©2022-2023 Arthur J. Gallagher & Co. All rights reserved.
Electronic Disclosure of Required Health & Welfare
Plan Notices
This resource provides the electronic disclosure rules for health & welfare related
federal notices for both ERISA and non-ERISA plans.
Fundamentally, employers and plans must provide notices related to their health and
welfare plans that fall into six categories – ERISA; Patient Protection and Affordable
Care Act (ACA); COBRA; HIPAA (both Portability and Privacy and Security); Internal
Revenue Code (IRC) disclosures; and Other Notices required under several different
federal laws. Following is a summary of the types of notices that fall into each of the six
categories and how those notices may be provided electronically.
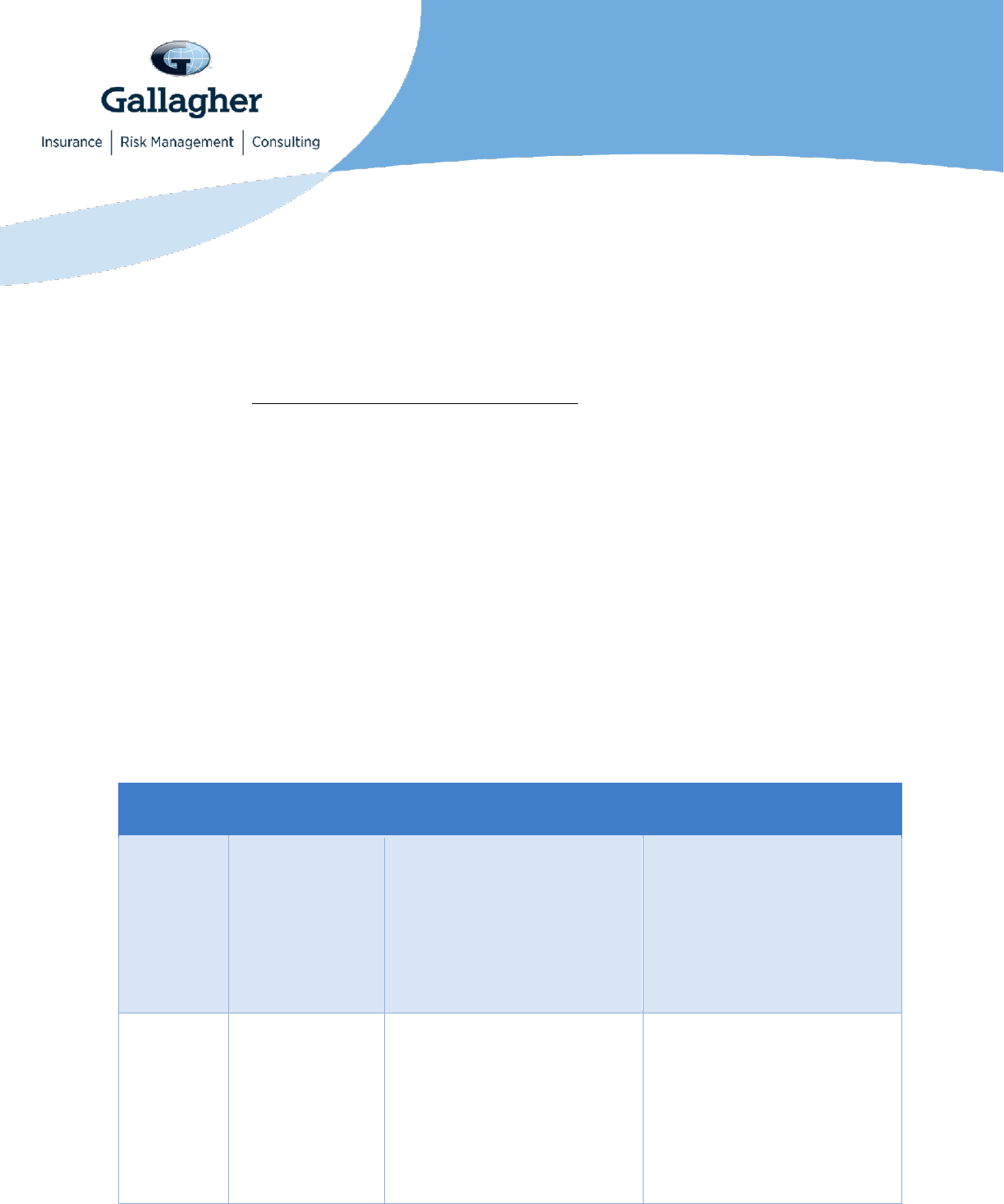
Summary of Required Participant Notices by Type
As discussed below, the rules regarding electronic delivery of required information vary
by the type of plan and notice. Employers have a variety of options to deliver materials
electronically depending on the circumstances. However, some notices require prior
consent from the recipient before electronic distribution. The below chart summarizes
which types of notices require prior consent. The specific rules are explained further in
separate sections below the chart.
Applicable
Law
Notice
ERISA Consent
Requirements
Non-ERISA Consent
Requirements
ERISA
All notices
required by
ERISA (SPDs,
SMMs, SMRs,
SARs)
Prior consent only required
for individuals without
worksite access to electronic
materials
Prior consent is not required
for individuals with worksite
access to electronic materials
Not applicable to non-ERISA
plans; however, these rules
may be used by non-ERISA
plans to prove disclosure, as
noted below.
ACA
Marketplace
Use the ERISA disclosure
rules:
• Employees with worksite
access do not have to
provide consent to
receive Marketplace
notice if using ERISA
disclosure rules.
Non-ERISA plans may use
the ERISA rules.
Non-federal governmental
plans may also follow the
electronic disclosure rules
that apply in the individual
insurance market.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
2
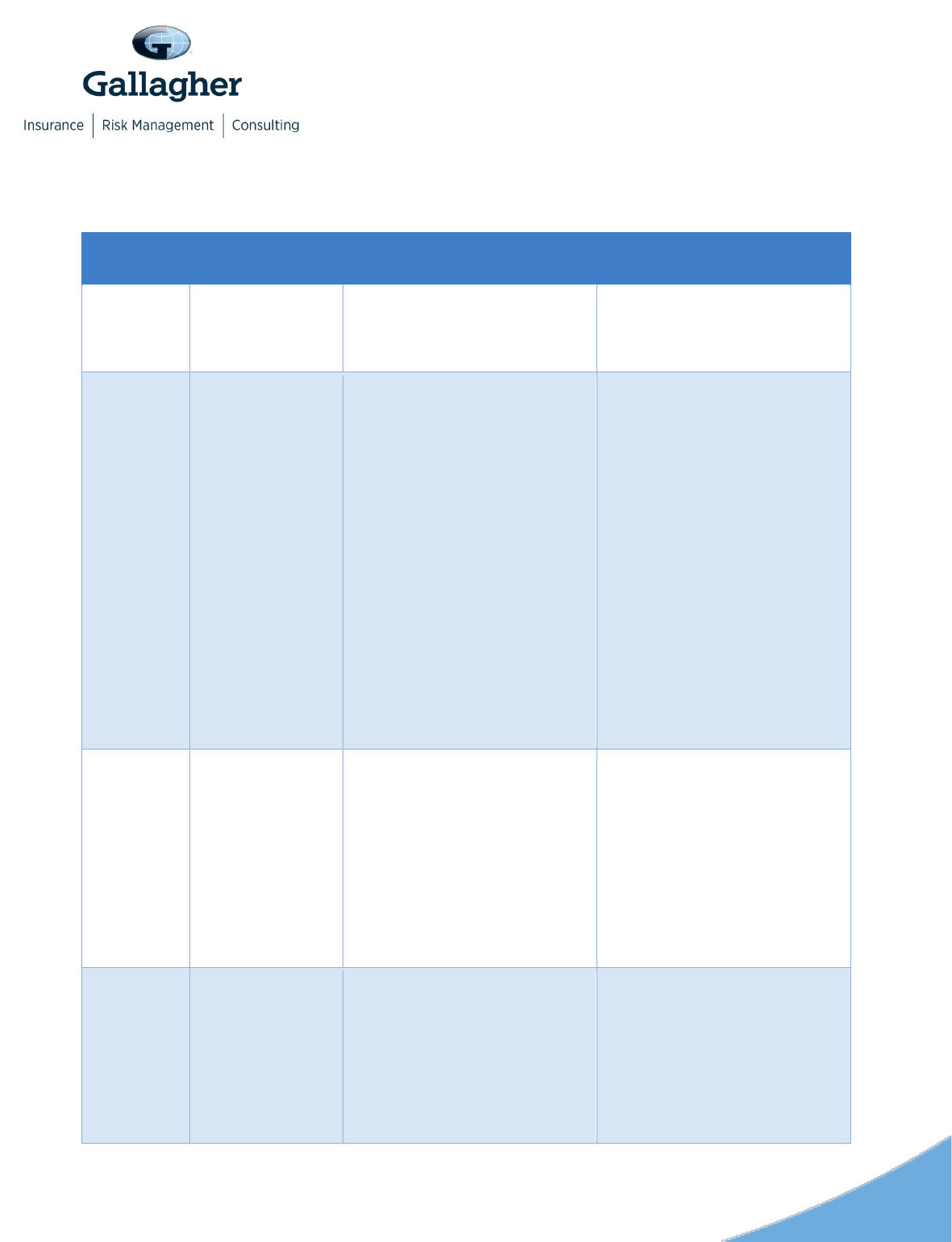
Applicable
Law
Notice
ERISA Consent
Requirements
Non-ERISA Consent
Requirements
• Employees without
worksite access may only
receive electronically after
providing consent.
Summary of
Benefits and
Coverage (SBC)
• Electronic delivery
permitted for participants
who enroll online or who
request the SBC online.
• Individuals with worksite
access do not have to
provide consent to
receive SBC.
• Individuals without
worksite access may
receive only after
providing consent using
ERISA disclosure rules.
• Internet posting permitted
as long as employees
notified in writing that
material available and
internet address provided.
Non-ERISA plans may use
the ERISA rules.
Self-insured non-federal
governmental plans may also
use the state’s rules for
individual medical insurance.
Grandfather
Status
Use the ERISA disclosure
rules:
• Prior consent only
required for individuals
without worksite access to
electronic materials
• Prior consent is not
required for individuals
with worksite access to
electronic materials.
Non-ERISA plans may use
the ERISA rules.
Patient
Protection
Notice
Use the ERISA disclosure
rules:
• Prior consent only
required for individuals
without worksite access to
electronic materials
• Prior consent is not
required for individuals
Non-ERISA plans may use
the ERISA rules.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
3
Applicable
Law
Notice
ERISA Consent
Requirements
Non-ERISA Consent
Requirements
with worksite access to
electronic materials.
No Surprises Act
Post notice on public website
of the plan. No requirement to
disclose individually except
on EOBs.
Post notice on public website
of the plan. No requirement to
disclose individually except
on EOBs.
COBRA
COBRA
general/initial
notice
Election notice
Notice of
unavailability
Notices of early
termination
Electronic disclosure may be
problematic. Read the
COBRA section below for
more detail.
For electronic disclosure, use
the ERISA disclosure rules:
• Prior consent only
required for individuals
without worksite access to
electronic materials
• Prior consent is not
required for individuals
with worksite access to
electronic materials.
Non-ERISA plans may use
the ERISA rules.
Church plans are not subject
to COBRA.
HIPAA
Children’s
Health
Insurance
Program
Reauthorization
Act (CHIP)
Use the ERISA disclosure
rules:
• Prior consent only
required for individuals
without worksite access to
electronic materials
• Prior consent is not
required for individuals
with worksite access to
electronic materials.
Non-ERISA plans may use
the ERISA rules.
HIPAA Special
Enrollment
Rights
Use the ERISA disclosure
rules:
• Prior consent only
required for individuals
without worksite access to
electronic materials
• Prior consent is not
required for individuals
Non-ERISA plans may use
the ERISA rules.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
4
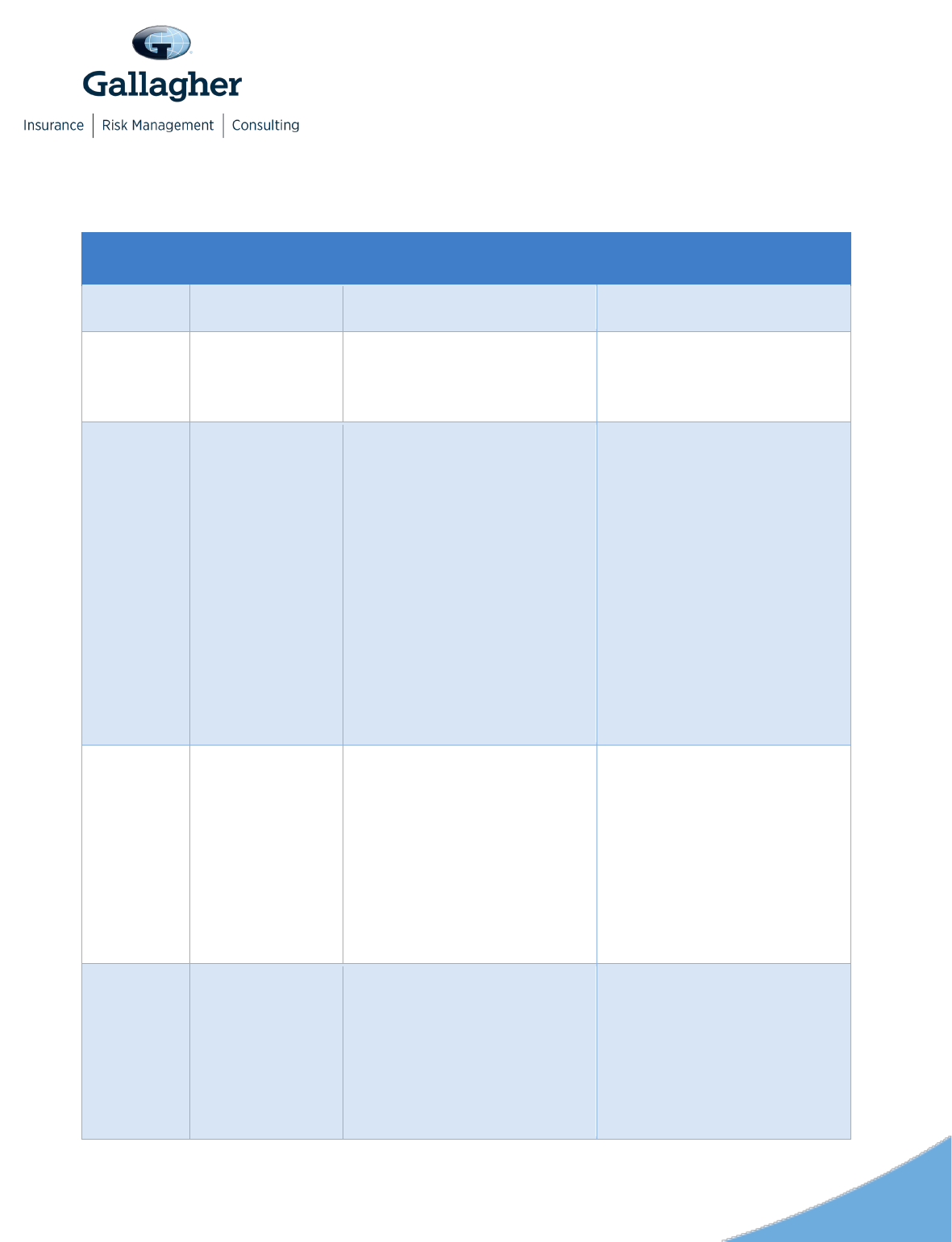
Applicable
Law
Notice
ERISA Consent
Requirements
Non-ERISA Consent
Requirements
with worksite access to
electronic materials.
Self-insured
non-federal
government plan
HIPAA Opt-Out
Election Notice
Not applicable to ERISA
plans.
Notices may be sent via
email if ERISA disclosure
rules are satisfied.
Notice of Privacy
Practices and
Reminder
Prior consent required for all
recipients. Notice may only
be distributed via email when
distributing electronically.
Prior consent required for all
recipients. Notice may only
be distributed via email when
distributing electronically.
IRS
Forms
1095-B or -C
May be provide electronically
if employee has consented
electronically and not
withdrawn the consent before
the statement is furnished.
The consent may be provided
via paper provided the
employee confirms consent
electronically in a way that
shows that the employee can
access the Form in the
electronic format in which it
will be furnished.
Same rules apply for non-
ERISA plans. See column to
the left for specific rules.
Evergreen
cafeteria plan
election notice
Prior consent not required for
those with effective access to
electronic materials
Prior consent only required
for individuals without
effective access to electronic
materials.
The consent may be provided
via paper provided the
employer confirms consent
electronically in a way that
shows that the employee can
access the Form in the
Same rules apply to non-
ERISA plans. See column to
the left for specific rules.
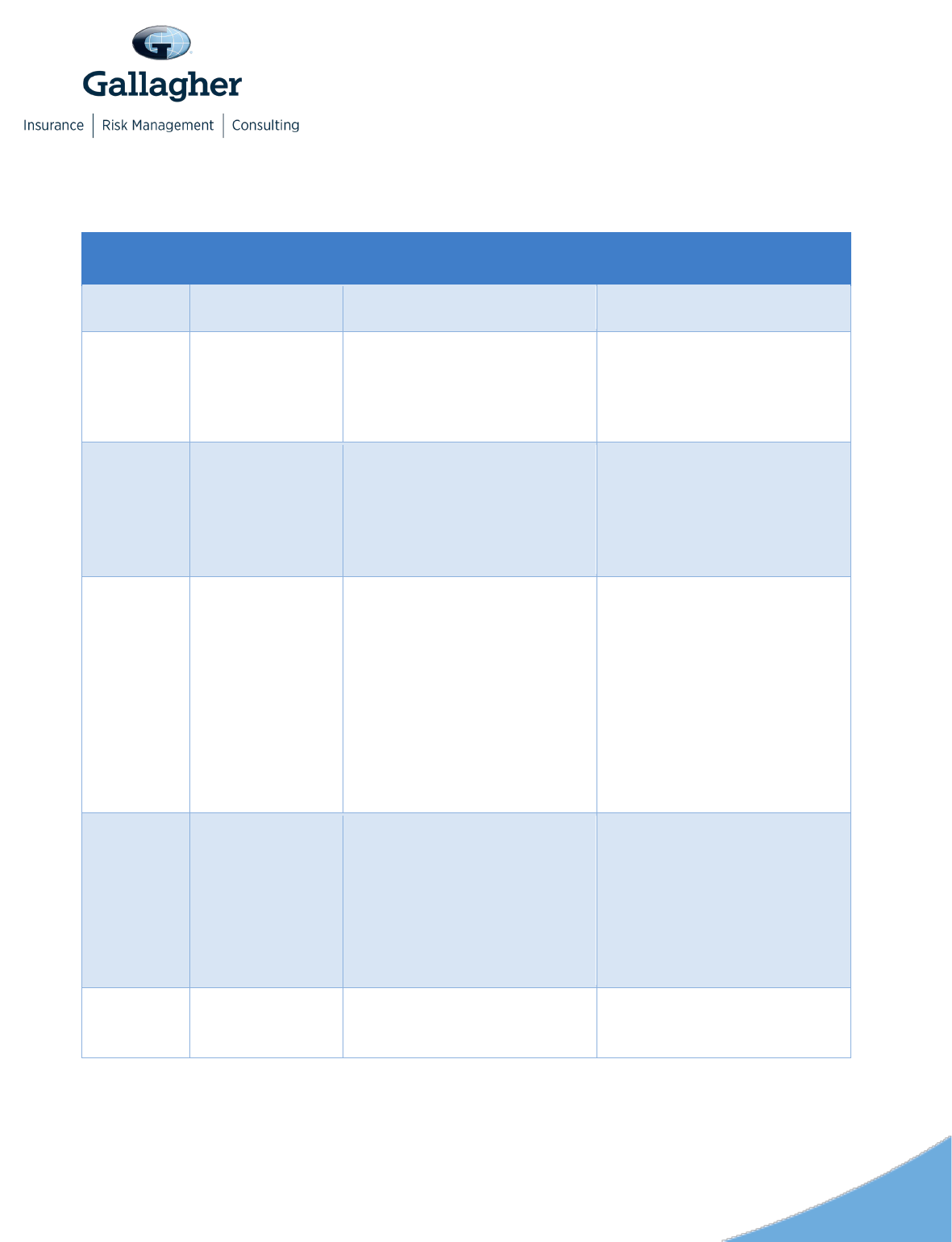
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
5
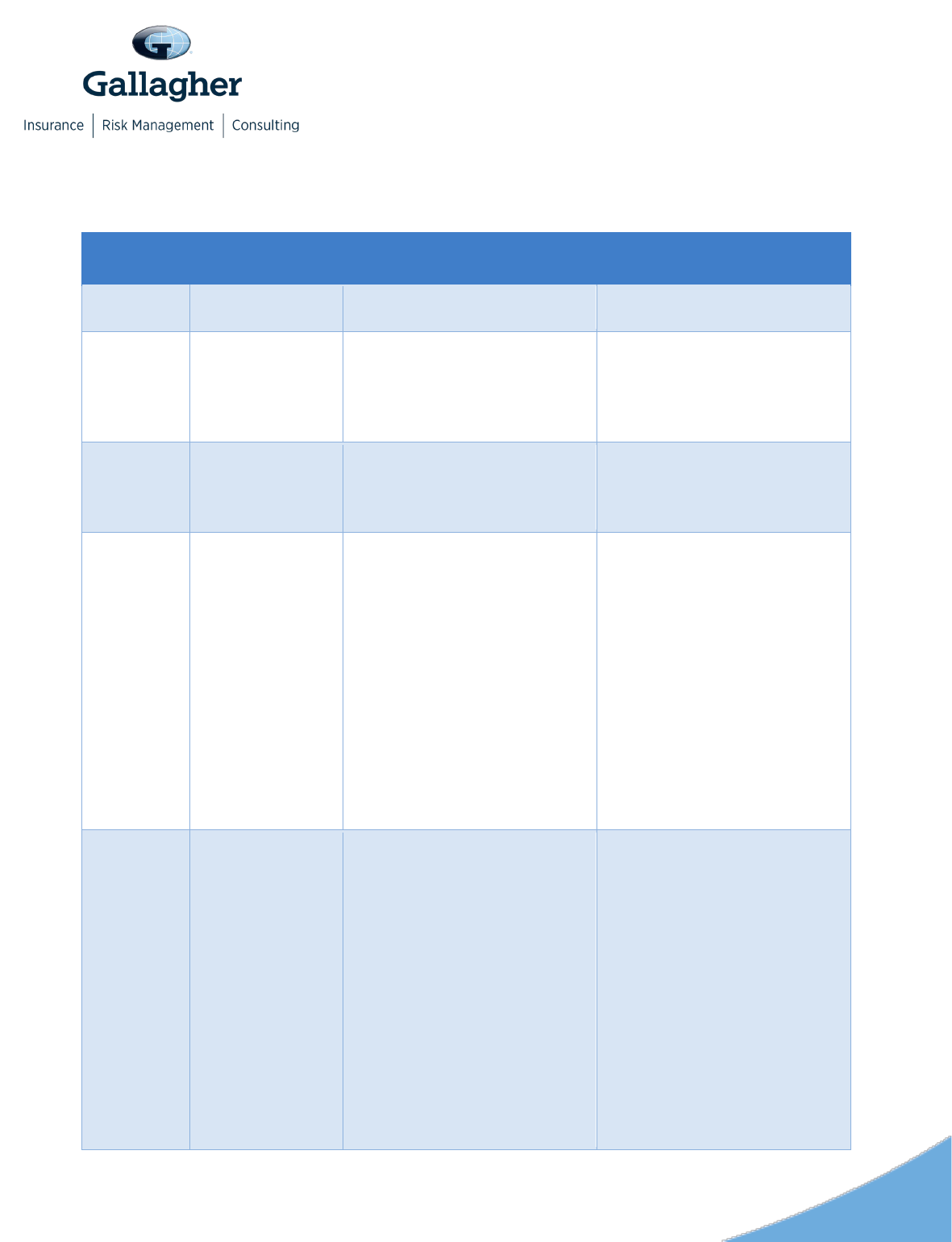
Applicable
Law
Notice
ERISA Consent
Requirements
Non-ERISA Consent
Requirements
electronic format in which it
will be furnished.
Other
Notices
Part D
Certificate of
Creditable (or
Non-Creditable)
Coverage
May be sent electronically
using the ERISA disclosure
rules.
Non-ERISA plans may use
the ERISA rules.
Michelle’s Law
May be sent electronically
using the ERISA disclosure
rules.
Limited applicability. See
Michelle’s Law section below.
Non-ERISA plans may use
the ERISA rules.
Limited applicability. See
Michelle’s Law section below.
Wellness
Program notices
required by
HIPAA/ACA,
ADA, & GINA
HIPAA/ACA Notice: ERISA
plans may use the ERISA
disclosure rules.
ADA & GINA Notices: may be
sent electronically in any
format that will be effective in
reaching employees. Email
may be used if the subject
line refers to the wellness
program.
HIPAA/ACA Notice: non-
ERISA plans may use the
ERISA disclosure rules.
ADA & GINA Notices: may be
sent electronically in any
format that will be effective in
reaching employees. Email
may be used if the subject
line refers to the wellness
program.
Newborns’ and
Mothers’ Health
Protection Act
Disclosure
Plans subject to ERISA will
generally include the
Newborns’ and Mothers’
Health Protection Act notice
in their SPDs.
ERISA plans should follow
the ERISA disclosure rules.
Non-ERISA plans will provide
the notice in their plan
documents.
Plans may follow the ERISA
disclosure rules.
Women’s Health
and Cancer
Rights Act
ERISA plans should follow
the ERISA disclosure rules.
Non-ERISA plans may use
ERISA disclosure rules.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
6
Requirements by Type of Notice
ERISA
Information that needs to be provided to newly eligible employees (returning employees
and newly hired employees) includes:
•
A Summary Plan Description (SPD) – or comparable document for non-ERISA plans
– for health and welfare and cafeteria plans
• Summaries of Material Modification (SMMs) or Material Reduction (SMRs) that have
not been incorporated into an SPD, and
• Summary Annual Report (SAR) for insured and funded plans required to file Form
5500
There are additional notices required by ERISA, such as a HIPAA special enrollment
rights notice, a CHIP notice, and the Women’s Health and Cancer Right Act Notice.
These notices are also required for non-ERISA plans and are discussed below. Each
section indicates which notices are subject to the ERISA disclosure rules.
The SPD must be provided within 90 days for newly covered participants and within 120
days for new plans. Updated SPDs are also required every five years if material
changes are made, or within 10 years if no material changes are made.
An SMM is provided within 210 days after the plan year in which a material modification
occurs. An SMR is required for material reductions to the plan and must be provided
within 60 days after the plan sponsor amends the plan. There is no model form for the
SMM or SMR, so employers are generally free to choose the content of those notices.
As a best practice, the notice should communicate what plan is affected by the change,
when the change is effective, a contact information for questions, and that the SMM or
SMR should be kept with the most recently issued SPD to provide a complete summary
of the plan. Practically, it is typically easier to align changes with annual enrollment and
use the annual enrollment guide as the SMM or SMR by inserting language in the
annual enrollment guide that designates it as an SMM or SMR.
Applies to: private employers, including for profit and non-profit (e.g., corporations,
S-Corporations, LLCs, etc.) that sponsor health or welfare benefits for their
employees and electing church plans (i.e., church plans that have made an IRC
410(d) election to be subject to ERISA).
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
7
The SAR must be provided to participants if the employer has a plan that is insured or
funded and is required to file Form 5500. Self-insured health and welfare plans with 100
or more participants on the first day of the plan year are required to file Form 5500, but
are not required to provide an SAR. The content that must be included in the SAR is
provided in the Department of Labor (DOL) SAR template.
Employers may also distribute additional materials such as enrollment guides or
workbooks used to help employees understand the employers’ plans and make benefit
selections.
Given the complexities involved in using different methods for different types of notices,
many employers (including those not subject to ERISA) use the ERISA requirements for
electronic disclosure for the majority of their notices. Employers who use this approach
will want to make sure that they are complying with all of the requirements for the
ERISA requirements for electronic disclosure, which can be burdensome.
For individuals who do not have worksite access, the ERISA requirements provide that
the individual must consent in a manner intended to demonstrate the individual’s ability
to access the materials. While individuals may be willing to provide their personal email
address to receive the materials, employers often find that many employees do not
consent in a manner that demonstrates the individual’s ability to access information in
the electronic format used thereby causing the delivery to fail to satisfy all of the
electronic disclosure requirements.
Employers have found the following approaches to be useful for some of their
employees who do not have worksite access.
• Requesting consent when employees are newly hired. Some employers have
addressed this challenge by asking individuals to consent when they are newly hired
as employees, as they are more likely to consent in a manner that demonstrates the
individual's ability to access information in the electronic form that will be used.
• Requesting consent as part of open enrollment. Employers can often increase
the number of employees who can be provided materials electronically by requesting
consent annually as part of open enrollment for those who have not previously
consented in accordance with the requirements.
• Providing materials in person. As an alternative to electronic disclosures, some
employers bring copies of the required notices to in-person open enrollment
meetings. Employees are provided with the materials and sign an acknowledgment
that the materials have been provided to them. Employees who do not wish to retain
these materials often leave them at the meetings and employers can provide these
paper copies to other employees. Under this approach, employers will typically also

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
8
have these materials available electronically and also provide them to employees
who request them in the future.
Please note that the following approaches do not satisfy the ERISA requirements
unless additional conditions are satisfied.
• Posting materials on a company website or in a benefits administration system.
Under this approach, the employer must also notify employees that the materials are
available. If the employees do not have worksite access, the employer would also
need the employee’s consent for electronic distribution.
• Sending a postcard with a link to a company website or benefits administration
system.
• Putting materials in a break room for employees to take if wanted.
• Having materials available at open enrollment meetings (unless the conditions
described above are satisfied).
• Having a kiosk where employees can print materials.
Given the challenges that can arise with electronic distributions of materials, employers
will want to work closely with their consultants to make sure that they are satisfying all of
the requirements.
For plans subject to ERISA, the DOL guidelines specify how plan materials may be
distributed electronically. In general, electronic disclosures must satisfy four general
requirements:
• The plan must use reasonable measures to insure receipt of the materials, such as
an automatic notice of non-delivery from an email system or periodic surveys to
confirm receipt.
• The style, format, and contents requirements for ERISA disclosures applies.
• Paper copies of the documents must be available upon request, generally at no
charge.
• The plan must take reasonable and appropriate steps to safeguard the
confidentiality of the information when a disclosure includes personal information
relating to an employee’s accounts and benefits.
The DOL regulations contain different requirements for distributing materials to
individuals who have worksite access to electronic materials, and others who do not
have worksite access, as well as a safe harbor for use of the employer’s website.
Below, we address each set of rules.

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
9
Individuals with Worksite Access may receive ERISA notices without
providing prior consent
Documents may be provided electronically automatically (i.e., without prior consent) to
an employee who regularly accesses the employer’s electronic system as an integral
part of the employee’s job. Access may be an employer’s worksite, or it may be from
home for workers who telework.
To determine whether individuals have worksite access, employers should consider: (1)
the individual’s ability to access documents at any location where he or she is
reasonably expected to perform job duties; (2) the frequency with which an individual
uses a computer to perform his or her daily job duties; and (3) the likelihood an
individual would be able to access documents if provided electronically. Traditionally,
workers such as assembly line workers or cashiers would likely not have worksite
access. Workers who report to an employer’s office regularly and use their computers to
access the employer’s electronic system on a daily basis generally have access.
Recent changes in the way employers conduct business may result in fewer employees
with worksite access. Some employees who reported to a worksite where they had
regular computer access may not be able to go to their worksites. Others may be
working remotely such as from home, but may only be able connect with work via phone
or email using their home computers. In other cases, the employer may have enabled
more employees to telework and as a result, more employees have regular, albeit
remote, access to the employer’s electronic system.
So long as an employee has worksite access as described above, then an employer
may disclose appropriate notices electronically without prior consent from the employee.
Individuals without Worksite Access may only receive ERISA notices
after providing consent
Documents may be provided electronically to an individual without worksite access only
if the individual receives a pre-consent statement with specific information, and
affirmatively consents to receiving the electronic material in a manner that demonstrates
the individual’s ability to access information in the electronic form that will be used.
Individuals without worksite access may include the following:
• Employees who do not access the employer’s electronic information system as an
integral part of their job duties – whether from a worksite or teleworking from home;

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
10
• Employees on a leave of absence such as Family Medical Leave Act (FMLA) leave;
• COBRA Qualified Beneficiaries;
• Former employees such as retirees;
• Alternate recipients under Qualified Medical Child Support Orders (QMCSOs); and
• Other individuals covered under the plan who may need to receive an SPD, such as
surviving spouses.
The pre-consent statement may be provided in electronic or non-electronic form;
however, individuals must consent “in a manner that reasonably demonstrates the
individual’s ability to access information in the electronic form that will be used.” For
example, if the employer plans to send electronic material through e-mail, the individual
should consent electronically through email. The pre-consent statement must include all
of the following information:
• The hardware and software requirements for receiving and viewing the material.
• Identification of the documents available with a description of the significance of
those documents.
• A description of the procedures for withdrawing consent with a statement that
consent may be withdrawn at any time.
• The process for updating contact information such as an email address.
• How to obtain a paper copy of the information at no charge.
If there is a change in either the hardware or software requirements that may materially
affect the transmission of the electronic information, the employer must notify
participants about the change in the requirements, remind individuals about their right to
withdraw consent without penalty, and obtain a new consent form using the modified
system.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
11
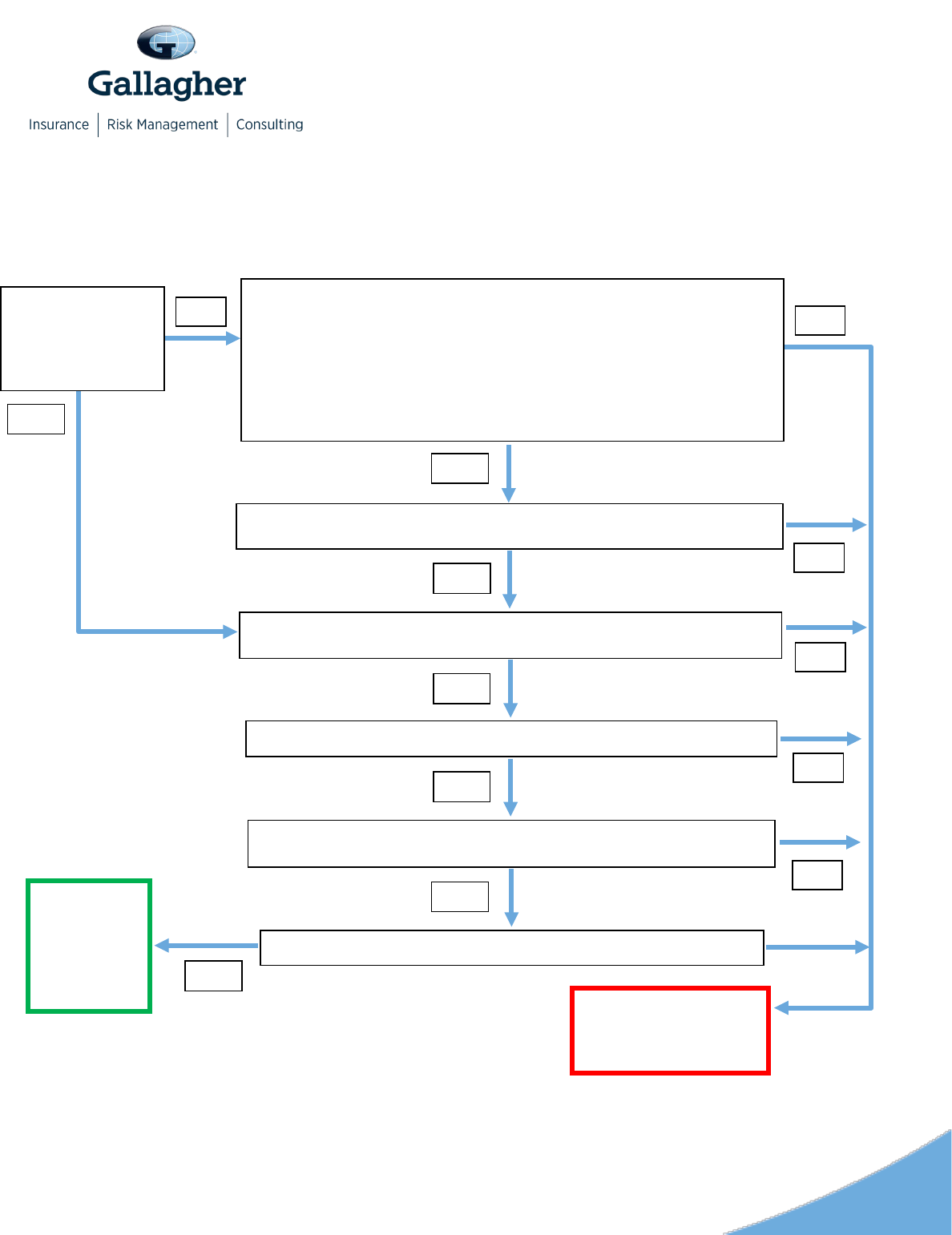
ERISA Requirements for Electronic Disclosure Flow Chart
*The DOL regulations indicate that “actual receipt” could include: (1) Adding a prominent link from the website's homepage to the
separate section that contains the material; (2) Providing directions on the website for how to replace a lost or forgotten password to
the extent one is needed; and/or (3) Maintaining the material on the website for a reasonable period of time following notice to
employees of their availability.
Does the employee
regularly access his or
her employer’s
electronic system as an
integral part of his or her
job?
Has the individual received a pre-consent statement that includes:
• Hardware and software requirements for material;
• Identification of available documents and their significance;
• Description of procedures for withdrawing consent and statement that consent may be
withdrawn at any time;
• Process for updating contact information; and
• How to obtain a paper copy of the information at no charge?
NO
Has the individual affirmatively consented in a manner that reasonably demonstrates the
individual's ability to access information in the electronic form that will be used?
YES
Has the individual been provided with a notice indicating where the material is located, the
nature of the material, and the significance of the information?
YES
Has the employer taken appropriate measures to ensure actual receipt of the material?*
Is a paper copy provided upon request and without charge?
Are the materials prepared and furnished in accordance with all applicable requirements
(e.g., timing and format requirements)?
YES
YES
YES
YES
The information
can be provided
electronically to
this individual in
accordance with
the ERISA
requirements.
YES
The information cannot be
provided electronically to this
individual under the ERISA
requirements.
NO
NO
NO
NO
NO

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
12
Posting on Employer’s Website
Employers can provide ERISA required disclosures on their websites provided that the
four general requirements (e.g., the style, format and contents for ERISA disclosures
applies) listed on page 6 are satisfied, and:
• The individual is provided with a notice indicating where the material is located, the
nature of the material, and the significance of the information. For example, the
employer may send an email or a postcard alerting the participant to the material
that is being posted to the website.
• The employer takes appropriate measures to ensure actual receipt of the material.
• The materials are prepared and furnished in accordance with all applicable
requirements (e.g., timing and format requirements).
• A paper copy is provided upon request and without charge.
The DOL regulations indicate that “actual receipt” could include:
• Adding a prominent link from the website's homepage to the separate section that
contains the material.
• Providing directions on the website for how to replace a lost or forgotten password to
the extent one is needed.
• Maintaining the material on the website for a reasonable period of time following
notice to employees of their availability.
Employers that choose to post material on their websites that may include confidential
information must take additional steps to safeguard any personal information.
The DOL regulations include an example of material contained in a separate section of
an employer’s website, which is easily accessible from the employer’s home page. The
separate section is restricted with access based on the use of either a password or PIN.
However, no formal guidance has been provided on what constitutes adequate
safeguards.
Note: Posting information to a website without also sending a separate notification such
as an email or post-card alerting the participant will not be sufficient. Failure to provide
notice of the posting is similar to just putting materials in a breakroom where they are
available to employees which is not an acceptable method of distributing materials
under the DOL regulations.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
13
Gallagher’s article “Electronic Communication Rules and Sample Language” contains a
description of the rules, sample language, and a sample consent that may be modified
and used when distributing ERISA disclosures electronically. In some cases, an
employer may not be able to provide materials electronically. In those situations,
employers will need to provide paper materials via the U.S. mail.
ACA
With the exception of the Marketplace notices, these notices must be provided when an
employee becomes eligible for the plan and annually. The SSBC must also be provided
when there is a mid-plan year material change that affects the contents of the SBC.
Notices include the following:
• Marketplace notice
• SBC for each medical plan option
• Notice of grandfathered status (if applicable)
• Patient protection notice
• No Surprises Act notice
Marketplace Notice
The Marketplace Notice must be provided by all employers subject to the Fair Labor
Standards Act (FLSA) to all newly hired employees within 14 days of hire. Two model
notices are available; one for employers that offer a medical plan and one for employers
that do not offer a medical plan.
SBC
The SBC must be created using the DOL’s template. The DOL website contains the
template with specific instructions for creating the SBC. For some fully insured plans,
the insurer may create the SBC, but it will generally be the employer that must distribute
the SBC. Employers with self-insured plans must both create and distribute an SBC.
ERISA plans must follow the DOL rules for electronic disclosure of the SBC.
Applies to: all group health plans sponsored by private employers, non-federal
governmental employers, and church plans that are not excepted benefits
1
or
retiree-only plans.

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
14
Non-ERISA plans such as non-federal governmental and church plans may satisfy the
notice requirement by using the ERISA rules. Alternatively, non-federal governmental
plans may satisfy the distribution requirement by following the rules for electronic
disclosure that apply in the individual insurance market.
The SBC must be provided to the participant; separate notices for other family members
are not required unless the plan is aware of the fact that a family member has a different
address.
Grandfathered Notice
For grandfathered medical plans, the notice of grandfathered status must be provided
annually and may be provided in the SPD or similar document for non-ERISA plans.
Sample language is available. In addition, plans that lose grandfathered status must
notify employees that the plan’s grandfathered status has been lost.
Patient Protection Notice
All group health plans must provide a Patient Protection Notice. This notice summarizes
the rules for the selection of a Primary Care Physician (PCP) (including pediatrician)
where designation of a PCP is required by the plan, coverage for routine obstetrical and
gynecological services, and a description of minimum coverage of services in an out-of-
network hospital emergency room. The notice must be provided annually and may be
provided via the SPD (or similar document for non-ERISA plans). The DOL has
provided sample language.
Prior to 2022, only non-grandfathered group health plans were required to provide this
notice.
No Surprises Act Notice
Beginning in plan years on or after January 1, 2022, a group health plan must make
publicly available, post on a public website of the plan, and include in the explanations
of benefit (EOBs) the protections against surprise billing under both the federal No
Surprises Act and any applicable state surprise billing laws. There is no requirement to
disclose this notice annually. A model notice is available.
Electronic Distribution Rules
Marketplace Notice
The Marketplace Notice may be provided electronically as long as the ERISA
requirements for electronic disclosure are satisfied.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
15
Summary of Benefits and Coverage (SBC)
Gallagher has created a summary of the electronic distribution requirements for
providing the SBC, which includes a flowchart and describes separately the rules for
private, non-federal governmental and church plans.
Electronic delivery is permitted for participants who enroll online and for individuals
(employees or family members) who request the SBC online. In either case, the plan
must provide a paper copy if requested. For employees covered under the plan who do
not enroll online, the SBC may be distributed using the ERISA rules for electronic
disclosure. For employees eligible, but not enrolled, the SBC may be provided
electronically if the format used is readily accessible and a paper version is provided
upon request at no charge. In addition, an Internet posting is permitted as long as
employees are notified in a paper form such as a postcard or via email that the material
is available on the Internet along with the Internet address. In all cases, paper copies
must be provided upon request at no charge.
Self-insured non-federal governmental plans may either use the ERISA rules or the
rules required for individual health insurance.
Grandfathered Notice
Grandfathered medical plans subject to ERISA must use the DOL’s rules for electronic
disclosure for distribution of the grandfather plan status notice. Non-ERISA plans may
also use the DOL’s rules.
Patient Protection Notice
Group health plans subject to ERISA must use the DOL’s rules for electronic disclosure.
Non-ERISA plans may also use the DOL’s rules.
No Surprises Act
There is no requirement to individually disclose this notice except on EOBs. Employers
sponsoring group health plans should post the notice on the public website of the plan.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
16
COBRA
The COBRA rules apply to all health coverage including excepted benefits such as
dental, vision, hearing, health FSA, EAP, wellness programs, and onsite clinics. The
primary required notices are:
• General/initial notice
• Election notice
• Notice of unavailability
• Notices of early termination
The COBRA general/initial notice must be distributed to the employee upon enrollment,
or the employee and the employee’s spouse if the spouse is covered. The election
notice or notice of unavailability of COBRA continuation must be provided when the plan
receives a notice of a qualifying event such as termination of employment or divorce.
The notice of early termination of COBRA coverage must be sent if coverage will be
terminated before the end of the 18, 29, or 36 month maximum period. Model
general/initial and election notices are available on the DOL’s website. The DOL has not
provided samples for the other two notices. However, Gallagher has sample language
that you may wish to use.
Electronic Distribution Rules
For all plans subject to ERISA, COBRA notices may be sent electronically using the
DOL’s rules described earlier. Non-ERISA plans may also use those rules.
While allowed, electronic distribution may be problematic. For example, the initial
COBRA notice must be provided to the employee and, if enrolled, to the spouse. In
many cases, the employer can provide the initial notice to the employee using the
employer’s email system or intranet, but will not be able to provide the notice to the
employee’s spouse using the same system. The employer would need to provide a pre-
consent notice and obtain an electronic consent from the spouse to use electronic
delivery. When there is a qualifying event, the plan must provide an election notice to
each qualified beneficiary. Providing election notices to other COBRA qualified
beneficiaries, such as the employee’s spouse and any adult dependents, would also
require following the electronic notice and consent rules for each qualified beneficiary.
Applies to: all group health plans sponsored by private and public employers that
have at least 20 employees. Church plans are exempt from COBRA.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
17
Provision of the election notice using the employer’s intranet or email may not work
where the qualifying event is the termination of employment. Sending an election notice
to the employee under other circumstances – such as a loss of coverage when the
employee’s hours are reduced – may be feasible.
HIPAA Portability
HIPAA portability regulations contain several requirements applicable to medical plans
including special enrollment rights for employees in the event of marriage, birth, or
adoption (including placement) of a child, loss of other medical coverage, gain of
eligibility for premium assistance under Medicaid or CHIP, or loss of eligibility under
Medicaid or CHIP. HIPAA Privacy regulations contain specific rules designed to protect
the privacy of an employee and beneficiary’s protected health information (PHI). PHI
includes the employee’s (or a beneficiary’s) individually identifiable health information
that is received, maintained, or transmitted by a health plan.
HIPAA rules require employers sponsoring medical plans (portability rules) to provide
the following notices to employees enrolled in the plan:
• Children’s Health Insurance Program Reauthorization Act (CHIP)
• HIPAA Special Enrollment Rights
• HIPAA Opt-Out Election Notice (Self-insured non-federal governmental plans only)
CHIP
The CHIP notice provides contact information for State Children’s Health Insurance
Program in the employee’s state. Employers must provide this notice to employees
eligible for their medical plan on an annual basis. A model notice, which is available on
the DOL’s website, is updated annually.
Special Enrollment Rights
Employers are required to provide employees with a notice explaining their HIPAA
special enrollment rights in the event of marriage, birth or adoption (including
placement) of a child, the loss of other medical coverage, gain of premium assistance
under Medicaid or CHIP, or loss of eligibility under Medicaid or CHIP.. Employees must
Applies to: all group health plans that are not excepted benefits or a retiree-only
plan. Self-insured, non-federal governmental plans that choose to opt-out of certain
HIPAA portability requirements use the Self-Insured Non-Federal Governmental
Plan HIPAA Opt-Out Election Notice below.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
18
be given a notice when they first become eligible to enroll in the medical plan.
Appropriate language must also be contained in an ERISA plan’s SPD (or similar
document for non-ERISA plans). Sample language is available.
Self-Insured Non-Federal Governmental Plan Opt-Out Election Notice
Self-insured medical plans sponsored by non-federal governmental employers are
permitted to opt-out of several of HIPAA’s portability requirements.
1
However, in order to
make an election to opt-out the plan must notify the Consumer Information and
Insurance Oversight (CCIIO), which is part of the Centers for Medicare and Medicaid
Services, and plan participants both when the election is made and on an annual basis.
Gallagher has a page dedicated to the Self-Insured Non-Federal Governmental Plan
Opt-Out.
The employer must provide initial and annual notices before the first day of the plan
year to which the election applies. The notice should be provided to enrollees and
identify the provisions for which the plan is electing the exemption, that the federal law
provides the right to elect an exemption and that the plan has elected the exemption,
identify which parts of the plan are subject to the election, and identify which provisions
continue to apply to the plan. A model notice is available. The plan will be in compliance
if it prints the notice prominently in a benefits summary provided at the time of
enrollment and annually.
Electronic Distribution Rules
CHIP and HIPAA special enrollment right notices may be provided electronically. Plans
subject to ERISA need to follow the DOL’s requirements for electronic distribution
discussed earlier. Non-ERISA plans may also choose to use those rules.
Non-federal governmental employers with self-insured medical plans that have elected
to opt-out of one or more of the HIPAA portability requirements may notify affected
enrollees electronically via email if the CCIIO’s requirements for electronic distribution
are satisfied. Initial notices must be provided prior to the first day of the plan year, and
renewal notices must be provided no later than the last day of each plan year. A model
notice is available.
1
These plans may opt out of the requirements under the Mental Health Parity and Addiction Equity Act, Michelle’s
Law, the Women’s Health and Cancer Rights Act, and the Newborns’ and Mothers’ Health Protection Act.

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
19
HIPAA Privacy Notices
Health plans are required to provide the following privacy notices:
• Notice of Privacy Practices
• Notice of the availability of the Notice of Privacy Practices
Employers with self-insured health plans, and insured health plans with access to PHI,
must distribute a Notice of Privacy Practices (NPP) to employees when they enroll in
any of the employer’s health plans. The NPP describes how the plan may use and
disclose PHI and includes information about the plan’s legal obligation to safeguard
employees’ (and other covered individuals’) PHI. Every three years the employer must
provide a notice to covered employees about the availability of the NPP. Finally, the
employer must provide a new NPP when the contents of the NPP have been changed.
Electronic Distribution Rules
The NPP may be provided electronically via email if (and only if) the employee has
agreed to receive the notice electronically and the agreement has not been withdrawn
before the NPP is sent. Note that the NPP may only be distributed via email. It is not
sufficient simply to post a copy of the NPP on an electronic enrollment portal or link to
the NPP from an enrollment platform landing page. The NPP or a link to the NPP must
be provided via email.
If the plan knows that the email transmission did not reach the employee, the plan must
provide a paper copy to the employee. The NPP does not have to be provided as a
separate document; it may be included with other materials such as an SPD or
enrollment materials, but if it is provided electronically with those materials, the prior
consent standard must be met. If the health plan has a website, the NPP must be
posted on the health plan’s website. If the employer maintains a website for its
business, it does not have to post the NPP on that site. Gallagher created a sample
consent form that may be modified, as appropriate, and used to obtain consent to
provide the HIPAA NPP electronically.
Applies to: all health plans, with an exception for self-administered plans with less
than 50 participants
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
20
IRS Required Forms and Notice
Several types of IRS Notices are not necessarily required when an employee first
enrolls in benefits, but for purposes of easing an employer’s administrative burdens, the
employer may wish to obtain consent to provide those notices electronically in
conjunction with enrollment for the following categories of notices:
• Forms 1095 (coverage and/or offers of coverage)
• Evergreen election notice under a cafeteria plan
Forms 1095-B and 1095-C
Employers that are applicable large employers subject to ACA’s Employer Mandate and
employers with self-insured medical plans must provide Forms 1095, which may be
either statements of self-insured medical coverage provided to employees and family
members or statements about offers of coverage to full-time employees (Forms 1095-B
or 1095-C). Statements for the previous calendar year must be provided by January 31
of the subsequent year. Beginning with tax years beginning after December 31, 2020,
proposed regulations an automatic 30-day extension, requiring the notice to be provided
by March 2 of each year.
Cafeteria Plan Evergreen Election Notice
Some cafeteria plans are limited to pre-tax employee contributions for coverage under a
single plan. Employers offering these plans may not have a formal annual enrollment.
Once an employee makes his or her choice, that election remains in effect until the
employee affirmatively changes it – often called an “evergreen” election. For cafeteria
plans that use an evergreen election, IRS rules require that the employer distribute a
notice to employees annually advising employees of their right to make an election
change.
Electronic Distribution Rules
Employers may furnish copies of statements – Forms 1095-B or 1095-C – electronically
if the employee consents to electronic distribution. The employer must obtain the
employee’s consent in a way that demonstrates that the employee can effectively
access the statement. Gallagher has created a sample procedure with sample language
that can be used as a starting point to create a compliant procedure.
Applies to: all employers, although variations exist within each type of disclosure.
See below for more detail.

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
21
The required annual notice for cafeteria plans that use an evergreen election may be
provided electronically if the employee has consented electronically. Employee consent
is not required if the employee has the effective ability to access the electronic medium
(for example, the employer’s own email system) that will be used to provide the notice.
The electronic confirmation must be accompanied by a statement that the employee
may request a paper copy at no charge.
Employee Consent Requirements
Where employee consent is required, the employee must consent to electronic delivery
and before consenting must be provided with a statement that includes the following:
• The employee has the right to receive the notice in a paper document rather than
electronically.
• The employee still has the right to receive a paper copy after consenting and
receiving the electronic notice. The plan may charge a reasonable fee for the paper
document. The amount of the fee must be disclosed in the pre-consent statement.
• The employee may withdraw consent (to receive any notice electronically) on a
prospective basis.
• The scope of the consent the employee is being asked to provide. For example,
whether the consent is just for this notice, or whether it also applies to future notices.
• Procedures for updating his/her electronic confirmation information (e.g., email
address).
• The hardware and software needed to access and retain the notice.
The employee’s consent to receiving these documents electronically must be obtained
using one of two methods:
• the employee consents electronically in a manner that demonstrates that he or she
can access the material in the electronic medium that will be used to send the
material; or
• the employee consents using a paper document if the employee confirms consent
electronically in a manner that reasonably demonstrates that the employee can
access the electronic confirmation in the electronic format that will be used.
Employee Enrollment in a Cafeteria Plan
In addition, when a plan uses electronic enrollment the following additional requirements
apply:

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
22
• The employee must be able to effectively able to access the electronic medium
being used to make the elections.
• The electronic system must be reasonably designed to prevent any person other
than the employee (or other participant such as a COBRA qualified beneficiary) from
making an election such as by use of a password or PIN.
• The system must give the participant making the election a reasonable opportunity
to review, confirm, modify or rescind the election before it becomes effective.
• The employee must receive a confirmation notice of the election. The confirmation
can be provided electronically or as a paper document. The confirmation must be
delivered within a reasonable period. For example, the participant should have
enough time after receiving the confirmation to correct mistakes.
• The employee must have the right to receive the confirmation in a paper document
rather than electronically.
The employer will need to track participant elections and consolidate the results of both
paper and electronic elections into files – either electronic or paper – and transmit
enrollment data to claim administrators and other vendors, such as Pharmacy Benefit
Managers, who will need to upload the enrollment data into their systems. Human
Resources will also need to share the information with payroll so that salary reduction
(pre-tax) and/or deduction (after-tax) amounts can be entered into the payroll system.
To the extent that an employer is able to conduct enrollment electronically, these final
stages of the enrollment process will be much easier to manage.
Other Required Notices
Several additional notices are required for many, but not all, employers under several
different federal laws. The following notices are required for both ERISA and non-ERISA
plans:
• Part D Certificate of Creditable (or Non-Creditable) Coverage
• Michelle’s Law Notice
2
• Wellness Program notices required by HIPAA/ACA, ADA, and GINA
• Newborns and Mothers Health Protection Act Disclosure (NMHPA)
3
• Women’s Health and Cancer Rights Act
3
2
Non-federal governmental employers with self-insured medical plans may elect to opt out of these requirements
subject to the notice requirements that apply to HIPAA opt-outs. (See HIPAA section for more information.)

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
23
Part D Creditable Coverage Notice
Employers are required to provide a notice to Medicare-eligible employees that
indicates if the employer’s drug plan provides “creditable” coverage (i.e., the coverage is
at least as valuable as Medicare Part D drug coverage) or if the coverage is “non-
creditable.”
This notice must be provided when an employee joins the plan and annually prior to the
beginning of Medicare’s open enrollment period each year. Model notices and
instructions are available on the CMS website.
Michelle’s Law
Michelle’s law requires continuation of health coverage when coverage for children is
based on student status. Under the ACA, medical plans must continue coverage until an
employee’s natural, adopted, step, or foster child attains age 26 and may not require
student status. Some plans may provide coverage beyond age 25, but condition
coverage at older ages on student status. Plans that include a student status
requirement for older children should provide a description of the terms of continuation
coverage available during medically necessary leaves of absence. ERISA employers
should consider including in their SPD and in the plan’s open enrollment materials. No
model notice exists.
Wellness Program Notices
Wellness programs may be subject to rules under HIPAA/ACA, the Americans with
Disabilities Act (ADA), and/or the Genetic Information Nondiscrimination Act (GINA). For
assistance in determining which wellness rules may apply to a particular type of
wellness plan, please see Gallagher’s Flowchart: Navigate Wellness Regulations.
Applies to: employers sponsoring medical plans that include coverage for
prescription drugs
Applies to: group health plans that require school enrollment for dependent
eligibility. Self-insured non-federal governmental plans may opt-out of this
requirement by using the opt-out process and notice as described in the HIPAA
Portability section.
Applies to: employer-sponsored wellness plans that feature certain designs as
described below.
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
24
The HIPAA wellness notice rules apply to all participants in wellness programs that are
related to a health plan or are themselves a health plan. Under HIPAA/ACA rules, a
reasonable alternative standard must be provided for individuals who cannot satisfy a
standard under a health-contingent wellness program. Notice regarding the availability
of a reasonable alternative standard must be disclosed in plan materials such as the
SPD and to individuals who fail to satisfy the standard.
The ADA applies if the wellness program includes disability-related inquiries or medical
exams including biometric testing. The ADA applies only to employees. Sample ADA
language is available.
GINA applies if the wellness program involves genetic information, for example a
wellness program that includes a Health Risk Assessment that asks about family
medical history. GINA applies to all participants. Sample GINA language is available.
Under the EEOC’s rules for ADA and GINA, the notice may be given in any format that
will be effective in reaching employees.
Newborn and Mothers Health Protection Act
The NMHPA requires medical plans to cover minimum hospital stays for delivery of a
child. Employers sponsoring medical plans are required to provide a disclosure of the
NMHPA coverage rights. Sample language is available.
ERISA plans must include this information in the plan’s SPD. Non-ERISA plans are
required to include appropriate language in the plan document.
If a self-insured non-federal governmental plan has opted out of this requirement, a
notice must be provided to participants when an employee enrolls and at each annual
enrollment. (See HIPAA Portability section for more detail) The notice must be printed
prominently in the SPD (or equivalent document) provided at initial and annual
enrollment
Women’s Health and Cancers Rights Act
Applies to: all group health plans. Self-insured non-federal governmental plans
may opt-out of this requirement by using the opt-out process and notice as
described in the HIPAA Portability section.
Applies to: all group health plans. Self-insured non-federal governmental plans
may opt-out of this requirement by using the opt-out process and notice as
described in the HIPAA Portability section.

©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
25
WHCRA requires medical plans to cover breast reconstruction following a mastectomy.
Employers that sponsor medical plans must provide employees with a notice when the
employee enrolls in the medical plan. Sample language is available.
Electronic Distribution Rules
For each of these notices, plans subject to ERISA must use the DOL’s disclosure rules
for these notices. Non-ERISA plans may use the DOL’s disclosure rules.
With regard to the creditable coverage notice, CMS has indicated that it prefers that
these notices be provided in paper format; however, electronic distribution is permitted if
the DOL’s rules for electronic disclosure are satisfied.
For the ADA and GINA wellness notices, EEOC FAQs state that it may be provided in
hard copy or as part of an email as long as the subject lime of the email indicates that
the information being communicated relates to the wellness program. In addition,
employees with a disability may need to have a notice in another format – such as a
large print version for employees with vision impairments. In addition, if notices are
distributed electronically, they should be formatted so that employees who use screen-
reading programs can read them.
Although electronic disclosure is permissible for alternate recipients under a QMCSO or
a NMSN, it may often be impractical. Alternate recipients will not have access to the
employer’s email system or intranet. Materials provided to an alternate recipient will
require a pre-consent notice and consent using the electronic method that will be used
to provide plan and enrollment materials. Employers will need to follow the DOL’s rules
for providing materials to individuals who do not have worksite access. Because the
materials to be provided to alternate recipients are different from those for active
employees, and the rules for providing materials electronically are more complicated
than for active employees, many employers will provide these materials on paper using
U.S. mail.
Employer Action Steps
In the near future, and in some cases for the longer term, employers may need or want
to distribute information about their health and welfare benefits plans electronically.
Employers that have conducted annual enrollments in person or on paper in the past
may want or need to move to an electronic system to the extent possible. Some
employers may be in a position to make this a gradual change. Others may not have
that option, but may need to move to electronic methods now. Employers facing a
change to electronic distribution will want to:
©2020-2022 Arthur J. Gallagher & Co. All rights reserved.
26
• Create a list of materials that will be distributed electronically,
• Identify groups of individuals for whom is it not practical to use electronic disclosure
and determine how materials will be provided,
• Obtain employee consents to provide materials electronically,
• Where feasible obtain consents from other individuals,
• Determine how to provide materials to employees (and others) who do not provide
consent,
• Create the electronic versions of materials to be distributed, and
• Determine to what extent enrollment can be performed electronically.
The intent of this analysis is to provide general information regarding the provisions of current federal
laws and regulation. It does not necessarily fully address all your organization’s specific issues. It should
not be construed as, nor is it intended to provide, legal advice. Your organization’s general counsel or an
attorney who specializes in this practice area should address questions regarding specific issues.
