Progress in the International
Health Partnership & Related
Initiatives (IHP+)
2014
Performance
Report
UNIVERSAL
HEALTH COVERAGE
FOR SEXUAL AND REPRODUCTIVE
HEALTH IN THE ASIA-PACIFIC
REGION
Lorem ipsum
UNIVERSAL
HEALTH COVERAGE
FOR SEXUAL AND REPRODUCTIVE
HEALTH IN THE ASIA-PACIFIC
REGION
September 2017

hera
right to health & development
Laarstraat 43
B-2840 Reet Belgium
Tel +32 3 844 59 30
hera@hera.eu
www.hera.eu

ACKNOWLEDGEMENTS
Pr
epared under contract to UNFPA Asia-Pacific Regional Office
Contributors
Aminur Rahman Shaheen, icddr,b (Bangladesh)
Aroonsri Mongkolchati, Mahidol University (Thailand)
Chean Men (Cambodia)
Josef Decosas, hera (team leader)
Leo Devillé, hera (quality assurance)
Luvsan Munkh-Erdene (Mongolia)
Marieke Devillé, hera (core team)
Marta Medina, hera (core team)
Rita Damayanti, Universitas Indonesia (Indonesia)
Vu Cong Nguyen, PHAD (Viet Nam)
The team acknowledges the valuable support provided by the UNFPA Country
Offices i n B angladesh, C ambodia, I ndonesia, M ongolia, T hailand a nd V iet
Nam, as well as by the UNFPA Regional Office for Asia-Pacific.
Disclaimer
The study of universal health coverage for sexual and reproductive health in
the Asia-Pacific Region was undertaken by hera under contract by the
United Nations Population Fund Asia and Pacific Regional Office. The views
expressed herein can in no way be taken to reflect the official opinion of
UNFPA. The contents of this publication are the sole responsibility of hera.
ACRONYMS AND ABBREVIATIONS
ANC
Antenatal Care
AP
Asia-Pacific
ART
Antiretroviral Therapy
AFPPD
Asian Forum of Parliamentarians
on Population and Development
CBHI
(Bangladesh) Community-based
Health Insurance
CHD
(Mongolia) Centre for Health
Development
CPA
(Cambodia) Complementary
Package of Activities
CPR
Contraceptive Prevalence Rate
CSMBS
(Thailand) Civil Servants’ Medical
Benefit Scheme
DHS
Demographic and Health Survey
DS
Satisfied Demand for Family
Planning
DSF
(Bangladesh) Demand-side
Financing (voucher scheme)
EmONC
Emergency Obstetric and Neonatal
Care
ESCAP
(UN) Economic and Social
Commission for Asia and the
Pacific
GBV
Gender-based Violence
HC
(Cambodia) Health Centre
Health
BPJS
(Indonesia) (social security agency
for health
HEF
(Cambodia) Health Equity Fund
HMIS
Health Management Information
System
HPV
Human Papillomavirus
IAEG
Inter-Agency and Expert Group
ICPD
International Conference on
Population and Development
IDR
Indonesian rupiah
MDG
Millennium Development Goal
MHI
(Thailand) Migrant Health
Insurance
MICS
Multiple Indicator Cluster Survey
MOH
Ministry of Health
MOHFW
(Bangladesh) Ministry of Health
and Family Welfare
MOLSP
(Mongolia) Ministry of Labour and
Social Protection
MOPH
(Thailand) Ministry of Public
Health
MPA
Minimum Package of Activities
MR
Menstrual Regulation
MRM
Medical Menstrual Regulation
(Bangladesh)
NCCD
(Mongolia) National Centre for
Communicable Diseases
NHSO
(Thailand) National Health Security
Office
NIPORT
(Bangladesh) National Institute of
Population Research and Training
NSO
(Mongolia, Thailand) National
Statistical Office
OOP
Out-Of-Pocket (payment for health
services)
OSCC
One-Stop Crisis Centre
PMTCT
Prevention of Mother to Child
Transmission (of HIV)
PNC
Postnatal Care
RH
(Cambodia) Referral Hospital
SBA
Skilled Attendance at Birth
SDG
Sustainable Development Goal
SHI
(Mongolia / Viet Nam) Social
Health Insurance
SHPS
(Bangladesh) Social Health
Protection Scheme
SRH
Sexual and Reproductive Health
SSK
(Bangladesh) (subsidised social
health insurance)
SSS
(Thailand) Social Security Scheme
STI
Sexually Transmitted Infection
THE
Total Health Expenditure
UCS
(Thailand) Universal Coverage
Scheme
UHC
Universal Health Coverage
UNGA
UN General Assembly
UNSTAT
UN Statistics Division
TABLE OF CONTENTS
Summary .............................................2
Effective coverage of sexual and reproductive health services
. 2
Equitable access to sexual and reproductive health services
..3
Financial risk protection for sexual and
reproductive health services
.............................3
Key issues
............................................4
The UN Agenda for Sustainable Development
...............5
Sexual and reproductive health services in Asia-Pacific
......6
The scope of the study of UHC for SRH
....................8
Bangladesh
...........................................9
Cambodia
...........................................13
Indonesia
............................................17
Mongolia
............................................21
Thailand
............................................. 25
Viet Nam
............................................29
Universal health coverage for sexual
and reproductive health
................................33
Effective coverage of SRH services
.......................34
Equitable access to SRH services
........................43
Financial risk protection for sexual and reproductive
health services .......................................47
Conclusions and recommendations
......................53
References
..........................................59

SUMMARY
The study reviewed the progress in six countries of the Asia-Pacific region towards
the achievement of the UN Sustainable Development Goals 3.7 and 3.8.
SDG Goal 3.7: By 2030, ensure universal access to sexual and reproductive
healthcare services, including for family planning, information
and education, and the integration of reproductive health into
national strategies and programmes
SDG Goal 3.8: Achieve universal health coverage, including financial risk
protection, access to quality essential health-care services
and access to safe, effective, quality and affordable essential
medicines and vaccines for all
Progress towards the achievement of universal access to sexual and reproductive
healthcare (SRH) was assessed according to a framework proposed in 2010 that
lists 11 key services for comprehensive SRH. Some services, for instance infertility
treatment, were not included in the assessment after consultation with the UNFPA
Regional Office.
Bangladesh, Cambodia, Indonesia, Mongolia, Thailand and Viet Nam have made
national policy commitments to achieve universal health coverage, each starting
from a different baseline of health service development and health financing, but
each working towards a system of a unified mechanism to pool resources for a
health financing system that would protect households from high levels of payment
for healthcare at the point of service.
Initiatives started in Mongolia in 1994 with the introduction of a mandatory social
health insurance, followed by Thailand in 2002, Indonesia in 2004, Viet Nam in 2008,
Cambodia in 2011 and Bangladesh in 2012. By 2015, the six countries had achieved
different levels of service coverage and financial risk protection. Thailand had
reached a high level of coverage for sexual and reproductive health services with
low point-of-service charges to clients, while Bangladesh was among the Asia-
Pacific countries with the lowest service coverage levels and the highest direct
user charges.
EFFECTIVE COVERAGE OF SEXUAL AND
REPRODUCTIVE HEALTH SERVICES
The Asia-Pacific region achieved significant progress in increasing the coverage
of effective sexual and reproductive health services. The maternal mortality ratio
declined by two thirds between 1990 and 2015, the contraceptive prevalence rate at
87.4 percent was three percent above the global level in 2015, and the adolescent
birth rate of 35/1,000 was considerably lower than the global average of 52/1,000.
The coverage of antiretroviral therapy for HIV was however five percent below the
estimated global average of 46 percent. While the HIV prevalence in the region is
low, the incidence of other sexually transmitted infections is higher than the global
average.
These regional statistics, however, hide many details. Some countries in the region
still record very high maternal mortality ratios, low contraceptive prevalence rates,
and very high adolescent fertility. Only a small proportion of sexually active adolescent
girls in Asia-Pacific are unmarried, but access to effective female-controlled methods
of contraception for these girls is particularly low. Furthermore, in four of the six
study countries, adolescent birth rates in 2014 were higher than the levels recorded
in 2005. Among the six study countries, the coverage of HIV antiretroviral treatment
ranged from nine percent in Indonesia to 74 percent in Cambodia.
Access to safe termination of pregnancy and post-abortion care varies among the
countries, depending on the national abortion laws. However even countries with
relatively unrestricted access to pregnancy termination still register large numbers
of unsafe abortions, especially among adolescents. Only Bhutan, Malaysia and
several Pacific Island States have introduced HPV immunisation in their national
immunisation programmes, while in the other countries this service is still in a pilot
phase.
2

National screening programmes for cervical cancer
exist in all six study countries, but only Thailand
records a significant coverage at 60 percent.
Several countries in the region have established
comprehensive one-stop crisis centres for girls
and women who are survivors of gender-based
violence. The centres are integrated in the national
health systems in four countries of the region, in
others they exist as pilots or in an early scale-up
phase.
EQUITABLE ACCESS
TO SEXUAL AND
REPRODUCTIVE HEALTH
SERVICES
The social equality gap in the use of family planning
and maternal health services has narrowed over
time. In the six study countries, there are no
inequalities in the use of modern contraceptives
among married women, but the gap in adolescent
fertility has not narrowed. Regionally, the difference
in the adolescent birth rate between women in the
lowest and the highest wealth groups increased
between 1998 and 2008. For skilled attendance
at birth, the gap between high and low-income
groups narrowed in Indonesia and Cambodia,
but it increased in Bangladesh. Women resident
in rural areas, remote regions and some island
provinces have lower access and utilisation rates
for reproductive health services, often because of
irregular supplies and stock-outs of contraceptive
commodities. Ethnic minority groups and the large
population of international migrants in Asia-Pacific
(estimated at 27.6 million) face numerous barriers
of access to health services, but information about
utilisation rates and reproductive health outcomes
among these groups is limited.
FINANCIAL RISK
PROTECTION
FOR SEXUAL AND
REPRODUCTIVE HEALTH
SERVICES
A mix of different financial protection schemes exist
in the six study countries. Efforts to consolidate
them into a single national social health insurance
scheme are furthest developed in Mongolia
and Viet Nam, and relatively far advanced in
Indonesia. In Thailand, however, three parallel
health insurance schemes continue to coexist and
achieve the highest levels of insurance benefit and
population coverage among the six study countries.
Some sexual and reproductive health services in
the other five countries are not included among
the health insurance benefits, but are provided in
public health facilities with varying levels of user-
charge exemptions.
Bangladesh has a fragmented system with a
demand-side financing (voucher) scheme for
maternal health services in 53 sub-districts and
public health provision of family planning services
throughout the country. In Cambodia, financial risk
protection is primarily provided through user-fee
subsidies in public health facilities for poor people,
and through health equity funds that reimburse the
cost of healthcare for the poor. Both countries are
in the early stages of developing a national social
health insurance.
With the exception of Thailand, and more recently
Indonesia, social health insurance schemes do not
provide benefits for family planning services. They
are provided free of charge to targeted populations
through public health services; in Viet Nam, for
instance, to ethnic minority populations; in Mongolia
and Cambodia to poor and vulnerable groups.
Population surveys in Bangladesh document that
many women bypass free public family planning
services in favour of buying services in the private
sector. In all study countries except Thailand, there
is a tendency to focus social health insurance
benefits on medical treatment and hospital
services, while prevention services, including for
sexually transmitted infections, are provided by
public health systems with varying service coverage
and varying levels of user-charge exemptions.
Services that require multi-sector interventions, for
instance services for the prevention and response
to gender-based violence, are generally not covered
by social health insurance. Migrant populations are
excluded from national financial risk protection
schemes in most countries. Only Thailand operates
a health insurance schemes for unregistered
migrant workers, which however only covers about
40 percent of the estimated target population of 3.4
million.
3

KEY ISSUES
• Without questioning the potential of the global UHC goals to contribute to
better services and improved health for all, there is a risk that the UHC
goals will focus decision-makers at national level, as well as international
development partners, on improving treatment services at the expense of
prevention and health promotion. The exclusion of family planning services
from many national UHC schemes is a concern, especially as they affect the
sexual and reproductive health and rights of adolescent girls.
• Improving sexual and reproductive health requires changes in social norms
to protect the rights of girls, promote gender equality, and improve the
access to information on health and rights among adolescents. Preventing
and responding to gender-based violence requires the participation of many
sectors, including education, justice, social affairs and health. Such multi-
sector responses cannot be wrapped up under a single UHC agenda.
• A history of international, national and local initiatives has left traces
of different types of health financing arrangements in most countries.
Consolidating several initiatives under a single UHC umbrella can create
efficiencies that allow an expansion of coverage and level of financial
protection. Consolidations that are relatively less selective of the type of
beneficiaries are less likely to make errors of omission, without necessarily
generating revenue losses from foregone insurance premiums. Consolidation
should, however, be approached with caution to assure that no essential SRH
service nor any vulnerable population group lose their coverage. By including
prevention and health promotion among the UHC benefits, future costs
for treatment can be reduced and the sustainability of the UHC schemes
consolidated.
• Sexual and reproductive health service coverage for adolescents is lagging
behind the general trend of improved service coverage in the region.
Insufficient financial risk protection may not be the most important reason.
In the development of financial risk protection schemes, however, the
special situation of adolescents should be kept in mind. Adolescents do not
necessarily have ready access to the financial resources of the economic
group in which they are categorised.
• Although there are examples of SRH programmes and financial risk
protection schemes that target vulnerable groups such as ethnic minority
populations, migrant workers or refugees, they are the exception rather
than the rule. There are major service coverage gaps that are reflected in
health statistics. Meeting national targets for sexual and reproductive health
will require that equity gaps be narrowed, including the gaps that separate
migrants from citizens and ethnic minorities from the majority.
• Assessments of progress towards UHC in sexual and reproductive health
that can generate actionable information for national decision-makers are
constrained by important information gaps. They include information about
service quality and about reasons why clients do not always take advantage
of public services provided free of charge; information about the cost-drivers
for out-of-pocket expenditures; information about coverage of migrant
populations; and information about the households among whom out-of-
pocket expenditures for health constitute a serious financial risk.
4

THE UN AGENDA FOR SUSTAINABLE DEVELOPMENT
On September 25
th
2015, the UN General Assembly adopted the Agenda for Sustainable Development entitled ‘Transforming
our World’. [1] It includes 17 Sustainable Development Goals (SDGs) to be achieved by 2030. The third goal is focused on
health and well-being and includes two sub-goals:
3.7 By 2030, ensure universal access to sexual and reproductive health-
care services, including for family planning, information and
education, and the integration of reproductive health into national
strategies and programmes
3.8 Achieve universal health coverage, including financial risk
protection, access to quality essential health-care services and
access to safe, effective, quality and affordable essential medicines
and vaccines for all
An Inter-Agency Expert Group (IAEG) developed the monitoring framework for the SDGs. It presented its final list of
232 indicators in March 2017, including two indicators each for SDG 3.7 and SDG 3.8. [2]
3.7.1 Proportion of women of reproductive age (aged 15-49 years) who have their need for family
planning satisfied with modern methods
3.7.2 Adolescent birth rate (aged 10-14 years; aged 15-19 years) per 1,000 women in that age group
3.8.1 Coverage of essential health services (defined as the average coverage of essential services
based on tracer interventions that include reproductive, maternal, newborn and child health,
infectious diseases, non-communicable diseases and service capacity and access, among the
general and the most disadvantaged population)
3.8.2 Proportion of population with large household expenditures on health as a share of total
household expenditure or income
The two SDG goals are closely linked. Sexual and reproductive health (SRH) services are essential services and
therefore also included under universal health coverage (UHC). The components of a comprehensive package of essential
SRH services were proposed in 2010:[3]
• Family planning and birth spacing services
• Antenatal care, skilled attendance at delivery, and postnatal care
• Management of obstetric and neonatal complications and emergencies
• Prevention of abortion and management of complications resulting from unsafe abortion
• Prevention and treatment of reproductive tract infections and sexually transmitted
infections including HIV
• Early diagnosis and treatment for breast and cervical cancer
• Promotion, education and support for exclusive breast feeding
• Prevention and appropriate treatment of sub-fertility and infertility
• Active discouragement of harmful practice such as female genital cutting
• Adolescent sexual and reproductive health
• Prevention and management of gender-based violence
The priority SRH needs differ among populations, and the list of essential SRH services must therefore be adapted to
the country context. Furthermore, some of the services in the list are highly aggregated, for instance ‘adolescent sexual
and reproductive health’. When conceptualised within a rights-based framework, the package of activities to promote
and protect the sexual and reproductive health of adolescents expands into many components that extend well beyond
services in the health sector.
The UHC indicator 3.8.1 for monitoring service coverage is based on 16 tracer health services, including three SRH
services, namely family planning, antenatal and delivery care, and cervical cancer screening. But with a total of 126
sub-goals in the SDG agenda, global indicators to monitor any one goal have to be highly aggregated. At the country and
regional level, there is a need for disaggregation, to understand the extent to which commitments to achieve universal
health coverage of essential sexual and reproductive health services are met, including those that are not captured by
the global monitoring system.
5

SEXUAL AND REPRODUCTIVE HEALTH
SERVICES IN ASIAPACIFIC
The UNFPA Asia-Pacific (AP) region comprises 37 nation states, including 14 Pacific
Island countries. With a total population of about four billion, it is home to more than
half of the world’s population. The region includes countries that rank in the low,
medium and high range of the UNDP human development index table. Averaging
indicators to establish a regional profile would therefore not be very informative.
Many countries in the Asia-Pacific region are experiencing large international
population movements. The 2015 Asia-Pacific Migration Report estimated that
more than 18 million migrants lived in five countries that are among the ten top
destination countries for international migration in the region (India, Pakistan,
Thailand, Iran and Malaysia). [5] A large proportion of the migrants are young
people whose needs for health care are mostly for sexual and reproductive health.
The extent to which they have access to SRH services and to financial protection at
the same level as the national population is a key equity dimension in the universal
health coverage profile of each country.
A general overview of the situation of universal health coverage of sexual and
reproductive health services can be presented in a scatter diagram, plotting an
index of SRH coverage on the vertical axis and a financial risk protection index
on the horizontal axis. The SRH service coverage index is calculated from three
indicators that are included among the global indicators for monitoring the SDGs:
• Adolescent birth rate per 1,000 women aged 15 to 19
• Proportion of family planning demand satisfied with modern methods
(women aged 15 to 49)
• Proportion of births attended by skilled health personnel
The financial risk protection index should ideally reflect the SDG indicator of
‘proportion of population with large household expenditures on health as a share of total
household expenditure or income’. Data for this indicator, however, are not widely
available. Instead, the proportion of total health expenditure that is paid by patients
and clients out of pocket is used. This is not an ideal indicator, because cash-for-
service requirements differ by type of service. They may be particularly high for
some SRH services that are excluded from health insurance coverage, including
family planning. The indicator also does not reflect uneven coverage for adolescents,
migrants and minority groups who may be uninsured to a much higher degree than
the rest of the population.
• Afghanistan
• Bangladesh
• Bhutan
• Cambodia
• China
• Cook Islands
• D.P.R. Korea
• Federated States
of Micronesia
• Fiji
• India
• Indonesia
• Iran
• Japan
• Kiribati
• Lao P.D.R
• Malaysia
• Maldives
• Marshall Islands
• Mongolia
• Myanmar
• Nauru
• Nepal
• Niue
• Pakistan
• Palau
• Papua New Guinea
• Philippines
• Samoa
• Solomon Islands
• Sri Lanka
• Thailand
• Timor-Leste
• Tokelau Islands
• Tonga
• Tuvalu
• Vanuatu
• Viet Nam
THE UNFPA ASIA-PACIFIC REGION
6
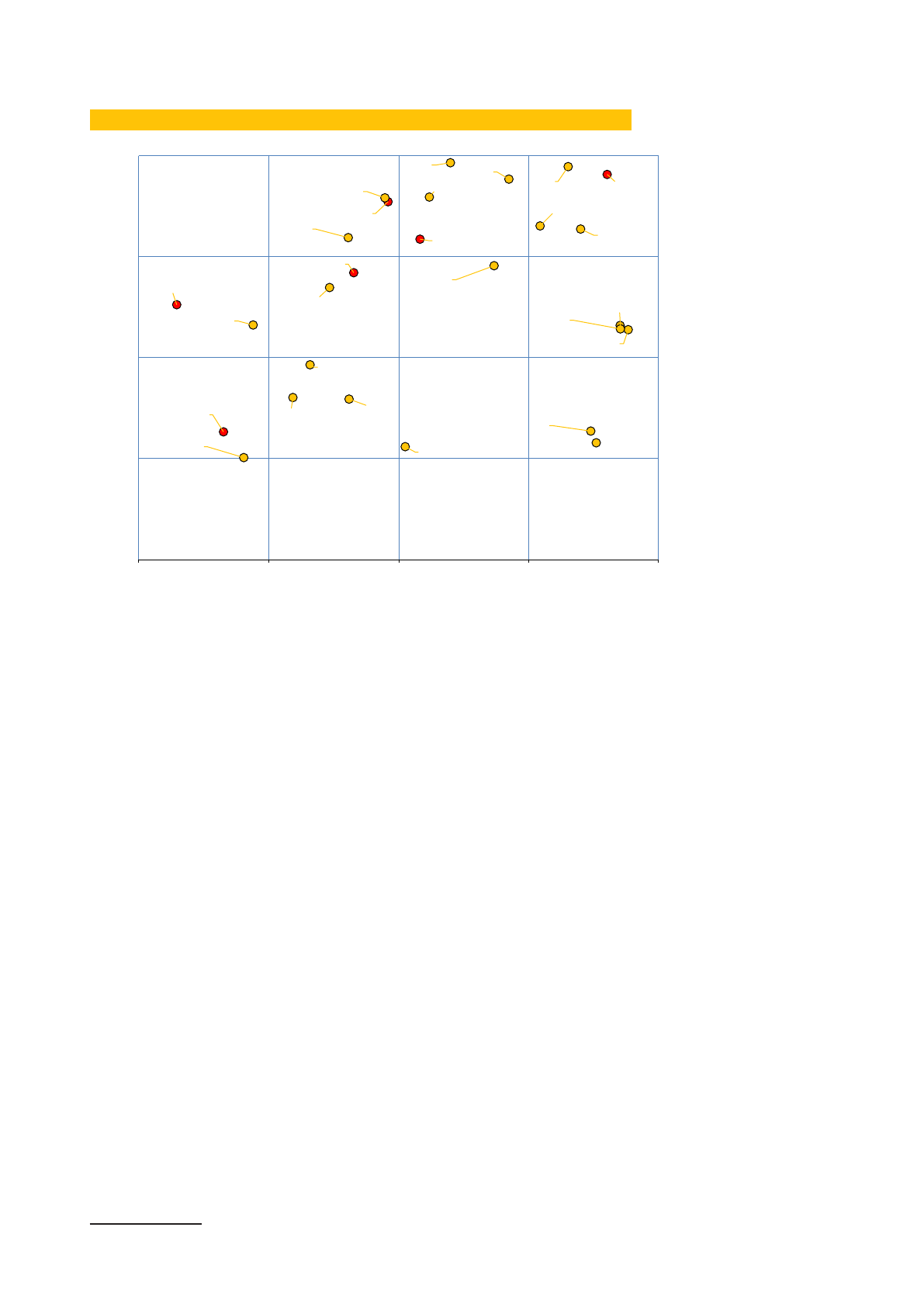
OVERVIEW OF SRH SE
RVICE COVERAGE AND FINANCIAL PROTECTION IN ASIA-PACIFIC
1
Data sources: Ref [6], [7]
An overview as presented in this graphic is useful for orientation. It shows that the
countries in the region map out across a broad range, some with low SRH service
coverage and minimal financial protection and some with high coverage and a high
level of financial protection. Details, however, are lost. Sexual and reproductive health
services range from sexuality education for adolescents to the treatment of cancers
of the reproductive system. The scope is wide, and not all services are provided in
the health sector. Financial risk protection can also take different forms, including
direct public financing of health services; third party payment for services by a
social insurance scheme that may be financed from general tax revenues, insurance
premiums, or a combination of both; a variety of financial risk pooling arrangements
including private health insurance or community mutual funds; and cash transfer or
voucher schemes, typically to offset indirect costs of seeking health care. A detailed
review that covers the range of services, the financial risk reduction schemes, and
the equity of access can only be done at the level of each country.
1 DPR Korea and 9 Pacific Island Countries are not included because of incomplete data
Afghanistan
Bangladesh
Bhutan
Cambodia
China
Fiji
India
Indonesia
Iran
Japan
Lao PDR
Malaysia
Maldives
Mongolia
Myanmar
Nepal
Pakist …
PNG
Philippines
Samoa
Solomon Isl.
Sri Lanka
Thailand
Timor-Leste
Tonga
Vanuatu
Viet Nam
20 40 60 80 100
SRH Service Coverage Index
Financial Risk Protection Index
Low
High
40
Low
Low
High
60
80
7

THE SCOPE OF THE STUDY OF UHC FOR
SRH
For the study, six countries with documented commitments to UHC were selected as
a focus:
Bangladesh
adopted a health financing strategy in 2012 with a roadmap
to achieve universal health coverage by 2032. [8]
Cambodia
adopted the ‘National Social Protection Strategy for the
Poor and Vulnerable’ in 2011 followed by the ‘National Social
Protection Policy Framework 2016-2025’. The long-term
vision presented in these documents is a comprehensive
system of universal health coverage. [9], [10]
Indonesia
initiated a national social security reform in 2004, with
national health insurance as the first of five social security
programmes to be introduced. [11] The national health
insurance programme was launched in 2014.
Mongolia
introduced mandatory social health insurance in 1994, and
in 2013 adopted a long-term strategy for the development of
social health insurance (2013-2022).[12]
Thailand
committed in the National Health Security Act of 2002 to
establish a National Health Security Fund ‘to encourage
access by persons to universal and efficient health service’.
[13]
Viet Nam
introduced a health insurance law in 2008 and revised it in
2014 with a target to reach universal health coverage by
2020. [14], [15]
The six countries are low or middle-income countries with a combined population of
about 600 million, which is almost half of the population of the Asia-Pacific region
excluding China and India.
The scope of sexual and reproductive health services reviewed in the study is
wide but not fully comprehensive. Some essential SRH services are not included,
for instance treatment of breast cancer, infertility treatment, support for exclusive
breast feeding, and health services for the prevention, diagnosis and treatment of
sexually transmitted infections (STI) among populations other than adolescents and
pregnant women. This leaves out STI and HIV services for men, transgender and
intersex persons.
Four countries, Indonesia, Mongolia, Thailand and Viet Nam introduced national
health insurance schemes, aiming to achieve a single third-party payment system for
all essential health services. For these countries, the study aimed at documenting
the sexual and reproductive health services that are covered by the insurance, as
well as the inclusiveness and equity of coverage. In Bangladesh and Cambodia,
efforts to establish a national social health insurance are still at an early stage, and
the purchasing arrangements for health services are more fragmented. Several
public and private schemes coexist, together with a public health system that
provides certain services free of charge to users. In these countries, the study aimed
at documenting the different types of schemes and their interactions, including only
those that aim at national coverage and that have a clear objective to protect users
from social hardship. Data were collected in November and December 2016 through
document reviews and interviews with key informants in the six countries.
8

BANGLADESH
9
BANGLADESH
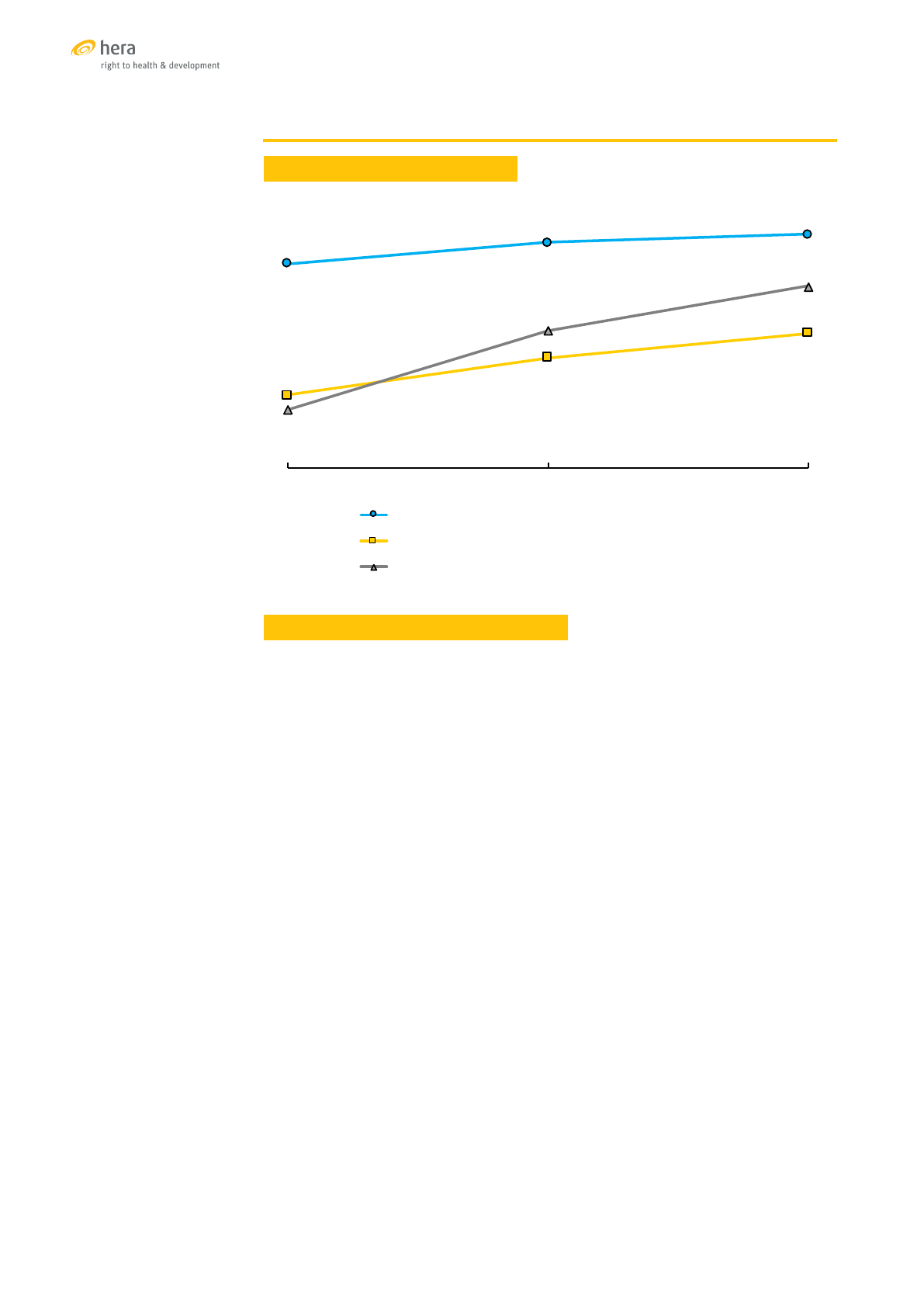
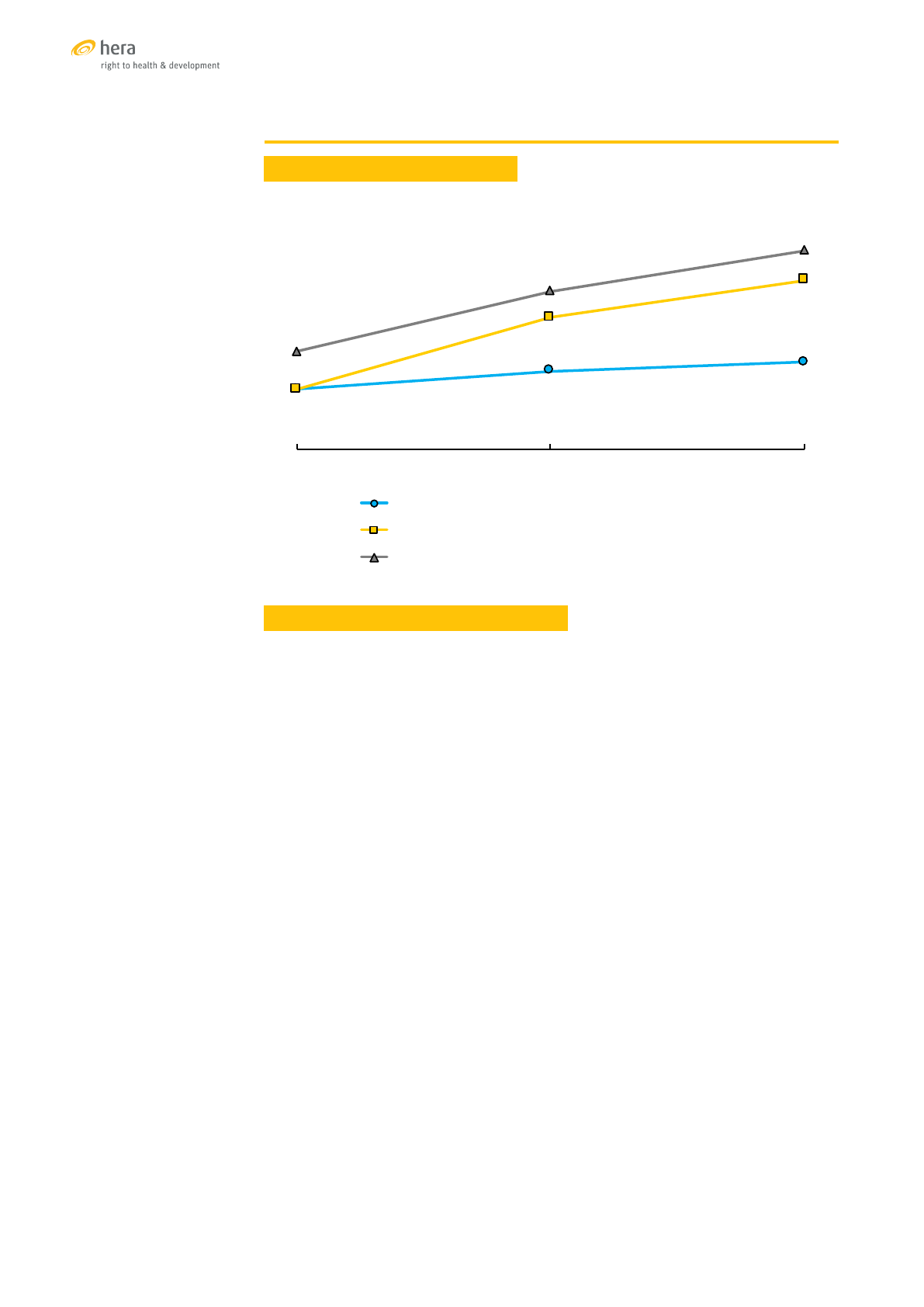
TRENDS OF SELECTED SRH INDICATORS
Sources: [16], [17], [18]
SEXUAL AND REPRODUCTIVE HEALTH SERVICES
Health services in the public sector in Bangladesh are delivered by the Ministry of
Health and Family Welfare (MOHFW) through a network of health centres and hospitals
from the primary to the tertiary level. The private health sector is large and has been
growing at approximately 15 percent per year since 2000. In 2013, approximately
half of registered clinic and hospital beds in the country were in the private sector,
and 62 percent of medical doctors were engaged in private practice. [19] Private
for-profit health facilities are concentrated in the urban areas. In addition, a large
number of health facilities for primary and secondary care are operated by NGOs and
confessional organisations, primarily in rural and in high density urban areas.
Although public facilities provide health services without charge to clients or at
subsidised user fees, the proportion of health expenditures covered by out-of-pocket
payments has continued to increase. At 67 percent, it is one of the highest in the
region. Two reasons are cited to explain this trend. Limitations of service quality and
availability in the public sector motivates clients to seek care in the private sector and
accept to pay for services that are perceived to be of better quality. At the same time,
the service offer of public facilities has contracted because of financial shortages.
Medicines and services that were previously provided free of charge are now often
only available at private pharmacies or laboratories. [19]
Contraception: The uptake of family planning was one of the early successes of
population programmes in Bangladesh. Between 1975 and 2014, the total fertility
decreased from 6.3 to 2.3 births per woman. In 2014, about 73 percent of the demand
for modern family planning was satisfied, with small differences between geographic
or socially stratified groups. The adolescent fertility rate, however, did not follow the
trend. After a sharp increase in the 1980s it decreased slowly, but in 2014 it was still at
the high level of 113 births per 1,000, about the same level as in 1975. The main reason
is the early age of marriage among girls in Bangladesh. In 2014, more than half (59%)
of young women were married before the age of 18, with even higher proportions in
rural areas. [18]
Menstrual regulation by vacuum extraction of uterine content to re-establish
menstrual flow in case of a delayed menstrual period has been part of the Bangladesh
national family planning programme since 1979. Menstrual regulation is available free
47%
52%
54%
17%
26%
31%
13%
32%
42%
2004 2011 2014
% married women (15-49) currently using modern contraception
% women with at least 4 ANC visits during their last pregnancy
% of births attended by a skilled provider
10

of charge in public clinics which provide about two thirds of these services. Medical
menstrual regulation through the induction of uterine bleeding by pharmaceutical
means was added more recently in some facilities.
Termination of pregnancy is illegal in Bangladesh under the 1860 Penal Code unless
performed to save a woman’s life. Despite the wide availability of contraceptive
services, including menstrual regulation, the use of induced unsafe abortions is
prevalent. The estimated rate of complications following induced abortions (6.5/1,000)
is comparable to other countries with restrictive abortion laws. [20] Post abortion care
is available in most public and private hospitals.
Maternal health services, including antenatal, obstetric and postnatal care, are
provided in public and private health facilities. A maternal health voucher system
has stimulated uptake of services. The vouchers can be redeemed in public and in
accredited private facilities.
The use of antenatal care has increased, but in 2014 it was still low, with only 31 percent
of women reporting that they had attended four or more antenatal consultations
during their last pregnancy. All increases in antenatal care between 2011 and 2014
were due to an increasing use of the private sector which accounted for 52 percent
of antenatal consultations in 2014. [18] HIV screening, syphilis screening and malaria
prevention are not routinely provided as part of antenatal care.
Deliveries in health facilities increased from 12 percent in 2004 to 37 percent in 2014.
The majority of deliveries, however, still take place in the home. Private hospitals
and maternity homes have become by far the most favoured places of delivery, with
almost twice as many births as in public sector facilities. There have been major
investments under the 2011-2016 health strategy to achieve national coverage of
basic and comprehensive emergency obstetric and neonatal care services, however
not all established centres are able to provide the full range of service, and coverage
in several provinces is still below the recommended minimum density.
The national incidence of delivery by caesarean section of 23 percent of births is very
high. Among women in the higher socio-economic strata, caesarean sections account
for half of all deliveries. A study among 500,000 women who gave birth between 2005
and 2011 found that 73 percent of deliveries in the private sector were by caesarean
section, suggesting that the private sector is driving a high caesarean section rate that
is not always medically indicated. [21]
Diagnosis and treatment of sexually transmitted infections are provided in public
facilities and NGO clinics. Statistics about the prevalence of sexually transmitted
infections in key populations such as sex workers and truck drivers are available,
but there is little information about the prevalence of STIs in the general population.
Reports of syphilis screening among pregnant women are scarce. The only available
data come from three tertiary hospitals where one third of the antenatal clients were
tested for syphilis. Among 626 women, two were found to be infected and one received
treatment. [22]
The prevalence of HIV infection is low in Bangladesh. Among people who inject drugs,
female sex workers, and men who have sex with men the prevalence is estimated
at 0.7 percent. HIV programmes primarily focus on prevention among these groups.
Almost all services for HIV, including antenatal testing and PMTCT, are provided by
programmes that rely on international funding. They are not covered by the public
health service. [23] PMTCT services are available in three government tertiary care
hospitals and in a few private facilities. The number of women tested is small, only 13
percent of those who tested positive received anti-retroviral treatment (ART) during
delivery, and only 1.4 percent during breastfeeding. [22]
Immunisation against Human Papillomavirus (HPV) is currently being piloted in
one district, aiming to immunise about 33,000 adolescent girls. The cervical cancer
burden in Bangladesh is estimated at 29.8 per 100,000 women per year. Cancers are
usually diagnosed in advanced stages as access to screening and early treatment is
limited. [24]
Services for the treatment and support of women survivors of sexual violence are
provided by the Ministry of Social Welfare.
11

FINANCIAL RISK PROTECTION
Public health services are nominally free or provided
at subsidised rates. The high level of out-of-pocket
expenditures for health indicates that the public health
service model is not working as intended. A survey in an
urban area of Bangladesh in 2013 reported that between
10 and 18 percent of households experienced an incidence
of catastrophic health costs within the three-month study
period. [25] Two public financial risk protection schemes
are meant to reverse the trend of increasing out-of-pocket
expenditures. In addition, there are a large number of
community-based or micro insurance schemes.
Shasthya Shurokkha Kormoshu (SSK) (subsidised social
health insurance) is the first and only social health insurance
scheme under the MOHFW. It is fully financed from general
government revenues. The long-term vision for SSK is of a
scheme combining risk pooling with a purchaser-provider
split under the stewardship of the MOHFW. In a first phase,
only the poor are covered, and the government pays their
insurance premiums. In the long run, other groups will be
included as paying members. A three-year pilot SSK scheme
opened in March 2016, targeting a population of about 95,000.
It is expected to increase access to hospitals and improve
the quality of services by generating income for the facilities
which they can use for improvements. [26]
The SSK benefits include inpatient care for fifty specified
health conditions in selected public facilities. They do not
include contraceptive and menstrual regulation services; HIV
testing and treatment; cervical cancer prevention, detection
and treatment; and services for survivors of gender-based
violence, child abuse or rape. The main challenges faced
during the pilot phase of SSK include coping with the increased
demand for services while developing reliable procedures to
manage an efficient third-party payment system for providers.
The Maternal Health Voucher / Demand Side Financing
scheme (DSF) started in 2007 as a pilot programme of the
MOHFW in 21 sub-districts. It was scaled up in 2010 to cover
53 sub-districts in 41 districts and a target population of about
26.5 million. At inception, the beneficiaries of the DSF scheme
were pregnant women during their first or second pregnancy
who were considered poor after a formal means test. In nine
sub-districts, ‘universal intervention’ was piloted, extending
the DSF benefits to all women. Vouchers provide a range of
benefits, including comprehensive coverage of antenatal,
delivery and postnatal care, transport subsidies and cash
incentives for mothers who deliver with the attendance of
a skilled provider. Public, NGO and private sector health
facilities that are accredited are reimbursed at a fixed rate for
the vouchers they collect. The total cost of the programme
per voucher distributed was estimated at US$ 41 in 2010.
[27] The programme is primarily financed by international
development partners. Technical assistance is provided by
WHO. Evaluations of the programme in 2011 and 2014 found
that the scheme increased the demand for reproductive
health care among poor women, and that it reduced the
average out-of-pocket costs for normal deliveries from US$
25 to US$ 21 and for caesarean sections from US$ 103 to US$
65. [28],[29]
Community-based and micro health insurance schemes are
managed by NGOs. The schemes are funded with insurance
premiums, cross-subsidisation from other NGO programmes,
and international and national donations. The schemes
target poor and disadvantaged groups as well as members
of the micro-credit groups operated by the same NGO.
Benefits differ among the micro-insurance schemes. Most
of them cover basic and preventive health services including
immunisation, family planning, out-patient consultations, and
normal deliveries. [30]
UNIVERSAL COVERAGE FOR SEXUAL AND REPRODUCTIVE HEALTH
B
angladesh is in the early stages of moving from a public health
service model under which health care is provided by government
and free of charge to users, to a social insurance model under which
health services in the public and private sector are purchased by a
health insurance provider who is funded with insurance premiums
and general government revenues.
Out-of-pocket payments for health care have continued to
increase and there has been a continued drift of patients to
the private sector. This gave rise to the emergence of multiple
community and micro-insurance schemes that provide a limited
amount of financial protection to some. The voucher scheme for
maternity care is a more ambitious initiative, documenting that the
equity and coverage of health services can be increased by offering
payments for services to providers, while protecting users from
expenditures. A large proportion of the increased coverage was
achieved by the private sector, indicating the limitations in service
capacity and quality of the public health sector. The high caesarean
section rates among private sector deliveries, however, suggest
that the scheme generates incentives for performing caesarean
sections without medical indication.
Beyond maternity care, the coverage of SRH services, for instance
for HPV immunisation, cervical cancer screening, or syphilis and
HIV testing in pregnancy, is limited. For services that are available
and provided free of charge in the public sector, for instance for
family planning and menstrual regulation, an increasing number
of women consult private sector providers and pay for the
service. This suggests that these services also face issues about
declining availability and acceptance, despite the substantial
public delivery infrastructure that was established.
The long-term goal pursued in Bangladesh is national coverage
of the entire population with the SSK social health insurance
scheme. SRH services, other than maternity care, are, however,
not included in the benefit package of SSK as it is currently being
piloted. While these services will for now still be offered through
special projects or by the public health service, the offer is limited
and the drift to the private sector will likely continue. This means
that user charges for SRH services will not disappear and may
even rise, as more and more of these services are pushed into
the private sector.
Because the systems for financial risk protection in Bangladesh
are fragmented, the equity of coverage is difficult to determine.
The SSK scheme protects the poor, but only as a pilot programme
with small coverage. The voucher scheme also has a pro-poor
focus, but it covers only about 20 percent of the population. Public
health services theoretically offer universal financial protection,
but they are bypassed by more and more people at all levels of
the socio-economic scale, with the result that they do not deliver
equitable protection from catastrophic health expenditures.
12

CAMBODIA
Creative Commons Photo credit: Clear Path International
https://www.flickr.com/photos/cpi/16775850/
13
CAMBODIA
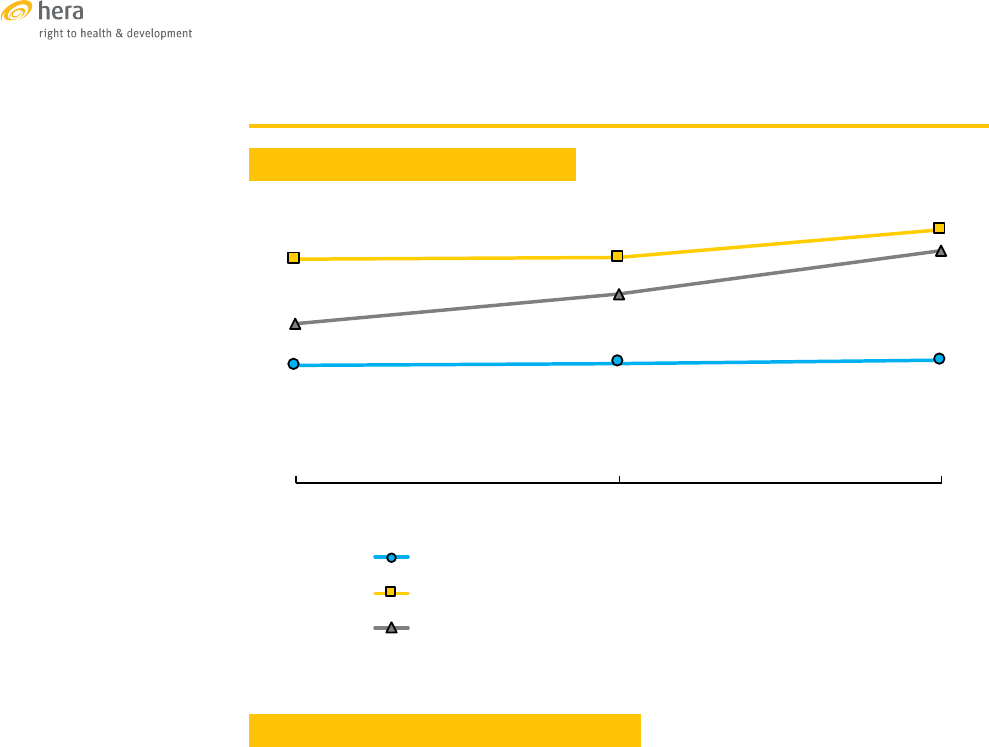
TRENDS OF SELECTED SRH INDICATORS
Sources: [31],[32],[33]
SEXUAL AND REPRODUCTIVE HEALTH SERVICES
Health services in Cambodia are provided in the public and private sector, including
by a variety of NGO-operated not-for-profit health facilities. Two packages of services
have been defined for public sector facilities, the Minimum Package of Activities
(MPA) provided primarily at the health centre level and the Complementary Package
of Activities (CPA) which is available in hospitals. [34]
Contraception, including family planning counselling, provision of implants, IUDs,
pills, condoms, male and female sterilisation, are included in the MPA and CPA.
Utilisation and availability of modern contraception is slowly increasing. The most
widely used methods are contraceptive pills. The uptake of long-acting contraceptive
methods remains limited, but availability in public health facilities is increasing
annually. Emergency contraception was introduced in the public sector in 2012 and
is reported to be available, although there is little information about access and use.
[35],[36] The total fertility rate in Cambodia declined from 3.4 births per woman in
2005 to 2.7 in 2014. The adolescent fertility rate at 57 births per 1,000 women aged 15
to 19 is comparable to other countries in South-East Asia, but shows an increasing
trend over the past years. [33]
Termination of pregnancy in the first trimester was legalised in Cambodia in 1997.
Between 2005 and 2015 the proportion of women who had at least one abortion
within the past five years doubled from 3.5 to 6.9 percent, however deaths related to
unsafe abortions decreased dramatically. In 2005, at least one death was reported
by 10 percent of hospitals, falling to one percent in 2009. [37] Most terminations
(44%) are performed in private health facilities and about 61 percent under the care
of a qualified provider. Vacuum aspiration is the most common method followed
by medical termination. The public sector has a secondary role in the provision of
abortion services. [33],[38]
27%
35%
39%
27%
59%
76%
44%
71%
89%
2005 2010 2014
%married women(1549)currently usingmodern contraception
%women with atleast4ANCvisitsduring theirlast pregnancy
%of births attended byaskilled provider
14

Maternal health services are provided under MPA and CPA. Public sector facilities
dominate in the provision of maternity services with little difference in use according
to social group or residence. Antenatal care consultations, including tetanus
immunisation, provision of folic acid and iron and micro-nutrient supplementation
are available at health centre level through MPA, but laboratory analyses and
ultrasound examinations are only available at referral hospitals. Normal deliveries
and post-natal care consultations are also conducted at health centres, whereas
assisted deliveries, caesarean sections and blood transfusion are only performed in
hospitals. Treatment for fistula and other in-patient hospital services are available at
the referral hospital, covered by the CPA. In 2014, 76 percent of Cambodian women
attended four or more ANC consultations and 89 percent of births were attended by
a skilled health care provider. [33]
Prevention and treatment of malaria during pregnancy is included among the
antenatal services, however the coverage is low. A recent study estimated that 21
percent of the population is at risk of malaria in 20 out of 24 provinces. However,
malaria tests are not routinely conducted during ANC visits as malaria is often not
suspected. Laboratory services are still not strong enough to ensure diagnosis by
quality assured microscopy or rapid diagnostic tests. [39]
Services for sexually transmitted infections are available for pregnant women and
adolescents at health centre level, including HIV testing, counselling, and prevention
of HIV transmission from mother to child. Laboratory analysis of STIs as well as
provision of ARVs are only available at referral hospitals. There are counselling and
testing sites in almost every referral hospital. They are not integrated into general
outpatient services, but they are provided as integral part of antenatal care. [36]
Immunisation against Human Papillomavirus and comprehensive services for
cervical cancer prevention, detection and treatment should be available at the
referral hospitals through the CPA, however, the availability of these services remains
severely limited. There are currently pilot projects for screening and treating cervical
cancer in the provinces but treatment remains concentrated at the district hospital
level. The availability of treatment options for those already diagnosed with cervical
cancer remains limited. Cambodia’s first national cancer centre is expected to be
operational by 2017. [34]
Currently, services available for survivors of gender-based violence are limited to
HIV post-exposure prophylaxis, emergency contraception and STI screening and
treatment. Following the adoption of the national guidelines for the management of
violence against women and children in 2014, the Ministry of Health is undertaking
efforts to build capacity, improve access to forensic services, strengthen referral
systems, and reduce delays in providing care to women who experienced violence.
[40]
15

FINANCIAL RISK PROTECTION
Per person out-of-pocket expenditures for health in
Cambodia are high. They increased three-fold between
2000 and 2014 from US$ 14 to US$ 45, while they
fluctuated as a proportion of total health expenditures
between 60 and 80 percent. [6]
In 2016, Cambodia adopted the ‘National Social
Protection Policy Framework 2016-2025’ with the two
main pillars of social assistance and social insurance.
[10] It is expected to eventually replace a fragmented
system of health financing and financial risk protection
that includes government subsidised and user-fee
financed services provided in public and contracted NGO
health facilities, community-based health insurance,
health equity funds, and voucher schemes. [41]
• Public sector health facilities provide services
defined in the CPA and MPA packages at fixed user
fees with exemptions for the poor. The service
packages include all medical services for sexual
and reproductive health, but the use of public
facilities for these services is variable, ranging
from 16 percent for termination of pregnancy to
76 percent for female sterilisation. [33]
• Health Equity Funds cover approximately 18
percent of the population. They are financed from
a pool of shared government and development
partner contributions. Beneficiaries are identified
according to their household economic situation
through a formal participatory mechanism. The
benefits include partial or full reimbursement of
expenditures for services included in the MPA and
CPA packages, food, transport and funerals.
• Several community-based health insurance
schemes provide similar benefits as the health
equity funds, but target primarily informal
sector workers above the national poverty line.
The coverage is less than one percent of the
population.
• Voucher schemes for reproductive health services
for poor women are operated by a number of
NGOs, but coverage is also very low.
• Social health insurance was recently introduced
to combine existing health insurance schemes
for civil servants and formal sector workers. The
insurance benefits are in line with MPA and CPA
packages.
UNIVERSAL COVERAGE FOR SEXUAL AND REPRODUCTIVE
HEALTH
Cambodia has adopted policies and programmes in key
areas to improve delivery of sexual and reproductive
health services. Laws, standards and guidelines have
focused on supporting universal coverage of maternal
health services and contributed to a rapid increase
in facility-based births and skilled birth attendance.
The provision of family planning improved only slowly.
Although the gap between wanted fertility and observed
fertility closed from 0.6 children per woman in 2005 to
0.3 in 2015, it was still at the level of 0.6 among women in
the poorest segment of the population in 2015, indicating
that they had not achieved the desired access to family
planning. Adolescent fertility rates are increasing,
although this is more related to early marriage than
to access to contraception. The unmet family planning
need for limiting fertility among adolescent women
aged 15 to 19 is quite low at 1.4 percent. [31],[33] Service
coverage for prevention and treatment of cervical cancer
and for addressing violence against women and girls is
still insufficient and requires attention. [37]
Fixed and transparent user fees for sexual and
reproductive health services provide some level of
protection against financial hardship, especially as the
fee levels are set in consultation with communities, and
provisions are made for fee exemptions for the poor. All
SRH services are included in the MPA or the CPA service
packages provided at health centre or hospital level. The
Health Equity Funds provide additional financial risk
protection for the poor. The protection, however, does not
extend to the private sector which delivers the majority
of some sexual and reproductive health services, for
instance for short-term family planning methods and
for termination of pregnancy. The cost of health services
is considered by two thirds of women as a barrier to
access. There is little difference among age groups,
but the financial barrier is higher for rural women and
as high as 79 percent for women in the lowest wealth
quintile. [33]
While Cambodia has achieved impressive progress in
expanding the service offer for sexual and reproductive
health after the almost complete break-down of health
services under the Khmer Rouge regime in the 1970s
and 80s, it has not yet achieved a high level of coverage
of financial risk protection. Social equity instruments
such as user fee exemptions and the current nationwide
expansion of the health equity funds have contributed
to narrowing some of the gaps in service utilisation
between poor and rich. But since health equity funds
are reimbursement mechanisms for health service
expenditures, an important financial barrier to service
utilisation remains.
16

INDONESIA
17
INDONESIA
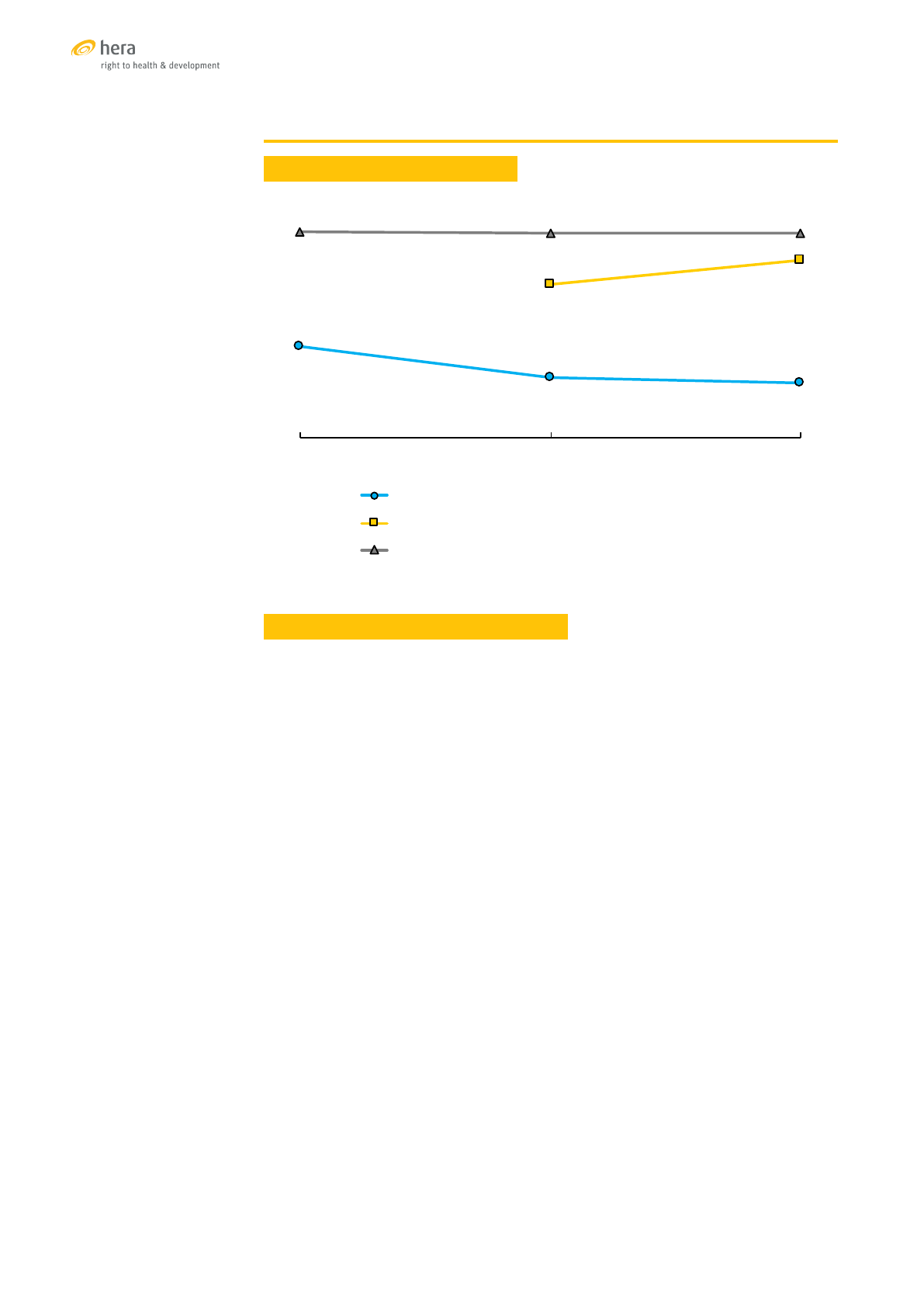
TRENDS OF SELECTED SRH INDICATORS
Sources: [42],[43],[44]
SEXUAL AND REPRODUCTIVE HEALTH SERVICES
The population of Indonesia is served by a mix of public and private health care
providers. Public health centres provide health promotion, immunisation, sanitation
and health care services. The Indonesian health policy requires local governments
to establish one public health centre for every 30,000 inhabitants and one sub-health
centre for every 10,000. There are, however, large differences in service provision
among provinces. A report in 2011 found that 25 percent of health centres country-
wide were without a medical doctor, most of them in remote, poor provinces. [45]
Contraceptive prevalence rates in Indonesia are high and have been for many
years. According to the most recent estimate, 81 percent of married women aged
15-49 have satisfied their need for family planning with the use of a modern method.
[46] The difference between wanted and observed fertility in 2012 was 0.6 children
per woman with little difference according to residence and social status. The
total fertility rate of 2.6 has not changed since 2002. Family planning services are
delivered by the Ministry of Health, and since 2016 they are included among the
National Health Insurance benefits. Contraceptive commodities are supplied by
the National Family Planning Board. Stock-outs of contraceptive supplies in health
facilities and poor quality of family planning services have, however, become an
issue of concern during the past three years. [47]
In 2003, the Ministry of Health started a programme to roll out the provision of
youth-friendly services in primary health centres. About a quarter of health
facilities are currently implementing the programme. However, the access of
adolescents to sexual and reproductive health services remains limited. Guidelines
for health providers stipulate that family planning services should only be provided
to married couples. Adolescent fertility rates have remained unchanged over three
rounds of DHS surveys between 2002 and 2012, each reporting that between nine
and ten percent of women aged 15-19 had started childbearing. [44]
57%
57%
58%
81%
82%
88%
66%
73%
83%
2002 2007 2012
%married women(1549)currently usingmodern contraception
%women with atleast4ANCvisitsduring theirlast pregnancy
%of births attended byaskilled provider
18
According to estimates by the FP2020 programme, there are approximately 2.6
million unintended pregnancies yearly. [46] Indonesia revised its general prohibition
of termination of pregnancy in 2009 under the Law 36 on Health. In Article 75
the prohibition was lifted in case of a threat to the life of mother or foetus and for
pregnancies due to rape. Among the requirements is the consent of both partners
except in cases of rape. [48] The law continues to be restrictive and statistics about
terminations of pregnancy are not available.
Indonesia made significant progress towards expanding maternal health services,
however the 2015 Demographic and Health survey estimated a very high maternal
mortality ratio of 359 deaths per 100,000 live births, an increase of more than 50
percent over the estimate in 2007. [44] In the subsequent strategic health plan (2015-
2019), sexual and reproductive health was therefore flagged as a priority area. [49]
There is evidence that with the launching of the National Health Insurance in 2014,
health service usage and outcomes improved greatly, but available population-
based data mostly predate the health insurance reform. Three subsequent DHS
surveys documented relatively high coverage of some key reproductive and
maternal health services with an increase in skilled attendance at delivery over
the five years preceding the 2012 survey. The surveys document that between 2007
and 2012 about two thirds of women delivered their infants in a health facility. Most
women chose private facilities, but the proportion of deliveries in public facilities
already started to increase prior to 2012 (from 22% in 2002 to 27% in 2012). It is
anticipated that the 2017 DHS will document further increases in deliveries in public
health facilities.
Coverage rates of services for sexually transmitted infections are not known,
however coverage of HIV positive pregnant women with anti-retroviral therapy for
the prevention of mother to child HIV transmission (PMTCT) is low and has been
falling. According to UNAIDS statistics it was 16 percent in 2012, falling to 9 percent
in 2015. Indonesia is not a high HIV incidence country, but because of its large
population there are an estimated 70,000 new HIV infections per year. [50] According
to the 2013 Global STI Surveillance Report, syphilis testing during pregnancy was
reported to be very low in Indonesia, at only 0.1 percent, in the context of a relatively
high rate of positivity of 1.2 percent reported in 2009. [51]
Immunisation programmes against Human Papillomavirus exist only in a pilot
phase. There is no information about the coverage rate. Indonesia has a national
cervical cancer screening programme with a quality assurance structure and a
mandate to supervise and to monitor screening. It does, however, not include an
active invitation for screening, and coverage statistics are not provided. A small
survey between 2007 and 2011 reported that 24 percent of participating women had
undergone cervical cancer screening within the last five years. [52]
19

FINANCIAL RISK PROTECTION
In 2004, Indonesia launched a national social
security reform with the development of a mandatory
national health insurance as the first of five social
security programmes. [11] In 2012, the ‘Road Map
towards National Health Insurance 2012-2019’ was
jointly developed by 14 national ministries and state
agencies with a target to cover the entire population
of Indonesia by 2019. [53] In 2014 a social security
agency for health (BPJS) was established with the task
of merging existing social protection and risk pooling
schemes under a single National Health Insurance
(JKN). Implementation started in January 2014 with
121.6 million members. The majority among them
were social insurance beneficiaries whose premiums
were paid by the State. Since then, there has been an
increasing proportion of contributing members who
joined the JKN through mergers of their civil servant,
military, formal sector or private insurance scheme.
By November 2016, membership was reported at
171 million, about two thirds of the population of
Indonesia. Insurance claims in the 2015 calendar year
were about 18 percent higher than in the first year of
operation in 2014. [54]
Insurance benefits differ among different membership
types and premium rates, but there are plans to
gradually abolish these differences. Premiums start
at 23,000 IDR per month (about 17 US$) which is the
subsidised rate paid by the State for the poor, and are
set at five percent of family earnings for civil servants
and other waged workers. For the self-employed
and those working in the informal economy, three
premium classes exist depending on the level of
services subscribed.
The benefits of the National Health Insurance scheme
launched under the BPJS-Health in January 2014 are
generous, covering most of sexual and reproductive
health services, and also covering some non-clinical
costs such as ambulance referrals and hospital
accommodation. Family planning services were
included in 2016. Not covered are services for the
termination of pregnancy except in special situations.
Care for spontaneous abortion and post-abortive care
are however included.
The JKN scheme is still in the process of expansion,
undergoing adjustments of tariffs, benefit packages
and premiums. According to key informants, it
concluded its first year of operation with a negative
balance, a deficit that increased in the second year.
There are well-founded concerns about the capacity
of government to fund the expansion. Some of the
wealthier cities and districts have introduced pro-
poor programmes to cover additional financial risks,
for instance transport costs.
UNIVERSAL COVERAGE FOR SEXUAL AND REPRODUCTIVE
HEALTH
Between 2014 and 2015, health service utilisation
increased by 60 percent, but changes in service
coverage for sexual and reproductive health are
only just starting to be documented. While coverage
for maternity-related services was already high or
increasing prior to the introduction of the universal
health insurance scheme, some services such as
syphilis screening during pregnancy are lagging
behind.
Access to SRH services for adolescents is restricted
despite the launching of a youth-friendly service at
the primary health care level. The restrictions are
primarily related to service provider regulations and
not to regulations of the National Health Insurance
system.
One of the main obstacles to overcome will be the
regional inequity in service coverage. While the
Capital Region of Jakarta recorded a satisfied demand
for family planning of 82 percent and a rate of skilled
assistance at birth of 99 percent, the corresponding
metrics for the Province of Papua are 48 and 40
percent. [44]
20

MONGOLIA
21
MONGOLIA
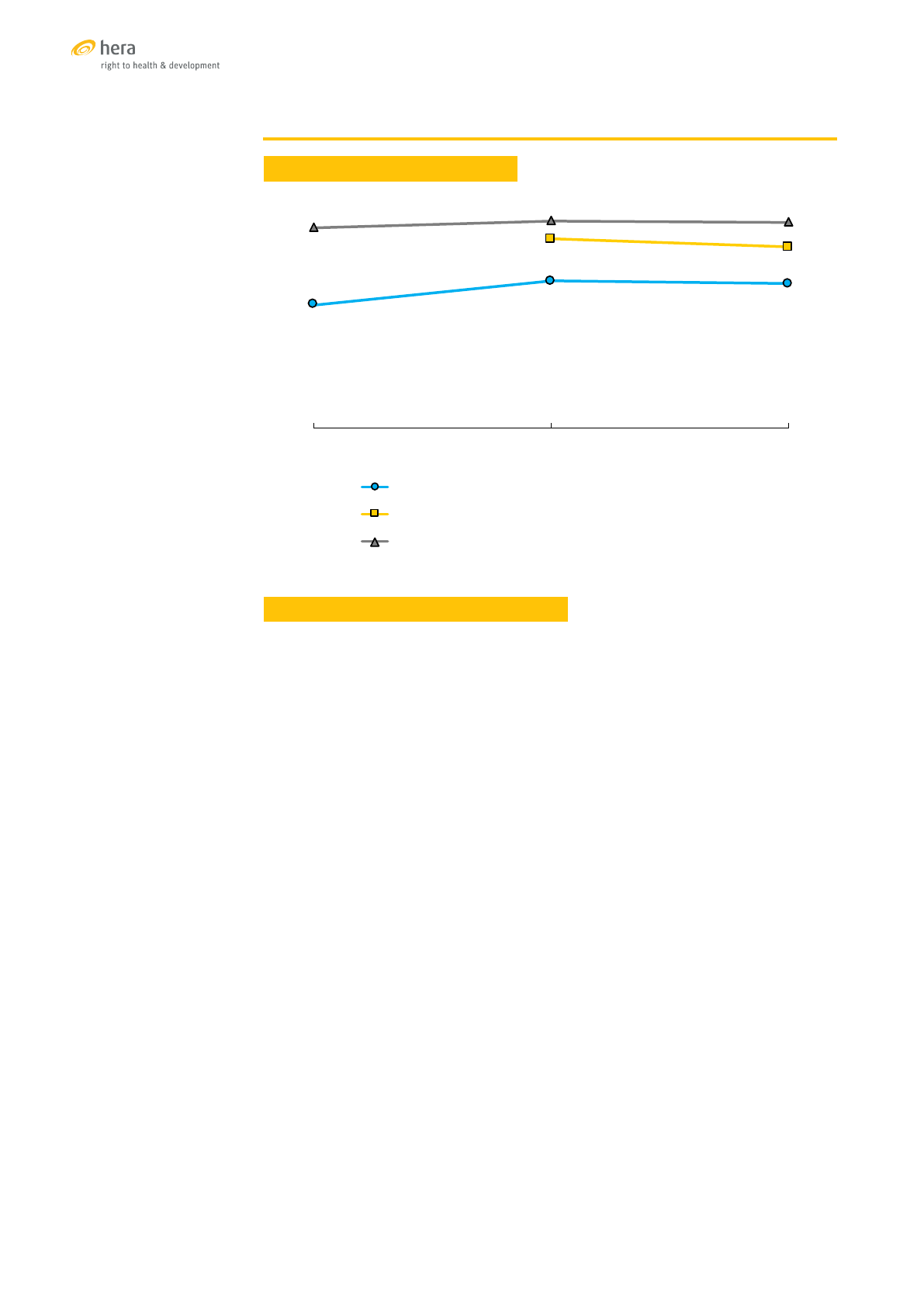
TRENDS OF SELECTED SRH INDICATORS
Sources: [55] ,[56],[57]
SEXUAL AND REPRODUCTIVE HEALTH SERVICES
Health care at the primary level in Mongolia is provided by private and public health
centres, secondary care by public hospitals and private clinics, and tertiary care
by multispecialty central hospitals and specialised centres located in the capital
Ulaanbaatar.
Contraceptive services in the public sector are provided at the primary and secondary
level. In line with a national policy to promote population growth, the service delivery
has deteriorated over the last ten years. Stock-outs of family planning commodities
are common. Even in Ulaanbaatar, all facilities reported stock-outs of family planning
commodities in 2015. The quality of service provision is low, with only 42 percent of
those attending family planning services reporting that they received any counselling.
[58] Contraceptive prevalence with modern methods has been decreasing since 2005,
while the unmet need for contraception also started to decrease in 2010.
In parallel to the decreasing availability and use of contraceptives, the adolescent
birth rate increased from 38 to 40 births per 1000 adolescent girls between 2010
and 2013. In contrast to the general decrease in the unmet need for family planning,
the unmet need among adolescent more than doubled from 14 to 36 percent. The
recently established adolescent health centres that provide counselling and services
for sexual and reproductive health to young people also experienced shortages of
contraceptive supplies. [58]
Termination of pregnancy in the first trimester is legal if performed in a health
facility by a licensed medical specialist. Second trimester terminations require the
permission of a medical committee. Between 2012 and 2013, an estimated 14 percent
of pregnancies ended with an induced abortion. Among never married women the
rate was 30 percent. [57]
61%
50%
48%
81%
90%
99%
99%
99%
2005 2010 2013
%married women(1549)currently usingmodern contraception
%women with atleast4ANCvisitsduring theirlast pregnancy
%of births attendedbyaskilled provider
22

Primary care facilities provide antenatal care and, in rural areas, also attend to
normal deliveries. About 80 percent of deliveries, however, are attended in secondary
level hospitals. Antenatal care coverage (90%) and skilled attendance at delivery
(98%) are high, however the provision of services to migrants and mobile populations
remains a challenge. [57] Mongolia made impressive progress in reducing maternal
mortality from 199 deaths per 100,000 live births in 1990 to 26 deaths in 2015.[59] The
national average, however, masks wide geographic and ethnic disparities. Seventy-
five percent of all maternal deaths occur among herdswomen, the unemployed and
unregistered migrants.
HIV testing is mandatory for antenatal care. More than 90 percent of women are
tested, however only 32 percent reported that they were counselled. [57] By 2014, only
seven HIV positive pregnant women had been diagnosed. Coverage rates for PMTCT
services can therefore not be calculated. All anti-retroviral drugs are provided by the
government and dispensed free of charge.
STI services are provided by public and private clinics. STI screening, including syphilis
testing, is mandatory in antenatal care. The high incidence of sexually transmitted
infections is a major concern. Between 2001 and 2013, the syphilis notification rate
increased threefold from 71 to 222 per 100,000. Approximately one third of all cases
of syphilis are diagnosed among pregnant women. One of the challenges of STI
control is the high rate of self-treatment, often with inappropriate medications or
doses. Despite MOH efforts, antibiotics are still dispensed without prescription. [60]
Cervical cancer ranks as the second leading cancer among women in Mongolia
and is the most common cancer in women aged 15 to 44 years. About 320 new
cervical cancer cases are diagnosed annually. [61] A national screening programme
was launched in 2007 and reached a coverage of 29.7 percent in 2008. [62] HPV
immunisation is being piloted in two provinces and two districts of Ulaanbaatar. [63]
Services for survivors of violence against women and girls are limited in the health
sector. UNFPA has piloted the provision of integrated services for victims of violence
through model one-stop centres in Ulaanbaatar and three provinces. [64]
FINANCIAL RISK PROTECTION
The health sector is financed from government resources, Social Health Insurance
(SHI) premiums and out-of-pocket payments. With coverage almost consistently at 90
percent, the SHI has contributed to a stable financing source for the health sector. As
a proportion of total health expenditures, however, government and SHI expenditures
decreased between 1995 and 2014 from 82 to 55 percent, while the proportion of out-
of-pocket expenditures increased from 17 to 41 percent. [6] The long-term health
financing strategy is to reach universal health coverage with a mix of financing
sources of public funds, health insurance funds, and out-of-pocket payments which
are targeted to contribute about 25 percent to total health expenditure.
Health insurance in Mongolia is mandatory. The government fully subsidises the
insurance premiums for about 60 percent of members. About 90 percent of SHI
revenues are through payroll deductions and employer contributions for salaried
employees. The premiums for children under 16, pensioners, mothers of children up
to two years of age, and the poor are paid by government. All others pay a minimum
monthly premium. Government subsidisation of the SHI premiums for students was
removed in 2016. While the system is effective in collecting premium payments in
the formal sector, it is not effective in raising contributions from people who are not
formally employed. [65]
23

The government budget covers prevention activities, primary level health care
services including for maternal and child health, treatment of cancer and diabetes
and treatment of tuberculosis and HIV. The Social Health Insurance benefit package
covers predominantly outpatient and inpatient care in secondary and tertiary public
hospitals, traditional medicine clinics, sanatoriums and rehabilitation centres. Co-
payment requirements at the secondary and tertiary level of care are 10 and 15
percent respectively. Accredited private hospitals can invoice services to SHI and
are allowed to charge user fees at established rates. Outpatient medicines including
contraceptives, diagnostic services above a monthly limit established by SHI, and a
number of specified services, including therapeutic termination of pregnancy, are
not covered by government or SHI and have to be paid for by patients.
This high share of out-of-pocket expenditures in health financing negatively affects
equity, access and use of health services. The poor have difficulties accessing
specific health services, including diagnostic tests and ultrasonography for
pregnant women, even if they are insured by SHI. [66] Among the poorest quintile
of the population, about 95 percent of household health expenditures are for the
purchase of outpatient medicines. [67]
In 2009, an estimated 3.8 percent of households experienced catastrophic health
care costs at more than 40 percent of their household subsistence income. [68] A
more recent study found that this proportion had dropped to 1.1 percent in 2012, but
an estimated 20,000 people were still forced into poverty by the cost of health care.
[69]
UNIVERSAL COVERAGE FOR SEXUAL AND REPRODUCTIVE HEALTH
Mongolia has made impressive advances in reducing maternal mortality, increasing
antenatal care and facility-based deliveries. However declining access and use
of family planning, stock-outs of family planning commodities in public facilities,
rising adolescent birth rates, high abortion rates, a high incidence of sexually
transmitted infections and limited services for survivors of gender-based violence
remain important challenges.
The government subsidises the health insurance contribution for poor and vulnerable
groups, including mothers of children up to two years old and adolescents up to 16
years. There are, however, groups such as the former nomadic households, that are
still uninsured.
Maternity care is provided free of charge at primary health facilities. More
specialised services are covered by the Social Health Insurance at secondary
and tertiary level facilities. Family planning services for most of the population,
ultrasound and other advanced tests during pregnancy, termination of pregnancy,
and out-patient prescription drugs are excluded from the SHI benefits, with the
result that the individuals and families have to pay directly for many SRH services.
The access to SRH services by young people has increased with the creation of the
adolescent health centres, but the initiative has yet to translate into documented
SRH outcomes. Furthermore, the cancellation of government subsidies for the SHI
premiums of students in 2016 may lead to an increase in the loss of health insurance
coverage by young people over the age of 16 years.
24

THAILAND
25
THAILAND
TRENDS OF SELECTED SRH INDICATORS
Sources: [70],[71],[72]
SEXUAL AND REPRODUCTIVE HEALTH SERVICES
Health care in Thailand is provided by the public and private sectors. The public
sector expanded rapidly in the 1960s under the National Economic and Social
Development Plans, which emphasised the coverage of the entire country with
a system of provincial hospitals, district hospital, and sub-district health centres.
Private hospitals are primarily located in urban centres.
Thailand charted early advances in family planning. The contraceptive prevalence
rate increased from 15 percent in 1969 to 74 percent in 1995 and reached a level of
78 percent in 2015. The total fertility rate fell from 6.8 children per woman in 1970 to
1.5 in 2015. Contraceptives are readily available, but a study in 2011 found that only a
small number of public health facilities provided long-term reversible contraceptives
such as IUDs and implants. [73]
Adolescent fertility is an area of concern in Thailand. Between 2000 and 2015, the
adolescent birth rate increased from 30 to 51 births per 1,000 girls aged 15 to 19. It
is considerably higher than the Asia-Pacific region’s average of 35 per 1,000. One of
the reasons are the marriage laws in Thailand that allow marriage at age 17. In 2015,
14 percent of adolescent girls aged 15-19 were married or in union, and four percent
of them before the age of 15. [72] In July 2016, the ‘Act for Prevention and Solution of
the Adolescent Pregnancy Problem’ came into force after approval by the National
Legislative Assembly in February. It stipulates, among others, that adolescents aged
between 10 and 20 years must be given access to reproductive health information
and services. Furthermore, schools must offer age-appropriate sexuality education
and provide counselling, support and protection for pregnant students to enable
them to complete their education.
Termination of pregnancy is legal in Thailand if performed by a physician for the
health of the woman, including her mental health, as well as in case of a pregnancy
resulting from rape. The combination of Misoprostol and Mifepristone for medical
termination of pregnancy was registered in 2015. Prescription is strictly controlled
by Department of Health. [74] Each year, however, an estimated 300,000 to 400,000
illegal abortions are performed in Thailand. The continued high prevalence of unsafe
abortions is thought to be due to a misconception in Thai society, including among
health workers, that abortion is illegal in all circumstances, and due to personal and
religious beliefs concerning termination of pregnancy. [75]
72%
79%
78%
93%
91%
97%
100%
99%
2005/06 2012 2015/16
%married women(1549)currently usingmodern contraception
%women with atleast4ANCvisitsduring theirlast pregnancy
%of births attended byaskilled provider
26

Thailand reached the MDG targets for maternal health well before the 2015
target date. In 2016, WHO certified that Thailand had eliminated mother-to-child
transmission of HIV and syphilis. [76] Between January and October 2016, Thailand
confirmed 392 cases of Zika virus infection, including 39 among pregnant women.
Systematic testing of pregnant women for Zika virus infection is under consideration.
[77]
Regulations requiring parental consent for HIV testing of adolescents under the age
of 18 were revised in 2014 improving the access of young people to HIV prevention.
Screening for HIV in antenatal care is universal. New infections with HIV have
declined since 2000, and the HIV epidemic has become increasingly concentrated
among key populations. Nevertheless, the prevalence of HIV among young people
(15-24) has not decreased as anticipated. In 2014, it was estimated at 0.52 percent,
compared to 0.58 percent in 2009. AIDS-related deaths declined sharply after the
introduction of antiretroviral therapy (ART) in 2000, and have since stabilised. In 2013,
about 80 percent of people living with HIV who were eligible for treatment received
ART. In 2014, the eligibility criteria changed, and ART was offered to all people with
HIV infection. The coverage rate, according to the new criteria, was 61 percent. [78]
Cervical cancer is the second most prevalent cancer among females in Thailand.
[79] Screening was introduced in 1999 in a pilot project using a ‘single visit approach’
consisting of visual inspection with acetic acid and immediate treatment with
cryotherapy if indicated. In 2003, the programme was scaled up country-wide. A study
of coverage of the screening programme in 49 districts in 2008 reported an average
coverage of 26 percent of eligible women, with some districts achieving a coverage
of 45 percent. [80] Early detection of cervical cancer is increasing in Thailand with
increasing diagnoses of in situ stage 1 and stage 2 cancers, and decreasing incidence
of advanced disease.
The introduction of Human Papillomavirus (HPV) vaccine has been under discussion
since 2008. Studies were conducted on the cost-effectiveness of the vaccine as well
as on more efficient ways to deliver it. Current pilot immunisation programmes are
planned to be gradually scaled up to nationwide coverage by 2020. [81]
Thailand adopted a law for the protection of victims of domestic violence in 2007
and established crisis centres in public hospitals at tertiary and community level. In
2013, the then Prime Minister officially launched a national network of 22,000 crisis
centres and 1,300 mobile units managed by the Ministry of Social Development and
Human Security. [82]
FINANCIAL RISK PROTECTION
In a major health sector reform in 2001, Thailand created the National Health
Security Office [13] which became the central public purchaser of health services,
allocating funds to public sector health facilities on the basis of catchment population
and service provision. At the same time the Universal Coverage Scheme (UCS) was
launched, a social health insurance aiming for national coverage. About 70 percent
of Thais were already covered by one of four existing insurance or welfare schemes:
the Social Security Scheme (SSS) for formal sector employees; the Civil Servants’
Medical Benefit Scheme (CSMBS) for active and pensioned civil servants; the Medical
Welfare Scheme which covered the poor, elderly, disabled and children under twelve
years; and the Voluntary Health Card Scheme, a contributory health insurance with
public subsidy for people in the informal sector. However, 18 million people, primarily
informal sector workers in lower income groups, had no coverage. Out-of-pocket
expenditures for health accounted for 33 percent of total health expenditure. UCS
replaced the Medical Welfare and Voluntary Health Card schemes, and at the same
time extended the coverage to all previously uninsured persons. It is fully tax-funded,
offering a comprehensive benefits package with a focus on the primary care level.
27

By 2014, all Thai citizens were covered by a social or
contributory health insurance scheme. Less than one
percent of the population were not covered because they
were foreigners or their citizen status was uncertain.
[83] Out-of-pocket expenditure as a proportion of
total health expenditure fell to eight percent in 2014.
A review of the first ten years of UCS estimated that
between 2004 and 2009 a total of 291,790 households
were protected from impoverishment by the scheme.
[84]
The Social Security Scheme (SSS) is a compulsory
health insurance for employees in the formal private
sector with contributions shared equally between
employees, employers, and the government. In 2014,
it covered approximately 11 million people. [83] The
scheme provides a comprehensive health services
package, including ambulatory care, medicines, dental
care, hospital care, and maternity care. Contracted
public and private hospitals are paid by capitation with
additional payments according to utilisation rates.
For services outside the contract hospitals, such as
emergency care or dental care, beneficiaries are
reimbursed according to established tariffs.
The Civil Servant Medical Benefit Scheme (CSMBS)
is a fully tax funded fringe benefits for government
employees, pensioners, and their dependents. In 2014,
it covered approximately five million people. [83] The
scheme provides a comprehensive health services
package, including ambulatory care, medicines, dental
care, and hospital care. Beneficiaries have free choice
of public facilities. They can access private hospitals
for inpatient care only in case of emergency and will
be reimbursed up to a ceiling. Providers are paid on a
fee for service basis.
The Universal Coverage Scheme (UCS) covers most
of the remaining population, or about 48 million
people. It provides a comprehensive health services
package, including ambulatory care, medicines,
dental care, and hospital care in registered facilities.
HIV treatment services were added in 2009, and a
programme for chronic disease care in 2010. The
budget to finance the UCS has grown steadily from 46
billion Baht (1.1 billion US$) in 2002 to 154 billion Baht
(4.7 billion US$) in 2014. Because of the overall growth
of the government budget, proportional expenditures
on UCS have been relatively stable in the region of
six percent of the national budget. The total annual
expenditure per registered beneficiary in 2014 was
2,895 Baht (approximately 89 US$). [83]
Thailand is home to about 3.7 million migrant workers
from neighbouring countries. [5] Migrants who work
in formal sector employment and who are registered
with the Social Security Office by their employer are
insured under SSS. A much larger group of migrants
are registered in the Migrant Health Insurance
(MHI) scheme at a cost of 600 Baht (approximately
17 US$) for an annual medical exam and 2,200 Baht
(approximately 61 US$) for the annual insurance
premium. Undocumented migrants, i.e. those without
a work permit, are encouraged to join the MHI
voluntarily. The scheme is managed by the MOPH. In
2014, there were 1.4 million migrants registered with
the MHI. The benefits under MHI are comprehensive,
and since 2013 also include anti-retroviral treatment
for HIV infection. However, they are not portable,
and tied to the hospital at which the annual medical
examination was performed. [85] Undocumented
migrants face barriers to enrol, such as the restricted
portability of the coverage, the cost of the annual
medical examination and policy renewal, and their
general reluctance to identify themselves as migrants
to the authorities. [86]
UNIVERSAL COVERAGE FOR SEXUAL AND REPRODUCTIVE
HEALTH
Thailand achieved a high level of service coverage for
health and for sexual and reproductive health with
policies and programmes that started in the 1970s. The
launching of the UCS social health insurance scheme in
2001 accelerated the progress and significantly closed
the equity gap between social groups and regions.
Impressive results were recorded in population
and health indicators, including in family planning,
maternal health, and the response to HIV. Three main
health insurance schemes and an additional scheme
for migrant workers provide financial risk protection for
the entire population. Practically all SRH services are
covered under the schemes, including HIV treatment
and HPV immunisation which is planned to be scaled
up to nationwide coverage. Universal coverage for
sexual and reproductive health in Thailand is a reality
today, financed primarily with general government
revenues.
There are some areas that still require attention.
Early marriage is common in Thailand and adolescent
birth rates are higher than the regional average. The
incidence of unsafe abortion is high despite relatively
unrestrictive laws about termination of pregnancy
and a social insurance system that covers the costs of
therapeutic abortions. These are issues that cannot be
addressed by the health sector alone.
Although health services and insurance coverage
for migrant workers in Thailand have improved
greatly, there are still cultural, societal and financial
barriers that prevent undocumented migrants from
accessing SRH services. Migrant work is an important
contributor to Thailand’s economic growth, but the
protection of the sexual and reproductive health and
rights of the large number of undocumented migrants
is lagging behind the rights that are enjoyed by Thai
citizens and documented migrants. Further progress
to ensure universal coverage for undocumented
migrants will require collaboration with government
sectors addressing migration and labour policies.
28

VIET NAM
29
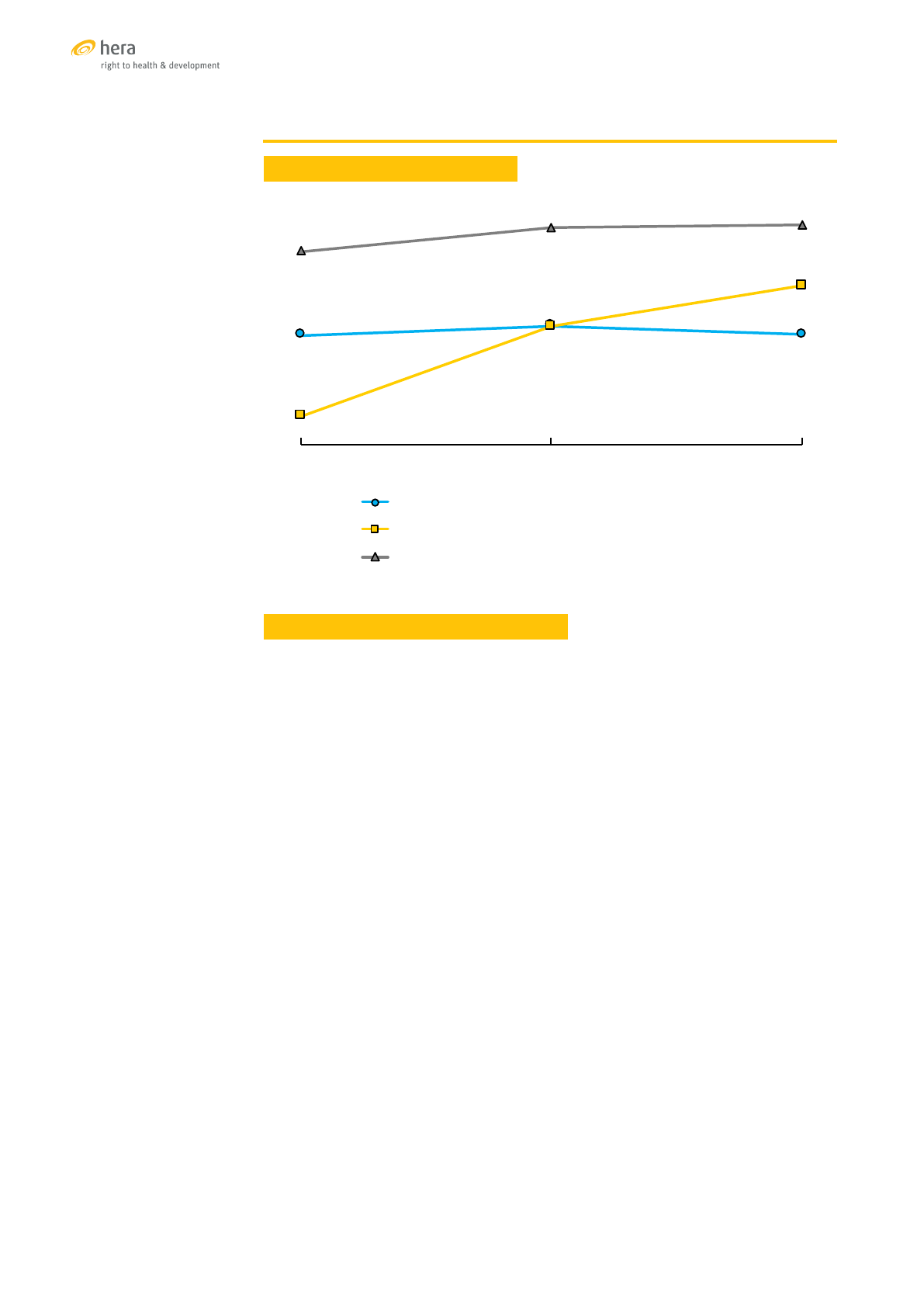
VIET NAM
TRENDS OF SELECTED SRH INDICATORS
Sources: [87],[88],[89]
SEXUAL AND REPRODUCTIVE HEALTH SERVICES
Ambulatory health services in Viet Nam are to 60 percent provided by the private
sector, while inpatient care is to 96 percent in the public sector. [90] The public sector
has a tiered structure from commune health centres at the primary level to national
specialised hospitals at the tertiary level. While the quality and coverage of services
for sexual and reproductive health have been increasing, the tertiary-level hospitals
are overcrowded, and the service quality is under pressure. Provincial hospitals
received significant government investments to improve the infrastructure, but they
are experiencing bottlenecks of qualified human resources. Census and population
survey data collected between 2000 and 2011 document a positive trend in the
utilisation of sexual and reproductive health services, although there are persistent
inequalities. [91]
Services for contraception, including family planning and emergency contraception
are provided at all levels of the Viet Nam health care system. Adolescents and adults
have access to these services. Services provided at the commune health centre level
are limited, but more services are generally available in the district and provincial
hospitals. Family planning services are not covered by the Social Health Insurance.
Ethnic minority and poor families living in remote mountainous provinces, however,
receive free family planning services funded by the National Population Programme.
The contraceptive prevalence (any modern method) increased during the 1980s and
90s, but has been stable around 60 percent since the turn of the century. [92] It is
higher among poorer women and among women in ethnic minority groups. The 2014
MICS reported a low unmet need for modern contraception of six percent among
women who are married or in union, although the unmet need among married
adolescent girls was considerably higher at 11 percent. [89] A national survey of
adolescent sexual and reproductive health in 2016 reported a much higher unmet
need of 24 percent among ever-married and 48 percent among never-married
adolescents and women aged 15 to 24. [93]
57%
60%
57%
29%
60%
73%
85%
93%
94%
2002 2011 2014
%married women(1549)currently usingmodern contraception
%women with atleast4ANCvisitsduring theirlast pregnancy
%of births attendedbyaskilled provider
30

The adolescent birth rates in Viet Nam in 2014 were 45 births per 1,000 girls aged
15 to 19 which is lower than in many neighbouring countries. The rate has, however,
increased steadily from a low of below 30 prior to 2005. It is more than twice as high
among girls in ethnic minority groups. [89]
There are no regulations prohibiting the termination of pregnancy before 12 weeks.
After the 12th week, termination must be done in a hospital with surgical facilities
and requires a prescription by a physician. Abortion rates in Viet Nam are high,
but according to unpublished data of the national health management information
system, they have recently fallen from 25 abortions per 100 deliveries in 2011 to 18
in 2014. This database may, however, miss a proportion of pregnancy terminations
that are performed in the private sector. According to a survey among adolescents
and young adults, six percent of pregnancies among adolescent girls aged 15-18, and
nine percent among women aged 19 to 24 resulted in a termination. Among the 14
unmarried young women in the sample who had ever been pregnant, five terminated
the pregnancy. More than half of the termination were performed in a private clinic
or hospital. [93]
Maternal health services including antenatal, obstetric, and postnatal care, as well
as treatment of obstetric fistulas and other health problems that may arise on the
basis of pregnancy and delivery are provided at the appropriate level health care
facilities. Micronutrient supplementation is provided as part of regular antenatal
services but it is not covered by health insurance unless a deficiency is diagnosed. In
2014, the coverage of skilled attendance at birth was estimated at 99 percent among
women from the main ethnic groups, but only at 68 percent among women from
ethnic minority populations. The difference in antenatal care was even greater, with
82 percent of women of Kinh and Hoa ethnicity reporting four or more antenatal
visits, while the proportion was only 33 percent among ethnic minority women.
Pregnant women who are at risk for HIV infection receive HIV testing and PMTCT
services under the National HIV Prevention Programme (funded by government or
international partners). Malaria is generally not a major public health problem in
Viet Nam, but multi-drug resistant malaria was detected in the border region to
Cambodia. Malaria prevention during pregnancy is not a routine service. Zika is an
emerging infectious disease in Viet Nam. By November 2016, a total of 70 cases had
been diagnosed. The National Institute of Hygiene and Epidemiology covers the cost
for Zika testing, if required.
Specialised centres for STI diagnosis and treatment have been established in all
provinces, providing treatment free of charge under the Social Health Insurance
scheme. User charges apply to diagnosis and treatment of STIs in other public-
sector facilities. Most patients, however, prefer to consult private practitioners. Since
they do not report to the national health information system, data on the incidence
and prevalence of STIs are limited.
The Ministry of Health has recommended to include immunisation against Human
Papillomavirus in the list of regular public health services, but this has not yet been
approved. Vaccines are available in most provincial immunisation centres. Cytology-
based cervical cancer screening (PAP tests) is only available in district and provincial
hospitals, and a small number of national and provincial hospitals offer screening
by use of HPV DNA tests. [94] Cervical cancer treatment is provided in tertiary level
facilities.
The health services have limited medical treatments options for women and girls
who are survivors of gender-based violence, child abuse, and rape. They include
emergency contraception and termination of pregnancy. There is no provision for
psychological or social support. The Women’s Union and the Ministry of Labour,
Invalid and Social Affairs operates some pilot projects for survivors, funded by
international organisations. However, these services are generally very limited.
31

FINANCIAL RISK PROTECTION
Universal health coverage was officially introduced
in Viet Nam with the 2008 Health Insurance Law and
updated in 2014 when membership in the national Social
Health Insurance (SHI) scheme was made compulsory.
SHI premiums for people in formal employment are paid
through payroll deductions and employer contributions,
for pensioners by the Social Security System, and
for the poor, children under six and persons over 80
years of age by government. Others have to buy SHI
membership which is subsidised in a range from 30 to
70 percent depending on income. In 2016, 82 percent of
the population was covered by SHI. [95]
Health services for carriers of SHI cards are to 80
percent paid by SHI, with an out-of-pocket co-payment
of 20 percent at the commune and district hospital
level. Many patients, however, directly access provincial
hospitals for primary care, with co-payment rates of
up to 70 percent. Registered private health facilities
can sign a contract with the SHI to offer services to SHI
members, but individual private practitioners are not
yet allowed to participate in the SHI scheme. Provider
payment mechanisms vary according to the type of
facility, including capitation and fee for service payment.
Payment according to diagnostic-related groups is
being piloted in some provinces. [95] The list of the SHI
services and tariffs are developed and published by the
Ministry of Health.
According to WHO estimates, out-of-pocket expenditures
for health as a proportion of total health expenditures
decreased steeply from 68 percent in 2005 to 37 percent
in 2012, but have since stagnated around this level. [6]
According to one study, out-of-pocket payments in state
hospitals varied between 45 and 78 percent in 2014. [96]
National experts interviewed for this report stated that
a further decrease of out-of-pocket expenditures was
unlikely, and an increase may even be seen in the near
future, because SHI tariffs are not keeping pace with
increasing costs of services.
In addition to SHI, a number of demand-side financing
and provider performance incentive schemes are being
piloted in Viet Nam. These are, however, implemented on
a small scale, often in the private sector, and do not have
a major impact on the overall delivery of SRH services.
UNIVERSAL COVERAGE FOR SEXUAL AND REPRODUCTIVE
HEALTH
The Social Health Insurance benefits in Viet Nam
focus on curative clinical services and therefore do not
cover many services for SRH. Almost all reproductive
health services related to pregnancy and delivery are
covered by SHI with a 20 percent out-of-pocket co-
payment, which is higher when primary levels of care
are bypassed. Pregnancy-related or co-existing health
conditions are covered according to the existing tariff
structure of the SHI.
Family planning services, termination of pregnancy,
cervical cancer screening, HPV immunisation, malaria
prevention, HIV treatment, Zika virus screening and
micro-nutrition supplementation during pregnancy
are not included among the SHI benefits. Some of
these services are covered by special programmes
or initiatives. These include the family planning
programme for ethnic minority women and poor
women living in remote provinces, as well as the
HIV and malaria control programmes. Most of the
specialised national programmes receive financial
support from international partners. In recent years,
this support has started to decrease. There are
concerns that the programmes will start collecting
user fees unless the services can be included among
the SHI benefits.
Increasing adolescent birth rates and high rates
of pregnancy termination should be a signal for
an increased effort to provide access to effective
contraception, especially to young people. The
decision to exclude family planning services from
the list of Social Health Insurance benefits therefore
appears counterintuitive.
The diagnosis and treatment of sexually transmitted
infections is covered by Social Health Insurance, but
only if delivered by a specialised STI centre. Most
individuals with STI symptoms, however, consult a
private medical practitioner or a primary level public
health facility and therefore have to pay for the service.
The success of targeted family planning programmes
for ethnic minority populations documents that SRH
service inequities for minority populations can be
overcome, however they continue to exist in other
areas of sexual and reproductive health, and especially
for maternity care.
Considerable progress towards universal health
coverage has been achieved in Viet Nam, but the
coverage of sexual and reproductive health services
is lagging behind. The Social Health Insurance is
implemented in a very tight fiscal space, and choices
have to be made about the coverage it can afford to
provide. However, a more comprehensive coverage of
SRH and preventive services would, in the longer run,
avoid future costs of expensive clinical services and
thereby contribute to consolidating and sustaining
universal coverage.
32

UNIVERSAL HEALTH COVERAGE FOR SEXUAL AND
REPRODUCTIVE HEALTH
As the six country profiles document, there has been significant progress towards achieving the goal of universal
health coverage for sexual and reproductive health services in the Asia-Pacific Region. Not surprisingly,
progress is not achieved at the same speed and in the same components of the UHC goal in all countries. There
are major cultural, social, economic and political differences, including among low- and lower-middle income
countries. In order to analyse the differences and generate common lessons, the goal was disaggregated into
its three components: Effective service coverage, equitable access to services, and financial risk protection for
users of the services.
CONCEPTUAL FRAMEWORK FOR UHC IN SEXUAL AND REPRODUCTIVE HEALTH
Adapted from [97]
The conceptual framework describes the necessary elements for achieving universal coverage for sexual and
reproductive health. It has major limitations because sexual and reproductive health is not only dependent
on health services. It is to an even greater degree dependent on the social context, the general level of social
protection, social cohesion, gender equality, and the respect of human rights, including children’s rights. The
extent to which people are able to realise their right to sexual and reproductive health depends on policies
and their implementation in many sectors, including education, justice, family, women, welfare, labour and
immigration. This cannot be fully captured in a framework that focuses on health services. Nevertheless,
universal coverage of sexual and reproductive health services is a goal that contributes significantly to sexual
and reproductive health and the realisation of sexual and reproductive rights.
Health Financing
System
Revenue
Collection
Pooling
Purchasing
Benefits
Financing Arrangements
Intermediate
Objectives
Payment
Public and private service
providers deliver
comprehensive quality
SRH services
SRH service provision is
inclusive and respectful
of the right to health for
all
SRH service delivery is
publicly financed or
included in equitable risk
pooling mechanisms
Goals
Equitable access to
SRH services
Effective coverage of
SRH service provision
Financial risk
protection for SRH
service users
33
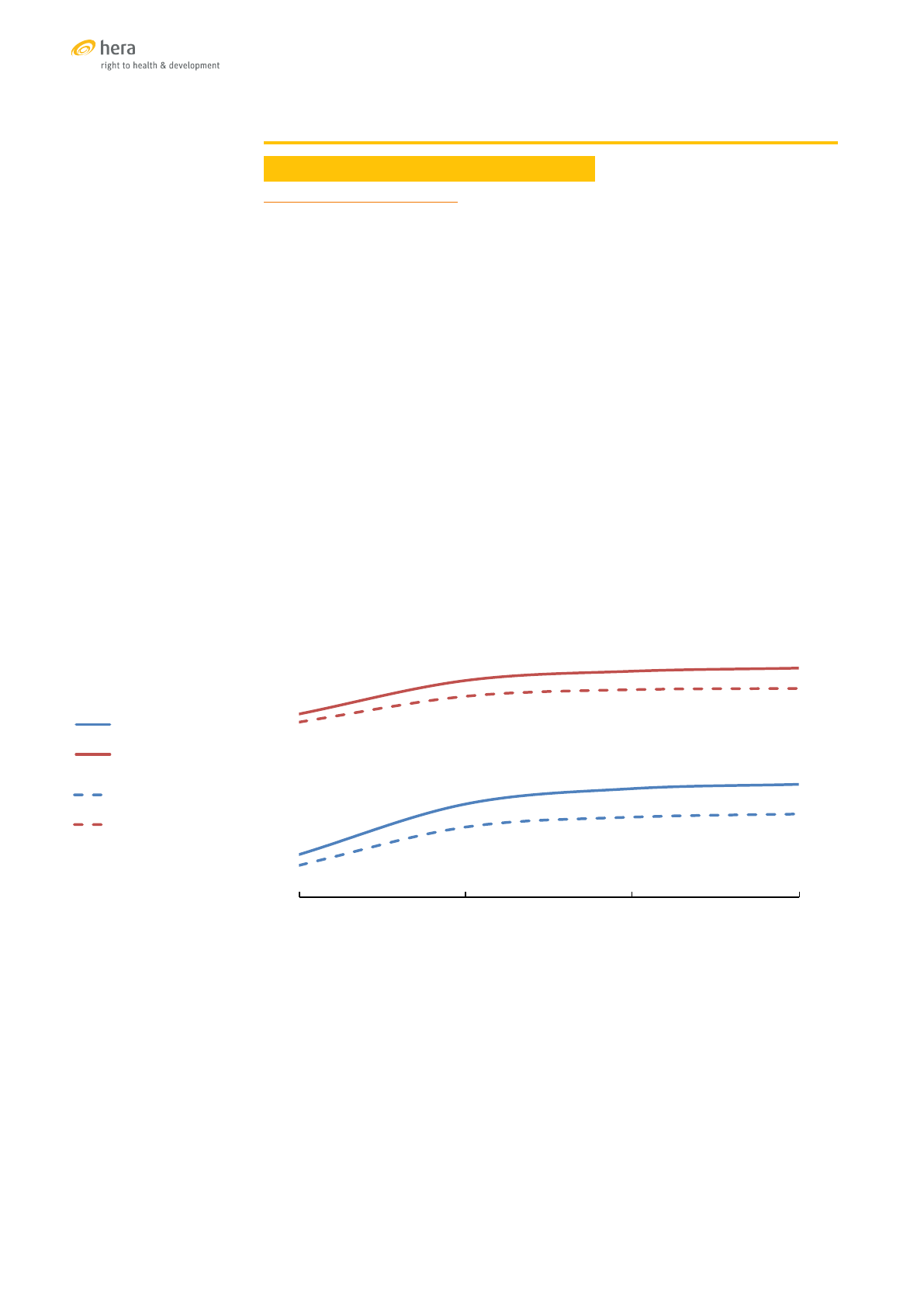
EFFECTIVE COVERAGE OF SRH SERVICES
CONTRACEPTION AND TERMINATION OF PREGNANCY
Fertility and contraception
Between 2010 and 2015, after four decades of steady decline, the global total fertility
rate (TFR) was estimated at 2.5 children per woman. The decline has even been
faster in the Asia-Pacific Region. Starting from a TFR of above 5.5 in 1970-1975,
the region achieved a rate of about 2.2 by 2010-2015. Several populous countries
in the region are now experiencing fertility rates that are lower than the population
replacement level of 2.1, notably Thailand (1.5), China (1.6), Iran (1.7), Malaysia (2.0)
and Viet Nam (2.0). The region does, however, also include countries with fertility
rates that are well above the global average, such as Afghanistan (5.1), Pakistan (3.7)
and several of the Pacific Island States. [98] In Mongolia, the total fertility rate has
been increasing steadily from 2.5 in 2003 to 3.1 in 2014, consistent with government
policy to encourage population growth. [58]
The region’s success in addressing the challenges of rapid population growth can
primarily be attributed to the expansion and promotion of family planning services.
While these were primarily motivated by population control objectives, they also
contributed to an increased realisation of sexual and reproductive health and rights.
The contraceptive prevalence rates (CPR) and the proportion of satisfied demand for
family planning (DS) among women in Asia-Pacific aged 15-49 who are married or
in union have been consistently higher than the global average since the 1990s. [99]
Contracepve prevalence rate and sased demand for family planning in the
Asia-Pacic Region and globally 1990 - 2015
Source: [99]
Some countries are left behind in meeting the demand for contraception. They include
Afghanistan (52% of demand satisfied), Timor Leste (53%), the Pacific Island States
(between 43% in Samoa and 64% in the Solomon Islands), and Pakistan (65%). The fact
that 84 percent of women in Bangladesh can satisfy their demand for contraception
is remarkable, considering that it is among the economically most disadvantaged
countries in the region. It should, however, also be kept in mind that despite the high
level of coverage achieved in Bangladesh and in the other populous countries such
as China (96%), Indonesia (85%) and India (82%), the number of women who are not
able to meet their demand for family planning in these countries is very high because
of the large population size. [99]
68.5%
63.6%
87.4%
84.2%
1990 2000 2010 2015
CPR Asia Pacific CPR World
DS Asia Pacific DS World
68.5%
63.6%
87.4%
84.2%
1990 2000 2010 2015
CPR Asia Pacific
CPR World
DS Asia Pacific
DS World
68.5%
63.6%
87.4%
84.2%
1990 2000 2010 2015
CPR Asia Pacific
CPR World
DS Asia Pacific
DS World
34
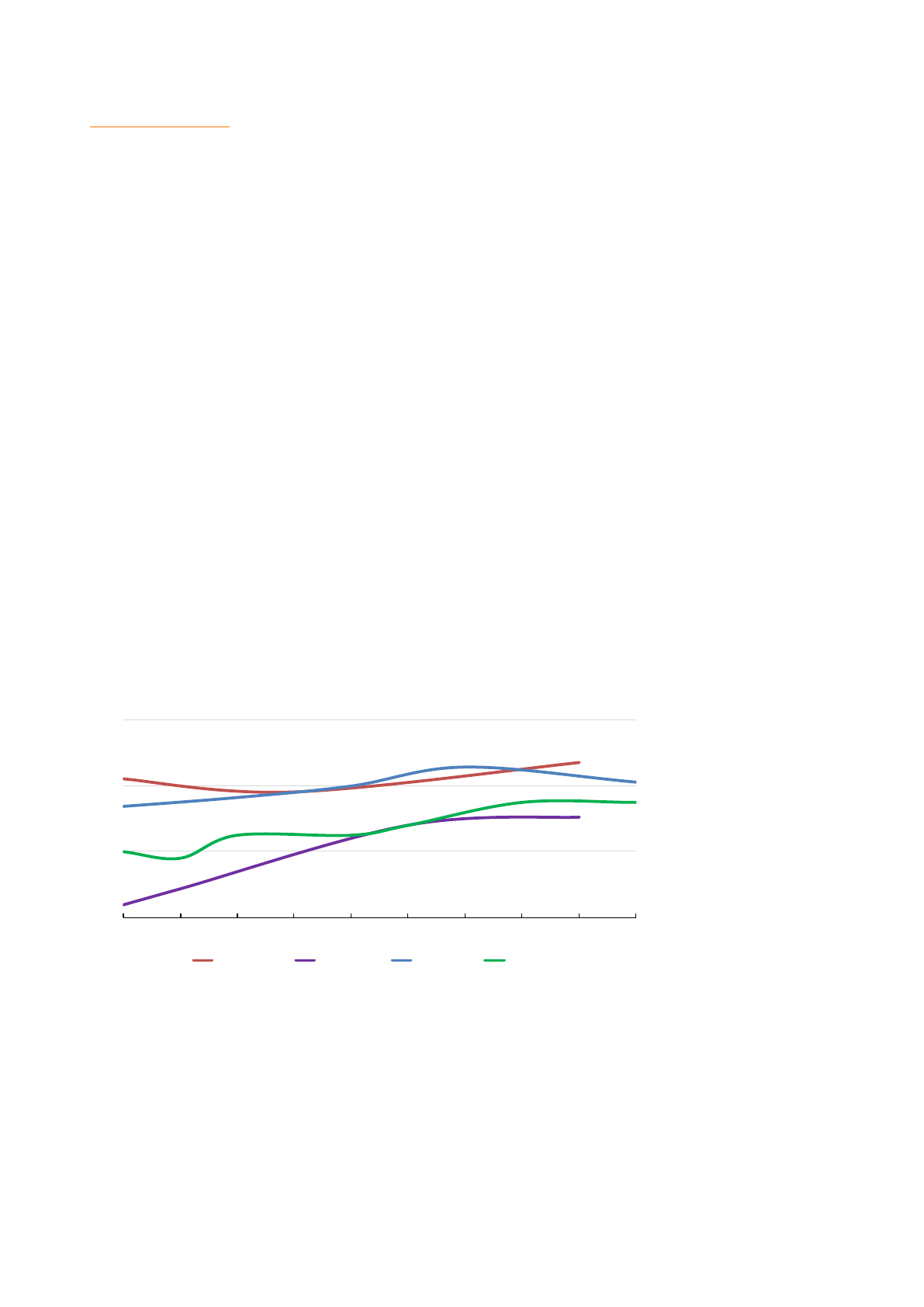
Adolescent fertility
The age of physical, sexual and mental maturity varies greatly among individuals.
Pregnancy at young age, however, often deprives girls of opportunities to fully develop
their potential in social, economic and emotional terms, and generates higher than
average risks of experiencing untoward outcomes, including stillbirths and maternal
deaths. Pregnancies among adolescent girls are also more likely to be unintended,
often resulting in unsafe abortions and adding an additional risk to the reproductive
health of young women. When discussing adolescent fertility, a distinction must be
made between girls who are married and in union, and those who are unmarried
and sexually active. The two groups have different reproductive health needs, require
different types of services, and different prevention strategies. These strategies are,
to a very large extent, outside the remit of the health sector. Early pregnancy and
child bearing are issues that concern women’s and children’s rights, child protection,
gender equality, sexuality education, and civil registration of births and marriages.
Health services, where the risks of early pregnancy become evident through the
complications at birth or after abortion, can contribute to prevention by providing
adolescents access to contraception, safe termination of unintended pregnancies
and post-abortion care, and they can reduce the risks of childbirth by providing
maternity services that are adapted to the needs of adolescents.
According to the most recent survey data between 2005 and 2014, an estimated 24
percent of adolescent girls in Asia-Pacific were sexually active, slightly less than the
global average of 26 percent. The great majority among them (99%) were married
or in union. The regional adolescent birth rate between 1991 and 2015 of 35 births
per 1,000 girls aged 15 to 19 was considerably lower than the global estimate of 52.
However, because of the large population, the region accounted for one third of all
births to adolescents in 2015, an estimated 5.2 million out of a total of 15.2 million.
[99] While globally, and especially in Asia-Pacific, adolescent birth rates have been
falling for two decades, survey data from the last ten years in four of the six sampled
countries show increasing trends.
Adolescent birth rates (per 1,000) in selected countries
10
30
50
70
2005 2007 2009 2011 2013
Cambodia Mongolia Thailand Viet Nam
Source: [100]
According to UNFPA estimates, only about one percent of sexually active adolescent
girls in Asia-Pacific are unmarried, but only one in five of these girls are protected
from unintended pregnancy, most of them by the use of male condoms. Only six
percent of them use a female-controlled method of contraception. [99] This points
to a major gap in coverage of contraceptive services for this group of adolescents
which is at high risk for resorting to unsafe terminations of their pregnancy. A review
of induced abortions in Thailand published in 2004 reported that among the women
who had resorted to an illegal abortion, the proportion of adolescents was 30 percent.
One third of these abortions had resulted in serious complications. [101]
35
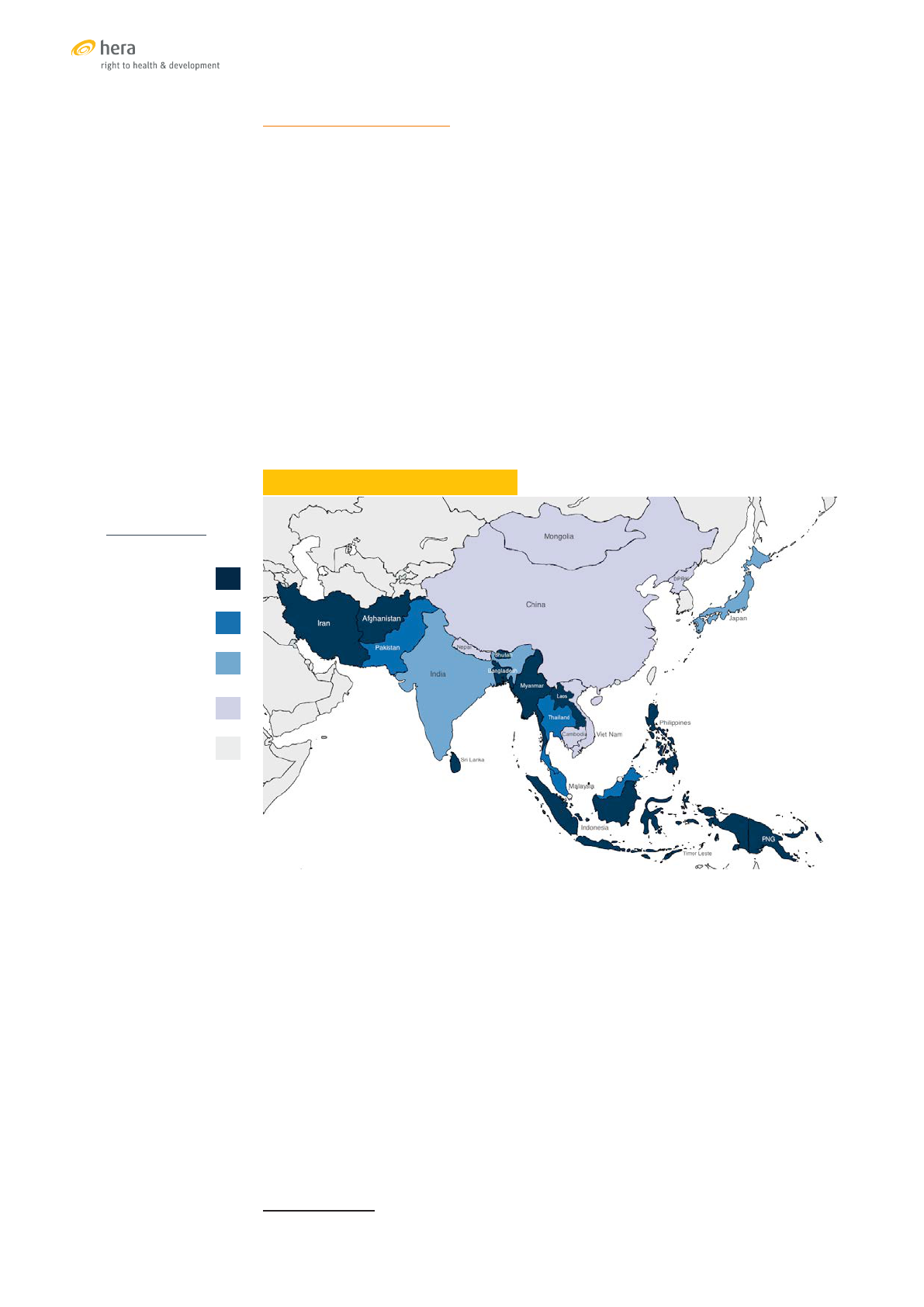
Termination of pregnancy
In many countries of the Asia-Pacific regions, the laws on the termination of
pregnancy are restrictive as illustrated in the map.
• The laws in the countries coloured in dark blue prohibit abortion, with
the exception to save a woman’s life although this may not be explicitly
mentioned in the legal text. These countries also include the Maldives and
the Pacific Island States which are not marked on the map.
• In Pakistan, Thailand and Malaysia abortion is permitted to preserve a
woman’s health, whereby this also includes mental health in Thailand and
Malaysia
• Additional legal permissions for social and economic reasons are granted in
Japan and India
• Only six countries, Mongolia, China, DPR Korea, Nepal, Viet Nam and
Cambodia permit unrestricted access to abortion within gestational limits
that vary among countries.
ABORTION LAWS IN ASIA-PACIFIC 2014
Source: [102]
In Bangladesh, termination of pregnancy is illegal except to save a woman’s life,
however menstrual regulation (MR) has been part of Bangladesh’s national family
planning programme since 1979. MR does not require a confirmation of pregnancy and
involves the manual vacuum aspiration of uterine content or the oral administration
of a combination of mifepristone and misoprostol to provoke menstrual bleeding
(MRM). Government regulations allow MR up to 10–12 weeks and MRM up to nine
weeks after a woman’s last menstrual period. [103]
While access to medical termination of pregnancy can contribute to women’s
realisation of their sexual and reproductive health and rights, sex-selective abortions
are performed because of social preferences for male offspring and are a practice
that violates women’s rights. Although they are illegal in many countries, including
in China and India, they are practiced widely as documented by the higher than
biologically plausible ratio of male to female births
2
, especially in China (116/100),
Viet Nam (112/100), India (110.9/100) and Pakistan (108.7/100). [98]
2 The biological sex ratio at birth is around 104 to 106 boys per 100 girls
To save the woman’s
life or prohibited
altogether
To preserve health
Socioeconomic
grounds
Without restriction
as to reason
Unavailable
Map colour key
36
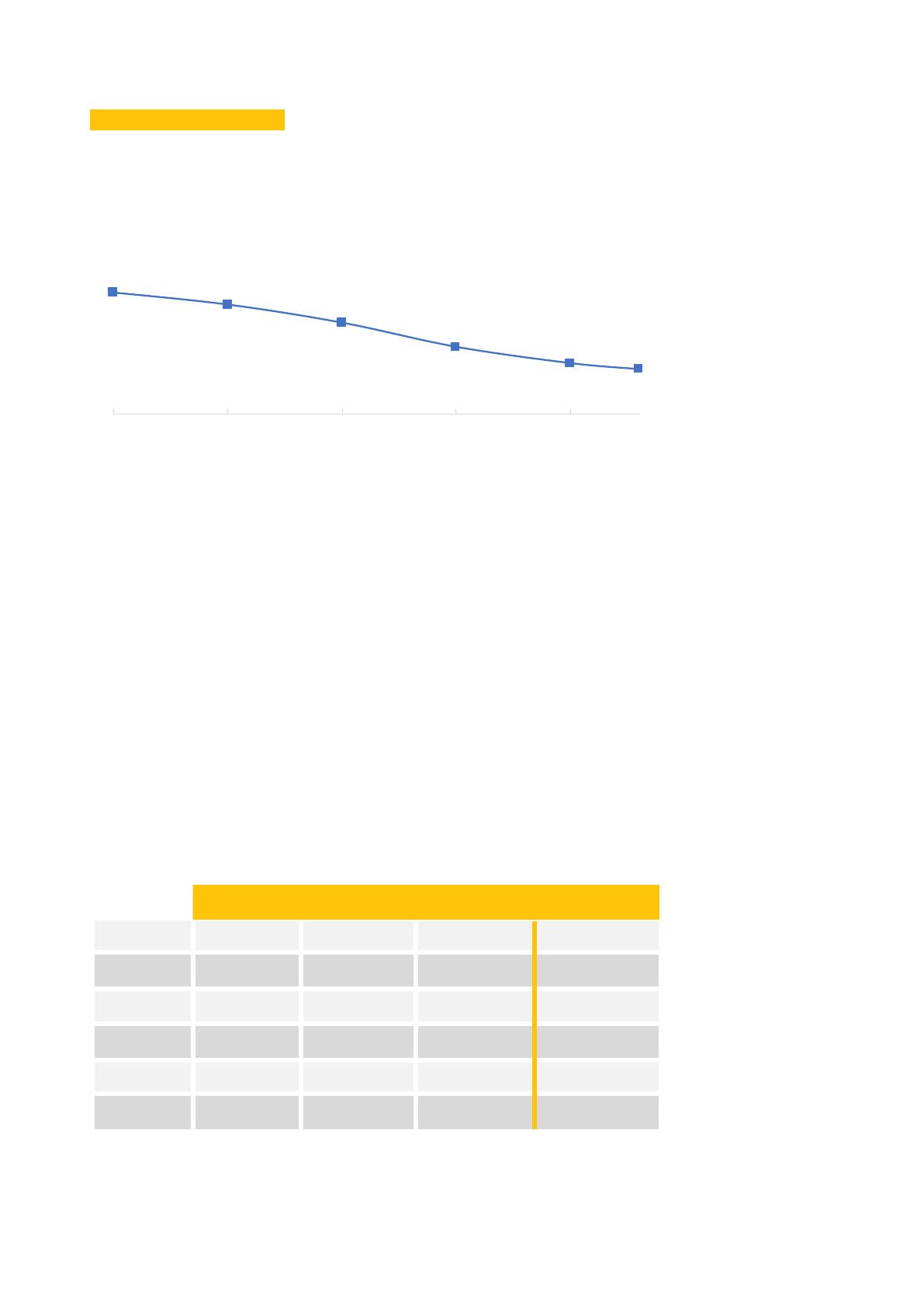
MATERNAL HEALTH SERVICES
The Asia-Pacific Region made significant progress in expanding access and utilisation
of maternal health services. This is best documented in the trend of the maternal
mortality ratio (MMR). Although the achievements fell short of the MDG target of a 75
percent reduction between 1990 and 2015, the ratio did decline by about two thirds.
Maternal deaths per 100,000 live births in South East Asia, East Asia & Oceania
1990-2013*
*largely congruent with the UNFPA Asia-Pacific Region
Source: [104]
The summary statistic, however, hides very large differences among countries. Among
the six countries included in the study, for instance, there is almost a nine-fold difference
between the estimated maternal mortality ratios in Thailand and in Bangladesh.
The quality, access and use of antenatal, obstetric, and postpartum care are key
determinants of maternal mortality. Additional determinants of equal importance are not
within the remit of the health sector. They include, for instance, the status of women, the
level of gender violence and the level of adolescent fertility. Recent survey statistics on the
coverage of maternal health services in the six study countries show that the countries
with high service coverage generally have low maternal mortality ratios. But there is no
direct correlation and there are exceptions. Cambodia and Viet Nam, for instance, have a
similar level of maternal health service coverage, but a three-fold difference in maternal
mortality. Improvements in services will not immediately be reflected in maternal
mortality statistics which are usually calculated over a period of several years. Other
reasons may be related to uneven quality of services provided. But these differences are
also a reminder that health is not just an issue of health service coverage.
Antenatal care (at least 4 contacts), skilled aendance at birth, postnatal care
within 48 hours of delivery and esmated maternal mortality rao (maternal
deaths per 100,000 live births)
*estimates of the UN Maternal Mortality Estimation Inter-Agency Group
#
the estimate of the 2012 DHS survey is considerably higher than the estimate of the
UN Inter-Agency Group
200
180
150
110
83
73
1990 1995 2000 2005 2010
ANC x 4 SBA PNC (48 hrs.) MMR*
Bangladesh 31.2 % 42.1 % 36.4 %
176
Cambodia 75.6 % 89.0 % 90.3 %
161
Indonesia 87.8 % 83.1 % 80.1 %
126* / 359
#
Mongolia 89.6 % 98.9 % 95.4 %
44
Thailand 90.8 % 99.1 % N/A
20
Viet Nam 73.7 % 93.8 % 89.8 %
54
37

Antenatal care
In 2016, the WHO replaced its recommendation for at least four antenatal visits during
pregnancy with a recommendation for a minimum of eight contacts. [105] However only
the coverage of four or more ANC contacts is currently being monitored. In developing
countries globally, it increased slowly between 1990 and 2014, from 35 percent to 52
percent. South East Asia, however, took a leap forward from 45 percent to 84 percent,
while South Asia lagged behind with an increase from 23 percent to only 36 percent.
[106] This split within the Asia-Pacific Region is also reflected in the statistics of the
six sampled countries. But national statistics hide significant inequities in coverage
among regions and social groups within the country.
Statistics about the frequency of antenatal care contacts do not provide information
about the content and quality of care. Comprehensive assessments of the quality
of care are only available from occasional evaluations of geographically limited
programmes. In Demographic and Health Surveys (DHS) women are asked whether
they received iron supplements during their pregnancy. Affirmative responses
recorded in recent surveys range from less than 50 percent in Pakistan to more than
95 percent in Cambodia. [107], [33]
One component of antenatal care is the prevention and management of pregnancy-
related or concurrent diseases. Comparable national statistics are only collected
for health conditions that are covered by international programmes or global health
initiatives. These include malaria, HIV infection and syphilis. Increasingly Zika virus
infection is receiving attention, but screening for Zika virus is not systematically
included in national ANC protocols of the six countries in the sample.
According to data collected by UNAIDS, about 7,500 pregnant women in five of the
six sampled countries received antiretroviral treatment for HIV infection during
pregnancy in 2015. [50] Most of these women were in Thailand, which achieved
more than 95 percent coverage of antiretroviral treatment among pregnant women
living with HIV. In June 2016, WHO certified that Thailand had eliminated mother-
to-child transmission of HIV and syphilis. [76] Viet Nam achieved about 58 percent
coverage, but in Indonesia the coverage was only estimated at nine percent and in
Bangladesh at 14 percent. In Mongolia, only two women were reported on treatment,
but because of the low HIV prevalence this was estimated to represent a coverage of
50 to 95 percent. Data from Cambodia were available for 2013 only, with 691 women
on treatment and an estimated coverage of about 60 percent. [108]
Data on coverage of syphilis screening and treatment at first ANC contact are
available from the WHO Global Health Observatory database for most countries of
the region. [109] Coverage rates above 95 percent were recorded for China, Mongolia,
Bhutan, Thailand and several Pacific Island States. Some countries in Asia-Pacific,
however, had very low coverage rates such as Indonesia (0.5%), Myanmar (12.4%),
Bangladesh (31.6%), and Cambodia (41.2%).
Obstetric and emergency obstetric care
Skilled attendance at birth (SBA), i.e. the attendance of a doctor, nurse or midwife
at the time of delivery, can potentially prevent obstetric complications and adverse
outcomes. It is, of course, also essential that professionals who are classified as
‘skilled’ are trained in the management of labour and delivery, and have the necessary
medicines and equipment to deal with obstetric emergencies. The SBA coverage
more than doubled over the past five to seven years in some Asia-Pacific countries,
for instance in Bangladesh, Cambodia and Nepal, but it is still less than 50 percent
according to the most recent surveys in Afghanistan, Bangladesh and Laos, and it is
only a first step towards improved maternal care.
38

The next important step is the access and use of emergency services in case
of complications. The extent to which health systems are equipped to respond to
obstetric emergencies is assessed in national surveys of emergency obstetric and
neonatal care (EmONC). Ministries of Health often have statistics on the number of
facilities that are classified as providing basic or comprehensive EmONC. Studies
of the functionality of these facilities, however, usually report significantly lower
numbers.
3
Cambodia assessed emergency obstetric care facilities in 2015 in preparation of the
EmONC Improvement Plan 2016-2020. The country had made significant progress
during the implementation of the preceding plan. The number of functional facilities
providing basic emergency care had increased from 19 to 110, and for comprehensive
emergency care from 25 to 37. The proportion of births in functional facilities had
more than doubled since 2008. However, the facilities providing comprehensive
care were primarily concentrated in urban hospitals, while the overall density of
emergency care facilities was still less than half of the recommended level of one per
100,000 population. Furthermore, an in-depth assessment of basic EmONC facilities
revealed that of the 110 listed facilities, only 28 were fully functional according to the
established criteria. [110]
Postnatal care
Postnatal care is recognised as a key intervention to save the lives of newborn infants.
The evidence for its impact on maternal health is less clear, but about 40 percent
of maternal deaths occur between the second and the seventh day after delivery,
primarily from infection and postpartum haemorrhage. [111] Postpartum check-ups
within the first 48 hours after delivery that focus on the mother and not only on her
newborn infant are therefore considered important interventions for maternal health.
Recent DHS and MICS surveys have included questions about postnatal check-ups of
mothers within 48 hours after delivery. Survey data from the Asia-Pacific Region are
only available from a few countries, and there are even fewer data on trends. As can
be expected, an increase in deliveries in health facilities also resulted in increased
coverage of post-partum check-ups. The coverage of post-partum care for mothers
in each country is therefore comparable to the proportion of births in health facilities.
PREVENTION AND TREATMENT OF SEXUALLY TRANSMITTED INFECTIONS
The global prevalence, incidence and treatment of HIV infection is monitored by
UNAIDS through regular reports submitted by countries to the global AIDS response
reporting mechanism. For four other sexually transmitted infections, gonorrhoea,
chlamydia, trichomonas and syphilis, the global situation is estimated every five
years by WHO based on national studies and surveillance reports. The latest available
regional estimates of STI incidence are for 2012. [51]
According to UNAIDS, there were 300,000 new HIV infections in Asia-Pacific in 2015.
[112] In 2012, the combined incidence of the four other STIs in the WHO regions of
South-East Asia and Western Pacific
4
was 181 million. [113] The incidence rate of
HIV infections in the region has always been low compared to other regions, and has
fallen by more than 50 percent since the late 1990s. The incidence rate of the other
four STIs, however, was generally above the global average and does not show the
same declining trend. In Mongolia, for instance, the syphilis notification rate more
than doubled between 2001 and 2011. [114] Because of its large population size, the
Asia-Pacific Region accounted for 14 percent of global HIV incidence in 2015, and for
51 percent of the combined global incidence of gonorrhoea, chlamydia, trichomonas
and syphilis. [113],[50]
3 Functionality for a basic care facility is defined as having performed each of seven ‘signal functions’ at least once within the last three
months, with the addition of surgery and blood transfusion for a comprehensive care facility (WHO, 2009)
4 The two WHO Regions combined correspond roughly with the UNFPA Asia-Pacific Region
39
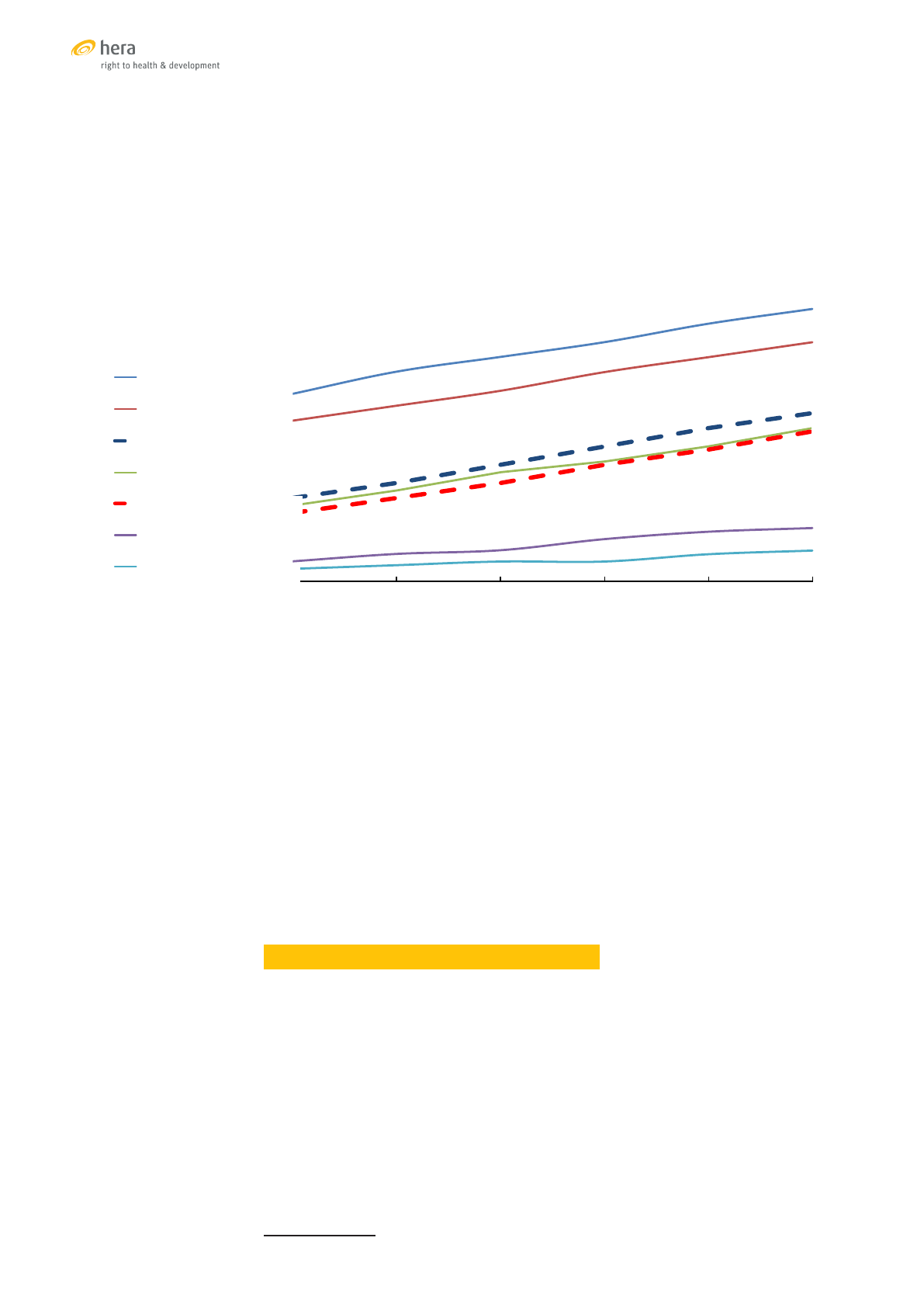
An estimated 41 percent of people living with HIV in the Asia-Pacific Region received
anti-retroviral treatment in 2015, less than the global average of 46 percent but
within the same estimation range. In the countries of the study, as well as regionally
and globally, there has been an almost linear increase in the proportion of people on
treatment, albeit at different speeds and levels. There is a large spread in treatment
coverage, with 74 percent of the estimated number of people living with HIV on
antiretroviral treatment in Cambodia and only nine percent in Indonesia in 2015.
Esmated anretroviral treatment coverage (% on treatment) in selected APR
countries
Source: [50]
The offer of health services for diagnosis and treatment of STIs has also greatly
expanded since the 1990s, aided by the introduction of syndromic management in
many countries of the region. Syndromic management allowed a decentralisation
of STI services to the primary health care level and the provision of diagnosis and
treatment in a single consultation. [e.g.115] There are, however, still barriers of access
to treatment that are related to societal attitudes or to the way the treatment services
are organised.
In 2010, for example, a survey of young people at risk
5
in Cambodia found that only 36
percent of young women and 41 percent of young men with symptoms of a sexually
transmitted infection sought treatment in a public or private clinic. Most of them
did not seek any treatment, and a smaller number resorted to self-medication or
traditional medicine. [116] In Viet Nam, treatment for STIs that is covered by social
health insurance is only available at specialised Venereal Prevention and Control
Centres. Many people, especially adolescents, avoid these centres and instead pay for
services or resort to self-medication.
PREVENTION AND TREATMENT OF CERVICAL CANCER
Cervical cancer is the fourth most common cancer in women with an estimated
528,000 new cases and 266,000 deaths globally in 2012. About half of the incidence,
269,000, and half of the deaths, 137,000, occurred in the Asia-Pacific Region. [117]
The lifetime risk of cervical cancer among women aged 15 to 79 varies greatly, from
below one percent in the Maldives, China, Sri Lanka and Pakistan to between three
and six percent in the Pacific Island States. [118]
The role of health services in the prevention and treatment of cervical cancer
comprises three interventions:
• Primary prevention: Immunisation against Human Papillomavirus (HPV)
• Secondary prevention: Screening and treatment of precancerous lesions
• Tertiary prevention: Treatment of invasive cancers and palliative care
5 including sex workers and clients, injecting drug users, and men who have sex with men
51
74
44
65
23
46
21
42
19
41
6
15
4
9
2010 2011 2012 2013 2014 2015
Cambodia
Thailand
Global
Viet Nam
Asia Pacific
Bangladesh
Indonesia
51
74
44
65
23
46
21
42
19
41
6
15
4
9
2010 2011 2012 2013 2014 2015
Cambodia
Thailand
Global
Viet Nam
Asia Pacific
Bangladesh
Indonesia
40
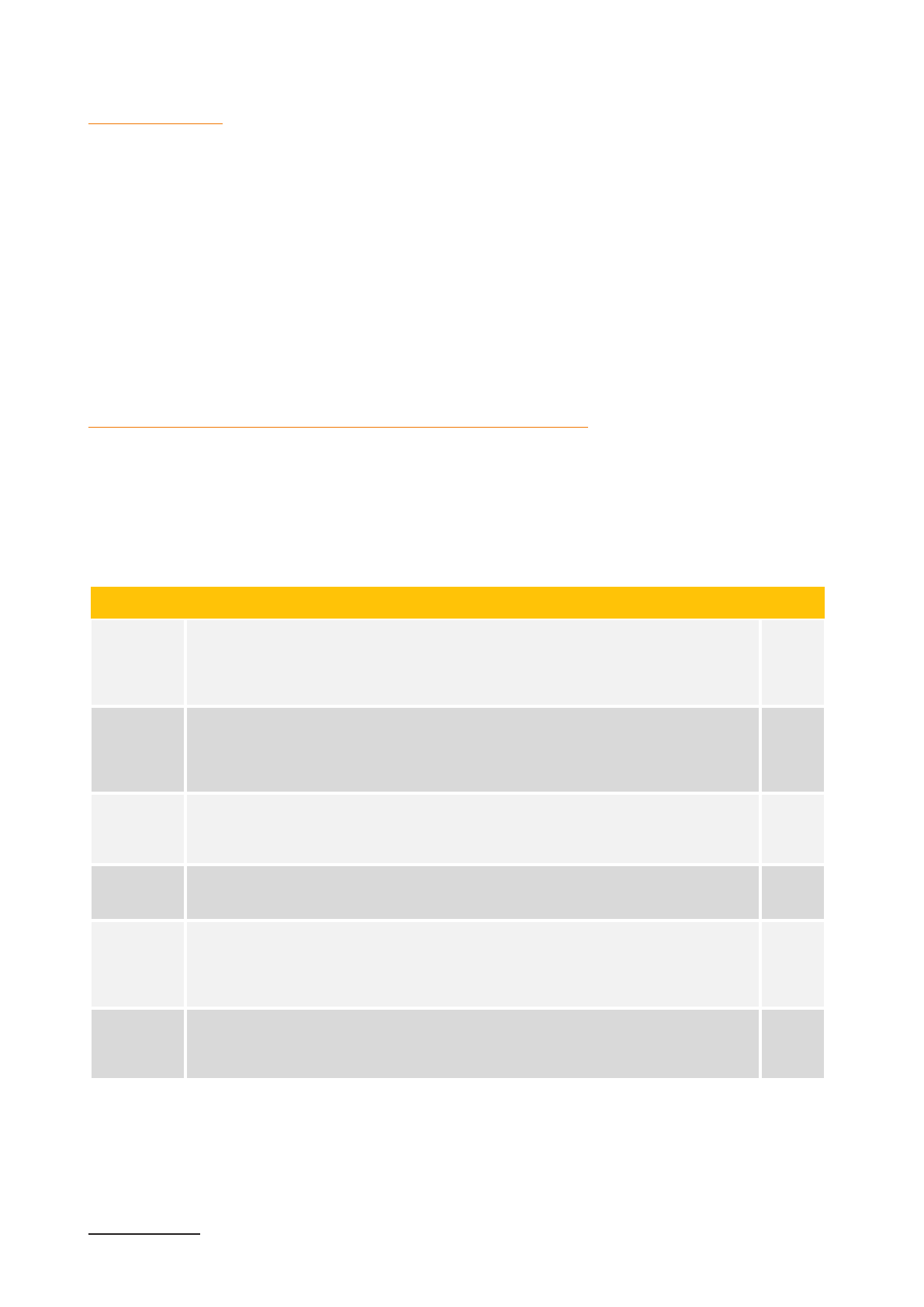
HPV immunisation
Infection with Human Papillomavirus is one of the most common sexually transmitted infection in the world.
A study in 2007 estimated that 291 million women were carriers of HPV DNA. [119] Three HPV vaccines have
been licensed since 2006, all protecting against HPV16 and HPV18, the types of HPV that are associated with
70 percent of invasive cervical cancers in Asia. [120] Since 2014, WHO recommends a two-dose vaccination
regime for girls aged 9 to 13, but many countries still apply the older three-dose regime. [121] In the Asia-
Pacific Region, only Bhutan, Malaysia and several Pacific Island States have introduced HPV vaccination in
their national immunisation programmes.
6
[122]
The Gavi Alliance provides financial support for the introduction of HPV immunisation to low and lower-
middle income countries that have met defined capacity criteria. By 2015, Bangladesh, Lao PDR, Nepal and
the Solomon Islands had applied for Gavi support. In other countries, pilot initiatives for HPV immunisation
were implemented with other international support, for instance in India and Viet Nam with support from
PATH International. In a demonstration project in four districts in Viet Nam, 6,358 eleven-year-old girls (91%
of eligible girls) were immunised during a two-year period. [123] The introduction of HPV vaccine in the
national immunisation schedule in Viet Nam is under discussion.
Screening for cervical cancer and treatment of precancerous lesions
Screening programmes for cervical cancer using cytological testing or visual inspection after acetic acid
application (VIA) have been launched in many countries, and more advanced methods such as HPV DNA
testing are being piloted. Many countries also introduced a single-visit approach for diagnosis and treatment,
combining VIA screening with cryotherapy, especially in rural health facilities. Networks of colposcopy centres
for referral and further treatment of women with abnormal cytology or VIA results have been established.
The status of development of these services varies from country to country.
Cervical cancer screening in selected APR countries
Programme Source
Bangladesh
National screening programme launched in 2005. Recommendation to screen
women over 30 every three years with VIA. Screening centres in 238 health
facilities country-wide. Colposcopy centres in medical college hospitals.
Participation is moderate with about 100,000 women screened each year. Recent
information on screening coverage is not available.
[125]
Cambodia
National programme in planning. Several pilot projects in operation using VIA
and single-visit VIA/cryotherapy approach. A screening programme linked to the
reproductive health voucher project screened 30,000 women between October
2014 and May 2016. A study of a small sample of 309 women in 2013 estimated a
national coverage of 19.7%
[125]
Indonesia
National screening programme launched in 2007. Recommendation to screen
women aged 30-50 every five years. Services for single-visit VIA screening and
cryotherapy are currently available in 347 primary health centres in 23 provinces.
Coverage between 2007-2011 was estimated at 24.4%.
[124]
[126]
[127]
Mongolia
National screening programme launched with the National Cancer Control
Programme 2007-2017. Objective to screen women aged 30-60 every year using
VIA. Coverage in 2008 was estimated at 29.7%.
[62]
[128]
Thailand
National screening programme launched in 2005. Recommendation to screen
women aged 30-60 ever five years using cytological screening. VIA, including
the single-visit approach, is used in remote districts. HPC DNA testing is being
piloted. Screening centres are linked to colposcopy services. Coverage in 2009
was estimated at 60.2%
[124]
[127]
[129]
Viet Nam
National screening programme launched in 2011. Recommendation to screen
women every two to three years with focus on the 30-50 age group. VIA and
cytology are used. HPV DNA testing is available in only a few national and
provincial hospitals. Recent information on screening coverage is not available
[130]
[94]
Services for cervical cancer screening as well as for treatment of pre-invasive and invasive cervical cancers
are only just starting to be scaled up into national programmes in most Asia-Pacific countries. Overall, the
health service coverage for the prevention and treatment of cervical cancer in Asia-Pacific has major gaps
at all levels. Very few countries are providing acceptable levels of services for primary prevention and early
detection through their public health system.
6 Marshall Islands (2008); Federated States of Micronesia, Palau (2009); Bhutan, Malaysia (2010); Cook Islands, Kiribati (2011); Fiji (2013)
41
Health services for gender-based violence
Gender-based violence (GBV) is based on gendered
role expectations and unequal power relationships.
Although it can be directed against men and boys
who do not comply with social gender norms, it is
overwhelmingly violence directed against women
and girls. [131] Like many issues of sexual and
reproductive health it is not just a health sector issue.
The responsibility for policies to prevent GBV is rarely
within the mandate of Ministries of Health. Services
to respond to violence, once it has happened, may be
located at health facilities, but are not always under
the authority of the Ministries of Health. However,
after an incidence of violence, health facilities are
most often the first contact points where the physical
and psychological consequences can be established
and addressed.
Gender-based violence as a public health issue is a
complex theme that has been discussed in great detail
in numerous fora and publications. In 2010, UNFPA
published a detailed assessment of the situation in
the Asia-Pacific Region, describing the laws, policies,
their application, as well as policy and service
initiatives to strengthen the health sector response to
GBV. [132]
Public health initiatives to prevent GBV, however, are
not activities that generate personal user charges. An
assessment of universal health coverage for sexual
and reproductive health can only provide a sketch
of service availability and access, and review the
systems for protecting women from financial risks
when accessing them. Although there are occasional
reports that injured women are charged for health
services in some countries, [e.g. 133] cost is not
the most formidable barrier to services for women
who have experienced violence. The availability and
comprehensiveness of services and referral networks,
the attitudes of providers, and the protection of the
woman’s safety and dignity are of much greater
importance.
Several countries in the region have established
One-Stop Crisis Centres (OSCCs) in public hospitals.
In addition to medical care and counselling, they
offer social and legal assistance and referral to
shelter. These centres have been well integrated in
the national health systems in Indonesia, Malaysia,
the Philippines and Thailand, and they are being
scaled up in Bangladesh, India and Sri Lanka.
In the six study countries, information obtained in
interviews conducted with key informants indicate
that medical care for physical injuries, post-exposure
prophylaxis for HIV infection, and emergency
contraception are generally available in health
facilities. Only Thailand has scaled up the coverage of
OSCCs nationwide. In Mongolia, the approach is still
only piloted in a few locations with UNFPA support. The
other countries are at different stages of developing
comprehensive services under the leadership of
different authorities such as the Ministry of Social
Welfare in Bangladesh, or the Ministry of Labour,
Invalid and Social Affairs in Viet Nam.
Papua New Guinea is a country that has captured
international attention because of the well-
documented high incidence of gender-based violence.
In 2005 PNG started a programme of creating Family
Support Centres offering medical care, forensic
examination, counselling, social support, legal
advice, short-term shelter and referral. In 2010,
family and sexual violence was included as a strategic
area in the national health strategy. [132] A detailed
account of the experience of a Family Support Centre
supported by Médecins Sans Frontières in Lae, PNG
was published in 2016. [133] The centre provided
medical care for victims of violence in 6,860 cases over
a period of 30 months. During this period, almost five
percent of women in the catchment area presented
at least once to the centre. About 90 percent required
treatment for physical injuries.
In 2013, the chair of PNG’s Family and Sexual Violence
Action Committee outlined the scale of the situation
and the need for support in a speech at the Australian
National University.
Right now, we have established Family Support Centres
(FSCs) where battered women and children can go
for immediate medical treatment and psychosocial
support. There are now about 15 of these centres in the
country and we have seen around 12,000 women come
through them in six years. … We are getting support to
roll out FSCs and [safe houses] across the country, but
what is really lacking are our skills to manage cases so
that good and proper assistance is given to survivors.
We have stories of so many of our women who have
been treated at FSCs and kept at safe houses, and then
when we send them home they have been murdered.
That is because we lack the facilities and skills to
manage the cases properly so that proper assistance is
given to these women before they are resettled in their
communities.
(quoted from: Betteridge A, Lokuge K (2014).
Combatting the family and sexual violence epidemic
in Papua New Guinea. Australian National University
Development Policy Centre)
42
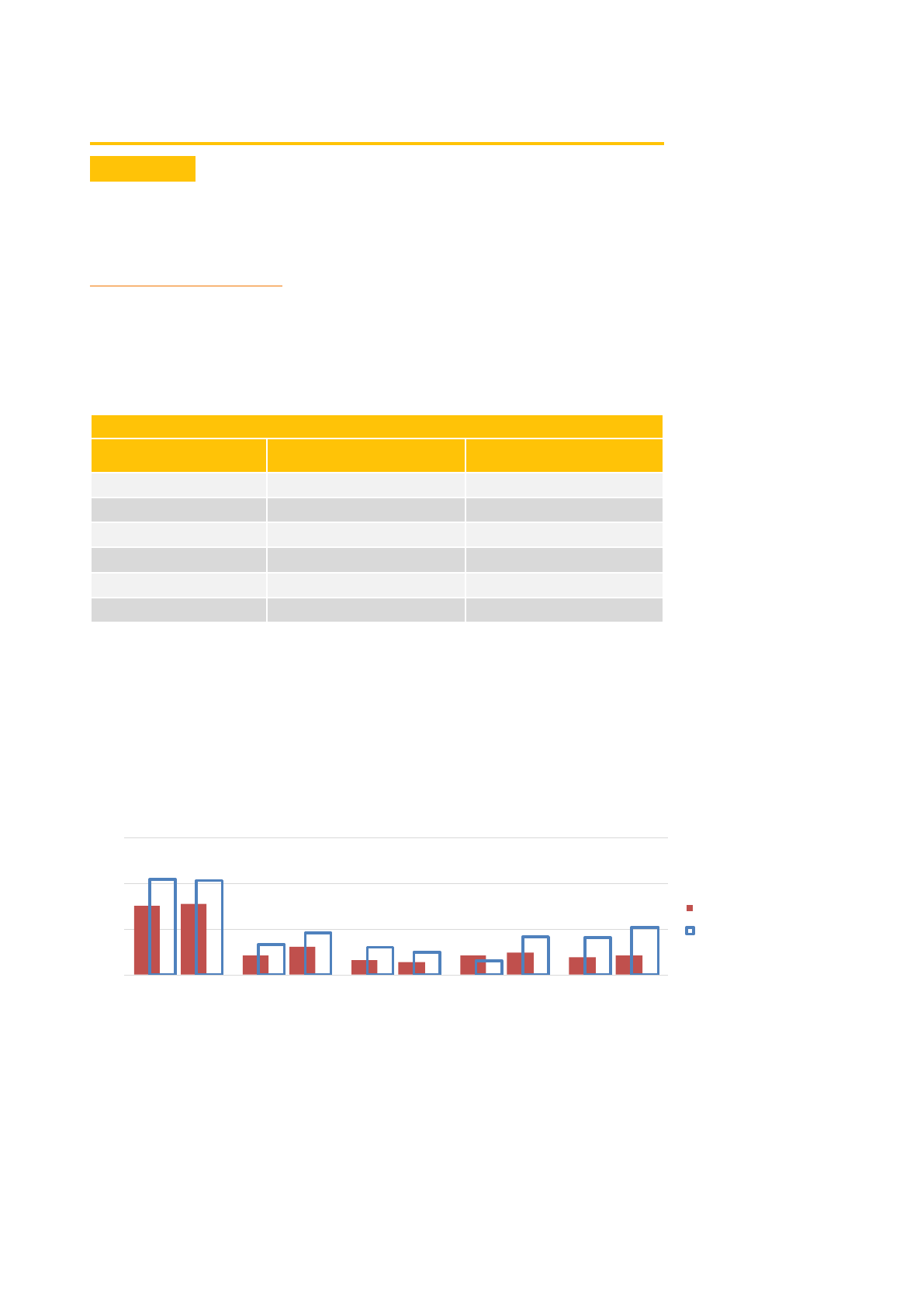
EQUITABLE ACCESS TO SRH SERVICES
SOCIAL STATUS
Inequities in access and use of sexual and reproductive health services according to
wealth and educational attainment persist in Asia. [134] While more of the poor are
reached with basic health services, large equity gaps remain in terms of access and
outcomes.
Contraception and fertility
Available trend data for the study countries document that inequities in contraceptive
prevalence and satisfied demand have decreased over time. In five of the six countries
(all except Indonesia) women in the lowest wealth quintile are today more likely to
use modern contraceptives than women in general.
Use of modern contraceptives (married women 15-49)
Use of modern contracepves (married women 15-49)
All women Poorest wealth quinle
Bangladesh 54.1 % 55.1 %
Cambodia] 38.8 % 39.4 %
Indonesia 57.9 % 53.0 %
Mongolia 48.2 % 57.8 %
Thailand 76.9 % 81.0 %
Viet Nam 57.0 % 61.2 %
Trends and equity gaps in adolescent birth rates, however, show a somewhat different
picture. Recent successive population-based estimates of the proportion of girls
aged 15 to 19 who have started childbearing are available from five of the six study
countries. The overall proportion increased in all countries except in Mongolia, but
the gap between the richest and the poorest group did not change significantly in
three countries. It increased in Viet Nam, and a major increase was reported by the
surveys in Indonesia, which does, however, raise questions of plausibility.
Proporon of adolescents (15-19) who have started childbearing: all adolescents,
and adolescents in the poorest wealth quinle
In a regional analysis that aggregated the results of two consecutive population
surveys in Asia-Pacific countries, the first conducted between 1998 and 2008, and
the second conducted between 2004 and 2014, the adolescent birth rate increased
among women in the lowest two wealth quintiles, while it decreased in the three
higher quintiles. The gap in the adolescent birth rate between women in the poorest
and the richest group increased from about 41/1,000 to 68/1,000. [135]
2011
2010
2010
2007
2011
2014
2014
2013
2012
2014
0%
20%
40%
60%
Bangladesh
DHS 2011 - 2014
Cambodia
DHS 2010 - 2014
Mongolia
MICS 2010 - 2013
Indonesia
DHS 2007 - 2012
Viet Nam
MICS 2011 - 2014
All
Poorest
43

Maternal health services
In surveys conducted between 2007 and 2011, the proportion of women who received
antenatal care by a skilled provider for their last birth (at least one consultation)
was already in the range of 90 percent in the six countries except for Bangladesh. In
follow-up surveys between 2013 and 2014, not much change was detected beyond a
small increase in coverage. The equity gap of coverage, comparing the coverage of
women of the poorest wealth quintile with the total coverage, decreased in Indonesia
and Cambodia, while it increased in Bangladesh.
Antenatal care by a skilled provider: all women and women in the poorest wealth
quinle
For delivery with the attendance of skilled personnel, the pattern was similar, although
the coverage rates were somewhat lower and the equity gaps larger. Between the
latest two surveys the equity gap increased in Bangladesh and Cambodia, and it
remained virtually unchanged in the other three countries.
Skilled aendance at birth: all women and women in the poorest wealth quinle
In Thailand (not included in the graphic analysis), the latest survey conducted
in 2015/16 reported that both the coverage of antenatal care and of skilled birth
attendance were almost universal (98.1% and 99.1%). This high level of coverage
was already observed in 2005/06, with very minor equity gaps. [70], [72] Data from
Thailand and Mongolia confirm that high coverage rates are related to smaller equity
gaps. [136]
RESIDENCE
According to a survey conducted by ESCAP and UNFPA on the implementation of
ICPD beyond 2014, the main barrier to increasing women’s access to comprehensive
SRH services in the Asia-Pacific Region was poor access in remote and rural areas.
People living in remote rural areas or on remote islands face difficulties in accessing
a variety of services because of poor transportation, communication barriers and a
tendency of national policies to concentrate service provision in the cities. [137]
When disaggregating the satisfied demand for family planning by residence,
large rural/urban differences are seen in Pakistan (17.9%), Nepal (12.2%), Timor-
Leste (12.1%) and India (7.6%). Limited availability of and access to a wide range
of contraceptive services remains a major challenge throughout the region.
Contraceptive stocks in rural and remote areas may be depleted for months at a time.
2011
2010
2010
2007
2011
2014
2014 2013 2012 2014
0%
20%
40%
60%
80%
100%
Bangladesh
DHS 2011 - 2014
Cambodia
DHS 2010 - 2014
Mongolia
MICS 2010 - 2013
Indonesia
DHS 2007 - 2012
Viet Nam
MICS 2011 - 2014
All
Poorest
2011
2010
2010
2007
2011
2014
2014
2013
2012
2014
0%
20%
40%
60%
80%
100%
Bangladesh
DHS 2011 - 2014
Cambodia
DHS 2010 - 2014
Mongolia
MICS 2010 - 2013
Indonesia
DHS 2007 - 2012
Viet Nam
MICS 2011 - 2014
All
Poorest
2011
2010
2010
2007
2011
2014
2014
2013
2012
2014
0%
20%
40%
60%
80%
100%
Bangladesh
DHS 2011 - 2014
Cambodia
DHS 2010 - 2014
Mongolia
MICS 2010 - 2013
Indonesia
DHS 2007 - 2012
Viet Nam
MICS 2011 - 2014
All
Poorest
2011
2010
2010
2007
2011
2014
2014
2013
2012
2014
0%
20%
40%
60%
80%
100%
Bangladesh
DHS 2011 - 2014
Cambodia
DHS 2010 - 2014
Mongolia
MICS 2010 - 2013
Indonesia
DHS 2007 - 2012
Viet Nam
MICS 2011 - 2014
All
Poorest
44
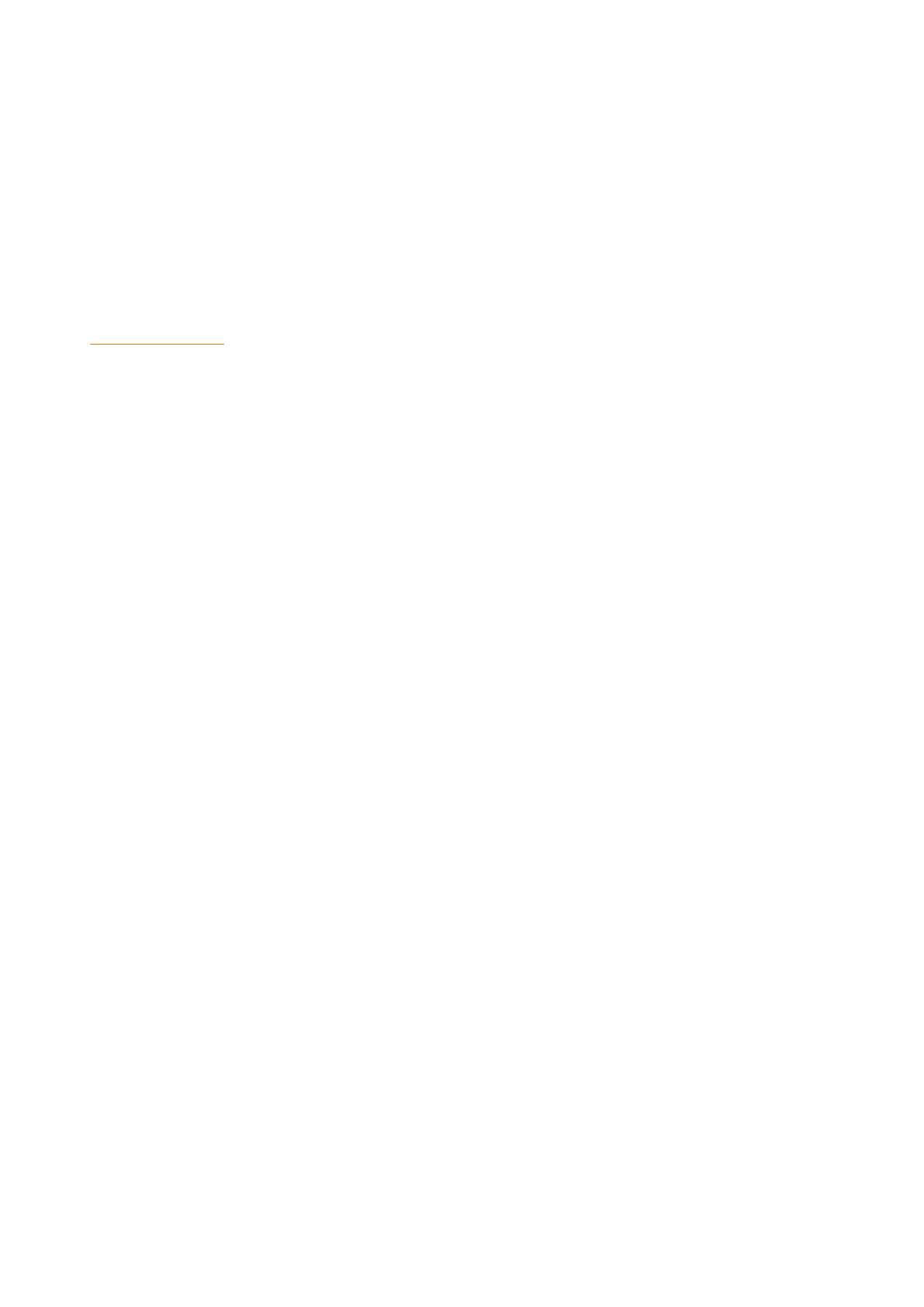
There are also significant disparities in terms of access and uptake of antenatal care.
The greatest disparities are in South and South-West Asia: ranging from a 25 percent
difference between women in rural and urban areas in Bangladesh and Pakistan, to
a 33 percent difference in Nepal.[137]
In the large countries of the Asia-Pacific Region that extend over many widely
dispersed islands, the inequity gaps may not be across the rural/urban divide,
but rather between regions with high and low service coverage. In Indonesia, for
instance, the 2012 Demographic and Health Survey reported only a small difference
in the contraceptive prevalence between rural and urban areas, with higher coverage
among rural women (58.7% / 57.0%). The regional contraceptive prevalence rates,
however, ranged from 19 percent in Papua to 62 percent in East Java. [44]
Vulnerable groups
Undocumented migrants, internally displaced persons, ethnic minorities, refugees,
older persons and persons with disabilities are the groups least frequently targeted
by SRH programmes.
Ethnic minorities are among the most vulnerable, disadvantaged and marginalised
groups across the Asia-Pacific Region. They are often excluded from decision-making
processes, and experience high rates of unemployment as well as low education and
health outcomes. [137]
A recent study in Viet Nam explored barriers of access to SRH services among ethnic
minorities. Compared to national estimates, antenatal care coverage (at least four
consultations) was 58 percentage points lower among respondents from ethnic
minority groups than the national average (16% vs 74%). The gap for delivery in a
health facility was 53 percentage points (41% vs 94%), and for births attended by
skilled personnel it was 45 percentage points (49% vs 94%). [138] Several qualitative
studies have tried to explain why ethnic minority groups are disadvantaged in terms
of health care in Viet Nam. Among the identified barriers are cultural preference for
home deliveries, perceived negative attitudes by health care personnel, language
barriers and high transport costs.[139]
Although Viet Nam’s poorest populations are covered by social health insurance,
co-payments and other indirect costs must be paid out of pocket, which may be a
further barrier. The study by the University of Toronto found that 81 percent of ethnic
minority women had valid health insurance cards, but only 52 percent used them
for ANC services, and 45 percent for delivery at a health facility. Misinterpretation
and misunderstanding among community members regarding eligibility for health
insurance, and lower coverage among the most disadvantaged families demonstrate
an apparent failure of local authorities to communicate the use and benefits of health
insurance. [138]
According to ILO estimates, countries in the Asia-Pacific Region host approximately
27.6 million migrants over 15 years of age of whom 47 percent are female. An
estimated 20.4 million among them are migrant workers, and 2.7 million are migrant
domestic workers. Female migrant workers are vulnerable to sexual violence,
economic exploitation, physical and verbal abuse and labour rights violations. The
flow of undocumented migrants in Asia-Pacific is larger than in all other regions of
the world, and it is mainly between neighbouring countries. [140]
The 1990 United Nations Convention on the Protection of the Rights of All Migrant
Workers and Members of their Families stipulates that migrant workers are entitled
to equal access to social and health services, and have the right to receive any urgent
medical services, regardless of their legal status. So far, only Bangladesh, Indonesia,
the Philippines, Sri Lanka and Timor-Leste have ratified this convention. [141] In
addition, Afghanistan, Bangladesh, China, India, Indonesia, Nepal, Pakistan, the
Philippines, Sri Lanka, Thailand, and Viet Nam adopted the 2011 Dhaka Declaration
to promote migrant-inclusive health policies ensuring equitable access to health
services as well as occupational safety and health. [142]
45

Migrants face various informal barriers to accessing
health services, such as language differences,
irregular migration status, lack of information
about health and insurance services, the need for
permission from the employer to seek health care,
employer reluctance to provide health care benefits,
and the fact that health facilities might be open only
during working hours. [137]
Some health policies discriminate against
registered migrant workers. In Malaysia, the policy
of mandatory testing requires migrant workers to
undergo at least three medical examinations in
order to renew their employment permit in the
first three years. Those who are HIV positive are
deported within three days. A similar policy is
also found in Singapore. [143], [144]
Migrants in an irregular situation often find it
difficult to access health services because of fear
of detection by the authorities. National labour
regulations for domestic work also affect the rights
of the mostly female migrant workers in domestic
employment. Thailand´s labour laws, for instance,
do not cover domestic workers. [145] In Malaysia,
domestic work is not officially recognised as a
form of work, and migrant domestic workers are
therefore excluded from the Social Security and
the Workmen’s Compensation schemes. Malaysia
also prohibits the entry into the country and the
employment of any person who lives or lived off
the proceeds of prostitution. Yet sex workers and
domestic workers are among the groups of women
who are most in need of SRH services. [143]
Little information is available about the access
and use of SRH services by migrants. A study
among rural-to-urban migrant beer promoters
in Cambodia, Laos, Thailand and Viet Nam found
that although they were often covered by health
insurance, their access to reproductive health
services was limited by health care provider stigma,
cost, and availability of services, in addition to
personal factors such as lack of time and shyness
to access services. [146]
A study conducted among local and migrant women
in Sabah (Malaysia) found that pregnant migrants
started to attend ANC services much later than
local women (7 months pregnancy compared to
3 months). Cost was a significant barrier, given
their low wages and Malaysia’s double-fee policy,
which requires foreigners to pay almost double
the amount for treatment than Malaysians. Some
undocumented migrants prefer to attend private
health care despite high costs, as they are not
required to present their identification cards. [143]
Conversely, two studies looking at internal migration
among garment workers in Cambodia and female
internal migration in Myanmar found that access to
SRH services among migrant women was relatively
high, and higher than among non-migrants. In
Cambodia, female garment workers had reasonably
high rates of antenatal care and skilled attendance at
birth, with most delivering in a public health facility.
Knowledge and use of contraception was also
consistent with the general population, however, the
abortion rate was higher and knowledge about the
legality of abortion was low. The study highlighted
that garment workers have limited time to access
health services, in particular public services. Cost
and the distance to health facilities also act as
barriers to access SRH services. [147] In Myanmar,
female internal migrants were more likely to be of
higher socioeconomic status and had better access
and use of SRH services than non-migrants. They
were 1.6 times more likely to use a modern method
of contraception and 1.3 times more likely to use
antenatal services and to deliver with a skilled
attendant compared to non-migrant women. These
findings suggest that social, economic and residence
factors may outweigh the effect of migration status
among internal migrants. [148]
In 2011, the Asia-Pacific Region hosted 54 percent of
the global refugee population. Most of the refugees
were those who crossed the Afghan border to
neighbouring Pakistan and the Islamic Republic of
Iran. The region also hosts one of the world’s largest
populations of internally displaced persons, mainly
in Myanmar, Indonesia and India. The right to seek
asylum and the right to nationality are verifiably not
guaranteed in the majority of the region’s countries
and territories. There is a significant gap between the
right to social protection and the access to services
because of legal and administrative barriers. [5]
Very little information is available on the access
to SRH services for refugees. A small study of
reproductive health issues and quality of life of
young people in two refugee camps in Thailand,
found that the health services do not target young
people. According to the camps’ official data, family
planning was used by only 12 percent on average,
however the pregnancy rate among girls aged 15-
19 was 60 per 1,000 and 80 per 1,000 in the two
camps. Access to reproductive health information,
education and services was limited, and the level
of knowledge about sexual and reproductive health
and contraception among young people was very
low. [149]
46
FINANCIAL RISK PROTECTION FOR
SEXUAL AND REPRODUCTIVE HEALTH
SERVICES
The increase of SRH service coverage and the reduction of inequity are two closely
related strategic pillars of UHC. The third pillar is the reduction of financial risk.
The objective of this pillar is to remove payment at the point of service as a barrier
against accessing and receiving needed SRH services. The services, of course, have
a cost that cannot be made to disappear. Financial risk protection thereby becomes
an issue of health financing.
Health financing is the process of raising revenues, collecting them into a pool of
funds to be spent on health services, and using them to purchase the services from
providers. In the most inequitable form of health financing, the resources are raised
by households when needed, and used to pay for health care at the point of service
delivery. Health services in Afghanistan, Bangladesh, Cambodia and India are financed
to more than 60 percent in this manner. It is, however, not certain that summary
statistics about sources of health financing also apply to sexual and reproductive
health services. On the one hand, user fees for maternal health services may have
been abolished, on the other hand, family planning services may be excluded from
subsidies applied to other health services.
National health accounts studies sometimes also analyse reproductive health sub-
accounts. They face a challenge of boundary definition because of overlaps with
other sub-accounts such as for HIV and malaria prevention and care. In addition,
expenditures on prevention and on services that are not provided by the health
sector, for instance for the prevention and response to gender-based violence, are
not included. A methodology to define the boundaries of health expenditures has
been developed, [150] but the sector boundaries for service provision in sexual and
reproductive health are more difficult to draw than for other health services. The
main challenge, however, is the fact that reproductive health sub-account studies
are expensive and are not done very frequently. An on-line search for recent
published reports of reproductive health sub-account studies found only three that
were published since 2010: Afghanistan, Tanzania and Malawi. The out-of-pocket
contribution to financing reproductive health services in Afghanistan and Tanzania
was higher than the general out-of-pocket contribution to total health expenditure,
but it was lower in Malawi. The question on whether SRH services are financed to a
greater degree by direct payments of households than health services in general,
and whether they therefore carry a higher financial risk for individual users, can
therefore not be answered with the available evidence.
Out-of-pocket expenditures for health and for reproducve health
Sources: [151] [152] [153]
UHC strategies direct their focus on developing more equitable mechanisms of pooling
funds. While the attention is focused on pooling, the other two functional components
of health financing, raising funds and paying providers should not be forgotten. Funds
can be allocated from national health budgets, raised from insurance premiums
or received as development assistance by international partners. Sufficient funds
have to be raised through these channels, or progress towards UHC will be slowed.
Equally, SRH services that are not included in the list of benefits to be purchased with
the pooled funds have to be purchased directly by the clients as documented in two
study countries:
Afghanistan
(2011/12)
Tanzania
(2010)
Malawi
(2011/12)
OOP expenditure as % of THE 73.3% 31.9% 11.1%
OOP expenditure for RH as % of
THERH
78.5% 47.7% 4.9%
47

• In Viet Nam, rising costs of health services and decreasing international funding have contributed to a gap in
resourcing the pooled funds of the Social Health Insurance. While health insurance is mandatory and coverage
rates are high, the proportion of health expenditures that are covered by out-of-pocket payments has not
decreased because the tariffs paid to providers from pooled resources do not cover their costs. [154]
• In Mongolia, the government procures reproductive health commodities for vulnerable groups. According to
an interview with a nurse at a health centre, free contraceptives are provided to ‘vulnerable and high-risk
women such as the poor, women with mental disorders and severe chronic diseases’. Meanwhile, sexually
active adolescent girls have a rising unmet need for contraception, estimated at 36 percent in 2013. Yet they
have to pay for contraceptive commodities. [58]
INCLUSION OF SRH IN FINANCIAL RISK PROTECTION SCHEMES
In all six countries of the study, universal social health insurance is an identified goal of the UHC policy. The aim is
to create a single pool of funds from all sources to finance health services: insurance premiums paid by members,
general government revenues and international development funds. In Mongolia, this system exists for many years
and has reached a high level of national coverage. In Bangladesh, it is only in a pilot phase with a very small population
coverage. In Cambodia, it is still in the planning phase, and premiums, tariffs and benefits are still under discussion.
The existing and planned universal social health insurance schemes are not the only system by which States provide
financial risk protection for users of sexual and reproductive health services. In some countries in this study social
health insurance is the least important system. However, on the assumption that plans to create single unified systems
will be pursued in these countries, the current coverage and benefits are presented in the table. The information was
not available for the planned social health insurance scheme in Cambodia.
Benets for selected services covered by the social health insurance scheme
Bangladesh Indonesia Mongolia Thailand Viet Nam
Name of SHI scheme SSK JKN SHI UHC SHI
Targeted population
95,000
Pilot
258 million
Total population
3 million
Total population
48 million
Sub-population*
94 million
Total population
Coverage of target N/A 66%
100% 82%
Insured Benefits
Family Planning No Yes Limited Yes No
Emergency
contraception
No No No Yes No
Menstrual regulation No No No Yes No
Termination of
pregnancy
No No No Yes Limited
Post-abortion care Yes Yes No Yes No
Antenatal care Yes Yes Yes Yes Yes
- Laboratory/
Diagnostics
Yes Yes Partial Yes Yes
- Micronutrients Yes No Yes Yes No
- Malaria prevention No No Not applicable Yes Not applicable
- PMTCT No No Yes Yes Planned for 2017
Obstetric services Yes Yes Yes Yes Yes
Post-natal care Yes Yes Yes Yes Yes
STI Diagnosis Yes Yes Partial Yes Yes
STI Treatment Yes Yes Partial Yes Limited
HPV immunisation No No Yes Yes No
Cervical cancer screening No Yes Yes Yes No
Cervical cancer
treatment
Yes Yes Yes Yes Yes
Services for GBV No No Yes Yes No
* The remaining population is insured under parallel schemes with similar benefits for nearly 100% coverage
48
>95%

The fact that some services are not covered as benefits under the national social health insurance scheme
does not mean that there is no financial risk protection. In many cases, these services are fully or partially
provided without user fees under the public health service delivery system or under a special programme,
for instance for malaria or HIV control. This applies, for instance, to family planning services and for malaria
control during pregnancy in Bangladesh. Limited or partial coverage means that services are provided
under the SHI only to selected populations such as family planning commodities provided only to vulnerable
groups in Mongolia; that they are only covered under specific conditions, such as STI treatment in Viet Nam
that is only covered if dispensed by a specialised clinic; or that only some of the services in the category
are insured, such as the exclusion of ‘expensive’ diagnostics for antenatal care in Mongolia. The fact that
a service is marked in green as being covered by social health insurance, on the other hand, does not
necessarily mean that it is widely available. This applies, for instance to cervical cancer screening in several
countries.
The status of financial risk protection coverage for sexual and reproductive health in the six study countries
can be summarised as follows:
• Maternal health care, including antenatal and postnatal care, is covered everywhere. Policies for the
removal of user charges for maternity services were adopted in many countries as part of acceleration
plans to reach national Millennium Development Goal targets.
• Treatment services for sexually transmitted infections have a long history of public funding for the
purpose of epidemic control. This focus on epidemic control, however, entails that services in some
countries are not client-friendly, especially for unmarried adolescents, and push many of them into
the private sector where they have to pay for receiving care. Examples among the study countries are
Cambodia and Viet Nam.
• There has been a long-standing and very effective international effort to pool funds for HIV care
by the Global Fund for AIDS, Tuberculosis and Malaria. Many countries are still depending on this
internationally pooled support, but some, for instance Thailand, have completely transferred the
costs of HIV care to the national pool of financial resources for health.
• Prevention has a major role in sexual and reproductive health. Prevention objectives include, for
instance, the reduction of adolescent births, the elimination of violence against women, and
micronutrient supplementation during pregnancy. Many of the activities to address such issues are
not fully within the remit of the health sector, and they are therefore not receiving much attention by
the emerging UHC schemes. A general neglect of prevention by the social health insurance in Viet
Nam, for instance, was mentioned by several key informants interviewed for this study.
• The main health service areas in which there are differences in financial risk protection are those
related to fertility regulation: contraception, termination of pregnancy, and post-abortion care. The
availability of pooled funds for pregnancy termination and post abortion care is linked to the abortion
laws of the country. Less restriction generally means higher probability of financial coverage,
although there are exceptions. In Viet Nam, a country with a relatively unrestrictive abortion policy,
no services related to termination of pregnancy are included in the UHC schemes. In Bangladesh,
a country with restrictive abortion laws, menstrual regulation is not included in the social health
insurance scheme, but services are widely available without user charges under the national family
planning programme.
• Among the six countries included in this study, the UHC schemes in Thailand and Indonesia provide
full cost coverage for contraceptive services, while in Bangladesh publicly funded contraception is
provided by the network of primary health facilities operated by the Directorate General for Family
Planning. However, 43 percent of family planning users in Bangladesh are procuring their services
in the private sector, a proportion that has been rising steadily over the past ten years. In Thailand,
the civil servant health insurance plan excludes implants and intra-uterine devices from coverage.
In Indonesia, contraceptive counselling, except emergency contraception, is included in the National
Health Insurance benefits and commodities are provided by the National Family Planning Board.
In Cambodia, the full range of contraceptive services are included in the Ministry of Health service
packages, however only the poor are exempted from user fees. In Mongolia, the services are provided
free of charge to vulnerable groups only. The Social Health Insurance in Viet Nam does not cover any
contraceptive services, but family planning services are provided free of charge to ethnic minority
populations by the National Population Programme.
49
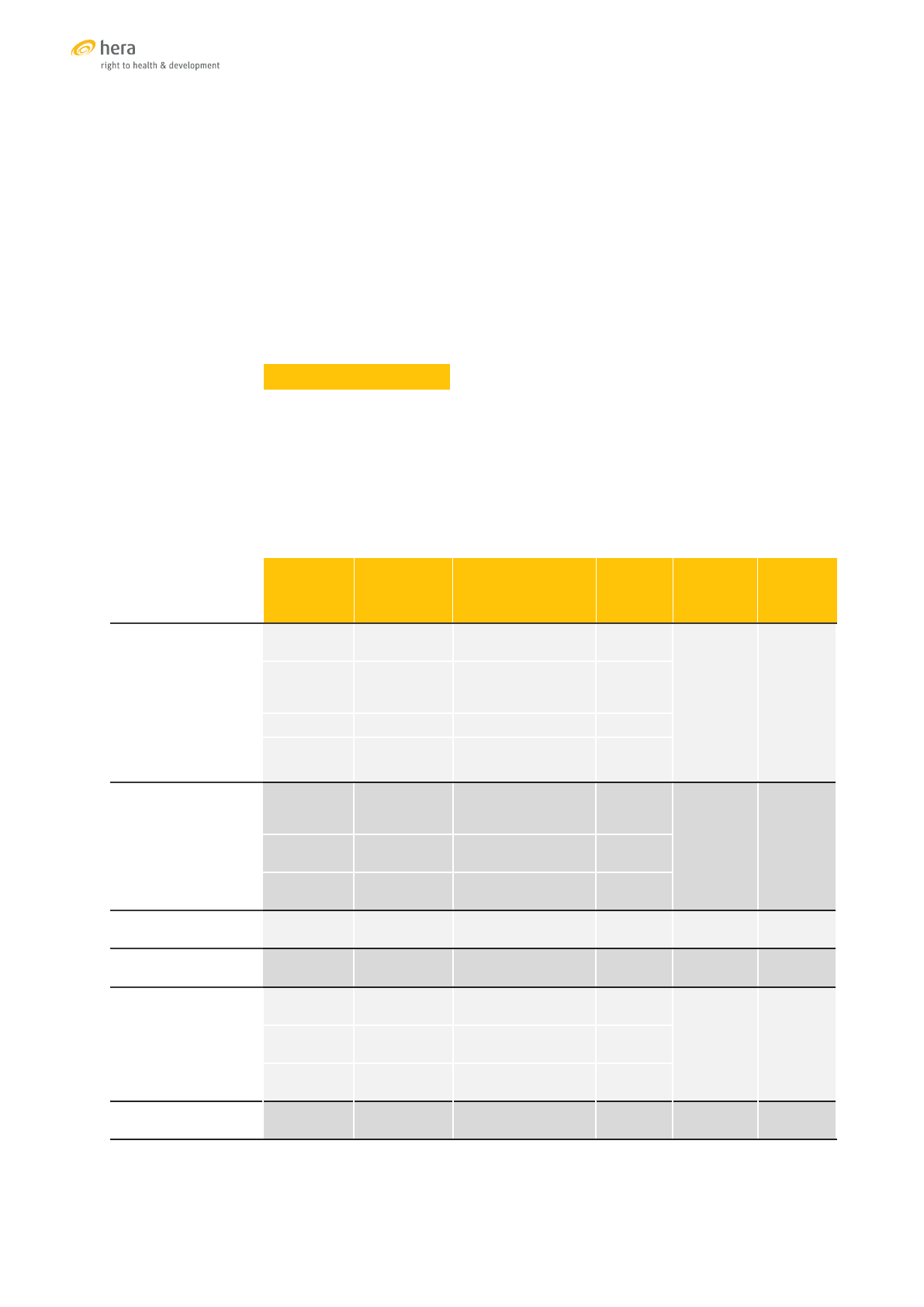
• Differences also exists in the coverage of primary and secondary prevention of
cervical cancer, although the main differences are in service coverage rather
than in the cost coverage. Nationwide HPV immunisation programmes do
not yet exist in any of the six study countries. Although most countries have
a national cervical cancer screening programme, only the programme in
Thailand reaches a significant coverage with 60 percent of the target, while
the next best coverage, in Mongolia, is only at 30 percent. HPV immunisation
is only included among the social health insurance benefits in Thailand and
Mongolia, and cervical cancer screening only in Thailand, Mongolia and
Indonesia. Bangladesh, however, provides the service without user charges
when it is available, and user-fee waiver programmes for the poor in Cambodia
may also apply to cervical cancer services.
POOLING OF FUNDS FOR UHC
While all six countries included in the study have a declared goal of a universal social
health insurance, other financial risk protection schemes exist. They all involve
some form of government subsidisation of health insurance funds to cover the poor,
vulnerable populations, and workers in the informal sectors. According to a recent
study, such initiatives exist in eight low- and middle-income countries in Asia with
a total of 14 different subsidisation schemes. [155] The current situation in the six
study countries is summarised in the table.
Financial risk protecon schemes and per person health expenditures
* Source: [6]
Scheme Start Targets
%
covered
Govt. per
person
health
expend.*
Per person
OOP
expend.*
Bangladesh
Maternal
Vouchers
2010
53 sub-districts
(26.5 million)
n/a
9 $ 21$
Micro
health
insurance
variable n/a n/a
SSK 2016 95,000 (pilot) n/a
Public FP
services
1970s All n/a
Cambodia
HEF 2000
Below naonal
poverty line
(2.7 million)
≈ 76%
14 $ 45 $User-fee
subsidies
2006 n/a n/a
SHI Just starng
Civil servants and
formal sector
n/a
Indonesia NHI 2014
Total populaon
(258 million)
≈ 66% 38 $ 47 $
Mongolia SHI 1995
Total populaon
(3 million)
> 95% 108 $ 81 $
Thailand
UCS 2001
≈ 73% of populaon
(48 million)
100%
177 $ 27 $SSS/CSMBS
≈ 24% of populaon
(16 million)
100%
MHI 2013
Migrants
(3.4 million)
≈ 40%
Viet Nam SHI 2008
Total populaon
(93.5 million)
70-
80%
77 $ 52 $
50

The contribution of insurance premiums to the funding pool differs from country
to country, with several schemes cross-subsidising health insurance membership
across income divides. But collecting premiums other than in the form of payroll
deductions is proving to be a challenge as demonstrated by the Viet Nam social health
insurance and the migrant health insurance in Thailand. For people who are not in
formal employment, the payment of insurance premiums is an important barrier of
access to financial protection.
Fragmentation is primarily an issue in Bangladesh and Cambodia. In both countries,
health services that are not paid by patients at the point of service are financed by
a mix of direct financing from the national health budget, as for instance the family
planning services in Bangladesh, and by third-party payment agents with or without
government budget support, such as the NGOs operating the health equity funds in
Cambodia or the micro-insurance plans in Bangladesh. Attempts to streamline the
purchasing function are being undertaken in Cambodia, although these are not as
extensive as the on-going initiative in Indonesia to create a single agency to pay for
all health services.
Relatively long-established social insurance pooling mechanisms that are financed
from a mix of premiums and government transfers exist in Viet Nam and Mongolia.
Both are acting in a tight fiscal space and are responding to this situation by limiting
the tariffs paid to service providers (in Viet Nam), or by eliminating premium subsidies
(for instance for students in Mongolia). The system in Mongolia has not been able
to chart any progress in reducing the role of out-of-pocket expenditures in health
financing, while the initially encouraging progress in Viet Nam has stalled over the
past three years.
Among the six sampled countries, Thailand is the only one that has achieved a
level of out-of-pocket financing for health comparable to established industrialised
economies through a non-selective system of enrolling all persons who cannot be
reached through their payroll in a government-funded insurance pool. Migrants are
the only exceptions, and a separate pooling system was established for them which
suffers some of the weaknesses of other premium-based systems, i.e. the difficulty
of registering and collecting premiums among people who are not fully integrated in
the formal economy.
Thailand also has the highest per capita income among the six countries. Government
expenditures in health are 13 times higher than in Cambodia and 20 times higher
than in Bangladesh. Thailand’s choice of using the national budget to finance a
universal coverage scheme that does not select by the type of service, nor by the
type of beneficiary, has clear equity and efficiency benefits, but it also has a cost. It
is difficult to conceive how such a high level of social protection could be achieved in
the poorer countries such as Bangladesh and Cambodia.
The relationship between a county’s economic wealth and the social protection
provided to its citizens, however, is not linear. This applies equally to universal
coverage of sexual and reproductive health services. In 2013, the ADB published
an assessment of the social protection index in Asia-Pacific in 2009. [156] The
numerator of the index is the sum of all public social protection expenditures for
social insurance, social assistance and labour market programmes per targeted
beneficiary. Social insurance, and especially social health insurance, dominates this
expenditure envelope. The denominator is calculated as one quarter of the GDP per
capita in local currency. This approximates the national poverty line in most countries
of the region and makes the index comparable across countries with different
economic core indictors.
51
Social Protecon Index 2009 in six APR countries
SPI
Mongolia
0.206
Viet Nam
0.137
Thailand
0.119
Indonesia
0.044
Bangladesh
0.043
Cambodia
0.020
Source: [156]
In the index, all public investments in social protection mechanisms, including social
health insurance, are aggregated. The data are quite old, dating back to 2009, and
predate major national UHC initiatives. Nevertheless, the table indicates the level
of government commitment to social spending. It was highest in the countries with
socialist political traditions, namely Mongolia and Viet Nam, where government
spending on social protection was equivalent to 21 and 14 percent of poverty level
incomes respectively. It was lowest in Indonesia, Bangladesh and Cambodia where
social insurance mechanisms were underdeveloped, a situation that has since
changed, especially in Indonesia.
Economic wealth and political commitment are main drivers for public investment
in social protection, but coverage is also determined by the efficiency of the system.
This is illustrated by an example from the Republic of Korea. Prior to 2000, three
types of health insurance funds existed in Korea with identical benefit schemes and
provider payments, but different levels and systems of premium contributions. In
2000, the three funds were merged into a single risk pool. An analysis in 2012 found
that the total administrative cost of social health insurance decreased from eight
percent in 1996 to less than 2.5 percent in 2008. Meanwhile, the coverage increased
from 90 percent of the population in 2000 to 96 percent in 2009. The savings in
administrative costs allowed an expansion of benefits, including for instance cancer
screening programmes, reduction of co-insurance rates for certain conditions, and
the establishment of a cumulative six-monthly ceiling for out-of-pocket expenditures.
[157]
While many countries in the region are striving towards the establishment of a
national social health insurance system that covers the entire population and
provides equitable financial risk protection, the situation of international migrants
remains precarious, including in countries that have achieved major progress towards
universal health coverage. In Malaysia, for instance, employers are required to provide
health insurance to all foreign workers, but many employers do not comply with this
regulation. Fully documented migrant workers in Thailand are entitled to be enrolled
in the Social Security Fund, as well as in the Workmen’s Compensation Fund, which
covers work-related injuries and illnesses. Despite this, among the approximately
one million documented migrants in 2013, only about one third were enrolled. [5]
Documented and undocumented migrants not enrolled in the Social Security Fund
have an option to join the Migrant Health Insurance scheme. Membership in this
scheme has been increasing, but in 2016 had only reached about one third of the
estimated number of migrants in the country. [158]
52

CONCLUSIONS AND RECOMMENDATIONS
The study sampled six countries in the region and does not claim to be representative.
It nevertheless generated a number of findings and recommendations that are
relevant for all countries in Asia-Pacific that are committed to achieving the UN
Sustainable Development Goals 3.7 (universal access to sexual and reproductive
health-care services) and 3.8 (universal health coverage, including financial
risk protection). Universal access to SRH services was explored according to an
existing framework of comprehensive services [3] with some modifications. Some
services listed in the framework, for instance infertility treatment and promotion
of breastfeeding were not included, as well as sexual health services for men who
have sex with men, transgender and intersex persons. Greater emphasis was placed
on a rights-based analysis, and on the acknowledgment of the limits of the health
sector contribution to sexual and reproductive health. This arose primarily from an
early analysis of data, showing major gaps in adolescent sexual health and in the
response to violence against women and girls. The study arrives at seven major
conclusions and recommendations that were discussed with the UNFPA Regional
and Country Offices, but for which the study team assumes full responsibility. They
do not necessarily reflect the views of UNFPA.
1. The health sector focus of UHC is too narrow to capture the SRH agenda
The agenda for sexual and reproductive health and rights extends beyond
the health sector. Addressing high levels of adolescent fertility, for instances,
requires changes in social norms to promote the rights and equality of girls
and to improve the access to information on sexual and reproductive health
and rights among adolescents. Preventing and responding to gender-based
violence requires the participation of many sectors, including education,
justice, social affairs and health. Such multi-sector responses cannot be
wrapped up under a single UHC agenda.
Universal health coverage is a health sector goal, a fact that is reinforced by the set
of indicators that have been adopted for its monitoring framework. The UHC lens on
the availability, quality, accessibility and affordability of health care is useful because
it focuses efforts within the sector. But the achievement of sexual and reproductive
health goals requires a wider lens. There are many priorities for achieving sexual
and reproductive health that cannot be pursued solely as part of a health sector
strategy. Health service providers and administrators need to know how to respond
to adolescent pregnancy and to gender-based violence, but most of the activities that
are necessary to confront these issues are not within their remit and competence.
Sexual and reproductive health is not a sub-goal within a UHC strategy, it is a separate
strategic domain with a potential for mutual reinforcement. A strategy to promote
sexual and reproductive health must also include many policies and programmes
that are not within the health sector and that should not be neglected in the pursuit
of health sector goals.
Recommendation 1: In defining and setting priorities for sexual
and reproductive
health at national and international level,
governments and development partners should acknowledge and
address the overlap and complementarity between UHC and SRH
strategies, as well as the areas that are out-of-scope for UHC. Issues
of sexual and reproductive health, especially for adolescents and key
population groups, should be addressed through actions in the health
sector and through actions outside the health sector.
53

2. Family planning services are excluded from social health insurance
schemes
There is a risk that the in pursuing UHC goals, decision-makers at national and
international level focus on improving curative health services at the expense of
prevention and health promotion. The exclusion of contraceptive services from
several national UHC schemes reviewed in this study is a concern, especially
as it affects the sexual and reproductive health and rights of adolescent girls.
An obstetric emergency can push a family into poverty if the health services have to
be pur
chased at the point of delivery. If the money is not available, the woman and/
or newborn child may die. The need of a 17-year old high school student to obtain an
effective contraceptive will not push anybody into immediate poverty. If there is no
money to pay for it, it will just be foregone. The consequence may be a pregnancy and
illegal abortion, and therefore, in the end, also a pregnancy-related death. While in
the first case a very direct relationship can be established between a mechanism that
pays for a life-saving service and the life saved, in the second case the relationship is
equally strong but less directly and immediately measurable.
National authorities who are monitoring household health expenditures may ask
why they should include contraceptive services and commodities among the
benefits of social health insurance or other financial risk protection schemes.
Purchasing contraceptives will never be a catastrophic health expenditure for an
individual or household. However, an unmet contraceptive need because of a
foregone expenditure has an impact in the short term on the realisation of sexual
and reproductive rights, in the medium term on increasing the probability of an
adverse reproductive outcome, and in the longer term on the sustainability of UHC
schemes by increasing future costs of covering health care expenditures related to
such outcomes.
Recommendation 2: Governments developing social health insurance
schemes under the UHC agenda should acknowledge the importance of
contraceptive services and act on it by including these services among
the insurance benefits. This is especially important for adolescents who
generally have a high unmet need for contraceptives, as well as a high rate
of unsafe termination of pregnancy. In the longer term, this will not only
contribute to meeting commitments to the sexual and reproductive rights of
young people, but also to the long-term sustainability of UHC schemes.
3. Insucient aenon is given to prevenon and ambulatory services
Emerging social health insurance schemes are not giving sufficient attention
to preventive services for sexual and reproductive health such as HPV
immunisation, cervical cancer screening and early treatment, micronutrient
supplementation during pregnancy, and HIV counselling and testing. Increasing
the offer and quality of prevention services and including them among the
social insurance benefits will contribute to the realisation of sexual and
reproductive health and rights as well as to the sustainability of UHC schemes.
UHC schemes like the social health insurance in Viet Nam or the SSK scheme that
is being piloted in Bangladesh, focus very strongly on covering in-patient hospital
services. These services are the most likely to generate catastrophic health
expenditures, and thereby produce immediately measurable effects on household
economies. Meanwhile, prevention services are continuing to be provided under
parallel financing arrangements, receiving more or less attention, often depending
on the availability of international funding.
As the move towards UHC also includes a move towards defragmentation of health
financing systems, there is a risk that the UHC agenda will leave important ambulatory
and preventive health services behind. They are, however, important components of a
comprehensive sexual and reproductive health strategy. Furthermore, when quality
prevention services are widely available and used, future savings on catastrophic
health expenditures will be realised, increasing the sustainability of UHC schemes.
54

Recommendation 3: As a part of a longer-term strategy under the UHC
agenda, governments should emphasise preventive services for sexual and
reproductive health, such as quality services for cervical cancer prevention,
prevention of micronutrient malnutrition among adolescent girls and
pregnant women, and prevention of HIV infection. These services should
be included among the social health insurance benefits, even if they are
currently funded by international partners or special programmes.
4. There is scope to improve the eciency and sustainability of UHC schemes
A history of international, national and local initiatives has left traces of different
types of social protection and health service purchasing arrangements in most
countries. Consolidating several initiatives under a single UHC umbrella can
create efficiencies that may be invested in the expansion of coverage and level
of protection. Schemes that aim at providing comprehensive and universal
coverage are less likely to make errors of omission without necessarily
generating major additional costs or revenue losses. Comprehensive and
universal coverage means providing a broad range of benefits while minimising
processes that control or limit access.
Fragmented financial risk pooling systems, social protection initiatives and provider
payment arrangements
were
observed in several countries included in the study, as
well as initiatives to gain efficiencies through defragmentation. All six countries in the
study have a number of parallel financial risk reduction schemes that predate their
commitment to UHC. These include directly government-funded health services,
demand-side financing programmes, community-based mutual funds, targeted user
fee exemptions, social and commercial health insurance.
Under the commitment to UHC, all six countries have started processes to
consolidate these schemes under a single coverage scheme. Consolidation and risk
pooling can generate efficiency savings that can then be applied to expanding
services and coverage. Despite mandatory health insurance coverage, more than
one in five Viet Namese citizens are uninsured because they cannot afford the
insurance premiums or gain access the government subsidy. In contrast, all
Thai citizens who are not insured through their place of employment are
automatically covered under a fully subsidised universal coverage scheme. Means
testing to decide on subsidy levels is avoided, as well as the difficult task of
collecting insurance premiums in the informal employment sector. The insurance
scheme may forego some premium revenue, but the amount is negligible
compared to the gain in efficiency, while 100 percent coverage is assured.
Parallel and sometimes overlapping systems to pay providers of maternity care,
family planning, STI control and HIV treatment exist in several countries, creating
inefficiencies and distortions. For instance, in some areas of Bangladesh with demand-
side financing schemes, excessively high caesarean section rates are recorded.
Several social insurance schemes are gradually expanding their range of benefits.
Indonesia added family planning services in 2016, Thailand gradually included all
HIV prevention and treatment services. The moves towards more comprehensive
coverage are likely to create efficiency savings and eliminate distortions.
Recommendation 4: Go
vernments should consider a bol
d approach to
creating universal access to financial risk reduction schemes without
complex eligibility requirements, premium structures and tiered subsidies
in order to achieve high coverage levels at minimal transaction costs. At
the same time, they should consider including all health services that
are currently funded through other domestic and international financing
mechanisms under a single financial risk reduction scheme, in order to
eliminate health systems distortions and avoid potential service gaps.
55

5. The coverage and nancial risk protecon for adolescent SRH services
needs more aenon
In several study countries, there is evidence that the sexual and reproductive
health service coverage for adolescents is lagging behind the general trend
of improved coverage. This applies especially to unmarried sexually active
adolescents. Gaps in availability, quality and acceptability of services are often
more important than insufficient financial risk protection. In the development
of UHC schemes, the special situation of adolescents should be kept in mind.
Adolescents do not necessarily have ready access to the financial resources of
the economic group in which they are categorised.
UHC initiatives and policies in the six study countries do not exclude adolescents that
otherwise are eligible for subsidised access to services or for insurance premium
subsidies. Nevertheless, adolescents in most countries are left behind in terms of
access and utilisation of contraception and other SRH services. Many countries have
started initiatives to make services more acceptable and accessible to adolescents.
It may still be too soon to see results. Yet, consideration should be given to the fact
that adolescents may not necessarily have full access to the financial resources of
the social and economic group in which they are classified. A young girl in a ‘rich’
household, whether in the position of wife or daughter, does not necessarily control
any financial resources herself. Adolescents therefore need special consideration
when subsidy schemes for services or insurance premiums are developed. Mongolia,
for instance, abolished its health insurance subsidy for students, a move that seems
counterintuitive in view of survey reports that point to significant gaps in the uptake
of services by adolescents.
Unmarried adolescents who are sexually active or whose sexual behaviour does
not fit cultural or social norms are often excluded from access to SRH services,
primarily for reasons related to how the services are being organised or delivered.
A survey among young people in Cambodia who were considered to belong to an ‘at
risk’ group, reported that only one third of young women and less than half of young
men with symptoms of a sexually transmitted infection sought medical treatment. A
study of women with complications following illegal abortions in Thailand reported
that one third of them were under the age of 19 years. Unmarried adolescents have
a particularly high unmet need for SRH services such as STI treatment, emergency
contraception, safe termination of pregnancy and post-abortion care.
Recommendation 5: Governments and development partners should be
reminded that providing SRH services for adolescents will, in the long run,
have a major impact on national SRH outcomes because they address key
issues at a time of highest vulnerability. They should therefore prioritise the
service offer and the financing of HPV immunisation, sexuality education and
access to contraception, including emergency contraception, that is provided
in a way that is acceptable and accessible to adolescents without social and
financial barriers.
6. Universal coverage of sexual and reproducve health care is not always
universal
The study documented several examples of SRH programmes and financial
risk protection schemes that target key populations and vulnerable groups
such as ethnic minorities, migrant workers or refugees. These examples,
however, document the exception rather than the rule. There are major
service coverage gaps that are reflected in health statistics, even in Thailand,
the country with the UHC system that has achieved the widest and most
comprehensive coverage among the countries in this report. Meeting national
targets for sexual and reproductive health will require that equity gaps are
narrowed, including the gaps that separate migrants from citizens and ethnic
minorities from the majority.
56

Some countries included in the study have developed and implemented schemes
to protect vulnerable populations from financial risks when seeking health care.
Thailand offers voluntary Migrant Health Insurance, even to undocumented migrants.
Viet Nam provides family planning services without charge to ethnic minority
communities. But statistics on service coverage and SRH outcomes collected among
such populations continue to show large differences to the national mean throughout
the region. Insufficient financial risk protection is usually not the only reason, and
also not the main reason. Structural issues of service delivery, culture, language,
geography and a distrust of authorities may be more important. A study in Viet Nam
reported that less than half of ethnic minority women who were in the possession
of a National Health Insurance card actually used it to access maternity services.
Addressing inequalities in SRH within countries requires a comprehensive targeted
approach to overcome all structural and cultural barriers, and that also includes
equitable access to financial risk protection schemes.
Recommendation 6: Governments that are rolling out national UHC schemes
should be fully aware of the SRH needs and the barriers to services among
groups and communities that have the longest way to travel towards
reaching the national SRH goals. Among others, they include the very large
populations of ethnic minorities, migrant workers and refugees in the Asia-
Pacific region. Closing the equity gap through inclusive and targeted health
programming should be a high priority.
7. Gaps in the evidence base constrain informed decision-making for UHC
and SRH
Assessments of progress towards UHC in sexual and reproductive health to
generate actionable information for decision-makers are constrained in most
countries by important information gaps. These include information about
service quality, and about reasons why clients do not always take advantage
of public services provided free of charge; information about the cost-drivers
for out-of-pocket expenditures; information about coverage of migrants and
other marginalised populations; and information about the households among
whom out-of-pocket expenditures for health constitute a serious financial risk.
The country studies documented that in several countries, public services provided
without charge are bypassed in favour of services by private, faith-based or NGO
providers that raise direct user charges. Quality and acceptability of services may
differ, but more information is required to understand why people are avoiding or
bypassing public sector SRH services.
Additional information gaps include the coverage of health services and social
protection mechanisms for international migrants and refugees. Furthermore, the
metric of ‘percent out-of-pocket expenditure of total health expenditure’ is a rough
measure that does not provide much actionable information. A breakdown of what
is purchased (consultations, surgery, laboratory services, medications, etc.) is often
available for general health services, but not for SRH. The proposed UHC indicator of
‘proportion of households with large household expenditures on health as a share of
total household expenditure or income’, is more informative. In future, data for this
indicator are likely to be collected more frequently and systematically, but they will
not provide information about user payments for SRH services.
The study documents that several countries in the Asia-Pacific region are pursuing
similar policies and goals in health financing and SRH service provision. Some have
embarked on this road many years ago, others have started more recently. A national
social health insurance, for instance, exists in Mongolia since 1994, was introduced
in Indonesia in 2014, and is currently being piloted in a small area of Bangladesh. In
a region that is characterised by increasing regional cooperation in many fields, this
provides an opportunity for south-south technical cooperation in order to learn from
each other in the development of national health systems.
57

Recommendation 7: To meet the information needs fo
r decision-making
governments partners should consider increasing the evidence-base for
UHC and SRH, including:
• Collecting evidence about the effect of out-of-pocket payments for SRH
services that are not covered by financial protection schemes because
the costs are not considered to be ‘catastrophic’, but that may constitute
significant financial barriers for individuals with little access to money,
including adolescents, migrants, and the very poor.
• Collecting evidence for reasons why even poor people in some countries
bypass public SRH services that are offered free of charge or that are
covered by social health insurance, and instead pay for services in the
private sector. Research questions should focus on the quality of public
services and on barriers of access for specific groups or populations of
users.
• Consider to systematically analyse SRH sub-accounts to identify specific
cost-drivers, such as consultation, laboratory services or commodities in
order to optimise the coverage of financial risk protection schemes.
• Expand regional partnerships and south-south technical cooperation
networks in order to maximise the potential of learning from the
experience of neighbouring countries.
58
REFERENCES
1. UN General Assembly (2015). Transforming our world: the 2030 Agenda for Sustainable
Development. (A/RES/70/1)
2. UN Statistics Division (20170. Report of the Inter-Agency and Expert Group on Sustainable
Development Goal Indicators (E/CN.3/2017/2), Annex III
3. Williams K, Warren C, Askew I (2010). Planning and Implementing an Essential Package of
Sexual and Reproductive Health Services. UNFPA and Population Council
4. UNFPA. asiapacific.unfpa.org/where-we-work (accessed 5/11/2016)
5. Economic and Social Commission for Asia and the Pacific (2015). Asia-Pacific Migration Report
2015: Migrants’ Contribution to Development. Bangkok, Thailand
6. WHO Global Health Expenditure Database (data for 2014) apps.who.int/nha/database (accessed
22/01/2017)
7. UNFPA World Population Dashboard (data for 2016) www.unfpa.org/world-population-
dashboard (accessed 22/01/2017)
8. Ministry of Health and Family Welfare (2012). Expanding Social Protection for Health: Towards
Universal Coverage - Health Care Financing Strategy 2012-2032. Dhaka, Bangladesh
9. Royal Government of Cambodia (2011). National Social Protection Strategy for the Poor and
Vulnerable. Phnom Penh, Cambodia
10. Royal Government of Cambodia (2016). National Social Protection Policy Framework 2016-2025.
Phnom Penh, Cambodia (unofficial translation as of August 03, 2016)
11. Republic of Indonesia (2004). Law 40 of 2004 Concerning the National Social Security System.
Jakarta, Indonesia
12. Ministry of Population Development and Social Protection Mongolia (2013). Long Term Strategy
for the Development of the Health insurance of Mongolia. Ulaanbaatar, Mongolia
13. National Health Security Office, Thailand (2002). National Health Security Act B.E. 2545.
Bangkok, Thailand
14. Viet Nam National Assembly (2008). Health Insurance Law of Viet Nam. Hanoi, Viet Nam
15. Viet Nam National Assembly (2014). Revised Health Insurance Law. Hanoi, Viet Nam
16. National Institute of Population Research and Training (NIPORT), Mitra and Associates, and
ORC Macro (2005). Bangladesh Demographic and Health Survey 2004. Dhaka, Bangladesh and
Calverton, Maryland, USA
17. National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF
International (2013). Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh and
Calverton, Maryland, USA
18. National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF
International (2016). Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh, and
Rockville, Maryland, USA
19. Ahmed S et al. (2015). Bangladesh health system review. Health Systems in Transition. 5 (3)
20. Guttmacher Institute (2012). Fact Sheet: Menstrual Regulation and Induced Abortion in
Bangladesh. New York, USA
21. Neuman et al. (2014). Prevalence and determinants of caesarean section in private and public
health facilities in underserved South Asian communities: cross-sectional analysis of data from
Bangladesh, India and Nepal. BMJ Open 2014; 4:e005982.doi:10.1136/bmjopen-2014-005982
22. Government of Bangladesh (2014). 2014 Progress Report on the status and response to HIV
submitted to UNAIDS. Dhaka, Bangladesh
23. ARROW (2016). Country profile on universal access to sexual and reproductive health:
Bangladesh. Dhaka, Bangladesh
59

24. Gavi Alliance (2015). Decision letter for the Bangladesh HPV demonstration vaccine project.
Geneva, Switzerland
25. Rahman M, et al. (2013). Health-related financial catastrophe, inequality and chronic illness in
Bangladesh. PLoS ONE 8(2): e56873. doi:10.1371/journal.pone.0056873
26. Ministry of Health and Family Welfare, Health Economics Unit (n.d). Shasthyo Suroksha
Karmasuchi (SSK): Step towards Universal Health Coverage. Dhaka, Bangladesh
27. Ministry of Health and Family Welfare, Health Economics Unit (2010). Economic Evaluation of
Demand-Side Financing (DSF) for Maternal Health in Bangladesh. Dhaka, Bangladesh
28. Ahmed S, Khan MM (2011). A maternal health voucher scheme: what have we learned from the
demand-side financing scheme in Bangladesh? Health Policy and Planning, 26(1), 25-32
29. Noor FR, Rob U (2014). Does maternal health voucher scheme have an impact on out-of-
pocket expenditure and utilization of delivery care services in rural Bangladesh? In Population
Association of America, 2014 Annual Meeting Program, May 1-3, 2014. Boston, MA
30. Giedion U, Alfonso EA, Diaz Y (2013). The impact of universal coverage schemes in the
developing world: a review of the existing evidence. UNICO Studies Series 25. Washington DC:
The World Bank Group
31. National Institute of Public Health, National Institute of Statistics and ORC Macro (2006).
Cambodia Demographic and Health Survey 2005. Phnom Penh, Cambodia and Calverton,
Maryland, USA
32. National Institute of Statistics, Directorate General for Health, and ICF Macro (2011). Cambodia
Demographic and Health Survey 2010. Phnom Penh, Cambodia and Calverton, Maryland, USA
33. National Institute of Statistics, Directorate General for Health, and ICF International (2015).
Cambodia Demographic and Health Survey 2014. Phnom Penh, Cambodia, and Rockville,
Maryland, USA
34. Annear LP (2015). Executive Summary. In Annear LP, et. al.: The Kingdom of Cambodia Health
System Review. Health Systems in Transition Vol. 5 No. 2 2015; Asia-Pacific Observatory on
Public Health Systems and Policies
35. Ministry of Health (2012). National Strategy for Reproductive and Sexual Health in Cambodia
2012-2016. Phnom Penh, Cambodia
36. Reproductive Health Association of Cambodia (2015). Country profile on universal access to
sexual and reproductive health: Cambodia. Phnom Penh, Cambodia
37. Liljestrand L, Sambath MR (2012). Socio-economic improvements and health system
strengthening of maternal care are contributing maternal mortality reduction in Cambodia.
Reproductive health matters 20(39):62-72; Doi: 10.1016/SO968-8080(12)39620-1
38. Petitet PH, et al. (2015). Toward safe abortion access: an exploratory study of medical abortion
in Cambodia. Reproductive Health Matters, Supplement (44):47–55; Doi: 10.1016/S0968-
8080(14)43826-6
39. Malaria Consortium (2013). Rapid Assessment of Malaria in Pregnancy in the Greater Mekong
Sub-Region Cambodia, Thailand and Myanmar (Burma). London, UK
40. Ministry of Health Cambodia (2014). National Guidelines for Managing Violence Against Women
and Children in the Health System. Phnom Penh, Cambodia
41. Chhun ER, Nachtnebel M (2015). Financing. In Annear L. P, et. al., The Kingdom of Cambodia
Health System Review. Health Systems in Transition Vol. 5 No. 2 2015; Asia-Pacific Observatory
on Public Health Systems and Policies
42. Badan Pusat Statistik-Statistics Indonesia and ORC Macro (2003). Indonesia Demographic and
Health Survey 2002-2003. Calverton, Maryland, USA
43. Badan Pusat Statistik-Statistics Indonesia and Macro International (2008). Indonesia
Demographic and Health Survey 2007. Calverton, Maryland, USA
44. Badan Pusat Statistik-Statistics Indonesia, National Population and Family Planning Board,
Kementerian Kesehatan, and ICF International (2013). Indonesia Demographic and Health
Survey 2012. Jakarta, Indonesia
60

45. Hodge A, Firth S, Marthias T, Jimenez-Soto E (2014). Location matters: Trends in inequalities in
child mortality in Indonesia. Evidence from repeated cross-sectional surveys. PLoS ONE 9(7).
e103597
46. Data from FP 2020 database: www.familyplanning2020.org/ (accessed 17/12/2016)
47. Information provided by UNFPA Country Office, Indonesia (January 2017)
48. Republic of Indonesia (2009). Law 36 of 2009: Health Law. Jakarta, Indonesia
49. Ministry of Health (2015). Rencana Strategis Kementerian Kesehatan (Health Strategic Plan)
Tahun 2015-2019. Jakarta, Indonesia
50. Data from UNAIDS: aidsinfo.unaids.org/ (accessed 17/12/2016)
51. WHO (2014). Report on global sexually transmitted infection surveillance 2013. Geneva,
Switzerland
52. HPV Info Centre (2016). Human Papillomavirus and Related Diseases Report: Indonesia
Summary Report 15 December 2016
53. Republic of Indonesia (2012). Roadmap toward the National Health Insurance 2012-2019. (Brief
Edition). Jakarta, Indonesia
54. Badan Penyelenggara Jaminan Sosial: bpjs-kesehatan.go.id/bpjs/ (accessed 17/12/2016)
55. National Statistical Office, UNICEF (2007). Mongolia Child and Development 2005 survey (MICS-
3), Final Report. Ulaanbaatar, Mongolia
56. National Statistical Office, UNICEF (2013). Mongolia Child and Development 2010 survey (MICS-
4), Final Report. Ulaanbaatar, Mongolia
57. National Statistical Office, UNICEF (2015). Mongolia Social Indicator Sample Survey-2013
(Multiple Indicator Cluster Survey), Final Report. Ulaanbaatar, Mongolia
58. Ministry of Health and UNFPA (2016). Situation analysis of family planning in Mongolia.
Ulaanbaatar, Mongolia
59. Centre for Health Development (2015). Health Indicators for 2015. Ulaanbaatar, Mongolia
60. National Center for Communicable Diseases (2014). Narrative Country Report for Global AIDS
Response Progress Reporting 2014. Ulaanbaatar, Mongolia
61. HPV Information Centre (2016). Human Papillomavirus and Related Diseases Report in
Mongolia. Summary Report 7 October 2016
62. Bruni L, et al. (2016). Human Papillomavirus and related diseases report: MONGOLIA. Summary
Report. ICO HPV Information Centre, Barcelona, Spain
63. WHO WPRO www.wpro.who.int/mongolia/mediacentre/vaccine/en/ (accessed 14/1/2017)
64. UNFPA Mongolia (2016). Annual Report 2015. Ulaanbaatar, Mongolia
65. Bayarsaikhan D, et al. (2016). Social health insurance development in Mongolia: Opportunities
and challenges in moving towards Universal Health Coverage. International Social Security
Review, 68(4)
66. Asian Development Bank. (2010). Access to health services for disadvantaged groups in
Ulaanbaatar, Situation analysis report, JFPR 9115-MON. Ulaanbaatar, Mongolia
67. World Health Organisation (2010). Policy brief on Financial Burden of Health Payments.
Ulaanbaatar, Mongolia
68. Bredenkamp C, et al. (2012) Mongolia - Health equity and financial protection report. Health
equity and financial protection report. World Bank Group, Washington DC, USA
69. Javkhlanbayar D, et al. (2016). Catastrophic health expenditure and impoverishment in
Mongolia. International Journal for Equity in Health, 15:105. DOI 10.1186/s12939-016-0395-8
70. National Statistical Office and UNICEF (2006). Thailand Multiple Indicator Cluster Survey 2005-
2006, Final Report. Bangkok, Thailand
71. National Statistical Office and UNICEF (2013). Thailand Multiple Indicator Cluster Survey 2012,
Final Report. Bangkok, Thailand
61

72. National Statistical Office and UNICEF (2016). Thailand Multiple Indicator Cluster Survey 2015-
2016, Final Report. Bangkok, Thailand
73. Department of Health (2011). Study on Family Planning Management System in Thailand.
Bangkok, Thailand
74. Ekachai S (2016). Hypocrisy holds back use of abortion pills. Bangkok Post, September 28, 2016.
Bangkok, Thailand
75. Chaturachinda K (2014). Unsafe Abortion in Thailand: Roles of RTCOG. Thai Journal of Obstetrics
and Gynaecology. 22:1
76. Sidibé M, Singh PK (2016). Thailand eliminates mother-to-child transmission of HIV and syphilis
(commentary). Lancet online doi.org/10.1016/S0140-6736(16)30787-5
77. Reuters News October 3, 2016. www.reuters.com/article/us-health-zika-thailand-
idUSKCN1230HX
78. National AIDS Management Center (2015). Thailand AIDS Response Progress Report 2015.
Bangkok, Thailand
79. Wilailak S, et al, (2016). The epidemiologic status of gynecologic cancer in Thailand. Journal of
Gynecologic Oncology.27, 6: doi.org/10.3802/jgo.2016.27.265
80. Sanghvi H, et al. (2008). Scale-Up, Performance and Quality in the Cervical Cancer Prevention
Program in Thailand: Results from the Outcomes Research Study. Baltimore, Maryland, USA
81. Klinsupa W (no date). HPV Vaccine introduction in Thailand. Expanded Program on
Immunization, Ministry of Health Thailand. Available at www.eiseverywhere.com/file_
uploads/7a51c93d87fa9a3600be1cc8 05d5941a_WorrawanKlinsupa.pdf
82. UN Women. www.unwomen.org/en/news/stories/2013/4/thailand-launches-one-stop-crisis-
centre-to-respond-to-violence-against-women (accessed 17/12/2016)
83. National Health Security Office (2015). Annual Report: Fiscal Year 2014. Bangkok, Thailand
84. Health Insurance Research Office (2012). Thailand’s Universal Coverage Scheme: An
independent assessment of the first 10 years (20012010) Synthesis report. Bangkok, Thailand
85. Guinto RLLR, et al. (2014). Universal health coverage in ‘One ASEAN’: are migrants included?
Global Health Action, 8, 25749
86. McMichael C, Healey J (2017). Health equity and migrants in the Greater Mekong Sub region.
Global Health Action, 10, 1271594
87. Committee for Population, Family and Children and ORC Macro (2003). Viet Nam Demographic
and Health Survey 2002. Calverton, Maryland, USA
88. General Statistical Office and UNICEF (2011). Viet Nam Multiple Indicator Cluster Survey 2011,
Final Report, Hanoi, Viet Nam
89. General Statistics Office and UNICEF (2015). Viet Nam Multiple Indicator Cluster Survey 2014,
Final Report. Hanoi, Viet Nam
90. Tuan PL (2015). Vietnam health system and health infrastructure: achievements, challenges
and orientation. www.designandhealth.com/upl/files/122262/pam-le-tuan-2015.pdf (accessed
17/01/2017)
91. Duc NHC, Nakamura K, Kizuki M, Seino K, Rahman M (2015). Trends in inequalities in utilization
of reproductive health services from 2000 to 2011 in Viet Nam. Journal of Rural Medicine, 10(2),
65–78
92. UN DESA (2017). World Contraceptive Use 2017. www.un.org/en/development/desa/population/
publications/dataset/contraception/wcu2017.shtml (accessed 14/7/2017)
93. UNFPA, CCIHP, ISMS (2016). National survey on sexual and reproductive health among
Vietnamese adolescents and young adults aged 10-24. Hanoi, Viet Nam
62

94. Ministry of Health (2017). National Action Plan for Cervical Cancer Prevention and Control, 2016-
2025, Hanoi, Viet Nam
95. Viet Nam Social Security (2017). National Social Health Insurance Report 2016. Hanoi, Viet Nam
96. Vuong DA, et al. (2014). Determining the impacts of hospital cost-sharing on the uninsured
near-poor households in Viet Nam. International Journal for Equity in Health, 13, 40
97. Kutzin J (2013). Health financing for universal coverage and health system performance:
concepts and implications for policy. Bulletin World Health Organisation, 91, 602–611
98. UN Department of Economic and Social Affairs (2015). World Fertility Patterns 2015: Data
Booklet. New York, USA
99. UNFPA (2016). Universal access to reproductive health: Progress and challenges. New York, USA
100. UNSTAT MDG Indicators. mdgs.un.org/unsd/mdg/default.asp (accessed 20/01/17) (updated with
more recent reports)
101. Warakamin S, Boonthai N, Tangcharoensathien V (2004). Induced abortion in Thailand: Current
situation in public hospitals and legal perspectives. Reproductive Health Matters, 12(24
Supplement), 147-156
102. Centre for Reproductive Rights. www.worldabortionlaws.com (accessed 18/1/2017)
103. Guttmacher Institute (2017). Fact Sheet: Menstrual regulation and unsafe abortion in
Bangladesh. www.guttmacher.org/fact-sheet/menstrual-regulation-unsafe-abortion-
bangladesh
104. Institute for Health Metrics and Evaluation. vizhub.healthdata.org/mdg/ (accessed 14/07/2017)
105. World Health Organization (2016). WHO recommendations on antenatal care for a positive
pregnancy experience. Geneva, Switzerland
106. United Nations (2015). The Millennium Development Goals Report 2015. New York, USA
107. National Institute of Population Studies and ICF International (2013). Pakistan Demographic and
Health Survey 2012-13. Islamabad, Pakistan, and Calverton, Maryland, USA
108. National AIDS Authority of Cambodia (2014). 6th Country Report on Global AIDS Response
Progress Reporting. Phnom Penh, Cambodia
109. WHO Global Health Observatory Database. apps.who.int/gho/data/node.main.A1358STI?lang=en
(accessed 20/1/2017)
110. Ministry of Health of Cambodia (2016). Emergency Obstetric and Newborn Health Improvement
Plan 2016-2020. Phnom Penh, Cambodia
111. World Health Organization (2010). Technical consultation on postpartum and postnatal care.
Geneva, Switzerland
112. UNAIDS (2016). Global AIDS update 2016. Geneva, Switzerland
113. World Health Organization (2016). Global health sector strategy on sexually transmitted
infections 2016-2020. Geneva, Switzerland
114. Baigalmaa J, et al. (2012). Increasing syphilis notifications in Mongolia: results from national
surveillance for 2001–2011. Western Pacific Surveillance and Response Journal, 3(4),86–93
115. World Health Organization (1997). Management of sexually transmitted diseases at district and
primary health care level. Regional Office for South East Asia, New Delhi, India
116. Ministry of Education, Youth and Sports (2011). Cambodia Most at Risk Young People Survey
2010. Phnom Penh, Cambodia
117. WHO IARC. globocan.iarc.fr/old/FactSheets/cancers/cervix-new.asp (accessed 27/01/2017)
(Combined statistics for the WHO Southeast Asia and Western Pacific Regions which roughly
correspond to the UN Asia-Pacific Region)
63

118. Forouzanfar MH, et al. (2011). Breast and cervical cancer in 187 countries between 1980 and 2010: A
systematic analysis. Lancet, 378, 1461-1484
119. de Sanjosé S, et al. (2007). Worldwide prevalence and genotype distribution of cervical human
papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infectious Diseases, 7,
453-459
120. TreatAsia, amfAR (2016). Cervical cancer, Human Papillomavirus and HPV Vaccines in Southeast Asia.
Bangkok, Thailand
121. World Health Organization (2014). Meeting of the Strategic Advisory Group of Experts on immunization,
April 2014 – conclusions and recommendations. Weekly epidemiological record, 89, 221-236
122. Bruni L, et al. (2016). Global estimates of human papillomavirus vaccination coverage by region and
income level: a pooled analysis. Lancet Global Health, 4, e453–63
123. PATH International (2012). HPV vaccination in Southeast Asia: Lessons learned from a pilot program in
Viet Nam. Seattle, USA
124. World Health Organization (2015). Strategic framework for the comprehensive control of cancer cervix
in South-East Asia Region. Regional Office for South East Asia, New Delhi, India
125. EPOS (2016). Cambodia: Positive Impact of Cervical Cancer Screening Programme. On-line publication.
www.epos.de/news/current-news/cambodia-positive-impact-cervical-cancer-screening-programme
(accessed 27/1/2017)
126. Bruni L, et al. (2016). Human Papillomavirus and related diseases report: INDONESIA. Summary
Report. ICO HPV Information Centre, Barcelona, Spain
127. Centres for Disease Control and Prevention (2015). Increasing cervical cancer screening coverage in the
United States and abroad. Atlanta, USA
128. Ministry of Health of Mongolia (2007). National Cancer Control Program 2007-2017. Ulaanbaatar,
Mongolia
129. Bruni L, et al. (2016). Human Papillomavirus and related diseases report: THAILAND. Summary Report.
ICO HPV Information Centre, Barcelona, Spain
130. Huy NVC (2014). Establishing cervical cancer screening programs in low-resource settings: experiences
from Vietnam. Presentation, World Cancer Congress 2014, Melbourne Australia
131. WAVE, UNFPA (2014). Strengthening Health System Responses to Gender-based Violence in Eastern
Europe and Central Asia: A Resource Package. Istanbul, Turkey
132. UNFPA (2010). Health sector response to gender-based violence: An assessment of the Asia-Pacific
Region. Bangkok, Thailand
133. Lokuge K, et al. (2016) Health Services for Gender-Based Violence: Médecins Sans Frontières
Experience Caring for Survivors in Urban Papua New Guinea. PLoS ONE 11(6): e0156813
134. Grundy J, et al. (2013). Improving average health and persisting health inequities—towards a justice and
fairness platform for health policy making in Asia. Health Policy and Planning, 29, 873–882
135. UNFPA (2016). Universal access to reproductive health: Progress and challenges. New York, USA
136. Kongsri (2011). Equity of access to and utilization of reproductive health services in Thailand: national
Reproductive Health Survey data, 2006 and 2009
137. Economic and Social Commission for Asia and the Pacific (2016). Sustaining Progress on Population and
Development in Asia and the Pacific: 20 years after ICPD. Bangkok, Thailand
138. University of Toronto, Mekong Development Research Institute (2016). Exploring Barriers to Accessing
Maternal Health and Family Planning Services in Ethnic Minority communities in Viet Nam. Hanoi, Viet
Nam
139. Goland E, et al. (2012). Inequity in maternal health care utilization in Viet Nam. International Journal for
Equity in Health, 11(1), 1
140. International Labour Organisation (2015). Global estimates of migrant workers and migrant domestic
workers: results and methodology. Geneva, Switzerland
64

141. UN Human Rights Office of the High Commissioner. Status of ratification. https://indicators.
ohchr.org/ (accessed 25/8/2017)
142. Low WY, Tong WT, Binns C (2015). Migrant Workers in Asia-Pacific and Their Rights to Health.
Asia-Pacific Journal of Public Health, 27(6), 584–587
143. Lasimbang H.B, et al. (2016). Migrant workers in Sabah, East Malaysia: The importance of
legislation and policy to uphold equity on sexual and reproductive health and rights. Best
Practice & Research Clinical Obstetrics and Gynaecology 32 (2016) 113:123
144. ILO Sub-regional Office for East Asia. (2009). Mandatory HIV testing for employment of migrant
workers in eight countries of South-East Asia: From discrimination to social dialogue. Bangkok,
Thailand
145. Huguet J, Chamratrithirong A, Natalie C (2012). Thailand at a crossroads: challenges and
opportunities in leveraging migration for development. IOM Migration Policy Institute Issue in
Brief No.6
146. Webber GC, et al. (2016). Migrant Beer Promoters’ Experiences Accessing Reproductive Health
Care in Cambodia, Laos, Thailand, and Viet Nam: Lessons for Planners and Providers. Asia-
Pacific Journal of Public Health, 27(2)
147. UNFPA Cambodia. (2015). Sexual and reproductive health and rights: Migrant garment factory
workers in Cambodia. Phnom Penh Cambodia
148. Sudhinaraset M, et al (2016). Influence of internal migration on reproductive health in Myanmar:
results from a recent cross-sectional survey. BMC Public Health (2016) 16:246
149. Benner (2010). Reproductive health and quality of life of young Burmese refugees in Thailand.
Conflict and Health 2010, 4:5
150. OECD, Eurostat, WHO (2017). A system of health accounts 2011: Revised edition March 2017.
Paris, France
151. Ministry of Public Health of Afghanistan (2013). National health accounts with subaccounts for
reproductive health 2011/12. Kabul, Afghanistan
152. Ministry of Health and Social Welfare of Tanzania (2012). National health accounts with
subaccounts for HIV/AIDS, malaria, reproductive health, and child health 2010. Dar es Salaam,
Tanzania
153. Ministry of Health of Malawi (2014). National heath accounts with subaccounts for HIV/AIDS,
malaria, reproductive health, and child health 2009/10, 2010/11, and 2011/12. Lilongwe, Malawi
154. Somanathan A, et al. (2014). Moving toward universal coverage of social health insurance in Viet
Nam: Assessment and options. World Bank, Washington, USA
155. Vilcu I, Probst L, Bayarsaikhan D, Mathauer I (2016). Subsidized health insurance coverage of
people in the informal sector and vulnerable population groups: trends in institutional design in
Asia. International Journal for Equity in Health, 15, 165
156. Asian Development Bank (2013). The Social Protection Index: Assessing Results for Asia and the
Pacific. Mandaluyong City, Philippines
157. Yip W, Hafez R (2015). Reforms for improving the efficiency of health systems: Lessons from ten
country cases. WHO, Geneva, Switzerland
158. Tangcharoensathien V, Thwin AA, Patcharanarumol W (2017). Implementing health insurance
for migrants, Thailand. Bulletin of the World Health Organisation, 95, 146–15
65

Progress in the International
Health Partnership & Related
Initiatives (IHP+)
2014
Performance
Report
PRODUCED BY:
hera
Laarstraat 43, 2840 Reet, Belgium
Tel. +32 38445930
www.hera.eu
UNIVERSAL
HEALTH COVERAGE
FOR SEXUAL AND REPRODUCTIVE
HEALTH IN THE ASIA-PACIFIC
REGION
Lorem ipsum
UNIVERSAL
HEALTH COVERAGE
FOR SEXUAL AND REPRODUCTIVE
HEALTH IN THE ASIA-PACIFIC
REGION
September 2017
