in both social and
work situations, by putting you back in control of a bodily function that if
neglected, can cause embarrassment.
If you do not or are unable to establish a proper bowel management
programme this may contribute to or result in various unpleasant side
effects or potential health problems:
• Headaches
• Bad breath
• Abdominal discomfort
• Flatulence
• Constipation
• Increased risk of Autonomic dysreflexia
• Infections e.g. bladder
• Bowel accidents and or leakage
• Diarrhoea
• Pressure ulcers (if you are leaking)
• Haemorrhoids, if constipation
becomes chronic.
How does my bowel work after my SCI?
After a spinal cord injury, the messages sent by the nerves located in
your bowel are not able to reach your brain as they did before your
injury. This means that stool will pass more slowly through your gut
which can lead to constipation and you will not get the message that
tells you your bowel is full and it’s time to go to the toilet.

3 Bowel Management (Part 1)
Another change is that you may not be able to move the muscle at the
opening of your back passage that controls when you have a bowel
movement.
The degree of loss of control will depend upon the level of your injury and
the extent of damage to your spinal cord.
Two words you may hear to describe bowel type
following spinal cord injury are reflex and flaccid
Reflex bowel
If your spinal cord injury is above T12 your bowel will usually continue to
empty when stimulated. The normal sensation which indicates that the
bowel is full is lost. The vital messages needed telling you the bowel is full
do not reach the brain. Reflexes which partly control bowel movement are
still present so the muscles in your lower bowel, rectum and anal
sphincter are still active and you or your carer may be able to trigger them
to empty your bowel at a convenient time. Care must be taken to ensure
that the rectum is properly empty as this will avoid a bowel accident later
in the day.
Flaccid bowel
If your spinal cord injury is at or below T12 your bowel will not fully empty,
even when stimulated. The nerves between your bowel and spinal cord
have been damaged therefore reflexes are lost. Your rectum will continue
to fill with faeces which may leak out as the anal muscles stay relaxed.
Incomplete injuries
If your injury is incomplete or is around T12, you may find that your bowel
takes on a mix of both the above.
Designing a Bowel Programme
How will my bowel function be assessed
Early in your rehabilitation an assessment of your impairment will be
carried out and this will help the medical team to identify your individual
bowel function and which is the best type of programme for you to follow.
Usually this assessment will not require any special tests, though
sometimes a physiological test, such as a colon transit time study is
needed.
To find what works best for you, your healthcare professional may ask you
to keep a bowel diary, or a bowel record, over two to three weeks. It is
most helpful to keep a bowel diary in the first weeks after you leave the

4 Bowel Management (Part 1)
hospital or whenever you are having problems and a few weeks before
your annual check-up.
What is a bowel diary?
A bowel diary is the precise recording of your daily bowel function. It is
designed to collect information on your bowel habit.
Every time you do your bowel care you will be asked to record details
such as:
• Assistive techniques (gastrocolic response, bending, lifting, push-
ups).
• Stimulation method used (digital or chemical rectal stimulation).
• The scheduling and exact timing of your bowel habit (start time of
stimulation; time the first stool begins to come out of the anus; time
when the last stool comes out).
• Stool amount, consistency (hard, firm, soft, liquid) and colour
(especially anything unusual for you).
Also, list any problems with your bowel such as unplanned bowel
movements, abdominal cramps, unexplained pain, rectal bleeding, gas or
bloating.
You should also give comments about your diet, especially the amount of
fibre you eat and your daily fluid intake. Also it is important to record your
activity level and list all of your current medications. All this information
will help to precisely assess your bowel programme.
A sample Bowel Diary is shown in Appendix 1.
What is a bowel programme?
A bowel programme is a personalised plan designed to help you regain
control of your bowel after your spinal cord injury and improve your
quality of life.
Consideration is given to several aspects in establishing your own bowel
program:
• Time of day
• Position; for example on the bed, over the toilet
• Skin care
• Diet and fluid intake
• Level of activity
• Assistive techniques
• Current medications
• If you can guarantee privacy.
Your bowel programme should be reviewed at least once a year to make
sure it is working well for you.
A bowel care diary is a key part of this review. Keep your completed bowel
care records in a notebook, folder, or other handy place and take them with
you when you visit your healthcare professional.

5 Bowel Management (Part 1)
What is bowel care?
Bowel care is the term for assisted evacuation of stools and is a part of
your bowel programme. It begins with starting a bowel movement, which
is done with digital stimulation and/or the use of a rectal stimulant
(suppository or mini-enema).
Digital stimulation is used to stimulate the bowel to pass a stool. A
lubricated gloved finger is inserted into the rectum and slowly rotated
maintaining contact with the rectal wall at all times. This is normally done
for 15-20 seconds then the finger is removed to see if any stools come with
it. Stimulation can be repeated every 3-5 minutes until a bowel movement
has been achieved.
Bowel care can include a variety of techniques. In addition, medications
taken both orally and / or suppositories help to achieve a satisfactory stool
evacuation.
You need to be able to perform the bowel care yourself or direct an
attendant or other carer on when and how you need help.
Why is it important to carry out good bowel care?
• To maximise your independence
• To help maintain good health
• To prevent complications such as constipation and diarrhoea but of
which may necessitate disruption of your daily routines
• Help prevent pressure ulcers and infections by maintaining dry /
intact skin
• Minimise damage to the bowel
• Help prevent an episode of Autonomic Dysreflexia
• Maintain self-esteem.
Can I be independent in my bowel care?
Independence in performing bowel care depends on many factors such
as the level and completeness of your SCI, your general health, how
strong you are, your weight and how much you want to be independent.
For complete independence, your arms, hands and fingers need to be
strong enough to manage your clothes, get you into a proper position,
place stimulant medication and carry out digital stimulation. Most people
with a thoracic, lumbar, or sacral injury are strong enough and have
sufficient balance.
If you have a cervical injury at C6, C7 or C8, you may not have enough
hand strength or sitting balance to do digital stimulation, insert a
suppository or a mini-enema independently. Special devices like digital
stimulators and suppository inserters can help with these activities.
Even if they can carry out bowel care themselves, some people choose to
have a carer do it for them. They find that it takes too long, or it simply
takes too much energy they would rather use doing other things. Whether
or not you do perform your own bowel care, you still need to manage your
bowel programme. That means watching what you eat and drink, your

6 Bowel Management (Part 1)
activity level, your medication, and the results of your bowel care routine.
If you need assistance with your bowel care, learn the process so that you
can teach it to carers and supervise your own care.
Why is timing important for my bowel management?
Once you are discharged from hospital you will perform your bowel care
in the morning or the evening to fit in with your daily life, your individual
arrangements, or with carers if you use them. A regular and consistent
time to perform your bowel care will train your bowel and help you to be
more confident in your bowels and not be ruled by them.
Choose a set time of day for your bowel routine. If possible, establish a
plan in which you empty your bowels daily or every other day. Regularity
is vital, if the schedule is more than three days this can cause fluid to be
absorbed from your stools and result in hard stools, causing constipation
and impaction.
Work out the time of day most convenient to fit into your lifestyle, in terms
of job, school, or general social needs. For instance, if you have to rise
early to go to work and have little time, you may find it best to arrange
your routine in the evenings. If you need to alter the time of your routine,
a changeover can be made, for instance, from evening to morning or vice
versa. Be aware that you should allow for a two to four week readjustment
period as during this time your routine may not be so reliable.
If possible, use the gastrocolic response. The gastrocolic response is a
natural reflex of the bowel when food or fluid is taken. This stimulates
waves of peristalsis, speeding up the movement of waste matter in your
bowel. Drinking warm liquids or eating a meal shortly before your bowel
care may help to stimulate a bowel movement. This can be useful when
organising a convenient time for your bowel emptying.
You may have to take a laxative approximately 8-12 hours prior to bowel
evacuation. Everyone’s body changes over time, even if you have kept a
regular bowel programme for years, it may stop working as well as it did
and you may have to adapt your scheduling.
How can I perform my bowel care?
If you have a reflex bowel, the aim of your bowel management programme
is to produce a soft, formed stool that can be passed easily with minimal
rectal stimulation. The bowel management routine usually starts with
digital stimulation or a stimulant medication.
If you have a flaccid bowel, the aim of your bowel management
programme is to produce a firm, formed stool that can be removed
manually with ease and doesn’t pass accidentally between bowel care
routines. Bowel care doesn’t usually require chemical stimulants because
the response would be very sluggish.

7 Bowel Management (Part 1)
What is manual evacuation?
Manual evacuation aims to empty the rectum with a lubricated gloved
finger, more properly described as "the digital removal of faeces". This
procedure can be carried out either on the bed, commode or toilet. This
procedure will be taught by a healthcare professional to suit your individual
needs.
What is digital stimulation?
Digital stimulation is a way to start the action of peristalsis within the colon,
to start a bowel movement and to keep it going. This method uses a
finger or a stimulant tool to relax and open the anal sphincter and to
trigger peristalsis. Most SCI people need to start bowel care by
stimulating the rectum to evacuate the stools, but if you have a high lesion
you might need assistance in doing so. There is another method of rectal
stimulation which relies on a pharmacological agent (a suppository or a
mini-enema) to trigger the emptying of the left colon.
Are digital stimulation and manual evacuation dangerous?
Digital stimulation and manual evacuation may trigger autonomic dysreflexia.
The first time that either procedure is performed careful attention should be
given to any signs suggesting autonomic dysreflexia and appropriate
measures be taken. Manual evacuation that is performed forcefully on a
person with impaired sensation can be associated with injury to the anal
sphincters and in some people this may contribute to sphincter weakness.
At every stage of digital stimulation it is important to use plenty of lubricant
and to be gentle, as pushing or rotating a finger too roughly can irritate or
tear the rectal lining. Make sure you have short nails. Both techniques
should be learned under supervision and performed by fully-trained
people. If performed carefully these techniques are very efficient and they
are not dangerous.
Are there other ways to manage my bowel care?
Your healthcare professional may suggest a number of tips or assistive
techniques to improve your bowel care results.
The most common are:
Abdominal massage
May help move stool through the colon to the rectum. Massage with the
heel of the hand applying gentle but firm pressure in a clockwise direction
firmly over your stomach may help to stimulate your bowel. Before
carrying out a bowel care routine you could try massage of your abdomen
starting from the lower right side across the top and down to the lower left
side, in a clockwise motion.

8 Bowel Management (Part 1)
What should I know about side effects of medications?
Medications can affect your bowel function and you should be aware of
the possible side effects of any medication that you are prescribed. Some
can help your body pass stool regularly, but others can make regular
bowel movements more difficult e.g. painkillers and sleeping tablets will
slow down bowel movements and may cause you to become constipated.
Some antibiotics can have the directly opposite effect, giving loose
motions and often causing diarrhoea. If you have any concerns about your
medication you must consult your GP, they may be able to offer an
alternative.
Why is activity level relevant?
Try to keep as physically active as possible, even when in bed for long
periods: this increases abdominal muscular tone and stimulates
peristalsis. Abdominal muscle exercises may help peristalsis, if you can
do them. Try to contract and relax your abdominal muscles by breathing
in deeply and pushing or bearing down. Being as independent as
possible in activities of daily living such as bathing, dressing, transferring
from your wheelchair etc. will help in providing regular exercise.
Why should I watch what I eat?
Diet plays a very important role in establishing a good bowel routine.
Frequency of bowel emptying and stool consistency is directly related to
the quantity and quality of foods eaten. What you eat and drink will affect
your bowel movements. Stool consistency is often a key factor in the
success or failure of a bowel programme. An important part of your diet is
the amount of fibre you eat. Foods that have a lot of fibre can absorb and
retain liquids and help make your stool more soft and easy to pass. Try to
eat well-balanced meals at regular times each day. Once the right balance
is established, the need for medication might be reduced and bowel
management can become easier.
For more information about diet and healthy bowels read our fact sheet on
Diet and Exercise.
9 Bowel Management (Part 1)
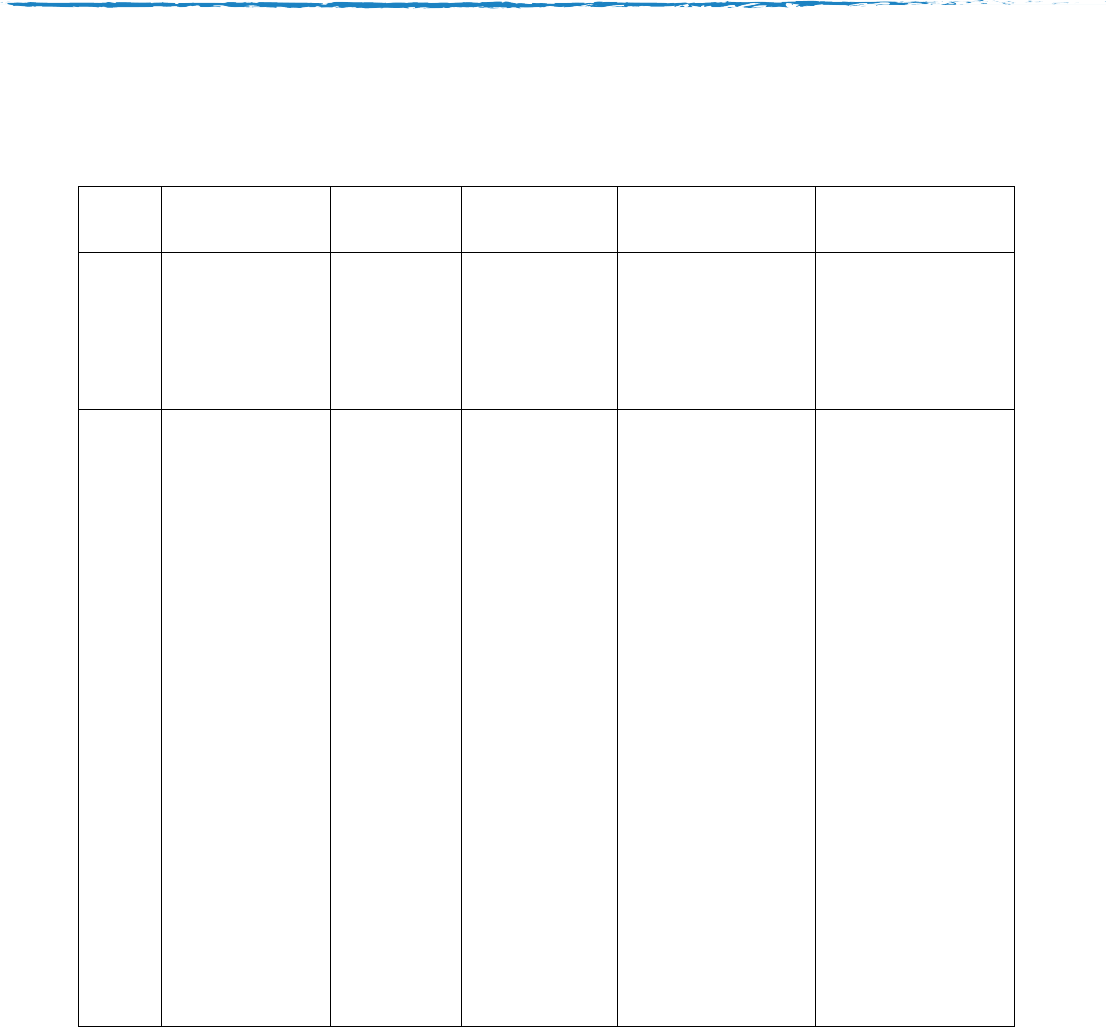
Appendix 1 - Sample Bowel Diary
Date
Aperients
Start time
Finish Time
Bowel result
Comments
Time, dose;
Bulking agent
Rectal
stimulation
Laxative
Circle appropriate
answer
Assistive
technique
Diet, fluid intake
Current
medications
Planned
Accidental
Result:
Very good
Adequate
Unsatisfactory
Amount:
Small
Medium
Large
Consistency:
Rock-hard
Normal
Loose
Watery

10 Bowel Management (Part 1)
Disclaimer
This factsheet has been prepared by SIA and contains general advice only
which we hope will be of use to you. Nothing in this factsheet should be
construed as the giving of specific advice and it should not be relied on as a
basis for any decision or action. SIA does not accept any liability arising
from its use. We aim to ensure the information is as up-to-date and accurate
as possible, but please be warned that certain areas are subject to change
from time to time. Please note that the inclusion of named agencies,
companies, products, services or publications in this factsheet does not
constitute a recommendation or endorsement by SIA.
Revised April 2017

11 Bowel Management (Part 1)
About SIA
The Spinal Injuries Association (SIA) is the leading national user-led charity
for spinal cord injured (SCI) people. Being user led, we are well placed to
understand the everyday needs of living with spinal cord injury and are here
to meet those needs by providing key services to share information and
experiences, and to campaign for change ensuring each person can lead a
full and active life. We are here to support you from the moment your spinal
cord injury happens, and for the rest of your life.
For more information contact us via the following:
Spinal Injuries Association
SIA House
2 Trueman Place
Oldbrook
Milton Keynes
MK6 2HH
T: 01908 604 191 (Mon – Fri 9am – 5pm)
T: 0800 980 0501 (Freephone Advice Line, Mon – Fri, 11am – 1pm/2pm – 4.30pm)
W: www.spinal.co.uk
Charity No: 1054097
Brought to you by:
12 Bowel Management (Part 1)
Please support SIA
SIA relies on fundraising, donations and gifts in wills to provide
services that help spinal cord injured people rebuild their lives.
With your help, we can provide the right support to spinal cord injured people and
their families and friends so they can enjoy a full and independent life after injury.
Your donation today will go towards changing someone’s life.
I would like to give: £15 £20 £53 other amount £………….
Method of payment
I enclose a cheque/postal order/CAF voucher made payable to Spinal Injuries
Association.
I would like to pay by Mastercard/Visa/Maestro/Switch (delete as appropriate)
Card number
Start date Expiry Date Security Code
Signature Date
……../……../..…….
Name…………………………………………………………………………………….
Address …………………………………………………………………………….......
……………………………………………………………………………………….......
Postcode …………………………… Tel no………………………………...............
Email address…………………………………………………………………………..
Please gift aid my donation
If you tick the box it means for every £1 you donate we can claim an extra 25p
from the taxman, at no extra cost to you. You need to pay an amount of income
tax or capital gains tax at least equal to the tax we reclaim from HM Revenue and
Customs – currently 25p in every £1 you give.
Please send your donation to: FREEPOST SPINAL INJURIES ASSOCIATION or
you can donate online at www.spinal.co.uk
Thank you for your support!
