
COMMUNITY HEALTH NEEDS ASSESSMENT
IMPLEMENTATION STRATEGY PLAN
2019

ABOUT THE IMPLEMENTATION STRATEGY PLAN
This Implementation Strategy Plan for NYC Health + Hospitals has been prepared to comply with federal
tax law requirements set forth in Internal Revenue Code section 501(r) requiring hospital facilities owned
and operated by an organization described in Code section 501(c)(3) to conduct a Community Health Needs
Assessment (CHNA) at least once every three years and adopt an Implementation Strategy Plan to meet the
community health needs identied in the CHNA. This Implementation Strategy Plan is intended to satisfy
each of the applicable requirements set forth in proposed regulations.
The following hospitals, organized by county, serve the communities addressed in this Implementation
Strategy Plan:
Bronx
• NYC Health + Hospitals/Jacobi
• NYC Health + Hospitals/Lincoln
• NYC Health + Hospitals/North
Central Bronx
Brooklyn
• NYC Health + Hospitals/Coney Island
• NYC Health + Hospitals/Kings County
• NYC Health + Hospitals/Woodhull
Manhattan
• NYC Health + Hospitals/Bellevue
• NYC Health + Hospitals/Harlem
• NYC Health + Hospitals/Henry J. Carter
Long-Term Acute Care
• NYC Health + Hospitals/Metropolitan
Queens
• NYC Health + Hospitals/Elmhurst
• NYC Health + Hospitals/Queens
A digital copy of the Community Health Needs Asessment is available: https://www.nychealthandhospitals.org/publications-re-
ports/2019-community-health-needs-assessment
A digital copy of this Implementation Strategy Plan is available: https://www.nychealthandhospitals.org/publications-reports/2019-implemen-
tation-strategy-plan
Community input is encouraged. Please address CHNA ISP feedback to [email protected]g
For additional information on available services visit http://www.nychealthandhospitals.org
For information on insurance coverage visit: http://www.nychealthandhospitals.org/insurance

TABLE OF CONTENTS
INTRODUCTION ...............................................................................................................................................................................................6
IMPLEMENTATION STRATEGY ........................................................................................................................................................................ 7
APPROACH…… ........................................................................................................................................................................................7
STRATEGIC FRAMEWORK .......................................................................................................................................................................7
ADDRESSING PRIORITY HEALTH NEEDS...............................................................................................................................................8
REDUCING THE BURDEN OF LIFE CYCLE-DRIVEN ILLNESS AND HEALTH EQUITY CHALLENGES ......................................8
REDESIGNING HEALTH CARE FOR COMMUNITIES
RETHINKING HEALTH CARE SYSTEMS .................................................................................................................................10
AN INFRASTRUCTURE FOR SCALING ..................................................................................................................................12
LOOKING FORWARD .....................................................................................................................................................................................14
BUILDING HEALTHY COMMUNITIES ....................................................................................................................................................14
RESOURCE COMMITMENT ...................................................................................................................................................................14
EVALUATION............................................................................................................................................................................................14
NOTES AND REFERENCES…. ........................................................................................................................................................... 15
ACKNOWLEDGMENTS ...................................................................................................................................................................... 16
APPENDICES
GLOSSARY OF NYC HEALTH + HOSPITALS TRANSFORMATIVE INITIATIVES AND PROGRAMS ........................................... 18
NYC HEALTH + HOSPITALS TRANSFORMATIVE INITIATIVES AND PROGRAMS BY BOROUGH ............................................ 28
PROPOSED SOLUTIONS FOR CONSIDERATION ..................................................................................................................... 33

4
About NYC Health + Hospitals
As the largest public health care system in the U.S., NYC Health + Hospitals’
mission is to deliver high-quality health care services to all New Yorkers with
compassion, dignity and respect, without exception. The system is an anchor
institution for the ever-changing communities it serves, providing hospital
and trauma care, neighborhood health centers, skilled nursing facilities and
community care, including care coordination and home care. NYC Health
+ Hospitals serves as a preeminent teaching facility and as a designated
treatment center for the U.S. President.
4

5
11
hospitals
+70
community centers
5
skilled nursing
facilities
1
long-term acute
care hospital
Over
1.1 million
New
Yorkers
served
annually
+40K
employees
correctional
health services
OneCity Health
OneCity Health is the largest Performing
Provider System (PPS) in New York State,
formed under the auspices of the Delivery
System Reform Incentive Payment (DSRIP)
program, comprising hundreds of
health care providers, community-based
organizations and health systems.
HHC ACO
The HHC Accountable Care Organization
(ACO) is a collaborative venture including
physician afliate organizations, NYC
Health + Hospitals acute care, outpatient
and skilled nursing facilities, as well as
teaching administration, quality assurance
and supervisory services.
MetroPlus
The NYC Health + Hospitals health
plan, MetroPlus, provides low to no-cost
health insurance to eligible New Yorkers
across the ve boroughs. Earning 5 out
of 5 stars, MetroPlus is a top health plan
in New York State.
+750k Medicaid lives
+200 partners
+10k Medicare lives
8 partners
+500k lives
5
5
level I trauma centers
1
level II trauma center
1
level II pediatric
trauma center

6
INTRODUCTION
As the largest public health care system in the United States and
an anchor institution in communities throughout New York City,
NYC Health + Hospitals delivers high-quality health services with
compassion, dignity and respect to all, without exception. Many
of the people served by NYC Health + Hospitals experience an
outsized chronic and behavioral disease burden, as reected in
previous community health needs assessments (CHNAs). These
health outcomes are partly driven by long standing structural
inequities such as entrenched racism and sexism, neighborhood
income, access to quality, affordable housing, access to healthy,
affordable food, safe places for physical activity and social
support.
1-6
As a leading health care provider and employer,
NYC Health + Hospitals directly responds to these issues
through investments in services to unite and elevate
communities. As a result of strategic investments through the
system’s transformation plan and New York State’s Delivery
System Reform Incentive Payment (DSRIP) program, health
trajectories of the communities served by NYC Health +
Hospitals have improved. These investments have strengthened
primary and preventive care, boosted health coverage for
New Yorkers, modernized health care delivery system-wide and
enabled crucial innovative partnerships with community-based
providers and organizations. However, challenges persist.
In 2019, NYC Health + Hospitals completed a CHNA to
identify, better understand and prioritize the health needs of
the communities served. The CHNA process was conducted
by OneCity Health, the NYC Health + Hospitals Performing
Provider System (PPS). OneCity Health utilized a multi-
stakeholder approach to identify system-wide population health
needs as well as the local needs of the diverse neighborhoods
served. Findings from the CHNA were driven by a combination
of quantitative and qualitative data from over 450 community
surveys, 16 inclusive community forums held at NYC Health
+ Hospitals facilities and more than 60 expert interviews with
system leadership and community stakeholders.
Two priority health needs were identied in the 2019 CHNA:
1. Reducing the burden of life cycle-driven illness and
health equity challenges
2. Redesigning health care for communities:
a) Rethinking health care systems
b) An infrastructure for scaling
The CHNA was approved and adopted by the NYC Health +
Hospitals Board of Directors in June 2019.
This Implementation Strategy Plan (ISP) describes the
transformative initiatives and programs NYC Health + Hospitals
and its community partners have or will implement to address
the priority health needs identied in the 2019 CHNA.
Continuous evaluation and monitoring of these initiatives and
programs and NYC Health + Hospitals’ overall strategic focus
will be developed to ensure they are improving health equity in
communities served. This report can also be used as a starting
point for individuals to understand the breadth of resources
available to the community.
NYC Health + Hospitals, the largest public health
care system in the United States, serves over
1 million people annually and offers comprehensive,
accessible and affordable health care to all, without
exception. The system’s 11 acute care hospitals and
long term acute care hospital provide top-ranked
trauma care, offer dozens of inpatient specialties
and mental health services and keep communities
healthy through a robust network of primary and
specialty care for children and adults. NYC Health +
Hospitals facilities have earned numerous special
designations for quality and culturally responsive
care and have received top ranks by U.S. News and
World Report.
COMMUNITY DEFINITION
NYC Health + Hospitals serves over 1.1 million
New Yorkers every year across the city’s ve boroughs
and empowers them to live their healthiest life.
The community is dened by vibrant and diverse
neighborhoods.
NYC Health + Hospitals has historically served as the
health care safety net for New Yorkers and cares for
all without exception. In fact, 70% of NYC Health +
Hospitals’ patients are insured by Medicaid or have no
insurance (compared to 40% for voluntary hospitals
throughout New York City).
The system offers 60% of behavioral health services
city-wide while voluntary hospitals have closed or
reduced services in recent years.
7
IMPLEMENTATION STRATEGY
The ISP outlines how NYC Health + Hospitals will address
the priority health needs identied in the 2019 CHNA at both
a system and local level. The report inventories transformative
initiatives and programs underway, as well as solutions the
system will consider moving forward to address the priority
health needs.
APPROACH
To address the priority health needs identied in the 2019
CHNA, OneCity Health brought together interdisciplinary
stakeholders including NYC Health + Hospitals’ system
leadership and front-line facility staff, city agencies and PPS
partners. The ISP was developed through the following
approach:
1. NYC Health + Hospitals catalogued transformative
initiatives and programs underway system-wide and at
each hospital that address the priority health needs of
the communities served.*
2. OneCity Health facilitated multi-stakeholder planning
through three working groups with over 50 participants
representing NYC Health + Hospitals, PPS partner
organizations and city agencies. Working group members
designed and pitched solutions to address the priority
health needs based on their daily experiences serving the
community. Members then prioritized solutions that will be
reviewed by NYC Health + Hospitals executive leadership
through the system’s clinical and business strategic
planning processes.**
3. Looking forward, NYC Health + Hospitals will continue
to invest in programs, services and partnerships that
address the priority health needs of the community. To
ensure services and programs are truly designed through
the lens of the patient and community, NYC Health +
Hospitals will engage community members, including
through its existing Community Advisory Boards (CABs)
and Patient and Family Advisory Councils (PFACs),
and OneCity Health’s growing network of over 200
community-based partners.
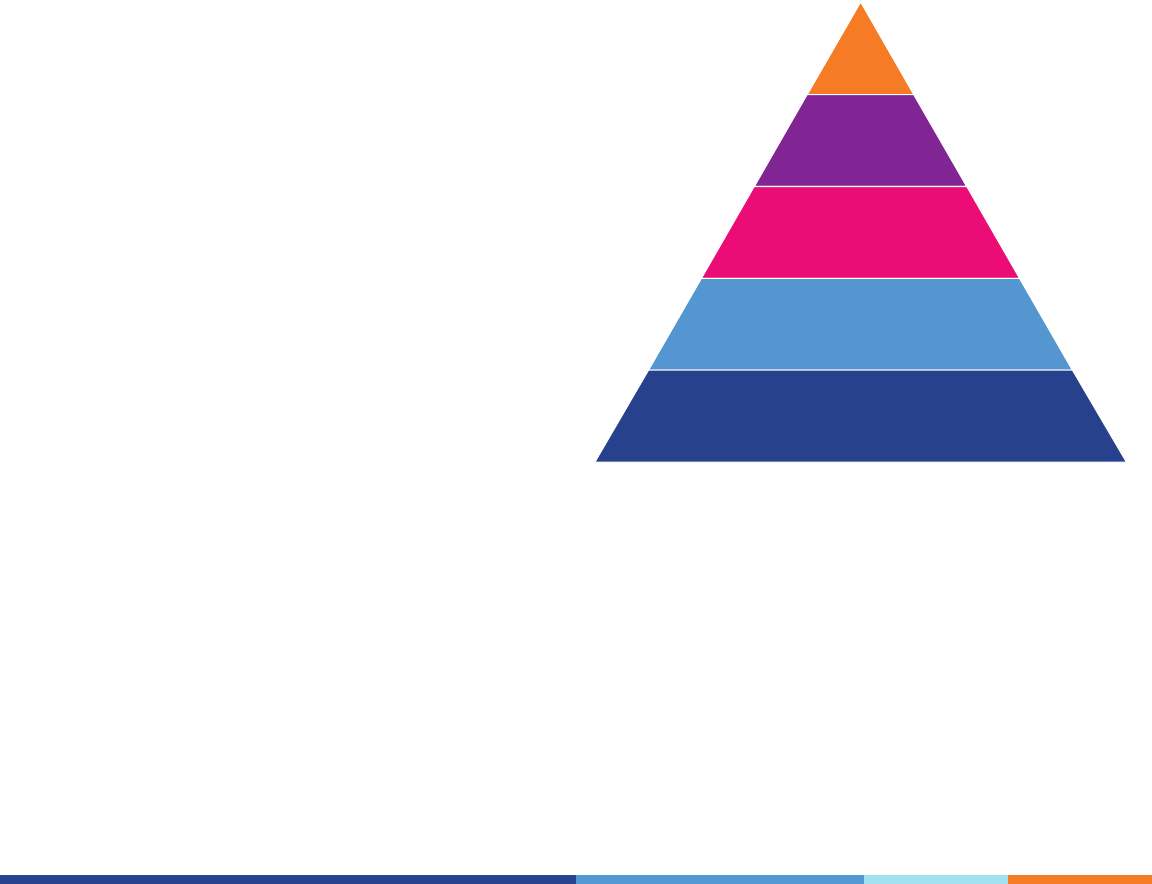
STRATEGIC FRAMEWORK
The NYC Health + Hospitals Strategic Framework demonstrates
how the system’s vision, mission, values and strategic
framework aim to support the patient, family and community
(Figure 1). The goals and tactics in this report are guided
by the strategic framework, which consist of: quality and
outcomes, care experience, nancial sustainability, access to
care and culture of safety. The framework is the foundation
of the system’s vision to be a fully integrated health system,
which requires effective organization of its community assets
and partners including MetroPlus, its health plan, OneCity
Health and the HHC ACO, its Accountable Care Organization,
to improve the overall health of the communities served in a
nancially sustainable manner.
PATIENT,
FAMILY AND
COMMUNITY
VISION
To be a fully integrated
health system that enables
New Yorkers to live their
healthiest lives.
MISSION
To deliver high quality health services
with compassion, dignity, and respect to all,
without exception.
OUR VALUES
ICARE: Integrity, Compassion, Accountability,
Respect and Excellence.
STRATEGIC PILLARS
QUALITY AND CARE FINANCIAL ACCESS CULTURE
OUTCOMES EXPERIENCE SUSTAINABILITY TO CARE OF SAFETY
Figure 1: NYC Health + Hospitals Strategic Framework
*See Appendix: Glossary of NYC Health + Hospitals Transformative Initiatives and Programs on page 18.
**See Appendix: Proposed Solutions for Consideration on page 33.
8
ADDRESSING PRIORITY HEALTH NEEDS
REDUCING THE BURDEN OF LIFE CYCLE-DRIVEN
ILLNESS AND HEALTH EQUITY CHALLENGES
The environmental conditions into which someone is born, plays,
lives, works and ages present social and economic risk factors
that impact health and life expectancy. These factors combined
with the evolution of one’s health throughout their life cycle can
lead to poor health outcomes including airway diseases, heart
disease and diabetes. To ensure every New Yorker has the same
opportunity to live a healthy life, life cycle-driven illness must be
addressed and social and economic risk factors reduced.
Goal: Reduce the burden of life cycle-driven illness and
address health equity challenges
Tactic: Manage the health of patients throughout their
life cycle by engaging them in services to improve health
outcomes across life stages
NYC Health + Hospitals is poised to build long-term relationships
with the community and its patients that can improve health
outcomes throughout the life cycle. The system and its over
70 neighborhood health center, hospital and skilled nursing
facility locations can help community members to build a
strong foundation for life at birth and infancy, establish healthy
behaviors at adolescence and achieve quality of life through
adulthood. By designing structurally competent health care
services embedded with person-centered values and delivered
with cultural humility,patients are better able to engage in their
health on an ongoing rather than episodic basis.
7,8
Further,
providing medical staff with implicit bias training ensures that
all patients receive the same level of care. This approach aims to
signicantly reduce the burden of life cycle-driven illness.
To do this, NYC Health + Hospitals is developing comprehensive
programs, coordinated through primary care, including
integration with specialty care for higher risk patients. For
example, patients with behavioral health needs (e.g. mental
health and substance use disorders) will be able to receive
integrated primary and behavioral health care at a single site
to eliminate the stigma traditionally associated with behavioral
health needs and their treatments. YouthHealth and Pride
Health Centers offer tailored health and social services for
adolescents and patients who identify as LGBTQ to meet their
unique health needs. Further, patients living with or at-risk of
developing diet-related illness or airway diseases can receive a
full range of services through their primary care provider, who
is able to escalate specialty care needs upward through the
interdisciplinary care team.
SPOTLIGHT
DSRIP Home-Based Environmental
Asthma Program
Priority health need addressed: Reducing the burden of life
cycle-driven illness and health equity challenges:
Airway diseases (asthma, COPD)
Since 2017, NYC Health + Hospitals, with the support of OneCity
Health, has provided an integrated home-based asthma program
to pediatric patients with uncontrolled asthma. Starting in 2019,
services expanded to adult patients with asthma and COPD. The
program aims to reduce avoidable hospital visits and improve
patient care by connecting patients to primary and specialty
care, social services and home remediation. In this model,
community health workers partner with patients and providers to
provide a home and environmental asthma assessment, disease-
management education and referrals to social services. Success
is measured by a reduction in avoidable hospital inpatient and
Emergency Department use, increased medication adherence
and connections to primary and specialty care.
.
SPOTLIGHT
Comprehensive Maternal Care and
Pregnancy Prevention Program
Priority health need addressed: Reducing the burden of
life cycle-driven illness and health equity challenges:
Pregnancy and birth outcomes
NYC Health + Hospitals, in partnership with the Mayor’s Ofce,
is implementing a comprehensive maternal care program with
the focus of identifying and responding to pregnancy-related
morbidity and mortality for women of color.
In the Maternal Medical Home, Maternal Care Coordinators
and social workers enhance care by assisting patients who
are at higher risk of developing health problems during their
pregnancy. They help patients to navigate their appointments
and receive supportive services.
#safemomsnyc is a simulation-based program that trains doctors,
nurses and others on the delivery team to respond to the highest
risk emergency situations in the Labor and Birthing suites.
The Interval Pregnancy Optimization program helps to improve
maternal health by training providers to ask patients specically
about pregnancy intention. In this way, the health of the woman
may be optimized before she becomes pregnant.
The Mother-Baby Coordinated Visit program aims to increase
adherence to the postpartum visit by having the patient
scheduled with the baby’s visit.
Further, NYC Health + Hospitals is adopting implicit bias
and anti-racism training and is focusing on a culture that
emphasizes safe and respectful care. Success will be measured
by a reduction in maternal morbidity and mortality outcome
disparities and improved prenatal and postpartum care.
9
Populations facing unique health equity challenges
9
• Adolescent and young adult
• Survivors of domestic violence
• Individuals with food insecurity
• Homeless or individuals with housing instability
• Immigrant
• Incarcerated or previously incarcerated
• LGBTQ
• Pregnant women of color
Tactic: Partner with the community to offer programs and
services that reduce health equity challenges
High-quality clinical care is critical to improving health
outcomes, but this alone cannot close the health equity gaps
often faced by communities served by NYC Health + Hospitals.
Partnerships that enable connections between the health care
and other systems (e.g. criminal justice, foster care, public
housing, shelter, food etc.) are essential to address poor health
outcomes. These services are made available to patients
through the co-location and optimization of referrals. To identify
patients who could benet from these services, NYC Health +
Hospitals offers benets screening and enrollment for health
insurance, food and social services and support for housing
services, legal assistance and income tax ling.
In partnership with real estate developers, the system has
repurposed unused space to offer over 1,300 units of supportive
and affordable housing. In addition, NYC Health + Hospitals
provides clinical care at one-stop NYC Family Justice Centers,
which offers comprehensive care for survivors of domestic
violence. Through DSRIP funding, OneCity Health is investing in
partnerships and programs to address health equity challenges
including food and housing insecurity and health literacy.
SPOTLIGHT
Woodhull Residence | Comunilife
Priority health need addressed: Reducing the burden of
life cycle-driven illness and health equity challenges:
Populations facing unique health equity challenges
NYC Health + Hospitals, in partnership with Comunilife, a
not-for-prot community-based organization specializing in
supportive housing development, launched the Woodhull
Residence in 2019. The brand new 89-unit supportive and
affordable housing residence was converted from a parking lot
located on the NYC Health + Hospitals/Woodhull campus. The
residence provides 54 studio apartments for formerly homeless
adults living with special needs and 35 studio apartments for
low income community residents. Comunilife aims to combat
the outsized chronic and behavioral disease burden among
individuals living with housing instability. Success will be
measured through health outcomes and patient satisfaction.
SPOTLIGHT
Correctional Health Services
Priority health need addressed: Reducing the burden
of life cycle-driven illness and health equity challenges:
Populations facing unique health equity challenges
NYC Health + Hospitals/Correctional Health Services (CHS)
operates one of the nation’s largest correctional health care
systems and provides patients with medical and mental health
care, substance use treatment, dental care and social work
services. Since joining the NYC Health + Hospitals system in
2016, CHS has expanded access to care through telehealth
services, decentralized care services to local detention centers
and enhanced community reentry support services.
10
REDESIGNING HEALTH CARE FOR COMMUNITIES:
RETHINKING HEALTH CARE SYSTEMS
By redesigning the health care system around communities and
patients, providers can more easily treat patients holistically, rather
than treat diseases alone. An empowered patient experience
is one where the patient and provider can build a long-term
relationship and jointly establish clear goals, resulting in a more
approachable, meaningful and personalized health care encounter.
Goal: Improve ease of access to and navigation through
the health system
Tactic: Design services around the end user, the patient –
this includes services that are easy and convenient to access,
structurally competent and delivered with cultural humility
By designing services that respond directly to patient and
provider needs, health care systems can deliver services that
make it easier for patients to engage in care and achieve better
health outcomes. NYC Health + Hospitals has and continues to
expand high-quality preventive and primary health care to more
convenient locations, including plans for three comprehensive
health centers to be opened by the end of 2020. In addition,
over 70 health centers offer after-hours options and new
ExpressCare centers provide walk-in and after-hours urgent care.
The individuals served by NYC Health + Hospitals come from
the different cultures that comprise New York City. The system
continues to be an industry leader in providing structurally
competent health care delivered with cultural humility – including
providing language appropriate services in patients’ preferred
modality. To prevent the chilling effect of Public Charge, NYC
Health + Hospitals continues to assure immigrant communities
that the system remains steadfast in its mission to deliver health
care to all New Yorkers without exception and regardless of
income, immigration or insurance status.
SPOTLIGHT
Expanding access to community-based care
and the Caring Neighborhoods Initiative
Priority health need addressed: Rethinking health care systems:
Ease of access and navigation
Through initial support from the Mayor’s Caring Neighborhoods
Initiative, NYC Health + Hospitals has expanded access to primary
and specialty care in underserved communities at eight new or
renovated sites across New York City. NYC Health + Hospitals
plans to open three new full-service ambulatory care sites by
the end of 2021, which will offer comprehensive, one-stop
ambulatory care and wellness support services. This expansion
will allow the system to serve over 50,000 more New Yorkers.
Success will be measured by patient satisfaction and the number
of patients served.
SPOTLIGHT
ExpressCare
Priority health need addressed: Rethinking health care systems:
Ease of access and navigation
ExpressCare provides the community with a new and
convenient way to access health care through walk-in urgent
care centers. Through ExpressCare, patients are promptly seen
by a provider, connected to primary care and other services
and enrolled in insurance when applicable. The clinical model,
designed in partnership with OneCity Health, supports the
goal of the DSRIP program to reduce avoidable hospital usage,
including unnecessary Emergency Department visits, by 25
percent by 2020. Success is measured through several metrics
including wait times in ExpressCare and number of linkages to
primary care. ExpressCare centers are open at NYC Health +
Hospitals/Lincoln and Elmhurst with plans to expand centers to
other NYC Health + Hospitals sites in the next three years.
SPOTLIGHT
NYC Care
Priority health need addressed: Rethinking health care systems:
Ease of access and navigation
NYC Care ensures that all New Yorkers have access to care
through low and no-cost services offered by NYC Health +
Hospitals. Individuals who cannot afford or are ineligible for
insurance can enroll in NYC Care regardless of immigration
status or ability to pay. NYC Care provides patients and
families with a dedicated primary care provider, connection
to a 24/7 customer service line and access to affordable
medication. The program launched in August 2019 in the
Bronx with plans to expand to all boroughs.
In the rst two months alone, over 5,000 patients were
enrolled. Success is measured by the number of patients
enrolled in and seeking care through the program.
11
Goal: Optimize the patient-provider relationship
Tactic: Improve patient continuity of care with primary care
providers
When patients and providers are able to develop long-term
relationships and achieve continuity of care, patients experience
higher quality care and achieve better health outcomes.
Historically, patients have entered NYC Health + Hospitals
through the Emergency Department, but investments in primary
care providers, stronger linkages to primary care for patients
and enrolling patients in insurance and NYC Care means that
patients can more easily access primary care services and build
relationships with their interdisciplinary care team.
NYC Health + Hospitals is making scheduling easier for patients
by implementing a patient-centered scheduling system,
providing patient continuity with their interdisciplinary care
team and “open access” scheduling options for same-day
appointments. This model accounts for the unpredictable
and busy schedules of individuals served by NYC Health +
Hospitals. Through Epic and eConsult,* the system is enhancing
communication and optimizing access between primary care
providers and specialists and their patients.
Goal: Increase transparency of health care costs for
patients and providers
Tactic: Enable shared decision making between patients
and providers guided by clinical need and value-based care
options rather than nancial constraints
Through the system-wide implementation of Epic H2O, NYC
Health + Hospitals providers will have access to decision
support tools so they can help patients make decisions informed
by clinical effectiveness and costs. Simultaneously, through
Epic MyChart, patients are able to understand how much a
procedure or medication costs and can access easy-to-read
medical bills.
All patients, including those with health care through NYC
Care, can connect to a 24/7 customer service line to understand
how and where to access their dedicated interdisciplinary care
team as well as the cost of care. Access to this level of service is
unprecedented among historically uninsured communities.
SPOTLIGHT
ICARE and person-centered care
Priority health need addressed: Rethinking health care systems:
Patient-provider relationships
ICARE is a system-wide employee value system that aims
to integrate Integrity, Compassion, Accountability, Respect
and Excellence into service delivery, rounding and leadership
development. Through ICARE trainings, this initiative is
increasing staff awareness and engagement in the mission and
vision of NYC Health + Hospitals, with the ultimate goal of
enhancing the patient experience. Success is measured by the
percentage of staff trained in ICARE.
New person-centered care initiatives aim to involve patients, the
interdisciplinary care team and other stakeholders in actively co-
designing solutions specic to local and individual needs.
SPOTLIGHT
Epic
Priority health need addressed: Information sharing
Epic H20, the NYC Health + Hospitals electronic health
record, serves as a unifying platform for communication and
collaboration across NYC Health + Hospitals’ more than 70
locations and partner sites enabling coordinated care as a single
integrated system. Further, Epic H2O improves patient care
through clinicians’ timely access to patients’ complete health
records. Simultaneously, Epic MyChart enables patients access
to their health records allowing them to actively participate in
health care decision-making with their interdisciplinary care
team. Success will be measured by patient satisfaction and
quality of care.
* See page 12.

12
REDESIGNING HEALTH CARE FOR COMMUNITIES:
AN INFRASTRUCTURE FOR SCALING
NYC Health + Hospitals must take advantage of its scale
and reach while tailoring services to the diverse needs of the
communities served. Health care systems should be designed
around the individual patient journey and information should
ow seamlessly between a patient and their interdisciplinary
care team, especially when transitioning between care settings.
To realize the benets of being a system, NYC Health +
Hospitals should continue to build an engaged workforce,
enable information sharing and provide services in a nancially
sustainable way. If systems operate as a system in name-only,
clinical staff have to spend more time navigating separate
entities rather than focusing on patient care and patients have
to navigate fragmented services.
Goal: Build and optimize workforce capacity
Tactic: Increase recruitment and retention of a talented
workforce
With the goal of increasing the preventive and primary care-
focused workforce, NYC Health + Hospitals launched two clinical
recruitment campaigns to identify, recruit and retain clinicians:
Docs4NYC and Nurse4NYC.
NYC Health + Hospitals offers a range of professional
development opportunities to staff including leadership
development and research opportunities to ensure continued
career development. NYC Health + Hospitals also launched
Health Care Administration Scholars and Clinical Leadership
Fellowship programs to develop the next generation of clinical
leaders in the areas of administration, population health
and quality. Through the New York State Care Restructuring
Enhancement Pilot program, administrative and clinical hospital
staff are being trained to serve patients in community-based
settings.
Tactic: Ensure the workforce can work to their highest level
of experience, skills and licensure
NYC Health + Hospitals is maximizing roles within the
interdisciplinary care team to ensure clinicians and support
staff can practice at the top of their licenses to maximize time
spent in direct patient care, population health management
and system-wide quality improvement efforts. The system has
also expanded the use of community health care workers and
peers to support patient navigation and act as extensions of
the interdisciplinary care team by offering communication and
health coaching support in communities. These new care team
members help to build trust, promote information sharing and
optimize time at each clinical visit.
Tactic: Support providers in managing their emotional health
Through the Arts in Medicine and Helping Healers Heal
programs, NYC Health + Hospitals is responding to compassion
fatigue and physician burnout, common in health care providers
and jobs with high emotional stress. These programs help
clinicians continue to connect with patients and offer high-quality,
compassionate care.
SPOTLIGHT
Clinical recruitment campaigns
including Docs4NYC and Nurse4NYC
Priority health need addressed: An infrastructure for scaling:
State of the workforce
To expand access to care, NYC Health + Hospitals launched
two targeted recruitment campaigns for doctors and nurses:
Docs4NYC and Nurse4NYC. The Nurse4NYC campaign focuses
on four high need specialty areas where nurses are needed the
most: ambulatory department; behavioral health; correctional
health services; Emergency Department/Trauma; home care.
These campaigns are supported by social media advertising
on Google, LinkedIn, Facebook and Instagram. Since 2018,
through Docs4NYC, Nurse4NYC and other recruitment efforts,
37 primary care physicians, 426 registered nurses, 229 nursing
support staff and revenue staff were hired. Success will be
measured by the number of patients served.
Goal: Improve communication and information sharing
across patients and providers
Tactic: Ensure more effective communication between
providers and with patients through technology-enabled
platforms
With the system-wide implementation of Epic H2O, patients
and providers will have transparency into the full picture of a
patient’s health and can participate jointly in making health
care decisions. Through Epic MyChart, patients can review
their medical history, book appointments, request prescription
rells and communicate with their interdisciplinary care team.
NYC Health + Hospitals also offers health care maintenance
and appointment reminders via their preferred language and
modality. With eConsult, primary care providers can connect
with specialists and advise patients on a timely basis. Community
providers can also connect to Epic H2O, which fosters patient
access and care coordination beyond the four walls of the
hospital.
13
Goal: Provide services in a way that are nancially
sustainable
Tactic: Enhance revenue opportunities and reduce
administrative expenses
NYC Health + Hospitals is implementing a ve-year nancial
plan consisting of signicant revenue generating and cost-saving
initiatives that aim to bolster the system’s nancial position while
expanding health care services. To date, NYC Health + Hospitals
has closed almost two-thirds of its $1.8 billion projected budget
gap.
Tactic: Prepare the system for a value-based payment
environment
Investments in transformation efforts and the DSRIP program,
which aims to improve access and quality and promote
community-based care, are preparing the system for the shift to
a value-based payment environment. This means increased and
easier access to high-quality holistic care designed to improve
health outcomes at a lower cost and with a better patient
experience.
Tactic: Boost health care and insurance coverage to all
New Yorkers
New York City and NYC Health + Hospitals are guaranteeing
health care for all New Yorkers through NYC Care and efforts
to expand enrollment in MetroPlus. More New Yorkers have
access to primary care providers, integrated clinical services,
coordinated care, prescription drugs and 24/7 customer service
than ever before. This is possible through expanded access to
nancial counselors and to GetCoveredNYC and MetroPlus
health plan enrollers based in facilities and in the community.
SPOTLIGHT
HHC ACO
Priority health needs addressed: An infrastructure for scaling:
Financial sustainability
NYC Health + Hospitals’ Accountable Care Organization (ACO) –
a group of doctors and other providers who coordinate care for
patients under the Medicare Shared Savings Program
(MSSP) – is the only MSSP ACO based in New York State to
earn shared savings for six consecutive years and one of only
18 ACOs around the country to have earned that distinction.
The ACO’s performance demonstrates NYC Health + Hospitals’
ability to provide quality patient care at a lower cost. The
ACO performed highest in the Preventive Health area, which
includes screening for patients with depression, helping patients
quit smoking and proper use of aspirin for patients with heart
disease. Success is measured by shared savings earned.
SPOTLIGHT
OneCity Health
Priority health needs addressed: An infrastructure for scaling:
Financial sustainability
OneCity Health, the largest PPS in New York state, is
prototyping innovative solutions through new collaborations
across hospital, community and managed care organization
partners that meet the goals of DSRIP and will be sustained
through new value-based payment arrangements. Investments
aim to provide streamlined, person-centered care to address
upstream social risk factors for poor health and to reduce
avoidable hospital utilization by redesigning care models
supported by robust data analytics capabilities.
Through OneCity Health’s $5 million DSRIP Innovation Fund,
the largest statewide, partners prototyped new food and
wellness delivery models, community based organization-led
peer outreach, health education programs and developed the
“Ask Me, AsthMe!” asthma health literacy app. OneCity Health
has achieved signicant reductions in avoidable hospital use
and nancial savings and is awaiting nal performance results.
Success is measured by DSRIP performance, earned value-based
payment incentives and a reduction in avoidable utilization rates.
Goal: Optimize the integration of assets across the system
Tactic: Promote coordination and integration of clinical,
nancial and social services to deliver a seamless and
streamlined patient experience
As the largest public health care system in the United States,
NYC Health + Hospitals operates a robust network of acute-
care hospitals, a long-term care hospital, neighborhood-based
primary care centers, nursing homes and post-acute centers, a
home care agency and a health plan, MetroPlus. To support this
network, the system is dedicated to building an infrastructure
that optimizes efciency, reliability and integration with the
ultimate goal of increasing access to primary care as well as
tailored delivery of high-quality, clinical services. This includes
enhancing data sharing, standardized high-quality clinical
services and seamless communication across the network.
Further, OneCity Health has provided technical assistance for
capacity building and other supportive services to prepare its
growing PPS partner network for successful partnerships with
NYC Health + Hospitals and health plans, including MetroPlus.

14
LOOKING FORWARD
BUILDING HEALTHY COMMUNITIES
The priority health needs identied in the 2019 CHNA are
structural and complex. Addressing them requires continued
collaboration between NYC Health + Hospitals, city agencies,
community partners and, crucially, patients. To ensure continued
alignment with community members, NYC Health + Hospitals
will continue to engage community members, including through
its existing CABs and PFACs. The following strategic elements
inform the transformative initiatives and programs NYC Health +
Hospitals will implement to strengthen the health system for all
New Yorkers.
• Tailor clinical services for populations facing health equity
challenges to reduce health disparities
• Repurpose unused space for preventive care services to
address life cycle-driven illness and health equity challenges
• Implement new care models to expand patient access
to convenient and appropriate health care including
expanding virtual care and enhancing care coordination
within the NYC Health + Hospitals unied call center
• Leverage real-time data and analytics, digital health
tools and Epic H2O to engage patients, families and
interdisciplinary care teams for a streamlined health care
experience – these data could support community-wide
health promotion, quality improvement and evaluation
efforts
• Connect patients, interdisciplinary care teams and social
service providers through health information exchange
networks to foster patient access to community resources
and promote shared decision making, to support
community health promotion and quality and evaluation
efforts
• Increase awareness of tools to identify needed clinical
services and increase understanding around health care
costs and billing for both patients and providers
• Test high-value care models at NYC Health + Hospitals and
scale sustainable solutions
RESOURCE COMMITMENT
NYC Health + Hospitals will commit both nancial and in-kind
resources during FY 2019–2021 to implement transformative
initiatives and programs. Resources include clinical and
nonclinical services, partnerships and innovative solutions
prototyping through OneCity Health PPS Partners and NYC
Health + Hospitals, including its ACO, as well as staff time
devoted to advance collective work, charitable contributions and
employee volunteerism.
EVALUATION
NYC Health + Hospitals will continue to disseminate ndings
from the CHNA to system staff and community members alike.
Additionally, NYC Health + Hospitals will promote and raise
awareness of transformative initiatives and programs identied
in this report. Evaluation plans will be established or continued.
Further, OneCity Health has invested in the Institute for People,
Place and Possibility (IP3) Assess, a data analytics platform that
helps to identify health needs and areas of opportunity to inform
place-based investments. NYC Health + Hospitals will use the
platform to support continuous monitoring and evaluation of
NYC Health + Hospitals and community-level impact in making
progress towards the system’s overall strategic focus and in
closing health equity gaps.

15
1. Ludwig J, Sanbonmatsu L, Gennetian L, et al.
Neighborhoods, obesity, and diabetes—a randomized
social experiment. Engl J Mede. 2011;365(16): 1509-1519.
doi:10.1056/NEJMsa1103216.
2. Schootman M, Andresen EM, Wolinsky FD, et al. The Effect
of Adverse Housing and Neighborhood Conditions on the
Development of Diabetes Mellitus among Middle-aged
African Americans. Am J Epidemiol. 2007;166(4):379–387.
doi:10.1093/aje/kwm190.
3. Christine PJ, Auchincloss AH, Bertoni AG, et al.
Longitudinal Associations Between Neighborhood Physical
and Social Environments and Incident Type 2 Diabetes
Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA).
JAMA Intern Med. 2015;175(8):1311–1320. doi:10.1001/
jamainternmed.2015.2691.
4. Strodl E,Kenardy J. Psychosocial and non-psychosocial
risk factors for the new diagnosis of diabetes in elderly
women. Diabetes Res and Clin Pract. 2006;74(1) :57-65.
doi: 10.1016/j.diabres.2006.02.01.
5. Rimm, E. B., Chan, J., Stampfer, M. J., Colditz, G. A.,
& Willett, W. C. (1995). Prospective study of cigarette
smoking, alcohol use, and the risk of diabetes in men.
BMJ, 310(6979), 555-559.
6. Rotella, F., & Mannucci, E. (2013). Depression as a risk
factor for diabetes: a meta-analysis of longitudinal studies.
The Journal of Clinical Psychiatry.
7. Structural competency can be dened as the trained
ability to discern how a host of issues dened clinically
as symptoms, attitudes or diseases (e.g., depression,
hypertension, obesity, smoking, medication “non-
compliance,” trauma, psychosis) also represent the
downstream implications of a number of upstream
decisions about such matters as health care and
food delivery systems, zoning laws, urban and rural
infrastructures, medicalization or even about the very
denitions of illness and health. See also www.ncbi.nlm.nih.
gov/pmc/articles/PMC4269606.
8. Practicing cultural humility goes beyond being respectful
and responsive to health beliefs and practices and
cultural and linguistic needs of individuals – it requires
acknowledgment and celebration of an individual’s identity
and agency over their own experience. See also www.
rwjf.org/en/blog/2018/06/practicing-cultural-humility-to-
transform-healthcare.html.
NOTES AND REFERENCES

16
THANK YOU TO COMMUNITY MEMBERS AND NYC HEALTH + HOSPITALS STAFF
WHO CONTRIBUTED TO THIS REPORT
Paul Albertson
Dr. Machelle Allen
Dr. Charles Barron
Dr. Leon
Boudourakis
Dr. Sheila Brocavich
Kaushal Challa
Dr. Dave Chokshi
Natalia Cineas
Dr. Susan Cohen
Andrea Cohen
Frederick Covino
Dr. Nichola Davis
Dr. Robert Faillace
Christine Flaherty
Kenra Ford
Benjamin
Goldsteen
Dr. Rajneesh Gulati
Dr. Patrick Hammill
Dr. Jennifer Havens
Bridgette Ingraham
Noah Isaacs
Alexander Izaguirre
Dr. Mitchell Katz
Marji Karlin
Dr. Norma Keller
Dr. Stuart Kessler
Marielle Kress
Rebecca
Linn-Walton
Dr. Justin List
Dr. Theodore Long
Kevin Lynch
Ana Marengo
Michelle Martelle
Dr. Joseph Masci
Maureen McClusky
Dr. Mary McCord
Kim Mendez
Alina Moran
Dr. Marisa Nadas
Dr. Jeremy
O’Connor
Dr. Manish Parikh
Dr. Joan Reibman
Israel Rocha
Matilde Roman
Dr. Talya Schwartz
Dr. Warren Seigel
Matthew Siegler
Vivian Sun
Dr. Sheldon
Teperman
Megan Thompson
John Ulberg
Dr. Amit Uppal
Yvette Villanueva
Dr. John Wagner
Dr. Andrew Wallach
Dr. Eric Wei
Roslyn Weinstein
Meryl Weinberg
Dr. Wendy Wilcox
Christopher Wong
Patricia Yang
NYC Health + Hospitals
Stakeholders
Steven Banks
Dr. Oxiris Barbot
Josephine Bolus
Dr. Vincent Calamia
Gordon Campbell
Dean Fuleihan
Sally Hernandez-
Piñero
Dr. Mitchell Katz
Anita Kawatra
Dr. Hillary Kunins
Helen Arteaga
Landaverde
Barbara Lowe
Robert Nolan
José Pagán
Feniosky Peña-
Mora
Freda Wang
BELLEVUE
Elvis Durazzo
William Hicks
Dr. Nathan Link
Justin Chin
Evelyn Hernandez
Linda Lombardi
CARTER
Floyd Long
Dr. David Margolis
Nyron McLeish
CONEY ISLAND
William Brown
Dr. Terence Brady
Maureen McClusky
Rosanne Mottola
Patricia Roman
Lakeisha Weston
ELMHURST
Israel Rocha
Dr. Jasmin
Moshirpur
Atiya Butler
Claire Patterson
Pierre Pham
Carol White
HARLEM
Eboné Carrington
Dr. Maurice Wright
Philip Cooke
Jeanette McGill
JACOBI
Christopher
Mastromano
Dr. Michael
Zinaman
Barbara Deiorio
NYC Health + Hospitals
Facility Leaders
KINGS COUNTY
Sheldon McLeod
Mikael Philip
Dr. Steven Pulitzer
Desiree Thompson
Steven Ritzel
LINCOLN
Milton Nunez
Dr. Akinola Fisher
Colette Barrow
METROPOLITAN
Michael Lettera
Alina Moran
Dr. John Pellicone
Noel Alicea
NORTH CENTRAL
BRONX (NCB)
Cristina Contreras
Dr. Chinyere
Anyaogu
QUEENS
Christopher Roker
Dr. Jasmin
Moshirpur
Cleon Edwards
WOODHULL
Gregory Calliste
Dr. Edward Fishkin
Maria Riccio
NYC Health + Hospitals
Board of Directors
17
Community Stakeholders Implementation Strategy Plan Working Group Members
AUTHORS
Molly Chidester
Michaela Mallow
Chris Philippou
Jeet Rangnekar
Lola Simpson
Georgia Sleeth
Wilbur Yen
BRIGHTPOINT
HEALTH
Jessica Diamond
Paul Vitale
COMMUNITY
HEALTHCARE
NETWORK
David Gross
FOX ROTHSCHILD
LLP
Margaret Davino
HEALTHFIRST
Dr. Susan Beane
Selena Pitt
Theresa Riordan
THE JEWISH
BOARD
Ellen Josem
MAKE THE ROAD
NEW YORK
Rebecca Telzak
NADAP
Gary Stankowski
NEW YORK
IMMIGRATION
COALITION
Claudia Calhoon
Seongeun Chun
Max Hadler
NEW YORK LEGAL
ASSISTANCE
GROUP
Elizabeth Breslin
Randye Retkin
PLANNED
PARENTHOOD
Carmina Bernardo
SERVICES
FOR THE
UNDERSERVED
Donna Colonna
ALL METRO
HEALTH CARE
Richard Keller
Mary Lorthioir
SUNY DOWNSTATE
HEALTH SCIENCES
UNIVERSITY
Richard Miller
Dr. Dilip Nath
Patricia Winston
COMUNILIFE
Beverley Raudales
FOX ROTHSCHILD
LLP
Margaret Davino
HEALTHFIRST
Nora Chaves
Ronald Sanchez
NEW YORK
IMMIGRATION
COALITION
Claudia Calhoon
Seongeun Chun
NEW YORK
CITY HOUSING
AUTHORITY
Andrea Mata
Kim Truong
NYC DEPARTMENT
FOR THE AGING
Meghan Shineman
NYC DEPARTMENT
OF HEALTH AND
MENTAL HYGIENE
Ana Gallego
Vidushi Jain
Dr. William Jordan
NYC DEPARTMENT
OF HOUSING
PRESERVATION
AND
DEVELOPMENT
Jenna Breines
Jennifer Jacobs
Guzmán
NYC HEALTH +
HOSPITALS
Noel Alicea
Dr. Chinyere
Anyaogu
Colette Barrow
William Brown
Kaushal Challa
Cristina Contreras
Dr. Nichola Davis
Dr. Robert Faillace
Dr. Edward Fishkin
Dr. Anjna Ganatra
Dr. Laura Iavicoli
Dr. Kelly Jarrett
Marji Karlin
Dr. Daran Kaufman
Dr. Ross Kristal
Michael Lettera
Jim Mancari
Dr. Joseph Masci
Mary Anne Marra
Kim Mendez
Dr. Mary McCord
Dr. Aaron Miller
Dr. Shaw Natsui
Dr. Olayinka
Oluwole
Claire Patterson
Mikael Phillip
Dr. Steven Pulitzer
Dr. Joan Reibman
Gabrielle Rivera
Dr. Madden Rowell
Lisa Scott-McKenzie
Katherine Redfern-
Shaw
Oli Sigurdsson
Hrafn
Dr. Mark Sinclair
Desiree Thompson
Megan Thompson
John Ulberg
Dr. Amit Uppal
Dr. Andrew Wallach
Carol White
Dr. Wendy Wilcox
William Hicks
Meryl Weinberg
PLANNED
PARENTHOOD OF
NYC
Carmina Bernardo
SUNY DOWNSTATE
HEALTH SCIENCES
UNIVERSITY
Susan Fraser-
McCleary
THANK YOU TO COMMUNITY MEMBERS AND NYC HEALTH + HOSPITALS STAFF
WHO CONTRIBUTED TO THIS REPORT
18
As of October 2019, the following initiatives and programs throughout NYC Health + Hospitals most clearly address the priority
health needs identied in the 2019 CHNA. Please note: this list is not exhaustive.
For a current list of services, visit NYC Health + Hospitals’ website and connect with NYC Health + Hospitals and OneCity Health
on social media.
APPENDIX: GLOSSARY OF NYC HEALTH +
HOSPITALS TRANSFORMATIVE INITIATIVES
AND PROGRAMS
PRIORITY HEALTH NEED: REDUCING THE BURDEN OF LIFE CYCLE-DRIVEN ILLNESS AND
HEALTH EQUITY CHALLENGES
Pregnancy and birth outcomes
Initiative Description
Comprehensive family planning services Programming and services focused on family planning including, but not limited to:
family planning counseling, long acting reversible contraception (LARC) expansion,
termination of pregnancy up to 24 weeks gestational age and medication abortion.
Comprehensive maternal health
programming
Programming and services focused on maternal health including, but not limited to:
Baby-friendly designation, Centering Pregnancy, Centering Parenting, maternal
depression screening, on-site reproductive psychiatry, social work and collaborative care.
Maternal homeless support program Partnership between NYC Health + Hospitals/Kings County and NYC Department of
Homeless Services (DHS) that links patients to health care services, community based
organizations and transportation.
Maternal Medical Home This program provides care management and screening for depression, clinical
conditions, trauma, social determinants of health and psychosocial conditions to
individuals predisposed to or at high risk for poor or adverse pregnancy outcomes.
Patients are also linked to community-based care programs and NYC Health +
Hospitals.
QINCA program This program provides education for physicians on LARC insertions and services
through community providers.
RELIAS RELIAS is a web-based, self-paced learning program with modules focused on fetal
heart rate interpretation, shoulder dystocia, obstetric hemorrhage and other obstetric
emergencies.
Simulation training Sometimes referred to as IMSAL, this training focuses on obstetric emergencies
including: hypertensive disorders in pregnancy, maternal hemorrhage, shoulder
dystocia and cardiac arrest.
Stork’s Nest Stork’s Nest is a combined partnership with NYC H+H/Kings County, Zeta Phi Beta
Sorority and March of Dimes. Stork’s Nest aims to increase the number of women
receiving early and regular prenatal care to prevent cases of low birth weight,
premature births and infant deaths.
Airway diseases (asthma, COPD)
Initiative Description
“Ask Me, AsthMe!” program This asthma smartphone application is designed for children and families with low
health literacy to increase their understanding of pediatric asthma and disease
self-management.
Asthma-Free Bronx This City Hall initiative, run by the NYC Department of Health and Mental Hygiene,
NYC Health + Hospitals and the NYC Department of Education, provides a suite
of personalized interventions aimed at reducing Emergency Department visits and
inpatient admissions of asthmatic pediatric patients in the South Bronx. As a part of
this program, community health workers also provide asthma education including self-
management education, environmental assessments and pest-remediation services.
19
Airway diseases (asthma, COPD), continued
Initiative Description
DSRIP Home-Based Environmental
Asthma Program
This program assigns a community health worker to support patients with frequent
or severe asthma attacks. Community health workers conduct home assessments
and provide services including self-management education and pest-remediation
services. This program was launched in 2017 for children and is expanding to
include adult patient populations.
Remote medication management The remote medication management program ensures asthmatic patients are in
compliance with medications prescribed by physicians.
Smoking Cessation This six-week program is designed to help individuals quit smoking. The program
includes group counseling and education, telephone counseling and Nicotine-
Replacement Therapy (NRP) in the adult medicine and behavioral health settings.
Behavioral health (mental health, substance use disorder)
Initiative Description
Assertive Community Treatment (ACT) The ACT program functions as a “clinic without walls,” providing multidisciplinary,
exible treatment and 24/7 support to individuals with severe mental illness in their
homes and communities. This evidenced-based practice uses a person-centered,
recovery-based approach.
Behavioral health critical time interventions OneCity Health invested in Coordinated Behavioral Care’s Pathway Home
program, which provides multidisciplinary care transition services such as
accompanying patients home, arranging for immediate needs such as food and
lling prescriptions, ensuring transport is arranged for health care visits and
providing ongoing communication and support.
Community Advisory Board (CAB)
community forums on opioids
NYC Health + Hospitals CABs continue to hold open community forums on the
impact of opioids in the community, including hosting opioid overdose prevention
trainings (Naloxone) for community members.
Comprehensive Psychiatric Emergency
Program (CPEP)
CPEP is an inpatient service that facilitates children and adults with mental health
disorders receiving emergency observation, evaluation and care in a supportive
environment. This program has expanded to include telehealth services at select
facilities and a crisis-outreach mobile intervention, which together extend the
program into the community.
Emergency Department Addiction Leads
and Inpatient Consult for Addiction
Treatment and Care in Hospitals (CATCH)
The Emergency Department Addiction Leads program engages peer counselors
to provide support to patients with substance use disorder in the Emergency
Department. This program launched in 2019 and is currently expanding to include
social workers.
The CATCH Program consults patients with substance use disorder and initiates
Medication Assisted Therapy (MAT) for interested patients. These consults include
linkages to treatment post-discharge.
Integrated care centers and collaborative
care model
Integrated care clinics co-locate primary care, behavioral health and care for
substance use disorder in one location. In addition to allowing for coordination
of care, these clinics administer a universal behavioral health screening tool and
perform patient outreach to engage patients.
20
Behavioral health (mental health, substance use disorder), continued
Initiative Description
Medication Assisted Therapy (MAT)
expansion
Services for patients with substance use disorder have now expanded to all ve
boroughs. These services include MAT, the distribution of naloxone kits and
screening for substance use disorder.
Partial Hospitalization (PHP) PHP is a short-term alternative to an Inpatient Psychiatric Unit stay. The step-down
program provides an intensive, structured treatment environment ve days a
week, ve hours a day for mentally-ill and mentally-ill/chemically dependent adults
experiencing severe psychiatric symptoms. The program decreases the patient’s
length of stay.
School program for behavioral health
adolescent inpatients
Public School 35 is a hospital-based public school providing educational and
behavioral services for children aged 5-19 years with mental health disorders.
3-2-1 IMPACT! 3-2-1 IMPACT! integrates a specially trained child development professional, called
a “Healthy Steps Specialist,” within the primary care team. This specialist partners
with families during well-child visits, coordinates screening efforts and problem-
solves with parents for common and complex child-rearing and other challenges.
Diet-related diseases (diabetes, hypertension)
Initiative Description
BlueStar app Through this app, patients receive individualized coaching, reminders, education
and support to help manage their Type 2 diabetes.
Diabetes cooking classes Diabetes cooking classes are held at select NYC Health + Hospitals locations to
provide culturally competent cooking classes tailored for patients with Type 2
diabetes.
Diabetes Prevention Program An evidence-based lifestyle change model based on the National Diabetes
Prevention Program led by the CDC, this program is for patients who are either at-
risk of diabetes or diagnosed with pre-diabetes. Programming includes coaching
patients in areas including healthy eating, physical activity and stress management.
Digital peer mentoring program This pilot program with InquisitHealth pairs patients with diabetes with a peer
mentor. Peer mentors offer guidance and support to patients on how to live with
and manage their diabetes.
Food and nutrition resources A hospital-community partnership where patients are connected to a variety of
on-site and community-based food and nutrition services. Food-insecure patients
are enrolled in eligible food benets, assisted with access to fresh produce or
medically tailored meals and electronically referred to food pantries and group
meals.
Plant-Based Lifestyle Medicine
Program
This pilot program began at Bellevue in 2018 with the goal to help patients access
a healthy lifestyle that includes a whole-foods, plant-based diet to improve, and in
some cases reverse, diet-related chronic illness.
Primary care-centered diabetes
management initiative
Programming includes: clinical pharmacists, teleretinal screening, digital peer
mentoring and digital coaching.

21
Diet-related diseases (diabetes, hypertension), continued
Initiative Description
Shape Up NYC classes Led by the New York City Department of Parks & Recreation, Shape Up NYC is a free,
drop-in tness program offering classes such as aerobics, yoga, Pilates and Zumba.
Class registration is not required.
30-day care transitions OneCity Health is investing in community partners to support seamless transition
for patients after a hospital discharge by assisting with access to healthy food, lling
prescriptions and providing transportation to and from primary care visits.
Treat-to-Target (T2T) Hypertension
Program
This program – recognized by The American Heart Association and the American
Medical Association – connects patients with hypertension with chronic disease nurses
to support them in controlling their blood pressure.
Aging and frailty
Initiative Description
Acute Care for the Elderly
(ACE) Unit
The ACE Unit is comprised of an interdisciplinary care team that supports older adults
in maintaining their independence and preventing physical and mental decline during
treatment for acute illness. The ultimate goal is to return patients to their everyday
routines and living situations.
Community Services, Inc. partnership This partnership between NYC Health + Hospitals/Queens and CBO Sunnyside
Community Services, Inc. addresses caregiver support for patients suffering from
Alzheimer’s disease and dementia.
Geriatrics practice Provides care to adults over the age of 65 by working with a specialized team to
understand the unique needs of patients. These practices coordinate throughout
the spectrum of care through a single provider, who helps manage screenings,
assessments and social services.
NICHE certication NICHE (Nurses Improving Care for Healthsystem Elders) is the leading nurse-driven
program designed to help hospitals and health care organizations improve care for
older adults through the provision of sensitive and exemplary care.
Palliative care Palliative care provides inpatient and outpatient services to help relieve pain and
discomfort in patients with chronic or advanced illnesses.
Senior community engagement
efforts
Ongoing efforts throughout several NYC Health + Hospitals facilities that include
activities such as Harlem’s Annual Senior Health Festival, where community partners
engage with attendees and provide outreach to local senior centers.
Homeless or individuals with housing instability
Initiative Description
Housing assistance Assistance includes, but is not limited to: referrals to Homebase housing, Breaking
Ground partnerships, Roomnders and outreach.
Hospital-housing developer partnerships Selected NYC Health + Hospitals facilities convert clinical space for on-site housing
through community initiatives and programs with partners including CAMBA, SKA
Marin and Comunilife.

22
Homeless or individuals with housing instability, continued
Initiative Description
Respite and transitional housing Investments in transitional supportive housing with respite providers to provide
three different respite programs to patients with medical needs, mental health
needs and intellectual and development disabilities who cannot be discharged to
a home.
Incarcerated or previously incarcerated
Initiative Description
Point of reentry/transition clinic for
correctional health
Includes the Port Clinic, which was recently established to provide primary care
services to previously incarcerated patients from Rikers Island and other New York
City detention centers.
Immigrants
Initiative Description
Interpreter services, any modality Interpreter services might include language lines, remote interpretation devices,
rovers for American Sign Language (ASL), live interpreters, etc.
NYLAG clinics New York Legal Assistance Group (NYLAG) clinics are available to patients to help
address health-harming legal needs.
Program for Survivors of Torture This program offers medical, mental health and social/legal services to survivors of
torture and persecution overseas.
LGBTQ
Initiative Description
Leader in LGBTQ Healthcare Equality
designation
The Leader in LGBTQ Healthcare Equality designation is awarded to hospitals
who exemplify LGBTQ-inclusive policies of delivering equitable care to LGBTQ
communities, creating an inclusive and supportive environment for employees and
demonstrating public support for the community.
The Pride Health Centers Community health centers that offers services for women’s health, men’s health,
gender transition, hormone therapy, HIV and STI prevention, screening and
treatment services, adolescent care, social work and behavioral health services and
general primary care.
Adolescents and young adults
Initiative Description
KIDs Ride A program that introduces youth to cycling as a safe and effective means of
transportation and as recreation, encouraging them to incorporate regular physical
activity into their lives.
23
Adolescents and young adults, continued
Initiative Description
100 Schools Project A city-wide health-system and community partnership launched to meet the needs
of students with emotional, behavioral and addiction challenges in middle and high
schools and city colleges. This program trains school staff to identify early signs of
mental illness and substance misuse and to promote wellness and prevention.
Union Settlement Youth Opportunity Hub In partnership with the District Attorney’s Ofce, Youth Opportunity Hubs knit
together community-based providers to provide coordinated services in new or
updated physical spaces for young people in target neighborhoods. The Hubs
provide attractive social spaces and link neighborhood service providers to provide
one-stop, comprehensive support for at-risk children, teens and young adults in
order to prevent them from becoming involved in the criminal justice system.
YouthHealth centers Centers that offer primary care, Plan B, STI testing, birth control, PrEP and
comprehensive physical examinations in a compassionate, condential and safe
environment.
Survivors of domestic violence
Initiative Description
Family Justice Centers The New York City Family Justice Center (FJC) provide free, condential assistance
for survivors of domestic and gender-based violence. NYC Health + Hospitals
provides on-site mental health services, including direct care, mental health
support, skill-building opportunities and mentoring to Family Justice Center staff.
SAFE program State-designated hospital program that provides specialized care to survivors of
sexual assault and/or torture.
Individuals with food insecurity
Initiative Description
Access to food and nutrition resources,
including farmers markets, food
coordinators, local food partnerships and
medically-tailored meals
Programs established across NYC Health + Hospitals that help combat food
insecurity by providing patients with increased access to food through farmers
markets and local food partnerships. Food coordinators assist patients with
enrolling in food benets and connecting patients to additional community
resources.
Other
Initiative Description
East Harlem Community Alliance NYC Health + Hospitals/Metropolitan is a leader in this consortium of over 185
nonprots, businesses, religious organizations and government agencies working
together to enhance the vitality and well-being of the East Harlem community.
Expand health care, health insurance and
benets enrollment
Initiative to support patients in insurance, NYC Care and other benets enrollment.
Includes support through food coordinators and tax ling counselors.
The Global Health Institute The Global Health Institute at NYC Health + Hospitals/Elmhurst supports and
advances groundbreaking research, grows existing relationships with community
and global partners, hosts educational events for the community and helps to
improve clinical and patient experiences.
24
Other, continued
Initiative Description
Tax preparation services As part of NYC Free Tax Prep, led by the NYC Department of Consumer Affairs, NYC
Health + Hospitals offers free tax preparation services at many of its sites for New
Yorkers earning $66,000 or less last tax year.
Violence prevention programs (e.g.
Guns Down Life Up (GDLU), Kings
Against Gun Violence (KAVI))
GDLU prevents violence by offering after school and summer hospital-based youth
development programs, underpinned by mentoring and scholastic support. The purpose
of the hospital-based youth development program is to involve at-risk young people in
positive activities before they become involved with violence.
KAVI, a non-prot organization started by an Emergency Medicine physician, provides a
holistic approach to violence intervention to communities of color in Central Brooklyn.
In hospitals, KAVI connects with youth who are both perpetrators and victims of violence
to help them cope with trauma, deescalate violence and serve as active leaders in their
community.
PRIORITY HEALTH NEED: REDESIGNING HEALTH CARE FOR COMMUNITIES:
RETHINKING HEALTH CARE SYSTEMS
Ease of access and navigation
Initiative Description
Expansion of primary care access
in underserved and high-need
neighborhoods
Expanding on Mayor de Blasio’s Caring Neighborhoods initiative, “One New York:
Health Care for Our Neighborhoods,” there are eight new or renovated health centers
across New York City in Bedford Stuyvesant, Brownsville, Bushwick, Crown Heights,
East Tremont, Jackson Heights, Lower East Side and North Shore Staten Island. Three
additional comprehensive health centers in Bushwick, Jackson Heights and Tremont will
open in 2020.
Expansion of telehealth and digital
coaching and monitoring
NYC Health + Hospitals is offering a variety of digital health platforms to promote
access, health engagement and chronic disease self-management. These platforms
include: a multi-modal appointment reminder system, a diabetes self-management app,
a telephone based peer mentorship app and an asthma self-management app.
ExpressCare ExpressCare provides the community with a new and convenient way to access health
care through urgent care walk-in centers. Through ExpressCare, patients are promptly
seen by a provider, connected to primary care and other services and enrolled in
insurance when applicable.
Imaging Centers of Excellence NYC Health + Hospitals is upgrading its medical imaging technology to provide patients
with modernized, state-of-the-art technology that will produce faster and better image
quality and lead to quicker diagnoses and treatment.
NYC Care NYC Care ensures that all New Yorkers have access to care through no- and low-cost
services offered by NYC Health + Hospitals. Individuals who cannot afford or are
ineligible for insurance can enroll in NYC Care regardless of immigration status or ability
to pay. NYC Care provides patients and families with a dedicated primary care provider,
connection to a 24/7 customer service line and access to affordable medication.
Retail pharmacy Through pharmacy expansion, all patients will have 24/7 access to comprehensive
retail pharmacy services, including specialty pharmacy and central lling services.
Single call center Through a new 24/7 customer service center (844-NYC-4NYC), patients can make
appointments and gain assistance navigating services.
25
Optimizing patient-provider relationships
Initiative Description
Arts in Medicine The Arts in Medicine program aims to reduce stress, support emotional health and
help address compassion fatigue, historically known as physician burnout in staff.
eConsult eConsult allows primary care providers to give their patients access to the advice of
specialty care providers before the patient visits a specialty clinic, enabling primary
care providers and their patients to immediately focus on a plan of action.
Helping Healers Heal A “second victim program,” Helping Healers Heal is a peer-led employee wellness
program offering emotional rst aid to health care providers who experience
demanding circumstances in the workplace that can lead to stress, anxiety or
depression.
ICARE The ICARE values promote NYC Health + Hospitals’ mission and vision and guide staff
to offer the highest-quality, safest and most patient-centered care.
Patient-centered scheduling and
open access
NYC Health + Hospitals is implementing patient-centered scheduling in conjunction
with the system’s call center to ensure patient-provider continuity. In addition, open
access scheduling allows for more walk-in slots for patients with their interdisciplinary
care team.
Health care cost and transparency
Initiative Description
Epic H2O MyChart consolidated billing
and pre-payment options
With H2O MyChart, patients can view consolidated billing information, make payments
and set up payment plans. In addition, patients can see expected drug and treatment
costs.
NYC Health + Hospitals’
‘Find Your Insurance’ tool
NYC Health + Hospitals has made it easier for New Yorkers to understand whether
their health insurance is accepted at NYC Health + Hospitals locations. The tool is
accessible in many languages on NYC Health + Hospitals’ website.
PRIORITY HEALTH NEED: REDESIGNING HEALTH CARE FOR COMMUNITIES:
AN INFRASTRUCTURE FOR SCALING
State of the workforce
Initiative Description
CityDoctors Scholarship CityDoctors Scholarship awardees commit to practicing primary care medicine for at
least two years at one of NYC Health + Hospitals’ acute care facilities. This partnership
was launched in 2012 to help address the shortage of primary care physicians and to
increase educational and career opportunities for local graduates.
Clinical Leadership Fellowship This one-year fellowship is designed for post-residency graduates interested in
administrative roles. Fellows are placed in one of NYC Health + Hospitals’ Central
Ofce locations to acquire hands-on, practical work experience including participation
in leadership meetings and developing and leading a substantial quality improvement
or population health-oriented project.
Clinician recruitment programs and
campaigns
Includes DOCS4NYC and Nurse4NYC, Mental Health Service Corps, CityDoctors
Scholarship, Healthcare Administration Scholars and Clinical Leadership Fellows.
26
State of the workforce, continued
Initiative Description
Healthcare Administration Scholars This two-year leadership training and management program is shaping the
next generation of leaders. The program requires scholars to develop quality
improvement projects across the health system.
Nursing Career Ladder NYC Health + Hospitals is offering full tuition to qualied registered nurses to earn
a bachelor’s degree in nursing.
Nurse Residency Program This residency program provides newly-hired, rst-time nurses with on-the-job
training focused on topics including ethics, decision making, clinical leadership
and the incorporation of evidence-based research into practice. The program
also provides new nurses with support and mentorship proven to enhance nurse
satisfaction, performance and retention.
Professional development programs for
clinical and non-clinical staff
NYC Health + Hospitals and OneCity Health are offering new training and
development programs including: Care Restructuring Enhancement Pilot workforce
development efforts, Leadership Academy, Revenue Cycle Institute, Quality
Academy and educational partnerships offering scholarships and continuing
education credits.
Information sharing
Initiative Description
EpicCare Link As NYC Health + Hospitals transfers to Epic, NYC Health + Hospitals is transferring
to EpicCare Link as the primary referrals platform for community providers. This
web-based platform allows providers to review their patients’ charts and test and
lab results, receive notications on their care and communicate with NYC Health
+ Hospitals’ providers. NYC Health + Hospitals is offering providers a training
program as a part of the transition.
Epic Community Connect OneCity Health is offering PPS partners a sophisticated instance of Epic
(OneConnect) that includes a unied patient record across NYC Health + Hospitals
and the OneCity Health PPS network.
Epic H2O and MyChart Epic H2O unies electronic health records from over 70 locations to support
clinicians in delivering high-quality, efcient care and allowing patients easy access
to their records through a secure patient portal called MyChart. The new electronic
health record also enables the system to better coordinate high-value care for
patients.
Epic Healthy Planet Epic Healthy Planet is a population health platform designed to identify, engage
and treat high-risk and high-cost patient populations in a coordinated manner
across the NYC Health + Hospitals and OneCity Health PPS networks.
Patient appointment reminders Patient appointment reminders and other health communications are sent through
an automated system based on the patient’s preferred communication modality,
including text, email or phone.
27
Financial sustainability
Initiative Description
MetroPlus and GetCoveredNYC
Enrollment Expansion
With the assistance of MetroPlus Health plan and GetCoveredNYC enrollers, NYC
Health + Hospitals is enrolling more New Yorkers in insurance across NYC Health +
Hospitals facilities.
NYC Health + Hospitals’ Financial
Transformation Plan through revenue and
expense improvement opportunities
NYC Health + Hospitals adopted a seven-point plan to close the $1.8 billion
nancial gap. The plan includes efforts to improve billing, contracting, coding and
documentation; investing in patient and revenue increases; increasing health plan
enrollments and reducing administrative expenses.
Value-based payment contracting NYC Health + Hospitals and OneCity Health are designing its transformative
initiatives and programs to achieve system-wide transformation to perform in
value-based purchasing environments, encouraging service innovation, care model
redesign and clinical quality improvements.
System complexity and scale
Initiative Description
OneCity Health CBO capacity building OneCity Health has invested in capacity building to help community-based
organization partners develop infrastructure to contract their services to hospitals
and health plans based on value. As a culmination of this work, OneCity Health
provided funding to community-based organizations through its Hospital-
Community Partnerships initiative.
OneCity Health primary care
capacity building
OneCity Health, in partnership with Primary Care Development Corporation (PCDC),
offered community provider practices expert coaching with the aim of improving
chronic disease prevention and management, behavioral health integration and
care coordination. The aim of this work is to prepare NYC Health + Hospitals and
community practices for evidence-based chronic disease management to provide
sustainable mechanisms for high-value care.

28
As of October 2019, the following initiatives and programs throughout NYC Health + Hospitals and organized by borough most
clearly address the priority health needs identied in the 2019 CHNA. Please note: this list is not exhaustive. For a description of each
initiative and program, refer to Appendix: Glossary of NYC Health + Hospitals Transformative Initiatives and Programs.
For a current list of services, visit NYC Health + Hospitals’ website and connect with NYC Health + Hospitals and OneCity Health on
social media.
APPENDIX: NYC HEALTH + HOSPITALS
TRANSFORMATIVE INITIATIVES AND
PROGRAMS BY BOROUGH
PRIORITY HEALTH NEED: REDUCING THE BURDEN OF LIFE CYCLE-DRIVEN ILLNESS AND
HEALTH EQUITY CHALLENGES
Initiative Bronx
Brooklyn,
Staten Island
Manhattan Queens
Pregnancy and birth outcomes
Comprehensive family planning services
Bellevue,
Metropolitan
Comprehensive maternal health programming System-wide
Maternal homeless support program Kings County
Maternal Medical Home Kings County
QINCA program Kings County
RELIAS Bellevue
Simulation training System-wide
Stork’s Nest Kings County
Airway diseases (asthma, COPD)
“Ask Me, AsthMe!” program Kings County
Asthma-Free Bronx Lincoln
DSRIP Home-Based Environmental Asthma Program
Jacobi, Lincoln,
North Central
Bronx
Kings County,
Woodhull
Bellevue,
Harlem,
Metropolitan
Elmhurst,
Queens
Remote medication management Elmhurst
Smoking Cessation
Jacobi, Lincoln,
North Central
Bronx
Woodhull Harlem
Elmhurst,
Queens
Behavioral health (mental health, substance use disorder)
Assertive Community Treatment (ACT)
Jacobi,
North Central
Bronx
Coney Island,
Woodhull
Bellevue,
Metropolitan
Elmhurst,
Queens
Behavioral health critical time interventions Lincoln Coney Island
Harlem,
Metropolitan
Community Advisory Board (CAB) community forums
on opioids
Metropolitan
Comprehensive Psychiatry Emergency Program
(CPEP)
Jacobi, Lincoln,
North Central
Bronx
Kings County,
Woodhull
Bellevue,
Harlem
Elmhurst,
Queens
29
Initiative Bronx
Brooklyn,
Staten Island
Manhattan Queens
Behavioral health (mental health, substance use disorder), continued
Emergency Department Addiction Leads System-wide
Healthy Steps Coney Island
Inpatient Consult for Addiction Treatment and
Care in Hospitals (CATCH)
Lincoln
Coney Island,
Woodhull
Bellevue,
Metropolitan
Elmhurst
Integrated care centers and collaborative care model System-wide
Medication Assisted Therapy (MAT) expansion System-wide
Partial Hospitalization (PHP)
North Central
Bronx
Kings County Bellevue
Elmhurst,
Queens
School program for behavioral health adolescent
inpatients
Metropolitan
3-2-1 IMPACT! Bellevue Queens
Diet-related diseases (diabetes, hypertension)
BlueStar app Metropolitan
Diabetes cooking classes Kings County Metropolitan
Diabetes Prevention Program System-wide
Digital Peer Mentoring Program Kings County
Food and nutrition resources System-wide
Plant-Based Lifestyle Medicine Program Bellevue
Primary Care-Centered diabetes management initiative System-wide
Shape Up NYC classes
Jacobi,
Lincoln
Kings County
Harlem,
Metropolitan
Elmhurst
30-day care transitions System-wide
Treat-to-Target (T2T) Hypertension Program System-wide
Aging and frailty
Acute Care for the Elderly (ACE) Unit Woodhull
Community Services, Inc. partnership Queens
COMPACT Model Woodhull
Geriatrics practice Woodhull
NICHE certication System-wide
Palliative care
Jacobi,
Lincoln
Bellevue, Harlem,
Henry J. Carter,
Metropolitan
Elmhurst,
Queens
Senior community engagement efforts Metropolitan
30
Initiative Bronx
Brooklyn,
Staten Island
Manhattan Queens
Homeless or individuals with housing instability
Housing assistance
North Central
Bronx
Kings County,
Woodhull
Bellevue,
Harlem,
Metropolitan
Elmhurst
Hospital-housing developer partnerships
Kings County,
Woodhull
Metropolitan Queens
Respite and transitional housing
Jacobi,
Lincoln
Kings County,
Woodhull
Bellevue
Elmhurst,
Queens
Incarcerated or previously incarcerated
Point of reentry/transition clinic for correctional health Kings County Bellevue
Immigrants
Interpreter services, any modality System-wide
NYLAG Clinics System-wide
Program for Survivors of Torture Bellevue Elmhurst
LGBTQ
Leader in LGBTQ Healthcare Equality designation System-wide
The Pride Health Centers
Bellevue,
Metropolitan
Adolescents and young adults
100 Schools Project System-wide
KIDs Ride Program Woodhull
Union Settlement Youth Opportunity Hub Metropolitan
YouthHealth centers System-wide
Survivors of domestic violence
Family Justice Centers System-wide
SAFE program System-wide
Individuals with food insecurity
Access to food and nutrition resources, including farmers
markets, food coordinators, local food partnerships and
medically-tailored meals
System-wide
Other
East Harlem Community Alliance Metropolitan
Expand health care, insurance and benets enrollment System-wide
The Global Health Institute Elmhurst
Tax preparation services Kings County Elmhurst
Violence prevention programs (e.g. Guns Down Life Up
(GDLU), Kings Against Gun Violence (KAVI))
Jacobi, Lincoln,
North Central
Bronx
Coney Island,
Kings County,
Woodhull
Bellevue,
Harlem
Queens
31
PRIORITY HEALTH NEED: REDESIGNING HEALTH CARE FOR COMMUNITIES:
RETHINKING HEALTH CARE SYSTEMS
Initiative Bronx
Brooklyn,
Staten Island
Manhattan Queens
Ease of access and navigation
Expansion of primary care access in underserved and
high-need neighborhoods
System-wide
Expansion of telehealth and digital coaching and
monitoring expansion
System-wide
ExpressCare Lincoln Elmhurst
Imaging Centers of Excellence System-wide
NYC Care
Jacobi, Lincoln
North Central
Bronx
Coney Island,
Kings County,
Woodhull
Retail pharmacy System-wide
Single call center System-wide
Optimizing patient-provider relationships
Arts in Medicine System-wide
eConsult System-wide
Helping Healers Heal System-wide
ICARE System-wide
Patient-centered scheduling and open access System-wide
Health care cost and transparency
Epic H2O MyChart consolidated billing and
pre-payment options
System-wide
NYC Health + Hospitals’ ‘Find Your Insurance’ tool System-wide
PRIORITY HEALTH NEED: REDESIGNING HEALTH CARE FOR COMMUNITIES:
AN INFRASTRUCTURE FOR SCALING
Initiative Bronx
Brooklyn,
Staten Island
Manhattan Queens
State of the workforce
CityDoctors Scholarship System-wide
Clinical Leadership Fellowship System-wide
Clinician recruitment programs and campaigns System-wide
Healthcare Administration Scholars System-wide
Nursing Career Ladder System-wide
32
Initiative Bronx
Brooklyn,
Staten Island
Manhattan Queens
State of the workforce, continued
Nurse Residency Program System-wide
Professional development programs for clinicians
and staff
System-wide
Information sharing
Epic Care Link System-wide
Epic Community Connect (OneConnect) System-wide
Epic H2O and MyChart System-wide
Epic Healthy Planet System-wide
Patient appointment reminders System-wide
Financial sustainability
MetroPlus and GetCoveredNYC Enrollment Expansion System-wide
Revenue and expense improvement opportunities System-wide
NYC Health + Hospitals’ Financial Transformation
Plan through revenue and expense improvement
opportunities
System-wide
System complexity and scale
OneCity Health CBO capacity building System-wide
OneCity Health primary care capacity building System-wide
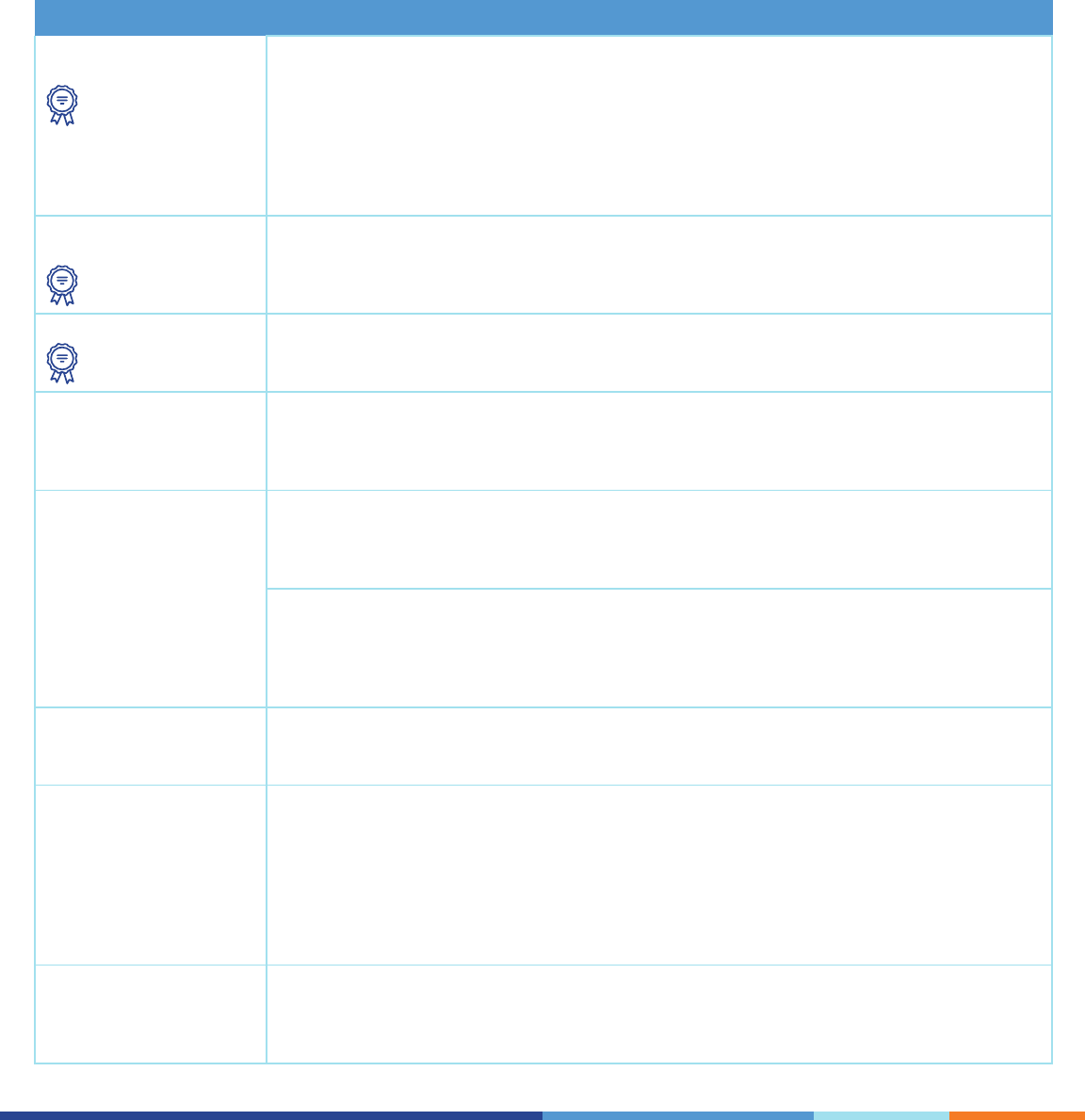
33
Below is a complete list of proposed solutions designed collaboratively during Implementation Strategy Plan working group
meetings to address the needs identied in the 2019 CHNA.
Solutions voted on by Implementation Strategy Plan working group members as highest priority are indicated below with an icon.
APPENDIX: PROPOSED SOLUTIONS FOR
CONSIDERATION
Priority health need: Reducing the burden of life cycle-driven illness and health equity challenges
Health and wellness of
all populations
Wellness University: The Wellness University would be an innovative, patient-centered model
integrating physician care plans, wellness and health promotion activities. Community health
workers would partner with patients and their physicians at a community-based site to support
populations in accessing a healthy life cycle and achieving optimal health outcomes. Recognizing
the limitations of a 20 minute visit with primary care providers, community health workers and
patients, working together in the Wellness University, would have sufcient opportunities in a
respectful, shame-free venue to master the elements of their care plans and become empowered to
take charge of their health.
Pregnancy and birth
outcomes
E-Mom program for pregnant individuals with housing insecurity: The E-Mom program would
allow pregnant individuals with housing insecurity easy access to coordinated care visits with
multi-disciplinary collaboration with the following focus areas: healthy babies, safe, stable housing,
nurturing relationships and economic sustainability.
Airway diseases Expansion of telehealth and health monitoring devices: Digital health innovations integrated
with inhalers can give providers access to real-time patient data to better support management of
treatment plans for patients with airway diseases.
Behavioral health Expanded co-location and integration of primary care, behavioral health and substance use
disorder services: Patients suffering from substance use disorders must be able to seamlessly
access coordinated, integrated care in one location, across NYC Health + Hospitals. Through
co-location of services, the model can alleviate existing regulatory barriers around data sharing.
Diet-related diseases New models for on-site food markets: Food markets (sometimes referred to as food pharmacies)
provide supplemental foods to patients based on clinical and social need through a prescription
from their interdisciplinary care team. Expansion would continue positive success measures
experienced thus far.
SEA Change: The Screening, Education and Access (SEA) Change program would utilize volunteer
community advocates in the community including places of worship, employment, residence,
refuse and recreation to screen, educate and promote access to health care in communities
where individuals face high rates of diet-related diseases such as hypertension, diabetes and
cardiovascular disease.
Aging and frailty Coordinated referral process for aging populations: A coordinated network of services tailored
to aging populations is critical to address their needs holistically. Coordinating the referral process
would support in providing this essential care.
Populations with health
equity challenges
Health Advocacy Partners program: The Department of Health and Mental Hygiene’s Harlem
Health Advocacy Partners (HHAP) program partners residents living in New York City Housing
Authority (NYCHA) developments with community health workers, organizers and health advocates
to support them to access needed services, enable healthy behavior change, support disease
management and build a community. The program has demonstrated HbA1C reductions in
individuals with diabetes, improved blood pressure control in persons with hypertension and
reduced hospital and Emergency Department visits for persons with asthma. Expansion would
further address the needs of populations with these health equity challenges.
Other Data integration across child welfare and health care systems: Enhanced integration between
NYC Health + Hospitals electronic health records system and the State Welfare Case Management
system would allow health care providers and child protective service workers to promote
bidirectional information sharing and coordinated care.

34
Priority health need: Rethinking health care systems
Ease of access and
navigation
Ease of clinical and community referrals: Enabling closed loop referrals between clinical
providers and community partners through Epic would enhance care coordination through
two-way communication.
Improve interpreter services: Expanded access to interpreter services using varied
communication modalities (e.g. video chat) and through the use of high-quality medical
interpreters.
Augment patient call center: A patient access care center would augment existing patient call
center functions and support the patient and interdisciplinary care team around communication
and information sharing, cost transparency, clinical needs and prescription rells through Epic
H2O.
Patient-provider
relationships
Facilitation of discharge: Modications to the discharge process, especially for patients who
require equipment, home care services or placement in post-acute care facilities would improve
the patient experience as well as health outcomes. Many patients don’t have coverage for
these services and thus remain in the acute care setting, representing suboptimal care for the
patients and an enormous cost to the health system. This expansion would promote patient
understanding of their health action plan and ease access to coordinated follow-up care.
Health care cost and
transparency
Patient engagement and activation programs: This type of program would aim to encourage
patients, possibly through incentives, to regularly engage with their interdisciplinary care team
and in other health promotion and wellness services.
Training on billing: This training would expand provider and staff education around billing and
health care costs in support of patient-centered care.
Priority health need: An infrastructure for scaling
State of the workforce Career development program: A comprehensive workforce development program would
create clear career ladders through increased training opportunities towards obtainment
of certicates, degrees and licenses, tuition reimbursement, mentorship programs and
establishment of joint practice/teaching positions with local, public colleges and universities
(e.g. CUNY).
Information sharing Improve information sharing and communication across provider entities and care teams:
Through Epic, collaboration and information sharing across interdisciplinary care teams, the
OneCity Health PPS partner network and city agencies would continue to promote coordinated,
longitudinal relationships between patients and providers.

36
19MISC0100
