Title Page
Title of Project: Patient Reminders and Notifications
Principal Investigator:
James D. Ralston, MD MPH
Other team members:
Jennifer McClure, PhD
Paula Lozano, MD MPH
Linda Kiel, MA
Luesa Jordan
Zoe Bermet
Wanda Pratt, PhD
Jordan Eschler, PhD
Katie O’Leary
Logan Kendall, PhD
Lisa Vizer, PhD
Leslie Liu, PhD
Organization: Kaiser Permanente Washington Health Research Institute, formerly Group Health
Cooperative
Inclusive Dates of Project:
Initial grant period: 08/01/2013 – 05/31/2016
No cost extension: 06/01/2016 – 05/31/2017
Federal Project Officer:
Shafa Al-Showk, AHRQ
Acknowledgement of Agency Support:
The project described was supported by grant number
1R01HS021590-01A1 from the Agency for Healthcare Research and Quality (AHRQ). Thank you to
AHRQ for their support. The contents of this report are solely the responsibility of the authors and do
not represent the official views of AHRQ.
Grant Award Number:
4R01HS021590-03
1
Structured Abstract
Purpose:
To describe patient needs and preferences for a comp
rehensive system of care healthcare reminders
and notifications. This work will inform future development and testing of patient-centered reminder and
notification systems.
Scope:
This study id
en
tified user needs, preferences and capabilities for a health reminder and notification
system by focusing on two populations of patients with disparate chronic and preventive care needs.
One population was women who also manage care for their child under age 12 who had asthma. The
second is patients with diabetes and other chronic health conditions including hypertension and
coronary artery disease.
Methods:
Content and functional specification of reminders and notifications were developed with techniques of
user-centered design and based on the Chronic Care Model conceptual framework.
Results:
User
needs assessment and prototype testing established core design features for improving
healthcare reminders and notifications including minimizing the extensive work of integrating healthcare
reminders into the home environment; accommodating the variation of reminder tools in the home;
tying reminders and notifications to individual’s values and where they carry emotional meaning, like
the memory of hard time or the support of a relationship; matching the design of persuasive reminding
to the individual and task; ensuring that reminders reflect and support collaboration with healthcare
providers: and enabling reminders to support shared tasks and interpersonal ties within social
networks. These design principles can help guide healthcare providers and health information
technology developers towards more effective and patient-centered care.
Key
Words:
patient-pr
ovider communication, chronic illness care, care management
2
!
PURPOSE
The overall goal of the project was to describe patient needs and preferences for a comprehensive
syst
em of care notifications and reminders in two patient groups. The results of this study provide
design specifications needed for further study and development of patient reminder and notification
systems across health care systems.
We had two specific Aims:
• Aim 1: Establish the needs and preferences of patients for notifications and reminders by
stu
dying patient workflow models, user requirements, personal communication patterns, and
contextual factors.
• Aim 2: Build and test a prototype of a patient-con
trolled health reminder and notification
system using iterative rapid prototyping and other user-centered design methods to clarify core
design elements and establish the feasibility of integration with the patient-centered medical
home.
3
!
&
&
&
&
SCOPE
Background
Patient reminders and notifications are effective at helping people reach health goals. They alert people
to schedule medical visits and screenings, remind people how to take complex medical regimens, and
provide a liaison between patients, providers, and the health care system. When combined with fully
functional electronic health records, new communication technologies are an opportunity to contact
patients more often with a more comprehensive set of reminders and notifications than previously
possible.
Despite their promise, reminders and notifications, if poorly designed, can overwhelm or annoy patients
and undermine their effectiveness. Questions also remain about patients’ preferences for receiving
more comprehensive reminders and notifications or using newer communication channels to interact
with their health care providers. Moreover, the effectiveness of such enhanced communication systems
is unclear.
Context
Most studies of reminders have focused on a single health care need or condition and a single delivery
mode, such as postal mail or the telephone. We know little about real-world use of reminder and
notification systems for multiple chronic and preventive health care needs targeting a diverse
population in varied settings. We also know little about how to use new communication tools such as
patient websites linked to electronic health records (EHRs), text messaging, or mobile phone
applications for reminders and notifications. In combination with EHRs, these technologies offer
opportunities for more frequent contact with patients and a more comprehensive set of messages.
However, we do not know the ideal attributes of reminders and notifications including the frequency and
timing of contact or the extent to which patients prefer straightforward reminders versus notifications
designed to encourage and support behavioral action. In addition, reminder and notification systems
have the potential to annoy, overwhelm, or frustrate patients. The impact of individual reminders may
diminish as patients receive multiple reminders and notifications. User needs and preferences must
also be balanced against threats to the integrity, security, and privacy of health care information
involved with newer communication technologies, such as text messaging and social network sites.
Designing optimal systems will involve addressing user needs and preferences for reminders and
notifications, being sensitive to patient confidentiality, and incorporating the capacity of newly emerging
communication technologies such as social media, text messaging, and mobile applications to interact
daily with patients.
Settings&
This study was conducted at Kaiser Permanente Washington (formerly Group Health), an integrated
care delivery system with over 660,000 members in Washington and North Idaho. The proposed study
was restricted to the 391,749 members who receive primary care at one of Kaiser Permamente
Washington’s 28 owned-and-operated clinics. At the time of the study, Kaiser Permanente
Washington’s membership includes 55,239 Medicare members, 19,089 Medicaid members, and 11,623
covered by the Basic Health Plan (a state supported insurance program for low-income families). The
Kaiser Permanente Washington’s population is generally similar to that of the surrounding area. Kaiser
Permanente Washington had a slightly higher proportion of women (53%) than the regional community
(50%) and the nation (51%). Kaiser Permanente Washington’s members are also older (46% ≥45
years) than the regional community (38%) and the nation (39%). Compared to the rest of the country,
Kaiser Permanente Washington members are more likely to be Asian or Pacific Islanders (9% versus
4%), but less likely to be African American (4% versus 12%) or report Hispanic ethnicity (4% versus
15%). The Kaiser Permanente Washington racial and ethnic composition broadly represents the Puget
Sound region. In this study, we purposively sampled the Kaiser Permanente Washington population to
simulate the educational status of the U.S. population when possible (approximately 50% with high
school or less educational level) and oversampled racial and ethnic minorities (see Study Population
below for details). Kaiser Permanente Washington uses an ambulatory EHR system (EpicCare) that
4
&
Aim 1:
Aim 2:
N
%
20
N
%
includes clinical decision support features, secure provider-to-provider messaging, and an EHR-
integrated online medical record shared with patients (
www.ghc.org
). Features include secure patient-
provider electronic messaging and online patient access to medical record elements, including results
of medical tests,
af
ter-vi
sit summaries,
and mobile
extensions of the
integrated personal
health record for
iPhone and Android
smart phones.
Currently, at Kaiser
Permanente
Washington, several
reminders are part of
the annual birthday
letter sent out to each
enrollee. Some
reminders also
appear on the patient
website. Like many
US healthcare
systems, notifications
of medical test results
are sent through US
mail letters and email
ticklers
recommending going
to the new test results
on the patient website
or mobile application.
Email notifications are
also sent if a new
secure message from
a provider is present
on the patient's
website.
Table 1: Characteristics of Patient Participants in Needs Assessment
Total
N
40
Asthma
100
Diabetes
20
100
Median Age (Years)
Me
an Age (Years)
54.5
54.
5
37.0
37.
5
64.0
64.
5
Race & ethnicity
Asian
2
0
0
2
10
Black
12
6
30
6
30
Hawaiian
1
1
5
0
0
Indian
0
0
0
0
0
Mixed
1
0
0
1
5
Other
2
1
5
1
1
Unknown
2
2
10
0
0
White
20
10
50
10
50
Hispanic*
2
1
5
1
5
Online health portal use
User
No
n-user
27
13
17
3
85
15
10
10
50
50
Education
>High school
Hi
gh school or less
28
12
16
4
80
20
12
8
60
40
*Hispanic ethnicity designation overlapped with other designations of race; total is > 100%
Participants
Table 1 shows the characteristics of the 40 individuals in our needs assessment. As shown in
the table, we purposively sampled individuals with minority racial and ethnic backgrounds in order to
more closely align our participant group with the demographics of the overall US population.
Participants with high school or less formal education level were difficult to recruit, particularly for the
mothers of children with asthma. We were still, though, able to recruit 30% of the overall population with
a high school or less educational level. Since portal use in the KP Washington population had also
grown to over 70% of members overall with even higher use among those with healthcare needs such
as diabetes and asthma, we also changed our initial sampling plan from half portal users to just under
70% portal users.
Aim 2 had four stages of patient and provider engagement in design. In the first stage, we engaged
thre
e cohorts of patients in two sequential sets of futures workshops to help envision ideal reminder
and notification systems; cohorts consisted of patients with diabetes and mothers of children with
asthma. In the second stage, we engaged three cohorts of participants in two sequential participatory
design sessions; cohorts consisted of a mix of patients, mothers of children with asthma and healthcare
5
Study Design
African American
Nat. Amer/Alask.
Hispanic
White
High Sch. or less
Some College
4YR College
+4YR College
providers. Table 2 shows the demographics of patient participants in participatory design sessions.
Providers involved in these sessions included 6 primary care providers, 3 medical assistants and 3
nurses
In the third stage of Aim 2, we held two
sequential prototype testing sessions
with 15 patients. Prototypes for the
second session were iterated based on
feedback from the first session. We also
held 2 separate prototype testing
sessions with 15 providers (7 PCPs, 7
MAs, 1 nurse). In stage four, we tested a
series of designs specifically focusing on
new reminder and notification
functionality in the patient portal. This
final stage included prototype testing with
19 patients.
1
Incidence and Prevalence
Measuring incidence and prevalence
was not part of t
his study.
Methods
We used mixed met
hods grounded in a
user centered design approach. Specific
methods included ethnographic
interviews, Q methodology, photo
elicitation, participatory design
workshops, and prototype testing.
Table 2: Aim 2: Participant Demographics for Participatory Design
Mothers of
children with
Asthma
Older adults with
Diabetes
N=11
N=12
Age
Range (yrs)
31-45
54-89
Mean (yrs)
38
73
Race
5
0
0
6
6
0
0
6
Education
2
5
1
3
4
2
2
4
Statistical Analysis
Statistical analysis was only applicable for Q-methodology. All other analyses were qualitative. For Q-
methodology, we used PQMethod software in factor analysis to help identify clusters of individuals with
shared attitudes towards self-management of chronic illness and use of communication technologies.
2
Data Sources/Collection
Data sources included the follo
wing: transcribed interviews; photos by participants; surveys of attitudes
towards communication technologies and self-management of chronic illness; Q data sets; recordings,
artifacts, transcripts and notes from participatory design workshops; audio and video recordings,
transcripts and notes from prototype testing sessions.
Measures and Surv
ey Items
Survey measures were used only for Q meth
odology where we adapted self-reported survey questions
from Davis’ measure of the perceived usefulness, ease of use, and user acceptance of technology
3
; the
patient assessment of chronic illness care (PACIC) and measures of autonomous support.
4,5
Limitations
Our comprehensive approach to remind
ers and notifications did not permit us to target all redesign
processes and follow-up activities involved in chronic care and preventive care. We were also
challenged to make the reminder and notification system simple and visible to a large population of
patients. To address this, we engaged the most diverse set of patients allowed by our methods and
resources.
6
Results
Principal Findings
We su
mmarize our prin
ciple findings by Aim below and then by core design principles. Further details
are in peer reviewed publications (9 published, 2 in process). Results not yet published or in
submission have more detail below.
Aim 1: Establish the needs and preferences of patients for notifications and reminders by studying
pati
ent workflow models, user requirements, personal communication patterns, and contextual factors.
Methods Development:
To begin our work, we published two methods papers to more effectively, efficiently and respectfully
elic
it patient stakeholder input on needs and preferences for designing better healthcare reminders and
notifications. We also published a third paper on the development of Q methodology to help understand
design tradeoffs for tailoring health technologies to different populations. These methods can also be
applied for eliciting patient and family needs for other health information technology applications.
1. Systematic inquiry for design of health care information systems: an example of elicitation of the
patient stakeholder perspective (published).
6
This paper describes the application of the
Vicente theoretical framework to organize qualitative data during our multistage study into
patient engagement with health information technology. The framework helped us develop
interview probes for encouraging patient narratives of engaging with reminders in task cycles in
their home. This approach allowed a more full description of individual and family work rather
only on positive or negative aspects of experiences with reminders systems.
2. Opportunities for empathetic responses in field interview scenarios investigating home health
routines (published).
7
This paper sought to identify and describe effective interview approaches
for fostering empathy with participants during the design process. Empathy with participants
who were living with chronic health conditions was considered essential for building trust and
engaging participants in the design process. The study was performed at midpoint in the data
collection from patient and family interviews in the first phase of Aim 1, which allowed
application of the findings to follow up interviews and other study activities. We identified factors
valuable for enhancing empathy during participant interviews including active listening methods
during expressions of frustration about a diagnosis and feelings of guilt or failure in treatment
and prevention of health conditions.
3. Understanding design tradeoffs for health technologies: a mixed methods approach
(published).
8
In order to better tailor reminder and notification systems, we sought to understand
how participants’ attitudes towards use of communication technologies intersected with their
attitudes towards self-management of chronic illness. In this paper, we describe an approach
involving a novel application of the Q-method, a mixed methods approach providing a few key
advantages for health design science including: a structured framework to guide data collection
and analysis; enhanced coding of unstructured data with statistical patterns of polarizing and
consensus view; and elicitation of participants active expression and weighting of competing
values relevant to healthcare design(see below for separate paper on Q method results).
Patient Work, Men
tal Models and Motivation
In a series of analyses, we developed
an understanding of how participants remember what to do
during daily life to inform better design of healthcare reminders and notifications. For these studies, we
viewed healthcare reminders and notifications within the larger context of self-management of chronic
illness.
1. Shared calendars for home health management (pub
lished).
9
Our home visits and interviews
quickly established that home calendars were a central tool for helping participants and families
remember tasks to do each day. This paper described the how 40 of our adult participants (20
each of mothers of children with asthma and individuals with type 2 diabetes) used shared
calendars to support home management. We report on both the diverse systems of home
calendar management, including the common use of multiple calendars within a home, and
failures experienced. We then describe implications for schedule management strategies for
7
individuals and families who need to remember and incorporate the common tasks of caring for
chronic illness.
2. Engineering for reliability in at-home
chronic disease management (published).
10
In this paper,
we examined remembering to perform healthcare tasks in the home from the perspective of
prospective memory theory and systems reliability engineering. Based on participants’
experiences, failures in remembering to perform self-management activities should be viewed
as system failures rather individual failures. Participants also described several design
strategies used to enhance the reliability of systems designs for remembering to perform self-
management tasks. We discuss how these results can be used to improve the reliability and
experience of healthcare reminder systems.
3. Understanding patients’ health and technology attitudes for tailoring self-man
agement
interventions (published).
2
In this publication, we used mixed methods approach (described in
publication #3 under Methods Development) and maximum variation sampling to describe the
intersection between attitudes towards communication technologies and attitudes towards self-
management of chronic illness in 40 of our participants. We found three participant clusters,
“Proactive Techies”, “Indie Self Managers” and “Remind Me! Non-techies” which were
independent of education level, race and age. These results are valuable for informing tailored
design of reminder and notification systems.
4. Designing Asynchronous Communication Tools for Optimization of Patient-Cli
nician
Coordination (published).
2
Since an increasing number of healthcare reminders and notifications
are communicated asynchronously between provider visits, either electronically or through US
mail, we sought to understand how designers can avoid pitfalls and optimize new opportunities
in this growing and evolving form of communication. Key themes emerged associated with both
unsatisfactory and satisfactory asynchronous communication. For good communication, these
themes included the following: enhancing care with followup; reducing uncertainty in plan of
care; and providing an automatic health archive to reference later. Themes of unsatisfactory
asynchronous communication included failing to track issues, including closing the loop on
reminder and notification communications, and exposing patients to inconsistent communication
patterns. Key design recommendations for asynchronous health communications included
incorporating patient preferences for non-urgent information exchange and incorporating status
indicators in asynchronous communications including reminder and notifications.
5. Finding Reminders in the World: How Individuals Support Motivation and Tasks in Managing
Chronic Illness (in revision for submission).
11
In our home visits, we heard clearly that day to day
remembering and performing health self-management tasks can be a tremendous burden for
patients. Motivation to complete these tasks is often a big challenge. After sending our
participants home with Polaroid cameras in the followup phase of the study, we discovered
participants were often appropriating everyday things to both remember and motivate
themselves to perform healthcare tasks. These included artifacts in the home, such as the
display of a cane that prompted a memory of former disability associated with lack of self-
management; and emblems of motivating relationships, such as pictures of loved ones. These
were the most potent reminders we found and highlight new opportunities for providers to
engage patients in identifying and developing a motivating and effective environment for health
in the homes.
Aim 2: Build and test a prototype of a patient-co
ntrolled health reminder and notification system using
iterative rapid prototyping and other user-centered design methods to clarify core design elements and
establish the feasibility of integration with the patient-centered medical home.
1. Persuasive Reminders for Health Self-Man
agement (published).
12
During participatory design
sessions, patients used a combination of storyboards, collages and cultural probes to describe
future reminder systems that could support fulfillment of tasks of managing chronic illness.
Participant’s ideas and prototypes for these idealized reminder systems identified four key types
of persuasive healthcare reminders: introspective, socially supportive, adaptive and symbolic.
Including these features in reminder design can help support patients to understand why and
8
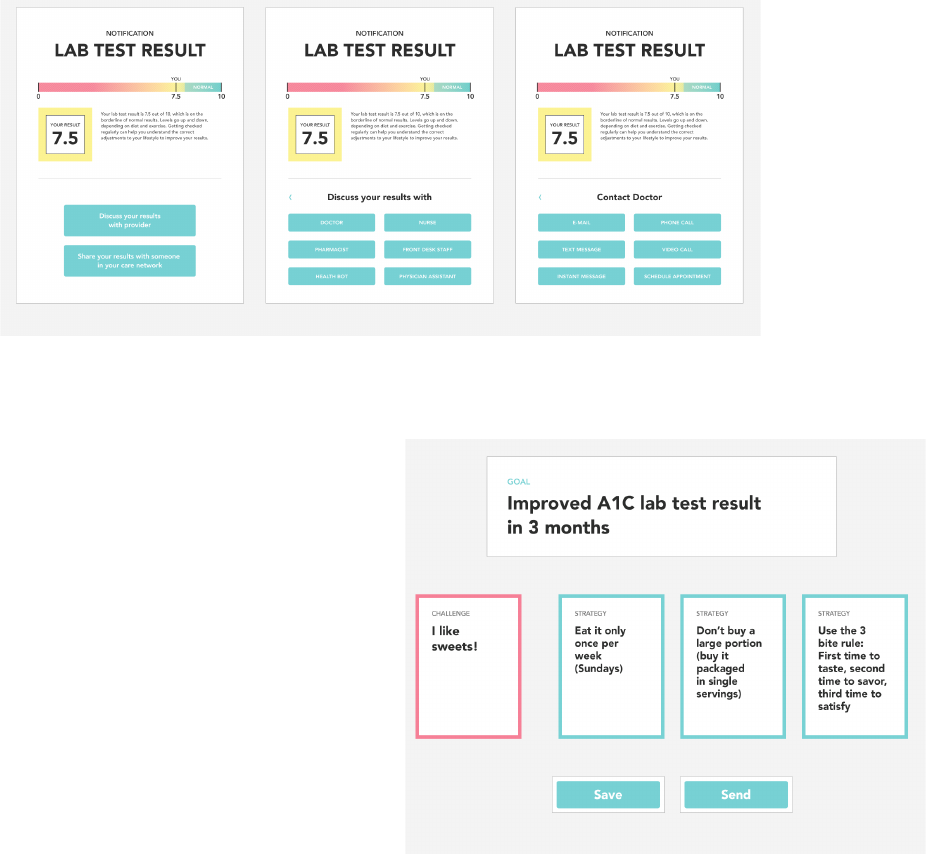
Figure XX: Discovery Tool for Notifications
how to complete healthcare tasks ahead of time.
2. Collaborative Health Reminders and Notifications (drafted for submission). During this final
phase of the project, we iteratively designed and tested prototype reminder and notification
systems in two iterative phases. To develop prototypes, we began with a synthesis of needs
analysis from Aim 1. This needs analysis then fed into value scenarios which were used with
designers in an inspiration workbook. Based on the results, we developed and tested with
participants low fidelity prototypes including a Symbolic Reminder Band, Social Reminder App,
a Reminder Invitation, a Discovery Tool (figure 1) and a Conversational Tool (Figure 2). We
show picture of two of these tools below. The discovery tool was created to explore how
patients gain clarity around their healthcare and how they communicate their need for that
clarity with their provider from outside of the clinic after receiving a notification.
Figure 1: Discovery Tool for Reminders
The conversational tool was created to explore how patients and providers might collaborate in
the clinic on creating reminders around unique patient challenges and strategies to overcome
those challenges.
Preliminary analysis of the results of
prototype testing found that participants
emphasized the importance of
designing collaborative health
reminders and notifications with
particular attention to three domains:
(1) Enable the p
atient-provider
relationship; (2) Support shared action
on health tasks; and (3) Promote
interpersonal ties based on shared
health tasks and goals. Participants
also reported on the potential
challenges of collaborative reminders,
including administering reminders
across social networks.
Figure 2: Conversational Tool for Reminders
3. Integrating the Patient Portal into
Health Management Work Ecosystems User Acceptance of a Novel Prototype (published):
1
. In
this paper, we built on our earlier to work to elicit feedback about reminder and notification
features in patient portals. We used a patient centered approach to design and test prototypes
of new features for managing health tasks within an existing portal tool. We iteratively tested
three prototypes with 19 patients and caregivers. Implications for design based on our findings
included building on the positive aspects of clinician relationship to enable engagement in the
portal including patient reminders; using face to face visits to promote clinical collaboration in
portal use including reminders for healthcare tasks and notifications of test results; and allowing
9
customization of portal modules to support tasks based on user roles.
4. Prototype Feasibility within the Primary Care Setting: In two
group sessions with primary care
team members including PCPs, RNs and MAs, we evaluated the feasibility of three prototypes
developed with patients and described above. We focused on prototypes most amenable
patients and with the most significant potential to impact primary care workflow. The first
prototype focused on a new reminder for getting a retinal screening exam in a patient newly
diagnosed with diabetes, who did not remember why an exam was needed. The prototype
allowed for different options to contact the healthcare provider. Most of the providers
emphasized the value of the reminder existing within an ongoing relationship that includes
educating patients on the importance of recommended healthcare tasks including retinal exams.
While participants endorsed the prototype’s overall concept of easily sending questions to
providers from a reminder, participants were concerned that the patient didn’t sufficiently
remember the value of the exam and identified a missed opportunity for the team to inform the
patient during prior in person visits. In the second reminder, a patient is notified of a medical test
result online and has a followup question. Multiple options for reaching different members of the
care team or a health bot are provided. Primary care team members were concerned about
being overwhelmed with messages from patients in this prototype and liked the possibility of an
automated health bot being the first stop to provide patients with a potential answer. The third
prototype was the conversational reminder tool described above. Overall, providers liked this
tool the most and thought it had potential, as long as the patient was excited to use it. Providers
struggled some, though, with how the tool could be integrated into current primary care staffing
and roles. Several providers thought using a health coach or similar new role would enable use
of the tool rather than adding to the existing roles of nurses or MAs.
Core Design Principles
Based on the combined analyses and publications above, we outline below the study’s core principles
for d
esigning better patient reminders and notifications. We have grouped these principles within four
broad categories of our findings: reminding and notifying within patient and family workflow;
opportunistic reminding; persuasive reminding; and collaborative reminding. Further details describing
these principles are included in our publications.
Reminders and Notifications within Patient and Famil
y Workflow. To integrate with the broad ecology of
calendaring and scheduling, reminder tools in the home should
• Incorporate patient preferences for modality of non-urgent i
nformation exchange.
• Enhance patient followup on reminders and communicate with providers about questions or
conce
rns relating to the healthcare recommendation in the reminder.
• Incorporate status indicators into reminders and other asynchronous communication. Thes
e
indicators would help build shared understanding and accountability between patients, providers
and family members for healthcare tasks and communication.
• Support need for some redundancy in home reminder systems including repeated reminders
and div
ersity of systems used in the home (e.g. paper and electronic)
Opportunistic Reminders. To en
able the most potent reminders we identified in our study,
• Healthcare providers should engage patients in identifying or developing artifacts, activities or
routines that can both remind and motivate for healthful behaviors.
• Heath IT developers should work to move the power of the opportunistic reminders outside of
the h
ome environment and onto mobile applications and into communications with patients and
families.
Persuasive reminders. To help reminders be more meaningful and persuasive, tailor reminder design to
one of
four types to match the task:
• Introspective reminders to trigger reflection goals.
• Socially supportive reminders to enhance motivation and mentoring relation
ships.
10
• Adaptive health reminders that change to meet the shifts in health status, task status and
modality preference.
• Symbolic reminders reminding of personally significant reasons for health behaviors (e.g.
images of a child, dog, garden)
Collaborative Reminders. To
support collaboration and relationships with healthcare providers, family
and friends, reminders should
• Enable the patient-provider relationship. Participants expressed a strong need for reminder to
reflect collaboration with healthcare providers on health goals and tasks and the reminders
themselves should in turn enable the patient-provider relationship.
• Support shared action on health tasks acr
oss social networks including family and friends.
• Promote interpersonal ties based on shared heal
th tasks and goals including both weak and
strong ties.
Discussion
The findings of this project helped address a critical junction in the design and use of patient
noti
fications and reminders. We developed several core design recommendations that can be used by
healthcare providers and policy makers as well as health information technology developers. The value
of our work was emphasized by the enthusiasm received in its publication including nomination of two
of our papers for the outstanding paper award at the Annual American Medical Informatics
Conference
2,12
with one paper winning the award.
2
During and after our presentations, we were also
sought out by health information technology companies for our results and how they might be applied to
current EMRs and patient facing health information technologies. We expect that our results will
continue to help guide both health information technology developers and the design of healthcare
delivery.
Grounding our project in the appro
ach and methods of user centered design allowed us to identify
unexpected challenges and opportunities for designing reminders. We entered the grant believing the
main challenges facing patients related to incorporating multiple reminders across an increasing
number of platforms of communication into daily workflow and management. We came out of the grant
recognizing that the biggest challenges and opportunities focused on designing reminders which better
reflected each patient’s values and goals developed within collaboration with healthcare providers. We
expanded our design probes and prototypes to accommodate this broader set of patient and family
needs.
Our study had
a few limitations. Due to our use of in depth investigation with individual patients, families
and providers, we had a limited number of subjects, all of whom lived in the greater Puget Sound area.
We sought to mitigate this limitation by recruiting a sample which better reflected the overall
demographics of the United States, including greater representation from those with minority racial and
ethnic background and lower formal educational levels. The needs, preferences and abilities for
healthcare reminders and notifications, however, may still be different among populations in other
regions of the United States. Our participants may also have expressed needs and preferences which
may not persist if we had built and deployed a fully functional reminder and notification system within
the patient centered medical home. Although our prototype testing helped attenuate the potential for the
well-known discordance that can occur between expressed and realized needs and preferences, only a
real world testing over months to years would fully clarify the system requirements.
Conclusions
Current healt
hcare reminders and notifications are not sufficiently meeting patients’ needs, preferences
and capabilities. Improving healthcare reminders and notifications will require minimizing the extensive
work of integrating healthcare reminders into the home environment; accommodating the variation of
reminder tools in the home; tying reminders and notifications to individual’s values and where they carry
emotional meaning, like the memory of hard time or the support of a relationship; matching the design
of a persuasive reminding to the individual and task; ensuring that reminders reflect and support
11
collaboration with healthcare providers: and enabling reminders to support shared tasks and
interpersonal ties within social networks. These design principles can help guide healthcare providers
and health information technology developers towards making care more effective and patient
centered.
Significance
This project addressed a
c
ritical junction in the design and use of patient notifications and reminders.
The increasing engagement of patients in care outside of office visits, including through using patient
websites and mobile communication technologies, offers new opportunities to improve care. The
number of potential reminders and patient notifications and the variety of delivery mechanisms also
risks overwhelming and alienating patients. In this study we identified key design principals that can
help keep reminders and notifications meaningful and effective for patients and families. Many of our
findings challenge current approaches to how we remind patients for common health care tasks and
notify them of medical test results and other health information.
Implications
Many of our findings can be applied immediately to the design of both healthcare del
i
very and health
information technology. Simple design changes, such as status indicators on a reminder for a task
received over a patient website or mobile application could substantially improve communication with
patients and may improve the effectiveness of care. Other findings, such as the collaborative reminder
tool, have strong potential to improve how we currently deliver self-management support programs for
chronic conditions including diabetes. These implementations could be done with little impact on
provider workflow and would not require significant changes in staffing or the delivery of care.
The results of our study, h
owever, also highlight many of the larger challenges remaining for the design
of better healthcare reminders and notifications. We heard consistently that reminders for healthcare
tasks need to reflect a patients values and a shared understanding of healthcare goals and tasks
established during collaboration with a personal healthcare provider. Even our best healthcare systems
are ill equipped to create and maintain this level of personalized care. The depth of detail needed for
individual patient and family engagement in this approach to care is beyond the current structure and
financing of healthcare in the United States. These challenges will only grow as the number of
healthcare tasks recommended for individuals continues to rise along with the increasing complexity of
many patients’ care. No health information technology can address these needs on its own. If we are
to build more effective and patient centered reminders and notifications that help patients achieve
better health, we must invest in better staffing and models of primary care.
List of Publications and Products
Publications:
1. O’Leary KO, Liu L, McClure JB, Ralston JD, & Pratt W. Persuasive reminders for health self-
management. Proceedings of the American Medical Information Association, Nov 12-16, 2016.
Chicago, IL.
2. Eschler J, Meas PL, Lozano P, McC
lure JB, Ralston JD, and Pratt W. Integrating the patient
portal into the health management work ecosystem: user acceptance of a novel prototype.
Proceedings of the American Medical Information Association, Nov 12-16, 2016. Chicago, IL.
3. O’Leary K, Vizer L, Eschler J, Ralston J, Pratt W. Understanding patients’ health and tec
hnology
attitudes for tailoring self-management interventions. AMIA Annu Symp Proc. 2015 Nov
5;2015:991-1000. PMC4765611.
4. Eschler J, Liu LS, Vizer L, McClure J, Lozano P, Pratt W, Ralston J. Designing asynchronous
com
munication tools for optimization of patient-clinician coordination. AMIA Annu Symp
Proc. 2015 Nov 5;2015:543-52. PMC4765629.
5. O’Leary K, Eschler J, Vizer LM, Ralston JD, Pratt W. Und
erstanding design tradeoffs for health
technologies: a mixed-methods approach. Proceedings of CHI (Human Computer Interaction).
April 2015.
12
6. Eschler J, O’Leary K, Kendall L, Ralston JD, Pratt W. Systematic inquiry for design of health care
information systems: an example of elicitation of the patient stakeholder perspective. In
Proc
eedings of the Hawaii International Conference on System Sciences. January, 2015.
7. Kendall L, Eschler J, Lozano
P, McClure JB, Vizer LM, Ralston JD, Pratt W. Engineering for
reliability in at-home chronic disease management. AMIA Annu Symp Proc. 2014 Nov
14;2014:777-86. PMC4419963.
8. Eschler J, Kendall L, O’Leary K, Vizer LM, Lozano P, McClure JB, Pratt W, Ralston JD. Shared
cale
ndars for home health management. In Proceedings of the 18th ACM conference on
Computer-Supported Cooperative Work and Social Computing. March, 2015.
Posters and Presentations:
1. Designing Reminders and Notifications for Patients: AHRQ National Webinar. May 7
th
, 2015
Manuscripts in Preparation:
1. Liu L, O’Leary K,
Pratt W, Ralston JD. Opportunistic Reminders in the World: How Older Adults
Design Everyday Reminders to Manage their Chronic Illness.
2. O’Leary K, Tenghe D, Pratt W, Ralston JD. Designing Reminders for Socialable Use.
References:
1. Eschler J, Meas PL, Lozano P, McClure JB, Ralston JD, Pratt W. Integrating the patient portal
into
the health management work ecosystem: user acceptance of a novel prototype. AMIA Annu
Symp Proc. 2016;2016:541-50. PMCID: PMC5333335.
2. O'Leary K, Vizer L,
Eschler J, Ralston J, Pratt W. Understanding patients' health and technology
attitudes for tailoring self-management interventions. AMIA Annu Symp Proc. 2015;2015:991-
1000. PMCID: PMC4765611.
3. Davis F. Perceived Usefulness, Perceived Ease of Use, and
Us
er Acceptance of Information
Technology. MIS Quarterly. 1989;13:319-39.
4. Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and
vali
dation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care. 2005;43:436-
44. Epub 2005/04/20.
5. Ryan RM, Deci EL. Self-det
erm
ination theory and the facilitation of intrinsic motivation, social
development, and well-being. Am Psychol. 2000;55:68-78.
6. Eschler J, O'Leary K, Kendall L, Ralston JD, Pratt W. Systematic inquiry for design
of health
care information systems: an example of elicitation of the patient stakeholder perspective. In
Proceedings of the Hawaii International Conference on System Sciences. 2015.
7. Eschler J, Ralston J. Opportunities for Empathetic Responses in Fiel
d Interview Scenarios
Investigating Home Health Routines. 2014.
8. O'Leary K, Eschler J, Kendall L, Vizer LM, Ralston JD, Pratt W. Understanding Design
Trad
eoffs for Health Technologies: A Mixed-Methods Approach. Proceedings of the 33rd
Annual ACM Conference on Human Factors in Computing Systems; Seoul, Republic of Korea.
2702576: ACM; 2015. p. 4151-60.
9. Eschler J, Kendall L, O’Leary K, Vizer LM, Lozano P, McClure JB, Pratt W, Ralston JD. Shared
cale
ndars for home health management. In Proceedings of the 18th ACM conference on
Computer-Supported Cooperative Work and Social Computing. 2015.
10. Kendall L, Eschler J, Lozano P, McClure JB, Vizer LM, Ralston JD, Pratt W. Engineering for
reli
ability in at-home chronic disease management. AMIA Annu Symp Proc. 2014;2014:777-86.
PMCID: PMC4419963.
11. Liu L. Finding Reminders in the World: How Individuals Support Motivation and Tasks in
Mana
ging Chronic Illness. 2017.
12. O'Leary K, Liu L, McClure JB, Ralston J, Pratt W. Persuasive Reminders for Health Self-
Management.
AMIA Annu Symp Proc. 2016;2016:994-1003. PMCID: PMC5333289.
13
