Medical Policy:
Cosmetic and Reconstructive Surgery Procedures
Proprietary information of EmblemHealth/ConnectiCare. © 2022 EmblemHealth & Affiliates
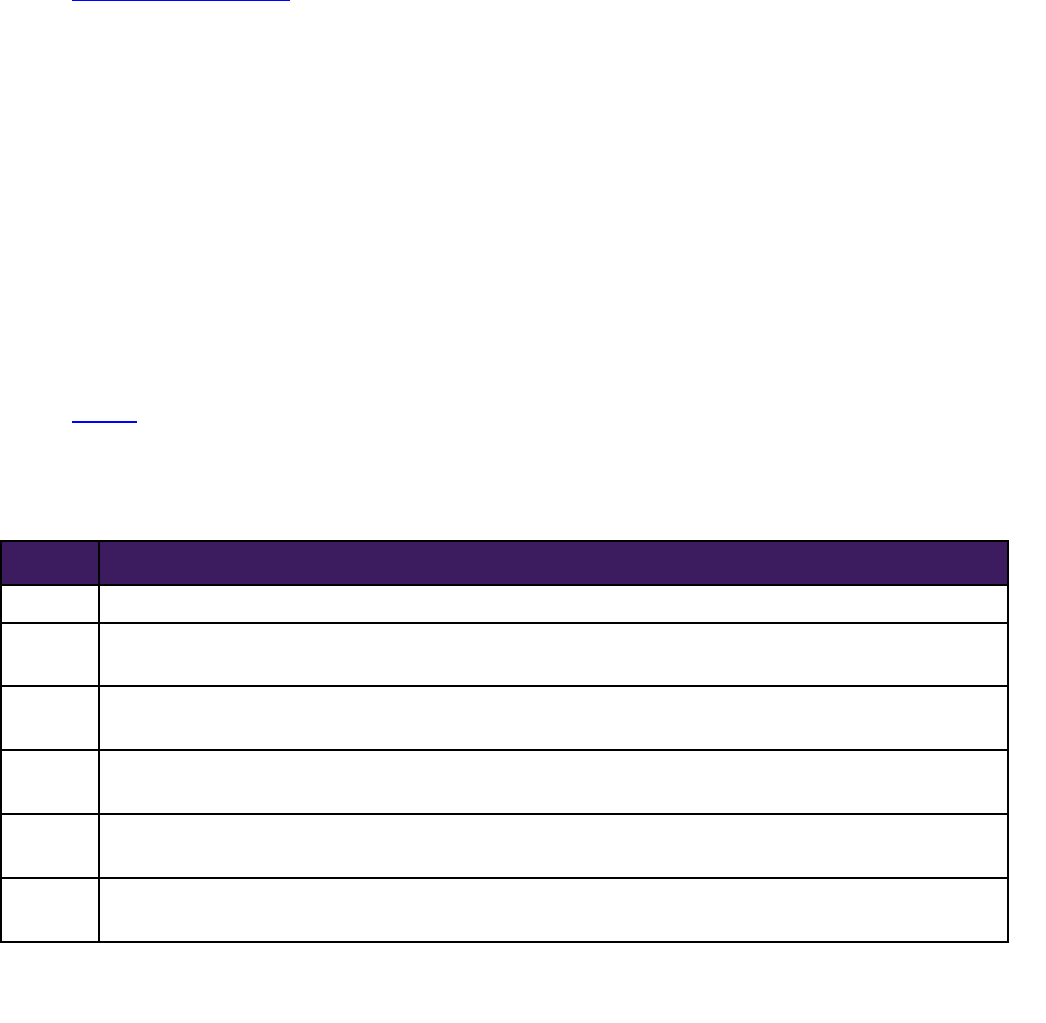
POLICY NUMBER LAST REVIEW APPROVED BY
EH.CCI.AD.01a August 12, 2022 Medical Policy Committee (MPC)
Medical Guideline Disclaimer Property of EmblemHealth. All rights reserved.
The treating physician or primary care provider must submit to EmblemHealth, or ConnectiCare, as applicable (hereinafter jointly referred to as
“EmblemHealth”), the clinical evidence that the member meets the criteria for the treatment or surgical procedure. Without this documentation and
information, EmblemHealth will not be able to properly review the request preauthorization or post-payment review. The clinical review criteria expressed
below reflects how EmblemHealth determines whether certain services or supplies are medically necessary. This clinical policy is not intended to pre-empt
the judgment of the reviewing medical director or dictate to health care providers how to practice medicine. Health care providers are expected to exercise
their medical judgment in rendering appropriate care. Health care providers are expected to exercise their medical judgment in rendering appropriate
care.
EmblemHealth established the clinical review criteria based upon a review of currently available clinical information (including clinical outcome studies in
the peer reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research
agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical
areas, and other relevant factors). EmblemHealth expressly reserves the right to revise these conclusions as clinical information changes and welcomes
further relevant information. Each benefit program defines which services are covered. The conclusion that a particular service or supply is medically
necessary does not constitute a representation or warranty that this service or supply is covered and/or paid for by EmblemHealth, as some programs
exclude coverage for services or supplies that EmblemHealth considers medically necessary.
If there is a discrepancy between this guideline and a member's benefits program, the benefits program will govern. Identification of selected brand names
of devices, tests and procedures in a medical coverage policy is for reference only and is not an endorsement of any one device, test or procedure over
another. In addition, coverage may be mandated by applicable legal requirements of a state, the Federal Government or the Centers for Medicare &
Medicaid Services (CMS) for Medicare and Medicaid members. All coding and web site links are accurate at time of publication.
EmblemHealth may also use tools developed by third parties, such as the MCG™ Care Guidelines, to assist us in administering health benefits. The MCG™
Care Guidelines are intended to be used in connection with the independent professional medical judgment of a qualified health care provider and do not
constitute the practice of medicine or medical advice. EmblemHealth Services Company, LLC, has adopted this policy in providing management,
administrative and other services to EmblemHealth Plan, Inc., EmblemHealth Insurance Company, EmblemHealth Services Company, LLC, and Health
Insurance Plan of Greater New York (HIP) related to health benefit plans offered by these entities. ConnectiCare, an EmblemHealth company, has also
adopted this policy. All of the aforementioned entities are affiliated companies under common control of EmblemHealth Inc.
Applicable to: EmblemHealth/ConnectiCare Commercial and EmblemHealth Medicaid Plans
Overview
EmblemHealth/ConnectiCare regard the surgical procedures listed in Applicable Coding Table(s) as cosmetic
(unless substantiating documentation is received that would otherwise indicate that the purpose of the procedure
is to restore or improve bodily function or is otherwise medically necessary).
The plan reserves the right to deny coverage for other procedures that are cosmetic and not medically necessary.
Benefit coverage for health services is determined by the member-specific benefit plan document and applicable
laws that may require coverage for a specific service. Please check benefit plan descriptions for details. If there is
a discrepancy between this policy and a member’s plan of benefits, then the provision of the benefits will prevail.
Indications for Coverage
For plans that include benefits for the procedures listed below, the following are eligible for coverage as
reconstructive and medically necessary when all of the following criteria are met:
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 2 of 3
There is documentation that the physical abnormality and/or physiological abnormality is causing
a functional impairment that requires correction; and
The proposed treatment is of proven efficacy and is deemed likely to significantly improve or
restore the patient’s physiological function.
Limitations and Exclusions
The Plan does not cover cosmetic procedures under the following circumstances, including but not limited
to:
Procedures that correct an anatomical Congenital Anomaly without improving or restoring
physiologic function (i.e, procedures that do not meet the reconstructive criteria in the
Indications for Coverage
section).
Pharmacological regimens, nutritional procedures, or treatments.
Scar or tattoo removal or revision procedures (such as salabrasion, chemosurgery and other such
skin abrasion procedures).
Skin abrasion procedures performed as a treatment for acne.
Treatment for skin wrinkles or any treatment to improve the appearance of the skin.
Treatment for spider or varicose veins outside of varicose vein medical policy.
Ancillary services related to cosmetic procedures that are not considered medically necessary.
Hair removal or replacement by any means (except when performed in conjunction with
approved services pertaining to gender dysphoria).
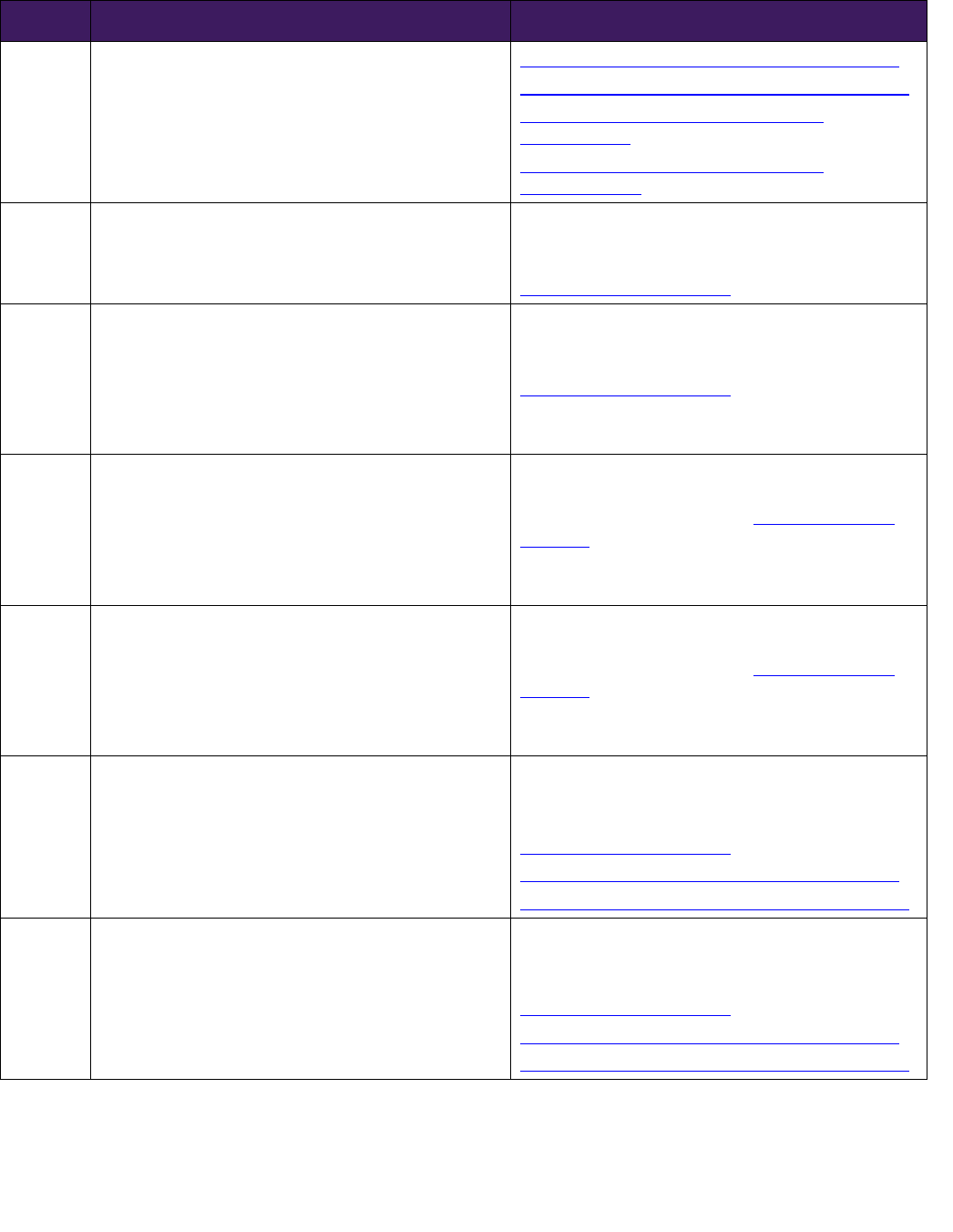
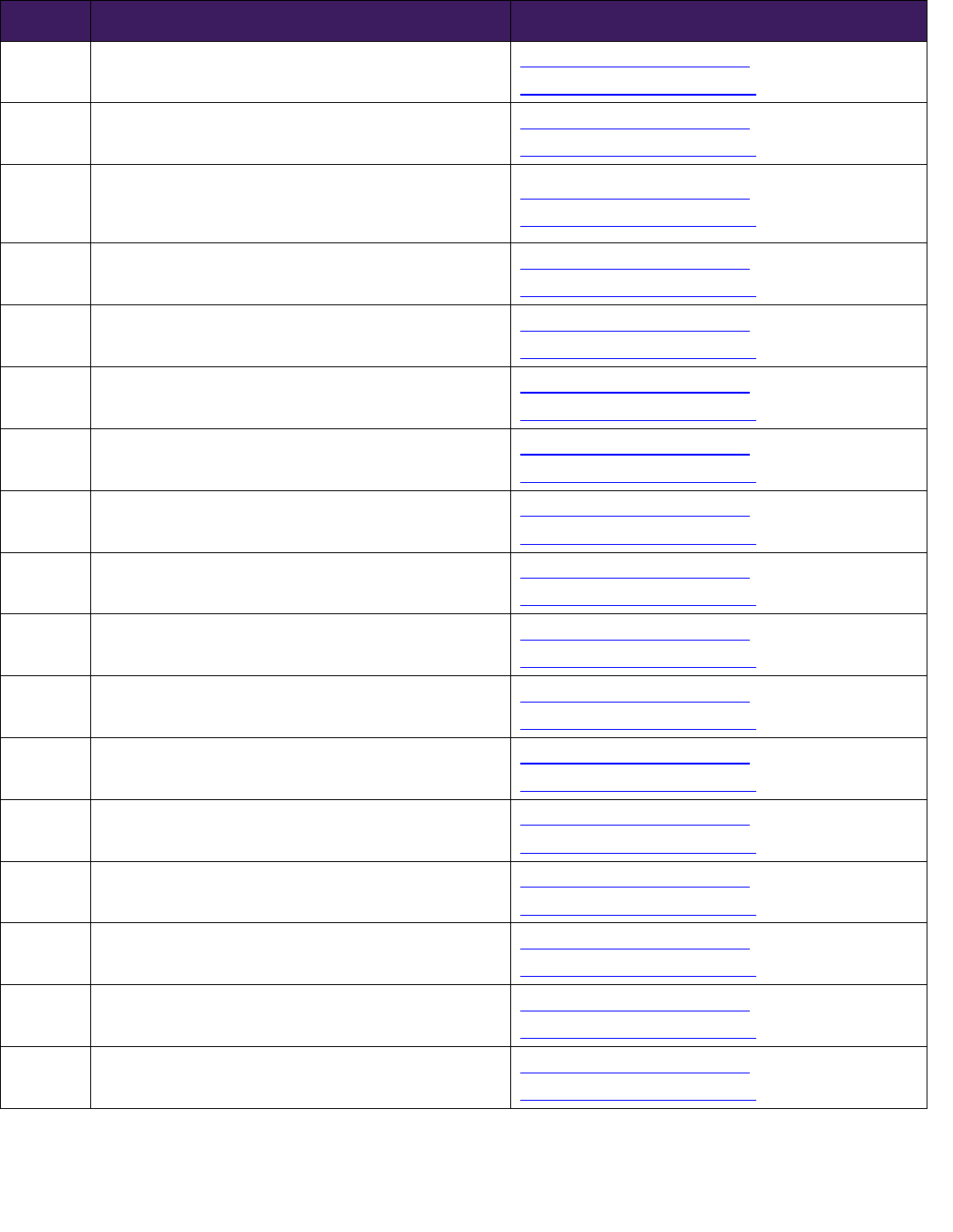
Applicable Coding Table(s)
Table 1: Medical procedures deemed always cosmetic
Table 2
: Medical procedures that may be cosmetic (review may be required to determine if the
service is cosmetic or reconstructive)
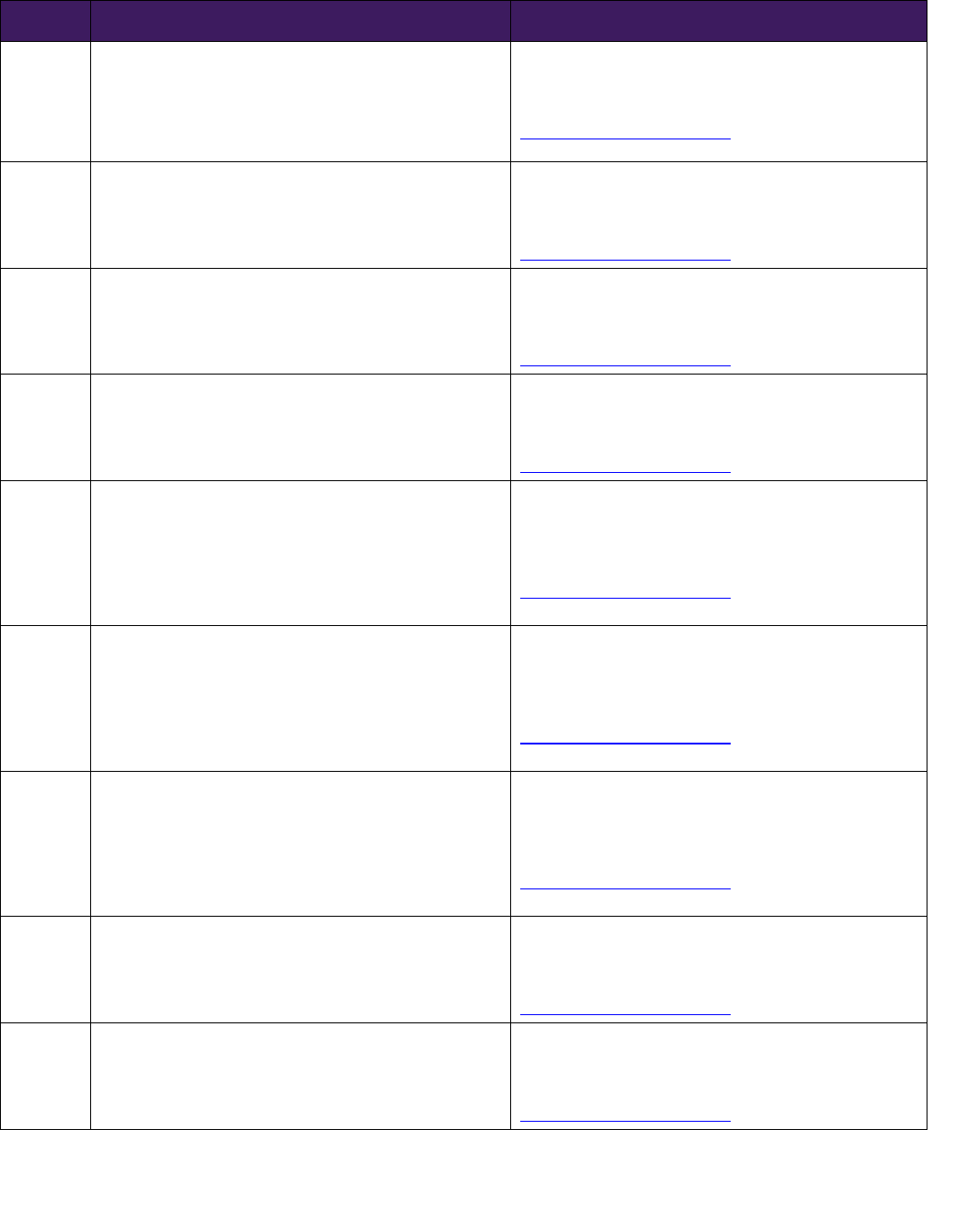
Table 1: Procedure codes deemed always cosmetic
Code Description
11200 Removal of skin tags, multiple fibrocutaneous tags, any area; up to and including 15 lesions
11201
Removal of skin tags, multiple fibrocutaneous tags, any area; each additional 10 lesions, or part thereof (List
separately in addition to code for primary procedure)
11950
Subcutaneous injection of filling material (eg, collagen)
Exception: NY and Mass HIV-related lipodystrophy mandate
11951
Subcutaneous injection of filling material (eg, collagen)
Exception: NY and Mass HIV-related lipodystrophy mandate
11952
Subcutaneous injection of filling material (eg, collagen)
Exception: NY and Mass HIV-related lipodystrophy mandate
11954
Subcutaneous injection of filling material (eg, collagen)
Exception: NY and Mass HIV-related lipodystrophy mandate
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 3 of 4
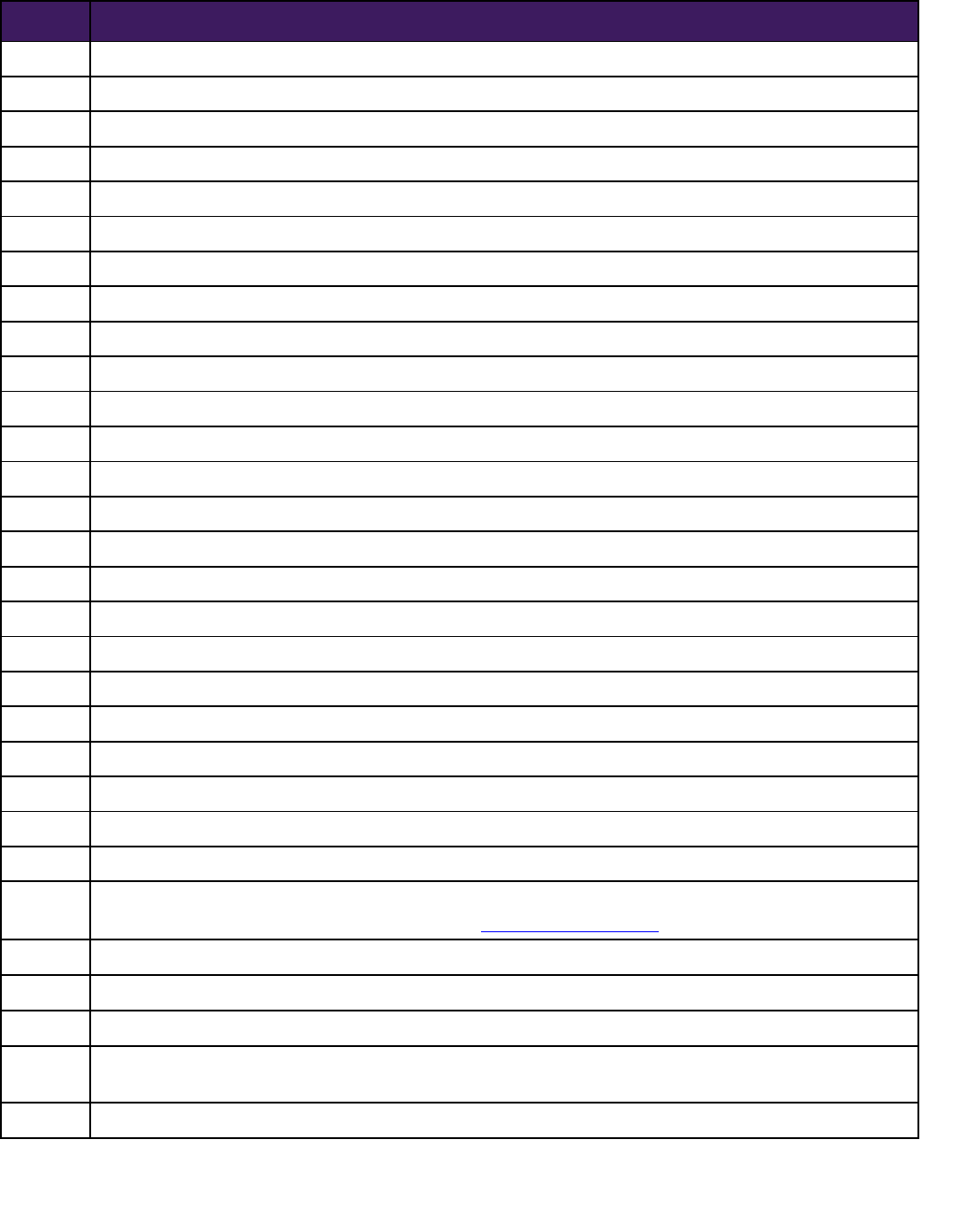
Code Description
15775 Punch graft for hair transplant
15776 Punch graft for hair transplant: more than 15 punch grafts
15786 Abrasion; single lesion (eg, keratosis, scar)
15787 Abrasion; each additional 4 lesions or less (List separately in addition to code for primary procedure)
15819 Cervicoplasty
15824 Rhytidectomy; forehead
15825 Rhytidectomy; neck with platysmal tightening (platysmal flap, P-flap)
15826 Rhytidectomy; glabellar frown lines
15828 Rhytidectomy; cheek, chin, and neck
15829 Rhytidectomy; superficial musculoaponeurotic system (SMAS) flap
15832 Excision, excessive skin and subcutaneous tissue (includes lipectomy); thigh
15833 Excision, excessive skin and subcutaneous tissue (includes lipectomy); leg
15834 Excision, excessive skin and subcutaneous tissue (includes lipectomy); hip
15835 Excision, excessive skin and subcutaneous tissue (includes lipectomy); buttock
15836 Excision, excessive skin and subcutaneous tissue (includes lipectomy); arm
15837 Excision, excessive skin and subcutaneous tissue (includes lipectomy); forearm or hand
15838 Excision, excessive skin and subcutaneous tissue (includes lipectomy); submental fat pad
15839 Excision, excessive skin and subcutaneous tissue (includes lipectomy); other area
15876 Suction assisted lipectomy; head and neck
15877 Suction assisted lipectomy; trunk
15878 Suction assisted lipectomy; upper extremity
15879 Suction assisted lipectomy; lower extremity
17340 Cryotherapy (CO2 slush, liquid N2) for acne
17360 Chemical exfoliation for acne (eg, acne paste, acid)
17380
Electrolysis epilation, each 30 minutes
Exception, see Gender Affirming/Reassignment medical policies (ConnectiCare, EmblemHealth)
21120 Genioplasty; augmentation (autograft, allograft, prosthetic material)
19355 Correction of inverted nipples
21121 Genioplasty; sliding osteotomy, single piece
21122
Genioplasty; sliding osteotomies, 2 or more osteotomies (eg, wedge excision or bone wedge reversal for
asymmetrical chin)
21123 Genioplasty; sliding, augmentation with interpositional bone grafts (includes obtaining autografts)
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 4 of 5
Code Description
65760 Keratomileusis
65765 Keratophakia
65767 Epikeratoplasty
65771 Radial keratotomy
69090 Ear piercing
69300 Otoplasty, protruding ear, with or without size reduction
96902
Microscopic examination of hairs plucked or clipped by the examiner (excluding hair collected by the patient)
to determine telogen and anagen counts, or structural hair shaft abnormality
S0800 Laser in situ keratomileusis (LASIK)
S0810 Photorefractive keratectomy (PRK)
S0812 Phototherapeutic keratectomy (PTK)
S0596 Phakic intraocular lens for correction of refractive error
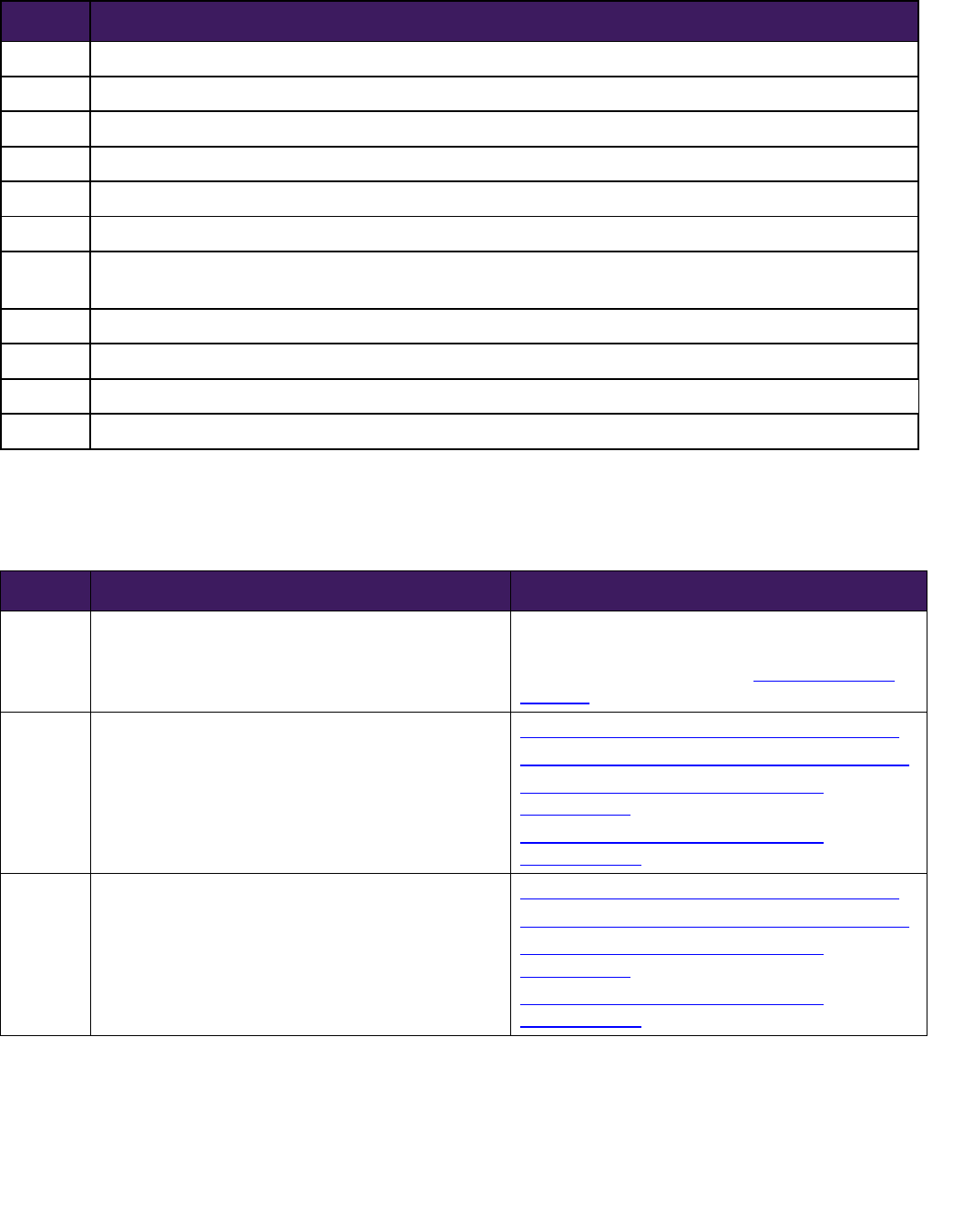
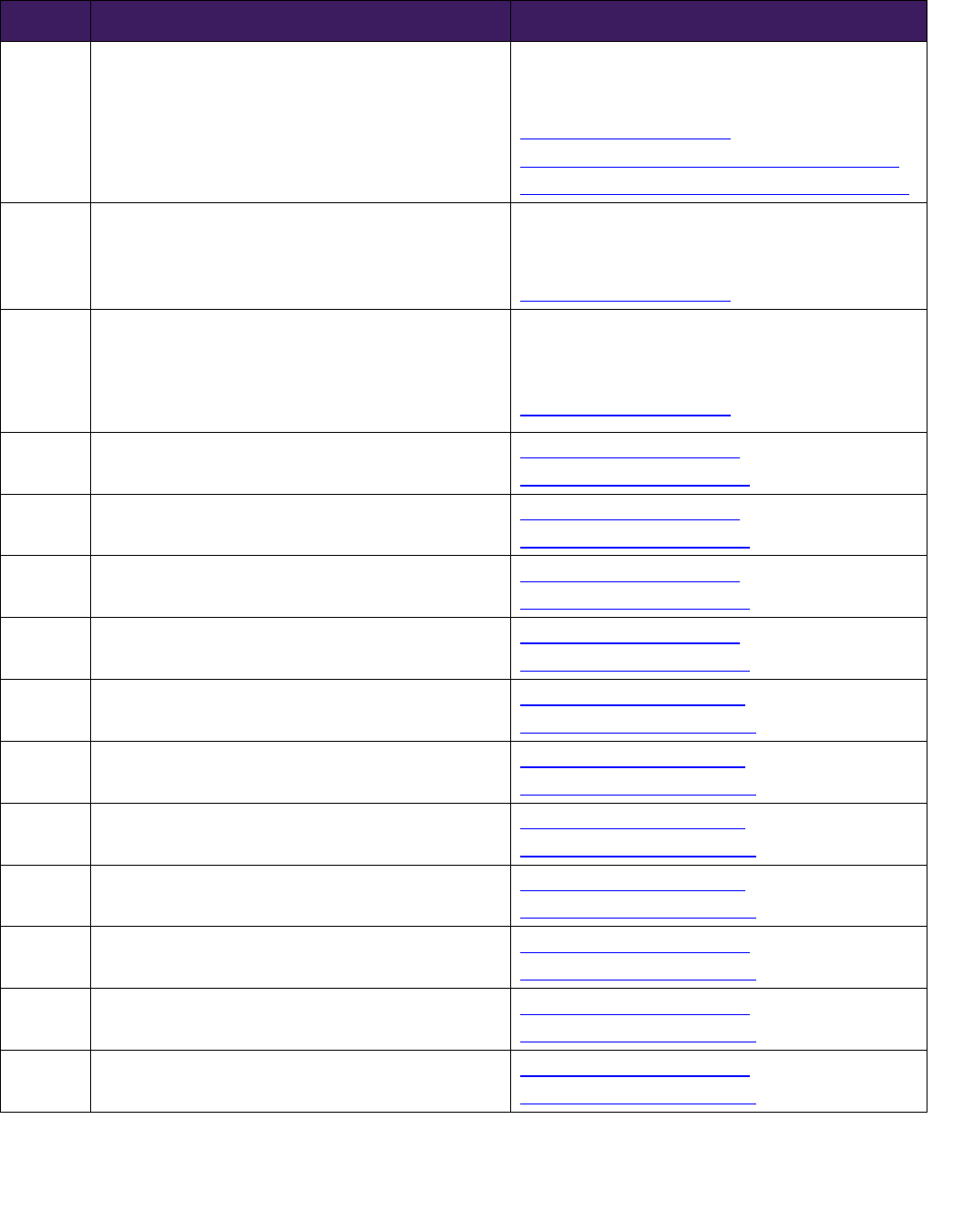
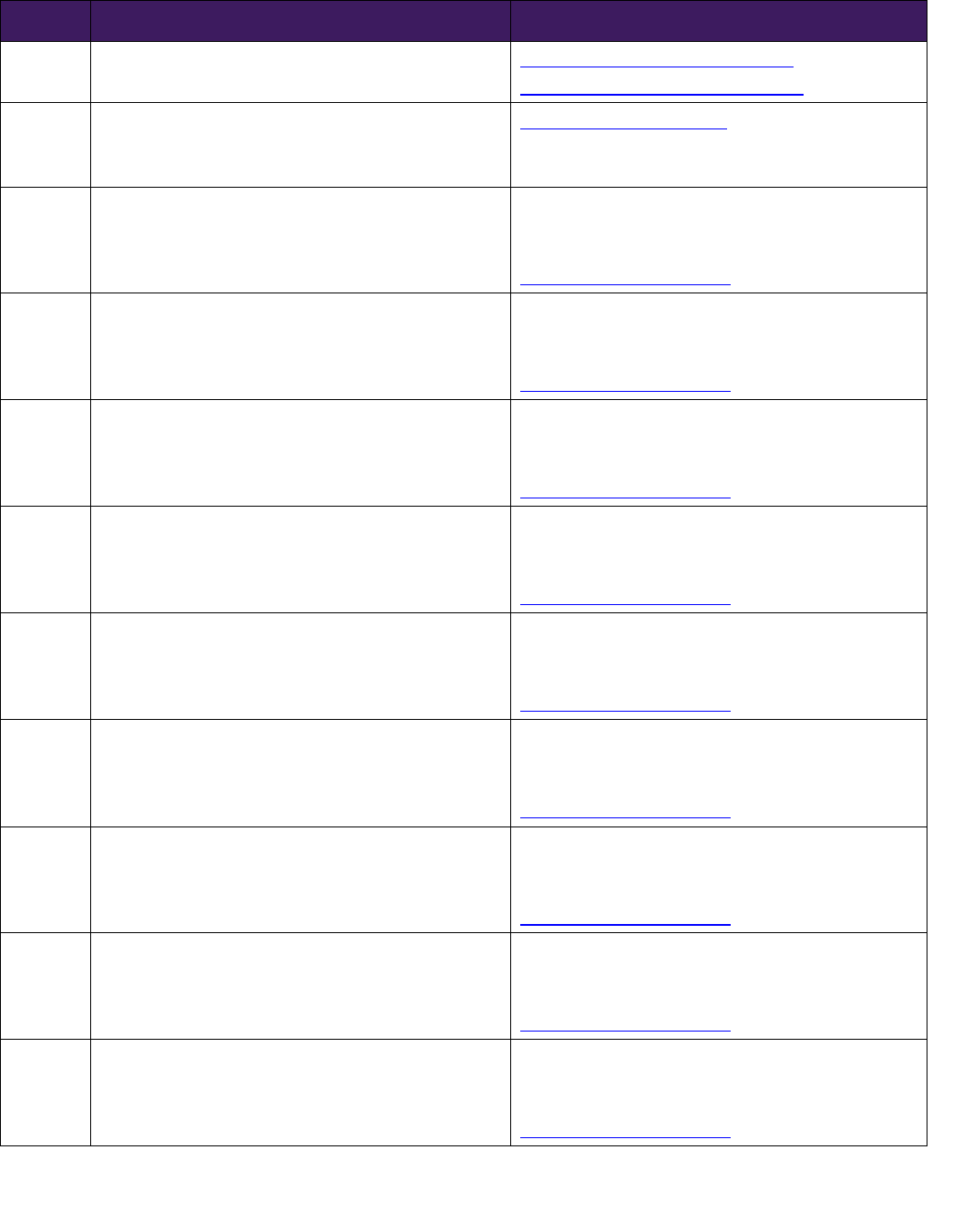
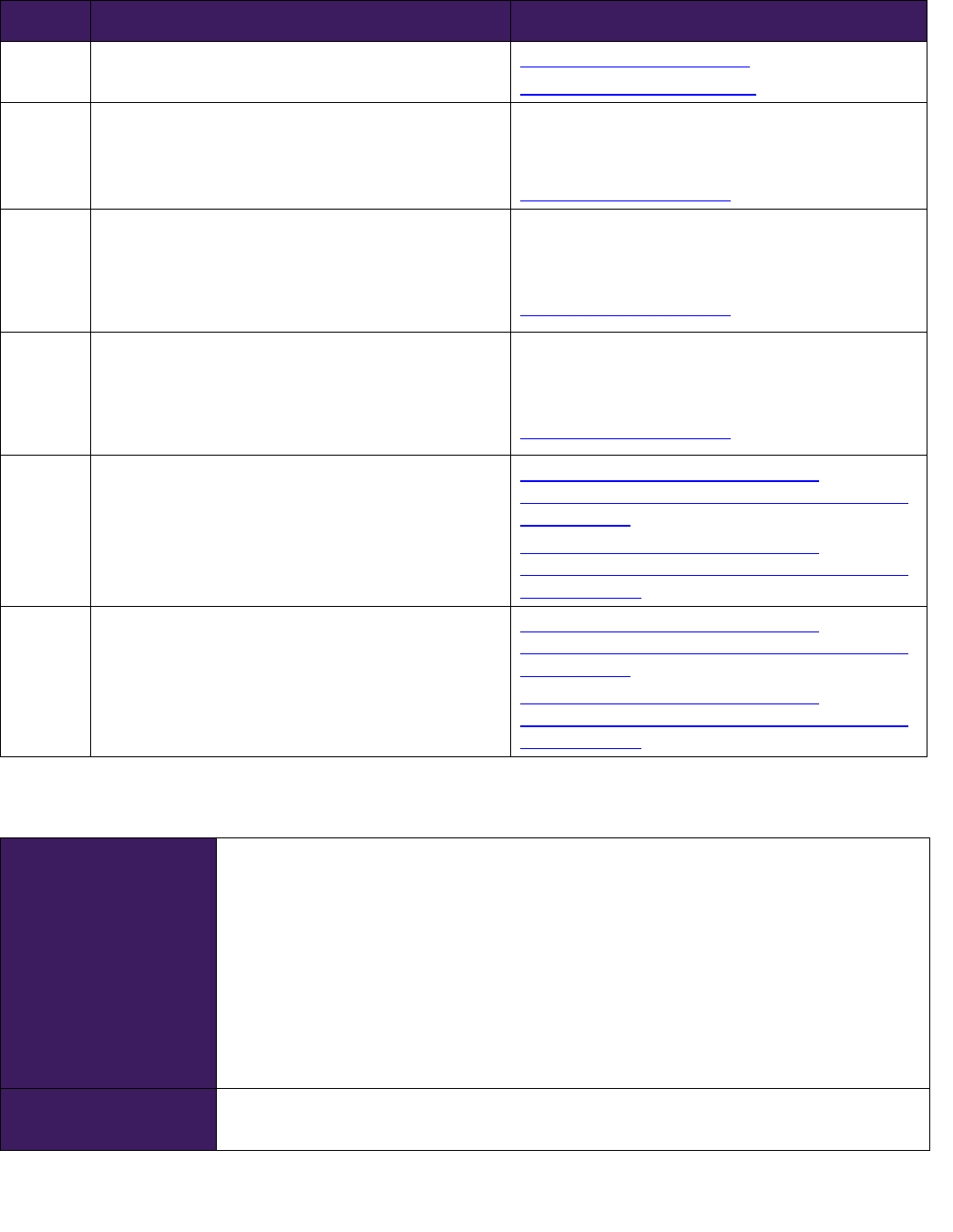
Table 2: Procedure codes generally deemed cosmetic (review may be required to
determine if the service is cosmetic or reconstructive)
Code Description Comments/Related Policy Links
10040
Acne surgery (eg, marsupialization, opening or
removal of multiple milia, comedones, cysts,
pustules)
May be considered medically necessary when
causing significant impairment of physical or
mechanical function.
See Indications for
Coverage
11920
Tattooing, intradermal introduction of insoluble
opaque pigments to correct color defects of skin,
including micropigmentation
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
11921 Tattooing, intradermal introduction
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 5 of 6
Code Description Comments/Related Policy Links
11922 Tattooing, intradermal introduction
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
11960
Insertion of tissue expander(s) for other than breast,
including subsequent expansion
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
11971
Removal of tissue expander(s) without insertion of
prosthesis
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Also applicable — MCG General Surgery or Procedure
GRG (SG-GS)
15730
Midface flap (ie, zygomaticofacial flap) with
preservation of vascular pedicle(s)
May be considered medically necessary when
causing significant impairment of physical or
mechanical function.
See Indications for
Coverage
Also applicable — MCG Wound and Skin
Management GRG (PG-WS)
15733
Muscle, myocutaneous, or fasciocutaneous flap; head
and neck with named vascular pedicle (ie,
buccinators, genioglossus, temporalis, masseter,
sternocleidomastoid,levator scapulae)
May be considered medically necessary when
causing significant impairment of physical or
mechanical function.
See Indications for
Coverage
Also applicable — MCG Wound and Skin
Management GRG (PG-WS)
15769
Grafting of autologous soft tissue, other, harvested
by direct excision (eg, fat, dermis, fascia)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
15771
Grafting of autologous fat harvested by liposuction
technique to trunk, breasts, scalp, arms, and/or legs;
50 cc or less injectate
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 6 of 7
Code Description Comments/Related Policy Links
15772 Grafting of autologous fat harvested by liposuction
technique to trunk, breasts, scalp, arms, and/or legs;
each additional 50 cc injectate, or part thereof (List
separately in addition to code for primary procedure)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
15773
Grafting of autologous fat harvested by liposuction
technique to face, eyelids, mouth, neck, ears, orbits,
genitalia, hands, and/or feet; 25 cc or less injectate
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
15774
Grafting of autologous fat harvested by liposuction
technique to face, eyelids, mouth, neck, ears, orbits,
genitalia, hands, and/or feet; each additional 25 cc
injectate, or part thereof (List separately in addition
to code for primary procedure)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
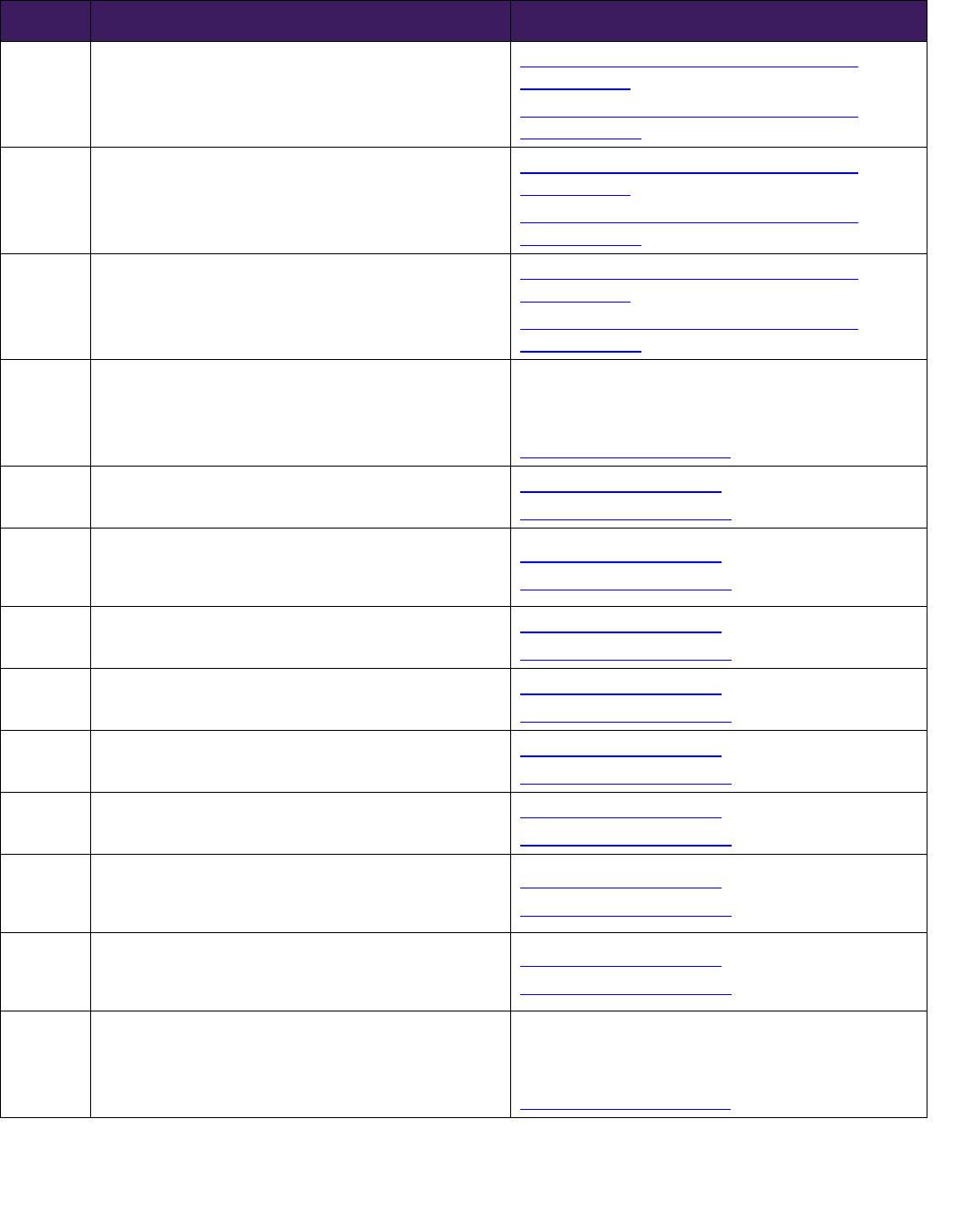
15780
Dermabrasion; total face (eg, for acne scarring, fine
wrinkling, rhytids, general keratosis)
Dermabrasion (ConnectiCare)
Dermabrasion (EmblemHealth)
15781 Dermabrasion; segmental, face
Dermabrasion (ConnectiCare)
Dermabrasion (EmblemHealth)
15782 Dermabrasion; regional, other than face
Dermabrasion (ConnectiCare)
Dermabrasion (EmblemHealth)
15783
Dermabrasion; superficial, any site (eg, tattoo
removal)
Dermabrasion (ConnectiCare)
Dermabrasion (EmblemHealth)
15788 Chemical peel, facial; epidermal
Chemical Peels (ConnectiCare)
Chemical Peels (EmblemHealth)
15789 Chemical peel, facial; dermal
Chemical Peels (ConnectiCare)
Chemical Peels (EmblemHealth)
15792 Chemical peel, nonfacial; epidermal
Chemical Peels (ConnectiCare)
Chemical Peels (EmblemHealth)
15793 Chemical peel, nonfacial; dermal
Chemical Peels (ConnectiCare)
Chemical Peels (EmblemHealth)
15820 Blepharoplasty, lower eyelid;
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
15821
Blepharoplasty, lower eyelid; with extensive
herniated fat pad
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
15822 Blepharoplasty, upper eyelid;
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
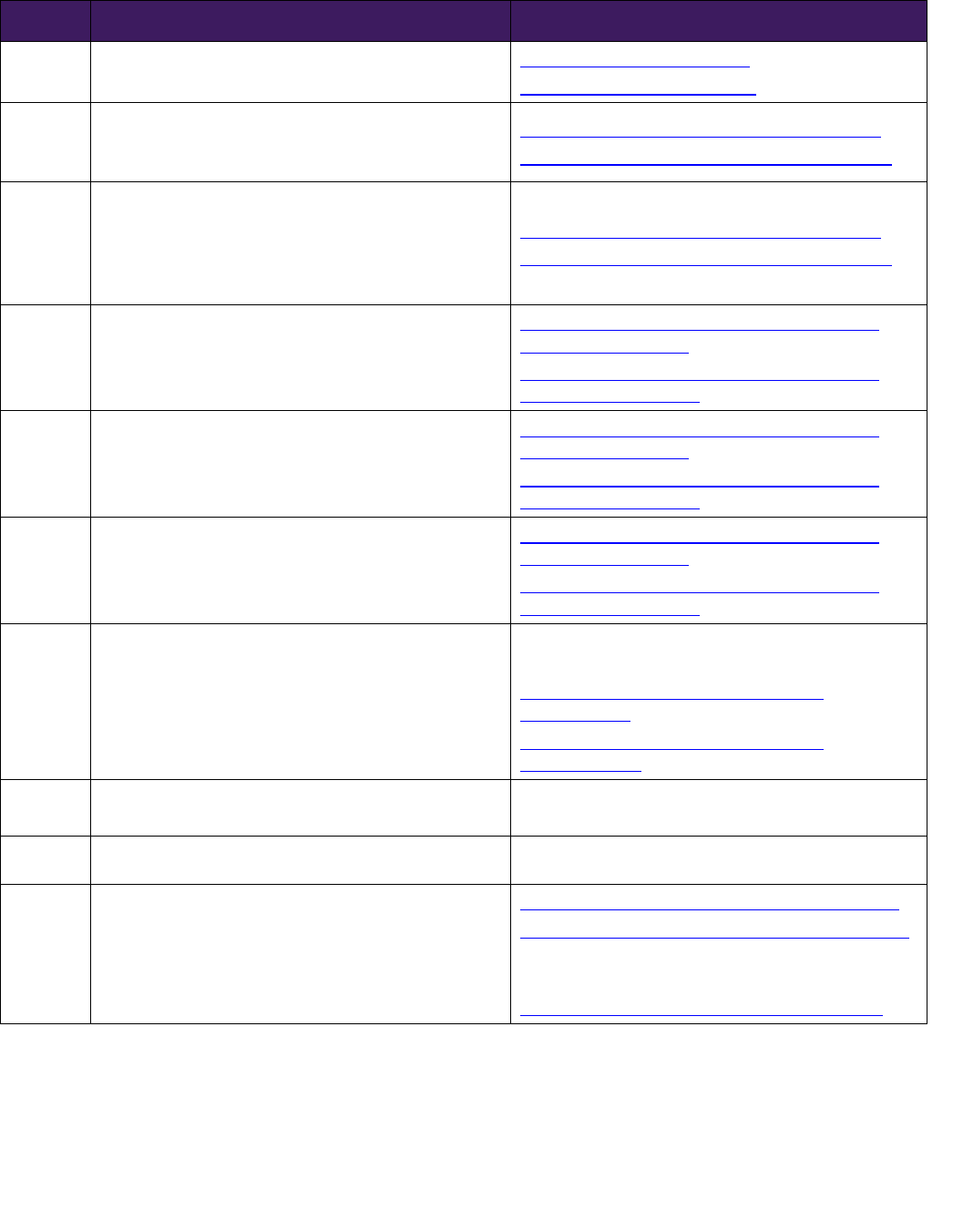
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 7 of 8
Code Description Comments/Related Policy Links
15823
Blepharoplasty, upper eyelid; with excessive skin
weighting down lid
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
15830
Excision, excessive skin and subcutaneous tissue
(includes lipectomy); abdomen, infraumbilical
panniculectomy
Abdominoplasty/Panniculectomy (ConnectiCare)
Abdominoplasty/Panniculectomy (EmblemHealth)
15847 Excision, excessive skin and subcutaneous tissue
(includes lipectomy), abdomen (eg, abdominoplasty)
(includes umbilical transposition and fascial plication)
(List separately in addition to code for primary
procedure)
Abdominoplasty/Panniculectomy (ConnectiCare)
Abdominoplasty/Panniculectomy (EmblemHealth)
17106
Destruction of cutaneous vascular proliferative
lesions (eg, laser technique); less than 10 sq cm
Pulse Dye Laser Therapy for Cutaneous Vascular
Lesions (ConnectiCare)
Pulse Dye Laser Therapy for Cutaneous Vascular
Lesions (EmblemHealth)
17107
Destruction of cutaneous vascular proliferative
lesions (eg, laser technique); 10.0 to 50.0 sq cm
Pulse Dye Laser Therapy for Cutaneous Vascular
Lesions (ConnectiCare)
Pulse Dye Laser Therapy for Cutaneous Vascular
Lesions (EmblemHealth)
17108
Destruction of cutaneous vascular proliferative
lesions (eg, laser technique); over 50.0 sq cm
Pulse Dye Laser Therapy for Cutaneous Vascular
Lesions (ConnectiCare)
Pulse Dye Laser Therapy for Cutaneous Vascular
Lesions (EmblemHealth)
17380 Electrolysis epilation, each 30 minutes
Considered always cosmetic except in conjunction
with gender affirming/reassignment.
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
17999
Unlisted procedure, skin, mucous membrane and
subcutaneous tissue
Medical records required for review of unlisted codes
19300 Mastectomy for gynecomastia MCG #A-0273 Mastectomy for Gynecomastia
19316 Mastopexy
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
MCG #A-0274 Reduction Mammaplasty
(Mammoplasty) (ConnectiCare)
Breast Reduction Mammoplasty (EmblemHealth)
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 8 of 9
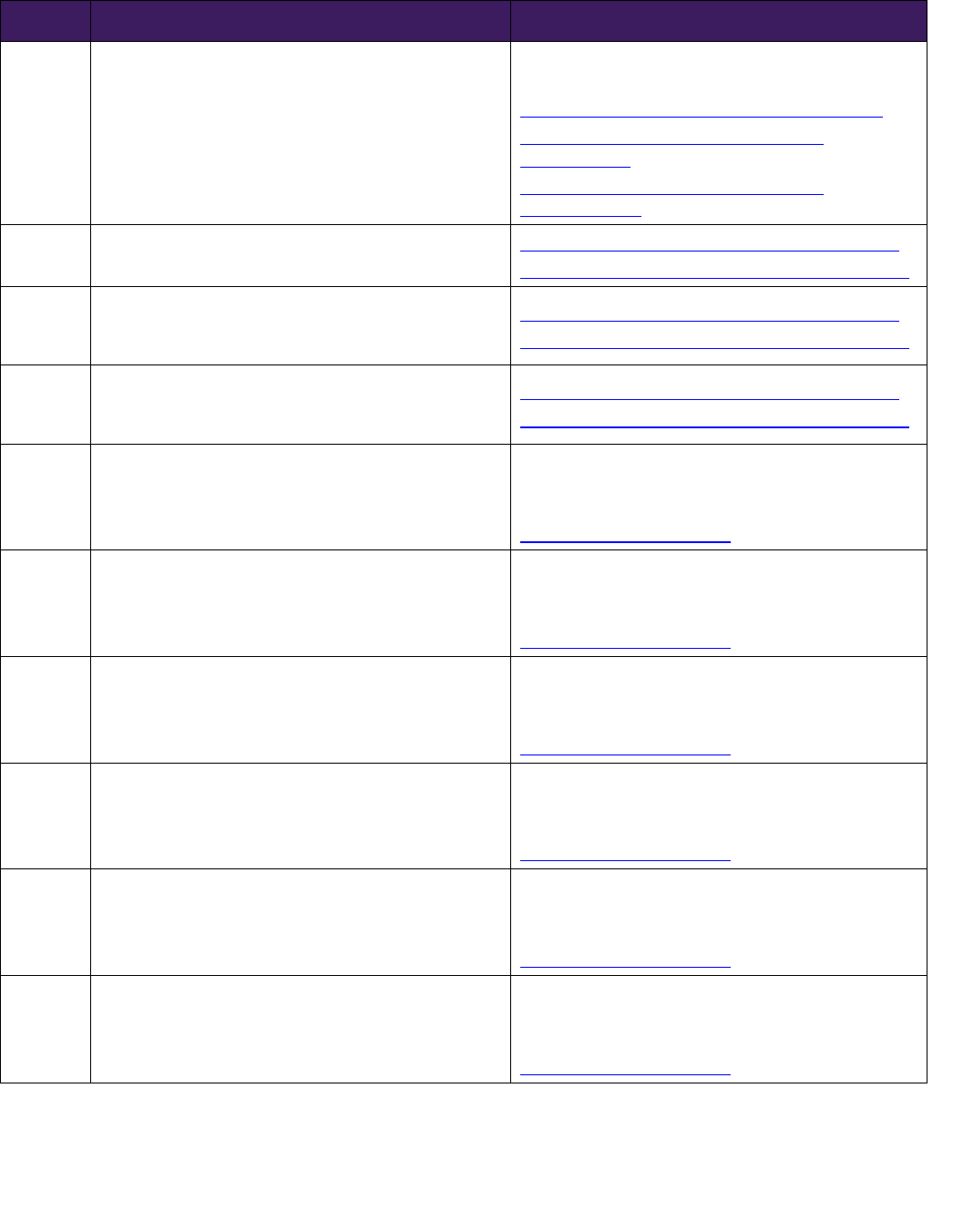
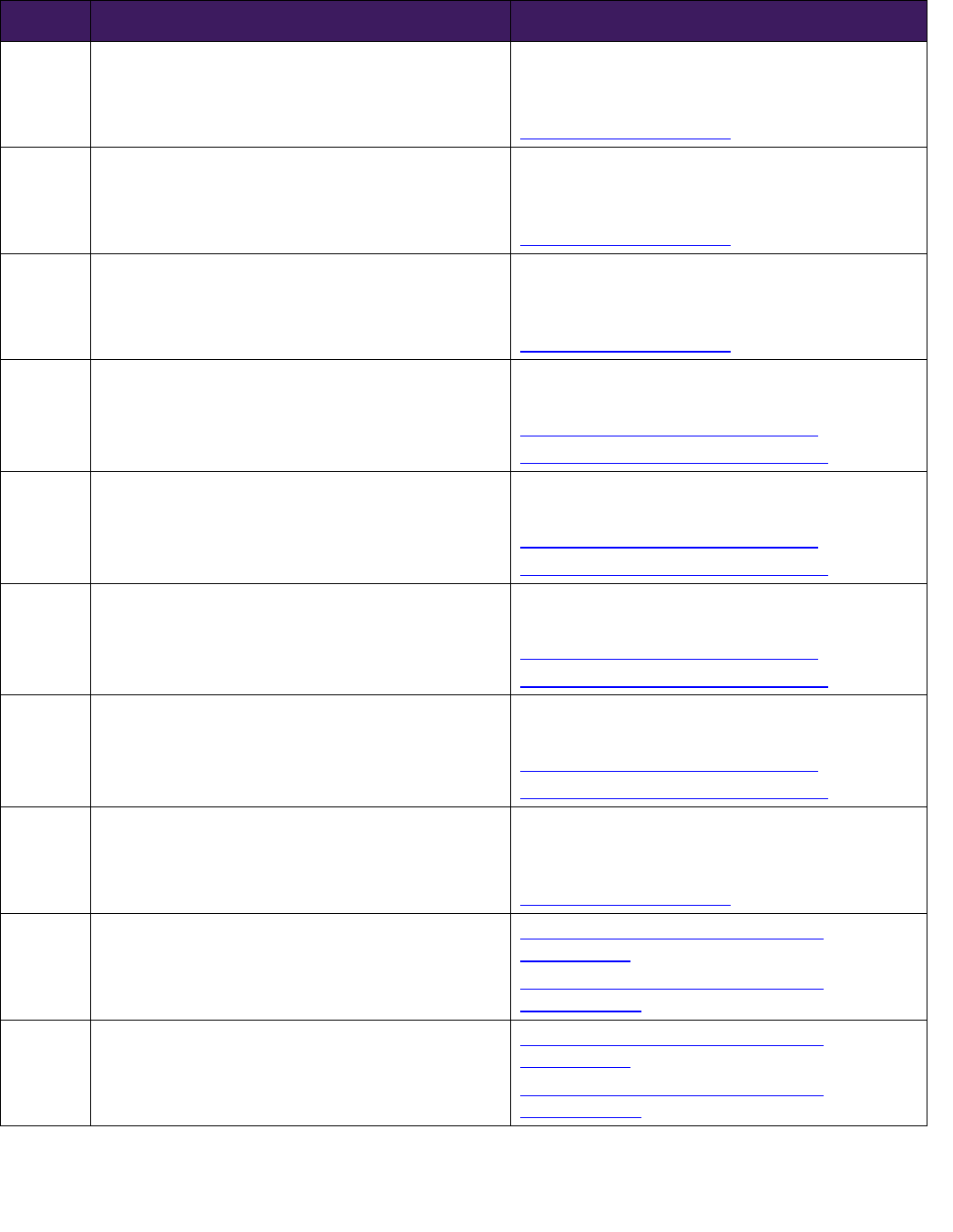
Code Description Comments/Related Policy Links
19318 Reduction mammaplasty
MCG #A-0274 Reduction Mammaplasty
(Mammoplasty) (ConnectiCare)
Breast Reduction Mammoplasty (EmblemHealth)
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
19325
Mammaplasty, augmentation; with prosthetic
implant
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
19340
Immediate insertion of breast prosthesis following
mastopexy, mastectomy or in reconstruction (unless
diagnosis of breast cancer is reported)
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
19342
Delayed insertion of breast prosthesis following
mastopexy, mastectomy or in reconstruction (unless
diagnosis of breast cancer is reported)
Breast Implants and Reconstruction (ConnectiCare)
Breast Implants and Reconstruction (EmblemHealth)
21086
Impression and custom preparation; auricular
prosthesis
May be considered medically necessary when
causing significant impairment of physical or
mechanical function.
See Indications for Coverage
21087 Impression and custom preparation; nasal prosthesis
May be considered medically necessary when
causing significant impairment of physical or
mechanical function.
See Indications for Coverage
21137 Reduction forehead; contouring only
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21138
Reduction forehead; contouring and application of
prosthetic material or bone graft (includes obtaining
autograft)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21139
Reduction forehead; contouring and setback of
anterior frontal sinus wall
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21172
Reconstruction superior-lateral orbital rim and lower
forehead, advancement or alteration, with or without
grafts (includes obtaining autografts)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 9 of 10
Code Description Comments/Related Policy Links
21175
Reconstruction, bifrontal, superior-lateral orbital rims
and lower forehead, advancement or alteration (eg,
plagiocephaly, trigonocephaly, brachycephaly), with
or without grafts (includes obtaining autografts
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21179
Reconstruction, entire or majority of forehead and/or
supraorbital rims; with grafts (allograft or prosthetic
material)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21180
Reconstruction, entire or majority of forehead and/or
supraorbital rims; with autograft (includes obtaining
grafts)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21181
Reconstruction by contouring of benign tumor of
cranial bones (eg, fibrous dysplasia), extracranial
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21182
Reconstruction of orbital walls, rims, forehead,
nasoethmoid complex following intra- and
extracranial excision of benign tumor of cranial bone
(eg, fibrous dysplasia), with multiple autografts
(includes obtaining grafts); total area of bone grafting
less than 40 sq cm
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21183
Reconstruction of orbital walls, rims, forehead,
nasoethmoid complex following intra- and
extracranial excision of benign tumor of cranial bone
(eg, fibrous dysplasia), with multiple autografts
(includes obtaining grafts); total area of bone grafting
greater than 40 sq cm but less than 80 sq cm
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21184
Reconstruction of orbital walls, rims, forehead,
nasoethmoid complex following intra- and
extracranial excision of benign tumor of cranial bone
(eg, fibrous dysplasia), with multiple autografts
(includes obtaining grafts); total area of bone grafting
greater than 80 sq cm
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21230
Graft; rib cartilage, autogenous, to face, chin, nose or
ear (includes obtaining graft)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21235
Graft; ear cartilage, autogenous, to nose or ear
(includes obtaining graft)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 10 of 11
Code Description Comments/Related Policy Links
21242 Arthroplasty, temporomandibular joint, with allograft
Orthognathic Surgery (ConnectiCare)
Orthognathic Surgery (EmblemHealth)
21243
Arthroplasty, temporomandibular joint, with
prosthetic joint replacement
Oral Surgery (ConnectiCare)
MCG #A-0523 Temporomandibular Joint Arthroplasty
(EmblemHealth)
21256
Reconstruction of orbit with osteotomies
(extracranial) and with bone grafts (includes
obtaining autografts) (eg, micro-ophthalmia)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21260
Periorbital osteotomies for orbital hypertelorism,
with bone grafts; extracranial approach
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21261
Periorbital osteotomies for orbital hypertelorism,
with bone grafts; combined intra- and extracranial
approach
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21263
Periorbital osteotomies for orbital hypertelorism,
with bone grafts; with forehead advancement
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21267
Orbital repositioning, periorbital osteotomies,
unilateral, with bone grafts; extracranial approach
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21268
Orbital repositioning, periorbital osteotomies,
unilateral, with bone grafts; combined intra- and
extracranial approach
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21275
Secondary revision of orbitocraniofacial
reconstruction
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21280 Medial canthopexy (separate procedure)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
21282 Lateral canthopexy
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 11 of 12
Code Description Comments/Related Policy Links
21740
Reconstructive repair of pectus excavatum or
carinatum; open
Surgical Correction of Chest Wall Deformities
(ConnectiCare)
Surgical Correction of Chest Wall Deformities
(EmblemHealth)
21742
Reconstructive repair of pectus excavatum or
carinatum; minimally invasive approach (Nuss
procedure), without thoracoscopy
Surgical Correction of Chest Wall Deformities
(ConnectiCare)
Surgical Correction of Chest Wall Deformities
(EmblemHealth)
21743
Reconstructive repair of pectus excavatum or
carinatum; minimally invasive approach (Nuss
procedure), with thoracoscopy
Surgical Correction of Chest Wall Deformities
(ConnectiCare)
Surgical Correction of Chest Wall Deformities
(EmblemHealth)
28344 Reconstruction, toe(s); polydactyly
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
30400
Rhinoplasty, primary; lateral and alar cartilages
and/or elevation of nasal tip
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30410
Rhinoplasty, primary; complete, external parts
including bony pyramid, lateral and alar cartilages,
and/or elevation of nasal tip
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30420 Rhinoplasty, primary; including major septal repair
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30430
Rhinoplasty, secondary; minor revision (small amount
of nasal tip work)
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30435
Rhinoplasty, secondary; intermediate revision (bony
work with osteotomies)
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30450
Rhinoplasty, secondary; major revision (nasal tip work
and osteotomies)
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30460
Rhinoplasty for nasal deformity secondary to
congenital cleft lip and/or palate, including columellar
lengthening; tip only
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30462
Rhinoplasty for nasal deformity secondary to
congenital cleft lip and/or palate, including columellar
lengthening; tip, septum, osteotomies
Rhinoplasty (ConnectiCare)
Rhinoplasty (EmblemHealth)
30540 Repair choanal atresia; intranasal
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 12 of 13
Code Description Comments/Related Policy Links
30545 Repair choanal atresia; transpalatine
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
30560 Lysis intranasal synechia
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
30620
Septal or other intranasal dermatoplasty (does not
include obtaining graft)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
36468
Injection of sclerosant for spider veins
(telangiectasia), limb or trunk
See Varicose Vein Treatment Limitations and
Exclusions
Varicose Vein Treatment (ConnectiCare)
Varicose Vein Treatment (EmblemHealth)
36469
Single or multiple injections of sclerosing solutions,
spider veins (telangiectasia); face
See Varicose Vein Treatment Limitations and
Exclusions
Varicose Vein Treatment (ConnectiCare)
Varicose Vein Treatment (EmblemHealth)
36470
Injection of sclerosant; single incompetent vein
(other than telangiectasia)
See Varicose Vein Treatment Limitations and
Exclusions
Varicose Vein Treatment (ConnectiCare)
Varicose Vein Treatment (EmblemHealth)
36471
Injection of sclerosing solution sclerosant; multiple
incompetent veins, (other than telangiectasia), same
leg
See Varicose Vein Treatment Limitations and
Exclusions
Varicose Vein Treatment (ConnectiCare)
Varicose Vein Treatment (EmblemHealth)
40500
Vermilionectomy (lip shave), with mucosal
advancement
May be considered medically necessary when
causing significant impairment of physical or
mechanical function.
See Indications for Coverage
55970 Intersex surgery; male to female
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
55980 Intersex surgery; female to male
Gender Affirming/Reassignment Surgery
(ConnectiCare)
Gender Affirming/Reassignment Surgery
(EmblemHealth)
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 13 of 14
Code Description Comments/Related Policy Links
67900
Repair of brow ptosis (supraciliary, mid-forehead or
coronal approach)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67901
Repair of blepharoptosis; frontalis muscle technique
with suture or other material (eg, banked fascia)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67902
Repair of blepharoptosis; frontalis muscle technique
with autologous fascial sling (includes obtaining
fascia)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67903
Repair of blepharoptosis; (tarso) levator resection or
advancement, internal approach
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67904
Repair of blepharoptosis; (tarso) levator resection or
advancement, external approach
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67906
Repair of blepharoptosis; superior rectus technique
with fascial sling (includes obtaining fascia)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67908
Repair of blepharoptosis; conjunctivo-tarso-Muller's
muscle-levator resection (eg, Fasanella-Servat type)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67909 Reduction of overcorrection of ptosis
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67911 Correction of lid retraction Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67912
Correction of lagophthalmos, with implantation of
upper eyelid lid load (eg, gold weight)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67914 Repair of ectropion; suture
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67915 Repair of ectropion; thermocauterization
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67916 Repair of ectropion; excision tarsal wedge
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67917
Repair of ectropion; extensive (eg, tarsal strip
operations)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67921 Repair of entropion; suture
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67922 Repair of entropion; thermocauterization
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67923 Repair of entropion; excision tarsal wedge
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 14 of 15
Code Description Comments/Related Policy Links
67924
Repair of entropion; extensive (eg, tarsal strip or
capsulopalpebral fascia repairs operation)
Blepharoplasty (ConnectiCare)
Blepharoplasty (EmblemHealth)
67950 Canthoplasty (reconstruction of canthus)
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
67961
Excision and repair of eyelid, involving lid margin,
tarsus, conjunctiva, canthus, or full thickness, may
include preparation for skin graft or pedicle flap with
adjacent tissue transfer or rearrangement; up to one-
fourth of lid margin
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
67966
Excision and repair of eyelid, involving lid margin,
tarsus, conjunctiva, canthus, or full thickness, may
include preparation for skin graft or pedicle flap with
adjacent tissue transfer or rearrangement; over one-
fourth of lid margin
Medical record review required. May be considered
medically necessary when causing significant
impairment of physical or mechanical function.
See Indications for Coverage
96912
Photochemotherapy; psoralens and ultraviolet A
(PUVA)
Phototherapy, Photochemotherapy and
Photodynamic Therapy for Dermatologic Conditions
(ConnectiCare)
Phototherapy, Photochemotherapy and
Photodynamic Therapy for Dermatologic Conditions
(EmblemHealth)
96913
Photochemotherapy (Goeckerman and/or PUVA) for
severe photoresponsive dermatoses requiring at least
four to eight hours of care under direct supervision of
the physician (includes application of medication and
dressings)
Phototherapy, Photochemotherapy and
Photodynamic Therapy for Dermatologic Conditions
(ConnectiCare)
Phototherapy, Photochemotherapy and
Photodynamic Therapy for Dermatologic Conditions
(EmblemHealth)
Definitions
Cosmetic surgery Cosmetic surgery procedures are those intended solely to refine or reshape structures or
surfaces that are not functionally impaired. They are performed to improve appearance or
self-esteem, or for other psychological, psychiatric, or emotional reasons.
Cosmetic surgery is differentiated from reconstructive surgery, which is generally designed to
improve function, but will usually include an improvement in appearance of the body area
involved.
Cosmetic surgery procedures are usually not considered eligible for coverage. This includes,
but is not limited to, treatments, drugs, products, hospital/facility charges, anesthesia,
pathology/lab fees, radiology fees and professional fees by the surgeon, assistant surgeon,
consultants and attending physicians.
Congenital Anomaly
A physical developmental defect that is present at the time of birth, and that is identified
within the first twelve months of birth
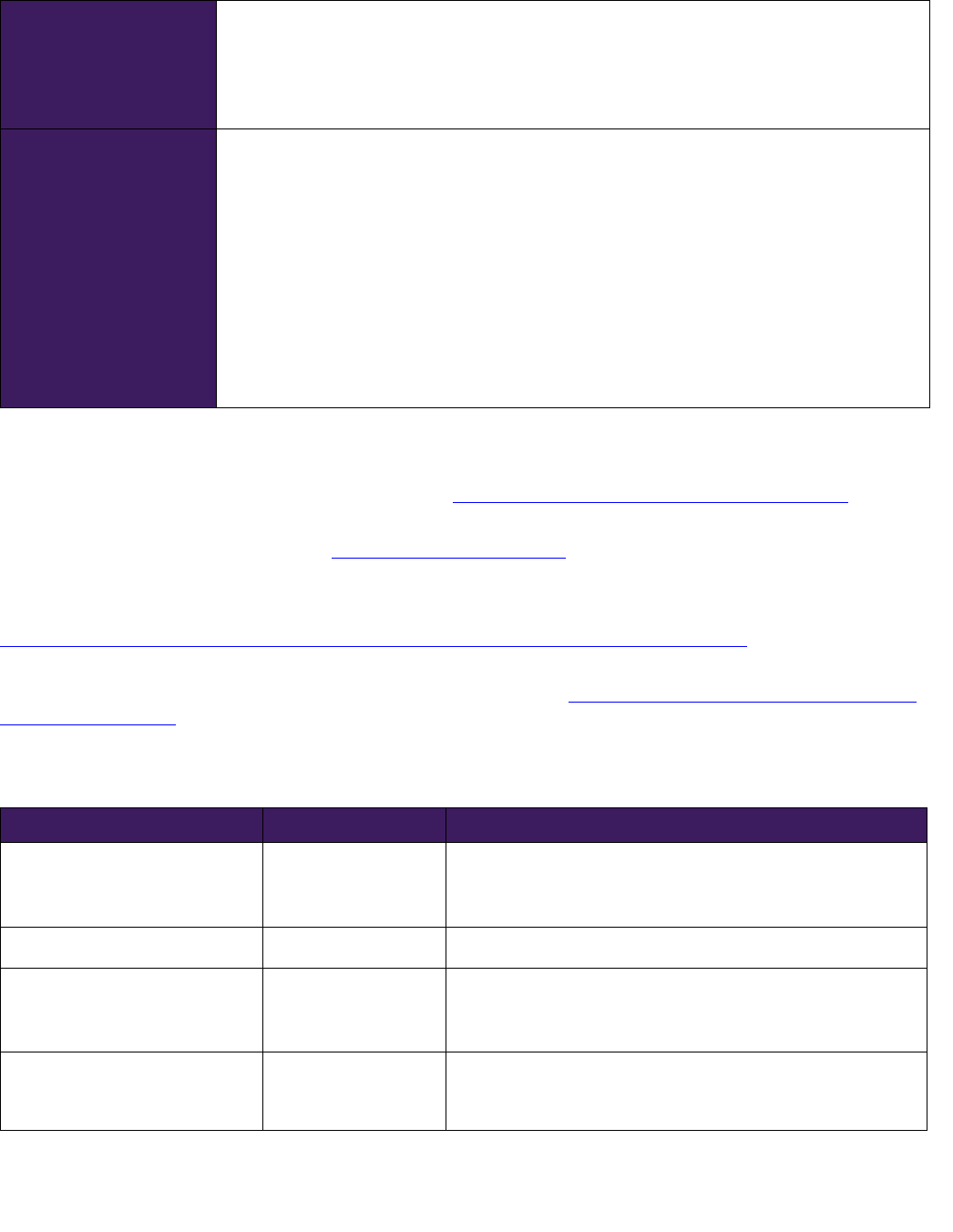
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 15 of 16
Functional or Physical
Impairment
A functional or physical or physiological impairment causes deviation from the normal
function of a tissue or organ. This results in a significantly limited, impaired, or delayed
capacity to move, coordinate actions, or perform physical activities and is exhibited by
difficulties in one or more of the following areas: physical and motor tasks; independent
movement; performing basic life functions.
Reconstructive
Procedures
Reconstructive Procedures when the primary purpose of the procedure is either of the
following:
Treatment of a medical condition
Improvement or restoration of physiologic function
Reconstructive Procedures include surgery or other procedures which are related to an
Injury, Sickness or Congenital Anomaly. The primary result of the procedure is not a changed
or improved physical appearance. Procedures that correct an anatomical Congenital Anomaly
without improving or restoring physiologic function are considered Cosmetic Procedures.
The fact that you may suffer psychological consequences or socially avoidant behavior
because of an Injury, Sickness or Congenital Anomaly does not classify surgery (or other
procedures done to relieve such consequences or behavior) as a Reconstructive Procedure.
References
American Medical Association (AMA). CPT® Assistant Online. https://www.ama-assn.org/practicemanagement/cpt. Accessed
August 24, 2022.
American Society of Plastic Surgeons (ASPS). https://www.plasticsurgery.org. Accessed August 24, 2022.
EmblemHealth/ConnectiCare Certificates of Coverage
Centers for Medicare & Medicaid Services. Women's Health and Cancer Rights Act (WHCRA).
https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/whcra_factsheet
. Accessed August 24,
2022.
U.S. Department of Labor. Women’s Health and Cancer Rights Act (WHCRA). https://www.dol.gov/agencies/ebsa/laws-and-
regulations/laws/whcra. Accessed August 24, 2022.
Revision History
Company(ies) DATE REVISION
EmblemHealth/ConnectiCare Aug. 12, 2022 Moved the following CPT codes to always cosmetic table:
11200, 11201, 15832, 15833, 15834, 15835, 15836, 15837,
15838, 15839, 15876, 15877, 15878, 15879 and 65771
EmblemHealth/ConnectiCare Jun. 29, 2022 Removed CPT codes 17110 and 17111
EmblemHealth/ConnectiCare May 31, 2022 Added CPT codes 21806 and 21807 to generally cosmetic table
Removed medical record review requirement for CPT codes
10040, 15730, 15733, 40500
EmblemHealth/ConnectiCare Apr. 20, 2022 Re-listed CPT codes 21120–21123 in always cosmetic table to
coincide with NYS Department of Financial Services list of
cosmetic codes
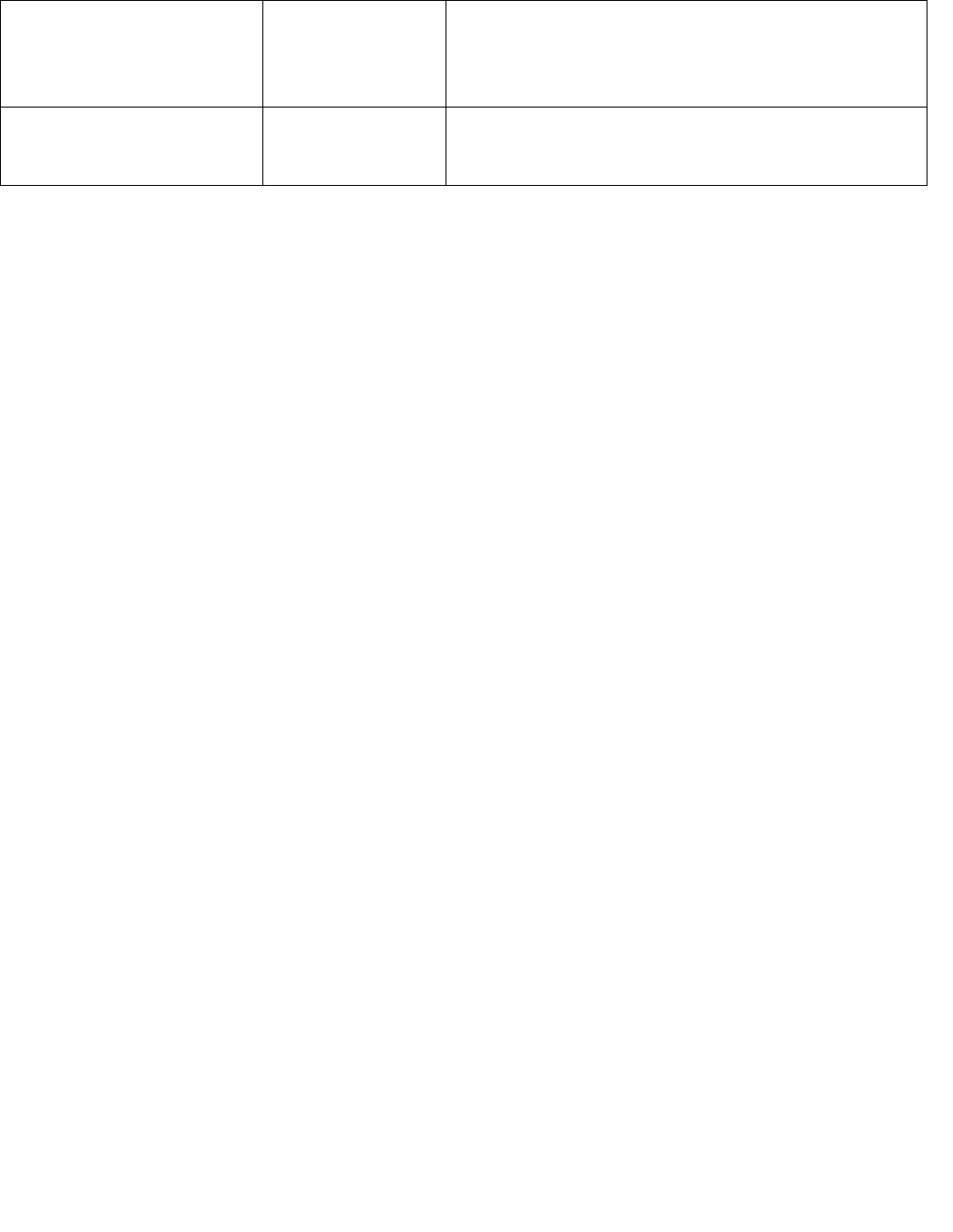
Proprietary information of EmblemHealth/ConnectiCare, Inc. © 2022 EmblemHealth & Affiliates
Page 16 of 16
EmblemHealth/ConnectiCare Feb. 15, 2022 Added CPT 15829 to always cosmetic table
Moved CPT codes 21120–21123 from always cosmetic table to
generally cosmetic table with redirect links added to
Obstructive Sleep Apnea Diagnosis and Treatment policies
EmblemHealth/ConnectiCare Nov. 12, 2021 Reformatted/reorganized policy. Consolidated the Individual
ConnectiCare and EmblemHealth Cosmetic Surgery policies
into a co-branded Cosmetic and Reconstructive Surgery policy
