February 16, 2024
Provider Relief Programs:
Provider Relief Fund and ARP Rural Payments
Frequently Asked Questions
General Information
Overview
Attestation
Rejecting or Returning Payments
Provider Relief Fund Terms and Conditions
ARP Rural Payments Terms and Conditions
Ownership Structures and Financial Relationships
Auditing and Reporting Requirements
Use of Funds
Calculating Eligible Expenses and Lost Revenue
Supporting Data
Change of Ownership
Non-Financial Data
Extensions
Miscellaneous
COVID-19 Vaccine Distribution and Administration
Balance Billing
Publication of Payment Data
Provider Relief Fund General Distribution and ARP Rural Payments
Phase 4 and ARP Rural Payments
Phase 4 Overview and Eligibility
ARP Rural Payments Overview and Eligibility
Targeted Distributions
Nursing Home Infection Control Distribution
1
February 16, 2024
2
General Information
Overview
Who was eligible to receive payments from the Provider Relief Fund? (Modified
12/4/2020)
Provider Relief Fund payments were disbursed via both “General” and “Targeted” Distributions.
To have been eligible for the General Distribution, a provider must have billed Medicare fee-
for-service in 2019, been a known Medicaid and CHIP or dental provider and provided after
January 31, 2020 diagnoses, testing, or care for individuals with possible or actual cases of
COVID-19. HHS broadly views every patient as a possible case of COVID-19.
A description of the eligibility for the announced Targeted Distributions can be found here.
All providers retaining funds must have signed an attestation and accepted the Terms and
Conditions associated with payment.
Was this a loan or a grant that I will need to pay back?
(Added 4/25/2020)
Retention and use of these funds are subject to certain terms and conditions. If these terms and
conditions are met, payments do not need to be repaid at a later date. These Terms and
Conditions can be found here.
Were Provider Relief Fund recipients required to notify HRSA if they have filed a
bankruptcy petition? (Added 12/9/2021)
Yes. Provider Relief Fund recipients must immediately notify HRSA about their bankruptcy
petition or involvement in a bankruptcy proceeding so that the Agency may take the appropriate
steps. When notifying HRSA about a bankruptcy, please include the name that the bankruptcy is
filed under, the docket number, and the district where the bankruptcy is filed. You must submit
this information to PRFbankruptc[email protected]. If a Provider Relief Fund recipient has filed a
bankruptcy petition or is involved in a bankruptcy proceeding, federal financial obligations will
be resolved in accordance with the applicable bankruptcy process, the Bankruptcy Code, and
applicable non-bankruptcy federal law.
What was the Assistance Listing (AL) (formerly the Catalog of Federal Domestic Assistance
(CFDA)) number for the Provider Relief Fund program? (Added 9/29/2021)
The AL number is 93.498.
Why would a provider not have been eligible for a General or Targeted Distribution
Provider Relief Fund payment? (Modified 6/30/2022)
In order to be eligible for a payment under the Provider Relief Fund, a provider must have met
the eligibility criteria for the distribution and complied with the Terms and Conditions for any
previously received Provider Relief Fund payments. Additionally, a provider must not have
been terminated from participation in Medicare or precluded from receiving payment through
Medicare Advantage or Part D; must not have been excluded from participation in Medicare,
Medicaid, and other Federal health care programs; and must not have had Medicare billing
privileges revoked as determined by either the Centers for Medicare &
February 16, 2024
3
Medicaid Services or the HHS Office of Inspector General in order to have been eligible to
receive a payment under the Provider Relief Fund.
How should providers classify the Provider Relief Fund payments in terms of revenue type
for cost reports? (Modified 9/3/2020)
Please refer to CMS FAQs on how Provider Relief Fund payments should be reported on cost
reports.
Can providers who have ceased operation due to the COVID-19 pandemic still receive this
funding? (Modified 2/16/2024)
If a provider ceased operation as a result of the COVID-19 pandemic, they are still eligible to
receive Provider Relief Fund payments so long as they provided on or after January 31, 2020,
diagnoses, testing, or care for individuals with possible or actual cases of COVID-19. HHS
broadly views every patient as a possible case of COVID-19, therefore, care does not have to be
specific to treating COVID-19. Recipients of funding must have complied with the Terms and
Conditions related to permissible uses of Provider Relief Fund payments.
In addition, if the Reporting Entity has ceased operation, they will still be responsible for
reporting on funds received. Reporting entities must also indicate whether their business has
ceased operation. If they have ceased operation, they will be required to enter the business cease
date and indicate whether the business was operational on 01/01/2020.
Were Provider Relief funds accessible in whole or in part to bankruptcy creditors and other
creditors in active litigation? (Added 6/8/2020)
Payments from the Provider Relief Fund shall not have been subject to the claims of the
provider’s creditors and providers were limited in their ability to transfer Provider Relief Fund
payments to their creditors. A provider may have utilized Provider Relief Fund payments to
satisfy creditors’ claims, but only to the extent that such claims constitute eligible health care
related expenses and lost revenues attributable to coronavirus and were made to prevent,
prepare for, and respond to coronavirus, as set forth under the Terms and Conditions.
May a health care provider that received a payment from the Provider Relief Fund exclude
this payment from gross income as a qualified disaster relief payment under section 139 of
the Internal Revenue Code (Code)? (Added 7/10/2020)
No. A payment to a business, even if the business is a sole proprietorship, does not qualify as a
qualified disaster relief payment under section 139. The payment from the Provider Relief Fund
was includible in gross income under section 61 of the Code. For more information, visit the
Internal Revenue Services’ website at https://www.irs.gov/newsroom/frequently-asked-
questions-about-taxation-of-provider-relief-payments.
Was a tax-exempt health care provider subject to tax on a payment it received from the
Provider Relief Fund? (Added 7/10/2020)
Generally, no. A health care provider that was described in section 501(c) of the Code is exempt
from federal income taxation under section 501(a). Nonetheless, a payment received by a tax-
exempt health care provider from the Provider Relief Fund may be subject to tax under section
511 if the payment reimbursed the provider for expenses or lost revenue attributable to an
unrelated trade or business as defined in section 513. For more information, visit the Internal
Revenue Services’ website at https://www.irs.gov/newsroom/frequently-asked-questions-about-
taxation-of-provider-relief-payments.

February 16, 2024
4
Will I receive a Form 1099?
(Modified 2/16/2024)
Yes, you will receive a Form 1099 if you received and retained within the calendar year 2023 a
total net payment from either or both of the Provider Relief Fund and/or COVID-19 Claims
Reimbursement to Health Care Providers and Facilities for Testing, Treatment, and Vaccine
Administration for the Uninsured that is in excess of $600.
When will my Form 1099 be available?
(Modified 2/16/2024)
Form 1099s will be mailed by January 31, 2024. If you have previously established an account
with UnitedHealth Group and elected to receive electronic copies of documents and notices, you
will not receive a mailed copy.
Who do I contact if I have questions regarding my Form 1099? (Modified 1/30/2023)
Please call the Provider Support Line (866) 569-3522 (for TTY, dial 711) for any questions you
may have regarding your Form 1099. If you have questions about filing your taxes generally,
seek guidance from your accountant and/or tax professional.
Which sections of 45 CFR 75 – UNIFORM ADMINISTRATIVE REQUIREMENTS,
COST PRINCIPLES, AND AUDIT REQUIREMENTS FOR HHS AWARDS are
applicable to the General and Targeted Distributions of the Provider Relief Fund?
(Added 12/28/2020)
Recipients (both non-federal entities and commercial organizations) of the General and Targeted
Distributions of the Provider Relief Fund are subject to 45 CFR 75 Subpart A (Acronyms and
Definitions) and B (General Provisions), subsections §75.303 (Internal Controls), and §75.351-
.353 (Subrecipient Monitoring and Management), and Subpart F (Audit Requirements). In
addition, the terms and conditions of the PRF payments incorporate by reference the obligation
of recipients to comply with the requirements to maintain appropriate financial systems at
§75.302 (Financial management and standards for financial management systems) and the
requirements for record retention and access at §75.361 through §75.365 (Record Retention and
Access).
Attestation
What action did a provider need to take after receiving a Provider Relief Fund payment?
(Modified 10/28/2020)
The CARES Act required Provider Relief Fund payment recipients to meet certain terms and
conditions if a provider retained a payment. If a provider chose to retain the funds, they had to
attest to have met the terms and conditions of the payment. Not returning the payment within 90
days of receipt would have been viewed as acceptance of the Terms and Conditions. A provider
must have attested for each of the Provider Relief Fund distributions received.
Did the Provider Relief Fund attestation portals require payment recipients to attest that
the payment amount was received? (Modified 10/28/2020)
Yes. The attestation portals required payment recipients to (1) confirm they received a payment
and the specific payment amount that was received; and (2) agree to the Terms and Conditions of
the payment.
February 16, 2024
5
Rejecting or Returning Payments
If a provider rejected a payment and the associated Terms and Conditions in the
attestation portal but decided to keep the funds after rejecting it in the attestation portal,
what should the provider have done in order to report on the use of funds kept? (Modified
10/27/2022) Providers who rejected one or more Provider Relief Fund and/or ARP Rural
payments exceeding $10,000, in aggregate, and kept the funds were required to report on these
funds during the applicable reporting period per the Terms and Conditions associated with the
payment(s). In order to be able to report on the use of funds, a provider must have contacted the
Provider Support Line at (866) 569-3522 (for TTY, dial 711) to request a change to their
attestation from “rejected” to “accepted.” Once the attestation status has been updated in the
attestation portal, the Provider Relief Fund Reporting Portal will subsequently be updated to
accurately reflect the kept payment that the provider was required to report on during the
applicable reporting period.
How can I return a payment I received under the Provider Relief Fund? (Modified
2/16/2024)
If you received an invoice from the U.S. Department of Treasury Centralized Receivables Service or Cross-
Servicing, please refer to the payment options found in your invoice. For more information, see
https://www.hrsa.gov/provider-relief/compliance/returning-funds.
The following instructions are to return the full payment amount:
If the provider received payment via electronic transfer, the provider needs to contact their
financial institution and ask the institution to initiate a “R23 - Credit Entry Refused by Receiver"
code on the original Automated Clearing House (ACH) transaction.
If a provider was paid via paper check, the provider should have destroyed the check if it is not
deposited or mail a paper check to UnitedHealth Group with notification of their request to
return the funds. Mail a refund check for the full amount payable to “UnitedHealth Group” to
the address below.
UnitedHealth Group
Attention: Provider Relief Fund
PO Box 31376
Salt Lake City, UT 84131-0376
Returning the payment in full or not depositing the payment received by paper check within 90
days without taking further action in the attestation portal is considered a de facto rejection of the
terms and conditions associated with the payment.
The following instructions were to return a partial payment amount:
Entities can return partial payments via Pay.gov. For more information on this process, please
review the instructions available at
https://na3.docusign.net/Member/PowerFormSigning.aspx?PowerFormId=45c01db6-78db-403a-
baa3-480c1950f596&env=na3&acct=dd54316c-1c18-48c9-8864-0c38b91a6291&v=2.
February 16, 2024
6
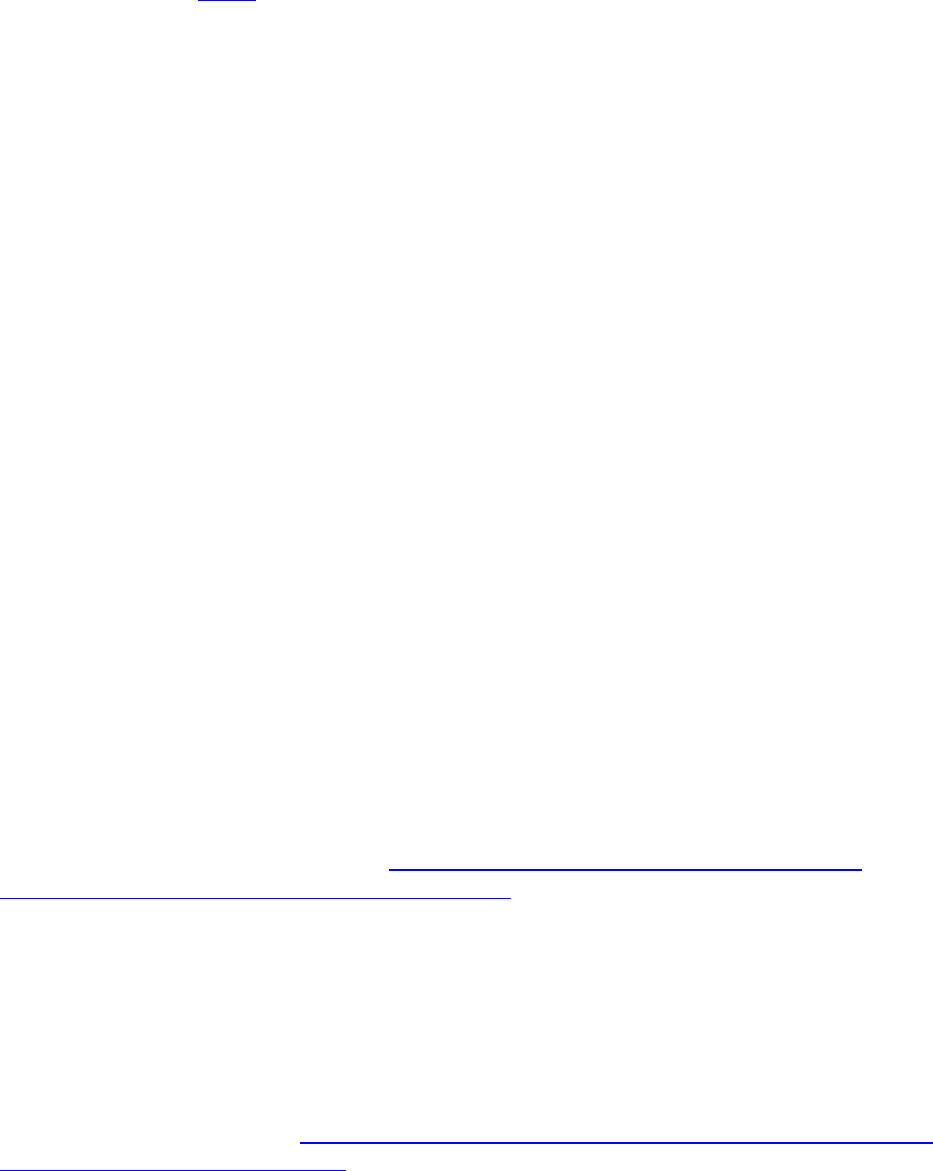
How can a provider return unused Provider Relief Fund payments that it has partially
spent? (Modified 2/16/2024)
Providers that have Provider Relief Fund payments that they cannot expend on allowable
expenses or lost revenues attributable to coronavirus by the Period of Availability that
corresponds to the Payment Received Period were required to return such funds to the
federal government.
Please note regarding the return of unused funds: The instructions on ‘PRF Return of Unused Funds
Portal’ explain the two-part process to return funds. There may be a delay in processing the return,
especially if repaying by paper check. If you have additional questions, please call the Provider
Support Line at (866) 569-3522 (for TTY, dial 711).
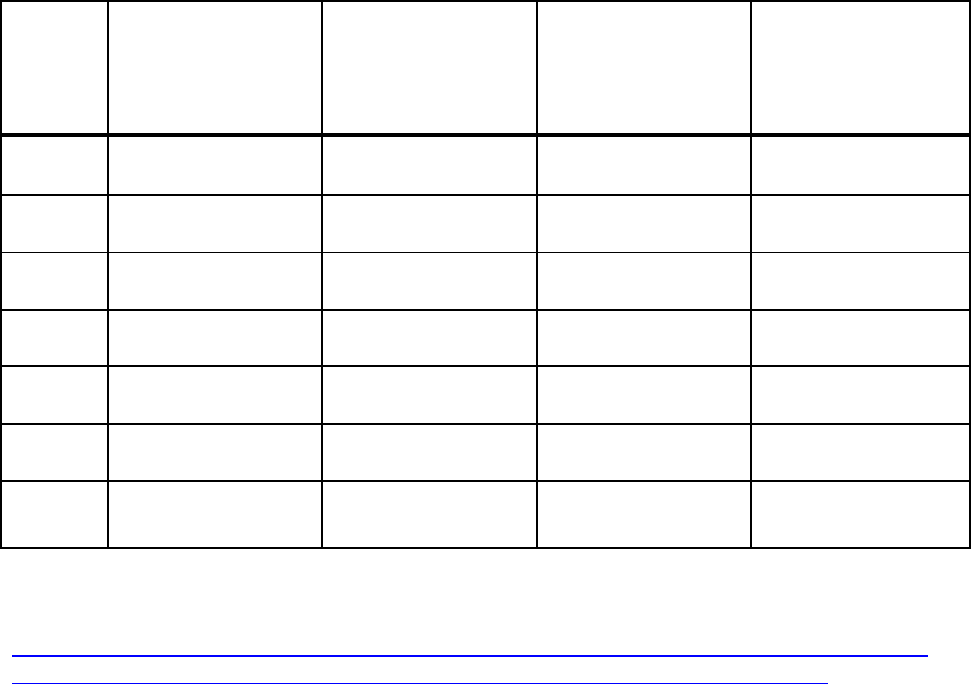
Period
Payment Received
Period
Period of
Availability for
Eligible Expenses
Period of
Availability for Lost
Revenues
Reporting Time
Period
1
April 10, 2020, to June
30, 2020
January 1, 2020, to
June 30, 2021
January 1, 2020, to
June 30, 2021
July 1, 2021, to
September 30, 2021
2
July 1, 2020, to
December 31, 2020
January 1, 2020, to
December 31, 2021
January 1, 2020, to
December 31, 2021
January 1, 2022, to
March 31, 2022
3
January 1, 2021, to
June 30, 2021
January 1, 2020, to
June 30, 2022
January 1, 2020, to
June 30, 2022
July 1, 2022, to
September 30, 2022
4
July 1, 2021, to
December 31, 2021
January 1, 2020, to
December 31, 2022
January 1, 2020, to
December 31, 2022
January 1, 2023, to
March 31, 2023
5
January 1, 2022, to
June 30, 2022
January 1, 2020, to
June 30, 2023
January 1, 2020, to
June 30, 2023
July 1, 2023, to
September 30, 2023
6
July 1, 2022, to
December 31, 2022
January 1, 2020, to
December 31, 2023
January 1, 2020, to
June 30, 2023
January 1, 2024, to
March 31, 2024
7
January 1, 2023, to
June 30, 2023
January 1, 2020, to
June 30, 2024
January 1, 2020, to
June 30, 2023
July 1, 2024, to
September 30, 2024
To return any unused funds, use the Return Unused PRF Funds Portal. Instructions for returning
any unused funds are available at:
https://na3.docusign.net/Member/PowerFormSigning.aspx?PowerFormId=45c01db6-78db-403a-
baa3-480c1950f596&env=na3&acct=dd54316c-1c18-48c9-8864-0c38b91a6291&v=2.
The Provider Relief Fund Terms and Conditions and applicable laws authorized HHS to
audit Provider Relief Fund recipients now or in the future to ensure that program
requirements are/were met. HHS is authorized to recover any Provider Relief Fund payment
amounts that were made in error, exceed lost revenue or expenses due to coronavirus, or do
not otherwise meet applicable legal and program requirements.

February 16, 2024
7
If a provider rejected the payment in the attestation portal but did not return the payment
within 15 calendar days, was the provider still subject to the Terms and Conditions? (Added
8/30/2021)
Yes. If the provider did not return the payment within 15 calendar days of rejecting the
payment in the attestation portal, the provider would have been considered to have accepted the
payment and must abide by the Terms and Conditions associated with the distribution. The
government may pursue collection activity to collect the unreturned payment.
If a provider returned a Provider Relief Fund payment to HHS, must it also return any
accrued interest on the payment? (Modified 12/11/2020)
Yes, for Provider Relief Fund payments that were held in an interest-bearing account, the
provider must return the accrued interest associated with the amount being returned to HHS.
However, if the funds were not held in an interest-bearing account, there is no obligation for the
provider to return any additional amount other than the Provider Relief fund payment being
returned to HHS. HHS reserves the right to audit Provider Relief Fund recipients in the future to
ensure that payments that were held in an interest-bearing account were subsequently returned
with accrued interest.
To return accrued interest, visit pay.gov. On the webpage, locate “Find an agency,” and select
“Health and Human Services (HHS) Program Support Center HQ.” Verify that the description
is “PSC HQ Payment” and form number is “HHSHQ,” then click continue. You will then need
to complete the following steps:
Step 1: Preview the form, then click “Continue.”
Step 2: Indicate whether you are completing on behalf of an individual or business and enter
the following information.
Business Name Field: Legal name of organization that received the payment
Invoice or Ticket Number Field: “HHS-COVID-Interest”
Contract/Agreement Number Field: Tax Identification Number (TIN) of organization
or provider that received the payment
Point of contact: Business contact information
Payment Amount: (The payment amount must match the interest earned on the payment
received.)
Step 3: Verify the interest return payment amount and select to pay by ACH or debit/credit
card, then select “Continue.”
Step 4: Enter the required information to complete the payment, then select “Review and
Submit.”
Step 5: Ensure that all information is correct and select “Submit.”
How should a provider return a payment it received via check? (Modified 10/28/2020)
If the provider received a payment via check and had not yet deposited it, destroy, shred, or
securely dispose of it. If the provider had already deposited the check, mail a refund check for the
full amount, payable to “UnitedHealth Group” to the address below via United States Postal
Service (USPS); mailing services such as FedEx and UPS cannot be used with this PO box.
Please list the check number from the original Provider Relief Fund check in the memo. Mail a
refund check for the full amount payable to “UnitedHealth Group” to the address below.
UnitedHealth Group
Attention: Provider Relief Fund
PO Box 31376
Salt Lake City, UT 84131-0376
February 16, 2024
8
How did a provider who received an electronic payment return funding if their financial
institution did not allow them to return the payment electronically? (Added 5/12/2020)
Contact UnitedHealth Group’s Provider Support Line at (866) 569-3522 (for TTY, dial 711).
Provider Relief Fund Terms and Conditions
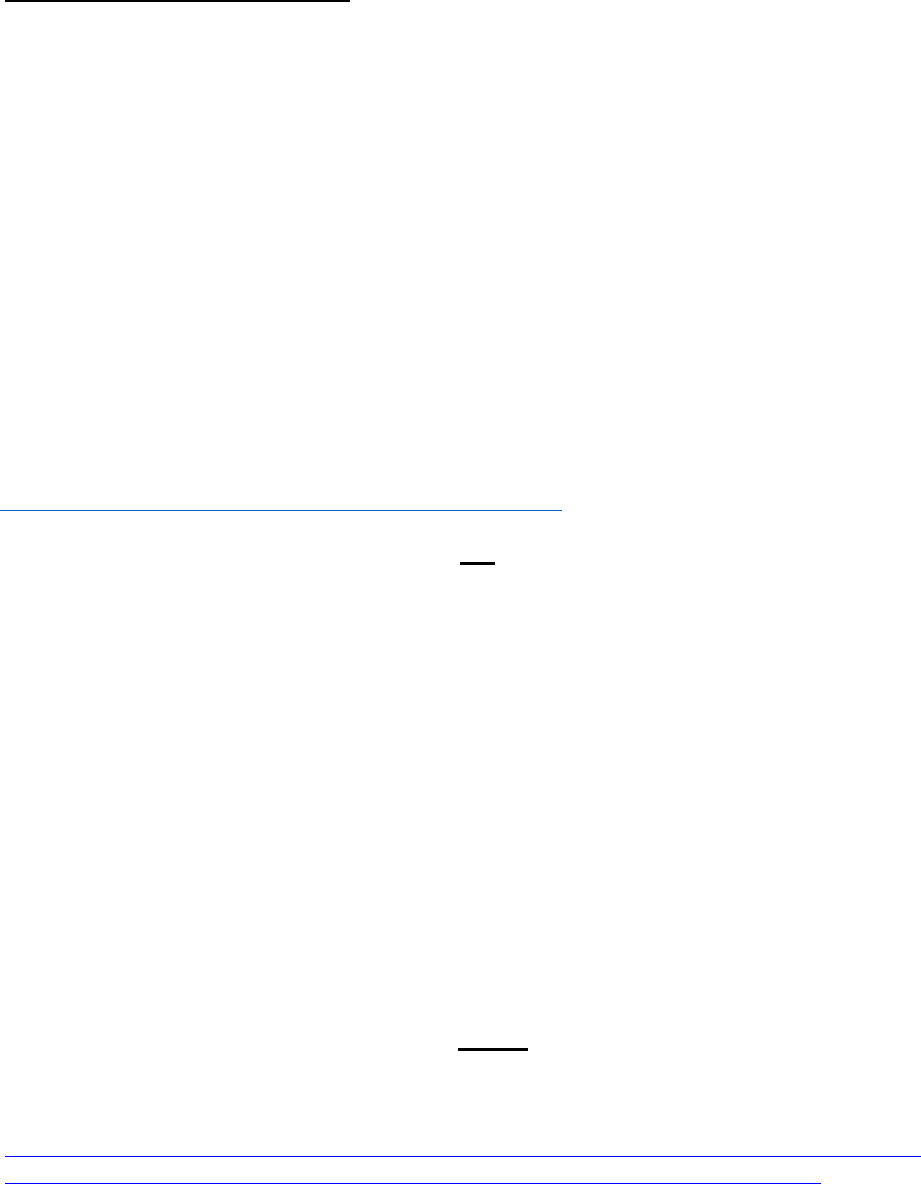
Was there a set period of time in which providers must use the payments to cover
allowable expenses or lost revenues attributable to COVID-19? (Modified 2/16/2024)
Yes. PRF and ARP Rural recipients must use payments for eligible expenses, including services rendered during
the period of availability, as outlined in Table 1 below. PRF and ARP Rural recipients may also use payments
for lost revenues attributable to COVID-19 incurred within the period of availability, but only up to June 30,
2023, the end of the quarter in which the COVID-19 Public Health Emergency ends.
The period of availability of funds was based on the date the payment was received. The payment was received
on the deposit date for automated clearing house (ACH) payments or the check cashed date. Providers must
follow their basis of accounting (e.g., cash, accrual, or modified accrual) to determine expenses.
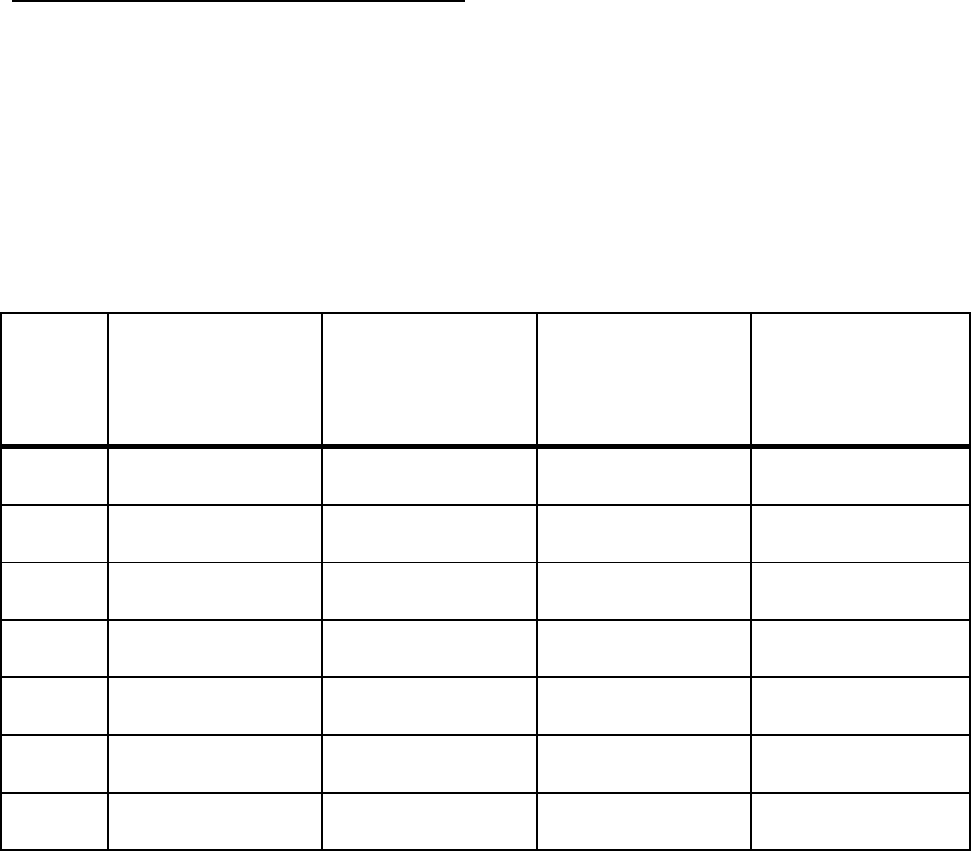
Period
Payment Received
Period
Period of
Availability for
Eligible Expenses
Period of
Availability for Lost
Revenues
Reporting Time
Period
1
April 10, 2020, to June
30, 2020
January 1, 2020, to
June 30, 2021
January 1, 2020, to
June 30, 2021
July 1, 2021, to
September 30, 2021
2
July 1, 2020, to
December 31, 2020
January 1, 2020, to
December 31, 2021
January 1, 2020, to
December 31, 2021
January 1, 2022, to
March 31, 2022
3
January 1, 2021, to
June 30, 2021
January 1, 2020, to
June 30, 2022
January 1, 2020, to
June 30, 2022
July 1, 2022, to
September 30, 2022
4
July 1, 2021, to
December 31, 2021
January 1, 2020, to
December 31, 2022
January 1, 2020, to
December 31, 2022
January 1, 2023, to
March 31, 2023
5
January 1, 2022, to
June 30, 2022
January 1, 2020, to
June 30, 2023
January 1, 2020, to
June 30, 2023
July 1, 2023, to
September 30, 2023
6
July 1, 2022, to
December 31, 2022
January 1, 2020, to
December 31, 2023
January 1, 2020, to
June 30, 2023
January 1, 2024, to
March 31, 2024
7
January 1, 2023, to
June 30, 2023
January 1, 2020, to
June 30, 2024
January 1, 2020, to
June 30, 2023
July 1, 2024, to
September 30, 2024
Provider Relief Fund recipients must use payments only for eligible expenses, including services
rendered, and lost revenues attributable to coronavirus, incurred by the end of the Period of
Availability that corresponded to the Payment Received Period. Providers were required to
maintain supporting documentation that demonstrated that costs were incurred during the Period
of Availability, as required under the Terms and Conditions. However, providers were not
required to submit that documentation when reporting. Providers must promptly submit copies of
such supporting documentation upon the request of the Secretary of HHS. Examples of costs
incurred for an entity using accrual accounting, during the Period of Availability include:

February 16, 2024
9
• Services that were received
• Renovation or construction that was completed
• Tangible property ordered, but need not have been delivered
For purchases of tangible items made using PRF payments, the purchase did not need to be in the
provider’s possession (i.e., back ordered PPE, ambulance, etc.) to be considered an eligible
expense but the costs must have been incurred by the end of the Period of Availability.
Providers must follow their basis of accounting (e.g., cash, accrual, or modified accrual) to
determine expenses. For projects that are a bundle of services and purchases of tangible items
that cannot be separated, such as capital projects, construction projects, or alteration and
renovation projects, the project costs cannot be reimbursed using Provider Relief Fund
payments unless the project was fully completed by the end of Period of Availability associated
with the Payment Received Period.
Recipients may use payments for eligible expenses or lost revenues incurred prior to receipt of
those payments (i.e., pre-award costs) so long as the were to prevent, prepare for, and respond to
coronavirus. However, HHS expects it would be highly unusual for providers to have incurred
eligible expenses or lost revenues before January 1, 2020. Additionally, the opportunity to apply
Provider Relief Fund payments (excluding the Nursing Home Infection Control Distribution) and
ARP Rural payments for lost revenues will be available up to June 30, 2023, the end of the quarter
in which the COVID-19 Public Health Emergency ends.
HHS reserves the right to audit Provider Relief Fund recipients now or in the future, and may
pursue collection activity to recover any Provider Relief Fund payment amounts that have not
been supported by documentation or payments not used in a manner consistent with program
requirements or applicable law. All payment recipients must have attested to the Terms and
Conditions, which required maintaining documentation to substantiate that these funds were
used for health care-related expenses or lost revenues attributable to coronavirus.
What financial transactions are Reporting Entities required to report in order to satisfy the
requirement in the Terms and Conditions for Phase 4 that recipients must notify HHS of a
merger with or acquisition of any other health care provider during the Payment Received
Period within the Reporting Time Period? (Added 12/9/2021)
The Terms and Conditions for Phase 4 required that recipients that received payments greater than
$10,000 notify HHS during the applicable Reporting Time Period of any mergers with or
acquisitions of any other health care provider that occurred within the relevant Payment
Received Period. HRSA considered changes in ownership, mergers/acquisitions, and
consolidations to be reportable events.
If a merger or acquisition was planned before receiving Phase 4 General Distribution
payments, will health care providers still need to report these activities? (Modified
12/9/2021)
If a Reporting Entity that received a Phase 4 General Distribution payment underwent a merger
or acquisition during the Payment Received Period, as described in the the Reporting Entity must
report the merger or acquisition during the applicable Reporting Time Period.
What type of review will HRSA do after a merger or acquisition has been reported by
recipients of a Phase 4 General Distribution payment? (Modified 12/9/2021)
If a Reporting Entity that received a Phase 4 General payment indicates when they report on the
use of funds that they have undergone a merger or acquisition during the applicable Payment
February 16, 2024
10
Received Period, this information will be a component that is factored into whether an entity is
audited.
Does HHS intend to recover any payments made to providers not associated with specific
claims for reimbursement, such as the General or Targeted Distribution payments?
(Modified 10/20/2021)
The Provider Relief Fund Terms and Conditions required that recipients be able to demonstrate
that lost revenues or expenses attributable to coronavirus, excluding expenses and losses that have
been reimbursed from other sources or that other sources are obligated to reimburse, meet or
exceed total payments from the Provider Relief Fund. Provider Relief Fund payment amounts that
have not been fully expended on health care expenses or lost revenues attributable to
coronavirus by the deadline to use funds that corresponds to the Payment Received Period must
be returned to HHS. The Provider Relief Fund Terms and Conditions and applicable legal
requirements authorized HHS to audit Provider Relief Fund recipients now or in the future to
ensure that program requirements are met. Provider Relief Fund payments that were made
incorrectly, or exceed lost revenues or expenses due to coronavirus, or do not otherwise meet
applicable legal and program requirements must be returned to HHS, and HHS is authorized to
recover these funds.
What should providers do if they had remaining Provider Relief Fund payments that they
cannot expend on allowable expenses or lost revenues by the relevant deadline? (Modified
10/20/2021)
Providers that had Provider Relief Fund payments that they cannot expend on allowable
expenses or lost revenues by the deadline to use funds that corresponds to the Payment Received
Period, as outlined in the Post-Payment Notice of Reporting Requirements, will return this
money to HHS. The Provider Relief Fund Terms and Conditions and legal requirements
authorize HHS to audit Provider Relief Fund recipients now or in the future to ensure that
program requirements are met. HHS is authorized to recover any Provider Relief Fund amounts
that were made incorrectly or exceed lost revenues or expenses due to coronavirus, or do not
otherwise meet applicable legal and program requirements.
What oversight and enforcement mechanisms did HHS use to ensure providers meet the
Terms and Conditions of the Provider Relief Fund? (Modified 10/20/2021)
Providers receiving payments from the Provider Relief Fund must comply with the Terms and
Conditions and applicable legal and program requirements. Failure by a provider that received a
payment to comply with any term or condition can result in action by HHS to recover some or all of the
payment. Per the Terms and Conditions, all recipients were required to submit documents to
substantiate that these funds were used for health care-related expenses or lost revenues attributable to
coronavirus, and that those expenses or lost revenues were not reimbursed from other sources and
other sources were not obligated to reimburse them. HHS monitored the funds distributed, and
oversaw payments to ensure that Federal dollars were used in accordance with applicable legal and
program requirements. In addition, the HHS Office of the Inspector General fights fraud, waste and
abuse in HHS programs, and may review these payments.
What if my payment was greater than expected or received in error? (Modified
10/14/2021) If HHS identified a payment made incorrectly, HHS recovered the amount paid
incorrectly or overpaid. If a provider received a payment that was greater than expected and
believed the payment was made incorrectly, the provider should contact the Provider Support
Line at (866) 569-3522 (for TYY, dial 711) and seek clarification.

February 16, 2024
11
Certain recipients are required to notify HHS of a merger with or acquisition of any other
health care provider during the Payment Received Period (as defined in the Provider Relief
Fund Post Payment Notice of Reporting Requirements). How will recipients report this
information to HHS/HRSA? (Added 9/29/2021)
To streamline the process and minimize provider burden, this information will be collected in the
Provider Relief Fund Reporting Portal as part of the regular reporting process. Additional
reporting information will be forthcoming for impacted providers.
If a provider cannot expend its Provider Relief Fund payment by the applicable deadline to
use funds, what was the deadline to return the unused funds to the government? (Modified
9/29/2021)
The provider must return any unused funds to the government within 30 calendar days after the
end of the applicable Reporting Time Period or any associated grace period.
Can providers use Provider Relief Fund distributions to repay payments made under the
CMS Accelerated and Advance Payment (AAP) Program? (Added 10/9/2020)
No, this was not a permissible use of Provider Relief Fund payments.
For how long are the Terms and Conditions of the Provider Relief Fund applicable? (Added
6/19/2020)
All recipients receiving payments under the Provider Relief Fund will be required to comply
with the Terms and Conditions. Some Terms and Conditions relate to the provider’s use of the
funds, and thus they apply until the provider has exhausted these funds. Other Terms and
Conditions apply to a longer time period, for example, regarding maintaining all records
pertaining to expenditures under the Provider Relief Fund payment for three years from the date
of the final expenditure.
What was the definition of individuals with possible or actual cases of COVID-19? (Added
5/6/2020)
Unless the payment was associated with specific claims for reimbursement for COVID-19
testing or treatment provided on or after February 4, 2020 to uninsured patients, under the
Terms and Conditions associated with payment, providers were eligible only if they provided or
provided after January 31, 2020, diagnoses, testing or care for individuals with possible or
actual cases of COVID-19. HHS broadly viewed every patient as a possible case of COVID-19.
Not every possible case of COVID-19 was a presumptive case of COVID 19.
What was the definition of Executive Level II pay level, as referenced in the Terms and
Conditions? (Added 5/29/2020)
The Terms and Conditions stated that none of the funds appropriated in this title shall be used to
pay the salary of an individual, through a grant or other mechanism, at a rate in excess of
Executive Level II. The salary limitation was based upon the Executive Level II of the Federal
Executive Pay Scale. Effective January 5, 2020, the Executive Level II salary is $197,300. For
the purposes of the salary limitation, the direct salary was exclusive of fringe benefits and
indirect costs. The limitation only applied to the rate of pay charged to Provider Relief Fund
payments and other HHS awards. An organization who received Provider Relief Fund payments
may pay an individual’s salary amount in excess of the salary cap with non-federal funds.
February 16, 2024
12
ARP Rural Payments Terms and Conditions
Was there a set period of time in which providers must use ARP Rural payments to
cover allowable expenses or lost revenues attributable to COVID-19? (Modified
2/16/2024i) Yes. Providers have at least 12 months, and as much as 18 months, based on the
payment received date, to control and use the payments for expenses and lost revenues
attributable to coronavirus incurred during the Period of Availability.
The payment was considered received on the deposit date for automated clearing house
(ACH) payments, or the check cashed date for all other payments.
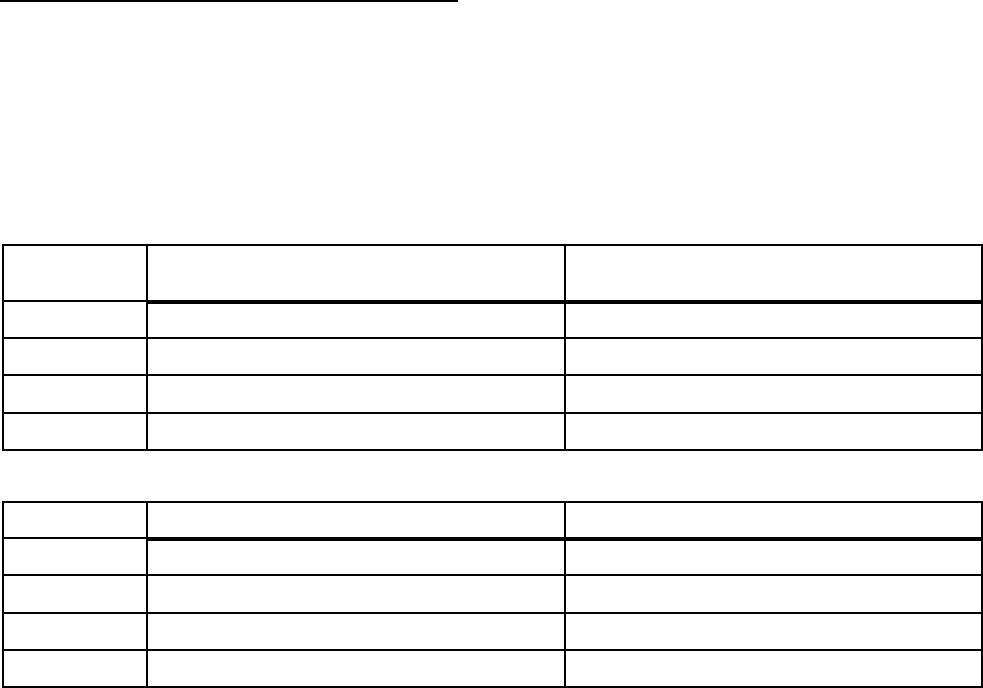
Period Payment Received Period
Period of Availability for Eligible
Expenses
Period 4
July 1, 2021 to December 31, 2021
January 1, 2020 to December 31, 2022
Period 5
January 1, 2022 to June 30, 2022
January 1, 2020 to June 30, 2023
Period 6 July 1, 2022 to December 31, 2022 January 1, 2020 to December 31, 2023
Period 7
January 1, 2023 to June 30, 2023
January 1, 2020 to June 30, 2024
Period
Payment Received Period
Period of Availability for Lost Revenues
Period 4
July 1, 2021 to December 31, 2021
January 1, 2020 to December 31, 2022
Period 5 January 1, 2022 to June 30, 2022 January 1, 2020 to June 30, 2023
Period 6
July 1, 2022 to December 31, 2022
January 1, 2020 to June 30, 2023
Period 7
January 1, 2023 to June 30, 2023
January 1, 2020 to June 30, 2023
ARP Rural recipients must use payments only for eligible expenses, including services rendered,
and lost revenues attributable to COVID-19, incurred by the end of the Period of Availability that
corresponds to the Payment Received Period. HRSA began distributing ARP Rural
payments on November 23, 2021. Providers were required to maintain supporting
documentation that demonstrated that costs were incurred during the Period of Availability, as
required under the Terms and Conditions. However, providers were not required to submit that
documentation when reporting. Providers must promptly submit copies of such supporting
documentation upon the request of the Secretary of HHS. Examples of costs incurred for an entity
using accrual accounting, during the Period of Availability include:
• Services that were received
• Renovation or construction that was completed
• Tangible property ordered, but need not have been delivered
For purchases of tangible items made using ARP Rural payments, the purchase did not need to be
in the provider’s possession (i.e., back ordered PPE, ambulance, etc.) to be considered an eligible
expense but the costs must be incurred by the end of the Period of Availability.
Providers must follow their basis of accounting (e.g., cash, accrual, or modified accrual) to
determine expenses. For projects that were a bundle of services and purchases of tangible items
that cannot be separated, such as capital projects, construction projects, or alteration and
renovation projects, the project costs cannot be reimbursed using Provider Relief Fund payments
unless the project was fully completed by the end of Period of Availability associated with the
Payment Received Period.
February 16, 2024
13
Recipients may use payments for eligible expenses or lost revenues incurred prior to receipt of
those payments (i.e., pre-award costs) so long as they were to prevent, prepare for, and respond
to coronavirus. Additionally, the opportunity to apply Provider Relief Fund payments
(excluding the Nursing Home Infection Control Distribution) and ARP Rural payments for lost
revenues were available up to June 30, 2023, the end of the quarter in which the COVID-19 Public
Health Emergency ended.
HHS reserved the right to audit Provider Relief Fund recipients now or in the future, and may
pursue collection activity to recover any ARP Rural payment amounts that have not been
supported by documentation or payments not used in a manner consistent with program
requirements or applicable law. All payment recipients must have attested to the Terms and
Conditions, which required maintaining documentation to substantiate that these funds were used
for health care-related expenses or lost revenues attributable to COVID-19.
What financial transactions were Reporting Entities required to report in order to satisfy
the requirement in the Terms and Conditions for ARP Rural payments that recipients
must notify HHS of a merger with or acquisition of any other health care provider during
the Payment Received Period within the Reporting Time Period? (Modified 12/9/2021)
The Terms and Conditions for ARP Rural payments required that recipients that received
payments greater than $10,000 notify HHS during the applicable Reporting Time Period of any
mergers with or acquisitions of any other health care provider that occurred within the Payment
Received Period. HRSA considered changes in ownership, mergers/acquisitions, and
consolidations to be reportable events.
If a merger or acquisition was planned before receiving ARP Rural payments, will health
care providers still need to report these activities? (Modified 12/9/2021)
If a Reporting Entity that received an ARP Rural payment undergoes a merger or acquisition
during the Payment Received Period, the Reporting Entity must report the merger or acquisition
during the applicable Reporting Time Period.
What type of review will HRSA do after a merger or acquisition has been reported by
recipients of an ARP Rural payment? (Modified 12/9/2021)
If a Reporting Entity that received an ARP Rural payment indicates when they report on the use
of funds that they have undergone a merger or acquisition during the applicable Payment
Received Period, this information will be a component that is factored into whether an entity is
audited.
Can an applicant allocate ARP Rural payments to its non-rural subsidiaries? (Added
9/29/2021)
No. As required by the Terms and Conditions, control and use of the ARP Rural payment must
be delegated to the provider associated with the billing TIN that was eligible for the ARP Rural
payment. The provider cannot not transfer or allocate the ARP Rural payment to another entity
not associated with the billing TIN.
What can ARP Rural payment recipients use funds for?
(Added 9/29/2021)
Payment recipients must have certified that the payment were only be used to prevent, prepare
for, and respond to COVID-19, and that the payment shall reimburse the Recipient only for
health care related expenses or lost revenues that were attributable to coronavirus not
reimbursed by other sources or that other sources are obligated to reimburse.
February 16, 2024
14
Lost revenues attributable to the coronavirus may include other income not derived from
delivery of health care services that was customarily used to support the delivery of health care
services by the recipient. Examples include, but were not limited to, decreases in tax revenue
and non-federal, government grant funding. In accounting for such lost revenues, the recipient
must document the historical sources and uses of these revenues. For more information about
lost revenues, please review HRSA’s Lost Revenues Guide available at
https://www.hrsa.gov/sites/default/files/hrsa/provider-relief/prf-lost-revenues-guide.pdf.
Additionally, expenditures to prevent, prepare for, and respond to coronavirus may include those
incurred expenses necessary to maintain health care delivery capacity by the recipient or to
increase health care delivery capacity in the future as informed by community health needs. This
may include outreach and education about the vaccine for the provider’s staff, as well as the
general public.
Ownership Structures and Financial Relationships
If, as a result of the sale of a healthcare facility, the TIN that received a Provider Relief Fund
payment is no longer providing health care services as of January 31, 2020, is it required to
return the payment? (Modified 7/1/2021)
Yes. If, as a result of the sale of a healthcare facility, the TIN that received a Provider Relief
Fund payment did not provide diagnoses, testing, or care for individuals with possible or actual
cases of COVID-19 on or after January 31, 2020, the provider must reject the payment. The
Provider Relief Fund Payment Attestation Portal guides providers through the attestation
process to reject the attestation and return the payment to HRSA.
Can a parent organization transfer General Distribution Provider Relief Fund payments to
its subsidiaries? (Modified 3/31/2021)
Yes, a parent organization can accept and allocate General Distribution funds at its discretion to
its subsidiaries, as long as the Terms and Conditions were met. Eligible health care entities,
including those that were parent organizations must substantiate that these funds were used for
health care-related expenses or lost revenue attributable to COVID-19, and that those expenses
or losses were not reimbursed from other sources and other sources were not obligated to
reimburse them.
Can a parent organization allocate Provider Relief Fund General Distribution to
subsidiaries that do not report income under their parent’s employee identification number
(EIN)? (Modified 3/31/2021)
Yes, as long as the Terms and Conditions were met. The parent organization (an eligible health
care entity) must substantiate that these funds were used for health care-related expenses or lost
revenue attributable to COVID-19, and that those expenses or losses were not reimbursed from
other sources and other sources were not obligated to reimburse them.
Must a parent organization that received a Provider Relief Fund Targeted Distribution on
behalf of a subsidiary in which it is has a direct ownership relationship remit the payment
to the subsidiary? (Modified 2/16/2024)
No. The parent organization may allocate the Targeted Distribution to any of its subsidiaries that
were eligible health care providers in accordance with the Consolidated Appropriations Act,
2021.
February 16, 2024
15
Can a parent organization with a direct ownership relationship with a subsidiary that
received a Provider Relief Fund Targeted Distribution payment control and allocate that
Targeted Distribution payment among other subsidiaries that were not themselves eligible
and did not receive a Targeted Distribution (i.e., Skilled Nursing Facility, Safety Net
Hospital, Rural, Tribal, High Impact Area) payment? (Modified 2/16/2024)
Yes, in accordance with the Consolidated Appropriations Act, 2021. The parent organization
may allocate the Targeted Distribution up to its pro rata ownership share of the subsidiary to any
of its other subsidiaries that were eligible health care providers. To determine whether an entity
is the parent organization, the entity must follow the methodology used to determine a subsidiary
in their financial statements. If none, the entity with a majority ownership (greater than 50
percent) will be considered the parent organization.
Auditing and Reporting Requirements
Were Provider Relief Fund payments to commercial (for-profit) organizations subject to
Single Audit in conformance with the requirements under 45 CFR 75 Subpart F? (Modified
2/16/2024)
Commercial (for-profit) organizations that expend $750,000 or more in annual awards have two
options under 45 CFR §75.216(d) and §75.501(i): 1) a financial related audit of the award or
awards conducted in accordance with Government Auditing Standards; or 2) an audit in
conformance with the requirements of 45 CFR 75 Subpart F (single or program-specific audit).
Non-Federal entities that expended $750,000 or more must have a single audit conducted in
accordance with §75.514 except when it elects to have a program-specific audit conducted in
accordance with §75.501(c).
To determine whether an audit in accordance with 45 CFR 75 Subpart F is required (i.e., annual total
awards expended are $750,000 or more), Provider Relief Fund and American Rescue Plan Rural
Distribution (93.498) and HRSA COVID-19 Claims Reimbursement for the Uninsured Program and
the COVID-19 Coverage Assistance Fund (93.461) must be included. Additionally, the Provider
Relief Fund payments included in the $750,000 was based on when the payment was received, the
specific period of availability, and aligned with the Provider Relief Fund Reporting Portal timelines.
Review the applicable Compliance Supplement at https://www.hrsa.gov/provider-relief/reporting-
auditing/audit-requirements for detailed information.
Commercial organizations subject to single audit requirements that received Provider Relief
Fund payments are highly encouraged to submit their audits electronically to the Commercial
Audit Reporting Portal at https://commercialaudit.hrsa.gov/s/login/. Commercial organizations
subject to single audit requirements not registered in the PRF Reporting Portal must submit their
Can my organization get an extension to the submission due date for Single Audits
conducted under 45 CFR Part 75? (Modified 2/16/2024)
HRSA followed federal guidelines set by the Office of Management and Budget (OMB) and did
not set requirements or provided extensions for the submission of the Single Audits. The due date
for an Audit was the earlier of 30 days after receipt of the auditor’s report(s), or 9 months after
the end of the audit period, which was likely your organization’s fiscal year end. (45 CFR 75.512).

February 16, 2024
16
OMB granted on October 20, 2022, under the Stafford Act, a six-month extension for all
single audits that covered recipients in the following areas declared as major disaster-
affected areas impacted by Hurricanes Fiona and Ian as well as the record storm occurring in
the following areas: Puerto Rico (September 18, 2022), Alaska (September 23, 2022),
Florida (September 29, 2022), South Carolina (September 29, 2022) and North Carolina
(October 1, 2022). Consistent with these declarations, OMB has granted a six-month
extension for all single audits that cover recipients in the affected areas and have due dates
between September 18, 2022 and December 31, 2022.
Additionally, OMB waived the 30-day deadline for any 2023 submissions with fiscal periods ending
between January 1, 2023 and September 30, 2023 and any 2022 submissions with fiscal periods ending
between January 1, 2022 and October 31, 2022. Requirement 2 CFR 200.512(1) stating that single
audits were due 30 days after receipt of the auditor’s report(s) was waived and considered on time if
they were submitted within nine months after their fiscal period end date.
If you have questions about this extension or want to inform HRSA you will be taking advantage
of this flexibility, please email HRSA's Division of Financial Integrity at [email protected]v.
If you have questions about the Single Audit for Provider Relief Fund, please email your
questions to Pr[email protected].
If a Reporting Entity had unallowable costs identified during an audit, can these
unallowable or offset costs be accounted for in a subsequent reporting period?
(Modified 10/18/2022)
Yes. Due to the cumulative nature of lost revenues, any lost revenues adjustments may be made
in subsequent reporting periods. If an unallowable expense was “replaced” by unreimbursed lost
revenues for use of funds purposes, the Reporting Entity should ensure that the lost revenues
reported in subsequent reports are deducted to avoid “double dipping.” Reporting Entities should
maintain appropriate documentation to support the deduction from the report.
If a Reporting Entity received a finding during an audit (including Single Audit), may it
amend its previously submitted report to resolve the finding? (Modified 2/16/2024)
No. The Reporting Entity may not amend its report after the reporting period has passed. However,
providers have the following options available:
• For providers required to report in subsequent reporting periods and that chooses to replace its
unallowable expense with its unreimbursed lost revenues in the reporting period in question.
o Providers would update their previously entered lost revenues information in the next
available reporting period.
o Providers are required to enter a justification for the change with a description
(including the notation that they were making this change to replace an unallowable
expense as part of their audit finding corrective action plan, adding the audit and/or
finding number).
• For providers that were not required to report in subsequent reporting period and chose to
replace its unallowable expenses with its unreimbursed lost revenues in the reporting period
in question.
In the corrective action plan, the provider would indicate that the unallowable expense was “replaced”
by unreimbursed lost revenues.
February 16, 2024
17
If a Reporting Entity had unallowable costs identified during an audit, can auditors
replace the unallowable costs (e.g. questioned costs) with unreimbursed lost revenues
noted in the submitted report being audited? (Added 2/16/2024)
No. Questioned cost per 45 CFR §75.2, means a cost that was questioned by the auditor because
of an audit finding:
1) Which resulted from a violation or possible violation of a statute, regulation, or the terms
and conditions of a Federal award, including for funds used to match Federal funds;
2) Where the costs, at the time of the audit, are not supported by adequate documentation; or
3) Where the costs incurred appear unreasonable and do not reflect the actions a prudent
person would take in the circumstances.
It was the responsibility of the Reporting Entity to address questioned costs through its corrective action
plan and HRSA to evaluate the Reporting Entity’s corrective action plan to determine its
appropriateness. Auditors must associate questioned costs with the specific award number(s) (AL) in the
audit finding detail and must not perform any offset, which results in the reduction of questioned costs.
I am having trouble submitting my commercial audit report in the Commercial Audit
Reporting Portal. (Added 2/16/2024)
The Provider Relief Bureau (PRB) Commercial Audit Reporting Portal had two user groups: 1) Provider
and 2) Audit Report Submitter.
1) The "Provider" user group contained all Provider Relief Fund (PRF) Reporting Portal users that
registered on behalf of their respective commercial entities. Providers used the same login
credentials (i.e., username, password, two-factor authentication) as the PRF Reporting Portal to
access the portal.
2) The "Audit Report Submitter" user group contained users created by the Provider user group to
allow audit report submissions on their commercial entity's behalf.
Commercial entities can only submit their audit reports using the Audit Report Submitters user group
login credentials. The Provider user group must create an Audit Report Submitter user account to
submit an audit report. Instructions to create an Audit Report Submitter are located in Section 3.6 STEP
2 – MANAGE AUDIT REPORT SUBMITTER ASSIGNMENT. Once the Audit Report Submitter user
account was created, the Audit Report Submitter user can follow the instructions in Section 4 USING
THE PORTAL – AUDIT REPORT SUBMITTER USER GROUP EXPERIENCE to submit an audit
report in the portal. Note, an Audit Report Submitter user profile must be associated with an email
address not used previously for PRF reporting purposes. A different email address must be used
to successfully add the Audit Report Submitter, which would then allow for audit report
submittal.
February 16, 2024
18
Do commercial organizations that did not submit their audit through the Federal Audit
Clearinghouse get an extension to the submission due date for their audit? (Modified
2/16/2024)
HRSA followed federal guidelines set by the Office of Management and Budget (OMB).
Both commercial organizations and non-federal entities are granted a six-month extension to the
submission of audits that have a fiscal-year end through June 30, 2021. As a reminder, audits are
due 30 calendar days after receipt of the audit report or nine months after the end of the audit period
– whichever is earlier. On March 19, 2021, the Office of Management and Budget (OMB) Memo
(M-21-20) extended the deadline for Single Audit submissions to six months beyond the normal
due date, and on October 28, 2021, HHS granted the same extension to commercial
organizations.
OMB granted on October 20, 2022, under the Stafford Act, a six-month extension for all
single audits that cover recipients in the following areas declared as major disaster-affected
areas impacted by Hurricanes Fiona and Ian as well as the record storm occurring in Alaska:
Puerto Rico (September 18, 2022), Alaska (September 23, 2022), Florida (September 29,
2022), South Carolina (September 29, 2022) and North Carolina (October 1, 2022).
Consistent with these declarations, OMB has granted a six-month extension for all single
audits that cover recipients in the affected areas and have due dates between September 18,
2022 and December 31, 2022. HHS granted the same extension to commercial organization.
Additionally, OMB waived the 30-day deadline for any 2023 submissions with fiscal periods
ending between January 1, 2023 and September 30, 2023 and any 2022 submissions with fiscal
periods ending between January 1, 2022 and October 31, 2022.
Requirement 2 CFR
§200.512(1) stating that single audits were due 30 days after receipt of the auditor’s report(s) was
waived and considered on time if they were submitted within nine months after their fiscal period
end date.
If you have questions about this extension or want to inform HRSA you will be taking advantage
of this flexibility, please email HRSA's Division of Financial Integrity at [email protected].
If you have questions about the audit in accordance with 45 CFR §75.501 for Provider Relief Fund
payments, please email your questions to ProviderReliefContact@hrsa.gov.
A non-profit corporation has multiple subsidiaries, including a for-profit subsidiary, that
were consolidated for financial reporting purposes. Can the Single Audit of the non-
profit corporation include the expenditures of federal awards of the for-profit subsidiary?
(Added 9/13/2021)
Yes, the non-profit corporation can include the expenditures of federal awards of its for-profit
subsidiary in its Single Audit. Federal regulations at 45 CFR §75.501 or “Uniform
Administrative Requirements, Cost Principles, and Audit Requirements for HHS Awards”
(Uniform Guidance) permitted a for-profit subsidiary to be included in the Single Audit, as long
as the for-profit subsidiary’s operations were included in the consolidated financial statements
and program expenditures were included in the Schedule of Expenditure of Federal Awards
(SEFA). The inclusion of the for-profit subsidiary in the consolidated entity’s Single Audit
would have met the for-profit entity’s responsibility for an audit under 45 CFR §75.501(i).
February 16, 2024
19
A for-profit corporation had multiple subsidiaries that were consolidated for financial
reporting purposes, and some of the subsidiaries also reported separately. Can the for-
profit entity fulfill the 45 CFR §75.501 audit requirements by having one financial-related
audit of all HHS awards in accordance with Government Auditing Standards that
incorporates all entities that are consolidated under Generally Accepted Accounting
Principles (GAAP)? (Added 9/13/2021)
Yes, the for-profit entity can have one financial-related audit of all HHS awards that incorporates
all entities. 45 CFR §75.501(i) audit requirements permit this approach.
Multiple for-profit entities under common control issue combined financial statements.
Can each of the for-profit entities fulfill the 45 CFR §75.501 audit requirements by having
one financial-related audit of all HHS awards in accordance with Government Auditing
Standards that incorporates each of the entities? (Added 9/13/2021)
Yes, multiple for-profit entities under common control that issue combined financial statements
can have one financial-related audit of all HHS awards that incorporated each of the entities. 45
CFR §75.501(i) audit requirements permit this approach.
When should Provider Relief Fund expenditures and/or lost revenue be reported on a for-
profit entity’s Schedule of Expenditures of Federal Awards (SEFA) or other schedules
prepared for the financial-related audit option conducted in accordance with Government
Auditing Standards? (Added 8/30/2021)
Similar to non-federal entities, for-profit entities included Provider Relief Fund expenditures
and/or lost revenues on their SEFAs or other schedules for fiscal year ends (FYEs) ending on or
after June 30, 2021.
How did a for-profit entity determine the amount of expenditures and/or lost revenues to
report on its SEFA or other schedules prepared for the financial-related audit option
conducted in accordance with Government Auditing Standards (for FYEs ending on or
after June 30, 2021)? (Modified 2/16/2024)
Similar to non-federal entities, a for-profit entity’s SEFA (or other schedules) was linked to its
report submissions to the Provider Relief Fund Reporting Portal. Therefore, the timing of
reporting of Provider Relief Fund payments on the SEFA (or other schedules) were as follows:
•
For a FYE of June 30, 2021, and through FYEs of December 30, 2021, recipients were
to report on the SEFA, the total expenditures and/or lost revenues from the PRF
Reporting Portal Period 1 PRF report submission.
•
For a FYE of December 31, 2021, and through FYEs of June 29, 2022, recipients were
to report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 1 and Period 2 PRF report submissions.
•
For a FYE of June 30, 2022, and through FYEs of December 30, 2022, recipients were
to report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 2 and Period 3 PRF report submission.
•
For a FYE of December 31, 2022, and through FYEs of June 29, 2023, recipients were
to report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 3 and Period 4 PRF report submissions.
•
For a FYE of June 30, 2023, and through FYEs of December 30, 2023, recipients were
to report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 4 and Period 5 PRF report submission.

February 16, 2024
20
•
For a FYE of December 31, 2023, and through FYEs of June 29, 2024, recipients were
to report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 5 and Period 6 PRF report submissions.
For FYEs on or after June 30, 2024, reporting guidance for the SEFA or other schedules will be
provided at a later date.
When should Provider Relief Fund expenditures and/or lost revenue be reported on a non-
federal entity’s Schedule of Expenditures of Federal Awards (SEFA)? (Modified 2/16/2024)
Non-federal entities must begin including Provider Relief Fund expenditures and/or lost
revenues on their SEFAs for fiscal year ends (FYEs) on or after June 30, 2021. Please refer to
the Office of Management and Budget Compliance Supplement, available at
https://www.whitehouse.gov/wp- content/uploads/2021/08/OMB-2021-Compliance-
Supplement_Final_V2.pdf, for additional information.
How will a non-federal entity determine the amount of expenditures and/or lost revenues to
report on its SEFA for FYEs ending on or after June 30, 2021? (Modified 2/16/2024)
A non-federal entity’s SEFA reporting is linked to its report submissions to the Provider Relief
Fund (PRF) Reporting Portal. Therefore, the timing of SEFA reporting of PRF will be as
follows:
•
For a FYE of June 30, 2021, and through FYEs of December 30, 2021, recipients are to
report on the SEFA, the total expenditures and/or lost revenues from the PRF
Reporting Portal Period 1 PRF report submission.
•
For a FYE of December 31, 2021, and through FYEs of June 29, 2022, recipients are to
report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 1 and Period 2 PRF report submissions.
•
For a FYE of June 30, 2022, and through FYEs of December 30, 2022, recipients are
to report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 2 and Period 3 PRF report submission.
•
For a FYE of December 31, 2022, and through FYEs of June 29, 2023, recipients are to
report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 3 and Period 4 PRF report submissions.
•
For a FYE of June 30, 2023, and through FYEs of December 30, 2023, recipients are to
report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 4 and Period 5 PRF report submission.
•
For a FYE of December 31, 2023, and through FYEs of June 29, 2024, recipients are to
report on the SEFA, the total expenditures and/or lost revenues from both the PRF
Reporting Portal Period 5 and Period 6 PRF report submissions. For FYEs on or after
June 30, 2024, SEFA reporting guidance will be provided at a later date.
February 16, 2024
21
Will HHS provide guidance to certified public accountants and those organizations that
providers will rely on to perform audits? (Modified 2/16/2024)
The only guidance HHS provided to auditors was through the Office of Management and
Budget Compliance Supplement. Entities subject to Single Audit requirements can find
guidance in the applicable Compliance Supplement, which is available at
https://www.whitehouse.gov/omb/office-federal-financial-management/.
The applicable
AL numbers include 93.498 [Provider Relief Fund] and 93.461 [HRSA COVID- 19 Uninsured
Program].
Were Provider Relief Fund payments to non-Federal entities (states, localgovernments,
Indian tribes, institutions of higher education, and nonprofit organizations) subject to
Single Audit? (Modified 2/16/2024)
Provider Relief Fund General and Targeted Distribution payments (AL 93.498) and Uninsured
Testing and Treatment reimbursement payments (AL 93.461) to non-Federal entities are
Federal awards and must be included in determining whether an audit in accordance with 45
CFR Part 75, Subpart F is required (i.e., annual total federal awards expended are
$750,000 or more). Additionally, the Provider Relief Fund payments included in determining whether
an audit was required were based on when the payments were received, the specific period of
availability, and aligned with the Provider Relief Fund Reporting Portal timelines. Review the
applicable Compliance Supplement at https://www.hrsa.gov/provider-relief/reporting-auditing/audit-
requirements for detailed information.
Effective October 1, 2023, audit reports must be submitted through the new Federal Audit Clearinghouse
(FAC) hosted by the General Services Administration (GSA), including all single audits for entities with
2023 fiscal year end dates.
Audit data submitted by non-Federal entities in 2022 and prior will be available via the Census Bureau
through the end of 2023. Beginning January 2024, historic single audit data will be available on the new
FAC, and the Census Bureau will close down the distribution of historical data at that time. Visit
https://www.fac.gov/ for more information.
(Requirements for audit of payments to commercial organizations are discussed in a separate
question.)
Use of Funds
Can Reporting Entities continue to put Provider Relief Fund and/or ARP Rural payments
toward lost revenues attributable to coronavirus or COVID-19 once the Public Health
Emergency ends? (Modified 5/5/2023)
The opportunity to apply Provider Relief Fund payments (excluding the Nursing Home Infection
Control Distribution) and ARP Rural payments for lost revenues will be available up to June 30,
2023, the end of the quarter in which the COVID-19 Public Health Emergency ends.
How did a Reporting Entity determine whether an expense was eligible for reimbursement
through the Provider Relief Fund or ARP Rural Distribution? (Modified 5/5/2023)
To be considered an allowable expense under the Provider Relief Fund or ARP Rural
Distribution, the expense must be used to prevent, prepare for, and respond to coronavirus.
Provider Relief Fund and ARP Rural payments may also be used for lost revenues attributable to
the coronavirus up to June 30, 2023, the end of the quarter in which the COVID-19 Public

February 16, 2024
22
Health Emergency ends. Reporting Entities are required to maintain adequate documentation to
substantiate that these funds were used for health care-related expenses or lost revenues
attributable to coronavirus or COVID-19, and that those expenses or losses were not reimbursed
from other sources and other sources were not obligated to reimburse them.
Reporting Entities were not required to submit that documentation when reporting. Providers
were required to maintain supporting documentation which demonstrated that costs were
incurred during the Period of Availability. The Reporting Entity was responsible for ensuring
that adequate documentation was maintained.
How did cost-based reimbursement relate to my Provider Relief Fund and/or ARP Rural
payment? (Modified 10/27/2022)
Recipient must follow CMS instructions for completion of cost reports available at
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Paper-Based-Manuals-
Items/CMS021935.
Under cost-based reimbursement, the payer agreed to reimburse the provider for the costs
incurred in providing services to the insured population. If the full cost were reimbursed based
upon this method, there is nothing eligible to report as a Provider Relief Fund or ARP Rural
expense attributable to coronavirus because the expense was fully reimbursed by another source.
Provider Relief Fund and/or ARP Rural payments cannot be used to cover costs that were
reimbursed from other sources or that other sources are obligated to reimburse. Therefore, if
Medicare or Medicaid made a payment to a provider based on the provider’s Medicare or
Medicaid cost, such payment generally was considered to fully reimburse the provider for the
costs associated with providing care to Medicare or Medicaid patients and no payment from the
Provider Relief Fund or ARP Rural Distribution would be available for those identified Medicare
and Medicaid costs. Per its authorizing statutes, Provider Relief Fund resources may only be
used for allowable expenses and lost revenues attributable to coronavirus, and may only be
reimbursed once. Reporting Entities should work with their accountants and maintain
documentation demonstrating that any reported health care expenses that Provider Relief Fund
and/or ARP Rural payments were applied to were not reimbursed by any other source, or
obligated to be reimbursed by another source.
However, in cases where a ceiling is applied to the cost reimbursement, or the costs were not
reimbursed under cost-based reimbursement (such as costs for care to commercial payer
patients), and the reimbursed amount by Medicare or Medicaid does not fully cover the actual cost,
those non-reimbursed costs were eligible for reimbursement under the Provider Relief Fund or
ARP Rural Distribution.
Must HRSA Health Center Program-funded health centers and look-alikes fully draw down
Health Center Program COVID-19 Supplemental grant funding received from HRSA
before using Provider Relief Fund or ARP Rural payments for eligible expenses and lost
revenues attributable to coronavirus? (Modified 10/27/2022)
Yes, Health Center Program COVID-19 Grants awarded to FQHCs and FQHC Look-Alikes for
costs for expenses or losses that were potentially eligible for payments under the Provider Relief
Fund and/or ARP Rural Distribution would need to be fully drawn down before Provider Relief
Fund or ARP Rural payments could be used during the applicable period of availability. The
Provider Relief Fund and ARP Rural Distribution required that payments not be used to
reimburse expenses or lost revenues that have been reimbursed from other sources or that other
February 16, 2024
23
sources are obligated to reimburse. If FQHCs or FQHC Look-alikes have incurred expenses or
lost revenues attributable to coronavirus that these grant awards do not cover, they may use
Provider Relief Fund or ARP Rural payments towards those expenses or losses. Grant funding
may be awarded to support either broad or specific allowable uses, depending on the terms and
conditions of the award. Recipients must use grant funding awarded by HRSA for the purposes
(as budgeted) approved by HRSA. Should those costs also be eligible for payment under the
Provider Relief Fund or ARP Rural Distribution, a Health Center Program-funded health center
or look-alike must use their grant funds before utilizing Provider Relief Fund or ARP Rural
payments.
If rent or mortgages were paid during the applicable period of availability but staff worked
remotely, could those expenses be claimed as eligible expenses? (Modified 10/27/2022) Health
care-related operating expenses were limited to costs incurred to prevent, prepare for, and respond
to coronavirus. The amount of mortgage or rent eligible for Provider Relief Fund or ARP Rural
reimbursement was limited to that which was incurred to prevent, prepare for, and respond to
coronavirus or COVID-19. Providers are required to maintain documents to substantiate that these
funds were used for health care-related expenses attributable to coronavirus, and that those
expenses or losses were not reimbursed from other sources and other sources were not obligated
to reimburse them. The burden of proof is on the provider to ensure that documentation is
maintained to show that expenses are to prevent, prepare for, and respond to coronavirus.
If a Reporting Entity anticipated that it would receive coronavirus-related assistance, such
as from FEMA, but that assistance was not received, should that be accounted for in its
Provider Relief Fund and ARP Rural reporting? (Modified 10/27/2022)
Provider Relief Fund and ARP Rural payments may have been applied to expenses or lost
revenues attributable to coronavirus, after netting the other funds received or obligated to be
received which offset those expenses. If a provider submitted an application to FEMA, but had not
yet received the FEMA funds, the provider should not have reported the requested FEMA
amounts in the Provider Relief Fund and/or ARP Rural report. If FEMA funds were received
during the same Payment Received Period in which provider reported on use of Provider Relief
Fund and/or ARP Rural payments, the receipt and application of each payment type is required in
the Provider Relief Fund and/or ARP Rural reporting process. If an entity received a retroactive
payment from FEMA that overlapped with the period of availability, the entity must not use the
FEMA payment on expenses or lost revenues already reimbursed by Provider Relief Fund or ARP
Rural payments.
Must the Reporting Entity have been in receipt of purchases made using Provider Relief
Fund Payments and/or ARP Rural in order for the expense to be considered eligible for
reimbursement? (Modified 10/27/2022)
No. For purchases of tangible items made using Provider Relief Fund and/or ARP Rural
payments, the purchase does not need to be in the Reporting Entity’s possession (i.e.,
backordered personal protective equipment, capital equipment) to be considered an eligible
expense. However, the costs must have been incurred before the Deadline to Use Funds.
Providers must follow their basis of accounting (e.g., cash, accrual, or modified accrual) to
determine expenses.
Could providers have allocated parent overhead costs to the entities that received Provider
Relief Funds and/or ARP Rural? (Modified 10/27/2022)
Yes, providers that already had a cost allocation methodology in place at the time they received
February 16, 2024
24
funds, may allocate normal and reasonable overhead costs to their subsidiaries, which may be an
eligible expense if attributable to coronavirus or COVID-19 and not reimbursed from other
sources.
How would I have determined if expenses should be considered “expenses attributable to
coronavirus not reimbursed by other sources?” (Modified 10/27/2022)
Expenses attributable to coronavirus may include items such as supplies, equipment, information
technology, facilities, personnel, and other health care-related costs/expenses for the period of
availability. The classification of items into categories should align with how Provider Relief Fund
and/or ARP Rural payment recipients maintain their records. Providers can identify their expenses
attributable to coronavirus, and then offset any amounts received through other sources, such as
direct patient billing, commercial insurance, Medicare/Medicaid/Children’s Health Insurance
Program (CHIP); other funds received from the federal government, including the Federal
Emergency Management Agency (FEMA); the Provider Relief Fund COVID-19 Claims
Reimbursement to Health Care Providers and Facilities for Testing, Treatment, and Vaccine
Administration for the Uninsured (Uninsured Program); the COVID-19 Coverage Assistance Fund
(CAF); and the Small Business Administration (SBA) and Department of the Treasury’s Paycheck
Protection Program (PPP). Provider Relief Fund and/or ARP Rural payments may be applied to
the remaining expenses or costs, after netting the other funds received or obligated to be received
which offset those expenses. The Provider Relief Fund and ARP Rural Distribution permitted
reimbursement of expenses related to coronavirus provided those expenses have not been
reimbursed from other sources or that other sources are not obligated to reimburse.
Could Reporting Entities have claimed the time spent by staff and director-level resources
on COVID-19-specific matters, such as participating in task forces or preparing their
health care organization’s COVID-19 response, that they would not have otherwise spent
time on in the absence of the pandemic? (Modified 10/27/2022)
Time spent by staff on COVID-19-specific matters may be an allowable cost attributable to
coronavirus so long as it was not reimbursed or obligated to be reimbursed by other sources. If
the personnel salaries were reimbursed by any other source of funding they cannot be also
reimbursed by the Provider Relief Fund or ARP Rural Distribution. In addition, no one individual
may be allocated as greater than one full-time equivalent (FTE) across all sources of funding. All
costs must have been tangible expenses (not opportunity costs) and supported by documentation.
The Reporting Entity must maintain appropriate records and cost documentation including, as
applicable, documentation described in 45 CFR §75.302 – Financial management and 45 CFR §
75.361 through §75.365 – Record Retention and Access, and other information required by future
program instructions to substantiate the reimbursement of costs under this award. The Recipient
must promptly submit copies of such records and cost documentation upon the request of the
Secretary, and the Reporting Entity agrees to fully cooperate in all audits the Secretary, Inspector
General, or Pandemic Response Accountability Committee conducts to ensure compliance with
these Terms and Conditions.
Were there any restrictions on how hospitals that received Medicaid disproportionate share
hospital (DSH) payments could use Provider Relief Fund General and Targeted Distribution
payments or ARP Rural payment? (Modified 10/27/2022)
Yes. Providers may not use Provider Relief Fund or ARP Rural payments to reimburse expenses
or losses that have been reimbursed from other sources or that other sources are obligated to
reimburse. Therefore, if a hospital has received Medicaid DSH payments for the uncompensated

February 16, 2024
25
costs of furnishing inpatient and/or outpatient hospital services to Medicaid beneficiaries and to
individuals with no source of third party coverage for the services, these expenses would be
considered reimbursed by the Medicaid program and would not be eligible to be covered by
money received from a General or Targeted Distribution or ARP Rural payment. For more
information on the calculation of the Medicaid hospital-specific DSH limit, see
https://www.medicaid.gov/state-resource-center/downloads/covid-19-faqs.pdf.
Was the interest earned on Provider Relief Fund or ARP Rural payments considered a
reportable revenue source to HHS? (Modified 10/27/2022)
Yes, if funds were held in an interest-bearing account, they would be considered reportable
revenue. If interest was earned on Provider Relief Fund disbursements that the Reporting Entity
expended in full, the interest amounts may be retained and applied toward a reportable use of funds.
If interest is earned on funds that are only partially expended, the interest on remaining unused
funds must be calculated, reported, and returned.
Recipients of ARP Rural and PRF Phase 4 payments are required to hold those payments in an
interest-bearing account per the Terms and Conditions. Reporting Entities must report on the
dollar value of interest earned on all retained ARP Rural payments, separately from Provider
Relief Fund Distributions. The total reportable amount of ARP Rural and Provider Relief Fund
payments will include the interest earned.
Were expenses related to securing and maintaining adequate personnel reimbursable
expenses under the Provider Relief Fund and/or ARP Rural? (Modified 10/27/2022)
Yes, expenses incurred by providers to secure and maintain adequate personnel, such as offering
hiring bonuses and retention payments, child care, transportation, and temporary housing, were
deemed to be COVID-19-related expenses if the activity generating the expense was newly
incurred after the declaration of the Public Health Emergency and the expenses were necessary to
secure and maintain adequate personnel.
Were outsourced or third-party vendor services that enabled access to health care services
reimbursable expenses under the Provider Relief Fund or ARP Rural Distribution?
(Modified 10/27/2022)
Yes, outsourced or third-party vendor services that enable sustained access to health care services
and daily operations, such as food/patient nutrition services, facilities management, laundering, and
disinfection/anti-contamination services, were considered reimbursable expenses if they are
attributable to coronavirus.
Could providers have used Provider Relief Fund or ARP Rural payments to pay taxes? (Modified
10/27/2022)
Yes. HHS considers taxes imposed on Provider Relief Fund or ARP Rural payments to be
“healthcare related expenses attributable to coronavirus” that are reimbursable with Provider
Relief Fund or ARP Rural money, except for Nursing Home Infection Control Distribution
payments.
Funds from the Federal Emergency Management Administration (FEMA) are generally
intended to be the last source of reimbursement, however, the Post-Payment Notice of
Reporting Requirements indicated that FEMA funds would be applied prior to the
February 16, 2024
26
Provider Relief Fund and ARP Rural distributions. In which order should governmental
funding sources be applied and reported? (Modified 10/27/2022)
As it relates to expenses, providers identify their health care-related expenses, and then apply any
amounts received through other sources (e.g., direct patient billing, commercial insurance,
Medicare/Medicaid, reimbursement from the Provider Relief Fund COVID-19 Claims
Reimbursement to Health Care Providers and Facilities for Testing, Treatment, and Vaccine
Administration for the Uninsured, or funds received from FEMA or SBA/Department of
Treasury’s Paycheck Protection Program) that offset the health care-related expenses. Provider
Relief Fund and/or ARP Rural payments may be applied to the remaining expenses or cost, after
netting the other funds received or obligated to be received which offset those expenses.
Would the Provider Relief Fund and/or ARP Rural Distribution have limited qualifying
expenses for capital equipment purchases to 1.5 years of depreciation, or could providers
fully expense capital equipment purchases? (Modified 10/27/2022)
Expenses for capital equipment and inventory could be fully expensed only in cases where the
purchase was directly related to prevent, prepare for and respond to the coronavirus. Examples of
these types of equipment and inventory expenses include:
• Ventilators, computerized tomography scanners, and other intensive care unit- (ICU)
related equipment put into immediate use or held in inventory
• Masks, face shields, gloves, gowns
• Biohazard suits
• General personal protective equipment
• Disinfectant supplies
What was included in use of funds for salaries and employee compensation? (Modified
10/27/2022)
Direct employee (full and part-time), contract labor, and temporary worker expenses are eligible
expenses provided they are not reimbursed from other sources, or only the incremental
unreimbursed amounts are claimed.
The Terms and Conditions associated with Provider Relief Fund and ARP Rural payment do not
permit recipients to use Provider Relief Fund and/or ARP Rural payments to pay any salaries at a
rate in excess of Executive Level II which is currently set at $197,300 (2020), $199,300 (2021),
$203,700 (2022), $212,100 (2023) For the purposes of the salary limitation, the direct salary is
exclusive of fringe benefits and indirect costs. The limitation only applies to the rate of pay
charged to Provider Relief Fund and/or ARP Rural payments and other HHS awards. An
organization receiving Provider Relief Fund and/or ARP Rural payments may pay an individual’s
salary amount in excess of the salary cap with non-federal funds.
An example of how this Executive Level II Salary cap is applied to aggregated personnel
expenses is shown below. Reimbursement from other sources is applied in Step Two. Providers
should apply reasonable assumptions when estimating the portion of personnel costs that are
reimbursed from other sources.
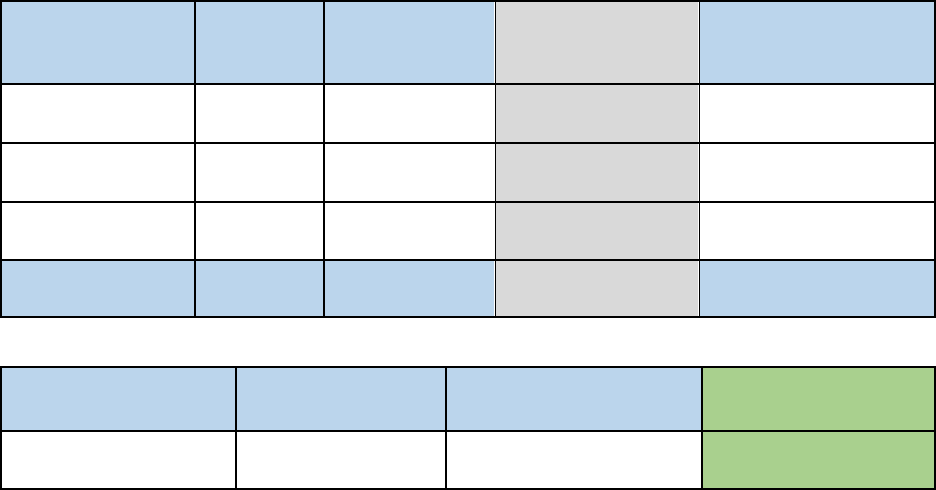
February 16, 2024
27
Step One
Personnel
Category
Number of
Personnel
Personnel
Expenses
Personnel
Expenses (Below
Salary Cap)
Ineligible for Federal
Reimbursement
Medical Director 1 $250,000 $197,300 $52,700
Registered
Nurses
25 $1,250,000 $1,250,000 0
Security 2 $80,000 $80,000 0
28 $1,580,000 $1,527,300 $52,700
Step Two
Personnel Expenses
(Below Salary Cap)
Less FEMA
Reimbursement
Less Reimbursement
from other sources
Eligible Personnel
Expenses
$1,527,300 $(50,000) $(1,000,000) $477,300
Were fringe benefits for both patient care staff and General and Administrative (G&A) staff
considered Provider Relief Fund and/or ARP Rural eligible expenses under the “expenses
attributable to coronavirus not reimbursed by other sources”? (Modified 10/27/2022)
Yes, fringe benefits associated with both types of personnel may have been eligible if not
reimbursed by other sources.
If a provider received Provider Relief Fund payments and ARP Rural payments, could they
have used these payments for the same eligible expenses or lost revenues? (Modified
4/6/2022) No.
Provider Relief Fund payments and ARP Rural payments must be used for
different expenses or lost revenues attributable to coronavirus or COVID-19. A provider may not
use an ARP Rural payment to cover eligible health care expenses or lost revenues attributable to
coronavirus or COVID-19 if the provider has already reported that their Provider Relief Fund
payment(s) have covered the eligible expense or lost revenues. If a provider received both types of
payments, the provider should have applied their ARP Rural payment towards eligible health care
expenses and lost revenues attributable to COVID-19 before utilizing Provider Relief Fund
payments to cover eligible health care expenses or lost revenues attributable to coronavirus. One
way to ensure funds are not used for the same expenses or lost revenues attributable to coronavirus
or COVID-19 may be to use them for different time periods.
Can providers include the entire cost of capital facilities projects as eligible expenses, or will
eligible expenses be limited to the depreciation expense for the period? (Modified 8/30/2021)
Expenses for capital facilities could have been fully expensed only in cases where the
purchase was directly related to preventing, preparing for and responding to the coronavirus.
Examples of these types of facilities projects include:
• Upgrading a heating, ventilation, and air conditioning (HVAC) system to support
negative pressure units
• Retrofitting a COVID-19 unit
• Enhancing or reconfiguring ICU capabilities
• Leasing or purchasing a temporary structure to screen and/or treat patients
February 16, 2024
28
• Leasing a permanent facility to increase hospital or nursing home capacity
In order for the capital facilities projects’ costs to have been expensed, the project must have been
fully completed by the end of the Period of Availability associated with the Payment Received
Period.
My state or territorial Medicaid or Children’s Health Insurance Program (CHIP) agency
directed providers to use Provider Relief Fund dollars before applying Medicaid or CHIP
reimbursement, as well as Medicaid COVID-19 supplemental payments, to cover health
care-related expenses or lost revenues attributable to coronavirus. Was this permissible?
(Added 12/28/2020)
No. As it relates to expenses, providers identify their health care-related expenses, and then apply
any amounts received through other sources (e.g., direct patient billing, commercial insurance,
Medicare/Medicaid/CHIP, reimbursement from the Provider Relief Fund COVID-19 Claims
Reimbursement to Health Care Providers and Facilities for Testing, Treatment, and Vaccine
Administration for the Uninsured, or funds received from FEMA or SBA/Department of
Treasury’s Paycheck Protection Program) that offset the health care-related expenses. Provider
Relief Fund payments may be applied to the remaining expenses or cost, after netting the other
funds received or obligated to be received which offset those expenses.
Did providers need to report total purchase price of capital equipment or only the
depreciated value? (Modified 12/11/2020)
Providers who used accrual or cash basis accounting may report the relevant depreciation amount
based on the equipment useful life, purchase price and depreciation methodology otherwise
applied.
For additional information on capital depreciation, please refer to the other Frequently Asked
Questions related to capital equipment and capital facility projects.
A parent TIN with multiple subsidiary TINs each received a General Distribution payment.
The subsidiary TINs attested to and accepted the General Distribution payments they
received. Could the subsidiary TINs have allocated the General Distribution payments up
to the parent TIN or to another subsidiary TIN? How does the parent TIN formally
acknowledge acceptance of those payments that were attested and accepted by the
subsidiary TIN? (Added 10/28/2020)
HHS initially advised providers that once a subsidiary TIN attested to and accepted a General
Distribution payment, the money must stay with, and be used by, the subsidiary TIN. However,
HHS has received feedback indicating that some subsidiary TINs accepted a General Distribution
payment prior to the release of this guidance, and that they would have had their parent TIN
accept the money, had they known earlier of HHS’s position. In light of these timing concerns,
HHS is revising its prior guidance and clarifying that, for General Distribution payments only, a
subsidiary TIN can transfer its General Distribution payment to a parent TIN; this is true even if a
subsidiary TIN initially attested to accepting a General Distribution payment. Consistent with
other longstanding guidance, the parent TIN may use the money and/or allocate the money to
other subsidiary TINs, as it deems appropriate.
Regardless of which entity (the parent or subsidiary) attested to the receipt of the General
Distribution payments, the parent entity can report on the use of the General Distribution
payment as part of the HHS reporting process.
February 16, 2024
29
Calculating Eligible Expenses and Lost Revenue
If a Reporting Entity has more lost revenues for a “Payment Received Period” than it
received Provider Relief Fund and/or ARP Rural payments for the same period, can those
lost revenues be carried forward and applied against payments received during later
“Payment Received Periods” and included in the lost revenues reported during later
reporting periods? (Modified 5/5/2023)
Yes. Provider Relief Fund and/or ARP Rural payments may be applied to expenses and lost
revenues according to the period of availability of funding. However, expenses and lost revenues
may not be duplicated. Specifically, payments received may not be applied to the same expenses
and lost revenues that Provider Relief Fund or ARP Rural payments received in prior payment
periods already reimbursed. The Payment Received Periods described in the Post-Payment Notice
of Reporting Requirements determine the period of availability of funding and when reports are
due. The opportunity to apply Provider Relief Fund payments (excluding the Nursing Home
Infection Control Distribution) and ARP Rural payments for lost revenues will be available up to
June 30, 2023, the end of the quarter in which the COVID-19 Public Health Emergency ends.
If a Reporting Entity experienced quarterly patient care revenue losses during some, but not
all, of the quarters during the period of availability of funds, could the Provider Relief Fund
and/or ARP Rural payments have been used to cover losses during those quarters only?
(Modified 5/5/2023)
Yes, lost revenues were calculated for each quarter during the period of availability, as a
standalone calculation. Provider Relief Fund and/or ARP Rural payments may be used to cover
those quarters where patient care revenue losses occurred as long as those losses were attributable
to coronavirus. The opportunity to apply Provider Relief Fund payments (excluding the Nursing
Home Infection Control Distribution) and ARP Rural payments for lost revenues will be
available up to June 30, 2023, the end of the quarter in which the COVID-19 Public Health
Emergency ends.
What was the maximum allotment of my organization’s Provider Relief Fund and/or ARP
Rural amount that can be allocated to lost revenues during the period of availability of
funds? (Modified 10/27/2022)
There was not a maximum or minimum that can be allocated. Reporting Entities will see the
reporting system asks for unreimbursed expenses attributable to coronavirus first in the overall use
of funds calculation; it is possible for a Reporting Entity to enter “0”. Provider Relief Fund and/or
ARP Rural payment amounts not fully expended on unreimbursed health care-related expenses
attributable to coronavirus during the period of availability are then applied to lost revenues. Lost
revenues or expenses must only have been incurred during the Period of Availability correlating to
the Payment Received Period as described in the Post-Payment Notice of Reporting Requirements.
For Option i (Comparison of Actual Lost Revenues), lost revenues are calculated for each quarter
during the Period of Availability, as a standalone calculation, with 2019 quarters serving as a
baseline. For Option ii (Comparison of Budgeted to Actual Lost Revenues), Reporting Entities
may use budgeted revenue if the budget(s) and associated documents covering the Period of
Availability were established and approved prior to March 27, 2020. For each calendar year of
reporting, the applicable quarters where lost revenues are demonstrated are totaled to determine an
annual lost revenues amount. There is no offset. Option iii provides maximum flexibility to
providers by allowing providers to calculate lost revenues using an alternate reasonable
methodology.
February 16, 2024
30
How will HRSA use the net unreimbursed expenses attributable to coronavirus in the
calculation of expenses or lost revenues? (Modified 10/27/2022)
The net unreimbursed expenses attributable to coronavirus reported to HRSA will not be used in
the calculation of expenses or lost revenues. Reporting Entities are expected to determine their
net unreimbursed expenses attributable to coronavirus after taking into consideration the
application of Other Assistance Received and all Provider Relief fund payments. HRSA expects
that Provider Relief Fund and/or ARP Rural payments would be applied to unreimbursed
expenses attributable to coronavirus that are not obligated to be reimbursed by other sources
before Provider Relief Fund and/or ARP Rural payments are used for lost revenues. Reporting
Entities will see the reporting system asks for unreimbursed expenses attributable to coronavirus
first in the overall use of funds calculation; it is possible for a Reporting Entity to enter “0”.
Was patient care revenue counted against a Reporting Entity twice if the entity reported in
“Other Assistance Received” and in the “Patient Care/Lost Revenue” sections of the
Reporting Portal? (Modified 10/27/2022)
Patient care revenue should not be reported as part of “Other Assistance Received” as it is a
source of revenue, not a source of other assistance as defined by Provider Relief Fund and ARP
Rural reporting requirements. The “Other Assistance Received” reported to HRSA will not be
used in the calculation of expenses applied to Provider Relief Fund and/or ARP Rural payments
or lost revenues.
Can a Reporting Entity use a different lost revenues methodology for each reporting
period? (Added 1/27/2022)
Yes. However, it is important to note that due to the overlapping periods of availability, each
time a Reporting Entity changes the method used to calculate lost revenues, the system will
recalculate total lost revenues for the entire period of availability. It is important to note that due
to the overlapping periods of availability, if a Reporting Entity changes the method used to
calculate lost revenues, the system will recalculate total lost revenues for the entire period of
availability, which may impact the previously reported unreimbursed lost revenues. The system
will also require that the Reporting Entity submit a written justification to support and explain the
change in lost revenues methodology. Please refer to the Post-Payment Notice of Reporting
Requirements for information on the three available methodologies for calculating lost revenues.
In subsequent reporting periods, will Reporting Entities be able to change the lost revenues
methodology used in a previous reporting period? (Added 1/27/2022)
Yes. Reporting Entities that previously reported will be able to choose a different methodology for
calculating lost revenues during Reporting Period 2 and any subsequent reporting periods.
However, if the Reporting Entity decides to use a different methodology, they must then use the
new methodology to calculate lost revenues for the entire period of availability. The Reporting
Entity will be required to submit a justification for the change. If a Reporting Entity chooses a
different methodology, lost revenues by quarter will not pre-populate from the previous reporting
period. It is important to note that due to the overlapping periods of availability, if a Reporting
Entity changes the method used to calculate lost revenues, the system will recalculate total lost
revenues for the entire period of availability, which may impact the previously reported
unreimbursed lost revenues. Please refer to the Post-Payment Notice of Reporting Requirements
for information on the three available methodologies for calculating lost revenues.

February 16, 2024
31
In a previous reporting period, a Reporting Entity reported lost revenues that were greater
than the PRF payments it received. How will the system account for the unused lost
revenues previously reported?
(Added 1/27/2022)
The PRF Reporting Portal was designed so that each subsequent report will build from the
previous completed and submitted report. The Reporting Portal will calculate remaining unused
lost revenues that can be reimbursed by PRF payments received during future payment periods.
If a Reporting Entity had more lost revenues for the overlapping period of availability than the
Entity was able to demonstrate in a previous reporting period, then the Reporting Entity will be
able to reimburse the unused lost revenues with payments issued in subsequent periods. It is
important to note that due to the overlapping periods of availability, if a Reporting Entity
changes the method used to calculate lost revenues from one reporting period to another, the
system will recalculate total lost revenues for the entire period of availability, which may impact
the previously reported unreimbursed lost revenues.
Could choosing a different methodology from one reporting period to another result in
having unused funds to return because the method to calculate lost revenues has now
changed? (Added 1/27/2022)
Yes. The Reporting Portal is designed to track changes in the calculation of lost revenues. This
includes any changes in the baseline used for comparison, and changes to the inputs for each
quarter. The system will also calculate and track unreimbursed lost revenues that may fluctuate
as a result of the methodology change. If as a result of the change to the method, a Reporting
Entity was previously reimbursed for more lost revenues than they had for the period of
availability, they may be required to return more funds than they received during the applicable
“Payment Received Period.”
What happens when a Reporting Entity changes the lost revenues methodology from one
reporting period to the next? (Added 1/27/2022)
When a Reporting Entity chooses a different lost revenues methodology from one reporting
period to the next, the system requires confirmation of the change by the Reporting Entity. If the
lost revenues methodology changes, data submitted in the prior reporting period is not pre-
populated into the current report (as it would be if the same methodology was used from one
reporting period to the next). After a change in methodology is saved in the current report, the
portal user will not be able to retrieve data entered in the previously submitted report. Lost
revenues data for the current reporting period must cover the entire period of availability.
The reporting portal tracks changes in the calculation of lost revenues from one reporting period
to the next. The changes tracked include any changes in the baseline used for comparison, that is,
changes to 2019 actuals for a provider that elected to use option 1, changes in the budgeted
numbers for providers who elected to use option 2, and any inputs used for providers who
elected to use option 3. The system will also calculate and track unreimbursed lost revenues that
may fluctuate as a result of the methodology change.
Please refer to the Reporting Portal Resources section of the Reporting Resources page for additional
information.

February 16, 2024
32
Could Nursing Home Infection Control payments have been used to reimburse lost
revenues attributable to coronavirus? (Added 1/27/2022)
No. Per the payment Terms and Conditions, the Nursing Home Infection Control Distribution
(including any Quality Incentive Program payments) may not be used to reimburse lost
revenues.
If a nursing home or skilled nursing facility received Nursing Home Infection Control
Distribution payments in addition to General Distribution payments and other Targeted
Distribution payments, how may these payments be applied toward expenses and lost
revenues?
(Added 1/27/2022)
PRF recipients have the flexibility to identify how to use their multiple payments toward
expenses and lost revenues, but must abide by the Terms and Conditions associated with each of
the payments and follow the requirements for determining allowable expenses and lost revenues.
The Nursing Home Infection Control Distribution, which includes the Quality Incentive Program
payments, may only be used to reimburse infection control expenses. This type of Targeted
Distribution payment may not reimburse lost revenues.
PRF payments may be used as described in the relevant payment Terms and Conditions for
expenses and lost revenues, as appropriate, dating back to January 1, 2020. Because of the
overlapping periods of availability, providers have the flexibility to identify which payments
they will use to reimburse allowable expenses and lost revenues incurred during the period of
availability. Duplication of reimbursement for expenses and lost revenues is not permitted.
When completing a report, were Reporting Entities required to submit documentation
to support Nursing Home Infection Control Distribution expenses? (Added 1/27/2022)
No. Documentation to support Nursing Home Infection Control Distribution expenses is not
required to be uploaded to the PRF Reporting Portal at the time of reporting. However,
Reporting Entities are required to maintain supporting documentation, per the Terms and
Conditions, that demonstrates that any allowable expenses were incurred during the period of
availability. Supporting documentation must be made available upon the request of the Secretary
of the Department of Health and Human Services.
How should reimbursements received from the HRSA COVID-19 Claims Reimbursement
to Health Care Providers and Facilities for Testing, Treatment, and Vaccine
Administration for the Uninsured (Uninsured Program) and the HRSA COVID-19
Coverage Assistance Fund (CAF) be reported in the Provider Relief Fund Reporting
Portal? (Added 9/13/2021)
Reimbursements received fromthe Uninsured Program and CAF should be included as “other” in the
“Total Revenues/Net Charges from Patient Care Related Sources” section of the reporting portal.
Reimbursements from theseprograms shouldnot be included as “HHS CARES Act Testing” or
“other assistance” under the “Other Assistance Received” section of the reporting portal.
How should providers that require separate reporting on behalf of parent entities and/or
subsidiaries have calculated lost revenue across these entities? (Added 9/13/2021)
The Provider Relief Fund payment recipient has discretion in allocating the payments to support
its subsidiaries’ health care-related expenses or lost revenues attributable to coronavirus, so long
as the payment is used to prevent, prepare for, or respond to coronavirus and those expenses or
February 16, 2024
33
lost revenues are not reimbursed from other sources or other sources were not obligated to
reimburse.
Option iii, from the Post-Payment Notice of Reporting Requirements, provides Reporting
Entities flexibility in the reconciliation of lost revenues. Lost revenues may then be applied as
the reporting entity sees fit. Reporting Entities should work with their accounting firms to
determine an appropriate way to allocate expenses and lost revenues. The Reporting Entity is
responsible for ensuring that adequate documentation is maintained. Provider Relief Fund
payments may be applied to expenses and lost revenues attributable to coronavirus according to
the Period of Availability of funding. However, expenses and lost revenues may not be
duplicated: payments may not be applied to the same expenses and lost revenues that were
reported on in prior reporting periods.
Should grants awarded to FQHCs under the Health Center Program and COVID-specific
grants to FQHC Look-Alikes be factored into the lost revenue calculation? (Added
8/30/2021)
No. Grants awarded to Health Center Program-funded health centers and look-alikes are used to
support specific operating costs of the FQHC, as approved by HRSA through the annual
budgeting process, and are not considered to be patient services revenue. Therefore, such grants
should not be factored into the lost revenues calculation.
How will HRSA calculate lost revenues for providers that select Option i (Comparison of
Actual Lost Revenues) at the time of reporting? (Modified 8/30/2021)
For Option i, lost revenues are calculated for each quarter during the Period of Availability, as a
standalone calculation, with 2019 quarters serving as a baseline. For each calendar year of
reporting, the applicable quarters where lost revenues are demonstrated are totaled to determine
an annual lost revenues amount. The annual lost revenues are then added together. There is no
offset.
How will HRSA calculate lost revenues for providers that select Option ii (Comparison of
Budgeted to Actual Lost Revenues) at the time of reporting? (Added 8/30/2021)
For Option ii, lost revenues are calculated for each quarter during the period of availability, as a
standalone calculation, with budgeted quarters serving as a baseline. For each calendar year of
reporting, the applicable quarters where lost revenues are demonstrated are totaled to determine
an annual lost revenues amount. The annual lost revenues for the years included in the period of
availability are then added together. There is no offset. Reporting Entities may use budgeted
revenues if the budget(s) and associated documents covering the Period of Availability were
established and approved prior to March 27, 2020.
When reporting on lost revenues, how should Reporting Entities treat “contractual
adjustments from all third party payers” and “charity care adjustments” when
determining patient care-related revenue sources? (Modified 8/30/2021)
Patient care-related revenue should be reported net of adjustments for all third party payers,
charity care adjustments, bad debt, and any other discounts or adjustments, as applicable when
reporting patient care-related revenue sources. For example, if a provider’s gross patient revenue
was $5,000, and the contractual adjustment from the third-party payer or charity care
adjustments was $3,000, the provider should report on the PRF report $2,000 in patient care-
related revenue.
February 16, 2024
34
What was the baseline comparison period for providers that report on patient care revenue
using Option i (Comparison of Actual Lost Revenues) or Option ii (Comparison of
Budgeted to Actual Lost Revenues)? (Modified 8/30/2021)
Actual revenue from quarters in 2019 will serve as the baseline period of comparison for the
Period of Availability for Option i. Budgeted revenue from the quarters reported in 2020 or 2021
will serve as the baseline period of comparison for Option ii. For Option ii, Reporting Entities
may use budgeted revenues if the budget(s) and associated documents covering the Period of
Availability were established and approved prior to March 27, 2020.
Can recipients use 2020 budgeted revenues as a basis for reporting lost revenues? (Modified
7/1/2021)
Yes. When reporting use of Provider Relief Fund payments toward lost revenues attributable to
coronavirus, Reporting Entities may use budgeted revenues if the budget(s) and associated
documents covering calendar year 2020 were established and approved prior to March 27, 2020. To
be considered an approved budget, the budget must have been ratified, certified, or adopted by the
Reporting Entity’s financial executive, executive officer or other responsible representative as of
that date, and the Reporting Entity will be required to attest that the budget was established and
approved prior to March 27, 2020. Documents related to the budget, including the approval, must
be maintained in accordance with the Terms and Conditions.
How will HRSA use “Other Assistance Received” when calculating expenses or lost
revenues? (Added 7/1/2021)
The Other Assistance Received reported to HRSA will not be used in the calculation of expenses
or lost revenues. Reporting Entities are expected to make a determination of their expenses
applied to Provider Relief Fund payments after considering “Other Assistance Received” and
taking into account that Provider Relief Fund payments may not be used for expenses or lost
revenues that other sources have reimbursed or that other sources are obligated to reimburse.
Reporting Entities have varying fiscal year ends (e.g., June 30, September 30, or December
31). How should providers report lost revenues if their fiscal year does not align with the
calendar year? (Added 7/1/2021)
All Reporting Entities that opt to report lost revenues using Option i (Comparison of Actual
Revenue) or Option ii (Comparison of Budgeted Revenue to Actual Revenue) must enter their
patient care revenue for each quarter within the entire period of availability. Reporting Entities
using Option iii must enter their lost revenues, calculated by any reasonable method, for each
quarter during the period of availability.
Supporting Data
What documentation was required for reporting?
(Modified 6/11/2021)
Supporting worksheets were available to assist Reporting Entities with completion of reports. In
addition, Reporting Entities who are using a portion of their funds for lost revenues may be
required to upload supporting documentation when reporting on their calculation of lost
revenues. The documentation required is dependent upon which method of calculating lost
revenues providers select. Please review the most recently published Post-Payment Notice of
Reporting Requirements for additional details.

February 16, 2024
35
What was the documentation retention requirements for the Provider Relief Fund? (Added
10/28/2020)
Providers need to retain original documentation for three years after the date of submission of the
final expenditure report, in accordance with 2 CFR 200.333.
Change of Ownership
Who was responsible for reporting use-of-funds in the event of a change of ownership after
receipt of a Provider Relief Fund payment? (Modified 6/11/2021)
In the case of a change in ownership after receipt of a Provider Relief Fund payment, the
responsibility for reporting in the Provider Relief Fund Reporting Portal is dependent on whether
funds were from the General or Targeted Distribution.
For General Distribution payments: A parent entity may report on its subsidiaries’ General
Distribution payments regardless of whether the subsidiary TINs received the General
Distribution payments directly or whether General Distribution payments were transferred to
them by the parent entity. The parent entity may report on these General Distribution payments
regardless of whether the parent or the subsidiary attested to the Terms and Conditions.
For Targeted Distribution payments: The original recipient of a Targeted Distribution payment is
always the Reporting Entity. A parent entity may not report on its subsidiaries’ Targeted
Distribution payments as part of its consolidated report. The original recipient of a Targeted
Distribution must report on the use of funds in accordance with the Coronavirus Response and
Relief Supplemental Appropriations (CRRSA) Act. This is required regardless of whether the
parent or subsidiary received the payment or whether that original recipient subsequently
transferred the payment. A Reporting Entity that is a subsidiary must indicate the payment
amount of any of the Targeted Distributions it received that were transferred to/by the parent
entity, if applicable.
Non-Financial Data
Why did HRSA require Reporting Entities to report patient metrics? (Modified
10/27/2022)
HRSA required Reporting Entities to report patient metrics to gather information on the number
of patients treated by Provider Relief Fund and/or ARP Rural recipients. Depending on recipient
type, these patients may be treated in either inpatient, outpatient, or residential settings. These
metrics enable HRSA to quantify respective volumes of inpatient, in-person, and virtual
outpatient visits, as well as emergency visit patients.
What if a Reporting Entity does not believe their patient encounters align with one of the
patient visit type options? (Added 12/9/2021)
If a Reporting Entity cannot identify a fitting patient visit type for their patient encounters, the
entity should count the distinct encounters or visits in the category that is the most fitting
category available.
Should dialysis chairs have been counted as staffed beds if a patient is admitted as an inpatient?
(Added 9/13/2021)
No.
Further, only the facility that owns the bed should report on the staffed beds.

February 16, 2024
36
What were the categories for patient metrics?
(Modified 7/1/2021)
Patient metric categories include a) inpatient admissions; b) outpatient visits (in-person and
virtual); c) emergency department visits; and d) facility stays (for long-term and short-term
residential facilities). The definitions are included below.
a) Inpatient Admissions: number of hospital admissions on a clinician’s order (i.e., direct
admit) or formally admitted from the emergency department to the hospital (i.e.,
emergency admission).
b) Outpatient Visits: number of in-person or virtual patient encounters with a clinician in an
office-based, clinic, or hospital outpatient department setting that do not require an
inpatient admission.
c) Emergency Department Visit: number of emergency department encounters for care or
treatment. This may include patients on observation status who are cared for no longer
than 72 hours but not formally admitted to a hospital.
d) Facility Stays: number of stays (defined as unique admissions) for patients residing in a
long-term or short-term care or treatment facility.
A comprehensive user guide with definitions will be made available when the first reporting
period begins.
What were the categories for classifying personnel?
(Modified 6/11/2021)
Personnel will be classified as either “clinical” or “non-clinical” staff using the following
categories: a) full-time; b) part-time; c) contractor; d) furloughed; e) separated; and f) hired.
a) Full-time: number of personnel employed on average 30 hours of service per week, or
130 hours for a calendar month.
b) Part-time: number of personnel employed any time between 1 and 34 hours per week,
whom may or may not qualify for benefits.
c) Contractor: number of personnel employed as an individual or under organizational
contracts and do not receive direct benefits or compensation from the Reporting Entity.
d) Furloughed: number of personnel on involuntary and unpaid leave of absence.
e) Separated: number of personnel who 1) voluntarily submitted a written or verbal notice of
resignation or 2) the Reporting Entity decided to terminate its relationship with the
employee(s) (includes lay-offs and expired contracts).
f) Hired: number of personnel 1) not previously employed by the Reporting Entity or 2) that
left a company due to voluntary or involuntary separation and are brought back to work by
employer.
What was considered a “staffed bed” for reporting facility metrics? (Modified 6/11/2021)
A staffed bed is licensed and physically available with staff on hand to attend to patients;
includes both occupied and available beds.
Extensions
Will HRSA allow late report submissions?
(Modified 4/6/2022)
In general, HRSA will not accept late report submissions after the applicable deadline associated
with the Payment Received Period. There are two instances where HRSA has provided flexibility
for providers.
In light of the challenges that providers across the country faced due to natural disasters and the
Delta variant, HRSA authorized a 60-day grace period for the first reporting period only, in order
to help providers adhere to their Provider Relief Fund reporting requirements, for those that failed
February 16, 2024
37
to meet the September 30, 2021 reporting deadline. This grace period ended on November 30,
2021, at 11:59pm Eastern Standard Time (EST).
HRSA will also provide an opportunity based on extenuating circumstances for Reporting Entities
to complete reports and come into compliance in order to retain the funds received during the
applicable Payment Received Period. Extenuating circumstances may include, but are not limited
to, natural disasters, death or serious illness of the individual(s) responsible for reporting, or not
receiving HRSA reporting notifications. This opportunity will be available for all reporting
periods. Providers should monitor their email and the Provider Relief Fund webpage for
additional information on the process for late report submission due to extenuating circumstances
at https://www.hrsa.gov/provider-relief. Reporting entities must follow the stated process to
request the opportunity. HRSA will review the requests for late report submissions due to an
extenuating circumstance. If the late submission is approved, the provider must complete the
report within the specified timeframe.
Providers who do not submit reports by the applicable deadline for the relevant reporting period,
or are granted additional reporting time due to an extenuating circumstance and do not submit as
instructed, will be considered out of compliance with program Terms and Conditions. Providers
that are out of compliance with the Terms and Conditions must return Provider Relief Fund
payments associated with the missed Reporting Time Period.
Were providers able to request extensions on submissions of their required reports for any of
the required reporting periods? (Modified 4/6/2022)
Generally, no. Providers that received one or more payments exceeding $10,000, in the aggregate,
during a Payment Received Period were required to report by the stated deadline for each
applicable Reporting Time Period. However, HRSA provided an opportunity based on
extenuating circumstances for Reporting Entities to complete reports and come into compliance in
order to retain the funds received during the applicable Payment Received Period. Extenuating
circumstances may include, but are not limited to, natural disasters, death or serious illness of the
individual(s) responsible for reporting, or not receiving HRSA reporting notifications. This
opportunity will be available for all reporting periods. Providers should monitor their email and
the PRF webpage for additional information on the process for late report submissions due to
extenuating circumstances at https://www.hrsa.gov/provider-relief. Reporting entities must follow
the process to request the opportunity. HRSA reviewed the requests for late report submissions due
to an extenuating circumstance. If the late submission was approved, the provider must
complete the report within the HRSA communicated timeframe.
Providers who were granted additional reporting time due to an extenuating circumstance and did
not submit as instructed will be considered out of compliance with program Terms and
Conditions. Providers that were out of compliance with the Terms and Conditions must return
Provider Relief Fund payments associated with the missed Reporting Time Period.
Were providers able to request extensions on the deadline to use funds? (Modified 9/29/2021)
No. HRSA will not approve extensions on the use of funds for any providers. Any unused funds
must be returned to the government within 30 calendar days after the end of the relevant
Reporting Time Period or any associated grace period.
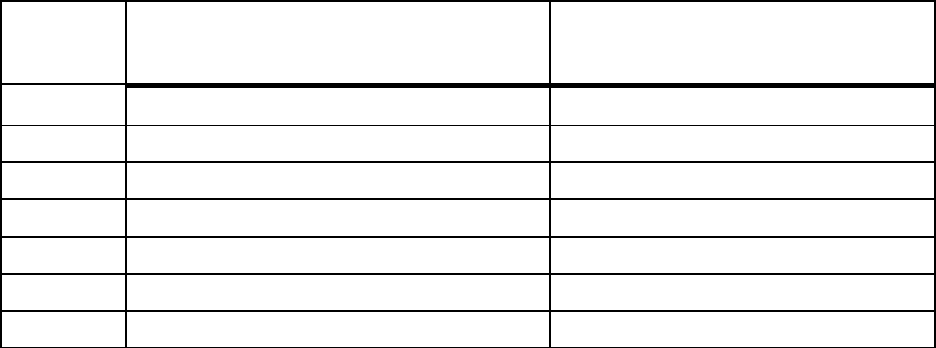
February 16, 2024
38
Miscellaneous
What were the required timelines for reporting? (Modified 5/5/2023)
Provider Relief Fund and/or ARP Rural recipients were required to report in each Payment
Received Period in which they received one or more payments exceeding, in the aggregate,
$10,000, as indicated in the table below. Reporting must be completed and submitted to HRSA
by the last date of the relevant Reporting Time Period. Provider Relief Fund and/or ARP Rural
recipients that do not report within the respective Reporting Time Period are out of compliance
with payment Terms and Conditions and funds may be subject to repayment and/or recovery
activities.
Period
Payment Received Period
(Payments Exceeding $10,000 in
Aggregate Received)
Reporting Time Period
Period 1 April 10, 2020 to June 30, 2020 July 1, 2021 to September 30, 2021*
Period 2
July 1, 2020 to December 31, 2020
January 1, 2022 to March 31, 2022
Period 3
January 1, 2021 to June 30, 2021
July 1, 2022 to September
30, 2022
Period 4 July 1, 2021 to December 31, 2021 January 1, 2023 to March 31, 2023
Period 5
January 1, 2022 to June 30, 2022
July 31, 2023 to September 30, 2023
Period 6
July 1, 2022 to December 31, 2022
January 1, 2024 to March 31, 2024
Period 7
January 1, 2023 to June 30, 2023
July 1, 2024 to September 30, 2024
* Grace period until November 30, 2021.
Were Intergovernmental Transfers (IGTs) related to state provider taxes allowable G&A
expenses? (Modified 10/27/2022)
A portion of a Provider Relief Fund and/or ARP Rural recipient’s state provider taxes may be
eligible expenses, but only to the extent the Provider Relief Fund recipient owes incrementally
increased state provider taxes, where the incremental increase is attributable to coronavirus.
If an entity received Provider Relief Fund and/or American Rescue Plan (ARP) Rural
payment(s) totaling over $10,000, but returned some, did they still have to report? (Modified
4/6/2022)
A Reporting Entity must report on their Provider Relief Fund and/or ARP Rural payment(s), only
when they have retained, as of the end of the Reporting Time Period, over $10,000 in aggregated
Provider Relief Fund and American Rescue Plan (ARP) Rural payments received during a
Payment Received Period. Entities that do not return a portion of the funds that places them below
the $10,000 threshold, or report on the use of funds by the end of the applicable Reporting Time
Period, must return all funds received during the Payment Received Period.
February 16, 2024
39
If the original recipient of a Targeted Distribution payment is a subsidiary, and the
recipient transferred that payment to a parent entity, how does the original recipient (i.e.,
subsidiary) demonstrate the use of funds in its report? Was it sufficient for the subsidiary to
report the amount transferred to the parent entity? (Added 1/27/2022)
For any subsidiary that was the original recipient of a Targeted Distribution payment reporting on
a payment spent by a parent entity, the expense worksheet(s) in the subsidiary report must include
any expenses applied to the payment, whether those were the expenses of the subsidiary or the
entity to which the payments were transferred. For any subsidiary Reporting Entity reporting on
how a payment was used to reimburse lost revenues, the subsidiary Reporting Entity can use the
alternative method for calculating lost revenues and demonstrate in their method how the lost
revenues of the parent or other subsidiary entity to which the payment was transferred was
considered in the lost revenues calculation.
Using the alternative reasonable methodology will allow Reporting Entities to reduce the parent
entity’s report by the amount of lost revenues accounted for by the Targeted Distribution
payment originally received by the subsidiary. The subsidiary Reporting Entity that originally
received the Targeted Distribution should report the exact amount of lost revenues as the
Targeted Distribution payment and the same dollar amount by which the parent entity’s lost
revenues were reduced. The deductions and reconciliations must be accounted for in each
methodology calculation for the parent and subsidiary that originally received the Targeted
Distribution payment. Both reports together should be sufficient for audit purposes.
If a Reporting Entity planned to report on General Distribution payments that were
transferred from a subsidiary that received the initial payment, how should patient care
revenue or lost revenues be aggregated and reported in the portal? (Added 1/27/2022)
HRSA does not prescribe which method Reporting Entities should use to calculate lost revenues.
However, Option iii, “alternate reasonable methodology,” provides the greatest flexibility in
unique circumstances.
If a Reporting Entity returned funds and the returned funds were not reflected in the
“Payments to Recipients” page in the PRF Reporting Portal, what should the Reporting
Entity do? (Added 1/27/2022)
There may be a delay between the time a payment is returned by a PRF recipient and the time the
payment is reconciled by HRSA. If a Reporting Entity does not see a returned payment reflected
in the Payments to Recipients page of the PRF Reporting Portal, the Reporting Entity should
contact the Provider Support Line at 866-569-3522 (for TTY, dial 711) to provide information about
the return (e.g., original payment date, amount returned, date of return, method of return) to assist
HRSA in the reconciliation of the returned payment amount.
If a Reporting Entity returned unused funds in excess of the amount owed, will HRSA repay
the Entity the difference between what was owed and returned? (Added 1/27/2022)
HRSA will not repay Reporting Entities the difference in unused funds that were owed and the
amount that was returned.
Should state and federal tax credits (e.g., employee retention tax credits) have been
reported as “other assistance received?” (Added 12/9/2021)
No. Tax credits were not considered a revenue source for purpose of reporting within the Provider
Relief Fund report.

February 16, 2024
40
How would a Reporting Entity know if HRSA determines if its revenue estimation approach
was considered reasonable? (Added 7/1/2021)
HRSA will notify a Reporting Entity if their proposed methodology is not reasonable, including if
it does not demonstrate with a reasonable certainty that claimed lost revenues were caused by
coronavirus. If HRSA determines that a Reporting Entity’s proposed alternate methodology is not
reasonable, the entity will be asked to resubmit its report within 30 days of notification using either
Option i or Option ii to calculate lost revenues attributable to coronavirus.
Providers may have significant fluctuations in year-over-year net patient revenues due to
settlements or payments made to third parties relating to care delivered outside the
reporting period (2019 and beyond). Should Provider Relief Fund recipients exclude from
the reporting of net patient revenue payments received for care not provided in 2019 and
beyond (Modified 12/07/2023)
Provider Relief Fund recipients shall exclude from the reporting of net patient revenue payments
received or payments made to third parties relating to care not provided in 2019 and beyond.
Who was required to report?
(Modified 2/16/24)
Recipients who received one or more General and Targeted Distributions and/or ARP Rural Distribution
payments exceeding $10,000 in the aggregate during a Payment Received Period are required to report
in each applicable Reporting Time Period.
What was the process to return unused funds? (Modified 6/11/2021)
When the first reporting period begins, providers will be able to return unused funds through the
Reporting Portal.
If a parent organization received a Provider Relief Fund Targeted Distribution on behalf of a
subsidiary, which organization should report on the use? (Added 1/28/2021)
The parent organization as the original recipient of the payment must report on the use of funds in
accordance with the Consolidated Appropriations Act, 2021.
If a subsidiary organization received a Provider Relief Fund Targeted Distribution, and
subsequently transferred it to its parent organization, which organization should report on
the use? (Modified 2/16/24)
The subsidiary as the original recipient of the payment must report on the use of funds and
any amount that was transfer to the parent organization in accordance with the Consolidated
Appropriations Act, 2021. For information on returning funds, visit the How to Return
Unused PRF Funds page.
Were Reporting Entities required to report each General and/or Targeted Distribution
payment separately? (Added 1/28/2021)
Reporting Entities that received General and Targeted Distribution payments were to submit a
consolidated report through the Provider Relief Fund Reporting Portal.
If all funds were expended to cover unreimbursed healthcare related expenses attributable to
coronavirus, were Reporting Entities still required to submit lost revenue information?
(Modified 1/28/2021)
Reporting Entities were required to submit actual patient care revenue for calendar years 2019 up
to June 30, 2023, the end of the quarter in which the COVID-19 Public Health Emergency ends ,
in order to inform program integrity and HRSA’s audit strategy.

February 16, 2024
41
What does “primary Tax Identification Number (TIN)” and “subsidiary TIN” refer to?
(Added 10/28/2020)
Primary TIN refers to the TIN of the parent company, and subsidiary TIN refers to the TIN of an
entity that is a subsidiary of the parent company. Providers may have received payments directly to
a parent and/or its subsidiary entities.
What was meant by “For some recipients, this may be analogous to Social Security number
(SSN) or Employer Identification Number (EIN)” with respect to the TIN? (Added
10/28/2020)
Some recipients may be individual providers for whom their TIN will be their SSN; similarly, for
some entities the TIN will be the EIN.
Should entrance fee amortization be excluded from patient care? (Added 10/28/2020) If
the provider includes entrance fee amortization as operating revenue on its financial
statements, it should be considered as revenue associated with patient services. Entrance fee
amortization must be handled in a consistent manner in both 2019 and 2020.
How do shareholder or partnership payments impact the lost revenue calculation? (Added
10/28/2020)
“Lost revenue attributable to coronavirus” was calculated based on operating revenue from patient
care sources. Shareholder and partnership payments are not eligible to be included in the lost
revenue calculation.
COVID-19 Vaccine Distribution and Administration
If a provider administered a COVID-19 vaccine to a patient that had Medicare Part A, but
not Part B, coverage, could the provider use Provider Relief Fund payments to cover the
unreimbursed costs associated with vaccine administration? (Added 1/28/2021)
Yes. The costs associated with administering a vaccine to a patient with Medicare Part A, but not
Part B, coverage would be considered unreimbursed under the Provider Relief Fund, and
payments could have been used to cover incurred expenses.
Could Provider Relief Fund payments have been used to support COVID-19 vaccine distribution?
(Modified 1/28/2021)
Provider Relief Fund payments may be used to support expenses associated with distribution of a
COVID-19 vaccine licensed or authorized by the Food and Drug Administration (FDA) that have
not been reimbursed from other sources or that other sources are not obligated to reimburse. Funds
may also be used ahead of an FDA-licensed or authorized vaccine becoming available.
This may include using funds to purchase additional refrigerators or freezers, personnel costs to
provide vaccinations, and transportation costs not otherwise reimbursed.
Could Provider Relief Funds have been used to cover the cost of vaccination, including doses
and administration fees, for Medicare, Medicaid, or CHIP beneficiaries? (Modified
12/11/2020)
In line with the Terms and Conditions, funds may not be used to reimburse expenses or losses that
have been reimbursed from other sources or that other sources are obligated to reimburse, which
include, but is not limited to, Medicare, Medicaid, and CHIP. If reimbursement does not cover the
full expense of administering vaccines, Provider Relief Funds may be used to cover the remaining
associated costs.
February 16, 2024
42
Balance Billing
How would a provider know the in-network rates to be able to comply with the requirement
to bill a presumptive or actual COVID-19 patient for cost-sharing at the in-network rate?
(Modified 4/6/2022)
Providers accepting the Provider Relief Fund payment should submit a claim to the patient’s health
insurer for their services. Most health insurers have publicly stated their commitment to reimbursing
out-of-network providers that treat health plan members for COVID-19-related care at the insurer’s
prevailing in-network rate. If the health insurer is not willing to do so, the out-of-network provider
may seek to collect from the patient out-of-pocket expenses, including deductibles, copayments, or
balance billing, in an amount that is no greater than what the patient would have otherwise been
required to pay if the care had been provided by an in-network provider. Generally, HRSA expects
that it would be highly unusual for providers to collect from an out-of-network presumptive or
actual COVID-19 patient an amount that exceeds the individual plan out-of-pocket maximum for
the calendar year.
The Terms and Conditions require recipients to attest that for all care for a presumptive or
actual case of COVID-19 the recipient will not seek to collect from the patient out-of-pocket
expenses in an amount greater than what the patient would have otherwise been required to
pay if the care had been provided by an in-network recipient. How should dental
providers have complied with this requirement? (Added 7/22/2020)
The prohibition on balance billing applies to “all care for a presumptive or actual case of
COVID-19.” A presumptive case of COVID-19 is a case where a patient’s medical record
documentation supports a diagnosis of COVID-19, even if the patient does not have a positive in
vitro diagnostic test result in his or her medical record. Dental providers who are not caring for
patients with presumptive or actual cases of COVID-19 would not be subject to this provision.
Did the Terms and Conditions for the General and Targeted Distributions require
attesting to a ban on balance billing for all patients and/or all care, because “HHS broadly
views every patient as a possible case of COVID-19”? (Added 5/6/2020)
No. As set forth in the Terms and Conditions, the prohibition on balance billing applies to “all
care for a presumptive or actual case of COVID-19.”
The Terms and Conditions provision related to balance billing suggested that providers
that provide out-of-network care to an insured, presumptive or actual COVID-19 patient
can bill the patient’s insurer any amount, as long as they do not bill the patient directly.
Was that correct? (Added 5/6/2020)
The Terms and Conditions do not impose any limitations on the ability of a provider to submit a
claim for payment to the patient’s insurance company. However, an out-of-network provider
delivering COVID-19-related care to an insured patient may not seek to collect from the patient
out-of-pocket expenses, including deductibles, copayments, or balance billing, in an amount
greater than what the patient would have otherwise been required to pay if the care had been
provided by an in-network provider.
February 16, 2024
43
The Terms and Conditions require that “for all care for a presumptive or actual case of
COVID-19, Recipient certifies that it will not seek to collect from the patient out-of-pocket
expenses in an amount greater than what the patient would have otherwise been required
to pay if the care had been provided by an in-network Recipient.” How did HHS define a
presumptive case of COVID-19? (Modified 6/12/2020)
A presumptive case of COVID-19 is a case where a patient’s medical record documentation
supports a diagnosis of COVID-19, even if the patient does not have a positive in vitro
diagnostic test result in his or her medical record.
Publication of Payment Data
Was there a publicly available list of providers and the payments they received through
the Provider Relief Fund? (Modified 2/16/2024)
HHS has posted a public list of providers and their payments once they attest to receiving the
money and agree to the Terms and Conditions. All providers that received a payment from the
Provider Relief Fund and retain that payment for at least 90 days without rejecting the funds are
deemed to have accepted the Terms and Conditions. The amounts reflect the net of funds
distributed excluding any monies that have been returned or recovered. .
What providers were included in the Provider Relief Fund data file on the CDC website?
(Modified 6/12/2020)
The data that are posted in the public list represent providers that received one or more payments
from the Provider Relief Fund and that have attested to receiving at least one payment and
agreed to the associated Terms and Conditions.
Why might a provider not be listed or listed with a different address than their service
location? (Added 5/12/2020)
Provider Relief Fund payments are being made to providers or groups of providers that are
organized within a Tax Identification Number (TIN). The information displayed is of providers
by billing TIN that have received at least one payment, which they have attested to, and the
address associated with that billing TIN. Providers will not be listed if they have not yet attested
to the payment terms and conditions or if they are within a larger billing entity that received
payment. In addition, the address listed for the billing TIN often corresponds with the billing
location (based on the Center for Medicare & Medicaid Services’ Provider Enrollment, Chain,
and Ownership System (PECOS)), and may not align with the physical location of a health care
practice site.
Will HHS release additional data elements, such as provider types, payment amount per
distribution, or payment recipients’ NPIs, on the public list of providers and payments?
(Added 5/12/2020)
HHS does not have plans to include additional data fields in the public list of providers and
payments.
Can a provider choose to have its payment data omitted from the Provider Relief Fund
public list on the CDC’s website? (Modified 2/16/2024)
No. To ensure transparency, HHS will publish the names of payment recipients.

February 16, 2024
44
Provider Relief Fund General Distribution and ARP Rural Payments
Phase 4 and ARP Rural Payments
Phase 4 Overview and Eligibility
Who was eligible for Phase 4 – General Distribution?
(Added 9/29/2021)
To be eligible to apply, the applicant must have met all of the following requirements:
1. Must have fallen into one of the following categories:
a. Must have either directly billed, or owned (on the application date) an included
subsidiary that has directly billed, their state/territory Medicaid program (fee-for
service or managed care) or Children’s Health Insurance Program (CHIP) for
health care-related services during the period of January 1, 2019 to December 31,
2020; or
b. Must have been a dental service provider who has either directly billed, or
owned (on the application date) an included subsidiary that has directly billed,
health insurance companies or patients for oral health care-related services
during the period of January 1, 2019 to December 31, 2020;
c. Must have either directly billed, or owned (on the application date) an included
subsidiary that has directly billed, Medicare fee-for-service (Parts A and/or B) or
Medicare Advantage (Part C) for health care-related services during the period of
January 1, 2019 to December 31, 2020;
d. Must have been a state-licensed/certified assisted living facility on or before
December 31, 2020;
e. Must have been a behavioral health provider who has either directly billed, or
owned (on the application date) an included subsidiary that has directly billed,
health insurance companies or patients for health care-related services during the
period of January 1, 2019 to December 31, 2020;
f. Must have received a prior Targeted Distribution payment.
2. Must have either (i) filed a federal income tax return for fiscal years 2018, 2019, or 2020,
or (ii) be an entity exempt from the requirement to file a federal income tax return and
have no beneficial owner that is required to file a federal income tax return (e.g. a state-
owned hospital or health care clinic); and
3. Must have provided patient care after January 31, 2020; and
4. Must not have permanently ceased providing patient care directly, or indirectly through
included subsidiaries; and
5. If the applicant was an individual that was providing patient care, had gross receipts or
sales from providing patient care reported on Form 1040, Schedule C, Line 1, excluding
income reported on a W-2 as a (statutory) employee.

February 16, 2024
45
Were providers that received payments under Phase 4 of the General Distribution limited to
using these funds to cover coronavirus-related losses or expenses experienced during the third
and fourth quarters of calendar year (CY) 2020 or first quarter of CY2021?
(Modified 2/16/24)
No. Providers may use these payments for eligible expenses, including services rendered during the
period of availability. Providers may also use payments for lost revenues attributable to COVID-19
incurred within the period of availability, but only up to June 30, 2023, the end of the quarter in which
the COVID-19 Public Health Emergency ended. For more information, please refer to the Post-Payment
Notice of Reporting Requirements (PDF).
ARP Rural Payments Overview and Eligibility
Who was eligible for ARP Rural payments?
(Added 9/29/2021)
In accordance with the statutory requirements, to be eligible to apply for ARP Rural Payments,
the applicant or at least one subsidiary TINs must have been:
1. A rural health clinic as defined in section 1861(aa)(2) of the Social Security Act; or
2. A provider treated as located in a rural area pursuant to section 1886(d)(8)(E), such as
critical access hospitals; or
3. A provider or supplier that:
a. Has directly billed for health care-related services between January 1, 2019 and
September 30, 2020:
i. Medicare fee-for-service (Parts A and/or B);
ii. Medicare Advantage (Part C)
iii. Their state/territory Medicaid program (fee-for service or managed
care); or
iv. Their state/territory Children’s Health Insurance Program (CHIP); and
b. Operated in or served patients living in the HHS Federal Office of Rural
Health Policy’s (FORHP) definition of a rural area:
i. All non-Metro counties;
ii. All Census Tracts within a Metropolitan county that have a Rural-Urban
Commuting Area (RUCA) code of 4-10. The RUCA codes allow the
identification of rural Census Tracts in Metropolitan counties;
iii. 132 large area census tracts with RUCA codes 2 or 3. These tracts are at
least 400 square miles in area with a population density of no more than
35 people per square mile; and
iv. 295 outlying Metropolitan counties with no Urbanized Area population.
Must control and use of the ARP Rural payment be delegated to the entity that was eligible
for and received the payment? (Added 9/29/2021)
Yes. To ensure the funds reach providers serving rural communities, control and use of the ARP
Rural payment must be delegated to the entity that was eligible for and received the Payment.
Unlike Phase 4 of the Provider Relief Fund, ARP Rural payment recipients must certify that they
will allocate the ARP Rural payment to the provider(s) associated with the applicable subsidiary
or billing TIN.

February 16, 2024
46
HRSA recently updated its definition of “rural.” Will the updated definition be used?
(Added 9/29/2021)
Yes. HRSA will use the most current definition of “rural” to calculate ARP Rural payments. The
HHS Federal Office of Rural Health Policy recently expanded the definition of “rural.” For more
information, please visit https://www.hrsa.gov/rural-health/about-us/definition/index.html.
Targeted Distribution
Nursing Home Infection Control Distribution
Were there different permissible uses of funds received as quality incentive payments
compared to those for the funds distributed previously under the $2.5 billion Nursing
Home Infection Control Distribution? (Modified 12/4/2020)
No. The same Terms and Conditions and restrictions on use of funds applied to the quality
incentive payments received by nursing homes as under the Nursing Home Infection Control
Distribution. Quality incentive payments could only be used for the infection control expenses,
as that term is defined in the Terms and Conditions. These include costs associated with
administering COVID-19 testing for both staff and residents; reporting COVID-19 test results to
local, state, or federal governments; hiring staff to provide patient care or administrative support;
incurring expenses to improve infection control, including activities such as implementing
infection control “mentorship” programs with subject matter experts, or changes made to
physical facilities; and providing additional services to residents, such as technology that permits
residents to connect with their families if the families are not able to visit in person.
Which nursing home providers received a payment under the Nursing Home Infection
Control Targeted Distribution? (Added 8/27/2020)
Nursing homes and skilled nursing facilities that were not revoked, had an active CMS
certification, and had at least 6 certified beds, were deemed eligible to receive payments.
What were the permissible uses for this distribution? (Added 8/27/2020)
The Nursing Home Infection Control Distribution could only be used for the infection control
expenses defined in the Terms and Conditions. These include costs associated with
administering COVID-19 testing for both staff and residents; reporting COVID-19 test results to
local, state, or federal governments; hiring staff to provide patient care or administrative support;
incurring expenses to improve infection control, including activities such as implementing
infection control “mentorship” programs with subject matter experts, or changes made to
physical facilities; and providing additional services to residents, such as technology that permits
residents to connect with their families if the families are not able to visit in person.
