Monitoring the
Nation’s Health
SAFE
Instruction Manual
Part 20
ICD-10 Cause-of-Death Querying, 2010
R ● HEALTHIER ● PEOPLE
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
Instruction Manual
Part 20
ICD-10 Cause-of-Death Querying, 2010
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
Hyattsville, Maryland
December 2009
Acknowledgments
This instruction manual update was prepared by the Division of Vital Statistics (DVS) under the
general direction of Robert N. Anderson, Ph.D., Chief of the Mortality Statistics Branch (MSB).
Donna Glenn and Julia Raynor (DVS) provided review of the original version of the instruction
manual; Donna L. Hoyert, Ph.D. (MSB) updated the content.
Questions regarding this manual and related processing problems should be directed to the
Mortality Statistics Branch, 3311 Toledo Road, Room 7318, Hyattsville, Maryland 20782 or the
Mortality Medical Classification Branch, Division of Vital Statistics, National Center for Health
Statistics, P.O. Box 12214, Research Triangle Park, North Carolina 27709. Questions concerning
interpretation of mortality data should be referred to the Mortality Statistics Branch as well.
Major Revisions from Previous Manual
1. Made changes in Appendix C to reflect the current infrequent and rare cause list in
Instruction manual part 2a.
2. Added a few infrequent and rare causes from Appendix C to Table 1.
3. Made changes in Table 1 related to footnote 2.
4. Modified Table 2 to make it consistent with current Instruction manual part 2a section on
the interpretation of highly improbable.
5. Update url’s referenced in the text.

Contents
Section Page
I. Introduction 1
Basics of medical certification 3
Completing a cause-of-death statement 8
Additional aids 8
II. Who Carries Out the Query 11
III. Use of Querying 12
IV. How Much to Query 13
V. Levels of Querying 14
Priority Level 1 16
Priority Level 2 18
Priority Level 3 18
Priority Level 4 19
Priority Level 5 19
Priority Level 6 20
Fetal death 20
Sample letters 21
VI. Evaluation of the Query Program 22
References 23
Appendix A- Specific Guidelines for When to Query
Table 1. Priority Levels for querying by ICD-10 Category 24
Order of entry of causes of death
Table 2. Priority Levels for improbable sequences in Part I of the death certificate 57
Table 3. Priority Levels for durations 63
Table 4. Priority Levels for placement and numbering of conditions 65
Appendix B- Sample Query Letters
Query Letter 1 68
Query Letter 2 72
Query Letter 3 78
Query Letter 4 84
Query Letter 5 90
Query Letter 6 96
Query Letter 7 102
Query Letter 8 108
Query Letter 9 114
Cause-of-death Querying
I. Introduction
Cause-of-death querying is a process by which the State health department contacts the medical
certifier who completed the cause-of-death statement and asks for clarification or further
information so that resulting mortality statistics may be as complete and accurate as possible.
The purpose of querying is two-fold: 1) to obtain information needed to properly code and
classify the cause of death and 2) to educate the certifier about the proper method of completing
medical certifications of death. Querying is one of the most important ways to improve the
quality of cause-of-death data. It must therefore, be viewed as an integral part of any State’s
vital statistics activity.
This manual has been revised for use with the 2003 U.S. Standard Certificate of Death and to
accommodate some updates to the International Classification of Diseases (ICD-10). The
general principles and procedures outlined in this manual are the same as in the previous manual
for the Tenth Revision of the ICD. While there are new items on the certificate related to
tobacco, pregnancy, and transportation injuries that relate to cause, the suggested queries in this
manual are built around the cause-of-death codes. Suggestions intended to minimize item non-
response for the tobacco, pregnancy, and transportation items are described in the Edit
Specifications for the Death Certificate posted at http://www.cdc.gov/nchs/vital_certs_rev.htm.
Querying is an essential part of the vital registration process (1-2), so both local registrars and
registration personnel in the State health department should be thoroughly knowledgeable of the
laws, procedures, and other requirements for death registration, querying, and death certificate
amendment. This manual is for those who have the responsibility for the acceptance and
- 1 -
registration of death certificates, primarily at the State level, and any key staff who have been
designated as responsible for communicating with medical certifiers about the accuracy and
completeness of the cause-of-death statement. The manual is restricted to the medical
certification portion of the record. Querying procedures for the demographic items on the death
certificate are addressed in a companion manual entitled “Guidelines for Implementing Field and
Query Programs for Registration of Births and Deaths” (Part 18).
Several levels of querying (levels 1 through 6) are offered in this manual; a minimal level of
querying (Priority Level 1) is necessary to produce cause-of-death statistics. It is estimated that
Level 1 querying would involve about five percent of a State’s death records. However, higher
levels of querying are desirable to ensure specificity and completeness in the physicians’
statements of cause of death. Not every State will be able to devote the same amount of effort to
querying; however, it is hoped that each registration area will elect to query at the maximum
level consistent with their resources and that all registration areas will query at least at Priority
Level 1. We believe that previous versions of this manual were of assistance to the States in
developing their own query programs, and we hope that this will as well.
In developing query procedures, consideration must also be given to the various uses of the death
certificate. Cause-of-death data are important for statistical uses in the following ways:
surveillance, research, design of public health and medical interventions, and funding decisions
for research and development. Cause-of-death data also have legal and administrative uses. For
example, in the case of accidents, the additional information requested such as the time and place
and the manner in which the injury occurred can be important in court cases, insurance claims,
etc. The Priority Levels in this manual focus on improving the usefulness of the data for
2

statistical purposes. States may wish to query other items that are legally or administratively
important in the particular State.
Normally, cause-of-death queries are directed to the certifier (attending physician, medical
examiner, coroner) who originally provided the information in the medical section of the death
certificate. However, if the death occurred in a hospital, it is also possible to obtain additional
information from the hospital files to further clarify the cause of death. For legal reasons, no
changes or additions should be made on the face of the original record without the approval of
the legally designated certifier. If the cause-of-death statement is substantially changed, the
certifying physician should be encouraged to file an amended certificate. The procedures for
filing amended certificates vary by State.
While querying has an immediate goal of clarifying the cause of death for individual records, it
has a broader goal of educating physicians on how to complete a medical certification. The
following section addresses some basics on medical certification.
Basics of medical certification
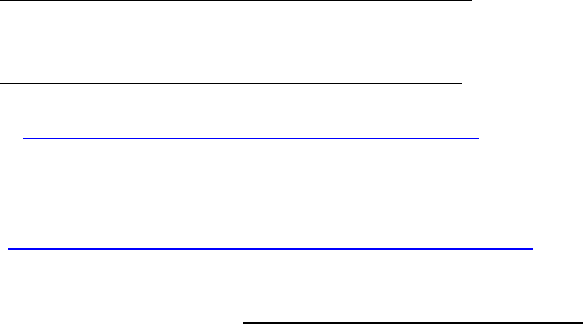
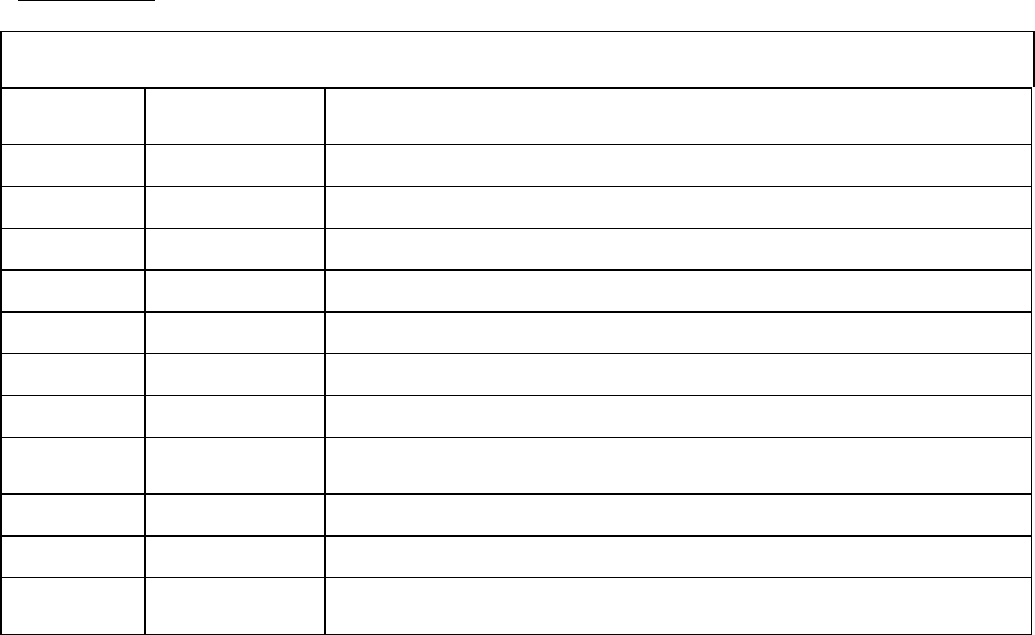
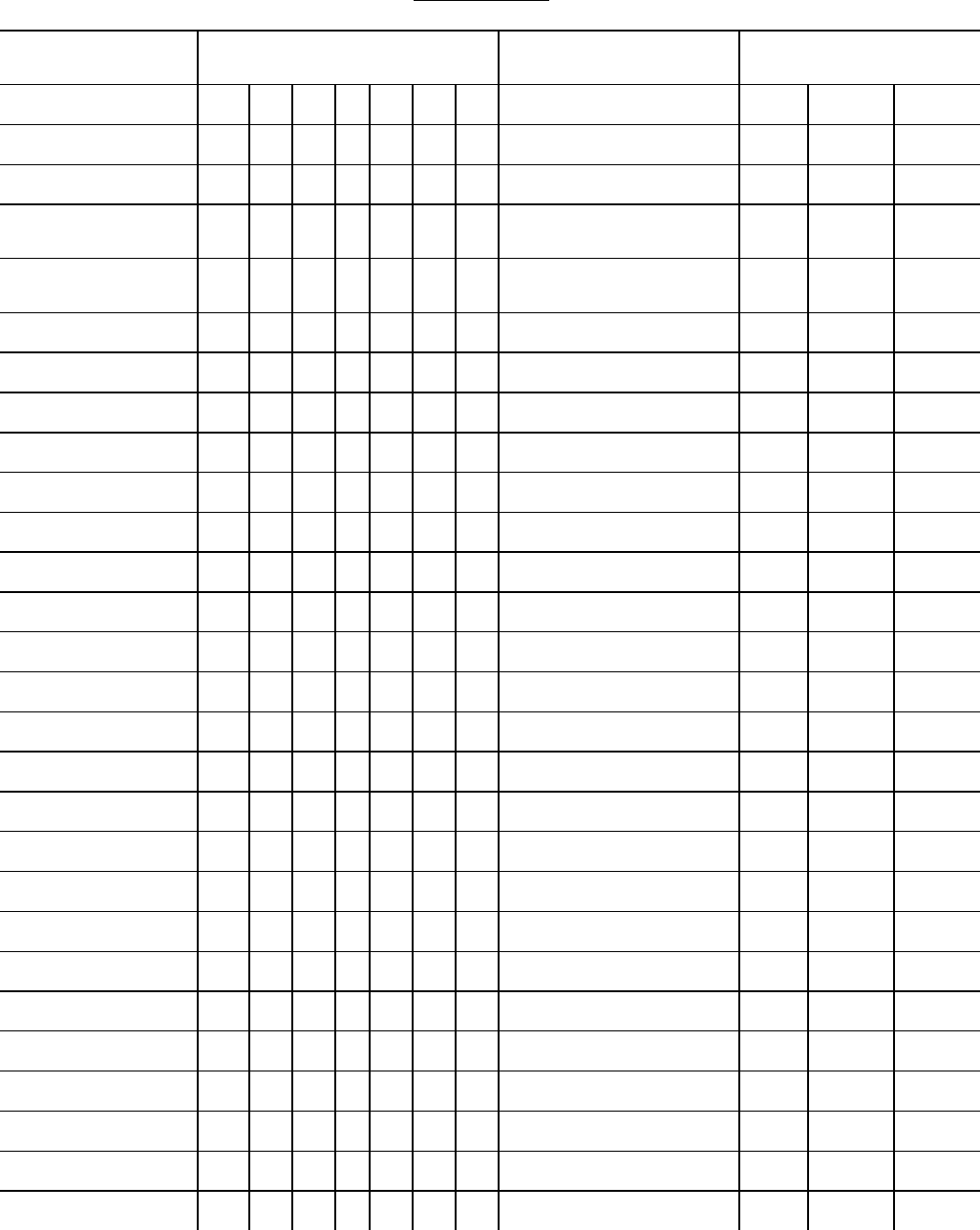
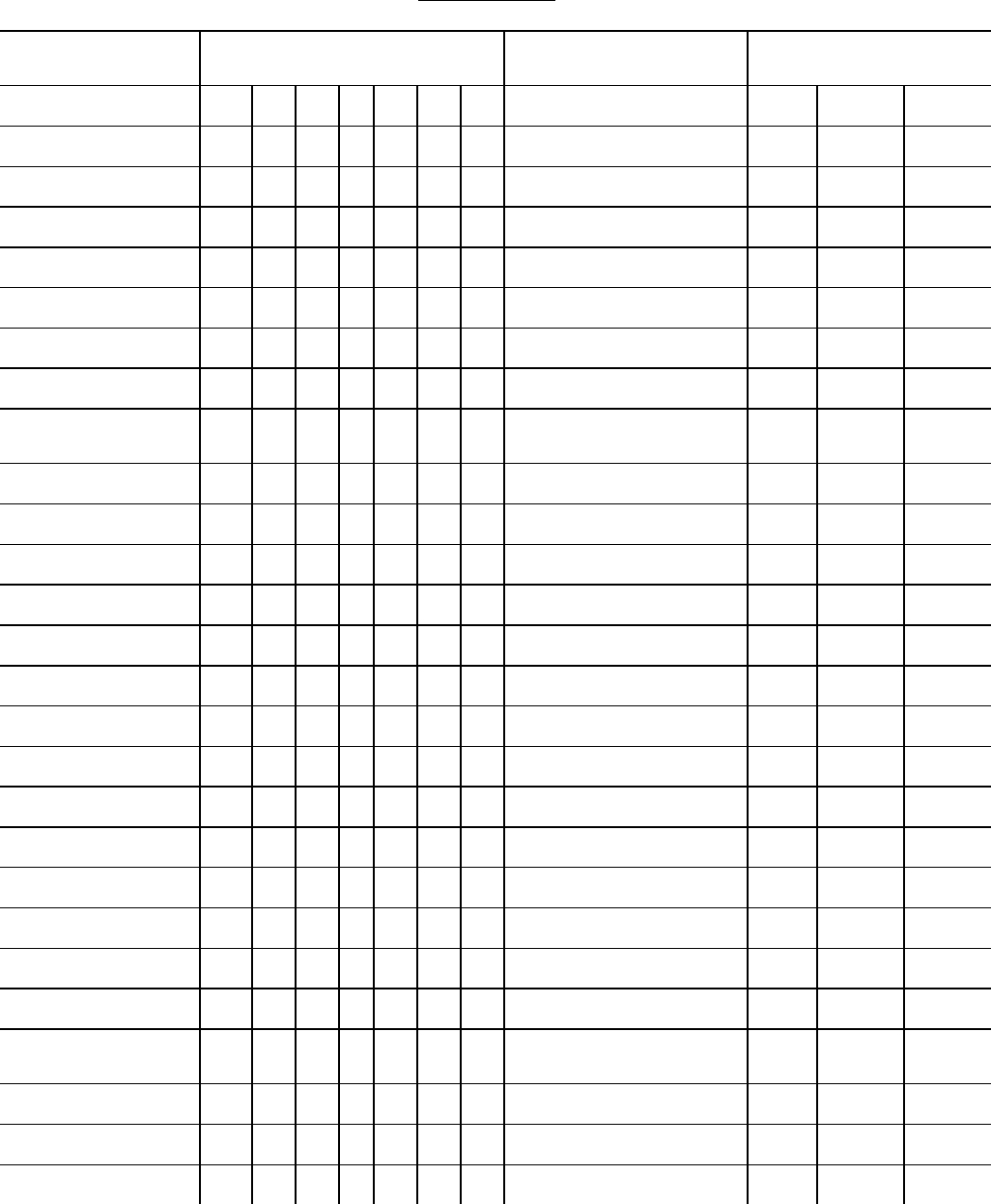
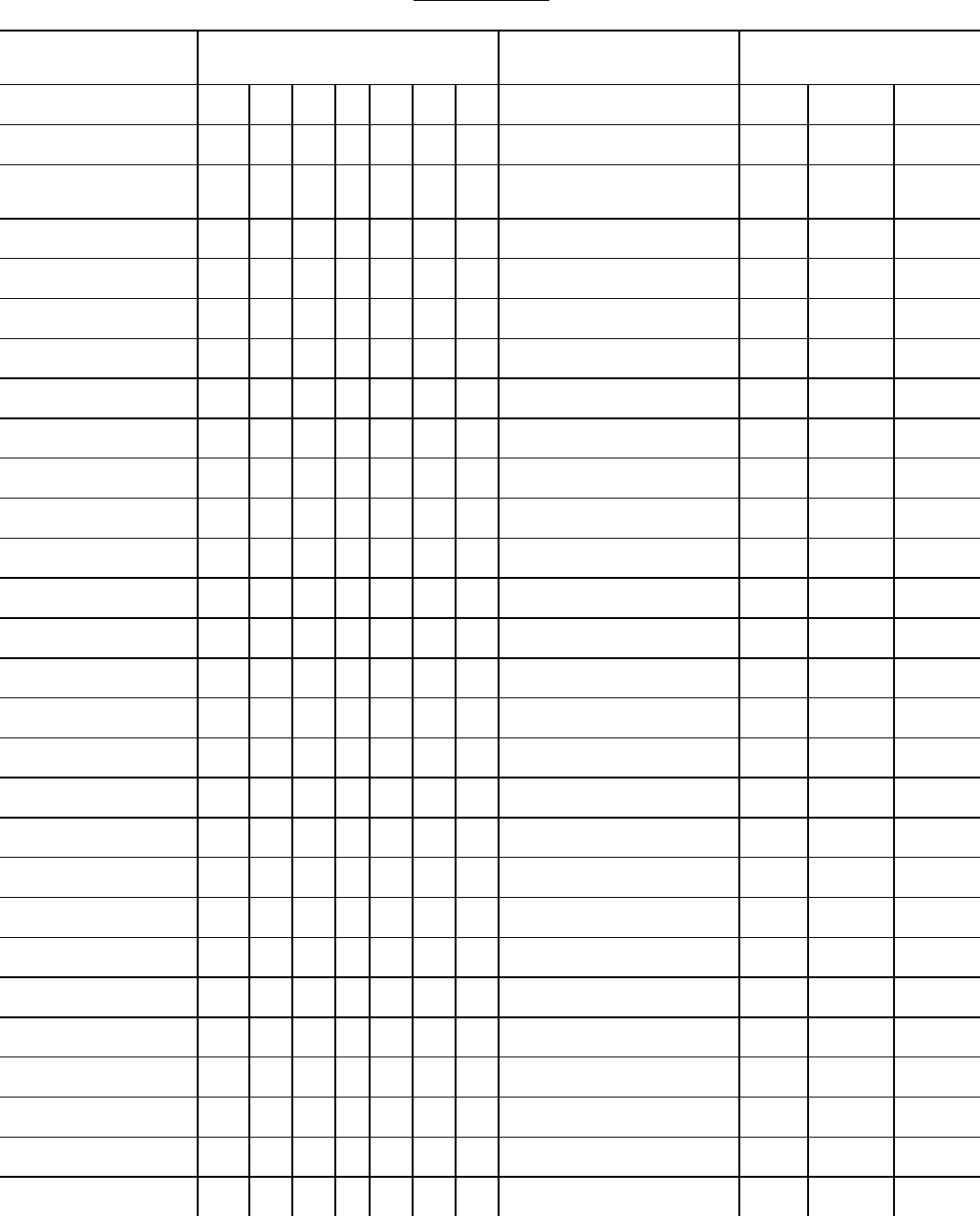
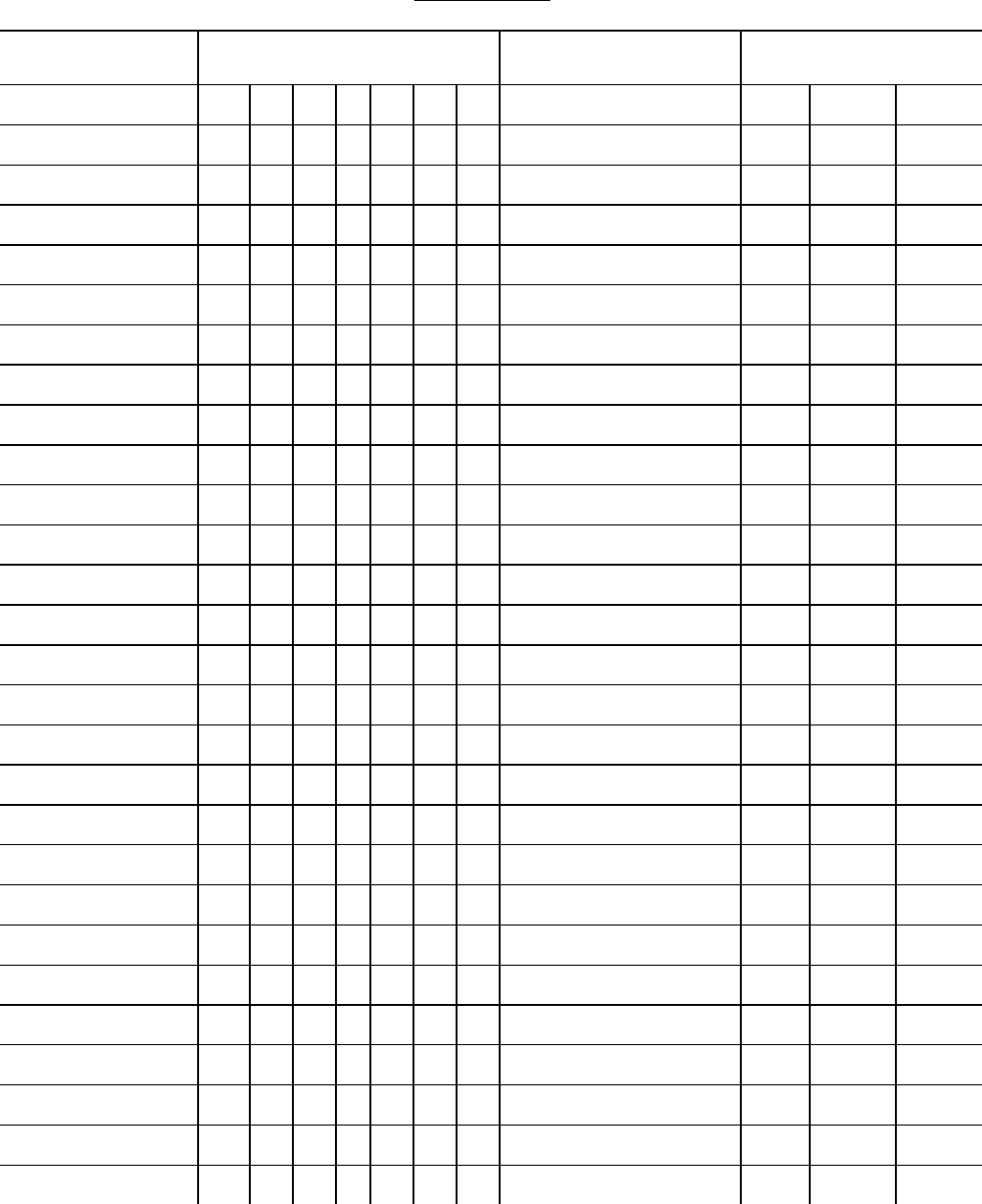
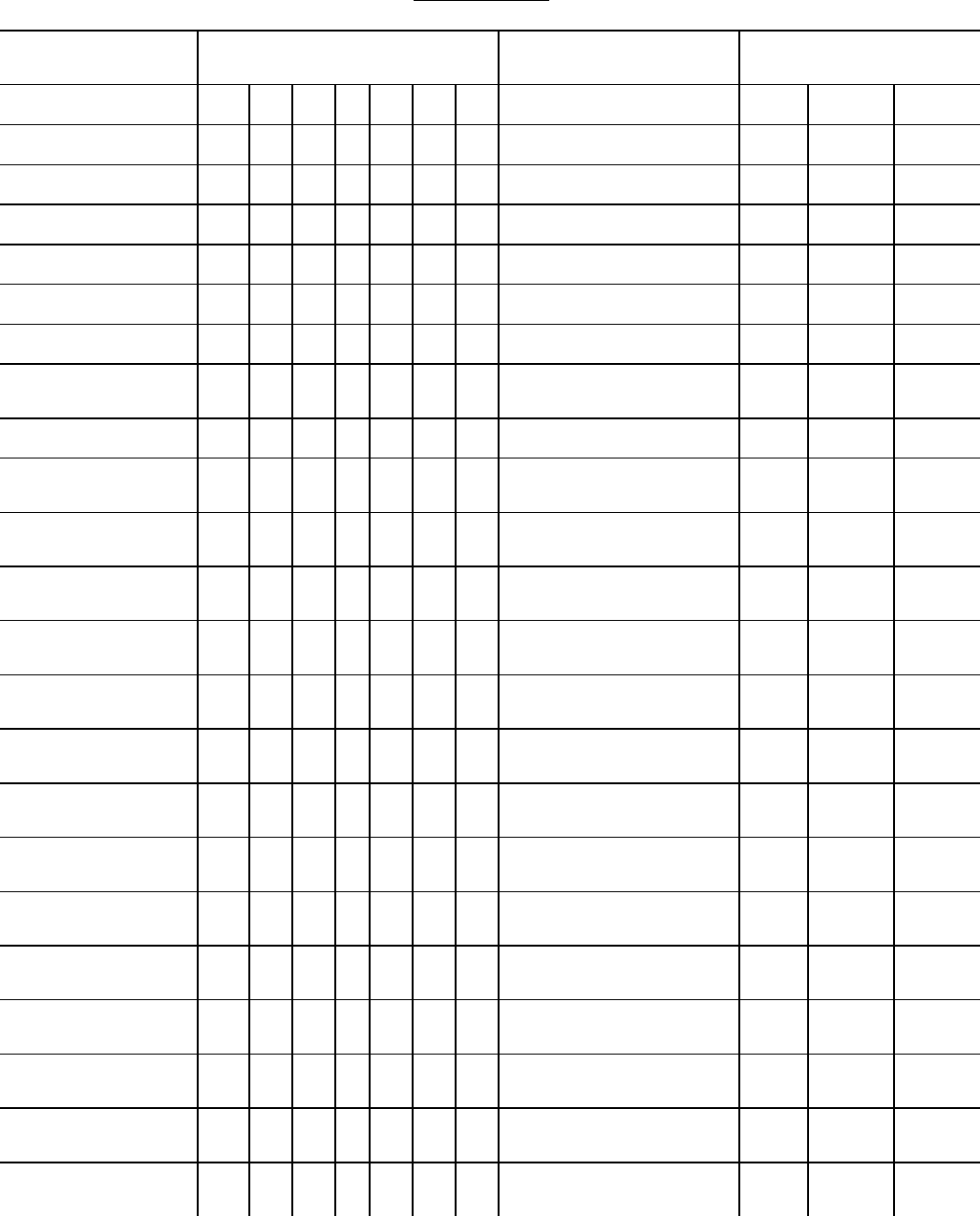
The medical certification section of the U.S. Standard Certificate of Death (Figure 1) is designed
to collect an underlying cause of death; that is, the disease or injury which initiated the train of
morbid events leading directly to death or the circumstances of the accident or violence which
produced the fatal injury. The certification section of the death certificate follows the format
recommended by the World Health Organization in the International Classification of Diseases
to facilitate reporting of the underlying cause of death by listing the immediate cause of death on
the top line of Part I followed by antecedent causes in proper sequence, with the reported
underlying cause being the last entry in Part I (Figure 2). Part II (Other Significant Conditions)
3
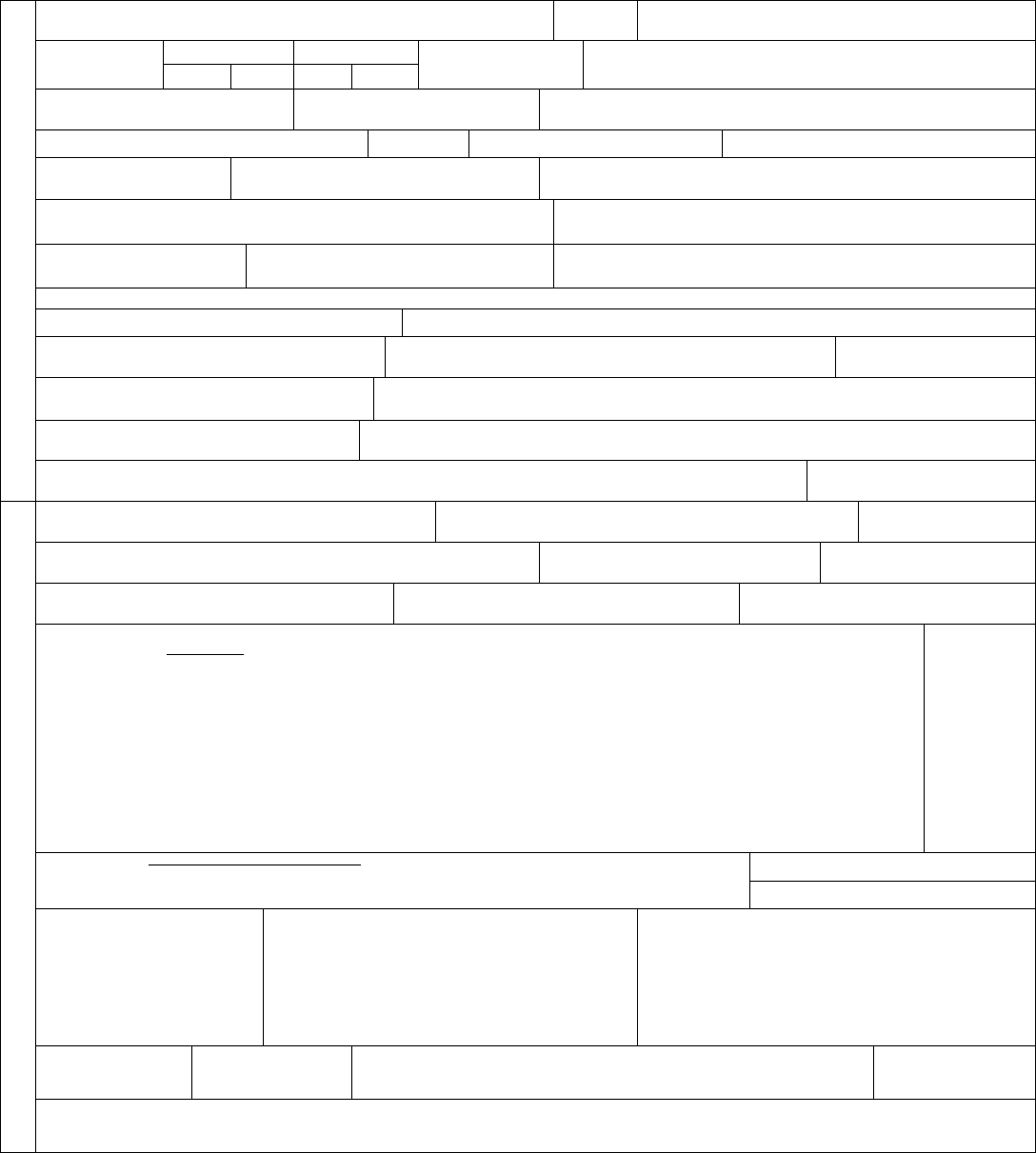
Figure 1. U.S. STANDARD CERTIFICATE OF DEATH
LOCAL FILE NO. STATE FILE NO.
NAME OF DECEDENT
For use by physician or institution
To Be Completed/ Verified By
FUNERAL DIRECTOR
1. DECEDENT’S LEGAL NAME (Include AKA’s if any) (First, Middle, Last)
2. SEX
3. SOCIAL SECURITY NUMBER
4a. AGE-Last Birthday
(Years)
4b. UNDER 1 YEAR 4c. UNDER 1 DAY 5. DATE OF BIRTH
(Mo/Day/Yr)
6. BIRTHPLACE (City and State or Foreign Country)
Months Days Hours Minutes
7a. RESIDENCE-STATE 7b. COUNTY 7c. CITY OR TOWN
7d. STREET AND NUMBER
7e. APT. NO.
7f. Z P CODE
7g. INSIDE CITY L MITS? Yes No
8. EVER N US ARMED FORCES?
Yes No
9. MARITAL STATUS AT TIME OF DEATH
Married Married, but separated Widowed
Divorced Never Married Unknown
10. SURVIV NG SPOUSE’S NAME (If wife, give name prior to first marriage)
11. FATHER’S NAME (First, Middle, Last)
12. MOTHER’S NAME PRIOR TO FIRST MARRIAGE (First, Middle, Last)
13a. INFORMANT’S NAME 13b. RELATIONSHIP TO DECEDENT 13c. MA L NG ADDRESS (Street and Number, City, State, Zip Code)
14. PLACE OF DEATH (Check only one: see instructions)
IF DEATH OCCURRED N A HOSPITAL:
Inpatient
Emergency Room/Outpatient
Dead on Arrival
IF DEATH OCCURRED SOMEWHERE OTHER THAN A HOSPITAL:
Hospice facility
Nursing home/Long term care facility
Decedent’s home
Other (Specify):
15. FACILITY NAME (If not institution, give street & number)
16. CITY OR TOWN , STATE, AND Z P CODE
17. COUNTY OF DEATH
18. METHOD OF DISPOSITION: Burial Cremation
Donation Entombment Removal from State
Other (Specify):_____________________________
19. PLACE OF DISPOSITION (Name of cemetery, crematory, other place)
20. LOCATION-CITY, TOWN, AND STATE 21. NAME AND COMPLETE ADDRESS OF FUNERAL FACILITY
22. SIGNATURE OF FUNERAL SERVICE LICENSEE OR OTHER AGENT
23. LICENSE NUMBER (Of Licensee)
To Be Completed By
MEDICAL CERTIFIER
ITEMS 24-28 MUST BE COMPLETED BY PERSON
WHO PRONOUNCES OR CERTIFIES DEATH
24. DATE PRONOUNCED DEAD (Mo/Day/Yr)
25. TIME PRONOUNCED DEAD
26. SIGNATURE OF PERSON PRONOUNCING DEATH (Only when applicable) 27. LICENSE NUMBER 28. DATE SIGNED (Mo/Day/Yr)
29. ACTUAL OR PRESUMED DATE OF DEATH
(Mo/Day/Yr) (Spell Month)
30. ACTUAL OR PRESUMED TIME OF DEATH
31. WAS MEDICAL EXAM NER OR
CORONER CONTACTED? Yes No
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a._____________________________________________________________________________________________________________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b._____________________________________________________________________________________________________________
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c._____________________________________________________________________________________________________________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d._____________________________________________________________________________________________________________
Approximate
interval:
Onset to death
_____________
_____________
_____________
_____________
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY F NDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. D D TOBACCO USE CONTRIBUTE
TO DEATH?
Yes Probably
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF NJURY
(Mo/Day/Yr) (Spell Month)
39. T ME OF INJURY
40. PLACE OF NJURY (e.g., Decedent’s home; construction site; restaurant; wooded area)
41. INJURY AT WORK?
Yes No
42. LOCATION OF INJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
4

43. DESCRIBE HOW NJURY OCCURRED:
44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
45. CERT FIER (Check only one):
Certifying physician-To the best of my knowledge, death occurred due to the cause(s) and manner stated.
Pronouncing & Certifying physician-To the best of my knowledge, death occurred at the time, date, and place, and due to the cause(s) and manner stated.
Medical Examiner/Coroner-On the basis of examination, and/or investigation, in my opinion, death occurred at the time, date, and place, and due to the cause(s) and manner stated.
Signature of certifier:_____________________________________________________________________________
46. NAME, ADDRESS, AND ZIP CODE OF PERSON COMPLETING CAUSE OF DEATH (Item 32)
47. TITLE OF CERTIF ER 48. LICENSE NUMBER 49. DATE CERTIFIED (Mo/Day/Yr)
50. FOR REGISTRAR ONLY- DATE FILED (Mo/Day/Yr)
To Be Completed By
FUNERAL DIRECTOR
51. DECEDENT’S EDUCATION-Check the box
that best describes the highest degree or level of
school completed at the time of death.
8th grade or less
9th - 12th grade; no diploma
High school graduate or GED completed
Some college credit, but no degree
Associate degree (e.g., AA, AS)
Bachelor’s degree (e.g., BA, AB, BS)
Master’s degree (e.g., MA, MS, MEng,
MEd, MSW, MBA)
Doctorate (e.g., PhD, EdD) or
Professional degree (e g., MD, DDS,
DVM, LLB, JD)
52. DECEDENT OF HISPANIC ORIGIN? Check the box
that best describes whether the decedent is
Spanish/Hispanic/Latino. Check the “No” box if
decedent is not Spanish/Hispanic/Latino.
No, not Spanish/Hispanic/Latino
Yes, Mexican, Mexican American, Chicano
Yes, Puerto Rican
Yes, Cuban
Yes, other Spanish/Hispanic/Latino
(Specify) __________________________
53. DECEDENT’S RACE (Check one or more races to indicate what the
decedent considered himself or herself to be)
White
Black or African American
American Indian or Alaska Native
(Name of the enrolled or principal tribe) _______________
Asian Indian
Chinese
Filipino
Japanese
Korean
Vietnamese
Other Asian (Specify)__________________________________________
Native Hawaiian
Guamanian or Chamorro
Samoan
Other Pacific Islander (Specify)_________________________________
Other (Specify)___________________________________________
54. DECEDENT’S USUAL OCCUPATION (Indicate type of work done during most of working life. DO NOT USE RETIRED).
55. KIND OF BUSINESS/INDUSTRY
allows the physician to list any other medically important disease or condition that was present at
the time of death and which may have contributed to death but was not a direct link in the chain
of events directly leading to death. Multiple causes of death include each of the causes reported
on the death certificate in Parts I or II.
Underlying cause is the item most commonly used in tabulation and analysis. As stated earlier,
underlying cause data are important for surveillance, research, design of public health and
medical interventions, and funding decisions for research and development. Multiple cause data
are an important supplement to underlying cause data and can provide additional analytical
information.
It is very important that all physicians, medical examiners, or coroners who may be certifying
deaths be properly oriented to the principles of medical certification, the manner in which the
statements are to be entered, and the importance of completeness, accuracy, and specificity in
5
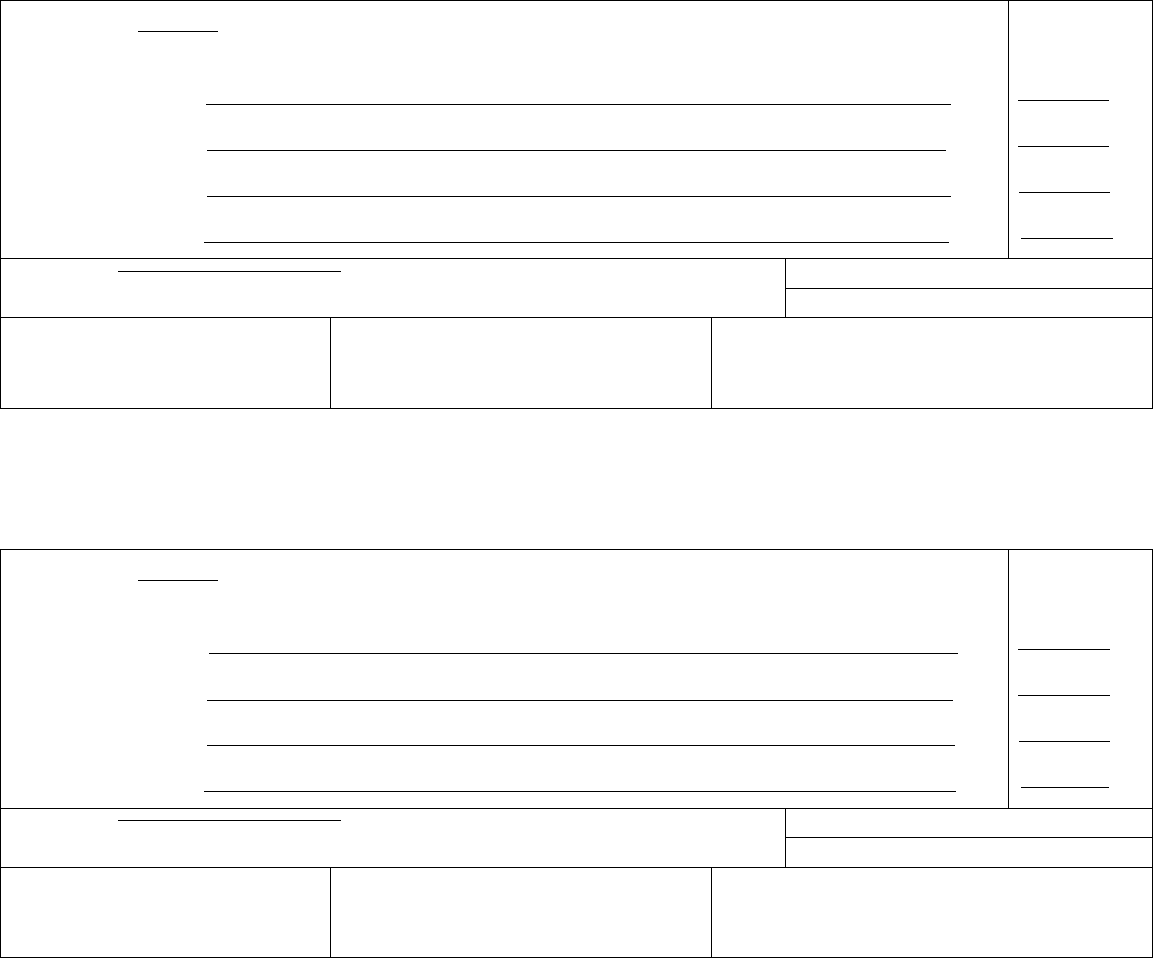
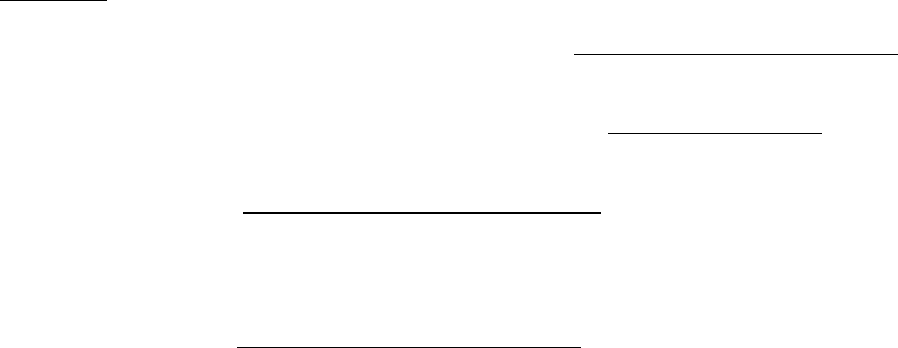
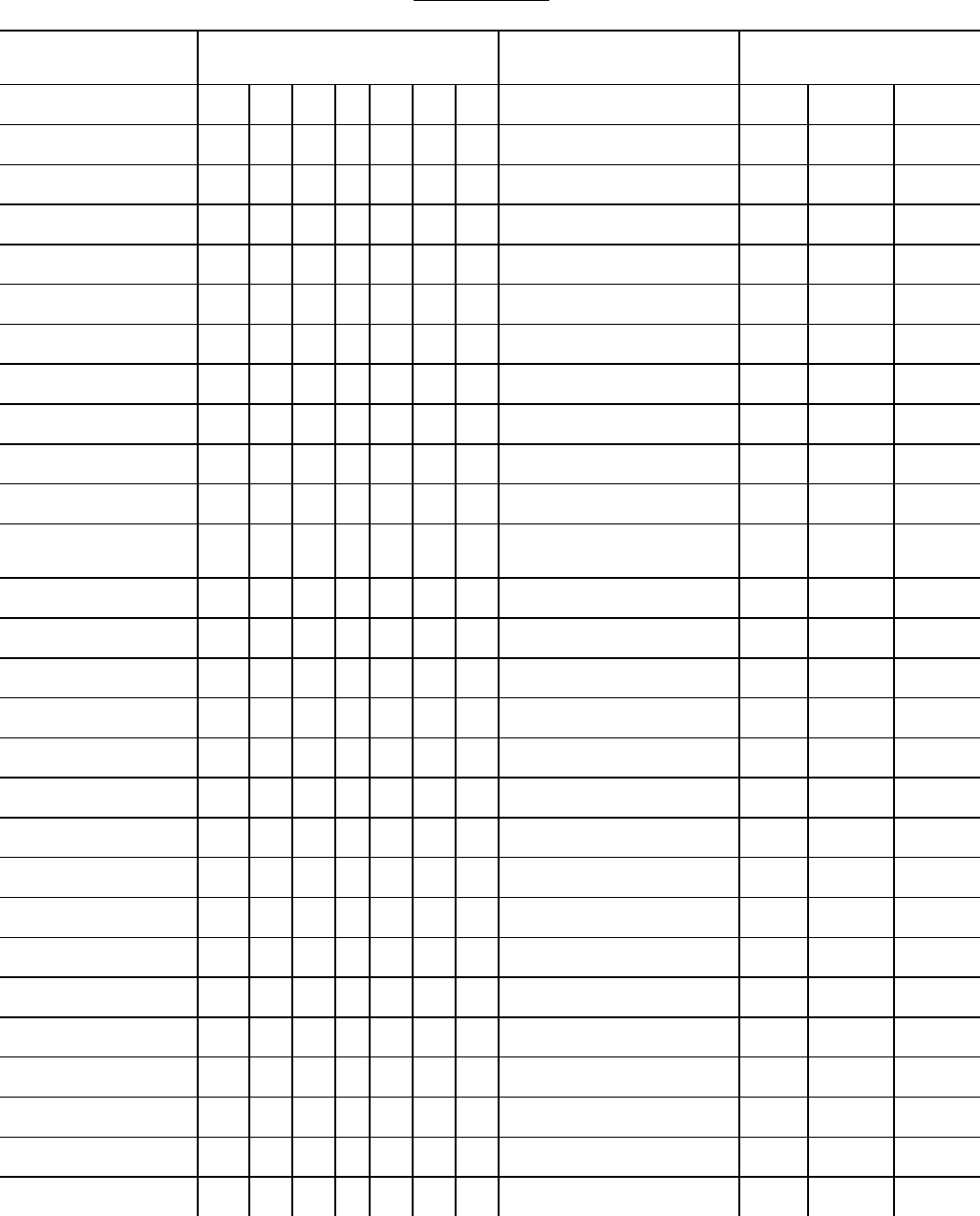
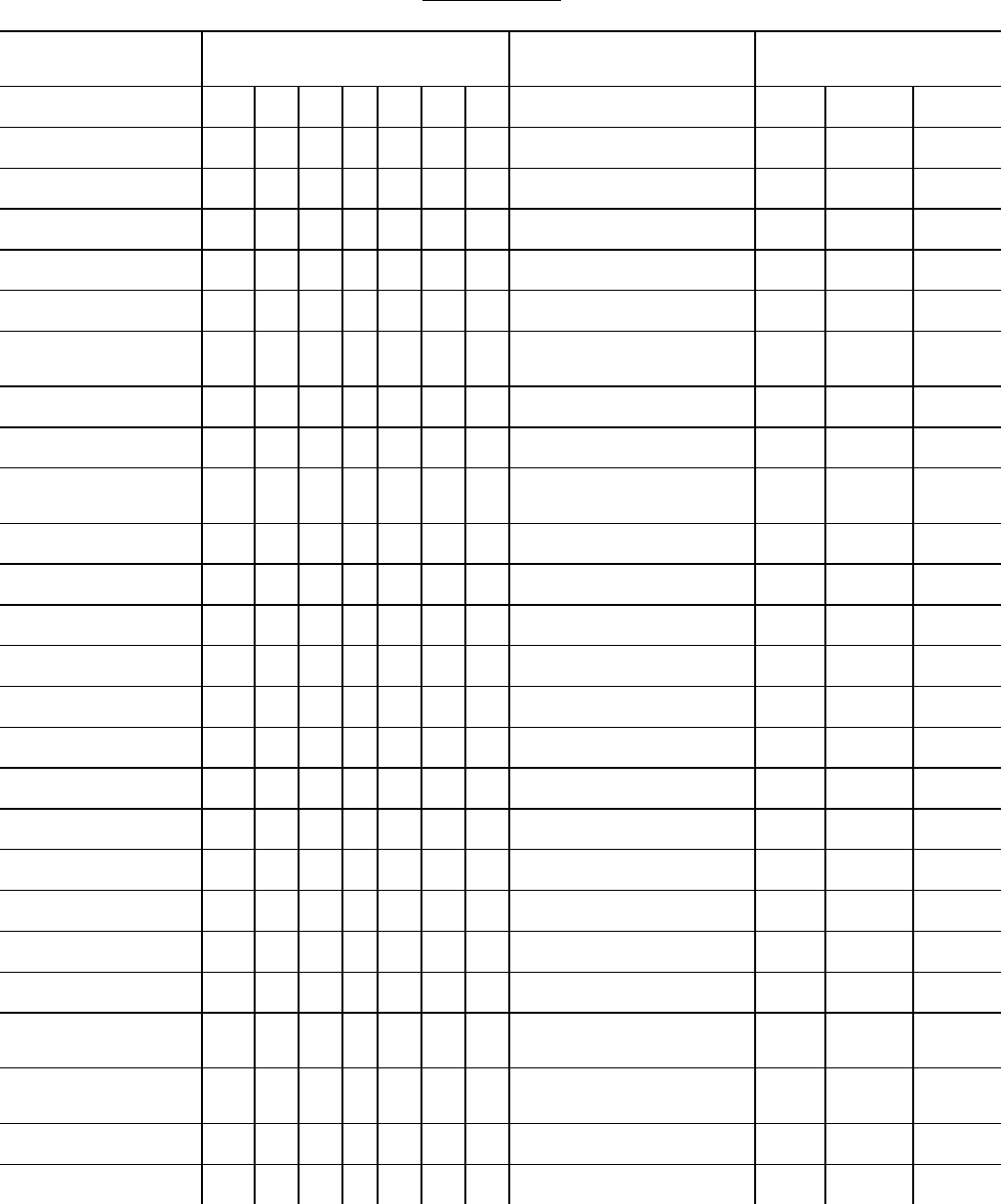
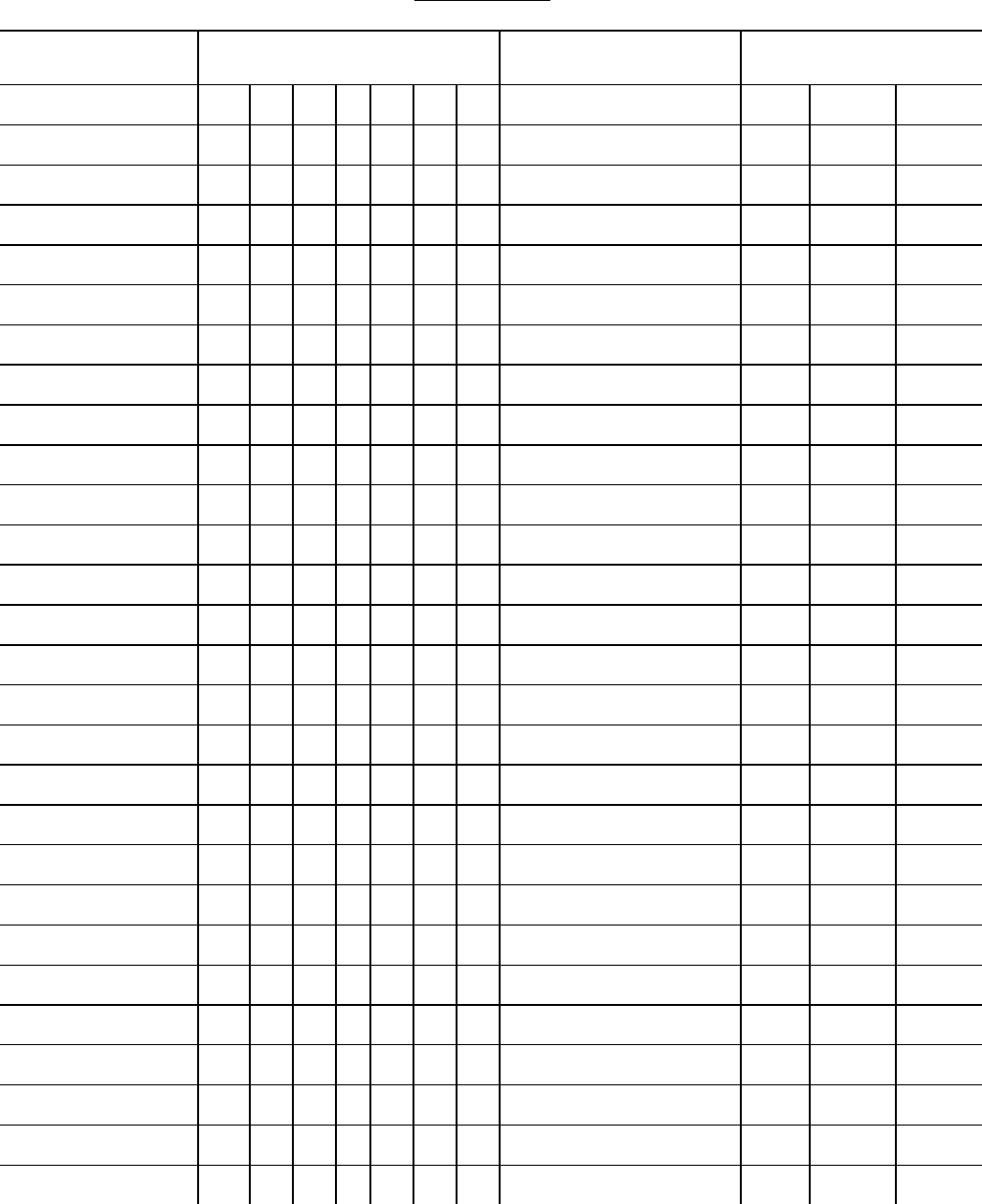
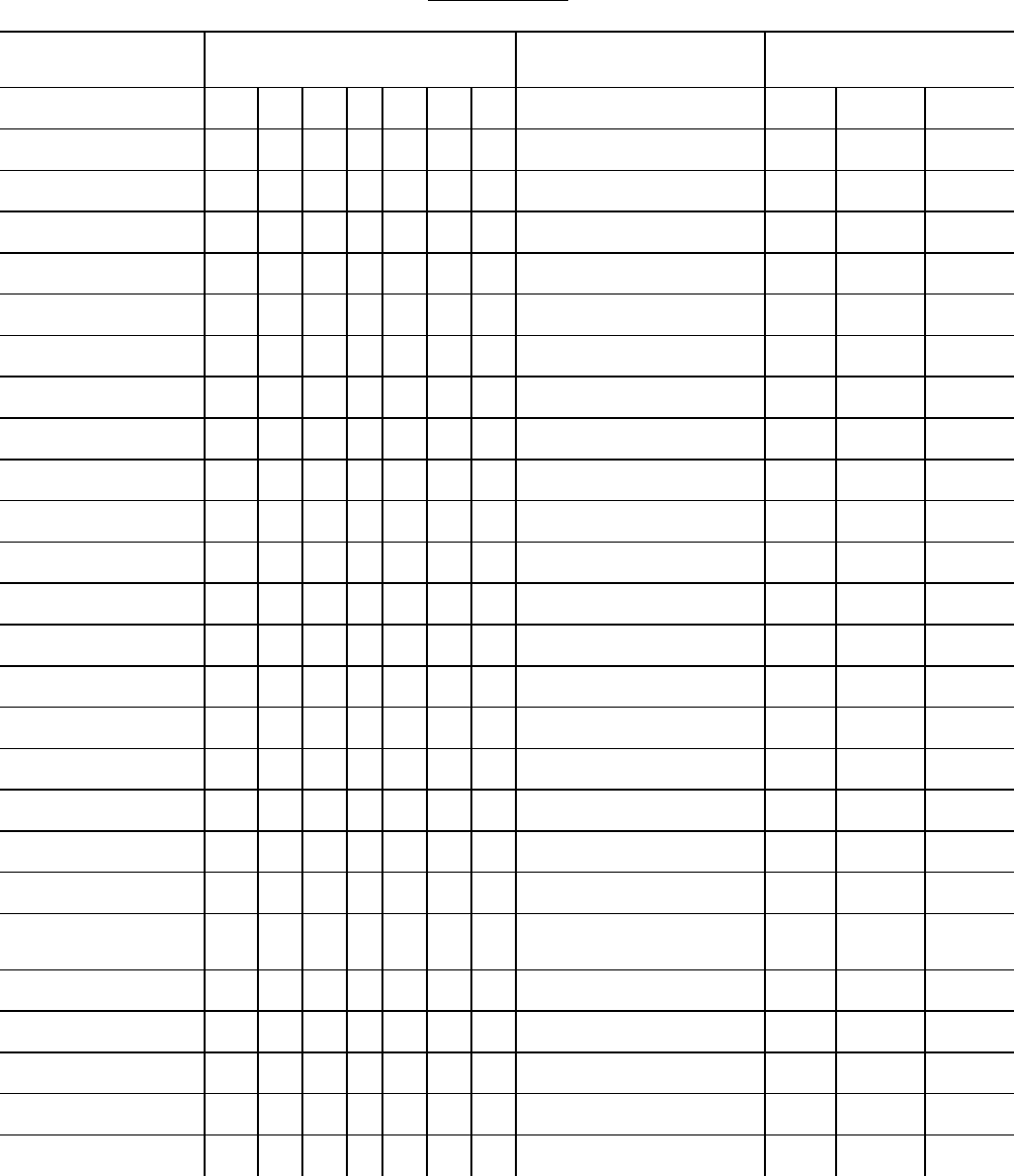
Figure 2.
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Immediate cause of death
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Intermediate cause
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Intermediate cause
initiated the events resulting
in death) LAST d. Underlying cause _______________________________________________________________________________
Approximate interval:
Onset to death
Time interval
Time interval
Time interval
Time interval
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Contributory cause(s), if any
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY F NDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Rupture of myocardium
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Acute myocardial infarction
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Coronary artery thrombosis
initiated the events resulting
in death) LAST d. Atherosclerotic coronary artery disease
Approximate interval:
Onset to death
Minutes
6 days
6 days
7 years
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Diabetes, Chronic obstructive pulmonary disease, smoking
33. WAS AN AUTOPSY PERFORMED?
■
Yes
No
34. WERE AUTOPSY F NDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
■
Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
■
Yes Probably
No Unknown
36. F FEMALE:
■
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
listing the causes of death. Even the most conscientious physician sometimes has a difficult time
in distinguishing between those conditions that should be included in the causal chain versus
those conditions not in the chain but medically important and relevant. The cause-of-death
6
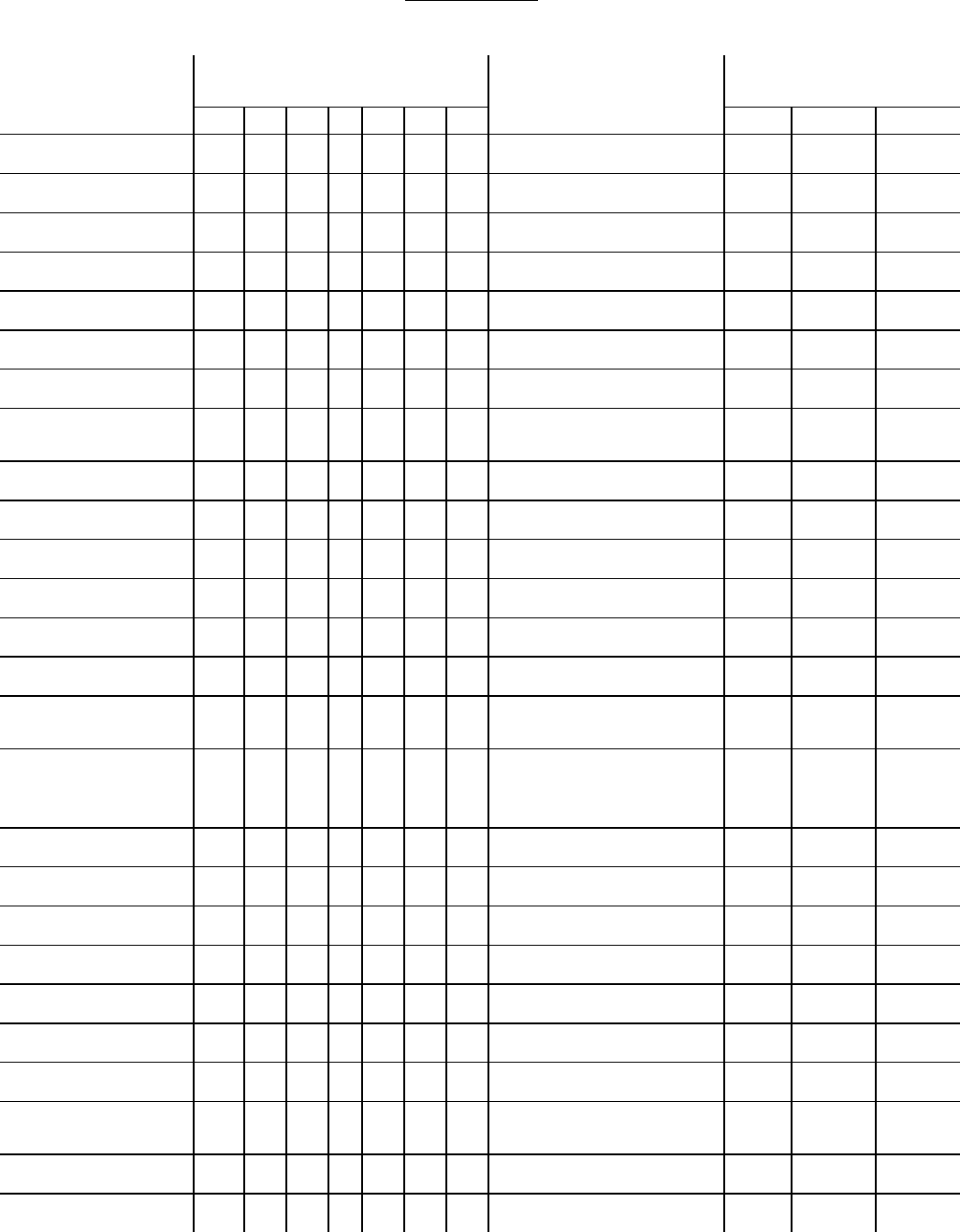
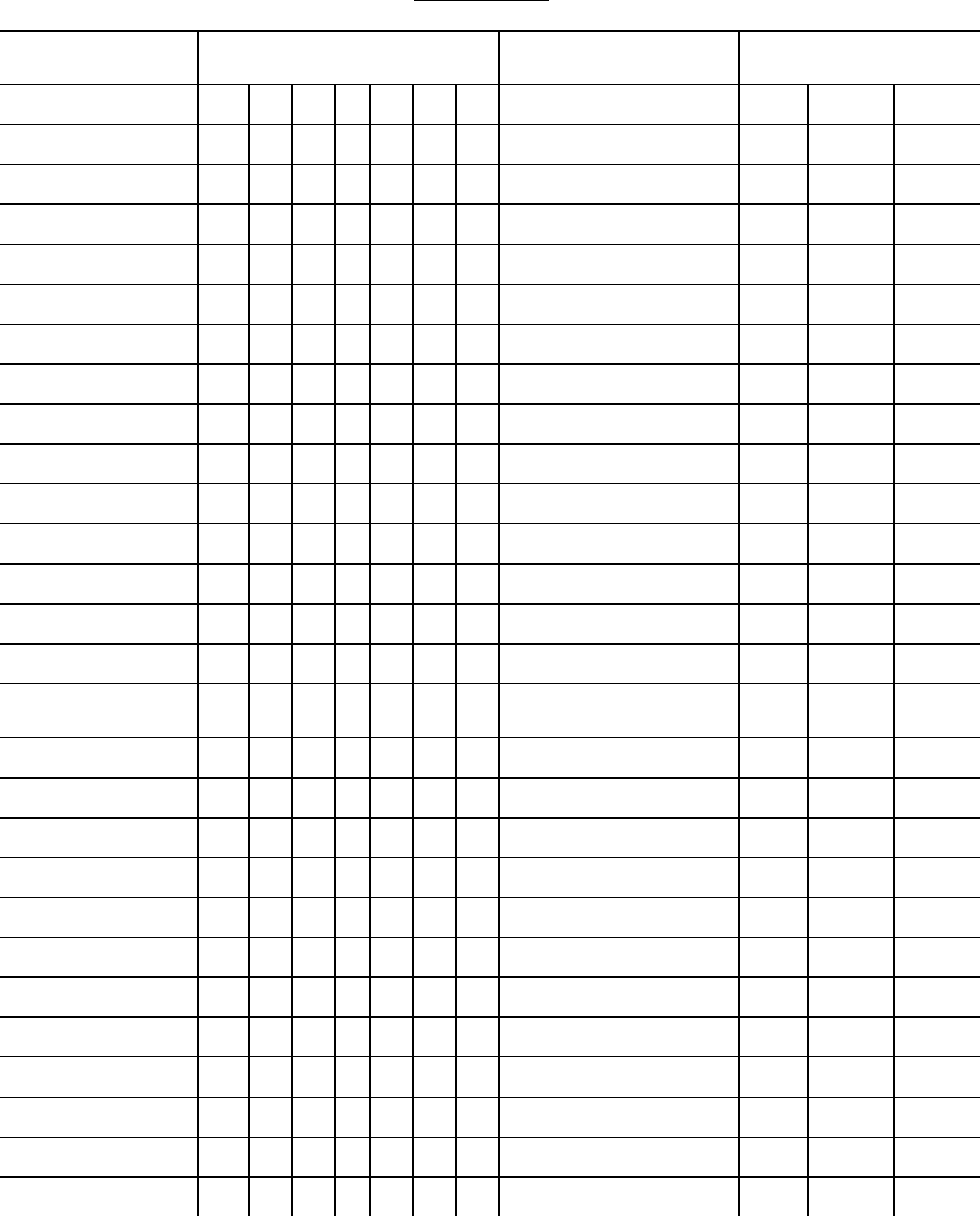
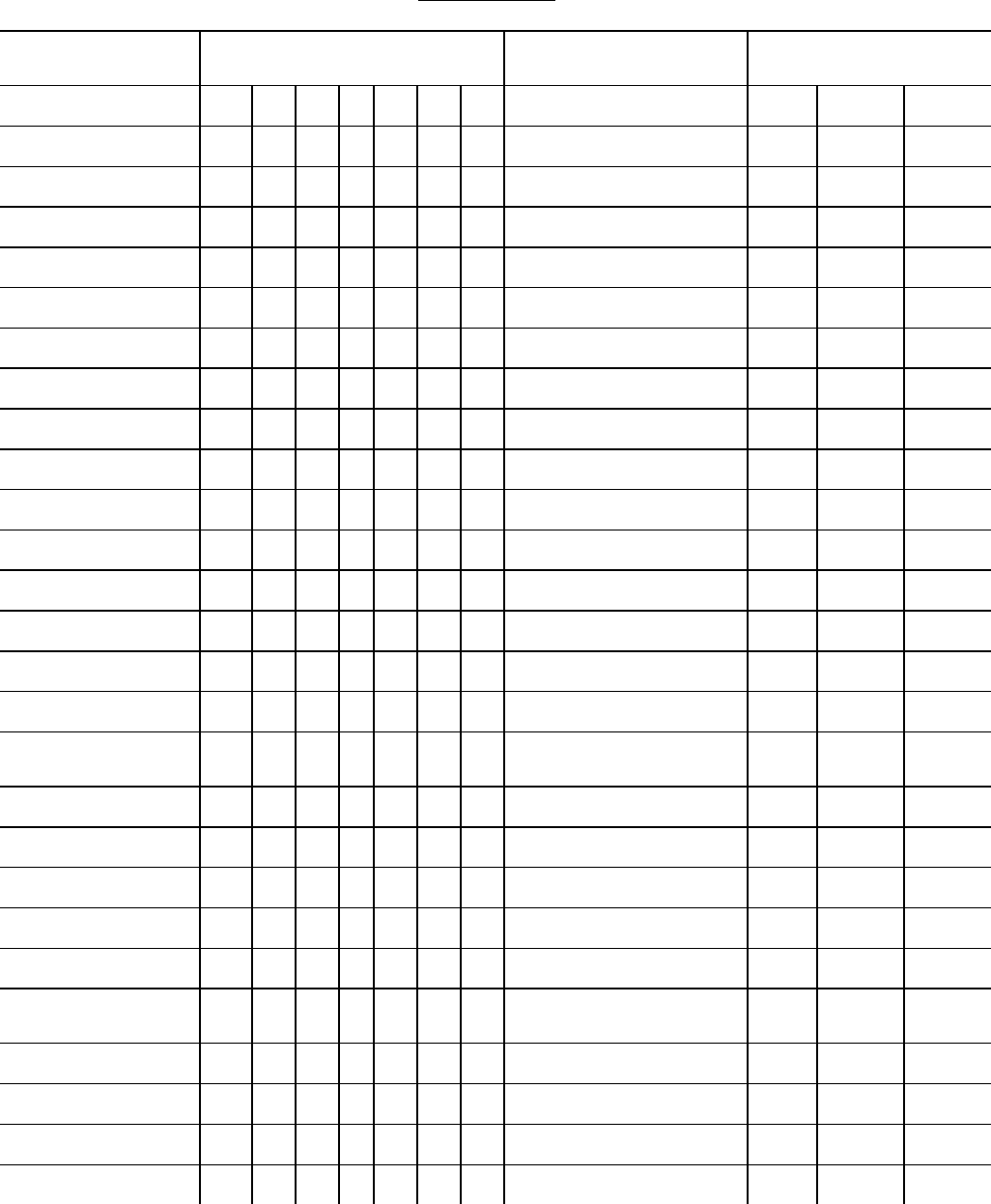
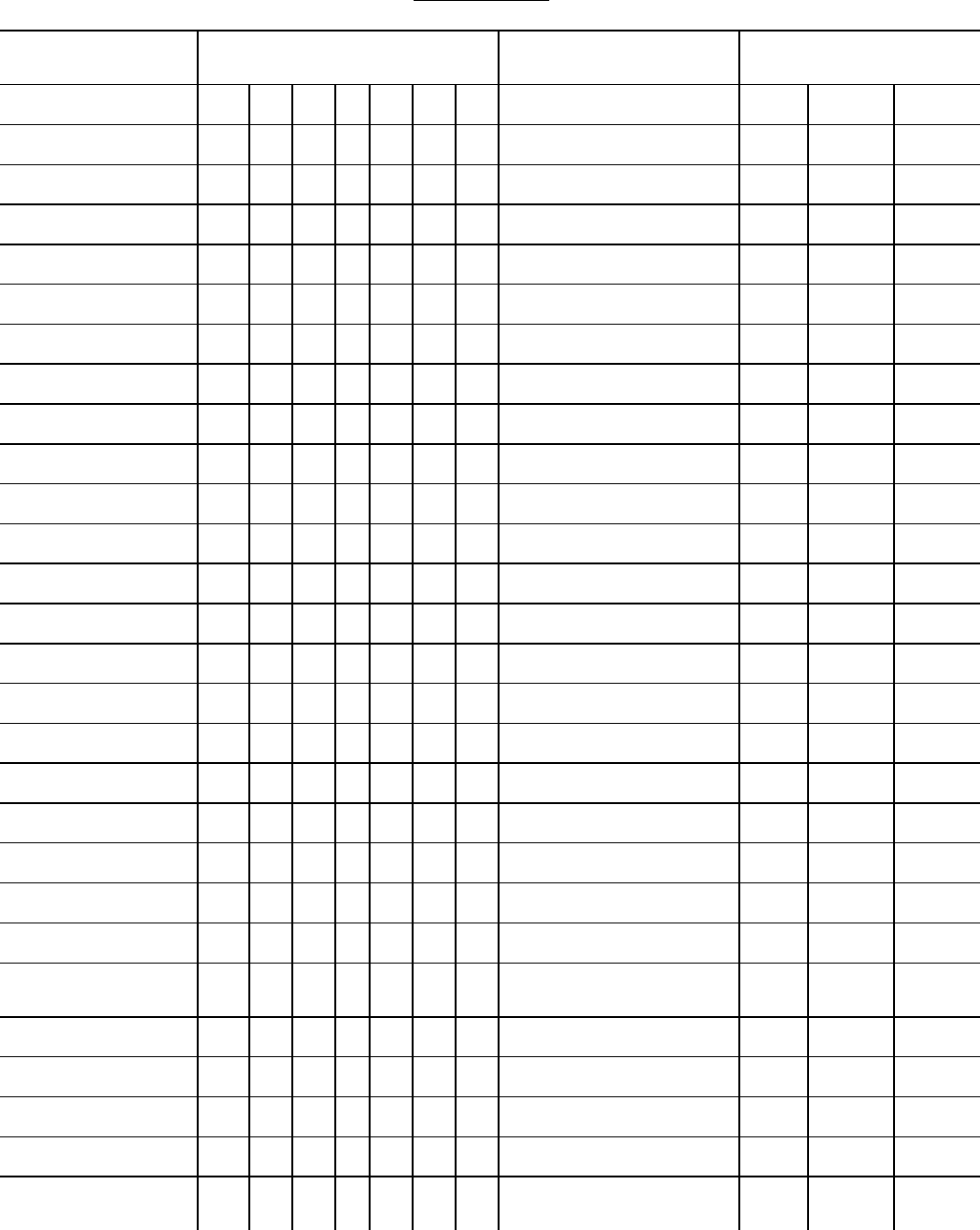
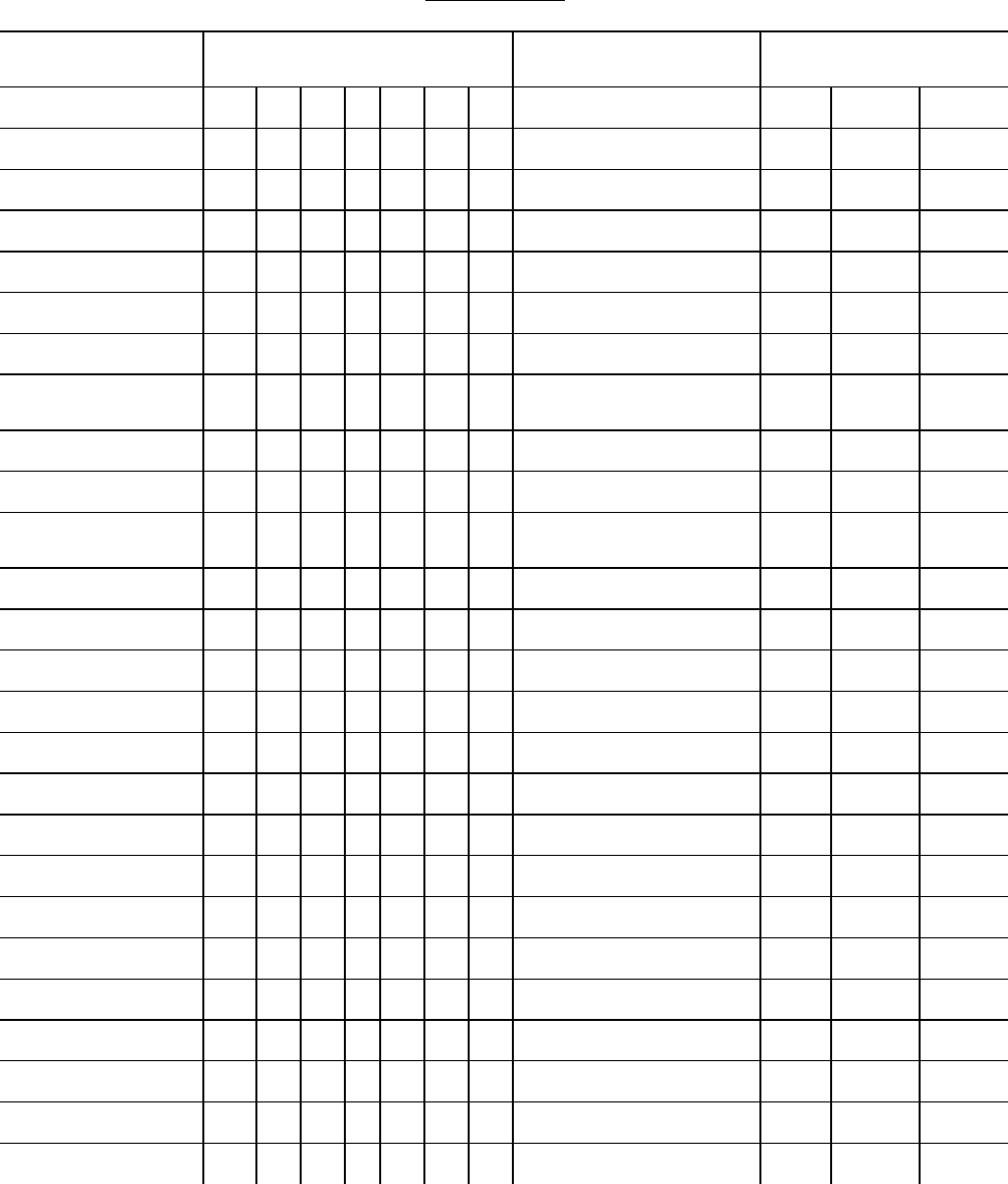
Figure 3. Completing a cause-of-death statement: Basic concepts
1) Deaths known or suspected of having been caused by injury or poisoning should be reported to the medical examiner or coroner,
and you will complete the death certificate if the medical examiner or coroner doesn’t accept the case.
2) The cause-of-death information should be your best medical opinion.
3) Only one condition should be listed per line in Part I. Additional lines may be added if necessary.
4) Each condition in Part I should cause the one above it.
5) Abbreviations and parentheses should be avoided in reporting causes.
6) Provide the best estimate of the interval between the presumed onset of each condition and death. The terms “approximately” or
“unknown” may be used. Do not leave the interval blank; if unknown, indicate that it is unknown.
7) If additional medical information or autopsy findings become available that would change the cause of death originally reported,
the original death certificate should be amended by the certifying physician by following the procedures in place in your State.
8) Report each disease, abnormality, injury, or poisoning that you believe adversely affected the decedent. A condition can be listed
as “probable” even if it has not been definitively diagnosed.
9) A complete sequence should be reported in Part I that explains why the patient died. The sequence may be an etiological or
pathological sequence as well as a sequence in which an earlier condition is believed to have prepared the way for a subsequent
cause by damage to tissues or impairment of function.
10) No entry is necessary on lines (b), (c), and (d) if a single cause of death reported on line (a) describes completely the train of events
resulting in death.
11) If two or more possible sequences resulted in death, report in Part I the one that, in your opinion, most directly caused death.
Report in Part II the other conditions or diseases.
12) A specific cause of death should be reported in the last entry in Part I so there is no ambiguity about the etiology of this cause.
13) Conditions or diseases in Part II should contribute to death but not result in the last entry in Part I.
14) Mechanistic terminal events such as respiratory arrest, asystole, cardiac arrest, cardio-respiratory arrest, ventricular fibrillation, and
electromechanical dissociation should not be the only condition included in the cause-of-death statement and are unlikely to be the
underlying cause.
15) Always report an etiology for organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory
failure on the lines beneath it.
16) If, in your opinion, the use of alcohol, tobacco, other substance by the decedent, or a recent pregnancy or injury caused or
contributed to death, then this condition should be reported.
17) A primary site and/or histological type should be specified for neoplasms or specify that site and type are unknown.
18) For deaths resulting from injuries, always report the fatal injury event, the trauma, and the impairment of function.
19)
Injury items (38-43 in Figure 1) should have some sort of entry if the manner has been reported as accident, homicide, or suicide.
7
certification constitutes a medical-legal opinion, not necessarily an absolute fact, since it is not
always possible to make a precise determination of interacting diseases or conditions. Thus, “to
the best of my knowledge” is included in the certification statement, since the certifier is
considered to be in a better position than anyone else to make a judgment as to the chain of
events leading to death, but he/she cannot always be presumed to have a clear cut “absolute
answer”.
In certifying causes of death, several kinds of errors or oversights are frequently made, often due
to the physicians not understanding how to complete the certification of death. One of the most
common errors is the listing of causes in incorrect or illogical order, or the listing of more than
one disease or condition on the same line. Another frequent error is omitting the interval
between onset and death, the hour of death, and whether an autopsy was performed.
Completing a cause-of-death statement
Figure 3 shows some basic guidelines to certifying physicians on how to complete a cause-of-
death statement.
Additional Aids
On occasion, it may be beneficial for the certifier physician to discuss medical certification of
death with a member of the State health department staff before certifying a cause of death. It is
helpful to provide a telephone number and the name of an individual who can provide answers to
the certifier’s questions. Needless to say, the person to whom such calls are referred must have a
familiarity with medical terminology and of the pathology and etiology of morbid conditions.
Additional instructional material on writing cause-of-death statements is available; widespread
knowledge and use of these materials by physicians could reduce many reporting problems and
8
the need for extensive querying. The sample letters include a very short reference to the
resources, but maximum benefit would probably be gained by providing the certifying physician
a packet of instructional material including, at least, items 2, 3, and 4 below:
1. Applicable State resources
2. Instructions for completing the cause-of-death section of the death certificate
(laminated plastic card or pocket size folder available from NCHS, also at
http://www.cdc.gov/nchs/data/dvs/blue form.pdf )
3. Instructions for completing the cause-of-death section of the death certificate for injury
and poisoning (laminated plastic card or pocket size folder available from NCHS, also at
http://www.cdc.gov/nchs/data/dvs/red_form.pdf )
4. Physicians’ Handbook on Medical Certification of Death (available from NCHS, also
at http://www.cdc.gov/nchs/data/misc/hb cod.pdf)
5. Medical examiners’ and coroners’ handbook on death registration and fetal death
reporting (available from NCHS, also at http://www.cdc.gov/nchs/data/misc/hb_me.pdf)
6. Possible solutions to common problems in death certification
(http://www.cdc.gov/nchs/about/major/dvs/handbk.htm)
7. Tutorial from the National Association of Medical Examiners under Death
Certificate Completion heading
(http://www.thename.org/CauseDeath/COD_main_page.htm)
8. The Medical Cause of Death Manual (3) edited by Randy Hanzlick: can be ordered
from the College of American Pathologists (800-323-4040 ext. 7531 for information and
credit card orders). The product code number is B260.
9. Cause-of-Death Statements and Certification of Natural and Unnatural Deaths edited
by Randy Hanzlick: can be ordered from the College of American Pathologists (800-323-
4040 ext. 7531 for information and credit card orders). The product code number is
BK7261.
Enlisting the cooperation of the State and local medical societies to conduct some
instructional/educational sessions on completing death certificates should be considered,
especially if a local region makes a disproportionate number of errors. Local medical schools
should also be approached about the possibility of including training on death certification as
part of their curriculum.
Training physicians in the proper completion of a death certificate will work best when the
physicians feel that they have a vested interest in the death certification process. One way of
improving the sense of being vested is to explain how the data is used for health programs and
9
II. Who Carries Out the Query
States must decide who can best carry out querying. Historically, nosologists have done the
querying, but with the advent of automated processing, fewer States have nosologists. These
States must develop different mechanisms for querying, perhaps by training other staff to query.
The person who queries records needs to be someone who understands the content and purpose
of the querying manual, which in turn implies an understanding of coding rules and medical
causality. That person could be an experienced nosologist or a trained statistician or a medical
officer with an understanding of how death certificates should be completed. Consideration
might be given to identifying a physician on staff in the State health department or under contract
who could provide assistance with the querying process. It is critical that the person doing the
querying have good communication skills as well as an understanding of why the certificate is
being queried (e.g., to obtain more information or to correct obvious inadequacies).
An area for future development is to develop automated procedures for querying. NCHS is
incorporating Priority Level 1 queries into the automated mortality medical software, specifically
SuperMICAR. Initially, the system will identify the certificate number, the query level, and the
recommended letter. The State staff can then pull the record and review the record to determine
if a query is needed. Eventually, the automated system will produce a letter that may be used to
query the record.
11
III. Use of Querying
If employed correctly, the query procedure can be a very effective method of acquainting
physicians with the proper methods for certifying a cause of death. Unfortunately, most
physicians do not receive training on completing death certificates during their formal education;
therefore, querying can help provide them with information to enable them to certify a death
correctly. Many common errors or omissions can be avoided by consistent querying, if sufficient
explanation is furnished to the certifier to help them modify their approach with future medical
certifications.
The design and wording of form letters used in querying is very important, not only for obtaining
the necessary information for the death being queried, but to convey to the certifier enough
information so that he/she can correctly certify future cases of the same or similar types.
Questions in query letters need to be specific enough to indicate what is missing or incorrect and
what information is being requested. The more explicit the letter, the better the response that can
be expected. Examples illustrating the correct certification of specific causes are shown on the
back of the sample form letters in Appendix B; these examples may serve as guides to the
certifier.
12

IV. How Much to Query
Querying is a critical part of maintaining and improving data quality. The official responsible
for vital registration and vital statistics should make a careful appraisal of the type and extent of
querying that has taken place on the cause-of-death statements in his/her own registration area.
Then, a better decision can be made about possible revisions in current query procedures and
practices. Such decisions should take into account:
1) The importance of querying in improving physicians’ practices in completing cause-
of-death statements
2) The importance of querying in improving the particular death record under review
3) The extent to which staff resources can be devoted to querying versus other office
activities
4) The query method that will be most effective in accomplishing 1) and 2) above.
Some records with questionable conditions or situations are easily identified as good candidates
for querying or further investigation. Situations that need clarification are described in general
terms in the description of the query levels and in specific terms in the four tables of
Appendix A. The query manual provides general guidelines to what should be queried but
informed judgment must be applied on a case-by-case basis before sending out a query to a
physician.
13
V. Levels of Querying
Recognizing that the availability of staff and resources to be utilized for querying varies from
State to State, the following levels of querying have been designed to aid decision makers in
developing the query program for the specific State vital statistics program. The categories are
in priority order ranging from “1" indicating cases that should always be queried, to “6" which is
an optional category. To facilitate referencing, Priority Level 1 is subdivided into categories a-g.
Those categories requiring no querying are indicated by “0". For systematic data improvement,
the manager should elect to query up to the highest Priority Level commensurate with the
registration area’s needs and resources. Intervening levels should not be skipped. NCHS
recommends that every registration area conduct, as a minimum, the Priority Level 1 queries.
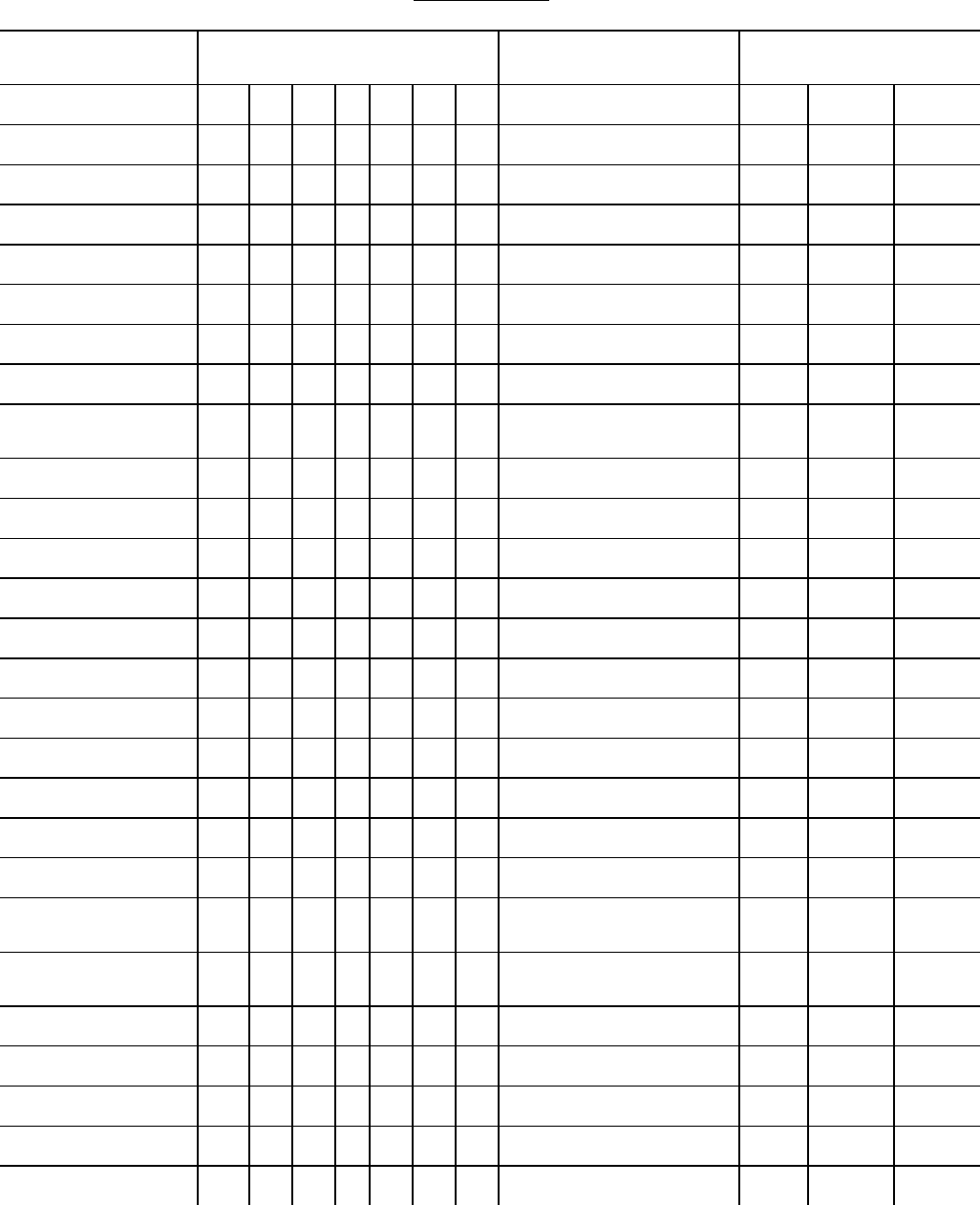
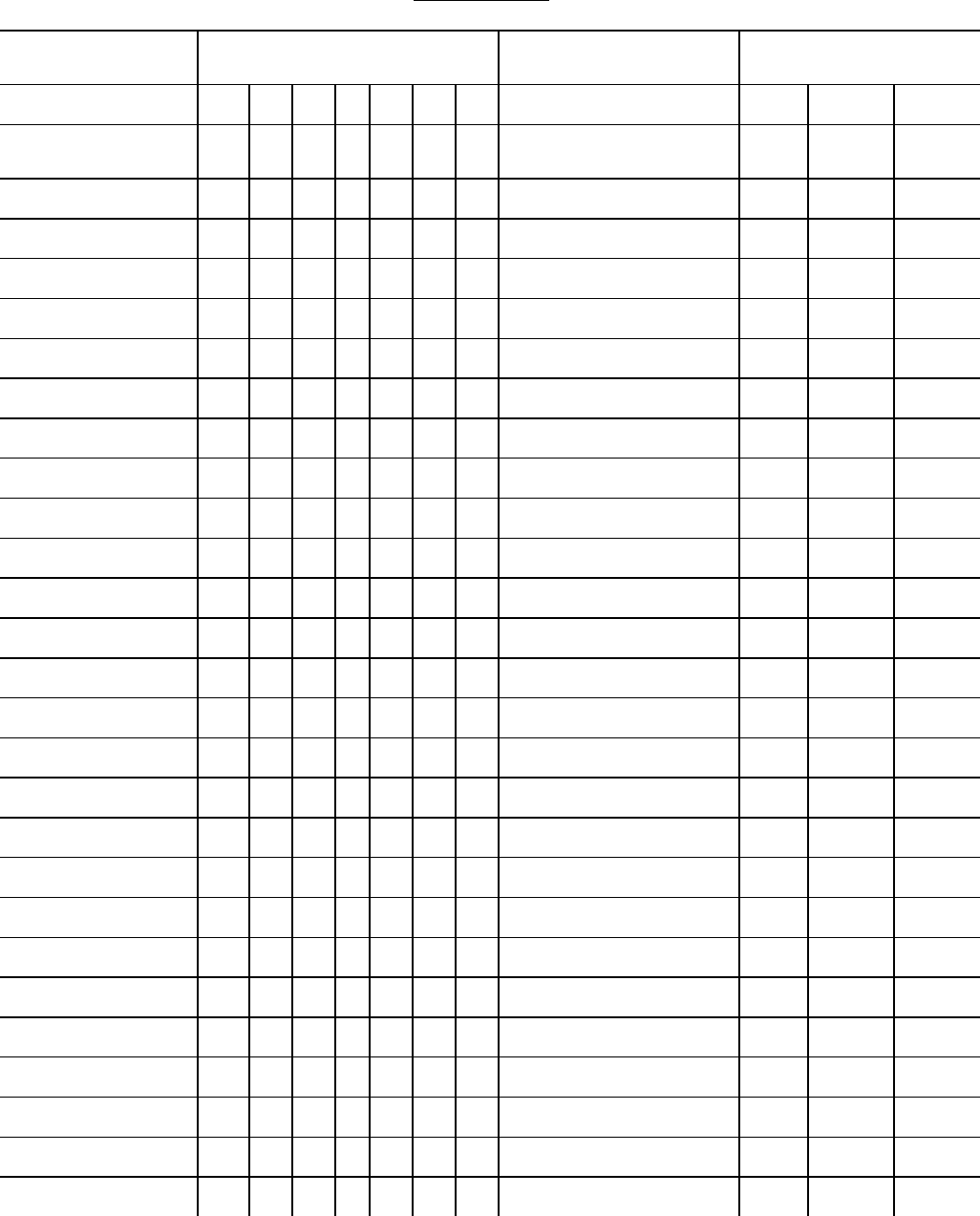
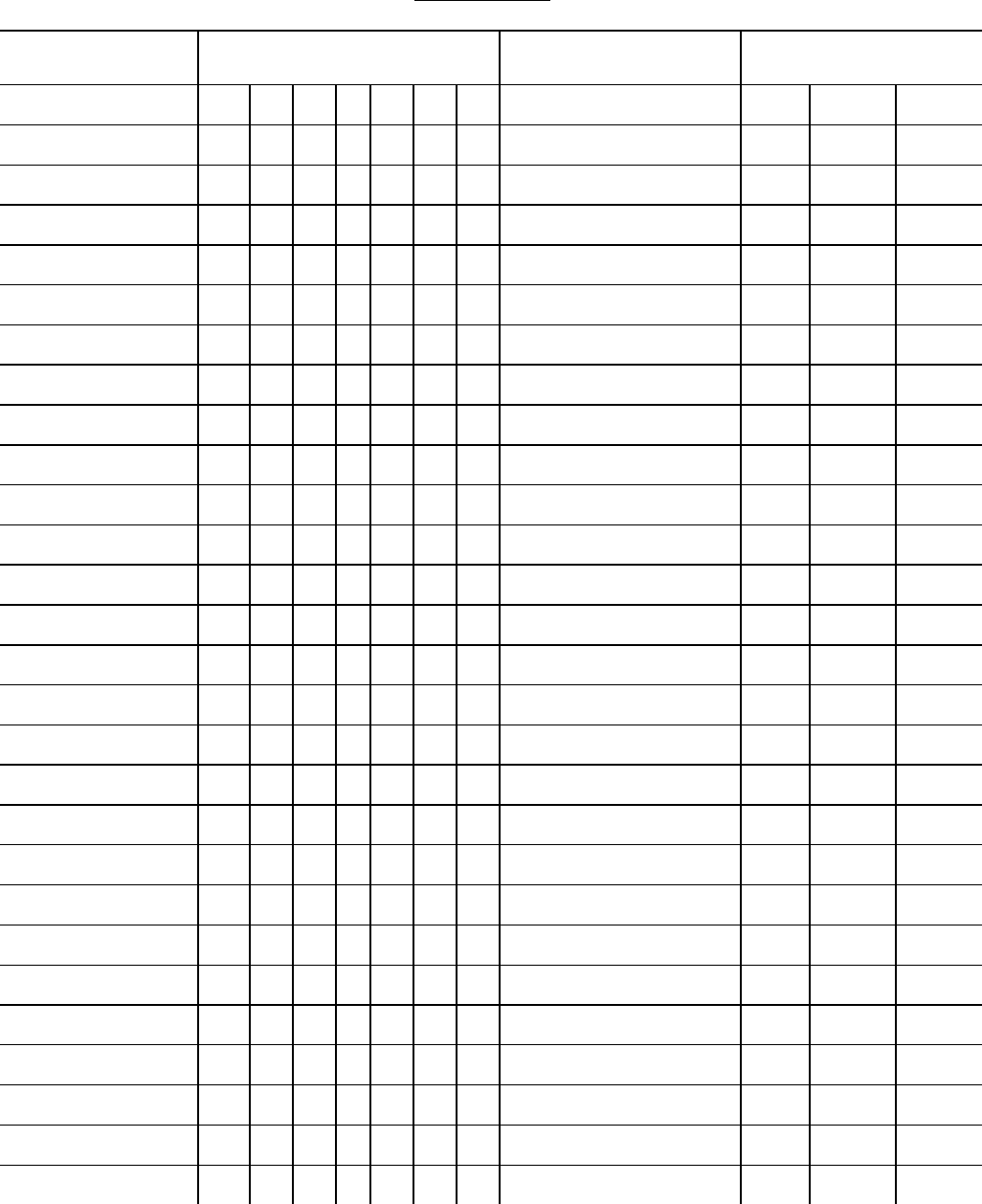
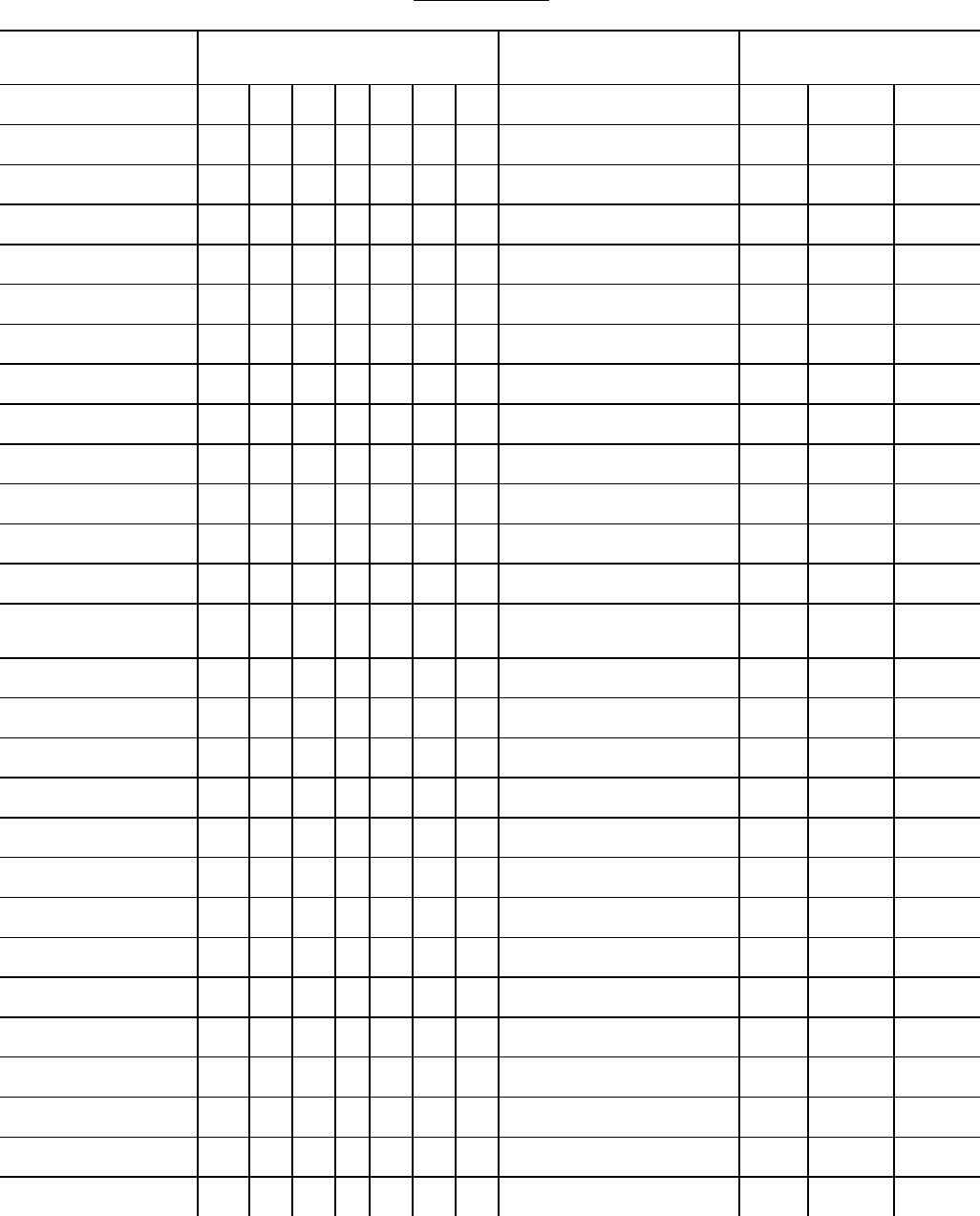
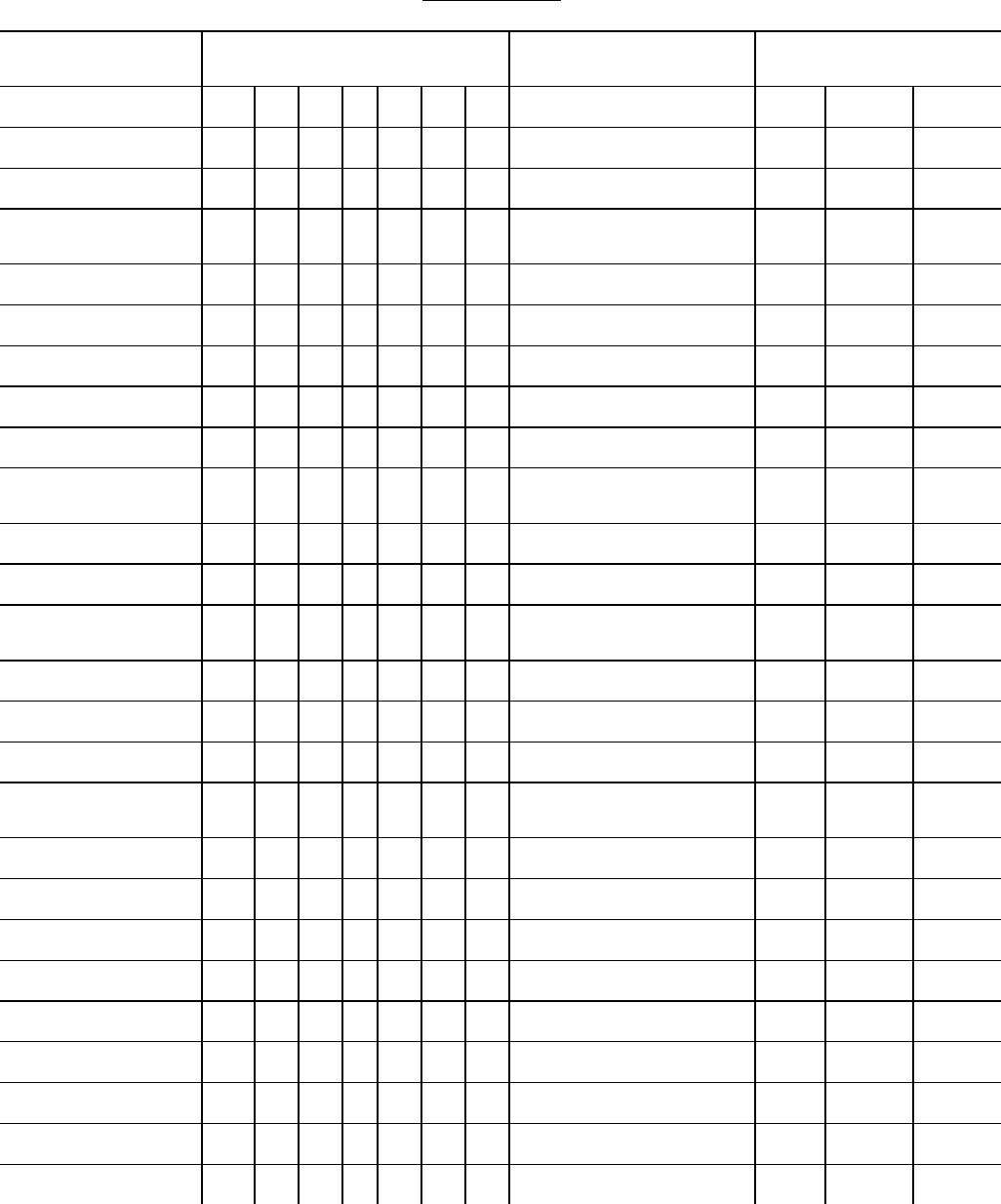
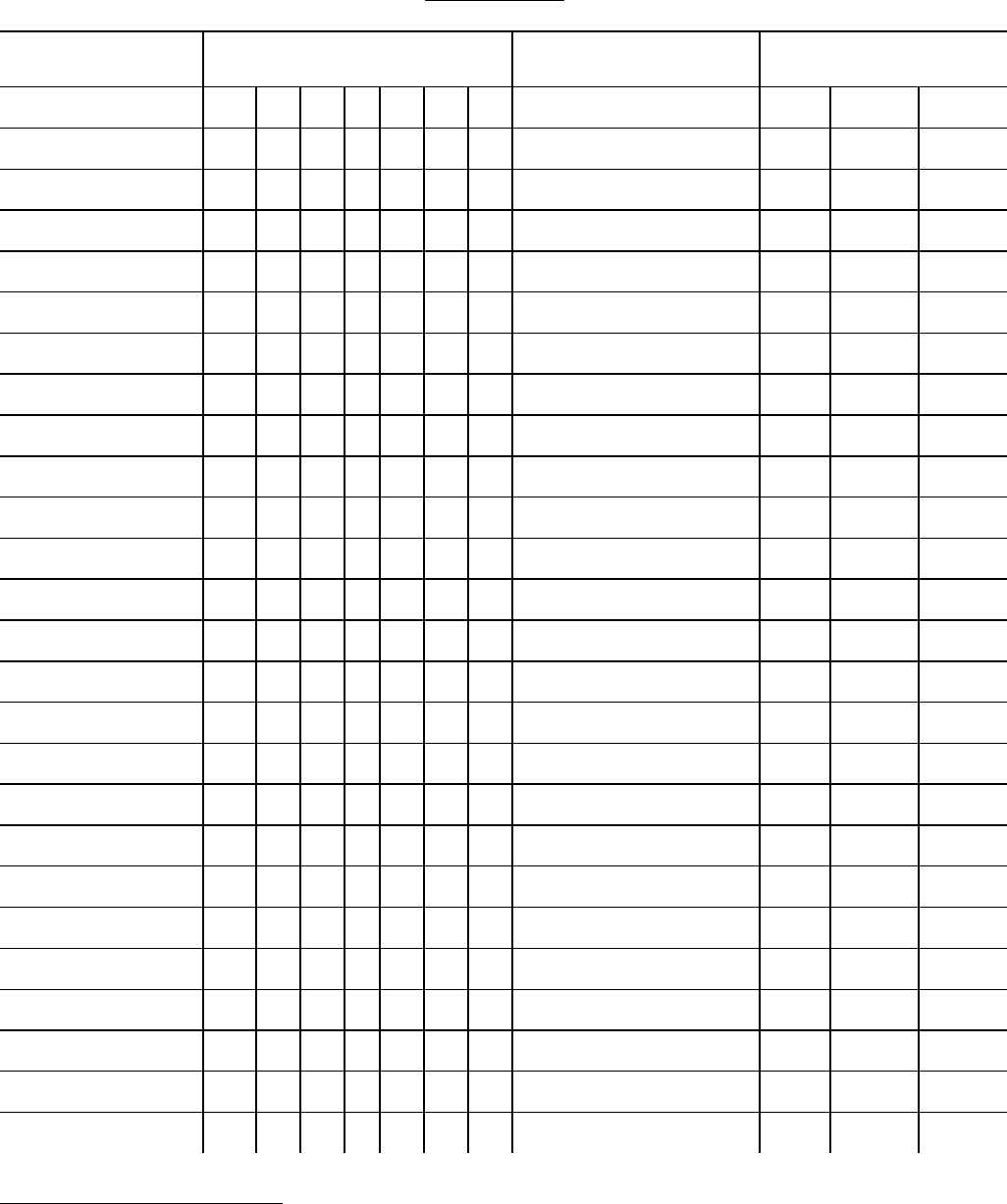
Appendix A presents an operationalization of the recommended Priority Levels. Table 1 shows
specific ICD-10 categories along with a querying Priority Level and a reference to a sample
query letter to use in querying (Appendix B contains the sample query letters). Table 2 presents
specific improbable sequences that should always be queried. Table 3 lists recommendations for
situations in which the duration for a specified cause is not clear. Table 4 presents selected
situations in which the certifier has reported causes in a way that conflict with the format of the
medical certification section along with a recommended query level and a reference to a sample
query letter. The following examples illustrate how Appendix A may be used.
I (a) Pain in joints
(b)
(c)
The ICD code for this condition is M25.5. Referring to this category in table 1 of
Appendix A, it specifies that a query should be initiated under Priority Level 1c for
14
conditions coded to M15-M25. Also, it shows that Query Letter No. 8 on page 107 can
be used.
I (a) Pharyngeal cancer
(b)
(c)
This condition would be coded C14.0. Referring to Appendix A, the Priority Level is
shown as 5 and Query Letter No. 2 on page 71 could be used. If, however, the State
queries only through Priority Level 4, no letter would be initiated in this case.
Appendix A provides guidelines for querying. Automatic or manual screening may be used to
identify certificates for possible querying. However, the State should review the certificate more
carefully to determine if the record really should be queried. For example, querying is not
necessary when terms such as “probable,” “unknown etiology,” and “unknown site” are stated.
In the case of SIDS or SUDI, querying is also not necessary when a complete investigation has
been conducted (www.cdc.gov/SIDS/TrainingMaterial.htm
reproductivehealth/SIDS/deathscene.htm) and the National Institute of Child Health and Human
Development criteria have been met for diagnosing SIDS. In these cases, it is clear that the
physician made an effort to provide a clear and complete etiological sequence.
While the form letters shown in Appendix B are adequate to cover most situations, there may be
times when an original letter should be written, or additional statements or questions should be
included. When two or more different query levels are applicable for the same record, the
attachments for each query level may be used. It may be clearer to keep the questions on
separate attachments rather than combining questions from multiple attachments.
15

Priority Level 1
Priority Level 1 contains the minimum level of querying that all State vital statistics programs
should use to promote basic integrity of State and national mortality data. This category is
designed to reduce the frequency with which assumptions must be made to properly assign
multiple cause or underlying cause-of-death codes because of missing or incorrect information.
Level 1a: Always query if an infrequent or rare cause appears anywhere in the medical
certification section.
Appendix C contains a list of infrequent and rare causes of death in the United States.
These causes of death occur rarely and/or present threats to public health in the United
States. As a result, each case should be verified to make sure there was no error in
certification. When NCHS requests confirmation of a rare cause of death, the VSCP
project director should work with staff to verify that the cause-of-death coding is correct
and obtain corroboration from the State Health Officer before signing the confirmation
letter. A notation of confirmation should also be recorded on the copy of the certificate
sent to NCHS. In the absence of this notation, the disease will be coded as stated; the
VSCP project officer will be contacted to confirm the accuracy of the certification.
Examples: “Cholera”, “plague”, “acute poliomyelitis”
See sample query letter number 1.
Level 1b: Always query neoplasm for a primary site and to determine if benign or
malignant. When a malignant neoplasm is stated to be the underlying cause of
death, it is important to determine the primary site.
Example: I (a) Carcinomatosis
(b)
(c)
Query to determine primary site.
Example: I (a) Breast tumor
(b)
(c)
Query to determine if benign or malignant.
See sample query letter number 2.
16
Level 1c: Always query when the following are reported alone or as the underlying cause
on the death certificate:
• conditions that would rarely cause death by themselves (e.g., trivial
conditions)
• symptoms and signs
• ill-defined conditions
• mechanisms of death
Example: I (a) Myopia
(b)
(c)
Example I (a) Senility
(b)
(c)
See sample query letter numbers 4, 6, 8, 9, and 10.
Level 1d: Always query for the reason for the “surgery or medical care” when the
underlying disease or condition is not reported anywhere on the death record.
Example: I (a) Hemorrhage
(b) Surgery
(c)
In the above example, the disease or condition requiring the surgery should be queried,
and also the specific type of surgery performed.
See sample query letter numbers 5 and 10.
Level 1e: Always query for an external cause when only nature of injuries, that is, codes
classifiable to S00-T98, are reported alone on the death certificate.
Example: I (a) Internal injuries
(b)
(c)
See sample query letter number 10.
17

Level 1f: Query when the sequence arrangement of the reported entries is questionable.
Improbable sequences in part I of the death certificate are shown in tables 2-4 of
Appendix A, pages 56-66, and in the instructions on “highly improbable” sequences
in section III of the NCHS Instruction manual part 2A.
Example: I (a) Pneumonia
(b) Hypertension
(c) Cardiac hypertrophy due to above
In this example, it is difficult to determine the intent of the certifier; therefore, more
information is needed.
See sample query letter number 11.
Level 1g: When any of the selected conditions in Appendix D is reported, whether in part I
or part II on the death certificate, and there is no mention of HIV (Human
immunodeficiency virus) infection, query for HIV.
See sample query letter number 3.
Priority Level 2
Priority Level 2 includes conditions not usually considered as the underlying cause for
which querying will help classify the underlying cause of death more specifically.
Example: I (a) Peritonitis
(b)
(c)
In this example, it is necessary to determine what led to or caused the peritonitis- - was it
a ruptured appendix, ruptured peptic ulcer, so-called “spontaneous peritonitis”, other?
See sample query letter numbers 4 and 8.
Priority Level 3
Priority Level 3 provides more detailed information that would enable the cause of death to
be classified more accurately and to a more detailed ICD category.
Example: I (a) Chronic liver disease
(b)
(c)
18

In this case, the specific type of disease is needed (alcoholic cirrhosis, biliary cirrhosis,
chronic (or recurrent) hepatitis, etc.)
See sample query letter numbers 4, 7, 8, 9, and 10.
Priority Level 4
Priority Level 4 includes:
• those cases in which the certifier may already provide a logical chain of events
leading to death but determining the site or location of stated diseases or conditions
will lead to a more precise code (see example below).
• entries which are unclear and need further explanation (e.g., situations related to
placement and numbering of conditions). For a list of examples, refer to table 4,
Appendix A, beginning on page 64.
Example: I (a) Embolism
(b)
(c)
A specific site is needed (e.g., brain, lung, coronary arteries), as is the source, if known.
See sample query letter numbers 4 and 11.
Priority Level 5
Priority Level 5 contains queries which would enable the cause of death to be coded to a
more precise subcategory within the three-digit category. This level of detail is frequently
required for specified special studies or research projects within a defined reporting area,
but may not be necessary for general querying.
Example: I (a) Carcinomatosis
(b) Cancer of pancreas
(c)
In this case, a query for a more specific site of the pancreas would be in order (e.g., body,
head, duct, etc.), as well as a query for the histologic type of tumor, such as
“Adenocarcinoma”.
See sample query letter numbers 4 and 10.
19

Priority Level 6
Priority Level 6 reflects the most thorough recommended level of querying. The conditions
in this category are queried for the purpose of obtaining even more explicit statements,
thus eliminating the necessity of using the assumptions which are allowed under ICD rules.
Example: I (a) Tuberculosis
(b)
(c)
Tuberculosis of the lung is assumed if not otherwise specified.
Example: I (a) Lupus
(b)
(c)
Systemic lupus is assumed if not otherwise specified.
See sample query letter numbers 4 and 11.
Fetal death
The principles and procedures described in this manual are applicable to fetal deaths. Since
many of the same causes may be stated on the fetal death report, the querying priorities in
Appendix A may be followed. The cause P95 is invalid for mortality records but is valid for
fetal deaths. This cause, P95, is shown in Appendix A for those wanting to use this manual to
query fetal deaths. While the causes of many fetal deaths are unknown, it is important to capture
results from pathological or histological examinations completed after the fetal death report or
certificate was filed and to remind physicians that casual reporting of “unknown” as a cause of
fetal death is not acceptable.
20
Sample letters
Guide to Sample Query Letters Shown in Appendix B
Letter
number
Query level
General reason for querying
1
1a
Rare causes
2
1b
Cancer
3
1g
HIV (also see Appendix D)
4
1c,2,3,4,5,6
Etiology, for specific site, and type of disease
5
1d
Reason for treatment (medical, surgical, therapy, medicaments)
6
1c
Mental disorders
7
3
Type of drug or exposure
8
1c,2,3
Signs, symptoms, non-specific conditions, trivial conditions, fetal
death code P95, mechanism of death, etc.
9
1c,3
Pregnancy-related conditions
10
1c,1d,1e,3,5
Manner of death and external causes
11
1f,4,6
Improbable sequence, duration, placement and numbering of
conditions
21
VI. Evaluation of the Query Program
To assure that the desired results are being obtained, a periodic evaluation of the query program
should be made. By keeping records of all queries sent out and returned, it is possible to
measure the overall effectiveness of the program, and also to pinpoint areas in need of a more
concentrated effort.
A rough measure of the improvement in certification may be obtained by comparing the percent
of records requiring a query at the beginning of the program with the percent required afer the
program has been in effect for several months. Ideally there should be a gradual decline in the
proportion of queries needed as the certifiers become educated as to the requirements. However,
there will always be a need for education since new physicians will start practicing in the State
and physicians who rarely complete a certificate may need assistance. The rate of response to
the queries and the time lag involved will also make it possible to determine how much follow-
up is needed, either by mail or by telephone.
A more detailed measure of the effectiveness of the program is made possible by keeping a
record of the types of questions asked. This information can reveal which types of situations
require the most querying, and also indicates which physicians may require special attention such
as a personal visit. This type of information can be very valuable when used in conjunction with
a field or training program, especially with the cooperation of the State and/or local medical
society In addition, it is helpful to ascertain the impact of querying by measuring the difference
in the records over time.
The following are illustrations of the types of information that can be recorded and tabulated
periodically for purposes of evaluating the query program:
A. Number and percent of queries sent, showing:
22
1. Adequate response
A. Changed the underlying cause
B. Did not change the underlying cause
C. Did not change the underlying cause, but resulted in additional cause-
of-death information
2. Inadequate response (e.g., response doesn’t address question)
3. No response
A. Number and percent of follow-up queries, by type of follow up and result.
B. Number and percent of queries sent, by ICD category and Priority Level.
C. Number and percent of queries sent, by individual physician, type of certifier, and type of
letter.
D. Number and percent of inadequate or non-responses by type of letter used.
E. Number and rate of ICD code changes made as a result of queries, by Priority Level.
In Oregon and Washington, systematic evaluation of the State query program has confirmed the
value of an overall program, identified effectiveness of querying specific causes, and helped
refine specific wording that works best in query letters (4-5).
References
1. Rosenberg, HM. 1989. Improving cause-of-death statistics. American Journal of Public Health.
79(5): 563-4.
2. Rosenberg, HM. 1991. The impact of cause-of-death querying. IIVRS Technical Paper, No. 45.
International Institute for Vital Registration and Statistics [IIVRS]: Bethesda, Maryland.
3. Hanzlick, R (Ed.) 1994. The Medical Cause of Death Manual. Northfield, IL: College of American
Pathologists.
4. Hopkins, DD, Grant-Worley, JA, and Bollinger, TL. 1989. Survey of cause-of-death query criteria
used by State vital statistics programs in the U.S. and the efficacy of the criteria used by
the Oregon
vital statistics program. American Journal of Public Health. 79(5): 570-574.
5. Hoyert, DL, and Lima A. 2005. Querying of death certificates in the United States. Public Health
Reports. 120: 1-9.
23
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
A00-A01
1a
1
67
A02-A04
0
A05 (.1)
1a
1
67
A05 (.0, .2-.8)
0
A05 (.9)
5
4
4/5
83
A06
0
A07 (.0-.1)
1a
1
67
A07 (.2)
1a
1g
1
3
67
77
A07 (.3)
1g
3
77
A07 (.8-.9)
1a
1
67
A08-A09
0
A16 (.2-.8)
1g
3
77
A16 (.9)
1g
6
3
77
A17
1g
3
77
A18 (.0-.3,
.5-.8)
1g
3
77
A18 (.4)
1g
3 Query Lupus, NOS (for
query level 3)
3
4 4/5
77
83
A19
1g
3
77
A20-A25
1a
1
67
A26
0
A27
1a
1
67
A28
0
A30
1a
1
67
A31 (.0, .8-.9)
1g
3
77
A31 (.1)
1c
1g
8
3
1
107
77
A32
0
A33-A37
1a
1
67
24
25
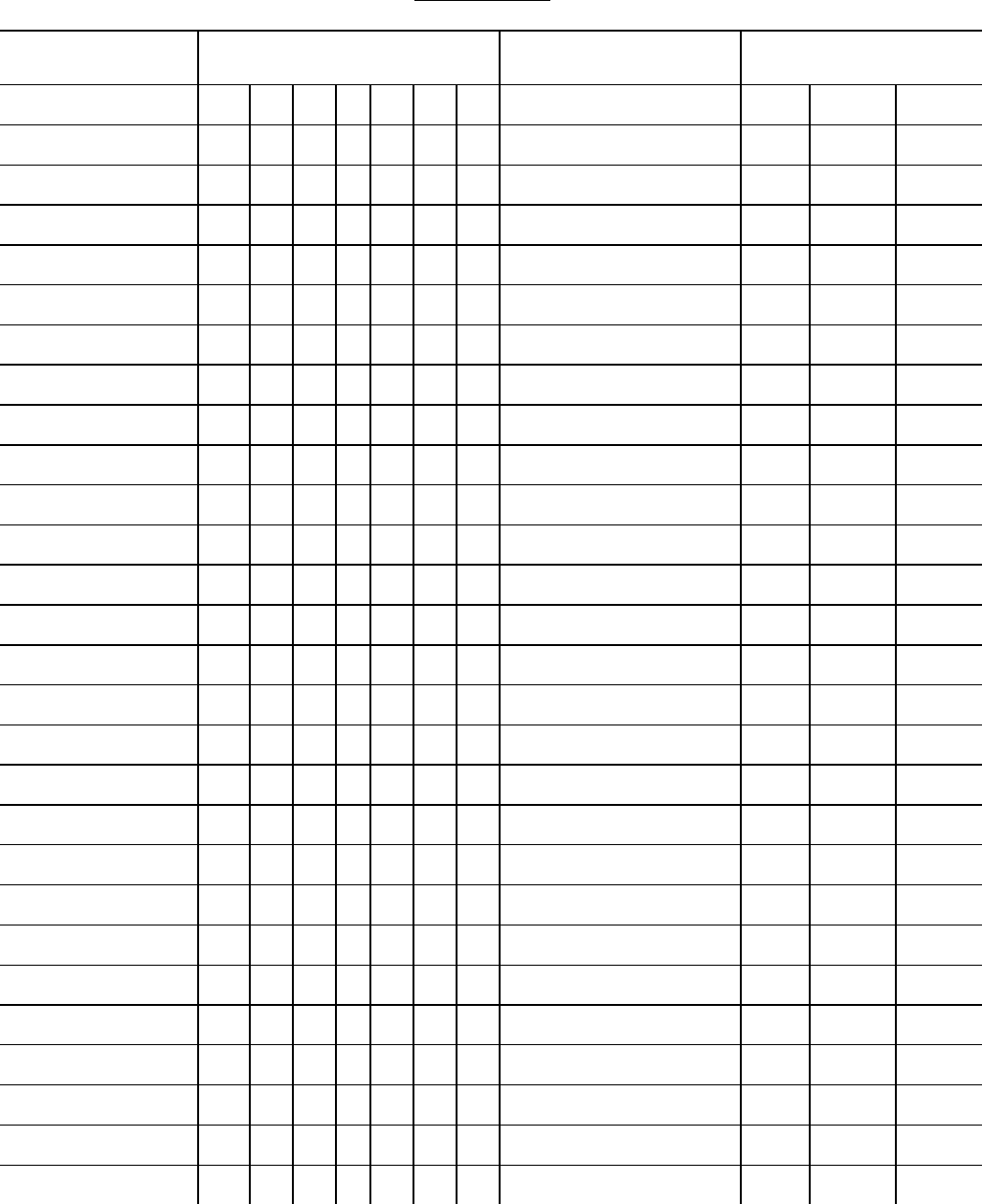
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
A38-A39
0
A40 (.0-.8)
0
A40 (.9)
5
4
5
83
A41 (.0-.8)
0
A41 (.9)
5
4
4
83
A42-A43
1g
3
77
A44
1a
1
67
A46, A48(.0-.2,
.4-.8)
0
A49
4
4
2
83
A50
0
A51
1c
8
2
107
A52-A55
0
A56-A64
1c
8
1,2
107
A65-A70
1a
1
67
A71-A74
1c
A75
1a
1
67
A77 (.0)
0
A77 (.1-.9)
1a
1
67
A78-A80
1a
1
67
A81 (.0-.1,
.8-.9)
1a
1
67
A81 (.2)
1a
1g
1
3
67
77
A82
1a
1
67
A83
0
A84
1a
1
67
A85 (.0-.1, .8)
0
A85 (.2)
1a
1
67
25
26
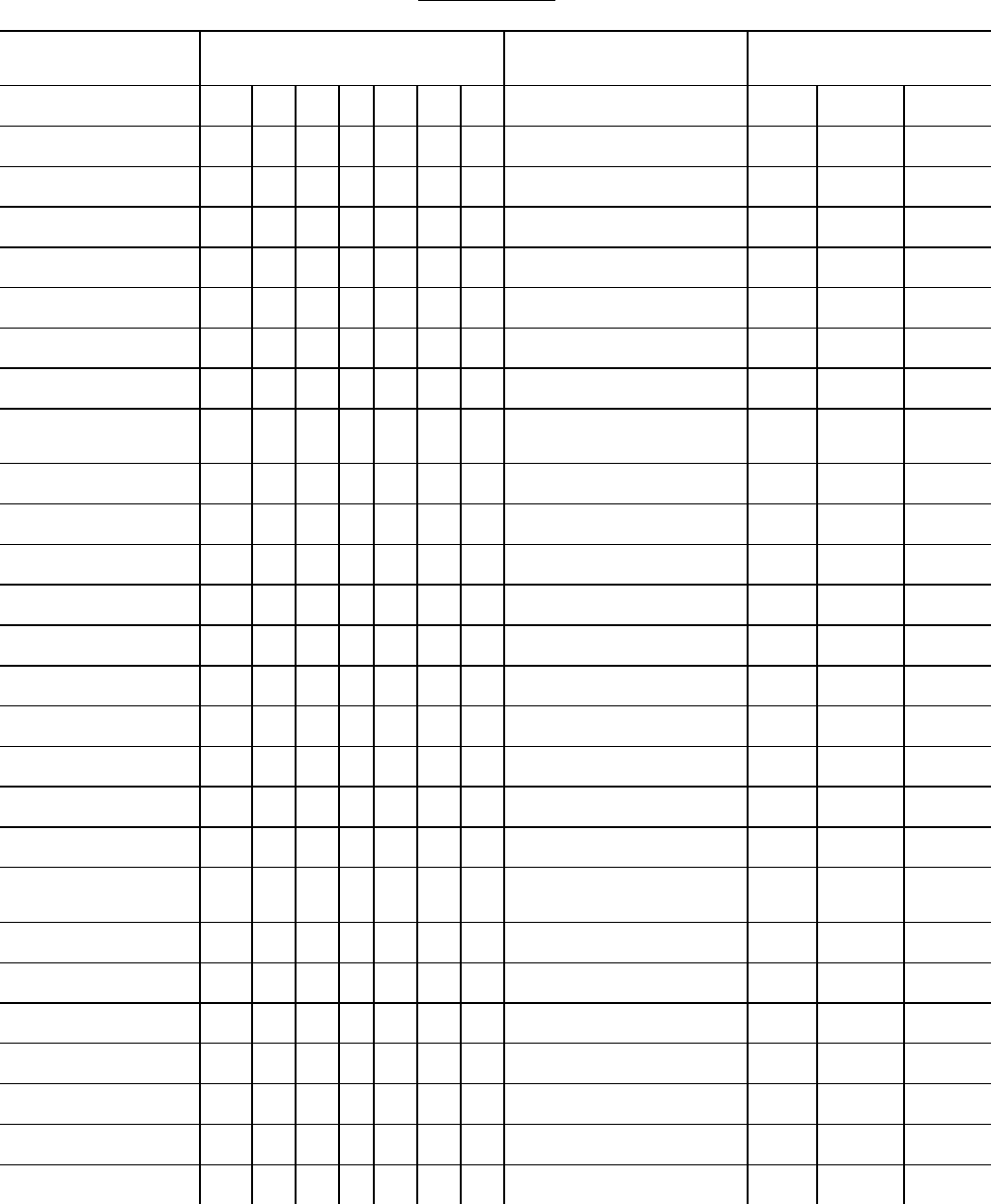
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
A86-A89
0
A90-A99
1a
1
67
B00 (.0, .3-.4,
.7, .9)
1g
3
77
B00 (.1-.2,
.5,.8)
1c
1g
8
3
1,2
107
77
B01
1a
1
67
B02
0
B03-B06
1a
1
67
B07
1c
8
1
107
B08 (.0)
1a
1
67
B08 (.1-.8)
1c
8
1
107
B09
1c
8
1
107
B15-B19
0
B20-24
0
B25
1g
3
77
B26
1a
1
67
B27
0
B30
1c
1
67
B33 (.0)
1a
1
67
B33 (.1-.3,.8)
0
B33 (.4)
1a
1
67
B34
0
B35-B36
1c
8
1,2
107
B37-B39
1g
3
77
B40-B43
0
B44-B45
1g
3
77
B46-B47
0
B48 (.0-.4, .8)
0
26
27
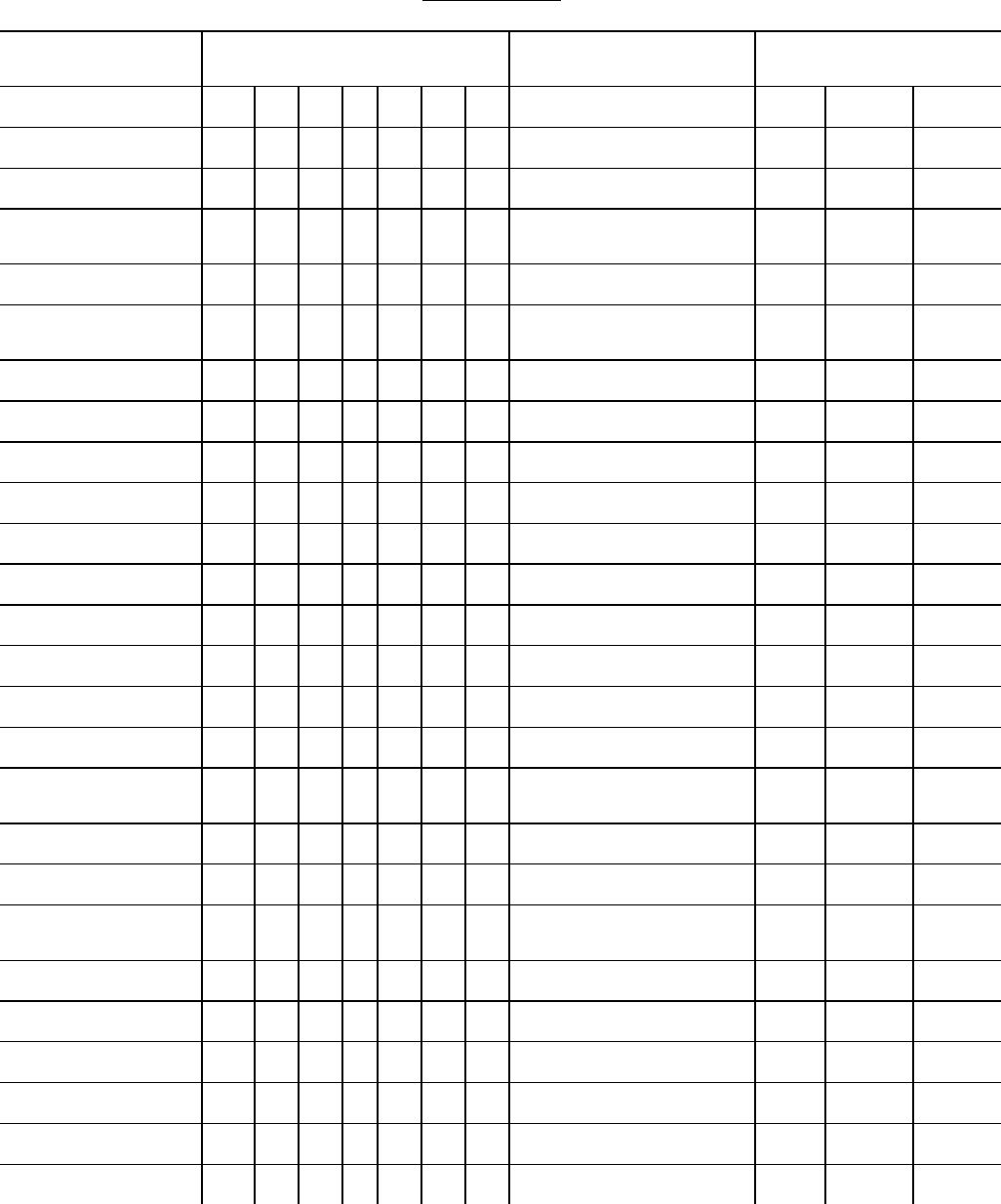
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
B48 (.7)
1c
8
1
107
B49
0
B50-B57
1a
1
67
B58-B59
1g
3
77
B60-B64
0
B65-B74
1a
1
67
B75-B83
0
B85-B86
1c
8
1,2
107
B87-B94
0
B99
0
C00 (.0-.4,
.6-.8)
0
C00 (.5, .9)
5
2
71
C01-C05
0
C06 (.0-.8)
0
C06 (.9)
4
2
71
C07-C09
0
C10 (.0-.8)
0
C10 (.9)
5
2
71
C11 (.0-.8)
0
C11 (.9)
5
2
71
C12
0
C13 (.0-.8)
0
C13 (.9)
5
2
71
C14 (.0)
5
2
71
C14 (.2-.8)
0
C15-C23
0
C24 (.0-.8)
0
27
28
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
C24 (.9)
5
2
71
C25 (.0-.8)
0
C25 (.9)
5
2
71
C26 (.0-.8)
0
C26 (.9)
4
2
71
C30
0
C31 (.0-.8)
0
C31 (.9)
5
2
71
C32 (.0-.8)
0
C32 (.9)
5
2
71
C33
0
C34 (.0-.8)
0
C34 (.9)
5
2
71
C37
0
C38 (.0-.2,
.4-.8)
0
C38 (.3)
5
2
71
C39
4
2
71
C40
0
C41 (.0-.8)
0
C41 (.9)
5
2
71
C43 (.0-.8)
0
C43 (.9)
5
2
71
C44 (.0-.8)
0
C44 (.9)
5
2
71
C45 (.0-.7)
0
C45 (.9)
5
2
71
C46 (.0-.8)
1g
3
77
28
29
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
C46 (.9)
1g
5
3
2
77
71
C47 (.0-.8)
0
C47 (.9)
5
2
71
C48 (.0-.1, .8)
0
C48 (.2)
5
2
71
C49 (.0-.8)
0
C49 (.9)
5
2
71
C50-C56
0
C57 (.0-.8)
0
C57 (.9)
4
2
71
C58-C62
0
C63 (.0-.8)
0
C63 (.9)
4
2
71
C64-C67
0
C68 (.0-.8)
0
C68 (.9)
4
2
71
C69 (.0-.8)
0
C69 (.9)
5
2
71
C70
0
C71 (.0-.8)
0
C71 (.9)
5
2
71
C72 (.0-.8)
0
C72 (.9)
5
2
71
C73-C74
0
C75 (.0-.8)
0
C75 (.9)
5
2
71
C76
3
2
71
29
30
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
C77-C80
1b
2
71
C81-C82
0
C83
1g
3
77
C84
0
C85
1g
3
77
C88-C94
0
C95
3
2
71
C96
0
C97
1b
2
71
D00-D07
0
D09 (.0-.7)
0
D09 (.9)
4
2
71
D10-D12
0
D13 (.0-.7)
0
D13 (.9)
5
2
71
D14 (.0-.3)
0
D14 (.4)
5
2
71
D15 (.0-.7)
0
D15 (.9)
5
2
71
D16 (.0-.8)
0
D16 (.9)
5
2
71
D17 (.0-.7)
0
D17 (.9)
5
2
71
D18
0
D19 (.0-.7)
0
D19 (.9)
5
2
71
D20
0
30
31
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
D21 (.0-.6)
0
D21 (.9)
5
2
71
D22 (.0-.7)
0
D22 (.9)
5
2
71
D23 (.0-.7)
0
D23 (.9)
5
2
71
D24-D27
0
D28 (.0-.7)
0
D28 (.9)
5
2
71
D29 (.0-.7)
0
D29 (.9)
5
2
71
D30 (.0-.7)
0
D30 (.9)
5
2
71
D31 (.0-.6)
0
D31 (.9)
5
2
71
D32
0
D33 (.0-.7)
0
D33 (.9)
5
2
71
D34
0
D35 (.0-.8)
0
D35 (.9)
5
2
71
D36 (.0-.7)
0
D36 (.9)
5
2
71
D37 (.0-.7)
0
D37 (.9)
5
2
71
D38 (.0-.5)
0
D38 (.6)
5
2
71
31
32
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
D39 (.0-.7)
0
D39 (.9)
5
2
71
D40 (.0-.7)
0
D40 (.9)
5
2
71
D41 (.0-.7)
0
D41 (.9)
5
2
71
D42
0
D43 (.0-.1,
.3-.7)
0
D43 (.2, .9)
5
2
71
D44 (.0-.8)
0
D44 (.9)
5
2
71
D45-D46
0
D47 (.0-.7)
0
D47 (.9)
5
2
71
D48 (.0-.7)
0
D48 (.9)
1b
2
71
D50-D58
0
D59 (.0,.2,.4,.6)
3
7
101
D59 (.1,.3,.5,
.8-.9)
0
D60
0
D61 (.0,.3-.8)
0
D61 (.1-.2)
3
7
101
D62
0
D64 (.0,.3-.8)
0
D64 (.1)
2
4
1
83
D64 (.2)
3
7
101
32
33
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
D64 (.9)
3
4
4
83
D65-D67
0
D68 (.0-.2,
.4-.9)
0
D68 (.3)
3
7
101
D69 (.0-.4,
.6-.8)
0
D69 (.5)
3
4
1
83
D69 (.9)
3
D70-D73
0
D74 (.0,.9)
0
D74 (.8)
3
4
4
83
D75-D84
0
D86 (.0-.8)
0
D86 (.9)
5
4
2
83
D89
0
E00-E02
0
E03 (.0-.1,
.5-.9)
0
E03 (.2-.4)
3
7
101
E04-E05
0
E06 (.0-.3,
.5-.9)
0
E06 (.4)
3
7
101
E07
0
E10-E14
0
E15
3
7
101
E16 (.0)
3
7
101
E16 (.1, .3-.9)
0
33
34
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
E16 (.2)
1c
8
1
107
E20-E22
0
E23 (.0,.2-.7)
0
E23 (.1)
3
7
101
E24 (.0-.1, .3-.9)
0
E24 (.2)
3
7
101
E25-E26
0
E27 (.0-.2,
.4-.9)
0
E27 (.3)
3
7
101
E28-E32
0
E34 (.0-.8)
0
E34 (.9)
1c
4
3
83
E40-E46
0
E50-E64
0
E65
1c
8
2
107
E66 (.0, .2-.9)
0
E66 (.1)
3
7
101
E67-E88
0
E89
1d
5
1
89
F01-F09
1c
6
95
F10-F19
0
F20-F48
1c
6
95
F50 (.0-.3,
.5-.9)
0
F50 (.4)
1c
6
95
F51-F53
1c
6
95
F54-F55
0
34
35
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
F59-F99
1c
6
95
G00
0
G03 (.0-.8)
0
G03 (.9)
3
4
4
83
G04 (.0-.8)
0
G04 (.9)
1g
3
3
4
4
77
83
G06-G41
0
G43-G45
1c
8
2
107
G47 (.0-.2,
.4, .9)
1c
8
2
107
G47 (.3, .8)
0
G50-G51
1c
8
2
107
G52 (.0)
1c
8
2
107
G52 (.1-.8)
0
G52 (.9)
3
4
3
83
G54
1c
8
1,2
107
G56-G58
1c
8
1,2
107
G60-G72
0
G80
0
G81-G83
2
8
1,2
107
G90-G92
0
G93 (.0, .7-.8)
0
G93 (.4)
1g
2
3
4
1
77
83
G93 (.1-.3,
.5-.6)
2
4
1
83
G93 (.9)
3
4
3
83
G95 (.0-.8)
0
35
36
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
G95 (.9)
1g
3
77
G96 (.0-.8)
0
G96 (.9)
3
4
3
83
G97
1d
5
1
89
G98
0
H00-H02
1c
8
2,3
107
H04-H05
0
H10-H57
1c
8
2
107
H59
1d
5
1
89
H60-H61
1c
8
2,3
107
H65-H74
0
H80-H83
1c
8
2,3
107
H90-H93
1c
8
2
107
H95
1d
5
1
89
I00-I22.9
0
I24.1 - I25 (.0-.1,
.3-.9)
0
I26-I42
0
I44-I45
2
4
3
83
I46
1c
8
1
107
I47-I50
2
4
3
83
I51 (.0, .5-.7)
0
I51 (.1-.4,
.8-.9)
3
4
1
83
I60-I64
0
I67 (.0-.8)
0
I67 (.9)
3
4
3
83
I69-I71
0
36
37
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
I72 (.0-.8)
0
I72 (.9)
4
4
2
83
I73
0
I74 (.0-.8)
0
I74 (.9)
4
4
2
83
I77-I78
0
I80 (.0-.8)
0
I80 (.9)
5
4
2
83
I81
0
I82 (.0-.8)
0
I82 (.9)
4
4
2
83
I83
0
I84 (.0-.1,
.3-.5, .7-.8)
0
I84 (.2,.6,.9)
1c
8
2
107
I85 (.0)
2
8
1
107
I85 (.9)
1c
8
1,2
107
I86-I89
0
I95
2
8
1
107
I97
1d
5
89
I99
0
J00
1c
8
1,2
107
J01-J05
0
J06
1c
8
1,2
107
J09
1a
1
67
J10-J22
0
J30
1c
8
1,2
107
J31-J32
0
37
38
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
J33
1c
8
2
107
J34 (.0-.1,
.3-.8)
0
J34 (.2)
1c
8
1
107
J35
1c
8
2
107
J36-J38
0
J39 (.0-.8)
0
J39 (.9)
3
4
3
83
J40-J63
0
J64
3
4
3
83
J65-J69
0
J70
3
7
1,2
101
J80
0
J81
2
4
1
83
J82-J94
0
J95
1d
5
1
89
J96
1c
8
1
107
J98 (.0, .2-.8)
0
J98 (.1)
2
8
1
107
J98 (.9)
3
4
3
83
K00-K01
1c
8
1,2
107
K02
0
K03
1c
8
1,2
107
K04-K05
0
K06-K14
1c
8
1,2
107
K20-K30
0
K31 (.0-.8)
0
K31 (.9)
3
4
3
83
38
39
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
K35-K51
0
K52 (.0-.8)
0
K52 (.9)
6
4
4
83
K55-K61
0
K62 (.0-.4)
1c
8
2
107
K62 (.5-.8)
0
K62 (.9)
3
4
4
83
K63 (.0-.3, .5, .8)
0
K63 (.4)
1c
8
2
107
K63 (.9)
3
4
4
83
K65
2
4
1
83
K66-K71
0
K72
1c
4
1
83
K73
3
4
1
83
K74-K75
0
K76 (.0)
1c
8
2
107
K76 (.1-.8)
0
K76 (.9)
3
4
4
83
K80-K81
0
K82 (.0-.8)
0
K82 (.9)
3
4
3
83
K83-K85
0
K86 (.0-.8)
0
K86 (.9)
4
4
3
83
K90 (.0-.8)
0
K90 (.9)
3
4
3
83
K91
1d
5
89
39
40
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
K92 (.0-.2)
2
4
1
83
K92 (.8)
0
K92 (.9)
3
4
3
83
L00
0
L01-L02
1c
8
2
107
L03-L04
0
L05-L08
1c
8
2
107
L10-L13
0
L20-L25
1c
8
2
107
L26
0
L27-L30
1c
8
2
107
L40-L41
0
L42-L44
1c
8
2
107
L50
1c
8
2
107
L51-L53
0
L55 (.0, .8-.9)
1c
8
2
107
L55 (.1, .2)
0
L56-L87
1c
8
2
107
L88-L89
0
L90-L95
1c
8
2
107
L97
0
L98
(.0-.1, .5-.9)
1c
8
2
107
L98 (.2-.4)
0
M00-M13
0
M15-M25
1c
8
1,2
107
M30-M34
0
M35 (.0-.2,
.4-.6, .8-.9)
0
40
41
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
M35 (.3, .7)
1c
8
1,2
107
M40-M45
1c
8
2
107
M46 (.0-.1, .4,
.8-.9)
1c
8
2
107
M46 (.2-.3, .5)
0
M47-M54
1c
8
2
107
M60 (.0)
3
7
101
M60 (.1-.9)
1c
8
2
107
M61
0
M62 (.0-.1,
.4-.9)
1c
8
2
107
M62 (.2-.3)
0
M65-M79
1c
8
2
107
M80 (.0, .2,
.5-.9)
0
M80 (.1, .3)
3
5
1
89
M80 (.4)
3
7
101
M81
1c
8
2
107
M83 (.0-.4,
.8-.9)
0
M83 (.5)
3
7
101
M84
1c
8
2
107
M85-M88
0
M89
1c
8
2
107
M91-M94
0
M95
1c
8
2
107
M96
1d
5
1
89
M99
1c
8
2
107
N00-N07
0
41
42
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
N10-N13
0
N14
3
7
101
N15
0
N17 (.0-.8)
0
N17 (.9)
2
4
2
83
N18 (.0-.8)
0
N18 (.9)
2
4
3
83
N19
2
4
3
83
N20-N23
0
N25-N27
0
N28 (.0-.8)
0
N28 (.9)
3
4
3
83
N30
0
N31
1c
8
1,2
107
N32 (.0-.8)
0
N32 (.9)
3
4
3
83
N34
0
N35
2
8
2
107
N36
0
N39 (.0, .8)
0
N39 (.1-.4)
1c
8
2
107
N39 (.9)
3
4
3
83
N40-N45
0
N46-N47
1c
8
2
107
N48-N50
0
N60
1c
8
2
107
N61
0
42
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
N62-N64
1c
8
2
107
N70-N76
0
N80-N83
0
N84-N91
1c
8
2
107
N92 (.0-.2, .4)
2
8
1
107
N92 (.3, .5-.6)
1c
8
2
107
N93-N97
1c
8
2
107
N98
0
N99
1d
5
89
O00-O02
0
003-O05 (.0-.8)
0
003-O05 (.9)
1c
9
1
113
O06 (.0-.8)
3
9
1
113
O06 (.9)
1c
9
1,2
113
O07 (.0-.8)
0
O07 (.9)
1c
9
1,2
113
O08
1c
9
1,3
113
O10-O21
0
O22 (.0-.1, .4)
1c
9
1
113
O22 (.2-.3,
.5-.9)
0
O23-O26
0
O28
1c
8
2
107
O29-O43
0
O44 (.0)
1c
9
1
113
O44 (.1)
0
43
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
O45-O46
0
O47-O48
1c
9
1
113
O60-O69
0
O70 (.0)
1c
9
1
113
O70 (.1-.9)
0
O71-O74
0
O75 (.0-.4,
.8-.9)
0
O75 (.5-.7)
1c
9
1
113
O85-O86
0
O87 (.0-.1,
.3-.9)
0
O87 (.2)
1c
8
2
107
O88-O91
0
O92
1c
8
2
107
O95-O99
0
P00-P15
0
P20-P29
0
P35 (.0)
1a
1
67
P35 (.1-.9)
0
P36-P38
0
P39 (.0-.8)
0
P39 (.9)
3
4
4
83
P50-P53
0
P54 (.0-.8)
0
P54 (.9)
1c
4
4
83
P55-P61
0
44
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
P70-P74
0
P76-P78
0
P80-P81
0
P83 (.0-.3, .8)
0
P83 (.4-.6, .9)
1c
8
1,2
107
P90-P92
1c
8
1
107
P93
3
7
101
P94
0
P95
1
1c
4
4
83
P96 (.0-.8)
0
P96 (.9)
1c
4
3
83
Q00-Q07
0
Q10-Q18
1c
8
2
107
Q20-Q28
0
Q30-Q34
0
Q35-Q37
1c
8
2
107
Q38 (.0-.3)
1c
8
2
107
Q38 (.4-.8)
0
Q39-Q45
0
Q50-Q54
1c
8
2
107
Q55-Q56
0
Q60-Q64
0
Q65-Q84
1c
8
2
107
Q85 (.0)
1c
8
2
107
Q85 (.1, .8)
0
1
P95: this code is valid only for fetal deaths
45
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
Q85 (.9)
3
4
3
83
Q86-Q87
0
Q89 (.0-.8)
0
Q89 (.9)
3
4
3
83
Q90-Q99
0
R00-R63
1c
8
1
107
R64
1c
1g
8
3
1
107
77
R68-R99
1c
8
1
107
S00
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
S01-S03
S04 (.0-.8)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S04 (.9)
1e
4
1e if external cause is
not stated on the record
10
4
1:A,B
3
119
83
S05 (.0-.1)
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
S05 (.2-.9)
S06-S09
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S10
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
S11-S19
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S20
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
S21-S29
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S30
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
S31-S39
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S40
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
S41-S49
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S50
1c
1e
1e if external cause is
not stated on the record
8
10
1
1:A,B
107
119
46
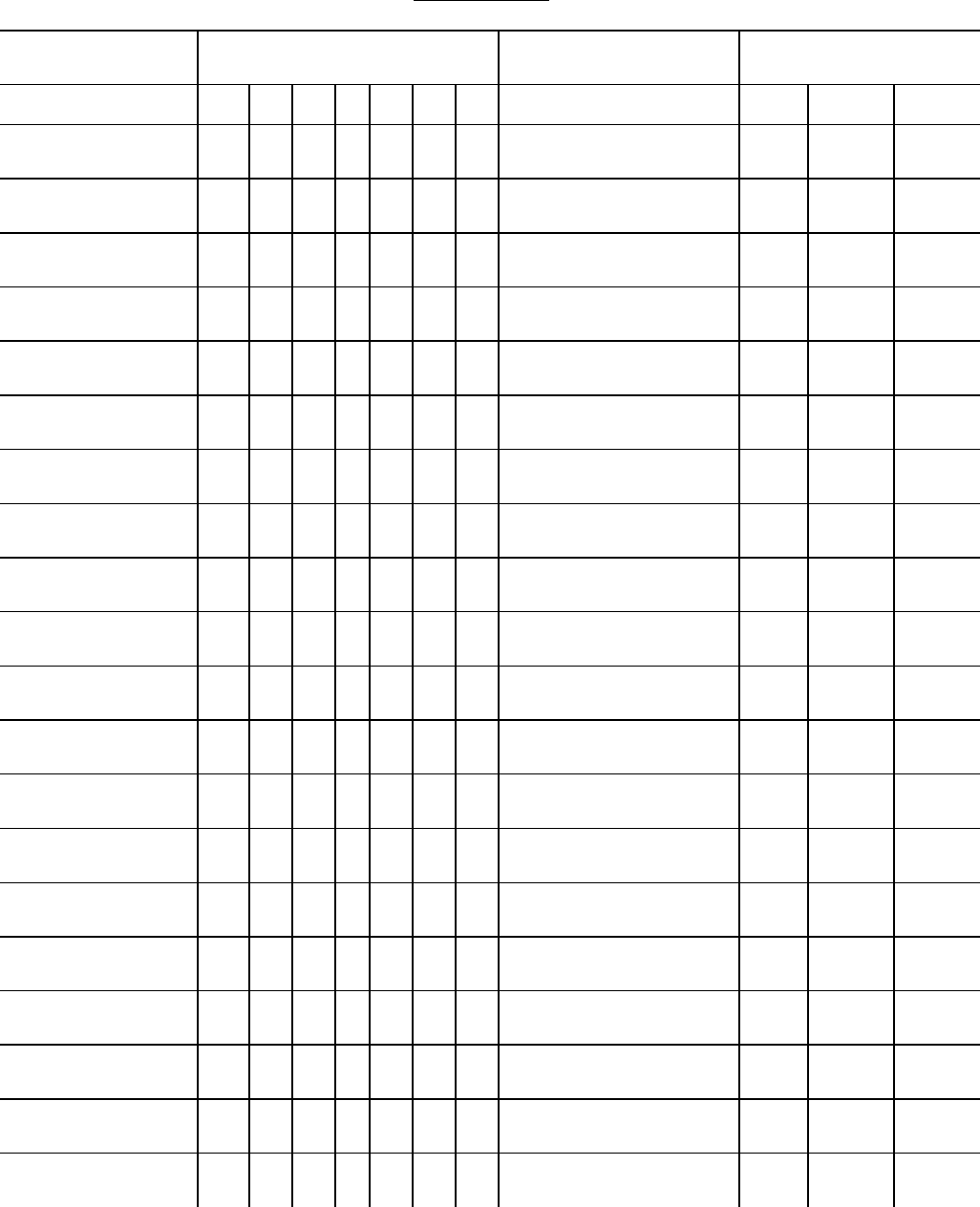
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
S51-S59
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S60
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
S61-S69
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S70
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
S71-S79
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S80
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
S81-S89
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
S90
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
S91-S99
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T00
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
T01-T05 (.0-.8)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T01-T05 (.9)
1e
4
1e if external cause is
not stated on the record
10
4
1:A,B
3
119
83
T06
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T07
1e
3
1e if external cause is
not stated on the record
10
4
1:A,B
2,3
119
83
T08
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T09 (.0)
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
T09 (.1-.9)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T10
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T11 (.0)
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
T11 (.1-.9)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
47
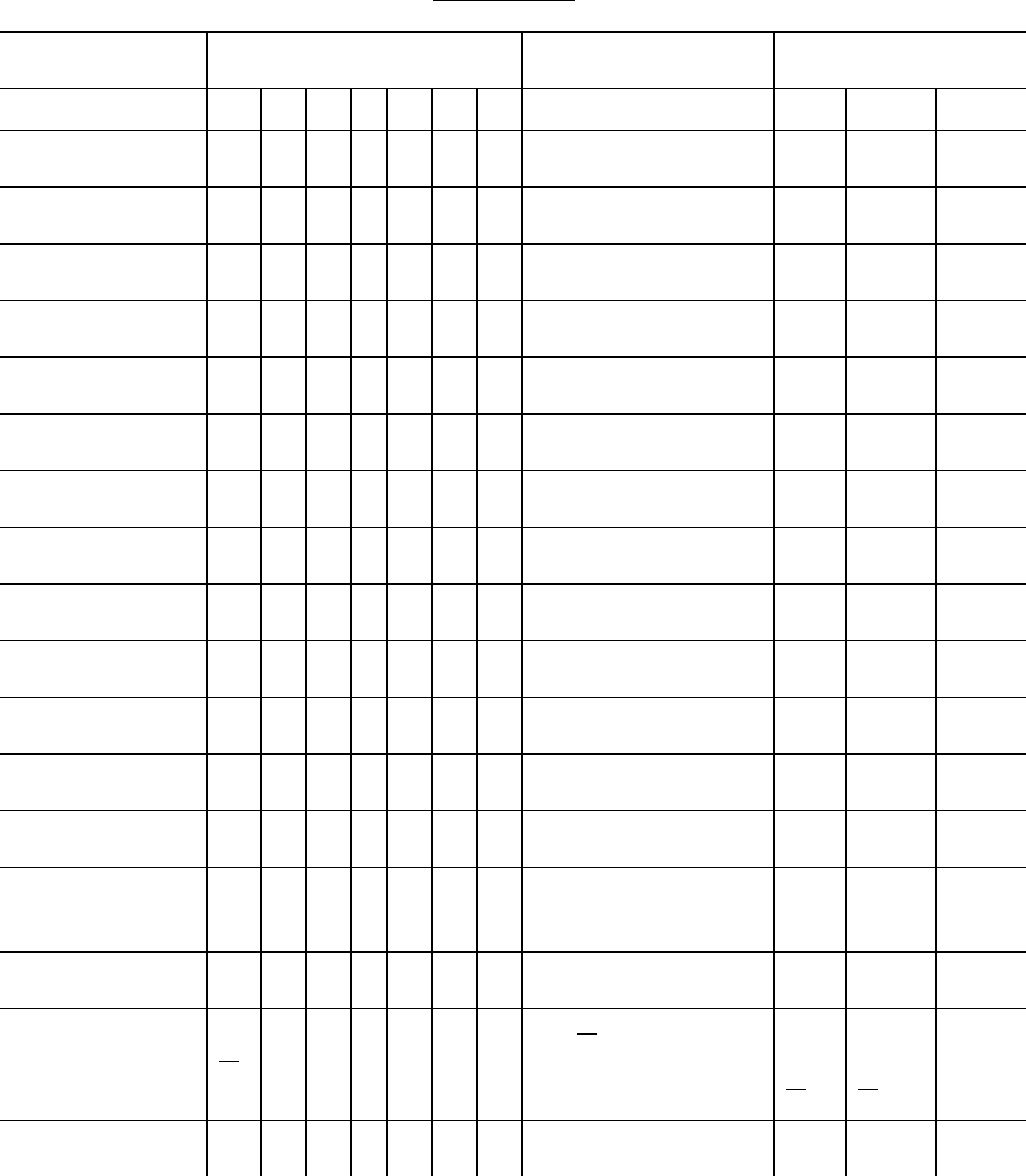
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
T12
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T13 (.0)
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
T13 (.1-.9)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T14 (.0)
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
T14 (.1-.9)
1e
4
1e if external cause is
not stated on the record
10
4
1:A,B
2
119
83
T15-T19
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T20-T25
(.0,.2-.7)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T20-T25 (.1)
1c
1e
1e if external cause is
not stated on the record
8
10
2
1:A,B
107
119
T26-T35
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T36-T37 (.0-.8)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T36-T37 (.9)
1e
5
1e if external cause is
not stated on the record
10
10
1:A,B
1:D
119
T50-T75
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T78 (.0-.8)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T78 (.9)
1e
3
1e if external cause is
not stated on the record
10
10
1:A,B
1:C
119
T79
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
T80-T88
1d
1e
or
0
1d or 1e if reason for
treatment, or external
cause is not stated on
the record respectively
10
10
or
1:C
1:A,B
or
119
T90-T97
T98 (.0-.2)
1e
0
1e if external cause is
not stated on the record
10
1:A,B
119
48
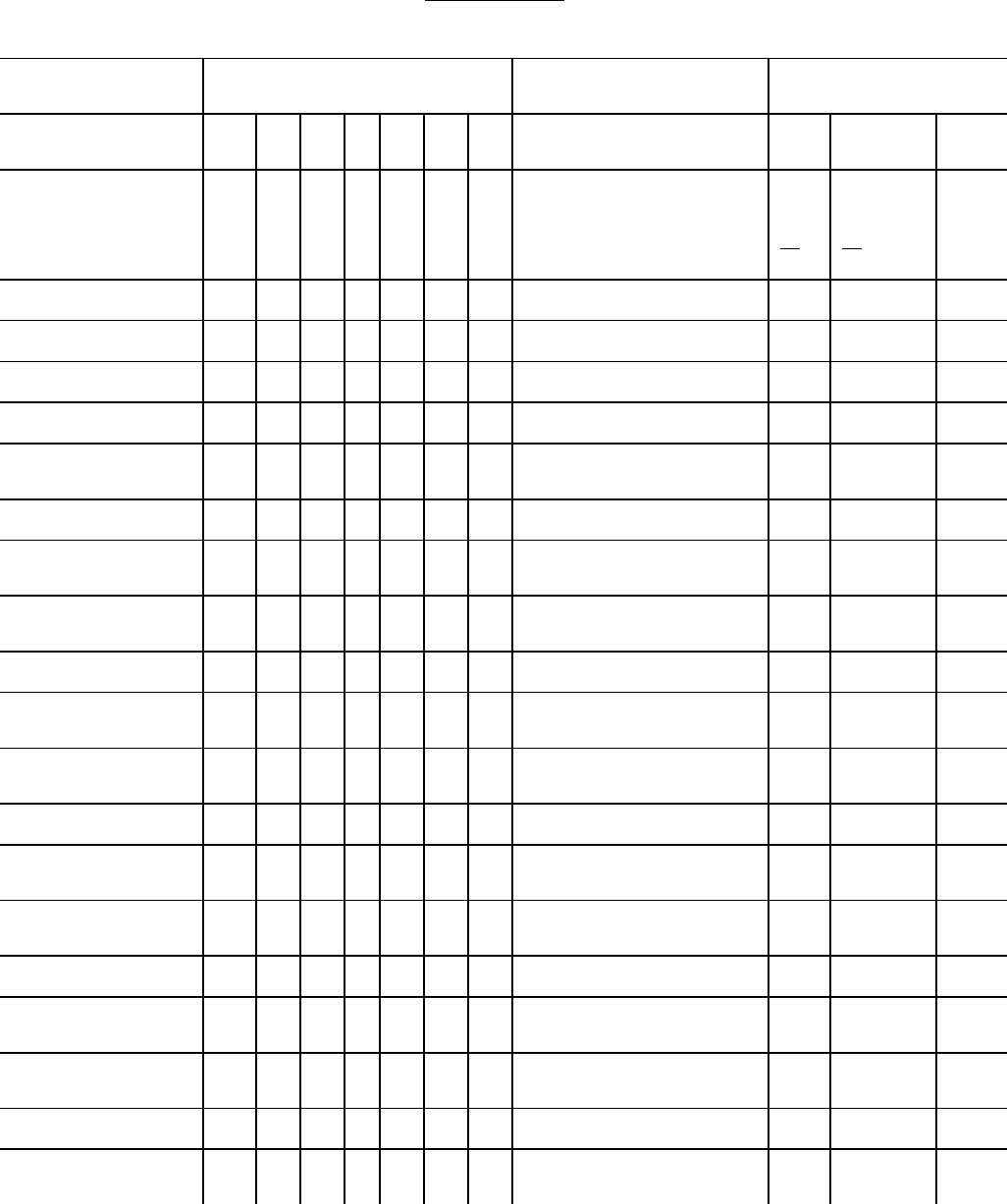
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
T98 (.3)
1d
or
1e
0
1d or 1e if reason for
treatment, or external
cause is not stated on
the record respectively
10
10
or
1:C
1:A,B
or
119
*
U04(.9)
1a
1
67
V01-V06 (.0-.1)
0
V01-V06 (.9)
3
10
4:B
119
V09
3
10
4:B/C
119
V10-V18
(.0-.1, .3-.5)
0
V10-V18 (.2,.9)
3
10
4:D)3)a
119
V19
3
10
4:C
4:D)3)a
119
V20-V28
(.0-.1, .3-.5)
0
V20-V28 (.2,.9)
3
10
4:D)3)a
119
V29
3
10
4:C
4:D)3)a
119
V30-V38
(.0-.2, .4-.7)
0
V30-V38 (.3,.9)
3
10
4:D)3)a
119
V39
3
10
4:C
4:D)3)a
119
V40-V48
(.0-.2, .4-.7)
0
V40-V48 (.3,.9)
3
10
4:D)3)a
119
V49
3
10
4:C
4:D)3)a
119
V50-V58
(.0-.2, .4-.7)
0
V50-V58 (.3,.9)
3
10
4:D)3)a
119
V59
3
10
4:C
4:D)3)a
119
49
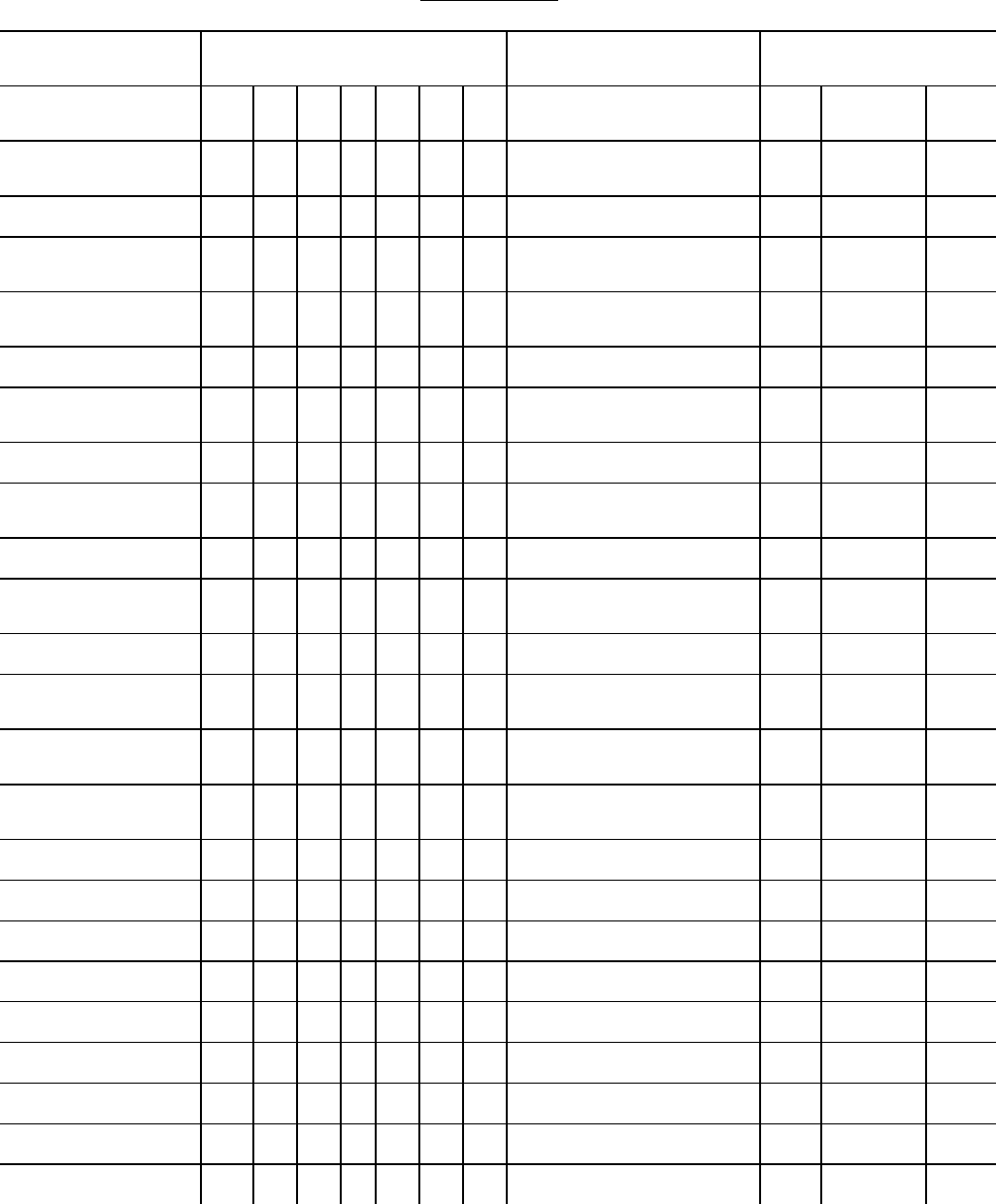
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
V60-V68
(.0-.2, .4-.7)
0
V60-V68 (.3,.9)
3
10
4:D)3)a
119
V69
3
10
4:C
4:D)3)a
119
V70-V78
(.0-.2, .4-.7)
0
V70-V78 (.3,.9)
3
10
4:D)3)a
119
V79
3
10
4:C
4:D)3)a
119
V80 (.0-.8)
0
V80 (.9)
3
10
4:C
4:D:2,3a
119
V81 (.0-.8)
0
V81 (.9)
3
10
4:C
4:D:1,2
119
V82 (.0-.8)
0
V82 (.9)
3
10
4:C
4:D:2,3
119
V83-V86
(.0-.2, .4-.7)
0
V83-V86 (.3,.9)
3
10
4:D:2,3,
4
119
V87-V88
3
10
4:D)3
119
V89
3
10
4:A,C,D
119
V90-V93 (.0-.8)
0
V90-V93 (.9)
5
10
4:A
119
V94
3
10
4:A,D
119
V95-V96 (.0-.8)
0
V95-V96 (.9)
5
10
4:A
119
V97-V98
0
V99
1e
10
4
119
50
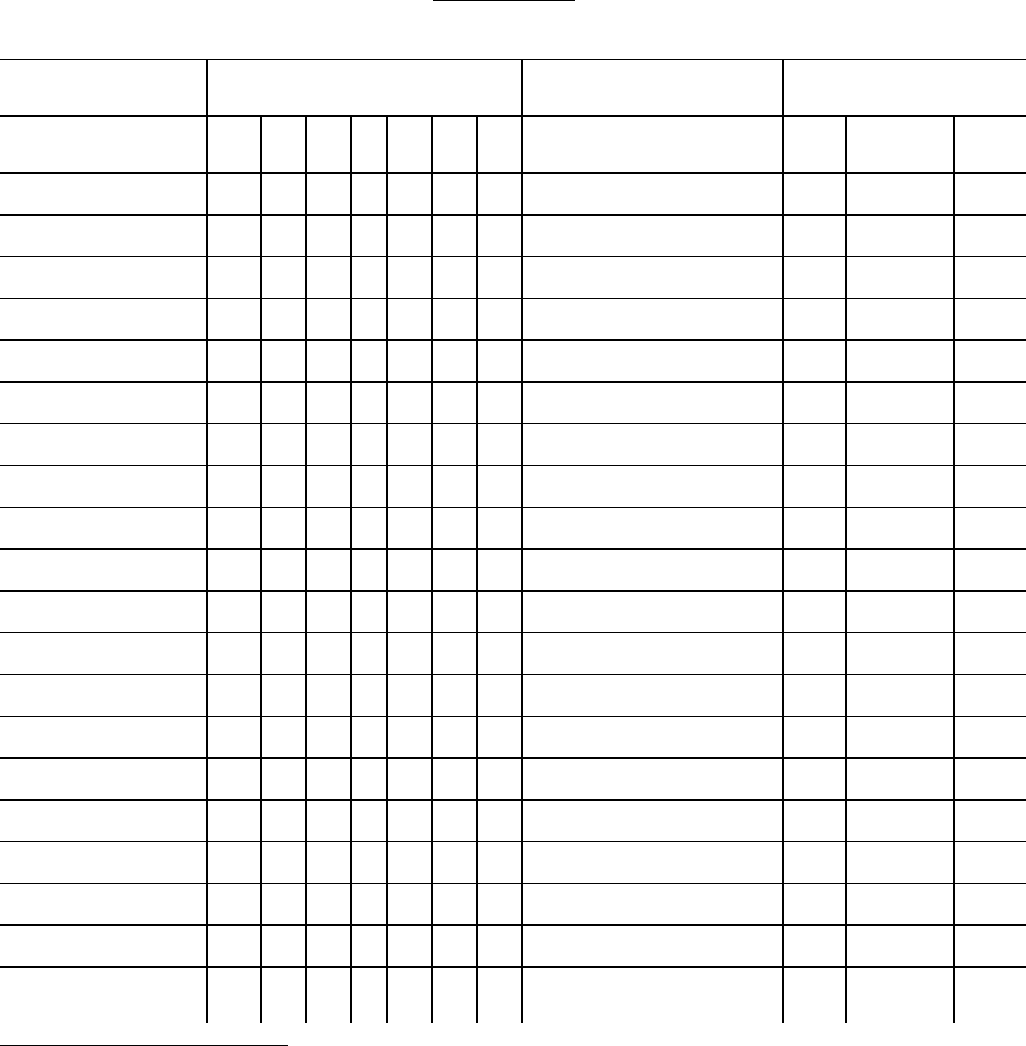
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
W00-W18 [.0-.8]
2
0
W00-W18 [.9]
2
5
10
119
W19
2
3
10
3
119
W20-W46 [.0-.8]
2
0
W20-W46 [.9]
2
5
10
119
W49
2
3
10
119
W50-W60 [.0-.8]
2
0
W50-W60 [.9]
2
5
10
119
W64
2
5
10
119
W65-W73 [.0-.8]
2
0
W65-W73 [.9]
2
5
10
119
W74
2
5
10
119
W75-W83 [.0-.8]
2
0
W75-W83 [.9]
2
5
10
119
W84
2
10
119
W85-W86 [.0-.8]
2
0
W85-W86 [.9]
2
5
10
119
W87
2
5
10
119
W88-W90 [.0-.8]
2
1a
1
67
W88-W90 [.9]
2
1a
5
1
10
67
119
2
W00-Y34, except Y06._, and Y07._: The “place-of-occurrence” codes indicated within brackets within
this table are to be treated as separate codes that have their own data tape field. They are not part of the
ICD-10 cause-of-death codes; however, priority levels for querying this information is provided.
51
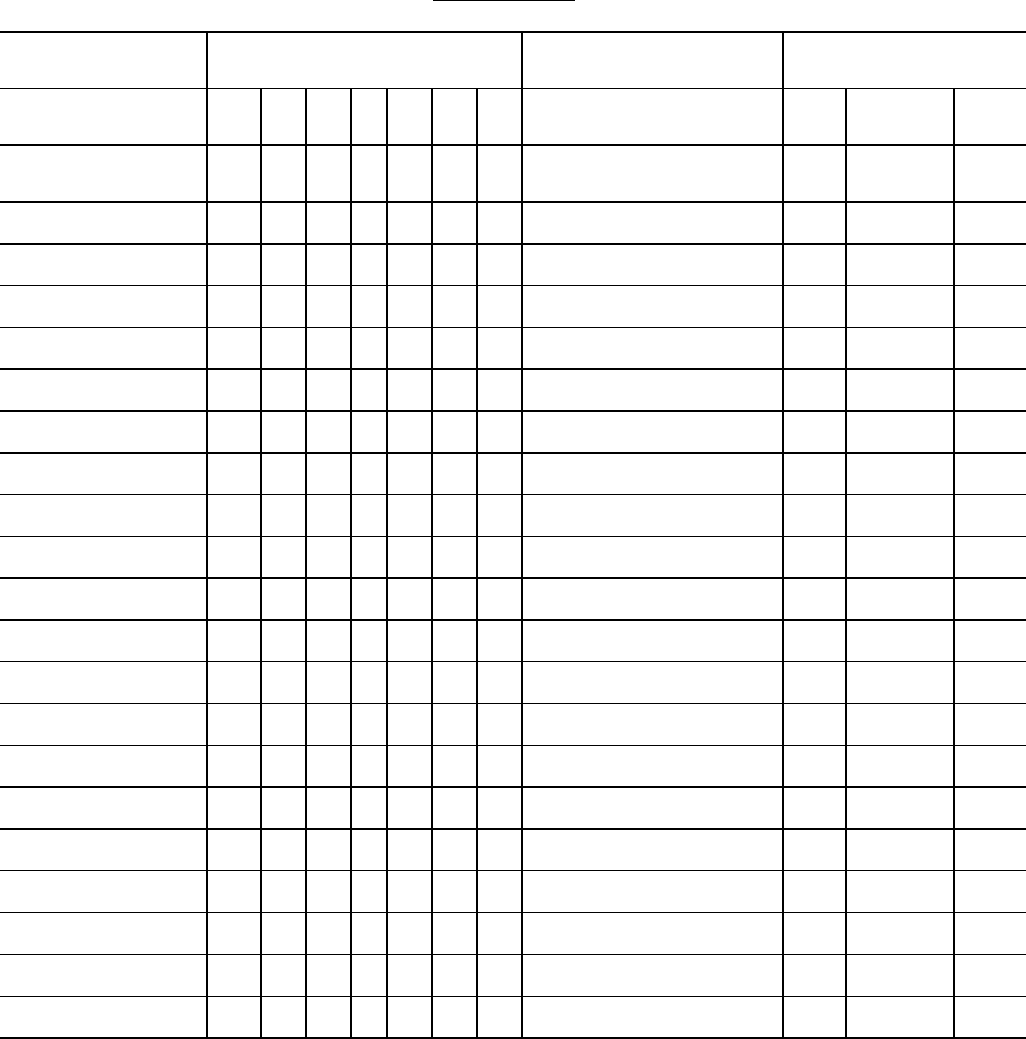
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
W91
2
1a
5
1
10
67
119
W93-W94 [.0-.8]
2
0
W93-W94 [.9]
2
5
10
119
W99
2
3
10
119
X00-X08 [.0-.8]
2
0
X00-X08 [.9]
2
5
10
119
X09
2
3
10
2
119
X10-X18 [.0-.8]
2
0
X10-X18 [.9]
2
5
10
119
X19
2
5
10
119
X20-X28 [.0-.8]
2
0
X20-X28 [.9]
2
5
10
119
X29
2
5
10
119
X30-X38 [.0-.8]
2
0
X30-X38 [.9]
2
5
10
119
X39
2
3
10
119
X40-X48 [.0-.8]
2
0
X40-X48 [.9]
2
5
10
119
X49
2
5
10
1D
119
X50-X58 [.0-.8]
2
0
X50-X58 [.9]
2
5
10
119
2
W00-Y34, except Y06._, and Y07._: The “place-of-occurrence” codes indicated within brackets
within this table are to be treated as separate codes that have their own data tape field. They are not part
of the ICD-10 cause-of-death codes; however, priority levels for querying this information is provided.
52
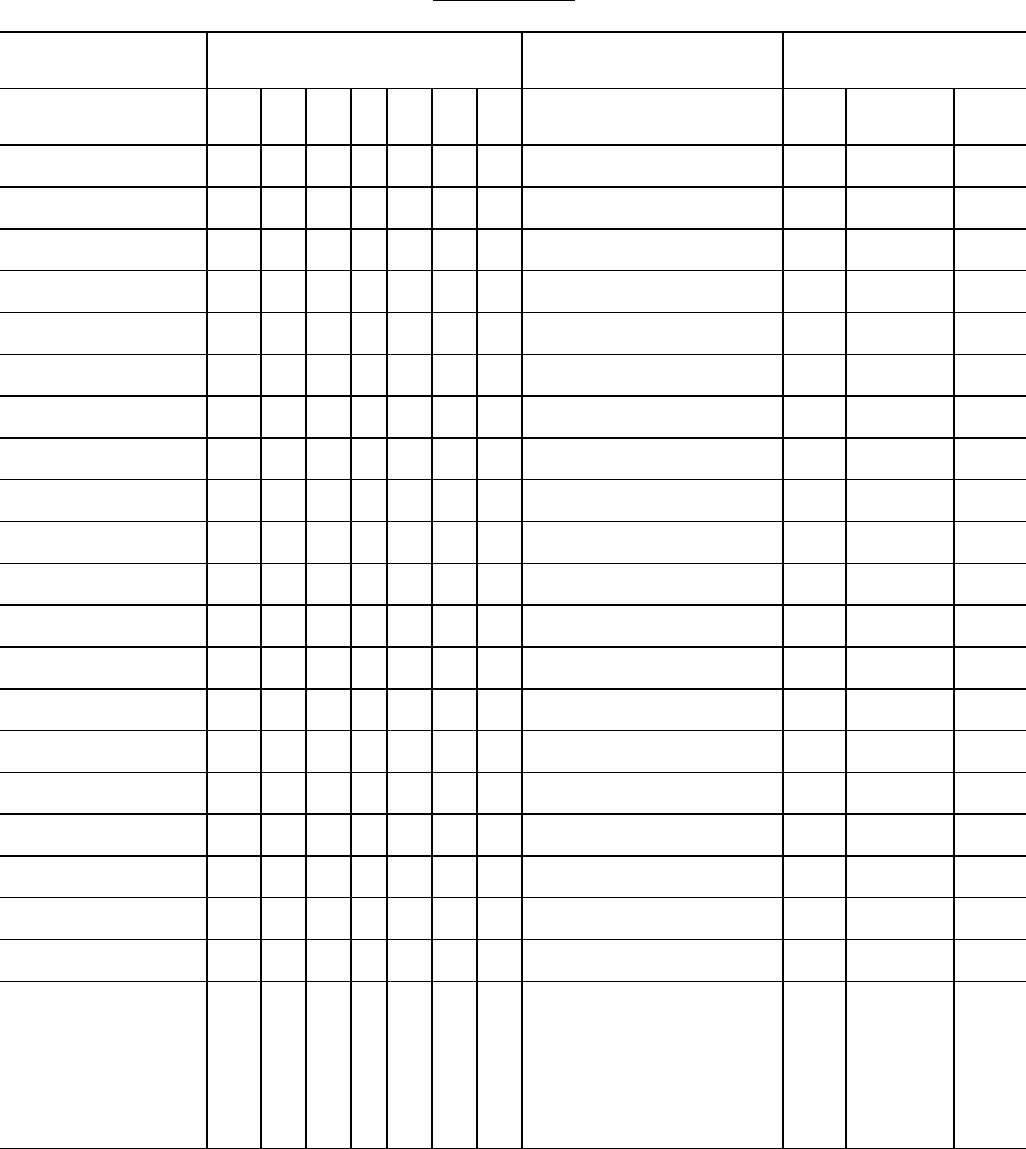
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
X59
2
3
10
1D
119
X60-X73 [.0-.8]
2
0
X60-X73 [.9]
2
5
10
119
X74
2
5
10
3
119
X75-X83 [.0-.8]
2
0
X75-X83 [.9]
2
5
10
119
X84
2
1e
10
3
119
X85-X89 [.0-.8]
2
0
X85-X89 [.9]
2
5
10
119
X90
2
5
10
1D
119
X91-X94 [.0-.8]
2
0
X91-X94 [.9]
2
5
10
119
X95
2
5
10
3
119
X96-Y05 [.0-.8]
2
0
X96-Y05 [.9]
2
5
10
119
Y06-Y07(.0-.8)
0
Y06-Y07 (.9)
5
10
119
Y08 [.0-.8]
2
0
Y08 [.9]
2
5
10
119
Y09
2
3
10
2
119
Y10-Y18 [.0-.8]
2
3
Y10-Y34:
Query for mannner of
death
(accident,homicide,
suicide,natural)
10
1A
119
2
W00-Y34, except Y06._, and Y07._: The “place-of-occurrence” codes indicated within brackets
within this table are to be treated as separate codes that have their own data tape field. They are not part
of the ICD-10 cause-of-death codes; however, priority levels for querying this information is provided
in this table.
53
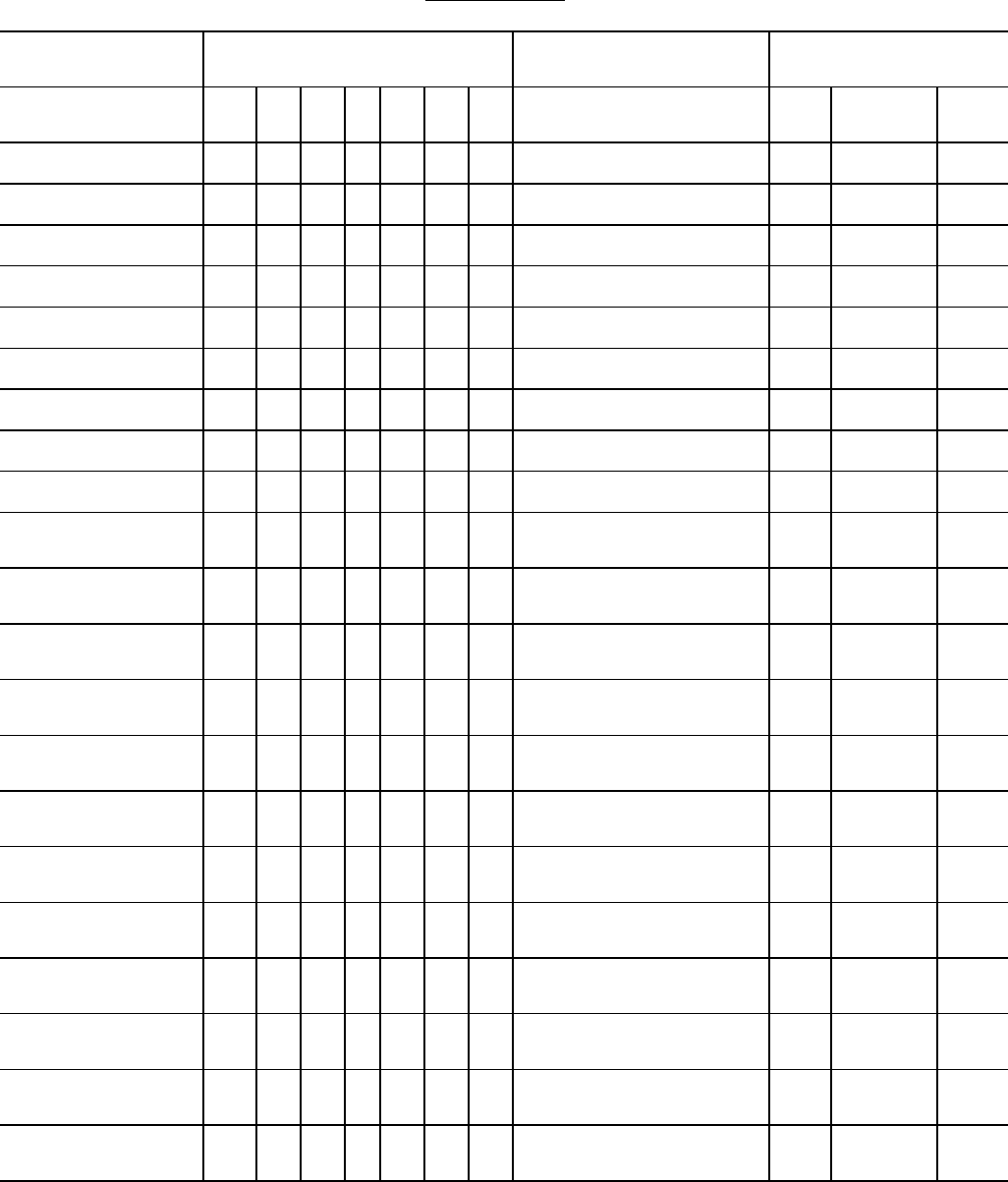
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
Y10-Y18 [.9]
2
3
10
1A
119
Y19
2
3
10
1:A,D
119
Y20-Y33 [.0-.8]
2
3
10
1A
119
Y20-Y33 [.9]
2
3
10
1A
119
Y34
2
1e
10
1:A,B
119
Y35
0
Y36
(.0-.4,.6-.8)
0
Y36 (.5)
1a
1
67
Y36 (.9)
5
10
119
Y40-Y43 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y40-Y43 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y44 (.0-.7)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y44 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y45 (.0-.7)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y45 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y46
(.0-.5,.7-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y46 (.6)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y47 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y47 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y48
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y49-Y53 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
2
W00-Y34, except Y06._, and Y07._: The “place-of-occurrence” codes indicated within brackets
within this table are to be treated as separate codes that have their own data tape field. They are not part
of the ICD-10 cause-of-death codes; however, priority levels for querying this information is provided
in this table.
54
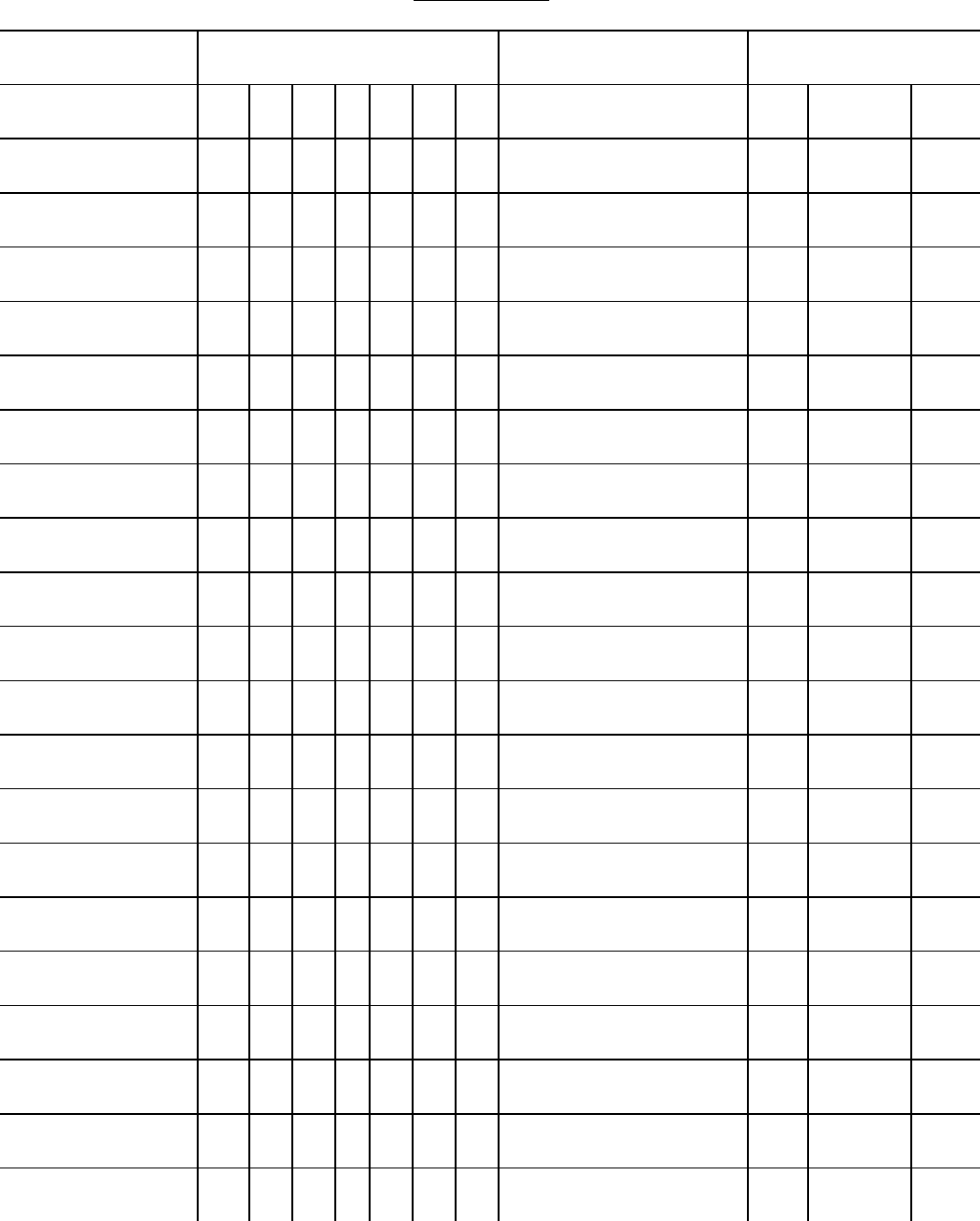
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
Y49-Y53 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y54
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y55 (.0-.6)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y55 (.7)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y56-Y57 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y56-Y57 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y58 (.0-.8)
1a
1d
1d if reason for medical
care not stated on record
10
1C
119
Y58 (.9)
1a
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y59 (.0-.3)
1a
1d
1d if reason for medical
care not stated on record
10
1C
119
Y59 (.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y59 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y60-Y62 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y60-Y62 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y63
(.0-.1,.4-.9)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y63 (.2-.3)
1a
1d
1d if reason for medical
care not stated on record
1
10
1C
67
119
Y64 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y64 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1C,9
119
Y65-Y66
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y69
1d
3
1d if reason for medical
care not stated on record
10
1C,9
119
Y70-Y81
1d
0
1d if reason for medical
care not stated on record
10
1C
119
55
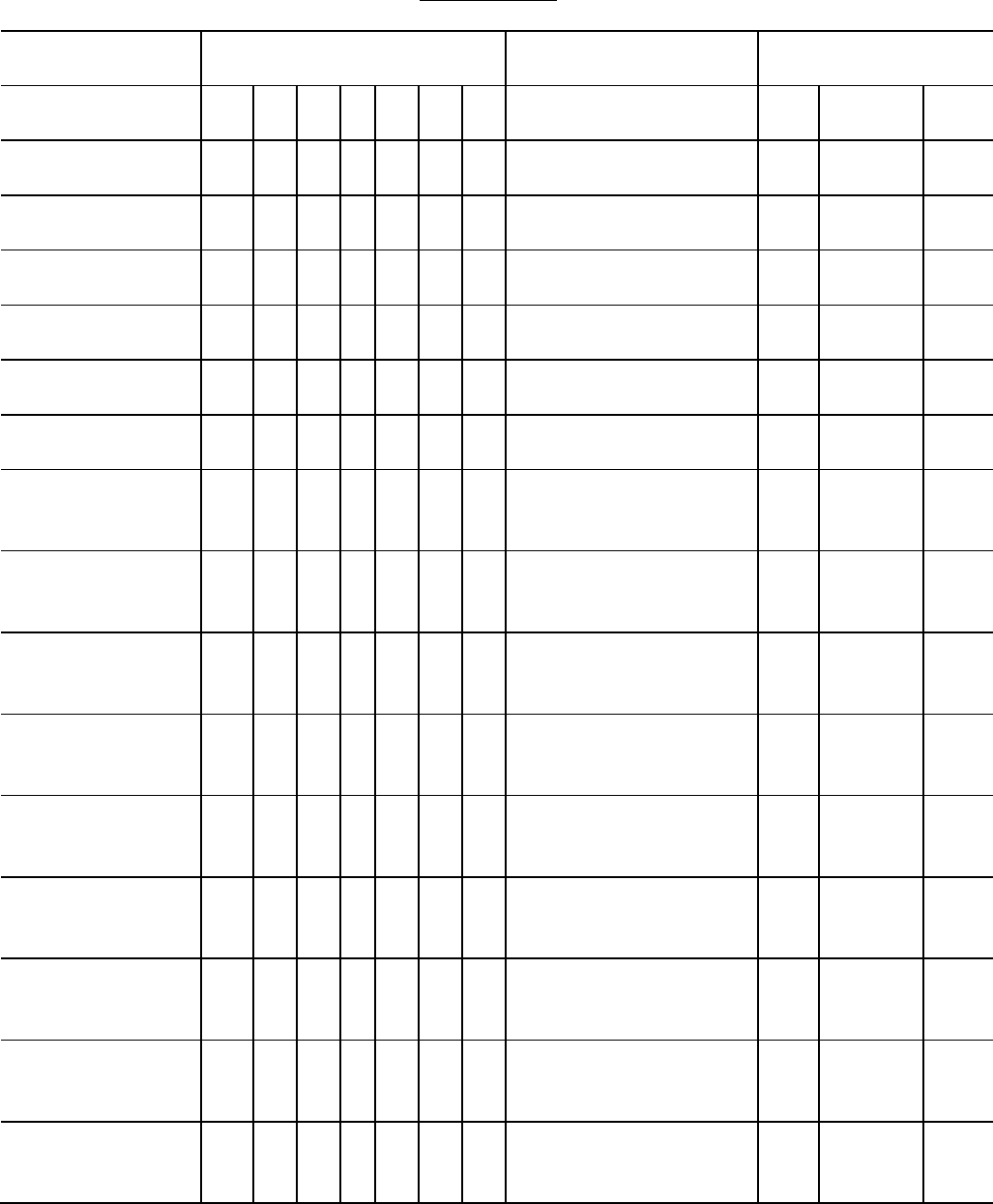
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
ICD
Category
Priority Levels
Comments
Query Form
1
2
3
4
5
6
0
Ltr
#
Ques#
Pg#
Y82
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y83 (.0-.8)
1d
0
1d if reason for medical
care not stated on record
10
1:C,D
119
Y83 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y84
(.0-.1, .3-.8)
1d
0
1d if reason for medical
care not stated on record
10
1C
119
Y84 (.2)
1a
1d
1d if reason for medical
care not stated on record
1
10 1C
67
119
Y84 (.9)
1d
5
1d if reason for medical
care not stated on record
10
1:C,D
119
Y85-Y86
1e
0
1e if nature of external
cause not stated on
record
10
2 and/or
4
119
Y87 (.0)
1e
0
1e if nature of external
cause not stated on
record
10
119
Y87 (.1)
1e
0
1e if nature of external
cause not stated on
record
10
119
Y87 (.2)
1e
0
1e if nature of external
cause not stated on
record
10
119
Y88 (.0)
1e
0
1e if nature of external
cause not stated on
record
10
4 and/or
1D
119
Y88 (.1)
1e
0
1e if nature of external
cause not stated on
record
10
4 and/or
1C
119
Y88 (.2)
1e
0
1e if nature of external
cause not stated on
record
10
4 and/or
1D
119
Y88 (.3)
1e
0
1e if nature of external
cause not stated on
record
10
4 and/or
1C
119
Y89 (.0-.9)
1e
0
1e if nature of external
cause not stated on
record
10
119
56
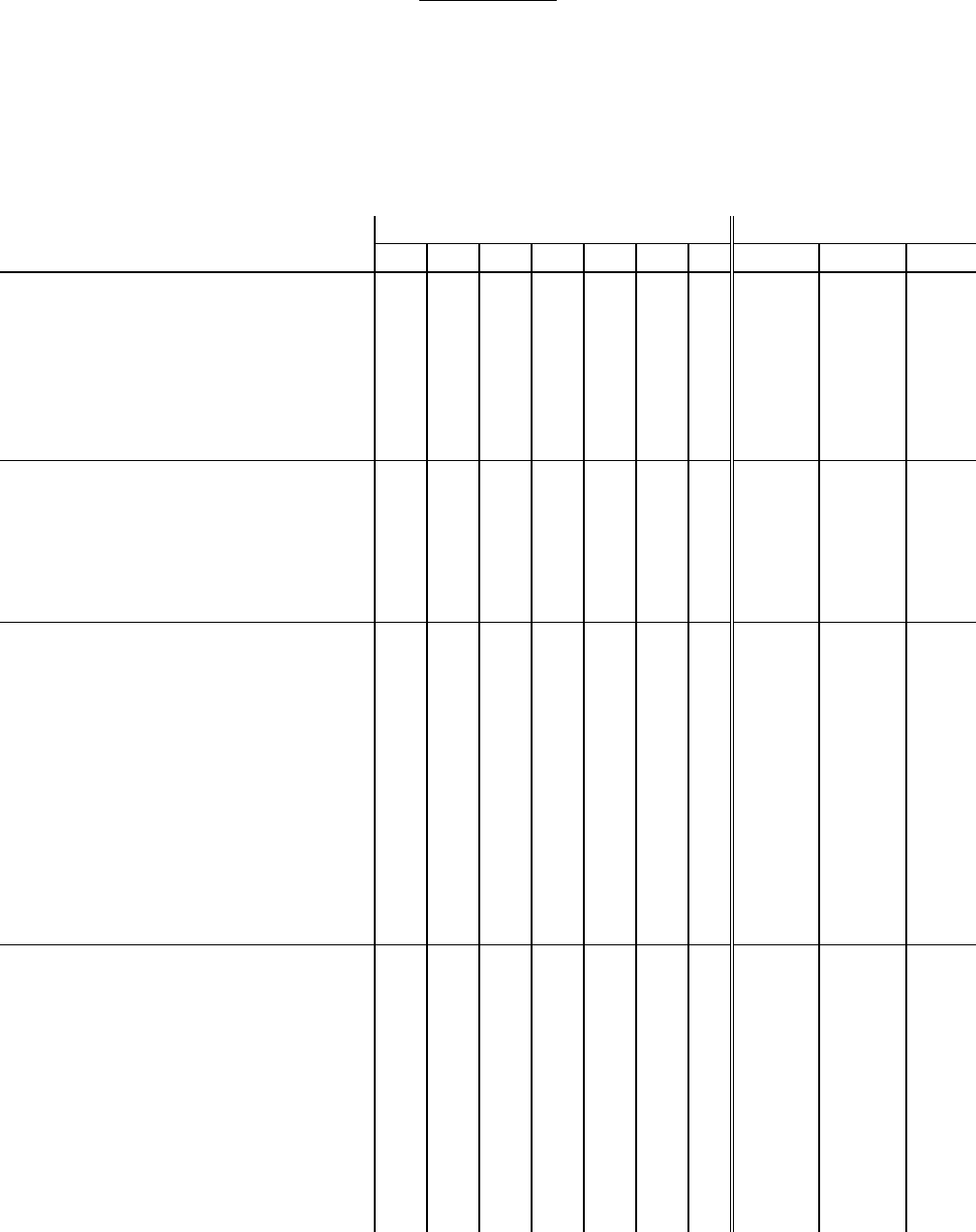
APPENDIX A
Table 1. Priority Levels for Querying by ICD-10 Category
For an interpretation of the ‘highly improbable’ rule, refer to Instruction manual part 2A, section III.
Items 14 and 15 below exclude a few additional codes according to NCHS coding procedures (see
Instruction Manual part 2a).
Improbable Sequence
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
1. Hemophilia classifiable to D66,
D67, D68.0-D68.2 reported due to
any other disease.
Example:
I (a) Hemophilia B
(b) ASHD
1f
11
145
2. Influenza classifiable to J10-J11
reported due to any other disease.
Example:
I (a) Influenza
(b) Acute pancreatitis
1f
11
145
3. Rheumatic fever (I00-I02) or
rheumatic heart disease (I05-I09)
reported due to any disease other
than scarlet fever (A38),
streptococcal septicemia (A40.-),
streptococcal sore throat (J02.0) and
acute tonsillitis (J03.-).
Example:
I (a) Heart failure
(b) Rheumatic fever
(c) Cancer of the lung
1f
11
145
4. Any cerebrovascular disease
(I60-I69) reported due to a disease of
the digestive system (K00-K92),
except Cerebral hemorrhage (I61.-)
due to Diseases of liver (K70-K76).
Example:
I (a) Respiratory failure
(b) Cerebrovascular insufficiency
(c) Acute appendicitis
1f
11
145
57
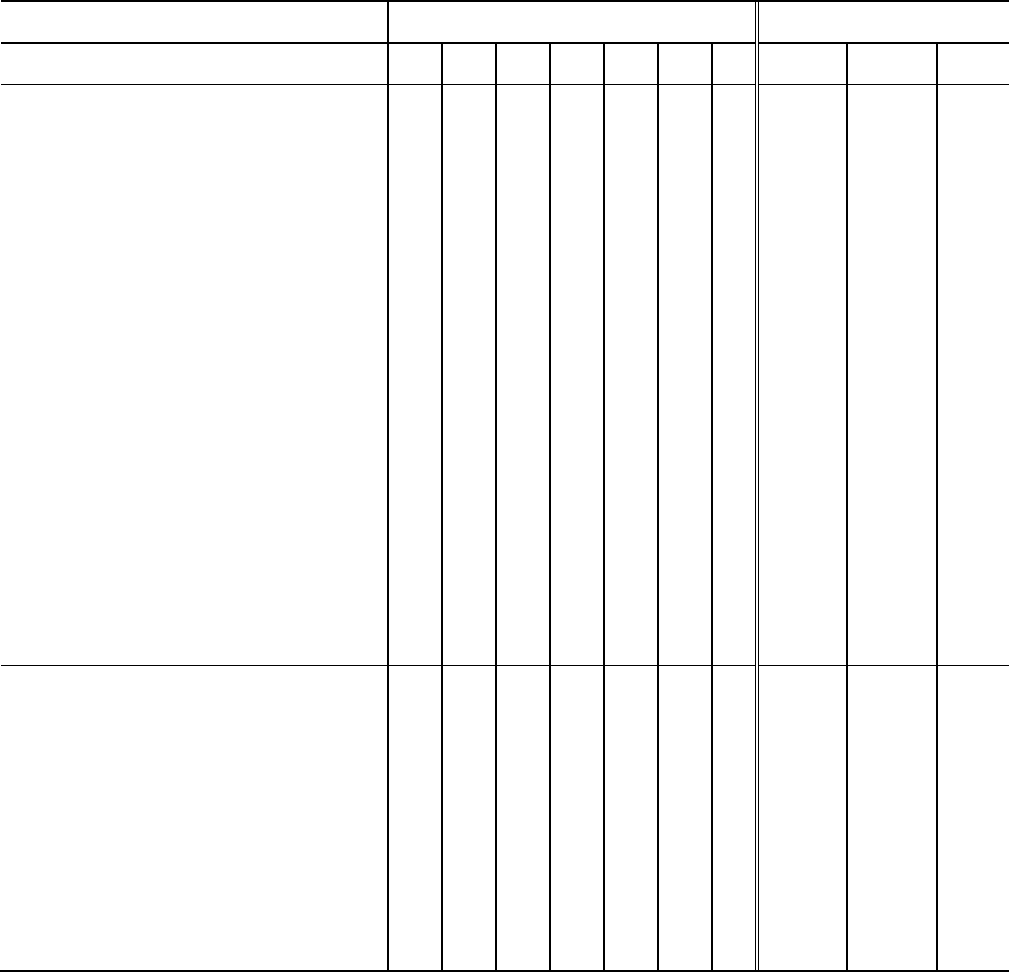
Appendix A
Table 2. Priority Levels for Improbable Sequences in Part I of the Death Certificate
(Order of Entry of Causes of Death)
Improbable Sequence
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
5. Cerebral infarction due to:
thrombosis of precerebral arteries
(I63.0); unspecified occlusion of
precerebral arteries (I63.2);
thrombosis of cerebral arteries
(I63.3); unspecified occlusion of
cerebral arteries (I63.5); cerebral
venous thrombosis, nonpyogenic
(I63.6); other cerebral infarction
(I63.8); cerebral infarction,
unspecified (I63.9); stroke, not
specified as hemorrhage or infarction
(I64); other cerebrovascular disease
(I67); sequela of stroke, not specified
as hemorrhage or infarction (I69.4);
sequela of other and unspecified
cerebrovascular diseases (I69.8)
reported as “due to” endocarditis
(I05-I08, I09.1, I33-I38).
1f
11
145
6. Occlusion and stenosis of
precerebral arteries, not resulting in
cerebral infarction (I65), except
embolism occlusion and stenosis of
cerebral arteries, not resulting in
cerebral infarction (I66) except
embolism sequela of cerebral
infarction (I69.3), except embolism
reported as “due to” endocarditis
(I05-I08, I09.1, I33-I38).
1f
11
145
58
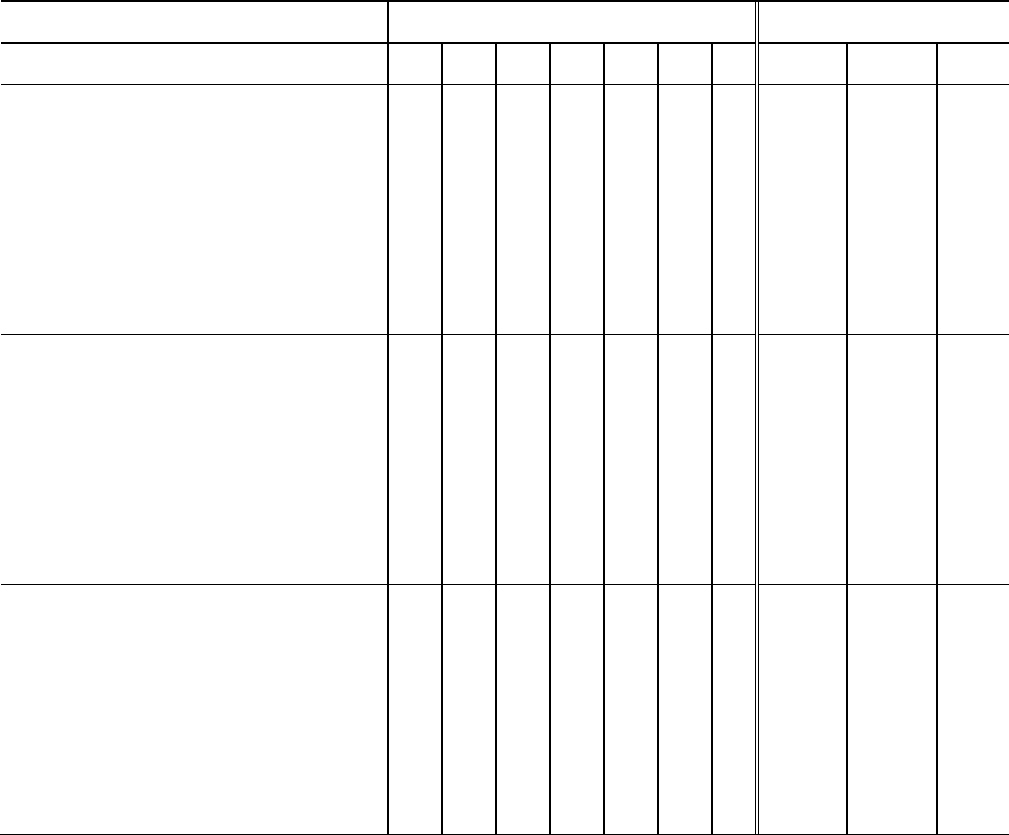
Appendix A
Table 2. Priority Levels for Improbable Sequences in Part I of the Death Certificate
(Order of Entry of Causes of Death)
Improbable Sequence
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
7. Chronic ischemic heart disease
(I20, I25) reported due to any
neoplasm (C00-D48).
Example:
I (a) Coronary artery disease
(b) Carcinomatosis
(c) Carcinoma of the face
1f
11
145
8. Any condition described as
arteriosclerotic [atherosclerotic]
reported due to any neoplasm (C00-
D48).
Example:
I (a) ASHD
(b) Acute myeloid leukemia.
1f
11
145
9. Any hypertensive disease reported
due to any neoplasm (C00-D48)
except carcinoid tumors or endocrine
and renal neoplasms.
Example:
I (a) Hypertension
(b) Malignant neoplasm of the throat
1f
11
145
59
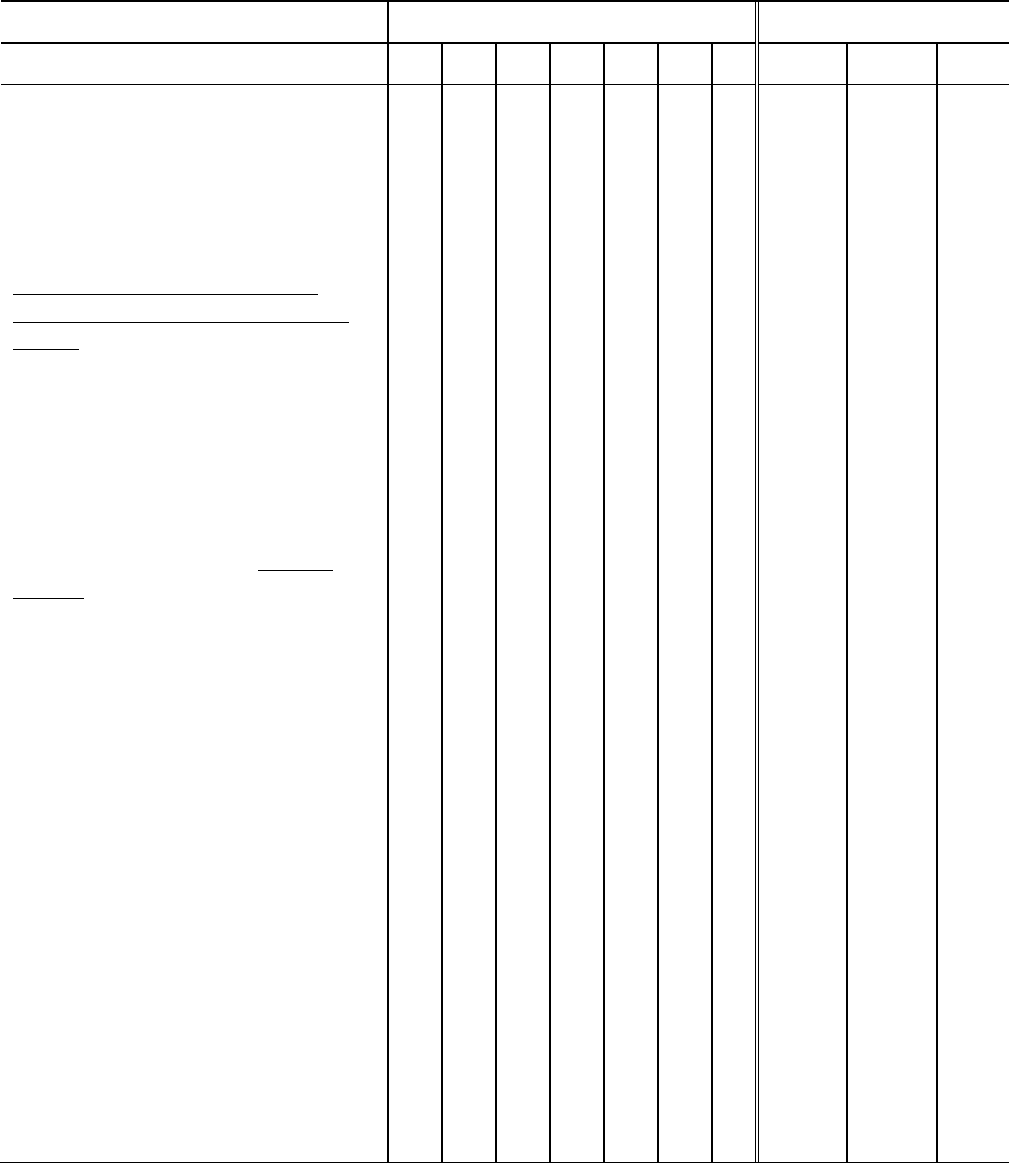
Appendix A
Table 2. Priority Levels for Improbable Sequences in Part I of the Death Certificate
(Order of Entry of Causes of Death)
Improbable Sequence
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
10. An infectious or parasitic disease
(A00-B99) reported due to any
disease outside this chapter, except
situations I, II, III, and IV:
I. The following may be accepted as
due to any other disease.
* diarrhea and gastroenteritis of
presumed infectious origin (A09,
B94.8)
* septicemia (A40-A41, B94.8)
* erysipelas (A46, B94.8)
* bacteremia (A49.0-A49.9, B94.8)
* gas gangrene (A48.0, B94.8)
* Vincent's angina (A69.1, B94.8)
* mycoses (B35-B49, B94.8)
II. Any infectious disease, except
A81.1, may be accepted as "due to"
immunosuppression by chemicals
(chemotherapy) and radiation; and
infectious diseases classified to A00-
A09.0, A16.2-B19, or B25-B64
reported as due to malignant
neoplasms.
III. Any infectious disease due to
disorders of immune mechanism
such as HIV or AIDS.
IV. Varicella and zoster infections
(B01-B02) may be accepted as "due
to" diabetes, tuberculosis and
lymphoproliferative neoplasms.
Example:
I (a) Cholera
(b) Myocarditis
1f
11
145
60
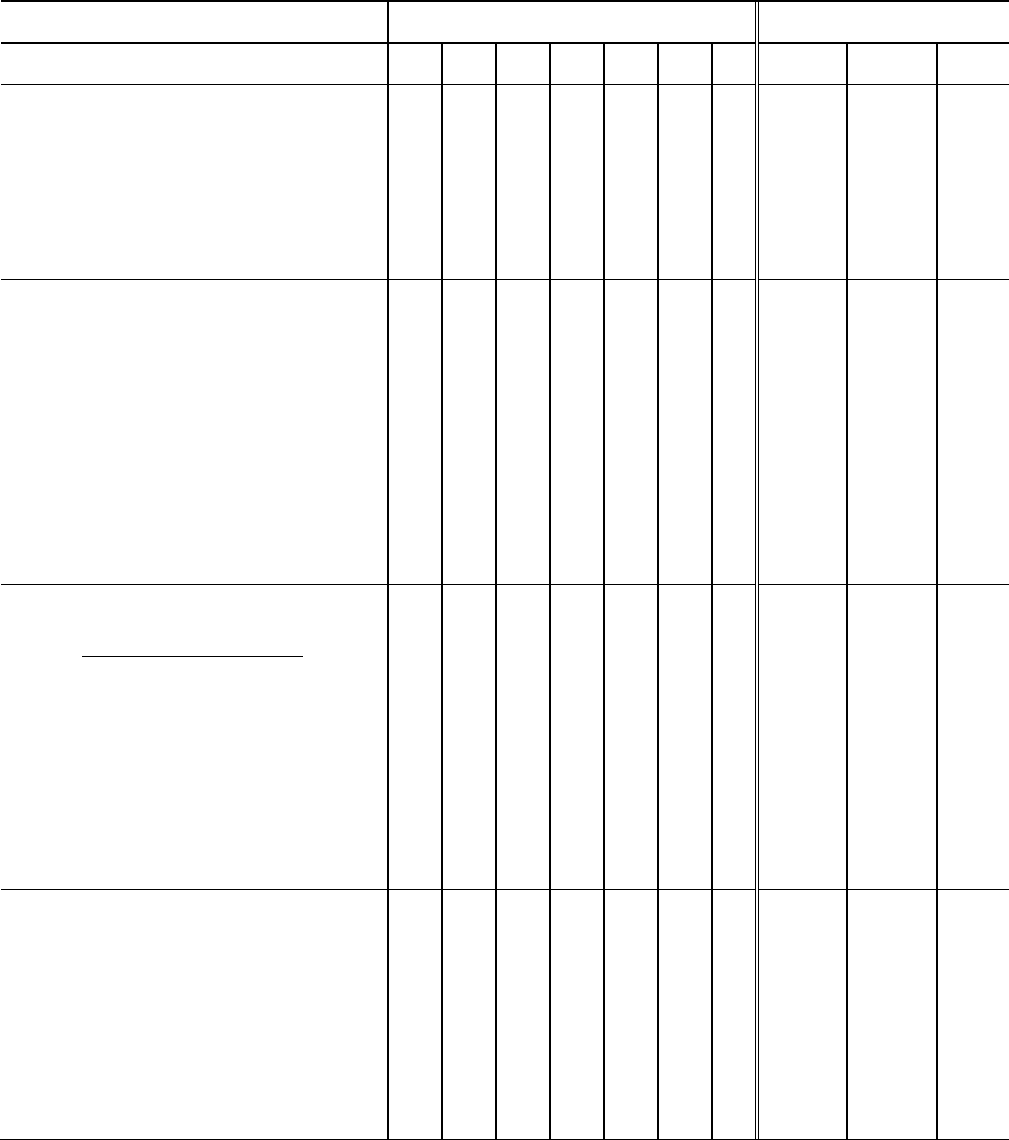
Appendix A
Table 2. Priority Levels for Improbable Sequences in Part I of the Death Certificate
(Order of Entry of Causes of Death)
Improbable Sequence
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
11. A malignant neoplasm
classifiable to C00-C97 reported due
to any disease, except HIV
Example:
I.(a) Multiple myeloma
(b) Emphysema
1f
11
145
12. Diabetes (E10-E14) reported due
to any other disease except
hemochromatosis (E83.1), diseases
of pancreas (K85-K86), pancreatic
neoplasms (C25.-, D13.6, D13.7,
D37.7), and malnutrition (E40-E46).
Example:
I.(a) Heart failure
(b) Diabetes with coma
(c) Gastric ulcer
1f
11
145
13. Congenital malformations (Q00-
Q99) reported due to any other
disease, including immaturity, except
chromosome abnormality or
congenital malformation syndrome;
pulmonary hypoplasia due to
congenital anomaly.
Example:
I.(a) Spina bifida
(b) Pneumonia
1f
11
145
14. An injury classifiable to Chapter
19 (S00-T98) except T17.2-T17.9
(foreign body in respiratory tract),
reported due to a disease condition
(A00-R99).
Example:
I.(a) Fracture of the neck
(b) Influenza
1f
11
145
61
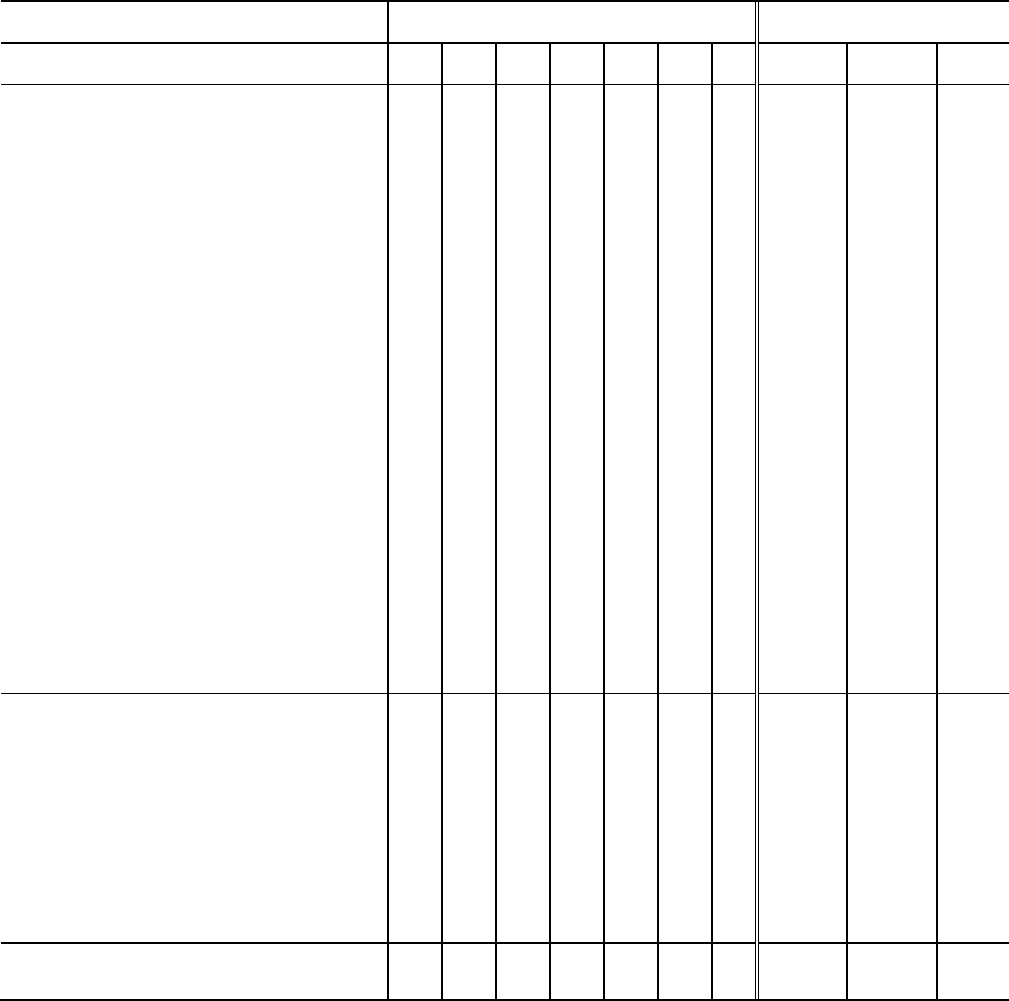
Appendix A
Table 2. Priority Levels for Improbable Sequences in Part I of the Death Certificate
(Order of Entry of Causes of Death)
Improbable Sequence
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
15. Accidents (V01-X59) is reported
due to any cause outside this chapter
except:
a) any accident (V01-X59) reported
as due to epilepsy (G40-G41),
b) Fall (W00-W19) due to a disorder
of bone density (M80-M85),
c) Fall (W00-W19) due to a
(pathological) fracture caused by a
disorder of bone density,
d) Asphyxia reported as due to
aspiration of mucus, blood (W80) or
vomitus (W78) as a result of disease
conditions,
e) Aspiration of food (liquid or solid)
of any kind (W79) reported as due to
a disease which affects the ability to
swallow.
Example:
I.(a) Heat stroke
(b) Myocardial infarction
1f
11
145
16. An injury is reported due to a
disease condition AND an external
cause that could result in the injury is
reported elswhere on record.
Example:
I.(a) Subdural hematoma
(b) Hypertension
II. Fell and struck head
1f
11
145
17. Suicide (X60-X84) due to any
cause
1f
11
145
62
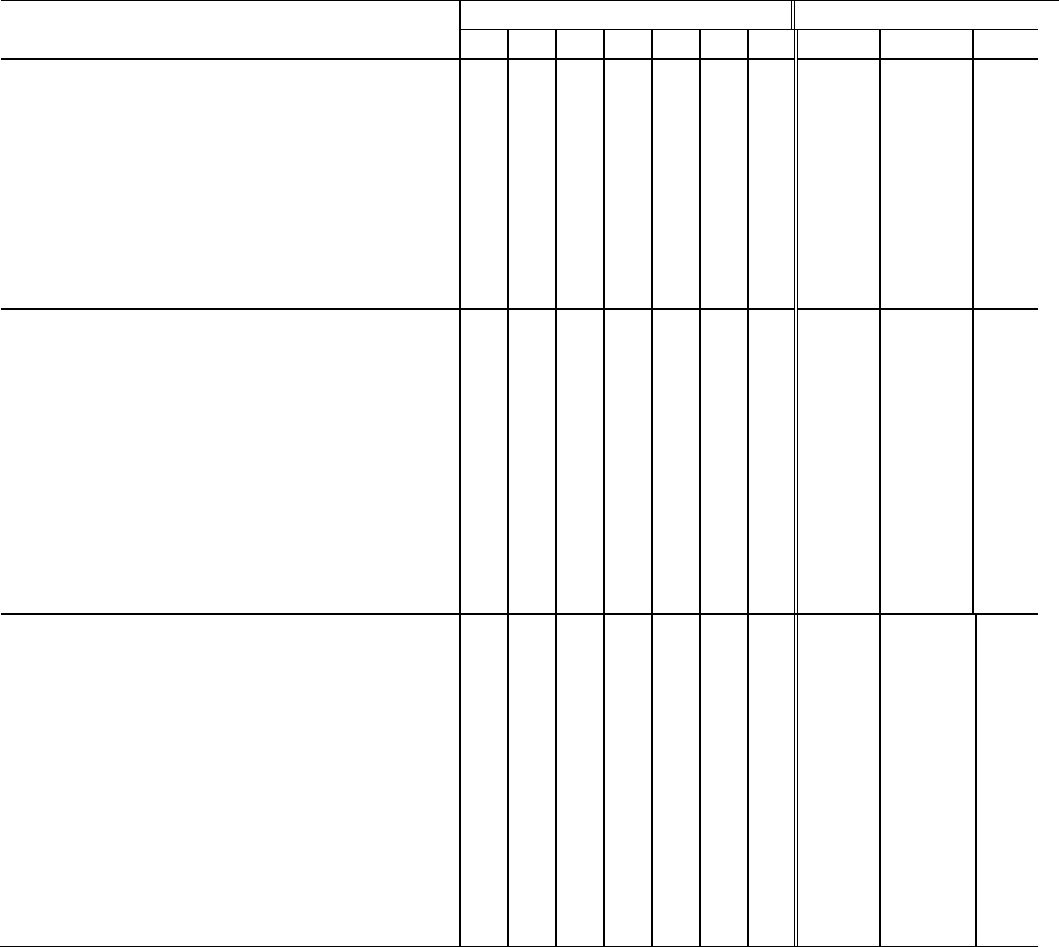
Appendix A
Table 3. Priority Levels for Durations
(Order of Entry of Causes of Death)
If resource permits, we recommend querying the following types of cause-of-death statements. When
querying is not feasible, refer to the coding instructions for these situations in Instruction Manual part
2B.
Problem With Duration
1. When a congenital malformation
classifiable to Q00-Q99 is reported with a
duration less than the age of the decedent.
Example: Age - 50 years
I(a) Heart failure
(b) Polycystic kidney disease 5 yr
(c)
II
2. When more than one condition is entered
on a single line in Part I with only one
duration.
Examples:
I(a) ASHD with M.I. 2 yrs.
(b)
(c)
I(a) Coma
(b) Gen. A.S. with CVA 5 yrs.
3. When the duration of an entity in a due to
position is shorter than that of an entity
reported on a line above it.
Examples:
I(a) Pneumonia days
(b) CVA 2 yrs.
(C) ASHD 1 yr.
I(a) Arteriosclerosis 5 yrs.
(b) Cerebral arterio 3 yrs.
(c) Hypertension 2 yrs.
1
2
Priority Levels
3
4
5
6
6
6
6
0
Query Form
Ltr#
Ques#
11
11
11
Pg#
145
145
145
63
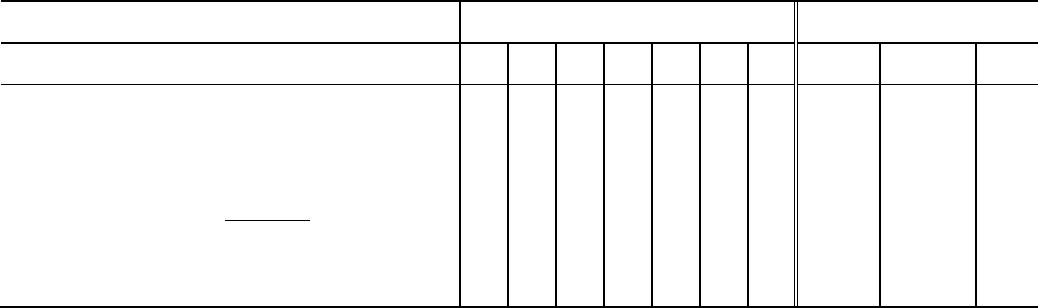
64
Appendix A
Table 3. Priority Levels for Durations
(Order of Entry of Causes of Death)
Problem With Duration
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques#
Pg#
4. When the certifier enters conflicting
durations for a single condition on a line in
Part I.
Example:
I(a) Coronary occlusion weeks|6 mos.
Duration
(b)
(c)
6
11
145
64
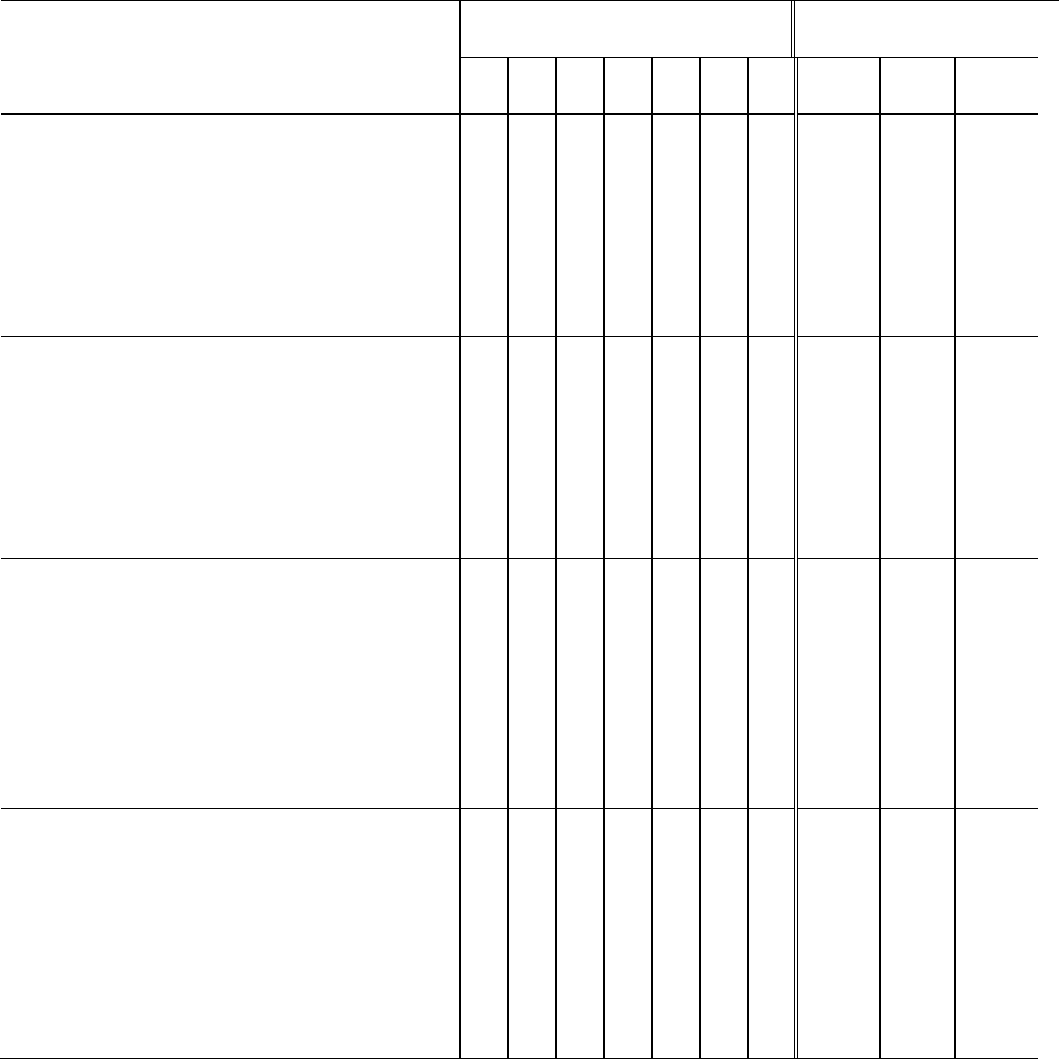
Appendix A
Table 4. Priority Levels for Placement and Numbering of Conditions
(Order of Entry of Causes of Death)
If resource permits, we recommend querying the following types of cause-of-death statements. When
querying is not feasible, refer to the coding instructions for these situations in Instruction Manual part 2B.
Problem with Placement and Numbering of
Conditions
1. When a condition is reported on the
certificate above line (a).
Example:
Cardiac arrest
I(a) ASHD
(b) A.S.
(c) Hypertension
2. When conditions are reported between
lines I(a) and I(b) or I(b) and I(c).
Example:
I(a) Cardiac arrest
(b) Pulmonary edema, Pneumonia
CHF
(c) Hypertension
3. When the certifier has entered conditions
on lines (a), (b), and (c) and has made a
statement that (c) was “due to above”.
Example:
I(a) Pneumonia
(b) Hypertension
(c) Cardiac hypertrophy due to
above
4. When the certifier has reported that a
condition in Part II was “caused by above”.
Example:
I(a) Hypotension
(b) Arteriosclerosis
(c)
II Mesenteric thrombosis caused by
Above
1
2
Priority Levels
3
4
5
4
4
4
6
6
0
Query Form
Ltr#
Ques
#
11
11
11
11
Pg#
145
145
145
145
65
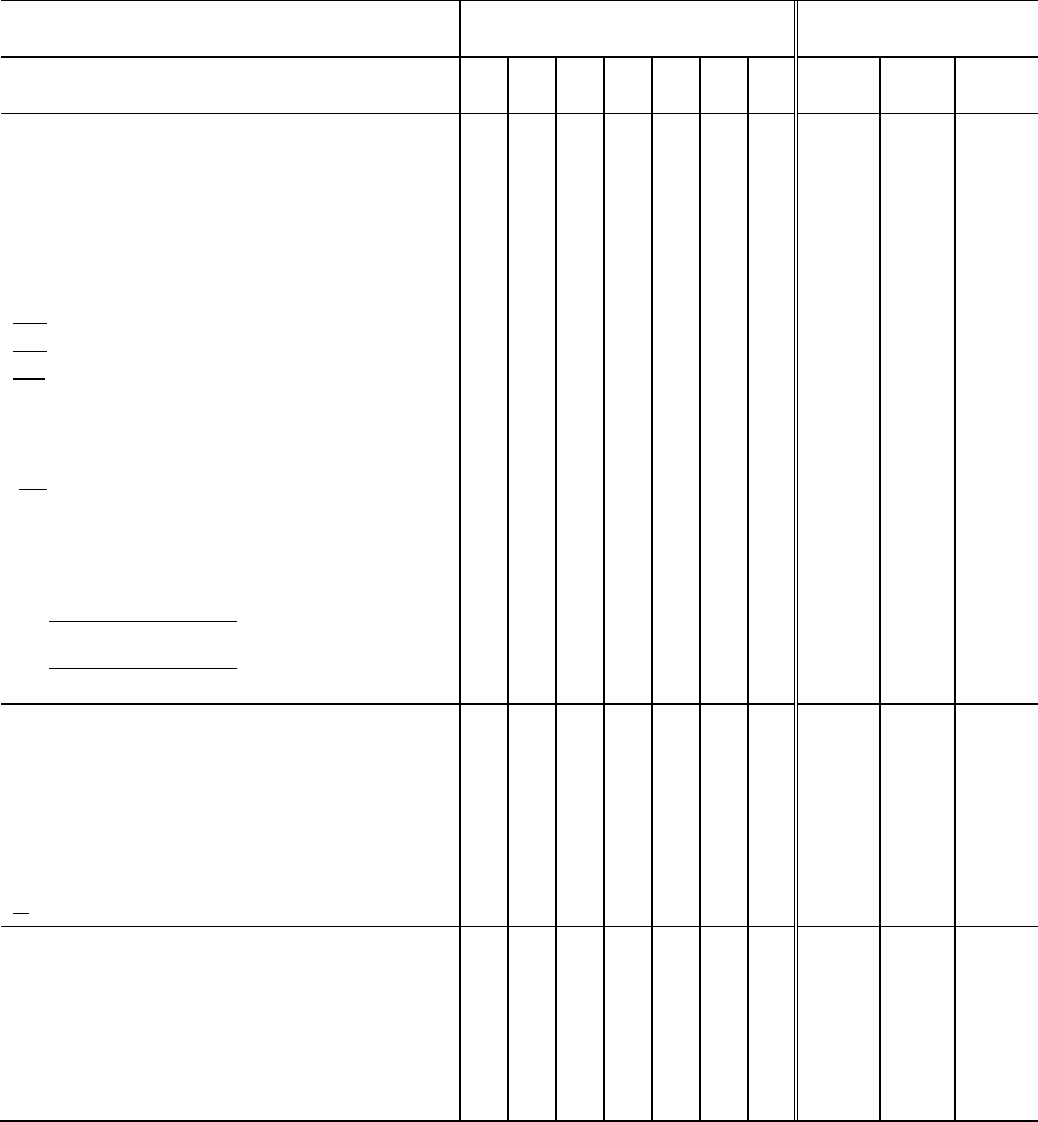
Appendix A
Table 4. Priority Levels for Placement and Numbering of Conditions
(Order of Entry of Causes of Death)
Problem with Placement and Numbering of
Conditions
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques
#
Pg#
5. When the certifier has marked through
lines (a), (b), and (c) or the printed “due to or
as a consequence of” which is interpreted to
mean that none of the conditions in Part I are
causally related.
Examples:
I(a) Gastrointestinal hemorrhage
(b) Gastric ulcer
(c)
II Arteriosclerosis
I(a) Congestive heart failure
(b) ASHD
(c)
II Pneumonia
I(a) Malnutrition
due to or as a consequence of
(b) Carcinoma of liver
due to or as a consequence of
(c) Carcinoma of pancreas
6
11
145
6. When the certifier has marked through the
printed “Part II”.
Example:
I(a) Pulmonary embolism
(b) Heart disease
(c)
II Hypertension
6
11
145
7. When the certifier has numbered all
causes on lines in Part I (i.e., 1, 2, 3, etc.).
Example:
I(a) 1.Pneumonia 2.C.H.F.
(b) 3.Pulmonary edema
(c) 4.Myocarditis
4
11
145
66
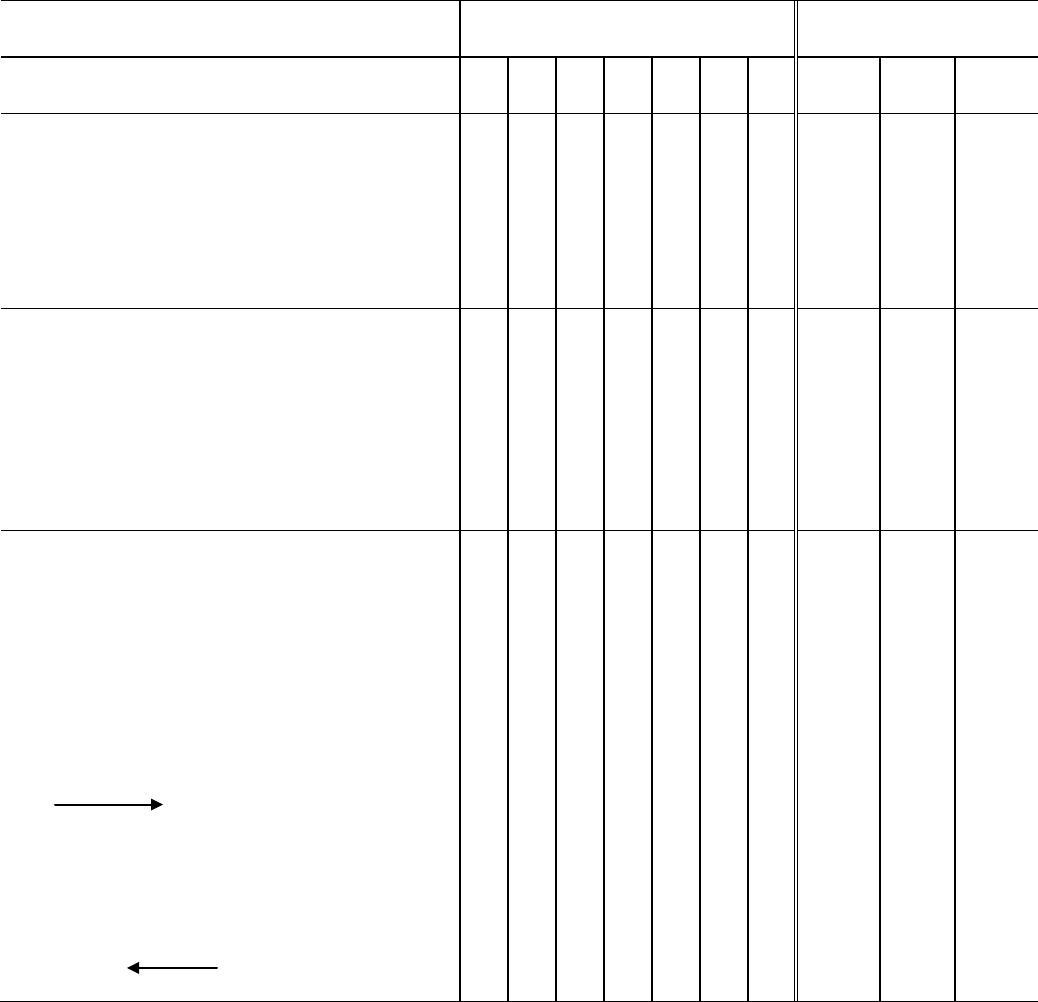
Appendix A
Table 4. Priority Levels for Placement and Numbering of Conditions
(Order of Entry of Causes of Death)
Problem with Placement and Numbering of
Conditions
Priority Levels
Query Form
1
2
3
4
5
6
0
Ltr#
Ques
#
Pg#
8. When the certifier has numbered part of
4
11
145
the causes in Part I.
Example:
I(a) 1.Acidosis
(b) 2.Coma
(c) Cerebral arteriosclerosis
9. When the causes in Part I are numbered
4
11
145
and one of the numbered causes is stated or
implied as due to another cause.
Example:
I(a) 1.Uremia due to nephritis
(b) 2.Hypertension
(c) 3.Arteriosclerosis
10. When the certifier has used arrows to
4
11
145
indicate moving conditions from Part I to
Part II and more than one condition is
entered on the line.
Examples:
I(a) ASHD
(b) Gen. Art.
(c) Parkinson dis. Encephalopathy
II |
I(a) Cardiorespiratory failure
(b) CVA
(c) G.I. hemorrhage gastric ulcer
II |
67

Appendix B
Query Letter 1
(Rare Causes)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________. Please answer the questions shown in the attachment.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical research,
funding, and resource allocation in our State and at the national level.
In this particular death, we wish to ensure that the cause of death is correct. The reported cause is one of the causes that
we always try to verify, either because the cause is rarely reported on a death certificate or may present threats to public
health in the United States. We appreciate your help in verifying the condition on this death certificate and look
forward to your prompt reply.
If you have any questions, please contact ____________________________.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
68
69
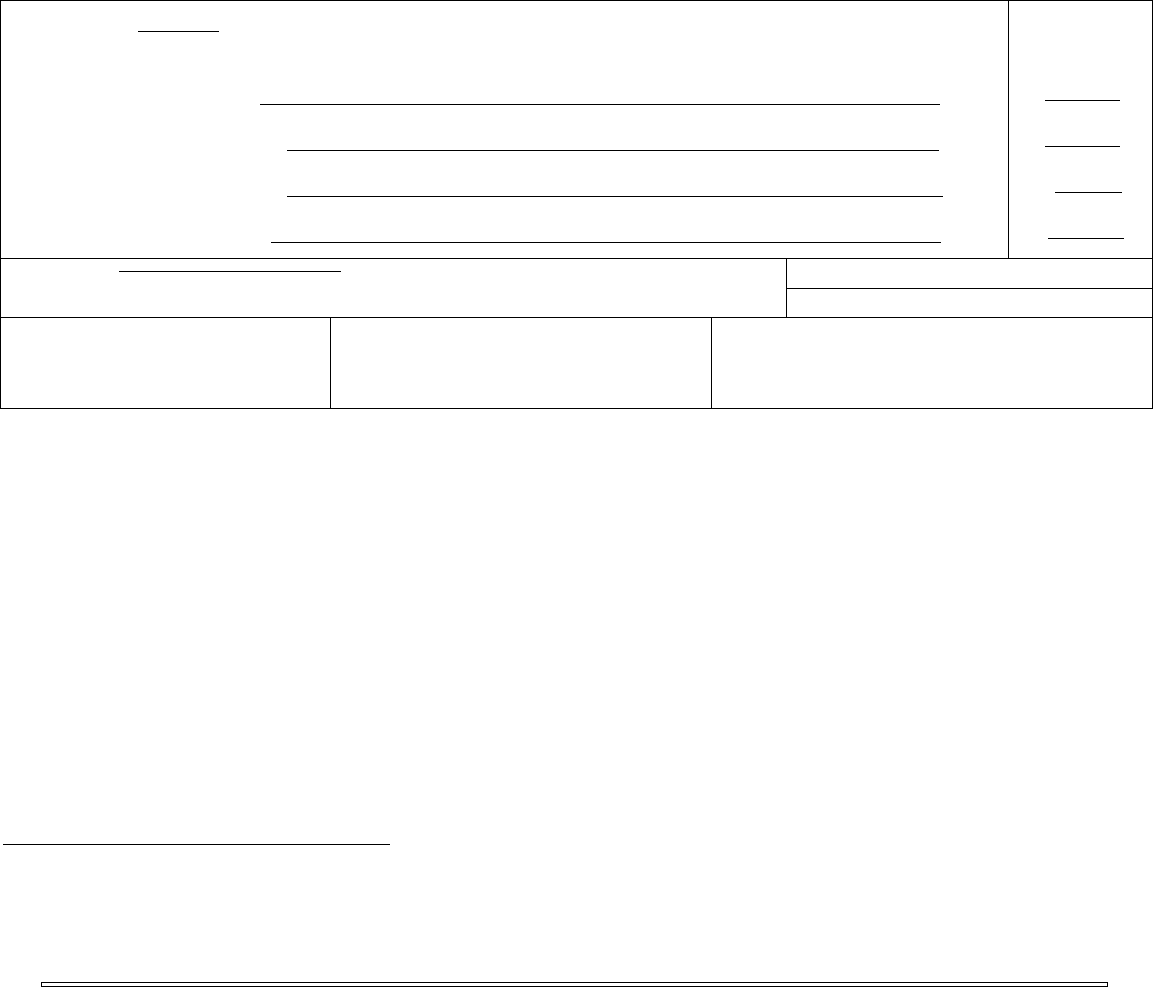
______________________________________________________________________________________________
______________________________________________________________________________
Rare Cause Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
_____ __ _____
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
_____
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
_____
initiated the events resulting
in death) LAST d. __________ _____
Approximate interval:
Onset to death
____ ________
____ ________
____
____ ________
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FIND NGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. D D TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
1. Is the stated cause of death, ____________________________________, correctly reported?
Yes_______ No_________
2. If yes, please state how the stated disease was confirmed: ______________________________________________
(laboratory test, history, clinical evidence, and/or others. If applicable, please state name of laboratory test, and/or source of evidence)
3. If no, please state the correct cause of death:
4. Was this condition active or current? Yes_______ No_________
5. Was the condition cured, old, or healed? Yes_______ No_________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
Available Resources to Assist With Medical Certification of Causes of Death
Your State vital statistics office should be able to assist with questions related to writing cause-of-death statements.
Additional instructional material on writing cause-of-death statements including handbooks, summary instructions, and
tutorials are available online at www.thename.org or www.cdc.gov/nchswww/about/major/dvs/handbk.htm, or by
request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003 (301-458-4333).
70
71
Query Letter 2
(Neoplasms)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical
research, funding, and resource allocation in our State and at the national level.
In this particular cancer death, we wish to ensure that sufficient information is available on the nature of the
neoplasm. In order to classify this death properly in our statistics, would you please supply the information on the
attachment? We want to assure you that the information you provide us is confidential and will be handled
accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death
statement, please contact __________________________________________. Instructions and an example of a
properly completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
72
73
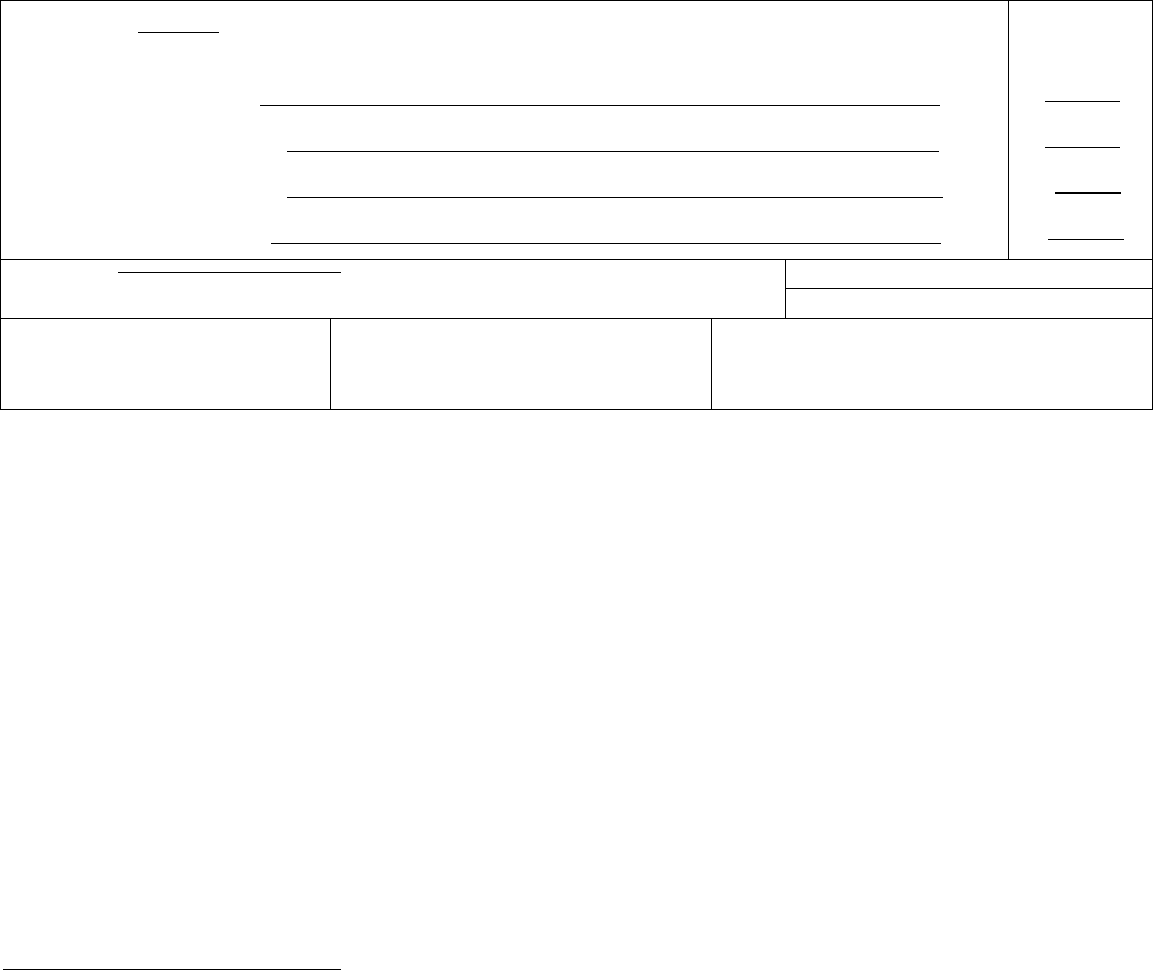
Neoplasm query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. __________
Approximate interval:
Onset to death
____
____
____
____
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FIND NGS AVA LABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
Was the neoplasm, ________________________________________________
1. Malignant___, Benign___, Undetermined___
2. Primary site __________________________
3. More detailed site or part of organ __________________________________
4. Histologic type, if known__________________________________________
5.Other __________________________________________________________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
74
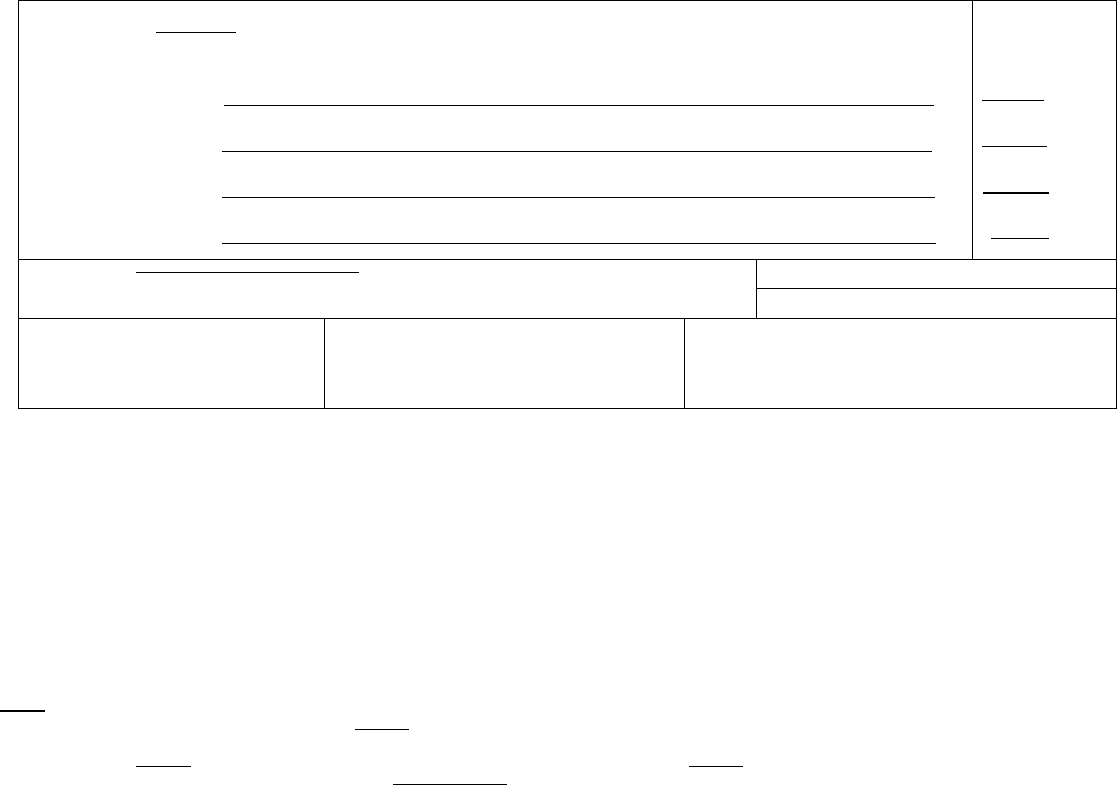
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Pneumonia
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Metastatic carcinoma to the liver
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Adenocarcinoma of the head of the pancreas
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
25 hours
3 months
7 months
_
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
■
No Unknown
36. IF FEMALE:
■
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the
final disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of
events that led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that
contributed to death but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best
medical OPINION. A condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print leg bly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if
necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may
be used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line
(a), then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to
blunt impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its
etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type
or that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell
carcinoma, lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for
example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most
directly caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
75

Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with
another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If
a certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the
body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour
clock; estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical
studies of injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit
for filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury
may differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example,
enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents.
This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years
of age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in
the course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or
type of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent
was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as
bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age,
and advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions
resulted in death, the physician should choose the single sequence that, in his or her opinion, best descr bes the process leading to death, and place any
other pertinent conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or
coroner should be consulted about conducting an investigation or providing assistance in completing the cause of death.
76
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without
explaining the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal
causes should be reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks
due to placental abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no
cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as
Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Abdominal hemorrhage
Carcinomatosis
Cardiac arrest
Disseminated intra vascular
coagulopathy
Hyponatremia
Hypotension
Pulmonary arrest
Pulmonary edema
Adhesions
Adult respiratory distress syndrome
Cardiac dysrhythmia
Cardiomyopathy
Dysrhythmia
End-stage liver disease
Immunosuppression
Increased intra cranial pressure
Pulmonary embolism
Pulmonary insufficiency
Acute myocardial infarction
Altered mental status
Cardiopulmonary arrest
Cellulitis
End-stage renal disease
Epidural hematoma
Intra cranial hemorrhage
Malnutrition
Renal failure
Respiratory arrest
Anemia
Anoxia
Cerebral edema
Cerebrovascular accident
Exsanguination
Failure to thrive
Metabolic encephalopathy
Multi-organ failure
Seizures
Sepsis
Anoxic encephalopathy
Arrhythmia
Cerebellar tonsillar herniation
Chronic bedridden state
Fracture
Gangrene
Multi-system organ failure
Myocardial infarction
Septic shock
Shock
Ascites
Aspiration
Cirrhosis
Coagulopathy
Gastrointestinal hemorrhage
Heart failure
Necrotizing soft-tissue infection
Old age
Starvation
Subdural hematoma
Atrial fibrillation
Bacteremia
Compression fracture
Congestive heart failure
Hemothorax
Hepatic failure
Open (or closed) head injury
Paralysis
Subarachnoid hemorrhage
Sudden death
Bedridden
Biliary obstruction
Bowel obstruction
Convulsions
Decubiti
Dehydration
Hepatitis
Hepatorenal syndrome
Hyperglycemia
Pancytopenia
Perforated gallbladder
Peritonitis
Thrombocytopenia
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown,
undetermined, probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Epidural hematoma
Hip fracture
Pulmonary emboli
Subdural hematoma
Bolus
Choking
Exsanguination
Fall
Hyperthermia
Hypothermia
Seizure disorder
Sepsis
Surgery
Thermal burns/chemical burns
Drug or alcohol overdose/drug or
alcohol abuse
Fracture Open reduction of fracture Subarachnoid hemorrhage
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-
death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
77
QUERY LETTER 3
(Query for HIV)
(Letterhead)
Dear Doctor _______________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical research,
funding, and resource allocation in our State and at the national level.
In this particular death, we are requesting additional information on HIV status. Certain conditions are frequently
associated with HIV infection. In order to classify this death properly in our statistics, would you please supply the
information on the attachment? We want to assure you that the information you provide us is confidential and will be
handled accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death statement,
please contact __________________________________________. Instructions and an example of a properly
completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
78
79
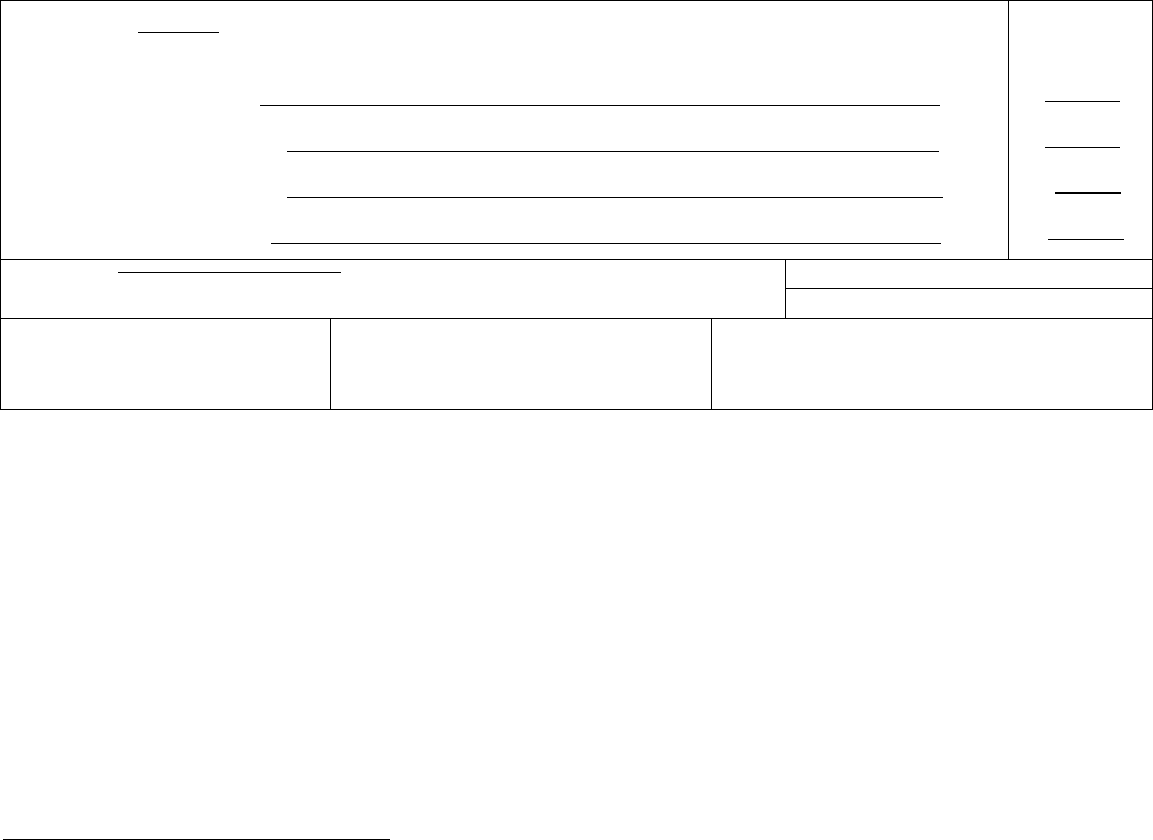
HIV Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. __________
Approximate interval:
Onset to death
____
____
____
____
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FIND NGS AVA LABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
1. Please check all that apply.
Was there any evidence of HIV infection? Yes___, No___
Was there any evidence of HIV disease? Yes___, No___
HIV status is not known. ______
Provide any other pertinent information _________________________________________
2. Other ____________________________________________________________________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
80
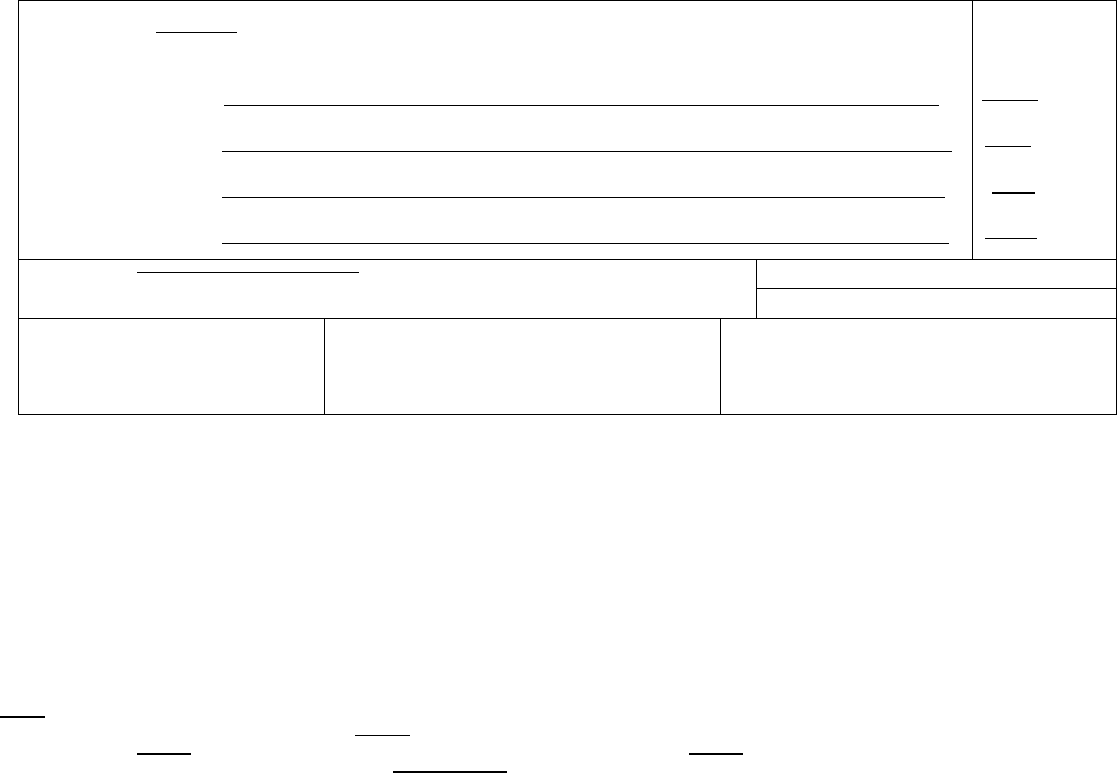
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Bilateral pneumothoraces
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Pneumocystis carinii pneumonia
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Acquired immunodeficiency
initiated the events resulting
in death) LAST d. Human immunodeficiency virus infection
Approximate interval:
Onset to death
Minutes
weeks
2 years
7 years
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FIND NGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
■
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
■
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that
led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death
but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A
condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry legible. Use a computer printer with high resolution, typewriter with good black r bbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt
impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its
etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for
example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contributing to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more poss ble sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
81

ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with
another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a
certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the
body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock;
estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contr bute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contr bute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is imposs ble to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example,
enter “factory”, not “Standard Manufacturing, Inc.”)
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents.
This includes all motor vehicle deaths. The item
mus t be completed for decedents ages 14 years or over and may be completed for those less than 14 years of
age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the
course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type
of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as
bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in
death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent
conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should
be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental
abruption due to blunt trauma to mother’s abdomen).
82
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no
cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as
Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Abdominal hemorrhage
Carcinomatosis
Cardiac arrest
Disseminated intra vascular
coagulopathy
Hyponatremia
Hypotension
Pulmonary arrest
Pulmonary edema
Adhesions
Adult respiratory distress syndrome
Cardiac dysrhythmia
Cardiomyopathy
Dysrhythmia
End-stage liver disease
Immunosuppression
Increased intra cranial pressure
Pulmonary embolism
Pulmonary insufficiency
Acute myocardial infarction
Altered mental status
Cardiopulmonary arrest
Cellulitis
End-stage renal disease
Epidural hematoma
Intra cranial hemorrhage
Malnutrition
Renal failure
Respiratory arrest
Anemia
Anoxia
Cerebral edema
Cerebrovascular accident
Exsanguination
Failure to thrive
Metabolic encephalopathy
Multi-organ failure
Seizures
Sepsis
Anoxic encephalopathy
Arrhythmia
Cerebellar tonsillar herniation
Chronic bedridden state
Fracture
Gangrene
Multi-system organ failure
Myocardial infarction
Septic shock
Shock
Ascites
Aspiration
Cirrhosis
Coagulopathy
Gastrointestinal hemorrhage
Heart failure
Necrotizing soft-tissue infection
Old age
Starvation
Subdural hematoma
Atrial fibrillation
Bacteremia
Compression fracture
Congestive heart failure
Hemothorax
Hepatic failure
Open (or closed) head injury
Paralysis
Subarachnoid hemorrhage
Sudden death
Bedridden
Biliary obstruction
Convulsions
Decubiti
Hepatitis
Hepatorenal syndrome
Pancytopenia
Perforated gallbladder
Thrombocytopenia
Uncal herniation
Bowel obstruction
Brain injury
Dehydration
Dementia (when not
Hyperglycemia
Hyperkalemia
Peritonitis
Pleural effusions
Urinary tract infection
Ventricular fibrillation
Brain stem herniation
Carcinogenesis
otherwise specified)
Diarrhea
Hypovolemic shock Pneumonia Ventricular tachycardia
Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia Epidural hematoma Hip fracture Pulmonary emboli Subdural hematoma
Bolus Exsanguination Hyperthermia Seizure disorder Surgery
Choking Fall Hypothermia Sepsis Thermal burns/chemical burns
Drug or alcohol overdose/drug or Fracture Open reduction of fracture Subarachnoid hemorrhage
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-
death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
83
Query Letter 4
(More Specific Information)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical research,
funding, and resource allocation in our State and at the national level.
In this particular death, we are requesting more specific information. In order to classify this death properly in our
statistics, would you please supply the information on the attachment? We want to assure you that the information
you provide us is confidential and will be handled accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death statement,
please contact __________________________________________. Instructions and an example of a properly
completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
84
85
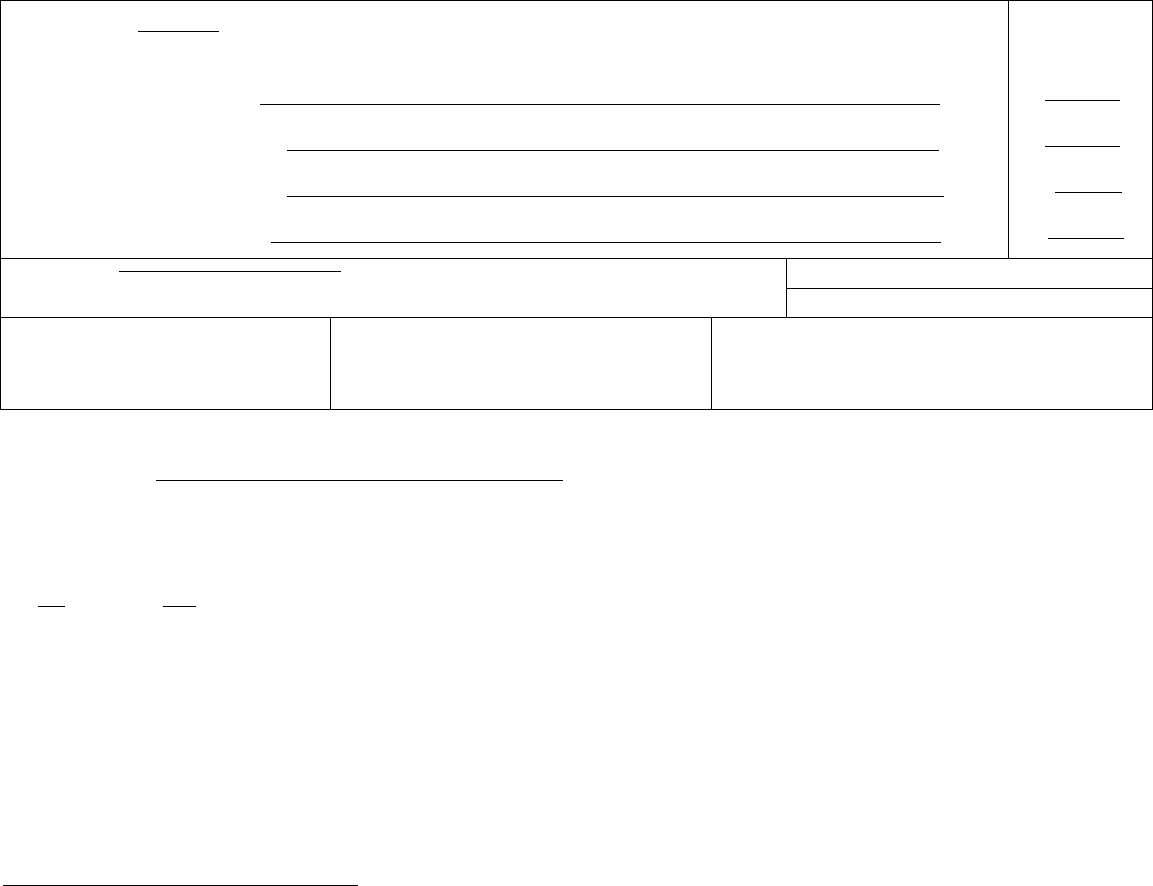
_____________________________________________________________
______________________________________________
Query for Additional Information
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
MMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
_____ __ _____
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
_____
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
_____
initiated the events resulting
in death) LAST d. __________ _____
Approximate interval:
Onset to death
____ ________
____ ________
____
____ ________
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
Is this condition,
, secondary to another condition?
Yes___, No___
If Yes, please indicate the primary condition ___________________________
2. Is there a known specific site of the condition, ____________________________________ ?
Yes , Unknown
If Yes, please state ______________________________________________________________
3. If known, please state a more specific type of the condition, ___________________________, or part of this organ or site.
4. If known, please state the type or etiology of this condition, __________________________________,
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
86
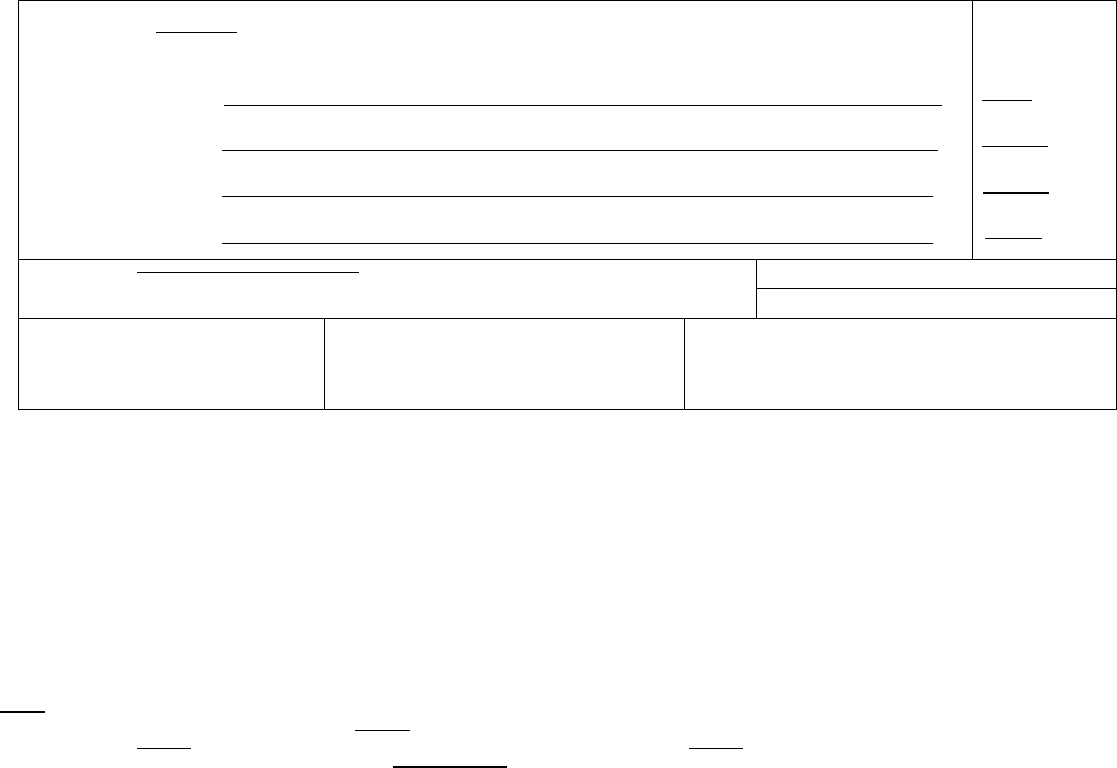
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Pneumonia
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Right Hemiplegia
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Cerebral thrombosis
initiated the events resulting
in death) LAST d. Cerebral artery atherosclerosis
Approximate interval:
Onset to death
1 week
6 months
6 months
years
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Hypertension
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FIND NGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
■
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that
led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death
but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A
condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry legible. Use a computer printer with high resolution, typewriter with good black r bbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt
impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its
etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for
example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contributing to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more poss ble sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
87

ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with
another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a
certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the
body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock;
estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contr bute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contr bute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is imposs ble to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example,
enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents.
This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of
age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the
course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type
of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as
bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in
death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent
conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should
be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental
abruption due to blunt trauma to mother’s abdomen).
88
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no
cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as
Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Abdominal hemorrhage
Carcinomatosis
Cardiac arrest
Disseminated intra vascular
coagulopathy
Hyponatremia
Hypotension
Pulmonary arrest
Pulmonary edema
Adhesions
Adult respiratory distress syndrome
Cardiac dysrhythmia
Cardiomyopathy
Dysrhythmia
End-stage liver disease
Immunosuppression
Increased intra cranial pressure
Pulmonary embolism
Pulmonary insufficiency
Acute myocardial infarction
Altered mental status
Cardiopulmonary arrest
Cellulitis
End-stage renal disease
Epidural hematoma
Intra cranial hemorrhage
Malnutrition
Renal failure
Respiratory arrest
Anemia
Anoxia
Cerebral edema
Cerebrovascular accident
Exsanguination
Failure to thrive
Metabolic encephalopathy
Multi-organ failure
Seizures
Sepsis
Anoxic encephalopathy
Arrhythmia
Cerebellar tonsillar herniation
Chronic bedridden state
Fracture
Gangrene
Multi-system organ failure
Myocardial infarction
Septic shock
Shock
Ascites
Aspiration
Cirrhosis
Coagulopathy
Gastrointestinal hemorrhage
Heart failure
Necrotizing soft-tissue infection
Old age
Starvation
Subdural hematoma
Atrial fibrillation
Bacteremia
Compression fracture
Congestive heart failure
Hemothorax
Hepatic failure
Open (or closed) head injury
Paralysis
Subarachnoid hemorrhage
Sudden death
Bedridden
Biliary obstruction
Convulsions
Decubiti
Hepatitis
Hepatorenal syndrome
Pancytopenia
Perforated gallbladder
Thrombocytopenia
Uncal herniation
Bowel obstruction
Brain injury
Dehydration
Dementia (when not
Hyperglycemia
Hyperkalemia
Peritonitis
Pleural effusions
Urinary tract infection
Ventricular fibrillation
Brain stem herniation
Carcinogenesis
otherwise specified)
Diarrhea
Hypovolemic shock Pneumonia Ventricular tachycardia
Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia Epidural hematoma Hip fracture Pulmonary emboli Subdural hematoma
Bolus Exsanguination Hyperthermia Seizure disorder Surgery
Choking Fall Hypothermia Sepsis Thermal burns/chemical burns
Drug or alcohol overdose/drug or Fracture Open reduction of fracture Subarachnoid hemorrhage
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-
death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
89
Query Letter 5
(Reason for Treatment)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you
certified for _________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also
for medical research, funding, and resource allocation in our State and at the national level.
In this particular death, we need to know the condition that required the treatment in order to
classify the cause of death correctly in our statistical records. In order to classify this death
properly in our statistics, would you please supply the information on the attachment? We want
to assure you that the information you provide us is confidential and will be handled accordingly.
If you have any question or would like to know more about various methods for certifying a
cause-of-death statement, please contact __________________________________________.
Instructions and an example of a properly completed death certificate are provided with the
attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
90
91
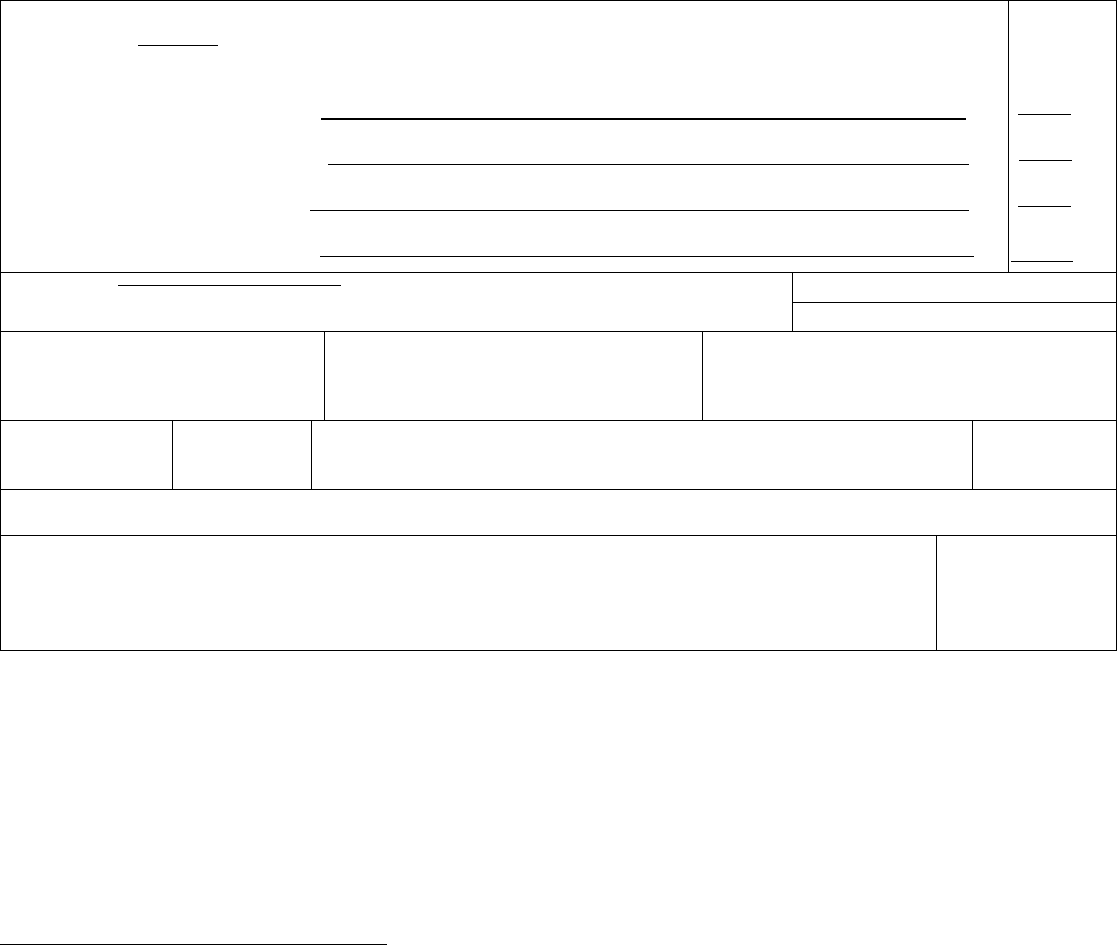
_______________________________________________________________________________________
_______________________________________________________________________________________
Reason for treatment query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. _____________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b. ______________
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. _____________
Approximate
interval:
Onset to death
______
______
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
39. TIME OF NJURY 40. PLACE OF NJURY (e.g., Decedent’s home; construction site; restaurant; wooded area)
41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED:
44. IF TRANSPORTATION
INJURY, SPEC FY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
1. State the medical condition or injury that necessitated the treatment, ______________________________
2. Other _____________________________________________________________________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
92
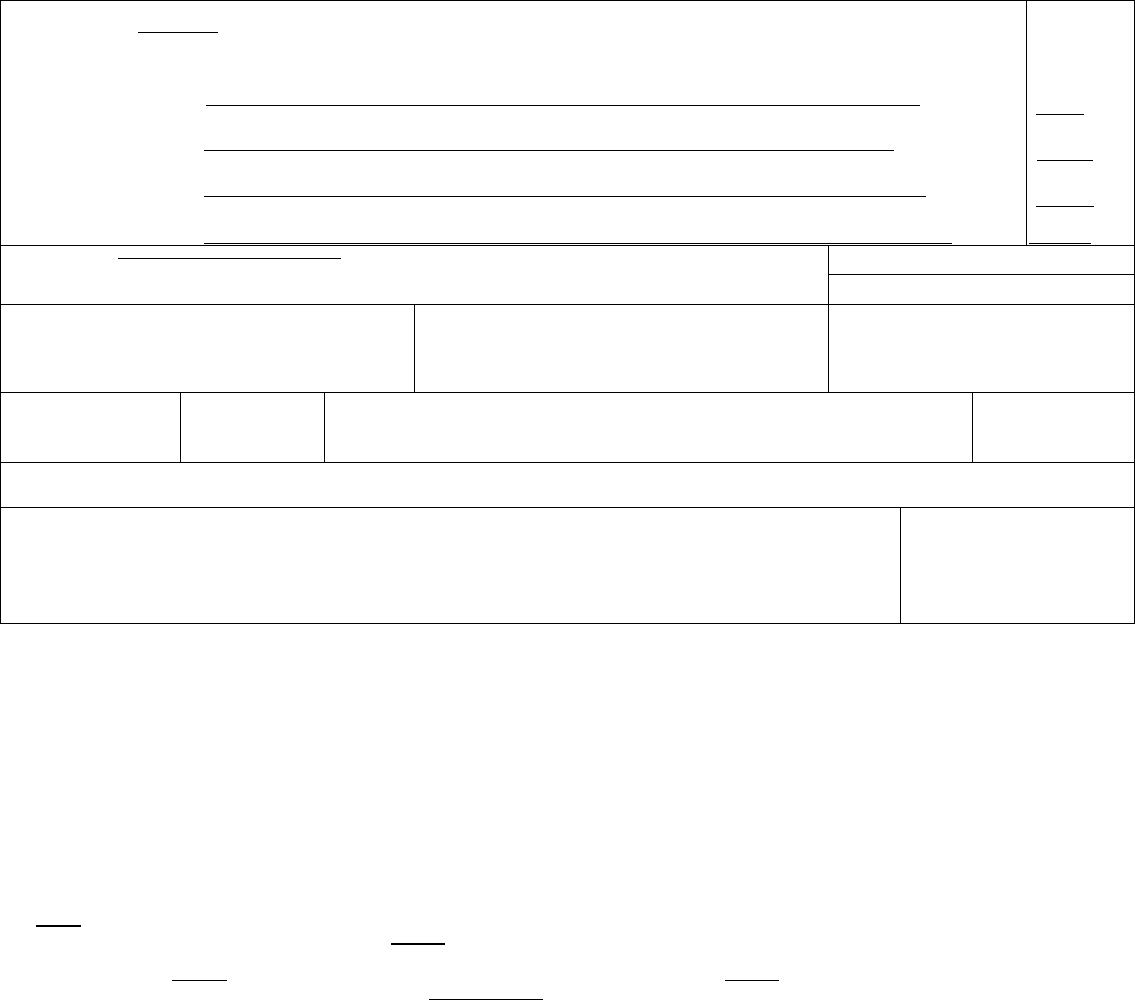
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Pulmonary embolism
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Cholelithotomy
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Calculus of gallbladder
initiated the events resulting
in death) LAST d.
Approximate
interval:
Onset to death
1 day
4 days
6 weeks
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Arteriosclerotic heart disease – Emphysema
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
■
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
■
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
39. TIME OF INJURY
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED: 44. IF TRANSPORTATION INJURY,
SPEC FY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death
(the final disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the
chain of events that led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or
injuries that contributed to death but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be
YOUR best medical OPINION. A condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if
necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately”
may be used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for
line (a), then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest
due to blunt impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report
its etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
93

•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell
type or that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous
cell carcinoma, lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function
(for example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying
cause of death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion,
most directly caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place
with another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items
24-28. If a certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date
the body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-
hour clock; estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for
example, tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check
“no” if, in your clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical
studies of injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time
limit for filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of
injury may differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For
example, enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and
accidents. This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those
less than 14 years of age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of
whether the injury occurred in the course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
94

•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun
or type of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle
decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such
as bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and
laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old
age, and advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of
conditions resulted in death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death,
and place any other pertinent conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the
medical examiner or coroner should be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without
explaining the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal
causes should be reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28
weeks due to placental abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age,
no cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be
reported as Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Abdominal hemorrhage
Carcinomatosis
Cardiac arrest
Disseminated intra vascular
coagulopathy
Hyponatremia
Hypotension
Pulmonary arrest
Pulmonary edema
Adhesions
Adult respiratory distress syndrome
Cardiac dysrhythmia
Cardiomyopathy
Dysrhythmia
End-stage liver disease
Immunosuppression
Increased intra cranial pressure
Pulmonary embolism
Pulmonary insufficiency
Acute myocardial infarction
Altered mental status
Cardiopulmonary arrest
Cellulitis
End-stage renal disease
Epidural hematoma
Intra cranial hemorrhage
Malnutrition
Renal failure
Respiratory arrest
Anemia
Anoxia
Cerebral edema
Cerebrovascular accident
Exsanguination
Failure to thrive
Metabolic encephalopathy
Multi-organ failure
Seizures
Sepsis
Anoxic encephalopathy
Arrhythmia
Cerebellar tonsillar herniation
Chronic bedridden state
Fracture
Gangrene
Multi-system organ failure
Myocardial infarction
Septic shock
Shock
Ascites
Aspiration
Cirrhosis
Coagulopathy
Gastrointestinal hemorrhage
Heart failure
Necrotizing soft-tissue infection
Old age
Starvation
Subdural hematoma
Atrial fibrillation
Bacteremia
Compression fracture
Congestive heart failure
Hemothorax
Hepatic failure
Open (or closed) head injury
Paralysis
Subarachnoid hemorrhage
Sudden death
Bedridden
Biliary obstruction
Convulsions
Decubiti
Hepatitis
Hepatorenal syndrome
Pancytopenia
Perforated gallbladder
Thrombocytopenia
Uncal herniation
Bowel obstruction
Brain injury
Dehydration
Dementia (when not
Hyperglycemia
Hyperkalemia
Peritonitis
Pleural effusions
Urinary tract infection
Ventricular fibrillation
Brain stem herniation
Carcinogenesis
otherwise specified)
Diarrhea
Hypovolemic shock Pneumonia Ventricular tachycardia
Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown,
undetermined, probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia Epidural hematoma Hip fracture Pulmonary emboli Subdural hematoma
Bolus
Choking
Exsanguination
Fall
Hyperthermia
Hypothermia
Seizure disorder
Sepsis
Surgery
Thermal burns/chemical burns
Drug or alcohol overdose/drug or
alcohol abuse
Fracture Open reduction of fracture Subarachnoid hemorrhage
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-
of-death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-
2003.
95
Query Letter 6
(Mental Disorders)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical
research, funding, and resource allocation in our State and at the national level.
In this particular death, we need to know whether a specific life threatening condition was associated with the
reported mental disorder. In order to classify this death properly in our statistics, would you please supply the
information on the attachment? We want to assure you that the information you provide us is confidential and
will be handled accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death
statement, please contact __________________________________________. Instructions and an example of a
properly completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
96
97
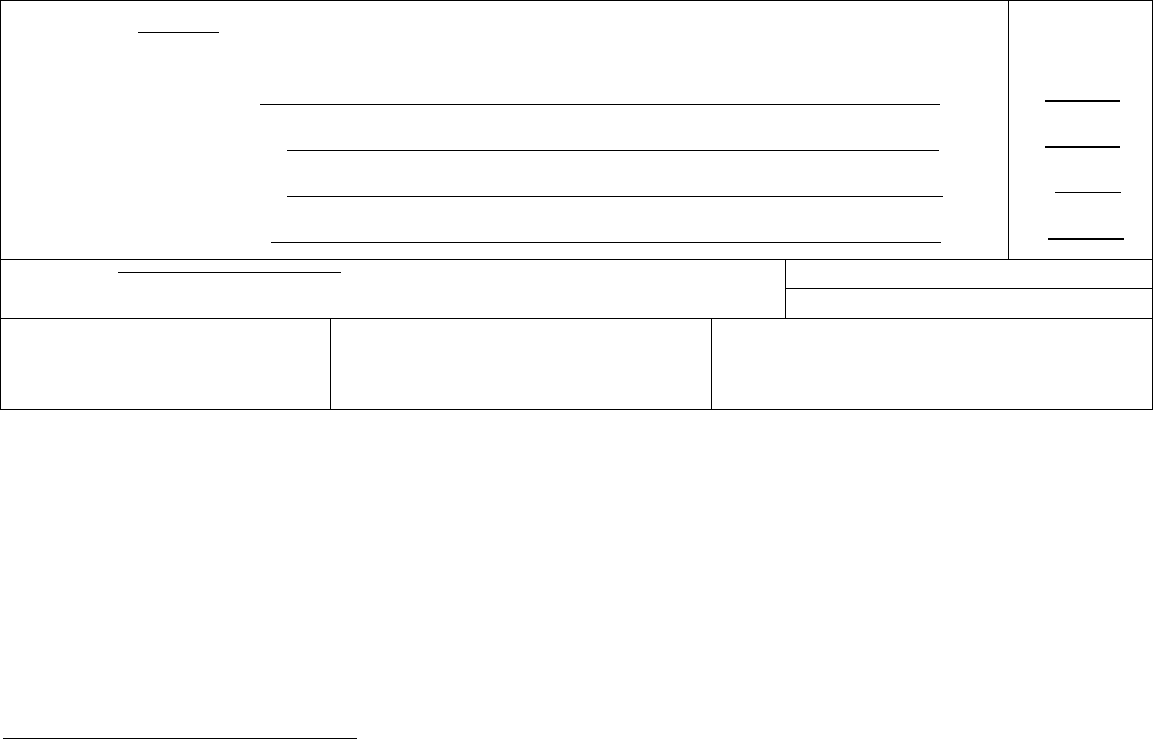
__________________________________________________________________________________________________
__________________________________________________________________________________________________
____________________________________________________________________________
___________________________________________
Mental Disorder Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
_____ __ _____
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
_____
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
_____
initiated the events resulting
in death) LAST d. __________ _____
Approximate interval:
Onset to death
____
____
____
____
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FIND NGS AVA LABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
If death did result from a mental disorder, please state the condition that resulted from the mental disorder and that caused
death:
Otherwise, please state the underlying cause of death that initiated the chain of events leading to death:
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
98
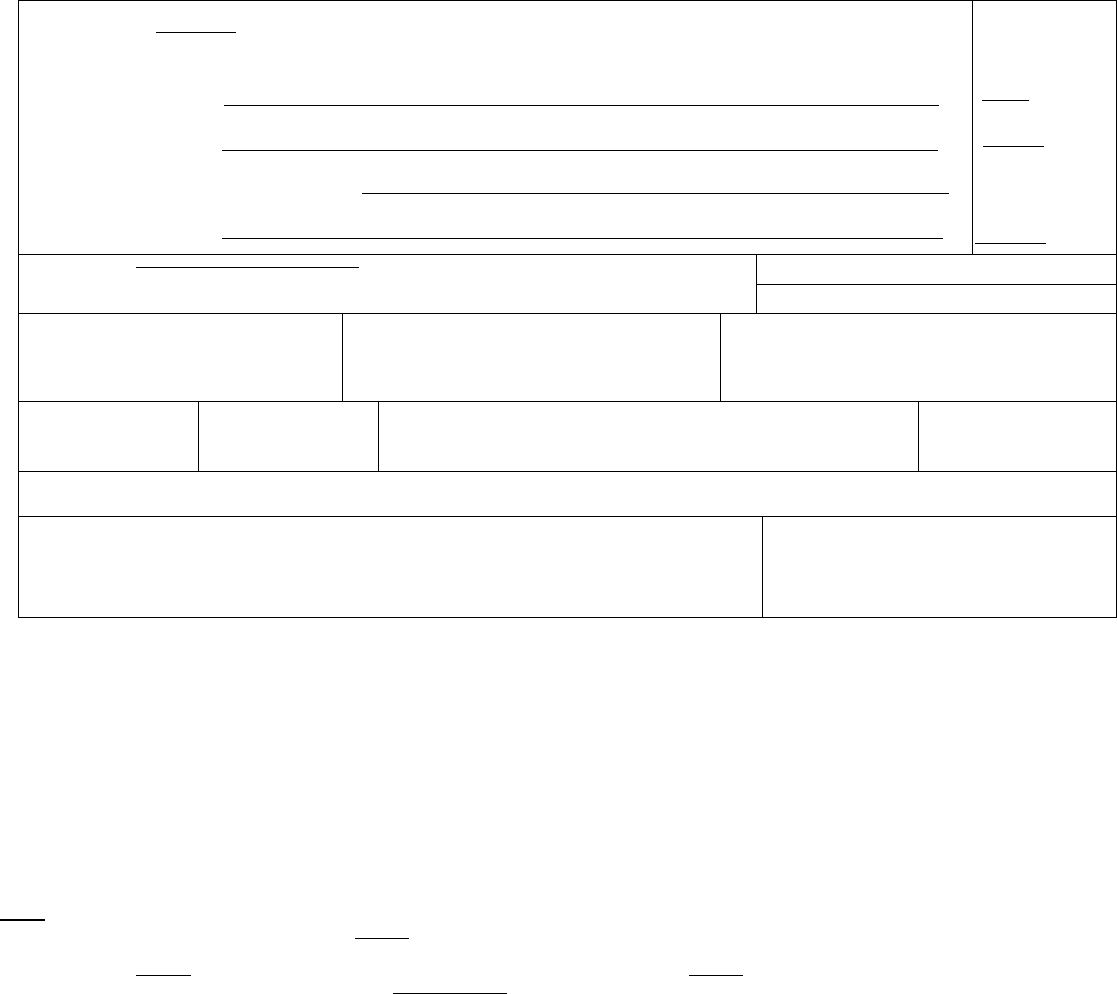
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Aspiration pneumonia
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Mental retardation
listed on line a. Enter the
UNDERLYING CAUSE c. _____________________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. __________________
Approximate interval:
Onset to death
3 days
15 years
_________
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
■
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
■
No Unknown
36. IF FEMALE:
■
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
39. TIME OF INJURY
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED: 44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death
(the final disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the
chain of events that led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or
injuries that contributed to death but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be
YOUR best medical OPINION. A condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if
necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately”
may be used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for
line (a), then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest
due to blunt impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report
its etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
99

•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell
type or that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous
cell carcinoma, lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function
(for example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying
cause of death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion,
most directly caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place
with another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items
24-28. If a certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date
the body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-
hour clock; estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for
example, tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check
“no” if, in your clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical
studies of injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time
limit for filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of
injury may differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For
example, enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and
accidents. This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those
less than 14 years of age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of
whether the injury occurred in the course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
100

•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun
or type of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle
decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such
as bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and
laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old
age, and advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of
conditions resulted in death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death,
and place any other pertinent conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the
medical examiner or coroner should be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without
explaining the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal
causes should be reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28
weeks due to placental abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age,
no cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be
reported as Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Abdominal hemorrhage
Carcinomatosis
Cardiac arrest
Disseminated intra vascular
coagulopathy
Hyponatremia
Hypotension
Pulmonary arrest
Pulmonary edema
Adhesions
Adult respiratory distress syndrome
Cardiac dysrhythmia
Cardiomyopathy
Dysrhythmia
End-stage liver disease
Immunosuppression
Increased intra cranial pressure
Pulmonary embolism
Pulmonary insufficiency
Acute myocardial infarction
Altered mental status
Cardiopulmonary arrest
Cellulitis
End-stage renal disease
Epidural hematoma
Intra cranial hemorrhage
Malnutrition
Renal failure
Respiratory arrest
Anemia
Anoxia
Cerebral edema
Cerebrovascular accident
Exsanguination
Failure to thrive
Metabolic encephalopathy
Multi-organ failure
Seizures
Sepsis
Anoxic encephalopathy
Arrhythmia
Cerebellar tonsillar herniation
Chronic bedridden state
Fracture
Gangrene
Multi-system organ failure
Myocardial infarction
Septic shock
Shock
Ascites
Aspiration
Cirrhosis
Coagulopathy
Gastrointestinal hemorrhage
Heart failure
Necrotizing soft-tissue infection
Old age
Starvation
Subdural hematoma
Atrial fibrillation
Bacteremia
Compression fracture
Congestive heart failure
Hemothorax
Hepatic failure
Open (or closed) head injury
Paralysis
Subarachnoid hemorrhage
Sudden death
Bedridden
Biliary obstruction
Convulsions
Decubiti
Hepatitis
Hepatorenal syndrome
Pancytopenia
Perforated gallbladder
Thrombocytopenia
Uncal herniation
Bowel obstruction
Brain injury
Dehydration
Dementia (when not
Hyperglycemia
Hyperkalemia
Peritonitis
Pleural effusions
Urinary tract infection
Ventricular fibrillation
Brain stem herniation
Carcinogenesis
otherwise specified)
Diarrhea
Hypovolemic shock Pneumonia Ventricular tachycardia
Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown,
undetermined, probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia Epidural hematoma Hip fracture Pulmonary emboli Subdural hematoma
Bolus
Choking
Exsanguination
Fall
Hyperthermia
Hypothermia
Seizure disorder
Sepsis
Surgery
Thermal burns/chemical burns
Drug or alcohol overdose/drug or
alcohol abuse
Fracture Open reduction of fracture Subarachnoid hemorrhage
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-
of-death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-
2003.
101
Query Letter 7
(Drugs and Other Agents)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical
research, funding, and resource allocation in our State and at the national level.
In this particular death, we need additional information about the drugs associated with the death. In order to
classify this death properly in our statistics, would you please supply the information on the attachment? We
want to assure you that the information you provide us is confidential and will be handled accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death
statement, please contact __________________________________________. Instructions and an example of a
properly completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
102
103
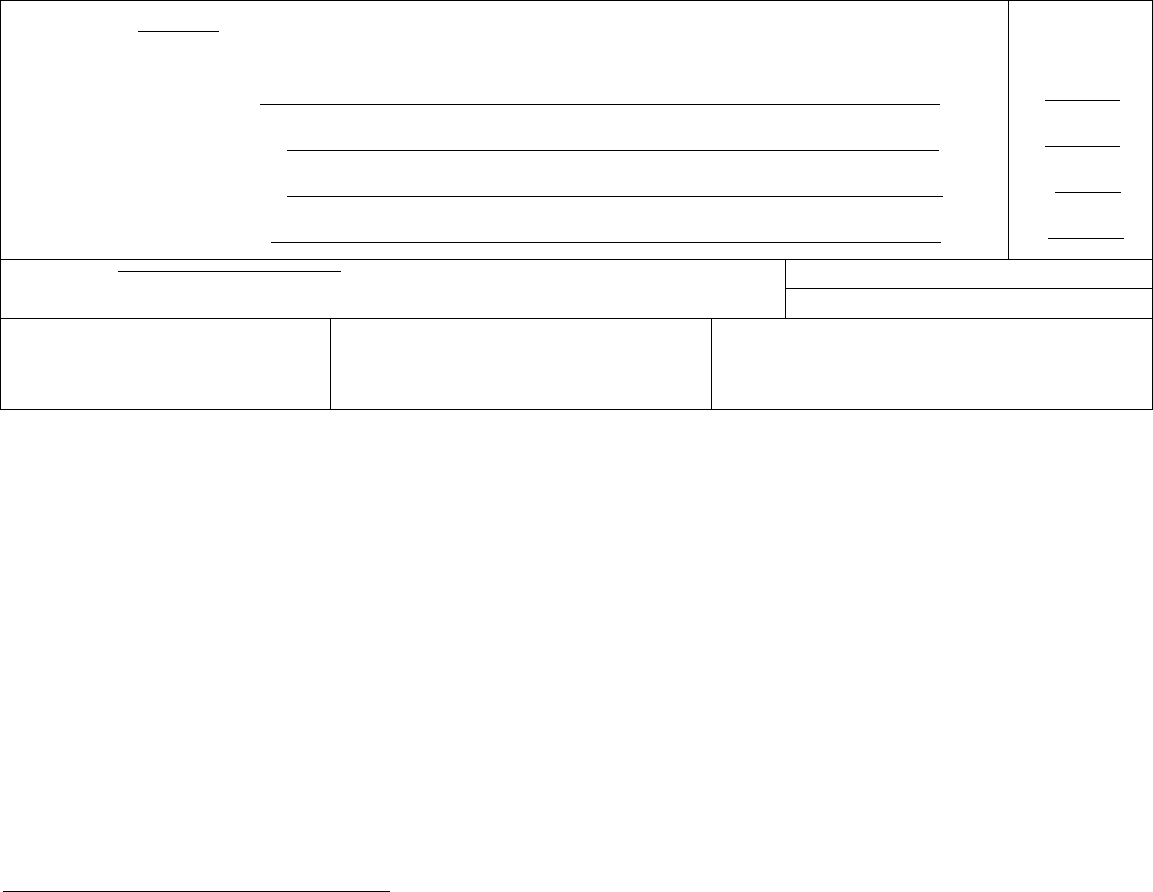
__________________________________________________________________________
Drugs and Other Agents Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. __________
Approximate interval:
Onset to death
____
____
____
____
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FIND NGS AVA LABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
1. Please state the type or name of drug(s) that brought about the medical complications which led to death.
2. Please state the type or name of other agent(s) or exposure that brought about the medical complications
which led to death. ______________________________________________________________________
3. Other ___________________________________________________________________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
104
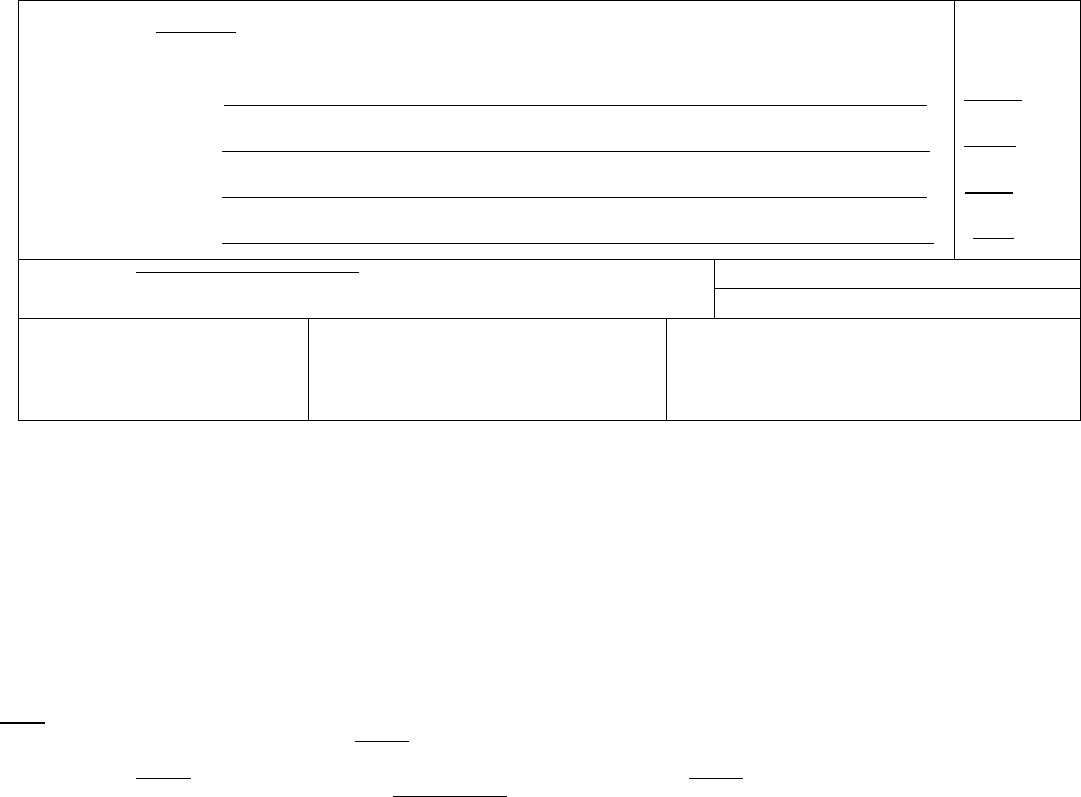
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Staphylococcus endocarditis
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Chronic intravenous heroin use
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Opiate addiction
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
2 weeks
7 years
7years
_
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTRIBUTE TO
DEATH?
Yes Probably
■
No Unknown
36. IF FEMALE:
■
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death
(the final disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the
chain of events that led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or
injuries that contributed to death but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be
YOUR best medical OPINION. A condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if
necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately”
may be used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for
line (a), then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest
due to blunt impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report
its etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell
type or that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous
cell carcinoma, lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function
(for example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying
cause of death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion,
most directly caused death. Report in Part II the other conditions or diseases.
105

CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place
with another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items
24-28. If a certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date
the body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-
hour clock; estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for
example, tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check
“no” if, in your clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical
studies of injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time
limit for filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of
injury may differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For
example, enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and
accidents. This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those
less than 14 years of age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of
whether the injury occurred in the course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun
or type of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle
decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such
as bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and
laws.
Common problems in death certification
106
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old
age, and advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of
conditions resulted in death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death,
and place any other pertinent conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the
medical examiner or coroner should be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without
explaining the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal
causes should be reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28
weeks due to placental abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age,
no cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be
reported as Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Abdominal hemorrhage
Carcinomatosis
Cardiac arrest
Disseminated intra vascular
coagulopathy
Hyponatremia
Hypotension
Pulmonary arrest
Pulmonary edema
Adhesions
Adult respiratory distress syndrome
Cardiac dysrhythmia
Cardiomyopathy
Dysrhythmia
End-stage liver disease
Immunosuppression
Increased intra cranial pressure
Pulmonary embolism
Pulmonary insufficiency
Acute myocardial infarction
Altered mental status
Cardiopulmonary arrest
Cellulitis
End-stage renal disease
Epidural hematoma
Intra cranial hemorrhage
Malnutrition
Renal failure
Respiratory arrest
Anemia
Anoxia
Anoxic encephalopathy
Cerebral edema
Cerebrovascular accident
Cerebellar tonsillar herniation
Exsanguination
Failure to thrive
Fracture
Metabolic encephalopathy
Multi-organ failure
Multi-system organ failure
Seizures
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown,
undetermined, probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Epidural hematoma
Hip fracture
Pulmonary emboli
Subdural hematoma
Bolus
Choking
Exsanguination
Fall
Hyperthermia
Hypothermia
Seizure disorder
Sepsis
Surgery
Thermal burns/chemical burns
Drug or alcohol overdose/drug or
alcohol abuse
Fracture Open reduction of fracture Subarachnoid hemorrhage
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-
of-death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-
2003.
107
Query Letter 8
(Ill-defined, Trivial, Etc.)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical
research, funding, and resource allocation in our State and at the national level.
In this particular death, we need to know if a more serious condition gave rise to the reported cause of death. In
order to classify this death properly in our statistics, would you please supply the information on the
attachment? We want to assure you that the information you provide us is confidential and will be handled
accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death
statement, please contact ____________________________. Instructions and an example of a properly
completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
108
109
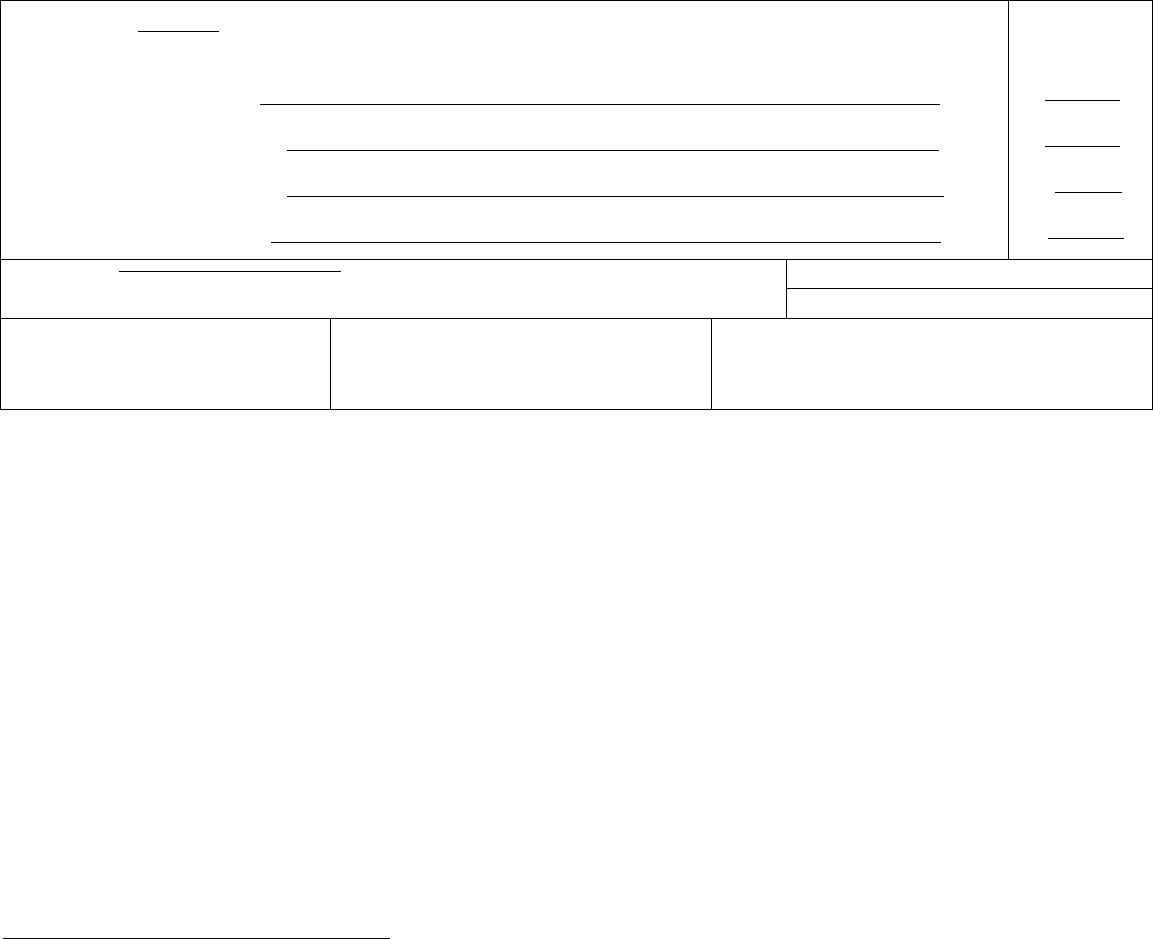
___________________________________________________________________________
_____________________________________________________________________________
Ill-defined or Trivial Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
MMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
_____
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. __________
Approximate interval:
Onset to death
____
____
____
____
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
1. In your opinion, what was the underlying cause of this condition?
OR
2. Did this condition give rise to another more serious condition which led to death?
If so, please state ______________________________________________________________
3.Other ______________________________________________________________________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
110
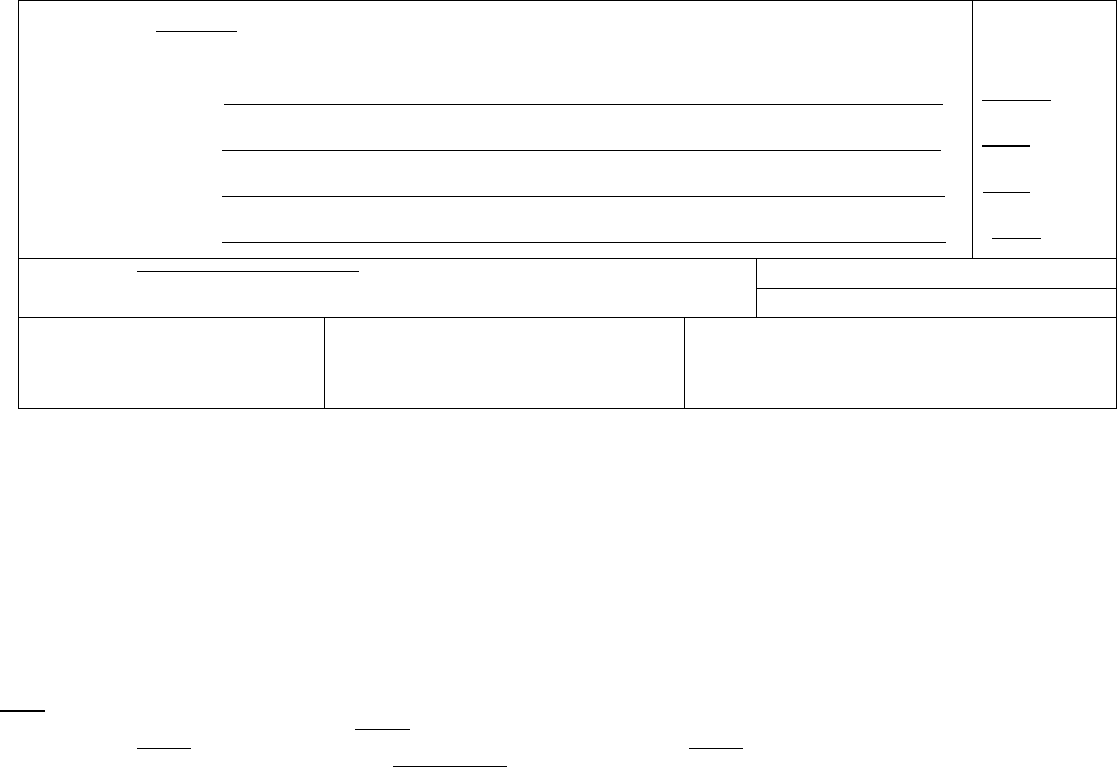
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Convulsion__________
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Fever _____ ___
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Influenza__________________________
initiated the events resulting
in death) LAST d. ______________________________ ________
Approximate interval:
Onset to death
3 minutes
1 day
6 days
_
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Arteriosclerosis, gout
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FIND NGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes
■
Probably
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that
led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death
but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A
condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry legible. Use a computer printer with high resolution, typewriter with good black r bbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt
impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its
etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for
example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contributing to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more poss ble sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
111

Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with
another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a
certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the
body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock;
estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contr bute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contr bute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is imposs ble to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example,
enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents.
This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of
age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the
course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type
of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as
bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in
death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent
conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should
be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
112
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental
abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no
cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as
Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess Carcinomatosis Disseminated intra vascular Hyponatremia Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-
death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
113
Query Letter 9
(Pregnancy Related)
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical research,
funding, and resource allocation in our State and at the national level.
In the case of this particular death, we need additional information to properly classify the maternal death. In order to
classify this death properly in our statistics, would you please supply the information on the attachment? We want to
assure you that the information you provide us is confidential and will be handled accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death statement,
please contact __________________________________________. Instructions and an example of a properly
completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
114
115
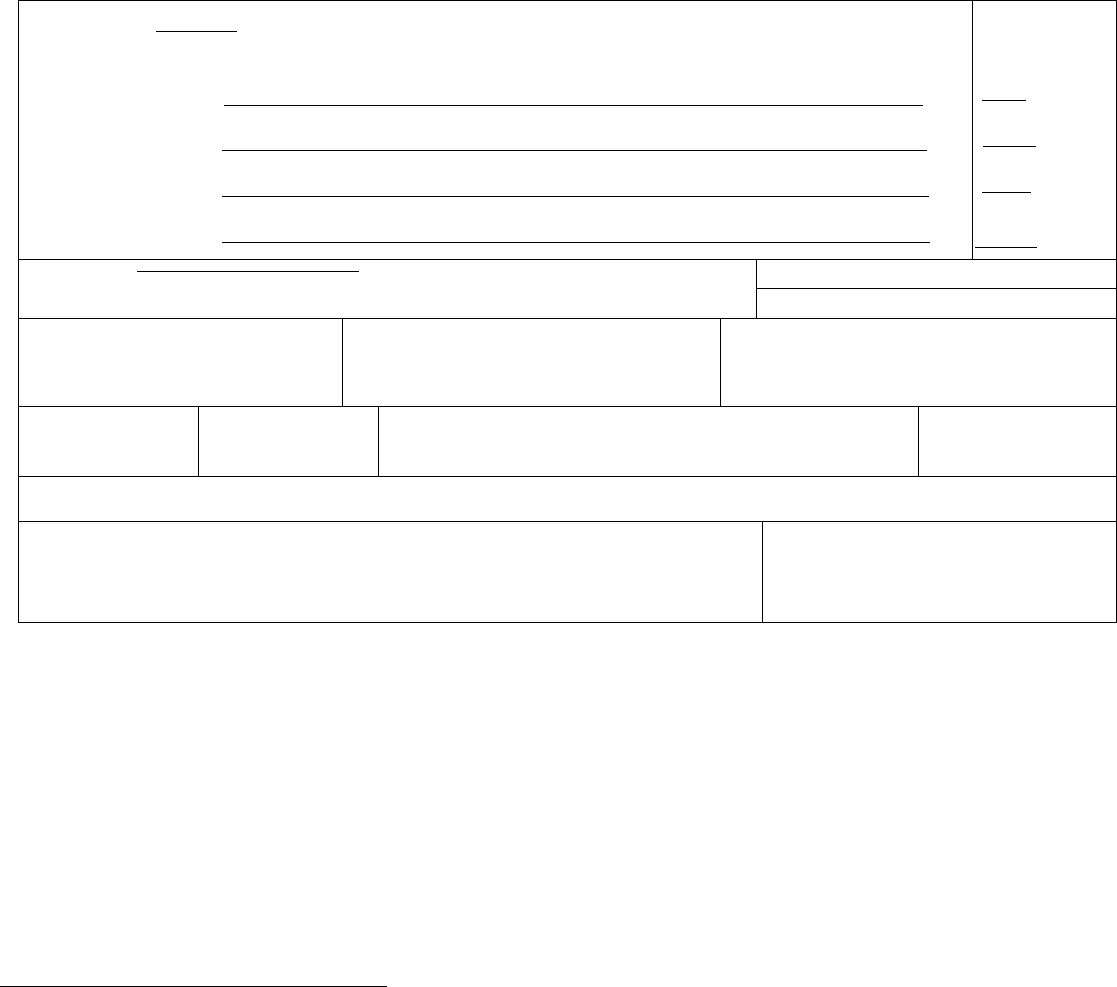
__________________________________________________________________________
Pregnancy-related Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FIND NGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF NJURY
(Mo/Day/Yr) (Spell Month)
39. T ME OF INJURY 40. PLACE OF INJURY (e.g., Decedent’s home; construction site; restaurant; wooded area) 41. NJURY AT WORK?
Yes No
42. LOCATION OF INJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCR BE HOW NJURY OCCURRED: 44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
1. What was the complication of the pregnancy (or a concomitant disease or injury) that initiated the chain of events
leading to death?
2. Was the abortion spontaneous ___?, legally induced___?, therapeutic ___? other___?
3. Other ___________________________________________________________________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
116
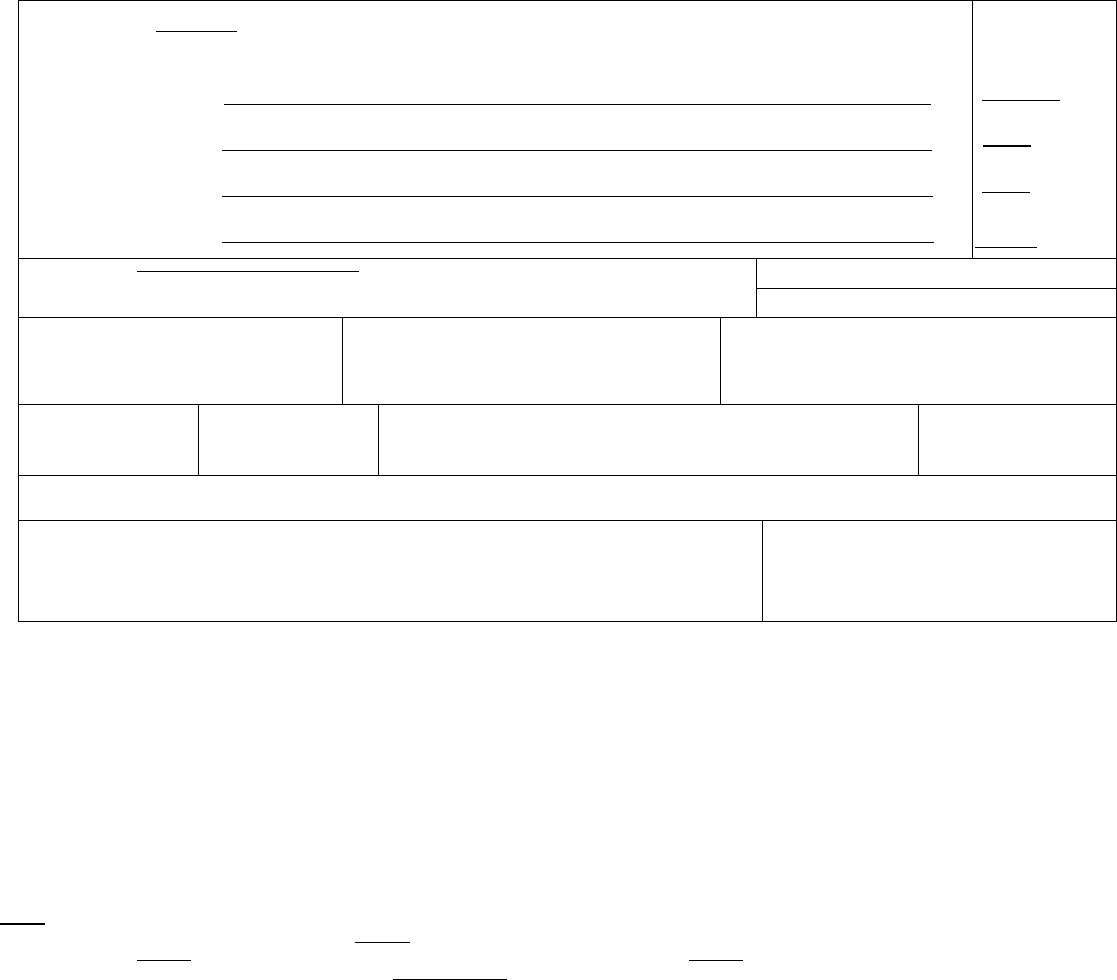
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Intestinal hemorrhage
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Ruptured intestine __
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Non-medically induced abortion
initiated the events resulting
in death) LAST d. _________________
Approximate interval:
Onset to death
10 minutes
1 day
1 day
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FIND NGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
■
No Unknown
36. F FEMALE:
Not pregnant within past year
Pregnant at time of death
■
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF NJURY
(Mo/Day/Yr) (Spell Month)
August 15, 2003
39. T ME OF INJURY
Approx. 2320
40. PLACE OF INJURY (e.g., Decedent’s home; construction site; restaurant; wooded area)
41. NJURY AT WORK?
Yes No
42. LOCATION OF INJURY: State: Missouri City or Town: near Alexandria
Street & Number: mile marker 17 on state route 46a Apartment No.: Zip Code:
43. DESCR BE HOW NJURY OCCURRED: 44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that
led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death
but which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A
condition can be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry legible. Use a computer printer with high resolution, typewriter with good black r bbon and clean keys, or print legibly using
permanent black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported.
ALWAYS enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt
impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its
etiology on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
117

•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for
example, air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contributing to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more poss ble sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death
certificate should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with
another person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a
certifier completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the
body is found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock;
estimates may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contr bute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contr bute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is imposs ble to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example,
enter “factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents.
This includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of
age if warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the
course of the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises
Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home
Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc.
Student in school
Injury while traveling on business, including to/from business contacts
Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type
of vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as
bicycles. Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
118

Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in
death, the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent
conditions in Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should
be consulted about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if poss ble. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental
abruption due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no
cause of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as
Sudden Infant Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Carcinomatosis
Disseminated intra vascular
Hyponatremia
Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be
complications of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-
death statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
119
Query Letter 10
(External Causes)
The following sample query letter consists of a lengthy series of questions even though the attachments have been
separated into four. The questions are designed to address a variety of problems in certification. We would suggest
that specific query letters list only the questions that are relevant for the specific case. This will improve the
appearance of the query letter.
(Letterhead)
Dear Doctor ________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical research,
funding, and resource allocation in our State and at the national level.
In this particular death, we need additional information to properly classify the death. In order to classify this death
properly in our statistics, would you please supply the information on the attachment? We want to assure you that the
information you provide us is confidential and will be handled accordingly.
If you have any question, please contact_____________________________________________. Instructions and an
example of a properly completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
4 Attachments
120
121
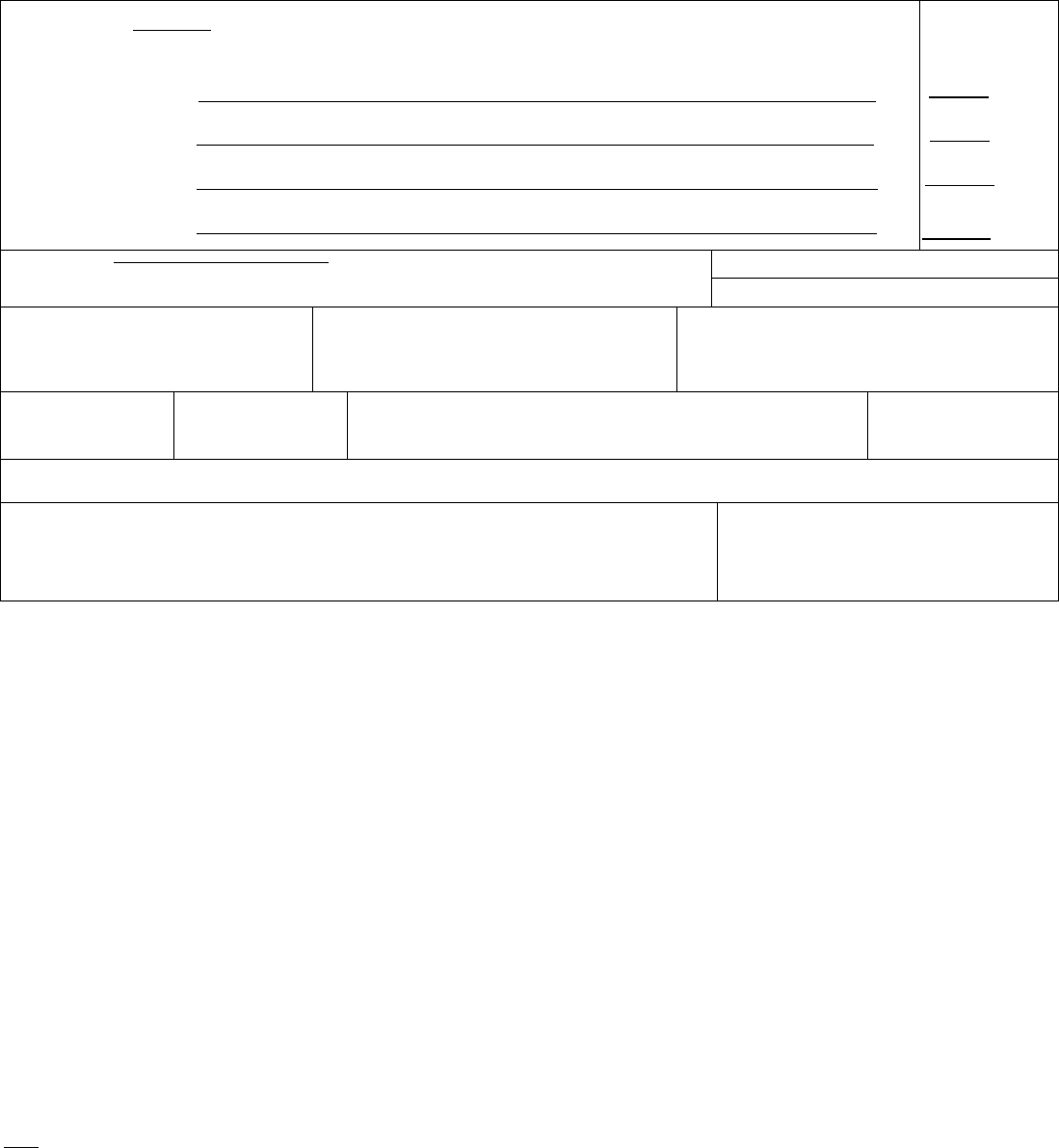
_________________________________________________________________________________________________________
_____________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
___________________________________________________
_________________________________________________________________________________________________________
_____________________________________________________________________
Query for Accidents Not Involving Transportation
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
MMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
______________
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
________
initiated the events resulting
in death) LAST d. ____________
Approximate interval:
Onset to death
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
39. TIME OF INJURY 40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area) 41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED:
44. IF TRANSPORTATION INJURY, SPEC FY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
1A. Please state if the manner of death was accidental, homicidal, suicidal, natural, or undetermined. __________________.
If undetermined, was there a pending investigation? _______________________________________________.
1B. State what happened to the decedent, describe in detail the external event that caused the death.
1C. State the medical condition(s) that required the treatment (medical, surgical, medicaments)
1D. Describe in detail the treatment (medical, surgical, name of medicaments) or the exposure (name of chemicals, type of medical
devices, or other applicable external factors)
2.
Fire
A. Origin of fire (blowlamp, candle, match, torch, fireplace etc.)___________________
122
_______________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
______________________________________________________________________________________________
B. If fire was caused by explosion, indicate agent (aerosol, gasoline, bomb etc.)_________________________________
C. Fire located in: Private dwelling___ Other building or structure ___ Not in building or structure (stationary vehicle, forest
etc)___ Other________________________________
D. Resulted in large uncontrolled fire: Yes___ No___
E. Fire ignited: Explosive material (specify type) ______ Clothing (type) ___________Other ________
F. Victim: Burned ___ Incinerated, cremated ___ Asphyxiated by (smoke, flame,
fumes, etc.) _________________ Other ___________________
3.
Fall (state how it happened, e.g. fall from/on/into/out of name of structure )
4. Describe in detail the external event (__________________________________ ) that eventually brought about the medical
complications which caused the death.
___________________________________________________.
5. Place of occurrence (home, residential institution, public administrative area, sports area, street and highway, trade and service
areas, industrial and construction area, farm, other -please specify-)
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
123
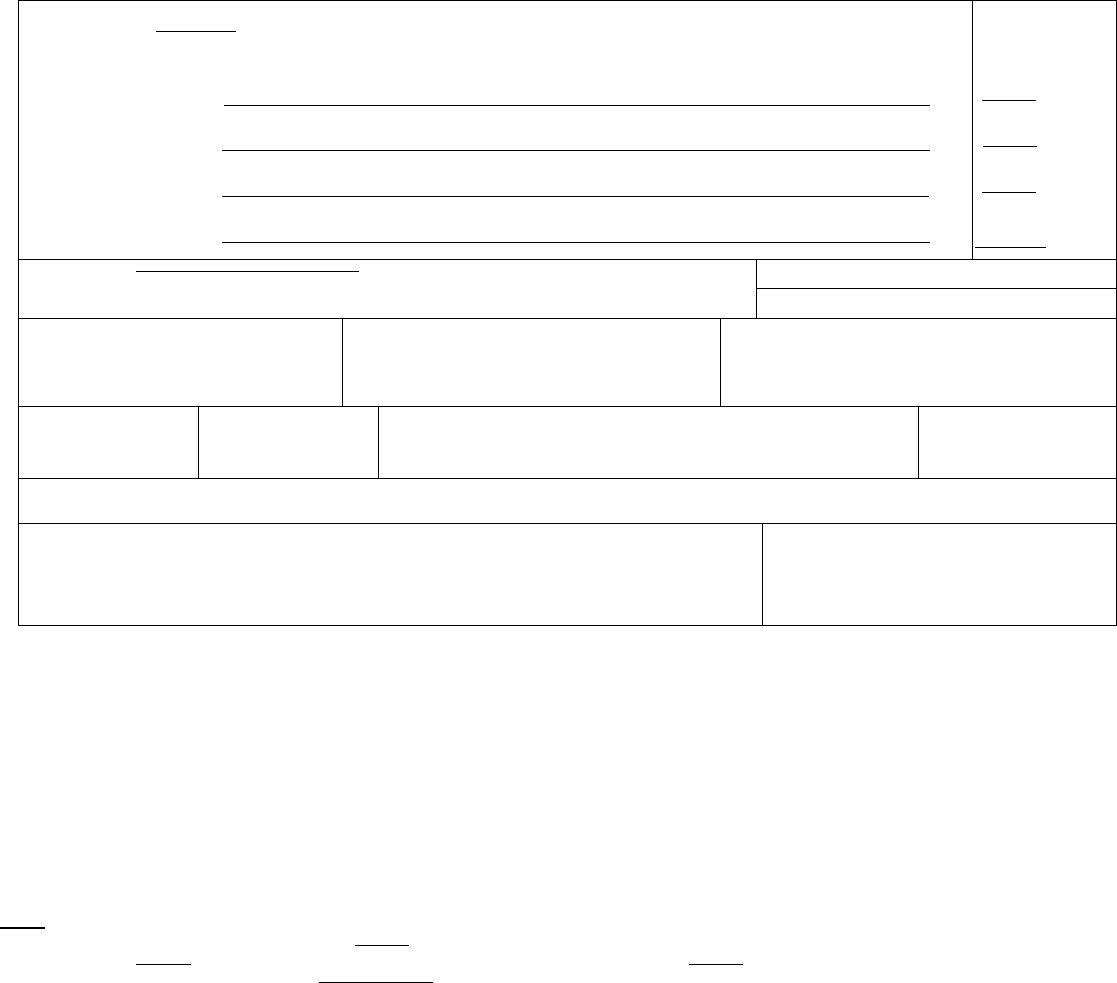
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Epidural hemorrhage
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Fractured skull
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Fall on stairway
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
1 hour
1 hour
1 hour
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Chronic rheumatic endocarditis
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
■
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
■
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
June 30, 2006
39. TIME OF INJURY
1500
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
decedent’s home
41. INJURY AT WORK?
Yes
■
No
42. LOCATION OF NJURY: State: North Carolina City or Town: Cary
Street & Number: 1426 May Drive Apartment No.: Zip Code: 27512-0004
43. DESCRIBE HOW INJURY OCCURRED: 44. IF TRANSPORTATION INJURY, SPECIFY:
Fell down basement stairs onto a cement floor
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that led
directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contr buted to death but
which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A condition can
be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using permanent
black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported. ALWAYS
enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt impact
to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its etiology
on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
124

•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for example,
air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death certificate
should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with another
person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a certifier
completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the body is
found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock; estimates
may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example, enter
“factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents. This
includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of age if
warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the course of
the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type of
vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
125

•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as bicycles.
Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in death,
the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent conditions in
Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should be consulted
about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental abruption
due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no cause
of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as Sudden Infant
Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess Carcinomatosis Disseminated intra vascular Hyponatremia Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Brain injury
Decubiti
Dehydration
Dementia (when not
Hepatorenal syndrome
Hyperglycemia
Hyperkalemia
Perforated gallbladder
Peritonitis
Pleural effusions
Uncal herniation
Urinary tract infection
Ventricular fibrillation
Brain stem herniation
Carcinogenesis
otherwise specified)
Diarrhea
Hypovolemic shock Pneumonia Ventricular tachycardia
Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be complications
of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-death
statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
126
127
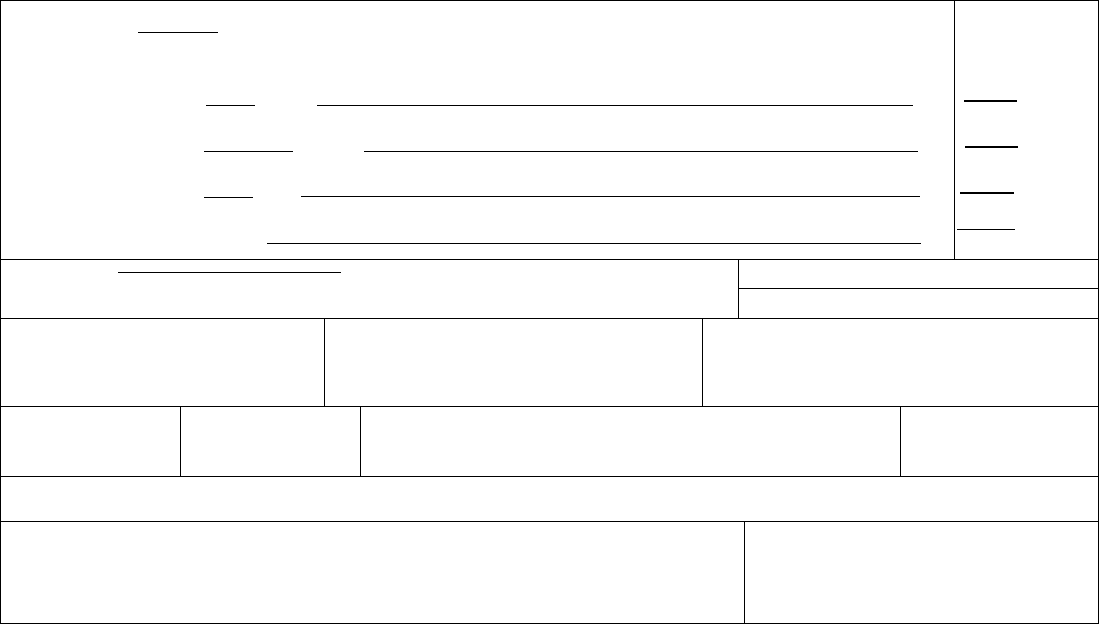
_________________________________________________________________________________________________________
_____________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________
Query for Accidents Involving Transportation
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. _______
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b. ________
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c. _____
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. _______
Approximate interval:
Onset to death
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
August 15, 2003
39. TIME OF INJURY
Approx. 2320
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
road side near state highway
41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED:
44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
1A. Please state if the manner of death was accidental, homicidal, suicidal, natural, or undetermined. __________________.
If undetermined, was there a pending investigation? _______________________________________________.
1B. State what happened to the decedent, describe in detail the external event that caused the death.
2. Describe in detail the external event (__________________________________ ) that eventually brought about the medical
complications which caused the death.
___________________________________________________.
3. Place of occurrence (home, residential institution, public administrative area, sports area, street and highway, trade and service
areas, industrial and construction area, farm, other -please specify-)
4A. Type of vehicle, e.g. automobile, motorcycle, 3-wheeled motor vehicle for on road use, van, pick-up truck, heavy transport
vehicle, bus, vehicle mainly used on industrial premises within buildings (e.g., forklift), vehicle mainly used in agriculture (e.g.,
tractor, combine), construction vehicle (e.g., bulldozer), all-terrain vehicle or other vehicle designed for off-road use, bicycle, train,
streetcar, animal, powered fishing boat, water-skis, helicopter, private airplane
4B. Location at time of accident. On highway ___ Off highway___ Stationary (parked car)___ Railway yard, track, railroad___ In
flight, midair___ At airport, on runway___ In water___ Other____________________________
4C. Collision: Yes___ No___.
128

_____________________________________________
If Yes, collision with what type of vehicle ________________ and location at time of collision
4D.1) Involving vehicle: Loss of control ___ Sinking ___ Explosion, fire___ Object thrown on__ Excessive heat___
Other _______________________________________
2) What happened to decedent? Fell___ Injured while boarding ___Inhaled smoke ___Fell from vehicle___
Run over by___ Hit by moving part___ Crushed___ Thrown from___ Other _________________________
3) Status of decedent: (check a. or b.)
a. If IN or ON vehicle:
Driver___ Passenger___ Occupant___ Rider___ Crew of vehicle___ Other ________________
b. If NOT in or on vehicle:
Pedestrian___ Outside of vehicle___ Water skier___ Swimmer___ Person on ground injured in air transport accident__
Airline ground crew ___ Dock worker___ Other_________________________________
4) If decedent was occupant of vehicle, please specify type of vehicle ______________
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
129
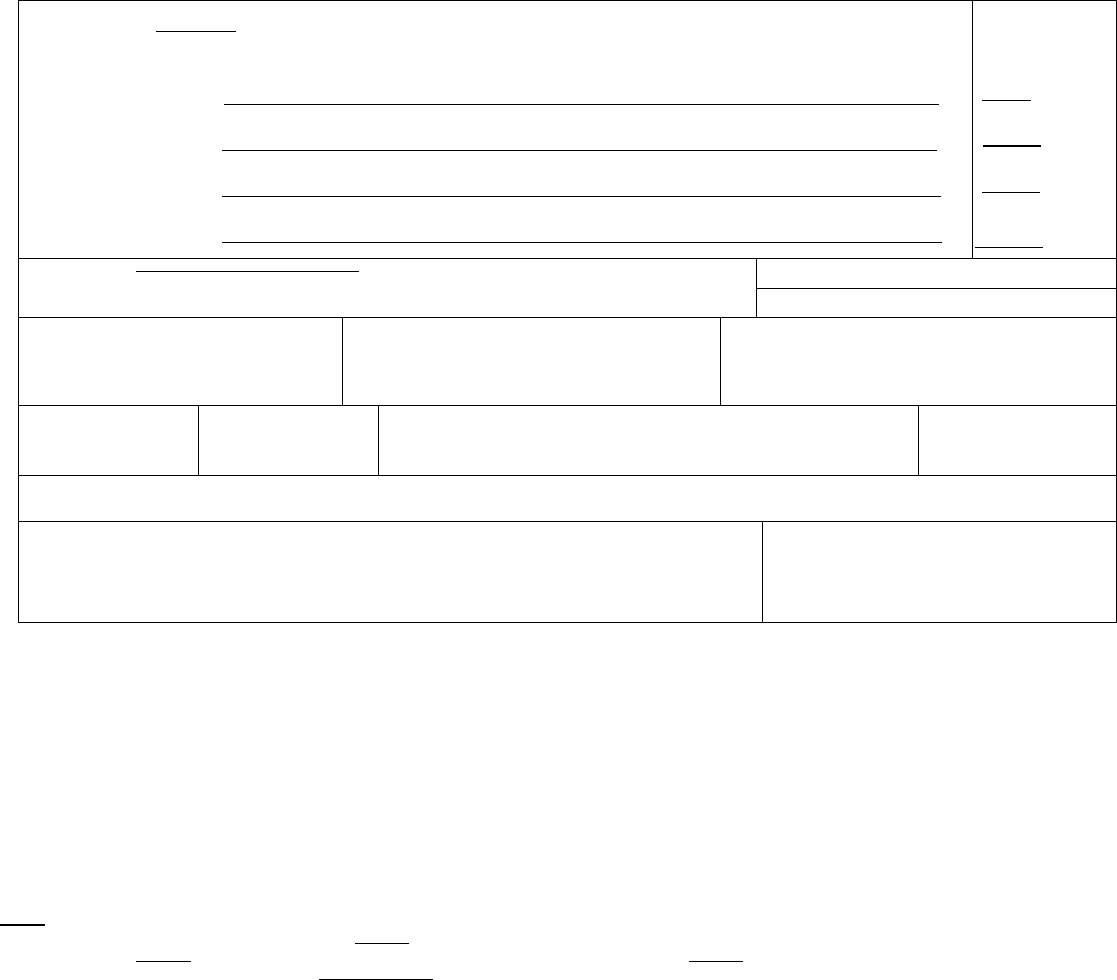
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Aspiration pneumonia
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Complications of coma
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Blunt force injuries
initiated the events resulting
in death) LAST d. Motor vehicle accident
Approximate interval:
Onset to death
2 Days
7 weeks
7 weeks
7 weeks
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
August 15, 2005
39. TIME OF INJURY
Approx. 2320
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
road side near state highway
41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: Missouri City or Town: near Alexandria
Street & Number: mile marker 17 on state route 46a Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED:
44. IF TRANSPORTATION INJURY, SPECIFY:
Decedent driver of van, ran off road into tree
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that led
directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contr buted to death but
which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A condition can
be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using permanent
black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported. ALWAYS
enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt impact
to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its etiology
on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
130

•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for example,
air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death certificate
should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with another
person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a certifier
completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the body is
found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock; estimates
may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example, enter
“factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents. This
includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of age if
warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the course of
the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises
Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home
Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc.
Student in school
Injury while traveling on business, including to/from business contacts
Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type of
vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as bicycles.
Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
131

Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in death,
the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent conditions in
Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should be consulted
about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental abruption
due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no cause
of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as Sudden Infant
Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Carcinomatosis
Disseminated intra vascular
Hyponatremia
Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be complications
of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-death
statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
132
133
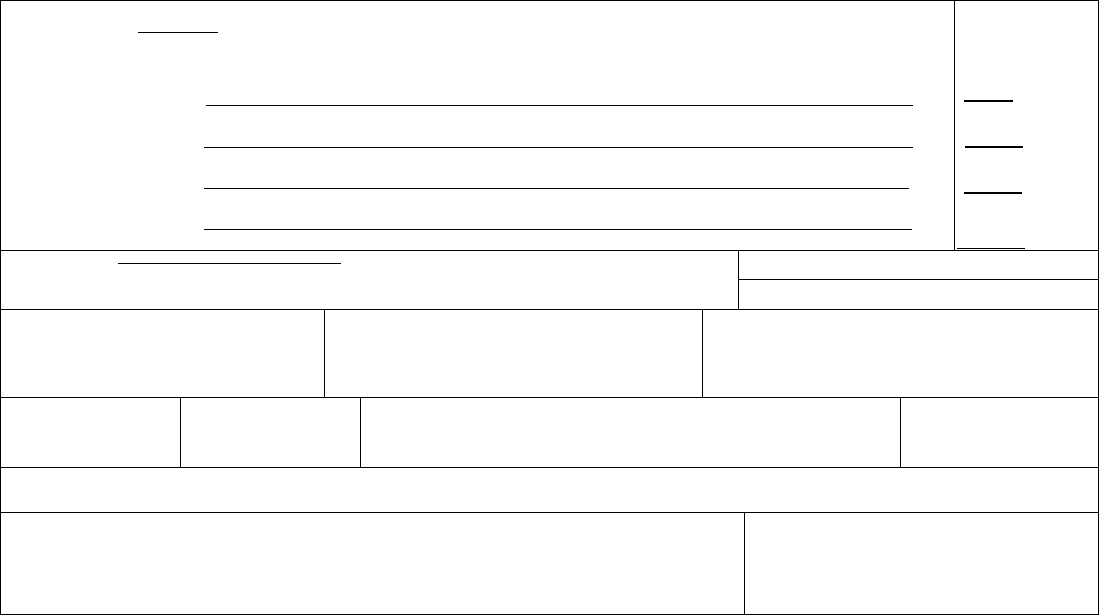
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_______________________________________________________________________________________
_________________________________________________________________________________________________________
_____________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
______________________________________________________________________________________________
Suicide Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
_____________________________________________________________________________________________
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
2 Days
7 weeks
7 weeks
7 weeks
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
39. TIME OF INJURY
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: Missouri City or Town:
Street & Number: mile marker 17 on state route 46a Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED: 44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
1A. Please state if the manner of death was accidental, homicidal, suicidal, natural, or undetermined. __________________.
If undetermined, was there a pending investigation? _______________________________________________.
1B. State what happened to the decedent, describe in detail the external event that caused the death.
2. How did the decedent commit suicide? (If applicable, state type of weapon, poison, medication etc.)
3. Describe in detail the external event (__________________________________ ) that eventually brought about the medical
complications which caused the death.
___________________________________________________.
4. Place of occurrence (home, residential institution, public administrative area, sports area, street and highway, trade and service
areas, industrial and construction area, farm, other -please specify-)
134

, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
135
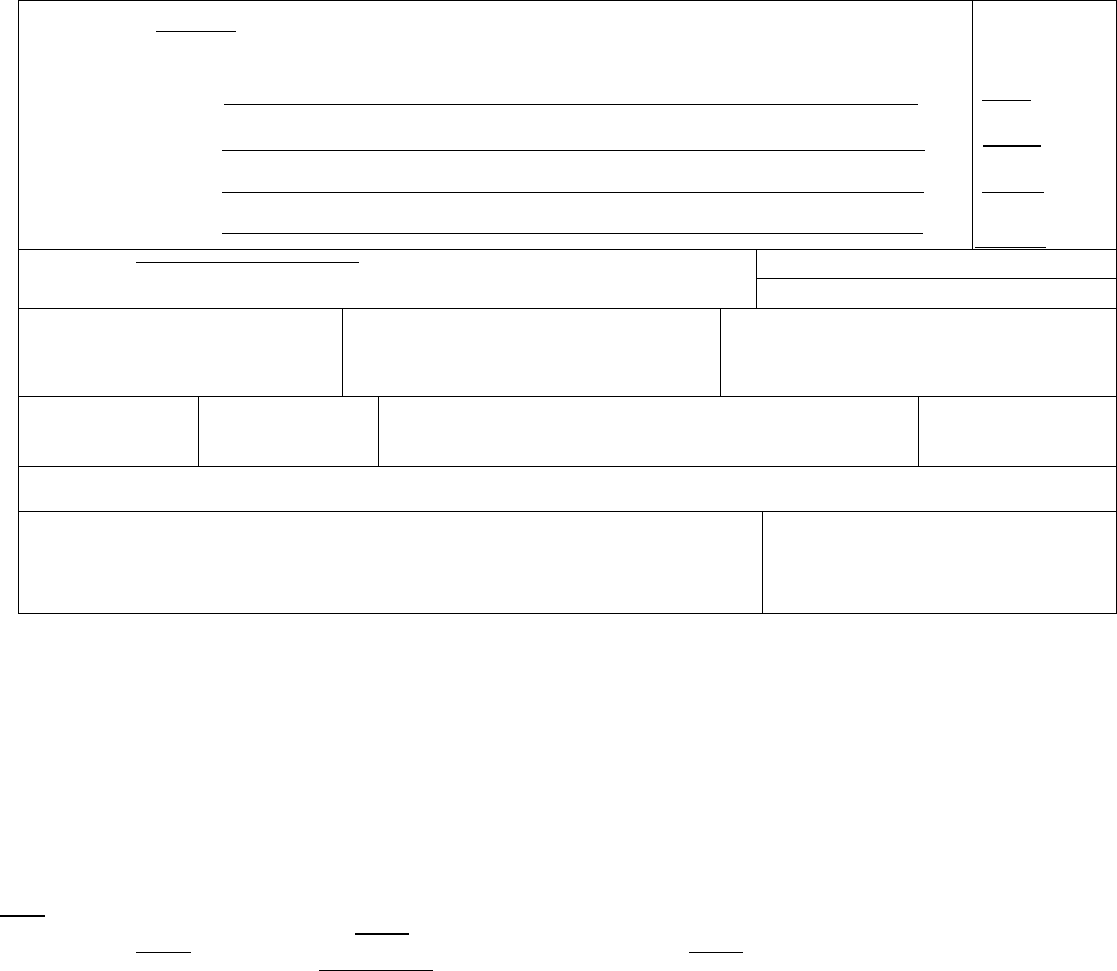
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Penetration brain injury
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Gunshot wound to head
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
2 Days
7 weeks
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
■
Yes
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
■
Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
■
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
■
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
May 10, 2005
39. TIME OF INJURY
2100
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
decedent’s home
41. INJURY AT WORK?
Yes
■
No
42. LOCATION OF NJURY: State: Alabama City or Town: near Alexandria
Street & Number: 3129 Discus Avenue Apartment No.: Zip Code: 36102-8888
43. DESCRIBE HOW INJURY OCCURRED:
Cleaning gun but had contact wound to right temple
44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that led
directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contr buted to death but
which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A condition can
be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using permanent
black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported. ALWAYS
enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt impact
to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its etiology
on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
136

•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for example,
air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death certificate
should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with another
person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a certifier
completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the body is
found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock; estimates
may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example, enter
“factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents. This
includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of age if
warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the course of
the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises
Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home
Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc.
Student in school
Injury while traveling on business, including to/from business contacts
Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type of
vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as bicycles.
Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
137

Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in death,
the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent conditions in
Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should be consulted
about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental abruption
due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no cause
of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as Sudden Infant
Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Carcinomatosis
Disseminated intra vascular
Hyponatremia
Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be complications
of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-death
statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
138
139
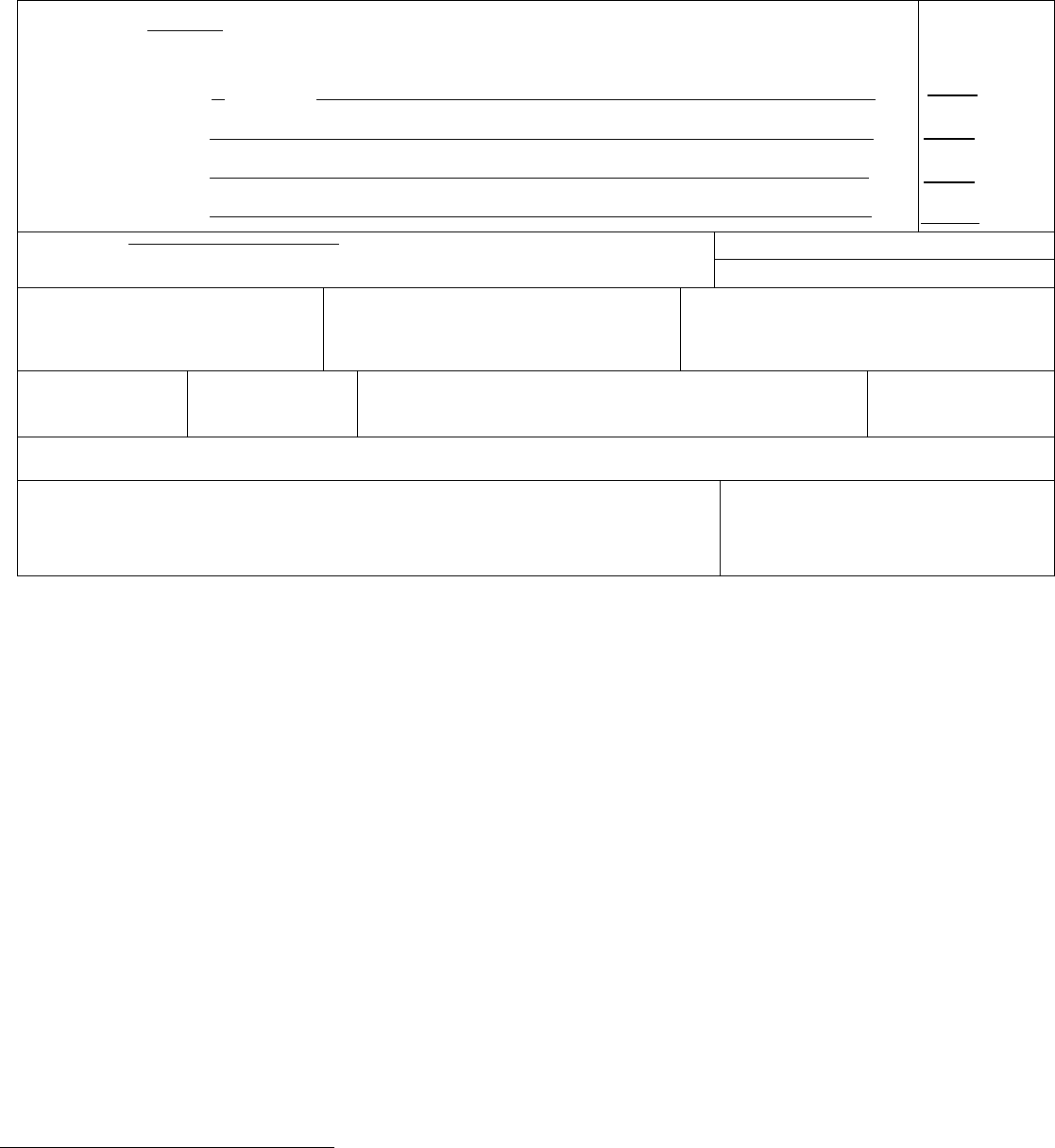
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
________________________________
_________________________________________________________________________________________________________
_____________________________________________________________________
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________
______________________________________________________________________________________________
Homicide Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ___________
resulting in death) Due to (or as a consequence of):
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
____________________________________________________________________________________________
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
39. TIME OF INJURY 40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area) 41. INJURY AT WORK?
Yes No
42. LOCATION OF NJURY: State: City or Town:
Street & Number: Apartment No.: Zip Code:
43. DESCRIBE HOW INJURY OCCURRED:
44. IF TRANSPORTATION INJURY, SPECIFY:
Driver/Operator
Passenger
Pedestrian
Other (Specify)
1A. Please state if the manner of death was accidental, homicidal, suicidal, natural, or undetermined. __________________.
If undetermined, was there a pending investigation? _______________________________________________.
1B. State what happened to the decedent, describe in detail the external event that caused the death.
2. How was the decedent assaulted? (If applicable, state type of weapon, poison, medication etc.)
3. Describe in detail the external event (__________________________________ ) that eventually brought about the medical
complications which caused the death.
___________________________________________________.
4. Place of occurrence (home, residential institution, public administrative area, sports area, street and highway, trade and service
areas, industrial and construction area, farm, other -please specify-)
, M.D.
140
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
141
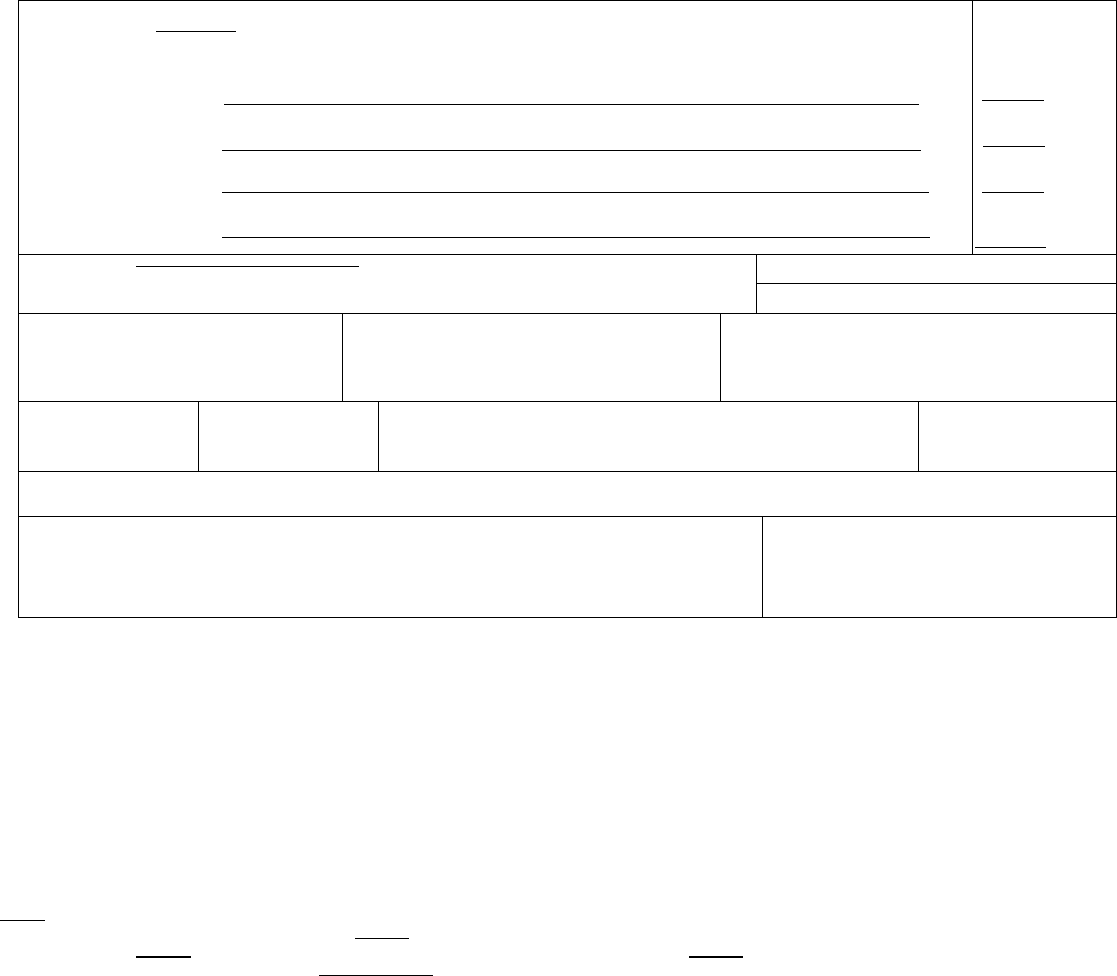
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Intrathoracic hemorrhage
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Stab wound of lung
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
________________________________________________________________________________________
initiated the events resulting
in death) LAST d.
Approximate interval:
Onset to death
15 hours
15 hours
_______
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Several stab wounds of abdomen and extremities
33. WAS AN AUTOPSY PERFORMED?
■
Yes
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH?
■
Yes No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
Yes Probably
■
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural
■
Homicide
Accident Pending Investigation
Suicide Could not be determined
38. DATE OF INJURY
(Mo/Day/Yr) (Spell Month)
August 23, 2006
39. TIME OF INJURY
0330
40. PLACE OF INJURY (e g., Decedent’s home; construction site; restaurant; wooded area)
Alley
41. INJURY AT WORK?
Yes
■
No
42. LOCATION OF NJURY: State: Maryland City or Town: Davidsonville
Street & Number: alley between 331 & 333 Smith Street Apartment No.: Zip Code: 21035-3330
43. DESCRIBE HOW INJURY OCCURRED: 44. IF TRANSPORTATION INJURY, SPECIFY:
Stabbed by a sharp instrument
Driver/Operator
Passenger
Pedestrian
Other (Specify)
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that led
directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contr buted to death but
which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A condition can
be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print legibly using permanent
black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported. ALWAYS
enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt impact
to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its etiology
on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
142

•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for example,
air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death certificate
should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with another
person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a certifier
completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the body is
found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock; estimates
may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example, enter
“factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents. This
includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of age if
warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the course of
the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises
Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home
Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc.
Student in school
Injury while traveling on business, including to/from business contacts
Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type of
vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as bicycles.
Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
143

Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in death,
the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent conditions in
Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should be consulted
about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental abruption
due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no cause
of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as Sudden Infant
Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess
Carcinomatosis
Disseminated intra vascular
Hyponatremia
Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be complications
of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-death
statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
144
145
Query Letter 11
(Format)
(Letterhead)
Dear Doctor _________
We are writing this letter to obtain additional information about the cause of death that you certified for
_________________________, who died _____________.
Accurate cause-of-death information is essential, not only to the family of the decedent, but also for medical research,
funding, and resource allocation in our State and at the national level.
In this particular death, we would appreciate your review of the reported sequence of conditions for completeness and
logic. In order to classify this death properly in our statistics, would you please supply the information on the
attachment? We want to assure you that the information you provide us is confidential and will be handled accordingly.
If you have any question or would like to know more about various methods for certifying a cause-of-death statement,
please contact __________________________________________. Instructions and an example of a properly
completed death certificate are provided with the attached material.
We appreciate your attention and prompt reply.
Sincerely,
State Registrar/Vital Statistics Cooperative Program
Attachment
146
147
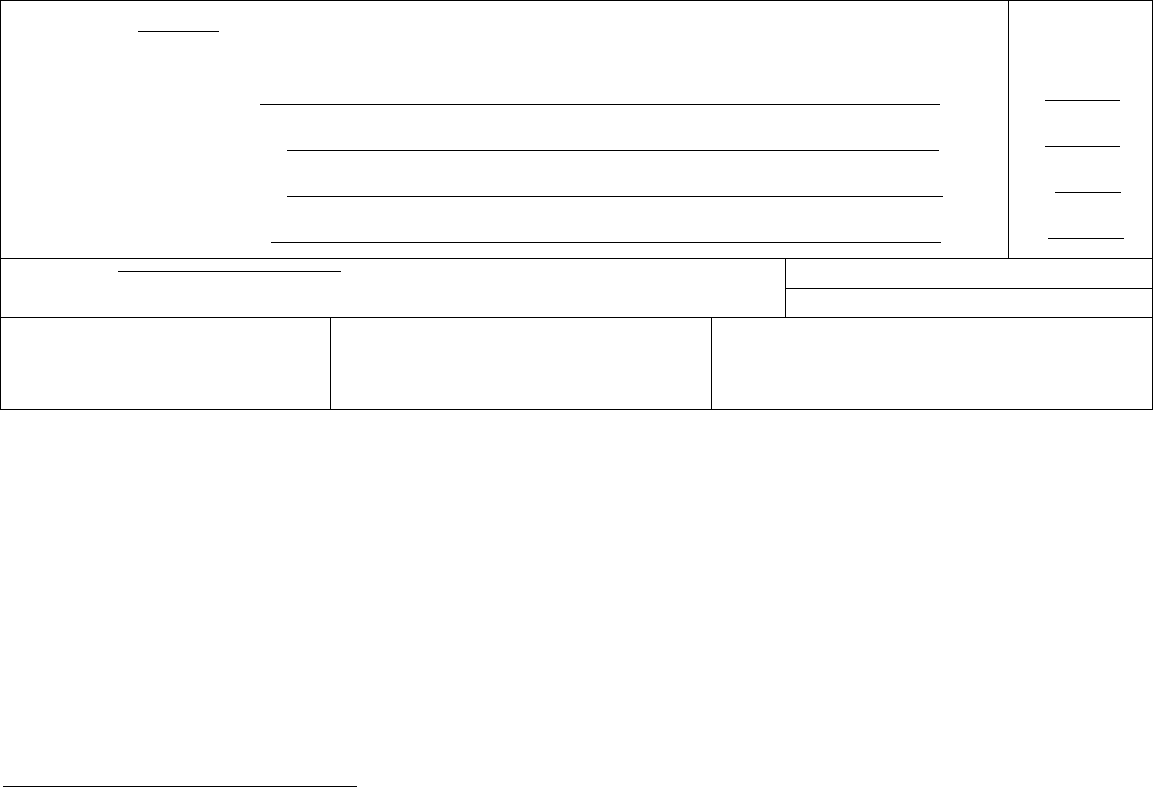
_____________________________________________________
_____________________________________________________
_____________________________________________________
_____________________________________________________
Format Query
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
IMMEDIATE CAUSE (Final
disease or condition ---------> a. ________
resulting in death) Due to (or as a consequence of):
____________________________________________________________________________________
Sequentially list conditions, b. ____________
if any, leading to the cause Due to (or as a consequence of):
_____________________________________________________________________________________
listed on line a. Enter the
UNDERLYING CAUSE c. ____________
(disease or injury that Due to (or as a consequence of):
initiated the events resulting
in death) LAST d. __________ _______________________________________________________________________________
Approximate interval:
Onset to death
____
____
____
____
PART II.
Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
33. WAS AN AUTOPSY PERFORMED?
Yes
No
34. WERE AUTOPSY FIND NGS AVA LABLE TO
COMPLETE THE CAUSE OF DEATH?
Yes
No
35. DID TOBACCO USE CONTR BUTE TO DEATH?
Yes Probably
No Unknown
36. IF FEMALE:
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
1. Is the reported sequence of conditions correct (i.e., condition on line a results from condition on line b)? Yes___ No___
If not, please indicate the correct order with the most recent condition on the top line and the condition starting the sequence on
the lowest line:
2. Is the duration for condition________ correct? Yes___ No____
If not, the duration should be _______________.
, M.D.
(Signature of Certifying Physician)
Please provide your office phone:_____________________ fax:________________________
(Please see other side)
148
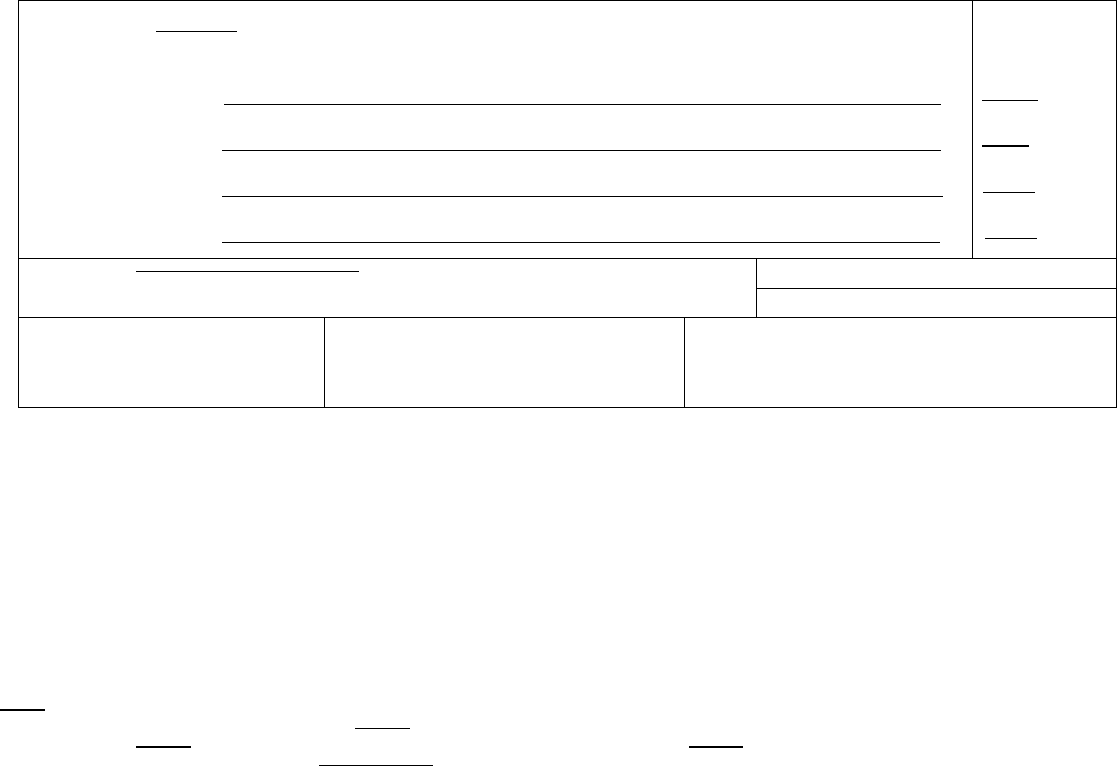
Instructions on Medical Certification of Causes of Death
Example of properly completed medical certification
CAUSE OF DEATH (See instructions and examples)
32. PART I. Enter the chain of events
arrest, respiratory arrest, or ventricular fibrillation without showing the etiology. DO NOT ABBREVIATE. Enter only one cause on a line. Add additional
--diseases, injuries, or complications--that directly caused the death. DO NOT enter terminal events such as cardiac
lines if necessary.
MMEDIATE CAUSE (Final
disease or condition ---------> a.
resulting in death) Due to (or as a consequence of):
Rupture of myocardium
Sequentially list conditions, b.
if any, leading to the cause Due to (or as a consequence of):
Acute myocardial infarction
listed on line a. Enter the
UNDERLYING CAUSE c.
(disease or injury that Due to (or as a consequence of):
Coronary artery thrombosis
initiated the events resulting
in death) LAST d. Atherosclerotic coronary artery disease
Approximate interval:
Onset to death
Minutes
6 days
5 years
7 years
PART II. Enter other significant conditions contributing to death but not resulting in the underlying cause given in PART I
Diabetes, Chronic obstructive pulmonary disease, smoking
33. WAS AN AUTOPSY PERFORMED?
Yes
■
No
34. WERE AUTOPSY FINDINGS AVAILABLE TO
COMPLETE THE CAUSE OF DEATH? Yes
■
No
35. DID TOBACCO USE CONTRIBUTE TO DEATH?
■
Yes Probably
No Unknown
36. IF FEMALE:
■
Not pregnant within past year
Pregnant at time of death
Not pregnant, but pregnant within 42 days of death
Not pregnant, but pregnant 43 days to 1 year before death
Unknown if pregnant within the past year
37. MANNER OF DEATH
■
Natural Homicide
Accident Pending Investigation
Suicide Could not be determined
ITEM 32 – CAUSE OF DEATH (See example above)
Accurate cause of death information is important
•to the public health community in evaluating and improving the health of all citizens, and
•often to the family, now and in the future, and to the person settling the decedent’s estate.
The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final
disease, injury, or complication directly causing death) on line a and the underlying cause of death (the disease or injury that initiated the chain of events that led
directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death but
which did not result in the underlying cause of death given in Part I. The cause-of-death information should be YOUR best medical OPINION. A condition can
be listed as “probable” even if it has not been definitively diagnosed.
Take care to make the entry leg ble. Use a computer printer with high resolution, typewriter with good black ribbon and clean keys, or print leg bly using permanent
black ink in completing the CAUSE OF DEATH Section. Do not abbreviate conditions entered in section.
Part I (Chain of events leading directly to death)
•Only one cause should be entered on each line. Line (a) MUST ALWAYS have an entry. DO NOT leave blank. Additional lines may be added if necessary.
•If the condition on Line (a) resulted from an underlying condition, put the underlying condition on Line (b), and so on, until the full sequence is reported. ALWAYS
enter the underlying cause of death on the lowest used line
in Part I.
•For each cause indicate the best estimate of the interval between the presumed onset and the date of death. The terms “unknown” or “approximately” may be
used. General terms, such as minutes, hours, or days, are acceptable, if necessary. DO NOT leave blank.
•The terminal event (for example, cardiac arrest or respiratory arrest) should not be used. If a mechanism of death seems most appropriate to you for line (a),
then you must always list its cause(s) on the line(s) below it (for example, cardiac arrest due to coronary artery atherosclerosis or cardiac arrest due to blunt
impact to chest).
• If an organ system failure such as congestive heart failure, hepatic failure, renal failure, or respiratory failure is listed as a cause of death, always report its etiology
on the line(s) beneath it (for example, renal failure due to Type I diabetes mellitus).
•When indicating neoplasms as a cause of death, include the following: 1) primary site or that the primary site is unknown, 2) benign or malignant, 3) cell type or
that the cell type is unknown, 4) grade of neoplasm, and 5) part or lobe of organ affected. (For example, a primary well-differentiated squamous cell carcinoma,
lung, left upper lobe.)
•Always report the fatal injury (for example, stab wound of chest), the trauma (for example, transection of subclavian vein), and impairment of function (for example,
air embolism).
Part II (Other significant conditions)
•Enter all diseases or conditions contr buting to death that were not reported in the chain of events in Part I and that did not result in the underlying cause of
death.
•If two or more possible sequences resulted in death, or if two conditions seem to have added together, report in Part I the one that, in your opinion, most directly
caused death. Report in Part II the other conditions or diseases.
CHANGES TO CAUSE OF DEATH
149
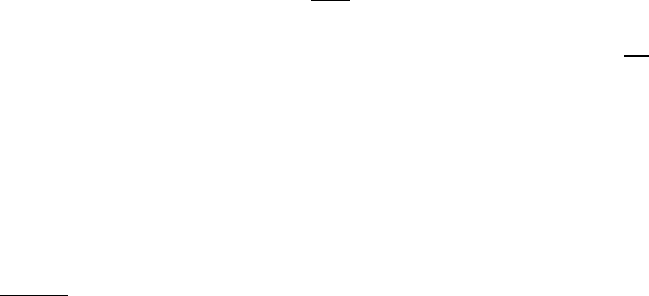
Should additional medical information or autopsy findings become available that would change the cause of death originally reported, the original death certificate
should be amended by the certifying physician by immediately reporting the revised cause of death to the State Vital Records Office.
ITEMS ON WHEN DEATH OCCURRED
Items 24-25 and 29-31 should always be completed. If the facility uses a separate pronouncer or other person to indicate that death has taken place with another
person more familiar with the case completing the remainder of the medical portion of the death certificate, the pronouncer completes Items 24-28. If a certifier
completes Items 24-25 as well as items 29-49, Items 26-28 may be left blank.
ITEMS 24-25, 29-30 – DATE AND TIME OF DEATH
Spell out the name of the month. If the exact date of death is unknown, enter the approximate date. If the date cannot be approximated, enter the date the body is
found and identify as date found. Date pronounced and actual date may be the same. Enter the exact hour and minutes according to a 24-hour clock; estimates
may be provided with “Approx.” placed before the time.
ITEMS 33-34 - AUTOPSY
•33 - Enter “Yes” if either a partial or full autopsy was performed. Otherwise enter “No.”
•34 - Enter “Yes” if autopsy findings were available to complete the cause of death; otherwise enter “No”. Leave item blank if no autopsy was performed.
ITEM 35 - DID TOBACCO USE CONTRIBUTE TO DEATH?
Check “yes” if, in your opinion, the use of tobacco contributed to death. Tobacco use may contribute to deaths due to a wide variety of diseases; for example,
tobacco use contributes to many deaths due to emphysema or lung cancer and some heart disease and cancers of the head and neck. Check “no” if, in your
clinical judgment, tobacco use did not contribute to this particular death.
ITEM 36 - IF FEMALE, WAS DECEDENT PREGNANT AT TIME OF DEATH OR WITHIN PAST YEAR?
This information is important in determining pregnancy-related mortality.
ITEM 37 - MANNER OF DEATH
•Always check Manner of Death, which is important: 1) in determining accurate causes of death; 2) in processing insurance claims; and 3) in statistical studies of
injuries and death.
•Indicate “Pending investigation” if the manner of death cannot be determined whether due to an accident, suicide, or homicide within the statutory time limit for
filing the death certificate. This should be changed later to one of the other terms.
•Indicate “Could not be Determined” ONLY when it is impossible to determine the manner of death.
ITEMS 38-44 - ACCIDENT OR INJURY – to be filled out in all cases of deaths due to injury or poisoning.
•38 - Enter the exact month, day, and year of injury. Spell out the name of the month. DO NOT use a number for the month. (Remember, the date of injury may
differ from the date of death.) Estimates may be provided with “Approx.” placed before the date.
•39 - Enter the exact hour and minutes of injury or use your best estimate. Use a 24-hour clock.
•40 - Enter the general place (such as restaurant, vacant lot, or home) where the injury occurred. DO NOT enter firm or organization names. (For example, enter
“factory”, not “Standard Manufacturing, Inc.” )
•41 - Complete if anything other than natural disease is mentioned in Part I or Part II of the medical certification, including homicides, suicides, and accidents. This
includes all motor vehicle deaths. The item
must be completed for decedents ages 14 years or over and may be completed for those less than 14 years of age if
warranted. Enter “Yes” if the injury occurred at work. Otherwise enter “No”. An injury may occur at work regardless of whether the injury occurred in the course of
the decedent’s “usual” occupation. Examples of injury at work and injury not at work follow:
Injury at work
Injury
not at work
Injury while working or in vocational training on job premises Injury while engaged in personal recreational activity on job premises
Injury while on break or at lunch or in parking lot on job premises Injury while a visitor (not on official work business) to job premises
Injury while working for pay or compensation, including at home Homemaker working at homemaking activities
Injury while working as a volunteer law enforcement official etc. Student in school
Injury while traveling on business, including to/from business contacts Working for self for no profit (mowing yard, repairing own roof, hobby)
Commuting to or from work
•42 - Enter the complete address where the injury occurred including zip code.
•43 - Enter a brief but specific and clear description of how the injury occurred. Explain the circumstances or cause of the injury. Specify type of gun or type of
vehicle (e.g., car, bulldozer, train, etc.) when relevant to circumstances. Indicate if more than one vehicle involved; specify type of vehicle decedent was in.
•44 -Specify role of decedent (e.g. driver, passenger). Driver/operator and passenger should be designated for modes other than motor vehicles such as bicycles.
Other applies to watercraft, aircraft, animal, or people attached to outside of vehicles (e.g. surfers).
Rationale: Motor vehicle accidents are a major cause of unintentional deaths; details will help determine effectiveness of current safety features and laws.
Common problems in death certification
The elderly decedent should have a clear and distinct etiological sequence for cause of death, if possible. Terms such as senescence, infirmity, old age, and
advanced age have little value for public health or medical research. Age is recorded elsewhere on the certificate. When a number of conditions resulted in death,
the physician should choose the single sequence that, in his or her opinion, best describes the process leading to death, and place any other pertinent conditions in
Part II. If after careful consideration the physician cannot determine a sequence that ends in death, then the medical examiner or coroner should be consulted
about conducting an investigation or providing assistance in completing the cause of death.
The infant decedent should have a clear and distinct etiological sequence for cause of death, if possible. “Prematurity” should not be entered without explaining
the etiology of prematurity. Maternal conditions may have initiated or affected the sequence that resulted in infant death, and such maternal causes should be
150
reported in addition to the infant causes on the infant’s death certificate (e.g., Hyaline membrane disease due to prematurity, 28 weeks due to placental abruption
due to blunt trauma to mother’s abdomen).
When SIDS is suspected, a complete investigation should be conducted, typically by a medical examiner or coroner. If the infant is under 1 year of age, no cause
of death is determined after scene investigation, clinical history is reviewed, and a complete autopsy is performed, then the death can be reported as Sudden Infant
Death Syndrome.
When processes such as the following are reported, additional information about the etiology should be reported:
Abscess Carcinomatosis Disseminated intra vascular Hyponatremia Pulmonary arrest
Abdominal hemorrhage
Adhesions
Cardiac arrest
Cardiac dysrhythmia
coagulopathy
Dysrhythmia
Hypotension
Immunosuppression
Pulmonary edema
Pulmonary embolism
Adult respiratory distress syndrome
Acute myocardial infarction
Cardiomyopathy
Cardiopulmonary arrest
End-stage liver disease
End-stage renal disease
Increased intra cranial pressure
Intra cranial hemorrhage
Pulmonary insufficiency
Renal failure
Altered mental status
Anemia
Cellulitis
Cerebral edema
Epidural hematoma
Exsanguination
Malnutrition
Metabolic encephalopathy
Respiratory arrest
Seizures
Anoxia
Anoxic encephalopathy
Cerebrovascular accident
Cerebellar tonsillar herniation
Failure to thrive
Fracture
Multi-organ failure
Multi-system organ failure
Sepsis
Septic shock
Arrhythmia
Ascites
Chronic bedridden state
Cirrhosis
Gangrene
Gastrointestinal hemorrhage
Myocardial infarction
Necrotizing soft-tissue infection
Shock
Starvation
Aspiration
Atrial fibrillation
Coagulopathy
Compression fracture
Heart failure
Hemothorax
Old age
Open (or closed) head injury
Subdural hematoma
Subarachnoid hemorrhage
Bacteremia
Bedridden
Congestive heart failure
Convulsions
Hepatic failure
Hepatitis
Paralysis
Pancytopenia
Sudden death
Thrombocytopenia
Biliary obstruction
Bowel obstruction
Decubiti
Dehydration
Hepatorenal syndrome
Hyperglycemia
Perforated gallbladder
Peritonitis
Uncal herniation
Urinary tract infection
Brain injury
Brain stem herniation
Dementia (when not
otherwise specified)
Hyperkalemia
Hypovolemic shock
Pleural effusions
Pneumonia
Ventricular fibrillation
Ventricular tachycardia
Carcinogenesis Diarrhea Volume depletion
If the certifier is unable to determine the etiology of a process such as those shown above, the process must be qualified as being of an unknown, undetermined,
probable, presumed, or unspecified etiology so it is clear that a distinct etiology was not inadvertently or carelessly omitted.
The following conditions and types of death might seem to be specific or natural but when the medical history is examined further may be found to be complications
of an injury or poisoning (possibly occurring long ago). Such cases should be reported to the medical examiner/coroner.
Asphyxia
Bolus
Epidural hematoma
Exsanguination
Hip fracture
Hyperthermia
Pulmonary emboli
Seizure disorder
Subdural hematoma
Surgery
Choking
Drug or alcohol overdose/drug or
Fall
Fracture
Hypothermia
Open reduction of fracture
Sepsis
Subarachnoid hemorrhage
Thermal burns/chemical burns
alcohol abuse
Contact your State vital statistics office for questions related to writing cause-of-death statements. Additional instructional material on writing cause-of-death
statements including handbooks, summary instructions, and tutorials are available online at www.thename.org or
www.cdc.gov/nchswww/about/major/dvs/handbk htm, or by request from NCHS, Room 7318, 3311 Toledo Road, Hyattsville, Maryland 20782-2003.
151
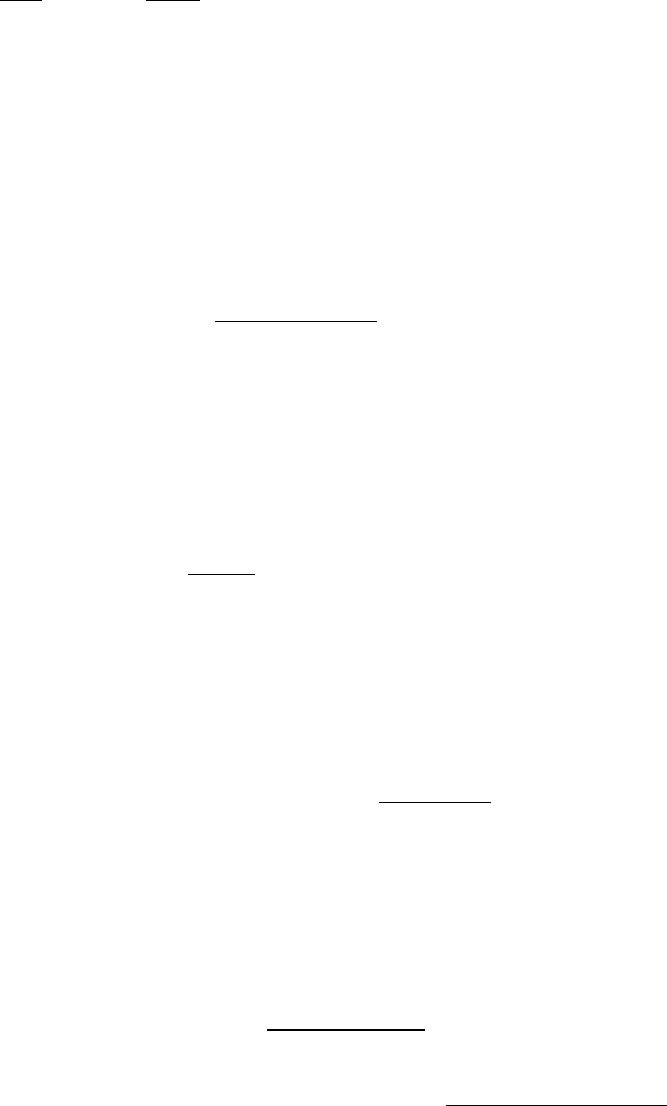
Appendix C
Infrequent and Rare Causes of Death
ICD-10
code Cause
A00 Cholera
A01 Typhoid and paratyphoid fevers
A05.1 Botulism (including infant and wound botulism)
A07.0-.2,.8-.9 Other protozoal intestinal diseases (excluding coccidiosis)
A20 Plague
A21 Tularemia
A22 Anthrax
A23 Brucellosis
A24.0 Glanders
A24.1-.4 Melioidosis
A25 Rat-bite fever
A27 Leptospirosis
A30 Leprosy [Hansen's disease]
A33 Tetanus neonatorum
A34 Obstetrical tetanus
A35 Other tetanus (Tetanus)
A36 Diphtheria
A37 Whooping cough
A44 Bartonellosis
A49.1 Streptococcus pneumoniae - less than 5 years of age
A65 Nonvenereal syphilis
A66 Yaws
A67 Pinta [carate]
A68 Relapsing fever
A69 Other spirochaetal infection
A70 Chlamydia psittaci infection (ornithosis)
A75 Typhus fever
A77.1 Spotted fever due to Rickettsia conorii (Boutonneuse fever)
A77.2 Spotted fever due to Rickettsia siberica (North Asian tick fever)
A77.3 Spotted fever due to Rickettsia australis (Queensland tick typhus)
A77.8 Other spotted fevers (Other tick-borne rickettsioses)
A77.9 Unspecified Spotted fevers, unspecified (unspecified tick-borne rickettsioses)
A78 Q fever
A79 Other rickettsioses
A80 Acute poliomyelitis
A81 Atypical virus infections of central nervous system
A82 Rabies
A84 Tick-borne viral encephalitis
A85.2 Arthropod-borne viral encephalitis, unspecified (Viral encephalitis
transmitted by other and unspecified arthropods)
A90 Dengue fever [classical dengue]
A91 Dengue hemorrhagic fever
A92 Other mosquito-borne viral fevers
A93 Other arthropod-borne viral fevers, not elsewhere classified
(including Oropouche fever, sandfly fever, Colorado tick fever
and other specified fevers)
152
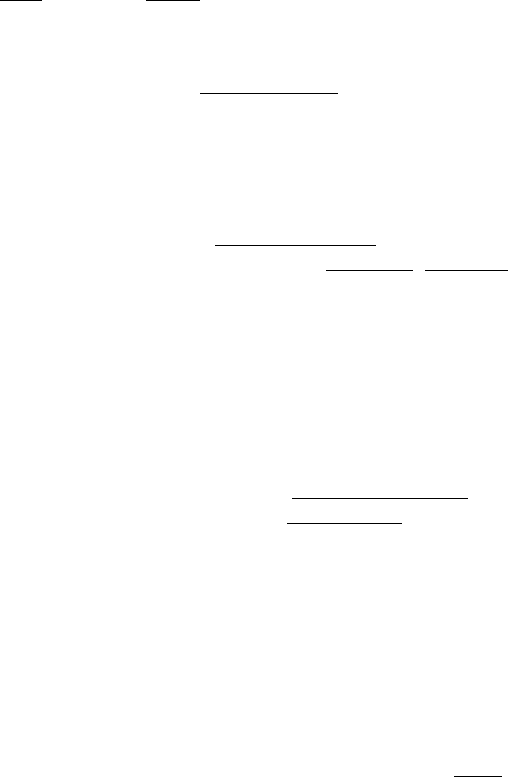
Appendix C
Infrequent and Rare Causes of Death
ICD-10
code Cause
A94 Unspecified arthropod-borne viral fever
A95 Yellow fever
A96 Arenaviral hemorrhagic fever
A98-A99 Other and unspecified viral hemorrhagic fevers (including
Crimean-Congo, Omsk, Kyasanur Forest, Ebola virus, Hanta virus)
B01 Varicella [chickenpox]
B03 Smallpox
B04 Monkeypox
B05 Measles
B06 Rubella [German measles]
B08.0 Other orthopoxvirus infections (including cowpox and paravaccinia)
B15 Acute hepatitis A – less than 20 years of age
B16 Acute hepatitis B – less than 20 years of age
B26 Mumps
B33.0 Epidemic myalgia (epidemic pleurodynia)
B33.4 Hantavirus (cardio)- pulmonary syndrome [HPS][HCPS]
B50-B54 Malaria
B55 Leishmaniasis
B56 African trypanosomiasis (trypanosomiasis)
B57 Chagas' disease (including American trypanosomiasis)
B65 Schistosomiasis [bilharziasis]
B66 Other fluke infections (including other trematode infections)
B67 Echinococcosis
B68 Taeniasis
B69 Cysticercosis
B70 Diphyllobothriasis and sparganosis
B71 Other cestode infections
B72 Dracunculiasis (Dracontiasis)
B73 Onchocerciasis
B74 Filariasis (Filarial infection)
J09 Influenza due to certain identified avian influenza virus
P35.0 Congenital rubella syndrome
*U04.9 Severe acute respiratory syndrome [SARS], unspecified
W88-W91 Exposure to radiation
Y36.5 War operation involving nuclear weapons
Causing adverse effects in therapeutic use:
Y58 Bacterial vaccines
Y59.0 Viral vaccines
Y59.1 Rickettsial vaccines
Y59.2 Protozoal vaccines
Y59.3 Immunoglobulin
153
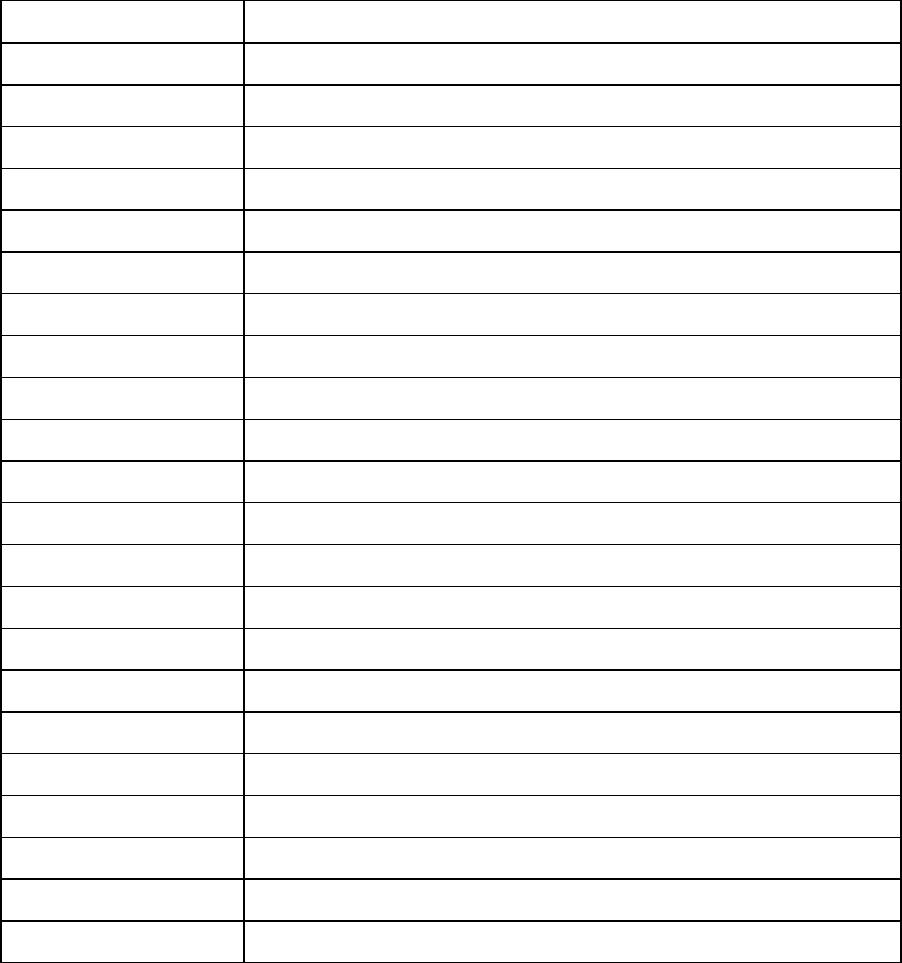
Appendix D
ICD-10 Codes Selected for Querying for HIV Under Priority Level 1g
ICD-10 code
Abbreviated title
A07.2
Cryptosporidiosis
A07.3
Isosporiasis
A16.2-A19
Tuberculosis
A31
Nontuberculous mycobacteriosis
A42
Actinomycosis
A43
Nocardidosis
A812
Progressive multifocal leukoencephalopathy
B00
Herpes simplex
B25
Cytomegalovirus
B37
Candidiasis
B38
Coccidioidomycosis
B39
Histoplasmosis
B44
Aspergillosis
B45
Cryptococcosis
B58
Toxoplasmosis
B59
Pneumocystosis
C46
Kaposi's sarcoma
C83, C85
Non-Hodgkin's Lymphoma
G049
Encephalitis, myelitis, and encephalomyelitis, unspecified
G934
Encephalopathy, unspecified
G959
Disease of spinal cord, unspecified
R64
Cachexia
154
