A
Cost-Effectiveness
Analysis
of
Exercise
as
a
Health
Promotion
Activity
EVRIDIKI
1.
HATZIANDREU,
MD,
MPH,
JEFFREY
P.
KOPLAN,
MD,
MPH,
MILTON
C.
WEINSTEIN,
PHD,
CARL
J.
CASPERSEN,
PHD,
AND
KENNETH
E.
WARNER,
PHD
Abstract:
We
used
cost-effectiveness
analysis
to
estimate
the
health
and
economic
implications
of
exercise
in
preventing
coronary
heart
disease
(CHD).
We
assumed
that
nonexercisers
have
a
relative
risk
of
2.0
for
a
CHD
event.
Two
hypothetical
cohorts
(one
with
exercise
and
the
other
without
exercise)
of
1,000
35-year-old
men
were
followed
for
30
years
to
observe
differences
in
the
number
of
CHD
events,
life
expectancy,
and
quality-adjusted
life
expectancy.
We
used
jogging
as
an
example
to
calculate
cost,
injury
rates,
adherence,
and
the
value
oftime
spent.
Both
direct
and
indirect
costs
associated
with
exercise,
injury,
and
treating
CHD
were
considered.
We
estimate
that
exercising
regularly
results
in
78.1
fewer
CHD
Introduction
Regular
aerobic
exercise
is
increasingly
being
viewed
by
health
professionals
as
a
key
behavioral
ingredient
in
reduc-
ing
the
risk
of
illness,
particularly
illness
associated
with
heart
disease.
The
"fitness
craze"
has
emerged
as
an
integral
component
of
the
broader
concern
with
health
promotion,
with
exercise
explicitly
recognized
in
the
US
Public
Health
Service's
health
promotion
and
disease
prevention
objectives
for
the
nation.1
In
recent
years
the
presumed
cardiovascular
benefits
of
exercise
have
received
convincing
empirical
support.2"
Accordingly
and
increasingly,
the
medical
pro-
fession
has
come
to
recognize
and
prescribe
exercise
as
a
preventive
and
rehabilitative
therapy.
Many
health
promotion
advocates
emphasize
also
the
economic
benefits
of
exercise,
in
addition
to
its
contribution
to
better
health.5
Because
both
the
economic
and
medical
dimensions
of
exercise
are
subjects
of
substantial
interest,
we
examine
the
cost-effectiveness
of
exercise
as
a
primary
prevention
medical
technology.
Our
interests
are
in
the
health
and
economic
implications
of
exercise
as
compared
with
its
absence
and
in
using
exercise
as
an
alternative
to
common
medical
interventions
designed
to
address
potential
or
existing
heart
disease.
In
addition,
we
examine
the
issue
of
whether
exercise
consumes
more
or
less
time
than
it
saves
in
increased
life
expectancy.
Methods
We
used
decision
analysis
and
cost-effectiveness
anal-
ysis
to
compare
a
regular
exercise
regimen
with
its
absence
in
cohorts
of
1,000
35-year-old
men,
followed
for
30
years.
We
defined
exercise
as
leisure
time
physical
activity
that
consumes
2,000
kcal
per
week.
Jogging
was
used
as
an
Address
reprint
requests
to
Jeffrey
P.
Koplan,
MD,
MPH,
Office
of
the
Director,
Centers
for
Disease
Control,
Bldg.
1,
Rm
2047
(D22),
Atlanta,
GA
30333.
Dr.
Hatziandreu
is
affiliated
with
that
office
also,
as
well
as
the
Departments
of
Epidemiology
and
Health
Policy
&
Management,
Harvard
School
of
Public
Health;
Dr.
Weinstein
is
with
the
Department
of
Health
Policy
&
Management,
Harvard
SPH;
Dr.
Caspersen
is
with
the
Center
for
Health
Promotion
and
Education,
CDC,
Atlanta;
Dr.
Warner
is
with
the
Department
of
Public
Health
Policy
&
Administration,
University
of
Michigan
SPH,
Ann
Arbor.
This
paper,
submitted
to
the
Journal
December
23,
1987,
was
revised
and
accepted
for
publication
June
9,
1988.
Editor's
Note:
See
also
related
editorial
p
1413
this
issue.
events
and
1,138.3
Quality
Adjusted
Life
Years
(QALYs)
gained
over
the
30-year
study
period.
Under
our
base
case
assumptions,
which
include
indirect
costs
such
as
time
spent
in
exercise,
exercise
does
not
produce
economic
savings.
However,
the
cost
per
QALY
gained
of
$11,313
is
favorable
when
compared
with
other
preventive
or
therapeutic
interventions
for
CHD.
The
value
of
time
spent
is
a
crucial
factor,
influencing
whether
exercise
is
a
cost-saving
activity.
In
an
alternative
model,
where
all
members
of
the
cohort
exercise
for
one
year,
and
then
only
those
who
like
it
or
are
neutral
continue,
exercise
produces
net
economic
savings
as
well
as
reducing
mor-
bidity.
(Am
J
Public
Health
1988;
78:1417-1421.)
example
to
calculate
costs,
injury
rates,
adherence,
and
the
value
of
the
time
spent.
Exercise
was
considered
to
be
a
prescriptive
medical
intervention,
analogous
to
chronic
anti-
hypertensive
or
hypoglycemic
treatment.
Cost-effective
is
a
relative
and
subjective
concept
defined
as
"having
an
addi-
tional
benefit
worth
the
additional
cost."6
Beneficial
pro-
grams
that
yield
net
cost
savings
are
automatically
cost-ef-
fective,
but
net
cost
saving
is
not
necessary
for
a
program
to
be
judged
cost-effective.
Using
epidemiologic
data,
we
estimated
the
number
of
fatal
and
nonfatal
coronary
heart
disease
(CHD)
events
that
would
be
expected
to
occur
over
time
in
each
cohort.
We
considered
the
consequences
of
CHD
events
to
be
their
direct
medical
care
cost
and
their
effects
on
life
expectancy
and
reduced
quality
of
life.
Thus,
our
measures
of
the
health
effectiveness
of
exercise
were
reductions
in
the
numbers
of
CHD
events,
gains
in
life
expectancy,
and
gains
in
quality-
adjusted
life
expectancy.
These
effectiveness
measures
served
as
denominators
in
our
cost-effectiveness
ratios.
The
numerators
of
the
ratio
represent
various
measures
of
the
difference
between
the
incurred
costs
of
the
two
strategies.
We
considered
both
direct
costs
and
savings
associated
with
an
exercise
regimen
(direct
costs,
including
equipment
and
clothing,
as
well
as
the
medical
cost
of
injuries,
and
savings
consisting
of
the
avoidance
of
treatment
for
CHD
events)
and
indirect
costs
and
benefits,
respectively
(time
spent
in
the
exercise
program
and
healthy
time
gained
as
a
result
of
CHD
events
prevented).
Our
outcome
measures
are
cost
(direct
or
direct
plus
indirect)
per year
of
life
saved,
cost
per
quality-
adjusted
life
year
(QALY)
saved,
and
cost
per
CHD
death
averted.
All
future
costs
and
years
of
life
saved
were
discounted
at
a
real
annual
rate
of
3
per
cent
to
determine
their
present
value.
We
chose
to
discount
health
benefits
(future
years
of
life
saved
and
cases
averted)
to
maintain
a
common
perspective
on
the
value
of
both
future
costs
and
future
health
effects.
Costs
were
measured
at
1985
price
and
wage
levels.
Definitions
and
Rates
Health
events
for
which
rates
were
required
in
the
analysis
were
exercise-related
injuries,
CHD
events,
and
non-CHD
mortality.
Injury
was
defined
as
an
adverse
health
effect
severe
enough
for
the
injured
person
to
seek
medical
consultation.
We
estimated
the
annual
probability
of
such
injury
to
be
5
per
cent,
with
17
per
cent
of
those
injured
AJPH
November
1988,
Vol.
78,
No.
11
1417
HATZIANDREU,
ET
AL.
quitting
jogging
permanently
because
of
the
injury.7
We
assumed
that
the
rate
of
injuries
and
quitting
remained
constant
throughout
the
30-year
study
period.
CHD
events
were
considered
to
be
death
(sudden
or
nonsudden),
myocardial
infarction,
or
other
CHD
(angina
pectoris
and
coronary
insufficiency).
Age-specific
incidence
rates
for
men
were
derived
from
the
Framingham
Heart
Study.8'9
These
rates,
however,
represent
combined
popu-
lation
rates,
which
include
those
who
do
and
those
who
do
not
exercise.
We
calculated
separate
rates
for
exercisers
and
nonexercisers
by
assuming
that
10
per
cent
of
all
men
exercise
as
defined
previously
and
that
exercise
reduces
the
risk
of
CHD
by
50
per
cent.
'0
Age-specific
death
rates
for
men
for
1980
from
all
other
causes
except
CHD
were
used.
In
both
the
exercise
and
nonexercise
cohorts,
we
sepa-
rated
those
who
experienced
nonfatal
CHD
into
subgroups
and
tracked
them
to
determine
the
number
of
additional
deaths
occurring
during
the
follow-up
period.
Annual
mor-
tality
rates
in
these
subgroups
of
persons
with
CHD
histories
were
based
on
data
from
the
American
Heart
Association
(age-specific
CHD
deaths
and
prevalence
of
CHD).
Persons
injured
due
to
exercise
and
unable
to
continue
jogging
were
considered
"quitters"
(dropouts).
We
assumed
that
they
did
not
engage
in
other
forms
of
aerobic
activity
and
that
they
experienced
the
CHD
rates
of
non-exercisers
from
the
year
of
quitting.
Costs
Exercise-The
direct
cost
of
exercise,
the
cost
of
equip-
ment
(running
shoes,
clothes,
etc.),
is
estimated
at
$100
annually.
Considering
exercise
to
be
a
prescriptive
medical
intervention,
we
have
included
the
cost
of
counseling
a
patient
to
undertake
an
exercise
regimen
as
a
direct
cost.
We
assumed
that
this
counseling
would
occur
during
a
routine
periodic
examination
and
would
represent
10
per
cent
of
a
45-minute
visit.
We
estimated
the
average
cost
of
the
history
and
examination
portion
of
a
routine
physician
visit
to
be
$75.
To
determine
the
indirect
cost,
we
assumed
five
hours
per
week,
including
exercise
time
(nine
minutes
per
mile,
20
miles
per
week)
and
preparation
time
(24
minutes,
five
times
a
week).
In
deriving
the
monetary
value
of
this
time,
we
used
the
results
of
a
telephone
survey
of
six
exercise
experts
who
estimated
the
proportions
of
participants
in
an
exercise
program
who
like
it
(55
per
cent),
dislike
it
(35
per
cent),
or
are
neutral
(10
per
cent).
We
assumed
that
those
who
are
neutral
toward
exercise
would
value
their
time
at
$4.50
per
hour
(half
the
1985
hourly
wage.
")
Those
who
dislike
exercise
would
value
their
time
at
$9
per
hour,
the
average
hourly
wage,
-whereas
those
who
like
exercise
would
view
it
as
costless,
the
"enjoyment
value"
exactly
canceling
out
the
opportunity
cost
of
time
expended.
Multiplying
these
mon-
etary
values
by
the
survey
proportions
produced
an
average
value
of
$3.57
per
hour
of
exercise
for
the
cohort.
Injury-For
the
direct
medical
cost
of
injury,
we
as-
sumed
that
an
average
office
visit
costs
$40,
and
50
per
cent
of
the
injured
have
an
x-ray
taken,
at
an
average
cost
of
$50.
For
the
indirect
cost,
we
estimated
the
average
hours
of
work
lost
because
of
injury.7
Work
time
lost
is
less
than
one
hour
per
injured
person
per
year,
which
then
multiplied
by
the
average
hourly
wage,
yields
an
estimate
of
$8
per
injured
person
per
year.
Coronary
Heart
Disease-We
used
published
direct
and.
indirect
lifetime
cost
estimates
for
CHD.9
Direct
costs
are
emergency
assistance,
hospitalization,
follow-up
care,
in-
cluding
office
visits,
tests,
and
medications,
and
possible
coronary
angiography
and
coronary
artery
bypass
grafting.
Indirect
costs
are
losses
of
earnings
due
to
disability
and
premature
death.
All
costs
were
adjusted
from
1980
to
1985
dollars.
Measures
of
Effectiveness
To
measure
the
health
effects
of
exercise
programs,
we
calculated
the
expected
number
of
CHD
events
and
the
gain
in
years
of
life
saved
to
allow
comparison
with
other
preventive
or
therapeutic
measures.'2
The
gains
in
years
of
life
expectancy
were
adjusted
for
changes
in
the
quality
of
life
due
to
decreased
morbidity
from
nonfatal
CHD.
We
calcu-
lated
QALYs
by
assuming
that
each
year
which
follows
the
onset
of
a
nonfatal
form
of
CHD
is
equal
to
.8
of
a
healthy
year.
12
We
calculated
QALYs
for
exercise-related
injuries
by
assuming
that
the
quality
of
the
time
spent
while
injured
was
.9
of
an
equivalent
uninjured
time
period.
Sensitivity
Analysis
We
performed
sensitivity
analyses
to
test
several
of
our
assumptions.
First,
we
varied
the
relative
risk
for
a
CHD
event
from
1.5
to
2.5.
In
addition,
we
varied
the
prevalence
of
those
who
exercise
from
10
per
cent
to
20
per
cent;
the
discount
rate
from
0
per
cent
to
5
per
cent;
the
direct
cost
of
exercise
from
$100
to
$200;
the
indirect
cost
of
exercise
from
$2
to
$13.50;
and
the
QALY
weight
from
.7
to
.9.
Alternative
Model
We
have
also
considered
an
alternative
(voluntary)
approach,
which
ultimately
would
target
the
exercise
pro-
gram
at
those
who
consider
it
to
be
enjoyable,
or
are
at
least
neutral.
We
assumed
that
persons
who
start
exercising
do
so
for
a
one-year
trial.
After
that,
those
who
like
it
or
are
neutral
continue,
whereas
those
who
do
not
like
it
quit
permanently.
We
used
probabilities
of
liking
or
disliking
exercise
derived
from
the
expert
survey
and
applied
the
same
cost
assump-
tions.
Analysis
of
Time
Trade-Off
Recent
critiques
of
analysis
of
the
life
expectancy
benefits
of
exercise
have
commented
that
exercisers
con-
sume
as
much
time
in
exercise
as
they
gain
in
life
expectancy.'3
To
examine
this
issue
and
to
provide
another
perspective,
we
determined
the
balance
between
time
spent
on
exercise
and
injuries
and
that
gained
from
CHD
preven-
tion.
In
effect,
this
approach
constitutes
a
time
cost-benefit
analysis
of
exercise.
We
used
the
same
assumptions
as
in
the
base
case
cost-effectiveness
analysis.
Results
Health
Benefits
of
Exercise
Under
the
base
case
assumptions
there
were
78.1
fewer
CHD
events
in
the
exercise
cohort
than
in
the
nonexercisers
(Table
1).
Furthermore,
because
of
gains
in
life
expectancy
and
quality
of
life,
there
were
1,138.3
QALYs
saved
in
the
same
cohort
(529.8
if
discounted)
(Table
2).
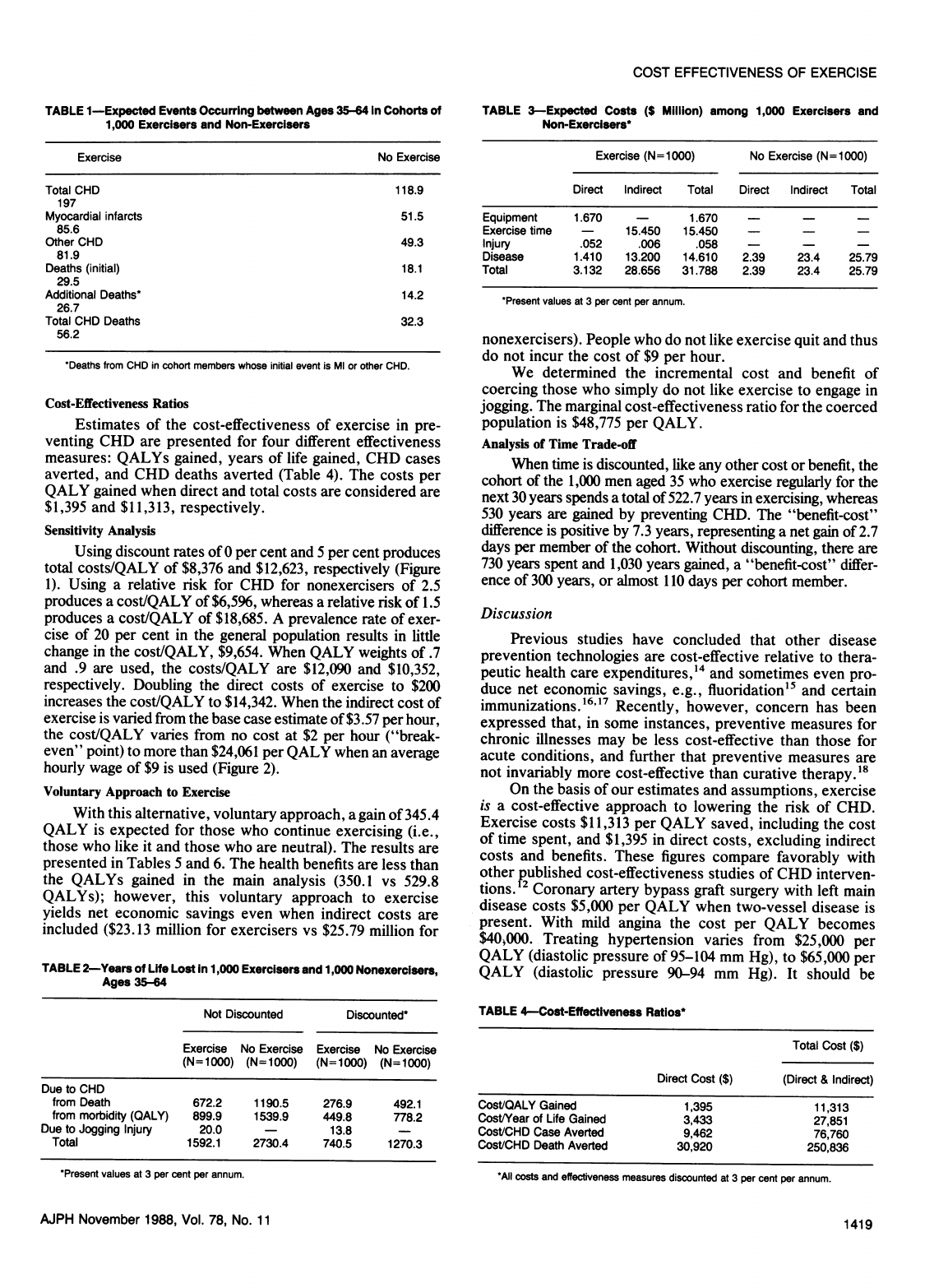
Costs
The
expected
costs
under
the
two
alternatives
are
displayed
in
Table
3.
Accounting
for
the
indicated
direct
and
indirect
costs
of
exercise,
injury,
and
disease,
exercise
does
not
produce
economic
savings.
It
costs
$740,000
more
in
direct
costs
and
$6
million
more
in
total
(direct
and
indirect)
costs
for
the
cohort
of
exercisers.
AJPH
November
1988,
Vol.
78,
No.
11
1418
COST
EFFECTIVENESS
OF
EXERCISE
TABLE
1-Expected
Events
Occurring
between
Ages
35-64
In
Cohorts
of
1,000
Exercisers
and
Non-Exercisers
Exercise
No
Exercise
Total
CHD
118.9
197
Myocardial
infarcts
51.5
85.6
Other
CHD
49.3
81.9
Deaths
(initial)
18.1
29.5
Additional
Deaths*
14.2
26.7
Total
CHD
Deaths
32.3
56.2
*Deaths
from
CHD
in
cohort
members
whose
initial
event
is
Ml
or
other
CHD.
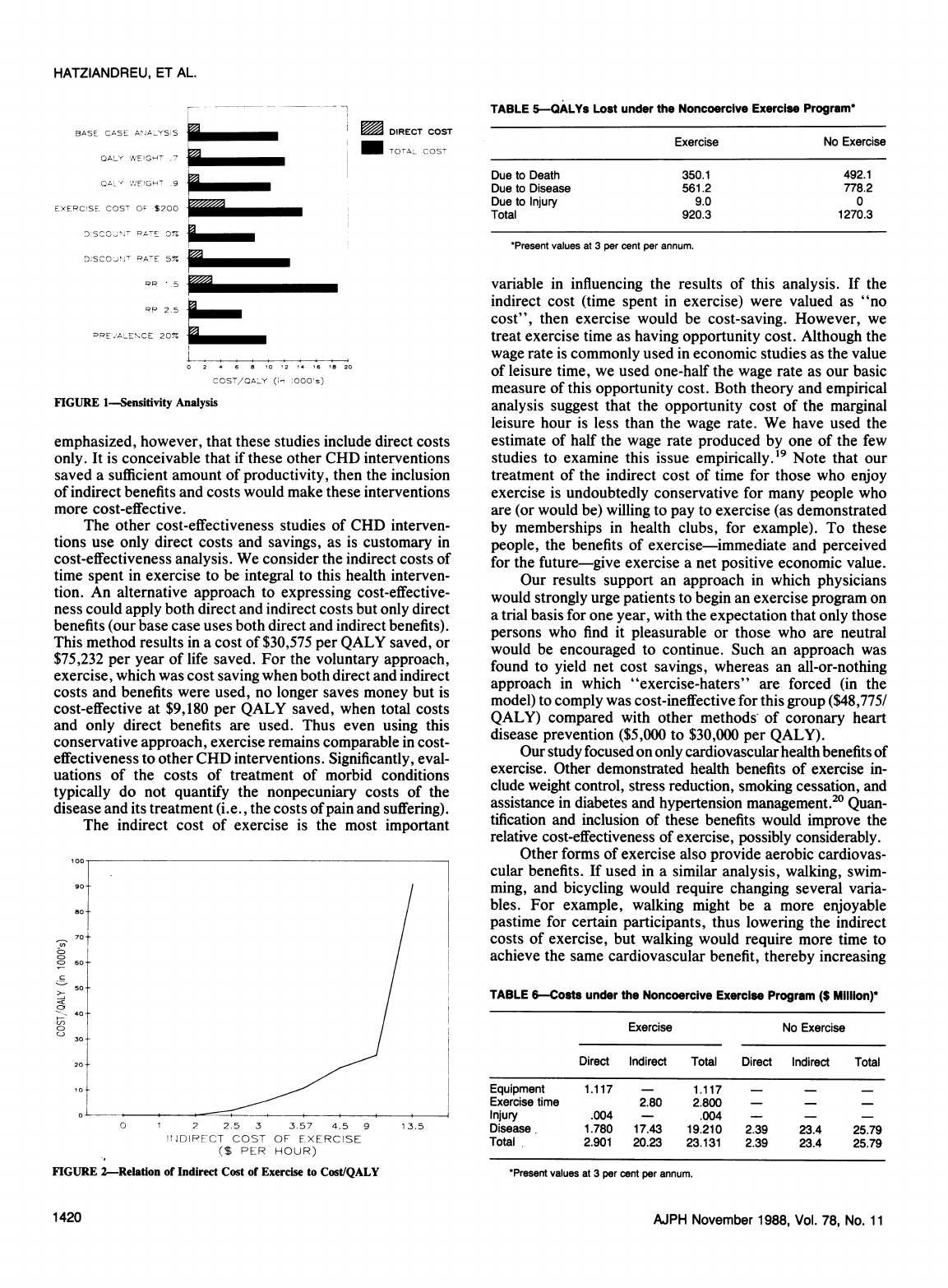
Cost-Effectiveness
Ratios
Estimates
of
the
cost-effectiveness
of
exercise
in
pre-
venting
CHD
are
presented
for
four
different
effectiveness
measures:
QALYs
gained,
years
of
life
gained,
CHD
cases
averted,
and
CHD
deaths
averted
(Table
4).
The
costs
per
QALY
gained
when
direct
and
total
costs
are
considered
are
$1,395
and
$11,313,
respectively.
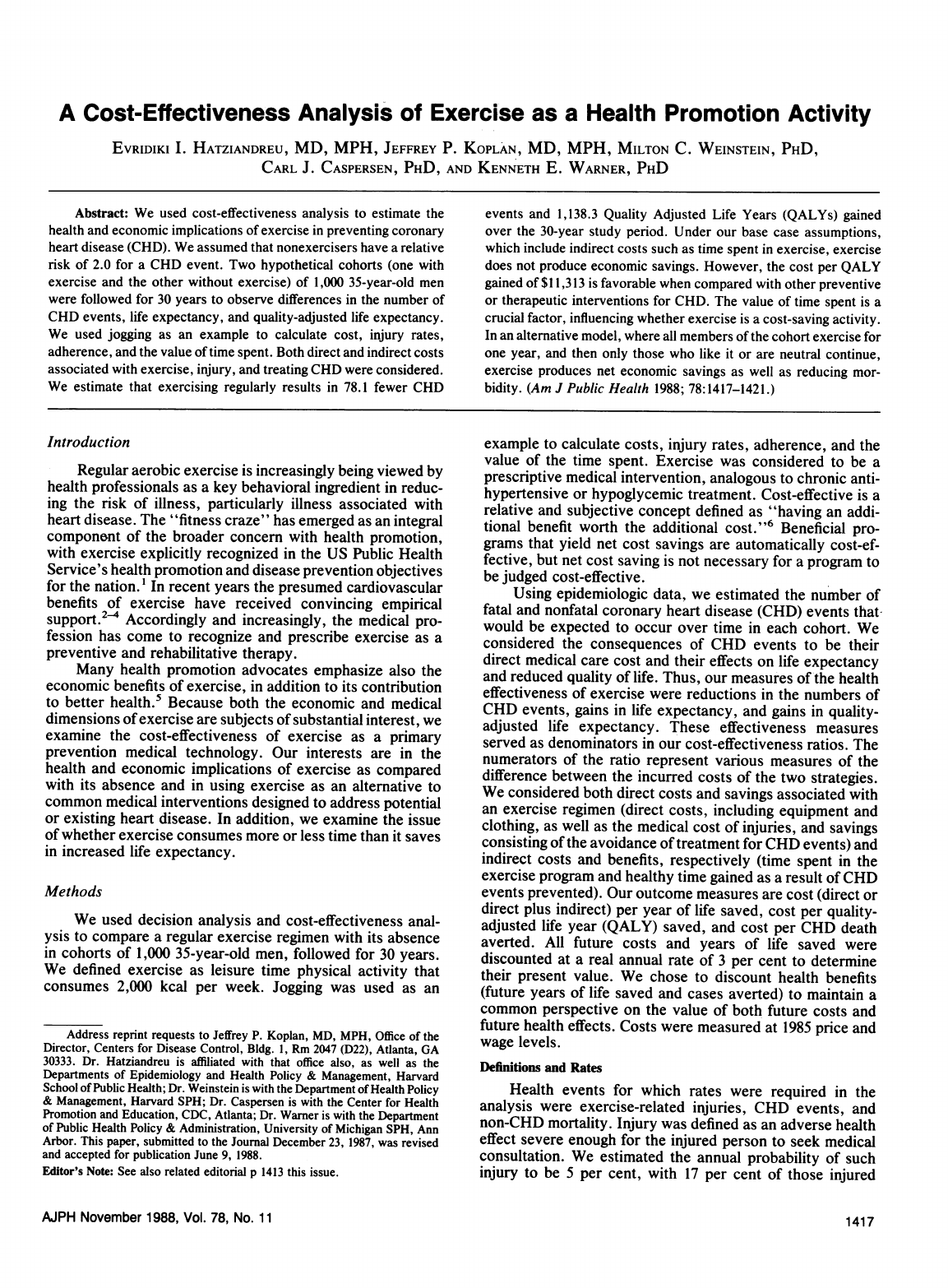
Sensitivity
Analysis
Using
discount
rates
of
0
per
cent
and
5
per
cent
produces
total
costs/QALY
of
$8,376
and
$12,623,
respectively
(Figure
1).
Using
a
relative
risk
for
CHD
for
nonexercisers
of
2.5
produces
a
cost/QALY
of
$6,596,
whereas
a
relative
risk
of
1.5
produces
a
cost/QALY
of
$18,685.
A
prevalence
rate
of
exer-
cise
of
20
per
cent
in
the
general
population
results
in
little
change
in
the
cost/QALY,
$9,654.
When
QALY
weights
of
.7
and
.9
are
used,
the
costs/QALY
are
$12,090
and
$10,352,
respectively.
Doubling
the
direct
costs
of
exercise
to
$200
increases
the
cost/QALY
to
$14,342.
When
the
indirect
cost
of
exercise
is
varied
from
the
base
case
estimate
of
$3.57
per
hour,
the
cost/QALY
varies
from
no
cost
at
$2
per
hour
("break-
even"
point)
to
more
than
$24,061
per
QALY
when
an
average
hourly
wage
of
$9
is
used
(Figure
2).
Voluntary
Approach
to
Exercise
With
this
alternative,
voluntary
approach,
a
gain
of
345.4
QALY
is
expected
for
those
who
continue
exercising
(i.e.,
those
who
like
it
and
those
who
are
neutral).
The
results
are
presented
in
Tables
5
and
6.
The
health
benefits
are
less
than
the
QALYs
gained
in
the
main
analysis
(350.1
vs
529.8
QALYs);
however,
this
voluntary
approach
to
exercise
yields
net
economic
savings
even
when
indirect
costs
are
included
($23.13
million
for
exercisers
vs
$25.79
million
for
TABLE
2-Years
of
Life
Lost
in
1,000
Exercisers
and
1,000
Nonexercisers,
Ages
35-64
Not
Discounted
Discounted*
Exercise
No
Exercise
Exercise
No
Exercise
(N=
1000)
(N=
1000)
(N=
1000)
(N=
1000)
Due
to
CHD
from
Death
672.2
1190.5
276.9
492.1
from
morbidity
(QALY)
899.9
1539.9
449.8
778.2
Due
to
Jogging
Injury
20.0
-
13.8
-
Total
1592.1
2730.4
740.5
1270.3
'Present
values
at
3
per
cent
per
annum.
TABLE
3-Expected
Costs
($
Million)
among
1,000
Exercisers
and
Non-Exercisers*
Exercise
(N=1000)
No
Exercise
(N=1000)
Direct
Indirect
Total
Direct
Indirect
Total
Equipment
1.670
-
1.670
-
Exercise
time
-
15.450
15.450
-
-
-
Injury
.052
.006
.058
-
-
-
Disease
1.410
13.200
14.610
2.39
23.4
25.79
Total
3.132
28.656
31.788
2.39
23.4
25.79
'Present
values
at
3
per
cent
per
annum.
nonexercisers).
People
who
do
not
like
exercise
quit
and
thus
do
not
incur
the
cost
of
$9
per
hour.
We
determined
the
incremental
cost
and
benefit
of
coercing
those
who
simply
do
not
like
exercise
to
engage
in
jogging.
The
marginal
cost-effectiveness
ratio
for
the
coerced
population
is
$48,775
per
QALY.
Analysis
of
Time
Trade-off
When
time
is
discounted,
like
any
other
cost
or
benefit,
the
cohort
of
the
1,000
men
aged
35
who
exercise
regularly
for
the
next
30
years
spends
a
total
of
522.7
years
in
exercising,
whereas
530
years
are
gained
by
preventing
CHD.
The
"benefit-cost"
difference
is
positive
by
7.3
years,
representing
a
net
gain
of
2.7
days
per
member
of
the
cohort.
Without
discounting,
there
are
730
years
spent
and
1,030
years
gained,
a
"benefit-cost"
differ-
ence
of
300
years,
or
almost
110
days
per
cohort
member.
Discussion
Previous
studies
have
concluded
that
other
disease
prevention
technologies
are
cost-effective
relative
to
thera-
peutic
health
care
expenditures,'4
and
sometimes
even
pro-
duce
net
economic
savings,
e.g.,
fluoridation15
and
certain
immunizations.
16"7
Recently,
however,
concern
has
been
expressed
that,
in
some
instances,
preventive
measures
for
chronic
illnesses
may
be
less
cost-effective
than
those
for
acute
conditions,
and
further
that
preventive
measures
are
not
invariably
more
cost-effective
than
curative
therapy.'8
On
the
basis
of
our
estimates
and
assumptions,
exercise
is
a
cost-effective
approach
to
lowering
the
risk
of
CHD.
Exercise
costs
$11,313
per
QALY
saved,
including
the
cost
of
time
spent,
and
$1,395
in
direct
costs,
excluding
indirect
costs
and
benefits.
These
figures
compare
favorably
with
other
published
cost-effectiveness
studies
of
CHD
interven-
tions.'2
Coronary
artery
bypass
graft
surgery
with
left
main
disease
costs
$5,000
per
QALY
when
two-vessel
disease
is
present.
With
mild
angina
the
cost
per
QALY
becomes
$40OOO.
Treating
hypertension
varies
from
$25,000
per
QALY
(diastolic
pressure
of
95-104
mm
Hg),
to
$65,000
per
QALY
(diastolic
pressure
90-94
mm
Hg).
It
should
be
TABLE
4-Cost-Effectiveness
Ratios*
Total
Cost
($)
Direct
Cost
($)
(Direct
&
Indirect)
CosVQALY
Gained
1,395
11,313
Cost/Year
of
Life
Gained
3,433
27,851
CosVCHD
Case
Averted
9,462
76,760
CosVCHD
Death
Averted
30,920
250,836
*All
costs
and
effectiveness
measures
discounted
at
3
per
cent
per
annum.
AJPH
November
1988,
Vol.
78,
No.
11
1419
HATZIANDREU,
ET
AL.
BASE
CASE
ANIALYSIS
OALY
WNEIGHT
.7
Q
AY
',W
E
IGHT
9
EXEPCISE
COST
OF
S200
O'SCO_"'J7
RATE
0%,
DISCO,J>T
PATE
5%
PP
7.5
m
DIRECT
COST
M
TOTAL
COST
RP2.5
-
PREVALENCE
20%
C
A
000
)I
0
2
4
6
8
no
12
14
16
18
20
COS7/C;A'Y
(in
lOOO
s)
FIGURE
1-Sensitivity
Analysis
emphasized,
however,
that
these
studies
include
direct
costs
only.
It
is
conceivable
that
if
these
other
CHD
interventions
saved
a
sufficient
amount
of
productivity,
then
the
inclusion
of
indirect
benefits
and
costs
would
make
these
interventions
more
cost-effective.
The
other
cost-effectiveness
studies
of
CHD
interven-
tions
use
only
direct
costs
and
savings,
as
is
customary
in
cost-effectiveness
analysis.
We
consider
the
indirect
costs
of
time
spent
in
exercise
to
be
integral
to
this
health
interven-
tion.
An
alternative
approach
to
expressing
cost-effective-
ness
could
apply
both
direct
and
indirect
costs
but
only
direct
benefits
(our
base
case
uses
both
direct
and
indirect
benefits).
This
method
results
in
a
cost
of
$30,575
per
QALY
saved,
or
$75,232
per
year
of
life
saved.
For
the
voluntary
approach,
exercise,
which
was
cost
saving
when
both
direct
and
indirect
costs
and
benefits
were
used,
no
longer
saves
money
but
is
cost-effective
at
$9,180
per
QALY
saved,
when
total
costs
and
only
direct
benefits
are
used.
Thus
even
using
this
conservative
approach,
exercise
remains
comparable
in
cost-
effectiveness
to
other
CHD
interventions.
Significantly,
eval-
uations
of
the
costs
of
treatment
of
morbid
conditions
typically
do
not
quantify
the
nonpecuniary
costs
of
the
disease
and
its
treatment
(i.e.,
the
costs
of
pain
and
suffering).
The
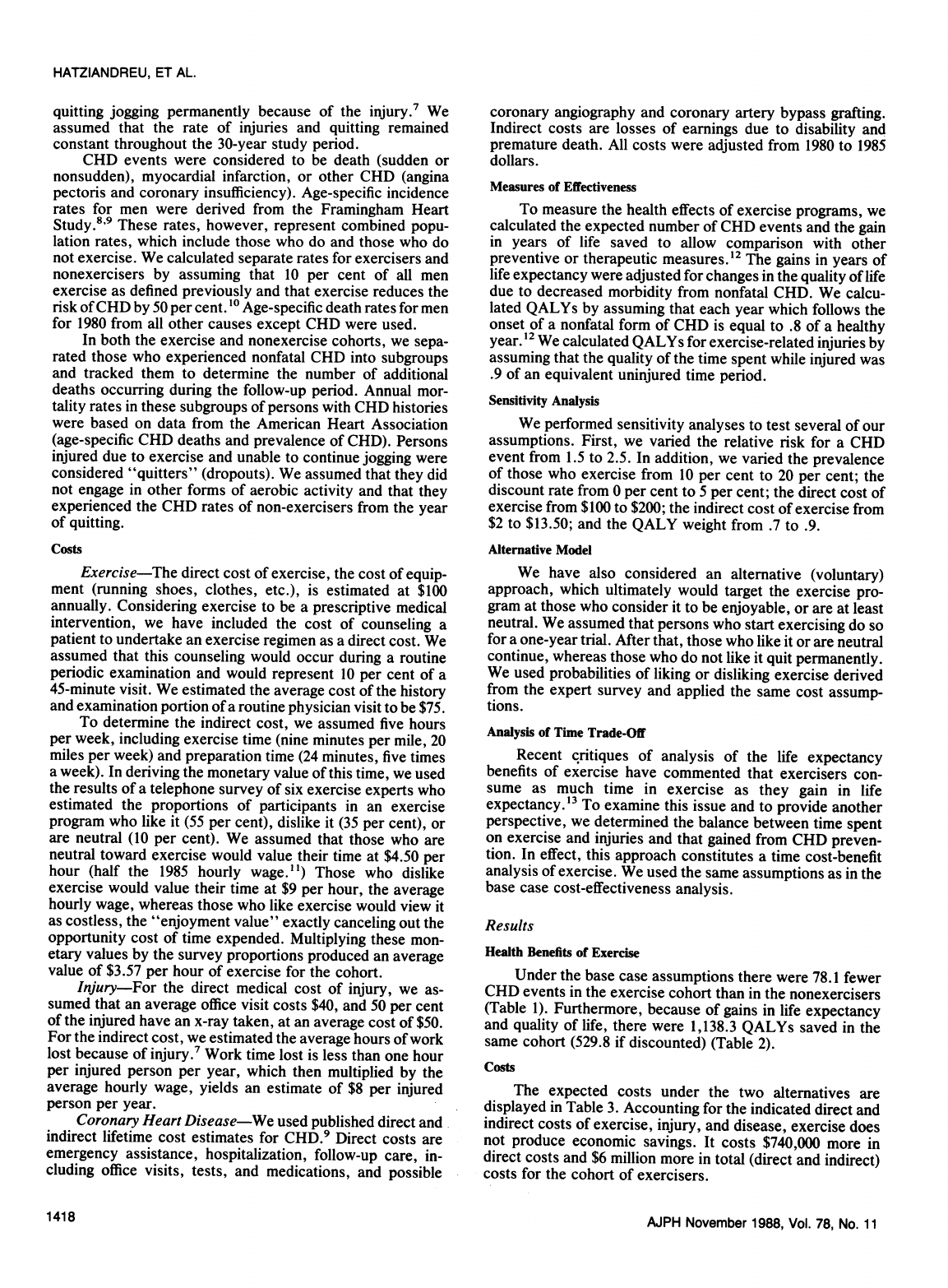
indirect
cost
of
exercise
is
the
most
important
100--
90-
/
70
s-
CD
60-
X
0
1
2
2.5
3
3.57
4.5
9
1
3.5
IIIDIRECT
COST
OF
EXERCISE
($
PER
HOUR)
FIGURE
-Relation
of
Indirect
Cost
of
Exercise
to
Cost/QALY
TABLE
5-QALYs
Lost
under
the
Noncoercive
Exercise
Program*
Exercise
No
Exercise
Due
to
Death
350.1
492.1
Due
to
Disease
561.2
778.2
Due
to
Injury
9.0
0
Total
920.3
1270.3
*Present
values
at
3
per
cent
per
annum.
variable
in
influencing
the
results
of
this
analysis.
If
the
indirect
cost
(time
spent
in
exercise)
were
valued
as
"no
cost",
then
exercise
would
be
cost-saving.
However,
we
treat
exercise
time
as
having
opportunity
cost.
Although
the
wage
rate
is
commonly
used
in
economic
studies
as
the
value
of
leisure
time,
we
used
one-half
the
wage
rate
as
our
basic
measure
of
this
opportunity
cost.
Both
theory
and
empirical
analysis
suggest
that
the
opportunity
cost
of
the
marginal
leisure
hour
is
less
than
the
wage
rate.
We
have
used
the
estimate
of
half
the
wage
rate
produced
by
one
of
the
few
studies
to
examine
this
issue
empirically.t9
Note
that
our
treatment
of
the
indirect
cost
of
time
for
those
who
enjoy
exercise
is
undoubtedly
conservative
for
many
people
who
are
(or
would
be)
willing
to
pay
to
exercise
(as
demonstrated
by
memberships
in
health
clubs, for
example).
To
these
people,
the
benefits
of
exercise-immediate
and
perceived
for
the
future-give
exercise
a
net
positive
economic
value.
Our
results
support
an
approach
in
which
physicians
would
strongly
urge
patients
to
begin
an
exercise
program
on
a
trial
basis
for
one
year,
with
the
expectation
that
only
those
persons
who
find
it
pleasurable
or
those
who
are
neutral
would
be
encouraged
to
continue.
Such
an
approach
was
found
to
yield
net
cost
savings,
whereas
an
all-or-nothing
approach
in
which
"exercise-haters"
are
forced
(in
the
model)
to
comply
was
cost-ineffective
for
this
group
($48,775/
QALY)
compared
with
other
methods
of
coronary
heart
disease
prevention
($5,000
to
$30,000
per
QALY).
Our
study
focused
on
only
cardiovascular
health
benefits
of
exercise.
Other
demonstrated
health
benefits
of
exercise
in-
clude
weight
control,
stress
reduction,
smoking
cessation,
and
assistance
in
diabetes
and
hypertension
management.20
Quan-
tification
and
inclusion
of
these
benefits
would
improve
the
relative
cost-effectiveness
of
exercise,
possibly
considerably.
Other
forms
of
exercise
also
provide
aerobic
cardiovas-
cular
benefits.
If
used
in
a
similar
analysis,
walking,
swim-
ming,
and
bicycling
would
require
changing
several
varia-
bles.
For
example,
walking
might
be
a
more
enjoyable
pastime
for
certain
participants,
thus
lowering
the
indirect
costs
of
exercise,
but
walking
would
require
more
time
to
achieve
the
same
cardiovascular
benefit,
thereby
increasing
TABLE
6-Costs
under
the
Noncoercive
Exercise
Program
($
Million)*
Exercise
No
Exercise
Direct
Indirect
Total
Direct
Indirect
Total
Equipment
1.117
-
1.117
-
Exercise
time
2.80
2.800
-
Injury
.004
-
.004
-
-
-
Disease.
1.780
17.43
19.210
2.39
23.4
25.79
Total
2.901
20.23
23.131
2.39
23.4
25.79
TPresent
values
at
3
per
cent
per
annum.
A1JPH
November
1988,
Vol.
78,
No.
11
1
1
420
m
..m
COST
EFFECTIVENESS
OF
EXERCISE
the
indirect
costs.
It
would
likely
also
reduce
the
direct
costs
of
injury
caused
by
the
exercise.
Our
study
focused
exclusively
on
35-year-old
men
fol-
lowed
for
30
years.
Further
studies
in
exercise
cost-effec-
tiveness
could
consider
women,
various
racial,
ethnic
or
socioeconomic
groups,
other
forms
of
exercise,
and
other
health
benefits.
Adherence
to
an
exercise
regimen
would
affect
the
results
of
this
analysis
just
as
would
adherence
to
a
drug
therapy.
Partial
adherence
would
reduce
the
cost
(indirect)
of
exercise
and
the
injury
rate
but
also
the
cardio-
vascular
benefits
conferred
by
exercis'e.
Thus,
additional
aspects
that
could
be
studied
would
be
to
vary
adherence
and
the
number
of
years
of
participation
in
an
exercise
program.
In
another
analysis
of
the
health
benefits
of
exercise,
Paffenbarger
et
al,2'
estimated
that
exercise
adds
2.15
years
to
the
life
expectancy.
If
we
change
some
of
the
assumptions
in
our
analysis
(no
discounting,
full
adherence,
and
no
QALY
adjustment),
the
total
years
gained
for
the
cohort
are
1,500,
which
is
1.5
years
per
person.
The
difference
can
be
attrib-
uted
to
the
fact
that
Paffenbarger,
et
al,
looked
at
mortality
from
all
causes
from
a
very
specific
cohort
(Harvard
alumni),
whereas
we
looked
at
increases
in
life
expectancy
by
pre-
venting
CHD
only,
using
national
estimates.
To
perform
this
analysis
we
have
had
to
make
several
assumptions
and
use
the
best
available
data.
The
analysis
can
be
improved
in
the
future
as
more
knowledge
is
gained
on
exercise
and
CHD,
and
then
applied
in
a
systematic
and
analytic
framework.
For
persons
who
enjoy
the
immediate
pleasure
and
benefits
of
exercise,
this
activity
is
probably
also
a
cost-
effective
measure
in
reducing
risks
of
CHD.
For
others
who
find
exercise
a
less
pleasant
activity,
its
cost-effectiveness
is
comparable
to
that
of
some
drug
therapies
and
surgical
interventions.
12
Most
persons
logically
would
prefer
to
pre-
vent
a
morbid
condition
rather
than
develop
it
and
have
it
treated.
However,
they
may
require
more
immediate
satis-
faction
to
undertake
and
maintain
a
regular
exercise
regimen
than
the
knowledge
that
it
will
reduce
their
long-term
risk
of
CHD
or
that
it
is
"cost-effective."
ACKNOWLEDGMENTS
We
thank
Gerald
Oster,
PhD,
Policy
Analysis,
Inc.,
and
Nancy
Haas
of
the
American
Heart
Association
for
providing
data
used
in
the
analysis.
This
study
was
presented
at
International
Society
for
Health
Technology
Assess-
ment
Meeting,
Boston,
June
1988.
REFERENCES
1.
US
Department
of
Health
and
Human
Services:
Promoting
Health/
Preventing
Disease.
Objectives
for
the
Nation.
Washington,
DC:
Govt
Printing
Office,
1980.
2.
Paffenbarger
RS
Jr,
Hyde
RT,
Wing
AL,
Steinmetz
CH:
A
natural
history
of
athleticism
and
cardiovascular
health.
JAMA
1984;
252:491-495.
3.
Salonen
JT,
Puska
P,
Tuomilento
J,
et
al:
Physical
activity
and
risk
of
myocardial
infarction,
cerebral
stroke
and
death:
A
longitudinal
study
in
Eastern
Finland.
Am
J
Epidemiol
1982;
115:526-537.
4.
Donahue
RP,
Abbott
RD,
Reed
DM,
Yano
K:
Physician
activity
and
coronary
heart
disease
in
middle-aged
and
elderly
men:
The
Honolulu
Heart
Program.
Am
J
Public
Health
1988;
78:683-685.
5.
Herzlinger
RE,
Calkins
D:
How
companies
tackle
health
care
costs:
part
III.
Harvard
Bus
Rev
1986;
64:70-80.
6.
Doubilet
P,
Weinstein
MC,
McNeil
BJ:
Use
and
misuse
of
the
term
"cost
effective"
in
medicine.
N
Engl
J
Med
1986;
314:253-256.
7.
Koplan
JP,
Powell
KE,
Sikes
RK,
et
al:
An
epidemiologic
study
of
the
benefit
and
risk
of
running.
JAMA
1982;
248:3118-3121.
8.
Shurtleff
D:
Section
30.
Some
characteristics
related
to
the
incidence
of
cardiovascular
disease
and
death.
Framingham
Study,
an
18
year
fol-
low-up.
In:
Kannel
WB,
Gordon
T
(eds):
The
Framingham
Study:
An
epidemiologic
investigation
of
cardiovascular
disease.
DHEW
Pub.
No.
(NIH)
74-599.
Bethesda,
MD:
Public
Health
Service,
1976.
9.
Oster
G,
Epstein
AM:
Primary
prevention
and
coronary
heart
disease:
The
economic
benefit
of
lowering
serum
cholesterol.
Am
J
Public
Health
1986;
76:647-656.
10.
Powell
KE,
Thompson
PD,
Caspersen
CJ,
Kendrick
JS:
Physical
activity
and
the
incidence
of
coronary
heart
disease.
Annu
Rev
Public
Health
1987;
8:253-287.
11.
Statistical
abstract
of
the
United
States:
1981,
ed
102.
Washington,
DC:
US
Bureau
of
the
Census,
1981.
12.
Weinstein
MC,
Stason
WB:
Cost-effectiveness
of
intervention
to
pre-
vent
or
treat
coronary
heart
disease.
Annu
Rev
Public
Health
1985;
6:41-
63.
13.
Jacoby
DB:
Letter
to
the
Editor.
N
Engl
J
Med
1986;
315:399.
14.
Eddy
DM:
The
economics
of
cancer
prevention
and
detection:
Getting
more
for
less.
Cancer
1981;
47(5
Suppl):1200-1209.
15.
Davies
GN:
Cost
and
benefit
of
fluoride
in
the
prevention
of
dental
caries.
WHO
pub.
No.
9.
Geneva:
WHO,
1974;
91.
16.
Koplan
JP,
Axnick
NW:
Benefits,
risks
and
costs
of
viral
vaccines.
Prog
Med
Virol
1982;28:180-191.
17.
Willems
JS,
Sanders
CR:
Cost-effectiveness
and
cost-benefit
analyses
of
vaccines.
J
Infect
Dis
1981;
166:486-493.
18.
Russell
L:
Is
prevention
better
than
cure?
Washington,
DC:
Brookings
Institution,
1986.
19.
Gramlich
EM:
Benefit-cost
analysis
of
government
programs.
Englewood
Cliffs,
NJ:
Prentice-Hall,
1981;
74.
20.
Mason
JO,
Powell
KE:
Physical
activity,
behavioral
epidemiology,
and
public
health.
Public
Health
Rep
1985;
100:113-115.
21.
Paffenbarger
RS
Jr,
Hyde
RT,
Wing
AL,
Hsieh
C:
Physical
activity,
all
cause
mortality,
and
longevity
of
college
alumni.
N
Engl
J
Med
1986;
314:
605-613.
Future
APHA
Meeting
Dates/Sites
1988
NOVEMBER
13-17
BOSTON,
MASSACHUSETTS
1989
OCTOBER
22-26
CHICAGO,
ILLINOIS
1990
SEPTEMBER
30-OCTOBER
4
NEW
YORK,
NEW
YORK
1991
NOVEMBER
10-14
ATLANTA,
GEORGIA
1992
NOVEMBER
8-12
WASHINGTON,
DC
1993
OCTOBER
24-28
SAN
FRANCISCO,
CALIFORNIA
1994
OCTOBER
30-NOVEMBER
3
WASHINGTON,
DC
1995
NOVEMBER
12-16
SEATTLE,
WASHINGTON
AJPH
November
1988,
Vol.
78,
No.
11
1421
