
Long-Term
Care Insurance
Multistate
Rate Review
Framework
April 2022
NAIC Long-Term Care Insurance (EX) Task Force of the
Executive (EX) Committee
Accounng & Reporng
Informaon about statutory accounng principles and the
procedures necessary for ling nancial annual statements
and conducng risk-based capital calculaons.
Consumer Informaon
Important answers to common quesons about auto, home,
health and life insurance — as well as buyer’s guides on annu-
ies, long-term care insurance and
Medicare supplement plans.
Financial Regulaon
Useful handbooks, compliance guides and reports on nancial
analysis, company licensing, state audit
requirements and receiverships.
Legal
Comprehensive collecon of NAIC model laws, regulaons
and guidelines; state laws on insurance topics; and other reg-
ulatory guidance on anfraud and consumer privacy.
Market Regulaon
Regulatory and industry guidance on market-related issues,
including anfraud, product ling requirements, producer
licensing and market analysis.
NAIC Acvies
NAIC member directories, in-depth reporng of state
regulatory acvies and ocial historical records of NAIC na-
onal meengs and other acvies.
Special Studies
Studies, reports, handbooks and regulatory research
conducted by NAIC members on a variety of insurance-
related topics.
Stascal Reports
Valuable and in-demand insurance industry-wide stascal
data for various lines of business, including auto, home,
health and life insurance.
Supplementary Products
Guidance manuals, handbooks, surveys and research
on a wide variety of issues.
Capital Markets & Investment Analysis
Informaon regarding porolio values and procedures for
complying with NAIC reporng requirements.
White Papers
Relevant studies, guidance and NAIC policy posions on
a variety of insurance topics.
© 1999-2022 National Association of Insurance Commissioners. All rights reserved.
ISBN: 978-1-64179-198-4
Printed in the United States of America
No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means,
electronic or mechanical, including photocopying, recording, or any storage or retrieval system, without written permission
from the NAIC.
NAIC Execuve Oce
444 North Capitol Street, NW
Suite 700
Washington, DC 20001
202.471.3990
NAIC Central Oce
1100 Walnut Street
Suite 1500
Kansas City, MO 64106
816.842.3600
NAIC Capital Markets
& Investment Analysis Oce
One New York Plaza, Suite 4210
New York, NY 10004
212.398.9000
The NAIC is the authoritave source for insurance industry informaon. Our expert soluons support the eorts of
regulators, insurers and researchers by providing detailed and comprehensive insurance informaon. The NAIC oers
a wide range of publicaons in the following categories:
For more informaon about NAIC
publicaons, visit us at:
hp://www.naic.org//prod_serv_home.htm

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS
PREFACE
The Long-Term Care Insurance Multistate Rate Review Framework (LTCI MSA Framework) was drafted by the Ad Hoc
Drafting Group of the NAIC Long-Term Care Insurance (EX) Task Force. The Ad Hoc Drafting Group consists of
representatives from state insurance departments in Connecticut, Minnesota, Nebraska, Texas, Virginia, and
Washington.
The LTCI MSA Framework was adopted by the NAIC Long-Term Care Insurance Multistate Rate Review (EX) Subgroup
and the Long-Term Care Insurance (EX) Task Force on Dec. 12, 2021, and the NAIC Executive Committee and Plenary
on April 8, 2022.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS
Table of Contents
I. INTRODUCTION ............................................................................................................................................. 1
A. PURPOSE ............................................................................................................................................................. 1
B. STATE PARTICIPATION IN THE MSA REVIEW ............................................................................................................... 1
C. GENERAL DESCRIPTION OF THE MSA REVIEW ............................................................................................................. 2
D. BENEFITS OF PARTICIPATING IN THE MSA REVIEW ....................................................................................................... 3
E. DISCLAIMERS AND LIMITATIONS ............................................................................................................................... 3
F. GOVERNING BODY AND ROLE OF THE NAIC LONG-TERM CARE INSURANCE (EX) TASK FORCE .............................................. 4
II. MSA TEAM .................................................................................................................................................... 5
A. QUALIFICATIONS OF AN MSA TEAM MEMBER ............................................................................................................ 5
B. DUTIES OF AN MSA TEAM MEMBER ......................................................................................................................... 5
C. PARTICIPATION OF AN MSA TEAM MEMBER .............................................................................................................. 6
D. MSA ASSOCIATE PROGRAM .................................................................................................................................... 6
E. CONFLICTS, CONFIDENTIALITY, AND AUTHORITY OF THE MSA TEAM ............................................................................... 6
F. REQUIRED NAIC AND COMPACT RESOURCES .............................................................................................................. 7
III. REQUESTING AN MSA REVIEW ...................................................................................................................... 7
A. SCOPE AND ELIGIBILITY OF A RATE PROPOSALS FOR MSA REVIEW .................................................................................. 7
B. PROCESS FOR REQUESTING AN MSA REVIEW .............................................................................................................. 8
C. CERTIFICATION ...................................................................................................................................................... 8
IV. REVIEW OF THE RATE PROPOSAL .............................................................................................................. 9
A. RECEIPT OF A RATE PROPOSAL ................................................................................................................................. 9
B. COMPLETION OF THE MSA REVIEW .......................................................................................................................... 9
C. PREPARATION AND DISTRIBUTION OF THE MSA ADVISORY REPORT................................................................................. 9
D. TIMELINE FOR REVIEW AND DISTRIBUTION OF THE MSA ADVISORY REPORT ................................................................... 10
E. FEEDBACK TO THE MSA TEAM ............................................................................................................................... 10
V. ACTUARIAL REVIEW ..................................................................................................................................... 11
A. MSA TEAM’S ACTUARIAL REVIEW CONSIDERATIONS .................................................................................................. 11
B. LOSS RATIO APPROACH ........................................................................................................................................ 12
C. MINNESOTA APPROACH ....................................................................................................................................... 13
D. TEXAS APPROACH ................................................................................................................................................ 14
E. RBOS ............................................................................................................................................................... 15
F. NON-ACTUARIAL CONSIDERATIONS ......................................................................................................................... 16
VI. APPENDICES ............................................................................................................................................ 16
A. APPENDIX A – MSA ADVISORY REPORT FORMAT ...................................................................................................... 16
B. APPENDIX B – INFORMATION CHECKLIST .................................................................................................................. 17
C. APPENDIX C—ACTUARIAL APPROACH DETAIL ........................................................................................................... 21
D. APPENDIX D—PRINCIPLES OF RBOS ASSOCIATED WITH LTCI RATE INCREASES ............................................................... 25
E. APPENDIX E—GUIDING PRINCIPLES ON LTCI RBOS PRESENTED IN POLICYHOLDER NOTIFICATION MATERIALS ...................... 26
VII. EXHIBITS .................................................................................................................................................. 31
A. EXHIBIT A—SAMPLE MSA ADVISORY REPORT ................................................................................................ 31

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 1
I. INTRODUCTION
A. Purpose
The NAIC charged the Long-Term Care Insurance (EX) Task Force with developing a consistent national approach for
reviewing current long-term care insurance (LTCI) rates that results in actuarially appropriate increases being
granted by the states in a timely manner and eliminates cross-state rate subsidization. Considering that charge and
the threat posed by the current LTCI environment both to consumers and the state-based system (SBS) of insurance
regulation, the Task Force developed this framework for a multi-state actuarial (MSA) LTCI rate review process (MSA
Review).
This framework is based upon the extensive efforts of the Long-Term Care Insurance Multistate Rate Review (EX)
Subgroup, including its experience with a pilot program conducted by the pilot program’s rate review team (Pilot
Team). As part of that pilot program, the Pilot Team reviewed LTCI premium rate increase proposals and issued MSA
Advisory Reports recommending actuarially justified state-by-state rate increases. This framework aims to
institutionalize a refined version of the Pilot Team’s approach to create a voluntary and efficient MSA Review that
produces reliable and nationally consistent rate recommendations that state insurance regulators and insurers can
depend upon. The MSA Review has been designed to leverage the limited LTCI actuarial expertise among state
insurance departments by combining that expertise into a single review process analyzing in force LTCI premium
rate increase proposals or rate proposal
1
and producing an MSA Advisory Report for the benefit and use of all state
insurance departments. Note that rate decrease proposals can be contemplated within the MSA Review. The same
concepts of this MSA Framework would be applied, if such a rate decrease proposal is received for MSA Review. The
goal of this framework is to create a process that will not only encourage insurers to submit their LTCI products for
multi-state review, but also provide insurance departments the requisite confidence in the MSA Review so they will
voluntarily utilize the Multistate Actuarial LTCI Rate Review Team’s (MSA Team’s) recommendations when
conducting their own state level reviews of in force LTCI rate increase filings.
2
Ultimately, the MSA Review is designed
to foster as much consistency as possible between states in their respective approaches to rate increases.
The purpose of this document is to function as a framework for the MSA Review that communicates to NAIC
members, state insurance department staff, and external stakeholders how the MSA Review works to the benefit of
state insurance departments and how insurers might engage in the MSA Review. This MSA framework is intended
to communicate the governance, policies, procedures, and actuarial methodologies supporting the MSA Review.
State insurance regulators can utilize the information and guidance contained herein to understand the basis of the
MSA Team’s MSA Advisory Reports. Insurance companies can access the information and guidance contained herein
to understand how to engage in the MSA Review, and how the MSA Advisory Report may affect the insurer’s in force
LTCI premium rate increase filing decisions and interactions with individual state insurance regulators.
This document will be maintained by NAIC staff under the oversight of the Task Force and be revised as directed by
the Task Force or an appointed subgroup. This document will be part of the NAIC library of official publications and
copyrighted.
B. State Participation in the MSA Review
The MSA Review of an insurer’s rate proposal will be available to state insurance departments who are both an
Impacted State and a Participating State. These are defined as follows.
• “Impacted State” is defined as the domestic state, or any state for which the product associated with the
insurer’s in force LTCI premium rate increase proposal is or has been issued.
1
“Premium rate increase proposal(s)” or “rate proposal(s)” in this document refers only to an insurer’s request for review of a proposed in force LTCI premium rate increase or
decrease under the MSA Review.
2
The term “rate increase filing” or “rate filing(s)” in this document refers only to the in force LTCI premium rate request(s) that is submitted to individual state departments of
insurance (DOI) for a regulatory decision. Filings refer to both rate increase filings and rate decrease filings.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 2
• “Participating State” is defined as any impacted state insurance department that agrees to participate in
the MSA Review. Participation is voluntary as described in Section IE(1) below. Participation may include
activities such as, but not limited to, receiving notifications of rate increase proposals in System for
Electronic Rate and Form Filing (SERFF), participation in communication/webinars with the MSA Team, and
access to the MSA Advisory Report.
Note that state participation is expected to increase in the future as the MSA Review process continues to be
developed and refined.
C. General Description of the MSA Review
The MSA Review provides for a consistent actuarial review process that will result in an MSA Advisory Report, which
state insurance departments may consider when deciding on an insurer’s rate increase filing or to supplement the
state’s own review process.
The MSA Review is conducted by a team of state’s regulatory actuaries with expertise in LTCI rate review. Each
review will be led by a designated member of the MSA Team. The review process is supported by NAIC staff and
Interstate Insurance Product Regulation Commission (Compact) staff, who will administratively assist insurers in
making requests to utilize the MSA process and facilitate communication between the insurer, the MSA Team and
[Participating/Impacted TBD
3
] States. The NAIC’s electronic infrastructure, SERFF, will be used to streamline the rate
proposal and review process. Although the administrative services of Compact staff and SERFF’s Compact filing
platform are utilized in the MSA Review, MSA rate proposals are reviewed, and MSA Advisory Reports are prepared
by the MSA Team. MSA rate proposals are not Compact filings, and Compact staff will not have any role in
determining the substantive content of the MSA Advisory Reports.
The MSA Review begins when an insurer expresses interest in an MSA Review being performed for an in force LTCI
rate proposal to the MSA Team through SERFF or supporting NAIC or Compact staff. The eligibility of the rate
proposal will be reviewed and determined by the MSA Team with assistance, as needed, from supporting staff.
The MSA Review of eligible rate proposals will resemble a state-specific rate review process utilizing consistent
actuarial standards and methodologies. The MSA Team will apply the Minnesota and Texas approaches to calculate
recommended, approvable rate increases. While aspects of the Minnesota and Texas approaches may result in lower
rate increases than those resulting from loss ratio-based approaches and are outside the pure loss ratio
requirements contained in many states’ laws and rules, the approaches fall in line with legal provisions that rates
shall be fair, reasonable, and not misleading. The MSA Team will review support for the assumptions, experience,
and projections provided by the insurer and perform validation steps to review the insurer-provided information for
reasonableness. The MSA Team will document how the proposal complies with the regulatory approach utilized by
the MSA Team for Participating States. See Section V for more details on the actuarial review.
Throughout the MSA Review, the MSA Team will provide updates to the insurer. The MSA Team will deliver the final
MSA advisory Report to the insurer and address any questions the insurer has about the results of the Review.
Additionally, the review will consider reduced benefit options (RBOs) that are offered in lieu of the requested rate
increases and factor in non-actuarial considerations.
At the completion of the review, the MSA Team will draft an MSA Advisory Report for Participating States and
insurers that provides both summary and detail information about the rate proposal, the review methodologies, the
analysis and other considerations of the team, and the recommendation for rate increases as outlined in Appendix
A. The MSA Advisory Report will also indicate whether the recommendation differs from the insurer’s proposal.
Participating States can utilize the MSA Advisory Report or supplement their own state’s rate review with it as
3
Certain processes for Impacted vs. Participating States are yet to be determined (TBD).
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 3
described in the following Section ID. Participating States may also utilize the information filed with the MSA Team
in addition to the Advisory Report as appropriate.
The rate proposal, review process, actuarial methodologies, and other review considerations are detailed within this
framework document and accompanying appendices.
D. Benefits of Participating in the MSA Review
Both state insurance regulators and insurers will benefit by participating in the MSA Review in multiple ways. For
state insurance regulators:
• First, they will be able to leverage the demonstrated expertise of the MSA Team in reviewing in force LTCI
rate increase filings in their state. It is recognized that multiple states may not have significant actuarial
expertise with LTCI, so participation in the MSA Review will allow those states to build on the specific,
dedicated LTCI actuarial expertise of the MSA Team.
• Second, state insurance regulators will be able to utilize the MSA Team to promote consistency of actuarial
reviews among filings submitted by all insurers to states and actuarial reviews across all states. Because the
MSA Team is using the same dedicated approach to in force LTCI rate increase reviews, states who utilize
the MSA Team will have the benefit of using the same consistent methodology that is relied upon by other
state insurance departments when reviewing in force LTCI rate increase filings in their state.
• Third, the MSA Review allows for more state regulatory actuaries to work with or under the supervision of
qualified actuaries, which affords them an opportunity to establish LTCI-specific qualifications in making
actuarial opinions. This is particularly important when we consider that requirements to be a qualified
actuary include years of experience under the supervision of another already qualified actuary in that
subject matter.
• Finally, participating in the MSA Review will allow all state insurance regulators to share questions and
information regarding a particular rate proposal or review methodologies; thus, increasing each state’s
knowledge base in this area and promoting a more consistent national approach to in force LTCI rate review.
Note that states’ use of and reliance on the MSA Advisory Report is expected to increase in the future as the MSA
Review continues to be developed and refined, and the benefits of the MSA Review described above become more
evident.
Long-Term Care (LTC) insurers will likewise see multiple benefits in participating in the MSA Review:
• First, by utilizing the MSA Review and through the receipt of MSA information and the MSA Advisory Report
from the MSA Team, insurers should see increased efficiency and reduced timelines for nationwide
premium rate increase filings. As the MSA Team delivers the MSA Advisory Report for a rate proposal to
Participating States, it has functionally reduced the review time for each state, meaning that LTC insurers
should see more efficient and timely reviews from these states.
• Second, participating in the MSA Review will provide LTC insurers with one consistent recommendation to
be used when making rate increase filings to all states, thus reducing the carrier’s workload in developing
often widely differing filings for states’ review.
E. Disclaimers and Limitations
State Authority Over Rate Increase Approvals
The MSA Advisory Report is a recommendation to Participating States based upon the methodologies adopted by
the MSA Review. The recommendations are not specific to, and do not account for, the requirements of any specific
state’s laws or regulations. The MSA Review is not intended, nor should it be considered, to supplant or otherwise
replace any state’s regulatory authority, responsibility, and/or decision making. Each state remains ultimately
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 4
responsible for approving, partially approving, or disapproving any rate increase in accordance with applicable state
law.
A Participating State’s use of the MSA Advisory Report’s recommendations with respect to one filing does not require
that state to consider or use any MSA Advisory Report recommendations with respect to any other filing. The MSA
Review in no way: 1) eliminates the insurer’s obligation to file for a rate increase in each Participating State; or, 2)
modifies the substantive or procedural requirements for making such a filing. While encouraged to adopt the
recommendations of the MSA Review in each of their state filings, insurers are not obligated to align their individual
state rate filings with the recommendations contained within the MSA Advisory Report.
The MSA Advisory Reports, including the recommendations contained therein, are only for use by Participating
States in considering and evaluating rate filings. The MSA Advisory Reports or their conclusions shall not be utilized
by any insurer in a rate filing submitted to a non-Participating State, nor shall the MSA Advisory Reports be used
outside of each state insurance regulator’s own review process or challenge the results of any individual state’s
determination of whether to grant, partially grant, or deny a rate increase.
Information Sharing Between State Insurance Departments
The MSA Review, including, but not limited to, meetings, calls, and correspondence on insurer-specific matters are
held in regulator-to-regulator sessions and are confidential. In addition, if certain information and documents related
to specific companies that are confidential under the state law of an MSA Team member or a Participating State
need to be shared with other state insurance regulators, such sharing will occur as authorized by state law, and
pursuant to the Master Information Sharing and Confidentiality Agreement (Master Agreement) between states that
governs the sharing of information among state insurance regulators. Through the Master Agreement, state
insurance regulators affirm that any confidential information received from another state insurance regulator will
be maintained as confidential and represent that they have the authority to protect such information from
disclosure.
Confidentiality of the Rate Proposal
Members of the MSA Team and Participating States affirm and represent that they will provide any in force LTCI rate
proposal, as discussed herein with the same protection from disclosure, if any, as provided by the confidentiality
provisions contained within their state’s laws and regulations.
Confidentiality of the MSA Reports
Likewise, members of the MSA Team and Participating States affirm and represent that they will provide any MSA
Advisory Report(s), as discussed herein with the same protection from disclosure, if any, as provided by the
confidentiality provisions contained within their state’s laws and regulations for rate filings.
F. Governing Body and Role of the NAIC Long-Term Care Insurance (EX) Task Force
The Long-Term Care Insurance (EX) Task Force is expected to remain in place for the foreseeable future to oversee
the implementation of the MSA Review, and related MSA Advisory Reports, and to provide a discussion forum for
MSA-related activities. The Task Force or any successor will continuously evaluate the effectiveness and efficiency
of the MSA Review for the benefit of state insurance regulators and provide direction, as needed. The Task Force
may create one or more subgroups to carry out its oversight responsibilities.
Membership and leadership of the Task Force will be selected by the NAIC president and president-elect as part of
the annual committee assignment meeting held in January. Selection of the membership and leadership may
consider a variety of criteria, including commissioner participation, insurance department staff competencies,
market size, domestic LTC insurers, and other criteria considered appropriate for an effective governance system.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 5
II. MSA TEAM
The MSA Team comprises state insurance department actuarial staff. MSA Team members are chosen by their skill
set and LTCI actuarial experience. The Long-Term Care Insurance (EX) Task Force, or its appointed subgroup, will
determine the appropriate experience and skill set for qualifying members for the MSA Team. It is expected that
state participants will provide expertise and technical knowledge specifically regarding the array of LTCI products
and solvency considerations. The desired MSA Team membership composition should include a minimum of five and
up to seven members.
Membership must follow the requirements below and be approved by the chair of the Task Force or the chair of an
appointed subgroup. The following outlines the qualifications, duties, participation expectations and resources
required for MSA Team members.
A. Qualifications of an MSA Team Member
To be eligible to participate as a member of the MSA Team, a state insurance regulator is required to:
• Hold a senior actuarial position in a state insurance department in life insurance, health insurance, or LTCI.
• Be recommended by the insurance commissioner of the state in which the actuary serves.
• Have over five years of relevant LTCI insurance experience.
• Hold an Associate of the Society of Actuaries (ASA) designation.
• Currently participates as a member of the Long-Term Care Insurance Multistate Rate Review (EX) Subgroup
(or an equivalent Subgroup appointed by the Long-Term Care Insurance (EX) Task Force) and the LTC Pricing
(B) Subgroup.
• Be a member of the American Academy of Actuaries (Academy) (at least one member).
Additionally, the following qualifications are preferred:
• Hold a Fellow of the Society of Actuaries (FSA) designation
• Have spent at least one year engaged in discussions of either the Task Force or its appointed Subgroup
As both state insurance regulators and the MSA Review may benefit by developing and expanding specific LTCI
actuarial expertise through participation in this process, having one or more suitably experienced and qualified
actuaries participate in and supervise the work of the MSA Team is critical to the viability of the MSA process.
Participation also provides opportunities for additional actuaries to meet the requirements of the U.S. Qualification
Standards applicable to members of the Academy and other U.S. actuarial organizations as they relate to LTCI.
Consideration will be given to joint membership where two actuaries within a state combine to meet the criteria
stated above.
Consultants engaged by the state insurance department would not be considered for MSA Team membership.
B. Duties of an MSA Team Member
• Active involvement with the MSA Team, with an expected average commitment of 20 hours per month (see
Section IV for details of the MSA Review and activities of a team member).
• Participate in all MSA Team calls and meetings (unless an extraordinary situation occurs).
• Review and analyze materials related to MSA rate proposals.
• Provide input on the MSA Advisory Reports, including regarding the recommended rate increase approval
amounts.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 6
• Maintain confidentiality of MSA Team meetings, calls, correspondence, and the matters discussed therein
to the extent permitted by state law and protect from disclosure any confidential information received
pursuant to the Master Agreement. MSA Team members should communicate any request for public
disclosure of MSA information or any obligation to disclose.
• Active involvement within NAIC LTCI actuarial groups.
• Willingness to provide expertise to assist other states.
C. Participation of an MSA Team Member
Except for webinars and other general communications with state insurance departments, participation in the MSA
Review conference calls and meetings related to the review of a specific rate proposal will be limited to named MSA
Team members, supporting NAIC or Compact staff members who will be assisting the MSA Team, and the chair and
vice chair of the Long-Term Care Insurance (EX) Task Force, or its appointed subgroup. Other interested state
insurance regulators (e.g., domiciliary state insurance regulators) may be invited to participate on a call at the
discretion of the MSA Team or the chair or vice chair of the Task Force or its appointed subgroup.
D. MSA Associate Program
The MSA Associate Program within the MSA Framework is intended to encourage and engage state insurance
regulators to become actively involved in the MSA process. Additionally, a benefit of the program is to provide an
educational opportunity for state insurance department regulatory actuaries that wish to gain expertise in LTCI.
Regulatory actuaries can participate with varying levels of involvement or for different purposes as described.
Regulatory actuaries may participate:
• As a mentee. The mentee would participate in aspects of the MSA Review. An MSA Team member will serve
as a mentor to another state regulatory actuary and provide one-on-one guidance.
• To gain more knowledge and understanding of the Minnesota and Texas actuarial approaches.
• To share their own expertise through feedback to the MSA Team on MSA Advisory Reports to better
enhance the overall MSA process.
• To participate on an ad hoc limited basis, i.e., where a regulatory actuary would like to participate but is
unable to make the required time commitment.
• To meet the U.S. Qualification Standards applicable to members of the Academy and other U.S. actuarial
organizations as they relate to LTCI by serving under the supervision of a qualified actuary on the MSA
Team.
• To serve as a peer reviewer of the MSA Advisory Reports.
E. Conflicts, Confidentiality, and Authority of the MSA Team
Authority of the MSA Team
Members of the MSA Team serve on a purely voluntary basis, and any member’s participation shall not be viewed
or construed to be any official act, determination, or finding on behalf of their respective jurisdictions.
Disclosures and Confidentiality Obligations, as Applicable
All members of the MSA Team acknowledge and understand that the MSA Review, including, but not limited to,
meetings, calls, and correspondence are confidential and may not be shared, transmitted, or otherwise reproduced
in any manner. Additionally, all members of the MSA Team affirm and represent that they will: a) provide any in
force LTCI rate proposal with the same protection from disclosure, if any, as provided by the confidentiality
provisions contained within their state’s laws and regulations; and, b) provide any MSA Advisory Report with the
same protection from disclosure, if any, as provided by the confidentiality provisions contained within their state’s
laws and regulations for rate filings.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 7
Conflict of Interest Avoidance Procedures and Certifications
No member of the MSA Team may own, maintain, or otherwise direct any financial interest in any company or its
affiliates subject to the regulation of any individual state, nor may any member serve or otherwise be affiliated with
the management or board of directors in any company or its affiliates subject to the regulation of any individual
state. All conflicts of interest, whether real or perceived are prohibited and no member of the MSA Team shall
engage in any behaviors that would result in or create the appearance of impropriety.
F. Required NAIC and Compact Resources
The MSA Team will require administrative and technical support from the NAIC. As the MSA Review develops, it is
expected that NAIC support resources will play an integral role in managing the overall program. Administrative staff
support will be needed to support MSA Team communications and manage record keeping for underlying
workpapers and final MSA Advisory Reports associated with each rate proposal, etc. Additionally, it is possible that
limited actuarial support will be needed for the analysis of rate proposals, including preparing data files, gathering
information, performing limited actuarial analysis procedures, drafting MSA Advisory Reports, and monitoring
interactions among the state insurance departments and the MSA Team. Dedicated staff support for the ongoing
work of the Long-Term Care Insurance (EX) Task Force will be needed as well. As more experience with rate proposal
volumes and average analysis time is gained, the full complement of human resources required will be better
understood.
The MSA Team and supporting NAIC and Compact staff will use the NAIC SERFF electronic infrastructure to receive
insurer rate increase proposals and correspond with insurers. As needed, the MSA Team or supporting NAIC and
Compact staff may communicate with the insurer outside of SERFF. The material substance of such communication
can be documented within SERFF. NAIC and Compact staff will communicate with insurers only at the direction of
the MSA Team. Compact staff will perform administrative work related to MSA rate increase proposals at the
direction of the MSA Team and as described in this framework.
III. REQUESTING AN MSA REVIEW
A. Scope and Eligibility of a Rate Proposals for MSA Review
The following are the preferred eligibility criteria for requesting an MSA Review of a rate proposal.
• Must be an in force LTCI product (individual or group).
• Must be seeking a rate increase in at least 20 states and must affect at least 5,000 policyholders nationwide.
• Includes any stand-alone LTCI product approved by states, not by the Compact.
• For Compact-approved products meeting certain criteria, the Compact office will provide the first-level
advisory review subject to the input and quality review of the MSA.
It is recognized that rate proposals vary from insurer to insurer. The above criteria and the timelines provided below
are general guidelines. The MSA Team has the authority to weigh the benefits of the MSA Review for state insurance
departments and the insurer against available MSA Team resources when considering the eligibility of rate proposals
and the timeline for completion. Based on these considerations, the MSA Team, at its discretion, may elect to
perform an MSA Review on a rate proposal that does not satisfy the above eligibility criteria.
The MSA Team reserves the right to deny a proposal that does not meet eligibility criteria. An insurer will be notified
if the proposal for an MSA Review is denied.
An insurer may ask questions for more information about a potential rate proposal through communication to
supporting NAIC and Compact staff and the MSA Team. This will be accomplished through a Communication Form

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 8
that will be available on the Compact web page. Supporting NAIC and Compact staff will work with the insurer to
complete the necessary steps to assess eligibility, discuss any technical or other issues, and answer questions.
The insurer will have access to primary and supplementary checklists in Appendix B that provide guidance to the
insurer for information that should be included in a complete MSA rate proposal requested through the NAIC’s SERFF
application.
B. Process for Requesting an MSA Review
As noted in Section IC above, the MSA Review will utilize the Compact’s multistate review platform within the NAIC’s
SERFF application and its format for in force LTCI rate increase proposals. Therefore, a state may participate in the
MSA Review without being a member of the Compact. The following describes a few key elements of the process
for insurers and state insurance regulators:
• The insurer will work with NAIC and Compact support staff and the MSA Team to make a seamless rate
increase proposal.
• Instructions containing a checklist for information required to be included in the rate increase proposal, as
reflected in Appendix B, will be available to insurers through the Compact’s web page or within SERFF.
• The insurer shall include in the rate proposal a list of all states for which the product associated with the
rate increase proposal is or has been issued. Participating States will have access to view the insurer’s rate
proposal and review correspondence in SERFF.
• Fee schedule for using the MSA Review [TBD].
• Rate increase proposals for MSA Review within SERFF will be clearly identified as separate from Compact
filings.
• The supporting NAIC and Compact staff through SERFF will notify the Impacted States upon receipt of the
rate increase proposal with the SERFF Tracking Number.
• The MSA Team may utilize a “queue” process for managing workload and resources for incoming rate
increase proposals through SERFF.
• The MSA Team may utilize Listserv or other communication means for inter-team communications.
• The MSA Team’s review of objections and insurer responses are completed through SERFF.
C. Certification
The insurer shall provide certifications signed by an officer of the insurer that it acknowledges and understands the
non-binding effect of the MSA Review and MSA Advisory Report. The certification shall also provide, and the insurer
shall agree, that it will not utilize or otherwise use the MSA Review and/or the resulting MSA Advisory Report to
challenge, either through litigation or any applicable administrative procedure(s), any state’s decision to approve,
partially approve, or disapprove a rate increase filing except when: 1) the individual state is a (Participating/Impacted
State [TBD]) that affirmatively relied on the MSA Review and/or the MSA Advisory Report in making its
determination; or 2) the individual state consents in writing to use of the MSA Review and/or the MSA Advisory
Report.
Failure to abide by the terms of the insurer’s certification will result in the insurer and its affiliates being excluded
from any future MSA Reviews, and it will permit the MSA Team to terminate, at its sole discretion, any other ongoing
review(s) related to the insurer and its affiliates.
Should the MSA Team exclude any insurer and its affiliates for failure to adhere to its certification, the MSA Team,
at its sole discretion, may permit the insurer and its affiliates to resume submitting rate proposals for review upon
written request of the insurer.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 9
IV. REVIEW OF THE RATE PROPOSAL
A. Receipt of a Rate Proposal
The MSA rate review process begins when an insurer expresses interest in an MSA Review being performed for a
rate proposal. This interest can be expressed through completion of a Communication Form, which will be available
through the Compact web page. The initial request will be reviewed by the MSA Team lead reviewer and/or
supporting NAIC and Compact staff. Once an insurer has completed this initial communication and meets the criteria
for requesting an MSA Review, the insurer will work with supporting NAIC and Compact staff and the MSA Team to
complete the rate increase proposal in SERFF. The MSA Team will be notified, via SERFF, when the rate increase
proposal is available for review.
The supporting NAIC and Compact staff will notify (Participating/Impacted States [TBD]) via SERFF or e-mail when
rate increase proposals are submitted, correspondence between the MSA Team and insurer is sent or received in
SERFF, the MSA Advisory Report is available, and other pertinent activities occur during the review.
B. Completion of the MSA Review
The MSA Team shall designate a lead reviewer to perform the initial review of each rate proposal. Once the rate
increase proposal is made through SERFF, the MSA Review will resemble a state-specific review process.
The MSA Team will meet periodically to discuss the review and determine any needed correspondence with the
insurer. Objections and communications with filers will be conducted through SERFF, like any state-specific filing or
Compact filing, to maintain a record of the key review items. Other supplemental communication between the
insurer and the MSA Team or supporting NAIC and Compact staff, may occur, such as conference calls or emails, as
appropriate.
The timeframe for completing the MSA Team’s review and drafting the MSA Advisory Report will be dependent upon
the completeness of the rate proposal and the size and complexity of the block of policies for which the rate increase
applies. The MSA Team may utilize a “queue” process for managing workload and resources for incoming rate
increase proposals through SERFF. The timeliness of any necessary communication between the MSA Team and the
insurer to resolve questions or request/receive additional information about the rate proposal will affect the
completion of the review.
As the MSA Team completes its review: 1) the insurer will receive initial communication of a completed review, and
a final MSA Advisory Report with recommendations will be drafted and communicated to state insurance
departments within the next month, which may serve as a signal for a potential ideal time for the insurer to prepare
to submit the state-specific filings to each state; and 2) the insurer will receive sufficient information regarding the
MSA Team’s recommendation to allow the insurer an opportunity to review the recommendation and in the event
that the MSA Team recommendation differs from the proposal submitted by the insurer, the insurer will be given
the opportunity to interact with the MSA Team in order to ask questions, and understand the MSA Team’s reasoning.
C. Preparation and Distribution of the MSA Advisory Report
Upon completion of the actuarial review, the MSA Team will prepare a draft MSA Advisory Report for the rate
proposal. The reports will be made available within SERFF “reviewer notes” for Participating States. Supporting NAIC
and Compact staff will maintain a distribution list and send notifications of the availability of reports to Participating
States. Consultants engaged by state insurance department staff to perform rate reviews would be given access to
the MSA Advisory Report, subject to the terms of the agreement between the consultant and the Participating State
insurance department.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 10
Consultants who are bound by the actuarial Code of Professional Conduct, adopted by the Academy of Actuaries,
the Society of Actuaries (SOA) and the Conference of Consulting Actuaries (CCA), should consider whether receipt
of the MSA Advisory Report is acceptable under Precept 7 regarding Conflicts of Interest. For other professions,
similar consideration should be made if bound by similar professionalism standards.
Prior to finalizing the MSA Advisory Report, the MSA Team will present the draft MSA Advisory Report to
Participating States on a regulatory-only call, as deemed necessary, to provide an overview of the recommendations
and respond to questions from Participating States.
The MSA Team will issue the final MSA Advisory Report to the Participating States and the insurer after consideration
of any comments and questions from Participating States.
The MSA Advisory Report will include standardized content, as reflected in Appendix A, with modifications, as
necessary, for any unique factors specific to the rate proposal. The content and format are based on feedback
received from state insurance departments and the Long-Term Care Insurance (EX) Task Force during the pilot
project.
The content and format of the MSA Advisory Report may be modified in the future under the direction of the Task
Force, or an appointed subgroup, as the MSA Team gains more experience in generating the reports and receives
more feedback from Participating states and the insurer, through this process.
D. Timeline for Review and Distribution of the MSA Advisory Report
The draft MSA Advisory Report will be made available to Participating States for a two-week comment period prior
to being finalized. The following timeline for this comment period and distribution of the final MSA Advisory Report
will be adhered to as close as possible, barring timing delays due to holidays or other unexpected events. Note that
the MSA Review is intended to occur before filings are made to the state insurance departments, therefore not
affecting state insurance departments’ required timelines for review. However, use of the MSA Advisory Report by
the state is expected to reduce the amount of time required for the state to complete its review.
Pre-Distribution - Share the draft MSA Advisory Report with the insurer. The insurer will be given the opportunity to
interact with the MSA Team to ask questions and understand the MSA Team’s reasoning.
Day 1 – Distribution of a draft MSA Advisory Report to all Participating States.
Day 5-7 – Regulator-to-regulator conference call of all Participating States during which the MSA Team will
present the recommendations in the MSA Advisory Report and seek comments from states.
Day 21 – Deadline for comments on the draft MSA Advisory Report.
• Day 35 – Distribution of the final MSA Advisory Report, with consideration of comments, to Participating
States and the insurer.
• Date TBD by the Insurer – Individual rate increase filings submitted to each state insurance department.
• Date TBD by each state’s DOI – Approval or disapproval of the rate increase filing submitted in each state.
E. Feedback to the MSA Team
At the direction of the Long-Term Care Insurance (EX) Task Force, or an appointed subgroup, state insurance
departments will be requested to periodically provide data and feedback on their state rate increase approval
amounts and their state’s use of and reliance on the MSA Advisory Reports. The following items may be considered
in a feedback survey:
1. The number of rate proposals made with the MSA Review Team.
2. The number of rate proposals reviewed by the MSA Review Team.
3. Information regarding states approval of MSA recommendations.
4. Feedback on additional information states requested.
5. Feedback regarding how the review process and methodology could be improved.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 11
State responses will be confidential pursuant to the Master Agreement, and aggregated results of feedback surveys
will not specifically identify state responses. The MSA Team and state insurance regulators welcome feedback from
insurers on their experience using the MSA Review Process. This collective feedback will aid the Task Force in
understanding the practical effects of the MSA Review in achieving the goal of developing a more consistent state-
based approach for reviewing LTCI rate proposals that result in actuarially appropriate increases being granted by
the states in a timely manner and eliminates cross-state rate subsidization. The feedback will also help refine the
review process, improve future reports to better meet participants’ needs, and make updates to this MSA
Framework. Finally, the feedback will assist NAIC leadership in making decisions regarding the technology and staff
resources needed for the continued success of the project. Aggregated feedback results will be shared with
Participating States and insurers as determined appropriate.
V. ACTUARIAL REVIEW
A. MSA Team’s Actuarial Review Considerations
In conducting its actuarial review of a rate proposal, the MSA Team will consider assumptions, projections, and other
information provided by the insurer as outlined in Appendix B. The MSA actuarial review process will be evaluated
and evolve over time as more rate proposals are reviewed.
The Minnesota and Texas approaches ensure remaining policyholders do not make up for losses associated with
past policyholders. Professional judgment is used to address agreed upon policy issues, including the handling of
incomplete or non-fully credible data. The Minnesota approach also considers adverse investment expectations
related to the decline in market interest rates, and a cost-sharing formula is applied. The Texas approach ensures
rate changes reflect prospective changes in expectations. More detail of each approach is provided in the following
sections.
The MSA Team will consider the following in performing their review, applying their expertise and professional
judgement to the review, and reviewing the actuarial formulas and results:
• Review insurer experience, insurer narrative explanation, and relevant industry studies.
• Assess reasonability of assumptions for lapse, mortality, morbidity, and interest rates.
• Validate and adjust or request new projections of claim costs and premiums by year.
o Validate that the patterns of claims and premium projections over time reasonably align those
reflected in the assumptions.
o Adjust or request new projections of claims and premium to the extent that any underlying
assumptions are deemed unreasonable or unsupported by the MSA Team. Any differences will initially
result in correspondence between the MSA Team and the insurer via SERFF.
o After verifying loss ratio compliance, apply both the Minnesota and Texas approaches for each rate
proposal submitted.
In developing a recommendation, the MSA Team will apply a balanced approach and professional judgement for
each rate proposal based on the characteristics of the block reviewed to determine the most appropriate method.
The MSA Team’s recommendation will not be the lowest or the highest percentage method just because it is the
lowest or the highest. Rather, the recommendation may be the result of either the Texas or Minnesota approach, a
blend of the two approaches: or using professional judgement, the MSA Team may recommend a rate increase
outside of these two approaches. Other methods may evolve over time that may be incorporated into the future
process that generate similar or unique results. In applying professional judgement, (e.g., when considering the
extent to which less-than-fully credible older-age morbidity should be projected to cause adverse experience), a
balanced approach is applied as opposed to denying a rate increase, which could lead to a spike in the future, or
approving the rate increase as if there was full credibility, which could lead to rates that could be too high. As the
MSA Team reviews more rate proposals, it will consider and evaluate the characteristics of the rate proposals as it
refines the blending of the two methods.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 12
The MSA Team will consider how to reflect the differences in the histories of states’ rate approvals. Current approach
includes:
• The MSA Team’s recommendation results in the same rate per unit in each state following the current rate
increase round, leading to higher percentage rate increases in states that approved lower rate increases in
the past.
• Analysis of state cost differences affecting justifiable rate increases will continue. As of May 2021, there
does not appear to be substantial evidence that policyholders who purchased policies in lower-cost states
should receive lower percentage rate increases. Part of the reason is that there was a tendency for people
in lower-cost areas to purchase less coverage. Their premium rates will continue to be lower than rates for
policyholders with more coverage, even if percentage rate increases are the same.
• Any recommendation from the MSA Team for a catch-up increase aims to achieve only current rate equity
between states and not lifetime rate equity between states.
Consideration of Solvency Concerns
If concerns exist regarding an insurer’s financial solvency and the impact of rate increases on future solvency, each
state DOI, by their authority over rate approval, has the flexibility to consider solvency adjustments in these rare
instances. In rare, non-typical circumstances, adjustments could be considered within the MSA Review, including
consultation with states as part of the MSA Advisory Report comment period.
Follow-Up Proposals on the Same Block
Any subsequent rate increase proposal to the MSA Team on a block of business previously reviewed by the MSA
Team needs to involve the development of adverse experience and/or expectations. In the absence of adverse
experience or expectation development, the MSA Team will consider a reasonable explanation from an insurer for
an increase in credibility of morbidity data of being the reason for a rate increase. Prior rate increases would need
to be implemented before the implementation of a subsequent rate increase. The MSA Team will not consider a
new rate increase proposal on a block that did not receive the full percentage rate increase requested without the
experience, expectation, or credibility criteria noted above. If an insurer did not receive the full percentage rate
increase and has no adverse changes in experience or expectations, the insurer should work directly with the
applicable state DOI.
B. Loss Ratio Approach
Key aspects of the loss ratio approach to the actuarial review of rate changes include:
1. At policy issuance, pricing based on a lifetime loss ratio target is typically established. A common target is
60%, which means the present value of claims is targeted to equal 60% of the present value of premiums.
In some instances, products may be priced with a projected lifetime loss ratio in excess of 60%. The
remainder goes towards sales-related costs, administrative expenses, expenses related to claims, and
profit. Note that 60% is a required minimum loss ratio under the pre-rate stability rules; newer policies may
be priced with lower expected loss ratios. Refer to state law or regulation modeled from the Long-Term
Care Insurance Model Regulation (#641), Section 19 for more details on compliance with loss ratio
standards.
2. As lapses and mortality have generally been lower than expected, more people have reached ages where
claims tend to occur than originally expected. In some cases, this has resulted in a substantial increase in
the present value of claims; thus, resulting in substantially higher expected lifetime loss ratios than
originally targeted. For companies where morbidity expectations have increased over original assumptions,
lifetime loss ratios would be even higher.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 13
3. The loss ratio approach increases future premiums to a level, referred to as make-up premium, such that
the original loss ratio target is once again attained.
4. The loss ratio approach, one of the minimum standards in many states’ statutes, is evaluated by the MSA
Team. However, there is general recognition that this approach produces rate increases that are too high
and do not recognize other typical statutory standards, such as fair and reasonable rates.
a. The loss ratio approach also does not recognize actuarial considerations such as the shrinking block
issue, where past losses being absorbed by a shrinking number of remaining policyholders would lead
to unreasonably high-rate increases. This concern was the main driver of the Minnesota, Texas, and
other approaches.
b. The loss ratio approach shifts all the risk to the policyholders. If the insurer is allowed to always return
to the 60% loss ratio, there may be a lower incentive for more appropriate initial pricing.
5. For rate-stabilized business, lifetime loss ratios are broken out, such as in a 58%/85% pattern, where the
58% reflects the portion of initial premiums and the 85% reflects the portion of the increased premium
available to pay the claims. For relevant blocks, this standard is analyzed by the MSA Team. If this standard
produced lower increases than the Minnesota and Texas approaches, it would produce the recommended
rate increase.
C. Minnesota Approach
Key aspects of the Minnesota approach to the actuarial review of rate changes include:
1. Blended if-knew / makeup approach to address the shrinking block issue.
a. The if-knew concept is to estimate a premium that would have been charged at issuance of the policy
if information we know now on factors such as mortality, lapse, interest rates, and morbidity was
available then.
b. The makeup concept is for a premium to be charged going forward to return the block to its original
lifetime loss ratio.
c. The blending method helps ensure concepts discussed in public NAIC Long-Term Care Pricing (B)
Subgroup calls from 2015 to 2019
4
are incorporated, including the concept that rates will not
substantially rise as the block shrinks, as policyholder persistency falls over time.
2. Cost-sharing formula that increases the insurer’s burden as cumulative rate increases rise.
a. This addition to the insurer’s burden moves rates away from a direction that could potentially be seen
as misleading. The insurer likely had or should have had more information on the likelihood of large
rate increases than the consumer had at the time the policy was issued.
3. Assumption review.
a. Verification that the insurer’s original and current assumptions are indeed drivers of the magnitude
increase in lifetime loss ratio presented by the insurer.
b. Verification of appropriateness of current assumptions.
i. A combination of credible insurer experience, relevant industry experience, and professional
judgement is applied.
ii. For areas of uncertainty, such as older-age morbidity, conservatism may be added to the insurer-
provided assumptions. This conservatism can be released as credible experience develops.
4. Interest rate / investment return component
4
NAIC Proceedings including meeting minutes are available from the NAIC Library, https://naic.soutronglobal.net/portal/Public/en-US/Search/SimpleSearch.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 14
a. The Minnesota approach considers changes in expectations regarding interest rates and related
investment returns in a manner consistent with how other key assumptions are considered. Reasons
include:
i. Changes in market interest rates are among the key factors driving profits and losses associated
with blocks of LTC business.
ii. In the Minnesota approach, all factors impacting the business are considered.
1. If interest rates rise, this would tend to lead to lower rate increase approvals. Note, in this
scenario, if interest rate changes were not considered, it is possible an insurer would get
approval for rate increases even when profits on the block were higher than expected.
2. If interest rates fall, this would tend to lead to higher rate increase approvals.
iii. To prevent shifting of “good assets” and “bad assets” to supporting LTC rates and prevent an
insurer from increasing rates based on risky investments turned into losses, an index of average
corporate bond yields (e.g., Moody’s) is relied on to reflect experience and current expectations.
iv. Original pricing typically includes an assumption on investment returns, for which premiums and
other positive cash flows are assumed to accumulate. This forms the interest component of the
original assumption.
v. The original pricing investment return in Section VC(4)iv is compared to the average corporate
bond yields in Section VC(4)iii to determine the adversity associated with the interest rate factor.
5. Original Assumption Adjustment
a. If original mortality, lapse, or investment return assumptions were out of line with industry-average
assumptions at the time of original pricing, the original premium is replaced by a “benchmark
premium.”
i. This results in a lower rate increase.
ii. This adjustment wears off over 20 years from policy issue.
1. The rationale for the wearing off of this adjustment is the assumption that no insurer would
intentionally underprice a product, knowing it would suffer losses for 20 years and then hope
to offset a portion of that loss with a rate increase.
iii. This adjustment is intended to prevent for example, an insurer underpricing a product, gaining
market share, and then immediately requesting a rate increase).
D. Texas Approach
The Texas approach to the actuarial review of rate changes was developed in response to the NAIC Long-Term Care
Pricing (B) Subgroup’s discussions regarding the recoupment of past losses in LTCI rate increases. The Texas approach
relies upon a formula intended to prevent the recoupment of past losses by calculating the actuarially justified rate
increase for premium-paying policyholders based solely on projected future (prospective) claims and premiums.
Key aspects of the Texas approach to the actuarial review of rate changes include:
1. Past losses are assumed by the insurer and not by existing policyholders. An approach that considers past
claims in the calculation of the rate increase, such as a lifetime loss ratio approach, permits, the recoupment
of past losses to some extent.
2. Calculates the rate increase needed to fund the prospective premium deficiency for active, premium-paying
policyholders based on an actuarially supported change in assumption(s). This ensures that active
policyholders do noy pay for the past claims of policyholders who no longer pay premium.
3. Data Requirements for Calculation:
a. The following calendar year projections, including totals, for current premium-paying policyholders
only, prior to the rate increase, all discounted at the maximum valuation interest rate:
i. Present Value of Future Benefits (PVFB) under current assumptions.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 15
ii. PVFB under prior assumptions (from prior rate increase filing, or if no prior increase, from original
pricing).
iii. Present Value of Future Premiums (PVFP) under current assumptions.
iv. PVFP under prior assumptions (from prior rate increase filing, or if no prior increase, from original
pricing).
1. Note that for all four projections above, the projection period is typically 40–50 years:
although, some companies project for 60 or more years.
To emphasize, these projections should only include active policyholders currently paying premium and
should not include any policyholders not paying premium (e.g., policies on wavier, on claim, or paid up)
regardless of the reason. Projections under current actuarial assumptions must not include
policyholder behavior as a result of the proposed premium rate increase, such as a shock lapse
assumption.
Also, the insurer should identify and explain any estimates or adjustments to the data, as applicable.
4. Assumptions
a. Rate increases are commonly driven by a change to the persistency, morbidity, mortality assumption,
or a combination of the three.
b. Verification that assumption change(s) are supported by credible data.
c. The interest rate is the same for all four projections. This ensures that interest rate risk is assumed by
the insurer, not the policyholder.
The formula used in the Texas approach is provided in Appendix C.
E. RBOs
In 2020, the Long-Term Care Insurance Reduced Benefit Options (EX) Subgroup of the Long-Term Care Insurance (EX)
Task Force, developed a list of RBO principles to provide guidance for evaluating RBO offerings in Appendix D.
RBOs in the MSA Advisory Report
As part of the MSA Review, the MSA Team will perform a limited review of the reasonableness of RBOs included in
the rate proposal that are extracontractual. The MSA Advisory Report will highlight how the insurer demonstrates
the proposed RBOs’ reasonableness. Note that the MSA Team will not perform an assessment of RBOs in relation to
individual state specific requirements for RBOs. The purpose of the guidance in the MSA Advisory Report is to provide
initial information about the RBOs with which the state insurance regulators can then utilize to perform a more
detailed assessment specific to their state’s requirements. As the MSA Review develops and as the Subgroup
continues its work, this area of review may evolve.
Future RBOs
As the industry continues to innovate new RBOs for consumers, the MSA Review will likewise develop and evolve to
consider the reasonableness of RBOs. Additionally, as the MSA Review evolves, additional regulatory expertise with
RBOs may be added to the MSA Team in the future. To achieve more consistency across states in their understanding
and consideration of RBOs, the Task Force will encourage its appointed Subgroup and/or an appropriate NAIC
actuarial committee or group to collectively consider new RBOs as they arise. This process will provide for input and
technical advice from actuaries and non-actuarial experts to the state insurance departments as they exercise their
authority in considering RBOs as part of rate filings. States and insurers are therefore encouraged to discuss new
and developing RBOs through this process.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 16
F. Non-Actuarial Considerations
The Long-Term Care Insurance (EX) Task Force continues to review and consider non-actuarial considerations
affecting states’ approval or disapproval of LTCI rate changes to develop consensus among jurisdictions and develop
recommendations for application of these considerations. These considerations include such topics as:
1. Caps or limits on approved rate changes.
2. Phase-in of approved rate changes over a period of years.
3. Waiting periods between rate change requests.
4. Considerations of prior rate change approvals and disapprovals.
5. Limits or disapproval on rate changes based solely or predominately on the number of policyholders in a
particular state.
6. Limits or disapproval on rate changes based on attained age of the policyholder.
7. Fair and reasonableness considerations for policyholders.
8. The impact of the rate change on the financial solvency of the insurer.
Considerations in the MSA Advisory Report
As part of the MSA Review, the MSA Team will identify relevant aspects of the insurer’s rate proposal, based on the
information provided by the insurer, which may be affected by a state’s non-actuarial considerations. Note that the
MSA Team will not perform a state-by-state review of each state’s non-actuarial considerations, statutes, or
practices. Instead, the MSA Team will highlight in the MSA Advisory Report those aspects of the rate proposal that
relate to or that may be affected by non-actuarial considerations. The purpose of this guidance in the MSA Advisory
Report is to prompt state insurance regulators to contemplate those affected aspects of the rate proposal when
completing their individual state’s rate review. For example, the MSA Advisory Report may highlight:
• If cumulative rate increases are high, as this may affect the cost-sharing formula.
• If a rate proposal is for a block of business where the average policyholder age is predominately 85 or above,
as this may affect states that consider age caps.
• If it is determined that the block of business will likely continue to incur substantial financial losses and
impose a potential solvency concern, as this may affect the potential need for adjustments to the cost-
sharing formula.
• Aspects of the coordination of rate and reserving review, as this may signify adjustments to the
methodology assumptions used by the MSA Team in its review.
Future Non-Actuarial Considerations
The MSA Review will continue to develop and evolve as it is implemented. To achieve more consistency and minimize
the number of differences across states in their application of other non-actuarial considerations in rate review
criteria for LTCI rate filings, the Task Force will encourage its appointed Subgroup, or an appropriate NAIC actuarial
committee or group, to collectively consider new future non-actuarial considerations as they arise. This process will
provide for input and technical advice from actuaries to states as they exercise their authority in considering non-
actuarial factors. States are therefore encouraged to discuss new and developing practices and/or recommendations
in this area.
VI. APPENDICES
A. Appendix A – MSA Advisory Report Format
The MSA Advisory Report that is distributed to Participating State insurance departments and the insurer will
generally follow a template that includes the following information. Note that degree of rigor in the review and the
details and content of the MSA Advisory Report will depend on the magnitude of rate increase and the complexity
of the rate proposal and the insurer’s financial condition. See also the sample MSA Advisory Report in Exhibit A.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 17
1. Executive Summary.
a. Overall recommended rate increase, before consideration of different states’ history of approvals.
2. Disclaimers.
a. Purpose and intent of how states should use the MSA Advisory Report.
b. Disclaimer that the MSA Review and findings shall not be considered an approval of the rate schedule
increase filing, nor shall it be binding on the states or the insurer.
c. Statement that the in force rate increase filing submitted to the respective states shall be subject to
the approval of each state, and each state's applicable state laws and regulations shall apply to the
entire rate schedule increase filing.
3. Background on the MSA Review.
4. Explanation of the insurer’s Proposal.
a. The explanation will be based on the aspects of the insurer’s rate proposal, which may include details
as to whether the rate increase submitted for review involved different types of coverages or
groupings.
5. Summary of the MSA Team’s rate review analysis, including these aspects:
a. Actuarial review.
i. The summary of the review and the MSA Team’s recommendation will be based on the aspects of
the insurer’s rate proposal, and may include specific details of the review, for example analysis of
projections, assumptions, margins, or other aspects.
b. Summary of consideration of differences in the history of state’s rate increase approvals.
c. Non-actuarial considerations and findings.
d. Financial solvency-related aspects and adjustments.
e. Review for reasonableness and clarity of RBOs.
f. Summary information about the mix of business.
6. Appendices.
a. Summary of the drivers of the rate proposal.
b. Details regarding the Minnesota and Texas approaches as applied to the rate proposal.
c. Summary of rate proposal correspondence.
d. Examples of rate increases if an RBO is not selected.
e. Potential cost–sharing formula for typical circumstances.
B. Appendix B – Information Checklist
At the request of the former Long-Term Care Insurance (B/E) Task Force, the Long-Term Care Pricing (B) Subgroup
developed a single checklist that reflects significant aspects of LTCI rate increase review inquiries from all states. In
this context, “checklist” means the list or template of inquiries that states typically send at the beginning of reviews
of state-specific rate increase filings.
This document contains aspects of the NAIC Guidance Manual for Rating Aspect of the Long-Term Care Insurance
Model Regulation
5
(Guidance Manual) and checklists developed by several other states. This consolidated checklist
is not intended to prevent a state from asking for additional information. The intent is to take a step toward moving
away from 50 states having 50 different checklists to a more efficient process nationally to provide the most
important information needed to determine an approvable rate increase. To keep the template at a manageable
length, it is anticipated that this template will result in states attaining 90–100% of the information necessary to
5
https://www.naic.org/documents/committees_b_senior_issues_160609_ltc_guidance_manual.pdf

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 18
decide on approvable rate increases. State and block specifics will generate the other 0-10% of requests. As states
apply this checklist, it or an improved version may be considered for a future addition to the Guidance Manual.
Information Required for an MSA Review of a Rate Proposal
The following provides a checklist of information necessary for a complete rate proposal to the MSA Review. This
checklist is consistent with the “Consolidated, Most Commonly Asked Questions – States’ LTC Rate Increase
Reviews”
6
as adopted by the Health Actuarial (B) Task Force on March 23, 2018.
1. Identify all states for which the product associated with the rate proposal is or has been issued.
2. New premium rate schedule, percentage increase for each rating scenario such as issue age, benefit period,
elimination period, etc., from the existing and original rates.
a. Provide rate increase percentages by policy form number and clear mapping of these numbers to any
alternative terminology describing policies stated in the actuarial memorandum and other supporting
documents.
b. Provide the cumulative rate change since inception, after the requested rate increase, for each of the
rating scenarios.
3. Rate increase history that reflects the filed increase.
a. Provide the month, year, and percentage amount of all previous rate revisions.
b. Provide the SERFF MSA numbers associated with all previous rate revisions.
4. Actuarial memorandum justifying the new rate schedule, which includes:
a. Lifetime loss ratio projection, with earned premiums and incurred claims discounted at the maximum
valuation interest rate.
i. The projection should be by year.
ii. Provide the count of covered lives and count of claims incurred by year.
iii. Provide separate experience summaries and projections for significant subsets of policies with
substantially different benefit and premium features. Separate projections of costs for significant
blocks of paid-up and premium-paying policies that should be provided.
iv. Provide a comparison of state versus national mix of business. In addition, a state may request
separate state and national data and projections. The insurer should accompany any state-specific
information with commentary on credibility, materiality, and the impact on requested rate
increase.
5. Reasons for the rate increase, including which pricing assumptions were not realized and why.
a. Attribution analysis - presents the portion of the rate increase allocated to and the impact on the
lifetime loss ratio from each change in assumption.
b. Related to the issue of past losses, explain how the requested rate increase covers a policyholder's own
past premium deficiencies and/or subsidizes other policyholders' past claims.
c. Provide the original loss ratio target to allow for comparison of initially assumed premiums and claims
and actual and projected premiums and claims.
d. Provide commentary and analysis on how credibility of experience contributed to the development of
the rate proposal.
6. Statement that policy design, underwriting, and claims handling practices were considered.
a. Show how benefit features (e.g., inflation and length of benefit period) and premium features (e.g.,
limited pay and lifetime pay) impact requested increases.
6
https://content.naic.org/sites/default/files/inline-files/cmte_b_ltc_price_sg_180323_ltc_increase_reviews%20%289%29.docx

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 19
b. Specify whether waived premiums are included in earned premiums and incurred claims, including in
the loss ratio target calculation; provide the waived premium amounts and impact on requested
increase.
c. Describe current practices with dates and quantification of the effect of any underwriting changes.
Describe how adjustments to experience from policies with less restrictive underwriting are applied to
claims expectations associated with policies with more restrictive underwriting.
7. A demonstration that actual and projected costs exceed anticipated costs and the margin.
8. The method and assumptions used in determining projected values should be reviewed considering
reported experience and compared to the original pricing assumptions and current assumptions.
a. Provide applicable actual-to-expected ratios regarding key assumptions.
b. Provide justification for any change in assumptions.
9. Combined morbidity experience from different forms with similar benefits, whether from inside or outside
the insurer, where appropriate to result in more credible historical claims as the basis for future claim costs.
a. Explain the relevance of any data sources and resulting adjustments made relevant to the current rate
proposal, particularly regarding the morbidity assumption.
b. A comparison of the population or industry study to the in force related to the rate proposal should be
performed, if applicable.
c. Explain how claims cost expectations at older ages and later durations are developed if data is not fully
credible at those ages and durations.
d. Provide the year of the most recent morbidity experience study.
10. Information from the Guidance Manual Question and Answer (Q&A): Morbidity, Lapse, Mortality, Interest.
a. Comparison with asset adequacy testing reserve assumptions.
i. Explain the consistency regarding actuarial assumptions between the rate proposal and the most
recent asset adequacy (reserve) testing.
ii. Additional reserves that the insurer is holding above Health Insurance Reserves Model Regulation
(#10) formula reserves should be provided, (such as premium deficiency reserves and LI—The
Application of Asset Adequacy Testing to Long-Term Care Insurance Reserves (AG 51) reserves.
b. Assumptions Template in Appendix 6 of the Guidance Manual for policies issued after 2017, where
applicable.
c. Provide actuarial assumptions from original pricing and most recent rate increase proposal and have
the original actuarial memorandum available upon request.
11. Provide the following calendar year projections, including totals, for current premium paying nationwide
policyholders only, prior to the rate increase, all discounted at the maximum valuation interest rate*:
a. Present value of future benefits (PVFB) under current assumptions
b. PVFB under prior assumptions (from prior rate increase filing, or if no prior increase, from original
pricing).
c. Present value of future premiums (PVFP) under current assumptions.
d. PVFP under prior assumptions (from prior rate increase filing, or if no prior increase, from original
pricing).
*To emphasize, these projections should include only active nationwide policyholders currently paying
premium, and they should not include any policyholders not paying premium, regardless of the reason.
Projections under current actuarial assumptions must not include policyholder behavior as a result of the
proposed premium rate increase, such as a shock lapse assumption or benefit reduction assumption.
b. Also, please identify the maximum valuation interest rate and ensure that it is the same for all four
projections.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 20
12. The Guidance Manual checklist items: 1) summaries (including past rate adjustments); 2) average premium;
3) distribution of business, including rate increases by state; 4) underwriting; 5) policy design and margins;
6) actuarial assumptions; 7) experience data; 8) loss ratios; 9) rationale for increase; and 10) reserve
description.
13. Assert that analysis complies with Actuarial Standards of Practice (ASOPs), including 18 and 41.
14. Numerical exhibits should be provided in Microsoft Excel spreadsheets with active formulas maintained,
where possible.
15. Rate Comparison Statement of renewal premiums with new business premiums, if applicable.
16. Policyholder notification letter should be clear and accurate.
a. Provide a description of options for policyholders in lieu of or to reduce the increase.
b. If inflation protection is removed or reduced, is accumulated inflation protection vested?
c. Explain the comparison of value between the rate increase and policyholder options.
d. Are future rate increases expected if the rate increase is approved in full? If so, how is this
communicated to policyholders?
e. How are partnership policies addressed?
17. Actuarial certification and rate stabilization information, as described in the Guidance Manual, and
contingent benefit upon lapse information, including reserve treatment.
Supplemental Information
As part of the Long-Term Care Insurance (EX) Task Force’s pilot project in 2020–2021, the following supplemental
information was identified by the MSA Team as beneficial; and, therefore, the Task Force may be requested to assist
in the MSA Review.
1. Benefit utilization:
a. Provide current, prior rate increase, and original assumptions, including first-projection year through
ultimate utilization percentages for 5% compound inflation, lesser inflation, and zero inflation cells.
b. Explain how benefit utilization assumptions vary by maximum daily benefit.
c. Provide the cost of care inflation assumption implied in the benefit utilization assumption.
2. Attribution of rate increase
a. Provide the attribution of rate increase by factor: morbidity, mortality, lapse, investment, and other.
b. For the morbidity factor, break down the attribution by incidence, claim length, benefit utilization, and
other.
c. Provide information on the assumptions that are especially sensitive to small changes in assumptions.
3. RBOs
a. Provide the history of RBOs offered and accepted for the block.
b. Provide a reasonability analysis of the value of each significant type of offered RBO.
4. Investment returns:
a. Provide original and updated / average investment return assumptions underlying the pricing.
b. Explain how the updated assumption reflects experience.
5. Expected loss ratio:

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 21
a. With respect to the initial rate filing and each subsequent rate increase filing, provide the target loss
ratio.
b. Provide separate ratios for lifetime premium periods and non-lifetime premium periods and for
inflation-protected and non-inflation-protected blocks.
6. Shock lapse history:
a. Provide shock lapse data related to prior rate increases on this block.
7. Waiver of premium handling:
a. Explain how policies with premiums waived are handled in the exhibits of premiums and incurred
claims.
b. Explain how counting is appropriate (as opposed to double counting or undercounting).
8. Actual-to-expected differences:
a. Explain how differences between actual and expected counts or percentages (in the provided exhibits)
are reflected or not reflected in assumptions.
9. Assumption consistency with the most recent asset adequacy testing:
a. Explain the consistency or any significant differences between assumptions underlying the rate
increase proposal and those included in Actuarial Guideline 51 testing.
C. Appendix C—Actuarial Approach Detail
Minnesota Approach
Details on the key aspects of the Minnesota approach to the actuarial review of rate changes include:
1. Review of current assumptions for appropriateness, reasonableness, justification, and support.
a. A combination of credible insurer experience, relevant industry experience, and professional
judgement is applied.
2. If-knew premium and makeup premium aspects – aggregate application.
a. Makeup percentage:
i. {[PV (claims) / original LLR] - PV (past premium)} / PV (future premium) – 1.
ii. To ensure past increases are not doubled counted, past premiums in the formula in 2.a.i should
reflect actual rate level, including past increases; while PV (future premium) in 2.a.i. should be
based upon the original rate level.
iii.
b. If-knew percentage:
i. [PV (claims) / PV (premiums)] / original LLR – 1.
ii. Premiums in the formula are at the original rate level.
iii. The concept is to estimate a premium that would have been charged at issuance of the policy if
information we know now on factors such as mortality, lapse, interest rates, and morbidity was
available then.
c. Definitions and explanations:
i. PV means present value.
ii. LLR means lifetime loss ratio.
iii. Interest rates underlying PVs and LLRs are based on:
1. For original PVs and LLRs, the interest rate is the investment return assumed in original pricing.
Note that this rate is typically different than the statutory LLR discount rate.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 22
2. For current PVs, the interest rates are the average corporate bond yields over time for each
year minus 0.25% (to account for expected defaults). For projections beyond the current year,
phasing over five years of the current rate to a target rate (currently 4%) is assumed.
iv. PV calculations are based on actual, current experience and expectations for persistency,
morbidity, and interest rate.
v. Insurer-provide premium and claim cash flows may be adjusted based on assumption review.
vi. Makeup percentage is similar to that attained by the loss ratio approach.
3. If-knew premium and makeup premium aspects – sample policy-level verification.
a. Over a range of issue years, issue ages, benefit periods, and inflation protection:
i. Calculate an estimate of the original premium.
1. Based on original pricing assumptions for persistency, morbidity, investment returns, and
expenses.
2. Apply first principles.
a. For each policy year, calculate PV of claims and expenses, applying mortality, lapse,
morbidity, and expenses, discounting at original investment rates.
b. Add the PV of claims expenses for each policy year to attain PV of claims & expenses at
issue.
c. Divide by the sum of the PV of an annuity of 1 per year.
d. Multiply {b / c] times (1 + originally assumed profit percentage) to attain the original
premium.
e. This premium provides the basis for comparison against the makeup and if-knew
premium.
3. Replace the original premium with a benchmark premium.
a. If the benchmark premium is higher than the original premium and original pricing
(reflected in mortality, lapse, and investment return assumptions) was out of line with
industry-average assumptions at the time of original pricing.
b. The benchmark premium is phased back into the original premium proportionally over 20
years from issue.
c. The benchmark aspect is intended to prevent for example, an insurer underpricing a
product, gaining market share, and then immediately requesting a rate increase.
ii. Calculate an estimate of the makeup premium.
1. Calculate the original dollar PV of profits for the sample policy using original pricing
assumptions.
2. Calculate an updated dollar PV of profits for the sample policy using:
a. Actual history of premiums and claims.
b. Expectations of future claims.
c. “Backed into” makeup premium.
3. Note that attaining the same dollar PV of profits for a sample policy leads to a lower makeup
premium than attaining the same percentage PV of profits (as a percentage of premium).
a. The reason for targeting the dollar instead of percentage is to avoid the dollar amount of
profit being higher as premium rates increase.
iii. Calculate an estimate of the if-knew premium.
1. The calculation is the same as for the original premium, except it is based on current
assumptions instead of original pricing assumptions.
b. Verifying the impact on expectation changes on rates
i. While lapse, mortality, and interest rate experience and assumptions are fairly
routine to track (for determination of the rate impact), morbidity experience and
assumptions tend to be difficult to track.
ii. A combination of information is relied up to estimate the impact of morbidity
expectation deviations (from original pricing) on rates. This information includes:

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 23
1. Original and current claim incidence and claim length by age and other factors.
Incidence and length are tracked separately for some companies and combined
for others.
2. Experience
3. Impact on LLR of changes in expectations of morbidity.
4. Industry information and trends (for reasonableness checks).
c. Assumptions underlying the calculations of estimates of premiums may be adjusted as
part of the review. For instance:
i. If sample policy verification shows less impact on rates due to changes in lapse,
mortality, interest rate, and morbidity expectations than demonstrated in the
insurer’s aggregate projections, past or projected premiums or claims may be
adjusted in the original, makeup, or if-knew premium calculations.
ii. If there is wide variance in practice among companies in morbidity assumptions at
ages where data is of low credibility, adjustments may be made to help ensure similar
situations resulting in similar rate increase approval amounts.
1. A balanced approach is pursued, recognizing that providing full or zero credit for
partially credible experience may result in harmful consequences (excessive
rates or later rate shocks).
2. Any reductions to rate increases caused by lack of credible experience can
potentially be reversed in subsequent rate increase requests as credibility
increases.
iii. Similar adjustments may apply when incomplete or inconsistent information is
provided by the insurer (after initial attempts to resolve significant differences or
gaps).
4. Reconciliation of aggregate and sample policy applications.
a. In many cases, the aggregate and sample policy applications will result in similar current LLRs.
b. In other cases, some steps are taken to understand the difference, including additional requests for
information.
c. Because the sample policy application considers information only related to premium-paying
policyholders, it is possible that differences between the aggregate and sample policy application are
caused by inclusion of past premiums and all claims related to non-premium payers in the aggregate
information.
d. When reconciliation occurs after rounds of communication, decisions will be made based on the
information provided.
5. Blending – same for aggregate and sample policy applications.
a. The weighting towards the makeup premium is the percentage of original policyholders remaining.
b. The weighting towards the if-knew premium is the percentage of original policyholders no longer
having active policies, or 1 minus the percentage in ii.
c. The blending of the if-knew premium and makeup premium helps ensure remaining policyholders are
not held responsible for paying for adverse experience associated with past policyholders.
d. The blending also helps limit cumulative rate increases at later durations; as the percentage of
remaining policyholders approaches zero, the blended approval amount approaches the if-knew
premium.
6. Cost-sharing formula that increases the insurer burden as cumulative rate increases rise.
a. The cumulative-since-issue, weighted if-knew / makeup premium-based increase is reduced by:
i. No haircut for the first 15%.
ii. 10% for the portion of cumulative rate increase between 15% and 50%.
iii. 25% for the portion of cumulative rate increase between 50% and 100%.
iv. 35% for the portion of cumulative rate increase between 100% and 150%.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 24
v. 50% for the portion of cumulative rate increase in excess of 150%.
7. Reduction for past rate increase:
a. Take 1 plus the cost-sharing-adjusted blend amount and divide by 1 plus the previous, cumulative rate
increases, then subtract 1. This is the approvable rate increase.
8. Summary.
a. Review current assumptions.
b. Calculate aggregate if-knew premium and makeup premium amounts. Calculate the blended amount.
c. Calculate the sample policy estimated original premium, if-knew premium, and makeup premium.
Calculate the blended amount.
d. Reconcile aggregate and sample policy blended amounts. Set this blended amount aside.
e. Apply the cost-sharing formula to the blended amount.
f. Deduct past rate increases.
g. Example – if:
i. The original premium is $1,000
ii. Makeup premium is $3,000.
iii. If-knew premium is $1,500.
iv. 60% of policyholders remain.
v. Past rate increases are 50%:
vi. Blended amount is:
1. $3,000 / $1,000 * 0.60 +
2. $1,500 / $1,000 * 0.40
3. – 1 =
4. 180% + 60% – 1 = 240% – 1 = 140%
vii. Cost sharing is:
1. 100% * 0.15 +
2. 90% * 0.35 +
3. 75% * 0.5 +
4. 65% * 0.4 =
5. 110%
viii. Deduction for past rate increases results in:
1. (1 + 1.1) / (1 + 5) – 1 =
2. 40%
Texas PPV Formula
Details on the PPV Formula of the Texas approach to the actuarial review of rate changes include the following. To
reiterate, the formula is limited to active, premium-paying policyholders.
For rate stabilized policies:
premiums) earned future(85.
premiums) earned future(
1
85.58.
c
laims) incurred future(
% increase rate
current
PV
PV
C
C
PV ∆
+
+
−∆
=
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 25
Where:
Δ indicates the change in PV due to the change in actuarial assumptions between the time of the last rate
increase (or original pricing if no prior rate increase) and the current assumptions.
C is the cumulative % rate increase to date. For example, if the current rate (prior to the proposed rate
increase) is 50% higher than the rate at initial pricing, then C = 0.5.
The current subscript in the denominator indicates that the PV should be computed using current assumptions. The
future earned premiums in the formula are based on the current premiums prior to the proposed rate increase.
(State insurance regulators may wish to consider the addition of margin to the rate increase. For example, the
ΔPV(future incurred claims) term in the above formula could be multiplied by (1 + margin).
For pre-rate stabilized policies, we use 0.6 in place of 0.58 and 0.8 in place of 0.85:
premiums) earned future(8.
premiums) earned future(
1
8.6.
claims) incurred future(
% i
ncrease rate
current
PV
PV
C
C
PV ∆
+
+
−∆
=
Prior to the time that Texas adopted the PPV approach, a past requested rate increase may have been reduced by
the state insurance regulator by a method other than the PPV approach. In this situation, for a current filing, the
state insurance regulator may make adjustments to the current approvable amount based on what would have been
approved had PPV been used in the prior filing.
D. Appendix D—Principles of RBOs Associated with LTCI Rate Increases
In 2020, the Long-Term Care Insurance Reduced Benefit Options (EX) Subgroup of the Long-Term Care Insurance (EX)
Task Force, was charged to “Identify options to provide consumers with choices regarding modifications to long-term
care insurance (LTCI) contract benefits where policies are no longer affordable due to rate increases.” In completing
this charge, the Subgroup developed the following list of RBO principles to provide guidance for evaluating
RBO offerings.
Principles and Issues
As related to:
1. Fairness and equity for policyholders who elect an RBO:
• If some policyholders facing a rate increase are being offered an RBO but not others, an adequate
explanation is needed.
• Each RBO should provide reasonable value relative to the default option of accepting the rate increase
and maintaining the current benefit level.
2. Fairness and equity for policyholders who choose to accept rate increases and continue LTCI coverage at
their current benefit level:
• The extent of potential anti-selection should be analyzed, with consideration of the impact on the
financial stability of the remaining block of business and the resulting effect on the remaining
policyholders.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 26
3. Clarity of communication with policyholders eligible for an RBO:
• Policyholders should be provided with maximum opportunity and adequate information to make
decisions in their best interest.
• Companies should present RBOs in clear and simple language, format, and content, with clear
instructions on how to proceed and whom to contact for assistance.
4. Consideration of encouragement or requirement for an insurer to offer certain RBOs:
• State insurance regulators should evaluate legal constraints, the impact on remaining policyholders
and insurer finances, and the impact on Medicaid budgets if encouraging or requiring reduced LTCI
benefits.
5. Exploration of innovation, particularly where an outcome of improved health and lower claim costs
are possible:
• Regulators and interested parties should continue to study the idea of offerings being made by insurers
including potentially being tied to rate increases (e.g., providing hand railings for fall prevention in high-
risk homes) and identifying the pros and cons of such an approach.
Widely Established RBOs in Lieu of Rate Increases
1. Reduce inflation protection going forward, while preserving accumulated inflation protection.
2. Reduce daily benefit.
3. Decrease benefit period/maximum benefit pool.
4. Increase elimination period.
5. Contingent nonforfeiture (CNF).
i. Claim amount can be the sum of past premiums paid.
ii. Only receive that benefit if the policyholder qualifies for a claim.
Less Common RBOs for Potential Discussion
1. Cash buyout.
2. Copay percentage on benefits.
As the industry continues to innovate new RBOs for consumers, such as the two listed above, the MSA Review will
likewise develop and evolve to consider the reasonableness of these RBOs. The Task Force will encourage its
appointed Subgroup or an appropriate NAIC actuarial committee or group, to collectively consider new RBOs, as
they arise, that provides for input and technical advice from actuaries to states as they exercise their authority in
considering RBOs as part of rate filings.
E. Appendix E—Guiding Principles on LTCI RBOs Presented in Policyholder Notification Materials
In 2020, the Long-Term Care Insurance Reduced Benefit Options (EX) Subgroup of the Long-Term Care Insurance (EX)
Task Force adopted the following guiding principles to ensure quality of consumer notices of rate increases and
RBOs. This section seeks to provide guiding principles in answering this question: “What are the recommendations
for ensuring long-term care insurance policyholders have maximized opportunity to make reduced benefit decisions
that are in their best interest?”
To complete the charge, the Subgroup 1) evaluated the quality of consumer notices and RBO materials presented to
policyholders; 2) considered the relevant lessons learned and consumer focus group studies from the liquidation of
LTC insurer Penn Treaty Network America; 3) reviewed existing RBO consumer notice checklists or principles from
multiple states (i.e., Nebraska, Pennsylvania, Texas, and Vermont); and 4) addressed stakeholder comments on RBO
principles.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 27
This document is intended to establish consistent high-level guiding principles for LTCI RBOs presented in
policyholder notification materials. These principles are guidance and do not carry the weight of law or impose any
legal liability.
Recognizing that each component outlined in these principles will not apply in all circumstances, this section:
• RECOMMENDS that insurance companies recognize these fundamental principles.
• CALLS ON all insurance companies to consider the following principles in communicating RBOs available to
consumers in the event of a rate increase.
• UNDERLINES that the following principles are complementary and should be considered as a whole
Filing Rate Action Letters
Insurers should consider:
• Sending rate actions after the state has approved the rate action filing.
• Making the rate action effective on a policy anniversary date, recognizing that the Long-Term Care
Insurance Model Regulation (#641) allows for the next anniversary date or next billing date.
• Mailing rate increase notification letters at least 45 days prior to the date(s) a rate action becomes effective,
consistent with any applicable state laws and/or regulations.
• Sending rate increase notifications each year for rate increases that are phased-in over multiple years.
• Disclosing all associated future planned rate increases approved by state insurance regulators in the initial
and phased-in rate increase notification letters.
• Filing rate action letter templates in the NAIC SERFF rate increase filing to include statements of variability
and sample letters highlighting the differences between the communications, consistent with any
applicable state laws and/or regulations.
• Presenting innovative options to state insurance regulators prior to filing new RBOs.
o This enables state insurance regulators to evaluate potential anti-selection, adverse morbidity, and
implications to consumers and future claims experience.
Readability and Accessibility
Insurers should consider:
• Drafting a rate action letter that is easy to follow, flows logically, and displays the essential information
and/or the primary action first, followed by the nonessential information.
• Presenting the RBOs in a way that is comprehensible, memorable, and adjusted to the needs of the
audience.
• Using cover pages, a table of contents, glossaries, plain language, headers, maximized white space, and
appropriate font size and reading level for the intended audience.
• Using illustrative tools, such as bullet points or illustrations, as appropriate, and graphs or charts enabling
a side-by-side comparison.
• Including definitions of complex terms; and if a term, subject, or warning is repeated throughout the
communication, consider making the language consistent throughout the document.
• Including a Q&A section that is succinct but answers the commonly asked questions in plain language.
• Providing appropriate accommodations for policyholders with disabilities or policyholders for whom English
is not a first language.
Identification
Insurers should consider drafting the RBO communication in a way that helps policyholders understand:
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 28
• What is happening.
• Why it is happening to them.
o Ensure the letter does not negatively reference the state insurance department.
• When it is happening.
• What they can do about it.
• How they take action.
Communication Touch and Tone
Insurers should consider:
• Drafting the communication in a way that helps policyholders envision or reflect on the reason(s) why they
purchased an LTCI policy.
• Conveying as much empathy as possible regarding the impact a rate action(s) may have on policyholders.
• Presenting RBOs fairly, refraining from the use of bolding, repeating, or emphasizing one option over
another.
• Displaying the policyholder’s ability to maintain current benefits by paying the increased premium.
• Using word choices that appreciate how those words could influence a policyholder’s decision.
o For instance, consider using “now” instead of “must”; or consider using “mitigation options,” “offset
premium impact” or “manage an increase” instead of “avoid an increase.”
Consultation and Contact Information
The insurer should consider listing multiple contacts in the communication in an easy-to-identify location to include
phone number, email address, and website when available. For example:
• Customer service.
• Lapse notifier.
• Insurance producer.
• State insurance department.
• State Health Insurance Assistance Program (SHIP).
The insurer should consider suggesting policyholders consult a family member or other trusted advisor, such as:
• Lapse notifier.
• Insurance producer.
• Financial advisor.
• Certified personal accountant or tax advisor (in the event cash buyouts are offered).
Understanding Policy Options
Insurers should consider the presentation of the communication by:
• Identifying what necessitated the communication on the first page.
o For example, the header could say, “Your Long-Term Care Premiums Are Increasing.”
• Including the RBOs with the rate action letter.
• Limiting the number of options displayed on the letter to no more than four or five.
• Identifying which RBO(s) have limited time frames.
• Advising policyholders that they can ask about reducing their benefits at any time, regardless of a
rate increase.
• Providing enough information in the communication to make a decision.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 29
o If supplemental materials (e.g., insurer’s website) are provided, they would enhance the policyholder’s
understanding, but not be necessary to use when making a decision.
Insurers should consider indicating the window of time to act by:
• Clearly indicating what the policyholder’s premium will increase to and by when.
• Displaying the due date(s) in an easy-to-identify location and repeating it multiple times throughout
the document.
• Clearly differentiating due date(s) for each RBO, if available for a limited time.
Insurers should consider including disclosures regarding rate increase history by:
• Disclosing that future rate actions could occur.
• Advising if prior rate actions have or have not occurred to include:
o Policy form(s) impacted.
o Calendar year(s) the policy form(s) was available for purchase.
o Percentage of increase approved to include the minimum and maximum if they vary by benefit type.
• Reminding policyholders that their policy is guaranteed renewable.
Insurers should consider advising policyholders of their current benefits:
• For example, the communication could disclose the policyholder’s current benefits to include:
o Daily maximum amount.
o Inflation option.
o Current pool of benefits for policies with a limited pool of benefits.
Insurers should consider personal needs decision-making by:
• Only listing RBOs that are available to the policyholder.
• Calling on policyholders to reflect on how each option could impact them personally.
• Prompting policyholders to consider their unique situation to include their current age, health conditions,
financial position, availability of caregivers, spouse or partner impacts, and the potential need for
institutionalized care.
• Reminding policyholders to consider the cost of care in the area and setting where they expect to
receive care.
• Informing policyholders of factors that impact LTC costs, such as:
o The average cost of care for in-home care, assisted living, and nursing home care in their area.
o The inflation rate of the cost of care for in-home and nursing home care in their area.
o The average age and duration of an LTC claim for in-home and nursing home care.
o Factors that influence the age, duration, and cost of a claim.
• Disclosing to policyholders when an RBO falls below the cost of care in their area.
• Calculating for policyholders the number of days or months a paid-up option could cover based on the cost
of care in their area.
o Buyout or cash-out disclosures.
The cash offerings, if any, should disclose to policyholders that the option could result in a taxable
event, and they should consult with their certified personal accountant and/or tax advisor before
electing this option.
Insurers should consider the value of each option by:
• Disclosing if the RBOs may not be of equal value and are dependent on the unique situation of
each policyholder.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 30
Insurers should consider communicating the impact of options by:
• Displaying the options in a way that enables policyholders to compare options, including details such as:
o Daily/monthly benefit.
o Benefit period.
o Inflation option.
o Maximum lifetime amount.
o Premium increase percentage and/or new premium.
o Nonforfeiture (NFO) or contingent nonforfeiture (CNF) amount.
o If the policy is Partnership qualified, changes to benefits may impact Partnership status.
o Current premium.
• Providing a series of questions to help policyholders contemplate the implications of each action, such as:
o What will happen if they take no action?
o What will happen if they make no payment before the policy anniversary date?
o If they accept the full increase without reducing their benefits, how will they handle potential future
rate increases?
o If they elect the cash buyout, there could be tax implications.
o If they elect a paid-up NFO, how long will the reduced benefit last if they had a claim?
o If they were to increase their elimination period from 30 days to 100 days, do they have enough funds
to cover those expenses?
o Partnership policies: Will reducing the benefits remove Partnership qualification? If so, the letter
should explain that their asset protection may be removed or reduced.
When rate actions span over multiple years, insurers should consider:
• Disclosing the full rate increase amount, how it is spread out across multiple years, and all associated future
planned rate increases approved by state insurance regulators.
• Specifying if the premium increase referenced is the first, second, third, last, etc.
• Offering CNF based on the full increase amount and offered with each phase of the rate action.
• Notifying policyholders at least 45 days in advance of each phase of the rate increase, consistent with any
applicable state laws and/or regulations.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 31
VII. EXHIBITS
A. EXHIBIT A—SAMPLE MSA ADVISORY REPORT
7
FROM: Long-Term Care Insurance (LTCI) Multistate Actuarial Rate Review Team
DATE: [Date]
RE: ABC Insurance Company – Block LTC1 – Draft of Initial MSA Advisory Report
Executive Summary
The LTCI Multistate Actuarial Rate Review Team (MSA Team) recommends a rate increase of 35% to be approved
for inflation-protected products and 20% to be approved for products with no inflation, related to ABC Company’s
block.
Higher rate increases are recommended for states where past cumulative rate increases below 55% have been
approved. Reduced benefit options (RBOs) may be selected to help manage the impact of the rate increase.
Analysis by the MSA Team resulted in the recommended rate increase being consistent with that resulting from the
actuarially justified Texas and Minnesota approaches. The recommended rate increases are below the increases that
would have resulted from the lifetime loss ratio approach and the rate stability rules.
Background
The MSA Team was formed to assist the Long-Term Care Insurance (EX) Task Force in developing a consistent
national approach for reviewing LTCI rates, which results in actuarially appropriate increases being granted by the
states in a timely manner and eliminates cross-state rate subsidization.
The members are: [List names and state of members]. Starting in the first half of 2020, the MSA Team accepted rate
increase proposals as part of a pilot program. The MSA Review became operational on [insert date].
This MSA Advisory Report is related to the rate increase proposal filed by ABC Company for its LTC 1 block sold
between 2003 and 2006. The MSA Team’s actuarial analysis is provided below. The intention is that states can utilize
this analysis and feel comfortable accepting the MSA Advisory Report recommendation when taking action on the
upcoming ABC filings that will be made to the states.
The MSA Review and findings shall not be considered an approval of the rate schedule increase filing, nor shall it be
binding on the states or the insurer. As this is a state-approved product, each state will ultimately be responsible for
approving, partially approving, or disapproving the rate increase. A goal of the Task Force is for as much consistency
as possible to occur between states in the rate increase approvals.
Insurer’s Proposal
ABC Company requests a rate increase of 60% to be approved for inflation-protected products and 40% to be
approved for products with no inflation.
In addition, ABC Company is requesting higher rate increases for states that did not grant full approval of prior rate
increase requests.
7
Information contained in this sample report is an example only and is not derived from any actual rate filing.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 32
Workstream-Related Review Aspects
Actuarial Review
At the direction of the Long-Term Care Insurance Multistate Rate Review (EX) Subgroup, the MSA Team applied the
Minnesota and Texas approaches to calculate the recommended, approvable rate increases. Aspects of the
Minnesota approach that result in lower rate increases than those resulting from loss ratio-based approaches
contained in many states’ laws and rules include:
- Reduction in rate increases at later policy durations to address shrinking block issues.
- Elimination of rate increases related to inappropriate recovery of past losses.
Minnesota also has additional unique aspects: 1) consideration of adverse investment expectations related to the
decline in market interest rates, 2) adjustments to projected claim costs to ensure the impact of uncertainty is
adequately borne by the insurer; and 3) a cost-sharing formula applied in typical circumstances.
Even though these additional aspects are outside the pure loss-ratio requirements, they fall in line with legal
provisions that rates shall be fair, reasonable, and not misleading.
The Minnesota approach, including application of the typical-circumstance cost-sharing formula, results in an
approvable rate increase of 35% for inflation-protected products and 20% for products with no inflation protection.
The Texas approach results in an approvable rate increase of 29% in aggregate.
The MSA Team’s recommendation, in consideration of the Minnesota and Texas approaches, is to approve a rate
increase of 35% for inflation-protected products and 20% for products with no inflation protection.
Higher rate increases are recommended for states where past cumulative rate increases below 55% have been
approved.
The MSA Team reviewed support for the assumptions, experience, and projections provided by the insurer and
performed validation steps to review the insurer-provided information for reasonableness. Details regarding the
actuarial review are provided in Appendix 1. Also, the initial submission and subsequent correspondence between
the insurer and the MSA Team are available on SERFF. The SERFF tracking number is ABCC-123456789.
Consideration of Differences in Histories of States’ Rate Increase Approvals
According to the Historical Rate Level Summary, Appendix D in the insurer proposal, past rate increase approvals by
state have varied and can be categorized as follows:
• 25 states have granted full or near-full approval of ABC Company’s past requests (at or near 55%,
cumulative).
• 18 states have granted cumulative approvals averaging 45%.
• Five states have granted cumulative approvals averaging 27%.
• Two states have granted cumulative approvals averaging 15%.
The insurer’s stated goal is to bring rates in all states up to an equivalent rate level. Currently, the average annual
premium rates for a policyholder range from below $1,700 in some states (with the lowest past approvals) to over
$2,200 in other states (with the highest past approvals).
The MSA Team’s recommendation is based on a goal of rates per benefit unit being uniform between states going
forward.
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 33
A table of examples of recommended rate increases based on past cumulative approval history is provided in
Appendix 2.
Non-actuarial & Valuation/Solvency Considerations
Non-actuarial considerations, including flexibility regarding the phase-in of rate increases, waiting periods between
rate increases being coordinated with phase-in periods, and other issues are being discussed at the Task Force and
the Subgroup.
Even with future claims potentially being reduced due to COVID-19-related behavioral impact, ABC Company will
continue to experience substantial losses on this block.
Regarding coordination of rate and reserving reviews, the insurer states that assumptions underlying the rate
increase proposal are consistent with assumptions underlying the reserve adequacy testing.
RBOs – Review for Reasonableness
Unless a rider was purchased, ABC Company policyholders facing a rate increase will be offered the following
applicable options in lieu of a rate increase:
1) Extending the elimination period.
2) Decreasing the benefit period.
3) Reducing future inflation accumulation.
The insurer produced rate tables which demonstrate that the RBOs provide reasonable value in relation to a case of
a policyholder retaining full benefits and paying the full rate increase.
Financial Impact for Insurer
The requested rate increase associated with recent adverse development would result in around $50 million of
reduced losses for this block according to information contained in the actuarial memorandum.
Mix of Business
From the insurer’s actuarial memorandum:
Enrollees:
• Total enrollees as of date of proposal: 15,000
• Inflation protection: 9,000 (inflation protection) and 6,000 (no inflation)
• Benefit period: 8,500 (lifetime benefits) and 6,500 (limited benefits)
Product type: Expense reimbursement:
• Average issue age: 58
• Average attained age: 75
• Annualized premium: $30 million; $2,000 average per policyholder
Appendix 1
Drivers of Rate Increase Proposal – Summary
The primary drivers, summarized in the insurer actuarial memorandum, were lower lapses and longer average claim
length. The insurer assumptions were based on actual-to-expected adjustments, based in part by insurer experience
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 34
that has become more credible in recent years. The assumptions were determined to be reasonable and in line with
industry and actuarial averages.
Details Regarding Minnesota Approach
For an average (in terms of benefit period and issue age), 5% compound inflation-protected cell:
• Makeup cumulative rate increase: 177% (the increase from original rates needed going forward to get the
block to the financial position contemplated at original pricing)
o This increase is equal to the increase that would result from a pure loss ratio approach.
• If-knew cumulative rate increase: 36% (the increase from original rates needed if the insurer could go back
to the past and reprice the product given information it knows now)
• Proportion of original policyholders remaining in force, based on insurer original and updated assumptions:
62%
• Blended if-knew / makeup rate cumulative rate increase since issue: 123%
o = 0.62 * 177% + (1 - 0.62) * 36%, adjusted for rounding
• Insurer cost share based on Minnesota formula (see Appendix 3): 12%
• Recommended cumulative rate increase since issue: 109%
o = (1 - 0.12) * 1.23, adjusted for rounding
• Past cumulative rate increases: 55%
• Actuarial recommended rate increase from current rates: 35%
o = (1 + 1.09) / (1 + 0.55) – 1, adjusted for rounding
• Final actuarial recommended rate increase from current rates (for the inflation-protected cell): 35%
o Minimum of calculated approval rate of 35% and insurer proposal of 60%.
• Using the same methodology, the final actuarial recommended rate increase from current rates (for the
non-inflation-protected cell): 20%
Note that the Minnesota approach includes the reflection of declining interest rates which tends to lead to adverse
investment returns compared to expectations in original pricing. Also, where applicable, insurer morbidity
assumptions are adjusted downward due to a lack of credible support at extremely high ages, and a general lack of
complete support for aspects of morbidity assumptions, including uncertainty regarding future benefit utilization.
Details Regarding Texas Approach
• Insurer Calculation (aggregate): 52%
PPV calculations
• Texas Life & Health Actuarial Office (LHAO) PPV Calculation (aggregate): 29%
LHAO Comments
• For the purposes of the MSA report, and as a component of the calculation of the approvable rate increase,
Texas recommends an actuarially justified PPV calculated amount of 29%.
Texas rate stabilized PPV Formula:
Reconciliation of Minnesota and Texas Approaches
The Texas PPV calculated amount of 29% aligns well with the Minnesota approach’s recommended rate increase of
35% for inflation-protected policies and 20% for non-inflation-protected policies when the distribution of inflation-

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 35
protected vs. non-inflation-protected cells is applied. The MSA Team’s recommended rate increase is 35% for
inflation-protected policies and 20% for non-inflation-protected policies.
Recommended rate increases by state, in consideration of various histories of rate increase approvals, are listed in
Appendix 2.
Correspondence Summary
• Template information request for multi-state rate increase filings, based on the list adopted by the Health
Actuarial (B) Task Force on March 23, 2018.
• New premium rate schedule, percentage increase for each rating scenario such as issue age, benefit period,
elimination period, etc., from the existing and original rates.
• Rate increase history that reflects the filed increase.
• Actuarial Memorandum justifying the new rate schedule, which includes:
o Lifetime loss ratio projection, with earned premiums and incurred claims discounted at the maximum
valuation interest rate.
o Reasons for the rate increase, including which pricing assumptions were not realized and why.
o Statement that policy design, underwriting, and claims handling practices were considered.
o A demonstration that actual and projected costs exceed anticipated costs and the margin.
o The method and assumptions used in determining projected values should be reviewed in light of
reported experience and compared to the original pricing assumptions and current assumptions.
o Combined morbidity experience from different forms with similar benefits, whether from inside or
outside the insurer, where appropriate to result in more credible historical claims as the basis for future
claim costs.
o Information (from NAIC Guidance Manual for Rating Aspect of the Long-Term Care Insurance Model
Regulation, “Guidance Manual” Q&A): Morbidity, Lapse, Mortality, Interest.
Comparison with asset adequacy testing reserve assumptions.
Provide actuarial assumptions from original pricing and most recent rate increase filing, and,
have the original actuarial memorandum available upon request.
o Guidance Manual Checklist items: summaries, including past rate adjustments; average premium;
distribution of business, including rate increases by state; underwriting; policy design and margins;
actuarial assumptions; experience data; loss ratios; rationale for increase; and reserve description.
o Assert that analysis complies with Actuarial Standards of Practice, including No. 18 and No. 41.
o Numerical exhibits should be provided in Microsoft Excel spreadsheets with active formulas
maintained, where possible.
• Rate Comparison Statement of renewal premiums with new business premiums, if applicable.
• Policyholder notification letter – should be clear and accurate.
o Provide a description of options for policyholders in lieu of or to reduce the increase.
o If inflation protection is removed or reduced, is accumulated inflation protection vested?
o Explain the comparison of value between the rate increase and policyholder options.
o Are future rate increases expected if the rate increase is approved in full? If so, how is this
communicated to policyholders?
o How are partnership policies addressed?
• Supplementary information, based on a list developed by the MSA Team following the review of initial pilot
program proposals:
o Information on benefit utilization.
o Attribution of rate increase by factor.
o RBO history and reasonability analysis.
o Investment returns.
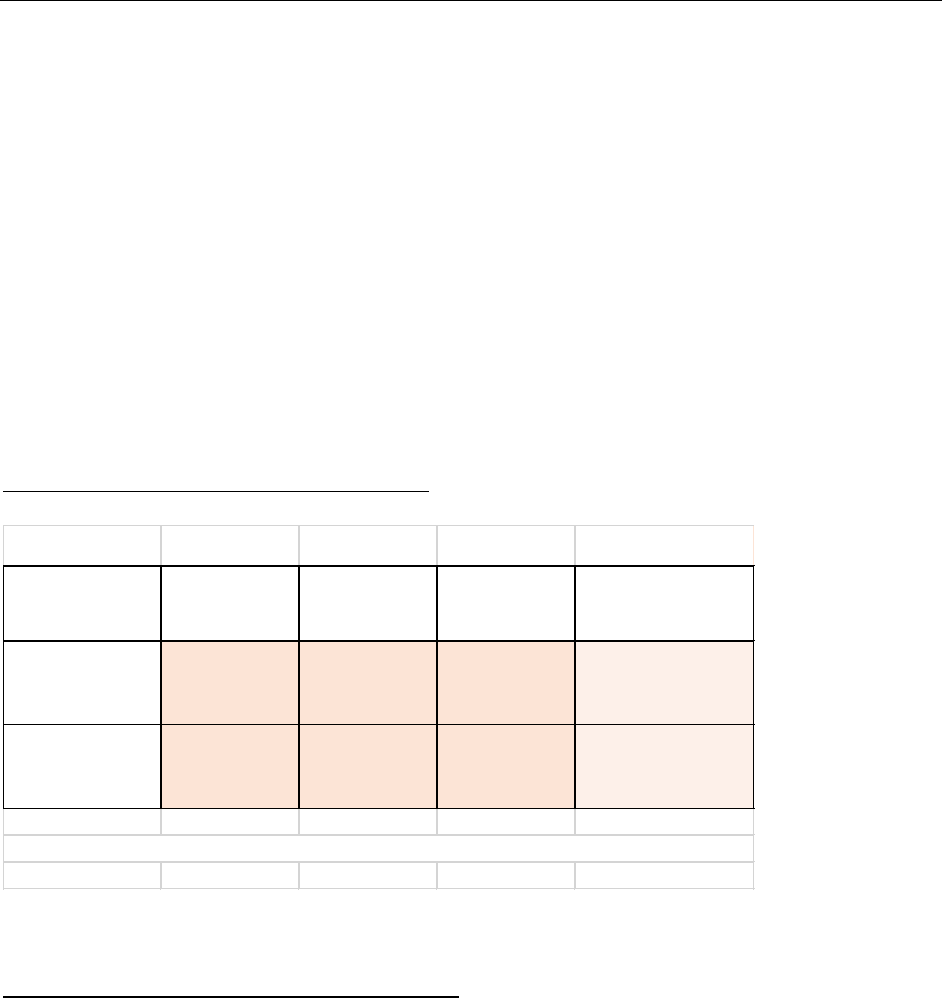
LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 36
o Expected loss ratio.
o Shock lapse history.
o Waiver of premium handling.
o Actual-to-expected differences.
o Assumption consistency with Actuarial Guideline 51 asset adequacy testing.
• Following initial review of the proposal, additional information was requested by the MSA Team related to:
o Original pricing assumptions.
o Lapse assumption by duration.
o Premiums and incurred claims by calendar year based on original assumptions.
o Distribution of in force by inflation protection.
o Loss ratios by lifetime/non-lifetime benefit period and with/without inflation protection.
o Description of waiver of premium handling in premium and claim projections.
o Commentary on COVID-19 short-term and long-term LTC impact.
Appendix 2
Examples of Rate Increases If an RBO is Not Selected
Appendix 3
Potential Cost-Sharing Formula for Typical Circumstance
Cumulative rate increase since issue date is haircut by:
• No haircut for the first 15%.
• 10% for the portion of cumulative rate increase between 15% and 50%.
• 25% for the portion of cumulative rate increase between 50% and 100%.
• 35% for the portion of cumulative rate increase between 100% and 150%.
• 50% for the portion of cumulative rate increase in excess of 150%.
Example: if the pre-cost sharing Minnesota approach results in a cumulative 210% rate increase since issue:
• Break 210% into the following components: 15%, 35%, 50%, 50%, 60%
• Post haircut approval is 100% of 15% + 90% of 35% + 75% of 50% + 65% of 50% + 50% of 60%
• = 15% + 32% + 38% + 33% + 30%
• = 147%
ABC Company
Jurisdiction
Example*
Past Cumulative
Approved
Increases
Increase to catch
up
Recommended
New
2021 Recommended
Rate Incr
Example: state with
average past
approvals
55% 0% 35% 35%
Example: state with
lower than average
past approvals
27% 22% 35% 65%
*The recommendation for each state is based on the actual past cumulative approved increases
in that state.

LTCI MSA Framework
©
2022 NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS 37
Justification for the cost-sharing formula is that the insurer should have had more information about the possibility
of triple-digit rate increases than the consumer had.
Adjustments to the formula may be desired when an insurer’s solvency position is dependent on a certain level of
rate increase approval. That is not the case with this insurer or proposal.

The National Association of Insurance Commissioners (NAIC)
is the U.S. standard-setting and regulatory support organization
created and governed by the chief insurance regulators from
the 50 states, the District of Columbia and five U.S. territories.
Through the NAIC, state insurance regulators establish
standards and best practices, conduct peer review, and
coordinate their regulatory oversight. NAIC staff supports these
efforts and represents the collective views of state regulators
domestically and internationally. NAIC members, together with
the central resources of the NAIC, form the national system of
state-based insurance regulation in the U.S.
For more information, visit www.naic.org.
