No part of this document may be reproduced or transmitted in any form or by
any means, electronic or mechanical, for any purpose, without the express
written permission of
U.S. Career Institute.
Copyright © 2012-2013, Weston Distance Learning, Inc. All Rights Reserved.
0201693TB01B-43
Acknowledgments
Editorial Staff
Trish Bowen
Elizabeth Munson
Bridget Tisthammer
Kathy DeVault
Georgia Chaney
Brenda Blomberg
Chris Jones
Joyce Jeckewicz
Stephanie MacLeod
Kelly Brown
Carrie Williams
Meloney Biggerstaff
Design/Layout
Connie Hunsader
Leslie Ballentine
Sandy Petersen
D. Brent Hauseman
FOR MORE INFORMATION CONTACT:
U.S. Career Institute
Fort Collins, CO 80525 • 1-800-347-7899
Lesson 1—The World of Health Care
Step 1 Learning Objectives for Lesson 1
Step 2 Lesson Preview
Step 3 Daily Activities in the Medical Office
A Day in the Life of the Medical Office Manager
The Doctor’s Point of View
Step 4 A Little Teamwork Goes a Long Way
Physicians
Nurses
Nurse’s and Physician Assistants
Support Staff
Emergency Personnel
Office Professionals
Step 5 Welcome to Your Career as a Medical Coding Specialist!
But Where Will I Work?
Step 6 Personal Qualities of a Medical Coder
Professionalism
Presentation
Adaptability
Step 7 Medical Records
Parts of a Medical Record
The Flow of Medical Information
Step 8 Lesson Summary
Lesson 2—Medical Insurance
Step 1 Learning Objectives for Lesson 2
Step 2 Lesson Preview
Step 3 The Life Cycle of a Medical Bill
Processing the Bill
Step 4 Insurance
Step 5 Common Insurance Terms
Provider
Claim Form
Deductible
Copayment
Reasonable and Customary
Explanation of Benefits
Electronic Claims
Step 6 Types of Health Insurance
Government Insurance
Private, Traditional Insurance
Managed Care
Blue Cross/Blue Shield
Step 7 Diagnostic Codes—A Piece of the Insurance Puzzle
How Important Is Diagnostic Coding?
Step 8 Procedure Coding—Another Piece of the Puzzle
Step 9 Looking Ahead
Step 10 Lesson Summary
Lesson 3—Introduction to Medical Terminology:
Word Parts
Step 1 Learning Objectives for Lesson 3
Step 2 Lesson Preview
Step 3 Word Parts
Step 4 Root Words
Step 5 Medical Terms
The Combining Vowel
Step 6 Root Words
The Functions of Root Words
Step 7 Pronounce Root Words
Step 8 Write Root Words
Step 9 Meanings of Root Words
Step 10 Prefixes
Step 11 Pronounce Prefixes
Step 12 Write Prefixes
Step 13 Meanings of Prefixes
Step 14 Suffixes
Step 15 Pronounce Suffixes
Step 16 Write Suffixes
Step 17 Meanings of Suffixes
Step 18 Lesson Summary
Just for Fun
Lesson 4—Medical Terminology:
Dividing and Combining Terms
Step 1 Learning Objectives for Lesson 4
Step 2 Lesson Preview
Step 3 Dividing Medical Terms
Consonants, Vowels and the Role They Play
A Little Practice
Word Meanings
Step 4 Pronounce Word Parts
Step 5 Write Word Parts
Step 6 Meanings of Word Parts
Step 7 Combining Medical Terms
Consonants, Vowels and the Role They Play
Step 8 Pronounce Word Parts
Step 9 Write Word Parts
Step 10 Meanings of Word Parts
Step 11 Lesson Summary
Lesson 5—Medical Terminology: Abbreviations,
Symbols and Special Terms
Step 1 Learning Objectives for Lesson 5
Step 2 Lesson Preview
Step 3 Abbreviations
Abbreviations in Hospitals
Office Records
Doctors
Pharmacies
Step 4 Learn Abbreviations
Step 5 Meanings of Abbreviations
Step 6 Slang
Medical Slang
English Slang
Step 7 Slang Terms
Step 8 Meanings of Slang Terms
Step 9 Symbols
Step 10 Special Terms
Eponyms
Brand Names
Acronyms
Step 11 Pronounce Acronyms
Step 12 Sound-Alikes and Opposites
Homophones (Sound-Alikes)
Antonyms (Opposites)
Step 13 Medical Plurals
Medical Rules for Plurals
Step 14 Lesson Summary
Lesson 6—Documenting Medical Records
Step 1 Learning Objectives for Lesson 6
Step 2 Lesson Preview
Step 3 Documentation—The Key Component of Medical Records
Types of Documentation
Commonly Used Narrative Formats
Step 4 The Business of Managing Medical Records
Good Recording Practices
Step 5 Lesson Summary
Lesson 7—Ethics and Legal Issues
Step 1 Learning Objectives for Lesson 7
Step 2 Lesson Preview
Step 3 Confidentiality
Guidelines for Confidentiality of Medical Records
Guidelines for Faxing Medical Records
Step 4 Medical Ethics
Step 5 Health Insurance Portability and Accountability Act
Step 6 Fraud and Abuse
Preventing Fraud and Abuse
Consequences of Committing Fraud
Step 7 Liability Insurance
Insurance Audits
Step 8 Recovery Audit Contractors
Step 9 Legal Concerns
Subpoenas
Arbitration
Medical Testimony
Step 10 Lesson Summary
Endnotes
Lesson 8—Introduction to Anatomy
Step 1 Learning Objectives for Lesson 8
Step 2 Lesson Preview
Step 3 Human Biology
What Is Human Biology?
Anatomy
Physiology
Step 4 Pathology
How Do Anatomy, Physiology and Pathology Relate to One Another?
Step 5 Beginning Anatomy and Physiology Concepts
The Anatomic Position
Planes and Sections of the Human Body
Transverse Planes and Sections
Sagittal Planes and Sections
Coronal Planes and Sections
Planes and Sections
Step 6 Location Terms
Step 7 Pronounce New Terms
Step 8 Write New Terms
Step 9 Meanings of New Terms
Step 10 Organ and Organ Systems
Respiratory System
Circulatory/Cardiovascular System
Nervous System
Muscular System
Skeletal System
Integumentary System
Endocrine System
Digestive System
Urinary System
Reproductive System
The Immune System
Step 11 Lesson Summary
Lesson 9—Anatomy: Landmarks and Divisions
Step 1 Learning Objectives for Lesson 9
Step 2 Lesson Preview
Step 3 Gross Anatomy
Landmarks and Divisions
Step 4 Pronounce New Terms
Step 5 Write New Terms
Step 6 Meanings of New Terms
Step 7 Adjective Forms for Landmark Names
Step 8 Divisions of the Abdomen
An Alternative Division of the Abdomen
Step 9 Internal Landmarks: The Body Cavities
Step 10 Membranes That Line the Body Cavities
Epithelial Tissue Membranes
Connective Tissue Membranes
Step 11 Retroperitoneal Organs
Step 12 Pronounce New Terms
Step 13 Write New Terms
Step 14 Meanings of New Terms
Step 15 Organization of the Body
Step 16 Lesson Summary
Just for Fun
Lesson 10—Cell and Tissue Anatomy and Pathology
Step 1 Learning Objectives for Lesson 10
Step 2 Lesson Preview
Step 3 Cell Components and Their Primary Functions
Cell Membrane
Cilia
Flagella
Villi
Step 4 More Cell Components and Their Functions
Cytoplasm
Step 5 The Nucleus
DNA
RNA
Nucleoli
Step 6 Pronounce New Terms
Step 7 Write New Terms
Step 8 Meanings of New Terms
Step 9 Cell Pathology
Step 10 Etiologies
Developmental Abnormality
Inflammatory Disease
Hyperplasia and Neoplasia
Metabolic Disease
Vascular Disease
Immunologic Disease
Idiopathic Abnormality
Iatrogenic Abnormality
Nosocomial Disease
Step 11 Cell Damage
Hypoxia and Anoxia
Toxic Agents
Microbial Infection
Allergic/Immune Reactions
Metabolic and Genetic Disturbances
Step 12 Cell Response
Atrophy
Hypertrophy
Hyperplasia
Metaplasia
Intracellular Accumulations
Aging
Step 13 Tissue Response
Inflammation
Repair
Damage or Death
Step 14 Pronounce New Terms
Step 15 Write New Terms
Step 16 Meanings of New Terms
Step 17 Lesson Summary
Lesson 11—Diagnostic Coding
Step 1 Learning Objectives for Lesson 11
Step 2 Lesson Preview
Step 3 History of the International Classification of Diseases
The WHO
ICD-9-CM
Step 4 Why Code?
Step 5 ICD-10
Impact for Coders
Step 6 ICD-9-CM vs. ICD-10-CM
Step 7 Lesson Summary
Endnotes
LESSON 1
The World of Health Care
Step 1 Learning Objectives for Lesson 1
When you have completed the instruction in this lesson, you will be trained to do
the following:
Explain an average day in a medical office.
List the different types of medical personnel and explain how each role
helps to ensure quality health care.
Describe your role as a medical coding specialist.
Discuss the job opportunities available in your new career.
Identify several types of medical records found in the healthcare world.
Step 2 Lesson Preview
Chances are that you’ve been to the doctor’s office and maybe even your local
hospital a few times in your life (though hopefully not too often!). You’ve seen
doctors, nurses, and office administrators hard at work in these settings, but how
much do you really know about what they do? Well, in this first lesson, we’ll
introduce you to the activities that go on in doctors’ offices.
We’ll introduce you to the activities that go on in doctors’ offices.
You’ll also see where you, the medical coding specialist, fit in! You’ll learn
about your future job duties and see how you will interact with other
healthcare professionals. We’ll also discuss a few of your many job
opportunities. Lastly, you’ll get a look at the medical records that coding
specialists handle on a daily basis.
Did you know that medical coding specialists are in demand throughout
the country because of the vast numbers of doctors and patients? More
doctors are needed now more than ever to take care of our aging
population. This is where you, the medical coder, come into play.
According to the U.S. Bureau of Labor Statistics, medical coding is one
of the 10 fastest-growing allied health occupations. Doctors need coding
specialists and are willing to pay well for the services they provide.
Well-trained medical coders make a lot of money. Medical coders often
make $35,000 per year or more. And in time, with practice, patience,
and hard work, you could earn more than $50,000 per year!
You are off to a terrific start by choosing this course as your education for
your exciting new career. In fact, the American Academy of Professional
Coders (AAPC), the renowned coding association, recognizes the
comprehensive quality of this course. This means the AAPC allows graduates
of this recommended program to waive one of the two years of coding
experience needed to become a Certified Professional Coder.
As you go through this program, you can feel confident that you are learning
from the experts. The school has been providing quality home
study
education for more than 30 years. We pride ourselves on our students’
accomplishments! People just like you are working in exciting jobs today
because of the investment they made in their education—we are here when
you need us. If you have a question, contact your instructor. It’s that easy.
Now let’s take those first steps on the path to your new career.
Step 3 Daily Activities in the Medical Office
To fully understand what a medical coding specialist does, you first must
understand how medical office personnel gather information. This information
includes patient data; insurance company information; and doctors’ procedures,
diagnoses and other actions.
To illustrate all of this, let’s take a look at a typical day in a medical office, or
an outpatient setting. (Outpatient settings include clinics, physicians’ offices,
outpatient surgery facilities and hospital emergency departments. Inpatient
settings include hospitals—or facilities where patients are admitted for an
overnight stay.) We’ll get the point of view of the first person to see patients
—the office manager or receptionist—and then we’ll look at the doctor’s
perspective.
A Day in the Life of the Medical Office Manager
Hannah is the office manager for Mercy Medical Center, a busy, family
medical clinic that has three doctors. As the first person to see patients, she
tracks them as they arrive and check in for their appointments. Today, each
doctor is scheduled to see about 15 patients. Hannah’s appointment book
contains a different page for each doctor’s schedule. Her day begins with the
8 a.m. appointments. Each doctor has a bright-and-early patient scheduled.
By 7:55 a.m., two of the three patients are in the waiting room. One is a new
patient at the clinic, and she is filling out the “New Patient Questionnaire.”
The other is an established patient.
Hannah pulls out the medical files for the established patient. The
medical files are thick, manila folders and are coded on the tab according
to the patient’s last name. She prints an encounter form or super bill for
the established patient and uses a paperclip to attach it to his folder. She
then places the files in the “Patients to See” stack for the nurse of one of
the doctors.
The new patient brings up her completed questionnaire, and Hannah spends
the next few minutes creating medical files for this new patient. Hannah
makes a new folder for the patient, labels it appropriately and places a copy
of the questionnaire in it. Then she takes the original questionnaire and types
the information from it into her computer. This creates two files for the
patient—one in the computer and one on paper. After Hannah has entered
the information about the patient into the computer, she prints an encounter
form or super bill. She then clips the encounter form to the appropriate folder
and places it in the “Patients to See” stack for the appropriate nurse.
It is now 8 a.m., and one appointment has yet to arrive. At 8:04 a.m.,
Hannah receives a call from the missing patient. He is having car trouble and
can’t make it today. Hannah assures the man he can reschedule. She sets up
a new appointment for him and logs it into the doctor’s appointment book. By
8:06 a.m., both of the other appointments are back in the examination
rooms. The 8:15 a.m. appointments begin to arrive. The routine is similar to
the first group of patients except that this time all three appointments arrive.
They all are established patients, so Hannah pulls their files, prints out
encounter forms, and distributes the folders to the correct nurses.
Medical office managers handle multiple tasks.
At 8:10 a.m. the first doctor is finished with his 8 a.m. appointment—
a man named Jim Burgess. Mr. Burgess walks out of the examination

room and gives the encounter form or super bill to Hannah.
Hannah looks at the procedures that the doctor circled and quickly fills in
an amount next to each one. She totals the bill—$187.50—and has Mr.
Burgess sign it. At Mercy Medical Center, most patients are covered by
insurance. In Mr. Burgess’s case the medical office will send the bill to the
insurance company without him paying an initial copayment or the entire
amount of the bill. Therefore, Mr. Burgess signs the bill to give the
insurance company permission to pay the clinic directly and returns it to
Hannah. She rips off the back copy for him.
As Mr. Burgess picks out a lollipop from the basket on the counter, Hannah
quickly files the completed and signed encounter form in her “To Submit,
Current” folder. The nurse has returned Mr. Burgess’s file, so Hannah puts
it in the “To Be Updated” basket. The folders in this basket are waiting for
the doctors’ dictation to be transcribed. Just then the telephone rings. It is
Mercy Medical Center’s medical transcriptionist calling to verify a patient’s
information. Hannah explains she will have to look up that information and
call the transcriptionist back.
Hannah’s day continues this way until she leaves at 5 p.m. During that time,
she continually checks in patients, enters new questionnaires on the
computer, creates files, retrieves files, completes encounter forms, answers
the telephone, and schedules and reschedules appointments.
Now let’s look at the same day’s events from a physician’s perspective.
The Doctor’s Point of View
Dr. Green is one of the physicians for whom Hannah works. He sees his
first patient at 8 a.m. He examines the patient, a woman in her mid-30s,
and determines the cause of her ailment. Dr. Green’s patient has a broken
arm. When she sees Dr. Green, he listens while she tells him what’s wrong
—this is called the chief complaint. Then Dr. Green looks at her arm and
recommends that x-rays be taken. Finally, since the x-rays show a
fracture, Dr. Green puts her arm in a cast.
This sequence began with a chief complaint—“my arm hurts”—and was
followed by a diagnosis aided by tests—a broken arm as seen on the x-
ray. The sequence is completed with a treatment or procedure—the
fracture care. Doctors perform one or more of these steps with every
patient they see.
Doctors perform many steps when they see patients.
And every time a doctor or nurse performs these duties, the steps must
be recorded into the patient’s history, which is a folder usually called a
chart. The diagnosis and treatment or procedure, along with any tests
done, eventually are coded by you, the medical coding specialist! You will
learn all about coding diagnoses, tests, and treatments as you move
through this course. For now, you just need to understand where you will
gather that information.
After Dr. Green examines the patient, he records some notes about the
encounter. The office’s medical transcriptionist will use this dictation to
transcribe the encounter into a formatted medical report. Dr. Green also
makes some notes on the patient’s history or chart. Now, he is ready to see
his second patient.
Please pause and complete online Practice Exercise 1-1.
Step 4 A Little Teamwork Goes a Long Way
Now you know how information flows in medical settings. You have a basic
understanding as to what some healthcare employees, such as office managers
and doctors, do in a typical day in a medical office. But before we talk about your
role in the healthcare team, let’s identify some of the key players in hospitals and
doctors’ offices and elaborate on what they do.
In most professions, teams of people work together to accomplish goals, and
this is true of physicians as well. In medicine, doctors certainly cannot
perform their jobs alone. Many people work hard, some behind the scenes,
others more visibly, to ensure that the healthcare system runs properly.
When you go to see the doctor, you don’t just see the doctor. You might see
a number of professionals, including a receptionist, an office manager, and a
nurse. Throughout a visit, a doctor may talk to several staff people, including
the medical coding specialist. All of these people are essential members of
the medical care team.
All of these people are essential members of the medical care team.
Physicians
Physicians or doctors are the most prominent members of the medical
care team. They perform life-saving procedures. They cure the sick and
help heal wounds. Becoming a doctor of medicine is one of the most
challenging career paths a person can choose. Not only do doctors earn
four
year college degrees, but they also must complete medical school
and one or more residency assignments. During residency, 85- to 100-
hour work weeks are common. Because of this huge commitment,
doctors deservedly receive much of the attention in the medical field.
Physicians diagnose illnesses and injuries. They prescribe drugs to alleviate
symptoms, treat conditions, and ease pain. They rely on their training to
make quality, accurate decisions. However, as good as physicians are, their
staff ultimately supports them as they provide quality treatment. Nurses are
one essential part of the medical staff.
Nurses
Nurses can give injections.
As professionals who perform a variety of tasks in the medical world, nurses
often must follow through with treatments physicians prescribe. Nurses can
give injections and check a patient’s vital signs, as well as assist in surgery.
It’s also true that nurses must often do the thankless jobs—cleaning up exam
rooms and organizing supplies.
Without nurses, the number of patients a doctor sees in a day would drop
dramatically. Because of their nurses, doctors see more patients and are able
to focus on those patients who require the most care.
Nurse’s and Physician Assistants
Two other categories of personnel in the medical field are nurse’s and
physician assistants. Nurse’s assistants, or nursing aides, help nurses with
daily duties, such as paperwork, general organization and taking a patient’s
temperature, weight, and blood pressure. Some nurse assistants also talk to
patients and make sure they’re comfortable.
Physician assistants or PAs normally are under the supervision of a
doctor, and can perform some of the same functions as a doctor. PA duties
might include stitching up a cut, taking a patient history, and even
performing lab work.
Support Staff
Doctors and nurses rely heavily on support staff to keep a medical office or
clinic running smoothly. As you might guess, each of these positions plays an
important role in the medical world.
Medical Billing Specialists
Medical billing specialists are a perfect example of how interrelated one job is
to the next in a medical office. Remember, coding specialists code what
occurs during a patient’s medical visit, while medical billing specialists use
the codes that a medical coder assigns. Billing specialists then complete the
insurance forms necessary to collect payment from the insurance companies.
These specialists know that the doctor doesn’t get paid unless the form is
completed and filed correctly. Billing specialists have training in medical
terminology, medical records handling, and some basic coding.
Medical Transcriptionists
Do you remember when the doctor in our previous example recorded some
notes about a patient encounter? Well, a medical transcriptionist who
listened to the doctor’s dictation typed what she heard. This then was added
to the patient’s medical record. By using transcriptionists, doctors save time
by speaking their notes.
Medical transcriptionists type the doctor’s dictation.
While you don’t need to know every aspect of medical transcription, you
should be aware as to what transcribed reports look like. As a medical coder,
you often will work from these transcribed reports. Two examples of
transcribed reports follow: one for Laura Brown and one for Johnny Cruz.
Study these reports so that you have a better understanding of a
transcriptionist’s role in the medical records process.
Transcribed Report Example One
Name: Laura Brown
#030311
PROBLEM

Upset stomach with vomiting and fever.
SUBJECTIVE
The patient is a 22-year-old female. She went to breakfast with her friends earlier this
morning. She ordered a cream-filled pastry with her coffee. She stated that no one else had a
pastry. About 4 hours later, she started having an abrupt onset of nausea, vomiting,
abdominal cramps, diarrhea, headache and a slightly elevated fever. Since she had the
symptoms for over three hours, she called her family physician and was able to see him this
afternoon.
OBJECTIVE
Physical examination reveals a well-developed, well
nourished female in acute distress.
Blood pressure: 125/85. Temperature: 99.6 ˚F. Pulse: 88. Respirations: 24. Chest is clear.
Cardiovascular examination: Regular rate and rhythm. Abdomen: Positive bowel sounds.
Diffuse tenderness with slight pain. Laboratory results indicated a slightly elevated white
blood cell count. Abdominal x-ray: Normal.
ASSESSMENT
Staphylococcus toxin gastroenteritis.
PLAN
The patient was sent home and told to get plenty of bed rest and begin clear fluids when
nausea and vomiting cease. If the symptoms continue for more than 3 more hours, she should
contact the office.
_________________________________
Robert Snow, MD
D:02-08-20xx
T:02-08-20xx
RS:CJL
Transcribed Report Example Two
Name: Johnny Cruz
#030315
PROBLEM
Sore throat with fever.
SUBJECTIVE
Johnny, a 5 year old, presents to his pediatrician with a sore throat, fever, loss of appetite
and a headache. His mother said that he has been on the couch all morning and refuses to
eat or play.
OBJECTIVE
After examining the patient, the doctor reports enlargement of the lymphatic glands and a
temperature of 103 ˚F. The oral exam reveals a swollen, bright-red throat. A throat culture is
postitive for strep throat.
ASSESSMENT
Acute follicular pharyngitis.
PLAN
Take erythromycin as directed. Temperature to be taken frequently. Children’s Tylenol every
4-6 hours as needed for fever. Encourage bed rest, modify activities and increase fluid
intake. All citrus juices should be avoided until symptoms subside. Call office if symptoms
persist.
_________________________________
Marikit Makabuhay, MD
D:09-15-20xx
T:09-15-20xx
MM:BDD
Medical Record Technologists
Certified medical record technologists control the flow of medical
records to the various people who need to see those records. These
technologists take a certification test that ensures they have the knowledge
to determine what records are needed, who is authorized to see the records,
and how these records are organized. You may find that medical record
technologists, who are certified, are also called Registered Health
Information Technicians or RHITs.
Emergency Personnel
Emergency personnel are a group of professionals with the sole responsibility
of providing immediate medical assistance and transporting the patient to the
hospital for treatment. When someone is hurt and needs an ambulance,
these people respond. Police officers, firefighters, and other rescue
professionals all have some level of medical training.
EMTs can be ambulance crew members.
You probably have heard of emergency medical technicians (EMTs) and
paramedics. EMTs take classes that enable them to stabilize patients who
have a wide variety of emergency medical conditions. They often are
members of ambulance crews and volunteer firefighting organizations.
Paramedics have more training than EMTs. Paramedics are not only able to
stabilize patients, but they can begin treatments to cure patients, such as
administering medication.
Office Professionals
Do you remember Hannah, the office manager from our previous example?
Hannah is an example of an office professional. Without office managers and
receptionists, many medical offices would grind to a halt! These people
organize schedules, record appointments, and answer patient questions.
Office staff members have terrific communication and organization skills.
They also must make a good first impression. The office manager may be the
first person a patient sees upon entering a medical office, and the manager’s
attitude can mean the difference between a pleasant visit and a nightmare
for the patient.
Please pause and complete online Practice Exercise 1-2.
Step 5 Welcome to Your Career as a Medical Coding
Specialist!
Now that you know the job duties of many of those in the healthcare world, let’s
talk about the role that you, the medical coding specialist, will play in the
healthcare picture. From the scenario you read at the beginning of this lesson, you
know that you will be responsible for assigning medical codes to the information
obtained from a patient’s visit to a medical facility. As the coding specialist, you get
the medical record the physician dictated that we talked about previously. You look
over the complaint, the diagnosis and the treatment performed, and then you code
appropriately. To code, you look up the information in a reference book and find
the right set of numbers that describes exactly what occurred.
You can code at home or work in a doctor’s office or hospital, and some
doctors use independent coding specialists. In fact, there are even companies
that hire coding specialists across the country. These remote coders work
online in distant locations, and the company finds work for them to code. So
much depends on where and when you want to work. What’s exciting is that
you’re in control—just as you are in this course, working toward your new
career!
As you already know, medical coding specialists are in demand. Just by
looking at the number of patients doctors see every day, you can imagine
how many coders are needed. Every appointment needs a code attached!
Experienced medical coding consultants can earn impressive salaries.
Surveys indicate that many medical coding specialists earn $35,000 per year
or more. In fact, some medical coding consultants make more than $100,000
per year. Of course, you shouldn’t expect to make $100,000 your first year.
But with work and dedication, you can earn a tremendous salary in a short
time.
But Where Will I Work?
Someone with the knowledge you’re gaining in this course will not be limited
to simply filling out forms. No, the world of medical coding is very diverse
and, as you already know, it offers full- or part-time job opportunities, at
home or in offices.
Medical Coding Specialist
Mercy Medical Center is looking for a part-time Medical Coding Specialist to accurately assign codes to records.
One year of coding experience is preferred, but those who can show they have real-world training in medical
coding also will be considered. Mercy Medical Center is an equal opportunity employer.
Please send cover letter, resume and references to:
Mercy Medical Center
111 Main Street Suite 1
Avery, Ohio 44444
Find Your Future as our Next Medical Coder!
Hart Family Practice is looking for a full-time medical coder to code medical records. Applicant must have
knowledge of medical terminology, anatomy and medical codes. The position offers a generous benefit
package, and salary is based upon experience. EOE
If interested in applying, please send a cover letter and resume to:
Hart Family Practice
222 Skinner Road
Pittman, Louisiana 23232
Medical coding specialists no longer are restricted to the doctor’s office but
now work in hospitals, pharmacies, nursing homes, mental healthcare
facilities, rehabilitation centers, insurance companies, consulting firms, health
data organizations, and their homes. And remember, if you decide you want
to work at home, you set your own work schedule and save on items such as
child daycare and transportation. So how is it possible that one career offers
so many choices? Let’s take a closer look at two different jobs available to
you in this career.
Medical Coding Specialist
A coding specialist typically works in an office or hospital. In some cases the
physician assigns the code, and the coding specialist simply verifies that
these codes are consistent with what the physician has documented. In other
cases the doctor does not assign codes. Instead, the medical coding specialist
translates the doctor’s written diagnosis and treatment into codes. Then the
coder often routes the codes to a medical billing specialist who sends the
claim to the insurance company.
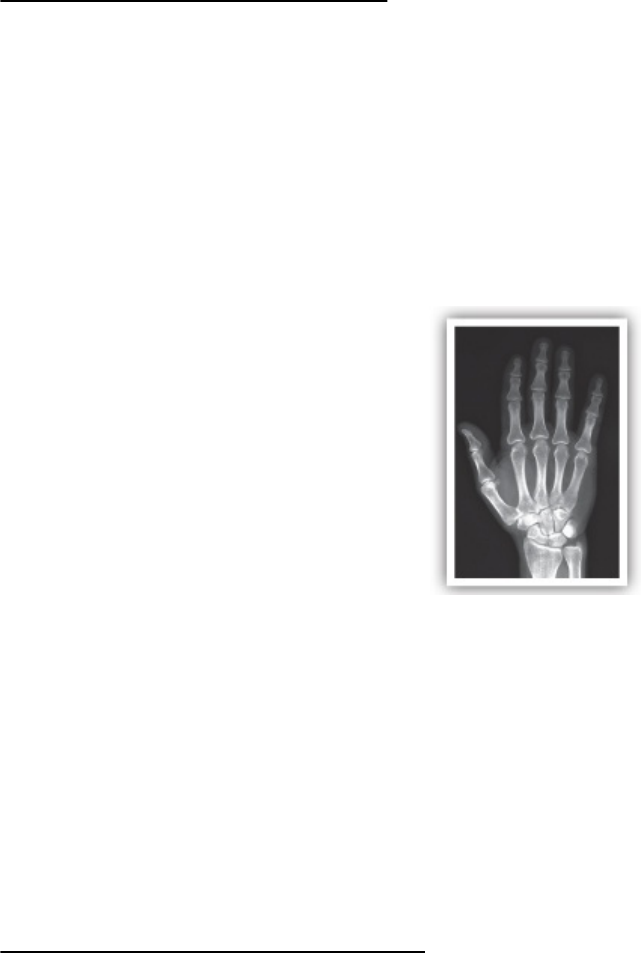
Medical coders apply codes for x-rays.
For example, a medical coder working for a radiologist might have a super bill
indicating a patient came in for a broken finger, as well as transcription
documenting how the x-ray was performed and the radiologist’s reading of
the x-ray. The medical coder would apply the correct codes for the diagnosis
and the procedure, and the medical billing specialist then would send these
codes to the insurance company.
The Medical Coding Service
A medical coding service is the most common at-home employment
opportunity for a medical coding specialist. Medical coding service
providers use a computer to complete the necessary forms and submit them
to the office manager or medical billing specialist. Typically, the self-
employed medical coding specialist charges by the medical record and has
more than one provider as a client.
The work of an independent medical coder doesn’t vary much from that of
those who work in offices and hospitals. The biggest difference involves how
the work gets to and leaves the medical coding specialist. If the coding
service does work for local providers, the work could be picked up and
dropped off every 24 to 48 hours. The medical coding specialist simply takes
the information home, codes it and then returns it to the physician’s office. If
the physician is having his transcription done online, he is set up for online
communication of all work. The coding work can be exchanged online. The
great thing about this route is the medical coding specialist isn’t limited to
clients in her town or even state!
If you’re going to do your medical coding work from home, there are several
items to consider. You’ll have to purchase equipment and set up a home
office, as well as market yourself to find clients. Consult the Medical Coding
Specialist Career Starter Kit included in this course for more guidance in
setting up a home-based business. For now, let’s talk a bit about the personal
qualities that medical coding specialists should possess.
Step 6 Personal Qualities of a Medical Coder
If you think about it, there are a large number of potential clients available in most
towns. Even small towns usually have one or two doctor’s offices and a hospital.
Many times qualified help is hard to find, and because you have a skill that is in
great demand, you have the opportunity to make good money. Though salaries
vary depending on experience, the number of hours worked, and location, we think
you’ll be pleased to discover the amount of money you can earn as a medical
coding specialist. And remember that as your experience builds, you can add to
your earnings while being a vital part of a medical team and doing work that helps
people.
As a part of the healthcare team, medical coders do much of their work
alone; however, coders still are a vital part of that team. The main
thing to remember when you approach a potential client or employer is
that you are the best medical coding specialist for the job. Your
competence means money—their livelihoods—to your employers!
Coders should remember and practice three qualities: professionalism,
presentation and adaptability.
Professionalism

As with any business, the
image you project
is important.
Professionalism is the conduct, aim or qualities that characterize a
profession or a professional person. As with any business, the image you
project is important. You must be professional. This includes how you dress,
talk, and interact with your clients. When you have an initial meeting with
potential clients, your level of professionalism will affect their impression of
you.
When you select what to wear, be conservative but not bland.
When you select what to wear, be conservative but not bland. Your attire
should be clean, wrinkle free and professional. Try to choose something you
feel comfortable wearing. If you are comfortable, you will be able to
concentrate on other important things such as your presentation and
answering any questions your potential client may have. An uncomfortable
outfit, whether in style, color or both, will distract you.
Another facet of professionalism is delivering what you promise. You’ve
probably heard the saying, “Five minutes early is 10 minutes late.” Basically,
this means if you have a meeting at 10 a.m., be 15 minutes early. Never be
late, especially for a first-time interview. Such promptness shows you are
responsible and considerate. If your client is a little late, be understanding.
Just make sure you aren’t the tardy one. When you are asked for work
samples, be prepared. Explain what you know and how you gained your
knowledge. If you ever are asked to complete a test task, do so promptly.
Presentation
Presentation is the act of bringing or introducing something into the
presence of someone else. Often your initial presentation will decide whether
you gain a client or employer. In addition to being on time and dressed
properly for the meeting, your presentation can go a long way in influencing
your client-to-be—both positively and negatively.
Be sure to present a confident image. Your attitude should say, “I know what
I’m doing” without being arrogant or condescending. Remember, this is the
client’s money you’re talking about. Confidence is a must!
Adaptability
Adaptability is the ability to be modified or changed. To be successful,
you must be able to adapt for each client. Some people want tasks done
a certain way. Others may have exactly the opposite requirements.
Insurance regulations change. Forms are altered. If you get too set in
your ways, you might lose clients who require slightly different
approaches.
Step 7 Medical Records
We’ve all had experiences with a doctor’s office. You’ve probably been asked to fill
out a new patient questionnaire in a doctor’s waiting room, or maybe you’ve called
to reschedule a dentist appointment. But you may not be familiar with the contents
of a medical record. Let’s clear up some of these mysteries. As a coder, you’ll
become a pro at explaining these contents.
A medical record is generated when a patient receives medical care. This
record usually begins its life as a questionnaire or patient data sheet—like
the one the new patient filled out in our example. The questionnaire asks
about a patient’s medical history, insurance coverage, and other important
facts. After the patient completes the form, the office administrator takes it
and any applicable insurance information and enters all of this into the
office’s database, either on a computer or manually in a file cabinet. Then a
medical file or record is created.
What is a medical record?
The medical record contains all of a patient’s medical history related
to that doctor and his office. The medical file includes charts, notes, and
information to identify the patient, support the diagnosis or reason for
the appointment, justify the treatment, and accurately document the
results. The record also contains past and present illnesses and
treatments. Every aspect of a patient’s treatment at a healthcare facility
is documented in this file. In other words, the medical record provides a
complete picture of the health care the patient has received.
Parts of a Medical Record
The most common parts of a medical record include: The patient
questionnaire, registration/admission form, consent for treatment form,
patient history form, plan of treatment form, and progress report form. Let’s
take a moment to discuss each of these briefly, as well as look at a few
examples.
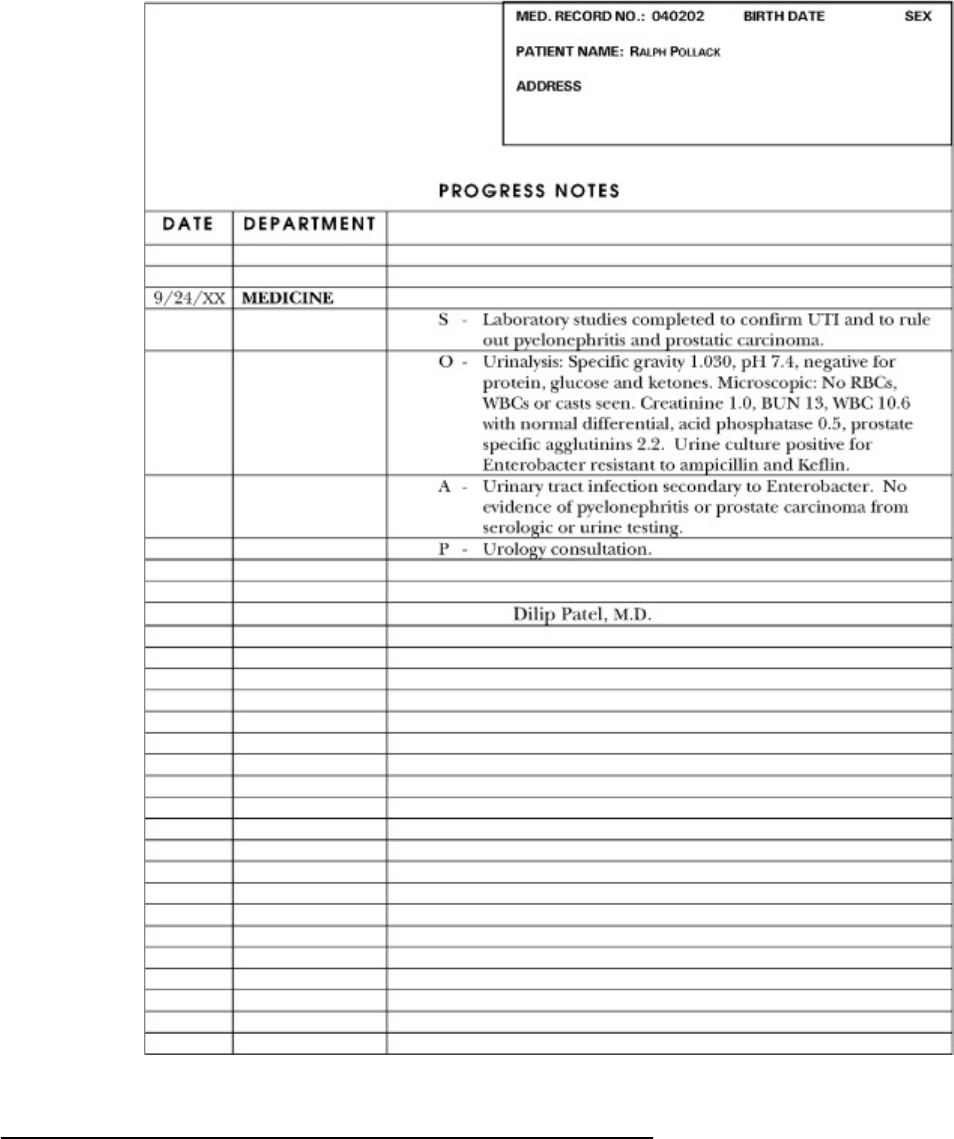
Questionnaire
A medical record is generated when a patient receives medical care. This
record usually begins its life as a questionnaire or patient data sheet. The
questionnaire asks about a patient’s medical history, insurance coverage
and other important facts.
Let’s take a look at an example questionnaire.
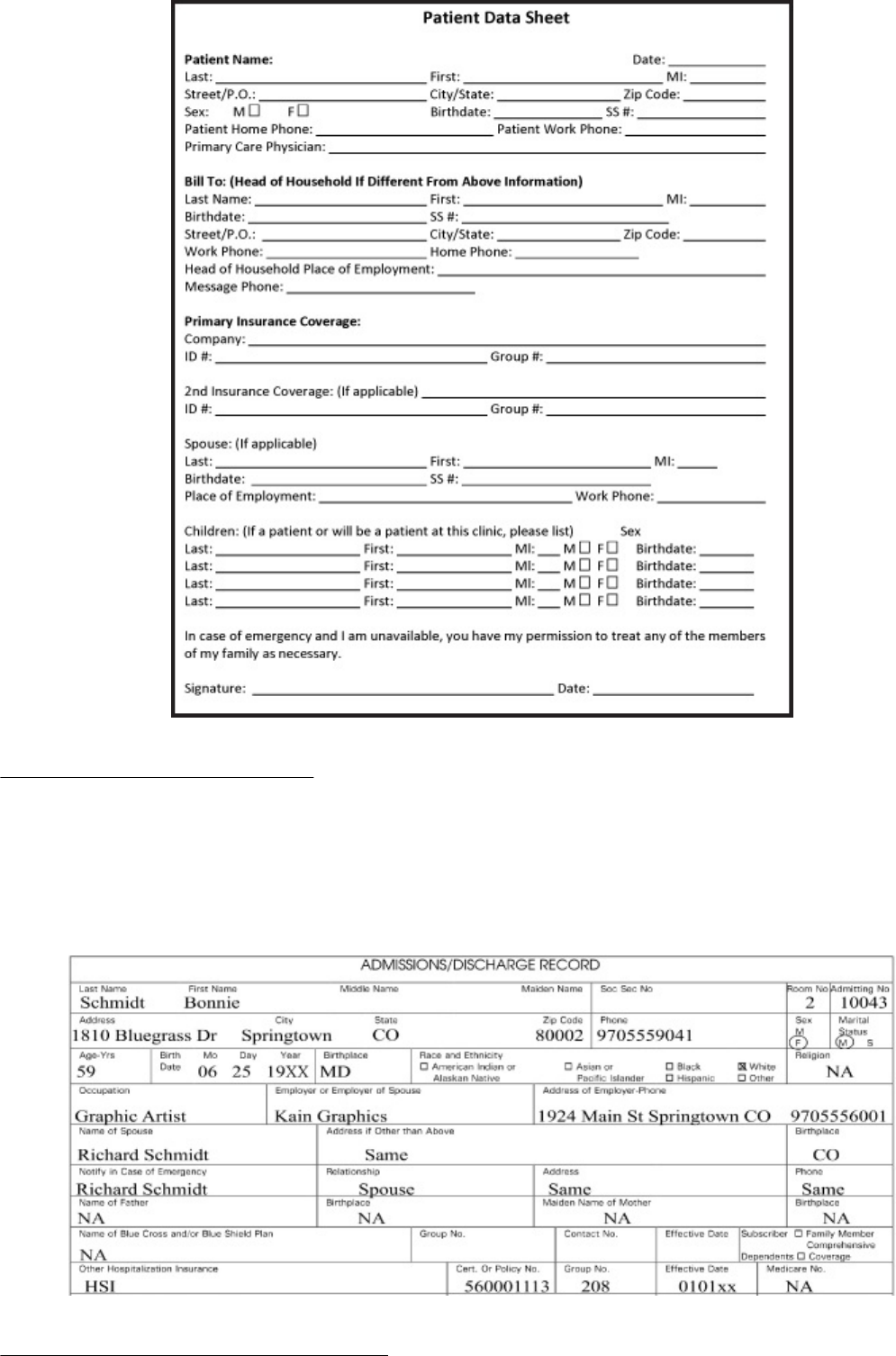
Registration/Admission
The registration/admission form is used to record important information,
such as the patient’s name, address and insurance information. This form
may be completed every time a patient sees the provider, or the practice
may keep one on file and update it as necessary.
Consent for Treatment Form
Whenever a patient agrees to a suggested treatment, the patient must
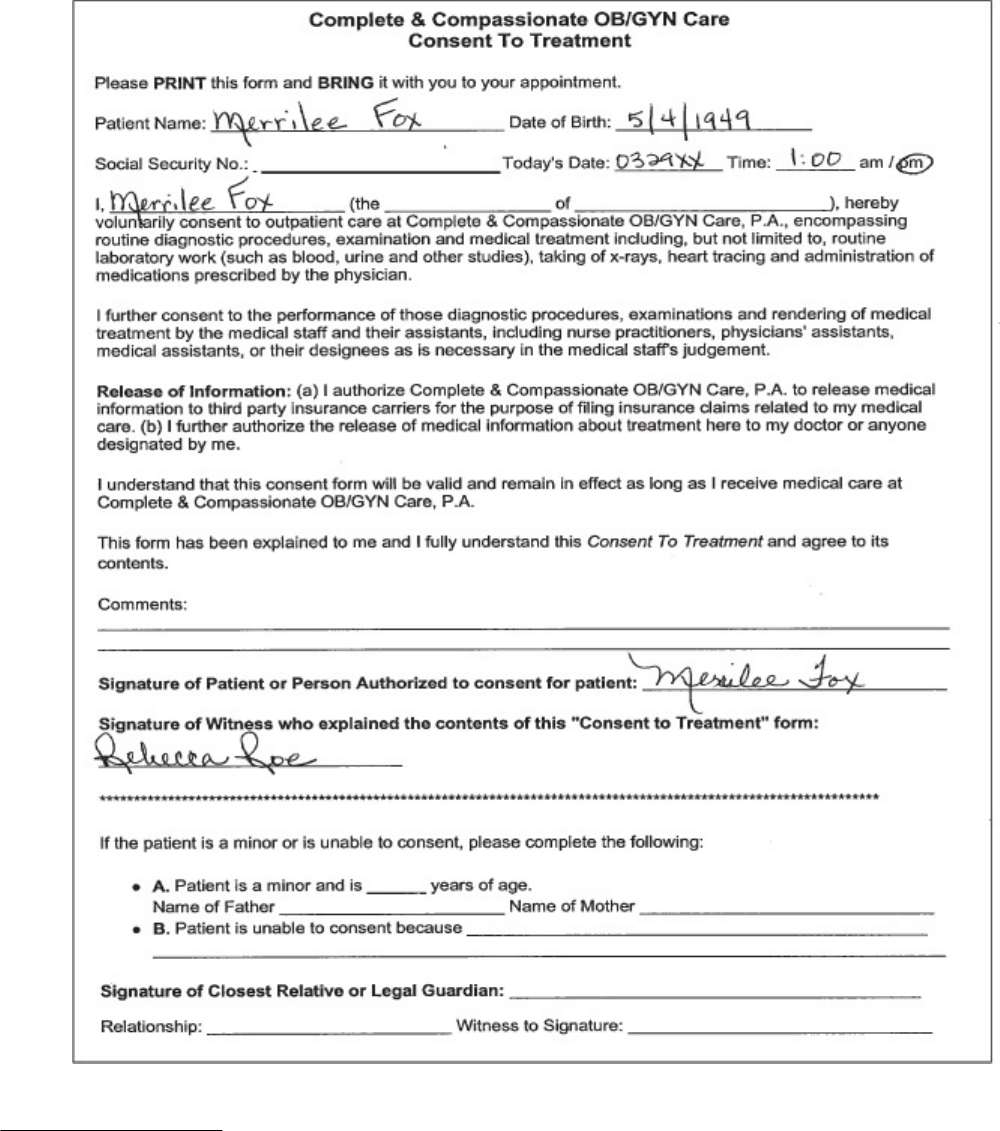
complete a consent for treatment form. The consent for treatment form
includes a statement indicating the patient has been informed of the
treatment plan, including possible side effects and negative outcomes. The
patient signs the form, indicating agreement to the treatment and awareness
of all possible consequences resulting from the treatment.
Patient History
When a patient sees a provider for the first time or hasn’t seen a
particular doctor for a long period of time, the patient is asked to fill out a
patient history form. The patient history contains critical questions
regarding the patient’s health history. The patient’s responses to these
questions enable the doctor and medical staff to give the patient the best
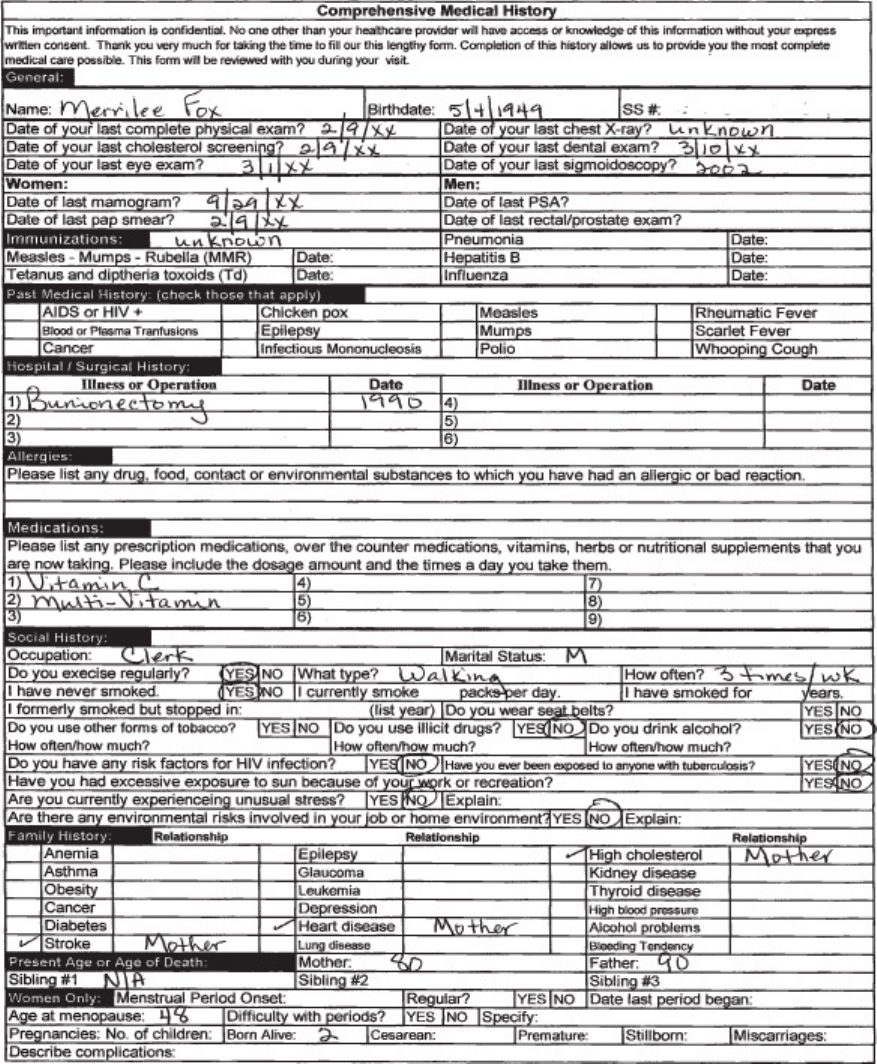
possible care.
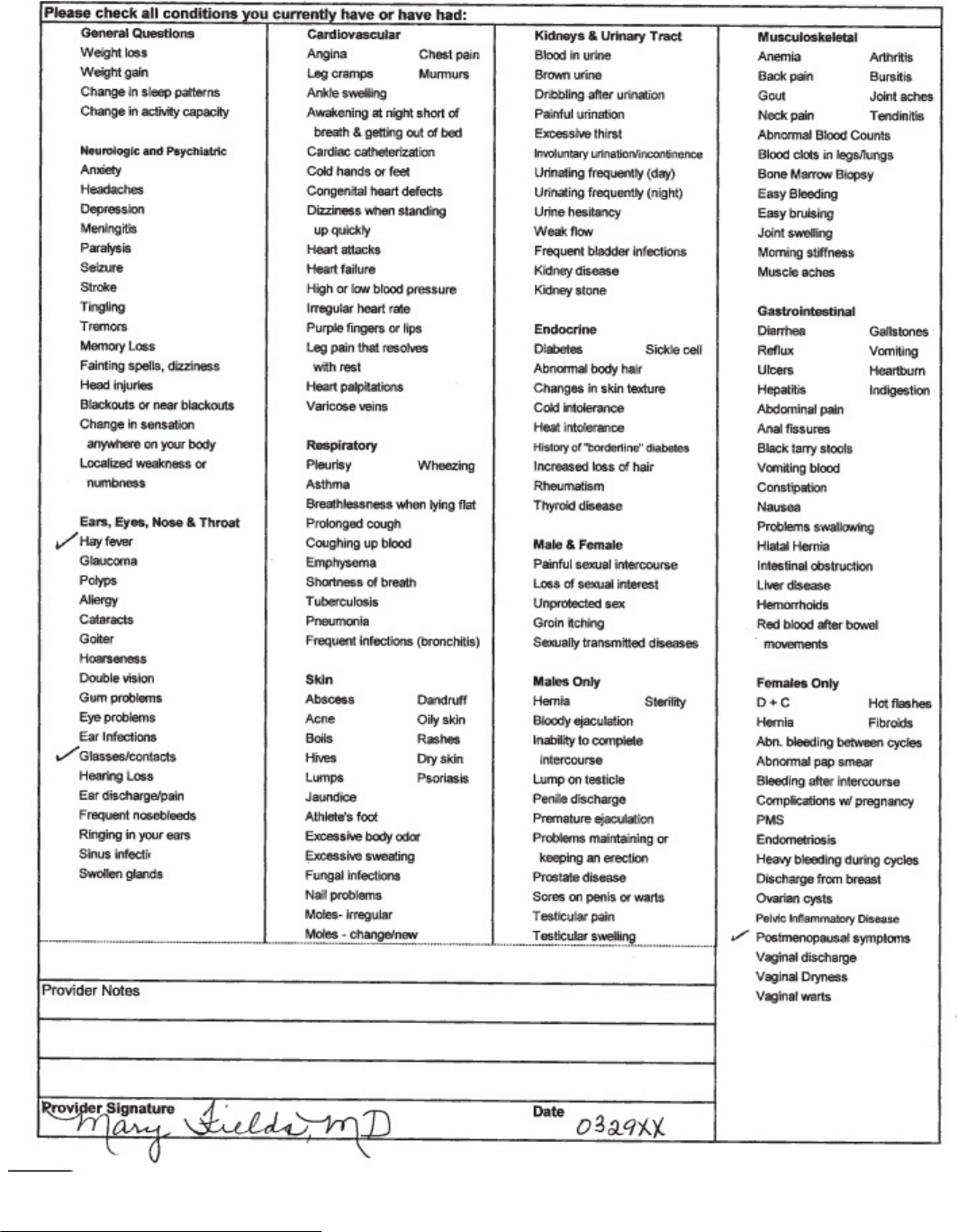
Plan of Treatment Form
The doctor records the orders given to the patient regarding treatment on the
plan of treatment form. In our example, the physician’s instructions are for
discharging the patient. Completion of this form helps establish a plan for
recovery and provides the patient with clear instructions to follow.
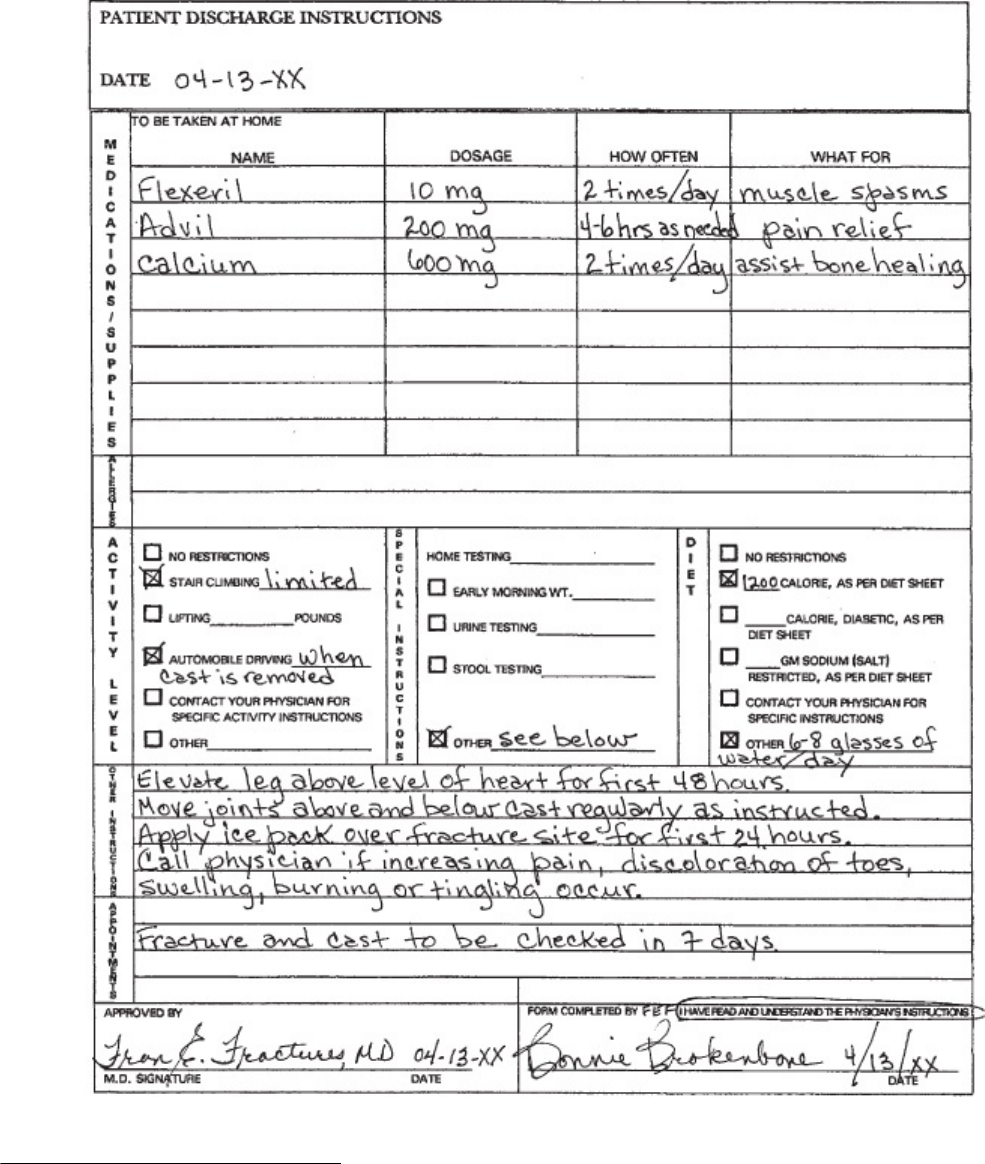
Progress Report Form
As a treatment plan moves along, or as a patient’s condition changes, the
information is recorded on the progress report form. Providers use this
form to chart changes of all kinds in their patients’ conditions. Changes can
include worsening conditions as well as improvements. Every patient has a
progress report form.
The Flow of Medical Information
Doctors, nurses, and other health professionals use the medical record
to provide patient information for the different segments of the patient’s
care. The record helps the various practitioners involved in treating the
patient to communicate with one another. It’s not necessary for a
doctor to individually speak with each healthcare professional. The
medical record keeps the current healthcare providers abreast of the
patient’s treatment and progress. In addition, the record depicts for
future providers an accurate picture of the patient’s previous care. It
enables one doctor who takes over for another to continue to treat the
patient without interrupting care.

Another important use of the medical record is for reimbursements. The
patient’s file supplies information so the patient and third-party payers
can be billed for services and expenses. The medical record
substantiates laboratory tests, medications, and other services listed on
an insurance claim.
The medical record serves other purposes as well. It’s a legal business record
for the healthcare provider. It gives the patient documentation with which to
make legal claims—for example, the extent of injuries from an auto- or
work
related accident. The record can be used to analyze and review the
quality of patient care. It also can be used for research and education and for
healthcare facility planning and market research. And medical records help
determine problems that the healthcare delivery system needs to address,
such as increases in the occurrence of heart disease or breast cancer.
Medical records first were kept in hospitals. Now, virtually every healthcare
provider maintains such records because complete files are necessary to
verify medical expenses, validate the healthcare provided, and meet
government requirements. Although different types of healthcare providers
maintain medical records, all records still are patterned after the hospital
medical record. The format used, and the information recorded in each record
is similar from one facility to another. The box that follows summarizes the
purpose of the information that medical records provide.
Medical Records:
• Identify the patient
• Record results of tests and treatments
• Justify diagnoses and treatments
• Offer information to all providers involved in the patient’s care
• Detail the patient’s previous care for future providers
• Maintain a record of services for billing third-party payers
• Provide the healthcare facility with a legal business record
• Provide tools for evaluating patient care
• Provide documentation for study and research
• Give healthcare providers data for planning delivery of services and
marketing
Please pause and complete online Practice Exercise 1-3.
Step 8 Lesson Summary
Medical coders are an important part of any medical setting, and the scenario at
the beginning of this lesson showed you how information flows through such
settings. This lesson also gave you a firm understanding as to what each member
of the healthcare team does. Coders work with physicians, nurses, office managers,
and others to contribute to the best possible patient care. You learned that this
care occurs in a three
part sequence: chief complaint, diagnosis, and treatment.
The diagnosis and treatment eventually are coded by you, the medical coding
specialist!
We also discussed a few important points for you to remember as you move
toward your new career. You learned about possible employment
opportunities and settings. You also learned the importance of
professionalism, presentation, and adaptability.
Lastly, this lesson discussed medical records. The medical coding specialist
works closely with medical records to assign the correct codes for the
diagnosis and procedure determined during a patient visit. The accuracy of
the codes determines correctly completed insurance forms, thereby obtaining
the proper reimbursement for the doctor.
As you continue this course, you’ll see in greater detail just how important
medical coding specialists are to those who work in and rely on medical
facilities. Medical coding specialists are in demand! The entire field is
expected to grow by more than 46 percent, and the projected growth for
those coders working directly for physicians is 94 percent! By choosing this
course, you have started on an exciting path toward success.
LESSON 2
Medical Insurance 101
Step 1 Learning Objectives for Lesson 2
When you have completed the instruction in this lesson, you will be trained to do
the following:
Explain how insurance works.
Define the terms common to most insurance carriers.
List the types of insurance programs available today.
Discuss how diagnostic and procedure codes apply to insurance.
Determine the basics of filing electronic claims.
Step 2 Lesson Preview
Most people in America qualify for some sort of medical insurance. In addition to
the various government programs available, hundreds of private companies also
provide medical insurance. Fortunately, a few common threads tie all insurance
companies together, for example, the terminology used and the forms required.
These common threads make the medical coding specialist’s job easier.
A few common threads tie all insurance companies together.
It is important to understand medical insurance concepts. With this
knowledge you will be able to communicate effectively with medical billing
specialists. You will work closely with them to secure the highest
reimbursement for the provider’s services. This is why medical coders are a
vital part of the provider’s support staff.
Additionally, the codes you use play a very important role in health data and
research. Did you know that medical codes help track diseases—and cures—
in our country? These codes are entered into a national database, which is
tracked by health researchers. Much government funding for cancer, AIDS,
and other diseases comes from the codes that you will assign. Not only are
you helping health care providers, but your coding work advances research
and treatment development of many illnesses.
In this lesson we will introduce you to the language of the insurance
world. After that, we’ll move into the different programs available. You’ll
be introduced to the various insurance programs. There are government
insurance programs such as Medicare and Medicaid, the managed care
approaches of health maintenance organizations and preferred provider
organizations.
This lesson will introduce two important concepts—diagnostic coding and
procedure coding—and you’ll learn how these codes relate to medical
insurance. And we’ll discuss electronic claims. Chances are you already know
a little about these terms and programs. If you don’t, fear not! We’ll cover
them here. So let’s get started!
Step 3 The Life Cycle of a Medical Bill
You’ve just started the medical bill’s life cycle.
Let’s first review a little about what you learned in the first lesson. Imagine you are
a patient at a doctor’s office. This is the first time you’ve been to this particular
doctor. When you check in with the front desk, the office manager hands you a
questionnaire to complete. This form asks for your name, address, telephone
number, medical history, and insurance information. After you complete the form,
you give it back to the receptionist. With this process, you’ve just started the
medical bill’s life cycle.
Now the office manager enters your information into the computer. The
computer might then produce a patient encounter form, also known as the
super bill. Remember, this is a standard form that contains a list of the most
common procedures the doctor performs at that office. An encounter form
typically lists many types of procedures and diagnoses, such as office visits,
physical exams, x-rays, blood tests, and common illnesses or conditions.
Based on the information you provided on the questionnaire, the computer
prints your name, billing address, insurance company, and policy number on
the encounter form. When you go back to the examination room, your
encounter form is part of the medical file the doctor works with as she
examines you.
When your examination is complete, the doctor circles on the encounter form
the procedures she performed. Usually, more than one procedure is involved.
For example, the doctor might circle the physical exam—new patient
procedure and the x-ray—lower leg procedure if you had to have x-rays
taken. The circled items let the office manager know what to charge you or
your insurance company for your visit. This form is now your bill.
After the bill is created, the next step in its life cycle is processing. Let’s look
at the details involved in that step.
Processing the Bill
Once the medical bill exists, it goes through several steps on its way to being
paid. A patient and medical facility handle bills for medical care in one of
three common ways:
The insurance company might require the patient to pay the entire bill at the time of service.
1. The insurance company might require the patient to pay the entire bill at
the time of service, before the patient leaves the medical facility. Then the
patient submits a claim to the insurance company for reimbursement.
2. The patient might pay a copayment—a flat amount, such as $10,
determined by the patient’s insurance policy—before he leaves the doctor’s
office. Then the doctor’s office submits a claim to the patient’s insurance
company for the remainder of the bill.
3. The patient might pay nothing at the time of the visit to the doctor’s office.
Following the patient’s visit, the medical facility submits a claim to the
patient’s insurance company for the bill. The doctor’s office is reimbursed
by the insurance company for the charges the patient’s insurance policy
covers. The doctor’s office then sends a bill to the patient for the remaining
costs that the insurance doesn’t cover.
How a medical bill is processed varies slightly depending on whether the
patient pays the bill before or after the insurance company pays its portion. If
the patient must pay the entire bill on the day of the treatment, then it also
is up to the patient to send the bill, together with a completed claim form, to
their insurance company. The insurance company then will pay the patient for
whatever charges the insurance covers. For example, if the bill is $100 and
the insurance policy pays 80 percent of those charges, the patient will be
reimbursed for $80 from the insurance company, leaving the out
of pocket
cost for the bill at $20.
If the doctor’s office bills the insurance company first, then the patient can
leave the office either without paying any of the bill or after paying only the
copayment. The insurance company receives the doctor’s request for
payment and pays the covered amount to the doctor’s office. So if the bill
was $100, and the insurance policy covered 80 percent of that, then the
insurance company would pay the doctor $80. The doctor would bill the
patient for the other $20 or for the difference between the $20 and what the
patient already paid as the copayment.
When the insurance company pays for services, whether it pays the patient
directly or pays the doctor’s office, it is reimbursing the patient or the office.
Reimbursement is the process of paying someone back for services already
performed or payments already made.
This entire process—from the initial questionnaire completed in the doctor’s
office all the way through reimbursement—represents the life cycle of the
medical bill. As you’ve probably guessed, a big part of the medical bill’s life
cycle has to do with the insurance part of the process.
Step 4 Insurance
Medical insurance is a contract between an insurance company or carrier and an individual or a group.
In the first lesson we talked briefly about how the medical codes you assign are
sent to insurance companies so that doctors can be paid. But what exactly is
insurance? Well, the terms medical insurance, health insurance, health care
coverage or some other similar phrase all refer to the same thing. Medical
insurance is a contract between an insurance company or carrier and an
individual or a group—the insured. This contract or policy states that in the case of
certain injuries or illnesses, the insurance carrier will pay some or all of the medical
bills of the insured.
In exchange for this coverage, the insurance carrier collects payments or
premiums from the insured. Premiums are paid in advance—they are paid
monthly, quarterly, semi-annually or annually, depending on the contract
between the carrier and the insured. When an insurance carrier pays for
medical treatment, it pays benefits.
It seems like insurance companies pay out lots of benefits, right? Well,
typically the insurance carrier collects premiums from many people and only
has to pay benefits to relatively few. Therefore insurance companies are
generally profitable and are able to provide their services. Every insurance
company requires an itemized list of procedures, pharmaceuticals, and other
materials before they pay benefits. Every procedure and pharmaceutical has
its own code. This is where you, as a medical coding specialist, enter the
picture. You know from what you read in the previous lesson that you must
code what happens during each patient’s visit. When you’ve completed this
course, you will be able to accurately assign diagnostic and procedure codes
for outpatient services.
But first you need to know the language insurance carriers and medical
coding specialists use to communicate. In the next section, you will learn
some of this language.
Step 5 Common Insurance Terms
Liz is an office manager for Dr. Grant. She is great at making appointments and
keeping track of patients. Yesterday, Dr. Grant’s insurance specialist was out sick,
and Dr. Grant asked Liz to check on some insurance information for him. He asked
her to compare the explanation of benefits for three different patients and see how
much each patient needed to pay. Then he asked if any of the three had a
copayment not yet made. Finally, he asked Liz to check the explanation of benefits
to see whether any of the three patients had met deductibles yet.
Liz understands English very well, but these questions all sounded like another language to her.
Liz understands English very well, but these questions all sounded like
another language to her. She dug through some insurance forms, but she
didn’t have a clue about any of the items Dr. Grant had requested. Finally,
she gave up and asked Dr. Grant to wait until the next day when the claims
specialist returned.
Imagine you were Liz. Could you ask someone from an insurance company

questions—and understand the answers? In this section, you will study some
basic insurance concepts that will help you function intelligently when you
come across insurance terminology in your medical coding work. Let’s review
some of the most frequently used terms and what they mean.
Provider
The provider is the person or organization that provides medical services.
Doctors are an example of providers.
Claim Form
The claim form is the completed document that a provider submits to
an insurance carrier. The medical coder’s job is to assign diagnostic and
procedure codes to each claim. The most common insurance forms are
the CMS-1500 and UB-04.
Deductible
The amount of money an individual must pay before insurance benefits
begin is called the deductible. Usually a policy will pay nothing of the
first $250, $500 or $1,000 of medical charges. They then will pay a
percentage of everything above that amount each year.
Any amount that is “applied to deductible” is a covered charge that is
subtracted from the total deductible amount. The insurance carrier does
not pay any money on “applied to deductible” charges.
For example, imagine that Toby has a medical policy that has a $250
deductible and, after the deductible is paid, 80 percent coverage. So far
this year, Toby has spent $200 of his own money on medical care, and
that medical care has been defined as covered under his insurance
policy. For the insurance company to begin to pay 80 percent of Toby’s
covered medical care costs, he must still pay out $50 more for covered
charges. After he has met the $250 deductible, Toby’s medical insurance
benefits will begin, and the carrier now will pay 80 percent of each claim
submitted for covered charges for the rest of the calendar year.
Copayment
A copayment is a flat amount of money paid by the patient at each visit
or for each prescription. Many policies have a copayment for prescription
drugs or office visits to a doctor. That means every time a person fills a
prescription or visits the doctor, it costs her no more than her copayment;
however, she must pay that copayment every time she fills a prescription
or goes to the doctor. Some policies require copayments even after the
deductible has been met. Other policies have no deductible, but a
copayment is required every time any type of medical care is received.
Copayments are paid at the time of service.
Reasonable and Customary
The phrase reasonable and customary or R&C refers to price
guidelines that insurance carriers use for different procedures. Usually a
carrier only will pay up to the maximum on their reasonable and
customary fee, regardless of the actual cost of a procedure to the patient.
For example, if a patient has knee surgery and the doctor charges
$1,000, the insurance company compares that fee to its reasonable and
customary scale.
If the R&C scale gives a $900 limit for that particular procedure, then the
patient may be responsible for the extra $100, depending on the agreement
the physician has with the insurance company. The physician may accept the
R&C scale amount. Fees that exceed the reasonable and customary scale are
disallowed by the carrier.
How much will he have to pay?
Many private insurance carriers have adopted the reasonable and customary
guidelines for their coverage. Many government insurance programs, which
we’ll discuss momentarily, also use reasonable and customary guidelines.
Explanation of Benefits
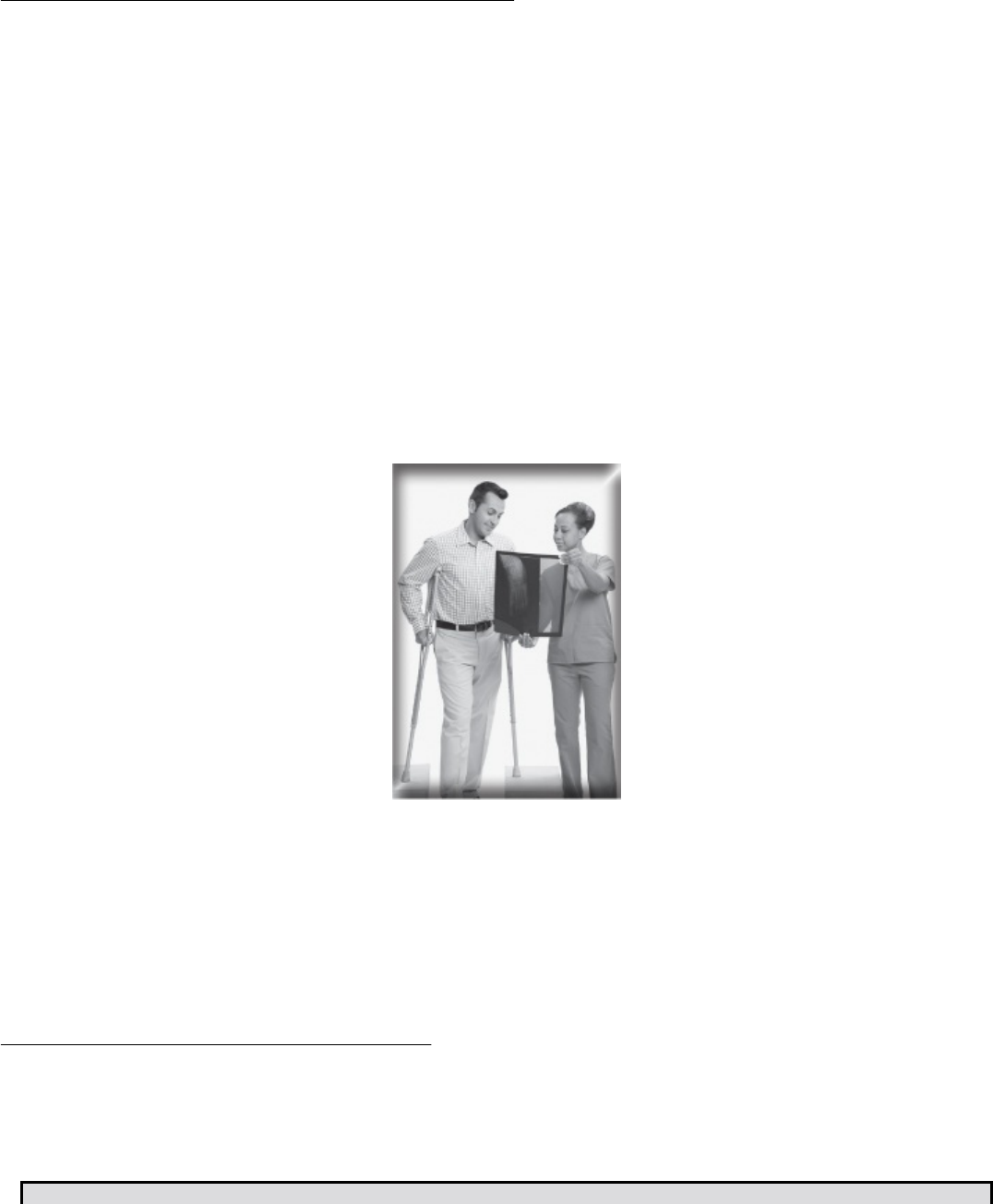
The explanation of benefits or EOB is a document that explains how much
the insurance company paid and how much it disallowed. Let’s look at two
samples of EOBs.
Bill from Doctor: $50
Disallowed: $6
Allowable Charge: $44
Applied to Deductible: $15
Amount due from Carrier: $29
The insurance company sends an explanation of benefits every time you
submit a claim. Even if the carrier is paying nothing on the claim, it still
sends this statement explaining why. As you can see from the example
above, the insurance carrier is paying $29 of a $50 charge, which means the
patient is responsible for the remaining $21.
The following table represents a breakdown of the EOB with a line-by-line
explanation of terms and amounts for the above example:
Electronic Claims
Before you dive into specifics, let’s first take a look at how electronic claims
processing works.
The Internet is used to determine eligibility.
Marissa enters her doctor’s office for her appointment. First, the office
manager uses the Internet to visit Marissa’s health plan Web site to
determine Marissa’s insurance eligibility. Next, the office manager prints out
an encounter form for the visit. The doctor sees Marissa, gives her a
prescription, and notes the diagnosis and procedure in her medical record.
Marissa then checks out with the office manager and pays her
copayment. The office manager begins the life of an electronic claim.
During the past several years, electronic claims submission rapidly has
gained popularity. But what exactly is an electronic claim? An
electronic claim is a digitized insurance claim form transmitted from a
computer using a modem and received by an insurance company or
clearinghouse. What does digitized mean? Well, after you, the coder,
code the items for the service, the data is entered into the computer.
Medical billing specialists use computer software to enter patient and
billing information into a claim format. When the data is entered into a
computer record, the information is digitized. That information then is
transmitted to a clearinghouse or insurance company using computer
software and a modem that allows the medical billing specialist’s
computer to communicate with the clearinghouse’s computer.
A clearinghouse is a company that facilitates the processing of claims
information into standardized formats and then submits the claims to the
appropriate insurance companies. Some insurance companies can receive
electronic submission of claims without going through a clearinghouse.
The clearinghouse downloads reports to the medical billing specialist
indicating how many claims it received, and then the electronic claims
are forwarded to the payers. The insurance carriers or payers will report
to the clearinghouse when they receive the claims.
After the insurance company receives the claim from the clearinghouse,
the claim is processed and paid or rejected. As you can imagine,
electronic insurance claims get paid much faster than paper claims.
The Health Insurance Portability and Accountability Act or HIPAA
regulates electronic claims, though this is just one of the many services
the act provides. The goal of HIPAA is that all healthcare workers have
similar ease and efficiency in their own communications. Later in this
course we’ll discuss HIPAA and its other facets in a bit more detail. You’ll
also learn exactly how it regulates electronic healthcare transactions.
Please pause and complete online Practice Exercise 2-1.
Step 6 Types of Health Insurance
Hundreds of private insurance companies provide medical coverage for individuals
and groups. These private insurance companies generally follow standards similar
to the government programs we will cover here. This next part of the lesson is
designed to introduce you to the many types of government-sponsored insurance
programs and each program’s requirements for coverage, along with the basic
types of private insurance.
Government Insurance
Unless otherwise noted, these programs are administered by the federal
government.
There are many types of government-sponsored insurance programs.
Medicare
Medicare is a federal health plan that covers people aged 65 and older and
people with disabilities.
Medicaid
Medicaid is a state-sponsored insurance program for low-income people
who otherwise wouldn’t be able to afford health insurance.
CHAMPUS
Until recently, CHAMPUS, which stands for Civilian Health and Medical
Program of the Uniformed Services, provided medical coverage for the
families of the various uniformed government services, including the armed
forces. Many changes have taken place in the military healthcare system in
the past several years. The most important of these changes is the transition
from CHAMPUS to the TRICARE healthcare system.
TRICARE
TRICARE is the name of the Department of Defense’s regional managed
healthcare program for military service families. TRICARE provides healthcare
options for the families of active-duty service members. These family
members are called beneficiaries. The service member is called the sponsor.
A sponsor can be active-duty, retired, or deceased. As its name suggests,
TRICARE has three options: TRICARE Standard, TRICARE Extra, and TRICARE
Prime.
TRICARE Standard
This is the new name for CHAMPUS. TRICARE Standard pays a share of the

cost of covered healthcare services obtained from authorized civilian hospitals
and doctors.
TRICARE Extra
This is a PPO-type option that provides healthcare services for eligible
participants on a visit-by-visit basis.
TRICARE Prime
This is an HMO-type option and is currently the least costly healthcare option
offered through TRICARE. Eligible persons must enroll for a year at a time
and agree to seek healthcare from the network of healthcare providers,
hospitals, and clinics. There is a fee for enrollment for retirees; active-duty
service members are enrolled automatically.
CHAMPVA
CHAMPVA, which stands for Civilian Health and Medical Program of the
Veterans Administration, provides medical coverage for veterans with
permanent, service-related disabilities. If a service member dies from a
service
related disability, CHAMPVA also provides coverage to the service
member’s family. Although very similar to TRICARE Standard in terms of
benefits, CHAMPVA is a separate program, distinctly different from
TRICARE Standard.
Workers’ Compensation
Workers’ compensation, a state-run program, pays the medical bills for
people with job-related illnesses or injuries.
Workers can be injured on the job.
In addition to the preceding government programs, many private insurance
companies exist. Private insurance companies can be categorized as either
traditional or managed care. In addition, there is Blue Cross/Blue Shield,
which represents a special case.
Private, Traditional Insurance
Twenty-five years ago, the traditional insurance concept was the only one.
The insurance company contracted with an individual to pay his or her
medical bills based on a fee-for-service concept—that is, whatever the
physician or medical provider charged was the amount on which the
insurance company based its reimbursement.
Private insurance companies are in business to earn profits. They pay out
benefits but also take in much more in premiums.
Managed Care
As healthcare costs skyrocketed, many businesses that held group insurance
policies for their employees began looking for ways to save money and still
provide excellent healthcare coverage. The solution was managed care.
Born in the 1980s, managed care introduced the concepts of Health
Maintenance Organizations, or HMOs, and Preferred Provider
Organizations, or PPOs. In both, groups of doctors contract with the
organization to charge set amounts for procedures. These amounts do
not change, and the patient cannot be charged an additional fee beyond
a copayment.
In HMOs, patients pay a fixed periodic rate monthly, quarterly or
annually. Patients then receive whatever health care they need, but they
must see a physician or medical provider who is part of that HMO. HMOs
encourage their members to practice preventive health care, often paying
for routine physicals and tests designed to catch signs of illness before
the person actually becomes sick. The patient is assigned a primary
physician when she joins the HMO. This primary physician then oversees
that patient.
Patients pay a fixed rate monthly, quarterly or annually.
PPOs contract with many doctors who agree to charge rates according to
the PPO scale. These doctors are not “employed” by the PPO. Instead,
they are independent offices, hospitals, and clinics that have joined the
PPO. When patients in a PPO go to a doctor or clinic who is not part of
the PPO, that patient sees a large reduction in benefits.
Blue Cross/Blue Shield
The oldest and largest prepaid insurance carrier is Blue Cross/Blue
Shield. Blue Cross provides hospital, outpatient, and home-care
coverage. Blue Shield covers physician services and provides dental and
vision-care coverage.
Blue Cross/Blue Shield differs from the other private insurance providers in
that it is not a commercial insurance company. Blue Cross/Blue Shield is a
federation of nonprofit community insurance corporations. Even though Blue
Cross/Blue Shield is not technically a government program, it must receive
state-level government approval before it can raise its rates.
Just as the HMO and PPO managed-care companies do, Blue Cross/Blue
Shield contracts with doctors who agree to charge a set fee for procedures
performed. Blue Cross/Blue Shield then reimburses the doctor directly for all
charges.
Step 7 Diagnostic Codes—A Piece of the Insurance
Puzzle
Now that you know about the different types of insurance programs, let’s take a
moment to discuss medical codes and how they apply to insurance.
After a patient’s office visit, tests, and other procedures, the medical billing
specialist fills out a claim form, which we discussed previously in this lesson.
These forms require special codes—diagnostic codes for diagnoses and
procedure codes for procedures performed. When you write a code on an
insurance form, a bill or a patient’s chart, you are “coding that entry.”
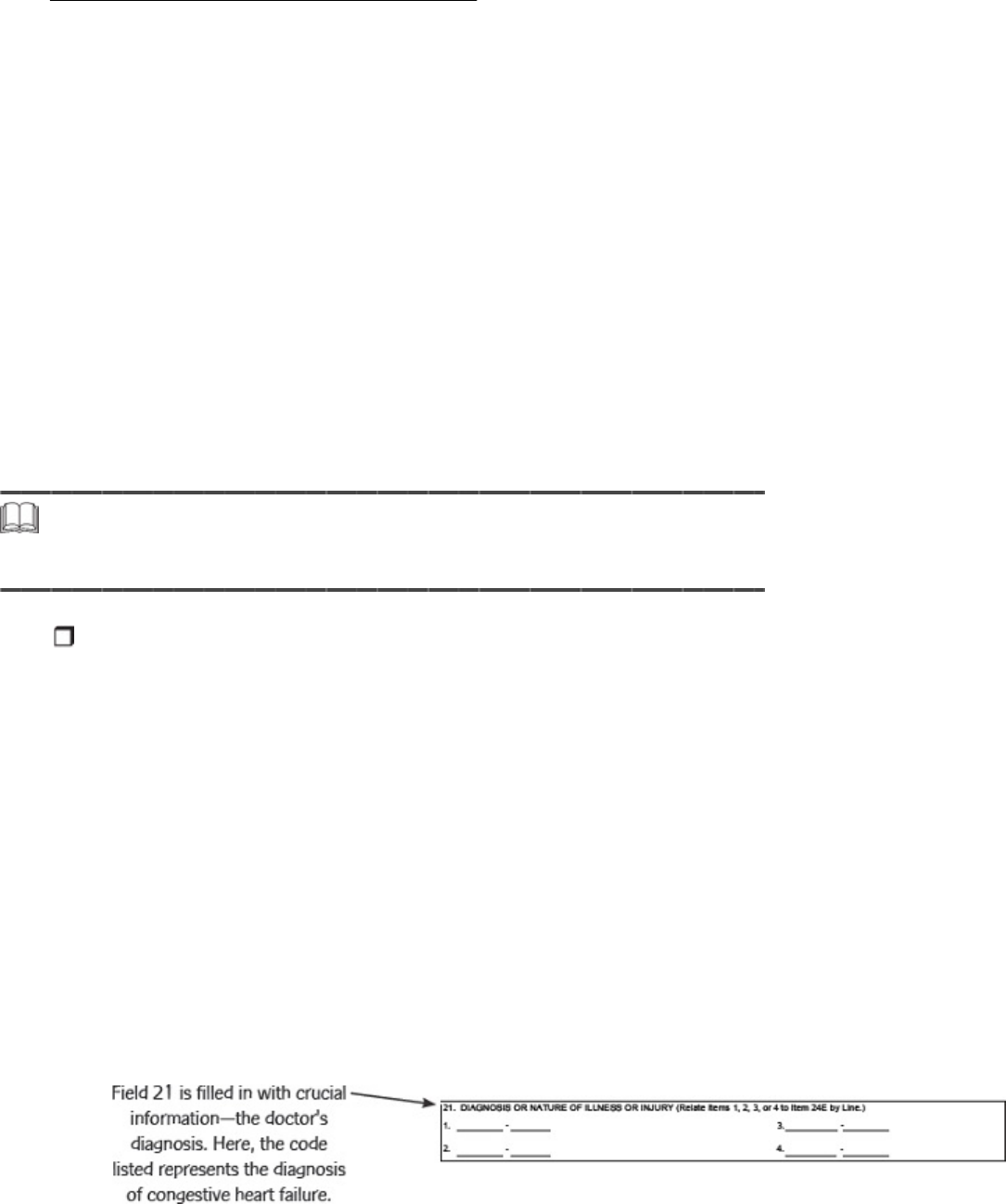
When you look at the CMS-1500 form, there are many fields to be filled.
One of the most important fields is Field 21—Diagnosis or Nature of
Illness or Injury. In this field, you must enter some crucial information.
But what information? Do you write in the doctor’s diagnosis? No. You
must use a diagnostic code.
Field 21 is filled in with crucial information—the doctor’s diagnosis. Here, the code listed represents the diagnosis of
congestive heart failure.
Diagnostic codes are numbers that identify the physician’s opinion
about what is wrong with the patient. This is the physician’s diagnosis.
These codes are not random numbers; they are based on a system called
the International Classification of Diseases or ICD. Hospitals, doctors’
offices, and medical coding specialists use ICD codes.
Often a patient is suffering from more than one symptom. In this case,
multiple diagnoses may apply. The doctor will determine a principal
diagnosis—usually the main cause of the symptoms or the main health
problem. When you code, you always enter the principal diagnosis code
first.
When a physician diagnoses more than one condition, the ones that aren’t principal are called concurrent conditions.
When a physician diagnoses more than one condition, the ones that aren’t
principal are called concurrent conditions. That means these conditions
happen at the same time as the principal diagnosis and might affect how the
patient recovers. For example, if Luke comes to the doctor suffering from a
broken leg—both the lower leg bones in his left leg are fractured—and a
sprained ankle.
How Important Is Diagnostic Coding?
It is your accurate and complete coding that ensures maximum
reimbursement to the provider and provides meaningful statistics to
assist our nation with its health needs. You probably think this seems like
a lot of responsibility, but don’t worry! You are not alone in this.
You know the whole process starts with the doctor and the patient. The
doctor has the responsibility to examine, test, and treat the patient as
needed and then document the services, supplies, and diagnosis.
Following the patient’s appointment, a medical transcriptionist types up
all of the information, and a medical coder then translates that
information into codes that support the procedures performed.
The codes and patient data then are transferred to a claim form and sent
to the insurance carrier for reimbursement to the provider based on the
medical necessity, diagnosis, and procedures involved. The types,
frequency of treatments, and diagnoses gathered from the patient
information provide the statistics necessary to depict health care in this
country. The government and insurance companies use these statistics to
establish guidelines to develop the rates of reimbursement paid to
medical practices in the future.
So you see, it’s the analysis of diagnostic codes that determines whether
insurance carriers will provide coverage for a particular procedure or
service. However, in the past, the diagnostic information that insurance
carriers gather has not been consistent. Therefore, the government now
is developing newer methods for collecting this information.
Now you have a bit of an idea as to how your new role affects insurance
reimbursement. Without your coding skills, doctors would not get
reimbursed for their services! We will cover diagnostic coding concepts
later in the course. Now, let’s look at procedure coding.
Step 8 Procedure Coding—Another Piece of the Puzzle
Diagnosis coding is not the only kind of coding you will do. If you look at the
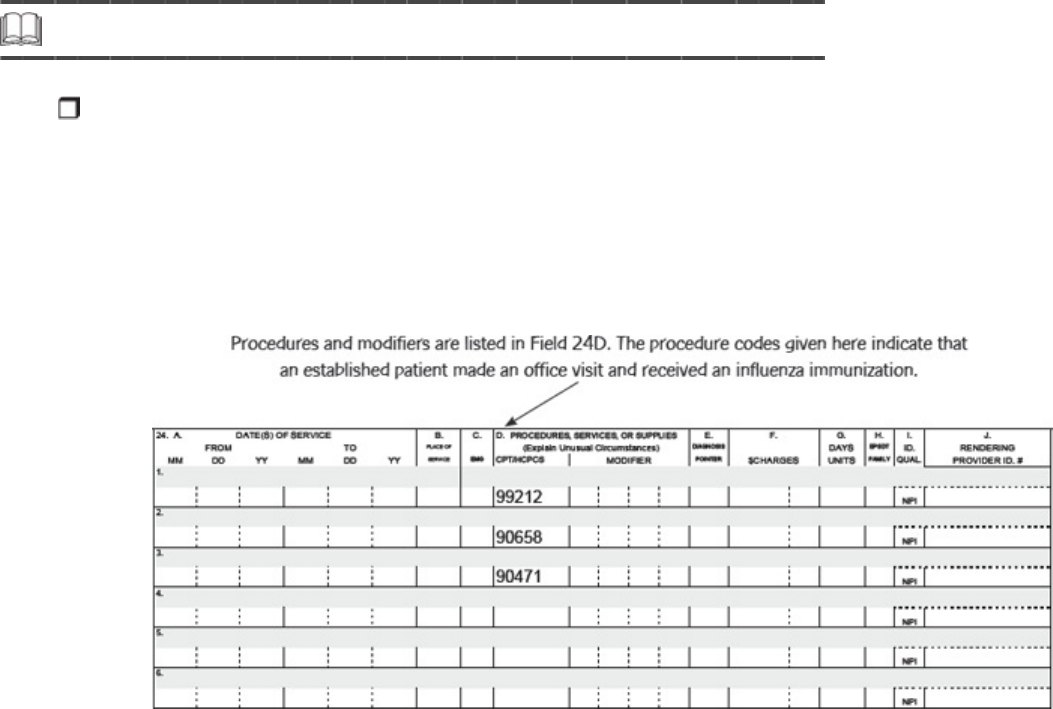
portion of the CMS-1500 form that follows, you will see Field 24D—a column for
Procedures, Services, or Supplies. This column is divided into halves. The first half
is labeled CPT/HCPCS, and the second is labeled Modifier. It is in this field that you
write down the code for the procedures and any modifications of those procedures
or treatments and tests that the doctor performed.
You might be called upon to double check records as they come through your
coding service. Usually double checking means checking to be sure the
diagnosis matches the procedures. Insurance companies use box 24D to
check the procedures and make sure they are consistent with the diagnosis.
If they aren’t consistent, reimbursement from the insurance company may be
delayed, denied or reduced.
Like diagnoses, procedures have their own numerical language. The language
of procedure codes is either the Current Procedural Terminology, CPT, or
the Healthcare Common Procedure Coding System, HCPCS—pronounced
“Hick-Picks.”
CPT coding is the most commonly used set of procedure codes. The CPT
codes, which the American Medical Association produces annually, are divided
into six sections.
CPT Procedure Coding Divisions
Evaluation and Management
Anesthesiology
Surgery
Radiology
Pathology and Laboratory
Medicine
Most procedures the doctor performs will have a code. You will enter the
correct code in the correct column of the CMS-1500 form. We’ll show you
exactly how to find this code later. For now, all you need to know are the
fields that codes go in on the CMS-1500 form.
Please pause and complete online Practice Exercise 2-2.
Step 9 Looking Ahead
Before we conclude this lesson, let’s take a moment to discuss the organization of
this course. You may be wondering why we are introducing you to insurance and
claims processing or why you will be learning medical terminology. You may be
asking, “Why can’t I just start coding?” Medical coding is an integral part of the
healthcare industry. Professionals in this field learn medical terms and language to
be able to communicate with each other effectively. Think about how many
different classes a doctor takes during her college education to practice the
profession. Doctors are the primary care providers you will be supporting in your
role as a medical coding specialist!
As you move through the course, you will learn medical terminology, medical
ethics, medical records handling, anatomy, and physiology. Medical
terminology is the first step to coding accurately. You must understand
medical terms to decide which code is best for each medical record you
receive. Accurate coding supports top-dollar insurance reimbursement for
your employer. If you are doing a good job for your employer, you will be
rewarded for your excellent coding skills. And remember, the job demand for
coders is expected to keep growing, so finding work should be a snap! In no
time you could be earning as much as $40,000 a year.
Have fun as you discover different aspects of the healthcare field! It won’t be
long before you are learning to use your coding manuals and actually coding
medical records. In that part of the course, we will include many examples
and Practice Exercises to help you understand the process. And your
instructors will be just a telephone call or e-mail away if you have questions.
We want you to feel prepared and confident as you enter into this exciting
field of medical coding!
Step 10 Lesson Summary
Medical insurance is a necessary part of America’s health care. Insurance coverage
comes from both government and private sources. Regardless of who provides the
coverage, insurance companies use a specific language to refer to different
insurance concepts.
In this lesson you learned that the different insurance programs available fall
into three categories: government, traditional, and managed care. The
federal government manages programs such as Medicare, TRICARE, and
CHAMPVA. State governments manage Medicaid and workers’ compensation.
In managed care, HMOs and PPOs contract with groups of doctors to provide
care at certain set amounts. These types of healthcare programs were
developed to help control the rising cost of medical care in America. This
lesson also gave you an understanding of diagnostic and procedure codes as
well as how electronic claims are filed.

As you move through this course you will see the important role you’ll play as a medical coder.
Keep in mind that this lesson was a brief overview of insurance programs and
how insurance works. As you move through this course you will see the
important role you’ll play as a medical coder. Your employer will depend on
you to submit the proper coding for filing claims to insurance companies and
federal agencies for reimbursement. The specialized training you get in these
lessons will make you and those for whom you work successful!
Please pause and complete an online Quiz. Good luck!
LESSON 3
Introduction to Medical Terminology: Word
Parts
Step 1 Learning Objectives for Lesson 3
When you have completed the instruction in this lesson, you will be trained to do
the following:
Explain word parts.
Define root word, and describe how the term is used.
Form terms with prefixes, suffixes, and root words.
Use an online medical dictionary.
Step 2 Lesson Preview
Medical coding specialists are in demand, so finding a job should be a snap.
In the first two lessons you learned about the day-to-day procedures in healthcare
settings. You also saw how medical professionals, including coding specialists, work
together as a team. You also became familiar with medical records, insurance and
the role both will play in your new career. Hopefully these lessons also taught you
that medicine is a very rewarding field. You will experience its satisfactions and live
up to its challenges every day that you work as a medical coding specialist. And
you know that skilled medical coding specialists are in high demand. Providers and
clinics all need qualified medical coding specialists. In fact, many such positions
remain unfilled due to a lack of qualified candidates. Most employers look for
coding specialists who have schooling and experience, and with the training you
receive in this course, you can count on learning everything you need to know
about this medical field. Finding the position you want should be a snap!
In the next three lessons, you’re going to focus on one very important
part of medicine—its language. Doctors, nurses and other healthcare
personnel, including coding specialists, communicate in specialized terms
that, at first, might sound like a foreign language. You’ve no doubt
overheard medical conversations in your own visits to the doctor. As a
coding specialist, you’ll hear medical terminology in daily conversation.
More importantly, you’ll use this knowledge as you review medical
records for diagnoses and procedures. Once you determine the correct
diagnoses and procedures, you’ll research those terms in your coding
manuals to find the correct medical code. Just think—you’ll soon be a
medical terminology guru! What used to sound like a foreign language
will someday become as familiar as your everyday conversation.
Doctors communicate in specialized terms.
Fear not—learning medical terminology is a lot easier than learning a foreign
language. Medical terms can be broken down into easy-to-understand parts.
In this lesson, we will introduce you to your new language—the language of
medicine. In these next few lessons, you’ll learn the building blocks you’ll
need so that you can break down any medical term. We’ll discuss root words,
prefixes, and suffixes and explain how these word parts come together to
form medical terms. Throughout the lesson, be sure to have your flashcards
handy as you will need to consult them as you study.
Step 3 Word Parts
Words are all around us. You use them every day to communicate. You use long
words and short words, complex words and simple words. And there always will be
words that are new to you. As a medical coding specialist, you often will be faced
with medical terms. These terms might seem complex at times, but you can
simplify them. In every sentence you speak, every letter you write, the words are
constructed of parts. These parts give clues to the words’ meanings. Because you
know this, you can break words down and figure out their meaning from their word
parts.
Words are all around us.
Look at these words you already know:
telephone
microwave
television
microscope
telescope
It’s easy to split these words into parts:
telephone = tele + phone
microwave = micro + wave
television = tele + vision
microscope = micro + scope
telescope = tele + scope
You see that some of these words contain some of the same parts. Tele/
is in three of the words. Telescope and microscope both have the word
part /scope.
So you see, words can be divided into smaller parts called word parts,
and they are very important in learning medical terminology. Word parts
are like building blocks. A child can take a dozen building blocks and make
many different things, combining the blocks in different ways. The same is
true of word parts. Many different words can be formed from a few word
parts.
Step 4 Root Words
The foundation for all words is the root word. The root word is the basic
component of the terms used to communicate. Many simple words contain only a
root word without any other word parts.
book
read
joy
cook
drive
Word parts are used together with root words to make new and different
words. This is usually done by adding either a prefix or a suffix. A prefix is
a word part added to the beginning of a root word. Conversely, a suffix is a
word part added to the end of a root word.
When other word parts are added to root words, a new word is formed, and
this new word means something slightly different. Below are some new
words that were formed from the root words we just mentioned. A prefix or
suffix has been added to each root word. Remember, a prefix is a word
beginning. A suffix is a word ending.
booklet a little book
reread to read again
joyful having the quality of joy
cooked to cook sometime in the past
driver a person who drives
In addition to prefixes and suffixes, different root words come together to
form new words. Words made up of two or more root words are called
compound words. Here are some examples:
book + shelf = bookshelf
drive + way = driveway
news + paper = newspaper
Understanding word parts helps you understand new words—even long and
complicated words.
You may not know the word recalculate. But if you know what calculate
means, and you know what the prefix re/ means, then you know that
recalculate means to calculate again.
In fact, you probably have made up some new words yourself just by
making new combinations of word parts.
Let’s review the word parts. Think of these word parts as the building blocks
of medical terms.
Word Parts
Root Word The root word is the foundation or cornerstone of the word.
Prefix A prefix is attached to the beginning of a root word to change its meaning.
Suffix
A suffix is attached to the end of a root word to change its word form or
meaning.
Now let’s take the basic concept of word parts and apply it to medical
terms.
Step 5 Medical Terms
Medical terms may appear to be long and complicated, but even the longest
medical term can be broken down into small, easy-to-understand parts. Once you
become familiar with the individual word parts, medical terminology becomes easy.
Try to look at medical terms like little puzzles. You’re putting together different
pieces (root words, prefixes, and suffixes) to form complete words.
Try to look at medical terms like little puzzles.
Understanding some essential word parts will help you recognize
medical terms. You will learn about each of these word parts, one at a
time, in a simple, logical, easy-to-understand sequence. This will make
it very easy for you to spell and understand even the longest and most
complicated terms.
The Combining Vowel
Many medical terms contain a fourth word part that we have not yet
discussed—the combining vowel. The combining vowel joins a root word to
other word parts.
Here is an example of how the combining vowel is used. As you can see, not
all terms have all four parts.
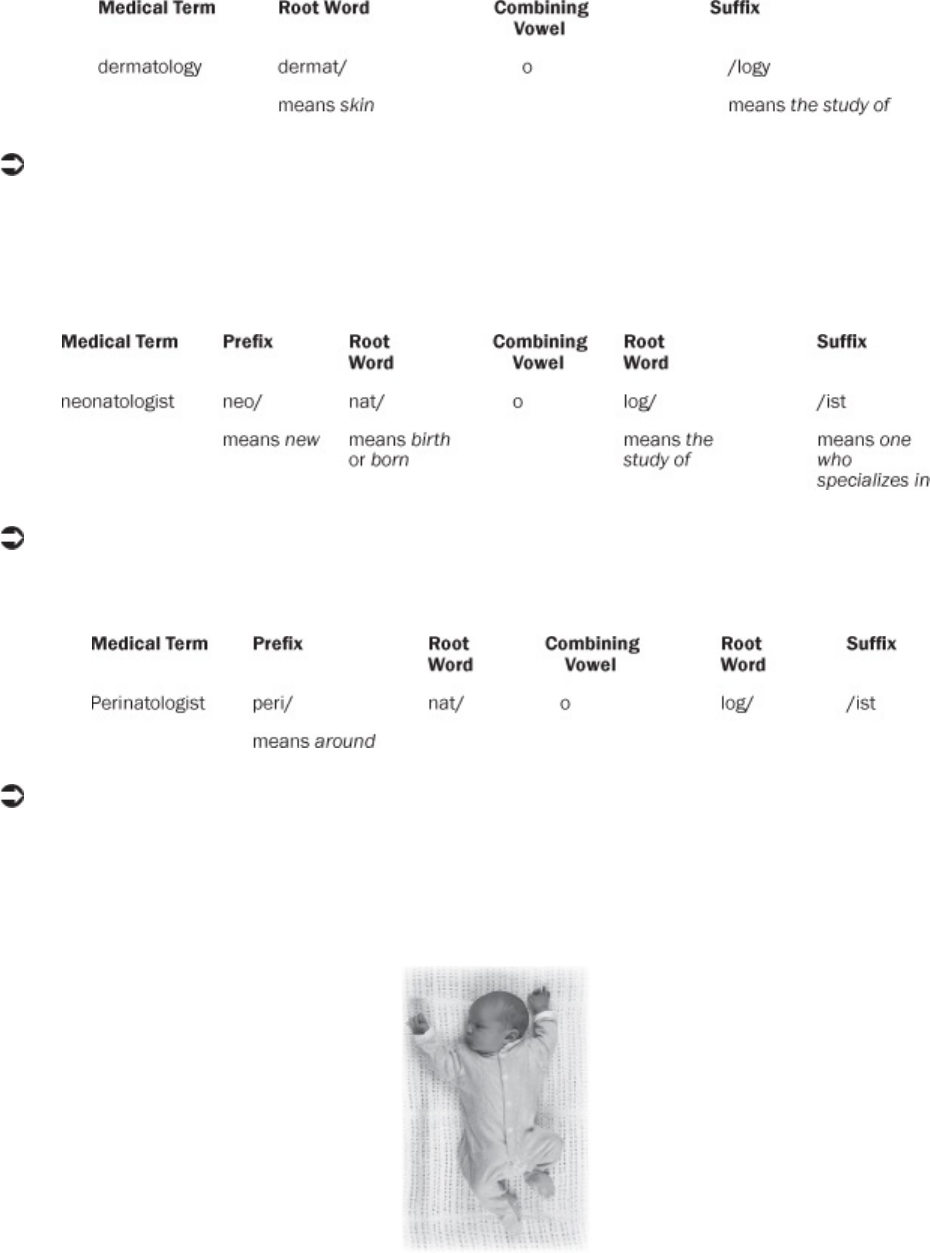
Dermatology means the study of skin.
On the following page are two more medical terms that show examples of
word parts. These are compound words because they contain more than one
root word.
A neonatologist is one who specializes in the study of the newborn.
If you use a different prefix, you will have the following term:
A perinatologist is someone who specializes in the study of the fetus and
newborn (the time around the birth).
These are two types of doctors you may find yourself working for as a
medical coding specialist!
A perinatologist is someone who specializes in the study of the fetus and newborn.
Before you move on, let’s take a moment to look up one of the new terms
you learned in your medical dictionary. Basically, a medical dictionary works
much the same way a regular dictionary does—you simply use it to look up
the spellings and definitions of medical terms. For example, if you came
across the term dermatology and wanted to know what it meant, you’d
thumb through your medical dictionary until you found the term. There is the

definition—the science that deals with the skin. If you find yourself having a
hard time understanding how to use your medical dictionary, feel free to
contact your instructor for guidance.
Tip
If you have access to a computer and the Internet, you can use an online
medical dictionary to look up terms. An online medical dictionary can be
found at http://www.online-medical-dictionary.org/. Feel free to check it out!
Please pause and complete online Practice Exercise 3-1.
Step 6 Root Words
As you previously learned in this lesson, word parts are the building blocks for all
words, including medical terms. Up to this point, word parts were described in a
general manner. Now you will take a closer look at root words—the foundation of
all words.
Root words are the foundation of all words.
You will find many of the root words in this lesson familiar because they are
used in everyday English, as well as in medical terminology. The words
covered in this lesson are the most common of all medical root words.
You may have wondered why medical terms are so long and
complicated. Well, it’s because these terms have very definite meanings.
In medicine, one complicated word takes the place of four or five
common words so that doctors can communicate exactly what they
mean to other health professionals. This prevents misunderstandings
that can interfere with the patient’s care. For example, the words
abdomen and stomach may mean the same thing to you, but they have
different meanings to a doctor. Because of this, doctors use different
words for the stomach and the abdomen. You will learn the root words
for these and other parts of the body in this lesson and in lessons to
come.
Doctors and other healthcare professionals use special medical terms
because they know it’s important to communicate precise information
about a patient’s condition. As you learn to build words, you will be
building your professional skills. You will be an important link in the
healthcare team. Without you, the medical coder, this patient
information would not make it to the insurance companies in the correct
format, meaning that your colleagues may not get properly reimbursed
for their expertise and services.
The medical codes you determine for each patient’s case serve an additional,
critical purpose. These codes enable government health agencies to track
and research life-threatening illnesses, such as various types of cancer, heart
disease, and AIDS. Your important role as a medical coder helps save lives!
The Functions of Root Words
There are three interesting facts about root words.
Facts About Root Words
• Root words are the foundation of medical terms.
• Root words name body parts or body functions that the terms represent.
• Most medical terms have at least one root word.
Look at these examples of root words:
Root Word English Meaning
neur/ nerve
gastr/ stomach
scop/ examine
log/ study of
cardi/ heart
path/ disease
These root words are in the medical terms that follow. Even though you may
not know the meaning of the medical term, you know the meaning of the
root word you saw just a moment ago.
Medical Term Meaning
neuritis inflammation of nerves
gastritis inflammation of the stomach
microscope an instrument to examine small things
logic a method of studying an area of thought
cardiac relating to the heart
pathology the process of the study of disease
Compound Words as Root Words
Some terms have two or more root words in them. They are called
compound words. In the examples below, you will use the same root
words you used previously.
Compound Word Meaning
neuropathy a disease process of nerves
gastroscope an instrument to examine the stomach
cardiologist one who studies the heart
pathologist one who studies disease
Notice that the combining vowel /o/ was used to join the root words.
Combining Forms of Root Words
Root words sometimes are awkward to pronounce. That is why you may see
the combining vowel—usually the letter /o/—between the root word and
other word parts. The combination of the root word and the combining vowel
is the combining form. Look at the combining forms for the root words you
saw previously.
Root Word Combining Form English Meaning
neur/ neur/o nerve
gastr/ gastr/o stomach
scop/ scop/o examine
log/ log/o study of
cardi/ cardi/o heart
path/ path/o disease
In this course, each new root word you learn will be in its combining
form.
Root Word + Combining Vowel = Combining Form
Now that you know the basics about root words, you’re ready to move ahead
and learn more about medical terms. First, you will practice pronouncing root
words using the following exercise.
Step 7 Pronounce Root Words
Follow these steps to learn how to pronounce root words.
a. Take your Quick-Learn Tutor and Set 1 flashcards out of your Quick-Learn
Kit. Each flashcard contains many flashterms.
b. Find the first flashcard. It begins with Flashterm 1-1. Insert the card into
the lower part of Side A of your Quick-Learn Tutor. Push the card up until
Flashterm 1-1 appears in the left window.
c. Access the online portion of your course. Go to the Lesson 3 book, and click
on Lesson 3 Listen to Root Words.
d. Listen to a root word as it is pronounced. After you hear a root word, pause
the audio.
e. Look at the root word in the left window of your Quick-Learn Tutor.
Practice pronouncing it out loud several times until you can pronounce it
correctly and easily. Push the flashcard up until the meaning of the root
word appears in the right window. Read the meaning of the root word.
f. Repeat steps d and e, continuing with all the flashterms on Flashcard 1.
g. When you have completed Flashcard 1, turn the card over for Flashcard 2.
Proceed until you have pronounced all the root words for Set 1.
h. Next, begin with Flashcard 1 and play the audio again. This time,
pronounce each root word in order but do not stop after each term.
i. As you pronounce each root word, look at it on the flashcard. Listen to your
own pronunciation of each root word. If you mispronounce one, put a check
mark next to it with your pencil.
j. Next, practice the root words you mispronounced by listening to the audio
again. Be sure you can pronounce each root word clearly and easily.
After you have finished pronouncing all of the root words for this lesson,
move on to the next exercise—learning to write root words.
Step 8 Write Root Words
Follow these steps to learn how to write root words.
a. Insert Flashcard 1 into Side A of your Quick-Learn Tutor.
b. Look at each root word as it appears in the window and say it out loud.
Write each root word on blank paper. Be sure to put a slash (/) between
the root word and the combining vowel, just as you see it on the flashcard.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the root word. Writing
these root words and meanings will help you learn them more easily. Here
is an example of the first flashterm.
aden/o gland
d. Do this for each flashterm for this set.
Finally, after you have pronounced and written each term, learn the
meanings of these root words in the next exercise.
Step 9 Meanings of Root Words
Follow these steps to learn the meanings of root words.
a. Again insert the flashcard for Set 1 into Side A of your Quick-Learn Tutor.
Beginning with Flashterm 1-1, pronounce each root word out loud. Before
you look at the meaning, see if you can remember it. Check yourself by
pushing the flashcard up until you can see the meaning in the right window.
Do this for each flashterm for this set.
b. Now insert Flashcard 1 into Side B of your Quick-Learn Tutor. Push the card
up until you see the meaning of Flashterm 1-1 in the right window. Read
each meaning out loud. Before you look, see if you can remember the word
part that goes with that meaning. Check yourself by pushing the flashcard
up until you can see the root word in the left window. Do this for each
flashterm for this set.
c. Practice with the flashcards several times until you are familiar with the
root words and their meanings. It’s not necessary to memorize all the
terms now. You will find that you begin to memorize medical terms as you
use them throughout this course.
You may use your flashcards for all Practice Exercises and Quizzes. However,
the time you spend reviewing the flashterms now will mean less time spent
looking them up later.
Tip
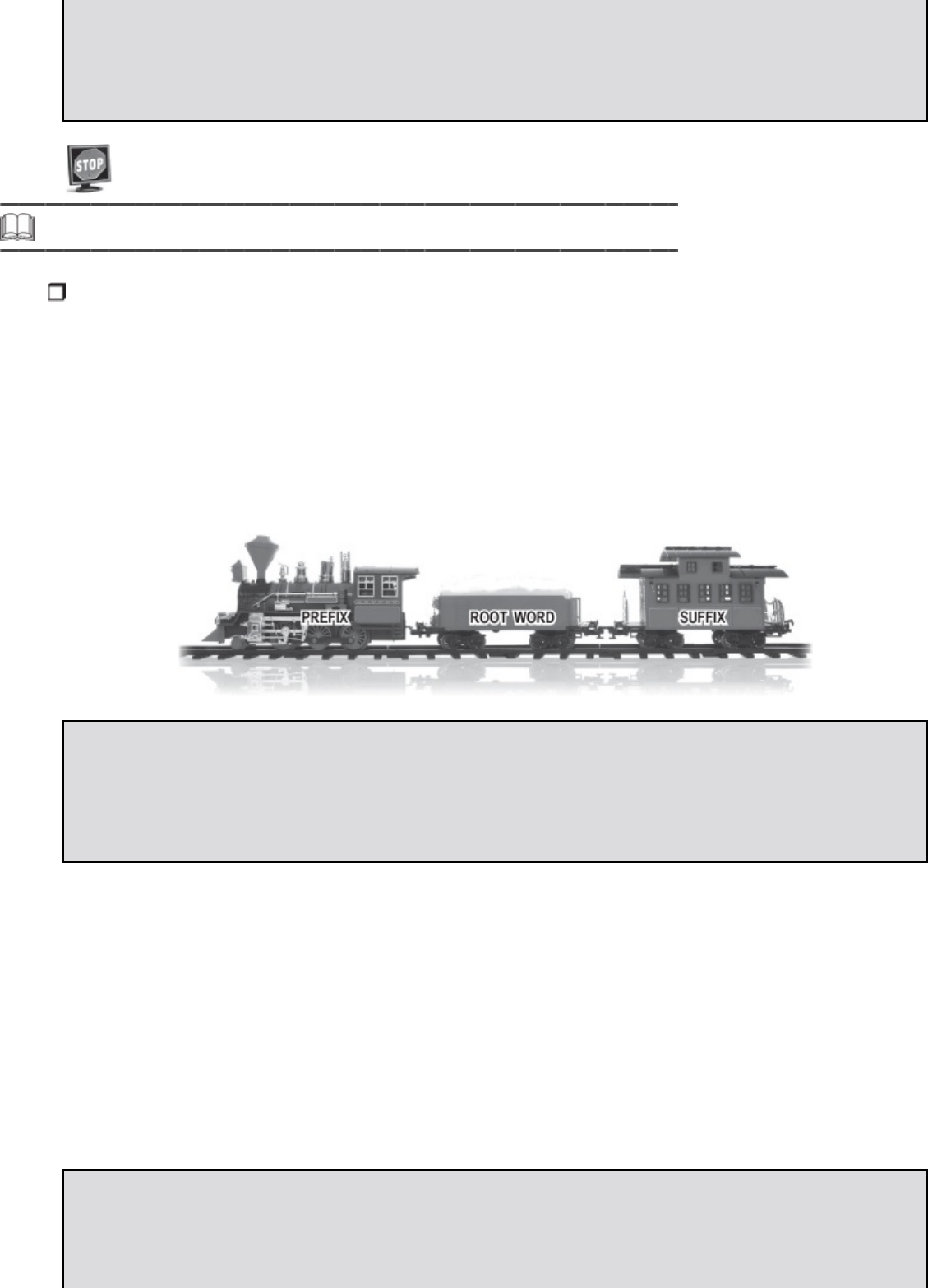
After you have finished your activities with a set of flashcards, return the
flashcards, in order, to your Quick-Learn Kit. You can easily refer to them
later, as needed, throughout the course.
Please pause and complete online Practice Exercise 3-2.
Step 10 Prefixes
Now that you’ve learned about root words, let’s learn about another word part—
prefixes. If you consider the root word to be the boxcar on a train, the prefix is the
engine, and the suffix is the caboose. You know that prefixes are added in front of
root words while suffixes are added at the end of root words.
A prefix changes the meaning of a medical term. While the root word names
a body part or body function, the prefix gives additional information about
the medical term.
Facts About Prefixes
• A prefix gives additional information about a medical term.
• A prefix usually tells where, when or how.
Let’s take a look at some examples of prefixes and their meanings. Notice
that prefixes do not have combining vowels.
Prefix Meaning
peri/ surrounding
brady/ slow
tachy/ fast
micro/ small, tiny
a/ without, absent
Now let’s learn more about prefixes.
Fact About Prefixes
A prefix does not change the meaning of a root word. A prefix does change
the meaning of the whole medical term.
In the following list, you see medical terms made from some of the root
words you studied earlier. Notice that the prefix does not change the
meaning of the root word. (Don’t worry about the vowel endings on the root
words for now. This will be explained shortly.)
Medical Term Meaning
renal relating to the kidney
perirenal relating to surrounding the kidney
cardia heart
bradycardia slow heart
tachycardia fast heart
glossa tongue
macroglossa large tongue
gastric relating to the stomach
hypogastric relating to below the stomach
leukocytosis condition of white cells
aleukocytosis condition of absence of white cells
Fact About Prefixes
Many terms do not begin with a prefix.
A prefix is attached to the root word. If there is no prefix, the first word part
you will see is the root word. Look at these examples.
perirenal starts with prefix
renal starts with root word
Remember, a prefix only tells where, when or how. A root word tells
what.
How do you tell if the beginning of the word is a prefix or a root? Well, one
way is to see what happens when you remove the first word part. Look at the
following example. You saw these terms a moment ago. The root word here
means heart.
Medical Term Meaning
cardia heart
bradycardia slow heart
When you take the prefix brady/ away, the meaning of the term changes
from slow heart to heart. However, the meaning of the root, heart, doesn’t
change, so you know that brady/ is a prefix.
Facts About Prefixes and Root Words
• If you take away a prefix, you take away only the where, when or how.
• If you take away a root word, you have taken away the what—the basic
meaning of the term.
Look at the next example. This term is a compound word. The “what” is a
white cell. A white cell is one kind of cell—it is not a red cell or a liver cell.
Look what happens to the meaning of the term when we remove one of the
two root words that make up the compound word.
Medical Term Meaning
leuk/o/cyt/osis condition of white cells
cyt/osis condition of cells
When the root word leuk/o is removed, the meaning of the term
changes from white cells to simply cells. The term cyt/osis means a
condition of any kind of cells: red cells, white cells, liver cells and so on.
The “what” of the term changed from white cells to cells. Therefore,
leuk/o is a root word.
For now, all the prefixes you learn are followed by a slash. Look at these
examples.
brady/ micro/ peri/
All the root words you learn have a slash between the root and the combining
vowel. Look at these examples.
cardi/o leuk/o cyt/o
Step 11 Pronounce Prefixes
Follow these steps to learn how to pronounce prefixes.
a. Take your Quick-Learn Tutor and your Set 2 flashcards out of your Quick-
Learn Kit.
b. Find the first flashcard for Set 2. Insert the card into Side A of your Quick-
Learn Tutor. Push the card up until the first prefix appears in the left
window.
c. Access the online portion of your course, and click on Lesson 3 Listen to
Prefixes.
d. Listen to each prefix as it is pronounced. After you hear a prefix, pause the
audio.
e. Look at the prefix in the left window of your Quick-Learn Tutor. Practice
pronouncing it out loud several times until you can pronounce it correctly
and easily. Push the flashcard up until the meaning of the prefix appears in
the right window. Read the meaning of the prefix.
f. Repeat steps d and e, continuing with all the flashterms on the flashcard.
g. When you have completed the flashcard, turn the card over. Proceed until
you have pronounced all the prefixes for Set 2.
h. Next, begin again with the first flashcard and play the audio. This time,
pronounce each prefix in order but do not stop after each term.
i. As you pronounce each prefix, look at it on the flashcard. Listen to your own
pronunciation of each prefix. If you mispronounce one, put a check mark
next to it with your pencil.
j. Next, practice the prefixes you mispronounced by listening again. Be sure
you can pronounce each prefix clearly and easily.
After you have finished pronouncing all the prefixes in this set, move on to
the next exercise—learning to write the prefixes.
Step 12 Write Prefixes
Follow these steps to learn how to write prefixes.
a. Insert the first flashcard for Set 2 into Side A of your Quick-Learn Tutor.
b. Look at each prefix as it appears in the window and say it out loud. Write
each prefix on blank paper. Remember to include the slash.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the prefix.
d. Do this for each prefix for this set.
Finally, after you have pronounced and written each term, learn the
meanings of these prefixes in the next exercise.
Step 13 Meanings of Prefixes
Follow these steps to learn the meanings of prefixes.
a. Again insert the flashcard into Side A of your Quick-Learn Tutor. Pronounce
each prefix out loud and then say the meaning. Check yourself by pushing
the flashcard up until you can see the meaning in the right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud and then say the prefix. Check yourself by
pushing the flashcard up until you can see the prefix in the left window. Do
this for each flashterm for this set.
c. Practice with the flashcards several times until you are familiar with the
prefixes and their meanings. Don’t struggle to memorize them. The more
times you review your flashcards, the more familiar they will be to you.
Tip
Remember to keep your flashcards in order even after you’re finished with
an activity so you can refer back to them easily.
A handy way to review flashcards from previous lessons is to read down the
flashcard without inserting it into the Quick-Learn Tutor.
Please pause and complete online Practice Exercise 3-3.
Step 14 Suffixes
A suffix is the word part that is attached to the end of a root word.
Why do we use suffixes? A suffix can change the word form or the meaning of
a term. The word form tells you how the word functions in the sentence.
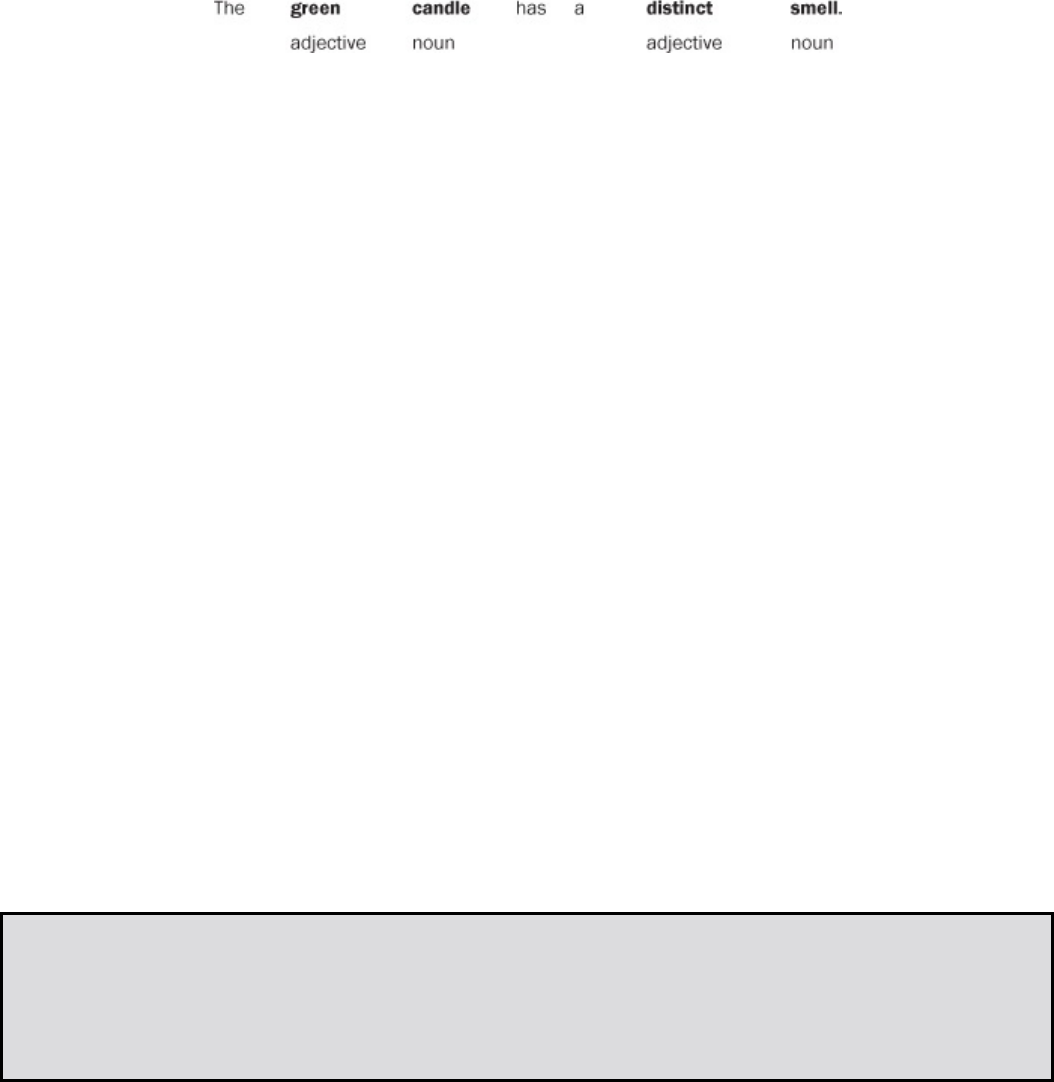
Word forms also are referred to as parts of speech.
Two important parts of speech are the noun and the adjective.
A noun is the name of a person, place or thing. An adjective is a word that
describes a noun. Here’s an example.
The words candle and smell are nouns because they name a person,
place or thing. The words green and distinct are adjectives because
they describe nouns.
Some root words can function as both nouns and adjectives. All you have to
do is change the suffix. Here’s an example.
Noun Adjective
courage courageous
Compare these two sentences:
Courage is an important quality for a soldier to have. The courageous man
saved the boy’s life.
In the first sentence, courage is a noun. It is a thing, a quality. In the second
sentence, the word man is the noun, and the word courageous describes the
man, making courageous an adjective.
Look at these examples of medical terms that can be changed from nouns to
adjectives just by changing the suffix.
Noun Adjective
cardi/a cardi/ac
gastr/ia gastr/ic
muc/us muc/ous
neur/osis neur/al
Fact About Suffixes
A suffix can change a root word to a noun or an adjective.
The suffix determines whether a word is a noun or an adjective. Suffixes
that make a word a noun are called noun suffixes. Suffixes that make
a word an adjective are called adjective suffixes. No matter what root
word they are joined to, a noun suffix always changes the word into a
noun, and an adjective suffix makes the word an adjective.
Here is a table of some common medical suffixes. Notice that some of the
suffixes are noun suffixes and some are adjective suffixes. Many noun suffixes
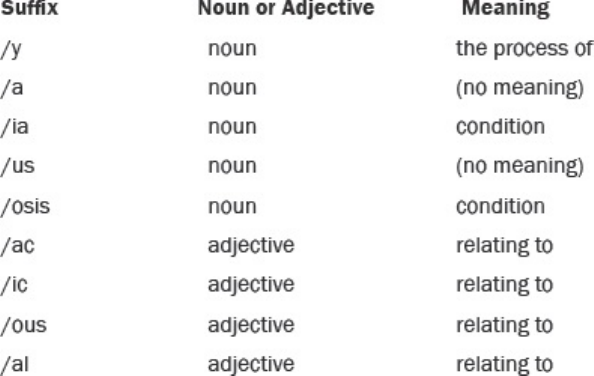
don’t really have a meaning. They are just used to show that the word is a
noun.
When you learn suffixes later in this lesson, the flashcard will tell you which
are noun suffixes and which are adjective suffixes.
Did you notice that many of the suffixes have the same meaning? If they
have the same meaning, how do you know which one to use? Well only
certain suffixes and certain root words can be combined. For example, each
root word generally can be combined with only one adjective ending. Cardi/o
is joined with /ac to form cardiac. Cardi/o is never joined with /ic, /al or /ous.
The words cardiic, cardial and cardious do not exist.
To help you learn which suffixes go with which root words, we have taken
many root words and combined them with the correct suffix. This will help
you remember which suffixes go with which roots.
In the next few lessons, you not only will be learning individual word parts
but also complete medical terms—both nouns and adjectives.
Often a root word + suffix combination can itself be used as a word ending.
You can think of this as a combined suffix. For example:
path/o + /y = /pathy
The combined suffix /pathy can be joined to many other words.
cardiopathy myopathy neuropathy
These combined suffixes will be written on your flashcards as regular suffixes,
but if you look closely, you’ll be able to see the root word + suffix
combination. Look at these examples.
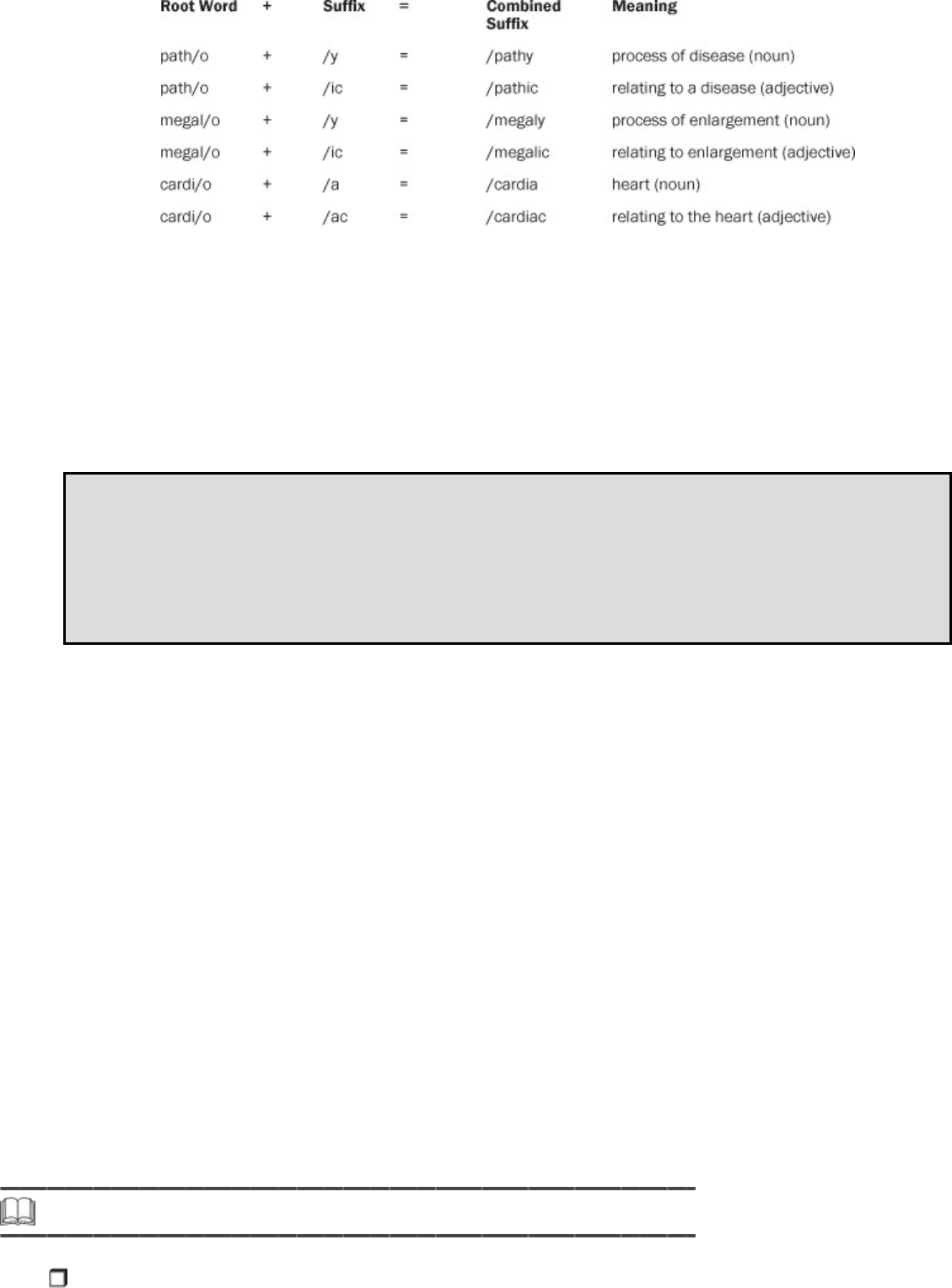
Before you move on, let’s pretend for a moment that you know the term
cardiopathy, which means heart disease, but you aren’t sure if
cardiopathy is in fact the correct spelling—you suspect it may be spelled
cardiapathy instead. So what should you do? Well, simply look in your
medical dictionary, following the terms until you find the correct spelling.
In your dictionary you see that you were right the first time. The term is
spelled cardiopathy!
Fact About Suffixes and Root Words
Most root words need either a noun suffix or an adjective suffix at the end of
them.
Most root words can’t stand alone as complete words—they need a suffix at
the end of them. But like everything else in life, there are exceptions. For
some root words, you don’t need a suffix of any kind to form a complete
word. These roots already are complete words. By dropping the combining
vowel, these root words stand alone. They also work as suffixes themselves.
Listed are three examples of root words that don’t need a suffix.
Root Word Suffix (Noun) Meaning
gram/o /gram picture, record, tracing
graph/o /graph
machine that creates a tracing or
recording
derm/o /derm skin
In this course you will be given more noun and adjective suffixes.
Whenever you learn a new term, look to see which suffixes are used with
which roots. That way you will begin to recognize which roots and
suffixes belong together.
Now let’s learn how to pronounce suffixes.
Step 15 Pronounce Suffixes
Follow these steps to learn how to pronounce suffixes.
a. Take your Quick-Learn Tutor and your Set 3 flashcards out of your Quick-
Learn Kit.
b. Insert the first flashcard for Set 3 into Side A of your Quick-Learn Tutor.
Push the card up until the first flashterm appears in the left window.
c. Access the online portion of your course, and click on Lesson 3 Listen to
Suffixes.
d. Listen to a suffix as it is pronounced. After you hear a suffix, pause the
audio.
e. Look at the suffix in the left window of your Quick-Learn Tutor. Practice
pronouncing it out loud several times until you can pronounce it correctly
and easily. Push the flashcard up until the meaning of the suffix appears in
the right window. Read the meaning of the suffix.
f. When you have completed the flashcard, turn it over for the next flashcard
for this lesson. Proceed until you have pronounced all the suffixes for Set 3.
g. Next, begin again with the first flashcard and play the audio again. This
time, pronounce each suffix in order but do not stop after each term.
h. As you pronounce each suffix, look at it on the flashcard. Listen to your
own pronunciation of each suffix. If you mispronounce one, put a check
mark next to it with your pencil.
i. Next, practice the suffixes you mispronounced by listening again. Be sure
you can pronounce each suffix clearly and easily.
Step 16 Write Suffixes
Follow these steps to learn how to write suffixes.
a. Insert the first flashcard for Set 3 into Side A of your Quick-Learn Tutor.
b. Look at each suffix as it appears in the window and say it out loud. Write
each suffix on blank paper.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the suffix.
d. Do this for each suffix for this lesson.
Finally, after you have pronounced and written each term, learn the
meanings of these suffixes in the next exercise.
Step 17 Meanings of Suffixes
Follow these steps to learn the meanings of suffixes.
a. Again insert the first flashcard for Set 3 into Side A of your Quick-Learn
Tutor. Pronounce each suffix out loud. Before you look at the meaning, see
if you can remember it. Check yourself by pushing the flashcard up until you
can see the meaning in the right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud. Before looking, see if you can remember the
suffix that goes with that meaning. Check yourself by pushing the flashcard
up until you can see the suffix in the left window.
c. Practice with the flashcards several times until you are familiar with the
suffixes and their meanings. You may use your flashcards for all Practice
Exercises and the Quizzes.
Please pause and complete online Practice Exercise 3-4.
Step 18 Lesson Summary
Understanding how to “decipher” medical terminology is a special link to becoming
an effective medical coding specialist. Understanding medical terminology will
allow you to find the correct diagnosis and procedure provides those healthcare
professionals and insurance companies with the information they need to get

properly reimbursed. Although medical terms might seem complex, you now know
that you can simplify them by breaking them down into word parts and then
figuring out the meanings of the parts. Word parts are like building blocks because
many different words can be formed from a few word parts.
You learned how to build medical terms, which will help you in your future career.
The foundation for all words is the root word, the basic component of terms.
The root word names the body part or body function that the term
represents. Most medical terms have at least one root word.
We use word parts together with root words to make new and different
words. This is usually done by adding either a prefix or a suffix. Prefixes
are word parts added to the beginning of a root word. A prefix gives
additional information about a medical term, and a prefix usually tells
where, when, or how. A prefix does not change the meaning of a root
word—but a prefix does change the meaning of the whole medical term.
A suffix is a word part added to the end of a root word. The suffix
determines whether a word is a noun or an adjective. Most root words
need either a noun suffix or an adjective suffix at the end of them.
Combining vowels are word parts that join a root word to another word
part. Combining vowels make terms easier to pronounce.
It’s important that you understand word parts as a medical coding
specialist. While this lesson may have strained your brain a little more
than the previous ones, you’ve now learned about the building blocks
you’ll need to “build” many medical terms! The Practice Exercises in this
lesson are important. If you skipped any or struggled to complete some
of them, take a few moments to go back and work on them again. Doing
so will prepare you for the upcoming Quiz and build upon your medical
foundation of knowledge.
Just for Fun
After a long day of helping people, most health professionals take a break to
smile and have fun. Having fun after working hard has four benefits.
It relieves stress.
It exercises your face muscles.
It isn’t fattening.
It is free.
If anything else in this world gave you these four benefits, you’d take as
much of it as you could get. So every once in a while we’ll take a fun break—
just like this.
Some Just for Fun pages are for enjoyment. Some will tell you interesting
things about language and the medical field. Some will give you a warm
smile.
Most people use words that come from Greek and Latin every day. Here are
some examples.
Greek Latin
telephone plumber
chemistry alibi
therapy medium
skeleton honor
The English language has more ways to say something than any other
language. That is because it contains words from so many languages. In fact,
there are a lot of words in English that come from French. Here are some
examples.
French
humility
liberty
image
The English language also uses words that are Anglo-Saxon. They are
usually three or four letters long. When you use a “four-letter word,” you

are probably using an Anglo-Saxon word. Look at these examples of
common three- and four-letter words.
Anglo-Saxon
cat
dog
free
Medicine has been around a long time. The word parts you are learning
come from Greek and Latin.
A long time ago, no one in England spoke English. The peasants spoke
Anglo
Saxon. Peasants couldn’t read or write. They could only speak their
language. It was very simple. Speaking Anglo-Saxon meant you hadn’t
been to school and didn’t have much in the way of gold and diamonds, or
even food, for that matter. Anglo-Saxon words became our everyday
words.
The only people who were educated were the clergy. They read and
wrote Latin. They studied Greek when they wanted to do something
really exciting. Therefore, anyone who spoke Latin or Greek was
considered educated. As science developed, scientists used Latin and
Greek so everyone would know they were educated. Greek and Latin
words became our professional terms.
In 1066, the French invaded England. The French ruled England and
owned the land. The French language gained importance. Eventually
French words became our elegant words.
After many years, the English language grew from these roots. That’s why
in English today, there are usually three words (at least) for everything. If
you consider where the different words come from, you can see why
different words for the same thing may sound everyday, scientific or
elegant. Look at these examples.
Anglo-Saxon Latin or Greek French
fire conflagration blaze
job profession affair
happy felicitous joyous
behind posterior derriere
Today, by choosing different words, English can still sound everyday,
professional or elegant. Don’t be afraid of long words. You soon will learn
easy, step-by-step ways of breaking them down to the building blocks
you have learned. In this section, you are learning the building blocks. In
future sections, you will learn what the terms mean. Soon you will be
using medical terms like a professional because you will be a
professional.
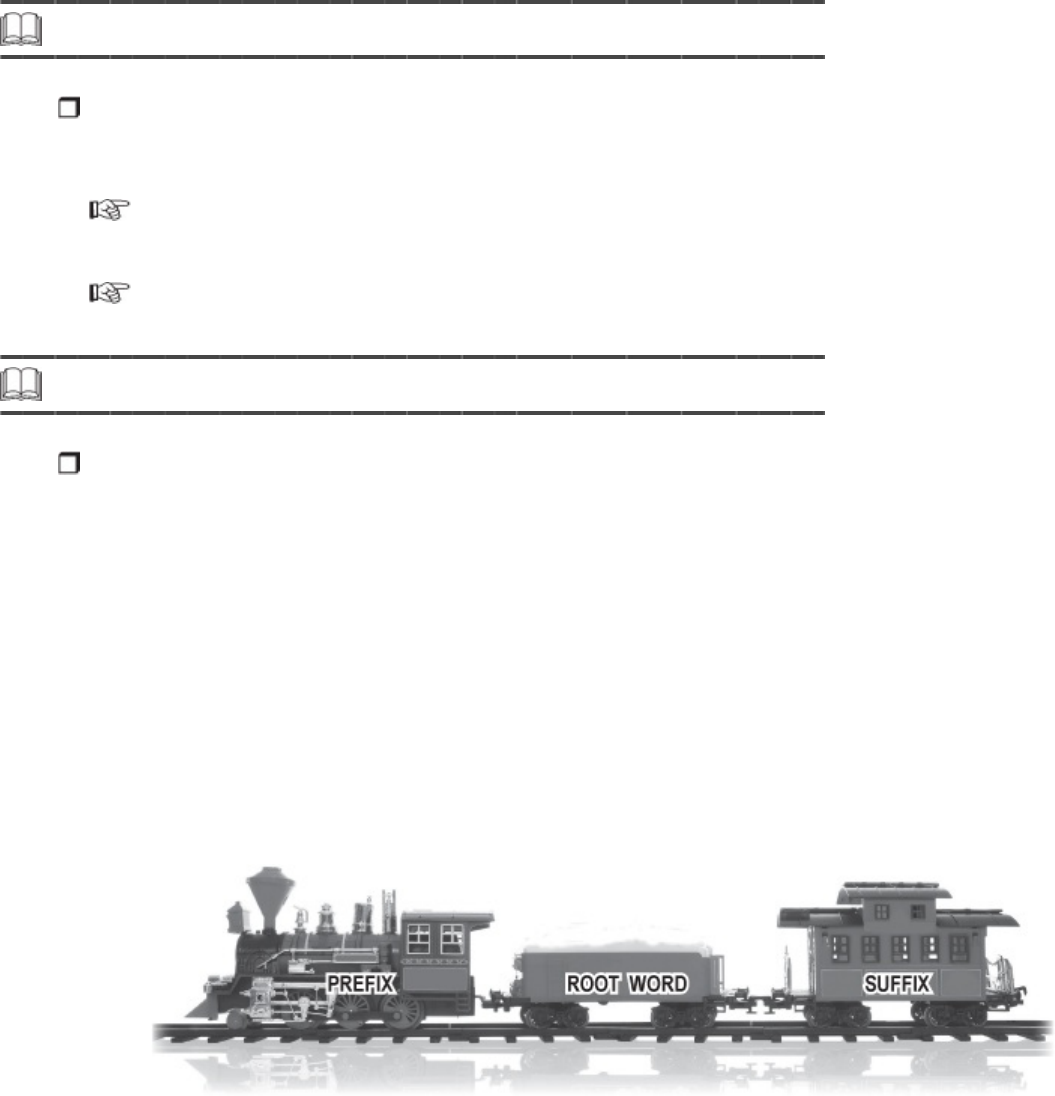
LESSON 4
Medical Terminology: Dividing and
Combining Terms
Step 1 Learning Objectives for Lesson 4
When you have completed the instruction in this lesson, you will be trained to do
the following:
Divide common medical terms into parts, and provide the meaning of
each part.
Properly combine prefixes, root words, and/or suffixes to form medical
terms that describe certain diagnoses and procedures.
Step 2 Lesson Preview
So far, you have learned the word parts that fit together to form medical terms:
prefixes, root words, and suffixes. In this lesson you’ll learn how to take complete
terms and divide them. You’ll also learn how to combine word parts correctly to
create new terms.
You may recall the train example in the last lesson—the root word is the
boxcar, the prefix is the engine and the caboose is the suffix. When you
divide medical terms, you can look at the entire train and determine the
prefix, suffix, and root word. This is important because you sometimes will be
faced with unfamiliar terms. If you can look at an unfamiliar word and divide
it properly, you then can determine its meaning based on the word parts.
As a medical coding specialist, you might review medical records that
don’t have the correct medical term spelled out for you. It will be your
job to determine the exact procedure or diagnosis—which we talked
about in the first two lessons—from the medical records. Without those
key terms coded, which you’ll soon learn how to do, the doctors for

whom you work could not get reimbursed by insurance companies for
their time and expertise. You are the link between the healthcare
provider and his salary! This lesson shows you how to take “plain
English” descriptions and combine word parts to form the correct
medical term. As you read this lesson, keep in mind that you are
learning both the meanings of and how to assemble words.
Throughout the lesson, be sure to have your flashcards handy as you will
need to consult them as you study the following material, do the Practice
Exercises, and take the Quiz. Your knowledge of medical terms will make you
a valuable resource in the medical field—you will be able to communicate
effectively with health care providers and insurance companies. Now, let’s get
started!
Step 3 Dividing Medical Terms
You have learned about word parts—the building blocks of medical terms—and you
can identify these building blocks in medical terms. By dividing these terms into
their word parts, you can recognize new or complicated medical terms. Then you
can look them up in a dictionary more easily and spell them correctly.
Fact About Dividing Words
When you are looking for the word parts in a medical term, read from the end of the
term to the beginning. This simple technique lets you “see” word parts more easily.
Let’s look at the following example.
thermometer
By dividing medical terms, you know the meaning of thermometer.
If you read from the end of the word, the first word part you see is the suffix
meter. Draw a slash to the left of meter.
thermo/meter
Continue reading from right to left. Next you see an o. This may be a
combining vowel. Put in another slash. Continue reading from right to left.
You see the root word therm.
therm/o/meter
Now give the meaning of thermometer starting with the suffix.
Word Part Starting with End of Word Meaning
/meter instrument to measure
o (combining vowels have no meaning)
therm/ heat
A thermometer is an instrument to measure heat.
The following three examples further show you how to divide a medical term,
reading from end to beginning, to find the meaning.
Word Part Starting with End of Word Meaning
/genesis creating
o (combining vowels have no meaning)
carcin/ cancer of gland tissue
Carcinogenesis means creating cancer of gland tissue.
Word Part Starting with End of Word Meaning
/plasty restore through surgery
o (combining vowels have no meaning)
maxill/ upper jaw
Maxilloplasty means restoring the upper jaw through surgery.
Of course, whenever you are pronouncing a term, you should read from the
beginning of the term to the end, just as you would read any new word in
English.
Consonants, Vowels and the Role They Play
When you divide medical terms it is important to remember that a
consonant is any letter of the alphabet except a, e, i, o, u and, for the
purposes of working with medical terms, y.
Fact About Dividing Medical Terms
When a suffix begins with a consonant, there is a combining vowel between the root
word and the suffix.
Let’s take a look at a few examples.
Term with Suffix Beginning with Consonant Meaning
cardi/o/ + gram tracing of the heart
thromb/o/ + plasty surgical repair of blood clot
thorac/o/ + centesis withdrawing fluid from the chest
gastr/o/ + megaly enlargement of the stomach
Because all the suffixes in these examples begin with a consonant, the
combining vowel is used. (Did you notice in these examples that dividing
slashes (/) were placed between each word part?)
Fact About Dividing Words
When the suffix begins with a vowel, there is no combining vowel between the root
word and the suffix.
You already learned that vowels are the letters a, e, i, o and u. Also, y is
considered a vowel when working with medical terms. Let’s look at some
examples.
Term with Suffix Beginning with Vowel Meaning
arthr/ + algia pain in joints
bi/ + opsy look at living (tissue)
cardi/ + ac relating to the heart
hemat/ + oma blood tumor (lump)
cardi/o/path/ + y disease of the heart
As you can see, the combining vowel was not used in the terms above
before the suffix. The last term, cardiopathy, ends with the suffix /y. The
suffix /y follows this vowel rule because it acts like a vowel here.
Fact About Dividing Words
There is a combining vowel between two root words in a compound word.
As you learned previously, a compound word has two or more root words in
it. Look at these examples. Notice the combining vowel between the root
words. Also notice that the combining vowel remains even if the second root
word begins with a vowel.
Compound Word with Combining Vowel Meaning
cardi/o/log/ist heart specialist
gastr/o/enter/o/logy study of the stomach and bowels
therm/o/meter instrument to measure heat
A Little Practice
Let’s get a little practice in dividing medical terms. Look for word parts in the
examples that follow. Read each term from the end of the term—from right
to left. Put in slashes between word parts. Pay special attention to whether
or not a combining vowel is present. Be careful. Not every o is a combining
vowel, so use your flashcards if you need help.
perirenal
hemostasis
neuritis
hepatitis
cranium
pararenal
appendectomy
paraneural
cardiology
hepatomegaly
Here is how you should divide these terms. Either way is correct as the
combined suffix does not always need to be divided.
peri/ren/al
hem/o/stasis
neur/itis
hepat/itis
crani/um
para/ren/al
append/ectomy or append/ec/tom/y
para/neur/al
cardi/o/logy or cardi/o/log/y
hepat/o/megaly or hepat/o/megal/y
Now give the meaning of these terms. Start at the end of the term and work
to the left. Write the meaning in the blank lines. (The meaning you give
doesn’t have to be exactly the same as the one provided. We will use the
meanings from your flashcards.)
peri/ren/al ____________________________________
hem/o/stasis ____________________________________
neur/itis ____________________________________
hepat/itis ____________________________________
crani/um ____________________________________
para/ren/al ____________________________________
append/ectomy ____________________________________
para/neur/al ____________________________________
cardi/o/logy ____________________________________
hepat/o/megaly ____________________________________
The meanings for each of the previous terms are listed here:
peri/ren/al around (surrounding) the kidney
hem/o/stasis control (hold in) blood
neur/itis inflammation of nerve(s)
hepat/itis inflammation of the liver
crani/um (structure of the) skull
para/ren/al beside (beyond) the kidney
append/ectomy (the process of) removal of the appendix
para/neur/al relating to beside a nerve
cardi/o/logy (the process of) the study of the heart
hepat/o/megaly (the process of) enlargement of the liver
The words “the process of” are enclosed in parentheses because they usually
are left off when the word is defined in common speech. For example,
hepatomegaly commonly is defined as enlargement of the liver, not the
process of enlargement of the liver.
Now that you know the meaning of hepatomegaly, would you like to see
what code you would assign for this diagnosis?
789.1 Hepatomegaly
See how a medical term is translated into a diagnostic code? This code would
be entered on the medial claim form required for the insurance company.
Without it, the insurance company processing the medical claim would not
know what is wrong with the patient. A medical coding specialist’s job is very
important!
Word Meanings
People who work in the medical field often use shorter and simpler
meanings of words to save time. As you become more familiar with
medical terms, you probably will use simpler meanings also. Sometimes
a simpler meaning of a word can be formed by reading the word from
beginning to end.
Compare these simpler meanings that were given by an experienced coding
specialist to the meanings derived from word parts.
Term
Meaning Derived from Word
Parts
Simpler Meaning
thermometer instrument to measure heat heat-measuring instrument
paraneural relating to beside a nerve next to a nerve
cardiology
(the process of) the study of the
heart
heart specialty
hepatomegaly
(the process of) enlargement of the
liver
liver enlargement
For now, simply start at the end of a word that is new to you. This will help
you look for word parts that you recognize and help you give meanings for
word parts. This is the easiest way to find word parts and give meanings. As
you become more familiar with various word parts, feel free to use simpler
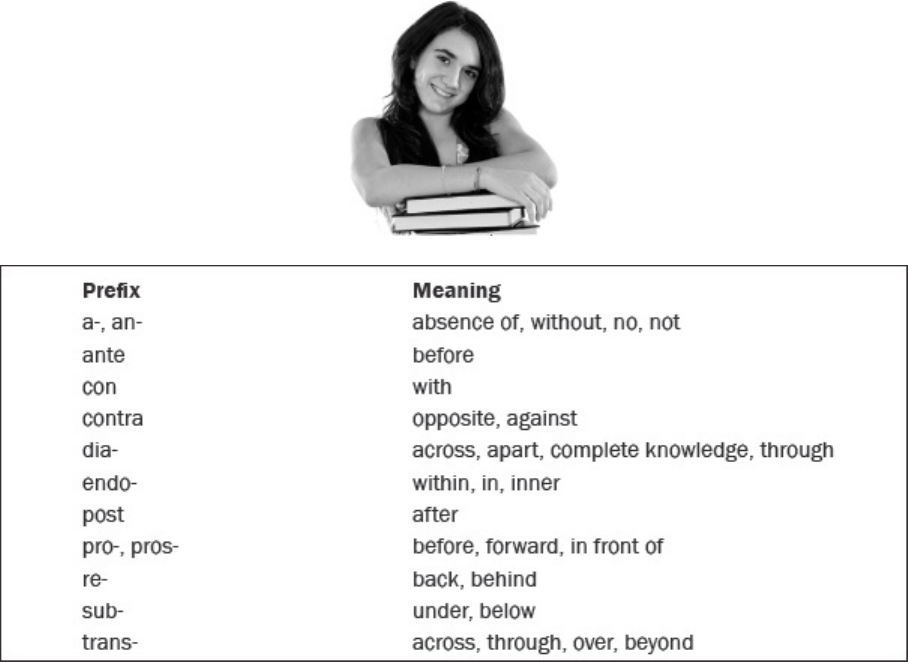
meanings.
Now let’s examine a few word parts and their meanings. Remember, you may
use your flashcards to find word part meanings, and as you learn more word
parts, dividing medical terms will become easier!
Word Part Meaning
bi/ two
/malacia softening
syn/, sym/ together with
gynec/o female
sarc/o nongland tissue, flesh
vit/o living, alive
chem/o chemical, drug
meta/ change, beyond
maxill/o upper jaw
nect/o bind
/oma tumor, mass
Examine the two boxes that follow. The boxes list common prefixes and
suffixes and their meanings. These boxes will help you as you divide and
combine terms.
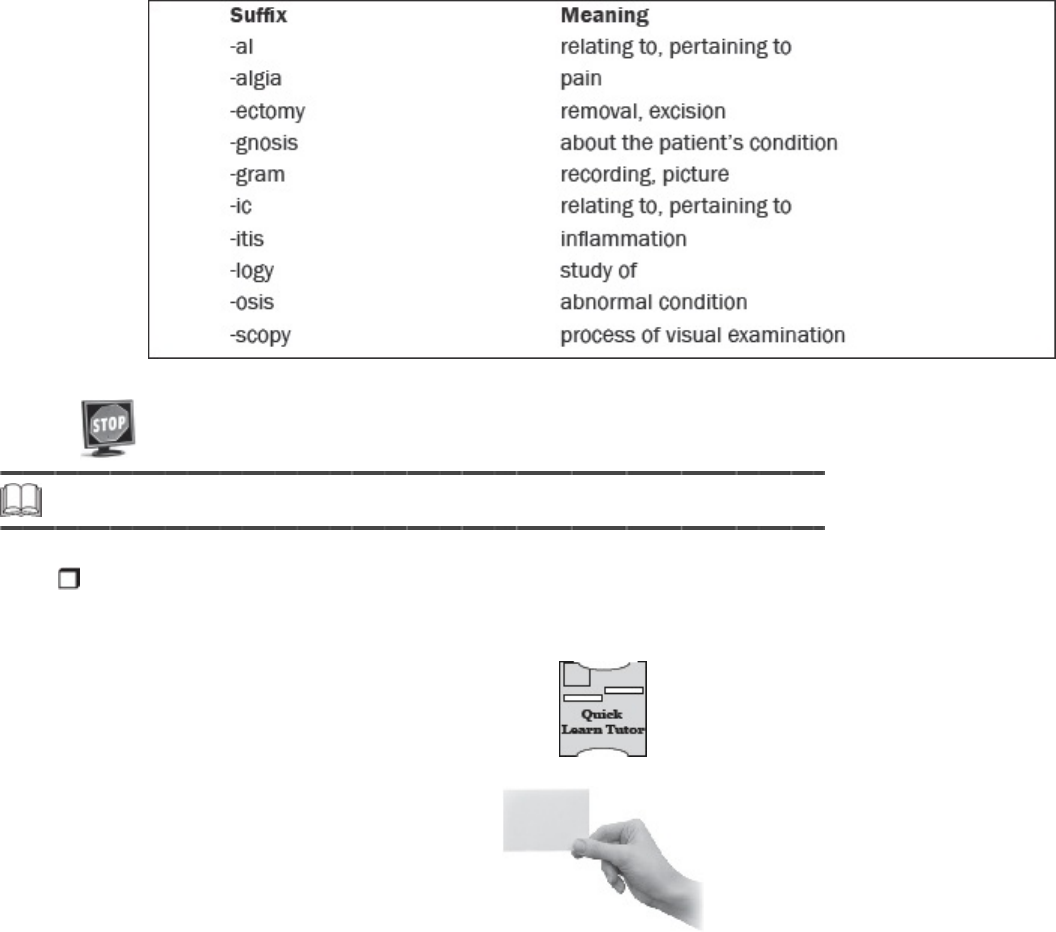
Please pause and complete online Practice Exercise 4-1.
Step 4 Pronounce Word Parts
Now that you know the basics about dividing medical terms, practice pronouncing
word parts using the following exercise.
a. Take your Quick-Learn Tutor and your Set 4 flashcards out of your Quick-
Learn Kit. Insert the first flashcard for Set 4 into Side A of the Tutor.
b. Access the online portion of your course, and click on Lesson 4 Listen to
Word Parts.
c. Listen to a word part as it is pronounced. After you hear a word part, pause
the audio.
d. Look at the word part in the left window of your Quick-Learn Tutor and
practice pronouncing it out loud several times until you can pronounce it
correctly and easily. Push the flashcard up and read the meaning of the
word part.
e. Continue this process for all the flashcards for this set.
f. Next, put the flashcards in order and play the audio again. This time,
pronounce each word part in order but do not stop.
g. As you pronounce each word part, look at it on the flashcard. Listen to your
own pronunciation of each word part. If you mispronounce one, put a check
mark next to that flashterm.
h. Next, practice the word parts you mispronounced by listening again. Be
sure you can pronounce each word part clearly and easily.
Step 5 Write Word Parts
The next step in your lesson is to practice writing the terms you have just learned.
Follow these instructions:
a. Insert the first flashcard for Set 4 into Side A of your Quick-Learn Tutor.
b. Look at each word part as it appears in the window and say it out loud.
Write each word part on blank paper. Remember to include the slash.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the word part.
d. Do this for each flashterm for this set.
Step 6 Meanings of Word Parts
Follow these steps to learn the meanings of the terms you have pronounced and
written.
a. Again insert the first flashcard for Set 4 into Side A of your Quick-Learn
Tutor. Pronounce each word part out loud and then say the meaning. Check
yourself by pushing the flashcard up until you can see the meaning in the
right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud. Before you look, see if you can remember the
word part that goes with that meaning. Check yourself by pushing the
flashcard up until you can see the word part in the left window. Do this for
each flashterm for this set.
c. Practice with the flashcards several times until you are familiar with the
word parts and their meanings. You may use the flashcards for the Practice
Exercises and the-in Quizzes.
Please pause and complete online Practice Exercises 4-2 and 4-
3.
Step 7 Combining Medical Terms
Combining word parts to form medical terms is just the reverse of dividing medical
terms into word parts.
When you learned to divide medical terms, you gained the skill of recognizing
long or complicated terms by dividing them into their word parts. Sometimes
when doctors fill out bills and charts, they may use a term unclearly or
incorrectly. If you know how to combine word parts, you can put together the
correct medical term from its everyday English meaning. This is the reason
for learning how to combine medical terms.
Knowing just a few word parts allows you to combine them into many
different medical terms. Look at this example of the number of new terms
you can form each time you add a new word part to your list.
Let’s see now. You only needed to learn eight word parts to build 16 medical
terms! Not bad. Just stick to the steps and before you know it, you will have
learned many word parts the easy way. Word parts, like nickels and dimes,
add up fast.
Would you like to see another example of a medical term that is coded? How
about gastritis? A patient visits the doctor because he has a stomachache.
After examination and testing, the doctor diagnoses him with acute gastritis.
You know that the meaning of gastritis is inflammation of the stomach. That
sounds painful!
535.00 Acute gastritis; without mention of hemorrhage
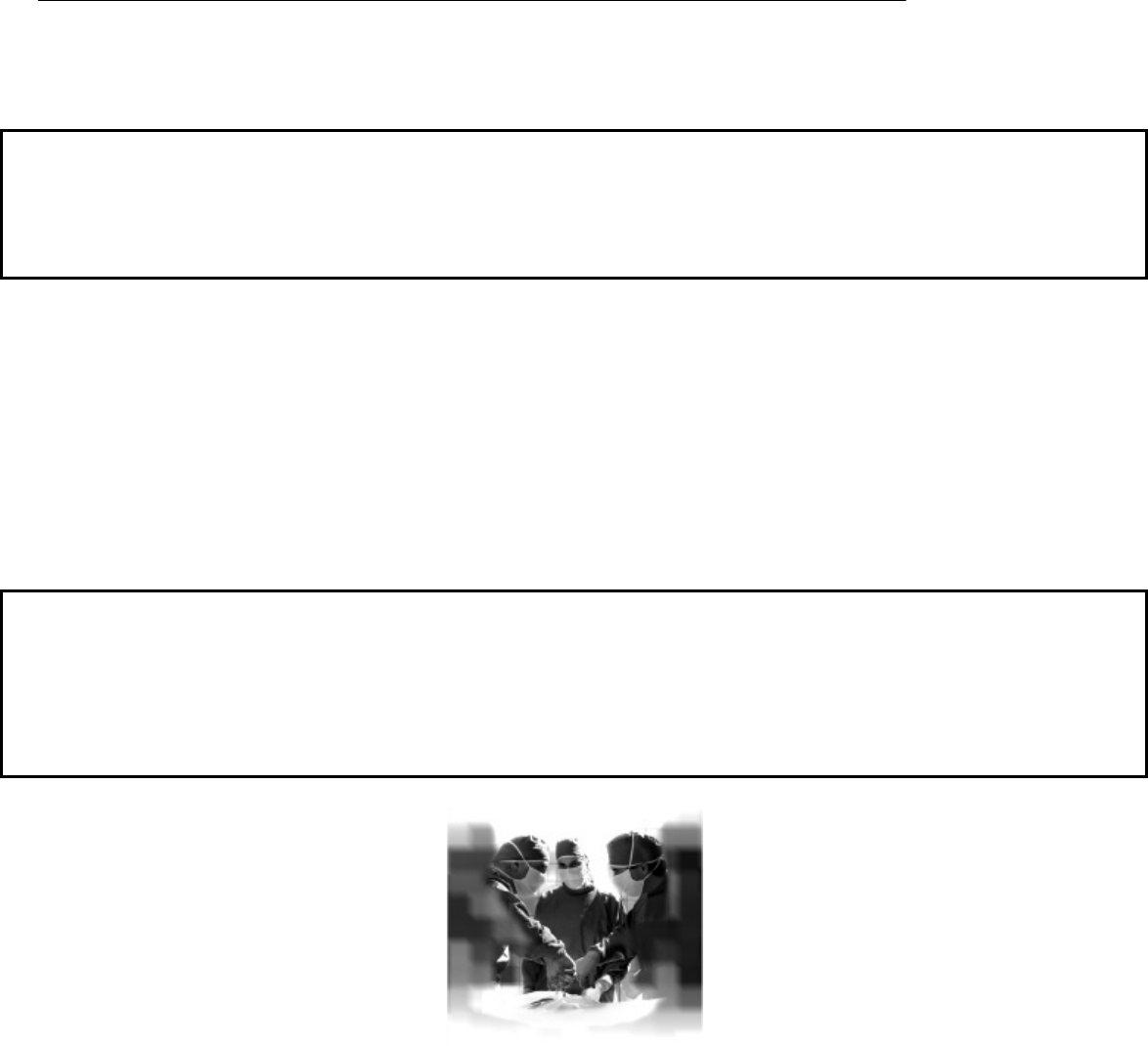
Isn’t it fun to see how what you are learning about combining medical terms
will later help you assign diagnostic and procedure codes? Keep working hard
and before you know it, you will be coding those medical records that we
learned about in the first lesson!
Consonants, Vowels and the Role They Play
Let’s go over the important things to remember when combining medical
terms. These rules will help you when combining most Latin terms.
Fact About Combining Word Parts
Use a combining vowel between a root word and a suffix that begins with a consonant.
Look at these examples of terms built from their English meanings. Each
suffix begins with a consonant. That’s why the combining vowel was used.
Meaning
Term with Suffix Beginning with
Consonant
Combined Term
tracing of the heart cardi/o/ + gram cardi/o/gram
surgical repair of a blood clot thromb/o/ + plasty thromb/o/plasty
to cut into the stomach gastr/o/ + tomy gastr/o/tomy
Facts About Combining Word Parts
• Do not use a combining vowel between a root word and a suffix that begins
with a vowel.
• Do not use a combining vowel between a prefix and a root word.
Thromboplasty is the surgical repair of a blood clot.
Look at these examples. The combining vowel is not used.
Meaning
Term with Suffix Beginning with
Vowel
Combined Term
blood tumor (lump) hemat/o/ + oma hemat/oma
look at living (tissue) bi/o/ + opsy bi/opsy
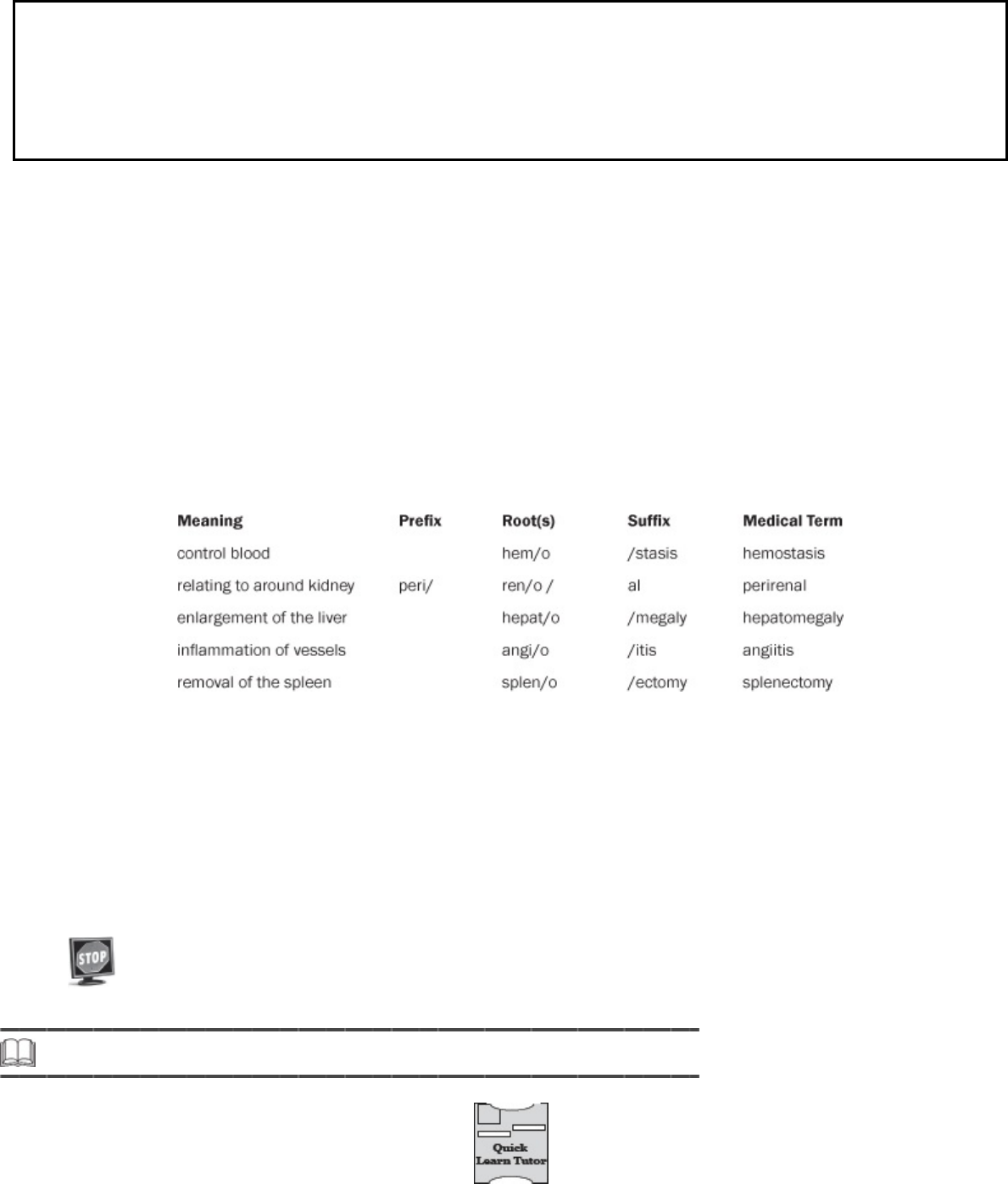
relating to the heart cardi/o/ + ac cardi/ac
Fact About Combining Word Parts
Use a combining vowel between two root words in a compound word even when the
second root word begins with a vowel.
Look at the following examples. The combining vowel is used between two
root words. All of the root words are in boldface type.
Meaning Compound Word Combined Term
heart specialist cardi/o/log/ist cardiologist
instrument to measure heat therm/o/meter thermometer
study of the stomach and intestines gastr/o/enter/o/log/y gastroenterology
relating to water electrical activity hydr/o/electr/ic hydroelectric
When dividing and combining terms in this course, it’s helpful to identify the
prefixes and suffixes in addition to the root words. For example:
Read from the beginning of the term to the end when you are
pronouncing a term you have created. And remember, read from the
end of the term to the beginning when you are checking the meaning of
a term you have created.
Now, let’s reinforce what you’ve learned so far with a few Practice
Exercises.
Please pause and complete online Practice Exercises 4-4 and 4-
5.
Step 8 Pronounce Word Parts
Follow these steps:
a. Take your Quick-Learn Tutor and your Set 5 flashcards out of your Quick-
Learn Kit. Insert the first flashcard for Set 5 into Side A of the Tutor.
b. Access the online portion of your course, and go to Lesson 4.
c. Listen to a word part as it is pronounced. After you hear a word part, pause
the audio.
d. Look at the word part in the left window of your Quick-Learn Tutor and
practice pronouncing it out loud several times until you can pronounce it
correctly and easily. Push the flashcard up and read the meaning of the
word part. Continue this process for all the flashcards for this set.
e. Next, put the flashcards in order and play the audio again. This time,
pronounce each word part in order but do not stop.
f. As you pronounce each word part, look at it on the flashcard. Listen to your
own pronunciation of each word part. If you mispronounce one, put a check
mark next to that flashterm.
g. Next, practice the word parts you mispronounced by listening to the audio
again. Be sure you can pronounce each word part clearly and easily.
Step 9 Write Word Parts
These are the steps to follow:
a. Insert the first flashcard for Set 5 into Side A of your Quick-Learn Tutor.
b. Look at each word part as it appears in the window and say it out loud.
Write each word part on blank paper. Be sure to include the slash.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside each word part.
d. Do this for each flashterm for this set.
Step 10 Meanings of Word Parts
Follow these steps:
a. Again insert the first flashcard for Set 5 into Side A of your Quick-Learn
Tutor. Pronounce each word part and then say the meaning. Check yourself
by pushing the flashcard up until you can see the meaning in the right
window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud, and then say the word part. Again, check
yourself by pushing the flashcard up until you can see the term in the left
window.
c. Practice with the flashcards several times until you are familiar with the
words and their meanings.
d. When you feel comfortable with the spelling, pronunciation, and meaning
of each word part, go on to the next step.
Please pause and complete online Practice Exercise 4-6.
Step 11 Lesson Summary
Previously, you saw that medical terms are constructed of root words, prefixes, and
suffixes. By learning these word parts, you can divide a medical term into its word
parts and derive its meaning. You can take an unfamiliar medical term, separate its
root word from any prefixes or suffixes, and determine what that word means. This
is important because you cannot—and should not—memorize every single medical
term healthcare providers use. But you can learn to divide and combine medical
terms, and this skill will enable you to become a competent, professional medical
coding specialist. You’ll be able to break up unfamiliar medical terms so that you
can look them up in your medical dictionary and coding manuals to determine the
correct spelling and meaning.
Now don’t get discouraged if you found this lesson a little challenging. The
Practice Exercises in this lesson are important. If you skipped any or
struggled to complete some of them, go back and work on them again. Doing
so only will help you with the upcoming Quiz. U.S. Career Institute
successfully has graduated thousands of men and women from its program,
and we want you to be one of these success stories! If you need a helping
hand, call your instructor. And remember that we offer support even after you
graduate and as you advance in your new career.
LESSON 5
Medical Terminology: Abbreviations,
Symbols and Special Terms
Step 1 Learning Objectives for Lesson 5
When you have completed the instruction in this lesson, you will be trained to do
the following:
Recognize common medical abbreviations.
List and explain common symbols.
Describe eponyms and acronyms.
Differentiate between terms that sound alike.
Determine terms that are opposites.
Convert singular medical terms to plurals, and recognize medical plurals.
Step 2 Lesson Preview
Imagine you run into a good friend who has a hard time keeping in touch with his
family. When you ask him, “Did you write that e-mail to your brother?” he shakes
his head no. Now look closely at the question you asked. The sentence, “Did you
write that e-mail to your brother?” illustrates the complexity of the English
language.
You (not ewe) also will learn some common medical abbreviations and symbols.
Your question contained three sound-alikes—the words you, write, and to
sound the same as other words (ewe, right or rite, and too or two).
Sound
alikes, medical plurals, and opposites are just three types of medical
terms we’ll cover in this lesson. You (not ewe) also will learn some common
medical abbreviations and symbols.
As a medical coder, you will often encounter terms that may sound or look
alike, such as hypertension and hypotension. Not only do these terms sound
alike, but they’re also opposites. Hypertension refers to high blood pressure,
and hypotension refers to low blood pressure. It will be your job to determine
if the term you see is, indeed, the correct term. Additionally, as you’ll soon
find out, healthcare providers use many abbreviations and symbols. It seems
only natural since many medical terms are long and complex! If you are
familiar with these abbreviations and symbols, you’ll easily be able to convert
them into the correct medical terms so that you can code them properly.
Hypertension refers to high blood pressure, and hypotension refers to low blood pressure.
It’s amazing how much you already know about medical terminology from the
previous two lessons. This knowledge will allow you to understand all the
facets of your new career in medical coding. Healthcare providers will
appreciate your knowledge. So let’s get started with this lesson about special
terms!
Step 3 Abbreviations
Doctors frequently use shortened versions of longer words or phrases. These
shortened versions of words and phrases are called abbreviations. Abbreviations
are extremely useful to a doctor because they save valuable time. However,
abbreviations are not helpful unless you, the coding specialist, can determine the
names for the procedures the doctor performed. Because it is important to be
completely accurate, doctors and hospitals get together and produce lists of
approved abbreviations—abbreviations they all agree on and understand.
Abbreviations in Hospitals
The Joint Commission is an independent, not-for-profit organization that
regulates hospitals and other healthcare facilities. Hospitals are required by
the Joint Commission on Accreditation of Healthcare Organizations (also
known as The Joint Commission) to keep a list of acceptable abbreviations.
Only the accepted abbreviations may be used in the medical records for that
hospital.

Office Records
The rules for abbreviations are more relaxed for the records in individual
offices. However, any bills or insurance forms that are typed must follow the
hospital’s list of abbreviations.
Doctors
Doctors sometimes have their own personal abbreviations. As a medical
coding specialist, you will need to learn these personal abbreviations. This
will help you communicate more effectively with your clients or employer.
Pharmacies
Lists of medications and treatments that a pharmacy prepares are included in
the medical bill, and they appear on the insurance forms filed by the doctor’s
office or hospital. Usually Latin abbreviations are used for these medications
and treatments.
On your flashcards, beside each Latin lower case abbreviation you will see
the full Latin phrase. You will not need to learn the Latin words—just the
punctuation and the everyday meaning.
Step 4 Learn Abbreviations
It’s important to be familiar with common medical abbreviations, so take some
time to practice saying and writing medical abbreviations using the following
exercise. Because pronunciation is not an issue with abbreviations, there is no
audio to go with this flashcard set.
a. Take your Quick-Learn Tutor and your Set 6 flashcards out of your Quick-
Learn Kit. Insert the first flashcard into Side A of the Tutor.
b. Look at each abbreviation as it appears in the window and say it out loud.
Write each abbreviation on blank paper.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside each abbreviation.
d. Do this for each flashterm for this set.
Step 5 Meanings of Abbreviations
Follow these steps:
a. Again insert the first flashcard for Set 6 into Side A of your Quick-Learn
Tutor. Pronounce each abbreviation and look at how it is spelled. Then say
the meaning. Check yourself by pushing the flashcard up until you can see
the meaning in the right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud and then say the abbreviation. Again, check
yourself by pushing the flashcard up until you can see the meaning in the
left window.
c. Practice with the flashcards several times until you are familiar with the
abbreviations and their meanings. Don’t struggle to memorize them. You
may always look up abbreviations.
Please pause and complete online Practice Exercise 5-1.
Step 6 Slang
There are two types of slang you may encounter in the medical field—medical
slang and English slang.
Medical Slang
The laboratory is the lab.
Medical slang words are informal abbreviations for longer medical terms.
For example sedimentation rate is called sed rate. The laboratory is the lab.
Doctors use medical slang frequently for the same reason they use
abbreviations—to save time.
Fact About Medical Slang
If you encounter slang on a medical form, use the full term the slang represents. For
example: If the doctor wrote, “The patient was prepped for appy,” you would know to code
for an appendectomy.
Some medical slang terms are used so frequently that they become accepted
medical terms. Exam and prep are two examples of this.
What code would you use for appendectomy? An appendectomy is a surgical
procedure and is coded from a different manual than a diagnosis. The code
would look like this:
44950 Appendectomy
This code would be entered on the medical claim form to tell the insurance
company exactly what procedure the doctor performed for the patient.
Remember, the diagnosis is the reason the patient sees the doctor, and the
procedure is what the doctor decides to do to help the patient.
English Slang
English slang words are highly informal words not often used in
professional writing.
Facts About English Slang
Obscene or offensive statements are never put in any medical report, including patient
files, insurance forms, and patient charts, unless the patient is being quoted (in this
case, use quotation marks around the quoted statement). If the patient is not being
quoted, the offensive or obscene statement would be deleted.
• Correct: The patient said, “I fell down and hurt my ass.”
• Incorrect: The patient is a pain in the ass. (Leave out this entire sentence.)
Step 7 Slang Terms
Follow these steps:
a. Take out your Quick-Learn Tutor and your Set 7 flashcards. Insert the first
flashcard into Side A of your Quick-Learn Tutor.
b. Look at each slang term as it appears in the window and say it out loud.
Write the slang term on blank paper.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside each slang term.
d. Do this for each flashterm for this set.
Step 8 Meanings of Slang Terms
Follow these steps:
a. Again insert the first flashcard for Set 7 into Side A of your Quick-Learn
Tutor. Pronounce each slang term and then say the meaning. Check
yourself by pushing the flashcard up until you can see the meaning in the
right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud; then say the slang term. Again, check
yourself by pushing the flashcard up until you can see the meaning in the
left window.
c. Practice with the flashcards several times until you are familiar with the
words and their meanings.
Step 9 Symbols
The symbols used in medicine are no different from those used in everyday life.
When you use symbols, you must be sure the symbol is well known. To give you a
better understanding of which symbols are acceptable, we will go through the main
rules you need to remember.
Facts About Using Symbols
• When you use symbols, do not leave a space between the symbol and the numeral.
• However, do leave a space between a numeral and the symbol x. This symbol means “by” in
dimensions, as in 6 x 9.
Let’s take a look at the following list of symbols, what they mean, and how
they are used.
Symbol Meaning Example
o
C
degrees Celsius
32
o
C
o
F
degrees Fahrenheit
98.6
o
F
& and (between capital letters only) D&C
x times, by x 3 days, 2 x 3 x 5
+ plus (urine; reflexes) 3+
: ratio; ___ to ___ 1:2
/ per, vision test 2/day; 20/20
/ over (blood pressure) 120/80
– minus, ___ to ___ (range), through –2, 4–5, II–XII
- suture size 3-0 (000) silk
# number #16 Fr, #3-0 silk
Please pause and complete online Practice Exercises 5-2 and 5-
3.
Try the online Practice Exercises to test your knowledge of slang words.
Step 10 Special Terms
In medical terminology, just as in the rest of the English language, there are
special terms that have specific rules. These special terms include proper nouns
and other capitalized words, sound-alikes, and opposites. Now we’re going to talk
about which words require special treatment, such as capitalization. You also will
learn about two special classes of terms: eponyms and acronyms.
Eponyms
In addition to the medical terms you learned to combine and divide in
previous lessons, medical reports contain other information, such as
laboratory test results, special medical abbreviations, and the names of
medical equipment and procedures. Often these words include proper
names—that is, brand names or the names of people. You must capitalize
proper names.
It was the custom in the past to use a person’s name to identify the
medical inventions or discoveries. The kinds of things named for people
include:
a new disease; a symptom or sign of disease
an anatomical structure
a new instrument, test or examination method
An eponym is a term that is formed from a person’s name. The person’s
name is given to the name of his or her discovery or invention to indicate
that person did the research and made the discovery. One example is
Bell’s palsy.
Fact About Eponyms
An eponym has two parts:
1. The person’s name as an adjective.
2. The type of invention or discovery as a noun.
Eponym Adjective Eponym Noun Meaning
Bell’s palsy facial paralysis
Pott’s clamp surgical instrument
Chiba needle long biopsy needle

McBurney’s point examination location
for the
appendix
Kaposi’s sarcoma unusual skin cancer
Because an eponym includes a person’s name, you won’t be able to divide it
into medical word parts. You do, however, capitalize the proper name in the
term, but not the noun.
If you use an eponym frequently enough, you probably will memorize how it
is spelled. Otherwise, you will have to look in your medical dictionary for the
proper spelling of eponyms.
Because it is difficult to remember the meanings of eponyms, it is becoming
less common for medical discoveries or inventions to be named for people. It
is now considered more professional to use a properly combined medical
term rather than an eponym. Nonetheless, doctors use eponyms frequently.
Brand Names
In the past, an eponym told you the name of the person who took credit for a
discovery or an invention. Some names of medical products indicate that a
company owns the patent for an invention or discovery. Brand names are
like eponyms because they demonstrate who discovered the procedure,
diagnosis, or disease. The kinds of new brand name eponyms you see today
are for the following:
General Electric CT scanner
a genetic cell line or tissue culture product
equipment or instruments
drugs or therapy methods
Look at these examples: General Electric CT scanner, Pen.Vee K penicillin and
Phillips’ milk of magnesia.
Don’t worry if you can’t pronounce some eponyms. All you need to be
able to do is to find the correct spelling in the dictionary. Before you

move on to acronyms, let’s take one more look at some common
eponyms.
Common Eponyms
Babkin reflex Halsted suture
Cantor tube Hodgkin’s disease
Charcot’s syndrome Hodgkin’s sarcoma
Colles’ fracture Kaposi’s sarcoma
Cooley’s anemia Legg’s disease
Epstein-Barr virus McBurney’s point
Erb’s palsy Miller-Abbott tube
Gordon’s reflex Pauley’s point
Laennec’s cirrhosis West Nile virus
Acronyms
An acronym is a word formed using the initials from a group of words or
from word parts. Here are some acronyms you probably already know:
Acronym Stands for
IRS Internal Revenue Service
USA United States of America
DMV Department of Motor Vehicles
Acronyms are a special kind of abbreviation. Doctors use acronyms because
they save time. Instead of writing the very long names of some diseases and
procedures, the doctor simply uses the acronym. Here are some examples of
some common medical term acronyms.
Medical Term or Phrase Acronym
cardiopulmonary resuscitation CPR
complete blood count CBC
USA is the acronym for United States of America.
Acronyms are formed by taking the first letter of each word in a phrase or by
taking the first letter of the word parts. For example, FTD stands for Florist
Telegraph Delivery, and NG stands for nasogastric. Not every word in the
phrase has to be represented in the acronym. Small, nonessential words are
usually omitted. For example, EENT stands for eye, ear, nose, and throat.
Acronyms usually are pronounced by saying the letters one by one. However,

if the letters of the acronym spell a word or can be pronounced as a word,
then the acronym may be pronounced as if it were a word. Let’s take a look
at a few examples.
Acronym Pronounced
EEG Say the letters—Ee-ee-gee
ELISA Pronounce the word—El-ee-sah
Scuba stands for self-contained underwater breathing apparatus.
In fact, some acronyms that are pronounced like words actually become
words if they are used often enough. The word laser began as an acronym for
the phrase Light Amplification by Stimulated Emission of Radiation. No one
bothers to say the whole phrase any more because laser is an accepted word.
The same is true of the word scuba, which stands for self
contained
underwater breathing apparatus.
Fact About Acronyms
Write acronyms in capital letters with no periods or spaces between the letters. For example,
CBC stands for complete blood count, and NSVD stands for normal spontaneous vaginal
delivery.
When you hear a new acronym, be sure to look it up and find out for what it
stands. This helps you write, type, and spell acronyms correctly. Most
common acronyms can be found in a medical dictionary.
Please pause and complete online Practice Exercise 5-4.
Step 11 Pronounce Acronyms
Follow these steps:
a. Access the online portion of your course, and click on Lesson 5. Listen to
Flashcard Set 8.
b. Put the first flashcard for Set 8 into Side A of your Quick-Learn Tutor.
c. Listen to each acronym as it is pronounced. Pause after each acronym.
d. Practice pronouncing each acronym until you can pronounce it clearly and
easily. You do not need to memorize the meaning of an acronym—only be
able to form it and look up its meaning on the flashcard.
e. Do this for each flashcard for this set.
Step 12 Sound-Alikes and Opposites
Two types of word pairs occasionally may present challenges for the medical
coding specialist. They are homophones and antonyms.
Homophones (Sound-Alikes)
At the beginning of this lesson, we called the words “to” and “too” sound-
alikes. Well, the more technical term for words that sound alike is
homophone. These words are not spelled alike, and they have different
meanings, but when homophones are pronounced, they sound the same. The
English language is full of homophones.
Look at these examples:
principle—principal
seen—scene
two—too
meddle—medal
As you can see, each of these four pairs of words looks different, but they
sound the same. As you work with medical records, doctors, insurance

companies, and others be careful that you distinguish between homophones
when you hear information. You certainly wouldn’t want to meddle in the
business’s principle scene when you really needed to know if the principal had
seen the medal. Okay, so that’s a stretch, but you get the idea!
Antonyms (Opposites)
Antonyms are words or word parts that have opposite meanings.
Sometimes these words sound similar to each other, which can cause
problems for someone with no training. Let’s take a look at these two
antonyms:
hypotension (low blood pressure)
hypertension (high blood pressure)
In your work as a medical coding specialist, make sure the terms you see
used make sense. Did the doctor mean what she wrote? If you have a
question, call the doctor’s office and check. Insurance companies will deny
claims for inaccurate codes!
Consider the following situation. If you know that normal blood pressure is
120/80, which term below is correct?
The patient has hypertension with a blood pressure of 90/60.
The patient has hypotension with a blood pressure of 90/60.
In this context, hypotension is correct because 90/60 is lower than 120/80.
The patient has hypotension with a blood pressure of 90/60.
The codes for hypotension and hypertension are different. You can see by the
following example how important it is to pay attention to the medical terms
and interpret the information in the coding manuals correctly.
458.9 Hypotension unspecified
401.9 Hypertension unspecified
Step 13 Medical Plurals
Many medical terms follow special medical plural rules. Some medical words even
have two plural forms, one which follows the normal English rule and one which
follows the medical rule. When there are two ways to make a medical term plural,
generally doctors use English rules when dictating reports for patients or other non-
medical people, and they use medical rules when reports go to other doctors or
into the medical chart. Since medical plurals and English plurals sound very
different, it will be easy for you to tell which rule the doctor is following.
Medical terms follow special medical plural rules.
Medical Rules for Plurals
In some cases, medical plurals are formed by changing suffixes. In other
cases, letters in the root word must be changed in addition to changes in the
suffix. The following chart shows you how to form medical plurals. Follow this
chart to form medical plurals.
Ending With Change To Example
/um /a medi/um—medi/a (mee-dee-uh)
/us /i calcul/us—calcul/i (cal-cue-lie)
/a /ae lamin/a—lamin/ae (lam-in-ee)
/is /es diagnos/is—diagnos/es (dy-ag-no-seez)
/itis /itid/es arthr/itis—arthr/itid/es (ar-thrit-a-deez)
i/on i/a criteri/on—criteri/a (cry-teer-ee-ah)
ax ac/es thorax—thorac/es (thore-a-seez)
ix ic/es cervix—cervic/es (serv-eh-seez)
ex ic/es index—indic/es (in-deh-seez)
yx yc/es calyx—calyc/es (kay-luh-seez)
Please pause and complete online Practice Exercises 5-5 and 5-
6.
Step 14 Lesson Summary
Congratulations! You’ve almost completed the last of three lessons that have
introduced you to the language of medicine—medical terminology you need to
effectively and professionally perform your job as a medical coding specialist. You
learned about word parts (root words, prefixes, and suffixes), and how to divide
and combine a medical term and derive its meaning using its word parts. In this
lesson, we talked about how to use abbreviations and symbols in your work. This
lesson also presented information about such special medical terms as eponyms,
acronyms, homophones (sound-alikes), antonyms (opposites), and plurals.
Now that you have learned the essential building blocks of medical
terminology, you’re one step closer to coding medical records. All of this
knowledge will make your coding job that much easier. You’ll be able to
figure out and research complex or unfamiliar medical terms, abbreviations,
and symbols so that you can assign the correct code to medical records.
Healthcare providers view those codes as extremely valuable information.
Without them, without you, healthcare providers could not get reimbursed.
Nor could government healthcare agencies track serious or terminal illnesses,
which in turn leads to research funding dollars that help save lives!
Please pause and complete an online Quiz. Good luck!
LESSON 6
Documenting Medical Records
Step 1 Learning Objectives for Lesson 6
When you have completed the instruction in this lesson, you will be trained to do
the following:
Describe the importance of documentation in medical records.
Identify the various types of medical record formats.
Explain how healthcare personnel manage medical records.
Step 2 Lesson Preview
Previously in this course, you learned about medical records and what they mean
to healthcare facilities, as well as your new career! You know how these records
are created, why they exist, and their key components. But there is one part of the
medical record that we have not yet discussed—the physician dictation.
Doctors record notes about patient encounters.
In this lesson, we’ll look in detail at physician dictation, a primary component
of a patient’s healthcare records. Do you remember our example with Dr.
Green in that first lesson? At the end of the patient’s appointment, Dr. Green
recorded some notes about the encounter. This is called physician
dictation. This lesson also will address how medical records are documented
and managed. You’ll come to understand just how significant all of this is to
your job as a coder! So let’s get started by discussing the importance of
documentation.
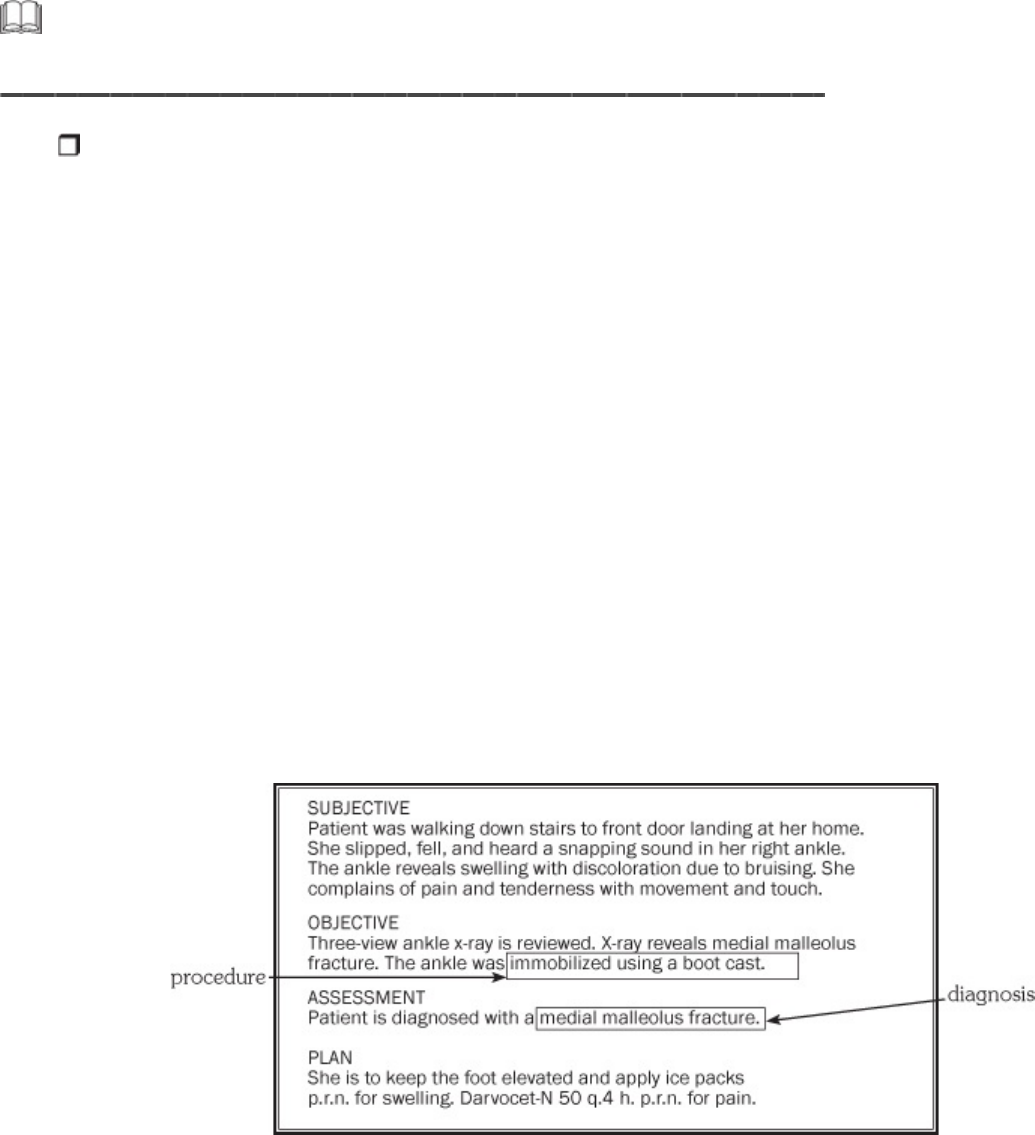
Step 3 Documentation—The Key Component of
Medical Records
You know from a previous lesson that medical records serve as a valuable source
of communication. In addition, medical records act as an important resource for
legal protection, financial reimbursement, education, quality assurance, and
medical research.
As a medical coding specialist, you’ll use doctor’s dictation to substantiate the
charges on a medical bill. You see, patients are charged for services received
based on what the physician documents. Documentation is the written
record of the services that the provider performs. When the physician dictates
the diagnosis and procedure for the medical records, these eventually end up
on the medical bill.
A physician’s dictation substantiates the charges on the medical bill. Because
dictation records diagnoses and procedures, it contains a lot of the
information that ends up on medical bills. This is the information you will use
to assign the correct medical codes for reimbursement purposes.
Look at the following example of dictation that notes the diagnosis and
procedure of Becky Johnson’s physician visit.
Don’t worry if you didn’t understand everything in the previous example. Just
remember that the diagnosis, or problem, and procedure, or what was done
about the problem, are what you will use to assign codes in your work as a
medical coding specialist.
Physician documentation has another important function; it represents a
database for reimbursement decisions for Medicare, Medicaid, third-party
insurance coverage, workers’ compensation, and pension payments. If
services are provided but not documented, the healthcare provider will not be
reimbursed. In other words, if it’s not documented, it didn’t happen. Let’s
take a look at a quick example.

Dr. Green biopsies a skin lesion on a patient’s face and removes two skin
tags. A biopsy means to remove and examine a living tissue sample. Dr.
Green documents the biopsy but fails to document the removal of the skin
tags. The insurance company receives a claim indicating both procedures and
then requests the medical record to confirm the procedures performed. But
remember, the doctor only documented the biopsy. Because Dr. Green failed
to document the removal of the skin tags, the insurance company only will
reimburse for the biopsy procedure. Ah! Not a pleasant outcome for the
doctor! However, as a coder, you’ll be trained to notice that the physician left
off the procedure in his dictation.
Doctors document exams performed.
Let’s look at another example—this one also illustrates the importance of
documentation. A new patient comes to a local clinic with a complaint of ear
pain. The physician takes the patient’s history, and he then performs an
exam. He circles the level of service on the encounter form and discharges
the patient with a prescription for antibiotics. After the patient leaves, the
doctor dictates the service; however, he is interrupted and ends the dictation
after documenting the patient’s history.
This dictation goes to the medical transcriptionist, whom you learned about
in our first two lessons. She transcribes the dictation and then gives this
document to the medical coder. The coder reads the dictation and notes that
the level of service that the physician circled on the encounter form does not
match what was documented. In this case, the coder will contact the
physician to correct this error. Later in this lesson when we discuss how to
handle medical records, you’ll learn the proper procedures healthcare
professionals use to correct an error.
So as a medical coding specialist, you can see how important the
accuracy of documentation—written and verbal—is to everyone working
in the healthcare field. Now let’s move on to study the different types of
documentation and narrative formats you may encounter in your daily
work.
Types of Documentation
The type and format of a physician’s dictation vary among facilities, but all
dictation contains the date and time the entry was written, the patient’s
complaint, the problem, and what the physician did during the service.
Study the following sample of traditional dictation.
Name: Yasuyo Mora
#030601
Dr. Anne Jones
HISTORY
CHIEF COMPLAINT
Exacerbation of CLL and lymphoma.
HISTORY OF PRESENT ILLNESS
This is a 78-year-old Asian woman who presented with symptoms of chronic lymphocytic
leukemia and was treated with chemotherapy. She went into complete remission and then
relapsed into a lymphomatous state. She has received chemotherapy on an intermittent basis.
The last chemotherapy was three months ago. Now she is seen in the office because of
increasing general malaise, leukocytosis, weight loss, cough, multifocal adenopathy and right
pleuritic chest pain. History of prior aortic aneurysm repair.
REVIEW OF SYSTEMS
Appetite and weight have been poor. Denies nausea, abdominal pain or changes in bowel
habits. No genitourinary or musculoskeletal complaints.
PHYSICAL EXAMINATION
GENERAL: Skin was normal in color and turgor.
HEENT: Normocephalic. Good dental hygiene.
NECK: The neck is supple, but there is submandibular adenopathy.
CHEST: The chest is clear to percussion and auscultation. The heart has regular sinus rhythm
without murmurs or gallops.
ABDOMEN: Abdomen is soft and nontender with inguinal and femoral adenopathy. There is
no hepatosplenomegaly. There is fullness in the left iliac fossa.
IMPRESSION
Exacerbation of chronic lymphocytic leukemia, lymphomatous type.
PLAN
Admit to hospital for chemotherapy including VP-16, Oncovin, bleomycin and methotrexate.
____________________________________
Anne Jones, MD
D:02/04/XX
T:02/04/XX
AJ:BM
Commonly Used Narrative Formats
Providers use a common dictation format with some variations, of course.
Aside from the loosely structured traditional narrative, the frequently used
format is identified by the acronym—SOAP.
The SOAP format stands for subjective, objective, assessment, and plan. If
you see dictation that includes something like “S: Pt. has no burning on
urination...,” then the doctor or nurse is using a SOAP format.
Subjective means the patient’s point of view or complaint.
Objective refers to the clinical findings.
Assessment is the examiner’s diagnosis based on the clinical
findings.
Plan refers to the doctor’s order.
You might encounter other dictation formats as well. For example, you might
see dictation with the following headings:
CC, which stands for chief complaint and is the same as Subjective in
the SOAP format.
Px, which stands for physical examination and is the same as Objective
in the SOAP format.
Dx, which stands for diagnosis and is the same as Assessment in the
SOAP format.
Rx, which stands for prescription and is the same as Plan in the SOAP
format.
Rx stands for prescription.
Before you move on, let’s look at an example of SOAP dictation:
Name: Sheryl Brown
#030314
PROBLEM
Acute chest pain.
SUBJECTIVE
The patient has long-standing osteoporosis and rheumatoid arthritis, under treatment with
prednisone 40 mg p.o. daily. Yesterday she experienced the onset of severe left chest pain in
the left midaxillary line. She has had pleuritic pain and dyspnea since that time. There is no
history of trauma. In addition, there is pain in the right ankle.
OBJECTIVE
There is pinpoint tenderness in the midaxillary line over ribs 4-6. There is 3/5 limitation of
motion of right ankle secondary to pain. Inversion-eversion motion 3/5. The femoral, popliteal,
posterior tibial, dorsalis pedis pulses are full and equal bilaterally. The Achilles tendon
reflexes are equal bilaterally. There is pronation deformity of the right ankle and minimal
swelling of the right ankle. The tibiotalar joint appears to be well maintained. The
taloscaphoid area has more swelling.
ASSESSMENT
1. Rule out spontaneous rib fractures secondary to prednisone therapy.
2. Rheumatoid arthritis with destructive disease of the subtalar joint.
3. Osteoporosis.
PLAN
Rib series and rib taping if fractures are present. Bone survey with attention to the right ankle
and foot. Orthopedic consultation for evaluation of right ankle and foot.
____________________________________
Ryo Miyamoto, MD
D:12/20/XX
T:12/20/XX
RM:JEF
Step 4 The Business of Managing Medical Records
Different medical facilities manage medical records in various ways—each method
is designed to promote good recording practices. Good recording practices
include those activities and procedures that the medical facility and staff do to
ensure that a patient’s medical record is legible, understandable, timely, error free,
and reproducible. Let’s look more closely at the medical-records-handling elements
that are likely to affect you as a medical coding specialist.
The doctor might have to rewrite the entry if key elements of the health record actually cannot be deciphered.
Good Recording Practices
Every medical record must be:
Legible. The doctor might have to rewrite the entry if key elements of
the health record actually cannot be deciphered. This action should be
reserved for only the critical elements of the health record, and the
request must be made very diplomatically. If the illegible part of the
record has been documented legibly elsewhere, or is clear on the
dictation, no rewrite should be requested.
Understandable. For medical records to be understandable,
abbreviations and arrangement of forms in the medical record must be
consistent with the medical facility’s standards and procedures. Everyone
on the medical staff should know the facility’s rules for the use of
abbreviations in the medical record. In fact, personnel should have an
official list of acceptable abbreviations and their meanings.
Timely. Timeliness of entries is critical to the accuracy of the health
record. The medical coder must return the coded document in a timely
manner, and the bill must be submitted in a reasonable amount of time.
This way if information is lacking or incorrect, the sooner it gets to the
provider, the sooner the situation can be remedied.
Error free. How errors are corrected is extremely important in terms of
patient care, as well as for legal purposes. When an error is made in the
medical record, several protocols should be taken:
Timeliness of entries is critical to the accuracy of the health record.
• The entry should be crossed out with a single line.
• The source of the error should be noted, such as indicating that the
entry pertains to another patient or noting another specific reason for
the error.
• The initials of the person making the correction should be noted.
• The date and time the error was discovered should be noted.
Let’s look at an example of how an error would be corrected. The original
dictation indicates the arm was cut. It was discovered the leg, not the arm,
was cut. The dictation would be corrected as follows. You’ll see the initials of
the person making the corrections at the top of the record, with the time in
military format and the date.
JL, 1547,
12/07/XX
SUBJECTIVE leg
Jeff complains of a 3.5 cm wound on his arm that he received while cutting wood.
OBJECTIVE
Superficial wound measuring approximately 3.5 cm. The wound is cleaned and then repaired
with a simple closure.
ASSESSMENT leg
The patient is diagnosed with a 3.5 cm simple arm laceration.
PLAN
Patient to watch for signs of infection such as redness or oozing. He is to return in a week for
Patient to watch for signs of infection such as redness or oozing. He is to return in a week for
the removal of the sutures.
Correcting an Electronic Health Record
Correcting an error in an EHR should follow the same basic principles as
correcting a written medical record. The system must have the ability to track
corrections or changes to the entry once the entry has been entered or
authenticated. When correcting or making a change to an entry in an EHR, the
original entry should be viewable, the current date and time should be
entered, the person making the change should be identified, and the reason
should be noted. In situations where there is a hard copy printed from the
electronic record, the hard copy must also be corrected.
Reproducible. A medical record must be correctly formatted and clear.
Medical records may be photocopied, microfilmed, or even scanned
electronically for storage. Consequently, handwritten entries must be
made in black ink, and computer-generated reports must be reproducible.
Computer-generated reports must be reproducible.
Well, now you have an idea of what types of documentation you’ll primarily
use to “get your facts” on each patient. Don’t worry if you didn’t recognize
some of the terminology in the reports; you’ll continue to add to that
knowledge throughout your course and throughout your career!
Please pause and complete online Practice Exercise 6-1.
Step 5 Lesson Summary
In this lesson you learned how important doctor dictation and accurate
documentation are to medical records. You know that you, the medical coding
specialist, will use doctor dictation to ensure that providers get reimbursed for the
services they provide. We also talked about the different types of documentation,
and you studied examples of the types of documentation that you might encounter
in your work.
You also know how essential it is that all medical facilities have standardized
processes and procedures in place to ensure that patient healthcare records
are legible, understandable, timely, error free, reproducible, complete, and
confidential. In our next lesson we’ll talk further about medical records and
the lengths taken to protect the information they contain.
And, by the way, keep up the great work!
LESSON 7
Ethics and Legal Issues
Step 1 Learning Objectives for Lesson 7
When you have completed the instruction in this lesson, you will be trained to do
the following:
Explain the importance of confidentiality in the healthcare profession.
Describe the concept of ethics.
Outline the main purposes of the federal HIPAA regulations.
Explain fraud, and determine some common fraudulent situations that
you must avoid.
Explain the development of and need for Recovery Audit Contractors.
Discuss the basic ideas surrounding liability and malpractice, including
insurance coverage.
Step 2 Lesson Preview
Legal issues include confidentiality and ethics—concepts you need to keep in mind
always. No matter how well you do your job as a medical coding specialist, you
must also be ethical. A big part of that code of ethics is ensuring that a patient’s
private health information remains private.
Confidentiality and ethics are concepts you always need to keep in mind.
Patients depend on workers in the healthcare field to protect their privacy
from creditors, employers, insurers and others. If an employer learns of a
potential employee’s family history of diabetes, would the employer refuse to
hire the person? Would a life insurance company that learned of a client’s
transfer to hospice care find a loophole to terminate coverage? Questions like
these are certainly on the minds of many people today.
Step 3 Confidentiality

Do you remember the last time that you went to the doctor? Even if it was just a
regular check up, you wouldn’t want your doctor to discuss your appointment at
dinner with his friends, would you? As a healthcare professional, you have access
to many medical records. It is essential that you understand that these records are
confidential.
Confidential originates from the Latin word meaning with trust.
When something is confidential, it means that it is kept secret.
Confidentiality goes hand in hand with ethics, which will be detailed shortly.
You have learned a bit about medical records, and you’ve probably guessed
that because of their sensitivity, these records are confidential. That means
you can only release them to authorized persons. A medical facility must
consider a wide range of factors to ensure confidentiality of patient records.
These factors include:
hiring trustworthy, responsible staff;
ensuring information stored on computerized systems is secure and
available only to authorized individuals; and
having standardized, secured procedures in place for transferring patient
information within the facility, between facilities and to outside
individuals.
Guidelines for Confidentiality of Medical Records
Beginning with the people it employs, a hospital, physician’s office or
other healthcare facility must ensure that sensitive patient information is
only accessible to reliable people. It’s important that all the policies and
procedures that relate to confidentiality and release of all medical
records be written down and available for reference.
Review the following security procedures that help ensure confidentiality
of medical records and information:

Employees are prohibited from working on records of acquaintances.
New employees are required to sign confidentiality pledges before
they can access confidential information, and a system must be in
place to ensure that such statements are signed.
Security procedures are in place for accessing medical record
storage areas that aren’t under continuous supervision by
authorized staff.
All computerized patient information must only be accessible with a
unique password, and information system users must not share their
passwords.
A written plan is developed to deal with suspected breaches of
confidentiality.
All physicians who use the computer system should agree, in writing,
to keep their ID codes confidential and be responsible for
authenticating their dictation.
Guidelines for Faxing Medical Records
Procedures help ensure confidentiality when faxing medical records.
In addition to following the guidelines previously mentioned, it is
important to guard against unauthorized access to records in situations
where a fax machine is used. Even if the information is sent to an
authorized person, it is possible for someone else to receive the
information. Procedures that help ensure the confidentiality of faxed
medical records include the following:
Always follow the rules set out by the provider or client with whom
you are working. If there is a policy that prohibits sending records by
fax, then do not do it. If there are no such restrictions, follow the next
guideline.
Always have an original release form on file before sending any
patient records via fax. Do not accept a faxed copy of a patient
release form; although the form appears to be signed, you have no
way of knowing if that signature is valid because you are looking at a
copy of the form and not the form itself.
Send faxes only to a secure fax machine. This means you have to
verify with the receiving person that the fax either will be picked up
immediately or that the fax is in a secure area away from people who
are not authorized to see what you are sending.
Never send sensitive test information via fax. This includes HIV and
pregnancy test results.
Always use a fax cover sheet. The cover sheet must list your name,
company name, telephone number, fax number and the number of
pages sent.
Now that you have a better understanding of the sensitivity of medical
records, let’s talk about being ethical.
Step 4 Medical Ethics
Medical ethics include confidentiality, accuracy, integrity and completeness of
medical records and the proper storage of these records. Medical ethics also
involve guarding against fraud and misleading claims.
Being ethical means that you strive to do what’s right and that you are
dependable and trustworthy. As a medical coding specialist, you will have
access to confidential information regarding patients, physicians, insurance
companies and government insurance programs. Handling this information
correctly and appropriately establishes your credibility and level of
professionalism. To work in the medical field, you must maintain your
credibility and have a very high level of professionalism.

It’s important to maintain your credibility and have a high level of professionalism.
Most organizations have a code of ethics, which is a document that
outlines specific ethical guidelines. This statement usually is posted where
it easily can be read and lists specific behaviors and efforts that members
or employees are expected to uphold. A code of ethics helps the
employees of a company know what is expected of them but also helps
patients or consumers relax and know that they are dealing with a
credible, responsible office or business. Take a look at the sample code of
ethics from the American Academy of Professional Coders that follows.
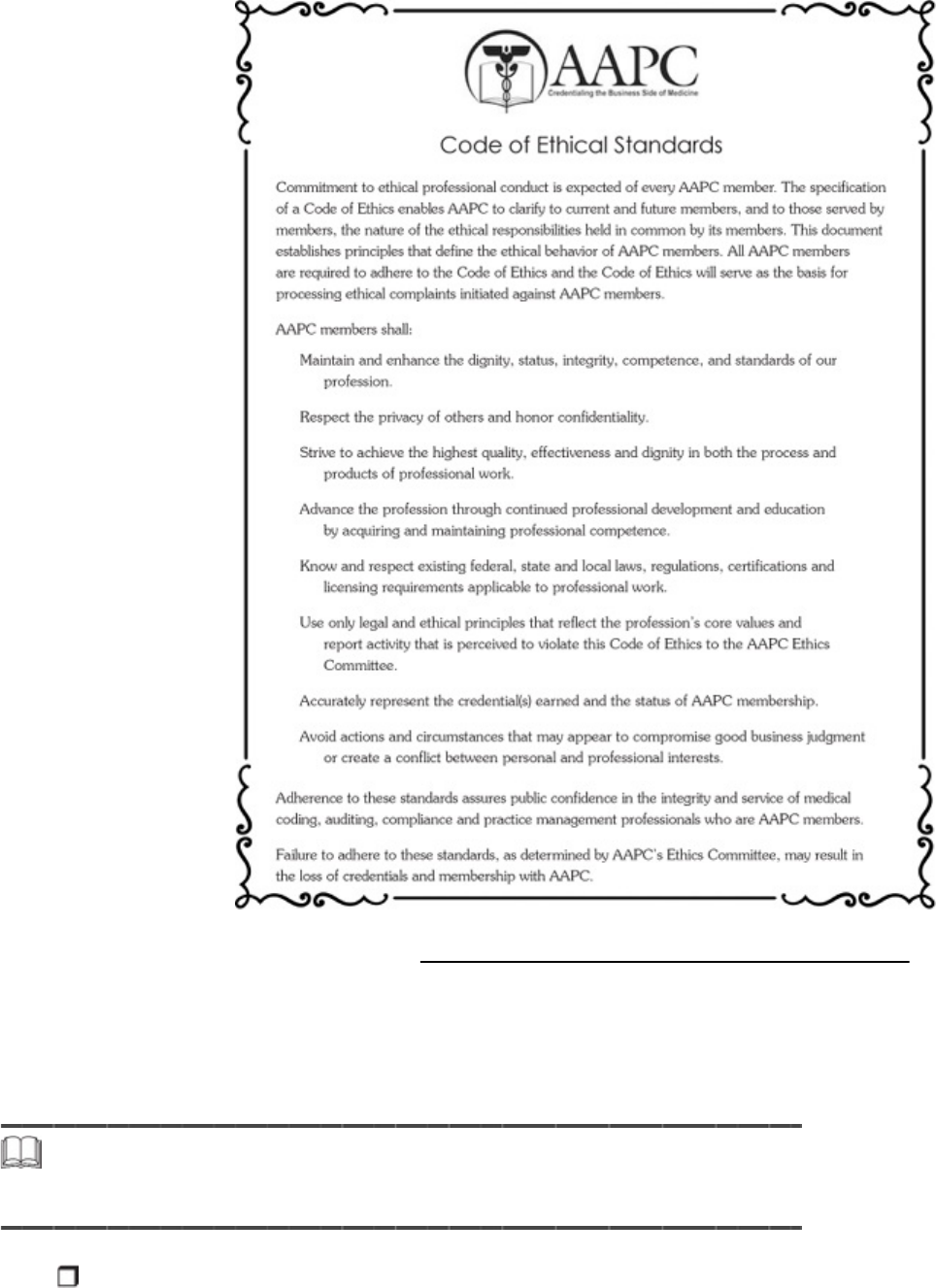
Source: AAPC Code of Ethics: http://www.aapc.com/AboutUs/code-of-ethics.aspx 19 July 2012
Confidentiality and ethics go hand in hand with the Health Insurance
Portability and Accountability Act, which you’ll learn about next. You’ll
learn who must abide by the act, the details of the act and how the act
applies to you as a medical coding specialist.
Step 5 Health Insurance Portability and Accountability
Act
In 1996, Congress enacted the Health Insurance Portability and
Accountability Act (HIPAA). This bill has two main objectives. The first
objective is portability, which is to ensure the continuation of health insurance
coverage for workers and their families during times of job change or loss. The
second, accountability, is to increase the effectiveness of the healthcare system
while protecting health data integrity, confidentiality and availability, as well as
preventing fraud and abuse. We’ll focus on the second objective, accountability.
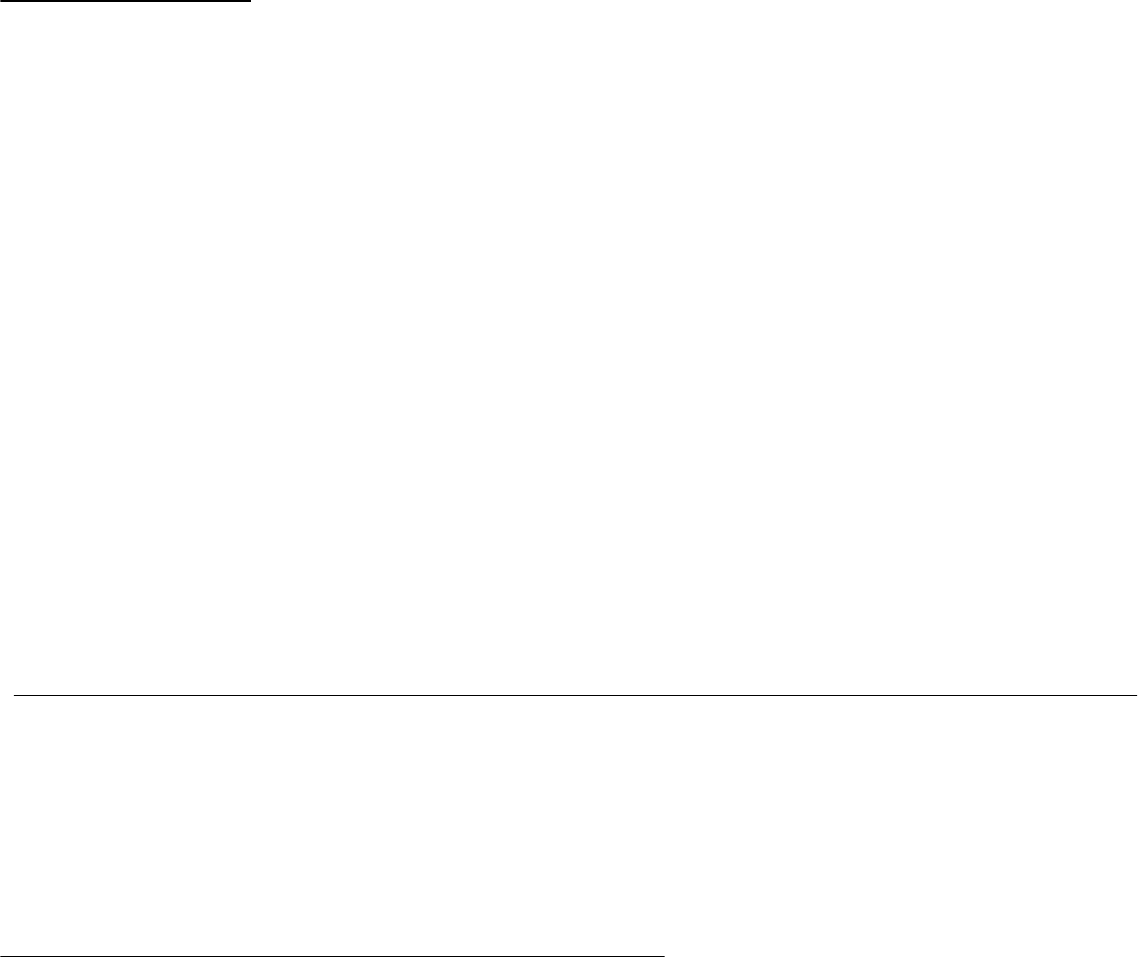
The Health Information Technology for Economic and Clinical
Health (HITECH) Act, enacted as part of the American Recovery and
Reinvestment Act (ARRA) of 2009, was signed into law on February 17,
2009, to promote the adoption and meaningful use of health information
technology.
1
HIPAA (as modified by the HITECH Act of 2009) requires
compliance to privacy standards and security in the maintenance and
electronic exchange of administrative and financial healthcare
information.
Many experts call HIPAA the most sweeping healthcare legislation in
years. Its provisions touch nearly everyone who works in health care.
Providers, payers and clearinghouses—anyone who deals with
confidential patient information is affected.
Covered Entities
Those that must follow HIPAA regulations are called covered entities.
Covered entities include health plans, healthcare clearinghouses and
healthcare providers who transmit any health information in electronic
form. A medical coding specialist who is a member of the covered entity’s
workforce is also known as a covered entity.
However, a medical coding specialist who is, for example, an
independent consultant providing coding services to a physician is not a
covered entity, but a business associate. A business associate is a
person that performs, or assists in the performance, of a function or
activity involving the use or disclosure of individually identifiable health
information. This includes claims processing or administration, data
analysis, utilization review, quality assurance, billing, benefit
management and practice management.
2
The contract between a
covered entity and a business associate must contain specific elements
describing the permitted and required uses of protected health
information. A sample business associate contract can be found at the
Department of Health and Human Services Web site at
www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/businessassociates.html
Now that you know who must comply with HIPAA, let’s look at the rules
that covered entities and their business associates must follow. Keep in
mind that when covered entities are referred to, it’s assumed that
business associates are included in the rule, as well, due to the contract
between covered entities and business associates.
Administrative Simplification Compliance Act
The different sections of HIPAA are known as titles. It is Title II, Subtitle

F that is probably the most important to the healthcare professional. This
part is called the Administrative Simplification Compliance Act. When
healthcare professionals talk about HIPAA and being HIPAA compliant,
they are usually referring to this section. The Administrative
Simplification Compliance Act (ASCA) sets up nationally consistent
regulations in four main areas:
Transaction and Code Sets Standards
Privacy Standards
Security Standards
Unique Identifier Standards
We’ll examine each of these standards in more detail and explain how it
affects you as a medical coding specialist. Let’s begin with transaction and
code sets standards.
Transaction and Code Sets Standards
According to HIPAA, a transaction is an electronic exchange involving the
transfer of information between two parties for a specific purpose.
3
A
transaction is electronic if it is transmitted with an electronic medium,
which includes Internet, Extranet, leased lines, dial-up lines and private
networks. Information physically moved from one location to another with
storage media, such as magnetic tapes, disks or CDs, is also considered an
electronic transaction. Telephone voice response or faxback systems are
not electronic transactions, according to HIPAA.
Transaction and Code Sets Standards simply outline the format and
codes used for electronic transmissions. At one time, there were about 400
formats for electronic health claims being used in the United States. This
lack of standardization made it difficult and expensive to develop and
maintain software to process claims. Today, it’s required that all covered
entities doing business electronically use the same transactions and code
sets. Let’s look at the standard code sets first.
Under HIPAA, specific code sets were adopted for diagnoses and
procedures to be used in all healthcare transactions. These code sets
include HCPCS (ancillary services/procedures), CPT (physician
services/procedures), CDT (dental terminology), ICD-9 (diagnoses and
hospital inpatient procedures), ICD-10 (replacement of the ICD-9) and
NDC (National Drug Codes). You’ll become more familiar with the HCPCS,
CPT and ICD-9 coding manuals later in the medical coding specialist
program. For now, it’s just important to know that these are the
recognized code sets used in the industry.
Now, let’s look at the standard transactions. You know about the CMS-1500
and UB-04 claim forms; however, when claim information is transmitted
electronically, it’s not submitted in the same format as you see on the paper
claim. Electronic data interchange (EDI) is the electronic transfer of
information in a standard format between trading partners. Basically, EDI is
the process of submitting a claim electronically in a standard format to an
insurance company for reimbursement for the provider’s services. Here is an
example of a claim submitted to an insurance carrier for Robert Daly seen
at the Medical Care Center:
4
Wow! That looks like gibberish, doesn’t it? As a medical coding specialist, it’s
not your responsibility to understand, describe or maintain this information.
You simply need to know that the claim information sent to an insurance
carrier is not transmitted in the same format as the paper CMS-1500 or UB
04
claim forms but in a standard form that HIPAA requires.
Finally, it’s helpful to recognize the terminology associated with these
electronic transactions. Since October 16, 2003, all healthcare businesses
that submitted claims electronically have been required to use version
4010. In 2012, version 5010 replaced version 4010 with improvements,
such as correcting technical issues, accommodating new business needs
and eliminating inconsistencies in reporting requirements.
All of this technical information may seem overwhelming to you.
However, keep in mind that it’s not the specifics that you need to know,
but the big picture. There are standards in the healthcare industry. These
standards define the codes you use, the forms you complete and how
information is submitted electronically. You may hear the term 5010 in
your work, and now you know that 5010 refers to the current standard
version of electronic transmissions!

Privacy Rule
The HIPAA Privacy Rule establishes national standards to protect
individuals’ medical records and other personal health information that
applies to covered entities.
5
The Privacy Rule addresses the use and
disclosure of a patient’s protected health information. Protected Health
Information (PHI) is individually identifiable health information, or
information that can be used to identify an individual, that is held or
transmitted by a covered entity or its business associate in any form,
whether electronic, paper or oral.
6
We’ll be talking about protected
health information a lot in this section, as it’s the foundation of the
privacy rule.
HIPAA requires that covered entities provide patients a notice of
privacy practices, which is a form that defines how the provider can
use PHI. A notice of privacy practice in plain language that describes the
following is necessary.
7
How the covered entity may use and disclose PHI about an individual.
The individual’s rights with respect to the information and how the
individual may exercise these rights, including how the individual may
complain to the covered entity.
The covered entity’s legal duties with respect to the information,
including a statement that the covered entity is required by law to
maintain the privacy of PHI.
Whom individuals can contact for further information about the covered
entity’s privacy policies.
In addition, the notice must include an effective date, and providers are
required to provide the notice on a patient’s first visit.
The basic principal of the Privacy Rule is to define and limit the
circumstances in which PHI may be used or disclosed by covered entities.
This rule allows healthcare providers to obtain a consent, or written
permission, to use or disclose a patient’s health information for
treatment, payment and healthcare operations, often referred to as TPO.
Written authorization is required for any use or disclosure of PHI that is
not for TPO or not otherwise specified in the Privacy Rule.
Authorization to disclose information forms must contain:
A specific description of the health information that will be used

The name or specific identification of the person or people to whom
the healthcare facility may disclose the information
The name or specific identification of the person or people who are
authorized to use the information
An expiration date that pertains to the individual or purpose of the
disclosure of the health information
A statement of a person’s right to rescind the authorization in writing
A statement that outlines the exceptions to the right to rescind
A statement that outlines how a person may rescind the
authorization right
A statement that the Privacy Rule would no longer protect health
information that the recipient redisclosed, even if authorization
disclosed it previously
The individual’s signature and the date
The following results in an invalid authorization:
The expiration date on the authorization to disclose information has
passed
The authorization to disclose information form is not completely filled
out
The authorization to disclose information form lacks one or more
required elements
The authorization to disclose information form covers more than one
request
The healthcare facility knows the patient or the patient’s legal
representative has rescinded authorization
The healthcare facility knows that some or all of the information in the
form is false
There are only two instances in which the patient may not rescind
authorization to disclose healthcare information: when the person or
people to whom the healthcare facility disclosed the information have
already taken action or when the authorization was given so that a
patient could receive insurance coverage, and the insurance company
contests a claim under the policy.
The Privacy Rules states that healthcare providers must make reasonable
efforts to use, disclose and request the minimum necessary amount of
PHI needed to accomplish the purpose of the authorization. Minimum
necessary limits unnecessary or inappropriate access to and disclosure
of PHI. Let’s look at an example to clarify this point.
A medical billing specialist that processes the billing for Weston Medical
Clinic does not require the entire documentation (medical record) to
submit a claim. The patient name and insurance information, as well as
the medical codes, are needed to create a claim for the reimbursement
process. Meanwhile, a medical transcriptionist does not need to know the
patient’s insurance information; she just needs to know who the patient
was, when the service was performed and what the provider did during
the service.
So, aside from our previous example, how does the Privacy Rule affect
you as a medical coding specialist? Well, in your healthcare profession,
you probably won’t be checking for consents or authorization, but you do
need to protect the patient’s medical record. Look at the following
scenario, and think about how the medical coding specialist should have
handled the situation differently.
Elizabeth does medical coding from home. Elizabeth’s home office is in the
living room of her townhome. She begins her day by connecting to an EHR to
pull the dictation that was transcribed the previous day. As she’s working on
assigning codes, Elizabeth’s neighbor, Alice, knocks on the door. Elizabeth
invites Alice in the living room for a cup of coffee. Forgetting to log off of the
EHR, Elizabeth runs to the kitchen to make the coffee. While alone in the
living room, Alice notices the name of a co
worker on the screen. Her
curiosity gets the best of her, and Alice inches closer to read the details on
the screen.
This is a violation of the Privacy Rule. It’s important that you, as the
medical coding specialist, keep the patient’s protected health information
private. After all, consider how you would feel if you were the patient in
one of these examples!
Security Rule
While the Privacy Rule focuses on protected health information in general,
the Security Rule deals with electronic protected health information
(ePHI). The Security Rule establishes a national set of security
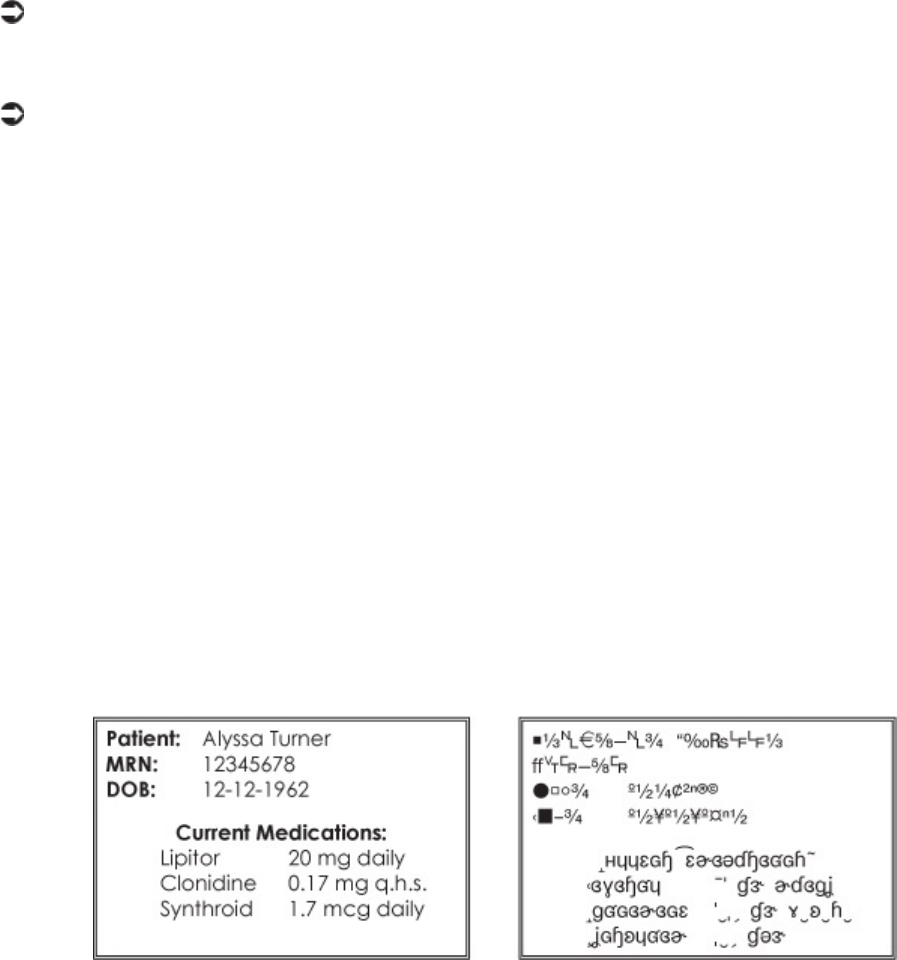
standards for protecting health information that is held or transferred in
electronic form. This rule does not apply to PHI transmitted orally or in
writing.
8
Prior to HIPAA, no formal security standards or requirements
existed for protecting health information. As technology evolved,
computers became standard in the healthcare profession, allowing medical
information to become more mobile and efficient, but also increasing the
potential security risk. Computer hackers and viruses can wreak havoc on
computer systems; they can corrupt files, make information public and
change critical data.
The Security Rule has two primary purposes:
Require appropriate security safeguards to protect ePHI that may be
at risk.
Promote access and use of ePHI while protecting an individual’s health
information.
Specifically, HIPAA notes: A covered entity must have in place appropriate
administrative, technical and physical safeguards to protect the privacy of
protected health information. This includes any intentional or unintentional
use or disclosure of ePHI. HIPAA requires each covered entity to assess its
own security needs and implement the measures that best meet those
needs. Administrative, physical and technical concerns must be examined
when these entities protect privacy. This doesn’t mean that every employee
must now have top-secret clearance. Some changes can be simple. For
example, a good security step is to ensure that unauthorized people cannot
view computer monitors and faxed pages. Other security measures are more
complicated, such as using proper electronic data encryption. Encryption
means the electronic information is put into a coded form while transmitted.
The encrypted electronic information cannot be understood without the
appropriate decryption equipment. Take a look at the example that follows.
In your career as a medical coding specialist, you will have access to
protected health information. While electronic health records provide ease
of access, you must have in place appropriate administrative, technical
and physical safeguards to protect the privacy of protected health
information. How will you do this? Passwords, key cards and encryption
are a few ways.
Healthcare organizations must control access to their files. A small
physician’s office might simply provide passwords for its personnel to
meet this requirement. The medical coding specialist working from home
could log onto the computer system to access coding information with her
password, while the nurse practitioner at the office could renew
prescriptions and view and modify health histories with her password.
In a large hospital, the access requirements have a more complex set of
tools. Key cards might be used for personnel to access particular rooms
that house information databases within the multi-building complex. A
security officer might view daily printouts that detail who accessed
certain files with their passwords. She also might require password
changes every few months. The feature of the security standards may
vary to ensure that compliance is economically feasible for organizations
of every shape and size.
Using encryption software is a simple safeguard for the healthcare profession
to ensure patient privacy. When PHI is encrypted, even if a hacker is able to
gain access to medical records, he won’t be able to read or interpret the
information. The patient’s privacy is protected because a key is required to
unscramble the information.
Let’s look at the final standard in the Administrative Simplification
Compliance Act, which is the Unique Identifier Standard.
Unique Identifier Standard
The Unique Identifier Standard establishes the implementation
specifications for obtaining and using the standard unique health identifier
for health care providers. At this time, there are two standards when it
comes to unique identifier: the Employer Identification Number and the
National Provider Identifier.
In 2002, HIPAA adopted the Employer Identification Number (EIN),
which was issued by the Internal Revenue Service (IRS) to identify employers
on standard transactions, which includes CMS-1500 and UB-04 claims, as well
as all electronic transmissions of claims. The billing provider includes his EIN
on the claim to be used for 1099 taxable income reporting purposes.
HIPAA mandated the adoption of a standard unique identifier for
healthcare providers in 2007. The National Plan and Provider
Enumeration System (NPPES) collects identifying information on
healthcare providers and assigns each a unique National Provider
Identifier (NPI). The NPI regulation seeks to eliminate multiple
identifiers. At one time, health care providers, such as Medicare and

Medicaid, assigned identifiers for providers to submit with claims. These
identifiers were known as UPIN, OSCAR and PIN. The identifiers were not
standardized, resulting in one provider having multiple identification and
billing numbers. These legacy numbers complicated the claims
submission processes and resulted in the assignment of the same
identification number to different health care providers by different health
plans.
According to CMS, the NPI is a 10-position, intelligence-free numeric
identifier (10-digit number). This means that the numbers do not carry
other information about healthcare providers, such as the state in which
they live or their medical specialty. Once assigned, NPI is associated with
the same provider forever; it will not change, regardless of job or location
changes.
The use of standard identifiers is expected to ease the administrative
challenges associated with all aspects of patient healthcare records. These
challenges include documentation, maintenance and billing requirements.
These standard identifiers will allow the various entities within the
healthcare system to most effectively and efficiently perform their respective
financial, clinical, preventive and research functions. To put it simply, a
healthcare entity can devote more time to its own particular business and
patients and less to general paper pushing when using an NPI.
Now that you have a better understanding of the standards associated with
the Administrative Simplification Compliance Act, let’s look at what happens
when patient privacy is breached, which means there was a violation or
infraction of a standard.
Breach of Privacy
What happens when there is an intentional or unintentional use or
disclosure of ePHI? The HITECH Act requires covered entities to provide
notification in the event of a breach of unsecured protected health
information. Unsecured means the information hasn’t been encrypted.
For instance, if a computer hacker gained access to patient information
that hasn’t been encrypted, the practice would have to inform all patients
and the Department of Health and Human Services (HHS) of that breach.
In some cases, the practice is also required to notify the media. However,
if the ePHI is encrypted, patients do not need to be notified.
Following are two examples of data breach notifications. The first is a
notice from TRICARE posted to its Web site alerting the public of the
breach. The second is a news article, also notifying the public of the
breach, as required by HIPAA.
Letters are being mailed from Science Applications International Corporation
(SAIC) to affected military clinic and hospital patients regarding a data
breach involving personally identifiable and protected health information
(PII/PHI). On Sept. 14, 2011, SAIC reported the loss of backup tapes
containing electronic health care records used in the military health system
(MHS) to capture patient data from 1992 through Sept. 7, 2011 in San
Antonio area military treatment facilities (MTFs), including filling pharmacy
prescriptions and other patients whose laboratory workups were processed
in these same MTFs, even if the patients were receiving treatment
elsewhere. The data may include Social Security numbers, addresses and
phone numbers, and some personal health data such as clinical notes,
laboratory tests and prescriptions. There is no financial data, such as credit
card or bank account information, on the backup tapes
ref: http://www.tricare.mil/breach/
This breach affected nearly 5 million patients, making it the largest medical
data breach since the HHS began tracking incidents in 2009.
On May 14, 2012 federal prosecutors charged one of the hospital’s medical
technicians with violating the Health Insurance Portability and Accountability
Act, or HIPAA. Prosecutors say that over a 17-month period Laurie Napper
used her position at the hospital to gain access to patients’ names,
addresses and Medicare numbers in order to sell their information.
ref: http://www.kaiserhealthnews.org/Stories/2012/June/04/electronic-health-
records-theft-hacking.aspx
The first case was an example of an unintentional breach of ePHI, while it
was clearly an intentional violation in the second.
Now, let’s look at the organization that has the right to enforce, audit,
fine and charge covered entities for violations of HIPAA, such as those
you just examined.
Office for Civil Rights
HIPAA and HITECH are administered by the HHS in the Office of the Civil
Rights (OCR). The OCR enforces the Privacy and Security Rules by
investigating complaints and conducting compliance reviews, as well as
performing education and outreach to foster compliance with the rules’
requirements. Since the compliance date in April 2003, HHS has received
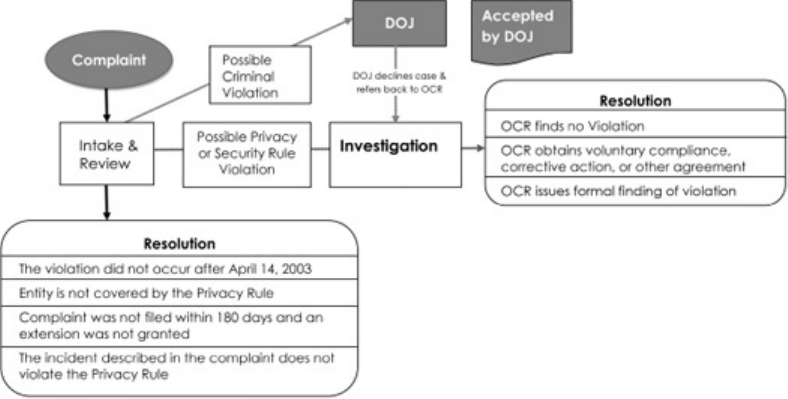
more than 71,849 HIPAA complaints. The OCR has resolved 91 percent of
complaints received (more than 65,460). The OCR has investigated and
resolved more than 16,708 cases by requiring changes in privacy
practices and other corrective actions by the covered entities. Of the
remaining complaints, 8,514 were investigated, and no violation was
found; 40,238 complaints were resolved through closure of cases that
were not eligible for enforcement because the entity wasn’t covered
under the Privacy Rule, the complaint was not filed in a timely fashion or
the incident described wasn’t in violation of the Privacy Rule.
HIPAA Privacy & Security Rule Compliant Process
The HIPAA complaint process includes possible criminal violations being
reported to the Department of Justice (DOJ).
Let’s look at those complaints that were resolved through investigation and
enforcement. If the evidence indicates that the covered entity was not in
compliance, the OCR will attempt to resolve the case with the covered
entity by obtaining voluntary compliance, corrective action and/or a
resolution agreement.
9
A resolution agreement is a contract signed by HHS and a covered
entity in which the covered entity agrees to perform certain obligations
(e.g., staff training) and make reports to HHS, generally for a period of
three years.
10
The HHS monitors the covered entity during these three
years to ensure that the entity is in compliance with the obligation.
According to the OCR, most Privacy and Security Rule investigations are
concluded to the satisfaction of the OCR. However, if the covered entity
does not take action to resolve the matter in a way that is satisfactory,
the OCR may decide to impose civil money penalties (CMPs) on the
covered entity. Under the HITECH Act, mandatory penalties have been
and will be imposed for willful neglect. According to HIPAA, willful
neglect means conscious, intentional failure or reckless indifference to
the obligation to comply with the administrative simplification provision
violated. Civil money penalties for willful neglect can extend up to
$250,000, with repeat or uncorrected violations extending up to $1.5
million.
You’ve learned a lot in this section! You studied the basics of HIPAA and
the HITECH Act. You know the standards associated with the
Administrative Simplification Compliance Act and understand how they
apply to your career as a medical coding specialist. And you found that
the OCR has the right to enforce, audit, fine and charge covered entities
for violations of HIPAA.
The last section about the violations of HIPAA may have seemed a bit
daunting, but it’s important to know that there will be ramifications for
willful neglect. However, the key is remembering to act in an ethical
manner and keep patient information private. As a medical coding
specialist, you know not to share a chart note you’ve reviewed earlier
that day with your family during dinner. You understand that coding a
chart of a close friend isn’t the best idea; it should be coded by someone
else! And you would never share your neighbor’s medical conditions with
another neighbor. These safeguards will keep you from breaking any of
the rules you’ve just learned about! Now, let’s pause for a quick review.
Please pause and complete online Practice Exercise 7-1.
Step 6 Fraud and Abuse
One of the government’s top priorities is to eliminate healthcare fraud.
Unfortunately, investigations of fraud and abuse are on the rise. Fraud occurs
when inaccurate information is used to wrongfully gain compensation. Fraud is a
crime. In the medical field, this often can occur in the medical record itself. For
example, a patient’s insurance coverage becomes effective June 15. The patient
receives service from a provider on June 1. The medical record is altered to
indicate the date of service as June 20 to allow the treatment to be covered by
insurance. This is fraud.
To guard against fraud, you must do one simple thing: Be accurate. Don’t
be tempted to change information on medical records if that information
already is correct. If you do change correct information, you are
committing fraud, and the consequences can be severe.
The U.S. General Accounting office estimates that $1 out of every $10
spent on Medicare and Medicaid is lost to fraud and abuse. With the
increasing costs associated with health care, the reduction of fraud and
abuse has become a point of focus for CMS.
Fraud examples:
Billing for services or supplies that were not provided
Altering claims to obtain higher payments
Soliciting, offering or receiving a kickback, bribe or rebate
Provider providing services for fictitious patients
Using another person’s Medicare card to obtain medical care
Abuse examples:
Excessive charges for services or supplies
Claims for services that are not medically necessary
Breech of the Medicare participation or assignment agreements
Improper billing practices including billing Medicare when Medicare is not
primary
Fraud and abuse can be reported to the federal Office of Inspector General,
OIG. This governing body then makes a decision as to the penalty. The
penalty can be monetary, criminal, administrative or a combination of any of
the three. The Office Inspector General is also responsible for notifying the
state intermediaries of any new scams.
As a medical coding specialist, you need to be sure you are coding properly,
that you are not coding for medically unnecessary services, that the Medicare
patient is who she says she is and that you are using an appropriate fee
schedule. Keep in mind you are human and may make a mistake from time to
time. Medicare is not after you; they are looking for those who are purposely
defrauding the system.
Preventing Fraud and Abuse
The Federal False Claims Act (FCA) was signed into law in 1863 by
Abraham Lincoln and is the basis for prosecution of healthcare fraud and
abuse claims. The FCA prohibits anyone from presenting a false or
fraudulent claim to be paid by the government, using a false record or
statement to conceal or avoid paying money to the government or
conspiring to defraud the government.
The FCA was not originally intended to investigate healthcare providers,

but in recent years, this has become increasingly necessary, as well as
very costly. In 1986, Ronald Reagan signed amendments into law that
significantly strengthened the government’s ability to successfully
prosecute for fraud. Damages increased from double to triple, and the
FCA was extended to include unintentional misconduct.
To prevent fraud and abuse, many healthcare providers have created
corporate compliance plans. Compliance plans are formalizations of
processes that identify, investigate and prevent violations in various
healthcare services.
In addition, the government has created model compliance plans for hospitals
and clinics. These include structure, standards, oversight, education,
monitoring and enforcement.
Insurance rates increase when an insurance company pays fraudulent
claims. When codes are not correct, the insurance company will not pay
the correct amount, which delays doctors’ payments and leads to
increased healthcare costs. Thus, insurance companies often try to collect
damages when they discover fraudulent claims.
Consequences of Committing Fraud
Fraud is a crime and, therefore, punishable by law. If the fraud was
intentional and systematic, and if the effects of the fraud were far-
reaching, the justice system can impose harsh penalties, including jail
time.
The criminal side of fraud is only half of the picture. There are also civil
consequences to fraud. Fraud affects us every day. When insurance
companies pay fraudulent claims, rates increase unnecessarily. Insurance
companies often try to collect damages when they discover fraudulent
claims. These damages include compensatory damages and punitive
damages.
Compensatory damages are damages directly related to the fraud. For
example, if a claim submitted to an insurance company with charges for
$700 worth of procedures that were not performed, the civil courts might
award the insurance company $700 in compensatory damages.
Compensatory damages represent the compensation a plaintiff receives
from a defendant for the actual damage caused (in our example, $700 in
overcharges). The plaintiff is the person who files the claim and initiates
a lawsuit, while the defendant is the person named in the claim or
charged with the crime. However, if the insurance company feels the
fraud was intentional or perhaps negligent, it might ask for punitive
damages.

Doctors and other healthcare professionals can be liable for damages in some situations.
Punitive damages are damages awarded to the plaintiff to punish the
defendant and, theoretically, deter the defendant from repeating the fraud in
the future. Punitive damages can far exceed compensatory damages. In our
$700 example above, a court might award punitive damages for five times
that amount ($3,500) if the fraud was intentional. Punitive damages are
awarded above and beyond any compensatory damages. That means our
original $700 judgment has now swelled to $4,200! This is a high cost for a
lapse in judgment. In addition, whoever committed the fraud is responsible
for paying all damages.
Doctors and other healthcare professionals can be liable for damages in some
situations, whether their actions were intentional or not. To help protect
healthcare professionals, insurance companies offer a variety of liability
insurance coverage.
Step 7 Liability Insurance
When you drive a car, you run the risk of being in an accident. Obviously, you don’t
set out to intentionally hit another car, but accidents happen. To protect yourself
and the other drivers on the road, you carry some form of automobile insurance.
No doubt you’ve heard of people being awarded thousands of dollars by courts for
damages suffered in accidents. If you have insurance, then your insurance
company pays for these damages. (After all, that’s what insurance is for.) If you
aren’t covered by insurance, then you pay the entire amount!
Doctors and other healthcare professionals can be covered by medical
liability insurance. The physician you work with usually carries this
insurance. In case there are damages suffered as a result of an accident or
negligence, the insurance covers the doctor, the doctor’s staff and anyone
the doctor contracts with for services relating to the practice.
In the medical world, physicians are legally responsible for their actions,
as well as the actions of their employees and anyone they contract with
for services relating to their practice. This protects you, the medical
coding specialist, as long as you stay within the scope of your duties,
which means as long as you are doing the job you were hired to do.
However, if you knowingly submit fraudulent claims or break the law in
some other manner, you are liable, and insurance won’t cover you. Let’s
look at two situations.
Example 1 While coding from a complex dictation, Julia accidentally
transposes two numbers, causing an error that results in overpayment by
the insurance company.
Example 2 Hillary works with Dr. Gregg. Dr. Gregg hands her his
dictation and says, “Don’t use the surgical package code. I never do
because I get more money if I code everything separately.” Hillary does
as Dr. Gregg asks.
Which example represents fraud? The answer is Example 2. When Hillary
knowingly goes along with Dr. Gregg, she is submitting codes she realizes
are false. This should be reported, not complied with. How do insurance
companies catch fraudulent claims? They conduct company-auditing
procedures.
Insurance Audits
Insurance companies guard very closely against fraud. Even with
safeguards, some fraudulent claims sneak through. However, through
insurance audits, many of these claims are caught. An insurance audit
is a thorough review by the insurance company of a claim and all related
documentation. Auditors compare and search the records for
inconsistencies and alterations.
What triggers an insurance audit? Well, the insurance company might find
the claim suspicious or notice that the doctor files an unusual number of
similar claims. On the other hand, the patient might bring a questionable
claim to the attention of the insurance company.
Many insurance companies encourage their clients to review medical
records and bills to ensure that the procedures listed were performed and
the diagnosis is accurate. If a patient has a question, the insurance
company has a toll-free number to call for that purpose. If there is an
overcharge on a claim that a patient notified the insurance company
about, that patient usually gets some kind of cash reward from the
insurance company. This encourages patients to review their records.
As a medical coding specialist, you may be interested in an auditing
position. Auditing ensures medical necessity, correct coding and
compliance. The knowledge you learn in this program will provide you the
skills for an entry
level position.
Step 8 Recovery Audit Contractors
According to the OIG, it is estimated that $16.4 billion in improper payments and
error rates were made in 2000.
11
The Medicare Modernization Act of 2003 created
a three-year project to recover Medicare overpayments and identify
underpayments. The three-year project focused on California, Florida, New York,
South Carolina and Massachusetts. In March 2008, the program ended with more
than $1.03 billion recovered from improper payments. Approximately 96 percent of
the improper payments were overpayments collected from providers, and the
remaining four percent were underpayments paid to providers.
12
The Tax Relief and Health Care Act of 2006 expanded this project to all 50
states, creating a permanent and nationwide program by 2010. CMS
contracted Recovery Audit Contractors (RACs) to recover overpayments.
RACs are paid on a contingency fee basis, receiving a percentage of the
improper payments they collect from providers.
13
RACs may review the last
three years of provider claims for the following types of services: hospital
inpatient and outpatient, skilled nursing facility, physician, ambulance and
laboratory, as well as durable medical equipment.
In 2011, CMS reported that it has collected more than $313 million in
Medicare overpayments through its recovery audit program since October
2009.
14
However, RAC decisions can be appealed. Look at the following
report:
The Centers for Medicare & Medicaid Services (CMS) has released appeals
data for Medicare fee-for-service Recovery Audit Contractors (RACs). For
claims originating in fiscal year 2011 (Oct. 1, 2010-Sept. 30, 2011),
providers appealed 56,620 repayment demands, over 6.25 percent of the
903,372 claims with overpayment determinations. Of these, 24,548 (43.4
percent) were decided in providers’ favor. Approximately 2.7 percent of all
claims with overpayment determinations were overturned on appeal.
ref: http://www.aapcps.com/news-articles/RAC-appeals-won.aspx
As with liability concerns, there are several legal concerns to consider when
working with medical records. Let’s take a closer look.
Step 9 Legal Concerns
The legal system in the United States is very complex. Attorneys study it for years
and still may not understand everything there is to know about law. While we will

cover some of the basic concepts regarding medical records and the law, you
should always consult an attorney if you have to deal with the legal system. By
doing so, you receive expert advice from someone who knows the system. This
section gives you an overview of some very basic concepts, which will enable you
to effectively communicate with other medical professionals.
Subpoenas
A subpoena is a legal document issued by the court requiring the person
named on the subpoena to appear in court or to supply certain
documents or both. A subpoena can authorize the legal release of
confidential medical records.
A subpoena cannot be mailed. Instead, it is served personally by an
authorized person. If you are served with a subpoena and fail to respond,
you can be arrested and charged with a crime. A subpoena is a legal
document and must never be ignored.
When you follow the directions contained in the subpoena, you have
complied with it. To comply with a subpoena for medical records, you
generally have a specified amount of time to produce the records. You
make copies of the appropriate records, and supply the copies to
whoever is named on the subpoena. Usually, this is an attorney.
If you receive a subpoena to testify, it means you must appear at the
designated court on the assigned day and time. You cannot be late, and
you cannot ignore the subpoena. Sometimes you are paid for your time,
and the fee is included with the subpoena. Remember not to get angry
with the person serving the subpoena. The server is usually neutral, not
involved with the case at all and “just doing a job.”
When a subpoena is issued, it usually means someone is headed to court and
needs the medical records for a case. Sometimes, however, disputes don’t
end up in court. Instead, they may be heard in arbitration.
Arbitration
Arbitration is an alternative to a court of law. In arbitration, two disputing
parties meet with an arbitrator, or a person chosen to decide a dispute or
settle differences. Each party tells its side of the situation, and the arbitrator
issues a ruling. In binding arbitration, the ruling is final and must be
obeyed. In nonbinding arbitration, the ruling is merely a suggestion from
an objective person. Many contracts now specify that disputes must be
settled in binding arbitration rather than in court. Arbitration is much less
expensive and usually resolves problems faster than the court system.
Medical Testimony
If arbitration is not an option, or if someone insists on going to court, then
people may have to provide testimony. Testimony is the sworn statements
of witnesses and experts given while on the witness stand in court. Witnesses
give statements under an oath of truth, and people who lie during testimony
can be charged with perjury, a serious crime.
In medical cases, doctors are sometimes called to testify. Often, doctors
testify as expert witnesses—people who know about the circumstances
surrounding a case, but not necessarily about the case itself. For example,
imagine a trial involving physical evidence, such as DNA. The DNA is analyzed
and the results brought to court. The side presenting the evidence might
have an expert talk about DNA in general. That expert is someone who
knows about DNA but has no other connection to the case. This person is an
expert witness.
Now it’s time to review what you’ve learned about fraud and abuse with the
following Practice Exercise.
Please pause and complete online Practice Exercise 7-2.
Step 10 Lesson Summary
We covered a lot of information in this lesson. Ethics and credibility are interwoven
like threads in a rug. When you are in business, whether it is your own or someone
else’s, you must always keep a strong code of ethics foremost in your mind. If you
follow the principles of these ethics, you can relax and do your job. You have
credibility. People can count on you.
Privacy and security are major concerns as more and more healthcare
data is transmitted and maintained electronically. The Health Insurance
Portability and Accountability Act is, in part, is federal legislation that
governs health information in electronic form. Here, legal and ethical
issues are joined. As a medical coding specialist, you must be sure that
you follow strict guidelines in protecting the confidentiality of the patient
information entrusted to you. A signed patient consent, obtained by the
physician, permits you to release information for purposes of treatment,
payment and healthcare operations. You must not make any other
release of information unless the patient has provided a signed
authorization allowing such release.
Even the most ethical person can make a mistake. Mistakes can be
covered by liability insurance carried by the physician with whom a
person works. Fraud, however, is an intentional misrepresentation of
facts. Fraud usually is committed to try to gain more money or some
other undeserved benefit. Fraud is illegal. When illegal acts are
committed or if two parties have a disagreement that cannot be settled,
the legal system might come into play.
The legal system, as you’ve learned, settles disputes and upholds laws.
Subpoenas are often used to present all the facts. A subpoena is a
document that is served to a person who is in possession of vital
information. This information might be in the form of medical records, or
it might be in the form of expertise in the field. If you are in charge of
records that are listed on a subpoena, you should make sure you are
authorized to release the records to the appropriate party, and then you
may do so.
Arbitration is used when two parties disagree and cannot settle their
disagreement. Binding arbitration means the arbitrator’s decision is final and
must be followed. In nonbinding arbitration, the decision of the arbitrator is
treated as a suggestion. Finally, you learned that sometimes a physician has
to go to court to provide medical testimony.
Now, let’s test your understanding of this lesson with a Quiz.
Please pause and complete online Quiz. Good luck!
Endnotes
1
HITECH Act Enforcement Interim Final Rule, U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/administrative/enforcementrule/hitechenforcementifr.html
2
The Definition of Business Associate, Health Insurance Portability and Accountability Act, http://www.hipaa.com/
2009/05/the-definition-of-business-associate/, 2009
3
Transaction & Code Sets Standards, Centers for Medicare & Medicaid Services, http://www.cms.gov/Regulations-
and-Guidance/HIPAA-Administrative-Simplification/TransactionCodeSetsStands/index.html?
redirect=/TransactionCodeSetStands/, March 22, 2012
4
The Evolution of the ANSI ASC X12N 837 format from the UB-92 Flat file format, Public Health Data Standards
Consortium, http:/www.phdsc.org/standards/pdfs/EvolutionofANSI.pdf, Jan. 13, 2004
5
The Privacy Rule, U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/administrative/privacyrule/index.html
6
Summary of the HIPAA Privacy Rule, U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/understanding/summary/privacysummary.pdf, May 2003
7
Notice of Privacy Practices for Protected Health Information,U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/notice.html, April 3, 2003
8
Summary of the HIPAA Security Rule, U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/understanding/srsummary.html
9
How OCR Enforces the HIPAA Privacy Rule, U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/enforcement/process/howocrenforces.html
10
Case Examples and Resolution Agreements, U.S. Department of Health & Human Services,
http://www.hhs.gov/ocr/privacy/hipaa/enforcement/examples/index.html
11
Centers for Medicare & Medicaid Services’ Use of Medicare Fee-for-Service Error Rate Data to Identify and Focus on
Error-Prone Providers, U.S. Department of Health & Human Services,
http://oig.hhs.gov/oas/reports/region5/50800080.pdf, Oct. 29, 2010
12
Recovery Audit Contractors (RAC), American Health Information Management Association,
http://www.ahima.org/resources/rac.aspx
13
Recovery Audit Contractor (RAC) Program, American Hospital Association, http://www.aha.org/advocacy-
issues/rac/index.shtml
14
CMS collects $162 million in overpayments in first three months of 2011, Modern Healthcare, March 14, 2012
LESSON 8
Introduction to Anatomy
Step 1 Learning Objectives for Lesson 8
When you have completed the instruction in this lesson, you will be trained to do
the following:
Explain the basic components of human biology.
Describe the human body, including how it works and how it is put
together.
Define the terms used to locate parts of the body.
Step 2 Lesson Preview
Leonardo da Vinci’s human form
When Leonardo da Vinci drew his sketches of the human body back in the 15th
century, he probably didn’t anticipate just how important the study of the human
body would become. In this lesson, you will be introduced to the basic components
of human biology, including anatomy, physiology and pathology. Keep in mind that
we do not expect you to memorize every term. The more familiar you are with your
terminology, the quicker and easier it will be to complete some of your tasks as a
medical coding specialist. However, it is important you use your research tools. If
you don’t remember a word while completing your lessons or while working, use
your materials or flashterms to help.
Today many people use anatomy daily in their professions. Athletic coaches
must be well versed in anatomy because their knowledge of muscles and
bones helps their players achieve top performance and avoid injury. Doctors
must know vast amounts of anatomy, from the top of the human head down
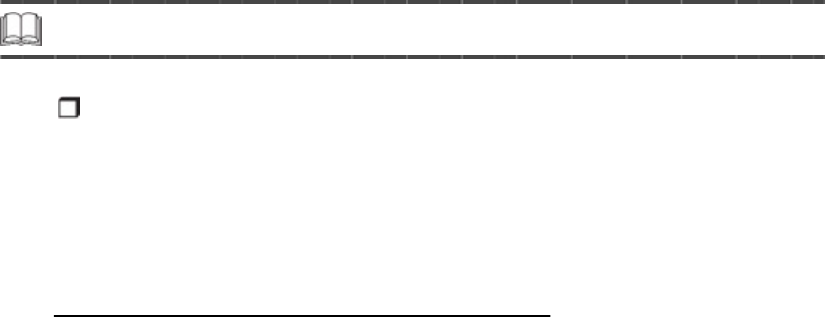
to the little toe, and all the nerves, blood vessels, and organs in between.
Medical coding specialists must know anatomy to understand the terms they
see in their work. Your knowledge of medical terms, as well as anatomy,
work together to make you a competent coder.
In this lesson, you will see how anatomy affects our everyday lives. We’ll
begin with an introduction to the science of life—biology. After you learn
about basic human biology, we will move into the more specific science of
anatomy, including physiology—the study of how the body works. Don’t
worry! We will move at a comfortable pace, and we’ll carefully cover each
detail you must know.
Step 3 Human Biology
For the next several lessons, you will learn about the study of human living things.
Because you are a human, you’ll learn a lot about yourself. In doing your Practice
Exercises and studying your flashterms, you’ll grow in your understanding of the
human body and the specialized terms doctors use to talk about the body.
What Is Human Biology?
Human biology is the study of how the body is put together and how
it works in health and disease. As a medical coding specialist, you do
not need to become an expert in biology. However, understanding the
basics of biology gives you a good background for the terms doctors
use, such as those you learned about in your medical terminology
lessons!
Human biology in the healthy state covers two basic concepts: anatomy and
physiology. Human biology in disease deals with pathology. Look at how
these concepts are related in the diagram on the following page.
We will discuss each of these topics in more detail. Remember, the idea is
not to become an expert in biology, but to understand the context of the
terms you might see in your daily work.
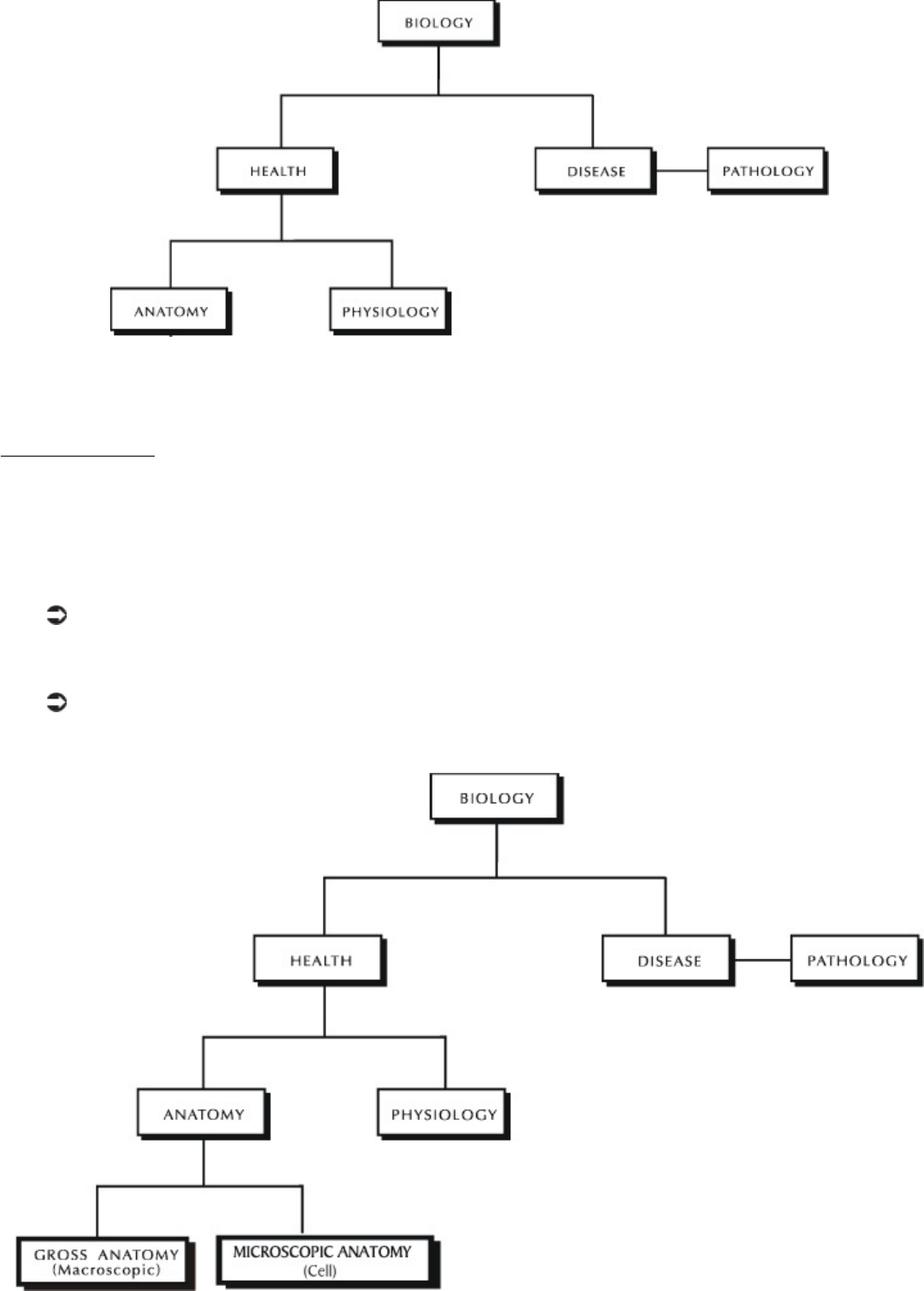
Biology deals with health and disease.
Anatomy
Anatomy is the science of the structure of the body—the appearance and
relationships of body parts. The two kinds of anatomy are gross anatomy and
microscopic anatomy.
Gross anatomy includes parts of the body that we can see with our
eyes. It is also called macroscopic anatomy.
Microscopic anatomy, or cell anatomy, includes parts of the body
that are too small to be seen with the naked eye.
The two kinds of anatomy are gross anatomy and microscopic anatomy.
Gross Anatomy
Gross anatomy focuses on the presence and appearance of a body
part. The study of the form of body parts is called morphology. The
form of a body part includes its size, shape, color, contour, and texture.
For example, when a kidney is normal in size, shape, color, contour, and
texture, it has normal morphology.
There is a morphologic difference between a jockey and a basketball player.
A basketball player and a jockey both have the same anatomic structure;
both have five fingers on each hand. However, there is a morphologic
difference between them. For example, the hand of the basketball player is
larger than the hand of the jockey.
Gross anatomy also deals with the location and position of the organs and
body parts. For example, not only should the heart be in the chest, but it
should be in the left side of the chest.
Fact About Gross Anatomy
The terms used to describe gross anatomy include:
• The names of the body parts
• Where the body parts are located
• How the locations of two body parts are related
Microscopic Anatomy
Microscopic anatomy is the science of the body’s individual cells and
tissues. This study is done with a microscope. The microscopic study of
cells is called cytology. The microscopic study of tissues is called
histology.
Fact About Microscopic Anatomy
The terms used to describe microscopic anatomy include:
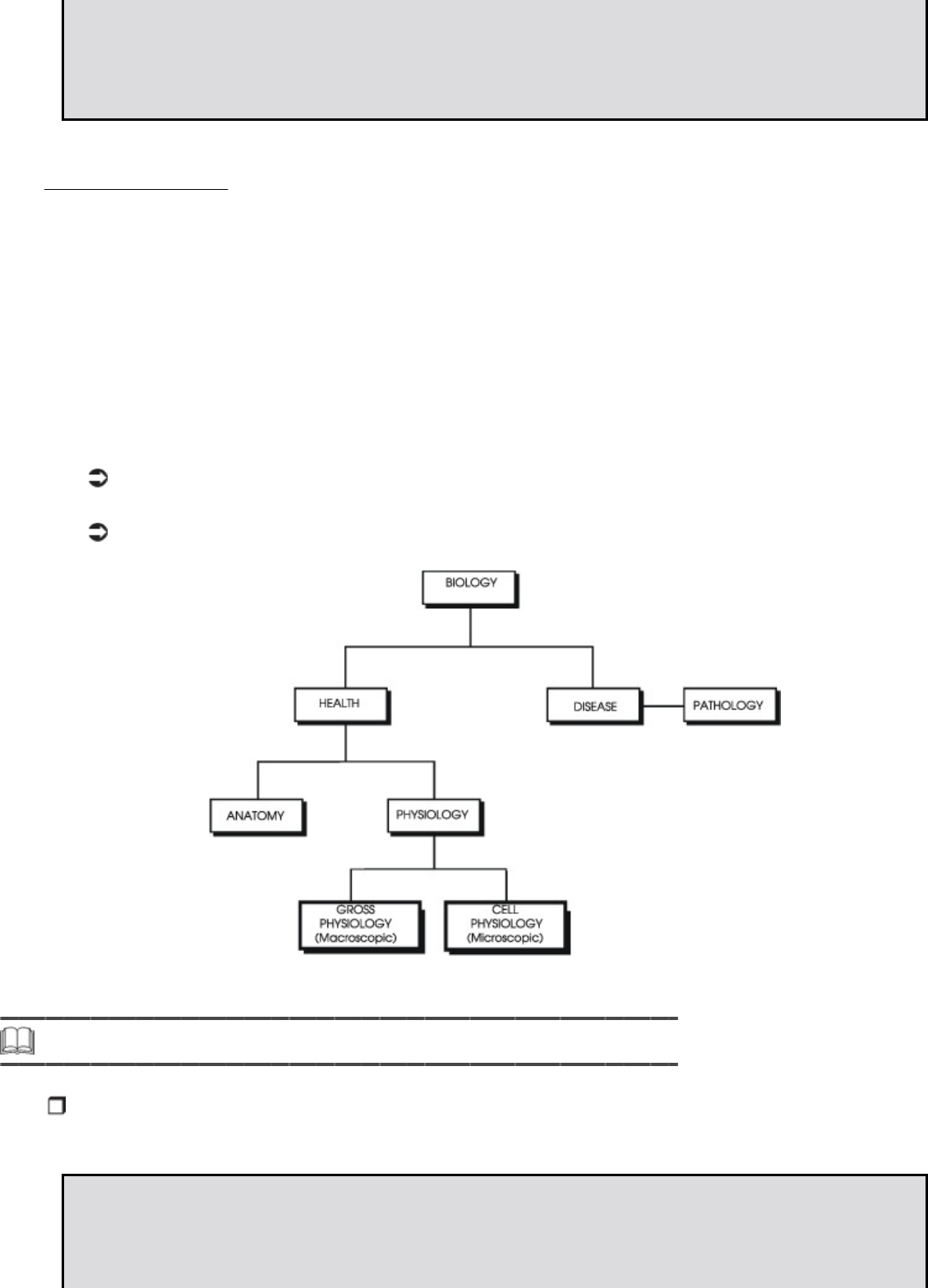
• The names of different cell parts and cell types
• The colors cells become when they are dyed for microscopic examination
• The ways cells are arranged in different types of tissue
Physiology
Physiology is the study of how the body works; it describes the function of
the body, and its organs, tissues, and cells.
Each organ, cell or tissue has its own special physiologic function. For
example, kidneys make urine, but they cannot think. The brain thinks, but it
cannot make urine.
Physiology also can be divided into macroscopic physiology and microscopic
physiology.
Macroscopic physiology usually is called gross physiology.
Microscopic physiology usually is called cell physiology.
Physiology can be broken into gross physiology and cell physiology.
Step 4 Pathology
Pathology is the study of human biology when anatomy and/or physiology are
abnormal.
Facts About Pathology
• Abnormal physiology sometimes is called pathophysiology.
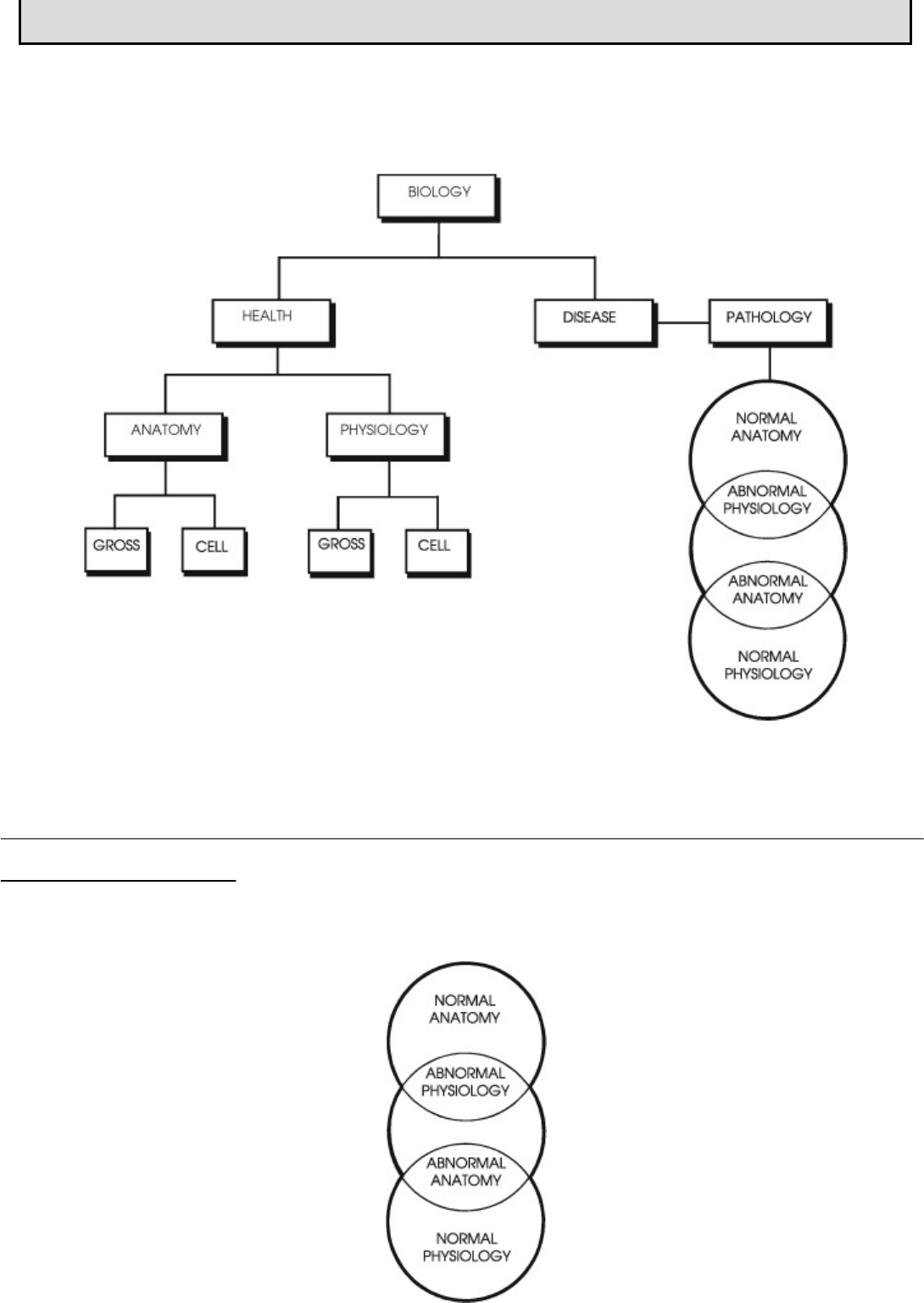
• Abnormal anatomy is called pathology or pathologic anatomy.
Pathology deals with abnormal anatomy and abnormal physiology. Look at
the relationships in the chart that follows. In the next section, we will
describe the relationships represented by the circles.
Pathology deals with abnormal anatomy and abnormal physiology.
How Do Anatomy, Physiology and Pathology Relate to
One Another?
In this section, we’ll examine normal anatomy and physiology.
Normal Anatomy/Abnormal Physiology
A person can have abnormal physiology but normal anatomy. For
example, a diabetic has abnormal physiology—the person cannot make
insulin—but the diabetic may have normal anatomy. The insulin-making
function is abnormal but the appearance and location of the organ that
makes the insulin is normal.
Abnormal Anatomy/Normal Physiology
A person can have abnormal anatomy but normal physiology. For
instance, a healthy dwarf has abnormal anatomy but normal physiology.
The anatomy is abnormal, but it functions normally.
Abnormal Anatomy/Abnormal Physiology
When an anatomic abnormality lasts long enough, it may lead to a
physiologic abnormality. For example, in early alcoholism, the liver changes
by containing more fat and enlarging. These are anatomic abnormalities. The
function is normal. If alcoholism continues long enough, the liver slowly stops
functioning. This is a physiologic abnormality.
The effects of a cold are physiologic abnormalities.
On the other hand, when a physiologic abnormality lasts long enough, it may
lead to an anatomic abnormality. For example, at the start of a cold, you
have sniffles and a loss of smell. These are physiologic abnormalities. The
function of the nose is abnormal. The anatomy of the nose, its size and color,
is normal. Later, you may have a swollen, red nose from the cold. Swelling
and redness are pathologic changes in anatomy. Because swelling and
redness are changes in size and color, they also can be called morphologic
changes.
For most disease processes, anatomy and physiology both are abnormal by
the time a diagnosis is made. For example, in the early stages of alcoholism,
the liver functions well, and the liver function tests are normal. The diagnosis
of alcoholic liver disease usually is not made. The patient feels fine and
cannot believe that the liver is abnormal. When both the anatomy and
physiology are pathologic, the patient feels sick, and the liver function tests
are abnormal. So you can see that the diagnosis is not usually made until
both the anatomy and physiology are pathologic.
Likewise, in the early stages of a cold, when you just have sniffles, you say,
“I think I’m getting a cold.” When your nose is red, swollen, stuffy, and runny,
you say, “I have a cold.” Again, the diagnosis isn’t usually made until both
anatomy and physiology are abnormal.
So even though diseases can be divided into anatomic pathology and
pathophysiology, medicine often deals with both anatomic and physiologic
pathology at the same time.
Please pause and complete online Practice Exercise 8-1.
Step 5 Beginning Anatomy and Physiology Concepts
Now that you have a basic understanding of human biology, you are ready to move
on to the more specific science of anatomy and physiology. Anatomy and
physiology are two key components in the medical world. Remember:
Anatomy refers to the structure of the body—the appearance and
relationships of body parts, such as muscles, bones, organs, and other
systems.
Physiology is the study of how these body parts work together to
sustain life—the functions of the body and its organs, tissues, and
cells.
The Anatomic Position
Doctors use a system to describe the location of anatomical parts. This
system assures that there is no confusion about the location of any body
parts. The location of body parts is always described as if the patient were in
the position shown in the following figure. This body position is called the
anatomic position.
Notice the position of the hands in the figure. The palms face forward, and
the thumbs face outward. No matter what the position of the patient, the
doctor describes the location of anatomic parts as if the patient were in this
position. Stand up and put your body in the anatomic position.
The anatomic position
Be sure you remember the anatomic position. The terms you learn in this
lesson are based on the relationships of body parts when the body is in this
position. When you are working as a medical coding specialist, understanding
the anatomical position and the relationship to body parts will help you
assign correct diagnostic and procedure codes.
Planes and Sections of the Human Body
The human body has three dimensions: height, width and depth.
Fact About Dividing the Body
The body can be divided in three different ways:
• Superior and inferior (top and bottom) sections
• Right and left sections
• Anterior and posterior (front and back) sections
Dividing the body like this helps you understand where organs or parts are
located. You can divide the body into these sections by making a mental
“slice” or “cut.”
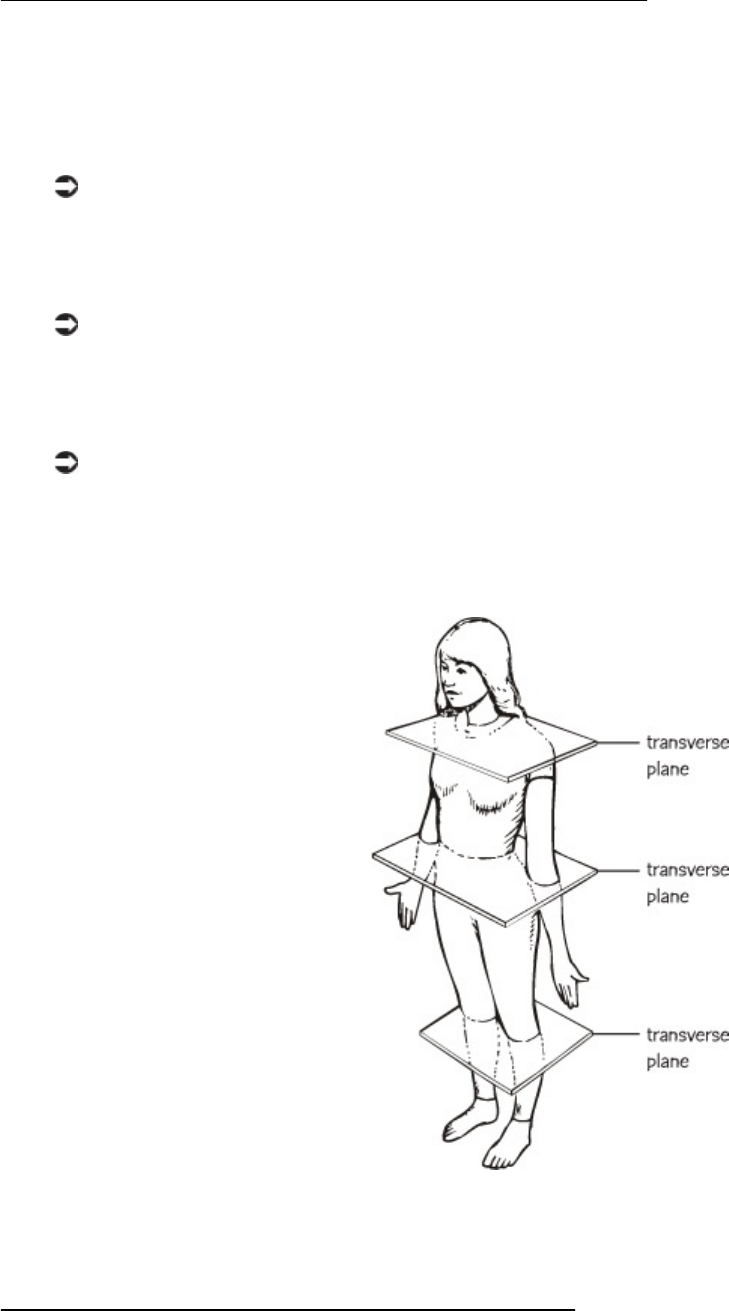
Transverse Planes and Sections
The transverse or horizontal plane divides the body into superior (above)
and inferior (below) sections. A transverse plane can be made anywhere in
the body from the feet to the head.
A transverse plane made at the neck divides the body into superior and
inferior sections. The head is superior to the plane. The chest, arms,
abdomen, and legs lie inferior to the plane.
A transverse plane made at the waist also divides the body into superior
and inferior portions. The head, chest, and arms are superior to the
plane. The pelvis and legs are inferior to the plane.
A transverse plane made at the level of the knees divides the body into
superior and inferior sections, too. The thighs, abdomen, chest, arms,
and head are superior to the plane. The calves and toes are inferior to
the plane.
Transverse sections
Sagittal Planes and Sections
A sagittal or longitudinal plane divides the body into right and left
sections. A midsagittal or median plane divides the body into equal
right and left sections. A midsagittal plane is the midline of the body. A
parasagittal plane divides the body into unequal right and left sections.
A sagittal plane can be made at any point of the body from the right side
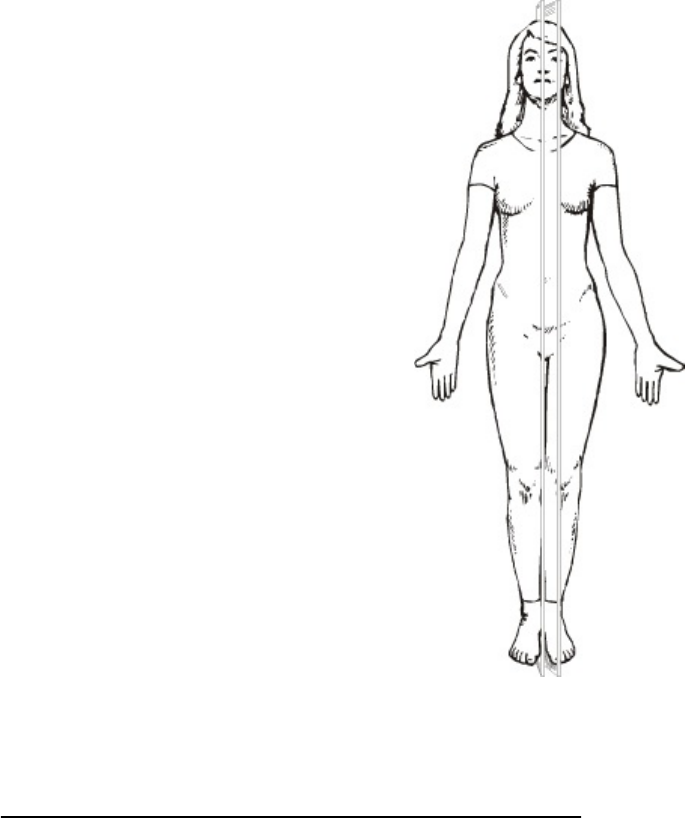
to left side.
Sagittal sections
Coronal Planes and Sections
A coronal or frontal plane divides the body into anterior (front) and
posterior (back) sections. A coronal plane can be made at any point from the
front of the body to the back of the body.
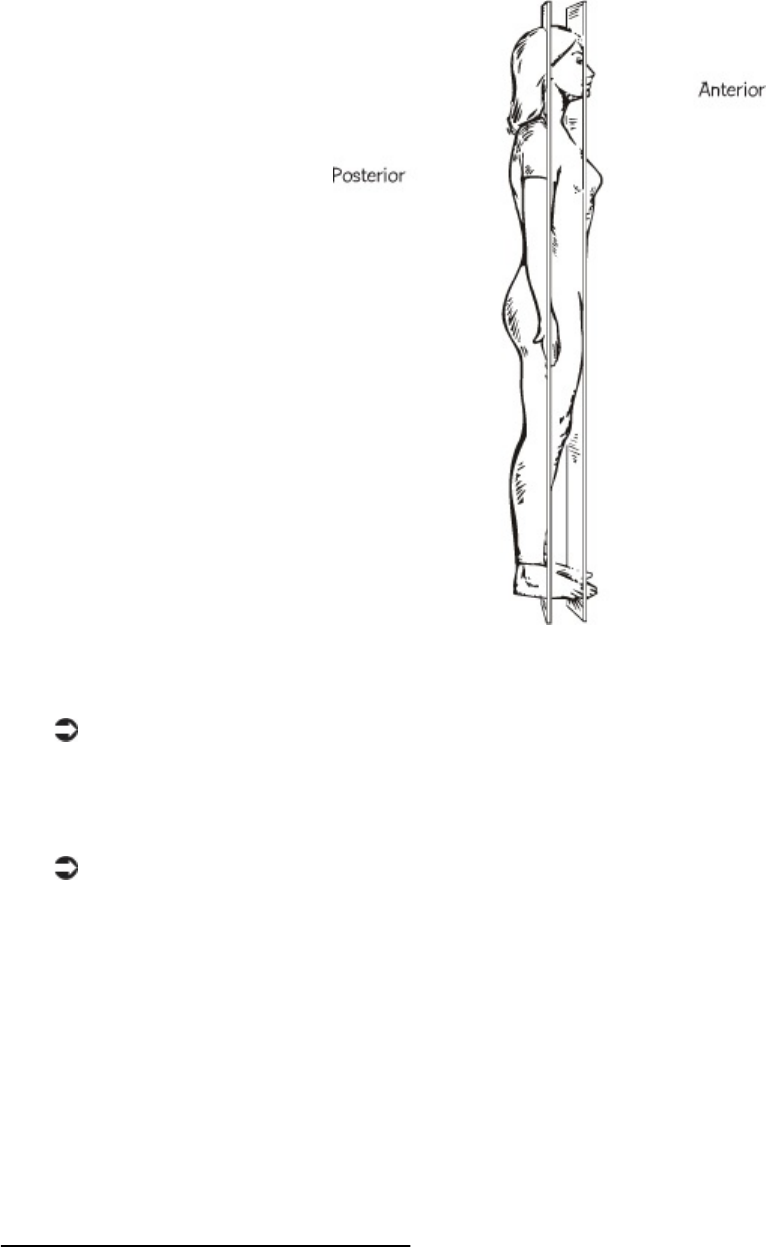
Coronal sections
A coronal plane at the level of the ears divides the body into anterior and
posterior sections. The face, abdomen, and knees are anterior to the
plane. The back, buttocks, and ankles are posterior to the plane.
A coronal plane at the level of the nose divides the body into anterior
and posterior sections. Almost everything else is posterior to the plane.
You can divide the body and each organ using planes. For example, a
midsagittal plane of the liver divides the liver into equal left and right
sections.
Study the definitions of these planes until you can form a mental image of
them. You’ll remember these concepts more easily if you picture the planes
using your own body.
Planes and Sections
You can divide the body and each organ using planes. For example, a
parasagittal plane of the liver divides the liver into unequal left and right
sections.
A parasagittal plane of the liver
Please pause and complete online Practice Exercise 8-2.
Step 6 Location Terms
The location terms you learn in this lesson are important to you, the coder,
because doctors use them to describe what they see when they examine a patient.
You will learn how to pronounce the terms later in this lesson.
Providers use location terms to document the examination.
When doctors describe the location of anatomic parts, they use terms that
compare the location of one part to another part. A number of terms describe
the relative location of body parts and organs. These terms rely on the
anatomical position and the anatomic sections you just learned.
Fact About Location Terms
These terms usually come in antonym pairs. Each word of an antonym pair
means the opposite of the other word, such as the antonym pairs above and
below or left and right.
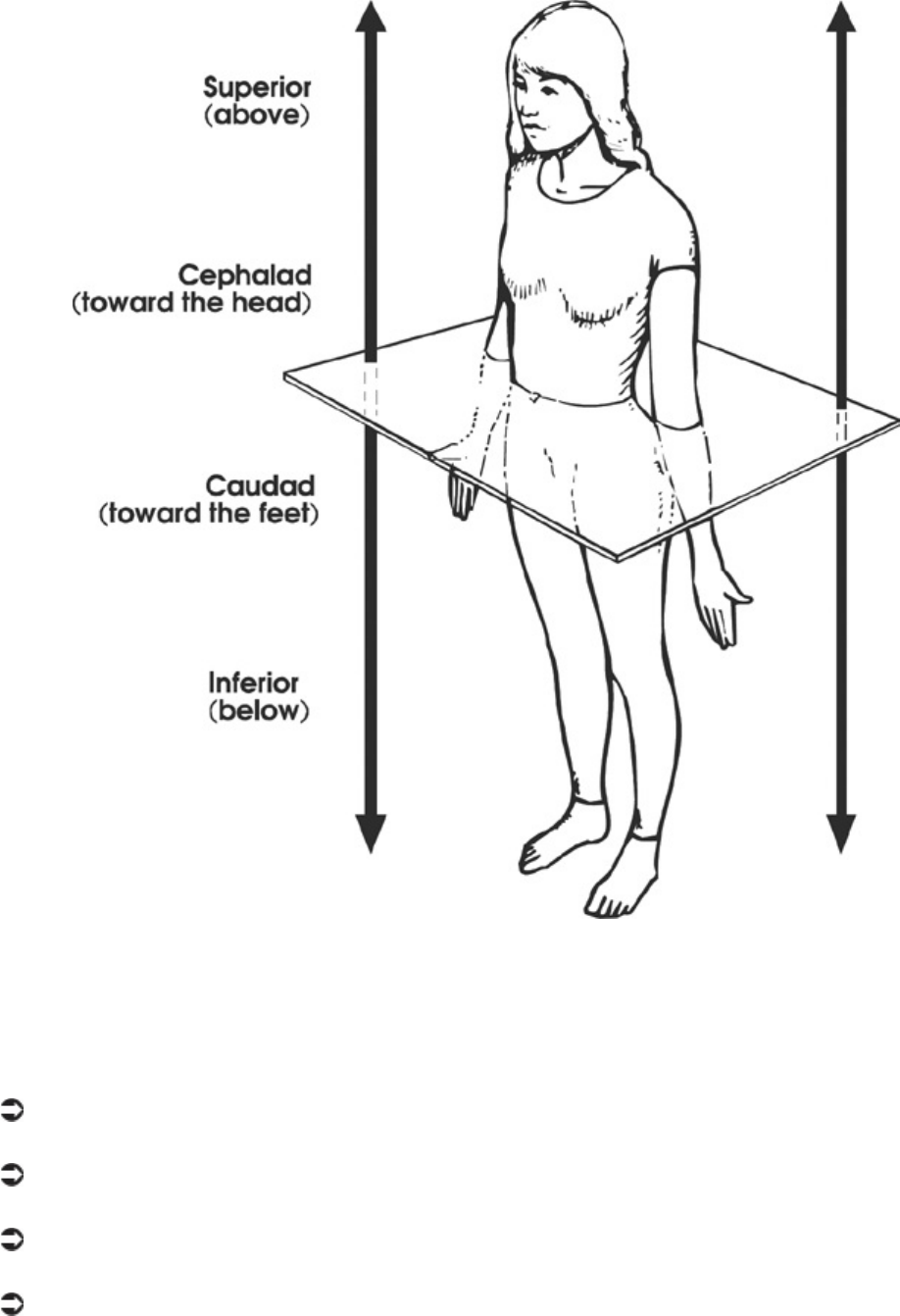
Transverse plane
If you draw a transverse plane through the body or an organ, these words
describe anything above or below that plane.
Superior means above.
Inferior means below.
Cephalad means toward the top of the head.
Caudad means toward the soles of the feet.
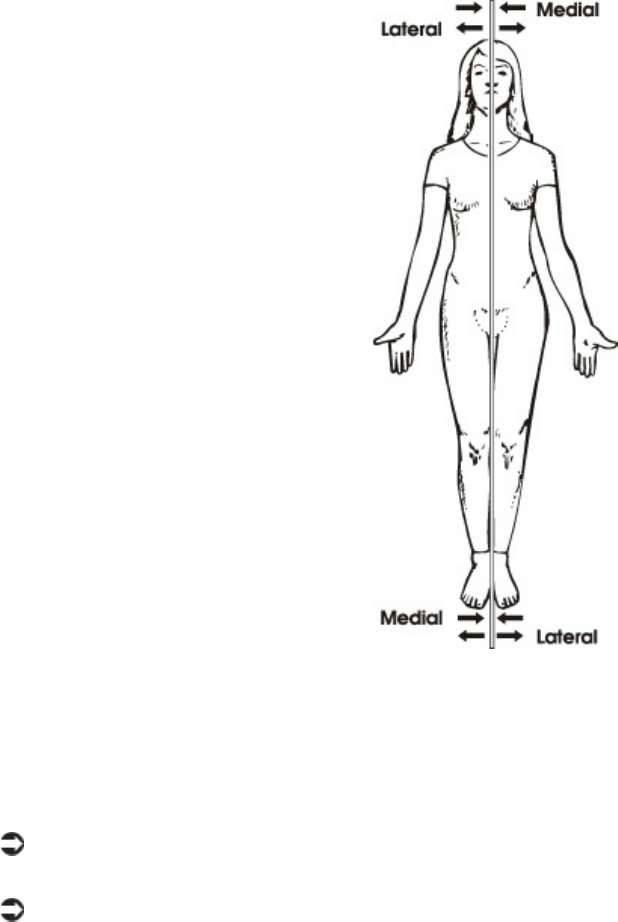
Sagittal plane
If you draw a midsagittal plane through the body or an organ, these words
describe anything closer to or farther away from that plane.
Medial means closer to the midsagittal plane or middle.
Lateral means farther away from the midsagittal plane or middle.
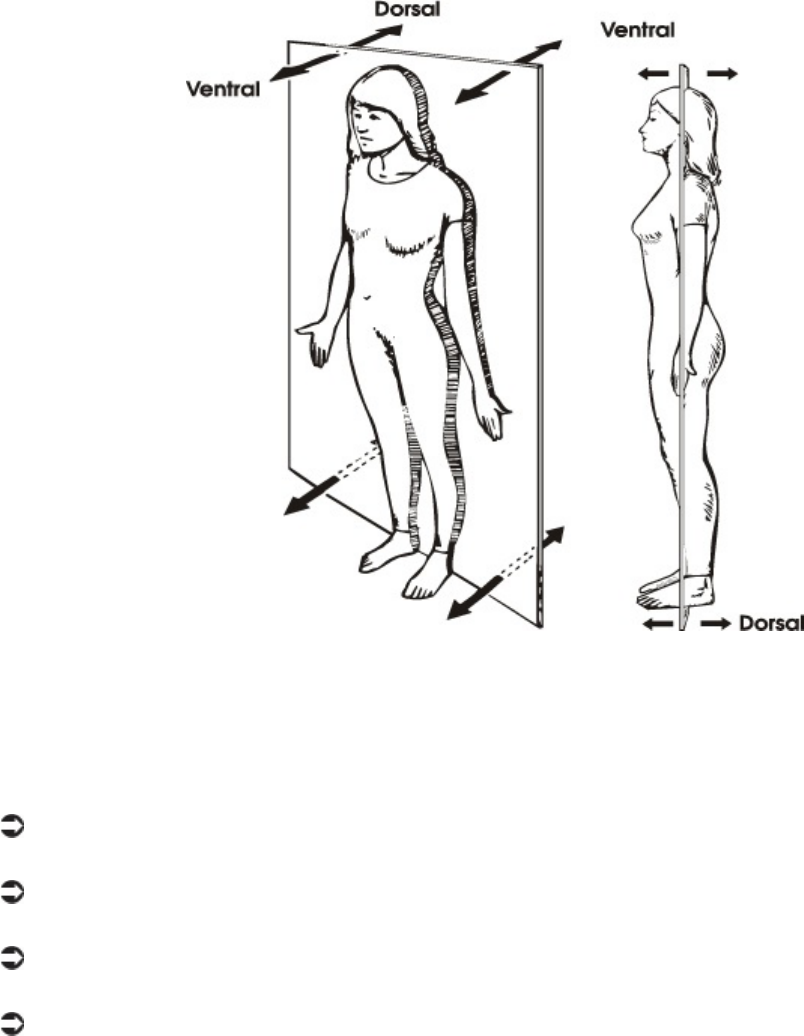
Coronal plane
If you draw a coronal plane through the body or an organ, these words
describe anything in front of or behind that plane.
Anterior means in front of.
Posterior means in back of.
Ventral means on the belly side.
Dorsal means on the back side.
The following chart summarizes these location terms and how they
are used.

Look at some sentences showing how these words are used. Compare these
statements to your own body. Be sure your body is in the anatomic position
when you do so.
The lungs are superior to the liver.
The liver is inferior to the heart.
The incision was made in a cephalad direction.
The arteries for the lower extremities travel in a caudad direction.
The nose is medial to the eye.

The right thumb is lateral to the right index finger.
The sternum is anterior to the heart.
The lungs are posterior to the sternum.
The ventral hernia was repaired.
The spine is dorsal to the stomach.
The following terms are used for the body or an organ as a whole. They
describe parts that are nearer the center or parts that are nearer the
surface of the body or an organ. Examples of how these words are used
follow the terms.
Proximal means nearer to the center of the body or organ.
The knee is proximal to the foot.
Distal means farther away from the center of the body or organ. The
foot is distal to the knee.
Superficial means on or closer to the skin or surface of an organ.
The wound was superficial, not involving the muscles, and did not
require sutures.
Deep means under or farther away from the skin or surface of an organ.
The wound was deep and penetrated the liver.
Central means within or near the center.
The heart is central within the rib cage.
Peripheral means at or near the rim or edge.
The peripheral veins of the arms and hands can be seen easily.
Parietal means the outer wall of a body cavity.
The parietal pleura forms the outer layer that surrounds the lungs.
Visceral means the covering of an organ.
The visceral pleura covers the lungs.
External means outside or closer to the skin or surface of an organ.
The pericardium is external to the heart.
Internal means inside or farther away from the skin or surface of an
organ.
The lungs are internal to the ribs.
Ipsilateral means situated on or affecting the same side of the body.
The left leg and left arm are ipsilateral.
Contralateral means situated on or affecting the opposite side of the
body.
The right leg and left arm are contralateral.
The lungs are internal to the ribs.
Some things in the body, like blood cells, fluid or nerve messages, can move.
The next two terms describe body parts that carry things that move.
Afferent means carrying toward a body part or the center of an organ.
An afferent neuron is a nerve that carries nerve messages to the brain
from a muscle.
Efferent means carrying away from a body part or the center of an
organ.
An efferent neuron is a nerve that carries nerve messages away from
the brain to a muscle.
An afferent neuron is a nerve that carries nerve messages to the brain from a muscle.
Step 7 Pronounce New Terms
Follow these steps:
a. Take your Quick-Learn Tutor and your Set 9 flashcards out of your Quick-
Learn Kit. Insert the first flashcard for Set 9 into Side A of the Tutor.
b. Access the online portion of your course and go to Lesson 8.
c. Listen to the flashterm. Pause the audio.
d. Practice pronouncing the term out loud. Take your time. Push the flashcard
up and read the meaning of the word part or term.
e. Do this for each term in this set.
f. Put the flashcards in order and play the audio again, pronouncing each
word part or term after you hear it. Don’t forget to listen to your own
pronunciation of each term. If you mispronounce one, put a check mark
next to that flashterm.
g. Practice the terms you mispronounced by listening again. Be sure you can
pronounce the terms clearly and easily.
Step 8 Write New Terms
Follow these steps:
a. Insert the first flashcard for this set into Side A of your Quick-Learn Tutor.
b. Look at each term as it appears in the window and say it out loud. Write
the flashterm on blank paper. Remember to include the slash if it is a word
part.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the flashterm.
d. Do this for each term.

Step 9 Meanings of New Terms
Follow these steps:
a. Again insert the first flashcard into Side A of your Quick-Learn Tutor.
Pronounce each word part or term and then say the meaning. Check
yourself by pushing the flashcard up until you can see the meaning in the
right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud, and then say the term. Again, check yourself
by pushing the flashcard up until you can see the term in the left window.
c. Practice with the flashcards several times until you are familiar with the
flashterms and their meanings. You may use the flashcards for the Practice
Exercises and Quizzes.
d. When you feel comfortable with the spelling, pronunciation, and meaning
of each flashterm, go on to the next step.
Step 10 Organ and Organ Systems
Now that you’ve laid a foundation in basic anatomy concepts, let’s take a look at
the body’s major organs and organ systems.
Tissues are grouped together to form an organ. In an organ, all the tissues
work as a team. Each type of tissue has its own job to do, but together the
tissues have a common purpose: the function of the organ.

Organ tissues work as a team.
Each type of tissue does its own job. For example, the liver contains tissues
from each of the basic tissue groups (epithelium, connective, muscle,
nervous). The epithelium covers and protects the organ and makes the
glands of the organ. Connective tissue holds the organ together and provides
support or repair. Muscle tissue provides motion, contraction or pressure in
ducts and vessels. Nervous tissue provides connection to the brain and
warning of danger. Then, all the groups of tissues in the liver work together
to perform the functions of the liver.
In the same way, the heart contains tissues from each of the tissue groups,
all acting together to perform the function of the heart. However, from a
practical point of view, when a patient has a problem, the problem is not with
a tissue type but with a particular organ, such as the liver or the heart.
An organ usually interacts with other organs that help it perform its
function. For example, the liver, pancreas, stomach and bowel are
organs that all work together to digest food. Thus, organs with similar
functions or physiology are grouped together in organ systems. In fact,
the different specialties of medicine represent the various organ
systems. You can probably recognize some of these systems and areas
of specialization already.
Respiratory System
The respiratory system is the gas exchange system that provides
oxygen to the body while removing the by-product of oxygen
metabolism, carbon dioxide. The body as a whole cannot do without
oxygen for more than three to five minutes because a lack of oxygen to
the most sensitive parts of the body—the brain and the heart—can
cause permanent, if not fatal, damage.
Circulatory/Cardiovascular System
The cardiovascular system is the supply transportation system for the
body. It brings nutrients like oxygen, glucose, amino acids and
hormones to all the cells in the body and carries off the waste products
of cell metabolism. The cardiovascular system includes the heart, blood
vessels, lymph vessels and the blood or lymph they contain.
The heart is like the dispatcher, sending blood out in regular shipments
through all the organs and cells of the body. The vascular system
includes arteries, veins, capillaries and lymph channels, which are like
highways and city streets. They provide a well-planned flow to and from
delivery and pick up points. The blood and lymph do the actual
transporting of all these materials to and from their destinations. Each
type of cell specializes in the supplies and waste materials it transports.
Nervous System
The nervous or neurological system includes the central nervous system,
which is made up of the brain and spinal cord, and the peripheral nervous
system, which includes the nerves that reach each organ in the body.
Because this system includes the mind, it can also be called the
neuropsychiatric system.
Muscular System
The muscular system consists of organs that produce movement as they
contract and relax. Muscles are not only in the extremities, such as the
biceps muscle that bulges when you flex your elbow, but also in almost
every other organ system in the body except the neurological system. The
muscular system also includes the tendons and aponeuroses, which is
connective tissue that attaches the ends of muscles to bones.
Skeletal System
The skeletal system includes bones, joints, cartilage and spine. Since it is
so difficult to separate the functions of the voluntary muscles and bones,
some people combine the muscular and skeletal organ systems into one
system, the musculoskeletal system. Most people think bones aren’t living
tissue, but rather something hard, like a rock. But each bone in your body is a
living organ, just like your heart.
Integumentary System
The integumentary system includes skin, nails, hair, sweat and sebaceous
glands. Integument means in the covering or in the skin. The skin and the
organs the skin contains are part of this system. The skin is the largest single
organ in the body! This fact explains why a large skin injury, such as a burn,
can be fatal.
Endocrine System
The endocrine system includes the glands that don’t have ducts. These
glands secrete within themselves directly into their blood vessels. Endocrine
glands are made of epithelium tissue. They secrete hormones. Endocrine
glands include the thyroid, parathyroid, pituitary, and adrenal glands as well
as the hypothalmus, pancreas, testes and ovaries. The testes and ovaries are
also part of the reproductive system.
Digestive System
The digestive system is concerned with digestion of food. This system begins
with the mouth and ends at the anus. The stomach, intestines, liver,
pancreas, mouth and esophagus all belong to the digestive system. This
system is also called the gastrointestinal system.
Urinary System
The urinary system filters the blood and produces urine. It includes the
kidneys, ureters, urinary bladder and urethra.
Reproductive System
This organ system involves the organs for reproduction. The reproductive
system includes such organs as the ovaries, uterus, vagina, breasts, testes
and penis.
The Immune System
One system you may not have heard about is the immune or
immunologic system. That is because this system that defends the
body from disease is not clearly understood. The immune system appears
to use parts of the cardiovascular system, the nervous system and the
endocrine system to provide defense against some kinds of disease. The
immune system provides immunity, or resistance, to diseases caused by
stress, viruses and degeneration. This system helps fight cancer and tries
to kill any foreign substance in the body, even a transplanted organ.

Please pause and complete online Practice Exercise 8-3.
Step 11 Lesson Summary
This lesson brings you along in your journey to become an effective and
professional medical coding specialist. Anatomy is an integral part of every aspect
of medicine, so the ability to recognize terms and their medical context makes you
a valuable member of the healthcare team.
This lesson explained the basics of human biology—the study of how the
body is put together and how it works in health and disease. Human biology
in the healthy state includes anatomy and physiology. Human biology in
disease deals with pathology.
You learned that anatomy is the science of the structure of the body,
including the appearance and relationships of body parts. The two kinds of
anatomy are macroscopic anatomy and microscopic anatomy. Physiology is
the study of how the body works; it describes the function of the body and its
organs, tissues, and cells. Physiology also can be divided into macroscopic
physiology, which usually is called gross physiology, and microscopic
physiology, which usually is called cell physiology.
We explained that pathology is the study of human biology when anatomy
and/or physiology are abnormal. Abnormal physiology sometimes is called
pathophysiology. Abnormal anatomy is called pathology or pathologic
anatomy. When doctors describe the location of anatomic parts, they refer to
the anatomic position and the anatomic sections with the corresponding
anatomic planes. There also are specific location terms that doctors use to
describe the relative locations of body parts and organs.
As you continue with the next few lessons, keep in mind that everything you
learn about the human body will help you in your new career as a medical
coding specialist! You are learning terms you will see in your daily work with
physicians and other healthcare professionals.
Please pause and complete an online Quiz. Good luck!
LESSON 9
Anatomy: Landmarks and Divisions
Step 1 Learning Objectives for Lesson 9
When you have completed the instruction in this lesson, you will be trained to do
the following:
Discuss landmarks and divisions as they apply to anatomy.
Talk about the basic body cavities.
Explain how the body is organized.
Step 2 Lesson Preview
In previous lessons you learned some of the language that goes along with the
medical field. In this lesson, we’ll talk about the body—how it works, how it is
organized and how its systems are connected.
In this lesson, we’ll talk about the body.
Don’t worry if you don’t remember everything about this lesson. It is an
introduction designed to give you a knowledge base. This base enables you
to understand what medical providers face every day. As a medical coding
specialist, you need this basic understanding to communicate with doctors
and other healthcare professionals in your work just as you need to
understand the medical terminology we talked about in previous lessons.
Step 3 Gross Anatomy
Contrary to what you might think, gross anatomy does not mean disgusting
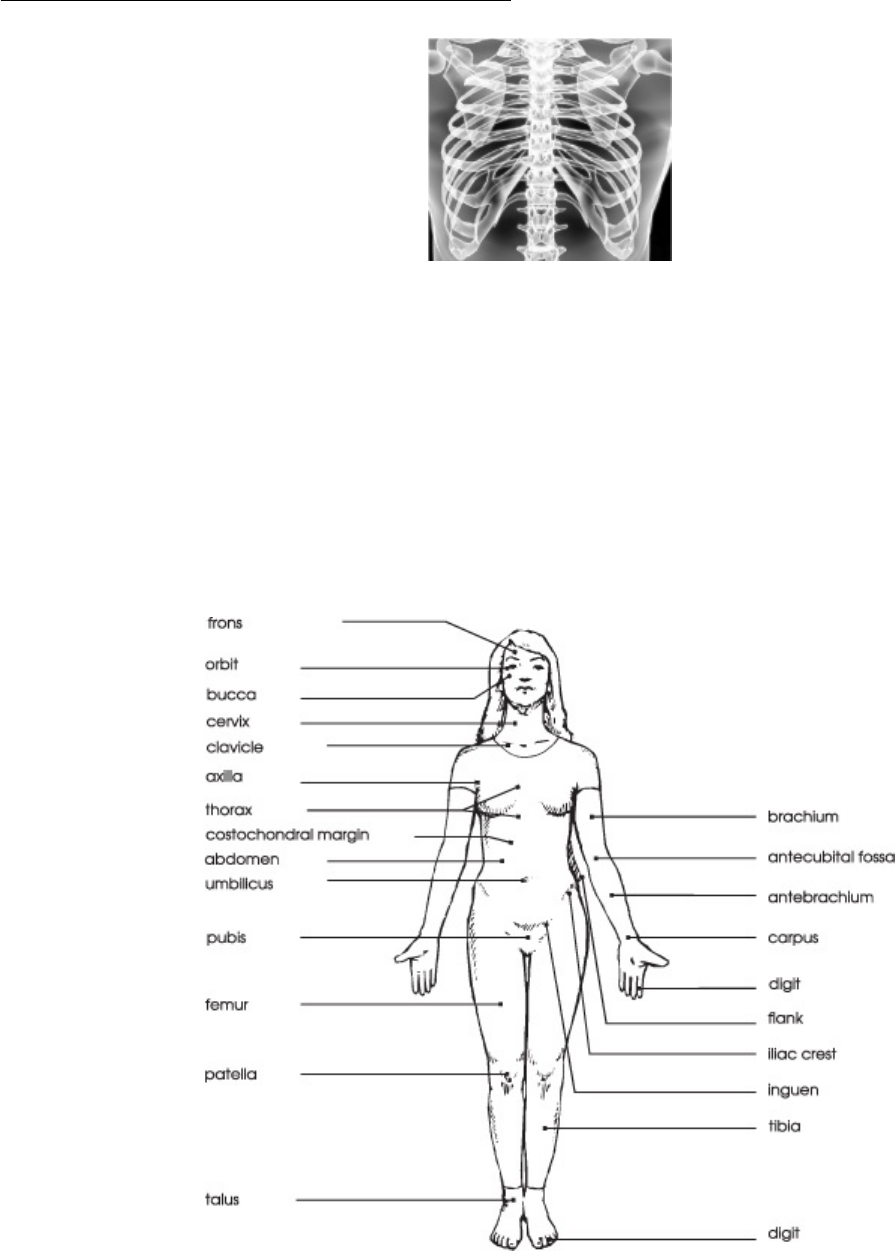
anatomy! Instead, as you learned in the previous lesson, it refers to the study of
body parts and systems that can be seen without the aid of a microscope. In this
context, the word gross means large.
Landmarks and Divisions
Location terms have been used for hundreds of years, long before providers could see inside the body with x-ray.
When a doctor examines the surface of the body, he uses several gross
anatomy terms to describe location. The study of the surface of the body
often is called superficial anatomy. These location terms, or landmarks, have
been used for hundreds of years, long before providers could see inside the
body with x-ray or ultrasound machines. These terms are used every day in
physical examinations, medical histories, and surgery reports. As a medical
coding specialist, you’re likely to encounter these terms often.
Surface landmarks, supine

Superficial Landmarks, Face Up
When the body is supine, which means lying flat on the back, the doctor sees
the anterior or ventral side of the body. Let’s look at the terms used for
superficial landmarks on the anterior surface. The following figure shows the
surface landmarks in the supine position. The surface landmarks are
labeled. Can you find these parts on your own body? Check off each landmark
after you find it. If you are not sure what a new term means, consult the list
of meanings that follows the picture.
Surface Landmarks, Supine Meaning
frons forehead
orbit eye
bucca cheek
cervix neck
clavicle collarbone
axilla armpit
thorax chest
costochondral margin rib and cartilage
abdomen trunk
umbilicus navel, bellybutton
pubis front pelvic bone
femur thigh
patella kneecap
talus ankle
brachium upper arm
antecubital fossa front of elbow
antebrachium forearm
carpus wrist
digit finger/toe
flank side from ribs to hip bone
iliac crest top rim of hip bone
inguen groin
tibia shin
digit toe/finger
Superficial Landmarks, Face Down
When the body is lying prone, or face down, the doctor sees the posterior or
dorsal side of the body. The following drawing shows the surface landmarks
in the prone position. The surface landmarks are labeled. Can you find
these parts on your own body? You may not be able to reach all of them.
Check off each landmark after you find it. If you need help, consult the list of
meanings that follows the picture.
Surface landmarks, face down
Surface Landmarks, Prone Meaning
cubitus elbow
occiput back of head
cervix neck
scapula shoulder blade
dorsum upper back
lumbus lower back
sacrum spinal bones located between the buttocks
gluteus buttock
popliteal fossa back of knee
sura calf
calcaneus heel
plantar surface sole of foot
Step 4 Pronounce New Terms
Follow these steps:
a. Take your Quick-Learn Tutor and your Set 10 flashcards out of your Quick-
Learn Kit. Insert the first flashcard for this set into Side A of the Tutor.
b. Access the online portion of your course and go to Lesson 9.
c. Listen to the flashterm. Pause the audio.
d. Practice pronouncing the term out loud. Take your time. Push the flashcard
up and read the meaning of the word part or term.
e. Do this for each term in this set.
f. Put the flashcards in order and play the audio again, pronouncing each
word part or term after you hear it. Don’t forget to listen to your own
pronunciation of each term. If you mispronounce one, put a checkmark next
to that flashterm.
g. Practice the terms you mispronounced by listening again. Be sure you can
pronounce the terms clearly and easily.
Step 5 Write New Terms
Follow these steps:
a. Insert the first flashcard into Side A of your Quick-Learn Tutor.
b. Look at each term as it appears in the window and say it out loud. Write
the flashterm on blank paper. Remember to include the slash if it is a word
part.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the flashterm.
d. Do this for each term in this set.
Step 6 Meanings of New Terms
Follow these steps:
a. Again insert the first flashcard into Side A of your Quick-Learn Tutor.
Pronounce each word part or term and then say the meaning. Check
yourself by pushing the flashcard up until you can see the meaning in the
right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud and then say the term. Again, check yourself
by pushing the flashcard up until you see the term in the left window.
c. Practice with the flashcards several times until you are familiar with the
word parts and terms and their meanings. You may use the flashcards for
your Practice Exercises and Quizzes.
d. When you feel comfortable with the spelling, pronunciation, and meaning
of each flashterm, go on to the next step.
Step 7 Adjective Forms for Landmark Names
Some of the landmark names you just learned probably were unfamiliar to you, but
you may have heard these terms in their adjective form. Read the following chart:
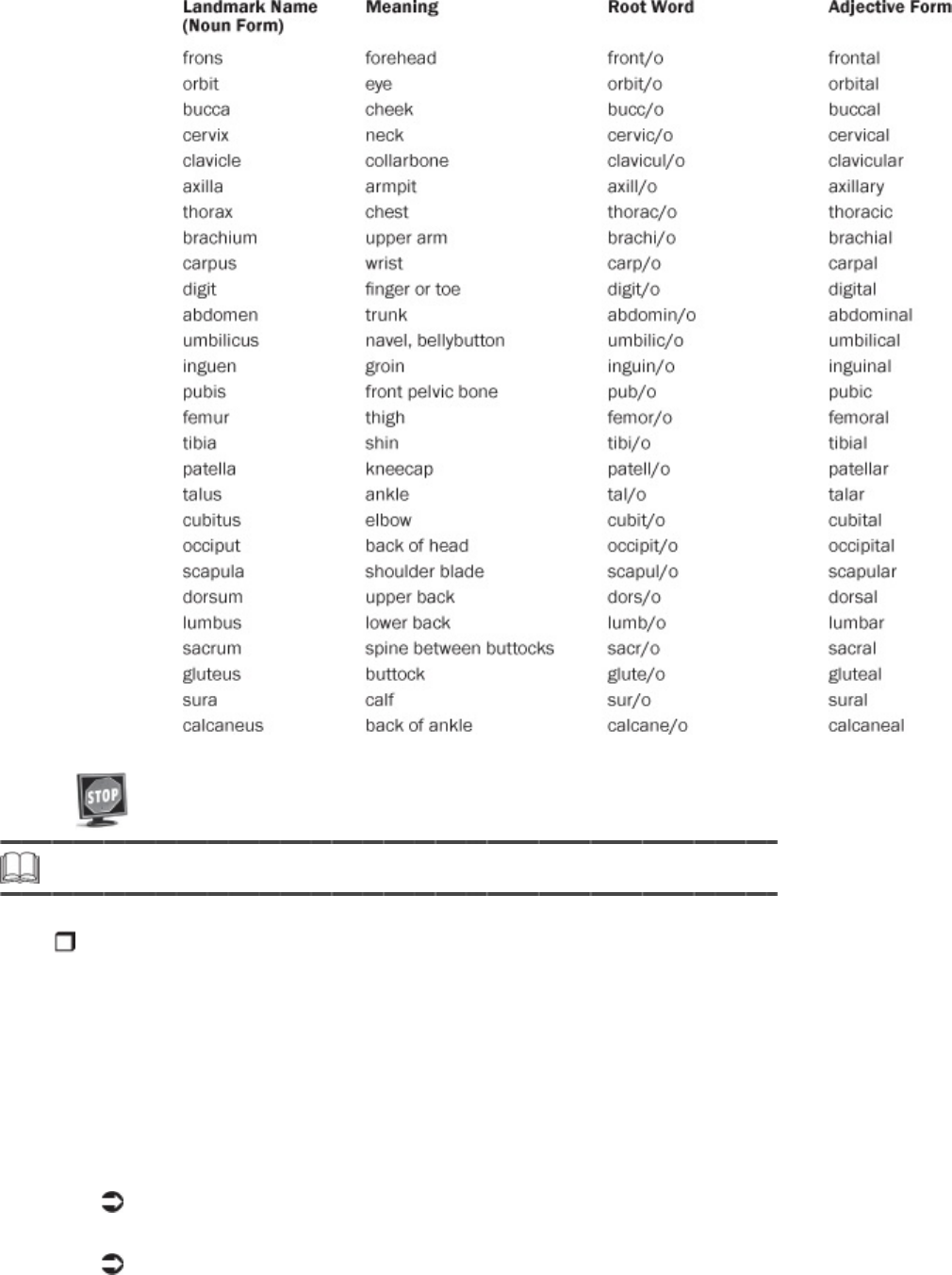
Please pause and complete online Practice Exercise 9-1.
Step 8 Divisions of the Abdomen
When a provider examines the abdomen, she mentally divides the abdomen into
nine areas or regions. When providers, especially surgeons, refer to these areas,
certain organs in the abdominal cavity are assumed to be in each region.
As a medical coder, you will hear these regions used to describe the
location of symptoms, abnormalities, and procedures. Look at these
examples.
An incision was made in the right hypochondriac region.
There are stretch marks in the hypogastric region.
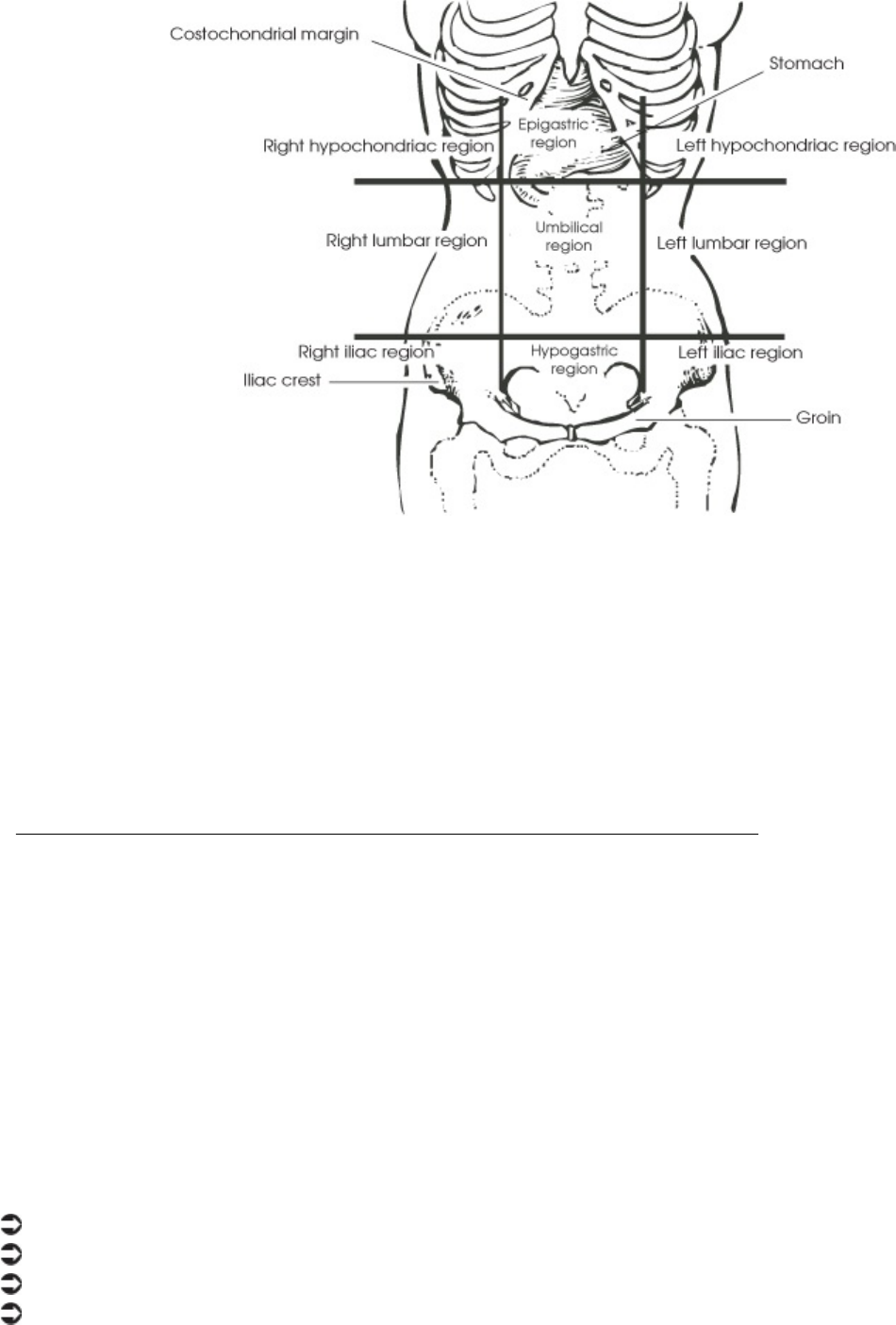
Divisions of the abdomen
These divisions are shown in the drawing that follows. Notice how the names
of some regions describe the superficial landmarks where they are located.
For example, two regions are named for their relationship to the location of
the stomach: the epigastric region and the hypogastric region. As you look at
the drawing, point out each region on your own abdomen.
An Alternative Division of the Abdomen
Some providers use a simpler way to divide the abdomen. The abdomen is
divided into fourths. Each of these areas is called a quadrant, which means
a one-fourth section.
The divisions are made by drawing a line along the midsagittal plane
(dividing left and right) and a line along the transverse plane (dividing
top and bottom) at the level of the umbilicus. This is shown in the
drawing that follows.
The four abdominal quadrants are named using the following words. The
acronym for each quadrant also is listed.
Right upper quadrant: RUQ
Left upper quadrant: LUQ
Right lower quadrant: RLQ
Left lower quadrant: LLQ
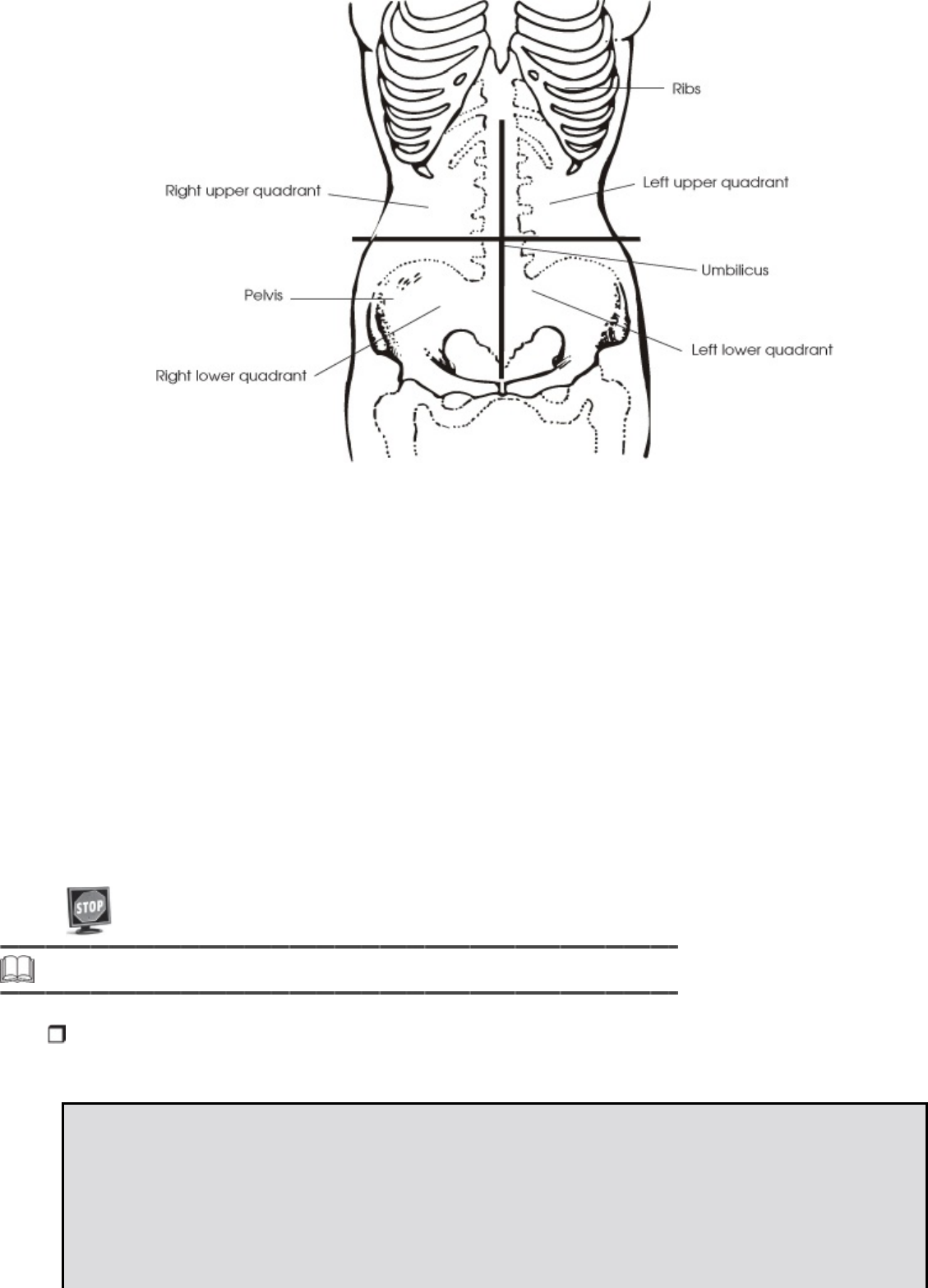
Quadrants of the abdomen
These terms are very important in assigning medical codes. Look at the
coding example for abdominal pain in the left upper quadrant:
789.02 Abdominal pain, left upper quadrant
Now look at the coding example for abdominal pain in the right lower
quadrant:
789.03 Abdominal pain, right lower quadrant
The location of the abdominal pain changes the code number! As you can
see, medical coding specialists must be aware of the four abdominal
quadrants to code correctly.
Please pause and complete online Practice Exercise 9-2.
Step 9 Internal Landmarks: The Body Cavities
The spaces within the body that contain the various internal organs are called
body cavities.
Facts About Body Cavities
Body cavities have two functions:
• Body cavities protect the organs they contain.
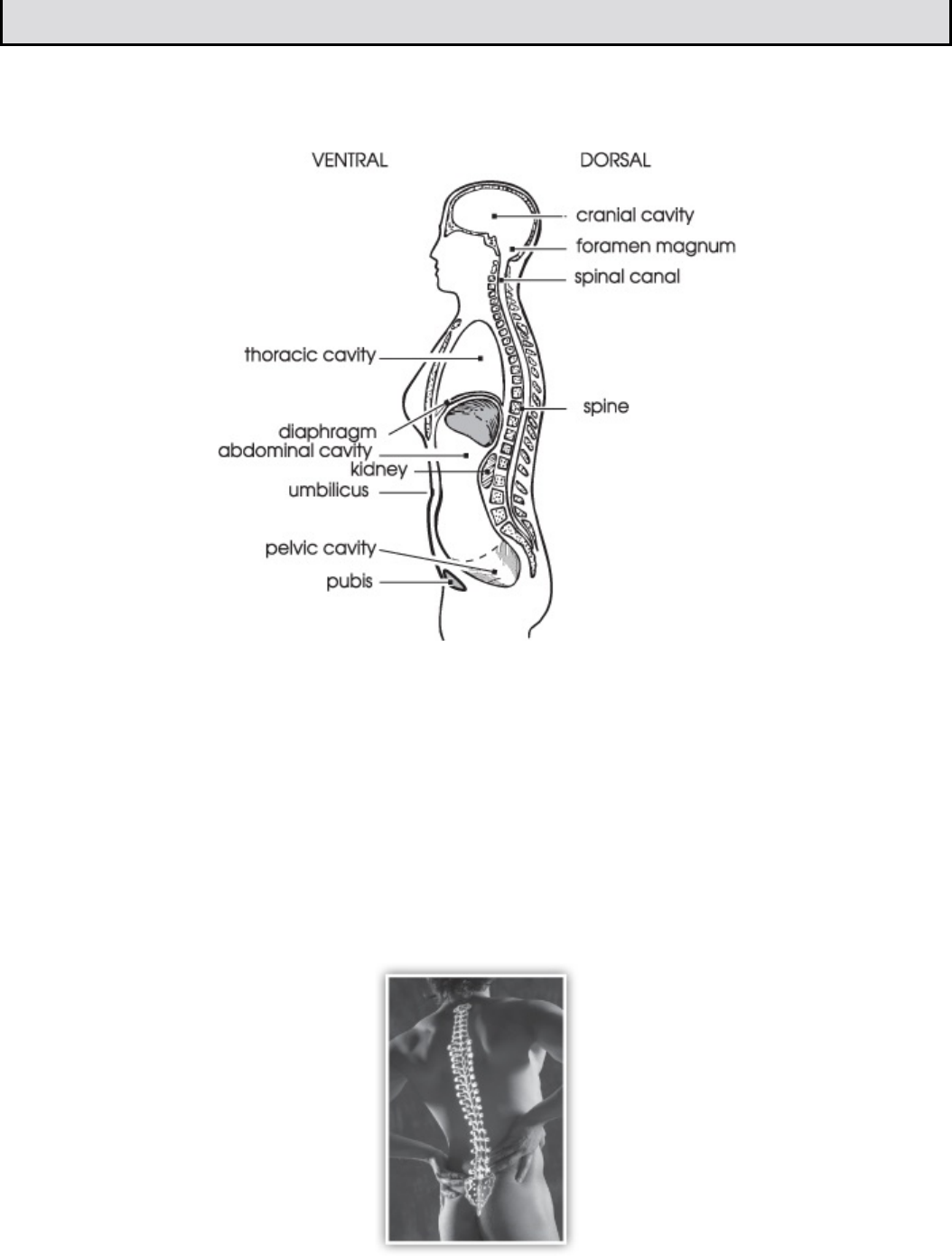
• Body cavities keep the organs in a fairly constant location.
The two principal body cavities are the dorsal body cavity and the ventral
body cavity. The major body cavities are shown in this drawing.
Body cavities
The dorsal body cavity is subdivided into the cranial cavity and the spinal
canal. The cranial cavity is the space inside the skull that contains the
brain. The spinal canal is the cavity formed by the vertebrae. The spinal
canal contains the spinal cord and the beginning of the spinal nerves. There
is no real boundary between the cranial cavity and the spinal canal. The
foramen magnum is the opening of the occipital bone that interconnects
the two cavities.
The spinal canal is the cavity formed by the vertebrae.
The ventral body cavity also is subdivided into the thoracic cavity and the
abdominopelvic cavity. The thoracic cavity contains smaller cavities and
subdivisions. The mediastinum is a mass of tissue between the lungs
extending from the sternum to the vertebral column. Included in the
mediastinum is the pericardial cavity, which encloses the heart. The two
pleural cavities each contain a lung. The boundary between the thoracic
cavity and the abdominopelvic cavity is the muscular diaphragm, a dome-
shaped muscle.
The abdominopelvic cavity consists of upper and lower portions. The
upper portion is called the abdominal cavity. It contains the gallbladder,
liver, spleen, stomach, small intestine, most of the large intestine, kidneys,
pancreas, and the ureters. The lower portion, called the pelvic cavity,
contains the bladder, colon, rectum, and the internal reproductive organs.
There is no physical boundary between the abdominal cavity and the pelvic
cavity. The imaginary boundary lies at the level of the rim of the pelvic bone.
There is no physical boundary between the abdominal cavity and the pelvic cavity.
Step 10 Membranes That Line the Body Cavities
Membranes are layers of tissue that cover organ surfaces, line body cavities, and
form tubes. Body membranes come from two basic tissue groups:
epithelial tissue
connective tissue
Epithelial Tissue Membranes
Epithelial membranes are classified by where they are located in the body.
Epithelial membranes include cutaneous membrane, mucous membrane,
and serous membrane.
Cutaneous Membrane
The outer layer of the skin is a cutaneous membrane. It is made of
stratified squamous epithelium. The surface of the skin, the outer layer of the
stratified squamous epithelium, dries to a tough, nonliving, keratinized layer
of squamous cells that waterproofs the skin.
Mucous Membrane
Mucous membranes, or mucosa, line every tube or cavity that connects to
the surface of the body. The mucous membranes often secrete mucus, which
prevents body cavities from drying out. The digestive, respiratory,
reproductive, and urinary tracts all are covered with mucous membranes.
Serous Membrane
Serous membranes (serosa) line the major body cavities that do
not connect to the surface of the body. Serous membranes occur in
pairs—the visceral layer lines the organ, and the parietal layer lines
the cavity. The serous membranes secrete serous fluid or serum,
which lubricates the organs and reduces friction as they glide across
each other and the cavity walls.
Serous membranes (serosa) line the major body cavities that do not connect to the surface of the body.
The Thoracic Cavity Membranes
The thoracic cavity is protected by a serous membrane lining called the
pleura. The serous membrane lining the pericardial cavity is the parietal
pericardium. The visceral pericardium is the thin, transparent serous
membrane covering the heart itself. The lungs are protected by two layers of
serous membranes—the parietal pleura lines the pleural cavities, and the
visceral pleura covers the lungs themselves.
The Abdominopelvic Cavity Membrane
The abdominopelvic cavity is protected by the largest serous membrane of
the body, which is called the peritoneum. Unlike other membranes, the
peritoneum contains large folds that bind organs to each other and to the
cavity wall. The parietal peritoneum lines the cavity wall. The visceral
peritoneum covers some of the organs within the cavity.
Connective Tissue Membranes
In this section, let’s review two types of connective tissue membranes.
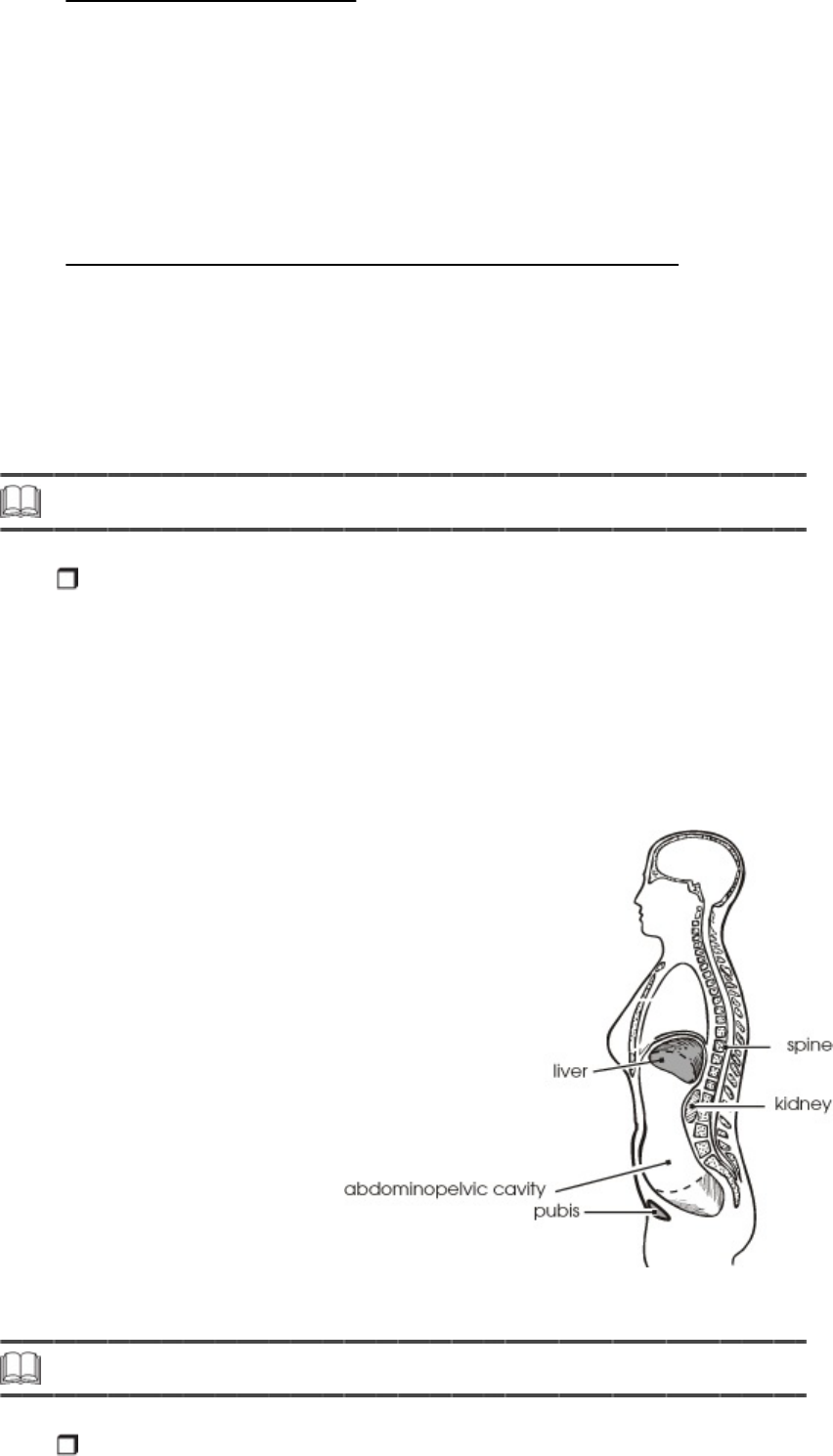
Synovial Membrane
The synovial membrane is composed of a gel-like material. It usually
contains different types of connective tissue elements. The synovial
membranes line the joints of the shoulders, knees, hips, fingers, and
toes. They secrete a fluid to cushion the motion of these joints so that
the bone surfaces do not rub against each other.
The Cranial and Spinal Canal Membranes
The brain and spinal cord are protected by meninges. The cranial
meninges line the cranial cavity and are continuous with the spinal
meninges that line the spinal canal. The meninges consist of three layers,
each called a meninx. The outer meninx is called the dura mater. The
middle meninx is the arachnoid, and the inner meninx is the pia mater.
Step 11 Retroperitoneal Organs
Sometimes an organ lies outside a cavity. When you look at this type of organ from
inside the cavity, its location is considered to be behind the parietal serosa. For
example, in the following graphic, you can see that the kidney is outside the
abdominal cavity.
Viewed from inside the abdomen, this kidney is behind the peritoneal serosa.
Organs in this location are called retroperitoneal organs.
The kidney is a retroperitoneal organ.
Step 12 Pronounce New Terms
As a medical coding specialist you will need to be able to understand a healthcare
professional’s pronunciation of terms, and you will need to pronounce anatomical
terms yourself. This exercise will help you understand and pronounce the terms
you just learned.
a. Take your Quick-Learn Tutor and your Set 11 flashcards out of your Quick-
Learn Kit.
b. Access the online portion of your course, and go to Lesson 9.
c. Listen to the flashterm as it is pronounced. After you hear a term, pause
the audio.
d. Practice pronouncing the term out loud. Take your time. Push the flashcard
up and read the meaning of the word part or term.
e. Continue this process for each flashcard in this set.
f. Put the flashcards in order and play the audio again, pronouncing each
word part or term after you hear it. Don’t forget to listen to your own
pronunciation of each term. If you mispronounce one, put a check mark
next to that flashterm.
g. Practice the terms you mispronounced by listening again. Be sure you can
pronounce each term clearly and easily.
Step 13 Write New Terms
The next step in your lesson is to practice writing the terms you learned. Follow
the instructions.
a. Insert the first flashcard for this set into Side A of your Quick-Learn Tutor.
b. Look at each term as it appears in the window and say it out loud. Write
the flashterm on blank paper. Remember to include the slash if it is a word
part.
c. Push the card up until the meaning appears in the right window and read

the meaning out loud. Write the meaning beside the flashterm.
d. Do this for each flashcard.
Step 14 Meanings of New Terms
Follow these steps to learn the meanings of the terms you have pronounced and
written.
a. Again insert the first flashcard into Side A of your Quick-Learn Tutor.
Pronounce each word part or term out loud and then say the meaning.
Check yourself by pushing the flashcard up until you can see the meaning in
the right window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud. Before you look, see if you can remember the
term that goes with that meaning. Check yourself by pushing the flashcard
up until you can see the term in the left window.
c. Practice with the flashcards several times until you are familiar with the
terms and their meanings. You may use the flashcards for the Practice
Exercises and Quizzes.
d. When you feel comfortable with the spelling, pronunciation and meaning of
each flashterm, go on to the next step.
Step 15 Organization of the Body
So far, you’ve discovered about how the body is organized anatomically. You
learned the locations of different body parts and how the internal parts of the body
are divided into cavities. Now you will study how the body is organized
physiologically, that is, how the body is organized to do its work.
Your body should work like an army.
Your body has many tasks to perform to keep you alive. These tasks often
must be performed simultaneously, and this requires great organization. Your
body has to work efficiently, like an army. In any army, there are many
individual soldiers, and these individuals must be organized so that various
tasks can be completed. Soldiers are grouped into squads, squads are
grouped into platoons, platoons are grouped into regiments, then divisions.
The whole unit is called an army. The army then works with other groups,
just as the U.S. Army works with the Navy, Marines, and Air Force to
accomplish tasks.
The smallest unit in your body is the cell. In fact, your body is composed
of millions of cells. The work of the body, although it appears to be the
work of large parts, is really the combined work of all the different types
of cells in the body.
Similar types of cells group together to form tissues. There are four types of
tissues:
Epithelial tissue covers every body surface, including the outer surface,
body cavities, and organs.
Connective tissue connects other types of tissues, helps support the
body and has its own blood supply.
Muscle tissue can extend and contract, allowing movement.
Nervous tissue transmits electrical impulses and makes up the brain,
spinal cord, and peripheral nerves.
For example, muscle cells group together to form muscle tissue. Liver cells
group together to form liver tissue. Nerve cells form nerve tissue.
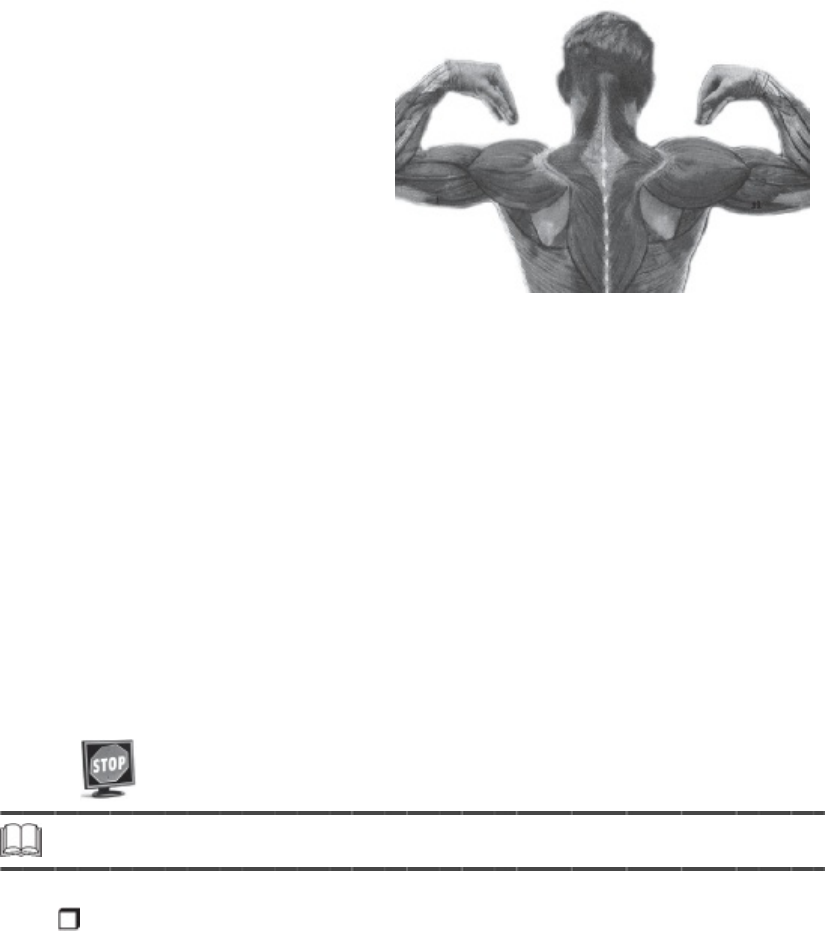
Muscle cells group together to form muscle tissue.
Different types of tissue group together to form organs. For example, liver
tissue, blood vessel tissue, nerve tissue, and bile tissue group together to
form the liver. Muscle tissue, connective tissue, nerve tissue, and blood
vessel tissue group together to form a muscle, such as the biceps muscle.
Body organs with similar functions can be grouped into organ systems. For
example, the liver, stomach, intestines, and pancreas are all organs whose
function is digestion. As a group, they form the digestive system.
As you can see, body organization begins with the cell and progresses to
tissues, organs and organ systems.
Please pause and complete online Practice Exercise 9-3.
Step 16 Lesson Summary
This lesson continued your introduction to anatomy—how the body works, how it is
organized, and how its systems are connected. Providers use terms, called
landmarks, to describe locations on the body. These include superficial, or surface,
landmarks for the body in the supine and prone positions. To accurately describe
locations on the abdomen, surgeons divide the abdomen into nine areas that refer
to certain organs in the abdominal cavity in each region. A simpler way to describe
locations on the abdomen is by dividing the abdomen into fourths, or quadrants.
The body is organized into a complex structure that enables it to work
effectively. The smallest unit is the cell. Cells group together to form tissues,
tissues group together to form organs, and organs form organ systems.
These systems function as a whole to operate the amazing mechanism we
call the body.
Everything you learned in this lesson is a base to help you understand the
context of terminology used in medical coding and to help you communicate
effectively with healthcare professionals.You don’t need to memorize the
terms, but being familiar with anatomical terms will help you in your medical
coding career. You’re ready for your next Quiz!
Please pause and complete an online Quiz. Good luck!
Just for Fun
Whew! You need to relax after all this. Relaxation does not come
automatically for many of us—often we are terrible at it. We may not
realize that we are stressed mentally or physically until a problem
develops.
When your body is relaxed, your mind works more efficiently. There are
some very simple physical relaxation exercises you can do as you work.
Give your eyes a rest as you work. Try the 20, 20, 20 method.
Every 20 minutes, let your eyes rest on an object at least 20
feet away, and look at that object for 20 seconds.
Every hour or so, get up out of your chair and walk. Slowly
stretch your arms up over your head. Then let your head and
hands hang toward the ground. Get that blood circulating!
Watch your posture. Are you slumped over? It’s harder for your
body to breathe when in a poor position. Sit up straight and take
a few long, slow breaths.
Let other areas of your body have a chance to move. Tense and
then relax various muscle groups in your body as you sit. For
example, tighten your gluteus maximus, hold for a few seconds
and then relax. Rotate your shoulders and head. If your work
area allows, stretch your legs out. Rotate your feet at the
ankles.
There are many paths to relaxation and reduction of stress. Some are
quite simple, others very sophisticated. A common element to all is that
they be practiced regularly and that work and worries be left behind. Do
any of these ideas appeal to you?
Going for a walk
Meditation
Visualization exercises
Long hot bath
Physical exercise
Massage
Yoga
Guided relaxation using audiotapes or CDs
Friends also can be great stress relievers. Plan fun times. Laugh.
Laughter benefits the heart, lungs, stomach, and other organs. Above all,
make sure you are kind to yourself. Have some fun every day. Give
yourself time off—and don’t feel guilty about it! Work when you work and
then leave it. Give your mind some time off, too.
LESSON 10
Cell and Tissue Anatomy and Pathology
Step 1 Learning Objectives for Lesson 10
When you have completed the instruction in this lesson, you will be trained to do
the following:
Describe the components of a cell.
Understand the primary functions of each cell component.
Determine the different categories of etiologies.
Explain cell damage and how cells respond to injury.
Determine how the body reacts to injury through inflammation, repair,
and damage or death.
Step 2 Lesson Preview
From a previous lesson you already know that the cell is the smallest unit in the
human body; it’s the basic unit of life. Humans started with one cell. That one cell
changed to many different kinds of cells. But what makes up a cell? How does it
function? As a medical coding specialist it’s important you understand this basic
component of the body and that you see how it works to allow the human body to
do all of which it is capable.
The cell is the smallest unit in the human body. It’s the basic unit of life.
In this lesson you’ll also learn about what happens when the body isn’t
operating at peak efficiency. You will study the concepts of pathology
and the disease process. Why is this important? You must understand
how the body defends itself from disease and what mechanisms are at
work in the body to promote health. Knowing why people seek medical
care in the first place also will help you as you assign accurate codes to
those medical records you learned about in earlier lessons.
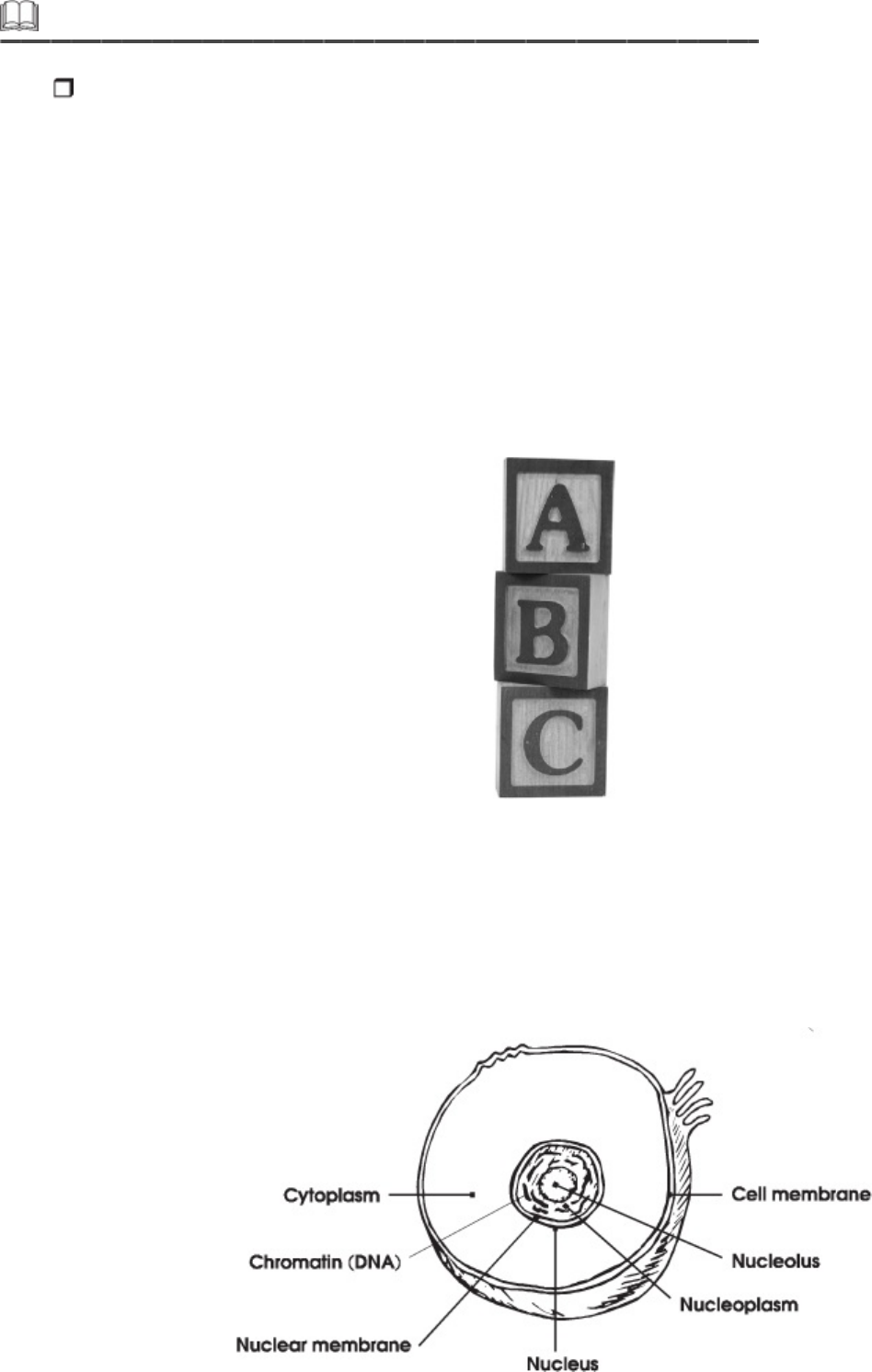
Step 3 Cell Components and Their Primary Functions
As you know, the human body is composed of an extraordinarily large number of
minute elements known as cells. Cells are the building blocks of the body. Every
structure in the body is made of cells. There are, of course, different types of cells.
But regardless of the type and function, all cells consist of the same basic
components.
In your previous anatomy lessons you learned that a large number of
combined cells with special properties form tissues. For example, certain cells
form muscle tissue, and others with quite different properties form nervous
tissue. These and other tissues, called connective tissues, combine to form
organs, such as the heart and brain.
Cells are the building blocks of the body.
Now you’ll learn about the parts of the cell. All cells contain a nucleus, cell
membrane, cytoplasm, mitochondria, endoplasmic reticulum, lysosomes, and
Golgi apparatus. The following illustration shows some of these parts. Each of
these structures has unique functions that are critical to the life of the cell.
Basic parts of a cell
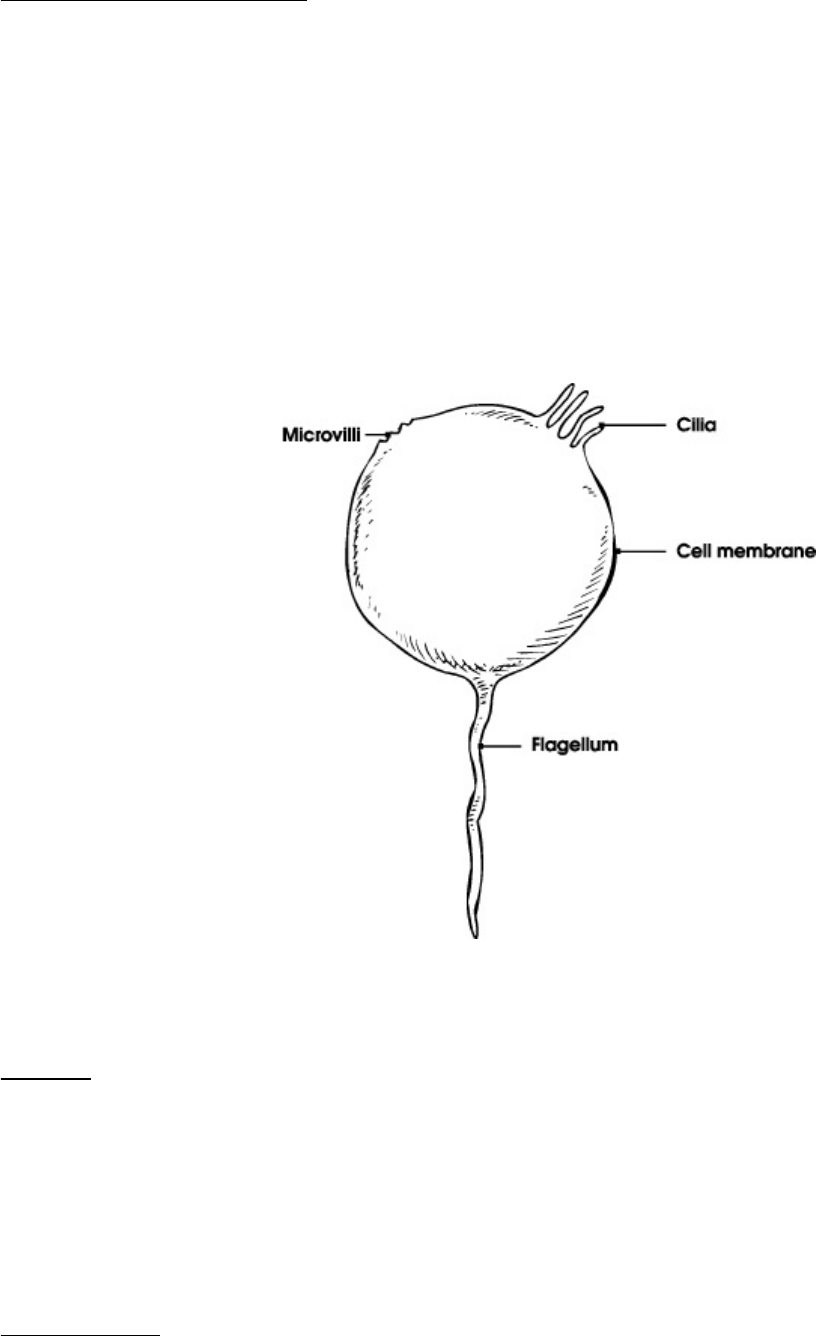
Cell Membrane
The cell membrane or plasma membrane forms the outer surface of
the cell. This membrane is made up of proteins, lipids, and
carbohydrates that provide energy to the cell, assist other cellular
particles in moving through the cell, and assure balance. The membrane
serves as the site of contact between the cell and its environment. The
cell membrane’s role in the structure and integrity of the cell is
invaluable because this membrane is responsible for the maintenance of
all essential cellular functions. If rupture or major damage to the cell
membrane occurs and cannot be repaired, the cell will die.
Cell surface
Cilia
Cilia are like hairs that wave in the fluid around a cell. They move the
fluid and anything it contains past the cell. Cells that have cilia are called
ciliated cells. For example, ciliated cells lining the trachea move mucus
up and out of the lungs.
Flagella
Flagella are long single projections, like rat tails. They move a cell in the
body fluids. Very few cells have flagella. The sperm cell is one that does. It
has one flagellum, like a tail, to help it move in body fluids.
Flagella are long single projections, like rat tails.
Villi
Villi are short projections of the cell membrane that look like fingers
projecting from the cell membrane. Only some cells have villi. On the other
hand most cells form microvilli, which are very small villi or wrinkles in the
cell membrane. Because microvilli are only wrinkles in the cell membrane,
they are no different than the rest of the cell membrane. Cells form microvilli
when they need them. Microvilli act like the webbing of a sponge to absorb
materials transported across the cell membrane.
Step 4 More Cell Components and Their Functions
Now that you know a little about the features on the outside of the cell, let’s talk
about what goes on inside these little building blocks.
Cytoplasm
The cytoplasm does most of a cell’s everyday work. Cytoplasm surrounds
the nucleus, which we’ll discuss in detail in a bit, and contains other cellular
structures such as mitochondria and the endoplasmic reticulum. These
structures, called organelles, provide energy and nutrients and are
imperative to the life of the cell.
In addition to organelles, the cytoplasm contains supplies of food and water,
called inclusions or inclusion bodies. Inclusions are like little bubbles
floating through the cytoplasm.
The drawing that follows shows the organelles that lie in the cytoplasm. After
you read about each organelle, look at the organelle in the drawing.
Sometimes organelles are named for how they look.
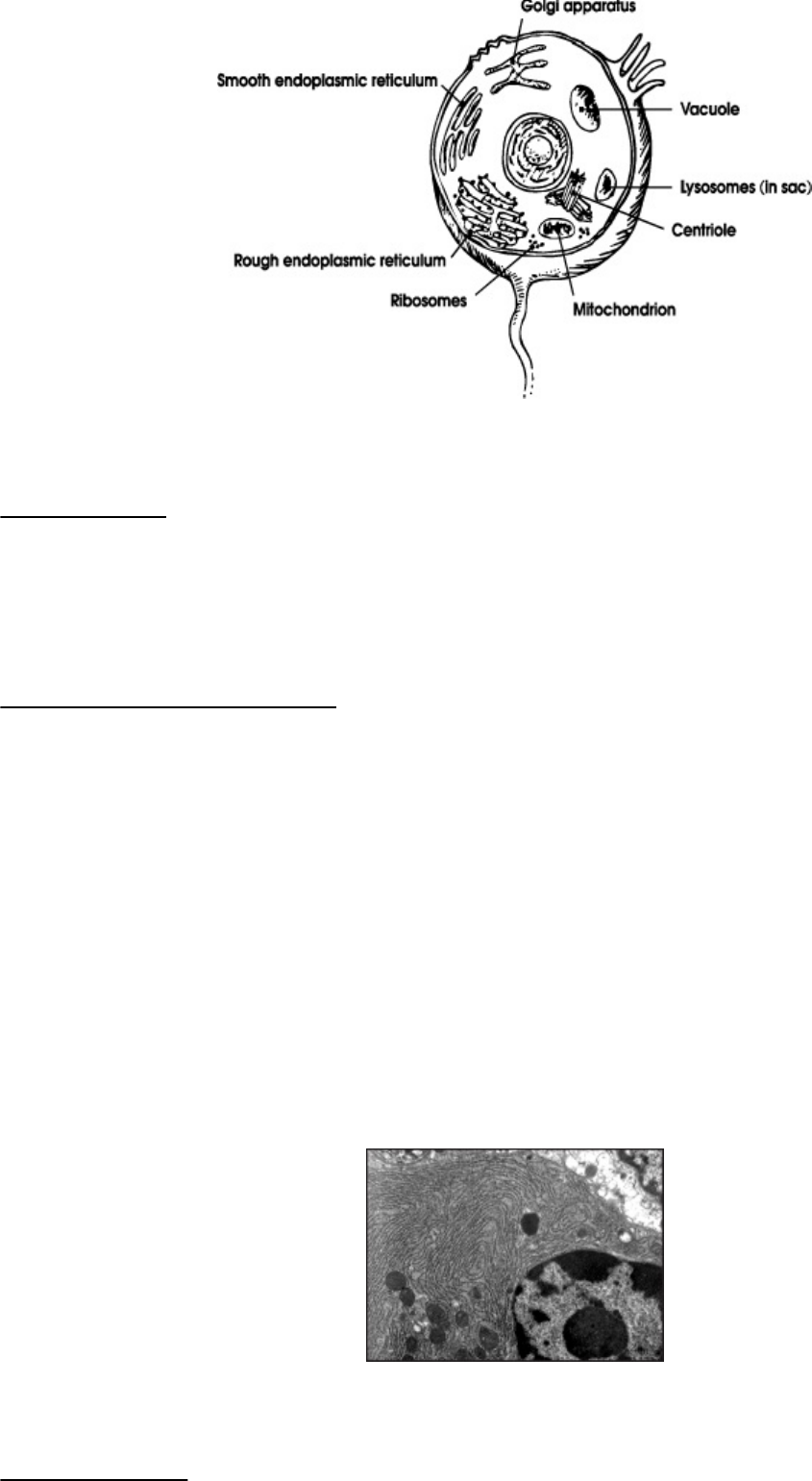
Organelles in the cytoplasm
Ribosomes
The ribosomes are where protein is made. Ribosomes either float freely
in the cytoplasm or attach to the membrane called the endoplasmic
reticulum.
Endoplasmic Reticulum
The endoplasmic reticulum (ER) is a spider web-type membrane inside
the cytoplasm. This structure is a series of little tubes called tubules or canals
that work like a subway to move materials around the cell.
There are two types of ER. Differentiated cells have either one or both types
of ER. Granular ER, also called rough ER, is covered with ribosomes on its
surface. This gives the ER a grainy appearance. The ribosomes use the
granular ER to store and transport protein. The more protein a cell makes,
the more granular ER it has to store and move the protein. Agranular ER,
also called smooth ER, does not have ribosomes on its surface, so it is not
grainy. It transports fatty materials called lipids. The more lipids a cell makes
or handles, the more agranular ER it has to handle this job.
The endoplasmic reticulum is a spider web-type membrane inside the cytoplasm.
Mitochondria
Mitochondria are thread-like bodies within the cytoplasm responsible for
the cell’s use of oxygen, a required element for all cells of the body to
function normally. Mitochondria use oxygen to digest food in the cell. This
process is called oxidation. When food is digested, there are two products:
heat and energy. The energy is stored in molecules called adenosine
triphosphate, or ATP. ATP provides the fuel, the energy, for all of the
activities in the cell.
Mitochondria are regarded as the power plants of the cell because they exist
in large numbers in those human cells that require an enormous amount of
energy to do their work, such as nerve and liver cells.
Mitochondria are regarded as the power plants of the cell.
Lysosomes
Lysosomes are membrane-bound bodies, or sacs of enzymes, in the
digestive part of the cell. These enzymes digest living material like debris and
old organelles and allow them to enter the cytoplasm. If the lysosome sac
breaks, the cell itself can be digested.
Centrioles
Centrioles only are active during reproduction. They become the
mitotic spindles, which pull the nucleus of a dividing cell apart to form
two new cells.
Golgi Apparatus
The Golgi apparatus is an organelle that packages proteins and other
products of a cell for delivery to the rest of the body. Enzymes or other
products of a cell are delivered to the Golgi apparatus. A sac is formed
around the product and sealed off, like a heat-sealed storage bag. This sac is
called a vesicle. The vesicle moves to the surface of the cell membrane,
fuses with it, and bursts. The contents of the vesicle are distributed outside
the cell. A vesicle acts just like a bubble in a pot of boiling water. The bubble
forms, rises to the top and bursts to let the steam out of the water.
A vesicle acts just like a bubble in a pot of boiling water.
Vacuole
A vacuole is any small cavity in the cytoplasm of a cell.
Step 5 The Nucleus
You’ve already learned about the cell membrane, which forms the outside surface
of the cell. Now let’s talk about the nucleus. The nucleus lies inside the cell and is
surrounded by a nuclear membrane.
Both the cell and nuclear membranes are separate compartments filled with
a gelatin-like material called protoplasm. In the cell compartment,
protoplasm is called cytoplasm. Inside the nucleus, protoplasm is called
karyoplasm or nucleoplasm. The suffix /plasm means “growth.”
DNA
The nucleus contains deoxyribonucleic acid, or DNA, which is the material
that directs how the cell will run and how it will reproduce. It is made up of
genes, the code for making proteins. DNA looks like a spiral staircase. Each
gene is a many-stepped segment of the DNA staircase. During reproduction,
the DNA coils tightly and is called a chromosome. Human cells have 23
pairs of chromosomes.
DNA looks like a spiral staircase.
When the cell is not reproducing, the DNA is scattered throughout the
nucleoplasm like pieces of lint. In this form, the DNA is called chromatin.
RNA
Ribonucleic acid, or RNA, is a messenger and helper for the DNA. It
shuttles the instructions for making protein from the nucleus to the
cytoplasm, where the proteins actually are made.
Nucleoli
Nucleoli are small, round bodies that make ribosomes. The ribosomes are
sent out of the nucleus to the cytoplasm.
You now know about the basic components of the cell; however, before you
move on, let’s take a moment to review what you’ve learned so far.
Please pause and complete online Practice Exercise 10-1.
Step 6 Pronounce New Terms
Follow these steps:
a. Take your Quick-Learn Tutor and your Set 12 flashcards out of your Quick-
Learn Kit. Insert the first flashcard for this lesson into Side A of the Tutor.
b. Access the online portion of your course and go to Lesson 10.
c. Listen to the flashterm, and pause the audio.
d. Practice pronouncing the term out loud. Take your time. Push the flashcard
up and read the meaning of the word part or term.
e. Do this for each term in this set.
f. Put the flashcards in order and play the audio again, pronouncing each
word part or term after you hear it. Don’t forget to listen to your own
pronunciation of each term. If you mispronounce one, put a check mark
next to that flashterm.
g. Practice the terms you mispronounced by listening again. Be sure you can
pronounce the terms clearly and easily.
Step 7 Write New Terms
Follow these steps:
a. Insert the first flashcard into Side A of your Quick-Learn Tutor.
b. Look at each term as it appears in the window and say it out loud. Write
the flashterm on blank paper. Remember to include the slash if it is a word
part.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the flashterm.
d. Do this for each term in this set.
Step 8 Meanings of New Terms
Do the following steps:
a. Again insert the first flashcard into Side A of your Quick-Learn Tutor.
Pronounce each word part or term and then say the meaning. Check
yourself by pushing the flashcard up until you see the meaning in the right
window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right window.
Read each meaning out loud and then say the term. Again, check yourself
by pushing the flashcard up until you see the term in the left window.
c. Practice with the flashcards several times, until you are familiar with the
word parts and terms and their meanings. You may use the flashcards for
your Practice Exercises and Quizzes.
d. When you feel comfortable with the spelling, pronunciation and meaning of
each term or word part, go on to the next step.
Step 9 Cell Pathology
Now that you have read about cell anatomy and know how cells function when
they are healthy, let’s talk about pathology. From a previous lesson, you know that
pathology is the study of human biology when anatomy and/or physiology are
abnormal.
Even though pathology means the process of studying disease, disease does
not cause all pathologic processes. Instead, pathology may be a result of an
injury. In some cases, pathology may be due to an abnormality of growth.
The type of abnormality seen in tissues and organs is determined by two
factors.
Pathology is the study of abnormal human anatomy or physiology.
The cause of the abnormality
For example, diseases injure tissue. Trauma can injure tissue. Growth or
development abnormalities don’t injure tissue but can cause a tissue to
look or act differently than normal. The cause of an abnormality or injury
is called the etiology.
How a tissue responds to injury
Each type of tissue only can respond to injury in a few limited ways. For
example, bone can break, but it doesn’t swell. Muscle tissue can’t break,
but it can be torn, and it can swell. Both bone and fat can develop pus in
an infection.

Step 10 Etiologies
Etiologies, the causes of pathology, can be put into categories. Doctors use these
categories to help themselves remember the kinds of etiologies there are for each
abnormality they find. When doctors don’t know the exact cause of an abnormality,
they may use the name of the category.
The basic categories follow.
Developmental Abnormality
This category includes abnormalities in the growth or development of a
particular tissue or organ. Developmental abnormalities have etiologies
that are either hereditary, congenital or acquired.
Hereditary etiologies are genetic. They exist because there is an
abnormality in one of the genes that was passed down from a parent. The
abnormality is inherited. For example, some dwarves have abnormal bone
development caused by an abnormal gene.
Congenital etiologies exist from birth. They are not inherited but
exist because of an abnormality that occurred while the fetus was
developing. An example is hydrocephalus, which means “water on the
brain.”
An abnormal gene can cause abnormal bone development.
An acquired etiology is an abnormality that the person “got” after birth and
did not inherit from a parent. An example of an acquired developmental
abnormality is childhood rickets, which is caused by a diet that does not have
enough vitamin D.
Inflammatory Disease

Inflammation is a common tissue response to any kind of tissue injury:
infection, trauma or disease. However, if the cause or etiology of a
widespread inflammation is not known, the condition is classified as an
inflammatory disease. Rheumatoid arthritis would fall into this category
because it is not caused by infection, trauma or another disease.
Infection is caused by the action of bacteria, viruses, and parasites.
These living organisms and viruses invade the body and cause disease as
long as they are alive and reproducing in the human body. Antibiotics only
work on infectious diseases caused by bacteria. They do not work for viral
infections or parasitic infestations.
Trauma is injury caused by the inappropriate application of force or toxic
agents. An automobile accident can cause traumatic injuries. A chemical
burn is trauma. For example, swallowing lye causes traumatic injury. The
word trauma is used to mean that the tissue or organ injury was not due
to infection or disease.
Hyperplasia and Neoplasia
This category includes conditions that have an abnormal increase in the
number of cells in a tissue or an organ. Hyperplasia means an increase
in the number of normal cells, usually due to a reaction from an outside
irritation. The anatomy and physiology of hyperplastic cells is normal.
Neoplasia is a new growth of cells whose anatomy is very abnormal.
These cells are bizarre versions of normal cells. Neoplastic cell
physiology is abnormal, especially the rate of reproduction. If a neoplasm
grows slowly and does not spread or destroy normal organ function, it is
called a benign neoplasm. If neoplasms grow rapidly, spread quickly, and
destroy normal organ function, they are called malignant neoplasms
or cancers.
As a medical coding specialist you must know if a neoplasm is benign or
malignant to arrive at the correct code. This information will be
documented in the patient’s medical record.
Look at these coding examples of a benign and malignant breast neoplasm
for a woman:
217 Benign neoplasm of breast
174.9 Malignant neoplasm of breast (female) unspecified
Do you see the importance in knowing the difference between a benign
and malignant neoplasm? Good! You are developing the skills needed to
become a successful medical coding specialist.
Metabolic Disease
Abnormalities in the function, or physiology, of cells and tissues cause these
diseases or conditions. They are due to abnormal metabolism of cells or
tissues. Unlike neoplasia, the rate of cell reproduction is normal. Sometimes
metabolic diseases are genetic or congenital. Sometimes they occur later in
life and are called acquired, meaning the body was normal at birth and up to
the time the patient developed the abnormality. Diabetes mellitus is a
disease caused by abnormal sugar metabolism.
Abnormal sugar metabolism caused diabetes mellitus.
Vascular Disease
Conditions that cause bleeding, blood vessel blockage or abnormal blood flow
fall in the category of vascular disease. Atherosclerosis, or hardening of the
arteries, is a good example. Diabetes mellitus, even though it has a
metabolic etiology, causes abnormalities of the blood vessels. It can be
categorized as a vascular disease for this reason.
Immunologic Disease
Immunologic diseases include abnormalities of the immune system. An
allergy is a good example. Allergies like hayfever and drug reactions are
included in this category. Some patients are allergic to their own tissues,
which causes tissue injury. This condition is called an autoimmune disease.
Idiopathic Abnormality
Idiopathic is a term used for any diseases or conditions where the etiology
is unknown. For example, the causes of many cancers or diabetes are
unknown. The idiopathic category is for a pathology that doesn’t have a
known etiology or won’t fit into any other category.
Iatrogenic Abnormality
Iatrogenic pathology is caused by the actions of a doctor, treatment,
procedure or medication. Have you ever had an allergic reaction to
medication prescribed by a doctor? This is an example of iatrogenic
pathology. Every side effect listed for a drug is an iatrogenic abnormality.
In other words, if the patient had not seen a doctor or taken a
medication, he wouldn’t have the iatrogenic abnormality. Iatrogenic
diseases and conditions can be the same conditions found in other
categories. The difference here is that the patient acquired them as a
result of a medical treatment.
Nosocomial Disease
Nosocomial diseases are diseases acquired in a hospital environment. A
number of factors account for this. You can catch a disease from someone
who already has it. Some hospital patients have lowered resistance to
disease and catch things a healthy person wouldn’t normally catch. Bacteria
that grow on the metal instruments in a hospital but rarely grow outside a
hospital can cause unusual infections.
Step 11 Cell Damage
You’ve read about the categories of etiologies or the causes of pathology. Now,
let’s look more closely at five specific ways in which cells can be damaged.
Hypoxia and Anoxia
Hypoxia is the decreased availability of oxygen to the cells. Anoxia is the
complete lack of oxygen. These two conditions are the most common causes
of cell injury.
All humans breathe, and while breathing, oxygen is brought into the body.
Other body functions serve to distribute this vital gas throughout the body,
feeding the cells. When this process is interrupted, either because breathing
has stopped or the body’s oxygen distribution process malfunctions, the cells
immediately suffer.
Hypoxia or anoxia occurs in many circumstances, including obstruction of the
respiratory tubes, such as in suffocation or drowning; reduced intake of
oxygen across the respiratory surfaces of the lung, such as when one has
pneumonia; inadequate transport of oxygen in the blood, such as when one
has anemia; or the inability of the cell to use oxygen for respiration, such as
in cyanide poisoning.
Of course, not all cells respond the same way to injury, and the final outcome
of anoxia will depend on many factors. Brain cells, for example, cannot
survive without oxygen for more than a few minutes, heart cells can survive
one to two hours and kidney cells can survive for several hours.
Obstruction of respiratory tubes can cause hypoxia or anoxia.
Toxic Agents
Toxic agents can damage cells. Poisons are toxic agents. Poisons are
substances that adversely affect the body and its functions. Some poisons act
by directly destroying cells. Others coat the outside of cells and keep them
from interacting in their required manner. If enough poison is ingested, the
cells suffer permanent injury. If enough cells are killed, then the person dies.
Poisons are often compounds and chemicals. Toxic injury is caused by
substances known for their direct toxic effects on cells and by substances that
are not directly toxic but that destroy cells after the body metabolizes the
substances.
For example, a heavy metal, such as mercury, is directly toxic because it
immediately destroys the cytoplasm of the cell. Carbon tetrachloride, a
component of metal cleaning solutions (metal polish), is an indirect toxin
because when digested, this poison changes characteristics and eventually
affects the cell membranes.
Drugs prescribed for medical conditions are not usually considered poisons;
however, it is important to note that drugs can be toxic and can cause cell
injury, especially if they are given in large amounts. Most drugs taken in large
amounts are toxic, and many are even lethal. Suicide by drug overdose is
probably the best example of drug-induced toxicity. However, while medical
treatments for cancer, such as chemotherapy, kill the cancerous cells, they
also might kill healthy cells, and they often cause toxic effects on the body.
Certain drugs have side effects that might cause organ shutdown or other
medical problems.
Microbial Infection
Microbial pathogens or bacteria cause cell injury in several ways. Bacteria
often produce toxins, which interfere with various cell functions such as
respiration or protein synthesis.
Have you ever been instructed not to consume food contained in dented
cans? The reason is that when a can is dented, microscopic breaks in the seal
can occur, allowing bacteria to grow. This bacteria, known as a microbial
pathogen, is harmful to humans.
Bacteria may grow in dented cans.
Food poisoning is one example of how the microbes can infect human cells
and damage them. A familiar scare that has occurred throughout the country
in recent years is the result of E coli bacteria, a form of which can be found in
meat that is not thoroughly cooked.
Another type of microbial pathogen is the virus. Certain viruses invade cells
and destroy them either by disturbing various cellular processes or by
changing the cell’s makeup in the nucleus or plasma membrane.
Allergic/Immune Reactions
When the body produces antigens to fight infections or other invasions, the
body’s own immune system can damage cells. This process often is harmless
because the body regenerates new cells to replace the damaged and dead
cells. However, in some rare disorders, the body’s defense mechanisms try to
kill off its own cells. In such instances, these people become allergic to
themselves, which is called immunopathy.
Metabolic and Genetic Disturbances
Some metabolic disorders damage cells. Metabolic disturbances such as
diabetes mellitus, a disease caused by insulin deficiency, produce changes in
the small blood vessels of the body that cause vessel wall injury. Such injury
often leads to tissue death or pathologic changes in many, if not all, body
organs.
Genetic problems exist, whereby parents pass along defective genes to children.
In addition to metabolic problems, genetic problems exist, whereby
parents pass along defective genes to children. Some genetic problems can
be dramatic and devastating. For example, Tay-Sachs disease, a genetic
deficiency of a certain hormone, causes destruction of the lysosomes of nerve
and eye cells. Severe mental deficiency and blindness develop, and death
usually occurs in early childhood.
Please pause and complete online Practice Exercise 10-2.
Step 12 Cell Response
In this step, you’ll look at how cells adapt to injury and how the cell structure
might change in this healing process. You’ll also learn the natural aging process of
cells that ultimately leads to cell death.
The term for when the body is not injured and cells are balanced with
their environment is homeostasis. However, prolonged exposure of
cells to adverse stimuli causes the cells to change. When the cause of
the injury is removed, the cells often are able to heal and revert to their
normal state. These minor injuries are reversible. On the other hand,
some forms of adaptation, especially those associated with cell loss due
to aging, such as bone loss in osteoporosis, are irreversible. Other forms
of adaptation cause permanent changes in the cell size—changes that
affect organ function after the cell has regenerated. Cell adaptation, a
necessary process the cell undergoes to survive injury, also often causes
secondary medical problems.
Aging is a type of cell adaptation.
Types of cell adaptation include the following:
Atrophy
Hypertrophy
Hyperplasia
Metaplasia
Intracellular Accumulations
Aging
Atrophy
A type of adaptation that causes a decrease in the size of a cell, tissue, organ
or the entire body is called atrophy. There are two types of atrophy:
physiologic and pathologic.
Physiologic atrophy is age related and involves changes in the entire body.
For example, the bones of elderly people are thin and more prone to fracture.
Also, as the body ages, the muscles atrophy and become weak.
Normal cell and one that has undergone atrophy
Another form of cell atrophy, pathologic atrophy, occurs as a result of
inadequate nutrition or stimulation. As nutrients are withheld, the cell
shrinks, and its functions decrease.
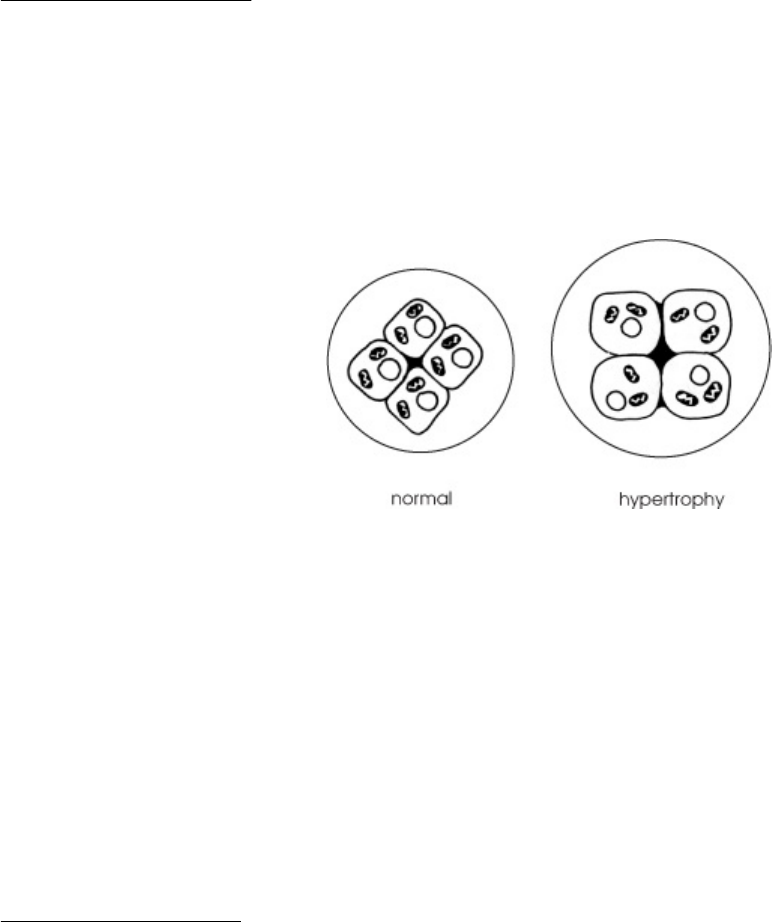
Hypertrophy
Hypertrophy is an increase in size of tissues or organs due to an
enlargement of individual cells. An example of hypertrophy is the
enlargement of the heart due to heart disease or an increased workload on
the heart. Hypertrophy of the skeletal muscles is usually caused by exercise
and typically is found in body builders.
Normal cell and one that has undergone hyperplasia
Would you like to see a coding example for hypertrophy of the heart?
429.3 Cardiomegaly
If you think back to your lessons on word parts, you probably can figure
out that cardiomegaly means enlargement of the heart. You know that
hypertrophy increases the size of tissues or organs, so this is an accurate
code.
Hyperplasia
In contrast to hypertrophy, hyperplasia is an increase in the size of the
tissues and organs caused by an increased number of cells, usually brought
about by hormonal stimulation. Examples of hyperplasia are the thickening of
the lining of a woman’s uterus due to an increase in cells (endometrial
hyperplasia) and the enlargement of the prostate in elderly men.
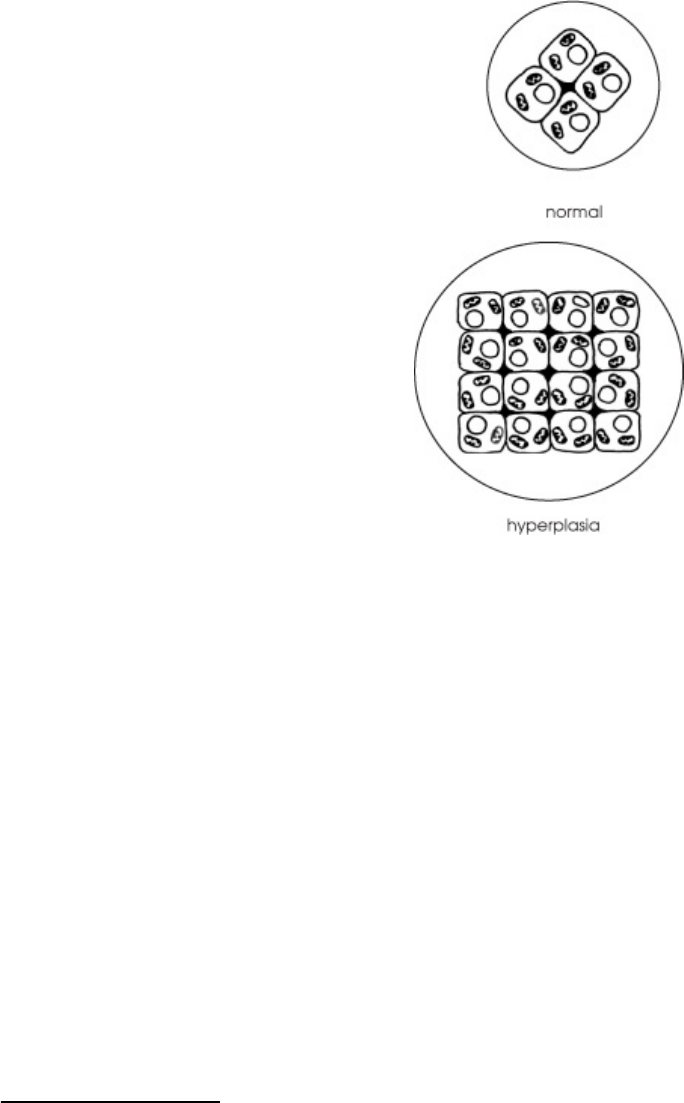
Normal cell and one that has undergone hypertrophy
Hyperplasia also can occur in cases of chronic injury. Sometimes the cause of
hyperplasia is obvious: Chronic irritation of the foot from tight shoes causes
the cells to undergo hyperplasia and form a callous or corn. Other hyperplasic
lesions have no obvious cause, such as polyps or benign growths in the large
intestine.
Now that you understand hyperplasia, let’s look at the diagnosis code for
endometrial hyperplasia.
621.30 Endometrial hyperplasia, unspecified
As a medical coding specialist, your knowledge of cell anatomy and responses
will help you code accurately.
Metaplasia
Another example of cellular adaptation is metaplasia. Metaplasia occurs
when cells change from one type to another. For example cigarette smoke
causes the bronchial tissues to change. Metaplasia often is reversible. For
example, if a person who smokes cigarettes stops smoking, their damaged
lung cells can revert to their original, normal structure.

Smoking causes the bronchial tissues to change.
Intracellular Accumulations
Intracellular accumulations might be the result of an overload of various
metabolites or external materials such as a disease-producing agent, or they
might be the result of metabolic disturbances. Intracellular accumulations
are materials that lie immediately near the cell. These cells are attached to
one another by junctions, and they communicate across these junctions. The
main products of intracellular accumulations are collagen and complex
sugars, which are extremely important in repairing damage to tissue and
maintaining the balance of the inner cell complex.
Aging
The last cell adaptation process we will talk about is the natural process of
aging and death of cells. Cell aging includes many forms of adaptation and,
unfortunately, many cell changes that are irreversible. Aging cannot be
avoided or prevented, and the best you can do is try to lessen aging’s
adverse effects on the body.
Because cells represent the basic living units of all tissues and organs,
scientists know that age-related illness and eventual death are the result of
cells being unable to regenerate and provide the specialized body functions
necessary to sustain life.
Aging cannot be avoided or prevented.
Pathologic changes associated with aging vary from person to person. Most
organs undergo atrophy and have a reduced functional reserve—that is, they
cannot reproduce new cells as needed. Resistance to infection declines with
advancing age, and the incidence of cancer and heart disease increases.
Before you move on, take a few minutes to complete the following Practice
Exercise to review what you’ve learned so far.
Please pause and complete online Practice Exercise 10-3.
Step 13 Tissue Response
You know how cells adapt to injury and how the cell structure might change in this
healing process. But how can you tell when cellular damage has occurred? Well,
let’s get started by discussing the body’s reaction to injury.
Injury to cells, tissues, or organs means that their physiology is interrupted or
they are anatomically changed. When the body is injured, there are three
ways tissues can respond.
Inflammation
Repair
Damage or death
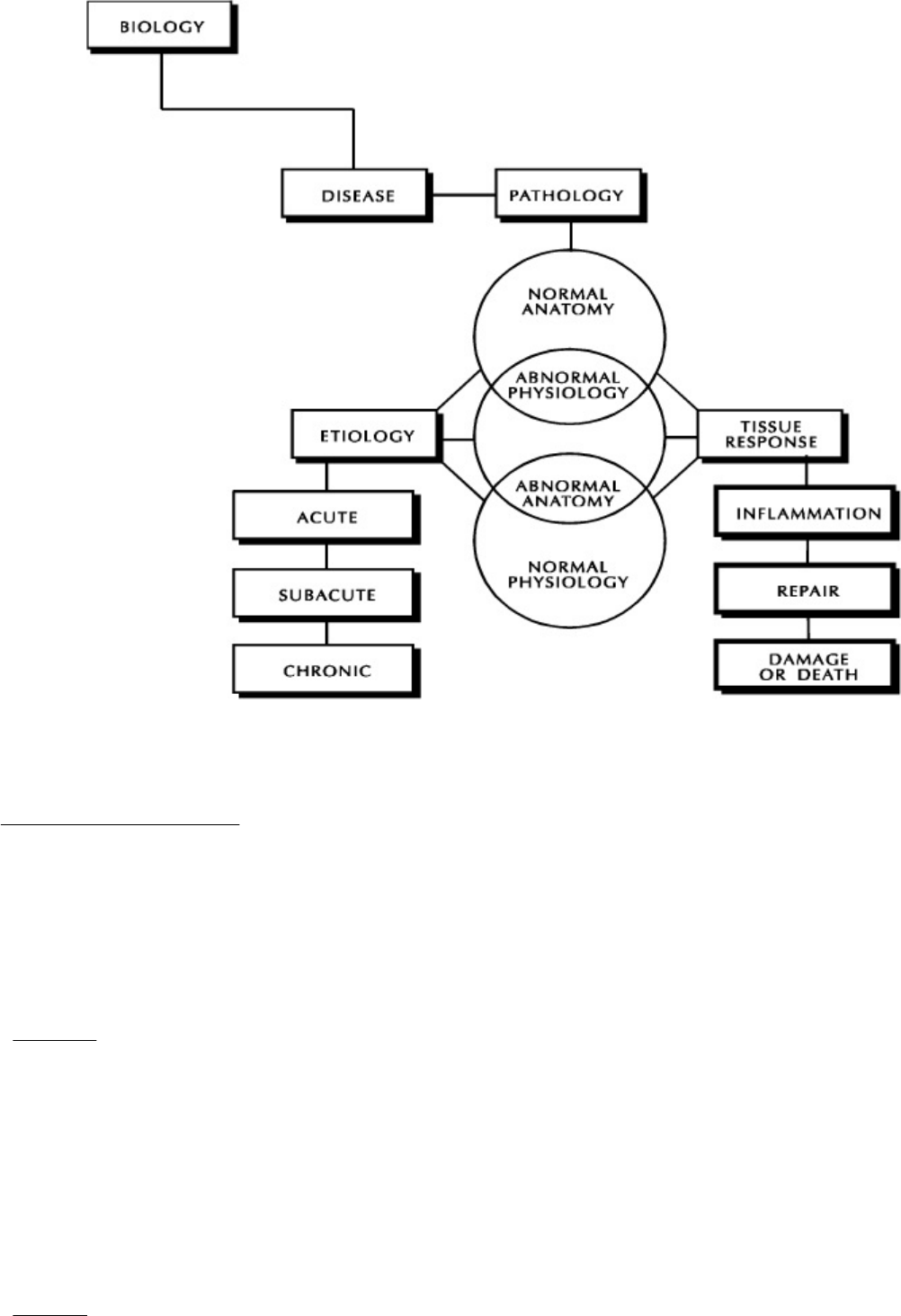
Tissue response
Inflammation
Inflammation is the response of the body to injury in cells, tissues or
organs. The function of the inflamed area decreases while it is inflamed.
Inflammation has four symptoms or signs. A symptom is what a patient feels;
a sign is what a doctor observes.
Rubor
Rubor means redness. Increased blood flow in the area causes this redness.
The medical term for this is hyperemia. The blood flow increases to bring
leukocytes to fight infection. Neutrophils and monocytes are two
leukocytes that eat foreign materials and bacteria. Neutrophils also are called
polymorphonuclear leukocytes. The slang term for neutrophils is polys;
the slang term for monocytes is monos.
Calor
Calor means heat. Hyperemia creates heat. Sometimes heat can kill bacteria
or viruses.

Calor means heat.
Tumor
Tumor means swelling. Increased fluid in the area causes swelling. The
medical term for this swelling is edema, and this can occur when cells are
damaged and lose water abnormally into the space surrounding the tissues. A
swollen area is edematous. Tumor also means a lump. Because cancers
feel like lumps, they are called tumors. But tumor only means a lump. Just
because something feels tumorous, it is not necessarily a cancer.
Dolor
Dolor means pain. Pain is caused when swelling of the tissues pinches nerve
cells. There is no pain if the nerve cells have died from the injury.
Which of the four symptoms of inflammation are present or which are most
noticeable depends on the severity of the injury and when it occurred.
The terms you have learned for injury also apply to the types of inflammatory
response.
Acute Inflammation
Acute inflammation is what most people think of as inflammation. The
changes usually are very dramatic. It is a response to acute injury, pyogenic
infection or severe allergy. The distinguishing feature of acute
inflammation is the fluid that is produced, which is what causes swelling.
Acute inflammation also may have redness, heat, and pain.
Acute inflammation may cause pain.
The fluid of inflammation is called an exudate. An exudate is cloudy and
contains protein, which leaked from damaged cells and bacteria. By
comparison, a transudate is clear fluid that doesn’t contain protein. It is

related to vascular disease, not inflammation.
There are several types of exudate. Serous exudate is the clear yellow fluid
that oozes from burns. It has more fluid than protein.
Fibrinous exudate has a blood clotting material called fibrin, which traps
bacteria in its net. Fibrinous exudate forms scabs.
Purulent exudate is commonly referred to as pus. It gets its appearance
from dead bacteria and neutrophils. Pyogenic means forming pus. A
pyogenic infection is one that forms a purulent exudate in the acute
inflammatory response. When an inflammatory response has a large amount
of pus, it is called a suppurative infection. When a collection of pus is
closed off in a sac by fibrous connective tissue, it is called an abscess. A
small abscess is called a carbuncle.
Ulcerative and pseudomembranous inflammation are two types of acute
inflammation.
Ulcerative inflammation is inflammation of the body surfaces or the
mucosa of hollow organs, such as the stomach or intestines, that
results in ulceration.
Pseudomembranous inflammation is a form of ulcerative
inflammation combined with fibrinopurulent drainage. That is, the fluid
contains fibrin, pus, cellular debris, and mucus. This fluid forms a type
of membrane on the surface of the ulcers.
Chronic Inflammation
Infections that don’t completely heal, slow injury and slow allergic irritation
cause chronic inflammation. The symptoms of chronic inflammation are
not as dramatic as the symptoms of acute inflammation. In chronic
inflammation, there is less exudate or fluid and more fibrous tissue repair.
Pain is more prominent than redness or heat. Arthritis is a good example of a
disease with chronic inflammation as the body’s response to disease.
Subacute Inflammation
Subacute inflammation is a “flare-up” of a chronic inflammation. The pain,
redness, heat, and/or edema are suddenly more noticeable than in the
chronic state.
Granulomatous Inflammation
Granulomatous inflammation forms tumors rather than heat, redness or
pain. The tumor that is formed is more like a lump than swelling. The tumor
is called a granuloma. In this type of inflammation, the cells that come to
clear out the infection are called macrophages.
Granulomatous inflammation has special causes. It is seen with fungus
infections, tuberculosis and foreign bodies, like popcorn in the trachea. Any
disease that causes a granulomatous inflammatory response is called a
granulomatous disease.
Repair
There are two ways tissues can repair damage: regeneration and repair.
Regeneration
Normally, tissue replaces itself as old cells degenerate and die. For example,
the lining of the stomach replaces itself every three days or so. Red blood
cells are replaced every 120 days. When your skin flakes, you can see the
dead cells that are removed. They are replaced by new young cells.
Your skin flakes much more after the trauma of sunburn.
Regeneration is a normal process. However, in disease, this process is sped
up to replace damaged cells. Your skin flakes much more after the trauma of
sunburn, for example.
Repair
Repair is the response to injury when regeneration won’t repair the damage
that disease caused. Here the damaged tissues cannot regenerate, so they
are replaced by fibrous connective tissue. This is called fibrous connective
tissue repair. This also is called scarring or fibrosis.
Fibrous tissue doesn’t have the function of the tissue it replaced and usually
is firmer. A wound will heal with fibrous tissue repair whether it is secondary
to trauma or to surgery. The body doesn’t know the difference.
A wound that is sewn shut by surgery will heal with a smaller scar than one
that is not sewn shut. When the wound is sewn shut, there is less damaged
tissue to replace with fibrous tissue. That is why large cuts are closed with
“stitches.” This is called healing by primary intention or primary union.
When a wound heals with the borders separated, there is more inflammatory
response, and the tissue that forms during healing is called granulation
tissue. The tissue is friable, meaning it breaks easily. It takes longer for the
fibrous tissue to repair the wound. The scar is larger. This is called healing by
secondary intention or secondary union.
Damage or Death
When cells, tissues or organs are injured, there is damage. When cells
are damaged, there is degeneration, and the function decreases. The
body can do one of the following: repair the damage, not repair the
damage or allow the tissue to die. If there is no repair, the following
things can happen.
Morbidity
Morbidity means damage to a whole organism, like the human body. This
damage usually is not a desired outcome of treatment. For example, after a
stroke the human body doesn’t die, but it may not return to normal function.
This loss of function is a morbid change.
Atrophy and Hypertrophy
Remember these terms from earlier in the lesson? You know that atrophy
means cells slowly have decreased in size and/or number over a long time.
Atrophic changes are caused by chronic injury.
Hypertrophy means that cells enlarge or swell but don’t increase in number.
Chronic injury can do this. In hypertrophic change, the swelling is in the cells.
In inflammation, the swelling is in the fluid surrounding the cells. Hypertrophy
is one of two ways that tissues or organs become bigger. The other way
tissues enlarge is hyperplasia, an increase in the number of cells, although
the cells are not larger in size.
Accumulated Compounds
Chronic injury usually leads to increased collections of abnormal, unwanted or
waste materials in cells. This will increase the size of cells and organs and
change their color and texture as well.
For example, when the liver is damaged, it can accumulate fat. This is called
fatty metamorphosis. The liver is becoming larger and more yellow in color
because it contains more fat than normal; it is changing from a
morphologically normal liver to a morphologically abnormal liver.
Death
Necrosis is death of cells, tissues or organs in a living body. The change is
not reversible. That is, death cannot be reversed to life. Death occurs when
cells are so damaged that they cannot repair or regenerate; the tissues are
necrotic. Necrosis often results from an acute injury.
Mortality means death of an organism, like the human body. Anything that
kills is called lethal. For example, if a gene causes a genetic or congenital
abnormality that kills the body, the gene is called a lethal gene.
Mortality means death of an organism.
Different types of necrosis are seen microscopically. They include coagulation
necrosis, liquefaction necrosis, and caseous necrosis. The type of necrosis
tells you its cause. Interruption of the blood supply causes coagulation
necrosis. Liquefaction necrosis is the result of infection. The liquid pus
you see is the debris left by the inflammatory response, including dead tissue
cells and white blood cells. Caseous necrosis, which is seen in
granulomatous inflammation, looks like cheese and contains dead tissue with
tuberculosis bacteria in it.
Step 14 Pronounce New Terms
Follow these steps:
a. Take your Quick-Learn Tutor and the flashcards labeled Set 13
out of your Quick-Learn Kit. Insert the first flashcard into Side A
of the Tutor.
b. Access the online portion of your course, and go to Lesson 10.
c. Listen to the term, and pause the audio.
d. Practice pronouncing each term out loud. Take your time. Push
the flashcard up and read the meaning of the term.
e. Do this for each term in this set.
f. Put the flashcards in order and play the audio again,
pronouncing each word part or term after you hear it.
g. Don’t forget to listen to your own pronunciation of each term. If
you mispronounce one, put a check mark next to that flashterm.
h. Practice the terms you mispronounced by listening again. Be
sure you can pronounce the terms clearly and easily.
Step 15 Write New Terms
Follow these steps:
a. Insert the first flashcard into Side A of your Quick-Learn Tutor.
b. Look at each term as it appears in the window and say it out loud. Write
the term on blank paper.
c. Push the card up until the meaning appears in the right window and read
the meaning out loud. Write the meaning beside the term.
d. Do this for each flashcard.
Step 16 Meanings of New Terms
Follow these steps:
a. Again insert the first flashcard into Side A of your Quick-Learn Tutor.
Pronounce each term out loud and then say the meaning. Check yourself
by pushing the flashcard up until you can see the meaning in the right
window.
b. Now insert the flashcard into Side B of your Quick-Learn Tutor. Push the
card up until you see the meaning of the first flashterm in the right
window. Read each meaning out loud. Before you look, see if you can
remember the term that goes with that meaning. Check yourself by
pushing the flashcard up until you can see the term in the left window.
c. Practice with the flashcards several times until you are familiar with the
terms and their meanings. You may use the flashcards for the Progress
Checks and the Mail-In Quizzes.
Please pause and complete online Practice Exercise 10-4.
Step 17 Lesson Summary

Wow! We’ve covered a lot of information here! If you’re feeling a little
overwhelmed, just relax. It’s not necessary that you memorize all the new terms
you’ve just learned. As a medical coding specialist, you won’t be asked to describe
ribosomes or give an example of chronic inflammation. However, it’s important that
you have an understanding of cells, how they work properly, and what happens
when they aren’t operating at their peak.
Let’s do a quick review before you move on to your Quiz. This lesson taught
you the basic components of a cell and each component’s function. You
learned about everything from cytoplasm to the nucleus. You studied
etiologies, or the cause of abnormalities and injuries. You also looked at how
cells adapt to injury and how the cell structure might change in the healing
process. Lastly, you learned the body reacts to injury through inflammation,
repair, and damage or death.
Hopefully, you found parts of this lesson fascinating. Learning about
how the human body responds to damage can be an interesting read.
Perhaps you’ve experienced your own body healing in a way we’ve
discussed here. If there were parts of this lesson that you found
particularly confusing, go back and reread those sections before
moving on. A little extra studying will pay off!
Please pause and complete an online Quiz. Good luck!
LESSON 11
Diagnostic Coding 101
Step 1 Learning Objectives for Lesson 11
When you have completed the instruction in this lesson, you will be trained to do
the following:
Describe the history and development of the diagnostic coding system.
Explain the role of medical coding and its uses.
Compare and contrast the ICD-9-CM and the ICD-10-CM coding systems.
Step 2 Lesson Preview
So far in this course, you’ve learned about everything from medical facilities and
healthcare professionals to how insurance works. You’ve also gained a strong
foundation in medical records, ethics, terminology and anatomy. You’re probably
wondering when you’ll get to code. Well, here you go! This lesson will introduce
you to diagnostic coding.
When a provider makes a diagnosis, it is you, the medical coding specialist, who codes it.
Whenever a patient sees a provider for a health-related problem, the
patient is asking for a diagnosis. We’ve talked quite a bit about diagnoses
in previous lessons, and you already know a bit about diagnosis codes.
You also know that when a provider makes a diagnosis, it is you, the
medical coding specialist, who codes it. The diagnosis codes that you
assign are then used to determine the medical necessity. This helps the
payer, such as the insurance companies, to determine reimbursement for
the provider’s services.
This lesson will discuss the history and development of the ICD coding
system and explain the future of diagnostic coding. So, let’s get started!
Step 3 History of the International Classification of

Diseases
We spoke briefly of the International Classification of Diseases in a previous
lesson. The history of the ICD dates back to the 1600s in England! The system
came to the United States in the mid-1700s. This classification of diseases
originally was used to track mortality statistics to determine how many people died
of different diseases.
London Bills of Mortality.
In the seventeenth century, the statistical study of diseases began with the
work of John Graunt on the London Bills of Mortality. The Bills was initially a
list of only the number of burials. Graunt had added to the Bills, which now
included the cause of deaths. He tabulated and studied the data from the
annual bills from 1629 through 1660 and published Natural and Political
Observations Made upon the Bills of Mortality in 1662. This publication is
considered one of the forerunners of today’s international mortality
classifications.
In 1837, the General Register Office of England and Wales found its first
medical statistician, William Farr. Farr labored to secure an improved
classification, as well as international uniformity. In 1853, the first
International Statistical Congress (ISC) asked Farr to prepare an
internationally applicable, uniform classification of causes of death.
1
Although this classification was never universally accepted, the general
arrangement survived as the basis of the International List of Causes of
Death.
The International Statistical Institute created a committee, chaired by Dr.
Jacques Bertillon, to prepare a classification of causes of death. The report
was presented in 1893, and the Bertillon Classification of Causes of Death,
as it was first called, received general approval. Several countries adopted
it at that point. Jesus E. Monjaras first used the classification in the
Americas for the statistics of San Luis de Potosi, Mexico.
2
In 1900, the first international conference for the revision of the Bertillon or
International List of Causes of Death convened. Representatives from 26
countries attended and adopted the first of the ICDs or International
Classification of Diseases. It was determined that the classifications should
be revised every 10 years; therefore, the succeeding conferences were
held in 1909, 1920, 1929 and 1938, and a new version of the ICD was
adopted at each.
3
The WHO
The World Health Organization (WHO) is the directing and coordinating
authority for health within the United Nations system. It is responsible for
providing leadership on global health matters, shaping the health research
agenda, setting norms and standards, articulating evidence-based policy
options, providing technical support to countries and monitoring and
assessing health trends.
4
In 1946, the United Nations gave the responsibility
of the ICD to the WHO, which issued the sixth and subsequent revisions in
1948, 1958 and 1967.
The ICD is the international standard diagnostic classification. It classifies
diseases and other health problems recorded on many types of health and
vital records, including death certificates and health records.
5
ICD-9-CM
The World Health Organization published the 9
th
Revision, International
Classification of Diseases (ICD-9) in 1977. In 1979, the United States
adopted the International Classification of Diseases, 9
th
Revision,
Clinical Modification (ICD-9-CM) based on the ICD-9. The Clinical
Modification expanded the number of diagnosis codes and developed
a procedural coding system.
ICD-9-CM manual
The ICD-9-CM consists of:
Tabular List
Alphabetical Index
Procedure Index and Tabular List
Please pause and complete online Practice Exercise 11-1.
Step 4 Why Code?
Through the years, the number of people who go to the doctor has increased. This
increase has occurred for several reasons:
People live longer and require more health care.
Technological advances offer more options for better health care.
People have better access to health care than ever before.
Your role as the medical coding specialist is to translate the provider’s written
diagnoses for all of these patients into numeric, or number codes, and
alphanumeric, or combined letter and number, codes. The provider’s office
uses this coded information for a number of purposes. A primary use of
medical codes is to communicate to the insured the reason for a patient’s
medical visit. Thus, the diagnosis code communicates to the insurance payer
the reason the provider required medical services.
Coded information is used for numerous purposes.
Another use for medical coding is as a statistics-gathering tool for research,
grants and financial analysis. Hospitals use coding to index hospital records
according to diseases and operations. By indexing—or organizing—records
this way, they consistently can store and retrieve data. Coding is useful for
reporting medical diagnostic trends to agencies that track this information.
For instance, the American Cancer Society can access accurate cancer
statistics thanks to coding.
As you can see, the coding system is a common language that the medical
community uses as a standard communications device. Using this coding
system correctly is important. You know by now that if a code is used that
does not match the services performed, the claim will be rejected. In
addition, for government claims, such as to Medicaid or Medicare, the correct
code is required by law.
Originally, medical coding was used to allow access to medical records for
easy retrieval of information for medical research, education and
administration. Today, coding is used to:
Facilitate payment of medical services.
Study patients’ use of healthcare facilities.
Study the cost of health care.
Research the quality of health care.
Determine healthcare trends.
Plan for future healthcare needs.
Step 5 ICD-10
After 30 years, the ICD-9 needs to be replaced. The terminology and classification
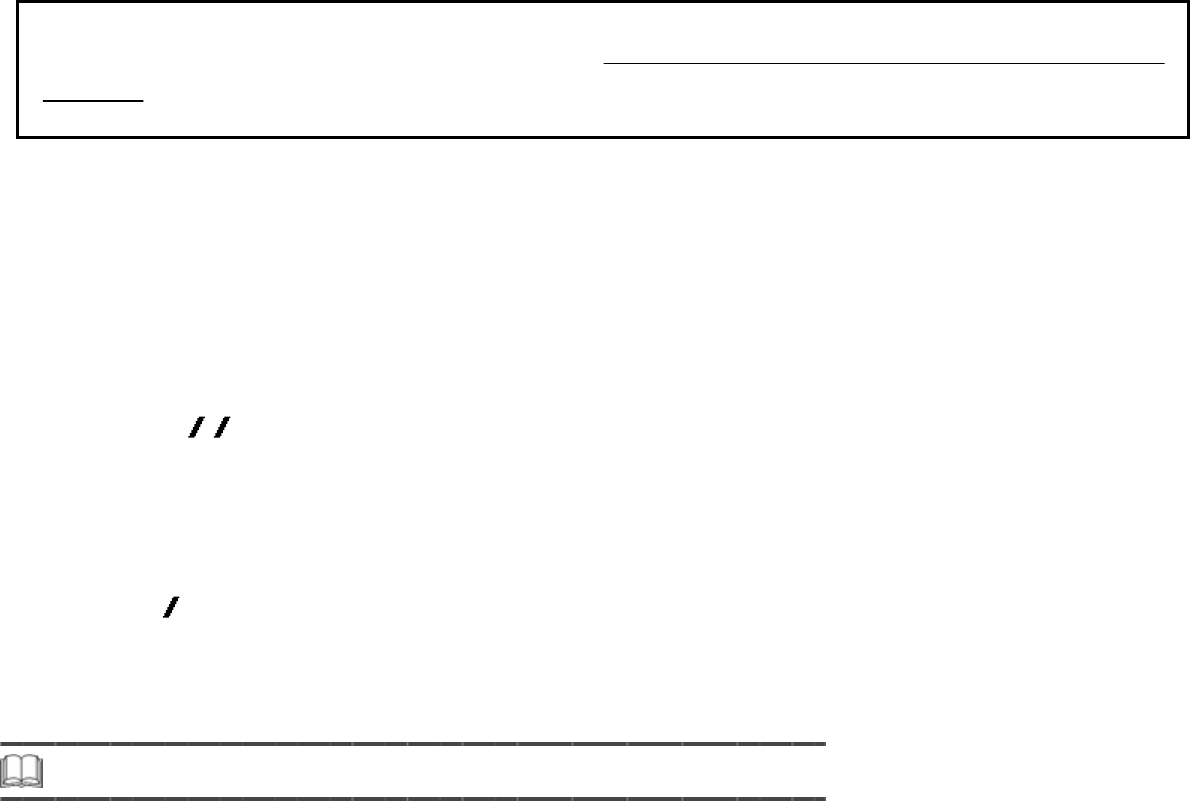
of some conditions are outdated and/or obsolete. These outdated codes produce
inaccurate and limited data. And, the limits of the categories result in increasing
lack of specificity. Finally, the ICD-9-CM hinders comparisons with international
data. It’s clear that the ICD must be flexible enough to adjust for emerging
diagnoses and procedures and exact enough to identify precise diagnoses and
procedures.
In 1989, the WHO prepared the International Statistical Classification of
Diseases and Related Health Problems, 10
th
Revision (ICD-10), which was
released in 1994. The United Kingdom adopted it in 1995, followed by the
Nordic countries of Denmark, Finland, Iceland, Norway and Sweden from
1994 through 1997. Each year, another country adopted the ICD-10: France
(1997), Australia (1998), Belgium (1999), Germany (2000) and Canada
(2001). On January 15, 2009, the Department of Health and Human Services
(HHS) released the final rule for the implementation of the International
Classification of Diseases, 10
th
Revision, Clinical Modification (ICD-10-CM)
and the International Classification of Diseases, 10
th
Revision, Procedural
Classification System (ICD-10-PCS). The final rule pushed the ICD-10 (both
ICD-10-CM and ICD-10-PCS) implementation date to October 1, 2013.
To read about the ICD-10 Final Rule, visit: http:edocket.access.gpo.gov/2009/pdf/E9-
743.pdf
On April 17, 2012, a proposed rule was released that would delay, for one
year, implementation of the ICD-10 data sets until October 1, 2014.
Impact for Coders
How does this affect you as a medical coder? Is it a waste of time to learn
coding from the ICD-9-CM? Absolutely not! Per U.S. government mandate,
the ICD
9 CM will be used by all medical service providers up until midnight
on September 30, 2014. The ICD-10-CM will be implemented on October 1,
2014. To make sure you have the information about the current industry
standard, we will focus on discussing the ICD-9-CM in your course for the
immediate future. Once you are familiar with the coding process with the
ICD-9 CM, it’ll be a smooth transition to the ICD-10-CM. You can get
reference material, in the format of an ICD-10-CM supplement, available for
purchase online through our bookstore. This supplement is optional and is not
a required part of your course.
Step 6 ICD-9-CM vs. ICD-10-CM
Let’s briefly review the two different code sets and compare them. The format and
structure will be examined in detail in later lessons. For now, just compare and
contrast the diagnosis code sets.
Now you understand the need for the ICD-9-CM update and when that will
happen.
Please pause and complete online Practice Exercise 11-2.
Step 7 Lesson Summary
Congratulations! You’ve made it through diagnostic coding 101. You have a
good understanding of the history behind the development of the ICD-9-CM
coding system. You can explain your role as a medical coding specialist, as
well as other uses for coding today. Finally, you know why the transition to
the ICD-10 is necessary and when to expect the implementation of this new
coding system. A background in the similarities and differences between the
coding systems will result in a smooth transition.
Please pause and complete an online Quiz. Good luck!
Endnotes
1
World Health Organization. The WHO Family of International Classifications. 2010.
http://www.who.int/classifications/icd/en/HistoryOfICD.pdf. Accessed 1 February 2010.
2
Bertillon J. Classification of the causes of death (abstract). In: Transactions of the 15th International
Congress on Hygiene Demography. Washington, 1912.
3
World Health Organization. The WHO Family of International Classifications. 2010.
http://www.who.int/classifications/icd/en/HistoryOfICD.pdf. Accessed 1 February 2010.
4
World Health Organization. About WHO. 2010. http://www.who.int/about/en/. Accessed 1 February 2010.
5
World Health Organization. International Classification of Diseases. 2010.
http://www.who.int/classifications/icd/en/. Accessed 1 February 2010.
Table of Contents
Title Page 2
Copyright 3
Table of Contents 5
Acknowledgments 4
Lesson 1—The World of Health Care 12
Step 1 Learning Objectives for Lesson 1 12
Step 2 Lesson Preview 12
Step 3 Daily Activities in the Medical Office 13
A Day in the Life of the Medical Office Manager 13
The Doctor’s Point of View 15
Step 4 A Little Teamwork Goes a Long Way 16
Physicians 17
Nurses 17
Nurse’s and Physician Assistants 18
Support Staff 18
Emergency Personnel 21
Office Professionals 22
Step 5 Welcome to Your Career as a Medical Coding Specialist! 22
But Where Will I Work? 23
Step 6 Personal Qualities of a Medical Coder 26
Professionalism 26
Presentation 28
Adaptability 28
Step 7 Medical Records 28
Parts of a Medical Record 29
The Flow of Medical Information 35
Step 8 Lesson Summary 37
Lesson 2—Medical Insurance 38
Step 1 Learning Objectives for Lesson 2 38
Step 2 Lesson Preview 38
Step 3 The Life Cycle of a Medical Bill 39
Processing the Bill 40
Step 4 Insurance 41
Step 5 Common Insurance Terms 42
Provider 43
Claim Form 43
Deductible 43
Copayment 43
Reasonable and Customary 44
Explanation of Benefits 44
Electronic Claims 45
Step 6 Types of Health Insurance 46
Government Insurance 47
Private, Traditional Insurance 49
Managed Care 49
Blue Cross/Blue Shield 50
Step 7 Diagnostic Codes—A Piece of the Insurance Puzzle 50
How Important Is Diagnostic Coding? 51
Step 8 Procedure Coding—Another Piece of the Puzzle 52
Step 9 Looking Ahead 53
Step 10 Lesson Summary 54
Lesson 3—Introduction to Medical Terminology: Word Parts 56
Step 1 Learning Objectives for Lesson 3 56
Step 2 Lesson Preview 56
Step 3 Word Parts 57
Step 4 Root Words 59
Step 5 Medical Terms 61
The Combining Vowel 61
Step 6 Root Words 63
The Functions of Root Words 64
Step 7 Pronounce Root Words 65
Step 8 Write Root Words 66
Step 9 Meanings of Root Words 67
Step 10 Prefixes 68
Step 11 Pronounce Prefixes 70
Step 12 Write Prefixes 71
Step 13 Meanings of Prefixes 72
Step 14 Suffixes 72
Step 15 Pronounce Suffixes 75
Step 16 Write Suffixes 76
Step 17 Meanings of Suffixes 77
Step 18 Lesson Summary 77
Just for Fun 78
Lesson 4—Medical Terminology: Dividing and Combining Terms 81
Step 1 Learning Objectives for Lesson 4 81
Step 2 Lesson Preview 81
Step 3 Dividing Medical Terms 82
Consonants, Vowels and the Role They Play 83
A Little Practice 84
Word Meanings 86
Step 4 Pronounce Word Parts 88
Step 5 Write Word Parts 89
Step 6 Meanings of Word Parts 89
Step 7 Combining Medical Terms 90
Consonants, Vowels and the Role They Play 91
Step 8 Pronounce Word Parts 92
Step 9 Write Word Parts 93
Step 10 Meanings of Word Parts 93
Step 11 Lesson Summary 94
Lesson 5—Medical Terminology: Abbreviations, Symbols and Special Terms 96
Step 1 Learning Objectives for Lesson 5 96
Step 2 Lesson Preview 96
Step 3 Abbreviations 97
Abbreviations in Hospitals 97
Office Records 98
Doctors 98
Pharmacies 98
Step 4 Learn Abbreviations 98
Step 5 Meanings of Abbreviations 99
Step 6 Slang 99
Medical Slang 100
English Slang 100
Step 7 Slang Terms 101
Step 8 Meanings of Slang Terms 102
Step 9 Symbols 102
Step 10 Special Terms 103
Eponyms 104
Brand Names 105
Acronyms 106
Step 11 Pronounce Acronyms 107
Step 12 Sound-Alikes and Opposites 108
Homophones (Sound-Alikes) 108
Antonyms (Opposites) 109
Step 13 Medical Plurals 110
Medical Rules for Plurals 110
Step 14 Lesson Summary 110
Lesson 6—Documenting Medical Records 112
Step 1 Learning Objectives for Lesson 6 112
Step 2 Lesson Preview 112
Step 3 Documentation—The Key Component of Medical Records 113
Types of Documentation 114
Commonly Used Narrative Formats 116
Step 4 The Business of Managing Medical Records 118
Good Recording Practices 118
Step 5 Lesson Summary 120
Lesson 7—Ethics and Legal Issues 122
Step 1 Learning Objectives for Lesson 7 122
Step 2 Lesson Preview 122
Step 3 Confidentiality 122
Guidelines for Confidentiality of Medical Records 123
Guidelines for Faxing Medical Records 124
Step 4 Medical Ethics 125
Step 5 Health Insurance Portability and Accountability Act 127
Step 6 Fraud and Abuse 139
Preventing Fraud and Abuse 140
Consequences of Committing Fraud 141
Step 7 Liability Insurance 142
Insurance Audits 143
Step 8 Recovery Audit Contractors 144
Step 9 Legal Concerns 144
Subpoenas 145
Arbitration 145
Medical Testimony 146
Step 10 Lesson Summary 146
Endnotes 147
Lesson 8—Introduction to Anatomy 149
Step 1 Learning Objectives for Lesson 8 149
Step 2 Lesson Preview 149
Step 3 Human Biology 150
What Is Human Biology? 150
Anatomy 151
Physiology 153
Step 4 Pathology 153
How Do Anatomy, Physiology and Pathology Relate to One Another? 154
Step 5 Beginning Anatomy and Physiology Concepts 156
The Anatomic Position 156
Planes and Sections of the Human Body 157
Transverse Planes and Sections 158
Sagittal Planes and Sections 158
Coronal Planes and Sections 159
Planes and Sections 160
Step 6 Location Terms 161
Step 7 Pronounce New Terms 167
Step 8 Write New Terms 168
Step 9 Meanings of New Terms 169
Step 10 Organ and Organ Systems 169
Respiratory System 170
Circulatory/Cardiovascular System 170
Nervous System 171
Muscular System 171
Skeletal System 171
Integumentary System 171
Endocrine System 172
Digestive System 172
Urinary System 172
Reproductive System 172
The Immune System 172
Step 11 Lesson Summary 173
Lesson 9—Anatomy: Landmarks and Divisions 174
Step 1 Learning Objectives for Lesson 9 174
Step 2 Lesson Preview 174
Step 3 Gross Anatomy 174
Landmarks and Divisions 175
Step 4 Pronounce New Terms 177
Step 5 Write New Terms 178
Step 6 Meanings of New Terms 178
Step 7 Adjective Forms for Landmark Names 179
Step 8 Divisions of the Abdomen 180
An Alternative Division of the Abdomen 181
Step 9 Internal Landmarks: The Body Cavities 182
Step 10 Membranes That Line the Body Cavities 184
Epithelial Tissue Membranes 184
Connective Tissue Membranes 185
Step 11 Retroperitoneal Organs 186
Step 12 Pronounce New Terms 186
Step 13 Write New Terms 187
Step 14 Meanings of New Terms 188
Step 15 Organization of the Body 188
Step 16 Lesson Summary 190
Just for Fun 191
Lesson 10—Cell and Tissue Anatomy and Pathology 193
Step 1 Learning Objectives for Lesson 10 193
Step 2 Lesson Preview 193
Step 3 Cell Components and Their Primary Functions 194
Cell Membrane 195
Cilia 195
Flagella 195
Villi 196
Step 4 More Cell Components and Their Functions 196
Cytoplasm 196
Step 5 The Nucleus 199
DNA 199
RNA 200
Nucleoli 200
Step 6 Pronounce New Terms 200
Step 7 Write New Terms 201
Step 8 Meanings of New Terms 201
Step 9 Cell Pathology 202
Step 10 Etiologies 203
Developmental Abnormality 203
Inflammatory Disease 203
Hyperplasia and Neoplasia 204
Metabolic Disease 205
Vascular Disease 205
Immunologic Disease 205
Idiopathic Abnormality 205
Iatrogenic Abnormality 206
Nosocomial Disease 206
Step 11 Cell Damage 206
Hypoxia and Anoxia 206
Toxic Agents 207
Microbial Infection 208
Allergic/Immune Reactions 208
Metabolic and Genetic Disturbances 208
Step 12 Cell Response 209
Atrophy 210
Hypertrophy 211
Hyperplasia 211
Metaplasia 212
Intracellular Accumulations 213
Aging 213
Step 13 Tissue Response 214
Inflammation 215
Repair 218
Damage or Death 219
Step 14 Pronounce New Terms 220
Step 15 Write New Terms 221
Step 16 Meanings of New Terms 221
Step 17 Lesson Summary 221
Lesson 11—Diagnostic Coding 223
Step 1 Learning Objectives for Lesson 11 223
Step 2 Lesson Preview 223
Step 3 History of the International Classification of Diseases 223
The WHO 225
ICD-9-CM 225
Step 4 Why Code? 226
Step 5 ICD-10 227
Impact for Coders 228
Step 6 ICD-9-CM vs. ICD-10-CM 228
Step 7 Lesson Summary 229
Endnotes 229
