
2023
UnitedHealthcare
Care Provider
Administrative Guide for
Commercial and Medicare
Advantage

i
2023 UnitedHealthcare Care Provider Administrative Guide
Welcome to UnitedHealthcare
Welcome to the UnitedHealthcare Care Provider Administrative Guide for Commercial and Medicare Advantage (MA) products.
This guide has important information on topics such as claims and prior authorizations. It also has protocol information for
health care professionals. This guide has useful contact information such as addresses, phone numbers and websites. More
policies and online solutions are available on uhcprovider.com.
• If you are looking for information about Surest, please see the Surest supplement to this guide.
• If you are looking for a Community and State manual, go to uhcprovider.com/guides > Community Plan Care Provider
Manuals By State and select the state.
• If you are a UnitedHealthcare or Optum® participating health care provider or facility with an active Department of Veterans
Affairs Community Care Network (VA CCN) agreement, you can find more information about VA CCN on the Optum VA
Community Care Network UnitedHealthcare Provider Portal at VACommunitycare.com/provider.
You may easily find information in this guide using these steps:
1. Hold keys CTRL+F.
2. Type in the key word.
3. Press Enter.
This 2023 UnitedHealthcare Care Provider Administrative Guide (this “guide”) applies to covered services you provide to our
members or the members of our affiliates
1
through our benefit plans insured by or receiving administrative services from us,
unless otherwise noted.
This guide is effective April 1, 2023, for physicians, health care professionals, facilities and ancillary health care providers
currently participating in our commercial and MA networks. It is effective now for health care providers who join our network
on or after Jan. 1, 2023. This guide is subject to change. We frequently update content in our effort to support our health care
provider networks.
Terms and definitions as used in this guide:
• “Member” or “customer” refers to a person eligible and enrolled to receive coverage from a payer for covered services as
defined or referenced in your Agreement.
• “Commercial” refers to all UnitedHealthcare medical products that are not MA, Medicare Supplement, Medicaid, CHIP,
workers’ compensation or other government programs. “Commercial” also applies to benefit plans for the Health Insurance
Marketplace, government employees or students at public universities.
• “You,” “your” or “provider” refers to any health care provider subject to this guide. This includes physicians, health care
professionals, facilities and ancillary providers, except when indicated. All items are applicable to all types of health care
providers subject to this guide.
• “Your Agreement,” “Provider Agreement,” “Agreement” or ”your contract” refers to your Participation Agreement with us.
• “Us,” “we” or “our” refers to UnitedHealthcare on behalf of itself and its other affiliates for those products and services
subject to this guide.
• Any reference to “ID card” includes both a physical or digital card.
MA policies, protocols and information in this guide apply to covered services you provide to UnitedHealthcare MA members,
including Erickson Advantage members and most UnitedHealthcare Dual Complete members, excluding UnitedHealthcare
Medicare Direct members. We indicate if a particular section does not apply to such MA members.
If there is a conflict or inconsistency between a Regulatory Requirements Appendix attached to your Agreement and this guide,
the provisions of the Regulatory Requirements Appendix controls for benefit plans within the scope of that appendix.
If there is inconsistency between the terms of your Agreement and this guide, your Agreement controls. The exception to this
rule is when your Agreement defines a protocol that is specific to one of our affiliates and is inconsistent with a protocol in the
corresponding affiliate supplement to this guide. In that situation, the protocol in the applicable affiliate supplement to this
guide controls.
Per your Agreement, you must comply with protocols. Payment will be denied, in whole or in part, for failure to comply with
a protocol.
1
UnitedHealthcare affiliates offering commercial and Medicare Advantage benefit plans and other services, are outlined in Chapter 1: Introduction.
Quick reference guide
ii
2023 UnitedHealthcare Care Provider Administrative Guide
Quick reference guide
Join our Network
and Credentialing
If you are interested in joining our network, visit uhcprovider.com/join. To view our credentialing
policies and procedures.
Credentialing application: Check on your application status by emailing [email protected].
Digital Solutions uhcprovider.com: uhcprovider.com is your home for health care provider information with 24/7
access to the UnitedHealthcare Provider Portal, medical policies and news bulletins. The website
offers great resources to support administrative tasks including eligibility, claims, referrals, and prior
authorizations and notifications.
uhcprovider.com/digitalsolutions: Going digital means less paper and more automation, faster
workflow between applications and quicker claims submission process to get you paid faster. Our
three digital solutions, Electronic Data Interchange (EDI), Application Programming Interface (API)
and the UnitedHealthcare Provider Portal, help to make that a reality, and it’s not a one-size-fits-all
approach. There’s flexibility to choose the best approach for your practice, and there’s the ability to
integrate with the practice management systems you use today. This webpage will help you choose the
right solution to fit your practice’s needs.
uhcprovider.com/portal: Our portal allows you to quickly get the answers you need to claims
information like status updates, reconsiderations and appeals. You can also submit prior authorization
requests, check eligibility and benefits information, access items in Document Library (including
virtual card payment statements) and even track your work, all at no cost to you and without having to
make a phone call. To log in, click Sign In in the top right corner of uhcprovider.com.
uhcprovider.com/edi: Submit and receive data using HIPAA Electronic Data Interchange (EDI) X12
transactions for claim submissions, eligibility and benefits, claim status, authorizations, referrals,
hospital admission, discharge and observation stay notifications, and electronic remittance advice.
You can submit single or batch transactions for multiple members and payers without manual data
entry or logging into multiple payer websites.
uhcprovider.com/api: Our Application Programming Interface (API) solutions allow you to access
comprehensive real-time data on a timetable you set. Data can be distributed to your practice
management system, proprietary software or any application you prefer. We have APIs for claim status
and payment, eligibility and benefits, reconsiderations and appeals, documents, and referrals.
Healthcare
Professional
Education and
Training
We provide a full range of training resources including interactive self-paced courses and instructor-
led sessions at uhcprovider.com/training. The training content is organized by categories to make it
easier to find what you need.
Provider Portal
Access and New
User Registration
In order to access the UnitedHealthcare Provider Portal, you’ll need to create a One Healthcare ID.
Visit uhcprovider.com/access.
UnitedHealthcare
Communications
Network News: Find health care provider news and updates for national and state commercial,
Medicare and Medicaid plans at uhcprovider.com/news.
Policy and Protocol Updates: News and updates regarding policy, product or reimbursement
changes are posted online at uhcprovider.com/news. Updates are posted at the beginning of each
month. Sign up to receive notification of these updates by email at uhcprovider.com/subscribe.
Quick reference guide
iii
2023 UnitedHealthcare Care Provider Administrative Guide
Contact
UnitedHealthcare
Most questions can be answered using one of our online solutions at
uhcprovider.com/digitalsolutions. If you need to speak with someone, we’re here to help. For state-
specific contact information, visit uhcprovider.com > Contact us.
UnitedHealthcare Web Support 1-866-842-3278
providertechsuppor[email protected]
Provider Services 1-877-842-3210
Provider Services (Individual Exchange Plans) 1-888-478-4760
Prior Authorizations 1-877-842-3210
Prior Authorizations (Individual Exchange Plans) 1-888-478-4760
Optum Pay
TM
Helpdesk 1-877-620-6194
Participation Agreement questions: Contact your Network Management representative. To identify
your Network Management representative, go to uhcprovider.com > Contact us > State-specific
health plan and network support and select your state.
Provider Advocate: To find your health care provider advocate, go to uhcprovider.com > Contact us >
State-specific health plan and network support and select your state.
Find a health care
provider
uhcprovider.com > Our network > Find a provider.
• Search for doctors, clinics or facilities by plan type.
• Find dental providers by state, network or location.
• Locate mental health or substance abuse services.
Eligibility Access benefit, coverage and identification card information:
Online: uhcprovider.com/eligibility and click Sign In in the top right corner.
EDI: 270/271 transaction | uhcprovider.com/edi270
For Individual Exchange Plans, call 1-888-478-4760.
Advance
Notification/Prior
Authorization,
Admission
Notification,
Discharge
Notification,
Observation Stay
Notification and
Referrals
To notify us or request prior authorization:
EDI: Transactions 278 and 278N
• Submit prior authorization requests and referrals using EDI 278 transactions. Go to uhcprovider.
com/edi278 for more information.
• Submit hospital admission, discharge and observation stay notifications using EDI 278N
transactions. Go to uhcprovider.com/edi278n for more information.
• Check the status of prior authorization requests and notifications at uhcprovider.com/edi278i.
Online: uhcprovider.com/paan
Use the Prior Authorization and Notification tool in the UnitedHealthcare Provider Portal to:
• Determine if notification or prior authorization is required.
• Complete the notification or prior authorization process.
• Upload medical notes or attachments.
• Check request status.
Information: uhcprovider.com/priorauth (information and advance notification/prior
authorization lists)
Phone: Call Care Coordination at the number on the member’s ID card (self-service available after
hours) and select “Care Notifications.”
Quick reference guide
iv
2023 UnitedHealthcare Care Provider Administrative Guide
Claims EDI: uhcprovider.com/edi837 View our Claims Payer List to determine the correct payer ID.
Online: uhcprovider.com/claimstool > Click Sign In in the top right corner.
Information: uhcprovider.com/claims (policies, instructions and tips)
Phone: 1-877-842-3210 (follow the prompts for status information)
1-888-478-4760 (Individual Exchange Plans)
Reimbursement Policies:
uhcprovider.com > Resources > Plans, policies, protocols and guides > For Commercial Plans >
Reimbursement Policies for UnitedHealthcare Commercial Plans
uhcprovider.com > Resources >Plans, Policies, protocols and guides > For Exchange Plans >
Reimbursement Policies for UnitedHealthcare Individual Exchange Plans
uhcprovider.com > Resources > Plans, policies, protocols and guides > For Medicare Advantage
Plans> Reimbursement Policies for Medicare Advantage Plans
uhcprovider.com > Resources > Plans, policies, protocols and guides > For Community Plans >
Reimbursement Policies for Community Plan
Reimbursement policies may be referred to in your Agreement as “payment policies.” Refer to the
Medicare Advantage policies for DSNP members.
Claim
Reconsiderations
and Appeals
API: Submit reconsiderations and appeals with attachments using our API solution. Get more
information online at uhcprovider.com/api.
Online: uhcprovider.com. Click Sign In in the top right corner.
Report escalated or unresolved issues to your Provider Advocate by email. Submit an appeal as a
final resolution.
Medical Policies: Get copies of the medical policies and guidelines at uhcprovider.com/policies.
Timely Filing
Guidelines
Refer to your internal contracting contact or Participation Agreement for timely filing information.
Care Provider
or Group
Demographic
Information
Update Forms
Care Provider or Group Demographic Information Update forms:
• uhcprovider.com/mpp > My Practice Profile
• uhcprovider.com/getconnected > Step 3: Verify your demographic and tax ID information
Preferred Lab
Network
uhcprovider.com > Our network > Preferred Lab Network
Specialty
Pharmacy
Program
(Commercial and
Exchange)
Specialty Pharmacy Program provides focused support to help better manage rare and complex
chronic conditions. Find details about the Specialty Pharmacy Program online at uhcprovider.com >
Resources > Drug Lists and Pharmacy > Specialty Pharmacy - Medical Benefit Management
(Provider Administered Drugs).
Commercial medical benefit specialty prior authorizations are managed under the
Specialty Guidance Program (SGP).
Phone: 1-888-397-8129
Email: [email protected]
v
2023 UnitedHealthcare Care Provider Administrative Guide
Contents
Welcome to UnitedHealthcare ........................................................i
Quick reference guide ii
Chapter 1: Introduction 1
Manuals and benefit plans referenced in this guide ...................................... 1
Online/interoperability resources and how to contact us .................................5
Online resources and how to contact us ...............................................8
Chapter 2: Provider responsibilities and standards 11
Verifying eligibility, benefits and your network participation status .........................11
Health plan identification (ID) cards ..................................................11
Access standards ................................................................14
Network participating health care provider responsibilities ...............................16
Civil rights .......................................................................16
Confidentiality, Use of Licensed Marks, Publicity .......................................17
Consolidated Appropriations Act, 2021 (CAA) requirements .............................18
Cooperation with quality improvement and patient safety activities ........................19
Demographic changes ............................................................19
Notification of practice or demographic changes (applies to Commercial benefit plans in
California) .......................................................................21
Administrative terminations for inactivity ..............................................22
Member dismissals initiated by a PCP (Medicare Advantage) ............................23
Medicare opt-out .................................................................23
Additional MA requirements ........................................................23
Filing of a lawsuit by a member .....................................................25
Chapter 3: Commercial products 27
Commercial product overview table .................................................27
Benefit plan types ................................................................31
PCP selection ...................................................................31
Consumer-driven health benefit plans ................................................31
Chapter 4: Individual Exchange plans 33
UnitedHealthcare participation in Exchanges ..........................................33
Plan coverage and metal levels .....................................................36
UnitedHealthcare benefit plans for Individual Exchanges ................................38
Understanding your network participation ............................................40
Verifying eligibility and benefits .....................................................41
Plan requirements/features ........................................................41
Patient care coordination and case management ......................................43
Government Inspections and Audits .................................................44
Telemedicine and Virtual Care .....................................................44
Pharmacy .......................................................................45
Specialty services (hearing, vision, dental, transplant, behavioral health, chiropractor, skilled
nursing facility) ...................................................................45
Claims process ..................................................................45
Policies and protocols ............................................................46
Quick reference guide .............................................................46
Contents
vi
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 5: Medicare products 53
Medicare product overview tables ...................................................54
PCP selection ....................................................................60
Coverage summaries and policy guidelines for MA members ............................60
Special needs plans managed by Optum .............................................61
Medicare supplement benefit plans .................................................63
Free Medicare education for your staff and patients ....................................64
Chapter 6: Referrals 65
Commercial products referrals ......................................................65
Non-participating health care providers (all Commercial plans) ...........................68
Individual exchange referral required plan ............................................69
Medicare Advantage (MA) referral required plans ......................................69
Chapter 7: Medical management 71
Advance notification/prior authorization protocol ......................................71
Advance notification/prior authorization requirements ..................................72
Advance notification/prior authorization list ...........................................73
Facilities: Standard notification requirements* .........................................74
How to submit advance notification/prior authorization, admission notification, discharge
notification and observation stay notification ..........................................77
Updating advance notification or prior authorization requests ............................78
Coverage and utilization management decisions .......................................78
Clinical trials, experimental or investigational services ..................................80
Medical management denials/adverse determinations ..................................81
Pre-service appeals ...............................................................82
MA Part C reopenings .............................................................83
Outpatient cardiology notification/prior authorization protocol ............................84
Outpatient radiology notification/prior authorization protocol .............................91
Medication-assisted treatment ......................................................98
Trauma services .................................................................. 98
Air ambulance licensure ...........................................................99
Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy 100
Commercial pharmacy ...........................................................100
Specialty pharmacy requirements for certain medical benefit specialty medications (commercial
plans – not applicable to UnitedHealthcare West) .....................................100
Medicare Advantage pharmacy ....................................................102
Drug utilization review program ....................................................106
Drug management program ......................................................106
Medication therapy management. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 107
Transition policy .................................................................108
Chapter 9: Specific protocols 109
Non-emergent ambulance ground transportation .....................................109
Interoperability protocol ..........................................................109
Laboratory services protocol ......................................................109
Nursing home and assisted living plans .............................................111
Social determinants of health protocol ..............................................112
Telehealth services protocol .......................................................113
Contents
vii
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 10: Our claims process 114
Optum Pay™ ...................................................................115
Virtual card payments ............................................................115
Enroll and learn more about Optum Pay .............................................116
Claims and encounter data submissions ............................................116
Risk adjustment data – MA, commercial and exchange ................................118
NPI ...........................................................................119
MA claim processing requirements .................................................119
Claim submission tips ............................................................120
Pass-through billing ..............................................................122
Special reporting requirements for certain claim types .................................122
Overpayments ..................................................................124
Subrogation and COB ............................................................125
Claim correction and resubmission .................................................126
Claim reconsideration and appeals process ..........................................127
Resolving concerns or complaints ..................................................129
Member appeals, grievances or complaints ..........................................130
Medical claim review .............................................................131
Chapter 11: Compensation 132
Reimbursement policies ..........................................................132
Charging members ..............................................................132
Member financial responsibility ....................................................135
Preventive care ..................................................................135
Extrapolation ...................................................................136
Audit services. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 136
Audit failure denials .............................................................137
Notice of Medicare Non-Coverage ..................................................137
Chapter 12: Medical records standards and requirements 138
Chapter 13: Health and disease management 141
Health management programs .....................................................141
Case management ..............................................................141
Commercial health services, wellness and behavioral health programs ...................142
Commercial consumer transparency tools ...........................................143
Medicare Advantage .............................................................143
Commercial and MA behavioral health information ....................................144
Chapter 14: Quality Management program 146
UnitedHealth Premium® program (commercial plans) ..................................147
Star ratings for MA and prescription drug plans .......................................148
Members’ experience of care ......................................................148
Imaging accreditation protocol .....................................................148
Chapter 15: Credentialing and recredentialing 149
Credentialing/profile reporting requirements .........................................149
Health care provider rights related to the credentialing process ..........................150
Credentialing committee decision-making process (non-delegated) ......................150
Monitoring of network providers and health care professionals ..........................151
Chapter 16: Member rights and responsibilities 152
Contents
viii
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 17: Fraud, Waste and Abuse 154
Medicare compliance expectations and training ......................................154
Exclusion checks ................................................................155
Preclusion list policy .............................................................155
Examples of potentially fraudulent, wasteful or abusive billing ...........................156
Prevention and detection .........................................................156
Corrective action plans ...........................................................157
Beneficiary inducement law .......................................................157
Reporting potential FWA to UnitedHealthcare ........................................157
Chapter 18: Provider communication 158
Email communication ............................................................158
Online resources ................................................................158
All Savers supplement 160
How to contact All Savers .........................................................160
Surest supplement 163
Surest plan resources ........................................................163
Surest health plan ID card. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 164
Our claims process ..............................................................165
Claim reimbursement (adjustments) ................................................165
How to submit your reconsideration or appeal ........................................165
Still have questions? .............................................................165
Capitation and/or Delegation Supplement 166
What is Capitation? ..............................................................166
What is Delegation? ..............................................................166
How to contact us ...............................................................167
Verifying eligibility and effective dates ...............................................167
Commercial eligibility, enrollment, transfers and disenrollment ..........................167
Medicare Advantage (MA) enrollment, eligibility and transfers, and disenrollment ..........172
Authorization guarantee (CA Commercial only) .......................................175
Health care provider responsibilities ................................................175
Delegated credentialing program ...................................................181
Virtual Care Services (Commercial HMO plans – CA only) ..............................183
Referrals and referral contracting ..................................................184
Medical management ............................................................188
Pharmacy ......................................................................197
Facilities .......................................................................198
Claim delegation oversight .......................................................203
Claims disputes and appeals ......................................................213
Contractual and financial responsibilities ............................................216
Customer service requirements between UnitedHealthcare and the delegated entity
(Medicare) .....................................................................221
Capitation reports and payments ...................................................222
CMS premiums and adjustments ...................................................226
Delegate performance management program ........................................229
Appeals and grievances ..........................................................230
Contents
ix
2023 UnitedHealthcare Care Provider Administrative Guide
Empire Plan supplement 231
Referrals .......................................................................231
ID cards .......................................................................231
Prior authorization and notification requirements ......................................232
Online resources and how to contact us .............................................234
Leased Networks 235
Level2 supplement 236
How to contact us ...............................................................236
Health plan ID cards .............................................................237
Claims process .................................................................237
Mid-Atlantic Regional supplement 239
Provider responsibilities ..........................................................240
Referrals .......................................................................242
Prior authorizations ..............................................................242
Claims process .................................................................244
Capitation ......................................................................245
Neighborhood Health Partnership supplement 247
How to contact NHP .............................................................247
Discharge of a member from participating provider’s care ..............................250
Laboratory services ..............................................................250
Referrals .......................................................................251
UM ............................................................................252
Claims reconsiderations and appeals ...............................................253
Capitated health care providers ...................................................253
New Mexico Supplement 254
OneNet PPO/Workers’ Compensation supplement 256
Who to contact ..................................................................257
Bill process .....................................................................258
Referrals .......................................................................263
Provider responsibilities and workflows .............................................264
Medical records standards and requirements ........................................264
Quality management and health management programs ...............................264
Participant rights and responsibilities ...............................................265
Oxford Commercial supplement 266
Oxford Commercial product overview ...............................................266
Oxford commercial products contact information .....................................266
Health care provider responsibilities and standards ...................................270
Referrals ......................................................................275
Utilization management ..........................................................277
Using non-participating health care providers or facilities ...............................279
Radiology and cardiology procedures ...............................................283
Emergencies and Urgent Care .....................................................288
Utilization reviews ...............................................................290
Claims process .................................................................298
Member billing ..................................................................301
Claims recovery, appeals, disputes and grievances ....................................302
Quality assurance ...............................................................307
Contents
x
2023 UnitedHealthcare Care Provider Administrative Guide
Case management and disease management programs ...............................308
Clinical process definitions ........................................................308
Member rights and responsibilities .................................................311
Medical/clinical and administrative policy updates ....................................311
Oxford Level Funded plans (CT, NJ and NY) 312
Oxford Level Funded product contacts ..............................................312
Our claims process ..............................................................312
How to submit your reconsideration or appeal ........................................313
Preferred Care Network supplement 314
How to contact us ...............................................................314
Confidentiality of Protected Health Information (PHI) ...................................318
Referrals .......................................................................318
Prior authorizations ..............................................................319
Appeal and reconsideration processes ..............................................323
Member rights and responsibilities .................................................324
Documentation and confidentiality of medical records .................................324
Provider reporting responsibilities ..................................................328
Preferred Care Partners supplement 329
About Preferred Care Partners .....................................................329
How to contact us ...............................................................329
Confidentiality of Protected Health Information (PHI) ...................................333
Prior authorizations ..............................................................333
Clinical coverage review ..........................................................335
Appeal and reconsideration processes ..............................................337
Member rights and responsibilities .................................................338
Documentation and confidentiality of medical records .................................339
Case management and disease management program information ......................340
Special needs plans .............................................................341
Health care provider reporting responsibilities ........................................342
River Valley Entities supplement 343
Eligibility .......................................................................343
How to contact River Valley .......................................................344
Reimbursement policies ..........................................................346
Referrals .......................................................................346
Utilization Management (UM) ......................................................347
Claims process .................................................................351
UMR supplement 355
How to contact UMR .............................................................355
Health plan identification cards ....................................................357
Prior authorization and notification requirements ......................................357
Clinical trials, experimental or investigational services .................................358
Pharmacy and specialty pharmacy benefits ..........................................358
Specific protocols ...............................................................358
Our claims process ..............................................................359
Health and disease management ...................................................360
Frequently asked questions .......................................................360

Contents
xi
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare FlexWork™ supplement 363
How to contact FlexWork™ ........................................................363
Health plan ID card ..............................................................364
Our claims process ..............................................................364
UnitedHealthcare Level Funded supplement 366
How to contact us ...............................................................366
Our claims process ..............................................................367
UnitedHealthcare West supplement 369
UnitedHealthcare West information regarding our health care provider website ............372
How to contact UnitedHealthcare West resources .....................................372
Health care provider responsibilities ................................................375
Utilization and medical management ................................................379
Hospital notifications .............................................................383
Home delivery pharmacy .........................................................387
Claims process .................................................................388
Health care provider claims appeals and disputes .....................................392
California language assistance program (California commercial plans). . . . . . . . . . . . . . . . . . . . 396
Member complaints and grievances ................................................397
California Quality Improvement Committee ..........................................397
UnitedHealthOne Individual Plans supplement 398
How to contact UnitedHealthOne resources ..........................................398
Claims process .................................................................399
Member complaints and grievances ................................................401
Glossary 404
1
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 1: Introduction
Manuals and benefit plans referenced in this guide
Some benefit plans included under your Agreement may be subject to requirements found in other health care provider guides
or manuals or to the supplements found in the second half of this guide.
This section provides information about some of the most common UnitedHealthcare products. Your Agreement may use
“benefit contract types,” “benefit plan types” or a similar term to refer to our products.
Visit uhcprovider.com/plans for more information
about our products and Individual Exchange
benefit plans offered by state.
If a member presents a health plan ID card with a product name you are not familiar with, use the UnitedHealthcare Provider
Portal > Eligibility to quickly find information on the plan. You may also call us at 1-877-842-3210 or Exchange Provider Services
at 1-888-478-4760.
You are subject to the provisions of additional guides when providing covered services to a member of those benefit plans, as
described in your Agreement and in the following table. We may make changes to health care provider guides, supplements
and manuals that relate to protocol and payment policy changes.
We may change the location of a website, a benefit plan name, branding or the health plan ID card. We inform you of those
changes through one of our health care provider communications resources.
Benefit plans subject to this guide
Plan Name Location of most members
subject to additional guides
Location of plan information
All Savers:
All Savers Insurance Company
All markets All Savers supplement to this
guide
myallsaversconnect.com
Empire Plan All markets outside of NY* and national health
care providers; Primary concentrations in: AZ,
CA, CT, DE, FL, GA, MA, MD, NC, NJ, NV, PA,
SC, TN, TX, VA
Health plan ID card indicates NYSHIP, The
Empire Plan and references UnitedHealthcare
logo on the back
* In the NY markets, there are a limited number
of health care providers with the Empire Plan
specifically added to their UnitedHealthcare
Agreement. Otherwise, we have a separate
health care provider network for Empire Plan
members in NY.
Empire Plan supplement to this
guide
uhcprovider.com
Exchanges AL, AZ, FL, GA, IL, KS, LA, MD, MI, MS, MO, NC,
OH, OK, TN, TX, VA, WA
Chapter 4: Individual Exchange
Plans to this guide.
Chapter 1: Introduction
2
2023 UnitedHealthcare Care Provider Administrative Guide
Plan Name Location of most members
subject to additional guides
Location of plan information
MDIPA:
MD Individual Practice
Association, Inc.
DC, DE, MD, VA, WV
Some counties in: Southeastern PA
Mid-Atlantic Regional Supplement
to this guide.
uhcprovider.com
Capitated and/or Delegated
Providers (Commercial and
MA) Supplement
All markets Capitation and/or Delegation
Supplement to this guide.
NHP:
Neighborhood Health
Partnership, Inc.
FL Neighborhood Health Partnership
Supplement to this guide.
uhcprovider.com
OCI:
Optimum Choice Inc.
DC, DE, MD, VA, WV
Some counties in: PA
Mid-Atlantic Regional Supplement
to this guide.
uhcprovider.com
OneNet PPO DC, DE, FL, GA, MD, NC, PA, SC, TN, VA, WV OneNet PPO Supplement to this
guide.
uhcprovider.com
Oxford:
• Oxford Health Plans, LLC
• Oxford Health Insurance, Inc.
• Investors Guaranty Life
Insurance Company, Inc.
• Oxford Health Plans (NY), Inc.
• Oxford Health Plans (NJ), Inc.
• Oxford Health Plans (CT), Inc.
• Oxford Level Funded Plans
(NJ, CT)
CT, NJ, NY (except upstate)
Some counties in: PA.
Oxford Commercial Supplement
to this guide.
For commercial benefits:
uhcprovider.com
For Medicare benefits:
uhcprovider.com
Preferred Care Network
Supplement
FL counties: Broward and Miami-Dade Preferred Care Network
Supplement to this guide.
uhcprovider.com
Preferred Care Partners FL counties: Broward, Miami-Dade and
Palm Beach
Preferred Care Partners
Supplement to this guide.
uhcprovider.com
Chapter 1: Introduction
3
2023 UnitedHealthcare Care Provider Administrative Guide
Plan Name Location of most members
subject to additional guides
Location of plan information
River Valley:
• UnitedHealthcare Services
Company of the River
Valley, Inc.
• UnitedHealthcare Plan
of the River Valley, Inc.
• UnitedHealthcare Insurance
Company of the River Valley
Parts of AR, GA, IA, IL, TN, VA, WI
Your UnitedHealthcare contract specifically
references River Valley or John Deere Health
protocols or guides; and
You are located in AR, GA, IA, TN, VA, WI
or these counties in Illinois: Jo Daviess,
Stephenson, Carroll, Ogle, Mercer, Whiteside,
Lee, Rock Island, Henry, Bureau, Putnam,
Henderson, Warren, Knox, Stark, Marshall,
Livingston, Hancock, McDonough, Fulton,
Peoria, Tazewell, Woodford, McLean; and
You are providing services to a River Valley
Commercial member and not a River Valley
Medicare Advantage, Medicaid or CHIP member.
Note: River Valley also offers benefit plans in LA,
NC, OH and SC, but the River Valley Additional
Guide does not apply to those benefit plans.
River Valley Entities Supplement
to this guide.
uhcprovider.com
Sierra or Health Plan of
Nevada:
• Sierra Health and Life
Insurance Co., Inc.
• Health Plan of Nevada, Inc.
• Sierra Healthcare Options,
Inc.
Outside NV only:
The health plan ID card identifies the Sierra or
Health Plan of Nevada members who access the
UnitedHealthcare network outside of Nevada,
and includes the following reference:
UnitedHealthcare Choice Plus Network
Outside Nevada.
Services rendered outside of
Nevada to Sierra or Health Plan of
Nevada members with the ID card
reference described in this row are
subject to your UnitedHealthcare
Agreement and to this guide unless
you are in Arizona or Utah and have
a contract directly with Sierra or
Health Plan of Nevada.
UMR:
• UMR
• UnitedHealthcare Shared
Services (UHSS)
All markets UMR supplement to this guide.
umr.com
UnitedHealthcare Level
Funded
(Previously sold under the
name All Savers® Alternate
Funding)
December 2020: AL, SD, ND, DE
September 2021: All markets
UnitedHealthcare Level Funded
supplement to this guide.
uhcprovider.com

Chapter 1: Introduction
4
2023 UnitedHealthcare Care Provider Administrative Guide
Plan Name Location of most members
subject to additional guides
Location of plan information
UnitedHealthcare West:
(Formerly referenced in this
guide as “PacifiCare”)
• UHC of California dba
UnitedHealthcare of California
(hereinafter referred to
as UnitedHealthcare of
California)
• UnitedHealthcare of
Oklahoma, Inc.
• UnitedHealthcare of
Oregon, Inc.
• UnitedHealthcare Benefits of
Texas, Inc.*
* PacifiCare of Arizona,
PacifiCare of Colorado
and PacifiCare of Nevada
are now referenced as
UnitedHealthcare Benefits of
Texas, Inc.
AZ, CA, CO, NV, OR, TX, WA UnitedHealthcare West
Supplement to this guide.
uhcprovider.com
UnitedHealthOne:
• Golden Rule
Insurance Company
Group #705214
• Oxford Health Insurance, Inc.
Group #908410
All markets
New Jersey
UnitedHealthOne Individual Plans
Supplement to this guide.
uhcprovider.com and
myuhone.com
UnitedHealthcare Freedom
Plans
NH, ME, VT uhcprovider.com
Chapter 1: Introduction
5
2023 UnitedHealthcare Care Provider Administrative Guide
Benefit plans not subject to this guide
Plan name Location of most
members subject to
additional guides
Additional guide/website
Rocky Mountain Health Plan (RMHP) CO rmhp.org
Sierra:
Sierra Health and Life Insurance Co., Inc.
Sierra Healthcare Options, Inc.
Health Plan of Nevada, Inc.
Health Plan of Nevada Medicaid/
Nevada Check Up
NV Benefit plans for Sierra Health and Life Insurance
Company, Inc.
sierrahealthandlife.com/provider
Benefit plans for Sierra Healthcare Options, Inc:
sierrahealthcareoptions.com
Benefit plans for Health Plan of Nevada, Inc:
healthplanofnevada.com/provider
myhpnmedicaid.com/provider
UnitedHealthcare Community Plan
Medicaid, CHIP and Uninsured
Multiple states UnitedHealthcare Community Plan Physician, Health
Care Professional, Facility and Ancillary Administrative
Guide for Medicaid, CHIP, or Uninsured.
uhcprovider.com/communityplan and
uhcprovider.com
Online/interoperability resources and how to contact us
Going digital means less paper and more automation, faster workflow between applications and a quicker claims submission
process to help you get paid faster. Learn the differences by viewing our Digital Solutions Comparison Guide. You will conduct
business with us electronically. This means using electronic means, where allowed by law, to submit claims and receive
payment, and to submit and accept other documents, including prior authorization requests and decisions, and reconsideration
and appeal requests and decisions. Using electronic transactions is fast, efficient, and supports a paperless work environment.
The UnitedHealthcare Provider Portal has tools such as EDI (uhcprovider.com/edi) and API (uhcprovider.com/api) that
provide maximum efficiency in conducting business electronically.
Application Programming Interface (API)
API is becoming the newest digital method in health care to distribute information to health care professionals and business
partners in a timely and effective manner. API is a common programming interface that interacts between multiple applications.
Our API solutions allow you to electronically receive detailed data on claims status and payment, eligibility and benefits, claim
reconsiderations and appeals (with attachments), referrals and documents. Information returned in batch emulates data in the
UnitedHealthcare Provider Portal and complements EDI transactions, providing a comprehensive suite of services. It requires
technical coordination with your IT department, vendor or clearinghouse. The data is in real time and can be programmed to be
pulled repetitively and transferred to your practice management system or any application you prefer. For more information, visit
uhcprovider.com/api.
Electronic Data Interchange (EDI)
EDI is a self-service resource using your internal practice management or hospital information system to exchange transactions
with us through a clearinghouse.
The benefit of using EDI is it permits health care providers to send batch transactions for multiple members and multiple payers
in lieu of logging into different payer websites to manually request information. This is why EDI is usually health care providers’
first choice for electronic transactions.
• Send and receive information faster.
• Identify submission errors immediately and avoid processing delays.
Chapter 1: Introduction
6
2023 UnitedHealthcare Care Provider Administrative Guide
• Exchange information with multiple payers.
• Reduce paper, postal costs and mail time.
• Cut administrative expenses.
The following are EDI transactions available to health care providers:
• Claims (837)
• Eligibility and benefits (270/271)
• Claims status (276/277)
• Referrals and authorizations (278)
• Hospital admission, discharge and observation stay notifications (278N)
• Electronic remittance advice (ERA/835)
Visit uhcprovider.com/edi for more information. Learn how to optimize your use of EDI at uhcprovider.com/optimizeEDI.
Getting started
• If you have a practice management or hospital information system, contact your software vendor for instructions on how to
use EDI in your system.
• Contact clearinghouses to review which electronic transactions can interact with your software system.
Read our Clearinghouse Options page for more information.
Point of Care Assist
TM
When made available by UnitedHealthcare, you will do business with us electronically. Point of Care Assist integrates members’
UnitedHealthcare health data within the Electronic Medical Record (EMR) to provide real-time insights of their care needs,
aligned to their specific member benefits and costs. This makes it easier for you to see potential gaps in care, select labs,
estimate care costs and check prior authorization requirements, including benefit eligibility and coverage details. This helps you
to better serve your patients and achieve better results for your practice. For more information, go to uhcprovider.com/poca.
uhcprovider.com
This public website is available 24/7 and does not require registration to access. You’ll find valuable resources including
administrative and plan-specific policies, protocols and guides, health plans by state, regulatory and practice updates, quality
programs, network news and more. You’ll also find information about our electronic workflow solutions, including Electronic
Data Exchange (EDI), Application Programming Interface (API), and the UnitedHealthcare Provider Portal.
UnitedHealthcare Provider Portal
This secure portal is available at uhcprovider.com. It allows you to access patient information such as eligibility and benefit
information and digital ID cards. You can also perform administrative tasks such as submitting prior authorization requests,
checking claim status, submitting appeal requests, and find copies of PRAs and letters in Document Library. All at no cost to
you and without needing to pick up the phone.
To access the portal, you will need to create or sign in using a One Healthcare ID. To use
the portal:
• If you already have a One Healthcare ID (formerly known as Optum ID), simply go to
uhcprovider.com > Sign In to access the portal.
• If you need to set up an account on the portal, follow these steps to register.
Use the UnitedHealthcare Provider Portal to access information for the following:
• UnitedHealthcare Commercial
• UnitedHealthcare Medicare Advantage
• UnitedHealthcare Community Plan (as contracted by state)
• UnitedHealthcare West
• UnitedHealthcare of the River Valley
Chapter 1: Introduction
7
2023 UnitedHealthcare Care Provider Administrative Guide
• UnitedHealthcare Oxford Commercial
• UnitedHealthcare Individual Exchange Plans
Available benefit plan information varies for each of our UnitedHealthcare Provider Portal tools.
Here are the most frequently used tools:
• Eligibility and Benefits — View patient eligibility and benefits information for most benefit plans. For more information, go to
uhcprovider.com/eligibility.
• Claims — Get claims information for many UnitedHealthcare plans, including access letters, remittance advice documents and
reimbursement policies. For more information, go to uhcprovider.com/claims.
• Prior Authorization and Notification — Submit notification and prior authorization requests. For more information, go to
uhcprovider.com/paan.
• Specialty Pharmacy Transactions — Submit notification and prior authorization requests for certain medical injectable drugs
by selecting the Prior Authorization dropdown in the UnitedHealthcare Provider Portal landing page. You will be directed to
Prior Authorization and Notification capability to complete your requests.
• My Practice Profile — View and update
1
your health care provider demographic data that UnitedHealthcare members see for
your practice. For more information, go to uhcprovider.com/mpp.
• Document Library — Access reports and correspondence from many UnitedHealthcare plans for viewing, printing or
download. For more information on the available correspondence, go to uhcprovider.com/documentlibrary.
• Paperless Delivery Options — Eliminate paper mail correspondence. In Document Library, you can set up daily or weekly
email notifications to alert you when we add new letters to your Document Library. With our delivery options, you decide when
and where the emails are sent for each type of correspondence. This tool is available to One Healthcare ID Primary Access
Administrators only.
You can learn more about the portal and access self-paced user guides for many of the
tools and tasks available in the portal.
UnitedHealthcare Web Support:
providertechsuppor[email protected] or 1-866-842-3278, option 1. Monday-Friday, 7 a.m. – 9 p.m. CT.
1
For more instructions, visit uhcprovider.com/training.
Chapter 1: Introduction
8
2023 UnitedHealthcare Care Provider Administrative Guide
Online resources and how to contact us
Online resources and how to contact us Where to go
How to Join Our Network For instructions on joining the UnitedHealthcare provider network, go to
uhcprovider.com/join. There you will find guidance on our credentialing
process, how to sign up for online tools and other helpful information.
UnitedHealthcare Provider Website uhcprovider.com
Resources:
• Administrative guides for network health care providers
• Plan-specific policies, protocols and guidelines
• Health plans by state
• News, regulatory and practice updates
• Guidance on common member- and claim-related tasks, including
eligibility and benefit verification, prior authorization and referral
requirements, and claims submissions and payments
• Information on our electronic workflow solutions, including Electronic
Data Interchange (EDI), Application Programming Interface (API) and the
UnitedHealthcare Provider Portal.
Advance Notification, Prior Authorization and
Admission, Discharge and Observation Stay
Notification
(To submit and get status information)
EDI: See EDI transactions and code sets on uhcprovider.com/edi
Online: Go to the UnitedHealthcare Provider Portal: uhcprovider.com >
Sign In to get started.
Information: Go to uhcprovider.com/priorauth and select the specialty
you need.
Phone: 1-877-842-3210 (Provider Service Voice Portal)
1-888-478-4760 (Individual Exchange Plans)
See ID card for specific service contact information.
Air Ambulance Non-Emergency Transport Online: uhcprovider.com/findprovider
Appeal – (Clinical) Urgent Submission
(Commercial members)
(Medicare Advantage – follow the directions in
the customer decision letter)
All Savers, Golden Rule Insurance Company
and UnitedHealthcare Oxford Navigate
Individual
An expedited appeal may be available if the time needed to complete a
standard appeal could seriously jeopardize the member’s life, health or
ability to regain maximum function.
Urgent medical fax: 1-801-994-1083
Urgent pharmacy fax: 1-801-994-1058
Urgent appeal fax: 1-866-654-6323
For Individual Exchanges:
Urgent medical fax: 1-888-808-9123
Application Programming Interface (API) Online: uhcprovider.com/api
Cardiology and Radiology
Notification/Prior Authorization
–Submission and Status
Online: Go to the UnitedHealthcare Provider Portal: uhcprovider.com >
Sign In to get started.
Information: Go to uhcprovider.com/priorauth and select the specialty
you need.
Phone: 1-866-889-8054
Chapter 1: Introduction
9
2023 UnitedHealthcare Care Provider Administrative Guide
Online resources and how to contact us Where to go
Chiropractic, Physical Therapy, Occupational
Therapy and Speech Therapy Providers
(Contracted with Optum Physical Health, a
UnitedHealth Group company)
Online: myoptumhealthphysicalhealth.com
Phone: 1-800-873-4575
Claims
(Filing, payments, reconsiderations)
EDI: uhcprovider.com/edi837 Learn more about the types of claims you
can file using EDI and view our claims payer list to identify the correct
payer ID.
Online: Go to UnitedHealthcare Provider Portal: uhcprovider.com > Sign
In to get started.
Information: uhcprovider.com/claims for policies, instructions and tips.
Phone: 1-877-842-3210 (follow the prompts for status information)
1-888-478-4760 (Individual Exchange Plans)
Optum Pay Online: optum.com/optumpay
Help Desk: 1-877-620-6194
Electronic Data Interchange (EDI)
and EDI Support
Online: uhcprovider.com/edi
Help: uhcprovider.com/edicontacts
Phone: 1-800-842-1109 (Monday–Friday, 7 a.m.–9 p.m. CT)
UnitedHealthcare EDI Support
Online: EDI Transaction Support Form
Email: suppor[email protected]
Phone: 1-800-842-1109
UnitedHealthcare Community Plan EDI Support
Online: EDI Transaction Support Form
Email: [email protected]
Phone: 1-800-210-8315
Fraud, Waste and Abuse
(Report potential fraud, waste
or abuse concerns)
Online: uhc.com/fraud, select the “Report a concern” icon.
Phone: 1-844-359-7736
Phone: 1-877-842-3210 (United Voice Portal)
For more information on fraud, waste and abuse prevention efforts, refer
to Chapter 17: Fraud, Waste and Abuse.
Genetic and Molecular Testing Online: Go to the UnitedHealthcare Provider Portal: uhcprovider.com >
Sign In to get started.
Information: Go to uhcprovider.com/priorauth and select the specialty
you need.
Member/Customer Care Online: myuhc.com
Phone: 1-877-842-3210 or the number listed on the back of the ID card
Mental Health and Substance Use Services See ID card for carrier information and contact numbers.
Chapter 1: Introduction
10
2023 UnitedHealthcare Care Provider Administrative Guide
Online resources and how to contact us Where to go
Outpatient Injectable Chemotherapy and
Related Cancer Therapies
Online: Go to the UnitedHealthcare Provider Portal: uhcprovider.com >
Sign In to get started.
Information: Go to uhcprovider.com/priorauth and select the specialty
you need.
Phone: 1-888-397-8129
Pharmacy Services Online: professionals.optumrx.com
Phone: 1-800-711-4555
Provider Advocates
For participating hospitals, health care, and
ancillary providers; locate your physician or
hospital advocate
Online: uhcprovider.com > Contact us > State-specific health plan and
network support
Provider Directory uhcprovider.com/findprovider
Radiation Therapy Prior Authorization For members:
Online:
1. Go to the UnitedHealthcare Provider Portal: uhcprovider.com > Sign
In to access the Prior Authorization and Notification tool.
2. Select Radiology, Cardiology, Oncology and Radiation Oncology
Transactions.
3. Select the service type Radiation Oncology
4. Select one of the product types: Commercial, Exchanges, Medicaid,
Medicare, or Oxford.
Phone: 1-888-397-8129 (8 a.m. – 5 p.m. local time Monday-Friday)
Referral Submission and Status
You can determine if a member’s benefit
plan requires a referral when you view their
eligibility profile.
EDI: 278 transaction
API: Referral API details are online at uhcprovider.com/api
Online: Go to the UnitedHealthcare Provider Portal: uhcprovider.com >
Sign In to get started.
Information: uhcprovider.com/referrals
Note: Submitted referrals are effective immediately but may not be
viewable for 48 hours.
Skilled Nursing Facilities
(Free-standing)
Online: uhcprovider.com/skillednursing
Phone: 1-877-842-3210 (Provider Service)
1-888-478-4760 (Individual Exchange Plans)
Subrogation Online: subroreferrals.optum.com
Fax: 1-800-842-8810
Mail: Optum
11000 Optum Circle
MN102-0300
Eden Prairie, MN 55344
Transplant Services See ID card for carrier information and contact numbers.
Vision Services See ID card for carrier information and contact numbers.

11
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 2:
Provider responsibilities and standards
Verifying eligibility, benefits and your network
participation status
Check the member’s eligibility and benefits prior to providing care. Doing this:
• Helps ensure you submit the claim to the correct payer.
• Allows you to collect copayments.
• Determines if a referral, prior authorization or notification is required.
• Reduces denials for non-coverage.
One of the primary reasons for claims rejection is incomplete or inaccurate eligibility information.
There are 4 easy ways to verify eligibility and benefits as shown in the Online/interoperability resources and how to contact
us section in Chapter 1: Introduction.
Eligibility grace period for Individual Exchange Plan members
When individuals enroll in a health benefit plan through the Health Insurance Marketplace (also known as Individual Exchange),
the plans are required to provide a 3-month grace period before terminating coverage. The grace period applies to those who
receive federal subsidy assistance in the form of an advanced premium tax credit and who have paid at least 1 full month’s
premium within the benefit year. Additionally, for individuals who do not receive federal subsidy assistance, plans are required
to provide a grace period consistent with state law (typically 30 or 31 calendar days) before terminating coverage.
You can verify if the member is within the grace period when you verify eligibility.
Refer to the Chapter 4: Individual Exchange Plans for more information.
Understanding your network participation status
Your network status is not returned on 270/271 transactions. Know your status prior to submitting 270 transactions. As our
product portfolio evolves and new products are introduced, it is important for you to confirm your network status for the medical
or pharmacy benefit plan (and tier status for commercial tiered benefit plans) while checking eligibility and benefits in the
UnitedHealthcare Provider Portal or by calling us at 1-877-842-3210 or 1-888-478-4760 (Individual Exchange Plans). If you
are not participating in the member’s benefit plan or are outside the network service area for the benefit plan, the member may
have higher costs or no coverage.
Commercial only
For more information about tiered benefit plans, visit uhcprovider.com/plans > Select your state > Commercial >
UnitedHealthcare Tiered Benefit Plans.
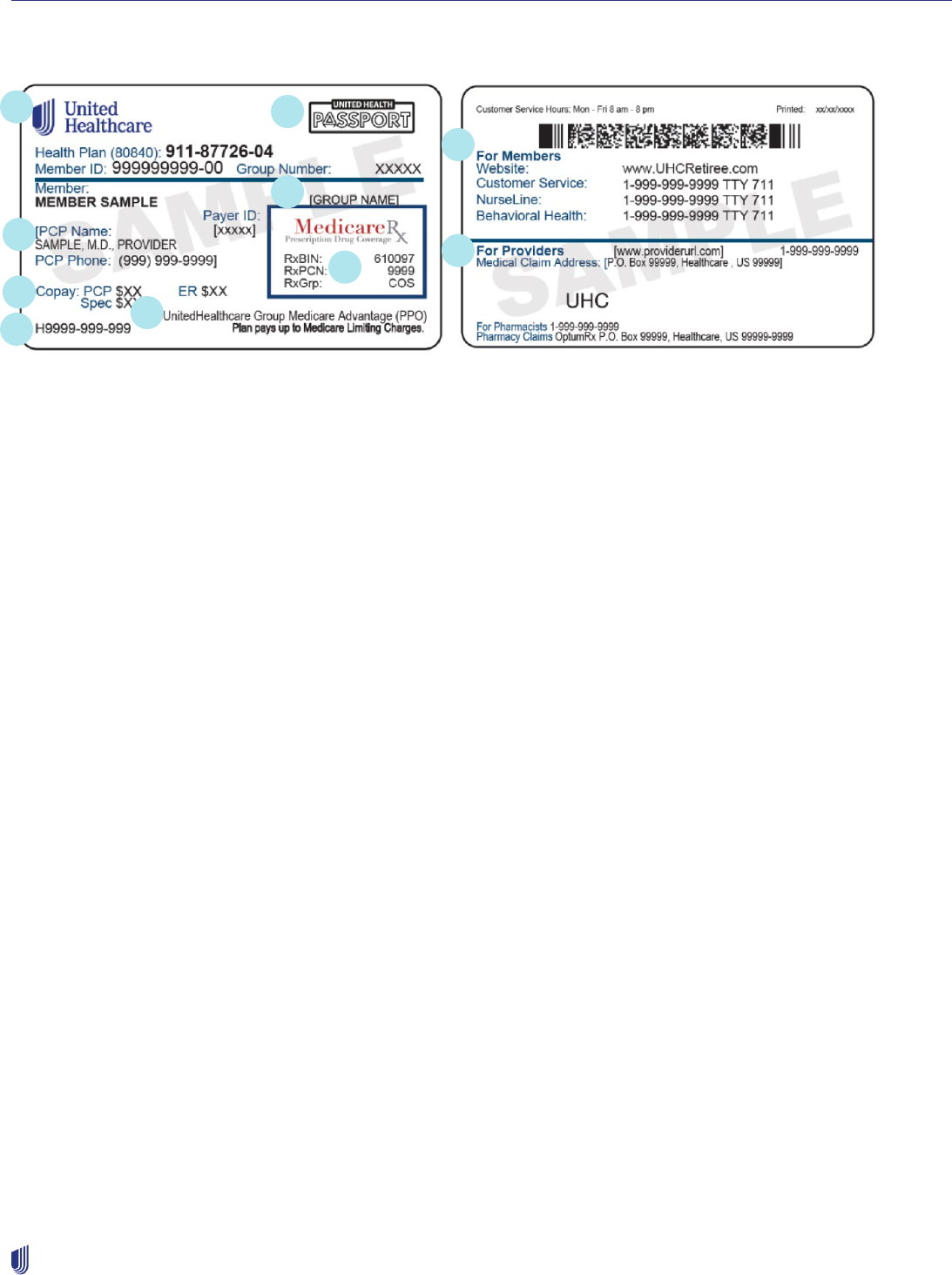
Health plan identification (ID) cards
We are moving towards eliminating physical ID cards, and members may not have one if not required by law. Use the Eligibility
and Benefits tool in the UnitedHealthcare Provider Portal to see a digital version of the ID card. You’ll also be able to access
member-specific information around plan benefits and requirements. Sample member ID cards are for illustration only; actual
information varies depending on payer, plan and other requirements.
Chapter 2: Provider responsibilities and standards
12
2023 UnitedHealthcare Care Provider Administrative Guide
View and download current ID cards for most
members using the Eligibility and Benefits tool in the
UnitedHealthcare Provider Portal. You can also view
member eligibility and benefits through an API solution.
You may download and keep a copy of both sides of the health plan ID card for your records. Possession of a physical ID card
is not proof of eligibility.
Commercial health plan ID card legend
Front Back
Member ID: Group Number:
Member:
Office: $99
Referrals Required
UrgCare: $99
Rx Bin:
610279
Rx PCN:
9999
Rx Grp:
UHEALTH
UnitedHealthcare Navigate
Underwritten by UnitedHealthcare Insurance Company
DOI-0508
ER: $99
Payer ID 87726
Copays:
999999999 999999
Customer Name Line 1
PCP:
FIRSTNAME LASTNAME
PCP Phone: (999) 999-9999
Spec: $99
MEMBER SMITH
Customer Name Line 2
INN: $99999/$99999 $99999/$99999
Tier 1: $99999/$99999 $99999/$99999
OON: $99999/$99999 $99999/$99999
Coins 99%
Ded IND/FAM OOPM IND/FAM
Ded IND/FAM
OOPM IND/FAM
$99999/$99999
$99999/$99999
$99999/$99999
$99999/$99999
INN:
OON:
Printed: 10/17/21
Members: We're here to help. Check benets, view claims, nd
a doctor, ask a question and more.
Web:
myuhc.com
Phone:
Providers:
UHCprovider.com 877-842-3210 or
Medical Claims:
555-555-5555
Pharmacy Claims: OptumRx PO Box 650540 Dallas, TX 75265-0540
Pharmacists:
888-290-5416
PO Box 740825, Atlanta GA 30374-0825
1. UnitedHealthcare brand: This includes UnitedHealthcare, All Savers, UnitedHealthcare Level Funded, UnitedHealthcare
Oxford Level Funded, Golden Rule, UnitedHealthcare Oxford, UnitedHealthOne, UMR and UnitedHealthcare Shared
Services (UHSS), UnitedHealthcare Freedom Plans.
2. Member Plan Identifier: This is a customized field to describe the member’s benefit plan (i.e., Individual Exchange, Tiered
Benefits, ACO).
3. Payer ID: Indicates claim can be submitted electronically using the number shown on card. Contact your vendor or
clearinghouse to set up payer in your system, if necessary.
4. PCP name and phone number: Included for benefit plans that have PCP selection requirements. For Individual Exchange
Members “PCP required” is listed in place of the PCP name and number. This section may also include Laboratory (LAB),
Preferred Lab Network (PLN) and Radiology (RAD) participant codes.
5. Copay information: If this area is blank, the member is not required to make a copay at the time of service.
6. Benefit plan name: identifies the applicable benefit plan name.
7. Referral requirements identifier: Identifies plans with referral requirements. Requires PCP to send electronic referrals.
8. For members section: Lists benefit plan contact information and, if applicable, referrals and notifications information.
9. For providers section: Includes the prescription plan name.
1
5
3
4
2
9
6
8
7
Chapter 2: Provider responsibilities and standards
13
2023 UnitedHealthcare Care Provider Administrative Guide
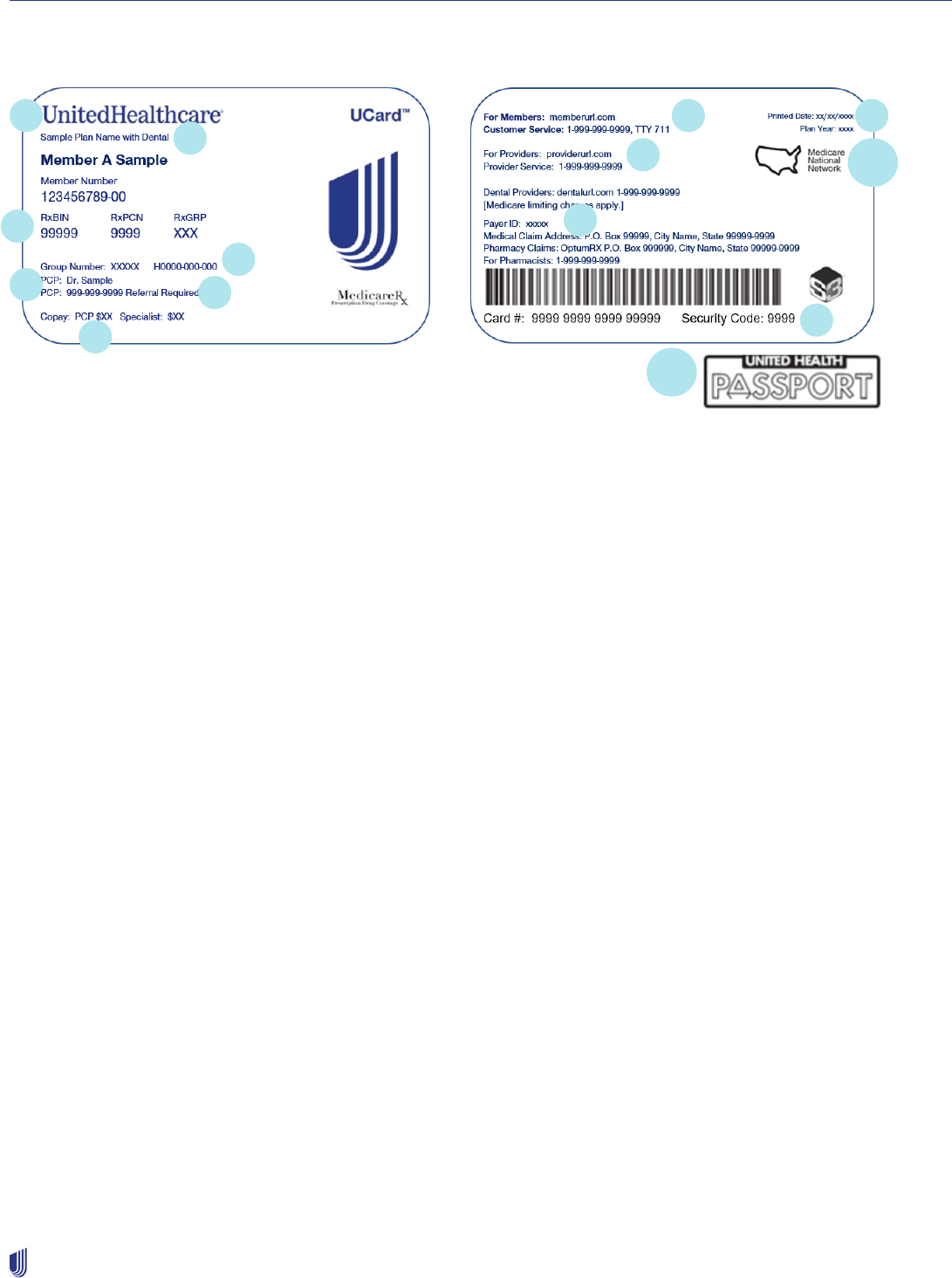
Medicare Advantage (MA) member ID card legend
Front Back
1. Benefit plan name: Identifies the applicable benefit plan name.
2. Dental benefits: Included if routine dental benefits are part of the benefit plan and/or if the member purchased an
optional supplemental dental benefit rider.
3. Prescription information: If the benefit plan includes Part D prescription drug coverage, the Rx BIN, PCN and Group
code are visible. If Part D coverage is not included, this area lists information for Medicare Part B Drugs.
4. Plan ID number: Identifies the plan ID number that corresponds to Centers for Medicare & Medicaid Services (CMS)
filings.
5. PCP: Included for benefit plans that require a PCP selection.
6. Referrals required: Identifies benefit plans with referral requirements. Refer to the Medicare Advantage (MA) Referral
Required Plans section in Chapter 6: Referrals for more detailed information.
7. Copay information: Select plans do not list copay information or may have a variance.
8. For members: Lists benefit plan contact information for the member.
9. For providers: Lists benefit plan contact information for the health care provider.
10. Plan Year: The year (1/1-12/31) during which plan benefits apply.
11a. Network Logo: If the Medicare National Network logo is present, the member has access to the national network.
11b. UnitedHealth Passport Logo: If the UnitedHealth Passport logo is present, the member’s plan has the Passport travel
benefit.
12. Payer ID: Indicates claim can be submitted electronically using the number shown on card. Contact your vendor or
clearinghouse to set up payer in your system, if necessary.
13. S3 Bar code, logo, card number and security code: S3 technology allows UnitedHealthcare to direct members to
approved products for in-store purchase.
1
2
3
4
5
6
7
8
12
10
11a
9
13
11b
Chapter 2: Provider responsibilities and standards
14
2023 UnitedHealthcare Care Provider Administrative Guide
Medicare Advantage (MA) Group Retiree member ID card legend
Front Back
1. UnitedHealthcare brand: Present on a UnitedHealthcare ID card.
2. Network Logo: If the UnitedHealth Passport logo is present, the member’s plan has the Passport travel benefit.
3. Group name: Identifies the name of the employer group.
4. PCP: Included for benefit plans that require a PCP selection.
5. Prescription information: If the benefit plan includes Part D prescription drug coverage, the Rx Bin, PCN and Group code
are visible. If Part D coverage is not included, this area lists information for Medicare Part B Drugs.
6. Copay information: Includes PCP, specialist and ER copays.
7. Plan ID number: Identifies the plan ID number that corresponds to Centers for Medicare & Medicaid Services (CMS)
filings.
8. Benefit plan name: Identifies the applicable benefit plan name.
9. For members: Lists benefit plan contact information for the member.
10. For providers: Lists benefit plan contact information for the health care provider.
Access standards
Covering physician
As a PCP, you must arrange for 24 hours a day, 7 days per week coverage of our members. If you are arranging a substitute
health care provider, use those who are in-network with the member’s benefit plan.
You must alert us if the covering health care provider is not in your medical group practice to prevent claim payment issues.
Use modifiers for substitute physician (Q5), covering physician (CP) and locum tenens (Q6) when billing services as a covering
physician. Collect the copay at the time of service.
To find the most current directory of our network physicians and health care professionals, go to
uhcprovider.com/findprovider.
2
3
4
5
6
7
8
9
10
1
Chapter 2: Provider responsibilities and standards
15
2023 UnitedHealthcare Care Provider Administrative Guide
Appointment standards
We have appointment standards for access and after-hours care to help ensure timely access to care for members. We use
these to measure performance annually. Our standards are shown in the following table.
Type of service Standard
Preventive care Within 30 calendar days
Regular/routine care appointment Within 30 calendar days
Urgent care appointment Same day
Emergency care Immediate
After-hours care 24 hours/7 days a week for PCPs
These are general UnitedHealthcare guidelines. State or federal regulations may require standards that are more stringent.
Contact your Network Management representative for help determining your state or federal regulations.
After-hours phone message instructions
If a member calls your office after hours, we ask that you provide emergency instructions, whether a person or a recording
answers. Tell callers with an emergency to do one of the following:
• Hang up and dial 911 or local equivalent.
• Go to the nearest emergency room.
When it is not an emergency, but the caller cannot wait until the next business day, advise them to do one of the following:
• Go to a network urgent care center.
• Stay on the line to connect to the physician on call.
• Leave a name and number with your answering service (if applicable) for a physician or qualified health care professional to
call back within specified time frames.
• Call an alternative phone or pager number to contact you or the physician on call.
Timely access to non-emergency health care services (applies to Commercial in California)
• The timeliness standards require licensed health care providers to offer members appointments that meet the California time
frames. The applicable waiting time for a particular appointment may be extended if the referring or treating licensed health
care provider, or the health professional providing triage or screening services, as applicable, is:
– Acting within the scope of their practice and consistent with professionally recognized standards of practice.
– Has determined and noted in the relevant record that a longer waiting time will not have a detrimental impact on the
member’s health.
• Licensed staff must triage or screen services by phone 24 hours a day, 7 days a week. Unlicensed staff shall not use the
answers to those questions in an attempt to assess, evaluate, advise or make any decision regarding the condition of a
member or determine when a member needs to be seen by a licensed medical professional.
• UnitedHealthcare of California managed care members and covered persons under UnitedHealthcare benefit plans have
access to free triage and screening services 24 hours a day, 7 days a week by calling the Optum NurseLine number on the
back of their ID card. If a member is unable to obtain a timely referral to an appropriate health care provider, refer to the Out-
of-Network Provider Referrals (Commercial HMO and Medicare Advantage) section for further details. If still unable to
obtain a timely referral to a health care provider after following these steps, contact the following:
– For members with Department of Managed Healthcare regulated plans: 1-888-466-2219
– For members with California Department of Insurance regulated plans: 1-800-927-4357

Chapter 2: Provider responsibilities and standards
16
2023 UnitedHealthcare Care Provider Administrative Guide
Telehealth services
Under certain benefit plans, we provide coverage for telehealth services regardless of whether the member is located at a CMS-
designated originating site. For more information on telehealth services, see the Telehealth services protocol in Chapter 9:
Specific protocols.
Provider privileges
You must have privileges at participating facilities or an arrangement with another participating health care provider to admit
and offer facility services. This helps our members have access to appropriate care and lower their out-of-pocket costs.
Cultural competency
Provide services in a culturally competent manner. This includes members with limited English proficiency, those with diverse
backgrounds and/or disabilities. For more information, go to uhcprovider.com > Resources > Resource Library > Patient Health
and Safety Resources > Cultural Competency
Translation/interpretation/auxiliary aide services
You must provide language services and auxiliary aides, including, but not limited to, sign language interpreters to members as
required, to provide members with an equal opportunity to access and participate in all health care services.
If the member requests translation/interpretation/auxiliary aide services, you must promptly arrange these services at no cost to
the member.
Members have the right to a certified medical interpreter or sign language interpreter to accurately translate health information.
Friends and family of members with limited English proficiency, or members who are deaf or hard of hearing, may arrange
interpretation services only after you have explained our standard methods offered, and the member refuses. Document the
refusal of professional interpretation services in the member’s medical record.
Any materials you have a member sign, and any alternative check-in procedures (like a kiosk), must be accessible to an
individual with a disability.
If you provide Virtual Visits, these services must be accessible to individuals with disabilities. Post your Virtual Visits procedures
for members who are deaf or hard of hearing so they receive them prior to the Virtual Visit.
Network participating health care provider responsibilities
Primary care providers (PCP)
As a PCP, you are responsible to provide medically necessary primary care services. You are the coordinator of our members’
total health care needs. You are responsible for seeing all members on your panel who need assistance, even if the member has
never been in for an office visit. Some benefit plans require PCPs to submit electronic referrals for the member to see another
network physician. Go to Chapter 6: Referrals for detailed information on referral requirements.
Civil rights
Non-discrimination
You must not discriminate against any patient with regard to quality of service or accessibility of services because they are our
member. You must not discriminate against any patient on the basis of any of the following:
• Type of health insurance
• Race
• Ethnicity

Chapter 2: Provider responsibilities and standards
17
2023 UnitedHealthcare Care Provider Administrative Guide
• Color
• National origin
• Religion
• Sex or gender
• Age
• Mental or physical disability or medical condition
• Sexual orientation
• Gender identity
• Claims experience
• Medical history
• Genetic information
• Type of payment
You must maintain policies and procedures to demonstrate you do not discriminate in the delivery of services and must provide
treatment for any members who need your service.
Complying with laws and regulations for individuals with disabilities
You must comply with applicable laws which include, but are not limited to, the Americans with Disabilities Act (ADA) and
Section 504 or 508 of the Rehabilitation Act.
Participating health care providers must have practice policies showing they accept any patient in need of the health care
they provide. The organization and its health care providers must make public declarations (i.e., through posters or mission
statements) of their commitment to non-discriminatory behavior in conducting business with all members. These documents
should explain that this expectation applies to all personnel, clinical and non-clinical, in their dealings with each member.
In this regard, you must undertake new construction and renovations, as well as barrier reductions required to achieve program
accessibility, following the established accessibility standards of the ADA guidelines. For complete details go to ADA.gov >
Featured Topics > A Guide to Disability Rights Laws.
We may request any of the following ADA-related descriptions of:
• Accessibility to your office or facility.
• The methods you or your staff use to communicate with members with disabilities. This may also include any electronic
communications.
• The training your staff receives to learn and implement these guidelines.
Care for members who are deaf or hard of hearing
You must provide a sign language interpreter if a member requests one. You must also have written office procedures for taking
phone calls or providing Virtual Visits to members who are deaf or hard of hearing.
Confidentiality, Use of Licensed Marks, Publicity
Consolidated Appropriations Act, 2021 (CAA) Prohibition on Gag Clauses
Your participation agreement may include a confidentiality provision that describes information that neither party may disclose
to a member, other health care provider or other third party except as required by an agency of the government, court order
or other third party. You agree the CAA constitutes such a requirement by an agency of the government, and nothing in your
participation agreement will be interpreted to supersede or conflict with the CAA. Specifically, your participation agreement will
not be interpreted to directly or indirectly restrict us (as a health insurance issuer offering group and individual health insurance
coverage) or a group health plan from:
1. Providing provider-specific cost or quality of care information to referring health care providers or current and potential
members.

Chapter 2: Provider responsibilities and standards
18
2023 UnitedHealthcare Care Provider Administrative Guide
2. Electronically accessing de-identified claims and encounter information for each member in the plan or coverage,
upon request and consistent with the privacy regulations related to section 264(c) of the Health Insurance Portability
and Accountability Act (HIPAA), the amendments made by the Genetic Information Nondiscrimination Act of 2008 and
American with Disabilities Act of 1990. This includes, on a per claim basis, the following:
a. Financial information
b. Provider information
c. Service codes
d. Any other data included in claim or encounter transactions.
3. Sharing information with a business associate as defined in section 160.103 of title 45, Code of Federal Regulations (or
successor regulations), consistent with HIPAA, the amendments made by the Genetic Information Nondiscrimination Act of
2008 and the Americans with Disabilities Act of 1990.
Use of Licensed Marks, Publicity
Except as required by applicable law or as provided herein, you will not have any right to use the names, logos, trademarks,
trade names or other marks of United (collectively, “United Marks”), including in connection with any advertising, sales
promotions, press releases and other publicity matters.
During the term of the Agreement, you are granted a limited, non-sublicensable, non-transferable, and non-exclusive license to
use within the United States the UNITEDHEALTHCARE name and logo (the “Licensed Marks”) solely for the limited purposes of
(i) using or displaying the Licensed Marks alongside names or logos of other insurance carriers with whom you have a network
participation agreement, or (ii) communicating verbally or in writing to your prospective or existing patients that you have an
agreement with us to provide health care services to our members. The use of the Licensed Marks cannot be expanded beyond
what is allowed under the Agreement or this guide. You will only utilize the trademark and logo files provided to you by the
United Brand Team (you must contact the United Brand Team at [email protected]). You will comply with all requirements
made available by United regarding use of United Marks and Licensed Marks. We may at any time withdraw our permission
for you to use any Licensed Marks, effective upon written notice to you, and you shall promptly comply with our instructions
provided in such notice. All other uses of United Marks will require our advance written consent.
If either you or we intend to issue a press release or other public disclosure pertaining to our business relationship, the issuing
party will ensure the material does not:
a. Mischaracterize the nature of the relationship between us,
b. Suggest any endorsement or promotion of the other party, or
c. Disclose or describe information subject to the confidentiality obligations embedded in our Agreement.
You will not issue a press release or other public disclosure pertaining to our Agreement without receiving our advanced written
consent.
Consolidated Appropriations Act, 2021 (CAA) requirements
Continuity of Care
Health insurance issuers, plan sponsors and/or health care providers are required to comply with the Continuity of Care
requirements under the CAA unless your participation agreement states otherwise.
Continuity of Care is provided in the following circumstances:
1. Your participation agreement with us or between you and a downstream provider is terminated by us, a payer, you or a
downstream provider.
2. The terms of your network participation with us or a payer changed, and that change leads to certain members no longer
receiving in-network coverage for your care.
3. A fully insured group contract between us and a group health plan terminated and that termination leads to members no
longer receiving in-network coverage for your care.
Chapter 2: Provider responsibilities and standards
19
2023 UnitedHealthcare Care Provider Administrative Guide
Under the CAA, Continuity of Care must be offered to members in your care or the care of your downstream contracted
providers who are:
1. Undergoing treatment for a serious and complex medical condition.
2. Undergoing inpatient or institutional treatment.
3. Scheduled to undergo nonelective surgery, including receipt of postoperative care with respect to such a surgery.
4. Pregnant and receiving treatment related to the pregnancy.
5. Terminally ill per the Social Security Act and receiving treatment for the terminal illness.
In accordance with the CAA, you must accept payment from us or a payer based on your participation agreement and
negotiated rates for any services rendered pursuant to the Continuity of Care requirements under the CAA. Any care you render
to a member under Continuity of Care is subject to our or any payer’s applicable policies, procedures and quality standards.
You also acknowledge additional rights for Continuity of Care may be required under state or local law or as specifically
required in your participation agreement with us.
Provider directory
Consistent with the CAA, we will verify information in our provider directory. You will provide us with accurate information and
respond to our questions when you receive them. You will respond within any time period listed in the communication we send
to you. We may remove health care providers and facilities from the provider directory if we can’t verify information.
Cooperation with quality improvement and patient
safety activities
You must follow our quality improvement and patient safety activities and programs. These include:
• Quick access to medical records when requested.
• Timely responses to queries and/or completion of improvement action plans during quality of care investigations.
• Participation in quality audits, including site visits and medical record standards reviews, and Healthcare Effectiveness Data
and Information Set (HEDIS®) record review.
• Allowing use of practitioner and health care provider performance data.
• Notifying us when you become aware of a patient safety issue or concern.
Demographic changes
If you have access to My Practice Profile and have editing rights, you can access the My
Practice Profile tool to make many of the updates required in this section. Facilities can use
the UnitedHealthcare Facility/Practice Profile tool. For more information, go to uhcprovider.
com/mypracticeprofile.
Physician/health care professional verification outreach
We are committed to providing our members with the most accurate and up-to-date information about our network. We are
currently undertaking an initiative to improve our data quality. This initiative is called Professional Verification Outreach (PVO).
Your office may receive a call from us asking to verify your data currently on file in our provider database. This information is
confidential and updated immediately in our database.
Provide official notice
Notify us, at the address in your Agreement, within 10 calendar days if any of these situations occur:
• Material changes to, cancellation or termination of liability insurance

Chapter 2: Provider responsibilities and standards
20
2023 UnitedHealthcare Care Provider Administrative Guide
• Bankruptcy or insolvency
• Any indictment, arrest or conviction for a felony or any criminal charge related to your practice or profession
• Any suspension, exclusion, debarment or other sanction from a state or federally funded health care program
• Loss, suspension, restriction, condition, limitation, or qualification of your license to practice (for physicians, any loss,
suspension, restriction, condition, limitation or qualification of staff privileges at any licensed hospital, nursing home, or
other facility)
• Relocation or closure of your practice, and, if applicable, transfer of member records to another physician/facility
• External sanctions or corrective actions levied against you by a government entity
Provide timely notice of demographic changes
Primary care physicians
As a PCP, you are responsible for monitoring your office capacity based on member assignments and for notifying us if you
have reached your maximum capacity. A self-reporting tool is available for you to generate a PCP panel roster report using
uhcprovider.com/reports.
We have developed specific definitions for open, closed or existing-only practices to promote consistency throughout the
participating health care provider network related to acceptance of new or transferring members. For purposes of this section, a
new member may be a member who has switched health plans and/or coverage plans, such as a member who switches from a
Fee-For-Service (FFS) plan to a Commercial HMO/MCO plan.
Follow these definitions:
• Open status – the PCP’s practice is open to additional new members and transferring members.
• Closed status – the PCP’s practice is closed to all new members and transferring members.
• Existing-only status – the PCP’s practice is only open to new or transferring members who have an established chart with the
health care provider’s office.
Notification of changes must be proactive
Every quarter, you, or an entity delegated to handle credentialing activities on behalf of us (a “delegate”), are expected to
review, update and attest to the health care provider information available to our members. If you or the delegate cannot attest
to the information, you must correct it online or through the Provider Service Center. You or the delegate must tell us of changes
to the information at least 30 calendar days before the change is effective. This includes adding new information and removing
outdated information, as well as updating the information listed in the following paragraph.
You and the delegates are required to update all health care provider information, such as the following:
• Patient acceptance status
• Address(es) of practice location(s)
• Office phone number(s)
• Email address(es)
• Health care provider groups affiliation
• Facility affiliation
• Specialty
• License(s)
• Tax identification number
• NPI(s)
• Languages spoken/written by staff
• Ages/genders served
• Office hours
Delegates are responsible for notifying us of these changes for all of the participating health care providers credentialed by
the delegate. If you or a delegate fails to (1) update records, or (2) give 30 days prior notice of changes, or (3) attest to the
information, you, or the participating health care providers credentialed by the delegate, may be subject to penalties. Penalties

Chapter 2: Provider responsibilities and standards
21
2023 UnitedHealthcare Care Provider Administrative Guide
may include a delay of processing claims or the denial of claims payment, until the records are reviewed and attested to or
updated.
If a health care provider leaves your practice, notify us immediately. This allows us to timely notify impacted members.
When you submit demographic updates, list only those addresses where a member may make an appointment and see the
health care provider. On-call and substitute health care providers who are not regularly available to provide covered services at
an office or practice location should not be listed at that address.
California Commercial: The penalties do not apply to benefit plans issued or administered by UnitedHealthcare Benefit Plans
of California.
To change panel status (open/closed/existing-only)
If you wish to change your panel status (i.e., open to new patients, open to existing patients only, or closed), the request
must be made in writing 30 days in advance. Changes to panel status apply to all patients for all lines of business (LOB) and
products for which a health care provider is participating. If you feel that exceptional circumstances exist, you may request to
have a different panel status for an LOB or product. Include the exception in the written request. Approval is at our discretion.
We may notify you in writing of changes in our panel status including closures based on state and/or federal requirements,
current market dynamics and patient quality indicators. Access My Practice Profile in the UnitedHealthcare Provider Portal at
uhcprovider.com/mpp to update your information.
To change an existing TIN or to add a physician or health care provider
To submit the change, complete and email the Provider Demographic Change Form to the appropriate email address listed on
the form.
The Provider Demographic Change Form is available on uhcprovider.com/findprovider.
You can also submit detailed information about the change and the effective date of the change on your office letterhead. Send
it to us using the email address on the bottom of the demographic change request form.
To update your practice or facility information
You can make demographic updates every 90 days to your practice information by:
1. Using Provider Directory Snapshot within CAQH ProView.
2. Accessing the UnitedHealthcare Provider Portal and using My Practice Profile for health care providers; UnitedHealthcare
Facility/Practice Profile for facilities.
3. Emailing the completed Provider Demographic Change Form to the appropriate email address listed on the bottom of the
form.
4. Calling our Enterprise Voice Portal at 1-877-842-3210.
For Preferred Care Network and Preferred Care Partners, you must contact their Network
Management department by email, pcp-NetworkManagementServices@uhcsouthflorida.
com, or call 1-877-670-8432. Changes should not be made in the UnitedHealthcare Provider
Portal.
Notification of practice or demographic changes (applies to
Commercial benefit plans in California)
California Senate Bill 137 requires us to perform ongoing updates to our health care provider directories, both online and hard
copy. As a participating medical group, IPA or independent physician, you are required to update UnitedHealthcare within 5
business days if there are any changes to your ability to accept new patients.

Chapter 2: Provider responsibilities and standards
22
2023 UnitedHealthcare Care Provider Administrative Guide
As a participating medical group, IPA or independent physician, if a member or potential enrollee seeking to become a patient
contacts you, and you are no longer accepting new patients, you must direct them to report any inaccuracy in our health care
provider directory to:
• UnitedHealthcare for additional assistance in finding a health care provider, and, as applicable.
• Either the California Department of Managed Health Care or the California Department of Insurance.
You shall cooperate with and provide the necessary information to us so we may meet the requirements of Senate Bill 137.
We are required to contact all participating health care providers, including but not limited to, contracted medical groups or
IPAs on an annual basis and independent physicians every 6 months. This outreach includes a summary of the information
that we have on record and requires you to respond by either confirming your information is accurate or providing us with
applicable changes.
If we do not receive a response from you within 30 business days, either confirming that the information on file is correct,
or providing us with the necessary updates, we have an additional 15 business days to make attempts for you to verify the
information. If these attempts are unsuccessful, we will notify you that, if you continue to be nonresponsive, we will remove you
from our health care provider directory after 10 business days.
If the final 10-business-day period lapses with no response from you, we may remove you from the directory. If we receive
notification that the provider directory information is inaccurate, the health care provider group, IPA, or physician may be
subject to corrective action.
In addition to outreach for annual or bi-annual attestations, we are required to make outreach if we receive a report of
inaccuracy for any health care provider data in the directories. We are required to confirm your information is correct. If we
attempt to contact you and do not receive a response, we will provide you a 10-business-day notice that we will suppress your
information from our health care provider directory.
Medical groups, IPAs, or independent physicians can submit applicable changes to:
For delegated providers: Email changes to P[email protected] or delpro[email protected].
For non-delegated providers: Visit uhcprovider.com for further instructions.
Administrative terminations for inactivity
Up-to-date directories are a critical element of providing our members with the information they need to take care of their health.
To offer more exact and up-to-date directories, we:
• Administratively terminate Agreements for health care providers who have not submitted claims for 1 year.
• Inactivate any TIN under which there have been no claims submitted for 1 year.
When health care providers tell us of practitioners leaving a practice, we make multiple attempts to get documentation of that
change.
We administratively terminate a health care provider if:
• We get oral notice that a practitioner is no longer with a practice.
• We make 3 attempts to obtain documentation confirming the practitioner’s departure, but do not receive the requested
documentation.
• The practitioner has not submitted claims under that practice’s TIN(s) for 6 months prior to our receipt of oral notice the
practitioner left the practice, or the effective date of departure provided to us, whichever is sooner. This does not apply to
Preferred Care Network and Preferred Care Partners.
Continuity of care following termination of your participation
If your Agreement ends for any reason, you may be required to help our members find another participating health care
provider. You may need to provide services at our contracted rates during the continuation period, per your Agreement and any
applicable laws. We are ready to help you and our members with the transition. We tell affected members at least 30 calendar
days prior to the effective date of your participation termination, or as required under applicable laws.

Chapter 2: Provider responsibilities and standards
23
2023 UnitedHealthcare Care Provider Administrative Guide
Member dismissals initiated by a PCP (Medicare Advantage)
We recognize there are certain instances a PCP may choose to terminate a patient relationship. While we will not interfere with
the PCP’s decision, we will:
• Remind the PCP of their obligation to terminate the relationship in accordance with applicable requirements.
• Help ensure the PCP provides us a reason for making the decision.
• Require documentation that they have communicated this decision to the member.
Each dismissal should be carefully considered based on the facts and circumstances specific to the member.
In addition, PCPs who wish to terminate their relationship with a Medicare Advantage (MA) member and have a member
reassigned must:
• Comply with all applicable legal and regulatory requirements.
• Send a certified letter to the member (evidence that the letter was mailed is acceptable even if a letter comes back as
“undeliverable as addressed”).
• Provide continuity of care as required by applicable laws and regulations.
• Provide us written notice.
Required Information from the PCP
For member reassignment, we require the following information from the PCP:
• The reason for reassignment or termination.
• Member’s name, date of birth, address and member ID number.
• PCP’s name, NPI and TINs.
• Copy of certified letter the PCP sent to the member notifying them of the termination.
We use good faith efforts to reassign the member to another PCP within 90 days of receipt of request. Changes will not be
applied retroactively.
Medicare opt-out
We follow, and require our health care providers to follow, Medicare requirements for physicians and other practitioners who opt
out of Medicare. If you opt out of Medicare, you may not accept federal reimbursement. Health care providers who opt out of
Medicare (and those not participating in Medicare) are not allowed to bill Medicare or its MA benefit plans during their opt-out
period for 2 years from the date of official opt-out. For our MA membership, we and our delegated entities do not contract with,
or pay claims to, health care providers who have opted-out of Medicare. Exception: In an emergency or urgent care situation, if
you have opted out of Medicare, you may treat an MA beneficiary and bill for the treatment. In this situation, you may not charge
the member more than what a non-participating health care provider is allowed to charge. You must submit a claim to us on the
member’s behalf. We pay Medicare-covered items or services furnished in emergency or urgent situations.
Additional MA requirements
As an MA organization, UnitedHealthcare and its network providers agree to meet all laws and regulations applicable to
recipients of federal funds.
If you participate in the network for our MA products, you must comply with the following additional requirements for services
you provide to our MA members.
• You may not discriminate against members in any way based on health status.
• You must allow members direct access to screening mammography and influenza vaccination services.
• You may not impose cost-sharing on members for the influenza vaccine or pneumococcal vaccine or certain other preventive
services. For additional information, refer to the Preventive Health Services and Procedures available on uhcprovider.com/
policies > Medicare Advantage Policies > Coverage Summaries for Medicare Advantage Plans.

Chapter 2: Provider responsibilities and standards
24
2023 UnitedHealthcare Care Provider Administrative Guide
• You must provide female members with direct access to a women’s health specialist for routine and preventive health
care services.
• You must make sure members have adequate access to covered health services.
• You must make sure your hours of operation are convenient to members.
• You must make sure medically necessary services are available to members 24 hours a day, 7 days a week.
• PCPs must have backups for absences.
• You must adhere to CMS marketing regulations and guidelines. This includes, but is not limited to, the requirements to remain
neutral and objective when assisting with enrollment decisions, which should always result in a plan selection in the Medicare
beneficiary’s best interest. CMS marketing guidance also requires that providers must not make phone calls or direct, urge,
or attempt to persuade Medicare beneficiaries to enroll or disenroll in a specific plan based on the health care provider’s
financial or any other interest. You may only make available or distribute benefit plan marketing materials to members in
accordance with CMS requirements.
• You must provide services to members in a culturally competent manner taking into account adjustments for members who
use English as a second language, hearing or vision impairment, and diverse cultural and ethnic backgrounds.
• You must cooperate with our procedures to tell members of health care needs that require follow-up and provide necessary
training to members in self-care.
• You must document in a prominent part of the member’s medical record whether they have executed an advance directive.
• You must provide covered health services in a manner consistent with professionally recognized standards of health care.
• You must make sure any payment and incentive arrangements with subcontractors are specified in a written agreement, that
such arrangements do not encourage reductions in medically necessary services, and that any physician incentive plans
comply with applicable CMS standards.
• You must comply with all applicable federal and Medicare laws, regulations, and CMS instructions, including but not limited
to: (a) federal laws and regulations designed to prevent or ameliorate fraud, waste, and abuse, including but not limited
to, applicable provisions of federal criminal law, the False Claims Act, and the Anti-Kickback Statute; and (b) HIPAA
administrative simplification rules at 45 CFR Parts 160, 162 and 164.
• The payments you receive from us or on behalf of us are, in whole or in part, from federal funds and you are therefore subject
to certain laws applicable to individuals and entities receiving federal funds.
• You must cooperate with our processes to disclose to CMS all information necessary for CMS to administer and evaluate
the MA program and disclose all information determined by CMS to be necessary to assist members in making an informed
choice about Medicare coverage.
• You must comply with our processes for notifying members if your participation agreement terminates.
• You must submit all Risk Adjustment Data (see definition in glossary), and other MA program and commercial insurance
related information we may request, within the time frames specified and in a form that meets MA program requirements
as well as state and federal commercial insurance requirements. By submitting data to us, you represent to us, and upon
our request you shall certify in writing, that the data is accurate, complete, and truthful, based on your best knowledge,
information and belief.
• You must comply with our MA policy guidelines, coverage summaries, quality improvement programs, and medical
management procedures.
• You must cooperate with us in fulfilling our responsibility to disclose to CMS quality, performance, and other indicators as
specified by CMS.
• You must cooperate with our procedures for handling grievances, appeals and expedited appeals. This includes, but is not
limited to, providing requested medical records within 2 hours for expedited appeals and 24 hours for standard appeals,
including weekends and holidays.
• You must comply with the Medicare Advantage Regulatory Requirements Appendix (MARRA) in your Provider Agreement.
Member communication (CMS approval required)
Member communications require CMS approval. This includes:
• Anything with the MA and/or the AARP name or logo, including MA Dual Special Needs Plans.

Chapter 2: Provider responsibilities and standards
25
2023 UnitedHealthcare Care Provider Administrative Guide
• Correspondence that describes benefits.
• Marketing activities.
Approval is not necessary for communications between health care providers and patients that discuss:
• Their medical condition.
• Treatment plan and/or options.
• Information about managing their medical care.
Once CMS approves, we send the letter to the member.
In addition to making sure the letter is approved by the governing regulatory body, we direct the letter to the correct audience.
For example, we may need to distinguish a mailing to MA plan individual members versus Medicare group retiree members, as
their benefits are distinctly different.
Part C reporting requirements
MA organizations are subject to additional reporting requirements. We may request data from you. This data is due by 11:59
p.m. PT on our established reporting deadline.
Some measures are reported annually, while others are reported quarterly or semi-annually. This includes, but is not limited to:
• Grievances.
• Organization determinations/reconsiderations including source data for all determinations and reopenings.
• Special needs plans care management.
• Rewards and incentive programs.
• Payments to health care providers.
• Telehealth benefits.
Filing of a lawsuit by a member
Lawsuits against a health care provider
We do not automatically move the member to another medical group/IPA because of a lawsuit.
We consider a transfer if:
• The complaint is about problems with quality of care or inappropriate behavior AND the health care provider requests
removal from their care.
• The transfer would not affect the member’s current treatment.
– The treating health care provider must confirm this.
– The treating health care provider must cooperate in the transfer of medical records and information to the new health care
provider.
• The member wants another health care provider who is part of the same medical group/IPA but located in a different office.
Lawsuits against a medical group/IPA
We do not deny the member access to health care providers within a medical group/IPA because of a lawsuit. We consider a
transfer if the member’s complaint is about problems with the general practices and procedures of the medical group/IPA.
Note: If you receive notification of a member’s plan to sue, notify your health care provider advocate online at uhcprovider.com
> Contact us > State-specific health plan and network support.

Chapter 2: Provider responsibilities and standards
26
2023 UnitedHealthcare Care Provider Administrative Guide
New York (NY) Domestic and Sexual Violence Hotline (only applicable to NY health care
providers who see Commercial and Oxford Health Plan members)
New York state law requires that all NY health care providers post the Domestic and Sexual Violence Hotline information in
their office. You can download the information at uhc.com/legal > New York > Members with a New York UnitedHealthcare
insurance policy who may be in danger from another family member (pdf).

27
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 3: Commercial products
We create new commercial products and networks to meet member needs for affordable and quality care. We offer a variety
of fully insured and self-funded commercial products for small and large groups. We also have individual benefit plans. These
products vary by network size and make-up, gated or non-gated requirements, and benefit structure.
Individual Exchange Plans
We offer commercial products on the Individual or Small Business Health Options Program (SHOP) Exchange in some states.
Commercial products on the Individual and SHOP Exchange follow the same policies and protocols within this guide, unless
otherwise stated in your Agreement.
For Individual Exchange in AL, AZ, FL, GA, IL, KS, LA, MD, MI, MS, MO, NC, OH, OK, TN, TX, VA and WA, refer to Chapter 4:
Individual Exchange Plans.
Understanding your network participation status
You are contracted to see all commercial members (including Exchange), unless your Agreement excludes you. This includes
new benefit plans brought into your market after the effective date of your Agreement. UnitedHealthcare Individual Exchange
Benefit Plans require you to have a location in a limited geographic market called the Individual Exchange Benefit Plans network
service area. Verify the current Individual Exchange Benefit Plans network service area at uhcprovider.com/plans.
Commercial networks
Each commercial product has a network of health care providers we work with to provide more affordable, quality health care.
Our commercial benefit plans include a subset of our commercial network providers: Navigate, Charter, Core, Compass,
Doctors Plan and NexusACO. A list of participating health care providers by benefit plan is on uhcprovider.com/findprovider.
Your Agreement requires you to coordinate care with other participating network providers. Do not engage non-network
providers in a member’s care.
Commercial product overview table
Product Name
1
How do members access physicians and health care
professionals?
2
Is a referral
required from the
member’s PCP
to the network
specialist?
Is the treating
network physician
and/or facility
required to give
notification when
providing certain
services?
UnitedHealthcare
Choice and
Choice Plus
Members can choose any Choice network physician
or health care professional without a referral and
without designating a PCP.
UnitedHealthcare Choice Plus provides out-of-network
benefits. UnitedHealthcare Choice does not cover out-
of-network services (except for emergency services).
No, members have
open access to a
national network
of Choice health
care providers.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
Chapter 3: Commercial products
28
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name
1
How do members access physicians and health care
professionals?
2
Is a referral
required from the
member’s PCP
to the network
specialist?
Is the treating
network physician
and/or facility
required to give
notification when
providing certain
services?
UnitedHealthcare
Doctors Plan and
Doctors Plan Plus
Members choose, or are assigned, a Doctors Plan
network PCP for each family member. Members are
encouraged to see their PCP to coordinate their care,
but are not required to see that PCP, or to obtain a
referral from a PCP when accessing a Doctors Plan
network specialist or facility for care.
UnitedHealthcare Doctors Plan Plus provides out-
of-network benefits. UnitedHealthcare Doctors Plan
does not cover out-of-network services (except for
emergency services).
No, members have
open access to a
limited network of
Doctors Plan health
care providers
available nationally.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
Select and
Select Plus
Members choose, or are assigned, a Select
network PCP for each family member. Members are
encouraged to see their PCP to coordinate their care,
but are not required to see that PCP, or to obtain a
referral from a PCP when accessing a Select network
specialist or facility for care.
UnitedHealthcare Select Plus provides out-of-network
benefits. UnitedHealthcare Select does not cover out-
of-network services (except for emergency services).
No, members have
open access to a
national network of
Select health care
providers.
Yes, on selected
procedures, as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
Options PPO
Members can choose any network physician or
health care professional without a referral and without
designating a PCP.
Options PPO provides out-of-network benefits.
No, members have
open access to a
national network of
Options PPO health
care providers.
This may be the
obligation of the
provider or the
member and will
depend on the
member’s benefit
plan.
UnitedHealthcare
Indemnity
Members can choose any physician or health
care professional.
No, members have
open access to
any health care
provider.
No, members are
responsible for
notifying us using
the phone number
on their health plan
ID card.
UnitedHealthcare
Core and Core
Essential
Members can choose any Core network physician or
health care professional without a referral and without
designating a PCP.
Core provides out-of-network benefits. Core Essential
does not (except for emergency services).
No, members have
open access to a
limited network
of health care
providers available
nationally.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
Freedom Plans
Members can choose any physician or health plan,
however they must choose a PCP for the EPO plan.
No, referrals are not
required.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
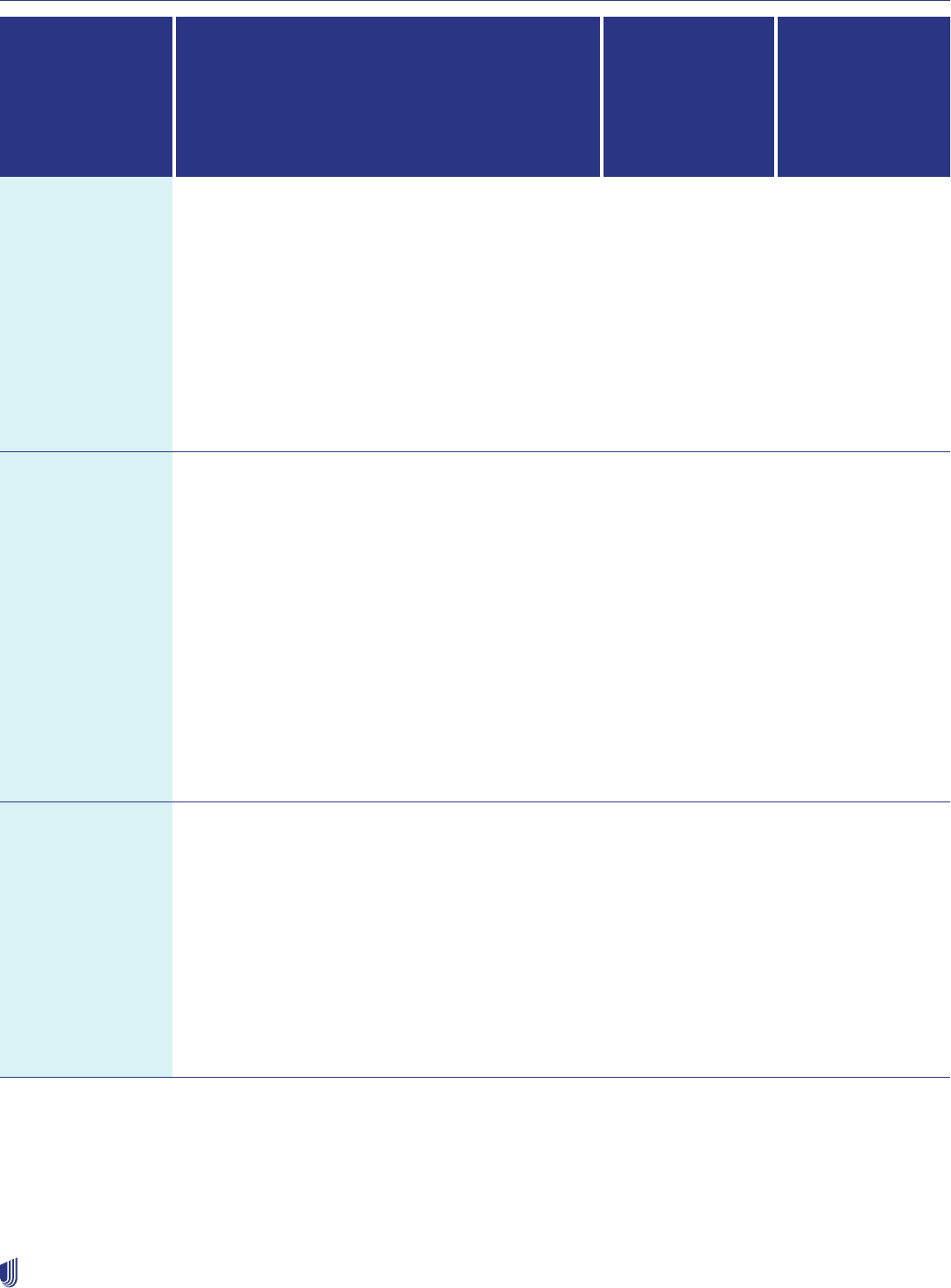
Chapter 3: Commercial products
29
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name
1
How do members access physicians and health care
professionals?
2
Is a referral
required from the
member’s PCP
to the network
specialist?
Is the treating
network physician
and/or facility
required to give
notification when
providing certain
services?
UnitedHealthcare
Navigate®,
Navigate
Balanced®
Navigate Plus®
Members must see their PCP and have electronic
referrals submitted to UnitedHealthcare by their PCP
before seeing another Navigate network physician.
Navigate Balanced and Plus benefit plans provide
additional network coverage, at a higher member
cost-share, for services from a Navigate network
physician other than the member’s PCP without
a referral.
Navigate Plus provides out-of-network benefits
3
.
Navigate and Navigate Balanced do not (except for
emergency services).
Yes, an electronic
referral from
the member’s
PCP is required
prior to receiving
services from a
Navigate physician
participating
in this limited
Navigate network.
See Chapter 6:
Referrals of this
guide.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
NavigateNOW
NavigateNOW
Balanced
NavigateNOW Plus
Subject to specific benefit designs, a member in
NavigateNOW must choose a care team/PCP at
the time of their enrollment. If not, we assign one.
NavigateNOW members must see their virtual care
team or selected PCP, and have electronic referrals
submitted to UnitedHealthcare by their care team
or PCP before seeing another Navigate network
physician.
NavigateNOW Balanced and Plus benefit plans
provide additional network coverage, at a higher
member cost-share, for services from a Navigate
network physician other than the member’s PCP
without a referral.
NavigateNOW Plus provides out-of-network benefits
3
.
NavigateNOW and NavigateNOW Balanced do not
(except for emergency services).
Yes, an electronic
referral from
the member’s
PCP is required
prior to receiving
services from a
Navigate physician
participating
in this limited
Navigate network.
See Chapter 6:
Referrals of this
guide.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
Charter®, Charter®
Balanced,
Charter® Plus
Members must see their PCP and have electronic
referrals submitted by their PCP before seeing another
Charter network physician to receive the highest
level of coverage. Charter Balanced and Charter Plus
benefit plans provide additional network coverage,
at a higher member cost-share, for services from a
Charter network physician other than the member’s
PCP without a referral.
Charter Plus provides out-of-network benefits. Charter
and Charter Balanced do not (except for emergency
services).
Yes, an electronic
referral from the
member’s PCP is
required prior to
receiving services
from a Charter
health care provider
participating
in this limited
Charter network.
See Chapter 6:
Referrals of this
guide.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
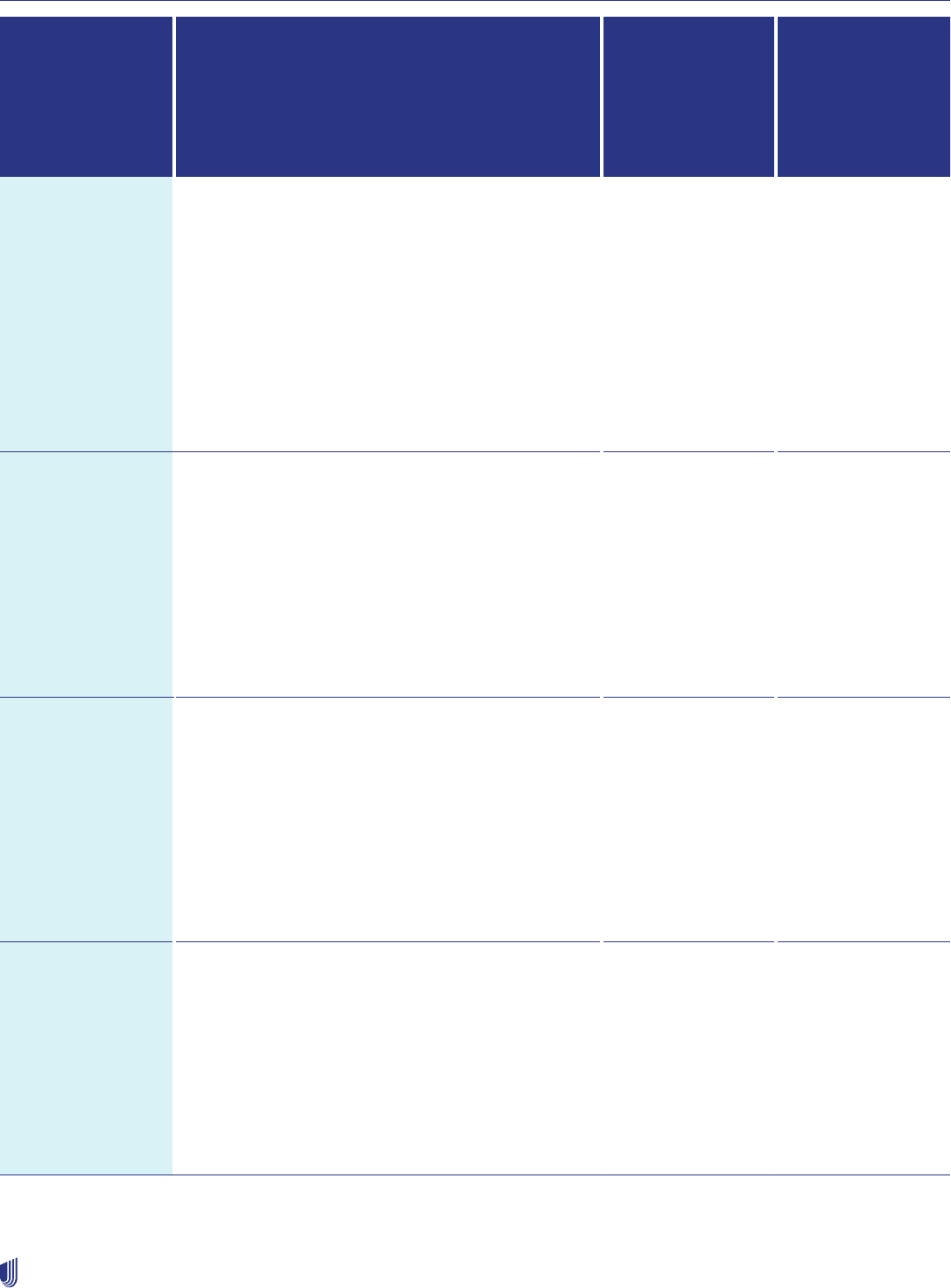
Chapter 3: Commercial products
30
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name
1
How do members access physicians and health care
professionals?
2
Is a referral
required from the
member’s PCP
to the network
specialist?
Is the treating
network physician
and/or facility
required to give
notification when
providing certain
services?
UnitedHealthcare
Compass,
Compass
Balanced,
Compass Plus
Members must see their PCP and have electronic
referrals submitted by their PCP before seeing another
Compass network physician within the Compass
network service area to receive the highest level of
coverage
4
. Compass Balanced and Plus benefit plans
provide network coverage at a higher member cost-
share for services from a network physician other than
the member’s PCP without a referral.
Compass Plus provides out-of-network benefits.
Compass and Compass Balanced do not (except for
emergency services).
Yes, an electronic
referral from the
member’s PCP is
required prior to
receiving services
from a health
care provider
participating
in this limited
Compass network.
See Chapter 6:
Referrals of this
guide.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
Individual
Exchange Plans
Plans are sold on the Exchange marketplace.
Members choose, or are assigned, a network PCP for
each family member. Members must see a network
PCP to coordinate care. In some states, members
must obtain a referral from a PCP when accessing a
network specialist for care.
Individual exchange plans do not provide out-of-
network benefits (except for emergency services) and
members must stay within a defined service area to
access care. See Chapter 4 for more information on
Individual Exchange Plans.
Referrals are
required in some
states.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
NexusACO OA®
NexusACO OAP®
NexusACO OA is a tiered benefit plan where members
choose, or are assigned, a network PCP for each
family member. The member is encouraged to see
their PCP to coordinate their care but is not required
to see that PCP or obtain a referral when accessing
other network providers.
NexusACO OAP is a tiered benefit plan and
provides out-of-network benefits. NexusACO OA
does not cover out-of-network services (except for
emergency services).
All NexusACO benefit plans are tiered
No, members have
open access to a
national network
of health care
providers.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
UnitedHealthcare
NexusACO R®
UnitedHealthcare
NexusACO RB®
NexusACO RP®
NexusACO R is a tiered benefit plan where members
must see their assigned network PCP and have
electronic referrals submitted by their PCP before
seeing another network specialist to receive the
highest level of coverage.
NexusACO RB benefits are reduced without a referral.
NexusACO RP provides out-of-network benefits.
3
NexusACO R and RB do not (except for
emergency services).
All NexusACO benefit plans are tiered.
Yes, an electronic
referral from the
member’s PCP is
required prior to the
member receiving
specialist services.
See Chapter
6: Referrals of
this guide.
Yes, on selected
procedures as
described in
Chapter 7: Medical
management of
this guide.
1
The UnitedHealthcare Network may be different among commercial products in your local market. Refer to your contract to determine whether you are part of that local network.
2
Physicians and health care professionals must be licensed for the health services provided and the health care services provided must be covered under the member’s benefit contract.
3
The benefit level for non-emergency services from out-of-network physicians and other health care providers is generally less than that for services from network physicians and other health care providers.
4
For more information about the Compass service area, go to uhcprovider.com/plans.

Chapter 3: Commercial products
31
2023 UnitedHealthcare Care Provider Administrative Guide
Benefit plan types
Open access benefit plans: No referral or PCP approval is required for members to see other network providers. Prior
authorization and notifications are required for certain services, described in Chapter 7: Medical management, with the
exceptions noted in the previous table. Benefit plans vary in the type of coverage offered based on network and tier status (for
tiered benefit plans only).
Gated benefit plans: Members must select and see their assigned PCP. The PCP must submit electronic referrals before a
member sees another network physician; this helps ensure the highest level of coverage. Benefit plans vary in type of coverage
offered based on PCP and referral requirements, network status, and tier status (for tiered benefit plans only).
Tiered benefit plans: Plans define tier 1 health care providers differently. Check your tier status when verifying eligibility and
benefits in the UnitedHealthcare Provider Portal. Some of our commercial products feature tiered benefits. NexusACO is
always offered as a tiered benefit plan. Members may have lower out-of-pocket costs for services provided by a tier 1 health
care provider or facility. Members with a tiered benefit plan have a “Tiered Benefits” identifier on the front of their ID card.
W500 additional network benefits
Some benefit plans include additional network benefits referred to as W500 Emergent Wrap. We contract with network
providers, whose agreements exclude them from some products, to provide network coverage for urgent, emergent and
network gap exception services. This extends the network of health care providers available to members outside their primary
network for these services. Members with additional network benefits display W500 on the back of their ID card.
PCP selection
Members in a gated plan
1
, and the open access products of Doctors Plan, NexusACO OA and Select choose a network PCP
at the time of their enrollment. If a PCP is not selected by a member, we assign one. A PCP is a physician in family practice,
internal medicine, pediatrics, or general practice. Other specialties may be included if required by state law.
The PCPs designated by the member and enrolled dependent(s) do not need to be the same person or affiliated with the same
group. The member and enrolled dependent(s) must select a PCP within the geographic area where the subscriber lives.
You can verify a member’s PCP when you verify their eligibility, as shown in the Verifying eligibility, benefits and your network
participation status section in Chapter 2: Provider responsibilities and standards.
Consumer-driven health benefit plans
Consumer-driven health benefit plans are made to help members:
• Become more informed and careful about their health care choices.
• Take control over their health and health care purchases.
These benefit plans are listed on the ID card and by checking eligibility and benefits in the UnitedHealthcare Provider Portal.
These plans include an account that helps members pay their out-of-pocket costs on a pre-tax basis. The account can either be
a health savings account (HSA) or a health reimbursement account (HRA).
HRAs and HSAs are similar in many ways:
• They are both a type of medical savings account.
• The medical benefit includes a deductible. Members typically use their HSA or HRA to pay out-of-pocket expenses until they
meet the deductible or after they meet the deductible. The benefit plans include an out-of-pocket maximum and, once met,
they pay 100% of covered services, including pharmacy.
• They cover routine preventive care under the basic medical benefit. These services are not subject to the deductible.
1
Subject to specific benefit designs.

Chapter 3: Commercial products
32
2023 UnitedHealthcare Care Provider Administrative Guide
HRAs and HSAs differ in that:
• Employers most often fund HRAs.
• Employees most often fund HSAs.
• With HSAs, if members do not have sufficient funds in their account, or choose to save those funds for a later date, they pay
any remaining cost-share out-of-pocket. The HSA belongs to the account holder even if they change employers. The Internal
Revenue Service allows annual deposits that can equal the benefit plan’s deductible.
33
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 4: Individual Exchange plans
UnitedHealthcare offers plans both on and off the Health Insurance Marketplace (Exchange). This chapter applies to the plans
we offer on the Health Insurance Marketplace for the states listed in the following table. Individual Exchange Benefit Plans are
also referred to as Individual and Family Plans. Additional plans may be offered in Nevada (administered by Sierra/Health Plan
of Nevada) and Colorado (administered by Rocky Mountain Health Plans). Those plans follow a separate administrative guide,
as indicated in the Benefit plans not subject to this guide section in Chapter 1: Introduction. Individual Exchange plans
offered in New York (Compass) and Massachusetts (Navigate) will follow the commercial plan guidelines in this guide.
UnitedHealthcare participation in Exchanges
UnitedHealthcare evaluates each Exchange opportunity according to our ability to provide value and honor commitments to our
existing local customers, members and health care providers. In 2020, UnitedHealthcare participated in the Individual Exchange
Marketplace in 4 states: Colorado, Massachusetts, Nevada and New York. In 2022, we participated in Alabama, Arizona,
Colorado, Florida, Georgia, Illinois, Louisiana, Maryland, Michigan, North Carolina, Oklahoma, Tennessee, Texas, Virginia and
Washington. In 2023, we will be adding 4 additional states: Kansas, Mississippi, Missouri, Ohio.
2023 Exchange footprint
State Service Area Network Marketplace
Alabama Baldwin, Bibb, Blount, Chilton,
Colbert, Coosa, Etowa, Geneva,
Henry, Houston, Jefferson,
Lauderdale, Lawrence,
Limestone, Madison, Mobile,
Morgan, Shelby, St Clair,
Talladega and Walker counties
Individual
Exchange
Benefit
Plan
Individual Exchange
Arizona Maricopa, Pinal and Pima
counties
Individual
Exchange
Benefit
Plan
Individual Exchange
Florida 21 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Chapter 4: Individual Exchange plans
34
2023 UnitedHealthcare Care Provider Administrative Guide
State Service Area Network Marketplace
Georgia 53 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Illinois Cook, Dupage, Kane,
Kankakee, Kendall, Lake,
Macon, Madison, Monroe,
Sangamon, Shelby, St. Clair
and Will counties
Individual
Exchange
Benefit
Plan
Individual Exchange
Kansas 21 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Louisiana 39 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Maryland Statewide Individual
Exchange
Benefit
Plan
Individual Exchange
Michigan Calhoun, Genesee, Kalamazoo,
Kent, Macomb, Monroe*,
Oakland, Shiawassee and
Wayne counties
*Monroe is a partial county,
and includes the following zips
only: 48144, 49267, 48179,
48182, 48133, 48177, 48157,
48117, 48166, 49270, 48145,
48140, 48162, 48161, 48131,
48159, 48110
Individual
Exchange
Benefit
Plan
Individual Exchange
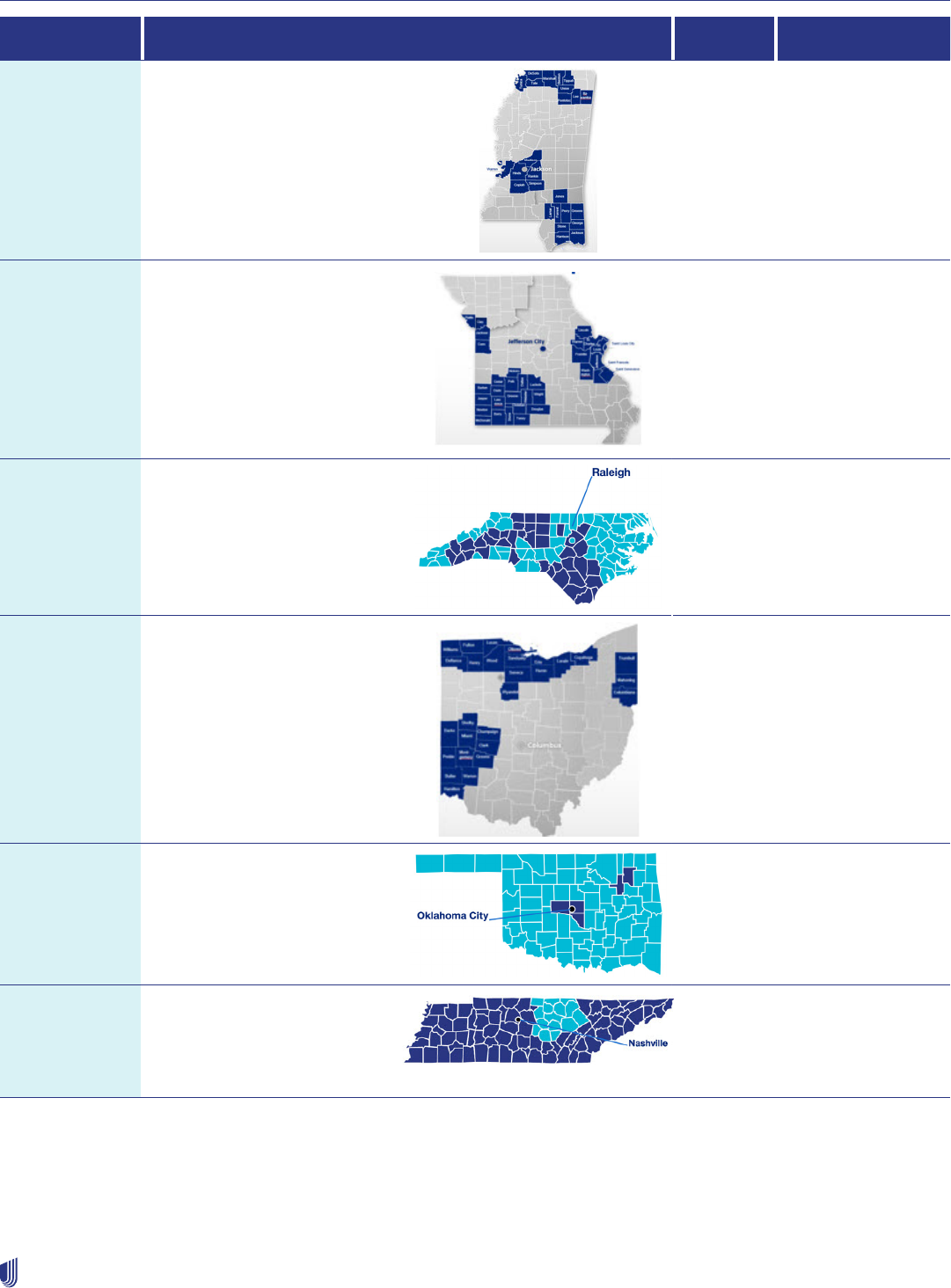
Chapter 4: Individual Exchange plans
35
2023 UnitedHealthcare Care Provider Administrative Guide
State Service Area Network Marketplace
Mississippi 25 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Missouri 33 counties Individual
Exchange
Benefit
Plan
Individual Exchange
North Carolina 39 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Ohio 28 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Oklahoma Canadian, Oklahoma, Rogers,
Tulsa and Cleveland counties
Individual
Exchange
Benefit
Plan
Individual Exchange
Tennessee 73 counties Individual
Exchange
Benefit
Plan
Individual Exchange
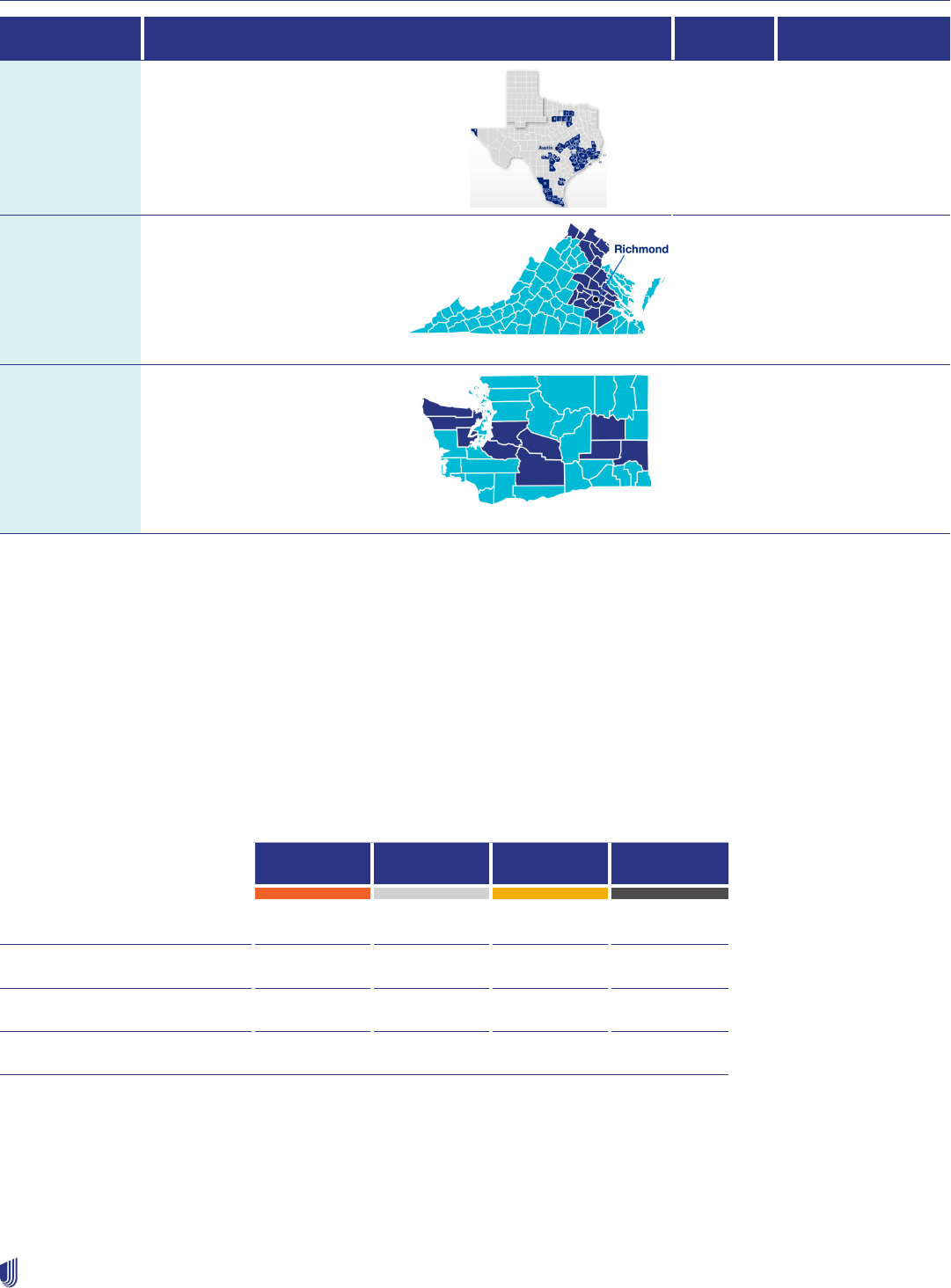
Chapter 4: Individual Exchange plans
36
2023 UnitedHealthcare Care Provider Administrative Guide
State Service Area Network Marketplace
Texas 48 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Virginia 36 counties Individual
Exchange
Benefit
Plan
Individual Exchange
Washington Adams, Clallam, Jefferson,
King, Kittitas, Lincoln, Mason,
Pierce, Whitman and Yakima
counties
Charter Individual Exchange
Plan coverage and metal levels
Essential health benefits
Individual Exchange health insurance plans are required to cover essential health benefits or essential care and services as
defined by each state. To learn more about essential health benefits, go to healthcare.gov.
Metal level plans
Plans offered on the Exchange are grouped into 4 metal levels based on the actuarial value: Bronze, Silver, Gold, and Platinum.
Each level covers the same set of essential health benefits, but differs by how much the member pays in premium and total cost
share. UnitedHealthcare offers Bronze, Silver and Gold plans. We do not offer Platinum plans.
Bronze Silver Gold Platinum
Monthly premium $ $$ $$$ $$$$
Cost per visit/prescription $$$$ $$$ $$ $
Plan pays 60% 70% 80% 90%
Member pays 40% 30% 20% 10%
Identifying metal levels
The ID card will identify the metal level and plan name. See the Health plan ID card section of this chapter.

Chapter 4: Individual Exchange plans
37
2023 UnitedHealthcare Care Provider Administrative Guide
Premium tax credits and cost-sharing reduction subsidies
People who purchase coverage on the Individual Exchange may qualify for financial assistance to help lower their premium or
cost-share amounts depending on their household income. As a member’s qualifications change, so does eligibility for financial
assistance or other government programs like Medicaid. These changes can occur within the same calendar year. Individuals
must inform their state Exchange when financial changes occur, so the government can adjust their subsidy accordingly. You
should verify eligibility at the point of service to confirm coverage and benefits.
3-month grace period
Individual Exchange members will have a monthly premium they are responsible to pay each month to maintain coverage. The
Patient Protection and Affordable Care Act (ACA) requires health insurers to provide a 3-month grace period before terminating
coverage for people who have not paid their premium. The grace period applies to those who receive an advanced premium
tax credit and have paid at least 1 full month’s premium within the benefit year. Members are required to pay the first month’s
premium before coverage goes into effect. Additionally, for individuals who do not receive federal subsidy assistance, plans are
required to provide a grace period consistent with state law (typically 30 or 31 days) before terminating coverage.
How the 3-Month Grace Period Works
Month 1 UnitedHealthcare processes the claims.
Month 2 UnitedHealthcare pends the claims and sends a letter to the health care provider advising them of
the delinquency. The member receives a copy of the letter. You may not balance bill the member at
this time. Reminders are sent to the member to complete payment.
Month 3 UnitedHealthcare pends the claims and sends a letter to the health care provider advising of the
delinquency. The member receives a copy of the letter. You may not balance bill the member at this
time. If the premium is paid in full by the end of the grace period, claims are released.
OR
If the premium is not paid in full by the end of the grace period, the member’s coverage will
terminate to the end of the first month. Any claims received during the second and third month will
be processed and denied. You may bill the member for any unpaid amounts at the end of the grace
period.
Identifying members in a grace period
There are 3 ways to verify if the member is in a grace period:
1. EDI 271 Response Transactions - We will return the following information:
• Coverage Status
– 1st month: Active
– 2nd month: Active – Pending Investigation
– 3rd month: Active – Pending Investigation
• Period Start – First day of the first month of the grace period
• Period End – Last day of the third month of the grace period
• MSG – Individual Exchange Grace Period
If the service date is 1 month after the
claim eligible through date, the member
is in the second grace period month.
Chapter 4: Individual Exchange plans
38
2023 UnitedHealthcare Care Provider Administrative Guide
2. UnitedHealthcare Provider Portal
The online secure UnitedHealthcare Provider Portal will indicate if the member is within a grace period and at what
month. The portal also includes an informational icon message where the user can hover to understand what each period
means to them and the member.
3. Contact Us
Verify member eligibility by calling Provider Services at 1-888-478-4760.
UnitedHealthcare benefit plans for Individual Exchanges
Plans are grouped into 4 product families
Plan Name Description Plan sub-type
Essential Lean plan design, offered in most markets, low-cost offering, with
higher deductible and lower premium
Bronze plans
Value Standard plan design. $0 PCP visits, unlimited virtual care with
Optum Everycare Now, HSA available, offered in all markets
Bronze, Silver and Gold plans
Advantage Richest plan design, options with embedded adult dental and vision
coverage, A “+” sign indicates plan includes embedded adult dental
and vision
Silver and Gold plans
Virtual First Offered in IL, FL, GA, TX, VA, MI, OH and MD, broad spectrum virtual
PCP care delivered through a mobile application, including specialty
urgent care
Bronze, Silver and Gold (MD
only) plans
Plan Requirements
State PCP Required Referral Required Prior Auth
Required
Out-of-Network/
Area Coverage
Alabama
1
Yes No, not required
for member to have
coverage.
Yes No*
Arizona Yes Yes, for the member
to have coverage
Yes No*
Florida
2
Yes Yes, for the member
to have coverage
Yes No*
Georgia Yes Yes, for the member
to have coverage
Yes No*
Illinois
3
Yes Yes, for the member
to have coverage
Yes No*
Kansas
4
Yes No, not required for
the member to have
coverage
Yes No*
Chapter 4: Individual Exchange plans
39
2023 UnitedHealthcare Care Provider Administrative Guide
Louisiana
5
Yes No, not required for
the member to have
coverage
Yes No*
Maryland
6
Yes Yes for gated plan; No
for non-gated plan
Yes No*
Michigan
7
Yes Yes, for the member
to have coverage
Yes No*
Mississippi
8
Yes No, not required for
the member to have
coverage
Yes No*
Missouri
9
Yes No, not required for
the member to have
coverage
Yes No*
North Carolina Yes No, not required for
the member to have
coverage
Yes No*
Ohio
10
Yes Yes, for the member
to have coverage
Yes No*
Oklahoma Yes No, not required for
the member to have
coverage
Yes No*
Tennessee
11
Yes No, not required for
the member to have
coverage
Yes No*
Texas Yes Yes, for the member
to have coverage
Yes No*
Virginia
12
Yes Yes for gated plan; No
for non-gated plan
Yes No*
Washington Yes Yes, for the member
to have coverage
Yes No*
*Except for emergency services and related authorized admissions.
1 Alabama Individual Exchange will have access to participating providers in the following counties in the state of Tennessee: Bedford,
Giles, Lawrence, Lewis, Lincoln, Marshall, Maury, Moore and Wayne. In addition, Alabama Individual Exchange members will have
access to participating providers in Escambia County, Florida. Alabama Individual Exchange members will also have access to
participating providers located in the following counties in the state of Mississippi: George, Jackson, Stone, Harrison. However, they
must select a PCP in the state of Alabama.
2 Florida Individual Exchange members will have access to participating providers in the following counties in the state of Alabama:
Baldwin and Mobile. However, they must select a PCP in the state of Florida.
3 Illinois Individual Exchange members will have access to participating providers in the following counties of Missouri: St Charles, St
Louis County, St Louis City, Jefferson, Sainte Genevieve. However, they must select a PCP in the state of Illinois.
4 Kansas Individual Exchange members will have access to participating providers in the following counties of Missouri: Cass, Clay,
Jackson, Platte. However, they must select a PCP in the state of Kansas.
5 Louisiana Individual Exchange members will have access to participating providers located in Warren county in Mississippi. However,
they must select a PCP in the state of Louisiana.
Chapter 4: Individual Exchange plans
40
2023 UnitedHealthcare Care Provider Administrative Guide
6 Maryland Individual Exchange members will have access to participating providers in the following counties in the state of Virginia:
Fairfax, Fairfax City, Loudoun and Arlington. However, they must select a PCP in the state of Maryland.
7 Michigan Individual Exchange members will have access to participating providers in the following counties of Ohio: Lucas. However,
they must select a PCP in the state of Michigan.
8 Mississippi Individual Exchange members will have access to participating providers located in the following counties of Alabama:
Mobile and Baldwin. They will also have access to participating providers in the following counties in the state of Tennessee: Shelby,
Tipton, Fayette, Hardeman, McNairy. In addition, they will be able to access participating providers in Madison, Franklin and Tensas
counties in the state of Louisiana. However, they must select a PCP in the state of Mississippi.
9 Missouri Individual Exchange members will have access to participating providers in the following counties of Kansas: Johnson,
Leavenworth, Miami, Wyandotte as well as the following counties in Illinois: Madison, St Clair, Monroe. However, they must select a PCP
in the state pf Missouri.
10 Ohio Individual Exchange members will have access to participating providers in the following counties of Michigan: Monroe. However,
they must select a PCP in the state of Ohio.
11 Tennessee Individual Exchange members will have access to participating providers in the following counties in the state of Alabama:
Colbert, Lauderdale, Lawrence, Limestone, Madison and Morgan. In addition, Tennessee Individual Exchange members will have
access to participating providers in the following counties in state of Mississippi: DeSoto, Tunica, Tate, Sharshall, Benton, Tippah,
Union. However, they must select a PCP in the state of Tennessee.
12 Virginia Individual Exchange members will have access to participating providers in the following counties in the state of Maryland:
Frederick, Montgomery and Prince Georges. However, they must select a PCP in the state of Virginia
Understanding your network participation
You may already participate in benefit plans offered on the Individual Exchange if you participate in UnitedHealthcare’s
commercial benefit plans, unless the network is listed as an excluded benefit plan in your Agreement. For Individual Exchange
Benefit Plan and Charter Exchange networks, you must also have a location in the network service area to be eligible for in-
network coverage.
As a participating health care provider, you agree to give UnitedHealthcare members equal access to the treatment they need.
This includes service or treatment for any Exchange member with plans in which you participate.
Reimbursement
Reimbursement for Individual Exchange plans is the same as your commercial rates, unless your Agreement includes a specific
Payment Appendix for the network name (Individual Exchange Benefit Plan, Charter).
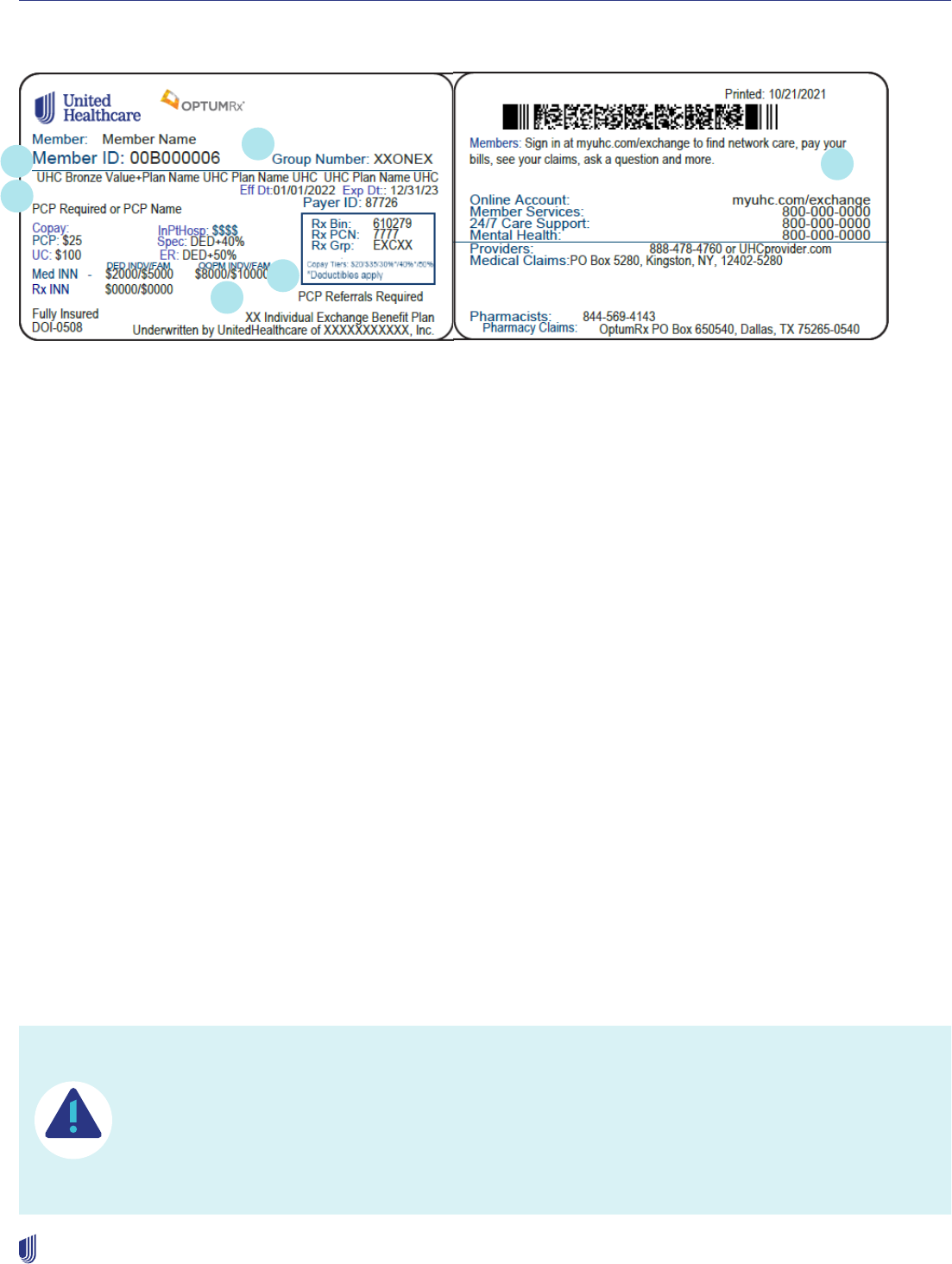
Chapter 4: Individual Exchange plans
41
2023 UnitedHealthcare Care Provider Administrative Guide
Health plan ID card
Front Back
This sample ID card is for illustration only. Actual information varies depending on payer, plan and other requirements.
1. Plan name – includes the metal level – bronze, silver, gold, platinum
2. Group number – “ONEX” – plans offered on the Exchange, “OFEX”
3. PCP Required indicator – all Exchange plans require a PCP
4. Referral required indicator (if applicable)
5. Member’s network name - Individual Exchange Benefit Plan
6. The word “exchange” indicates an exchange plan
Verifying eligibility and benefits
Check the member’s eligibility and benefits before providing care. Health plans and coverage can change within a single
enrollment year.
When checking eligibility, be sure you:
1. Verify your network participation in the member’s health plan using the UnitedHealthcare Provider Portal.
2. Confirm whether the member is in the grace period.
3. Know the member’s financial liabilities at the time of service.
Plan requirements/features
PCP selection
Members enrolled in Individual Exchange benefit plans, otherwise known as Individual and Family Plans, must select a PCP at
the time of enrollment to manage their health care needs. If the member does not select a PCP within the first month, one will
be assigned for them. Members may change their PCP by calling the member services number listed on the back of their ID
card or through their online account at myuhc.com/exchange. This process is outlined in Chapter 3: Commercial products.
Out-of-network/out-of-area benefit coverage
Individual Exchange Benefit Plan members do not have out-of-network or out-of-area benefit coverage,
except for emergency services and related admissions, unless specifically approved by UnitedHealthcare.
Members must receive eligible services at participating health care provider locations within the service area
to be covered. Members may be responsible for full cost of services rendered by out-of-network or out-of-
area providers. Members can search for in-network health care providers by logging into their online account
at myuhc.com/exchange.
3
1
2
4
5
6

Chapter 4: Individual Exchange plans
42
2023 UnitedHealthcare Care Provider Administrative Guide
Specialist referral requirements
Many Individual Exchange Benefit Plans will require a specialist referral. Where applicable, the PCP must submit referrals on
uhcprovider.com when the member needs additional care by a network specialist. Any eligible service provided by a specialist,
in any setting, requires a referral to a participating network specialist¹. Once the referral end date has passed, or the number of
visits is exhausted, the member must contact their PCP to request a new referral before receiving additional care. Specialists
should confirm a valid referral is on file before each office visit. Members seen without a valid referral on file may have
no coverage. Refer to the Benefit Plan grid for specific plan details by state.
Referral impacts on hospital claims
Individual Exchange benefit plans that require specialist referrals also apply to planned inpatient and outpatient procedures
where the specialist is the admitting physician. The member must have a referral on file to see a network specialist for planned
services in any setting, including in the hospital. The specialist referral requirement is in addition to notification requirements.
Members without a valid referral on file with the admitting physician for planned inpatient or outpatient services will have no
coverage for both the admitting physician’s claim and the hospital claim. This does not apply to non-physician hospital services,
such as radiology and lab testing.
Eligible services that do not require a referral
• Services from PCPs within the same tax ID as the member’s assigned PCP. Note: Specialists within the same TIN as the
member’s assigned PCP require referrals.
• Services from network OB/GYNs, including perinatologists.
• Services rendered in network urgent care centers or convenience care clinics.
• Routine refractive eye exams performed by a network provider.
• Mental health disorders/substance use services from network behavioral health clinicians.
• Services from a network pathologist, network radiologist or network anesthesiologist.
• Services performed by a designated virtual care network provider for primary or urgent care needs.
• Emergency room or emergency ambulance.
• Physician services for emergency/unscheduled admissions or emergency ambulance services.
• Services from network, facility-based inpatient/outpatient consulting physicians, assisting surgeons, co-surgeons or team
surgeons.
• Indian Health Services.
• Non-physician services, including but not limited to durable medical equipment (DME), home health, prosthetic devices,
hearing aids, outpatient lab, X-ray or diagnostics, physical therapy, speech therapy, occupational therapy, chiropractic care,
pulmonary rehabilitation services, cardiac rehabilitation services, post cochlear implant aural therapy, cognitive rehab - with
the exception of vision therapy (e.g., physician services). Services performed by a specialist will require a referral.
• Other network services for which applicable laws do not require a referral.
Important facts about referrals
1. Unless otherwise allowed by law, electronic referrals are required.
2. Referrals can be backdated up to 5 days prior to the date of entry.
3. Referrals are valid for up to 6 months or 6 visits, whichever comes first.
4. The PCP may submit up to 6 visits. Unused visits expire after 6 months. For members with the following chronic conditions,
the PCP may submit up to 99 visits per 6 month referral: AIDS/HIV, Anemia, Cancer, Cystic Fibrosis, Schizophrenia
spectrum and other psychotic disorders, Parkinson’s Disease, Amyotrophic Lateral Sclerosis, Multiple Sclerosis, Epileptic
Seizure, Myasthemia Gravis, Glaucoma.
1
Referrals are NOT required for Individual Exchange Benefit Plans in AL, KS, LA, MS, MO, NC, OK, TN. The following states may offer plans with and without referral requirements: MD, VA.

Chapter 4: Individual Exchange plans
43
2023 UnitedHealthcare Care Provider Administrative Guide
Prior authorizations
Prior authorization and notification requirements apply to Individual Exchange members and are posted at uhcprovider.com.
Click Prior Authorization > Prior Authorization and Notification > Advance Notification and Plan Requirements Resources >
Exchange Plans Advanced Notification / Prior Authorization Requirements. Make sure you and your staff are familiar with the
Exchange-specific prior authorization list.
Unless otherwise allowed by law, you must submit prior authorizations electronically. We will not accept them by phone or fax.
We will not accept prior authorization or notification requests that also require a referral unless a completed referral is on file. If
you do not meet the referral requirements, we may deny the physician’s and hospital’s claim for planned inpatient admissions.
Additionally, admission notification and authorization is not a guarantee of coverage or payment (unless mandated by law).
Note: Prior authorization is not required for chiropractic services. Go to uhcprovider.com/exchanges for state-specific
information. In addition, submit behavioral health services from in-network health care providers requiring prior authorization on
providerexpress.com, or you can call the provider services phone number on the back of the ID card.
Patient care coordination and case management
Complex Care Management (CCM) and Transitional Case Management (TCM)
UnitedHealthcare case managers are registered nurses who engage the appropriate internal, external or community-based
resources to support the specific Individual Exchange member’s needs. Our complex care nurses are trained to identify and
assist individuals with complex medical conditions who need long-term care support, have unmet access or who have care
plan, psycho-social, or knowledge needs.
Our transitional case managers will collaborate, evaluate and coordinate post-hospitalization needs for Individual Exchange
members who are at risk of re-hospitalization or frequent users of high-cost services.
To refer Individual Exchange members to CCM or TCM, complete the referral form at uhcprovider.com and email it
toprovider_ref[email protected]. You will receive a status update on the referral within 7 business days. Members must meet
program criteria to receive complex care management.
Helping members stay in the network
You play a leading role in helping members stay within their plan’s network. This helps members get the best level of coverage
for the highest quality of care. Remember to:
• Use the online provider directory to find other in-network providers when members require additional care. Go to uhcprovider.
com > Our network > Find a provider.
• Submit electronic referrals at uhcprovider.com/referrals.
• Refer patients to participating lab providers. For more information, go to uhcprovider.com > Resources > News > Article: Help
your patients save money.
• Search for in-network health care providers at myuhc.com/exchange.
Coordinating care for new patients
We understand there can be challenges when a member changes their plan or PCP assignment while undergoing treatment.
Here is how you can help:
• Help the individual become an established patient in your practice.
• Issue referrals for care that requires immediate attention, especially for those undergoing treatment or who have previously
scheduled procedures.
• Check online to confirm network participation status for the member’s plan.
• Secure valid referrals and/or prior authorizations before each visit.

Chapter 4: Individual Exchange plans
44
2023 UnitedHealthcare Care Provider Administrative Guide
• Partner with UnitedHealthcare regarding member referrals, requests for information or case management opportunities.
• An out-of-network provider may continue to treat the patient under certain circumstances if pre-approved
by UnitedHealthcare.
Coordinating care between medical and behavioral health care
To support coordination of medical and behavioral services, our CCM nurses are trained to identify and assist individuals
with complex medical conditions who may also have behavioral health conditions that need follow-up with a behavioral
health provider. Additionally, our Live and Work Well website is available to all members as a resource to support individual
self-management and to educate and assist members in accessing medical and behavioral services. Learn more at
liveandworkwell.com.
Health Risk Assessments (HRA)
Upon enrollment in our Individual Exchange plan, we will ask members to complete an annual health risk assessment (HRA).
The purpose of the HRA is to identify and engage members with high-risk needs or conditions to connect them with programs
and benefits that will help them navigate care and manage their health. Encourage your patients to complete their HRA. They
can do so by phone, email or online.
Government Inspections and Audits
You must permit access by the Secretary of the U.S. Department of Health and Human Services (HHS) and the Office of
Inspector General or their designees, in the case of Federally Facilitated Exchange business, or comparable State regulators,
in the case of State Exchange business, in connection with their right to evaluate through audit, inspection, or other means,
your books, contracts, computers, or other electronic systems, including medical records and documentation, relating to
UnitedHealthcare’s obligations as a QHP Issuer in accordance with Federal standards under 45 CFR §156.340, as it may be
amended from time to time, until 10 years from the final date of your Agreement period or such lesser or greater period which
may be specified in State law for State Exchanges.
You agree to cooperate with these entities and to allow access to and the right to audit, inspection, or other means, your books,
contracts, computers, or other electronic systems, including medical records and documentation. If you refuse to allow access,
this will constitute a breach of your Agreement.
Telemedicine and Virtual Care
The term Telemedicine refers specifically to the treatment of various medical conditions without seeing the member in person.
Providers will use telehealth platforms like live video, audio or instant messaging to address a patient’s concerns and diagnose
their condition remotely. Virtual Care is a broad term that encompasses all of the ways that healthcare providers remotely
interact with their patients. It encompasses all of the ways that patients and doctors can use digital tools to communicate in real
time.
Individual Exchange plans include access to telehealth and virtual care. Members can use virtual visits for urgent or primary
care services. The virtual visit benefit has a separate defined cost share. Members may access virtual visits from their online
account at myuhc.com/exchange or by connecting with local in-network health care providers who offer virtual care.
Individual Exchange members may also use virtual visits to access behavioral health services. With this benefit, members can
talk to an Optum participating licensed therapist or psychiatrist for the evaluation and treatment of behavioral health conditions
such as depression and anxiety. Members can schedule their appointment online with some providers or call the health care
provider directly to schedule.

Chapter 4: Individual Exchange plans
45
2023 UnitedHealthcare Care Provider Administrative Guide
Billing for telehealth or virtual care services
UnitedHealthcare will consider reimbursement for eligible virtual care services when they are given by audio and video with a
place of service POS 02 or POS 10. The Distant Site is where the rendering health care provider is housed during a virtual care
encounter and is reported on the claim with POS 02 or POS 10 in Box 24B on the 1500 claim form.
We do not require you to report one of the virtual care-associated modifiers (GT, GQ, G0 or 95) when performing a service, but
modifiers are accepted as informational if reported on a claim with eligible virtual services. For additional coding guidelines,
refer to Telehealth and Telemedicine Policy, Professional - Exchange (uhcprovider.com). Additional modalities may be
allowed for virtual behavioral health services. Please refer to Optum’s Telemental Health policy located on Optum - Provider
Express.
Pharmacy
For information about pharmacy benefits for the Exchanges, go to uhcprovider.com/exchanges.
• View and search the Prescription Drug List (PDL).
• Learn about prior authorization, step therapy protocols and utilization management edits.
• Learn how to request a prior authorization or exception.
To request authorization for outpatient self-administered medications, call 1-800-711-4555 or online at professionals.optumrx.
com.
For authorization for provider-administered medications, go to uhcprovider.com/paan.
Members can access pharmacy benefit information, including PDLs, drug costs and in-network pharmacies within their online
account at myuhc.com/exchange.
Specialty services (hearing, vision, dental, transplant,
behavioral health, chiropractor, skilled nursing facility)
Follow the standard processes for specialty services for Individual Exchange members. See the following Quick Reference
Guide for contact information.
Claims process
Refer to Chapter 10: Our claims process for more information about our claims process, including claim submission tips,
claim reconsiderations and appeals processes and more. For the Individual Exchange plans included in this chapter, use the
following claim addresses and electronic payer ID.
Initial Submissions:
Please submit claims electronically using Electronic Payer ID: 87726
Provider Appeals and Reconsiderations:
Please submit electronically using the process outlined in Chapter 10: Our Claims Process. If you are unable to submit
electronically, use the following fax numbers.
Fax: 1-888-404-0940 (standard requests)
1-888-808-9123 (expedited requests)
Chapter 4: Individual Exchange plans
46
2023 UnitedHealthcare Care Provider Administrative Guide
Policies and protocols
For policies and protocols, go to uhcprovider.com > Resources > Plans, policies, protocols and guides > For Exchange Plans.
Quick reference guide
Resource Where to Go
Ambulatory Infusion Suites National
Providers
Alera Care
Phone: 1-602-334-1232
aleracare.com
Infusion Express (IVX Health)
1-800-746-8147
Infusionexpress.com
Metro Infusion Center
1-877-448-3627
metroinfusioncenter.com
Palmetto Infusion Services
1-615-367-1444
palmettoinfusion.com
Vivo Infusion (AKA MPP Infusion
Centers)
Phone: 1-855-478-1528
mppinfusion.com
Breast Pump National Providers
†
Acelleron Breast Pumps
Phone: 1-877-932-6327
Fax: 1-978-738-9801
acelleron.com
AdaptHealth
1-844-PCS-MOMS (727-6667)
adapthealth.com
AeroflowHealthcare
1-844-867-9890
aeroflowbreastpumps.com
Byram Healthcare
1-877-773-1972
byramhealthcare.com (mail order)
Edgepark Medical Supplies
1-855-504-2099
edgepark.com (mail order)
Medline Industries
1-800-633-5463
medline.com
Pumping Essentials
1-866-688-4203
pumpingessentials.com
Cardiology
Diagnostic catheterization, electrophysiology
implants, echocardiogram and stress
echocardiogram
Online: uhcprovider.com/paan
Phone: 1-866-889-8054
Request prior authorization in the Outpatient cardiology notification/prior
authorization protocol section of Chapter 7: Medical management.
Claims Submission Electronic Claims Submission
Payer ID: 87726
Reconsideration and Appeals
Please submit electronically as per process outlined in Chapter 10.
Convenience Care Clinics National
Providers
The Little Clinic (located in Kroger
stores)
solvhealth.com/company/the-
little-clinic
Minute Clinic
Phone: 1-866-389-2727
cvs.com/minuteclinic
Walmart Clinics (TX Only)
walmarthealth.com
Chapter 4: Individual Exchange plans
47
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Dental uhcdental.com
Provider Services: 1-800-822-5353
Electronic Payer ID: 521337971
Claims Address:
UnitedHealthcare Dental - Claims Unit
P.O. Box 30567
Salt Lake City, UT 84130-0567
Dialysis (National Providers) American Renal Associates (ARA)
Phone: 1-978-922-3080
innovativerenal.com/about-ara/
DaVita Dialysis
Phone: 1-800-424-6589
davita.com
Dialysis Clinic, Inc
Phone: 1-833-602-2199
www.dciinc.org
Fresenius
Phone: 1-866-434-2597
fmcna.com
Home Dialysis Service (HDS)
Phone: 1-608-833-8033
homedialysis.org/
Chapter 4: Individual Exchange plans
48
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
DME/Cardiac, Respiratory and
Commodity Services National Providers
†
Advanced Respiratory
Respiratory high frequency chest
compression vest
1-800-426-4224
respiratorycare.hill-rom.com
Apria Healthcare
Standard DME
1-800-277-4288
apria.com
Bioventus
Bone growth stimulator
1-800-396-4235
bioventus.com
Cranial Technologies
Cranial helmets
1-844-447-5894
cranialtech.com
DJO
Bone growth stimulator
1-800-321-9549
djoglobal.com
DynaSplint Systems
Dynamic splinting, braces, orthotics
1-800-638-6771
dynasplint.com
EBI
Bone growth stimulator
1-800-526-2579
biomet.com
ElectroMed
Respiratory high frequency chest
compression vest
1-800-462-1045
smartvest.com
Electrostim Medical Svcs
TENS units
1-800-588-8383
wecontrolpain.com
Gordian Medical
Wound care supplies (SNF only)
1-800-568-5514
amtwoundcare.com
Hoveround Corp.
POV and power wheelchairs
1-800-701-5781 or 1-800-771-6565
hoveround.com
InfuSystem, Inc.
Ambulatory infusion pumps
1-800-962-9656
infusystem.com
Insulet Corporation
Omnipod and supplies
1-800-591-3455, #4
myomnipod.com
KCI USA
Negative pressure wound pump
1-800-275-4524
acelity.com/about-kci
Kinex Medical
CPM, ThermoComp, TENS
1-800-845-6364
kinexmedical.com
Liberator Medical Supply
Incontinence, ostomy and urologic
supplies
liberatormedical.com
Lincare
Standard DME
1-727-530-7700
lincare.com
Linkia Orthotics and Braces (aka
Hanger)
Orthotics/Braces
1-877-754-6542
linkia.com
MDINR (a Lincare company)
Home PT/INR monitor
1-800-877-4910
mdinr.com
Medline Industries
Enterals – adults and children
1-833-718-2229
medline.com
Medtronic
Diabetic insulin pump
1-800-646-4633
medtronicdiabetes.com
National Biological Corporation
Ultraviolet light therapy
1-216-831-0600
natbiocorp.com
Chapter 4: Individual Exchange plans
49
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
DME/Cardiac, Respiratory and
Commodity Services National Providers
†
(continued)
National Seating and Mobility
Technology mobility products,
custom wheelchairs
nsm-seating.com/findus
Novocure
Optune brain stimulator
novocure.com
Numotion
Mobility products, custom
wheelchairs
1-888-232-1333
numotion.com/locations
Orthofix
Bone growth stimulator
1-800-535-4492
orthofix.com
Otto Bock Healthcare
CPM
1-800-736-8276
ottobockus.com
PHM Logistics (aka Quipt Home
Medical)
Standard DME and Respiratory
Equipment
1-859-441-8876
quipthomemedical.com
Prentke Romich
Speech generating devices
1-800-268-5224
prentrom.com
RespirTech
Respiratory high frequency chest
compression vest
1-800-793-1261
respirtech.com
Rotech Healthcare
Standard DME
1-877-254-1725
rotech.com
Tactile Systems
Pneumatic compression devices
1-866-435-3948
tactilemedical.com
Tandem Diabetes Care
Tandem diabetic insulin pump
1-877-801-6901
tandemdiabetes.com
Tobii Dynavox
Speech generating device
1-866-588-4548
tobiidynavox.com
Wound Care Concepts (aka
Gentell)
Wound care devices
1-800-840-9041
ZOLL LifeVest
AED – wearable defibrillator
1-800-543-3267
zoll.com
EDI Support Online: uhcprovider.com/edi
Phone: 1-800-842-1109
Eligibility and Benefits EDI: Transactions 270 and 271
Online: uhcprovider.com
Phone: 1-800-210-5315
Enteral Providers AdaptHealth
1-844-727-6667
adapthealth.com
APRIA Healthcare
1-800-277-4288
apria.com
Aveanna Healthcare Medical
Solutions
1-713-956-5288
aveannamedicalsolutions.com
Byram Healthcare
1-877-773-1972
byramhealthcare.com
Edgepark Medical Supplies
1-800-321-0591
edgepark.com
Lincare
1-727-530-7700
lincare.com
Medline Industries
1-866-356-4997
medline.com
PHM Logistics (aka Quipt Home
Medical)
1-859-441-8876
quipthomemedical.com
Hearing Provider Services: 1-888-478-4760
Chapter 4: Individual Exchange plans
50
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Home Health Services National Providers
†
Bayada Home Health Care
1-800-305-3000
bayada.com
Brookdale Home Health
brookdaleliving.com
Encompass Health Home Health
encompasshealth.com
Heartland Healthcare
1-800-736-4427
hcr-manorcare.com
Maxim Health Care Services
1-800-899-9525
maximhomecare.com
PSA Healthcare
1-770-441-1580
psahealthcare.com
Home Infusion and Specialty Pharmacy
National Providers
†
*Ambulatory Infusion Suites
Accredo
1-800-803-2523
accredo.com
Avella (part of Optum Pharmacy;
Specialty Pharmacy)
1-877-342-9352
specialty.optum.com
Basic Home Infusion
1-888-822-7428
basichomeinfusion.com
Biologics
1-800-856-1984
biologicsinc.com
Caremark
1-877-287-1234
cvsspecialty.com
Diplomat Specialty Infusion Group
1-877-306-4036
specialty.optumrx.com/infusion
Eversana
1-866-336-1336
eversana.com
Freedom Fertility Pharmacy
1-800-660-4283
freedomfertility.com
Genoa Healthcare
1-800-519-1139
genoahealthcare.com
Kroger Specialty Pharmacy
1-855-802-3230
krogerspecialtypharmacy.com
Option Care Health
1-866-827-8203
optioncare.com
Optum Infusion Services
1-877-306-4036
briovarxinfusion.com
Optum Pharmacy
1-866-218-7398
briovarx.com
Optum Women’s and Children’s
Health
1-800-950-3963
alere.com
Orsini Pharmaceutical
1-800-672-0869
orsinihealthcare.com
PANTHERx
1-855-726-8479
pantherspecialty.com
U.S. Bioservices
1-888-518-7246
usbioservices.com
Walgreen’s Specialty Pharmacy
1-888-282-5166
walgreenshealth.com
Insulin Pumps and Supplies National
Providers
†
Insulte Corporation
1-800-591-3455
myomnipod.com
MiniMed Distribution Group (Medtronic)
1-800-933-3322
minimed.com
Chapter 4: Individual Exchange plans
51
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Medical Supply National Providers
†
Disposable supplies, ostomy, urological,
incontinence supplies
180 Medical
1-877-688-2729
180medical.com
Byram Medical
1-877-902-9726
byramhealthcare.com
Edgepark Medical
1-888-394-5375
edgepark.com
Liberator Medical Supply
1-888-244-0789
liberatormedical.com
Medline
1-800-633-5463
medline.com
Medline Industries
1-866-356-4997
medline.com
Mental Health and Substance Use
Prior Authorization
Online: providerexpress.com
Phone (Provider Services): 1-888-478-4760
Optum Care Solutions
Physical, occupational, speech therapy and
chiropractic services
Online: myoptumhealthphysicalhealth.com
Phone: 1-800-873-4575
Fax: 1-248-733-6070
Optum Rx
Pharmacy services and self-administered
medications benefit information
Phone: 1-800-711-4555
Online: professionals.optumrx.com
Preferred Lab Network Online: uhcprovider.com > Our network > Find a provider > Preferred Lab
Network
Prior Authorization and Notification
(Includes provider-administered
medications)
Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth
Provider Advocates
For participating hospitals, health care and
ancillary providers
Online: uhcprovider.com > Contact us > State-specific health plan and
network support
Provider Services Online: uhcprovider.com
Phone: 1-888-478-4760
Confirm member eligibility, provide
care coordination notification,
check claim status, update facility/
practice data
Radiation Therapy Prior Authorization Online: uhcprovider.com/paan
Information: Visit uhcprovider.com/paan and log in, select Radiology,
Cardiology, Oncology and Radiation Oncology Transactions. Select the
service type: Radiation Oncology
Select one of the product types: Commercial, Exchanges, Medicaid,
Medicare, or Oxford
Phone: 1-888-397-8129 8a.m. - 5p.m. local time, Monday-Friday
Radiology/Advanced Outpatient Imaging
Procedures
CT scans, MRIs, MRAs, PET scans and
nuclear medicine studies including nuclear
cardiology
Online: uhcprovider.com/paan
Phone: 1-866-889-8054
Request prior authorization for
services as described in the
Outpatient radiology notification/
prior authorization protocol
section in Chapter 7: Medical
management
Chapter 4: Individual Exchange plans
52
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Referrals
(If plan requires)
EDI: Transaction 278R
Online: uhcprovider.com/referrals
Skilled Nursing Facilities
(Free-standing)
Online: uhcprovider.com/skillednursing
Phone: 1-888-478-4760
Transplant Resource Services and
Ventricular Assist Devices
Phone: 1-888-936-7246
Fax: 1-855-250-8157
Request prior authorization
Urgent Care (National Providers) Concentra (American Current Care)
www.concentra.com/urgent-care-
centers
Dispatch Health (mobile urgent
care)
dispatchhealth.com
MedExpress
medexpress.com
Vision Online: spectera.com
Electronic Payer ID: 00773
Phone: 1-800-638-3120 (Monday–Friday, 8 a.m.–11 p.m. ET;
Saturday 9 a.m.–4:30 p.m. ET)
Claims Address:
UnitedHealthcare
P.O. Box 30978
Salt Lake City, UT 84130
†
May be subject to change without notice.

53
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 5: Medicare products
Visit uhcprovider.com, AARPMedicarePlans.com or
UHC.com/Medicare for more information about our
Medicare products in your area.
UnitedHealthcare Medicare products offer Medicare Advantage (MA) benefit plans for Medicare eligible individuals and
employer group retirees. If a member presents a ID card with a product name with which you are not familiar, verify the
member’s eligibility and benefits in the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Use the My Practice
Profile tool in the UnitedHealthcare Provider Portal to view your practice’s accepted health insurance plans and effective
dates. For more information and to login, visit uhcprovider.com/mpp. Product lists provided for your convenience are subject
to change at any time.
This guide does not apply to UnitedHealthcare MedicareDirect, our MA Private Fee-for-Service product. UnitedHealthcare
MedicareDirect does not use a contracted Medicare health care provider network. For information about UnitedHealthcare
MedicareDirect, go to: uhcprovider.com/plans > Select your state > Medicare > UnitedHealthcare® MedicareDirect (PFFS).

Chapter 5: Medicare products
54
2023 UnitedHealthcare Care Provider Administrative Guide
Medicare product overview tables
MA – Products for individuals
Product Name Medicare
Member’s
Eligibility
How do members
access physicians
and health care
professionals?
Does a primary
care physician
have to make
a referral to a
specialist?
Is the treating
physician
and/or facility
required to give
notification
when providing
certain services?
HMO and HMO-POS plans:
HMO
• Medicare Advantage Assure
• MedicareMax
• Preferred Choice Broward
• Preferred Choice Dade
• Preferred Choice Palm Beach
HMO-POS
• AARP Medicare Advantage
• AARP Medicare Advantage
SecureHorizons
• UnitedHealthcare Medicare
Advantage
(Each of the plan names above may
have one of the following at the end:
Access, Ally, Flex, Flex Plus, Focus,
Freedom Plus, Harmony, Navigate,
Patriot, Plus, Premier, Premier Value,
Prime, Profile, Rebate, Value, Value
Care, Walgreens, Walmart Flex)
• Sharp SecureHorizons Plan by
UnitedHealthcare
• Sharp Walgreens by UnitedHealthcare
• UnitedHealthcare Canopy Health
Medicare Advantage
• UnitedHealthcare Northern Light
Health Flex
• UnitedHealthcare The Villages
Medicare Advantage
• UnitedHealthcare The Villages
Medicare Focus
Members who
are Medicare
eligible for
Part A and
B, and reside
in the plan’s
service area.
Members choose
a PCP from the
Medicare network
of providers
who can help
coordinate
their care.
HMO benefit
plans do not cover
out-of-network
services, except
for emergency
services, urgently
needed services
and out-of-area
renal dialysis.
HMO-POS benefit
plans provide
out-of-network
coverage for some
covered benefits.*
A referral may
or may not be
required to see
a specialist,
depending on the
benefit plan.**
For further
information,
go online to
see Medicare
Advantage
(MA) Referral
Required Plans,
or call 1-877-842-
3210.
Have the member
ID and your TIN
available.
PCPs should
coordinate
care with the
appropriate
Medicare network
specialists.
Yes, see
guidelines
in Chapter
7: Medical
management.
*The plan will cover services from in-network and out-of-network providers, as long as the services are covered benefits and medically necessary. However, a member’s cost-share may be higher for covered
out-of-network services. Some HMO-POS plans only cover out-of-network dental care.
** Most services rendered to members in referral-required benefit plans require referrals and/or authorizations from the PCP or Physician Hospital Organization, dependent upon contractual arrangement.
Chapter 5: Medicare products
55
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name Medicare
Member’s
Eligibility
How do members
access physicians
and health care
professionals?
Does a primary
care physician
have to make
a referral to a
specialist?
Is the treating
physician
and/or facility
required to give
notification
when providing
certain services?
Local PPO and Regional PPO (RPPO)
plans
• AARP Medicare Advantage
• UnitedHealthcare Medicare
Advantage
(Each of the plan names above may
have one of the following at the end:
Assure, Choice, Choice Flex, Choice
Premier, Choice Rebate, Focus,
Headwaters, Lakeshore, Mosaic
Choice, Open, Open Flex, Open
Premier, Patriot, Premier, Premier
Choice, Riverbank, Value Care,
Walgreens)
• UnitedHealthcare Northern Light
Health Choice
Members who
are Medicare
eligible for
Part A and
B, and reside
in the plan’s
service area.
Members should
choose a PCP
from the Medicare
network of
providers who can
help coordinate
their care.
PPO benefit plans
provide out-of -
-network coverage
for all covered
network benefits.*
No, a referral is
not needed.
Yes, see
guidelines
in Chapter
7: Medical
management.
Institutional Special Needs Plans
(HMO, HMO-POS, PPO)
• UnitedHealthcare Assisted Living Plan
• UnitedHealthcare Nursing Home Plan
Members reside
in a contracted
skilled nursing
facility (Nursing
Home Plan) or
they reside in
a community
setting and
require an
institutional level
of care (Assisted
Living Plan).
Members choose
a PCP from the
Medicare network
of providers
to coordinate
their care.
PPO and HMO-
POS benefit
plans provide
out-of-network
coverage.*
HMO benefit
plans do not cover
out-of-network
services, except
for emergency
services, urgently
needed services
and out-of- area
renal dialysis.
No, a referral is
not needed.
Yes, see
guidelines
in Chapter
7: Medical
management.
* The plan will cover services from in-network and out-of-network providers, as long as the services are covered benefits and medically necessary. However, a member’s cost-share may be higher for covered
out-of-network services. Some HMO-POS plans only cover out-of-network dental care.
Chapter 5: Medicare products
56
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name Medicare
Member’s
Eligibility
How do members
access physicians
and health care
professionals?
Does a primary
care physician
have to make
a referral to a
specialist?
Is the treating
physician
and/or facility
required to give
notification
when providing
certain services?
Dual Special Needs Plans
HMO
MedicareMax Plus
Preferred Medicare Assist
Preferred Medicare Assist Palm Beach
UnitedHealthcare Dual Choice One
UnitedHealthcare Dual Complete ONE
UnitedHealthcare Senior Care Options
(Massachusetts)
HMO POS:
UnitedHealthcare Dual Complete
(Plan name may have one of the
following at the end: Ally, Balance, LP,
LP1, ONE, ONE Plus, Select)
PPO, RPPO:
UnitedHealthcare Dual Choice
UnitedHealthcare Dual Choice Unity
UnitedHealthcare Dual Complete
(Plan name may have one of the
following at the end: Balance, Choice,
Choice LP, Choice Premier, Choice
Select, Choice Select LP, RP, Select)
UnitedHealthcare NorthernLightHealth
Dual Complete
Members
who are both
Medicare
and Medicaid
eligible.
Members choose
a PCP from the
Medicare network
of providers, to
coordinate their
care.
HMO-POS and
PPO benefit
plans provide
out-of-network
coverage.*
HMO benefit
plans do not cover
out-of-network
services, except
for emergency
services, urgently
needed services
and out-of-area
renal dialysis.
A referral may
or may not be
required to see
a specialist,
depending on the
benefit plan.**
For further
information, call
1-877-842-3210.
Have the member
ID card and your
TIN available.
PCPs should
coordinate
care with the
appropriate
Medicare network
specialists.
Yes, see
guidelines
in Chapter
7: Medical
management.
* The plan will cover services from in-network and out-of-network providers, as long as the services are covered benefits and medically necessary. However, a member’s cost-share may be higher for covered
out-of-network services. Some HMO-POS plans only cover out-of-network dental care.
** Most services rendered to members in referral-required benefit plans require referrals and/or authorizations from the PCP or Physician Hospital Organization, dependent upon contractual arrangement.
Chapter 5: Medicare products
57
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name Medicare
Member’s
Eligibility
How do members access
physicians and health
care professionals?
Does a primary care
physician have to
make a referral to a
specialist?
Is the treating
physician
and/or facility
required
to give
notification
when
providing
certain
services?
Chronic Special Needs Plans
HMO:
MedicareMax Chronic
Preferred Special Care Miami-
Dade
UnitedHealthcare Chronic
Complete Focus
HMO-POS:
UnitedHealthcare Chronic
Complete
UnitedHealthcare Chronic
Complete Ally
UnitedHealthcare Chronic
Complete Focus
UnitedHealthcare Medicare
Advantage Ally
UnitedHealthcare Medicare
Advantage Assist
UnitedHealthcare Medicare
Advantage Walgreens
PPO:
UnitedHealthcare Chronic
Complete
UnitedHealthcare Chronic
Complete Assure
UnitedHealthcare Medicare
Advantage Assist
RPPO:
UnitedHealthcare Medicare Gold
UnitedHealthcare Medicare Silver
Members
who have 1
or more of
the following
qualifying
chronic
conditions:
diabetes,
chronic heart
failure, and/or
cardiovascular
disorders.
Members choose a
PCP from the Medicare
network of providers who
can help coordinate their
care.
HMO-POS and PPO
benefit plans provide out-
of-network coverage.*
HMO benefit plans do
not cover out-of-network
services, except for
emergency services,
urgently needed
services and out-of-area
renal dialysis.
A referral may or
may not be required
to see a specialist,
depending on the
benefit plan.**
For further
information, call
1-877-842-3210.
Have the member
ID card and your
TIN available.
PCPs should
coordinate care
with the appropriate
Medicare network
specialists.
Yes, see
guidelines
in Chapter
7: Medical
management.
* The plan will cover services from in-network and out-of-network providers, as long as the services are covered benefits and medically necessary. However, a member’s cost-share may be higher for covered
out-of-network services. Some HMO-POS plans only cover out-of-network dental care.
** Most services rendered to members in referral-required benefit plans require referrals and/or authorizations from the PCP or Physician Hospital Organization, dependent upon contractual arrangement.
Chapter 5: Medicare products
58
2023 UnitedHealthcare Care Provider Administrative Guide
Product Name Medicare
Member’s
Eligibility
How do members access
physicians and health
care professionals?
Does a primary care
physician have to
make a referral to a
specialist?
Is the treating
physician
and/or facility
required
to give
notification
when
providing
certain
services?
Erickson Advantage Plans
(HMO-POS)
Erickson Advantage Freedom
Erickson Advantage Liberty with
Drugs
Erickson Advantage Liberty
without Drugs
Erickson Advantage Signature
with Drugs
Special Needs Plans:
Erickson Advantage Champion
(Chronic)
Erickson Advantage Guardian
(Institutional)
Members
who reside in
an Erickson
Retirement
Community.
Members are assigned
a PCP from the Erickson
Health Medical Group
network of providers. The
PCP coordinates their
care.
These HMO-POS benefit
plans provide out-of-
network coverage for
all covered network
benefits.*
No, a referral is
not needed.
Yes, see
guidelines
in Chapter
7: Medical
management.
* The plan will cover services from in-network and out-of-network providers, as long as the services are covered benefits and medically necessary. However, a member’s cost-share may be higher for covered
out-of-network services. Some HMO-POS plans only cover out-of-network dental care.
Chapter 5: Medicare products
59
2023 UnitedHealthcare Care Provider Administrative Guide
Medicare products for groups
Product Name Member’s
Eligibility
How do members access
physicians and health care
professionals?
Does a primary care
physician have to make a
referral to a specialist?
Is the treating
physician and or
facility required
to give notice
when providing
certain services?
UnitedHealthcare
Group Medicare
Advantage (HMO)
Members
must meet
all Medicare
eligibility
requirements
as well as the
employer’s
requirements.
Members choose a PCP
from the Medicare network of
providers. The PCP coordinates
their care.
HMO benefit plans do not cover
out-of-network services, except
for emergency services, urgently
needed services and out-of-area
renal dialysis.
A referral may or may
not be required to see a
specialist based on the
benefit plan.**
For further information,
go online to see
Medicare Advantage
(MA) Referral Required
Plans, or call the number
on the member ID card.
Have the ID card and
your TIN available.
PCPs should
coordinate care with the
appropriate Medicare
network specialists.
Yes, see
guidelines
in Chapter
7: Medical
management of
this guide.
UnitedHealthcare
Group Medicare
Advantage
(Regional PPO)
Members
must meet
all Medicare
eligibility
requirements
as well as the
employer’s
requirements.
Members may choose a PCP
from the Medicare network of
providers. If a PCP is chosen, the
PCP coordinates their care.
Regional PPO plans provide out-
of-network coverage.*
No, a referral is
not needed.
Yes, see
guidelines
in Chapter
7: Medical
management of
this guide.
UnitedHealthcare
Group Medicare
Advantage (PPO)
Members
must meet
all Medicare
eligibility
requirements
as well as the
employer’s
requirements.
Members are encouraged
but not required to see a PCP
from the Medicare network of
providers to help coordinate
their care.
No, a referral is
not needed.
Yes, see
guidelines
in Chapter
7: Medical
management of
this guide.
* The plan will cover services from in-network and out-of-network providers, as long as the services are covered benefits and medically necessary. However, a member’s cost-share may be higher for covered
out-of-network services. Some HMO-POS plans only cover out-of-network dental care.
** Most services rendered to members in referral-required benefit plans require referrals and/or authorizations from the PCP or Physician Hospital Organization, dependent upon contractual arrangement.
MA products
Individual HMO, HMO-POS and PPO plans
These plans provide all of the benefits covered under Original Medicare and more. Our plans do not have limits for pre-existing
conditions, and they do not require physical exams. The member may have multiple choices of health plans depending on
where they live.
While exact benefits may vary, these plans may give:
• Access to medical care through a trusted network of health care providers.
• Coverage for many preventive services with no copays.

Chapter 5: Medicare products
60
2023 UnitedHealthcare Care Provider Administrative Guide
• Help with financial protection with annual out-of-pocket limits.
• Worldwide emergency care coverage.
• Medicare Part D prescription drug coverage.
• Coverage for additional benefits like routine dental, vision and hearing care.
Some plans do not require an additional monthly premium for this coverage. The member simply continues to pay the Medicare
Part B premium unless the member has coverage through Medicaid or another third party.
Dual special needs plan
This Special Needs Plan (SNP) meets the needs of individuals enrolled in Medicare who also qualify for Medicaid (called dual
eligible). This plan combines the benefits of Medicare and Medicaid.
Chronic special needs plan
This SNP is for members who have 1 or more severe or disabling chronic conditions. We help members manage their condition
as well as their overall health and well-being.
Institutional special needs plans
These SNPs are for members who reside in a contracted skilled nursing facility (institutional SNP) or who live in a community
setting and require an institutional level of care (Institutional-Equivalent SNP).
UnitedHealthcare Group MA
We offer these plans to employer groups for their retired Medicare-eligible employees. They have benefits similar to the
individual plans. (Note: We do not currently offer Group special needs plans.) The ID card has the employer group name and
number on it.
PCP selection
For most plans, members are required to select a Medicare network PCP (some plan exclusions may apply). If not, we assign
one automatically.
Changing PCP
Members may change their network PCP at any time. Changes are generally effective on the first day of the following month.
The change does not affect referrals previously submitted by their PCP as long as the member remains in the same network.
Coverage summaries and policy guidelines for MA members
Hierarchy of references/resources
We develop our MA Coverage Summaries and Policy Guidelines with the help of:
• National Coverage Determination (NCD) or other Medicare guidance, e.g., Medicare Policy Benefit Manual, Medicare
Managed Care Manual, Medicare Claims Processing Manual, Medicare Learning Network (MLN) Matters Articles.
• Local Coverage Determination (LCD) and Local Policy Articles (A/B MAC and DME MAC).
• UnitedHealthcare Commercial Medical Policies/Coverage Determination Guidelines.

Chapter 5: Medicare products
61
2023 UnitedHealthcare Care Provider Administrative Guide
Coverage summaries and policy guidelines
Our MA plan Evidence of Coverage (EOC) and Summary of Benefits (SOB) list the member’s covered benefits, limitations and
exclusions. We use our MA Coverage Summaries and Policy Guidelines to interpret benefits for our members. The policies are
subject to change based on Medicare’s coverage requirements, clinical evidence, technology and evolving practice patterns.
You are responsible for reviewing the CMS Medicare coverage guidance documents. If there is a conflict between our policies
and the guidance documents, the CMS information controls. Our MA Coverage Summaries and Policy Guidelines are available
on: uhcprovider.com/policies > Medicare Advantage Policies.
Coverage summary and policy guideline updates
We publish monthly editions of the Medicare Advantage Coverage Summary and Policy Guideline Update Bulletins. These
online resources provide notice to our network providers of changes to MA Coverage Summaries and Policy Guidelines. The
bulletins are posted on the first calendar day of every month on:
• uhcprovider.com/policies > Medicare Advantage Policies > Coverage Summaries for Medicare Advantage Plans > Medicare
Advantage Coverage Summary Update Bulletins
• uhcprovider.com/policies > Medicare Advantage Policies > Policy Guidelines for Medicare Advantage Plans > Medicare
Advantage Policy Guideline Update Bulletins
A supplemental link to the policy updates announced in the Medicare Advantage Coverage Summary and Policy Guideline
Update Bulletins is also available at uhcprovider.com/news.
Special needs plans managed by Optum
UnitedHealthcare Dual Special Needs Plans (DSNPs) and Chronic Condition Special Needs Plans (CSNPs) are two types
of Medicare Advantage Special Needs Plans. These protocols establish the guidelines and process for clinical integration,
cooperation, and collaboration of, and with respect to, the care of members of UnitedHealthcare DSNPs and CSNPs managed
by Optum.
These protocols are applicable to PCPs in UnitedHealthcare’s network for DSNPs and/or CSNPs, who are treating DSNP or
CSNP members managed by our affiliate Optum.
These protocols do not apply to DSNP or CSNP members who are assigned to an Accountable Care Organization based upon
the member’s PCP or whose PCP participates in a global capitation or risk-sharing arrangement with UnitedHealthcare.
Optum’s management of UnitedHealthcare DSNP and CSNP members includes the UnitedHealthcare At Home (UAH)Program,
which is an integrated care delivery program that coordinates the delivery and provision of clinical care of members in their
place of residence. When members participate in this program, their health care providers must follow a communications
structure that helps ensure better coordination of their medical care.
To promote the best possible outcomes, the program supports:
• Sharing information between care team members, including performance reviews.
• Tracking clinical outcomes.
• Communicating evidence-based guidelines.
The UnitedHealthcare At Home Program’s Interdisciplinary Care Team includes an Optum-trained advanced practice clinician
(ARNP/PA), the member’s PCP and other health care providers as appropriate, in addition to the member and the member’s
family. Together, they provide care customized to the member’s needs and goals of care. As part of this program, Optum
clinicians will:
• Conduct annual evaluations.
• Provide longitudinal care management for high-risk members to address medical, behavioral and socioeconomic concerns.
• Help ensure care coordination for members experiencing a care transition.
Chapter 5: Medicare products
62
2023 UnitedHealthcare Care Provider Administrative Guide
The UnitedHealthcare At Home Program supplements care provided by our members’ PCPs. It is not intended to replace the
care provided by our members’ PCPs. If these protocols differ from, or conflict with, other protocols in connection with any
matter pertaining to members of UnitedHealthcare DSNP or CSNP plans managed by Optum, these protocols govern unless
statutes and regulations dictate otherwise.
Protocols for UnitedHealthcare DSNPs members managed by Optum
As the PCP for UnitedHealthcare DSNP members managed by Optum, you agree to:
• Collaborate and cooperate with the UAH program, including UAH advanced practice clinicians and other staff assigned to
UnitedHealthcare DSNP members managed by Optum.
– Work with applicable members of the Interdisciplinary Care Team (designated by UAH) and other treating clinicians to
provide, and arrange for, the provision of covered services to UnitedHealthcare DSNP members managed by Optum.
– Identify preferred process(es) for bidirectional communication with the UAH Interdisciplinary Care Team, including member
care needs/concerns, facilitation of scheduling, social determinate issues, responding to acute clinical and/or mental
health needs, home health certifications, etc. via the appropriate communication channel (phone or secure email).
– Initiate proactive communication to UAH, as appropriate, regarding patient needs identified in previous bullet.
• Attend quality meetings as requested by UAH; this includes monthly/quarterly/ad-hoc meetings focused on
comprehensiveness of patient care and ongoing coordination of such. Review information provided by UAH, including
Provider Performance Reviews and tracking of clinical outcomes.
– Develop and execute action plans, targeting continuous quality improvement.
• Review and adhere to Evidence Based Guidelines to develop care plans, close gaps in care, and respond to deficiencies
identified in care monitoring.
• Assist with care transitions – including (but not limited to) medication reconciliation, follow up visits, home health needs and
prescription management.
• Assess and refer patients with unmet Social Determinants of Health (SDOH) needs and notify UAH when unmet needs are
identified.
• Make every effort to accept new patients who do not have an attributed PCP relationship, as patient capacity permits.
• Coordinate with the UAH team to identify and engage patients who are difficult to reach and/or unable to engage.
• Share up-to-date patient contact information with the UAH team.
Protocols for UnitedHealthcare CSNP members managed by Optum
As the PCP for UnitedHealthcare CSNP members managed by Optum, you agree to:
• Comply with all of the requirements of Protocols for UnitedHealthcare DSNP members managed by Optum (previous section).
• Complete a Chronic Condition Attestation, annually, for each applicable member.
– Assess each suspected or previously coded chronic condition (listed on attestation) by indicating “yes” or “no” to confirm
or reject each specific diagnosis.
– List all additional chronic conditions diagnosed.
– Document all chronic conditions to the highest level of specificity, linking manifestations when applicable, per ICD-10
guidelines.
– Submit supporting documentation (progress notes, visit summary, etc.) specifically addressing each chronic condition
assessed.

Chapter 5: Medicare products
63
2023 UnitedHealthcare Care Provider Administrative Guide
Medicare supplement benefit plans
AARP Medicare Select benefit plans
This Medicare Supplement product is available only to eligible AARP members who reside within the service area of a
participating hospital in our Medicare Select network.
What is Medicare Select?
Medicare was not designed to cover all health care expenses incurred by older adults.
• Medicare Supplement plans cover many of the out-of-pocket costs that Original Medicare (Part A and B) does not cover,
which can provide consumers with a greater sense of security.
• Medicare Select plans offer consumers the benefits of a standard Medicare Supplement plan at a lower price. Unlike a
standard Medicare Supplement plan, Medicare Select requires members to use a Medicare Select network hospital to
receive their full benefits.
Members must use a Medicare Select network hospital for inpatient services. They can seek services from any physician of
their choice that accepts Medicare and retain full Medicare benefits.
Network hospitals agree to waive the Part A Inpatient Hospital Deductible ($1,556 in 2022). While a network hospital waives
the Part A deductible, the hospital still receives the remaining reimbursement from Medicare. UnitedHealthcare reimburses all
other Medicare-eligible expenses not paid by Medicare other than the Part A deductible amounts waived under the terms of the
hospital Agreement. Hospitals can arrange for automatic deposits or reimbursements.
UnitedHealthcare uses these savings to offer a Medicare Supplement plan with a lower premium. If an insured member receives
inpatient services outside of the Medicare Select network, the member is responsible for the Part A deductible, unless:
• The services were emergency related.
• The service was not available from a participating hospital.
• The member was more than 100 miles from home.
No prior authorization for medical services is required.
Medicare Select plans C, F, G and N
These Medicare plans reduce member expenses by covering some or all of the following:
• Part A inpatient hospital deductible
• Part A inpatient hospital coinsurance for days 61-90 in a Medicare benefit period
• Part A inpatient hospital coinsurance for days where lifetime reserve days are used
• Part A eligible expenses for a lifetime maximum of 365 days after all Medicare Part A benefits are exhausted
• Part B coinsurance
• Part B deductible (Select Plans C and F only)
• Daily coinsurance for days 21-100 for Skilled Nursing Facility stays
• Part A and B blood deductible for the first 3 pints of un-replaced blood
• Foreign travel emergencies
• Hospice and respite care copayments and coinsurance
• Part B excess charges for Medicare approved services (Select Plans F and G only)
Claims submission information
To submit a claim electronically, contact your Clearinghouse and provide our electronic payer ID (36273). This number is
specific to Medicare Select Plans and other AARP Supplemental and Personal Health Plans.

Chapter 5: Medicare products
64
2023 UnitedHealthcare Care Provider Administrative Guide
To submit a Part A or Part B claim by mail, send a standard billing form along with a Part A or B Remittance Advice to:
UnitedHealthcare
P.O. Box 740819
Atlanta, GA 30374-0819
To promote timely processing on all claim submissions, follow standardized Medicare billing practices. Be sure to include the
member’s 11-digit AARP membership ID number. If you have questions or need more information please call UnitedHealthcare
Customer Service at 1-800-523-5800
Free Medicare education for your staff and patients
Medicare Made Clear (MMC) is our public service campaign that gives consumers the information they need to select a
Medicare benefit plan that is right for them. Consumers can easily access important information on topics such as the parts
of Medicare, enrollment timing, what’s covered (and what’s not) and what they need to know to make good choices on our
reference website MedicareMadeClear.com.

65
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 6: Referrals
Referrals vs. advance notification and/or prior authorization
The referral process, advance notification process and prior authorization process are separate processes. You must follow the
requirements when providing a service that requires a notification and/or prior authorization.
A referral does not replace the notification and/or prior authorization process.
Referral submission requirements
1
Referrals must be submitted by the member’s PCP or by a PCP within the same provider group and tax ID number. Specialists
can’t enter referrals in our system. They must ask the member’s PCP to enter a referral. Referrals are accepted to network
physicians only.
The member’s assigned PCP must:
• Submit referrals electronically, prior to the service being rendered, using:
– API | uhcprovider.com/api.
– EDI Transaction 278 | uhcprovider.com/edi278.
– UnitedHealthcare Provider Portal | Click Sign In in the top right corner of uhcprovider.com.
– Delegated entity’s website listed on the member’s ID card.
• Enter a start date within 5 calendar days of submission date.
– Referrals are effective immediately but may take up to 2 business days to be viewable in the portal system. They may be
backdated up to 5 calendar days before the date of entry.
• Follow all requirements.
– If you provide services when a referral is not on file, see the product-specific details in the following section for the impact
to your reimbursement and the member benefits, as this varies by product.
If you need to refer a member to an out-of-network provider because there are no available network providers in the area,
request prior authorization by calling the Provider Services number on the member’s ID card. You can also sign into the
UnitedHealthcare Provider Portal by going to uhcprovider.com and clicking on Sign In in the top right corner. Then, select Prior
Authorizations from the drop-down menu in the portal.
Maximum referral visits
The PCP determines the number of visits, up to the allowed max, needed for each referral in a 6-month period. They may submit
another referral after the member uses the visits or they expire.
Commercial products referrals
These referral requirements apply to covered services given to commercial members enrolled in the following plans:
• Navigate, Navigate Balanced, Navigate Plus
• NavigateNOW
• Charter, Charter Balanced, Charter Plus
• Compass, Compass Balanced, Compass Plus
• Most Individual Exchange Plans (for more information, refer to Chapter 4: Individual Exchange Plans)
• NexusACO R, NexusACO RB, NexusACO RP
1
Delegated may follow different referral submission requirements.
Chapter 6: Referrals
66
2023 UnitedHealthcare Care Provider Administrative Guide
Not obtaining a referral for a required service means that:
Navigate, NavigateNOW, Charter, Compass and NexusACO R NexusACO RB, NexusACO RP, and Balanced and Plus
versions of Navigate, NavigateNOW, Charter and Compass
The service is not covered, and the member is responsible for
the charges.
There is a higher out-of-pocket cost for the member.
Commercial members of gated benefit plans have “PCP to send electronic referral” printed on the back of their ID card and
“Referrals Required” on the front of the ID card.
Specialist referrals
The member’s assigned PCP manages their care. The member’s PCP needs to submit electronic referrals to us before the
member sees another network provider (a network provider that is not within the same provider group and tax ID number as
the member’s PCP). Referrals are valid for any health care provider within the same provider group and tax ID number as the
specialist listed. It is best practice to communicate clinical findings to the referring PCP. For tiered benefit plans, members will
have a lower out-of-pocket cost when referred to a tier 1 specialist.
Direct PCP referrals (ME only)
If a member needs covered health care services, you must accept a referral from a direct PCP; they are treated the same
regardless of whether the referring physician is a PCP or DPC provider. UnitedHealthcare may require a direct PCP making a
referral (who is not a member of the carrier’s provider network) to provide information demonstrating the health care provider is
a direct PCP through a written attestation or a copy of a direct primary care agreement with a member. To request a referral to
an in-network health care provider, call the member phone number on the member health plan ID card.
Referral submission and status verification
There are multiple ways to submit referrals electronically to UnitedHealthcare:
1. API | uhcprovider.com/api
2. EDI: Transaction 278 | uhcprovider.com/edi278
3. Online: UnitedHealthcare Provider Portal | Click Sign In in the top right corner of uhcprovider.com
Managing referrals
Specialists and facilities must check the status of a referral for the admitting physician’s TIN before each visit. For planned
admissions and health care provider outpatient services, facilities must check that the servicing physician has a referral to
see the member. If not, the facility claim may not be covered, or the member may have a higher cost-share. Referrals are
for the specialist rendering the service or for the facility. You should review a list of referrals related to the member in the
UnitedHealthcare Provider Portal when verifying the member’s eligibility.
• Referrals are only valid for the authorized number of visits or through the indicated referral end date. Any unused visits are not
valid after the end date.
• If a referral is no longer valid, but the member requires additional care, the member or specialist must contact the member’s
PCP to request a new referral. The PCP then decides whether to issue an additional referral.
• If a network specialist sees a need for a member to go to another specialist, the specialist must ask the member’s PCP to
issue an additional referral.
Online submissions of referrals
Referral submissions are separate from both notification and
prior authorization requests. Use the Referrals tool on the
UnitedHealthcare Provider Portal to submit referrals.

Chapter 6: Referrals
67
2023 UnitedHealthcare Care Provider Administrative Guide
Commercial benefit plan services not requiring a referral
Members in these plans do not need a referral for:
• Services from network physicians in the same provider group and TIN as the member’s PCP or their covering network
physicians.
• Services from network OB/GYN specialists, nurse practitioners, nurse midwives and physicians assistants.
• Routine refractive eye exam from a network provider.
• Network optometrists.
• Mental health/substance use services with network behavioral health clinicians.
• Services rendered in any emergency room, network urgent care center or network convenience care clinic.
• Services performed by a designated virtual care network provider (e.g., Teladoc) for primary or urgent care needs.
• Services billed as observation.
• Admitting physician services for emergency/unscheduled admissions.
• Services from facility-based inpatient/outpatient network consulting physicians, network assisting surgeons, network co-
surgeons or network team surgeons.
• Services from a network pathologist, network radiologist or network anesthesia physician.
• Outpatient network lab, network X-ray or network diagnostic services.
– Services billed by a network specialist require referral.
• Network rehabilitative services with exception of manipulative treatment and vision therapy (physician services).
– Services billed by a network specialist require referral.
• Other services for which applicable law does not allow us to impose a referral requirement.
• Newborn hospital stay, either routine or extended stay.
• Pediatric vision and dental for routine services.
• Immunization services at a network pharmacy.
Refer to Chapter 4 for individual exchange plans.
Referral submission requirements
• Submit electronic referrals to UnitedHealthcare before rendering services.
• Referrals are effective immediately.
• They are viewable online within 48 hours.
• We do not accept referrals by phone, fax or paper, unless state law requires us to.
• The PCP can backdate them up to 5 calendar days from the date of submission.
• Web users must have access to the Referral Submission role on their user profile to submit and verify referrals.
• Only the member’s PCP, or other PCP practicing under the same provider group and TIN, can submit referrals for the
member to see a network specialist. A specialist cannot enter a referral.
Maximum referral visits
The PCP may submit up to 6 visits on a referral. Unused visits expire after 6 months. For members with the following chronic
conditions, the PCP may submit up to 99 visits for up to 6 months per referral:
• AIDS/HIV
• Anemia
• Cancer
• Cystic Fibrosis
• Schizophrenia spectrum and other psychotic disorders
• Parkinson’s Disease
• Amyotrophic Lateral Sclerosis

Chapter 6: Referrals
68
2023 UnitedHealthcare Care Provider Administrative Guide
• Multiple Sclerosis
• Epileptic seizure
• Myasthenia Gravis
• Glaucoma
• Retinal detachment
• Thrombotic Microangiopathy
• Allergic Rhinitis
• Renal failure (acute)
• Seizure
• Fracture care
Non-participating health care providers (all Commercial
plans)
In non-emergent circumstances, you are required to refer our members to an in-network provider. You can confirm if a health
care provider is in our network at uhcprovider.com, or call 1-877-842-3210 or 1-888-478-4760 (Individual Exchange Plans).
For an exception to this requirement, you must do one of the following:
1. Follow the prior approval process outlined in the next paragraph.
2. Get the member’s written consent to involve an out-of-network provider.
To get prior approval to involve an out-of-network provider, submit a request by calling the number on the back of the member’s
ID card. We review the request and network providers available. If approved, we will apply the network benefits to the services
done by the out-of-network provider. We will mail our decision to the requesting health care provider and the member.
To get a member’s written consent to involve an out-of-network provider, you must use the Member Consent for Referring Out-
of-Network form. This form is located on uhcprovider.com > Resources > Plans, policies, protocols and guides > Protocols >
Member Consent for Referring Out-of-Network form. The member must acknowledge that you:
1. Summarized the reason you are referring them to an out-of-network provider.
2. Disclosed whether you have a financial interest in, or relationship with, the health care provider to whom you are referring
the member.
3. Explained the member may have no coverage or additional costs as a result of your referral.
– Some members may have additional costs for services they receive from out-of-network providers. Some members don’t
have any out-of-network benefits, which means the out-of-network provider will bill the member for the entire cost of the
referred service.
For referrals to an out-of-network laboratory, go to eligibility and benefits in the UnitedHealthcare Provider Portal to provide us
with the completed Member Consent for Referring Out-of-Network form.
If you violate this protocol, and do not confirm the member’s consent for the referral, you will be in violation of our Agreement.
As a result, we may:
1. Disqualify you from any rewards or incentive program.
2. Decrease your fee schedule.
3. Hold you financially responsible for any costs collected from a member by a non-participating healthcare provider and
hold you financially responsible for any payments made to a non-participating health care provider(s) as a violation of this
protocol.
4. Terminate your agreement.

Chapter 6: Referrals
69
2023 UnitedHealthcare Care Provider Administrative Guide
Before submitting a request for network benefits for services from a non-participating
health care provider:
1. See if there is a network provider available by searching on the Physician Directory.
2. If a network provider is not available, see if the W500 icon appears on the back of the member’s ID card.
– If W500 is indicated, search for a network provider in the W500 Emergent Wrap directory.
› If you find a W500 Emergent Wrap health care provider, submit a request for coverage for the member to see that
health care provider.
– If W500 is not on the member’s ID card or you cannot find a network provider in the W500 Emergent Wrap Directory,
continue submitting your request.
To find a list of health care providers participating in the W500 network, go to uhcprovider.com/findprovider > Search for Care
Providers in the General UnitedHealthcare Plan Directory > Medical Directory > Employer and Individual Plans > Shopping
Around > W500 Emergent Wrap.
Individual exchange referral required plan
Refer to Chapter 4: Individual Exchange Plans for referral requirements for Exchanges in AL, AZ, FL, GA, IL, LA, MI, MD, NC,
OK, TN, TX, VA and WA.
Medicare Advantage (MA) referral required plans
Some UnitedHealthcare Medicare Advantage benefit plans require referrals for specialty care. These plans emphasize the
role of the member’s primary care provider (PCP). The PCP will manage referrals when a member seeks care from a network
specialist or other health care professional. The PCP will also determine the appropriate number of visits and the timing for the
referral and can submit additional referrals if a referral expires. If the specialist doesn’t verify that a referral is in place, claims
will be denied and the member can’t be billed. Coverage, cost-share and benefits will be determined based on the member’s
benefit plan for services provided by a specialist.
Check the member’s ID card for referral language to see if the plan requires referrals. You can also check eligibility and benefits
or referrals in the UnitedHealthcare Provider Portal to see if referrals are required.
For more detailed information and to see a sample ID card, refer to the Health plan identification (ID) cards section of Chapter
2: Provider responsibilities and standards.
MA services not requiring a referral
1
These services do not require a referral. However, they may require notification and/or prior authorization. For information on
authorization requirements, refer to uhcprovider.com/priorauth.
• Any service provided by a network PCP
• Any service provided by a network physician practicing under the same tax ID as the member’s PCP
• Any service from a network OB/GYN, chiropractor, optometrist, ophthalmologist, optician, podiatrist, audiologist, oncologist,
nutritionist or disease management and infectious disease specialist
• Services performed while in an observation setting
• Allergy immunotherapy injections
• Mental health/substance use services with behavioral health clinicians
• Any service from a pathologist or anesthesiologist
• Any service from an inpatient consulting physician including hospitalists
• Services rendered in an emergency room, emergency ambulance or a network urgent care center or convenience clinic
• Telehealth (virtual visits) for medical and mental health services
1
Delegated benefit plans may follow a separate referral exclusion list. For Preferred Care Network and Preferred Care Partners of Florida plans, refer to the Preferred Care Network and Preferred Care Partners
supplements.

Chapter 6: Referrals
70
2023 UnitedHealthcare Care Provider Administrative Guide
• Medicare-covered preventive services, kidney disease education or diabetes self-management training
• Routine annual physical exams, vision or hearing exams
• Any lab services and radiological testing service, excluding radiation therapy
• DME, home health, prosthetic/orthotic devices, medical supplies, diabetic testing supplies and Medicare Part B drugs
• Additional benefits that may be covered by some MA benefit plans but are not covered by Medicare, such as hearing aids,
routine eyewear, fitness memberships or outpatient prescription drugs
• Services obtained while accessing the UnitedHealthcare Medicare National Network or UnitedHealth Passport®, which allows
for services while traveling
71
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 7: Medical management
The purpose of the UnitedHealthcare Medical Management Program is to determine if medical services are:
• Covered under the member’s benefit plan.
• Clinically necessary and appropriate.
• Performed at the most appropriate setting for the member.
Advance notification/prior authorization protocol
For additional details on prior authorization requirements and processes unique to the Surest plan, see the Surest supplement
to this guide.
Benefit plans not subject to this protocol
Some benefit plans may have separate notification or prior authorization requirements. Refer to the Benefit plans subject
to this guide table in Chapter 1: Introduction and to the supplements of this guide for additional information for the plans
listed.
• UnitedHealthcare Options PPO: Depending on the member particular benefit plan, UnitedHealthcare Options PPO
health care providers may not be required to follow this protocol for Options PPO benefit plans unless members enrolled
in these benefit plans are responsible for providing notification/requesting prior authorization.
• UnitedHealthcare Indemnity
• UnitedHealthOne - Golden Rule Insurance Company (“GRIC” group number 705214) only
• M.D.IPA, Optimum Choice or OneNet PPO
• Benefit plans subject to the Neighborhood Health Partnership (NHP) Supplement
• Benefit plans subject to the Oxford Commercial Supplement, except for UnitedHealthcare Oxford Navigate Individual
benefit plans (group number 908410)
• Benefit plans subject to the River Valley Entities Supplement
• Benefit plans subject to the UnitedHealthcare West Supplement
• Medicare Advantage (MA) plans that have delegated arrangements with medical groups/IPAs - in these arrangements, the
delegate’s protocols must be followed. Submit prior authorizations as directed on the member’s ID card.
• Benefit plans subject to an additional guide or supplement (refer to the Benefit plans subject to this guide table).
• Other benefit plans such as Medicaid, CHIP and Uninsured that are neither Commercial nor MA.
The advance notification requirements outlined in this protocol do not apply to services subject to the following protocols:
• Outpatient cardiology notification/prior authorization protocol
• Outpatient radiology notification/prior authorization protocol
• Laboratory services protocol
Each are addressed in separate sections later in this guide.
Advance notification vs. prior authorization
Advance notification is the first step in determining coverage. We also use it for case and condition management program
referrals. The information we receive about planned medical services helps support the pre-service clinical coverage review and
care coordination. Advance notification helps assist members from pre-service planning to discharge planning.
Advance notification is required for services listed on the Advance Notification/Prior Authorization List located at uhcprovider.
com/priorauth > Advance Notification and Plan Requirement Resources.
We require prior authorization for all MA benefit plans and some commercial benefit plans. Prior authorization requests allow
us to verify if services are medically necessary and covered. After you notify us of a planned service listed on the Advance
Notification/Prior Authorization List, we tell you if a clinical coverage review is required, as part of our prior authorization
process, and what additional information we need to proceed. We notify you of our coverage decision within the time required
Chapter 7: Medical management
72
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare Web Support
providertechsuppor[email protected]
1-866-842-3278, Option 1, Monday–Friday, 7 a.m. – 9 p.m. CT
Prior Authorization
and Notification tool
uhcprovider.com
Enhanced functionality in the Prior
Authorization and Notification tool in the
UnitedHealthcare Provider Portal that may
provide improved response times for all
plans.
Resources:
Access and New User Registration
• uhcprovider.com/access and new user registration
Interactive Guide for Prior Authorization and Notification in the
UnitedHealthcare Provider Portal
• Use this guide for more details on how to verify requirements,
create submissions and check status.
Resource Page
• Go to uhcprovider.com/paan for more resources. You’ll
find self-paced modules, live-webinar training registration
information and more.
No need to call, fax or mail
information so you can
spend time on other things.
Save time Reduce costs
Online solutions are the most
efficient and cost-effective
way to manage these
transactions.
Get information
Check if prior authorization
or notification is required by
member or procedure code.
Intuitive and accurate
Required information is
highlighted, and fields
automatically adjust as data
is entered. Error messages
alert corrections needed
before submitting.
Superior
documentation
Obtain a Decision ID for
inquiries and a reference
number for submissions.
Save PDF confirmation files
or print records as you wish.
Find and check status
Many search options are
available to check the
status of your submissions,
regardless of the submission
method you used.
• Check requirements by
member or procedure
• Submit requests
• Upload medical notes
• Check status
• Update cases
• Radiology, cardiology and
oncology transactions
• Specialty pharmacy
transactions
• Admission notification,
discharge notification and
observation stay notification
by law. Just because we require notification for a service does not mean
it is covered. We determine coverage by the member’s benefit plan.
If there is a conflict or inconsistency between applicable regulations and
the notification requirements in this guide, the applicable regulations
govern.
Advance notification/prior
authorization requirements
Physicians, health care professionals and ancillary health care providers
are responsible for:
• Providing advance notification or requesting prior authorization for
services on the Advance Notification/Prior Authorization List, including
for non-emergent air transport services.
• Directing members to use health care providers within their network.
Members may be required to obtain prior authorization for out-of-
network services.
Facilities are responsible for:
• Obtaining prior authorization for non-emergent, fixed-wing
transportation services and using in-network, fixed-wing air
ambulance providers.
• Obtaining prior authorization for inpatient admission to skilled nursing
facility, acute inpatient rehabilitation and/or long-term acute care.
• Confirming coverage approval is on file (for services requiring advance
notification/prior authorization) prior to the date of service.
• Providing admission and discharge notification for inpatient services,
even if coverage approval is on file.
If you perform multiple procedures for a member in 1 day, and at least 1
service requires prior authorization, you must obtain prior authorization
for any of the services to be paid.
If you do not follow these requirements, we may deny claims. In
that case, you cannot bill the member. Advance notification or prior
authorization is valid only for the date of service or date range listed on
it. If services have not been rendered and the specified date of service
or date range has passed, you must contact us to update the date of
service or date range. When you contact us, we will advise if we will
require a new submission.
• Giving us advance notification, or receiving prior authorization from
us, is not a guarantee of payment, unless required by law or Medicare
guidelines. This includes regulations about health care providers on a
sanctions or excluded list, the Medicare preclusion list and/or health
care providers not included in the Medicare Provider Enrollment Chain
and Ownership System (PECOS)
1
list. Payment of covered services is
based on:
– The member’s benefit plan.
– Your eligibility for payment.
1
PECOS is the CMS online enrollment system where health care providers and health care entities are required to
register so they can manage their Medicare provider file and establish their Medicare specialty as eligible to order and
refer services/items.

Chapter 7: Medical management
73
2023 UnitedHealthcare Care Provider Administrative Guide
– Claim processing requirements.
– Your Agreement.
See Coverage and utilization management decisions section for additional details.
Information required for advance notification/prior authorization requests
Your request must have the following information:
• Member name and member health plan ID number
• Ordering health care provider name and TIN or NPI
• Rendering health care provider name and TIN or NPI
• ICD-10-CM diagnosis code
• All applicable procedure codes
• Anticipated date(s) of service
• Type of service (primary and secondary) procedure code(s) and, if relevant, the volume of service
• Place of service
• Facility name and TIN or NPI where service will be performed (when applicable)
• Original start date of dialysis (End Stage Renal Disease [ESRD] only)
If the member’s benefit plan requires a clinical coverage review, we may request additional information, as described in more
detail in the Clinical coverage review section.
Advance notification/prior authorization list
The list of services that require advance notification and prior authorization is the same. The process for providing notification
and submitting a prior authorization request is the same. Services that require prior authorization require a clinical coverage
review based on medical necessity.
View the most current and complete advance notification requirements,
including procedure codes and associated services, at uhcprovider.com/
priorauth > Advance Notification and Plan Requirement Resources.
Advance notification/prior authorization lists are subject to change. We will inform you of changes on uhcprovider.com/news.
Sign up to receive email updates at uhcprovider.com/subscribe.
If you need a paper copy of the requirements, contact your UnitedHealthcare Network Management representative or
provider advocate at uhcprovider.com > Contact us.
When to submit advance notification or prior authorization requests
We recommend that you submit advance notification with supporting documentation as soon as possible, but at least 2 weeks
before the planned service (unless the Advance Notification Requirements states otherwise). Following a facility discharge,
advance notification for home health services and DME is required within 48 hours after the start of service.
After submitting your request, you get a service reference number. This is not an authorization. When we make a coverage
determination, we issue it under this reference number.
It may take up to 15 calendar days (14 calendar days for standard MA requests and 72 hours for expedited requests) for us to
make a decision. We may extend this time if we need additional information. Submitting requests through the Prior Authorization
and Notification tool in the UnitedHealthcare Provider Portal assists in timely decisions.
We prioritize case reviews based on:
• Case specifics.
• Completeness of the information received.

Chapter 7: Medical management
74
2023 UnitedHealthcare Care Provider Administrative Guide
• CMS requirements.
• State or federal requirements.
If you require an expedited review, call the number listed on the member’s ID card. You must explain the clinical urgency. You
will need to provide required clinical information the same day as your request.
We expedite reviews upon request when the member’s condition:
• Could, in a short period of time, put their life or health at risk.
• Could impact their ability to regain maximum function.
• Causes severe, disabling pain (as confirmed by a physician).
DME
DME provides therapeutic benefits to a member because of certain medical conditions and/or illnesses. DME consists of items
which are:
• Primarily used to serve a medical purpose.
• Not useful to a person in the absence of illness, disability or injury.
• Ordered or prescribed by a health care provider.
• Reusable.
• Repeatedly used.
• Appropriate for home use.
• Determined to be medically necessary.
Refer to the following policies pertaining to DME for more information:
• Commercial Coverage Determination Guideline: uhcprovider.com > Resources > Plans, policies, protocols and guides >
For Commercial Plans > Medical & Drug Policies and Coverage Determination Guidelines for UnitedHealthcare Commercial
Plans > Durable Medical Equipment, Orthotics, Medical Supplies and Repairs/Replacements - Commercial Coverage
Determination Guideline
• Individual Exchange Coverage Determination Guideline: uhcprovider.com > Resources > Plans, policies, protocols and guides
> For Exchange Plans > Medical & Drug Policies and Coverage Determination Guidelines for UnitedHealthcare Individual
Exchange Plans > Durable Medical Equipment, Orthotics, Medical Supplies and Repairs/Replacements - Individual
Exchange Coverage Determination Guideline
• Coverage Summaries for Medicare Advantage Plans: uhcprovider.com > Plans, policies, protocols and guides > For Medicare
Advantage Plans > Coverage Summaries for Medicare Advantage Plans >
– Durable Medical Equipment (DME), Prosthetics, Corrective Appliances/Orthotics (Non-Foot Orthotics), Nutritional
Therapy and Medical Supplies Grid - Medicare Advantage Coverage Summary
– Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) Prosthetics, Corrective Appliances/
Orthotics and Medical Supplies - Medicare Advantage Coverage Summary
Facilities: Standard notification requirements*
Confirming coverage approvals
Before providing a service on the Advance Notification/Prior Authorization List, the facility must confirm coverage approval is
on file. This promotes an informed pre-service discussion between the facility and member. If the service is not covered, the
member can decide whether to receive and pay for the service.
If the facility performs the service without confirming a coverage approval is on file, and we decide the service is not a covered
benefit, we may deny the facility claim.
The facility may not bill the member or accept payment from the member due to the facility’s non-compliance with our
notification protocols.
*For state-specific variations, refer to uhcprovider.com/priorauth > Advance Notification and Plan Requirement Resources.
Chapter 7: Medical management
75
2023 UnitedHealthcare Care Provider Administrative Guide
Admission notification requirements
Benefit plans not subject to this protocol
Some benefit plans may have separate notification or prior authorization requirements. Refer to the Benefit plans subject
to this guide table in Chapter 1: Introduction and to the supplements of this guide for additional information for the plans
listed.
• UnitedHealthcare Options PPO: Depending on the member particular benefit plan, UnitedHealthcare Options PPO
health care providers may not be required to follow this protocol for Options PPO benefit plans unless members enrolled
in these benefit plans are responsible for providing notification/requesting prior authorization.
• UnitedHealthcare Indemnity
• M.D.IPA, Optimum Choice or OneNet PPO
• Benefit plans subject to the Neighborhood Health Partnership (NHP) Supplement
• Benefit plans subject to the Oxford Commercial Supplement, except for UnitedHealthcare Oxford Navigate Individual
benefit plans (group number 908410)
• Benefit plans subject to the River Valley Entities Supplement
• Benefit plans subject to the UnitedHealthcare West Supplement
• Medicare Advantage (MA) plans that have delegated arrangements with medical groups/IPAs - in these arrangements, the
delegate’s protocols must be followed. Submit prior authorizations as directed on the member’s ID card.
• Erickson Advantage
• Benefit plans subject to an additional guide or supplement (refer to the Benefit plans subject to this guide table).
• Other benefit plans such as Medicaid, CHIP and Uninsured that are neither Commercial nor MA.
Facilities are responsible for admission notification for the following inpatient admissions. We need admission notification, even
if the physician provided advance notification and pre-service coverage approval is on file:
• Planned/elective admissions for acute care
• Acute inpatient rehabilitation
• Long-term acute care
• Unplanned admissions for acute care
• SNF admissions
• Admissions following outpatient surgery
• Admissions following observation
• Newborns admitted to Neonatal Intensive Care Unit (NICU)
• Newborns who remain hospitalized after the mother is discharged
– Notice is required within 24 hours of the mother’s discharge.
Weekday admissions, you must notify us within 24 hours, unless otherwise indicated.
Weekend and holiday admissions, you must notify us by 5 p.m. local time on the next business day.
Emergency admissions (when a member is unstable and not capable of providing coverage information), you must:
• Notify us within 24 hours, or the next business day if on a weekend/holiday, from the time coverage information is known.
• When notifying us, you must communicate the extenuating circumstances.
Payment is not reduced due to notification delay in an emergency.
Receipt of an admission notification does not ensure payment. Payment for covered services depends on the member’s
benefits, facility’s contract, claim processing requirements and eligibility for payment.
You must include these details in your admission notification:
• Member name, health plan ID number and date of birth
• Facility name and TIN or NPI
• Admitting/attending physician name and TIN or NPI
• Description for admitting diagnosis or ICD-10-CM diagnosis code
• Actual admission date
• Extenuating circumstances, if an emergency admission

Chapter 7: Medical management
76
2023 UnitedHealthcare Care Provider Administrative Guide
All SNF admissions for UnitedHealthcare Nursing Home plan members must be authorized by an Optum nurse practitioner
or physician’s assistant. Claims may be denied if authorizations are not coordinated through Optum. All SNF admissions for
UnitedHealthcare Assisted Living plan members must be authorized by naviHealth. Claims may be denied if authorizations are
not coordinated through naviHealth. Submit prior authorization for SNF, acute inpatient rehabilitation and long-term acute care
through the UnitedHealthcare Provider Portal, naviHealth Access Provider Portal or by calling naviHealth at 1-855-851-1127.
SNF admissions directly from the member’s home setting may be authorized and coordinated by an Optum nurse practitioner
or physician’s assistant.
Discharge notification requirements
Hospitals must notify us of discharge from acute facility stays within 24 hours after weekday discharge (or by 5 p.m. local time
on the next business day if the 24-hour limit would require notification on a weekend or holiday). For weekend and holiday
discharges, we must receive the notification by 5 p.m. local time on the next business day.
Emergency services
Decisions regarding whether services met the definition of an “emergency” may be made by our Medical Director (or designee)
or another process. This determination is subject to appeal. You can find a definition of “emergency” in the Glossary.
Reimbursement reductions for lack of timely admission notification
Facilities must provide timely admission notification (even if the physician provided advance notification and pre-service
coverage approval is on file) or claims payments are denied in full or in part:
Notification time frame Reimbursement reduction
Admission notification received after it was due,
but not more than 72 hours after admission.
100% of the average daily contract rate
1
for the
days preceding notification.
Admission notification received after it was due,
and more than 72 hours after admission.
100% of the contract rate (entire stay).
No admission notification received. 100% of the contract rate (entire stay).
1
The average daily contract rate is calculated by dividing the contract rate for the entire stay by the number of days for the entire length of stay.
Note: We do not apply reductions for maternity admissions. We apply reductions for post-acute inpatient admissions on our
Commercial plans, but we do not apply them on our MA plans.
Maryland state-specific notification requirements for facilities
If advance notification or prior authorization is required for an elective inpatient procedure, the physician must get the approval.
The facility must notify us within 24 hours (or the following business day if the admission occurs on a weekend or holiday) of
the elective admission. If the physician gets the approval, but the facility does not get theirs within a timely manner, we reduce
payment to only room and board charges.
If the physician received coverage approval, we pay the initial day of the inpatient admission unless any of the following are true:
1. The information submitted to us regarding the service was false or intentionally misrepresentative.
2. Critical information requested by us was missing and our determination would have been different had we known
the information.
3. A planned course of treatment approved by us was not followed.
4. On the date the preauthorized or approved service was delivered: (i) the individual was not covered by UnitedHealthcare,
(ii) a member eligibility verification system was available to the health care professional by phone or internet, and (iii) the
member eligibility verification system in the UnitedHealthcare Provider Portal shows no coverage.
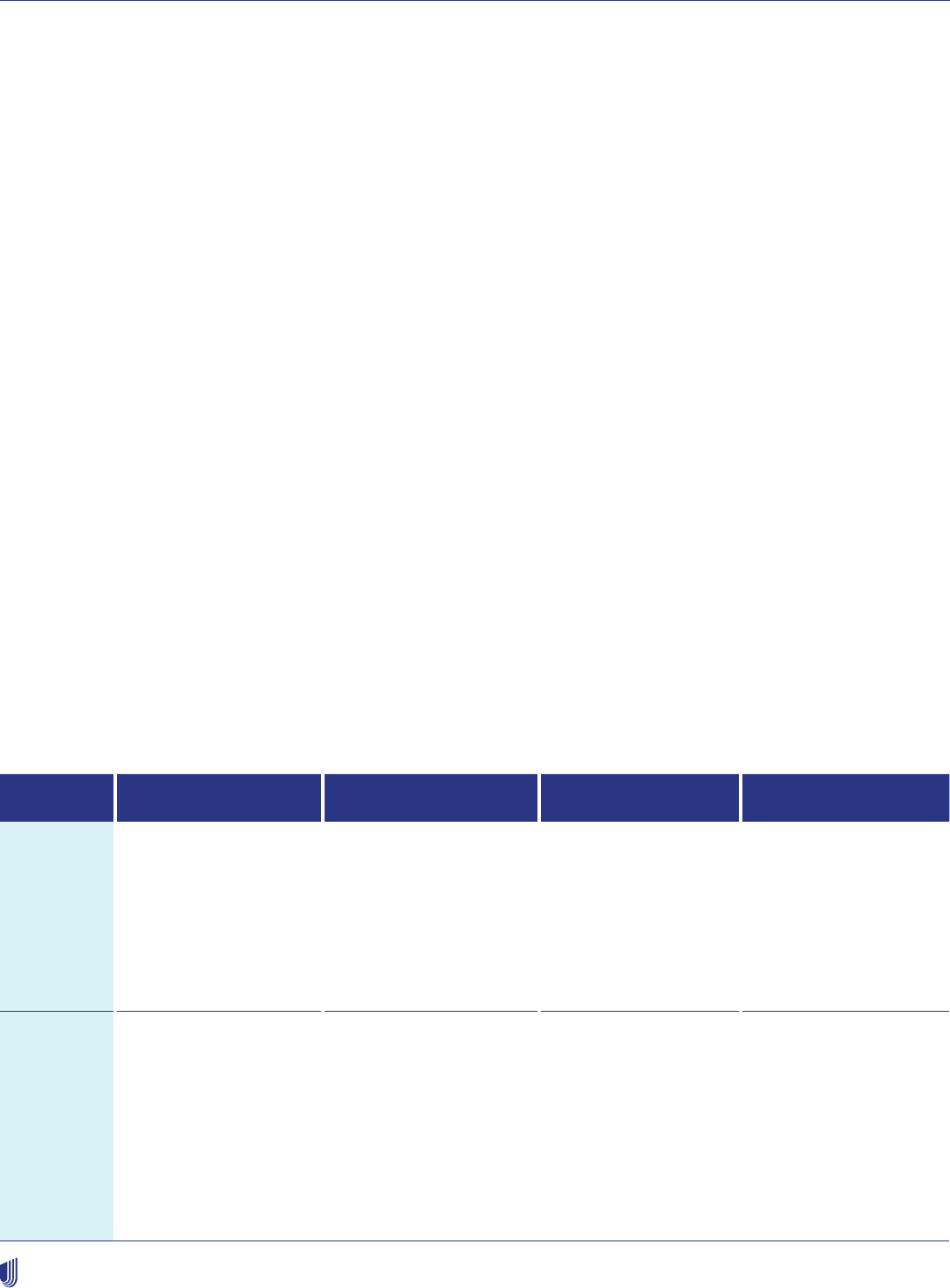
Chapter 7: Medical management
77
2023 UnitedHealthcare Care Provider Administrative Guide
Inpatient review: clinical information
We determine the medical necessity of inpatient admissions through either concurrent or retrospective review. We require you
to comply with our requests:
• For information, documents or discussions related to our reviews and discharge planning. This includes primary and
secondary diagnosis, clinical information, treatment plan, admission order, patient status, discharge planning needs, barriers
to discharge and discharge date. When available, provide access to electronic medical records (EMR).
• From our interdisciplinary care coordination team and/or Medical Director. This includes our requests that you help us
engage our members directly face-to-face or by phone.
– If you receive the request before 1 p.m. local time:
› Supply all requested information within 4 hours
– If you receive our request after 1 p.m. local time:
› Provide the information within the same business day, but no later than 12 p.m. local time the next business day
Facility denial process
We issue a denial letter if the level of care or any inpatient bed days are not medically necessary. We decide this through
concurrent or retrospective review. We use nationally recognized criteria and guidelines to determine if the service/care was
medically necessary under the member’s benefit plan. We can provide the criteria to you upon request.
A facility denial letter is sent to the member and copied to the admitting physician, the PCP (if applicable) and the facility, as
required.
How to submit advance notification/prior authorization,
admission notification, discharge notification and
observation stay notification
You can submit notifications and prior authorizations many ways. After receiving confirmation, do not resubmit your request.
Submit prior authorization for SNF, acute inpatient rehabilitation and long-term acute care through the UnitedHealthcare
Provider Portal (preferred) or phone. For markets where naviHealth manages post-acute care, notification and prior
authorization follows the naviHealth process.
API EDI 278 transactions Online
uhcprovider.com
Live call
Method Electronic
uhcprovider.com/api
Electronic
uhcprovider.com/edi278
Advance Notification
and Prior Authorization
(278) and uhcprovider.
com/edi278n Admission
Notification, Discharge
Notification, Observation
Stay Notification (278N).
Electronic
uhcprovider.com/paan
Non-Electronic
Advance notification
and prior authorization,
admission and
discharge notification
and observation stay
notification; notification
status for previously
submitted notifications.
Description Referral submission and
status is available.
12 different EDI
submissions
available directly to
UnitedHealthcare or
through a clearinghouse.
Submit, update or
check the status of an
advance notification,
prior authorization or
admission notification,
discharge notification
or observation stay
notification request.
Phone submission
directly to
UnitedHealthcare through
1-877-842-3210 (option
3) or dial the number
provided on member’s ID
card.
For Erickson Advantage,
call Erickson Campus
customer service number
on the member’s ID card.
Chapter 7: Medical management
78
2023 UnitedHealthcare Care Provider Administrative Guide
API EDI 278 transactions Online
uhcprovider.com
Live call
Business
hours
(all times
Eastern)
uhcprovider.com:
Generally available 24
hours per day, 7 days a
week. Maintenance is
scheduled outside of the
following hours:
Monday–Friday:
6:30 a.m.–12 a.m.
Saturday: 7 a.m.–6 p.m.
Sunday: 7 a.m.–5 p.m.
Holidays: Same as above
Monday–Friday:
7 a.m.–2 a.m.
Saturday: 7 a.m.–6 p.m.
Sunday: 7 a.m.–6 p.m.
Holidays: Same as above
uhcprovider.com:
Generally available 24
hours per day, 7 days a
week. Maintenance is
scheduled outside of the
following hours:
Monday–Friday:
6:30 a.m.–12 a.m.
Saturday: 7 a.m.–6 p.m.
Sunday: 7 a.m.–5 p.m.
Holidays: Same as
above
Monday–Friday: 7 a.m.–
8 p.m.
Saturday: 9 a.m.–6 p.m.
Sunday: 9 a.m.–6 p.m.
Holidays: 9 a.m.–6 p.m.
Some plans have a state requirement for fax capability for prior authorization requests and will continue to use their existing fax number for their members. However, you can still use the Prior Authorization and
Notification tool in the UnitedHealthcare Provider Portal to submit requests for those plans. A listing of active fax numbers as well as information regarding retired and retiring fax numbers can be found at
uhcprovider.com/priorauth.
Updating advance notification or prior authorization requests
Before services are rendered, you may make certain updates to your notification/prior authorization request, depending on the
status of the request and whether the service date has passed.
You may contact us at uhcprovider.com/paan, by phone at 1-877-842-3210, 1-888-478-4760 (Individual Exchanges) or the
number provided on the member’s ID card, and we will let you know whether we updated your notification/prior authorization
request.
If, during the service, you perform an additional or different procedure than what was originally approved, you are not required
to modify the existing notification/prior authorization request, or request a new notification/prior authorization record for code
combinations on the Prior Authorization Crosswalk table available at uhcprovider.com.
For code combinations not listed on the Prior Authorization Crosswalk table, you must contact us within 5 business days of
rendering the service to advise of the changed or added procedure. If you do not contact us within 5 business days to advise of
the changed or added procedure for code combinations not listed on the Prior Authorization Crosswalk table, and if the added
or changed service is reduced or denied for lack of pre-service notification, you can request a clinical review by submitting
records indicating why the original procedure code was changed or a new procedure code was added.
If we do not approve the notification/prior authorization request, you cannot make updates to it. You may submit an appeal by
following the instructions listed in the adverse determination letter we send you.
This section applies to Commercial members only. It does not apply to notification/prior authorization requests for genetic and
molecular testing, BRCA, oncology, radiology, cardiology and injectable medications.
Coverage and utilization management decisions
We base coverage decisions, including medical necessity decisions, on:
• Member’s benefits.
• State and federal requirements.
• The contract between us and the plan sponsor.
• Medicare guidelines including national coverage determination (NCD) and local coverage determination (LCD) guidelines.
• Medicare Benefit Policy Manual (MA members).
• UnitedHealthcare medical policies, medical benefit drug policies, coverage determination guidelines, utilization review
guidelines and MA coverage summaries.

Chapter 7: Medical management
79
2023 UnitedHealthcare Care Provider Administrative Guide
Our employees, contractors and delegates do not receive financial incentives for issuing non-coverage decisions or denials.
We and our delegates do not offer incentives for underutilization of care/services or for barriers to care/service. We do not hire,
promote or terminate employees or contractors based on whether they deny benefits.
We use tools such as UnitedHealthcare medical policies and third-party resources (such as InterQual® criteria and other
guidelines), to assist us in administering health benefits and determining coverage.
These tools and resources are not equivalent to the practice of medicine or medical advice, and you should use them in
addition to independent, qualified medical judgment.
Clinical coverage summaries and policy guidelines for Medicare Advantage
We follow CMS guidance (including NCD and LCD guidelines) if the tools and resources we use contradict CMS guidance. If we
do not perform a pre-service clinical coverage review, we may use Medicare guidelines, including NCD and LCD guidelines, to
perform a clinical review when we receive the claim.
The complete libraries of our MA policy guidelines and coverage summaries are on uhcprovider.com/policies > Medicare
Advantage Policies.
Coverage decisions
Some plans require prior authorization through a pre-service clinical coverage review. Once you notify us of any planned
service, item or drug on our Advance Notification/Prior Authorization List, we will inform you of any required information
necessary to complete the clinical coverage review as part of our prior authorization process. We will notify you of the coverage
decision within the time frame required by law.
You and our member must be aware of coverage decisions before you render services. If you provide the service before a
coverage decision is made, and we determine the service is not covered, we may deny the claim. The member cannot be billed.
If you provide services prior to our decision, the member cannot make an informed decision about whether to pay for and
receive the non-covered service.
Clinical coverage review
You can review a list of required information by service on uhcprovider.com/protocols > Medical Record Requirements for
Pre-Service Reviews. If you submit required information with the advance notification/prior authorization, your review will go
faster. You must:
• Return calls from our care management team and/or Medical Director.
• Submit the most correct and specific code available for the services.
• Comply with our request for additional information or documents and discussions, including requests for medical records
and imaging studies/reports.
– If you receive our request before 1 p.m. local time, provide the information within 4 hours.
– If you receive our request after 1 p.m. local time, provide the information no later than 12 p.m. local time the next
business day.
Medical & drug policies and coverage determination guidelines for commercial members
A complete library of our medical policies and guidelines is available
on uhcprovider.com/policies > Commercial Policies > Medical & Drug
Policies and Coverage Determination Guidelines.
We develop medical policies, medical benefit drug policies, coverage determination guidelines and utilization review guidelines
to support the administration of medical benefits. You may request a copy of our medical policies and guidelines by calling
our care management team at 1-877-842-3210 or 1-888-478-4760 (Individual Exchange Plans). They are only for informational
purposes; they are not medical advice. You are responsible for deciding what care to give our members. Members should
talk to their health care providers before making medical decisions. Drug policies for commercial members covered under the
pharmacy benefit are on uhcprovider.com/pharmacy.

Chapter 7: Medical management
80
2023 UnitedHealthcare Care Provider Administrative Guide
Benefit coverage is determined by the following:
• Laws that may require coverage
• The member’s benefit plan document
– Summary Plan Description
– Schedule of Benefits
– Certificate of Coverage
The member’s benefit plan document identifies which services are covered, which are excluded and which are subject to
limitations. If there is a conflict, the member’s benefit plan document supersedes our policies and guidelines.
We develop our policies and guidelines as needed. We regularly review and update them. They are subject to change. We
believe the information in these policies and guidelines is accurate and current as of the publication date. We also use tools
developed by third parties, such as InterQual criteria, to help us manage health benefits. If you believe we should consider new
or additional clinical evidence pertaining to a specific medical policy, complete this form for UnitedHealthcare medical policy
review. Do not submit protected health information using this form. If you have questions or concerns about a specific service
for a member, refer to the appropriate benefits, claims or prior authorization/notification process.
Medical policy updates
For more information on medical policy updates, refer to Chapter 18: Provider communications.
Clinical trials, experimental or investigational services
Experimental items and medications have limited coverage. We do not delegate utilization management for experimental or
investigational services or clinical trials.
Commercial
Members with cancer may have coverage for routine costs related to the cancer clinical trial. It depends on the state. You
should consider recommending the clinical trial if there is a potential for the member to benefit.
Medicare Advantage (MA)
Experimental and investigational procedures, items and medications are not a covered MA benefit. Call us at 1-877-842-3210
or 1-888-478-4760 (Individual Exchanges) for a clinical coverage review.
Certain clinical trials are a benefit of MA plans. You should bill Medicare directly. Members can get additional information on
clinical trials by calling 1-800-MEDICARE.
Approval or denial of clinical trials
After a clinical review, we send a determination notice to the member and health care provider. An experimental/investigational
denial requires a disclosure of additional rights. It also requires information regarding the independent external review process.
This includes:
• An Independent Medical Review (IMR) packet.
• Physician certification form (commercial only).
• One-page application form and addressed envelope that the member returns to the Department of Managed Health Care to
request the IMR (CA only).
Evaluations prior to entry into a clinical trial
Evaluations, tests and consultations are benefits of both the commercial and MA plans. Coverage for these does not change
if the member does not qualify for a clinical trial. For capitated health care providers, the member’s health care provider is
responsible for these tests, unless stated differently in your contract.

Chapter 7: Medical management
81
2023 UnitedHealthcare Care Provider Administrative Guide
You can find more information on clinical trials and experimental procedures in:
• Commercial: The Coverage Determination Guideline for Clinical Trials available on uhcprovider.com/policies > For
Commercial Plans > Medical & Drug Policies and Coverage Determination Guidelines for UnitedHealthcare Commercial Plans
> [search for] Clinical Trials.
• MA: The Coverage Summary for Experimental Procedures and Items, Investigational Devices and Clinical Trials is available
on uhcprovider.com/policies > For Medicare Advantage Plans > Coverage Summaries for Medicare Advantage Plans.
• Individual Exchange Plans: The Coverage Determination Guide for Clinical Trials is available on uhcprovider.com/policies
> For Exchange Plans > Medical & Drug Policies and Coverage Determination Guidelines for UnitedHealthcare Individual
Exchange Plans > [search for] Clinical Trials.
Medical management denials/adverse determinations
We may issue denials/adverse determinations. We issue these when:
• The service, item or drug is not medically necessary.
• The service, item or drug is not covered.
• We receive no supporting (or incomplete) information.
If you disagree with our determination, you may appeal on behalf of the member. Appeal information is on the determination
letter we send you. Our medical reviewers are able to discuss the denial with the treating or attending health care provider.
We make our authorization determination and communicate it based on the member’s medical condition and following state
and federal law.
We base our decisions on sound clinical evidence. This includes:
• Medical records review.
• Consultation with the treating health care providers.
• Review of nationally recognized criteria; for example, Medicare Coverage Criteria.
Denials, delays or modifications
Requests that do not meet the criteria for immediate authorization are reviewed by the Medical Director or the Utilization
Management Committee (UMC), designated health care provider or presented to the collective UMC or subcommittee.
Only a health care provider (MD or DO, psychiatrist, doctoral level clinical psychologist or certified addiction medicine specialist,
as appropriate) may delay, modify or deny services to a member for reasons of medical necessity. We use board-certified
licensed health care providers from appropriate specialty areas to help determine medical necessity.
• Health care providers will not review their own referral requests.
• Our qualified staff members review referral requests being considered for denial.
• Any referral request where the medical necessity or the proposed treatment plan is not clear can be clarified by discussion
with the health care provider thereafter. Complex cases go to the UMC/Medical Director for further discussion and decision.
• Individual(s) who meet the qualifications of holding financial ownership interest in the organization may not influence the
clinical decision making regarding payment or denial of a service.
• Prior authorization determinations may include the following decision:
– Approved as requested — No changes.
– Approved as modified — Referral approved, but the requested health care provider or treatment plan is modified. Denial
letter must be sent if requested health care provider is changed or specific treatment modality is changed (e.g., requested
chiropractic, approved physical therapy).
– Extension — Delay of decision regarding a specific service (e.g., need additional documentation, information, or require
consultation by an expert reviewer).

Chapter 7: Medical management
82
2023 UnitedHealthcare Care Provider Administrative Guide
– CMS allows delays of decision (extensions) for MA members when the extension is justified and in the member’s interest:
› Due to the need for medical evidence from a non-contracted health care provider that may change the decision to deny
an item or service.
› Due to extraordinary, exigent or other non-routine circumstances and is in the member’s interest.
– Delay in Delivery — Access to an approved service postponed for a specified period or until a specified date will occur. This
is not the same as a modification. A written notification in the denial letter format is required.
– Denied — Non-authorization of a request for health care services. Reasons for denials of requests for services include, but
are not limited to, the following:
› Not a covered benefit — the requested service(s) is a direct exclusion of benefits under the member’s benefit plan — you
must note a specific benefit exclusion.
› Not medically necessary or benefit coverage limitation — specify criteria or guidelines used in making the determination
as it relates to the member’s health condition.
› Member not eligible at the time of service.
› Benefit exhausted — include specific information as to what benefit was exhausted and when.
› Not a network provider — a network provider/service is available.
› Experimental, investigational or unproven procedure/treatment.
› Self-referred/no prior authorization (for non-emergent post-service).
› Services can be provided by the PCP.
We have aligned reimbursement policy on Wrong Surgical or Other Invasive Procedure Events Professional Reimbursement
Policy to be consistent with CMS.
We do not reimburse for a surgical or other invasive procedure when the health care provider performs:
• A different procedure altogether.
• The correct procedure, but on the wrong body part.
• The correct procedure, but on the wrong member.
We do not reimburse facilities or professional services related to these wrong surgical or other invasive procedures.
Pre-service appeals
A pre-service appeal is a request to change a denial of coverage for a planned health care service. The member’s rights in the
member’s benefit plan govern this process. To submit a normal pre-service appeal request, follow the information in the pre-
service denial letter. A peer-to-peer review is highly recommended before you file a pre-service appeal.
Expedited or urgent appeals
If you have already provided the service, an expedited or urgent appeal is not available. Submit a claim based on the service
provided. See the appeal section for more information.
To request an urgent pre-service appeal on behalf of the member, follow the information in the pre-service denial letter. We
consider requests urgent when:
• The standard review time frame risks the life or health of the member.
• The member’s ability to regain maximum function is jeopardized.
• The member’s severe pain is not able to be managed without the care or treatment requested.
Medical records request submission time frame
If we request medical records to process an appeal, you must provide the information within the following time frames. This
includes providing a copy of the denial notice.
• Expedited appeal: Within 2 hours
1
of receipt of request
• Standard appeal: Within 24 hours
1
of receipt of request
1 Time frames may change based on applicable law or your Agreement.

Chapter 7: Medical management
83
2023 UnitedHealthcare Care Provider Administrative Guide
MA Part C reopenings
CMS requires us to adhere to the appropriate handling of reopenings of our determination. A reopening is a remedial action
taken to change a final determination or decision, even though the determination or decision was correct based on the evidence
of record.
Reopening reason categories:
• New and Material Evidence — documentation not previously available or known during the decision making process that
could possibly result in a different decision.
• Clerical Error — includes such human and mechanical errors as mathematical or computational mistakes, inaccurate coding
and computer errors, inaccurate data entry and denial of claims as duplicates.
• Fraud or Similar Fault — post-service decision when reliable evidence shows the decision was procured by fraud or similar
fault when the claim is auto-adjudicated in the system.
Reopening requests made by a member, member’s authorized representative or a non-contracted health care provider must be:
• Clearly stated.
• Include the specific reason for the reopening.
• In writing or verbal.
• Filed within the prescribed periods.
The request does not have to use the actual term “reopening.” We must process a clerical error as a reopening, instead of
an appeal.
A request for a reopening may occur under the following conditions:
• A binding determination or decision has been issued.
• The 60-calendar-day time frame for filing a reconsideration has expired.
• There is no active appeal pending at any level.
Types of determinations or requests that cannot be reopened are as follows:
• A pre-service determination cannot be reopened for any reason other than for a clerical error, unless the 60-calendar-day
period to file a reconsideration has expired.
• Upon receipt of previously requested documentation for a pre-service determination denied due to lack of information, the
delegate must consider and submit to us as a reconsideration, unless there is a clerical error.
• A pre-service determination made as part of the appeals process.
• Upon request for a peer-to-peer review following an adverse pre-service determination, if the member, member’s
representative or non-contracted health care provider provides new and material evidence not previously known or available,
which changes the decision or the rationale for the prior decision, we will not review as a reopening and will provide
instructions on how to file a reconsideration.
Impact on peer-to-peer requests
We offer a peer-to-peer discussion with the medical director that made the pre-service determination. Once a pre-service
adverse determination has been made, Medicare does not allow the decision to be changed as a result of the peer-to-peer
discussion. You must submit any additional information from the post decision discussion if you want to submit a Medicare
appeal.
To allow for a change in decision as a result of a peer-to-peer discussion, we have a pre-decision peer-to-peer window for
standard clinical denials (excludes expedited and administrative denials). This is for outpatient and inpatient pre-service
requests. We reach out to offer a 24-hour window, prior to finalizing a potential adverse determination, to allow for the
discussion between the physician and the medical director. If we receive additional information during this pre-decision peer-
to-peer window, it can change the final decision of the determination. If the discussion does not happen before the end of the
24-hour window, the decision is finalized and any peer-to-peer discussion that follows is informational only.
Chapter 7: Medical management
84
2023 UnitedHealthcare Care Provider Administrative Guide
Outpatient cardiology notification/prior authorization protocol
This protocol applies to commercial members and MA members. It does not apply to the following commercial or MA benefit
plans, or other benefit plan types including Medicaid, CHIP or uninsured benefit plans. The following benefit plans may
have separate cardiology notification or prior authorization requirements. Refer to Chapter 1: Introduction for additional
supplements or health care provider guides that may be applicable.
Commercial benefit plans not subject to these requirements
UnitedHealthcare Options PPO: Depending on the member particular benefit plan, UnitedHealthcare Options PPO health
care providers may not be required to follow this protocol for Options PPO benefit plans unless members enrolled in these
benefit plans are responsible for providing notification/requesting prior authorization.
UnitedHealthOne – Golden Rule Insurance Company
(“GRIC”) group number 705214 only
M.D.IPA, Optimum Choice, (See the Mid-Atlantic Regional Supplement) or OneNet PPO
Oxford (USA, New Jersey Small Group, certain NJ public Sector groups, CT public Sector, Brooks Brothers [BB1627] and
Weil, Gotshal and Manages [WG00101], any member at VAMC facility)
UMR and UnitedHealthcare Shared Services (UHSS)
UnitedHealthcare Indemnity/Managed Indemnity
Benefit plans sponsored or issued by certain self-funded employer groups
MA benefit plans may not be subject to these requirements
In some instances, we have delegated prior authorization services to a provider group. Call the number listed on the member’s
ID card. If you are a network provider who is contracted directly with a delegated medical group/IPA, then you must follow the
delegate’s protocols. Delegates may use their own systems and forms. They must meet the same regulatory and accreditation
requirements as UnitedHealthcare. Delegated plans include:
Arizona: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Group
92004; AARP Medicare Advantage Choice Plan 2 (PPO) - Group 92007; AARP Medicare Advantage Patriot (PPO) - Groups:
92008, 92015; AARP Medicare Advantage Patriot (PPO) - Group 90108; AARP Medicare Advantage Walgreens Plan 1
(PPO) - Groups 92001, 92002; AARP Medicare Advantage Walgreens Plan 2 (PPO) - Group 92006, 92009; AARP Medicare
Advantage Walgreens Plan 3 (PPO) - Group 92010
Arizona: The following groups are delegated to P3 Health Partners: AARP Medicare Advantage (HMO-POS) - Group 90192;
AARP Medicare Advantage Choice Plan 1 (PPO) - Groups 90196, 90601; AARP Medicare Advantage Choice Plan 2 (PPO)
- Groups 90197, 90602; AARP Medicare Advantage Patriot (PPO)- Groups 90198, 90603; AARP Medicare Advantage Plus
(HMO-POS) - Group 90191; AARP Medicare Advantage Walgreens Plan 1 (PPO) - Group 90195; AARP Medicare Advantage
Walgreens Plan 2 (PPO) - Group 90199; UnitedHealthcare Chronic Complete Assure (PPO C-SNP) - Groups 90303, 90600
Colorado: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Groups
90091, 90092, 90093, 90094, 91014, 91015, 91016, 91017; AARP Medicare Advantage Choice Plan 2 (PPO) - Groups
90039, 90057, 91012, 91013; AARP Medicare Advantage Choice Rebate (PPO) - Groups 90097, 90133; 90134, 90135,
91018, 91019, 91020, 91021; AARP Medicare Advantage Walgreens (PPO) - Groups 90095, 90096, 91010, 91011
Connecticut: The following groups are delegated to Advantage Plus Network: AARP Medicare Advantage Choice (PPO)
- Group 90125; AARP Medicare Advantage Choice (Regional PPO) - Groups 90150, 90151; AARP Medicare Advantage
Choice Flex (PPO) - Group 90223; UnitedHealthcare Medicare Advantage Patriot (HMO-POS) - Groups -27155, 27156,
27062, 27151, 27064, 27153, 27100, 27150
Chapter 7: Medical management
85
2023 UnitedHealthcare Care Provider Administrative Guide
Florida: The following groups are delegated to WellMed: AARP Medicare Advantage (HMO-POS) - Groups 82958,
82960, 82969, 82977, 82980, 90028, 90078, 90079; AARP Medicare Advantage Choice (PPO) - Groups 70342, 70343,
70344, 70345, 70346 ,70347, 70348, 80192 ,80193, 80194, 90086 ,90089; AARP Medicare Advantage Choice Plan 2
(Regional PPO) - Group 72811; AARP Medicare Advantage Focus (HMO-POS) - Groups 70341, 82970; AARP Medicare
Advantage Patriot (Regional PPO) - Group 72790; AARP Medicare Advantage Plan 2 (HMO-POS) - Group 82962; AARP
Medicare Advantage Premier (HMO-POS) - 82978; UnitedHealthcare Medicare Advantage Walgreens (HMO-POS C-SNP)
- Groups 95115, 95116, 95117, 95118; UnitedHealthcare The Villages Medicare Advantage (HMO-POS) - Group 82940;
UnitedHealthcare The Villages Medicare Focus (HMO-POS) - Group 40199
Florida: The following groups are delegated to WellMed Pf: Preferred Care Network: MedicareMax (HMO) - Groups 98151,
98152; MedicareMax Chronic (HMO C-SNP) - Groups 90215, 98153, 98154, 98155; Preferred Care Partners: Preferred
Choice Broward (HMO) - Group 99791; Preferred Choice Dade (HMO) - Group 99790; Preferred Choice Palm Beach (HMO)
- Group 99797; Preferred Medicare Assist (HMO D-SNP) - Groups 99792, 99793, 99796; Preferred Medicare Assist Palm
Beach (HMO D-SNP) - Groups 99798, 99799, 99800; Preferred Special Care Miami-Dade (HMO C-SNP) - Group 99795
Georgia: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Rebate (PPO) - Groups
92107, 92108; AARP Medicare Advantage Plus Plan 1 (HMO-POS) - Group - 92104; AARP Medicare Advantage Plus Plan 2
(HMO-POS) - Group 92105; AARP Medicare Advantage Walgreens (HMO-POS) - Group 92103; UnitedHealthcare Medicare
Advantage Choice (Regional PPO) - Group - 92109, 9211; UnitedHealthcare Medicare Advantage Choice Plan 1 (PPO) -
Group 92106; UnitedHealthcare Medicare Advantage Patriot (Regional PPO) - Group 92113; UnitedHealthcare Medicare
Advantage Patriot (Regional PPO) - Group 92115
Hawaii: The following groups are delegated to MDX: AARP Medicare Advantage Choice (PPO) - Group 77026; AARP
Medicare Advantage Choice Plan 1 (PPO) - Groups 77000, 77007; AARP Medicare Advantage Choice Plan 2 (PPO) - Group
77024; AARP Medicare Advantage Choice Patriot (PPO) - Groups 77003, 77008
Idaho: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Group 90219; AARP
Medicare Advantage Choice Plan 1 (PPO) - Group -90216; AARP Medicare Advantage Choice Plan 2 (PPO) - Group 90217;
AARP Medicare Advantage Choice Plan 3 (PPO) - Group 90218; AARP Medicare Advantage Patriot (HMO-POS) - Group
90221; AARP Medicare Advantage Plan 1 (HMO-POS) - Groups 38014, 90220; AARP Medicare Advantage Plan 2 (HMO-
POS) - Groups 44016, 90222; UnitedHealthcare Chronic Complete Assure (PPO C-SNP) - Groups 90305
Indiana: The following groups are delegated to OptumCare/American Health Network Indiana: AARP Medicare Advantage
(HMO-POS) - Groups 00744, 00748, 00749, 00750, 00755, 00758; AARP Medicare Advantage Choice (PPO) - Group -
90103; AARP Medicare Advantage Choice Plan 1 (PPO) - 67026, 67030, 67034, 90101; AARP Medicare Advantage Choice
Plan 2 (PPO) - Groups 90126, 90127, 92018, 92020, 92021; AARP Medicare Advantage Focus (PPO) - Group 74000; AARP
Medicare Advantage Patriot (PPO) - Group 90041; AARP Medicare Advantage Profile (HMO-POS) - Group 00746
Kansas: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Group
90193; AARP Medicare Advantage Choice Plan 2 (PPO) - Group 90326; AARP Medicare Advantage Patriot (PPO) - Group
90328; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 90167; AARP Medicare Advantage Plan 2 (HMO-POS) -
Group 90088
Kentucky: The following groups are delegated to WellMed: AARP Medicare Advantage Choice (PPO) - Groups 90137,
90139; AARP Medicare Advantage Flex Plan 1 (HMO-POS) - Group 90076; AARP Medicare Advantage Flex Plan 2 (HMO-
POS) - Group - 90077; AARP Medicare Advantage Flex Plan 6 (HMO-POS) - Groups - 90002, 90141; AARP Medicare
Advantage Plan 2 (HMO-POS) - Group - 90047; AARP Medicare Advantage Plan 3 (HMO-POS) - Group 90044
Missouri: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Groups
90194; AARP Medicare Advantage Choice Plan 2 (PPO) - Groups 90327; AARP Medicare Advantage Patriot (PPO) - Group
- 90168; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 90152; UnitedHealthcare Medicare Advantage Choice Plan
2 (Regional PPO) - Group 99932, 99936; UnitedHealthcare Medicare Advantage Choice Plan 3 (Regional PPO) - Group -
90053, 90054
Nevada: The following groups are delegated to Intermountain Healthcare Group (IHC): AARP Medicare Advantage (HMO-
POS) - Group 90204; AARP Medicare Advantage Premier (HMO-POS) - Group 90206; AARP Medicare Advantage Walgreens
Plan 1 (HMO-POS) - Group 90213; UnitedHealthcare Dual Complete (HMO-POS D-SNP) - Group - 90011; UnitedHealthcare
Medicare Advantage Assist (HMO-POS C-SNP) - Group 90211
Chapter 7: Medical management
86
2023 UnitedHealthcare Care Provider Administrative Guide
Nevada: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Group 90202;
AARP Medicare Advantage Choice (PPO) - Group 92011; AARP Medicare Advantage Patriot (PPO) - Group 92012; AARP
Medicare Advantage Plan 1 (HMO-POS) - Group - 90209; AARP Medicare Advantage Plan 2 (HMO-POS) - Group 90214;
AARP Medicare Advantage Premier (HMO-POS) - Group 90205; AARP Medicare Advantage Walgreens Plan 1 (HMO-POS)
- 90212; AARP Medicare Advantage Walgreens Plan 2 (PPO) - Groups 90027, 92013; UnitedHealthcare Dual Complete
(HMO-POS D-SNP) - Group 90008, 90009; UnitedHealthcare Medicare Advantage Assist (HMO-POS C-SNP) - Group 90210;
UnitedHealthcare Medicare Advantage Focus (HMO-POS) - Group 90207
New Jersey: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Groups 92014,
92016; AARP Medicare Advantage Choice Premier (PPO) - Groups 90330; AARP Medicare Advantage Patriot (HMO-POS)
- Groups 09100; AARP Medicare Advantage Plan 1 (HMO-POS) - Groups 09102, 09103; AARP Medicare Advantage Plan 2
(HMO-POS) - Group 90068, 90069;AARP Medicare Advantage Plan 3 (HMO-POS) - Groups 90071, 90072
New Mexico: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Groups 17087,
38011, 38013, 38018; AARP Medicare Advantage Choice Plan 1 (PPO) - Groups - 90035, 90037; AARP Medicare Advantage
Choice Plan 2 (PPO) - Groups 79710, 79711; AARP Medicare Advantage Choice Rebate (PPO) - Groups 79751, 79752;
79755; 79756; AARP Medicare Advantage Patriot (PPO) - Group - 74062; UnitedHealthcare Chronic Complete Assure (PPO
C-SNP) - Group 90132
New Mexico: The following groups are delegated to WellMed: AARP Medicare Advantage Choice (PPO) - Groups 79718,
79735
New York: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Groups 90189,
90190, 90179, 90180, 90183, 90184, 90185, 90186, 90188; AARP Medicare Advantage Choice (PPO) - Groups 90316,
90318, 90319, 90320, 90321, 90322, 90323, 90324;AARP Medicare Advantage Mosaic Choice (PPO) - Groups 09000,
09001; AARP Medicare Advantage Patriot (HMO-POS) - Groups 90175, 90176; AARP Medicare Advantage Plan 1 (HMO-
POS) - Group 90169, 90170. 90171, 90172; AARP Medicare Advantage Plan 2 (HMO-POS) - Groups 90177, 90178, 90181,
90182; AARP Medicare Advantage Premier Choice (PPO) - Groups 09002, 09003; AARP Medicare Advantage Prime (HMO-
POS) - Groups - 90173, 90174; AARP Medicare Advantage Value Care (HMO-POS) - Groups 41034, 90187; AARP Medicare
Advantage Value Care (PPO) - Groups 09117, 09118; UnitedHealthcare Medicare Advantage Choice Plan 1 (Regional PPO)
- Groups 90142, 90143; UnitedHealthcare Medicare Advantage Choice Plan 3 (Regional PPO) - Groups 90146, 90147;
UnitedHealthcare Medicare Advantage Choice Plan 4 (Regional PPO) - Groups 90148, 90149; UnitedHealthcare Medicare
Advantage Patriot (Regional PPO) - 90144, 90145
Ohio: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Groups 90138, 90140;
AARP Medicare Advantage Choice Flex (PPO) - Group 90049; AARP Medicare Advantage Choice Plan 4 (PPO) - Groups
92017; AARP Medicare Advantage Flex Plan 6 (HMO-POS) - Groups 90074; AARP Medicare Advantage Flex Plan 8 (HMO-
POS) - Groups 90063; AARP Medicare Advantage Patriot (PPO) - Groups 90001; AARP Medicare Advantage Plan 1 (HMO-
POS) - Groups 90007; AARP Medicare Advantage Plan 2 (HMO-POS) -Groups 90046, 90048; AARP Medicare Advantage
Plan 3 (HMO-POS) - Group 90045; AARP Medicare Advantage Plan 5 (HMO-POS) - Group 90043; AARP Medicare
Advantage Plan 7 (HMO-POS) - Group 90005
Oregon: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Group 90081; AARP
Medicare Advantage Patriot (PPO) - Group 90085; AARP Medicare Advantage Walgreens (PPO) - Groups 90083, 90084;
UnitedHealthcare Chronic Complete Assure (PPO C-SNP) - Group 90304
Chapter 7: Medical management
87
2023 UnitedHealthcare Care Provider Administrative Guide
Texas: The following groups are delegated to WellMed: AARP Medicare Advantage (HMO-POS) - Groups 00300, 00304,
00306, 00309, 90312, 90315; AARP Medicare Advantage Ally (HMO-POS) - Group 90129; AARP Medicare Advantage
Choice (PPO) - Groups 17064, 17065, 17066, 72806, 72807, 72814, 72815, 77018, 77019, 79717, 79730, 90112, 90113,
90114, 90115; AARP Medicare Advantage Patriot (HMO-POS) - Groups 00308, 96000; AARP Medicare Advantage Plan 1
(HMO-POS) - Groups 90122, 90123; AARP Medicare Advantage Plan 2 (HMO-POS) - Groups 90116, 90117; AARP Medicare
Advantage Walgreens (PPO) - Groups 90110, 90111; UnitedHealthcare Chronic Complete (HMO-POS C-SNP) - Groups
90117, 90119, 90120, 90121; UnitedHealthcare Chronic Complete Ally (HMO-POS C-SNP) - Group 90130; UnitedHealthcare
Dual Complete (HMO-POS D-SNP) - Groups 00307, 90165; UnitedHealthcare Dual Complete (HMO-POS D-SNP) - Groups
TX99TXDSNPF1, TX99TXDSNPF2, TX99TXDSNPF3, TX99TXDSNPP1, TX99TXDSNPP2, TX99TXDSNPP3,TX99TXSNH2FW,
TX99TXSNH2PW; UnitedHealthcare Dual Complete Ally (HMO-POS D-SNP) - Groups 90131, 90164; UnitedHealthcare Dual
Complete Choice (Regional PPO D-SNP) - Group 99952; UnitedHealthcare Dual Complete Choice Premier (PPO D-SNP) -
Groups TX99TXSNPF1W, TX99TXSNPP1W; UnitedHealthcare Dual Complete Select (HMO-POS D-SNP) - Groups 00012,
00303,00305, 00310, 90029, 9031, 90032, 90166, 90313, 90314, TX99TXDSNP5F, TX99TXDSNP5P; UnitedHealthcare
Medicare Advantage Choice (Regional PPO) - Groups 99953, 99955; UnitedHealthcare Medicare Gold (Regional PPO
C-SNP) - Groups 99951, 99954; UnitedHealthcare Medicare Silver (Regional PPO C-SNP) - Group 99950
Utah: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Group 90034; AARP
Medicare Advantage Choice Rebate (PPO) - Groups 92101, 92102; AARP Medicare Advantage Patriot (HMO-POS) - Group
42004; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 42000; AARP Medicare Advantage Plan 2 (HMO-POS) -
Group 42030; UnitedHealthcare Dual Complete Choice (PPO D-SNP) - Group 90064; UnitedHealthcare Dual Complete
Select (PPO D-SNP) - Group 90065; UnitedHealthcare Medicare Advantage Assist (HMO-POS C-SNP) - Group 90055
Washington: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Groups 90158,
90162; AARP Medicare Advantage Choice (PPO) - Group 90160; AARP Medicare Advantage Choice Plan 2 (PPO) - Group
90059; AARP Medicare Advantage Patriot (HMO-POS) - Group 90156; AARP Medicare Advantage Patriot (PPO) - Group
90058; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 90153; AARP Medicare Advantage Plan 2 (HMO-POS) -
Group 90155
Excluded Plans
The UnitedHealthcare Prior Authorization Protocol does not apply to the following excluded benefit plans. However, these
benefit plans may have separate notification or prior authorization requirements.
For the Preferred Care Network and Preferred Care Partners of Florida groups, refer to the Preferred Care Network and
Preferred Care Partners Prior Authorization Requirements located at uhcprovider.com > Prior Authorization > Advance
Notification and Plan Requirement Resources > Plan Requirements and Procedure Codes.
UnitedHealthcare® MedicareDirect (PFFS)
Erickson Advantage Plans
This protocol applies to all participating health care providers who order or render any of the following cardiology procedures:
• Diagnostic catheterizations
• Electrophysiology implant procedures
• Echocardiograms
• Stress echocardiograms
Notification/prior authorization is required for certain cardiology procedures. See the final paragraph of this section for
information on locating the most current listing of CPT codes that require notification/prior authorization.
A cardiology procedure for which notification/prior authorization is required is referred to as a “Cardiac Procedure.”
Notification/prior authorization is required under this protocol for outpatient and office-based services only.
Cardiology procedures done in and appropriately billed with any of the following places of service do not require notification/
prior authorization:
• Emergency room visits
• Observation unit

Chapter 7: Medical management
88
2023 UnitedHealthcare Care Provider Administrative Guide
• Urgent care
• Inpatient stays
If you do not complete the entire notification/prior authorization process before you do the procedure, we will reduce or deny
the claim. You cannot bill the member if claims are denied in this instance.
For the most current listing of CPT codes for which notification/prior authorization is required based on this protocol, refer to
uhcprovider.com/cardiology > Specific Cardiology Programs. Note: For MA benefit plans, prior authorization is not required
for echocardiograms.
Prior authorization and notification process for Cardiac Procedures
Ordering health care provider
The health care provider ordering the Cardiac Procedure must contact us prior to scheduling the procedure. Once we receive
procedure notification and if the member’s benefit plan requires medical necessity to cover services, we conduct a clinical
coverage review, based on our prior authorization process, to determine if the service is medically necessary. You do not need
to determine if a clinical coverage review is required because once we receive notification, we will let you know if a clinical
coverage review is required.
You must notify us, or request prior authorization, by contacting us:
• Online: UnitedHealthcare, UnitedHealthcare West, UnitedHealthcare Oxford Navigate Individual, All Savers, UnitedHealthcare
Level Funded, UnitedHealthcare Oxford Level Funded, Neighborhood Health Partnership, UnitedHealthcare of the River Valley
Commercial and Medicare Advantage benefit plans subject to this protocol: uhcprovider.com/paan.
• Phone: 1-866-889-8054
Non-participating health care providers can provide notification, and complete the prior authorization process if applicable,
either through the UnitedHealthcare Provider Portal (once registered) at uhcprovider.com, or by calling 1-866-889-8054.
We may request the following information at the time you notify us:
• Member’s name, address, phone number and date of birth
• Member’s health plan ID number and group number
• The examination(s) or type of service(s) being requested, with the CPT code(s)
• The working diagnosis with the appropriate ICD code(s)
• Ordering health care provider’s name, TIN/NPI, address, phone and fax number and email address
• Rendering health care provider’s name, address, phone number and TIN/NPI (if different)
• The member’s clinical condition, which may include any symptoms, treatments, dosage and duration of drugs, and dates for
other therapies
• Dates of prior imaging studies performed
• Any other information the ordering health care provider believes would be useful in evaluating whether the service ordered
meets current evidence-based clinical guidelines, such as prior diagnostic tests and consultation reports
MA benefit plans and certain commercial benefit plans require covered services be medically necessary.
If the member’s plan requires covered services to be medically necessary, and if the service is determined to be medically
necessary, we issue an authorization number to the ordering health care provider. To help ensure proper payment, the ordering
health care provider must communicate the authorization number to the rendering health care provider.
If it is determined the service is not medically necessary, we issue a clinical denial. If we issue a clinical denial for lack of
medical necessity, the member and health care provider receive a denial notice outlining the appeal process.
Certain commercial benefit plans do not require covered health services to be medically necessary.
If the member’s benefit plan does not require covered health services to be medically necessary and:
• If the service is consistent with evidence-based clinical guidelines, we issue a notification number to the ordering
health care provider.

Chapter 7: Medical management
89
2023 UnitedHealthcare Care Provider Administrative Guide
• If the service is not consistent with evidence-based clinical guidelines, or if we need additional information to assess the
request, we will let the ordering health care provider know what we need from them, including whether a physician-to-
physician discussion is required.
• If a physician-to-physician discussion is required, you must complete that process to help ensure eligibility to receive
payment. Upon completion of the discussion, the health care provider confirms the procedure ordered and we issue a
notification number. The purpose of the physician-to-physician discussion is to support the delivery of evidence-based health
care by discussing evidence-based clinical guidelines. This discussion is not a prior authorization, precertification or medical
necessity determination unless applicable state law dictates otherwise.
Receipt of a notification number or authorization number does not guarantee or authorize payment unless state regulations
(including regulations pertaining to a health care provider’s inclusion in a sanction and excluded list and non-inclusion in the
Medicare Provider Enrollment Chain and Ownership System [PECOS] list, or Medicare Preclusion List) and MA guidelines
require it. Payment for covered services depends upon:
• Coverage with an individual member’s benefit plan.
• If you are eligible for payment.
• Claims processing requirements.
• Your participation with UnitedHealthcare.
The notification/prior authorization number is valid for 45 calendar days. It is specific to the Cardiac Procedure requested, to be
performed 1 time, for 1 date of service within the 45-day period. When we enter a procedure notification/authorization number,
we use the date issued as the starting date for the 45-day period. The procedure must be performed within the 45 days. If you
do not do the procedure within 45 calendar days, you must request a new notification/authorization number.
Urgent requests during regular business hours
The ordering health care provider may make an urgent request for a notification/prior authorization number if they determine
the service is medically urgent. Make urgent requests by calling 1-866-889-8054 or online at uhcprovider.com/paan. The
ordering health care provider must state the case is clinically urgent and explain the clinical urgency. We respond to urgent
requests within 3 hours of our receipt of all required information.
Retrospective review process for urgent requests outside of regular business hours
If the ordering health care provider determines a Cardiac Procedure is medically required on an urgent basis, and the ordering
health care provider cannot request a notification/prior authorization number because it is outside of our normal business
hours, they must make a retrospective notification/authorization request using the following guidelines:
• Within 2 business days of the date of service for:
– Echocardiograms.
– Stress echocardiograms.
• Within 15 calendar days of the date of service for:
– Diagnostic catheterizations.
– Electrophysiology implants.
Request the retrospective review by calling 1-866-889-8054 based on the following process:
• Documentation must explain why the procedure had to be done on an urgent basis and why a notification/authorization
number could not have been requested during our normal business hours.
• Once we receive Cardiac Procedure retrospective notification, and if the member’s benefit plan requires medical necessity for
services to be covered, we will conduct a clinical coverage review to determine whether the service is medically necessary. If
we determine the service was not medically necessary, we will issue a denial and we will not issue an authorization number.
The member and health care provider will receive a denial notice outlining the appeal process.
• Once we receive Cardiac Procedure retrospective notification and if the member’s benefit plan does not require medical
necessity for services to be covered:
– We issue a notification number to the ordering health care provider if the service is consistent with evidence-based
clinical guidelines.
Chapter 7: Medical management
90
2023 UnitedHealthcare Care Provider Administrative Guide
– If the service is not consistent with evidence-based clinical guidelines, or if we need additional information to assess the
request, we will let the ordering health care provider know if they must have a physician-to-physician discussion to explain
the request, to give us more clinical information and to discuss alternative approaches. After the discussion is completed,
the ordering health care provider will confirm the procedure ordered and we will issue a notification number.
Rendering health care provider
Prior to performing a Cardiac Procedure, the rendering health care provider must confirm a notification/authorization number is
on file. If the member’s benefit plan requires medical necessity to cover health services, the rendering health care provider must
validate the ordering health care provider completed the prior authorization process and was issued a coverage determination.
If the rendering health care provider finds a coverage determination has not been issued, and the ordering health care provider
does not participate in our network and is unwilling to complete the notification/prior authorization process, the rendering
health care provider is required to complete the notification/prior authorization process. The rendering health care provider
must verify we have issued a coverage decision based on this protocol, prior to performing the service. Contact us at the
online address or phone number listed in the previous Ordering health care provider section if you need to notify us, request
prior authorization, confirm that a notification number has been issued or confirm whether a coverage determination has been
issued.
If the member’s benefit plan does not require that services be medically necessary to be covered and:
• If you render a Cardiac Procedure and submit a claim without a notification number, we will deny or reduce payment. You
cannot bill the member for the service in this instance.
• If you determine there is no notification number on file, and the ordering health care provider participates in our network, we
use reasonable efforts to work with you to urge the ordering health care provider to complete the notification process and
obtain a notification number prior to the rendering of services.
• If you determine there is no notification number on file, and the ordering health care provider does not participate in our
network, and is not willing to obtain a notification number, you are required to obtain a notification number.
• If you do not obtain a notification number for the procedure ordered by a non-participating health care provider, we will deny
or reduce payment for failure to provide notification. You cannot bill the member for the service in this instance.
If the member’s benefit plan does require services to be medically necessary to be covered and:
• If you determine we have not issued a coverage determination, and the ordering health care provider participates in
our network, we use reasonable efforts to work with you to urge the ordering health care provider to complete the prior
authorization process and obtain a coverage decision prior to the rendering of services.
• If you determine we have not issued a coverage determination, and the ordering health care provider does not participate in
our network and is not willing to complete the prior authorization process, you are required to complete the prior authorization
process and verify that we have issued a coverage decision prior to rendering the service.
• If you provide the service before a coverage decision is issued, we may deny or reduce your claim payment. You cannot bill
the member for the service in this instance.
• Services not medically necessary are not covered under the member’s benefit plan. When we deny services for lack of
medical necessity, we issue the member and ordering health care provider a denial notice with the appeal process outlined.
We do not issue an authorization number if we determine the service is not medically necessary. We issue an authorization
number to the ordering health care provider if the service is medically necessary.
Crosswalk table
You are not required to modify the existing notification/prior authorization request, or request a new notification/prior
authorization record for the CPT code combinations in the Cardiology Notification/Prior Authorization CPT Code List and
Crosswalk table available online on uhcprovider.com/cardiology > Specific Cardiology Programs.
For code combinations not listed on the Cardiology Notification/Prior Authorization CPT Code List and Crosswalk table, you
must follow the Cardiology Notification/Prior Authorization Protocol process.
Chapter 7: Medical management
91
2023 UnitedHealthcare Care Provider Administrative Guide
Outpatient radiology notification/prior authorization protocol
This protocol applies to commercial members and MA members. It does not apply to the following commercial or MA benefit
plans or other benefit plan types including Medicaid, CHIP or uninsured benefit plans. The following benefit plans may have
separate radiology notification or prior authorization requirements. Refer to Chapter 1: Introduction for additional supplements
or health care provider guides that may be applicable.
Commercial benefit plans not subject to these requirements
UnitedHealthcare Options PPO: Depending on the member particular benefit plan, UnitedHealthcare Options PPO health
care providers may not be required to follow this protocol for Options PPO benefit plans unless members enrolled in these
benefit plans are responsible for providing notification/requesting prior authorization.
UnitedHealthOne – Golden Rule Insurance Company
(“GRIC”) group number 705214 only
M.D.IPA, Optimum Choice, (See the Mid-Atlantic Regional Supplement), or OneNet PPO
Oxford Health plans
UMR and UnitedHealthcare Shared Services (UHSS)
UnitedHealthcare Indemnity/Managed Indemnity
Benefit plans sponsored or issued by certain self-funded employer groups
MA benefit plans may not be subject to these requirements
In some instances, we have delegated prior authorization services to a provider group. In these cases, the “For Providers”
section on the member’s ID card will list the delegated group managing the prior authorization process. Call the number listed
on the member’s ID card. If you are a network provider who is contracted directly with a delegated medical group/IPA, then you
must follow the delegate’s protocols. Delegates may use their own systems and forms. They must meet the same regulatory and
accreditation requirements as UnitedHealthcare. Delegated plans include:
Arizona: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Group
92004; AARP Medicare Advantage Choice Plan 2 (PPO) - Group 92007; AARP Medicare Advantage Patriot (PPO) - Groups:
92008, 92015; AARP Medicare Advantage Patriot (PPO) - Group 90108; AARP Medicare Advantage Walgreens Plan 1
(PPO) - Groups 92001, 92002; AARP Medicare Advantage Walgreens Plan 2 (PPO) - Group 92006, 92009; AARP Medicare
Advantage Walgreens Plan 3 (PPO) - Group 92010
Arizona: The following groups are delegated to P3 Health Partners: AARP Medicare Advantage (HMO-POS) - Group 90192;
AARP Medicare Advantage Choice Plan 1 (PPO) - Groups 90196, 90601; AARP Medicare Advantage Choice Plan 2 (PPO)
- Groups 90197, 90602; AARP Medicare Advantage Patriot (PPO) - Groups 90198, 90603; AARP Medicare Advantage Plus
(HMO-POS) - Group 90191; AARP Medicare Advantage Walgreens Plan 1 (PPO) - Group 90195; AARP Medicare Advantage
Walgreens Plan 2 (PPO) - Group 90199; UnitedHealthcare Chronic Complete Assure (PPO C-SNP) - Groups 90303, 90600
Colorado: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Groups
90091, 90092, 90093, 90094, 91014, 91015, 91016, 91017; AARP Medicare Advantage Choice Plan 2 (PPO) - Groups
90039, 90057, 91012, 91013; AARP Medicare Advantage Choice Rebate (PPO) - Groups 90097, 90133; 90134, 90135,
91018, 91019, 91020, 91021; AARP Medicare Advantage Walgreens (PPO) - Groups 90095, 90096, 91010, 91011
Connecticut: The following groups are delegated to Advantage Plus Network: AARP Medicare Advantage Choice (PPO)
- Group 90125; AARP Medicare Advantage Choice (Regional PPO) - Groups 90150, 90151; AARP Medicare Advantage
Choice Flex (PPO) - Group 90223; UnitedHealthcare Medicare Advantage Patriot (HMO-POS) - Groups -27155, 27156,
27062, 27151, 27064, 27153, 27100, 27150
Chapter 7: Medical management
92
2023 UnitedHealthcare Care Provider Administrative Guide
Florida: The following groups are delegated to WellMed: AARP Medicare Advantage (HMO-POS) - Groups 82958,
82960, 82969, 82977, 82980, 90028, 90078, 90079; AARP Medicare Advantage Choice (PPO) - Groups 70342, 70343,
70344, 70345, 70346 ,70347, 70348, 80192, 80193, 80194, 90086, 90089; AARP Medicare Advantage Choice Plan 2
(Regional PPO) - Group 72811; AARP Medicare Advantage Focus (HMO-POS) - Groups 70341, 82970; AARP Medicare
Advantage Patriot (Regional PPO) - Group 72790; AARP Medicare Advantage Plan 2 (HMO-POS) - Group 82962; AARP
Medicare Advantage Premier (HMO-POS) - 82978; UnitedHealthcare Medicare Advantage Walgreens (HMO-POS C-SNP)
- Groups 95115, 95116, 95117, 95118; UnitedHealthcare The Villages Medicare Advantage (HMO-POS) - Group 82940;
UnitedHealthcare The Villages Medicare Focus (HMO-POS) - Group 40199
Florida: The following groups are delegated to WellMed Pf: Preferred Care Network: MedicareMax (HMO) - Groups 98151,
98152; MedicareMax Chronic (HMO C-SNP)- Groups 90215, 98153, 98154, 98155; Preferred Care Partners: Preferred
Choice Broward (HMO) - Group 99791; Preferred Choice Dade (HMO) -Group 99790; Preferred Choice Palm Beach (HMO)
- Group 99797; Preferred Medicare Assist (HMO D-SNP) - Groups 99792, 99793, 99796; Preferred Medicare Assist Palm
Beach (HMO D-SNP) - Groups 99798, 99799, 99800; Preferred Special Care Miami-Dade (HMO C-SNP) - Group 99795
Georgia: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Rebate (PPO) - Groups
92107, 92108; AARP Medicare Advantage Plus Plan 1 (HMO-POS) - Group - 92104; AARP Medicare Advantage Plus Plan 2
(HMO-POS) - Group 92105; AARP Medicare Advantage Walgreens (HMO-POS) - Group 92103; UnitedHealthcare Medicare
Advantage Choice (Regional PPO) - Group - 92109, 9211; UnitedHealthcare Medicare Advantage Choice Plan 1 (PPO) -
Group 92106; UnitedHealthcare Medicare Advantage Patriot (Regional PPO) - Group 92113; UnitedHealthcare Medicare
Advantage Patriot (Regional PPO) - Group 92115
Hawaii: The following groups are delegated to MDX: AARP Medicare Advantage Choice (PPO) - Group 77026; AARP
Medicare Advantage Choice Plan 1 (PPO) - Groups 77000, 77007; AARP Medicare Advantage Choice Plan 2 (PPO) - Group
77024; AARP Medicare Advantage Choice Patriot (PPO) - Groups 77003, 77008
Idaho: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Group 90219; AARP
Medicare Advantage Choice Plan 1 (PPO) - Group - 90216; AARP Medicare Advantage Choice Plan 2 (PPO) - Group 90217;
AARP Medicare Advantage Choice Plan 3 (PPO) - Group 90218; AARP Medicare Advantage Patriot (HMO-POS) - Group
90221; AARP Medicare Advantage Plan 1 (HMO-POS) - Groups 38014, 90220; AARP Medicare Advantage Plan 2 (HMO-
POS) - Groups 44016, 90222; UnitedHealthcare Chronic Complete Assure (PPO C-SNP) - Groups 90305
Indiana: The following groups are delegated to OptumCare/American Health Network Indiana: AARP Medicare Advantage
(HMO-POS) - Groups 00744, 00748, 00749, 00750, 00755, 00758; AARP Medicare Advantage Choice (PPO) - Group 90103;
AARP Medicare Advantage Choice Plan 1 (PPO) - 67026, 67030, 67034, 90101; AARP Medicare Advantage Choice Plan
2 (PPO) - Groups 90126, 90127, 92018, 92020, 92021; AARP Medicare Advantage Focus (PPO) - Group 74000; AARP
Medicare Advantage Patriot (PPO) - Group 90041; AARP Medicare Advantage Profile (HMO-POS) - Group 00746
Kansas: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Group
90193; AARP Medicare Advantage Choice Plan 2 (PPO) - Group 90326; AARP Medicare Advantage Patriot (PPO) - Group
90328; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 90167; AARP Medicare Advantage Plan 2 (HMO-POS) -
Group 90088
Kentucky: The following groups are delegated to WellMed: AARP Medicare Advantage Choice (PPO) - Groups 90137,
90139; AARP Medicare Advantage Flex Plan 1 (HMO-POS) - Group 90076; AARP Medicare Advantage Flex Plan 2
(HMO-POS) - Group 90077; AARP Medicare Advantage Flex Plan 6 (HMO-POS) - Groups 90002, 90141; AARP Medicare
Advantage Plan 2 (HMO-POS) - Group 90047; AARP Medicare Advantage Plan 3 (HMO-POS) - Group 90044
Missouri: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice Plan 1 (PPO) - Groups
90194; AARP Medicare Advantage Choice Plan 2 (PPO) - Groups 90327; AARP Medicare Advantage Patriot (PPO) - Group
90168; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 90152; UnitedHealthcare Medicare Advantage Choice Plan 2
(Regional PPO) - Group 99932, 99936; UnitedHealthcare Medicare Advantage Choice Plan 3 (Regional PPO) - Group 90053,
90054
Nevada: The following groups are delegated to Intermountain Healthcare Group (IHC): AARP Medicare Advantage (HMO-
POS) - Group 90204; AARP Medicare Advantage Premier (HMO-POS) - Group 90206; AARP Medicare Advantage Walgreens
Plan 1 (HMO-POS) - Group 90213; UnitedHealthcare Dual Complete (HMO-POS D-SNP) - Group 90011; UnitedHealthcare
Medicare Advantage Assist (HMO-POS C-SNP) - Group 90211
Chapter 7: Medical management
93
2023 UnitedHealthcare Care Provider Administrative Guide
Nevada: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Group 90202;
AARP Medicare Advantage Choice (PPO) - Group 92011; AARP Medicare Advantage Patriot (PPO) - Group 92012; AARP
Medicare Advantage Plan 1 (HMO-POS) - Group 90209; AARP Medicare Advantage Plan 2 (HMO-POS) - Group 90214;
AARP Medicare Advantage Premier (HMO-POS) - Group 90205; AARP Medicare Advantage Walgreens Plan 1 (HMO-POS)
- 90212; AARP Medicare Advantage Walgreens Plan 2 (PPO) - Groups 90027, 92013; UnitedHealthcare Dual Complete
(HMO-POS D-SNP) - Group 90008, 90009; UnitedHealthcare Medicare Advantage Assist (HMO-POS C-SNP) - Group 90210;
UnitedHealthcare Medicare Advantage Focus (HMO-POS) - Group 90207
New Jersey: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Groups 92014,
92016; AARP Medicare Advantage Choice Premier (PPO) - Groups 90330; AARP Medicare Advantage Patriot (HMO-POS)
- Groups 09100; AARP Medicare Advantage Plan 1 (HMO-POS) - Groups 09102, 09103; AARP Medicare Advantage Plan 2
(HMO-POS)- Group 90068, 90069; AARP Medicare Advantage Plan 3 (HMO-POS) - Groups 90071, 90072
New Mexico: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Groups 17087,
38011, 38013, 38018; AARP Medicare Advantage Choice Plan 1 (PPO) - Groups 90035, 90037; AARP Medicare Advantage
Choice Plan 2 (PPO) - Groups 79710, 79711; AARP Medicare Advantage Choice Rebate (PPO) - Groups 79751, 79752;
79755; 79756; AARP Medicare Advantage Patriot (PPO) - Group 74062; UnitedHealthcare Chronic Complete Assure (PPO
C-SNP) - Group 90132
New Mexico: The following groups are delegated to WellMed: AARP Medicare Advantage Choice (PPO) - Groups 79718,
79735
New York: The following groups are delegated to OptumCare: AARP Medicare Advantage (HMO-POS) - Groups 90189,
90190, 90179, 90180, 90183, 90184, 90185, 90186, 90188; AARP Medicare Advantage Choice (PPO) - Groups 90316,
90318, 90319, 90320, 90321, 90322, 90323, 90324;AARP Medicare Advantage Mosaic Choice (PPO) - Groups 09000,
09001; AARP Medicare Advantage Patriot (HMO-POS) - Groups 90175, 90176; AARP Medicare Advantage Plan 1 (HMO-
POS) - Group 90169, 90170. 90171, 90172; AARP Medicare Advantage Plan 2 (HMO-POS) - Groups 90177, 90178, 90181,
90182; AARP Medicare Advantage Premier Choice (PPO) - Groups 09002, 09003; AARP Medicare Advantage Prime (HMO-
POS) - Groups - 90173, 90174; AARP Medicare Advantage Value Care (HMO-POS) - Groups 41034, 90187; AARP Medicare
Advantage Value Care (PPO) - Groups 09117, 09118; UnitedHealthcare Medicare Advantage Choice Plan 1 (Regional PPO)
- Groups 90142, 90143; UnitedHealthcare Medicare Advantage Choice Plan 3 (Regional PPO) - Groups 90146, 90147;
UnitedHealthcare Medicare Advantage Choice Plan 4 (Regional PPO) - Groups 90148, 90149; UnitedHealthcare Medicare
Advantage Patriot (Regional PPO) - 90144, 90145
Ohio: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Groups 90138, 90140;
AARP Medicare Advantage Choice Flex (PPO) - Group 90049; AARP Medicare Advantage Choice Plan 4 (PPO) - Groups
92017; AARP Medicare Advantage Flex Plan 6 (HMO-POS) - Groups 90074; AARP Medicare Advantage Flex Plan 8 (HMO-
POS) - Groups 90063; AARP Medicare Advantage Patriot (PPO) - Groups 90001; AARP Medicare Advantage Plan 1 (HMO-
POS) - Groups 90007; AARP Medicare Advantage Plan 2 (HMO-POS) - Groups 90046, 90048; AARP Medicare Advantage
Plan 3 (HMO-POS) - Group 90045; AARP Medicare Advantage Plan 5 (HMO-POS) - Group 90043; AARP Medicare
Advantage Plan 7 (HMO-POS) - Group 90005
Oregon: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Group 90081; AARP
Medicare Advantage Patriot (PPO) - Group 90085; AARP Medicare Advantage Walgreens (PPO) - Groups 90083, 90084;
UnitedHealthcare Chronic Complete Assure (PPO C-SNP) - Group 90304
Chapter 7: Medical management
94
2023 UnitedHealthcare Care Provider Administrative Guide
Texas: The following groups are delegated to WellMed: AARP Medicare Advantage (HMO-POS) - Groups 00300, 00304,
00306, 00309, 90312, 90315; AARP Medicare Advantage Ally (HMO-POS) - Group 90129; AARP Medicare Advantage
Choice (PPO) - Groups 17064, 17065, 17066, 72806, 72807, 72814, 72815, 77018, 77019, 79717, 79730, 90112, 90113,
90114, 90115; AARP Medicare Advantage Patriot (HMO-POS) - Groups 00308, 96000; AARP Medicare Advantage Plan 1
(HMO-POS) - Groups 90122, 90123; AARP Medicare Advantage Plan 2 (HMO-POS) - Groups 90116, 90117; AARP Medicare
Advantage Walgreens (PPO) - Groups 90110, 90111; UnitedHealthcare Chronic Complete (HMO-POS C-SNP) - Groups
90117, 90119, 90120, 90121; UnitedHealthcare Chronic Complete Ally (HMO-POS C-SNP) - Group 90130; UnitedHealthcare
Dual Complete (HMO-POS D-SNP) - Groups 00307, 90165; UnitedHealthcare Dual Complete (HMO-POS D-SNP) - Groups
TX99TXDSNPF1, TX99TXDSNPF2, TX99TXDSNPF3, TX99TXDSNPP1, TX99TXDSNPP2, TX99TXDSNPP3,TX99TXSNH2FW,
TX99TXSNH2PW; UnitedHealthcare Dual Complete Ally (HMO-POS D-SNP) - Groups 90131, 90164; UnitedHealthcare Dual
Complete Choice (Regional PPO D-SNP) - Group 99952; UnitedHealthcare Dual Complete Choice Premier (PPO D-SNP) -
Groups TX99TXSNPF1W, TX99TXSNPP1W; UnitedHealthcare Dual Complete Select (HMO-POS D-SNP) - Groups 00012,
00303,00305, 00310, 90029, 9031, 90032, 90166, 90313, 90314, TX99TXDSNP5F, TX99TXDSNP5P; UnitedHealthcare
Medicare Advantage Choice (Regional PPO) - Groups 99953, 99955; UnitedHealthcare Medicare Gold (Regional PPO
C-SNP) - Groups 99951, 99954; UnitedHealthcare Medicare Silver (Regional PPO C-SNP) - Group 99950
Utah: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Group 90034; AARP
Medicare Advantage Choice Rebate (PPO) - Groups 92101, 92102; AARP Medicare Advantage Patriot (HMO-POS) - Group
42004; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 42000; AARP Medicare Advantage Plan 2 (HMO-POS) -
Group 42030; UnitedHealthcare Dual Complete Choice (PPO D-SNP) - Group 90064; UnitedHealthcare Dual Complete
Select (PPO D-SNP) - Group 90065; UnitedHealthcare Medicare Advantage Assist (HMO-POS C-SNP) - Group 90055
Washington: The following groups are delegated to OptumCare: AARP Medicare Advantage Choice (PPO) - Groups 90158,
90162; AARP Medicare Advantage Choice (PPO) - Group 90160; AARP Medicare Advantage Choice Plan 2 (PPO) - Group
90059; AARP Medicare Advantage Patriot (HMO-POS) - Group 90156; AARP Medicare Advantage Patriot (PPO) - Group
90058; AARP Medicare Advantage Plan 1 (HMO-POS) - Group 90153; AARP Medicare Advantage Plan 2 (HMO-POS) -
Group 90155
Excluded Plans
The UnitedHealthcare Prior Authorization Protocol does not apply to the following excluded benefit plans. However, these
benefit plans may have separate notification or prior authorization requirements.
For the Preferred Care Network and Preferred Care Partners of Florida groups, refer to the Preferred Care Network and
Preferred Care Partners Prior Authorization Requirements located at uhcprovider.com > Prior Authorization > Advance
Notification and Plan Requirement Resources > Plan Requirements and Procedure Codes.
UnitedHealthcare® MedicareDirect (PFFS)
Erickson Advantage Plans
This applies to all participating health care providers that order or render any of the following advanced imaging procedures:
• Computerized Tomography (CT)
• Magnetic Resonance Imaging (MRI)
• Magnetic Resonance Angiography (MRA)
• Positron-Emission Tomography (PET)
• Nuclear medicine
• Nuclear cardiology
Notification/prior authorization is required for certain advanced imaging procedures. See the final paragraph of this section for
information on locating the most current listing of CPT codes that require notification/prior authorization.
An advanced imaging procedure for which notification/prior authorization is required is called an “Advanced Outpatient
Imaging Procedure.”
Notification/prior authorization is required for outpatient and office-based services only.
Chapter 7: Medical management
95
2023 UnitedHealthcare Care Provider Administrative Guide
Advanced imaging procedures done in and appropriately billed with any of the following places of service do not require
notification/prior authorization:
• Emergency room
• Observation unit
• Urgent care
• Inpatient stay
If you do not complete the entire notification/prior authorization process before you do the procedure, we will reduce or deny
the claim. You cannot bill the member if denied claims are denied in this instance.
For the most current listing of CPT codes for which notification/prior authorization is required based on this protocol, refer to:
uhcprovider.com/radiology > Specific Radiology Programs. Note: For MA benefit plans, prior authorization is not required for
CT, MRI or MRA.
Prior authorization and notification process for Advanced Outpatient Imaging Procedures
Ordering health care provider
The health care provider ordering the Advanced Outpatient Imaging Procedure must contact us before scheduling the
procedure. Once we receive procedure notification and if the member’s benefit plan requires covered health services to
be medically necessary, we conduct a clinical coverage review, based on our prior authorization process, to determine if
the service is medically necessary. You do not need to determine if a clinical coverage review is required. Once we receive
notification, we will let you know if we require a clinical coverage review.
You must notify us, or request prior authorization, by contacting us:
• Online: UnitedHealthcare, UnitedHealthcare West, UnitedHealthcare Oxford Navigate Individual, All Savers, UnitedHealthcare
Level Funded, UnitedHealthcare Oxford Level Funded, Neighborhood Health Partnership, UnitedHealthcare of the River
Valley, commercial and MA benefit plans subject to this protocol: uhcprovider.com/paan.
• Phone: 1-866-889-8054
Non-participating health care providers can provide notification, and complete the prior authorization process if applicable,
either through the UnitedHealthcare Provider Portal (once registered) at uhcprovider.com or by calling 1-866-889-8054.
We may request the following information at the time you notify us:
• Member’s name, address, phone number and date of birth
• Member’s health plan ID number and group number
• The examination(s) or type of service(s) requested, with the CPT code(s)
• The working diagnosis with the appropriate ICD code(s)
• Ordering health care provider’s name, TIN/NPI, address, phone and fax number, and email address
• Rendering health care provider’s name, address, phone number and TIN/NPI (if different)
• The member’s clinical condition, including any symptoms, treatments, dosage and duration of drugs, and dates for
other therapies
• Dates of prior imaging studies performed
• Any other information the ordering health care provider believes would be useful in evaluating whether the service ordered
meets current evidence-based clinical guidelines, such as prior diagnostic tests and consultation reports
MA benefit plans and certain commercial benefit plans require covered health services to be medically necessary.
If the member’s plan requires covered services to be medically necessary, and if the service is medically necessary, we issue
an authorization number to the ordering health care provider. To help ensure proper payment, the ordering health care provider
must communicate the authorization number to the rendering health care provider.
If it is determined the service is not medically necessary, we issue a clinical denial. If we issue a clinical denial for lack of
medical necessity, the member and health care provider receive a denial notice outlining the appeal process.
Certain commercial benefit plans do not require covered health services to be medically necessary.

Chapter 7: Medical management
96
2023 UnitedHealthcare Care Provider Administrative Guide
If the member’s benefit plan does not require health services to be medically necessary to be covered and:
• If the service is consistent with evidence-based clinical guidelines, we issue a notification number to the ordering
health care provider.
• If the service is not consistent with evidence-based clinical guidelines, or if we need additional information to assess the
request, we let the ordering health care provider know what we need from them, including whether a physician-to-physician
discussion is required.
• If a physician-to-physician discussion is required, you must complete that process to help ensure eligibility to receive
payment. Upon completion of the discussion, the health care provider confirms the procedure ordered and we issue a
notification number. The purpose of the physician-to-physician discussion is to support the delivery of evidence-based health
care by discussing evidence-based clinical guidelines. This discussion is not a prior authorization, precertification or medical
necessity determination unless applicable state law dictates otherwise.
Notification or authorization number receipt does not guarantee or authorize payment unless state regulations (including
regulations pertaining to a health care provider’s inclusion in a sanction and excluded list and non-inclusion in the Medicare
PECOS* list) and MA guidelines require it. Payment for covered services depends upon:
• Coverage with an individual member’s benefit plan.
• The health care provider being eligible for payment.
• Claims processing requirements.
• The health care provider’s participation with UnitedHealthcare.
The notification/authorization number is valid for 45 calendar days. It is specific to the Advanced Outpatient Imaging Procedure
requested, to be performed 1 time, for 1 date of service within the 45-day period. When we enter a notification/authorization
number for a procedure, we use the date we issued the number as the starting date for the 45-day period you must perform the
procedure. If you do not do the procedure within 45 calendar days, you must request a new notification/authorization number.
Urgent requests during regular business hours
The ordering health care provider may make an urgent request for a notification/prior authorization number if they determine
the service is medically urgent. Make urgent requests by calling 1-866-889-8054 or online at uhcprovider.com/paan. The
ordering health care provider must state the case is clinically urgent and explain the clinical urgency. We respond to urgent
requests within 3 hours of our receipt of all required information.
Retrospective review process for urgent requests outside of regular business hours
If the ordering health care provider determines an Advanced Outpatient Imaging Procedure is medically required on an urgent
basis and they cannot request a notification/prior authorization number because it is outside of our normal business hours, they
must make a retrospective notification/prior authorization request within 2 business days after the date of service.
Request the retrospective review by calling 1-866-889-8054, based on the following process:
• Documentation must explain why the procedure had to be done on an urgent basis and why a notification/authorization
number could not have been requested during our normal business hours.
• Once we receive retrospective notification of an Advanced Outpatient Imaging Procedure, and if the member’s benefit plan
requires medical necessity for services to be covered, we conduct a clinical coverage review to determine medical necessity.
If we determine the service was not medically necessary, we issue a denial and do not issue an authorization number. The
member and health care provider receive a denial notice outlining the appeal process.
• Once we receive retrospective notification of an Advanced Outpatient Imaging Procedure and if the member’s benefit plan
does not require medical necessity for services to be covered:
– We issue a notification number to the ordering health care provider if the service is consistent with evidence-based
clinical guidelines.
– If the service is not consistent with evidence-based clinical guidelines, or if we need additional information to assess the
request, we let the ordering health care provider know if they must have a physician-to-physician discussion to explain the
request, to give us more clinical information, and to discuss alternative approaches. After the discussion is completed, the
ordering health care provider will confirm the procedure ordered and we will issue a notification number.

Chapter 7: Medical management
97
2023 UnitedHealthcare Care Provider Administrative Guide
Rendering health care provider
Before performing an Advanced Outpatient Imaging Procedure, the rendering health care provider must confirm a notification/
authorization number is on file. If the member’s benefit plan requires medical necessity for health services to be covered, the
rendering health care provider must validate that the ordering health care provider completed the prior authorization process
and was issued a coverage determination. If the rendering health care provider finds a coverage determination has not been
issued, and the ordering health care provider does not participate in our network and is unwilling to complete the notification/
prior authorization process, the rendering health care provider is required to complete the notification/prior authorization
process. The rendering health care provider must verify we have issued a coverage decision based on this protocol before
performing the service. Contact us at the online address or phone number listed in the previous Ordering health care provider
section if you need to notify us, request prior authorization, confirm that a notification number has been issued or confirm
whether a coverage determination has been issued.
If the member’s benefit plan does not require covered services be medically necessary and if you:
• Render an Advanced Outpatient Imaging Procedure and you submit a claim without a notification number, we will deny or
reduce payment. You cannot bill the member for the service in this instance.
• Determine there is no notification number on file, and the ordering health care provider participates in our network, we will
use reasonable efforts to work with you to urge the ordering health care provider to complete the notification process and
obtain a notification number before rendering services.
• Determine there is no notification number on file, and the ordering health care provider does not participate in our network,
and is not willing to obtain a notification number, you are required to obtain a notification number.
• Do not obtain a notification number for the procedures ordered by a non-participating health care provider, we will deny or
reduce payment for failure to provide notification. You cannot bill the member for the service in this instance.
If the member’s benefit plan does require medical necessity for covered services and:
• If you determine we did not issue a coverage determination and the ordering health care provider participates in our network,
we will use reasonable efforts to work with you to urge the ordering health care provider to complete the prior authorization
process and obtain a coverage decision before rendering services.
• If you determine we did not issue a coverage determination, and the ordering health care provider does not participate in our
network and is not willing to complete the prior authorization process, you are required to complete the prior authorization
process and verify that we issued a coverage decision before rendering services.
• If you provide the service before we issue a coverage decision, we may deny or reduce your claim payment. You cannot bill
the member for the service in this instance.
• Services not medically necessary are not covered under the member’s benefit plan. When we deny services for lack of
medical necessity, we issue the member and ordering health care provider a denial notice with the appeal process outlined.
We do not issue an authorization number if we determine the service is not medically necessary. We issue an authorization
number to the ordering health care provider if the service is medically necessary.
Provision of an additional or modified Advanced Outpatient Imaging Procedure
If, during the delivery of an Advanced Outpatient Imaging Procedure, the rendering health care provider determines an
additional Advanced Outpatient Imaging Procedure should be delivered above and beyond the approved service(s) assigned
a notification/prior authorization number, then the health care professional who determined the need for the additional or
modified outpatient imaging procedure must request a new notification/prior authorization number before scheduling the
procedure, based on this protocol.
If, during the delivery of an Advanced Outpatient Imaging Procedure for which the health care provider completed the
notification/prior authorization processes, the physician modifies the Advanced Outpatient Imaging Procedure, and if the CPT
code combination is not on the CPT Code Crosswalk Table, then follow this process:
• Contiguous body part – If the procedure is for a contiguous body part, the ordering or rendering health care provider must
modify the original notification/authorization number request online or by calling within 2 business days after rendering the
procedure.
• Non-contiguous body part – If the procedure is not for a contiguous body part, the ordering health care provider must submit
a new notification/authorization number request and must have a coverage determination before the procedure takes place.

Chapter 7: Medical management
98
2023 UnitedHealthcare Care Provider Administrative Guide
Crosswalk table
You are not required to modify the existing notification/prior authorization request or request a new notification/prior
authorization record for the CPT code combinations in the UnitedHealthcare Radiology Notification/Prior Authorization
Crosswalk Table available online at uhcprovider.com/radiology > Specific Radiology Programs.
For code combinations not listed on the UnitedHealthcare Radiology Notification/Prior Authorization Crosswalk Table, you must
follow the Radiology Notification/Prior Authorization Protocol process.
Medication-assisted treatment
Medication-assisted treatment (MAT) combines behavioral therapy and medications to treat opioid use disorders (OUD). The
Food and Drug Administration (FDA) approved medications for OUD including Buprenorphine, Methadone and Naltrexone.
To prescribe Buprenorphine, you must complete the waiver through the Substance Abuse and Mental Health Services
Administration (SAMHSA) and obtain a unique identification number from the United States Drug Enforcement
Administration (DEA).
As a medical health care provider, you may provide MAT services even if you don’t offer counseling or behavioral health
therapy in-house. However, you must refer your patients to a qualified health care provider for those services. If you need help
finding a behavioral health provider, call the number on the member’s ID card or search for a behavioral health provider on
liveandworkwell.com.
To find a medical MAT provider in a state:
1. Go to uhcprovider.com.
2. Select “Resources > Find a Provider” in the top right corner of the home page.
3. Select “Search for Care Providers in the General UnitedHealthcare Plan Directory.”
4. Click on “Medical Directory.”
5. Choose a type of plan.
6. Select applicable plan.
7. Refine the search by typing “Medication Assisted Treatment” in the search bar.
For more SAMHSA waiver information:
samhsa.gov
If you have questions about MAT, call Provider Services at 1-877-842-3210, enter your TIN, then say “Representative’” then
“Representative” a second time, then “Something Else” to speak to a representative.
Trauma services
Trauma services are medically necessary, covered services given at a state-licensed, designated trauma facility or a facility
designated to receive trauma cases. Trauma services must meet identified county or state trauma criteria.
We may retrospectively review trauma service claims and medical records to verify that they met the trauma criteria. We may
also confirm the trauma facility has an active trauma license.
We consider these criteria when authorizing trauma services:
• Trauma team activated.
• Trauma surgeon is the primary treating health care provider.
• Member’s clinical status meets the county’s current EMS protocols for designating a trauma member.
• Trauma services, once rendered, apply to the first 48 hours post-facility admission, unless there is documented evidence of
medical necessity indicating that trauma level services are continuing delivery.

Chapter 7: Medical management
99
2023 UnitedHealthcare Care Provider Administrative Guide
• Trauma service status should no longer apply when, based on medical necessity, the member is stable and/or medically
appropriate for transfer out of the critical care area.
• Clinical management of a member(s) by the trauma team is not the sole criterion used to determine and authorize continued
trauma services care.
Air ambulance licensure
UnitedHealthcare may request licensure for in-network and out-of-network air ambulance and all servicing medical personnel.
To help ensure timely and proper air ambulance claim review and processing, submit this information with the claim.
You must obtain prior authorization for air ambulance service. See the Advance notification/prior authorization requirements
section for more information.

100
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 8: Specialty pharmacy and Medicare
Advantage pharmacy
Commercial pharmacy
For information related to commercial pharmacy benefits:
Online: uhcprovider.com/pharmacy
• View and search the prescription drug list (PDL) and a current list of participating specialty pharmacy providers that apply to
the use of certain pharmaceuticals.
• Learn about pharmaceutical management procedures for prior authorization requirements, supply limits and step
therapy protocols.
For pharmacy notification, prior authorization or questions on utilization management procedures, call:
Phone: 1-800-711-4555
Specialty pharmacy requirements for certain medical benefit
specialty medications (commercial plans – not applicable to
UnitedHealthcare West)
The Optum specialty medication guidance program manages the prior authorization process
for certain outpatient medical benefit specialty medications
Optum manages prior authorization requests for certain medical benefit injectable medications for these commercial plan
members. This includes the affiliate plans UnitedHealthcare of Mid-Atlantic, Inc., Neighborhood Health Partnership, Oxford
Health Plan, UnitedHealthcare Freedom Insurance Company, and UnitedHealthcare of the River Valley. You will be notified when
other commercial plans and lines of business migrate to this new process.
How the process works
Click on the Specialty Pharmacy Transactions tool in the Prior Authorization and Notification Tool from within the
UnitedHealthcare Provider Portal. The system will document clinical requirements during the intake process and prompt you
to provide responses to the clinical criteria questions. Attach medical records, if requested. For additional questions, call 1-888-
397-8129.
Coverage of self-infused/injectable medications under the pharmacy benefit
This protocol applies to the provision and billing of self-infused/injectable medications, such as hemophilia factor products,
under the pharmacy benefit.
Under most UnitedHealthcare products, self-infused/injectable medications are generally excluded from coverage under
the medical benefit. A pharmacy benefit rider can provide coverage for a self-infused/injectable medication. This exclusion
from the medical benefit does not apply to self-infused/injectable medications due to their characteristics, as determined by
UnitedHealthcare, that are typically administered or directly supervised by a qualified physician or licensed/certified health care
professional in an outpatient setting.
If medications are subject to this exclusion, participating physicians, health care professionals, home infusion providers,
hemophilia treatment centers or pharmacies fulfilling, distributing and billing for the provision of self-infused/injectable
medications to members are required to submit claims for reimbursement under the member’s pharmacy benefit.

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
101
2023 UnitedHealthcare Care Provider Administrative Guide
Prohibition of provision of non-contracted services
• This protocol applies to the provision and billing of specific specialty pharmacy medications covered under a member’s
medical benefit.
• Specialty pharmacy or home infusion health care providers may not provide non-contracted services for a therapeutic
category, even if the specialty pharmacy or home infusion health care provider is contracted for other medical benefit
medications and services, and is billing us as a non-participating or non-contracted specialty pharmacy or home infusion
health care provider.
• This protocol does not apply when a physician or other health care professional, who procures and bills us directly for
specific specialty medications, administers specialty medications in an office setting.
Requirement of specialty pharmacy and home infusion providers to be a network provider
We have contracted with a network of specialty pharmacy and home infusion health care providers by therapeutic category
to distribute specialty medications covered under a member’s medical benefit. Inclusion in this network is based on their
distribution, contracting, clinical capabilities and member services. This national network provides fulfillment and distribution
of the specialty medications on a timely basis to meet the needs of our members and our network. Full program participation
requirements are identified in the contracted specialty pharmacy or home infusion health care provider’s Agreement.
Requirement to use a participating specialty pharmacy health care provider for certain
medications
This requirement applies to the specialty medications listed on uhcprovider.com > Resources > Drug Lists and Pharmacy >
Specialty Pharmacy - Medical Benefit Management (Provider Administered Drugs) > Medication Sourcing > Drugs that require
sourcing. The drug list identifies those drugs for which sourcing requirements apply to all outpatient health care providers and
those for which the requirements only apply to outpatient facilities.
The medications subject to our sourcing requirement are subject to change. The requirement does not apply when Medicare or
another health benefit plan is the primary payer, and we are the secondary payer.
We have contracted health care providers for the distribution of these specialty medications. Our participating specialty
pharmacy health care providers give fulfillment and distribution services to meet the needs of our members and our health
care providers. Our participating specialty pharmacy health care providers provide reviews consistent with our drug policies
for these drugs. They work directly with the clinical coverage review unit to determine whether treatment is covered. Our
National Pharmacy & Therapeutics Committee (NPTC) periodically reviews and updates our drug policies for these drugs.
The committee helps ensure the policies are consistent with published clinical evidence and professional specialty society
guidance. Our participating specialty pharmacy health care providers report clinical data and related information and are
audited on an ongoing basis to support our clinical and quality improvement activities. You must acquire these specialty
medications from a participating specialty pharmacy health care provider, except as otherwise authorized by us.
Overview of submission, administration and billing processes
To fill a prescription through a contracted specialty pharmacy health care provider, submit an enrollment form (uhcprovider.
com > Resources > Drug Lists and Pharmacy > Specialty Pharmacy Program - Commercial > Pharmacy Enrollment Forms)
and a prescription request directly to the specialty pharmacy. The specialty pharmacy will advise the member of any medication
cost-share responsibility and arrange for collection of any amount due before dispensing the medication to the service location.
The specialty pharmacy will dispense these medications to you in compliance with the UnitedHealthcare Drug Policy and
the member’s benefit plan and eligibility. It will bill UnitedHealthcare for the medication. You may bill for administration of the
medication. You cannot bill us or the member for the medication itself.
For a list of the medications and participating specialty pharmacy provider(s), refer to the Drugs that Require Sourcing list.
For more information about the sourcing requirement and participating specialty pharmacies, go to uhcprovider.com >
Specialty Pharmacy Program > Specialty Pharmacy - Medical Benefit Management (Provider Administered Drugs) >
Medication Sourcing.

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
102
2023 UnitedHealthcare Care Provider Administrative Guide
Administrative actions for acquisition of certain specialty medications from
non-participating pharmacies
We anticipate that all health care providers will be able to procure certain medications from a participating specialty
pharmacy health care provider.
We may deny, in whole or in part, any claim from non-participating specialty pharmacy health care providers, wholesalers or
direct purchase from the manufacturers by you or any other health care professional without prior approval from us. You may
also be subject to other administrative actions as provided in your Agreement.
Contact your local UnitedHealthcare network management representative if you have any questions.
Medicare Advantage pharmacy
Pharmacy network
A member may fill prescriptions from any Medicare Advantage (MA) network pharmacy in the pharmacy directory or online at
optumrx.com.
Reimbursement for prescriptions from a non-network pharmacy is available to some members in limited circumstances.
MA prescription drug formulary
We use the United States Pharmacopoeia’s drug classification system for development of the Formulary for MA.
The Pharmacy & Therapeutics Committee conducts formulary development and oversight. The committee is also responsible
for identifying safe, cost-effective and medically appropriate drug therapies that reflect community and national standards
of practice.
MA formulary tier structure
The MA Prescription Drug Formulary is a list of drugs covered as a pharmacy plan benefit for MA members.
For non-group plans, we categorize medications into 5 tiers:
• Tier 1: Preferred generic drugs
• Tier 2: Generic drugs
• Tier 3: Preferred brand-name drugs
• Tier 4: Non-preferred drugs
• Tier 5: Specialty drugs
Note: Tiers 2-4 may include higher-cost generic drugs as well.
For group plans, several formularies are available. Medications are often categorized into 4 tiers:
• Tier 1: Preferred generic drugs
• Tier 2: Preferred brand-name drugs
• Tier 3: Non-preferred drugs
• Tier 4: Specialty drugs
Note: Tiers 2 and 3 may include higher-cost generic drugs as well.
For MA Prescription Drug Formulary information, see aarpmedicareplans.com, UHC.com/Medicare or uhcprovider.com. If a
drug is not on our formulary, you might be able to switch the member to a different drug that we do cover, or you can request a
formulary exception. While we are evaluating the exception, we may provide members with a temporary supply.

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
103
2023 UnitedHealthcare Care Provider Administrative Guide
MA prescription drug benefit
UnitedHealthcare offers several prescription drug coverage plans based on the member’s county of residence and the
member’s prescription drug needs. The benefit structure follows the CMS model:
• Prescription drug deductible — Some benefit plans have a deductible the member must meet before getting access to the
prescription drug benefit. In some plans, this deductible will only apply to specific drug tiers (e.g., Tier 3, Tier 4 and Tier 5
only).
• Initial coverage limit — During this period, the member is responsible for a specific copayment or coinsurance for
prescription drugs.
• Coverage gap — While in the coverage gap, the member will pay 25% of the total cost of brand-name and generic drugs in
2023. Coverage plans vary, and the member may pay a different amount.
• Catastrophic coverage level — Members who reach this level may have a significantly lower copayment/coinsurance for
prescription drugs until the end of the year. Coverage plans vary, and the member may pay a different amount.
Prescriptions for a non-formulary or non-covered drug are not covered unless the member or the member’s health care provider
requests and receives an approved formulary exception through the prior authorization process.
The member pays 100% of our contracted rate with the pharmacy if this amount is less than the member’s applicable
copayment/coinsurance for the prescription. This process does not apply to excluded medications.
Refer to the exceptions process included in the following section for the coverage criteria of a non-formulary or non-covered
drug.
MA Part D members
Prior authorization requests
OptumRx® follows the coverage determination timelines as established by CMS. We must complete standard coverage
determinations within 72 hours of receipt of request or prescriber’s supporting statement for exceptions. OptumRx must
complete expedited coverage determinations within 24 hours of receipt of request or prescriber’s supporting statement
for exceptions.
OptumRx may ask for more information from the prescriber or their designee. We may also ask the member and send them
notification of the resulting case decision.
Different types of requests include:
• Prior authorization (PA).
• Medicare Part B vs Medicare Part D.
• Non-formulary exception (NF).
• Step therapy (ST).
• Quantity limit (QL).
• Opioid safety edits.
• Tier cost-sharing exception (TCSE).
TCSE rules vary by specific benefit plans and available alternatives. Criteria for copayment reduction TCSE are:
• The requested drug is FDA-approved for the condition being treated.
• One of the following:
– Diagnosis is supported as a use in American Hospital Formulary Service (AHFS), under the Therapeutic Uses section.
– Diagnosis is supported in the Therapeutic Uses section in DRUGDEX Evaluation with a Strength of Recommendation rating
of IIb or better.
– Diagnosis is listed in the Therapeutic Uses section in DRUGDEX Evaluation and carries a Strength of Recommendation of
III or Class Indeterminate, and Efficacy is rated as “Effective” or “Evidence Favors Efficacy.”
– History of failure, contraindication or intolerance to all applicable formulary alternatives in the lower qualifying tiers.

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
104
2023 UnitedHealthcare Care Provider Administrative Guide
Coverage limitations
For some drugs, we may require authorization before the drug can be prescribed (prior authorization), limit the quantity that can
be prescribed per prescription (quantity limits) or require that you prescribe drugs in a sequence (step therapy), trying one drug
before another drug.
We provide an exception process to allow for the chance the formulary may not accommodate the member’s unique
medical needs. To make an exception to these restrictions or limits, or to initiate a prior authorization, submit a coverage
determination request:
Online: professionals.optumrx.com/prior-authorization
Phone: 1-800-711-4555
More information about requirements is available at professionals.optumrx.com > Resources > Formulary Lists or by calling the
OptumRx Prior Authorization department at the previously listed number.
Part B covered drugs
Drugs covered under Part B are typically administered and obtained at the health care provider’s office (e.g., certain cancer
drugs administered by a physician in their office as buy and bill). Some drugs covered under Part B are dispensed by
outpatient pharmacies (e.g., injections, specialty medications, certain oral cancer drugs, insulin when administered by a pump,
immunosuppressants for Medicare-covered transplants, diabetic test supplies).
MA diabetes monitoring supplies
Some plans have a Preferred Diabetic Supply program for members who have diabetes (insulin and non-insulin users). Covered
services include supplies to monitor blood glucose (blood glucose monitor, blood glucose test strips, lancet devices and
lancets) and glucose control solutions for checking the accuracy of test strips and monitors.
UnitedHealthcare only covers the following brands of blood glucose monitors and test strips:
• Blood glucose monitors: OneTouch Verio Flex®, OneTouch Verio Reflect®, OneTouch® Verio, OneTouch®Ultra 2, Accu-Chek®
Guide Me and Accu-Chek® Guide. Test strips: OneTouch Verio®, OneTouch Ultra®, Accu-Chek® Guide, Accu-Chek® Aviva
Plus and Accu-Chek® SmartView.
Other brands are not covered.
The Preferred Diabetic Supply program is a Part B covered benefit. It is also available through OptumRx as well as through
some of our DME providers.
Drugs covered under Part B or Part D
Some drugs can fall under either Part B or Part D. We base our coverage determination on if the drug is Part B or Part D on
several factors, such as diagnosis, route of administration and method of administration. UnitedHealthcare may coordinate
Part D vaccine submitted charges with the member’s prescription benefit plan. For a list of medications in each category, refer
to cms.gov > Medicare > Prescription Drug Coverage - General Information > Downloads. Select the appropriate document.
You may also call 1-800-711-4555.
Long-term care facility (includes mental health facilities) pharmacies
We provide convenient access to network long-term care (LTC) pharmacies for all members residing in LTC and mental
health facilities. For a list of network pharmacies covering LTC facilities, refer to the provider directory on uhcprovider.com/
findprovider.
Home infusion
Our plan will cover home infusion therapy drugs for home infusion services provided by a home infusion therapy network
pharmacy. However, Medicare Part D does not cover the supplies and equipment needed for administration. For information on
home infusion therapy, call our Pharmacy department at 1-877-306-4036.

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
105
2023 UnitedHealthcare Care Provider Administrative Guide
Vaccines
Part D covers most vaccines and the associated administration fees. Our plan provides coverage of a number of vaccines.
Some vaccines are medical benefits (Part B medications) and others are Part D drugs.
Part D covers most preventive vaccines. Part B covers flu, pneumococcal, hepatitis B (for intermediate or high-risk individuals),
and some other vaccines (e.g., rabies) for intermediate or high-risk individuals when directly related to the treatment of an injury
or direct exposure to a disease or condition.
The rules for coverage of vaccinations are complex and depend on a number of factors. If you are unsure of the member’s
benefit coverage for vaccines, contact the member’s drug plan to discuss the cost share and allowable Part D vaccine charges
as part of the drug plan’s out-of-network access and/or to ask about other vaccine access options.
• Many network pharmacies can both dispense and administer vaccines at the pharmacy.
• The member may obtain the vaccine from an in-network pharmacy and take it into their physician visit for administration. The
physician may bill UnitedHealthcare for the vaccine administration fee. $20 is the maximum reimbursable amount.
• The physician or member may request that the pharmacy ship the vaccine directly to the physician’s office for administration.
The physician may bill UnitedHealthcare for the vaccine administration fee. $20 is the maximum reimbursable amount.
If the member has been informed about coverage and elects to receive the Part D vaccine and administration from the
physician, do not charge any upfront costs where the Part D vaccine claim will be submitted to UnitedHealthcare along with any
other medical services provided during the visit.
You may choose to enroll with TransactRx for real-time Part D claims’ adjudication, allowing you to collect the copay from the
member at point of service.
For approved claims where a payment is due, a paper check and remittance advice will be issued by OptumRx soon after. As a
contracted UnitedHealthcare entity, providers must refrain from collecting anything more than the copay from the member (i.e.
balance billing) for any UnitedHealthcare approved claim, which includes Part D vaccine out-of-network claims.
If you have questions about claims’ status, payments or need additional information, contact UnitedHealthcare Provider
Services at 1-877-842-3210. Passing costs onto the member without first contacting the plan to discuss their liability and
balance billing are strictly prohibited by UnitedHealthcare and may result in corrective action.
You may access the TransactRx application to submit claims electronically and receive real-time claim adjudication, which
allows you to communicate cost shares to your patient at point of service. It eliminates the need to manually bill pharmacy
claims and prevents the need for the patient to seek reimbursement. Refer to the TransactRx section for details or enroll for
TransactRx at www.transactrx.com/enrollment for real-time Part D vaccine claim adjudication.
For a current list of vaccines and how they are covered, visit professionals.optumrx.com > Resources > Formulary.
Part D vaccines administered in a physician’s office, clinic or hospital
Check the member’s eligibility and benefits prior to providing care to verify which plan covers the vaccine, and communicate
any out-of-pocket cost to the UnitedHealthcare member prior to dispensing and administering a vaccine in a medical outpatient
setting. Check your network status to ensure the member responsibility communicated with the patient reflects the correct
contracted or non-contracted rate. Medical benefit plans and pharmacy benefit plans have separate networks.
Specialty or injectable medications
We may require prior authorization for specialty or injectable medications administered in your office or self-administered
medications from a specialty pharmacy supplier. Refer to the Drug Utilization Review Program section for more information.
Request these authorizations 1‒2 weeks in advance of the service date to allow for eligibility, coverage review and shipping.
For specialty or injectable medications provided and administered in the office (i.e., buy and bill), you must call 1-877-842-
3210 prior to rendering services to understand coverage and/or to obtain an exception. CMS deems some medications as
self- administered (SAD). To prevent the member from having unnecessary out-of-pocket costs, they may need to obtain the
SAD drug from a network pharmacy instead. Providers who fail to follow UnitedHealthcare buy and bill protocols for specialty or
injectable medications or SAD drugs cannot bill the member nor pharmacy benefit for reimbursement.
Call 1-800-711-4555 for details on the rules governing injectable medications or to submit a prior authorization request for
injectable medications obtained by the pharmacy. Optum manages prior authorization requests for medical benefit injectable

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
106
2023 UnitedHealthcare Care Provider Administrative Guide
medications for MA plan members. To initiate a request, click on the Specialty Pharmacy Transactions tool from within the
UnitedHealthcare Provider Portal. The system will display the clinical requirements during the intake process and prompt you
to provide responses to the clinical criteria questions. Attach medical records, if requested. For additional questions, call 1-888-
397-8129.
TransactRx
TransactRx is an online application allowing providers to bill the member’s Part D prescription benefit plan for all Part D covered
vaccines (such as Shingrix and TDAP) and the vaccine administration fee.
This resource helps you submit claims electronically and receive real-time claim adjudication, which lets you communicate and
collect cost shares at point of service. It eliminates the need to submit a claim to the medical plan or Part D prescription drug
plan.
Once enrolled you will be able to:
• Verify member’s eligibility and benefits
• Submit Part D vaccine claims electronically
• Advise members of their cost share and collect this amount at point of service (reducing the potential to balance bill)
• Apply claim adjustments appropriately
• Manage multiple provider billing addresses
• Receive electronic payments
• Receive payments and remits directly from TransactRx twice a month. You have the flexibility to use patient IDs or chart
numbers when submitting a claim, making it easier to reconcile to the remit and payment received.
If interested, please contact TransactRx at 1-866-522-3386 or enroll at: transactrx.com/enrollment.
Drug utilization review program
We conduct drug utilization reviews to help ensure members are getting safe and appropriate care. These reviews are
especially important for members who have more than one doctor prescribing their medications.
As part of the program, we review member drug utilization each time members fill a prescription and by regularly reviewing our
records. We look for medication errors such as:
• Unnecessary drugs because the member is taking another drug to treat the same medical condition.
• Drugs that are inappropriate because of age.
• Possible harmful interactions between drugs.
• Drug allergies.
• Drug dosage errors.
If we identify any problems, we share our findings with you and discuss other alternatives. You may receive calls or faxes from
our pharmacy department following up on findings. If you have questions, contact the pharmacy department.
Drug management program
Our drug management program (DMP) helps ensure members safely use their prescription opioid medications and other
medications that are frequently abused. If members use opioid medications from several doctors or pharmacies, we may talk
to you to make sure opioid medications are appropriate and medically necessary. Working with you, if we decide the use of
prescription opioid medications is not safe, we may limit how the member can get those medications. The limitations may
include:
• Requiring the member to get all prescriptions for opioid medications from certain providers or pharmacies.
• Limiting the amount of opioid medications we will cover for the member.

Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
107
2023 UnitedHealthcare Care Provider Administrative Guide
The DMP may not apply to members who have certain medical conditions, such as cancer. It may not apply to members
receiving hospice, palliative or end-of-life care or who live in an LTC facility.
If you have questions about the program, contact Optum Case Management at 1-855-218-3456.
Electronic prescribing of controlled substances
To help address the misuse and abuse of opioids and other controlled substances, OptumRx home delivery pharmacy requires
electronic prescribing for controlled substances. Several resources are available at professionals.optumrx.com/epcs to help
you get started.
This only affects OptumRx home delivery services. If electronic prescribing is not an option, members still have access to the
retail pharmacy network.
Exceptions process
We offer a formulary exception process to allow for cases where the formulary or its restrictions may not accommodate a
member’s unique medical needs. To request an exception, submit a prior authorization request online or by phone. You must
include a supporting statement explaining why you are requesting an exception.
Generally, we will only approve your request for an exception if alternative drugs included on our formulary list, a lower-tiered
drug or additional utilization restrictions would not be as effective in treating the member’s condition or would cause the
member to have adverse medical effects.
New members taking drugs not on our formulary list, or for which there are restrictions, should talk with you to decide if they
should switch to another appropriate drug we do cover, or if you should request an exception.
You can request an authorization or exception by:
• Online: professionals.optumrx.com/prior-authorization
This online service enables health care providers to submit a real-time prior authorization request 24 hours a day, 7 days a
week. After logging on at optumrx.com with a unique NPI number and password, a physician or health care provider can
submit patient details securely online, enter a diagnosis and medical justification for the requested medication. In many cases,
you can receive authorization instantly.
• Phone: 1-800-711-4555
(We delegate prior authorization services to OptumRx. OptumRx staff adhere to CMS requirements, NPTC practice guidelines
and other professionally recognized standards.)
Generic substitution
Our network pharmacies may recommend or give members the generic version of a drug unless you tell us otherwise. Brand-
name drugs may require our approval if the generic equivalent is covered.
Therapeutic interchange
The pharmacy may contact you by phone, letter or fax to request a member be switched to a preferred alternative drug.
Medication therapy management
The medication therapy management (MTM) program is a free service we offer to members. We conduct reviews on
members who:
• Have multiple chronic conditions.
• Are taking multiple Part D drugs.
• Incur an annual cost of at least $4,935 for all covered Part D drugs.
• Are locked into a specific pharmacy or health care provider in the drug management program.
Chapter 8: Specialty pharmacy and Medicare Advantage pharmacy
108
2023 UnitedHealthcare Care Provider Administrative Guide
We use the MTM program to help ensure our members are using appropriate drugs to treat their medical conditions and to
identify possible medication errors. We educate members about drugs currently on the market, making recommendations for
lower-cost or generic drugs where applicable. In addition, we inform members in the MTM program about the safe disposal of
unused medications, including controlled substances.
We may relay this information to you as well with the option to change drug therapies, as appropriate. You may receive calls or
faxes from our pharmacy department following up on any interventions discussed with your patient.
Transition policy
Our transition policy allows for a 1-month coverage for members who have an immediate need for a drug not on our formulary,
subject to restriction or no longer covered. You should switch the member to a different drug or request a formulary exception.
We may provide the member with a temporary transition supply while you pursue an exception. The drug must be a Part D drug
purchased at a network pharmacy.
The following table summarizes the rules for receiving a transition supply of a drug. Members should read their plan’s evidence
of coverage (EOC) for details.
Transition eligible situations Temporary transition supply amount
New members: During the first 90 days of membership in the plan
Continuing members: During the first 90 days of the calendar year if the drug
encountered a negative formulary change
At least a 1-month supply, as
described in member’s EOC.
For members who have been in the plan for more than 90 days and reside in a LTC
facility and need a supply right away
At least a 31-day supply, as described
in the member’s EOC.
Members who have unplanned transitions such as hospital discharges (including
psychiatric hospitals) or level of care changes (i.e., changing long-term care
facilities, exiting and entering a long-term care facility, ending Part A coverage
within a skilled nursing facility, ending hospice coverage and reverting to Medicare
coverage) at any time during the plan year
At least a 1-month supply, as
described in member’s EOC.
To request a formulary exception, you may use the online tool at professionals.optumrx.com or call our Pharmacy Department
at 1-800-711-4555.

109
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 9: Specific protocols
Non-emergent ambulance ground transportation
Non-emergent ambulance transportation is appropriate with documentation that the member’s condition is such that other
means of transportation could endanger the member’s health, and ambulance transportation is medically required.
There is no referral required for in-network health care providers.
Interoperability protocol
To help encourage the exchange of real-time health information, you are required to communicate with us electronically through
the use of near real-time data exchange services, based on Health Level Seven (HL7) standards inside your Electronic Health
Record (EHR) workflow. This includes:
• Eligibility inquiries: HL7 Fast Healthcare Interoperability Resources (FHIR).
• Patient care opportunities.
• Admission, discharge and transfer (ADT) notifications: HL7 ADT.
• High-performing provider referral with cost estimation.
• Identification of preferred labs and/or diagnostic radiology locations.
• Prior authorization for medical and pharmacy services.
As a result of this protocol, we are expanding our medical records standards and requirements. If asked, you’ll work with us to
develop a clinical data exchange and integration plan within 60 days of outreach to provide us with remote access to your EHR
for UnitedHealthcare members. This clinical data exchange and integration plan will support near real-time data exchanges with
UnitedHealthcare in an automated fashion. To support this initiative, we’ll work with you to establish EHR access to decrease
administrative burden for programs that aren’t currently supported by interoperability standards. These capabilities are in
addition to the medical records requirements in your Participation Agreement. If we can’t access the medical records in your
EHR system, or the information contained in your EHR system is unclear or insufficient, you’ll need to submit paper copies of
medical records for UnitedHealthcare members upon request.
For more information, go to uhcprovider.com > Resources > Plans, policies, protocols and guides. Under Additional
Resources, choose Protocols.
Laboratory services protocol
Clinical information submission
To comply with state and federal data collection and reporting requirements, we require clinical data from you. It helps us
measure quality of care for our members. It also helps us collaborate with you to address gaps in care. You must submit all
clinical data including laboratory test results. Give us this data within 30 calendar days from the date of service or within the
time specified by law.
When giving us clinical data, you must follow state and federal laws, and obtain prior consent to give us the clinical data when
state or federal law requires it. We need to provide the source of the data to satisfy National Committee for Quality Assurance
(NCQA) audits or other compliance requirements. You must confirm that the information given to us is accurate and complete.
We verify that security measures, protocols and practices are compliant with:
• HIPAA regulations.
• UnitedHealthcare data usage, governance and security policies.

Chapter 9: Specific protocols
110
2023 UnitedHealthcare Care Provider Administrative Guide
We use the clinical data to:
• Perform treatment.
• Payment.
• Follow state and federal law.
• Health care operations, as defined in HIPAA.
Health care operations may include:
1. Compliance with state and federal data collection and reporting requirements, such as:
– Healthcare Effectiveness Data and Information Set (HEDIS).
– Consumer Assessment of Healthcare Providers and Systems (CAHPS).
– Health Outcomes Survey (HOS).
– NCQA accreditation.
– Centers for Medicare and Medicaid Services (CMS) or Star Ratings.
– CMS and HHS Hierarchical Condition Category Risk Adjustment System.
2. Care coordination and other care management and quality improvement programs such as:
– Physician performance.
– Pharmaceutical safety.
– Member health risks using predictive modeling and the subsequent development of disease management programs
used by UnitedHealthcare.
– Other member and health care provider health awareness programs.
3. Quality assessment and benchmarking data sets.
We will work with you to help ensure all clinical data values are being transmitted effectively. This allows for lawful identification
and use of the clinical data.
We define the HIPAA minimum necessary data requirements defined in specific documents related to the method of clinical
data acquisition. The companion guides that contain these requirements are on uhcprovider.com/edi.
Self-referral and anti-kickback
This protocol applies to all participating physicians and health care professionals. It also applies to all laboratory services,
clinical and anatomic, ordered by physicians and health care professionals.
We do not allow our health care providers to earn money from referring members to a lab. This includes profits from:
• Investments in an entity where the referring health care provider generates business.
• Profits from collection, processing and/or transporting of specimens.
• Cost reductions such as:
– Free Wi-Fi.
– Free urine cups.
If you do not follow this rule, we may:
• Decrease your fee schedule.
• Terminate your network participation.
• Prosecute.
Structured exchange of clinical data
Our protocols require electronic submission of lab results within 30 days of a lab test. This supports HEDIS closure rates and
significantly reduces the burden of manual chart requests for our health care providers.
Health care providers are required to submit an expanded set of clinical data following a physician visit, as well as a discharge
summary within 7 days of an inpatient discharge. Failure to comply with this clinical data exchange may result in penalties to
your practice.

Chapter 9: Specific protocols
111
2023 UnitedHealthcare Care Provider Administrative Guide
When you share this data with us electronically, we can:
• Promote timely engagement between you and our members.
• Reduce the administrative burden of manual information sharing.
• Drive quality outcomes for you and our members by closing gaps and improving coordination of care.
To begin sharing the required information, visit uhcprovider.com/ediconnect to find the best solution for your practice. Health
care providers have different data transfer capabilities, and we will work with you to find the best method of data transmission.
Nursing home and assisted living plans
UnitedHealthcare nursing home plans and assisted living plans are Medicare Advantage Institutional Special Needs Plans.
These protocols are only applicable to PCPs, nurse practitioners (NP) and physician assistants (PA) who participate in the
network for the nursing home plan and/or the assisted living plan care team, which may include both an onsite advance
practice clinician (ARNP/PA) and a registered nurse (RN) who cooperate with and are bound by these additional protocols.
If these protocols conflict with other protocols in connection with any matter pertaining to UnitedHealthcare Nursing Home Plan
or Assisted Living Plan members, these protocols apply, unless statutes and regulations dictate otherwise.
Nursing home plan PCP protocols
As the PCP, you cooperate with and are bound by these additional protocols:
1. Attend PCP orientation session and annual PCP meetings.
2. Conduct face-to-face initial and ongoing assessments of the medical needs of our members, including those mandated by
regulatory requirements.
3. Deliver health care to our members at their residence with the primary care team.
4. Participate in family care conferences with responsible parties, family and/or legal guardian to discuss the member’s
condition; care needs; overall plan of care; and goals of care, including advance care planning.
5. Collaborate with other members of the primary care team designated by us and other treating professionals to provide and
arrange for the provision of covered services to our nursing home plan members. This includes making joint visits with
other primary care team members and participating in formal and informal conferences with primary care team members
and/or other treating professionals following a scheduled member reassessment, significant change in plan of care and/or
condition.
6. Collaborate with us when a change in the primary care team is necessary.
7. Give us at least 45 calendar days prior notice when stopping services at a facility where our members live.
8. When admitting our member to a hospital, immediately notify the PCP and UnitedHealthcare nursing home plan or payer of
the admission and reasons for the admission.
Nursing home plan and assisted living plan protocols for other provider types
The nursing home plan NP, PA and/or assisted living plan care team member (i.e., RN or ARNP/PA), must follow these
additional protocols:
1. Attend training and orientation meetings as scheduled by the plan.
2. Deliver health care to our members at their place of residence in collaboration with a PCP.
3. Communicate with the member’s responsible parties, family and/or legal guardian on a regular basis. Participate in
conferences with responsible parties to discuss the member’s condition, care needs, overall plan of care and goals of care.
4. Collaborate with other members of the primary care team and other health care providers to provide and arrange for the
provision of covered services for our members. This includes:
– Making joint visits with others on the primary care team to our members.
– Participating in conferences with primary care team members and/or other treating professionals following a scheduled
member reassessment, significant change in plan of care and/or condition.

Chapter 9: Specific protocols
112
2023 UnitedHealthcare Care Provider Administrative Guide
5. Collaborate and communicate with the Director of Clinical Operations to coordinate all inpatient, outpatient and facility care
for our members. Forward copies of the required documentation to our office. Work with the director to develop a network
of health care providers who are aware of the special needs of the frail elderly.
6. Conduct a complete initial assessment for all of our nursing home plan members within 30 calendar days of enrollment (90
days for assisted living plan members), that includes:
• History and physical examination, including mini-mental status and functional assessment.
• Review previous medical records.
• Prepare problem list.
• Review medications and treatments.
• Review lab and X-ray results.
• Review current therapies (e.g., physical therapy, occupational therapy, speech therapy).
• Update treatment plan.
• Review advance directive documentation including Do Not Resuscitate: Do Not Intervene (DNR/DNI) and use of other
life-sustaining techniques.
• Contact the family/responsible party within 30 calendar days of enrollment to:
– Schedule a meeting at the facility, if possible.
– Obtain further history.
– Agree on type and frequency of future contacts.
– Discuss advance directives.
• Perform clinical and quality initiative documentation as directed.
7. Provide care management services to coordinate all the covered services outlined in our member’s benefit plan.
Examples include:
• All medically necessary and appropriate facility services.
• Outpatient procedures and consultations.
• Inpatient care management.
• Podiatry, audiology, vision care and mental health care provided in the facility:
– When a member is admitted, notify the PCP and UnitedHealthcare or payer immediately if it is for an emergency or
observation.
– If contact information is not available, call the local office or coordinate communication through the nursing facility
clinical staff.
8. Give us at least 45 calendar days’ notice when discontinuing services at any facility where our members live.
Social determinants of health protocol
We strongly encourage you to document social determinants of health (SDoH) using ICD-10 diagnostic code(s) (or successor
diagnostic codes) in the member’s medical record. Unless prohibited by federal or state law, this protocol applies to all
UnitedHealthcare members, including MA and individual and group market plans.
As a result of this protocol, we strongly encourage you to routinely screen, document and submit the corresponding ICD-10
code(s). Although the list of ICD-10 codes is not comprehensive of all social determinants, it is a step we can take together in
improving the lives of our members. We encourage you to remain current on the utilization of these SDoH ICD-10 codes, as they
may be updated.
For more information, go to uhcprovider.com > Resources > Plans, policies, protocols and guides > Under Additional
Resources, choose Protocols > Social Determinants of Health ICD-10 Coding Protocol.

Chapter 9: Specific protocols
113
2023 UnitedHealthcare Care Provider Administrative Guide
Telehealth services protocol
UnitedHealthcare will consider reimbursement for telehealth services performed while the member was at home or another
originating site under certain commercial and MA benefit plans.
To be eligible for payment, you must meet the following telehealth service requirements:
• Comply with the American Medical Association (AMA) and Federation of State Medical Board guidelines, which require all
telemedicine visits use live interactive audio and video as well as visual transmission of a physician-patient encounter. For
UnitedHealthcare individual and fully insured group market plans, some state-specific variations may apply.
• Use a secure technology platform that meets federal and state requirements for security and confidentiality of electronic
member information.
• Comply with all applicable federal and state laws concerning the security and confidentiality of member information, including
HIPAA and its governing regulations.
• Maintain member records related to telehealth services in a secure medium that meets federal and state requirements for
encryption and security of electronic member information. Additionally, records should include the application/service used
to conduct the telehealth visit.
• Offer telehealth services in a clean, private space and not in vehicles or public spaces.
• Code the telehealth services in accordance with applicable reimbursement policies.
114
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 10: Our claims process
For information on submitting claims using Electronic Data Interchange (EDI), go to uhcprovider.com/edi837.
You can learn more about the many tools available to help you prepare, submit and manage
your UnitedHealthcare claims on uhcprovider.com/claims. These include Claim Estimator
with bundling logic, training tools and resources such as frequently asked questions
(FAQs), quick references, step-by-step instructions and tutorials.
Prompt claims processing
We know you want prompt payment. We work hard to process your claims timely and accurately. This is what you can do to
help us:
1. Submit the claim to the correct payer by reviewing the member’s eligibility as outlined in Verifying eligibility, benefits and
your network participation status.
Note: When we give you eligibility and benefit information, we are not guaranteeing payment or coverage in any specific
amount. Actual reimbursement depends on many factors, such as compliance with administrative protocols, date(s) of
services rendered, and benefit plan terms and conditions. For Medicare Advantage (MA) benefit plans, reimbursement
also depends on CMS guidance and claims processing requirements.
2. Follow the instructions in the How to submit advance notification/prior authorization, admission notification, discharge
notification and observation stay notification section.
3. Prepare complete and accurate claims. (See Claims and Encounter Data Submissions section or use our reference
guides found on uhcprovider.com/claims.)
4. Submit claims electronically with EDI for fast delivery and confirmation of receipt.
• Electronic submissions are preferred for sending claims to UnitedHealthcare. View our Claims Payer List to determine the
correct payer ID to use.
• Our contracts generally require you to conduct business with us electronically. They contain specific requirements
for electronic claim submission. Review your Agreement and follow the requirements. While some claims may require
supporting information for initial review, we have reduced the need for attachments. We request additional information
when needed.
• For helpful resources and tips on submitting claims electronically, visit uhcprovider.com/edi.
• Check the status of a claim using EDI 276/277 Claim Status Inquiry and Response transactions. Contact your vendor or
clearinghouse if these transactions are not available or activated in your system.
• Learn how to elevate your productivity and savings using EDI at uhcprovider.com/optimizeedi.
• If you need assistance using EDI, visit our EDI Contacts page.
• For EDI connectivity options, go to uhcprovider.com/ediconnect to learn more. You can use Claim Submission in the
UnitedHealthcare Provider Portal to submit claims online. View uhcprovider.com/claims for more information.
HIPAA claim edits and Smart Edits
When claims are submitted using EDI, HIPAA edits are applied by the clearinghouse to help ensure claims contain specific
information. Any claims not meeting requirements are rejected and returned back to the health care provider to make
corrections and resubmit electronically.
Smart Edits are an EDI capability that auto-detects claims with potential errors. Smart Edits may also be applied to help reduce
claim denials and improve the claim processing time. You have 5 calendar days to correct claims flagged or identified by Return
and Documentation Smart Edits before they are automatically processed. Rejection Smart Edits require you to take action in for
your claims to make it into our claim processing system.

Chapter 10: Our claims process
115
2023 UnitedHealthcare Care Provider Administrative Guide
For more information on HIPAA claim edits, go to uhcprovider.com/claimedits. For more information on Smart Edits, go to
uhcprovider.com/smartedits.
Optum Pay™
Optum Pay™ offers electronic funds transfer (ACH)/direct deposit and electronic remittance advice (ERA) services. Optum Pay
is the preferred method of receiving ACH/direct deposit payments from us. Printable and downloadable provider remittance
advice (PRA) documents related to those ACH/direct deposit payments are also accessible in the Optum Pay portal.
Optum Pay delivers electronic payments and provides online remittance advice and 835 files to health care providers, hospitals
or facilities.
If you use a billing service company, Optum Pay created a new portal just for third-party billing service companies. The billing
service first needs to enroll for access to Optum Pay.
After your billing service enrolls, it can set up users on its Optum Pay account and then associate its Optum Pay account with
your practice. This enables the service to access the claim payment information needed to post and close claims.
You may choose to receive electronic payments by direct deposit/ACH into your organization’s bank account. The ACH initial
setup or a change in banking information will take approximately 10 business days for processing and bank account validation.
If ACH/direct deposit is not chosen, a virtual card payment (VCP) will be issued. This method does not require bank account
information, as you would process your payments using your credit card point of sale terminal. Your current credit card
processing fees apply. You can confirm those rates with your merchant processor directly.
In certain unique situations or where required by applicable law, you may be entitled to request payment by paper check. For
a list of health care providers who may qualify for an exemption, and how to request one, go to uhcprovider.com/claims >
Electronic Payment Solutions > EPS Frequently Asked Questions.
Optum Pay posting and balancing with direct deposit
We will not mail PRAs once you enroll in Optum Pay and consent to electronic delivery of your remittance and PRA documents.
However, there are a few options for you to access them electronically:
1. With the basic level of Optum Pay, you can access the last 13 months of your PRAs in PDF format on Optum Pay.
2. You can also access the last 24 months of most UnitedHealthcare commercial, Medicare and Medicaid PRAs from the
Document Library at no cost.
3. PRAs from UnitedHealthcare-affiliated networks are generally available at no cost on their portals, such as OxfordHealth
and UMR.
4. If you are using the premium level of Optum Pay, you can access the last 36 months of your PRAs on Optum Pay.
To sign up, visit uhcprovider.com/payment.
Virtual card payments
Process virtual card payments (VCPs) using the same method your organization uses to process credit card payments. Your
current credit card processing fees apply. You can confirm those rates with the merchant processor directly. If your practice
does not want to receive VCPs, you can register for ACH/direct deposit as described previously. The VCP process does not
require that you share your banking information.
Posting and balancing with VCP
1. A single-use VCP will be issued and provided with each payment you receive.
2. If you are receiving paper correspondences, you will receive a paper remittance and paper virtual card statement in the
mail.
Chapter 10: Our claims process
116
2023 UnitedHealthcare Care Provider Administrative Guide
3. Process your payment the same way you process a “card not present” transaction from a member. Enter:
– The exact amount of the payment.
– The 16-digit account number found on your virtual card statement.
– The expiration date.
– The card validation code (CVC).
– The payer’s ZIP code if prompted by your point of sale terminal.
All the information you’ll need to process your VCP can be found on the virtual card statement.
Credit card processing fees may apply to virtual cards. Contact your merchant processor or financial institution for information
on specific costs.
Unspent funds for VCPs are subject to state unclaimed property laws. OptumHealth Financial Services, a UnitedHealthcare-
affiliated company, provides payment services to the health care industry and offers various claim payment options.
UnitedHealthcare-affiliated companies may receive transaction fees or other compensation related to some payment options.
Enroll and learn more about
Optum Pay
To enroll with Optum Pay to receive direct deposit payments,
visit myservices.optumhealthpaymentservices.com. To
complete the enrollment, upload an image of a voided check
and an image of your organization’s Internal Revenue Service
(IRS) Form W-9, Request for Taxpayer Identification Number
(TIN) and certification.
If you have questions about Optum Pay or direct deposit, call us
at 1-877-620-6194 to speak with an Optum Pay representative.
Claims and encounter data
submissions
You must submit a claim and/or encounter for your services,
regardless of whether you have already collected the
copayment, deductible or coinsurance from the member. If you
have questions about submitting claims to us, call us at the
phone number listed on the member’s ID card.
It is important to accurately code the claim because a
member’s level of coverage under their benefit plan may vary
for different services. To help correctly code your claims, use
Claim Estimator in the UnitedHealthcare Provider Portal. It
includes a feature called Professional Claim Bundling Logic.
This helps you determine allowable bundling logic and other
commercial claims processing edits for a variety of procedure
codes. This is not available for all products.
Pricing and payment calculations for professional commercial
claims are available under the Pre-Determination of Benefits
option. Allow 45 calendar days for us to process your claim,
unless your Agreement says otherwise. Check claims in the
UnitedHealthcare Provider Portal before sending second
Learn more:
For more information — including quick reference guides
and videos — go to uhcprovider.com > Resources > The
UnitedHealthcare Provider Portal resources.
UnitedHealthcare Web Support
providertechsuppor[email protected]
1-866-842-3278, Option 1, Monday–Friday, 7 a.m. – 9 p.m. CT
Get the most up-to-date claims status and
payment information, and submit your claim
reconsideration and appeal requests.
View claims information
for multiple
UnitedHealthcare® plans
Access letters, remittance
advice documents and
reimbursement policies
Flag claims for
future viewing
Submit additional
information requested
on pended claims
Submit claim
reconsideration and
appeal requests
Receive instant
printable confirmation
for your submissions
Simplify your administrative workflow with
Claims in the
UnitedHealthcare
Provider Portal
Chapter 10: Our claims process
117
2023 UnitedHealthcare Care Provider Administrative Guide
submissions or tracers. If you do need to submit a second submission or a tracer, submit the claim electronically no sooner
than 45 days after original submission.
Complete claims by including the information listed under the Requirements for complete claims and encounter data
submission section. We prefer to receive claims electronically.
If we receive a claim electronically with missing information or invalid codes, we may reject the claim, not process it or, if
applicable, not submit it to CMS for consideration in the risk adjustment calculation.
Requirements for complete claims and encounter data submission
We may pend or deny your claim if you do not include the following information:
• Member’s name, address, gender, date of birth or relationship to subscriber (policy owner).
• Subscriber’s name (enter exactly as it appears on the member’s ID card), ID number, employer group name and employer
group number.
• Rendering health care provider’s name, signature or representative’s signature, address where service was rendered, “Remit
to” address, phone number, NPI, taxonomy and federal TIN.
• Referring health care provider’s name and NPI, as well as TIN (if applicable). All laboratory, DME, imaging and home health
claims and/or encounters must include the referring health care provider’s name and NPI number in addition to the other
elements of a complete claim and/or encounter described in this guide.
• Complete service information, including date of service(s), place of service(s), number of services (days/units) rendered,
Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) procedure codes,
with modifiers where appropriate, and current ICD-10-CM diagnostic codes by specific service code to the highest level of
specificity. You must communicate the primary diagnosis for the service performed, especially if more than one diagnosis is
related to a line item.
• Charge per service and total charges.
• Itemized bill – There may be times when we request an itemized bill to help adjudicate the claim. In an effort to avoid
unnecessary delays, submit itemized bills upon request.
• Detailed information about other insurance coverage.
• Information regarding job-related, auto or accident information, if available.
• Retail purchase cost (or a total retail rental cost) greater than $1,000 for DME.
• Current National Drug Code (NDC) 11-digit number, NDC unit of measure (F2, GR, ML, UN, ME) and NDC units dispensed
(must be greater than 0) for all claims submitted with drug codes. Enter the NDC information for the drug(s) administered
in the 24D field of the CMS-1500 Form, field 43 of the UB-04 form, or the LIN03 and CTP04-05 segments of the HIPAA 837
Professional or institutional electronic form.
• Method of administration (self or assisted) for hemophilia claims – note the method of administration and submit with the
claim form with applicable J-CODES and hemophilia factor, to enable accurate reimbursement. Method of administration is
either noted as self or assisted.
Submission of unlisted medical or surgical codes
Include a detailed description of the procedure or service for claims submitted with:
• Unlisted medical/surgical CPT.
• “Other” revenue codes.
• Experimental services.
• Reconstructive services.
Additional information needed for a complete UB-04/CMS-1450 Form
Your claim may be pended or not processed if you do not include:
• Date and hour of admission.
• Date and hour of discharge.
• Member status-at-discharge code.
Chapter 10: Our claims process
118
2023 UnitedHealthcare Care Provider Administrative Guide
• Type of bill code (3 digits).
• Type of admission (e.g., emergency, urgent, elective, newborn).
• Current 4 digit revenue code(s).
• Attending physician ID number.
• For inpatient and outpatient services/procedures, the specific CPT or HCPCS codes, line item date of service and
appropriate revenue codes (e.g., laboratory, radiology, diagnostic or therapeutic).
• Complete box 45 for physical, occupational or speech therapy services (revenue codes 0420-0449).
• Any special billing instructions that are in your Agreement.
• On an inpatient hospital bill type of 11x, use the actual time the member was admitted to inpatient status.
• If charges are rolled to the first surgery revenue code line on hospital outpatient surgery claims, report a nominal monetary
amount ($10 or $100) on all other surgical revenue code lines to assure appropriate adjudication.
• The condition code designated by the National Uniform Billing Committee (NUBC) on claims for outpatient preadmission non-
diagnostic services that occur within 3 calendar days of an inpatient admission and are not related to the admission.
Timely Filing
Your claim must be filed within your timely filing limits, or it may be denied. If you disagree with a claim that
was denied due to timely filing, you will be asked to show proof you filed the claim within your timely filing
limits.
Timely filing limits vary based on state requirements and contracts. Refer to your internal contracting contact
or Agreement for your specific timely filing requirements.
Risk adjustment data – MA, commercial and exchange
U.S. Department of Health and Human Services (HHS) requires risk adjustment for commercial small group and individual
benefit plans. Similar to the CMS risk adjustment program for MA benefit plans, HHS uses Hierarchical Condition Categories
(HCCs) to calculate an annual patient risk score that represents the specific patient’s disease burden. Every year, CMS and
HHS require demographic and health information about our members. Diagnoses do not carry forward to the following year and
must be assessed and reported every year.
The risk adjustment data you give us, including clinical documentation and diagnosis codes, must be accurate and complete. It
is critical for you to refer to the ICD-10-CM coding guide to code claims accurately. To comply with risk adjustment guidelines,
specific ICD-10-CM codes are required.
• Medical records must support all conditions coded on the claims or encounters you submit using clear, complete and
specific language.
• Code all conditions that co-exist at the time of the member visit and require or affect member care, treatment or management.
• Never use a diagnosis code for a “probable” or “questionable” diagnosis. Code only to the highest degree of certainty for the
encounter/visit. Include information such as symptoms, signs, abnormal test results and/or other reasons for the visit.
• Specify whether conditions are chronic or acute in the medical record and in coding. Only choose diagnosis code(s) that fully
describe the member’s condition and pertinent history at the time of the visit. Do not code conditions that no longer exist.
• Carry the diagnosis code all the way through to the correct digit for specificity. For example, do not use a 3-digit code if a
5-digit code more accurately describes the member’s condition.
• Check the diagnosis code against the member’s gender.
• Sign chart entries with credentials.
• All claims and/or encounters submitted to us for risk adjustment consideration are subject to federal and/or UnitedHealthcare
audit. Audits may come from CMS, HHS or us, where we may select certain medical records to review to determine if the
documentation and coding are complete and accurate. Give us any requested medical records quickly. Provide all available
medical documentation for the services rendered to the member.
• Notify us immediately about any diagnostic data you have submitted to us that you later determine may be erroneous.

Chapter 10: Our claims process
119
2023 UnitedHealthcare Care Provider Administrative Guide
CMS HCC risk adjustment
We offer an alternate method of reporting CMS risk adjustment data in addition to the normal claim/encounter submission
process. All encounter submissions are required to process 837 Claim Encounter in a HIPAA 5010-compliant format. To
supplement a previously submitted 837 Claim/Encounter, you may submit an 837 replacement claim/encounter or send
additional diagnosis data related to the previously submitted 837 through the Optum ASM Operations FTP process. If you
choose to submit by ASM, you will first need to contact the Optum ASM Operations team at [email protected] to start the
onboarding process.
NPI
HIPAA, federal Medicare regulations and many state Medicaid agencies require health care providers to obtain and use a
standardized NPI. You are required to use an NPI as identification on electronic transactions as outlined in the instructions for
HIPAA electronic transaction X12N Implementation Guides.
State-specific regulations may also require you to submit your NPI on claims. To avoid payment delays or denials, you must
submit a valid billing NPI, rendering NPI and relevant taxonomy code(s) on all claims and encounters. In addition, we encourage
you to submit the referring health care provider’s NPI.
The NPI information you report on your claims and encounters helps us to efficiently process claims and encounters and to
avoid delays or denials.
We accept NPIs submitted through:
• UnitedHealthcare Provider Portal: In My Practice Profile, under Practice Management, select the Provider Demographics or
Group Demographics tab to make health care provider updates. In the UnitedHealthcare Facility/Practice Profile, select the
View/Update NPI Information tab to make facility updates.
• Fax: Using the fax form on uhcprovider.com/mypracticeprofile > Go to My Practice Profile.
• Phone: United Voice Portal (UVP) at 1-877-842-3210. Select the Health Care Provider Services prompt. Say “Demographic
Changes,” and your call will go to the service center to collect your NPI, health care provider taxonomy codes and other NPI-
related information.
• Credentialing/Contracting: NPI and National Uniform Claim Committee (NUCC) taxonomy indicators are collected as part of
credentialing, recredentialing, new provider contracting and re-contracting efforts.
How to submit NPI, TIN and taxonomy on a claim or encounter
Information is provided for the location of NPI, TIN and taxonomy on claims on uhcprovider.com/mypracticeprofile.
MA claim processing requirements
Section 1833 of the Social Security Act prohibits payments to a care provider if there is not sufficient information to determine
the “amounts due to such provider.” We apply various claims processing edits based on:
• National and local coverage determinations.
• The Medicare Claims Processing Guide.
• National Correct Coding Initiative (NCCI).
• Other applicable guidance from CMS, including the Official ICD-10-CM Guidelines for Coding and Reporting.
These edits provide us with information to determine:
• The correct amount to pay.
• If you are authorized to perform the service.
• If you are eligible to receive payment.
• If the service is covered, correctly coded and correctly billed to be eligible for reimbursement.

Chapter 10: Our claims process
120
2023 UnitedHealthcare Care Provider Administrative Guide
• If the service is provided to an eligible beneficiary.
• If the service was provided in accordance with CMS guidance.
Health care providers in our MA network must follow CMS guidance regarding billing, coding, claims submission and
reimbursement. For example, you must report serious adverse events by having the Present on Admission (POA) indicator on all
acute care inpatient hospital claims and ambulatory surgery center outpatient claims. If you do not report the serious adverse
event, we try to determine if any charges filed with us meet the criteria as a Serious Reportable Adverse Event or Never Event. If
you do not follow these requirements, we will deny the claim. You cannot bill the member.
There may be situations when we implement edits, and CMS has not issued any specific coding rules. In these cases, we
review the available rules in the Medicare Coverage Center. We find those coding edits that most align with the applicable
coverage rules.
Due to CMS requirements, you are required to use the 837 version 5010 format. We reject incomplete submissions.
Hospice – MA
UnitedHealthcare is participating in the CMS Value-Based Insurance Design (VBID) hospice pilot in AL, OK, IL (Chicago metro)
and WellMed in Corpus Christi, TX. Refer to uhcprovider.com/mahospice to review protocol for those states. All other states
will adhere to the following protocol.
When an MA member elects hospice, bill claims for:
• Hospice-related services to CMS.
• Services covered under Medicare Part A and B (unrelated to the terminal illness) to the Medicare administrative contractor.
We are not financially responsible for these claims. We may be financially responsible for additional or optional supplemental
benefits under the MA member’s benefit plan such as eyeglasses and hearing aids. Medicare does not cover additional and
optional supplemental benefits.
Medicare Crossover
Medicare Crossover is the process by which Medicare, as the primary payer, automatically forwards Medicare Part A (hospital)
and Part B (medical) claims to a secondary payer. Medicare Crossover is a standard offering for most Medicare-eligible
members covered under our commercial benefit plans. Enrollment is automatic for these members.
• For more information on Medicare Crossover, refer to EDI Quick Tips for Claims > Secondary/COB or Tertiary Claims >
Medicare Crossover.
• More information on Medicare/Crossover can be found on the 837 Claims page of uhcprovider.com/edi.
Claim submission tips
Do not use a claim form to resubmit claims that were denied or pended for additional information. Use the Claims tool in the
UnitedHealthcare Provider Portal.
The payer ID is an identification number that instructs the clearinghouse where to send your electronic claims or encounters.
In some cases, the payer ID listed on our Claims Payer List may be different from the number issued by your clearinghouse.
Validate any errors with your clearinghouse to avoid delays.
• Before submitting your EDI claims to us, refer to the member’s ID card for the payer ID.
• If no payer ID is listed, or you do not have access to the member’s ID card, refer to our Claims Payer List for the correct payer
ID number.
Submit professional and institutional claims and/or encounters electronically. We accept primary and secondary claims
electronically. Find specific information about secondary claims submissions, such as coordination of benefits (COB) electronic
claim requirements and EDI specifications, on uhcprovider.com/ediclaimtips > Secondary/COB or Tertiary Claims.
The HIPAA ANSI X1 25010 837 format is the only acceptable format for submitting claims and encounter data.

Chapter 10: Our claims process
121
2023 UnitedHealthcare Care Provider Administrative Guide
We support other HIPAA EDI transactions to assist you with your revenue cycle process. For a complete list of EDI transactions
available to our health care providers, go to uhcprovider.com/edi. Locate specific claims with your provider ID or a specific
member’s ID. You can get a claim summary or line-item detail about claims status.
Estimating treatment costs
The Claim Estimator tool (not available for all products) is a fast and simple way to get your commercial professional claim
predeterminations through uhcprovider.com/claims > Get a Claim/Procedure Cost Estimate. With Claim Estimator, you
receive an estimate on whether a procedure will be covered, at what percentage, if any, and what the claim payment will be.
Claim Estimator gives you expense information you can share with your patient before treatment.
HRA and HSA benefit plans claims submission tips
For faster claims turnaround and more accurate reimbursement with UnitedHealthcare HRAs or HSAs, verify member eligibility
and benefits coverage as an EDI 270/271 transaction, or use the UnitedHealthcare Provider Portal. You can also call the
member service number on the back of your patient’s ID card.
For our HRA members: Once logged into the Patient Eligibility & Benefits, the “HRA Balance” field will display if the member is
enrolled in any of our consumer-driven health plans. When there are funds available in an HRA account, the current balance will
display. The current balance is also returned if you are using EDI.
This amount is based on the most recent information available and is subject to change. The actual balance may differ from
what is displayed if there are outstanding claims or adjustments that have not yet been submitted or processed.
Balances for HSA members are not available through the UnitedHealthcare Provider Portal or EDI.
Most UnitedHealthcare HRA and HSA benefit plans do not require copayments. Do not ask those members to pay a copayment
at the time of service unless indicated on their ID card.
Submit claims electronically as an 837 EDI transaction or through the Claims Submission tool in the UnitedHealthcare Provider
Portal, or to the address on the back of the member’s ID card.
Wait until after a claim is processed and you receive your explanation of benefits (EOB)/remittance advice before collecting
funds from our members with an HRA/HSA benefit plan. The member responsibility may be reimbursable through their HRA
account and paid to you. The remittance advice displays any remaining member balance. We will not automatically transfer
the HSA balance for payment. However, the member can pay with their HSA debit card or convenience checks linked to their
account balance.
Consumer account cards and qualified medical expenses
You may only charge our HRA or FSA consumer account cards for qualified medical expenses incurred by the cardholder, the
cardholder’s spouse or their dependent. Qualified medical expenses are expenses for medical care that provide diagnosis,
cure, mitigation, treatment or prevention of any disease; or for affecting any structure or function of the body.
Examples of non-qualifying expenses include:
• Cosmetic surgery/procedures (i.e., procedures directed at improving a person’s appearance that do not meaningfully
promote the proper function of the body or prevent or treat illness or disease), such as:
– Face lifts.
– Liposuction.
– Hair transplants.
– Hair removal (electrolysis).
– Breast augmentation or reduction.
› Surgery or procedures necessary to improve a defect from a congenital abnormality, and reconstructive surgery following
a mastectomy for cancer, may qualify.
• Teeth whitening and similar cosmetic dental procedures.
• Advance expenses for future medical care.

Chapter 10: Our claims process
122
2023 UnitedHealthcare Care Provider Administrative Guide
• Weight loss programs (Disease-specific nutritional counseling may be covered.)
• Illegal operations or procedures.
An expense may be a qualified medical expense even if not covered under a member’s benefit plan. For updated information
regarding qualified medical expenses, go to irs.gov or call the IRS at 1-800-TAX-FORM (1-800-829-3676).
Pass-through billing
You may only bill for services that you or your staff perform. You may not bill on behalf of another provider who actually
performed the services.
Pass-through billing is not permitted and may not be billed to our members.
Clinical Laboratory Improvement Amendments requirements/reimbursement policy
requirements/reimbursement policy
We only reimburse for laboratory services that you are certified to perform through the federal Clinical Laboratory Improvement
Amendments (CLIA). You must not bill our members for any laboratory services and respective procedure codes if you don’t
have the applicable CLIA certification.
In-office laboratory tests and CLIA waived tests
Health care provider offices granted a CLIA Certificate of Waiver may conduct a limited number of tests in-house.
As defined by CLIA, waived tests are simple tests with a low risk of an incorrect result. Sites that perform only waived testing
must have a CLIA Certificate of Waiver and follow the manufacturer’s instructions; other CLIA requirements do not apply to
these sites. To determine if the test being performed has been approved for Certificate of Waiver status, make sure the test is on
the CLIA Waived Test List.
All other laboratory tests require a referral to a participating or capitated laboratory. You can find a list of approved codes on
cms.gov > Regulations & Guidance > Legislation > Clinical Laboratory Improvement Amendments. Participating laboratories
are listed on uhcprovider.com.
Note: Some plans are capitated for laboratory services. The capitated laboratory health care provider must be used to perform
services not allowed in the health care provider’s office.
Claim payment is subject to our payment policies and medical policies, which are available at uhcprovider.com/policies or
upon request to your network management contact.
Special reporting requirements for certain claim types
Anesthesia services
For detailed instructions, refer to uhcprovider.com/policies > Commercial (or Medicare Advantage) Policies > Reimbursement
Polices > Anesthesia Services.
Laboratory claims
Many benefit plan designs exclude outpatient laboratory services if they were not ordered by a participating health care
provider. Our benefit plans may also cover such services differently when a portion of the service (e.g., the draw) occurs in the
health care provider’s office, but an independent laboratory performs the analysis. A licensed health care provider must order
laboratory services.
All laboratory claims and/or encounters must include the referring health care provider’s name and NPI number, in addition to
the other elements of a complete claim and/or encounter described in this guide. All claims for laboratory services must include

Chapter 10: Our claims process
123
2023 UnitedHealthcare Care Provider Administrative Guide
the CLIA number for the servicing health care provider. We reject or deny laboratory claims that do not include the identity of
the referring health care provider.
This requirement applies to claims and/or encounters for both anatomic and clinical laboratory services. It also applies to
claims and/or encounters received from both participating and non-participating laboratories, unless otherwise provided under
applicable law. It does not apply to claims for laboratory services done by health care providers in their offices.
Report the AMA Claim Designation code or Abbreviated Gene Name in loop 2400 or SV101-7 field for electronic claims or
Box 24 for paper claims. When submitting code 81479, unlisted molecular pathology, report the Genetic Test Registry (GTR)
unique ID.
Claims that have complied with notification or prior authorization requirements in UnitedHealthcare’s Genetic Testing and
Molecular Prior Authorization program satisfy the policy’s requirements without further provider action, as long as they meet our
GTR requirements. When requesting notification or prior authorization, include the codes and services that will be performed
and only the authorized procedure code(s) that should be billed.
Laboratory genetic test registry protocol
For more information on the UnitedHealthcare Genetic and molecular testing prior authorization/advance notification program,
go to uhcprovider.com > Prior Authorization > Genetic and Molecular Testing.
Physical medicine and rehabilitation services
Physical medicine and rehabilitation (PM&R) services are eligible for reimbursement if provided by a physician or therapy health
care provider duly licensed to perform those services.
Assistant surgeons or surgical assistants claim submission requirements
The practice of using non-participating health care providers significantly increases the costs of services for our members. We
require our participating health care providers to use reasonable efforts to find network providers, including network surgical
assistants or assistant surgeons, for our members. The use of a non-participating assistant surgeon practice, in which our
participating health care provider has an ownership interest or other financial arrangement, is prohibited unless the participating
health care provider discloses that interest or arrangement to us in advance.
Submission of claims for services subject to medical claim review
We have the right to review claims to confirm a health care provider is following appropriate and nationally accepted coding
practices. Health care providers must cooperate by providing access to requested claims information, all supporting
documentation (such as medical records) and other related data and information that we may request, including itemized bills
and manufacturer invoices. We may adjust payment to the health care provider at the revised allowable amount based on our
review of this information. If such information is not submitted following our request, we may deny the claim or adjust payment
to the health care provider at a revised allowable amount as we determine appropriate.
We may pend or deny a claim and request medical records to determine whether the service rendered is covered, including
medically necessary and eligible for payment. In these cases, we send a letter explaining what we need.
To help claim processing and avoid delays due to pended claims, resubmit only what is requested in our letter. The claim letter
will state specific instructions for required information to resubmit, which may vary for each claim. You must also return a copy
of our letter with your additional documents.
For MA benefit plans, if you are not eligible for payment, but the service is covered, we will deny payment. You may not bill the
member for the amount denied.
Erythropoietin (for commercial members)
For Erythropoietin (EPO) claims, you must submit the Hematocrit (HCT) level for us to determine coverage under the member’s
benefit plan. For claims submitted by paper to UnitedHealthcare on a Form 1500, you must enter the HCT level in the shaded
area of line 24a in the same row as the J-code. Enter HCT and the lab value (HCTxx).

Chapter 10: Our claims process
124
2023 UnitedHealthcare Care Provider Administrative Guide
For electronic claims, the HCT level is required in the (837P) Standard Professional Claim Transaction, Loop 2400 – Service
line, segment MEA, Data Element MEA03.
Report the MEA segment as follows:
• MEA01 = qualifier “TR”, meaning test results
• MEA02 = qualifier “R2”, meaning hematocrit
• MEA03 = hematocrit test result (Example: MEA*TR*R2*33~)
The following J codes require an HCT level on the claim:
• J0881 Darbepoetin alfa (non-ESRD use)
• J0882 Darbepoetin alfa (ESRD on dialysis)
• J0885 Epoetin alfa (non-ESRD use)
• J0886 Epoetin alfa, 1,000 units (for ESRD on Dialysis)
• Q4081 Epoetin alfa (ESRD on dialysis)
For EPO claims submitted on a UB-04 claim form, an HCT level is not required.
Overpayments
If we inform you of an overpaid claim, and you do not disagree, send us the refund check or recoupment request within 30
calendar days (or as required by law or your Agreement) from the date of notification. We may apply the overpayment against
future claim payments unless your Agreement states otherwise or as required by law. If you find we overpaid for a claim, use the
Overpayment Refund/Notification Form. Call 1-800-727-6735 with questions related to overpayments. Send refunds to:
Regular mail
UnitedHealthcare Insurance Company
P.O. Box 101760
Atlanta, GA 30392-1760
Overnight mail
UnitedHealthcare Insurance Company – Overnight Delivery
Lockbox 101760
3585 Atlanta Ave
Hapeville, GA 30354
Include documentation that shows the overpayment, including member’s name, health plan ID number, date of service and
amount paid. If possible, also include a copy of the provider remittance advice (PRA) that corresponds with our payment. If
the refund is owed because of COB with another carrier, provide a copy of the other carrier’s EOB/remittance advice with
the refund.
If we find a claim was paid incorrectly, we may make a claim adjustment. You will see the adjustment on the EOB or PRA.
Disagreement
If you disagree with the claim adjustment, or request for an overpayment refund or recoupment, you may submit a notice of
disagreement within 30 calendar days (or as required by law or your Agreement) from the date of receipt of notification. You
must clearly state the basis for your disagreement and include any relevant and supporting documentation. The notification
letter will include instructions on how to submit a notice of disagreement.

Chapter 10: Our claims process
125
2023 UnitedHealthcare Care Provider Administrative Guide
Direct Connect
Direct Connect is a no-cost, web-based platform that helps payers and health care providers communicate effectively, automate
workflows and drive resolutions. This portal can replace previous methods of letters, faxes, phone calls and spreadsheets. It
also helps:
• Track and manage certain types of overpayments in a controlled process; some inventory restrictions apply.
• Create a transparent view between health care provider and payer.
• Avoid duplicate recoupment and returned checks.
• Decrease resolution time frames.
• Track inventories in resolution process through real-time reporting.
• Provide control over financial resolution method.
• Manage and review overpayment disagreements.
• Attach images for quick reference.
For more information, contact the Optum Direct Connect Team at directconnectacce[email protected].
Subrogation and COB
Our benefit plans are subject to subrogation and COB rules.
1. Subrogation — We have the right to recover benefits paid for a member’s health care services when a third party causes
the member’s injury or illness to the extent permitted under state and federal law and the member’s benefit plan. For
subrogation/reimbursement matters, contact:
Optum
11000 Optum Circle
MN102-0300
Eden Prairie, MN 55344
subroreferrals.optum.com
Fax: 1-800-842-8810
2. COB — COB is administered according to the member’s benefit plan and in accordance with law. We accept secondary
claims electronically. To learn more, go to uhcprovider.com/edi > EDI Quick Tips for Claims > Secondary/COB or Tertiary
Claims. You can also contact EDI Support at uhcprovider.com/edicontacts.
3. Workers’ Compensation — In cases where an illness or injury is employment-related, workers’ compensation is primary. If
you receive notification that the workers’ compensation carrier has denied a claim for services, submit the claim to us. It is
also helpful to send us the workers’ compensation denial statement with the claim.
4. Medicare — If the health care provider accepts Medicare assignment, all COB types coordinate up to Medicare’s allowed
amount. Medicare Secondary Payer (MSP) rules dictate when Medicare pays secondary.
Other coverage is primary over Medicare in the following instances:
• Aged employees: For members who are entitled to Medicare due to age, commercial is primary over Medicare if the employer
group has 20 or more employees.
• Disabled employees (large group health plan): For members who are entitled to Medicare due to disability, commercial is
primary over Medicare if the employer group has 100 or more employees.
End-stage renal disease
If a member has or develops end-stage renal disease (ESRD) while covered under an employer’s group benefit plan, the
member must use the benefits of the employer’s group plan for the first 30 months after becoming eligible for Medicare.
After the 30 months, Medicare is the primary payer. However, if the employer group benefit plan coverage was secondary to
Medicare when the member developed ESRD, Medicare is the primary payer, and there is no 30-month period.

Chapter 10: Our claims process
126
2023 UnitedHealthcare Care Provider Administrative Guide
Continuation of Benefits — Consolidated Omnibus Budget Reconciliation Act
Continuation of Benefits — Consolidated Omnibus Budget Reconciliation Act (COBRA) provides continued group health benefits
to workers and families who lost coverage. COBRA generally requires group health plans with employers who have 20 or more
employees, in the prior year, to offer continuation of coverage in certain instances where coverage would end. This coverage
is available at the group premium rates. Coverage benefits and limitations for COBRA members are the same to those of the
group.
• We are not responsible for initiating a terminated member’s election of continuation coverage.
• Interested members should contact the subscriber’s human resources office for eligibility information.
• Members eligible for COBRA may elect to convert to an individual health plan, where available.
• Additional information on COBRA is available at dol.gov > Topics > Continuation of Health Coverage - COBRA.
Coverage begins on the date that coverage would otherwise have been lost and ends at the end of the maximum period. It may
end earlier if:
• Premiums are not paid.
• The employer ceases to maintain any group health plan.
• After the COBRA election, the member obtained coverage with another employer-group health plan that does not contain
any exclusion or limitation with respect to any pre-existing condition of such beneficiary. However, if the member obtains
other group health coverage prior to electing COBRA, COBRA coverage may not be discontinued, even if the other coverage
continues after the COBRA election.
• If a beneficiary becomes entitled to Medicare benefits after electing COBRA. However, if Medicare is obtained prior to
COBRA election, COBRA coverage may not be discontinued, even if the other coverage continues after the COBRA election.
COBRA specifies certain periods of time that continued health coverage must be offered. It does not prevent plans from
offering more health coverage beyond the COBRA period.
Note: In some cases, there may be an extensive period where a continuing member does not appear on the eligibility list. If this
occurs, contact your network provider account manager or provider advocate for assistance.
Claim correction and resubmission
Electronic process:
• Submit corrected claims electronically as an EDI 837 transaction with the appropriate frequency code. For more details, go to
uhcprovider.com/ediclaimtips > Corrected Claims.
• Use the claims tool in the UnitedHealthcare Provider Portal to resubmit corrected claims that have been paid or denied.
• If you received a letter asking for additional information, submit it using the Claims tool in the UnitedHealthcare Provider
Portal.
• When correcting or submitting late charges on 837 institutional claims, use bill type xx7, Replacement of Prior Claim. Do not
submit corrected or additional charges using bill type xx5, Late Charge Claim.
• When correcting or submitting late charges on a 1500 professional claim, use the following frequency code in Box 22 and use
left justified to enter the code. Include the 12-digit original claim number under the Original Reference Number in this box.
– Frequency code 7 Replacement of Prior Claim: Corrects a previously submitted claim.
– Frequency code 8 Void/Cancel of Prior Claim: Indicates this bill is an exact duplicate of an incorrect bill previously
submitted. This code will void the original submitted claims.

Chapter 10: Our claims process
127
2023 UnitedHealthcare Care Provider Administrative Guide
Claim reconsideration and appeals process
Claim reconsideration does not apply in some states, such as MD, based on applicable state law. Refer to Health care provider
dispute resolution (CA Commercial HMO, OR HMO claims, OR and WA commercial plans) section for more information on
similar prohibitions in those jurisdictions.
Note: For non-network providers claim appeals and dispute process, refer to uhcprovider.com/plans > Choose your state >
Medicare > Select plan name >Tools & Resources > Non-Contracted Care Provider Dispute and Appeal Rights.
Step 2: Appeals
If you disagree with the outcome of
the claim reconsideration in Step1,
you may use one of the following
processes to submit an appeal.
Attach all supporting materials
to the appeal, including member-
specific treatment plans or clinical
records. We make our decision
based on the materials available at
the time of appeal review.
Submit your appeal electronically
using the Claims tool in the
UnitedHealthcare Provider
Portal.
Submit your appeal (with
attachments) using API. Go to
uhcprovider.com/api for more
information.
OR
PROOF OF CLAIM TIMELY FILING
To show the date of the claim submission, please include confirmation we received and
accepted your claim within your filing limit or include a screen print from your accounting
software to show the date of submission. Timely filing limits vary based on state
requirements and contracts. Refer to your Agreement for your specific timely filing
requirements.
If you disagree with the outcome of a processed claim
(payment or denial), you can request reconsideration
of the decision by first submitting a Claim
Reconsideration Request. Follow one of the processes
outlined below:
Submit your Claim Reconsideration Request electronically
using the Claims tool in the UnitedHealthcare Provider
Portal.
Submit your Claim Reconsideration Request (with
attachments) using API. Go to uhcprovider.com/api for more
information.
If you are submitting medical documentation we
requested for a pended claim, use the Claims tool in the
UnitedHealthcare Provider Portal.
Call the number on the back of the member’s ID card to
request an adjustment to a claim that does not require
written documentation.
Step 1: Claim
Reconsideration
OR
OR
You must submit both your reconsideration and appeal to us within 12 months (or as required by law or your Agreement) from
the date of the EOB or PRA. The 2-step process, as outlined in the following graphic, allows for a total of 12 months for timely
submission for both steps (Step 1: Reconsideration and Step 2: Appeals). For more information and necessary forms, visit
uhcprovider.com/claims.

Chapter 10: Our claims process
128
2023 UnitedHealthcare Care Provider Administrative Guide
20 or more claims (research request)
If you have a request to reconsider 20 or more paid or denied claims for the same administrative issue (and attachments are not
required), you may submit these in bulk online. Use the Claims Research Project tool in the UnitedHealthcare Provider Portal.
Attachments
If you are submitting medical documentation we requested for a pended claim, use the Claims tool in the UnitedHealthcare
Provider Portal.
Go to the UnitedHealthcare Provider Portal to submit a Claim Reconsideration Request for a claim denied because filing was
not timely.
Provide one of the following documents:
• EDI report—and include confirmation that it was received and accepted within your filing limit.
• A submission report from your accounting software to include a screen print to show the date the claim was submitted.
• A billing software statement to show the claim was submitted timely to the clearinghouse (if rejected proof is not acceptable).
• A resubmission form or letter with a statement that you billed the wrong insurance, or the member gave you the wrong
insurance information. If available, include any other evidence you may have such as the other insurance carrier’s denial or
rejection, EOB, letter indicating coverage terminated or member not eligible.
All proof must include documentation that the claim is for the right patient and the correct date of service. For electronic claims,
include confirmation that we received and accepted your claim.
Response details
If the claim then requires an additional payment, the EOB or PRA will serve as notification of the outcome on the review. If the
original claim status is upheld, you will be sent a letter outlining the details of the review.
Retroactive eligibility changes
Eligibility under a benefit plan may change retroactively if:
• We receive information an individual is no longer a member.
• The member’s policy/benefit contract has been terminated.
• The member decides not to purchase continuation coverage.
• The member fails to pay their full premium within the 3-month grace period established by the Affordable Care Act (and
applicable regulations) for subsidized Individual Exchange members.
• The eligibility information we receive is later determined to be incorrect.
If you have submitted a claim affected by a retroactive eligibility change, a claim reconsideration may be necessary, unless
otherwise required by state and/or federal law. We list the reason for the claim reconsideration on the EOB or PRA. If you are
enrolled in electronic payment system, you will not receive an EOB. However, you will be able to view the transaction online or in
the electronic file. If we implement a claim reconsideration and request a refund, we notify you at least 30 business days prior to
any adjustment, or as required by law or your Agreement.
MA hospital discharge appeal rights protocol
MA members who are hospital inpatients have the statutory right to request an immediate review by the Quality Improvement
Organization (QIO) when UnitedHealthcare and the hospital, with physician concurrence, determine that inpatient care is no
longer necessary. The QIO notifies the facility and UnitedHealthcare of an appeal.
• When UnitedHealthcare completes the Detailed Notice of Discharge (DND), UnitedHealthcare delivers it to the facility and
the QIO. The facility will give the DND, on behalf of UnitedHealthcare, to the MA member or their representative as soon as
possible but no later than 12 p.m. local time of the day after the QIO notification of the appeal. The facility will also fax a copy
of the DND to the QIO.
• When the facility completes the DND, the facility will give the DND on behalf of UnitedHealthcare to the MA member or their
representative as soon as possible but no later than 12 p.m. local time of the day after the QIO notification of the appeal.

Chapter 10: Our claims process
129
2023 UnitedHealthcare Care Provider Administrative Guide
The facility will fax a copy of the DND to the QIO and UnitedHealthcare. If the MA member fails to make a timely request
to the QIO for immediate review and remains in the hospital, they may ask for an expedited reconsideration (appeal)
by UnitedHealthcare.
Resolving concerns or complaints
If you have a concern/complaint regarding:
• Claim payments – You must complete the claim reconsideration and appeal process as set forth in this guide before you can
initiate the dispute resolution process set forth in your Agreement.
• Your relationship with us – Follow the notice procedures set forth in your Agreement to send a letter containing the details,
and a representative will look into your complaint and try to resolve it through an informal discussion. If you disagree with the
outcome of this discussion, you can initiate the dispute resolution process set forth in your Agreement.
For further information on resolving concerns related to your relationship with us, including decisions on appeals, refer to the
dispute resolution section of your Agreement.
Arbitration locations:
Unless your Agreement states differently, the following list contains locations where arbitration proceedings will be held, based
on the locations where you provide care:
AL Jefferson County, AL
AK Anchorage, AK
AZ Maricopa County, AZ
AR Pulaski County, AR
CA Los Angeles County, CA; San Diego County, CA;
San Francisco County, CA
CO Arapahoe County, CO
CT Hartford County, CT; New Haven County, CT
DE Montgomery County, MD
DC Montgomery County, MD
FL Broward County, FL; Hillsborough County, FL;
Orange County, FL
GA Gwinnett County, GA
HI Honolulu County, HI
ID Boise, ID; Salt Lake County, UT
IL Cook County, IL
IN Marion County, IN
IA Polk County, IA
KS Johnson County, KS
KY Fayette County, KY
LA Jefferson Parish, LA
ME Cumberland County, ME
MD Montgomery County, MD
MA Hampden County, MA; Suffolk County, MA
MI Kalamazoo County, MI; Oakland County, MI
MN Hennepin County, MN
MS Hinds County, MS
MO St Louis County, MO; Jackson County, MO
MT Yellowstone County, MT
NE Douglas County, NE
NV Clark County, NV; Washoe County, NV;
Carson City County, NV
NH Merrimack County, NH; Hillsboro County, NH
NJ Essex County, NJ
NM Bernalillo County, NM
NY New York County, NY; Onondaga County, NY
NC Guilford County, NC
ND Hennepin County, MN
OH Butler County, OH; Cuyahoga County, OH;
Franklin County, OH
OK Tulsa County, OK
OR Multnomah County, OR
PA Allegheny County, PA; Philadelphia County, PA
RI Kent County, RI
SC Richland County, SC
SD Hennepin County, MN
TN Davidson County, TN
TX Dallas County, TX; Harris County, TX; Travis
County, TX
UT Salt Lake County, UT
VT Chittenden County, VT; Washington County, VT;
Windham County, VT
VA Montgomery County, MD
WA King County, WA
WV Montgomery County, MD
WI Milwaukee County, WI; Waukesha County, WI
WY Laramie County, WY
Chapter 10: Our claims process
130
2023 UnitedHealthcare Care Provider Administrative Guide
Member appeals, grievances or complaints
Members may be unhappy with health care providers or with us. We respect the members’ rights to express dissatisfaction
regarding quality of care/services and to appeal any denied claim/service. All members receive instructions on how to file a
complaint/grievance with us in their Combined Evidence of Coverage and Disclosure Form, Evidence of Coverage or Certificate
of Coverage, as applicable.
When there is a member grievance or appeal, you are required to comply with the following requirements:
1. Assist the member with filing an Appeal or Grievance upon request from the member. This form is located by logging onto
myuhc.com > Claims and Accounts > Medical Appeals and Grievances > Medicare and Retirement Member Appeals and
Grievance Form.
Note: An appeal, grievance or complaint process may differ based on product. See the applicable benefit plan supplement
to verify the process for those plan members. Encourage the member to contact UnitedHealthcare Customer Service for
assistance in filing an appeal or grievance.
2. Immediately forward all member grievances and appeals (complaints, appeals, quality of care/service concerns) in writing
for processing to:
Individual Exchange Plans Member and Provider Appeals and Reconsiderations:
UnitedHealthcare
P.O. Box 6111
Cypress, CA 90630
Fax: 1-888-404-0940 (standard requests)
1-888-808-9123 (expedited requests)
Medicare Advantage (MA) and
Medicare Advantage Prescription
Drug (MAPD) Plans
UnitedHealthcare
P.O. Box 6106
Mail Stop CA 124-0157
Cypress, CA 90630
Medicare and Retirement
Prescription Drug Plans (PDP)
UnitedHealthcare
P.O. Box 6106
Mail Stop CA 124-0197
Cypress, CA 90630
Commercial Plans UnitedHealthcare
P.O. Box 30573
Salt Lake City, UT 84130-0573
All Savers supplement ASIC Members:
Grievance Administrator
P.O. Box 31371
Salt Lake City, UT 84131-0371
Standard Fax: 1-801-478-5463
Expedited Fax: 1-866-654-6323
Phone: 1-800-291-2634
UnitedHealthcare Level Funded
and UnitedHealthcare Oxford Level
Funded
Appeals Review
P.O. Box 31393
Salt Lake City, UT 84131
UnitedHealthOne Individual
Plans Supplement (Golden
Rule Insurance Company,
UnitedHealthcare Oxford Navigate
Individual benefit plans offered by
Oxford Health Insurance, Inc.)
Grievance Administrator
P.O. Box 31371
Salt Lake City, UT 84131-0370
Standard Fax: 1-801-478-5463
Expedited Fax: 1-866-654-6323
Phone: 1-800-657-8205
Chapter 10: Our claims process
131
2023 UnitedHealthcare Care Provider Administrative Guide
UMR and UnitedHealthcare Shared
Services
Appeals
(Pre-Service)
UMR
Fax: 1-888-615-6584
Phone: 1-800-808-4424 x 15227
(Note: This is a voicemail line. We return
calls within 1 business day).
Mail: UHC Appeals - CARE
P.O. Box 400046
San Antonio, TX 78229
UHSS
Fax: 1-866-427-7703
Mail: P.O. Box 30783
Salt Lake City, UT 84130-0783
Reconsiderations and Appeals
(Post-Service)
UMR
Fax: 1-877-291-3248
Phone: Call the number listed on the
back of the member’s ID card.
Mail: UMR - Claim Appeals
P.O. Box 30546
Salt Lake City, UT 84130-0546
(or send to the address listed on
the provider ERA)
UHSS
Fax: 1-866-427-7703
Mail: P.O. Box 30783
Salt Lake City, UT 84130-0783
3. Respond to our requests for information within the designated time frame. You must supply records as requested within 2
hours for expedited appeals and 24 hours for standard appeals. This includes weekends and holidays.
4. For Medicare member appeal requests, CMS regulation states once an appeal is received, within 60 calendar days of the
denial, it must be reviewed under the appeal process. A request to review a post-service determination will not be reopened
for any reason (i.e., New and Material Evidence, Fraud or Similar Fault, Other) other than for a clerical error, unless the
60-calendar-day time frame to file a reconsideration has expired.
5. Cooperate with our external independent medical review organization and us. This includes:
– Promptly forwarding all medical records and information relevant to the applicable health care service to the external
review organization
– Providing newly discovered relevant medical records or any information in the participating medical group’s/IPA’s
possession to the external review organization
6. Provide us with proof that reversals of adverse determinations were done within the stated time frames. You must supply
proof within:
– Expedited appeals — 2 hours of overturn notice.
– Standard appeals — 24 hours of overturn notice. This applies to all calendar days (no exceptions or delays allowed for
weekends or holidays).
Medical claim review
We have the right to review claims. This helps ensure that health care providers follow nationally accepted coding practices and
that we pay correctly. Please cooperate with our review of claims and payments. We may request access to claim information
and supporting documentation.

132
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 11: Compensation
Reimbursement policies
We apply reimbursement policies. Our reimbursement policies are available online at:
• uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans.
• uhcprovider.com/policies > For Medicare Advantage Plans > Reimbursement Policies for Medicare Advantage Plans.
• uhcprovider.com/policies > For Exchange Plans > Reimbursement Policies for UnitedHealthcare Individual Exchange
Plans.
We use the terms “reimbursement policies” and “payment policies” interchangeably.
Charging members
Members are responsible for copayments, deductibles and coinsurance. You may collect copayments at the time of service.
Once we process the claim, the final member financial responsibility is listed on the provider remittance advice (PRA) and the
member’s explanation of benefits (EOB).
Individual and family annual deductibles and out-of-pocket maximums (commercial)
Annual individual and family out-of-pocket maximums are equal to the combined total of deductible, copayment and
coinsurance amounts the member pays as shown on their Schedule of Benefits. Cost-share is the amount the member is
financially responsible for, such as copayments, coinsurance and deductibles according to their plan benefits. Cost-sharing for
certain types of covered services may not apply toward the annual individual or family out-of-pocket maximums. Refer to the
member’s Schedule of Benefits to determine if a cost-share amount, for a particular covered service, applies to the member’s
annual individual and/or family out-of-pocket maximums.
When an individual member’s out-of-pocket expenses have reached the individual out-of-pocket maximum, the member will not
have any additional cost-share for services that apply to the annual individual out-of-pocket maximum for the rest of that plan
year.
When a family’s out-of-pocket expenses have reached the annual family out-of-pocket maximum, the family members will not
have any additional cost-share for services that apply to the annual family out-of-pocket maximum for the rest of that plan year.
Some services may not be covered until the member meets the annual individual deductible. Only amounts incurred for covered
services that are subject to the annual individual deductible will count toward the annual individual deductible. Benefit plans
may have an annual individual deductible only or both an annual individual and annual family deductible. No further deductible
will be required for any individual family member when the individual deductible amount has been satisfied for the rest of the
plan year. For plans with both annual individual and family deductibles, no further deductible will be required from any covered
family member for the rest of the plan year when the annual family deductible has been met.
As previously indicated, only certain covered services apply to the annual individual and family deductibles. Covered services
that do not apply to the annual individual and family deductibles may incur a member cost-share that is considered separate
from, and not included in, the annual individual and family deductibles. The annual individual and family deductibles apply to
the annual individual and family out-of-pocket maximums. The amounts applied are based upon UnitedHealthcare’s contracted
rates, copayments and coinsurance.
Annual out-of-pocket maximum (Medicare Advantage)
Annual out-of-pocket maximum is equal to the member’s annual copayment maximum (if any), as shown on the member’s
Evidence of Coverage (EOC).

Chapter 11: Compensation
133
2023 UnitedHealthcare Care Provider Administrative Guide
Cost-sharing for certain types of covered services may not apply toward the annual out-of-pocket maximum. Refer to the
member’s EOC to determine applicability to the benefit plan. When an individual member’s out-of-pocket expenses has reached
the individual annual out-of-pocket maximum, no further cost-share amounts will be due by the member for those services that
apply to the annual out-of-pocket maximum. Plans with benefits that do not apply to the annual out-of-pocket maximum will still
require cost-sharing for those excluded benefits after the annual out-of-pocket maximum reached.
Cost-share is defined as amounts paid by the member such as copayments, coinsurance and deductibles according to their
plan benefits.
Coinsurance calculation
For all Medicare Advantage (MA) products, coinsurance is calculated as follows:
1. For services reimbursed on a service-specific contracted rate, or on a fee-for-service basis, the coinsurance is based on the
contracted rate or billed amount, whichever is less or as agreed upon in your Agreement with us.
2. For services reimbursed under a downstream capitation Agreement between your organization and a health care provider
of the service, and where payment is not issued for each specific service rendered, coinsurance is based on Medicare’s
allowance for the location at which the service is rendered.
This coinsurance calculation is consistent with the definition of coinsurance as the amount a member pays as their share of
the cost for services or prescription drugs. The methodology is used for all UnitedHealthcare MA plans nationwide. Ensure you
have the correct system setup and use consistent coinsurance calculations to help reduce member appeals and complaints.
Additional fees for covered services
Do not charge additional fees for:
• Covered services beyond their copayments, coinsurance or deductible.
• Retainers or administrative fees.
• Services/claims that were denied because you failed to follow our protocols and/or reimbursement policies.
• Reductions applied to services/claims resulting from our protocols and/or reimbursement policies.
You may charge members for missed appointments. (CMS does not allow you to charge MA members for missed appointments
unless the member was aware of that policy.)
Concierge/boutique medical practices
Concierge/boutique medical practices charge members a service fee in exchange for longer visits, a commitment from the
practices for shorter wait times or, in many cases, access to the provider’s cell phone number and email address to get in touch
with their health care provider quickly.
We will allow our contracted network providers to charge concierge/boutique medicine fees with the following restrictions:
• You must give members the choice of paying the concierge membership fee; if the member chooses not to pay the fee, the
member may continue seeing your medical practice.
• You must be transparent with the member about what they will receive as part of the concierge membership and fees.
• If you cannot meet the criteria because you are requiring all members to pay the fees, you will need to consider changing your
concierge program to comply with our requirements, or you will be terminated from our network.
• We must have the opportunity to review and approve the services included with the concierge membership fee. The
concierge services should not consist of any covered services that are already included in your Participation Agreement with
us.
Charging members for non-covered services
You may collect payment from our commercial members for services not covered under their benefit plan if you first get
the member’s written consent. The member must sign and date the consent before the service is done. Keep a copy in the
Chapter 11: Compensation
134
2023 UnitedHealthcare Care Provider Administrative Guide
member’s medical record. If you know or have reason to suspect the member’s benefits do not cover the service, the consent
must include:
• An estimate of the charges for that service.
• A statement of reason for your belief the service may not be covered.
• When we determine the planned services are not covered services, a statement that we have determined the service is not
covered and that the member knows our determination and agrees to be responsible for those charges.
For MA members, in addition to obtaining the member’s written consent before the service is done, you must do the following:
• If you know or have reason to believe that a service or item you are providing or referring may not be covered, request a pre-
service determination from us prior to rendering services.
• If we determine the service or item is not covered, we issue an Integrated Denial Notice (IDN) to the member and you. The
IDN gives the member their cost for the non-covered service or item and appeal rights. You must make sure the member has
received the IDN prior to rendering or referring for non-covered services or items to collect payment. Per CMS requirements,
for you to hold a MA member financially liable for the non-covered service or item, the member must first have an IDN, unless
the Evidence of Coverage, or other related materials, clearly excludes the item or service.
• A pre-service organization determination is not required to collect payment from a MA member where the EOC or other
related materials issued to a MA member is clear that a service or item is not covered.
Use our Provider Authorization and Notification (PAAN) tool in the UnitedHealthcare Provider Portal to submit an advance
notification request. The PAAN tool does not issue denials. It tells you if a procedure code requires a review or not. For more
information, go to uhcprovider.com/paan.
You should know or have reason to suspect that a service or item may not be covered if:
• We have provided notice through an article on uhcprovider.com, including clinical protocols and/or medical policies.
• We have made a determination that the planned service or item is not covered and have communicated that determination.
• For MA benefit plans, CMS has published information to help you determine if the service or the item is covered. You are
required to review the Medicare Coverage Center. If you do not follow this protocol, you cannot bill our member.
If you followed this protocol and requested a pre-service organization determination, and an IDN was issued before the non-
covered service was rendered, you must include the GA modifier on your claim for the non-covered service. Including the GA
modifier on your claim helps ensure your claim for the non-covered service is appropriately adjudicated as member liability.
Do not bill the member for non-covered services in cases where you do not follow this protocol. If you don’t follow the terms
of this protocol (such as requesting a pre-service organization determination for a MA member or rendering the service to a
MA member before we issue the pre-service organization determination), you may receive an administrative claim denial. You
cannot bill the member for administratively denied claims.
Balance billing
You cannot bill members for covered services beyond their normal cost-sharing amounts (copayment, deductible
or coinsurance).
You cannot:
• Bill.
• Charge.
• Collect a deposit.
• Seek compensation.
• Seek remuneration.
• Seek reimbursement.
• Have recourse against our members, their representative or the MA organization.
You must either:
• Accept payment made by or on behalf of us as payment in full.
• Bill the appropriate state source for such cost-sharing amount.

Chapter 11: Compensation
135
2023 UnitedHealthcare Care Provider Administrative Guide
Billing for dual-eligibles
Dual-eligible members qualify for both Medicare and Medicaid. If you are a participating health care provider in our MA
network, you cannot refuse to see these members. For dual-eligibles for whom the state is responsible for covering Medicare
cost-sharing, our contract requires that you accept payments made by or on behalf of our MA plans for covered Part A and B
services as payment in full. You can bill the appropriate state Medicaid source for the balance.
Cost-sharing for Qualified Medicare beneficiary
Qualified Medicare beneficiaries (QMBs) are not responsible for Medicare cost-sharing under CMS regulations. Medicare
cost-sharing includes the deductibles, coinsurance and copays associated with covered Part A and B services included under
MA plans. You cannot bill, charge, collect a deposit from or seek compensation from any MA member who is eligible for both
Medicare and Medicaid. You can accept payment from us as payment in full or bill Medicaid for the remaining amount.
Member financial responsibility
Members are responsible for paying their copayments, deductibles and coinsurance. You can collect copayments at the time of
service.
To determine the exact member responsibility, submit claims first and refer to the EOB or PRA before billing our members.
If you prefer to collect payment at time of service, you must make a good faith effort to estimate the member’s responsibility
and collect no more than that amount at the time of services. You must help ensure the member has not exceeded their annual
out-of-pocket maximum. Several tools on our website can help you determine member and health benefit plan responsibility,
including the UnitedHealthcare Claim Estimator at uhcprovider.com/claims > Get a Claim/Procedure Cost Estimate and by
checking eligibility and benefits in the UnitedHealthcare Provider Portal, which shows HRA balances. The Claim Estimator is
available only for professional commercial claims.
If the member pays you more than the amount indicated on the EOB/PRA, you must refund the member.
Preventive care
The Department of Health and Human Services requires most benefit plans to include certain preventive care services to be
covered without any out-of-pocket costs as long as a participating health care provider provides the service.
We update our Coverage Determination Guidelines (CDG) for Preventive Care Services to help you identify and correctly
code preventive services. This CDG is on uhcprovider.com/policies > For Commercial Plans > Medical & Drug Policies and
Coverage Determination Guidelines for UnitedHealthcare Commercial Plans or at uhcprovider.com/policies > For Exchange
Plans > Medical & Drug Policies and Coverage Determination Guidelines for UnitedHealthcare Individual Exchange Plans.
We update the CDG when we receive new guidance about preventative services and revised codes. The United States
Preventive Services Task Force is one of the primary references driving changes to the CDG. We must cover items that have
an “A” or “B” rating without cost-share by non-grandfathered benefit plans. This applies to both fully insured and self-funded
benefit plans. While grandfathered benefit plans are not required to implement these changes, some grandfathered benefit
plans have chosen to cover preventive care services at no cost-share.
This does not apply to members enrolled in government health benefit plans (Medicare/Medicaid) including our MA benefit
plans. For information on Medicare coverage of preventive services, go to uhcprovider.com/policies > Medicare Advantage
Policies > Coverage Summaries for Medicare Advantage Plans > Preventive Health Services and Procedures. For more
information visit:
• Benefit Verification: Check the Eligibility and Benefits tool in the UnitedHealthcare Provider Portal.
• Health Care Reform: uhc.com/united-for-reform.

Chapter 11: Compensation
136
2023 UnitedHealthcare Care Provider Administrative Guide
Extrapolation
We may review paid claims to help ensure payment integrity. If reviewing all medical records for a procedure would burden
you, we may select a statistically valid random sample (SVRS) or smaller subset of the SVRS. This gives an estimate of the
proportion of claims we paid in error. The estimated proportion, or error rate, can be projected across all claims to determine
overpayment. You may appeal the initial findings. You must supply all requested medical records. Failure to do so may result in
a failure of the entire SVRS and all claims submitted within the review.
You must handle overpayment disagreements as outlined in this guide and in your Agreement.
Provider claim reviews may be conducted through a phone call, on-site visit, internal claims review, client-directed/regulatory
investigation and/or compliance reviews. We ask that you provide us, or our designee, during normal business hours, access to
examine, review, scan and copy any and all records necessary to determine compliance.
If you refuse to allow access to your facilities, we reserve the right to recover the full amount paid or due to you.
Audit services
Audit services develops and implements audits designed to identify billing and coding inaccuracies. (See Chapter 17: Fraud,
Waste and Abuse (FWA) for examples of potentially fraudulent, wasteful or abusive billing.) Audit programs are developed
in response to identified overpayment risk and include comprehensive research of critical claim elements, such as medical
records, itemized bills and manufacturer invoices. We conduct audits in conjunction with applicable federal or state regulations,
national guidelines and contract terms.
UnitedHealthcare may use external vendors to conduct the audits. Audits may be conducted onsite or remotely.
Not all requests for records are considered an audit. We also request documents to conduct claim reviews to help ensure
proper reimbursement. Refer to Chapter 10: Our claims process of the guide for information on claim reviews.
Access
Our auditors notify you of our intent to audit a claim by notifying your appropriate representative. As the health care provider,
you are responsible for:
• Sending a copy of the medical record, itemized bill, bill breakdown and/or other requested documentation within the time
frame specified in the intent to audit letter.
• Obtaining the member authorization to release their medical information.
– In many cases, the member signs this authorization at the time of admission.
• Waiving the fee associated with the audit or copying of records, unless otherwise specified in your Agreement.
In addition, for onsite audits, you are responsible for:
• Cooperating in a timely manner to allow audit scheduling within 30 calendar days of the scheduling request.
• Coordinating the audit location.
• Providing the auditor access to the medical records, department charge sheets, itemized bills, other documentation and any
applicable policy and procedure (if requested).
• Providing our audit vendors the same access as our employee auditors.
– Vendors authorized by us are bound to our obligations under the Agreement.
• Not imposing time limitations on our right or ability to audit, unless otherwise stated in the Agreement or by state/federal law.
Audit findings
When the audit is complete, the auditor notifies you of any findings. If an overpayment has been identified, the auditor will
request an overpayment refund.
• Refund Remittance ‒ You must remit the overpayment amount within 30 calendar days of receipt of the overpayment refund
request, or as required by state or federal law.

Chapter 11: Compensation
137
2023 UnitedHealthcare Care Provider Administrative Guide
• Audit Findings – If you disagree with the findings, you may submit notification of the disagreement within the time frame
outlined in the overpayment refund request. The notification must clearly identify the items of disagreement and include any
relevant documentation to support your position.
• Disagreement Resolution – We respond to audit disagreements in writing, according to the terms of your contract and/or
applicable state law. If you are not satisfied with our response, you may use other applicable dispute resolution procedures
outlined in your contract or Chapter 10: Our Claims Process - Claim reconsideration and appeals process in this guide.
• Offsets ‒ When we issue a refund request in connection with an audit, we recoup or offset the identified overpayment and/or
disallowed charge amounts after 45 calendar days from the date of the refund request, except when:
– You have already remitted the amount due.
– You have provided written notification of disagreement with the audit findings within the 45-calendar-day repayment period.
– Your Agreement or state law says otherwise.
Audit failure denials
You are required to submit, or provide access to, medical records upon our request. Failure to do so in a timely manner may
result in an audit failure denial, creating an overpayment. Medical record requests that do not comply with the guidelines in the
Overpayments section of Chapter 10: Our claims process follow the auto failure denial process.
Notice of Medicare Non-Coverage
You must deliver required notice to members at least 2 calendar days before termination of skilled nursing care, home health
care or comprehensive rehabilitation facility services. If the member’s services are expected to be fewer than 2 calendar days
in duration, the notice should be delivered at the time of admission or commencement of services in a non-institutional setting.
In a non-institutional setting, if the span of time between services exceeds 2 calendar days, the notice should be given no later
than the next to last time services are furnished.
Delivery of notice is valid only upon signature and date of member or their authorized representative, if the member is
incompetent. You must use the most current version of the standard CMS approved notice titled Notice of Medicare Non-
Coverage (NOMNC).
The standardized form and instructions regarding the NOMNC may be found on the CMS website at cms.gov > Medicare >
Beneficiary Notices Initiative (BNI) > MA ED Notices or contact your Quality Improvement Organization (QIO) for information.
There can be no modification of this text, and all required elements must be present, including instructions on how to contact
the QIO and the member’s MA benefit plan.
Any appeals of such service terminations are called fast track appeals and are reviewed by the QIO. You must provide
requested records and documentation to us or the QIO, as requested, no later than by close of calendar day of the day you are
notified by us or the QIO if the member has requested a fast track appeal. This includes weekends and holidays.

138
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 12: Medical records standards
and requirements
Access to records
Unless otherwise stated in your Agreement, you are required to:
• Send copies of our members’ medical, financial, administrative, or purchasing and leasing records.
• Provide electronic medical records (EMR) access to UnitedHealthcare on a 24 hours a day, 7 days per week basis.
• Supply records to UnitedHealthcare within 14 days upon request, free of charge.
– Supply records faster in certain circumstances.
• Maintain and protect records for 10 years.
• Give access to records for all dates of service that occurred when you were a contracted provider.
• Assist us, or our designee, in completing chart reviews for MA members.
Medical record standards
You may access medical record tools, templates and patient safety resources on uhcprovider.com/patient.
Member encounters
For every visit, document the:
• Member’s complaint or reason for the visit.
• Physical assessment.
• Unresolved problems from previous visit.
• Diagnosis and treatment plans.
• Member education, counseling or coordination of care with other health care providers.
• Date of return visit or other follow-up care, including phone calls.
• Review by the PCP (initialed) on consultation, lab, imaging and special studies, as well as ancillary, outpatient and inpatient
records.
• Follow-up care plans.
When coding the encounter, pick the Evaluation and Management level that reflects the member’s condition at the time of
the visit.
Monitoring the quality of medical care through review of medical records
A well-documented medical record reflects the quality of care delivered to patients. Accreditation and regulatory groups review
medical records as part of their oversight activities. Maintain your medical records in a manner that is current, detailed and
organized. This allows for effective and confidential patient care and quality reviews.
Correspondence from the Quality of Care Department is considered privileged and confidential. The involved health care
provider cannot share or discuss correspondence with the patient, member or any member representative. You may not file the
communication in the patient’s medical record.
Medical records duplication
• Medical Record Copies for Specialist Referrals — The PCP office pays for the cost of duplicating and shipping the records
due to a referral. You cannot charge the member for records used during the member’s course of treatment.
• Member Transfer to Another PCP — Do not charge the member if they need records sent to another PCP.

Chapter 12: Medical records standards and requirements
139
2023 UnitedHealthcare Care Provider Administrative Guide
• Member Request for Medical Records — The member, or member’s representative, may request copies of records from
your office. You can charge a fee of up to 25 cents per page plus any reasonable clerical costs incurred, unless state laws
indicates otherwise.
Medical record guidelines
Medical records must have all information necessary to support claims for your services. You are expected to have written
policies for the following:
• Medical records guidelines including maintenance of a single, permanent medical record that is legible, current and detailed
• Process for handling missed appointments
• Non-discrimination of health care delivery
• Staff training on confidentiality and safe record keeping
• Release of information
• Medical record retention
• Availability of medical records if housed in a different location
• Coordination of care between medical and behavioral health care providers
• Process for notifying UnitedHealthcare upon becoming aware of a patient safety issue or concern
General documentation guidelines
We expect you to follow guidelines for medical record information and documentation including the following:
• Date all entries, and identify the author and their credentials. The documentation should show which individual performed a
given service.
• Clearly label or document changes to a medical record entry by including the author and date of change. You must keep a
copy of the original entry.
• Generate documentation at the time of service or shortly thereafter. Clearly label any documentation generated at a previous
visit as previously obtained, if it is included in the current record.
• Gather demographic information including name, gender, date of birth, member number, emergency contact name,
relationship, phone numbers and insurance information.
• Transcribe family and social history, including marital status and occupational status or history.
• Prominently place information on whether the member has executed an advance directive. This is critical.
• List medical history, chronic conditions and significant illnesses, accidents and operations. Include the chief complaint,
diagnosis and treatment plan at each visit.
• List medication allergies and adverse reactions. Also note if the member has no known allergies or adverse reactions. This is
critical.
• Include name of current medications, dosages and over-the-counter drugs.
• Reflect all services provided, ancillary services/tests ordered and all diagnostic/therapeutic services referred by the health
care provider.
• Document member history and health behaviors such as:
– Tobacco habits, including advice to quit, alcohol use and substance use (age 11 and older).
– Immunization record.
– Preventive screenings/services and risk screenings.
– Screenings for depression and evidence of coordination with behavioral health care providers.
– Blood pressure, height and weight and body mass index.
– Physical assessment for each visit.
– Growth charts for children and developmental assessments.
– Physical activity and nutritional counseling.

Chapter 12: Medical records standards and requirements
140
2023 UnitedHealthcare Care Provider Administrative Guide
• Clinical decision and safety support tools in place to help ensure evidence-based care and follow-up care. Examples include:
– Lab, X-ray, consultation reports, behavioral health reports, ancillary health care providers’ reports, facility records and
outpatient records show health care provider review by signature or initials.
– Report from eye care specialist related to medical eye examinations.
Record accuracy goals
• 90% of medical records will contain documentation of critical measures.
• 80% of medical records will contain documentation of all other elements when those elements are included in quality
improvement medical record assessments.
• 100% of medical records will contain documentation of allergies and adverse reactions.
Chart assessments and failure to comply
We have the right to assess health care provider records to determine the accuracy of ICD-10-CM and CPT coding. We notify
you of the results. We may charge a penalty if you fail to submit the information.
Risk adjustment and medical records
Medical records are important for both CMS reimbursement for our members and to accurately calculate an annual patient risk
score that represents the specific patient’s disease burden for the Department of Health and Human Services (DHHS). Every
year, CMS and DHHS require information about the demographic and health of our members. Diagnoses do not carry forward
to the following year and must be assessed and reported every year. Records must show all conditions evaluated during
the visit. It is important to evaluate all medical conditions, both chronic and acute, at least annually. Report the appropriate
diagnosis code for all documented conditions that coexist at the time of the visit that require or affect care.
For accurate reporting on ICD-10-CM diagnosis codes, the medical record documentation must describe the member’s
condition. This should include specific diagnosis, symptoms, problems or reasons for the visit. You are responsible for making
sure ICD-10-CM coding adheres to ethical standards. Member charts are subject to review. We may review the charts to identify
conditions not coded on claims.
CMS conducts audits to confirm that the Hierarchical Condition Categories (HCCs) triggered for payment based on ICD-10-CM
coding and supported by chart documentation. CMS works through us to obtain these records for the MA program. The DHHS
requests this data from us for the Commercial Risk Adjustment Program. Since our legal obligation is to provide this information
to federal agencies, we appreciate and require your cooperation with this as well.

141
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 13: Health and disease management
Clinical and preventive health guidelines
We use evidence-based clinical and preventive health guidelines from nationally recognized sources to guide our quality and
health management programs. We hope you use this information for our members. A complete list of clinical guidelines is on
uhcprovider.com/policies > Additional Resources > Clinical Guidelines.
Health management programs
We offer case and disease management programs to support your treatment plans. They also assist members in managing
their conditions. By using medical, pharmacy and behavioral health claims data, we can identify members who are high-risk
and a good fit for our programs. A referral from a health risk assessment, the NurseLine or a member/caregiver can also
help identify these high-risk members. You can refer these members to the appropriate program by calling the number on
the member’s health plan ID card. Participation in these programs is voluntary. Upon referral, we assess members for the
appropriate level of care for their individual needs. The programs vary based on the member’s benefit plan.
Case management
Our case managers are registered nurses. They engage the appropriate internal, external or community-based resources to
support the member’s needs. When applicable, we refer to other internal programs such as:
• Disease management.
• Complex condition management.
• Behavioral health employee assistance.
• Disability.
Case management services are voluntary. The member can opt out at any time.
Transitional Case Management (TCM): The collaboration of evaluating and coordinating post-hospitalization needs for
members who are at risk of re-hospitalization or frequent users of high-cost services.
General Condition Management: Serves members:
• With chronic conditions.
• In need of long-term care support.
• Who have unmet access.
• Who have care plan, psycho-social or knowledge needs.
Commercial complex medical conditions programs
Transplant Resource Services: Members eligible for this program have access to the Optum Center of Excellence (COE)
transplant network.
Congenital Heart Disease Program: Members 18 and younger who have a clinical diagnosis of CHD can join. It offers
them clinical management and support throughout the process of selecting a facility, being inpatient and experiencing post-
discharge.
Cancer Resource Services: Members eligible for this program have access to the COE cancer network.
Cancer Support Program: Covers all types of cancer and provides case management support from an experienced cancer
nurse.

Chapter 13: Health and disease management
142
2023 UnitedHealthcare Care Provider Administrative Guide
Bariatric Resource Services: Helps achieve positive results by using evidence-based guidelines and access to a COE/
designated health care provider network of quality bariatric centers to help improve clinical and economic outcomes. It also
offers clinical case management by a dedicated nursing staff.
Women’s Health Services: We offer integrated, connected care strategies to positively influence pregnancy outcomes for both
mother and the baby.
• Our fertility, maternity and neonatal care management programs support members with appropriate guidance, education and
counseling. Members with unique health needs and high-risk pregnancies receive personalized case management support to
minimize pregnancy complications.
• Our easy-to-access, multimodal channels allow members to remain engaged with their care team. The new UnitedHealthcare
Healthy Pregnancy App delivers personalized content, helps determine risks, and facilitates maternity nurses’ support and
care during pregnancy.
Kidney Resource Services: Our specialized chronic kidney disease (CKD) Stage 4-5 and end-stage renal disease (ESRD) care
management programs focus on patients who have experienced a severe decrease in kidney function, are transitioning into
renal replacement therapy or are already on dialysis. We engage and support our members to identify gaps in care and utilize
evidence-based guidelines to close those gaps.
Decision support programs
NurseLine: This program uses a call model and Integrated Clinical User Experience (ICUE) to help facilitate better health
outcomes. Each call becomes an opportunity to address a symptom and to connect members with the right care, right health
care provider, right medication and right lifestyle.
Emergency Room Decision Support (ERDS): This is a program that helps identify, educate and assist members whose
emergency room visits are preventable, avoidable or treatable in a lower-care non-emergency setting.
Commercial health services, wellness and behavioral
health programs
We offer many types of programs for members. They focus on delivering skilled resources to support members as they seek
their personal best health. To access these programs, have the member call the phone number listed on the back of their ID
card. Programs and health services may vary based on the member’s coverage.
Tobacco Cessation: We offer a comprehensive tobacco cessation solution that uses an evidence-based combination of
physical, psychological and behavioral strategies to help members overcome their tobacco addiction, including use of
electronic nicotine delivery systems (ENDs) or e-cigarettes.
Wellness Coaching: This is an online or phone-based program. It helps members identify and prioritize unhealthy behaviors
and set personalized goals that focus on positive, healthy behavior change.
Real Appeal: Real Appeal is a health service that takes an evidence-based approach to support weight loss. This service
helps people make small changes necessary for larger, long-term health results. It is based on weight-loss research studies
commissioned by the National Institutes of Health.
Biometrics: Health Screening Solutions allow employers to offer wellness screenings to onsite, remote and mobile employees,
as well as spouses and adult dependents. Broad access is achieved by offering both onsite and offsite screening options.
These delivery options include offering Know Your Numbers onsite screening events, at-home screening materials, lab
screening visits or health provider results forms.
Wellness Incentive Programs: These programs reward employees with financial incentives when they complete wellness
activities and/or achieve targeted health outcomes.
UnitedHealthcare Motion: A digital wellness program designed to promote physical activity with compatible activity trackers
enabling members to earn incentives for meeting certain daily walking goals.

Chapter 13: Health and disease management
143
2023 UnitedHealthcare Care Provider Administrative Guide
Behavioral Health Programs: We offer specialized mental health and substance use disorder benefits delivered by our affiliate
company United Behavioral Health, operating under the brand Optum. This may be available to members depending on their
health benefit plan. To access these programs, have the member call the phone number listed on the back of their ID card.
Employee Assistance Programs (EAP): The EAP provides confidential support and short-term counseling for individuals who
may be struggling with those everyday challenges or for more serious personal concerns such as:
• Depression.
• Stress and anxiety.
• Relationship difficulties.
• Financial and legal advice.
• Parenting and family problems.
• Child and elder care support.
• Dealing with domestic violence.
• Substance use disorder and recovery.
Commercial consumer transparency tools
An online cost estimator tool is available in some markets at myuhc.com. The tool is designed to assist members in making
informed health care choices based on cost and quality. It displays health care provider-specific cost estimates together with
UnitedHealth Premium physician designations. Information can be found on myuhc.com. Once logged in, select Find Care &
Costs.
If you would like to review your cost data, contact your UnitedHealthcare Network Management representative or hospital or
provider advocate at uhcprovider.com/contactus.
Medicare Advantage
Note: Medicare Advantage (MA) may include Dual Special Needs Plans (DSNP).
Clinical programs: Condition management and care management
Our MA plans provide a full spectrum of care management programs as part of our standard plan offerings. Clinical programs
include inpatient care management, care and condition management, specialty care management (e.g., transplant and ESRD
management), behavioral health care management, Advanced Illness, HouseCalls, (not all members are eligible for this
program), and Solutions for Caregivers (available on select MA plans). Participation by the member is encouraged but voluntary.
Condition management programs
These programs help members with chronic conditions—such as diabetes, heart failure and ESRD—to be their healthiest. We
offer education and resources to support optimal health of members actively treated for chronic conditions. Members receive
case management and can attend workshops to help manage their condition.
Care management programs
• Inpatient Care Management: Nurses review the clinical information that outlines the clinical treatment plan for the member.
They evaluate appropriateness for admission based on evidence-based medicine and discharge planning needs, including
identifying members for post-discharge follow-up and referral to outpatient programs.
• Behavioral Health: Led by experienced psychiatrists and licensed behavioral health clinicians, our program integrates with
our medical team to identify, engage and manage a member’s behavioral health concerns.
• Community Transitions Program: Designed to reduce complications by smoothing the transition from hospital to home,
program staff coordinate transitions in care or changes in member health status to avoid potential adverse outcomes and
unnecessary readmissions.

Chapter 13: Health and disease management
144
2023 UnitedHealthcare Care Provider Administrative Guide
• High-Risk Care Management: Nurses support members who have complex care needs by helping them access care,
coordinate services and learn to better manage their chronic conditions.
• Advanced Illness: Provides comprehensive care for members facing life-limiting illness generally defined as the last 12
months of life.
• Transplant Resources: Our transplant management program drives positive clinical outcomes by addressing the complex
needs of members who are facing transplants.
• Post-Acute Transition Program: Uses an individualized, whole-person approach to remove barriers to discharge from post-
acute care, such as SNF so the member can safely return to the least restrictive setting possible.
Special Needs Plans Model of Care
The Model of Care (MOC) is the framework for care management processes and systems that enable coordinated care for
Special Needs Plans (SNP) members. The MOC includes descriptions of the following:
• SNP population (including health conditions)
• Care coordination
• Provider network
• Quality measurement
• Performance improvement
The MOC helps ensure the unique needs of the population are identified and addressed through care management practices.
We evaluate MOC goals on an annual basis to determine effectiveness.
To learn more, contact us at: snp_moc_provider[email protected].
CMS requires annual SNP MOC training for all health care providers who treat SNP members. The training is reviewed and
updated annually to reflect current practices related to care coordination. This includes communication of the Individualized
Care Plan (ICP) for each member. The Annual SNP MOC Provider Training is available at uhcprovider.com/training. Updates
about the annual training can be found at uhcprovider.com/news. To receive news updates by email, sign up at uhcprovider.
com/subscribe.
Commercial and MA behavioral health information
The U.S. Preventive Services Task Force (USPSTF) recommends that PCPs screen patients for depression, substance use
disorder and alcohol misuse. If left untreated, these disorders can adversely affect quality of life and clinical outcomes.
Screening for these disorders is critical to treatment since it can contribute to the patient’s readiness to change.
You can help by screening all patients, including adolescents. To assist, we recommend the following screenings:
Depression Patient Health Questionnaire (PHQ-9)
†
CPT 99420
Alcohol Misuse Alcohol Use Disorders Identification Test
(AUDIT) or CAGE
CPT 99420
† PHQ-9 was developed by Drs. Robert L Spitzer, Janet B. Williams, Kurt Kroenke and colleagues, with an educational grant from Pfizer Inc.
When doing a screening for depression in adults, remember to include the 99420 CPT Code and the ICD-10-CM Z13.89 code.
Find these screening tools and other resources online at uhcprovider.com > Resources > Resource library > Behavioral
Health Resources.
For more information on depression, alcohol use disorders, opioid use disorders and other behavioral conditions, access the
Optum website providerexpress.com > Clinical Resources > Behavioral Health Toolkit for Medical Providers. You may also
email your request to BHInfo@uhc.com.
To refer a member to an Optum network provider for assessment and/or treatment, call the number on the back of the
member’s ID card. A link to the Optum Clinician Directory is on providerexpress.com > Our Network > Directories.

Chapter 13: Health and disease management
145
2023 UnitedHealthcare Care Provider Administrative Guide
The UnitedHealthcare Preventive Medicine and Screening Reimbursement Policy notes that counseling services are included
in preventive medicine services. This policy is available on uhcprovider.com/policies > Commercial (or Medicare Advantage
Policies). The Preventive Care Services Coverage Determination Guideline is on uhcprovider.com/policies > Commercial
Policies > Medical & Drug Policies and Coverage Determination Guidelines for UnitedHealthcare Commercial Plans.
For information on coverage of mental health services and preventive health services for MA members, see the Medicare
Advantage Coverage Summary for Preventive Health Services and Procedures, and the Medicare Advantage Coverage
Summary for Mental Health Services and Procedures, available on uhcprovider.com/policies > Medicare Advantage Policies
> Coverage Summaries for Medicare Advantage Plans. Optum Health Education offers continuing education courses for
providers on patient treatment, best practices, trends and other key information regarding behavioral health. Continuing
education opportunities are available at optumhealtheducation.com.
Depression, substance use disorder/addiction and Attention Deficit Hyperactivity Disorder
preventive health program information
Optum has developed online preventive health resources that offer up-to-date information and tools to support treatment of
major depressive disorder, alcohol and drug use disorder and Attention Deficit Hyperactivity Disorder (ADHD). The preventive
health website, prevention.liveandworkwell.com, includes:
• A screening tool to help you decide whether to seek care.
• Articles about behavioral health conditions and how they are treated.
• A list of organizations you can contact if you want more information about a condition and its treatment.
• Contact information for self-help groups if you want to talk with others who can provide support and encouragement.
• Information on how to contact us if you have questions or concerns.
Substance use disorder helpline
Optum offers a 24/7 helpline for health care providers and patients to:
• Identify local medication-assisted treatment (MAT) and behavioral health care providers.
• Provide targeted referrals for evidence-based care.
• Educate members/families about substance use.
• Find community support services.
• Assign a care advocate to provide ongoing support for up to 6 months, when appropriate.
Health care providers and patients can call 1-855-780-5955. More information is available at liveandworkwell.com > Mind &
Body > Substance Use Disorder/Addiction.
Collaboration between primary physicians and behavioral health clinicians
When a member receives services from more than one health care provider, collaborate and coordinate effectively to help
ensure care is comprehensive, safe and effective. Lack of communication may negatively affect quality patient care. For
example, members with medical illnesses may also have mental health or substance use disorders. Continuity and coordination
of care is important for members with severe and persistent mental health and/or substance use disorders. This is especially
true when the member is prescribed medication and has:
• Coexisting medical/psychiatric symptoms.
• Been hospitalized for a medical or psychiatric condition.
Talk to your patients about the benefits of sharing essential clinical information.
Psychiatric and behavioral therapy consults for medical patients
Contact Optum if you:
• Want to arrange a psychiatric consultation for a member in a medical bed.
• Are unclear whether a behavioral health consultation is needed.
• Want assistance with any needed behavioral health authorization.
Reach Optum by calling the phone number on the back of the member’s ID card.

146
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 14: Quality Management program
The Quality Management (QM) program helps ensure access to health care and services with a review using established quality
improvement principles.
We use our QM program to:
• Identify the type of care and services given.
• Use clinical guidelines and service standards to monitor clinical performance.
• Review the quality and appropriateness of services given to our members.
• Review the medical qualifications of participating health care professionals.
• Continue to improve member health care and services.
• Improve patient safety and confidentiality of member medical information.
• Resolve identified quality issues.
Our board of directors oversees the QM program. The vice president of quality and chief medical officer are in charge of day-to-
day QM operations.
QM committee structure
Committee structure for Medicare and commercial product lines may include the following:
• The National Quality Oversight Committee (NQOC) directs the QM Program for UnitedHealthcare at the national level and
interfaces with other national and regional committees, as applicable. The board of directors has delegated responsibility for
the oversight of health plan QM activities to NQOC and Regional Quality Oversight Committee (RQOC).
• The Medical Advisory Committee (MAC) oversees, reviews and provides recommendations on QM activities. These include:
– Clinical indicators monitoring.
– Analysis of potential/actual barriers to improve clinical performance.
– Medical policies.
– Pharmacy updates.
– Service standards.
This committee suggests quality improvement activities based on a review of potential/actual barriers to improving clinical
performance found in their regions. They create and implement regional components of the QM work plan.
• The RQOC oversees these quality improvement activities.
• When there are significant concerns about quality of care, the Regional Peer Review Committee (RPRC) is a forum for
physicians to investigate, talk about and take action on these cases. The RPRC can make decisions on behalf of the National
Peer Review and Credentialing Policy Committee (NPRCPC).
– The NPRCPC is a forum for physicians to talk about and take disciplinary action on member cases involving quality of care
concerns that were unresolved through Improvement Action Plans administered by the RPRC.
• The National Practitioner Sanctions Committee (NPSC) is a forum for physicians to discuss and act on sanction reports
about compliance with our credentialing plan and/or patient safety concerns. Sanctions related to licensed independent
practitioners are monitored by government agencies and authorities. These include:
– Centers for Medicare & Medicaid Services (CMS).
– Medicaid agencies
– State licensing boards.
– The Office of the Inspector General within the federal Department of Health and Human Services.
– The Office of Personnel Management (OPM).

Chapter 14: Quality Management program
147
2023 UnitedHealthcare Care Provider Administrative Guide
Program scope
The QM program:
• Identifies high-volume and/or high-risk areas of care and service affecting our members.
• Develops clinical practice guidelines for preventive screening, acute and chronic care, and appropriate drug usage. These are
based on available national guidelines.
• Identifies clinical areas for quality improvement activities using claims and other data analyses. These include frequency and
cost breakdown by member’s age, sex and line of business. It also includes groupings like episode treatment groups, major
medical procedure categories and diagnosis-related groups (DRGs).
• Reviews preventive care delivered using health care audit results.
• Surveys members, health care providers and employers to track satisfaction and reason for voluntary health care provider
disenrollment.
• Measures results against physician service standards like wait times for appointments, in-office care, practice size and
availability. We use information from members, Consumer Assessment of Healthcare Providers and Systems (CAHPS)
member survey information and GeoAccess analysis.
• Checks to help ensure providers perform QM-related activities as our contracts require.
• Audits records to see if medical record standards and preventive care guidelines were met. This is not the only reason we
audit medical records. Other audits may have different purposes and processes.
• Helps to ensure medical record documentation provides the plan for member care. This includes continuity and coordination
of care with other physicians, facilities and health care professionals.
• The RPRC and NPRCPC investigates and resolves member complaints about medical care and services. The investigation
may include contact with the member, physician and/or other health care professionals. It may also review medical records
and your responses to potential concerns.
UnitedHealth Premium® program (commercial plans)
The UnitedHealth Premium® program provides physician designations based on quality and cost-efficiency criteria. This helps
members make more informed choices for their medical care.
This program includes both quality care and cost-efficient care evaluations. Quality is the primary measurement. The emphasis
on quality demonstrates our commitment to evidence-based medicine as only those physicians who meet quality are evaluated
for cost efficiency. The results of these evaluations are used to determine a designation that we publicly display. Quality is
evaluated using national standardized measures. Cost efficiency is evaluated using 2 measures: patient total cost and patient
episode cost.
Physicians receive one of these designations:
Premium Care Physician
The physician meets the UnitedHealth Premium program quality and cost-efficient care criteria.
Quality Care Physician
The physician meets the UnitedHealth Premium program quality care criteria but does not meet the program’s cost-
efficient care criteria or is not evaluated for cost-efficient care.
Does Not Meet Premium Quality Criteria
The physician does not meet the UnitedHealth Premium program quality criteria, so the physician is not eligible for a
Premium designation.
Not Evaluated for Premium Care
The physician’s specialty is not evaluated in the UnitedHealth Premium program or the physician’s program evaluation
is in process; or if the physician does not have enough claims data to be evaluated for UnitedHealth Premium program
quality, then the physician is not eligible for a Premium Care Physician designation.

Chapter 14: Quality Management program
148
2023 UnitedHealthcare Care Provider Administrative Guide
Physicians may use these designations when referring patients to other physicians and to support their efforts to provide quality
and cost-efficient care to their patients. In markets where tiered benefit plans are available, employers may offer employees a
tiered benefit plan with a lower member cost share for using Premium Care Physicians.
Some health care provider directories may display quality evaluation results only. In those directories, physicians who have met
the Premium program’s quality care criteria may be displayed as a Quality Care Physician.
For more information regarding the UnitedHealth Premium program, including measures, measurement methodology and how
we use the results, go to UnitedHealthPremium.uhc.com. To contact us, go to UnitedHealthPremium.uhc.com > Help and
Support > Contact Premium.
Star ratings for MA and prescription drug plans
CMS Star Ratings provide external validation of our MA and Part D benefit plan performance and quality progress. For
information on CMS Star Ratings, go to uhcprovider.com/starratings.
Members’ experience of care
A certified National Committee for Quality Assurance (NCQA) vendor conducts our annual survey of member experience of
care using the CAHPS survey. Members rate their experience and satisfaction in multiple areas:
• The health plan
• Their health care and providers
• Access
• Referral process
• Specialty care
• Benefits
• Member service
For more information on CAHPS or other quality improvement programs, go to uhcprovider.com/reports.
Imaging accreditation protocol
The imaging accreditation protocol promotes compliance with nationally recognized quality and safety standards.
Accreditation is required for the following advanced imaging studies:
• CT scan
• Echocardiography
• MRI
• Nuclear medicine/cardiology
• PET scan
If you fail to obtain accreditation, your reimbursement may be affected. We may do an administrative claim reimbursement
reduction for global and technical service claims.
Additional information on this protocol and the required accreditation agencies is on uhcprovider.com/join >
Imaging Accreditation.

149
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 15: Credentialing and recredentialing
Credentialing/profile reporting requirements
Credentialing program
We credential physicians, health care providers and facilities who want to join our network and be listed in our Provider
Directory. We recredential at least every 36 months. Our credentialing program helps us maintain and improve the quality
of care and services delivered to our members. Our credentialing standards are fully compliant with and go beyond the
National Committee for Quality Assurance (NCQA), Centers for Medicare and Medicaid Services (CMS) and applicable state
requirements. We have a thorough, written credentialing program, outlined in our Credentialing Plan on uhcprovider.com/join.
We review and revise our credentialing program at least every 2 years, or as NCQA, state or federal requirements change.
When we contract with a delegate to carry out credentialing activities, they must meet our standards as outlined in:
• This Administrative Guide.
• The Credentialing Plan.
• The Delegation Agreement.
We use the Council for Affordable Quality Healthcare (CAQH) process for credentialing application submissions, unless state
law requires differently. Health care providers applying to join our network, and those scheduled for recredentialing, must use
CAQH ProView. Instructions are provided on uhcprovider.com/join > Credentialing for Care Providers. Minnesota and western
Wisconsin health care providers may submit applications to the Minnesota Credentialing Collaborative (MCC), also known
as ApplySmart. Log into credentialsmart.net/mcc to select UnitedHealthcare as a Preference, complete your application
and submit to us. Washington health care providers are required to complete the ProviderSource application by logging into
onehealthit port.com.
As a participating health care provider, you are responsible for verifying your clinical staff have required licenses and
other credentials.
Non-discrimination
Credentialing and recredentialing decisions are not based on a health care provider’s or professional’s:
• Race or ethnic/national identity.
• Gender.
• Age.
• Sexual orientation.
• Types of procedures they specialize in.
• Specialties that serve high-risk populations or conditions that require costly treatment.
We may however choose to include health care providers in our network because they meet certain demographic, specialty or
cultural needs of our members.
Network providers and business needs
When we decide to approve or deny an application/reapplication, we consider:
• Our current network of health care providers.
• Our business needs.
• The health care provider’s credentials and qualifications.

Chapter 15: Credentialing and recredentialing
150
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare’s discretion
Our credentialing criteria, standards and requirements do not limit our discretion in any way or create rights on the part of health
care providers who seek to provide health care services to our members. We retain the right to approve, suspend and terminate
individual health care providers and sites in situations where we have delegated credentialing decision-making authority.
Confidentiality
Our staff treats information obtained in the credentialing process as confidential. We and our delegates maintain mechanisms
to properly limit review of confidential credentialing information. Our contracts require delegated entities to maintain the
confidentiality of credentialing information. Credentialing staff or representatives will not disclose confidential health care
provider credentialing information to any persons or entity except with the express written permission of the health care provider
or as otherwise permitted or required by law.
Health care provider rights related to the credentialing
process
Health care providers applying for participation in our network have the right to:
• Review the information submitted for your application. This excludes personal or professional references or peer review
protected materials.
• Correct erroneous information. We let applicants know in writing, by fax or email, if we find any information that varies
substantially from the information they provided. Applicants must submit corrections, in writing, directed by the credentialing
entity within 30 days of the notification of the discrepancy.
• Be given the status of your credentialing or recredentialing application, upon request. Check the status of your application by
emailing [email protected].
Additional information on our credentialing program can be found by clicking the following links:
• UnitedHealthcare Credentialing Plan
• UnitedHealthcare Credentialing Plan State and Federal Addendum
• Join our Network & Credentialing
• Credentialing FAQs
Credentialing committee decision-making process
(non-delegated)
Determination and notice of approval or denial
After it completes the review and evaluation of all of the credentialing information, the National Credentialing Committee
approves or denies participation in our network.
For initial credentialing, all health care providers are notified of initial credentialing decisions within 60 calendar days of the
National Credentialing Committee’s decision or as required by state law, though we are generally able to notify health care
providers within 14 days of the National Credentialing Committee’s decision. For recredentialing, we notify health care providers
within 60 calendar days of the decision or as required by law if the National Credentialing Committee determines they are no
longer eligible to participate in our network. We send written notice of recredentialing approvals to health care providers as
required by state law.

Chapter 15: Credentialing and recredentialing
151
2023 UnitedHealthcare Care Provider Administrative Guide
Right to see members
Approved for participation does not mean “active.” Health care providers may not begin seeing our members until they and we
have signed a contract and are in our systems, or they receive the effective date of their active status. We send written notice
that the contract is active.
Monitoring of network providers and health
care professionals
We monitor sanction activity from state licensing boards, CMS, Office of Inspector General (OIG) and other regulatory bodies.
If we find a health care provider has a sanction that results in loss of license or governmental authorization, we terminate them
from our network.
Health care provider office site quality review
We have office site standards that you must follow, including:
• Physical accessibility, such as handicapped accessible.
• Physical appearance and cleanliness of the site.
• Adequacy of waiting and examining room space.
• Availability of appointments.
• Adequacy of treatment record keeping (e.g., secure/confidential filing system).

152
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 16: Member rights and responsibilities
Our members have certain rights and responsibilities to help uphold the quality of care and services they receive from you. We
list the rights and responsibilities in the member materials for commercial and MA benefit plans.
• You can request a copy of the Member Rights and Responsibilities by calling your provider advocate at 1-877-842-3210.
• An online version of member rights is on uhc.com > Featured Links > About Us > Member Rights & Responsibilities. These
apply to all members.
• Member Rights and Responsibilities specifically for MA members can be found on:
– UHC.com/Medicare
– AARPMedicarePlans.com
– uhcRetiree.com
• Find provider news and updates at uhcprovider.com/news. Subscribe to receive updates by email at uhcprovider.com/
subscribe.
• Members have a right to a second opinion. Members should be referred to their benefit plan for specific steps to obtain the
second opinion.
Member appeals and grievance complaints
We maintain a system of logging, tracking and analyzing appeals and grievance issues received from members and health care
providers consistent with state and federal regulatory requirements. We use the information to measure and improve member
and health care provider satisfaction. This system helps us fulfill the requirements and expectations of our members and our
network providers. In addition, it supports compliance with the Centers for Medicare & Medicaid Services (CMS), the National
Committee for Quality Assurance (NCQA), The Joint Commission, and other accrediting and/or regulatory requirements.
Members have the right to appeal the determination of any denied services or claims by filing an appeal. Time frames for filing
an appeal vary depending on applicable state or federal requirements.
We track and trend health care provider complaints and use the information during recredentialing. We conduct an annual
analysis of the complaint data to look for opportunities for improvement. Health care provider and member complaints are
important to the recredentialing process because they help us attract and retain health care providers, employer groups and
members.
Member’s request for confidentiality
The state and federal government allows an individual, other than the subscriber, to request confidential treatment as it
relates to the following:
• Referrals
• Authorizations
• Denials
• Claims payments
We require our members to submit written requests for confidential status to you. The request must include their current
address, private phone number, and date and time you received it. Having a written request prevents disagreements regarding
the accuracy of their personal contact information. Members are responsible for resubmitting new confidentiality forms if their
information changes.
Privacy regulations
HIPAA privacy regulations provide federal protection for the privacy of health care information. These regulations control the
internal and external uses of health information. They also create certain individual patient rights. Information related to our
privacy practices can be found on uhc.com > Privacy.

Chapter 16: Member rights and responsibilities
153
2023 UnitedHealthcare Care Provider Administrative Guide
Advance directives
The federal Patient Self-Determination Act (PSDA) gives patients the legal right to make choices about their medical care prior
to a severe illness or injury through an advance directive. Under the federal act, health care providers and facilities must:
• Not discriminate against an individual based on whether the individual has executed an advance directive.
• Document in a prominent part of the individual’s current medical record whether the individual has executed an advance
directive.
• Educate its staff about its policies and procedures for advance directives.
• Provide for community education regarding advance directives.
• Give patients written information on state laws about advance treatment directives, patients’ rights to accept or refuse
treatment, and their own policies regarding advance directives.
We also inform members about state laws on advance directives through our member’s benefit material. We encourage these
discussions with our members.
Information is also available from the Robert Wood Foundation, Five Wishes. The information there meets the legal
requirements for an advance directive in certain states and may be helpful to members. Five Wishes is available on
AgingWithDignity.org.

154
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 17: Fraud, Waste and Abuse
The purpose of our Fraud, Waste and Abuse (FWA) program is to protect the ethical and fiscal integrity of our health care
benefit plans and programs. Our program has 2 main functions:
• UnitedHealthcare Payment Integrity, Optum entities and others perform our payment integrity functions to help:
– Ensure reimbursement accuracy.
– Keep up to date on new and emerging FWA schemes.
– Discover methodologies and technologies to combat FWA.
• Special Investigations Units (SIUs) perform prospective and retrospective investigations of suspected FWA committed against
our benefit plans and programs.
This program is part of our Compliance Program led by our chief compliance officer. Our Compliance Department works
closely with internal business partners in developing, implementing and maintaining the program.
For definitions of fraud, waste, or abuse, refer to the Glossary at the back of this guide.
If you identify compliance issues and/or potential FWA, report it to us immediately so we can investigate and respond
appropriately. Refer to the Online/interoperability resources and how to contact us section in Chapter 1: Introduction for
contact information. UnitedHealthcare prohibits any form of retaliation against you if you make a report in good faith.
Medicare compliance expectations and training
The Centers for Medicare & Medicaid Services (CMS) requires Medicare Advantage (MA) organizations and Part D plan
sponsors, including UnitedHealthcare, to annually communicate specific Compliance and FWA requirements to their “first
tier, downstream and related entities” (FDRs). FDRs include contracted physicians, health care professionals, facilities and
ancillary providers as well as delegates, contractors and related parties. As a delegate that performs administrative or health
care services, CMS and other federal or state regulators require that you and your employees meet certain FWA and general
compliance requirements.
FDRs are expected to have an effective compliance program, which includes training and education to address FWA and
compliance knowledge. UnitedHealthcare’s expectation remains that FDRs and their employees are sufficiently trained to
identify, prevent and report incidents of non-compliance and FWA. This includes temporary workers and volunteers, the CEO,
senior administrators or managers and sub delegates who are involved in or responsible for the administration or delivery of
UnitedHealthcare MA or Part D benefits or services.
We have general compliance training and FWA resources available at unitedhealthgroup.com. The required education, training
and screening requirements include the following:
Standards of conduct awareness
What you need to do
Provide a copy of your own code of conduct, or the UnitedHealth Group’s Code of Conduct at unitedhealthgroup.com > Who
We Are > Our People & Culture > Ethics & Integrity > Code of Conduct to your employees. Provide the materials annually and
within 90 days of hire for new employees.
Maintain records of distribution standards (i.e., in an email, website portal or contract) for 10 years. We may request
documentation to verify compliance.

Chapter 17: Fraud, Waste and Abuse
155
2023 UnitedHealthcare Care Provider Administrative Guide
Fraud, waste, and abuse and general compliance training
What you need to do
Provide FWA and general compliance training to employees and contractors of the FDR working on MA and Part D programs.
Administer FWA and general compliance training annually and within 90 days of hire for new employees.
Exclusion checks
Prior to hiring or contracting with employees, you must review federal (HHS-OIG and GSA) and state exclusion lists, as
applicable. This includes the hiring of temporary workers, volunteers, the CEO, senior administrators or managers, and sub
delegates who are involved in or are responsible for the administration or delivery of UnitedHealthcare MA and Part D and
Medicaid benefits or services.
What you need to do
• Make sure potential employees are not excluded from participating in federal health care programs. For more information or
access to the publicly accessible excluded party online databases, use the following links:
– Department of Health and Human Services – Office of the Inspector General (OIG) List of Excluded Individuals and Entities
(LEIE) at oig.hhs.gov
– General Services Administration (GSA) System for Award Management at sam.gov
• Review the exclusion lists every month and disclose to UnitedHealthcare any exclusion or any other event that makes an
individual ineligible to perform work directly or indirectly on federal health care programs.
• Maintain a record of exclusion checks for 10 years. We or CMS may request documentation of the exclusion checks to verify
they were completed.
Preclusion list policy
The CMS has a Preclusion List effective for claims with dates of service on or after April 1, 2019. The Preclusion List applies to
MA plans as well as Part D plans.
The Preclusion List is comprised of a list of prescribers and individuals or entities who:
• Are revoked from Medicare, are under an active re-enrollment bar and CMS has determined that the underlying conduct that
led to the revocation is detrimental to the best interests of the Medicare program.
• Have engaged in behavior for which CMS could have revoked the prescriber, individual or entity to the extent possible if they
had been enrolled in Medicare and that the underlying conduct that would have led to the revocation is detrimental to the
best interests of the Medicare program.
• Have been convicted of a felony under federal or state law within the previous 10 years and that CMS deems detrimental to
the best interests of the Medicare program.
Health care providers receive a letter from CMS notifying them of their placement on the Preclusion List. They have the
opportunity to appeal with CMS before the preclusion is effective. There is no opportunity to appeal with UnitedHealthcare.
CMS updates the Preclusion List monthly and notifies MA and Part D plans of the claim-rejection date, the date upon which
we reject or deny a health care provider’s claims due to precluded status. Once the claim-rejection date is effective, a
precluded health care provider’s claims will no longer be paid, pharmacy claims will be rejected and the health care provider
will be terminated from the UnitedHealthcare network. Additionally, the precluded health care provider must hold Medicare
beneficiaries harmless from financial liability for services provided on or after the claim-rejection date.
As contracted health care providers of UnitedHealthcare, you must ensure that payments for health care services or items are
not made to individuals or entities on the Preclusion List, including employed or contracted individuals or entities.
For more information on the Preclusion List, visit cms.gov.

Chapter 17: Fraud, Waste and Abuse
156
2023 UnitedHealthcare Care Provider Administrative Guide
Examples of potentially fraudulent, wasteful or abusive
billing
Back filling: Billing for part of the global fee before the claim is received for the actual global code.
Billing for services not rendered: Billing for services or supplies that were not provided to the member.
Billing for unauthorized services or equipment: Billing for ancillary, therapeutic or other services without a required
physician’s order.
Billing while ineligible: Billing for services after health care provider’s license has been revoked/restricted or after a health care
provider has been debarred from a government benefits program for fraud or abuse.
Double billing: Billing more than once for the same service.
Falsified documents: Submitting falsified or altered claims or supporting claims with falsified or altered medical records and/or
supporting documentation.
Looping: Submitting claims for various family members when only one member is receiving services.
Misrepresentation: Misrepresenting the diagnoses and/or services provided to obtain higher payment or payment for non-
covered services.
Patient brokering: Using “brokers” who offer money to subscribers for the use of their ID cards.
Phantom billing: Billing by a “phantom” or non-existent health care provider for services not rendered.
Unbundling: Billing each component of a service when one comprehensive code is available.
Up-coding: Billing at a higher level of service than was actually provided.
Waiver of copay: Choosing not to collect copayments or deductibles as part of the payment Agreement.
Prevention and detection
We help prevent and detect potential FWA through many sources. These include the following:
• UnitedHealthcare payment integrity functions
• Optum companies within UnitedHealth Group
• Health care providers
• Health plan members
• Federal and state regulators and task forces
• News media
• Professional anti-fraud and compliance associations
• CMS websites: sam.gov/SAM
We also monitor and audit prevention and detection by:
Prospective detection:
• Prepayment data analytics
• Data mining queries
• Abnormal billing patterns
• Other activities to determine if we need additional prospective activities
Chapter 17: Fraud, Waste and Abuse
157
2023 UnitedHealthcare Care Provider Administrative Guide
Retrospective detection:
• Post-payment data analytics
• Payment error analytics
• Industry trend analysis
• Health care provider audits
Corrective action plans
As a part of our payment integrity responsibility we evaluate the appropriateness of paid claims. We may initiate a formal
corrective action plan if a provider does not comply with our billing guidelines or performance standards. We will monitor the
plan to confirm that it is in place and address any billing/performance problems.
Beneficiary inducement law
The Beneficiary Inducement Law is a federal health care program created in 1996 as part of the Health Insurance Portability
Accountability Act (HIPAA). The law makes it illegal to offer money, or services that are likely to influence a member to select a
particular health care provider, practitioner or supplier. Examples include:
• Offering gifts or payments to induce members to come in for a consultation or treatment.
• Waiving copayments and deductibles.
Health care providers who violate this law may be fined up to $10,000 for each item or service for which payment may be made,
and $5,000 for each individual violation. Fines may be assessed for up to 3 times the amount claimed. Violators may also be
excluded from participating in Medicare and Medicaid programs.
Allowable gratuities: Items or services offered to members for free must be worth less than $15 and total less than $75 per
year per beneficiary. Never give cash or gift cards to members.
Reporting potential FWA to UnitedHealthcare
When you report a situation you believe is FWA, you are doing your part to protect patients, save money for the health care
system and prevent personal loss for others. Taking action and making a report is an important first step. After your report is
made, UnitedHealthcare works to detect, correct and prevent FWA in the health care system.
You can report to UnitedHealthcare online on uhc.com/fraud or by calling 1-844-359-7736.

158
2023 UnitedHealthcare Care Provider Administrative Guide
Chapter 18: Provider communication
UnitedHealthcare is on a multi-year effort to enhance our digital delivery channels and transition paper transactions to
electronic, whenever possible. Our goal is to make it easier for you to work with us and reduce the time it takes for you to
perform claim and clinical activities UnitedHealthcare may provide electronic notice of policy, protocol and payment policy
changes; news and other important updates in the following ways:
• Network News email briefs to the email address you provide when you subscribe to the alerts
• On the first of month at uhcprovider.com/news
Email communication
Required email contact information
Health care professionals and facilities in the UnitedHealthcare network are required to do business with us electronically. We
must have a valid email address on file to send you required notifications and important information.
Submit your email address in one of the following ways:
1. Sign up for a One Healthcare ID, which also gives you access to the UnitedHealthcare Provider Portal
• Already have an ID? To review or update your email, simply sign in to the portal and click your user name in the upper
menu and then click Account Information to manage your email.
2. Subscribe to Network News email briefs to receive regular email updates
• Need to update your information? It takes just a few minutes to manage your email address and content preferences.
Network News email briefs
Subscribe today to receive a regular summary of the latest news, policy and reimbursement updates that we’ve posted on our
news webpage. You can tailor your subscription to help ensure that you only receive updates relevant to your state, specialty
and point of care.
These email briefs include:
• Monthly notification of policy and protocol updates, including medical and reimbursement policy changes
• Announcements of new programs and changes in administrative procedures
• Enhancements and additions to our suite of digital tools
Online resources
There are a number of ways clinicians, practice managers, administrative staff, facilities and hospitals can stay up to date on
items of interest from UnitedHealthcare.
uhcprovider.com
This public website is available 24/7 and does not require registration to access. You’ll find valuable resources including
administrative and plan-specific policies, protocols and guides, health plans by state, regulatory and practice updates, quality
programs and more.
Chapter 18: Provider communication
159
2023 UnitedHealthcare Care Provider Administrative Guide
We encourage you to bookmark the following frequently referenced pages for quick access:
Policies and Protocols
This library includes UnitedHealthcare Community Plan policies and protocols. Go to uhcprovider.com > Resources > Plans,
policies, protocols and guides.
Health plans by state
This is the fastest way to review all of the health plans UnitedHealthcare offers in each state. Go to uhcprovider.com >
Resources > Health Plans > Choose a Location > View Plans to review specific plans offered in that market.
UnitedHealthcare Provider Portal
This secure portal allows you to access patient information such as eligibility and benefit information and digital ID cards. You
can also perform administrative tasks such submitting prior authorization requests, checking claim status, submitting appeal
requests, and find copies of PRAs and letters in Document Library. Go to uhcprovider.com > Sign In.
To access the portal, you will need to create or sign in using a One Healthcare ID. To use
the portal:
• If you already have a One Healthcare ID (formerly known as Optum ID), simply go to
uhcprovider.com > Sign In to access the portal.
• If you need to set up an account on the portal, follow these steps to register.
You can learn more about the portal in Chapter 1 of this guide or by visiting uhcprovider.com/portal. You can also access self-
paced user guides for many of the tools and tasks available in the portal by visiting uhcprovider.com > Resources > Education
and training.
UnitedHealthcare Network News
Bookmark the Network News page on uhcprovider.com > Resources > News. It’s the home for updates across our commercial,
Medicare Advantage and Community Plan (Medicaid) health plans. You’ll find contractual and regulatory updates, process
changes and reminders, program launches and resources to help manage your practice and care for patients. This includes the
communication formerly known as the Network Bulletin.
Subscribe today to receive personalized Network News emails twice a month. They’ll
summarize the latest news, policy and reimbursement updates that we’ve posted on our
news webpage. These email briefs include:
• Monthly notification of policy and protocol updates, including medical and reimbursement
policy changes
• Announcements of new programs and changes in administrative procedures
You can tailor your subscription to help ensure that you only receive updates relevant to your
state, specialty and point of care.
160
2023 UnitedHealthcare Care Provider Administrative Guide
All Savers supplement
Applicability of this supplement
You are subject to both the main guide and this supplement. This supplement controls if it conflicts with information in the main
guide. If there are additional protocols, policies or procedures online, you will be directed to that location. Refer to the main
guide for anything not found in this supplement.
Employer groups who were previously sold under the name All Savers®Alternate Funding, are now sold under the new product
name UnitedHealthcare Level Funded. See the UnitedHealthcare Level Funded supplement for more information.
How to contact All Savers
Group Numbers: 908867, 908868, 921728
Resource Where to go Requirements and Notes
Cardiology
Diagnostic catheterization,
electrophysiology implants,
echocardiogram and stress
echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/
cardiology
Phone: 1-866-889-8054
Request prior authorization for
services as described in the
Outpatient cardiology notification/
prior authorization protocol
section of Chapter 7: Medical
management
Claims Submission Electronic Claims Submission:
Payer ID 81400
Genetic and Molecular Testing Online: uhcprovider.com/priorauth and
select the specialty you need.
Outpatient Injectable Chemotherapy
and Related Cancer Therapies
Online: uhcprovider.com/priorauth >
Oncology
Phone: 1-888-397-8129
Policies and instructions
Pharmacy Services Prior Authorizations Phone:
1-800-711-4555
Benefit Information:
Call the number on the back of the
member’s ID Card.
For information on the PDL,
myallsaversconnect.com
Prior Authorization and Notification Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth
(policies and instructions)
Phone: 1-800-999-3404
Prior authorization and notification
is required as described in Chapter
7: Medical management. EDI 278A
transactions are not available.

All Savers supplement
161
2023 UnitedHealthcare Care Provider Administrative Guide
Radiology/Advanced Outpatient
Imaging Procedures
CT scans, MRIs, MRAs, PET scans and
nuclear medicine studies, including
nuclear cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/radiology
Phone: 1-866-889-8054
Request prior authorization for
services as described in the
Outpatient radiology notification/
prior authorization protocol
section of Chapter 7: Medical
management
Health plan ID card
ASIC members receive health plan ID cards with information that helps you to submit claims. The cards list the claims address,
copayment information, and phone numbers.
A sample ID card and more information is in the Health plan identification (ID) cards section in Chapter 2: Provider
responsibilities and standards.
Our claims process
Follow these steps for fast payment:
1. Notify ASIC.
2. Prepare a complete and accurate claim form.
3. For ASIC members, submit claims using payer ID number 81400.
4. For contracted health care providers who submit electronic claims and would like to receive electronic payments and
statements, call Optum Financial Services Customer Service line at 1-877-620-6194 or visit optumbank.com > Partners >
Providers.
Claim reimbursement (adjustments)
If you think your claim was processed incorrectly, call the number on the ID card. If you find a claim where you were overpaid,
send us the overpayment within 30 calendar days. If we find a claim was overpaid, payment is due within 30 calendar days.
If you disagree with our decision regarding a claim adjustment, you may appeal.
Claim reconsideration, appeals and disputes
Claim reconsideration does not apply to some states based on applicable state legislation (e.g., Arizona, California, Colorado,
New Jersey or Texas). For states with applicable legislation, any request for dispute will follow the state specific process.
There is a 2-step process available for review of your concern. Step 1 is a Claim Reconsideration. If you disagree with the
outcome of the Claim Reconsideration, you may request a Claim Appeal (step 2).
How to submit your reconsideration or appeal
If you disagree with claim payment issues, overpayment recoveries, pharmacy, medical management disputes, contractual
issues or the outcome of your reconsideration review, send a letter requesting a review to:
ASIC members:
Grievance Administrator
P.O. Box 31265
Salt Lake City, UT 84131-0371
Standard fax: 1-801-478-5463
Phone: 1-800-291-2634

All Savers supplement
162
2023 UnitedHealthcare Care Provider Administrative Guide
If you feel the situation is urgent, request an expedited appeal by phone, fax or writing:
Grievance Administrator
2020 Innovation Dr.
DePere, WI 54115
Expedited Fax: 1-866-654-6323
Phone: 1-800-291-2634
Time frame
You must submit your claim reconsideration and/or appeal to us within 12 months (or as required by law or your Agreement),
from the date of the original EOB or denial. The 2-step process allows for a total of 12 months for timely submission, not 12
months for step 1 and 12 months for step 2.
What to submit
As the health care provider of service, you submit the dispute with the following information:
• Member’s name and health plan ID number
• Claim number
• Specific item in dispute
• Clear rationale/reason for contesting the determination and an explanation why the claim should be paid or approved
If you disagree with the outcome of the claim appeal, you may file for an arbitration proceeding. A description of this process is
in your Agreement.
Refer to Claim reconsideration and appeals process section in Chapter 10: Our claims process, for more information.
Notice to Texas health care providers
To verify ASIC members’ benefits, call the number on the back of the ID card.
ASIC uses tools developed by third parties, such as InterQual Care Guidelines, to help manage health benefits and to assist
clinicians in making informed decisions.
As an affiliate of UnitedHealthcare, ASIC may also use UnitedHealthcare’s medical policies as guidance. These policies are
available on uhcprovider.com/policies.
Notification does not guarantee coverage or payment (unless mandated by law). We determine the member’s eligibility. For
benefit or coverage information, call the phone number on the back of the ID card.
Michigan law regarding diabetes
Michigan law requires us to provide coverage for some diabetic expenses. It also requires us to establish and provide a
program to help prevent the onset of clinical diabetes. We have adopted the American Diabetes Association (ADA) Clinical
Practice Guidelines.
The program focuses on best practices to help prevent the onset of clinical diabetes and to treat diabetes, including, but not
limited to, diet, lifestyle, physical exercise and fitness, and early diagnosis and treatment. Find the Standards of Medical Care in
Diabetes and Clinical Practice Recommendations at care.diabetesjournals.org.
Subscription information for the American Diabetes Journals is available on the previous website or by calling 1-800-232-3472,
8:30 a.m.–8 p.m. ET, Monday–Friday. Journal articles are available without a subscription at the website previously listed.
163
2023 UnitedHealthcare Care Provider Administrative Guide
Surest supplement
Surest, a UnitedHealthcare company, offers fully-insured and self-funded health plans with an innovative and personalized
benefit design. Surest plans have neither deductibles nor coinsurance. Members, who have access to the UnitedHealthcare and
Optum networks, can check costs and care options in advance. In addition, some plans have a feature called flexible coverage.
This means—for a small set of plannable tests, procedures or treatments—the member must activate coverage at least three
business days in advance.
Applicability of this supplement
You are subject to both the main guide and this supplement. This supplement controls if it conflicts with information in the
main guide. If there are additional protocols, policies or procedures online, you will be directed to that location. Refer to the
Surest Provider Information Guide at uhcprovider.com/guides > Surest Administrative Guide for information not found in this
supplement.
Surest plan resources
Resources to help prepare for Surest members and claims.
Group numbers available at surest.com/provider-resources.
Resource Where to go Requirements and notes
UnitedHealthcare Shared Services
(UHSS) and uhcprovider.com portal
Online: uhcprovider.com
Phone: 1-844-368-6661
Information:
• surest.com/providers
• uhcprovider.com/surest
Real Time Eligibility (270/271):
25463 and/or Surest
Verify Surest member eligibility and
benefits with UHSS Provider Services.
Use subscriber IDs when prompted.
Claims submission Electronic claims submission
Payer ID: 25463
Paper claims submission
Mail to the address listed on the back
of the member’s ID card.
Send claims directly to Surest payer ID
25463. Always include the subscriber
ID and rendering address on the claim.
This confirms the copay/member
price. If not included, the copay/
member price may be incorrect from
what was originally quoted. One of
the most common billing errors is
easy to correct—inaccurate payer
ID or mailing address for paper
claims. Claims should be submitted
to Surest with the Surest payer ID,
not to UnitedHealthcare with the
UnitedHealthcare payer ID
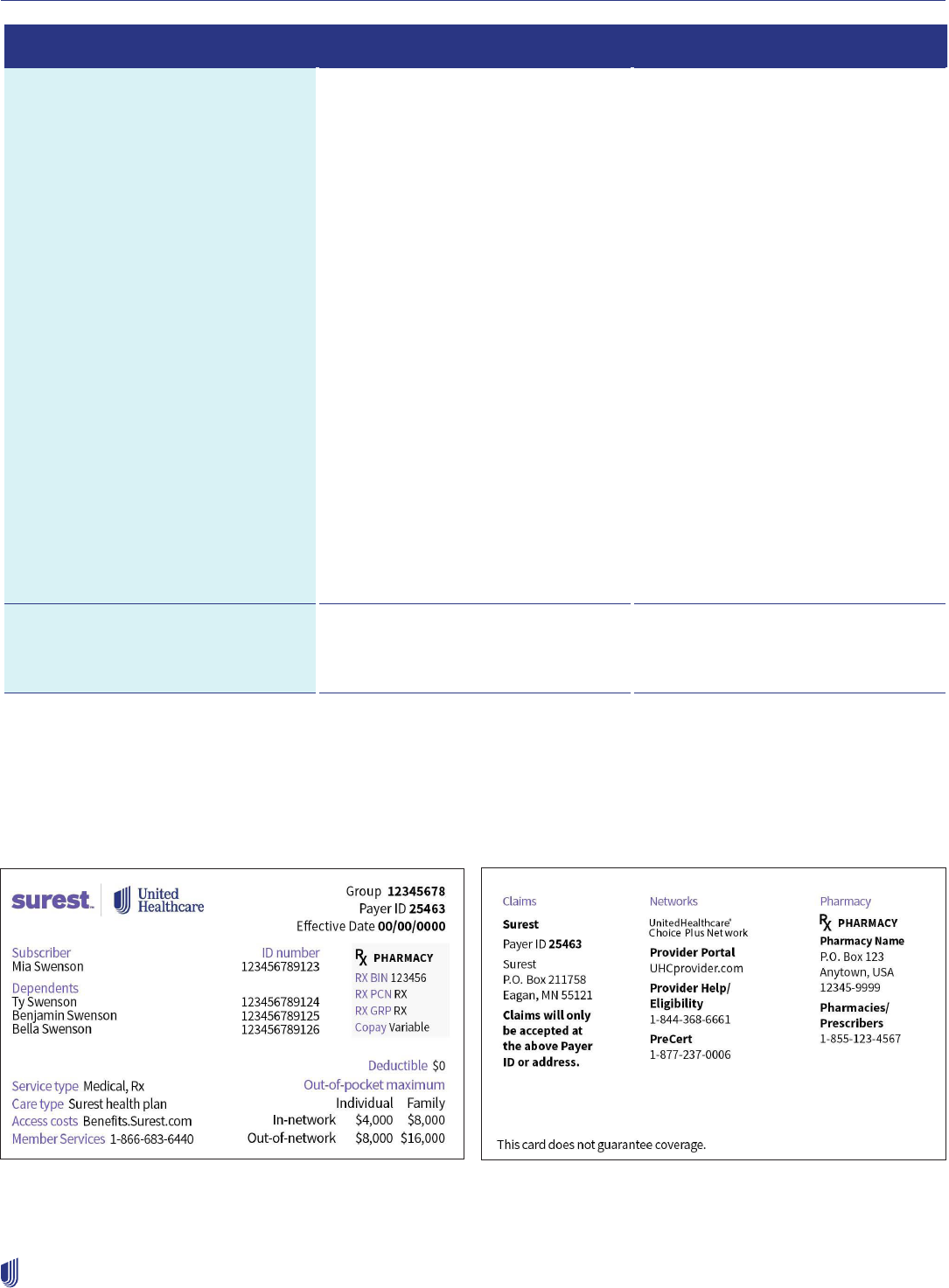
Surest supplement
164
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go Requirements and notes
Prior authorization and notification Online: uhcprovider.com/paan
Phone: 1-877-237-0006
Information:
• surest.com/providers
• uhcprovider.com/surest
Prior authorization and notification
is required as described in Chapter
7: Medical Management, except
for Flexible Coverages that must
be activated in advance. No prior
authorization is required for these
procedures.
We recommend that you submit
advance notification with supporting
documentation as soon as possible,
but at least 2 weeks before the
planned service (unless the Advance
Notification Requirements state
otherwise).
Just because a service does not
require prior authorization, it does not
mean that a service is covered. Please
contact UHSS Provider Services at
1-844-368-6661 to verify eligibility and
coverage. Learn more at uhcprovider.
com/guides > Surest Provider
Information Guide.
Claim status Online: uhcprovider.com
Phone: 1-844-368-6661
Please enter subscriber ID when
prompted. For dependents, you will still
enter subscriber ID.
Surest health plan ID card
Surest members receive health plan ID cards with information that helps you submit claims. The cards list the claims address,
provider portal information and phone numbers.

Surest supplement
165
2023 UnitedHealthcare Care Provider Administrative Guide
Our claims process
Follow these steps for fast payment:
1. Prepare a complete and accurate claim form according to UnitedHealthcare guidelines. Be sure to include subscriber ID and
accurate rendering address on all submissions.
2. For Surest plan members, submit electronic claims using payer ID 25463. Submit paper claims to the address listed on the
back of the member’s ID card.
3. For contracted health care providers who submit electronic claims and would like to receive electronic payments and
statements, call Optum Financial Services at 1-877-620-6194 or go to optumbank.com > Partners > Providers.
Claim reimbursement (adjustments)
If you think your claim was processed incorrectly, call UHSS Provider Services at 1-844-368-6661. If you find a claim where you
were overpaid, send us the overpayment within 30 calendar days. If we find a claim was overpaid, payment is due within 30
calendar days.
If you disagree with our decision regarding a claim adjustment, you may appeal.
How to submit your reconsideration or appeal
For claim reconsiderations (pricing or other), you can submit one of the following ways:
Mail: UHSS
Attn: Claims
P.O. Box 30783
Salt Lake City, UT 84130
Fax: 1-866-427-7703
Please remember to send to the attention of a person you have spoken to, if applicable.
For clinical appeals (prior authorization or other), you can submit one of the following ways:
Mail: UnitedHealthcare Appeals-UHSS
P.O. Box 400046
San Antonio, TX 78229
Fax: 1-888-615-6584
Phone: 1-800-808-4424 ext. 15227
You must submit all supporting materials to the appeal request, including member-specific treatment plans or clinical records.
Please note: Clinical appeals are only for services that received a medical necessity review and were determined to lack
medical necessity.
Still have questions?
Go to surest.com/providers for more information about Surest.
Additional resources
• Surest Provider Information Guide
• Surest self-paced educational course
• Surest provider survey

166
2023 UnitedHealthcare Care Provider Administrative Guide
Capitation and/or Delegation Supplement
This supplement is for capitated participating physicians, health care providers, facilities and ancillary providers as well as
delegated accountable care organizations (ACOs) for certain UnitedHealthcare products. It applies to all benefit plans for
members who:
1. Have been assigned to or have chosen a health care provider who receives a capitation payment from us for that member,
and
2. Are covered under an applicable benefit plan under UnitedHealthcare.
This supplement controls if it conflicts with the main guide. For protocols, policies and procedures not referenced in this
supplement, refer to the main guide.
What is Capitation?
Capitation is a payment arrangement for health care providers. If you have a capitation agreement with us, we pay you a set
amount for each member assigned to you per period of time. We pay you whether or not that person obtains care. In most
instances, a capitated health care provider is a medical group or an Independent Practice Association (IPA). Sometimes, the
capitated health care provider is an ancillary health care provider or hospital.
For this supplement, we use the term “medical group/IPA” interchangeably with “capitated health care providers” and
“Managed Care Risk Entity (MCRE).”
Also, capitated health care providers may be subject to the protocols, policies and procedures related to any or all delegated
activities. Refer to your Delegation Grids within the Agreements to determine which delegated activities, if any, you perform on
behalf of UnitedHealthcare.
What is Delegation?
Delegation is a process that gives another entity the authority to perform specific functions on our behalf. We may delegate:
1. Medical management.
2. Credentialing.
3. Claims.
4. Complex case management.
5. Other clinical and administrative functions.
When we delegate any of these responsibilities to you, you are a delegated health care provider. This is also called a “delegated
entity” or “delegate.” We are responsible to external regulatory agencies and other entities for the performance of the delegated
activities. To become a delegate, the provider/ACO must be in compliance with our established standards and best practices.
To remain a delegate, the provider/ACO must continue to comply with our standards and best practices. If the delegate is non-
compliant with our standards and best practices, we may revoke any or all delegated activities.
If you are associated with a delegated medical group, IPA, or other entity, use their office policies and protocols.
This supplement is intended for use by participating physicians, health care providers, facilities and ancillary providers who are
delegated for certain UnitedHealthcare activities. This supplement applies to all benefit plans for members whose:
1. Medical group, IPA or other health care provider performs any of the previous functions on behalf of UnitedHealthcare.
2. Health care provider is a member of an ACO, where the ACO performs any of the previous functions on behalf of
UnitedHealthcare.

Capitation and/or Delegation Supplement
167
2023 UnitedHealthcare Care Provider Administrative Guide
How to contact us
For phone numbers and websites related to specific products, refer to Online/interoperability resources and how to contact
us in Chapter 1: Introduction or in the appropriate supplement.
For specific product information, refer to the appropriate supplement.
Verifying eligibility and effective dates
For information on ways to verify eligibility, refer to Verifying eligibility, benefits and your network participation status in
Chapter 2: Provider responsibilities and standards. This helps ensure you:
• Submit the claim to the correct payer.
• Collect copayments.
• Determine if a referral, prior authorization or advance notification is required.
• Reduce denials for non-coverage.
We can provide you with daily and/or monthly member eligibility information using an electronic file. You must coordinate
initiation of electronic eligibility files with your software vendor and us. Advantages of receiving electronic eligibility are:
• Lower cost and effort required to maintain eligibility manually.
• Faster updates loaded into your system.
Refer to ASC X12 Technical Report Type 3/Companion Guides or ask your health care provider advocate for more
information.
Commercial eligibility, enrollment, transfers
and disenrollment
Members must meet all eligibility requirements established by the employer group and us. We may request proof of
eligibility requirements.
Enrollment
To enroll, an applicant must complete a UnitedHealthcare enrollment form or an employer enrollment form approved by us.
Some larger member accounts may provide open enrollment through electronic means rather than enrollment forms.
Newly eligible members may present a copy of the enrollment form as proof of eligibility. Make a copy of the enrollment form.
If unable to verify member eligibility online or through our voice response systems, follow up with member services the next
business day. The capitated medical group/IPA is responsible for making sure its contracted network of health care providers
accepts the enrollment form as temporary proof of eligibility.
Enrollment periods
Each employer group typically has an annual open enrollment period where current employees elect their health insurance
choices for the following benefit year. Jan. 1 is a commonly used benefit start date. However, many employers select different
dates throughout the year. Benefit plan codes change throughout the year on your eligibility reports.
Effective date
Coverage begins at 12:01 a.m. on the effective date.

Capitation and/or Delegation Supplement
168
2023 UnitedHealthcare Care Provider Administrative Guide
Selection of PCP or medical group/IPA
Members enrolled in some commercial benefit plans, such as HMO or Managed Care Organization (MCO) plans, must choose
a PCP. This process is outlined in the PCP Selection section in Chapter 3: Commercial products.
Newborn dependents coverage
Coverage of the subscriber’s newborn children begins at birth. The subscriber must submit an enrollment application to the
employer group or UnitedHealthcare, as applicable, within 30 calendar days from the date of birth to continue coverage, unless
the subscriber’s benefit plan says otherwise.
If the mother is the subscriber’s dependent, but not their spouse, domestic partner or common law spouse, we will not cover
any services provided to the newborn grandchild beginning upon delivery unless coverage is stated in the subscriber’s
benefit plan.
We do not cover medical or facility services for surrogate mothers who are not our members.
California Commercial: Eligible newborns have coverage for the first 30 days, beginning on their date of birth. If the newborn is
not enrolled as a dependent on the subscriber’s plan, the newborn has 30 days eligibility with the subscriber’s medical group/
IPA following birth. However, COB may be applied as determined by the birthday rule. (The “birthday rule” applies to dependent
children covered by parents who are not separated or divorced. The coverage of the parent whose birthday falls first in the
calendar year is the primary carrier for the dependent[s].)
Newborn enrollment policy
Unless the subscriber’s benefit plan dictates otherwise:
If the mother (subscriber, spouse or domestic partner) is our member, the newborn remains with the mother’s medical group/
IPA until another PCP or medical group/IPA is selected following the 15/30 rules.
When the father is primary for the newborn per the birthday rule, his plan covers the newborn for the first 30 days, even if the
newborn is not enrolled on his plan.
If both the mother’s and the father’s insurance plans provide coverage for the newborn, coordination of benefit rules apply once
the mother is discharged. The medical group/IPA must make sure they handle care coordination appropriately.
If both the mother and father of a dependent newborn are eligible under separate UnitedHealthcare benefit plans, we add the
dependent newborn to both plans as determined by the subscribers.
Any subsequent PCP or medical group/IPA transfer of a dependent newborn will follow the 15/30 rules.
Adopted dependents coverage
Coverage begins on the first day of physical custody if the subscriber submits an enrollment application to the employer group
within 30 calendar days of physical custody of the child, unless the subscriber’s benefit plan dictates otherwise.
Surrogate (newborn coverage)
We may provide coverage for a surrogate when the surrogate is the subscriber or eligible dependent. Refer to the
UnitedHealthcare benefit plan. However, the newborn dependent(s) may not have coverage at birth. Surrogate cases need
individual review. We make decisions on a case-by-case basis. We may issue newborn coverage denials to the facility before the
newborn’s birth. Contact your Provider Relations representative if a surrogate case comes to your attention.
California: Under California rescission rules, if UnitedHealthcare or the member’s health care provider or medical group/
IPA authorizes surrogate newborn care (beyond 30 days from birth), and the facility relies upon such authorization to render
treatment, those claims must be paid.
We may seek recovery of our actual costs from a member receiving reimbursement for medical expenses for maternity services
while acting as a surrogate.

Capitation and/or Delegation Supplement
169
2023 UnitedHealthcare Care Provider Administrative Guide
Member transfers
A member may select a new medical group/IPA or PCP by calling Member Service or accessing myuhc.com.
Members may change their PCP within the same medical group/IPA. The change is effective the first day of the following month
after the member calls requesting the change, unless the benefit plan says otherwise.
If a member requests a transfer out of the member’s medical group/IPA entirely, and the change request is received prior to or
on the 15th of the month, we will change the member’s medical group/IPA effective the first day of the following month. If the
request to transfer to another medical group/IPA is received after the 15th of the month, the change is effective the first day of
the second month following receipt of the request.
If the member expresses dissatisfaction with the proposed effective date, we, in our discretion, may process the member’s
request as a “Forward Primary Care Provider Change Request,” (if our contract with requested network provider allows for a
“retroactive” transfer). Based on the contract, you may have the right to refuse to accept the member until the first day of the
second month following the request receipt. Some health care provider groups may only accept new members during an open
enrollment period. If the member meets all eligibility requirements, the change becomes effective the first day of the following
month, even though the change request was received after the 15th of the month. If the 15th of the month falls on a weekend or
holiday, we will allow transfer requests received on the first business day after the 15th to become effective the first day of the
following month.
Transfers from one participating medical group/IPA to another, or PCP transfers initiated outside a member’s open enrollment
period, will not be effective until the first day of the month following the member’s discharge from care, if at the time of the
request for transfer or on the effective date of transfer, the member is currently:
• Receiving inpatient care at an acute care facility.
• Receiving inpatient care at a skilled nursing facility (SNF), at a skilled level.
• Receiving other acute institutional care.
• In the third trimester of her pregnancy (defined as when the member reaches the 27th week of pregnancy).
• Experiencing a high-risk pregnancy (not applicable to California members).
Retroactive member transfers
Members may retroactively change their medical group/IPA or PCP within the same month if the member calls to request a
change within 30 calendar days:
• Of their effective date and has not received services with the originally assigned health care provider.
• Due to a household move over 30 miles, and the member has not received services with the originally assigned health care
provider.
If the member received services during the current month from you, other than the month requested, a current month change is
not permitted.
Transfer due to termination of medical group/IPA, facility or health care provider
If the member’s medical group/IPA, PCP, or facility is terminated, we give prior written notice to members as applicable or when
required by state or federal law. In such event, the member may qualify for continuation of care as outlined in the Continuity
of care section of this supplement or the main guide under the CAA requirements. For individual physician terminations, the
medical group/IPA is responsible for providing the notice to commercial members in the following circumstances:
• PCP terminations in medical groups/IPAs where medical group/IPA assigns members to the PCPs
• All specialist terminations
Each commercial member has at least 30 calendar days (exception: 60 calendar days in California) to select another medical
group, IPA, PCP or facility.
When a member needs care, and their PCP terminated without proper notice, we transfer the member to another PCP. The new
PCP will be in the same medical group/IPA with an effective date retroactive to the first of the current month.

Capitation and/or Delegation Supplement
170
2023 UnitedHealthcare Care Provider Administrative Guide
Member removal
The medical group/IPA agrees we may move a medically stable member to another medical group/IPA or health care provider
due to a strained relationship between the medical group/IPA and member.
Commercial members
When commercial members refuse treatment or prevent you from delivering care, the medical group/IPA may consider the
health care provider-member relationship as unworkable. In these cases, the medical group/IPA may believe they need to
dismiss the member from their panel.
The medical group/IPA may request a member change medical groups/IPAs in these cases. We evaluate requests based
on the interest of the member and accessibility of another medical group/IPA. If we approve the transfer request, we ask the
member to choose another medical group/IPA within 30 calendar days. The primary medical group/IPA is responsible for
directing and managing all care until the change or transfer is effective.
If the member does not select another medical group/IPA, we select another medical group/IPA for them.
If no professionally acceptable alternatives exist, neither UnitedHealthcare nor the medical group/IPA are responsible to provide
or arrange for the medical care or pay for the condition under treatment.
Areas of concern for requesting removal of a commercial member from the medical group/IPA include:
• Repeated disruptive behavior or dangerous behavior exhibited in the course of seeking/receiving care.
• Failure to pay required copayments (minimum dollar amount of $200 outstanding).
• Fraudulently applying for any UnitedHealthcare benefits.
Once you send us a completed Incident Report for Removal of Members and related documentation, we respond to the
member. We copy the PCP or medical group/IPA on all correspondence.
If you receive notification of a member’s intent to sue, tell your health care provider advocate.
Send copies of all notification letters, request for removal and supporting documentation to your health care provider advocate.
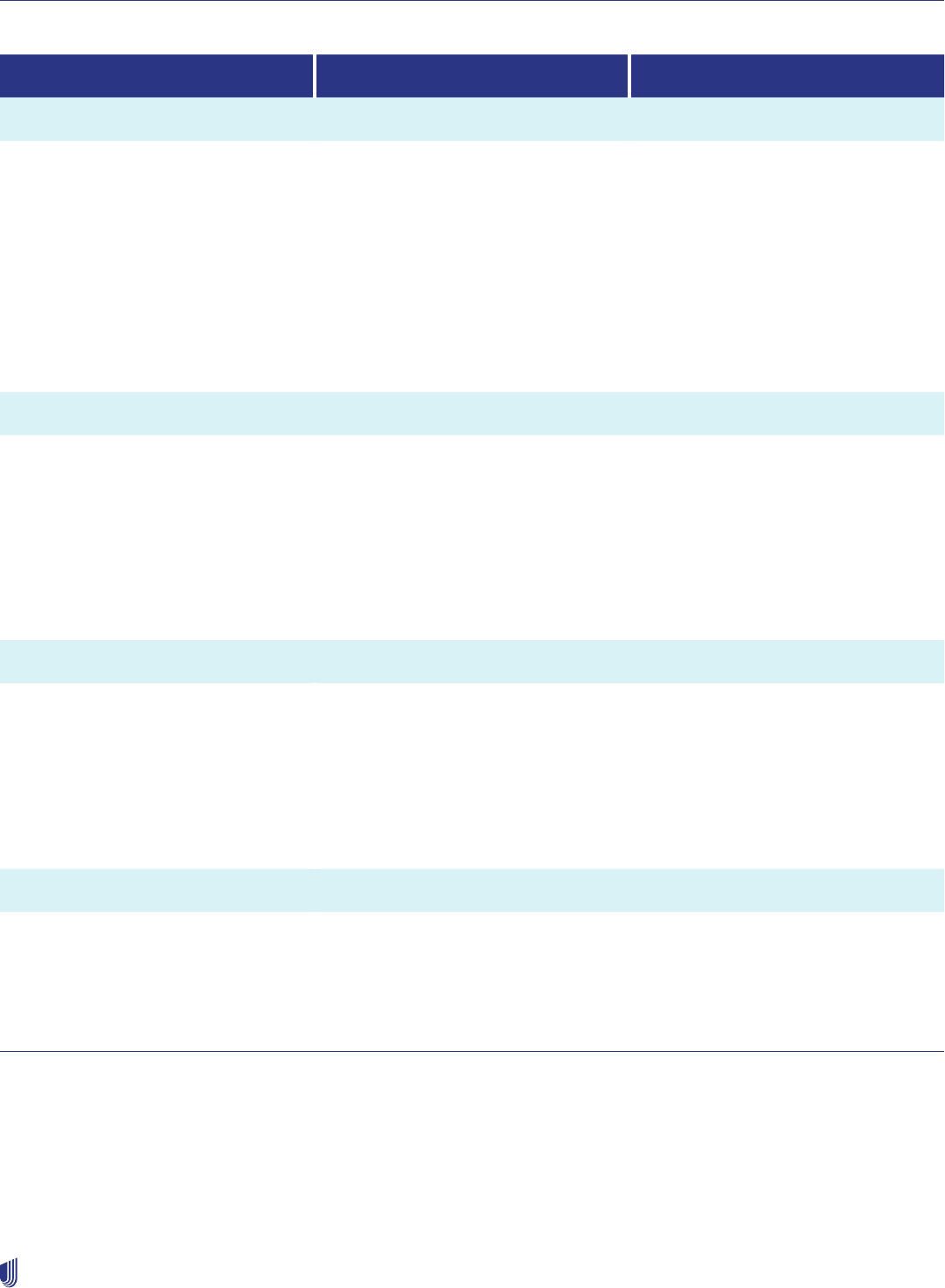
Capitation and/or Delegation Supplement
171
2023 UnitedHealthcare Care Provider Administrative Guide
Criteria and procedure for removal of commercial members from the medical group/IPA
Level I Level II Level III
Criteria
Demanding a payment from medical
group/IPA for non-authorized services
Minor disruptive behavior*
Failure to pay required copayments**
3 or more missed appointments within
6 consecutive months without 24-hour
prior notice
Refusal to follow recommended
treatment or procedures by health care
provider resulting in deterioration of
member’s medical condition.
Disruptive behavior, verbal threats of
bodily harm toward medical group/
IPA personnel and/or other members,
provided the conduct is not a direct
result of the member’s medical
condition or prescribed medication.+
Member fraudulently applies for any
UnitedHealthcare benefits.
Dangerous behaviors exhibited in
the course of seeking or receiving
care provided the conduct is not a
direct result of the member’s medical
condition or prescribed medication.
Need an eyewitness willing to formally
document the incident in writing. For
example: law enforcement involvement,
police report.
First occurrence:
Medical group/IPA must counsel with
and send the member a certified letter
saying such behavior is unacceptable.
Discussions need documentation.
Send copies to UnitedHealthcare,
which sends a warning letter outlining
behavior and possible consequences.
Medical group/IPA must counsel with
and send the member a certified letter
saying such behavior is unacceptable.
Discussions need documentation.
Send copies to UnitedHealthcare,
which will send warning letter outlining
behavior and possible consequences.
Medical group/IPA requests immediate
removal of subscriber/member from
medical group/IPA. Incident must
be, formally documented by medical
group/IPA.
Send written notification to member
in a certified letter. Mail copies of
documentation and member letter to
UnitedHealthcare for review.
Second occurrence:
Medical group/IPA must counsel with
and send second letter to member
expressing concern regarding their
unacceptable behavior.
Send copies to UnitedHealthcare,
which sends warning letter outlining
continued behavior and possible
consequences.
Send UnitedHealthcare a request to immediately remove subscriber/member
from the medical group/IPA. UnitedHealthcare reviews the medical group/IPA
documentation outlining continued unacceptable behavior.
Third occurrence:
Send us a request to immediately
remove a subscriber/member from
the medical group/IPA. We review the
medical group/IPA documentation,
which outlines continued unacceptable
behavior.
* Minor disruptive behavior: Unruly behavior, use of abusive and/or profane language directed toward medical group/IPA and/or other members.
** UnitedHealthcare West will not consider the removal of a member unless the unpaid copayment balance exceeds $200.00.
+ Disruptive behavior: Physical or verbal threat of bodily harm toward medical group/IPA personnel and/or other members or property, and/or use of unacceptable behavior relative to drug and/or alcohol misuse.
# Dangerous behavior such as attempted physical abuse, display of weapon or damage to property, use of unacceptable behavior relative to drug and/or alcohol misuse, and/or chronic demands for
unreasonable services.

Capitation and/or Delegation Supplement
172
2023 UnitedHealthcare Care Provider Administrative Guide
Notification of platform transitions or migrations
A delegated entity agrees to provide at least 270 days advance written notice to UnitedHealthcare and its contract administrator
or health care provider advocate of its intent to:
1. Change administrative platforms for impacted delegated functions or upgrade current platform, including migrations
or versions.
2. Make material changes in existing administrative platforms impacting delegated functions.
If you are unsure of what a material change is, contact your delegation oversight representative. Most changes will require pre-
cutover evaluation by UnitedHealthcare delegation oversight team(s) and integrated testing with UnitedHealthcare. Failure to
adhere to these notification requirements may result in financial penalties or loss of delegation responsibilities.
Medicare Advantage (MA) enrollment, eligibility and
transfers, and disenrollment
For more information and instructions for confirming eligibility refer to Verifying eligibility and effective dates.
Eligibility lists
Eligibility reports are available electronically. We send them to the capitated health care provider through a file transfer protocol.
You may view them on uhcprovider.com. We provide full eligibility file information once per month consisting of all active
members for the month at the time the file was run. We also provide daily or weekly update files that include member change
transactions for prior and future periods, upon request. Weekly update files are the preferred frequency by most groups.
Upon request, we send each medical group/IPA a monthly eligibility list of all its assigned members. This list contains the
members’ identification information, their enrollment date, and benefit plan information. This includes benefit plan type and
effective date and any member cost-sharing.
Eligibility (MA)
Medicare beneficiaries who join an MA plan must:
• Be entitled to Medicare Part A and enrolled in Medicare Part B.
• Reside in our MA service area. To maintain permanent residence, the beneficiary must not continuously reside outside the
applicable service area for more than 6 months (9 months if using the UnitedHealth Passport® benefit).
MA plans include a Contract ID, Plan ID (the plan benefit package, or PBP) and Segment ID from CMS that corresponds to CMS
filings. This will be on the individual member ID card or eligibility file.
You may identify a capitation/delegation plan or member by referring to the member ID card.
Change of membership status (MA)
If a Medicare beneficiary is an inpatient at these facilities when their membership becomes effective, the previous carrier pays
for Part A services (inpatient facility care) until the day after the member is discharged to a lower level of care:
• Acute facility
• Psychiatric facility
• Long–term care (LTC) facility
• Rehabilitation facility
The member’s assigned medical group/IPA pays for Part B services (medical care) on their membership effective date. If a
member’s coverage terminates while the member is an inpatient at any of these facilities, the medical group/IPA is no longer
financially responsible for Part B (medical care) services. If the facility is a capitated health care provider, a ‘capitated facility’,
the facility remains financially responsible for Part A (inpatient facility care) services until the day after the member’s discharge
to a lower level of care (e.g., home health). If the member is an inpatient at a SNF at the time of their effective date, the medical
group/IPA and capitated facility is financially responsible for Part A and Part B services on the member’s effective date.

Capitation and/or Delegation Supplement
173
2023 UnitedHealthcare Care Provider Administrative Guide
Refer to the UnitedHealthcare MA Coverage Summary titled Change in Membership Status while Hospitalized (Acute, LTC
and SNF) or Receiving Home Health on uhcprovider.com/policies > Medicare Advantage Policies > Coverage Summaries for
Medicare Advantage Plans.
Benefit plan changes
A benefit plan change occurs when the member:
• Moves from one service area to another. If an MA member permanently moves outside of the service area (regardless of
state), or the plan receives indication that the member may have moved outside the service area, the plan will disenroll the
member at:
1. The end of the month in which they report/confirm the move.
2. The end of the month in which they move (if they report the move in advance).
– If a member fails to respond to an address confirmation request, the plan will disenroll the member at the end of the
sixth month following notification of potential move from the service area. See Chapter 2, sections 50.2-50.2.1.5 in the
CMS Medicare Managed Care Manual for more information.
• Changes from one benefit plan to another. If the member does not return a completed form, they remain on the existing plan.
The member may only change benefit plans using their CMS-defined annual enrollment period from Oct. 15–Dec. 7, or during
the open enrollment period from Jan. 1–March 31 each year.
– If the member has exhausted these elections and does not qualify for a Special Election Period, they are locked in the
current benefit plan for the remainder of the calendar year.
CMS requires us to treat a member whose benefit plan changes as a new member, rather than as an existing member, for the
purpose of determining the new plan’s effective date. Therefore, the member’s enrollment to another PCP or medical group/IPA
is effective the first of the month following receipt of the completed form.
Enrollment
An applicant must enroll in a UnitedHealthcare MA plan. Completing an enrollment form does not ensure enrollment in a
Medicare Advantage (MA) prescription drug plan. Enrollment may be denied for either the UnitedHealthcare MA plan and/or the
MA prescription drug plan if eligibility requirements are not met. See Chapter 2, section 20 of the CMS Medicare Managed
Care Manual or Chapter 3, section 20 of the CMS Prescription Drug Benefit Manual for eligibility information.
Enrollment periods
Individual
CMS has specific enrollment periods during which individual plan members may enroll in a health plan, change to another
health plan, change benefit plans, or return to Medicare. Details on the types of enrollment periods and the requirements of
each type are outlined on cms.hhs.gov.
Group retiree plans
Enrollment periods for UnitedHealthcare Group MA members are dictated by the employer group’s annual renewal date with us.
Employers may establish their own enrollment dates. See Chapter 2, section 30.4.4, item 1 - SEPs for Exceptional Conditions
in the CMS Medicare Managed Care Manual for more information. A group retiree annual enrollment period aligns with the
employer’s annual enrollment cycle.
Selection of PCP or medical group/IPA
For most plans, the member must select a PCP or medical group/IPA as outlined in Chapter 5: Medicare products, Medicare
Product Overview Tables.

Capitation and/or Delegation Supplement
174
2023 UnitedHealthcare Care Provider Administrative Guide
Transfer of members (MA)
According to CMS guidelines, a member may not change medical groups/IPAs or PCPs if:
• The member is an inpatient in a facility, a SNF or other medical institution at the time of the transfer request.
• The change may have an adverse effect on the quality of the member’s health care.
• The member is an organ transplant candidate.
• The member has an unstable, acute medical condition for which they are receiving active medical care.
In the following instances, a member may request a medical group/IPA or PCP change, outside the 15/30 rule, that will be
effective the first of the following month:
• The member calls to request a change within 30 calendar days of the effective date with UnitedHealthcare due to the wrong
medical group/IPA or PCP being assigned.
• The member calls to request a change within 30 calendar days of the effective date with UnitedHealthcare and has not
received services with the originally assigned health care provider.
• The member calls to request a change within 30 calendar days due to a household move over 30 miles, and the member has
not received services with the originally assigned health care provider.
If a member changes their medical group/IPA or PCP while an inpatient at any of the following facilities, the capitated entity at
risk for Part A services at the time of the admission will retain financial risk until discharge to home or another care setting:
• Acute care facility
• Critical access facility
• LTC facility
• Psychiatric facility
• Inpatient rehabilitation facility
Financial responsibility for Part B services will be the responsibility of the new medical group/IPA or PCP on the effective date
of the transfer.
For more information about ambulance transfers due to a medical group/IPA change while the member is an inpatient, go to
uhcprovider.com/policies > For Medicare Advantage Plans > Coverage Summaries for Medicare Advantage Plans.
Transfer due to termination of medical group/IPA, facility or health care provider
If the member’s medical group/IPA, PCP, or facility is terminated, we give prior written notice to members as applicable or when
required by state or federal law. In such event, the member may qualify for continuation of care as outlined in the Continuity of
care section of this supplement. For individual physician terminations, the medical group/IPA is responsible for providing the
notice in the following circumstances:
• PCP terminations in medical groups where the medical group assigns members to the PCPs
• All specialist terminations
Each Medicare member has at least 14 calendar days to select another medical group/IPA, PCP, or facility within the member’s
current medical group/IPA. The member receives a new member ID card prior to the first of the month in which the transfer is
effective.
When a member needs care, and their PCP terminated without proper notice, we transfer the member to another PCP. The new
PCP will be in the same medical group/IPA with an effective date retroactive to the first of the current month.
Member removal (MA)
For information on PCPs removing MA members from rosters, refer to Member dismissals initiated by a PCP (Medicare
Advantage) in Chapter 2: Provider responsibilities and standards. The medical group/IPA is responsible for directing and
managing all care until the change or transfer is effective.

Capitation and/or Delegation Supplement
175
2023 UnitedHealthcare Care Provider Administrative Guide
Disenrollments
Member-elected disenrollment
If a member requests disenrollment from our benefit plan through you, refer them to Member Services. Once we process the
disenrollment, we send the member a letter with the effective date. If the member submits a request for disenrollment during
the month, the disenrollment is effective the first day of the following month.
Authorization guarantee (CA Commercial only)
Authorization guarantee procedure
Authorization guarantee procedure limits the medical group’s/IPA’s risk of incurring financial risk for services provided
to ineligible members where the individual’s lack of eligibility is only determined after services are provided. It offers
reimbursement to the medical group/IPA providing covered services to a member who:
1. We identified as eligible before the date of service through our eligibility determination and verification processes and is
later determined to be ineligible for benefits on the date of service.
2. We provided an authorization to whom we confirmed as eligible prior to the date of service but later determined to have
been ineligible on the date of service (“authorization guarantee”).
Authorization guarantee billing procedures
Medical group/IPA provides or arranges for health care services for an eligible member through our eligibility determination
and verification processes. If authorization is provided, and the individual was not a member when the health care services were
provided, medical group/IPA may seek reimbursement for such services.
The medical group/IPA must submit the following information to our health care provider dispute team for reimbursement
consideration. Their address is in the UnitedHealthcare West Bulk Claims Rework Reference Table. Include:
• Cover sheet.
• Copy of authorization and the itemized bill for services rendered.
• A record of any payment received from any other responsible payer.
• Amount due based on medical group’s/IPA’s cost of care rate, less any payment received from any other responsible payer.
Authorization guarantee reimbursement
The medical group/IPA must follow the authorization guarantee billing procedures. Eligible services must be reimbursed within
45 business days of receipt of information. Reimbursement should be at the cost of care rates listed in the contract, no greater
than the full uncollected balance. The medical group/IPA must reimburse the health care provider.
Health care provider responsibilities
Demographic updates
To help ensure we have your most current directory information, submit any changes to:
For Delegated Health Care Providers: Submit monthly provider roster changes or additions to your local network account
manager or health care provider advocate.
For Non-Delegated Health Care Providers: Visit uhcprovider.com > Our network > Find a provider for the Provider
Demographic Change Submission Form and further instructions.
For delegated MA health care providers, if you expect any significant changes to your network, notify your health care provider
advocate of changes per your agreement. Additionally, please notify your health care provider advocate prior to the third quarter
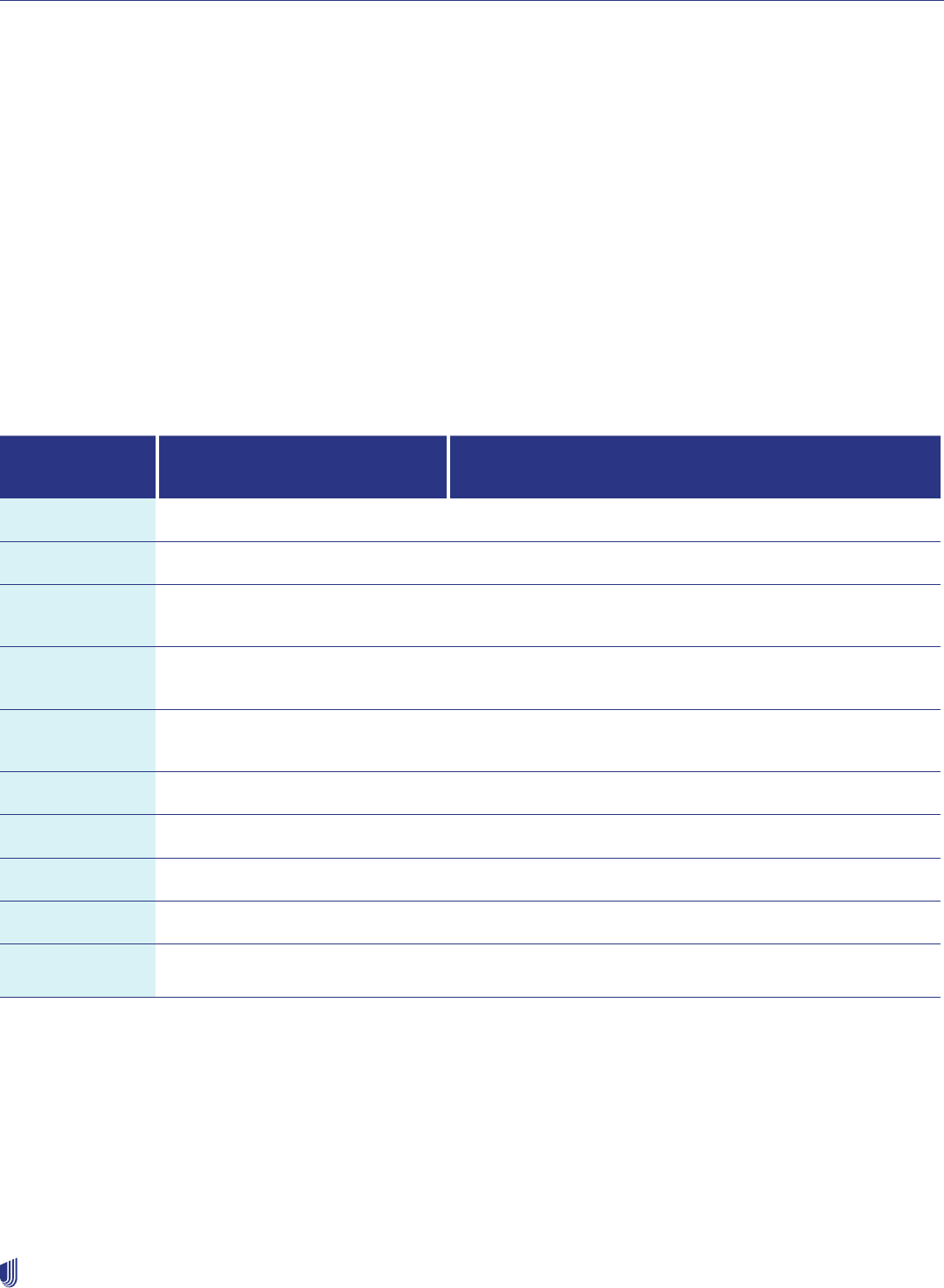
Capitation and/or Delegation Supplement
176
2023 UnitedHealthcare Care Provider Administrative Guide
of the calendar year. This helps our members select the correct health care provider during the annual enrollment period from
October–December. It also reduces health care provider directory errors.
Electronic Data Interchange (EDI)
EDI is our preferred choice for conducting business transactions with health care providers and health care industry partners.
We accept EDI claims submission for all our product lines. Find information and help with EDI on uhcprovider.com/edi. Also
see the EDI section of Chapter 2: Provider responsibilities, which includes information about ASC X12 Technical Report Type
3 publications, companion guides, and a list of standardized HIPAA-compliant EDI transactions.
ASC X12 technical report type 3/companion guides
The ASC X12 Technical Report Type 3 (TR 3 also known as HIPAA Implementation Guides) publications are the authoritative
source for EDI Transactions. You may purchase the ASC X12 Technical Report Type 3 publications from Washington Publishing
at wpc-edi.com.
We developed guides to provide transaction specific information we require for successful EDI submissions. These companion
guides are available at uhcprovider.com/edi.
The following table includes standardized HIPAA-compliant EDI transactions available at UnitedHealthcare:
ANSI ASC X12N*
Transactions
HIPAA EDI Transactions Acceptable
UnitedHealthcare Versions
Available at UnitedHealthcare Transaction Descriptions
270/271 005010X279A1 Eligibility Benefits Inquiry and Response (Real Time and Batch)
276/277 005010X212 Claim Status Inquiry and Response (Real Time and Batch)
278 005010X278
Health Care Services Review - Request for Review and
Response (Real Time and Batch)
278 005010X216
Health Care Services Review - Notification and
Acknowledgment (Real Time and Batch)
278 005010X215
Health Care Services Review - Inquiry and Response (Real
Time and Batch)
820 005010X218 Premium Payment
834 005010X220A1 Benefit Enrollment and Maintenance
835 005010X221A1 Claims Payment and Remittance Advice
837 005010X222A1 Healthcare Claim/Encounter Professional
837 005010X223A2 Healthcare Claim/Encounter Institutional
Changes in capacity
The medical group/IPA must provide us with at least 90 calendar days written notice prior to any changes to the medical group/
IPA or network providers. Include the following in the notice:
• Inability of medical group/IPA to properly serve more members due to lack of PCPs
• Closing or opening the PCP’s practice to more members
• Closure of any office or facility the medical group/IPA, PCPs or other network provider and health care professional uses
The medical group/IPA, its health care providers and other licensed independent health care professionals must continue to
accept members during the 90-day notice. For purposes of this section, a new member may be a member who has switched
Capitation and/or Delegation Supplement
177
2023 UnitedHealthcare Care Provider Administrative Guide
health plans and/or coverage plans. This includes a member who switches from a Fee-For-Service (FFS) plan to a Commercial
HMO/MCO plan.
California requirements for capacity reporting
We require capitated health care providers to give us updates within 5 business
days if capacity changes affect your ability to accept new members. If we receive
notification your information is inaccurate, you will be subject to corrective action.
Privacy
You must make reasonable efforts to limit Protected Health Information (PHI) as defined under the Health Insurance Portability
and Accountability Act (HIPAA) Privacy Rule to the minimum necessary when using or disclosing PHI. The minimum necessary
standard should not affect treatment, payment or health care operations (TPO). The Privacy Rule requires written member
authorization for uses and disclosure that fall outside of the TPO.
Member Communication Scope
The Managed Care Risk Entity (MCRE) is responsible for member communication that pertains to care providers.
UnitedHealthcare retains the responsibility to provide timely and efficient member communication surrounding Explanations of
Benefits (EOBs) and other product and plan-based communications.
Non-discrimination
You must not discriminate against any patient with regard to quality of service or accessibility of services because they are our
member. You must not discriminate against any patient on the basis of any of the following:
• Race
• Gender identity
• Ethnicity
• National origin
• Religion
• Sex and gender
• Age
• Mental or physical disability or medical condition
• Sexual orientation
• Claims experience
• Medical history
• Evidence of insurability
• Disability
• Genetic information
• Source of payment
• Medicaid status for Medicare members
You must maintain policies and procedures to demonstrate you do not discriminate in the delivery of service and accept for
treatment any members in need of your service.
Inclusion of notice of availability of language assistance in non-standard vital documents
issued by delegated health care provider groups (CA commercial members only)
The delegated health care provider group must include the California Department of Managed Health Care’s (DMHC) approved
Notice of Availability of Language Assistance with each vital document containing member-specific information issued to
UnitedHealthcare’s Language Assistance Program (LAP) members. The notice must be included in UnitedHealthcare’s
threshold languages (English, Spanish and Chinese). Vital documents include UM modification, delay, or denial letters issued
to our members by the delegated health care provider group. We review compliance with this requirement during the annual
assessment of delegated medical management.
UnitedHealthcare worked with Industry Collaborative Effort (ICE) to standardize the inclusion of the required notice.
Contact your UnitedHealthcare clinical delegation oversight consultant for current UnitedHealthcare letter templates.
Hospital Incentive Program (HIP) professional capitation
In a professional capitation agreement, the medical group/IPA receives capitation for medical services. We pay selected
facility services out of the HIP. The HIP provides an incentive for the medical group/IPA to use facility services such as
inpatient activity, in-area emergency services and other selected outpatient services provided to our members efficiently. The

Capitation and/or Delegation Supplement
178
2023 UnitedHealthcare Care Provider Administrative Guide
HIP calculates overages and deficits based on an annual comparison of accumulated actual costs based on the terms of the
UnitedHealthcare medical group/IPA Agreement.
This section provides general information for a professional capitation arrangement on the following:
• How are HIP results calculated?
• What services are included in the HIP?
• What information is available to assess HIP performance?
Budget (CA only)
The Integrated Healthcare Association (IHA) P4P Value-Based Incentive Program for commercial members is not a component
of your Agreement. It is under a separate letter of agreement.
The budget for the Medicare Advantage Hospital Incentive Program (MAHIP) for Medicare members is based on a percent of
premium, less the reinsurance premium. Aside from the budget, all other aspects of the HIP apply to the MAHIP.
Reinsurance
Reinsurance is required to protect the HIP budget and medical group/IPA against catastrophic cases.
Actual costs
The Division of Financial Responsibility (DOFR) section of the Agreement defines the services that are included to make up the
HIP costs. The HIP costs typically include the following:
• Inpatient costs for facility services rendered to our members by network providers valued at the actual costs we incur
• Other facility services given to our members by network providers other than inpatient services, valued at actual costs we
incur
• The actual amount paid for facility services, which are rendered by non-network care providers
• A percentage of all facility services incurred during the period but not yet processed (for the interim calculation), minus:
– Reinsurance recoveries
– Third-party recoveries received during calculation
Monitoring performance
We monitor the medical group/IPA financial performance through:
• Records of authorized services.
• Claims paid/denied reports.
• HIP financial report for the settlement period. The report details:
– Total number of member months.
– Total budget allocation for the member months.
– Total expenses paid during the period.
– A description of each amount of expense allocated to the risk arrangement by member ID number, date of service,
description of service by claim codes, net payment, and date of payment.
– Risk determination accuracy as identified through review of issue resolution data of risk disputes and risk reconsiderations.
Settlement calculations
We perform interim settlements, the final settlement and reconciliation of the HIP.
We provide a quarterly incentive program report to the medical group/IPA within 45 calendar days of the close of each calendar
quarter. The incentive program report contains the monitored information.

Capitation and/or Delegation Supplement
179
2023 UnitedHealthcare Care Provider Administrative Guide
Split capitation
In a split capitation Agreement, the medical group/IPA receives capitation for the provision of medical services. The facility
receives capitation for facility services and selected outpatient services. The medical group/IPA and facility may create and
administer their own facility incentive program under a split capitation Agreement.
Monthly reporting
We either post online or distribute to each medical group/IPA, a monthly-shared risk claims report. It lists the actual costs
incurred and denied during the previous month for services included in the HIP. Review this report each month to make sure the
claims were processed and/or paid correctly.
The following tools will help the medical group/IPA analyze the Shared Risk Claims Report:
• Claims Code Sheet
• Place of Service Mapping
– This document cross-references the CMS place of service codes to UnitedHealthcare’s internal place of service codes.
Discrepancy report
Use the Discrepancy Report to request research of the payment or denial of a claim we processed. After reviewing the Monthly
Shared Risk Claims Report, complete all fields in the Discrepancy report. Submit it electronically to our Network Management
department. If all required fields are not completed, we return the files to the medical group/IPA. The required fields include:
• Member ID number (7-digit number).
• Member ID number suffix (2 digits).
• Claim number.
• Expected health care provider reimbursement.
• Health care provider comments — why the medical group/IPA is disputing the payment.
Discrepancy report timely filing
The medical group/IPA must submit discrepancy reports monthly. We do not pursue recoveries of overpayments you submit
late based on your Agreement with us or by state law.
We reserve the right to deny/reject any request for review submitted beyond the timely filing limit.
Individual stop loss and reinsurance programs (stop loss protection)
Individual Stop Loss (ISL)/Reinsurance (REI) limits the medical group’s/IPA’s/facility’s financial risk for medical and facility
services beyond a specified dollar amount per member, per calendar year. This program applies to services for which we
capitated the medical group/IPA/facility.
The ISL program is updated annually. Each medical group/IPA/facility may take part each year.
The medical group/IPA may purchase ISL/reinsurance from us or an outside carrier.
We determine our premium for ISL based on our experience. We convert the calculated premium for stop loss to either a
percentage of premium or flat per member per month (PMPM) rate based on the medical group’s/IPA’s Agreement. Every
month, we subtract the result from the total capitation.
We reimburse a medical group/IPA that purchases ISL through us for services that exceed the ISL deductible at the ISL
program rates specified in the Agreement or the ISL election letter for the applicable contract year, minus the medical group’s
ISL coinsurance amount.
We reimburse a facility that purchases reinsurance through us for services that exceed the reinsurance deductible at the
reinsurance program rates specified in the Agreement or the reinsurance election letter for the applicable contract year, less the
facility’s reinsurance coinsurance. The facility must identify all reinsurance claims before submission. The facility reinsurance
program is updated annually.

Capitation and/or Delegation Supplement
180
2023 UnitedHealthcare Care Provider Administrative Guide
The medical group/IPA or facility may elect to opt out of the UnitedHealthcare ISL/reinsurance program by purchasing ISL/
reinsurance coverage through a third-party insurance carrier. Such coverage must be through an entity we approve of and in the
amounts required by UnitedHealthcare and state and federal law. Refer to your Agreement for details.
Notification of ISL/reinsurance claims
The medical group/IPA or facility provides written notification to us when services for a member equal 50% of the ISL/
reinsurance deductible. The written notification submission needs to be to us no later than the 15th day of the month following
the month in which the claim amounts reach the 50% threshold.
ISL/reinsurance claims submission procedure
Submit all ISL/reinsurance claims having met the ISL/reinsurance deductible to us annually but no later than 90 calendar days
after the end of the calendar year.
To receive reimbursement under the ISL/reinsurance program, follow these steps:
• Submit the ISL/reinsurance claims by spreadsheet to [email protected]. Scan and email all hard-copy images.
Include these on the submission spreadsheet:
– Service health care provider name
– Date of service
– Service description
– Correct RBRVS or CPT codes and description of services if required
– Billed charges
– Place of service
– Medical group/IPA paid amount
– Other insurance information
– Discount adjustments
– ICD-10-CM diagnosis codes
– Proof of payment (copies of canceled checks)
• Each spreadsheet submission sheet must be for 1 member only. We do not accept combined submissions for a family or for
more than 1 member.
• For capitated services rendered outside the medical group/IPA/facility, we require copies of canceled checks showing actual
amounts paid. Upon request, submit copies of all referral bills and/or copies of consultation and operative reports.
• We may ask you to submit a brief member history (copy of a consultant report and/or history dictation). We do not require lab
results, X-ray results or records.
• These are excluded from the calculation of ISL/reinsurance claims:
– Member copayment amounts
– Non-covered services
– Services paid by Workers’ Compensation
– Services paid by other health plans
– Services paid through third-party reimbursement
Our Claims Production Unit reviews the claim for completeness and tells medical group/IPA/facility if it needs any other
information. It may need supporting records for ISL/reinsurance claim verification. After review, if the claim is accepted, we
make a payment within 60 calendar days. Submit ISL/Reinsurance claims to [email protected].

Capitation and/or Delegation Supplement
181
2023 UnitedHealthcare Care Provider Administrative Guide
Delegated credentialing program
Delegated credentialing requirements
This information is supplemental to the credentialing requirements outlined in Chapter 15: Credentialing and recredentialing.
Delegated entities and capitated health care providers are also subject to the following requirements.
We maintain standards, policies and procedures for credentialing and recredentialing of health care providers and other
licensed independent health care professionals, facilities and other organizational health care provider facilities that provide
medical services to our members. We may delegate credentialing activities to a medical group, IPA, PHO, hospital or other
entity that complies with our Credentialing and Recredentialing Plan. Delegation of credentialing may occur through a stand-
alone Delegation Credentialing Agreement or through a Delegation Grid within the capitation agreement.
The delegate must maintain a written description of its credentialing program that documents the following activities, in a format
that meets the Credentialing Entity’s standards:
• Credentialing
• Recredentialing
• Assessment of network providers and other licensed independent health care professionals
• Sub-delegation of credentialing, as applicable
• Review activities, including establishing and maintaining a credentialing committee
Confidentiality
Delegated entities must not share credentialing and recredentialing information with anyone without the health care provider’s
written permission or as required by law.
Delegate Fraud, Waste and Abuse
UnitedHealthcare is committed to protecting the integrity of the health care program and the efficiency of operations by
preventing, detecting, and investigating fraud, waste and abuse. During delegation, the MCRE is responsible for preventing,
detecting, and investigating fraud, waste and abuse and reacting in an ethical manner upon discovery.
Delegate Action
Delegates are to withhold payment to any providers they are investigating for fraud and notify UnitedHealthcare of their findings.
For a comprehensive resource, please see Chapter 17 of the 2022 Administrative Guide (Fraud, Waste and Abuse FWA).
Term of FWA Providers
Delegate is to submit terminations and appropriate legal and regulatory documentation for care providers who are investigated
and found guilty of Fraud, Waste and/or Abuse.
Initial credentialing process
When credentialing is delegated, applicants must use the medical group’s/IPA’s application form and process or as prescribed
by law.
Delegation oversight
We perform an initial assessment to measure the delegate’s compliance with the established standards for delegation of
credentialing. Every year after that, we assess the delegate to monitor its compliance with established standards. This includes
NCQA standards and state and federal requirements. If needed, we may conduct a focused assessment review based on
specific delegate activity.

Capitation and/or Delegation Supplement
182
2023 UnitedHealthcare Care Provider Administrative Guide
Improvement action plans
If delegates are not compliant, we may require an improvement action plan. If compliance is not reached within a determined
time frame, we continue oversight. We may revoke delegated functions if delegates remain non-compliant with our
credentialing standards.
Credentialing reporting requirements for delegates
In addition to complying with state and contractual requirements, we require all delegates to adhere to the following standards
for notification procedures. The delegate provides prior written notice to us of the addition of any new health care providers
or other licensed independent health care professionals. For all new and current health care providers with changes to
credentialing information, include these in your notice:
• Demographic information including name, gender, specialty and medical group/IPA address and locations
• Initial credentialing committee date
• Recredentialing committee date
• License
• DEA registration
• Education and training, including board certification status and expiration date
• Facilities with admitting privileges, or coverage arrangements
• Billing information — to include:
– Legal entity name
– Billing address
– TIN
• Product participation (e.g., Commercial, Medicare Advantage)
• Languages spoken and written by the health care provider or clinical staff
Reporting changes
Every month, the delegate must provide to the credentialing entity current demographics for their health care providers and/or
changes to a status. Changes include the following:
• Address
• Phone number a member can call to make an appointment
• TIN
• Status of accepting patients: open, closed or existing patients
• Directory display indicator
• Additional elements per roster template (e.g., office hours, languages spoken)
• Product participation (only applies if your group has the option to opt in/out of certain products)
The delegate must provide full roster submissions at least twice a year per NCQA requirements. Submit reports to delprov@
uhc.com or to the email address the Roster Manager provides to the Delegated Entity. UnitedHealthcare has a submission
template you can use, or you can make changes with CAQH ProView for Groups (requires approval from UnitedHealthcare).
When you submit demographic updates, list only those addresses where a member may make an appointment and see the
health care provider. On-call and substitute health care providers, who are not regularly available to provide covered services
at an office or practice location, should not be listed at that address. Report all demographic changes, open/closed status,
product participation or termination to your local network account manager, health care provider advocate or within My
Practice Profile in the UnitedHealthcare Provider Portal.
Delegate reporting of terminations
The delegate must notify us, in writing, of any terminations of health care providers or other licensed independent health care
professionals. Send notice 90 calendar days before the termination effective date. It is imperative we receive such notices on
a timely basis to comply with our regulatory obligations related to the terminations of health care providers and other licensed
independent health care professionals.

Capitation and/or Delegation Supplement
183
2023 UnitedHealthcare Care Provider Administrative Guide
Effective dates of termination must be the last day of the month to properly support group capitation. We do not accept mid-
month terminations.
Termination notice requires:
• Reason for termination.
• Effective date of termination.
• Direction for reassignment of members (for PCP terminations, if UnitedHealthcare does assignment).
When a PCP terminates affiliation with a delegate, our members have 2 options:
• Stay with their existing medical group/IPA and change health care providers.
• Transfer to another medical group/IPA to stay with the existing health care provider.
If the delegate fails to indicate the reassignment preference, we assign the member to another PCP within the same medical
group/IPA, based on the medical group’s/IPA’s direction for reassignment. We make exceptions to this policy on a case-by-
case basis. Members may change their health care provider as described in their benefit plan.
Negative actions reporting requirements
The delegate must notify us, in writing, of a change in a health care provider’s status that results in any restrictions, limitations,
suspension or termination.
Virtual Care Services (Commercial HMO plans – CA only)
Commercial HMO members can use Virtual Visits for 24/7 Virtual Visits (urgent care), Virtual Primary Care or through their
selected PCP or medical group/IPA. Virtual Visits provide communication of medical information in real time between the
member and a health care provider or health specialist, through use of interactive audio and video communications equipment
outside of a medical facility (e.g., home or work). When covered by a member’s benefit plan, the Virtual Visit benefit has a
separate defined copayment.
24/7 Virtual Visits: Commercial members can connect to a doctor by video through myuhc.com or the UnitedHealthcare app.
Doctors treat a wide range of health conditions (e.g., flu, pinkeye and migraines) and can even prescribe medication as needed.
24/7 Virtual Visits treats many of the same conditions as in-person urgent care and utilizes the Designated Virtual Network
Provider benefit. The network provider groups offering Virtual Visit services must comply with the service standards. If you
provide Virtual Visits, these services must be accessible to individuals with disabilities. Post your Virtual Visits procedures for
members who are deaf or hard of hearing so they receive them prior to their Virtual Visit.
Virtual Primary Care: Virtual Primary Care delivers many of the same services as traditional primary care, including preventive
and regular exams, management of chronic conditions and acute non-emergency needs. It combines convenience with the
potential advantages of seeing a doctor regularly who knows your employees’ health history. Virtual Primary Care uses the
Physician Office Benefit.
We prefer members to access Virtual Visits through their selected PCP or medical group/IPA (local care), if available.
Commercial HMO members may access Virtual Visits from a Designated Virtual Network Care Provider. If the member’s
medical group/IPA or PCP does not offer Virtual Visit services, we make a nationally contracted Virtual Visit health care provider
available. The Designated Virtual Network Care Provider groups offering Virtual Visit services must comply with the service
standards.
Service standards
Access — When the health care provider group develops Virtual Visit technology, it may offer services to assigned members
who have the coverage as a part of their benefit plan. We pay for Virtual Visit primary care services delivered by health care
providers covered under professional capitation. Not all benefit plans have the Virtual Visit benefit option. The health care
provider group must confirm member eligibility and cost-share for Virtual Visit service. This applies only if medical group/IPA
develops its own virtual visit technology.
24 Hour/7 day availability — Virtual Visit technology services are available 24 hours a day, 7 days a week.

Capitation and/or Delegation Supplement
184
2023 UnitedHealthcare Care Provider Administrative Guide
Staffing credentials — All professional staff are certified or licensed in their specialty or have a level of certification, licensure,
education and/or experience based on state and federal laws.
Staff orientation and ongoing training — The health care provider group must take part in a written orientation plan with
documented skill demonstrations. It must also have initial and ongoing training programs, including policies and procedures.
The health care provider group will pursue accreditation of its Virtual Visit program with the American Telemedicine Association.
Service response time — Within 30 minutes after a member requests a visit, the health care provider group contacts the
member to either schedule or hold a Virtual Visit.
Technology security — The health care provider group conducts all member Virtual Visits using interactive audio and/or video
telecommunications systems on a secure technology platform that meets state and federal law requirements for security and
confidentiality of electronic member information. It maintains member records in a secure medium that meets state and federal
law requirements for encryption and security of electronic member information.
Professional accreditation — The health care provider group pursues applicable accreditation by the American Telemedicine
Association (or other mutually agreed upon accreditation body) to become accredited within 1 year after the accreditation
program release date.
Continuous quality improvement (CQI) — The health care provider group must have a documented CQI program for identifying
data opportunities for time-measured improvement in areas of core competencies. There must be demonstrated ties between
CQI findings and staff orientation, training, and policies and procedures.
Member complaints — The health care provider group logs, by category and type, member complaints with specific
improvement action plans for any patterns. There should be complaints registered on less than 2% of member cases.
Regulatory assessment results — If we ask, the health care provider will allow access to any applicable regulatory audit results.
Utilization — The health care provider group submits Virtual Visit encounters with proper coding as part of its existing encounter
submission process.
Electronic billing/encounter coding — The health care provider group will submit Virtual Visit encounters or claims with proper
coding as part of its existing encounter submission process.
Eligibility verification — The health care provider group uses existing eligibility validation methods to confirm Virtual Visit
benefits.
Case communication — The health care provider group will support member records management for Virtual Visits using
existing EMR systems and standard forms. Keep required medical information in EMR records, including referrals and
authorizations.
Joint operating committee — The health care provider meets with us up to quarterly at our request to review data reports and
quality issues. We also address any administration issues.
Professional environment — The health care provider group helps ensure that, when conducting Virtual Visits with members,
the rendering health care provider is in a professional and private location. The health care provider group (rendering health
care providers) may not conduct member Virtual Visits in vehicles or public locations.
Medical director — The health care provider employs or engages a licensed health care provider as medical director. The
medical director is responsible for clinical direction.
Referrals and referral contracting
Direct access services
Members may receive certain services without prior authorization or referrals. Refer to Chapter 6: Referrals for details about
direct access services.
Access to participating eye health care providers (select health care providers in CA only)
If the medical group/IPA is delegated for vision services, it must allow the member direct access to any eye health care provider
participating and available under the plan. An eye health care provider is a licensed network optometrist or ophthalmologist.

Capitation and/or Delegation Supplement
185
2023 UnitedHealthcare Care Provider Administrative Guide
The medical group/IPA may require the eye health care provider to submit requests for approval of surgical vision-related
procedures.
Access to participating chiropractor (WA only)
If the medical group/IPA is delegated for chiropractic services, they must allow the member direct access to any participating
chiropractor available under the plan. The medical group/IPA may use managed care cost and containment techniques.
PCP and health care provider responsibilities
We assign each member a PCP at the time of enrollment if the member does not select one. The PCP coordinates the
member’s overall health care, including behavioral health care, and the appropriate use of pharmaceutical medications.
The delegated medical group/IPA sets its own policies regarding health care provider responsibilities.
Out-of-network provider referrals (Commercial HMO and Medicare Advantage)
When medically necessary, the PCP refers the member to in-network providers. If the needed health care provider is not
available in-network, not available within the needed time frame or too far away, the PCP needs to request an out-of-network
provider review. The delegated medical group/IPA reviews this request. If approved, the member is not responsible for costs
over their applicable in-network cost-sharing.
Referral contracts (Medicare Advantage)
We encourage the medical group/IPA to establish contracts with health care providers so they may refer our members for
specialty services. Each contract must have the specific parts described in this section. The medical group/IPA may establish
written contracts with health care providers. They may use existing UnitedHealthcare contracts unless they are delegated for
claims processing. Delegated medical groups/IPAs must negotiate their own contracts. These contracts must comply with this
guide:
• No contractual arrangement between the delegate and any subcontracting health care provider may violate any provision of
law.
• The delegate helps ensure all provisions of its agreement with any health care provider who provides services to MA
members includes all provisions required under the delegate’s MA Agreement and regulatory requirements and applicable
accreditation standards.
• If a health care provider has opted out of the Medicare program, the delegate does not contract with them to provide services
to MA members.
• Members enrolled in the AARP Medicare Advantage Freedom Plus plan do not need to obtain referrals for select OON
benefits and services.
Establishing contracts for specialty services
Any medical group/IPA delegated for claims processing must negotiate contracts with individual specialists or group practices
to facilitate the availability of appropriate services to members. All contracts must be in writing and comply with state and
federal law, accreditation standards and the MA Agreement.
Depending upon the delegate’s contract with us, this may include contracting for services with hospitals, home health agencies
and other types of facilities.
Subcontract review (MA)
CMS requires us to check the written agreements the medical group/IPA has with its health care providers. We check them
at least annually. We recommend the medical group/IPA reviews their subcontracts annually. These checks help ensure
compliance with federal law and CMS regulations. We require an Improvement Action Plan (IAP) for any medical group/IPA who
has non-compliant contracts. The IAP lists our findings and expected time frame to reach compliance.

Capitation and/or Delegation Supplement
186
2023 UnitedHealthcare Care Provider Administrative Guide
Referral authorization procedure
The delegated medical group/IPA may initiate the referral authorization process when asked to refer a member for services.
Refer to their Notification/Prior Authorization list. These capitated medical services may need a referral authorization:
• Outpatient services
• Laboratory and diagnostic testing (non-routine, performed outside the delegated medical group’s/IPA’s facility)
• Specialty consultation/treatment
• Facility admissions
• Out-of-network services
The medical group/IPA, PCP and/or other referring health care provider verifies eligibility and participating health care provider
listings on all referral authorization requests. This helps ensure they refer a member to the appropriate network provider. The
medical group/IPA must comply with the following procedures:
• When a member requests specific health care provider services, treatment or referral, the PCP or treating health care provider
reviews the request for medical necessity.
• If there is no medical indication for the requested treatment, the health care provider discusses an alternative treatment plan
with the member.
• If the member’s treatment option requires referral or prior authorization, the PCP or treating health care provider submits the
member’s request to the delegate’s Utilization Management Committee or its designee for a decision. The PCP or treating
health care provider includes appropriate medical information and referral notes about why the requested service is medically
necessary. Information should include results of previous treatment.
• If the request is not approved in whole, the medical group/IPA (or if not delegated, UnitedHealthcare) issues a denial
letter to the member. It states the requested services, treatment or referral and complies with applicable state and
federal requirements.
Standing referral/extended referral for care by a specialist
The delegated entity must have specialty care referral procedures. They need to explain standing and extended referrals for
specialists and specialty care centers. The entity needs a standing referral if the member requires:
• Continued care from a specialist or specialty care center for a prolonged time.
• Extended access to a specialist for a life-threatening, degenerative or disabling condition.
There may be a limit to the number of specialist visits or time authorized. The specialist may need to provide regular reports to
the PCP.
For an extended specialty referral, the PCP and specialist must determine which health care service each manages. The PCP
should handle primary care and keep records of the reason, diagnosis, and treatment plan for the referral.
HIV/AIDS extended referrals (CA commercial only)
The medical group/IPA must have a written process for extended referrals to HIV/AIDS specialists when the PCP and medical
group/IPA medical director agree the diagnosis and/or treatment of the member’s condition requires an HIV/AIDS specialist’s
expertise. To comply with the state laws and regulations, the delegated medical group/IPA must identify health care providers
within their group who qualify as HIV/AIDS specialists. If no such health care providers are in the medical group/IPA, the
medical group/IPA must have a way to refer members to a qualified HIV/AIDS specialist outside of the group. The qualification
of an HIV/AIDS specialist are outlined in the California Health and Safety Code 1374.16.
Referral and/or authorization forms
For commercial members, the delegate may design its own request for referral and/or authorization forms without our approval.
When the forms communicate approvals to the member, use at least 12-point Times New Roman font. If the form is not at least
12-point font, the delegate needs to send a written notification that is. For MA members, we provide an approval template letter.
At a minimum, include all the following components in the form or written notice:
• Member identification (e.g., member ID number and birth date)
• Services requested for authorization including appropriate ICD-10-CM and/or CPT codes
Capitation and/or Delegation Supplement
187
2023 UnitedHealthcare Care Provider Administrative Guide
• Authorized services including appropriate ICD-10-CM and/or CPT codes
• Name, address, phone number and TIN of the health care provider the member is referred to
• Proper billing procedures, including the medical group/IPA address
• Verification of member eligibility
The delegate provides copies of the referral and/or authorization form to the:
• Referral health care provider.
• Member.
• Member’s medical record.
• Managed care administrative office.
Looking for more information about notification requirements?
See section on Non-discrimination taglines for Section 1557 of
the Affordable Care Act in this supplement.
Member or health care provider requests for services carved-out of UnitedHealthcare or
outside vendors (Medicare and Commercial)
CMS regulations allow a member to make a direct request for services from either the MA plan or the entity making the
determination, which is the utilization management/medical management delegated medical group/IPA. This applies to both
standard and expedited pre-service Initial Organization Determinations (IODs). The established requirements for pre-service
standard and expedited IODs apply.
Delegated medical groups/IPAs handle the timely processing of all pre-service organization determination requests, including
the delegate’s requests that are UnitedHealthcare’s responsibility. The medical group/IPA must have explicit policies and
procedures for the following:
• Starting the referral or authorization processes when a member contacts the delegate to request services, or when a health
care provider requests a service of the delegate that is UnitedHealthcare’s responsibility. The medical group/IPA must use
the date and time the member or health care provider first called as the received date and time of the request to comply with
required turn-around times.
• Working with UnitedHealthcare on service referrals or authorizations where a member or health care provider has contacted
us to request services. The medical group/IPA must use the date and time of the request to UnitedHealthcare as the received
date and time of the request for compliance with turnaround times.
If the carved-out service is UnitedHealthcare’s responsibility, the delegated medical group/IPA will:
• Transfer member requests to the customer service number on the back of the member’s ID card.
• Transfer health care provider requests to Provider Services at 1-877-842-3210.
• Stay on the line and explain the request.
If the carved-out service is the responsibility of an outside vendor, the Primary Medical Group will locate Vendor contact
information through member Evidence of Coverage documentation or through uhcprovider.com, transfer member or provider
calls to the appropriate vendor contact or submit the carve-out request to the appropriate vendor if not a call and document
actions.
• Locate vendor contact information on uhcprovider.com or on the member’s Evidence of Coverage (EOC) and transfer
member or provider to the appropriate contact.
• Call 1-877-842-3210 to verify information to complete the request.
– Follow the IVR menu to reach correct department or obtain vendor information.
– Submit request directly to vendor and inform the member of vendor name and contact information.
Medicare Advantage and Commercial delegated medical groups/IPAs cannot send a carve-out letter.
• Delegates on the NICE platform may submit the carve-out services as a prior authorization submission using the
UnitedHealthcare Provider Portal Prior Authorization tool: uhcprovider.com > Sign In.

Capitation and/or Delegation Supplement
188
2023 UnitedHealthcare Care Provider Administrative Guide
Looking for more information on referrals?
Additional detailed information and requirements
for referrals can be found in Chapter 6: Referrals
Coordination of care between medical and behavioral health care
Medical groups/IPAs providing behavioral health services must collect information about how to improve coordination of care
with the behavioral health care providers. Based on the data collected, the medical group/IPA must work with those health
care providers to make improvements. The medical group/IPA submits this report annually to their quality improvement or
appropriate committee. The medical group/IPA must have procedures describing how it will complete this cycle. We look at the
process and report during our annual review of the medical group/IPA.
A medical group/IPA providing behavioral health services must also review members’ experiences at least annually. This
includes a member survey. Based on the survey results, the medical group/IPA identifies areas for improvement and makes
necessary changes. The medical group/IPA then measures the effectiveness of these changes. It submits this report to its
quality improvement or appropriate committee. We look at the process and report during our yearly review.
Medical management
The protocols in this section are unique to capitated and/or delegated medical management entities. The protocols in Chapter
7: Medical management may also apply if we are financially responsible for the service.
If we are financially responsible for the service, or responsible for processing the claim, ask us if we require an authorization.
Clinical delegation oversight
We monitor the performance of delegated activities. We hold our delegates to the requirements outlined in the main guide
and this supplement. We perform clinical assessments of those activities prior to the approval of delegation to make sure the
potential delegate meets those requirements. Once we approve the delegate, and they are implemented, we make sure they
remain compliant. We provide our delegates with information they need to meet regulatory and contractual requirements and
accreditation standards.
Pre-contractual or pre-delegation assessments
When an entity—usually a medical group/IPA—expresses interest in contracting to perform delegated activities, we begin an
assessment process to confirm the entity can perform those activities. Clinical reviewers request documented processes
(e.g., programs, policies and procedures, work flows or protocols) and supporting evidence prior to an onsite visit. Supporting
evidence may include materials (e.g., letter templates, scripts, brochures or website) and reports (or the demonstrated ability
to produce required reports). Clinical reviewers arrange an onsite visit to further assess systems and processes, staffing
and resources. We report assessment results and delegation recommendations to the Delegation Oversight Governance
Committee, which decides whether to proceed with delegation and determines any contingencies for delegation.
Post-contractual or post-delegation clinical assessments
We conduct another assessment within 90 calendar days after the contract or delegation effective date. Assessments are based
on documented processes, materials, reports and case records or files specific to the delegated activities. Further assessments
are performed at least quarterly. The quarterly review process includes:
• A review of all updated policies and/or procedures.
• File review (3-month look back from previous review period).
• Remediation plan, if appropriate.

Capitation and/or Delegation Supplement
189
2023 UnitedHealthcare Care Provider Administrative Guide
Quarterly review process
The quarterly review process includes new scoring guidelines for any deficiencies found. Total assessment scores will no longer
be provided. Any review items marked as not met will be placed into the following categories on your remediation plan:
• Immediate Corrective Action Required (ICAR)
– The issue requires immediate correction and may have impacted member’s health and safety or access to services.
– You have 2 business days to respond with root cause.
– You have 7 business days to remediate the issue.
• Corrective Action Required (CAR)
– The issue requires correction, but the member’s health and safety is not affected.
– You have 5 business days to respond with root cause.
– You have 14 business days to remediate the issue.
• Observations
– A non-systemic or one-off issue.
– You have 5 business days to respond with root cause.
– You have 21 business days to remediate the issue.
Criteria for determining medical necessity
UnitedHealthcare and medical groups/IPAs delegated for utilization/medical management review nationally recognized
evidence-based criteria to determine medical necessity and appropriate level of care for services whenever possible.
UnitedHealthcare and delegates use several resources and guidelines to determine medical necessity and appropriate level
of care.
Hierarchy of criteria use
When using criteria to make decisions about service requests, the delegate must use the following criteria appropriate to the
benefit plan:
Commercial
• Eligibility and benefits
• State/federal laws and regulations
• Summary Plan Description/Certificate of Coverage
• UnitedHealthcare clinical determination guidelines
• UnitedHealthcare medical policies and review guidelines
• For medical necessity only:
– Evidence-based criteria, such as InterQual guidelines
UHC West
• Eligibility
• Evidence of Coverage (EOC)/Schedule of Benefits (SOB)
• UnitedHealthcare West Benefit interpretation policies (BIP)
• UnitedHealthcare West Medical management guidelines (MMG)
• UnitedHealthcare West Medical/drug policies or review guidelines (when not addressed in MMG)
• MCG Care Guidelines/InterQual criteria
• Hayes
Medicare Advantage
• Eligibility
• Evidence of Coverage/Summary of Benefits
• Federal/States Mandates (e.g., WHCRA)

Capitation and/or Delegation Supplement
190
2023 UnitedHealthcare Care Provider Administrative Guide
• Medicare criteria:
– National Coverage Determination (NCD)
– Local Coverage Determination (LCD)
– Local Coverage Medical Policy Article (LCA)
– Medicare Benefit Policy Manual (MBPM)
• UnitedHealthcare Medical Policies/Coverage Determination Guidelines/UnitedHealthcare Commercial Medical Benefit Drug
Policy
– Note: UnitedHealthcare Medicare Advantage Coverage Summaries are not used as criteria but as a pathway to correct
criteria.
• For Step Therapy: UnitedHealthcare Medicare Part B Step Therapy Programs:
– Review for medical necessity, first using the Medicare hierarchy of review, then review for Step Therapy.
• MCG Care Guidelines/InterQual criteria
• Delegate policies if UHC policy/guidelines DO NOT exist. Delegate policy, if utilized, would be required to have appropriate
delegate committee approval(s) and cannot be more restrictive than Medicare.
• UHC Cardiology/Radiology Guidelines (Use restricted to UnitedHealthcare radiology/cardiology programs outlined in the
UnitedHealthcare Care Provider Administrative Guide.)
With limited exceptions, we do not reimburse for services that are not medically necessary, or when you have not followed
correct procedures (e.g., notification requirements, prior authorization, or verification guarantee process). Delegates may
institute the same policy.
Accreditation standards require all health care organizations, health benefit plans, and medical groups/IPAs delegated for
utilization/medical management to distribute a statement to all members, physicians, health care providers and employees who
make utilization management (UM) decisions stating:
• UM decision-making is based only on appropriateness of care and service and existence of coverage.
• Practitioners or other individuals are not rewarded for issuing denials of coverage or service.
• Financial incentives for UM decision-makers do not encourage decisions that result in under-utilization.
Regardless of the medical management program determination, the decision to render medical services lies with the member
and the attending physician.
If you and a member decide to go forward with the medical service once UnitedHealthcare or the delegate has denied prior
authorization (and issued a denial notice to the member and physician as appropriate), neither UnitedHealthcare nor the
delegate reimburse for the denied services. Medical directors are available to discuss their decisions and our criteria with you.
Find medical policies and guidelines on uhcprovider.com/policies or from the delegated medical group/IPA as applicable.
Level of specificity — use of codes
To track the specific level of care and services provided to its members, UnitedHealthcare requires you to use the most current
service codes (i.e., ICD-10-CM, UB and CPT codes). We also require you to make sure the documented bill type is appropriate
for the type of service provided.
Health care provider responsibilities for participation in medical management
You must participate, cooperate and comply with our medical management policies. You must render covered services at the
most appropriate level of care, based on nationally recognized criteria.
We may delegate medical management functions to a medical group/IPA or other entity that demonstrates compliance with
our standards. Health care providers associated with these delegates must use the delegate’s medical management office and
protocols. We may retain responsibility for some medical management activities, such as inpatient admissions and outpatient
surgeries. When a health care provider is not associated with a delegate, or when we are responsible for the specific medical
management activity, the health care provider must comply with our medical management procedures.
For medical management functions retained by us, you must receive authorization from us before rendering services for a
member. If you have not requested a prior authorization, submit the request within 3 business days before providing or ordering
the covered service. The exception is emergency or urgent services.

Capitation and/or Delegation Supplement
191
2023 UnitedHealthcare Care Provider Administrative Guide
To confirm prior authorization has been approved by UnitedHealthcare, use the Prior Authorization and Notification tool in the
UnitedHealthcare Provider Portal, or uhcprovider.com/paan. If the member is assigned to a delegated medical group/IPA,
check with that medical group/IPA for confirmation.
For urgent or emergent cases, we notify you within 24 hours of services rendered, or an admission.
If you don’t get prior authorization when required or tell us within the appropriate time frame, we may deny payment.
The delegated medical group/IPA sets its own policies about health care provider responsibilities.
If you do not get a prior authorization, neither us (or our delegate) nor our member can be held responsible to reimburse health
care providers for medical services, admissions, inappropriate facility days, and/or not medically necessary services. Receiving
an authorization does not affect the payment policies or determining reimbursement.
Continuity of care
Continuity of care provides a short-term transition period so members may temporarily continue to receive services from a non-
network provider. See general information under the CAA requirements detailed in Chapter 2: Provider responsibilities and
standards of this guide.
A condition that warrants a request for continuity of care requires prompt medical attention for a short time. It is not enough
that the member prefers receiving treatment from a former health care provider or other non-network care provider, even for
a chronic condition. A member should not continue care with a non-network provider without formal approval by us or the
delegate. Except for emergencies or urgent out-of-area (OOA) care, if the member does not receive prior authorization from us
or the delegate, the member pays for services performed by a non-network care provider.
We (or the medical group/IPA delegated for continuity of care) review and document all requests for continuity of care on
a case-by-case basis. We consider the severity of the member’s condition and the potential clinical effect on the member’s
treatment and outcome of the condition under treatment, which may result from a change of health care provider. Document
member specifics for consideration in case reviews as relevant clinical information.
Prior authorization protocol
For any service that requires a prior authorization, the health care provider initiates an authorization request online at least 3
business days prior to the scheduled date of service.
• You must complete and submit the appropriate prior authorization request forms as applicable to state and/or federal
regulatory requirements. We do not accept incomplete or incorrect forms, or submissions with incomplete medical records.
You may find the list of forms on uhcprovider.com/priorauth.
• Our medical management team documents the information, responds to the authorization request, and provides a decision
within required regulatory time frames. If approved, we issue an authorization number. If denied, we forward the reason for
denial to you and the member.
• In the case of a denial, you may speak with a medical director to discuss the case.
• The authorized health care provider who delivers care to the member should share documentation of the recommended
treatment with the member’s PCP.
• Exception for AARP Medicare Advantage Freedom Plus plan. Providers do not need to obtain prior authorizations for select
OON benefits and services.
The authorized health care provider submits a claim with the authorization number in the usual manner to the appropriate
address.
If you are a network care provider for a delegated medical group/IPA, follow the delegate’s protocols. Delegates may use their
own systems and forms. They must meet the same regulatory and accreditation requirements as UnitedHealthcare.

Capitation and/or Delegation Supplement
192
2023 UnitedHealthcare Care Provider Administrative Guide
Emergency services and/or direct urgent facility admissions
Tell us of a member’s emergency admission within 24 hours of admission, or as soon as the member’s condition has stabilized.
The medical management department receives admission notifications 24 hours a day, 7 days a week at:
EDI: Transaction 278N
Online: uhcprovider.com/paan
Phone: 1-800-799-5252
Document member specifics for consideration in case reviews as relevant clinical information.
The delegate sets its own policies regarding notification and authorization for these services.
Service area
The medical group/IPA/facility is financially responsible for providing all approved medical and facility services within a
designated service area as well as approved services rendered while a member is outside of the medical group’s/IPA’s
contracted service area. The contract service area is typically defined as being within 30 miles or less from medical group/IPA
site based on the shortest route using public streets and highways but can be based on other contractual terms. Refer to your
Agreement for your delegated entity service area. For MA members, refer to the CMS regulatory access requirements.
Urgent or emergency services provided within the medical group/IPA/facility service area are the financial risk of the capitated
entity regardless of whether services are rendered by the medical group’s/IPA’s/facility’s network of health care providers
unless your Agreement states otherwise.
OOA medical services
OOA medical services are emergency or urgently needed services that treat an unforeseen illness or injury while a member
is outside of the medical group’s/IPA’s contracted service area. These would have been the medical group’s/IPA’s financial
responsibility if they had been provided within the medical group/IPA service area.
• UnitedHealthcare is accountable for managing OOA cases unless otherwise contractually defined. Refer to the Division of
Financial Responsibility (DOFR) section of your Agreement to determine risk for OOA medical services.
• Medical services provided outside of the delegated medical group/IPA defined service area that the member’s medical
group/IPA arranges or authorizes are the delegate’s responsibility. They are not considered OOA medical services. This
includes out-of-network provider services referred by a health care provider affiliated with the delegated medical group/IPA,
whether or not that health care provider received appropriate authorization. In such cases, the delegated medical group/IPA
performs all delegated medical management activities, including issuing appropriate authorization and denials.
• Members referred by the delegated medical groups/IPA for out-of-network outpatient consultation, who are then found
through their evaluation to require medically necessary inpatient care, are the referring medical group’s/IPA’s responsibility.
They do not meet the OOA criteria.
• The delegated medical group/IPA must issue appropriate denials for member-initiated non-urgent, non-emergency medical
services provided outside the medical group’s/IPA’s defined service area.
• The medical group/IPA notifies UnitedHealthcare OOA department of all known OOA cases no later than the first business
day after receiving member notification of an OOA admission, procedure and/or treatment.
• Failure to notify us within this time frame may result in UnitedHealthcare holding the medical group/IPA financially responsible
for the OOA care and service.
• Once a UnitedHealthcare member’s PCP or medical group/IPA identified specialist speaks with the OOA attending health
care provider to determine the member’s stability for transport to an in-area facility, member’s PCP, or medical group/IPA
identified specialist:
– Determines the appropriate mode of transportation and obtains any required authorization.
– Determines the appropriate level of care or facility for the member’s care and obtains any required authorization.
– Arranges for a bed at the accepting in-area facility.
• If the member is found stable for transfer to an in-area facility, the medical group/IPA must collaborate with the health plan to
return the member to a network care provider and facility in a timely fashion.

Capitation and/or Delegation Supplement
193
2023 UnitedHealthcare Care Provider Administrative Guide
• The medical group/IPA facilitates the return of the member to a network care provider by making sure the following process
occurs in a timely fashion:
– The medical group is responsible for transfer and care coordination planning with the out-of-network care provider to an in-
network care provider, as medically appropriate, as soon as the medical group is aware of the OOA admission.
– If the medical group/IPA delays the transfer of a member considered medically stable for transfer to move, we may hold the
medical group/IPA financially responsible for any OOA charges incurred as a result of the delay.
– Ambulance transportation from OOA facility to in-area location.
– If an accident or illness occurs within the medical group/IPA contracted service area, and emergency personnel transport
the member to a facility outside the contracted service area for treatment, such services are not considered OOA and are
handled by the medical group/IPA in the same manner as in-area services. The medical group/IPA must authorize and
direct the member’s care as if the member were receiving services at the affiliated facility or health care provider facility.
Travel dialysis is not considered an OOA medical service unless contractually defined. Refer to your Division of Financial
Responsibility (DOFR) to determine if the medical group/IPA is responsible for travel dialysis.
Injectable medication used in a member’s home
The delegated medical group/IPA is responsible for authorizing and arranging medically necessary services. If the DOFR
assigns risk for injectable medications to a medical group/IPA, the medical group/IPA authorizes and pays for all injectable
medications, whether self-injected or given with the aid of a health professional in the home.
Trauma services
Trauma services are medically necessary, covered services rendered at a state-licensed, designated trauma facility or a
facility designated to receive trauma cases. Trauma services must meet county, state and/or federal regulatory requirements
as applicable.
The medical group/IPA reviews and authorizes trauma services using the applicable provision review criteria.
Transplant services/case management
Optum serves as our transplant network. For medical groups/IPAs that have risk for transplant services, notify the Optum case
management department when a member is referred for evaluation, authorized for transplant and admitted for transplant and/or
may meet criteria for service denial. Medical groups/IPAs that do not have risk for transplant services must refer members into
Optum transplant case management program who have been identified as:
• Requiring evaluation for a bone marrow/stem cell, including chimeric antigen receptor T-cell (CAR-T) therapy in certain
hematologic malignancies or solid organ transplant.
• Undergoing a transplant evaluation.
• Receiving a transplant.
• Receiving post-transplant care within the first year following the transplant.
You may submit referrals to Optum by:
• Phone: 1-888-936-7246
• Fax (Commercial): 1-855-250-8157
• Fax (Medicare): 1-855-250-7278
• Fax (Medicare Secure Horizon only): 1-888-361-0502
• Fax (Medicaid): 1-877-814-0488
• Fax (Dual Special Needs): 1-877-814-0488 and 1-855-250-7278
For UnitedHealthcare West members, you may submit referrals to Optum by:
• Phone: 1-866-300-7736
• Fax: 1-888-361-0502

Capitation and/or Delegation Supplement
194
2023 UnitedHealthcare Care Provider Administrative Guide
The transplant case manager works with the member’s transplant team, PCP, and other clinicians to assess the member’s
health care needs, develop, implement, and monitor a care plan. They also coordinate services and re-evaluate the member’s
care plan.
• Get prior authorization for transplant evaluations and transplant surgery, regardless of financial risk.
• Transplant evaluations and surgery must be performed at one of Optum Centers of Excellence or a facility approved by
UnitedHealthcare/Optum medical directors.
• For medical groups/IPAs who do not have risk for transplant services, Optum handles the authorization and management for
all transplant-related care and services. This includes the evaluation, transplant procedure, and 1 year post-transplant unless
dictated by the member’s benefit or federal/state law.
• Optum oversees the authorization and management of donor care and services related to transplants. This starts from the
date of stem cell/bone marrow collection or 24 hours prior to organ donation surgery. It ends 60 calendar days after the
transplant or as member’s benefit plan or state law dictates.
• Optum manages authorization and reimbursement of all travel expenses per the member’s benefit plan. If the medical group/
IPA has financial risk for transplants, they need to authorize and reimburse all travel expenses per the member’s benefit plan
in the same manner as Optum.
• Authorization and management of all non-transplant related services (e.g., medically necessary, covered services for the
member) is the delegated medical group’s/IPA’s responsibility. Non-transplant related services include those services needed
to treat the member’s underlying disease and maintain the member until transplant can be completed (e.g., ventricular assist
devices or mechanical circulatory support devices). Financial responsibility for non-transplant related, medically necessary
covered services remain as described in the DOFR.
• Medical groups/IPAs must comply with our transplant protocols, policies and procedures. We may modify these protocols,
policies and procedures from time to time.
Ventricular Assist Device (VAD)/Mechanical Circulatory Support Device (MCSD)
services/case management
Notify the case management department when you refer a member for evaluation for VAD/MCSD and admit a member for VAD/
MCSD.
Perform VAD/MCSD evaluations and surgery at a facility in Optum VAD Network, or a facility approved by our medical directors,
to align with heart transplant service centers.
Second opinions
Members have the right to second opinions. The delegate provides a second opinion when either the member or a qualified
health care professional requests it. Qualified health care professionals must provide the member with second opinions at no
cost. We also allow a third opinion.
When a member meets the following criteria, they may be authorized to receive a second opinion consultation from an
appropriately qualified health care professional:
• The member questions the reasonableness or necessity of a recommended surgical procedure.
• The member questions a diagnosis or treatment plan for a condition that threatens loss of life, limb, bodily function, or
substantial impairment (including a serious chronic condition).
• The clinical indications are not clear or are complex and confusing.
• A diagnosis is in doubt due to conflicting test results.
• The treating health care provider cannot diagnose the condition.
• The member’s clinical condition is not responding to the prescribed treatment within a reasonable period of time given the
condition, and the member is requesting a second opinion.
• The member attempted to follow the treatment plan or consulted with the initial health care provider and still has serious
concerns about the diagnosis or treatment plan.

Capitation and/or Delegation Supplement
195
2023 UnitedHealthcare Care Provider Administrative Guide
PCP second opinions
When the PCP is affiliated with a delegated medical group/IPA, and the member requests a second opinion based on care
received from that PCP, the medical group/IPA is responsible for authorizing and paying for the second opinion. If delegated for
claims, the medical group/IPA is responsible for claims payment.
A second opinion regarding primary care is provided by an appropriately qualified health professional of the member’s choice
from within the medical group/IPA group’s network of health care providers.
• California regulations allow SignatureValue HMO members to obtain second and third opinions from out-of-network care
providers. The delegate sends to UnitedHealthcare all requests for second and third opinions from health care providers not
participating in the delegate’s network.
If the request for a second medical opinion is denied, the medical group/IPA tells the member in writing and provides the
reasons for the denial. The member may appeal the denial. If the member gets a second medical opinion without prior
authorization from the delegate and/or UnitedHealthcare, the member is financially responsible for the cost of the opinion.
When the PCP is not affiliated with any participating medical group/IPA but is independently contracted with us, the member
may request a second opinion from a health care provider or specialist listed in our health care provider directory on
uhcprovider.com/findprovider.
The approved health care provider documents the second medical opinion in a consultation report, which they will make
available to the member and the treating participating health care provider. The second opinion health care provider reports
any recommended procedures or tests they believe are appropriate. If this second medical opinion includes a recommendation
for a particular treatment, diagnostic test or service covered by UnitedHealthcare, and the delegate or UnitedHealthcare (as
appropriate) determines if the recommendation is medically necessary, then the delegate or UnitedHealthcare arranges the
treatment, diagnostic test or service.
Note: Although a second opinion may recommend a particular treatment, diagnostic test or service, this does not mean the
recommended action is medically necessary or covered. The member is responsible for paying any applicable cost-sharing
amount to the health care provider who gives the second medical opinion.
Specialist care second opinions
The member has the right to request a second opinion consultation based on care received through an authorized referral to a
specialist within the medical group/IPA network.
The second opinion may be provided by any practitioner of the member’s choice from any medical group/IPA within the
UnitedHealthcare network care provider of the same or equivalent specialty.
• MA members: Second and third opinions, whenever possible, should be provided in-network. The delegate or we consider
authorizing health care providers outside of the delegate’s network if there is no available or appropriate network care
provider.
• California regulations allow commercial HMO members to obtain second and third opinions from out-of-network care
providers. The delegate sends to UnitedHealthcare all requests for second and third opinions from health care providers not
participating in the delegate’s network.
If the health care professional is part of the member’s assigned medical group/IPA, the medical group/IPA authorizes the
second opinion consultation. The medical group/IPA is also responsible to pay claims if it is delegated for claims.
If approved, we pay the claim for the non-participating health care professional’s second opinion consultation.
A second opinion consists of 1 office visit for a consultation or evaluation only. The health care provider’s opinion is included
in a consultation report after completing the examination. The member must return to their assigned medical group/IPA for all
follow-up care and authorizations.
If a second opinion consultation differs from the initial opinion, coverage for a third opinion must be provided if requested by
the member or health care provider, following the same process as for second opinions.
If the request for a second medical opinion is denied, the medical group/IPA tells the member in writing and provides the
reasons for the denial. The member may appeal the denial.
Capitation and/or Delegation Supplement
196
2023 UnitedHealthcare Care Provider Administrative Guide
Turnaround time for second or third opinions
We process requests for second opinions in a timely manner to support the clinical urgency of the member’s condition. We
follow established utilization management procedures and regulatory requirements. When a member’s health is seriously
threatened, we (or the delegate) make the second opinion decision within 72 hours after receipt of the request. An imminent
and serious threat includes the potential loss of life, limb, or other major bodily function. It can also exist when a delay would be
detrimental to the member’s ability to regain maximum function.
Clinical trials, experimental or investigational services
Experimental items and medications have limited coverage. We do not delegate coverage determinations for experimental/
investigational services or clinical trials.
For capitated care providers, the member’s health care provider is responsible for these tests, unless stated differently in your
contract.
We only cover experimental/investigational services when they meet Medicare requirements. Do not authorize or deny services.
Contact:
Cancer Resource Services/Cancer Support Program
Commercial:
• Phone: 1-866-936-6002
Medicare Advantage:
• Phone: 1-877-842-3210
Transplant Resource Services
• Phone: 1-888-936-7246
Commercial
• Fax: 1-855-250-8157
Medicare Advantage
• Fax: 1-855-250-7278
Medicaid
• Fax: 1-877-814-0488
Dual Special Needs
• Fax: 1-855-250-7278 and 1-877-814-0488
For all other clinical trials, contact the prior authorization department at 1-877-842-3210 or visit uhcprovider.com/paan.
Delegates on the NICE platform may also visit uhcprovider.com to submit carve-out services in the UnitedHealthcare Provider
Portal as a prior authorization submission, outlining commercial clinical trials request.
Looking for more information on clinical trials?
You can find additional information and requirements in the Clinical trials, experimental or
investigational services section in Chapter 7: Medical management, and on uhcprovider.com>
Resources > Plans, policies, protocols and guides > For Medicare Advantage Plans > Coverage
Summaries for Medicare Advantage Plans > Experimental Procedures and Items, Investigational
Devices and Clinical Trials.
Capitation and/or Delegation Supplement
197
2023 UnitedHealthcare Care Provider Administrative Guide
Commercial radiation therapy
(Commercial, for services carved out of capitation)
For certain radiation therapy services, such as intensity modulated radiation therapy (IMRT), proton beam therapy (PBT),
stereotactic body radiation therapy (SBRT) and Yttrium 90/Selective Internal Radiation Therapy (SIRT), prior authorization
is required. For certain commercial plans, Image Guided Radiation Therapy (IGRT), Special Services and Fractionation also
requires prior authorization. Use the Prior Authorization and Notification tool at uhcprovider.com/paan. You may also initiate
your request by calling the number on the back of the member’s ID card.
Prior authorization staff will not process the request or make a decision until they receive all necessary information from the
medical group/IPA. They make a decision and contact the medical group/IPA within the applicable time frame.
We authorize radiation therapy services following the member’s benefit design, provided the member has not exceeded their
benefit restrictions.
Looking for more information on radiation therapy?
Go to:
1. Go to the UnitedHealthcare Provider Portal by clicking the Sign In button in the top right corner of
uhcprovider.com.
– Go to Prior Authorization and Notification and select the Submission and Status link under the
Radiology, Cardiology and Radiation Oncology section.
– Select service type “Radiation Oncology.”
2. uhcprovider.com/policies > Commercial Policies > Reimbursement Policies or Medical & Drug Policies
and Coverage Determination Guidelines for UnitedHealthcare Commercial Plans.
Pharmacy
Pharmacy information and requirements for commercial and MA plans are in Chapter 8: Specialty pharmacy and Medicare
Advantage pharmacy.
Medications not covered under capitation (Medicare Advantage)
We may delegate decisions to authorize specific pharmacy services based on your Agreement.
A member or health care provider may request authorization from you for medication carved out of your Agreement terms.
Notify the member you are not responsible for the authorization of these services. Recommend the member refer to any Part D
coverage they may have.
Prior authorization is necessary for payment to be processed
The medical group/IPA must request prior authorization for select drugs. Get prior authorization forms on uhcprovider.com/
priorauth or by contacting your health care provider advocate or clinical contacts at UnitedHealthcare. Our staff will not process
the request until we receive all necessary information. Once we make a determination, we notify you within the correct time
frame compliant with state and federal law.
We make authorizations following benefit design, provided the member does not exceed benefit restrictions (applied to the
requested agents/therapeutic class, and the prior authorization process).
We fax the approval or denial back to you. For denials, we send a letter to the member and health care provider stating why we
denied the requested medication. The letter outlines the process for filing standard and expedited appeals.
Prior authorization process for medications carved out of capitation
If UnitedHealthcare has financial responsibility for medications currently covered under the commercial member’s medical
benefit, this policy applies to those medications listed in your Agreement.

Capitation and/or Delegation Supplement
198
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare uses a prior authorization process to review any medication carved out of capitation.
We review the administration of these medications for compliance with the National Comprehensive Cancer Network’s Drugs &
Biologics Compendium (NCCN Compendium®) recommended uses for the drug, as it pertains to treatment regimen and/or line
of therapy. Non-compliant services are not eligible for coverage or payment reimbursement by UnitedHealthcare. If the medical
group/IPA does not receive prior authorization from us before administering these drugs, we deny reimbursement. This policy
does not apply to bevacizumab (Avastin) used for non-oncological indications.
Prescription drug appeals process
Members may initiate an appeal for coverage of a prescription drug if the initial determination is adverse to them. They may start
an appeal in the following circumstances:
• The requested drug is not on the formulary.
• The drug is not considered medically necessary.
• The drug is furnished by an out-of-network provider pharmacy.
• The drug is not a drug for which Medicare will pay under Part D.
• A coverage determination is not provided in a timely manner.
• The delay would adversely affect the health of the member.
• A request for an exception is denied.
• The member is dissatisfied with a decision regarding the copayment required for a prescription drug.
Facilities
Notification requirements for facility admissions (delegated health care providers in shared
risk groups)
Contracted facilities must provide timely notification to both the delegate and UnitedHealthcare within 24 hours of admission for
all inpatient and observation status cases. This includes changes in level of care that affect billing category.
For maternity cases, provide notification before the end of the mandated period (48 hours for normal vaginal delivery or 96
hours for C-section delivery). We require notification if the newborn stays longer than the mother does. In all cases, we require
separate notification immediately when a newborn is admitted to the NICU.
The delegate must have a clearly defined process with the facility whereby it provides the medical group/IPA and
UnitedHealthcare with the facility information on all admissions, updates in member status, and discharge dates daily.
UnitedHealthcare and the medical group/IPA require timely notification of admission so we can verify eligibility, authorize care,
including level of care (LOC), and initiate concurrent review and discharge planning.
For emergency admissions, provide notification once the member’s condition is stabilized in the emergency department. For
timely and accurate payment of facility claims, we require proper notification on the day of admission.
Authorization log and denial log submission (delegated health care providers in shared risk
groups only)
Submit authorization logs for all inpatient acute, observation status, SNF cases and denial logs at least twice a week to the
Authorization Log Unit at [email protected] or EDI transmission.
We also require specific markets to submit Outpatient Prior Authorization and Denial Logs to include services where
UnitedHealthcare pays claims or where UnitedHealthcare is financially responsible for the services rendered. For new
submitters, arrange a log delivery schedule with the Authorization Log Unit prior to the first submission.
The Authorization Log Unit must agree in writing and in advance with changes to your submission schedule. Any medical
group/IPA undergoing a system change or upgrade that may affect delivery of authorization logs must notify the Authorization
Log Unit prior to change date and work with us to help ensure a seamless transition.

Capitation and/or Delegation Supplement
199
2023 UnitedHealthcare Care Provider Administrative Guide
Logs must be compliant with state and federal regulations and include all concurrent IP and SNF admissions between the
previous and current log submission:
• Cases generated upon admission
• Length of stay changes/extensions
• Discharged cases
• Submit completed outpatient authorization cases on a separate log:
– If there are no applicable cases to report, the medical group/IPA must submit a weekly authorization log indicating either
“no activity” or “no admissions” for each of the designated admission service types for the applicable reporting time.
• Logs must include the following:
– Member name
– Member ID
– Member date of birth
– Reason for denial
– Authorization/reference number
– Requesting health care provider (name, address, TIN or NPI)
– Attending/servicing health care provider (name, address, TIN or NPI)
– Facility health care provider (name, address, TIN or NPI)
– Admitting diagnosis (ICD-10-CM or its successor code)
– Actual admission date
– Actual discharge date
– Status (approved/denied)
– Service start date
– Service end date
– Clearly defined level of care description (i.e., Acute IP, mental health, acute rehabilitation, LTAC, skilled nursing,
observation, outpatient procedures at acute facilities, codes must be submitted with descriptions of LOC)
– Approved length of stay (number of days)
– Denied length of stay (number of days)
– Procedure/surgery (CPT Code)
– Discharge disposition
– Planned admission date
– Planned discharge date
– Service type
– Medical group/IPA
– Insurance (Commercial/Medicare)
The medical group/IPA must have a clearly defined process for determining medical necessity and authorizing outpatient
services. These services are paid as either shared risk or plan risk per the medical group/IPA contract.
The medical group/IPA must be capable of submitting, pursuant to our request, authorization or denials for all shared risk or
plan risk services for which the group has authorized or denied care on behalf of UnitedHealthcare.
Medical observation
Typically, observation status rules out a diagnosis or medical condition that responds quickly to care. Facility observation status
is generally designed to assess a member’s medical condition to determine the need for inpatient admission, or to stabilize a
member’s condition. UnitedHealthcare or our delegate will authorize facility observation status when medically indicated and
the case meets nationally recognized evidenced based guidelines. A member’s outpatient observation status may later be
changed to an inpatient admission if medically necessary and if appropriate criteria have been met.

Capitation and/or Delegation Supplement
200
2023 UnitedHealthcare Care Provider Administrative Guide
We expect our medical management delegates to support compliance with the review of criteria. The delegated medical group/
IPA must issue a facility denial when the inpatient stay does not meet nationally recognized evidence-based guideline. This
happens when:
1. It receives notification of the admission.
2. It receives a post-service request for admission authorization prior to claims submission. It determines the admission does
not meet medical necessity criteria, including relevant Medicare inpatient admission requirements and is not on the CMS
list of HCPCS codes that would be paid only as inpatient procedures.
3. There is no inpatient order matching the date of the inpatient admission for Medicare members.
Facility denial process
When we delegate services for authorization and concurrent review, we expect the delegate to issue a facility denial letter to
the contracted facility when the facility’s medical record or claim fails to support the LOC or services rendered. This may be
determined through concurrent or retrospective review.
There are 3 types of facility denial letters:
• Delay in inpatient services.
• Delay in change of LOC within the same facility.
• Delay in facility discharge.
The delegated medical group/IPA must comply with our protocols, policies and procedures for denials. This includes
turnaround times for issuing, delivering and submitting facility denial letters to UnitedHealthcare.
When UnitedHealthcare is responsible for paying facility services, the delegated medical group/IPA must comply with
UnitedHealthcare’s protocols, policies and procedures for submitting facility denial letters to UnitedHealthcare. Whether a
denial is issued by UnitedHealthcare or its delegate, the UnitedHealthcare care provider dispute resolution process manages
any facility disputes.
If the delegated medical group/IPA is responsible for paying inpatient facility services, then the delegate need not submit
copies of facility denials to UnitedHealthcare. Facility denials are sent to the facility and must specifically exclude the member
from liability for the denied LOC and/or services. Under these circumstances, the delegated medical group’s/IPA’s health care
provider dispute resolution process manages any health care provider facility disputes.
Delegate must provide a copy of the facility denial letter to the member, if requested.
Radiation therapy services (Medicare Advantage)
(For services carved out of capitation)
This policy applies if UnitedHealthcare has financial responsibility for the following outpatient MA services. Prior authorization is
required for:
• Intensity Modulated Radiation Therapy (IMRT).
• Proton Beam Therapy (PBT).
• Body Radiation Therapy (SBRT), including Stereotactic Radiosurgery (SRS).
• Image-Guided Radiation Therapy (IGRT).
• Special and associated services.
• Fractionation using IMRT, PBT and standard 2D/3D radiation therapy for prostate, breast, lung and bone metastasis cancers.
• Selective internal radiation therapy (SIRT), Yttrium 90 (Y90) and implantable beta-emitting microspheres for treatment of
malignant tumors.
We use National Coverage Decision (NCD), Local Coverage Decision (LCD) and UnitedHealthcare medical policies and
guidelines to determine eligibility of coverage. We require authorization before the start of therapy and each time a member
starts a new treatment regimen.

Capitation and/or Delegation Supplement
201
2023 UnitedHealthcare Care Provider Administrative Guide
Prior authorization required to process payment
Initiate a prior authorization request for outpatient radiation therapy services carved out of capitation on uhcprovider.com/
paan. We do not process the request or make a determination until we have received all necessary information. Then we make
a decision within the applicable time frame.
For MA plans, the time frame to review and render a decision begins upon receipt of the initial request.
We authorize radiation therapy services based on the member’s benefit design provided the member does not exceed their
benefit restrictions.
UnitedHealthcare may, at its sole discretion, use a nationally contracted vendor for utilization management to administer the
prior authorization program for all radiation therapy services. The nationally contracted vendor uses the NCDs, LCDs and the
UnitedHealthcare MA coverage summaries for managing the program.
We communicate the approval or denial via online to the medical group/IPA for each case serviced. For denials, an outbound
call is placed to schedule a peer to peer review. Denials also require a letter sent to both member and health care provider
stating why we denied the requested service. The letter outlines the process for filing standard and expedited appeals.
For a list of CPT and HCPCS codes requiring
authorization, refer to uhcprovider.com/paan >
Advance Notification and Plan Requirement
Resources > choose UnitedHealthcare Medicare
Solutions, UnitedHealthcare West Medicare
Advantage, and UnitedHealthcare Community
Plan (Dual Special Needs Plan) Prior Authorization
Requirements
Denials, delays or adverse determinations
Delegates that receive requests for services must make decisions and provide notification within applicable regulatory and
accreditation time frames. We hold the delegate to the most stringent requirements for approvals, extensions of decision
turnaround times, denials, delays, partial approvals and modification of requested services.
Find additional information in the Medical management denials/adverse determinations section in Chapter 7: Medical
management.
Qualifications of who can deny or make adverse determinations
Only physicians or appropriately licensed clinical personnel can deny or make adverse determinations based on medical
necessity. This reviewer may be a physician, doctoral level clinical psychologist or pharmacist as appropriate to the requested
service.
The reviewer must have a current unrestricted license. Delegates must provide evidence of verification according to
credentialing requirements.
For MA, the delegate must verify the reviewer has experience showing knowledge of Medicare coverage criteria. Evidence
of verification may include content of curriculum vitae, training as part of onboarding process, training after onboarding, or
interaction between our medical director and the delegate’s reviewers. Evidence may also include review of denial records or
files indicating appropriate use of criteria applicable to the request for services and member’s condition.
Oral or verbal notification
We have various requirements for oral or verbal notification of approvals or denials. This may vary from state to state or by
request type (such as pre-service, expedited or concurrent). The delegate must document efforts to provide oral notification
and meet written notification requirements as well.
Capitation and/or Delegation Supplement
202
2023 UnitedHealthcare Care Provider Administrative Guide
Written denial notice
The written denial is an important part of the member’s chart and the delegate’s records. Regardless of the form used, the
denial letter documents member and health care provider notification of:
• The denial, delay, partial approval or modification of requested services.
• The reason for the decision, including medical necessity, benefits limitation or benefit exclusion.
• Member-specific information about how the member did not meet criteria.
• Appeal rights.
• An alternative treatment plan, if applicable.
• Benefit exhaustion or planned discharge date, if applicable.
CMS requires the use of the CMS Integrated Denial Notice (IDN) for MA and Medicaid plan members. Do not alter this
template except to add text to the requested areas.
Most states require approved standardized templates for member notices, such as denial of services. UnitedHealthcare
provides appropriate and approved templates to the delegates.
Minimum content of written or electronic notification
A notice to deny, delay or modify a health care services authorization request must include:
• The requested services.
• A reference to the benefit plan provisions to support the decision.
• The reason for denial, delay, modification, or partial approval, including:
– Clear, understandable explanation of the decision.
– Name and description of the criteria or guidelines used.
– How those criteria were applied to the member’s condition.
• A statement the member can get a free copy with the benefit provision, guideline, protocol or other criterion used to make the
denial decision.
• Contractual rationale for benefit denials.
• Alternative treatments offered, if applicable.
• A description of additional information needed to complete that request and why it is necessary (for delay of decision).
• Appeal and grievance processes, including:
– When, how and where to submit a standard or expedited appeal.
– The member’s right to appoint a representative to file the appeal.
– The right to submit written comments, documents or other additional relevant information.
– The right to file a grievance or appeal with the applicable state agency, including information regarding the independent
medical review process (IMR), as applicable.
• The name and phone number of the health care professional responsible for the decision included in the health care
provider’s notice. This is not required in the member’s notification.
• Any state-mandated language (Commercial).
• ERISA information as applicable (Commercial).
• Ombudsman information (Commercial).
Find address and contact information for medical management
appeals in the Online/interoperability resources and how to
contact us table in Chapter 1: Introduction, or similar tables in the
applicable supplement.
CMS reasonable outreach
For information regarding reasonable outreach, refer to CMS.gov.

Capitation and/or Delegation Supplement
203
2023 UnitedHealthcare Care Provider Administrative Guide
Special Needs Plans (SNP) Model of Care (MOC)
The MOC is the framework for care management processes and systems that enable coordinated care for SNP members. The
MOC includes descriptions of the following:
• SNP population (including health conditions)
• Care coordination
• Provider network
• Quality measurement
• Performance improvement
The MOC helps ensure the unique needs of the population are identified and addressed through care management practices.
We evaluate MOC goals on an annual basis to determine effectiveness.
To learn more, contact us at [email protected].
CMS requires annual SNP MOC training for all providers who treat SNP members. The training is reviewed and uploaded
annually to ensure that it reflects current practices related to the core MOC elements in the preceding list. The Annual
SNP MOC Provider Training is available at uhcprovider.com/training. Updates about the annual training can be found at
uhcprovider.com/news. To receive news updates by email, sign up at uhcprovider.com/subscribe.
Delegation of complex case management and disease management
We may delegate the functions of complex case management (CCM) or disease management. Requirements are based on
Population Health Management (PHM) and NCQA accreditation standards.
If these functions are delegated to a medical group/IPA or other organization, we conduct pre-contractual and post-contractual
assessments. If assessments identify deficiencies, we require delegates to undergo improvement action. The oversight process
mirrors the delegation oversight process for medical management.
If these functions are not delegated to a medical group/IPA or other organization, you can refer members by submitting an
Optum Universal Referral form to provider_ref[email protected].
Non-discrimination taglines for Section 1557 of the Affordable Care Act
The U.S. Department of Health and Human Services published final non-discrimination rules from Section 1557 of the
Affordable Care Act. The final rule clarifies and codifies existing nondiscrimination requirements and sets standards for
including non-discrimination notices on significant communications sent to health plan members. This includes member-facing
letters (e.g., IDN, NOMNC, service denials), documents, notices, newsletters and brochures sent to the member.
April 2020: Medicare Tagline guidelines
To align with our clinical practices, delegates may use the short tagline for all significant written communications, regardless of
length, to all UnitedHealthcare Medicare members.
Please note the following:
• Using the short tagline is not a requirement, but an option to align with UnitedHealthcare clinical practices.
• You may continue to use the long taglines if it suits your clinical operations for communications of any length.
Claim delegation oversight
Pre-contractual claim delegation assessments
We may delegate claims processing to entities that have requested delegation and have shown through a pre-delegation
assessment they are capable of processing claims compliant with applicable state and/or federal regulatory requirements, and
health plan requirements for claim processing.

Capitation and/or Delegation Supplement
204
2023 UnitedHealthcare Care Provider Administrative Guide
Delegated entities must develop and maintain claims operational and processing procedures that allow for accurate and
timely claim payments. Procedures must properly apply benefit coverage, eligibility requirements, appropriate reimbursement
methodology and meet all applicable state and/or federal regulatory requirements, and health plan requirements for
claim processing.
Medical claim review (delegated medical groups/IPAs)
A delegated medical group/IPA must implement and maintain a post-service/retrospective review process consistent with
UnitedHealthcare processes.
We define a post-service/retrospective/medical claim review as the review of medical care treatments, medical documentation
and billing after the service has been provided.
We perform a medical claim review to provide fair and consistent means to review medical claims and confirm delegates meet
the following criteria:
• Medical necessity determinations
• Admission, length of stay and LOC are appropriate
• Eligibility was verified
• Follow-up for utilization, quality and risk issues was needed and initiated
• Billing is correct
• Claims-related issues as they relate to medical necessity and UnitedHealthcare claims payment criteria and/or guidelines are
identified and resolved
We also perform medical claim reviews on claims that do not easily allow for additional focused or ad-hoc reviews, such as:
• High-dollar claims.
• Claims without required authorization.
• Claims for unlisted procedures.
• Trauma claims.
• Implants not identified on our implant guidelines used by our claim department.
• Claim check or modifier edits based on our claim payment software.
• Foreign claims.
• Claims with level of service (LOS) or LOC mismatch.
The delegated medical group/IPA is accountable for conducting the post-service review of emergency department claims and
unauthorized claims. Review presenting symptoms, as well as the discharge diagnosis, for emergency services.
Post-contractual claim compliance assessments
We have policies and procedures designed to monitor the performance of delegated entities’ compliance with contractual state,
federal and UnitedHealthcare claims processing requirements. Our auditors perform ongoing claims processing compliance
monitoring in addition to comprehensive operational assessments which typically occur on an annual basis. Our auditors also
review for:
• Assessment results indicating non-compliance.
• Self-reported timeliness reports indicating non-compliance for 2 consecutive months.
• Non-compliance with reporting requirements.
• Lack of resources or staff turnover.
• Overall performance trends (claims appeal activity, claims denial letters or member and health care provider claims-related
complaints).
• Allegations of fraudulent activities or misrepresentations.
• Information systems changes or conversion.
• New management company or change of processing entity.
• Established Management Service Organization (MSO) acquires new business.

Capitation and/or Delegation Supplement
205
2023 UnitedHealthcare Care Provider Administrative Guide
• Significant increase in members or volume of claims.
• Regulatory agency request.
• Significant issues concerning financial stability.
As part of our ongoing claims processing performance monitoring, we require all delegated entities to submit a monthly
universal claims data extract file containing all processed claims during the month in addition to a claims data extract file of all
pended (open) claims inventory as of close of business on the last day of the month. These files must be in the format defined
by us and are due by the fifteenth calendar day of the following month. The delegate may be subject to the implementation of
an Improvement Action Plan (IAP) and/or financial consequences if it or any sub-delegated entity fails to submit or meet the
data requirements as outlined here in this guide and or the delegates contractual agreement with UnitedHealthcare. As part of
our comprehensive operational compliance assessment, we may request additional claims reporting to facilitate our review. The
auditor reviews the claims data and selects random claims for further review. The delegated entity must be ready for the auditor
at the time of assessment. Our procedures include an audit of the entire claims cycle, which includes validation/verification of
the claim date received, acknowledged, processed, and closed and a virtual walk-through of the delegated entity’s end-to-end
claim operations is conducted. During our procedures we review:
• Claims timeliness assessment for applicable claim element being reviewed.
• Financial accuracy (including proper benefit application, appropriate administration of member cost-share accumulation).
• Administrative accuracy.
• Customer denial accuracy and denial letter review.
• Health care provider denial assessment.
• Non-contracted and contracted health care provider payment dispute resolution (overturns and upholds) claims assessment.
• Fraud, waste and abuse inspection.
• Claim operational policies and procedures.
• Maximum out-of-pocket (MOOP) administration.
• Timely forwarding of misdirected claims.
• Significant decrease in membership and/or claim volume.
Non-compliant assessments
Either our ongoing operational monitoring or assessments may reveal that a delegated entity is not compliant with contractual
state and/or federal regulations, and/or UnitedHealthcare standards for claims processing.
Problems include, but are not limited to:
• Processing timeliness issues.
• Failure to pay interest or penalties.
• Failure to submit monthly/quarterly self-reported processing timeliness reports.
• Canceling assessments/audits.
• Failure to submit requested claims listings.
• Failure to have all documentation ready for a scheduled assessment.
• Failure to provide access to canceled checks or bank statements.
• Failure to submit accurate reporting.
When we put a delegated entity on a IAP, we place them on a cure period. A cure period is the time frame we give a delegated
entity to demonstrate compliance. The cure period is typically 30 to 60 days depending on the severity of the deficiency. The
delegate must provide a remediation plan describing how the deficiencies will be corrected and the time frame to complete
those efforts. We conduct frequent reviews during the cure period to ensure progress is being made. Should the delegate fail to
meet the compliance requirements, UHC Delegation Oversight will deploy its Claims Management Consulting Services (CMCS)
to assist with remediation of the IAP. CMCS may consist of conducting an on-site or virtual operational assessment, frequent
oversight, engagement and monitoring. We bill the delegated entity for all CMCS activities involving the remediation of the IAP.
UHC will charge the delegate for all CMCS activities with an initial fee of $2,500 plus $100/hour for the first month of the IAP
and $250 per hour after the first month of the IAP until the IAP is closed.

Capitation and/or Delegation Supplement
206
2023 UnitedHealthcare Care Provider Administrative Guide
If CMCS activities do not successfully correct the issues, additional actions such as revocation of delegation status and/or
enrollment freezes may occur. In addition, notwithstanding the previously mentioned, UnitedHealthcare reserves the right to
cancel the contract as defined in the Agreement.
Claim denial letters
When a delegated entity receives a claim for a commercial or MA member, they must assess the claim for the following before
issuing a denial letter:
• Member’s eligibility status with UnitedHealthcare on the date of service
• Responsible party for processing the claim (forward to proper payer)
• Contract status of the health care provider of service or referring health care provider
• Presence of sufficient medical information to make a medical necessity determination
• Covered benefits
• Authorization for routine or in-area urgent services
• Maximum benefit limitation for limited benefits
• Prior to denial for insufficient information, the medical group/IPA/capitated facility must document their attempts to get
information needed to make a determination
Member denials
When a member is financially responsible for a denied service, UnitedHealthcare or the delegated entity (whichever holds
the risk) must provide the member with written notification of the denial decision based on federal and/or state regulatory
standards.
For MA members, the delegated entity must issue a member denial notice within the appropriate regulatory time frame.
The delegated entity must use the most current CMS-approved Notice of Denial of Payment letter template. The letter must
accurately document the service health care provider, the service provided, the denial reason, the member’s appeal rights and
instructions on how to file an appeal.
For commercial members enrolled in a benefit plan subject to ERISA, a member’s claim denial letter must clearly state the
reason for the denial and provide proper appeal rights. The denial letter must be issued to the member within 30 calendar days
of claim receipt.
For all other commercial plans, the denial letter must comply with applicable state regulatory time frames. For instance, in CA,
denial letters must be sent within 45 working days.
The delegated entity remains responsible to issue appropriate denials for member-initiated, non-urgent/emergent medical
services outside their defined service area. For all members, the delegated entity must use the most current Language Access
Plan (LAP) document to accompany the denial letter.
Health care provider denials
When the member is not financially responsible for the denied service, the member does not need to be notified of the denial.
The health care provider must receive notification of the denial and their financial responsibility (i.e., writing the charges off for
the claims payment).
UnitedHealthcare or the delegated entity’s claims department (whichever holds the risk) is responsible for providing
the notification.
The denial notice (letter, EOP or PRA) issued to any non-contracted health care provider of service must state:
1. Their appeal rights.
2. The member is not to be balance billed.
When the member has no financial responsibility for the denied service, the denial notice issued to any health care provider of
service must clearly state the member is not billed for the denied or adjusted charges.

Capitation and/or Delegation Supplement
207
2023 UnitedHealthcare Care Provider Administrative Guide
Time limits for filing claims
For commercial claims, submit clean claims per the time frame listed in your Agreement or per applicable laws. We, or our
capitated care provider, allow at least 90 days for participating health care providers. For commercial plans, we allow up to 180
days for non-participating health care providers from the date of service to submit claims. For MA plans, we are required to
allow 365 days from the “through” date of service for non-contracted health care providers to submit claims for processing. If
we, or our capitated provider, are not the primary payer, we give you at least 90 days from the day of payment, contest, denial or
notice from the primary payer to submit the claim.
If a network care provider fails to submit a clean claim within the outlined time frames, we reserve the right to deny payment
for such claim. You cannot bill a member for claims denied for untimely filing. We have established internal claims processing
procedures for timely claims payment to our health care providers.
Timely filing
The claims “timely filing limit” is the calendar day period between the claims last date of service or payment/denial by the
primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim.
Determination of the date of UnitedHealthcare’s or its delegate’s receipt of a claim, the date of receipt shall be regarded as the
calendar day when a claim, by physical or electronic means, is first delivered to UnitedHealthcare’s specified claims payment
office, post office box, designated claims processor or to UnitedHealthcare’s capitated health care provider for that claim. We
use the following date stamps to determine date of receipt:
• UnitedHealthcare HMO claims department date stamp primary payer claim payment/denial date as shown on the Explanation
of Payment (EOP)
• Delegated health care provider date stamp
• Third-party administrator date stamp
• Confirmation received date stamp that prints at the top/bottom of the page with the name of the sender
• Electronic date stamp
MA claims must use the oldest received date on the claim. Refer to the official CMS website for additional rules and instructions
on timely filing limitations.
For commercial claims, refer to the applicable official state-specific website for additional rules and instructions on timely
filing limitations.
Date stamp
Delegated entities must have a clearly identifiable date stamp for all claims they receive. Electronic claims date stamps must
follow federal and/or state standards.
Date of receipt and date of service
“Date of receipt” means the working day when a claim, by physical or electronic means, is first delivered to either the plan’s
specified claims payment office, post office box, or designated claims processor or to UnitedHealthcare’s capitated health care
provider for that claim.
“Date of Service,” for the purposes of evaluating claims submission and payment requirements, means:
• For outpatient services and all emergency services and care: The date the health care provider delivered separately billable
health care services to the member.
• For inpatient services: The date the member was discharged from the inpatient facility. However, UnitedHealthcare or the
capitated health care provider must accept separately billable claims for inpatient services at least bi-weekly.
Misdirected claims
UHC West (Commercial and Medicare Advantage)
We identify, batch and forward misdirected claims to the appropriate delegated entity following state and/or federal regulations.
Our preferred method of forwarding claims is electronically; however, claims may also be forwarded via mail.
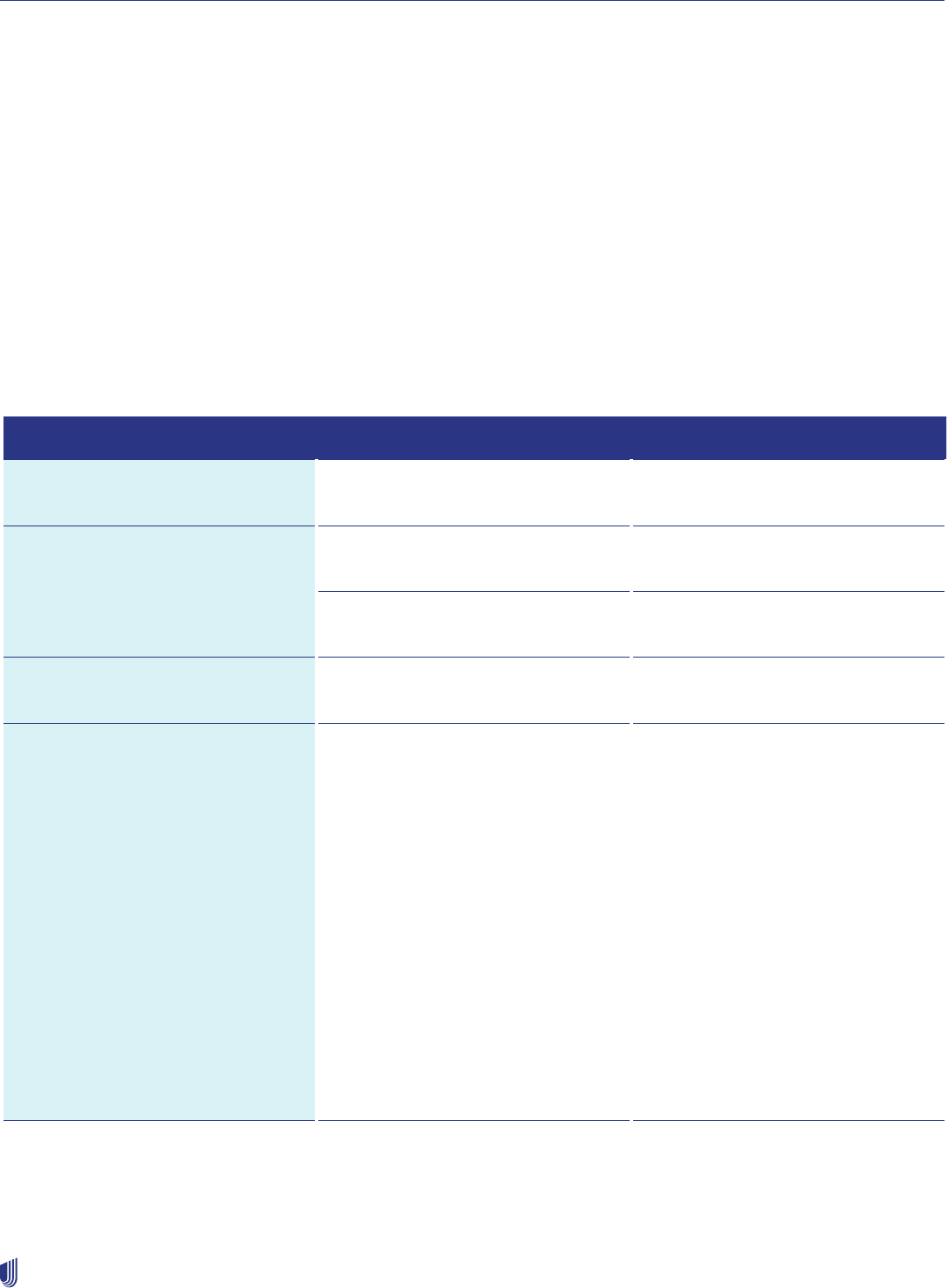
Capitation and/or Delegation Supplement
208
2023 UnitedHealthcare Care Provider Administrative Guide
We forward misdirected claims to the proper payer following state and federal regulations. If health care providers send claims
to a delegated entity, and we are responsible for adjudicating the claim, the delegated entity must forward the claim to us
within 10 working days of the receipt of the claim. Failure to comply with this requirement will lead to the implementation of an
Improvement Action Plan (IAP) and possible financial penalties.
The delegated entity must identify and track all claims billed to them received in error. Tracking must include, but is not limited
to, the received date of the claim by the delegate, the date forwarded, and the name of the entity where the claim was sent.
The delegated entity must then forward the claims to the appropriate payer and follow state and/or federal regulatory
time frames.
When the claim is adjudicated, the delegated entity must notify the health care provider of service who the correct payer is, if
known, using the EOP they give to the health care provider.
If you, the delegated entity, received a claim directly from the billing health care provider, and you believe that claim is the
health plan’s responsibility, forward it to your respective UHC Regional Mail Office P.O. Box, which is found on the back of
the member’s ID card. If the address on the back of the ID card is your (the delegate’s) address, refer to the following table to
identify where to send a copy of the claim along with any additional information received. If you are unsure which address is
applicable, reach out to your healthcare Provider Advocate. For MA member claims only, include the timestamp of your original
receipt date on the claim submission.
State Product Address
Arizona Medicare Advantage (MA) P.O. Box 30965
Salt Lake City, UT 84130-0965
California Commercial and MA P.O. Box 30968
Salt Lake City, UT 84130-0968
CALPERS Commercial only P.O. Box 30510
Salt Lake City, UT 84130-0510
Colorado MA P.O. Box 30983
Salt Lake City, UT 84130-0983
Nevada
UnitedHealthcare uses 2 delegated
payers in Nevada. Refer to the
member’s ID card to confirm which
delegate is assigned for that member’s
claims.
All HMO claims are processed by
delegated payers. Therefore, health
care provider appeals are reviewed
primarily by the delegated payer. Refer
to the member’s ID card to confirm
which delegate is assigned for that
member’s claims.
MA Claim Submission
• Intermountain Healthcare
P.O. Box 95638
Las Vegas, NV 89193-5638
• OptumCare - NV
P.O. Box 30539
Salt Lake City, UT 84130
Rework and Dispute Resolution
• Intermountain Healthcare
P.O. Box 95638
Las Vegas, NV 89193-5638
• OptumCare - NV
P.O. Box 30539
Salt Lake City, UT 84130
Capitation and/or Delegation Supplement
209
2023 UnitedHealthcare Care Provider Administrative Guide
State Product Address
Oregon MA P.O. Box 30974
Salt Lake City, UT 84130-0974
Texas MA P.O. Box 30975
Salt Lake City, UT 84130-0974
Washington MA P.O. Box 30976
Salt Lake City, UT 84130-0976
If you, the delegated entity, believe a claim we forwarded to you is the health plan’s financial responsibility, return the claim with
the appropriate Misdirected Claims cover sheet and provide a detailed explanation why you believe these claims are the health
plan’s responsibility.
You can download the cover sheet at uhcprovider.com/claims. Send all required information, including the claim and
Misdirected Claims cover sheet, to:
P.O. Box 30984
Salt Lake City, UT 84130-0984
In the event you, the delegate, change your payer ID (for electronic claims recipients) or physical mailing address where we
send misdirected claims, you must provide 90 calendar days advance written notice to your health care provider advocate.
If your address change is related to a claims/encounter processing platform or MSO change, refer to the Notification of
Platform Transitions or Migrations section of this supplement, as those notification timelines differ.
Non UHC West (Medicare Advantage ONLY)
When a claim has been determined to be the responsibility of the delegate, we will issue to the billing provider a provider
remittance advice (PRA) or 835 when billing provider associated with the claim is enrolled for 835, informing them their claim
has been forwarded to another entity. Claim charges that are determined to be the responsibility of the delegate will reflect
a disallow remark code (PRA), or CARC/RARC (835), explaining that the claim was forwarded to the delegate and payer ID
associated with the delegated entity. We forward misdirected claims to the proper payer following state and federal regulations.
If health care providers send claims to a delegated entity, and we are responsible for adjudicating the claim, the delegated entity
must forward the claim to us within 10 business days of the receipt of the claim. Failure to comply with this requirement will lead
to implementation of an Improvement Action (IAP) and possible financial penalties.
The delegated entity must identify and track all claims billed to them received in error. Tracking must include, but is not limited
to, the following relevant information:
1. The name of the entity to which the claim was sent.
2. The received date of the claim by the delegate, and the date sent/mailed (date of forwarding the misdirected claim).
The delegated entity must then forward the claims to the appropriate payer and follow state and/or federal regulatory time
frames.
When the claim is adjudicated, the delegated entity must notify the health care provider of service who the correct payer is, if
known, using the EOP they give to the health care provider.
In the event you, the delegate, change your payer ID (for electronic claims recipients) or physical mailing address where we
send misdirected claims, you must provide 90 calendar days advance written notice to your health care provider advocate.
If your address change is related to a claims/encounter processing platform or MSO change, refer to the Notification of
Platform Transitions or Migrations section of this supplement, as those notification timelines differ.
If you, the delegated entity, received a claim directly from the billing health care provider, and you believe that claim is the health
plan’s responsibility, forward it to your respective UHC Regional Mail Office P.O. Box, which is found on the member’s ID card.
If the address on the back of the ID card is your (the delegate’s) address, refer to the following table to identify where to send
a copy of the claim along with any additional information received. For MA member claims only, include the timestamp of your
Capitation and/or Delegation Supplement
210
2023 UnitedHealthcare Care Provider Administrative Guide
original receipt date on the claim submission. Please forward your claim to the respective addresses noted below, with the
required information.
Claim Benefit Category;la Product Address
Medical Medicare Advantage (MA) Forward claim with cover sheet to:
UnitedHealthcare
P.O. Box 31362
Salt Lake City, UT 84131
Transplant Member - Services related
to transplant
MA Forward claim with cover sheet to:
OptumHealth CMC
P.O. Box 30758
Salt Lake City, UT 84130
Transplant Member - Non-transplant
medical claim
MA Forward claim with cover sheet to:
UnitedHealthcare
P.O. Box 31362
Salt Lake City, UT 84131
Behavioral MA Forward claim with cover sheet to:
Optum Behavioral Health
P.O. Box 30760
Salt Lake City, UT 84130
Dental MA Dates forwarded <1/15/20: forward
claim without cover sheet to following
address.
Dates forwarded =>1/15/20: forward
claim with cover sheet to following
address.
UHC Dental
P.O. Box 30567
Salt Lake City, UT 84130
Vision MA Dates forwarded <1/15/20: forward
claim without cover sheet to following
address.
Dates forwarded =>1/15/20: forward
claim with cover sheet to following
address.
UHC Vision
P.O. Box 30978
Salt Lake City, UT 84130
Pharmacy MA Include OCN received date stamp on
the copy of the claim directly.
Optum Rx
ATTN: Escalated Claims
P.O. Box 650287
Dallas, TX 75265-0287
Capitation and/or Delegation Supplement
211
2023 UnitedHealthcare Care Provider Administrative Guide
Claim Benefit Category;la Product Address
Physical Health
(Chiropractic, Acupuncture, Physical
Therapy, Occupational Therapy,
Speech Therapy related services)
MA Forward claim with cover sheet to
Optum Physical Health - ACN
P.O. Box 30525
Salt Lake City, UT 84130-0525
Hearing Aids (hardware) MA Forward claim with cover sheet to:
UnitedHealthcare
P.O. Box 31362
Salt Lake City, UT 84131
Hearing Screening MA Forward claim with cover sheet to:
UnitedHealthcare
P.O. Box 31362
Salt Lake City, UT 84131
If you, the delegate, receive a misdirected claim from us that you believe to be the financial responsibility of the health plan, and
are requesting a reconsideration of the financial risk determination, please send a PDF image of the claim, with a COMPLETED
Risk Reconsideration form, in Microsoft Word format, along with any relevant information to us via secure email. It is important
to follow these instructions when submitting a financial risk reconsideration:
Please send the secure email to [email protected] with the subject line: COSMOS Delegated Claim
Reconsideration Submission. *Do not put any other information in the subject line.
For each request, please include the following documentation:
1. PDF copy of claim.
2. Completed Risk Reconsideration Form, including an explanation of why you, the delegate, believe the claim is not your
responsibility, but is the health plan’s responsibility. All fields must be completed on the template to be considered
complete. You can download the form at uhcprovider.com/claims.
NOTE: Send one email per claim when requesting a financial risk reconsideration. If you have more than one claim for the same
issue, please submit separate emails with separate completed forms. If you have 20 or more claims for the same issue, please
reach out to your Provider Advocate to discuss alternative submission solutions.
Out of Area (OOA) urgent or emergent claims
In several contractual arrangements, UnitedHealthcare has financial responsibility for urgent or emergent OOA medical and
facility services provided to our members. We follow laws and regulations regarding payment of claims related to access to
medical care in urgent or emergent situations. If we determine the claims are not emergent or urgent, we forward the claims to
the capitated/delegated health care provider for further review. Medical services provided outside the medical group’s/IPA’s
defined service area and authorized by the member’s medical group/IPA are the medical group’s/IPA’s responsibility and are
not considered OOA medical services.
Payment methodology
Health care provider delegates must ensure appropriate reimbursement methodologies are in place for non-contracted and
contracted health care provider claims.
For payment of non-contracted network provider services, the letter, EOP or PRA issued must notify them of their dispute rights
if they disagree with the payment amount. You may not bill members for the difference of the billed amount and the Medicare
allowed amount. MA contracted health care provider claims must be processed following contract rates and within state and
federal regulatory requirements.

Capitation and/or Delegation Supplement
212
2023 UnitedHealthcare Care Provider Administrative Guide
Interest payment
Health care provider delegates must automatically pay applicable interest on claims based on state and/or federal
requirements.
Maximum out-of-pocket (MOOP)
Delegated entities must have a method of tracking individual member out-of-pocket expenses in their claim processing system.
In addition, member cost-share may not be applied once a member has met their out-of-pocket maximum. This helps ensure
members pay their appropriate cost-sharing amount. For more information, see the Member out-of-pocket/deductible
maximum section of this supplement.
ERISA claims processing
For claims falling under the Department of Labor’s ERISA regulations, you must issue denials within 30 calendar days of receipt
of the complete claim. You must issue payments within 45 working days or within state regulation, whichever is more stringent.
The legislation does not differentiate between clean or unclean, or between participating and non-participating claims. Interest
must be automatically paid on all uncontested claims not paid within 45 working days after receipt of the claim. Interest accrues
at the rate established by state regulatory requirements, per annum, beginning with the first calendar day after the 45 working
day period. It must be included with the initial payment. If interest is not included, there is an additional penalty paid to the
health care provider in addition to the interest payment.
Submission of claims for medical group/IPA reimbursement
Insured services
Insured services are those service types defined in the Agreement to qualify for medical group/IPA reimbursement, assuming
the qualifications of certain designated criteria. The medical group/IPA pays the claim and submits it to UnitedHealthcare for
reimbursement. Examples of an insured service could include authorization guarantee or preexisting pregnancy.
Indemnified services
UnitedHealthcare may retain financial risk for services (or service categories) that cannot be submitted through the regular
claims process due to operational limitations. These limitations include ambiguous coding and/or system limitations which
may cause the claim to become misdirected. Misdirected claims are a risk to both organizations in terms of meeting regulatory
compliance and inflating administrative costs.
Claims for insured or indemnified services qualify for payment to the capitated entity as defined in the medical group/IPA
or facility Agreement. Should you have additional questions surrounding this process, speak with your health care provider
advocate.
Medicare Advantage claim processing
MA contracted health care provider claims must be processed based on agreed-upon contract rates and within applicable
federal regulatory requirements. Participating health care provider claims are adjudicated within 60 calendar days of oldest
receipt date of the claim.
Medicare Advantage non-contracted health care provider claims are reimbursed based on the current established locality-
specific Medicare Physician Fee Schedule, DRG, APC, and other applicable pricing published in the Federal Register. Non-
contracted, clean claims are adjudicated within 30 calendar days of oldest receipt date. Non-clean claims are adjudicated within
60 calendar days of oldest receipt date. Clean and unclean claim definition is based on CMS guidelines.
Medicare Advantage interest payment requirements
CMS requires an interest payment on clean claims submitted by non-contracted health care providers if the claim is not paid
within 30 calendar days. Find information on this requirement on CMS.gov.

Capitation and/or Delegation Supplement
213
2023 UnitedHealthcare Care Provider Administrative Guide
Medicaid reclamation claims
Entities with Dual Special Needs Plan (DSNP) delegation must develop and implement a Medicaid reclamation claims process
to help ensure compliance with state-specific reclamation requests.
Medicaid reclamation occurs when a state/agency contacts UnitedHealthcare to recover funds they believe they paid in error
and are now seeking reimbursement in the form of Medicaid reclamation claims.
Medicaid reclamation claims requirements are state-specific and vary by state.
Claims disputes and appeals
Contracted health care provider disputes
Contracted health care providers who have a claim dispute with a delegated medical group/IPA must make sure they have
followed all guidelines set forth by the medical group/IPA.
Overpayment reimbursement for a medical group/IPA/facility (CA only)
A request for reimbursement for any overpayment of a claim completed in compliance with state and/or federal
regulations must:
• Provide a clear, accurate, written explanation.
• Be issued within 365 calendar days from the last date of payment for the claim.
• Commercial claims — Give the health care provider 30 working days to send written notice contesting the request for
reimbursement for overpayment.
Medicare Advantage non-contracted health care provider disputes
Non-contracted health care provider disputes — CMS non-contracted health care provider payment dispute resolution
process (applicable to non-contracted MA paid claims)
A non-contracted health care provider can use the CMS non-contracted health care provider Payment Dispute Resolution
(PDR) process for any decision where they contend the amount paid by the organization (i.e., the delegated entity) for a
covered service is less than the amount which would have been paid under Original Medicare. This PDR process also includes
disagreements between a non-contracted health care provider and the delegate about the delegate’s decision to pay for a
different service than that billed (i.e., rate of payment, DRG payment dispute). The health care provider must submit a payment
dispute within 120 calendar days from the date of the original claim determination. At a minimum, the delegate must have the
following requirements and processes in place when handling claim payment disputes with an MA non-contracted health care
provider:
• Well-defined internal payment dispute process that includes:
– A system for receiving PDRs.
– Proper identification of payment disputes. Health care providers must clearly state what they are disputing and why,
supply relevant information that will help support their position, including description of the issue, copy of submitted claim,
supporting evidence to demonstrate what Original Medicare would have allowed for the same service, etc.
– A system for tracking disputes.
– Monitoring their PDR claims inventory.
• A requirement to communicate the time frame of 120 calendar days from the original claim determination to submit a
payment dispute to the non-contracted health care provider at time of claim payment.
• Information on how to submit an internal claim payment dispute to the organization communicated to the non-contracted
health care provider at time of claim payment, including their mailing address for submitting disputes and other dispute
information (e.g., email addresses, phone numbers).
• Requirements to process and respond (i.e., to finalize the PDR claim) to the non-contracted health care provider within 30
calendar days from the date the PDR claim is received (oldest received date of the PDR claim).

Capitation and/or Delegation Supplement
214
2023 UnitedHealthcare Care Provider Administrative Guide
• Help ensure correct calculation of interest payments on overturned PDRs. Interest payment is required on a reprocessed,
non-contracted health care provider clean claim if the group made an error on the original determination. Interest is only
applied on the additional amount paid if the original claim was clean and calculated from the oldest receive date of the
original claim until the check mail date of the additional amount paid.
• Provide a complete and clear rationale to the non-contracted health care provider for upheld PDRs.
• Help ensure the PRA, EOP and uphold PDR determination letter have the right information and meet requirements.
• Include information on how to contact the organization in notices of upheld or overturned payment disputes if the non-
contracted health care provider has questions.
• Include information in the notices of upheld or overturned payment disputes on how to contact the organization if the non-
contracted health care provider has questions.
• If the root-cause of overturned PDRs is system-related, have a process in place to update their claims system so future claims
will reimburse appropriately.
• Have a process in place that identifies trends that contract year for any non-contracted health care provider who submitted a
payment dispute to help ensure they are paid correctly.
• Have an ongoing training program in place for any piece of the internal claim PDR process that educates all areas of the
organization, such as customer service, claims, appeals.
• Monitor internal compliance to help ensure CMS requirements are met.
• Follow an end-to-end quality review process. It should start when a dispute is received from the non-contracted health care
provider until the dispute decision is sent to the non-contracted health care provider.
Excluded from the payment dispute resolution
The following are examples of issues excluded from the PDR process:
• Instances in which a member filed an appeal, and you filed a dispute regarding the same issue. In these cases, the member’s
appeal takes precedence. You can submit a health care provider dispute after the member appeal decision is made. If you are
appealing on behalf of the member, the appeal processes as a member appeal.
• An Independent Medical Review initiated by a member through the member appeal process.
• Any dispute filed outside of the timely filing limit applicable to you, and for which you fail to supply good cause for the delay.
• Any delegated claim issues not reviewed through the delegated payer’s claim resolution mechanism.
• Any request for a dispute, which involves reviews by the delegated medical group/IPA/payer or capitated facility/health care
provider and does not involve an issue of medical necessity or medical management.
Delegated claims reporting
All states: Use the most updated Medicare Advantage (MA) and Commercial Monthly Timeliness Report (MTR) you received
from the Claims Delegation Oversight Department.
1. MTR forms, both monthly and quarterly reports, are due by the 15th calendar day of each month or the following business
day if the due date falls on a weekend or holiday.
2. Claims Activity Reports/data files are due on the 15th calendar day of each month or the following business day if the due
date falls on a weekend or holiday.
3. PDR quarterly reports are due:
– First Quarter: April 30
– Second Quarter: July 31
– Third Quarter: Oct. 31
– Fourth Quarter: Jan. 31
If the due date for the PDR falls on a weekend or holiday, provide the following business day.
4. Submit Claims Activity Reports in the template or format UnitedHealthcare requests. This includes existing methods of
submitting reports and any enhancements made throughout the year to meet regulatory and/or health plan requirements.
Delegated entities must complete an Improvement Action Plan (IAP) and submit it to the health plan for submitting untimely
reports or reports containing inaccurate or incomplete information.

Capitation and/or Delegation Supplement
215
2023 UnitedHealthcare Care Provider Administrative Guide
All delegated entities must upload their Claims Activity Reports, claims data files and MTR forms to the ECG Connect Portal.
Upload monthly MTR forms to the ECG Connect Portal by the 15th calendar day of each month. Upload Claims Activity Reports
to the ECG Connect Portal by the 15th calendar day of each month.
Reporting due dates may change, and you must submit reports to the health plan by the established due date(s).
Based on either state regulatory requirements (CA), or other contractual requirements, UnitedHealthcare shall verify on a
quarterly basis that our delegated entities have the administrative and financial capacity to meet contractual obligations through
routine reviews of financial indicators and monitoring financial solvency deficiencies. UnitedHealthcare requires delegated
entities to provide copies of quarterly financial statements, including a balance sheet, income statement and statement of cash
flow. Prepare these based on generally accepted accounting principles within 45 calendar days of the end of each calendar
quarter.
Submit copies of assessed annual financial statements together with copies of all auditors’ letters to management in connection
with such reviewed annual financial statements submissions within 150 calendar days of the end of each fiscal year. If these
financial statement submissions have deficiencies in financial solvency grading criteria defined by state regulations, submit a
self-initiated CAP proposal in an electronic format (template may be found on the Iceforhealth.org website) to UnitedHealthcare
within 45 calendar days of the end of the reporting period for which the deficiency was reported. In addition, submit quarterly
progress reports to UnitedHealthcare within 45 calendar days of the end of each subsequent reporting period until compliance
with all financial grading criteria achievement.
Email financial statements and IAP to UnitedHealthcare at [email protected].
Both UnitedHealthcare and the delegated entity must provide compliance oversight of the delegated entity’s financial
reporting IAP.
CA Commercial NPI
The California Department of Managed Health Care (DMHC) Timely Access to Non-Emergency Health Care Services Regulation
applies to California Commercial HMO membership only. The regulation establishes time-elapsed standards or guidelines to
make sure members have timely and appropriate access to needed health care services, including a 24/7 telephonic triage
or screening requirement. Health plans must comply with certain provisions of the regulation and provide an annual report
detailing the status of the plan’s network care provider and enrollment, which includes the health care provider’s NPI. To comply
with this regulation, UnitedHealthcare requires all California Commercial HMO health care providers to include their NPI with all
health care provider additions or when submitting a claim.
PDR requirements for delegated commercial claims (CA only)
A delegated entity that is contractually delegated to process claims or approve referrals for service must have a fair, fast and
cost-effective dispute resolution mechanism. This process must help manage contracted and non-contracted health care
provider disputes based on state and federal regulations.
If the dispute request is for services payable by the delegated entity, we determine if the appropriate payer has reviewed
the request for dispute. If the appropriate payer has not reviewed the dispute request, we forward the dispute request to the
appropriate payer. We notify the health care provider of service of the forwarding dispute request to the delegated entity
for processing.
The delegated entity must submit all required information to us and the appropriate state agency based on state and federal
regulations. All delegated claims processing entities are required to report PDR processing compliance results quarterly based
on state and federal regulations. Submit quarterly reports no later than the 30th day following the end of the quarter.
We regularly conduct a compliance assessment of the PDR Process of each delegated entity, typically on an annual basis.
As part of the compliance assessment, we request data files and related reports of Delegated Entity Provider Disputes. The
auditor reviews the dispute data and randomly selects finalized disputes for review. The auditor also requires a copy of the
delegated entity’s PDR Policy and Procedures and evidence of the availability of the PDR mechanism. If the capitated medical
group/IPA or capitated facility is non-compliant with UnitedHealthcare, state or federal requirements, the delegated entities
must develop a IAP designed to bring them back into compliance. If the delegate entity does not achieve compliance, UHC will
employ its Claims Management Consulting Services (CMCS) model. The delegate is charged for all CMCS activities associated
with IAP remediation. For further details see the Non-compliant assessments section.

Capitation and/or Delegation Supplement
216
2023 UnitedHealthcare Care Provider Administrative Guide
If you continue to have a commercial claims dispute with the delegated entity related to medical necessity and utilization
management, forward all claim information and correspondence between the delegated entity and you to UnitedHealthcare for
review. We do not begin the review until we receive the supporting documentation.
Commercial health care provider claims must be processed based on agreed-upon contract rates or member benefit plan and
within state and federal requirements.
Note: Date stamps from other health plans or insurance companies are not valid received dates for timely filing determination.
Commercial interest rates and time frames for processing may vary, depending on the applicable state requirements. In some
states, an additional penalty for late claims payments may also apply and be paid by the delegated medical group/IPA/facility.
Contractual and financial responsibilities
Compliance with CMS
As an MA plan, UnitedHealthcare and its network providers agree to meet all laws and regulations applicable to recipients of
federal funds. The medical group/IPA and capitated facility acknowledge they must comply with certain laws applicable to
entities and individuals receiving federal funds.
Changes in risk status during inpatient admissions
An inpatient admission includes:
• Inpatient acute care.
• SNF.
• Detoxification.
• Medical rehabilitation.
• All related services.
Partial risk to shared risk
If a member’s assigned health care provider is partial risk at the time of admission and then changes to shared risk prior to the
member’s discharge, all claims related to this confinement from admission through discharge are processed according to the
partial risk DOFR in effect at the time of the admission.
Shared risk to partial risk
If a member’s assigned health care provider is shared risk at the time of admission and then changes to partial risk prior to
the member’s discharge, all claims related to this confinement from admission through discharge processed according to the
shared risk DOFR will be in effect at the time of the admission.
Collection of fees
When a member needs one of the following forms for reasons other than medical reasons, you may collect a fee, in
addition to the office visit copayment, for completion of these forms (unless the member’s benefit plan or applicable law
dictates otherwise):
• DMV forms
• Camp or school forms
• Employment or insurance forms
• Adoption form
You cannot collect an additional fee, copayment, or surcharge for:
• Completion of Prior Authorization form for non-formulary drugs.
• Completion of disability forms.

Capitation and/or Delegation Supplement
217
2023 UnitedHealthcare Care Provider Administrative Guide
• Missed appointments/no shows or late cancellations.
• Times when a member cannot pay office visit copayment at the time of visit for basic health care services. The medical
group/IPA may reschedule the member’s appointment. If the member requires urgently needed care or emergency care, the
medical group/IPA must render care.
You can collect copayments when professional services are rendered by a:
• Licensed medical doctor or doctor of osteopath as defined by the state.
• Physician assistant.
• Nurse practitioner.
Do not collect copayments when there is no actual office visit. For example:
• Injections administered by a nurse or medical assistant.
• Routine immunizations administered by a nurse or medical assistant.
Member out-of-pocket/deductible maximum
We are required to monitor and track each member’s annual individual out-of-pocket/deductible maximum amount. The
member’s annual individual out-of-pocket/deductible maximum accumulation is calculated through the member’s cost-share
data collected from all or some of the following sources:
• Medical group/IPA/capitated hospital encounters
• Prescription related encounters
• Behavioral health-related encounters
• Claims processed by UnitedHealthcare or its delegates
UnitedHealthcare and its capitated health care providers share responsibility to monitor the member’s individual out-of-pocket/
deductible maximum. For additional information on reporting available from UnitedHealthcare, see Chapter 11: Compensation
of this guide.
UnitedHealthcare monitors the capitated health care provider’s compliance with this policy to help ensure all requests for
claims reprocessing and member reimbursement are completed timely. Failure to comply with all requirements will result in an
Improvement Action Plan (IAP) that may lead to financial penalties and potential loss of delegation responsibilities if not cured.
If necessary, we work with the capitated health care provider to help ensure each member is reimbursed for any amounts
collected in excess of the member’s annual individual out-of-pocket/deductible maximum amounts as specified in the
member’s benefit plan.
If the capitated health care provider fails to reimburse a member for amounts collected in excess of the member’s annual
individual out-of-pocket/deductible maximum, we may reimburse the member directly and recover the payment by capitation
deduction as specified in your Agreement.
In the event a delegate is not meeting any one of the performance standards, we will send a formal notification to the delegate
and initiate a cure period. The cure period is the time frame we give the delegated entity to demonstrate compliance. The
cure period could be 30 to 60 days. If the performance standard(s) are not cured within the defined cure period, an IAP will be
issued, and financial consequences could be implemented. UHC MOOP Oversight will require regularly scheduled meetings
with the delegate to ensure progress is being made towards meeting those requirements. Should the delegate fail to meet those
requirements within the allotted time frame, UHC MOOP Oversight may bill the delegated entity for all activities surrounding the
remediation of the IAP. UHC MOOP Oversight will charge an initial fee of $2,500 plus $100/hour to assist the delegate for the
first month of the IAP, and $250 per hour after the first month of the IAP until the IAP is closed.
Member cost share operational overview
• Cost-share information comes from different sources derived through claims and encounter data submissions.
• Delegated entities can view up-to-date cost-share information including various reports that they can download on
uhcprovider.com. Reach out to your health care provider advocate for further details.
• Delegated entities can contact [email protected] for any member out-of-pocket inquiries.
Capitation and/or Delegation Supplement
218
2023 UnitedHealthcare Care Provider Administrative Guide
• Delegated entities are responsible for updating their systems within 2 business days of receiving the notification from
UnitedHealthcare that a member met their maximum out-of-pocket costs. This helps ensure members not charged for
copayments, coinsurance and deductibles once the annual maximum is met.
When a member meets their annual individual out-of-pocket/deductible maximum, UnitedHealthcare notifies the member’s
capitated health care provider. Delegated entities must work with UnitedHealthcare to address member issues related to out-of-
pocket balances. This includes:
• Responding to a UnitedHealthcare request for data on care services provided to a member:
– Within 24 to 48 hours for escalated issues.
– Within 5 calendar days on standard issues.
• For claims identified by UnitedHealthcare to be re-processed by the delegated entity:
– Within 7 calendar days, adjusting cost-share amounts, reprocessing the claims and confirming transactions with
UnitedHealthcare.
– Within 14 calendar days, submitting the corrected encounter data. The Delegate is responsible to refund the member any
cost share amounts collected in excess of the member’s annual individual out-of-pocket and deductible maximums and to
verify that the member received all appropriate reimbursements. Failure to comply with these requirements may result in an
improvement action plan that may lead to financial penalties and loss of delegation if not addressed appropriately. Please
refer to the Non-compliant assessments section for further information on the improvement action plan and the associated
employment of the CMCS model.
Financial risk disputes between UnitedHealthcare and the delegated entity
To help ensure timely processing of service health care provider claims, delegated entities are responsible for working with
UnitedHealthcare to address financial risk dispute issues. This includes:
• When UnitedHealthcare requests data from the delegated entity on claim processing status and/or clarification on claim
financial risk determinations, you must respond within:
– 24-48 hours for escalated issues (i.e., regulatory or urgent member/provider issues).
– 5 calendar days on standard issues.
• When UnitedHealthcare identifies claims to be re-processed by the delegated entity to resolve service health care provider or
member issues:
– Reprocess the claims and confirm transactions with UnitedHealthcare within 7 calendar days.
– Submit the corrected encounter data within 14 calendar days.
Failure to comply with these requirements may result in an improvement action plan that may lead to financial penalties and loss
of delegation if not addressed appropriately. Please refer to the Compliance assessments section for further information on
the policies and procedures in place to help ensure health care provider compliance with contractual state and federal claims
processing requirements. Please refer to the Non-compliant assessments section for further information on the improvement
action plan and the associated deployment of the Claims Management Consulting Services (CMCS) model.
Encounter data requirements
Professional and institutional encounter data consist of an itemization of medical group/IPA/capitated facility, capitated and
sub-capitated services provided to our commercial or MA members.
We require you to transmit your encounter data on a weekly basis, at a minimum. We also welcome your encounter submissions
more frequently. Frequent encounter submissions allows us to support various state and federal regulatory requirements for
reporting, such as risk adjustment reporting for Medicare reimbursement from CMS, member out-of-pocket costs, STARS
reporting and NCQA and HEDIS reporting.
We request that you use one of our preferred clearinghouses to transmit your
encounters. Contact [email protected] for this information.
Capitation and/or Delegation Supplement
219
2023 UnitedHealthcare Care Provider Administrative Guide
We continuously monitor encounter data submissions for quality and quantity. Our delegated groups should meet or exceed
current established thresholds, as defined by the UnitedHealthcare Encounter Operations Team. As you are processing claims
on our behalf, we expect all encounter submissions to accurately reflect the original claim received from the provider. Delegates
are required to send replacement or void encounters for both commercial and MA lines of business, if applicable. Delegates
send a replacement encounter when information on the original logged encounter at UnitedHealthcare needs to be corrected.
A void submission is required to eliminate a previously submitted logged encounter at UnitedHealthcare. Delegates should not
send replacements and voids when the original encounter is rejected by a clearinghouse or by UnitedHealthcare.
For examples of when a replacement or void encounter should be submitted and the required details on submitting
them within the 837P and 837I ASC X12 EDI format, refer to section 6.1 of the Electronic Claim Submission Guidelines
in the UnitedHealthcare Companion Guides or contact [email protected]. All encounter data submitted
to UnitedHealthcare are subject to state and/or federal audit. We have the right to perform routine medical record chart
assessments on any or all of the medical group’s/IPA’s network providers at such time or times as we may reasonably elect to
determine the completeness and accuracy of encounter data ICD-10-CM and CPT coding. We notify the medical group/IPA in
writing of audit results for coding accuracy.
The delegate may be subject to the implementation of a Improvement Action Plan (IAP) and/or financial consequences if it or
any sub-delegated entity fails to submit or meet encounter data element requirements as outlined here in this guide and or the
delegates contractual agreement with UnitedHealthcare.
In the event a delegate is not meeting any one of the performance standards, we will send a formal notification to the delegate
and initiate a cure period. The cure period is the time frame we give the delegated entity to demonstrate compliance. The cure
period could be 30 to 60 days depending on the severity of the deficiency. If the performance standard(s) are not cured within
the defined cure period, an IAP will be issued, and financial consequences could be implemented.
Encounter Operations will require regularly scheduled meetings with the delegate to ensure progress is being made towards
meeting those requirements.
Delegates will be held to the following performance standards. UHC Encounter Operations/Delegation Oversight will deploy its
Claims Management Consulting Services (CMCS) to assist with remediation of the IAP. CMCS may consist of conducting virtual
or on-site operational assessments, oversight and monitoring. UHC will charge the delegate for all CMCS activities with an initial
fee of $2,500 plus $100/hour for the first month of the IAP and $250 per hour after the first month of the IAP until the IAP is
closed.
Timeliness
• 90% of encounters received within 90 days of the date of service. If less than 90% for 3-consecutive months, cure period will
be enforced.
• 95% of encounters received within 14 calendar days of the delegate’s claim adjudication date. If less than 95% for
3-consecutive months, cure period will be enforced.
Accuracy
• <=2% of encounters rejected as a % of total encounter submissions based on the most current month’s submissions for
current year’s dates of service reporting period
• <= 10% edits aged over 90 days from the date of rejection for current year’s dates of service reporting period
Completeness
• >=95% of encounters received within 3 months from the initial month where it was identified that encounters were not
received based on monthly claims processed by the delegate.
System/software upgrades, change in claims platforms, change to new clearinghouse
When system/software upgrades occur, you will be required to test your encounter files. Changes/modifications to the
platforms and applications used to process claims and encounters will be required to complete testing with your clearinghouse
and UnitedHealthcare. Should you be required to test your files with your clearinghouse and UnitedHealthcare due to the
following:
• A brand new delegate
• Implementing a new claims platform

Capitation and/or Delegation Supplement
220
2023 UnitedHealthcare Care Provider Administrative Guide
• Software upgrades
• Change to a new clearinghouse
Our expectation is that the exchange of test files between the clearinghouse and UnitedHealthcare should not exceed three
months. Should you exceed the three-month testing window without approval to move to sending production files, we will
implement an Improvement Action Plan (IAP), which will include monthly financial penalties for non-compliance of encounter
data submission requirements until compliance is reached.
If changing to a new clearinghouse, you are required to obtain approval from the UnitedHealthcare Encounter Operations team.
There is special advance setup required at UnitedHealthcare and your new clearinghouse for encounters to be transmitted
and processed successfully at UnitedHealthcare. Please include your UnitedHealthcare provider advocate and encounter data
business analyst in your 270-day advance notification to UnitedHealthcare. Following these guidelines will ensure your data is
837 5010 EDI compliant and reduce gaps in your weekly encounter submissions.
Refer to the Notification of Platform Transitions or Migrations section for more information.
Commercial encounter data requirements
The capitated medical group/IPA, or other submitting entity, must certify the completeness and truthfulness of its encounter
data submissions as required by the state regulatory agency. The medical group/IPA, or other submitting entity, must submit all
professional and institutional encounter data for UnitedHealthcare members to:
• Comply with the Affordable Care Act for Essential Health Benefits (EHB) and NCQA-HEDIS® reporting requirements.
• Enhance member and health care provider service quality.
• Provide the medical group/IPA, or other submitting entity, with comparative data.
• Facilitate settlement calculations if applicable, and oversight of utilization management and quality management.
• Report member out-of-pocket maximums.
We require capitated medical groups/IPAs and capitated facilities to submit timely and compliant encounter data. Include
the member cost-share amount on the encounter data submissions based on the member’s benefit plan, not the amount the
member paid at the time of service. The encounter should clearly distinguish between copayment, coinsurance and deductible
amounts within the Claim Adjustment Segments (CAS) segment of Loop 2430, as indicated on the ANSI ASC X12N 837 Health
Care Claims transaction for each service line of your assigned commercial members.
Check with your clearinghouse to verify the appropriate payer ID to use to send your encounters to them, or contact
The Affordable Care Act dictates reporting requirements. To comply with those requirements, we require all contracted
health care providers to submit all diagnosis and procedure codes to the highest level of specificity relevant to the encounter
data submission. If the encounters do not include specific information, or data elements are invalid or missing, the
clearinghouse will reject them.
For more information on UnitedHealthcare encounter data submission requirements, refer to the UnitedHealthcare’s EDI
MA encounter data requirements
CMS reimburses all MA plans based on the member’s health status. They use the diagnosis codes from the MA claims and/
or encounter data (inpatient, outpatient and health care provider) to establish each member’s health status or Hierarchical
Condition Category (HCC). CMS uses the HCC to help calculate Medicare reimbursement payments for each member.
As a result, we are required to send all adjudicated claims and capitated encounter data for MA members to CMS.
These claims and encounters must pass all the edits CMS applies to its fee-for-service HIPAA 5010 837 and CMS-1500 and UB-
04 submissions.
To reduce rejected claims, delegates must process MA claims and encounters in the same manner as their Medicare Fee-For-
Service bills. Delegates are subject to the specific claims submission and other requirements stated in this guide.
CMS may at any time audit our submissions. The medical record must support the diagnoses you submit. Only the health care
provider can change or submit new CMS-1500 or UB-04 data, so your cooperation is required for us to submit the correct data.

Capitation and/or Delegation Supplement
221
2023 UnitedHealthcare Care Provider Administrative Guide
We require the medical group/IPA/capitated facility or other submitting entity to submit all professional and institutional claims
and/or encounter data for MA members to:
• Comply with regulatory requirements of the CMS Balanced Budget Act (BBA), and NCQA-HEDIS reporting requirements.
• Enhance member and health care provider service quality.
• Submit to us for risk adjustment reporting and accurate Medicare reimbursement so we can submit to CMS.
• Provide the submitting entity with comparative data.
• Facilitate utilization management oversight, quality management oversight and settlement calculation, if applicable.
• Support Services 75 FR 19709-Maximum Allowable Out-of-Pocket Cost Amount for Medicare Parts A and B.
To comply with the CMS regulation 75 FR 19709 to report member cost-sharing as well as out-of-pocket maximums, we require
contracted health care providers to submit current, complete and accurate encounter data. This includes member cost-sharing/
revenue, within the CAS segment of the ANSI ASC X12N 837 Health Care Claims transaction for each service line of your
assigned MA members. Check with your clearinghouse to verify the appropriate payer ID to use to send your encounters to
them, or contact [email protected].
CMS requires EOBs for Part C benefits to report total costs incurred by the health plans (UnitedHealthcare) for capitated and/or
delegated health care provider services.
Medicare Advantage organizations (MAOs) are required to report the total costs incurred for capitated and/or delegated health
care provider services. MAOs must populate dollar amounts for capitated and/or delegated health care providers in the “Total
cost” and “Plan’s share” columns in the monthly EOB. The “Total Cost” field on the member EOB includes what the member
pays (“Your Share” on the EOB) and what the health plan (“Plan Paid” on the EOB) pays.
The MAOs, capitated medical groups, facilities and ancillary health care providers must submit the payer amount paid at
the claim level, the Service Line Paid Amount, and the member cost-sharing for all professional and institutional Medicare
encounter data. The payer amount paid submitted in the encounter should not be a zero unless the claim was denied.
We also refer to the payer amount paid as the contracted rate, Medicare Fee Schedule Rate, or Calculated Capitation Rate less
any applicable member responsibility. For more information on CMS EOB requirements, refer to cms.gov > Medicare > Health
Plans.
All encounter data submitted to UnitedHealthcare are subject to state and/or federal assessment. We have the right to perform
routine medical record chart assessments on any or all of the medical group’s/IPA’s network providers at such time or times
as we may reasonably elect to determine the completeness and accuracy of encounter data, ICD-10-CM and CPT coding. We
notify the medical group/IPA in writing of audit results for coding accuracy.
For further details on UnitedHealthcare encounter data submission requirements, refer to the UnitedHealthcare EDI Companion
Customer service requirements between UnitedHealthcare
and the delegated entity (Medicare)
To help ensure timely support for member customer service requests, the delegated entity is responsible for working with
UnitedHealthcare to address member service requirements, member/patient communication, and data sharing requests.
This includes:
• Specific toll-free number (TFN) for service-related inquiries where you must respond with:
– An average monthly service level at 80% or higher.
– Average speed of answer (ASA) within 30 seconds or less.
• When UnitedHealthcare requests data from the delegated entity requiring additional research on claim processing status
and/or clarification on claim financial risk determinations and/or Utilization Management processing status, you must
respond within:
– 2 business days on escalated issues.
– 5 business days on standard issues.

Capitation and/or Delegation Supplement
222
2023 UnitedHealthcare Care Provider Administrative Guide
• Providing details related to specific member/patient communication on programs offered by the delegated entity. Failure to
comply with all requirements could result in financial penalties and/or loss of delegation responsibilities.
OptumCare Care Delivery Organization customer service specific requirements
The delegated entity is responsible for working with UnitedHealthcare to address member service requirements, member/
patient communication and data sharing requests.
This includes:
• Dedicated phone line for service-related inquiries where you must respond with:
– An average monthly service level at 80% or higher.
– ASA within 30 seconds or less.
– Weekly/monthly call metrics with UnitedHealthcare leadership including call volume, calls per 1,000 members, service
level, ASA, transfer rate and experience (post-call survey).
• Online chat capability between UnitedHealthcare member service advocates and OptumCare advocates.
– Sharing online chat metrics between UnitedHealthcare and OptumCare advocates.
• When UnitedHealthcare requests data from the delegated entity requiring additional research on claim processing status
and/or clarification on claim financial risk determinations and/or utilization management processing status, you must respond
within:
– 1 day on escalated issues.
– 2 days on standard issues.
• Providing details related to specific member/patient communication on programs offered by the delegated entity including
outbound call campaigns.
Capitation reports and payments
Capitation reports
UnitedHealthcare runs capitation reports by process month for both commercial and MA products. Typically, each month’s
capitation report and payment reflects all current activity and retroactivity up to the standard 6-month system window. The
Agreement may define a non-standard eligibility window for less than the standard 6-month system window. This non-standard
eligibility window will override the standard 6-month system window. For MA plans, the non-standard eligibility retro window will
not limit the retroactivity related to premium increases/decreases from CMS.
Capitation reports and first-of-the-month eligibility reports run from the same snapshot of membership data. The actual date of
this snapshot varies but typically occurs on or around the 15th calendar day of the prior month for commercial and during the
last week of the prior month for MA.
The reports mentioned throughout this section are available online and provide detailed information regarding each health care
provider’s capitation payments. The types of reports available include:
• Flat file — Contains approximately 198 data elements in CSV (comma separated value) format.
• Image reports — In PDF format and are at both the member and summary levels.
• Supplemental health care provider reports — Details any non-standard deductions from capitation (i.e., claims that are the
financial risk of the health care provider and paid by UnitedHealthcare).
Reports are available on uhcprovider.com/reports on the date specified in your Agreement. If the due date falls on a non-
business day, the reports are available the next business day.
• Reports —View image reports in a PDF format (Adobe Acrobat is required) or download the file.
• Data Files — Download the flat files from a zipped file format.
• All —Download image reports and flat files in 1 zipped file.

Capitation and/or Delegation Supplement
223
2023 UnitedHealthcare Care Provider Administrative Guide
Claims withhold reports and data files
Supplemental health care provider Reports for Claims Withhold are available online. These reports have 2 capitation reporting
options described in the following section: Reports and data files.
Medical drug benefit reports and data files
Medical Drug Benefit reports are available online.
The Claims Withhold and Medical Drug Benefits reports are 1 month behind the current Capitation Report month. For example,
all claims on the Claims Withhold and Medical Drug Benefit reports that paid in April will process in May capitation. To reconcile
May capitation, view the April Claims Withhold and April Medical Drug Benefits Reports.
The Shared Risk Claims Report is also dated 1 month behind the current Capitation Report month. For example, all Shared
Risk claims paid in May will process in the June capitation.
We maintain capitation and eligibility reports online for the current month and the previous 2 months.
We recommended you complete your capitation download in a timely manner to make sure you have complete and accurate
capitation information.
Hierarchical Condition Category and capitation reporting
CMS payments are based on the Hierarchical Condition Category (HCC) Reporting. This payment methodology requires MA
health plans to submit accurate diagnosis information at the greatest level of specificity available.
CMS HCC risk adjustment
We offer an alternate method of reporting CMS risk adjustment data in addition to the normal claim/encounter submission
process. All encounter submissions are required to process the 837 Claim/Encounter in a HIPAA 5010-compliant format. To
supplement a previously submitted 837 Claim/Encounter, submit an 837 replacement Claim/Encounter, or send additional
diagnosis data related to the previously submitted 837, through the Optum ASM Operations FTP process. If you choose
to submit via ASM, you first need to contact the Optum ASM Operations team at [email protected] to start the
onboarding process.
Access health care provider reports on uhcprovider.com/reports, or use Document Library in the
UnitedHealthcare Provider Portal.
Capitation processing
Capitation is typically a PMPM payment to a medical group/IPA or facility that covers contracted services for assigned
members. This is an alternative to the fee-for-service arrangement. Capitation payments made whether or not the member
seeks services from the capitated health care provider.
• Under a shared risk arrangement, the medical group/IPA receives capitation for professional services rendered to its
assigned members.
• Under a partial risk contract, the facility also receives capitation for institutional services rendered to their assigned members.
Refer to the Division of Financial Responsibility (DOFR) grid in your Agreement for a detailed listing of capitated services.
Services not specifically excluded from capitation are included in the capitation payment made to the medical group/IPA
or facility.
Facility and regulatory surcharges
The Managed Care Risk Entity (MCRE) is responsible for calculating all facility and regulatory surcharges that may be incurred
by their member panels.
Capitation and/or Delegation Supplement
224
2023 UnitedHealthcare Care Provider Administrative Guide
15/30 rule
The capitation system uses a 15/30 rule to determine whether capitation is paid for the full month or not at all. If the effective
date of a change falls between the first and 15th of the month, the change is effective for the current month, and capitation paid
for that month. However, if the effective date falls on the 16th or later, the change reflected the first of the following month and
capitation paid for the following month.
For capitation payments, we add members on the first day of the month or terminate on the last day of the month. Newborns are
added on their dates of birth. We pay or recoup commercial capitation for full months.
Retroactive add
A member added retroactively between the first and the 15th of the month would generate a capitation payment for the entire
month. However, a member added on the 16th or later would not generate a capitation payment for that month even though
they would be considered eligible for services.
Retroactive term
A member retroactively terminated between the first and 14th of the month would generate a capitation recoupment entry for
the capitation previously paid for the entire month. However, a member retroactively terminated on the 15th or later would not
generate a capitation recoupment entry for the capitation previously paid for the entire month.
Capitation payments
We make monthly capitation payments to the medical groups/IPAs and capitated facilities for providing and arranging covered
services to our members.
We deliver capitation payments through check or electronic funds transfer on the date listed in the Agreement. If the due date
falls on a non-banking day, we deliver the capitation payment the next banking day.
Electronic funds transfer (EFT)
To receive capitation payments through EFT, we require a signed EFT Payments form detailing the bank account and bank
routing information. It takes 3 weeks for the EFT initial setup, or a change in banking information, to take effect.
We deposit capitation payments through EFT by the end of the banking/business day on the date specified in the Agreement.
Note: Most financial institutions charge a per transaction fee on EFTs.
Use the UnitedHealthcare Provider Portal to access and submit Authorization Agreement Payments forms.
For detailed instructions on EFT enrollment, click here.
Additional information and requirements for claims payment
options can be found in Chapter 10: Our claims process.
Capitation calculation methods (Commercial)
Capitation calculation methods are detailed in your Agreement. For commercial products, we use 5 capitation
calculation methods:
Flat Rate Calculation: A flat rate (PMPM) capitation calculated by applying the flat rate for each member to yield the standard
services capitation amount. The flat rate is detailed in your Agreement. Both the flat file and the image reports display each
member-level transaction.
Fixed Rate Age/Gender Adjusted Calculation: Fixed rate age/gender adjusted capitation uses age/gender factors to modify
the flat base rate up or down to align standard services capitation with age-weighted risk. The flat base rate multiplied by the
age/gender factor yields the standard services capitation amount.
Age/gender factors work to weight for age/gender risk consideration with respect to the demographic population.
UnitedHealthcare actuarially develops age/gender factors. The age/gender factors may vary between medical groups/IPAs and
are included in the Agreement.

Capitation and/or Delegation Supplement
225
2023 UnitedHealthcare Care Provider Administrative Guide
We report the age/gender factors and standard services capitation amount at the member level on the flat file. Only the
standard services capitation amount is reported on the image reports.
Fixed Rate Age/Gender/Benefit Adjusted Calculation: Fixed rate age/gender/benefit adjusted capitation contains 3
components: flat base rate, age/gender factor and benefit factor.
Fixed Rate Age/Gender/Copayment Adjusted Calculation: Copayment adjustment works to evaluate the member’s
copayment made directly to the health care provider. We actuarially derive the copayment adjustment for each copayment level.
• We add or subtract the copayment adjustment from the flat base rate. The sum of flat base rate +/- copayment adjustment
multiplied by, the age/gender factor to yield the standard services capitation amount. We report the flat base rate, age/gender
factor, copayment adjustment and standard services capitation amounts at the member level on the flat file. The image
reports only show the standard services capitation amount.
Professional Risk Capitation Model: Base capitation rate × risk adjustment factor (Optum Symmetry Episode-Related Group
[ERGs]) × benefit plan factor × geographic factor).
Commercial capitation contracts with multiple rates
The capitation source system can administer a single commercial contract with multiple rates, if the contract requires a different
rate for members enrolled in a specific plan or in-network. These contracts are identified by the Primary Care Provider Network
Indicator (PCPNI). The 4 capitation calculation methods described in the Capitation Calculation Methods section apply. This
option is available for commercial contracts. It allows you to manage your capitation under 1 medical group/IPA number.
Capitation transactions reports can be summarized or detailed. All individual transactions are summarized by PNI code and
reported on several capitations image reports. There are also detailed health care provider PNI transactions reports on both the
flat file (CP7810, column U, field 21) and image reports (CP7210, CP7230). Member PNI is reported on the flat file (CP7810,
column AP, field 42).
Capitation calculation for Medicare Advantage
For MA products, we use 3 capitation calculation methods:
• Flat rate — A rate is paid PMPM. We calculate the flat rate capitation by applying the flat rate for each member to give us the
standard services capitation amount. The Agreement details the flat rate. Both the flat file and image reports display each
member level transaction.
• Percent of premium — The percent of CMS premium calculation begins with the premium identified from the CMS Monthly
Membership Report (MMR), less any premium adjustments, and multiplied by the contracted percentage.
The net of all adjustments is the CMS premium. The flat file (1 R record type), shows the CMS premium at the member level
with the field name Cap_Premium_Gross_Cap.
Medical groups/IPAs and capitated facilities with a percentage-of-premium contract receive their contracted percentage rate
of this cap premium gross cap amount as the standard services capitation amount for each member.
The flat file (1 R record type) shows the standard services capitation amount at the member level by summing the fields
Group_Capitation_Amt plus Facility_Capitation_Amt. Image reports also show the standard services capitation amount at the
member level.
• Risk adjusted fixed rate —We calculate capitation using the base rate detailed in the Agreement, multiplied by
various factors.
It contains 3 components:
1. Base rate — as detailed in the Agreement.
2. Risk Adjusted Factor (RAF) — the score for each MA plan member taken directly from CMS’ Monthly Membership Report
(MMR). This factor is reported on the flat file and image reports.
3. Health status variables are the base rate adjusted for members categorized as ESRD or Hospice by CMS on the MMR. For
details on the ESRD and Hospice adjustments, see your Agreement.
The risk-adjusted fixed rate capitation amount will vary monthly resulting in changes in the risk adjustment factor and
demographic factors for MA plan members for that month. Both the flat file and image reports show each member-level

Capitation and/or Delegation Supplement
226
2023 UnitedHealthcare Care Provider Administrative Guide
transaction. The risk-adjusted fixed rate capitation has the standard 6-month system retro window. Payments made by CMS
outside the 6-month retroactivity window are not included.
Medicare Advantage capitation contracts with multiple rates
The capitation source system can administer a single MA contract with multiple Percent of Premium rates, if the contract
requires a different rate for members enrolled in a specific plan or network. These contracts are identified by the Primary Care
Provider Network Indicator (PCPNI). The capitation calculation methods described in the capitation calculation section apply.
This option is available for MA contracts. It allows you to manage your capitation under 1 medical group/IPA number. Capitation
transactions reports can be summarized or detailed. All individual transactions are summarized by PNI code and reported on
several capitations image reports. There are also detailed health care provider PNI transactions reports on both the flat file
(CP7810, column U) and image reports (CP7010, CP7030). Member PNI is reported on the flat file (CP7810, column AP).
CMS premiums and adjustments
CMS premium
We use the premium reported on the MMR from CMS as the first step in development of the premium used for the percent of
premium calculation. The algorithm, methodology-blend percentage and rates/factors are posted on the CMS website at cms.
gov for all periods.
Unpaid CMS premium
If we do not receive payment from CMS for a particular member, we do not pay capitation for that member. Typically unpaid
CMS premiums occur in the first month of eligibility. The payment is usually received within 60 calendar days.
If the medical group/IPA has unpaid premiums, it must continue to arrange for the member’s medical care and pay for
services accordingly.
If CMS does not retroactively pay the premium within 120 calendar days, the medical group/IPA should notify its provider
advocate with specific information for that member. That way, the non-payment can be pursued with CMS.
Out-of-area premium
We receive premium from CMS based, in part, on the member’s State and County Code (SCC) as reported by CMS. We use the
premium CMS reports as a basis for percent of premium capitation.
CMS may report a member in a different state than the state their assigned medical group/IPA is located. As an example, CMS
may report a member’s SCC as Washington, yet their assigned medical group/IPA is in Oregon.
Once the CMS system updates SCC, CMS pays the correct SCC going forward. Typically, CMS does not retroactively adjust
premium for changes in SCC.
End Stage Renal Disease (ESRD) premium
ESRD premiums are paid using a risk-adjusted model. The model provides a 3-tier approach: dialysis status, receiving a
transplant, and functioning graft status. CMS communicates these tiers using the Customer’s Risk-Adjusted Factor Type Code.
In addition to the ESRD flag, the flat file reports the member-level risk-adjusted factor type code to help the medical group/IPA
identify their ESRD patient who is our member. The risk-adjusted factor type code is not reported on the image reports. Find
more information on CMS.gov.
Working aged premium adjustment
The working aged adjustment shows as a member-specific adjustment in the premium payment we receive from CMS. CMS
calculates the working aged adjustment based on a yearly Medicare Secondary Payer (MSP) factor CMS determines. We show

Capitation and/or Delegation Supplement
227
2023 UnitedHealthcare Care Provider Administrative Guide
this adjustment at the member level on the flat file (1 R record type for adjustments within the 6-month retro window and the 3M
record type for adjustments beyond the 6-month retro window). Find specifics on the CMS Working Aged Program on cms.gov.
CMS user fee premium adjustment
CMS deducts a user fee from all MA plans to fund various education programs for Medicare-eligible persons. The user fee
adjustment shows as a non-member specific adjustment in our payments from CMS. Every member is allocated the user fee
adjustment. CMS might modify the rate monthly, however, typically the percentage changes 3 times per year. We show this
adjustment at the member level on the flat file, 1 R record type, with the field name CMS_User_Fee.
Sequestration premium adjustment
UnitedHealthcare’s MA plans reduce health care provider capitation payments for MA membership by 2%.The 2% sequestration
reduction is reported at the member level on the flat file, 1 R record type, with the field name called the MSBP.
This is a result of the CMS-announced sequestration reductions of Medicare payments to health care providers, facilities and
other health care professionals and impacts health care provider, facility, ancillary health care provider and other professional
payments in our MA plans, including Medicare Advantage Dual Special Needs Plans (DSNP).
PART D buy-down adjustment
The exclusion/inclusion of the Part D Basic and Supplemental Rebate for UnitedHealthcare MA plans is based on the medical
group/IPA contract language. This information is included on the flat file (1R and 3M record type, column AT).
The following indicators are used:
• I - Part D Buy-Down Premium is included
• E - Part D Buy-Down Premium is excluded
• C - Part D Buy-Down PMPM rate as specified by the contract
Sample member capitation assessment
Capitation reports reflect the “cap premium gross cap” amount. A medical group/IPA and/or capitated facility with a percent of
premium contract can request a sample member capitation assessment.
For MA plans, the review reflects the premium received from CMS. It also shows the transactions outlined in the preceding CMS
premium sections to calculate the standard services capitation payment.
You may request a sample member capitation assessment no more than once a year.
A medical group/IPA or capitated facility may request 1 member capitation assessment, covering 1 month within the last
12-month period, for no more than 6 members per contract year.
Confidentiality
Sample member capitation review results include confidential and proprietary information. The medical group/IPA or capitated
facility must sign a confidentiality agreement before receiving a sample member capitation assessment. We only present
this information in one of our offices. The confidentiality agreement states that assessment results may not be removed from
the premises.
Capitation reconciliation
UnitedHealthcare produces capitation using 2 separate systems:
• Core transaction processing system — Information from this system reflected in the capitation flat file and on the image
reports. The summary reports, CP7030 or CP7010, go to the payment summary.
• Payment system — Information from this system reflects the sum of the core transaction system, system transaction plus any
non-system manual adjustments.

Capitation and/or Delegation Supplement
228
2023 UnitedHealthcare Care Provider Administrative Guide
We provide a capitation payment summary to each medical group/IPA to allow the medical group to reconcile the monthly
capitation payment. The payment amount is the sum of the amount from the core transaction processing system, plus any non-
system adjustments.
Capitation adjustment codes
We use capitation adjustments in a variety of circumstances. Each adjustment consists of a 3-character Capitation Adjustment
Code. Each adjustment code has a corresponding description. We use adjustment codes to administer a specific system-
generated payment or carve-out per your Agreement. We also use a code for a non-system adjustment.
The flat file contains only the capitation adjustment code. However, the CP7020 image report contains both the capitation
adjustment code and corresponding description.
We give health care providers documentation, as specified in this guide, in support of each capitation payment.
Non-system manual adjustments
An electronic format of non-system manual adjustments and corresponding backup documentation is available on
uhcprovider.com. Each adjustment is reported as a separate line item on the payment summary. To force these adjustments
through the system, we reverse them in the next processing-period, processed as a system adjustment and reported on the flat
file and image reports.
Provider remittance advice (PRA)
The invoice number on the PRA is an indication of the source system from which the transaction originated. Each transaction
originated from either the core transaction processing system (NICE) or payment system as a non-system manual adjustment
(ORACLE). Each of the source systems follows an invoice numbering convention as follows:
• Core transaction: YYMMPPNNNNSSDD (Example: 1701CO 00013301). This amount will foot to the CP7030 or CP7010
[image reports]:
– YY — last 2 [4] digits of the year (06)[(2006)]
– MM — month (06) PP — product type (CO) Commercial [(SH) Medicare]
– NNNN — computer generated sequential number (0001)
– SS — UnitedHealthcare State code (33)
– DD — UnitedHealthcare division code (01)
• Non-system manual adjustment: YYM M PPAAACTN N N N N N I IOSSDD (Example: 0606COALG 1101 [SHQMB] 2345JSC
[ZZC] 3301). This amount will not be included in the Capitation Reporting:
– YY — last 2 digits of the year (06) MM — month (06)
– PP — product type (CO) Commercial [(SH) Medicare]
– AAA — adjustment code (Example MBR would be for a member adjustment.)
– C — transaction count (1)
– T — contract type (1) values include; 1-Primary Care, 2-Facility, 3-Subcap, 4-Third Party
– NNNNNN — health care provider number (01 2345)
– II — internal document tracker (JS) [(ZZ)]
– ORACLE system indicator (C)
– SS — UnitedHealthcare State code (33)
– DD — UnitedHealthcare division code (01)
Retroactive term
The MA capitation process uses the member’s date of birth, as reported by CMS, as a basis for capitation calculations driven
by member age.

Capitation and/or Delegation Supplement
229
2023 UnitedHealthcare Care Provider Administrative Guide
Extended retro process (MA)
CMS sends MA premium payment adjustments to UnitedHealthcare that may span over a 72-month time frame on the Monthly
Membership Report (MMR). Our capitation processing engine can only process retroactivity up to 48 months, regardless of
contractual or eligibility limitations on retroactive changes. We apply the premium capitation calculation methodology. These
extended retro process adjustments appear on the capitation flat file, 3M record type with the following adjustment codes:
• MMR — Standard retroactive premium payment adjustments.
• MME — Adjustments represent transactions outside of the 6-month retro window that error out during the processing of
the MMR.
• MMX — Adjustments represent transactions for members that could not be identified during the processing of capitation or
are beyond the 48-month system limitation.
• The MME and MMX adjustments processed in subsequent months after they occur, due to the research involved to complete
these transactions.
Delegate performance management program
We conduct an analysis of clinical, quality and health outcomes to identify potential variations in care delivery to support
the best quality care and outcomes for our members. By comparing data, that is risk-adjusted when appropriate, identifying
variations from peer benchmarks and sharing that information with you, we can work collaboratively to improve value for
our members.
Together we get a clearer picture of measures that may provide opportunities for improving quality and care experiences for our
members. We account for standards of care, evidence-based guidelines and Choosing Wisely® recommendations from the
American Board of Internal Medicine Foundation, supported through partnerships with more than 70 national medical specialty
societies. Any changes to care programs not previously communicated to the Delegation Oversight Committee should be raised
during annual review.
Performance domains
Performance measurement supports practice improvement and provides delegates with access to information regarding how
their group compares to peer benchmarks for specific measures. This information provides a starting point for an ongoing
dialog regarding how we may best support your efforts to provide high-quality, cost-effective care to our members.
Delegate performance domains include:
• Clinical UM.
• Clinical quality including STARS, HEDIS and member satisfaction.
• Encounter data performance management.
• Financial performance management.
• Compliance with UnitedHealthcare, federal and state requirements.
Performance domains are evaluated regularly, compared to peer benchmarks, and communicated to the delegate in
performance reports.
Improvement action plans
We may require the delegate to develop an improvement action plan designed to bring the delegate into compliance with
performance standards.
Delegates who do not achieve compliance within the established time frames may require continued oversight until they
achieve compliance.
Continued non-compliance or failure to perform may result in removing the delegate from the services.
Notification of platform transitions or migrations
During our initial review of a delegate’s operational capabilities, we also review the delegate’s information systems or transaction
platforms to validate their ability to comply with our operational and regulatory requirements and connectivity standards.
Capitation and/or Delegation Supplement
230
2023 UnitedHealthcare Care Provider Administrative Guide
Therefore, we request the delegate provide at least 270 calendar days advance written notice to their UnitedHealthcare
delegation oversight representative and their UnitedHealthcare contract administrator or provider advocate of the intent to
either:
• Change administrative platform(s) for impacted delegated function(s), including migrations, version upgrades, or conversions.
• Make material changes in existing administrative platforms that might impact delegated functions.
If you are unsure of what a material change is, contact your delegation oversight representative.
Most changes require pre-cutover evaluation and testing by the UnitedHealthcare delegation oversight team(s) to ensure
continued compliance with all regulatory compliance and data sharing capabilities. Failure to adhere to these notification
requirements may result in financial penalties and/or loss of delegation responsibilities.
Appeals and grievances
Member grievance and appeals
Network providers are required to:
• Immediately, within 1 hour of receipt, forward all member grievances and appeals (complaints, appeal, quality of care/service
concern, whether oral or written) to us for processing to:
UnitedHealthcare
P.O. Box 6106
Mail Stop CA 124-0157
Cypress, CA 90630
• Respond to our requests for information about the member’s appeal or grievance within the designated time frame. For
expedited appeals, submit the requested information within 2 hours. For standard appeals, submit within 24 hours (no
exceptions or delays due to weekend or holidays). Time frames apply to every calendar day of the year.
• Comply with our final determinations regarding member appeals and grievances.
• Cooperate with us and the external independent medical review organization. This means promptly forwarding copies of
all medical records and information relevant to the disputed health care service in your possession to the external review
organization, and/or any newly discovered relevant medical records or any information in the your possession, requested by
an external review organization. Respond to our requests for proof of claim payment or a copy of the pre-service authorization
of overturned appeals: expedited appeals, within 2 hours, standard appeals, within 24 hours (no exceptions or delays due to
weekend or holidays). Time frames apply to every calendar day of the year.
• Provide us with proof of claim payment or a copy of the pre-service authorization within the stipulated time frames on
reversals of adverse determinations. Respond to requests for proof overturned appeals were resolved: expedited appeals,
within 2 hours, standard appeals, within 24 hours (no exceptions or delays due to weekend or holidays). Time frames apply to
every calendar day of the year.
UnitedHealthcare West member grievances
CA Commercial
Members may use a UnitedHealthcare West Grievance Form to file their grievance. We do not delegate authority or
responsibility for processing member grievances, appeals or complaints to our network providers. However, we do require our
network providers help resolve grievances, appeals or complaints.
For more information regarding disputes and grievance processes for
UnitedHealthcare West members (AZ, CA, CO, NV, OK, OR, TX, WA),
refer to the UnitedHealthcare West Supplement.

231
2023 UnitedHealthcare Care Provider Administrative Guide
Empire Plan supplement
Applicability of this supplement
The Empire Plan is a health insurance program developed by New York State and its employee unions, especially for employees
of New York State and their families. It is the most selected group health insurance option under the New York State Health
Insurance Program (NYSHIP), covering more than 1 million employees, retirees and eligible dependents from more than 740
participating employers and agencies. There are member populations nationwide with larger concentrations outside New York
in Arizona, California, Connecticut, Delaware, Florida, Georgia, Massachusetts, Maryland, North Carolina, New Jersey, Nevada,
Pennsylvania, South Carolina, Tennessee, Texas and Virginia.
Multiple carriers/vendors are involved in plan administration:
• Medical/Surgical Program is administered by UnitedHealthcare. It includes a PPO network for its Participating Provider
Program. Certain hospital services are included in this coverage.
• Hospitalization and Related Expense coverage is administered by Empire BlueCross.
• Mental Health and Substance Use Program is administered by Beacon Health Options, Inc.
• Prescription Drug Program is administered by CVS Caremark.
Referrals
The Empire Plan does not include requirements for a PCP to coordinate referrals for specialist care. Members may self-refer
to any health care provider for covered services and receive appropriate in-network or out-of-network benefits based on the
network status of the health care provider.
Anesthesia services
You will help ensure all covered anesthesia services rendered at your practice location are performed by participating health
care providers for as long as the Agreement is in effect.
Laboratory services
We only reimburse for laboratory services you are certified to perform through the Federal Clinical Laboratory Improvement
Amendments (CLIA). You must not bill our members for any laboratory services if you don’t have the applicable CLIA
certification.
Other services
If you determine a member requires treatment or services from another health care provider, you must use reasonable efforts to
refer them to a network provider.
ID cards
Empire Plan participants are given NYSHIP ID cards by the State of New York Department of Civil Service, the Empire Plan
policyholder. Current versions of NYSHIP ID cards are displayed on the following page. Prior versions also remain in circulation.
Some list the Empire Plan name and/or carriers involved in coverage; others do not. All are valid Empire Plan ID cards.
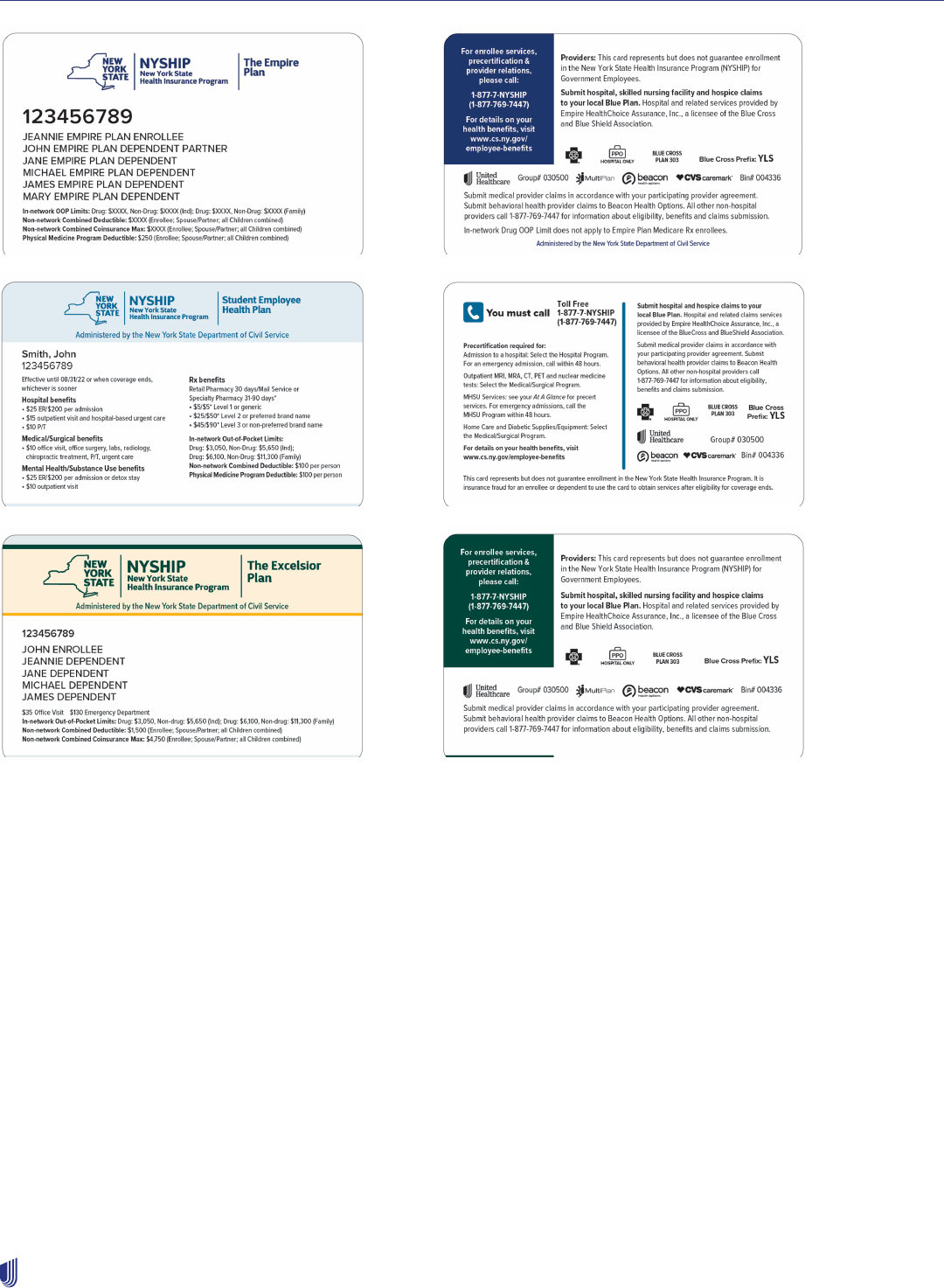
Empire Plan supplement
232
2023 UnitedHealthcare Care Provider Administrative Guide
Prior authorization and notification requirements
We require advance notification of the procedures and services listed in the following chart. These services are likely to identify
members with unmet health care needs who will benefit from UnitedHealthcare’s programs, or those of other Empire Plan
vendors. In general, depending on the program, members are responsible for either notifying Empire Plan program vendors of
certain services or for using network providers for these services.
Call 1-877-7-NYSHIP (1-877-769-7447) and follow the prompts to notify the appropriate program carrier/vendor as outlined on
the following page, or go to uhcprovider.com/paan.
This notification list may be modified. The presence or absence of a procedure or service on this list does not mean that benefit
coverage exists for that procedure or service. The member benefit contract will determine whether a procedure or service is
covered.
Empire Plan supplement
233
2023 UnitedHealthcare Care Provider Administrative Guide
Service Contact
Advanced diagnostic imaging services
• MRI
• MRA
• CT scan
• PET scan
• Nuclear medicine test
UnitedHealthcare
Benefits Management Program
Alcoholism treatment Beacon Health Options, Inc.
Behavioral Health Program
Chiropractic services Managed Physical Network, Inc. (MPN)
Managed Physical Medicine Program
DME and integral supplies
• Mastectomy prosthetics over $1,000
• Diabetic shoes (when the Empire Plan is primary coverage)
• DME items listed on the DME Notification List at uhcprovider.com/paan
> Advanced Notification and Plan Requirement Resources > Empire Plan
Notification Lists > Empire Plan Durable Medical Equipment (DME)
Notification List for Members with Primary Empire Plan Coverage.
UnitedHealthcare
Home Care Advocacy Program
Home health services that take the place of hospitalization UnitedHealthcare
Home Care Advocacy Program
Home infusion therapy and enteral formula
(Except administration of enteral formula through a tube for patients whose
primary coverage is Medicare)
UnitedHealthcare
Home Care Advocacy Program
Home nursing services UnitedHealthcare
Home Care Advocacy Program
Hospital admissions
• Elective
• Emergency/urgent (within 48 hours)
Empire BlueCross
Benefits Management Program
Mental health services Beacon Health Options, Inc.
Behavioral Health Program
Physical therapy MPN
Managed Physical Medicine Program
Prescription drugs
As noted in Preferred Drug List or Flexible Formulary List
CVS Caremark
Prescription Drug Program
Skilled nursing facility admissions Empire Blue Cross Blue Shield
Benefits Management Program
Substance use services Beacon Health Options, Inc.
Behavioral Health Program
Empire Plan supplement
234
2023 UnitedHealthcare Care Provider Administrative Guide
Online resources and how to contact us
The following outlines Empire Plan specific contact information that may differ from the standard contacts and tools outlined
earlier in this guide. For other topics such as contractual questions, demographic updates and credentialing of new providers,
use the standard contact information outlined earlier in this guide and at uhcprovider.com.
Resource Where to go
Advance Notification and Prior Authorization
(Submit and get status information)
EDI: See EDI transactions and code sets on uhcprovider.com/edi
Online: uhcprovider.com/paan
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Admission Notification Empire BlueCross
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Cancer Resource Services Phone: 1-866-936-6002
Claims
(Filing, payments, reconsiderations)
EDI: uhcprovider.com/edi. Payer ID: 87726
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In >
Claims & Payments.
Information: uhcprovider.com/claims (policies, instructions and tips)
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Infertility Services UnitedHealthcare / Home Advocacy Program.
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Kidney Resource Services Phone: 1-866-936-7246
Member/Customer Care Online: myuhc.com
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Mental Health and Substance Use services Beacon Health Options, Inc.
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Pharmacy Services CVS Caremark
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Provider Directory empireplanproviders.com
Skilled Nursing Facilities
(Freestanding)
Empire BlueCross
Phone: 1-877-7-NYSHIP (1-877-769-7447)
Transplant Services Empire BlueCross
Phone: 1-877-7-NYSHIP (1-877-769-7447)

235
2023 UnitedHealthcare Care Provider Administrative Guide
Leased Networks
This may apply to health care providers in Hawaii, Kentucky, Michigan, Puerto Rico and the U.S. Virgin Islands. Refer to your
Agreement.
Applicability of this supplement
The Leased Network Supplement applies to physicians, health care professionals, facilities and ancillary providers who
participate through a leased network for certain products accessed by UnitedHealthcare in an area where we do not have a
direct network.
These participating health care providers are subject to both the main guide and this supplement. This supplement controls if it
conflicts with information in the main guide. For topics not referenced in this supplement, refer to main guide.
Leased supplement
For these certain products, the mention of a health care provider’s “Agreement with us” refers to your agreement with the entity
operating the leased network (your “Master Contract Holder”).
For the following processes, follow your Master Contract Holder Agreement to:
• Update demographic information.
• Submit NPI information.
• Submit credentialing/re-credentialing information.
236
2023 UnitedHealthcare Care Provider Administrative Guide
Level2 supplement
Applicability of this supplement
You are subject to both the main guide and this supplement. This supplement controls if it conflicts with information in the main
guide. If there are additional protocols, policies or procedures online, you will be directed to that location. Refer to the main
guide for anything not found in this supplement.
How to contact us
Resources Where to go What you can do there
Cardiology
Diagnostic
catheterization,
electrophysiology
implants,
echocardiogram and
stress echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/cardiology
Phone: 1-866-889-8054
Request prior authorization for services
as described in the Outpatient cardiology
notification/prior authorization protocol section
of Chapter 7: Medical management
Claims Submission Online: UnitedHealthcare Provider Portal at
uhcprovider.com > Sign In
Payer ID: 87726
Information: uhcprovider.com/claims
Genetic and Molecular
Testing
Online: uhcprovider.com/priorauth >
Genetic and Molecular Testing
Verify eligibility and benefits of
enrolled members
Outpatient Injectable
Chemotherapy and
Related Cancer
Therapies
Online: uhcprovider.com/priorauth >
Oncology
Phone: 1-888-397-8129
Policies and instructions
Pharmacy Services Prior Authorizations
Phone: 1-800-711-4555
Benefit Information:
Call the number on the back of the
member’s ID Card.
For information on the Prescription Drug List
(PDL), myallsaversconnect.com
Prior Authorization and
Notification
Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth
Phone: 1-800-999-3404
Prior authorization and notification is required as
described in Chapter 7: Medical management.
EDI 278A transactions are not available.
Level2 supplement
237
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to go What you can do there
Radiology/Advanced
Outpatient Imaging
Procedures
CT scans
MRIs
MRAs
PET scans and nuclear
medicine studies,
including nuclear
cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/radiology
Phone: 1-866-889-8054
Request prior authorization for services
as described in the Outpatient radiology
notification/prior authorization protocol section
of Chapter 7: Medical management.
Health plan ID cards
Level2 members receive health plan ID cards with information that helps you to submit claims. The cards list the claims
address, copayment information and phone numbers.
A sample ID card and more information is in the Health plan identification (ID) cards section in Chapter 2.
Claims process
Follow these steps for fast payment:
1. Notify Level2.
2. Prepare a complete and accurate claim form.
3. For Level2 members, submit electronic claims using payer ID number 87726. Submit paper claims to the address on the
member’s ID card.
4. For contracted care providers who submit electronic claims and would like to receive electronic payments and statements,
call Optum Financial Services Customer Service line at 1-877-620-6194 or visit optumbank.com > Partners > Providers.
Claim reimbursement (adjustments)
If you think your claim was processed incorrectly, call the number on the member’s ID card. If you find a claim where you were
overpaid, send us the overpayment within 30 calendar days. If we find a claim was overpaid, payment is due within 30 calendar
days.
If you disagree with our decision regarding a claim adjustment, you may appeal.
Claim reconsideration, appeals and disputes
Claim reconsideration does not apply to some states based on applicable state legislation (e.g., Arizona, California, Colorado,
New Jersey or Texas). For states with applicable legislation, any request for dispute will follow the state-specific process.
There is a two-step process available for review of your concern. Step one is a Claim Reconsideration. If you disagree with the
outcome of the Claim Reconsideration, you may request a Claim Appeal (step 2).

Level2 supplement
238
2023 UnitedHealthcare Care Provider Administrative Guide
How to submit your reconsideration or appeal
Claims payment issues or outcome of a reconsideration review
If you disagree with claim payment issues or the outcome of your reconsideration review, submit your request using our
electronic tools:
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In.
API: Submit reconsiderations and appeals (with attachments) using API. Go to uhcprovider.com/api for more information.
Overpayment recoveries, pharmacy, medical management disputes or contractual issues
If you disagree with overpayment recoveries, pharmacy, medical management disputes, or contractual issues send a letter
requesting a review to:
UnitedHealthcare Level2 members:
Grievance Administrator
P.O. Box 31393
Salt Lake City, UT 84131-0371
Fax: 1-801-994-1416
Time frame
You must submit your claim reconsideration and/or appeal to us within 12 months (or as required by law or your Agreement),
from the date of the original EOB or denial. The two-step process allows for a total of 12 months for timely submission, not 12
months for step one and 12 months for step two.
What to submit
As the care provider of service, you submit the dispute with the following information:
• Member’s name and health plan ID number
• Claim number
• Specific item in dispute
• Clear rationale/reason for contesting the determination and an explanation why the claim should be paid or approved. If you
disagree with the outcome of the claim appeal, you may file for an arbitration proceeding. (A description of this process is in
your Agreement.)
Refer to Claim reconsideration and appeals process section in Chapter 10: Our Claims Process, for more information.
239
2023 UnitedHealthcare Care Provider Administrative Guide
Mid-Atlantic Regional supplement
Applicability of this supplement
This Mid-Atlantic Regional supplement applies to services provided to members enrolled in:
• MD-Individual Practice Association, Inc. (“M.D.IPA”) and M.D.IPA Preferred.
• Optimum Choice, Inc. (“Optimum Choice”), Optimum Choice Preferred and Optimum Choice Small Business Health Options
Program (“SHOP”).
It may apply to health care providers in Delaware, Washington, D.C., Maryland, Pennsylvania, Virginia and West Virginia;
reference your Agreement for applicability.
Health care providers are subject to both the main guide and this supplement. This supplement controls if it conflicts with
information in the main guide. For protocols, policies and procedures not referenced in this supplement refer to appropriate
chapter in the main guide.
A complete list of Mid-Atlantic Health plan protocols pertaining to M.D.IPA, M.D.IPA Preferred, Optimum
Choice, and Optimum Choice Preferred may be located on uhcprovider.com/plans > Choose Your State.
The term “prior authorization” referenced in this supplement is also referred to as “preauthorization.” We use both terms in this
supplement. They mean the same.
Product summary
This table provides information about M.D.IPA and Optimum Choice products for the Mid-Atlantic Region.
Attributes M.D.IPA and Optimum Choice M.D.IPA Preferred and Optimum Choice Preferred
How do
members access
physicians and
health care
professionals?
Members choose a PCP who arranges or
coordinates their care, except emergency
services, network OB/GYN, routine eye
refraction care and behavioral health care
services.
Network benefits: Members choose a PCP who arranges
or coordinates care, with the exception of emergency
services, network OB/GYN, routine eye refraction care and
behavioral health care services.
Out-of-network benefits: Members are not required to
have care arranged or coordinated by a PCP.
Does a PCP
have to write
a referral to a
specialist?
Yes; except for visits to a network
OB/GYN, routine eye refraction care,
emergency services and behavioral
health care services.
Network benefits: Yes, except for visits to a network OB/
GYN, routine eye refraction care, emergency services and
behavioral health care services.
Out-of-network benefits: No referral needed.
Is the treating
physician
required to
obtain prior
authorization for
procedures or
services?
Yes; view the section on Prior
Authorizations process located within
this supplement. Find a complete list of
codes requiring prior authorization on
uhcprovider.com/priorauth > Advance
Notification and Plan Requirement
Resources > UnitedHealthcare Mid-
Atlantic Plan Notification/Prior
Authorization Requirements.
Yes; view the section on Prior Authorizations process
located within this supplement. Find a complete list of
codes requiring prior authorization on uhcprovider.com/
priorauth > Advance Notification and Plan Requirement
Resources > UnitedHealthcare Mid-Atlantic Plan
Notification/Prior Authorization Requirements.
Mid-Atlantic Regional supplement
240
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare Optimum Choice SHOP
For more information, refer to Chapter 4: Individual Exchange Plans.
Key Points Optimum Choice SHOP Exchange
Product name Optimum Choice, Inc.
How do members access physicians
and health care professionals?
For each covered family member, members choose a network PCP, or are
assigned a PCP, to manage the member’s care and generate referrals to network
specialists when required.
Is a special referral required? Yes, on selected procedures. See guidelines in the referral requirements section
of this supplement.
Are treating physicians and/or facilities
required to request prior authorization
when providing certain services?
Yes, on selected procedures. See guidelines in the Prior Authorization List
located on uhcprovider.com/priorauth.
UnitedHealthcare Optimum Choice HSA Plan
The Optimum Choice and Optimum Choice Preferred HSA benefit plans are high-deductible medical benefit plans that combine
our traditional gated HMO benefit plans with an HSA option. Expenses under this benefit plan are the member’s responsibility
until their deductible is reached. HSA benefit plans require reimbursement for services provided to members are based on a
fee-for-service reimbursement methodology.
Key Points Optimum Choice, Inc. Health Savings Account
PCP requirement The Optimum Choice HSA product requires each UnitedHealthcare member to
choose a PCP.
PCP referrals to network specialists The member’s PCP generates referrals for specialty care and facility care.
Reimbursement Services for members enrolled in Optimum Choice HSA are excluded from your
capitation payment and are paid on a fee-for-service (FFS) basis per the All Payer
Payment Appendix included in the UnitedHealthcare physician Agreement.
Optimum Choice HSA member health
plan ID card
The Optimum Choice HSA product name and member’s PCP are indicated on the
member’s ID card. Specialist referral requirements are on the back of the ID card.
Check Eligibility and Benefits in the UnitedHealthcare Provider Portal.
Provider responsibilities
For detailed information and instructions on verifying eligibility, the choice and role of the PCP, and other health care provider
requirements, refer to Chapter 2: Provider responsibilities and standards.
Eligibility and health plan ID cards
Member ID card information may vary by health benefit plan. For example, some members may have ID cards which indicate
M.D.IPA Preferred or Optimum Choice Preferred benefits. You can see an image of the ID card specific to the member when
you verify the member’s eligibility. For more information on ID cards and to see a sample health plan ID card, refer to the Health
plan identification (ID) cards section of Chapter 2: Provider responsibilities and standards.
Before seeing a member, it is important you verify their eligibility and benefits in the UnitedHealthcare Provider Portal, as well
as the member’s PCP selection, to avoid payment issues. Go to uhcprovider.com and click Sign In in the top right corner. Then
click Eligibility from the drop-down menu.

Mid-Atlantic Regional supplement
241
2023 UnitedHealthcare Care Provider Administrative Guide
The following unique features are located on M.D.IPA and Optimum Choice health plan ID cards:
• Laboratory provider information is located on the front of the cards; see the Laboratory Requirements section of this
supplement.
• Radiology county information is located on the front of the cards; see the Radiology Services section of this supplement.
• Information regarding the necessity of referral and prior authorization requirements is now listed on the back of the cards.
Laboratory requirements
M.D.IPA and Optimum Choice members must use the medical laboratory noted on their ID card for medical laboratory services.
Any specimens collected in the office MUST be sent to the laboratory indicated on the member’s ID card. Depending on where
the member lives, the ID card shows:
• LAB = LABCORP (Laboratory Corporation of America).
• LAB = PAR (may use any participating outpatient commercial medical laboratory). Our online directory of health care
professionals is available on uhcprovider.com/findprovider.
Refer to uhcprovider.com/plans > Choose a location.
Radiology services
M.D.IPA and Optimum Choice members must use the radiology county noted on the ID card. Depending upon the member’s
PCP’s office location, the ID card shows:
• RAD = PAR (may use any office based participating provider). A complete list of these providers may be found on
uhcprovider.com/findprovider.
• RAD = County (the name of a county, i.e., “MONT [Montgomery County]” is listed on the card).
A complete list of county specific radiology vendors is found on uhcprovider.com/plans > Choose a location > Commercial >
Radiology Vendors.
Copays
Verify the member’s copayments when verifying their eligibility.
Member PCP requirements
A PCP is defined as a physician specializing in family practice, internal medicine, pediatrics or general practice. Other health
care providers will be included as primary physicians as required by state mandates. Members are required to see their PCP
or a covering physician at the address location that shares the same TIN listed on the Patient Eligibility screen. Some PCPs
have multiple TINs but may not participate under each of those TINs for the member’s benefit plan. Before scheduling an
appointment, verify the member’s assigned PCP and TIN (listed on the Patient Eligibility screen) matches the TIN address
where the member will be seen. Submit your address corrections through My Practice Profile in the UnitedHealthcare Provider
Portal, or call the phone number on the back of the member’s ID card before seeing the member.
For requests about panel status (i.e., Open/Closed to New/Existing Patients), contact your network account representative 30
calendar days before any action. To find your network account representative, go to uhcprovider.com > Contact us > State-
specific health plan and network support > Select your state. Members are required to select a network PCP, or a PCP is
auto-assigned.
Direct access services
Female members may receive OB/GYN physician services directly from a participating OB/GYN, family practice physician, or
surgeon identified by the medical group/IPA or UnitedHealthcare as providing OB/GYN physician services. This means the
member may receive these services without prior authorization or a referral from the member’s PCP. In all cases, the physician
must be affiliated with the member’s assigned medical group/IPA and participating with UnitedHealthcare.
Mid-Atlantic Regional supplement
242
2023 UnitedHealthcare Care Provider Administrative Guide
Referrals
For referral process information, check the Mid-Atlantic Health Plan Referral Protocol located on uhcprovider.com/plans
> Choose Your State > Commercial Plans > Mid-Atlantic Health Plan > Referral Protocol for M.D.IPA, M.D.IPA Preferred,
Optimum Choice, and Optimum Choice Preferred for:
• Referral submission requirements.
• Maximum number of referral visits.
• Exceptions for specific specialists or treatments.
Referrals are not required when M.D.IPA or Optimum Choice is the secondary carrier.
Find forms and specific referral processes for some treatments on uhcprovider.com/plans > Choose Your State >
Commercial Plans > Mid-Atlantic Health Plan. The referral form is hyperlinked within the protocol titled “Referral Protocol
for M.D.IPA, M.D.IPA Preferred, Optimum Choice and Optimum Choice Preferred.”
Prior authorizations
How to submit
There are multiple ways to submit prior authorization requests to UnitedHealthcare, including electronic options. To avoid
duplication, once a prior authorization is submitted and confirmation is received, do not resubmit.
• Online: uhcprovider.com/paan
• Phone: 1-877-842-3210. Clinical services staff are available during the business hours of 8 a.m.–8 p.m. ET.
• Information: uhcprovider.com/priorauth (for information and prior authorization lists)
Find the following forms referenced at uhcprovider.com/priorauth > Frequently searched > Advance
Notification and Plan Requirement Resources.
Radiology prior authorization requests and prior authorization list
Prior authorization requests for radiology may be submitted electronically using the Prior Authorizations tool in the
UnitedHealthcare Provider Portal. M.D.IPA and Optimum Choice are not part of the UnitedHealthcare Radiology Prior
Authorization Program. Refer to the uhcprovider.com/priorauth > Frequently searched > Advance Notification and Plan
Requirement Resources > UnitedHealthcare Mid-Atlantic Health Plan Notification/Prior Authorization Requirements.
Outpatient rehabilitation (physical, occupational and speech therapy) prior
authorization request
Prior authorization requests for physical, occupational, speech and other therapy-related service may not be submitted
electronically. Fax these prior authorization requests to the Clinical Care Coordination Department at 1-888-831-5080 using the
Rehabilitation Services Extension Request Form found at uhcprovider.com/plans > Choose a Location.
Chiropractic services prior authorization request
Prior authorization requests for chiropractic services may not be submitted electronically. Fax these prior authorization requests
to the Clinical Care Coordination Department at 1-888-831-5080 using the Chiropractic Services Extension Form, found on
uhcprovider.com/plans > Choose a Location > Commercial Plans > Mid-Atlantic Health Plan, along with a copy of the current
Consultant Treatment Plan (PCP Referral).
Allow 2 business days for extension request decisions. Missing information may result in a delayed response. Decisions are
based on the member’s plan benefits, progress with the current treatment program and submitted documentation.
Mid-Atlantic Regional supplement
243
2023 UnitedHealthcare Care Provider Administrative Guide
Exception requests
All exceptions to our policies and procedures must be preauthorized by submitting a request online at uhcprovider.com/paan
or by phone at 1-877-842-3210. The most common exception requests are:
• Immunizations (outside the scope of health benefit plan guidelines).
• Referral of an HMO member out-of-network to a non-participating physician, health care practitioner or facility.
Prior authorization is required for elective outpatient services. It is the physician’s responsibility to obtain any relevant prior
authorization. But the facility should verify prior authorization is obtained before providing the service. If the facility does not get
the required prior authorization, we may deny payment. Final coverage and payment decisions are based on member eligibility,
benefits and applicable state law.
If you have a question about a pre-service appeal, see the section on Pre-Service Appeals under Chapter 7: Medical
management.
Inpatient admission notification
It is the facility’s responsibility to notify UnitedHealthcare within 24 hours after weekday admission (or by 5 p.m. ET the next
business day if 24-hour notification would require notification on a weekend or federal holiday). For weekend and federal holiday
admissions, notification must be received by 5 p.m. ET the next business day.
For emergency admissions when a member is unstable and not capable of providing coverage information, the facility
should notify us as soon as they know the information and explain the extenuating circumstances. Facilities are responsible
for providing admission notification for inpatient admissions, even if advance notification was provided by the physician and
coverage approval is on file.
Prior authorization is required for all elective inpatient admissions for all M.D.IPA and Optimum Choice members. It is the
admitting physician’s responsibility to obtain the relevant prior authorization. But the facility should verify that prior authorization
is obtained before the admission. Payment may be denied to the facility and attending physician for services provided in the
absence of prior authorization. Prior authorization doesn’t guarantee coverage or payment. All final coverage and payment
decisions are based on member eligibility, benefits and applicable state law.
SNF placements do not require prior authorization. You must verify available benefit and notify us within 1 business day of SNF
admission.
Maryland facility variations from the standard notification requirements for facilities
For information specific to members in Maryland, refer to uhcprovider.com/priorauth > Prior Authorization and Notification
Program Summary > and scroll down.
Admission Notification Requirements
EDI: Transaction 278N
Online: Use the Prior Authorization and Notification tool at uhcprovider.com/paan.
Phone: 1-800-962-2174
Once we receive your notification, we begin a case review. If notification isn’t provided in a timely manner, we may still review
the case and request other medical information. We may retroactively deny 1 or more days based upon the case review. If
a member receiving outpatient services needs an inpatient admission, you must notify us as previously noted. Emergency
room services resulting in a covered admission are payable as part of the inpatient stay as long as you have notified us of the
admission as described.
Delay in service
Facilities that provide inpatient services must maintain appropriate staff resources and equipment to help ensure covered
services are provided to members in a timely manner. A delay in service is defined as any delay in medical decision-making,
test, procedure, transfer or discharge not caused by the member’s clinical condition. Services should be scheduled the same
day as the physician’s order. However, procedures in the operating room, or another department requiring coordination with
another physician, such as anesthesia, may be performed the next day unless emergent treatment was required. A service
delay may result in sanctions of the facility and non-reimbursement for the delay days, if permissible under state law.

Mid-Atlantic Regional supplement
244
2023 UnitedHealthcare Care Provider Administrative Guide
A clinical delay in service is assessed for any of these reasons:
• Failure to execute a physician order in a timely manner, resulting in a longer length of stay.
• Equipment needed to fulfill a physician’s order is not available.
• Staff needed to fulfill a physician’s order is not available.
• A facility resource needed to fulfill a physician’s order is not available.
• Facility doesn’t discharge the member on the day the physician’s discharge order is written.
Concurrent review
Review is conducted onsite at the facility or by phone for each day of the stay using criteria. Your cooperation is required when
we request information, documents or discussions such as clinical information on member status and discharge planning. If
criteria aren’t met, the case is referred to a medical director for assessment. We deny payment for facility days that don’t have a
documented need for acute care services. We require physicians’ progress notes be charted for each day of the stay. Failure to
document will result in denial of payment to the facility and the physician.
Facility post-discharge review
A post-discharge review is conducted when a member has been discharged before notification to UnitedHealthcare occurs
or before information is available for certification of all the days. A UnitedHealthcare representative will request the member’s
records from the Medical Records Department or assess a review by phone and review each non-certified day.
Inpatient days that don’t meet acuity criteria are referred to a medical director for determination and may be retrospectively
denied. Delays in service or days that don’t meet criteria for level of care may be denied for payment.
Facility-to-facility transfers
The facility must notify us of a facility-to-facility transfer request. In general, transfers are approved when:
• There is a service available at the receiving facility that isn’t available at the sending facility.
• The member would receive a medically appropriate level of care change at the receiving facility.
• The receiving facility is a network facility and has appropriate services for the member.
If any of the previous conditions aren’t met, transfer coverage is denied. Services at the receiving facility will be approved if:
• Medical necessity criteria for admission were met at the receiving facility.
• There were no delays in providing services at the receiving facility.
Clinical appeals
To appeal an adverse decision (a decision by us to not prior authorize a service or procedure, or a payment denial because
the service wasn’t medically necessary or appropriate), you must submit a formal letter that includes your intent to appeal,
justification for the appeal and supporting documentation. The denial letter will provide you with the filing deadlines and the
address to submit the appeal.
Urgent Appeal Submissions:
Medical fax: 1-801-994-1083
Pharmacy fax: 1-801-994-1058
Claims process
Refer to Chapter 10: Our claims process for detailed information about our claims process.
All claims that can be submitted electronically must be submitted to payer ID 87726.
Reconsideration and appeals processes
For claim reconsiderations for M.D.IPA and Optimum Choice, submit your request in the Claims tool in the UnitedHealthcare
Provider Portal at uhcprovider.com > Sign In.
Mid-Atlantic Regional supplement
245
2023 UnitedHealthcare Care Provider Administrative Guide
Capitation
Capitation payment will be paid to the practice for covered services PMPM. The PCP receives separate capitation payments for
members of M.D.IPA and Optimum Choice monthly, on the fifth day of each month.
The PMPM is calculated by multiplying the fixed monthly rates (detailed in the Capitation Rate Schedule contained in your
Agreement) by the number of members who have selected or been assigned to a PCP within the practice.
Payment rules
The capitation payment for a given month is calculated based on the 15/30 rule. This rule is used to determine whether a
capitation payment is made for the full month or not at all. If the effective date of member change falls between the first and
15th of the month, the change is effective for the current month. If the effective date of the member change falls on or after the
16th of the month, the capitation adjustment is reflected on the first of the following month. As such, retroactive adjustments to
capitation payments may be made based on the member’s eligibility on the 15th of the month.
15/30
Rule
For purposes of capitation payments, members are added on the first day of the month or terminated on the last
day of the month, with the exception of newborns, which are added on the date of their birth(s). Capitation is paid
for full months, and conversely recouped for full months if appropriate. For example:
Retroactive Add:
A member added retroactively on the 15h of the month would generate a capitation payment for the entire month.
However, a member added on the 16th or later would not generate a capitation payment, even though the member
would be considered eligible for services. To help you identify these members, the member’s standard services
capitation is reported as $0.
Retroactive Term:
A member retroactively terminated between the first and 14th of the month would generate a capitation recoup
entry for the capitation previously paid for the entire month. However, a member retroactively terminated on the
15th or later would not generate a capitation recoup entry for the capitation previously paid for the entire month.
UnitedHealthcare of the Mid-Atlantic region provides capitation reports to PCPs, as described as follows:
ECap Report Name ECap Report Purpose
7030-A01: Capitation Analysis Summary –
Provider Medical Group Report
High-level capitation information by current and retro periods for each
health care provider.
7010-A01: Capitation Paid ECap – Provider
Medical Group Report – Summary
A contract-level report that summarizes the capitation paid by current and
retro periods. The 3 sections of the report include amounts for:
1. Standard services.
2. Supplemental benefits and capitated adjustments.
3. Non-capitated adjustments and withholds.
7010-A02: Capitation Paid ECap – Primary
Care Provider Report – Detail
A PCP-level report that summarizes the capitation paid by current and
retro periods. The 3 sections of the report include amounts for:
1. Standard services.
2. Supplemental benefits and capitated adjustments.
3. Non-capitated adjustments and withholds.
7210-A01: Capitation Details – Primary
Care Provider Report for Standard Services
– (PMG)
Detailed capitation information for each current member assigned to a PCP.
Mid-Atlantic Regional supplement
246
2023 UnitedHealthcare Care Provider Administrative Guide
ECap Report Name ECap Report Purpose
7240-A01: Member Changes Capitation
Details – Primary Care Provider Report for
Standard Services – (PMG)
Detailed retroactive change information on added, changed and
terminated members. The 3 sections of the report include information on:
1. Member adds
2. Member demographic changes
3. Member terms
7290-A01: Capitation Adjustment Details –
Primary Care Provider Report – (PMG)
Capitation adjustment details for member and provider-level
guide adjustments. The 2 sections of the report include information on:
1. Current period
2. Retro period
The PCP practice should reconcile the capitation payment and report upon receipt. Requests for an adjustment or
reconciliation of the capitation payment must be made within 60 calendar days of receipt. If the PCP/medical group (practice)
does not request reconsideration of the capitation payment within 60 days, the capitation payment provided is accepted as
payment in full (as per contract). You may obtain copies of the previous reports by calling Provider Services at 1-877-842-3210.
Bill above
In addition to the capitation payments, certain covered services are eligible for reimbursement. To obtain a copy of this
information, contact your network representative. To locate your network representative, go to uhcprovider.com > Contact us >
State-specific health plan and network support > Select your state.
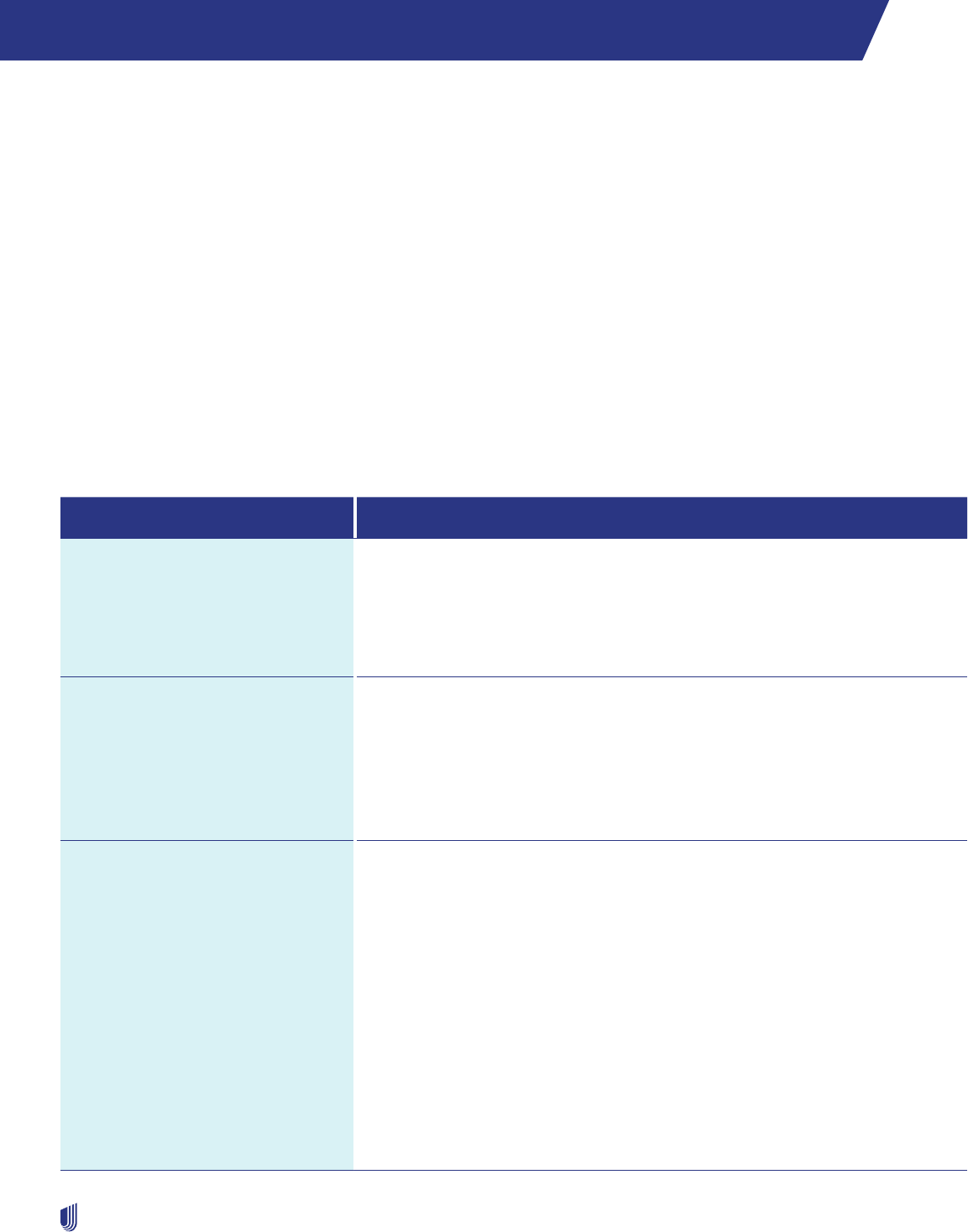
247
2023 UnitedHealthcare Care Provider Administrative Guide
Neighborhood Health Partnership supplement
Applicability of this supplement
The Neighborhood Health Partnership (NHP) supplement applies to covered services provided to members enrolled in NHP
benefit plans when you fit into these 2 categories:
1. Your Agreement with UnitedHealthcare includes a reference to the NHP protocols or guides, or you have directly contracted
with NHP to participate in networks maintained for NHP members.
2. You are located in the NHP service area, which is expanding.
NHP Flex Benefit Plans: This supplement does not apply to health care providers located outside the NHP service area.
NHP participating health care providers are subject to both the main guide and this supplement. This supplement controls if it
conflicts with information in the main guide. For protocols, policies and procedures not referenced in this supplement, refer to
appropriate chapter in the main guide.
The term “prior authorization” referenced in this supplement is also referred to as “precertification.” We use both terms in
this supplement.
How to contact NHP
Resource Where to go
Provider Website uhcprovider.com
Policies: uhcprovider.com/policies > Commercial Policies
Provider news and updates: uhcprovider.com/news
Note: You must register to access some of the features available to you. Go to
uhcprovider.com/access.
Advance Notifications, Prior
Authorizations, Admission
Notifications
EDI: See EDI transactions and code sets on uhcprovider.com/edi.
We accept EDI 278 submissions directly to UnitedHealthcare or through a
clearinghouse. Be sure to include the CPT codes for your request.
Online: uhcprovider.com/paan
Phone: 1-877-842-3210
See ID card for specific service contact information.
Appeals
Urgent Appeals
Standard Pre-Service Appeals
Post-Service Appeals
Urgent appeals fax:
Medical: 1-801-994-1083
Pharmacy: 1-801-994-1058
Standard pre-service appeals address:
UnitedHealthcare
P.O. Box 30559
Salt Lake City, UT 84130
Standard pre-service appeals fax:
Medical: 1-801-938-2100
Pharmacy: 1-801-994-1345
Post-Service appeals
Online: UnitedHealthcare Provider Portal: uhcprovider.com > Sign In
API:
Submit reconsiderations and appeals (with attachments) using API: uhcprovider.
com/api for more information.
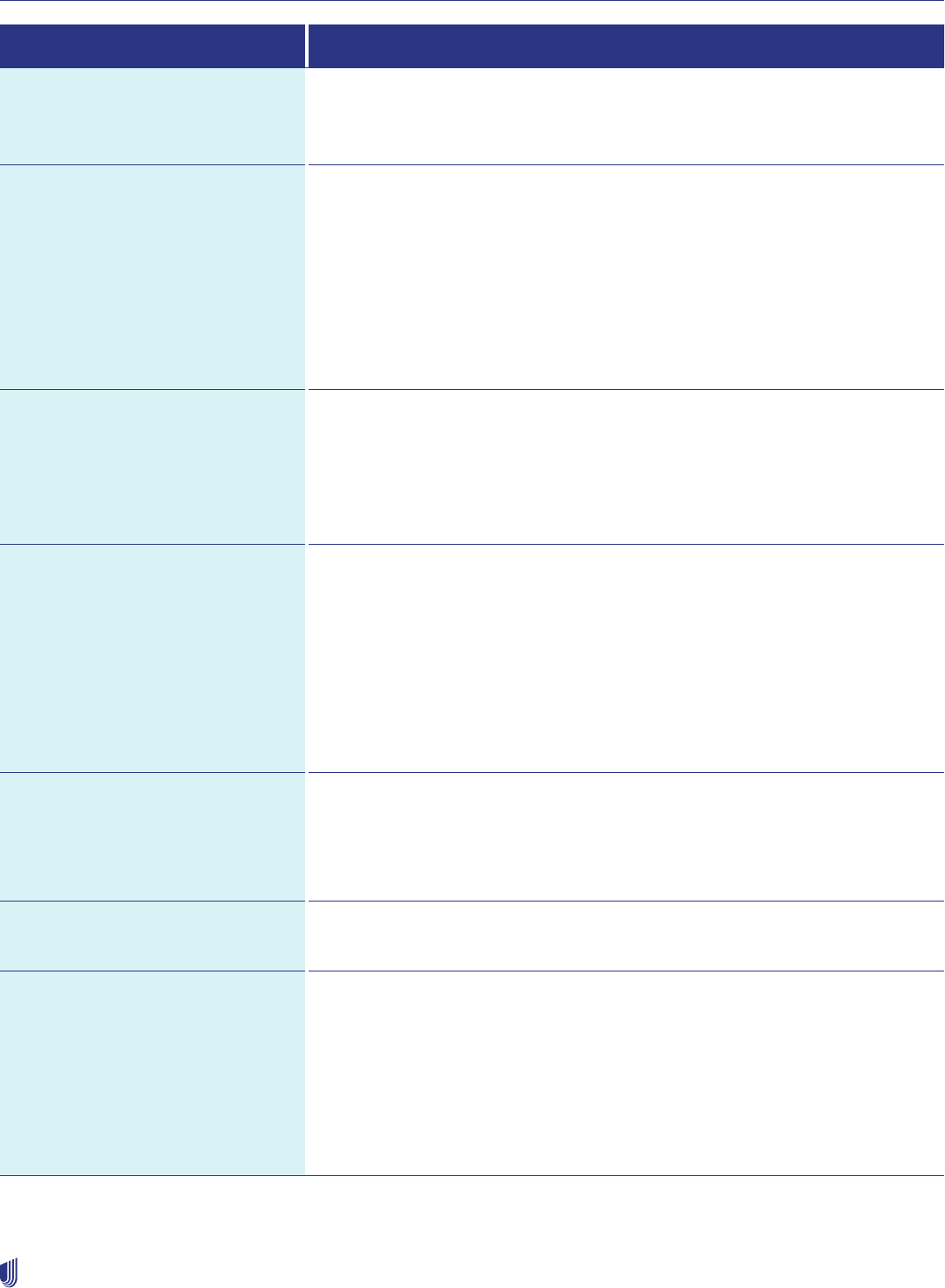
Neighborhood Health Partnership supplement
248
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Breast Pumps Lincare: 1-855-236-8277 lincare.com
Byram Medical: 1-877-902-9726 byramhealthcare.com
Edgepark Medical: 1-888-394-5375 edgepark.com
Cardiology: Request prior
authorization of cardiology services
as described in the Outpatient
cardiology notification/prior
authorization protocol section of this
guide.
• Diagnostic catheterization
• Electrophysiology implants
• Echocardiogram
• Stress echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/cardiology
Phone: 1-866-889-8054
Chiropractic Services Information ALIVI
3511 NW 91st Ave.
Doral, FL 33172
(Address ID 003138529)
Phone: 1-786-441-8500
Fax: 1-305-675-2353
Claims EDI: uhcprovider.com/edi (Payer ID: 87726)
The ERA payer ID number is also changing to 87726. If you would like to receive
835 ERA files for NHP, or if you currently receive 835 ERA files for NHP under
payer ID 95123 or 96107, contact your vendor to enroll under payer ID 87726. The
health plan ID card for members who have transitioned indicates payer ID 87726.
Online: UnitedHealthcare Provider Portal at uhcprovider.com/claims > Sign In >
Claims & Payments. Then select Look up a Claim from the menu.
Information: uhcprovider.com/claims (policies, instructions and tips)
Phone: 1-877-842-3210 (follow the prompts for status information)
Durable Medical Equipment/
Respiratory and Commodity
Services
(Oxygen, CPAP, hospital beds,
standard wheelchairs)
Apria: 1-855-613-8303 apria.com
Lincare: 1-855-236-8277 lincare.com
Rotech: 1-877-623-5272 rotech.com
EDI Support Online: uhcprovider.com/edi
Phone: 1-866-509-1593
Eligibility Verification
• Verify primary care physician
• Verify eligibility and benefits
• Check claim(s) status
• Obtain status of referrals
• Office visit copay
• Inpatient copay
• Prescription drug copay
(if applicable)
EDI: Transactions 270 (Inquiry) and 271 (Response) through your vendor
or clearinghouse
Online: UnitedHealthcare Provider Portal at uhcprovider.com/eligibility > Sign In.
Then, select Eligibility from the menu.
Phone: 1-877-842-3210
Neighborhood Health Partnership supplement
249
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Home Health Services Lincare: 1-855-236-8277 lincare.com
Byram Medical: 1-877-902-9726 byramhealthcare.com
Edgepark Medical: 1-888-394-5375 edgepark.com
Home Infusion Services
(Including enteral)
Orsini Health: 1-800-240-9572 orsinihealthcare.com
Express Scripts: 1-855-315-3590 accredo.com
OptionCare Infusion: 1-800-683-5252 optioncarehealth.com
Insulin Pumps and Supplies
National Vendors
MiniMed Distribution Group (Medtronic): 1-800-933-3322 minimed.com
Medical Supply Providers
(Disposable supplies, ostomy,
urological, incontinence supplies)
Byram Medical: 1-877-902-9726 byramhealthcare.com
Edgepark Medical: 1-888-394-5375 edgepark.com
Medline: 1-800-633-5463 medline.com
McKesson: 1-855-404-6727 mckesson.com
Mental Health Services
Prior Authorization
Optum
Phone: 1-800-817-4705
Outpatient Injectable Chemotherapy
and Related Cancer Therapies
Online: uhcprovider.com/oncology
Phone: 1-888-397-8129
Pharmacy (OptumRx) Online: professionals.optumrx.com > Prior Authorizations
Prior Authorization: 1-800-711-4555
Specialty Pharmacy Customer Service: 1-888-739-5820
Physical, Occupational and Speech
Therapy (OptumHealth)
Phone: 1-800-873-4575
Fax: 1-248-733-6070
Podiatry
Foot and Ankle Network (FAN)
ALIVI
3511 NW 91st Ave.
Doral, FL 33172
(Address ID 003138529)
Phone: 1-786-441-8500
Fax: 1-305-675-2353
Prior Authorization and Advance
Notification
EDI: Transactions 278A and 278N
Online: uhcprovider.com/paan
Phone: 1-877-842-3210 (if you do not have access to electronic services)
Information: uhcprovider.com/priorauth
Neighborhood Health Partnership supplement
250
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Radiology/Advanced Outpatient
Imaging Procedures:
Request prior authorization of
radiology services as described in the
Outpatient radiology notification/
prior authorization protocol section
of this guide
• CT scans
• MRIs
• MRAs
• PET scans
• Nuclear medicine studies, including
nuclear cardiology
Online: uhcprovider.com/paan
Phone: 1-866-889-8054
Information: uhcprovider.com/radiology
Radiation Therapy Online: UnitedHealthcare Provider Portal at uhcprovider.com/oncology > Sign In.
Then select Prior Authorizations from the menu.
– Select the Submission and Status link under the Radiology, Cardiology &
Radiation Oncology section
– Select service type: Radiation Oncology
Phone: 1-877-842-3210
Information: uhcprovider.com/oncology > Radiation Therapy Services
Substance Use Services Optum
Phone: 1-800-817-4705
Case Management Congenital Heart Disease: 1-877-842-3210
Kidney Resource Services: 1-877-842-3210
Ventricular Assist Devices: 1-877-842-3210 or fax 1-855-282-8929
Transplant Resource Services: 1-877-842-3210 or fax 1-855-250-8157
Discharge of a member from participating provider’s care
Refer to the section Member dismissals initiated by a PCP, Chapter 2: Provider responsibilities, for more information.
Laboratory services
Direct all NHP members to LabCorp, Inc. service centers for outpatient laboratory procedures. If a participating health care
provider draws the specimen in the office, send the specimen to LabCorp, Inc.
Home health care agencies are responsible for delivery of drawn specimens to one of the LabCorp, Inc. service centers.
We pay laboratory services according to your Agreement. They must be performed by a participating health care provider that
is a facility for:
• Emergency room services
• Chemotherapy
• Ambulatory surgery

Neighborhood Health Partnership supplement
251
2023 UnitedHealthcare Care Provider Administrative Guide
• Transfusions
• Hemodialysis
LabCorp, Inc. must process clinical laboratory specimens drawn at a skilled nursing facility.
Use of non-participating laboratory services
This applies to all participating health care providers. It also applies to laboratory services, clinical and anatomic, ordered by
any practitioner.
You are required to refer laboratory services to participating laboratories, except as otherwise authorized by NHP. To get more
information on participating laboratories:
• Go to LabCorp.com or call 1-800-833-3984, option 3, to determine how to conveniently access their services.
• Call Provider Services at 1-877-842-3210.
In the unusual circumstance you require a specific laboratory test for which you find no participating laboratory is available,
contact NHP UM at 1-877-842-3210.
LabCorp requires this information to make sure accurate testing and billing:
• Member’s NHP ID number
• LabCorp requisition forms with all required fields completed
• Specific test orders using test codes
• Diagnosis codes
Referrals
The PCP is responsible for determining when the member needs a referral. Only the PCP may make an initial referral. These
must be made to participating health care providers. We deny claims for services rendered without a proper referral. You may
not bill the member for those services unless, prior to receiving the service, the member agrees in writing:
1. That the referral is not in place or the service is not a covered service.
2. To be financially responsible for the cost of the service.
Referrals to a specialist may be necessary:
• When a member fails to respond to current medical treatment.
• To confirm or establish a member’s diagnosis and/or treatment modality.
• To provide diagnostic studies, treatments or procedures that range beyond the scope of the PCP. PCPs may make referrals to
a specialist according to the following Specialty Referral Guidelines section.
These specialty services do not require referral:
• Chiropractic (subject to benefit limitations)
• Dermatology
• Gynecology
• Podiatry*
• Substance use treatment*
• Mental health*
Out-of-network referrals
Out-of-network referrals are only approved when the services are not available from a participating health care provider.
Request out-of-network referrals by calling NHP at 1-877-842-3210. Once we receive the referral, the data will be reviewed and,
if approved, entered into the system to help ensure payment of the specialist claims.
* See the Prior Authorization section of this supplement.

Neighborhood Health Partnership supplement
252
2023 UnitedHealthcare Care Provider Administrative Guide
Specialty referral guidelines
• Once the specialty services have been properly authorized, the member or PCP may schedule an appointment with
the specialist.
• Submit specialist referrals in the Referrals tool in the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In.
• We mail an authorization letter to the specialist for the member’s medical record.
• We do not pay specialist claims without a referral.
• The specialist should re-verify the member’s eligibility at the time of visit by calling Provider Services at 1-877-842-3210. Refer
to the back of the ID card to help ensure the appropriate Provider Services department is contacted.
• Call 1-800-817-4705 for behavioral health service requests.
• All NHP HMO members require a referral before scheduling appointments for specialty services.
Obstetrics
A member may self-refer to an NHP obstetrician who is a participating health care provider for routine OB care. If the member is
referred to a non-participating specialist, the specialist must notify us through uhcprovider.com or by calling 1-877-842-3210 to
make sure accurate claims payment for ante- and postpartum care.
• Plain film radiography performed by an NHP participating health care provider or in the obstetrician’s office during an
authorized visit, does not require prior authorization.
• Routine labs performed in the obstetrician’s office, or that are provided by a participating health care provider in support of
an authorized visit, do not require prior authorization.
• Office procedures and diagnostic and/or therapeutic testing performed in the obstetrician’s office that do not require prior
authorization may be performed.
UM
Submit your request electronically using one of the methods outlined in the How to Contact NHP section.
Be sure to include the place of service and CPT codes in your request.
If you do not have electronic access, you may submit prior authorization requests by phone.
Prior authorization requirements
All NHP members require prior authorization for the services listed on the Prior Authorization List located on uhcprovider.com/
priorauth > Frequently searched > Advance Notification and Plan Requirement Resources > Neighborhood Health Partnership
Advance Notification Guide.
Except as otherwise provided, NHP requires prior authorization prior to these admissions:
• All hospital admissions*
• Inpatient rehabilitation facility
• Skilled nursing facility
• Long term acute care facility
• Special care unit
You must provide clinical information to support the medical necessity of the admission and/or observation stay, by the next
business day following the admission. Final determinations are made by a medical director, as appropriate.
* Admissions from the emergency room, to the ICU/CCU, or admission for emergency surgery must be Post-certified by the next business day following admission.

Neighborhood Health Partnership supplement
253
2023 UnitedHealthcare Care Provider Administrative Guide
Concurrent review
The continued stay for all inpatient admissions must be certified through the concurrent review process. Upon request, you
must submit to NHP, or its delegated entities, sufficient clinical information to:
• Certify the continued stay.
• Allow the review of the member’s medical status during an inpatient stay.
• Extend the member’s stay.
• Coordinate the discharge plan.
• Determine medical necessity at an appropriate level of care.
• Perform quality assurance screening.
All discharge planning and cases requiring comprehensive services for catastrophic or chronic conditions are coordinated
through NHP Case Management. This includes OB care. If the diagnosis or treatment of a member is delayed secondary to
the inability of the facility to provide a needed service, payment for these days is denied. This includes, but is not limited to, the
unavailability of diagnostic and/or surgical services on weekends and holidays, delays in the interpretation of diagnostic testing,
delays in obtaining requested consultations and late rounding by the admitting physician.
Reimbursement for continued stay that does not meet NHP medical necessity criteria is denied. The member may not be billed
for these services unless they have signed a waiver of liability or the services are denied as non-covered services. The member
is held harmless in these proceedings.
Claims reconsiderations and appeals
Claim reconsideration
Refer to Claim reconsideration and appeals process section located in Chapter 10: Our claims process for detailed
information about the reconsideration process.
Your documentation should clearly explain the nature of the review request.
If you are unable to use the online reconsideration and appeals process outlined in Chapter 10: Our claims process, fax
reconsideration or appeal information to 1-801-938-2100.
You have 1 year from the date of occurrence to file an appeal with the NHP. You will receive a decision in writing within 60
calendar days from the date we receive your appeal.
If you have a question about a pre-service appeal, see the Pre-Service Appeals section in Chapter 7: Medical management.
Capitated health care providers
Optum Pay is available to health care providers who participate under a capitated arrangement. You may enroll in EFT. To enroll
go to optum.com/optumpay. To sign in after enrollment, go to optumbank.com > Sign in.
You may access and download a capitation detail file. To learn how to access the report and view instructions for using it, go to
uhcprovider.com/reports.

254
2023 UnitedHealthcare Care Provider Administrative Guide
New Mexico Supplement
New Mexico commercial plans: Provider grievance process
In accordance with New Mexico law NMAC 13.10.16, providers have the right to file a grievance about health care insurer
operations, termination from a health plan, credentialing and timely claims payment.
Health plan operation grievances include grievances about quality of care or network adequacy issues. Grievances about denial
of a specific member’s access to a benefit should be filed pursuant to the member grievance plan found in the member’s health
plan language. You can send provider grievances to:
UnitedHealthcare
Attn: Provider Contract Appeals
P.O. Box 31376
Salt Lake City, UT 84131-0376
Here’s how the grievance process works:
Operational grievances
At the first level of an operational grievance, providers have the right to present their concerns to a committee responsible
for the area addressed by the grievance. The substance of the first-level grievance will also be conveyed to the health plan’s
governing body.
The health plan’s governing body must be provided the opportunity to direct the committee’s review and resolution of the
grievance. The governing body may also dictate who serves on the grievance review committee. The health plan must issue a
written decision to the provider within 20 days of receiving the operational grievance and all relevant information.
Termination for cause
For terminations based on cause, the health plan must allow the provider to appear in person before a fair hearing officer or
committee appointed by the health plan. Providers have the right to:
• Present a case to the fair hearing officer or committee
• Submit supporting materials to the hearing officer or committee
• Ask questions of any representative of the health plan
• Be represented by an attorney or other person of the provider’s choice
• Ask for an expedited hearing where the health plan has not provided written notice of the termination to the provider because
the health plan has reason to believe that further care by the provider would result in imminent and significant harm to
members
The health plan must issue a written decision within 20 days of the fair hearing and forward a copy of the decision to the
provider using the method of written communication chosen by the provider.
When the quality of care provided to members is the basis for termination and the health plan has reason to believe that further
care by the provider would result in imminent and significant harm to members, the health plan is not required to provide
advance written notice of termination for cause.
Other terminations
For all other terminations, the health plan will provide a written explanation to the provider at least 30 days in advance of the
termination.
Appeal rights for operational grievances and terminations
If the provider is dissatisfied with the results of the plan’s internal grievance procedure, they may file a written request for review
with the superintendent within 30 days from receipt of the written decision of the managed health care plan (MHCP) concerning
the grievance.
Complaints to the New Mexico Office of Superintendent of Insurance should be filed with the New Mexico Office of
Superintendent of Insurance. After appropriate investigation of a provider complaint, the superintendent may schedule a
hearing.

New Mexico Supplement
255
2023 UnitedHealthcare Care Provider Administrative Guide
Claims payments
In accordance with New Mexico law NMAC 13.10.16, providers also have the right to grieve the failure of the health plan to
pay clean claims. To initiate an internal review, providers should file an inquiry with the health plan about the status of the claim
as a clean claim and why the claim has not been paid. The health plan will respond to this inquiry in writing within 15 days of
receiving the inquiry. The health plan’s response will explain the plan’s failure or refusal to pay, or the expected date of payment
if payment is pending.
If a provider is not satisfied with the outcome of this grievance, the provider may file a complaint with the Office of
Superintendent of Insurance. The provider may file a complaint if the health plan doesn’t respond or the issue hasn’t been
resolved at the internal level within 45 days of initiation of the claims payment grievance.
Questions?
Contact your network management representative.

256
2023 UnitedHealthcare Care Provider Administrative Guide
OneNet PPO/Workers’ Compensation supplement
Applicability of this supplement
This supplement lists operational procedures and information applicable to services received by a OneNet Customer that are
covered under a Property or Casualty Benefit Plan sponsored, issued or administered by a OneNet Payer. (Terms defined in
the following section.) Such services are subject to both the main guide and this supplement. This supplement controls in the
event of any conflict with the main guide. For protocols, policies and procedures not referenced in this supplement, refer to the
appropriate chapter in the main guide. OneNet PPO, LLC (OneNet) is a wholly owned subsidiary of UnitedHealthcare Insurance
Company, a part of UnitedHealth Group, Inc. Because OneNet is a network only and not a payer, certain provisions of the main
guide will apply to OneNet with some variation. This supplement identifies these principal variations.
Terms used in the supplement
Adjuster: An adjuster works for an insurance company, third-party administrator (TPA) or directly for a self-insured employer.
This person coordinates with all parties on a workers’ compensation case or auto liability claim. They are responsible for,
among other things, the wage replacement and return-to-work coordination as well as all management of the funding for
medical services.
Clean Bill/Claim: “Bill” refers to the submitted UB or CMS1500 form. “Claim” represents the entire workers’ compensation or
auto accident, including all submitted bills.
Bill/Claim Pricing or Repricing: The process of applying the OneNet contracted rates to bills, including the application of
clinical edits, reimbursement policies and standard coding practices. It may include the application of state or federal workers’
compensation fee schedule rates, usual and customary or reasonable rate (UCR) or prevailing rate as defined by the state,
or other government-authorized pricing methodology or schedule. The terms “claim/bill pricing” and “repricing” are used
interchangeably. The process of applying contracted rates to bills from network care providers includes the application of the
lesser of the billed charges, contracted rate, state/federal schedule, UCR or other authorized fee schedule.
OneNet Client: An entity that has contractual authority to access the OneNet network of health care providers. OneNet Clients
may include, without limitation, insurance carriers, workers’ compensation insurance carriers, auto liability insurers, risk
management entities, claims management entities, TPAs and employers. A OneNet Client can access the OneNet network for
itself, on behalf of another entity that is a OneNet Payer or both. A OneNet Client may or may not be the OneNet Payer for a
particular OneNet Customer. A OneNet Client accessing the OneNet Network on behalf a OneNet Payer may perform some or
all of the OneNet Payer’s administrative services (e.g., eligibility verification, claims adjudication and bill payment).
OneNet Customer: A person whose coverage under a Property or Casualty Benefit Plan enables them to receive treatment
from OneNet participating health care providers. The term “OneNet Customer” means the same as “customer,” “member,”
“participant,” “primary participant,” “injured worker,” “subscriber,” “employee,” insured” and “claimant” as used this guide.
OneNet Payer: An entity that is obligated to reimburse services covered under a Property or Casualty Benefit Plan and that
has contractual authority to access the OneNet network of health care providers. References to “Participating Entity,” “Payer”
or “Alternate Payer” in the health care provider Agreement and in this guide also apply to OneNet Payers. OneNet, Procura and
UnitedHealthcare and its affiliates are not OneNet Payers. OneNet Payers may include, without limitation, insurance carriers,
workers’ compensation insurance carriers, auto liability insurers, risk management entities and employers. A OneNet Payer’s
access to the OneNet Network may be through its own contractual access to the OneNet network or through a OneNet Client’s
contractual access to the OneNet network. Some or all of a OneNet Payer’s administrative services (eligibility verification,
claims adjudication and bill payment) may be performed by a OneNet Client or other entity.
Property or Casualty Benefit Plan: A Benefit Plan sponsored, issued or administered by a OneNet Payer that is not a medical
Benefit Plan but that includes coverage for medical services and supplies. Property and Casualty Benefit Plans include, without
limitation, workers’ compensation programs and auto liability insurance.
Utilization Review: Utilization management or utilization review is the use of managed care techniques such as prior
authorization that allows payers to address clinical appropriateness using evidenced-based criteria or guidelines as defined by
each state. Procura may or may not provide utilization management services for their clients.
OneNet PPO/Workers’ Compensation supplement
257
2023 UnitedHealthcare Care Provider Administrative Guide
UCR/Prevailing Rate: The UCR rate (also known as prevailing rate) determined by the state or other governmental entity or
a database referenced by a state or governmental agency such as FAIR Health. The database is created using rates typically
charged by care providers in a geographic area.
OneNet PPO product overview
OneNet is a network of physicians, health care practitioners, hospitals and ancillary facilities whose Agreements with
UnitedHealthcare provide for participation in Property and Casualty Benefit Plans, including workers’ compensation programs
and auto liability insurance. Entities that are obligated to reimburse medical services under Property and Casualty Benefit
Plans contract directly or indirectly with Procura Management, Inc. (a UnitedHealthcare affiliate) to access OneNet providers at
negotiated rates.
OneNet may include health care providers within the OneNet service area, as well as those in other areas (e.g., states adjacent
to the service area or future expansion areas). Currently, the OneNet service area includes Delaware, Florida, Georgia,
Maryland, North Carolina, South Carolina, Pennsylvania, Tennessee (except for auto liability insurance), Virginia, Washington
D.C. and West Virginia.
Advantages that providers who participate in the OneNet Property and Casualty network may see include the following:
• Increased patient volume by referrals generated through published directories, workplace postings and online provider look-
up tools
• Efficient and consistent payment and adjudication of bills defined by your contract terms
• Hands-on Provider Relations staff
Who to contact
Resource Where to go
OneNet/Procura Clients and Payers
Responsible for the administration
and payment of Property and
Casualty programs (including workers’
compensation and auto liability)
accessing the OneNet PPO Network.
Responsibilities include:
• Determining bill eligibility.
• Processing bills.
• Providing EOB statements or
remittance advices.
• May also include case management
and utilization review services.
For questions related to these services, contact the payer identified on the EOR
or the payer provided by the patient. Procura and OneNet names will appear on
the EOR/EOB/remittance advice when the OneNet Network is being accessed.
Procura For OneNet PPO in-network referrals, OneNet contracted rate pricing inquiries/
appeals, or how to contact our clients.
Phone: 1-877-461-3750
Email: [email protected]
Contract Questions Contact your UnitedHealthcare Network Management representative. If you
require assistance determining who your representative is, or how to reach them,
visit uhcprovider.com > Contact us > State-specific health plan and network
support.
OneNet PPO/Workers’ Compensation supplement
258
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Appeals If you are disputing state pricing or services deemed not part of the workers’
compensation/auto illness or injury, contact the client at the number identified
on the EOR.
For all network-related concerns, contact Procura:
Phone: 1-877-461-3750
Email: [email protected]
Some states have formal dispute resolution or appeals processes. Follow the
appeal time frames and dispute resolution procedures outlined in your contract
and this guide. Contact Procura if you have questions about this requirement.
To Request a copy of the Decision
Point Review (DPR) Plan
Contact the payer identified on the EOR. DPR Plan provides specific
requirements for submitting an appeal for medical reconsideration of an auto
liability claim, but they are not required in all states.
Website OneNet pricing sheets are available in the UnitedHealthcare Provider Portal at
uhcprovider.com > Sign In > Claims & Payments > UnitedHealthcare OneNet
PPO Pricing. Final payment determination is the responsibility of our clients.
News, Information and Updates For information on policies, protocols, products, new initiatives, website
enhancements and online solutions, visit uhcprovider.com/news. Sign up for
email updates at uhcprovider.com/news.
Patient eligibility
Contact the claimant or injured worker’s employer, workers’ compensation carrier, auto liability insurer or administrator to verify
acceptance of an injury for purposes of coverage. ID cards are not usually issued or used for workers’ compensation and
auto liability programs. Injured workers and claimants accessing you through the OneNet PPO Network will not present an ID
card. Insurers, administrators and employers are instructed to advise you of network access, if known, when you call to verify
the injury and coverage. You may ask if the employer, carrier or administrator is contracted with Procura to access OneNet’s
workers’ compensation and auto liability networks.
Bill process
Bill submission
All bills should be sent directly to the applicable employer, worker’s compensation carrier, auto liability insurer or third-party
administrator (TPA). Do not submit bills directly to OneNet or Procura, except for pricing appeals.
When submitting a bill, it is important to submit complete bills and to accurately code all diagnoses and services in accordance
with national coding guidelines.
Additional information may be required for particular types of services, or based on particular circumstances or
state requirements.
Clean bills must be submitted within the time frame identified in your contract, or within 12 months of the date services are
provided, and in accordance with any applicable laws. Failure to submit bills correctly will result in the rejection and return of
bills. You will receive a notice from the applicable claimant or injured worker’s employer, workers’ compensation carrier, auto
liability insurer or TPA in the event your bills are being withheld from bill pricing and payment while compensability is being
determined.
If you have questions about submitting claims to us, call the claimant or injured workers’ employer, workers’
compensation carrier, auto liability insurer or TPA for instructions on how to submit a bill.

OneNet PPO/Workers’ Compensation supplement
259
2023 UnitedHealthcare Care Provider Administrative Guide
Complete bill requirements
Your bills may not be processed if you omit:
• Items identified under the Claims and Encounter Data Submissions section of the UnitedHealthcare Guide.
Additional requirements:
• Items identified under the Additional information needed for a complete UB-04/CMS-1450 Form section of the
UnitedHealthcare Guide.
• When billing late charges, indicate bill type 115 or 117 (inpatient), or 135 or 137 (outpatient), in form locator 4 of the
CMS-1450/UB-04.
• Bill all outpatient surgeries with the appropriate revenue and CPT codes if reimbursed according to ambulatory
surgery groupings.
Submit all bills for professional services or facility services on a CMS 1500 or UB-04 claim form or their electronic equivalents
and include all standard code sets that apply.
Bill review procedures
Our bill review procedures identify coding errors and coding irregularities. This helps provide better consistency during our
claims pricing.
Tips to expedite bill processing:
• Submit bills on a red CMS 1500 or a UB-04 form, using 11 or 12 point font size and black laser jet ink.
• Do not use a highlighter on the claim form or any attachments.
• Line up forms to print in the appropriate boxes.
• Submit bills on original forms, not photocopies.
• Complete all required fields on standard forms.
• Make sure attachments are complete and legible.
• Make sure information such as the health care provider’s name, telephone number, taxonomy code, NPI and other
information is accurate.
• Remember to sign and date all necessary forms; an electronic signature is acceptable.
Pricing of bills
OneNet pricing includes bill completeness, accuracy review and pricing, per your contracted rate.
Payment for covered services related to a workers’ compensation injury is the least of the following:
• The Property & Casualty Benefit Plan payment rate per your Agreement
• Your eligible billed charges
• The state’s workers’ compensation fee schedule
• The federal workers’ compensation fee schedule
• UCR or prevailing rate as determined by the state
• Other state, federal or government authorized fee schedule
Application of this reimbursement comparison is generally at the claim line (service code) level, unless state or federal
regulations applicable to the job-related injury specify comparisons must be done at claim-level aggregate values.
Payment for covered services of an auto liability bill is the least of the following:
• The Property & Casualty Benefit Plan Auto Liability payment rate per your agreement
• Your eligible billed charges
• UCR or prevailing rate as determined by the state
• Any state, federal or mandated rates applicable to auto
OneNet PPO/Workers’ Compensation supplement
260
2023 UnitedHealthcare Care Provider Administrative Guide
Bills subject to bill edits
For bills subject to code edits or line bundling and unbundling, the bill pricing resulting from these edits is allocated back to the
original submitted bill lines and codes (refer to the OneNet pricing sheet). Priced bills do not display the lines or codes added or
deleted by these bill edits. This is intended to assist physicians and OneNet’s clients and payers in bill reconciliation by having
priced bills match the originally submitted bills.
Allocation of global pricing to the bill line level
Certain bills are subject to global pricing, including case rates, flat rates and per diems. In these cases, a fixed percentage of
the overall global rate may be allocated to the applicable lines of the bill.
Example of global pricing distributed across lines
A health care provider has billed lines totaling $100 that are subject to a state fee maximum of $90 and a contracted global rate
of $80. A portion of the global rate is allocated to each line as a percentage of the state fee charges.
Billed Charges State Fee Allowed Amount
Line 1 $50 $45 $40
Line 2 $30 $27 $24
Line 3 $20 $18 $16
Total $100 $90 $80
These allocations occur because individual lines where global pricing has been distributed may not be processed
separately. This means if the payer finds a service line to be non-compensable, and a portion of a global rate has been
allocated to that line, that portion must still be considered when determining payment. Remark codes on the pricing sheet show
when we cannot process individual lines of a bill-level rate separately.
Bill inquiries
OneNet can verify our receipt, the OneNet contracted pricing and the date returned to our client. We cannot verify payment
status or questions related to anything outside of the network contract.
Bill inquires related to the status of payments and non-OneNet related pricing should be directed to the applicable claimant or
injured worker’s employer, workers’ compensation carrier, auto liability insurer or TPA.
The fastest way to locate a OneNet PPO pricing sheet is to access the UnitedHealthcare Provider Portal at uhcprovider.com
> Sign In > Claims & Payments > UnitedHealthcare OneNet PPO pricing. Pricing sheets show the allowed amount of your
bills after the application of OneNet bill pricing. They do not show the final bill adjudication by the payer, which could include
pricing for charges that the payer identifies as non-payable, ineligible or the patient’s responsibility. The EOB or remit created
by the applicable claimant or injured worker’s employer, workers’ compensation carrier, auto liability insurer or TPA will identify
charges deemed not payable for workers’ compensation or auto liability.
If you do not have internet access, or if you cannot find the information for the Procura client you need on our website, call
1-877-461-3750.
Bill payment
OneNet and Procura do not pay bills and do not have an obligation to pay for services rendered to an injured worker or
claimant authorized to access a OneNet PPO Network provider. We send the priced bill to the appropriate client or payer
for adjudication and payment determination. You are required to accept the OneNet contracted amount as payment in full for
covered services.
For compensable workers’ compensation-related services, the injured worker may not be billed. There are no copayments,
deductibles, or coinsurances. Balance billing is prohibited for all services covered by a workers’ compensation benefit plan.

OneNet PPO/Workers’ Compensation supplement
261
2023 UnitedHealthcare Care Provider Administrative Guide
A health care provider may not bill participants for non-professional services including charges for overhead, administration
fees, malpractice surcharges, membership fees, fees for referrals, or fees for completing bill forms or submitting additional
information. If OneNet rejects or denies a bill because a health care provider failed to follow policies and procedures, the patient
may not be billed.
For compensable auto claims, the claimant may have deductibles according to their policy. The claimant is responsible for
those deductibles. An auto liability policy may also contain limited benefits. Once those benefits are exhausted, the claimant is
responsible for all remaining charges or the services can be billed through their health insurance carrier if there are additional
benefits for the claimant to use.
OneNet payers are required to adjudicate and pay clean bills within 30 days of bill pricing, or within applicable state or federal
guidelines. If the OneNet payer fails to adjudicate and pay a bill within this time period, the health care provider may, at their
discretion, request the least of the full charges. In the case of workers’ compensation, the applicable state or federal maximums
will still apply. In these instances, the OneNet payer will pay the bill as it was priced by OneNet. After receiving payment, the
health care provider must notify the OneNet payer that payment of full charges or applicable state or federal maximums are
requested due to late bill payment. A health care provider cannot request full billed charges for failing to offer timely payment if
OneNet, Procura or the client or payer notifies the health care provider after receipt of the bill but before the expiration of the bill
payment’s time limit that the bill is denied, is missing required information, is deficient in some way or is being held to determine
auto or workers’ compensation compensability.
The claimant or injured worker’s employer, workers’ compensation carrier, auto liability insurer or TPA must send you an EOB
or remittance advice indicating that the OneNet PPO Network was accessed and the reimbursement amount for those services.
The EOB shows:
• The billed charges for services.
• The OneNet contracted amount.
• The reimbursement amount.
• The amount adjusted based on the Property or Casualty Benefit Plan contract/benefit plan.
• Services found to be non-payable.
Submit bills with services not payable under the Property or Casualty Benefit Plan to the injured worker or claimant’s health
plan. Do not assume that UnitedHealthcare is the claimant or worker’s health insurer. You can get this information by calling
their employer or from the claimant or injured worker directly.
Non-covered services and other participant protocols
Follow UnitedHealthcare’s protocols on compensation for care provided to OneNet participants with the following exceptions:
• Workers’ compensation and auto liability lines of business - When you perform a service that may not be covered under the
workers’ compensation/auto claim or the patient’s health insurance, you may balance bill the injured worker or claimant only
if the following conditions are met:
– You notified the injured worker or claimant at the time of service that the charge may not be compensable under their
workers’ compensation/auto injury or illness.
– The injured worker or claimant agrees at the time of service to be responsible for the charge.
– You obtained written consent from the patient to perform the service.
– You have submitted the bill to both the workers’ compensation/auto employer, carrier, insurer or TPA and the claimant
or injured worker’s health insurance, and the service is not compensable under either the workers’ compensation/auto
coverage or the injured worker or claimant’s health insurance.
• The claimant or injured workers’ employer, workers’ compensation carrier, auto liability insurer or TPA determines
compensability.
• You cannot use the online claim estimator on uhcprovider.com to estimate bills.
• You cannot submit OneNet bills for real-time processing on uhcprovider.com.
For hospital audit services, OneNet and OneNet clients or payers may conduct their own audits of hospital bills. They may
follow their own procedures, subject to mutual agreement of the OneNet client or payer and the audited facility. These
procedures vary from those of UnitedHealthcare’s Hospital Audit Service Department. OneNet or Procura may request copies
of medical records to comply with audits required by external accreditation agencies, the state, OneNet clients or payers or

OneNet PPO/Workers’ Compensation supplement
262
2023 UnitedHealthcare Care Provider Administrative Guide
for cause. OneNet clients and payers may conduct independent hospital or facility bill audits and request copies of medical
records to help ensure quality care. You must provide medical records when requested by OneNet or OneNet clients or payers
at no cost to OneNet, the OneNet client or payer, or the participant. UnitedHealthcare’s hospital bill audit protocol does not
apply to such audits or requests for medical records.
Bill appeals (post-service)
Email direct pricing appeals for Procura bills to [email protected], or call 1-877-461-3750. Questions about a state rate
allowance should be directed to the claimant or injured worker’s employer, workers’ compensation carrier, auto liability insurer
or TPA identified on the EOR.
Any bill pricing appeals must be submitted within 12 months of the bill process date, or within the time frame prescribed by
applicable law or your Agreement.
Utilize the following procedure for payment appeals related to OneNet PPO:
• Email your payment appeals to Procura at: [email protected].
• When resubmitting information, attach all applicable documentation, including any additional information requested.
• Include the UB/HCFA bill and EOB.
If you have any concerns about the appeal process or specific concerns about a Procura/OneNet client or payer, contact
Procura at [email protected] or call 1-877-461-3750.
Overpayments
Direct all questions or refunds of overpayments to the applicable OneNet client or payer using the phone number listed on the
claimant or injured worker’s EOB or remittance advice.
If you find a bill where you were overpaid or if we inform you of an overpaid bill that you do not dispute, you must send
the overpayment within 30 calendar days (or as required by law or your Agreement) from the date of your identification or
our request.
Attach appropriate documentation that outlines the overpayment, including the patient’s name, ID number, date of service and
amount paid. If possible, include a copy of the EOB that corresponds with the payment.
If you disagree with a request for an overpayment refund, notify the payer in writing as to why you do not believe overpayment
occurred and why you dispute the refund.
If the payer still believes a refund should be provided, the payer forwards the information to Procura and OneNet for further
review. Procura and OneNet will work with you and the payer to resolve the issue.
Bill pricing adjustments of $5 or less
We strive to accurately re-price all bills and make adjustments when an incorrectly priced bill results in significant underpayment
or overpayment for services.
Bill pricing resulting in either an overpayment or underpayment of $5 or less is not adjusted.
Appeals, grievances or complaints
OneNet injured workers and claimants direct appeals or grievances to their employer, workers’ compensation carrier, auto
liability insurer or TPA. They do not use the Appeals and Grievance Form used by UnitedHealthcare members. You are required
to support the payer’s appeals process by providing records as requested and complying with final determinations. In the
case of complaints or grievances related to a participating health care provider, the employer, workers’ compensation carrier,
auto liability insurer or TPA refers the information to UnitedHealthcare and OneNet. If you are disputing the state or services
deemed not part of the workers’ compensation/auto illness or injury, contact the employer, workers’ compensation carrier, auto
liability insurer or TPA at the number identified on the EOR. For all network-related concerns, call Procura at 1-877-461-3750.
Some states have formal dispute resolution or appeals processes. You must submit your appeal to Procura before using these
appeals processes for both workers’ compensation and auto bills.

OneNet PPO/Workers’ Compensation supplement
263
2023 UnitedHealthcare Care Provider Administrative Guide
Online services
Health care professionals can view pricing sheets in the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In >
Claims & Payments > UnitedHealthcare OneNet PPO Pricing. Pricing sheets show the allowed amount of your bill after the
application of OneNet pricing. Pricing sheets do not show the final bill adjudication by the payer. It may include billed charges
and pricing for charges that are not payable as identified on the EOB or remittance advice.
Because workers’ compensation and auto liability information is not stored on any UnitedHealthcare member system, many of
the online solutions on uhcprovider.com are unavailable for OneNet claims.
Some unavailable tools include the following:
• Eligibility or benefits
• View patient personal health records
• Submit advance notifications
• View your OneNet fee schedule
• Claim Estimator
• Claim submission
• Reprint EOBs
• Optum Pay
• Authorizations and referral information, submission and status
Similar limitations exist for other UnitedHealthcare systems designed to use or verify benefits and eligibility information, such as
the United Voice Portal.
Referrals
UnitedHealthcare’s requirements for health care provider referrals do not apply to the OneNet PPO Network. Do not use the
referral submission system online. However, in some states the injured worker or claimant may be required to use certain health
care providers to receive benefits. Contact the injured worker or claimant’s adjuster for guidance. Try to recommend another
participating health care provider, if requested. For assistance identifying participating health care providers, call Procura at
1-877-461-3750.
Air ambulance, fixed-wing non-emergency transport
UnitedHealthcare’s requirement to refer non-emergency fixed-wing air ambulance to a participating health care provider does
not apply. The injured worker or claimant may not receive benefits, depending on the state, unless an authorized health care
provider is used. If an in-network provider is not available, contact the adjuster to determine where to refer the injured worker or
claimant for authorized care.
Laboratory services
UnitedHealthcare’s requirement that participating laboratory providers must be used does not apply. The injured worker or
claimant may not receive benefits unless an authorized laboratory is used. Contact the adjuster for guidance. Try to refer to a
laboratory based on the information provided by the adjuster. The OneNet PPO Network includes national, regional and local
health care providers of laboratory services. The self-referral and anti-kickback provisions of UnitedHealthcare’s laboratory
services protocols apply to OneNet health care providers.
Pharmacy services
The OneNet PPO workers’ compensation and auto liability networks do not include a pharmacy network. Contact the adjuster
to determine where to refer the patient for care.

OneNet PPO/Workers’ Compensation supplement
264
2023 UnitedHealthcare Care Provider Administrative Guide
Specialty pharmacy and home infusion
UnitedHealthcare’s requirements on Designated Specialty Pharmacy or Home Infusion Providers for Specialty Medications, and
Specialty Pharmacy Requirements for Certain Specialty Medications do not apply to, and are not supported by, the OneNet
PPO Network. Contact the adjuster for the name of a specialty pharmacy provider, as the injured worker or claimant may be
required to use certain health care providers to receive benefits.
Provider responsibilities and workflows
OneNet health care providers follow Chapter 2: Provider responsibilities and standards with these noted exceptions:
• As part of transitions under continuity of customer care, participating health care providers should notify current patients
accessing them through the OneNet network of an effective date of termination of their Agreement at least 30 calendar days
prior, or as required under applicable laws. OneNet does not maintain participant names and addresses and may not notify
participants on your behalf.
• Additional exceptions related to benefits, eligibility, online tools and health plan ID cards are in other parts of this supplement.
Behavioral health services
Contact the adjuster if you believe an injured worker or claimant would benefit from mental health/substance use services
due to their job-related injury or auto accident. The OneNet network includes behavioral health care providers. Follow Official
Disability Guidelines (ODG) and requirements or other evidence-based requirements as defined by each state.
Case management
Payers may use their own internal case management services for injured workers or claimants. You are required to comply with
the case management programs used by Procura and its clients and payers. They will follow state-driven requirements or other
evidenced-based guidelines. OneNet health care providers must work with case managers and follow all applicable state laws,
regulations and rules.
Medical records standards and requirements
Standards and requirements described in Chapter 12: Medical records standards and requirements apply to OneNet health
care providers. Adhere to any state requirements that exceed the requirements as outlined.
Quality management and health management programs
The following exceptions apply to the Health and Disease Management procedures in how they apply to OneNet and OneNet
participants:
• UnitedHealthcare Case Management, Behavioral Health and Disease Management programs do not apply to OneNet
workers’ compensation or auto liability.
• Do not report OneNet participant information to the UnitedHealthcare Cancer Registry.
• OneNet encourages the use of the Clinical and Preventive Health Guidelines when treating OneNet participants. A complete
list of clinical guidelines located on uhcprovider.com/policies > Additional Resources > Clinical Guidelines.
• While OneNet encourages the use of resources available on uhcprovider.com related to mental health/substance use, the
processes described for behavioral health consults do not apply to the OneNet PPO Workers’ Compensation or Auto Liability.
Contact the case manager or adjuster for guidance if you believe a participant would benefit from mental health/substance
use services due to their job-related injury or auto accident. You must follow ODG guidelines and requirements or other
evidence-based requirements as defined by each state.

OneNet PPO/Workers’ Compensation supplement
265
2023 UnitedHealthcare Care Provider Administrative Guide
Participant rights and responsibilities
Get a copy of OneNet’s Participant Rights and Responsibilities, which vary from UnitedHealthcare’s Member Rights and
Responsibilities, by calling Procura at 1-877-461-3750.
Advance Directives
Follow the advance directive requirements provided in the UnitedHealthcare guide for the OneNet Network, if applicable.
OneNet does not produce benefit materials for injured workers or auto liability plans. We cannot inform OneNet participants of
state laws on advance directives. This is the responsibility of the employer, workers’ compensation carrier or other entities as
defined by the employer.
266
2023 UnitedHealthcare Care Provider Administrative Guide
Oxford Commercial supplement
Oxford Commercial product overview
Our Oxford commercial products are gated, non-gated and level funded. For information specific to level funded plans in New
Jersey and Connecticut, see the Oxford Level Funded plans section of this supplement.
Applicability of this supplement
This supplement applies to all covered services you provide to your patients who are Oxford members (insured by or receiving
administrative services from Oxford). Oxford commercial products are offered under the names of Freedom, Liberty and Metro,
as follows:
• Freedom products are offered in Connecticut, New Jersey and New York.
• Liberty products are offered in Connecticut, New Jersey and New York.
• Metro products are offered in New York and New Jersey.
You are subject to both the main guide and this supplement. This supplement controls if it conflicts with information in the main
guide. If there are additional protocols, policies or procedures online, we will direct you to that location when applicable. For
protocols, policies and procedures not referenced in this supplement, refer to the appropriate chapter in the main guide.
Benefit Plans not Subject to the Requirements in this Protocol
• UnitedHealthcare Medicare Advantage plans offered under the AARP® MedicareComplete®, AARP® MedicareComplete®
Mosaic and UnitedHealthcare Medicare Advantage brands on the Oxford health plan platform
• Oxford individual benefit plans underwritten by Oxford Health Insurance, Inc.
Oxford commercial products contact information
Resource Where to Go
Appeals, Administrative
(Claims)
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In
API: Submit reconsiderations and appeals (with attachments) using API. Go to
uhcprovider.com/api for more information.
Appeals, Clinical and Medical
Necessity
Pre-s ervice
Fax: 1-877-220-7537
Phone: 1-800-666-1353
Mail: Oxford Health Plans
Attn: Clinical Appeals
P.O. Box 31388
Salt Lake City, UT 84131
Post-s ervice
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In
API: Submit reconsiderations and appeals (with attachments) using API. Go to
uhcprovider.com/api for more information.
Behav ioral Health Appeals
Mail: Oxford Behavioral Health Appeals
P.O. Box 30512
Salt Lake City, UT 84130-0512
Phone: 1-800-999-9585
Fax: 1-855-312-1470
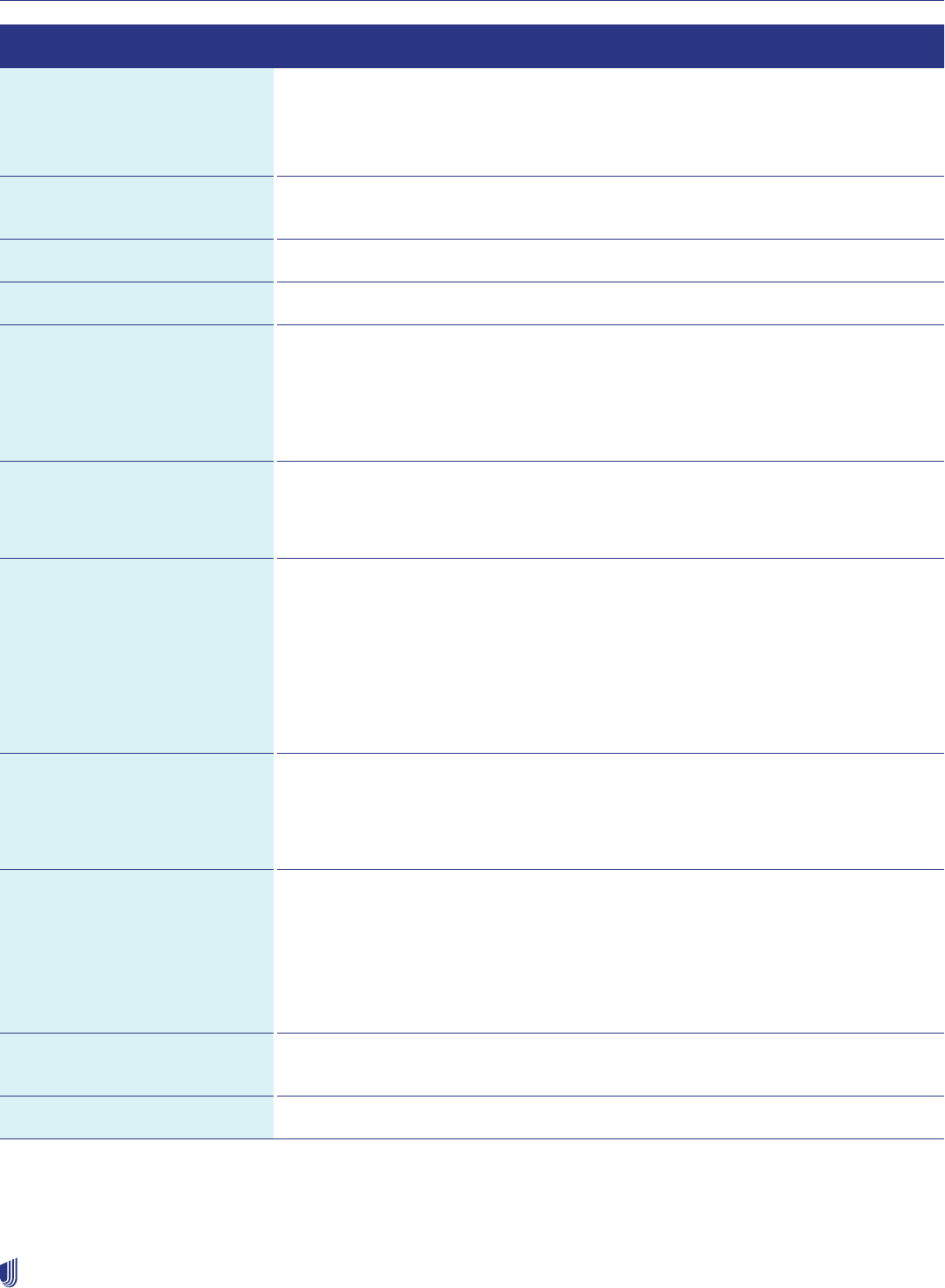
Oxford Commercial supplement
267
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Appeals (Members)
Second Level Member Appeals
uhcprovider.com > Claims and Payments
Mail: Oxford Grievance Review Board
P.O. Box 31387
Salt Lake City, UT 84131
Internal Appeals:
Claims Payment Disputes
uhcprovider.com > Claims and Payments
Appeals: Pharmacy (urgent) Fax: 1-801-994-1058
Behavioral Health Department Phone: 1-800-201-6991
Cardiology
Cardiac Catheterization
Echocardiogram
Stress Echocardiogram
Online: uhcprovider.com/priorauth > Cardiology (available 24 hours a day)
Policies: uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare®
Oxford Clinical and Administrative Policies
Phone (eviCore): 1-877-PREAUTH/1-877-773-2884
(Monday–Friday, 7 a.m.–7 p.m. ET)
Chiropractic Services: Optum Provider Services/Claims
Online: myoptumhealthphysicalhealth.com
Phone: 1-800-985-3293
Claim Submission EDI: Commercial Claims Payer ID: 06111
More information about EDI: optumpay.com/optumpay
You may also visit PNTdata.com to learn about a free submission tool that doesn’t
require practice management software.
Online: UnitedHealthcare Provider Portal at uhcprovider.com/claims > Sign In. Then
select Claims & Payments from the menu > Submit a Claim
Information: uhcprovider.com/claims
Claim Corrections and
Reconsiderations
EDI: Submit facility claim corrections electronically.
Online: UnitedHealthcare Provider Portal at uhcprovider.com/claims > Sign In. Then
select Claims & Payments from the menu > Look up a Claim.
Information: uhcprovider.com/claims
Claim Status EDI: 276/277
Claim Status Inquiry and Response transactions are available through your vendor or
clearinghouse.
Online: uhcprovider.com > Claims and Payments
Phone: 1-800-666-1353 and say “claims” when prompted. You may also speak with a
representative Monday–Friday, 8 a.m.–6 p.m. ET.
Clinical and Administrative
Policies
Online: uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare®
Oxford Clinical and Administrative Policies
Clinical Services Department Phone: 1-800-666-1353 (Monday–Friday, 8 a.m.–6 p.m. ET)
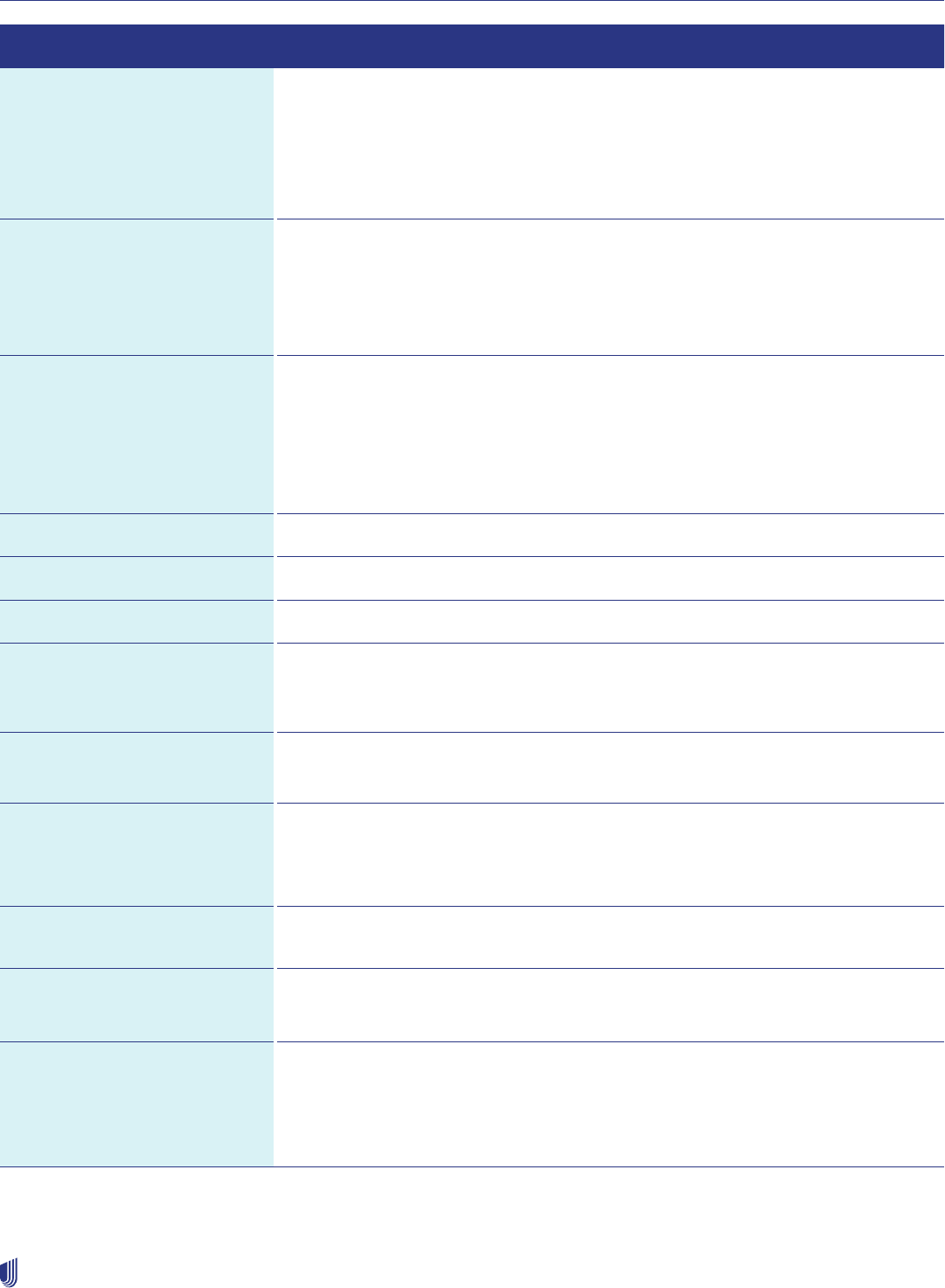
Oxford Commercial supplement
268
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Credentialing and
Recredentialing
Member of the Council for
Affordable Quality Healthcare
(CAQH)
Online: uhcprovider.com > Recredentialing
Phone: Voice Portal at 1-877-842-3210
New Jersey only
Online: State of New Jersey Department of Health: nj.gov/health or CAQH.org.
Phone: Provider Services at 1-800-666-1353 or CAQH Support at 1-888-599-1771
Electronic Data Interchange
(EDI)
Check status of referrals,
precertifications and claims;
member eligibility and benefits
Payer ID: 06111
Online:
• uhcprovider.com/edi
• uhcprovider.com > Eligibility
Phone: 1-800-842-1109, Monday–Friday, 8:30 a.m.–5 p.m. ET
Eligibility and Benefits EDI: 270/271 Eligibility and Benefits Inquiry and Response transactions are available
through your vendor or clearinghouse.
Online: uhcprovider.com > Eligibility
Voice Portal and Provider Services:
1-800-666-1353 and say “benefits and eligibility” when prompted.
You may also speak with a representative Monday–Friday, 8 a.m.–6 p.m. ET.
Forms Online: uhcprovider.com > Resources > Health plans > Health Plans by State
Fraud Hotline Phone: 1-866-242-7727
Genetic and Molecular Testing Online: uhcprovider.com/priorauth and select the specialty you need.
HIPAA Compliance and Security Online: uhc.com/privacy
For additional information on granting remote access to your EMR system: emrcdsa@
uhc.com.
Infertility Services: Optum Phone: 1-877-512-9340
Fax: 1-855-536-0491
Inpatient Admission EDI: Use your clearinghouse.
Online: uhcprovider.com > Prior Authorization
Phone: 1-800-666-1353
Inpatient and Outpatient:
Clinical Services
Phone: 1-800-666-1353
Laboratory Services Locate participating laboratories:
Online: uhcprovider.com > Our network > Find a provider > Preferred Lab Network
Optum Pay
Information and Enrollment
Online:
• optum.com/optumpay
• optumbank.com > Sign in
Helpdesk: 1-877-620-6194
Oxford Commercial supplement
269
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Outpatient Injectable
Chemotherapy and Related
Cancer Therapies
Online: uhcprovider.com/priorauth > Oncology
Phone: 1-888-397-8129
Pharmacy Customer Service Phone: 1-800-788-4863
TTY/TDD: 1-800-498-5428
Available 24 hours per day
Pharmacy Prior Authorization Phone: 1-800-711-4555
Available 24 hours per day
Physical and Occupational
Therapy Claims Submission and
Inquiry
Provider Services: 1-877-369-7564
Online: myoptumhealthphysicalhealth.com
For claims submitted electronically: Payer ID 06111
Phone: 1-800-873-4575
Mail (paper claims):
UnitedHealthcare
Attn: Oxford Claims Department
P.O. Box 31386
Salt Lake City, UT 84131
Prescription Mail Order OptumRx
P.O. Box 2975
Mission, KS 66201
Prior Authorization Submission EDI: Use your vendor or clearinghouse.
Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth
Phone: Provider Services 1-800-666-1353 (Monday–Friday, 8 a.m.–6 p.m. ET)
Prior Authorization Verification EDI: Use your vendor or clearinghouse.
Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth
Phone: Provider Services 1-800-666-1353 and say “precertification” when prompted.
You may also speak with a representative Monday–Friday, 8 a.m.–6 p.m. ET.
Radiation Therapy Online: UnitedHealthcare Provider Portal at uhcprovider.com/paan > Sign In
• Go to the Prior Authorizations tool and select the Radiology, Cardiology, Oncology
and Radiation Oncology Transactions box.
• Select service type: Radiation/Oncology and enter the member’s state and product
details.
• You will be directed to the Optum site to complete your request.
Fax: 1-844-284-8068
Mail: UnitedHealthcare
Attn: Oxford Clinical Coverage Review
1300 River Drive, Suite 200
Moline, IL 61265
Phone: 1-888-397-8129 (Monday–Friday, 7 a.m.–9 p.m. CT)
Oxford Commercial supplement
270
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to Go
Radiology Online: uhcprovider.com/priorauth > Radiology (available 24 hours per day, 7 days per
week)
Policies: uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare®
Oxford Clinical and Administrative Policies
Phone (eviCore): 1-877-PREAUTH (1-877-773-2884)
Monday–Friday, 7 a.m.–7 p.m. ET
Referral Submission or
Verification
EDI: Use your clearinghouse or vendor.
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In
Information: uhcprovider.com > Referrals
Phone: Provider Services 1-800-666-1353 and say “referral” when prompted. You may
also speak to a representative Monday–Friday, 8 a.m.–6 p.m. ET.
Search for Participating
Health Care Providers, Other
Health Care Professionals and
Facilities
Online: uhcprovider.com > Our network > Find a provider
Phone: 1-800-666-1353 (Monday–Friday, 8 a.m.–6 p.m. ET)
Termination Requests Phone: 1-800-666-1353 (Monday–Friday, 8 a.m.–6 p.m. ET)
Mail: Physicians and other health care professionals send by certified mail, return
receipt requested to:
UnitedHealthcare
Oxford Network Contract Support
Mail Route: TX023-1000
1311 W President George Bush Highway, Suite 100
Richardson, TX 75080-9870
Termination requests can be submitted in writing and emailed to
Behavioral health providers only
Phone: 1-877-614-0484
Health care provider responsibilities and standards
Compliance with quality assurance and utilization review
Physicians and other health care professionals agree to fully comply with and abide by the rules, policies and procedures that
we have or will establish. We provide written notice of any changes 30 days in advance, including, but not limited to:
• Quality assurance, such as onsite case management of members, incentive programs and notification compliance measures.
• Utilization management, including prior authorization procedures, referral processes or protocols and reporting of clinical
accounting data.
• Member, physician and other health care professional grievances.
• Timely provision of medical records when we or our contracted business associates request them.
• Cooperation with quality of care investigations, including timely response to queries and/or completion of improvement
action plans.
• Health care provider credentialing.
• Any similar programs developed by us.

Oxford Commercial supplement
271
2023 UnitedHealthcare Care Provider Administrative Guide
Advising members of their rights
Our members have the right to obtain complete, current information concerning diagnosis, treatment and prognosis in terms
they may understand. When it is not advisable to give such information to the member, make the information available to an
appropriate person acting on the member’s behalf.
Our members also have the right to receive information as necessary to give informed consent before the start of any procedure
or treatment. They may refuse treatment to the extent permitted by law. You must inform them of the medical consequences of
that action.
Office and access standards
Your office must adhere to policies regarding:
• Confidentiality of member medical records and related member information.
• Patient-centered education.
• Informed consent, including telling a member before initiating services when a particular service is not covered and
disclosing to them the amount they must pay for the service.
• Maintenance of advance directives.
• Handling of medical emergencies.
• Compliance with all federal, state and local requirements.
• Minimum standards for appointment and after-hours accessibility.
• Safety of the office environment.
• Use of physician extenders, such as physician assistants (PA), nurse practitioners (NP) and other allied health professionals,
together with the relevant collaborative agreements.
As a participating health care provider, you agree to certain access standards. You agree to arrange coverage for medical
services, 24 hours a day, 7 days a week, including:
1. Telephone coverage after hours: You must have either a constantly operating answering service or a telephone recording
directing members to call a special number to reach a covering medical professional. Your message must tell the caller
to go to the emergency room (ER) or call 911 if there is an emergency. The message should be in English and any other
relevant languages if your panel consists of members with special language needs.
2. Covering health care providers: You must provide coverage of your practice 24 hours a day, 7 days a week. Your covering
health care provider must be a participating health care provider unless there isn’t one in your area. We must certify any
non-participating health care professionals you use to provide coverage for your practice.
Americans with Disabilities Act (ADA) guidelines
You must have practice policies showing you accept for treatment any patient in need of the health care you provide. Your
organization and health care providers must make public declarations (i.e., through posters or mission statements) of their
commitment to non-discriminatory behavior in conducting business with all members. These documents should explain that
this expectation applies to all personnel, clinical and non-clinical, in their dealings with each member.
In this regard, you are required to undertake new construction and renovations, as well as barrier reductions required to achieve
program accessibility, following the established accessibility standards of the ADA guidelines. For complete details go to ADA.
gov > (search) A Guide to Disability Rights Laws.
We may request from a health care provider’s office
We may request any of the following ADA-related descriptions of:
• Accessibility to your office or facility.
• The methods you or your staff uses to communicate with members who have visual or hearing impairments.
• The training your staff receives to learn and implement these guidelines.
Oxford Commercial supplement
272
2023 UnitedHealthcare Care Provider Administrative Guide
Care for members who are hearing-impaired
Refusing to provide either care or the help of an interpreter while caring for a person with a qualifying disability is an ADA
violation. Members who are hearing-impaired have the right to use sign-language interpreters to help them at their doctor visits.
We will bear the reasonable cost of providing an interpreter. You must not bill the member for interpreter fees.* The health care
provider/facility pays the interpreters for their services, then bills us for these services by submitting a claim form with Current
Procedural Terminology (CPT) code 99199 with a description of the interpreter service.
If you provide Virtual Visits, these services must be accessible to individuals with disabilities. Post your Virtual Visits procedures
for members who are deaf or hard of hearing, so they receive them prior to the Virtual Visit.
Confirming eligibility and benefits
Checking the member’s eligibility and benefits before rendering services helps ensure you submit the claim to the correct
payer, collect correct copayments, determine if a referral is required and reduce denials for non-coverage. To check eligibility
and benefits, use any of the following methods:
• EDI: 270/271 Eligibility and Benefit Inquiry and Response transactions are available through your vendor or clearinghouse.
• Online: UnitedHealthcare Provider Portal at uhcprovider.com/eligibility > Sign In. Then select Eligibility from the menu.
• Information: uhcprovider.com/eligibility
• Phone: 1-800-666-1353 and say “benefits and eligibility” when prompted. You can also speak with a representative Monday–
Friday, 8 a.m.–6 p.m. ET.
For additional help with the website, Oxford Voice Portal and EDI solutions, go to uhcprovider.com > Our network > Contact us >
Technical Assistance. You will find quick reference guides and instructions to assist you.
Member health plan identification (ID) cards
Find Oxford-specific member information in the UnitedHealthcare Provider Portal to help you identify the member’s health
benefit plan. You can view current member ID cards when you verify eligibility and benefits in the UnitedHealthcare Provider
Portal. You may download and keep a copy of both sides of the ID card for your records.
For more detailed information and to see a sample ID card, refer to the Commercial Health Care ID Card Legend in Chapter
2: Provider responsibilities and standards. You may see a sample ID card image specific to the member when you verify
eligibility and benefits in the UnitedHealthcare Provider Portal.
Participating hospitals, ancillary providers and health care providers agree to:
• Verify a member’s status. We will not pay for services rendered to persons who are not our members.
• Obtain prior authorization from us or a delegated vendor for all hospital services requiring prior authorization before rendering
services. Generally, all hospital services require our prior authorization.
• Notify us of all emergency/urgent admissions of members upon admission or on the day of admission. If the facility is unable
to determine on the day of admission that the patient is our member, the facility must notify us as soon as possible after
discovering that the patient has coverage with us.
• Notify us of an ambulatory surgery performed due to an ER or urgent care visit within 24‒48 hours.
• Admit and treat our members the same way you treat all other facility patients (i.e., according to the severity of the medical
need and the availability of covered services).
• Render services to members in a timely manner. The services provided must be consistent with the treatment protocols and
practices used for any other facility patient.
• Work with the responsible PCP to help ensure continuity of care for our members.
• Maintain appropriate standards for your facility.
• Cooperate with our utilization review program and audit activities.
• Receive compensation only from us and adhere to our balance billing policies.
• Complete appeals process in a timely manner before proceeding to arbitration.
* 28 CFR Sect. 36.301(c) and 36.303(b)(1)-36.303(c)

Oxford Commercial supplement
273
2023 UnitedHealthcare Care Provider Administrative Guide
Standards of practice
Services you perform for members must be consistent with the proper practice of medicine and be performed following the
customary rules of ethics and conduct of the American Medical Association and other bodies, formal or informal, governmental
or otherwise, from which you seek advice and guidance or to which they are subject to licensing and control.
PCP selection
All HMO products require members to select a PCP to provide primary care services and coordinate their overall care.
Female members may also select an obstetrician/gynecologist (OB/GYN), which they may see without a referral from their
PCP. Members may only select a PCP within their network (e.g., a Liberty Plan member must select a Liberty Network
participating PCP).
Role of the PCP
As a PCP, you must deliver medically necessary primary care services. You are the coordinator of our members’ total health
care needs. Your role is to provide all routine and preventive medical services and coordinate all other covered services,
specialist care and care at our participating facilities or at any other participating medical facility where our members might
seek care (e.g., emergency care). You are responsible for seeing all members on your panel who need care, even if the member
has never been in for an office visit. You may not discriminate on the basis of race, ethnicity, national origin, religion, sex, age,
mental or physical disability, sexual orientation, genetic information, place of residence, health status or source of payment.
Some PCPs are also qualified to perform services ordinarily handled by a specialist. We will only pay claims submitted for
specialist services by such a PCP if they are listed as a participating specialist in the particular specialty.
HIV confidentiality
Per New York regulations, all health care providers must develop and implement policies and procedures to maintain the
confidentiality of HIV-related information. You must have the following procedures in place to comply with regulations specific to
the confidentiality, maintenance and appropriate disclosure of HIV patient information.
Office staff will:
• Receive initial and annual in-service education regarding the legal prohibition of unauthorized disclosure.
• Maintain a list containing job titles and specified functions for employees authorized to access such information.
• Maintain and secure records, including records which are stored electronically, and ensure records are used for the
purpose intended.
• Maintain procedures for handling requests by other parties for confidential HIV-related information.
• Maintain protocols prohibiting employees, agents and contractors from discriminating against persons having or suspected
of having HIV infection.
• Perform an annual review of the following policies and procedures:
– Perform HIV testing on all newborns.
– Prenatal health care providers should counsel expectant mothers regarding the required testing of newborns and the
importance of the mother getting tested.
– Advise expectant mothers of the counseling and services offered when results are positive. This includes psychosocial
support and case management for medical, social and addictive services.
Only employees, contractors and medical nursing or health-related students who have received such education on HIV
confidentiality shall have access to confidential HIV-related information while performing the authorized functions.
Specialists
As a participating specialist, you agree to:
• Provide referrals for specialty services.
• Provide results of medical evaluations, tests and treatments to the member’s PCP.
• Precertify inpatient admission.
• Receive compensation only from us and adhere to our balance billing policies.

Oxford Commercial supplement
274
2023 UnitedHealthcare Care Provider Administrative Guide
• Provide access to your records relating to services rendered to our members. If you believe consent is required from the
specific member, you must obtain their consent.
• Follow our authorization guidelines for those services requiring prior authorization.
We only reimburse you for services if:
• We have a referral on file, or the member has a non-gatekeeper benefit plan and the service is covered and
medically necessary.
• A referral is not on file, and the member has an out-of-network benefit (i.e., a POS benefit plan), and if the service is covered
and medically necessary, you are entitled to the contracted rate. However, the member is required to pay any deductible and/
or coinsurance based on their out-of-network benefits.
• If the member is enrolled in a benefit plan without an out-of-network benefit (i.e., an HMO benefit plan), we are not responsible
for payment (except in cases of emergency), nor may the member be balance billed.
Specialists as PCPs
We allow a member who has a life-threatening condition or a degenerative and disabling condition (i.e., complex medical
condition) or disease, either of which requires specialized medical care over a prolonged period of time, to elect a network
specialist as their PCP. We may grant a standing referral, and the specialist PCP becomes responsible for providing and
coordinating all of the member’s primary care and specialty care. The PCP, specialist and our established Oxford treatment
plan must all be aligned.
We may authorize a standing referral (see Standing Referrals and Specialty Care Centers) when the health care provider is
requesting more than 30 visits within a 6-month period or covered services beyond a 6-month period but within 12 months.
Under a standing referral, a member may seek treatment with a designated specialist or facility without a separate PCP referral
for each service.
If such an election appears to be appropriate, our Clinical Services department faxes the specialist a form to complete
and return.
We cover such services without a referral only after you complete the form and we accept it. Otherwise, a referral is required for
members with a gatekeeper benefit plan.
Transitional care
Continuity and coordination of care helps ensure ongoing communication, monitoring and overview by the PCP across each
member’s health care continuum. Documentation of services provided by specialists such as podiatrists, ophthalmologists and
mental health practitioners, as well as ancillary health care providers including home care and rehabilitation facilities, help the
PCP maintain a medical record supporting whole person care.
The NCQA and state departments in the tri-state area (New York, New Jersey and Connecticut) require elements of the chart to
indicate continuity and coordination of care among health care providers. We monitor the continuity and coordination of care
that members receive through the following mechanisms:
• Medical record reviews
• Adverse outcomes that may develop as the result of disruptions in continuity or coordination of care
• Health care provider termination
Newly enrolled members who need transitional care or continuity of care
When a new member enrolls with us, they may qualify for coverage of transitional care services rendered by their non-
participating health care providers.
For more information about transitional care, members may call us at the phone number on their health plan ID card or at 1-800-
444-6222.

Oxford Commercial supplement
275
2023 UnitedHealthcare Care Provider Administrative Guide
Reassignment of members who are in an ongoing course of care or who are being treated for pregnancy
We adhere to the following guidelines when notifying members affected by a health care provider termination:
• We notify all members who are patients of any terminated PCP’s panel — internal medicine, family practice, pediatrics, OB/
GYN — about our policy and what steps to follow should the member require transitional care. We follow the same policy for
members who regularly see a specialist who is terminated from our network or who is not (or no longer) in our network.
• We instruct members of a terminated PCP’s panel to call Member Service if they choose to select a new PCP or to request
transitional care from their current health care provider. We encourage them to request our Roster of Participating Physicians
and Other Health Care Professionals to make their new selection.
• We instruct members of a specialist terminated from our network to call Member Services if they need to request transitional
care from their current specialist. We also direct members to call their current PCP for an alternate specialist referral.
Transitional care when a health care provider leaves our network
We use the following rules when notifying members affected by a health care provider terminated from our network:
• Oxford members in New York qualify for transitional services on a network basis for a certain time period to be determined
based upon their clinical presentation.
• We tell all members who are patients of any terminated PCP, such as internal medicine, family practice, pediatrics and OB/
GYN, about our policy and what steps to follow should they need transitional care. We follow the same policy for members
being seen regularly by a specialist who is terminated from our network.
• We instruct members with PCPs who are not or no longer in our network to call Member Services whether they choose
to select a new PCP or to ask for transitional care from their current health care provider. We encourage them to visit
uhcprovider.com > Our network > Find a provider to make their new selection.
• We tell our members who are patients of a terminated specialist to call Member Service if they need to request transitional
care from their current specialist. Additionally, we tell them to call their current PCP to ask for a referral to a different
network specialist.
If the member has entered the second trimester of pregnancy at the effective date of enrollment, the transitional period includes
the provision of postpartum care directly related to the delivery. Our medical director must find the treatment by the non-
participating health care provider medically necessary. Transitional care is available only if the health care provider agrees to:
• Accept as payment our negotiated fees for such services before transitional care.
• Adhere to our quality management procedures and provide medical information related to the member’s care.
• Adhere to our policies and procedures regarding the delivery of covered services, including referrals and preauthorization
policies, and a treatment plan approved by us.
Referrals
Submitting and verifying referrals
A PCP or OB/GYN may issue a referral to participating health care providers using any of the methods outlined in the How to
Contact Oxford Commercial section.
Once you enter the referral, the referring health care provider may receive a reference number by fax. Provide the referral
reference number to the member. The member may bring this reference number to the specialist who can directly confirm a
referral is on file using our Provider Portal at uhcprovider.com > Sign In or call 1-877-842-3210.
Referral policies and guidelines
Our physician contracts require referrals be issued to participating physicians, hospitals, ancillaries and other health care
professionals within the applicable network of health care providers available to our members enrolled in gated health benefit
plans. The only exceptions to this are:
1. Emergency cases.
2. There are no participating health care providers who can treat the member’s condition.

Oxford Commercial supplement
276
2023 UnitedHealthcare Care Provider Administrative Guide
If you would like to direct a member to non-participating health care providers, you must request a network exception from
our Clinical Services department and receive approval before the member receives service. If the member requests to see a
specialist and is unable to reach their PCP or OB/GYN (after-hours, weekends or holidays), the PCP may issue a referral up to
72 hours after the member received services.
Prior authorization guidelines still apply to those covered services requiring prior authorization.
We must review and approve all referrals. A referral does not guarantee coverage of the services provided by the participating
specialist. Covered services are subject to:
• Medical necessity, as determined by Oxford clinical policies.
• Member eligibility on the date(s) of service.
• Member’s benefits as defined in the conditions, terms and limitations of their Summary of Benefits/Certificates/Contract.
Participating specialists may only issue referrals within the applicable network of health care providers available to the members
enrolled in gated health benefit plans for certain covered services as outlined in the Referrals policy. You may not refer a
member to a non-participating specialist. For more information, refer to the section on Using Non-Participating Health Care
Providers or Facilities.
Automated fax notification
When you submit a referral, we send a fax to the referred-to health care provider or other health care professional, usually within
24 hours. This fax serves as a confirmation notice of the referral.
You have the option to update your referral fax number or decline the auto-fax notification feature on our website in the My
Account section.
Member self-referrals
We have programs to improve outcomes for members and help us better manage the use of medical services. You may refer
members to these programs, or members may self-refer, to network specialists for the following services:
1. OB/GYN care, to include prenatal care, 2 routine visits per year and any follow-up care, or for care related to an acute
gynecological condition
2. One mental health visit and one substance use visit with a participating health care provider per year for evaluation
3. Vision services from a participating health care provider
4. Diagnosis and treatment of tuberculosis by public health agency facilities
5. Family planning and reproductive health from participating or Medicaid health care providers
Outpatient radiology self-referral procedures
We designed the Outpatient Imaging Self-Referral Policy to promote appropriate use of diagnostic imaging by network PCPs,
specialty physicians and other health care professionals in the office and outpatient setting.
This policy does not apply to radiology services performed during an inpatient stay, ambulatory surgery, ER visit or pre-
operative/pre-admission testing. See the How to Contact Oxford Commercial section for contact information.
The outpatient imaging self-referral list is applicable to commercial benefit plans. You may find more information in the Oxford
Outpatient Imaging Self-Referral Clinical Policy at uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare®
Oxford Clinical and Administrative Policies.
Standing referrals and specialty care centers
You may request a standing referral to a participating specialist, ancillary provider or specialty care center if a member
requires ongoing specialist treatment, has a life-threatening condition or disease or a degenerative and disabling condition or
disease. This referral is available only if the condition or disease requires specialized medical care over a prolonged period.
The participating specialist or ancillary provider must have the necessary medical expertise and be properly accredited or
designated (as required by state or federal law or a voluntary national health organization) to provide the medically necessary

Oxford Commercial supplement
277
2023 UnitedHealthcare Care Provider Administrative Guide
care required for the treatment of the condition or disease. We cover the services provided only to the extent outlined in the
member’s Certificate of Coverage.
Utilization management
Prior authorization (precertification)
We refer to the terms “prior authorization” and “precertification” in the supplement. You will notice both terms used throughout
this supplement.
You may submit prior authorization requests using any of the methods outlined in the How to Contact Oxford
Commercial section.
We urge you, facilities, ancillaries and other health care professionals to perform a prior authorization status check first to
determine if there is already a prior authorization on file.
Submit prior authorization as far in advance of the planned service as possible to allow for review. We require prior authorization
at least 14 business days before the planned service date.
• Submit authorization requests for obstetrical admissions for normal delivery as early as possible in the course of prenatal
care, based on the expected date of delivery.
• Participating health care providers and facilities are responsible for contacting us for:
– Procedures requiring prior authorization. However, an active referral must also be on file for services to be covered as
network benefits, depending on the member’s health benefit plan referral requirements.
– Any change of treating health care provider, location, CPT codes or dates of service for the authorized service.
– Member emergency admissions upon admission or on the day of admission. If the health care provider/facility is unable to
determine on the day of admission that the patient is our member, the health care provider/facility must notify us as soon as
possible after discovering that the patient has coverage with us.
• We notify participating health care providers of all determinations involving New York members by phone and in writing. All
participating health care providers are responsible for calling the member the same day the health care provider receives
notification of our determination.
• Neither prior authorization nor referral is required for members to access a participating women’s health specialist (i.e.,
gynecologists and/or certified nurse midwives) for routine and preventive health care services. Routine and preventive health
care services include screening breast exams, mammograms and pap tests.
• Members are responsible for notifying us of emergency facility admissions to a non-participating facility.
• We may require a member see a health care provider, selected by us, for a second opinion. We reserve the right to seek a
second opinion for any surgical procedure. There is no formal list of procedures requiring second opinions. Members may
also seek a second opinion when appropriate.
Status of a submitted authorization request
Verify the status of an authorization request by the following methods:
• Voice Portal: available 24 hours a day
• Online: available 24 hours a day
• Provider Services: speak to a service representative during business hours
Medically necessary services
Medically necessary services are services or supplies provided by a hospital, skilled nursing facility (SNF) or health care
provider that are required to identify or treat a member’s illness or injury, as determined by our medical director. These services
or supplies must be:
• Consistent with the symptoms or diagnosis and treatment of a member’s condition.
• Appropriate regarding standards of good medical practice.

Oxford Commercial supplement
278
2023 UnitedHealthcare Care Provider Administrative Guide
• Not solely for the member’s convenience or that of any health care provider.
• The most appropriate supply or level of service that may safely be provided.
• For inpatient services, it also means the member’s condition may not safely be diagnosed or treated on an outpatient basis.
Prior authorization list
1. Go to uhcprovider.com/priorauth > Advance Notification and Plan Requirement Resources > Commercial Advanced
Notification/Prior Authorization Requirements.
2. You may request a copy of the most current list by mail:
Oxford Policy Requests and Information
4 Research Drive
Shelton, CT 06484
Changes to the policies related to services appearing on this list are announced in the Oxford Policy Update Bulletin available
at uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare® Oxford Clinical and Administrative Policies > Policy
Update Bulletins.
• A member’s benefit plan may not cover certain services, regardless of whether we require advance notification.
• If there is conflict or inconsistency between applicable regulations and the supplement notification requirements, we follow
applicable regulations.
• Prior authorization requirements may differ by individual health care providers, ancillary providers and facilities. If additional
prior authorization requirements apply, we notify you before applying prior authorization rules.
eviCore healthcare prior authorizations online
eviCore healthcare (eviCore) provides a secure, interactive web-based program where prior authorization requests may be
initiated and determined in real time. If the program finds the request is medically necessary, it issues an authorization number
immediately. If the program cannot verify medical necessity through the online process, you may submit more information at the
session conclusion and print a procedure request summary page. If an online request for authorization doesn’t meet medical
necessity criteria, eviCore forwards it for clinical review. They may request more information for medical necessity review with a
medical director.
If the criteria have not been met, your office and the member are notified in writing of the denial. Use the Prior Authorizations
tool in the UnitedHealthcare Provider Portal, where the automated system guides you through a series of prompts to collect
routine demographic and clinical data. This eliminates the need to call eviCore and lets you enter multiple clinical certification
requests at your convenience. Learn more at uhcprovider.com/paan.
Prescription medications requiring prior authorization
Based on the member’s benefit plan design, some high-risk or high-cost medications require advance notification to be
eligible for coverage. This process is also known as prior authorization and requires you to submit a formal request and receive
advanced approval for coverage of certain prescription medications.
Learn more at uhcprovider.com/priorauth > Clinical Pharmacy and Specialty Drugs.
Prior authorization and referral guidelines when coordinating benefits
When we are the secondary or tertiary carrier, we modify normal requirements for prior authorization and referrals as follows:
• We defer to the requirements of the primary carrier and waive our referral and prior authorization guidelines. We do not
waive other requirements (e.g., itemized bills, student verification, consent for exchange of mental health or substance
use information).
• Exception: Referral and prior authorization guidelines apply:
– If the primary carrier does not cover a service or applies an authorization penalty.
– When a motor vehicle accident occurs or workers’ compensation is involved.
Oxford Commercial supplement
279
2023 UnitedHealthcare Care Provider Administrative Guide
Using non-participating health care providers or facilities
As a participating health care provider, you must use participating health care providers and facilities within the member’s
benefit plan network (i.e., Liberty Network). We have a compliance program to identify participating health care providers who
regularly use non-participating health care providers and facilities. We take appropriate measures to enforce compliance.
If a member asks you for a recommendation to a non-participating health care provider, you must tell the member you may
not refer to a non-participating health care provider. The member must contact us to obtain the required prior authorization by
calling us at the phone number on their health plan ID card or 1-800-444-6222.
If you contact us for authorization to perform a non-emergency procedure at a non-participating facility for a member who has
out-of-network benefits, we may authorize the procedure as out-of-network.
This means the reimbursement to the non-participating facility is subject to the member’s out-of-network deductible and
coinsurance obligations. The non-participating facility’s charges are only eligible for coverage up to the reimbursement levels
available under the member’s benefit plan, using either a usual, customary and reasonable (UCR) fee schedule or a Medicare
reimbursement system called the Out-of-Network Reimbursement Amount for our New York members.
Members are responsible for paying their out-of-pocket cost and the difference between the UCR fee or other out-of-network
reimbursement and the non-participating facility’s billed charges. Remind the member their expenses may be significantly
higher when using a non-participating health care provider.
If you contact us for authorization to perform a non-emergency procedure at a non-participating facility on a member who does
not have out-of-network benefits (HMO and EPO benefit plan members), we may deny the services based on the benefit plan.
If you ask for an exception, we may consider it only when our medical director determines in advance that:
1. Our network does not have an appropriate participating network provider who can deliver the necessary care.
2. Medically necessary services are not available through our network providers.
In such cases, we will approve the requested authorization. It must include a treatment plan approved by our medical director,
the PCP and the non-participating health care provider.
Exception process for the use of non-participating health care providers
(New York and Connecticut)
For participating health care providers, the use of participating health care providers is required unless:
1. We approved an in-network exception.
2. The member explicitly agrees prior to the service (no more than 90 days before the scheduled date of the procedure) to
receive services from a non-participating health care provider by signing the applicable consent form and understands that
the use of this health care provider is:
a. Out-of-Network: For members with out-of-network benefits, we pay non-care provider claims at the out-of-network benefit
level. Out-of-network cost-shares and deductibles apply.
b. Denied: For members without out-of-network benefits, we deny non-participating health care provider claims as not
covered because the member has no coverage for services provided by non-participating health care providers.
Members are therefore responsible for the entire cost of the service.
For more information, go to uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare® Oxford Clinical and
Administrative Policies.
Hospital services, admissions and inpatient and outpatient procedures
Facilities are responsible for providing admission notification for all of the following types of inpatient admissions, even if
advance notification was provided by the physician and coverage approval is on file:
• Planned/elective admissions for acute care
• Unplanned admissions for acute care (admission notification only)
• SNF admissions
• Admissions following outpatient surgery and observation

Oxford Commercial supplement
280
2023 UnitedHealthcare Care Provider Administrative Guide
• Newborns admitted to Neonatal Intensive Care Unit (NICU) and who remain hospitalized after the mother is discharged
• The facility must confirm a pre-service approval is on file for services requiring prior authorization
Health care providers and ancillary providers are responsible for obtaining prior authorization for outpatient surgical and major
diagnostic testing performed in an outpatient clinic or any ambulatory or freestanding surgical or diagnostic facility.
Concurrent review: clinical information
Upon admission, Clinical Services will accept concurrent review information provided by the admitting health care provider or
other health care professional and/or the hospital’s Utilization Review department. The hospital must also provide us with the
discharge plan on or before the discharge date. If a member requires an extended length of stay or more consultations, call our
Clinical Services department at 1-800-666-1353 for prior authorization instructions.
• For mental health/substance use, direct calls related to inpatient prior authorization to 1-800-201-6991.
• You must cooperate with all requests for information, documents or discussions for purposes of concurrent review and
discharge. When available, provide clinical information using electronic medical records (EMR).
• You must cooperate with all requests from the interdisciplinary care coordination team and/or medical director to engage our
members directly face-to-face or by phone.
• You must return/respond to inquiries from our interdisciplinary care coordination team and/or medical director. You must
provide complete clinical information and/or documents as required within 4 hours if you receive our request before
1p.m.ET. You must make best efforts to provide requested information within the same business day if you receive the
request after 1 p.m. ET (but no later than 12 p.m. ET the next business day).
• We use InterQual Care Guidelines with our Oxford members, which are nationally recognized clinical guidelines, to help
clinicians make informed decisions in many health care settings.
Inpatient maternity stay and subsequent home nursing
We follow federal mandates regarding the length of an inpatient maternity stay and the coverage of subsequent home nursing
visits. Home nursing visit regulations vary by state as outlined in the following.
Inpatient maternity length of stay
We will cover the Oxford member’s inpatient maternity stays for both mother and newborn as follows:
• 48 hours following a vaginal delivery
• 96 hours following a cesarean delivery
Post-discharge home nursing visits
• Connecticut Oxford Plans: We will approve 2 home nursing visits if both mother and newborn are discharged before the
mandated length of stay described previously.
• New Jersey and New York Oxford plans: We will approve 1 home nursing visit if both mother and newborn are discharged
before the mandated length of stay described previously.
Newborn coverage varies by benefit plan and state. For more details, refer to uhcprovider.com > Eligibility.
Neonatal Intensive Care Unit (NICU) level of care
We base NICU bed levels on the intensity of services and identifiable interventions received by the neonate. NICU bed levels are
linked to revenue codes defined by the National Uniform Billing Committee. Based on our medical necessity review, we assign
a bed day level for those facilities contracted with more than one level of NICU. Claims are reimbursed based on what has been
authorized per a medical necessity review of the NICU bed day per the facility contract.
Hospital responsibilities
The hospital is required to notify us of:
• Newborns admitted to NICU and who remain hospitalized after the mother is discharged.
• Concurrent inpatient stays (notification before discharge).

Oxford Commercial supplement
281
2023 UnitedHealthcare Care Provider Administrative Guide
• Any member who changes level of care. The member must be enrolled and effective with us on the date the services are
rendered. But, if CMS or an employer or group retroactively disenrolls the member up to 90 days following the dates of
service, we may deny or reverse the claim.
The hospital must also:
• Provide daily inpatient census log by 10 a.m. ET, including all admits and discharges through midnight the day prior.
• Provide notification of all admissions of our members at the time of, or before, admission. The hospital must notify us of all
emergencies (upon admission or on the day of admission), and of “rollovers” (i.e., any member who is admitted immediately
upon receiving a preauthorized outpatient service).
• Provide notification for any transfer admissions of members before the transfer unless the transfer is due to life-threatening
medical emergency.
• Communicate necessary clinical information daily, or as requested by our case manager.
If the hospital does not provide the necessary clinical information, we may deny the day for medical necessity. We give
reconsideration only if we receive clinical information within 48 hours (72 hours for New Jersey facilities).
If we conduct onsite utilization review, the hospital will provide our onsite utilization management personnel reasonable
workspace and access to the hospital, including access to members and their medical records. All health care providers must
deliver letters of non-coverage to the member before discharge. This includes hospitals, acute rehabilitation, SNFs and home
care.
We consider appeals if the hospital can show that the necessary clinical information was provided within 48 hours, but we failed
to respond in a timely manner.
Retrospective review of inpatient stays (notification of admission after discharge)
If we request it, the hospital will provide the necessary clinical information to perform a medical necessity review within 45 days
of discharge. If the hospital does not provide the necessary clinical information, we may deny the day for medical necessity. We
give reconsideration only if clinical information is received within 48 hours (72 hours for New Jersey members).
Our responsibilities for inpatient notifications
• We will maintain a system for verifying member eligibility/status and use reasonable efforts to transmit a decision regarding
an emergency/urgent admission to the hospital.
• We will request any necessary clinical information. If we do not ask for such information, the day’s services will be our liability.
• We agree to provide concurrent and prospective reviews for all services.
• We will assign a first day of review (FDOR) for all elective inpatient services, and we will certify all days up to and including
the FDOR.
• We will notify the hospital and attending health care provider or other health care professional verbally and in writing of all
denied days.
• We will perform clinical review of days that fall on the weekends and holidays for which we or the facility is closed, and
days upon which there are unforeseen interruptions in business on the following business day. Such reviews will be
considered concurrent.
• We will not deny services retrospectively or reduce the level of payment for services that have been preauthorized or received
concurrent review approval unless:
– The member is retroactively disenrolled.
– The certification or concurrent review approval was based on materially erroneous information.
– The services are not provided in accordance with the proposed plan of care.
– Hospital delays in providing an approved service to prolong the length of stay beyond what was approved.
Mental health, substance use and detoxification treatment
Inpatient care
All inpatient mental health/substance use treatment requires prior authorization.

Oxford Commercial supplement
282
2023 UnitedHealthcare Care Provider Administrative Guide
Partial hospitalization
Partial hospitalization always requires certification through the behavioral health department. If clinical criteria are met, the
case manager facilitates certification and management at a contracted facility with a partial hospitalization program. The case
manager continues to follow the member’s treatment while they are in the program.
Prior authorization outpatient mental health services (New York)
Covered services are those received on an outpatient basis from duly licensed psychiatrists or practicing psychologists,
certified social workers, or a facility-issued operating certificate by the commissioner of mental health, a facility operated by the
Office of Mental Health, a professional corporation or university faculty practice corporation. This includes:
• Diagnosis.
• Treatment planning.
• Referral services.
• Medication management.
• Crisis intervention.
We provide coverage to the maximum number of visits shown on the member’s Summary of Benefits.
Inpatient mental health services (New York)
Members receive covered services on an inpatient or partial hospitalization basis in a facility as defined by subdivision 10 of
section 1.03 of the Mental Hygiene Law, as well as by any other network provider we deem appropriate to provide the medically
necessary care.
We cover a required inpatient stay as a semi-private room. If we authorize partial hospitalization, 2 partial hospitalization visits
may be substituted for 1 inpatient day. We provide coverage for active treatment to the maximum number of days shown on the
member’s Summary of Benefits.
Visits for biologically based services will apply to this limit. Active treatment means treatment furnished together with inpatient
confinement for mental, nervous or emotional disorders, or ailments that meet standards prescribed within the regulations of
the commissioner of mental health.
Laboratory policies and procedures
Ancillary services
Our network of laboratory service providers consists of an extensive selection of walk-in patient service centers; many local,
regional and national laboratories.
Participating vs. non-participating laboratory provider referrals
Refer our members to participating service centers and laboratories to help them avoid unnecessary costs. Referrals are not
required. Only a health care provider’s prescription or lab order form is required.
We review laboratory ordering information periodically. If our data shows a pattern of out-of-network utilization for your practice,
we contact you to share this information and engage you to use the contracted network.
Participating provider laboratory and pathology protocol (New York)
You must follow specific guidelines when you are recommending the use of, making a referral to, or involving a non-participating
laboratory or pathologist in a member’s care.
For additional details and/or to get a copy of the Laboratory & Pathology Services Consent Form, refer to uhcprovider.com/
policies > For Commercial Plans > UnitedHealthcare® Oxford Clinical and Administrative Policies.
In-office laboratory testing and procedures list
The in-office laboratory testing and procedure list outlines the laboratory procedural/testing codes we reimburse to network
providers when performed in the office setting. For the most up-to-date list, refer to the In-Office Laboratory Testing and
Procedures List at uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare® Oxford Clinical and Administrative
Oxford Commercial supplement
283
2023 UnitedHealthcare Care Provider Administrative Guide
Policies. One of our network laboratories must perform laboratory procedures/tests not appearing on this list. See the How to
Contact Oxford Commercial section for contact information.
Specimen Handling and Venipuncture
Your prescription or lab order form is required when using participating laboratories to process specimen. If you bill specimen
handling and venipuncture codes along with a lab code on the In-Office Laboratory Testing and Procedures List, we only
reimburse the lab and venipuncture codes.
If you bill specimen handling and venipuncture codes without a lab code on our In-Office Laboratory Testing and Procedures
List or with other non-laboratory services, we reimburse the specimen handling and venipuncture codes per our fee schedule.
Radiology and cardiology procedures
We have engaged eviCore to perform initial reviews of prior authorization requests on behalf of our Oxford members.
eviCore has established an infrastructure to support the review, development and implementation of comprehensive outpatient
imaging criteria. The radiology and cardiology evidence-based guidelines and management criteria are available on the eviCore
website.
eviCore handles all prior authorization requests. To request prior authorization for radiology or cardiology, call eviCore or use
the Prior Authorization and Notification tool in the UnitedHealthcare Provider Portal:
• Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In
• Information: uhcprovider.com/paan
• Phone: 1-877-PRE-AUTH (1-877-773-2884)
Accreditation requirements
We require health care provider accreditation and certification requirements for various radiology and cardiology imaging
studies performed on our Oxford members.
Find more detailed information in the following policies found at uhcprovider.com/policies > For Commercial Plans >
UnitedHealthcare® Oxford Clinical and Administrative Policies:
• Accreditation Requirements for Radiology Services
• Credentialing Guidelines: Participation in the eviCore healthcare Network
• Oxford’s Outpatient Imaging Self-Referral Policy
• Radiology Procedures Requiring Prior Authorization for eviCore healthcare Arrangement
• Obstetrical Ultrasonography
• Cardiology Procedures Requiring Prior Authorization for eviCore healthcare Arrangement
Imaging requiring prior authorization
The referring health care provider is responsible for contacting eviCore to request prior authorization and to provide sufficient
history to verify the appropriateness of the requested services. Our policy does not permit prior authorization requests from
persons or entities other than referring health care providers.
Urgent requests during regular business hours
As the attending health care provider, you may make an urgent request for a prior authorization number if you determine the
service is medically urgent. Make urgent requests by calling 1-877-PRE-AUTH (1-877-773-2884). You must state the case
is clinically urgent and explain the clinical urgency. eviCore will respond to urgent requests within 24 hours of receiving all
required information.
Retrospective review process for urgent requests outside of regular business hours
If you determine an Advanced Outpatient Imaging Procedure is medically urgent, and you cannot request a prior authorization
number because it is outside of eviCore’s normal business hours, you must make a retrospective prior authorization request
Oxford Commercial supplement
284
2023 UnitedHealthcare Care Provider Administrative Guide
within 2 business days after the date of service. Request the retrospective review by calling 1-877-PRE-AUTH (1-877-773-2884)
according to the following process:
1. Documentation must explain why the procedure had to be done on an urgent basis and why you could not request an
authorization number during eviCore’s normal business hours.
2. Once eviCore receives retrospective notification of an Advanced Outpatient Imaging Procedure, and if the member’s
benefit plan requires services to be medically necessary to be covered, eviCore will conduct a clinical coverage review to
determine whether the service was medically necessary.
3. If eviCore determines the service was not medically necessary, they will issue a denial and will not issue an authorization
number. The member and health care provider will receive a denial notice outlining the appeal process.
Obtain prior authorizations for outpatient radiology or cardiology procedures using the Prior Authorization
tool in the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In.
For more information, go to uhcprovider.com/paan.
1-877-PRE-AUTH (1-877-773-2884)
Cardiology procedures
We engage eviCore to perform initial reviews of requests for prior authorization of echocardiogram, stress echocardiogram,
cardiac nuclear medicine studies, cardiac CT, PET and MRI and cardiac catheterizations procedures for our Oxford members.
Evidence-based criteria is used to determine medical necessity of cardiology services. The cardiology evidence-based criteria
and management criteria are available on the eviCore website at evicore.com. We continue to be responsible for decisions to
limit or deny coverage and for appeals.
The utilization review process involves matching the member’s clinical history and diagnostic information with the approved
criteria for each imaging procedure requested. Qualified health care providers make utilization review decisions for diagnostic
procedures. eviCore may assign data collection for clinical certification of imaging services to non-medical personnel working
under the direction of qualified health care providers. You receive communication of review determinations for non-urgent care
by fax/telephone within 2 business days of receiving all the necessary information.
Urgent requests during regular business hours
As the attending health care provider, you may make an urgent request for a prior authorization number if you determine the
service is medically urgent. Make urgent requests by calling 1-877-PRE-AUTH (1-877-773-2884). You must state the case
is clinically urgent and explain the clinical urgency. eviCore will respond to urgent requests within 24 hours of receiving all
required information.
Retrospective review process for urgent requests outside of regular business hours
If you determine that a Cardiac Procedure is medically urgent, and you cannot request a prior authorization number because
it is outside of eviCore’s normal business hours, you must make a retrospective authorization request using the following
guidelines:
• Within 2 business days of the date of service for:
– Echocardiograms.
– Stress echocardiograms.
• Within 15 calendar days of the date of service for:
– Diagnostic catheterizations.
Request the retrospective review by calling 1-877-PRE-AUTH (1-877-773-2884), according to the following process:
1. Documentation must explain why the procedure had to be done on an urgent basis and why you could not request an
authorization number during eviCore’s normal business hours.
2. Once eviCore receives retrospective notification of a Cardiac Procedure, and if the member’s benefit plan requires services
to be medically necessary to be covered, eviCore will conduct a clinical coverage review to determine whether the service
was medically necessary.
Oxford Commercial supplement
285
2023 UnitedHealthcare Care Provider Administrative Guide
3. If eviCore determines the service was not medically necessary, they will issue a denial and will not issue an authorization
number. The member and health care provider will receive a denial notice outlining the appeal process.
For a list of procedures requiring prior authorization through eviCore, refer to the Cardiology Procedures
Requiring Prior Authorization for eviCore healthcare Arrangement policy at:
uhcprovider.com > Resources > Plans, policies, protocols and guides > For Commercial Plans >
UnitedHealthcare® Oxford Clinical and Administrative Policies.
Claims processing
You may not balance bill the member if a claim is denied because medical necessity was not demonstrated. We will offer all
appropriate appeal rights for any service that is not approved for payment.
Prior authorization is not required when radiology or cardiology procedures are provided in the ER, observation unit, urgent
care facility or during an inpatient stay.
See a list of Services Requiring Prior Authorization at uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare®
Oxford Clinical and Administrative Policies.
The clinical criteria consistent with existing Oxford policies are available on evicore.com.
You can verify prior authorization requirements by:
1. Calling the number on the back of the member’s ID card to check eligibility.
2. Visiting uhcprovider.com/priorauth > Advance Notification and Plan Requirement Resources.
3. Using the Prior Authorization and Notification tool in the UnitedHealthcare Provider Portal.
Infertility utilization review process
Optum, a UnitedHealth Group company, is delegated to perform reviews for infertility services under the Managed Infertility
Program (MIP) for all Oxford commercial members with an infertility benefit. Optum uses MIP to promote both quality of care
and continuity of service by supporting members through every aspect of the infertility process. Optum infertility nurse case
managers provide support and help members make informed decisions about infertility treatment and care through treatment
education, considerations in choosing where to obtain care and assistance navigating the health care system.
For Oxford products, the rendering health care provider is required to request prior authorization and/or notification of services.
Make this request using the Managed Infertility Program (MIP) Treatment form. Provide sufficient information to determine the
medical necessity of the requested services.
Optum has been diligent in their research to help ensure the clinical policies and guidelines they use are consistent with best
practices and state mandates.
Get the Managed Infertility Program (MIP) Prior Authorization template by:
• Logging onto myoptumhealthcomplexmedical.com.
• Calling Optum at 1-877-512-9340.
• Sending an email to [email protected]
Musculoskeletal services
OrthoNet, a musculoskeletal disease management company, is our network manager for most musculoskeletal services.
OrthoNet’s orthopedic division performs utilization management review of requested services to help ensure they meet
approved clinical guidelines for medical necessity.
OrthoNet conducts the review by determining medical necessity and medical appropriateness, and initiates discharge planning,
as appropriate. OrthoNet will base the results on clinical information and some or all of the following criteria/tools:
• Member benefits
• Oxford medical and reimbursement policies
• InterQual Care Guidelines

Oxford Commercial supplement
286
2023 UnitedHealthcare Care Provider Administrative Guide
Services performed by the following specialties (participating and non-participating) are subject to utilization review by
OrthoNet’s orthopedic division regardless of the diagnosis:
• Orthopedic surgery
• Pediatric orthopedic surgery
• Podiatry
• Neurosurgery
• Hand surgery
• Physical medicine rehabilitation
OrthoNet’s orthopedic division manages services provided by the following facilities (participating and non-participating) when
billed together with certain ICD-10 codes:
• Acute care hospital
• Ambulatory surgery
• DME
• Other ancillary facility
• Home health care
• Physical rehabilitation hospital
• Physical rehabilitation facility
• SNF
For a complete list of orthopedic diagnosis codes, or for more information on our arrangement with OrthoNet, refer to the
Orthopedic Services policy at uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare® Oxford Clinical and
Administrative Policies.
Physical and occupational therapy
We have delegated certain administrative services related to outpatient physical and occupational therapy services for Oxford
members to OptumHealth Care Solutions, LLC (Optum). Hospital outpatient treatment facilities and outpatient facilities at or
affiliated with rehabilitation hospitals are considered outpatient settings for physical and occupational therapy.
All physical and/or occupational therapy visits require utilization review and an authorization, including the initial evaluation.
After registering on myoptumhealthphysicalhealth.com, click on the Forms link and locate the Patient Summary Form. The
treating health care provider or health care professional must submit a Patient Summary Form to Optum®. They may submit the
completed form through the Optum website at myoptumhealthphysicalhealth.com. Send the forms within 3 days of initiating
treatment. They must be received within 10 days from the initial date of service indicated on the form. Optum adjusts the initial
payable date when they receive the forms outside of the 10-day submission requirement.
The Patient Summary Form must include the initial visit. If Optum does not receive the required form(s) within this time frame,
they deny the claim. Optum reviews the services requested for medical necessity. After the initial approved visits have occurred,
if a member’s care requires additional visits or more time than was approved, you must submit a new Patient Summary Form
with updated clinical information.
Note: Prior authorization is not required for certain groups.
Chiropractic services
OptumHealth Care Solutions, LLC (Optum) manages our chiropractic benefit. To receive standard chiropractic benefit
coverage, members must obtain an electronic referral from their PCP. PCPs perform the customary initial comprehensive
differential diagnosis with the necessary and appropriate workup.
You may request a chiropractic referral for a maximum of 1 visit within 180 days (6 months). Participating chiropractors must
complete and submit Patient Summary Forms to Optum® for services performed.
They may submit the Patient Summary Forms through the Optum website at myoptumhealthphysicalhealth.com. They must
submit the form within 3 business days and no later than 10 business days following the member’s initial visit or recovery

Oxford Commercial supplement
287
2023 UnitedHealthcare Care Provider Administrative Guide
milestone. We must receive the patient summary form within 10 days from the initial date of service indicated on the form.
Optum adjusts the initial payable date when they receive the forms outside of the 10-day submission requirement.
Once they receive the forms, Optum reviews the services requested for medical necessity and makes denial determinations.
If a member’s care requires more visits or time than was approved, you must submit a new Patient Summary Form with updated
clinical information after the initially approved visits have occurred.
According to your contract with Optum, the member may not be balance billed for any covered service not reimbursed if you do
not submit the Patient Summary Form, or for those services which do not meet medical necessity or coverage criteria. However,
you may file an appeal.
Acupuncture services
Only members who have the alternative medicine rider have coverage for acupuncture. If a member does not have the
alternative medicine rider, we deny requests to cover acupuncture, even if a letter of medical necessity has been submitted.
Acupuncture services must be rendered in-network and performed by one of the following health care provider types:
• Participating licensed acupuncturist (LAC)
• Participating licensed naturopaths
• Participating health care provider (MD or DO) who is credentialed as physician acupuncturist
Pharmacy management programs
The pharmacy benefit plan includes a dynamic medication list, referred to as the PDL, and various clinical drug utilization
management programs. We base these programs on FDA-approved indications and medical literature or guidelines.
The PDL contains medications in 3 tiers. Tier 1 is the lowest cost option, and Tier 3 is the highest cost option. Some groups
have a 4-tier benefit design.
To help make medications more affordable, consider whether a Tier 1 or Tier 2 alternative is appropriate if the member is
currently taking a Tier 3 medication. We perform ongoing reviews of the PDL and make updates up to three times per year.
Medications requiring notification or prior authorization are noted with a “PA,” medications that require step therapy are noted
with “ST” and supply limits with “SL.”
PDL Management Committee and the Pharmacy and Therapeutics Committee
Our PDL Management Committee, a group of senior health care providers and business leaders, makes tier decisions and
changes to the PDL based on a review of clinical, economic and pharmacoeconomic evidence.
Our National Pharmacy and Therapeutics (P&T) Committee is responsible for evaluating and providing clinical evidence to the
PDL Management Committee to help assign medications to tiers on the PDL. The information provided by the P&T Committee
includes evaluation of a medication’s role in therapy, its relative safety and its relative efficacy.
The P&T Committee reviews and approves clinical criteria for prior authorization and step therapy programs and supply limits.
In addition to medications covered under the pharmacy benefit, the P&T Committee is responsible for evaluating clinical
evidence for medications, which require administration or supervision by a qualified, licensed health care professional.
The P&T Committee is comprised of internal and external physicians representing various specialties and pharmacists.
For more information regarding the Oxford pharmacy management program, go to uhcprovider.com/pharmacy.
Quality Management and Patient Safety Programs Drug Utilization Review (DUR)
We receive the majority of prescription claims electronically for payment. Within seconds, our systems record the member’s
claim and review past prescription history for potential medication-related problems. DUR helps review for potentially harmful
medication interactions, inappropriate utilization and other adverse medication events to maximize therapy effectiveness within
the appropriate medication usage parameters. There are 2 types of DUR programs: concurrent and retrospective.
Concurrent Drug Utilization Review (C-DUR)
The C-DUR program performs online, real-time DUR analysis at the point of prescription dispensing. This program screens
every prescription before dispensing for a broad range of safety and utilization considerations. C-DUR uses a clinical database

Oxford Commercial supplement
288
2023 UnitedHealthcare Care Provider Administrative Guide
to compare the current prescription to the member’s inferred diagnosis, demographic data and past prescription history.
The C-DUR program uses criteria to identify potential inappropriate medication consumption, medical conflicts or dangerous
interactions that may result if the prescription is dispensed.
If the C-DUR identifies a potential problem, it notifies the dispensing pharmacist by sending either a soft alert (warning
message) or a hard alert (a warning message also requiring the pharmacist to enter an override). The dispensing pharmacist
uses professional judgment to determine appropriate interventions, such as contacting the prescribing health care provider or
other health care professional, discussing concerns with the member and dispensing the medication.
Retrospective Drug Utilization Review (R-DUR)
The R-DUR program involves a daily review of prescription claims data to identify patterns in prescribing or medication
utilization suggesting inappropriate or unnecessary medication use. The program uses a clinical database to review member
profiles for potential over- or under-dosing as well as duration of therapy, potential drug interactions, drug-age considerations
and therapy duplications.
You and other prescribers receive a member-specific report outlining opportunities for intervention and asking them to respond
to specific issues and concerns.
Clinical programs
Prescription medications requiring prior authorization (subject to plan design)
Based on the member’s benefit plan design, selecting high-risk or high-cost medications may require advance notification to
be eligible for coverage. We may ask you to provide information explaining medical necessity and/or past therapeutic failures.
A representative will collect pertinent clinical data for the service requested. If we do not approve the prior authorization, a
pharmacist or medical director, in keeping with state regulations, makes the final coverage determination. We notify you and the
member of the decision.
Step therapy (subject to plan design)
Certain medications may be subject to step therapy, also referred to as First Start for members with a New Jersey plan. The
step therapy program requires a trial of a lower-cost, Step 1 medication before a higher-cost, Step 2 medication is eligible for
coverage. When a member presents a Step 2 medication at the pharmacy, our systems may automatically check the claims
history to see if a Step 1 medication is in the claims history. The medication may automatically process. If not, you may request
a coverage review. If we do not approve the medication, a pharmacist or medical director, in keeping with state regulations,
makes the final coverage determination. We notify you and the member of the decision.
Supply limits (subject to plan design)
Some medications are subject to supply limits. We base supply limits on FDA-approved dosing guidelines as defined in the
product package insert and the medical literature or guidelines and data supporting the use of higher or lower dosages than
the FDA-recommended dosage. This program focuses on select medications or categories of medications that are high cost
and/or are frequently used outside of generally accepted clinical standards.
When a pharmacist submits an online prescription claim, the online claims processing system compares the quantity entered
with the allowable limits.
If the prescription exceeds the established quantity limits, we reject the claim and the pharmacist receives a message. The
current supply limit for the medication is displayed in the message. For New York and New Jersey fully insured business, a
subset of medications has coverage criteria available to obtain quantities beyond the established limit, if medically necessary.
Emergencies and Urgent Care
Urgent Care
Urgent care is medical care for a condition that needs immediate attention to minimize severity and prevent complications but is
not a medical emergency. It does not otherwise fall under the definition of emergency care.

Oxford Commercial supplement
289
2023 UnitedHealthcare Care Provider Administrative Guide
Definition of a medical emergency
Connecticut: An “emergency condition” is defined as a medical condition, manifesting itself by acute symptoms of sufficient
severity, including severe pain, such that a prudent layperson with an average knowledge of health and medicine, acting
reasonably, would have believed that the absence of immediate medical attention would result in placing the health of such
person or others in serious jeopardy or serious impairment to bodily functions; or serious dysfunction of a bodily organ or
part; or would place the person’s health or, with respect to a pregnant woman, the health of the woman or her unborn child, in
serious jeopardy.
New Jersey: An “emergency condition” is defined as a medical condition, manifesting itself by acute symptoms of sufficient
severity including, but not limited to, severe pain, psychiatric disturbances and/or symptoms of substance use, and the absence
of immediate medical attention to result in placing the health of the individual (or, with respect to a pregnant woman, the health
of the woman or her unborn child) in serious jeopardy; serious impairment to bodily functions; or serious dysfunction of a bodily
organ or part. With respect to a pregnant woman who is having contractions, an emergency exists where there is inadequate
time to affect a safe transfer of the woman or unborn child to another hospital before delivery, or the transfer may pose a threat
to the health or safety of the woman or the unborn child.
New York: “Emergency condition” means a medical or behavioral condition, the onset of which is sudden, that manifests
itself by symptoms of sufficient severity, including severe pain, that a prudent layperson, possessing an average knowledge of
medicine and health, could reasonably expect the absence of immediate medical attention to result in (a) placing the health of
the person afflicted with such condition in serious jeopardy, or in the case of a behavioral condition, placing the health of such
person or others in serious jeopardy; (b) serious impairment to such person’s bodily functions; (c) serious dysfunction of any
bodily organ or part of such person; or (d) serious disfigurement of such person.
Emergency room visits
We cover ER services for medical emergencies. The member is responsible for paying their copayment. Follow-up ER visits
within our service areas are not covered. However, follow-up care, if appropriate, is coordinated through the member’s PCP and
is subject to the standard referral process.
• ER visits during which a member is treated and released without admission do not require notice to us.
• If an ambulatory surgery occurs because of an ER or urgent care visit, you must notify us within 24‒48 hours of when the
surgery is performed. Coordinate all follow-up needs related to such emergency services through the member’s PCP. They
are subject to the standard referral process.
• When a member is unstable and not capable of providing coverage information, the facility should submit the concurrent
authorization as soon as they know the information and communicate the extenuating circumstances.
In-area emergency services
You do not need to provide notification or obtain authorization for in-area ER treatment and subsequent release. However,
all emergency inpatient admissions and emergency outpatient admissions (i.e., for emergent ambulatory surgery) require
notification upon admission or on the day of admission (no later than 48 hours from the date of admission, or as soon as
reasonably possible).
Out-of-area emergency services
Out-of-area coverage for ER services are limited to care for accidental injury, unanticipated emergency illness or other
emergency conditions when circumstances prevent a member from using ER services within our service area.
Emergency admission review
If the member is admitted to a hospital due to an emergency (as previously defined), we review the hospital admission for
medical necessity and determine appropriate length of stay based on our approved criteria for concurrent review. Review
begins when we become aware of the admission. You must notify us of all emergency inpatient admissions no later than 48
hours from the date of admission, or as soon as reasonably possible. If the member is admitted to a contracted hospital, we use
reasonable efforts to transmit a decision about the admission to the hospital (to the fax number and contact person designated
by the hospital) within 24 hours of making the decision.
Oxford Commercial supplement
290
2023 UnitedHealthcare Care Provider Administrative Guide
Non-emergency hospitalization
Any hospitalization service that does not meet the criteria for an emergency or for urgent care requires prior authorization and is
subject to medical necessity review.
Coverage outside of the United States
We provide limited coverage for Oxford members outside of the United States, Mexico, Canada or the U.S. Territories.
New York (NY) and Connecticut (CT) products
The following applies to out-of-country health care providers.
• Claims received for services performed outside of the United States do not require an authorization if the services are
emergent in nature.
• We will not cover elective procedures outside of the United States, Mexico, Canada or the U.S. Territories for members who
reside in the United States unless an authorization exists specifically indicating that out-of-country services were authorized.
This includes prenatal care and delivery.
• All claims from out-of-country health care providers must be translated and the amount billed and calculated in American
dollars using the conversion rate as of the processing date.
New Jersey (NJ) products
The following applies to out-of-country health care providers.
• Claims received for services performed outside of the United States do not require an authorization if the services are
emergent or urgent in nature.
• Claims will not be covered for elective procedures outside of the United States, Mexico, Canada or the U.S. Territories for
members who reside in the United States unless an authorization exists specifically indicating that out-of-country services
were authorized. This includes prenatal care and delivery.
• All claims from out-of-country health care providers must be translated and the amount billed and calculated in American
dollars using the conversion rate as of the processing date.
Out-of-country resident members
NJ Small Group/PPO FP and Liberty
Services provided outside of the United States are excluded unless the covered member is outside of the United States for one
of the following reasons:
• Travel, provided the travel is for a reason other than securing health care diagnosis and/or treatment, is for a period of 6
months or less.
• Business assignment, provided the covered member is temporarily outside of the United States for a period of 6 months
or less.
• Eligibility for full-time student status (subject to pre-approval), provided the covered member is either enrolled and attending
an accredited school in a foreign country or is participating in an academic program in a foreign country, for which the
institution of higher learning at which the student matriculates in the United States grants academic credit.
Note: We deny charges in connection with full-time student status in a foreign country that we have not pre-approved as non-
covered charges.
Utilization reviews
Our UM represents a combination of different disciplines, including utilization review with benefit and eligibility requirements,
effective and appropriate delivery of medically necessary services, quality of care across the continuum, discharge planning
and case management.

Oxford Commercial supplement
291
2023 UnitedHealthcare Care Provider Administrative Guide
Our Clinical Services department monitors services provided to members to identify potential areas of over and underutilization.
UM decision-making is based only on appropriateness of care and service and the existence of coverage. We do not specifically
reward or offer incentives to practitioners or other individuals for issuing denials of coverage or service care. Financial
incentives for UM decision-makers do not encourage decisions that result in underutilization.
Criteria and clinical guidelines
We have adopted the InterQual Care Guidelines and criteria for inpatient and ambulatory care where no specific Oxford
policy exists. We also develop specific policies related to covered services. Each policy describes the service and its
appropriate utilization.
We employ several means to review the consistency and quality of clinical decision-making as directed through policies and
adopted guidelines. The following processes are in addition to those required by regulatory agencies and NCQA:
• Inter-rater reliability tests developed in conjunction with an external consultant
• Monthly medical director consistency meetings and case discussions
• Monthly blind reviews done by all medical directors on a common set of clinical factors
We employ a process for adopting and updating clinical practice guidelines for use by network providers and other health care
professionals. Clinical practice guidelines help practitioners and members make decisions about health care in specific clinical
situations. We develop guidelines for preventive screening, acute and chronic care, and appropriate drug usage based on:
• Availability of accepted national guidelines
• Ability to monitor compliance
• Projected ability to make a significant impact upon important aspects of care
Clinical practice guidelines are available on uhcprovider.com/policies > Clinical Guidelines.
Clinical review
We may perform clinical reviews for various reasons, including but not limited to, medical necessity determinations, member
eligibility and to validate accuracy of coding for services or procedures requested or rendered by participating or non-
participating health care providers and other qualified health care professionals. We consider medically necessary services
for reimbursement when rendered to eligible members, as reflected in the clinical information, provided the services are not
fraudulent or abusive.
We may review clinical information on an entire population of, or a subset of, health care providers, procedures or members, at
our discretion. We may review this information prospectively, concurrently and/or retrospectively. We define clinical information
as the member’s clinical condition, which may include symptoms, treatments, dosage and duration of drugs, and dates for
other therapies. Dates of prior imaging studies performed and other information the ordering health care provider believes is
useful in evaluating whether the service ordered meets current evidence-based clinical guidelines, such as prior diagnostic
tests and consultation reports, should be provided.
Clinical information reviewed prospectively may be reviewed again concurrently or retrospectively to confirm the accuracy of the
information available at the time of previous review. We will retrospectively deny an approval only in circumstances indicated in
the approval or in circumstances involving fraud, abuse or material misrepresentation.
The procedure and information required for review will depend on the circumstances of interest, as determined by us.
The process of selecting services for review, requests for clinical information concerning such services, review of clinical
information and action based on clinical information complies with all relevant federal and state regulations, laws and provisions
in your Oxford contract. We provide information on appeal rights for adverse determinations as required by law and regulation.
Utilization review of services provided to New York members
All adverse utilization review (UR) determinations (whether initial or on appeal) are made by a clinical peer reviewer. Appeals of
adverse UR determinations will be reviewed by a different clinical peer reviewer than the clinical peer reviewer who rendered the
initial adverse determination.

Oxford Commercial supplement
292
2023 UnitedHealthcare Care Provider Administrative Guide
Initial Utilization Review Determination Time Periods
We make UR decisions by the following methods and in the following time frames:
Prior Authorization - We make UR decisions and provide notice to you and the member, by phone and in writing, within 3
business days of receipt of necessary information.
Concurrent review - We make UR decisions and provide notice to the member or their designee by phone and writing within 1
business day of receipt of necessary information.
Retrospective - We will make UR decisions within 30 days of receipt of necessary information. We may reverse a preauthorized
treatment, service or procedure on retrospective review when all the following circumstances occur:
1. Relevant medical information presented to us or the UR agent during retrospective review is materially different from the
information presented during the preauthorization review.
2. The information existed at the time of the preauthorization review but was withheld or not made available.
3. We, or our UR agent, were not aware of the existence of the information at the time of the preauthorization review.
4. If we had been aware of the information, we would not have authorized the treatment, service or procedure requested.
If an initial adverse UR determination is rendered without attempting to discuss such matter with the member’s health
care provider or other health care professional who specifically recommended the health care service, procedure or
treatment under review, such health care providers and other health care professionals have the opportunity to request
reconsideration of the adverse determination. Except in cases of retrospective reviews, the medical director or other health
care professional conducts the review as the clinical peer reviewer and make the determination within 1 business day of
receipt of the request.
Failure to make an initial UR determination within the time periods described is deemed to be an adverse determination eligible
for appeal.
Components of an initial adverse determination
If the review results in an adverse determination, the initial adverse determination letter includes the following:
1. Reasons for the determination, including clinical rationale
2. Instructions on how to initiate internal appeals (standard and expedited appeals) and eligibility for external appeals
3. Clinical review criteria relied upon to make our decision is provided upon request from the member or the
member’s designee
4. Any other necessary information that must be provided to, or obtained by us, to render a decision on an appeal of
our determination
Appeal requirements for initial adverse utilization review determinations (New York
member appeals)
Member appeals must be submitted to us or our delegate within 180 days from the receipt of the initial adverse UR
determination. Standard (non-expedited) UR appeals may be filed by telephone or in writing by the member or their designee.
Member appeals may be initiated in writing or by calling our Member Service department at the number on the member’s ID
card or at 1-800-444-6222. However, we strongly recommend the appeal be filed in writing. Determinations concerning services
that have already been provided are not eligible to be appealed on an expedited basis. In the event that only a portion of such
necessary information is received, we request the missing information, in writing, within 5 business days of receipt of partial
information. If a determination is not made within 15 days of the filing of the appeal, we provide written acknowledgment to the
appealing party within 15 days of the filing of a standard appeal.
Expedited UR appeals
An expedited UR appeal may be filed for denials of:
• Continued or extended health care services, procedures or treatment.
• Additional services for member undergoing a course of continued treatment.
• Health care services for which the health care provider or other health care professional believes an immediate appeal is
warranted.

Oxford Commercial supplement
293
2023 UnitedHealthcare Care Provider Administrative Guide
We make a decision on expedited UR appeals within 2 business days of receipt of the information necessary to conduct such
appeal. If we require more information to conduct an expedited appeal, we immediately notify the member and their health
care provider by phone or fax to identify and request the necessary information. We follow up with a written notification. The
appealing party may re-appeal an expedited appeal using the standard appeal process or through the external appeal process.
We allow you to submit an expedited member appeal without a member’s written consent. All other appeals require the
member’s explicit written consent to appeal after our initial UR decision is made. A general assignment will not be accepted.
If we do not make a determination within 60 calendar days of receipt of the necessary information for a standard appeal
or within 2 business days of receipt of necessary information for an expedited appeal, we consider the initial adverse UR
determination to be reversed.
The law allows the member and us to jointly agree to waive the internal UR appeal process. Typically, we do not agree to this.
In those rare situations where we are willing to waive the internal UR appeal, we inform the appeal requester and/or member
verbally and/or in writing. If the member agrees to waive the internal UR appeal process, we provide them with a letter within 24
hours of the Agreement with information on filing an external appeal.
Internal utilization management appeals process
Retrospective review appeals (New York provider appeals)
A retrospective adverse determination is one where the initial medical necessity review is requested or initiated after the
services have been rendered. This process does not apply to services where precertification or concurrent review is required.
You may request an external appeal on your own behalf, by phone or in writing, when we have made a retrospective final
adverse determination on the basis that the service or treatment is not medically necessary or is considered experimental or
investigational (or is an approved clinical trial) to treat the member’s life-threatening or disabling condition (as defined by the
New York State Social Security Law).
All requests for such internal retrospective appeals must be made within 60 days of receipt of the initial retrospective medical
necessity or experimental/investigational determination. If we require more information to conduct a standard internal appeal,
we notify the member and their health care provider, in writing, within 15 days of receipt of the appeal, to identify and request
necessary information.
Once we make a decision about the retrospective review appeal, we notify the member and their health care provider in writing
within 2 business days from the date we make the decision.
If the decision is adverse, and you continue to dispute our decision, you may be eligible for an external appeal through the New
York external appeal process. Hospitals and other facilities may have alternate dispute mechanisms in place for review of these
issues instead of external appeal. Check your contract for more information.
Internal retrospective appeals submitted after the 60-day time frame is not handled through this process. If your appeal is still
submitted within the contractual deadlines for an appeal, we automatically handle it through the contractual appeal process
discussed in the following section.
Medical necessity internal appeals process for health care providers under your contract
If we make a decision that a requested service is not medically necessary, you may dispute our determination. Mail a written
request, with supporting clinical documentation showing why we should reverse the denial of services, to:
Oxford Clinical Appeals Department
P.O. Box 31388
Salt Lake City, UT 84131
The Clinical Appeals department makes a reasonable effort to render a decision within 60 calendar days of receiving the appeal
and supporting documentation. If the contractual appeal decision is adverse, and you continue to dispute the decision, the
dispute may be eligible for arbitration under your contract.
Note: There is a separate appeal process for internal member appeals and retrospective provider appeals under New York law.
These processes do not apply to contractual appeals.
Appeals not submitted within the contractual time frames are denied.

Oxford Commercial supplement
294
2023 UnitedHealthcare Care Provider Administrative Guide
Connecticut members
Utilization review appeals
UR occurs whenever judgments pertaining to medical necessity and the provision of services or treatments are rendered.
The UR appeals process should be used after you receive an initial adverse UR determination and you do not agree with our
decision. All appeals are subject to a review by us to evaluate the medical necessity of the services. You may use this process
to appeal adverse determinations relating to all UR determinations, regardless of whether the services requested by you or your
authorized representative have not yet been rendered (pre-service), are currently being rendered (concurrent) or have already
been rendered (post-service).
Note: This UR appeals process should not be used for appeals relating to benefit, network or administrative issues.
UR appeals must be initiated within 180 days from receipt of an adverse determination (i.e., receipt of the determination notice).
A decision may be rendered within the standard time frames or may be expedited as described in this section.
While a UR appeal may be filed by telephone or in writing, we strongly recommend you file your appeal in writing. The written
request will give us a clear understanding of the issues being appealed. In addition to your request for an appeal, you or your
authorized representative must send documentation/information already requested by us (if not previously submitted) and
additional written comments and documentation/information you would like to submit in support of the appeal. At the time of
our review, we will review all available comments, documentation and information.
Unless we already issued a written determination, we use our best efforts to provide written acknowledgment of the receipt of
your appeal within 5 business days but not later than 15 calendar days. Our decision to either uphold or reverse the adverse
determination is made and communicated to you as follows:
• Request for service (pre-service): Within 30 calendar days of our receipt of the appeal. However, if additional information is
requested, a determination is made within 3 business days of our receipt of the information, or the expiration of the period
allowed to provide the information (i.e., 45 days).
• Concurrent services for a member in an ongoing course of treatment (concurrent): Within 30 calendar days of our receipt of
the appeal. In this instance, treatment is continued without liability while your appeal is being reviewed. However, if additional
information is requested, a determination is made within 1 business day of our receipt of the information, or the expiration of
the period allowed to provide the information (i.e., 45 days).
• Coverage for services rendered (post-service): Within 60 calendar days of our receipt of the appeal. However, if additional
information is requested, a determination is made within 15 days of our receipt of the information, or the expiration of the
period allowed to provide the information (i.e., 45 days).
If we do not follow the process outlined in this section, you will have been deemed to have exhausted the internal appeals
process. You may then file a request for an external review (see the following section), regardless of whether we can assert
substantial compliance or de minimis error.
This will be our final adverse determination. If you are not satisfied with our decision, you have the option of filing an External
Appeal. Refer to the following External Appeals section.
Expedited/urgent Utilization Review (UR) appeals
You can expedite your UR appeal when:
• You receive an adverse determination involving continued or extended health care services, procedures or treatments or
additional services while you are undergoing a course of continued treatment (concurrent) prescribed by a health care
provider.
• The time frames of the non-expedited UR appeal process would seriously jeopardize your life, health or ability to regain
maximum function.
• In the opinion of a health care provider with knowledge of the health condition, the time frames of the non-expedited UR
appeal process would cause you severe pain that cannot be managed without care or treatment requested.
• Your health care provider believes an immediate appeal is necessary because the time frames of the non-expedited UR
appeal process would significantly increase the risk to your health.

Oxford Commercial supplement
295
2023 UnitedHealthcare Care Provider Administrative Guide
• For a substance use disorder, a co-occurring mental disorder or a mental disorder requiring inpatient services, partial
hospitalization, residential treatment or intensive outpatient services necessary to keep a covered person from requiring an
inpatient setting.
You have 2 available options for expedited reviews. These options are not available for health care services that have
already been rendered (post-service).
1. Internal Expedited UR Appeal: This process includes procedures to facilitate a timely resolution of the appeal including,
but not limited to, the sharing of information between your health care provider and us by telephone or fax. We provide
reasonable access to our clinical peer reviewer within 1 business day of receiving notice of an expedited UR appeal.
A decision is rendered and communicated for an internal expedited UR appeal within the following time frames:
• 24 hours from our receipt of the appeal when the service being appealed is for substance use disorder or co-occurring
mental disorder, and inpatient services, partial hospitalization, residential treatment or those intensive outpatient services
needed to keep the member from requiring an inpatient setting in connection with a mental disorder.
• 72 hours from our receipt of the appeal for all other types of services.
If you are not satisfied with the outcome of the expedited UR appeal, you may further appeal through the external appeal
process. If we do not make a determination within 72 hours of receipt of the necessary information, the adverse determination
is reversed.
The notice of an appeal determination includes reasons for the determination. If the adverse determination is upheld on
appeal, the notice will include the specific reason(s) and clinical rationale used to render the determination, a reference to the
specific health benefit plan provisions on which the decision is based, a statement you may receive from us (upon request
and free of charge) and reasonable access to and copies of all relevant documents. We also include a notice of your right to
initiate an external appeal. A description of each process and associated time frames is included.
If we do not follow the process outlined in this section, you will have been deemed to have exhausted the internal appeals
process. You may then file a request for an external review (see the following option), regardless of whether we can assert
substantial compliance or de minimis error.
2. External Expedited Appeal: You have the option to seek review by an independent review organization in emergency or
life-threatening circumstances. You may make a request to the Commissioner of Insurance for an expedited external appeal
without first completing the internal appeals process if:
• The time frame for completion of an expedited internal appeal may cause or exacerbate an emergency or life-threatening
situation; or
• For a substance use disorder, a co-occurring mental disorder or a mental disorder requiring inpatient services, partial
hospitalization, residential treatment or intensive outpatient services necessary to keep a covered person from requiring an
inpatient setting; and
• The member or you, acting on their behalf with their consent, filed a request for expedited internal review.
If you choose this option, you must submit the appeal by contacting:
Connecticut Insurance Department
P.O. Box 816
Hartford, CT 06142-0816
Phone: 1-860-297-3910
For more information on how to file an expedited external appeal, refer to the External UR Appeals section.
Final Adverse Determination Notice (FAD)
The contents of a FAD vary based on the state in which the member’s certificate of coverage was issued. Each notice of FAD is
in writing, dated and includes the following:
Connecticut:
1. Information sufficient to identify the benefit request or claim involved, including the date of service, the health care
professional and the claim amount, if known.

Oxford Commercial supplement
296
2023 UnitedHealthcare Care Provider Administrative Guide
2. The specific reason(s) for the adverse determination, including, upon request, a listing of relevant clinical review criteria
including professional criteria and medical or scientific evidence used to reach the denial and a description of the Oxford
standard, internal rule, guideline, protocol or other criterion, if applicable, used in reaching the denial.
3. Reference to the specific health benefit plan provisions we used to reach the denial.
4. A description of other material or information necessary for the covered person to perfect the benefit request or claim,
including an explanation of why the material or information is necessary to perfect the request or claim.
5. A description of the Oxford internal appeals process, which includes:
i. Oxford expedited review procedures,
ii. Limits applicable to such process or procedures,
iii. Contact information for the organizational unit designated to coordinate the review on behalf of the health carrier, and
iv. A statement the member or their authorized representative is entitled, following requirements of the Oxford internal
grievance process, to receive from us, free of charge upon request, reasonable access to and copies of all documents,
records, communications and other information and evidence regarding the request.
If the adverse determination is based on:
1. An internal rule, guideline, protocol or other similar criteria:
i. The specific rule, guideline, protocol or other similar criteria; or
ii. A statement that:
• A specific rule, guideline, protocol or other similar criteria was relied upon to make the adverse determination and a
copy of such rule, guideline, protocol or other similar criteria will be provided to the covered person free of charge
upon request;
• Provides instructions for requesting a copy; and
• The links to such rule, guideline, protocol or other similar criteria on the Oxford website.
2. Medical necessity or an experimental/investigational treatment:
i. A written statement of the scientific or clinical rationale used to render the decision that applies the terms of the
benefit plan to the member’s medical circumstance; and
ii. Notification of the member’s right to receive, free of charge upon request, reasonable access to and copies of all
documents, records, communications and other information and evidence not previously provided regarding the
adverse determination under review.
3. A statement explaining the right of the member to contact the Office of the Healthcare Advocate at any time for assistance
or, upon completion of the Oxford internal grievance process, to file a civil suit in a court of competent jurisdiction. Such
statement shall include:
i. The contact information for said offices; and
ii. A statement if the member or their authorized representative chose to file a grievance that:
• Appeals are sometimes successful;
• The member may benefit from free assistance from the Office of the Healthcare Advocate, which may assist them
with filing a grievance pursuant to 42 USC 300gg–93, as amended from time to time;
• The member is entitled and encouraged to submit supporting documentation for our consideration during the review
of an adverse determination, including narratives from the member or from their authorized representative and letters
and treatment notes from the member’s health care professional; and
• The member has the right to ask their health care professional for such letters or treatment notes.
4. A health carrier may offer a member’s health care professional the opportunity to confer with a clinical peer as long as a
grievance has not already been filed prior to the conference. This conference between the physician and the health care
professional peer will not be considered a grievance of the initial adverse determination.
New Jersey:
1. Information sufficient to identify the claim involved, including date of service, health care provider, claim amount (if
applicable) and a statement describing the availability, upon request, of the diagnosis code and its corresponding meaning
and the treatment code and its corresponding meaning. Any request for such diagnosis and treatment information following

Oxford Commercial supplement
297
2023 UnitedHealthcare Care Provider Administrative Guide
an initial adverse benefit determination shall be responded to as soon as practicable, and the request itself shall not be
considered a request for a stage 1, stage 2 or stage 3 appeal;
2. The reason(s) for the adverse benefit determination, including denial code and corresponding meaning, as well as a
description of the standard used by us in the denial;
3. Any new or additional rationale, which was relied upon, considered or used, or generated by us, in connection with the
adverse benefit determination; and
4. Information regarding the availability and contact information for the consumer assistance program at the Department
of Banking and Insurance, which assists covered persons with claims, internal appeals and external appeals, which shall
include the address and telephone number at N.J.A.C. 11:24-8.7(b).
New York:
1. The specific reason for denial, reduction or termination of services;
2. The specific health service that was denied, including the name of the facility/health care provider and developer/
manufacturer of service, as available;
3. A statement that the member may be eligible for an appeal, and a description of appeal procedures including a description
of the urgent appeal process if the claim involves urgent care;
4. A clear statement, in bold, that the member has 45 days from the FAD to request an external appeal, and that choosing the
second level internal appeal may exhaust the time limits required for filing an external appeal; and
5. A description of the external appeals process.
If we fail to adhere to these requirements for rendering decisions, the following rules apply to members enrolled in Connecticut
and New Jersey Oxford products.
Connecticut: The member is deemed to have exhausted the Oxford internal appeals process and may file an external review,
even if we could prove substantial compliance or minor (de minimis) error.
New Jersey: Members are not obligated to complete the internal review process and may proceed directly to the external
review process under the following circumstances:
• We fail to comply with any deadlines for completion of the internal appeals process without demonstrating good cause or
because of matters beyond our control while in the context of an ongoing, good faith exchange of information between
parties and it is not a pattern or practice of non-compliance;
• We, for any reason, expressly waive our rights to an internal review of any appeal; or
• The member and/or their health care provider applied for expedited external review at the same time as applying for an
expedited internal review.
In such a case where we assert good cause for not meeting the deadlines of the Oxford appeals process, members or their
designee and/or their health care provider may request a written explanation of the violation. We must provide the explanation
within 10 days of the request and must include a specific description of the basis for which we determine the violation should
not cause the internal appeals process to be exhausted. If an external reviewer or court agrees with us and rejects the request
for immediate review, the member has the opportunity to resubmit their appeal.
Member’s rights to external appeal
The member has a right to an external appeal of a FAD.
A FAD is a first-level appeal denial of an otherwise covered service where the basis for the decision is either a lack of medical
necessity, appropriateness, health care setting, level of care or effectiveness or the experimental/investigational exclusion.
The health care provider’s certification must include a statement of the evidence relied upon by the health care provider in
certifying their recommendation, and an external appeal must be submitted within 45 days upon receipt of the FAD, whether a
second-level appeal is requested or not. If a member chooses to request a second-level internal appeal, the time may expire for
the member to request an external appeal.
An external appeal may also be filed:
1. When the member had coverage of a health care service denied on the basis that such service is experimental or
investigational.

Oxford Commercial supplement
298
2023 UnitedHealthcare Care Provider Administrative Guide
2. The denial has been upheld on appeal or both us and the member have jointly agreed to waive any internal appeal.
3. The member’s attending health care provider certified that the member has a life-threatening or disabling condition or
disease:
• For which standard health services or procedures have been ineffective or would be medically inappropriate.
• For which there does not exist a more beneficial standard health service or procedure covered by their health care plan.
• For which there exists a clinical trial.
4. The member’s attending health care provider, who must be a licensed, board-certified or board-eligible health care provider
qualified to practice in the area of practice appropriate to treat the member’s life-threatening, or disabling condition or
disease, must have recommended either:
• A health service or procedure (including a pharmaceutical product within the meaning of PHL 4900(5)(b)(B)), that based
on 2 documents from the available medical and scientific evidence, is likely to be more beneficial to the member than any
covered standard health service or procedure.
• A clinical trial for which the member is eligible. Any health care provider certification provided under this section shall
include a statement of the evidence relied upon by the health care provider in certifying their recommendation.
5. The specific health service or procedure recommended by the attending health care provider that would otherwise
be covered under the policy except for our determination that the health service or procedure is experimental
or investigational. The member is not required to exhaust the second level of internal appeal to be eligible for an
external appeal.
External appeal process
If the Clinical Appeals department upholds all or part of such an adverse determination, the member or their designee has the
right to request an external appeal. An external appeal may be filed when:
1. The member had coverage of a health care service denied on appeal, in whole or in part, on grounds that such health care
service is not medically necessary but otherwise would have been a covered benefit.
2. We made a final adverse determination regarding the requested service.
3. We and the member both agreed to waive any internal appeal.
All external appeal requests may be sent to the following:
New York State Insurance Department
P.O. Box 7209
Albany, NY 12224-0209
Phone: 1-800-400-8882
Fax: 1-800-332-2729
Claims process
Time frame for claims submission
To be considered timely, health care providers, other health care professionals and facilities are required to submit claims within
the specified period from the date of service:
• Connecticut - 90 days
• New Jersey - 90 or 180 days if submitted by a New Jersey participating health care provider for a New Jersey line of
business member
• New York - 120 days
The claims filing deadline is based on the date of service on the claim. It is not based on the date the claim was sent or
received. Claims submitted after the applicable filing deadline will not be reimbursed; the stated reason will be “filing deadline
has passed” or “services submitted past the filing date” unless one of the following exceptions applies.

Oxford Commercial supplement
299
2023 UnitedHealthcare Care Provider Administrative Guide
Exceptions:
• If you have an Oxford agreement containing specific filing deadlines, the agreement will govern.
• If COB caused a delay, you have 90 days from the date of the primary carrier explanation of benefits to submit the claim to us.
• If the member has a health benefit plan with a specific time frame regarding the submission of claims, the time frame in the
member’s certificate of coverage will govern. If a claim is submitted past the filing deadline due to an unusual occurrence
(e.g., health care provider illness, health care provider’s computer breakdown, fire, flood) and the health care provider has a
historic pattern of timely submissions of claims, the health care provider may request reconsideration of the claim.
Clean and unclean claims, required information for all claim submissions
For complete details and required fields for claims processing, refer back to Chapter 10: Our claims process.
Time frame for processing claims
The state-mandated time frames for processing claims for our fully insured members are as follows. The time frames are
applied based upon the site state of the member’s product:
• Connecticut ‒ 45 days (paper and electronic)
• New Jersey ‒ 40 days (paper), 30 days (electronic)
• New York ‒ 45 days (paper), 30 days (electronic)
We strive to process all complete claims within 30 days of receipt. If you have not received an explanation of benefits (EOB)/
remittance advice within 45 days, and have not received a notice from us about your claim, verify we received your claim.
Hospitals and ancillary facilities
A member must be enrolled and effective with us on the date the hospital and ancillary service(s) are rendered. Once the
facility verifies a member’s eligibility with us, (we maintain a system for verifying member status) that determination will be final
and binding on us, unless the member or group made a material misrepresentation to us or otherwise committed fraud in
connection with the eligibility or enrollment.
If an employer or group retroactively disenrolls the member up to 90 days following the date of service, we may deny or reverse
the claim. If there is a retroactive disenrollment for these reasons, the facility may bill and collect payment for those services
from the member or another payer. A member must be referred by a participating health care provider to a participating facility
within their benefit plan’s network. Network services require an electronic referral or prior authorization consistent with the
member’s benefits.
Requirements for claim submission with COB
Under COB, the primary benefit plan pays its normal plan benefits without regard to the existence of any other coverage. The
secondary benefit plan pays the difference between the allowable expense and the amount paid by the primary plan, if the
difference does not exceed the normal plan benefits that would have been payable had no other coverage existed.
If Oxford coverage is secondary to that of a commercial payer, bill the primary insurance company first. When you receive the
primary carrier’s explanation of benefits (EOB)/remittance advice, submit it to us along with the claim information.
We participate in Medicare Crossover for all our members who have Medicare as their primary benefit plan. This means
Medicare will automatically pass the remittance advice to us electronically after the claim has been processed. We may process
these claims as secondary without a claim form or remittance advice from your office.
Note: If Medicare is the secondary payer, you must continue to submit the claim to Medicare. We cannot crossover in reverse.
Determining the primary payer among commercial plans
When a member has more than 1 commercial health insurance policy, primary coverage is determined based upon model
regulations established by the National Association of Insurance Commissioners (NAIC).
1. COB provision rule: The benefit plan without a COB provision is primary.

Oxford Commercial supplement
300
2023 UnitedHealthcare Care Provider Administrative Guide
2. Dependent/non-dependent rule: The benefit plan covering the individual as an employee, member or subscriber or retiree
is primary over the benefit plan covering the individual as a dependent.
3. Birthday rule: The “birthday rule” applies to dependent children covered by parents who are not separated or divorced.
The coverage of the parent whose birthday falls first in the calendar year is the primary carrier for the dependent(s).
4. Custody/divorce decree rule: If the parents are divorced or separated, the terms of a court decree determines which
benefit plan is primary.
5. Active or inactive coverage rule: The benefit plan covering an individual as an employee (not laid off or retired), or as that
employee’s dependent, is primary over the benefit plan covering that same individual as a laid off or retired employee or as
that employee’s dependent.
6. Longer/shorter length of coverage rule: If the preceding rules do not determine the order of benefits, the benefit plan that
has covered the person for the longer period of time is primary.
Coordinating with Medicare benefit plans
We coordinate benefits for members who are Medicare beneficiaries according to federal Medicare program guidelines.
We have primary responsibility if any of the following apply to the member:
• 65 years or older, actively working and their coverage is sponsored by an employer with 20 or more employees
• Disabled, actively working and their coverage is sponsored by an employer with 100 or more employees
• Eligible for Medicare due to end-stage renal disease (ESRD) and services are within 30 months of the first date of dialysis
Reimbursement claim components
Additional copies of EOBs/remittance advice: Should you misplace a remittance advice, you may obtain a copy by logging in
to the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In.
Ancillary facility reimbursement: We reimburse ancillary health care providers for services provided to members at rates
established in the fee schedule or in attachment or schedule of the ancillary contract.
Fee schedules: Although our entire fee schedule is proprietary and may not be distributed, upon request, we provide
our current fees for the top codes you bill. Provider Services may provide this information to answer questions regarding
claims payment.
Global surgical package (GSP): A global period for surgical procedures GSP may be found in the Global Days policy at
uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans.
Hospital reimbursement: We reimburse hospitals for services provided to members at rates established in the attachment of
the hospital contract.
Modifiers: Modified procedures are subject to review for appropriateness consistent with the guidelines outlined in our
policies. For complete details regarding the reimbursement of recognized modifiers, refer to the Modifier Reference policy at
uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans.
PCP/Specialist reimbursement: All PCPs and specialists agree to accept our fee schedule and payment and processing
policies associated with administration of these fee schedules.
Release of information: Under the terms of HIPAA, we have the right to release to, or obtain information from, another
organization to perform certain transaction sets.
Requests for additional information: There are times when we request additional information to process a claim. Submit the
requested information promptly as outlined in the request. If you don’t submit it within 45 days, you must submit an appeal with
the information.
Reimbursement address, phone or TIN changes: An accurate billing address is necessary for all claims logging, payment
and mailings. Notify us of any changes. For instructions and forms on how to do so, go to uhcprovider.com > Our network >
Demographics and profiles.

Oxford Commercial supplement
301
2023 UnitedHealthcare Care Provider Administrative Guide
New York Health Care Reform Act of 1996 (HCRA)
The enactment of the HCRA, in part, created an indigent care (bad debt and charity care) pool to support uncompensated
care for individuals with no insurance or who lack the ability to pay. Therefore, the New York Bad Debt and Charity (NYBDC)
surcharge is applied on a claim-by-claim basis. The NYBDC surcharge applies to most services of general facilities and most
services of diagnostic and treatment centers in New York. Your obligation is to:
• Understand your eligibility as it relates to HCRA.
• Know what services have a surcharge and bill those services accordingly.
For additional information on HCRA, reference the New York Department of Health’s website: health.ny.gov > Laws &
Regulations (on the bottom of the page under General Information) > Health Care Reform Act.
Member billing
Balance billing policy
Health care providers in our Oxford network are contracted with us to provide specific services to Oxford members. Health
care providers participating with the Oxford network must follow the Oxford referral, precertification and privileging policies
and procedures. You may not bill members for unpaid charges related to covered services except for applicable copays, co-
insurance or permitted deductibles. This includes balance billing a member for a covered service denied by us because there
was no referral or authorization on file with us when one was required.
Exceptions: The instances in which you are authorized to balance bill a member, after first getting the member’s written
consent, are as follows. You are still required to follow the Oxford privileging, referral and/or precertification requirements. In
these instances, you may balance bill the member billed charges. To the extent that the terms and conditions of your contract
conflict with these guidelines, the terms and conditions of your contract prevail. You may balance bill a member when any of the
following apply:
• A service or item is not a covered benefit (i.e., the service is excluded in the “Exclusions and Limitations” section of the
member’s certificate of coverage).
• A benefit limit is exceeded/exhausted.
• We denied a request for precertification, before the service was rendered, and the member proceeded to receive the service
anyway.
• We denied a concurrent certification request (i.e., the member is currently receiving the service).
• If you do not participate in a member’s Oxford network, and a member self-refers to you (i.e., Oxford Liberty Network member
self-refers to you, and you do not participate in the Oxford Liberty Network). In this instance, if you participate in our W500
network, you may only bill up to your contracted rate for emergent services.
If you are uncertain whether a service is covered, you must make reasonable efforts to contact us and obtain coverage
determination before seeking payment from a member. You are prohibited from balance billing the member for covered
services when claims are denied for administrative reasons (lack of referral or authorization when one was required, etc.). If
a member has been inappropriately balance billed by a health care provider, the member has the right to file a complaint or
grievance, verbally or in writing, regarding the balance billing. Participating health care providers who repeatedly violate these
restrictions will be subject to discipline up to and including termination of their provider Agreement. If you inappropriately
balance bill a member, we will hold the member harmless and pursue the matter directly with you.
Member out-of-pocket costs
Out-of-pocket amounts for outpatient and inpatient care vary by group, type of health care provider and type of benefit plan.
Check the member’s health plan ID for the out-of-pocket cost specific to their benefit plan.

Oxford Commercial supplement
302
2023 UnitedHealthcare Care Provider Administrative Guide
Claims recovery, appeals, disputes and grievances
See Claim reconsideration and appeals process found in Chapter 10: Our claims process for general appeal requirements.
Claims submission and status
To submit a claim, or verify the status of a claim, use any method outlined in the How to Contact Oxford Commercial section in
this chapter.
Claims recovery
The following information applies to health care providers but does not apply to facilities or ancillaries.
We periodically ask our participating health care providers to return overpayments due to either:
• Administrative reasons: Duplicate payments, payments relating to fee schedules or billing/bundling issues, payments made
where Oxford coverage was not the primary coverage
• Behavioral issues: Upcoding, misrepresentation of service provided, services not rendered at all, frequent waiver of member
financial responsibility
We may pursue such claim overpayments as permitted by law and following the applicable statute of limitations (usually
6 years). We use random sampling, examination by external experts and reliable statistical methods to determine claim
overpayments in situations involving large volumes of potentially overpaid claims.
Note: Once a health care provider is given notice, we initiate discussions and take action during the following 1 year period.
We do not pursue collection of overpayments from individual participating health care providers when overpayments are
identified as isolated mistakes or where the health care provider is not at fault if the overpayments were more than 1 year before
the date of notice of the overpayment or use extrapolation. Examples include overpayments related to duplicate claims, fee
schedule issues, isolated situations of incorrect billing/unbundling and claims paid when Oxford coverage was not the primary
coverage.
Exception: We will pursue collection of overpayments beyond 1 year and use statistical methods and extrapolation in situations
where:
1. We have a reasonable suspicion of fraud or a sustained or high level of billing errors related to:
• Extensive or systemic upcoding.
• Unbundling.
• Misrepresentation of services or diagnosis.
• Services not rendered.
• Frequent waiver of member financial responsibility.
• Misrepresentation of health care provider rendering the services or licensure of such health care provider, and similar
issues.
2. A health care provider affirmatively requests additional payment on claims or issues older than 1 year.
3. CMS makes a retroactive change to enrollment or to primary versus secondary coverage of a Medicare benefit plan
member.
Participating health care provider claims reconsiderations and appeals
Our administrative procedures for members with an Oxford product require facilities, and health care providers participating in
our network, to file a claim reconsideration and/or appeal before proceeding to arbitration under their contract.
Claim reconsideration
See Claim reconsideration and appeals process found in Chapter 10: Our claims process for general reconsideration
requirements and submission steps. Continue for Oxford-specific requirements.
1. Pre-Appeal Claim Review
Before requesting an appeal determination, contact us, verbally or in writing, and request a review of the claim’s payment.

Oxford Commercial supplement
303
2023 UnitedHealthcare Care Provider Administrative Guide
We make every effort to clarify or explain our actions. If we determine that additional payment is justified, we reprocess the
claim and remit the additional payment.
2. Who May Submit a Reconsideration or Appeal
• Participating health care providers appealing a decision on their own behalf, according to the terms of their Agreement
with us.
• Any health care provider or practitioner when appealing on behalf of the member, with signed member consent. You must
follow the process for member administrative claims appeals. Refer to the Member Administrative Grievance & Appeal
(Non UM) Process & Time frames policy at uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare®
Oxford Clinical and Administrative Policies.
3. Time frame for Submitting a Reconsideration or Appeal
a. Claim Reconsideration and Appeal Process
If you disagree with the way a claim was processed, or need to submit corrected information, you must file your
reconsideration and/or appeal request of an administrative claim determination within 12 months (or as required by
law or your Agreement) from the date of the original EOB or PRA. You must include all relevant clinical documentation,
along with a Participating Provider Review Request Form.
The 2-step process described here allows for a total of 12 months for timely filing – not 12 months for step 1 and 12
months for step 2. If an appeal is submitted after the time frame has expired, we uphold the denial.
Exceptions: There are separate processes for New Jersey Participating Providers and Unilateral Coding Adjustments
for New York Hospitals. Refer to the New Jersey Participating Provider Appeal Process and Unilateral Coding
Adjustments for New York Hospitals sections for additional information.
i. Step 1 – Reconsideration Level: Submit the reconsideration using the UnitedHealthcare Provider Portal Claims
tool: uhcprovider.com/claims > Sign In and then select Claims & Payments. If after reconsideration we do not
overturn our decision, the EOB or response letter includes next-level rights and where to submit a request for
further review.
ii. Step 2 – Appeal Level: Participating health care provider and practitioner appeals must be submitted in writing
within the same 12-month time frame. The appeal must include all relevant documentation, including a letter
requesting a formal appeal and a Participating Provider Review Request Form. If the appeal does not result in an
overturned decision, the health care provider must review their contract for further dispute resolution steps.
b. New Jersey Participating Provider Appeal Process
New Jersey (NJ) participating health care providers are subject to the NJ state-regulated appeal process. If a NJ
participating health care provider has a dispute relating to payment of a claim involving a NJ commercial member, the
dispute is eligible for an individual 2-step process.
i. First Level: The first-level appeal is made through the Oxford internal appeal process. A written request for appeal
must be submitted by the Health Care Provider Application to Appeal a Claims Determination Form created by the
NJ Department of Banking and Insurance. This appeal must be submitted within 90 days of the date on our initial
determination notice to:
UnitedHealthcare
Attn: Oxford Provider Appeals
P.O. Box 31387
Salt Lake City, UT 84131
We conduct the review and communicate the results to the health care provider in a written decision within 30
calendar days of receipt of all material necessary for such appeal.
ii. Second Level: The second-level appeal must be made through the external dispute resolution process. If a NJ
participating health care provider completed the internal appeal process and is not satisfied with the results of that
internal appeal, the health care provider has the right under their Oxford contract to arbitrate the dispute with us.
Health care providers should submit their request to:
MAXIMUS, Inc.
Attn: New Jersey PICPA
50 Square Drive, Suite 210
Victor, NY 14564
Requests may be submitted by fax to 1-585-425-5296. (MAXIMUS, Inc. requests that faxes be limited to 25 pages.)

Oxford Commercial supplement
304
2023 UnitedHealthcare Care Provider Administrative Guide
Consult your contract to determine the appropriate arbitration authority. Most such contracts provide for arbitration
before the American Arbitration Association (AAA). The costs of arbitration are borne equally by the participating
health care provider and us, unless the arbitrator determines otherwise. The decision in such arbitration depends
on the participating health care provider and us, pursuant to the terms of the Agreement. To commence arbitration,
the health care provider must file a statement of claim with the AAA.
c. Unilateral Coding Adjustments for New York Hospitals
If a New York hospital receives an Oxford remittance advice/payment indicating that we have adjusted payment based
on a particular coding (i.e., assignment of diagnosis and or CPT/HCPCS or other procedure code), the hospital has the
right to resubmit the claim, along with the related medical record supporting the initial coding of the claim, within 30
days of receipt/notification of payment. We must review the medical records within the normal review time frames (45
days). If our initial determination:
• Remains unchanged, the insurer’s decision must be accompanied by a statement providing the specific reasons why
the initial adjustment was appropriate.
• Changes, and the payment is increased based on the information submitted by the hospital, we must provide the
additional reimbursement within the 45-day review time frame.
If we fail to provide the additional reimbursement within the 45-day review time frame, we must pay to the hospital
interest on the amount of the increase. The interest must be computed from the end of the 45-day period after
resubmission of the additional medical record information.
Note: Neither the initial or subsequent processing of the claim by us may be considered an adverse determination if it
is based solely on a coding determination.
4. Method for Submitting a Reconsideration or Appeal
Find the correct mailing address on the Oxford Participating Provider Claim(s) Review Request Form. There are separate
processes for the following appeal types:
• Internal and external claims payment appeals for NJ participating health care providers who treat NJ commercial
members.
• The appeal of unilateral coding adjustments made to New York hospital claims.
5. Appeal Decision and Resolution
Full documentation of the substance of the appeal and the actions taken will be maintained in an appeal file (paper or
electronic). Written notification to the health care provider is issued by means of a letter or updated Remittance Advice (RA)
statement at the time of determination of the appeal. This decision constitutes our final internal decision. If the health care
provider is not satisfied with our decision, they may arbitrate the issue as set forth in their Oxford contract. Refer to the Time
frame Standards for Benefit Administrative Initial Decisions policy at uhcprovider.com/policies > For Commercial Plans >
UnitedHealthcare® Oxford Clinical and Administrative Policies.
6. Arbitration
If the health care provider wants to file for arbitration after the first-level appeal has been completed, the health care
provider must follow the terms of their participation agreement and file a statement of claim with the AAA at the following
address:
American Arbitration Association
Northeast Case Management Center
950 Warren Avenue 4th Floor
East Providence, RI 02914
Phone: 1-800-293-4053
Health care providers located outside of New York, New Jersey and Connecticut should refer to the AAA website at adr.
org for submission guidelines.
• Participating health care providers appealing an adverse determination are entitled under their health care provider
contract to bring the issue before the AAA consistent with the terms of their provider agreement. They have this right
only under the following circumstances:
– The first-level internal grievance process has been completed.
– The appeal is on their own behalf (not on behalf of the member).
Oxford Commercial supplement
305
2023 UnitedHealthcare Care Provider Administrative Guide
• Participating hospitals and ancillary facilities also have arbitration rights, but those rights vary depending on contracts.
If a hospital or ancillary facility calls to inquire about arbitration rights, they should be referred to their contract for the
specific arbitration entity. Hospitals and ancillary facilities still must use the first-level internal appeal process.
New York state-regulated process for external review
For participating health care providers and other health care professionals treating New York members, this external appeals
process applies only to services provided to commercial members who have coverage by virtue of an insurance benefit plan
licensed in the state of New York.
This appeals process does not apply to the self-funded line of business. Health care providers may use this process to appeal
concurrent and retrospective utilization review decisions. Other external appeals require written consent from the member.
In connection with retrospective decisions, if the health care provider’s Agreement includes arbitration language or alternate
dispute language, the health care provider must follow that process. The external review process is no longer an option for
dispute resolution.
Medical necessity appeals
Standard medical necessity appeals process
If members or their designees would like to file an appeal, they must hand-deliver or mail a written request within 180 days of
receiving the initial denial determination notice to:
Oxford Clinical Appeals Department
P.O. Box 31388
Salt Lake City, UT 84131
Expedited medical necessity appeals process for members
• Members have the right to request an expedited appeal.
• To request an expedited appeal, the member or health care provider or other health care professional must state specifically
that the request is for an expedited appeal.
• The Clinical Appeals department determines whether or not to grant an expedited request.
• If the Clinical Appeals department determines the request does not meet expedited criteria set by the Clinical Appeals
department, the member is notified.
Benefit Appeals
Appeals of benefit denials issued by the Clinical Services and Disease Management departments are handled by the Clinical
Appeals department.
Administrative appeals (grievances)
Administrative appeals without the Clinical Services department’s involvement are handled by the Member Appeals unit. If a
member would like to file an appeal on a claim determination, they must mail all administrative appeals to the Grievance Review
Board. See How to Contact Oxford Commercial section for address information.
Second-level member appeals
Members have the right to take a second-level appeal* to our Grievance Review Board (GRB). If they remain dissatisfied with
the first-level appeal determination, they may request a second-level appeal. Members with a Connecticut line of business do
not have the option of submitting a second-level appeal request for a benefit or administrative issue. The request for appeal and
any additional information must be submitted to the our GRB. See How to Contact Oxford Commercial section for address
information.
* In New York, a second-level appeal is not required by us to be eligible for an external appeal.
Oxford Commercial supplement
306
2023 UnitedHealthcare Care Provider Administrative Guide
External appeal process for members
New York, New Jersey and Connecticut members have the right to appeal a medical necessity determination to an external
review agent. They may file a consumer complaint with one of the following applicable regulatory bodies. The applicable
regulatory body is determined by the state in which the member’s certificate of coverage was issued, not where the
member resides.
Connecticut State of Connecticut Insurance Department
153 Market Street
P.O. Box 816
Hartford, CT 06142-0816
1-860-297-3800
New Jersey Division of Insurance Enforcement and Consumer Protection
20 West State Street
P.O. Box 329
Trenton, NJ 08625-0329
Consumer Protection Services Dept. of Banking and Insurance
P.O. Box 329
Trenton, NJ 08625-0329
1-800-446-7467 (in NJ)
1-609-292-7272
Fax: 1-609-545-8468
New York Consumer Services Bureau
State of New York Insurance Department
25 Beaver Street
New York, NY 10004-2349
1-212-480-6400
Office of Managed Care Certification and Surveillance
New York Department of Health
Corning Tower, Room 1911
Empire State Plaza
Albany, NY 12237
1-518-474-2121
New York notice of health care provider contract termination and appeal rights
We immediately remove any health care provider from the Oxford network who is unable to provide health care services due to
a final disciplinary action.
We may not prohibit, terminate or refuse to renew a contract with a health care provider solely for the following:
• Advocating on behalf of a member
• Filing a complaint against us
• Appealing a decision made by us
• Providing information or filing a report per PHL4406-c regarding prohibitions
• Requesting a hearing or review
We grant health care providers and certain health care professionals the right to appeal certain disciplinary actions imposed by
us.
The appeals process is structured so most appeals for terminations, not including non-renewal of the health care provider’s
contract with us, may be heard before disciplinary action is implemented.

Oxford Commercial supplement
307
2023 UnitedHealthcare Care Provider Administrative Guide
A health care provider or health care professional may request an appeal (fair hearing or review) after we take adverse action to
restrict, suspend or terminate a health care provider or health care professional’s ability to provide health care services to our
members for reasons relating to the professional competence or conduct that adversely affects or could adversely affect the
member’s health or welfare.
A notice is provided within 30 calendar days after the adverse action is taken. It includes the following:
1. We determined an adverse action is necessary, and the final action will be reported to the National Practitioner Data Bank
and appropriate state licensing board.
2. A description of and reason for the action.
3. Right to request an appeal in writing within 30 calendar days after receipt of the notice. Failure to file such request shall
constitute a waiver of all rights to the appeal process, unless such a right is provided under state law.
4. A summary of the health care provider’s or health care professional’s appeal rights provided.
We will notify the health care provider or health care professional of the fair hearing or review date within 30 calendar days of
our receipt of request for appeal, or within the time frame required by state law. The fair hearing or review takes place within 60
calendar days of the date we receive the request for appeal, or within the time frame required by state law.
The hearing panel will be composed of at least 3 persons appointed by UnitedHealthcare. At least 1 person on the panel will
have the same discipline or same specialty as the health care provider under review. The panel may consist of more than 3
members, provided the number of clinical peers constitutes one-third or more of the total panel membership.
The hearing panel will render a decision in a timely manner. Decisions will be provided in writing and include one of
the following:
1. Reinstatement
2. Provisional reinstatement with conditions set forth by us
3. Termination
Quality assurance
Medical records requirements
As a participating health care provider or other health care professional, you must provide us with copies of medical records
for our members within a reasonable time period following our request for the records. We may request records for various
reasons, including an audit of your practice. An audit may be performed at our discretion and for several different purposes as
we deem appropriate for our business needs.
Standards for Medical Records
A comprehensive, detailed medical record is vital to promoting high-quality medical care and improving patient safety. Our
requirements include, but are not limited to:
• Separate medical record for each member.
• The record verifies the PCP is coordinating and managing care.
• Medical record retention period of 6 years after date of service rendered and for a minor, 3 years after majority or 6 years after
the date of the service, whichever is later.
• Prenatal care only: A centralized medical record for the provision of prenatal care and all other services.
Transferring Member Medical Records
If you receive a request from a member to transfer their medical records, do so within 7 days to help ensure continuity of care.
To safeguard the privacy of the member’s records, mark them as “Confidential.” Be sure no part of the record is visible during
transmission.
Oxford Commercial supplement
308
2023 UnitedHealthcare Care Provider Administrative Guide
Electronic medical records
An electronic medical record (EMR) is any type of electronic concurrent medical information management system. This process
improves efficiency and quality inpatient care through integrated decision support that provides better information storage,
retrieval and data sharing capabilities. EMR systems allow health care providers, nurses and other health care staff to access
and share information smoothly and quickly, enable them to work more efficiently and make better-quality decisions.
Oxford credentialing and re-credentialing notifications
We follow New York and New Jersey requirements regarding notification of when we receive a credentialing application and
when credentialing has been completed. For more information, refer to our Credentialing Plan and the State and Federal
Addendum at uhcprovider.com > Resources > Resource library > Join our Network > Get Credentialed.
Healthcare provider performance evaluations
We are required to provide health care professionals with any information and profiling data used to evaluate your performance.
Periodically, and at your request, we provide the information, profiling data and analysis used to evaluate your performance. You
are given the opportunity to discuss the unique nature of your patient population, which may have bearing on your profile, and
we work with you to improve your performance as needed.
Healthcare effectiveness data and information set measures
The annual Healthcare Effectiveness Data and Information Set (HEDIS) was developed by the National Committee for Quality
Assurance (NCQA). NCQA is an independent group established to provide objective measurements of the performance of
managed health care benefit plans, including access to care, use of medical services, effectiveness of care, preventive services,
and immunization rates, and each benefit plan’s financial status.
CMS, state regulators (commercial) and prospective members use HEDIS measures to evaluate the value and quality of
different health plans.
Each year we collect data from a randomly selected sample of our members’ medical records for HEDIS. HEDIS is mandated by
the New York Department of Health, New Jersey Department of Health and Senior Services, Connecticut Department of Health
and CMS. The HEDIS medical record study measures our participating health care providers’ adherence to nationally accepted
clinical practice guidelines.
Case management and disease management programs
We created a number of programs designed to improve outcomes for our members and to allow us to better manage the use of
medical services. You may refer members to these programs, or members may self-refer.
For more information, go to uhcprovider.com/news > 10/2020: Case and Disease Management Programs or call Member
Services at 1-877-842-3210. You can also visit myuhc.com.
Case management and disease management programs referrals
You may refer members, or members may self-refer to several Case Management and Disease Management programs. These
programs are designed to improve outcomes for members and to help us better manage the use of medical services.
Clinical process definitions
Some services may be subject to prior authorization and/or ongoing medical necessity reviews.
Acute Hospital Day (AHD)
An AHD is any day when the severity of illness (clinical instability) and/or the intensity of service are sufficiently high, and care
may not reasonably be provided safely in another setting.

Oxford Commercial supplement
309
2023 UnitedHealthcare Care Provider Administrative Guide
Alternative Level of Care (ALC)*
We determine that an inpatient ALC applies in any of the following scenarios:
• An acute clinical situation has stabilized.
• The intensity of services required may be provided at less than an acute level of care.
• An identified skilled nursing and/or skilled rehabilitative service is medically indicated.
• ALC is prescribed by the member’s health care provider or other health care professional.
• Inpatient ALC must meet both the following criteria:**
– The skills of qualified technical or professional health personnel such as registered nurses, licensed practical (vocational)
nurses, physical therapists, occupational therapists and speech pathologists or audiologists are required.
– Such services must be provided directly by or under the general supervision of those skilled nursing or skilled rehabilitation
personnel to assure the safety of the patient and achieve the medically desired result.
New technology
New technology refers to a service, product, device or drug that is new to our service area or region. Any new technology
must be reviewed and approved for coverage by the Medical Technology Assessment Committee or the Clinical Technology
Assessment Committee for Behavioral Health technologies.
Potentially Avoidable Days (PAD)
A PAD arises in the course of an inpatient stay when, for reasons not related to medical necessity, a delay in rendering a
necessary service results in prolonging the hospital stay. PADs must be followed by a medically necessary service.
There are several types of PADs:
• Approved potentially avoidable day (AOPAD): We caused delay in service; the day will be payable.
• Approved health care provider or other health care professional potentially avoidable day (APPAD): The health care
provider or other health care professional caused delay in service; the day will be payable.
• Approved mixed potentially avoidable day (AMPAD): A delay due to mixed causes not solely attributable to us, the health
care provider, other health care professional or the hospital; the day is payable.
• Denied hospital potentially avoidable day (DHPAD): The hospital caused the delay in service; DHPAD is a non-certification
code, and the day is not payable.
We will not reverse any certified day unless the decision to certify was based on erroneous information supplied by the health
care provider or other health care professional, or a potentially avoidable day was identified.
When a member is readmitted to the hospital for the same clinical condition or diagnosis within 30 days of discharge, the
second hospital admission will not be reimbursed when any of the following conditions apply:
• The member was admitted for surgery, but surgery was canceled due to an operating room scheduling problem.
• A particular surgical team was not available during the first admission.
• There was a delay in obtaining a specific piece of equipment.
• A pregnant woman was readmitted within 24 hours and delivered.
• The member was admitted for elective treatment for a particular condition, but the treatment for that condition was not
provided during the admission because another condition that could have been detected and corrected on an outpatient
basis prior to the admission made the treatment medically inappropriate.
In any of these situations, the hospital may not bill the member for any portion of the covered services not paid for by us.
Diagnosis-Related Group (DRG) hospitals
DRG is a statistical system of classifying an inpatient stay into groups of specific procedures or treatments. When a hospital
contracts for a full DRG, we reimburse the hospital a specific amount (determined by the contract) based on the billed DRG
rather than paying a per diem or daily rate (DRG facility). A DRG is determined after the member has been discharged from
the hospital.
* ALC only applies if the facility has a contracted rate.
** Inpatient ALC must meet clinical criteria per clinical guidelines. Failure to satisfy these criteria may result in denial of coverage.

Oxford Commercial supplement
310
2023 UnitedHealthcare Care Provider Administrative Guide
When admission information is received through our website, we consider this to be notification only. First-day approval is
granted to hospitals with a DRG contract. When we receive notification of an admission to a hospital with a DRG contract, our
case manager reviews the admission for appropriateness. If the case manager cannot make a determination based on the
admitting diagnosis, the case manager requests an initial review to determine whether the admission is medically necessary.
The hospital is required to provide admission notification.
Prepayment DRG validation program
We may request a DRG hospital to send the inpatient medical record before claim payment so we may validate the submitted
codes. After review of all available medical information, the claim is paid based on substantiated codes following review of the
medical record. See the Claims Recovery, Appeals, Disputes and Grievances section of this supplement for Appeal Rights.
We may request hospital records to validate ICD-10-CM (or its successor codes) and/or revenue codes billed by participating
facilities for inpatient hospital claims. If the billed ICD-10-CM codes (or successor codes) or revenue codes are not
substantiated, we only pay the claim with the validated codes.
Disposition determination
A disposition determination is a technical term describing a process of care determination that results in payment as agreed at
specific contracted rates. It helps eliminate certain areas of contention among participating parties and allows processing of
claims. Specific instances where a disposition determination may apply:
• Delay in hospital stay
• APPAD/AMPAD when so contracted
• ALC determinations when so contracted, unless there is a separate ALC rate
• Discharge delays that prolong the hospital stay under a case rate
Late and no notification
Late notification is defined as notification of a hospital admission after the contracted 48-hour notification period and before
discharge. No notification is defined as failure to notify us of a member’s admission to a hospital after discharge, up to and
including at the time of submitting the claim.
Mental health and substance use services
The behavioral health department specializes in the administration of mental health and substance use benefits. The
department consists of a medical director who is licensed in psychiatry, facility care advocates (licensed RNs and licensed/
certified social workers) and intake staff who collectively handle certification, referrals and case management for our members.
We encourage coordination of care between our participating behavioral health clinicians and PCPs as the best way to achieve
effective and appropriate treatment. For this purpose, we developed a Release of Information (ROI) Form to help facilitate
member consent and share information with the PCP in the presence of their behavioral health clinician. See the How to
Contact Oxford Commercial section for telephone numbers.
Clinical definitions and guidelines
The behavioral health department uses the Optum Clinical Criteria when determining the medical necessity of inpatient
psychiatric, partial hospitalization substance use treatment and rehabilitation, and outpatient mental health treatment. For a
complete list of programs and detailed information on clinical criteria, visit the Optum network website at providerexpress.com.
Inpatient mental health
Inpatient (or acute) care for a mental health condition is indicated when it involves a sudden and quickly developing clinical
situation characterized by a high level of distress and uncertainty of outcome without intervention.
Partial hospitalization - mental health
Partial hospitalization for mental health treatment involves day treatment of a mental health condition at a hospital or ancillary
facility with the following criteria:
• The primary diagnosis is psychiatric.
Oxford Commercial supplement
311
2023 UnitedHealthcare Care Provider Administrative Guide
• The facility is licensed and accredited to provide such services.
• The duration of each treatment is 4 or more hours per day.
Residential treatment
Residential treatment services are provided in a facility or a freestanding residential treatment center that provides overnight
mental health services for members who do not require acute inpatient care but require 24-hour structure.
Outpatient mental health
Psychotherapeutic approaches to treatment of mental health conditions, including methods from different theoretical
orientations (e.g., behavioral, cognitive and interpersonal) may be administered to an individual, family or group on an outpatient
basis.
Inpatient detoxification
Inpatient detoxification is the treatment of substance dependence to treat a life-threatening withdrawal syndrome, provided on
an inpatient basis.
Outpatient substance use rehabilitation
Outpatient substance use rehabilitation is the treatment of a substance use disorder including dependence at an accredited,
licensed substance use treatment facility.
Member rights and responsibilities
For the entire list of Member Rights and Responsibilities, go to uhc.com > Legal > Annual Member Notices > Select Your Code.
Medical/clinical and administrative policy updates
We amend the contents of this supplement annually to reflect changes in policies or as required by regulation. A complete
library of the Oxford Clinical and Administrative Policies is available for your reference at uhcprovider.com/policies > For
Commercial Plans > UnitedHealthcare® Oxford Clinical and Administrative Policies.
You may also request a paper copy of a Clinical or Administrative Policy by writing to:
Oxford Policy Requests and Information
4 Research Drive
Shelton, CT 06484
Policy update bulletin
We publish monthly editions of the Oxford Policy Update Bulletin. This online resource provides notice to our network providers
of changes to our Clinical and Administrative Policies. The bulletin is posted on the first calendar day of every month on
uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare® Oxford Clinical and Administrative Policies > Policy
Update Bulletins. A supplemental link to the policy updates announced in the Oxford Policy Update Bulletin is posted monthly
at uhcprovider.com/news.
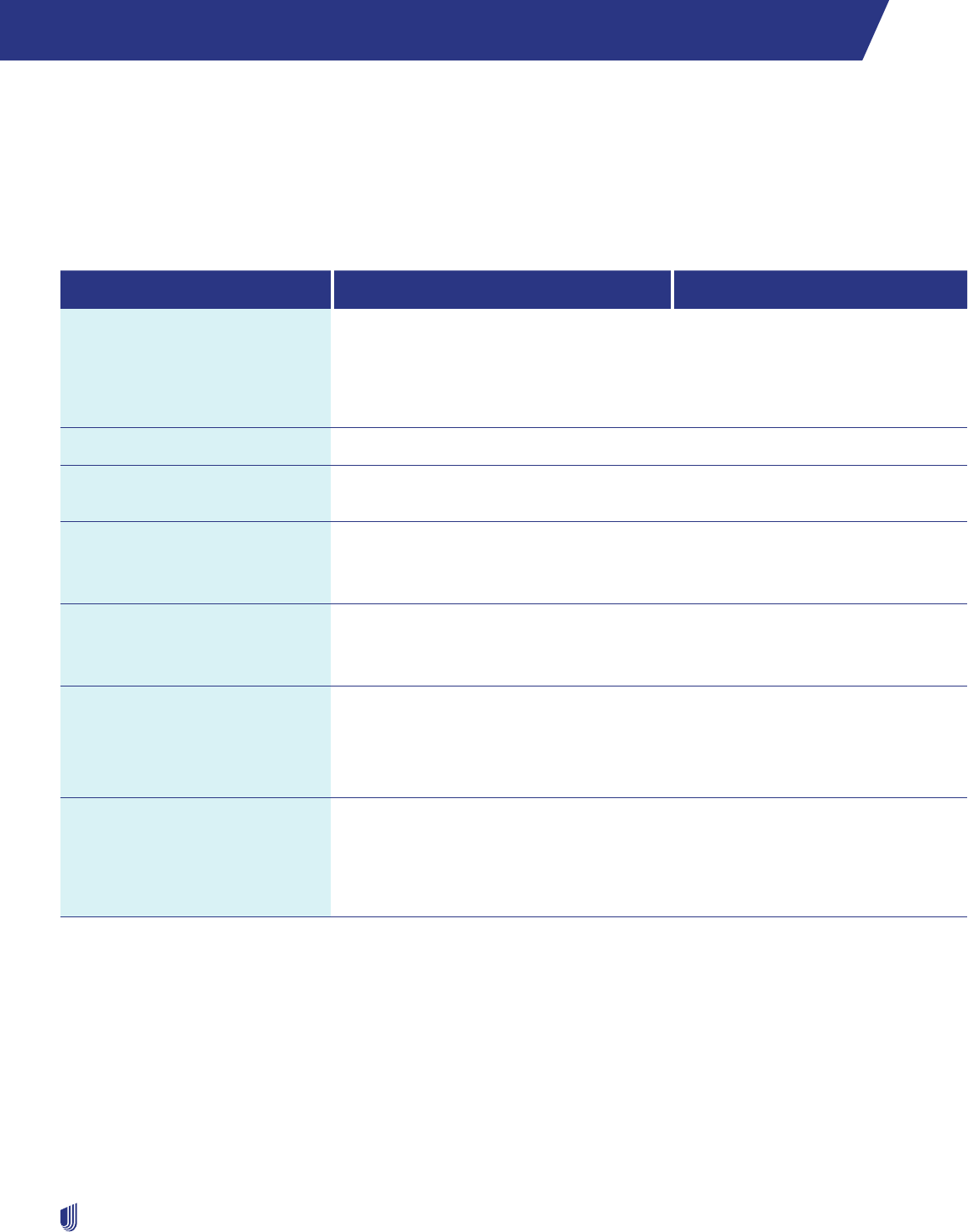
312
2023 UnitedHealthcare Care Provider Administrative Guide
Oxford Level Funded plans (CT, NJ and NY)
Applicability of this supplement
This supplement applies to all covered services you provide to your patients who have a Connecticut or New Jersey Oxford
Level Funded plan.
Oxford Level Funded product contacts
Resource Where to go Requirements/Notes
Cardiology
Diagnostic catheterization,
electrophysiology implants,
echocardiogram and stress
echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/cardiology
Phone: 1-877-773-2884
(Monday–Friday, 7 a.m.–7 p.m. ET)
Request prior authorization for
services as described in the
Outpatient Cardiology Notification/
Prior Authorization Protocol section
of Chapter 7: Medical management.
Claims submission Payer ID: 87726
Genetic and molecular testing Online: uhcprovider.com/priorauth and
select the specialty you need.
Outpatient injectable
chemotherapy and related
cancer therapies
Online: uhcprovider.com/priorauth >
Oncology
Phone: 1-888-397-8129
Polices and instructions
Pharmacy services Prior Authorization: 1-800-711-4555
Benefit Information: Call the number on the
back of the member’s ID card.
For information on the Prescription
Drug List, visit myallsaversconnect.
com.
Prior Authorization and
Notification
Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth
Phone: 1-800-999-3404
Prior authorization and admission
notification is required as described
in Chapter 7: Medical management.
EDI 278A transactions are not
available.
Radiology/Advanced Outpatient
Imaging Procedures
CT scans, MRIs, MRAs, PET scans
and nuclear medicine studies,
including nuclear cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/radiology
Phone: 1-877-773-2884
(Monday–Friday, 7 a.m.–7 p.m. ET)
Request prior authorization for
services as described in the
Outpatient Radiology Notification/
Prior Authorization Protocol section
of Chapter 7: Medical management.
Our claims process
Follow these steps for fast payment:
1. Notify Oxford Level Funded claims.
2. Prepare a complete and accurate claim form.
3. For Oxford Level Funded plan participants, submit electronic claims using payer ID number 87726.

Oxford Level Funded plans (CT, NJ and NY)
313
2023 UnitedHealthcare Care Provider Administrative Guide
Claim reimbursement (adjustments)
If you think your claim was processed incorrectly, call the number on the plan participant’s health plan ID card. If you find a
claim where you were overpaid, send us the overpayment within 30 calendar days. If we find a claim was overpaid, payment is
due within 30 calendar days.
If you disagree with our decision regarding a claim adjustment, you may appeal.
Claim reconsideration, appeals and disputes
Claim reconsideration does not apply to some states based on applicable state legislation (e.g., Arizona, California, Colorado,
New Jersey or Texas). For states with applicable legislation, any request for dispute will follow the state specific process.
There is a 2-step process available for review of your concern. Step 1 is a claim reconsideration. If you disagree with the
outcome of the claim reconsideration, you may request a claim appeal (step 2).
How to submit your reconsideration or appeal
Claims payment issues or outcome of a reconsideration review
If you disagree with claim payment issues or the outcome of your reconsideration review, submit your request using our
electronic tools:
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In.
API: Submit reconsiderations and appeals (with attachments) using API. Go to uhcprovider.com/api for more information.
Overpayment recoveries, pharmacy, medical management disputes or contractual issues
If you disagree with overpayment recoveries, pharmacy, medical management disputes or contractual issues, send a letter
requesting a review to:
Oxford Level Funded plan (CT, NJ and NY) members:
Grievance Administrator
P.O. Box 31393
Salt Lake City, UT 84131-0371
Fax: 1-801-994-1416
Time frame
You must submit your claim reconsideration and/or appeal to us within 12 months (or as required by law or your Agreement),
from the date of the original EOB or denial. The 2-step process allows for a total of 12 months for timely submission, not 12
months for step 1 and 12 months for step 2.
What to submit
As the health care provider of service, you submit the dispute with the following information:
• Plan participant’s name and health plan ID number
• Claim number
• Specific item in dispute
• Clear rationale/reason for contesting the determination and an explanation why the claim should be paid or approved. If you
disagree with the outcome of the claim appeal, you may file for an arbitration proceeding. A description of this process is in
your Agreement.
Refer to Claim Reconsideration and Appeals Process section in Chapter 10: Our claims process, for more information.
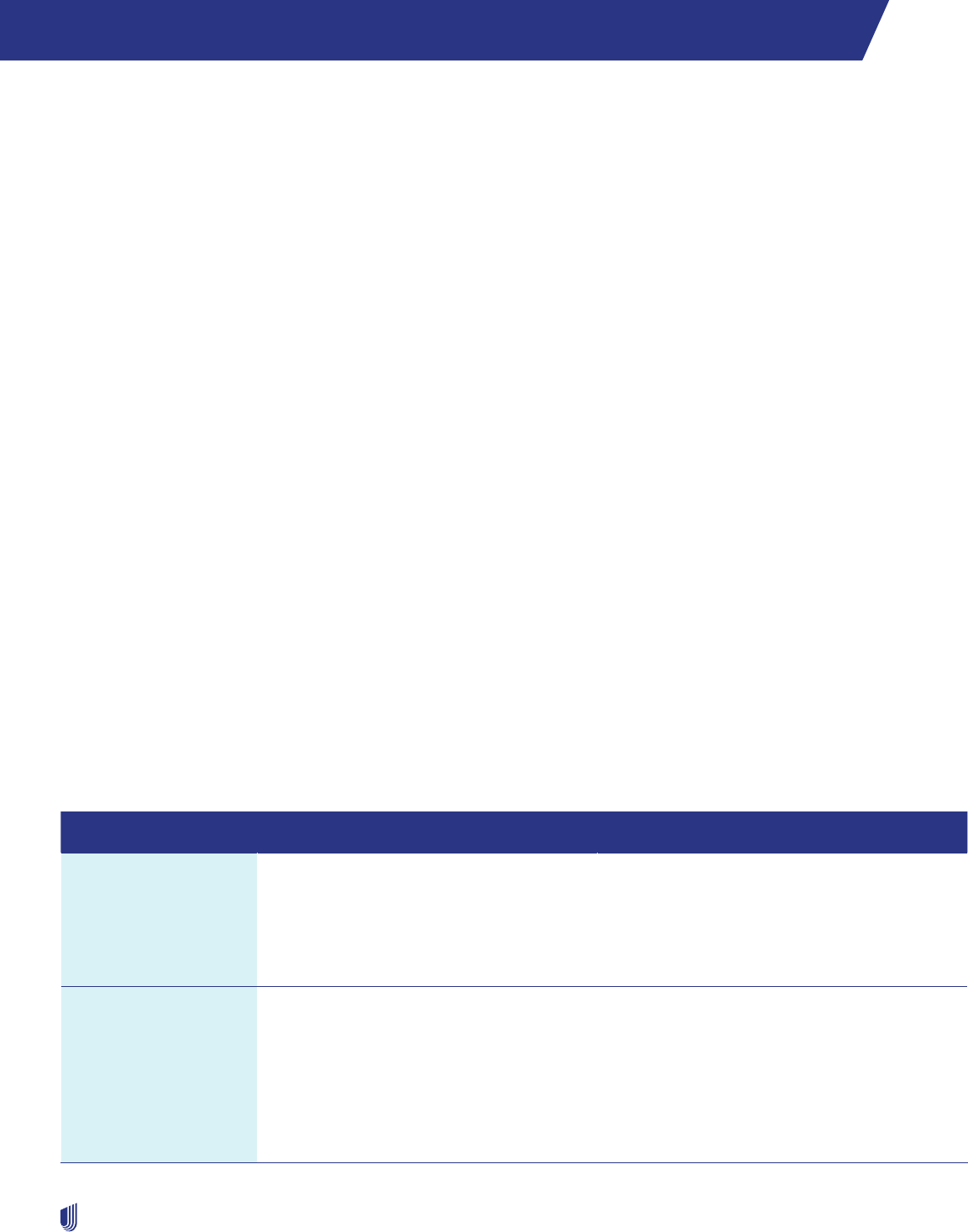
314
2023 UnitedHealthcare Care Provider Administrative Guide
Preferred Care Network supplement
About Preferred Care Network
Preferred Care Network, a wholly-owned subsidiary of UnitedHealthcare, is a Medicare Advantage (MA) health plan. We offer
MA plans in 2 Florida counties: Broward and Miami-Dade.
Preferred Care Network participating health care providers are subject to both the main guide and this supplement. This
supplement controls if it conflicts with information in the main guide. For protocols, policies and procedures not referenced in
this supplement, refer to the appropriate chapter in the main guide.
Mission statement
We work to improve the health of our members by providing:
• Access to health care services.
• Choices for their health care needs.
• Simplification of the health care delivery system.
We streamline authorization and referral processes. We build health care provider networks around the needs of our members.
This provides the best experience for our members and health care providers. We commit to give direct access to expert
customer service representatives who understand member needs and may help them make informed choices.
How to contact us
Questions or comments
Questions or comments about this Guide should be emailed to Network Management Services (NMS) at
pcp-NetworkManagementServices@uhcsouthflorida.com, or submitted by mail to:
Preferred Care Network
Network Management Services
9100 South Dadeland Blvd.
Suite 1250
Miami, FL 33156-6420
Resources Where to Go What you can do there
Authorizations and
Notifications
EDI: Transactions 278 and 278N
Online: uhcprovider.com/paan
Phone: 1-866-273-9444
8 a.m.–8 p.m. local time,
7 days a week
• Initiate requests for notifications and
authorizations electronically
• Submit notifications, prior authorizations,
referrals, admissions and discharge planning
• Submit after-hours or weekend emergencies,
notifications or hospital admissions
Authorizations and
Notifications (WellMed)
Online: eprg.wellmed.net
Outpatient Notifications
Phone:
1-877-299-7213
Inpatient Notifications
Phone:
1-877-490-8982
Fax:
1-877-757-8885
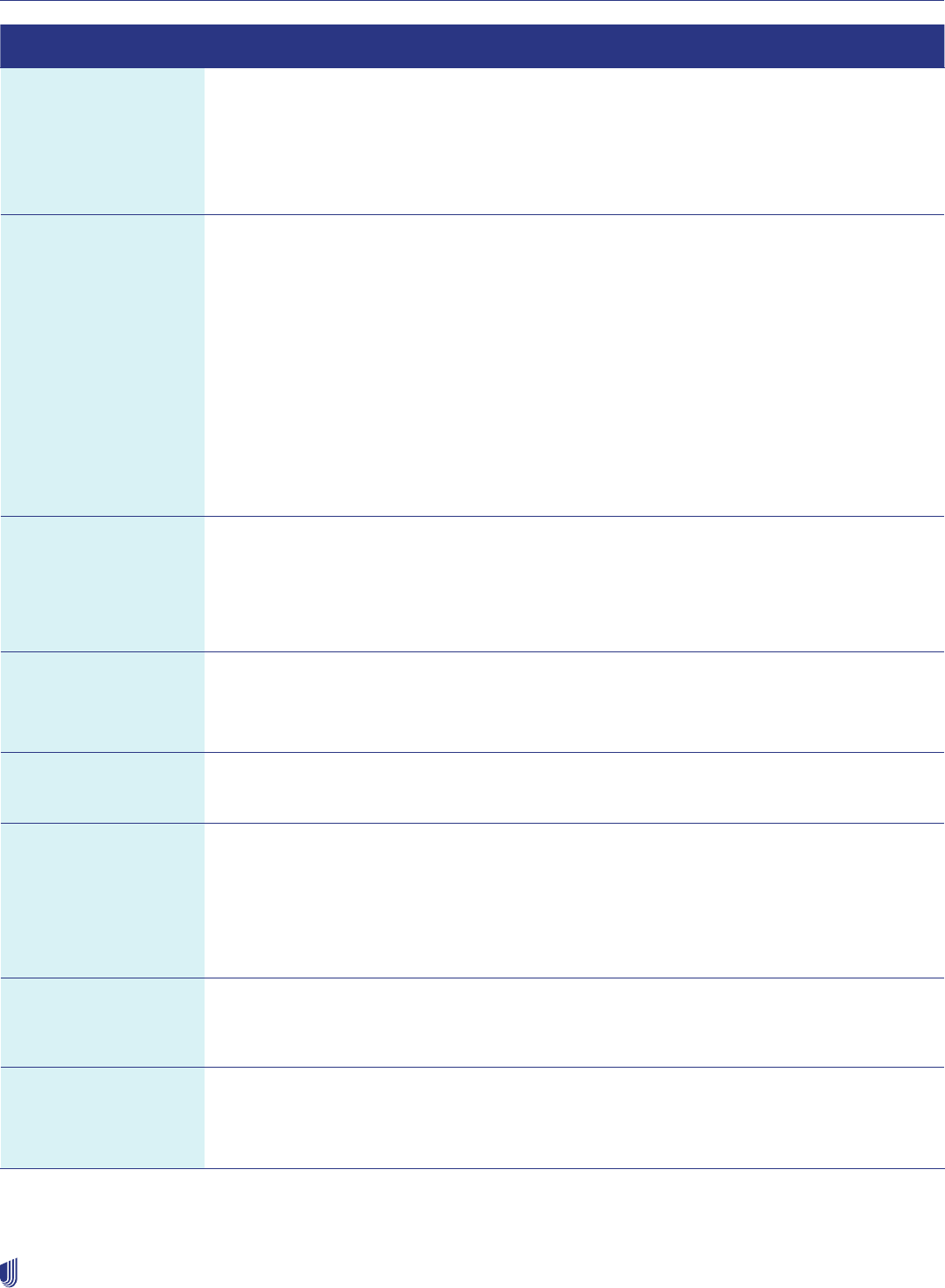
Preferred Care Network supplement
315
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to Go What you can do there
Eligibility and Benefits
Verification
Online: UnitedHealthcare Provider Portal at
uhcprovider.com/eligibility > Sign In. Then
select Eligibility from the menu.
Phone: 1-800-348-5548
8 a.m.–8 p.m. local time,
7 days a week
• Verify eligibility and benefits of
enrolled members
Claims Online: UnitedHealthcare Provider Portal
at uhcprovider.com/claims > Sign In. Then
select Claims & Payments from the menu.
Information: uhcprovider.com/claims
Phone: 1-800-348-5548
8 a.m.–8 p.m. local time,
7 days a week
Fax: 1-866-725-9337
Mail (Delegated providers only):
Preferred Care Network
P.O. Box 30448
Salt Lake City, UT 84130-0448
• Submit or review claims, encounters, inquiries,
status or review requests
• Check claims, eligibility and benefits
Claims (WellMed) Online: eprg.wellmed.net
Phone: 1-800-550-7691
Mail: WellMed Claims
P.O. Box 30508
Salt Lake City, UT 84130-0508
• Use payer ID WELM2
Technical Support for
Change Healthcare
Claims Submission
Network
Phone: 1-800-845-6592 • Obtain assistance with password or technical
support issues
Audit and Recovery Phone: 1-877-842-3210
Online: connect.werally.com
• Ask questions related to overpayments
Chiropractic, Physical
Therapy, Occupational
Therapy and Speech
Therapy Providers
Phone: 1-877-670-8432
Monday–Friday, 9 a.m.–5 p.m.
Fax: 1-888-659-0619
Email: pcp-
NetworkManagementServices@
uhcsouthflorida.com
• Access list of participating Physical Therapist
providers in our directory
Credentialing Phone: 1-800-963-6495
Monday–Friday, 9 a.m.–5 p.m.
Fax: 1-844-897-6352
• Update or complete credentialing, re-
credentialing, document changes, or recent
hires or terminations in your practice or facility
DME and Infusion
(MedCare)
Phone: 1-800-819-0751
Monday–Friday, 9 a.m.–5 p.m.
On call: 24 hours a day, 7 days a week
• Register for these services
• On call 24 hours a day
• You may also call Utilization Management or
Network Management
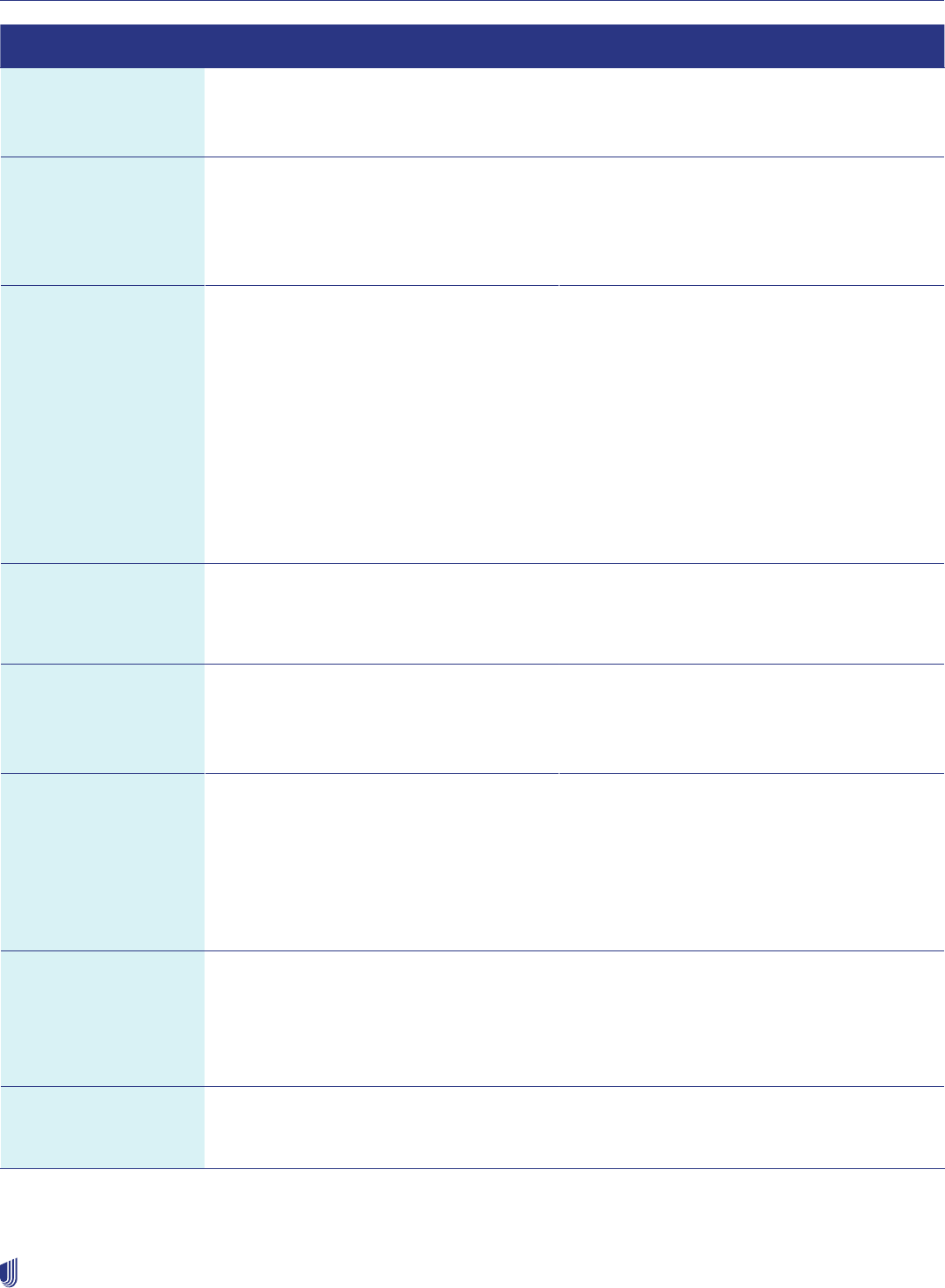
Preferred Care Network supplement
316
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to Go What you can do there
Electronic Remittance
(Facilitated by Change
Healthcare)
Phone: 1-800-845-6592
Online: changehealthcare.com
• Information and registration for electronic
payment services
Fraud, Waste, and
Abuse (FWA) Hotline
Online: uhc.com/fraud
Phone: 1-844-359-7736 (UHC Fraud
Hotline)
1-877-842-3210 (United Voice
Portal)
• Report concerns related to fraud, waste
or abuse
Grievances
and Appeals
MA and MA Prescription Drug (MAPD)
Plans:
Preferred Care Network
P.O. Box 6106
Mail Stop CA 124-0157
Cypress, CA 90630
Medicare and Retirement Prescription
Drug Plans (PDP):
Preferred Care Network
P.O. Box 6106
Mail Stop CA 124-0197
Cypress, CA 90630
• Obtain information about filing a grievance or
appeal on behalf of a member, status inquiries
or requests for forms
Home Health
(MedCare)
Phone: 1-305-883-2940 • Arrange for services
• On call 24 hours a day
• You may also call Utilization Management or
Network Management
Member Services Phone: 1-800-407-9069 - TTY 711
8 a.m.–8 p.m. local time,
7 days a week
• Assist our members with questions, help
locate specialists and perform other
related functions
• Also printed on the member’s ID card
Network Management
Services — Provider
Relations
and Contracting
Phone: 1-877-670-8432
Monday–Friday, 9 a.m.–5 p.m.
Fax: 1-888-659-0619
Email: pcp-NetworkManagementServices
@uhcsouthflorida.com
• Ask questions regarding your Agreement, in-
servicing and follow-up and outreaches
• Report demographic changes such as TIN
changes, health care provider terminations
and additions
• Submit informal complaints
• Find or request forms or other materials
• Panel status
Pharmacy
(OptumRx)
Online: professionals.optumrx.com
Phone: 1-800-711-4555
Mail: OptumRx
P.O. Box 650287
Dallas, TX 75265-0287
• Verify pharmacy benefits and eligibility,
adjudications or authorizations
Risk Management Phone: 1-877-504-1179
Email: [email protected]
• Report incidents involving all privacy issues
(potential breaches of PHI or PII) immediately
to our Risk Manager
Preferred Care Network supplement
317
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to Go What you can do there
24-Hour Nurse Hotline
Optum Nurse Line
Only available under
certain plans
Phone: 1-855-575-0293 • Speak to a nurse to triage to emergency or
urgent care, or to refer members to their
primary care physician
Optum
(Behavioral Health)
Online: providerexpress.com
Licensed clinicians available
24 hours.
Member Services – 24 hours.
Phone: 1-800-985-2596 No DSNP
1-800-496-5841 DSNP and iSNP
• Obtain information about behavioral health
and substance use services for all members
• Access a list of behavioral health practitioners
and health care providers in the provider
directory
Dental
(Solstice)
Online: SolsticeBenefits.com
Phone: 1-855-351-8163
• Access a list of Solstice dental providers in the
provider directory
Fitness
(Renew Active)
Online: uhcRenewActive.com
Phone: 1-800-407-9069
Hearing
(UHC Hearing)
Phone: 1-855-523-9355, TTY 711
Monday–Friday,
8 a.m.–8 p.m. CT
Laboratory
LabCorp
QUEST
Online: labcorp.com
Phone: 1-855-277-8669 Automated Line
Phone: 1-877-7831 Live Scheduling
Online: Questdiagnostics.com
Phone: 1-866-697-8378
• Find information on locations, to make an
appointment and to order lab tests and
view results
Mail Order Pharmacy
(OptumRx)
Online: optumrx.com
Phone: 1-877-889-6358
• Obtain mail-order medications
Podiatry - Network
Mgmt Services
(Foot and Ankle
Network)
Phone: 1-877-670-8432
Monday–Friday, 9 a.m.–5 p.m.
• Access a list of podiatrists in our
provider directory
Transportation
(ModivCare)
Phone: 1-888-774-7772
Monday–Friday, 8 a.m.–5 p.m.
• Request services
Vision - Network Mgmt
Services (iCare)
Phone: 1-877-670-8432
Monday–Friday, 9 a.m.–5 p.m.
• Access a list of vision providers in our
provider directory
WellMed Medical Management, Inc. (WellMed)
For members who belong to a Primary Care Physician (PCP) in the Preferred Care Network, their utilization management (UM)
and claim services are handled through WellMed. To identify these members, refer to the member ID card. The payer ID is listed
as WELM2, and “WellMed” is listed in the lower right corner of the card.

Preferred Care Network supplement
318
2023 UnitedHealthcare Care Provider Administrative Guide
Claims Processing for WellMed Members
Submit claims electronically to payer ID WELM2. If mailing, send to:
WellMed Claims
P.O. Box 30508
Salt Lake City, UT 84130-0508.
Confidentiality of Protected Health Information (PHI)
All employees, contracting health care providers and delegates of Preferred Care Network are required to maintain the
confidentiality of all PHI. We keep all UM information confidential, following federal and state laws and regulations. We limit PHI
access to the minimum necessary.
You must report all privacy issues immediately to Risk Management at 1-877-504-1179.
Examples of privacy incidents include:
• Reports and correspondence containing PHI or Personally Identifiable Information (PII) sent to the wrong recipient.
• Member or provider correspondence that includes an incorrect member’s information.
• Complaint received indicating PHI or PII may have been misused.
• Concern about compliance with a privacy or security policy.
• PHI or PII sent unencrypted outside of your office.
• Lost or theft of laptops, PDAs, CDs, DVDs, flash/USB drives and other electronic devices.
• Caller mentions they are a regulator (i.e., person is calling from the Office for Civil Rights, Office of E-Health Standards
& Services, State Insurance Departments, Attorney General’s Office, Department of Justice), or threatens legal action or
contacting the media in relation to a privacy issue.
• Caller advises your office of a privacy risk.
Physician extender responsibilities
Physician extenders are state-licensed health care professionals who are employed or contracted by physicians to examine and
treat Medicare members. These are advanced registered nurse practitioners (ARNPs) and physician assistants (PAs). When a
physician extender provides care, they must:
• Be supervised by a physician. The physician must be on the premises at all times when the physician extender is
seeing patients.
• Ensure the member is made aware of their credentials. The member should be aware they might not see a medical doctor.
• Get the sponsoring physician’s signature on all progress notes.
• Provide services as defined and approved by the sponsoring physician.
Referrals
Preferred Care Network’s Simple Referral Process helps PCPs coordinate patient care.
Referrals are needed for most participating specialists.* Requests for non-participating health care providers need
additional authorization.
• You may request a referral for 1 or multiple visits.
• The referral is good for the number of visits approved, valid for 6 months from the date issued.
• No supporting documentation is needed for referrals to specialists.
• Submit all requests for referrals in the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In > Referrals. For more
information on referrals, go to uhcprovider.com/referral.
* Contact Network Management Services for a complete list of specialty types that need referrals.

Preferred Care Network supplement
319
2023 UnitedHealthcare Care Provider Administrative Guide
• Upon submitting a referral request, the system automatically generates the referral number.
• For member convenience, you may also provide members with a copy of the referral confirmation.
• Specialists have the ability to view referrals via the UnitedHealthcare Provider Portal.
• For additional questions call us at 1-877-670-8432 or email us at pcp-NetworkManagementSer[email protected].
Prior authorizations
Preferred Care Network does not require prior authorization for certain services. Use the Enterprise Prior Authorization
List (EPAL) to see what services do require authorization on uhcprovider.com/priorauth > Frequently searched > Advance
Notification and Plan Requirement Resources > under Plan Requirements and Procedure Codes > Preferred Care Network
and Preferred Care Partners Prior Authorization Requirements.
WellMed and utilization management
Prior authorization requests for Preferred Care Network members assigned to a PCP belonging to Preferred Care Partners
Medical Group (PCPMG) can be done online at eprg.wellmed.net.
Authorization requirements
• You are responsible for getting prior authorization for all services requiring authorization before the services are scheduled
or rendered.
• Submit prior authorization for outpatient services or planned inpatient admissions, including skilled nursing facilities (SNF),
acute inpatient rehab (AIR) and long-term acute care hospital (LTACH) admissions, as far in advance of the planned service
as possible to allow for review. You are required to submit prior authorizations at least 7 calendar days prior to the planned
date of service.
• Prior authorizations for home health and home infusion services, durable medical equipment and medical supply items
should be submitted to MedCare Home Health at 1-305-883-2940 and Infusion/DME at 1-800-819-0751.
Note: Request an expedited (72 hours) review if waiting for a standard (14 calendar days) review could place the member’s
life, health or ability to regain maximum function in serious jeopardy. If the situation meets this definition, request a prior
authorization be expedited by placing ‘STAT’ or ‘urgent’ on the Prior Authorization Form.
• Prior authorizations are required for referrals to out-of-network providers when the member requires a necessary service
that is not within the Preferred Care Network. The referring physician must submit a completed prior authorization form for
approval.
• It is important you and the member are fully aware of coverage decisions before you render services.
• If you provide the service before a coverage decision is rendered, and we determine the service was not a covered benefit,
we may deny the claim and you must not bill the member. Without a coverage determination, a member does not have the
information needed to make an informed decision about receiving and paying for services.
Notification requirements
Prior to doing an inpatient or ambulatory outpatient service requiring prior authorization, the facility must confirm the coverage
approval is on file. This promotes conversations between the facility and the member about the cost for the procedure.
• Facilities are responsible for admission notification for inpatient services even if the coverage approval is on file.
• If a member is admitted through the emergency room, notification is required no later than 24 hours from the time the
member is admitted for purposes of concurrent review and follow-up care.
• If a member receives urgent care services, you must notify us within 48 hours of the services being rendered.

Preferred Care Network supplement
320
2023 UnitedHealthcare Care Provider Administrative Guide
Admission notification requirements
Facilities are responsible for admission notification for the following inpatient admissions, even if advance notification was
provided by the physician and coverage approval is on file:
• Planned elective admissions for acute care
• Unplanned admissions for acute care
• Admissions following observation
• Admissions following outpatient surgery
• SNF admissions
• LTACH
• AIR
• Unless otherwise indicated, admission notification must be received within 24 hours after actual weekday admission (or by 5
p.m. ET on the next business day if 24-hour notification would require notification on a weekend or federal holiday). For after-
hour, weekend and federal holiday admissions, call the Utilization Management department at 1-866-273-9444 for assistance.
• Even if the physician gave us the admission notification, the facility still needs to submit one.
• Receipt of an admission notification does not guarantee or authorize payment. Payment of covered services depends on:
– The member’s coverage
– The facility being eligible for payment
– Claim processing requirements
– The facility’s Agreement with us
• Admission notifications must contain:
– Member name and member health plan ID number
– Facility name
– Admitting/attending physician name
– Description for admitting diagnosis or ICD-10-CM (or its successor) diagnosis code
– Actual admission date
– Admission orders written by a physician
• For emergency admissions when a member is unstable and not capable of providing coverage information, the facility
should notify us as soon as the information is known and communicate the extenuating circumstances. We will not apply any
notification-related reimbursement deductions.
If the requirements described are not followed, the services may be denied. The member may not be billed.
A notification or prior authorization approval does not ensure or authorize payment, subject to state rules and MA policies.
Payment depends on the member’s coverage, the health care provider’s eligibility and Agreement and claim requirements.
How to request prior authorization
• Online: uhcprovider.com/paan
• Phone: If you do not have electronic access, call the number on the back of the members’ health plan ID card.
Required information for prior authorizations:
• Member information: Name, date of birth and membership ID number
• Requesting health care provider information: Name, specialty, designate par or non-par, address and phone and fax numbers
• PCP information, if different from the requesting health care provider: Name, phone and fax numbers
• Referral information: Name of referral health care provider, designate par or non-par, address, phone and fax numbers
• Diagnosis or symptoms: Include the diagnosis description and the corresponding ICD-10 code for each diagnosis to the
highest specificity

Preferred Care Network supplement
321
2023 UnitedHealthcare Care Provider Administrative Guide
• Service(s) requested:
– Identify each procedure and its corresponding CPT code
– Document any pertinent clinical summary information that would be helpful to that specialist or for the UM determination in
the additional comments field
– Enter the date of service and number of visits requested and sign where indicated
Where a clinical coverage review is required in the member’s benefit plan, we may request additional information.
• We may not cover certain services within an individual member’s benefit plan, regardless of whether prior authorization
is required.
• In the event of a conflict or inconsistency between applicable regulations and the advance notification requirements in this
manual, we follow the notification process in accordance with applicable regulations.
Time frames for processing prior authorization requests
We will make a determination within 14 calendar days of receipt, or within 72 hours for an expedited review.
It is important we have all necessary documentation at the time of your request to help with the decision.
Clinical coverage review
Certain services require prior authorization, which result in:
1. A request for clinical information.
2. A clinical coverage review based on medical necessity.
3. A coverage determination.
You must cooperate with our requests for information, documents or discussions for purposes of a clinical coverage review,
including providing pertinent medical records, imaging studies and reports and appropriate assessments for determining
degree of pain or functional impairment.
As a network provider, you must return calls from our UM staff or Medical Director. You must provide complete clinical
information as required within the time frame specified on the outreach form.
In addition:
• We may also use tools developed by third parties, such as the InterQual Care Guidelines, to assist us in administering health
benefits and to assist clinicians in making informed decisions in many health care settings. These tools are intended to
be used in connection with the independent professional medical judgment of a qualified health care provider and do not
constitute the practice of medicine or medical advice.
• For MA members, we use CMS coverage determinations, the National Coverage Determinations (NCD) and Local
Coverage Determinations (LCD) to determine clinical criteria for Medicare members. There is a hierarchy used in applying
clinical criteria.
Clinical coverage review criteria
We use scientifically based clinical evidence to identify safe and effective health services for members for inpatient and
outpatient services. For inpatient care management (ICM), we use evidence-based InterQual Care Guidelines. Clinical coverage
decisions are based on:
• The member’s eligibility.
• State and federal mandates.
• The member’s certificate of coverage, evidence of coverage or summary plan description.
• UnitedHealthcare medical policies and medical technology assessment information.
• CMS NCDs and LCDs, and other clinical-based literature (for Medicare and Retirement).

Preferred Care Network supplement
322
2023 UnitedHealthcare Care Provider Administrative Guide
Coverage determination decisions
We base coverage determinations for health care services upon the member’s benefit documents and applicable federal
requirements. Our UM staff, its delegates and the physicians making these coverage decisions are not compensated or
otherwise rewarded for issuing adverse non-coverage determinations.
Preferred Care Network and its delegates do not offer incentives to physicians to encourage underutilization of services or to
encourage barriers to receiving the care and services needed.
Coverage decisions are made based on the definition of “reasonable and necessary” within Medicare coverage regulations
and guidelines. We do not hire, promote or terminate physicians or other individuals based upon the likelihood or the perceived
likelihood the individual will support or tend to support the denial of benefits.
Prior authorization denials
We may deny a prior authorization request for several reasons:
• Member is not eligible.
• Service requested is not a covered benefit.
• Member’s benefit has been exhausted.
• Service requested is identified as not medically necessary (based upon clinical criteria guidelines).
We must notify you and the member in writing of any adverse decision (partial or complete) within applicable time frames. The
notice must state the specific reasons for the decision and reference the benefit provision and clinical review criteria used in the
decision making process. We provide the clinical criteria used in the review process for making a coverage determination along
with the notification of denial.
Peer-to-Peer (P2P) clinical review
For ICM, P2P requests may come in through the P2P support team by calling 1-800-955-7615.
P2P discussions may occur at different points during case activity in accordance with time frames once a medical director has
rendered an adverse determination. A P2P reconsideration request may only occur before you file a formal appeal.
UnitedHealthcare physicians conducting clinical review determinations are available by phone to discuss medical necessity
review determinations with the member’s physician requesting the service. We offer pre-denial P2P review. A clinician will
contact you to initiate the P2P call. Follow the time line provided by the nurse during the call.
Additional UM information
External agency services for members
Some members may require medical, psychological, social services or other external agencies outside the scope of their
benefits (for example, from Health and Human Services or Social Services). If you encounter a member in this situation,
you should either contact Network Management Services or have the member contact our Member Services department at
1-800-407-9069 for assistance with, and referral to, appropriate external agencies.
Technology assessment coverage determination
We use the technology assessment process to evaluate new technologies and new applications of existing technologies.
Technology categories include medical procedures, drugs, pharmaceuticals or devices. This information allows us to
support decisions about treatments that best improve member’s health outcomes, efficiently manage utilization of health
care resources, make changes in benefit coverage to keep pace with technology changes and to help ensure members have
equitable access to safe and effective care. If you have any questions regarding whether a new technology or a new application
of existing technologies are a covered benefit for our members, contact UM at 1-866-273-9444.
Hospitalist program for inpatient hospital admissions
The hospitalist program is a voluntary program for members. Hospitalists are physicians who specialize in the care of members
in an acute inpatient setting (acute care hospitals and skilled nursing facilities). A hospitalist oversees the member’s inpatient
admission and coordinates all inpatient care. The hospitalist is required to communicate with the member’s selected physician

Preferred Care Network supplement
323
2023 UnitedHealthcare Care Provider Administrative Guide
by providing records and information, such as the discharge summary, upon the member’s discharge from the hospital
or facility.
Discharge planning
Discharge planning is a collaborative effort between the inpatient care managers, the hospital/facility case manager, the
member and the admitting physician to ensure coordination and quality of medical services through the post-discharge phase
of care.
Although not required to do so, we may assist in identifying health care resources, which may be available in the member’s
community following an inpatient stay.
Utilization case management nurses conduct telephone reviews to support discharge planning, with a focus on coordinating
health care services prior to the discharge.
The facility or physician is required to contact us and provide clinical information to support discharge decisions under the
following circumstances:
• An extension of the approval is needed. Contact must be made prior to the expiration of the approved days.
• The member’s discharge plan indicates transfer to an alternative level of care is appropriate.
• The member has a complex plan of treatment that includes home health services, home infusion therapy, total parenteral
nutrition or multiple or specialized durable medical equipment identified prior to discharge.
• Addressing lifestyle-related health issues and referring to programs for weight management, nutrition, smoking cessation,
exercise, diabetes education and stress management, as appropriate.
• Helping members understand and manage their condition and its implications.
• Education for reducing risk factors, maintaining a healthy lifestyle and adhering to treatment plans and medication regimens.
Appeal and reconsideration processes
MA hospital discharge appeal rights protocol
MA members have the statutory right to appeal their hospital discharge to a Beneficiary Family Centered Care Quality
Improvement Organization (BFCC-QIO) for immediate review. The BFCC-QIO for Florida is KEPRO.
The BFCC-QIO notifies the facility and Preferred Care Network of an appeal and:
• Preferred Care Network facility onsite concurrent review staff completes the Detailed Notice of Discharge (DNOD) and
delivers it to the member or their representative as soon as possible but no later than 12 p.m. ET of the day after the BFCC-
QIO notification of the appeal is received. The facility faxes a copy of the DNOD to the BFCC-QIO.
• When there are not any Preferred Care Network facility onsite staff, the facility completes the DNOD, and delivers the DNOD
to the member or their representative as soon as possible but no later than 12 p.m. ET of the day after the BFCC-QIO
notification of the appeal is received. The facility faxes a copy of the DNOD to the BFCC-QIO and Preferred Care Network.
Facility (SNF, HHA, CORF) Notice of Medicare Non-Coverage (NOMNC) protocol
CMS requires SNFs, home health agencies (HHAs) and comprehensive outpatient rehabilitation facilities (CORFs) to deliver
the NOMNC notice to members at least 2 calendar days prior to termination of skilled nursing care, home health care or
comprehensive rehabilitation facility services. If the member’s services are expected to be fewer than 2 calendar days in
duration, the notice should be delivered at the time of admission, or commencement of services in a non-institutional setting.
In a non-institutional setting, if the span of time between services exceeds 2 calendar days, the notice should be given no later
than the next to last time services are furnished.
Delivery of notice is valid only upon signature and date of member or member’s authorized representative if the member is
incompetent. You must use the most current version of the standard CMS approved notice entitled Notice of Medicare Non-
Coverage form. The standardized form and instructions regarding the NOMNC are on the CMS website or contact KEPRO, the
BFCC-QIO for Florida, at keproqio.com. The NOMNC notification text may not be modified.

Preferred Care Network supplement
324
2023 UnitedHealthcare Care Provider Administrative Guide
Clinical appeals: Standard and expedited
To appeal an adverse decision (a decision to deny authorization of a service or procedure because the service is determined
not to be medically necessary or appropriate) on behalf of a member, you must submit a formal letter outlining the issues and
submit supporting documentation. The denial letter you received provides you with filing deadlines and the address to submit
the appeal. Medicare guidance allows the servicing health care provider to submit an appeal on behalf of the member.
When we make the final decision, we notify you via mail. If the decision is to overturn the original determination, we will
authorize the service. If the decision is to uphold the original denial determination, there will be no further action for you
to undertake.
Benefit summaries
For information on benefit plans, visit pcnhealth.com > Members.
Member rights and responsibilities
The Member Rights and Responsibilities Statement is published each year in the Evidence of Coverage (EOC) available on the
Preferred Care Network website at pcnhealth.com. You may get a copy of the Member Rights and Responsibilities Statement
by contacting Network Management Services at 1-877-670-8432. If your patient has questions about their rights as a MA
member, refer them to the Member Services phone number on the back of their ID Card.
Member participation in treatment options
Members have the right to freely communicate with their physician and participate in the decision-making process regarding
their health care, regardless of their benefit coverage. Physicians should encourage and provide active member communication
and participation in their treatment planning and course of care. This includes the member’s right to withhold resuscitative
services or to forgo or withdraw life-sustaining treatment in compliance with federal and state laws.
Each member has the right to receive information on available treatment options (including the option of no treatment) or
alternative courses of care and other information specified by law, as applicable. Physicians must communicate information,
regarding the risks, benefits and consequences of treatment or non-treatment, at a level the member may understand to decide
among the treatment options.
Competent members have the right to refuse a recommended treatment, counsel or procedure. The physician may regard such
refusal as incompatible with the continuance of the physician/patient relationship and provision of proper medical care. If this
occurs, and the physician believes that no professionally acceptable alternatives exist, the physician must inform the member in
writing by certified mail. The physician must give the member 30 calendar days to find another health care provider.
During this time, the physician is responsible for providing continuity of care to the member.
Advance directives
For information on advance directives, refer to Chapter 16: Member rights and responsibilities.
Documentation and confidentiality of medical records
You are required to maintain records, correspondence and discussions regarding the member in the strictest of confidence
and protection.
You must keep a medical records system that:
• Follows professional standards.
• Allows quick access of information.
• Provides legible information, accurately documented and available to appropriate health care providers.
• Maintains confidentiality.

Preferred Care Network supplement
325
2023 UnitedHealthcare Care Provider Administrative Guide
Our member should sign a Medical Record Release Form as a part of their medical record. Call Network Management Services
(1-877-670-8432) to request a copy of this form.
The following guidelines are applicable:
• Records that contain medical/clinical, social, financial or other data on a patient is treated as confidential and is protected
against loss, tampering, alteration, destruction or inadvertent disclosure.
• Release of information from your office requires you have the patient sign a Medical Record Release Form. Retain it in the
medical record.
• Release of records is in accordance with state and federal laws, including the Health Insurance Portability and Accountability
Act of 1996 (HIPAA).
• Records containing information on mental health services, substance use or potential chronic medical conditions that may
affect the member’s plan benefits are subject to additional specific waivers for release and confidentiality.
Exemption from release requirements
HIPAA regulations allow us to give PHI to government programs without member permission. We give this when it is necessary
to determine member eligibility.
Medical records requirements
You must ensure your medical records meet our standards. The following are expanded descriptions of some of
these requirements.
Patient Identifiers: Should consist of the patient name and a second unique identifier; they should appear on each page of the
medical record.
Advance Directives: It is your responsibility to provide the member with advance directive information and to encourage the
member to retain a copy for their personal records.
Biographical Information: Each record should contain the patient’s name, date of birth, address, home and work phone
numbers, marital status, sex, primary language spoken, name and phone number of emergency contact, appropriate consent
forms and guardianship information if relevant.
Signatures: For paper medical records, have all entries dated and signed or initialed by the author. Author identification may
be a handwritten signature or initials followed by the title (MD, DO, PA, ARNP, RN, LPN, MA or OM). There must be a written
policy requiring, and evidence of, physician co-signature for entries made by those other than a licensed practitioner (MD, DO).
Electronic signatures are acceptable for electronic medical records.
Family History: Document the family history no later than the first visit.
Past Medical History: Documentation should include a detailed medical, surgical and social history.
Immunizations: Documentation of immunizations performed by the office should include the date the vaccine was
administered, the manufacturer and lot number and the name and title of the person administering the vaccine. At a minimum,
you must have their vaccination history.
Medication List: List the member’s current medications, with start and end dates, if applicable. Reconcile within 30 days post
inpatient admissions.
Referral Documentation: If a referral was made to a specialist, the consultation report should be filed in the medical record.
There should be documentation the physician has discussed abnormal results with the patient, along with recommendations.
Chart Organization: You should maintain a uniform medical record system of clinical recording and reporting with respect to
services, which includes separate sections for progress notes and the results of diagnostic tests.
Preventive Screenings: You need to promote the appropriate use of age/gender specific preventive health services for
members to achieve a positive impact on the member’s health and better medical outcomes.
Required Encounter Documentation: For every visit, document the following:
• The date
• Chief complaint or purpose

Preferred Care Network supplement
326
2023 UnitedHealthcare Care Provider Administrative Guide
• Objective findings
• Diagnosis or medical impression
• Studies ordered (lab, X-ray, etc.)
• Therapies administered or ordered
• Education provided
• Disposition, recommendations, instructions to the member and evidence of whether there was follow-up
• Outcome of services
You must document you have a written policy in place regarding follow-up care and written procedures for recording results of
studies and therapies and appropriate follow-up.
As a part of their medical record, members should sign a Medical Record Release Form. They should sign a Refusal Form
when declining a preventive screening referral.
We recommend medical records include copies of care plans whenever you provide home health or skilled nursing services.
Case management and disease management program information
Optum provides case management (CM) and disease management (DM) services for Preferred Care Network.
Here are the criteria for referrals to Optum CM and DM programs:
• Complex Case Management — Special Needs Plan (SNP) members only
• Three or more unplanned admissions and/or emergency room (ER) visits in the last 6 months
• Multiple, complex co-morbid conditions
• Coordination of multiple community resources/financial supports to cover basic services
• Heart failure (HF) DM program
– Diagnosis of HF
– Has congestive heart failure (CHF) on an inpatient claim
– HF admission in last 3 months
• Diabetes DM program
– Diabetic with A1C 9% or greater
– An inpatient admission related to diabetes in the past 12 months
– Two or more ER visits related to diabetes
• Advanced Illness CM — Primary goal is to facilitate and support end-of-life wishes and services
– Life expectancy of 12–18 months
– Chronic, irreversible disease or conditions and declining health
– Reduce disease and symptom burden
• Transplant CM and network services bone marrow/stem cell including chimeric antigen receptor T-cell (CAR-T) therapy for
certain hematologic malignancies, kidney and kidney/pancreas, heart, liver, intestinal, multi-organs and lung transplants
– CM for 1 year post-transplant
• End stage renal disease CM — The member is diagnosed with end stage renal disease and is undergoing outpatient dialysis
including in-center or home hemodialysis, home peritoneal dialysis, etc.
If the member does not qualify for one of the previously listed programs, they do have 24/7, 365 days a year access to speak
with a nurse by calling the Optum NurseLine number on the back of their ID card.
Note: Preferred Care Network no longer provides social worker evaluations without skilled services. Direct your patient to their
local social services department or The Florida State Department of Elder Affairs Help Line at 1-800-963-5337.
To request CM or DM services for one of our members, select only one program that your member meets the criteria for, and
email the CM/DM referral form available on pcnhealth.com > Provider/Facility > Forms.

Preferred Care Network supplement
327
2023 UnitedHealthcare Care Provider Administrative Guide
When appropriate, we provide referrals to other internal programs such as disease management, complex condition
management, mental health, employee assistance and disability. Case management services are voluntary, and a member may
opt out at any time.
Optum (Behavioral Health)
We work with Optum to provide behavioral health care services for our members. For more information on how to access the
behavioral health care programs, you or our members may contact a representative through the phone number listed on the
back of their ID card.
Special Needs Plans (SNP)
SNP Model of Care (MOC)
The MOC is the framework for care management processes and systems to help enable coordinated care for SNP members.
The MOC contains specific elements that delineate implementation, analysis and improvement of care.
These elements include description of SNP population (including health conditions), care coordination, provider network and
quality measurement and performance improvement.
The MOC is a quality improvement tool, and MOC helps ensure the unique needs of our SNP members are identified and
addressed through care management practices. MOC goals are evaluated annually to determine effectiveness. To learn more,
contact us via email at: [email protected].
CMS requires annual SNP MOC training for all health care providers who treat SNP members. The annual SNP MOC provider
training is available at uhcprovider.com. Updates about training requirements are communicated annually on uhcprovider.
com/news as described in Chapter 18: Provider communication.
Risk management
Risk management addresses liability, both proactively and reactively. Proactive is avoiding or preventing risk. Reactive is
minimizing loss or damage after an adverse or bad event. Risk management in health care considers patient safety, quality
assurance and patients’ rights. The potential for risk is present in all aspects of health care, including medical mistakes,
electronic record keeping, provider organizations and facility management.
An adverse event is defined as an event over which health care personnel could exercise control rather than as a result of the
member’s condition. Identifying something as an adverse event does not imply “error,” “negligence” or poor quality care. It
simply indicates an undesirable clinical outcome resulted from some aspect of diagnosis or therapy, not an underlying disease
process. Examples of adverse events in health care include unexpected death, failure to diagnose or treat disease or surgical
mistakes or accidents. Adverse events interfere with a health care provider’s delivery of medical care and may result in litigation.
Agency for Healthcare Administration
The Florida Agency for Healthcare Administration (AHCA), as directed under F.S. 641 Parts I, II, III and other applicable state
laws, provides oversight and monitoring of health plans operating in the State of Florida as an HMO and their compliance to
applicable regulations. This includes implementation of a Risk Management Program (RMP) with the purpose of identifying,
investigating, analyzing and evaluating actual or potential risk exposures by a state licensed risk manager. The RMP also
corrects, reduces and eliminates identifiable risks through instruction and training to staff and health care providers.
Examples of adverse and serious incidents as defined by AHCA include:
• Death of a patient.
• Severe brain or spinal damage to a patient.
• Performance of a surgical procedure on the wrong patient.
• Performance of a wrong site surgical procedure.
• Performance of a wrong surgical procedure.
For more information, go to the AHCA website at ahca.myflorida.com.

Preferred Care Network supplement
328
2023 UnitedHealthcare Care Provider Administrative Guide
Provider reporting responsibilities
You are required to report all adverse events identified previously, whether actual or potential. To report such incidents, call
1-877-504-1179.
You must report incidents to AHCA within 24 hours of it happening. You must report all serious incidents, such as those listed,
immediately. This allows us to quickly assess the risk and address liability. Examples of serious incidents include:
• Death or serious injury.
• Brain or spinal damage.
• Performance of a surgical procedure on the wrong patient.
• Performance of a wrong site surgical procedure.
• Performance of a wrong surgical procedure.
• Medically unnecessary surgical procedure.
• Surgical repair of damage from a planned surgical procedure.
• Removal of unplanned foreign object remaining from a surgical procedure.
Our provider contracts include the obligation to participate in quality management inquiries upon request.
What are the responsibilities of physicians and providers?
You must report the ICD-10-CM diagnosis codes to the highest level of specificity and accurately. This requires accurate and
complete medical record documentation. You are required to alert the MA organization of wrong information submitted. You
must follow the MA organization’s procedures for correcting information.
Finally, you must report claims and encounter information in a timely manner, generally within 30 days of the date of service (or
discharge for hospital inpatient facilities).
Links to resources for the latest ICD guidelines and MRA resources are available online at pcnhealth.com.
CPT and HCPCS codes
The American Medical Association (AMA) and CMS update procedure codes quarterly, with the largest volume effective
January 1 of each year. CPT and HCPCS codes may be added, deleted or revised to reflect changes in health care and
medical practices.
If you submit your claim with an invalid or deleted procedure code, we will deny or return it. A valid procedure code is required
for claims processing.
We encourage you to access CPT, HCPCS and ICD-10 coding resources and materials at the AMA’s website at ama-assn.org,
or from another vendor.
329
2023 UnitedHealthcare Care Provider Administrative Guide
Preferred Care Partners supplement
About Preferred Care Partners
Preferred Care Partners (PCP), Inc., a wholly owned subsidiary of UnitedHealthcare, is a Medicare Advantage (MA) health plan.
We offer MA plans in 3 Florida counties: Broward, Miami-Dade and Palm Beach.
Mission statement
We improve the health of our members by providing:
• Access to health care services.
• Choices for their health care needs.
• Simplification of the health care delivery system.
We streamline authorization and referral processes. We build health care provider networks around the needs of our members.
This provides the best experience for our members and health care providers. We commit to giving direct access to expert
customer service representatives who understand member needs and helping them make informed choices.
How to contact us
Questions or comments
Email questions or comments to Network Management Services (NMS) at
PCP-NetworkManagementServices@uhcsouthflorida.com, or send mail to:
Preferred Care Partners Network Management Services
9100 South Dadeland Blvd. Suite 1250
Miami, FL 33156-6420
Contact Us Table
Resources Where to Go What you can do there
Authorizations
and Notifications
EDI: Transactions 278 and 278N
Online: uhcprovider.com/paan
Information: uhcprovider.com/priorauth (Policies,
instructions and tips)
Phone: 1-800-995-0480
Submit notifications, prior
authorizations, referrals, admissions and
discharge planning.
Initiate requests for notifications and
authorizations electronically. If the request
cannot be completed electronically, our staff
is available to answer questions or discuss
any issues with referrals, prior authorizations,
case management, concurrent review and
admission certification or notification.
Authorizations and
Notifications
(WellMed)
Online: eprg.wellmed.net
Outpatient Notifications
Phone: 1-877-299-7213
Inpatient Notifications
Phone: 1-877-490-8982
Fax: 1-877-757-8885
Preferred Care Partners supplement
330
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to Go What you can do there
Claims Online: UnitedHealthcare Provider Portal
at uhcprovider.com > Sign In. Then
select Claims & Payments from the
menu.
Information: uhcprovider.com/claims
Phone: 1-866-725-9334
8 a.m. - 8 p.m. local time, 7 days a
week
Fax: 1-866-725-9337
Delegated Providers Only:
Mail: Preferred Care Partners
P.O. Box 30448
Salt Lake City, UT 84130-0448
Check claims, eligibility, benefits.
Use payer ID 65088.
Claims
(WellMed)
Online: eprg.wellmed.net
Phone: 1-800-550-7691
Mail: WellMed Claims
P.O. Box 30508
Salt Lake City, UT 84130-0508
Check claims, eligibility, benefits.
Use payer ID WELM2.
Technical Support
for Change
Healthcare Claims
Submission
Network
Phone: 1-800-845-6592 Obtain assistance with password or
technical support issues.
Obtain information on electronic
claims submission.
Credentialing Phone: 1-800-963-6495
Monday–Friday, 9 a.m.–5 p.m. (ET)
Fax: 1-844-897-6352
Submit or update credentialing, re-
credentialing, document changes or recent
hires or terminations in your practice
or facility.
Electronic
Remittance
(Facilitated by
Change Healthcare)
Online: ChangeHealthcare.com
Phone: 1-800-845-6592
Get information and register for electronic
payment services.
Eligibility
and Benefits
Verification
Online: uhcprovider.com/eligibility
Phone: 1-866-725-9334
Verify eligibility and benefits of
enrolled members.
Access a summary of benefits for each
plan online.
Fraud, Waste,
and Abuse (FWA)
Hotline
Online: uhc.com/fraud
Phone: 1-844-359-7736 (UHC Fraud Hotline)
1-877-842-3210 (United Voice Portal)
Report concerns related to fraud, waste
or abuse.
Preferred Care Partners supplement
331
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to Go What you can do there
Grievances
and Appeals
MA and MA Prescription Drug (MAPD) Plans:
Preferred Care Partners, Inc.
P.O. Box 6106
Mail Stop CA 124-0157
Cypress, CA 90630
For Medicare and Retirement Prescription
Drug Plans (PDP):
Preferred Care Partners, Inc.
P.O. Box 6106
Mail Stop CA 124-0197
Cypress, CA 90630
For information about filing a grievance
or appeal on behalf of a member, status
inquiries or requests for forms.
Member Services Online: mypreferredcare.com
Phone: 1-866-231-7201, TTY 711
Monday–Friday, 8 a.m.–8 p.m. local time
Members may ask questions about health
care providers, benefits and claims.
This toll-free phone number is also printed
on the member’s plan ID card.
Network
Management
Services Provider
Relations and
Contracting
Phone: 1-877-670-8432
Monday–Friday, 9 a.m.–5 p.m. (ET)
Fax: 1-888-659-0619
Email: PCP-NetworkManagementServices@
uhcsouthflorida.com
Ask questions regarding your Agreement, in-
servicing and follow-up or outreaches.
Report demographic changes.
Submit informal complaints.
Request forms or other materials.
Pharmacy
(OptumRx)
Online: professionals.optumrx.com
Phone: 1-800-711-4555
Mail: OptumRx
P.O. Box 650287
Dallas, TX 75265-0287
Verify pharmacy benefits and eligibility,
adjudications or authorizations.
See pharmacy benefit updates.
Risk Management Phone: 1-877-504-1179
Email: [email protected]
Report incidents involving all privacy issues
(potential breaches of PHI or PII) immediately
to our risk manager.
Ancillary and Enhanced Benefit Providers
Optum
(Behavioral Health)
Online: providerexpress.com
Phone: 1-800-985-2596 No DSNP
1-800-496-5841 iSNP
Member Services available 24 hours.
Licensed clinicians are on call 24 hours a day, 7 days
a week.
Obtain information about behavioral health
and substance use services for all members.
Access a list of behavioral health care
providers in the provider directory.
Dental
(Solstice)
Online: SolsticeBenefit.com
Phone: 1-855-351-8163
Access a list of Solstice dental providers in
the provider directory.
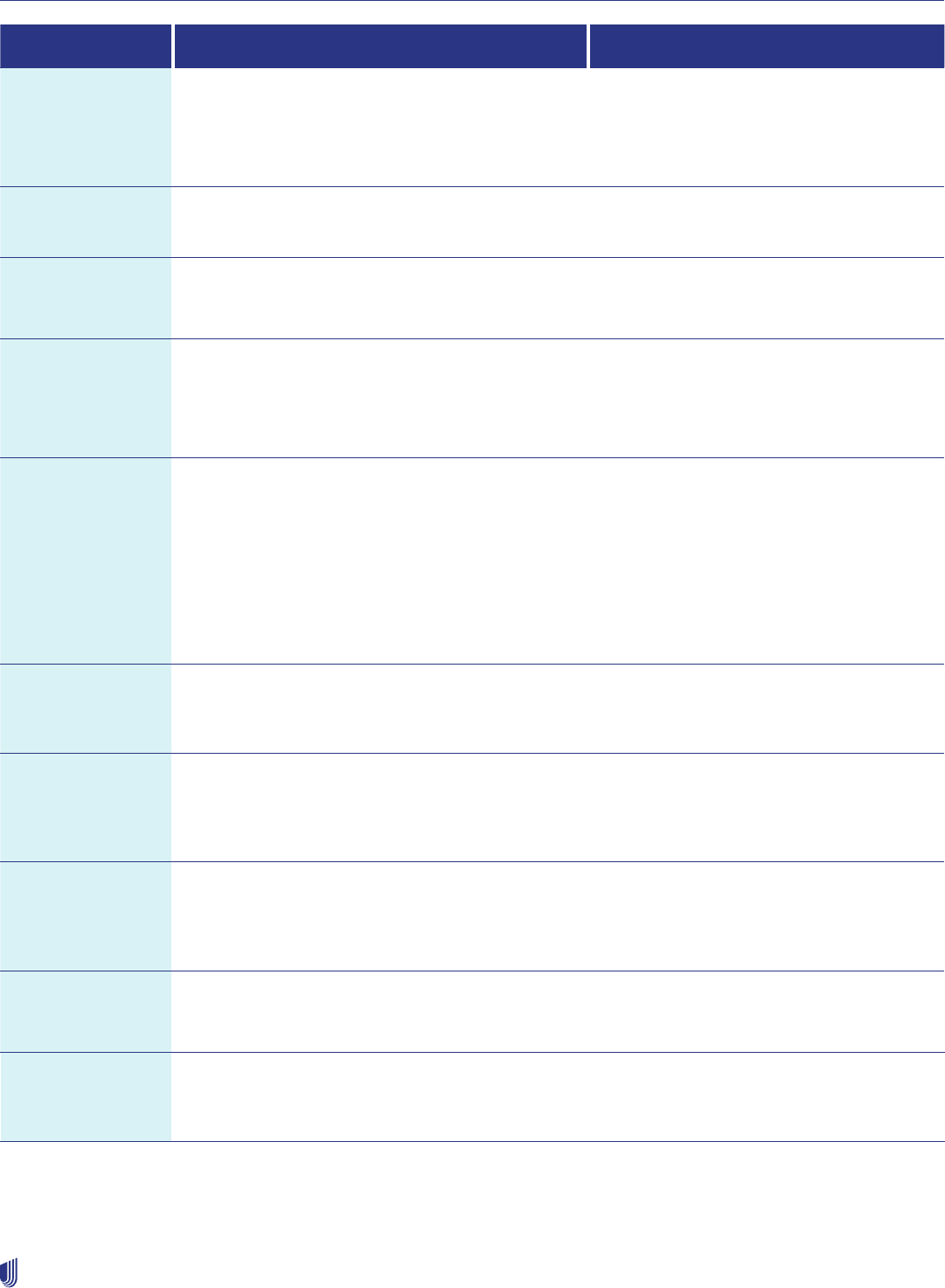
Preferred Care Partners supplement
332
2023 UnitedHealthcare Care Provider Administrative Guide
Resources Where to Go What you can do there
DME/Infusion
(MedCare)
Phone: 1-800-819-0751
Monday–Friday, 9 a.m.–5 p.m. (ET)
On call: 24 hours a day, 7 days a week
• Register for these services
• On call 24 hours a day
• You may also call Utilization Management
or Network Management
Fitness
(Renew Active)
Online: Preferredcare.myrenewactive.com
Phone: 1-866-231-7201
Hearing
(UHC Hearing)
Phone: 1-855-523-9355, TTY 711
Monday–Friday, 8 a.m.–8 p.m. (CT)
Home Health
(MedCare)
Phone: 1-305-883-2940
On call: 24 hours a day, 7 days a week
• Register for these services
• On call 24 hours a day
• You may also call Utilization Management
or Network Management
Laboratory
LabCorp
QUEST
Online: labcorp.com
Phone: 1-855-277-8669 Automated Line
Phone: 1-800-877-7831 Live Scheduling
Online: questdiagnostics.com
Phone: 1-866-697-8378
Find information on locations, make
an appointment, order lab tests and
view results.
Mail Order
Pharmacy
(OptumRx)
Online: optumrx.com
Phone: 1-877-889-6358
Obtain mail-order medications.
Nurse Hotline
(Optum NurseLine)
Phone: 1-855-575-0293
Available 24 hours a day,
7 days a week.
Only available under certain plans.
Speak to a nurse to triage emergency or
urgent care, or to refer them to their primary
care physician.
Podiatry — Network
Mgmt Services
(Foot and Ankle
Network)
Phone: 1-877-670-8432
Monday–Friday, 9 a.m.–5 p.m. (ET)
Access a list of podiatrists in our
provider directory.
Transportation
(ModivCare)
Phone: 1-888-774-7772
Monday–Friday, 9 a.m.–5 p.m. (ET)
Request services.
Vision - Network
Mgmt Services
(iCare)
Phone: 1-877-670-8432
Monday–Friday, 8 a.m.–5 p.m. (ET)
Access a list of vision providers in our
provider directory.

Preferred Care Partners supplement
333
2023 UnitedHealthcare Care Provider Administrative Guide
Confidentiality of Protected Health Information (PHI)
All employees, participating health care providers and delegates of Preferred Care are required to maintain the confidentiality of
PHI. All information used for UM activities is kept as confidential in accordance with federal and state laws and regulations. We
limit PHI access to the minimum necessary.
You must report all privacy issues immediately to Risk Management at 1-952-406-4806.
Examples of privacy incidents that must be reported include:
• Reports and correspondence containing PHI or Personally Identifiable Information (PII) sent to the wrong recipient.
• Member or health care provider correspondence that includes incorrect member information.
• Complaint received indicating that PHI or PII may have been misused.
• Concern about compliance with a privacy or security policy.
• PHI or PII sent unencrypted outside of your office.
• Lost or theft of laptops, PDAs, CDs, DVDs, flash or USB drives and other electronic devices.
• Caller mentions they are a regulator (i.e., person is calling from the Office for Civil Rights, Office of E-Health Standards
& Services, State Insurance Departments, Attorney General’s Office, Department of Justice) or threatens legal action or
contacting the media in relation to a privacy issue.
• Caller advises your office of a privacy risk.
Physician extender responsibilities
Physician extenders are state-licensed health care professionals who may be employed or contracted by physicians to examine
and treat Medicare members. Physician extenders are advanced registered nurse practitioners (ARNP) and physician assistants
(PA). When physician extenders provide care, they must:
• Be supervised by a physician. The physician must be on the premises at all times when the physician extender is
seeing patients.
• Help ensure the member knows of their credentials. Make the member aware they might not see a medical doctor.
• Get the sponsoring physician’s signature on all progress notes.
• Provide services as defined and approved by the sponsoring physician.
Prior authorizations
We do not require prior authorization for certain services. Use the Enterprise Prior Authorization List (EPAL) to see what services
do require authorization on uhcprovider.com/paan > Advance Notification and Plan Requirement Resources > under Plan
requirement resources – Preferred Care Network and Preferred Care Partners Prior Authorization Requirements.
WellMed and utilization management
Prior authorization requests for Preferred Care Partners members assigned to a PCP belonging to Preferred Care Partners
Medical Group (PCPMG) may be done online at eprg.wellmed.net.
WellMed members
WellMed requires a referral from the assigned PCP before rendering services for selected specialty health care providers.
The referral must be entered by the PCP in the WellMed provider portal at eprg.wellmed.net.
The WellMed Florida Specialty Protocol List gives more information about which specialties/services may be exempt from the
referral process. Providers may view the WellMed Specialty Protocol List in the WellMed Provider portal at eprg.wellmed.net in
the Provider Resource Tab.
Preferred Care Partners supplement
334
2023 UnitedHealthcare Care Provider Administrative Guide
Authorization requirements
• Obtain prior authorization for all services requiring authorization before the services are scheduled or rendered.
• Submit prior authorization for outpatient services or planned Acute Hospital Admissions and admissions to Skilled Nursing
Facilities (SNF), Acute Rehabilitation Hospital and Long-Term Acute Care (LTAC) as far in advance of the planned service as
possible to allow for coverage review. We require prior authorizations to be submitted at least 7 calendar days before the date
of service.
• Submit prior authorizations for home health and home infusion services, durable medical equipment (DME) and medical
supply items to MedCare Home Health at 1-305-883-2940 and Infusion/DME at 1-800-819-0751.
Note: Request an expedited (72 hours) review if waiting for a standard (14 calendar days) review could place the member’s
life, health or ability to regain maximum function in serious jeopardy.
• We require prior authorizations to out-of-network specialty or ancillary health care providers when the member requires a
necessary service that cannot be provided within the available Preferred Care network. The referring physician must submit a
completed Prior Authorization Form for approval.
• You and the member should be fully aware of coverage decisions before services are rendered.
• If you provide the service before the coverage decision is rendered, and we determine the service was not a covered benefit,
we may deny the claim. You must not bill the member. Without a coverage determination, a member does not have the
information needed to make an informed decision about receiving and paying for services.
Notification requirements
• For any inpatient or ambulatory outpatient service requiring prior authorization, the facility must confirm, before rendering the
service, that the coverage approval is on file. The purpose of this protocol is to enable the facility and the member to have an
informed pre-service conversation. If the service will not be covered, the member may decide whether to receive and pay for
the service.
• Facilities are responsible for admission notification for inpatient services, even if the coverage approval is on file.
• If a member is admitted through the emergency room, you must notify us no later than 24 hours from the time the member is
admitted for purposes of concurrent review and follow-up care.
• If a member receives urgent care services, you must notify us within 24 hours of the services being rendered.
Admission notification requirements
Facilities are responsible for admission notification for:
• Planned elective admissions for acute care.
• Unplanned admissions for acute care.
• Admissions following observation.
• Admissions following outpatient surgery.
• Skilled Nursing Facility (SNF) admissions.
• Long Term Acute Care Hospital (LTACH).
• Acute Inpatient Rehab (AIR).
• Unless otherwise indicated, admission notification must be received within 24 hours after actual weekday admission (or by 5
p.m. ET on the next business day if 24-hour notification would require notification on a weekend or federal holiday).
• Admission notification by the facility is required even if notification was supplied by the physician and a coverage approval is
on file.
• Receipt of an admission notification does not guarantee or authorize payment. Payment of covered services is contingent
upon coverage within an individual member’s benefit plan, the facility being eligible for payment, any claim processing
requirements and the facility’s Agreement with us.
• Admission notifications must contain the following:
– Member name and member health plan ID number
– Facility name
– Admitting or attending physician name
Preferred Care Partners supplement
335
2023 UnitedHealthcare Care Provider Administrative Guide
– Description for admitting diagnosis or ICD-10-CM (or its successor) diagnosis code
– Actual admission date
– Admission orders written by a physician
• For emergency admissions when a member is unstable and not capable of providing coverage information, the facility
should notify us as soon as the information is known and communicate the extenuating circumstances. We will not apply any
notification-related reimbursement deductions.
If the requirements are not followed, the services may be denied. You may not bill the member.
A notification or prior authorization approval does not ensure or authorize payment, subject to state rules and MA policies.
Payment is dependent upon the member’s coverage, the health care provider’s eligibility and Agreement and claim
requirements.
To initiate member discharge or to request authorization for transition to AIR and LTAC,
call 1-800-995-0480.
Clinical coverage review
Certain services require prior authorization, which results in:
1. A request for clinical information.
2. A clinical coverage review based on medical necessity.
3. A coverage determination.
You must cooperate with all requests for information, documents or discussions for purposes of a clinical coverage review
including providing pertinent medical records, imaging studies or reports and appropriate assessments for determining degree
of pain or functional impairment.
As a network provider, you must respond to calls from our UM staff or medical director. You must provide complete clinical
information as required within the time frame specified on the outreach form.
In addition:
• We may use tools developed by third parties, such as the InterQual Care Guidelines, to assist us in administering health
benefits. These tools assist clinicians in making informed decisions in many health care settings. These tools are intended to
be used in connection with the independent professional medical judgment of a qualified health care provider. They do not
constitute the practice of medicine or medical advice.
• For MA members, we use CMS coverage determinations, the National Coverage and Local Coverage Determinations (LCD)
to determine benefit coverage for Medicare members. If other clinical criteria, such as the InterQual Care Guidelines or any
other coverage determination guidelines, contradict CMS guidance, we follow the CMS guidance.
Clinical coverage review criteria
We use scientifically based clinical evidence to identify safe and effective health services for members for inpatient and
outpatient services. For Inpatient Care Management (ICM), we use evidence-based InterQual Care Guidelines. Clinical coverage
decisions are based on the member’s eligibility, state and federal mandates, the member’s certificate of coverage, evidence of
coverage or summary plan description, UnitedHealthcare medical policies and medical technology assessment information. For
Medicare Advantage members, we use CMS, NCDs and LCDs and other evidence-based clinical literature.
Coverage determination decisions
Coverage determinations for health care services are based upon the member’s benefit documents and applicable federal
requirements. Our UM staff, its delegates and the physicians making these coverage decisions are not compensated or
otherwise rewarded for issuing adverse non-coverage determinations. Preferred Care and its delegates do not offer incentives
to physicians to encourage underutilization of services or to encourage barriers to receiving the care and services needed.
Preferred Care Partners supplement
336
2023 UnitedHealthcare Care Provider Administrative Guide
Coverage decisions are made based on the definition of “reasonable and necessary within MA coverage regulations and
guidelines.” Hiring, promoting or terminating physicians or other individuals are not based upon the likelihood or the perceived
likelihood that the individual will support or tend to support the denial of benefits.
Prior authorization denials
We may deny a prior authorization request for several reasons:
• Member is not eligible.
• Service requested is not a covered benefit.
• Member’s benefit has been exhausted.
• Service requested is identified as not medically necessary (based upon clinical criteria guidelines).
We must notify you and the member in writing of any adverse decision (partial or complete) within applicable time frames. Our
notice states the specific reasons for the decision. It also references the benefit provision and clinical review criteria used in the
decision-making process. We provide the clinical criteria used in the review process for making a coverage determination along
with the notification of denial.
Peer-to-Peer (P2P) clinical review
For Inpatient Care Management Cases, P2P requests may come in through the P2P Support team by calling 1-800-955-7615.
P2P discussions may occur at different points during case activity in accordance with time frames, once a medical director has
rendered an adverse determination.
The post-decision consult process must conclude for the Medicare population. This requires establishing a pre-decision
medical director outreach for standard (14-day turnaround time) requests for both inpatient and outpatient adverse
determinations. It excludes expedited pre-service requests and administrative denials.
We must treat the following situations as reconsiderations or appeals:
• Clinical information received after notification is complete.
• Peer-to-peer requests received after notification is complete.
Additional UM information
External agency services for members
Some members may require medical, psychological and social services or other external agencies outside the scope of their
plan benefits (e.g., from Health and Human Services or Social Services). If you encounter a member in this situation, contact
Network Management Services. You may also have the member contact our Member Services Department at 1-866-231-7201
for assistance with, and referral to, appropriate external agencies.
Technology assessment coverage determination
The technology assessment process helps evaluate new technologies and new applications of existing technologies.
Technology categories include medical procedures, drugs, pharmaceuticals or devices. This information allows us to support
decisions about treatments that best improve member’s health outcomes, efficiently manage utilization of health care resources
and make changes in benefit coverage to keep pace with technology changes. It also helps ensure members have equitable
access to safe and effective care. If you have any questions regarding whether a new technology or a new application of existing
technologies are a covered benefit for our members, call Utilization Management at 1-800-995-0480.
Hospitalist Program for inpatient hospital admissions
The Hospitalist Program is a voluntary program for members. Hospitalists are physicians who specialize in the care of members
in an acute inpatient setting (acute care hospitals and SNFs). A hospitalist oversees the member’s inpatient admission and
coordinates all inpatient care. The hospitalist communicates with the member’s selected physician by providing records and
information, such as the discharge summary.

Preferred Care Partners supplement
337
2023 UnitedHealthcare Care Provider Administrative Guide
Discharge planning
Discharge planning is a collaborative effort between the inpatient care manager, the hospital/facility case manager, the member
and the admitting physician. It helps ensure coordination and quality of medical services through the post-discharge phase of
care.
Although not required to do so, we may help identify health care resources available in the member’s community following an
inpatient stay.
UM nurses conduct telephone reviews to support discharge planning, with a focus on coordinating health care services prior to
the discharge.
The facility or physician is required to contact us and provide clinical information to support discharge decisions under the
following circumstances:
• An extension of the approval is needed. Contact must be made before the expiration of the approved days.
• The member’s discharge plan indicates transfer to an alternative level of care is appropriate.
• The member has a complex plan of treatment that includes home health services, home infusion therapy, total parenteral
nutrition or multiple or specialized durable medical equipment identified before discharge.
To initiate patient discharge, update the case directly online at uhcprovider.com/paan or call us at 1-800-995-0480.
Appeal and reconsideration processes
MA hospital discharge appeal rights protocol
MA members have the right to appeal their hospital discharge to a Beneficiary Family Centered Care Quality Improvement
Organization (BFCC-QIO) for immediate review. The BFCC-QIO for Florida is KEPRO.
The BFCC-QIO notifies the facility and Preferred Care of an appeal and:
• Preferred Care facility onsite concurrent review staff completes the Detailed Notice of Discharge (DNOD) and delivers it to the
MA member or their representative as soon as possible but no later than 12 p.m. ET the day after the BFCC-QIO notification
of the appeal is received. The facility faxes a copy of the DNOD to the BFCC-QIO.
• When no Preferred Care facility onsite staff is available, the facility completes the DNOD and delivers it to the MA member or
their representative as soon as possible but no later than 12 p.m. ET the day after the BFCC-QIO notification of the appeal is
received. The facility faxes a copy of the DNOD to the BFCC-QIO and Preferred Care.
Facility (SNF, HHA, CORF) notice of Medicare Non-Coverage (NOMNC) protocol
CMS requires SNFs, HHAs and CORFs deliver the NOMNC-required notice to members at least 2 calendar days before
termination of skilled nursing care, home health care or comprehensive rehabilitation facility services. If a member’s services
are expected to be fewer than 2 calendar days in duration, deliver the notice at the time of admission or commencement of
services in a non-institutional setting. In a non-institutional setting, if the span of time between services exceeds 2 calendar
days, give the notice no later than the next to last time services are furnished.
Delivery of notice is valid only upon signature and date of the member or their authorized representative if the member is
incompetent. You must use the most current version of the standard CMS-approved form titled, “Notice of Medicare Non-
Coverage” (NOMNC). You may find the standardized form and instructions on the CMS website. You may also contact KEPRO,
the BFCC-QIO for Florida, at kepro.com for more information. You may not change the NOMNC notification text.
Clinical appeals: standard and expedited
To appeal an adverse decision (a decision to deny the authorization of a service or procedure because the service is
determined not to be medically necessary or appropriate) on behalf of a member, submit a formal letter outlining the issues.
Include supporting documentation. The denial letter you received provides you with the filing deadlines and the address to use
to submit the appeal.
Medicare guidance allows the servicing health care provider to submit an appeal on behalf of the member.

Preferred Care Partners supplement
338
2023 UnitedHealthcare Care Provider Administrative Guide
When we make a final decision, we notify you by mail. If we overturn the original determination, the service will be authorized. If
we uphold the original denial determination, there is no additional action.
Benefit summaries
For information on benefits, go to mypreferredcareprovider.com > Provider Resources > Summary of Benefits.
Member rights and responsibilities
The Member Rights and Responsibilities Statement is published each year in the Evidence of Coverage (EOC). It is available on
our website at mypreferredcare.com or by contacting the Network Management Department at 1-877-670-8432. If our member
has questions about their rights, refer them to the Member Services phone number on the back of their ID card.
Member participation in treatment options
Members have the right to freely communicate with their physician and participate in the decision-making process regarding
their health care, regardless of their benefit coverage. Each member has the right to receive information on available
treatment options (including the option of no treatment) or alternative courses of care and other information specified by law,
as applicable.
Competent members have the right to refuse recommended treatment, counsel or procedure. The physician may regard such
refusal as incompatible with the continuance of the health care provider/patient relationship and the provision of proper medical
care. If this occurs, and the physician believes that no professionally acceptable alternatives exist, they must so inform the
member in writing, by certified mail. The physician must give the member 30 calendar days to find another health care provider.
During this time, the physician is responsible for providing continuity of care to the member.
Advance directives
The federal Patient Self-Determination Act (PSDA) of 1990 gives individuals age 18 and older the legal right to make choices
about their medical care in advance of incapacitating illness or injury through an advance directive.
This law states that members’ rights and personal wishes must be respected, even when the member is too sick to make
decisions on their own. You may find the Patient Self-Determination Act at gpo.gov.
To help ensure a person’s choices about health care are respected, the Florida legislature enacted Chapter 765, Florida
Statutes. It requires all health care providers and facilities to provide their patients with written information regarding treatment
options.
Document this discussion at least once in the member’s record.
To comply with this requirement, we also inform members of state laws on advance directives through our members’ benefit
material. We encourage you to have these discussions with our members.
Online Resources: You may find the federal Patient Self-Determination Act at gpo.gov. You may download free forms from the
state at floridahealthfinder.gov/reports-guides/advance-directives.aspx.
Information is also available from the Robert Wood Foundation, Five Wishes. The information there meets the legal
requirements for an advance directive in Florida and may be helpful to members. Five Wishes is available on AgingWithDignity.
org.
Member financial responsibility
Members are responsible for the copayments, deductibles and coinsurance associated with their benefit plan. Collect
copayments at the time of service. To determine the exact member responsibility related to benefit plan deductibles and
coinsurance, we recommend you submit claims first. You will then receive the Summary of Benefits (SOB) to see what the
member needs to pay.
If you prefer to collect payment at the time of service, you must make a good faith effort to estimate the member’s responsibility
using our Claims tool in the UnitedHealthcare Provider Portal. Learn more at uhcprovider.com/claims.

Preferred Care Partners supplement
339
2023 UnitedHealthcare Care Provider Administrative Guide
Documentation and confidentiality of medical records
You are required to protect records, correspondence and discussions regarding the member.
You must keep a medical records system that:
• Follows professional standards.
• Allows quick access of information.
• Provides legible information that is correctly documented and available to appropriate health care providers.
• Maintains confidentiality.
Have our member sign a Medical Record Release Form as a part of their medical record. Contact Network Management
Services, 1-877-670-8432, to request a copy of this form. The member should sign a Refusal Form when declining a
preventative screening referral.
Follow these confidentiality guidelines:
• Records that contain medical, clinical, social, financial or other data on a patient are treated as confidential. They must be
protected against loss, tampering, alteration, destruction or inadvertent disclosure.
• Release of information from your office requires that you have the patient sign a Medical Record Release Form that is
retained in the medical record.
• Release of records is in accordance with state and federal laws, including the Health Insurance Portability and Accountability
Act of 1996 (HIPAA).
• Records containing information on mental health services, substance use or potential chronic medical conditions that may
affect the member’s plan benefits are subject to additional specific waivers for release and confidentiality.
Exemption from release requirements
HIPAA regulations allow us to give PHI to government programs without member permission. This is given to determine
member eligibility.
Medical records requirements
You must ensure your medical records meet the standards described in this section. The following are expanded descriptions
of these requirements:
Patient Identifiers: Consist of the patient name and a second unique identifier; they should appear on each page of the
medical record.
Advance Directives: Provide the member with advance directive information and encourage them to retain a copy for their
personal records. Document this conversation at least once in the member’s medical record.
Biographical Information: Include the member’s name, date of birth, address, home and work phone numbers, marital status,
sex, primary language spoken, name and phone number of emergency contact, appropriate consent forms and guardianship
information, if relevant.
Signatures: For paper medical records, have all entries dated and signed or initialed by the author. Author identification may be
a handwritten signature or initials followed by the title (e.g., MD, DO, PA, ARNP, RN, LPN, MA or OM). There must be a written
policy requiring, and evidence of, physician co-signature for entries made by those other than a licensed physician (e.g., MD,
DO). Electronic signatures are acceptable for electronic medical records.
Family History: Document the family medical history no later than the first visit.
Past Medical History: Include a detailed medical, surgical and social history.
Immunizations: Include the date the vaccine was administered, the manufacturer and lot number and the name and title of the
person administering the vaccine. At a minimum, you must have members’ vaccination history.
Medication List: List the member’s current medications, with start and end dates, if applicable. Reconcile within 30 days after
inpatient admissions.
Referral Documentation: If a referral was made to a specialist, file the consultation report in the medical record. Include
documentation that the physician has discussed abnormal results with the member, along with recommendations.

Preferred Care Partners supplement
340
2023 UnitedHealthcare Care Provider Administrative Guide
Chart Organization: Maintain a uniform medical record system of clinical recording and reporting with respect to services,
which includes separate sections for progress notes and the results of diagnostic tests.
Preventive Screenings: Promote the appropriate use of age- or gender-specific preventive health services for members to
achieve a positive effect on the member’s health and better medical outcomes.
Required Encounter Documentation: For every visit, document the following:
• Date
• Chief complaint or purpose
• Objective findings
• Diagnosis or medical impression
• Studies ordered (lab, X-ray, etc.)
• Therapies administered or ordered
• Education provided; disposition, recommendations or instructions to the member and evidence of whether there was follow-
up
• Outcome of services
You must document that a written policy regarding follow-up care and written procedures for recording results of studies and
therapies and appropriate follow-up is in place.
We recommend that medical records include copies of care plans whenever you provide home health or skilled
nursing services.
Case management and disease management
program information
Optum provides Case Management (CM) and Disease Management (DM) services for Preferred Care Partners.
Here is the criteria for referrals to Optum CM and DM Programs:
• Complex Case Management — (Special Needs Plan [SNP] members only)
– 3 or more unplanned admissions and/or emergency room (ER) visits in the last 6 months
– Multiple, complex co-morbid conditions
– Coordination of multiple community resources/financial supports to cover basic services
• Heart Failure (HF) Disease Management Program
– Diagnosis of HF
– Has CHF on an inpatient claim
– HF admission in last 3 months
• Diabetes Disease Management Program
– Diabetic with A1C 9% or greater
– An inpatient admission related to diabetes in the past 12 months
– Two or more ER visits related to diabetes
• Advanced Illness Case Management — The primary goal is to facilitate and support end-of-life wishes and services
– Life expectancy of 12‒18 months
– Chronic, irreversible disease or conditions and declining health
– Reduce disease and symptom burden
• Transplant Case Management and Network Services
– Bone marrow/stem cell, including chimeric antigen receptor T-Cell (CAR-T) therapy for certain hematologic malignancies,
kidney and kidney/pancreas, heart, liver, intestinal, multi-organs and lung transplants
– Case management for 1 year post-transplant

Preferred Care Partners supplement
341
2023 UnitedHealthcare Care Provider Administrative Guide
• End-Stage Renal Disease Case Management — The member is diagnosed with end-stage renal disease and is undergoing
outpatient dialysis including in-center or home hemodialysis, home peritoneal dialysis, etc.
If the member does not qualify for one of these programs, they have 24/7, 365 days a year access to speak with a nurse by
calling the Optum NurseLine number on the back of their ID card.
Note: South Florida Preferred Care Partners no longer provides social worker evaluations without skilled services. Direct your
patient to their local social services department or the Florida State Department of Elder Affairs Help Line at 1-800-963-5337.
To request CM or DM services for one of our members, select only 1 program based on the program criteria that most closely
matches the member’s medical condition. Then submit the CM/DM referral form, available on mypreferredprovider.com, to
Behavioral health care programs
We work with Optum to provide behavioral health care services for our members. For more information on how to access the
behavioral health care programs, you or our members may contact a representative through the phone number listed on the
back of their health plan ID card.
Special needs plans
Special Needs Plans (SNP) Model of Care (MOC)
The MOC is the framework for care management processes and systems to help enable coordinated care for SNP members.
The MOC contains specific elements that delineate implementation, analysis and improvement of care.
These elements include a description of SNP population (including health conditions), Care Coordination, Provider Network
and Quality Measurement and Performance Improvement.
The MOC is a quality improvement tool, and MOC helps ensure the unique needs of our SNP members are identified and
addressed through care management practices. MOC goals are evaluated annually to determine effectiveness. To learn more,
contact us by email at: snp_moc_provider[email protected].
The Centers for Medicare and Medicaid (CMS) requires annual SNP MOC training for all health care providers who treat
SNP members. The Annual SNP MOC Provider Training is available at uhcprovider.com. We communicate updates about
the training requirements annually on uhcprovider.com/news. Learn more about provider news in Chapter 18: Provider
communication.
Risk management
Risk management addresses liability, both proactively and reactively. Proactive is avoiding or preventing risk. Reactive is
minimizing loss or damage after an adverse or bad event. Risk management in health care considers patient safety, quality
assurance and patients’ rights. The potential for risk is present in all aspects of health care, including medical mistakes,
electronic record-keeping, health care provider organizations and facility management.
An adverse event is defined as an event over which health care personnel could exercise control rather than as a result of the
member’s condition. Identifying something as an adverse event does not imply “error,” “negligence” or poor quality care. It
indicates that an undesirable clinical outcome resulted from some aspect of diagnosis or therapy, not an underlying disease
process. Adverse events interfere with a health care provider’s delivery of medical care and may result in litigation.
Agency for Healthcare Administration
The Florida Agency for Healthcare Administration (AHCA), as directed under F.S. 641 Parts I, II, III and other applicable state
laws, provides oversight and monitoring of health plans operating in the State of Florida as an HMO and their compliance to
applicable regulations.

Preferred Care Partners supplement
342
2023 UnitedHealthcare Care Provider Administrative Guide
This includes implementation of a Risk Management Program (RMP). The program helps identify, investigate, analyze and
evaluate actual or potential risk exposures by a state licensed risk manager. The RMP also corrects, reduces and eliminates
identifiable risks through instruction and training to staff and health care providers.
For more information, go to the AHCA website at ahca.myflorida.com.
Health care provider reporting responsibilities
You are required to report all adverse events as identified in previous sections, whether actual or potential. To report such
incidents, call 1-952-406-4806.
You must report incidents to AHCA within 24 hours of it happening. You must report all serious incidents, such as those listed,
immediately. This allows us to quickly access the risk and address liability. Examples of adverse and serious incidents include:
• Death or serious injury.
• Brain or spinal damage.
• Performance of a surgical procedure on the wrong patient.
• Performance of a wrong site surgical procedure.
• Performance of a wrong surgical procedure.
• Medically unnecessary surgical procedure.
• Surgical repair of damage from a planned surgical procedure.
• Removal of unplanned foreign object remaining from a surgical procedure.
Health care provider contracts include the obligation to participate in quality management inquiries upon request.
What are the responsibilities of physicians and health care providers?
You must report the ICD-10-CM diagnosis codes to the highest level of specificity and accuracy. This requires accurate and
complete medical record documentation. You are required to alert the MA organization of wrong information submitted.
You must follow the MA organization’s procedures for correcting information. Finally, you must report claims and encounter
information in a timely manner, generally within 30 days of the date of service (or discharge for hospital inpatient facilities).
Links to resources for the latest ICD guidelines and MRA resources are available online at mypreferredprovider.com.
CPT and HCPCS codes
The American Medical Association (AMA) and the CMS update procedure codes quarterly, with the largest volume effective
January 1 of each year. CPT and HCPCS codes may be added, deleted or revised to reflect changes in health care and
medical practices.
If a claim is submitted with an invalid or deleted procedure code, it will be denied or returned. A valid procedure code is
required for claims processing.
We encourage you to purchase current copies of CPT and HCPCS reference guides. You may access CPT, HCPCS and ICD-10
coding resources and materials at the American Medical Association’s website, ama-assn.org.

343
2023 UnitedHealthcare Care Provider Administrative Guide
River Valley Entities supplement
Information regarding the use of this supplement
This supplement applies to covered services rendered to River Valley entities members. This supplement does not apply to
Medicare Advantage, Medicaid or CHIP benefit plans.
It also applies to health care providers who have the following:
1. A UnitedHealthcare Agreement with one of the following:
– A reference to the River Valley or John Deere Health protocols or guides
– A direct contract with 1 or more River Valley entities that participate in River Valley entities networks
2. Located in Arkansas, Georgia, Iowa, Tennessee, Virginia, Wisconsin or the following Illinois counties: Jo Daviess,
Stephenson, Carroll, Ogle, Whiteside, Lee, Mercer, Rock Island, Henry, Bureau, Putnam, Henderson, Warren Knox, Stark,
Marshall, Livingston, Hancock, McDonough, Fulton, Peoria, Tazewell, Woodford, McLean.
The following River Valley entities sponsor, issue and administer River Valley benefit plans:
• UnitedHealthcare Services Company of the River Valley, Inc.
• UnitedHealthcare Plan of the River Valley, Inc.
• UnitedHealthcare Insurance Company of the River Valley, Inc.
The River Valley entity is listed on the front of the member’s ID card (bottom left).
Health care providers who are not subject to this supplement (including health care providers in Louisiana, North Carolina, Ohio
and South Carolina) may disregard this information. You may work with us when providing services to River Valley members in
the same way as you do when providing services to other UnitedHealthcare members.
For protocols, policies and procedures not specified in this supplement, refer to appropriate chapter in the main guide.
For policies and procedures relating to the TennCare®, Iowa Medicaid/hawk-i® and Secure Plus Complete Medicaid Plans®,
refer to the UnitedHealthcare Community Plan administrative guides available on uhcprovider.com/guides.
Eligibility
Call the number on the back of the member’s ID card to get information about a River Valley member, such as eligibility
information and claims status information.
Member ID cards
When members enroll, they get a new ID card with a member ID number. The phone number, website and claims address for
our core UnitedHealthcare systems are listed on the back. Refer to the section titled Health plan identification (ID) cards in
Chapter 2: Provider responsibilities and standards, for more information about ID cards.
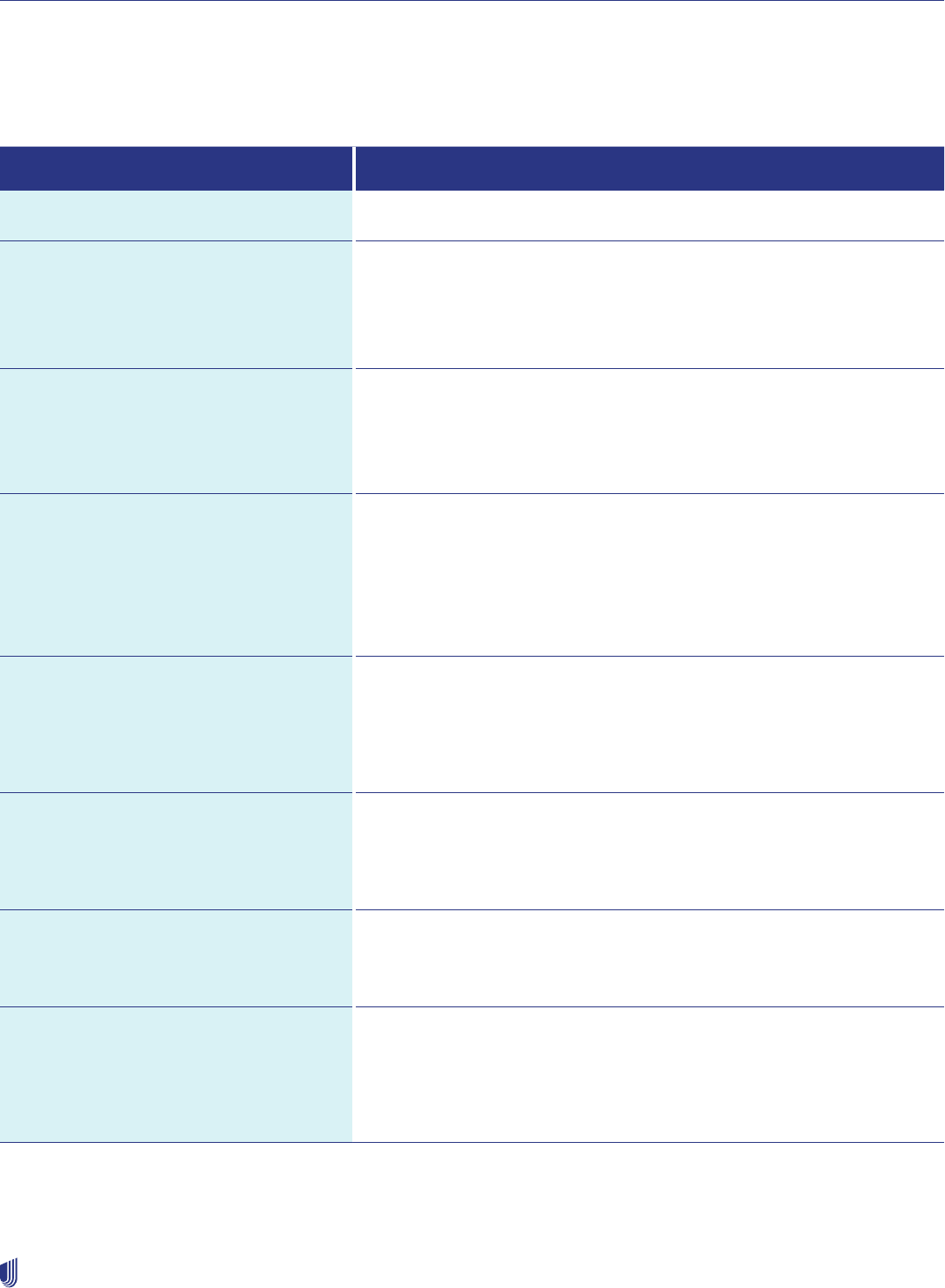
River Valley Entities supplement
344
2023 UnitedHealthcare Care Provider Administrative Guide
How to contact River Valley
Health care providers who practice in Illinois, Iowa and Wisconsin may refer to the “Midwest” references in the following grid.
Health care providers who practice in Arkansas, Georgia, Tennessee and Virginia may refer to the “Southeast” references in the
following grid.
Resource Where to go
UnitedHealthcare Provider Website uhcprovider.com
Cardiology
Diagnostic catheterization
Electrophysiology implants
Echocardiogram
Stress echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/cardiology
Phone: 1-866-889-8054
Case Management/UM
Initiate case management and UM
Congenital Heart Disease: Number on the back of the member’s ID card.
Kidney Resource Services: Number on the back of the member’s ID card.
Transplant Resource Services: Fax: 1-855-250-8157
Ventricular Assist Devices: Phone: 1-888-936-7246, option 2
Claims
(Information and submissions)
EDI: Medical claims payer ID: 87726
Dental claims payer ID: 95378
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In Then
select Claims & Payments from the menu.
Information: uhcprovider.com/claims (policies, instructions and tips)
Phone: 1-866-509-1593
Claims Reconsiderations and Appeals Online: uhcprovider.com > Sign In Then select Claims & Payments from the
menu.
Refer to the Claim reconsideration and appeals process section in
Chapter 10: Our claims process for more information, or:
Fax: 1-801-938-2100
Disease Management Phone: 1-800-369-2704, option 4
(Monday–Friday, 8 a.m.–4:30 p.m., CT)
Fax: 1-866-950-7759, Attn: CMT Coordinator
Email: MailW[email protected]
Electronic Data Interchange (EDI)
EDI Support
Online: uhcprovider.com/edi
Help: uhcprovider.com > Contact us > Technical Assistance
Phone: 1-800-842-1109 (Monday–Friday, 7 a.m.–9 p.m. CT)
Eligibility (Member) EDI: Transactions 270 (Inquiry) and 271 (Response)
through your vendor or clearinghouse
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In Then
select Eligibility from the menu.
Information: uhcprovider.com/eligibility
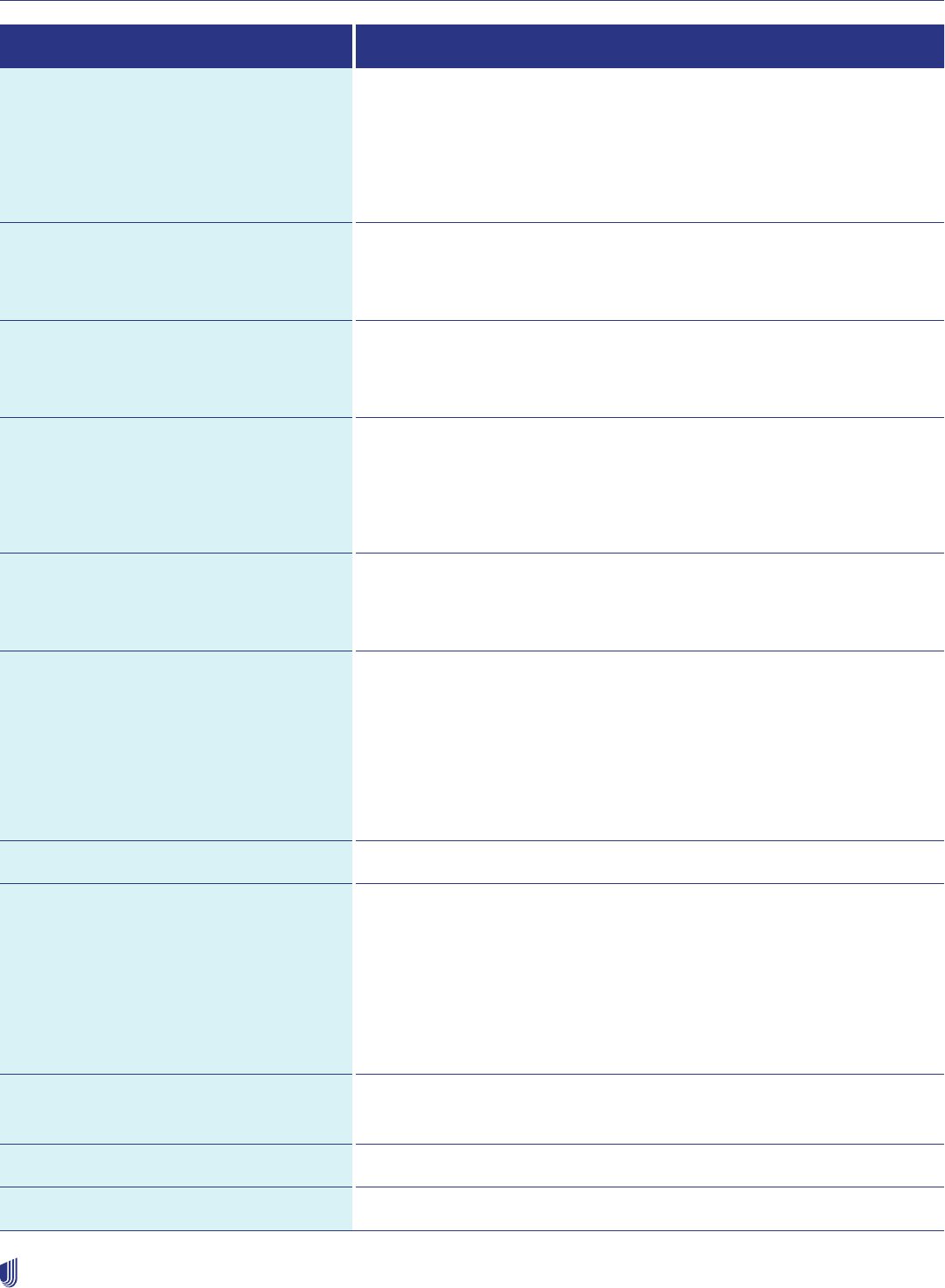
River Valley Entities supplement
345
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Eligibility for:
• End-of-life care
• Home health care
• Infusion services (prior authorizations)
Online: uhcprovider.com/paan
Phone: 1-877-842-3210
Mail: UnitedHealthcare
Attn: Clinical Coverage Review
1300 River Drive
Moline, IL 61265
Inpatient Admissions (notifications) EDI: Transactions 278N
Online: uhcprovider.com/paan
Phone: 1-877-842-3210
Mental Health/Substance Use
Vision
Transplant Services
Phone: 1-877-842-3210
Optum Pay Online:
• uhcprovider.com/optumpay
• optum.com/optumpay
• Optum Pay in the UnitedHealthcare Provider Portal
Help Desk: 1-877-620-6194
Pharmacy Services/Prescription Drugs
Requiring Preauthorization
Online: uhcprovider.com/pharmacy or professionals.optumrx.com
Phone OptumRx: 1-800-711-4555
Urgent Pharmacy Appeal Fax: 1-801-994-1058
Prior Authorization
Including preauthorization for certain
DME. See Cardiology, Radiology, Inpatient
Admissions and End-of-Life Care for specific
contact information
EDI: See EDI transactions and code sets on uhcprovider.com/edi.
We accept EDI 278 submissions directly to UnitedHealthcare or through a
clearinghouse.
Online: uhcprovider.com/paan
Phone: (Inpatient requests only) 1-877-842-3210, option 3, or the number on
the back of the member’s ID card
Information: uhcprovider.com/priorauth (policies, instructions and tips)
Appeals (Urgent) Fax: 1-801-994-1058 (urgent appeals only)
Radiology/Advanced Outpatient
Imaging Procedures:
CT scans
MRIs
MRAs
PET scans and nuclear medicine studies,
including nuclear cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/radiology
Phone: 1-866-889-8054
Skilled/Extended Care Online: uhcprovider.com/paan
Phone: 1-877-842-3210
United Voice Portal (Provider Services) Phone: 1-877-842-3210

River Valley Entities supplement
346
2023 UnitedHealthcare Care Provider Administrative Guide
Use the UnitedHealthcare Provider Portal at uhcprovider.com to perform secure transactions, check member eligibility and
benefits, and manage claims and prior authorization requests.
Reimbursement policies
Claim payment is subject to reimbursement policies on uhcprovider.com/policies > Commercial Policies > Reimbursement
Policies for Commercial. Claims Estimator tools are not available for River Valley members.
We will inform you of changes to these policies on uhcprovider.com/news.
Coding edits may also affect reimbursements. We apply coding edits based primarily on the NCCI edits developed by the
Centers for Medicare and Medicaid Services (CMS), as well as the CMS’ Outpatient Code Editor (OCE). You may find NCCI and
OCE edits on cms.gov > Medicare > Coding > National Correct Coding Initiative Edits.
Referrals
Network referrals
Primary Care Coordinator Plans (PCC Plans) do not require a referral.
Out-of-network referrals
An out-of-network referral means a written authorization provided by a participating health care provider and approved by us
for services to be received from a non-participating health care provider. Out-of-network referrals must be requested by the
member’s PCP. If an out-of-network referral is obtained, services received from a non-participating health care provider are
covered at a network level of benefits under the member’s benefit plan. An out-of-network referral is needed when services
are not available from a participating health care provider and may be needed for various services including, but not limited to,
podiatry, chiropractic and mental health/substance use services.
Out-of-network referral approval
A referral to an out-of-network provider must be approved by us before the services are rendered. We must also give prior
approval for modified or expired out-of-network referrals as described in this supplement. We may approve an out-of-network
referral when services are needed but not available from a participating health care provider. Prior approval of an out-of-network
referral is required for each follow-up visit unless we indicate otherwise. A medical director will review requests that do not meet
approval criteria.
In the case of emergencies, notify us the first business day following the referral.
Out-of-network referral process
To determine whether an out-of-network referral is necessary under a member’s benefit plan, contact us at the number on the
back of the member’s ID card.
Refer to the section Non-participating health care providers (all commercial plans), in Chapter 6: Referrals, for
more instructions.
• We will make decisions within the time frames required by state and federal law (including ERISA) and in accordance with
NCQA standards.
• We will send a letter confirming our approval or denial of a referral to the member and your office.
If a member requests approval after the fact, advise them this is against policy. Ask them to call 1-877-842-3210.
Participating health care providers may not refer their own family members to non-participating physicians/facilities due to
conflict of interest. If the health care provider denies a referral, the health care provider must refer the member to their benefit
document for any appeal rights, or have them call 1-877-842-3210.
River Valley Entities supplement
347
2023 UnitedHealthcare Care Provider Administrative Guide
Utilization Management (UM)
The term “prior authorization” is also referred to as “preauthorization.”
Our UM Program has several parts. These include but are not limited to:
• Preauthorization for various procedures, medical services, treatments, prescription drugs and DME.
• Review of the appropriateness of inpatient admissions and ongoing inpatient care coverage.
• Prior approval for referrals to non-participating health care providers, if applicable.
• Case management.
Our goal is to encourage the highest quality of care in the right place at the right time from the right health care provider.
Health care providers must cooperate with our UM program. You will allow us access, in the form we request, to data about
covered services provided to our members. You will allow us to collect data to conduct UM reviews and decisions.
Medical & drug policies and coverage determination guidelines
River Valley uses UnitedHealthcare’s Medical Policies, Medical Benefit Drug Policies, Coverage Determination Guidelines, and
Utilization Review Guidelines on uhcprovider.com/policies > Commercial Policies > Medical & Drug Policies and Coverage
Determination Guidelines for UnitedHealthcare Commercial Plans.
For more information refer to Medical & Drug Policies and Coverage Determination Guidelines for Commercial Members in
Chapter 7: Medical management.
Preauthorization
Services that require preauthorization
We require preauthorization for certain procedures, DME, prescription drugs and other services.
The list of services requiring preauthorization is available on uhcprovider.com/priorauth >
Advance Notification and Plan Requirement Resources > UnitedHealthcare of the River
Valley Advance Notification Procedure Codes.
Submit adequate clinical documentation
You must request preauthorization when required. Provide complete clinical information and supporting medical documentation
for each procedure, device, drug or service when you submit your request. That way, we may promptly determine whether the
services are covered and medically necessary. We consider additional information provided within the time period allowed for
review. However, delayed submissions increase administrative time.
Refer to our Medical & Drug Policies and Coverage Determination Guidelines for what information to provide.
How to request preauthorization
Refer to How to Contact River Valley in this supplement for how to submit a request for preauthorization.
If you do not get a required preauthorization, the claim may be denied. You may not bill the member for denied services.
Preauthorization review hours of operation
Staff may review your preauthorization requests Monday–Friday, 8 a.m.–4:30 p.m. CT. Medical directors are available to discuss
clinical policies or decisions by calling 1-877-842-3210. The office is closed for national holidays and the day after Thanksgiving.

River Valley Entities supplement
348
2023 UnitedHealthcare Care Provider Administrative Guide
Clinical review of a preauthorization request
When we receive a preauthorization request, our Clinical Coverage Review Department evaluates the information to determine
whether the procedures, devices, drugs or other services are medically necessary and appropriate. Our nursing staff makes
decisions to approve care based on specific criteria. Care and/or services that do not fall within the criteria are referred
to a medical director or other appropriate reviewer. This may include a board-certified specialty physician or a registered
pharmacist. Only physicians and other appropriate health care providers may issue a medical necessity denial.
River Valley’s staff and our delegates who make these decisions are not rewarded for denying coverage. We do not offer
incentives that encourage underutilization of care or services.
The treating physician has the ultimate authority for the member’s medical care. The medical management process does not
override this responsibility.
UM decisions
We make UM decisions within the time frames set by state and federal law (including ERISA). We make UM decisions in
accordance with National Committee for Quality Assurance (NCQA) standards.
We also tell health care providers and members our decisions according to applicable state and federal law, as well as to
NCQA standards and River Valley policy. Denial letters explain members’ applicable appeal rights, which may include the right
to an expedited and/or external review. They also explain the requirements for submitting an appeal and receiving a response.
A member may have a health care professional appeal a decision on their behalf. We require a copy of the member’s written
consent with the appeal.
Facility utilization review
Notification of inpatient admission required
Facilities must notify us of an inpatient admission within 24 hours of admission or on the next business day after a holiday or
weekend. We need the member’s name, ID number, admitting diagnosis and attending physician’s name.
Facilities are responsible for admission notification even if advance notification was provided by the physician and coverage
approval is on file.
Failure to notify
If the facility does not tell us about an admission as required, claims will be returned as not allowed. The facility may not bill the
member for the services. Retrospective reviews may be completed, and any approved services may be re-billed.
Inpatient review
Our UM activities include inpatient review. We usually begin our review on the first business day following admission. The
medical director and clinical staff review member hospitalizations for over- and under-utilization. Then they decide whether the
admission and continued stay are medically appropriate and align with evidence-based guidelines.
Where appropriate, River Valley also uses InterQual Care Guidelines. These are nationally recognized clinical guidelines that
help clinicians make informed decisions, on a case-by-case basis, in many health care settings. These settings include acute
and sub-acute medical, rehabilitation, SNF, home health care and ambulatory facilities. Other criteria may be used when
published peer-reviewed literature or guidelines are available from national specialty organizations that address the admission
or continued stay.
When the guidelines are not met, the medical director considers community resources and the availability of alternative care
settings. These include skilled facilities, sub-acute facilities or home care, and the ability of the facilities to provide all necessary
services within the estimated length of stay.
Inpatient review also helps us contribute to decisions about discharge planning and case management. In addition, we may
identify opportunities for quality improvement and cases appropriate for referral to one of our disease management programs.
If a nurse reviewer believes an admission or continued stay does not meet criteria, you may be asked for more information
about the treatment and case management plan. The nurse then refers the case to our medical director. If the medical

River Valley Entities supplement
349
2023 UnitedHealthcare Care Provider Administrative Guide
director determines an admission or continued stay at the facility, being managed by a participating physician, is not medically
necessary, we tell the facility and the health care provider.
You may speak with our medical director within 1 business day of the request. When decisions require expertise outside the
scope of the physician advisor, we have a board-certified physician of the relevant specialty (or similar specialty) review the
case. We use external independent review when we decide it is appropriate or by member request, according to applicable law.
Admission to rehabilitation units
We require prior authorization for admission for all rehabilitation confinements. We review them concurrently for continued
services. Refer to the Skilled/Extended Care row in the How to Contact River Valley section in this supplement for how to
submit a preauthorization request.
Admission to skilled nursing units
A member may require inpatient skilled nursing care due to acute illness, injury, surgery or exacerbation of a disease process.
• We require notification for all admissions to a SNF (or skilled level of care within an acute facility). Refer to How to Contact
River Valley in this supplement for how to submit a notification request.
• The facility must submit the care plan along with treatment goals, summary of services to be provided, expected length of
stay and discharge plan.
• We authorize admission consistent with the level of care required based on the treatment plan.
Concurrent review
• The skilled facility provider must provide appropriate documentation, including changes in the level of care.
• Approval for additional days of authorized coverage must be obtained before the authorization expires.
• Decisions about levels of care must consider not only the level of service but the member’s medical stability.
• Our medical director will speak with the physician managing the member in the skilled facility about disagreements
concerning the level of care required. The member or authorized representative may request an appeal when coverage is not
approved. We determine whether the admission, stay and care are covered and medically necessary based on the following
clinical guidelines, among others:
– Physicians must order services. The services must be necessary for treatment. They must align with the nature and severity
of the illness or injury, medical needs and accepted medical practice standards. The member must be stable. Clinical and
laboratory findings must have either improved or not changed for the last 24 hours. Diagnosis and initial treatment plan
must be established before admission. The services must be reasonable in terms of duration and quantity. The member
must require daily (i.e., available on a 24-hour basis, 7 days a week) skilled services. If skilled rehabilitation services are not
available on this basis, a member whose stay is based on the need for them would meet the daily basis requirement when
they need and receive those services at least 5 days a week. Skilled services, however, are required and provided at least 3
times per day. How often a service must be performed does not make it a skilled service.
– We consider the nature and complexity of a service and the skills required for safe and effective delivery when determining
whether a service is skilled. Skilled care requires trained medical personnel to frequently review the treatment plan for a
limited time. It ends when a condition is stabilized or a predetermined treatment plan is completed. Skilled care moves the
member to functional independence.
Observation
Observation helps health care providers determine whether a member needs to be admitted to a hospital. It may be needed to
monitor or diagnose a condition when testing or treatment exceeds usual outpatient care. Observation is used when physicians
need 48 hours or less to determine a member’s condition. In some cases, more than 48 hours may be necessary. Members
may be admitted when a condition is diagnosed requiring a long-term stay (e.g., acute MI). This condition may involve long-term
treatment or further monitoring (e.g., persistent severe asthma).

River Valley Entities supplement
350
2023 UnitedHealthcare Care Provider Administrative Guide
Notice of termination of inpatient benefits
We may determine that an admission, continued hospital stay, rehabilitation unit or SNF are not covered. These reasons include
but are not limited to:
• A medical director determines an admission or continued stay, which was not preapproved at an out-of-network facility, is not
medically necessary at the facility’s level of care.
• Preauthorization was not obtained for a procedure or service that needed it.
• A medical director determines the member’s condition is custodial and is not covered.
• A medical director, upon consulting with the attending physician, determines continued acute inpatient rehabilitation/SNF
level of care is no longer medically necessary, but the member refuses discharge.
• The member has used all inpatient or skilled care benefits under their benefit plan. If a non-coverage determination is made,
we provide written notification to the physician, the member and facility that day.
Services obtained outside the River Valley service area
• We process treatment authorizations as directed by you and the OOA attending physician.
• With you and the OOA attending physician, we coordinate a member’s transfer back to the service area when medically
feasible and appropriate.
• We cover OOA urgent or emergent stabilization services according to the member’s benefit plan. This includes the time they
are stabilized in the emergency room before admission as an inpatient and are discharged.
• We cover post-stabilization care services.
• We cover OOA inpatient services until the member is stable enough to be transferred to a participating hospital. Transfers
should happen within 48 hours of that point. Payment for preventive or non-emergent/urgent services performed outside the
network varies by benefit plan. Determinations on benefit coverage may include but are not limited to non-covered, covered at
a lower benefit level or covered at the network level with a referral. Call Member Services if you have questions.
Special requirements DME
Preauthorization is required for some DME. Refer to the How to Contact River Valley section of this supplement for how to
submit a preauthorization request.
Subject to the noted exceptions, members must get all DME, orthotics, prosthetics and supply items from a contracted vendor.
If an item is not available from a contracted vendor, whether or not preauthorization is required, you must get an out-of-network
referral. Otherwise, payment will be denied unless the member has an out-of-network DME benefit.
Note: Even when medically necessary, certain items (e.g., orthotic devices) may not be covered. Others (e.g., prosthetic
devices) may be subject to benefits limits.
Contact Member Services for information about a member’s plan and preauthorization requirements.
Prescription drugs
We require preauthorization for some prescription drugs. Refer to the How to Contact River Valley section of this supplement
for how to submit a preauthorization request
Some drugs have special rules and require special management services. These include drugs with therapy prerequisites,
quantity limitations and/or multiple copays.
• If you order and/or administer any medication that requires preauthorization or clinical management services, you may need
to get those medications from a participating specialty pharmacy unless we authorize a non-specialty pharmacy.
• Certain drugs are available in quantities up to 90- or 100-day supplies, depending on plan benefit design. A list of drugs on
the 3-month supply list is on uhcprovider.com/pharmacy.
• River Valley’s PDL is on uhcprovider.com/pharmacy.
Not all drugs on a PDL are covered under the pharmacy benefit.

River Valley Entities supplement
351
2023 UnitedHealthcare Care Provider Administrative Guide
Sleep studies to diagnose sleep apnea and other sleep disorders
We require preauthorization for laboratory-assisted and polysomnography treatment. We also require it for the site of service
(e.g., sleep lab v. portable home monitoring).
Home health care (including home infusion services)
• We require preauthorization for home health care. This may include home infusion services.
• If requested services are required after business hours, notify us within 24 hours or the next business day following a holiday
or weekend. Include the member’s name, ID number, diagnosis, the attending physician’s name and requested services.
• If you do not notify us, we will deny your claim. You may not bill the member for the service.
Assisted reproduction program
Most River Valley benefit plans exclude coverage for infertility evaluation or treatment. Some employer groups have a variation
or rider to cover these services. Some states, however, require fertility treatment coverage for some groups. Refer to How to
Contact River Valley section of this supplement for preauthorization contact information.
Transplants
• We require preauthorization for transplants. Call the Optum transplant case manager at 1-888-936-7246. They will request
medical records to see whether the transplant is appropriate for a member. We send all information to a physician expert in
the related transplantation field for review.
• If authorized, the case manager coordinates referrals and helps select a transplant center based on the member’s needs.
They also provide information about our transplant management program.
• If a transplant candidate needs home care or is involved with a participating center, the transplant care manager will arrange
service.
• Any post-transplant lab or pathology that cannot be performed or interpreted by a network physician may be sent to the
transplant center for interpretation. Tell the transplant case manager if you need help making arrangements. Most of these
services are covered under the transplant contract. The transplant center should be involved in the member’s continuing care.
Post-transplant care
• We require preauthorization for all follow-up care. Make requests using the standard River Valley preauthorization process.
• One year after the transplant, members are transferred to their local physician for any other needed care
management services.
End-of-life care
Some members have end-of-life care benefits, which may include hospice services. These services require preauthorization.
Approved care is coordinated by our care managers.
Claims process
EDI
Use EDI to submit claims and conduct other business with us electronically. To enroll, call EDI customer service at 1-866-509-
1593, or email RVI[email protected].
Claims Transmission
Tell your office software vendor that you want to begin transmitting electronic claims to the River Valley payer ID 87726 for
medical claims and 95378 for dental.
We receive all claims through our clearinghouse, OptumInsight. The clearinghouse sets up claims as commercial. Your
EDI software vendor must establish connectivity to the clearinghouse. They can make sure you meet the requirements to
transmit claims.

River Valley Entities supplement
352
2023 UnitedHealthcare Care Provider Administrative Guide
EDI acknowledgment and status reports
Your software vendor will give you a report showing an electronic claim left your office. It does not confirm we or the
clearinghouse received or accepted the claim.
Clearinghouse acknowledgment reports show the status of your claims. They are given to you after each transmission. This lets
you confirm whether a claim reached us, was rejected because of an error or needed additional information.
We will also send you status reports providing more data on claims. These include copies of EOBs/remittance advice and
denial letters that may request more information.
Carefully review all vendor reports, clearinghouse acknowledgment reports and the River Valley status reports when you
receive them.
Electronic claims submission and billing
We require you to submit claims electronically. For electronic claims submission requirements, refer to Requirements for
complete claims and encounter data submission section in Chapter 10: Our claims process.
Share this document with your software vendor. We update the Companion Guide regularly, so review it to help ensure you have
the most current information about our requirements.
For more information about electronic claims, refer to uhcprovider.com/claims.
Special rules for electronic submission
• Corrected Claims must include the words “corrected claims” in the notes field. Your software vendor may help you with
correct placement of all notes.
• Unlisted Procedure Code Claims must include details in the notes field. If you cannot, you must submit a paper claim.
• Claims for Occupational Therapy, Speech Therapy, Physical Therapy, Dialysis and Mental Health or Substance Use
Services must have the date of service by line item. We do not accept span dates for these types of claims.
• Secondary COB Claims must include the following fields:
– Institutional: Payer Prior Payment, Medicare Total Paid Amount, Total Non-Covered Amount, Total Denied Amount.
– Professional: Payer-Paid Amount, Line Level Allowed Amount, Patient Responsibility, Line Level Discount Amount
(contractual discount amount of other payer), Patient-Paid Amount (amount that the payer paid to the member, not the
health care provider).
– Dental: Payer Paid Amount, Patient Responsibility Amount, Discount Amount, Patient Paid Amount.
– Span Dates: We require exact dates of service when the claim spans a period of time. Put the dates in Box 24 of
the CMS 1500, Box 45 of the UB-04, or the Remarks field. This will prevent the need for an itemized bill and allow
electronic submission.
Requirements for claims reporting revenue codes
• We require the exact dates of service for all claims reporting revenue codes.
• If you submit revenue code 270 by itself on an institutional claim for outpatient services, we require a valid CPT or HCPCS
code or description.
• If you report revenue code 274, describe the services or include a valid CPT or HCPCS code.
• We require an itemized statement for claims with revenue codes 250-259 if the charges exceed $1,000.
• All claims reporting the revenue codes on the following list require you to report the appropriate CPT and HCPCS codes.
Revenue Codes Requiring CPT® and HCPCS Codes
260 IV Therapy (General Classification)
261 Infusion Pump
262 IV Therapy/Pharmacy Services
Revenue Codes Requiring CPT® and HCPCS Codes
263 IV Therapy/Drug/Supply Delivery
264 IV Therapy/Supplies
269 Other IV Therapy
290 DME (other than renal) (General Classification)
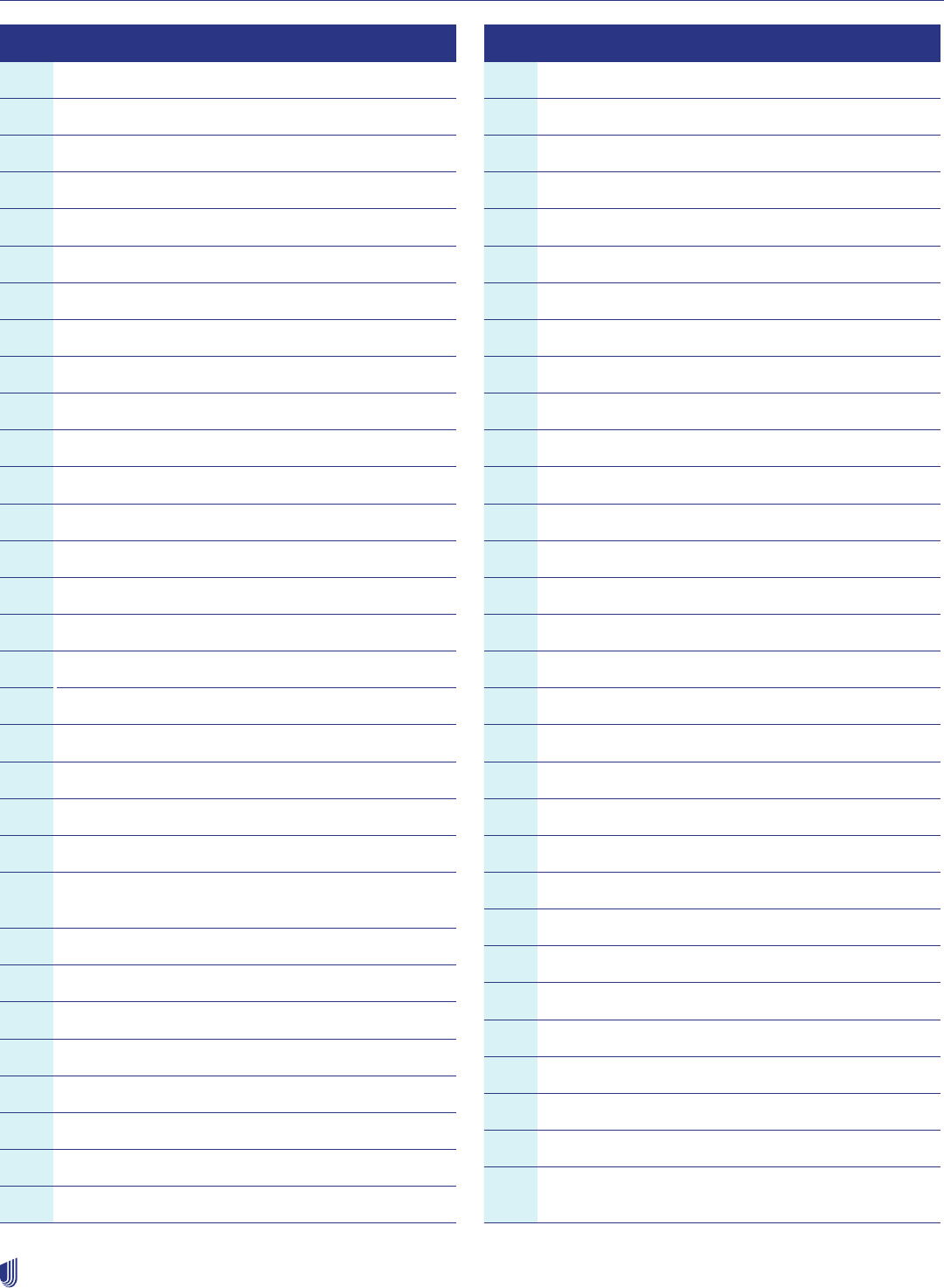
River Valley Entities supplement
353
2023 UnitedHealthcare Care Provider Administrative Guide
Revenue Codes Requiring CPT® and HCPCS Codes
291 DME/Rental
292 Purchase of New DME
293 Purchase of Used DME
300 Laboratory (General Classification)
301 Chemistry
302 Immunology
303 Renal Patient (Home)
304 Non-Routine Dialysis
305 Hematology
306 Bacteriology & Microbiology
307 Urology
309 Other Laboratory
310 Laboratory-Pathology (General Classification)
311 Cytology
312 Histology
319 Other Laboratory Pathological
320 Radiology-Diagnostic (General Classification)
321 Angiocardiography
322 Arthrography
323 Arteriography
324 Chest X-Ray
329 Other Radiology-Diagnostic
330 Radiology-Therapeutic and/or Chemotherapy
Administration (General Classification)
331 Chemotherapy Administration-Injected
332 Chemotherapy Administration-Oral
333 Radiation Therapy
335 Chemotherapy Administration-IV
339 Other Radiology-Therapeutic
340 Nuclear Medicine (General Classification)
341 Diagnostic Procedures
342 Therapeutic Procedures
Revenue Codes Requiring CPT® and HCPCS Codes
350 CT Scan (General Classification)
351 CT-Head Scan
352 CT-Body Scan
359 CT-Other
360 Operating Room Services (General Classification)
361 Minor Surgery
362 Organ Transplant-Other Than Kidney
367 Kidney Transplant
369 Other Operating Room Services
400 Other Imaging Services (General Classification)
401 Diagnostic Mammography
402 Ultrasound
403 Screening Mammography
404 Positron Emission Tomography
409 Other Imaging Services
410 Respiratory Services (General)
412 Inhalation Services
419 Other Respiratory Services
460 Pulmonary Function (General Classification)
469 Other-Pulmonary Function
470 Audiology (General Classification)
471 Audiology/Diagnostic
472 Audiology/Treatment
480 Cardiology (General Classification)
481 Cardiac Cath Lab
482 Stress Test
483 Echocardiology
489 Other Cardiology
490 Ambulatory Surgical Care (General Classification)
499 Other Ambulatory Surgical Care
610 Magnetic Resonance Technology (MRT) (General
Classification)
River Valley Entities supplement
354
2023 UnitedHealthcare Care Provider Administrative Guide
Revenue Codes Requiring CPT® and HCPCS Codes
611 Magnetic Resonance Imaging (MRI)-Brain/Brain
Stem
612 MRI-Spinal Cord/Spine
614 MRI-Other
615 Magnetic Resonance Anglogram (MRA)-Head and
Neck
616 MRA-Lower Extremities
618 MRA Other
618 Other MRT
623 Surgical Dressing
624 FDA Investigational Devices
634 Erythropoietin (EPO) < 10,000 units
635 Erythropoietin (EPO) > 10,000 units
636 Drugs Requiring Detail Coding
730 EKG/ECG (Electrocardiogram) (General
Classification)
731 Holter Monitor
732 Telemetry
Revenue Codes Requiring CPT® and HCPCS Codes
739 Other EKG/ECG
740 EEG (Electroencephalogram) (General
Classification)
750 Gastro-Intestinal (GI) Services (General
Classification)
790 Extra-Corporeal Shock Wave Therapy (formerly
Lithotripsy) (General Classification)
921 Peripheral Vascular Lab
922 Electromyogram
923 Pap Smear
924 Allergy Test
925 Pregnancy Test
929 Additional Diagnostic Services
940 Other Therapeutic Services (General
Classification)
941 Recreational Therapy
942 Education/Training (Diabetic Education)
949 Other Therapeutic Services (HRSA-approved
weight loss providers)
Claim reconsideration and appeals process and resolving disputes
Refer to Claim reconsideration and appeals process in Chapter 10: Our claims process and in the How to Contact River
Valley section of this supplement.
If you have a question about a pre-service appeal, see Pre-Service Appeals in Chapter 7: Medical management.
355
2023 UnitedHealthcare Care Provider Administrative Guide
UMR supplement
Applicability of this supplement
UMR is a wholly owned subsidiary of UnitedHealthcare, a part of UnitedHealth Group. UMR is a third-party administrator (TPA)
and not an insurance company.UMR delivers solutions for self-funded employer groups to ensure claims are paid correctly
according to the member’s benefit plan. In addition to offering self-funded employer groups access to the UnitedHealthcare
networks, UMR is a full-service TPA with a range of capabilities and solutions from medical claim administration to stop
loss coverage and pharmacy benefits administration, to proprietary care management and wellness programs. UMR has a
proprietary claims platform with dedicated customer service.
UnitedHealthcare Shared Services (UHSS) is a unique service model that allows plan sponsors who self-administer their benefit
plans or already have a TPA, to access the UnitedHealthcare network and clinical programs. UHSS is NOT a leased network
arrangement. It is a partnership between the customer/plan administrator and UnitedHealthcare designed to meet the needs of
the customer and member.
You are subject to both the UnitedHealthcare Care Provider Administrative Guide and this UMR supplement. This supplement
supersedes the main guide if there is conflicting information. If there are additional protocols, policies or procedures online, we
will direct you to that location when applicable. For protocols, policies and procedures not referenced in this supplement, refer
to the appropriate chapter in the main guide.
How to contact UMR
Contact Area Where to Go
Claims, Benefits, and Eligibility Online: umr.com
Phone: Call the number listed on the back of the member ID card or call
1-877-233-1800
Mail: Use the address listed on the back of the member ID card
For UHSS:
Contact information is listed on the back of the member ID card
Appeals (Pre-service) Fax: 1-888-615-6584
Mail:
UHC Appeals - CARE
P.O. Box 400046
San Antonio, TX 78229
Online: umr.com
For UHSS:
Mail:
P.O. Box 30783
Salt Lake City, UT 84130-0783
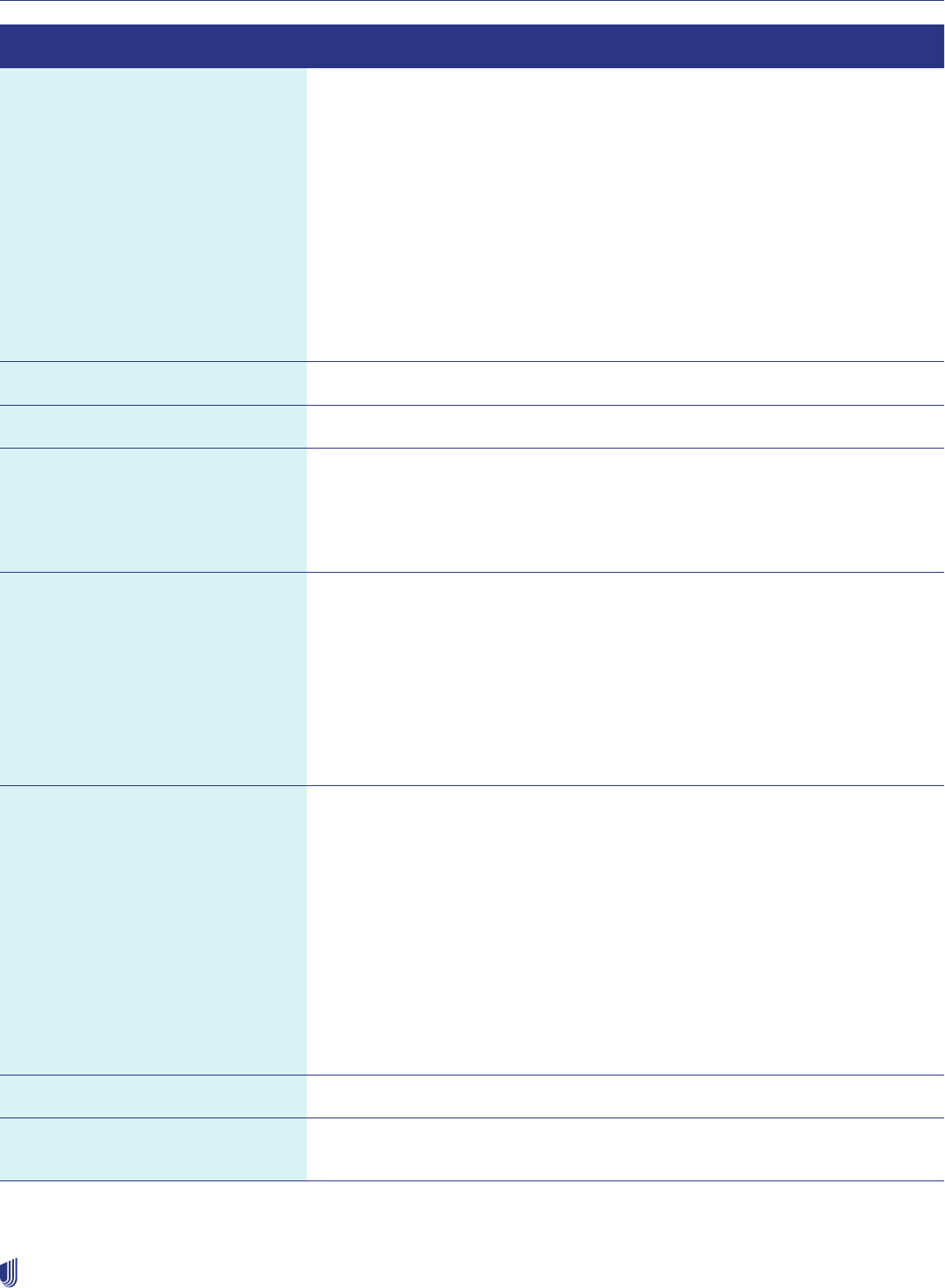
UMR supplement
356
2023 UnitedHealthcare Care Provider Administrative Guide
Contact Area Where to Go
Reconsiderations and Appeals
(Post-Service)
Fax: 1-877-291-3248
Mail:
UMR- Claim Appeals
P.O. Box 30546
Salt Lake City, UT 84130-0546
(or send to the address listed on the provider ERA)
Online: umr.com
Phone: Call the number listed on the back of the member ID card
For UHSS:
Mail:
P.O. Box 30783
Salt Lake City, UT 84130-0783
Electronic Data Interchange (EDI) See the back of the member ID card for the payer ID
Forms Online: umr.com
Prior Authorization (Request for
clinical decision, including inpatient
admission notification, advance
notification or medical specialty
injectable drug/medication)
Prior Authorization serviced by UMR
Online: umr.com
Fax: 1-866-912-8464
Phone: Call the number listed on the back of the member ID card
Pre-determination Fax: 1-877-442-1102
Mail:
UMR
P.O. Box 8023
Wausau, WI 54402-8023
For Overnight Mail Delivery:
UMR
115 W. Wausau Avenue
Wausau, WI 54401
Overpayment/Refund Regular Mail:
UMR
P.O. Box 30541
Salt Lake City, UT 84130-0541
Overnight Mail:
UMR
P.O. Box 8033
115 W Wausau Ave
Wausau, WI 54402
For UHSS:
UHSS
P.O. Box 30783
Salt Lake City, UT 84130-0783
Pharmacy or Specialty Pharmacy Phone: Call the number listed on the back of the member ID card
Online Technical Support
for umr.com
Phone: 1-866-922-8266
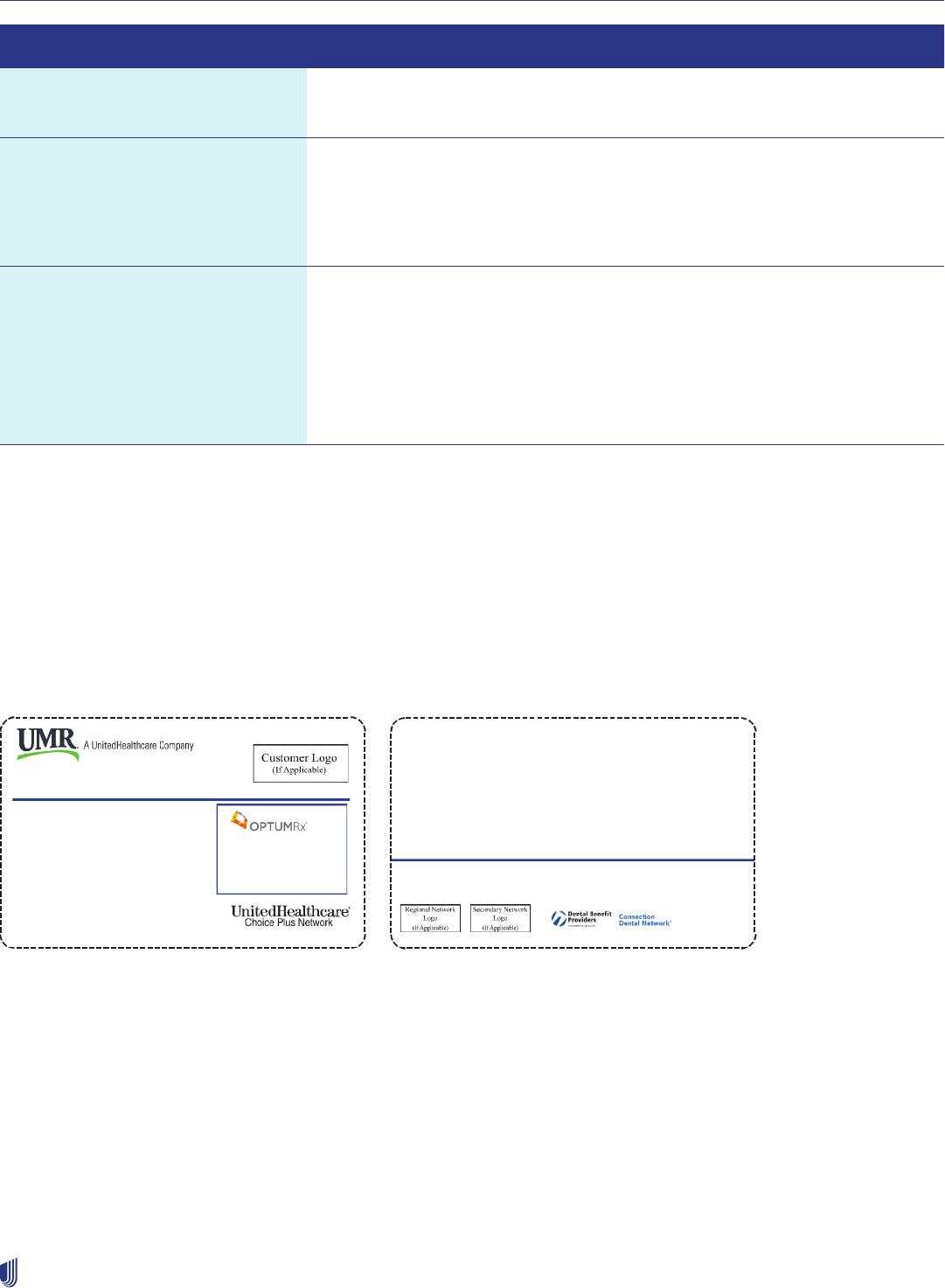
UMR supplement
357
2023 UnitedHealthcare Care Provider Administrative Guide
Contact Area Where to Go
Medical Record Submission Fax: Use fax number noted on the UMR medical record request letter
Mail: Use mailing address noted on the UMR medical record request letter
UnitedHealthcare Provider Pricing
and Participation Disputes
Phone: 1-844-598-7538
Mail:
UMR United Provider Advocacy Team
P.O. Box 30546
Salt Lake City, UT 84130-0546
Electronic Funds Transfer (EFT)
Vendors
Optum Financial Health
Help Desk: 1-877-620-6194
Online: optumbank.com
Zelis
Help Desk: 1-877-828-8770
Online: zelis.com
Health plan identification cards
Our members receive health plan identification (ID) cards that include information necessary for you to submit claims, such as
the payer ID for electronic claims submission. Information on the cards may vary by health benefit plan.
Check the member’s ID card at each visit. You may keep a copy of both sides of the ID card for your records. Having a health
plan ID card is not proof of eligibility and is not considered a guarantee of benefits.
UMR ID card sample
The primary network(s) can be found on the front of the ID card.
The member ID cards do not specify what service requires prior notification. However, they include information to begin the
notification process. (See previous sample ID card.) The care management vendor phone number is on the back of the ID card.
Use this number to initiate authorization and notification.
Prior authorization and notification requirements
UMR prior authorization capabilities are not available on uhcprovider.com. Instead, you can reference the How to contact
UMR section in this supplement for tools and resources.
Issuer (80840) 911-39026-02
Member ID: Group Number:
Member:
Rx BIN:
Rx PCN:
Rx GRP:
610127
CO-PAYS MAY APPLY
0730
01960000
0196XXXX
Self-funded plan administered by UMR
YOUR COMPANY NAME HERE
12345684 76-123456
JAMES A SAMPLE 00 MED DEN
INTENTIONALLY BLANK
03122 9977091 0000 0000001 0000001 082 9 117 03122 9977091 0000 0000001 0000001 082 9 117
RUN_DATE 20220323 14:56:41DATA_SEQ_NO 0000001CLIENT_NUMBER 003122UHG_TYPE DIG2SHRTDOC_ID DOC_SEQ_ID 0000001NAME SAMPLE ,JAMESMAILSET_NUMBER 0000001CUSTCPS_KEY1 1234568412345684_KEY0 CARD2CUSTCPS_KEY2 76123456CUSTCPS_KEY3 JAMESCUSTCPS_KEY4 UMR/MedicalCUSTCPS_KEY5 00CUSTCPS_KEY6 20220101CUSTCPS_KEY7 12345684~00CARD2CUSTCPS_KEY8 12345684CUSTCPS_KEY9 12345684~00CARD2
This card must be presented each time services are requested. Printed: 10-27-2021
Call UMR CARE at 866-494-4502 for plan required prior authorization.
FAILURE TO CALL FOR PRIOR AUTHORIZATION MAY REDUCE BENEFITS.
For Members: www.umr.com 8XX-XXX-XXXX
Nurseline: 8XX-XXX-XXXX
For Providers: www.umr.com 877-233-1800
Claims: EDI # 39026, UMR, PO Box 30541, Salt Lake City, UT 84130-0541
Pharmacists & Members: 877-559-2955
Medical: In-Net Out of Net
Ded: $750* $1,500
OOPM:
*includes pharmacy
$3,000* $6,000
Shipper ID: 00000000 Insert #1 Insert #2
Shipping Method: 2ND DAY Insert #3 Insert #4
CARRIER: UPS Insert #5 Insert #6
Address: Insert #7 Insert #8
TO: UMR
Insert #9 Insert #10
Insert #11 Insert #12
ATTN: KELLY PETERSON
115 W WAUSAU AVE
Cycle Date: 20220323
WAUSAU, WI 54401
PDF Date: Wed Mar 23, 2022 @ 14:56:41
MaxMover: N
Mailing/Meter Date: UHG JOB ID: 8100 GRP: 76123456 PV: 001 RC: EMP MKT:
MT: 00 SA: 90 OI: 02 FORM: K2H000 CPAY: PKG ID:
DALE BROWN: N LETTER NM: LETTER2 DIVISION : CARD TYPE:
TEMPLATE: TPA C30 : FAMILY T07 : 2SHRT
SORT HCN:
Issuer (80840) 911-39026-02
Member ID: Group Number:
Member:
Rx BIN:
Rx PCN:
Rx GRP:
610127
CO-PAYS MAY APPLY
0730
01960000
0196XXXX
Self-funded plan administered by UMR
YOUR COMPANY NAME HERE
12345684 76-123456
JAMES A SAMPLE 00 MED DEN
INTENTIONALLY BLANK
03122 9977091 0000 0000001 0000001 082 9 117 03122 9977091 0000 0000001 0000001 082 9 117
RUN_DATE 20220323 14:56:41DATA_SEQ_NO 0000001CLIENT_NUMBER 003122UHG_TYPE DIG2SHRTDOC_ID DOC_SEQ_ID 0000001NAME SAMPLE ,JAMESMAILSET_NUMBER 0000001CUSTCPS_KEY1 1234568412345684_KEY0 CARD2CUSTCPS_KEY2 76123456CUSTCPS_KEY3 JAMESCUSTCPS_KEY4 UMR/MedicalCUSTCPS_KEY5 00CUSTCPS_KEY6 20220101CUSTCPS_KEY7 12345684~00CARD2CUSTCPS_KEY8 12345684CUSTCPS_KEY9 12345684~00CARD2
This card must be presented each time services are requested. Printed: 10-27-2021
Call UMR CARE at 866-494-4502 for plan required prior authorization.
FAILURE TO CALL FOR PRIOR AUTHORIZATION MAY REDUCE BENEFITS.
For Members: www.umr.com 8XX-XXX-XXXX
Nurseline: 8XX-XXX-XXXX
For Providers: www.umr.com 877-233-1800
Claims: EDI # 39026, UMR, PO Box 30541, Salt Lake City, UT 84130-0541
Pharmacists & Members: 877-559-2955
Medical: In-Net Out of Net
Ded: $750* $1,500
OOPM:
*includes pharmacy
$3,000* $6,000
Shipper ID: 00000000 Insert #1 Insert #2
Shipping Method: 2ND DAY Insert #3 Insert #4
CARRIER: UPS Insert #5 Insert #6
Address: Insert #7 Insert #8
TO: UMR
Insert #9 Insert #10
Insert #11 Insert #12
ATTN: KELLY PETERSON
115 W WAUSAU AVE
Cycle Date: 20220323
WAUSAU, WI 54401
PDF Date: Wed Mar 23, 2022 @ 14:56:41
MaxMover: N
Mailing/Meter Date: UHG JOB ID: 8100 GRP: 76123456 PV: 001 RC: EMP MKT:
MT: 00 SA: 90 OI: 02 FORM: K2H000 CPAY: PKG ID:
DALE BROWN: N LETTER NM: LETTER2 DIVISION : CARD TYPE:
TEMPLATE: TPA C30 : FAMILY T07 : 2SHRT
SORT HCN:

UMR supplement
358
2023 UnitedHealthcare Care Provider Administrative Guide
We may refer to the terms “preauthorization,” “prior authorization” or “precertification” in the supplement and in our resources.
These terms are used interchangeably.
Advance notification/prior authorization lists
Services requiring advance notification and prior authorization vary by plan and can change. Services requiring prior
authorization require a clinical coverage review based on medical necessity.
Advance notification/prior authorization lists are available at umr.com through a lookup feature best used in the Google
Chrome web browser. You can view the most up-to-date plan-specific requirements. You must have the member’s ID card to
obtain accurate information.
How to submit advance notification or prior authorization requests
UnitedHealthcare’s prior authorization and notification (PAAN) tool does not access UMR membership. Instead, you may submit
an advance notification or prior authorization in 1 of 3 ways, all of which require the member’s ID card:
• Online: umr.com
– Watch this training for more information about online capabilities.
– After submitting a request online, you will receive a confirmation email with a transaction reference number. This is not
a determination. Once we process your request, you will receive a status email with the request reference number. You
can then login and view the status of your request using the member ID number and selecting “Transactions” from the
Welcome menu.
• Fax: 1-866-912-8464
• Phone: Call the number listed on the back of the member ID card.
– After submitting a request by fax or phone, you will be given a request reference number. This is not a determination. When
we make a coverage decision, we will issue the decision under the same request number.
Clinical request forms
Some clinical requests for predetermination or prior authorization (i.e., spinal surgery or genetic testing) require specific forms
that you must submit with the request. Find clinical request forms at umr.com > Provider > Find a Form.
Clinical trials, experimental or investigational services
Evaluations, tests and consultations coverage varies by plan. You must confirm benefit eligibility by calling the number on the
back of the member ID card.
Pharmacy and specialty pharmacy benefits
Pharmacy and specialty pharmacy vendors vary by UMR customer. You must confirm benefit eligibility by calling the number on
the back of the member ID card. Coverage may be available under the medical benefit plan or the pharmacy benefit plan.
Specific protocols
Benefits vary by UMR customer. For example, non-emergent ambulance transportation may not have the same protocols to
determine coverage. You must confirm the benefit eligibility by calling the number on the back of the member ID card.
UMR supplement
359
2023 UnitedHealthcare Care Provider Administrative Guide
Our claims process
UMR/UHSS claims, benefits and eligibility are not available on uhcprovider.com. Refer to the How to contact UMR section of
the UMR supplement for tools and resources.
UMR
• Online: umr.com
• Phone: Call the number listed on the back of the member ID card or dial 1-877-233-1800.
• Mail: Use the address listed on the back of the member ID card.
For UHSS
Contact information is listed on the back of the member ID card.
Overpayments for UMR
If we inform you of an overpaid claim that you do not disagree with, send us the refund check within 30 calendar days (or as
required by your Agreement) from the date of notification.
We may apply the overpayment against future claim payments, unless your Agreement states otherwise. If an overpayment is
eligible for recoupment, UMR will attempt to recoup the overpayment for 120 days. If recoupment is unsuccessful, there is no
activity within 120 days, or the customer and/or health care provider opted out of the recoupment process, the overpayment will
be sent to Payment Resolution Solutions for recovery assistance. In some situations, we may handle overpayment recoveries
internally, or the customer may use their own overpayment vendor for recoveries. If you identify an overpaid claim, send the
refund along with the Overpayment Refund/Notification Form to the following address:
UMR
P.O. Box 30541
Salt Lake City, UT 84130-0541
For overpayment questions, call 1-877-233-1800 or the customer service number listed on the back of the member ID card.
Claim reconsideration and appeals process
If you disagree with the outcome of a processed claim (payment, correction or denial), you can complete the Claim
Reconsideration Request Form and check “Previously denied/closed for additional information” as your reason for request.
Include the following information on the form to prevent processing delays:
• Member name
• Member ID number
• Date of service/claim information
• Provider name, address and TIN
• All supporting materials to the request, including member-specific treatment plans or clinical records (The decision is based
on the materials you provide.)
UMR
Online: umr.com > Provider > Provider Submission > Claim Appeals. Follow prompts for submitting the inquiry.
Fax: 1-877-291-3248
Mail:
UMR- Claim Appeals
P.O. Box 30546
Salt Lake City, UT 84130-0546
(or send to the address listed on the provider RA)
Phone: Call the number listed on the back of the member ID card.

UMR supplement
360
2023 UnitedHealthcare Care Provider Administrative Guide
For UHSS
Mail:
UHSS
P.O. Box 30783
Salt Lake City, UT 84130-0783
Health and disease management
Care management programs (CARE) vary by UMR customer. Locate a list of a member’s programs at umr.com using the
information on the member ID card.
Frequently asked questions
What are the timely filing requirements for UMR?
Timely filing requirements are determined by the self-funded customer, as well as the provider-contracted timely filing
provisions. You must file the claim within the timely filing limit, or it may be denied. If you dispute a claim that was denied due
to timely filing, you must submit proof that you filed the claim within the timely filing limits. Timely filing limits can vary based on
your contract and/or the self-funded benefit plan.
What are the major differences between customer benefit plans serviced by UMR?
Our process is similar to UnitedHealthcare. As a TPA, we work to customize the health care needs of the customer. Differences
are the types of services selected as part of the administration, the level of benefits at which covered services are processed
and the services covered. Examples of services available include medical and dental claim administration, FSA, PBM, stop loss
carriers, vision plans, care management, case management, utilization management and disease management.
Can I access a list of UMR denial codes and definitions?
We use the American National Standards Institute (ANSI) denial codes and definitions.
If I mistakenly call UnitedHealthcare customer service for UMR-related issues, will they
transfer me to the correct service agent?
We have a dedicated customer service line. UnitedHealthcare cannot transfer these calls.
What is the customer service number for physicians, facilities and other care professionals to
call for eligibility, benefits and follow-up on claim issues?
Our Interactive Voice Response (IVR) system number is 1-877-233-1800. The IVR system offers information through faxback. If
you have additional questions, the faxback contains a passcode and number to call to speak with a representative.
Visit umr.com to access claim information and obtain the phone number and passcode, which will allow you to speak with
a representative.
How do I obtain a passcode on umr.com to speak with a representative?
1. Log into umr.com > Enter the member ID number > Select the family member > Select summary view > Select search >
Click search.
2. Go to “Need additional information on this member?” > Click on “provider service center.” The passcode will be provided.
3. Call 1-877-233-1800, follow the prompts and enter the passcode to speak with a representative.
UMR supplement
361
2023 UnitedHealthcare Care Provider Administrative Guide
How do health care providers working with UMR members access online resources?
Go to umr.com. On the first visit, you will need to register your tax identification number (TIN). The website is an efficient way
to check claim status, obtain benefits and much more. Be sure all TINs used are registered. If you have trouble registering, call
Technical Support at 1-866-922-8266.
Note: This is a secure website for UMR member claim and benefit information.
What forms are available on umr.com?
• Preauthorization
• Dental claim
• Electronic remittance advice (ERA)
• Itemized statement
• UMR post-service appeal request
• Various clinical request forms
If we only have a member’s Social Security Number, can we verify member
information online?
You can search using the member’s Social Security Number, and the results will include the member’s unique health plan ID
number. Due to HIPAA requirements, we will not show the Social Security Number online.
Can UMR Customer First Representatives make claim adjustments over the phone?
UMR Customer First Representatives (CFRs) can address claim adjustments over the phone, depending on the claim details.
CFRs cannot change a claim if inappropriate modifiers or CPT/HCPCS codes are listed. Such issues require a resubmission of
the claim with corrected codes from the servicing health care provider. CFRs cannot advise you on how to bill.
How do I know what network the member uses?
The primary network(s) are listed on the front of the member’s ID card.
How can I check claim status?
Visit umr.com or call 1-877-233-1800.
If a payment is not received, how can I request a check tracer?
We can initiate the check tracer process 30 days after the check was issued. After the check tracer has been initiated, we work
with the employer group to verify if the check has been cashed. This process can take up to an additional 30 days.
A claim denied for medical records. What are the next steps?
Return the letter request with the medical records. This will help ensure the records are routed to the correct department for
review and prevent any potential delays. Do not re-submit the original claim with the medical records.
At UMR, claims are denied for additional information (not pended).
Medical records can be submitted using the following 3 options:
• Online: umr.com
• Fax: Use the fax number noted on the request letter.
• Mail: Use the mailing address noted on the request letter.

UMR supplement
362
2023 UnitedHealthcare Care Provider Administrative Guide
What should I do if a claim was denied as a duplicate to a Medicaid claim?
Medicaid is responsible to bill UMR for reimbursement of what was previously paid to you.
If Medicaid returns the UMR payment, we can reconsider your claim at that time. Our customer plan provisions will apply.
Where can I go on the website to display refund tracking?
Log into umr.com > Click “refund tracking” under myMenu > Enter financial control number (FCN).
All FCNs must be 11 digits long. The FCN is located on the remittance advice.
If a health care provider did not receive a remit with the paper check, what should they do?
Log into umr.com > Select Advanced claims under myMenu > Select Check number > Enter the 10 digit check number > Enter
the group number > Click Search.
The results will show all claims paid on the given check. You can call the customer service number on the back of the ID card to
request a copy or the remit sent to them.
What happens if a health care provider switched delivery from paper to electronic or wants to
keep both options?
UMR will keep the provider on dual delivery of paper and electronic for 6 months.
If the provider would like to stop the dual delivery, log into umr.com > Provider > Find a Form and select the electronic paper
remittance advices request form.
Electronic Funds Transfer/Electronic Remittance Advice
Electronic funds transfer (EFT) enrollment does not guarantee that all payments coming from UMR will be sent using this
electronic option. EFT approval must also be received from UMR customer groups. UMR is a TPA paying claims from each
customer’s bank account.
Note: There is no charge to the provider to enroll in the EFT/electronic remittance advance (ERA) process.
When UMR processes a claim, the check/EFT issue date will determine the date that the funds are sent to the electronic
vendor. The electronic vendor will make a deposit into the provider’s account. This is typically 3-7 days after UMR sends the
funds to the electronic vendor.
Important: The customer chooses which day of the week/month to release payment.
363
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare FlexWork™ supplement
Applicability of this supplement
You are subject to both the main guide and this supplement. This supplement controls if it conflicts with information in the main
guide. If there are additional protocols, policies or procedures online, you will be directed to that location. Refer to the main
guide for anything not found in this supplement.
How to contact FlexWork™
Group Numbers 928276, 924699*
*(Does not require prior authorization)
Resource Where to go Requirements and Notes
Cardiology
Diagnostic Catheterization,
Electrophysiology Implants, Echocardiogram
and Stress Echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/
cardiology
Phone: 1-866-889-8054
Request prior authorization
for services as described in
the Outpatient cardiology
notification/prior authorization
protocol section of Chapter 7:
Medical management
Claims Submission Online: UnitedHealthcare Provider
Portal at uhcprovider.com > Sign In.
Then select Claims & Payment from
the menu > Submit a Claim.
Payer ID: 81400
Paper Claims Submission: Mail to
the address listed on the back of the
member’s ID Card.
Information: uhcprovider.com/
claims
Genetic and Molecular Testing Online: uhcprovider.com/priorauth
and select the specialty you need.
Outpatient Injectable Chemotherapy and
Related Cancer Therapies
Online: uhcprovider.com/priorauth >
Oncology
Phone: 1-888-397-8129
Policies and instructions
Pharmacy Services Prior Authorizations:
1-800-711-4555
Benefit Information:
Call the number on the back of the ID
Card.
For information on the PDL,
myallsaversconnect.com
Prior Authorization and Notification Online: uhcprovider.com/paan
Information: uhcprovider.com/
priorauth (policies and instructions)
Phone: 1-800-999-3404
Prior authorization and admission
notification is required as
described in Chapter 7: Medical
management.
EDI 278A transactions are not
available.

UnitedHealthcare FlexWork™ supplement
364
2023 UnitedHealthcare Care Provider Administrative Guide
Radiology/Advanced Outpatient Imaging
Procedures:
CT scans, MRIs, MRAs, PET scans and
nuclear medicine studies, including nuclear
cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/
radiology
Phone: 1-866-889-8054
Request prior authorization for
services as described in the
Outpatient radiology notification/
prior authorization protocol
section of Chapter 7: Medical
management
Health plan ID card
UnitedHealthcare FlexWork™ members receive health plan ID cards with information that helps you to submit claims. The cards
list the claims address, copayment information and phone numbers.
A sample ID card and more information is in the Health plan identification (ID) cards section in Chapter 2.
Our claims process
Follow these steps for fast payment:
1. Notify UnitedHealthcare FlexWork™.
2. Prepare a complete and accurate claim form.
3. For UnitedHealthcare FlexWork™ members, submit electronic claims using payer ID number 81400. Submit paper claims to
the address on the member’s ID card.
4. For contracted health care providers who submit electronic claims and would like to receive electronic payments and
statements, call Optum Financial Services Customer Service line at 1-877-620-6194 or visit optumbank.com > Partners >
Providers.
Claim reimbursement (adjustments)
If you think your claim was processed incorrectly, call the number on the member’s ID card. If you find a claim where you were
overpaid, send us the overpayment within 30 calendar days. If we find a claim was overpaid, payment is due within 30 calendar
days.
If you disagree with our decision regarding a claim adjustment, you may appeal.
Claim reconsideration, appeals and disputes
Claim reconsideration does not apply to some states based on applicable state legislation (e.g., Arizona, California, Colorado,
New Jersey or Texas). For states with applicable legislation, any request for dispute will follow the state specific process.
There is a 2-step process available for review of your concern. Step 1 is a claim reconsideration. If you disagree with the
outcome of the claim reconsideration, you may request a claim appeal (step 2).
How to submit your reconsideration or appeal
If you disagree with claim payment issues, overpayment recoveries, pharmacy, medical management disputes, contractual
issues or the outcome of your reconsideration review, send a letter requesting a review to:
Grievance Administrator
P.O. Box 31265
Salt Lake City, UT 84131-0371
Standard Fax: 1-801-994-1416
Phone: 1-800-291-2634

UnitedHealthcare FlexWork™ supplement
365
2023 UnitedHealthcare Care Provider Administrative Guide
If you feel the situation is urgent, request an expedited appeal by phone, fax or writing:
Grievance Administrator
2020 Innovation Dr
DePere, WI 54115
Expedited Fax: 1-866-654-6323
Phone: 1-800-291-2634
Time frame
You must submit your claim reconsideration and/or appeal to us within 12 months (or as required by law or your Agreement),
from the date of the original EOB or denial. The 2-step process allows for a total of 12 months for timely submission, not 12
months for step 1 and 12 months for step 2.
What to submit
As the health care provider of service, you submit the dispute with the following information:
• Member’s name and health plan ID number
• Claim number
• Specific item in dispute
• Clear rationale/reason for contesting the determination and an explanation why the claim should be paid or approved.
If you disagree with the outcome of the claim appeal, you may file for an arbitration proceeding (a description of this process is
in your Agreement.)
Refer to Claim reconsideration and appeals process section in Chapter 10: Our claims process for more information.
Notice to Texas care providers
To verify UnitedHealthcare FlexWork™ members’ benefits, call the number on the back of the member’s ID card.
UnitedHealthcare FlexWork™ uses tools developed by third parties, such as InterQual Care Guidelines, to help manage health
benefits and to assist clinicians in making informed decisions.
As an affiliate of UnitedHealthcare, UnitedHealthcare FlexWork™ may also use UnitedHealthcare’s medical policies as
guidance. These policies are available on uhcprovider.com/policies.
Notification does not guarantee coverage or payment (unless mandated by law). We determine the member’s eligibility. For
benefit or coverage information, call the phone number on the back of the member’s ID card.
Michigan law regarding diabetes
Michigan law requires us to provide coverage for some diabetic expenses. It also requires us to establish and provide a program
to help prevent the onset of clinical diabetes. We have adopted the American Diabetes Association (ADA) Clinical Practice
Guidelines.
The program focuses on best practices to help prevent the onset of clinical diabetes and to treat diabetes, including, but not
limited to, diet, lifestyle, physical exercise and fitness, and early diagnosis and treatment. Find the Standards of Medical Care in
Diabetes and Clinical Practice Recommendations at diabetesjournals.org/care.
Subscription information for the American Diabetes Journals is available on the previous website or by calling 1-800-232-3472,
8:30 a.m. - 8 p.m. ET, Monday–Friday. Journal articles are available without a subscription at the previous website.
366
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare Level Funded supplement
Applicability of this supplement
You are subject to both the main guide and this supplement. This supplement controls if it conflicts with information in the main
guide. If there are additional protocols, policies or procedures online, you will be directed to that location. Refer to the main
guide for anything not found in this supplement.
How to contact us
Resource Where to go Requirements and Notes
Cardiology
Diagnostic Catheterization,
Electrophysiology Implants, Echocardiogram
and Stress Echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/
cardiology
Phone: 1-866-889-8054
Request prior authorization
for services as described in
the Outpatient cardiology
notification/prior authorization
protocol section of Chapter 7:
Medical management
Claims Submission Online: UnitedHealthcare Provider
Portal at uhcprovider.com > Sign In.
Then select Claims & Payment from
the menu > Submit a Claim.
Payer ID: 87726
Information: uhcprovider.com/
claims
Genetic and Molecular Testing Online: uhcprovider.com/priorauth
and select the specialty you need.
Outpatient Injectable Chemotherapy and
Related Cancer Therapies
Online: uhcprovider.com/priorauth >
Oncology
Phone: 1-888-397-8129
Policies and instructions
Pharmacy Services Prior Authorizations:
1-800-711-4555
Benefit Information:
Call the number on the back of the ID
card.
For information on the PDL,
myallsaversconnect.com
Prior Authorization and Notification Online: uhcprovider.com/paan
Information: uhcprovider.com/
priorauth (policies and instructions)
Phone: 1-800-999-3404
Prior authorization and admission
notification is required as
described in Chapter 7: Medical
management.
EDI 278A transactions are not
available.
Radiology/Advanced Outpatient Imaging
Procedures:
CT scans, MRIs, MRAs, PET scans and
nuclear medicine studies, including nuclear
cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/
radiology
Phone: 1-866-889-8054
Request prior authorization for
services as described in the
Outpatient radiology notification/
prior authorization protocol
section of Chapter 7: Medical
management

UnitedHealthcare Level Funded supplement
367
2023 UnitedHealthcare Care Provider Administrative Guide
Our claims process
Follow these steps for fast payment:
1. Notify UnitedHealthcare Level Funded.
2. Prepare a complete and accurate claim form.
3. For UnitedHealthcare Level Funded members, submit electronic claims using payer ID number 87726.
4. For contracted health care providers who submit electronic claims and would like to receive electronic payments and
statements, call Optum Financial Services Customer Service line at 1-877-620-6194 or visit optumbank.com > Partners >
Providers.
Claim reimbursement (adjustments)
If you think your claim was processed incorrectly, call the number on the ID card. If you find a claim where you were overpaid,
send us the overpayment within 30 calendar days. If we find a claim was overpaid, payment is due within 30 calendar days.
If you disagree with our decision regarding a claim adjustment, you may appeal.
Claim reconsideration, appeals and disputes
Claim reconsideration does not apply to some states based on applicable state legislation (e.g., Arizona, California, Colorado,
New Jersey or Texas). For states with applicable legislation, any request for dispute will follow the state specific process.
There is a 2-step process available for review of your concern. Step 1 is a claim reconsideration. If you disagree with the
outcome of the claim reconsideration, you may request a claim appeal (step 2).
How to submit your reconsideration or appeal
Claims payment issues or outcome of a reconsideration review
If you disagree with claim payment issues or the outcome of your reconsideration review, submit your request using our
electronic tools:
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In.
API: Submit reconsiderations and appeals (with attachments) using API. Go to uhcprovider.com/api for more information.
Overpayment recoveries, pharmacy, medical management disputes, or contractual issues
If you disagree with overpayment recoveries, pharmacy, medical management disputes, or contractual issues, send a letter
requesting a review to:
UnitedHealthcare Level Funded members:
Grievance Administrator
P.O. Box 31393
Salt Lake City, UT 84131-0371
Fax: 1-801-994-1416
Time frame
You must submit your claim reconsideration and/or appeal to us within 12 months (or as required by law or your Agreement),
from the date of the original EOB or denial. The 2-step process allows for a total of 12 months for timely submission, not 12
months for step 1 and 12 months for step 2.
What to submit
As the health care provider of service, you submit the dispute with the following information:
• Member’s name and health plan ID number
• Claim number

UnitedHealthcare Level Funded supplement
368
2023 UnitedHealthcare Care Provider Administrative Guide
• Specific item in dispute
• Clear rationale/reason for contesting the determination and an explanation why the claim should be paid or approved If you
disagree with the outcome of the claim appeal, you may file for an arbitration proceeding (a description of this process is in
your Agreement)
Refer to Claim reconsideration and appeals process section in Chapter 10: Our claims process for more information.
369
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare West supplement
Applicability of this supplement
This supplement is intended for use by physicians, health care professionals, facilities, ancillary health care providers and their
respective staff when seeing non-capitated or non-delegated members in their respective state. Unless otherwise specified, any
references to UnitedHealthcare West in this supplement are intended to apply to any or all of the following entities and benefit
plans. This information is subject to change.
Capitation is a payment arrangement for health care providers. If you have a capitation Agreement with us, you are paid a
set amount for each member assigned to you, whether or not that person seeks care. If you have a UnitedHealthcare West
capitation Agreement with us, refer to the Capitation and/or Delegation Supplement of the guide as this supplement does not
apply to you.
Health care providers who participate in the listed benefit plans are subject to both the main guide and this supplement. This
supplement controls if it conflicts with information in the main guide. If there are additional protocols, policies or procedures
online, you will be directed to that location when applicable. For protocols, policies and procedures not referenced in this
supplement, refer to appropriate chapter in the main guide.
You may identify a UnitedHealthcare West member by a reference to “WEST” on the back of their ID card. Information may vary
in appearance or location on the card due to unique benefit plan requirements.
You may see more detailed information on ID cards and a sample health plan ID card, in the section titled Health plan
identification (ID) cards in Chapter 2: Provider responsibilities and standards. You may see a sample ID card image specific
to the member when you verify eligibility and benefits in the UnitedHealthcare Provider Portal.
Benefit plans referenced in this supplement
We offer a wide range of products and services for employer groups, families and individual members. Benefit plan availability
may vary. Contact us for more information about benefit plan availability and service areas where each of these products and
supplemental benefits are available.
State Products Offered Benefits Plans
Arizona Medicare Advantage
(MA)
AARP® Medicare Advantage
UnitedHealthcare® Chronic Complete (Chronic SNP)
UnitedHealthcare® Group Medicare Advantage (HMO)
California Commercial and MA Commercial:
UnitedHealthcare SignatureValue® family of products including but not limited to:
• UnitedHealthcare SignatureValue
• UnitedHealthcare SignatureValue Advantage
• UnitedHealthcare SignatureValue VEBA
• UnitedHealthcare SignatureValue Alliance
• UnitedHealthcare SignatureValue Flex
• UnitedHealthcare SignatureValue Focus
• UnitedHealthcare SignatureValue Harmony
UnitedHealthcare West supplement
370
2023 UnitedHealthcare Care Provider Administrative Guide
State Products Offered Benefits Plans
California
(continued)
Commercial and MA Medicare:
• AARP® Medicare Advantage Focus
• AARP® Medicare Advantage Freedom Plus
• AARP® Medicare Advantage Harmony
• AARP® Medicare Advantage Patriot
• AARP® Medicare Advantage Rebate
• AARP® Medicare Advantage SecureHorizons®
• AARP® Medicare Advantage SecureHorizons® Focus
• AARP® Medicare Advantage SecureHorizons® Premier
• AARP® Medicare Advantage SecureHorizons® Value
• Sharp® SecureHorizons® Plan by UnitedHealthcare®
• Sharp® Walgreens® by UnitedHealthcare®
• UnitedHealthcare® Canopy Health Medicare Advantage
• UnitedHealthcare® Chronic Complete (Chronic SNP)
• UnitedHealthcare® Chronic Complete Focus (Chronic SNP)
• UnitedHealthcare® Group Medicare Advantage (HMO)
• UnitedHealthcare® Medicare Advantage Assure
California Commercial UnitedHealthcare Core Essential
SM
Refer to the main guide for regulations, processes and contact information
Colorado MA AARP® Medicare Advantage
AARP® Medicare Advantage Patriot
AARP® Medicare Advantage SecureHorizons®
UnitedHealthcare® Chronic Complete (Chronic SNP)
UnitedHealthcare® Chronic Complete Focus (Chronic SNP)
UnitedHealthcare® Group Medicare Advantage (HMO)
Nevada MA UnitedHealthcare® Group Medicare Advantage (HMO)
Oklahoma Commercial UnitedHealthcare SignatureValue®
Oregon Commercial and MA Commercial:
UnitedHealthcare SignatureValue®
Medicare:
AARP® Medicare Advantage
UnitedHealthcare® Group Medicare Advantage (HMO)
UnitedHealthcare West supplement
371
2023 UnitedHealthcare Care Provider Administrative Guide
State Products Offered Benefits Plans
Texas Commercial and MA Commercial:
UnitedHealthcare SignatureValue®
Medicare:
AARP® Medicare Advantage
AARP® Medicare Advantage Patriot
AARP® Medicare Advantage SecureHorizons®
UnitedHealthcare® Chronic Complete (Chronic SNP)
UnitedHealthcare Dual Complete® (Dual SNP)
UnitedHealthcare® Group Medicare Advantage (HMO)
UnitedHealthcare® Medicare Advantage Ally (Chronic SNP)
Washington Commercial and MA Commercial:
UnitedHealthcare® SignatureValue®
Medicare:
AARP® Medicare Advantage
AARP® Medicare Advantage Walgreens
UnitedHealthcare® Group Medicare Advantage (HMO)
Commercial products
Commercial benefit plans consist of Health Maintenance Organizations (HMOs) or Managed Care Organizations (MCOs).
Members access health services through a network primary care physician (PCP). PCPs manage the member’s medical
history and individual needs. HMOs/MCOs offer minimal paperwork and low, predictable out-of-pocket costs. Members pay a
predetermined copayment or a percentage copayment each time they receive health care services.
MA products
Refer to Chapter 5: Medicare products for a description of Medicare Advantage (MA) products offered. You may see a
complete list of health plans on uhcprovider.com/plans.
Administrative services are provided by the following affiliated companies: UnitedHealthcare Services, Inc., OptumRx or
OptumHealth Care Solutions, LLC.
Behavioral health products are provided by U.S. Behavioral Health Plan. California is doing business as OptumHealth Behavioral
Solutions of California or United Behavioral Health operating under the brand Optum.
Special Needs Plans (SNP) Model of Care (MOC)
The MOC is the framework for care management processes and systems to help enable coordinated care for SNP members.
The MOC contains specific elements that delineate implementation, analysis and improvement of care.
These elements include a description of SNP population (including health conditions), care coordination, provider network and
quality measurement, and performance improvement.
The MOC is a quality improvement tool, and MOC helps ensure the unique needs of our SNP members are Identified and
addressed through care management practices. MOC goals are evaluated annually to determine effectiveness. To learn more,
contact us by email at [email protected]. The Centers for Medicare & Medicaid Services (CMS) requires
annual SNP MOC training for all health care providers who treat SNP members. The annual SNP MOC Provider Training is
available at uhcprovider.com. We communicate updates about the training annually on uhcprovider.com/news. Learn more
about provider news in Chapter 18: Provider communication.
UnitedHealthcare West supplement
372
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare West information regarding our health
care provider website
This supplement is located at uhcprovider.com, our health care provider website. Visit uhcprovider.com/news for the latest
updates. Certain health care providers will also receive notices by mail, where required by state law.
To access the UnitedHealthcare Provider Portal online solutions, go to uhcprovider.com and click Sign In in the upper
right corner. Sign in with your One Healthcare ID. Information on all available tools is on uhcprovider.com > Resources > The
UnitedHealthcare Provider Portal resources. We offer several live webinar options; information and registration is available on
uhcprovider.com/training.
A One Healthcare ID is required to access the UnitedHealthcare Provider Portal and perform online transactions, such as
eligibility verification, claims status, claims reconsideration, referrals and prior authorizations. To get a One Healthcare ID, go to
uhcprovider.com/access to register for UnitedHealthcare Provider Portal.
For help with the UnitedHealthcare Provider Portal, contact UnitedHealthcare Web Support at providertechsupport@uhc.
com or 1-866-842-3278, option 1, Monday–Friday 9 a.m. – 11 p.m. Central Time (CT).
How to contact UnitedHealthcare West resources
Resource Where to go
Helpful Health Plan Service
Phone Numbers
uhcprovider.com > Contact us > Health Plans Support by State.
Benefit Interpretation Policies and
Medical Management Guidelines
Online:
Benefit Interpretation Policies: uhcprovider.com/policies > For Commercial Plans >
UnitedHealthcare West Benefit Interpretation Policies
Medical Management Guidelines: uhcprovider.com/policies > For Commercial
Plans > UnitedHealthcare West Medical Management Guidelines
Provider Website uhcprovider.com
Preauthorization EDI: Transaction 278
Online: uhcprovider.com/paan
Arizona and Colorado Medicare Advantage Phone: 1-800-746-7405
California, Oregon and Washington: SignatureValue, Medicare Advantage, direct
contract network and medical group/IPA carve-out
Phone: 1-800-762-8456
Texas: Medicare Advantage, Signature Value
Oklahoma: SignatureValue Inpatient Notification/Utilization Management
Phone: 1-800-668-8139
To view the most current and complete Advance Notification List, including
procedure codes and associated services, go to uhcprovider.com/priorauth.
Radiology/Advanced Outpatient
Imaging Procedures
CT scans, MRIs, MRAs, PET scans
and nuclear medicine studies,
including nuclear cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/radiology
Phone: 1-866-889-8054
Request prior authorization of radiology services as described in Outpatient
radiology notification/prior authorization protocol in Chapter 7:
Medical management.
UnitedHealthcare West supplement
373
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Cardiology
Diagnostic Catheterization,
Electrophysiology Implants,
Echocardiogram and Stress
Echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/cardiology
Phone: 1-866-889-8054
Request prior authorization of cardiology services as described in Outpatient
cardiology notification/prior authorization protocol in Chapter 7:
Medical management.
Hospital Inpatient Notification
(Non-delegated) Inpatient includes:
Acute Inpatient, Skilled Nursing
Admission, Long-Term Acute Care,
Inpatient Rehabilitation Places
of Service
EDI: Transaction 278N
Online: uhcprovider.com/paan
Phone: 1-800-799-5252
Mental Health (Medicare Advantage): 1-800-508-0088
Transplant
Phone: 1-866-300-7736 Fax: 1-888-361-0502
EDI Support
Encounter Collection, Submission
and Controls, including
ERA/835 transactions
Password and user ID are not required to review and access EDI information on
uhcprovider.com.
Online:
uhcprovider.com/edi > EDI Contacts > EDI Transaction Support Form
Phone: 1-800-842-1109 (For UnitedHealthcare West ERA/835 questions, select
option 4 and then option 2)
Email: suppor[email protected]
Payer IDs: UnitedHealthcare West encounters, 95958.
For claims, the payer ID is 87726.
For a complete list of payer IDs, refer to the Claims Payer List.
Eligibility EDI: Transactions 270 (Inquiry) and 271 (Response) through your vendor
or clearinghouse
Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In > Eligibility
Information: uhcprovider.com/eligibility
United Voice Portal
(Follow prompts to
access information)
Commercial and Medicare Advantage HMO/MCO:
California: 1-800-542-8789
Arizona (MA)/Colorado (MA)/Nevada (MA Group only): 1-888-866-8297
Oklahoma (Commercial)/Texas (Commercial, MA): 1-877-847-2862
Oregon: 1-800-920-9202
Washington MCO: 1-800-213-7356
UnitedHealthcare West supplement
374
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go
Standard Commercial Member
Appeals
(Applies only to Commercial
UnitedHealthcare Signature Value
HMO/MCO)
California, Oklahoma, Oregon, Texas, Washington
Mail:
Mailstop CA124-0160
P.O. Box 6107
Cypress, CA 90630
Phone:
California: 1-800-624-8822
Oklahoma/Texas: 1-800-825-9355
Oregon/Washington: 1-800-932-3004
Fax: 1-866-704-3420
Medicare Advantage
Member Appeals
Mailstop CA124-0157
P.O. Box 6106
Cypress, CA 90630
Fax: 1-888-517-7113
uhc.com/medicare
Expedited Commercial
Member Appeals
(Applies only to Commercial
UnitedHealthcare SignatureValue
HMO/MCO)
California, Oklahoma, Oregon, Texas, Washington
Phone: 1-888-277-4232
Fax: 1-800-346-0930
Urgent Clinical Appeals
(Medical or pharmacy appeals)
Fax: 1-800-346-0930
Pharmacy Services Commercial products: uhcprovider.com
uhcprovider.com/specialtyrx
uhcprovider.com/pharmacy
Medicare products: uhc.com/medicare > Shop For a Plan > Medicare
Prescription Drug Plans
Phone: 1-855-812-4301
Mental Health/Substance Use,
Vision or Transplant Services
See ID card for carrier information and contact numbers.
View the ID card when you verify eligibility on uhcprovider.com.
California Language Assistance
Program
(Applies only to commercial products
in California)
Online: uhcprovider.com > scroll to the very bottom > Language assistance
Phone: 1-800-752-6096
Health Management and Disease
Management Programs
Phone: 1-877-840-4085
Fax completed referral form to: 1-877-406-8212

UnitedHealthcare West supplement
375
2023 UnitedHealthcare Care Provider Administrative Guide
Health care provider responsibilities
Electronic Data Interchange
The fastest way for us to talk is electronically. Electronic Data Interchange (EDI) is the preferred method for doing business
transactions. Find more information on uhcprovider.com/edi.
Professional independence
The issues of confidentiality and objective medical observations are the key in the diagnosis and treatment of our members.
Therefore, a health care provider or other licensed independent health care professional who is also a UnitedHealthcare
member shall not serve as PCP for themselves or their dependents.
Monitor eligibility
You are responsible for checking member eligibility within 2 business days prior to the date of service. You may be eligible
for reimbursement under the Authorization Guarantee program described in the Capitation and/or Delegation Supplement
for authorized services if you have checked and confirmed the member’s eligibility within 2 business days before the date
of service.
Member eligibility
You must verify the member’s eligibility each time they receive services from you. We provide several ways to verify eligibility:
• Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Then select Eligibility from the menu.
• EDI: 270/271 transactions through your vendor or clearinghouse
• Phone: See How to contact UnitedHealthcare West resources for specific numbers
• Electronic eligibility lists (upon request)
Get more details regarding a specific member’s benefit plan in the member’s Combined Evidence of Coverage and
Disclosure Form, Evidence of Coverage or Certificate of Coverage. Benefit plans may be addressed in procedures/protocols
communicated by us. Details may include the following:
• Selection of a PCP
• Effective date of coverage
• Changes in membership status while a member is in a hospital or skilled nursing facility (SNF)
• Member transfer/disenrollment
• Removal of member from receiving services by a PCP
Health Plan Identification (ID) Cards
Each member receives a health plan ID card with information to help you submit claims accurately. Information may vary in
appearance or location on the card due to payer or other unique requirements. You may identify a UnitedHealthcare West
member by a reference to “WEST” on the back of their ID card. Information may vary in appearance or location on the card due
to unique benefit plan requirements. You can view and download current ID cards when you verify eligibility and benefits in the
UnitedHealthcare Provider Portal.
For more detailed information on ID cards and to see a sample ID card, refer to the Health plan identification (ID) cards
section of Chapter 2: Provider responsibilities and standards.
Services Provided to Ineligible Members (does not apply in CA)
If we provide eligibility confirmation indicating that a member is eligible at the time the health care services are provided, and
it is later determined that the patient was not eligible, we are not responsible for payment of services provided to the member,
except as otherwise required by state and/or federal law. In such event, you are entitled to collect the payment directly from the
member (to the extent permitted by law) or from any other source of payment.
UnitedHealthcare West supplement
376
2023 UnitedHealthcare Care Provider Administrative Guide
Eligibility verification guarantee (TX commercial)
We reimburse Texas health care providers who request a guarantee of payment through the verification process. The
verification is based on the Agreement and the guidelines in Texas Senate Bill SB 418.
We will guarantee payment for proposed medical care or health care services if you provide the services to the member within
the required time frame. We reduce the payment by any applicable copayments, coinsurance and/or deductibles.
You must include the unique UnitedHealthcare West verification number on the claim form (Field 23 of CMS 1500 or Field 63
of UB-04).
You must request eligibility prior to rendering a service. Otherwise, we are not responsible for payment of those services. You
are entitled to collect the payment directly from the member to the extent permitted by law or from any other source of payment.
Submit service verification requests to:
• Phone: 1-877-847-2862
or
• Mail: Care Provider Correspondence
P.O. Box 30975
Salt Lake City, UT 84130-0975
Access and availability: Standards and exceptions
We monitor members’ access to medical and behavioral health care to make sure that we have an adequate health care
provider network to meet the members’ health care needs. We use member satisfaction surveys and other feedback to assess
performance against standards.
Health plans in California must conduct an annual Provider Appointment and Availability Survey. The overall plan results are
available at myuhc.com.
We have established access standards for appointments and after-hours care. Exceptions or additions to those standards are
shown in the following table.
Type of Care Guideline
Regular or Routine UnitedHealthcare Standard: 14 calendar days
Exceptions:
California Commercial HMO: Members are offered appointments for non-urgent PCP within 10
business days of request, within 15 business days for non-urgent specialist request;
Texas: Within 3 weeks for medical conditions.
Preventive Care UnitedHealthcare Standard: 4 weeks
Exceptions:
As directed by PCP
Texas: Within 2 months for child and within 3 months for adult.
Medicare Advantage within 30 days.
Urgent Exam
(PCP or Specialist)
UnitedHealthcare Standard: Same day (24 hours)
Exceptions:
California Commercial Members: Within 48 hours when no prior authorization required, within 96
hours when prior authorization required.
In-Office Wait Time California: In-office wait time is less than 30 minutes.
UnitedHealthcare West supplement
377
2023 UnitedHealthcare Care Provider Administrative Guide
Type of Care Guideline
Referral Process Complete notification to the member in a timely manner, not to exceed 5 business days of a
request for non-urgent care or 72 hours of a request for urgent care.
Non-Urgent Ancillary
(Diagnostic)
15 business days
1. Our members must have access to all physicians and support staff who work for you and must not be limited to particular
physicians. We recognize that some substitution between physicians who work out of the same office/building may occur
due to urgent/emergent situations.
2. Members must have access to appointments during all normal office hours and not be limited to appointments on certain
days or during certain hours.
3. Members must have access to the same time slots as all other patients who are not our members.
4. You must work cooperatively with our Medical Management Department toward:
– Managing inpatient and outpatient utilization.
– Member care and member satisfaction.
5. Use your best efforts to refer members to our network providers. You must use only our network laboratory and radiology
health care providers unless specifically authorized by us.
Timely Access to Non-Emergency Health Care Services (Applies to Commercial in California)
For details on these access standards refer to Chapter 2: Provider responsibilities and standards, Timely access to non-
emergency health care services (applies to Commercial in California).
Notification of practice or demographic changes
Report all demographic changes, open/closed status, product participation or termination to us.
For complete information, refer to the Demographic changes section of Chapter 2: Provider responsibilities and standards.
Compliance with the medical management program
Compliance with the Medical Management Program includes:
• Allowing our staff to have onsite access to members and their families while the member is an inpatient.
• Allowing our staff to participate in individual case conferences.
• Facilitating the availability and accessibility of key personnel for case reviews and discussions with the medical director or
designee representing UnitedHealthcare West, upon request.
• Providing appropriate services in a timely manner.
Benefit Interpretation Policies and Medical Management Guidelines
A complete library of Benefit Interpretation Policies (BIPs), and Medical Management Guidelines (MMGs) is available
on uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare West Benefit Interpretation Policies or
UnitedHealthcare West Medical Management Guidelines.
We publish monthly editions of the BIP and MMG Update Bulletins. These online resources provide notice to our network
providers of changes to our BIPs and MMGs. The bulletins are posted on the first calendar day of every month on:
• uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare West Benefit Interpretation Policies > Benefit
Interpretation Policy Update Bulletins.
• uhcprovider.com/policies > For Commercial Plans > UnitedHealthcare West Medical Management Guidelines > Medical
Management Guideline Update Bulletins.
We post a supplemental link to the policy updates announced in the BIP and MMG Update Bulletins monthly on uhcprovider.
com/news.

UnitedHealthcare West supplement
378
2023 UnitedHealthcare Care Provider Administrative Guide
Continuity of care
Continuity of care is a short-term transition period, allowing members to temporarily continue to receive services from a
non-participating health care provider. Continuity of Care is detailed under the Consolidated Appropriations Act (CAA)
requirements section in Chapter 2: Provider responsibilities and standards of this guide. If the specific requirements in this
section expand the coverage for Continuity of Care, then this section applies for UnitedHealthcare West members.
Examples of an active course of treatment or condition considered for continuity of care
• An acute condition is a medical condition that involves a sudden onset of symptoms due to an illness, injury or other medical
problem that requires prompt medical attention and that has a limited duration. Completion of covered services provided for
the duration of the acute condition.
• A serious chronic condition is a medical condition due to disease, illness, medical problem, mental health problem, or
medical or mental health disorder that is serious in nature, persists without full cure, worsens over an extended period of
time, or requires ongoing treatment to maintain remission or prevent deterioration. Completion of covered services provided
for the period necessary to complete the active course of treatment and to arrange for a clinically safe transfer to a network
provider. The active course of treatment is determined by a UnitedHealthcare West or medical group/IPA medical director
in consultation with the member, the terminated health care provider or the non-network provider and as applicable, the
receiving network provider, consistent with good professional practice. Completion of covered services for this condition will
not exceed 12 months from the Agreement’s termination date, or 12 months after the effective date of coverage for a newly
enrolled member.
• A terminal illness is an incurable or irreversible condition that has a high probability of causing death within 1 year.
Completion of covered services may be provided for the duration of the terminal illness, which could exceed 12 months,
provided that the prognosis of death was made by the: (i) terminated health care provider prior to the Agreement termination
date, or (ii) non-network provider prior to the newly enrolled member’s effective date of coverage with UnitedHealthcare West.
• A pregnancy diagnosed and documented (i) by the terminated health care provider prior to termination of the Agreement, or
(ii) by the non-network provider prior to the newly enrolled member’s effective date of coverage with UnitedHealthcare West.
Completion of covered services provided for the duration of the pregnancy and immediate postpartum period.
• The care of a newborn service provided to a child between birth and age 36 months. Completion of covered services will
not exceed the earliest of: (i) 12 months from Agreement, termination date, (ii) 12 months from the newly enrolled member’s
effective date of coverage with UnitedHealthcare West, or (iii) the child’s third birthday.
• Surgery or other procedure
Performance of a surgery or other procedure that was authorized by UnitedHealthcare West or the member’s PCP. Parts of
a documented course of treatment have been recommended and documented by (i) the terminating health care provider
to occur within 180 calendar days of the Agreement’s termination date, or (ii) the non-network provider to occur within 180
calendar days of the newly enrolled member’s effective date of coverage with UnitedHealthcare West.
Continuity of care does not apply when a member initiates a change of PCP or medical group/IPA. Authorizations granted by
the previous medical group shall be invalid in such situations at the commencement of the member’s assignment to the new
PCP or medical group/IPA; members shall not be entitled to continuing care unless the member’s new PCP or medical group/
IPA authorizes that care.
Virtual Visits (commercial HMO plans CA only)
Some UnitedHealthcare of California HMO member benefit plans include Virtual Visits. We define Virtual Visits as primary care
services that include the diagnosis and treatment of low-acuity medical conditions for members through the use of interactive
audio and video telecommunication and transmissions, and audio-visual communication technology.
Virtual Visit primary care services are typically delivered by the capitated provider groups. Not all UnitedHealthcare West benefit
plans will have the Virtual Visit benefit option.
To read more about Virtual Visits, refer to the Capitation and/or Delegation Supplement.
UnitedHealthcare West supplement
379
2023 UnitedHealthcare Care Provider Administrative Guide
Utilization and medical management
Medical emergencies and emergency medical conditions
For benefit plan definitions of an emergency, refer to the
member’s Combined Evidence of Coverage and Disclosure
Form, Evidence of Coverage or Certificate of Coverage, as
applicable. Additional definitions are found in our glossary.
Direct the member to call 911, or its local equivalent, or to go to the nearest emergency room. Prior authorization or advance
notification is not required for emergency services. However, you should tell us about the member’s emergency by calling
1-800-799-5252 between 8 a.m. and 5 p.m. PT, Monday–Friday.
Provide after-hours and weekend emergency services as clinically appropriate; enter the notification online or call
1-800-799-5252 the next business day.
Urgently needed services
Check the member’s benefits with Member Services or at uhcprovider.com, as applicable, for the benefit plan definition of
urgent care. For our commercial members, you must contact the member’s PCP or hospitalist on arrival for urgently needed
services. Request these services by calling 1-800-799-5252 between 8 a.m. and 5 p.m. PT, Monday–Friday.
Routine authorizations
We consider all other services as routine. To request preauthorization for urgent or routine services, the PCP must enter all the
necessary information into uhcprovider.com/priorauth, contact the delegated medical group for approval, or complete and
submit the appropriate preauthorization request form to obtain approval. Routine and urgent requests are responded to within
the following time frames, if all required clinical information is received:
Product State Time frame
Medicare Advantage
(Urgent)
All 72 hours
Part B drugs (including step therapy drugs) are reviewed in 24 hours.
Medicare Advantage
(Routine)
All 14 calendar days
Part B drugs (including step therapy drugs) are reviewed in 72 hours.
Commercial
(Urgent)
OR, WA 2 business days
CA, OK 72 hours
TX 3 calendar days
Commercial
(Routine)
OR, WA 2 business days; exception: - A delay of decision (DOD) letter
CA 5 business days; exception: - A delay of decision (DOD) letter
OK 15 calendar days
TX 3 calendar days
Authorization status determination
Only a physician (or pharmacist, psychiatrist, doctoral-level clinical psychologist or certified addiction medicine specialist,
as applicable and appropriate) may determine whether to delay, modify or deny services to a member for reasons of
medical necessity.

UnitedHealthcare West supplement
380
2023 UnitedHealthcare Care Provider Administrative Guide
Prior authorization process
A list of services that require prior authorization is available on uhcprovider.com/priorauth.
We will deny payment for services you provide without the required prior authorization. Such services are the health care
provider’s liability, and you may not bill the member.
Primary care services
Most PCP services do not require prior authorization. However, if prior authorization is required, the following guidelines apply:
1. The PCP/requesting health care provider is responsible for verifying eligibility and benefits prior to rendering services.
2. To request prior authorization, use our online processes, contact the delegated medical group, or complete and submit
the appropriate prior authorization request form (unless the services are required urgently or on an emergency basis). The
completed form must include the following information:
– Member’s presenting complaint
– Physician’s clinical findings on exam
– All diagnostic and lab results relevant to the request
– Conservative treatment that has been tried
– Applicable CPT and ICD codes
3. The fastest way to check the status of a treatment request is by using the Prior Authorization and Notification tool in the
UnitedHealthcare Provider Portal.
4. If approved, the treatment request is given a reference number that may be viewed when you check the status, or by
contacting the delegated medical group, or faxed back to the physician office depending on how the PCP/servicing health
care provider submitted the form.
5. Notate the reference number on the claim when you submit it for payment.
6. All authorizations expire 90 calendar days from the issue date.
7. Participating health care providers should refer members to network providers. Referrals to non-network providers require
prior authorization.
8. Once the PCP refers a member to a network specialist, that specialist may see the member as needed for the referring
diagnosis. The specialist is not required to direct the member back to the PCP to order tests and/or treatment.
9. If a specialist feels a member needs other services related to the treatment of the referral diagnosis, the specialist may refer
the member to another participating health care provider.
We or our delegates conduct reviews throughout a member’s course of treatment. Multiple prior authorizations may be required
throughout a course of treatment because prior authorizations are typically limited to specific services or time periods.
Serious or complex medical conditions
The PCP should identify members with serious or complex medical conditions and develop appropriate treatment plans for
them, along with case management. Each treatment plan should include a prior authorization for referral to a specialist for an
adequate number of visits to support the treatment plan.
Specialty care (including gynecology) in an office-based setting
We send the status of the prior authorization request (approved as requested, approved as modified, delayed or denied) to the
specialist by fax or online. For those services that do not require prior authorization, the PCP sends a referral request directly to
the specialists.
1. All specialist authorizations will expire 90 calendar days from the date of issuance.
2. Plain film radiography rendered by a network provider, or in the specialist’s office in support of an authorized visit, does not
require prior authorization.
3. Routine lab services performed in the specialist’s office, or provided by a designated participating health care provider in
support of an authorized visit, do not require prior authorization.

UnitedHealthcare West supplement
381
2023 UnitedHealthcare Care Provider Administrative Guide
4. Members may self-refer to a gynecologist who is a participating health care provider for their annual routine gynecological
exams. For women’s routine and preventive health care services, female MA members may self-refer to a women’s health
specialist who is a participating health care provider.
5. Female MA members older than 40 years may self-refer to a participating radiology health care provider for a
screening mammogram.
Note: Mammograms may require prior authorization in California.
Obstetrics
1. A member may self-refer to an obstetrician who is a participating health care provider for routine obstetrical (OB) care. If the
member is referred by her PCP to a non-participating health care specialist, the specialist must notify us using online tools.
This helps ensure accurate claims payment for ante and postpartum care.
2. Routine OB care includes office visits and 2 ultrasounds.
3. Plain film radiography that is performed by a participating health care provider or in the obstetrician’s office in support of an
authorized visit, does require prior authorization.
4. Routine labs performed in the obstetrician’s office, or provided by a participating health care provider in support of an
authorized visit, do not require prior authorization. In-office tests must follow CMS in-office testing CLIA requirements.
Specimens collected in the physician’s office and sent out to a non-participating laboratory for processing must follow the
out-of-network member consent requirements.
Maternal mental health screening requirement (California commercial plans)
The California Department of Managed Health Care (AB 2193) requires licensed health care practitioners who provide prenatal
or postpartum care for a patient to offer maternal mental health screening during the second and/or third trimester and/or at
the postpartum visit. When screening pregnant and postpartum members for mental health issues, we recommend using the
Patient Health Questionnaire 9 (PHQ-9). You can request hard copies of the PHQ-9 by emailing uhccscaqualitydepartment_
[email protected] or download a copy on uhcprovider.com > Resources > Resource library > Behavioral Health Resources.
Second opinions (California commercial plans)
We authorize and provide a second opinion by a qualified health care professional for members who meet specific criteria. A
second opinion consists of 1 office visit for a consultation or evaluation only. Members must return to their assigned PCPs for all
follow-up care. For purposes of this section, a qualified health care professional is defined as a PCP or specialist who is acting
within the scope of practice and who possesses a clinical background, including training and expertise related to the member’s
particular illness, disease or condition.
The PCP may request a second opinion on behalf of the member in any of the following situations:
• The member questions the reasonableness or necessity of a recommended surgical procedure.
• The member questions a diagnosis or treatment plan for a condition that threatens loss of life, limb, or bodily function or
threatens substantial impairment, including, but not limited to, a serious chronic condition.
• The clinical indications are not clear or are complex and confusing.
• A diagnosis is in doubt due to conflicting test results.
• The treating health care provider is unable to diagnose the condition.
• The member’s medical condition is not responding to the prescribed treatment plan within an appropriate period of time, and
the member is requesting a second opinion regarding the diagnosis or continuance of the treatment.
• The member has attempted to follow the treatment plan or has consulted with the treating health care provider and has
serious concerns about the diagnosis or treatment plan.
Turnaround time for second opinion reviews
We process requests for a second opinion in a timely manner to accommodate the clinical urgency of the member’s condition
and in accordance with established utilization management procedures and regulatory requirements. When there is an
imminent and serious threat to the member’s health, we or our delegate will make the second opinion determination within 72
hours after receipt of the request.

UnitedHealthcare West supplement
382
2023 UnitedHealthcare Care Provider Administrative Guide
An imminent and serious threat includes the potential loss of life, limb or other major bodily function. It may also be when a
lack of timeliness would be detrimental to the member’s ability to regain maximum function. For more detailed information and
benefit exclusions, refer to uhcprovider.com/policies:
• UnitedHealthcare Medicare Advantage Coverage Summary titled Second and Third Opinions
• UnitedHealthcare West Benefit Interpretation Policy titled Member Initiated Second and Third Opinion: CA
• UnitedHealthcare West Benefit Interpretation Policy titled Member Initiated Second and Third Opinion: OK, OR, TX, WA
Ventricular Assist Device (VAD)/Mechanical Circulatory Support Device (MCSD) Services/
Case management
We request that you notify the case management department when a member is referred for evaluation and/or is authorized for:
• VAD/MCSD and admitted for VAD/MCSD and/or may meet criteria for service denial.
• VAD/MCSD evaluations and surgery should be performed at a facility in the Optum VAD network, or facility approved by
UnitedHealthcare West medical directors, to align with heart transplant service centers.
Extension of prior authorization services
The specialist must request an extension of prior authorization online or by contacting the delegated medical group/IPA if they
desire to perform services:
• Beyond the approved visits.
• Beyond the allotted time frame of the approval (typically 90 calendar days).
• In addition to the approved procedures, and/or diagnostic or therapeutic testing.
The extension must be authorized before care is rendered to the member. The request for extension of services must include
the following information:
• Member’s presenting complaint
• Health care provider’s clinical findings on exam
• All diagnostic and laboratory results relevant to the request
• All treatment that has been tried
• Applicable CPT and ICD codes
• Requested services (e.g., additional visits, procedures)
The existing authorization is reviewed by the receiving party, who mails or faxes a response to the health care provider and/or
makes the information available online There is no need to contact the member’s PCP.
Facility-based outpatient surgery (CA, OR, WA and NV)
Facility-based outpatient surgery services are defined using CMS Guidelines, CPT/HCPCS coding conventions, and clinical
and/or proprietary standards. The following denotes services considered facility-based outpatient surgery services under
this definition:
• A procedure with an ASC grouping assigned
• A procedure with a global period of 90 days (according to the health care provider fee schedule)
• Core needle biopsies
• Unlisted or new codes may be considered surgery in the following situation:
– Unlisted or new code is related to other codes in the same APC group that had an ASC assigned is considered facility-
based outpatient surgery.
• A procedure with surgical risk or anesthetic risk as determined by clinical review

UnitedHealthcare West supplement
383
2023 UnitedHealthcare Care Provider Administrative Guide
Hospital notifications
Independent from prior authorization, notification by the facility is required for inpatient admissions on the day of admission,
even if an advanced notification was provided prior to the actual admission date.
Hospitals, rehabilitation facilities and skilled nursing facilities (SNFs) are required to notify us daily of all admissions, changes in
inpatient status and discharge dates.
Facilities are responsible for admission notification, even if advance notification was provided by the physician and coverage
approval is on file.
Admission notification
Facilities are responsible for notifying us of all member inpatient admissions including:
• Planned/elective admissions for acute care.
• Unplanned admissions for acute care.
• SNF admissions.
• Admissions following outpatient surgery.
• Admissions following observation.
• Newborns admitted to Neonatal Intensive Care Unit (NICU).
• Newborns who remain hospitalized after the mother is discharged (notice required within 24 hours of the mother’s discharge).
We must receive the admission notification within 24 hours after actual weekday admission (or by 5 p.m. local time on the next
business day if 24 hour notification would require notification on a weekend or holiday). For weekend and holiday admissions,
we must receive the notification by 5 p.m. local time on the next business day.
Receipt of an admission notification does not guarantee or authorize payment. Payment of covered services is contingent
upon coverage within the member’s benefit plan, the facility being eligible for payment, compliance with claim processing
requirements, and the facility’s Agreement with UnitedHealthcare.
Admission notifications must contain the following details regarding the admission:
• Member name, health plan ID number and date of birth
• Facility name and TIN or NPI
• Admitting/attending physician name and TIN or NPI
• Description for admitting diagnosis or ICD-10-CM diagnosis code
• Actual admission date
• Primary medical group/IPA
For emergency admissions where a member is unstable and not capable of providing coverage information, the facility should
notify us online, by EDI or by phone within 24 hours (or the next business day, for weekend or holiday admissions) from the time
the information is known and communicate the extenuating circumstances.
The following reports must be faxed daily to our Clinical Information Department:
• Census report for all our members
• Discharge report
• Face sheets to report outpatient surgeries and SNF admissions
• Inpatient Admission Fax Sheet to report “no UnitedHealthcare West admissions” for that day
The census report or face sheets must include the following information:
• Primary medical group/IPA
• Admit date
• Member name (first and last) and date of birth
• Bed type/accommodation status/level of care (LOC)
• Expected length of stay (LOS)
• Admitting physician

UnitedHealthcare West supplement
384
2023 UnitedHealthcare Care Provider Administrative Guide
• Admitting diagnosis (ICD-10-CM)
• Procedure/surgery (CPT Code) or reason for admission
• Attending physician
• Facility
• Address/city/state
• Policy number/member health plan ID number
• Other insurance
• Authorization number (if available)
• Discharge report, including member demographic information, discharge date and disposition
Coordination of care
Facilities are required to assist in the coordination of a member’s care by:
• Working with the member’s PCP
• Notifying the PCP of any admissions
• Providing the PCP with discharge summaries
After hour admissions/SNF transfers
• For admissions or transfers after hours or on weekends, the member should be admitted to the appropriate facility at the
appropriate level of care. Authorization must be obtained on the next business day.
• Transfers/admissions to SNFs may be admitted directly from the emergency room or home to a SNF.
Out-of-network admissions
• A referral/transfer to a non-network facility requires prior authorization. However, in the case of an emergency, a non-
participating hospital may be used without prior authorization.
• After initial emergency treatment and stabilization, we may request that a member be transferred to a network hospital, when
medically appropriate.
• If a PCP directs a member to a non-network hospital for non-emergent care without prior authorization, the PCP may be
held responsible.
Consultation with providers during inpatient stays
Authorization is not required for a consultation with a participating health care provider during an inpatient stay. However,
consultation with a non-network provider requires prior authorization.
Concurrent review
We conduct concurrent review on all admissions from the day of admission through the day of discharge. Clinical staff perform
concurrent reviews by phone as well as onsite at designated facilities. We have established procedures for onsite concurrent
review which include: (a) guidelines for identification of our staff at the facility; (b) processes for scheduling onsite reviews in
advance; and (c) staff requirements to follow facility rules. If the clinical reviewer determines that the member may be treated at
a lower level of care or in an alternative treatment setting, we discuss the case with the hospital case manager and the admitting
physician. If a discrepancy occurs, our medical director or designee discusses the case with the admitting physician.
Variance days
Variance days are days that we determine, through inpatient care coordination and the review of diagnostic services, are
not medically necessary or are not provided in a timely manner contributing to delays in care. We adjust reimbursement
accordingly. Our concurrent review staff attempts to minimize variance days by working with the attending physicians and
hospital staff. If a variance is noted in the member’s acute care process, our concurrent review staff discusses the variance with
the hospital’s medical management/case management representative. If the variance exists after the discussion, our concurrent
review staff documents the variance in our utilization records and submits to a UnitedHealthcare concurrent review manager for

UnitedHealthcare West supplement
385
2023 UnitedHealthcare Care Provider Administrative Guide
review. If upheld, the variance is entered into our database as a denial of reimbursement for the variance time period. We mail a
letter to the facility stating the variance type and time period. The facility may appeal the variances in writing.
Our medical director will review the appeal and render a decision to overturn or uphold the decision.
Medical observation status
We authorize hospital observation status when medically appropriate. Hospital observation is generally designed to evaluate
a member’s medical condition and determine the need for actual admission, or to stabilize a member’s condition. For MA
members, we also follow any applicable CMS guidelines to determine whether observation services are medically appropriate.
Typical cases, when observation status is used, include rule-out diagnoses and medical conditions that respond quickly to care.
Members under observation status may later convert to an inpatient admission if medically necessary.
Emergency and/or direct urgent admissions
Commercial plans
If a hospital does not receive authorization from us within 1 hour of the initial call requesting authorization, the emergent and/
or urgent services prompting the admission are assumed to be authorized and should be documented as such to us until we
direct or arrange care for the member. Once we become involved with managing or directing the member’s care, all services
provided must be authorized by us.
Medicare Advantage plans
When we receive the notification of admission, we request clinical information and make a determination within 1 business day
of receiving complete clinical information from the facility. If complete clinical information is not received within the 3 business
days, the case is denied for lack of information.
Skilled nursing facilities
Before transfer/admit to a SNF, we must approve the member’s treatment plan. The member’s network physician must perform
the initial physical exam and complete a written report within 48 hours of a member’s admission to the SNF. We perform an
initial review and subsequent reviews as we deem necessary. Federal and state regulations require that members at SNFs be
seen by a physician at least once every 30 calendar days.
Discharge planning
The initial evaluation for discharge planning begins at the time of notification of inpatient admission. A comprehensive
discharge plan includes, but is not limited to, the following:
• Assessment and documentation of the member’s needs as compared to those upon admission, including the member’s
functional status and anticipated discharge disposition, if other than a discharge to home
• Development of a discharge plan, including evaluation of the member’s financial and social service needs and potential need
for post-hospital services, such as home health, DME, and/or placement in a SNF or custodial care facility
• Approved authorizations for necessary post-discharge plan
• Organization, communication and execution of the discharge plan
• Evaluation of the effectiveness of the discharge plan
• Referrals to population-based disease management and case management programs, as indicated
For after-hours or weekend discharges requiring home health and/or DME, facility should arrange the care and obtain
authorization on the next business day.
Retrospective review (medical claim review)
Medical claim review, also known as medical cost review, medical bill review and/or retrospective review, is the examination
of the medical documentation and/or billing detail after a service has been provided. Medical claim review is performed to
provide a fair and consistent means to retrospectively review medical claims and make sure medical necessity criteria are met,

UnitedHealthcare West supplement
386
2023 UnitedHealthcare Care Provider Administrative Guide
confirm appropriate level of care and length of stay, correct payer source, and identify appropriate potential unbundling and/or
duplicate billing occurrences.
The review includes an examination of all appropriate claims and/or medical records against accepted billing practices and
clinical guidelines as defined by entities such as CMS, AMA, CPT coding and InterQual Care Guidelines depending on the type
of claims submitted.
Claims that meet any of the following criteria are reviewed before the claim is paid:
• High-dollar claims
• Claims without required authorization
• Claims for unlisted procedures
• Trauma claims
• Claims for implants that are not identified or inconsistent with the UnitedHealthcare West’s Implant Guidelines
• Claim check or modifier edits based on our claim payment software
• Foreign country claims
• Claims with LOS or LOC mismatch
To help ensure timely review and payment determinations, you must respond to requests for all appropriate medical records
within 7 calendar days from receipt of the request, unless otherwise indicated in your Agreement.
We may review specific claims based on pre-established retrospective criteria to make sure acceptable billing practices
are applied.
For hospital and other institutional providers, we may reduce the payable dollars if line item charges have been incorrectly
unbundled from room and board charges.
Minimum content denials, delays, or modification requests
If we deny, delay delivery or modify a request for authorization for health care services, our written or electronic notices will, at a
minimum, include the following:
• The specific service(s) denied, delayed in delivery, modified or partially approved
• The specific reference to the benefit plan provisions to support the decision
• The reason the service is being denied, delayed in delivery, modified, or partially approved, including:
– Clear and concise explanation of the reasons for the decision in sufficient detail, using an easily understandable summary
of the criteria, so that all parties may understand the rationale behind the decision.
– Description of the criteria or guidelines used, and/or reference to the benefit provision, protocol or other similar criterion on
which the decision was based.
– Clinical reasons for decisions regarding medical necessity.
– Contractual rationale for benefit denials.
• Notification that the member may obtain a copy of the actual benefit provision, guideline, protocol or other similar criterion on
which the denial decision was based, upon request
• Notification that the member’s physician may request a peer-to-peer review
• Alternative treatment options offered, if applicable
• Description of any additional material or information necessary from the member to complete the request, and why that
information is necessary
• Description of grievance rights and an explanation of the appeals and grievances processes, including:
– Information regarding the member’s right to appoint a representative to file an appeal on the member’s behalf.
– The member’s right to submit written comments, documents or other additional relevant information.
– Information notifying the member and their treating health care provider of the right to an expedited appeal for time-
sensitive situations (not applicable to retrospective review).
– Information regarding the member’s right to file a grievance or appeal with the applicable state regulatory agency, including
information regarding the independent medical review process, as applicable.

UnitedHealthcare West supplement
387
2023 UnitedHealthcare Care Provider Administrative Guide
– Information that the member may bring civil action, under Section 502(a) of the Employee Retirement Income Security Act
(ERISA), if applicable (Commercial products).
– For the treating health care provider, the name and direct phone number of the health care professional responsible for
the decision.
Home delivery pharmacy
A member may fill prescriptions from any network provider pharmacy in the pharmacy directory or online at optumrx.com.
A member who obtains a prescription from a non-network pharmacy will not be eligible for reimbursement of any charges
incurred unless the prescription received was not available from a participating pharmacy (e.g., urgent or emergent
prescriptions, after hours, out of the service area or Part D-covered vaccines provided by the health care provider).
Home delivery service
Each UnitedHealthcare West member with a prescription drug benefit is eligible to use our prescription home delivery service.
When appropriate, you may write prescriptions for a 3-month, 90-calendar-day supply and up to 3 additional refills. Only
medications taken for chronic conditions should be ordered through the home delivery service. The member may obtain acute
prescription needs, such as antibiotics and pain medications, through a network pharmacy site to avoid delay in treatment.
You may also elect to discourage members from using the home delivery service for medications where large quantities
dispensed at one time to the member may pose a problem (e.g., tranquilizer).
Pharmacy prescription drug list
The UnitedHealthcare West prescription drug list includes most generic drugs/medications and a broad selection of brand
name drugs/medications. Prescription drugs and medications listed on the prescription drug list are considered a covered
benefit. However, select prescription drug list medications may require prior authorization to be covered.
Many members have a 3-tier pharmacy benefit plan with coverage of formulary generics, formulary brand name drugs and non-
formulary drugs. A prior authorization process may apply to certain non-formulary drugs.
We update the prescription drug list three times a year, in January, May and September. Health care provider requests for
formulary review of medications or preauthorization guidelines are welcome. Find formulary changes on uhcprovider.com/
pharmacy, or uhcprovider.com/priorauth > Clinical Pharmacy and Specialty Drugs.
Non-formulary medications
Non-formulary prescriptions/medications not provided as a plan benefit are the member’s financial responsibility, unless the
prescribing health care provider requests and receives prior authorization for the non-formulary medications and the member
meets criteria for coverage.
Commercial plan members may also have coverage when their employer purchases an Open Formulary or Buy-up Plan. The
member may be charged the usual and customary cost of the medication or the non-formulary copayment depending on the
member’s benefit design.
Drug utilization review program
UnitedHealthcare West is dedicated to working with our network providers to supply information and education needed for
effective management in growing cost of pharmaceutical care. Our clinical pharmacists can identify and analyze areas where
health care providers may be able to prescribe products considered effective as well as economical.
Additionally, our pharmacy staff can help identify when a more detailed review of therapy may improve member care, such as:
• Overuse of controlled substances.
• Duplicate therapies.
• Drug interactions.
• Polypharmacy.
UnitedHealthcare West supplement
388
2023 UnitedHealthcare Care Provider Administrative Guide
Through pharmacist review and information, health care providers are given the data needed to better manage the quality of
their members’ care while also managing pharmacy program costs.
Prior authorization process
We delegate prior authorization services to OptumRx®. OptumRx staff adhere to benefit plan-approved criteria, National
Pharmacy and Therapeutics Committee (NPTC) practice guidelines, and other professionally recognized standards.
Request authorizations:
• Online: professionals.optumrx.com > Prior Authorizations
• To simplify the prior authorization experience, health care professionals can submit a real-time prior authorization request
24 hours per day, 7 days per week, through one of the online services found at professionals.optumrx.com. After logging
on with your unique National Provider Identifier (NPI) number and password, you may submit member details securely
online, enter a diagnosis and medication justification for the requested medication and, in many cases, receive authorization
instantly. Otherwise, you may verbally submit a prior authorization request by:
• Phone: 1-800-711-4555
California Commercial products: Prescribing providers in California must use the Prescription Drug Prior Authorization
Request Form when submitting authorization requests to OptumRx.
Also, the California utilization management delegates may have contractual responsibilities for payment of certain prescription
medications. When the delegate requires prior authorization for use of those drugs prescribed by their health care providers,
the delegate must also require the use of Optum Prescription Drug Prior Authorization Request Form. The delegate must
have a policy and process in place and be able to demonstrate compliance.
You can call the OptumRx Prior Authorization department at 1-800-711-4555 to either submit a verbal prior authorization request
or to request a California state-mandated fax form.
Claims process
Find instructions and quick tips for EDI
on uhcprovider.com/edi.
Claims and encounters
EDI is the preferred method of claim submission for participating physicians and health care providers. Submit all professional
and institutional claims and/or encounters electronically for UnitedHealthcare West and Medicare Advantage HMO
product lines.
Do not resubmit claims using EDI or paper claims forms. Resubmit claims online using the UnitedHealthcare Provider Portal
at uhcprovider.com > Sign In > Claims & Payments.
Refer to our online Companion Guides for the data elements required for these transactions found on uhcprovider.com/edi.
For information on EDI claim submission methods and connections, go to EDI 837: Electronic Claims.
OptumInsight Connectivity Solutions, UnitedHealthcare’s managed gateway, is also available to help you begin submitting and
receiving electronic transactions. For more information, call 1-800-341-6141.
Submit your claims and encounters and primary and secondary claims as EDI transaction 837.
For UnitedHealthcare West encounters, the payer ID is 95958. For claims, the payer ID is 87726. For a complete list of payer IDs,
refer to the Claims Payer List.

UnitedHealthcare West supplement
389
2023 UnitedHealthcare Care Provider Administrative Guide
In some cases, the payer ID listed on uhcprovider.com/edi may be different from the numbers issued by your clearinghouse.
To avoid processing delays, you must validate with your clearinghouse for the appropriate payer ID number or refer to your
clearinghouse published Payer Lists.
Electronic Funds Transfer
You may enroll or make changes to Electronic Funds Transfer (EFT) and ERA/835 for your UnitedHealthcare West claims using
the UnitedHealthcare West EFT Enrollment tool in the UnitedHealthcare Provider Portal. Enrollment in UnitedHealthcare
West EFT currently applies to payments from SignatureValue and MA plans only. You’ll continue to receive checks by mail
until you enroll in UnitedHealthcare West EFT. View our ERA Payer List to determine the correct payer ID to use for ERA/835
transactions.
For more information, go to uhcprovider.com/claims > Electronic Payment Solutions.
Claims adjudication
We use industry claims adjudication and/or clinical practices, state and federal guidelines, and/or our policies, procedures
and data to determine appropriate criteria for payment of claims. To find out more, contact your network account manager,
physician advocate or hospital advocate or visit uhcprovider.com/claims.
Complete claims requirements
We follow the Requirements for complete claims and encounter data submission, as found in Chapter 10: Our claims
process.
National Provider Identification
We accept the National Provider Identification (NPI) on all HIPAA transactions, including the HIPAA 837 professional and
institutional claim submissions. A valid NPI is required on all covered claims in addition to the TIN. For institutional claims,
include the billing provider National Uniform Claim Committee (NUCC) taxonomy. We will accept NPIs submitted through any of
the following methods:
• Online: uhcprovider.com/mypracticeprofile
• Phone: 1-877-842-3210 through the United Voice Portal, select the “Health Care Professional Services” prompt. State
“Demographic changes.” Your call will be directed to the Service Center to collect your NPI, corresponding NUCC Taxonomy
Codes, and other NPI-related information.
Level-of-care documentation and claims payment
Claims are processed according to the authorized level of care documented in the authorization record, reviewing all claims to
determine if the billed level of care matches the authorized level of care.
If the billed level of care is at a higher level than the authorized level of care, we pay you the authorized level of care. You
may not bill the member for any charges relating to the higher level of care. If the billed level of care is at a lower level than
authorized, we pay you based on the lower level of care, which was determined by you to be the appropriate level of care for
the member.
Level of specificity — use of codes
To track the specific level of care and services provided to its members, we require health care providers to use the most
current service codes (i.e., ICD-10-CM, UB and CPT codes) and appropriate bill type.
Member financial responsibility
Verify the eligibility of our members before you see them and obtain information about their benefits, including required
copayments and any deductibles, out-of-pockets maximums or coinsurance that are the member’s responsibility.

UnitedHealthcare West supplement
390
2023 UnitedHealthcare Care Provider Administrative Guide
No balance billing
You may not balance bill our members. You may not collect payment from the member for covered services beyond the
member’s copayment, coinsurance, deductible and for non-covered services unless the member specifically agreed on
in writing before receiving the service. In addition, you shall not bill a UnitedHealthcare West member for missed office
visit appointments.
Claims status follow-up
We can provide you with an Explanation of Payment (EOP). If you don’t get one, you may follow-up on the status of a claim using
one of the following methods:
• EDI: 276/277 Claim Status Inquiry and Response transactions are available through your vendor or clearinghouse.
• Online: UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Then select Claims & Payments > Look up a Claim.
• Phone: See How to contact UnitedHealthcare West resources section for telephone numbers. This system provides a fax
of the claim status detail information that is available.
Claims submission requirements
Refer to the Prompt claims processing section of Chapter 10: Our claims process, for more information about electronic
claims submission and other EDI transactions. If your claim is the financial responsibility of a UnitedHealthcare West delegated
entity (e.g., PMG, MSO, Hospital), then bill that entity directly for reimbursement.
Claims submission requirements for reinsurance claims for hospital providers
If covered services fall under the reinsurance provisions set forth in your Agreement with us, follow the terms of the Agreement
to make sure:
• The stipulated threshold has been met.
• Only covered services are included in the computation of the reinsurance threshold.
• Only those inpatient services specifically identified under the terms of the reinsurance provision(s) are used to calculate the
stipulated threshold rate.
• Applicable eligible member copayments, coinsurance and/or deductible amounts are deducted from the reinsurance
threshold computation.
• The stipulated reinsurance conversion reimbursement rate is applied to all subsequent covered services and
submitted claims.
• The reinsurance is applied to the specific, authorized acute care confinement.
• Claims are submitted in accordance with the required time frame, if any, as set forth in the Agreement. In addition, when
submitting hospital claims that have reached the contracted reinsurance provisions and are being billed in accordance with
the terms of the Agreement and/or this supplement, you shall:
– Indicate if a claim meets reinsurance criteria.
– Make medical records available upon request for all related services identified under the reinsurance provisions (e.g., ER
face sheets).
If a submitted hospital claim does not identify the claim as having met the contracted reinsurance criteria, we process the
claim at the appropriate rate in the Agreement. An itemized bill is required to compute specific reinsurance calculations and to
properly review reinsurance claims for covered services.
Interim bills
We adjudicate interim bills at the per diem rate for each authorized bed day billed on the claim and reconcile the complete
charges to the interim payments based on the final bill.
The following process increases efficiencies for both us and the hospital/SNF business offices:
• 112 Interim – First Claim: Pay contracted per diem for each authorized bed day billed on the claim (lesser of billed or
authorized level of care, unless the contract states otherwise).

UnitedHealthcare West supplement
391
2023 UnitedHealthcare Care Provider Administrative Guide
• 113 Interim – Continuing Claim: Pay contracted per diem for each authorized bed day billed on the claim (lesser of billed or
authorized level of care, unless the contract states otherwise).
• 114 Interim – Last Claim: Review admits to discharge and apply appropriate contract rates, including per diems, case rates,
stop loss/outlier and/or exclusions. The previous payments will be adjusted against the final payable amount.
Reciprocity agreements
You shall cooperate with our participating health care providers and our affiliates and agree to provide services to members
enrolled in benefit plans and programs of UnitedHealthcare West affiliates and to assure reciprocity with providing health care
services.
If any member who is enrolled in a benefit plan or program of any UnitedHealthcare West affiliate, receives services or
treatment from you and/or your sub-contracted health care providers (if applicable), you and/or your subcontracted health
care providers (if applicable), agree to bill the UnitedHealthcare West affiliate at billed charges and to accept the compensation
provided pursuant to your Agreement, less any applicable copayments and/or deductibles, as payment in full for such services
or treatment.
You shall comply with the procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement
of such services or treatment.
Overpayments
Follow the instructions in the Overpayments section of Chapter 10: Our claims process.
ESRD
If a member has or develops ESRD while covered under an employer’s group benefit plan, the member must use the benefits of
the plan for the first 30 months after becoming eligible for Medicare due to ESRD. After the 30 months elapse, Medicare is the
primary payer. However, if the employer group benefit plan coverage were secondary to Medicare when the member developed
ESRD, Medicare is the primary payer, and there is no 30-month period.
Medicaid (applies only to MA): Follow the instructions in the Member financial responsibility section of Chapter 11:
Compensation.
The calendar day we receive a claim is the receipt date, whether in the mail or electronically. The following date stamps may be
used to determine date of receipt:
• Our claims department date stamp
• Primary payer claim payment/denial date as shown on the Explanation of Payment (EOP)
• Delegated provider date stamp
• TPA date stamp
• Confirmation received date stamp that prints at the top/bottom of the page with the name of the sender
Note: Date stamps from other health benefit plans or insurance companies are not valid received dates for timely
filing determination.
Time limits for filing claims
You are required to submit to clean claims for reimbursement no later than 1) 90 days from the date of service, or 2) the time
specified in your Agreement, or 3) the time frame specified in the state guidelines, whichever is greatest.
If you do not submit clean claims within these time frames, we reserve the right to deny payment for the claim(s). Claim(s) that
are denied for untimely filing may not be billed to a member.
We have claims processing procedures to help ensure timely claims payment to health care providers. We are committed to
paying claims for which we are financially responsible within the time frames required by state and federal law.
UnitedHealthcare West supplement
392
2023 UnitedHealthcare Care Provider Administrative Guide
Health care provider claims appeals and disputes
Claims research and resolution (OK and TX commercial plans)
The Claims Research & Resolution (CR&R) process applies:
• If you do not agree with the payment decision after the initial processing of the claim.
• Regardless of whether the payer was UnitedHealthcare West, the delegated medical group/IPA or other delegated payer, or
the capitated hospital/provider, you are responsible for submitting your claim(s) to the appropriate entity that holds financial
responsibility to process each claim.
UnitedHealthcare West researches the issue to identify who holds financial risk of the services and abides by federal and
state legislation on appropriate timelines for resolution. We work directly with the delegated payer when claims have been
misdirected and financial responsibility is in question. If appropriate, health care provider-driven claim payment disputes will be
directed to the delegated payer Provider Dispute Resolution process.
Claim reconsideration requests (does not apply to capitated/delegated claims in California)
You may request a reconsideration of a claim determination. These requests typically can be resolved with the appropriate
documents to support claim payment or adjustments (e.g., sending a copy of the authorization for a claim denied for no
authorization or proof of timely filing for a claim denied for untimely filing). All requests must be submitted within 365 calendar
days following the date of the last action or inaction, unless your Agreement contains other filing guidelines. Submit your
requests in the UnitedHealthcare Provider Portal. Learn more at uhcprovider.com/portal.
To mail your request, refer to the chart titled UnitedHealthcare West Provider Rework or Dispute Process Reference Table at
the end of this section.
Submission of bulk claim inquiries
The Claims Project Management (CPM) team handles bulk claim inquiries. Contact the CPM team at the address in the table to
initiate a bulk claim inquiry:
UnitedHealthcare West Bulk Claims Rework Reference Table
Provider’s state Contact information Notes
Arizona UnitedHealthcare
Attn: WR Claims Project Management
P.O. Box 52078
Phoenix, AZ 85072-2078
For requests with 20+ claims.
California Claims Research Projects CA120-0360
P.O. Box 30968
Salt Lake City, UT 84130-0968
For requests with 19+ claims.
Colorado Medicare Advantage Claims Department
Attn: Colorado Resolution Team
P.O. Box 30983
Salt Lake City, UT 84130-0983
For requests with 20+ claims.
UnitedHealthcare West supplement
393
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare West Bulk Claims Rework Reference Table
Provider’s state Contact information Notes
Nevada For Medicare Advantage claims:
UnitedHealthcare
Attn: WR Claims Project Management Claims
Research Projects
1) Intermountain Healthcare
P.O. Box 95638
Las Vegas, NV 89193-5638
2) OptumCare-NV
P.O. Box 30539
Salt Lake City, UT, 84130
UnitedHealthcare uses 2 delegated payers in Nevada.
Refer to the ID card to confirm which delegate is
assigned for that member’s claims.
The Nevada delegate handles bulk claim inquiries
received from providers of service. The provider of
service should submit the bulk claims with a cover
sheet indicating “Appeal” or “Review” to the Claims
Research Department at the designated address to
initiate a bulk claim inquiry.
For requests with 10+ claims.
Oklahoma Claims Research Projects
P.O. Box 30967
Salt Lake City, UT 84130-0967
For requests with 20+ claims.
Oregon Claims Research Projects
P.O. Box 30968
Salt Lake City, UT 84130-0968
For requests with 10+ claims.
Texas Claims Research Projects
P.O. Box 30975
Salt Lake City, UT 84130-0975
For requests with 20+ claims.
Washington Claims Research Projects
P.O. Box 30968
Salt Lake City, UT 84130-0968
For requests with 10+ claims.
UnitedHealthcare West’s response
We respond to issues as quickly as possible.
• Reworks/disputes requiring clinical determination: Individuals with clinical training/background who were not previously
involved in the initial decision review all clinical rework/dispute requests. We send a letter to you outlining our determination
and the basis for that decision.
• Reworks/disputes requiring claim process determination: Individuals not previously involved in the initial processing of the
claim review the rework/dispute request.
Response details: If claim requires an additional payment, the EOP serves as notification of the outcome on the review. If the
original claim status is upheld, you are sent a letter outlining the details of the review.
California: If a claim requires an additional payment, the EOP does not serve as notification of the outcome of the review.
We send you a letter with the determination. In addition, payment must be sent within 5 calendar days of the date on the
determination letter. We respond to you within the applicable time limits set forth by federal and state agencies. After the
applicable time limit has passed, call Provider Relations at 1-877-847-2862 to obtain a status.
Health care provider dispute resolution (CA Commercial HMO, OR HMO claims, OR and WA
commercial plans)
If you disagree with our claim determination, you must initiate and complete the PDR process before commencing arbitration on
a claim. You must submit a PDR in writing and with additional documentation for review. All disputes must be submitted within
365 calendar days following the date of the adverse payment determination on the claim, unless your Agreement or state law
dictate otherwise. This time frame applies to all disputes regarding contractual issues, claims payment issues, overpayment
recoveries and medical management disputes.
UnitedHealthcare West supplement
394
2023 UnitedHealthcare Care Provider Administrative Guide
The PDR process is available to provide a fair, fast and cost-effective resolution of health care provider disputes, in accordance
with state and federal regulations. We do not discriminate, retaliate against or charge you for submitting a health care provider
dispute. The PDR process is not a substitution for arbitration and is not deemed as an arbitration.
What to submit
As the health care provider of service, submit the dispute with the following information:
• Member’s name and health plan ID number
• Claim number
• Specific item in dispute
• Clear rationale/reason for contesting the determination and an explanation why the claim should be paid or approved
• Your contact information
Disputes are not reviewed if the supporting documentation is not submitted with the request.
Where to submit
State-specific addresses and other pertinent information regarding the PDR process may be found in the UnitedHealthcare
West Provider Rework or Dispute Process Reference Table at the end of this section.
Accountability for review of a health care provider dispute
The entity that initially processed/denied the claim or service in question is responsible for the initial review of a PDR request.
These entities may include, but are not limited to, UnitedHealthcare West, the delegated medical group/IPA/payer or the
capitated hospital/health care provider.
Excluded from the PDR process
The following are examples of issues excluded from the PDR process:
• A member has filed an appeal, and you have filed a dispute regarding the same issue. In these cases, the member’s appeal
is reviewed first. You may submit a health care provider dispute after we make a decision on the member’s appeal. If you are
appealing on behalf of the member, we treat the appeal as a member appeal.
• An Independent Medical Review initiated by a member through the member appeal process.
• Any dispute you file beyond the timely filing limit applicable to you, and you fail to give “good cause” for the delay.
• Any delegated claim issue that has not been reviewed through the delegated payer’s claim resolution mechanism.
• Any request for a dispute which has been reviewed by the delegated medical group/IPA/payer or capitated hospital/health
care provider and does not involve an issue of medical necessity or medical management.
UnitedHealthcare West Provider Rework or Dispute Process Reference Table
Provider’s state Contact information Notes
Arizona UnitedHealthcare Benefits of
Texas, Inc.
Attn: Claims Resolution Team
P.O. Box 52078
Phoenix, AZ 85072-2078
First Review: Request for reconsideration of a claim is considered
a grievance. Physicians and health care professionals are required
to notify us of any request for reconsideration within 1 year from the
date the claim was processed.
Second Review: Request for reconsideration of a grievance
determination is also considered a grievance. You are required
to notify us of any second level grievance within 1 year from the
date the first level grievance resolution was communicated to the
health care provider.
UnitedHealthcare West supplement
395
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare West Provider Rework or Dispute Process Reference Table
Provider’s state Contact information Notes
California Online: UnitedHealthcare
Provider Portal at uhcprovider.
com > Sign In
UnitedHealthcare West
Provider Dispute Resolution
P.O. Box 30764
Salt Lake City, UT 84130-0764
UnitedHealthcare acknowledges receipt of paper disputes within 15
business days and within 2 business days for electronic disputes. If
additional information is required, the dispute is returned within 45
business days. A written determination is issued within 45 business
days.
Colorado Medicare Advantage
Claims Department
Attn: Colorado Resolution Team
P.O. Box 30983
Salt Lake City, UT 84130-0983
Upon receipt of a dispute, Colorado Resolution Team:
Acknowledges receipt of the dispute within 30 calendar days of the
receipt of the dispute;
Conducts a thorough review of your dispute and all
supporting documentation;
Acknowledges receipt, including the specific rationale for the
decision, within 60 calendar days of receipt of the dispute;
Processes payment, if necessary, within 5 business days of the
written determination;
Replies to the health care provider of service within 30 calendar
days if additional information is required.
If additional information is required, we will hold the dispute request
for 30 additional calendar days.
Nevada For Medicare Advantage claims:
UnitedHealthcare
1) Intermountain Healthcare
P.O. Box 95638
Las Vegas, NV 89193-5638
2) OptumCare - NV
P.O. Box 30539
Salt Lake City, UT 84130
All Nevada Medicare Advantage HMO claims are processed by
delegated payers. Therefore, health care provider appeals are
reviewed primarily by the delegated payer. Refer to the ID card to
confirm which delegate is assigned for that member’s claims.
Oklahoma UnitedHealthcare West
Provider Dispute Resolution
P.O. Box 30764
Salt Lake City, UT 84130-0764
Oregon UnitedHealthcare West
Provider Dispute Resolution
P.O. Box 30764
Salt Lake City, UT 84130-0764
UnitedHealthcare of Oregon allows at least 30 calendar days for you
to initiate the dispute resolution process.
We render a decision on health care provider or facility complaints
within a reasonable time for the type of dispute.
In the case of billing disputes, we render a decision within 60
calendar days of the complaint.
Texas UnitedHealthcare West
Claims Department
P.O. Box 400046
San Antonio, TX 78229
UnitedHealthcare West supplement
396
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare West Provider Rework or Dispute Process Reference Table
Provider’s state Contact information Notes
Washington UnitedHealthcare West
Provider Dispute Resolution
P.O. Box 30764
Salt Lake City, UT 84130-0764
UnitedHealthcare of Washington allows at least 30 calendar days for
health care providers to initiate the dispute resolution process.
We render a decision on health care provider or facility complaints
within a reasonable time for the type of dispute.
In the case of billing disputes, we render a decision within 60
calendar days of the complaint.
California language assistance program (California
commercial plans)
UnitedHealthcare of California members who have limited English proficiency have access to translated written materials
and oral interpretation services, free of charge, to help them get covered services. For more program information, call
1-800-752-6096.
If the member’s language of choice is not English, or they have limited English proficiency, try to arrange for oral interpretive
services before the date of service.
Verbal interpreter/written translation services
The UnitedHealthcare West Call Center is a central resource for both health care providers and members. The following
information and services are accessible through the call center:
• How to access and facilitate oral interpretation services for members needing language assistance in any language
• Request for an in-person interpreter for a member by selecting the appropriate phone number (based on language
preference) to speak with a customer service representative and/or to conference in an interpreter
UnitedHealthcare SignatureValue (HMO/MCO):
1-800-624-8822; Dial 711 TDHI
Where to obtain the member’s language preference
The member’s preferences for spoken language, written language and eligibility for written language service is displayed when
checking eligibility and benefits in the UnitedHealthcare Provider Portal.
Documentation of member refusal of interpreter services
If a member refuses your offer of an interpreter, you must note the refusal in the medical record for that visit. Documenting
the refusal of interpreter services in the medical record not only protects you, it also helps ensure consistency. We verify
compliance with this documentation when we conduct site reviews of medical records.
If a member wants to use a family member or friend as an interpreter, consider offering a telephonic interpreter in addition to the
family member/friend to help ensure accuracy of interpretation. For all Limited English Proficiency (LEP) members, document
the member’s preferred language in the member’s medical record.

UnitedHealthcare West supplement
397
2023 UnitedHealthcare Care Provider Administrative Guide
Member complaints and grievances
Member satisfaction (California)
In addition to the NCQA CAHPS® survey, we conduct an annual California HMO member assessment survey using a sample of
members at the health care provider organization or medical group level. We summarize the results at the provider organization
or medical group level and use them to identify improvement opportunities. These results are important for the evaluation
of member perspectives about access to PCP, specialty and after-hours care. In addition to access, topics include care
coordination and interactions with the doctor and the office staff.
We use the results from this survey to support the Integrated Healthcare Association’s Pay-for-Performance Program.
Availability of grievance forms
Member disputes may arise from time to time with UnitedHealthcare West or with our participating health care providers.
UnitedHealthcare West respects the rights of its members to express dissatisfaction regarding quality of care or services and to
appeal any denied claim or service.
Find instructions on how to file a complaint or grievance with us in the member’s Combined Evidence of Coverage and
Disclosure Form, Evidence of Coverage or Certificate of Coverage.
California Commercial HMO members may access grievance forms online. Direct members to myuhc.com > Find a Form. The
form is accessible in 2 places: From the California member welcome page or, Library tab page, on the left side, and click on
Grievance Form. You and your staff are required to assist the member with obtaining a form if the member asks. You may print a
form from myuhc.com or by providing a number for the member to call Member Services to file the grievance orally. Grievance
forms are available in English, Spanish and Chinese.
California Quality Improvement Committee
The California Quality Improvement Committee (CA-QIC) oversees activities specific to members in health plans operating in
California to help ensure that state-specific interests are met. The CA-QIC activities are carried out in collaboration with the West
Regional Quality Oversight Committee (RQOC) to avoid duplication of effort.
The CA-QIC is chaired by the chief medical officer physician licensed in CA. The committee meets at least quarterly and reports
to the UHC of CA Board of Directors and, as needed, to the West RQOC.

398
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthOne Individual Plans supplement
Applicability of this supplement
UnitedHealthOne is the brand name of the UnitedHealthcare family of companies that offers individual personal health
products, including Golden Rule Insurance Company (GRIC), UnitedHealthcare Life Insurance Company, (UHCLIC),
UnitedHealthcare Insurance Company (UHIC) and UnitedHealthcare Oxford Navigate Individual plans offered by Oxford Health
Insurance, Inc.
This supplement applies to services provided to members enrolled in GRIC and UnitedHealthcare Oxford Navigate Individual
benefit plans offered by Oxford Health Insurance, Inc.
You are subject to the main guide, this supplement and the member’s benefit plan. This supplement and the member’s benefit
plan controls if it conflicts with information in the main guide. If additional protocols, policies or procedures are available online,
we direct you to that location when applicable. For protocols, policies and procedures not referenced in this supplement, refer
to appropriate chapter in the main guide.
How to contact UnitedHealthOne resources
Resource Where to go Requirements and Notes
GRIC- Group Number 705214;
Oxford- Group Number 908410
Notification
Admission notification is required for
all inpatient services as described in
Chapter 7: Medical management.
Call the number on the back of the
ID card, or go to uhcprovider.com/
priorauth.
Benefits and Eligibility Call the number on the back of the ID
card, or go to myuhone.com.
To inquire about a member’s plan
benefits or eligibility
Claims Go to myuhone.com. To view pending and processed claims
Pharmacy Services Prior Authorizations:
Online: professionals.optumrx.com
Benefit Information:
Call the pharmacy number on the back
of the ID card.
For information on the PDL, go to
uhcprovider.com.
Oxford – Group Number 908410
Behavioral Health Services Online: providerexpress.com
Phone: 1-855-779-2859
Submit admission notification or prior
authorization for behavioral health,
including substance use and autism.
Cardiology
Diagnostic catheterization,
electrophysiology implants,
echocardiogram and stress
echocardiogram
Online: uhcprovider.com/paan
Information: uhcprovider.com/
cardiology
Phone: 1-866-889-8054
Request prior authorization for services
as described in the Outpatient
cardiology notification/prior
authorization protocol section of
Chapter 7: Medical management.
Chiropractic, Physical and
Occupational Therapy
Online (clinical submission request):
myoptumhealthphysicalhealth.com
Phone: 1-888-676-7768
Follow the clinical submission
process for chiropractic, physical and
occupational therapy as described in
Chapter 7: Medical management.
UnitedHealthOne Individual Plans supplement
399
2023 UnitedHealthcare Care Provider Administrative Guide
Resource Where to go Requirements and Notes
Claims Submission Electronic Claims Submission:
Payer ID 37602
Pharmacy Services Prior Authorizations:
Online: professionals.optumrx.com
Benefit Information:
Call the pharmacy number on the back
of the ID card.
For information on the PDL, go to
uhcprovider.com/pharmacy.
Prior Authorization and Notification EDI: Transactions 278 and 278N
Online: uhcprovider.com/paan
Phone: 1-800-999-3404
Information: uhcprovider.com/
priorauth
Prior authorization and admission
notification is required as described in
Chapter 7: Medical management. EDI
278A transactions are not available.
Radiology/Advanced Outpatient
Imaging Procedures:
CT scans, MRIs, MRAs, PET scans and
nuclear medicine studies, including
nuclear cardiology
Online: uhcprovider.com/paan
Information: uhcprovider.com/
radiology
Phone: 1-866-889-8054
Request prior authorization for
services as described in the
Outpatient radiology notification/
prior authorization protocol section of
Chapter 7: Medical management.
Health plan ID card
Members receive health plan ID cards with information to help you submit claims accurately. Information varies in appearance
or location on the card. However, cards display the same basic information (e.g., claims address, copayment information,
phone numbers).
You can view and download current ID cards when you verify eligibility and benefits in the UnitedHealthcare Provider Portal.
For more detailed information and to see a sample ID card, refer to the Health plan identification (ID) cards section of Chapter
2: Provider responsibilities and standards.
Claims process
We know you want to be paid promptly for your services. To help prompt payment:
1. Notify us based on the notification requirements in this supplement.
– For Navigate referrals, refer to Chapter 6: Referrals.
2. Prepare a complete and accurate claim form. For facility (UB-04/8371) claims, see number 4.
3. Submit electronic claims using the electronic payer ID on the health plan ID card. GRIC payer ID is 37602.
4. Requirements for claims reporting revenue codes:
– All claims reporting revenue codes require the exact dates of service if there is a span of dates.
– If you report revenue codes 274, 275, 276, 277, 278, 279 with a billed amount of $500 or greater, you are required to
provide a valid CPT or HCPCS code.
– If you report revenue codes 25X with a billed amount of $1,000 or greater, and the codes are not billed with NDC, you are
required to provide a valid CPT/HCPCS code.

UnitedHealthOne Individual Plans supplement
400
2023 UnitedHealthcare Care Provider Administrative Guide
Claim adjustments
If you believe your claim was processed wrong, call the number on the back of the ID card. Request an adjustment as soon
as possible, in accordance with applicable statutes and regulations. If you identify a claim overpayment, or we notify you of an
overpayment, send us the overpayment within 30 calendar days from the date of identification or notification.
Claim reconsideration, appeals and disputes
If you disagree with a claim payment determination or adjustment, you may appeal. Request a review by mail, fax or phone:
Grievance Administrator
P.O. Box 31371
Salt Lake City, UT 84131-0371
Standard Fax: 1-801-478-5463
Phone: 1-800-657-8205
If you feel your situation is urgent, request an expedited (urgent) appeal by mail, fax or phone:
Grievance Administrator
2020 Innovation Drive
DePere, WI 54115
Expedited Fax: 1-866-654-6323
Phone: 1-800-657-8205
Your appeal must be submitted within 12 months from the date of payment shown on the EOB, unless your Agreement with us
or applicable law provide otherwise.
Refer to Claim reconsideration and appeals process section in Chapter 10: Our claims process.
If you disagree with the outcome of the claim appeal, you may file an arbitration proceeding as described in your Agreement.
Claim reconsideration does not apply to some states based on applicable state law (e.g., Arizona, California, Colorado, New
Jersey, Texas). For states with applicable law, dispute requests will follow the state-specific process.
New Jersey health care provider dispute process
Disputes involving New Jersey commercial members are subject to the New Jersey state-regulated health care provider dispute
process.
The state-regulated health care provider dispute process does not apply in the following situations:
• Our determination involves a UM denial. UM denials are refusals to pay a claim or to authorize a service or supply because we
have determined the service or supply is one of the following:
– Not medically necessary
– Experimental or investigational
– Cosmetic
– Dental rather than medical
– Treatment of a pre-existing condition.
UM denials include prescription quantity limit denials and requests for in-plan exception denials. You may appeal a UM denial
by going through the Internal UM Appeals Process described under the Member Complaints and Grievances section. You
must submit a completed Consent to Representation in Appeals of Utilization Management Determinations and Authorization
for Release of Medical Records in UM Appeals and Independent Arbitration of Claims form to begin the UM appeal process.
• Our determination indicates we denied the service or supply as not covered under the terms of the plan or because the
person is not our member.
• The dispute is due to COB.
• We have provided you notice that we are investigating this claim (and related ones, as appropriate) for possible fraud.
The process does apply for the following situations:
• The claim was not paid for any reason other than previously listed.

UnitedHealthOne Individual Plans supplement
401
2023 UnitedHealthcare Care Provider Administrative Guide
• The claim was paid at a rate you did not expect based on your network contract or the terms of the plan.
• The claim was paid at a rate you did not expect because of differences in our treatment of the codes in the claim from what
you believe is appropriate.
• We required additional substantiating documentation to support the claim, and you believe the required information is
inconsistent with our stated claims handling policies and procedures or is not relevant to the claim.
• You believe we failed to adjudicate the claim, or an uncontested portion of a claim, in a timely manner consistent with law and
the terms of your network contract, if any.
• Our denial was due to lack of appropriate authorization, but you believe you obtained appropriate authorization from us or
another carrier for the services.
• You believe we failed to appropriately pay interest on the claim.
• You believe our statement that we overpaid on 1 or more claims. A claim is erroneous or the amount we calculated as
overpaid is erroneous.
• You believe we have attempted to offset an inappropriate amount against a claim because of an effort to recoup for an
overpayment on prior claims.
If the dispute is eligible, the following process will apply:
Submit a written request for appeal using the Health Care Provider Application to Appeal a Claims Determination Form created
by the New Jersey Department of Banking and Insurance. Submit the request within 90 days following receipt of our initial
determination notice to:
UnitedHealthcare Oxford Navigate Individual
Grievance Administrator
P.O. Box 31371
Salt Lake City, UT 84131-0371
Standard Fax: 1-801-478-5463
We will review the request and tell you our decision in writing within 30 calendar days of receipt of the form.
If you are not satisfied with the decision, you may initiate the New Jersey Program for Independent Claims Payment Arbitration
(PICPA) process. Submit your requests to MAXIMUS, Inc. within 90 calendar days from receipt of the internal dispute decision.
A dispute is eligible if the payment amount in dispute is $1,000 or more. The arbitration decision is binding.
Member complaints and grievances
Member disputes may arise from time to time with UnitedHealthOne or with our participating health care providers. We respect
the rights of our members to express dissatisfaction regarding quality of care or services and to appeal any denied claim or
service. Instructions on how to file a complaint or grievance with us are in the member’s Combined Evidence of Coverage and
Disclosure Form, Evidence of Coverage, or Certificate of Coverage. Refer to Member Appeals, Grievances or Complaints
section in Chapter 10: Our claims process for detailed information about your role in the member appeal process.
UnitedHealthcare Oxford Navigate individual - internal utilization management
appeals process
You or the member should identify UM appeals 180 calendar days from initial adverse UM determination receipt. UM appeals
include denials as not medically necessary, experimental or investigational, cosmetic, dental rather than medical, prescription
quantity limit denial, denial of a request for an in-plan exception, or excluded as a pre-existing condition.
To initiate the standard internal UM appeal process, write to:
UnitedHealthcare Oxford Navigate Individual
Grievance Administrator
P.O. Box 31371
Salt Lake City, UT 84131-0371
Standard Fax: 1-801-478-5463

UnitedHealthOne Individual Plans supplement
402
2023 UnitedHealthcare Care Provider Administrative Guide
If you feel the situation is urgent, request an expedited (urgent) appeal by mail, fax or phone:
UnitedHealthcare Oxford Navigate Individual
Grievance Administrator
2020 Innovation Drive
DePere, WI 54115
Expedited Fax: 1-866-654-6323
Phone: 1-800-291-2634
All UM appeals are done by clinical peer reviewers other than the clinical peer reviewer who rendered the initial UM
determination.
Expedited appeal requests involving continued inpatient care in a network facility for a substance use disorder are determined
within 24 hours. Expedited appeal requests for urgent care, emergency care, an admission, availability of care, continued stay,
or health care services for which the member received emergency services, but has not been discharged from a facility, are
determined within 72 hours. Standard UM appeals are determined within 10 calendar days of appeal receipt.
If the member or designee is not happy with the results of the appeal process, they may pursue an external appeal through an
Independent Utilization Review Organization (IURO) for final internal UM determinations. You must complete an internal appeal
before you may request a review by an IURO, except when:
• We fail to meet the deadlines for completion of the internal appeals process:
– Without demonstrating good cause.
– Because of matters beyond our control.
– While in the context of an ongoing, good faith exchange of information between parties.
– It is not a pattern or practice of non-compliance.
• We, for any reason, expressly waive our rights to an internal review of an appeal.
• The treating health care provider and/or member have applied for expedited external review at the same time as applying for
an expedited internal review.
To initiate the external appeal, the member or designee must:
• File a written request with the New Jersey Department of Banking and Insurance within 4 months of receiving a final
determination on an appeal.
• Sign a release that allows the IURO to review all the necessary medical records related to the appeal.
• Send a check or money order in the amount of $25 made payable to New Jersey Department of Banking and Insurance with
the request. The form, release and check must be sent to:
Department of Banking and Insurance
Consumer Protection Services
Office of Managed Care
P.O. Box 329
Trenton, NJ 08625-1062
The IURO completes the review within 45 days of receipt.
The IURO completes its review within 48 hours if the appeal involves:
• Urgent or emergency care.
• An admission.
• Availability of care.
• Continued stay.
• Health care services for which the member received emergency services and not yet discharged.
• A medical condition that would put the member’s life or health in danger when waiting for the normal appeal process.
If UnitedHealthcare Oxford Navigate Individual has good cause for not meeting the appeal process deadlines, members or
their designee and/or their health care provider may request a written explanation of the delay. UnitedHealthcare Oxford
Navigate Individual must provide the explanation within 10 days of the request. If an external reviewer or court agrees with

UnitedHealthOne Individual Plans supplement
403
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare Oxford Navigate Individual and rejects the request for immediate review, the member has the opportunity to
resubmit their appeal.
Internal administrative appeal process
The administrative appeal process is used to appeal an initial determination concerning a claim for benefits or an administrative
issue. Issues include but are not limited to:
• Denials based on benefit exclusions or limitations not involving UM decisions.
• Claims payment disputes.
• Administrative issues concerning other requirements of the health plan. Administrative issues include but are not limited to
issues involving:
– Eligibility
– Enrollment issues
– Rescission of coverage
Note: Benefit and administrative issues do not include initial determinations that the service or supply is not medically
necessary, experimental or investigational, cosmetic, dental rather than medical, prescription quantity limit denials, denials of a
request for an in-plan exception, or treatment of a pre-existing condition. Those determinations are UM decisions.
You or the member must initiate administrative appeals in writing unless expedited.
Determinations concerning services that have already been provided are not eligible to be appealed on an expedited basis.
Expedited administrative appeals are determined within 72 hours from receipt of the appeal. All other appeals are determined
within 30 calendar days of receipt of the appeal.
Notice to Texas providers
To verify benefits for GRIC members, call 1-800-395-0923.
Tools have been developed by third parties, such as the InterQual Care Guidelines (formerly known as Milliman Care
Guidelines®), to assist in administering health benefits and making informed decisions in many health care settings, including
acute and sub-acute medical, rehabilitation, skilled nursing facilities, home health care and ambulatory facilities.
As affiliates of UnitedHealthcare, GRIC and Oxford Health Insurance, Inc. may also use UnitedHealthcare’s medical policies as
guidance. These policies are available on uhcprovider.com/policies.
Notification does not guarantee coverage or payment (unless mandated by law). The member’s coverage eligibility is
determined by the health benefit plan. For benefit or coverage information, call the insurer at the phone number on the back of
the member’s ID card.
To obtain a verification as required by 28 TAC §19.1719, call 1-800-842-1792.
Important information regarding diabetes (Michigan)
Michigan requires insurers to provide coverage for certain expenses to treat diabetes. It also requires insurers to establish and
provide members and participating health care providers with a program to help prevent the onset of clinical diabetes. We have
adopted the ADA Clinical Practice Guidelines.
The program for participating health care providers emphasizes best practice guidelines to help prevent the onset of clinical
diabetes and to treat diabetes, including diet, lifestyle, physical exercise and fitness, and early diagnosis and treatment. The
Standards of Medical Care in Diabetes and Clinical Practice Recommendations are on care.diabetesjournals.org.
Subscription information for the American Diabetes Journals is available on the website. You may also call 1-800-232-3472 and
select option 1, 8:30 a.m. to 8 p.m. ET, Monday–Friday. View journal articles without an online subscription.

404
2023 UnitedHealthcare Care Provider Administrative Guide
Glossary
Abuse: Actions that may, directly or indirectly, result in
unnecessary costs to the health insurance plan, improper
payment, payment for services that fail to meet professionally
recognized standards of care or medically unnecessary
services. Abuse involves payment for items or services when
there is no legal entitlement to that payment, and the provider
has not knowingly and/or intentionally misrepresented facts to
obtain payment. Abuse cannot be differentiated categorically
from fraud because the distinction between “fraud” and
“abuse” depends on specific facts and circumstances,
intent and prior knowledge, and available evidence, among
other factors.
Accreditation: A process that a health care provider goes
through to be recognized for meeting certain standards such
as quality.
Acute Inpatient Care: Care provided to persons sufficiently ill
or disabled requiring:
• Constant availability of medical supervision by attending
provider or other medical staff.
• Constant availability of licensed nursing personnel.
• Availability of other diagnostic or therapeutic services and
equipment available only in a hospital setting to help ensure
proper medical management by the health care provider.
Adjudication: The process of determining the proper payment
amount on a claim.
Ambulatory Care: Health services provided on an outpatient
basis. While many inpatients may be ambulatory, the term
“ambulatory care” usually implies that the patient has come to
a location other than their home to receive services and has
departed the same day. Examples include chemotherapy and
physical therapy.
Appeal: An oral or written request by a member or member’s
personal representative received by UnitedHealthcare for
review of an adverse action.
Authorization: Approval obtained by health care providers
from UnitedHealthcare for a designated service before
the service is rendered. Used interchangeably with
preauthorization or prior authorization.
Authorized Health Care Provider: A health care provider
who meets UnitedHealthcare’s licensing and certification
requirements and has been authorized by UnitedHealthcare to
provide services.
Benefit: The amount of money UnitedHealthcare pays for care
and other services.
Capitation: Per-person way of payment for medical services.
UnitedHealthcare pays a participating capitated provider a
fixed amount for every member they care for, regardless of the
care provided.
Claim: The documentation of the services that have occurred
during the course of a visit to a health care provider.
Clinical Laboratory Improvement Amendments of 1988
(CLIA): United States federal regulatory standards that apply
to all clinical laboratory testing performed on humans in the
United States, except clinical trials and basic research.
Clean Claim: A claim that has no defect, impropriety
(including lack of any required substantiating documentation)
or particular circumstance requiring special treatment that
prevents timely payment.
Centers for Medicare & Medicaid Services (CMS): A
federal agency within the U.S. Department of Health and
Human Services.
Coordination of Benefits (COB): Allows benefit plans that
provide health and/or prescription coverage for a person
with Medicare to determine their respective payment
responsibilities (i.e., determine which insurance benefit plan
has the primary payment responsibility and the extent to which
the other benefit plans will contribute when an individual is
covered by more than 1 benefit plan).
Coinsurance: The member’s share of the costs of a covered
health care service, calculated as a percent (for example,
20%) of the allowed amount for the service. Members may pay
coinsurance plus any deductibles owed.
Commercial: Refers to all UnitedHealthcare medical products
that are not Medicare Advantage, Medicare Supplement,
Medicaid, CHIP, workers’ compensation, TRICARE, or other
governmental programs (except that “Commercial” also
applies to benefit plans for the Health Insurance Marketplace,
government employees or students at public universities).
Copayment: A fixed amount members may pay for a covered
health care service, usually upon receiving the service.
Covered Services: Medically necessary services
included in the member’s benefit plan. Covered services
change periodically and may be mandated by federal or
state legislation.
Credentialing: The verification of applicable licenses,
certifications and experience to assure that provider status
is extended only to professional, competent providers
who continually meet the qualifications, standards and
requirements established by UnitedHealthcare.

Glossary
405
2023 UnitedHealthcare Care Provider Administrative Guide
Current Procedural Terminology (CPT) Codes: American
Medical Association (AMA)-approved standard coding for
billing of procedural services performed.
Deductible: The amount a member owes for health care
services the health insurance or benefit plan covers before the
health insurance or benefit plan begins to pay.
Delivery System: The mechanism by which health care is
delivered to a patient. Examples include, but are not limited
to, health care facilities, health care provider offices and home
health care.
Dependent: A child, disabled adult or spouse covered by the
health benefit plan.
Discharge Planning: Process of screening eligible candidates
for continuing care following treatment in an acute care
facility, and assisting in planning, scheduling and arranging for
that care.
Disease Management: A prospective, disease-specific
approach to improving health care outcomes by providing
education to members through non-physician.
Disenrollment: The discontinuance of a member’s eligibility
to receive covered services from a contractor.
Dual-Eligibles: Members who qualify for both Medicare
and Medicaid.
Durable Medical Equipment (DME): Medical equipment that
is all of the following:
• Ordered or provided by a physician for outpatient use
primarily in a home setting
• Used for medical purposes
• Not consumable or disposable except as needed for the
effective use of covered DME
• Not of use to a person in the absence of a disease
or disability
• Serves a medical purpose for the treatment of a sickness
or injury
• Primarily used within the home
Durable Medical Equipment, Prosthetics, Orthotics and
Supplies (DMEPOS): In November 2006, the Centers for
Medicare & Medicaid Services (CMS) approved 10 national
accreditation organizations that will accredit suppliers of
DMEPOS as meeting new quality standards under Medicare
Part B.
Electronic Data Interchange (EDI): The electronic exchange
of information between 2 or more organizations.
Electronic Funds Transfer (EFT): The electronic exchange of
funds between 2 or more organizations.
Electronic Medical Record (EMR): The electronic version of
a member’s health records.
Emergency Care: The provision of medically necessary
services required for immediate attention to evaluate or
stabilize a medical emergency (see definition to follow).
Employee Retirement Income Security Act of 1974
(ERISA): A federal law that sets minimum standards for most
voluntarily established pension and health benefit plans in
private industry to provide protection for individuals in these
benefit plans.
Encounter: An interaction between a patient and health care
providers, for the purpose of provider health care services or
assessing the health status of a patient.
Expedited Appeal: An oral or written request by a
member or member’s personal representative received by
UnitedHealthcare requesting an expedited reconsideration
of an action when taking the time for a standard resolution
could seriously jeopardize the member’s life, health or ability
to attain, maintain or regain maximum function; or would
subject the member to severe pain that cannot be adequately
managed without the care or treatment that is the subject of
the appeal.
Fee for Service: Health care providers are paid for each
service (like an office visit, test or procedure).
Fraud: Health care fraud is a crime that involves
misrepresenting information, concealing information or
deceiving a person or entity to receive benefits, or to make a
financial profit (18 U.S.C.§1347).
Grievance: An oral or written expression of dissatisfaction by
a member, or representative on behalf of a member, about any
matter other than an adverse action.
Health Care Provider: A person who provides medical or
other health care (doctor, nurse, therapist or social worker) or
office support staff. A health care provider may be a doctor
practicing alone, in a hospital setting or in a group practice. A
health care provider could work from a remote location, in a
public space or any combination of locations.
Health Insurance Portability and Accountability Act
(HIPAA) Act of 1996: A federal legislation that provides
data privacy and security provisions for safeguarding
medical information.
Health Plan Employer Data and Information Set (HEDIS):
Set of standardized measures developed by National
Committee for Quality Assurance (NCQA). Originally HEDIS
was designed to address private employers’ needs as
purchasers of health care. It has since been adapted for use
by public purchasers, regulators and consumers. HEDIS is
used for quality improvement activities, health management
systems, provider profiling efforts, an element of NCQA
accreditation and as a basis of consumer report cards for
managed care organizations.

Glossary
406
2023 UnitedHealthcare Care Provider Administrative Guide
Home Health Care or Home Health Services: Medical care
services provided in the home, often by a visiting nurse,
usually for recovering patients, aged homebound patients or
patients with a chronic disease or disability.
Managed Care: A system designed to better manage the
cost and quality of medical services. Managed care products
not only offer less member liability but also less member
control. Managed care aims to improve accessibility to health
care, reduce cost and improve quality of service. Many
managed care health insurance programs work with Health
Maintenance Organization (HMO) and Preferred Provider
Organization (PPO) boards to promote use of specific health
treatment procedures. Managed care health insurance benefit
plans also educate and work with consumers to improve
overall health by addressing disease prevention. The common
types of managed care products are HMO, PPO and Point of
Service (POS) benefit plans.
Medical Emergency: A medical condition manifesting itself
by acute symptoms of sufficient severity (including severe
pain) that a prudent layperson, who possesses an average
knowledge of health and medicine, could reasonably expect
the absence of immediate medical attention to result in
the following:
• Placing the health of the individual (or, with respect to a
pregnant woman, the health of the woman or her unborn
child) in serious jeopardy
• Serious impairment to bodily functions
• Serious dysfunction of any bodily organ or part
Medically Necessary: To determine medical necessity, we
use generally accepted standards of medical practice, based
on credible scientific evidence published in peer-reviewed
medical literature and generally recognized by the relevant
medical community. We may also use standards based on
physician specialty recommendations, professional standards
of care and other evidence-based, industry-recognized
resources and guidelines, such as InterQual® Care Guidelines.
For Medicare Advantage and Medicaid members, we
use Medicare guidelines, including National Coverage
Determinations and Local Coverage Determinations, to
determine medical necessity of services requested.
If other nationally recognized criteria contradict InterQual,
UnitedHealthcare and delegated medical groups/IPAs follow
the Medicare guidelines for Medicare Advantage members.
Individual criteria is provided to you upon request.
Member: Refers to an individual who has been
determined UnitedHealthcare-eligible and is enrolled
with UnitedHealthcare to receive services pursuant to the
Agreement. Other common industry terms: customer, patient,
beneficiary, insured, enrollee, subscriber, dependent.
National Provider Identification (NPI): NPI is a unique
10-digit identification number issued to health care providers
in the United States by CMS.
Network provider: A professional or institutional health
care provider who has an Agreement with UnitedHealthcare
member’s plan to provide care at a contracted rate. A network
provider agrees to file claims and handle other paperwork for
UnitedHealthcare member. A network provider accepts the
negotiated rate as payment in full for services rendered.
Non-Network Provider: A non-network provider does not
have an Agreement with UnitedHealthcare but is certified to
provide care to UnitedHealthcare members. There are 2 types
of non-network providers: non-participating and participating.
• Non-participating health care provider: A non-
participating health care provider is a UnitedHealthcare-
authorized hospital, institutional provider, physician or
other provider that furnishes medical services (or supplies)
to UnitedHealthcare members but who does not have an
Agreement and does not accept the UnitedHealthcare
allowable charge or file claims for UnitedHealthcare
members. A non-participating health care provider may only
charge up to 15% above the UnitedHealthcare allowable
charge.
• Participating health care provider: A health care provider
who has agreed to file claims for UnitedHealthcare
members, accept payment directly from UnitedHealthcare,
and accept the UnitedHealthcare allowable charge as
payment in full for services received. Non-network providers
may participate on a claim-by-claim basis. Participating
health care providers may seek payment of applicable
copayments, cost-shares and deductibles from the member.
Under the UnitedHealthcare outpatient prospective payment
system, all Medicare participating health care providers and
hospitals must, by law, also participate in UnitedHealthcare
for inpatient and outpatient care.
Nurse Practitioner: A registered nurse who has graduated
from a program that prepares registered nurses for advanced
or extended practice and who is certified as a nurse
practitioner by the American Nursing Association.
Optum: A UnitedHealth Group
TM
health services and
innovation company that designs and implements custom
information technology systems, and offers management
consulting, in the health care industry nationwide. Optum
offers behavioral health care programs including integrated
behavioral and medical programs, depression management,
employee assistance, work/life management, disability
support and pharmacy management programs.
Out-of-Area Care: Care received by a UnitedHealthcare
member when they are outside of their geographic territory.

Glossary
407
2023 UnitedHealthcare Care Provider Administrative Guide
Password Owners: Individuals at a health care provider’s
organization who set up and maintain co-workers’ access
to our health care provider websites, the UnitedHealthcare
Provider Portal and uhcprovider.com. Find your Primary
Access Administrator.
Physician Assistant: A health care professional licensed
to practice medicine with physician supervision. Physician
assistants are trained in intensive education programs
accredited by the Commission on Accreditation of Allied
Health Education Programs.
Policy: A contract between the insurer and the insured, known
as the policyholder, which determines the claims the insurer is
legally required to pay.
Primary Care Provider (PCP): A physician such as a family
practitioner, pediatrician, internist, general practitioner or
obstetrician, who serves as a gatekeeper for their assigned
members’ care. Other providers may be included as primary
physicians such as nurse practitioners and physician
assistants as allowed by state mandates.
Pre-Service Appeals: A pre-service appeal is a request to
change a denial of coverage for a planned health care service.
The member’s rights in the member’s benefit plan govern
this process.
Primary Care Team: A team comprised of a care manager, a
PCP and a nurse practitioner or physician assistant.
Prior Authorization and Notification: A unit under
the direction of the UnitedHealthcare Clinical Services
Department that is an essential component of any managed
care organization. Prior authorization is the process where
health care providers seek approval prior to rendering
services as required by UnitedHealthcare policy.
Provider Group: A partnership, association, corporation or
other group of providers.
Provider Manual: This document is referred to as a health
care provider manual or guide. It may also be referred to as
the provider administrative guide or handbook.
Qualified Medicare Beneficiary (QMB): A Medicaid program
for beneficiaries who need help paying for Medicare services.
Quality Management (QM): A methodology used by
professional health personnel to the degree of conformance
to desired medical standards and practices; and activities
designed to improve and maintain quality service and care,
performed through a formal program with involvement of
multiple organizational components and committees.
Reinsurance: The contract made between an insurance
company and a third party to protect the insurance company
from losses.
Risk Adjustment Data: All data used in the development and
application of a risk adjustment payment model, as defined in
42 CFR 422.310, 42 USC 18063 and 45 CFR Part 153.
Secondary Payer: A source of coverage that pays after the
primary insurance benefit has been applied.
Self-Funded Plan: Self-funded health care, also known
as Administrative Services Only (ASO), is a self-insurance
arrangement whereby an employer provides health or
disability benefits to employees with its own funds.
Self-Insured: A self-insured group health benefit plan is one
in which the employer assumes the financial risk for providing
health care benefits to its employees.
Service Area: A geographic area serviced by a
UnitedHealthcare contracted provider, as stated in the health
care provider’s Agreement with us.
Skilled Nursing Facility (SNF): A Medicare-certified nursing
facility that (a) provides skilled nursing services and (b) is
licensed and operated as required by applicable law.
Subrogation: A health plan’s right, to the extent permitted
under applicable state and federal law and the applicable
benefit plan, to recover benefits paid for a member’s health
care services when a third party causes the member’s injury
or illness.
Subscriber: Person who owns an insurance policy.
Supplemental Benefits: Supplemental insurance includes
health benefit plans specifically designed to supplement
UnitedHealthcare standard benefits.
Third-Party Administrator (TPA): An organization that
provides or manages benefits, claims or other services, but it
does not carry any insurance risk.
Transitional Care: A program that is designed for members
to help ensure a coordinated approach takes place across the
continuum of care.
UnitedHealthcare Assisted Living Plan: A Medicare
Advantage Institutional-Equivalent Special Needs Plan that:
• Exclusively enrolls special needs individuals who are living
in a community setting, have Medicare A and B and meet
the local state’s criteria for “institutional level of care.”
• Is issued by UnitedHealthcare Insurance Company or by
one of UnitedHealthcare’s affiliates.
• Is offered through our UnitedHealthcare Medicare
Advantage business unit, as indicated by a reference to
assisted living plan name listed on the face of the valid
member ID card.

Glossary
408
2023 UnitedHealthcare Care Provider Administrative Guide
UnitedHealthcare Nursing Home Plan: A Medicare
Advantage Institutional Special Needs Plan that:
• Exclusively enrolls special needs individuals who, for 90
calendar days or longer, have had or are expected to need
the level of service requiring an institutional level of care (as
defined in 42 CFR 422.2).
• Is issued by UnitedHealthcare Insurance Company or by
one of UnitedHealthcare’s affiliates.
• Is offered through our UnitedHealthcare Medicare
Advantage business unit, as indicated by a reference to
Nursing Home Plan or Erickson Advantage Guardian in the
benefit plan name listed on the face of the valid member
ID card.
Us: “Us,” “we” or “our” refers to UnitedHealthcare on behalf
of itself and its other affiliates for those products and services
subject to this guide.
Utilization Management (UM): The process of evaluating
and determining the coverage for and the appropriateness
of medical care services, as well as providing assistance
to a clinician or patient in cooperation with other parties,
to help ensure appropriate use of resources. UM includes
prior authorization, concurrent review, retrospective review,
discharge planning and case management.
Waste: The overutilization of services, or other practices that,
directly or indirectly, result in unnecessary costs to a health
care benefit program. Waste is generally not considered to
be caused by criminally negligent actions but rather misuse
of resources.
Workers’ Compensation: Workers’ compensation is a
form of insurance providing wage replacement and medical
benefits to employees injured in the course of employment
in exchange for mandatory relinquishment of the employee’s
right to sue their employer for the tort of negligence.
You: “You,” “your” or “provider” refers to any health care
provider subject to this guide, including physicians, health
care professionals, facilities and ancillary providers; except
when indicated, all items are applicable to all types of
providers subject to this guide.

01/23 © 2023 UnitedHealthcare Services, Inc.
