
Washington Apple Health (Medicaid)
Telemedicine
Policy and Billing
January 1, 2023

CPT® codes and descriptions only are copyright 2022 American Medical Association.
2 | Telemedicine Policy and Billing
Disclaimer
Every effort has been made to ensure this document’s accuracy. If an actual or
apparent conflict between this document and a Health Care Authority (HCA) rule
arises, the rule applies.
HCA will update this document on an as-needed basis. Due to the nature of
content change on the internet, we do not fix broken links in past versions of our
documents. If you find a broken link, please check the most recent version of the
document. If this is the most recent version, please notify us at
askmedicaid@hca.wa.gov.
About this document
This publication takes effect January 1, 2023, and supersedes earlier versions.
HCA is committed to providing equal access to our services. If you need an
accommodation or require documents in another format, please call 1-800-562-
3022. People who have hearing or speech disabilities, please call 711 for relay
services.
Washington Apple Health means the public health insurance
programs for eligible Washington residents. Washington Apple
Health is the name used in Washington State for Medicaid, the
children’s health insurance program (CHIP), and state-only
funded health care programs. Washington Apple Health is
administered by the Washington State Health Care Authority.
Note: Refer to Apple Health (Medicaid) program guides on
HCA’s website for program-specific telemedicine policy and
information.
How can I get HCA Apple Health provider documents?
To access provider alerts, go to HCA’s provider alerts webpage.
To access provider documents, go to HCA’s provider billing guides and fee
schedules webpage.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
3 | Telemedicine Policy and Billing
Copyright disclosure
Current Procedural Terminology (CPT) copyright 2022 American Medical
Association (AMA). All rights reserved. CPT® is a registered trademark of the
AMA.
Fee schedules, relative value units, conversion factors and/or related components
are not assigned by the AMA, are not part of CPT, and the AMA is not
recommending their use. The AMA does not directly or indirectly practice
medicine or dispense medical services. The AMA assumes no liability for data
contained or not contained herein.
Further billing guidance
The managed care organizations also have their specific billing instructions at the
links below:
• Molina Healthcare
• Coordinated Care
• United Health Care
• Community Health Plan of Washington
• Amerigroup
Confidentiality toolkit for providers
The Washington State Confidentiality Toolkit for Providers is a resource for
providers required to comply with health care privacy laws. To learn more about
the toolkit, visit the HCA website.
What has changed?
The table below briefly outlines how this publication differs from the previous
one. This table is organized by subject matter. Each item in the Subject column is
a hyperlink that, when clicked, will take you to the specific change summarized in
that row of the table.
Subject Change Reason for Change
Client eligibility Added section To conform to HCA billing
guide publishing
standards and improve
usability
Modifier 95 and
distinguishing
between
facility/nonfacility
Added a box stating that
using modifier 95 and
distinguishing between
facility/nonfacility are not
applicable for behavioral
health providers who use
the guides listed
Not a policy change.
Added to clarify policy.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
4 | Telemedicine Policy and Billing
Table of Contents
Definitions ............................................................................................................................................ 6
Telemedicine ....................................................................................................................................... 7
Introduction to telemedicine .................................................................................................. 7
Best Practices .................................................................................................................................. 7
Resources ......................................................................................................................................... 8
Client Eligibility................................................................................................................................... 9
How do I verify a client’s eligibility? .................................................................................... 9
Are clients enrolled in an HCA-contracted managed care organization (MCO)
eligible? .......................................................................................................................................... 10
Managed care enrollment ..................................................................................................... 11
Checking eligibility ............................................................................................................... 11
Clients’ options to change plans .................................................................................... 12
Clients who are not enrolled in an HCA-contracted managed care plan for
physical health services ...................................................................................................... 12
Integrated managed care (IMC) ..................................................................................... 12
Integrated Apple Health Foster Care (AHFC) ........................................................... 13
Fee-for-service Apple Health Foster Care .................................................................. 13
American Indian/Alaska Native (AI/AN) Clients ..................................................... 13
What if a client has third-party liability (TPL)? ............................................................. 14
Originating and Distant Sites .................................................................................................... 15
Introduction ................................................................................................................................. 15
Documentation requirements .............................................................................................. 15
Originating site ........................................................................................................................... 16
Payment..................................................................................................................................... 16
Billing .......................................................................................................................................... 17
Distant Site ................................................................................................................................... 17
Payment..................................................................................................................................... 17
Billing .......................................................................................................................................... 18
Audio-only telemedicine............................................................................................................. 20
Documentation requirements .............................................................................................. 20
Procedure codes ......................................................................................................................... 20
Billing .............................................................................................................................................. 20
Store and Forward ......................................................................................................................... 22
Requirements .............................................................................................................................. 22
Teledermatology ........................................................................................................................ 23

CPT® codes and descriptions only are copyright 2022 American Medical Association.
5 | Telemedicine Policy and Billing
Payment..................................................................................................................................... 23
Coverage ................................................................................................................................... 23
Billing .......................................................................................................................................... 24

CPT® codes and descriptions only are copyright 2022 American Medical Association.
6 | Telemedicine Policy and Billing
Definitions
This section defines terms used in this document.
Audio-only telemedicine – The delivery of health care services using audio-only
technology, permitting real-time communication between the client at the
originating site and the provider, for the purposes of diagnosis, consultation, or
treatment.
Distant site – The site at which a physician or other licensed provider, delivering
a professional service, is physically located at the time the service is provided
through telemedicine.
Face-to-face – The client could be receiving the care in person or via audio-
visual technology.
Facility – See the Site-of-Service Payment Differential section in HCA’s Physician-
related services/Health care professional services billing guide.
Hospital – A facility licensed under chapter 70.41, 71.12, or 72.23 RCW.
In person – The client and the provider are in the same location.
Medicaid agency or agency – The Washington State Health Care Authority.
Medically necessary – See WAC 182-500-0070.
Nonfacility – See the Site-of-Service Payment Differential section in HCA’s
Physician-related services/Health care professional services billing guide.
Originating site – The physical location of a client receiving health care services
through telemedicine.
Store and forward technology – Use of an asynchronous transmission of a
covered person's medical or behavioral health information from an originating
site to the health care provider at a distant site which results in medical or
behavioral health diagnosis and management of the covered person and does
not include the use of audio-only telephone, facsimile, or email.
Telemedicine – The delivery of health care services using interactive audio and
video technology, permitting real-time communication between the client at the
originating site and the provider, for the purpose of diagnosis, consultation, or
treatment. Telemedicine includes audio-only telemedicine, but does not include
any of the following services:
• Email and facsimile transmissions
• Installation or maintenance of any telecommunication devices or systems
• Purchase, rental, or repair of telemedicine equipment
• Incidental services or communications that are not billed separately, such as
communicating laboratory results

CPT® codes and descriptions only are copyright 2022 American Medical Association.
7 | Telemedicine Policy and Billing
Telemedicine
Introduction to telemedicine
Before 2020, the Health Care Authority (HCA) had been encouraging and
allowing healthcare providers to provide telemedicine options for HCA clients for
several years. In response to the COVID-19 pandemic, HCA, working with Apple
Health (Medicaid) managed care organizations, expanded the use of a variety of
telemedicine technologies to meet the health care needs of clients, families, and
providers. In the health care community, the words telehealth and telemedicine
are often used interchangeably. However, for Apple Health, telemedicine is
defined in a very specific way. See Definitions.
Best Practices
When conducting telemedicine services, it is important to ensure that the
standard of care for telemedicine is the same as that for an in-person visit,
providing the same health care service. Refer to the Department of Health for
requirements from various commissions (e.g., Medical Commission, Nursing
Commission, etc.).
Best practices may include, but are not limited to, the following:
• Consider the client’s resources when deciding the best platform to provide
telemedicine services.
• Test the process and have a back-up plan; connections can be disrupted with
heavy volume. Communicate a back-up plan in the event the technology fails.
• Introduce yourself, including what your credential is and what specialty you
practice. Show a badge when applicable.
• Ask the client their name and verify their identity. Consider requesting a photo
ID when applicable/available.
• Inform clients of your location and obtain the location of clients. Include this
information in documentation.
• Inform the client of how the client can see a clinician in-person in the event of
an emergency or as otherwise needed.
• Inform clients they may want to be in a room or space where privacy can be
preserved during the conversation. Explain that personal health information
may be disclosed.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
8 | Telemedicine Policy and Billing
Resources
There are many resources available for providers to get started with telemedicine.
The following are examples of resources:
• Telehealth Collaborative provider training (required)
• Telemental Health Toolkit from NRTRC
• Washington State Dental Association
• University of Washington Behavioral Health Institute
• Washington state Department of Health
Additionally, many professional societies have telemedicine guidelines that may
provide valuable care-specific information for health care professionals.
Note: Inclusion in the above list does not reflect an endorsement
or verification of complete accuracy by HCA.
CPT® codes and descriptions only are copyright 2022 American Medical Association.
9 | Telemedicine Policy and Billing
Client Eligibility
Most Apple Health clients are enrolled in an HCA-contracted managed care
organization (MCO). This means that Apple Health pays a monthly premium to an
MCO for providing preventative, primary, specialty, and other health services to
Apple Health clients. Clients in managed care must see only providers who are in
their MCO’s provider network, unless prior authorized or to treat urgent or
emergent care. See HCA’s Apple Health managed care webpage for further
details.
It is important to always check a client’s eligibility prior to
providing any services because it affects who will pay for the services.
How do I verify a client’s eligibility?
Check the client’s Services Card or follow the two-step process below to verify
that a client has Apple Health coverage for the date of service and that the
client’s benefit package covers the applicable service. This helps prevent
delivering a service HCA will not pay for.
Verifying eligibility is a two-step process:
Step 1. Verify the patient’s eligibility for Apple Health. For detailed
instructions on verifying a patient’s eligibility for Apple Health,
see the Client Eligibility, Benefit Packages, and Coverage Limits
section in HCA’s ProviderOne Billing and Resource Guide.
If the patient is eligible for Apple Health, proceed to Step 2. If the
patient is not eligible, see the note box below.
Step 2. Verify service coverage under the Apple Health client’s
benefit package. To determine if the requested service is a
covered benefit under the Apple Health client’s benefit package,
see HCA’s Program benefit packages and scope of services
webpage.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
10 | Telemedicine Policy and Billing
Note: Patients who are not Apple Health clients may apply for
health care coverage in one of the following ways:
• Online: Go to Washington Healthplanfinder - select the
"Apply Now" button. For patients age 65 and older or on
Medicare, go to Washington Connections select the “Apply
Now” button.
• Mobile app: Download the WAPlanfinder app – select “sign
in” or “create an account”.
• Phone: Call the Washington Healthplanfinder Customer
Support Center at 1-855-923-4633 or 1-855-627-9604 (TTY).
• Paper: By completing an Application for Health Care
Coverage (HCA 18-001P) form.
To download an HCA form, see HCA’s Free or Low Cost
Health Care, Forms & Publications webpage. Type only the
form number into the Search box (Example: 18-001P). For
patients age 65 and older or on Medicare, complete the
Washington Apple Health Application for Aged, Blind,
Disabled/Long-Term Services and Support (HCA 18-005) form.
• In-person: Local resources who, at no additional cost, can
help you apply for health coverage. See the Health Benefit
Exchange Navigator.
Are clients enrolled in an HCA-contracted managed
care organization (MCO) eligible?
Yes. Most Medicaid-eligible clients are enrolled in one of HCA’s MCOs. For these
clients, managed care enrollment will be displayed on the client benefit inquiry
screen in ProviderOne.
All medical services covered under an HCA-contracted MCO must be obtained
through the MCO’s contracted network. The MCO is responsible for:
• Payment of covered services
• Payment of services referred by a provider participating with the plan to an
outside provider
Note: A client’s enrollment can change monthly. Providers who
are not contracted with the MCO must receive approval from
both the MCO and the client’s primary care provider (PCP) prior
to serving a managed care client.
Send claims to the client’s MCO for payment. Call the client’s MCO to discuss
payment prior to providing the service. Providers may bill clients only in very
limited situations as described in WAC 182-502-0160.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
11 | Telemedicine Policy and Billing
Note: HCA continues to pay for the following through fee-for-
service (FFS):
- Professional fees for dental procedures using CDT® codes
- Professional fees using CPT® codes only when the provider’s
taxonomy starts with 12
See the Dental-Related Services Billing Guide or the Physician-
Related Services/Health Care Professional Services Billing
Guide, or both, for how to bill professional fees.
Managed care enrollment
Most Apple Health (Medicaid) clients are enrolled in HCA-contracted MCO the
same month they are determined eligible for managed care as a new or renewing
client. Some clients may still start their first month of MC eligibility in the FFS
program because their qualification for MC enrollment is not established until the
month following their Medicaid eligibility determination. Providers must check
eligibility to determine enrollment for the month of service.
New clients are those initially applying for benefits or those with changes in their
existing eligibility program that consequently make them eligible for Apple
Health managed care.
Checking eligibility
• Providers must check eligibility and know when a client is enrolled and with
which MCO. For help with enrolling, clients can refer to the Washington
Healthplanfinder’s Get Help Enrolling webpage.
• MCOs have retroactive authorization and notification policies in place. The
provider must know the MCO’s requirements and be compliant with the
MCO’s policies.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
12 | Telemedicine Policy and Billing
Clients’ options to change plans
Clients have a variety of options to change their plan:
• Available to clients with a Washington Healthplanfinder account:
Go to the Washington Healthplanfinder website.
• Available to all Apple Health clients:
o Visit the ProviderOne Client Portal website:
o Call Apple Health Customer Service at 1-800-562-3022. The automated
system is available 24/7.
o Request a change online at ProviderOne Contact Us (this will generate an
email to Apple Health Customer Service). Select the topic “Enroll/Change
Health Plans.”
For online information, direct clients to HCA’s Apple Health Managed Care
webpage.
Clients who are not enrolled in an HCA-contracted
managed care plan for physical health services
Some Medicaid clients do not meet the qualifications for managed care
enrollment. These clients are eligible for services under the fee-for-service (FFS)
Medicaid program. In this situation, each Integrated Managed Care (IMC) plan
will have Behavioral Health Services Only (BHSO) plans available for Apple Health
clients who are not in managed care. The BHSO covers only behavioral health
treatment for those clients. Eligible clients who are not enrolled in an HCA-
contracted managed care plan are automatically enrolled in a BHSO, except for
American Indian/Alaska Native clients. If the client receives Medicaid-covered
services before being automatically enrolled in a BHSO, the FFS Medicaid
program will reimburse providers for the covered services. Some examples of
populations that may be exempt from enrolling into a managed care plan are
Medicare dual-eligible, American Indian/Alaska Native, Adoption support and
Foster Care alumni.
Integrated managed care (IMC)
Clients qualified for enrollment in an integrated managed care plan receive all
physical health services, mental health services, and substance use disorder
treatment through their HCA-contracted managed care organization (MCO).
For full details on integrated managed care, see HCA’s Apple Health Managed
Care webpage and scroll down to “Changes to Apple Health managed care.”
CPT® codes and descriptions only are copyright 2022 American Medical Association.
13 | Telemedicine Policy and Billing
Integrated Apple Health Foster Care (AHFC)
Children and young adults in the Foster Care, Adoption Support and Alumni
programs who are enrolled in Coordinated Care of Washington’s (CCW) Apple
Health Foster Care program receive both medical and behavioral health services
from CCW.
Clients under this program are:
• Under the age of 18 who are in foster care (out of home placement)
• Under the age of 21 who are receiving adoption support
• Age 18-21 years old in extended foster care
• Age 18 to 26 years old who aged out of foster care on or after their 18th
birthday (alumni)
These clients are identified in ProviderOne as
“Coordinated Care Healthy Options Foster Care.”
The Apple Health Customer Services staff can answer general questions about
this program. For specific questions about Adoption Support, Foster Care or
Alumni clients, contact HCA’s Foster Care and Adoption Support (FCAS) Team at
1-800-562-3022, Ext. 15480.
Fee-for-service Apple Health Foster Care
Children and young adults in the fee-for-service Apple Health Foster Care,
Adoption Support and Alumni programs receive behavioral health services
through the regional Behavioral Health Services Organization (BHSO). For details,
see HCA’s Mental Health Services Billing Guide, under How do providers identify
the correct payer?
American Indian/Alaska Native (AI/AN) Clients
American Indian/Alaska Native (AI/AN) clients have two options for Apple
Health coverage:
• Apple Health Managed Care
• Apple Health coverage without a managed care plan (also referred to as fee-
for-service [FFS])
If an AI/AN client does not choose a managed care plan, they will be
automatically enrolled into Apple Health FFS for all their health care services,
including comprehensive behavioral health services. See the Health Care
Authority’s (HCA) American Indian/Alaska Native webpage.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
14 | Telemedicine Policy and Billing
What if a client has third-party liability (TPL)?
If the client has third-party liability (TPL) coverage (excluding Medicare), prior
authorization must be obtained before providing any service requiring prior
authorization. For more information on TPL, refer to HCA’s ProviderOne Billing
and Resource Guide.
CPT® codes and descriptions only are copyright 2022 American Medical Association.
15 | Telemedicine Policy and Billing
Originating and Distant Sites
Introduction
Telemedicine is an interaction between a healthcare provider who is physically
located at the distant site and a client who is physically located at the
originating site. This section provides more information on documentation,
payment, and billing requirements attributed to each type of site.
Documentation requirements
Billing site Documentation requirement
Distant site • Specification of the telehealth modality that was used (e.g.,
visit was conducted via HIPAA-compliant real-time
audio/visual)
• Verification that telemedicine was clinically appropriate for
this service
• Whether any assistive technologies (e.g., electronic
stethoscopes, mobile automatic blood pressure device, etc.)
were used
• The location of the client
• The location of the provider (such as billing office, home,
etc.). Include city/state.
• The names and credentials (e.g., MD, ARNP, PA, etc.) of all
provider personnel involved in the telemedicine visit
• The people who attended the appointment with the client
(family, friend, caregiver)
• The start and end times of the health care service provided
by telemedicine or the duration of service when billing is
based on time
• The consent for care via the modality that was used
Originating
site
• Specification of the telehealth modality that was used (e.g.,
visit was conducted via HIPAA-compliant real-time
audio/visual)
• If there are staff involved in providing the service list the
names and credentials (e.g., MD, ARNP, PA, etc.) of all
provider personnel involved in the telemedicine visit
• Any medical service provided (e.g., vital signs, weight, etc.)
• The start and end times of the health care service provided
by telemedicine

CPT® codes and descriptions only are copyright 2022 American Medical Association.
16 | Telemedicine Policy and Billing
Originating site
Payment
Originating sites that are enrolled with HCA to provide services to HCA clients
and bill HCA may be paid a facility fee for infrastructure and client preparation.
Note:
- An originating site must be located within the continental
United States, Hawaii, District of Columbia, or any United
States territory (e.g., Puerto Rico).
- HCA does not pay an originating site facility fee to the client
in any setting.
Additionally, HCA does not pay an originating site facility fee in the following
situations:
• Audio-only telemedicine
• Store and forward
• If the originating site is:
o The client’s home
o A hospital (inpatient services)
o A skilled nursing facility
o Any location receiving payment for the client’s room and board
o The same entity as the distant site or if the provider is employed by the
same entity as the distant site
CPT® codes and descriptions only are copyright 2022 American Medical Association.
17 | Telemedicine Policy and Billing
Billing
To bill for an originating site facility fee for an eligible service, please use the
appropriate billing codes as listed below:
Originating site Billing
Critical access hospital Use revenue code 0780 on the
same line as HCPCS code Q3014
FQHC or RHC Use HCPCS code Q3014
Home, or location determined appropriate
by the individual receiving service
Not eligible for an originating
site reimbursement
Hospital inpatient Not eligible for an originating
site reimbursement
Hospital outpatient Use revenue code 0780 on the
same line as HCPCS code Q3014
Other setting Use HCPCS code Q3014
Physician or other healthcare professional
office
Use HCPCS code Q3014
Skilled nursing facility Not eligible for an originating
site reimbursement
Distant Site
Payment
HCA reimburses medically necessary covered services through telemedicine when
the service is provided by a Washington Apple Health provider and is within their
scope of practice.
For kidney centers or ambulatory surgery centers to bill, either the client or the
provider must be physically present at the facility at the time the service was
rendered. See 42 CFR 440.90 for rules related to clinic services.
Note: A distant site must be located within the continental
United States, Hawaii, District of Columbia, or any United States
territory (e.g., Puerto Rico).
CPT® codes and descriptions only are copyright 2022 American Medical Association.
18 | Telemedicine Policy and Billing
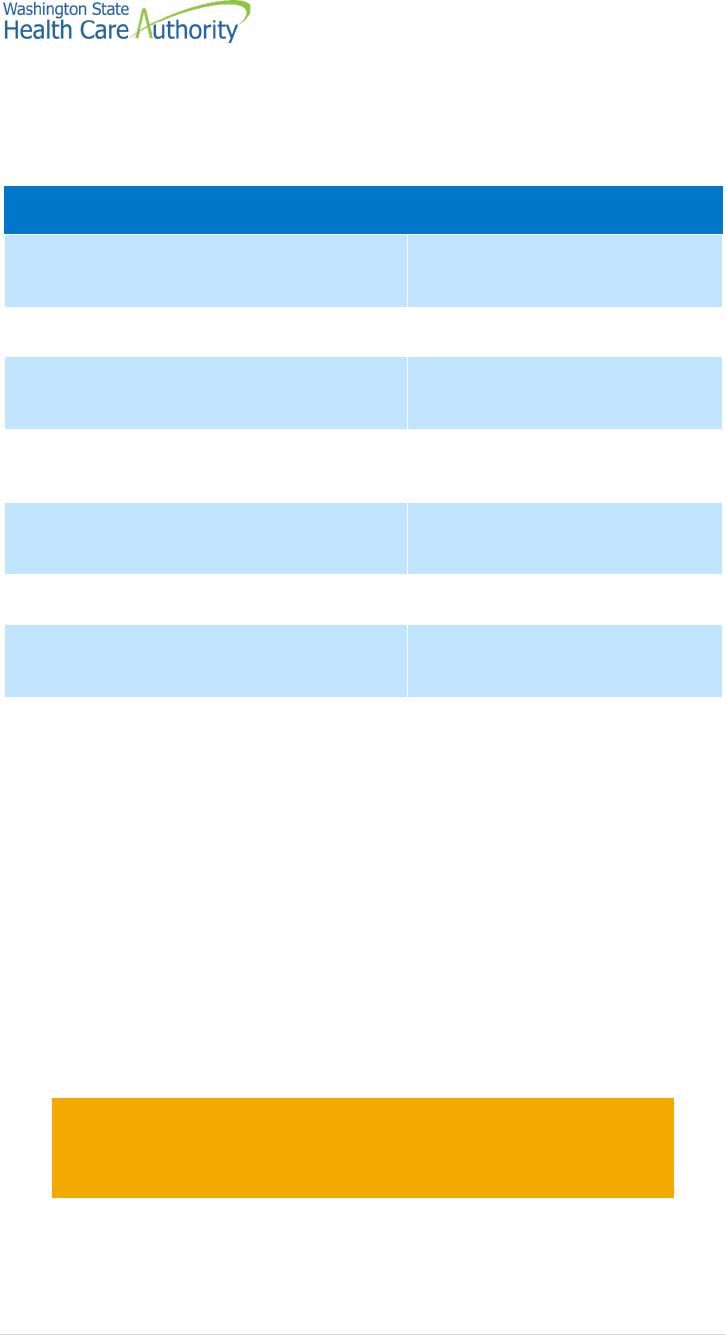
Billing
The payment amount for the professional service provided through telemedicine
by the provider at the distant site is equal to the current fee schedule amount for
the service provided. Submit claims for telemedicine services using the
appropriate CPT® or HCPCS code for the professional service.
Use place of service (POS) 02 or 10 to indicate that a billed service was furnished
as a telemedicine service from a distant site.
Place of
service Description
02 The location where health services and health related services are
provided or received through telecommunication technology.
Patient is not located in their home when receiving health services
or health-related services through telecommunication technology
10 The location where health services and health-related services are
provided or received through telecommunication technology.
Patient is in their home (which is a location other than a hospital or
other facility where the patient receives care in a private residence)
when receiving health services or health-related services through
telecommunication technology.
When billing with POS 02 or 10:
• Add modifier 95 if the distant site is designated as a nonfacility.
• Nonfacility providers must add modifier 95 to the claim to distinguish them
from facility providers and ensure that they receive the nonfacility rate.
Attention licensed behavioral health agencies (BHA)—Using
modifier 95 and distinguishing between facility/nonfacility are
not applicable for behavioral health providers who use the
following guides:
- Service encounter reporting instructions (SERI) guide
- Mental health billing guide (Part 2)
- Substance use disorder (SUD) billing guide

CPT® codes and descriptions only are copyright 2022 American Medical Association.
19 | Telemedicine Policy and Billing
HCA discontinued the use of modifier GT for claims submitted for professional
services (services billed on a CMS-1500 claim form, when submitting paper
claims). Distant site practitioners billing for telemedicine services under the
Critical Access Hospital (CAH) optional payment method must use modifier GT.
See HCA’s ProviderOne Billing and Resource Guide for more information on
submitting claims to HCA. See HCA’s Inpatient Hospital Services Billing Guide for
more information on billing for services under the CAH optional payment
method.
Follow CMS guidance for modifiers if Medicare is the primary insurance.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
20 | Telemedicine Policy and Billing
Audio-only telemedicine
Documentation requirements
In addition to the telemedicine requirements previously noted, providers must
obtain consent before rendering the service per RCWs 74.09.325 and 71.24.335.
Consent must be documented in the client record.
Procedure codes
Refer to HCA’s Provider billing guides and fee schedules webpage, under
Telehealth, for a complete list of audio-only telemedicine procedure codes, under
Audio-only telemedicine.
Billing
HCA requires providers to bill audio-only services with the appropriate audio-
only modifiers (93 or FQ). For services that are partially audio/visual and partially
audio-only, a service is considered audio-only if 50% or more of the service was
provided via audio-only telemedicine.
Modifier Description
93 Synchronous Telemedicine Service Rendered Via Telephone or
Other Real-time Interactive Audio-Only Telecommunications
System: Synchronous telemedicine service is defined as a real-time
interaction between a physician or other qualified health care
professional and a patient who is located away at a distant site
from the physician or other qualified health care professional. The
totality of the communication of information exchanged between
the physician or other qualified health care professional and the
patient during the synchronous telemedicine service must be of an
amount and nature that is sufficient to meet the key components
and/or requirements of the same service when rendered via a face-
to-face interaction.
FQ For counseling and therapy provided using audio-only
telecommunications
CPT® codes and descriptions only are copyright 2022 American Medical Association.
21 | Telemedicine Policy and Billing
Information related to specific service areas and billing guidelines includes the
following:
Billing guide/Resource Modifier
Service Encounter Reporting Instructions (SERI), Substance Use
Disorder (SUD) Billing Guide, and Part II of HCA’s Mental Health
Services Billing Guide
FQ
Part I of HCA’s Mental Health Services Billing Guide 93
All other physical health programs 93
Note: For more information, see the Apple Health (Medicaid)
behavioral health policy and billing during the COVID-19
pandemic (FAQ) under Telehealth on HCA’s Provider billing
guides and fee schedules webpage.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
22 | Telemedicine Policy and Billing
Store and Forward
Store and Forward is the transmission of medical information to be reviewed later
by a physician or practitioner at a distant site. A client’s medical information may
include, but is not limited to, video clips, still images, x-rays, laboratory results,
audio clips, and text. The physician or practitioner at the distant site reviews the
case without the client present.
Requirements
HCA pays for Store and Forward when all the following conditions are met:
• The visit results in a documented care plan that is communicated back to the
referring provider.
• The transmission of protected health information is HIPAA-compliant.
• Written informed consent is obtained from the client that Store and Forward
technology will be used and who the consulting provider is.
If the consultation results in a face-to-face visit in person or via telemedicine with
the specialist within 60 days of the Store and Forward consult, HCA does not pay
for the Store and Forward consultation.
Note: The originating site for Store and Forward is not eligible to
receive an originating site fee.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
23 | Telemedicine Policy and Billing
Teledermatology
Payment
HCA pays for Store and Forward for teledermatology. Teledermatology does not
include single-mode consultations by telephone calls, images transmitted via
facsimile machines, or electronic mail.
Coverage
HCA covers the following procedure codes for teledermatology:
E/M service
CPT® code Short description
99241-99243 Office consultation, new or established patient
99251-99253 Initial inpatient consultation
99211-99214 Office or other outpatient visit
99231-99233 Subsequent hospital care
Note:
- For information related to the public health emergency and
e-consults, see HCA’s Telehealth clinical policy and billing on
HCA’s Provider Billing Guides and Fee Schedules webpage,
under Telehealth.
- Teledermatology requires expedited prior authorization
(EPA) # 870001419.

CPT® codes and descriptions only are copyright 2022 American Medical Association.
24 | Telemedicine Policy and Billing
Billing
Teledermatology services provided via Store and Forward telecommunications
system must be billed with modifier GQ. Bill only the portion(s) rendered from
the distant site with modifier GQ. The sending provider bills as usual with the E/M
and no modifier. The use of modifier GQ does not alter reimbursement for the
CPT® or HCPCS code billed.
You must use POS 02 to indicate the location where health services are provided
through Store and Forward technology. POS 02 code does not apply to the
originating site.
Note: HCA denies claims submitted for Store and Forward
services with POS code 02 if modifier GQ is not included.
HCA may perform a post-pay review on any claim to ensure the above conditions
were met.
