
Nutrition Line: 617-732-8884*
Medical Line: 617-732-8882*
*Expect to leave a voicemail, calls returned within
48 hours M-F except holidays.
Message us through patient gateway!
www.patientgateway.org
Nutrition Guidelines for
Single Anastomosis-Duodeno-Ileostomy (SADI),
Duodenal Switch (DS),
& Type 1 Distalization
Brigham and Women’s Center for Weight Management and Wellness
75 Francis Street Boston, Massachusetts 02115
www.brighamandwomens.org/cwmw
This book is designed to help you, your family, and your friends understand how nutrition and eating will
change after surgery. It is important to commit to healthy lifestyle habits for the rest of your life to be
successful with surgery. It is still possible for people to overeat and gain weight after bariatric surgery. It is
encouraged to start practicing healthy lifestyle changes before surgery so they will become habits you can
sustain long-term!
We hope the guidelines in this book, and the support from our team, will help you to have a healthy life after
surgery.
Contents
Nutrition Class Worksheet .................................................................................................................................... 1
The Surgeries ........................................................................................................................................................ 5
Skills for Success ................................................................................................................................................... 6
Physical Activity .................................................................................................................................................... 7
Getting Ready for Surgery ..................................................................................................................................... 8
2-Week Pre-Surgery Diet ...................................................................................................................................... 9
Post-Op Diet Stage 1: Fluids ................................................................................................................................ 10
Post-Op Diet Stage 2: Full Liquids ....................................................................................................................... 11
Post-Op Diet Stage 3: Smooth Textures .............................................................................................................. 13
Post-Op Diet Stage 4: Soft Textures .................................................................................................................... 16
Post-Op Diet Stage 5: Regular Textures .............................................................................................................. 19
Serving Sizes ....................................................................................................................................................... 24
Possible Problems & Solutions ............................................................................................................................ 30
Frequently Asked Questions ............................................................................................................................... 33
Your Typical Dietitian Appointment Schedule
Individual appointments are 30 minutes; groups and classes are 45-60 minutes.
Before Surgery:
✓ Nutrition Class
Nutrition Assessment*
*Please have completed the “Nutrition Worksheet” prior to this appointment (pages 1-4 below)
Nutrition Follow-Ups as needed
After Surgery
2-3 weeks (group session)
3 months
6 months
9 months
1 year
After 1 year, meet with dietitian twice per year (every 6 months) forever

1 © Center for Weight Management & Wellness 2023
Nutrition Class Worksheet
After your nutrition class, keep a food log for 3 days (see example page 23) and complete the
questions below (pages 1-4) to review at your 1
st
individual nutrition visit.
This form is fillable or print / complete by hand.
1. 1. After surgery, when is your first nutrition appointment (hint: virtual, group)?
2.
☐ 2-3 weeks post-op
☐ 6-8 weeks post-op
☐ 3 months post-op
☐ 1-year post-op
3. 2. List 2 eating behaviors that will help food digest more easily /prevent feeling overly full after surgery?
4.
• __
• __
5. 3. List 2 signs of dehydration:
6.
• __
• __
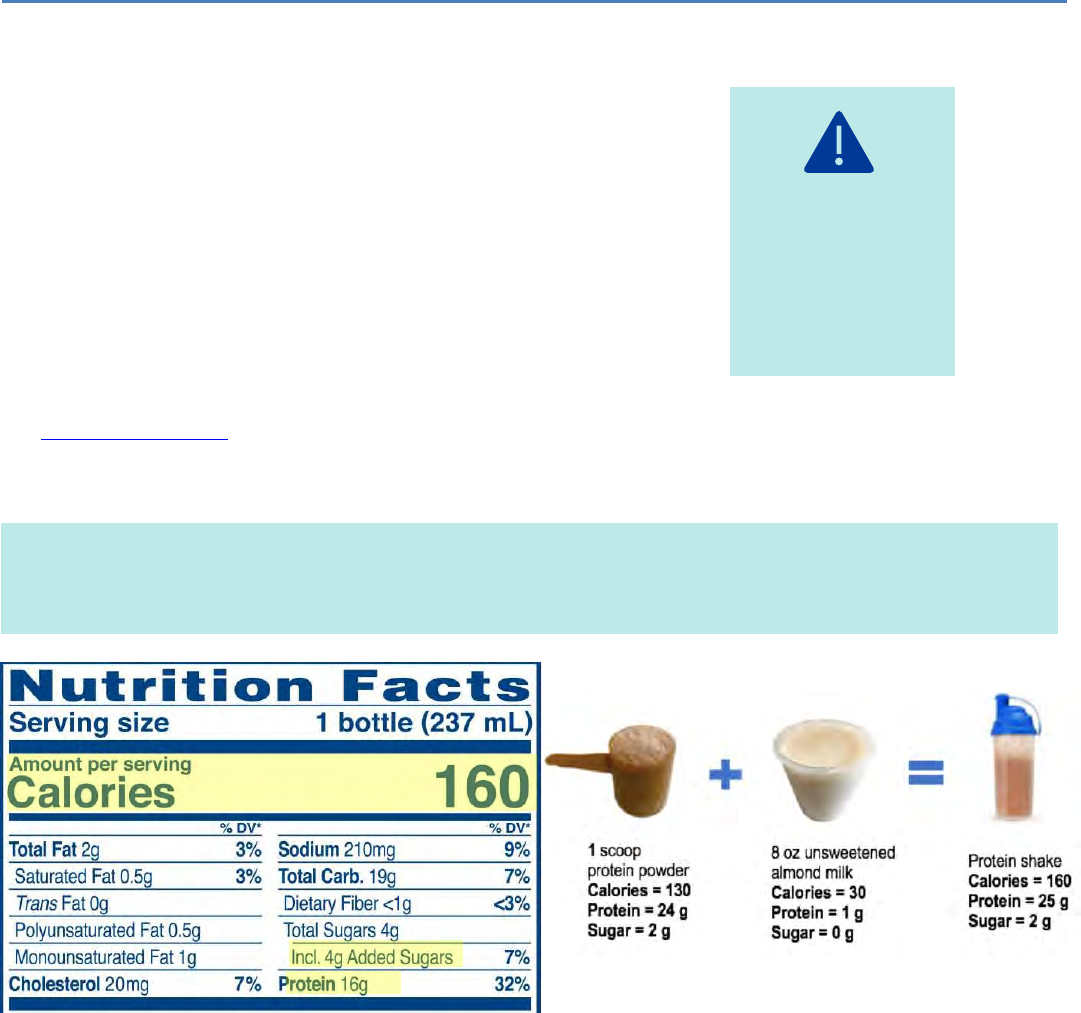
4. Name one recommended protein shake and list it’s calories, protein and added sugar amount:
_
_
7. 5. Circle all foods that are in the protein food group (hint: refer to page 24)
8.
☐Avocado
☐Banana
☐Chicken
☐Chickpeas
☐Eggs
☐Whole wheat bread
☐Green beans
☐Ground beef
☐Shrimp
☐Spinach Salad
2 © Center for Weight Management & Wellness 2023
9. 6. Circle all foods below that are allowed on the Stage 3: Smooth textures diet (see page 13)?
10.
☐Chili
☐Greek Yogurt
☐Pureed carrots
☐French fries
☐Oatmeal
☐Steak
☐Lentil or Bean Soup
☐Cottage Cheese
7. Rank these groups in order of most important after surgery, from 1-4: 1 is most important, 4 is least
important (hint: see stage 5, regular textures diet)
_____Starches _____Protein _____Vegetables/Fruits _____Fluids
8. After surgery, how many ounces of fluid should you drink every day?
_____ Ounces/day
9. After surgery, how many grams of protein should you eat every day?
_____ Grams /day
10. Which of the following vitamins and minerals should be taken after surgery to prevent vitamin and
mineral deficiencies? (Select all that apply)
☐Calcium citrate and vitamin D
☐Ginkgo Biloba
☐“Bariatric” Multivitamin (high in ADEK)
☐Calcium carbonate
☐Multivitamins without iron
☐ Iron
11. For best absorption, you should separate multivitamin w/ iron from calcium citrate by ____ hours
and each calcium dose by ____ hours.
12. Which of the following is the purpose of the 2-week before surgery diet? (Select all that apply):
☐It will prevent hair loss
☐It will shrink my liver
☐It will make my surgery safer
☐It will clean out my stomach before surgery

3 © Center for Weight Management & Wellness 2023
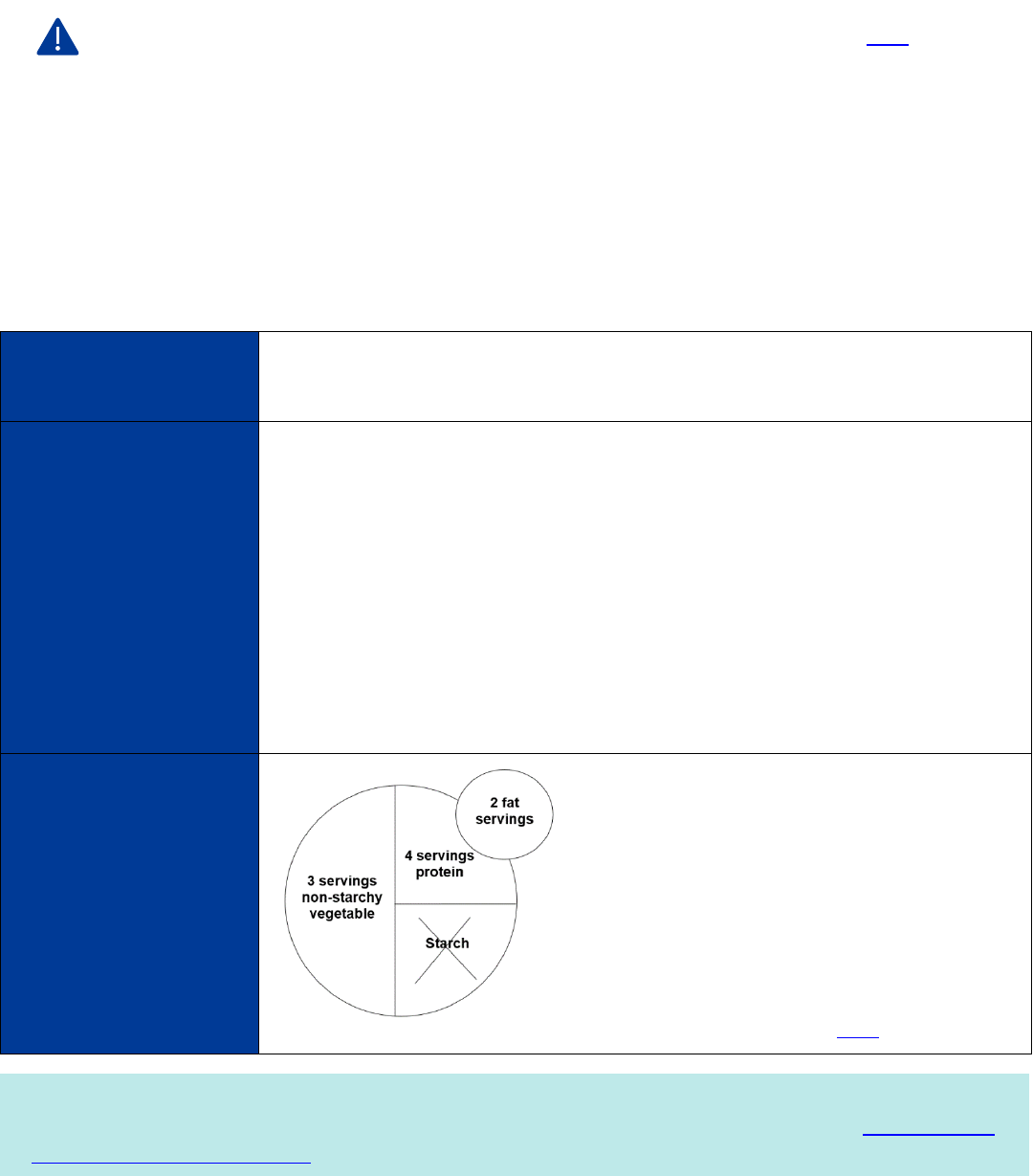
13. Plan a meal you would enjoy for your “1 daily meal” on the 2-week before surgery diet (page 9).
• Fill in the plate below with your food choices and list the serving amounts!
• Hint: use the Food group pages 24-29 to identify foods and serving sizes!)
3 servings non-starchy
vegetable:
___
4 servings protein:
__
Starch*
*If you take insulin or have been given the “2 week
before surgery diet for patients with diabetes” you can
add 1 starch serving at this meal.
1 starch serving: ________
2 fat servings:
__
4 © Center for Weight Management & Wellness 2023
14. Use page 32 to help you match the symptom to the possible vitamin deficiency:
_____ Bruising easily A. Iron
_____ Pale skin and increase tiredness/fatigue/weakness B. Vitamin A
_____ Vision changes (night blindness) C. Zinc
_____ Loss of or diminished smell or metallic taste in mouth D. Vitamin K
Questions to help you prepare for your nutrition appointments:
1. What do you need help with to be most successful after surgery?
_
2. Do you have any concerns following the guidelines or achieving your goals after surgery?
_
3. What do you need to do to ensure you have enough support and time to commit to the
recommended lifestyle changes?
_
4. Do you have any food allergies or intolerances we should know about?
_
5. Write one exercise goal you have before surgery.
_
6. What questions do you still want to address with the dietitian?
_
Please Start Keeping a Food Log and Bring to your Appointments
• There is a risk of malnutrition if you are unable to eat enough protein after surgery.
Keeping a food log will help you track your protein.
• We want to see that you can eat 80-100 grams or 11 servings of protein per day. If
you do not know how to track this, just start with writing down what you eat each day.
Food Log/Tracking: pick whatever method of tracking suites you best:
o Pen/Paper- see page 23 for an example tracking sheet
o Note taking app on your phone
o Calorie tracking apps: Baritastic, MyFitnessPal, LoseIt, MacroFactor
5 © Center for Weight Management & Wellness 2023
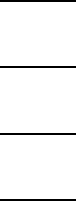
The Surgeries
SADI BPD-DS or DS
Single Anastomosis Duodeno-Ileostomy Biliopancreatic Diversion with Duodenal Switch
Digestive Changes
You will likely notice several changes to your digestion and bowel movements after surgery. Because not all your food is
being broken down it can cause more frequent bowel movements, loose stools and excess flatulence (gas). It is normal
to have between 2-4 bowel movements per day after SADI/DS. Excessive bowel movements or very smelly gas can be
caused by eating foods high in fat (fried food, greasy food, creamy sauces, oils) or eating too many simple carbohydrates
(sweets, cookies, cakes, candies, ice cream, white bread, white pasta, cereal, milk, protein shakes containing lactose).
Please see page 31 for more information and troubleshooting.
There are three main ways that the SADI, DS and Type 1 Distalization
surgeries will help you to lose weight and become healthier.
• Restriction – Your smaller stomach will limit how much food
you can eat at one time. The restriction will decrease over
time so you will need to rely on healthy lifestyle habits for
long-term portion control.
• Metabolic Changes – Stomach hormones and some other
signals in your body change after surgery. This can make
people feel less hungry and can help with health conditions
like diabetes. Your body can adapt to this change in gut
hormones over time and you will probably feel hunger again.
• Malabsorption—both surgeries divert the flow of bile acids
and pancreatic juices, so they have less contact with the food
you eat. This prevents the absorption of some vitamins,
nutrients, and calories to aid in additional weight loss.
You are usually in the hospital for 1 night after either surgery.
6 © Center for Weight Management & Wellness 2023
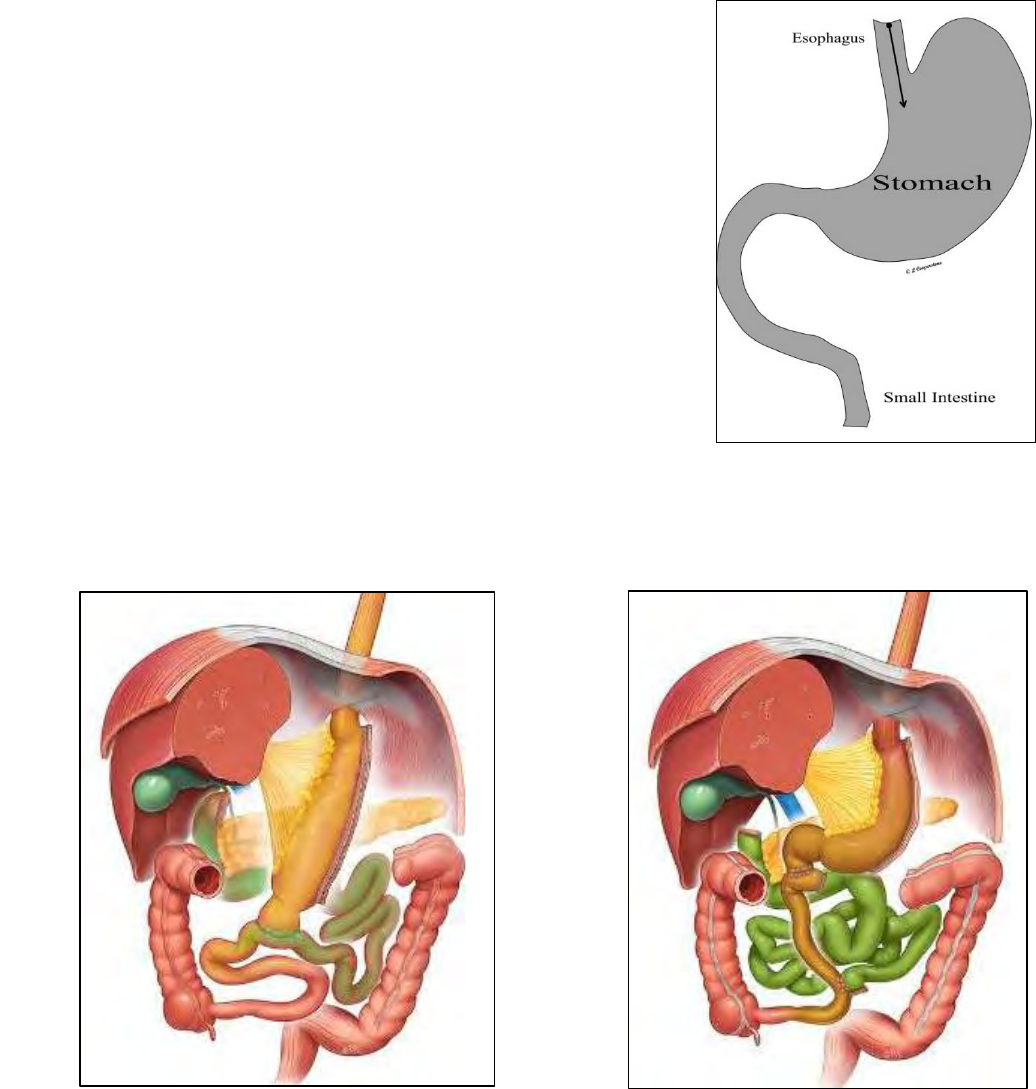
Skills for Success
Bariatric surgery is a tool. Below are 6 skills to start practicing now for long term success!
5. Plan ahead
Life will always be busy!
✓ Pack food and drinks for busy days
✓ Plan for social events
✓ Chop/peel ingredients in advance
✓ Buy pre-cut or ready to eat foods
✓
Include a protein source at every meal!
(See page 24 for ideas)
6. Stay accountable
Post-op Nutrition appointments:
✓ 2-3 weeks after surgery
✓ Every 3 months for first year
✓ Twice per year for life!
Stay engaged and meet other patients*
✓ Behavior + Nutrition support groups
✓ Private Facebook group
✓ Educational forums
*Ask a dietitian how to join!
1. Sip fluids throughout the day
No Caffeine
X 6 weeks
No Alcohol
X 12 months
✓ 48-64 ounces every day, no gulping
✓ Choose sugar-free, non-carbonated
beverages (see page 10 for ideas)
✓ Watch for signs of dehydration: Dark
colored urine, dizziness, nausea
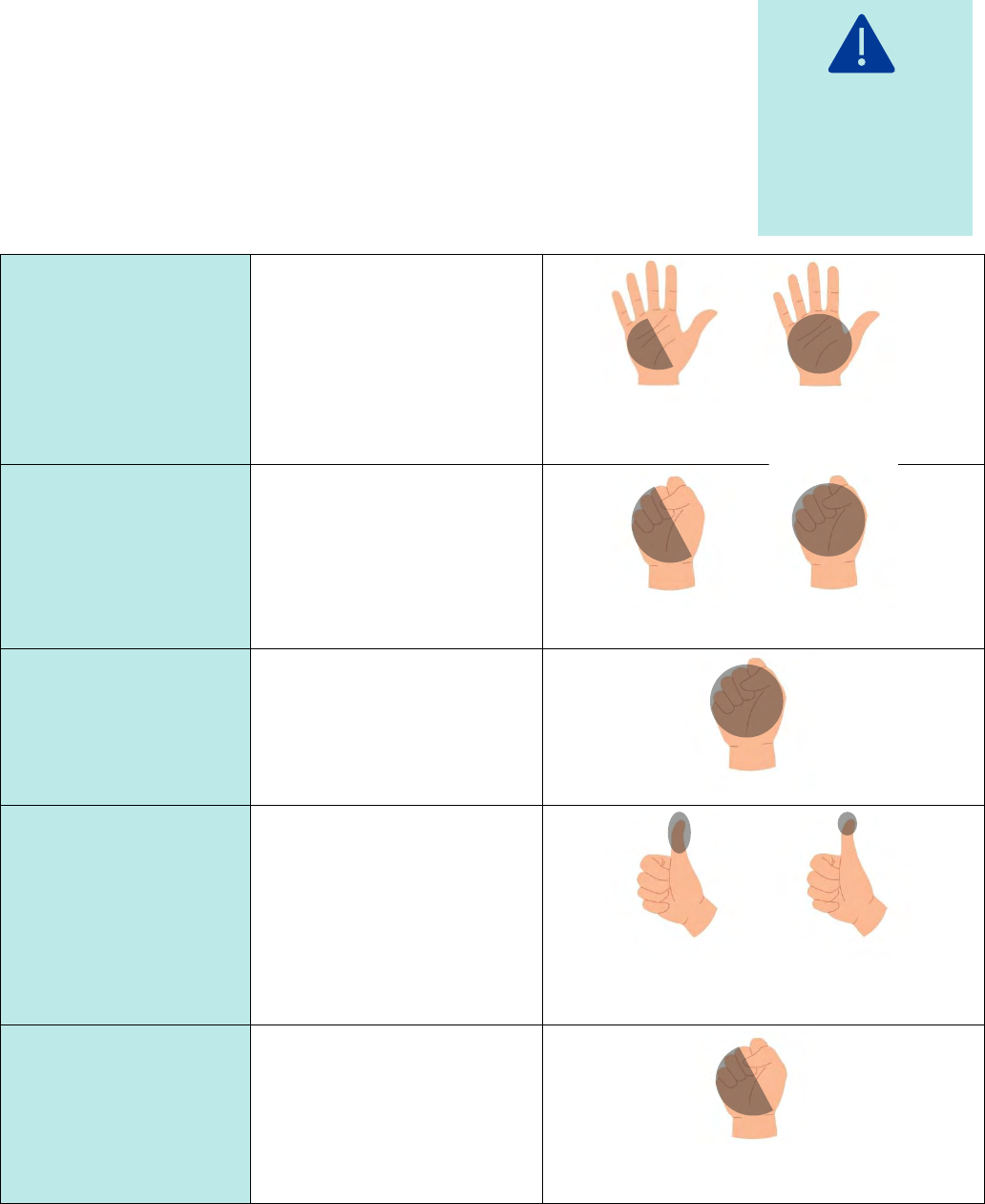
3. Eat slowly, take small bites,
chew to puree
Wait 30
seconds
Dime-sized bites
Chew 30-40
times
Pause, see
how your
stomach feels
Meals should
last 30-40
minutes
4. Eat every 2-3 hours
✓ Schedule eating events into your day
✓ Avoid grazing, nibbling, and picking
✓ Avoid going too long without eating
✓ Minimize distractions while eating,
engage all senses
Snack
Breakfast
Snack
Lunch
Dinner
2. Avoid eating and drinking at the
same time
✓ Prevents getting overly full, nauseas or sick
✓ Wait 30 mins after your meal to start
drinking again
Drink
Eat
Wait
Drink
7 © Center for Weight Management & Wellness 2023
Physical Activity
Before Surgery
Building a habit of physical activity is more important than the type or frequency. Start moving your body in a way that
feels comfortable. It’s okay to break up exercise into smaller amounts throughout the day (i.e. 10 mins, 3 times per
day). Remember, before beginning strenuous activities, check with your doctor.
Walk more! Try setting a
daily step goal.
Turn up the music and
dance.
Try chair exercises.
Make exercise a family
event. Go for a walk or hike
together.
Do yard work, gardening,
or household chores that
require brisk movement
Check out a new exercise
class, online or at your
local gym.
For low impact, try pool
exercises, water aerobics, or
a stationary bicycle.
Check out exercise apps on
your phone or videos
online.
Use resistance bands or
free weights to add
strength activities.
After Surgery
Key Points
Weekly Goal
Examples
Weeks 1-6
Recovery
Start slow. Listen to your body. Try and
move often to prevent blood clots and
promote healing. No weightlifting.
Drink plenty of fluids before, during,
after.
20-30 minutes of light
activity daily, broken up
throughout the day
• Take a walk around the
house every hour
• Light housework (dishes,
dusting, fold laundry)
• Leg lifts while sitting
• Short walks as tolerated
Weeks 6-8
Exercise Clearance
You need to receive clearance from
your surgeon or physician assistant
around this time before resuming
unrestricted exercise.
20-30 minutes of light
activity daily or more as
instructed by medical
team
Add more minutes or
frequency to exercise as able
Months 2-6
Make it a Habit
Work to build a consistent habit by
scheduling activity into your week.
Consider cardiovascular exercise (walk,
bike, elliptical, etc.) and strength
exercise (weights, bands, etc.).
30 minutes of low to
moderate intensity
exercise 5 days per week
or 150 minutes total per
week
• Walk, swim, or bike riding
• Dance, Zumba, Barre
• Yoga/Pilates
• Light weights, resistance
bands or chair exercise
• Gardening/Yardwork
Months 6-18
Build Strength &
Endurance
By 6 months you should have more
energy. Now you can start to SLOWLY
increase the time and intensity of
exercise. Listen to your body.
30-40 minutes of low to
moderate intensity
exercise 5 days per week
or 200 minutes total per
week. Include at least 2
days of strength training.
• Longer walks, swims, bike
rides
• Walking on hills or incline
• Aerobic or strength classes
• Weights or resistance
bands
Months 18+
Maintenance
Exercise after surgery may be the most
important factor in achieving long-
term maintenance. You need more
exercise in maintenance than you did
during the weight loss phase.
Aim for 250-300 minutes
(4 hours) weekly or as little
as 35-40 minutes per day.
Including at least 2 days of
strength training.
All of the above!

8 © Center for Weight Management & Wellness 2023
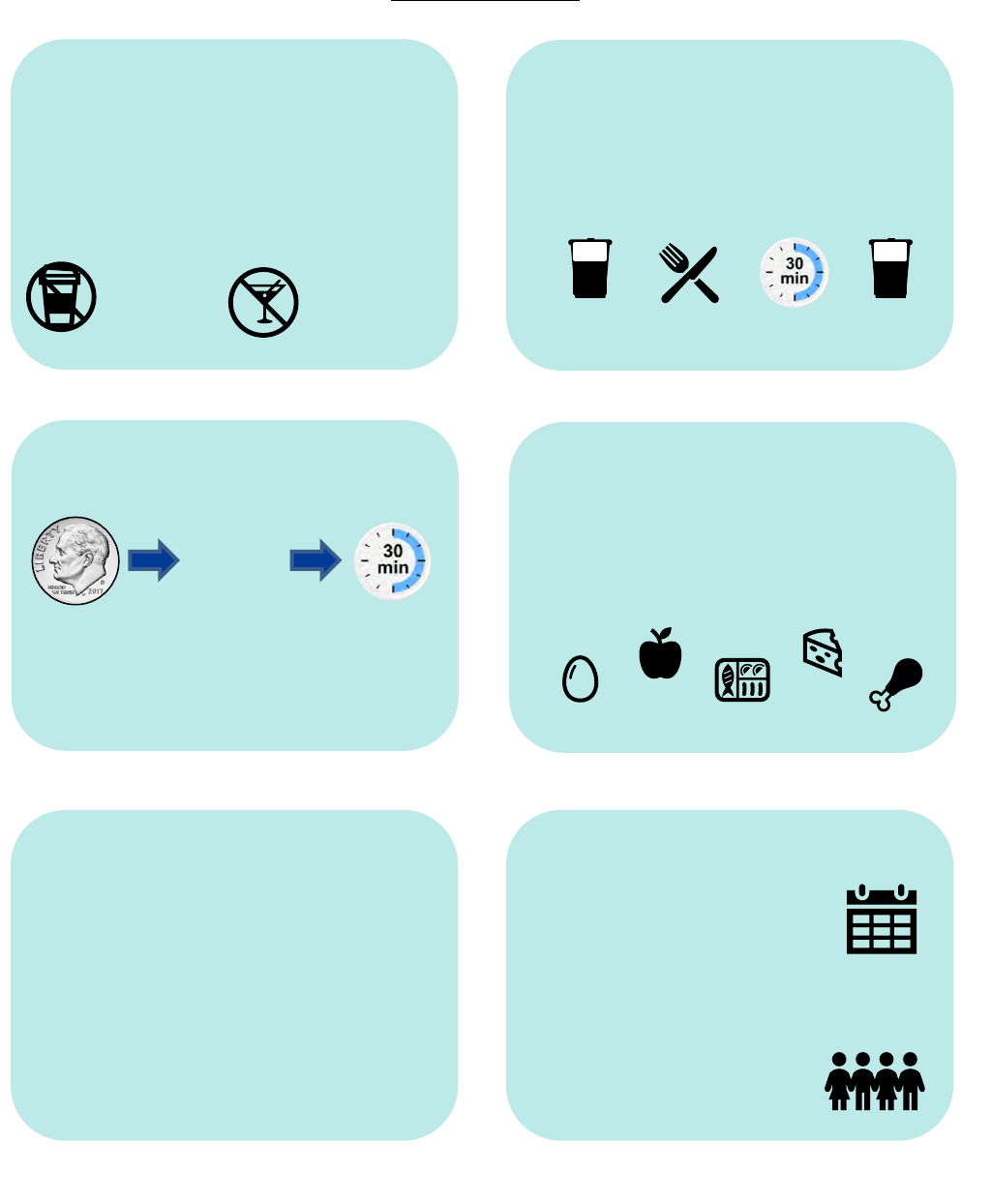
Getting Ready for Surgery
What to Buy
2-Week Pre-Surgery Diet— This diet helps shrink your liver and makes surgery safer. For 2 weeks
before surgery, eat 5 times daily from selected options and drink 64 ounces of sugar free fluid. For example:
See page 9 for more details on the 2-week pre-surgery diet.
After Surgery Diet- After surgery, follow a progressive textured diet while your stomach is healing. The
following pages provide more detail for each stage.
Measuring
Cups
Recommended
Vitamins
Food
Scale
Body Weight
Scale
Protein
Shakes
Sugar Free
Fluids
Shake
Snack
Shake
Snack
4 servings
protein
3 servings
non-starchy vegetables
No Starch
Meal
2 servings
fat
Stage 1:
Fluids
Stage 2:
Full
Liquids
Stage 3:
Smooth
Textures
Stage 4:
Soft
Textures
Stage 5:
Regular
Textures
Surgery
Day
Day 1
Day 7
Day 14
Day 35
9 © Center for Weight Management & Wellness 2023
2-Week Pre-Surgery Diet
Start this diet 2 weeks before your surgery date. This diet is considered low in carbohydrates, it is required and
will help shrink your liver, which makes a safer and easier surgery.
Instructions:
• Every day consume 2 protein shakes, 2 snacks and 1 meal from the choices below.
• Separate each eating event/shake by 3-4 hours and drink fluids in between
• Drink at least 64 oz of sugar-free beverages (water, crystal light, etc)
• Do not eat bread, rice, pasta, starchy vegetables (potatoes/peas/corn/squash), sweets nor drink alcohol
Pre-Op Diet Options:
Protein shakes:
Drink 2 daily
• Choose from protein shake options on page 12
• Mix powders with water, unsweetened almond /soy milk only
Snacks:
Eat 2 daily
• 1 fruit serving (i.e. 1 small apple) + 1 TBSP nut butter
• 1 fruit serving (i.e. 15 grapes) + 1 cheese stick
• 1/2 cup cottage cheese + 1 serving fruit (see page 26 for serving sizes)
• 1 Hard boiled egg + 1 serving fruit
• 1 container Zero Sugar Greek Yogurt + 14 almonds
• 1/2 cup red pepper strips + ½ cup carrot sticks + ¼ cup guacamole
• 1 cup raw veggies + 3 Tbsp hummus
• 1/4 cup dried Chickpea Snacks (e.g. Biena)
• Select Bars: Nature Valley Protein bar OR Pure Protein Bar OR Fiber One
Protein OR Power Crunch bar
1 Meal
Your daily meal should
include:
Use pages 24-29 for
serving size suggestions
4 servings of protein:
4 oz cooked/grilled chicken
3 servings of non-starchy
vegetables:
3 cups lettuce, tomatoes, onion
2 servings of fats
4 Tbsp Light Italian dressing
Find pre-op meal recipes here!
If you have been told to follow the pre-op diet for diabetes, see separate handout here!
On the day of surgery: Start drinking 1 carbohydrate drink (12oz Clearfast, or 10oz Ensure Pre-Surgery
Clear, or 12oz Gatorade) 3 hours before surgery and finish within 2 hours of surgery (See "Preparing for
your bariatric surgery guide").
10 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 1: Fluids
Starts: Day of surgery (“day 0”) or the day after surgery (“day 1”)
Lasts for: Up to 1 day
What to do:
1. Sip sugar-free, non-carbonated, non-caffeinated fluids throughout the day
2. Watch for signs of dehydration (dark color urine, headaches, dizziness)
Appropriate fluid choices:
• Water, still/flat only
• Crystal Light, MiO, or other sugar-free flavorings
• Decaf coffee and tea
• Broth
• Fruit-flavored water (Hint Water or homemade by floating fruit in water)
• Sugar-free Jell-o
• Sugar-free popsicles
• Sugar-free sports drinks (PowerAde Zero, Propel, Gatorade Zero)
o G2 only recommended with severe diarrhea and vomiting
Stage 1 Key Points:
• You will be in the hospital for this diet stage. The nurses will guide you to sip fluids during the day.
• Fluid intake is the number one priority after surgery.
• You will only be able to sip small amounts of fluid at one time. Pace yourself throughout the day.
• Gulping and chugging fluids will cause stomach pain.
• Avoid caffeine until Stage 5. It irritates the stomach.
• Carbonation can cause gas, belching, bloating, and stomach discomfort. Some people never tolerate
carbonation after surgery.
• You can use artificial sweeteners such as PureVia and Truvia (Stevia) and Nectresse (monk fruit), or
others: Equal (Aspartame), Sweet & Low (Saccharin), Splenda (Sucralose)
• If you are experiencing gas pain or discomfort, try walking around.
11 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 2: Full Liquids
Starts: Day of surgery (“day 0”) or the day after surgery (“day 1”)
Lasts for: 1 week
What to do:
1. Aim for 48-64 oz fluids every day. Prioritize hydration before protein.
• Avoid caffeine, added sugars, carbonation
• Signs of dehydration: dark urine color, lightheadedness or dizziness, and headaches
2. Have 80-100 grams of protein from protein shakes and allowed options below
• It may be challenging to get all your protein right away. Work toward this goal every day.
3. Monitor bowel movements. If concerned about constipation or diarrhea, please contact us.
Protein options:
• Protein shakes (lactose free)
• Egg whites/eggbeaters
• Low-fat, Greek yogurt*
• Low-fat Plain yogurt*
• Low-fat Soy yogurt*
*Choose yogurts with 5g or less added sugar per serving
Non-protein options
• No added sugar/unsweetened applesauce
• Sugar-free pudding
See Stage 2 meal ideas for specific texture, ingredient and recipe descriptions.
Choosing Protein Shakes
After Surgery, each protein shake / powder should have:
✓ Between 100-200 calories ✓ 15g or more protein ✓ 7g or less added sugar
To help you heal
and avoid
irritation, only
choose options
listed on this page.
12 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 2: Full Liquids (continued)
Protein Shake Shopping Guide
• We recommend taste-testing shakes before surgery
• Choose shakes from this list for your pre-op diet protein shake options too
Suitable for lactose intolerance:
Recommended for SADI/DS
Contains lactose:
NOT Recommended
Ensure Max*, Plant Protein Shake, High Protein*
Premier Protein* Ready-to-drink OR Powder
Fairlife Nutrition Plan* OR Core Power*
Muscle Milk “Genuine” powder
GNC Lean Shake 25* Ready-To-Drink
Pure Protein Ready-to-Drink or Powder
Orgain Plant Based Ready-to-drink
BOOST Max* (not regular BOOST)
Isopure Zero Carb* Powders
Quest* Ready-To-Drink
Premier plant protein Powder
Slim Fast High Protein* Ready-to-drink only
Muscle Milk “Zero” or “Genuine” Ready-to-drink
Syntrax Matrix Powders
* Certified Gluten Free- Please note, “cookies and cream” flavor protein shakes are not gluten free
Shopping Tips:
• Find protein shakes in grocery stores. Local pharmacies and online. See full shopping guide here.
• “Coffee” “latte” and “energy” flavors may have caffeine, avoid until post-op diet stage 5
• Look for sales on company websites and in weekly grocery ads, ask your dietitian for discount codes!
• Powders are usually cheaper per serving than ready-to-drink options
• Buying in bulk saves costs, but remember your tastes may change after surgery
Possible Stage 2 Problems: Call your dietitian if you need more help!
Lactose Intolerance:
Lactose is a natural sugar in milk. After surgery, your body may not digest lactose well which may cause
nausea, cramping, bloating, gas, or diarrhea. If you think you have lactose intolerance, try these tips:
• Stop drinking protein shakes for 24 hours. Keep hydrated with at least 48 oz or more stage 1 fluids.
• Use only ‘lactose free’ shakes:
o Shakes with ‘whey protein isolate’ or plant-based protein sources should not contain lactose
o Avoid cow’s milk and products with ingredients: “whey”, “milk concentrate” or, “whey blend”.
Taste changes may occur. Try adding your own flavors!
• Try extracts (vanilla, almond, mint etc.), sugar-free syrups (i.e. Da Vinci Gourmet or Torani brands),
spices (cinnamon, ginger, nutmeg, and cloves, even hot sauce, salt/pepper or Mrs. Dash). Mix shakes
or yogurts with unsweetened cocoa powder or powdered peanut butter.
• Consider unsweetened options: unflavored protein powder or chicken soup flavor (chicken broth!)
Smell-sensory changes:
• Drink your shake from a bottle with a small opening.
• Drink your shake using a straw.
• Drink your shake at a very cold temperature or mixed with ice.
13 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 3: Smooth Textures
Starts: Day 7
Lasts for: 1 Week
What to Do:
1. Keep sipping fluids; Goal: 48-64 ounces daily.
2. Choose protein foods first to reach your 80-100 gram daily goal. Then, may include non-protein foods.
3. Based on typical portion sizes, you will need to eat 6 times daily, including protein shakes.
4. Start taking chewable vitamin and mineral supplements (see page 15)
Only choose foods listed on this page. Your stomach is still healing and other foods may be irritating.
See Stage 3 meal ideas for specific texture, ingredient and recipe descriptions.
Protein Foods
• Egg whites or eggbeaters (no whole eggs)
• Low-fat Greek yogurt (blended or without fruit chunks) *
• Refried beans, no meat (black / pinto, low fat)
• Low-fat cottage cheese
• Tofu
• Part-skim ricotta cheese
• Protein shakes and powders
Other Foods
• Fat-free or light yogurt or soy-yogurts*
• Unsweetened applesauce, canned pears or peaches (in own juice or water/no syrup)
• Soft banana
• Oatmeal, cream of wheat, farina, maicena*
• Pureed vegetable (non-starchy: carrots, broccoli, cauliflower, green beans) without peel or seeds
• Sugar-free pudding
*Choose yogurts and oatmeal products with less than 5g added sugar/serving
How do I know how much protein I am eating?
It is important to keep track of how much protein you are eating. See page 24 and
read nutrition labels to adjust for the amount you ate.
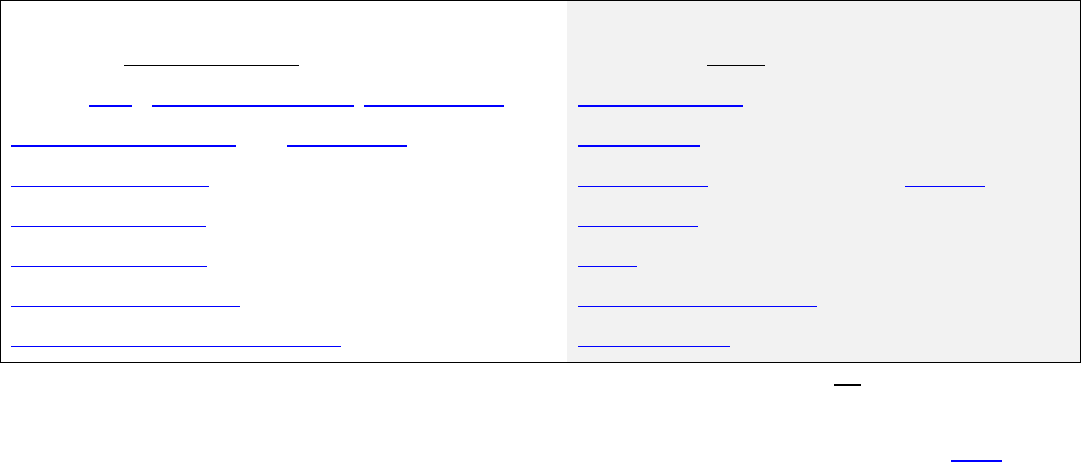
For example: Greek yogurt, individual container
▪ The serving size is “1 tub.”
▪ If you eat the whole container, you ate 15g protein.
▪ If you eat half, then you only ate half the protein
half of 15 = 7.5 grams.
15 g protein 7.5 g protein
14 © Center for Weight Management & Wellness 2023
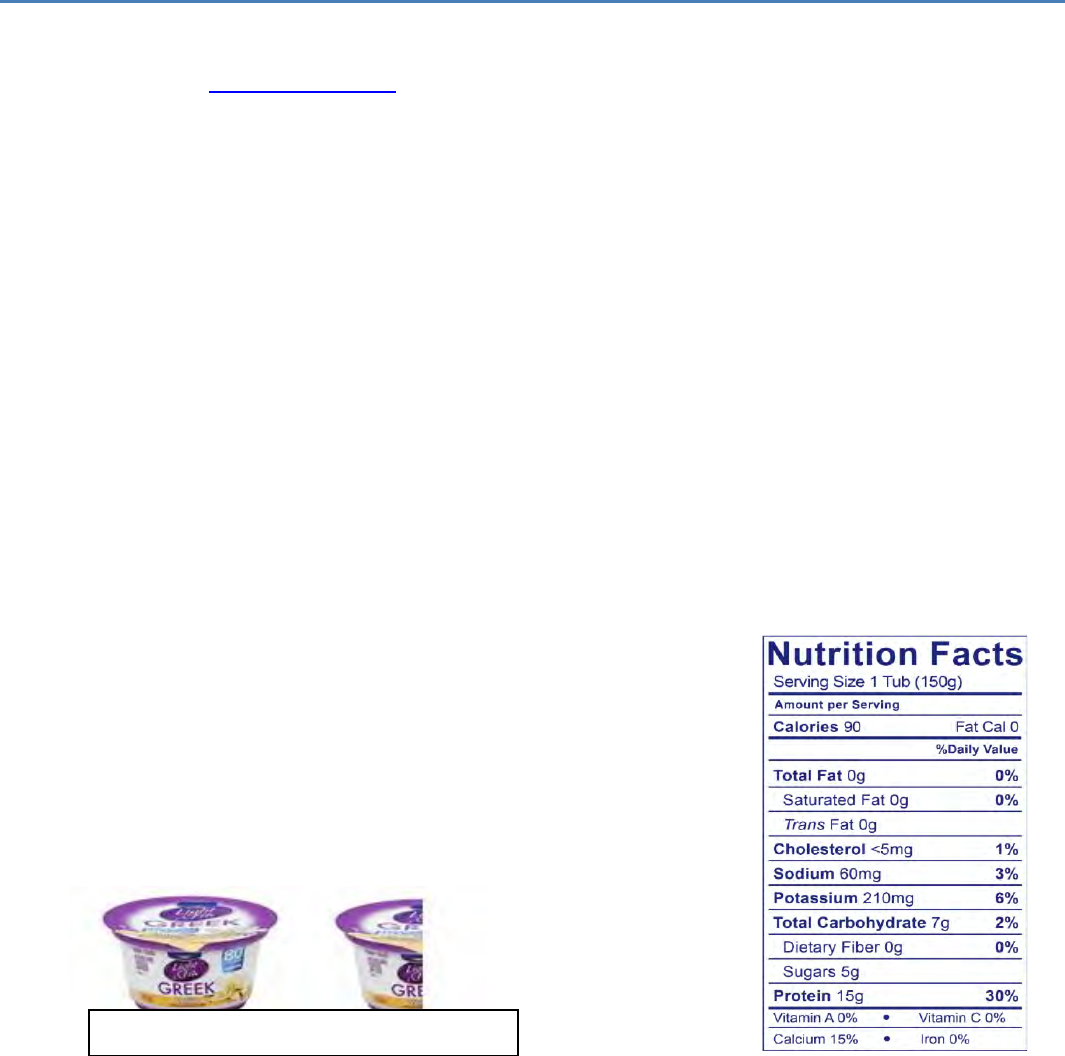
Post-Op Diet Stage 3: Smooth Textures (Example Day)
8am: Breakfast
Oatmeal with
¼ scoop protein powder
=7 grams protein
10am: Snack #1
Protein shake
= 30 grams protein
12pm: Lunch
2 Egg White
Omelet
= 6 grams protein
6pm: Dinner
1.5 ounces Tofu
=6 grams protein
3pm: Snack #2
¼ cup Cottage Cheese
with Chives
=7 grams protein
8pm: Snack #3
Protein shake
=25 grams protein
Foods do not
have to be bland.
Add seasonings
and spices.
You might not
be hungry but
still eat every
3-4 hours.
Stop eating at
the first sign of
fullness
(see right).
Remember to sip
fluids between
meals/snacks. Wait
30 minutes after
eating to drink.
Signs of Fullness
chest pressure
runny nose
hiccups
watery eyes
nausea
Daily Total
= 81 grams
protein
15 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 3: Vitamin Supplements
Both SADI and DS surgeries are malabsorptive procedures, therefore you will be on high doses of
specialty vitamins multiple times per day, for the rest of your life, to prevent serious vitamin and
mineral deficiencies. Learn more about signs and symptoms of deficiencies on page 31.
TAKE THESE VITAMINS DAILY, FOR LIFE:
• “Bariatric” multivitamin look for “high ADEK” formula
• Iron: 45-60 mg (may be in multivitamin)
• Calcium citrate+ vitamin D: 1500-1800 mg per day (SADI), 1800-
2400mg (DS). Do not take at same time as iron/multivitamin (see below)
• Chewable vitamins are recommended from week 1 after surgery until week 5
Chewable Multivitamin Options
Choose 1 below
Dose
Estimated cost / month
1. Bariatric Advantage Chewable High ADEK with Iron
2
$25
2. Celebrate Multi Chewable ADEK with Iron
2
$30
3. Bariatric Fusion Complete Chewable High ADEK
SADI: contains adequate calcium
DS: add one additional calcium per day
4
$36
Chewable Calcium Options: Each dose: 500-630 mg calcium citrate and >12 mcg/500 IU vitamin D
Choose 1 below
Dose
Estimated cost / month
1. Opurity Calcium Citrate Plus Chewable
2 tabs
3-4 times daily
$17
2. Calcium Citrate soft chews/chewy bites:
Bariatric Advantage, Bariatric Pal, Celebrate
1 chew
3-4 times daily
$25-35
3. Nature's Way liquid calcium citrate
At local pharmacies, supermarkets and online
1 Tbsp
3-4 times daily
$20
TIPS
• Separate each calcium dose from each other by 4 hours
and take 2 hours away from your iron/multivitamin.* (see
right)
>Try alarms, pill boxes and reminders to help you!
• Ask us about insurance coverage, discount codes and
vitamin samples!
• Having trouble with your chewable vitamin? You may
tolerate a small, non-chewable option earlier than week 5.
Talk to your dietitian for more information.
4hrs
4hrs
2hrs
8am: Calcium 500mg
12pm: Calcium 500mg
4pm: Calcium 500 mg
6pm: Multivitamin
8pm: Calcium 500 mg
Example Vitamin Schedule*
4hrs
16 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 4: Soft Textures
Starts: Day 14 / At week 2
Lasts for: 3 weeks
What to Do:
1. Keep sipping fluids. Goal: 48-64 ounces daily
2. Have a protein shake or eat a protein food 5-6 times per day (minimum 80-100 grams daily)
3. Keep taking vitamin and mineral supplements
Only choose foods listed on this page. Your stomach is still healing, other foods may be irritating.
See Stage 4 meal ideas for specific texture, ingredient and recipe descriptions.
Example Plate – it might be this small!
Protein Foods
• Egg, egg whites, or egg beaters
• Fat-free Greek yogurt (without fruit chunks)
• Low-fat cottage cheese
• Part-skim ricotta cheese
• Tofu
• Chicken or turkey (dark meat is fine)
• Fish (flaky fish like tuna, cod, haddock,
salmon, and tilapia)
• Veggie burger
• Beans and lentils
• Protein shakes or powders
Other Foods
• Well-cooked non-starchy or starchy vegetables
with no skins or peels
• Canned fruit/ applesauce (unsweetened, in own
juice or water, no syrup)
• Fresh fruits: try soft first, avoid skins & peels
• Tomato sauce
• Fat-free or light yogurt (non-Greek)
• Reduced-fat or light cheese
• Oatmeal, cream of wheat, or farina, maicena
Fats
• Light mayonnaise or salad dressing
• Hummus
• Avocado
• Smooth nut butter (not crunchy)
• Butter or oil
How to Count Grams of Protein
(if the food does not have a nutrition label)
7 grams of protein =
1 ounce chicken/turkey/fish
1 egg
¼ cup egg substitute
2 oz firm tofu / 3 oz soft tofu
½ cup beans
See page 24 for more details
Protein Foods
Non-protein
foods
1st
2nd
17 © Center for Weight Management & Wellness 2023
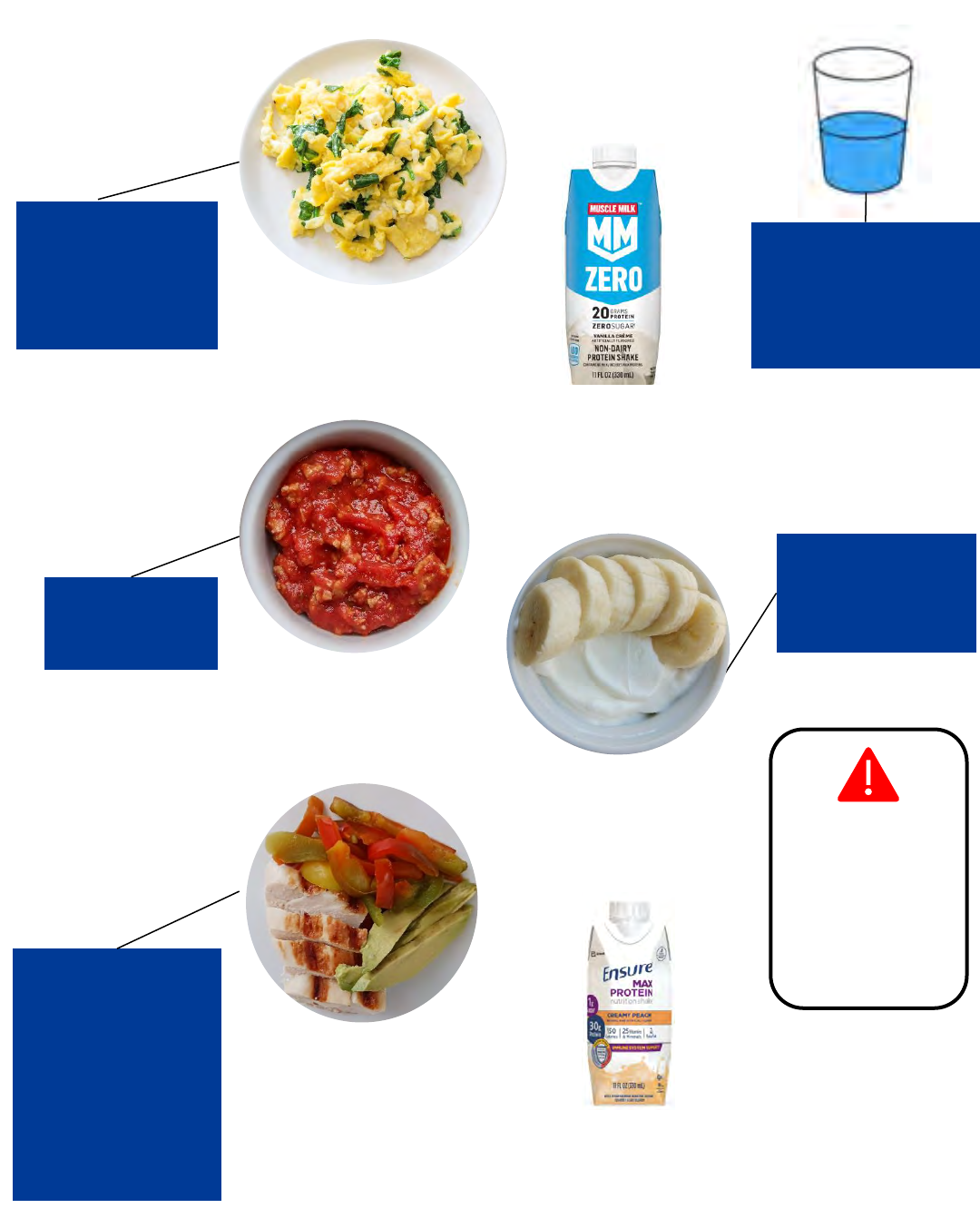
Post-Op Diet Stage 4: Soft Textures (Example Day)
8am: Breakfast
1 egg + 1 TBSP spinach
= 7 grams protein
10am: Snack #1
Protein shake
= 20 grams protein
12pm: Lunch
1.5 ounces Turkey Chili
= 6 grams protein
6pm: Dinner
1 oz chicken
+ ¼ cup peppers
+ 1 Tbsp avocado
=7 grams protein
3pm: Snack #2
1/2 cup Greek yogurt
+ ¼ banana
= 10 grams protein
Remember to sip
fluids between
meals/snacks. Wait 30
minutes after eating
to drink.
Eat foods that are
“fork mashable”–
foods that are too
tough or dry can
be hard to tolerate.
Eat slow– take 30
minutes for each
eating event, pause
after each bite
Keep meat tender
and moist– use a
slow cooker,
marinate meats,
cook in foil packets,
don’t over-cook.
Use broth when
reheating meat in
the microwave.
Chew until your
food is pureed
by your teeth.
Daily Total
= 80 grams
protein
Food Feel Stuck?
Do not panic.
Do NOT drink
water.
Stay calm, move
around, it will
pass.
8pm: Snack #3
Protein shake
= 30 grams protein
18 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 4: Soft Textures (Key Points)
• Think “fork-mashable” for the appropriate texture. If the food can be mashed easily with a fork, it’s
probably soft enough to eat in this stage.
• You might not feel hungry but you still need to eat regularly. Space eating events evenly during the
day, about every 2-4 hours. Set reminders or timers to help you remember to eat if helpful!
• Some days you won’t have room for everything. Do your best to reach your protein goal first.
• If food feels like it is “stuck”,
o Do not panic and do not drink water.
o Stay calm, move around, and it will pass.
After the sensation passes, think about what may have gone wrong…
o Ate too fast? Take 30 minutes for each eating event and pause after each bite.
o Didn’t chew enough? Chew until your food is pureed by your teeth.
o Food too tough? Make sure you are only eating foods from stages 4 and earlier.
o Food too dry? Dry foods may be hard to tolerate. Keep meat tender and moist.
▪ Use a slow cooker, marinate meats, cook in foil packets, avoid over-cooking.
▪ Add broth when reheating meat in the microwave to keep it moist.
o Too full? Try to stop before you get “over-full” which can feel like chest pressure or nausea.
• Dehydration can still happen. You are likely getting back to your daily routine and will be busy.
Remember to drink your fluids in between eating times. Be aware of possible foods that could cause
diarrhea and put you at risk for dehydration (see page 31 for more information)
• You may not tolerate certain textures the first time you try them. If you have trouble with a food even
when you are eating very carefully, avoid the food for 2-3 weeks before trying again.
• It’s normal to not.
19 © Center for Weight Management & Wellness 2023
Post-Op Diet Stage 5: Regular Textures
Starts: Day 35 / At week 5
Last for: Forever, but your meal plan may change over time.
What to Do:
1. Keep sipping at least 48-64 ounces daily (continue sugar free, non-carbonated choices)
2. Focus on protein at meals (protein goal is at least 80-100 grams daily)
3. Use this meal plan as a guide for a balanced diet; all food groups can be included over time
4. Keep taking vitamin and mineral supplements; you can change to pill form if you prefer
How do I start in Stage 5?
In Stage 5, you may not tolerate every food you try. Be patient with your stomach. Tolerance usually improves
over time. See below for possible ‘problem foods’ to help guide your choices. See Stage 5 Meal Ideas for more
ideas!
Remember to stay hydrated first!
At mealtimes, start with protein
and as you tolerate, add in other
food groups.
Follow this order of importance:
Fluids 1
st
Proteins 2
nd
Vegetable/fruits 3
rd
Starches, 4
th
1st
2nd
last
Possible ‘Problem Foods’
Your stomach can be sensitive for 3-6 months after surgery, sometimes longer. The following
foods have unique textures that may be difficult to tolerate if eaten too soon. Be cautious!
Protein: Tough red meat, hamburger, fatty meats (salami, sausage, chorizo), lobster, scallops,
clams, shrimp
Fruits: Stringy, thick skins, peels (like oranges, grapes, pineapple)
Vegetables: Stringy, fibrous (like asparagus, peapods, celery, lettuces, yuca)
Starches: Rice, pasta, doughy breads, popcorn
20 © Center for Weight Management & Wellness 2023
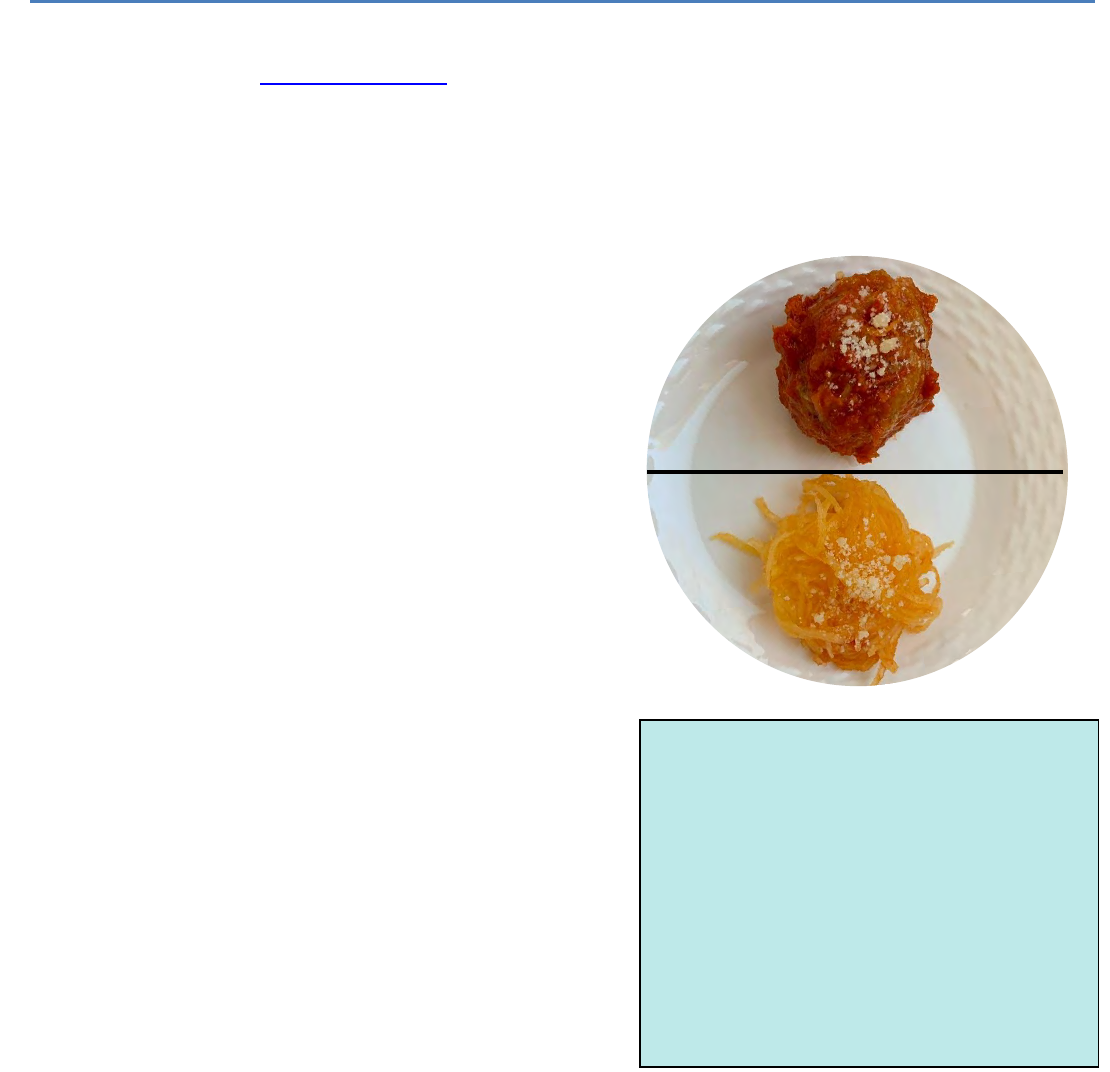
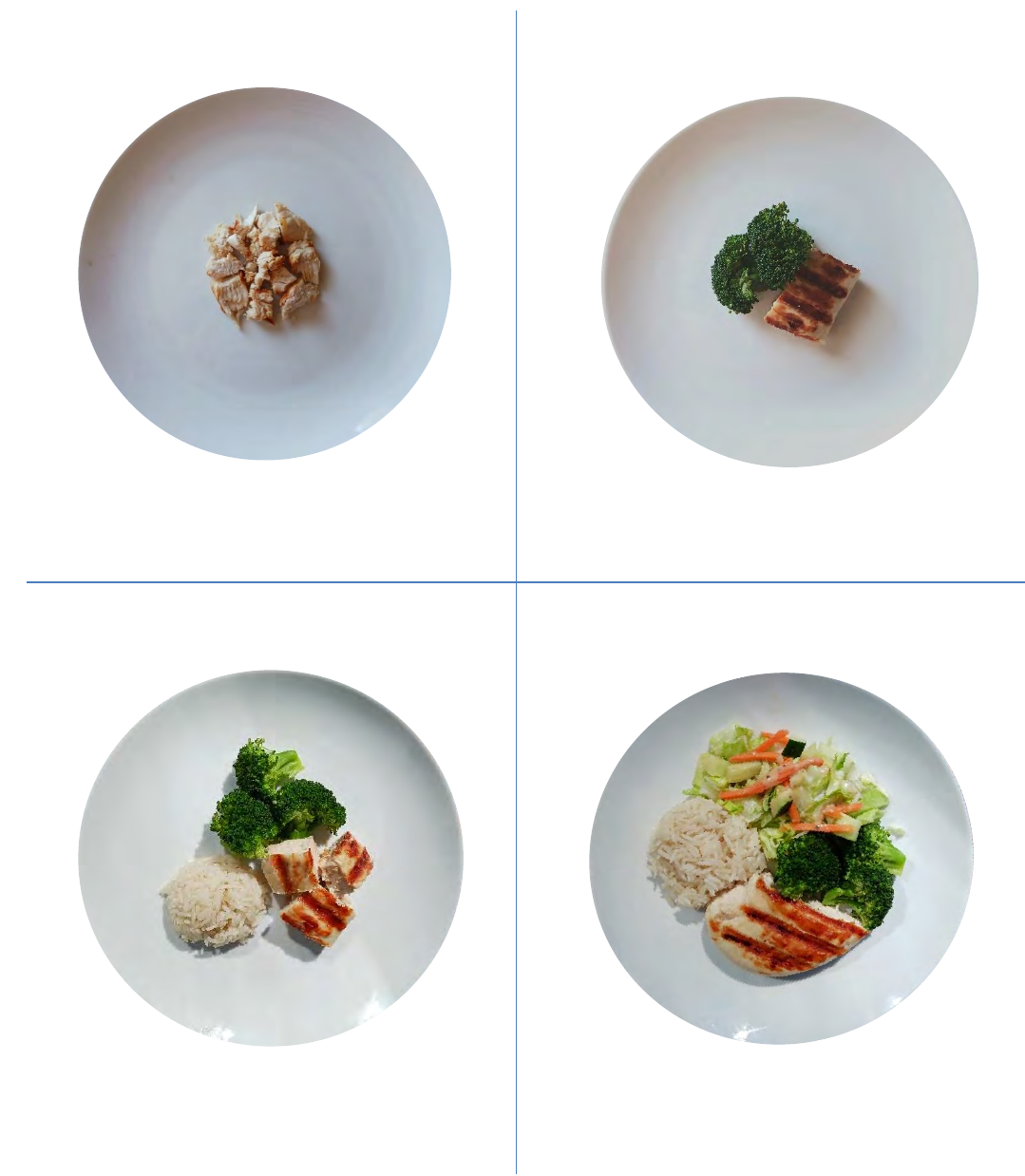
Post-Op Diet Stage 5: Portion Size Suggestions
As you heal, the amount of food you can eat at one meal will increase over time. Do not worry if you are
eating slightly more or less. Remember, stop eating before getting overly full or uncomfortable to create
healthy eating habits for long-term success!
Month 1
Month 3
Month 6
Month 12+
2-4 TBSP per meal
Shown: 1 ounce chicken
1/4- 1/3 cup per meal
Shown: 1 ounce chicken + ¼ cup broccoli
1/2-3/4 cup per meal
Shown: 2 ounces chicken + 1/2 cup broccoli
+ 2 tablespoons rice
1-1 ½ cup per meal
Shown: 3 ounce chicken + 1/2 cup broccoli
+ ½ cup salad + ¼ cup rice
21 © Center for Weight Management & Wellness 2023
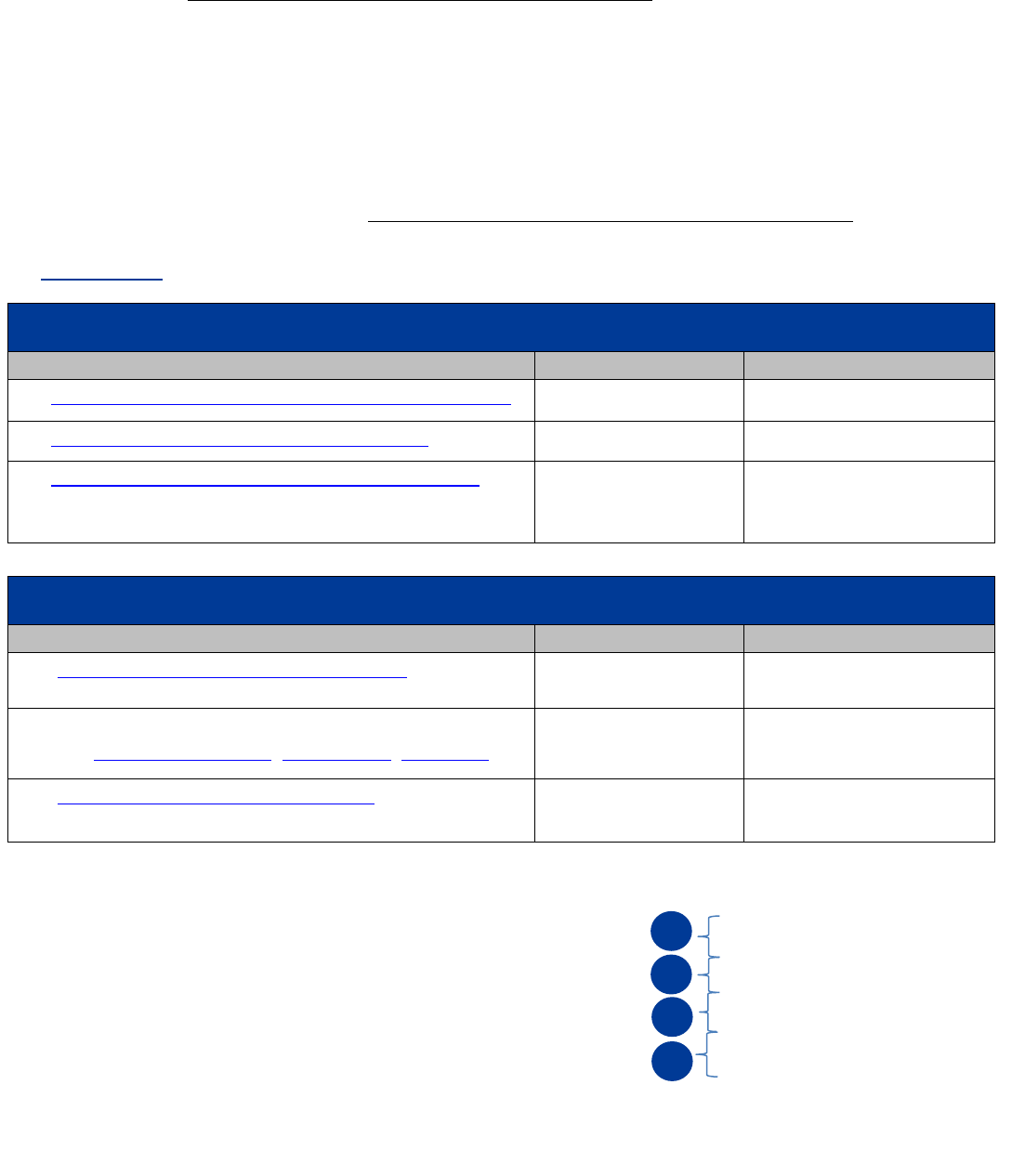
Post-Op Diet Stage 5: Meal Plan
Use the meal plan to guide your choices throughout the day. Each checkbox is a serving of food from that food
group. Use pages 24-29 for additional foods and serving sizes of each food group.
Serving Size Quick Guide
Protein
Chicken, fish, beef, pork,
tofu, etc.
Page 24
Vegetables
Broccoli, cauliflower, carrots,
peppers, green beans,
onions, zucchini, salad etc.
Page 25
Fruits
Apples, berries, oranges,
mango, melons, etc.
Page 26
Fats
Salad dressing, avocado,
peanut butter, nuts/seeds,
oils, butter, etc.
Page 28
Starch
Rice, pasta, quinoa,
potatoes, hot cereals, etc.
Page 29
2 ounces
(2 servings)
4 ounces
(4 servings)
*portion depends on tolerance
½ cup
Cooked vegetables
1 cup
Raw vegetables
1 cup
1 Tbsp
1 Tsp
Dressings, nut butter,
hummus, avocado
Oil, butter, mayo
½ cup
Cooked starch
11 protein servings
2 vegetable servings
2 fruit servings
1 dairy serving
2 fat servings
3 starch servings
This meal plan is
not one size fits all.
Ask your dietitian
to help
individualize!
22 © Center for Weight Management & Wellness 2023
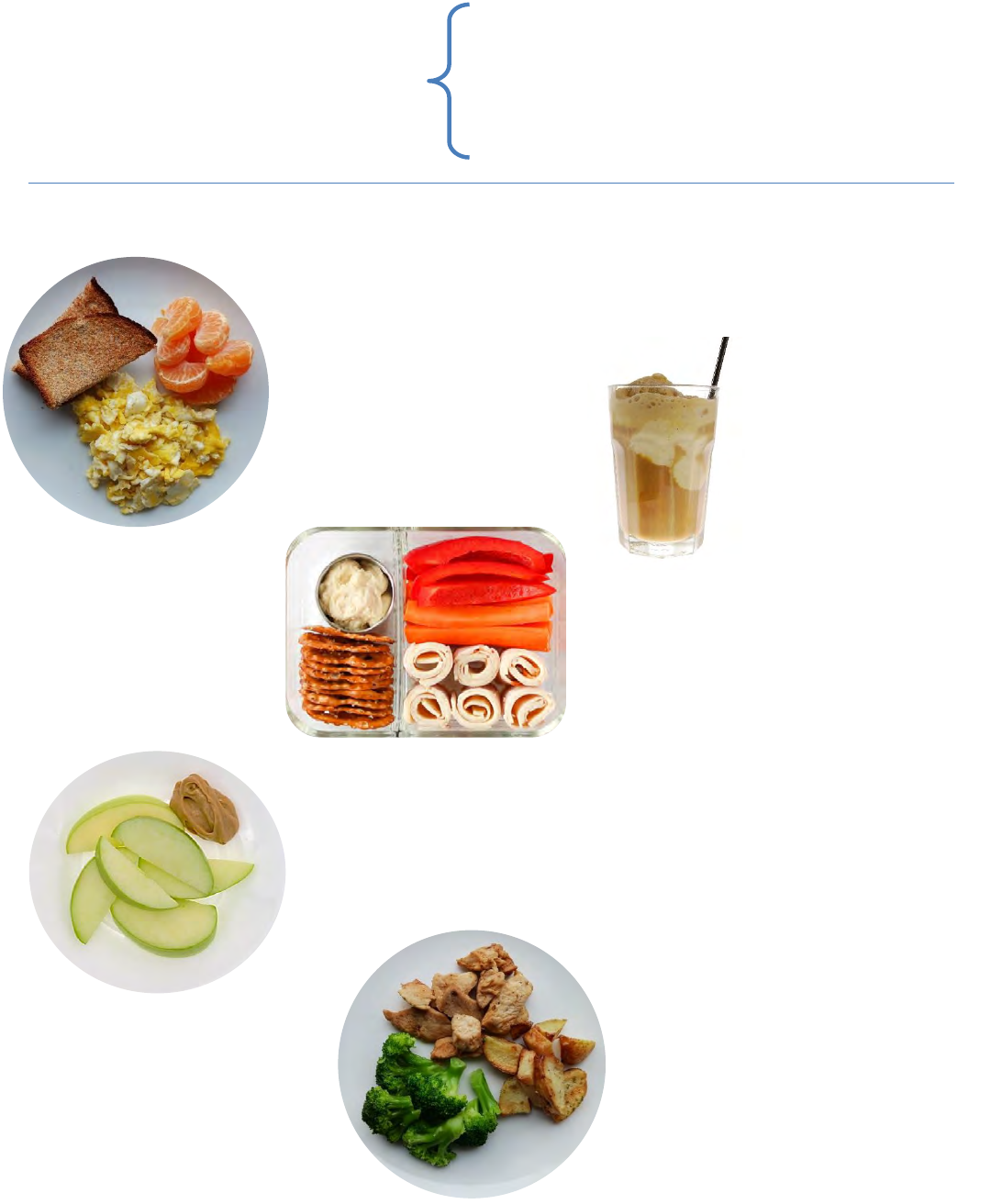
Post-Op Diet Stage 5: Example Day ~12 months post-op
BREAKFAST
2 eggs (2 protein serving)
1 clementine (1 fruit serving)
1 toast (1 starch serving)
1 ounce cheese (1 dairy serving
)
DINNER
4 ounces chicken (4 protein servings
)
½ cup broccoli (1 vegetable serving)
½ cup potato (1 starch serving)
SNACK
1 apple (1 fruit serving
)
2 Tsp peanut butter (1 fat serving
)
LUNCH
2 ounces deli turkey (2 protein servings
)
1 cup peppers (1 vegetable serving)
2 Tbsp hummus (1 fat serving)
1 ounce pretzels (1 starch serving)
SNACK
Protein shake in coffee
(25 grams= 3 protein
servings)
11 protein servings
2 vegetable servings
2 fruit servings
1 dairy serving
2 fat servings
3 starch servings
By 12 months, many people
can eat all the servings
provided in the meal plan but
this will vary based on your
individual stomach capacity.
23 © Center for Weight Management & Wellness 2023
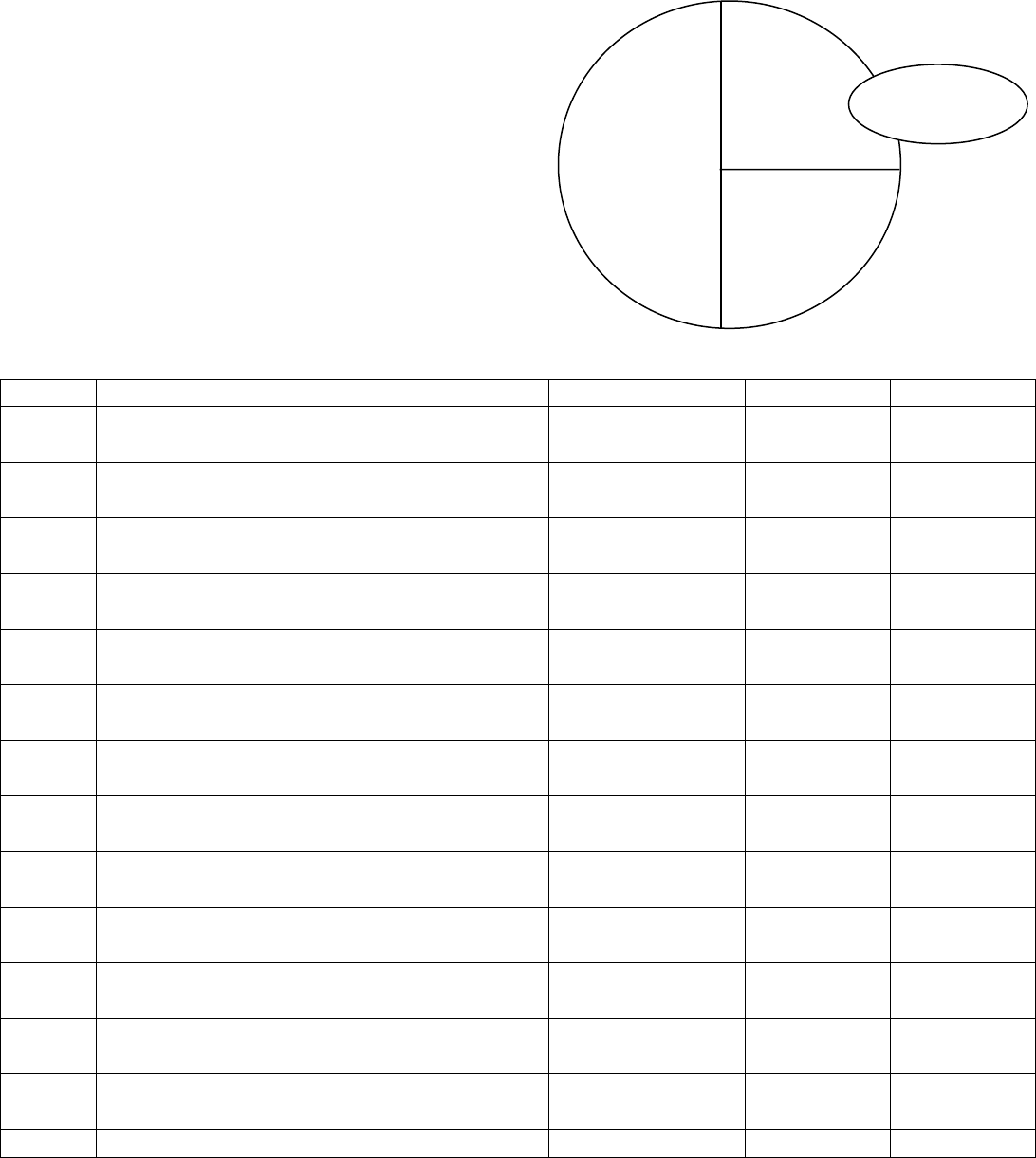
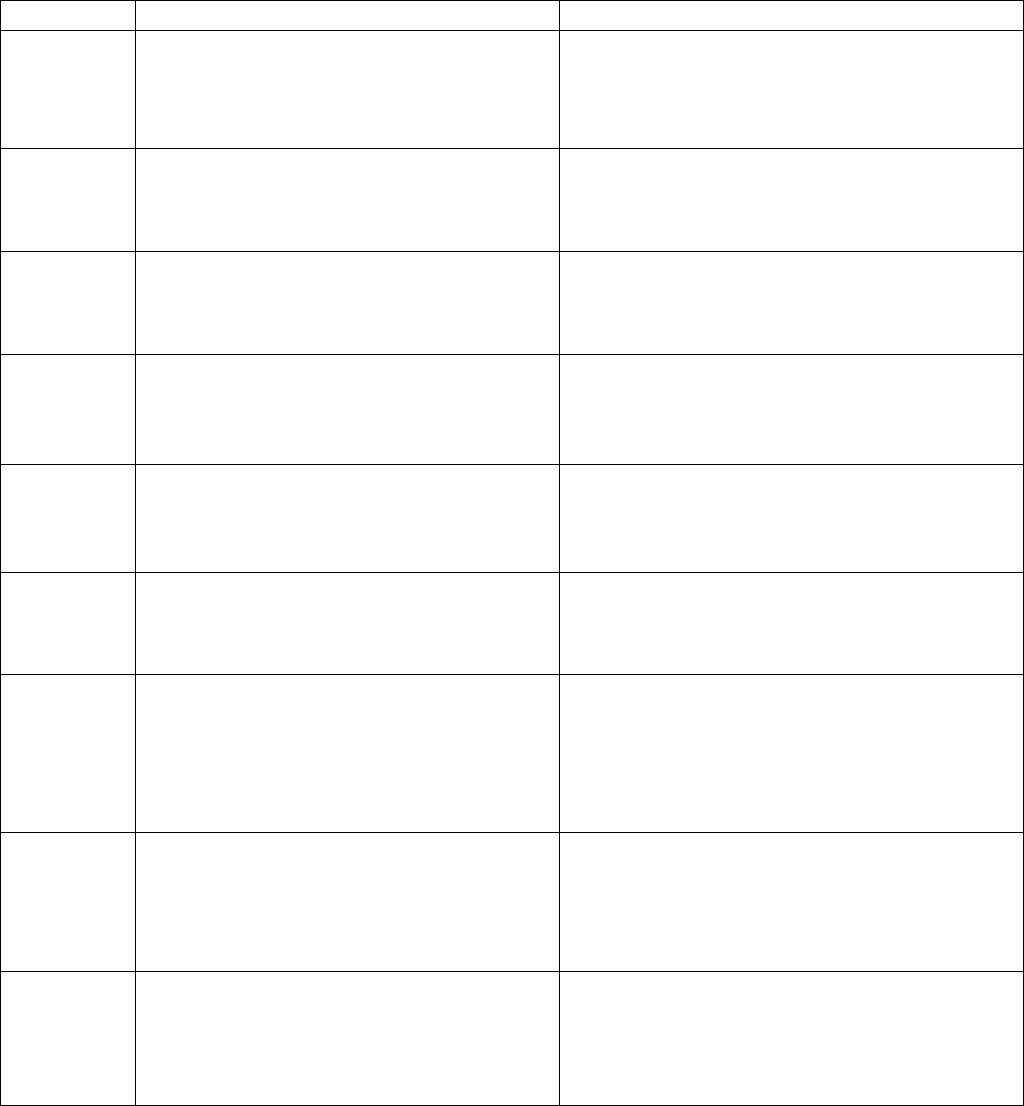
Post-Op Diet Stage 5: Regular Textures (Meal Planner)
Use this meal planning worksheet to plan your individual eating schedule or track your food intake. Keep track
of fluid and protein to help hit your minimum goals of 64 ounces fluid and 80-100 grams protein!
8 cups of fluid
11 protein servings
2 vegetable servings
2 fruit servings
1 dairy serving
2 fat servings
3 starch servings
Time
Food
Liquid (oz)
Protein (g)
Vitamins
Total
oz
g
Starch
#3
Vegetables
or Fruits
#2
Protein
#1
Fat/
Condiment
24 © Center for Weight Management & Wellness 2023
Serving Sizes
Protein Foods
Each protein food contains 7 grams of protein per serving. You may eat multiple servings at a time.
*1/2 cup beans is equal to 1 protein serving + 1 starch serving
1 ounce or 1 serving = about 7 grams of protein
2 ounces or 2 servings = about 14 grams of protein
3 ounces or 3 servings = about 21 grams of protein
• Choose lower fat protein foods (like skinless chicken breast, 99% fat free ground turkey).
• Limit red meat (beef, lamb, pork, goat,).
• Processed meats can increase a person’s risk of colorectal and stomach cancer. Processed meats
include hot dogs, pepperoni, salami, chorizo, sausages, corned beef, ham, bacon, pastrami, and any
other meats that have been cured, smoked, salted or treated with any chemical preservatives. The
dietitian can provide you with more information about processed meats.
1 ounce chicken
1 ounce turkey
1 ounce fish or shellfish
1 ounce beef
1 ounce pork
1 ounce duck
1 ounce lamb
1 ounce venison
1 ounce goat
2 oz firm tofu/3 oz soft tofu
¼ cup non-fat cottage cheese
¼ cup non-fat ricotta cheese
3 oz Greek yogurt (1/2 individual
container)
½ cup beans*
¼ cup egg substitute
1 egg
7 grams
of protein
=
1 serving
of protein
=
Aim to eat 11 protein servings every day
(Which is about 80-100 g of protein daily)!
25 © Center for Weight Management & Wellness 2023
Non-Starchy Vegetables
Each vegetable serving contains 5 grams or less of carbohydrates and 2-3 grams of fiber per serving.
Fresh and frozen vegetables are ready to eat! Rinse canned vegetables to remove some salt.
Examples of non-starchy vegetables:
Starchy vegetables: corn, peas, potatoes, plantains, yuca (manioc/cassava), winter squash
are on the Starches List (page 29).
Aim for at least 2 servings of
non-starchy vegetables every day!
½ cup cooked
vegetables
or
1 cup raw
vegetables
1 serving
of
vegetables
=
Green beans
Jicama
Kale
Kohlrabi
Lettuce
Mushrooms
Mustard greens
Okra
Onions
Peppers (bell and spicy)
Prickly Pear (Nopal cactus)
Radishes
Rutabaga
Artichoke
Asparagus
Beets
Broccoli
Brussels Sprouts
Cabbage
Carrots
Cauliflower
Celery
Chayote
Cucumber
Eggplant
Endive
Salad Greens
Sauerkraut
Scallion/chive
Spinach
Sprouts
Snap Peas
Summer Squash
Tomato
Turnips
Water Chestnuts
West Indian Pumpkin
(auyama)
Zucchini
26 © Center for Weight Management & Wellness 2023
Fruits
Each fruit serving contains 15 grams of carbohydrates and 2 or more grams of fiber.
Use fresh, frozen or canned fruits with no sugar added.
Eat fruit in its whole form instead of blending or juicing. Whole fruit will fill you up more!
Fresh, Frozen, & Unsweetened Canned Fruit
Apple (2 in. across) 1 apple
Applesauce (unsweetened) ½ cup
Apricots (canned) ½ cup or 4 halves
Apricots (medium, fresh) 4 apricots
Banana (8 in. long) ½ banana
Blackberries ¾ cup
Blueberries ¾ cup
Breadfruit …………………………….. ¼ cup
Cantaloupe 1 cup cubes
Cherries (canned) ½ cup
Cherries (fresh)....... 12 cherries
Chico fruit (like kiwi)…………………. ½ chico fruit
Figs (fresh) 2 figs
Grapefruit (medium) ½ grapefruit
Grapefruit (segments) ¾ cup
Grapes 15 grapes
Honeydew melon 1 cup cubes
Guava, guayaba……………………… ½ cup
Kiwi 1 kiwi
Mamey ………………………………... 2/3 cup
Nance fruit (cherry like) …………….. 1 cup, pitted
Mandarin oranges ¾ cup
Mango ½ mango
Nectarine (2 ½ in. across) 1 nectarine
Orange (2 ½ in. across) 1 orange
Papaya 1 cup
Passion fruit ………………………….. 1/3 cup pulp
Peach (fresh) 1 peach or ¾ cup
Peaches (canned) ½ cup (2 halves)
Pear (fresh) ½ large or 1 small
Pears (canned) ½ cup or 2 halves
Persimmon 2 persimmons
Pineapple (canned) 1/3 cup
Pineapple (fresh) ¾ cup
Plantain and green banana ………… ½ a plantain or ¾
cup small green banana
Plum 2 plums
Pomegranate ½ of fruit
Raspberries 1 cup
Soursop ………………………………. 1/3 cup pulp
Starfruit ………………………………. 3 cups cut up
Strawberries (whole) 1 ¼ cup
Tamarind ………………………… 11-12 raw tamarinds
Tangerine (clementines) 2 tangerines
Watermelon 1 ¼ cup cubes
Dried Fruit (no added sugar)
Serving sizes for dried fruits are small
because they are calorie-dense foods.
Apples 4 rings
Apricots 7 halves
Dates 2 ½ medium
Figs 1 ½
Prunes 3 medium
Raisins 2 Tablespoons
Dried cranberries 2 Tablespoons
Every fruit & amount
listed on this page
=
1 serving of fruit
Aim for 2 servings of
fruit every day!
27 © Center for Weight Management & Wellness 2023
Dairy / Non-Dairy Alternatives
Each serving of dairy contains 6-8 grams of protein.
Choose low sugar option! On a label look for products with less than 5g added sugar per serving.
8 oz skim / fat-free milk
8 oz 1% / low-fat milk
8 oz Lactaid / lactose-free milk
8 oz soy milk
½ cup evaporated skim milk
1/3 cup dry nonfat milk
1 cup nonfat yogurt (non-Greek)
1 oz cheese*
¼ cup shredded cheese*
1 string cheese*
* Choose reduced-fat, part-
skim, or light when possible
1 serving
of dairy
=
Aim for 1 serving of
dairy every day!
28 © Center for Weight Management & Wellness 2023
Fats
Each serving of fat contains 5 grams of fat. Conversion tip: 1 Tablespoon = 3 teaspoons
1 teaspoon oils (olive, canola…)
2 teaspoons of nut butter
1 teaspoon butter
1 teaspoon ghee
2 tablespoons low-fat cream cheese
1 tablespoon light tub margarine
1 tablespoon light mayonnaise
1 teaspoon mayonnaise
2 tablespoons light salad dressing
1 tablespoon oil-based dressing
2 teaspoons creamy salad dressing
1 tablespoon light creamy dressing
2 tablespoons of hummus
2 tablespoon avocado
2 Tbsp coconut, fresh/shredded
10 small or 5 large olives
6 almonds
2 whole pecans
10 small peanuts
2 whole walnuts
1 tablespoon seeds
1 serving
of fat
=
Limit to 2-3 servings of
fat every day!
29 © Center for Weight Management & Wellness 2023
Starches
Each serving contains 15 grams of carbohydrates.
Cereals/Grains/Pasta
Cold cereals (unsweetened) ¾ cup
Bran cereals 1/3 cup
Bran cereals (flaked) ½ cup
Granola 2 Tbsp
Shredded wheat ½ cup
Barley, cooked……………….1/3 cup
Bulgur (cooked) ½ cup
Hot cereals (unsweetened) ½ cup
Couscous ……………………. ½ cup
Grits (cooked) ½ cup
Masa arepa………………….. ¼ cup
Pasta (cooked) ½ cup
Rice (cooked) 1/3 cup
Quinoa (cooked) 1/3 cup
Crackers and ‘Snack Foods
Animal crackers 8
Graham crackers (2.5 in. square) 3
Matzo ¾ oz
Melba toast 5
Oyster crackers 24
Popcorn (popped, 94% fat free) 3 cups
Pretzels ¾ oz
Rye crisp (2 in. x 3 in.) 4
Saltine crackers 6
Soda crackers …………………………6
Wheat Thins 8
Triscuits 4
Breads
Bagel (from cafe) ¼ (1 oz)
Bagel (pre-packaged, grocery store) ½ (1 oz)
Bread sticks 2 (2/3 oz)
English muffin ½
Hamburger or hot dog bun ½ (1 oz)
Pita, 6 in. across ½
Plain roll, small 1 (1 oz)
Bread 1 slice (1 oz)
Injera bread………………………….. 1/3
Naan (3 oz commercially prepared). 1/3
Tortilla, 6 in. across……………………1
Sandwich thins/deli flats 1
Sweet bread (Pan dulce)……………. ½ bread roll
Cooked Beans/Peas/Legumes
(also count as 1 protein)
Beans and legumes (kidney, pinto, black, lentils,
chickpeas, black-eyed peas) ½ cup
Baked beans ¼ cup
Limit to 3 servings of
starch every day!
Starchy Vegetables
Corn ½ cup
Corn on the cob, 6 in. long 1
Green peas ½ cup
Plantain ½ cup
Potato, baked (medium) 1/2
Potato, mashed ½ cup
Taro, boiled/mashed ½ cup
Winter squash (acorn, butternut) ½ cup
Yam/sweet potato 1/3 cup
Every food &
amount listed on
this page
=
1 serving of starch
Choose 100% whole grain / whole
wheat options whenever possible!
30 © Center for Weight Management & Wellness 2023
Possible Problems & Solutions
We do not expect problems to occur, but if they do, we want you to know how to solve them. It is helpful to keep a
record of anything unusual that occurs and what you did before and after it happened to identify trends and help you
talk to your care providers more specifically.
Dizziness, Headaches, Lightheadedness, Dark Urine (Signs of Dehydration)
✓ Drink fluids with electrolytes (like Propel Zero or Powerade Zero).
✓ Add salt to your foods.
✓ Drink salty bouillon or soup broth.
✓ Call the Physician’s Assistant phone line at 617-732-8882 if you are unable to catch up on your fluids.
Nausea and/or Vomiting
✓ Tune into your eating behaviors. Take small bites, chew thoroughly and pause after each bite.
✓ Stop eating or drinking at the first sign of fullness, which may feel like pressure in your upper chest.
✓ Stay hydrated. Drink at least 48-64 ounces of fluids.
✓ Keep foods tender and moist.
✓ Determine whether you might have lactose intolerance (page 12).
✓ Avoid eating and drinking at the same time.
✓ If these suggestions do not work, or you vomit bright red or dark brown liquid, please call the PA line or your
surgeon’s office.
Heartburn
✓ Every person has different food and beverage triggers of heartburn. Make a list of the ones that trigger
heartburn for you and avoid them.
✓ Take your prescribed heartburn medication.
✓ Tune into your eating behaviors. Take small bites, chew thoroughly and pause after each bite.
✓ Avoid lying down for 3-4 hours after eating.
Hair Loss
✓ Hair loss after bariatric surgery is called ‘telogen effluvium’ and generally occurs around 3-6 months. This
happens because some of your hair follicles are in resting stage (telogen phase) during the time of surgery, and
the stress of significant weight loss can cause that hair to stay in the resting stage.
✓ There’s generally not much you can do about hair loss at 3-6 months post-op except minimize washing and
brushing to prevent extra fallout.
✓ If hair loss continues after month 6, speak to your dietitian. It could be related to iron, copper, zinc, or B vitamin
deficiencies or not eating enough protein.
✓ You can also try Nioxin shampoo.
Dental Health
✓ Because you won’t be eating and drinking together after surgery, you may be at a higher risk for dental carries.
Also, acid reflux may damage your teeth, so consider the following:
✓ Swish your mouth out with water/mouth wash (don’t swallow!) and spit after eating to remove food particles.
✓ Floss regularly.
✓ Consider brushing 3 times daily.
✓ Talk to your dentist about your bariatric surgery, especially if you have acid reflux.
✓ Consider adding a 3
rd
cleaning; instead of every 6 months, schedule a cleaning for every 4 months.
31 © Center for Weight Management & Wellness 2023
Possible Problems & Solutions (Bowel Movements)
Constipation
Short-term Solutions
✓ Increase your fluids – aim for 64 ounces daily.
✓ Try a laxative, such as Milk of Magnesia or Miralax, and take a stool softener up to 3 times daily.
✓ Try psyllium, a natural soluble fiber.
Long-term Solutions
✓ Increase your fluids – aim for 64 ounces daily.
✓ Increase your fiber intake.
o Eat more fruits, vegetables, legumes and whole grains if your diet stage permits.
o If you are unable to add more fiber through your diet, try a fiber supplement, such as Benefiber or
Metamucil.
o Slow and steady is the key to adding fiber to your diet. Start with a small amount, such as one serving of
fiber supplement or one extra serving of food with fiber. Stick with that amount for 1-2 weeks before
increasing as needed.
✓ Stay physically active.
✓ Continue taking a stool softener as needed.
Frequent Bowel Movements
✓ It is normal to have between 2-4 bowel movements per
day after SADI/DS.
✓ If having more frequent bowel movements, look for
potential food triggers (see right)
✓ Frequency and consistency of stools usually improve over
time as your intestines adapts in the months and years
after surgery but may be lifelong.
Diarrhea
✓ Loose stools and diarrhea are common after SADI/DS.
✓ Look for potential food triggers (see right)
✓ Eat slowly and chew thoroughly.
✓ Do not drink fluids with meals.
✓ Limit caffeinated beverages.
✓ Try a probiotic supplement – ask your dietitian for
suggestions.
✓ Try psyllium, a natural soluble fiber that can help thicken
stool.
✓ If you hare having more than 6-8 bowel movements per
day, contact your surgeon/PA.
Bloating/Gas/Cramping
✓ It is common to have a lot of gas that can be extremely
foul smelling after surgery.
✓ Look for potential food triggers like lactose, processed
carbs, sugar alcohols, and high fiber foods (see right)
✓ Avoid carbonated beverages.
✓ If drinking through a straw causes these problems, avoid
using one.
Oily Stool
✓ Stool that is loose but bulky, floats at the top, and droplets of oil on top of the water, can mean you are eating
too much fat in your diet (see right)
Possible Food Triggers
for Frequent Bowel Movements, Diarrhea,
Smelly Gas
Most Common:
• Lactose: dairy, cream, milk, soft cheese, ice
cream, protein shakes. See page 12 for
lactose free shake options.
• High sugar foods: sweets, cookies, cakes,
candies, ice cream, syrups.
• High fat foods: fried food, creamy sauces,
greasy food, oils, dressings, mayo, butter,
whole fat dairy, full fat cheese.
Additional triggers:
• Excess processed carbs: pasta, rice, cereal,
crackers, bread, chips, etc.
• Sugar alcohols: malitol, sorbitol, xylitol, etc.
found in sugar free candy, protein bars,
beverages, gum
• Fermentable fibers (add to diet slowly):
beans, lentils, legumes, broccoli, cauliflower,
cabbage, brussels, onion, garlic, fruits.
• Gastric irritants: alcohol, caffeine.
Tip: Keep a food journal and bring with you to
your next dietitian appointment so we can
review with you. You do not need to avoid all of
the foods on this list, only the ones that cause
you symptoms!
32 © Center for Weight Management & Wellness 2023
Possible Problems & Solutions (Vitamin Deficiencies)
Not all vitamin deficiencies have obvious symptoms, it is important to continue to take your
vitamins and have your bloodwork done, even when you are feeling well.
Vitamin
Function
Signs / Symptoms of Deficiency
Vitamin A
Important for eye health, immune system, lungs,
skin, digestive and urinary systems. Also
important in wound healing and reproductive
system.
• Vision changes (night blindness), dry eyes
• Dry, cracked lips, mouth or eye sores
• Dry hair, dry/itchy/bumpy skin
• Poor wound healing
Vitamin B1
Enables us to use carbohydrates and sugar as
energy and plays key roles in nerve, muscle and
heart function.
• Muscle weakness
• Short term confusion, memory loss
• Numbness of limbs; imbalance
• Nausea or loss of appetite
Vitamin
B12
Involved in nervous system functioning; red
blood cell formation and DNA synthesis
• Extreme weakness and fatigue
• Numbness/tingling of limbs
• Memory loss
• Swelling of the tongue
Vitamin D
Aids in calcium absorption for bone health,
important for immune system, growth and
development and cellular function.
• Muscle weakness or cramps
• Bone pain; unexplained bone fractures
• Depression/Seasonal affective disorder
• Fatigue
Vitamin E
Important for vision, reproduction and the health
of your blood, skin, brain and nervous system.
Also acts as an antioxidant-which protects cells
from toxins in the body.
• Muscle weakness
• Difficulties coordinating and walking
• Numbness or tingling in hands/feet
• Frequent infections (immune issues)
Vitamin K
Helps with blood clotting to prevent excessive
bleeding. May also help protect bones from
softening and/or fractures.
• Bruising easily
• Black, tar-like stool (contains blood)
• Excessive bleeding from wounds; bleeding gums
or frequent nose bleeds
Iron
Important mineral in the body that helps build
blood cells, carries oxygen and detoxifies. Also
helpful with immune and enzyme functioning as
well as in growth and development.
• Tiredness, fatigue, weakness
• Pale skin
• Frequently cold; shortness of breath
• Brittle nails and hair loss
• Ice eating or “pica” (cravings for non-food items
like dirt, paper)
Calcium
A very important mineral for healthy teeth and
bones. 99% of calcium in body is stored in teeth
and bones. Also helps the heart, brain, nerves,
muscles and circulatory system.
• Muscle spasm or cramping
• Tingling / burning in mouth and fingers
• Brittle nails, hair
• Unexpected fractures
• Loss of teeth / dental issues
Zinc
This mineral is the essential component of many
enzyme and plays a role in cell division and
formation of protein. It is important for immune
function, digestion, skin and hair health,
antioxidant activity and more!
• Loss of/diminished smell or taste
• Metallic taste in mouth
• Hair loss, rough skin/rash
• Fatigue
• Cracks on lips, sores around mouth
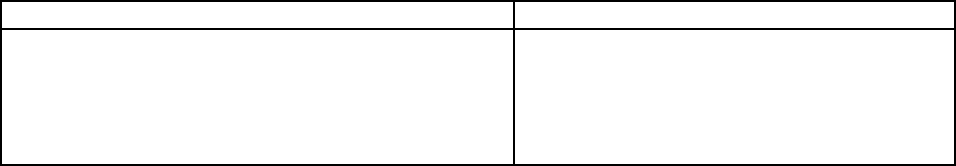
33 © Center for Weight Management & Wellness 2023
Frequently Asked Questions
Navigating Diet Stage 5 and Beyond
Q: How much should I be eating in stage 5?
A: Appropriate portion sizes will look a bit different for everybody and get a bit larger over time. About a ½ cup portion
is common at the beginning, leveling off at about 1-1.5 cups total volume per meal when your diet stabilizes. See page
20 for visual examples. Avoid distractions and eat slowly so you can start paying attention to your body’s cues for
fullness. Stop eating at the first sign of fullness. Fullness cues may now include nausea, runny nose, or hiccups.
Q: What will my meals look like?
A: Look at the Stage 5 meal plan to guide food choices and suggested portions. Remember, choose protein foods first,
then vegetables or fruits, and starches last. Use fats as flavorings or for moisture. Stay in touch with the dietitians too!
Q: Will my appetite return?
A: The hormone changes experienced after surgery might not last forever and it is normal for your appetite and hunger
cures to gradually return over time. It is important to establish healthy meal routines and avoid skipping meals. Foods
high in protein and fiber help control hunger. Avoid eating just because or from boredom, stress, and emotional triggers.
Q: Will I be able to enjoy my favorite foods again?
A: After the initial recovery period and in the long-term we would expect you to eat a wide variety of foods and no foods
are off limits completely. There may be foods that no longer agree with your new anatomy and can cause worsening
diarrhea, gas, bloating (see page 31) if eaten in large amounts. However, we will work with you to carefully plan meals
and snacks to help ensure you are your meeting your nutrition needs while including foods that you enjoy.
Q: How much weight will I lose?
A: Every patient will lose a different amount of weight, at different paces and places. It's important to never compare
your rate of weight loss with other patients because everyone is different. Most weight loss occurs in a "stair-case
fashion" where patients lose a certain amount of weight followed by a stall period. Try to look for non-scale indicators of
progress such as body composition changes, gains in energy levels and a reduction of medications.
Behavioral Considerations
Working with the Bariatric Psychologists
Your experience after surgery will most likely be very positive. There are many behavioral and lifestyle
changes needed after surgery. Our team will help you make changes and manage challenges both before and after
surgery. We are also happy to help provide referrals for additional behavioral support as necessary.
Common challenges after surgery…
Behavioral treatment to help…
• body image disturbance
• “mourning” the loss of food
• compulsive behaviors (e.g. gambling, excessive
shopping, promiscuous sex)
• difficulty noticing changes
• cognitive behavioral therapy (CBT)
• communication skills
• social support
• relaxation techniques
• coping skills training
Q. How can I expect to feel in the first month after surgery?
A. Patients often find that the first month after surgery can be a most challenging time. It is not unusual to experience
“buyer’s remorse”, or the sense of “why did I do this to myself?”. This may be natural when dealing with post-surgical
pain, impaired sleep, diet changes, and fatigue. However, mood and anxiety symptoms tend to improve quickly. Please
monitor your symptoms, you may notice mood returning to normal after you have settled into your new lifestyle.

34 © Center for Weight Management & Wellness 2023
Frequently Asked Questions (Continued)
Q. Will I need to change my psychotropic medications after surgery?
A. Our team will review all your medications and suggest changes, if needed. Extended release (ER) or sustained release
(SR) medications are often not absorbed as well after surgery. You may need to speak with your physician about making
a change to your prescription. Please do not make any changes to your medications unless approved by the
prescribing physician (PCP or psychiatrist).
Q. Will my sleep disorder improve after surgery?
A. Many patients’ sleep improves after surgery. However, while patients with sleep apnea sense they “snore less” or are
sleeping better, they often still have milder symptoms of sleep apnea. Therefore, they may still require ongoing
treatment. Please continue use of CPAP, BiPAP, or AutoPAP until otherwise advised by your physician.
Q. What can I expect to feel in social situations?
A. Patients report many positive and negative changes with others after surgery. Changes could include:
• increased positive attention
• feeling more comfortable in social situations
• decreased stigma/rejection
• improvements in body image
• improvements in sexual functioning
• disruptions of relationships
• insensitivity or jealousy from others
• increased irritability
• difficulty with increased sexual attention/navigating dating situations
It is worth noting there is a higher divorce rate in patients who have had weight loss surgery. This could be associated
with younger age, prior history of divorce, shorter time in marriage, and/or history of substance abuse. A key factor in
break ups of relationships appears to be one which was already unhealthy. It is strongly encouraged to discuss the
impact of weight loss on your relationship with your partner. We will continue to monitor your mood and social status
after surgery, and may recommend other psychological support including marital therapy or communication training.
Q. How long should I avoid alcohol after surgery?
A. It is recommended to avoid alcohol during the first year after surgery. This will allow for complete healing of your
procedure and prevent dangerous leaks from the surgical sites. After that time, it is still important to be careful with
how much you drink as your body will not metabolize alcohol in the same way.
As a result of the surgery, alcohol gets into the bloodstream at a higher rate than you have felt before, has a more
immediate effect, and takes longer to clear your system. These factors lead to a situation in which one glass of wine, a
beer, or a shot of liquor could lead you to be above the legal limit to drive within 15 minutes. An increase in rates of
alcohol use disorder have also been noted and presents numerous risks. If you (or a loved one or friend) feel you are
drinking more or more often, please contact us or your primary care doctor for help.
Q. How can I expect to the feel years after surgery?
A. Most patients are very happy they’ve had surgery and often report, “I wish I’d done it sooner.” While depressive
symptoms tend to improve initially after surgery, some patients do see a return of symptoms 2-5 years after
surgery. This is not necessarily a new symptom, but a return or worsening of depression/mood symptoms in patients
who have experienced this in the past. During your assessment your psychologist can identify risk factors and make
recommendations to aid in overall wellbeing even years after surgery. Our bariatric psychologists are ready to help you!
Please follow-up with your surgery team whenever you need.
35 © Center for Weight Management & Wellness 2023
Q: How can I be successful with keeping weight off?
A: Stay connected and in-control! We want to support you and your health goals. Research shows staying connected
with your program and providers will help you be more successful long term. The surgery is just a tool and your lifestyle,
eating, and exercise patterns will determine how successful you will be. Know that some weight regain can happen to
most patients, it is most likely to happen about a year and a half after surgery. Some patients can regain more than
others, possibly due to a return of problematic eating habits which can include emotionally triggered eating, grazing,
meal skipping, difficulty with portion control, restrictive eating, or even “binge” eating (feeling a loss of control). Please
keep in mind that these behaviors, while worrisome, can be addressed with our team!
Tips for Staying connected:
• Being active in support groups and/or attending individual appointments on a regular basis.
• After the first year of surgery, our time likes to see you at least every 6-12 months.
o Schedule these appointments in advance to avoid forgetting
Tips for staying in control:
• Remember your victories: log them, save them, and regularly remind yourself what you have achieved!
• Keep a “motivation” folder (virtual or physical location) to store before and after pictures, or your first airplane
ticket without a seatbelt extender or tickets to the amusement park ride you enjoyed with your kids after
surgery.
• Be aware of eating habits and try to identify if you have started picking or grazing.
• Avoid unplanned eating moments and try to control your environment to minimize these opportunities.
• Have scheduled and structured eating times.
• Meal planning can minimize unplanned eating events.
• Check yourself: use a food log or exercise tracker occasionally can help you spot emerging trends.
