Theme:
Financing
Marie Stopes
Evidence Brief
Country focus:
Ghana
Who pays for family planning? Taking a step
towards national health insurance coverage
IN BRIEF
Family planning is often
forgotten when countries
develop their national health
insurance systems.
In Ghana, provision was
made for “any relevant FP
packages” in the 2012 revised
National Health Insurance
Authority (NHIA) act – but it
has never been implemented.
So Marie Stopes Ghana
has been running a pilot to
demonstrate how it is possible
to integrate family planning
into the existing National
Health Insurance Scheme.
It will run for two years but
early results are already
shedding light on how best to
implement similar approaches
in the future.
THE CHALLENGE
Getting family planning in national
health insurance
In Ghana the NHIA is working with GHS and private providers to
make services available to the whole population, but FP is not
included in the package of services on offer and there is no clarity
on how to pay providers to make it available.
Marie Stopes International’s experience of nancing and delivering
family planning services has shown that, for effective provision of
family planning to happen, those nancing services need to take
into account the 4 Ps of:
We are gathering
valuable lessons
on how to integrate
family planning into
national insurance
schemes
WHAT WE DID
Integrating paid family planning
We are gathering valuable lessons on how to integrate family
planning into national insurance schemes to test the effective
integration of paid family planning services into the primary
health care package.
The pilot aims to demonstrate how best to integrate case-based
payments into existing systems, with a particular emphasis on
long acting reversible contraceptive (LARC) services.
People (who is included)
Provider (which are nanced)
Package (is each FP service addressed?)
Payment (how are services paid for)
WHAT WE DID
The early results
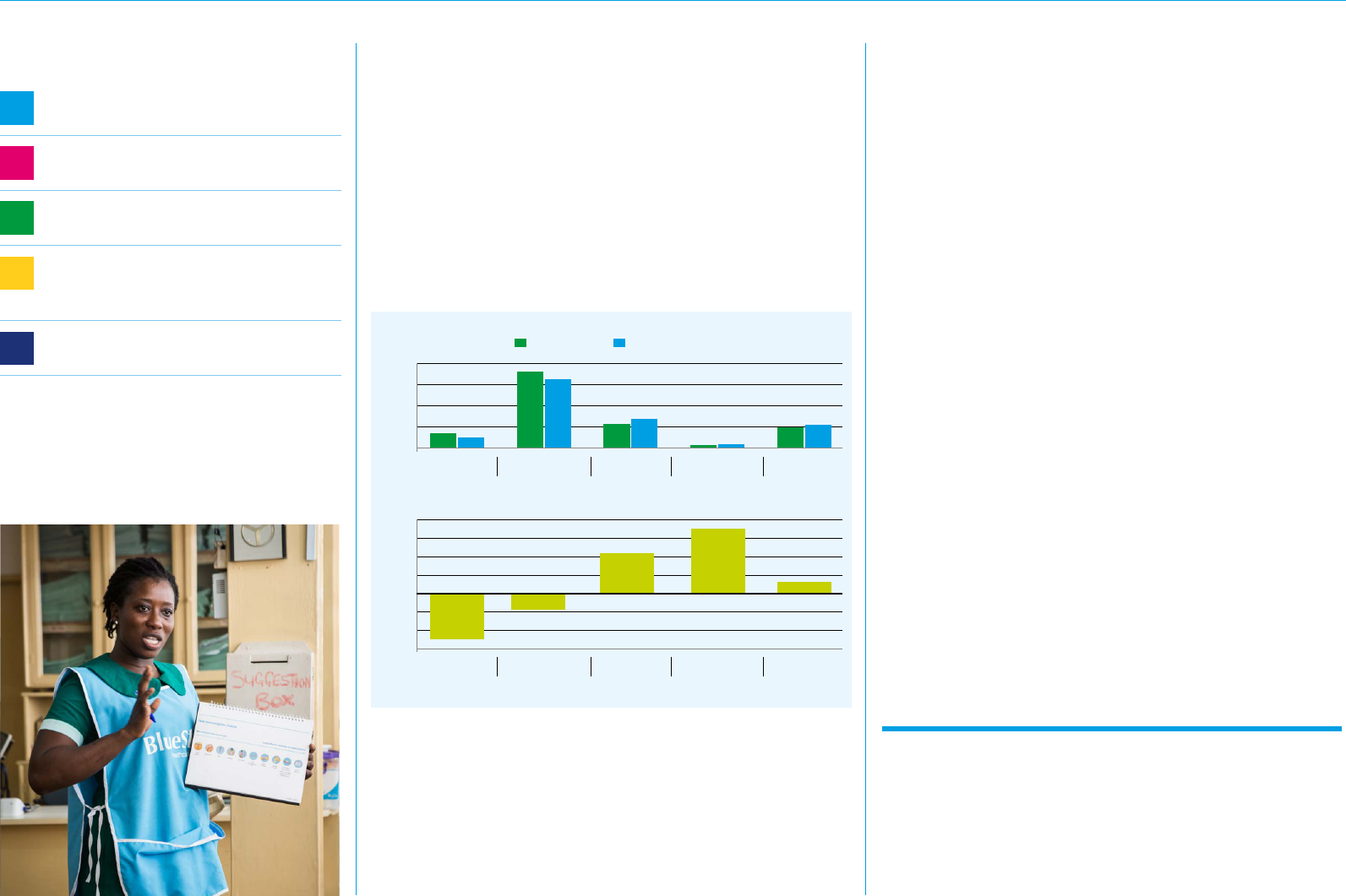
Although it is too early to address the overarching questions this pilot
attempts to answer, a monitoring team made up of NHIA, GHS, Population
Council and MSIG has identied some interesting initial ndings.The pilot
covered all NHIA accredited service providers and payments are made for
all contraceptive methods requiring clinical delivery. Participating public and
private providers are reimbursed through the NHIA payment systems for
each implant, IUD or injectable service provided. After just three months,
we’ve seen a net positive increase in uptake of long term methods. Clients
choosing these more effective methods over short-term methods, which
have decreased in the same period.
WHAT THIS MEANS
Where do we go from here?
The FP pilot experienced some initial operational challenges, but
there have been enough positives and gained insights that will help
shape a national roll-out.
We have seen that you need to have innovative approaches in order
to reach the poor with contraceptive services. In addition to the early
results described above we’ve learned some valuable lessons about
the ‘how’ of doing this type of work, such as:
• Include contraception from the start – to successfully
integrate family planning into a benets package, the ‘how’ of
including contraception should be thought through very carefully
by applying the 4Ps mentioned above at the design stage.
• Understand stakeholders’ views – to help anticipate
potential stakeholders interests and responses and strategise
on whether and how to address them.
• Be patient – the complexities of family planning, particularly
any cultural barriers, are not always understood so a level
of learning should be integrated as part of the pilot to inform
the national scale up plan.
• Be exible – key elements of a pilot project may not be fully
dened upfront; changes will continue to be made as new
information comes in.
This pilot still has some time to run before delivering the answers
to the questions it set out to address which, we hope, will help
shape the NHIA’s decision on formally integrating FP into the
NHIS package. In the meantime we hope that lessons learned
in Ghana can inform similar decisions that are being made as
health insurance packages are developed in countries across
the region and beyond.
Where can I nd more information?
For more information on Marie Stopes International and
the work that we do please contact:
T +44 (0)20 7636 6200 • [email protected]
Alternatively, visit our website: www.mariestopes.org
Registered charity number: 265543
© Marie Stopes International 2018
Who pays for family planning? Taking a step towards national health insurance coverage Ghana | Financing
During the development phase we
wanted to know:
1
Which FP methods should be included in the
National Health Insurance package?
2
What should be integrated in the case-based
reimbursement tariff?
3
How do we ensure contraceptive
commodity security?
4
How do we avoid perverse effects?
(e.g. providers leaning towards provision
of short term methods for nancial gains)
5
How do we ensure contraceptive choice
for clients?
— Feb-Apr 2018 — May-Jul 2018
500
-20%
0
-30%
1000
-10%
20%
1500
0%
30%
2000
10%
40%
Cumulative new FP uptake
Percentage change in new FP uptake
New acceptors
of Norigynon
New acceptors
of Norigynon
New Acceptors
of Depo Provera
New Acceptors
of Depo Provera
New Acceptors
of Implanon
New Acceptors
of Implanon
New acceptors of
Copper-T (IUD)
New acceptors of
Copper-T (IUD)
New acceptors
of Jadelle
New acceptors
of Jadelle
Although 3 months data is very early days yet to make any conclusive
inference, it does point to a shift from short acting methods (Norigynon
and Depo Provera) to long-acting reversible contraceptives (LARC) – even
though the case-based tariffs for injectables serve as an incentive for
providers to learn towards its provision. It further supports our assumption
that the removal of out-of-pocket cost will shift FP uptake from cheaper
but less effective methods (short acting methods) to expensive but more
effective methods (LARCs). However, with some of the challenges in the
start up it is too early to draw denite conclusions from this.
FP method results from 3 months after 1st May for 7 pilot districts
Participating public and private providers
are reimbursed through the NHIA payment
system for each implant, IUD or injectable
service provided – including payment for
comprehensive FP counselling and provision
of the chosen method.
