End of Proclamation & Public
Health Emergency –What Now?
For Adult Family Home Providers
1
Residential Care Services
Aging and Long-Term Support Administration
Learning Objectives
By the end of the presentation, participants will
• Know what rules are reinstated and which continue under emergency
or permanent rule creation after the end of the public health
emergency
• Identify what Infection Prevention and Control (IPC) regulations apply
to the Adult Family Home (AFH) setting
• Understand what to do to comply with AFH IPC regulations
2
Terminology
• CDC - Centers for Disease Control and Prevention
• DOH - Washington State Department of Health
• ICAR - Infection Control Assessment and Response (tools used to systematically
assess a healthcare facility’s IPC practices and guide quality improvement activities)
• IPC - Infection Prevention and Control
• IPC System - a collection of procedures and precautions to prevent the spread of
infection
• LTC QIP – Long-term Care Quality Improvement Program (RCS non-regulatory
program to help providers strengthen care and documentation systems, improve
regulatory compliance, and prevent harm to vulnerable adults in their care
• Source Control - use of well-fitting face coverings, facemasks, or respirators to cover
a person’s mouth and nose to prevent spread of potentially infectious respiratory
secretions when they are breathing, talking, sneezing, or coughing.
3
End of the State of Emergency by October 31
st
, 2022
Washington State
Proclamations & Requirements ending 10/27/2022
• LTC Covid Response Plans are no longer in effect
• Proclamations 20-36, 20-52, 20-65, and 20-66, which waived and
suspended rules and laws in long-term care settings.
• The Washington state vaccine requirement for health care workers ends
• Federal vaccination requirements for NH & ICF/IID continue
• Vaccine requirements remain in place for state employees
4
What Rules Are Reinstated?
No Emergency Rules in Place - Facilities must comply by 10/27/2022
5
Requirement
Resident Rights
- follow local health jurisdiction (LHJ) quarantine or isolation
guidance during outbreak
CPR and first aid training. Facilities must be in compliance with WAC 388
-112A-
0720
Food Handler Permit. Facilities must be in compliance with RCW 70.128.250. New
CE requirements apply
Please review updates to WAC 388-112A and Dear Provider Letter 22-037
GOVERNOR’S PROCLAMATIONS RELATED TO COVID-19 ENDING OCTOBER 27
What Emergency or Permanent Rules Are in Effect?
6
Requirement
Long
-term care worker training, including home care aide certification,
specialty training, and continuing education timelines.
Nursing assistant
– certified training timeline extended for people in an
approved training program based on date of hire.
GOVERNOR’S PROCLAMATIONS RELATED TO COVID-19 ENDING OCTOBER 27
https://www.dshs.wa.gov/sites/default/files/ALTSA/rcs/documents/multiple/022-09-09-1.pdf
What Emergency or Permanent Rules Are in Effect?
7
Requirement
Fingerprint
-based background checks. Long-
term care workers hired after
August 28, 2022, resume the 120
-day timeline to obtain results.
Permanent rules have been adopted that list the criteria used to
reestablish timelines for completing licensing inspections. These rules
went into effect September 11, 2022.
GOVERNOR’S PROCLAMATIONS RELATED TO COVID-19 ENDING OCTOBER 27
https://www.dshs.wa.gov/sites/default/files/ALTSA/rcs/documents/multiple/022-09-09-1.pdf
What Requirements Continue?
A Respiratory Protection Program (RPP) is Required by State and Federal law
when/if respirators are used in the workplace
• OSHA 1910.134 Respiratory Protection
• WAC 296-842 Respirators
NINE Key Requirements of an RPP:
1. Written program with policies & procedures
2. Program Administrator
3. Hazard Evaluation & Respirator Selection
4. Medical Evaluation for Respirator Wearers
5. Fit Testing: Initial, Annual, After Any Physical Changes That Affect Fit
6. Proper Respirator Use, Storage, Maintenance, Repair, Disposal
7. Training
8. Program Evaluation
9. Record Keeping
8
What Requirements Continue?
The Statewide Face Covering Order issued by the state Department of Health
(DOH) will remain in place for health care and long-term care settings. Staff in
long-term care facilities must continue to wear a face covering during resident
care encounters.
Exceptions - Face Coverings Are Not Required:
• While working in areas not generally accessible to the public
• When only employees are present
• But only if the employee is fully vaccinated* against COVID-19
• While working alone
• Isolated from interactions with others
• With little or no expectation of in-person interruptions
9
*The definition of
fully vaccinated
does not include
a COVID-19
booster.
What Requirements Continue?
• Eye protection will still be required in long-term care facilities,
according to CDC and DOH guidance.
• Centers for Disease Control and Prevention (CDC) guidance says that
facilities located in counties where Community Transmission is high should
also consider having HCP use PPE as described below: Eye protection (i.e.,
goggles or a face shield that covers the front and sides of the face) worn
during all patient care encounters.
• Washington State Department of Health (DOH) guidance says to wear eye
protection for all patient / client encounters if facility is in an area with high
Community Transmission
10
NOTE: Community Transmission (Healthcare Guidance) Community Level (Public Guidance)
CDC Data Tracker
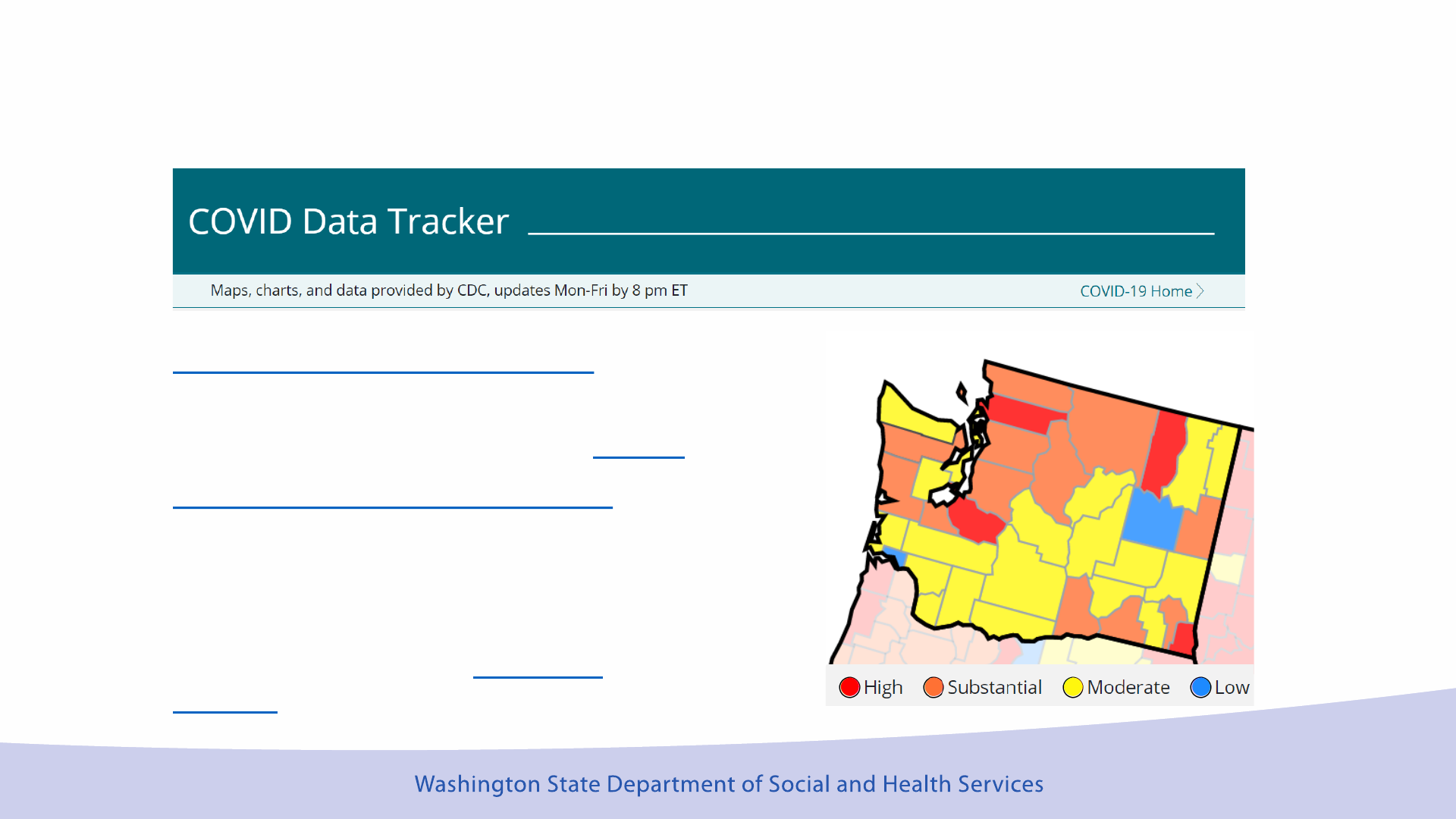
How do I Know the Community Transmission Level?
COVID-19 Community Levels
Determine the impact of COVID-19
on communities and to take action.
COVID-19 Transmission Levels
Describe the amount of COVID-19
spread within each county.
Healthcare facilities use Transmission
Levels to determine infection
control interventions.
11
https://covid.cdc.gov/covid-data-tracker/#datatracker-home
What is a Resident Care Encounter?
Resident Care Encounters Are Defined As:
• in-person, interactions between staff and residents
• when there is less than 6 feet between the staff and resident
• for any period of time.
Encounters May Involve: medical procedures, caregiving activities,
activities of daily living, medication administration, transportation, etc.
NOTE: Passing by a resident in a common area would not be considered a
resident encounter.
12
https://doh.wa.gov/sites/default/files/2022-06/420-391-HealthcareIPCCOVID.pdf
What if
Residents or
Visitors Refuse
to Wear Masks?
Providers should:
1. Follow Centers for Disease Control and Prevention and
Department of Health Source Control Guidance to have
policies, support and education for mask wearing.
• Ensure everyone is aware of the recommendation to wear
masks
• Put up signs and posters reminding staff, residents and
visitors of what to do
• Talk to residents, visitors and families about how masks
protect them
2. Respect Resident Rights
• Follow their process for when a resident refuses care. This
may include counseling, education, enlisting the aid of
family, significant others, and/or ombudsman. Document
efforts to engage the resident in wearing a mask.
• You may NOT require the resident to remain in their room
instead of wearing a mask.
13
Frequently Asked Questions
QUESTION: Does the end of the Public Health Emergency (PHE) mean that
no one has to use eye protection anymore?
ANSWER: Staff in facilities located in counties with high transmission
levels should wear eye protection during all resident encounters.
QUESTION: How do I know the Transmission Level?
ANSWER: Go to the CDC COVID Data Tracker Website and check
“Transmission Levels” NOT “COVID-19 Community Level”
https://covid.cdc.gov/covid-data-tracker/#datatracker-home
QUESTION: Do I have to wear eye protection if I am by myself in the office
or cooking in the kitchen when no residents are around?
ANSWER: No. Eye protection is required when engaged in resident
encounters (in-person interactions between staff & residents/clients, <
6 feet distance, for any length of time). NOTE: eye protection should be
cleaned each time it is taken off, before putting it back on.
14
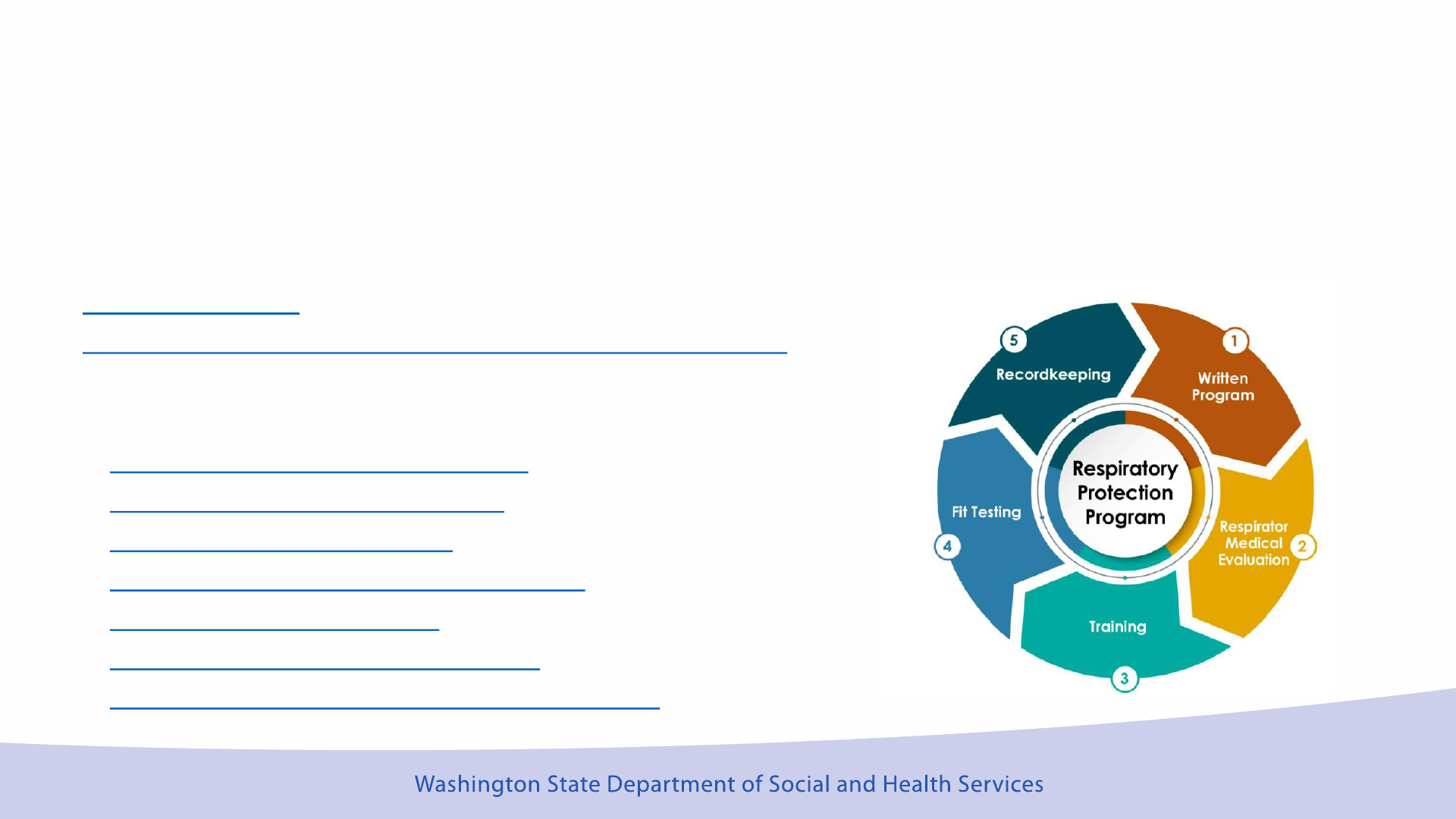
Where Can AFH Providers Get Help With Their RPP?
The Washington State Department of Health Obtained a Grant to Provide RPP
Support to LTC Settings. This includes:
Fit Testing Training
Respiratory Protection Program for Long-Term Care Facilities
• No-Cost for Online Respirator Medical Evaluations
Training program resources
• RPP N95 User Training (PowerPoint)
• N95 Respirator Fit-testing process
• OSHA Respirator Safety video (don, doff, and seal check)
• OSHA Donning and Doffing an N95 video (YouTube, 2:02)
• OSHA User Seal Check video (YouTube, 4:39)
• Facial hair/ facial jewelry guide (PDF)
• A close shave can save (facial hair poster) (PDF)
15
Department of Health Update
16
DOH Updates – Alignment with CDC Guidance
Screening – The AFH must establish a process to make sure everyone entering
the home is aware of what to do to prevent infection spread.
Universal eye protection and AGP. Implement when Community Transmission
levels are high
• N95 respirator in select situations (e.g., AGPs)
• Eye protection during all patient/resident/client care encounters
17
Aerosol Generating Procedures (AGP) are medical procedures that can produce small particles that
another person could breathe in and become infected
Common AGP are CPAP (continuous positive airway pressure) devices for sleep apnea
DOH Updates – Alignment with CDC Guidance
No Quarantine or Work Restriction After COVID-19 Exposure for Staff or
Residents
• Vaccination status does not matter
• If symptoms appear – the person must isolate
After Exposure Do These Things:
• Monitor for symptoms
• Test for COVID-19 on day 1, 3, 5 after exposure
• Wear a mask for 10 days following the exposure
• Prompt isolation or work restriction if symptoms develop or testing is positive for
COVID-19
18
DOH Updates – Different From CDC Guidance
Universal source control (Masks) for everyone in healthcare
settings.
• Masks must cover a person’s mouth and nose to prevent spread of
infection when they are breathing, talking, sneezing, or coughing
• Residents and visitors should wear their own well-fitting mask upon
arrival and throughout their stay in the AFH
• Residents may remove their mask when alone in their rooms but
should put it back on when around others (for example, when
visitors enter their room) or when leaving their room
19
DOH Updates – Different From CDC Guidance
Continue to follow DOH’s Interim recommendation for
SARS-CoV-2 infection prevention and control in healthcare
settings.
• Follow Community Transmission for Infection Control
Measures (not COVID-19 Community Level)
• Cohort and Isolate Residents who have COVID-19
• Everyone wears a mask
20
How Should the DOH Interim Guidance Be Used?
The interim DOH guidance helps you know what to do:
• To Prevent the Spread of COVID-19
• When Different Types of Personal Protective Equipment (PPE)
are Required
• When and How to Use Isolation and Quarantine
• When There are Healthcare Personnel Staffing Shortages
• When and How Often Testing is Needed
• How to Protect Staff During Aerosol Generating Procedures
When You Have Questions – Call Your Local Health
Jurisdiction for Help
http://www.doh.wa.gov/AboutUs/PublicHealthSystem/LocalHealthJurisdictions
21

Frequently Asked Questions
QUESTION: Is active screening (temperature checks, symptom
reporting) required for visitors?
ANSWER: Active screening is not required, but you must have a way to
tell people what to do to prevent the spread of infection in your home.
QUESTION: When is a DOH recommendation a requirement?
ANSWER: Providers must create a safe and healthy environment for
residents to prevent and control the spread of infection. Healthcare
standards and guidance are used so that all (providers, staff, residents,
families, surveyors) know what is to be done using known, established
and evidence-based practice.
QUESTION: When will the “Interim Guidance” go away?
ANSWER: There is not an end or sunset date on Interim COVID-19
guidance. When the Interim guidance is no longer needed, it will be
archived. What will remain is standard IPC practice, like standard
precautions and outbreak management.
22
AFH IPC Regulations
23
What Regulations Apply to Infection Prevention and
Control?
24
Regulation
WAC 388
-76-10255 Infection control.
The adult family home must develop and implement
an infection control system that: (1) Uses nationally recognized infection control standards;
(2) Emphasizes frequent hand washing and other means of limiting the spread of infection;
WAC 388
-76-10400 Care and services. (3) The care and services in a manner and in an
environment that: (b) Actively supports the safety of each resident;
WAC 388
-76-10225 Reporting requirement
. (3) Whenever an outbreak of suspected food
poisoning or communicable disease occurs, the adult family home must notify:
(a) The local public health officer; and
(b) The department's complaint toll
-free hotline number.
What Must Providers Do to Meet Regulations?
WAC 388-76-10255 Infection control.
• Emphasize handwashing and take action to prevent the spread of
infection based on the most current local, federal & state guidance
WAC 388-76-10400 Care and services.
• Provide a safe, clean environment that prevents the spread of infection
WAC 388-76-10225 Reporting requirement.
• Report communicable disease outbreak (infections that spread from one
person to another) to the local health jurisdiction (LHJ) and the
complaint resolution unit (CRU)
25
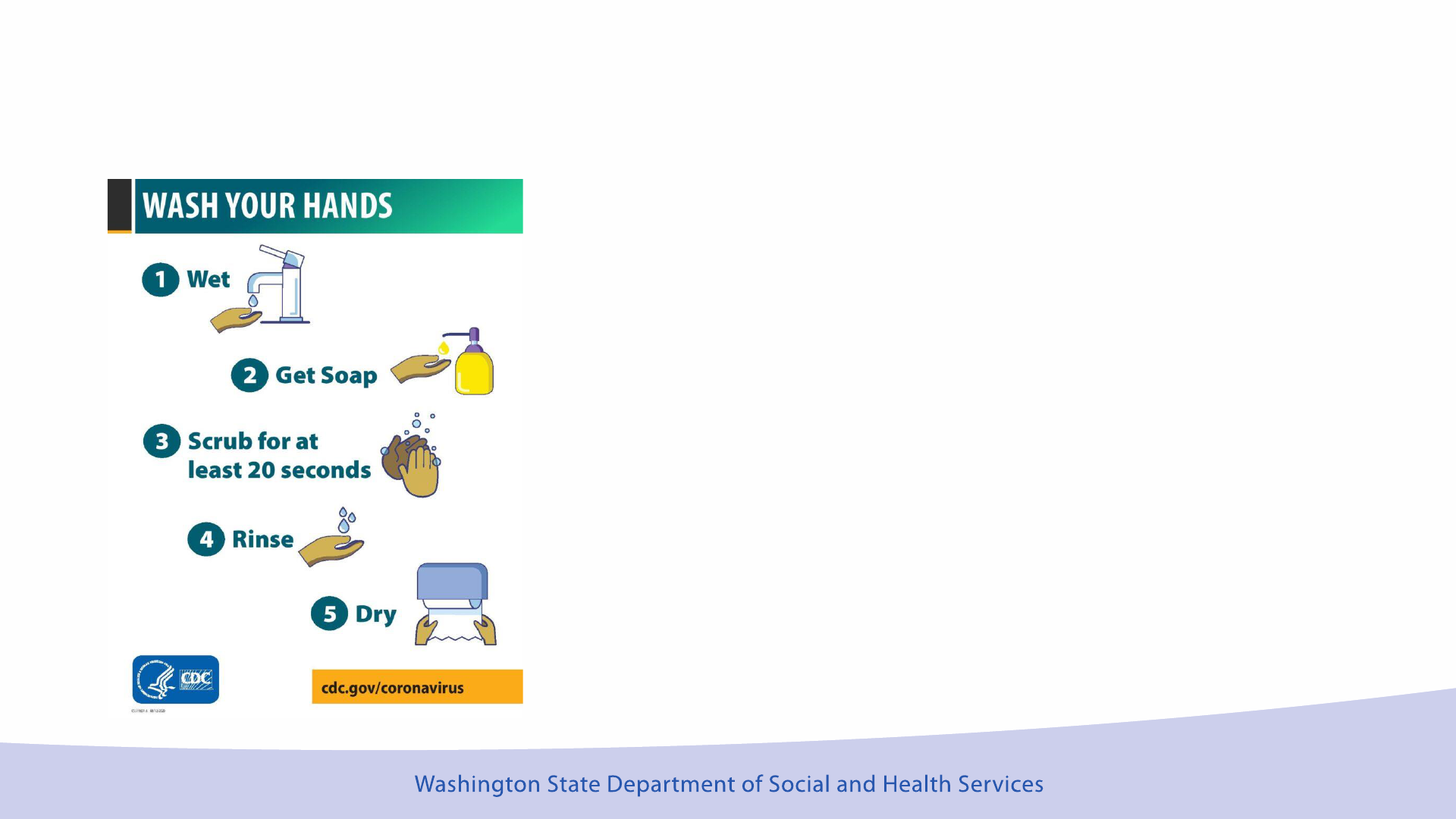
Limiting the Spread of Infection – Wash Hands
Frequent Hand Washing is emphasized
when you:
• Provide readily accessible hand washing
supplies, like alcohol-based hand rub
(ABHR), soap and sinks for hand washing
• Teach your caregivers how to perform
hand hygiene correctly
• Expect hand hygiene between resident
care and before preparing food or
medications
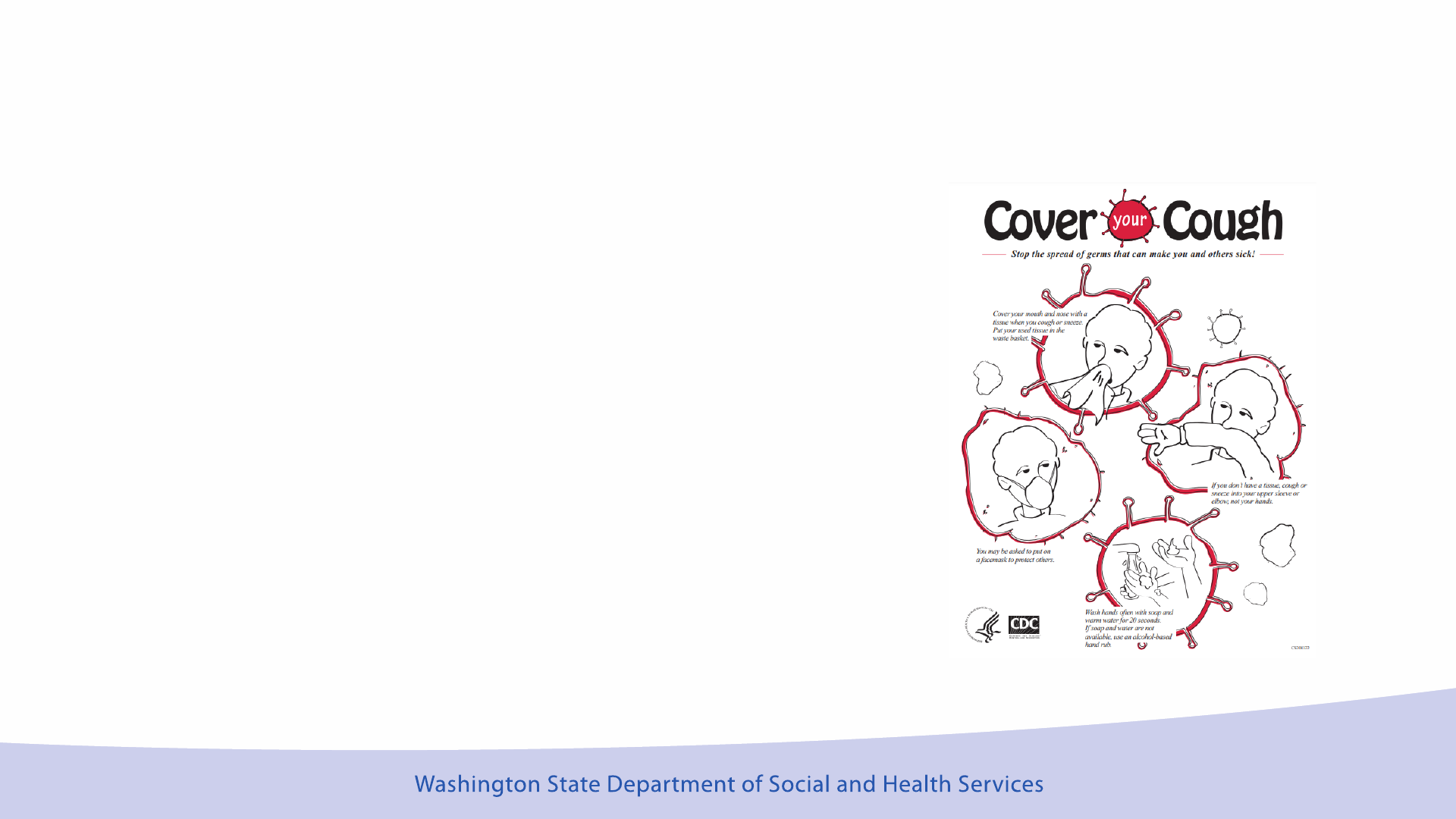
Limiting the Spread of Infection – Other Actions
Other actions that limit the spread of
infection:
• Respiratory Hygiene/Cough Etiquette
• Cleaning High Touch Surfaces With Proper
Cleaning Solution
• Exclusion of ill staff and visitors
• Early recognition and testing of suspected
infection
Nationally Recognized Standards
• Centers for Disease Control and Prevention
(CDC)
• Federal standards and guidance
• National Institute for Occupational Safety and Health
(NIOSH) is responsible for conducting research and
making recommendations for the prevention of work-
related injury and illness.
• Occupational Safety and Health Administration
(OSHA)
• Respiratory Protection Program
• Federal Drug Administration (FDA)
• Personal Protective Equipment (PPE) standards
• Environmental Protection Agency (EPA)
• Cleaning Solution Standards
28

Standard Precautions (CDC)
29
https://www.cdc.gov/infectioncontrol/basics/standard-
precautions.html
Hand hygiene
Use of personal protective equipment (e.g.,
gloves, masks, eyewear)
Respiratory hygiene / cough etiquette
Appropriate resident placement (Isolation)
Clean and Disinfect care equipment and
environment.
Safely handle textiles and laundry
Safe injection practices
Sharps safety (engineering and work practice
controls)

Infection Control System
Standard Precautions for All Resident Care
• Hand Hygiene (cleaning hands between resident
encounters, before preparing food or medications, after
providing personal care)
• Use Personal Protective Equipment (PPE) such as gloves,
gowns, masks if there is possible exposure to infectious
material
• Follow Respiratory hygiene/cough etiquette
• Separate ill residents until they are not contagious
• Environment: (Use proper product, avoid contamination)
• Clean & disinfect care equipment & environment
• Safely handle laundry
• Safe practice for injections & needle disposal
Do not work if ill, do not let employees work if ill
Infection Control System - Ask Yourself
Do I know the nationally recognized infection control standards?
How do I emphasize frequent hand washing in my home?
What do I do to limit the spread of infection in my home?
• Readily available tissues and garbage to dispose of contaminated
tissues?
• Readily available hand hygiene products?
• Regular surface cleaning with products that kill viruses and bacteria?
• Readily available gloves, gowns, masks?
• Do not allow staff or self to work when ill?
How Will Licensors and Complaint Investigators
Determine IPC Regulatory Compliance?
Complaints – RCS Complaint Investigators use the RCS Infection Prevention
and Control (IPC) Assessment when there is a complaint related to disease
transmission.
• Observation Examples: hand hygiene, masks, use of eye protection when
required, cleaning and disinfecting, appropriate use and availability of PPE
• Interview Example: Ask the provider how they know staff are following training
related to hand hygiene, cough etiquette, PPE use, laundry, safe sharps, and
injection practice
Licensors – Every licensing inspection includes review of IPC practice using
the RCS IPC assessment. May cite if IPC concerns are noted during
observation of care or review of practice.
32
Frequently Asked Questions
QUESTION: Why are IPC standards for AFH the same as a Nursing Home?
ANSWER: Nationally recognized IPC standards help prevent the spread
of infection from person to person. Any caregiver in any setting follows
standard precautions.
QUESTION: How will I know if I am meeting the regulation requirements?
ANSWER: Ask yourself “How am I preventing the spread of infection in
my home?” “Do the things I do to prevent the spread of infection align
with Standard Precautions?”
QUESTION: Who can help me improve my IPC system?
ANSWER: Department of Health and RCS LTC Quality Improvement
Program (QIP)
• DOH Respiratory Protection Program Site
• DOH Infection Control Assessment and Response (ICAR) Site
• RCS LTC QIP email RCSQIP@dshs.wa.gov
33
Resources
DOH ICAR Consultation
• Voluntary, Free & Confidential
• IPC Nurse comes to your home
for 1-2 hours
• Focus on your IPC needs and
systems
• Ongoing relationship if desired
To schedule an In-Person or Virtual Visit:
http://doh.wa.gov/ICAR
Contact: HAI-FieldTeam@doh.wa.gov
What to expect on your ICAR for Long Term Care
Facilities (PDF)
34
RCS LTC QIP Consultation
• Voluntary, Free & Confidential
• LTC QIP Nurse visit
• Off site conversation
• On-site visit 1 or more hours
• Follow up virtual visit
• Focus on your IPC goals and
meeting regulatory standards
To request an RCS LTC QIP Visit RCSQIP@dshs.wa.gov
Brochure
References
• Interim Recommendations for SARS-CoV-2 Infection Prevention and Control in Healthcare Settings 2022
https://doh.wa.gov/sites/default/files/2022-06/420-391-SARS-CoV-2-
InfectionPreventionControlHealthcareSettings.pdf
• Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus
Disease 2019 (COVID-19) Pandemic https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-
recommendations.html
• Interim Guidance for Managing Healthcare Personnel with SARS-CoV-2 Infection or Exposure to SARS-CoV-2
https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
• Frequently Asked Questions about COVID-19 Vaccination https://www.cdc.gov/coronavirus/2019-
ncov/vaccines/faq.html
• Secretary_of_Health_Order_20-03_Statewide_Face_Coverings.10-28-2022.pdf
• Respiratory Protection Program for Long-Term Care Facilities https://doh.wa.gov/public-health-healthcare-
providers/healthcare-professions-and-facilities/healthcare-associated-infections/respiratory-protection-program
35