Introduction
Background
Indonesia has made great progress in improving access to family planning (FP) services over the last three decades.
Beginning in 1976, under President Suharto, contraceptives were subsidized by the government and provided free of
charge, which increased public demand for the commodities. In 1987, the Government of Indonesia made eorts to
increase the private sector’s role in supplying FP services under the KB Mandiri (self-reliant) FP program.
i
Under the
“Blue Circle” campaign, the Government of Indonesia promoted use of FP services through private providers and
supplied these providers with contraceptives, leaving clients responsible only for covering the cost of services. Between
1987 and 1991, the percentage of FP users who received services from private sources increased from 12% to 22% while
the percentage of users who paid a fee for FP services increased from
36% to 62%.
i
The government’s eorts were successful in including
the private sector in addressing FP needs while instituting a norm of
consumers paying for FP services out-of-pocket in Indonesia.
Between 1976 and 2002, the total fertility rate (TFR) decreased from
5.6 to 2.6 lifetime births per woman in Indonesia.
ii
Estimates for 2015
indicate that unmet need for contraception is low, at 11%.
iii
Data from
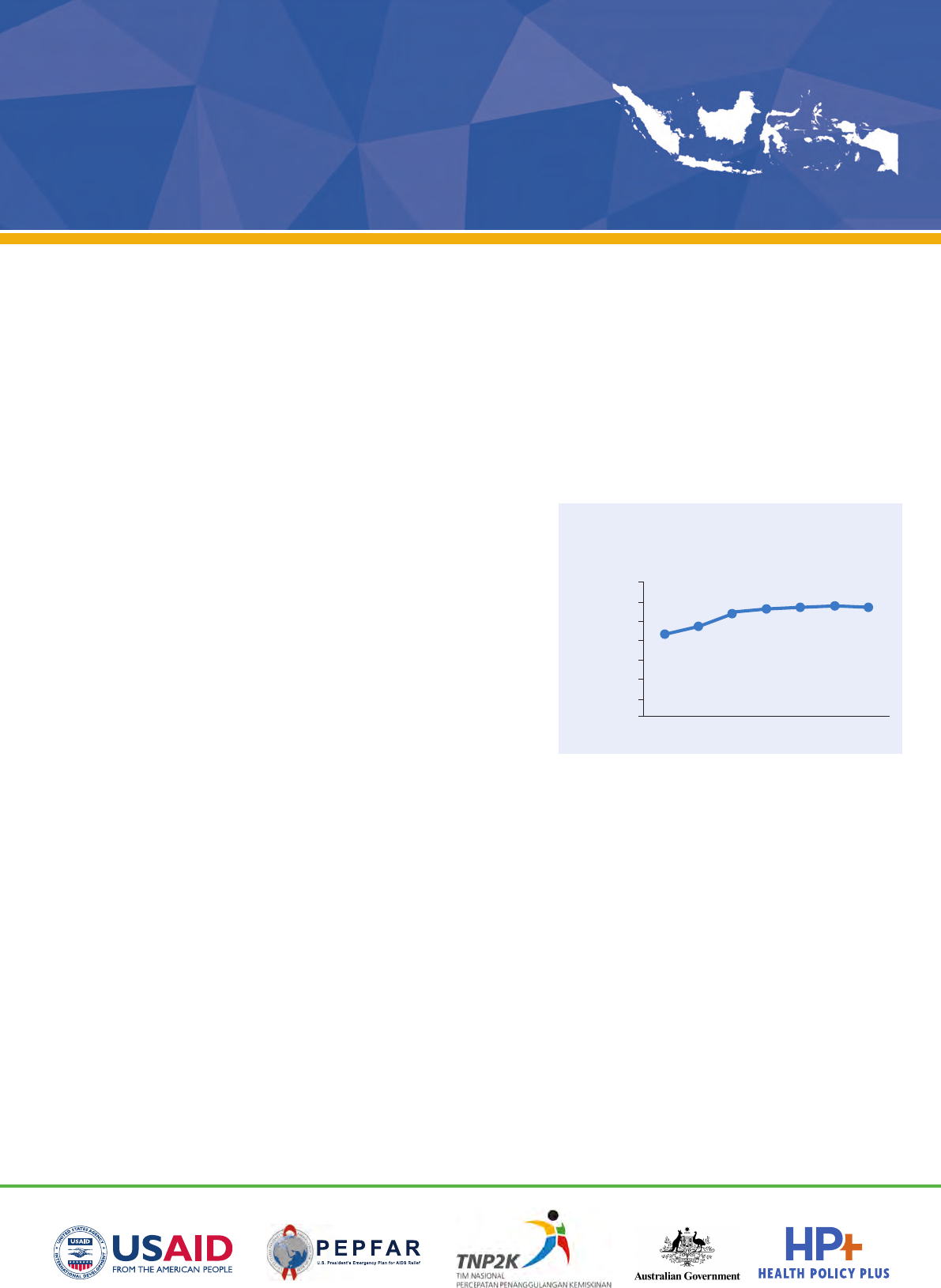
Indonesia Demographic and Health Surveys (IDHS) over time highlight
improvements in modern contraceptive prevalence rate (mCPR)
between 1987 and 2012 (see Figure 1). However, recent data indicates
that mCPR progress has stalled, decreasing from 57.9% in 2012 to
57.1% in 2017 among married Indonesian women.
Family Planning within National Health Insurance in Indonesia
In 2014, Indonesia launched Jaminan Kesehatan Nasional, or JKN, a national health insurance program that aims
to achieve universal health coverage (UHC) by 2019. The central purpose of the JKN scheme is to address existing
inequities in access to healthcare, with particular emphasis on ensuring that the poor and near-poor can access
quality care without facing financial hardship. The benefit package under JKN is a “negative list” whereby services must
be explicitly excluded to be considered not covered by the scheme. FP services are not explicitly excluded, though
contraceptive commodities for FP are not covered in practice under JKN reimbursements to primary or secondary
facilities. All FP service delivery costs are otherwise covered by JKN and reimbursed to providers in various ways.
Under Indonesia’s decentralized health system, both national and local government entities procure commodities
for FP, though this responsibility appears to be shifting to the latter. But much remains uncertain regarding how local
governments plan for, quantify, and submit procurement orders for FP commodities and define which population
groups they intend to cover.
Multiple agencies are involved in the oversight and provision of FP services, including the National Population and
Family Planning Board (Badan Koordinasi Keluarga Berencana Nasional, or BKKBN), the Ministry of Health (MOH), and
the national health insurance agency (Badan Pelaksana Jaminan Sosial-Kesehatan, or BPJS-K) that manages JKN.
BKKBN’s central role is to develop integrated programs across government sectors to meet the goals of the 2015–
2019 National Medium Term Development Plan (Rencana Pembangunan Jangka Menengah Nasional, or RPJMN) with
May 2018
Has Indonesia’s National Health
Insurance Scheme Improved
Family Planning Use?
Authors: Lyubov Teplitskaya, Rebecca Ross, and Arin Dutta
Percentage using a
modern method
10%
0%
1987 1992 1997 2007 2012 2017
20%
30%
40%
50%
60%
70%
2002
Figure 1. mCPR among Indonesian
married women in IDHS
relation to FP (see Box 1). Some overlap exists between the MOH
and BKKBN in FP service provision responsibility, in part because
the MOH manages a youth reproductive health program alongside
BKKBN’s eorts to increase FP coverage among adolescents.
BPJS-K is responsible for covering all FP service delivery
reimbursements to providers for long-acting reversible methods,
permanent methods, FP counseling, and other sexual and
reproductive health services, as well as short-acting FP commodities
such as pills and condoms (see Table 1). Until recently, BKKBN
was responsible for purchasing intrauterine devices (IUDs) and
injectables and coordinating these purchases with BPJS-K; this
responsibility will soon shift to local governments.
Challenges Surrounding Family Planning Under JKN
An Indonesia case study from 2016 indicated the potentially challenging nature of coordinating the many players
responsible for FP service provision in Indonesia with relation to JKN.
iv
Adequate coordination between BPJS-K
and BKKBN is needed to ensure FP service availability—for example, BKKBN was responsible for IUD and injectable
commodity procurement while BPJS-K has been responsible for payment of most individualized FP services. In
addition, coordination between BKKBN, local government, and health providers is needed to ensure that supply-side
constraints do not occur at the provider level. Box 2 summarizes the challenges related to FP service provision and
coordination noted in the literature.
Although FP services are oered at all healthcare levels, according to the Ministry of Health, most (46%) of BPJS-K-
contracted providers at the primary level consist of public centers (puskesmas). Currently, BPJS-K does not directly
contract with private midwives because they do not typically oer the full spectrum of primary healthcare services
Box 2: Summary of FP Challenges in Indonesia
• Coordination between BKKBN, MOH, and BPJS-K on FP services and reducing unmet need
• Coordination between BKKBN, local government, BPJS-K, and health providers on FP commodity needs
• Limitation of FP services to cohabiting couples in Indonesia
• Limited knowledge of the inclusion of FP services in JKN benefits packages
• Inadequate capacity of public and private facilities to provide quality FP services
• Preference of midwives to practice in urban areas/lack of sucient incentivization for healthcare providers to
work in the poorest rural areas
• Limited number of BPJS-K-contracted private providers
• Reliance on FP services at uncontracted private facilities leading to out-of-pocket payments
• Ineective referral mechanisms
Sources: Authors; Avenir Health (2016); Ensor et al. (2009); World Bank Group (2016).
Box 1: BKKBN’s Role
1. Purchase FP commodities, specifically
IUDs and injectables, in coordination
with BPJS-K
2. Coordinate with local government
3. Promote FP programs to young people
4. Increase FP coverage through various
means, including mobile provision of
FP services and increasing FP coverage
among the poor
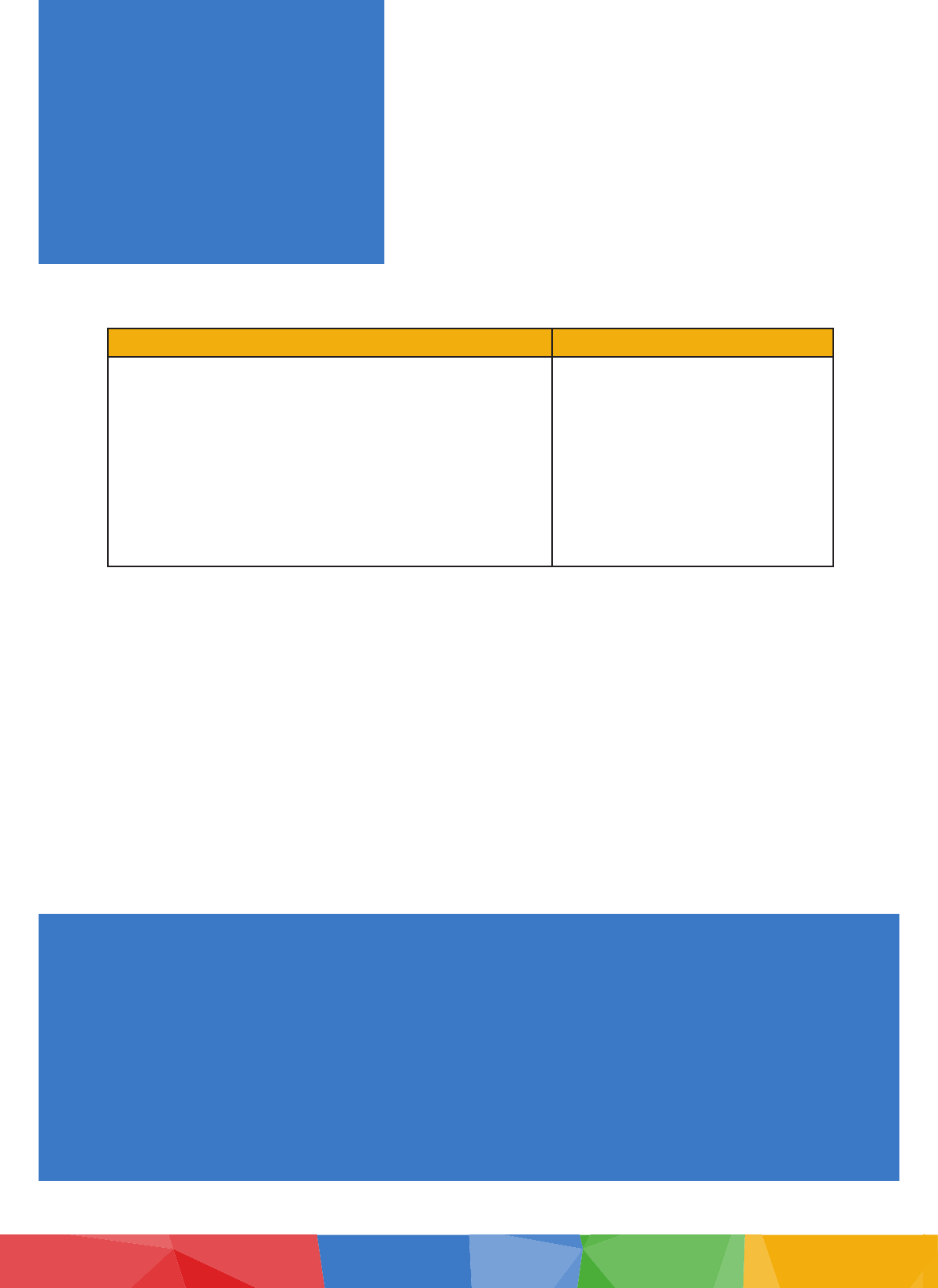
Table 1: Summary of FP Services Covered Under JKN
Services covered by primary healthcare facilities Services covered by hospitals
Capitation
• FP counseling
• Sexual and reproductive health services
• Other FP commodities such as pills and condoms
Fee-for-service*
• Insertion and/or removal of IUD/implant
• Injectables
• Treatment for FP complications
• Tubectomy/vasectomy
INA-CBGs**
• Post-partum sterilization
• Male sterilization
* Also referred to as “non-kapitasi” (non-capitation) fees, **INA-CBGs: Indonesia case-based groups
at their clinics.
v, 1
Data from the Ministry of Health indicate that there are an estimated 163,541 midwives in Indonesia,
constituting 16.3% of health personnel in 2016, with many leading their own clinics. These individual practitioners do
not typically employ electronic record keeping. From an administrative perspective, this lends to diculties in BPJS-K’s
ability to feasibly directly contract with midwives. Additional evidence indicates that midwives are not appropriately
incentivized to practice in rural areas, preferring to practice in urban areas for both financial and non-financial reasons.
vi
These issues are particularly problematic given that many Indonesian women, particularly the poor and those who
reside in rural areas, continue to access FP services through private sector midwives and pay out-of-pocket for such
services. This reliance on private providers for FP services extends beyond poor and rural—as of 2009, an estimated
40% of all women rely on private sector providers for FP services.
vii
From anecdotal sources, the capitation payments
currently instituted by BPJS-K are discouraging wide private primary provider involvement in the scheme.
Other challenges concern quality and supply of FP services at the facility level. Findings from the 2014 Indonesia Family
Life Survey noted deficiencies in the quality of FP services provided at both public and private facilities. An estimated
80% of puskesmas lacked a single sta member trained in FP services within the previous two years and an estimated
40% of private clinics lacked combined oral contraceptive pills while 20% lacked injectable contraceptives.
viii
Given the limited evidence available on trends in FP coverage since JKN’s introduction, this brief explores mCPR
and modern method mix over time using household survey data. Although IDHS and surveys such as Performance
Monitoring & Accountability 2020 (PMA2020) have explored mCPR and method mix by wealth quintile, such analyses
have not disaggregated these measures by insurance status. As part of the Government of Indonesia-led JKN
Comprehensive Assessment coordinated by the National Team for the Acceleration of Poverty Reduction (TNP2K) with
support from the U.S. Agency for International Development (USAID)-funded Health Policy Plus (HP+) project, this
analysis focuses on these disaggregated measures by insurance status, socioeconomic status (SES), and island grouping
using Indonesia’s National Socioeconomic Survey (Susenas) data. This approach allows for annual tracking of FP trends
over time, and before and after and after JKN. The study provides insight to the key policy question of whether JKN has
improved use of key interventions in Indonesia—specifically FP services—in the three years since its launch.
Methodology and Data Sources
We used Susenas datasets to examine mCPR and modern method mix prior and subsequent to JKN implementation,
and analyzed these measures using 2015 PMA2020 data. We expanded upon previously published PMA2020 data
analysis by exploring locations where modern contraceptive methods were procured by insured and uninsured FP users
and examined the average amount paid for FP services by insured and uninsured users. Table 2 further elaborates on
data sources, years, and key variables used in this analysis.
Results
Has utilization of FP services in Indonesia changed since 2011?
The mCPR progress has plateaued in recent years.
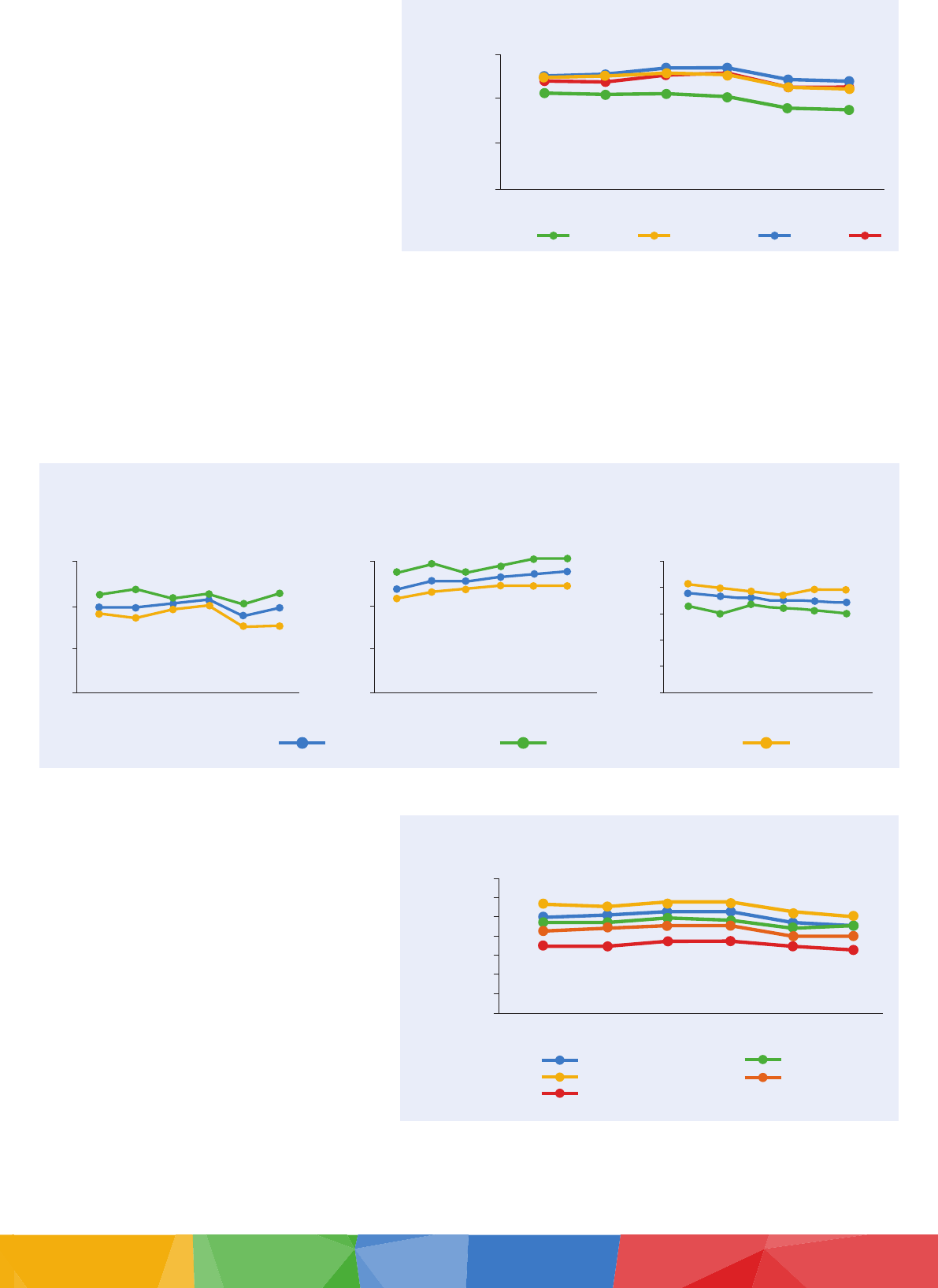
Susenas and IDHS results indicate that mCPR progress has stagnated in recent years. As Figure 2 shows, according to
Susenas, the mCPR among married women decreased from 50.2% in 2014 to 44.9% in 2016. This data is lower than the
rates found in PMA2020 data for 2015 (59.3%) and IDHS data for 2017 (57.1%).
1
Although BPJS-K does not directly contract midwives, there are three ways in which they may receive JKN funding. (1) Midwives can be staff within a BPJS-K-
contracted primary care facility; (2) they can develop an agreement with a BPJS-K-contracted primary care facility to have patients referred to them, and are paid
non-kapitasi fees from the contracted facility once they provide the services; (3) they can also hire a doctor to provide the full package of primary care services in
their clinics, thereby allowing them to be eligible for BPJS-K to contract with their facility directly.
Table 2: Summary of Datasets and Key Measures
Dataset Years Key Measures
Susenas 2011–2016 • mCPR
• Method mix (permanent, long-acting reversible, and short-acting methods)
PMA2020 2015 • mCPR
• Method mix (permanent, long-acting reversible, and short-acting methods)
• Amount paid for FP services at last FP visit
• Modern method source mix (public facility, private facility, or other [through
friends/relatives, at a shop, or other])
BPJS-K
INA-CBG
2014–2016 • JKN expenditure on male sterilization and female sterilization following delivery
• Male sterilization and female sterilization caseload through JKN
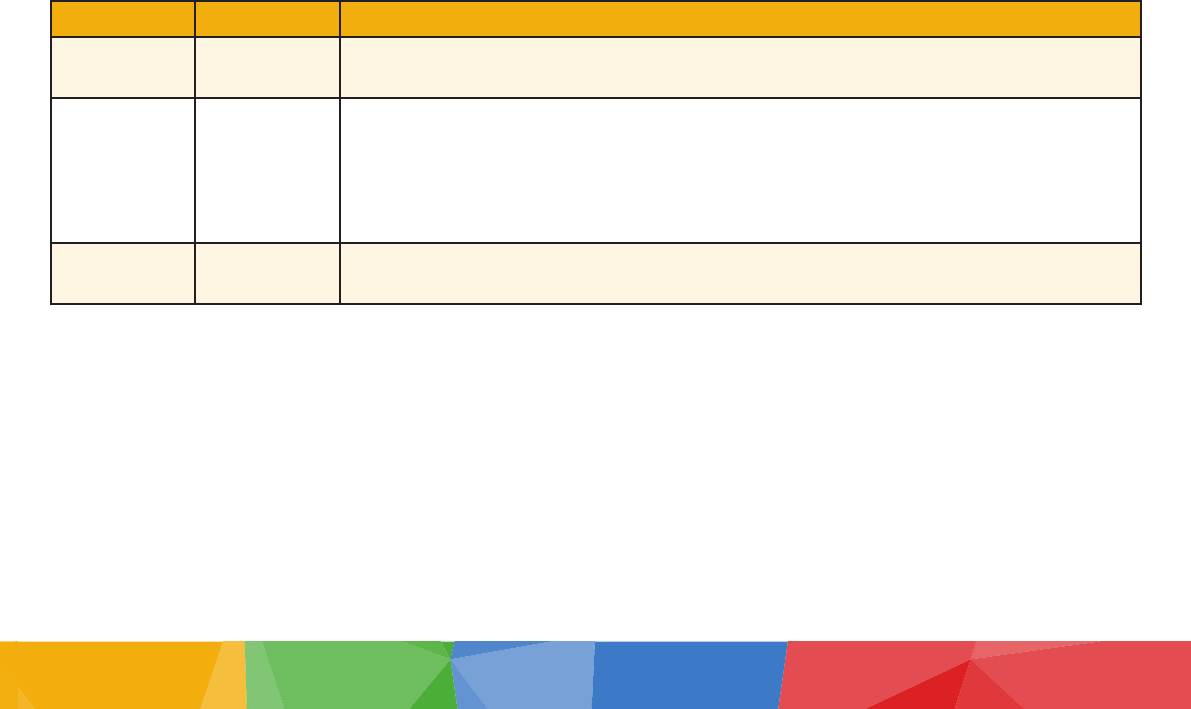
Rich married women use long-acting and permanent
contraceptive methods at much higher rates than do
other SES groups.
Use of long-acting reversible contraceptive methods
is increasing over time for all SES groups in Indonesia,
though a significantly higher proportion of rich married
FP users use permanent and long-acting reversible
contraceptive methods as compared to their poor,
near-poor, and middle-income counterparts (see Figure
3). Although these groups used short-acting methods at
rates much higher than the rich, the utilization of short-
acting methods has decreased between 2011 and 2016
nationwide. 2015 PMA2020 data substantiates these
general trends in method mix by wealth quintile.
Research incorporating data from twenty countries has shown that wealthier women are more likely than poorer
women to use long-acting and permanent methods in place of short-acting methods.
ix
Common reasons for using
short-acting methods include ease of access, lower cost, privacy, and freedom to discontinue use without involving a
health provider.
x
These reasons may help to explain the higher use of short-acting methods among poor Indonesian
women given the prevalent use of FP services in the private sector. If poor women prefer to seek FP services in the
private sector and cost is a factor, they are more likely to seek out lower-cost FP services, which mainly consist of short-
acting methods.
Has use of FP services changed since JKN
implementation?
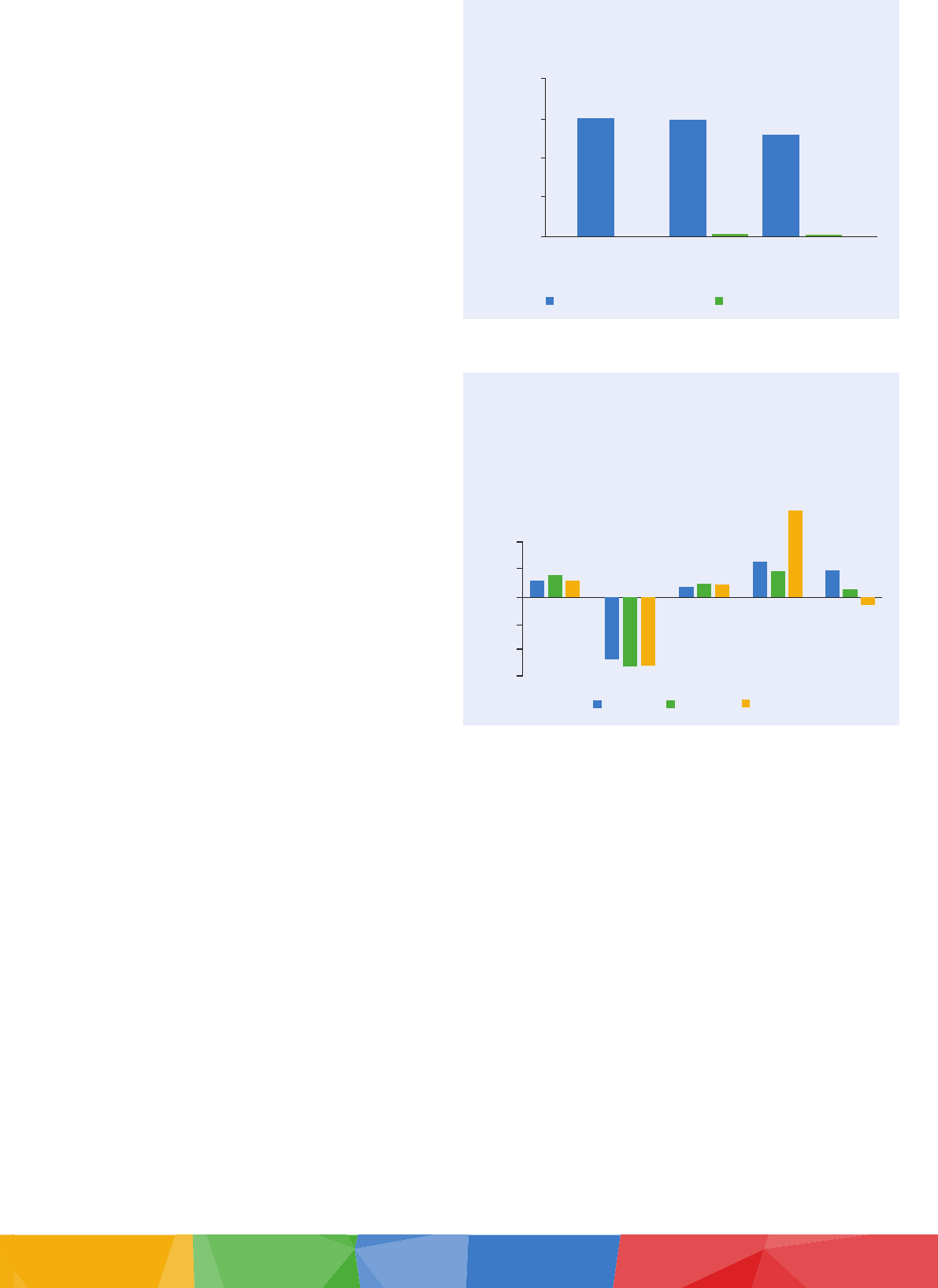
The mCPR declined for both insured and uninsured.
Susenas household survey data reveals that mCPR
had been increasing among the insured prior to 2014
and began to decline for both uninsured and insured
married women following JKN implementation (see
Figure 4). The data also show that with the exception
of one year (2013), mCPR is consistently higher
among the uninsured compared to the insured.
Trends indicate JKN is more important for FP use
among poor women compared to rich women.
Since JKN implementation, mCPR has consistently
decreased among all SES groups, though the trend is most pronounced for insured rich women (see Figure 5). The
mCPR among insured rich women decreased by 16.6% from 2011 to 2016, whereas mCPR among insured poor women
8%
6%
4%
2%
0
2011 2012 2013 2014 2015 2016
7%
5%
3%
1%
25%
20%
15%
5%
0%
2011 2012 2013 2014 2015 2016
10%
rich middle near-poor poor
100%
80%
60%
20%
0%
40%
2011 2012 2013 2014 2015 2016
Data source: Analysis using 2011–2016 Susenas data
Figure 3: Shifts in method mix nationwide among married women from 2011—2016, by SES
Use of permanent methods Use of long-acting methods Use of short-acting methods
Percentage using
modern method
55%
50%
45%
40%
2011 2012 2013 2014 2015 2016
Insured Uninsured
Figure 4: mCPR among insured and uninsured
married women
Data source: Analysis using 2011–2016 Susenas data
Percentage using a
modern method
10%
0%
2011 2012 2013 2015 2016
20%
30%
40%
50%
60%
2014
Susenas
49.4%
50.2%
50.4%
50.2%
46.0%
44.9%
IDHS PMA2020
Figure 2. Trends in mCPR among married women,
2011–2017
decreased by 5.7% during the same period. The
mCPR is significantly higher among the insured
poor compared to the insured rich throughout
the study period, and the gap widens between
2011 and 2016: in 2011, mCPR for the insured
poor was 48.6% compared to 43.4% (a 12%
dierence); by 2016, mCPR for the insured
poor was 46.0% compared to 36.2% (a 21%
dierence). These results indicate that JKN
insurance coverage may be more important for
FP use among the poor than the rich.
Trends indicate JKN is important for
insured women’s use of long-acting and
permanent methods.
Insured married women in Indonesia use permanent and long-acting reversible methods at higher rates compared to
uninsured married women (see Figure 6). Our Susenas analysis highlights an increase in use of permanent methods by
insured FP users after 2015 and a steady increase in use of long-acting reversible methods among insured FP users after
2013. The data likewise reveals a steady decline in insured married women’s use of short-acting methods since 2013.
These results suggest that JKN coverage may be important for insured women’s access to long-acting and permanent
methods of contraception.
Method mix trends for the insured compared
to the uninsured are consistent by SES, as
seen previously in Figure 3. For example, the
insured poor use short-acting methods at lower
rates compared to the uninsured poor, and
use of short-acting methods for the insured
poor continues to decline following JKN
implementation. Similarly, the insured rich use
long-acting reversible methods at higher rates
than the uninsured rich. These findings bolster
the finding that JKN insurance may serve as a
factor influencing method mix in Indonesia.
Method mix is improving by island group,
particularly in Eastern Indonesia.
Our analysis also explored FP trends by island
group (see Figures 7 and 8). We hypothesized that FP use may dier by geographical location and other influences, such
as supply-side factors. We found that mCPR is consistently highest in Kalimantan, the island grouping with the highest
55%
50%
45%
40%
2011 2012 2013 2014 2015 2016
rich middle near-poor poor
Percentage using
modern method
Figure 5: mCPR among insured married women, by SES
Data source: Analysis using 2011–2016 Susenas data
90%
85%
80%
70%
65%
2011 2012 2013 2014 2015 2016
75%
2011 2012 2013 2014 2015 2016
15%
10%
5%
0%
6%
4%
2%
0
2011 2012 2013 2014 2015 2016
All married FP users Insured women Uninsured women
Figure 6: Method mix among married FP users, by insurance status
Data source: Analysis using 2011–2016 Susenas data
Use of permanent methods Use of long-acting methods Use of short-acting methods
70%
50%
20%
0%
2011 2012 2013 2014 2015 2016
Java
Kalimantan
10%
Eastern Indonesia
Sumatra
Sulawesi
30%
40%
60%
Percentage using
modern method
Figure 7: mCPR among JKN-insured married women by
island grouping

use of short-acting methods and lowest use of long-acting and permanent methods. By contrast, mCPR is lowest in
Eastern Indonesia, where use of long-acting methods has increased and use of short-acting methods has significantly
decreased since 2013. These changes in method mix may be the result of community-level initiatives, such as the
Improving Contraceptive Method Mix (ICMM) Program, which have been implemented throughout Eastern Indonesia
to improve uptake of long-acting and permanent methods of contraception.
xi
Following JKN implementation, mCPR
decreased in Java to the levels seen in Sumatra. Use of permanent methods is highest in Java, where more than half
of Indonesians live. This method mix may be due to improved access to a variety of healthcare facilities that oer FP
services in Java.
Insured women obtain modern contraceptive methods at
public facilities at greater rates than do uninsured women.
PMA2020 data highlighted the source mix for married
Indonesian women in 2015 (see Figure 9). The results
indicate that a greater proportion of insured married women
acquire modern methods at public facilities (18%) compared
to uninsured women (13%). However, the most prevalent
modern method source was private facilities, where 55%
of insured and 63% of uninsured women obtained their
contraceptive methods in 2015.
Analysis of PMA2020 data indicated that, on average, the
wealthiest quintile (Q5) paid the most out-of-pocket for FP
services at their last visit (IDR 34,967, or US$2.59) whereas
the poorest quintile (Q1) paid the least (IDR 23,492, or
US$1.74). On average the insured wealthiest quintile paid
more than three times the cost for long-acting reversible
methods compared to the insured poorest quintile (see
Table 3). The uninsured poorest quintile paid more out-of-
pocket for short-acting and long-acting reversible methods compared to the insured poorest quintile. In the PMA2020
dataset, only one observation was noted for out-of-pocket payments made for permanent services.
8%
4%
2%
0
2011 2012 2013 2014 2015 2016
6%
2011 2012 2013 2014 2015 2016
25%
10%
5%
0%
15%
20%
95%
85%
80%
70%
65%
2011 2012 2013 2014 2015 2016
75%
90%
Java Sumatra Kalimantan Sulaweisi Eastern Indonesia
Figure 8: Shifts in method mix nationwide among married women from 2011–2016, by island group
Use of permanent methods Use of long-acting methods Use of short-acting methods
100%
50%
0
All Insured Uninsured
Public facility Private facility Other
26%
59%
15%
27%
55%
18%
25%
63%
13%
Figure 9: Modern method source mix among
married women
Data source: Analysis using 2015 PMA2020 data
Table 3: Average Amount Paid for FP Services at Last Visit (in Indonesian Rupiah)
Method mix
Insured Uninsured
Q1 Q5 Q1 Q5
Short-acting 20,525 21,329 21,540 20,803
Long-acting reversible 84,004 352,729 94,406 348,602
Permanent -- 250,000 -- --
Data source: Analysis using 2015 PMA2020 data
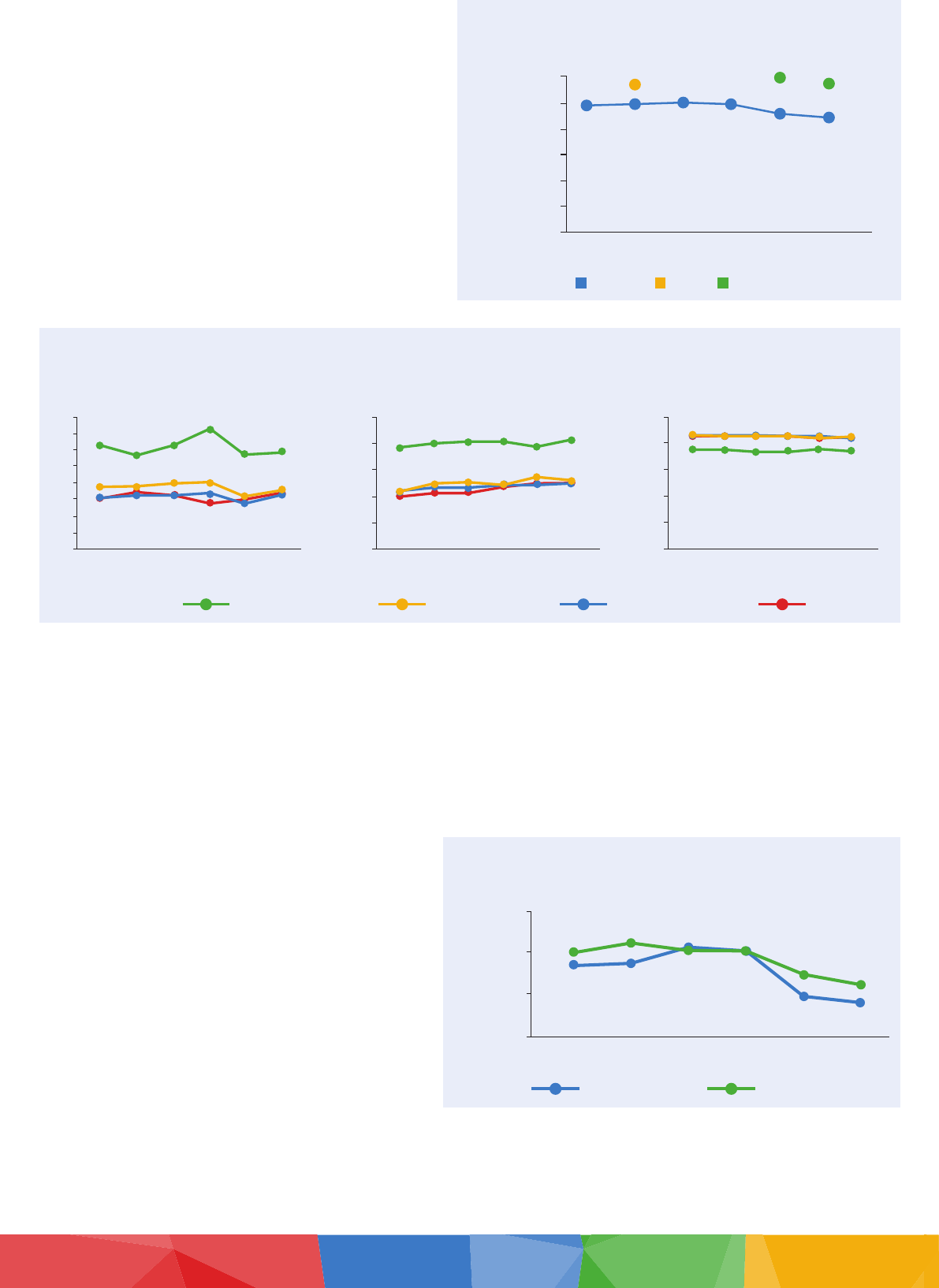
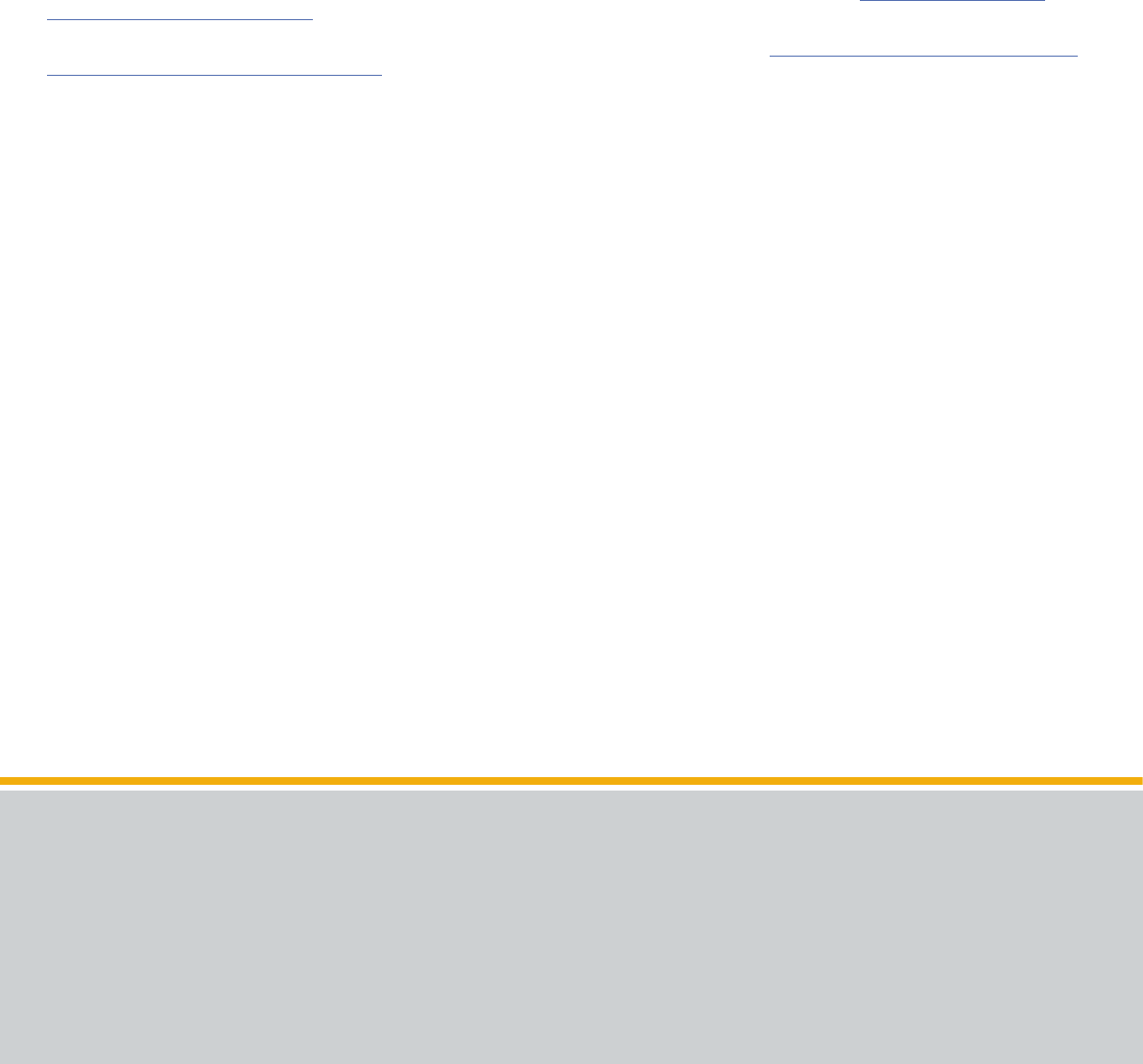
JKN expenditure on permanent methods at the
hospital level decreased between 2014 and 2016.
JKN expenditure on permanent methods decreased
from 2014 to 2016 and the majority was spent on female
sterilization following vaginal labor at the hospital level
(see Figure 10). Only four cases of male sterilization
were recorded between 2014 and 2016 while a total
of 76 outpatient and 10,849 inpatient cases of female
sterilization following labor took place during the same
period.
Analysis of JKN expenditure on female sterilization
compared to the share of female reproductive-aged
women by island grouping reveals that costs are
not equitable across islands (see Figure 11). Sulawesi
only accounts for 7% of Indonesia’s reproductive-
aged women but constitutes between 19% and 64%
of total JKN expenditure on post-partum sterilization
costs. Compared to Sulawesi, expenditure in Java and
Kalimantan is still over-represented compared to its
share of the reproductive-aged female population,
but by a smaller amount. By contrast, expenditure in
Eastern Indonesia shifted from being over- to under-
represented in the same time period. These shifts cannot
be interpreted as inherently positive or negative—for
instance, a shift toward under-represented expenditure
as a share of population could indicate greater use of
services at the primary healthcare level (data that are not
captured in this analysis).
Discussion and Conclusions
Although mCPR is quite high in Indonesia, echoing the
data captured in the IDHS, our results find that mCPR
is decreasing, indicating stalled FP progress. Since JKN
was launched in 2014, mCPR has been higher among
the uninsured compared to the insured. Many FP users
face far distances to and long wait times at puskesmas. As a result, many continue to access FP services in clinics
through private providers, which may not be BPJS-K-contracted. This arrangement may help to explain the discrepancy
in mCPR between the insured and uninsured. Furthermore, in our analysis of average mCPR by SES, we found that
the mCPR decrease was larger for the insured rich compared to the insured poor. These results indicate that being
covered by JKN insurance may be more important for accessing FP services among the insured poor compared to the
insured rich.
Short-acting methods have historically been most commonly used in Indonesia; however, our results highlight a shift
in method mix since JKN implementation among the insured toward long-acting and permanent methods. Given that
price can be a factor in the decision to choose short-acting methods, this shift in method mix indicates that JKN may
be alleviating some of the financial burden women face when accessing long-acting and permanent methods.
Our analysis by island grouping indicates that geographical disparities for FP access remain, with mCPR lowest in the
most rural island grouping, Eastern Indonesia. These geographical inequities highlight the possibility of other barriers
existing in the health system, such as lack of adequately trained health personnel and/or health facilities that do not
provide a broad method mix of FP services. Given that private midwives are not incentivized to work in rural areas,
higher FP uptake by more urban island groupings such as Java may at least be partially explained by this supply-side
deficiency. However, improvements in method mix in Eastern Indonesia highlight that community-level initiatives can
be eective in increasing long-acting and permanent method uptake.
40
20
0
2014 2015 2016
Female sterilization Male sterilization
30
10
30.2
25.9
29.7
Indonesian Rupiah, billions
Figure 10: JKN expenditure on permanent
methods at the hospital level
Data source: Analysis using BPJS-K data
40%
20%
0%
-20%
-40%
-60%
2014 2015
2016
Java Sumatra
Kalimantan Sulawesi
Eastern
Indonesia
Figure 11: Share of JKN post-partum sterilization
costs at the hospital level compared to share of
female population, by island
Data source: Analysis using BPJS-K data
Health Policy Plus (HP+) is a ve-year cooperative agreement funded by the U.S. Agency for International
Development under Agreement No. AID-OAA-A-15-00051, beginning August 28, 2015. The project’s
HIV activities are supported by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). HP+ is
implemented by Palladium, in collaboration with Avenir Health, Futures Group Global Outreach, Plan
International USA, Population Reference Bureau, RTI International, ThinkWell, and the White Ribbon
Alliance for Safe Motherhood. Funding for TNP2K was partially supported by the Australian Government.
This publication was produced for review by the U.S. Agency for International Development. It was
prepared by HP+. The information provided in this document is not ofcial U.S. Government information
and does not necessarily reect the views or positions of the U.S. Agency for International Development
or the U.S. Government.
CONTACT US
Health Policy Plus
1331 Pennsylvania Ave NW, Suite600
Washington, DC 20004
www.healthpolicyplus.com
policyinfo@thepalladiumgroup.com
To improve FP access through JKN, policymakers and health systems decision-makers should consider the
following recommendations:
• Prioritize facilitating the inclusion of more private providers as BPJS-K-contracted providers
• Improve coordination between BKKBN and BPJS-K as well as between BKKBN and health providers to ensure
the availability of FP methods at all health facilities
• Ensure necessary health facilities and adequately trained health providers are available nationwide, particularly in
the most geographically disadvantaged island groups such as Eastern Indonesia
Acknowledgments
This brief was developed as part of the government-led JKN Comprehensive Assessment, conducted from 2016–2018,
coordinated by TNP2K with technical assistance from HP+. The assessment would not have been possible without
continuous support of Prastuti Soewondo of TNP2K and her team. The brief merited from data analysis contribution
by Thomas Fagan of HP+. Authors greatly appreciate the review by Prastuti Soewondo, and Edhie Rahmat and Zohra
Balsara of USAID.
References
i
Robey, B., P.T. Piotrow, and C. Salter. 1994. “Family Planning Lessons and Challenges: Making Programs Work.” Population Reports. Series J, No. 40: 24.
ii
World Bank Group. n.d. “Fertility rate, total (births per woman); Indonesia.” World Development Indicators. Available at: https://data.worldbank.org/
indicator/SP.DYN.TFRT.IN?locations=ID
iii
Performance Monitoring & Accountability 2020 (PMA2020). 2015. PMA2015/INDONESIA-R1. Available at: https://www.pma2020.org/sites/default/les/
PMA2015-ID-WASH-2PG-Brief_en_2016-06-14.pdf
iv
Avenir Health. 2016. Supporting Family Planning Within National Health Financing Schemes: Indonesia Case Study.
v
Rajkotia, Y., J. Gergen, I. Djurovia, S. Koseki, M. Coe, et al. 2016. Re-envisioning Maternal and Newborn Health in Indonesia: How the Private Sector and Civil
Society Can Ignite Change. Washington, DC: Palladium, Health Policy Plus.
vi
Ensor T., Z. Quayyum, M. Nadjib, and P. Sucahya. 2008. “Level and Determinants of Incentives for Village Midwives in Indonesia.” Health Policy and
Planning. Nov 20;24(1):26-35.
vii
Wang, H., M. McEuen, L. Mize, C. Cisek, and A. Barraclough. 2009. Private Sector Health in Indonesia: A Desk Review. Bethesda, MD: Health Systems 20/20
project, Abt Associates Inc.
viii
World Bank Group. 2016. Indonesia Health Financing System Assessment: Spend More, Right and Better. World Bank, Washington, DC: World Bank.
ix
Ugaz, J., M. Chatterji, J. Gribble, and K. Banke. 2016. “Is Household Wealth Associated with Use of Long-Acting Reversible and Permanent Methods of
Contraception? A Multi-Country Analysis.” Global Health: Science and Practice. 4(1), 43-54.
x
Tibaijuka, L., R. Odongo, E. Welikhe, W. Mukisa, Ls. Kugonza, et al. 2017. “Factors Inuencing Use of Long-Acting Versus Short-Acting Contraceptive
Methods Among Reproductive-Age Women in a Resource-Limited Setting.” BMC Women’s Health. 17(1), 25.
xi
Titaley C., R. Wijayanti, R. Damayanti, A. Setiawan, D. Dachlia, et al. 2017. “Increasing the Uptake of Long-Acting and Permanent Methods of Family
Planning: A Qualitative Study with Village Midwives in East Java and Nusa Tenggara Barat Provinces, Indonesia.” Midwifery. Oct 1;53:55-62.
