OXFORDMEDICALPUBLICATIONS
OxfordHandbookofRheumatology
PublishedandforthcomingOxfordHandbooks
OxfordHandbookfortheFoundationProgramme3e
OxfordHandbookofAcuteMedicine3e
OxfordHandbookofAnaesthesia2e
OxfordHandbookofAppliedDentalSciences
OxfordHandbookofCardiology
OxfordHandbookofClinicalandLaboratoryInvestigation3e
OxfordHandbookofClinicalDentistry4e
OxfordHandbookofClinicalDiagnosis2e
OxfordHandbookofClinicalExaminationandPracticalSkills
OxfordHandbookofClinicalHaematology3e
OxfordHandbookofClinicalImmunologyandAllergy2e
OxfordHandbookofClinicalMedicine—MiniEdition8e
OxfordHandbookofClinicalMedicine8e
OxfordHandbookofClinicalPharmacy
OxfordHandbookofClinicalRehabilitation2e
OxfordHandbookofClinicalSpecialties8e
OxfordHandbookofClinicalSurgery3e
OxfordHandbookofComplementaryMedicine
OxfordHandbookofCriticalCare3e
OxfordHandbookofDentalPatientCare2e
OxfordHandbookofDialysis3e
OxfordHandbookofEmergencyMedicine4e
OxfordHandbookofEndocrinologyandDiabetes2e
OxfordHandbookofENTandHeadandNeckSurgery
OxfordHandbookofExpeditionandWildernessMedicine
OxfordHandbookofGastroenterologyandHepatology
OxfordHandbookofGeneralPractice3e
OxfordHandbookofGenitourinaryMedicine,HIV,andSexualHealth2e
OxfordHandbookofGeriatricMedicine
OxfordHandbookofInfectiousDiseasesandMicrobiology
OxfordHandbookofKeyClinicalEvidence
OxfordHandbookofMedicalSciences
OxfordHandbookofNephrologyandHypertension
OxfordHandbookofNeurology
OxfordHandbookofNutritionandDietetics
OxfordHandbookofObstetricsandGynaecology2e
OxfordHandbookofOccupationalHealth
OxfordHandbookofOncology3e
OxfordHandbookofOphthalmology
OxfordHandbookofPaediatrics
OxfordHandbookofPalliativeCare2e
OxfordHandbookofPracticalDrugTherapy2e
OxfordHandbookofPre-HospitalCare
OxfordHandbookofPsychiatry2e
OxfordHandbookofPublicHealthPractice2e
OxfordHandbookofReproductiveMedicineandFamilyPlanning
OxfordHandbookofRespiratoryMedicine2e
OxfordHandbookofRheumatology3e
OxfordHandbookofSportandExerciseMedicine
OxfordHandbookofTropicalMedicine3e
OxfordHandbookofUrology2e

OxfordHandbookof
Rheumatology
FourthEdition
GavinClunie
ConsultantRheumatologistandMetabolicBonePhysician,
Addenbrooke’sHospital,Cambridge,UK
NickWilkinson
ConsultantPaediatricandAdolescentRheumatologist,
EvelinaLondonChildren’sHospital,London,UK
ElenaNikiphorou
ConsultantRheumatologist,WhittingtonHospital;
ClinicalResearcher,AcademicRheumatologyDepartment,
King’sCollegeLondon,UK
DeepakJadon
ConsultantRheumatologistandDirectorofthe
RheumatologyResearchUnit,
Addenbrooke’sHospital,Cambridge,UK

GreatClarendonStreet,Oxford,OX26DP,UnitedKingdom
OxfordUniversityPressisadepartmentoftheUniversityofOxford.
ItfurtherstheUniversity’sobjectiveofexcellenceinresearch,scholarship,andeducationbypublishing
worldwide.OxfordisaregisteredtrademarkofOxfordUniversityPressintheUKandincertainother
countries
©OxfordUniversityPress2018
Themoralrightsoftheauthorshavebeenasserted
FirstEditionpublishedin2002
SecondEditionpublishedin2006
ThirdEditionpublishedin2011
FourthEditionpublishedin2018
Impression:1
Allrightsreserved.Nopartofthispublicationmaybereproduced,storedinaretrievalsystem,or
transmitted,inanyformorbyanymeans,withoutthepriorpermissioninwritingofOxfordUniversity
Press,orasexpresslypermittedbylaw,bylicenceorundertermsagreedwiththeappropriatereprographics
rightsorganization.Enquiriesconcerningreproductionoutsidethescopeoftheaboveshouldbesenttothe
RightsDepartment,OxfordUniversityPress,attheaddressabove
Youmustnotcirculatethisworkinanyotherformandyoumustimposethissameconditiononany
acquirer
PublishedintheUnitedStatesofAmericabyOxfordUniversityPress
198MadisonAvenue,NewYork,NY10016,UnitedStatesofAmerica
BritishLibraryCataloguinginPublicationData
Dataavailable
LibraryofCongressControlNumber:2017960672
ISBN978–0–19–872825–2
eISBN978–0–19–104394–9
OxfordUniversityPressmakesnorepresentation,expressorimplied,thatthedrugdosagesinthisbookare
correct.Readersmustthereforealwayschecktheproductinformationandclinicalprocedureswiththemost
up-to-datepublishedproductinformationanddatasheetsprovidedbythemanufacturersandthemost
recentcodesofconductandsafetyregulations.Theauthorsandthepublishersdonotacceptresponsibility
orlegalliabilityforanyerrorsinthetextorforthemisuseormisapplicationofmaterialinthiswork.
Exceptwhereotherwisestated,drugdosagesandrecommendationsareforthenon-pregnantadultwhois
notbreast-feeding
LinkstothirdpartywebsitesareprovidedbyOxfordingoodfaithandforinformationonly.Oxford
disclaimsanyresponsibilityforthematerialscontainedinanythirdpartywebsitereferencedinthiswork.

Foreword
I am pleased to introduce you to the 4th edition of the Oxford Handbook of
Rheumatology. This edition has increased in size, but continues to be just as
accessible. It presents the reader with a pragmatic approach to making a
differentialdiagnosis.Theapproachtothinkingabouthowtomakesenseofthe
history and clinical findings is clear. The common rheumatological conditions
are covered well, and the new edition incorporates relevant sections on
paediatricandadolescentrheumatology.
FromthedaysofSirWilliamOsler,theartoflisteningtoandobservingthe
patient has been a key focus of what defines a good doctor. Medicine has
advancedconsiderablysincehisday,butthecorevaluesofaphysicianhavenot
changed.
The focus on good clinical history taking and examination technique is a
reminderofthecoreskillsetthatweuseasphysicians.Whenallelsefails,go
backto thebasicprinciples,andback tothepatient.Thisbook showsushow
importantthatskillsetis.
ProfessorJaneDacreMD,PRCP
President
RoyalCollegeofPhysicians
London,UK

Preface
Rheumaticmusculoskeletalconditionsarecommonbothingeneralandhospital
practice.Musculoskeletalsymptomsareaprimaryfeatureofmanymultisystem
illnesses,not onlyintheautoimmunejointandconnective tissuediseases, but
alsometabolic,endocrine,neoplastic,andinfectiousconditions.Symptomsare
also common in the context of injury, age-related change, and psychological
distress.Manyconditionsinrheumatologyareamajorsourceofmorbidityand
mortality.
We have kept the format of the previous edition for this version but
importantly have updated the text to include paediatric and adolescent
rheumatology.
Part I remains as a guide to evaluation of rheumatic and musculoskeletal
disease from the point of referral and reflects the way clinical
problems/symptomspresenttotheclinicianinreallife.Wehaveconsideredhow
this happens for adults, and new in this version, for children and adolescents,
affected by rheumatological and musculoskeletal disease. The reader will find
detail on musculoskeletal anatomy and functional anatomy in this part of the
book.
PartIIremainsasthesectionofthebookwherethereadercanfinddisease-
specificinformation(e.g.spondyloarthritis,vasculitis,backpain,andsoon).We
have included paediatric sections in each chapter where there is relevance for
disease occurring in children and adolescents, noting the difference in disease
anditsmanagementinchildrenandadolescentscomparedwithadults.
PartIIIremainsasmedicinemanagementandcontainschaptersondrugsused
inrheumatologypractice,glucocorticoidinjectiontherapy,andrheumatological
emergencies.
Wehavetriedtoavoidduplicationbutcrossreferencebetweenchapters.We
hopethisbookishelpfulandinformativeforalldoctors,physiotherapists,and
specialistnursingpractitionerswhoarefacedwithmanagingpeopleandpatients
with undiagnosed musculoskeletal symptoms or established rheumatic
musculoskeletaldiseases.

Acknowledgements
Theauthorswouldliketoacknowledgetheworkoftheco-founderauthor-editor
of the textbook Dr Alan Hakim for his contribution, whom together with Dr
Clunie,devisedandwrotethebookfromthefirsteditionandco-author-editorDr
InamHaq(whojoinedforthe2ndand3rdeditions),inhelpingtoestablishthe
Oxford Handbook of Rheumatology as the market leader small textbook for
rheumatology.
Contents
Contributors
Symbolsandabbreviations
PartIThepresentationofrheumaticdisease
1 Evaluatingrheumatologicalandmusculoskeletalsymptoms
2 Musculoskeletalassessmentandpatternsofdisease:makingaworking
diagnosis
3 Regionalmusculoskeletalsymptoms:makingaworkingdiagnosis
4 Thespectrumofdisordersassociatedwithadultrheumaticand
musculoskeletaldiseases
PartIITheclinicalfeaturesandmanagementofrheumaticdiseases
5 Rheumatoidarthritis
6 Osteoarthritis
7 Crystal-inducedmusculoskeletaldisease
8 Thespondyloarthritidesincludingpsoriaticarthritis
9 Juvenileidiopathicarthritis
10 Systemiclupuserythematosus
11 Antiphospholipidsyndrome
12 Sjögren’ssyndrome
13 Systemicsclerosisandrelateddisorders
14 Idiopathicinflammatorymyopathiesincludingpolymyositisand
dermatomyositis
15 Primaryvasculitides
16 Metabolicbonediseases
17 Infectionandrheumaticdisease
18 Rareautoinflammatoryandmiscellaneousdiseases
19 Hereditarydisordersofconnectivetissue
20 Commonupperlimbmusculoskeletallesions
21 Spinaldisordersandbackpain
22 Chronicpainsyndromes
PartIIIMedicinemanagementandemergencies
23 Drugsusedinrheumatologypractice
24 Glucocorticoidinjectiontherapy
25 Rheumatologicalemergencies
Index

Contributors
DrEmmaDavies
SpecialistRegistrarinRheumatology,RoyalNationalHospitalforRheumatic
Diseases,Bath,UK
DrCatherineFairris
SpecialistRegistrarinRheumatology,RoyalNationalHospitalforRheumatic
Diseases,Bath,UK
DrShabinaHabibi
SeniorClinicalResearchFellow,RoyalNationalHospitalforRheumatic
Diseases,Bath,UK
DrPhilipHamann
PhDResearchFellow&SpecialistRegistrarinRheumatology,RoyalNational
HospitalforRheumaticDiseases,Bath,UK
DrDobrinaHull
SpecialistRegistrarinRheumatology,GuysandStThomas’HospitalNHS
FoundationTrust,London,UK
DrEiphyuHtut
SpecialistRegistrarinRheumatology,Addenbrooke’sHospital,Cambridge
UniversityHospitalsNHSFoundationTrust,Cambridge,UK
DrAnthonyIsaacs
SpecialistRegistrarinRheumatology,TheWhittingtonHospitalNHSTrust,
London,UK
DrRituMalayia
SpecialistRegistrarinRheumatology,GuysandStThomas’HospitalNHS
FoundationTrust,London,UK
DrSerainaPalmer
FellowinPaediatricRheumatology,Kinderspital,Zürich,Switzerland
DrElizabethReilly
SpecialistRegistrarinRheumatology,RoyalNationalHospitalforRheumatic
Diseases,Bath,UK
DrMalihaSheikh
SpecialistRegistrarinRheumatology,Addenbrooke’sHospital,Cambridge
UniversityHospitalsNHSFoundationTrust,Cambridge,UK
DrGiuliaVarnier
FellowinPaediatricRheumatology,EvelinaLondonChildren’sHospital,Guys
andStThomas’HospitalNHSFoundationTrust,London,UK
DrNatashaWeisz
SpecialistRegistrarinRheumatology,TheWhittingtonHospitalNHSTrust,
London,UK
DrCeeYiYong
SpecialistRegistrarinRheumatology,NorfolkandNorwichUniversityHospitals
NHSFoundationTrust,Norwich,UK
Symbolsandabbreviations
cross-reference
α alpha
β beta
↑ increased
↓ decreased
↔ normal
> greaterthan
< lessthan
~ approximately
∴ therefore
AAV ANCA-associatedvasculitis
ABA abatacept
AC adhesivecapsulitis
ACA anticentromereantibody
ACE angiotensin-convertingenzyme
AChA acrodermatitischronicumatrophicans
AC(J) acromioclavicular(joint)
ACL anticardiolipin
ACPA anticitrullinatedpeptideantibody(-ies)
ACR AmericanCollegeofRheumatology
AD autosomaldominant
ADM abductordigitiminimi
AFF atypicalfemoralfracture
AICTD autoimmuneconnectivetissuedisease
AIS autoinflammatorysyndrome
AKI acutekidneyinjury
ALNT anterolateralneospinothalamictract
ALP alkalinephosphatase
ALT alaninetransaminase
AMA amyloidA
AML amyloidL
ANA antinuclearantibody
ANCA antineutrophilcytoplasmicantibody
Anti-β2GP1 anti-β2glycoprotein-1
AOSD adult-onsetStill’sdisease
AP anteroposterior
APB abductorpollicisbrevis
APL abductorpollicislongus
APL antiphospholipid
APRIL aproliferationinducing-ligand
APS antiphospholipid(antibody)syndrome
APTT activatedpartialthromboplastintime
AR autosomalrecessive
ARA AmericanRheumatismAssociation
ARB angiotensinIIreceptorblocker
ARDS adultrespiratorydistresssyndrome
ARTEMIS AbataceptTreatmentinPolymyositisandDermatomyositistrial
AS ankylosingspondylitis
ASAS AssessmentofSpondyloarthritisInternationalSociety
AST aspartatetransaminase
ASOT antistreptolysinOtitre
ASU avocado/soybeanunsaponifiable
ATN acutetubularnecrosis
axSpA axialspondyloarthritis
AZA azathioprine
β2GP1 β2glycoprotein-1
BAFF B-cellactivatingfactor(seealsoBLyS)
BAL bronchoalveolarlavage
BCP basiccalciumphosphate(crystals)
BD Behçet’sdisease
bDMARD biologicdisease-modifyingantirheumaticdrug
BILAG BritishIslesLupusAssessmentGroup
BLyS B-lymphocytestimulator(seealsoBAFF)
BMC bonemineralcontent
BMD bonemineraldensity
BMI bodymassindex
BSR BritishSocietyofRheumatology
BVAS BirminghamVasculitisActivityScore
C cervical(e.g.C6isthesixthcervicalvertebra)
CA coracoacromial
CADM clinicallyamyopathicdermatomyositis
CAMPS CARD14-mediatedpsoriasis
CANDLE chronicatypicalneutrophilicdermatosiswithlipodystrophyand
elevatedtemperature
cAPS catastrophicantiphospholipidsyndrome
CAPS cryopyrin-associatedperiodicfeversyndromes
CARD caspaseactivationandrecruitmentdomain
CBT cognitiveandbehaviouraltherapy
CCP cycliccitrullinatedpeptide
CDAI ClinicalDiseaseActivityIndex
CHB congenitalheartblock
CHCC ChapelHillConsensusConference
CINCA chronic,infantile,neurological,cutaneous,andarticular
syndrome
CK creatinekinase
CKD chronickidneydisease
CMC(J) carpometacarpal(joint)
CMP comprehensivemetabolicpanel
CMV cytomegalovirus
CNO chronicnon-bacterialosteomyelitis
CNS centralnervoussystem
COMP cartilageoligomericmatrixprotein
COX cyclooxygenase
CPP calciumpyrophosphate
CPPD calciumpyrophosphatedeposition
CREST calcinosis,Raynaud’s,(o)esophagealdysmotility,sclerodactyly,
telangiectasia(syndrome)
CRMO chronicrecurrentmultifocalosteomyelitis
CRP C-reactiveprotein
CRPS complexregionalpainsyndrome
CS congenitalscoliosis
CSF cerebrospinalfluid
CT computedtomography
CTX collagenX-link
cTnC cardiactroponinC
cTnT cardiactroponinT
CTS carpaltunnelsyndrome
CWP chronicwidespreadpain
CXR chestradiograph
CYC cyclophosphamide
DAS DiseaseActivityScore
dcSScl diffusecutaneoussystemicsclerosis
DIC diffuseintravascularcoagulation
DILE drug-inducedlupuserythematosus
DIP(J) distalinterphalangeal(joint)
DIRA deficiencyofIL-1receptoragonist
DISH diffuseidiopathicskeletalhyperostosis
DITRA deficiencyofinterleukin36receptorantagonist
DLCO diffusioncapacityforcarbonmonoxide
DOMS delayed-onsetmuscularstrain
DM dermatomyositis
DMARD disease-modifyingantirheumaticdrug
DVT deepveinthrombosis
DXA dual-energyX-rayabsorptiometry
EA enteropathicarthritis
EANM EuropeanAssociationofNuclearMedicine
EBV Epstein–Barrvirus
ECG electrocardiogram
ECM erythemachronicummigrans
ECRB extensorcarpiradialisbrevis
ECRL extensorcarpiradialislongus
ECU extensorcarpiulnaris
ED extensordigitorum
EDL extensordigitorumlongus
EDM extensordigitiminimi
EDS Ehlers–Danlossyndrome
EED erythemaelevatumdictinum
EHL extensorhallucislongus
EI extensorindicis
EGPA eosinophilicgranulomatosisandpolyangiitis
ELISA enzyme-linkedimmunosorbentassay
ELMS Eaton–Lambertmyasthenicsyndrome
EM erythemamigrans
EMG electromyography
EN erythemanodosum
ENA extractablenuclearantigen
ENT ear,nose,andthroat
EPB extensorpollicisbrevis
EPL extensorpollicislongus
ERA enthesitis-relatedarthritis
ESR erythrocytesedimentationrate
ESSG EuropeanSpondyloarthropathyStudyGroup
EULAR EuropeanLeagueAgainstRheumatism
F female
FBC fullbloodcount
FCAS familialcoldautoinflammatorysyndrome
FCR flexorcarpiradialis
FCU flexorcarpiulnaris
FD fibrousdysplasia
FDA FoodandDrugAdministration
18
F-FDG
fluorine-18fluorodeoxyglucose
FDL flexordigitorumlongus
FDP flexordigitorumprofundus
FDS flexordigitorumsuperficialis
FENa fractionalexcretionofsodium
FFS Five-FactorScore
FGF fibroblastgrowthfactor
FHB flexorhallucisbrevis
FHH familialhypocalciurichypercalcaemia
FJ facetjoint
FLS FractureLiaisonService
FM fibromyalgia
FMF familialMediterraneanfever
FPL flexorpollicislongus
FR flexorretinaculum
FVSG FrenchVasculitisStudyGroup
GALS gait,arms,legs,spine(examination)
GARA gut-associatedreactivearthritis
GBS Guillain–Barrésyndrome
GC glucocorticoid
GCA giantcellarteritis
GFR glomerularfiltrationrate
GH(J) glenohumeral(joint)
GI gastrointestinal
GIO glucocorticoid-inducedosteoporosis
GLA gammalinoleicacid
GOA generalizedosteoarthritis
GORD gastro-oesophagealrefluxdisease
HA hydroxyapatite
HAQ HealthAssessmentQuestionnaire
HCQ hydroxychloroquine
HDCT hereditarydisorderofconnectivetissue
h-EDS hypermobility(type)Ehlers–Danlossyndrome
HELLP haemolysis,elevatedliverenzymes,andlowplatelets
HIDS hyperIgDsyndrome
HIV humanimmunodeficiencyvirus
HLA humanleucocyteantigen
HMG-COA 3-hydroxy-3-methyl-glutaryl-coenzymeA
HPOA hypertrophicpulmonaryosteoarthropathy
HPT hyperparathyroidism
HRT hormonereplacementtherapy
HSCT haematopoieticstemcelltransplantation
HSP Henoch–Schönleinpurpura
HUS haemolyticuraemicsyndrome
HTLV humanT-cellleukaemiavirus
IA intra-articular
IBD inflammatoryboweldisease
IBM inclusion-bodymyositis
ICD implantablecardioverterdefibrillator
IFN interferon
IgG4-RD immunoglobulinG4-relateddisease
IGRA interferongammareleaseassay
IIM idiopathicinflammatorymyopathy
IL interleukin
ILAR InternationalLeagueofAssociationsforRheumatology
ILD interstitiallungdisease
IM intramuscular(ly)
IMM idiopathicinflammatorymyopathy
INR internationalnormalizedratio
IP interphalangeal
ISCD InternationalSocietyofClinicalDensitometry
ISG InternationalStudyGroup
ISN InternationalSocietyforNephrology
ITB iliotibialband
IV intravenous(ly)
IVDU intravenousdruguser
IVIg intravenousimmunoglobulin
JAK Januskinase
JAS juvenileankylosingspondylitis
JCA juvenilechronicarthritis
JDM juveniledermatomyositis
JIA juvenileidiopathicarthritis
JIIM juvenileidiopathicinflammatoryarthritis
JIO juvenileidiopathicosteoporosis
JPM juvenilepolymyositis
JPsA juvenilepsoriaticarthritis
JRA juvenilerheumatoidarthritis
JSLE juvenilesystemiclupuserythematosus
JSpA juvenilespondyloarthritis
KD Kawasakidisease
KUB kidneyureterbladder
L lumbar(e.g.L5isthefifthlumbarvertebra)
LA lupusanticoagulant
LCL lateralcollateralligament
lcSScl limitedcutaneoussystemicsclerosis
LDA low-doseaspirin(75–150mg/day)
LDH lactatedehydrogenase
LE lupuserythematosus
LEF leflunomide
LFTs liverfunctiontests
LGL largegranularlymphocyte
LH luteinizinghormone
LHE lateralhumeralepicondylitis
LIP lymphocyticinterstitialpneumonitis
LLLT low-levellasertherapy
LMWH low-molecular-weightheparin
M male
MAA myositis-associatedautoantibodies
MAGIC mouthandgenitalulcerswithinflamedcartilage
MAS macrophageactivationsyndrome
MCL medialcollateralligament
MCP(J) metacarpophalangeal(joint)
MCTD mixedconnectivetissuedisease
MDI MyositisDiseaseIndex
MDP methylenediphosphonate
MDT multidisciplinaryteam
MEN mycophenolatemofetil
MEVK mevalonatekinase
MFS Marfansyndrome
MG myastheniagravis
MHC majorhistocompatibilitycomplex
MKD mevalonatekinasedeficiency
MMF mycophenolatemofetil
MMPI MinnesotaMultiphasicPersonalityInventory
MMT manualmuscletest
mNY modifiedNewYork
MPA microscopicpolyangiitis
MPO myeloperoxidase
MR magneticresonance
MRA magneticresonanceangiography
MRI magneticresonanceimaging
MSA myositis-specificautoantibodies
MSK musculoskeletal
MSU monosodiumurate
MTP(J) metatarsophalangeal(joint)
MTX methotrexate
MUA manipulationunderanaesthesia
MVA mevalonicaciduria
MVK mevalonatekinase
MWS Muckle–Wellssyndrome
MYOACT myositisdiseaseactivityindex
MYODAM myositisdamageindex
NAI non-accidentalinjury
NCS nerveconductionstudy
NICE NationalInstituteforHealthandCareExcellence(UK)
NLE neonatallupuserythematosus
NLRs NOD-likereceptors
NMS neuromuscularscoliosis
NO nitrousoxide
NOAC noveloralanticoagulant
NOD nucleotide-bindingoligomerizationdomain
NOMID neonatal-onsetmultisysteminflammatorydisease
NSAID non-steroidalanti-inflammatorydrug
NSF nephrogenicsystemicfibrosis
OA osteoarthritis
OI osteogenesisimperfecta
OMIN OnlineMendelianInheritanceinMan
ONFH osteonecrosisofthefemoralhead
OO osteoidosteoma
OT occupationaltherapist
PAH pulmonaryarteryhypertension
PAMPS pathogen-associatedmolecularpatterns
PAN polyarteritisnodosum
PAPA pyogenicarthritis,pyodermagangrenosum,andacne
PBC primarybiliarycirrhosis
PCR polymerasechainreaction
PDB Paget’sdiseaseofbone
PDE5 phosphodiesterasetype5
PE pulmonaryembolism
PET positronemissiontomography
PFAPA periodicfever,aphthousstomatitis,pharyngitis,adenitis
syndrome
PHP pseudohypoparathyroidism
PIN posteriorinterosseousnerve
PIP(J) proximalinterphalangeal(joint)
PL palmarislongus
PM polymyositis
PML progressivemultifocalleucoencephalopathy
PMN polymorphonuclearneutrophil
PMR polymyalgiarheumatica
PoTS posturalorthostatictachycardiasyndrome
PRR pattern-recognitionreceptor
Ps psoriasis
PsA psoriaticarthritis
PSA prostatic-specificantigen
PTH parathyroidhormone
PUO pyrexiaofunknownorigin
PV plasmaviscosity
PVNS pigmentedvillonodularsynovitis
RA rheumatoidarthritis
RAID rareautoinflammatorydisease
RAPS rivaroxabanforantiphospholipidantibodysyndrome
RCT randomizedcontrolledtrial
RD Raynaud’sdisease
ReA reactivearthritis
RF rheumatoidfactor
RhF rheumaticfever
RNA ribonucleicacid
RNP ribonuclearprotein
ROD renalosteodystrophy
RP relapsingpolychondritis
RPS RenalPathologySociety
RSD reflexsympatheticdystrophy(algo/osteodystrophy)
RSI repetitivestraininjury
RS
3
PE remittingseronegativesymmetricalsynovitiswithpittingoedema
RTA renaltubularacidosis
RTX rituximab
sACE serumangiotensinconvertingenzyme
SAI subacromialimpingement
SAA serumamyloidA
SADAI SimplifiedDiseaseActivityIndex
SAPHO synovitis,acne,palmoplantarpustulosis,hyperostosis,aseptic
osteomyelitis(syndrome)
SARA sexuallyacquiredreactivearthritis
SC subcutaneous
SC(J) sternoclavicular(joint)
Scl systemicscleroderma
SCS spinalcordstimulation
SD standarddeviation
sDMARD syntheticdisease-modifyingantirheumaticdrug
SERM selectiveoestrogenreceptormodulator
SHPT secondaryhyperparathyroidism
SI(J) sacroiliac(joint)
SIP SicknessImpactProfile
SLE systemiclupuserythematosus
SLEDAI SystemicLupusErythematosusDiseaseActivityIndex
SLICC SystemicLupusInternationalCollaboratingcriteria
SNRI serotonin-norepinephrinere-uptakeinhibitors
SoJIA systemic-onsetjuvenileidiopathicarthritis
SpA spondyloarthritis
SRC sclerodermarenalcrisis
SRP signalrecognitionpeptide
SS Sjögren’ssyndrome
SScl systemicsclerosis
SSRI selectiveserotoninreuptakeinhibitor
SSZ sulfasalazine
STIR shorttauinversionrecovery
SUA serumuricacid
SUFE slippedupperfemoralepiphysis
T thoracic(e.g.T5isthefifththoracicvertebra)
TA Takayasuarteritis
TB tuberculosis
TCZ tocilizumab
TENS transcutaneouselectricalnervestimulation
TFT thyroidfunctiontest
TGF transferringgrowthfactor
TIA transientischaemicattack
TLRs Toll-likereceptors
TM(J) temporomandibular(joint)
TNFα tumournecrosisfactor(alpha)
tPA tissueplasminogenactivator
TPMT thiopurineS-methyltransferase
TRAPS tumournecrosisfactor-associatedperiodicsyndrome
TSH thyroid-stimulatinghormone
TTP thromboticthrombocytopenicpurpura
U&E ureaandelectrolytes(inUKtestincludescreatinine)
UC ulcerativecolitis
uPCR urineprotein:creatinineratio
US ultrasound
UV ultraviolet
VAS visualanaloguescale
VDI VasculitisDamageIndex
vs versus
WBC whitebloodcell
WHO WorldHealthOrganization
WRD work-relateddisorder
XLHR X-linkedhypophosphataemicrickets

Chapter1
Evaluatingrheumatologicalandmusculoskeletal
symptoms
Introduction
Musculoskeletalpaininadults
Elicitedpainonexaminationinadults
Otherpresentingsymptomsinadults
Theadultgait,arms,legs,spine(GALS)screeningexamination
Painassessmentinchildrenandadolescents
Limpandgaitconcernsinchildrenandadolescents
Pyrexia, fatigue and unexplained acute-phase response in children and
adolescents
ThepaediatricGALSscreen
Introduction
Adultsandchildrencanpresentwithmusculoskeletal(MSK),inflammatory,and
autoimmunediseasesinvariedways.Symptomscanbesimpleandfocal,suchas
regionalpain,orgeneralandnon-specific,ofteninthecontextofageneralized
processsuchasfeverorfatigue.Thefollowingareimportantpointsinassessing
thetime,type,andnatureofpresentation:
• Whysomeonehaspresentedataparticulartime.
• Whatistheimpactofsymptoms,emotionallyandfunctionally.
• The individual’s perceptions, fears, or cultural references that might modify
(amplifyorsuppress)expressionofthesymptoms.
• What fears, beliefs, and factors might present a barrier to effective medical
engagement.
• The same pathological processes might present variably at different ages:
broadlyspeaking,theyoung,adults,andtheelderly.
Inthischapter,theassessmentofsymptomshasbeenseparatedintotwoparts.
First,theassessmentofsymptomsinadultsandsecond,thepatternsofdisease
presentationinchildrenandadolescents.
Musculoskeletalpaininadults
Introduction
Themostcommonpresentingsymptomtotherheumatologistisunexplainedor
ineffectivelytreatedMSKpain.
• Painisdefinedbyitssubjectivedescription,whichmayvarydependingonits
physical(orbiological)cause,thepatient’sunderstandingofit,itsimpacton
function,andtheemotionalandbehaviouralresponseitinvokes.
• Painisparticularlypronetobe‘coloured’bycultural,linguistic,andreligious
differences.Therefore,painisnotmerelyanunpleasantsensationtomany;it
is,ineffect,an‘emotionalchange’.
• Painexperienceisdifferentforeveryindividual.
Localizationofpain
Adultsusuallylocalizepainaccurately,althoughtherearesomesituationsworth
notinginrheumaticdiseasewherepaincanbepoorlylocalized(Table1.1):
• Adults maynotclearly differentiate between periarticularand articularpain,
referringtobursitis,tendonitis,andotherformsofsofttissueinjuryas‘joint
pain’.Therefore,itisimportanttoconfirmthepreciselocationofthepainon
physicalexamination.
• Pain maybewell localizedbut causedbya distantlesion, e.g.interscapular
pain caused by mechanical problemsinthecervicalspine,or right shoulder
paincausedbyacutecholecystitis.
• Paincausedbyneurologicalabnormalities,ischaemicpain,andpainreferred
fromvisceraisharderforthepatienttovisualizeorexpress,andthehistory
maybegivenwithvariedinterpretations.
• Bone pain is generally constant despite movement or change in posture—
unlikemuscular,synovial,ligament,ortendonpain—andoftendisturbssleep.
Fracture, tumour, and metabolic bone disease are all possible causes. Such
constant,local,sleep-disturbingpainshouldalwaysbeinvestigated.
• PatternsofpaindistributionareassociatedwithcertainMSKconditions.For
example,polymyalgiarheumatica(PMR)typicallyaffectstheshouldergirdle
andhips, whereasrheumatoidarthritis (RA)affectsthe jointssymmetrically,
withapredilectionforthehandsandfeet.
• Patternsofpaindistributionmayoverlap,especiallyintheelderly,whomay
have several conditions simultaneously, e.g. hip and/or knee osteoarthritis
(OA), peripheral vascular disease, and degenerative lumbar spine all may
causelowerextremitydiscomfort.
Table1.1Clinicalpointersinconditionsinadultswherepainispoorlylocalized
Diagnosis Clinicalpointer
Periarticular
shoulderpain
Referredtodeltoidinsertion—notspecificforlesion
buttypicalinrotatorcufflesions
Carpaltunnel
syndrome
Nocturnalparaesthesiasand/orpain,oftendiffuse—
patientsoftenreportsymptomsinallfingersbut
detailedassessmentthenisneededtodisclose5th
fingersparing
Insertionalgluteus
medius
tendonitis/enthesitis
Nocturnalpainlyingonaffectedside
Hipsynovitis Groin/outerthighpainradiatingtotheknee
Thequalityofpain
Someindividualsfindithardtodescribepainorusedescriptorsofseverity.A
description of the quality of pain can often help to discriminate the cause.
Certain pain descriptors in adults are associated with non-organic pain
syndromes(Table1.2):
• Burning pain, hyperpathia (i.e. an exaggerated response to painful stimuli),
andallodynia(i.e.painfromstimulithatarenormallynotpainful)suggesta
neurologicalorcentral‘painsensitization’cause.
• Achangeinthedescriptionofpaininapatientwithalong-standingcondition
isworthnoting,sinceitmaydenotethepresenceofasecondcondition,e.g.a
fractureorsepticarthritisinapatientwithestablishedRA.
• Repeated, embellished, or elaborate descriptions (‘catastrophizing’) may
suggest non-organic pain, but be aware that such a presentation may be
cultural. Such descriptions may associate with illness behaviour in the
consultationorduringtheexamination.
Painfromtrauma/damagetotissues(‘mechanical’)inadults
Ingeneral,mechanicaldisordersareworsenedbyactivityandrelievedbyrest.
Thisdoesnotmeanpainisnotpresentatrest;inseveremechanical/degenerative
disorders,paindisturbssleep.
• A good knowledge of anatomy and functional anatomy should allow
localization of affected structures though localization of pains in young
childrencanbedifficult.
• An appreciation of secondary muscle spasm is important as such pain can
mask,toadegree,localizationofamechanicalpain,particularlyintheback.
Inflammatorymusculoskeletalpaininadults
Inflammatorylesionscausingpaintypicallydosowithorafterimmobility,such
aswhengettingoutofbedorafteralongcarjourney.
• InflammatoryMSKpainisoftendescribedwith‘stiffness’.
• Inflammatory joint pains from RA, inflammatory OA and peripheral joint
diseaseinpsoriaticarthropathy(PsA)oraxialspondyloarthritis(axSpA)can
bepresentonwakingandeasewithjointmovement.
• Anassessmentofinflammatorybackpainisakeyassessmentinayoungadult
withbackpain(painatnight,pain/stiffnessintheearlymorningeasingwith
movement; resolution or significant improvement with non-steroidal anti-
inflammatory drugs (NSAIDs); associated posterior pelvic/buttock pains of
similarqualityanddescription);axSpAneedstoberuledout.
Table1.2TermsfromtheMcGillpainscalethathelpdistinguishbetweenorganicandnon-organicpain
syndromes(adults)
Organic Non-organic
Pounding Flickering
Jumping Shooting
Pricking Lancinating(‘shooting’)
Sharp Lacerating
Pinching Crushing
Hot Searing
Tender Splitting
Nagging Torturing
Spreading Piercing
Annoying Unbearable
Tiring Exhausting
Fearful Terrifying
Tight Tearing
Elicitedpainonexaminationinadults
In adults, eliciting pain or discomfort by the use of different examination
techniquesmaybeusedtoprovidecluestothediagnosis:
• Palpationandcomparisonofactiveandpassiverangeofmotioncanbeusedto
reproduce pain and localize pathology. This requires practice and a good
knowledgeofanatomy.
• Manyoftheclassicphysicalexamsignsandmanoeuvreshaveahighdegree
ofinter-observervariability.Interpretationshouldtakeintoaccountthecontext
inwhichtheexaminationisdoneandtheeffectsofsuggestibility.
• Palpation and passive range of motion exercises are performed while the
patientisrelaxed.
• Theconceptof‘passive’movementistheassumptionthatwhenthepatientis
completelyrelaxed,themusclesandtendonsaroundthejointareremovedas
potentialsourcesofpain;intheory,passiverangeofmotionislimitedonlyby
pain at the true joint. This assumption has its own limitations, however,
especially since passive movements of the joint will still cause some
movement of the soft tissues. In some cases (e.g. shoulder rotator cuff
disease),thejointmaybepainfultomovepassivelybecauseofsubluxationor
impingementduetoamusculotendinouslesion.
• The clinician should be aware of myofascial pain when palpating
musculotendinousstructures,especiallyaroundtheneckandshoulderregions.
Myofascialpainissaidtooccurwhenthereisactivationofatriggerpointthat
elicitspaininazonestereotypicalfortheindividualmuscle.Itisoftenaching
innature.
• Trigger points are associated with palpable tender bands. It is not clear
whether trigger points are the same as the tender points characteristic of
fibromyalgia.
• Some lesions may cause pain primarily on movement and may not be
amenabletodisclosurefromstaticpalpation(e.g.enthesitis).Donotdismiss
thereportoffocalpain(orthinkofitasreferredonly)ifthereisnotenderness
at the site on static examination. Pain may only occur with tissue
function/movement.
• Local anaesthetic infiltration at the site of a painful structure is sometimes
usedtohelplocalizepathology,e.g.injectionundertheacromionmayprovide
substantial relief from a ‘shoulder impingement syndrome’. However, the
technique is reliable only if localization of the injected anaesthetic can be
guaranteed. Few, if any, rigorously controlled trials have shown it to give
specificresultsforanycondition.
• Always complete a regional MSK examination by examining the adjacent
more proximal structures/joint. Typically, patterns of pain referral extend
distally so problems at one joint can cause symptoms in the area of the
adjacentdistaljoint.
Otherpresentingsymptomsinadults
Stiffness
StiffnessisacommonpresentingsymptomofMSKrheumatologicaldisease.It
may be a manifestation of inflammation or reduced movement due to
mechanicalpathologyincludingswelling,orbeusedbyanindividualtodescribe
reducedmovementduetopain
• Stiffness is often worse after a period of rest. Short periods (<30 min) of
stiffnessthatpersistaftermobilizingisnotameaningfulobservation.Stiffness
lasting>30minandoftenseveralhoursaftermobilizingisatypicalsymptom
ofinflammatoryarthritis.
• Stiffnesscanoccurinnormaljoints.Individualstypicallyclickorcracktheir
jointstostretchthetissuesandgainrelief.
• Stiffnessmaybeamanifestation of tissue fibrosis; in tendons, for example,
fibrosismaycausenodulestoformthatintheirmostextremeleadtolocking
ortriggering.
• Swelling may arise as a result of synovitis in a joint or tendon, oedema,
cellulitis,haematomaorvaricosities,ganglia(commonaroundthewrist),tophi
(fingers,toes),cysts,ornodules(e.g.RAnodulesoverelbows,ornodulesin
fasciaasinDupuytren’sinthehand).
Swelling
• Thereportofswellinghasshowntobeunreliableinmanyinstances.Regard
‘swelling’asasignonexaminationunlessthedescriptionofitasasymptomis
convincingandthestoryhasbeenelicitedverycarefully.
• Nerve compressionor irritationcan oftenbe perceivedasswelling(thinkof
howyourlipfeels—butisn’t—afteradentalanaesthetici.e.swollen!)andcan
colourthereportingofcarpaltunnelsyndromesymptom.
Clunks,snaps,andclicks
• ‘Clicks’areoftenthefocusofsymptomreportsandcancausesomeanxiety.
However, ‘clicks’ from many different structures are not specific for
‘pathology’.
• Inducedsnapslikecrackingknucklesareusuallynoisescreatedfromthequick
expansionofgas/airwithinaconfinedspace.
• ‘Clunks’, however, may denote structural loss of integrity (e.g.
femoroacetabular impingement, multidirectional instability of shoulder in
hypermobile Ehlers–Danlos syndrome (EDS)) and are arguably then more
likelytobeassociatedwith‘pathology’comparedwith‘clicks’.
Constitutionalsymptoms
Fatigue, fevers, sweats, and excessive sweating sometimes occur with many
differentrheumatologicaldiseases.
• Itiskeytoascertainwhatismeantbyfatigue,differentiatingitfromlackof
sleep,deconditioning,orspecificmuscleweakness.
• Fatigueisexperiencedbymanypatientsinassociationwithsystemicillness,
anaemia,endocrinopathy,ormetabolicpathologybutalsofrommoreinsidious
(psychosocialinfluenced)processessuchasfrustration,stress,andanxietyor
asaconsequenceofdisturbedsleep.
• Fatigue often has to be interrogated as sometimes patients won’t report it,
thinkingitispartofageing,orbecauseoftheirstageinlife(e.g.menopause),
orbecauseoftheirworkpattern.
• Feversandsweatscan,onthefaceofit,suggestsystemicinfection,butthese
symptoms can be associated with autoimmune connective tissue diseases
particularly systemic lupus erythematosus (SLE), and in systemic vasculitis
andseverecasesofcrystal-inducedinflammatorydisease(e.g.gout).
• Flushes are often drug induced but are often used to describe generalized
vascularreactivityoraresponsetotachycardiaorothersymptoms(secondary
effects).
• Excessive sweating is associated with glucocorticoid (GC) use, generalized
inflammatory diseases such as giant cell arteritis (GCA) and autoimmune
conditions such as SLE. True hyperhidrosis is associated with acne and
SAPHO (synovitis, acne, palmoplantar pustulosis, hyperostosis, aseptic
osteomyelitis)syndrome.
Rashes
Therearemanyrheumatologicalconditionsthataremanifestinpartbyrashes.
Theassociationmaybetemporallyrelatedorseparateintimesoabroadviewof
thehistoryoftherashneedstobetaken.Thelatterisexceptionallyimportantfor
thediagnosisofpsoriasisdisease.
• Erythematous rashes occur with viral arthritis, with SLE (as urticarias) and
adult-onsetStill’sdisease(AOSD)typically.
• Acne oracneiformrashescanoccurinSAPHOsyndrome,Behçet’s disease,
andpsoriasisdisease.
• Pustulesoccurinaformofpsoriasisdisease,candenotegonococcaldiseasein
the right clinical context, and are a hallmark lesion of vasculitides (with
palpablepurpura).
• LivedoreticularisisakeyfeatureofSLEbutmostnotablyantiphospholipid
syndrome(APS).Itcanbesevereenoughtocausealocalizedvasculitis.
• A brawny, violaceous, slightly raised, confluent, skin eruption is typical of
dermatomyositis(uppertrunk,periorbital,andbacksofhandstypically).
• Psoriasisisnotoriouslyvariedanddiffersparticularlyinrelationtowhereitis.
An atlas of typical psoriasis appearances is a very useful tool in the
rheumatologyclinic.
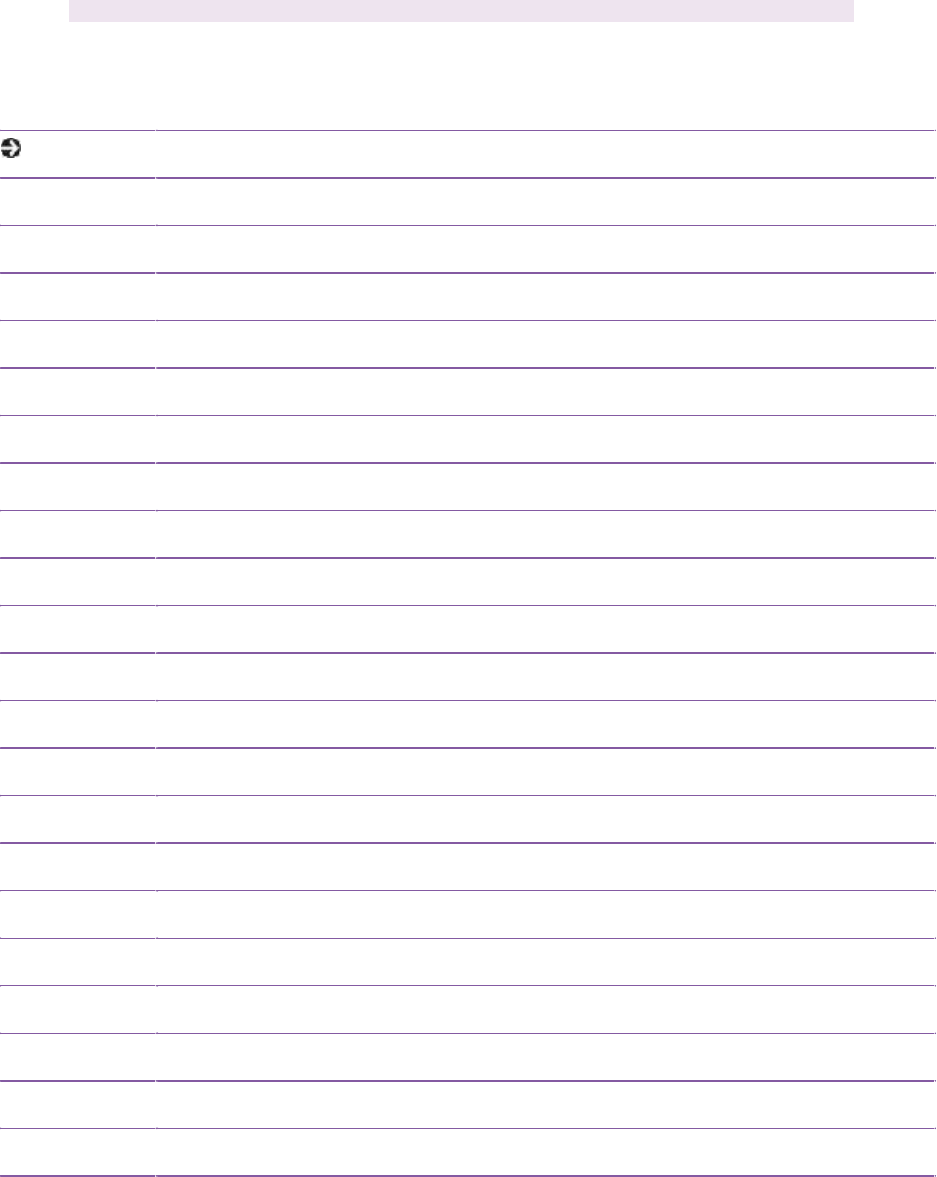
Theadultgait,arms,legs,spine(GALS)
screeningexamination
AsanintroductiontoageneralMSKexaminationitishelpfultobefamiliarwith
the GALS screen,
1
designed to quickly identify the regions of the body
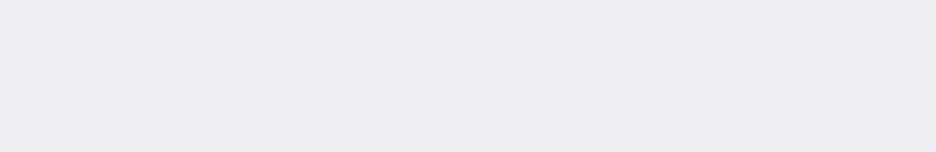
functionally affected. Table 1.3 and Fig. 1.1, and Table 1.4 and Fig. 1.2
demonstratethisprocessintextandvisualformat.
2
Table1.4Physicalexaminationscreeningtool—gait,arms,legs,andspine(GALS)inadults
Position Observation/action Cuetopatientforactive
movements
Gait and
spine
Patient
standing
Active
(patient-
initiated)
movements
Gait:smoothmovement,arm
swing,pelvictilt,normalstride
length,abilitytoturnquickly
‘Walktotheendofthe
room,turn,andwalkback
tome’
Lumbarspine:
Lumbarforwardflexion ‘Bendforwardandtouch
yourknees/ankles/toes’
Lumbarlateralflexion ‘Placeyourhandsbyyour
side;bendtotheside
runningyourhanddown
theoutsideofyourleg
towardyourknee’
Trendelenburgtest.Ifopposite
sideofthepelvisdropsbelow
thehorizontal,suggests
weaknessofthehipabductorson
theweight-bearingleg
‘Standononeleg...now
theother’
Neck and
thoracic
spine
Patient sitting
facingyou
Active
(patient-
initiated)
movements
Neck:smoothmovement,nopain/stiffness
Forwardflexion ‘Putyourchintoyour
chest’
Sideflexion ‘Tipyourearontoyour
shoulder’
Extension ‘Tiltyourheadback’
Rotation ‘Turnyourheadontoyour
shoulder’
Thoracicspine:smoothmovement,nopain/stiffness
1)Lateralchestexpansion
2)Rotation ‘Foldyourarms,turn
bodytothe...’
Hands,
wrists,
elbows,
and
shoulders
Patient sitting
facingyou
Active
(patient-
initiated)
movements
and
palpation
Hand,wrist,finger:swelling
deformity
‘Placebothhandsoutin
front,palmsdownand
fingersstraight’
Handpronation:observepalms
andgripfunction
‘Turnthehandsover,
palmsup’—‘makeafist’
GentlysqueezetheMCPjoints
bycompressingtherowofjoints
together.Assessforpain.Feel
forwarmth.Lookforoperation
scars
‘Placepalmsofhands
togetherasiftopray,with
elbowsouttotheside’
Wristextensionandflexion ‘Withtheelbowsinthe
samepositionplacethe
handsbacktobackwith
thefingerspointingdown’
Elbows:lookfornodules,rash ‘Bendyourelbows
bringingyourhandsupto
yourshoulders’
Shoulders:
Abductionto180°
‘Raisearmssideways,up
topointattheceiling’
Rotation ‘Touchthesmallofyour
back’
Hips, knees,
andankles
Patient supine
oncouch
Passive
examination
of hips and
knees
Some active
movements
Hips:liftleg(bendedknee)andpositionupperlegvertical.
Rotatelowerleg
Knees:
Flexandextendkneefeelingthe
patellawithpalmofhandfor
‘crepitus’andwithbackofhand
forwarmth
Feelbackoftheknee,calf,and
Achillestendonforpainand
swelling
Anklesandfeet:gentlysqueeze
theMTPjointsbycompressing
theforefoot.Assessforpain.
‘Turn your ankles in a
circular motion’ ‘Now
upanddown’
‘Wiggleyourtoes’
• ThenumberinginTable1.3correspondswiththatinFig.1.1.
• Table1.4documentstheverbalcommandsrequiredinFig1.2.
The adult GALS and paediatric GALS (pGALS) examination screens are
valuable, quick assessment tools for identifying sites of major MSK
abnormalities and function before entering into a more detailed physical
examination.
The adult GALS screen is summarized in Table 1.4. The pGALS screen
(video format) is detailed at: http://www.arthritisresearchuk.org/health-
professionals-and-students/video-resources/pgals.aspx
Table1.3Examinationinadults—generalinspection
Position Observation
Observefromthefront:
1 Neck Abnormalflexion(torticollis,effectofkyphosis)
2
Shoulder
Musclebulkacrossthechest,shoulderswelling,
acromioclavicularjointOA,chestdeformities
3 Elbow Full(orhyper)extension,jointswelling,nodules
4 Pelvis Level—tiltedlowerononesidemaybeleglengthdifferenceor
spinalcurvature(scoliosis)
5
Quadriceps
Musclebulk
6 Knee Alignment—bow-legged(varusdeformity)orknock-kneed
(valgusdeformity);swellingabovepatella(synovitis)
7 Midfoot Swelling,operationscars
Lossofmidfootarch—flatfeet
Observefromtheback:
8
Shoulder
Musclebulkacrossdeltoid,trapezius,andscapularmuscles
9 Spine
alignment
Scoliosis/kyphosis
10 Gluteal Musclebulk/pelvicasymmetry
11 Knee Swelling
12 Calf Musclebulk,swelling
13
Hindfoot
Out-turning(eversion)oftheheelassociatedwithflat-foot
Achillestendonswelling
Observefromtheside:
14 Spine
alignment
Cervical—normallordosis;dorsal/thoracic—normalkyphosis;
lumbar—normallordosis
15 Knee Excessiveextension—hypermobility
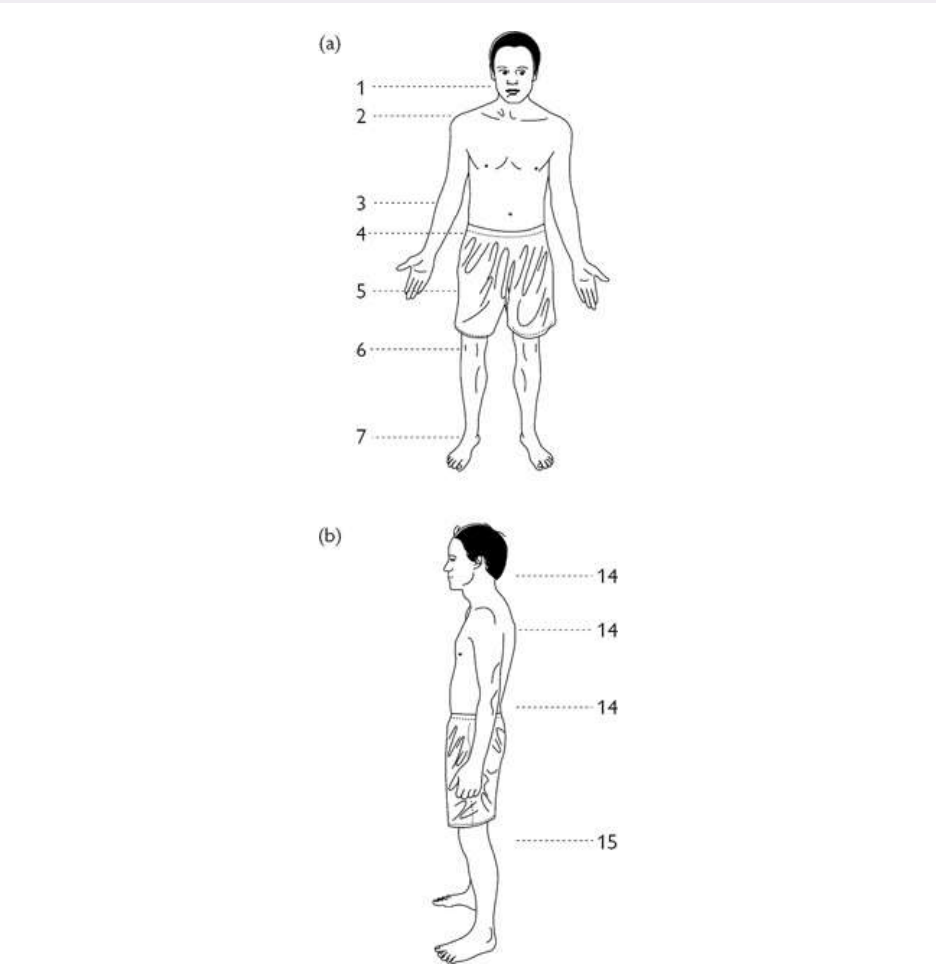
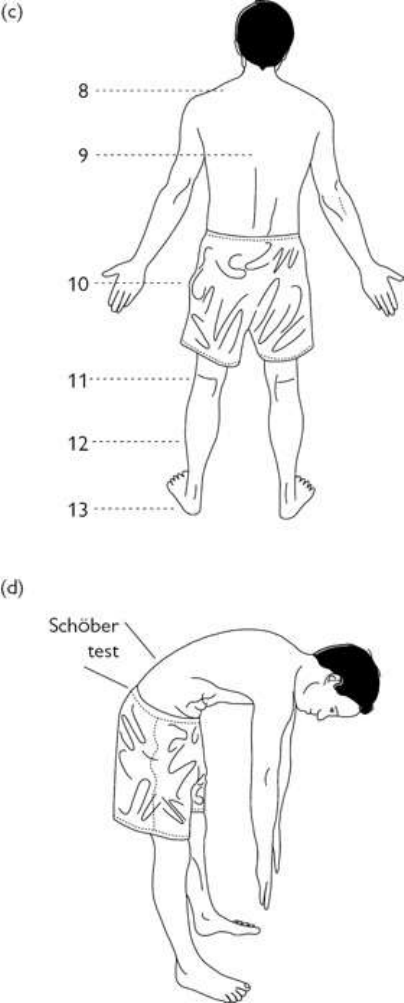
Fig.1.1Physicalexamination—generalinspection.MeasurelumbarflexionusingtheSchöbertest.With
thepatientstandingupright,makeahorizontalmarkacrossthesacraldimplesandasecondmarkoverthe
spine10cmabove.Thepatientthenbendsforwardasfaraspossible.Re-measurethedistancebetweenthe
marks.Itshouldincreasefrom10to>15cm;lesssuggestsrestriction.AdaptedfromHoughtonAR,Gray
D.(2010)Chamberlain’sSymptomsandSignsinClinicalMedicine:AnIntroductiontoMedicalDiagnosis,
13thedition.HodderArnold,London.
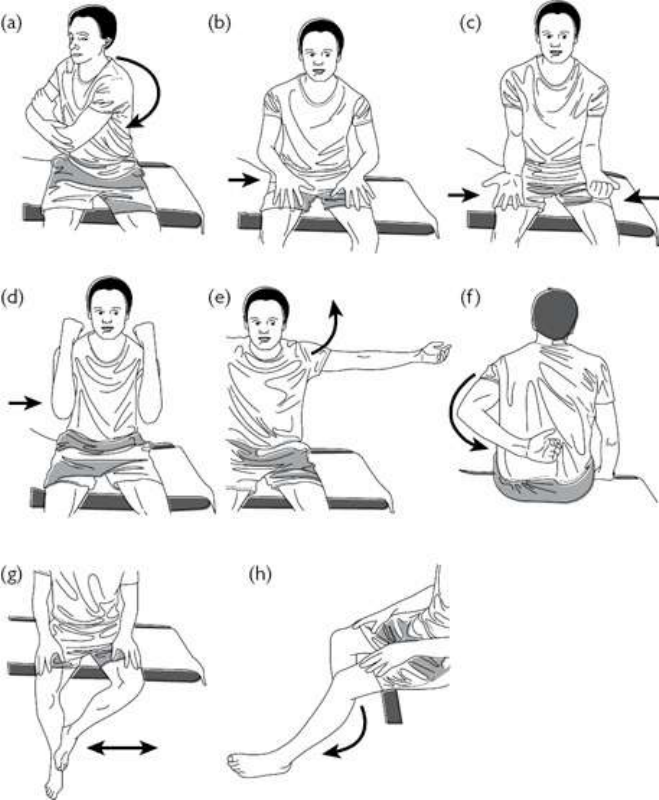
Fig.1.2Physicalexaminationscreeningmanoeuvres.AdaptedfromHoughtonAR,GrayD.(2010)
Chamberlain’sSymptomsandSignsinClinicalMedicine:AnIntroductiontoMedicalDiagnosis,13th
edition.HodderArnold,London.
References
1. Doherty M, Dacre P, Dieppe P, Snaith M. The ‘GALS’ locomotor screen. Ann Rheum Dis
1992;51:1165–9.
2. HakimAJ.Themusculoskeletalsystem.In:HoughtonAR,GrayD(eds),Chamberlain’sSymptomsand
SignsinClinicalMedicine,13ed.London:HodderArnold,2010.
Painassessmentinchildrenandadolescents
Introduction
Moreapparentinchildren,thanatotherages,isthatthelevelofdistressfrom
pain does not correlate well with the severity of the underlying or causative

pathology.
• Somechildrenwillcomplainlittleofpain,but‘silently’losethefunctionofa
limbduetoinflammationofajoint,muscle,orbone.
• Somechildren,perhapsfuelledbyconcernorlackofconcernofaparent,may
becomedistressedwithanessentiallynormalexamination.
• Allreportsofpainandwhatrelievespainshouldbebelieved.
• Thus, all childrenrequirethorough assessment, which here isguidedby the
ageanddevelopmentofthepatient.
Painassessmentinspecificscenarios
Thenon-orminimallyverbalchild
Intheveryyoung,orthosewithcognitiveoremotionalimpairment,thehistory
ofpainanditsimpactissoughtfromtheparentorcarerandcorrelatedwithan
astuteclinicalexaminationthatlooksfordistress.
• Parents mayvolunteer that,attimes ofdistress,sleep isdisturbed orcertain
activitiesormovementsareimpaired.
• Attentionshouldbepaidtospecificactivitiessuchasmovementofalegwhen
nappychangingorchangeinaffectwhenapartofthebodyistouched.Both
canbecarefullycorroboratedduringexaminationfeelingfor,butnottryingto
overcome, any resistance to joint movement and monitoring facial
expressions.Preciselocalizationofthe painortenderness, however, maybe
difficult.
• Babiesandtoddlersmaybebetterexaminedonaparent’slap,especiallyatthe
startoftheexamination.
Thetoddlerandschool-agedchild
• Childrenfrom<3yearsoldcanvolunteerhelpfulinformationandattemptsto
engage them in friendly discussion will provide reassurance before
examination.
• Engagement of the young child is also optimized with an appropriate
environmentthatincludesfreelyaccessibletoys,aplayspecialist,andrelaxed
parentswhofeeltheyhavebeenheard.
• Youngchildrenmightnotunderstandthewordpainandparentsmayhelpin
thechoiceoflanguage.Useofapictureorcuddlytoymayhelptolocalizethe
siteofpainandtheuseoftheFacesPainScaleisastandardtooltoindicate
pain intensity, see: http://www.iasp-pain.org/Education/Content.aspx?
ItemNumber=1519.
• Alotofinformationcanbegainedfromwatchingachildatplaywhilehistory
taking and thereafter all children and toddlers are best approached with

confidenceandease.
• BeginningwiththepGALSas aplayfulexerciseofcopying oftenfacilitates
cooperationwiththemoreformalregionalexam(see ‘ThepaediatricGALS
screen’andalsoat http://www.arthritisresearchuk.org/health-professionals-
and-students/video-resources/pgals.aspx).
• Look, feel, and move limbs and joints with careful facial observation and
appropriate reassurance. Swelling may arise from subcutaneous tissues,
tendons, or joints, and may include oedema, lymphoedema, cellulitis, and
haematoma.
• Clicking is common and normal unless associated with a jarring or locking
movement.
• Pain at end of range of joint movement typically indicates intra-articular
pathology.
Teenagers
• Byspeakingdirectlytotheyoungperson,amoreaccurateclinicalpicturewill
beacquiredthanfromspeakingtoparentsalone.
• Direct, friendly questioning willalsohelp engage and optimize examination
andanyfutureappointment.
• Supplemental information from parents may be helpful as may any
discordancebetweenhistories.
• Where possible, teenagers should be offered to be seen on their own, with
parents included fully in the consultation thereafter. This is now considered
bestpractice.
• Explainconfidentiality,andrespectforprivacyandmodestywillalsopromote
trustandoptimizeclinicalassessment.
• Avoidnon-verbalsignalsthatappeartojudgetheindividual.
• Identify problems with sleep. Early morning wakening with pain may be
associatedwithinflammatoryormalignantconditions,whereasdifficultywith
sleepinitiationormaintenancemaybeassociatedwithchronicpain.
• In particular, insufficient sleep is associated with pain amplification and
reducedresilience.
• In a study of chest pain, only 1 in 300 patients had associated cardiac
pathologywhichwasclearlyapparentonexamination.
• Over90%ofbackpainisbenignorbiomechanicalinnature.
• Frequent associations with chronic pain include bowel, bladder, and
psychologicaldisturbances.

Limpandgaitconcernsinchildrenand
adolescents
Most cases of limp (an asymmetric gait pattern) present acutely and so are
commonlyseeninA&E/emergencyroombyanorthopaedicsurgeontoruleout
infectionandmalignancyiftherearesystemicfeatures,orPerthesdiseaseand
slippedupperfemoralepiphysis(SUFE)iftherearenosystemicfeatures.Most
cases of acute limp, however, have a preceding illness and are diagnosed as
irritable hip or transient tenosynovitis. Subacute or long-standing limp or
concernsaboutgaitmaypresenttorheumatologists.
Age-specificassessment
Toddlersandpre-schoolchildren
• Review the child with reference to normal development and spend time
observingthegait,firstnotingnormalvariants(see pp.37–39).
• Enquireaboutageofonset(whenonsetisatthetimeoffirstwalking,consider
developmentalhipdysplasia).
• Noteanyprecedingillnessortrauma.
• Takecarenottosimplyascribelimptotraumainthepresenceofotherfeatures
andifthehistoryisincongruent,considernon-accidentalinjury(NAI)history.
• Immunosuppressionmaymasksepsis.
• Morningstiffnessistypicalofjuvenileidiopathicarthritis(JIA).
• Carefullyobservefootpositionwhenthechildiswalkingforfootandankle
involvementinJIA.
• Consider that referred pain from the abdomen or groin may be present and
avoidasimplefocusonthehip.
• Weaknesspredominatesinneuromuscularconditionsandtheremayhavebeen
sloworevenlossofgrossmotormilestones.
• Localizing pain or tenderness may be difficult for young children and the
youngchildshouldbeassessedaspreviouslydescribedforpain.
• Thesolesofthefeetshouldbeexamined.
School-agedchildrenandadolescents
• An insidious onset of limp is typical of Perthes disease and JIA, the latter
havingassociatedstiffnessafterprolongedrest.
• Otherosteochondrosesshouldalsobeconsidered(see Table16.11).
• Association with exercise and evening predominance is typical of
biomechanicalconditions.
• New-onset limp in adolescents raises concerns for chronic SUFE or bone
tumour.
• Hip restriction or pain at the limits of internal or external rotation requires
furtherinvestigation.
Pyrexia,fatigue,andunexplainedacute-phase
responseinchildrenandadolescents
Feverandpyrexiaofunknownorigin(PUO)
• Persistent or intermittent low-grade fever especially when associated with
failure to gain or loss of weight will raise suspicion of malignancy and
multisystemdisease,suchasSLE.
• Documentingtheperiodicityoffevermaybehelpful.
• AsubacutefeverorPUO(intermittentorpersistentfever>38°Cfor>3weeks)
may indicate contact with infectious diseases, travel, tick bite exposure,
medication use (‘drug fever’), and sexually acquired infection (in an
adolescent).
• A full systems enquiry should be backed up by a detailed examination
includingnailfoldcapillaries,lymphnodeassessment,fundoscopy,andcardiac
auscultation.
• ‘Phonephotos(takenbythechild,adolescent,orparent)ofrashescanhelpin
the assessment of relapsing–remitting rashes and ultimately as a record to
sharewithotherprofessionals,suchasadermatologist.
Unexplainedacute-phaseresponse
• An unexplained erythrocyte sedimentation rate (ESR) >15 mm/min has a
differentialdiagnosissimilartothatoffever/PUOandacompletehistoryand
examinationisrequired.
• Persistentincrease(over6–12weeks)inplateletcountandC-reactiveprotein
(CRP)increasesthelikelihoodofaninflammatorydiseasebeingfound.
• Biopsy of any suspected lesion can be helpful and whole-body magnetic
resonanceimaging(MRI)canbeahelpfulscreenformalignancyortolocate
sourcesoflocalizedinflammation.
• Other causes include renal disease especially when there is azotaemia,
multiple myeloma, and anaemia of chronic disease associated with iron
deficiency.
Fatigue
• Itisunclearfromwhatagechildrenreportnegativeexperiencesofgeneralized
exhaustion, which as in adults may accompany any illness, but it may be

reportedbyparentsasapresentingsymptom.
• Itiskeytoascertainwhatismeantbyfatigue,differentiatingitfromlackof
sleep,deconditioning,orspecificmuscleweakness.
• Itisimportanttounderstandspecificconcernsoftheparent(e.g.asenseofnot
beinglistenedto).
• Otherenquiriesshouldincludedetailsabouttheonsetoffatigue,medication,
andappetite.
• A full systems enquiry may raise suspicion of active inflammation;
malignancy; endocrine disorder; distress from pain, bowel, or bladder
dysfunction;skinsensitivities;andotherfunctionaldisorders.
• Investigations are usually directed by suspicion of any underlying disorder,
but, as in pain assessment, care should be taken to avoid unnecessary or
endless investigations that prevent effective engagement in a management
plan.
• Simplescreeningtestsincludeinflammatorymarkers,fullbloodcount(FBC),
thyroidfunction,andantinuclearantibody(ANA).
ThepaediatricGALSscreen
The adult GALS MSK disease screening examination has been modified to a
paediatricform(pGALS)tofacilitateengagementofpatientsasyoungas2years
and to account for subtleties in joint restriction of joints typically involved in
JIA.
• Limbs should be adequately exposed to permit full examination and the
pGALSisdemonstratedbythedoctorfacingthepatientandencouragingthem
tocopy.Inthisway,afullscreeningjointexaminationcanbeplayedoutasa
game without touching the patient initially, thereby building rapport and
patientconfidence.
• Gaitexaminationisdiscussedindetailin pp.37–39.
• Supplementaltoneckexaminationisrangeofmotionandasymmetryofjaw
opening.Temporomandibularjointmovementshouldallowthreefingersofthe
patient’shandtobeheldverticallyintheiropenmouth.
• JointmovementrestrictionisasignofdiseaseactivityinJIAconditions.Asa
result,whereJIAissuspected,increasedattentionshouldbepaidtoflexionat
allfingerjoints,extensionoftheelbow,andinversionandeversionofthefoot,
checkingsubtalarandmidfootjoints.
• A full demonstration of pGALS can be found at
http://www.arthritisresearchuk.org/health-professionals-and-students/video-
resources/pgals.aspx

Chapter2
Musculoskeletalassessmentandpatternsof
disease:makingaworkingdiagnosis
Introduction
Musculoskeletal(MSK)featuresnottobemissed
Assessmentofchildrenandadolescents
AssessmentofpatternsofMSKfeaturesinadults
Introduction
• Whenevaluatingaperson—childoradult—withfocalorwidespreadpain,itis
importanttoconsiderthatthepainmaybederivedfromjoints.Sometimesit
won’t be obvious. MSK pain may arise from joints (disease of synovium,
cartilage, or bone) but also entheses, tendons, muscles, or a combination of
structures,orcanbereferredfromsitetosite(usuallyfromproximaltodistal),
or can be associated with/secondary to neurogenic lesions. Patterns of
presentationofpaincanbeusefulpointerstodiagnosis.
• Morethanoneinfivegeneralpractitioner(GP)consultationsareforpatients
with MSK problems, with osteoarthritis (OA) the most common cause of
chronicpainandrestrictedactivityintheover50s.
• MSKpainisthepresentingsymptomin6–13%ofconsultationsinpaediatric
primarycarewith additionalconsultationsfor concernsaboutgait, swelling,
andweakness.
• MSKpaininthepaediatricpopulationiscommonanditsprevalenceincreases
withage.Chronicseverepain,lasting>3monthsandaffectingqualityoflife,
iscommontoo,withaprevalenceofupto16%insecondaryschool-agedgirls.
• The majority of causes (>80%) of MSK pains are self-limiting and have
minimalimpactonqualityoflife.Inthisrespect,painisnotasensitivemarker
of disease yet it is still important to provide reassurance to avoid symptom
amplificationandprolongeddisability.
• Butalso,MSKpaincanbeapresentingfeatureofconditionsnottobemissed
and other long-term conditions that may result in tissue damage or
significantlyaffectparticipationandqualityoflife.
• The challenge is to understand pain in the context of other symptoms and
signs.Manydiagnosescanbemadewithoutinvestigations.
• Tocategorizetheapproachtoassessment,wehavesubclassifiedthepatterns
ofpain/diseaseinto:
• features/conditionsnottobemissed.
• normalvariants.
• inflammatoryarthritis.
• non-inflammatoryMSKpain.
• To helpinthe assessmentofinflammatory arthritis,wehave categorizedby
age, numberofjoints,and by joint number. Although not the convention in
paediatrics, we have taken a threshold of 3 joints to define multi-articular
involvement:
• mono/oligoarticulararthritisinchildren(1–2joints).
• monoarthritisinadults.
• oligoarthritisinadults.
• poly-articulararthritisinchildren(≥3joints).
• poly-articulararthritisinadults.
• arthritisandsystemicfeatures(childrenandadolescents).
• Widespreadpainsarealsothepresentingfeatureofchronicpainsyndromes.
Musculoskeletal(MSK)featuresnottobemissed
(thatmaybeindicativeofseriousdisease)
Generalconsiderations
AmongthemanyMSK,inflammatory,andautoimmunediseasesthatpresentto
rheumatologists, some require prompt intervention including life-threatening
conditions: cancer, infection, and non-accidental injury (NAI) in children and
vulnerable adults (Box 2.1). Complex regional pain syndrome (CRPS) is
includedhereduetothelevelofassociatedincapacitationandearlyintervention
beingessential.
Box2.1Conditions‘nottobemissed’inchildrenandadolescents
Keyfeaturesthatmayindicatetheseconditionsincludesystemicsymptoms,a
historyoftraumathatdoesnotadequatelyexplainexaminationfindings,focal
unexplainedbonepainandtendernesslastingmorethanafewweeks,andin
childrenmarkeddisabilityorlossofdevelopmentalmilestones.
• Septicarthritis,osteomyelitis
• Acutelymphoblasticleukaemia,lymphoma
• Bonetumours(e.g.sarcoma)
• Neuroblastomainchildren
• NAI
• CRPS.
• Unexplainedandpersistentfocalpainandbonytendernessinchildrenisa‘red
flag’. Such pain lasting more than 2 weeks raises the suspicion of bone
cancers.
• ‘Focal’meansabletoclearlypointtothesiteofbonepainortendernessandis
often associated with a limp or disability, and where the pain cannot be
explainedbyosteochondroses,trauma,orinfection.
• Inchildren,bonecancersaretypicallyassociatedwithweightlossandfatigue.
Earlymetastasizationisassociatedwithincreasedmortalitynecessitatingearly
recognition.
Keyfeatureswhichshouldtriggerreferralforfurtherassessmentin
childrenandadolescents
• Limp(seealso ‘Assessmentofthelimpingchild’pp.37–39).
• Persistentlocalized(unilateral)painthroughthenight.
• Jointrestrictionorpersistentjointswelling.
• Impairedfunctionalability.
• Schoolabsenceorteacherconcern.
• Morning symptomsunexplainedby the previousday activities andtiredness
afterdisturbedsleep.
• Widespreadpain.
• Worryingthoughtsoranxietyofthepatientorparent.
• Systemic features such as fever, malaise, anorexia, weight loss, rash, raised
acute-phase response and abnormal growth or development. For example,
thesefeaturesmightleadtodisclosureof:
• septic arthritis or osteomyelitis (high fever, hot and tender joint, or limb
pain).
• leukaemia, lymphoma neuroblastoma, lupus, or vasculitis (persistent >2
weeksoflow-gradefevertypicallyassociatedwitharash).
• Kawasakidisease(highspikingfeverinunder6swithlimbpains).
• multisysteminflammatorydisorders.
• reactivearthritis.
• chronic infections including tuberculosis (TB) (travel history and contact
tracingisimportant).
• other reactive illnesseswith or without clearinfection (e.g. Lyme disease,
Streptococcus, Henoch–Schönlein purpura (HSP)); in all of these, the
presenceofrashmaybeindicativeofdiagnosis.
• Ahistoryoftraumaincongruentwithexamfindingscouldbeconsistentwith
NAIorCRPS.InNAI,themechanismofinjurymaynotexplainitsextentor
severity, and should be discussed with a paediatrician or lead clinician. In
CRPS,thereisfrequentlyahistoryofminortrauma.
• Reportedlossofmilestones.
• Loss of peer or social contact or significant reduction in physical activity.
These changes should not be dismissed as behavioural or anxiety induced
(whether parent or child) without plans for a timely review of resolution or
progression.
• Suspicion of neuromuscular disease. The onset of muscular dystrophies,
congenitalandmetabolicmyopathies,andneuropathiesareofteninsidiousin
onset.Muscleweakness,musclefatigue,numbness,anddelayeddevelopment
predominatebutmaybeassociatedwithwidespreadorfocalpainthatisthe
presentingfeature.
• Suspected problems with pain processing. Notably CRPS, juvenile
fibromyalgia,andsensoryintegration-autisticspectrumandanxietydisorders
can be associated with very high levels of disability due to altered pain
processing.Therecanbecompleteschoolabsenceandgrosslyabnormalsleep
routinesattributedtopain.
• Hypermobility with widespread pain. Hypermobility does not indicate the
causeofthepain.Caremustbetakenwhenusingtheterm‘hypermobility’as
it can be perceived as disabling with a poor outcome. The cause of pain is
often complex, but with effective communication and a range of integrated
strategies that includes a focus on self-management and resilience, the
outcomewillbeexcellentwithfullparticipationinanormalqualityoflife.
• Inconsideringtheabove-listedfeatures,whichshouldpromptfurtherreferral,
thereareotherkeypointswhichmaybehelpfulintheassessment:
• Attributingpaintonon-specifictraumaorsprainorinternaldisruptionofthe
jointcanbereassessedafter2–3weekstoseeifithasresolved.
• Arthritis is commonly associated with persistent and prolonged morning
stiffnessandjointrestriction.Painisnotamajorfeatureandanyreportof
jointswellingunreliable.
• Bonelesionsareindicatedbypainandfocaltendernessoftenwithconsistent
symptomsatnight.Painisoftenintense(e.g.osteoidosteomaorleukaemia
withmarrowinvolvement).
• Pain from muscle lesions localize well to the affected muscle. Functional
weakness,notattributabletofearofmovementfrompain,maybeindicated
bywalkingontiptoesanddifficultiesclimbingstairs,andputtingonT-shirts
orjumpers.
• Lesionsfromligaments,tendons,andenthesesmaybedifficulttoestablish
duetothesymptomstheycausecoexistingwithsymptomsfromassociated
muscleandbonelesions.
• Focal tenderness may be revealing, particularly at entheses including the
heel,patella,anteriorsuperioriliacspine,andplantarfascia.
• Entheseal and ligamentous pain can be intense and often seemingly
disproportionatetoexaminationfindings.
• Weight falling across centiles or unexplained weight loss >5% in an
adolescentneedsdetailedassessment.
Keyfeaturestoidentifypromptingfurtherurgentrheumatological
assessment—adults
For non-rheumatologists, generally the more systemic features present
associatedwithMSKsymptoms,themoretheneedtoobtainurgentassessment:
• Fevers and sweats canindicatesinister disease but candenoteinfection and
bothautoinflammatoryandautoimmunedisease.
• Feverandsweatscanaccompanyseveregoutorvasculitis,includingGCAin
theelderly.
• Arthralgiasandmyalgiascanbepartofaparaneoplasticsyndrome—however,
featuresarenotspecificandtheconditionisrare.
• Most rheumatologists would consider obtaining an extensive panel of lab
investigationsandchestX-ray(CXR)inpatientswithsevereMSKsymptoms
andsystemicfeatures.
• Systemic features in the context of a positive ANA require that a thorough
examination is done and urinalysis obtained to rule out renal disease
associatedwithSLE.
• Severepainandswellinginajointwithorwithoutsystemicfeaturesrequires
prompt assessment, and aspiration of fluid from the joint for Gram stain,
culture,andpolarizedlightmicroscopy(?crystals).
• Incipient cord compression can present with progressive stiffness and limb
weaknesswithoutpain.Such‘neurological’stiffnessreportedasasymptom,is
amimicofstiffnessfromsymptomsassociatedwithperipheralMSKlesions.
Keyfeaturesnecessitatingtimelyrheumatologicalreferral—adults
ManyhealthcaresystemsdooperateabasicMSKserviceinprimarycaresetting
tosupportprimarycaredoctorsinmanagingtheextensiveamountbenign/self-
limiting of MSK disease seen. However, all systems sensibly require triage
processestopromptlyidentifypatientsthatrequirepromptonwardreferraltoa
rheumatologist:
• Keysymptomstoidentifyandwhy:
• Multiple small joint pain/stiffness—might be RA which requires early
treatmenttoreducepermanentjointdamageanddisability.
• Inflammatorybackpain(see Chapter8)—whichcanpredictthepresence
ofaxSpA/AS.
• SystemicsymptomspluspositiveANAmightbeanautoimmuneconnective
tissue disease (e.g. SLE) which can in some patients cause serious organ
disease.
• Severe unexplained temporal head pain and/or scalp sensitivity and/or
amaurosisfugaxwithhighCRPorESR—mightbeGCAandrequireprompt
steroidtreatment.
• Apragmaticwayofscreeningforinflammatorysmalljointarthritishasbeen
adopted as an educational initiative by The UK Royal College of General
Practitioners.The3‘Ss’:Stiffness,Swelling,andapositiveSqueezetest(pain
elicitedbysqueezingtheknuckles).
• Insidious cord compression can present with progressive stiffness and limb
weakness without pain. Such ‘neurological’ stiffness is a mimic of ‘MSK’
stiffness.
• Goutandsepticarthritiscanlookexactlythesame—soaspirate!
• Polymyalgiarheumatica(PMR)-typesymptomscanbethepredominanttype
of MSK symptomology in a number of conditions including pyrophosphate
arthritis,psoriasis-relatedMSK disease,axSpA,and autoimmune connective
tissuediseases.AwiseGPconsiderstheconditionasymptom-complexwhich
mayhaveanunderlyingdiseaseexplanation.
Assessmentofchildrenandadolescents
Normalvariants
Effective reassurance that a child has a normal variant avoids unnecessary
referral,investigation,andintervention.SeeTable2.1.
Table2.1NormalMSKvariationinchildrenandadolescents
Normal Prevalence Notes
variant
Genuvarum
(bowlegs)
Verycommon<2yrsold IfprogressiveconsiderBlount’s
disease,rickets,skeletaldysplasia
Genu
valgum
(knock
knees)
Physiological4–7yrs;
andasamildconditionis
commonthereafter
Referifintermalleolardistance>8
cm,unilateral,gaitismodified,
deteriorating,ornewonsetin
adulthood
In-
toeing/out-
toeing
Commoninunder5s Usuallyresolvesby9yrs.Causes
includemetatarsusadductus,
femoralanteversion,andtibial
torsion.Refer>9yrsifgait
affected
Toewalking 7–24%ofchildren
(especiallyinautistic
spectrumdisorder)
Usuallyresolvesby3yrs.If
obligate,newonset,progressive,or
unilateralconsiderneuromuscular
andorthopaedicdisorders
Femoral
anteversion
Common4–7yrs Presentsasin-toeingand
occasionallylimbpain.Rarely
requiressurgicalintervention
Hypermobile
hands
Verycommon<5yrs.At
13yrsispresentin30%
boys,46%girls
Noclearassociationwithpain.
Maybeassociatedwith
developmentandcoordination
delayneedingwritingsupport
Hypermobile
knees
Common<5yrs.Affects
8–11%atage13yrs
Maybeassociatedwith
patellofemoralpainandassociated
biomechanicalimbalance
Flatfeet(pes
planus)
Universalinitially.
Affects>40%atages3–
6yrsand1in7adults.
Longitudinalarch
developsat3–5yrs
Shoeinsertsstabilizebutdonot
correctthefoot.Exerciseswill
addressbiomechanicalpain.Rigid
flatfootindicatesboneorneural
problem
Higharch
(pescavus)
Affects10%ofthe
population
Assessbiomechanicsandfor
neuromusculardisorderif
progressiveorconcern.Consider
spinaltumourifunilateral
Benign
nocturnal
limbpainof
childhood
Commoninchildren3–12
yrs.Peaksatage6yrs.
Occursinupto40%
under5s
Furtherassessmentifassociated
withdisability,focaltenderness,
systemicfeatures,significant
morningstiffness,swelling,
erythema,weakness
Inflammatoryarthritisinchildrenandadolescents
Thekeyfeaturesofrecognizinginflammatoryarthritisare:
• Consistentmorningstiffnesslasting>30min.
• Swellingwithjointrestriction.
• Associatedmuscleatrophy
• Involvementof>1–2joints(seeTable2.2).
Table2.2Typicalpatternsofjointinvolvementinthevariousinflammatoryjuvenileconditions
1–2
joints
≥3
joints
SepticarthritisincludingTB xx
JIA xx xx
Reactive/viralarthritis xx x
Post-streptococcalarthritis xx x
Rheumaticfever x
Inflammatoryboweldisease(IBD)-relatedarthritis x x
Henoch–Schönleinpurpura(HSP) x x
Haemophilia x
Lymedisease x
Foreignbodysynovitis x
Malignancy x x
Autoinflammatorydisease(e.g.familialMediterranean
fever(FMF))
x x
Multisystemautoimmunedisease x
Pigmentedvillonodularsynovitis(PVNS) x
Chronicrecurrentmultifocalosteomyelitis(CRMO) x x
Sarcoid x x
Non-inflammatoryconditions x
Infectiousfeatures
• Thefeaturesofareactivearthritismayincludeprecedingsymptomsofaviral
infectionsuchascoryzaornon-specificrash.
• Otherviralfeatures include‘slappedcheek’of parvovirus,awidespread and
facialmacularrashofrubella, andsorethroatof mumps,althoughtheseare
rarely seen due to vaccination. In this respect, a vaccination history is
required.
• Vaccinations may be associated with arthralgia and myalgia but are not
associatedwiththedevelopmentofJIA.
• A non-SpA reactive arthritis is usually short lived, typically 3–6 weeks in
duration although may be up to 8 weeks. However, a uniphasic reactive
arthritisinachildwhoishumanleucocyteantigen(HLA)-B27positive(with
related features such as conjunctivitis, urethritis, psoriasiform rash) may be
considerablylonger.Inthissituation,thereistypicallyahistoryofdiarrhoeain
children.
• Associateddiarrhoea,especiallybloodydiarrhoeaandafever,shouldalertto
entericorganismssuchasShigella,Yersinia,Campylobacter,andSalmonella,
whichmaybeculturedfromthestool.
• EscherichiacoliandClostridiumdifficilearealsoknowntotriggerareactive
arthritis.
• Post-streptococcal arthritis is typically associated with a sore throat without
cough and a very painful, marginally swollen, often flitting polyarthritis.
Mucocutaneous features may include rash of scarlet fever and strawberry
tongue.
• Acuterheumaticfever(RhF)shouldalsobeconsideredwiththeabove-listed
features (see Chapter 17) and additional clinical features may include
erythema marginatum, skin nodules, a pericardial rub or new-onset murmur
(andprolongedECGPRinterval),andchorea.
• In moderate- to high-risk incidence populations there are newly revised
internationalguidelinesforthediagnosisofRhF(2015StatementofAmerican

HeartAssociation).LowriskisanincidenceofRhF<2per100,000school-
aged children or all-age prevalence of rheumatic heart disease <1 per 1000.
New criteria include echocardiographic and Doppler findings and
monoarthritisandpolyarthralgiaasmajorcriteria.
Historyoftrauma
• Trauma is common and often the event that draws attention to an already
swollenjoint.
• Haemarthrosis from internal joint disruption or periarticular swelling from
quadricepscontusionortearoccurswithin2hoursoftrauma.
• Traumamayincludeapenetratinginjurywithapunctumfromablackthornor
similarforeignbody.
• A mechanism of injury incongruous with examination findings may raise
suspicionofNAIorCRPS(see Chapter22).
Systemsenquiryandpastmedicalhistory
• May indicate features of coeliac or IBD or raise suspicion of multisystem
inflammatorydisorderssuchasSLEorvasculitis.
• Other conditions associated with an increasedriskofarthritis include cystic
fibrosis,coeliacdisease,Down’ssyndrome,andothergeneticconditions.
Familyhistory
• EnquireaboutarthritidesincludingaxSpA/ASandrelatedconditionssuchas
IBD,psoriasis,andpreviousiritis.
• Patients may volunteer haemophilia, FMF, SLE, and other autoimmune
diseases.
• The familyhistoryis also veryhelpfulin raising parentalorpatient worries
about cancer or perceptions about arthritis or joint pains as witnessed in an
older family member who may have RA, osteoarthritis, or fibromyalgia or
otherconditions.
Travelhistoryandinfectiouscontacts
• Previous travel history may raise suspicion of TB, Salmonella, and other
entericorganisms.
• Travel history should incorporate enquiry about unusual infections such as
brucellosisandleishmaniosisfromendemicareas.Enquiryaboutconsumption
ofunpasteurizedmilkproductsmaybehelpful.
• Insectbitesandcontactwithticsincludingtraveltoendemicruralareasmay
leadtoconsiderationofLymedisease(see Chapter17)andotherconditions.
• Scratches from a cat and associated lymphadenitis or lymphangina is
suggestiveofBartonellainfection.
Responsetomedication
• Theoutcomeofmedicationusecanbeviewedasa‘test’initself.Resultsof
the‘test’willhelpguidefuturemanagement.
• Failure to respond to intra-articular steroids can raise the suspicion of
undiagnosedTBandPVNS.
Examination
• Routine examination should include height and weight and a well-practised
paediatricpGALS(see Chapter1).
• Observethechildatplayfirstandrespecttheprivacyofadolescents.
• Beattentiveofandreassuringaboutpainfulmovements.
• pGALSisaquick,excellentscreeningtoolforjointrestriction,oftenkeyto
finding multiple joint involvement when just 1 or 2 joints were initially
suspected.Itisalsoavaluableandplayfulwayofengagingayoungerchildin
examinationwithouttouchingthechildandavoidingdistress.
• Evensubtledifferencesinrangeofmotionmaysignifysynovialthickening.
• Anydoubtaboutthepresenceofsynovitiscanbeaddressedwithultrasound
(orMRI,asdirectedlaterinthissection).
RegionalMSKexamination
• Subsequent assessmentshould includecomparisonof bothsides,assessment
formusclewasting,scars,deformity,tenosynovitis,enthesitis,andspinaland
hipdisease.
• Muscle wasting, a clear sign of chronicity, typically affects vastus medialis
withkneeinvolvementand calfwithankleinvolvement.Upperlimbmuscle
wastingisusuallylessprominentthaninadults.
• Tenosynovitis is more commonly seen around the ankle, but may be
mechanical in origin rather than inflammatory. It is not associated with any
specificsubtypeofJIA.
• Involvementofthetendonsofthehandmayresultintriggerfinger.
• Enthesitis discriminates enthesitis-related arthritis from other forms of JIA;
areasoftendernessincludeAchilles’insertion,patellartendon,attachmentof
quadsandhamstringstopelvis,andplantarfascia.
• Examination of the spine should include the Schöber test of spinal drift in
enthesitis-related arthritis (ERA; see Chapter 9) and distraction of the
sacroiliac joints (with four quadrant test) to illicit any discomfort of these
joints.

Characteristicrashes
• Psoriasisandassociatednailpits(see Chapter8).
• PalmarpustulosisandacneofSAPHO(see Chapter8).
• Henoch–Schönleinpurpura(HSP;see Chapter18).
• ErythemachronicummigransofLymedisease(see Chapter17).
• Erythemamarginatum.
• Erythema nodosum of vasculitis and sarcoid (see Chapters 15 and 18,
respectively).
• Lipodystrophyand/orskinthickeningwithpinkhaloinscleroderma.
• Othervasculiticrashesespeciallyinvolvingthepalmorfingertips.
• Nailbedcapillarychangesofsystemicsclerosis(SScl),SLE,andautoimmune
overlapconditions.
Investigations:imaging
Itisrecommendedthatimagingshouldbediscussedwitharadiologistwhenever
possible:
• Ultrasound(US)canbehelpfulwhenexamfindingsareequivocal.
• But US is associated with a high false-negative rate in routine clinical
situationsespeciallyforfeet,ankles,andsmalljointsofthehand.
• UScanpickupearlyerosionsthatmayguidechangesinmedication.
• MRI may be less available or immediate but is better for demonstrating
chondral changes and bone and entheseal oedema. It has a very low false-
negativerateforsynovitisandlowfalse-positiveratewhenusinggadolinium
enhancement.
• MRI is the investigationofchoicefor pelvic and spinal assessmentandhas
characteristicfindingsforPVNS.
• Radiographscanbehelpfulwhensuspiciousofskeletaldysplasiaormetabolic
bone disease (including rickets and scurvy) and for assessing bone
mineralization.
• Radiographs may also demonstrate periarticular osteopenia, erosions, and
loosebodies ofosteochondritis althoughUS isthepreferredinvestigationin
thiscircumstance.
• DXA scanning grades bone mass (BMD) against average expected but data
needs adjustment for bone growth and pubertal changes (bone mineral
apparentdensity(BMAD)).Anumberofapproachestodatacorrectionexist,
butshouldbeinterpretedwithcaution.
• When malignancy or infection is suspected, a whole-body MRI (+fat
suppression sequences) may be helpful, and has replaced bone scintigraphy
andfluorine-18fluorodeoxyglucose(
18
FDG)positronemissiontomography–

computedtomography(PET-CT)scans,whichimparthighradiation.
• Whole-body MRI is also used when non-bacterial osteomyelitis (including
CRMO and SAPHO (see Chapter 18 and Chapter 8, respectively) is
suspected.
Laboratorytests
• Autoimmune serology is helpful in multisystem inflammatory disorders but
nottypicallyinJIA,forwhichtherearenodiagnostictests.
• ANAisnotdiagnostic.Itisnowconsideredariskfactorforuveitisalthough
eyeinflammationstilloccursinthosewhoareANAnegative.Furtherresearch
intothevalueoftestingANAisongoing.
• ESRandFBCmaybenormalinactiveJIA.
• Thrombocytosisiscommoninmostinflammatoryconditionsandcanbevery
highinsystemic-onsetJIA,alongwithneutrophilia.
• Platelet and lymphocyte counts are commonly low in juvenile SLE and
antiphospholipidsyndrome.
• A low platelet and neutrophil count in the presence of raised inflammatory
markersandarthritismayindicatemalignancy.
• A high neutrophil count—especially with ‘bands’ on film inspection—may
indicateinfection.
• Interpretation of antistreptolysin O titre (ASOT) can be difficult. The most
reliableclinicalfeatureforstreptococcalinfectionissorethroatwithoutcough.
Serial ASOT are required and combined measurement of anti-streptococcal
DNAseBandstreptozymemaybehelpful.
• Rheumatoidfactor(RF)-positivepolyarticularJIAoccursin<5%ofJIAand
has a characteristic symmetrical appearance. RF should not be considered a
routinetestandismorelikelytobemisinterpretedwhenfalselypositive.
• Lyme serology should only be requested in keeping with Lyme disease
diagnosticguidelines(see Chapter17).
• ForsuspectedTB,interferon-γassays(IGRA),CXR,andMantouxtestsare
importantifsynovialaspirationforcultureisnotdone.
Jointaspirationandsynovialbiopsy
Care should be taken to avoid psychological trauma when undertaking this
procedureasitmayleadtolossoftrustandfutureproblemswithvenesection,
routineexamination,aswellasrepeatsteroidinjection.
• Joint injections may be done under general anaesthesia or with the aid of
inhaledagentssuchasEntonox
®
.
• Joint aspirationforGram stain andcultureis the investigationofchoice for
septicarthritisandwhenconsideringTBsynovitis.
• Insomecentres,synovialfluidcelldifferentialscanbedeterminedwhichmay
behelpfulindifferentiatingbetweenlow-gradesepsisandautoimmunity.
• Bloody taps are common but if the blood runs through the whole of the
sample,haemarthrosisshouldbeconsideredandmaybeattributabletotrauma,
bleedingdiathesis,PVNS,orhaemangioma.
• Crystal arthropathy is very rare in children and adolescents and is not a
commonpresentationofhyperuricaemia.
• Synovial biopsy is helpful when considering PVNS, sarcoid, chronic
infections,andmalignancy.Arthroscopicbiopsyhasahigheryieldthanneedle
biopsy.
Assessmentofgaitandthelimpingchild
The normal gait is a complex automatic process that in a child requires
developmentofmuscles,bones,joints,andligamentseffectivelycontrolledand
coordinatedbytheneurologicalsystem.Imbalancesinanyofthisprocesswill
leadtoproblemsbutingeneral,adelayedgaitisusuallyattributabletoslower
cephalocaudal myelinization of normal development. It is inappropriate to
ascribe hypermobility or hypotonia to this delay or related problems with
balanceandcoordination.Slowerdevelopmentmaybeperceivedasaproblem,
but is not a medical disorder. Catch up with peers takes time and the finer
adjustmentstothegaitpatternmaynotoccuruntilthechildis8–10yearsofage.
Asimpleviewofnormalgaitincludesa:
• Stancephasestartingwiththeheelstrike,progressingthroughplantar-flexion
totoe-off.Assessmentalsolooksatbasewidthandsingle-limbsupporttime.
• Swingphasefromtoe-offtoheelstrikewithforwardrotationandtiltingofthe
pelvis and a stable lumbar spine and abdomen. Assessment also includes
cadenceandstridelength.
Assessmentofalimp
Alimpisanasymmetricgait,butmanypeopleinterpretotherabnormalitiesof
gait as a limp. Some abnormalities of gait are listed as follows. Examples of
causesoflimpinchildrenattendingA&EareshowninTable2.3.
• Antalgicgaitresultsfrompainorstiffnessleadingtoashorterstancephase.
• Trendelenburg limp or gait is attributable to weak hip abduction causing a
bodyswayinstancephaseandadroopofthehipintheswingphase.
• Waddlinggaitisattributabletoneuromuscularorarticularstiffnessaroundthe
pelvis.
• Stiff-legged(peg-leg)gaitresultsfromlossofkneeflexionandcircumduction
withpelvicelevationontheaffectedside.
• Toewalkingmaybehabitual,typicallyresolvingat3yearsormaybedueto
muscle contractures or spasticity. Check whether the child can heel strike
when concentrating. Unilateral toe walking may indicate a lower-extremity
lengthinequalityorbefromawoundtotheheel.
• Highsteppinggaitmayresultfromdifficultieswithdorsiflexionofthefoot,
usually associated with peroneal neuropathies lower motor neuron
neurologicaldisease(e.g.spinabifida,polio)andperipheralneuropathies(e.g.
hereditarymotorsensoryneuropathyI/II).
• Stoopedgaitmightindicateabdominalpathology.
• Clumsygait is often describedbutrarely seen in formal assessment.Itisin
part the result of inattention and may also be from subtle physiological
developmental delay (often associated with handwriting difficulties and
learningdelayordisability).Mayincludemorefrankneurodevelopmentalor
metabolicdisorders.
• Ataxicgait.
Table2.3CausesofalimpinchildrenseeninA&E;medianage4.4years(interquartilerange2.9–7.5
years)
Finaldiagnosis No.(%) Mediandaysto
presentation
‘Irritablehip’ 96(40%) 1
Nofinaldiagnosis 72(30%) 1
Musclestrain/overuse 42(17%) 3
Perthesdisease 5(2%) 30
Osteomyelitis 4(2%) 0.5
Localinfection 5(2%) N/A
JIA 2(1%) N/A
Trauma/fracture/toddlerfracture 4(1%) 2
Osteochondrosis 2(1%) N/A
Neoplasia 2(1%) N/A
Back/abdominal 3(1%) N/A
SlippedUpperFemoralEpiphysis
(SUFE)
1(0.5%) 30
Other 5(1.5%)
Total 243
(100%)
Furthergaitassessment
ShouldfollowgeneralMSKassessmentplus:
• Localizesiteofpathology(andincludebackandabdomen;see Chapter3)—
20%oflimpsarenotassociatedwithpain.
• Lookforbiomechanicalimbalances.
• Trivialinjuryortraumamaybeunwitnessedandtoddlerfracturesmissedon
conventionalradiographs.
• IncongruenceorinconsistencyinhistoryraisessuspicionofNAI.
• Considersports-relatedinjuriesandoverusesyndromes.
• Neurovascularstatus,includingstrength,sensation,andreflexes,canalsobe
assessedwhilethechildissittingorsupine.
• Measureandcomparelower-extremitylengths.
• Walk,run,andhopallowassessmentofcoordination,strength,andbringout
subtleabnormalityandprovidedevelopmentalassessment.
• Alsoassessskin,soleoffeet,nails,andshoes.
Assessmentofmusclepainandweaknessinchildrenandadolescents
Changesingait,anddifficultyclimbingstairsandputtingonjumpersorT-shirts
maybeattributabletomusclepainorweakness.
• In the history of acute muscle pain there should be enquiry about trauma,
previousbiomechanicalmusclepains,precedingviralinfection,andfeverand
site.
• Benignmyositisofchildhoodisatransientillnessthattypicallypresentswith
calf pain in the 4–10-year-old age range 3 days after onset of fever and is
associated with a high creatine kinase (CK). Guillain–Barré syndrome also
affectsdistalmusclesandfollowscertainviralorbacterialinfectionsbutwill
beassociatedwithgradualprogression,markedweakness,sensorysymptoms,
andnormalCK.
• Chronic myositis may also be associated with a low-grade fever, muscle
tendernessandhighCK.
• Juvenile dermatomyositis, SLE, pyomyositis, and some periodic fevers with
myalgiawillhavecharacteristicrashes.
• Non-inflammatory causes of muscle weakness include neuromuscular
conditions, such as muscular dystrophies, that are progressive with loss of
motor milestones; upper motor neuron lesions including spinal compression
with increased reflexes; or anterior horn cell conditions, neuropathies, and
metabolicmusclediseasewithabsentreflexes.Theseconditionsrarelycause
muscletenderness.
• MuscleweaknessandTrendelenburggaitarealsoseeningrossdeconditioning
fromsedentarybehaviourandchronicpainconditions.Tendernessiscommon
alongwithsymptomaticdeteriorationtowardstheendoftheday.
• Widespreadmyalgiasofjuvenilefibromyalgiaandenthesitismaybeconfused
witheachother.
Jointpainswithsystemicfeaturesinchildrenandadolescents
Wherethereisfever,rash,andarthritis,diagnosesotherthansystemic-onsetJIA
(SoJIA; previously known as Still’s disease) ought to be considered first and
beforeatrialofsteroidswhichwillmaskinfections,malignancy,andKawasaki
disease.
• Travel, infection contact, social, and family histories are vital in terms of
disclosingahistorysuggestiveofinfection.
• Thereshouldbeafullenquiryaboutsymptomsreferabletoeachorgansystem,
whichmaypointtoadiagnosisofmultisysteminflammatorydisease.
• Characterizingthefever,includingfluctuationthroughouttheday,periodicity,
and duration may be diagnostic of SoJIA, Kawasaki disease, and specific
periodicfevers(see Chapter18).
• A ‘quotidian’ fever occurring once or twice a day with return to baseline is
characteristicofSoJIA,Kawasakidiseasehasahighspikingfeverforatleast
5days.Forperiodicfeverssee Chapter18.
• Lookforandcharacterizeanyrash.ThismayfacilitatediagnosesofSoJIAfor
which there are multiple typical rashes, lupus, dermatomyositis, periodic
fevers and vasculitis. Other important rashes are those of pyoderma and
neutrophilic dermatoses, scleroderma, and Behçet’s disease; all may need
distinguishingfromviralexanthemsandfungalinfection.
• Ocular features may include red eye, pain, double vision, photophobia, and
blurring.
• Ear, nose, and throat (ENT) features may include sinusitis, crusting, bloody
discharge,tinnitus,hearingloss,facialweakness,oralulceration,sorethroat,
parotitis,anddrymouth.
Non-inflammatoryMSKconditionsinchildrenandadolescents
(SeealsoBox2.2.)
Principlesofdiagnosis
• Biomechanicalandnon-inflammatorypainisverycommoninhealthychildren
andadolescentsandisbyfarthecommonestcauseofMSKpain.
• Hypermobilityinthenormalpopulationiscommonandcareshouldbetaken
before ascribing focal or widespread MSK pain to the hypermobility
syndrome/Ehlers–Danlossyndrome(EDS)type3.Inappropriate/over-zealous
useofthediagnosticlabelcanreflectamisunderstandingofthemultifactorial
nature of MSK pain and project a ‘disabling’ rather than ‘enabling’
formulationontopatients.Inturn,thiscanleadtoparentalconfusion,alackof
flexibilityovertreatmentstrategies,andexcessdisability.
• Biomechanicalpaintypicallyincreaseswithactivityandoccursintheevening
or following morning or two after increased physical activity. It may be
associatedwithstiffnessatthesetimes.
• Biomechanicalpainmaybeassociatedwithminorswellingandtendernessand
may occur with inflammatory or other conditions. It commonly occurs with
chronicarthritisduetomuscleandjointinhibitionfromactiveinflammation
andsubsequentMSKimbalance.
• Focal bone pain occurs with osteochondroses and osteoid osteoma and
although very rare, osteosarcomas should be considered in the absence of
typicalfeaturesofanosteochondrosis.
• Neuromuscular conditions manifest by weakness may present with (often
initiallyfocal)pain.
Contributoryfactorstochronicnon-inflammatoryMSKpainsandtheir
impact
• MSK imbalance—from tight and/or weak musculature or ligaments
(patellofemoralsyndromeisanexample).
• General deconditioning—whether through overall lack of background
effectivephysicalactivity,excesssedentarybehaviour,oravoidanceofactivity
duetopain.
• Repetitivephysicalactivityinthepresenceofsuboptimalmuscularcontrol.
• Subchondralorotherbonystress.
• Features of gross motor development (including proprioception) which are
slower than global development or development of peers and siblings—
development requires nerve myelination and neuromuscular imprinting, so
practicewillnotimproverateofchange(asoccurswithnocturnalenuresis).
• The pace of proprioceptive movement programming, which continues to
developuntilpuberty.
• Suboptimalstrengthforrangeofjointmovement(aswithsomehypermobile
joints).
• Adversegaitorotherpatternsofmovementincludingtrackingofpatella.For
example, gaitmaturationand improvements in gait efficiency continue until
afterskeletalmaturity.
• A‘boomandbust’approachtophysicalactivity.
• Lossofconfidenceinspecificmovements.
• Difficultiesinpainself-appraisal.
• Centralandperipheralpainpathway(orneuromatrix)sensitization.
• Difficulties with background sensory processing as occurs in patients with
autisticspectrumdisorders.
• Ruminatingorattentivebehaviours.
• Reinforcingparentalorotherfamilymemberresponses.
• Socialandenvironmentalfactorsincludingthoseatschool.
Box2.2Typicalnon-inflammatoryMSKdisordersinchildrenand
adolescents
Painfulconditionsfromfocallesions
• Patellofemoralsyndrome
• Otherbiomechanicalimbalances
• Tendinopathyandenthesitis(includingERA)
• Perthesdisease(groin,thigh)
• SlippedUpperFemoralEpiphysis(SUFE)(groin,thigh)
• Osteochondroses
• Neuroblastoma
• Osteoidosteoma
• CRPS
• Osteosarcoma
• Stressfracture
• PVNS(usuallylargejoint).
ConditionsthatmaybeassociatedwithwidespreadMSKpain
• Haemophilia
• Juvenilefibromyalgia
• NAI
• Skeletaldysplasias
• Marfansyndrome
• Ehlers–Danlossyndrome
• Osteogenesisimperfecta(focalormultiplefractures)
• Musculardystrophiesandotherneuromuscularconditions
• Rickets
• VitaminCdeficiency-scurvy
• Hyperparathyroidism
• X-linkedhypophosphataemicrickets(fractures/bonepain).
Notablefeaturesinthehistory(‘pearls’)
• Osteochondroses develop gradually and are associated with pain and
tendernessattypicaltendoninsertionorjointsites.
• Lockingorgellingofajointmayindicateanosteochondritisdissecanslesion
(typicallyelbow,knee,ankle).
• Weakness may beindicated by difficulty climbingstairs, or gettingup from
thefloor(e.g.atschoolassembly).
• Non-participation in physical education lessons, extracurricular sport, and
otherphysicalactivitymayindicateeitherasignificantimpactofacondition
orgeneraldeconditioningandreflectcyclesofbehaviourinresponsetopain.
• Disruptionatthehipmaypresentasinsidiousonsetofkneepainorlimp.This
includes Perthes disease in childrenaged4–10yearsandsubacuteSUFE in
peripubertaladolescentswithanincreasedincidenceinthoseoverweight.
• Withrespecttokneejointpain/lesions:
• Meniscaltearsareassociatedwithanacuteevent.
• Cruciateligamenttearsarealsoassociatedwithacutetraumaandtheremay
beahistoryofpoppingwithinthekneeandimmediateswelling.
• Skeletal dysplasias may present with limb pain and deformity but usually
presentwithafamilyhistoryanddisproportionateshortstatureorinthecase
of osteogenesis imperfecta, fractures. Occasionally, suspicion arises when
polyarthropathy fails to respond to conventional treatments for arthritis and
bilateralhipdysplasiaorPerthesdisease.
Otheraspectsofthehistory
• Typical features which might suggest a functional disorder include irritable
bowelsyndrome,dizziness,paraesthesiae,headaches,andbladderdysfunction.
• Family history may indicate other painful conditions but these are very
unlikelytobegeneticallyrelatedotherthanthroughbodytypeandpatternsof
movementandbehaviour.
• Responsetomedicationwillhelptoguidefuturemanagement.
• Engagementwith,andresponseto,othertreatmentsincludingphysiotherapy,
osteopathy, and complementary therapies will also help guide future
management.
• Assessment of ‘engagement’ includes an understanding of the patient’s
cooperationwithhomeexercise programmesandthiscanbecorrelatedwith
exam findings (e.g. persistence of tight musculature or specific areas of
deconditioning).
Examination:general
• Routine examination should include measuring height and weight and a
pGALS(see Chapter1).
• There should be a general assessment of conditioning and posture, which
includes the presence of spinal contour noting any hyperlordosis or loss of
lordosis.
• Gaithaspredictivepatterns(seealso ‘Gaitassessment’,pp.37–39):
• Noteanyantalgicgaitfromtraumaorinflammation.
• A Trendelenburg or waddling gait can occur from hip abductor weakness
fromneuromusculardisordersorhipjointdisorders.
• Circumductiongaitfromhemiplegia orleglengthdiscrepancyattributable
tochronickneesynovitis(see Plate1).
• Ataxiaduetoneurologicalinvolvement.
• Toe walking—if unilateral or not correctable with advice, upper motor
neuronorlysosomaldisordersshouldbeconsidered.
• WeaknesscanbeassessedthoughtheGowersigninayoungerchild,risingout
of a chair without use of upper limbs, sustained neck flexor strength, and
wingingofscapulaewhenpushingagainstawall.
• RegionalMSKassessmentisdescribedin Chapter3andisusuallykeyto
diagnosisandmanagementofnon-inflammatoryconditions.
• Regionalexaminationshouldincludeassessmentofadjacentregionsgiventhe
functionalconnectionbetweenregions.
Investigations:imaging
Theprinciplesofimaginginyoungchildrenaretominimizeproceduretimeand
radiation exposure wherever possible and to request imaging judiciously
followingdiscussionwithapaediatricradiologist.
• Radiographs are often normal in early joint inflammation, but they are the
investigation of choice if considering periosteal lesions, traumatic or stress
fractures, mineralization defects (e.g. rickets), or major structural conditions
suchasskeletaldysplasia.
• ConsiderUSifthereislikelihoodofjoint/tendonsynovitis,anosteochondral
lesion,oraligament,enthesis,ortendonlesion.
• MRI and further radiological investigation may include assessment of any
organ,especiallyforfeetandankles,hips,andspine.
• Where there is a pyrexia of unknown origin or similar broad differential
diagnosis,whole-bodyMRI(withfatsuppressedsequences)maybehelpful.
Investigations:laboratorytests
• Allinvestigationsshouldbeperformedwithaclearunderstandingofhowto
interpret the results and specific tests (such as serology for multisystem
disorders,Streptococcus,Borrelia,etc.)shouldbeinterpretedaccordingtothe
pre-testprobability.
• Weakpositiveresultsforlupusanticoagulant,RF,ANA,ENA,andASOTmay
needrepeating.
• Serologicaltestsshouldalsobeinterpretedwithcautionafterimmunoglobulin
infusionsorseriousinfectionsandHIV.
ChronicpainwithoutidentifiableMSKabnormalitiesinchildrenand
adolescents
Keyconsiderations
Chronic pain is defined (for research purposes) as the presence of pain or
discomfort for >3 months. This may be continuous in the same location or
intermittent. This may be a useful definition for clinical purposes and to help
raisechronicpainsyndromesordisordersinthedifferentialdiagnosis.
• In most circumstances, there is a characteristic history and examination
findings and a positive diagnosis should be made. This does not require
investigation.
• Treating these conditions as diagnoses of exclusion tends to undermine the
diagnosis and raise suspicion in the patient or parent that sufficient
investigationhasnotbeendonetoruleoutalternativecausesofpain.
• Ifinvestigationsareordered,theexactpurposeofthisinvestigationshouldbe
explainedandshouldbeframedinthecontextofapositivediagnosis.
• In children and adolescents, both local, or regional, and widespread chronic
painoccurs.This includesthe currentterminologyof complexregional pain
syndrome (CRPS) and juvenile fibromyalgia (FM), both pain processing or
neuromatrixproblems.Thereshouldbeguardeduseoftheseterminologiesas
thereisafarbetterprognosisinchildrenandadolescentsthaninadultsanduse
ofsuchtermsmayleadtounintendedinterpretations.
• The commonest cause of regional and widespread pain, however, remains
biomechanical problems typically associated with growth and development.
Thisincludesbenignnocturnallimbpainsofchildhood.
• Itislikelythatpatientswillhaveseenotherprofessionalsandatthebeginning
thepatientorparentshouldbeaskedwhattheyhopefromtheconsultation.
• LocalizedpainsuchasCRPSistypicallyassociatedwithanepisodeofminor
trauma(majortraumaisusuallyassociatedwithhighlevelsofappraisaland
adjustment) in circumstances that may be challenging or alarming (e.g.
unanticipated summersault on a trampoline, unexpected fall, excessively
boisterousplay,roadtrafficaccident,orthepresenceofexhaustionfromlack
ofsleeporheatstroke).
• The pain often builds up over time and the source of pain is considered
mysterious and unexplained to patient and/or parent. This is frequently
compounded by inconsistent assessment and explanation by health
professionalsandbyagitatingfamilymembersorfriends.
• WidespreadidiopathicpainincludingjuvenileFMisusuallyinsidiousinonset
withgradualimpositiononqualityoflifeovertime.
• Thelevelsofdisabilityanddistressforbothlocalizedandwidespreadchronic
pain are usually well in excess of the clinical findings from history and
examination,butshouldnotbedismissed.
• The needs of patients with chronic pain should be clearly identified to help
direct an effective treatment strategy that often requires a multidisciplinary
approach (input from experienced physiotherapist, occupational therapist
(OT),andpsychologist).
• Theroleofmedicationisunclearandifused,medicineuseshouldbeclosely
monitoredforbenefitandsideeffects.Medicationtendstobemosteffective
when used to support engagement with other physical and psychological
therapeuticstrategies.
AssessmentofpatternsofMSKfeaturesinadults
Whenevaluating anadult withjoint, tendon,and muscleproblems, ithelps to
initiallyconsiderwhatisnormalvariationandwhatisabnormaland,inthecase
of jointpains,the likely number ofjointsinvolved. Whether monoarticular (1
joint),oligoarticular(2–3 joints),orpolyarticular(>3joints)willinfluencethe
initialdifferentialdiagnosisandworkingdiagnosis.
• Forexample,RAcanpresentwithmonoarthritisbutitwouldbeaveryunusual
presentation whereas gout in men typically presents as a single site of
inflammation.
• The differential diagnosis generates a working diagnosis which in turns

dictatestoadegreewhattestsaredoneandinwhatorder.
Normalvariants
NormalvariantfeaturesofMSKorigininchildrenareusuallydevelopmentalin
origin (see Table 2.1, p. 32). In adults, varied skeletal morphological
appearances are not usually associated with disease directly, though their
mechanical effects may lead to secondary MSK problems, notably early
degeneration.
• Inadults,asymmetricMSKappearances,however,aremorelikelytorepresent
relevantpathology.
• Adults can come to clinical attention, reporting noticeable change in MSK
appearance though invariably, such changes, if indeed present at all, but
without pain and other features, are not sinister and rarely indicate serious
disease.
• Adult MSK appearancesdovarynotably. Typical sites ofhighvariation are
neck length, kyphotic/hyperlordotic lumbar thoracolumbar spine contour,
degree of shoulder protraction, sloping shoulders, degree of elbow valgus,
pelviswidthandtilt,degreeoffemoralanteversionangle,Q-angleattheknee,
degreeoftibialtorsion,in-toeing/out-turn,and reducibleplano-valgusinthe
feet.
• Subtle appearances of some MSK structures, however, can indicate an
underlying condition and occasionally are not identified through childhood
and adolescenceand lead to(alate) diagnosis ofthecondition in adulthood
(e.g. trichorhinophalangeal syndrome, hypermobility syndrome/EDS3, and
Scheuermann’sdisease).
Monoarticularpaininadults
• Acute pain and swelling of a joint follows intra-articular trauma such as
cruciate or meniscus tears in the knee. History will be key indiscriminating
traumaorspontaneousinflammation;MRIisessentialtoidentifythecauseof
trauma.
• Acuteinflammatorymonoarthritisiscommonlyduetocrystalarthropathiesin
theolderpatient(see Chapter7), infection (particularly gonococcal in the
youngeradult; Chapter17) or haemarthrosis, the causes of which include
trauma,bleedingdisorder,vitaminCdeficiency,synovialhaemangioma,and
PVNS.
• AspirationoffluidforGramstain,culture,andpolarizedlightmicroscopyis
anearlypriorityofmanagement.
• Afractureacrossthejointlinemayalsocauseanacutemonoarthritis.Stress
fracturesoccuras theresultof repetitiveloadingof bone,andcan be found
withoccupational, recreational,or athleticactivities. Stressfractures maybe
small and therefore can be missed on plain radiographs; MRI may be more
sensitiveandshouldbeconsideredifthepatientisatrisk.
• Non-gonococcal septic arthritis is particularly important to consider in the
elderly, who may not present with the signs and symptoms expected with
infection.Non-gonococcalsepticarthritisisarheumatologicalemergency(see
Chapters 17 and 25), and should be treated with intravenous antibiotics
immediatelyonsuspicion.
• In the UK, although Staphylococcus aureus is the most common organism
causing septic arthritis in the elderly, it is prudent to consider atypical
infections(e.g.Gramnegative).
• SepticarthritispreferentiallyoccursinpatientswithRA,inpatientswithrenal
disease,andimmunocompromisedpatients.
• Thepresenceofcrystalsinmonoarticularjointfluidaspiratesdoesnotexclude
infection.
• Distinguishing a swollen digital joint from a swollen digit is important in
discriminating dactylitis—usually associated with PsA and other
spondyloarthritides.
• Not all great toe pain/swelling is gout. The great toe is very commonly
affectedinPsA—checkif digitisdactylitic andthereisnail disease—see
Chapter8.
• Boxing glove-type swellingofa hand is a typicalmanifestationof calcium-
containing crystal-induced inflammation, particularly calcium pyrophosphate
deposition(CPPD)-pseudogout—onhandradiographslookforthejointspace
lossandmarkedsclerosisofarticularsurfacesofbonesinCPPDofthecarpal
jointsandchondrocalcinosisinthewristtriangularfibrocartilagecomplex.
Oligoarticularpaininadults
(SeealsoTable2.4.)
Theassessmentofaninflamedjoint
• Theclinicalfeaturesofinflammationandpainatanygivensynovialjointand
the differential diagnosis in the context of other possible regional MSK
diagnosesarediscussedin Chapter3.
• Synovitis is the term given to inflammation of the synovial lining. This
inflammationmaybeaconsequenceofarangeofcellularprocesses,andisnot
specificforanyonediagnosis.Jointeffusionsoftenaccompanysynovitis.
• Inflammation of periarticular tissues may accompany synovitis. Enthesitis
(inflammation at a tendon or ligament insertion into bone) or tenosynovitis
(inflammationofthetendonitself)maybethemostprominentfeature.
History:generalpoints
• Pain and stiffness are typical features of synovitis and enthesitis. Both are
often worseinthemorning, or after periods of immobility. The presence or
absence of stiffness does not discriminate between different causes of
synovitis.
• Pain is often severe in acute joint inflammation. In chronic situations, pain
may be less severe (due to mechanisms that increase physical and
psychological tolerance). There are no specific descriptors that discriminate
painfromsynovitisorenthesitis.
• Swelling, either due to synovial thickening or effusion, often accompanies
synovitis.
• Apatient’sreportofswellingisnotalwaysreliable.Patientswithcarpaltunnel
syndrome, for example, will frequently report that their hands are swollen,
evenwhennoswellingisvisible.
• Reducedmobilityinajointaffectedbyenthesitis/synovitisisalmostuniversal
regardlessofitscause.
Examination:generalpoints
• Swellingmaybeobservedordetectedbypalpation.Itsabsencedoesnotrule
outsynovitisorenthesitis.Synovialswellingneedstobediscriminatedfrom
bonyswelling,fat,andotherconnectivetissueswellings(e.g.ganglia,nodules,
etc.).Withoutimagingorattemptingtoaspiratejointfluid,itmaybedifficult
todiscriminatesynovialthickeningfromeffusion.
• Skin erythema (implying periarticular inflammation) and warmth do not
alwaysaccompanyjointinflammation,buttheyarecommonwithcrystalline
and septic arthritis. Erythema can also occur in reactive arthritis, rheumatic
fever,andwithnascentHeberden’sorBouchard’snodesinosteoarthritis(OA;
see Chapter6).
Table 2.4 Common causes of monoarticular/oligoarticular joint inflammation and typical patterns of
presentation(adults)
Disease Typicalpattern
Gout
(see Chapter
7)
Age>40yrs.Initiallypresentsasanacutemonoarthritis.
Strongassociationwithhyperuricaemia,renal
impairment,anddiuretics.Possiblegeneralsymptoms
mimickingsepsis.Possiblefamilyhistory.Acute-phase
reactantsandserumwhitebloodcellsoftenhigh.Joint
fluiduratecrystalsseenbypolarizedlightmicroscopy.
Jointerosionsandtophioccurinchronicdisease
Spondyloarthritis
(see Chapter
8)
Age<40yrs,menmorethanwomen.Mostly
oligoarticularlowerlimbjointenthesitis/synovitis.May
occurwithsacroiliitis,urethritisorcervicitis,uveitis,gut
inflammation,psoriasis(scalyorpustular).Possible
familyhistory.ESR/CRPmaybenormal.Moresevere
courseifHLA-B27positive
CPPDarthritis
(see Chapter
7)
Meanage72yrs.Oligoarticular,acutemonoarticular
(25%),andoccasionallypolyarticularpatternsofsynovitis
Haemarthrosis Obvioustraumadoesnotalwaysoccur.Swellingusually
considerable.Causesincludetrauma(e.g.cruciaterupture
orintra-articularfracture),PVNS,bleedingdiatheses,and
chondrocalcinosis
Osteoarthritis
(see Chapter
6)
Softtissueswellingisusuallynotasobviousasbony
hypertrophy(osteophytes).Typicaldistribution(e.g.first
carpometacarpalandkneejoints)
Rheumatoid
arthritis(see
Chapter5)
Caninitiallypresentwithanoligoarthritisthatevolves
intoasymmetricalpolyarthritis.Canrarelypresentasan
acutemonoarthritis
Septic arthritis
(excluding
Neisseria
gonorrhoeae)
(see Chapter
17)
MostcommoncauseStaphylococcusaureus.Associated
withchronicarthritis,jointprostheses,andreducedhost
immunity.Peakincidenceinelderly.Systemicsymptoms
commonandsometimesovert.SynovialfluidisGram+ve
in50%ofcasesandculture+vein90%ofcases
Gonococcal
arthritis(see
Chapter17)
Age15–30yrsinurbanpopulationsandwithinherited
deficiencyofcomplementsC5toC9.Oneformpresentsas
anacutesepticmonoarthritis.OrganismdetectedbyGram
stainofjointfluidin25%andbyculturein50%inthe
secondgroup

• Tenderness of thickened synovium is common, but is not always present.
Severely tender swelling suggests joint infection, haemarthrosis, or an acute
inflammatoryreactiontocrystals.
• Inflammation of entheses results in ‘bony’ tenderness at joint margins, and
sitesoftendonorligamentinsertion.
• Decreasedrangeofmotionisalmostalwaysdemonstrableinajointaffected
by synovitis or enthesitis. The degree to which passive and active range of
motionisreduceddependsonanumberofofteninterdependentfactors(e.g.
pain,sizeofeffusion,periarticularmuscleweakness,orpain).
• Movementofajoint affectedby synovitisorenthesitiswillinducepainand
stiffness,althoughneitherisspecific.Affectedjointswilldemonstratereduced
rangeonactiveorpassiverangeofmotionexercises;movingthejointbeyond
thatpointwillelicitpain.
• The age,sex,and occupationofthe patient givenon-specific, but important
clues:
• Oligoarthritis is uncommon in young adults. SpA, especially reactive
arthritis, is likely to be the main cause; 75% of patients who develop
reactivearthritisare<40yearsold.
• Gouttypicallyoccursinthose>40yearsold,andisthemostcommoncause
ofinflammatoryarthritisinmen(self-reportedin1in74menand1in156
women).
• ThemeanageofpatientswithCPPDarthritisisabout72years(range63–93
years).
• Areas endemic for tick infection (forestation) with Borrelia are at risk of
Lymearthritis.
History:whichjointsareaffected?
Someprocessesaremorecommonincertainjointsthanothers:
• Shoulder synovitis is typical in hydroxyapatite arthritis (Milwaukee
shoulder/kneesyndrome)andALamyloidosis(see Chapter18).
• Involvementofashoulderorhipisextremelyunusualingout.
• CPPDarthritis(aspseudogout)occursrarelyinthesmallfingerjoints(see
Chapter7).
• Thekneeisthecommonlyinvolvedinacutecrystallinearthropathyandseptic
arthritis(bothgonococcalandnon-gonococcal).
• Large knee effusions are common with Lyme arthritis, but this is a non-
specific finding. Large effusions can also be seen with septic and psoriatic
arthritis(see Chapter8).
• In theory, there are many causes of synovitis in a single first
metatarsophalangeal(MTP)joint,butthemajorityofcaseswillbeduetogout;
50–70% of first attacks occur in this joint. Care is needed in not mistaking
dactylitisduetoPsAforgout.
History:precedingfactors
Factors preceding swelling of a single joint or oligoarthritis may be highly
relevant.Theseincludetraumaandinfection:
• Acutenon-traumaticmonoarticularsynovitisismostcommonlyduetocrystal-
inducedsynovitisorsynovitisassociatedwithSpA.
• A preceding history of trauma typically suggests intra-articular fracture
(with/without haemarthrosis), a meniscus tear (knee), or an intra-articular
loosebody,suchasanosteochondralfragment(whichmaycausethepatientto
complainabouta‘locking’knee).
• Twinges of joint pain often precede an acute attack of gout. Acute arthritis
(‘pseudogout’)occursin25%ofpatientswithCPPDarthritis.
• In hydroxyapatite arthritis, synovitis is usually mild to moderate, gradual in
onset,andtypicallyworseatnight.
• AnacutemonoarthritiswithfeverinFMF(see Chapter18)isamimicof
septicarthritis.Suchjointmanifestationsarepresentinupto75%ofcases.
• Septic arthritis should always be considered (and promptly ruled out) as a
causeofacutejointswelling(see Chapter25).
History:familyandsocialhistory
Theremaybeimportantcluesfromthefamilyandsocialhistory:
• Both gout and SpA have a familial component. Between 6% and 18% of
patientswithgoutalsohaveafamilyhistoryofgout.Theremaybeafamily
history of SpA or uveitis in patients who have reactive, psoriatic, or
enteropathicarthritisorankylosingspondylitis(AS).
• Gout in young adults suggests an inherited abnormality (usually increased
urate production from 5-phosphoribosyl-1-pyrophosphate synthetase ‘super’-
activity,sincetheotherenzymedeficienciespresentinchildhood).
• Excessive alcohol consumption is associated with gout. Alcohol can also
contributetolacticacidosisthatinhibitsuratebreakdown.
• ConsiderLymediseaseifpatientslive,work,orvisitendemicareas;outsideof
the United States, this includes Europe, Russia, China, and Japan. Peak
incidenceoccursduringthesummer.
• Brucella arthritis is generally monoarticular and occurs primarily in areas
where domesticated animals are infected and poor methods of animal
husbandry,feedinghabits,andhygienestandardscoexist.

History:askaboutotherassociatedfeatures
Associatedextra-articularfeaturesincludepreviouseye,gastrointestinal,cardiac,
andgenitourinarysymptoms:
• Low-grade fever, malaise, and anorexia occur commonly in both septic
arthritisandgout.Markedfevercanoccuringoutandonlyoccursinabouta
thirdofpatientswithsepticarthritis.
• AskaboutanycurrentorpreviousfeatureswhichmightsuggestSpA:
• backorbuttockpain(enthesitisorsacroiliitis).
• swellingofadigit(dactylitis).
• plantarheelpain(plantarfasciitis).
• redeyewithirritation(anterioruveitis).
• urethritis,balanitis,cervicitis,recurrentoracutediarrhoea(reactivearthritis)
—besuspiciousofpreviousdiagnosisofIBD—askaboutgettingupatnight
to open bowels and passing slime/mucus—both suggestive symptoms for
IBD.
• psoriasis.
• symptomsofinflammatoryboweldisease.
• Behçet’sdisease(see Chapter18)cancauseanoligoarthritis.Otherfeatures
includepainfuloralandgenitalulcers,anduveitis.
• Theinvolvementofmorethanonejointdoesnotruleoutsepticarthritis.Inup
to20%ofcases,multiplejointscanbecomeinfected.
Examination:general
• Always compare sides, to establish if the changes are symmetric or
asymmetric.
• Itisimportanttoestablishfromtheexaminationwhetherthereistruesynovial
swelling.Ahistoryofswellingisnotalwaysreliableandother,non-synovial,
pathologycanpresentwithsingleoroligoarticularjointpain.
Examinationofaffectedjoints
Examinethe affected jointsfor tenderness.Checkpassiverangeof motionfor
evidenceoflockingorinstability:
• Acuteprocessessuchascrystalarthritis,infection,andpost-traumaticeffusion
oftenleadtopainfulswelling,markedtendernessofswollensofttissues,and
painfullyrestrictedactiveandpassivemovementofthejoint.Thesefeatures
areusuallylessovertwithchronicarthritis.
• Instabilityofanacutelyinflamedjointortestsforcartilagedamageintheknee
maybedifficultto demonstrate.Further examinationwillbe necessaryafter
drainageofjointfluid.

• Detectionofenthesistendernessaroundtheaffectedjointsoratothersitesisa
usefulcluetothediagnosisofSpA.
Examinationofothermusculoskeletalstructures
• Examine the low back and typicalsitesofbonytenderness—sacroiliitis and
enthesitisarecommonfeaturesofSpA.
• Tendonitis is not specific and can occur in gout, CPPD arthritis, SpA, and
gonococcalinfection.
Examination:lookforskinrashesandanyinflammation
Oligoarthritismaybepartofasystemicinflammatoryorinfectiouscondition:
• Temperature and tachycardia can occur with some non-infectious causes of
acutearthritis(e.g.crystalarthritis),althoughtheirpresenceinthecontextof
oligoarticularjointswellingrequiresexclusionofjointinfection.
• Goutytophimaybeseeninthepinnaeandinotherperipherallocations.They
canbedifficulttodiscriminateclinicallyfromrheumatoidnodules.Polarized
lightmicroscopyofmaterialobtainedbyneedleaspirationwillbediagnostic
fortophi.
• Thehallmarkofrelapsingpolychondritis(see Chapter18) islobe-sparing,
full-thicknessinflammationofthepinna.
• Mouthulcersarecommon;however,cropsorlargepainfultongueandbuccal
lesionsassociatedwitholigoarticulararthritissuggestBehçet’sdisease.
• Atypicalsitefortheosteitis(tenderswellingofbone)ofSAPHOsyndrome
(see Chapter16)isaroundthesternumandclavicles.
• Skinerythemaoverajointsuggestscrystalarthritisorinfection.
• Associated skin rashes may include erythema nodosum (associated with
ankle/knee synovitis in acute sarcoid), purpuric pustular rashes (Behçet’s,
gonococcal infection, and SAPHO syndrome), erythema marginatum
(rheumaticfever),orkeratodermablennorrhagica(aggressive-lookingrashof
thesoleofthefootinsexuallyacquiredreactivearthritis).
• Psoriasismaybeassociatedwithbothsynovitisandenthesitis.
Investigations
ThepresenceofsynovitiscanbeconfirmedbyobtainingUSorMRIofthejoints
inquestion.Atlargerjoints,botharesensitiveforthedetectionofeffusionand
synovialthickening.Inflammationatperiarticularorcapsularenthesescanalso
beseen.
Laboratorytests:jointfluid
The most important investigation of a patient with monoarticular synovitis is
jointaspirationandpromptexaminationoffluid.Fluidshouldbesentinsterile
bottlesformicroscopyandculture:
• The appearance of synovial fluid is not specific; however, blood or
bloodstaining suggests haemarthrosis from trauma (including the aspiration
attempt),ahaemorrhagicdiathesis,haemangioma,PVNS,andsynovioma.
• Turbidity (decreased clarity) of fluid relates to cellular, crystal, lipid, and
fibrinouscontent.Synovialfluidinsepticarthritisandacutecrystalarthritisis
frequentlyturbidduetotheeffectsofahighnumberofneutrophils.
• Cell counts give some diagnostic guidance but are non-specific (Table 2.5).
Thereisahighprobabilityofinfectionorgoutiftheneutrophildifferentialis
>90%.
• Jointfluideosinophiliaisnotspecific.
• Polarizedlightmicroscopyoffluidcandiscriminateurate(3–20µminlength,
needle-shaped,andnegatively birefringent—blueandthen yellowasthe red
platecompensatorisrotatedthrough90°)andcalcium-containingcrystalssuch
ascalciumpyrophosphate(positivelybirefringentcrystals,typicallysmalland
rectangularorrhomboidinshape).
• Lipid and cholesterol crystals are not uncommon in joint fluid samples, but
theirsignificanceisunknown.
• Crystalsappearinginsynoviumlesscommonly,butintypicalsettingsinclude
hydroxyapatite associated with Milwaukee shoulder (and knee) syndrome
(alizarin red-S stain positive), calcium oxalate in end-stage renal failure on
dialysis (may need scanning electron microscopy to confirm), cystine in
cystinosis,andxanthineinxanthinosis.
• Thepresenceofcrystalsinjointfluiddoesnotexcludeinfection.
• The most common causes of non-gonococcal septic arthritis in Europe and
North America are Staphylococcus aureus (40–50%), Staphylococcus
epidermidis (10–15%), Streptococcal species (20%), and Gram-negative
bacteria(15%).
Table2.5Characteristicsofjointfluid
Characteristic Normal GroupI(non-
inflammatory)
GroupII
(inflammatory)
GroupIII
(septic)
Viscosity Very
high
High Low Variable
Colour None Straw Strawor
opalescent
Variable
with
organisms
Clarity Clear Clear Translucentor
opaque
Opaque
Leucocytes
(cells/mm
3
)
200 200–2000 2000–50,000 >50,000
Polymorphonuclear
neutrophils(%)
<25 25 Often>50 >75
Investigations:radiographs
Radiographs can confirm an effusion,showcharacteristicpatternsofchondral
and bone destruction (e.g. in infection or erosive gout), and can reveal intra-
articularcalcificationassociatedwithCPPDorhydroxyapatitearthritis.
• Septicarthritiscausespatchyosteopeniaandlossofbonecortex.
• ‘Punched-out’erosions(withinjointsoraroundmetaphyses;‘LulworthCove
erosions’),softtissueswellings(tophi),andpatchycalcificationarehallmarks
ofchronicgout.
• Intra-articular calcification may commonly be either chondrocalcinosis (fine
linear or punctate fibrocartilage calcification) or larger loose bodies (often
withprolificosteophytes)—bothareassociatedwithCPPDarthritis.
• Numerousregularlyshapedcalcificmassesinajointmaybeduetosynovial
chondromatosis(mostcommoninmiddle-agedmen;50%ofcasesaffectthe
knee).
• ThepresenceoferosionsdoesnotimplicateRA.Thearthritismaybedueto
an enthesitis associated with SpA or erosive OA. Discrimination of erosive
enthesitis,RAerosions,OA-associatedsubchondralcysts,andgouterosionsis
often poorly done by non-MSK radiologists and the unwary/unlearned
rheumatologist!
Investigations:furtherimaging
Furtherimagingshouldbediscussedwithyourradiologists:
• MRIconfirmationof traumatizedstructuressuchasmeniscusdamageinthe
kneeandlabraldamageintheshouldershouldbesoughtifsuspected.
• US of knee or shoulder might be first-line imaging depending on the
experience of the radiologist when considering periarticular lesions (e.g.
anteriorkneestructurelesionsaroundthepatellarligamentortherotatorcuff
oftheshoulder).
• MRI can confirm synovitis, although appearances are usually non-specific.
CharacteristicMRIappearancesofenthesitisandassociatedosteitisandPVNS
arerecognized.
Otherlaboratoryinvestigationstoconsider
• FBC, acute-phase response (ESR, CRP). Neutrophilia is not specific for
infectionandcanoccurincrystalarthritis.
• Bloodurea,electrolytes,creatinine,andurate(e.g. hyperuricaemiaandrenal
impairmentassociatedwithgout).
• Blood calcium, phosphate, albumin, alkaline phosphatase (±PTH), thyroid
functiontests,andferritintoscreenforhyperparathyroidism,thyroiddisease,
andhaemochromatosis,allofwhichcanbeassociatedwithCPPDarthritis.
• Autoantibodies: RF and anticitrullinated peptide antibody (ACPA) may help
identifyearlyRA.RFisnotspecificforRAandislessspecificthanACPA.Be
awareoftheassociationofRFwithprimarySjögren’ssyndrome.
• Immunoglobulin M (IgM) Borrelia burgdorferi serology may help diagnose
Lymediseaseinpatientsatrisk(e.g.acutearthropathyormigratoryarthritis).
• Antibodies to the streptococcal antigens streptolysin O (ASOT) DNAase B,
hyaluronidase,andstreptozymemaybeusefulinpatientswhohavehadsore
throat,migratoryarthritis,orfeaturesofrheumaticfever(see Chapter18).
Investigations:synovialbiopsy
• If there is a haemarthrosis or suspicion of PVNS, MRI of the joint is wise
beforebiopsytocharacterizethevascularityofalesion.
• Considerabiopsytoevaluateamonoarthritisofunclearaetiology.Biopsymay
be helpful to diagnose sarcoid arthropathy (see Chapter 18), infectious
arthritis,orcrystalarthropathywhentheusualdiagnostictestsarenegative.
• Formalinfixationofsamplesissufficientinmostcases.Samplesforpolarized
light microscopy are best fixed in alcohol (urate is dissolved by formalin).
Snapfreezinginnitrogenisessentialifimmuno-histochemistryisrequired.
• Arthroscopicbiopsywillyieldmoretissuethanneedlebiopsyandwillallow
jointirrigation.
• Congo red staining of synovium, ideally with polarized light microscopy,
shouldberequestedifAA,AL,orβ
2
-microglobulinamyloidisapossibility
(see Chapter18).Thisshouldbeconsideredinpatientswithmyeloma(AL)
and long-term dialysis patients (β
2
-microglobulin). AA amyloid is an
uncommon, but recognized complication of RA, AS, FMF, and Crohn’s
disease.
WidespreadMSKpainsinadults
Widespread MSK pain is a common reason for adults to seek medical advice
(Table 2.6). Although some patients will have a polyarticular arthritis, many
conditions are characterized by MSK symptoms which may be diffuse or
multicentric. In addition, the interpretation and reporting of symptoms varies
considerablyandcanbeasourceofconfusion.Thissectionreviewsimportant
aspectsofthehistory,examination,andinvestigationsintheinitialevaluationof
patientswhopresentwithnon-localized,multicentricpains.
Initialimpressions
• Thinkbroadlyaboutthepossiblediagnoses.
• Usewhatyouknowabouttheepidemiologyoflikelyconditions.Forexample,
a35-year-oldmanwithperipheraljointpainsismorelikelytohavepsoriatic
arthritis(see Chapter8)thanRAorgeneralizedOA(see Chapter6),SLE
(see Chapter10),orPMR.
Age,gender,andracialbackground
• Whatcluescanbedrawnfromtheage,sex,andracialbackground?
• The degree to which these factors influence the likelihood of disease varies
according to the prevalence of the disease in the local population. Review
whatyouknowaboutepidemiologyofdiseases.
Previousdiagnoses
PresentingfeaturesmaybeputincontextearlyifyouhaveknowledgeofMSK
associationsofdiagnosesthathavealreadybeenmade.Forexample:
• Synovitis in patients with (radiological) chondrocalcinosis (CPPD
disease/arthritis).
• Arthropathyinpatientswithhyperparathyroidismandhypercalcaemia(see
Chapter16,CPPDarthritis/pseudogout).
• Enthesitis/synovitisinpatientswithCrohn’sdiseaseorulcerativecolitis(see
Chapter8,Spondyloarthritis).
• Polyarticularsynovitisandmyalgiainpatientswithlymphoma.
• Crystal-induced orβ
2
-microglobulin deposition arthritis and osteodystrophy
inchronicrenaldisease(see Chapter16).
Takingahistory
First, establish whether pains arise from joints or tendons/entheses, muscles,
bone,orareneurologic.
• Althoughthepatientmayreport ‘jointpains’,taketimetoestablishwhether
thepainsaretrulyfromthejointorperiarticulartissues.
• Listencarefullytothedescriptionofthepains;trytodetermineifthepatient
hasasingleconditionoranumberofoverlappingcausesofpain.
Table2.6BroadcategoriesofconditionsthatmaypresentwithwidespreadMSKpain
Common Inflammatorypolyarthritis(e.g.RAorpsoriaticarthritis)
Generalized(nodal)OA(see Chapter6)
Fibromyalgia/chronicpainsyndromes(see Chapter22)
Non-specificmyalgiasandarthralgias*associatedwithinfection
(e.g.viruses)(see Chapter17)
Less
common
Myoarthralgias*inautoimmuneconnectivetissuediseases
Myalgias/muscleinflammation(e.g.polymyositis)(see Chapter
14)
Myoarthralgias*withneoplasiaand/orskeletalmetastases
PolyostoticPaget’sdisease(see Chapter16)
Rare Metabolicbonediseases(e.g.osteomalacia,see Chapter8)
Metabolicmyopathies(e.g.hypokalaemia;see Chapter14)
Neurologicaldisease(Parkinson’sdisease)
*Incertainsituations/conditionspatientsmaycomplainofbothmuscleandjointpains.Thisiseasily
appreciatedifyou’veeverhadinfluenza!
Obtainadetailedhistoryofthepainatdifferentsites
• Agoodhistoryshouldhelpnarrowthedifferentialdiagnosisconsiderably.For
example,a70-year-oldmanreferredwith‘widespreadjointpainsmostlyinhis
legs’couldhavemultipleweight-bearingjointOAorlumbosacralnerveroot
claudication symptoms (see Chapters 3 and 6 and Chapter 21,
respectively).Amiddle-agedwomanwith‘handandneckpain’couldhavean
arthropathyorradicularpainassociatedwithcervicalspondylosis.
• Widespread paindueto bone pathology could bedueto skeletal metastasis.
Bonypainisoftenunremitting,andchangeslittlewithchangesinpostureand
movement.
• Onepitfallistoassumethatallpainsarisefromasinglepathologicalprocess.
Forexample,inanolderpatient,multiplepathologiesfrequentlyexistandcan
becomplicatedtounravel.Thefollowingareallcommonintheelderly:
• osteoarthritis(any/multiplejoints).

• CPPDarthritis.
• rotatorcuffarthropathy.
• sarcopenia/fallsrisk.
• PMR.
• spinalstenosisoflumbarcanalwithlegsymptoms.
• primaryhyperparathyroidism.
• CKD-relatedMSKsymptoms.
• hypovitaminosisD/osteomalacia.
Jointpainatrest,afterrest,orwithjointuse?
Establishwhetherpainarisesfromjointsortendons/entheses.
• Pain occurring with inflammation is conventionally regarded as being
associatedwithmorningstiffnessorstiffnessafterperiodsofrest.Ittendsto
be prominent in conditions such as RA, SpA, PMR, and myositis.
Inflammatoryjointpainoftenimprovesintheday.
• Milddegreesofimmobility-associatedpainandstiffnessoccurinsomeother
conditions, such as OA and fibromyalgia, although such forms of stiffness
generallylastfor<1h.Stiffnessmayalsobeafeatureofmusclespasmand
soft-tissueoedema.
• Mechanical joint damage such as OA is also painful. Unlike inflammatory
jointpain,mechanicaljointpainisworsenedbyuse,andimproveswithrest.
Ask,anddocumentindetail,whichjointsareaffected
• AsymmetricpolyarthritisaffectingthesmalljointsistypicalforRA.RAcan
also present withcarpaltunnelsyndrome,tenosynovitis, tennis elbow, or an
asymmetric pattern of joint involvement, and can be preceded by a
palindromic pattern of joint pain (see ‘Ask about the pattern of joint
symptomsovertime’,pp.57–58).
• Arthritis from parvovirus B19 infection may also be polyarticular and
symmetricbutalsomaycausemyopathyandgeneralsymptoms.
• Small joint pain in the hands occurs in nodal generalized OA. Distal
interphalangeal joints (DIPJs), proximal interphalangeal joints (PIPJs), and
thumbjointsareusuallyaffected.OAisalsoassociatedwithpaininthespine,
hips,andknees.
• Thecombinationofsacroiliac(lowbackandbuttock),pelvic,andlowerlimb
joint/enthesis pain, typically in an asymmetric oligoarticular pattern, is
suggestive of SpA. Typical sites of involvement include anterior knee,
posteriorandinferiorheel(plantarfascia).
• Enthesitis can affect the wrists and small joints of the hand and feet (e.g.
plantarfasciaoriginandinsertionatmetatarsalheads)andmaybedifficultto
distinguishfromRAonclinicalgroundsalone.
• CPPD typically favours the large and medium-sized joints, but a picture of
multiple joint involvement similar to that in RA is possible (including
tenosynovitis).
• Widespreadarthralgias/arthritisoccursinpatientswithleukaemia,lymphoma,
myeloma,andcertaininfections.
Askaboutthepatternofjointsymptomsovertime
• Ashort,strikinghistoryofmarked,acutepolyarticularsymptomsoftenoccurs
withsystemicinfection(Table2.7).Prominentmalaiseandfevershouldraise
suspicionofinfection.
• There may be a longer history than is first volunteered. Autoimmune
rheumaticandconnectivetissuediseasesmayevolveoveraperiodoftimeand
often naturally relapse and remit; the first symptoms of disease may be
dismissedbythepatientasirrelevant.
• Conventionally,persistentinflammatoryjointsymptomsshouldbepresentfor
atleast6weeksbeforeRAisdiagnosed.
• Migratory arthralgias occur in 10% of RA patients initially: a single joint
becomesinflamedforafewdaysthenimprovesandadifferentjointbecomes
affected for a few days and so on. A similar pattern can occur in post-
streptococcalarthritis,granulomatosiswithpolyangiitis(previouslyknownas
Wegener’sgranulomatosis),sarcoidosis,Lymedisease,andWhipple’sdisease.
• RecurrentpainsfromvariousMSKlesions,whichhaveoccurredfrominjury
or have developed insidiously, are typical in patients with underlying
hypermobility(e.g.EDSincludinghypermobility-EDS,OI,MarfanSyndrome
etc)(see Chapter19).
• Theonsetofenthesopathymaybeinsidiousoracute.
Table2.7Commoninfectionsthatcanpresentwithacutepolyarthritisandaraisedacute-phaseresponse
Infection Commonextra-articular
clinicalfeatures
Keylaboratory
diagnostictestsin
acuteinfection
Rheumaticfever
(groupAhaemolytic
streptococci)
Acuteinfection1–2weeks
earlier,fever,rash,carditis
Positivethroatswab
culture.HighASOT(in
80%)
Post-streptococcal Acuteinfection3–4weeks Asabove
earlier,tenosynovitis
ParvovirusB19
(adults*)
Severeflu-likeillnessat
onset,variousrashes
Anti-B19IgM
Rubella(alsopost-
vaccine)
Fever,coryza,malaise,
briefrash
Culture.Anti-rubella
IgM
HepatitisB Fever,myalgia,malaise,
urticaria,abnormalliver
function
Bilirubin+,ALT+,
AST+,anti-HBsAg,
anti-HBcAg
Lymedisease(Borrelia
burgdorferi)
Tickbites,fever,
headache,myalgias,
fatigue,nervepalsies
Anti-BbIgM(ELISA+
immunofluorescence)
Toxoplasmagondii Myositis,paraesthesias Anti-ToxoIgM
*ThepresentationofparvovirusB19illnessmaybequitedifferentinchildren.
Evenifserologicaltestshavehighsensitivityandspecificity,thepositivepredictivevalueofthetestis
lowiftheclinicallikelihoodoftheinfectionislow.Therefore,donotuseserologicaltests
indiscriminately.
Istherewidespreadmusclepain?
Ifyouthinkthereiswidespreadmusclepain,considerthat:
• Themyalgiasmaybefibromyalgiaorenthesitis.
• Painlocatingtomusclegroupareasmaybeischaemicorneurologicinorigin,
andnotnecessarilyduetointrinsicmuscledisease.
• Thedifferentialdiagnosisofpolymyositis(PM)anddermatomyositis(DM)is
broad,butmanyoftheseconditionsarerare(Table2.8andsee Chapter14).
Askaboutthedistributionanddescriptionofmyalgiasandweakness
• True weakness may denote either myopathy or a neurological condition.
However, patients may report a feeling of weakness if muscles are painful,
therefore,relymoreonyourexaminationbeforedecidingmusclesareweak.
• PMR (rare in patients <55 years old), myositis, and endocrine or metabolic
myopathiestypicallypresentwithproximalweakness.
• PMR does not lead to objective weakness; instead, patients experience
proximal muscle pain and stiffness that is worse in the morning, and is
frequentlydescribedbythepatientas‘weakness’.
• Althoughrare,truncalmusclepain,andstiffnesscanbeapresentingfeatureof
Parkinson’sdisease.
• Cramp-like pains may be a presenting feature of any myopathy (e.g.
hypokalaemic) or even motor neuron disease. However, some patients may
interpretradicular(nerveroot)painsas‘cramp-like’.
• Inflammatory,endocrine,andmetabolicmyopathiesareoftennotpainful.
• Occasionally, some genetic muscle diseases (e.g. myophosphorylase, acid
maltase deficiency), can present atypically late (in adults) with progressive
weaknessthatmaybemistakenforPM.
Askaboutthepatternofmusclepainsovertime
• Severe,acutemusclepainoccursinavarietyofconditions.Themostcommon
causes are viral, neoplastic, and drugs. Some toxic causes may result in
rhabdomyolysis,myoglobinuria,andacutekidneyinjury(AKI).
• UsuallyPM/DMischaracterizedbyslowlyevolving butprogressivemuscle
painandweakness(e.g.weekstomonths).
• Low-grade episodic muscle pains may denote a previously undisclosed
hereditarymetabolicmyopathy.
• Fibromyalgia (see Chapter22) is a chronic pain syndrome and symptoms
mayhavebeenpresentforaconsiderabletimeatpresentation.
Arethepainsischaemic?
• Ischaemic muscle pain often occurs predictably in association with repeated
activityandeasesorresolvesonrest(‘claudication’).Considerthisespecially
ifpainsareconfinedtoasinglelimborbothlegs.
Table2.8Themajorcausesofmyopathiesandconditionsassociatedwithdiffusemyalgia
Infectiousmyositis Viruses(e.g.influenza,hepatitisBorC,Coxsackie,
HIV,HTLV-I)
Bacteria(e.g.Borreliaburgdorferi(Lymedisease))
Other(e.g.malariatoxoplasmosis)
Endocrineand
metabolic
Hypo/hyperthyroidism
Hypercortisolism
Hyperparathyroidism
Hypocalcaemic,hypokalaemic
Autoimmune
diseases
Polymyositis
Dermatomyositis
SLE
Systemicsclerosis(SScl)
Sjögren’ssyndrome
RA,Vasculitis(e.g.PAN,AAV,rheumatoidvasculitis)
Myastheniagravis
Eosinophilicfasciitis
Carcinomatousmyopathy
Idiopathic Fibromyalgia(musclesshouldnotbeweak)
Inclusionbodymyositis
Sarcoidmyositis
Drugs Lipid-loweringdrugs(e.g.fibrates,gemfibrozil,
niacin)
Anti-immune(e.g.colchicine,ciclosporin,
penicillamine*)
Rhabdomyolysis(e.g.alcohol,opiates)
TNFαinhibitors
Others(e.g.azathioprine,chloroquine*)
Muscular
dystrophies
Limbgirdle
Facioscapulohumeral
Congenital
myopathies†
Mitochondrialmyopathy
Myophosphorylasedeficiency
Lipidstoragediseases
*Drugsmostlikelytocausepainfulmyopathy.
†Becauseofvariableseverity,someconditionsmaynotpresentuntiladulthood.
Note:Guillain–Barrésyndromeandmotorneurondiseasemaybeconsideredinthedifferential
diagnosisofnon-painfulmuscleweakness
• Thedistributionofpainsmaygivecluesastositesofunderlyingpathology,
e.g.upperextremitiesareaffectedbysubclavianarterystenosisandthoracic
outlet syndrome; lower extremities are affected by atherosclerotic vascular
diseaseorlumbarnerverootstenosis.
• Ischaemic pains in the context of a highly inflammatory state may suggest
systemicvasculitis,suchaspolyarteritisnodosa.
Widespreadpainmaybeduetobonepathology
• Bone pains are unremitting and disturb sleep. They could denote serious
pathology—radiographicandlaboratoryinvestigationsareimportant.
• The major diagnoses to consider include disseminated malignancy, multiple
myeloma, metabolic bone disease (e.g. renal osteodystrophy,
hyperparathyroidism,osteomalacia),andpolyostoticPaget’sdisease.
Specificquestionsareoftenrequiredbecausepreviousproblemsmaynotbe
regardedasrelevantbythepatient.Forexample:
• Forthosewithjointpainsahistoryofthefollowingmaybeofhelp:
• otherautoimmunediseases(increasedriskofRA,SLE,etc.).
• Raynaud’sphenomenon(associationwithSScl,RA,andSLE).
• dryeyes(possibleSjögren’ssyndrome).
• uveitisoracute‘redeye’(associationwithSpA).
• recurrent injuries/joint dislocations (association with joint hypermobility
syndrome.
• genital,urine,orseveregutinfection(linkwithSpA).
• psoriasis(associationwithSpA).
• diabetes(cheiroarthropathy).
• Forthoseinwhommyalgias/myositisseemslikely:
• precedingviralillness(possibleviralmyositis).
• foreigntravel(tropicalmyositis).
• otherautoimmunedisease(associatedwithPM/DM).
• previouserythemanodosum(sarcoid).
• drugsandsubstanceabuse.
• Forallpatients:
• weightlossoranorexia(associationwithmalignancy).
• feversornightsweats(associationwithinfection).
• sorethroat(possiblepost-streptococcalcondition).
• persistentspinalpain(associationwithfibromyalgia).
• rashes(associationwithLymedisease,SLE,DM,vasculitis).
• Forthosewithwidespreadbonypain:
• historyofrickets(associationwithosteomalacia).
• chronicrenaldisease(willprecederenalosteodystrophyandmaypredispose
tocrystallinearthritisandosteoarticulardepositionofβ
2
-microglobulin).

Psychosocialandsexualhistory
• Precedingsexualactivityandgenitalinfectionisimportantprimarilybecause
of an association of Chlamydia trachomatis infection with reactive arthritis
andenthesitis/SpA(see Chapter8).
• ReactivearthritishasanassociationwithHIV.HIVisalsoassociatedwithPM,
andisariskfactorforpyomyositis.
• ThereisanassociationofanxietyanddepressionwithFM(see Chapter22).
Askabouttravel
• Residencein,ortravelto,ruralareaspopulatedbydeermightbeimportantin
indicating a risk of exposure to Borrelia burgdorferi and contracting Lyme
disease(the spirocheteis carriedby ticksthat colonizedeer,boar, andother
animalsandbiteothermammals).
• Plasmodium falciparum (intertropical areas), Trypanosoma (mainly South
America), Trichinella, and cysticerci (tapeworm larval cysts) infections are
associatedwithmyalgias/myositis.
Familyhistory
Askaboutfamilywitharthritisorautoimmunediseases:
• There is a hereditary component to psoriatic arthritis, SpA, large joint and
generalizednodalOA,andhyperuricaemia/gout.
• The risk of developing any autoimmune condition is higher in families of
patientswithautoimmunediseasesthangenerally.
• Hypermobilityperse(notnecessarilyjointhypermobilitysyndrome)andFM
showastrongheritabilityintwinstudies.
Drughistory
• Thefollowingdrugshavebeenreportedtocauseamyopathy(thosemarked
*
aremorelikelytobepainful):lithium,fibrates,statins,penicillin,colchicine,
penicillamine
*
, sulphonamides, hydralazine, ciclosporin, phenytoin,
cimetidine
*
(musclecramps), zidovudine, carbimazole,TNFαinhibitors, and
tamoxifen.
• The myositis that occurs with penicillamine is not dose dependent or
cumulativedosedependent.Itcanbelife-threatening.
• Drug-inducedSLE,whichischaracterizedcommonlybyarthralgias,aching,
andmalaise,andlesscommonlybypolyarthritis,canoccurwithanumberof
drugs including hydralazine, procainamide, isoniazid, minocycline, TNFα
inhibitiontherapy.Quinidine,labetalol,captopril,phenytoin,methyldopa,and
sulfasalazinemayalsocausesimilarsymptoms.
• Mildmyalgiasandarthralgiasmaybecausedbyanumberofcommonlyused
drugs,e.g.protonpumpinhibitorsandquinoloneantibiotics.
• Alcoholinexcessandsomeillegaldrugsareassociatedwithtoxicmyopathy
occasionallyresultinginrhabdomyolysis.
Askaboutchestpain,dyspnoea,palpitations,cough,andhaemoptysis
• Cardiac abnormalities are features of autoimmune rheumatic and connective
tissuediseases, butare infrequentat initialpresentation.Cardiacinfectionis
associated with widespread aches and pains (e.g. rheumatic fever/post-
streptococcalmyalgias/arthralgias,infectiveendocarditis).
• Chroniceffort-relateddyspnoeaduetointerstitiallungdiseaseoccursinmany
patients with autoimmune connective tissue and rheumatic diseases. Up to
40%ofRApatientsmayhaveCTevidenceoflungdisease.Inmanysedentary
patients,however,symptomsarenotprominent.Dyspnoeamaybepresentat
presentation.
• Respiratory failure and aspiration pneumonia can occur as a result of a
combinationoftruncalstriated,diaphragmatic,andsmoothmuscleweakness
inPM.
• ThereisanassociationbetweenbronchiectasisandRA.
• Themostcommonneoplasminpatientsdiagnosedwithmalignancy-associated
myositis,isofthelung.
Askspecificallyaboutdysphagia,abdominalpain,anddiarrhoea
• Patients may not mention gastrointestinal symptoms if they have resolved.
Therearemanylinksbetweenboweldiseaseandinflammatoryarthritis(SpA
linkedtoIBDisprobablythecommonest).
• Ask specifically about previous severe diarrhoeal or dysenteric erythema
migransinLymedisease.
• Erythemamarginatuminrheumaticfever.
• UVsensitiverashonface/armsinSLE.
• Violaceousrashonknuckles/aroundeyes/baseofneckinDM.
• LivedoreticularisinSLEandAPS.
• Purpuricrashinvasculitis(e.g.HSP).
• Erythemanodosuminsarcoidosis.
• Illnesses such as those caused by Campylobacter, Yersinia, Shigella, or
Salmonella,willberelevanttodiagnosingreactivearthritis/SpA.
• Gutsmoothmusclemaybeaffectedinpolymyositisandgiverisetodysphagia
andabdominalpain.
Examination
Inpatientswithwidespreadpain,afullmedicalexaminationisalwaysnecessary.
Skinandnails
Inallpatientslookcarefullyattheskinandnails:
• Nails may show prominent ridges or pits in psoriatic arthropathy, splinter
haemorrhages in infective endocarditis, systemic vasculitis or APS, or
periungualerythemainsclerodermaandtheinflammatorymyopathies.
• Look for skin rashes in conditions characterized by widespread pain. For
example, lymphadenopathy may be present with either infection or
inflammation and is non-specific. However, if prominent it may denote
lymphoma.
• Signs of anaemia are a non-specific finding in many chronic systemic
autoimmunediseases.
• ClubbingofthedigitsmaybepresentinCrohn’sdiseaseandulcerativecolitis
(associatedwithSpA)andbronchiectasis(associatedwithRA).
• Oedemacanoccurinbothupperandlowerextremitiesinasubsetofpatients
presenting with inflammatory polyarthritis/tenosynovitis. The condition has
beentermedRS
3
PE(remittingseronegativesymmetricsynovitis withpitting
oedema).Thisconditionisstrikinginthatitoccurssuddenly,ofteninpatients
60–80 years old and is very disabling. It may be associated with other
conditions.ItmaybeamanifestationofpseudogoutinCPPDdisease.
Examinationofthejoints
Importantpointstonotewhenexaminingjoints:
• Eachjointshouldbecomparedtothejointontheoppositeextremity,firstby
observation, then palpation, then by its active and passive range of motion
exercises.
• Useful examination tools include a tape measure to record swelling
(circumferential)andagoniometer(protractorwitharms)tomeasuretherange
ofjointmovement.
Patternsofabnormality
Notethespecificcauseofjointswellingandsiteoftenderness,distributionof
affectedsites,andhypermobility:
• InnodalgeneralizedOA,osteophytes(bonyswelling—maybetender)canbe
notedatDIPJs(Heberden’s nodes)andPIPJs(Bouchard’s nodes).Periosteal
newboneatsitesofchronicenthesitismaybepalpableandtender.
• Nodules may occur in nodal OA, RA, polyarticular gout, ANCA-associated
vasculitis,multicentricreticulohistiocytosis,orhyperlipidaemia(xanthomata).
• Soft tissue swelling with tenderness and painful restriction of the joint on
movementsuggestsaninflammatoryarthritis.Thereisoftenadjacentmuscle
wasting.Thisismosteasilyappreciatedintheinterosseousmusclesinpatients
withhandarthritis,orthequadricepsinpatientswithkneearthritis.
• The ‘painful joints’ may be inflamed tendons or entheses. Tender tendon
insertionsandperiarticularbonetenderness,oftenwithoutanyjointswelling,
maydenoteenthesisinflammationassociatedwithSpA.
• Tendonitismaybepartofmanyautoimmunerheumatic orconnective tissue
diseases.Lookspecificallyforthickeningofthedigitalflexorsandswellingof
thedorsalextensortendonsheathinthehand,andtenderness/swellingofboth
peronealandposteriortibialtendonsinthefoot.
• GrossswellingwithpainfulrestrictionofsmalljointsisunusualinSLE.Often
thereislittletofindonexaminationofjoints.
• Generaljointhypermobilitymayleadtojointandothersofttissuelesions.An
examinationscreenfor hypermobility maybe helpful (Table2.9; also see
Chapter19).Checkalsoforassociatedfeatures.
Table2.9Featuresofhypermobility.Thesearethe‘Brighton’criteria
Examinationscreen
(scoredoutof9)
Abilitytoextendfifthfinger>90°atMCPJ
(score1+1forR+L)
Abilitytoabductthumb(withwristflexion)to
touchforearm(score1+1)
Extensionofelbows>10°(1+1)
Extensionofknees>10°(1+1)
Abilitytoplacehandsflatonfloorwhenstanding
withkneesextended(1)
Associatedfeatures
Prolongedarthralgias
Skinstriae,hyperextensibility,andabnormal
scarring
Recurrentjointdislocations
Varicoseveins
Uterine/rectalprolapse
Recurrentsoft-tissuelesions
Marfanoidhabitus
Eyesigns:droopingeyelids,myopia,down-
slantingeyes
Examinationofpatientswithwidespreadmyalgia
• Check for muscle tenderness and weakness. Document the distribution. Is
thereevidenceofneurologicorvasculardisease?
• The characteristic sites of tenderness in fibromyalgia should be confidently
recognized(Fig.2.1;seealso Chapter22).Despitediscomfort,themuscles
shouldbestrong.
• Examinethestrengthofbothtruncalandlimbmusclegroups(Fig.2.2).Inthe
presenceofpain,itmaybedifficulttodemonstratesubtledegreesofmuscle
weakness.
• Patternsofmuscleweaknessarenotdiseasespecific;however,therearesome
characteristic patterns: symmetric proximal extremities in PM and DM;
quadriceps and forearm/finger flexors in inclusion body myositis; limb
musclesinmitochondrialmyopathy.(Note:usingspecificapparatusphysical
therapists can help document isometric muscle strength in certain muscle
groups.)
• MusclesinPMRarenotintrinsicallyweak.
• Muscle wasting is not specific. If wasting is profound and rapid, consider
neoplasia.Wastingwilloccurinmostlong-standingmyopathies.
• Check for increased limb tone and rigidity—most evident by passive
movement atajoint—consistent with extrapyramidal disease. Theremaybe
restingtremorinthehand,facialimpassivity,and‘stiff’gait.Musculartonein
the limbs may also be increased in motor neuron disease; however, if
presentingwithmuscle pains,thepatientwithmotorneurondiseaseismore
likely to have a lower motor neuron pattern of neuronal loss (progressive
muscular atrophy) with muscular weakness/wasting, flaccidity, and
fasciculations.
• The fatiguability of myasthenia gravis can be identified by determining the
lengthoftime the patientcankeep theirarmsextended in frontofthem, or
maintainanupwardgaze.
• Muscle pains or cramps due to large-vessel ischaemia are likely to be non-
tenderatrestandstrong.Demonstrateabsentpulsesandbruitsandsubstantiate
findingswithUSDopplerexamination.
• In suspected cases of PM and DM, examine for cardiopulmonary
abnormalities. Other associated signs in DM include periungual
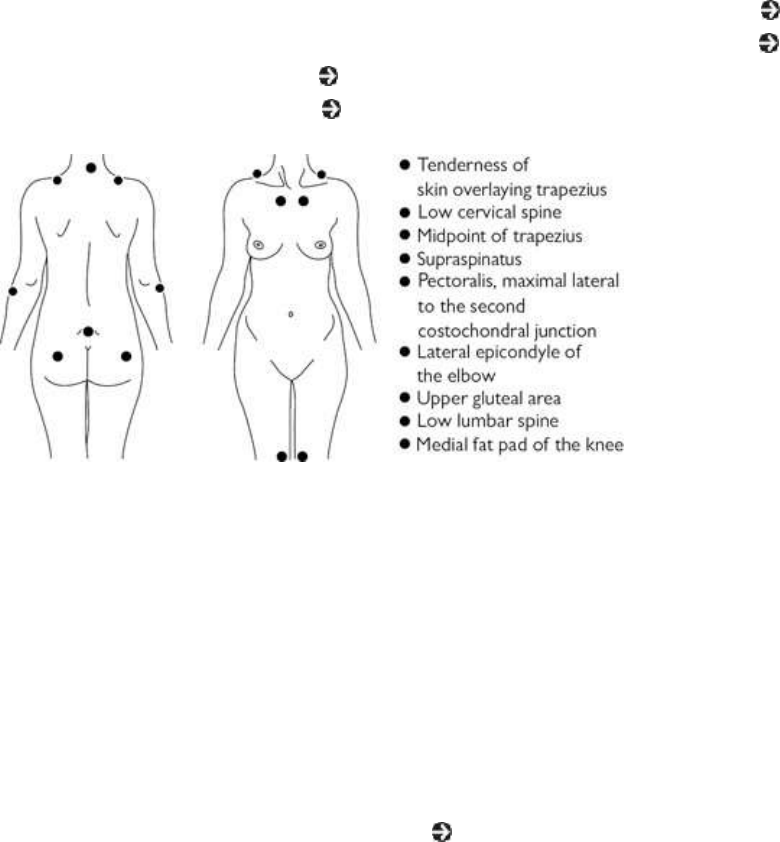
erythema/telangiectasia, erythematous violaceous rash and skin calcinosis.
DysphoniaandswallowingabnormalitiesoccurinbothPMandDM.
• Because of its associations, patients with myositis should be carefully
examinedforthefollowingsigns:dryeyes/mouth(Sjögren’ssyndrome;see
Chapter12), skin thickening/tendernessordiscoloration (scleroderma;see
Chapter 13), skin rashes (SLE; see Chapter 10), thyroid tenderness or
enlargement(endocrinemyopathy;see Chapter4).
Fig.2.1Typicalsitesoftendernessinfibromyalgia.
Investigations:generalpoints
• ESR and CRP may be higher than normal in the setting of infection,
malignancy,oractiverheumaticdisease.AslightlyelevatedESRisacommon
findinginhealthyelderlypeople.
• ApositiveANAmayoccurinassociationwithmanyautoimmuneconditions,
inotherdiseases(Table2.10),andinsomehealthypeople.Itis,therefore,not
diagnosticforSLEoranysinglecondition;however,high-titreANAmaybe
significantandconversely,ANA-negativeSLEisrare.
• ACPA is more specific for RA than RF (see Chapter 5), which can be
positiveinanumberofinflammatoryconditions.
• Controversy exists about the diagnosis of FM. It is prudent to only make a
diagnosisofFMwhenotherdisorderscanbeconfidentlyexcluded.Consider:
psoriasis-related MSK disease, SAPHO, sarcoid, autoimmune connective
tissuediseasesincludingAPS,vasculitides.
Basictestsinpatientswithpolyarthropathy
• Urinalysis (dipstick) may show proteinuria or haematuria. Both glomerular
and tubular damage are possible. Glomerulonephritis (in SLE, vasculitis, or
endocarditis, for example) is usually associated with significant proteinuria
andhaematuriasimultaneously.Thesepatientswillneedurgentevaluationby
anephrologist.
• ESRandCRParenon-specificandmaybenormalintheearlystagesofthese
conditions.Ifveryhigh,thenconsiderinfectionormalignancy.Thereisoften
no evidence of an acute-phase response in patients with enthesitis (even
though pain and bony tenderness may be widespread). A mild anaemia and
thrombocytosismayaccompanyinflammation.
• Throat swab, ASOT, anti-DNAaseB antibodies may be useful to identify a
recent post-streptococcal condition, but levels may remain mildly elevated
long-termandindicatepreviousinfection(IgG).
• Othertestswhichcanbeconsideredintheappropriatesetting:
• randombloodsugar(diabetes).
• TFTs/thyroidantibodies(hyper/hypothyroidism).
• prostatic-specificantigen(malignancy).
• fecalcalprotectin(screeningforinflammatoryboweldiseaseinSpA).
• Jointfluidaspirationandcultureismandatoryforpatientsinwhomsepsisisa
possibility. Fluid should be examined by polarized light microscopy in
suspectedcasesofcrystal-inducedsynovitis.
• InpatientswhoareANA-positive,testforextractablenuclearantigens(ENAs)
tohelpcharacterizethetypeofautoimmuneprocess.
• In many patients presenting with a short history of widespread joint pains,
radiographswillbenormal.Anearlysignofjointinflammationisperiarticular
osteopenia, but this is not specific. Recognized types of erosions, and bone
reactionlesionsandtheirdistributioncanbenotedbyexperiencedradiologists
inspecificconditions(e.g.RA,psoriaticarthritis,gout,CPPDarthritis).
• Referraltoasexualhealthclinicforfurtherdetailedinvestigationsifthereisa
suggestionofrecentorrecurrentgenitalinfectionmayhelptostrengthenthe
evidenceforadiagnosisofsexuallyacquiredreactivearthritis.
Laboratorytestsinpatientswithwidespreadmusclepain/weakness
• Dipstickurinalysis:toscreenforhaematuriaormyoglobinuria.
• FBC,ESR.
• Initial screening tests to consider: urea/electrolytes (U&E), creatinine,
TFTs/TSH, bone profile, and 25-hydroxyvitamin D, liver function tests
(LFTs), angiotensin-converting enzyme (ACE), CK, parathyroid hormone
(PTH),ANA/ENAs,RF,myositisspecificantibodypanelandconsiderrandom
cortisoland24-hoururinarycortisol.
Table 2.10. Examples of the prevalence of antinuclear antibodies (ANAs) in some diseases using
ELISA,orHep2cellsassubstrate
Populationgroup PrevalenceofANAs
(‘upto’)(%)
Normalpopulation 8
SLE 100
Otherautoimmunejoint,
vasculitis,orCTDs
Systemic
sclerosis
95
Sjögren’s
syndrome
70–80
Psoriatic
arthritis
50
Polymyositis 40
Polyarteritis
nodosa
18
Examplesfromotherdiseases Chronicactive
hepatitis
100
Drug-induced
lupus
100
Myasthenia
gravis
50
Sarcoidosis 30
Diabetes 25
• ElevatedCKoraldolaseoccursinmostcasesofPM.ALT,AST,andlactate
dehydrogenase(LDH)arenon-specificmarkersofmuscledamage.Notethat
specificmuscleisoenzymesofCKandLDHexistandthenormalrangeofall
enzymesmayvaryindifferentpopulations.Muscleenzymesmaybeelevated
afternon-inflammatorycausesofmuscledamage,e.g.exercise/trauma.
• Check for ANA and, if positive, screen for ENAs. Antibodies to certain
(cytoplasmic)tRNAsynthetases(e.g.Jo-1,SRP)aremyositis-specific.
• Think of checking for urinary myoglobin in cases where acute widespread
muscle pain may be associated with myolysis—causes include excessive

alcoholoringestionofcertaindrugs(cocaine,amphetamines,ecstasy,heroin),
exercise,ortrauma.Suchpatientsmaybeatriskofrenalfailure.
• PM can be a presenting feature of HIV. In HIV-positive patients, infections
causingmusclediseaseincludeTBandmicrosporidia.
• Viral myositis may be clinically indistinguishable from PM. Serology may
yielddiagnosticclues.
Electrophysiologyandimaginginpatientswithmuscleconditions
• Electromyography (EMG) abnormalitiesoccur in two-thirds ofpatientswith
muscleinflammation.Moreinformationislikelyifstudiedintheacuterather
than the chronic phase of the illness. In the acute phase, denervation and
muscledegenerationgivefibrillationpotentialsin74%ofPMand33%ofDM
patients (see Chapter 14). Other features include low-amplitude short-
durationmotorunitandpolyphasicpotentials.
• EMGispooratdiscriminatingongoingmuscleinflammationinmyositisfrom
steroid-inducedmyopathy.
• TherearecharacteristicMRIpatternsofabnormalityinPMandDM.MRIcan
beusedtoidentifypotentialmusclebiopsysitestoavoidfalse-negativeresults
associatedwithpatchymuscleinflammation.
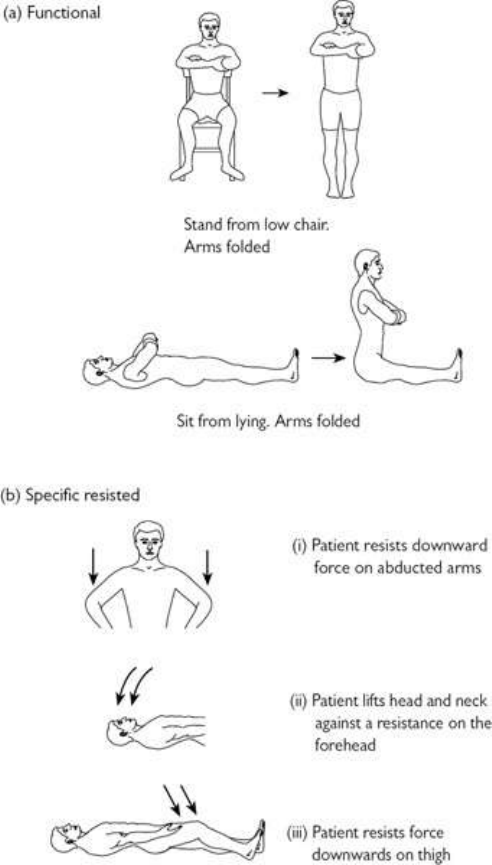
Fig.2.2Screeningexaminationforproximalmyopathy.(a)Functionalmovementsrequiringtruncaland
proximallowerlimbmusclestrength.(b)Resistedmovementtestingofdeltoid(i),longitudinalflexorsof
theneck(ii),andiliopsoas/quadriceps(iii)strength.
Musclebiopsy
• MusclebiopsyshouldbeconsideredinallpatientsevaluatedforPMorDM.
• In PM, inflammatory infiltrates predominate in the endomysial area around
muscle fibres without perifascicular atrophy. In DM, inflammation is more
prominentintheperimysialareaandaroundsmallbloodvesselsandthereis
typicallyperifascicularatrophy.
• Routine tests do not reliably distinguish PM from cases of viral myositis.
Some of the glycogen storage diseases will become apparent from light
microscopyofbiopsymaterial.
• An autoimmune myositis is unlikely in the absence of positive HLA
immunohistochemistryonbiopsymaterial.
Investigationsformalignancy
Investigations in adults with widespread bony pain should aim to rule out
malignancy, particularly myeloma, gonadal tumours, and malignancies from
breast,renal,andprostatecancers:
• Investigationsshouldincludemammography,urinecytology,PSA,renalUS,
serumandurinaryproteinelectrophoresis.
• Hypercalcaemia may accompany these conditions; check blood calcium,
phosphate,25-hydroxyvitamin-D,PTH,PTH-relatedprotein.
• PTHshouldalsobecheckedinsuspectedcasesofosteomalacia(raiseddueto
calcium/vitaminDdeficiency)togetherwith25-hydroxyvitaminDlevels(low
orlow/normal),alkalinephosphatase(high/normal),24-hoururinarycalcium
willbelow.
• Radiographsofaffectedsitesareimportant.IncludeaCXR.
• Bonescintigraphycanidentifysitesofneoplasia,Paget’sdisease,osteoporotic
fractures,severePTHbonedisease,orosteomalacia.Characteristicpatternsof
abnormalityexist.
• Whole-body CT scan is often the best single investigation to rule out deep
tissuemassesinabdomenandpelvis.
• Bonebiopsy(maintainedundecalcifiedbyplacingsamplein70%alcohol)of
affected sites will be diagnostic in some, but not all, cases of osteomalacia,
osteoporosis,andrenalosteodystrophy.Thebestsamplesareobtainedfroma
transiliacbiopsy.Bonemarrowcanbeaspiratedforexaminationatthesame
time.
• PET-CTisnowusedtoscreenforsuspectedsmalltumourswhereothertests
arenegative,forlocatinglymphomatissueforbiopsyandinidentifyingdeep
tissueinflammationorsepsiswherediagnosisisotherwiseunclear.

Chapter3
Regionalmusculoskeletalsymptoms:makinga
workingdiagnosis
Introduction
Neckpaininadults
Neckpaininchildrenandadolescents
Shoulderpaininadults
Shoulderpaininchildrenandadolescents
Painaroundtheelbowinadults
Elbowpaininchildrenandadolescents
Wristpaininadults
Symptomsinthehandinadults
Wristandhandpaininchildrenandadolescents
Upperlimbperipheralnervelesions
Thoracicbackandchestpaininadults
Thoracicbackandchestpaininchildrenandadolescents
Lowbackpaininadults
Lowbackpaininchildrenandadolescents
Pelvic,groin,andthighpaininadults
Pelvic,groin,andthighpaininchildrenandadolescents
Kneepaininadults
Kneepainandlowerlimbdevelopmentinchildrenandadolescents
Lowerlegandfootdisordersinadults
Lowerlegandfootdisordersinchildrenandadolescents
Introduction
Thischapteraimstoprovideaguidetoconstructingadifferentialdiagnosisin
the patient who presents with regional musculoskeletal (MSK) symptoms. It
doesnotmakereferencetoallpossiblediagnoses,onlythemostcommon.
Generalconsiderations(adults)
• Findings from conventional clinical examination and imaging of the MSK
systemusuallyoccurwhenthepatientisatrest,andthereforeonlyminimally
symptomatic.
• Examinationinthecontextoffunction(i.e.carrying,lifting,walking,bending,
etc.) is not easy, although it is arguably more appropriate. Therefore, a
thoroughhistoryutilizingagooddepthofknowledgeoffunctionalanatomyis
thebestalternativeandaninvaluablewayofobtaininggoodinformationabout
abnormalfunctionanditscauses.
• Time spent obtaining a detailed account of onset of symptoms is helpful
whetherornotthesymptomsareofrecentonset,orchronic,orassociatedwith
trauma.Patientsusuallyhaveaclearerconceptofinjury-induceddiseaseand
may try to rationalize the appearance of non-trauma-related symptoms by
associationwithaneventorinjury.
• Lay terms may reflect lay understanding. For example, the term ‘repetitive
straininjury’iscommonlyusedby thelaypersontodenoteadiagnosis.Itis
not a diagnosis, merely a description of a (unlikely!) mechanism by which
injuryhasoccurred.Itisimportanttoidentifyanatomicallywheretheproblem
liesandtothenenquireastoactivitiesthatmayhaveinducedorperpetuated
theproblem.
• Considerthepossibilitythattheproblemisa‘work-relateddisorder’(WRD).
A WRD may not just be MSK; consider the possibility of associated
respiratory (asthma, fibrosis), dermatological (dermatoses), neurological
(neuropathy, behavioural), psychosocial (anxiety, depression), and infective
(sewage, carcasses, needlestick) pathologies. Examples of MSK WRDs are
giveninthischapter.
• Withchildren,itisimportanttoobtainahistoryfromboththechildandacare
provider.Second-handinformation,evenifprovidedbyaparent,maybeless
reliable than direct information from someone who has the opportunity to
observethechildduringtheday.
• Regional MSK lesions may be a presenting feature of a systemic disorder,
suchasanautoimmunerheumaticdisease,malignancy,orinfection.Clinical
suspicionshouldguidetheevaluation.
• Screening for disseminated malignancy, lymphoma, myeloma, and infection
should at least include a FBC, metabolic screen, serum and urine protein
electrophoresiswithimmunofixation,ESR,andCRP.
• Weakness(asasymptom)maybeduetoaneuropathicormyopathiccondition
or it may be perceived according to the impact of other symptoms such as
pain.
Generalconsiderations(childrenandadolescents)
Regional MSK assessment in children and adolescents differs from adult
assessment, in the need to account for developmental variation, and motor
‘competence’.
• Though MSKproblemsfromcongenitaldeformities canpresent forthe first
time in adults—to adult rheumatologists—it is more likely that congenital
anomaliesaredisclosed initially inchildren.Regional MSK assessmentina
childrequiresconsiderationofthis.
• AlthoughMSKpainisanubiquitousexperienceinchildhood,responsetopain
by an individual child depends on various states of anxiety, stress, and past
experiences and can be influenced by the role of parents or other family
members.
Neckpaininadults
Backgroundepidemiology
• About 10%ofthe adultpopulationhas neckpainat any onetime, although
manypeopledonotseekmedicalhelp.
• About1%ofadultpatientswithneckpaindevelopneurologicaldeficits,but
overalllevelsofdisabilityarelowerthanforpatientswithlowbackpain.
• A continuum of radiological appearances exists in relation to age:
intervertebraldiscnarrowing,marginalend-plateosteophytes,andfacetjoint
changes. Appearances are often termed ‘degenerative’; however, the
correlationwithpresenceandseverityofpainispoor;Table3.1liststhemajor
causesofneckpaininadults.
Functionalanatomy
• Theneckisthemostmobile(37separatearticulations),butleaststablepartof
the spine. There are seven vertebrae (C1–C7) and five intervertebral discs
(C2/3–C6/7).TheC5/6discismostoftenassociatedwithradicularsymptoms.
If it occurs, cord compression is most likely in this region, although
atlantoaxial (C1–C2) subluxation may produce the same picture, especially
amongpatientswithRA.
• Minor congenital abnormalities are not infrequent and increase the risk of
degenerativechanges.
• NerverootsC2andC3coversensationoverthebackofthehead,thelower
jawline,andtheneck.
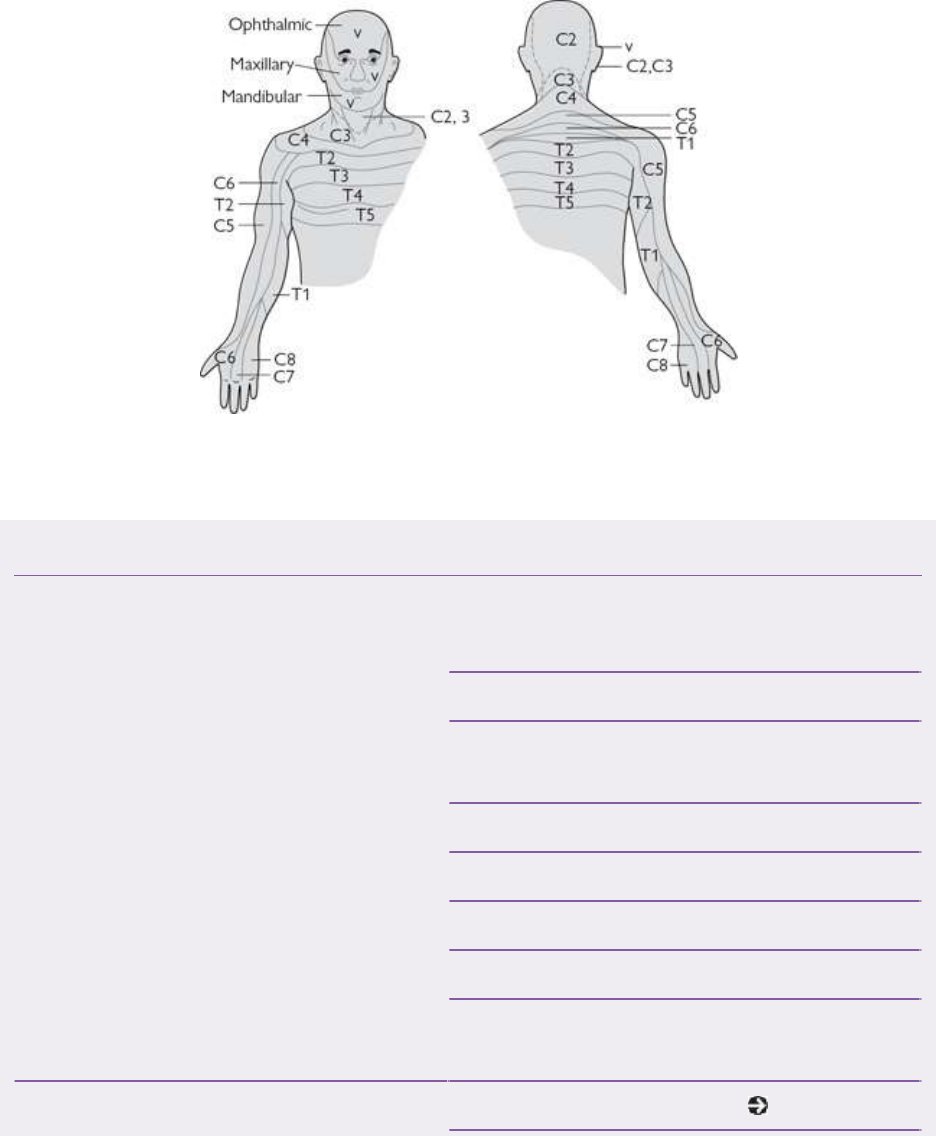
• Nerve roots (C4–T1) leave the spine in dural root sleeves, traverse the
intervertebralforamina,andformthebrachialplexus.
• Cervicalnerveshaveadermatomalrepresentation(Fig.3.1)andsupplyupper
limbmusculatureinapredictableway.
Fig.3.1Dermatomaldistributionofthecervicalandupperthoracicnervesreflectingtheradicularpatternof
nerverootlesions.
Table3.1Themajorcausesofneckpaininadults
Softtissuelesions(posture,
psychogenic,andoveruseas
modifiers)
Neckstrain
Torticollis
Myofascialpain
Trauma(e.g.acuteflexion-extension
injury(‘whiplash’))
Cervicothoracicinterspinousbursitis
Degenerativeandmechanical
lesions
Spondylosis
Discprolapse
Thoracicoutletsyndrome
Diffuseidiopathicskeletalhyperostosis
(DISH)
Inflammatoryconditions Rheumatoidarthritis(see Chapter5)
Spondyloarthropathy(±fracture
±inflammatorydiscitis)
Juvenileidiopathicarthritis(see
Chapter9)
Polymyalgiarheumatica(PMR)
Myelitis
Bonelesions Traumaticfracture
Osteomyelitis(e.g.TB)
Osteoporosis(fracture)(see Chapter
16)
Osteomalacia(bonediseaseormuscle
pain)
Paget’sdisease
Non-osseousinfections Generalsystemicinfection
(general/cervicalmyalgias)
Meningitis
Discitis
Malignancy Primary(rare)orsecondarytumours
(±pathologicalfracture)
Myeloma,lymphoma,leukaemia
Brachialplexuslesions Trauma
Thoracicoutletsyndrome(e.g.cervical
rib)
Referredpain Acromioclavicularor
temporomandibularjoint
Heartandmajorarteries(e.g.angina,
aortadissection)
Pharynx(e.g.infection,tumours)
Lunganddiaphragm(e.g.tumour,
subphrenicabscess)
Abdomen(e.g.gallbladder,stomach,
oesophageal,orpancreaticdisease)
Shoulder(e.g.adhesivecapsulitis)
Takingahistoryofneckpaininadults
Thesite,radiation,anddescriptionofpain
• Nerveroot(radicular)pain isusuallysharpandreasonablywelllocalized in
thearms.Itisoften‘burning’andassociatedwithparaesthesiaandnumbness.
• Nerve root irritation and compression by an intervertebral disc are common
causes of radicular pain. However, in older adults and those who suffer
recurrentboutsofpainitisusuallyduetoencroachmentofvertebralend-plate
or facet joint osteophytes, or thickened soft tissue or fibrosis on the nerve
leadingtostenosisoftheexitforamen.
• Painfromdeepcervicalstructuresiscommon.Itoftenlocalizespoorlyacross
theupperback.Itcanbereferredtotheupperarms,istypicallydescribedas
‘heavy’or‘aching’andismorediffusethannerverootpain.
• Musclespasmcanaccompanyanylesion.Itcanbeverypainful.
• Pain from the upper cervical spine (C1–C3) can be referred to the
temporomandibularjoint(TMJ)orretro-orbitalregions.Conversely,painfrom
bothTMJdisordersandasaresultofdentalmalocclusioncanbereferredto
theneck.
• Pain from the lower neck may be referred to the interscapular and anterior
thoracicwallregions.Thelattermaymimiccardiacischaemicpain.
• Floriddescriptionsofthepainandofitsextentandseverity(‘catastrophizing’)
areassociatedwithprominentpsychologicalmodulatorsofpain.
• Evaluation of the shoulder joint is often necessary as pathology there often
coexistsandsymptomsaroundtheshoulderoftencomplicateneckevaluation.
• Occipitalheadacheisacommonmanifestation.
Acuteneckpainwithtrauma
Acute neck pain with trauma requires urgent assessment, even if there are no
obviousneurologicalsymptoms:
• Acutetraumarequiresurgentevaluationforfracture,spinalcorddamage,and
vertebralinstability.About80%ofseriousinjuriesoccurfromanaccelerating
headhittingastationaryobject.
• An abrupt flexion injury may fracture the odontoid (less common with
extension); however, <1 in 5 injuries at C1/C2 produce neurological deficit
becauseofthewidecanalatthislevel.
• Ifnottraumaticorosteoporotic(thelatterbeingrelativelyrareinthecervical
spine),fracturesmayoccurinboneinvadedbymalignancy.
Newand/orassociatedsymptoms
Askaboutassociatedlegweakness,andnewbladderorbowelsymptoms.New-
onset acute neck pain with neurological features needs urgent evaluation.
Neurologicalsymptomsmayalsoaccompanychronicneckpain:
• Spinalosteomyelitis,meningitis,discitis(infectionorinflammation),myelitis,
andfracturemayallpresentwithacuteorsubacuteneckpain.Allmaycause
cord compression. Myelopathy due to spondylosis typically presents with a
slowlyprogressivedisabilityoverweekstomonths,althoughitcanbeacute,
particularlyifassociatedwithcentraldiscprolapse.
• Subacute pain,flaccidparalysis, andprofounddistal neurological signsmay
suggest myelitis, a condition caused mainly by infections and autoimmune
diseases.
• Tinnitus,gaitdisturbance,blurringofvision,anddiplopiaassociatedwithneck
painareallascribedtoirritationofthecervicalsympatheticnerves.
• The vertebralarteriespass close tothefacet joints justanteriorto emerging
nerveroots.Disruptionofvertebralbloodflowmaycausedizzinessinsevere
casesofneckspondylosis.
Previoustrauma
Askaboutprevioustrauma.Itcanprecedeandinfluencechronicpain:
• Acuteandoccupational(chronicoveruse)traumaisacommonantecedentof
chronicneckpain.
• Cervical dystonia (torticollis) can occur 1–4 days after acute trauma, it
respondspoorlytotreatment,andcanbelong-standing.Itmayalsocomplicate
arthropathy,suchasinRAorParkinson’sdisease.
• Whiplashinjuryisassociatedwithchronicmyofascialpain.
• Insomepatientswithchronicpainfollowing(sometimestrivial)trauma,there
may be dissatisfaction with the quality of care received at the time of the
injury.
• Unresolvedlitigationassociatedwithtraumacorrelateswiththepersistenceof
neckpainandreporteddisability.
Occupationalandleisureactivities
Someoccupations,sportsandactivitiesareassociatedwithrecurrentneckpain:
• Neck pain (andearlyspondylosis) is prevalentinpeople whose occupations
requirepersistentawkwardheadandneckpostures,e.g.professionaldancers.
• Although biomechanical factors may be an important influence in initiating
and aggravating neck pain, there may also be an underlying genetic
predispositiontoOAand/orhypermobility.
Otherpoints
Establishwhetherthepainstartedorvarieswithnon-MSKsymptoms:
• Cardiacischaemia,dyspepsia,orabdominalpaincanresultinreferredpainto
theneck(Table3.1).
Examinationoftheneck:adults
Theneckispartofthefunctionalupperlimbandsymptomsinthearmsandlegs
mayberelevant.Neurologicalexaminationofthearmsisimportant:
• Anadequateexaminationcannotbeperformedinaclothedpatient.Despitethe
inconvenience,itisimportanttohavethepatientchangeintoanexamination
gowntoavoidmissingrelevantclues.
• Inspectionfromfrontandbackmayrevealspecificmusclewastingorspasm
andpoorposture.
• Observing active movements reveals little if the patient has severe pain or
musclespasm.Inabilitytomovetheneckevensmalldistancesischaracteristic
inaxialspondyloarthritis(axSpA;see Chapter8).
• Tenderness often localizes poorly in degenerative disease. Exquisite
tendernessraisesthepossibilityofadisclesion,osteomyelitis,ormalignancy
(thelattertwoarerare).
• There may be ‘trigger points’ in neck stabilizer and extensor muscles.
Activation of a trigger point elicits myofascial pain in a zone that is
stereotypicalfortheindividualmuscle.
• Tender points (localized, non-radiating pain elicited by pushing with the
thumb), notably at the occipital origin of the trapezius, the medial scapular
border,andthemid-bellyofthetrapezius,arefeaturesoffibromyalgia(FM;
see Chapter 22). It is not clear whether tender and trigger points are the
same.
• Examinationofpassivemobility maybehelpfulprimarilyif itrevealsgross
asymmetry.Thenormalrangeofmovementvariesdependingonage,sex,and
ethnicity.Generally,atleast45°oflateralflexionand70°ofrotationshouldbe
achieved in a middle-aged adult. Global loss of passive mobility is non-
specific and occurs with increasing age. The range of movement that might
indicatehypermobilityhasnotbeenestablished.
• Care should be taken if neck instability is a possibility (e.g. fracture, RA).

Vigorouspassiveexaminationofforwardflexionmayexacerbatedisclesions.
• Examination of the shoulder is important to evaluate any referred pain or
associatedarticularlesion(e.g.adhesivecapsulitis).
• Neurologicalexaminationofupperandlowerlimbsisimportantinall cases
where pain is referred to the arms and/or the legs if cord compression is a
possibility:lookforincreasedtone,clonus,pyramidalweakness,andextensor
plantarresponse.Checkforacervicothoracicsensorylevel.
Investigationofneckconditionsinadults
Radiographs
Radiographsshouldberequestedwithspecificobjectivesinmind:
• A lateral neck film may demonstrate soft tissue thickening in infection or
synovium in RA (see Chapter 5), will document spondylitis
(syndesmophytes, discitis, and periosteal apposition in posterior elements
associatedwithpsoriasis),andtheseverityofspondylosis.
• Oblique viewscentred onthe suspectedlevelmayshownerve rootforamen
stenosisfrombonyencroachmentinpatientswithradiculopathy.Theremaybe
underlyingOA(see Chapter6).
• High cervical flexion and extension views and a ‘through-the-mouth’
(odontoid)viewareusefultoseeodontoidpathology.
• InanadultwithRA,ifthedistancebetweentheanteriorarchoftheatlasand
odontoidprocessis >3mm on alateral (flexion)image thereislikely tobe
C1/C2subluxationinthesagittalplane.
• Onalateralimage,superiorodontoidsubluxationinRAcanbejudgedfroma
reduced distance from the antero-inferior surface of C2 to a line drawn
between the hard palate and base of the occiput (McGregor’s line). The
distanceshouldbe>34mminmenand>29mminwomen.Lateralodontoid
subluxationisbestdemonstratedwithmagneticresonanceimaging(MRI).
• Stepwisevertebralsubluxationthroughoutthecervicalspinedemonstratedon
alateralimageischaracteristicofadvancedRA.
• Theremaybeonlyafew,butimportantsignsofspinalinfection,suchasasoft
tissuemassorisolatedlossofjointspace.
Magneticresonanceimagingandcomputedtomography(CT)
• MRI has largely superseded CT, arthrography, and CT arthrography in
assessing cervical spine/nerve, dural, vertebral, disc, and other soft tissue
lesionsintheneck.
• InmanycasestherelevanceofsomeMRIfindingsisstillbeingestablished—
patterns of signal abnormality do occur in asymptomatic people. The

frequencyoftheseeffectsincreaseswithage.
• MRIisthetechniqueofchoiceforimagingdiscprolapse,myelopathy(see
Plate2),myelitisandforexcludinginfectionortumours.MRIisusedtohelp
evaluate the need for, and plan, neurosurgical intervention in high cervical
instabilityinRApatients.
• MRI may show soft tissue swelling around the odontoid in calcium
pyrophosphatedeposition(CPPD)disease(see Chapter7),butthediagnosis
isbestmadewithCT,whichshowscalcificationaroundtheodontoidandof
adjacentligaments(‘crowneddenssyndrome’).
• In patients with the combination of unexplained radiographic signs and
generalized symptoms MRI is an important investigation. Cases of spinal
infectionsuchas tuberculosis(TB)orbrucellosisandlymphomaandcanbe
pickedup(see Chapter17).
Bonescintigraphy
• Despiteimprovedimagequalityandtomographicimages,theneckispoorly
imagedusingbonescintigraphy.
Treatmentofneckpaininadults
Fig.3.2showstheprinciplesoftreatingmechanicalcervicalsyndromesinadults
andthetimingofMRIscanning:
• Remember to review the diagnosis if pain persists despite treatment and
symptomsseemdisproportionatetotheresultsofimaging.
• In our experience, inflammatory spondyloarthritis (SpA)-related neck pains
canbemistakenasaresultof‘cervicalspondylosis’.Thismaybebecausethe
clinician too readily assumes the latter diagnosis and/or radiologists report
degenerativechangesonlyonradiographs.
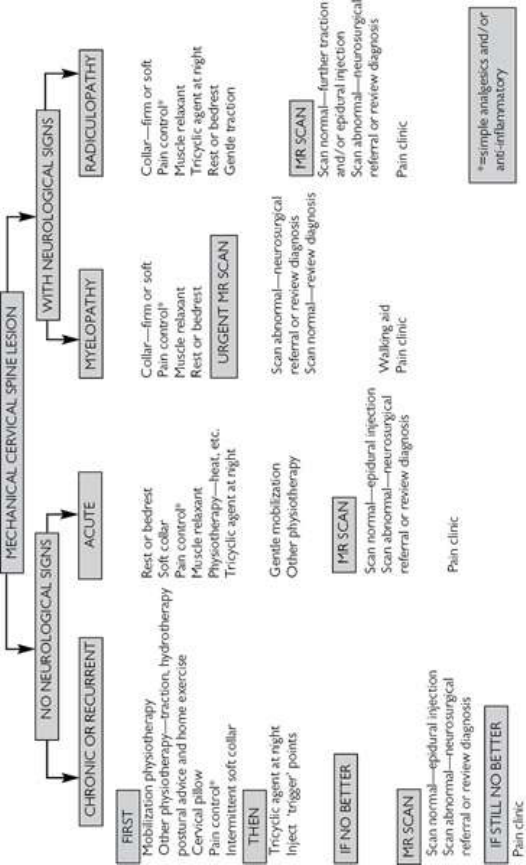
Fig.3.2TheprinciplesoftreatingmechanicalnecksyndromesinadultsandthetimingofMRIscanning.
Neckpaininchildrenandadolescents
Generalconsiderations
Neckpainin children iscommon.See Table3.2. Though there are conditions
specifictochildhoodbelow,thissectionshouldbereadinassociationwithneck
painassessmentin adultsp. 74includingfunctional anatomyand examination
(foradolescents).
• Theprevalenceofneckpaininsecondaryschool-agedchildrenis~11%.
• Inonestudy,60% ofchildrenexperiencedatleastoneepisodeofneckpain
overa2-yearperiodand9%experiencedneckpain‘often’.
• OfthosechildrenwithneckpainwhopresenttoA&E,62%havehadtrauma,
19% presented following infection, in 18% neck pain is related to adverse
posture,andjust1.2%hadneckpainassociatedwithotherconditions.Neck
painresolvesin96%within2weeks.
Clinicalfeatures
• Inyoungerchildren,neckproblemsaremostcommonlymanifestastorticollis
orstiffness.
• Subacute or chronic infectious aetiology includes lymphadenitis, including
tuberculousretropharyngealabscess,anddiscitis.
• Bonepathologyisveryrarebutcausesincludeeosinophilicgranuloma,non-
bacterialosteomyelitis,andosteoidosteoma.Malignancyisusuallyassociated
withcharacteristicMRIfindings.
• SystemiconsetandotherformsofJIAareassociatedwithneckstiffnessmore
thanwithpain.
• Studiesinadulthoodhaveindicatedcervicalspineinvolvementinupto80%
casesofpolyarticularJIA.
• InJIA,neckinvolvementisoftenassociatedwithTMJinvolvement.
Examinationoftheneck:childrenandadolescents
• Generalguidelinesfortheassessmentofpainshouldbefollowedasoutlined
in Chapter1.
• There should be full exposure of the spine for the examination and a
neurologicalexaminationundertakeninallcases.
• A full examination includes assessment of posture and biomechanics of the
shouldersandlowerspineandpelvis.
• Examinationoflymphnodes,pharynx,eyes,andjointsisimportant.
• ImagingofchoiceisMRI.
Table3.2Thecausesofneckpaininchildren
Softtissue
injury
Neckstrain,congenitaltorticollis,traumaincludingwhiplash,
andsportinginjury
Inflammatory
conditions
JIA,juvenileSpA,non-bacterialosteomyelitis,myelitis
Skeletal
conditions
Osteomyelitis(includingTB),osteoidosteoma,histiocytosis,
malignancy,insufficiencyfracture(e.g.idiopathicjuvenile
osteoporosis)
Non-skeletal
infection
Lymphadenitis,meningitis,discitis,retropharyngealabscess
Neurological
conditions
Posteriorfossatumour,benignparoxysmaltorticollis,syrinx
Other Oculartorticollis(Duanesyndrome,refractiveerror,
nystagmus,visualfielddefect),chronicpainsyndrome,
thoracicoutletsyndrome
Shoulderpaininadults
Anatomyoftheshoulder
(SeeFig.3.3.)
• Theglenohumeraljointisaballandsocketjoint.Theshallowglenoidcavity
permitsawiderangeofmovement.Thecircularfibrocartilaginouslabrumsits
on theglenoid,increases the articularsurfacearea, and acts asastatic joint
stabilizer.
• Normalglenohumeralmovementsincludedepression,thenglideandrotation
ofthehumeralheadunderthecoraco-acromial(CA)archtoenableelevation
ofthearm.Asthearmelevates,thereissmoothrotationandelevationofthe
scapulaonthethoracicwall.
• Shoulder movements are a synthesis of four joints: glenohumeral,
acromioclavicular(AC),sternoclavicular(SC),andscapulothoracic.
• Movements at AC and SC joints enable slight clavicular rotation, shoulder
elevation/depression,andprotraction/retraction.
• TherigidCAarchprotectstheglenohumeraljointfromtraumaandit,andthe
overlying deltoid, are separated from the capsule by the subacromial
(subdeltoid)bursa.
• A cuff of muscles surrounds the glenohumeral joint capsule. These ‘rotator
cuff ‘muscles are the supraspinatus, infraspinatus, teres minor, and
subscapularis.
• The supraspinatus initiates abduction by depressing the humeral head, then
elevating the arm alone for the first 10° of movement. The more powerful
deltoid then takes over abduction. Infraspinatus/teres minor and the
subscapularis externally and internally rotate the arm in the anatomical
positionrespectively(Fig.3.4).
• Production of powerful shoulder movements requires some degree of arm
elevation as the larger muscles, such as deltoid, latissimus dorsi (extensor),

andteresmajor(adductor),workinefficientlywiththearmintheanatomical
position. Rotator cuff muscles act synchronously as joint stabilizers through
therangeofshouldermovement.
• The long head of the biceps tendon originates above the glenoid usually
attached to the labrum and runs within the glenohumeral joint capsule
anteromediallyinabonygroove.
Painandshoulderlesionsinadults
(Seealso Chapter20.)
• Shoulderpainiscommonandmayhaveitsorigininarticularorperiarticular
structuresormaybereferredfromtheneckorthoracicspine,thoracicoutlet,
orsub-diaphragmaticstructures(Table3.3).
• Shoulderlesionsoftenproducepainreferredtothehumeraldeltoidinsertion
(patientpointstoupperarm).
• Periarticular disorders, mainly shoulder subacromial impingement (SAI)
disorders, are the most common cause of shoulder pain in adults (>90% of
cases).
• Traumaticorinflammatorylesionsofmanydifferentshoulderstructuresand
conditions that result in neuromuscular weakness of the rotator cuff or
scapularstabilizersmayresultinimpingementpain.
• Painfromsubacromialimpingementsyndromeisthoughttobegeneratedby
the‘squashing’ofsubacromialstructuresbetweenthegreatertuberosityofthe
humeralheadandtheCAarchduringrotation/elevationofthehumeralhead.
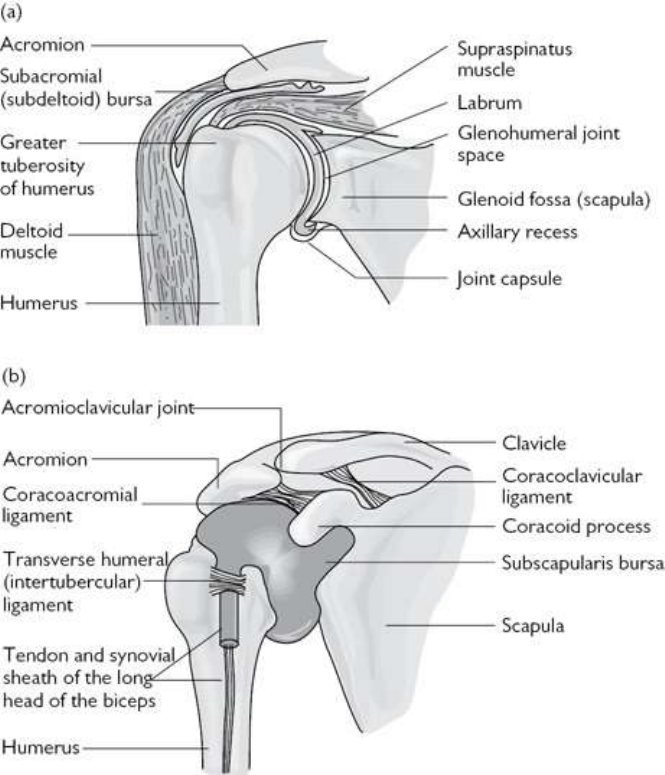
Fig.3.3(a)Majorshoulderstructures.(b)Therelationshipofthejointcapsuletoitsbonysurroundandthe
coracoacromialarch.
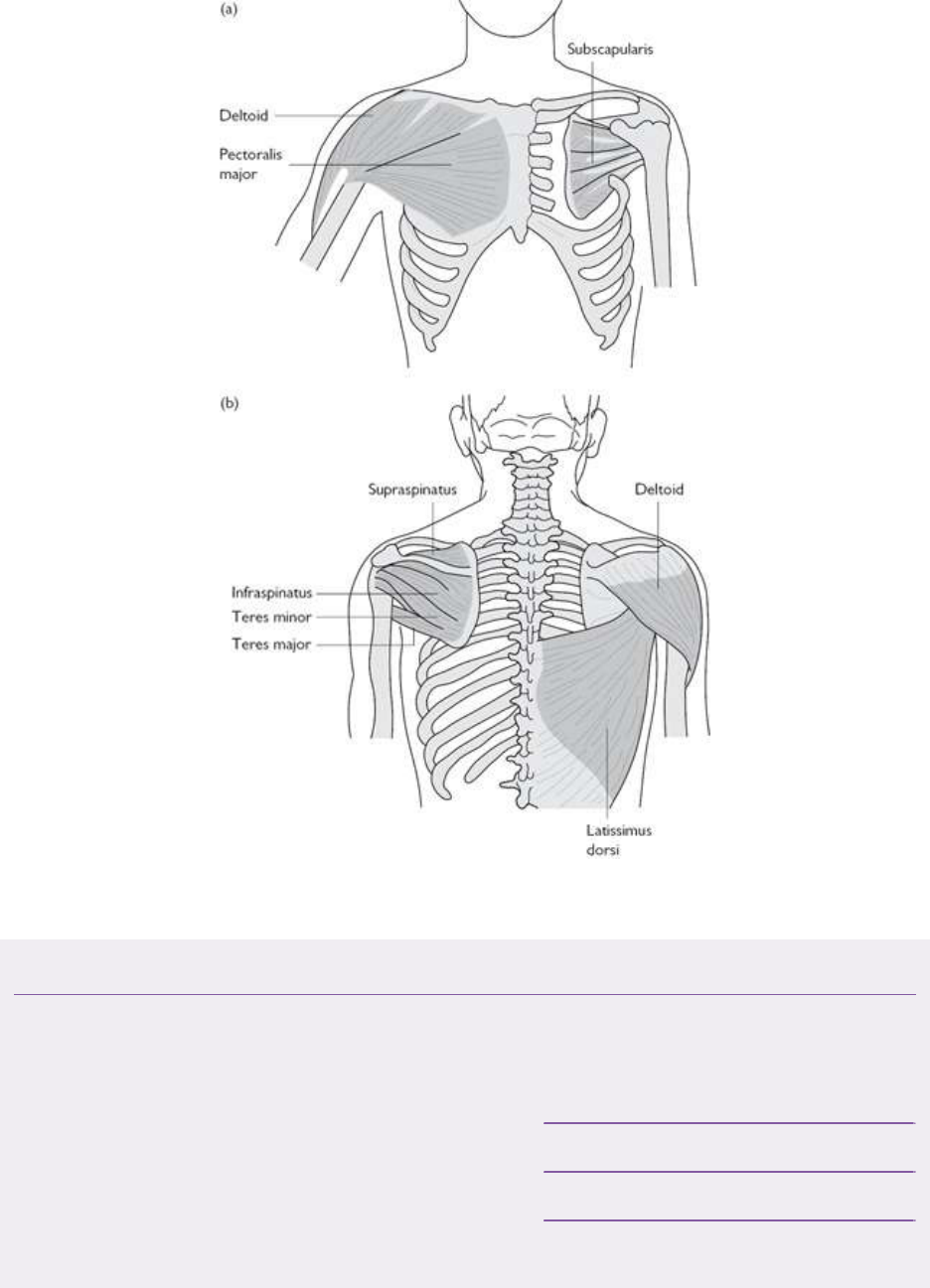
Fig.3.4Themusclesoftheshoulder:(a)anteriorview;(b)posteriorview.
Table3.3Themostcommoncausesofshoulderpaininadults
Periarticularlesions(oftenmanifestas
subacromialimpingementpain)
Rotatorcufftendonitis/tears
(common>40years)
Calcifictendonitis
Bicipitaltendonitis
Subacromialbursitis
Enthesopathyassociatedwith
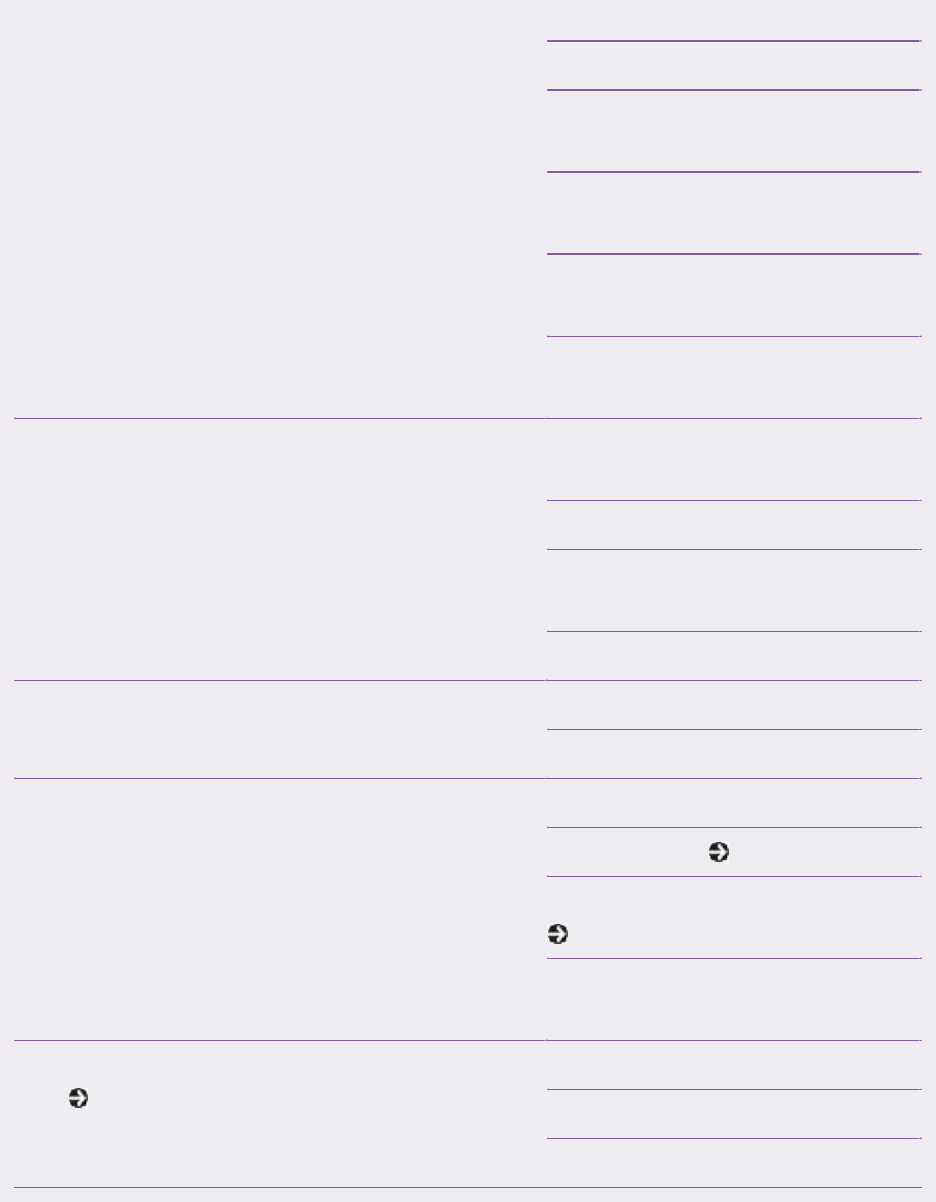
SpA,e.g.PsA
Periarticularmuscleweakness
Articularlesions
Synovitis(glenohumeralor
ACjoints)
OA(glenohumeralorAC
joints)
Glenohumeralinstability(e.g.
labraltears)
Adhesivecapsulitis(‘frozen
shoulder’)
Neurologic Cervicalnerverootand
radicularreferredpain
Neurologicalamyotrophy
Spinalcordlesions:tumours,
syringomyelia
Brachialneuromyopathy
Thoraciclesions(referredpain) Mediastinaltumours
Angina
Systemicanddiffuseconditions Polymyalgiarheumatica
Myositis(see Chapter14)
Chronicpainsyndromes(see
Chapter22)
Polyarticularinflammatory
arthritis
Bonedisorders
(see Chapter16)
Tumours
Osteonecrosis
Paget’sdisease
Takingahistoryaboutshoulderpaininadults
Whendidthepainstart?
Shoulderinjuriesarecommon,andmaybeacuteorchronic(overuse).
• Rotatorcufflesions(inflammation,degenerativeweakness,ortear)areoften
associated with activities and occupations that involve straining the arm in
abduction or forward flexion. A history of an acute injury, however, is not
always obtained. Subsequent calcification in the tendon following a
supraspinatusinjurycanbeasymptomaticorpresentwithacutepain.
• Manual labour is a risk factor for rotator cuff lesions. There is typically no
acute injury, but a history of repetitive movements over years that lead to
injury.
• Athleteswhotakepartinthrowingandracketsportsareatriskofrotatorcuff
tendinopathy and labral tears. Rugby and American Football players and
cyclistsareatriskofclaviclefracture,shoulderdislocationanddisruptionof
theACjoint.
• Pain from degenerative glenohumeral or AC joint arthritis might be a long-
termsequelaofaboneorjointinjury.
• Myofascial pain of the shoulder girdle is common and may mimic the
symptomsofcervicalradiculopathyandevenrefluxoesophagitisorischaemic
heartdisease.
• Severe,persistent,sleep-disturbingpainofrecentonsetmaybeindicativeof
avascularnecrosis,osteomyelitis,orbonytumours.
Whereisthepain?
• Painfromtheshouldermaybereferredtothedeltoidinsertion.
• Well-localized pain may occur with AC joint arthritis (e.g. patient places a
fingerontheaffectedjoint),butrememberthatreferredC4nerverootpainand
painfrombonelesionsofthedistalclavicleismaximalinthesamearea.
• Glenohumeral articular and capsulitis pain is not well localized (e.g. the
patientcoverstheirshoulderwiththeirhand).
• Pericapsular pain may be associated with SAI, but may also be myofascial
(typically)orreferredfromthecervicothoracicspine.
• Bilateral shoulder pain should increase suspicion of the presence of an
inflammatory polyarthritis such as RA (see Chapter 5), psoriatic arthritis
(see Chapter8) orCPPDarthritis (see Chapter 7)—but these would be
rarewithoutotherjointsymptoms.
• Diffusepainacrosstheshouldergirdlemusclesinthose>55yearsoldraises
thepossibilityofPMR.Painisoftenassociatedwithimmobilityandstiffness,
particularlyearlyintheday.
• A deep aching pain associated with stiffness is characteristic of adhesive
capsulitis (frozen shoulder). The useofthetermfrozenshoulderis popular,
butoftenincorrectlyapplied.Itisaconditionthatisrareinpatients<40years
of age. The condition occurs in three phase: a painful phase, an adhesive
(‘frozen’)phase,andaresolutionphase.Phasesoftenoverlapandtheduration
variesbutlong-termlimitationofshouldermovementremainsinupto15%of
patients.Itisassociatedwithdiabetes.
Doesthepainvary?
Movement-orposture-relatedpainmaybeacluetoitscause:
• Rotator cuff lesions often present to rheumatologists with a subacromial
impingementpatternofpain—thatis,painreproduciblyaggravatedbyspecific
movements during each day such as reaching up (overhead) with the arm.
Articular,bone,andadhesivecapsulitispainismorelikelytobepersistent.
• A history of recurrent bouts of shoulder pain in young adults may suggest
glenohumeralinstabilityduetohypermobilityorprevioustrauma,e.g.alabral
tear.
• In an unstable shoulder, pain may result from synovitis, subchondral bone
damage,oranSAIdisorder.Thefrequencyofrecurrentanteriorsubluxationis
inverselyproportionaltotheageatwhichtheinitialdislocationoccurs.
Aretherespinalsymptoms?
There is an association between neck conditions and shoulder pain. C4 nerve
root pain is referred to the shoulder, adhesive capsulitis is associated with
cervical nerve root symptoms (the nature of the link is unknown), and
inflammatoryconditions,suchasCPPDandpsoriaticspondylitisformscanbe
associatedwithbilateralshoulderpainreferralandcanmimicPMR.
Examinationoftheshoulderinadults
Visualinspection
Inspect the neck, shoulders, and arms from the front, side, and back with the
patientstanding.
• Abnormalityofthecontourofthecervicothoracicspinecouldindicatemuscle
imbalance/spasmormightbeassociatedwithanerverootoriginofpain.
• Scapularasymmetryatrestisespeciallyrelevantwhenexaminingchildrenand
may indicate a congenital bony deformity. Subtle degrees of asymmetry are
common and are not usually due to specific pathology, nor are they of
consequence.
• Diffuse swelling of the whole shoulder may suggest a shoulder
effusion/haemarthrosis or subacromial bursitis. In the elderly, Milwaukee

shoulder should be considered. Swelling of the AC joint occurs with joint
diastasis,arthritis,anddistalclavicularbonelesions.
• Armswellingandskinchangesdistallycouldindicateacomplexregionalpain
syndrome.
Elicitanytenderness
Elicitingtendernessofshoulderstructuresisoftenunrewarding:
• TendernessoftheACjoint,humeralinsertionofthesupraspinatustendon,and
thelongheadofbicepstendonmaybecluestopathology,butpalpationwill
notbespecificfordiagnosis.
• ThedeltoidoriginisatypicalenthesisinvolvedinactivePsA.
• Anappreciationoftriggerpointsassociatedwithmyofascialpainandtender
pointsinfibromyalgia(see Chapter22)isimportantintheinterpretationof
regionalsofttissuetenderness.
Documentbilateral(active)shouldermovements
This aids diagnosis but also gives an indication of the level of functional
impairmentandcanhelpinmonitoringchangesovertime.Themovementsare
first tested actively (the patient does the movement) and then passively (the
cliniciansupportsthelimb).Musclestrengthcanalsobeassessedwhiletesting
activemovement.
• Observe active arm elevation in the scapular plane from behind, noting
symmetryofscapularmovement,thepatternofpainduringelevation,andthe
range of elevation. Hunching of the shoulder at the outset of arm elevation
often occurs with an impingement problem. A painful arc may suggest a
rotator cuff lesion. Inability to lift the arm suggests a rotator cuff tear or
weakness, capsulitis, or severe pain, e.g. acute calcific supraspinatus
tendonitis.
• Observe and compare active internal rotation of shoulders, which can be
judgedbyhowfarupthebackthehandcanreach.Poorperformancemaybe
duetorotatorcuffweakness,weaknessofthescapularstabilizingmuscles,or
pain (generally from impingement syndrome). This manoeuvre assumes
normalelbowfunction.
• Observe theactive rangeof externalrotationofthehumerusfromthefront.
Ask the patienttoflex their elbows as if theywereholdinga tray and then
rotatethearmsoutwards.Minordegreesofrestrictioncausedbypainarenot
specific,butsevererestrictionischaracteristicofadhesivecapsulitis.
• Passiverangeofmotionshouldbetestedwithtwohands:onehandguidesthe
movement, while the second rests on the shoulder. Many patients will
subconsciouslyflexthespinetocompensateforrestrictedrangeofmotionat
theshoulder;usingbothhandscanhelpdetectthisandotherabnormalitiesin
movementatthejoint.
Testforsubacromialimpingement
• Always compare the affected with the non-symptomatic side and make
conservative judgements about muscle weakness if there is pain impeding
voluntaryeffort.
• Most tests rely on their ability to narrow the distance between the humeral
headandtheCAarch,bydrivingthegreatertuberosityundertheCAarchas
thehumerusrotates(Fig.3.5).
• Whetherthetestsarespecificforlesionsofthesubacromialstructuresorfor
thesiteofimpingementisunknown.
Movementoftheglenohumeraljoint
Movetheglenohumeraljointpassivelyinalldirectionsbymovingtheupperarm
with one hand and placing the other over the shoulder to feel for ‘clunks’,
crepitus,andresistancetomovement:
• Ifthehumeralheadcanbeslidanteriorly(oftenwitha‘clunk’)clearlywithout
rotationintheglenoiditsuggestsinstability.
• Grosslyreducedpassiveshouldermovement(notablyexternalrotation,withor
withoutpain)isthehallmarkofadhesivecapsulitis.
• Pull down on both (hanging) arms. If the humeral head moves inferiorly
(sulcussign)theremaybeglenohumeralinstability.
Stresstheacromioclavicularjoint
StressingtheACjointmayreproducethepain.Thisisconventionallydoneby
compressionorsheartests:
• These tests should not normally be painful. Although painful tests have not
provedtobespecificforACpathology(painfromSAImayalsobepresent),a
positive test may provide a clue that the AC joint is arthritic, dynamically
unstable,orthatimpingementofstructuresinthesubacromialspaceunderthe
ACjointisoccurring.
• Holdthepatient’sarminforwardflexion(90°)anddrawitacrossthetopof
the patient’s chest. The resulting compression of the AC joint may produce
pain.ACjointpaincanalsobeelicitedbypassivelyelevatingthearmthrough
180°,bringingthehandtotheceiling.Painisexperiencedintheupper10°or
soofmovement.
Gaugestrengthinrotatorandothershouldermuscles
Oncethepotentialactiverangeofmovementhasbeenascertainedinthecontext
ofpainandyouknowwhichmovementshurt(bytestingactivelyandpassively)
thenyoucanjudgethevalidityoftheexaminationofisolatedmuscleresistance
testing(Table3.4):
• Rotatorcuffmusclesneedtobetestedsub-maximallyinregardofstrengthfor
strengthagainst resistance—explaintothepatientnottopushtoohard—see
Table3.4.
• Knowledge of nerve supply is important to know whether there might be a
neuromyopathic cause for weakness and where a lesion might be (post-
infectivebrachialneuritis cancausefocalrotatorcuffneuromyopathyandis
notuncommon).
Table3.4Isolatedmuscletestingofshouldergirdlemuscles
Muscle:nerve
root,peripheral
nerve,supply
andmuscle
action
Muscleposition Isolatedmuscle
test
Pathology
affectingmuscle
strength/bulk
Supraspinatus:
C5/C6.
Suprascapular
nerve.Initial
humeral
abductionand
stabilityofraised
upperarm
Frombehind,
seenandfelt
abovethe
scapularspineat
restandwhen
activated
Abductarmfrom
neutralagainst
resistance
Tearordisuse
followingdamage,
e.g.afterafall,
chronicoveruse
stress,orin
athletes(throwing
arm)
Infraspinatus:
C5/C6.
Suprascapular
nerve.External
rotationand
stabilityof
humeralhead
Frombehind,
seenandfelt
arisingfrom
medialscapular
borderpassing
laterally(below
thescapular
spine)
Externalrotation
ofarminneutral,
elbowsupported
andflexedat90°
Tearordisuse
followingchronic
damage
Serratus
anterior:C5–C7.
Appreciatedfrom
behindwhen
Testbypushing
wallwithan
Damagetolong-
thoracicnerve
Long-thoracic
nerve.Pullsthe
scapulaforward
onthethoracic
wall(extends
forwardreachof
arm)
patientispushing
againstawall
witharms
outstretchedin
front,inthat
scapularemains
fixed
outstretchedarm
orpush-up.If
paralysedthere
willbeliftingand
lateralexcursion
ofthescapula
fromtrauma.
Patientmayalso
haveSAI
Deltoid:C5/C6.
Axillarynerve.
Flexion,extension
butmainly
abductionof
humerus
Arisesfromthe
scapularspine
andacromion,
thenswathesthe
shoulderinserting
intothehumerus
laterally
Wastingmaybe
obvious.
Weaknessin
isometricstrength
ofanarm
abductedto90°
Lesionsofaxillary
nervedamagedby
anteriorshoulder
dislocation
(externalrotation
mayalsobeweak
fromdenervationof
teresminor)
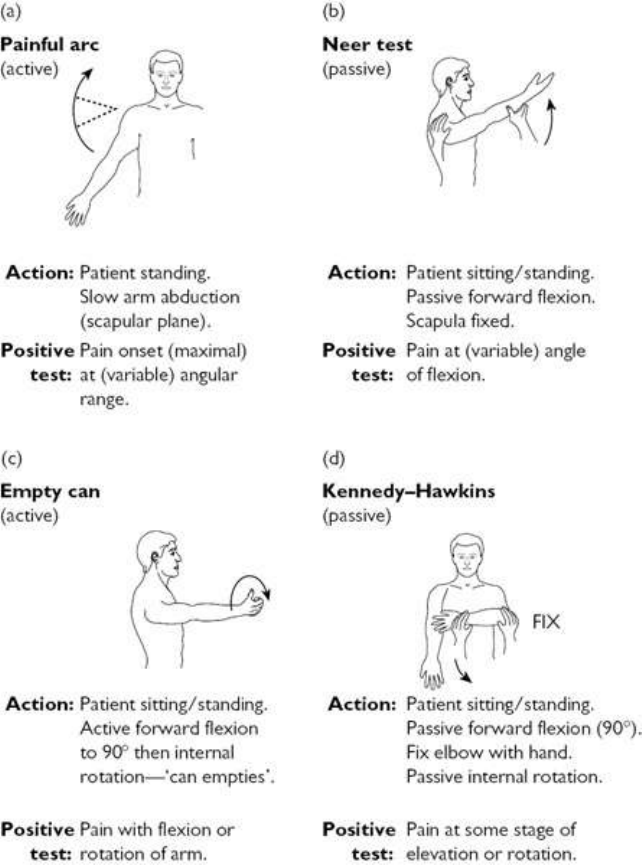
Fig.3.5Testsusefulforelicitingsubacromialimpingement.
Shoulderexaminationwiththepatientsupine
Examinetheshoulderswiththe patientsupineto testwhetherthereis anterior
cuff deficiency, glenohumeral joint laxity, or a labral tear: this is especially
important in young adults and adolescents to identify an ‘unstable shoulder’.
Holdandsupport the upper armheld in slightabductionand external rotation
(theelbowisflexed).Movethearmgently(craniallyinthecoronalplane)and
applygradualdegreesofexternalrotation.
• Deficiencyofanteriorstructuresissuggestedbypatientapprehensionthatpain
isimminentorthattheshoulderwillslipforward.Withalabraltear,theremay
beanaudibleorpalpable‘clunk’.

• Pressure down on the upper arm (taking the pressure off anterior shoulder
structures by an anteriorly translocated humeral head) may relieve
apprehensionorpainassociatedwithit(+verelocationtest).
• An unstable shoulder identified with the above tests may denote previous
traumaticinjury(e.g.shoulderdislocation)orahypermobilitydisorder.
Investigationsofshoulderdisordersinadults
Optimum initial imaging for investigating undiagnosed shoulder pain is
disputed.Managementofshoulderproblemsbasedonhistoryandexamination
alone isapracticalapproach to a common problem,sincemanyproblems get
betterintheshortterm.Thelong-termsequelaeofsuchmanagementstrategies,
however,areunknown.Studiesofshoulderpainprimarilysuggestthatchronic
shoulderproblemsarecommon,oftendespiteinitialimprovement.
Radiographs
• The standard projection for screening purposes is anteroposterior (AP),
although the AP axial–lateral view taken with the arm abducted may add
informationabouttherelationshipoftheglenoidandhumeralhead.Lookfor
calcific deposits in soft tissue basic calcium phosphate crystals: Milwaukee
shoulder(see Chapter7).
• Supraspinatusoutletviewsareoftenusedtoassessacromialconfigurationand
identifyinferioracromialosteophytesinpatientswithSAI.
• Ifrecurrentdislocationissuspected,associatedhumeralheaddefectsmaybe
identified by an AP film with internal humeral rotation or a Stryker view.
Bilateralfilmsdistinguishanomaly(invariablybilateral)fromabnormality.
• BilateralAPACjointviewswiththepatientholdingweightsmayidentify,and
gradedegreesof,ACjointdiastasis(separation).Distalclavicularerosionmay
be due to RA, hyperparathyroidism, myeloma, metastases, or post-traumatic
osteolysis.
• AlthoughcharacteristicpatternsofabnormalityareassociatedwithSAI(see
Plate3),minorage-relatedradiographicabnormalitiesarenormal.
Otherimaging:ultrasound,arthrography,CTarthrography,MRI,isotope
bonescan
• Ultrasound (US) scoring systems for locating and grading rotator cuff tears
now exist. US permits examination of the rotator cuff with the shoulder in
differentpositions,butishighlyoperatordependent.
• Patterns of rotator cuff abnormality and subacromial impingement are well
recognizedwithbotharthrographyandMRI.However,thereisnoconsensus
aboutwhichofultrasound,MRI,orarthrographyismostaccuratefordetecting
rotatorcufftears.
• Children, adolescents, and young adults suspected of having unstable
shoulders should have an MRI examination, since detailed views of the
humeral head, glenoid labrum, periarticular glenohumeral soft tissues, and
subacromialareaareimportant.
• MRIisthemodalityofchoiceinyoungadultswheninstabilityisdiagnosed.
Rotator cuff lesions and labral abnormalities are best assessed with MRI.
EnhancementwithIVcontrastmay increasethechanceofdetectingalabral
tear.
• No specific patterns of bone scan abnormality have been consistently
recognized for isolated shoulder lesions, although a phase study may be
diagnosticforcomplexregionalpainsyndromeinthearm.
Otherinvestigations
• Local anaesthetic injection may help disclose the site of shoulder pain,
although it is possible that by the time anaesthesia occurs, the injected
anaesthetichasspreadtoareasnotintendedasatarget.
• Jointaspirationisessentialifinfectionispossible.Fluidis usuallyaspirated
easily from a distended shoulder capsule. Haemarthroses can occur in
degenerateshoulders,with haemophilia, trauma,and pigmented villonodular
synovitis(PVNS).
• Electrophysiological tests (electromyography (EMG)/nerve conduction study
(NCS)) may confirm muscle weakness and help establish the presence of
neuromusculardisease,e.g.myositisorneurologicalamyotrophy.
• Bloodtestsarerequiredifconsideringinfectionorinflammation.
• A normal creatine kinase (CK) and aldolase will rule out myositis in the
majorityofcases.
• Bloodurea,electrolytes,creatinine,alkalinephosphatase,calcium,phosphate,
thyroidfunctiontests,andmyelomascreenshouldbeconsideredifmetabolic
boneormyopathicdiseaseisconsidered.
Treatmentofshoulderdisordersinadults
• Physicaltherapyshouldplay afocalpartinencouragingmobilizationofthe
joint,andearlyassessmentisprudent.
• Know whether there is an additional neck/spinal generated pain component
(physicaltherapistsareindependentdiagnosticiansandsomemayerroneously
aimtherapyatcervicothoracicsegmentsforindividualshoulderlesions).
• Donotrefertophysiotherapywithoutknowledgeofwhowillseethepatient,
andtheapproachthatwillbetakenforinstabilityandrotatorcuffweakness.

• Simpleanalgesicsareoftennecessary.
• Steroid injections can be considered in the following situations (see also
Chapter24):
• Tendonitisoftherotatorcuff.
• Adhesivecapsulitis(see Plate4).
• ACjointpain.
• Subacromialbursitis(see Plate5).
• The principles of steroid injection and rehabilitation are dealt with in
Chapter24.
• Thereareseveralsituationswherelocalsteroidsshouldbeavoided:
• Bicipitaltendonitis(rest,analgesia,physicaltherapy).
• Thefirst6weeksofanacuterotatorcufftear.
• When symptoms have become chronic and conservative therapy has not
helped for a presumptive clinical diagnosis (this requires reassessment,
imagingassurgerymayberequired).
• Surgical intervention may be: subacromial decompression arthroscopy,
synovectomyoftheSCjointandACjoint,orexcisionofthedistalendofthe
clavicle:
• Subacromial decompression may be necessary for chronic rotator cuff
tendonitis especially when imaging has shown inferior acromial
osteophytes.
• Otherinterventionsincluderepairofarotatorcufforbicepstendonrupture
andjointreplacement (forpain reliefratherthan improvementin function
mainly).
• Lithotripsy does not offer advantages over steroid injection and physical
therapyforcalcificsupraspinatustendonitis.
Shoulderpaininchildrenandadolescents
Generalconsiderations
Theprevalenceofchronicshoulderpaininadolescentsis7–11%.
• Theprincipalcauseofshoulderpainisbiomechanicalimbalanceeitherfrom
deconditioning, sporting injury (e.g. labral tear or rotator cuff lesions),
overuse,orsecondarytodirecttrauma.
• TheshouldercanbeinvolvedinJIA.
• Examinationfollowstheprinciplesofadultexaminationalreadydescribedand
paediatricguidelinesonexamination—see Chapter1.
Table3.5Causesofshoulderpaininchildrenandadolescents
Softtissue
injury
Biomechanicalimbalanceanddeconditioning:adverse
neuromuscularpatterning/glenohumeralorscapularinstability;
subacromialimpingement;bicepstendinopathy;rotatorcuff
tendinopathy;trauma;myositis
Joint
pathology
ACjointinjury;juvenileidiopathicarthritis;labraltear
Skeletal
lesions
Proximalhumeralstressinjurytophysis(includinglittle
leaguer’sshoulder);osteomyelitisandnon-bacterialosteomyelitis
(especiallyofclavicle);osteoidosteoma;osteosarcoma
(especiallyinadolescent);fracture;distalclavicularosteolysis
Other Brachialplexusinjury;chronicpainsyndrome;referredpain
(fromtheneck);thoracicoutletsyndrome;periphrenic
inflammation
Painaroundtheelbowinadults
Functionalanatomy
• The humero-ulnar articulation is the prime (hinge) joint at the elbow. The
radius also articulates with the humerus and allows forearm and hand
supination/pronation,withtheulnaattheelbow(Fig.3.6).
• Normalextensionresultsinastraightarm,butsomemuscularpeoplelackthe
last5–10°ofextensionandsome(especiallywomen)haveuptoanextra10°
ofextension(hyperextension).
• Normal flexion is to 150–160° and forearm supination/pronation range is
around180°.
• Duetoobliquityof thetrochlea,extension isassociatedwitha slightvalgus
thatcanbeaccentuatedinwomen(upto15°).
• Unilateral acute traumatic or chronic overuse lesions of the elbow are
common.Bilateralsymptomsmayoccurinthesesituations,butalsoconsider
the possibility of an inflammatory arthritis affecting the elbows or referred
painfromtheneck.
Takingahistoryofelbowpaininadults
Ispainexclusivelylocatedintheelboworreferredfromelsewhere?
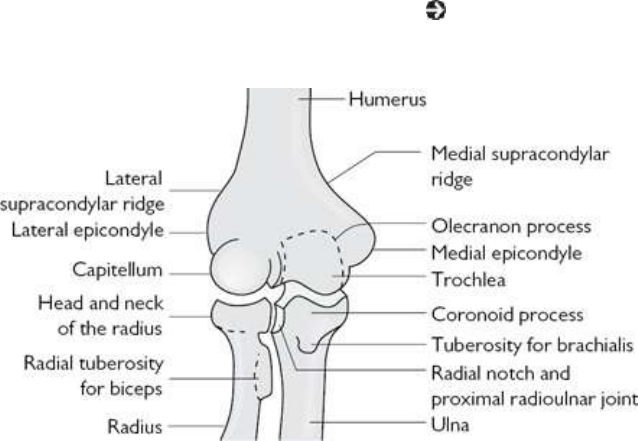
Establish whether the pain is associated with neck pain and whether it has
neurogenicqualitiesorisassociatedwithparaesthesiasornumbness.Painmay
bereferredfromproximalneurologiclesions(e.g.C6,C7)orfromdistallesions
suchascarpaltunnelsyndrome(CTS).
Isthereahistoryofacuteorchronic(overuse)trauma?
• Pain at the lateral epicondyle 1–2 weeks after a weekend of ‘home
maintenance’ might suggest lateral epicondylitis (tennis elbow) following
excessiveuseofascrewdriver,forexample.
• Othercommonsitesofpain,wherecharacteristicconditionsrelatedtooveruse
arerecognized,includethemedialhumeralepicondyle(‘golfer’selbow’)and
theolecranonbursa(repetitivepressure/friction).Althoughtypicallyacutein
onset,theseconditionsmaydevelopinsidiously.
• Fractures around the elbow and fractures/dislocations in the forearm are
common.
• Dislocation of the radial head alone is rare and is usually associated with
concurrentfractureoftheulna(radiographsmaynotidentifythefracture).If
notassociatedwith fracture(and especiallyifrecurrent), dislocationmay be
associatedwithgeneralizedhypermobility(see Chapter19)orshorteningof
theulnaduetobonedysplasia.
Fig.3.6Bonyconfigurationatthe(right)elbow(anteriorview).
Doesthepainradiatedistally?
• ForearmpainmaybeanadditionalcluetoC6orC7radicularpain,butmay
alsobedueto thespreadof MSKpainalongtheextensorgroupofmuscles
fromlateralepicondylitisorfromentrapmentofthemediannerveintheelbow
region.

• Peritendonitis crepitans is pain, tenderness, and swelling in the forearm
associatedwithoccupationaloveruse.Itisthoughttobeduetodamageofthe
longwrist/handflexorsandextensorsatthemuscle–tendonjunction.
• Diffusepainintheforearmcanoccurasaresultofoveruseinjury,particularly
in musicians and typists, although there is overlap with regional pain
syndromes.
• Painaroundtheforearmmayalsoarisefrominflammationatthewrist(see
‘Wrist pain in adults’, pp. 106–109) particularly in De Quervain’s
tenosynovitis.
Isthereprominentstiffnesswiththepain?
• Stiffnessisoftennon-specificbutmaydenoteinflammationsuchassynovitis
of the joint or olecranon bursa. It raises the possibility of an autoimmune
rheumaticorcrystaldepositiondisease.
• Inthemiddleagedandelderly,gout(see Chapter7)oftheolecranonbursa
andsurroundingsofttissues,particularlyoverlyingtheborderoftheulna,is
commonandisoftenmisdiagnosedasacellulitis.
Askaboutlocking
Locking of the elbow either in flexion or supination/pronation may be due to
loose intra-articular bodies. A single loose body is most commonly due to
osteochondritis dissecans of the capitellum and multiple loose bodies are
associatedwithOAorsynovialchondromatosis.
Isthepainunremittingandsevere?
Thistypeofpainsuggestsbonypathology:
• Althoughnon-fracturebonepathologyisrareintheelbowregion,localbony
painmightsuggestosteochondritisoravascularnecrosisor,ifpartofawider
patternofbonypain,metabolicbonedisease.
• Intheelderlyandothersathighriskforosteoporosis,supracondylar,andother
fracturesmayoccurwithsurprisinglylittletrauma.
Aretheresymptomsinotherjoints?
Askaboutotherjoints,lowback(sacroiliac)painsandrisksforgout:
• ElbowsynovitisisanuncommonpresentingfeatureofadultRA.
• Periarticularenthesitisisarecognizedfeatureofspondyloarthritis(SpA)(see
Chapter8)andmaymimictenniselbow.
• Theperiarticulartissuearoundtheelbowisacommonsiteforgout.
Examinationoftheelbowinadults

Lookforabnormalitythenpalpatewiththethumb.Observetheactive,passive,
andresistedactive rangeofjoint and relatedtendon movements, andconsider
examining for local nerve lesions. A complete assessment should include
examinationofneck,shoulder,andwrist.
Visualinspection
Lookforobviousdeformityorasymmetryintheanatomicalposition:
• Upto10°ofextensionfromastraightarmisnormal.Moreextensionmight
suggestahypermobilitydisorder.
• A child with an elbow lesion typically holds the extended arm close to the
body,ofteninpronation.
• Swellingduetojointsynovitisisdifficulttoseeintheantecubitalfossaunless
itisflorid:itismosteasilyseen(andmoreeasilyfelt)adjacenttothetriceps
tendoninsertion.
• Theolecranonbursa,whichmaybeinflamed,overliestheolecranonanddoes
not as a rule communicate with the joint. Overlying erythema, though non-
specific,maybeasignofinfectionorgout.
• NodulesovertheextensorsurfaceorulnabordermaybeassociatedwithRA
(see Chapter5).
• Psoriaticplaquesarecommonlyfoundattheelbowextensorsurface.
Observeactiveflexionandsupination/pronationwiththeelbowsheldin90°of
flexion
• Althoughtherangeofmovementmaybeaffectedbyextra-articularpain,loss
ofrangeusuallyimpliesanintra-articulardisorder.
Palpatethelateralepicondyleofthehumerus
• Inlateralepicondylitis(tenniselbow),thereistenderness,whichmayextend
distally. Resisted wrist and finger extension with the elbow in extension or
passivelystretchingthetendons (makefist,flexwrist,pronateforearm,then
extendelbow)mayreproducethepain.
• Lateralepicondyletendernessmaybeduetoinflammationoftheradiohumeral
bursathatliesundertheextensortendonaponeurosis.
• Notethattendernessoflateralandsometimesmedialepicondylescanoccurin
chronicpainsyndromes.Inthesecases,therelevantextensororflexortendon
provocationtestsarelikelytobenegative.
Palpatethemedialhumeralepicondyle
• Tenderness suggests traumatic medial epicondylitis (‘golfer’s elbow’), a
regionalorchronicpainsyndrome,orenthesitis.Confirmthesiteofthepain
by stretching the wrist flexors—supinate the forearm then passively extend
boththewristandelbowsimultaneously.Resistedpalmarflexionofthewrist
or forearm pronation with elbow extension may also cause pain. Tasks that
relyonthisrepetitivemovementareoftentheprovokingcause.
• Consider osteochondritis of the medial humeral epicondyle as a cause of
persistentpainfollowinganinjury.
Passivelyflexandextendtheelbowjoint
Passivelyflexandextendthejointand notetherangeof movementand‘end-
feel’(thefeelofresistanceattheendoftherangeofpassivejointmovement):
• ‘End-feel’maytell youwhetherthere isablock to fullflexion or extension
from a bony spur or osteophyte (solid end-feel) or from soft tissue
thickening/fibrosis(springy,oftenpainful).
• Noteanycrepitus(oftenassociatedwithintra-articularpathology)andlocking
(mayhaveloosebodiesinthejoint).
Supinateandpronatetheforearm
Passively supinate and pronate the forearm supporting the elbow in 90° of
flexionwithyourthumbovertheradioulnararticulation:
• There may be crepitus or instability/subluxation associated with pain.
Instabilitymightsuggestatear/damagetotheannularligament(duetotrauma
orchronic/aggressiveintra-articularinflammation).
Testperipheralnervefunctioniftherearedistalarmsymptoms
• Givenitscoursearoundthelateralepicondyle,theintegrityoftheradialnerve
shouldalwaysbetestedwhenalateralelbowlesionissuspected.
• The median nerve runs in the antecubital fossa and may be affected in
traumaticelbowlesions.Itisparticularlysusceptiblewhereitrunsbetweenthe
twoheadsofpronatorteres(frommedialepicondyleandthecoronoidprocess
oftheulna)andseparatesintoanteriorinterosseousandterminalmediannerve
branches.
• Theulnarnerveliesinthegroovebehindthemedialepicondyle.Bonyorsoft
tissueabnormalityinthisareamayaffectnervefunctionandleadtoreduced
sensationinthelittlefingerandweaknessinthesmallmusclesofthehand,the
flexorcarpiulnaris(FCU),theextensorcarpiulnaris(ECU),ortheabductor
digiti minimi (ADM). The median and ulnar nerves are dealt with in more
detailinthelatersectionsonwristandhanddisorders.
Investigationofelbowconditionsinadults
Radiographsandotherimaging

• Standard AP and lateral radiographs are the most straightforward way of
imagingtheelbowinitially.CTorMRImaythenbeneededifthediagnosisis
stillobscureandreferredpaincanberuledout.
• Look for periosteal lesions and enthesophytes (new bone spurs at clear
entheseslikethetricepsinsertion).Periostealnewboneandenthesophytesare
typicalinpsoriaticarthritis(see Chapter8).
• A lateral radiograph may identify displacement of the anterior fat pad
associatedwithajointeffusion(sailsign).
• Dislocations of the radial head and associated ulna fractures in children are
easilymissed.Tomakethisdiagnosisahighdegreeofsuspicionandfurther
imagingareoftenneeded.
Needlearthrocentesis/olecranonbursocentesis
• Arthrocentesis/bursocentesiswithfluidsentformicroscopyandcultureshould
alwaysbedoneinsuspectedcasesofsepsis.
• Fluid should be sent for polarized light microscopy in cases of bursitis that
maybeduetogout.Serumurateisworthrequestingbutmaynotberaisedin
acutegout.
• Examination of fluid for crystals should always be considered in cases of
monoarthritisintheelderlyorpatientsondialysis.
Electrophysiology
If nerve entrapment is suspected and there is some uncertainty after clinical
examination, then electrophysiological tests may provide useful information.
Testingcanhelpidentifythedegreeandlikelysiteofnervedamageandcanhelp
todiscriminatebetweenaperipheralandnerverootlesion(ifEMGofselected
musclesrequestedalso).
Treatmentofelbowconditionsinadults
• Themanagementoffracturesisbeyondthescopeofthistext.
• Epicondylitisisbestmanagedearlyonwithrest,splinting,analgesia,andlocal
steroidinjections.Theefficacyofphysicalmanipulationhasnotbeenproven,
although there are theoretical reasons why ultrasound therapy could be of
value (e.g. it passes through the myofascial planes and concentrates near
bone).Resistantcasesmaybenefitfromsurgery—a‘lateralrelease’.
• Steroid injections (see Chapter 24) may be of value in the following
situations:
• lateralormedialepicondylitis(hydrocortisone).See Plate6.
• inflammatoryarthritis(usuallylongactingsteroid).
• olecranonbursitis.
• ulnarnerveentrapment.
• Surgicalprocedures include excisionof nodules andbursae,transposition of
the ulnar nerve, synovectomy, excision of the head of the radius, and
arthroplasty.
• Arthroplasty in inflammatory arthritis is best reserved for severe pain and
shouldbeundertaken byan experiencedsurgeon. Lesserprocedures suchas
proximalradialheadexcisioncanbeeffectivetoimprovepainandfunctionif
forearmpronation/supinationarepoor.
• Radiation synovectomy of the elbow (Re-186) for inflammatory arthritis,
PVNS, or synovial chondromatosis requires ultrasound guidance (see
guidelinesavailableat http://www.eanm.org).
Elbowpaininchildrenandadolescents
Generalconsiderations
Theelbowisacommon siteof injuryin childrenandadolescents;thegrowth
plateandenthesealattachmentsarevulnerabletooveruseinjurybeforeskeletal
maturity.
• Characteristic injurious lesions are associated with specific activities (e.g.
baseballpitchingorthrowingsports,gymnasts).
• Thetwomainenthesesattheelbow—originoflongtendonstothefingersat
medial andlateralhumeral epicondyles—can become inflamed orpainfulin
peoplewithjuvenilePsAorSpA.
• Examinationoftheelbowinyoungpeopleisasforadultssee p.100.See
alsofunctionalanatomysee p.98.
Table3.6Causesofelbowpaininchildrenandadolescents
Lateral
elbow
Lateralhumeralepicondylitis/enthesitis(causedbytraumaorJSpA
orJPsA);osteochondritisandosteochondritisdissecans(adolescent
gymnasts);Panner’sdisease(osteonecrosisofcapitellumseenin
childrenaged5–10yearsandmayberelatedtothrowinginjuries)
Medial
elbow
Medialhumeralepicondylitis/enthesitiscausedbytrauma—seen
inchildren9–12yrsfromthrowingsportsincludingpitchingin
baseball—andenthesitisinJSpAandJPsA;medialcollateral
ligament(MCL)injury;ulnarneuritis;pronatorstrain
Posterior
elbow
Olecranonenthesitis;olecranonosteochondritis;olecranon
impingement(overheadarmuseinracketsports,swimming,
boxing,etc.);tricepsavulsion
Other JIA;fracture;loosecartilaginousbody;skeletaldysplasia
Wristpaininadults
Functionalanatomyofthewrist
• The wrist includes radiocarpal (scaphoid and lunate) and intercarpal
articulations.Theulnadoesnottrulyarticulatewiththelunate,butisjoinedto
it,thetriquetrum,andtheradius(ulnarsideofdistalaspect),bythetriangular
fibrocartilagecomplex.
• Theintercarpaljointsarejoinedbyintercarpalligamentsandaremoststable
whenthewristisinfullextension.Anteriorcarpalligamentsarestrongerthan
posterioronesandarereinforcedbytheflexorretinaculum.Wristandfinger
flexor tendons, the radial artery, and the median nerve enter the hand in a
tunnelformedbythecarpalbonesandtheflexorretinaculum(carpaltunnel).
• Flexion(70°),extension(70°),radialandulnardeviation(about20°and30°
frommidline,respectively)occuratthewristbutsupination/pronationofthe
wristandhandisduetoradiohumeralmovementattheelbow.
• Flexorcarpiradialis(FCR)andulnaris(FCU)arethemainflexorsofthewrist,
although palmarislongus(PL)also helps (Fig.3.7). They all arise from the
medialhumeralepicondyle.
• Allcarpalextensorsarisefromthelateralhumeralepicondyle(Fig.3.7).
• Radial deviation (abduction) occurs primarily when radial flexors and
extensors act together. Ulnar deviation (adduction) occurs primarily when
ulnarflexorsandextensorsacttogether.
Takingahistoryofwristpaininadults
Table 3.7 details the major diagnoses for painful conditions of the wrist and
hand.
Determinetheexactlocationofthepain
• Painlocalizingonlytothewristmostlikelycomesfromlocaltissuepathology.
CervicalnerverootpainasaresultofaC6,C7,orC8lesionandpainfrom
peripheralnervelesionsislikelytobelocatedchieflyinthehand.
• Painatthebaseofthethumb,aggravatedbythumbmovements,inmiddleand
oldageistypical ofOA (see Chapter6)ofthetrapezium-firstmetacarpal
joint.Paininthisareamightalsobeduetotenosynovitisofthumbtendons.
Traumahistory
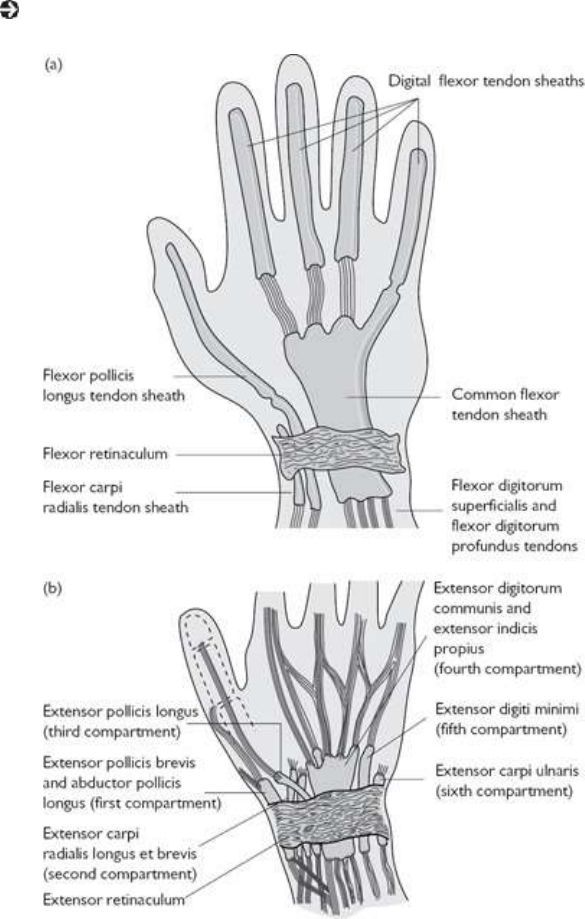
Injury/post-injury conditions are common. Taking a history of trauma is
important.
• Common fractures in adults are scaphoid and base of the first metacarpal
(Bennett’s),andheadoftheradius(Colles’).
• Post-traumatic chronic wrist pain following injuries may be due to
ligamentousinjuryandchroniccarpalinstabilityorosteonecrosis(lunate).
• Unusual or florid pain descriptors suggest a regional pain syndrome (e.g.
CRPS;see Chapter22).
Fig.3.7Flexor(a)andextensor(b)tendonsheathscrossingthewrist.Flexorcarpiradialis(FCR)inserts
intothesecondandthirdmetacarpals.Flexorcarpiulnaris(FCU)insertsintothepisiform,hamate,andfifth
metacarpal.Extensorcarpiradialislongus(ECRL)insertsintothebaseofthesecond,extensorcarpiradialis
brevis(ECRB)intothethird,andextensorcarpiulnaris(ECU)intothefifthmetacarpal,respectively.
Table3.7Painfulconditionsofthewristandhand(adults)
Articular Chronicinflammatoryarthritis(e.g.PsA,RA,JIA,CPPD)
Osteoarthritis
Septicarthritis
Carpalinstability(e.g.lunatedislocation)
Periarticular
DeQuervain’stenosynovitis
Tenosynovitisofcommonflexor/extensortendonsheath
Flexorpollicistenosynovitis
Distalflexorstenosingtenosynovitis(triggerfingerorthumb)
Ganglia,subcutaneousnodules,tophi
Diabeticcheiroarthropathy
Dupuytren’scontracture
Bone Fracture
Neoplasia
Infection
Osteochondritis( Chapter16)
Neurologic Mediannerveentrapment(carpaltunneloratpronatorteres)
Anteriorinterosseousnervesyndrome
Ulnarnervelesions(cubitaltunnelorinGuyon’scanalin
wrist)
Posteriorinterosseousnerveorradialnerveentrapment
Brachialplexopathyorthoracicoutletsyndrome
Cervicalnerverootirritationorentrapment
Complexregionalpainsyndrome
Spinalcordlesions,e.g.syringomyelia
Aretherefeaturestosuggestsynovitis?

• Pain due to wrist joint synovitis may be associated with ‘stiffness’ and be
worse at night or early morning. Stiffness ‘in the hand’ may have various
causes including multiple tendon/small joint synovitis, diabetic
cheiroarthropathyorsystemicsclerosis(SScl;see Chapter13).
• WristsynovitisoccurscommonlyinadultRAandPsA.
• Intheelderly,wristsynovitismaybeduetoCPPDarthritis(see Chapter7).
Thequalityofthepain
• Althoughprimarybonepathologyisrare,localbonypain(unremitting,severe,
sleepdisturbing)mightsuggestosteonecrosisor,ifpartofawiderpatternof
bonypain,metabolicbonedisease.
• Radicular pain may be burning in quality and is typically associated with
numbnessandparaesthesia.Suchneurogenicpainiscommonlyduetonerve
rootirritationorcompression.
Otherjoint/MSKsymptoms
• Wristandextensortendonsheathsynovitisisacommonpresentingfeatureof
adultRA.Otherjointsmaybeaffected.
• CPPD arthritis commonly involvesthewrist, and can mimic RA in its joint
distributionandpresentationintheelderly.
• Wrist synovitis and enthesitis occurs in SpA. Pain may be considerable,
althoughswellingisminimal.Theremaybeinflammatory-typesymptomsof
spinalpainandenthesitiselsewhere.
Askspecificallyaboutjob/leisureactivities
• Repetitivelateralandmedialwristmovementswiththumbadductedcancause
tenosynovitis of the abductor pollicis longus (APL) or the extensor pollicis
brevis(EPB),commonlycalledDeQuervain’stenosynovitis.
• Ifthereisnoobvioushistoryoftrauma,tendonitismaybeapresentingfeature
ofasystemicautoimmunerheumaticdiseaseorevengonococcalinfectionin
adolescentsandyoungadults.
• Overusepainsyndromesmayoccurasaresultofrepetitiveactivity.Theterm
‘repetitive strain injury’ is controversial. Objective assessment of pain,
location of swelling, etc., from the outset is invaluable in assessing the
response to treatment. Lack of objective findings (if imaging is normal)
suggestsaregionalpaindisorder.
Examinationofthewristinadults
Visualinspection
Inspectthedorsalsurfaceofbothwristslookingforswelling,deformity,orloss

ofmusclebulk(see Plate7a):
• Diffuseswellingmaybeduetowristjointorextensortendonsheathsynovitis
orboth.
• Aprominentulnastyloidmayresultfromsubluxationatthedistalradioulnar
jointowingtosynovitisorradioulnarligamentdamage.
• Prominence (‘squaring’) of the trapezoid–first metacarpal joint commonly
occursinOAofthisjoint.
• Loss of muscle bulk in the forearm may be due to a chronic T1 nerve root
lesionordisuseatrophy.
Flexion/extensionrangetestsformajorwristlesions
• The normal range of both flexion and extension in adults is about 70°.
Synovitisinvariablyreducesthisrange.
• Substantial common flexor or extensor tendon swelling will probably block
thefullrangeofwristmovements.
• There is normally an additional 20° of flexion and extension to the active
rangewithpassivemovement.
• Painandcrepitusareunlikelytobespecificforanytypeoflesion.
Examinethedorsumofthewristindetail
• Noteanyabnormalexcursionoftheulnarstyloidassociatedwithpainand/or
crepitussuggestingsynovitis.
• Post-traumatic carpal instability, particularly scapulolunate dissociation, is
relativelycommon.Thelatterisdemonstratedbyelicitingdorsalsubluxation
oftheproximalscaphoidpolebyfirmpressureonitsdistalpoleasthewristis
deviated radially from a startingpositionwiththeforearm pronated and the
wristinulnardeviation.Noteanygapbetweenscaphoidandlunate,andany
associatedtenderness.
• Noteanytendernessorthickeningofthecommonextensortendonsheathand
tendonsheathofAPLandEPB.
• Tendernessatthebaseofthethumbmaybeduetowristsynovitis,carpalor
carpometacarpalOA,tenosynovitis,aganglion,oraligamentlesion.
• Finkelstein’s test for De Quervain’s tenosynovitis may be used to elicit
APL/EPBtendonpain.Withthethumbadductedandopposed,thefingersare
curledtoformafist.Passiveulnardeviationatthewriststretchestheabnormal
tendons andelicitspain. Although it is asensitivetest, it is notspecificfor
tendonpain.
• Protrusionofthethumboutofthefistontheulnarsideofthehandduringthe
first part of this test is unusual and suggests thumb, and perhaps general,

hypermobility.
Testtheintegrityofthetendons
Many muscles/tendons that move both the wrist and digits originate at the
elbow; therefore, the quality of information gained from isolated tendon
resistancetests(eitherforpainorstrength)maybeaffectedbypainelsewhere
aroundthewrist,wristdeformity,orelbowlesions.
• Interpretfindingscautiously.
• Usefulinformationmightbeobtainedbypassivemovementofatendon,rather
than by resisted active movement, and also by feeling for thickening or
crepitusofthetendons.
Investigationandtreatmentofwristconditionsinadults
Theinvestigationandtreatmentofwristconditionsiscoveredin ‘Symptoms
inthehandinadults’,pp.112–121.
Symptomsinthehandinadults
Symptoms in the hand are a common presenting feature of some systemic
conditions,andlocalizedneurologicalandMSKlesionsarecommon,especially
in adults. Detailed knowledge of anatomy is beyond the scope of this text.
Functional anatomy is important and the more common abnormalities are
summarizedhere.
Functionalanatomyofthehand
Thelongtendons
• Digitalpowerisprovidedprimarilybyflexorandextensormusclesarisingin
theforearm.Theiractionissupplementedandmodifiedbysmallmusclesin
thehand.Precisemovementsofthehandaremainlyduetosmallmuscles.
• Powerful flexors (Fig. 3.7): flexor digitorum superficialis (FDS), flexor
digitorumprofundus(FDP),andflexorpollicislongus(FPL).
• FDS flexes proximal interphalangeal joints (PIPJs) and, more weakly,
metacarpophalangealjoints(MCPJs)/wrist.
• FDP flexes distal interphalangeal joints (DIPJs) and, increasingly weakly,
PIPJs,MCPJs/wrist.
• FPLflexes(at90°tootherdigits)mainlythePIPJ,butalsothewholethumbin
apowergrip(seelater).
• Powerful digital extensors (Fig. 3.7 and Fig. 3.8): extensor digitorum (ED)
arises from the lateral epicondyle splitting at the wrist to insert into each
digitaldorsalexpansion(digitstwotofive)thatattachestoallthreephalanges.
The fifth digit has an additional tendon, extensor digiti minimi (EDM) that
alsoarisesatthelateralepicondyle.
• APLabductsthethumbattheMCPJ,providedthewristisstable.
• EPBandEPLextendthethumb.
• Extensorindicis(EI)arisesfromtheulnaposteriorborderdistaltoEPLand
joinstheindexfingerEDtendon.
• Themusclesofthethenareminence(Table3.8)actsynchronously.Allexcept
adductorpollicis(ulnarnerve,C8/T1)aresuppliedbythemediannervefrom
C8/T1nerveroots.Allthreemusclesaresuppliedbytheulnarnerve(C8/T1).
Theintrinsicmuscles
• Thelongitudinalmusclesofthepalm(fourdorsalandfourpalmarinterossei
andfourlumbricals)allinsertintodigits.
• Palmarinterosseifrommetacarpals1,2,4,5,insertintodorsaltendons.
• Eachdorsalinterosseousarisesfromoriginsontwoadjacentmetacarpals.The
muscles abduct the second and fourth fingers and move the middle finger
eithermediallyorlaterally.
• Thefourlumbricals(Fig.3.9andTable3.9)arisefromtendonsofFDPinthe
palm passing to the lateral side of each MCPJ inserting into the dorsal
expansions.
• Theinterosseicombinewithlumbricalstofacilitatefinecontrolofflexionand
extensionofMCPJsandPIPJs.

Fig.3.8Extensorexpansionofafinger.
Table3.8Musclesofthethenareminence
Muscle Origin Insertion
Abductor
pollicis
brevis
Flexorretinaculum,scaphoid,and
trapezium
Thumbproximal
phalanxanddorsal
expansion
Flexor
pollicis
brevis
Flexorretinaculum,trapezium,
trapezoid,andcapitate
Thumbproximal
phalanx(baseofradial
side)
Opponens
pollicis
Flexorretinaculumandtubercleof
thetrapezium
Firstmetacarpal(lateral
border)
Adductor
pollicis
Capitate,basesofsecond/third
metacarpalsanddistalthird
metacarpal
Thumbproximalphalanx
(medialside)
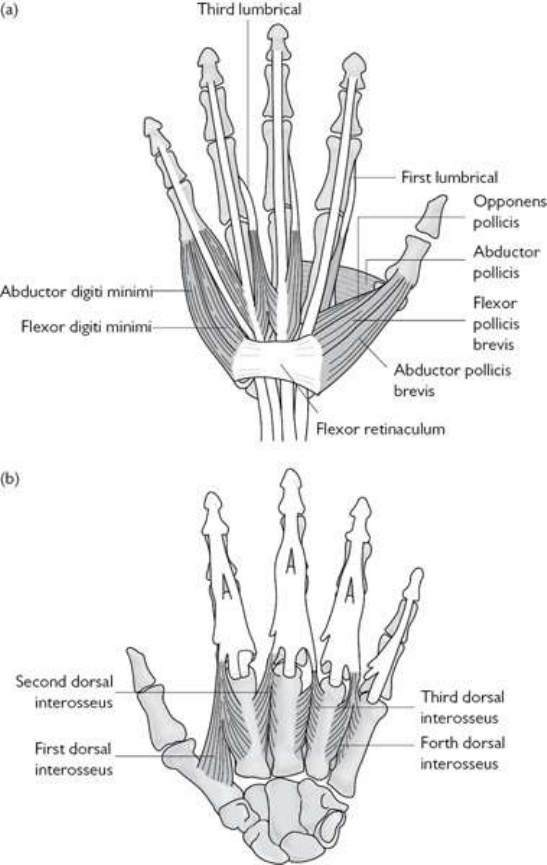
Grip
• Forpower,thewristextendsandadductsslightly,andthelongdigitalflexors
contract.
• A modified power grip, the hook grip,isusedtocarryheavy objects like a
suitcase. The thumb is extended out of the way and extension at MCPJs
accompaniesflexionatPIPJs/DIPJs.
• More precision in the grip can be obtained using varying degrees of thumb
adduction,abduction,andflexion.Thethumbcanbeopposedwithanyofthe
fourotherdigitsdependingontheshapeoftheobjecttobeheldandthetype
ofmanipulationrequired.
Fig.3.9(a)Lumbricalmusclesandmusclesofthethenarandhypothenareminences.(b)Dorsalinterossei.
Table3.9Musclesofthehypothenareminence
Muscle Origin Insertion
Abductor
digitiminimi
Flexorretinaculum(FR),
pisiform,andpisohamate
ligament
Baseofthefifthproximal
phalanxanddorsal
expansion
Flexordigiti
minimi
brevis
FlexorretinaculumandHook
ofhamate
Baseofthefifthproximal
phalanx
Opponens
digitiminimi
FlexorretinaculumandHook
ofhamate
Medialsideofthefifth
metacarpal
Takingahistoryofhandsymptomsinadults
A history of acute or overuse trauma with subsequent localized symptoms
requires a straightforward application of anatomical knowledge, precise
examination, and judicious choice of imaging techniques for diagnosis.
However,therearesubtlerorlesseasilydelineatedpatternsofsymptomsinthe
hand,particularlywhenpainisdiffuseorpoorlylocalized.
Isthepainassociatedwithimmobilityorstiffness?
• Stiffnessmaybeassociatedwithjointortendonsynovitisbutisnotspecific.
Promptingmayprovidemoreaccuratelocalizationofsymptoms.
• Ifunilateral,especiallyonthedominanthand,besuspiciousthatdiffusehand
painmaybeduetoaregionalpainsyndrome.
Isstiffnesslocalordiffuse?
• Patterns of joint involvement in autoimmune rheumatic disease and
polyarticulararthritisaresummarizedin Chapter2.
• Iflocalizedinthepalm,theremaybeDupuytren’scontracture(associatedwith
diabetes). If diffuse, there may be thickening of soft tissue from a systemic
process,e.g.hypothyroidism,SScl,diabeticcheiroarthropathy,ordisordersof
mucopolysaccharide metabolism (the latter especially in infants, although
Fabry’s disease can present in adulthood with acroparaesthesias and palmar
telangiectasia).
• Stiffnessduetoanuppermotorneuronlesion(aninterpretationofincreased
tone)isunlikelytobeconfinedtothehandandislikelytobeassociatedwith
weakness. The pattern of symptoms over time should give a clue to its
aetiology.
Arethereneurologicqualitiestothepainorcharacteristicstypicalofa
commonnervelesion?
• ‘Burning’ or‘deep’ episodicpainvarying with head, neck, andupperspinal
positionistypicalofcervicalnerverootpain.Askaboutoccupationandother
activitiesthatare associated withneckproblems, the relationshipwithsleep
posture,andfrequentheadaches.
• Pain on the radial side of the hand waking the patient at night and often
relieved, at least partially, by shaking the hand is typical of median nerve
entrapment in the wrist. However, pain in this condition is often poorly
localizedatinitialpresentation.Rememberotherlesionsthatproducepainin
the area around the thumb base: trapezoid–first metacarpal joint OA,
tenosynovitisofAPL/EPB(DeQuervain’s)orEPL,referredpainfromaC6
nerverootlesion,andligamentlesions(e.g.ulnarcollateralligamentoffirst
MCP—‘skier’sthumb’).
Tingling/pinsandneedles/numbness
Make sure bothyouandthepatient understand what you each mean by these
terms:
• Symptomsusuallydenotecervicalnerverootorperipheralnervecompression,
althoughtheycanreflectunderlyingischaemia.
• Tingling in the fingertips of both hands, however, is recognized to occur
commonlyinpatientsdiagnosedwithfibromyalgia.
• Symptomsassociatedprimarilywithspecificpositionsofthewholearmmay
beduetothoracicoutletcompressionofneurovascularstructures.
Painarisingfrombone
Pain in the hands arising from bones may be difficult to discriminate.
Radiographswilloftenleadtoconfirmationofthediagnosis:
• The most common tumour in the hand is an enchondroma. It is usually
painless.Iftheyarepainful,thenoneshouldsuspectinfarctionor malignant
change.
• Secondary metastases and malignant bone tumours in the hand are rare, but
must be ruled out in children, adolescents, and young adults with persistent
localizedbonepain.
• Paget’sdiseaseofhandbonescanoccur,butisrelativelyrare.
• Digital bone pain from osteomalacia/rickets occurs, but is unusual at
presentation.
• Digitalpainmayrarelybeduetosarcoidosis,hyperparathyroidbonedisease,

thyroid acropachy, hypertrophic (pulmonary) osteoarthropathy (HO), or
pachydermoperiostitis.Lookforclubbing.
Ischaemicpain?
A history suggestive of ischaemic pain in the hands is rare in rheumatologic
practice.Persistentischaemicdigitalpaincancomplicatesystemicsclerosisand
severeRaynaud’s(see Chapter13):
• Digitalvasomotorinstability(e.g.Raynaud’sdisease(RD);see Chapter13)
isepisodic,triggeredbycoldandemotion,andcharacterizedbydigitalcolour
changes:white/bluethenred.
• Pain fromvasculitis islikelyto bepersistent andassociatedwith apurpuric
rash,nailfoldinfarcts,orsplinterhaemorrhages.
• Ischaemic pain associated with cervicothoracic posture or prolonged arm
elevationmaybeduetoalesionofthethoracicoutlet.
• Pain may be due to thromboembolism (e.g. antiphospholipid syndrome),
infectiveendocarditis,orthromboarteritisobliterans(Buerger’sdisease).
‘Swelling’
Examinationismorereliablethanahistory:
• Apartfromisolatedlesions,suchasganglia,patients’descriptionofsofttissue
or joint swelling may be unreliable and should be substantiated by
examination.
• Nerve lesionscangive theimpression thatswellingis present(think whata
dentist’s local anaesthetic does for your lip!). Patients with carpal tunnel
syndrome,forexample,cancomplainofthehandswellingatnight.
‘Weakness’
Askabouttrauma,neck,andmediannerveentrapmentsymptoms:
• Acutetendoninjuriesarecommonindustrialaccidents.Chronicoccupational
overusemayalsoleadtorupture.
• If weaknessis profoundandtherehasbeen noobvious trauma,thecauseis
likelytobeneuromuscular.
• If not associatedwith pain, weaknessismore likely tobeneurological than
MSKinorigin.
• WeaknessassociatedwithpainmaybeduetoaneurologicorMSKlesion,the
lattersituationoftenduetoaninabilitytousethehand(orpartofit)because
of pain or an alteration in biomechanical function as a result of deformity,
whichmayonlybeslight.
• Trueweaknessassociatedwithstiffnessisassociatedwithmyelopathyoreven
motorneurondisease.
• Adetailedhistoryoftheprogressionofsymptomsisimportantandneurologic
examinationshouldbethorough.
Triggerfinger
Thismaydenotetenosynovitisofadigitalflexortendon.Damagetothetendon
anditssheathcanresultinafibrousnoduleattachedtothetendonthatmoves
andcatchesundertheproximalannularligamentjustdistaltotheMCPJ.Itmay
notbepainful.Thismostcommonlyaffectsthemiddleandringfingers,andis
prevalent among professional drivers, cyclists, and those in occupations
requiringrepeateduseofhand-heldheavymachinery.
Examinationofthehand:adults
Thefollowingsequenceiscomprehensive,butshouldbeconsideredifageneral
conditionissuspected.Oftenanexaminationonlyneedstobemorespecifically
directed.
Inspectionofthenailsandfingers
• Pits/ridgesanddactylitisareassociatedwithpsoriaticarthritis(see Plate8
and Chapter8).
• Splinter haemorrhages may be traumatic, but are associated with infective
endocarditisorvasculitis(see Chapter13).
• Obvious cuticle damage and punctate cuticle erythema (dilated capillary
loops)arefeaturesofsecondaryRDorSScl(see Plate9).
• Periungual erythema is associated with a number of autoimmune rheumatic
andconnectivetissuediseases.
• MultipletelangiectasiasareassociatedwithlcSScl(see Chapter13).
• Diffusefinger thickening(dactylitis) maybedue togrosstendon thickening
(e.g. SpA or sarcoid), or connective tissue fibrosis/thickening (SScl,
cheiroarthropathy). Bony or soft tissue DIPJ or PIPJ swelling should be
discriminated.
• Ashiny/waxyskinappearancemayindicatescleroderma/morphoea.
• Scattered, tiny, non-blanching dark red punctate lesions are typical of
cutaneousskinvasculitis.
• Erythematousorviolaceousscalypapules/plaquesoverMCPJsorPIPJsmay
suggestdermatomyositis(see Chapter14).
Noteanydiffuseswellingofthehand
• Diffuse soft tissue/skin swelling, may occur in association with RA, CPPD-
pseudogout,CRPS,andSScl.
• RS
3
PE (remitting seronegative symmetric synovitis with pitting oedema),

whichpresentsmainly in adultsintheir 70s, maybe a distincttypeof non-
erosivepolyarticular/tendonsynovitis,butmaybeassociatedwithother,often
haematological,conditions.
• SwellingassociatedwithCRPSmaybelocalizedordiffuse(see Plate10).
Skin may be shiny and later there is often a dark red or blue mottled
appearance.
• Typical skin appearances are critical to making a clinical diagnosis of
scleroderma. The skin may be initially puffy, but later shiny and tight and,
withprogression,atrophicwithcontractures.
Noteanymusclewasting
Wastingmaybeduetoadegreeofchronicdenervation(e.g.thethenareminence
in CTS), disuse atrophy (e.g. painful polyarthropathy, joint hypomobility), or
catabolismofmuscle(e.g.polymyositis,RA).Intheelderly,theremaybeage-
relatedmuscleloss(‘sarcopenia’).
Noteanydeformityofdigits
• Deformities tendto occurwith long-standingpolyarticular jointdisease, e.g.
OA,severeRA,andpsoriaticarthritis.
• Isolated deformities may be due to previous bone or tendon trauma, severe
neurological lesions and Dupuytren’s contracture. A mallet finger (loss of
active DIPJ extension) is due to rupture of the distal extensor tendon
expansionusuallyduetodirecttrauma.
Inspectthepalmanddorsumofthehand
• Palmarerythemaisnotspecific,butisassociatedwithautoimmunedisorders
ofconnectivetissueandjoints.
• CheckforDupuytren’sdisease(fascialthickeningonulnarside).
• On the dorsum of the hand, ganglia and swelling of the common extensor
tendonsheathareusuallyeasilynoted.Swellingoftheextensortendonsheath
iscommonlyassociatedwithRAinadults.
Palpationofjointsandnodules
Palpationofjointsandnodulesisbestdoneusingthumbpadswiththepatient’s
wristsupported:
• Swelling should be noted for site, consistency, tenderness, and mobility.
Osteophytes and exostosis are periarticular or at sites of pressure, may be
tender,butarealwaysfixed(see Plate7d).
• Gangliaarehardandusuallyquitemobile(canoccuranywhere).
• Rheumatoidnodules(occuranywhere,buttypicallyonthedorsumofthehand

andtheextensorsurfaceoftheelbow)andtophi(usuallydistal)arerubbery,
hard,relativelyfixed,butmaybemoved(see Plate7a).
• Synovitisisoftenrepresentedbysoft(‘boggy’),oftenspringy,swellingaround
ajoint.Itmaybetenderandwarmbutthisisnotinvariable.
• Synovitisinasinglejointmaybeduetoautoimmunerheumaticdisease,OA,
infection,orforeign-bodysynovitis(e.g.rosethornsynovitis).
Palpatetendonsinthepalmoronthevolaraspectofthephalanges
• Thickening,tenderness,andcrepitussuggesttenosynovitis,buttenosynovitis
canbehardtospotifitismild.
• Tethering and thickening of tendons in the palm associated with excessive
digitalflexionwhenthehandisatrestandablocktopassivefingerextension
suggestschronicflexortenosynovitis(takecaretonoteanycontributoryjoint
damage).
• Passive tendon movement by gently flexing/extending a proximal phalanx
maydisclosepalpabletendonnodules,crepitusandtenderness.
DiscriminateDupuytren’sdiseasefromflexortendinopathy
Dupuytren’sdisease(afasciacontracture)typicallyinvolvesthefourthandfifth
fingers (40% bilateral). It is common in males aged 50–70 years. The fascia
extendstothesecondphalanx,thus,ifsevere,theconditioncausesfixedflexion
ofMCPJsandPIPJs.Itisassociatedwithepilepsy,diabetes,andalcoholism,and
usuallyisnotpainful.
Investigationofwristandhanddisorders:adults
Radiographs
• An AP view of the hand and wrist is a useful screening investigation to
characterize a polyarthropathy and diagnose traumatic and metabolic bone
lesions(Table3.10).
• Radiographsmayrevealsofttissueswellingaroundjointscompatiblewitha
diagnosisofsynovitis.
• Radiographsareinsensitiveforidentifyingerosionsinearlyautoimmunejoint
disease.
• Anobliqueviewofthehandmayaddinformationaboutjointerosionsifan
erosiveMCPJarthritisisconsidered.
• Lateralandcarpaltunnelviewsofthecarpuscanbeobtainedbyvaryingthe
degreeofX-ray projectionangle; however, unlesssearchingfor evidenceof
fracturetheseviewsarerarelyneeded.
Table3.10Someconditions/featurestypicallydiagnosedonsimpleAPhand/wristradiographs
Bone
conditions
Fractures(e.g.scaphoid,baseoffirstmetacarpal)
Tumours
Metabolicbonediseases(e.g.rickets,hyperparathyroidism—
lookforcorticallossandtunnellinginphalanges)
Osteonecrosis(e.g.post-traumatic—lunate,sicklecelldisease)
Sarcoidosis( Chapter18)—typicallybonecysts
Specific
features
Cartilagedamage(jointspacelossandsubchondralbone
changes—primaryorsecondaryOA)
Articularerosions
Osteophytes
Infection(cortexloss,patchyosteolysis)
Calciumdepositioninjoint(e.g.triangularligament
chondrocalcinosisinCPPDdisease)
Softtissueswelling(e.g.overulnarstyloidinwristsynovitis)
Periarticularosteoporosis(associatedwithjointinflammation)
Carpaldislocation(e.g.lunatedisplacementinchroniccarpal
pain)
Polyarticular:
overall
patternsof
radiological
abnormality
OA(distributionofosteophytesandsubchondralbone
changes)
RA(e.g.deformities,erosionappearance/distribution)
Psoriaticarthritis(e.g.deformities,juxta-articularnewbone,
enthesophytes,erosionappearance—DIPJs)
CPPD:carpal—particularlyscapho-trapezial,trapezio-
metacarpaland2ndand3rdMCPJs—degenerativechanges,
intenselinearperiarticularsclerosisandosteophytes
Gout:erosionappearance—‘punchedout’bites,likeLulworth
Cove.Basesoferosionssclerosed

Furtherimaging:US,MRI,andbonescintigraphy
• Inexperiencedhands,UScanbeausefulwayoflookingforearlysynovitis
andpatternsofabnormalityinassociationwithmediannerveentrapment.
• MRImaydemonstrateatornoravulsedtriangularcartilageinpatientswitha
post-traumaticpainfulwristorwithcarpalinstability.
• MRI images of the carpal tunnel are useful in confirming median nerve
compression/tethering and soft tissue wrist pathology, particularly when
symptomsrecuraftercarpaltunnelreleasesurgery.
• MRI can provide valuable information about the degree and distribution of
inflammatory disease in joints and tendons, particularly in children and
patientswherehistoryandexaminationaredifficult.
• MRI is more sensitivethanradiography in identifying jointerosionsin RA.
ChoosingMRIoverUSdependsonavailabilityandsonographerexperience.
• Bonescintigraphyisnotspecificforanysinglecondition,butinyoungadults
(after closure of epiphyses and before OA is likely) it may be useful for
disclosingpatternsofinflammationatandaroundjointsandentheses.
99m
Tc-
labelled human immunoglobulin is more specific for detecting patterns of
synovitisinchildrenandadults.
Laboratoryinvestigations
• FBC, ESR, CRP: the characteristic, though non-specific, picture in patients
with a systemic inflammatory condition such as RA is mild anaemia with
normal (or slightly hypochromic, microcytic) red cell indices, high or
high/normalplatelets,andincreasedacutephase.
• Notably in PsA and in SpA the acute phase measures may be low, even
normal,evenwhenthereiswidespreadpain/diseaseactivity.
• Lymphopeniafrequentlyaccompaniesautoimmunedisease.
• Neutrophilsareraisedininfection,withsteroids,withcrystal-inducedarthritis,
andinadult-onsetStill’sdisease(see Chapter18).
• Bloodurea,electrolytes,creatinine,anduratewilldetecthyperuricaemiaand
renalimpairmentassociatedwithgout.
• Bloodcalcium,phosphate,albumin,vitaminD,alkalinephosphatase,andPTH
willscreenformetabolicbonedisease.Testallcomponentstointerpretfully
themetabolicpicture.
• Rheumatoid factor (RF) and anti-cyclic citrullinated peptide (ACPA) are
usefulfordiagnosingrheumatoidarthritis.
• Antinuclear antibody (ANA) and a screen of extractable nuclear antibodies
(ENAs)maybehelpfulfortheevaluationofanumberofdisorders,including
SLEandscleroderma.
• Otherinvestigationstoconsider:serumangiotensinconvertingenzyme(ACE)
for sarcoidosis, glycosylated haemoglobin in diabetics, serum, and urinary
proteinelectrophoresisformyeloma.
Otherinvestigations
• Neurophysiology (EMG/NCS) is a useful adjunct to clinical examination in
diagnosisofupperlimbneuropathies.
• Joint/bursa fluid aspiration is mandatory in suspected cases of sepsis and
shouldbesentforcultureandmicroscopy(requestGramstainandpolarized
lightmicroscopyoffluidfromthelab).
Treatmentofwristandhanddisordersinadults
TreatmentsforspecificdiseasesareconsideredintherelevantchaptersinPartII
ofthisbook.Managementofthesofttissuelesionsinthehandandwrist,like
elsewhere,combinesperiodsofrestandsplintingwithactivephysicaltherapy,
avoidanceofrepetitiveactivity,andanalgesia.Inmostcases,theconditionwill
resolvespontaneously,butsevereorpersistentpainanddisabilitymaywarrant
inputfromahandoccupationaltherapist,localsteroidinjections,oroccasionally
surgicalsofttissuedecompression:
• Conditionsthatrespondtolocalsteroidtherapy(see Chapter24):
• tenosynovitis,e.g.DeQuervain’s.
• tendonnodulesandganglia.
• flexortenosynovitis(andtriggerfinger).
• Dupuytren’scontracture.
• carpaltunnelsyndrome.
• synovitis: radiocarpal and radioulnar at the wrist, MCPJs and PIPJs, first
carpometacarpal.
• TheaccuracyofneedleplacementislikelytobeimprovedbyUSguidance;
however,greaterefficacyfromanUSprocedureversusblindinjectionhasnot
yetbeenshown.
• Theprinciplesofsteroidinjectionaredealtwithin Chapter24.
• Functionalevaluation(fromaphysicalandoccupationaltherapist)islikelyto
be of use in cases of polyarthropathy. Early use of splints, orthotics, and
exercisesmayleadtogreaterfunctionalabilityandadecreaseinsymptoms.
• Surgicaloptionsforthehandandwristmayinclude:
• fusionorresectionofthecarpalbones.
• ulnastyloidectomyandwristsynovectomy(RA).
• tendonrepairandtransferoperations(RA).
• synovectomyofjointsand/ortendons(RA).

• fusionofsmalljoints.
• PIP/MCPjointreplacements.
• Dupuytren’srelease/fasciectomy.
• carpaltunnelrelease.
• trapeziectomyforthumbCMCjointOA.
Manyoftheseproceduresprimarilyreducepain;functionmaynotberestored.
Wristandhandpaininchildrenandadolescents
Generalconsiderations
IsolatedMSKlesionsinthewristandhandsofchildrenarerare.Afewnotable
conditionsexist.
• Smallswellingsmaybeganglia—resolvespontaneouslyin50%.
• Congenitaltriggerthumborfingerisnotrareandcanaffect1in300children.
Spontaneousresolutionoccursinupto60%within2years.
• Swelling in wrists and fingers may denote JIA. US is a relatively easy and
acceptablewayofconfirmingsynovitisispresentinjointsinyoungchildren,
thougholderchildrenmaytolerateMRI.
• Wrist pain and swelling may be the key presenting feature of rickets,
especiallyinachildoradolescentwithaseverelyrestricteddiet.
• Digital vasomotor instability is more commonly seen in children with
neurologicalconditionsincludingcerebralpalsy.
• AssessmentofRaynaud’sDisease,typicallyinadolescents,issimilartothatin
adults(see Chapter13)anderythromelalgia,whichcausesmarkedredness
ofhandand feetassociated withdiffusepain,swelling anddistress, ismore
commonlyseenintoddlersthanolderchildren.
• Digitalulcersandischaemiclesions,Gottron’spatchesandnailbedvascular
changesmayindicateSLE,JDMorSScl.
• AlthoughCRPS(see Chapter22),isoccursinchildren,itislesscommon
thaninadults.
• Wrist pain may be the presenting feature of a skeletal dysplasia—a wrist
radiograph should be obtained. Specialist centre radiologist input can be
helpfulinsuchcases(e.g.dREAMS: http://www.d-reams.org)
• Assessment of the wrist and hand in children and adolescents is essentially
similartotheassessmentinadults.
• Forfunctionalanatomyofthewristsee pp.106–107,andforthehand,see
pp.112–115.
Upperlimbperipheralnervelesions
Background
• Upper limb peripheral nerve lesions are common. Most are entrapment
neuropathies. Occasionally, nerve trauma may present to primary care
providersorrheumatologistswith(primarily)regionalmuscleweakness.
• Althoughnotspecificforitsdiagnosis,thecombinationofpain,paraesthesia,
numbness,andweaknessissuggestiveofnerveentrapment.Featuresmaybe
consideredmorespecificfornerveentrapmentifthereisahistoryofacuteor
overusetraumaproximaltothedistributionofthesymptoms.
• Lesions may characteristically occur in association with specific activities,
occupations,orsports(e.g.ulnarneuropathyincyclists).
• Accuratediagnosisreliesondemonstrationoftheanatomiclesion.Usefulin
thisrespectisknowledgeoflikelysitesofentrapmentordamageand,inthe
case of entrapment, the ability to elicit a positive Hoffman–Tinel sign (i.e.
pressureorpercussionoverentrapednervecourseelicitingsensorysymptoms
inthenervedistribution).
• Alwayscompareexaminationfindingsinbothupperlimbs.
• Neurophysiologicexaminationisanadjuncttoclinicaldiagnosis.Itshouldnot
bereliedontomakeadiagnosisintheabsenceofgoodclinicalassessment.
• MRIofnerveroots/spineandpotentialsitesofdistalnerveentrapmentcanbe
used, with clinical assessment and neurophysiology, to pinpoint with high
accuracy,anynervelesionintheupperlimb.
Thelongthoracicnerve
• Entrapmentisinthedifferentialdiagnosisofpainlessshoulderweakness.The
nerve origin is at C5–C7, and its course runs beneath the subscapularis and
intotheserratusanterior.
• Muscleparalysisisoftenpainlessandimplieslossofthelast30°ofoverhead
arm extension, disrupted scapular rhythm, and scapula winging. Winging is
demonstrated by inspection from behind with the patient pressing against a
wallwithanoutstretchedarm.
• Damagetothenerveoccurstypicallyfromananteriordirectbloworbrachial
plexusinjury.Damagesometimesoccursaftercarryingheavybackpacks(e.g.
armyrecruits)oraftersurgicalresectionofacervicalrib.
• Itcanalsooccurspontaneouslyafterinfection.Thereisnospecifictreatment.
Thesuprascapularnerve
• The nerve origin is at roots C4–C6; its course is lateral and deep to the
trapezius, through the suprascapular notch, terminating in the supraspinatus
and posteriorly in the infraspinatus. It carries pain fibres from the
glenohumeraljointandACjoint.
• Impingementofthenerveatthesuprascapularnotchshouldbeconsideredina
patient complaining of shoulder pain despite a normal examination and
imagingtests.
• Injury to the nerve often gives diffuse shoulder pain, although painless
paralysisofthemusclescanoccur.
• Injury isoftenthought tooccurfrom repeatedstretchingof thenerveat the
notch.Weightliftersarepronetobilateralinjuryandvolleyballplayersprone
todominantsideinjury.
• Neuromyopathy (acute weakness, pain, CK+, muscle wasting on MRI?
secondarytoinfection)ofsupraspinatusorinfraspinatusisnotuncommon.
• Compressionbygangliaortumours(andevenpossiblygouttophi)occursand
canbeconfirmedbyMRI.
Ulnarnerve
TheulnarnerveoriginatesfromC8andT1.Itliesalongthemedialsideofthe
brachial artery in the upper arm, then above the medial humeral epicondyle
where it passes posteriorly, piercing the medial intermuscular septum. It then
runsbehindtheelbowinagroovebetweentheolecranonandmedialepicondyle,
coveredbyafibroussheathandarcuateligament(cubitaltunnel).Followingthe
lineoftheulnaintheflexorcompartmentoftheforearm,branchessupplythe
flexordigitorumprofundus(FDP)andtheflexorcarpiulnaris(FCU).Thenerve
entersthehandontheulnarsidedividingintosuperficial(palmarisbrevisand
skinoverthemedialoneandahalfdigits)anddeep(smallmusclesofthehand)
branches:
• Lesionsareusuallyduetoentrapment.
• The ulnar nerve is occasionally damaged in the relatively exposed cubital
tunnel(cubitaltunnelsyndrome)resultinginpainandparaesthesiaalongthe
medialforearm,wrist,andfourth/fifthdigits.Damagemayoccurfromdirect
trauma,compression,orrecurrentsubluxation.TheTineltestattheelbowmay
bepositiveandtheremightbesensorylossoverthepalmaraspectofthefifth
digit.
• Thereareanumberofsiteswhereentrapmentof theulnarnerve mayoccur
aroundthewrist,eitherproximaltothevolarcarpalligamentorbeneathitor
thepisohamateligament.Externalcompression,acuteorrecurrenttrauma,and
gangliaaretheusualcauses.Symptomshavebeennotedincyclists,usersof
pneumaticorvibratingtoolsandinavidvideogameplayers.Entrapmentofthe

purelysensorycutaneousbranchcanoccurfromexcesscomputermouseuse.
• Motorweaknessmaybemostevidentbyobservinggeneralmusclewastingin
the hand (hypothenar eminence, interossei, adductor pollicis) and flexion
deformityofthefourthandfifthdigits—thelattercausedbythirdandfourth
lumbricalweakness(see Plate11).
• Flexionofthewristwithulnardeviation(FCU)andthumbadductionmaybe
weak(adductorpollicisweaknesswillbeevidentifyouaskthepatientto‘run
the thumb across the base of the fingers’ as normally it can sweep across
touchingtheskin).
• Froment’s sign also signifies weakness of the adductor pollicis, and is
demonstrated by a weakness in holding paper between the thumb and the
indexfingerwhenbothareinthesagittalplane.
• Discriminationofawristsitefromanelbowsiteofnerveentrapmentishelped
by the site of a positive Hoffman-Tinel test, preservation of power of wrist
flexion/medialdeviation(FCU)inawristlesion,andelectrophysiology.
• Rest, analgesia, and occasionally local steroids are helpful. A review of
posture, repetitive activity, and a biomechanical assessment with changes in
activitiesandtechniquearerecommended.Surgicaldecompressionmayalso
benecessary.
Radialnerve
ThenerveoriginisatrootsC5–C8,anditscourserunsanteriortosubscapularis
then passes behind the humerus in a groove that runs between the long and
medialheadsoftriceps.Itthenwindsanteriorlyaroundthehumeralshafttolie
betweenbrachialisandbrachioradialis.Intheflexorcompartmentofthearmit
divides at the level of the lateral epicondyle into superficial branch
(cutaneous/sensory) and the posterior interosseous nerve (PIN), which runs
through the supinator muscle into the forearm to supply the extensor
compartmentmuscles:
• Entrapment needs to be considered in those cases of shoulder or upper arm
trauma,wheresubsequentpresentationincludesarmandwristweakness.
• Compressionoftheradialnerveintheupperarmcausesstiffnessinthedorsal
armandforearm,weaknessofthewrist,andlittlefingerextension.Thetriceps
isusuallyunaffectedasthenervesupplytothemuscleleavestheradialnerve
proximally.
• Transientcompressionofthenerveatthesiteofthemedialheadoftricepshas
beendescribedintennisplayers.
• Compressioncanoccurasthenervepiercesthelateralintermuscularseptum
justdistaltotheradialheadandalsowherethePINpiercesthesupinator.
• At this lower site, compression is often a consequence of trauma, may be
associated with a positive Hoffman-Tinel test and local tenderness, and the
painmaybereproducedbyextremepassiveforearmpronationcombinedwith
wrist flexion. Symptoms may mimic those of lateral epicondylitis. Surgical
explorationmaybenecessarytoconfirmadiagnosis.
Mediannerve
ThenerveoriginisfromC6–T1nerveroots.Itscoursefromthebrachialplexus
runstogetherwiththebrachialarteryintheupperarm(supplyingnothing)then
enterstheforearmbetweenthetwoheadsofpronatorteres(frommedialhumeral
epicondyle and coronoid process of the ulna). It runs deep in the forearm
dividing into median and anterior interosseous branches. The median branch
entersthehandbeneaththeflexorretinaculumontheradialsideofthewrist.All
pronatorandflexormusclesintheforearm(exceptFCUandthemedialhalfof
FDP)aresuppliedbythetwobranches.Themediansuppliessensorynervesto
theradialsideofthehand:
• Entrapmentsyndromeatthewristisverycommon;CTS.
• Intherarepronatorsyndrome,trauma, swelling,ormassesbetweenthe two
pronatorheadscancauseentrapmentgivinglowerarmpain,paraesthesias,and
weaknessofforearmpronation.Thereislocaltendernessandreproductionof
painfromresistedforearmpronationorwristflexion.
• Pain in CTS is often present at night and relieved by exercising the hand.
Daytimesymptomscan persist.Paincan bereferredup thearmeven tothe
shoulder.Sensorysymptomsareconfinedtotheradialthreeandahalfdigits.
• ClumsinessisacommonearlyfeatureofCTS.
• Symptoms reproduced by a positive Tinel’s sign (percussion over the volar
aspectofthewrist)andPhalen’smanoeuver(volaraspectofthewristrested
onthebackofachairandthehandallowedtofalllooselyundergravity,held
for1min)indicatesnervecompression.
• Asevereorchroniclesionisassociatedwithsensorytestingabnormality(Fig.
3.10) and motor weakness of the abductor pollicis brevis (APB), opponens
pollicis,andthefirstandsecondlumbricals.
• NCSsareindicatedifthediagnosisisuncertain,theconditionisprogressive,
motorneurondiseaseissuspected(thenarmusclewastingmarked/progressive
with minimal sensory symptoms), dual pathology is suspected, surgical
decompression is being considered, and in cases of surgical failure. False-
negativeresultsoccurin10%ofcases.
• MRI appears to be more sensitive than US for detecting abnormalities
involvingthemediannerveinoraroundthecarpaltunnel.

• Aetiology ofCTS isdebated,but probablymultifactorial. Thefollowingare
associated: Colles’ fracture, trauma, carpal OA, diabetes, inflammatory
joint/tendon disease (e.g. RA, SScl), ganglia, menopause and pregnancy.
Hypothyroidism,acromegaly,amyloid,andbenigntumoursarealsoassociated
withCTS.
Treatmentofcarpaltunnelsyndrome(CTS)
( Chapter24hasfurtherinformationonsteroidinjectiontechniques.)
• Nightsplintingmaybecurative,especiallyearlyinthecondition.
• NSAIDsarehelpfulifthereisunderlyinginflammatorydisease.
• Localsteroidinjectionsareofvalue.Ifpartialremissionisachieved,consider
repeatingtheinjection(see Chapter24).
• Surgical decompression is indicated when there is failure of conservative
therapy, progressive/persistent neurological changes, or muscle
atrophy/weakness.
• Failureofsurgicalreleaseofthecarpaltunnelrequiresfurtherconsiderationof
underlying causes such as a ganglion or other soft tissue lesion. Reconsider
alsowhethertherereallyisamechanical/localorperhapsasubtlercause(e.g.
mononeuritis or peripheral neuropathy, entrapment at the pronator or nerve
rootlesion).
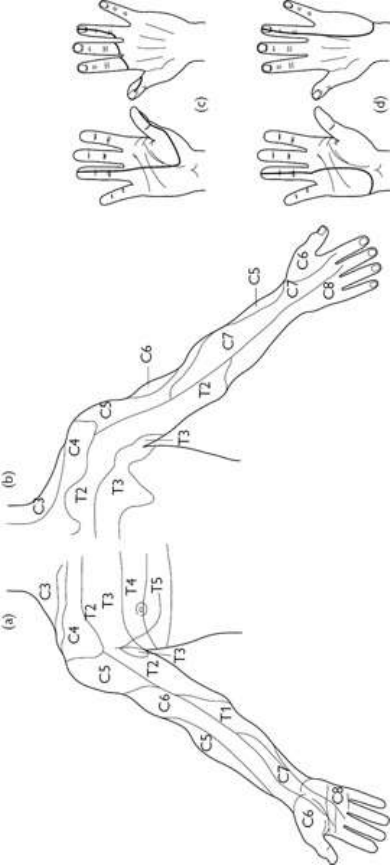
Fig.3.10Approximatedistributionofdermatomesontheanterior(a)andposterior(b)aspectsofthe(right)
upperlimb.Approximateareaofsensorychangeinlesionsofthemedian(c)andulnar(d)nerves.
Thoracicbackandchestpaininadults
Background
• Thethoracicsegment(T1–T12)moveslessthanthelumbarandcervicalspine.
Segmentalmovementinanydirectionisabout6°.However,giventhenumber
ofsegmentsthiscanadd upto appreciablemobility overall.Less segmental
movement results in reduced frequency of problems overall (only 6% of
patientsattendingaspinalclinichavethoracicspineproblems).
• Ribs (1–10) articulate posteriorly with vertebrae at two points: the articular
facetoftheribheadwiththecostovertebralfacetoneachvertebralbodyand
the articular facet of the rib tubercle with the costotransverse facet on each
vertebrallateralprocess.Thesearebothsynovialjoints.Ribs11and12donot
havecostotransversejoints.
• The ribs, each continuous with its costal cartilage, articulate anteriorly by a
synovialjointwiththemanubrium(1–2),sternum(2–7),eachcostalcartilage
above(8–10),ordonotarticulate(11/12‘floatingribs’).
• Amassiveblockofspinalextensormusclesisresponsibleformaintainingthe
body against gravity. Some extend over some distance (e.g. the spinalis
thoracisfromtheupperthoracictothemid-lumbarspinousprocesses).
• DermatomesarecircumferentialandextendfromT2attheclaviclestoT10at
theumbilicus.However,uptofivenerverootsmaycontributeinnervationof
anyonepointinatruncaldermatome.
Takingahistoryinadults
The interpretation of cardiac, oesophageal, or pleural chest pain as MSK in
origin can occur. It may result in missing a serious condition (Table 3.11 and
Table3.12). Similarly, theinterpretation of neurogenicorMSK chest pains as
cardiogenic, oesophageal, or pleural can occur and may lead to unnecessary
investigations.
Table3.11Characteristicsofchestpaininadults:fromnon-neurologicalandnon-MSKpathology
Process Characteristicsofpain
Angina Gradualonsetoftenrelatedtoexercise,aheavymeal,or
emotion.Squeezing,strangling,orconstrictioninchest,can
beachingorburninginnature.Commonlysubsternal,but
radiatestoanyofanteriorchest,interscapulararea,arms
(mainlyleft),shoulders,teeth,andabdomen.Reduceswith
restandsublingualnitrates
Myocardial
infarction
Similartoaboveregardingqualityanddistribution.Longer
duration.Lesseasilyrelieved
Pericardial
inflammation
Sharporsteadysubsternalpain.Canbereferredtoshoulder
tip,anteriorchest,upperabdomen,orback.Oftenhasa
pleuralcomponentandisalteredbychangeinposition—
sharpermoreleft-sidedwhensupinebuteasedbyleaning
forward
Aortic
dissection
Acuteonsetwithextremelyseverepeak.Feltincentreof
chestorback.Lastsforhours
Pleuritic
inflammation
Common.Sharp,knife-like,superficial.Aggravatedbydeep
inspiration,sneezing,orcoughing.Ifaccompaniedby
haemoptysisconsiderpulmonaryembolism
Mediastinal
conditions
Empyemaorsurgicalemphysemamaybeintenseandsharp
andradiatefromsubsternaltoshoulderarea.Associatedwith
crepitus.Mediastinitisandtumourpainresemblespleural
pain.Mayhaveconstantfeelingofconstriction/oppression
Peptic
disease
Penetratingduodenalulcerscancauseintense,persistentmid-
thoracicbackpain
Oesophageal
reflux
Persistentretrosternalburningistypical.Oftenpost-prandial,
whenlyingoratnight/earlymorning.Oesophagealspasmcan
besimilartoanginaandcancausemid-thoracicbackpain,but
refluxsymptomsoftencoexist
Table3.12PainfulneurologicalandMSKconditionsofthethoracicspineandchestwallinadults
Thoracic
vertebraldisease
Osteoporoticorpathologicalfracture
Tumours,e.g.osteoidosteoma,metastasis
Osteomyelitis
Paget’sdisease
Osteomalacia,rickets
Costovertebraljointdysfunction
Nerveirritation
Rootirritation/compressionfromdiscprolapseor
osteophyteatexitforamen,fromstructuredistaltoexit
foramen,orfromneuroma
Biomechanical/
degenerative
Scoliosis(non-structuralcompensatory,structural)
Diffuseidiopathicskeletalhyperostosis(DISH)
Calciumpyrophosphatedihydratedisease
Herpeszosterofintercostalnerve
Chest
wall/superficial
lesions
Ribfracture
Otherriblesions,e.g.tumours,fibrousdysplasia,
osteomalacia
Costochondritis/enthesitis(e.g.PsA)
Intercostalmuscletear/strain
Mastitisorfibrocysticdiseaseofthebreast
Myofascialpainandfibromyalgia
Parietalpleuralinflammation/infection/infiltration
Spondyloarthritis
(SpA)
Spinalinflammation
Acutediscitis
Chronicindolentdiscitis
Scheuermann’s
osteochondritis
Inadolescentsonly
• Areviewofthequalityandradiationofcardiacandoesophagealpaininthe
clinicalcontextshouldalwaysbeconsidered.
• Pleuriticpainiscommon.Chronicpulmonaryembolimaybeunderdiagnosed
and have serious consequences. Any inflammatory, infective, or infiltrative
pleurallesionwillbepainful.
• Lesionsconfinedtopulmonaryparenchymadonotproducepain.
• PericardialpaincanbemisinterpretedasMSKorpleuritic.
• Mediastinalabnormalitiescanproducepainthatisoftenreferred.
• Thoracicspinelesionscanresultinreferredanterolateralchestpain.
• Costovertebralandcostotransversejointdysfunctionisrelativelycommonand
isgenerallyage-related,butcanoccurinanyonewithspinaldeformity.Itmay
producethoracicspinepainaloneorresultinanextensivepatternofradiation
ofpainovertheback,lateral,andanteriorchestwall.
• Lowercervicalspinelesionscanreferpaintotheanteriorchestwall.
• Manypainfulchestconditionsareassociatedwithradiationofthepaindown
theleftarm.Thispatternisnotspecificformyocardialischaemia.
• Lowercervicalpainmaybereferredtotheinter-scapularregion.
• Inter-scapularpainmayalsobeassociatedwithmechanicallumbardisorders.
Unlikeinfection,tumours,andfracture,referredpainiseasedorabolishedby

changesinpositionorposture.
• If there is thoracic back pain alone and it is acute and/or severe consider
osteoporoticfracture,tumours,andinfection.
• Osteoporotic vertebral collapse is common in postmenopausal women. An
acute,non/minimal-trauma-associatedseverepainistypical.Fracturesoccurin
manyothersituations,e.g.ASoraneoplasticbonelesion.
• Spinalinfectionsshouldnotbemissed.ThemostcommonareStaphylococcus
aureus,Brucella,andMycobacteriumtuberculosis.
Askaboutthequalityofpain
• MSK pain (local or referred) generally associates with specific movements,
positions,orpostures,andisreproducible.
• Painthatincreaseswithcoughing,sneezing,ordeepinspiration,issuggestive
of pleural lesions. Rib and intercostal lesions or costovertebral joint
dysfunctionmayalsocausethissortofpain.
Askaboutothersymptomsandriskfactors
• Thepainfromafracture/lesion(osteoporotic,malignancy,infection)isoften
localizedandextreme,wakingthepatientatnight.
• Acute or chronic thoracic spine lesions may be associated with cord
compression.Askabout recent changein sphincter functionandprogressive
lowerlimbstiffnessorheaviness.
• Risksforosteoporosis(see Chapter16).
• Systemicsymptomsoffever(osteomyelitis).
• Bonepainelsewhere(metastases,osteomalacia,Paget’sdisease).
• Spinalpaininadolescence(foranadultwithkyphosis/spinalpain).
• A positive family history is recognized in idiopathic scoliosis, osteoporosis,
andgeneralizedosteoarthritis(see Chapter6).
• Depressionandanxietyareimportantmodulatorsofpain.However,although
thoracicbackandchestpainsmaybepsychogenic,itisunwisetosettleonthis
diagnosiswithoutexcludingMSKconditionsanddiseasesofviscerathatcan
causereferredpain.
Examinationofthe(MSK)thoraxinadults
Visualinspection
Observethepatient(whohasundresseddowntotheirunderwear)fromtheback
and front. Look for deformity, asymmetry, swellings, and note the respiratory
pattern:
• Any scoliosis should be noted. Non-structural scoliosis is frequently due to

posture, severe back or abdominal pain, leg length discrepancy, and, rarely,
canbepsychogenic.Structuralscoliosismaybeduetovariouslesionsatany
age.
• There is a normal mild thoracic kyphos; however, marked kyphos in adults
(particularly postmenopausal women) might suggest multiple osteoporotic
vertebralfracturesordegenerativediscdisease.Alossofnormalkyphosis(flat
spine)maybeseeninspondylitisorpossiblyseveremusclespasm.
• Loosefoldsofskinonthebackcandenoteheightlossfrommultiplevertebral
fractures.
• Costochondral swelling occurs in some cases of costochondritis or SAPHO
(synovitis, acne, pustulosis (palmoplantar), hyperostosis, and (aseptic)
osteomyelitis)syndrome.Lookforlesionsofcostosternalorsternoclavicular
joints(whicharealsofoundinPsA).
Palpation
Palpateoverthevertebrae,paravertebraljoints,andbackmusculaturewiththe
patientprone.Palpatetheanteriorchestwall:
• Spinal osteomyelitis may be associated with obvious skin swelling and
erythema,exquisitefocaltenderness,andextensorspasm.Tumoursmaygive
similarsigns,thoughskinerythemaisnotlikely.
• Costotransverse joints may be tender (4–5 cm from midline). Discomfort at
anycostovertebraljointanditsreferredpaincanbeelicitedbyindividualrib
manipulation(downwardpressureontheriblateraltoitsvertebraljointswhen
thepatientisprone).
• Identifyanytriggerpointsthatreproducemyofascialpaininbackmuscles.
• Tenderswellingofthesternoclavicular,costomanubrial,orsternocostaljoints
maysuggestspondyloarthritis(axSpA)orSAPHOsyndrome.See Chapter
8.
• Inflammationofcostalcartilagesisoftenassociatedwithpainfulswellingand
tenderness. Rib and intercostal lesions should be easily discriminated from
referredpainbyelicitinglocaltenderness.
Checkthoracicspinalmovement
Movementsofthethoracicspineshouldbechecked.Askthepatienttositonthe
couch with their arms folded in front of them. Guided by movements of the
spinousprocesses,gaugetherangeofthoracicspinemovement:
• Approximatenormalrangesofmovementintheabove-mentionedpositionare
extension30°,lateralflexion30°,flexion90°,androtation60°.
• Scoliosisisoftenassociatedwithrotationthatisaccentuated,onexamination,

onflexion.
• Abnormalmobilitywillnotbespecificforanyunderlyingcondition,butmay
draw attention to the major affected spinal segment. Painful segments are
‘guarded’andmayappearhypomobile.
• AxSpA/ankylosingspondylitis(AS)maybecomeobviousifthereisextensive
spinalhypomobility.
• Chest expansion should be measured from forced expiration to complete
inspiration measuring at expansion, with a tape, at the level of the
xiphisternum.
Otherexamination
• Given the range of serious conditions causing chest pains, a full medical
examinationisimportantandshouldalwaysbeconsidered.
• Neurologicalexaminationofthelegsshouldbeconsideredinanyonewhoisat
riskofspinalcordcompression.Lookforincreasedtone,weakness,andbrisk
reflexes.
• Breastandaxillarylymphnodeexaminationshouldbedone.
Investigationsofthoracicconditionsinadults
Radiographs
• Lateral view radiographs generally provide more information about thoracic
spinelesionsthananteroposteriorviews;however,together,bothviewsshould
confirm osteoporosis, degenerative disease (e.g. previous Scheuermann’s
osteochondritis,ochronosis,DISH),andPaget’sdisease(see Chapter16).
• Look for vertebral squaring (in axSpA/AS) and either marginal or non-
marginal syndesmophytes as in psoriatic spondylitis or other SpAs (see
Chapter8).
• DiscriminateenthesitisinSpAfromDISHatthecornersofvertebraebythe
presence of erosions with bone reaction (enthesitis) compared with bone
proliferation alone (DISH). Spondylodiscitis is part of the SpA spectrum of
diseases.
• Radiographsofthespine,orCTimages,areprobablyabetterindicatedofPsA
inthespinecomparedwithMRI.
• Normalradiographsdonotexcludemalignancy.
• BonelesionscanbewellcharacterizedbyCT(e.g.osteoidosteoma).
MRI
• MRIisimportantindiscriminatingtumourfrominfection.
• Disclesions,spinalcanal,andcordarewellvisualizedwithMRI.
• Fatsuppressedorcontrast-enhancedMRsequencesmaybenecessarytodetect
enthesitisorspondylodiscitisassociatedwithSpA.
Bonescintigraphy(
99m
Tc-diphosphonate-MDP)
• Bonescintigraphyisasensitivetestforinfectionandmalignancy.
• In suspected cases of malignancy, it is more sensitive than radiographs, can
often confirm the lytic or sclerotic nature of a lesion and will identify any
otherskeletalsitesofdisease.
• ThepatternofabnormalitiesinSAPHOsyndromearecharacteristic.
• Itisausefulinvestigationinpatientswithmalignancywhopresentwithback
pain. A lack of additional lesions strongly suggests against a single spinal
abnormalitybeingmalignancy-related.
• Scintigraphic tomography can detect abnormality in the pars interarticularis,
facetjoint,anddisc/vertebralbody.
• Scintigraphy sensitively identifies rib and, in most cases, inflammatory
intercostal lesions. The differential diagnosis is of a metastasis, primary
malignant or benign bone tumour, healed rib fracture, fibrous dysplasia,
Paget’sdisease,hyperparathyroidism,orinfection.
Otherinvestigationstoconsiderinpatientswithchestpain
• CXR, then consider pulmonary ventilation-perfusion scan and spiral CT to
evaluateforpulmonaryembolism.
• CTofthechestinpatientswithunexplainedpleuralpain.
• ECGandanexercisestresstestifpossiblecardiacischaemia.
• Transthoracicechocardiographytoshowthickenedpericardiumoraneffusion
associatedwithpericarditis.
• UpperGIendoscopyinsuspectedcasesofpepticulceration.
• Diagnostictrialofaprotonpumpinhibitorincasesofrefluxoesophagitis.
Thoracicbackandchestpaininchildrenand
adolescents
Generalconsiderations
Chest pain is a common paediatric presentation to primary care and A&E in
patientsaged10–21years.Acutechestpainiscardiacin<6%ofpatients.
• Chest pain is often alarming to parents and patients, but rarely caused by a
seriouscondition(Table3.13).
• Inastudyof300patientswithchronicchestpaintherewasacardiaccausein

justonepatient.
• Differentiating cardiac pain and other serious parenchymal pathology, from
musculoskeletalandotherbenignpainremainsimperative.
• PaediatricchestpaincanbeclassifiedintoMSK,respiratory,GI,cardiacand
otherconditions(seeTable3.13).
• For assessment of: thoracic back pain in children and adolescents see
Chapter 21 p. 618; low back pain in children see p. 154; and thoracic
assessmentinadults,see p.130.
Historyandexamination
Generalconsiderations
• Focalchestpaininchildrenisusuallychest-wall(MSK)orpleuralinorigin.
• Diffusechestpainismostlikelytobereferredfrominternalorganpathology.
• A third of adolescents with chest pains who present to outpatients have a
historyofstressfulevents.Theirchestpainsymptomsaretypicallyassociated
with other somatic complaints and sleep disturbance. Hyperventilation,
dyspnoea,dizziness,orparaesthesiamayindicatepanicattacks,unrecognized
bythepatientorparent.

Cardiachistoryandexamination
• Exertionalchestpainwithchesttightnessandsyncopemightbeduetoatrial
flutterortachycardia whichin turnmaybe duetostructuralcardiacdisease
(e.g.hypertrophicordilatedcardiomyopathy).
• Angina chestpain isusually associatedwithexertion,afeelingoftightness,
andradiatestotheneck,throat,jaw,teeth,orshoulder.
• Pericarditispresentsassharpretrosternalchestpainoftenradiatingtotheleft
shoulder,aggravatedbylyingsupineordeepbreathsandrelievedbybending
forward.
• Severeandtearingmidsternalchestpainradiatingtothebackmaybedueto
aorticdissectioninMarfansyndrome,Turner’ssyndrome,Ehlers–Danlostype
IV,andhomocystinuria.
• Though non-specific, chest pain with fatigue and exertional dyspnoea or
syncopecanindicatepulmonaryhypertension.
• PastmedicalhistoryshouldbetakentonoteanypreviousKawasakidiseaseor
cardiacsurgery.
• Takeafamilyhistoryforarrhythmias,tonotefamilialsuddendeath,genetic
conditionsorhyperlipidaemia.
• Cardiac signs on examination: a harshejectionsystolicmurmur radiating to
theneckin aorticstenosis; anejectionclick froma stenosedbicuspidaortic
valve;abnormalperipheralpulses(e.g.previousKawasakidisease).
Musculoskeletalfeatures
• Chestwallpainexacerbatedbydeepbreathinglastingsecondstominutesmay
be due to costochondritis (e.g. secondary to infection or intercostal muscle
enthesitis in ERA or JSpA). Chest-wall tenderness may be present (usually
unilateralalongtheuppertwoormorecontiguouscostochondraljoints).
• Tietzesyndromeisatermusedtodescribeanteriorchestwallpainusuallyina
singlejoint(commonlyatthesecondorthirdribarticulationatthesternumor
sternoclavicularjoint).DifferentialdiagnosisSAPHOsyndromeinadolescent
andenthesitis(see Chapter16).
• Intense pain in thelowerchest or upper abdomenmaydenote‘slipping-rib’
syndrome, which is secondary to trauma and dislocation of ribs 8, 9, 10.
Noting a history of physical strain, sports-related injury, or direct trauma is
important.
• Slipping ribsyndrome paincan bereproducedbyhookingfingers underthe
inferior rib margin and pulling the rib edge outward and upward (hooking
manoeuvre).Thismanoeuvremayproduceaclick.
• A history of sickle cell disease may be relevant given any MSK pains and
pulmonarydisease(e.g.thromboembolism).
Pulmonarydiseasefeatures
• Pulmonarydiseaseis chieflyidentifiablefromahistoryofdyspnoea,cough,
andconventionalrespiratorysymptoms.
• Severe pain, dyspnoea, and low oxygen saturations require both pulmonary
embolismandpneumothoraxtobeexcluded.
Other
• Abdominal pathology can present with chest pain (e.g. typical ‘heartburn’
symptomsinthethroat; cholecystitis-relatedchestpainradiatingto theright
shoulder).
• Throbbing or burning focal chest pain locating to breast tissue is typical of
mastitis,fibrocysticdisease,orpregnancy.
• Burningpainorparaesthesiainadermatomal pattern,precedinga rashbya
fewdayssuggestsherpeszoster.
Table3.13Causesofchestpaininchildrenandadolescents
Tissue/organ Diagnosis/syndrome Frequency
Musculoskeletal Trauma,injury
Costochondritis/Tietzesyndrome,xiphydynia
Slippingribsyndrome
Sicklecelldisease
15–30%
Cardiac Pericarditis,coronaryarteritis(Kawasaki
disease),aorticdissection,anginasecondaryto
structuralcardiacdisease
Veryrare
(<2%)
Respiratory Pleuralinflammation(infectionandsterile
pleuritis(SLE)),pneumonia,PE,asthma,acute
chestsyndrome
2–11%
Gastrointestinal GORD,IBD,cholecystitis 8%
Neurological Herpeszoster
Nerverootsymptoms
Rare
Other Idiopathic
Anxiety,panic-hyperventilation
Breast-relatedconditions
>50%
Lowbackpaininadults
(Seealso Chapter21.)
Epidemiology
• The lifetime prevalence of back pain is 58% and the greatest prevalence is
between45and64yearsofage.
• Most recent statistics report in the order of 12 million primary care
consultationsandover2.4millionadultspecialistconsultationsannuallyinthe
UKforlowbackpain(population64million).Lowbackpainisthefifthmost
commonreasonforallphysicianvisitsintheUSA.
• 2%oftheworkforceintheUSAiscompensatedforbackinjurieseveryyear.
• EstimatedannualcosttotheUKNationalHealthServiceis£500millionwith
over £5 billion lost annually due to absence from work. The financial
healthcare and indirect employment costs of low back pain in the USA are
estimatedtobemorethan$24billion.
Lumbarandsacralspineanatomy
• Therearenormallyfivelumbarvertebrae.Anomaliesarenotuncommonatthe
lumbosacraljunction.
• Thetransitionbetweenthemobilelumbarspine(flexion,extension,andlateral
flexion)andfixedsacrumtogetherwithhighweight-loadingcombinetomake
theregionhighlypronetodamage.
• The facet joints are sharply angled, effectively reducing rotation in lumbar
segments.
• Thesacroiliacjoints(synovial)areheldfirmlybyastrongfibrouscapsuleand
tough ligaments. The amount of normal movement (essentially rotation) is
normallyinverselyproportionaltoage.
• The spinal cord ends at L1/L2. Nerves then run individually, are normally
mobileinthespinalcanal,andtogetheraretermedthecaudaequine.
• Each nerve exits its appropriate lateral intervertebral exit foramen passing
initially superior and then laterally to the disc, e.g. L4 from L4/L5 exit
foramen. However, in the spinal canal each nerve descends immediately
posterior to the more proximal intervertebral disc before it exits. Thus, for
example, L4 root symptoms can occur from either lateral herniation of the
L4/5discorposteriorherniationoftheL3/L4disc(orfromboth).
• Facetjointinnervationisfromposteriorprimaryrami,eachofwhichsupplies
thecorrespondingjointatitslevel,onehigherandonelower.
Basicprinciplesofassessment
• Low back pain can arise from damage or inflammation of the thoracic or
lumbar spines or from the posterior pelvis. Pathology in retroperitoneal
abdominalandpelvicvisceracanresultinreferredpaintothelowback.
• A simple way of categorizing back pain is to consider its cause to be
mechanical, inflammatory, neurologic, referred, or due to bone pathology
(Table3.14).
• Over90%ofepisodesoflowbackpaininadultsaremechanical,self-limiting,
anddonotrequireinvestigation.
• Indicatorsforfurtherinvestigationincludeage>55years,stiffness,focalpain,
pain that disturbs sleep, nerve root symptoms, and chronic persistent (>6
weeks)pain.
• The low back is often a focus for those who may use pain (consciously or
unconsciously) as a protective deviceinthefaceofdomestic,emotional, or
occupational stress. These stresses commonly influence the description and
impact of pain but rarely act alone in causing pain—there is usually some
underlyingorganicpathology.
Table3.14Commonand/orseriouscausesoflowbackpaininadults
Mechanical/degenerative
(verycommon)
Intervertebraldiscdisease(annulartear,internal
disruption,prolapse)
Facetjointarthritis
Spondylolisthesis
Scoliosis/kyphosis
Spinalstenosis
Inflammatory(common)
AS/axSpA( Chapter8)includingsacroiliitis
DISH
Infection(rare) Osteomyelitis(e.g.Staphylococcusaureus,
TB,brucellosis)
Bonedisease(common) Osteoporoticfracture
Paget’sdisease
Osteomalacia
Neoplasia(rare) Secondarymetastases
Multiplemyeloma
Other Sicklecellcrisis
Renaldisease(e.g.tumours,infection)
Gynaecologicaldisease
Fibromyalgia( Chapter22)
Takingahistoryoflowbackpaininadults
Differentiate whether the pain is likely to be primarily mechanical or
inflammatory,duetobonepathologyorreferred:
• The site and extent of the pain does not easily discriminate the cause. All
disordersmaybeassociatedwithmechanicaldeformityand/ormusclespasm
thatmaycausepaininadiffusedistribution.
• Generally, pain due to mechanical lesions is often acute in onset, while
patients with pain from inflammatory lesions often present after symptoms
havebeenpresentforsometime.
• Inflammatorypainisoftenassociatedwithmorningstiffnessthatcanlastfor
severalhoursandiseasedbymovement.Mechanicallesionstendtoworsen
with use. Many ‘mechanical’ or ‘degenerative’ lesions may have an
inflammatorycomponent,e.g.internaldiscdisruptioncausingdiscogenicpain.
• Intrinsicbonepathologyoftencausessevere,unremitting,focalpain.Sleepis
disturbed.Paindoesnoteasesubstantiallywithmovement.
• About 3% of patients presenting with back pain have non-MSK causes. A
significantproportionofwomenhavepelvicconditionssuchasovariancysts
orendometriosis.Painmaybecyclical.
• For those aged >55 with no previous similar episodes of pain increase
suspicionofanunderlyingneoplasticlesion.Investigationisrequired.
• Associated systemic symptoms are common in osteomyelitis and may be
presentifamalignancyhasdisseminated.
Askaboutpainradiationandsymptomsinthelegs
• Progressiveneurologicallegsymptomssuggestaworsening/expandinglesion
suchasatumour,infection/vertebralcollapse,Paget’sdisease,orlumbosacral
spinalstenosis.
• Pressure on the cauda equina sufficient to cause a disturbance in perineal
sensationand/orbowel/bladderparalysisisaneurosurgicalemergency(cauda

equinasyndrome;see Chapter21).
• Legpaincausedbynerverootirritation/compressionisoftenclearlydefined
and sharp, often accompanied by numbness or paraesthesias. The most
commonlyinvolvednerverootsareL4,L5,orS1.Paingenerallyradiatesto
belowthekneeandoften,butnotalways,totheheelandbigtoe.
• Sciatic nerve entrapment at the piriformis muscle can produce identical
radicularsymptomstoL5orS1nerverootentrapment.
• Neurological symptoms in the distribution of the femoral nerve (primarily
anterior thigh musculature) might suggest a high lumbar nerve root lesion
(L1–L3,forexample).
• Disc prolapse is the most common cause of nerve root pain, but bony
encroachment at the nerve root exit foramen by vertebral end-plate or facet
joint osteophytes, and/or soft tissue thickening or fibrosis can cause similar
pain(foramenalstenosis).
• Annulardisctearsandinternaldisruption(i.e.microfracturesinvertebralend-
plates)cancauseapatternofpain,termeddiscogenicpain,characterizedby
lowbackandreferredbuttock/posteriorthighpainaggravatedbymovement.
• Generally, all mechanical lesions of the lumbar spine can result in referred
painaroundthepelvisandanteriorthighs.However,painfromlumbarfacet
jointsandprobablyothersegmentalstructurescanbereferredtothelowerleg.
• Aching in the back and posterior thighs after standing is typical of, but not
specific for, spondylolisthesis. There are often added spasms of acute pain,
especiallyifthereissegmentalinstability.
• The symptoms of spinal stenosis are often relieved by sitting bent slightly
forward,sincethespinalcanaldimensionsincreaseinthisposition.
• Sacroiliitis often causes referred pain to the buttocks and back of thighs. It
occurscommonlyinSpA(see Chapter8).
• Sacroiliac pain can occur in multiparous women—the condition may be
associatedwithhypermobility.
Notethedescriptionofthepain
• Painmaybe‘severe’whateverthecause;however,notewhetherthepatient’s
descriptorsofitsuggestnon-organicinfluences.
• Sharp, lancinating leg pains suggest nerve root irritation/compression
(radicular pain), whereas leg pain referred from other structures within a
lumbarsegmentisgenerallydeepandaching.Thedistributionmaybesimilar
(see earlier in section). More persistent, rather than episodic, radicular pain
maydenotestenosisofthenerverootexitforamen.
• A description of bilateral buttock/leg pain that worsens on walking is

consistent with spinal stenosis, especially in those with normal peripheral
pulsesandnobruits.
• A change in the description of pain in someone who has an established
diagnosismaybeimportant,e.g.subacute,severe,unremittinglocalizedpain
in a patient with axSpA who normally has mild inflammatory pain might
reflectasuperaddeddiscitis;or,acutesevereunremittingsleep-disturbingpain
inanelderlywomanwithknownchronicmechanicalpainassociatedwithOA
mightsuggestosteoporoticfracture.
• Florid descriptions of the pain and its severity are associated with
psychologicalmodulatorsofpain.
Previousbackpainandtrauma,occupation,andfamilyhistory
• Scheuermann’sdisease(whichisassociatedwithirregularvertebralendplates)
causes spinal pain in adolescence. It is a risk for spinal degeneration and
kyphosisinadults.See p.514.
• Previoustraumamayhavecausedparsinterarticularisfractures(anantecedent
of spondylolisthesis),vertebralfracture (risk offurthermechanical damage),
orligamentrupture(subsequentsegmentalinstability).
• Itisgenerallyacceptedthatthehighprevalenceofdiscdiseaseamongmanual
workers at a relatively young age provides some evidence for a causal
relationship.
• Itisoftenthecasethatpatientswithchronicpainfollowing(sometimestrivial)
traumamaybedissatisfiedwiththequalityofcarereceivedatthetimeofthe
injury.Beawarethatmanybelieve,andthereissomeevidencetosupportthis,
that the way in which spinal pain is handled at its onset significantly
influencesitssubsequentcourse.
• Sacroiliitis is an early part of Brucella arthritis (20–51% of patients). Poor
animal- or carcass-handling hygiene or ingestion of infected foodstuffs/milk
can lead to infection. Spondylitis is a late feature and is characterized by
erosions,discinfection,andabscesses.
• Apositivefamilyhistoryoflowbackpainmight,incontext,suggestSpAor
generalizedOA.
Examinationofanadultwithlowbackpain
Inspecttheundressedpatientfromthesideandbehind
• Notethefluidityofmovementwhenthepatientisundressing.
• Check the skin for redness, local swelling, and skin markings. Redness and
swellingoccasionallyaccompanyosteomyelitis.
• Lipoma, hairy patches, café-au-lait patches, or skin tags often reflect
underlying structural nerve or bone abnormality, e.g. spina bifida,
diastematomyelia,neurofibromatosis.
• Skinfolds often suggest an underlying significant structural change, such as
osteoporoticfractureorspondylolisthesis.
• Noteanydeformity:hyperlordosis(associatedwithL5/S1damageandweak
abdominal musculature), prominent thoracolumbar kyphosis (multiple disc
degeneration or vertebral fractures), scoliosis (degenerative, compensatory
musclespasmforunilateralpain).
• Look from the side. A gentle lordotic curve is normal. Flattening suggests
musclespasmorfusioninSpA.Withmajorspondylolisthesis,astepbetween
spinousprocessescansometimesbeseen.
Observeactivemovementswhilethepatientisstanding
Lumbarforwardflexion(‘...withyourlegsstraight,slowlyreachdowntotry
and touch your ankles . . .’), lateral flexion (‘. . . with your legs and back
straight,tipsidewaysandrunyourhanddownyourlegtowardsyourknee...’)
andextension(‘...withyourlegsstraight,slowlybendbackwards...’).Note:
flexion can be mediated by the hip joints; extension can be affectedbyslight
pelvic tilt and body sway. Ask what can be achieved normally and what is
painful:
• Abnormalmovementsarenotspecificforanyconditionthoughtheymayhelp
tolocalizeaproblem.
• Pain in extension is characteristic of retrolisthesis, facet joint arthritis, or
impingingspinousprocesses.Mayberelievedbyflexion.
• Failure of the spinous processes to separate in a patient who manages good
forward flexion would be consistent with permanent spinal stiffness, e.g.
axSpA/AS,withflexionmediatedbythehipjoints.
• ForwardflexioncanbemeasuredusingthemodifiedSchöbertest.Whenerect,
marktheskinatthepointmidwaybetweentheposteriorsuperioriliacspines
(Venus’ dimples) and again 10 cm above and 5 cm below. Measure the
increase in distance between the outer marks at full forward flexion—in a
youngadultthisisnormally>6cm.
• Ask the patient to stand on one foot then lift onto their toes a few times.
WeaknessmightimplyanL5nerverootentrapment(gastrocnemius/soleus).
Observethegaitpattern
Abnormalityofgaitmayreflectanyspinalorlowerlimbproblem:
• Anantalgicgait;aself-protectivelimpduetopain,typicallycharacterizedby
ashortstancephaseontheaffectedleg.Thecommonestcauseispathologyat
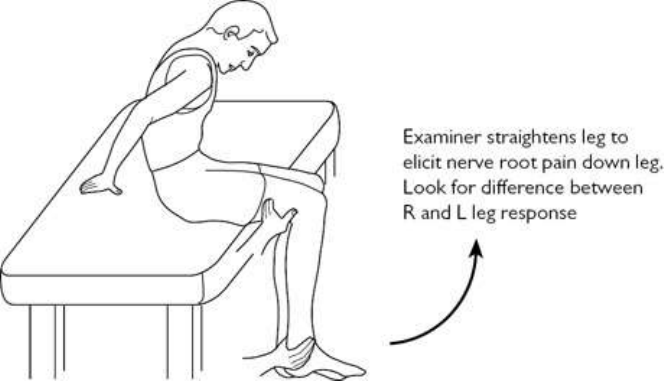
thehip.
• Awide-basedgaitsuggestsunsteadiness(duetodizziness,muscularweakness,
proprioceptive,orcerebellardeficit,etc.).
• Leaningforwards/stifflegged—althoughnotspecific,inolderpeoplethismay
denotespinalstenosis.
• Shuffling, which could suggest parkinsonism (back pain/stiffness is a
recognizedearlysign).
• Footdrop,whichcouldsuggestL5orS1nerverootcompression.
• Flat feet, hind feet valgus, and genu recurvatum on stance phase, might
suggestgeneralhypermobility—associatedwithvariouslowbacklesions.
Checkextensionandlumbarrotation(patientseated)
Withthepatientseatedonthecouch,checklumbarextensionandrotation(the
pelvisisnowfixed):
• Typically,combinedrotationandextensioncanelicitpainfromarthriticfacet
joints.Itisasensitivethoughnotspecifictest.
• Slumpingforwards(Fig.3.11)stretchesthedura.Increasedlumbarpainmay
be elicited in cases of disc prolapse, but more importantly, leg pain can be
elicitedincasesofnerverootentrapment.Amoreprovocativetestcanbedone
by gently extending each knee in turn in the slump position. Look for
asymmetry.
Fig.3.11The(passive)slumptestidentifiespainfromlumbardiscandnerverootirritationorcompression.
‘Active’legextensioncanalsotriggerpain.
Examinethesacroiliacjointsandhips(patientsupine)
Withthepatientsupine,examinationofthesacroiliacjointsandanexamination

ofthehipsshouldbedonetoexcludepainarisingfromthesestructures:
• Testflexionandtherotationalrangeofeachhipbyliftingtheleg,flexedatthe
knee,sothattheupperlegisvertical.Passivemovementshouldnormallybe
pain-free.
• NoSIjointstresstestisspecific.Testsaredesignedtoreproducepainincases
ofSIjointdysfunctionorsacroiliitis.Herearetwo:
• Pressdown/outreasonablyfirmlyoverbothanteriorsuperioriliacspinesat
thesametime.
• Liftoneleg,flex,andabductthehipslightly.Exertanaxialforceintothe
acetabulumattwoorthreedifferentangles.Thistestisconsideredbymany
tobemoreusefulandprobablystressesboththejointandmanyofthesacral
ligaments,butislessspecificifthehipjointisabnormal.
Testingnerveroottension
(Alsosee Chapter21.)Usestraightlegraisewiththepatientsupine,Lasegue’s
test,andtheslumptest.
• Thenormalvariationinstraightlegraiserangesfrom60°tomorethan90°in
adults.Comparesides:
• Discomfort from normal tightening of the posterior thigh or calf muscles
mustbediscriminatedfromapositivetest.
• Apositivetest(legraisingrestrictedto40°orlessbytheradicularpain)is
mostspecificinpatientsaged<30yearsandforL5orS1nerverootlesions.
• A crossed straightlegraise(pain elicited by raising theunaffected leg) is
evenmorespecificfornerverootentrapment.
• Lasegue’stestisdonebyliftingtheaffectedlegwithkneefullyflexedatfirst
thenwiththeupperpartofthelegvertical,slowlyextendingthepatient’sleg
attheknee(passiveexamination).
• ApositiveLasegue’stestiswhenpainistriggeredinbuttockorbackasinthe
straightlegraise.
• Slumptestisparticularlyusefulwhenthepatientisunabletoliesupinefora
straightlegraiseorLasegue’stest.Withthepatientsitting,andslumped(Fig.
3.11)andlegshangingfreeofftheground,graduallyextendthelowerlegand
askifbuttockorlowbackpainistriggered(apositivetest).
• To identify more subtle cases of nerve root entrapment with all three tests,
apply additional foot dorsiflexion at the maximum possible extent of leg
raise/kneeextension(pain-free).
Neurologicalexamination
Neurologicalexaminationofthelegsisessentialinsuspectedcasesofnerveroot
entrapment, cord compression, spinal stenosis, and cauda equina syndrome.
Table 3.15 lists tests for muscle strength in the lower limbs—weakness may
denotenerverootentrapment—andTable3.16liststheprincipalsignsoflumbar
nerverootlesions.
Examinationofthepronepatient
Askthepatienttoturntolieprone.Palpatelowbackandoversacrum:
• Diffusetendernessmaybeduetomusclespasm.
• Superficial tenderness over the spinous processes or interspinous interval
mightsuggestinterspinousligamentdisruptionorimpingingprocesses.
• Paravertebralbonytendernessmaysuggestfacetjointarthritis.
• Costovertebralangle/lointendernesscouldindicaterenalpathology.
• TendernessovertheSIjointsisnotspecificforsacroiliitis.
• ApositivefemoralstretchtestreproducesL1–L4(especiallyL3)radicularpain
intheanteriorormedialpartofthethigh.Flexthepatient’skneeto90°and
passivelyextendthehip.
Otherexamination
• Insuspectedcasesofspinalstenosisorcaudaequinasyndrome,itisessential
to check for sensory loss in the sacral nerve dermatomes. Also check anal
sphinctertonebyrectalexamination(S5).
• In suspected cases of spinal stenosis, the patient can be asked to walk until
limitedbypainthenre-examined.Ifthereisanyischaemiaofthecaudaequina
or of a nerve root (from foramenal stenosis), nerve root signs may become
moreobvious.
Investigationoflowbackpaininadults
(Alsosee Chapter21.)
Therearetwoimportantinitialstepsininvestigatinglowbackpain.
Firstdecidingwhetherradiographswillhelp.Second,althoughrelativelyrarein
practice, the possibility of infection, malignancy, and cauda equina
compressionalwaysneedstobeconsidered.
• Simpleradiographicviewsareinsensitiveindicatorsoftheseconditionsand,
inmostcases,arenotspecificalthoughmostradiologistswouldagreetheyare
desirable in addition to CT or MRI. Laboratory tests are mandatory in all
suspectedcasesofinflammation,infection,andmalignancy.
Table3.15Testingmusclestrengthinthelowerlimbs(patientsupineunlessotherwisestated).Weakness
maydenotenerverootentrapment
Muscleormuscle
group
Nerve
roots
Test
*
Hamstrings(knee
flexion)
L5,
S1,
S2
Askpatienttoflexthekneeto45°,hold
patient’sankleandaskthemtobendtheknee
furtheragainstyourhold
Iliopsoas(hip
flexion/internal
rotation)
L1,
L2,
L3
Askpatienttoliftthelegwithabentknee,
holduptheupperlegandresistyourpush.Try
topushthelegdownandslightlyoutwards
Quadricepsfemoris
(hipflexion,knee
extension)
L2,
L3,
L4
Holdthepatient’srelaxedupperlegabovethe
couch(holdunderneathabovetheknee).The
lowerlegshoulddroploosely.Askthemto
raisethelowerlegagainstyourresistance
Frompatientstandingtestrepetitivesquatting
formoresubtleweakness
Tibialisanterior
(ankledorsiflexion).
Tibialisposterior
(ankleinversionand
plantarflexion)
L4,
L5
Withthekneestraightaskthepatienttopull
backtheirfoot(showthemfirst)againstyour
pull.Resistdorsiflexion
Standingorwalkingonheelstestsformore
subtleweakness.Note:ifthehindfootrestsin
valgusorthepatientsignificantlyevertsthe
footduringdorsiflexion,thetestmayalso
recruitperonealmuscles(L5,S1)
Extensorhallucis
longus
L5,
S1
Askthepatienttopulltheirbigtoeback
againstyourfinger(atthebase)
Gastrocnemiusand
soleus(ankleplantar
flexion)
S1,
S2
Askthepatienttopointtheirtoes.Resist
movementbypressingtheballofthefoot
Standingorwalkingonthetoestestsformore
subtleweakness
*
Comparesides.Scoreaccordingtoscale,forexample:0=nomusclecontraction;1=contraction
visible;2=activemovement,gravityeliminated;3=activemovementagainstgravity;4–/4/4+=active
movementagainstslight/moderate/strongresistance;5=normalpower.
Table3.16Principalcombinationsofsignsusedforidentifyinglumbarnerverootlesions
Nerve
root
Paraesthesiasandsensory
change
Muscleweakness Tendon
reflex
changes
L2 Upperthigh:anterior,
medial,andlateralsurfaces
Hipflexionandadduction None
L3 Anteriorsurfaceoflower
thigh
Hipadductionandknee
extension
Kneejerk
possibly
reduced
L4 Anteromedialsurfaceof
lowerleg
Kneeextension,foot
dorsiflexion,andinversion
Kneejerk
decreased
L5 Anterolateralsurfaceof
lowerlegand
dorsum/medialsideof
foot/toe
Hipextensionand
abduction.Kneeflexion.
Foot/toedorsiflexion
None
S1 Lateralborderandsoleof
foot.Backofheelandcalf
Kneeflexion.Plantar
flexionandeversionoffoot
Anklejerk
decreased
Radiographs:decision-makinginrequestingthem
(SeeTable3.17.)
• Lumbarspineradiographsarenotalwayshelpful.Rememberthatnineoutof
ten cases of back pain in the primary care setting are mechanical and self-
limiting.Featuresonaplainradiographofthelumbarspinecorrelatepoorly
withthepresenceorpatternofpain.
• Spondylosisiscommon,age-related,andoftenisn’tsymptomatic.
• MRIbestidentifiesaparsinterarticularisfracture,anyassociatedboneoedema
and spondylolisthesis seen in young people and athletes (see p.620). CT
helpsclarifythehealingresponse(bridgingofboneacrossthedefect).
• Obtaining radiographs to help in the management of patients is a different
issuetoobtainingthemtoaiddiagnosisandonethatrequirescarefulthought,
e.g.isthepatientlikelytoperceivethattheyhavereceivedsuboptimalcareifa
radiographisnotrequested?
• Spondylolysis may be seen on a lateral view, but is seen better on oblique
view.Obliqueviewsmayalsoshowpediclestressfractures.
• Spondylolisthesismaybeidentifiedandgradedbyalateralfilm.
• Flexionandextensionviews maybe helpfulindelineating subtlecases,and
instability(spondylolytic).
• General osteopenia is a risk factor for low bone mass; however, it is not a
sensitiveindicatoroflowbonemass.
Table3.17Commonlyreportedpatternsofradiographicabnormalityinadultswithspinalsymptoms:the
interpretation,andsuggestedreaction
Radiographic
abnormalities
Lesion
suggested
Sensiblefurtheraction
Lumbosacral
anomalies
Riskforfuture
backpain
Maynotbeclinicallysignificant.Riskfor
lowbackpain(esp.ifhypermobile)
Generalized
osteopenia
Osteoporosis Measurementofbonedensity.Ruleout
secondarycauses,e.g.myeloma
Narrowed
discspace,
marginal
vertebralend-
plate
osteophytesor
both
Intervertebral
discdisruption
MRIifpersistentsymptomsorsignsof
samelevelnerverootentrapment,spinalor
nerverootexitforamenstenosis
Localized
lucentor
sclerotic
lesion,lossof
cortex
Tumour,
infection,or
fracture
Discusscasewithradiologist.MRIorCT
maybeadvised.Abonescanmaybe
helpful.Initiateappropriatelaboratorytests
immediately
Facetjoint
OA
Facetjoint
syndrome
Considerwhetherthereisassociated
spinal/nerverootexitforamenstenosis(?
radicularsymptoms)orsymptoms
suggestiveofspondylolisthesis.CTorMRI
isthenlikelytobeappropriate
Pars
interarticularis
defect
Spondylolysis/?
spondylolytic
Furtherobliquefilmcentredonsuspected
levelorCTshouldconfirm.Association
withsymptomsorsignsofdiscdiseaseor
spondylolisthesis.Flexionandextension
lateralviewradiographsmaydetailthe
lesionfurther.MRIcharacterizesbone
stress,softtissueinvolvementandnerve
impingment.
Shortlumbar
pedicles
Spinalstenosis ConsiderMRIifsymptomssuggestspinal
stenosis
Mixedpatchy
sclerosisand
lucencyin
entire
(enlarged)
vertebra(e)
Paget’sdisease Neurologicallegsymptomssuggest
spinal/exitforamenstenosisorvascular
‘steal’
• Lookforvertebralsquaring(inAS),non-marginalsyndesmophytes(inother
SpA,suchaspsoriatic—see Plate13),orflowingsyndesmophytes(inDISH
—atleastthreecontiguousvertebralbodies).
• Consider obtaining an AP view of the pelvis. Established (but not early)
sacroiliitiscanberuled-out.Afurther‘coned’viewisoftenhelpful.
• Sacroiliitis (periarticular osteoporosis, erosion, sclerosis of bone, widening
jointspace)occursinalltypesofSpA.Itcanbeunilateral.
• Sclerosis of the SI joint on the lower iliac side alone suggests osteitis
condensansilii.Jointspaceisnormalandjointmarginwelldefined.
• Patterns of metabolic bone disease, Paget’s disease and hip pathology are
usuallyreadilyidentifiableonapelvicfilm.
Bonescintigraphy(see Plate16)
• Bonescintigraphyisasensitivetestforinfectionormalignancy.Itisauseful
investigation in patients with previously diagnosed malignancy who present
with back pain, especially in those who have had no previous skeletal
metastases. No additional lesions strongly suggests against a single spinal
abnormalitybeingmalignancyrelated.
• Itisnotspecificforthevariousdegenerativelesions,butcanhelplocalizethe
siteofalesion.
• SI joint appearances can locate pathology but appearances may depend on
bothpreviouspathologyand/orcurrentinflammation.
CTorMR?
The choice of imaging depends on local availability and likely differential
diagnosis,althoughMRIispreferredinyoungpeople:
• For spondylolytic spondylolisthesis, CT shows bone bridging and size of
defectwhereasMRIshowsbonestressofanyrecentfracture.
• NerveimpingementcanbeshownbyCTorMRI.
• Intervertebraldiscprolapse,bothposteriorandposterolateral,canbeshownby
eithertechnique.ProlapsematerialisofsimilarCTdensityandMRsignalto
thedisc,andwell-definedagainstepiduralfat.
• Changesinthenormaldiscsignalpatternareassociatedwithage-relateddisc
degeneration. Discogenic pain has been associated with MRI abnormalities
classifiedaccordingtoModic.
• OnT2-weightedMRI,discmaterialisusuallyofhighersignalthan‘scar’(e.g.
fibrosisfromapreviouslesion),inwhichsignaldecreaseswithageing.Recent
scarring enhances immediately, but old scarring does so only slowly. This
discriminationrequiresgadolinium-enhancedMRI.
• CT or MRI shows early sacroiliitis in axSpA when radiographs are normal
thoughMRIwillshowcurrentinflammationbetterthan‘ever’involvementof
SIJs—forwhichCTisbetter.
• TheshapeandoutlineofthespinalcanalareideallyshownonCT,butarealso
seen withMRI.Itis difficultforMRI to distinguish fibrous structures from
sclerotic or cortical bone, though it shows intrathecal content more readily
whichisanadvantageinidentifyingintraduraltumours.
• Spondylodiscitis(partofaxSpA),ifchronic,maybedifficulttodiscriminate
from degenerative disc/vertebral end-plate disease. Fat-suppressed or
gadolinium-enhanced sequences may show high signal at the anterior disc
vertebralend-platejunctions.
Screeningforinfection,malignancy,ormetabolicbonedisease
• In cases where the history and examinationsuggestamechanical condition,
but where the clinician wishes to be more confident of excluding an
inflammatorycondition,ESR,andCRParesuggested.
• AraisedESRwouldpointtowardsfurtherlaboratoryinvestigation.
• An infection screen should include an FBC for anaemia and leucocytosis,
CRP,blood,andurinecultures.IfspinaltuberculosisissuspectedaplainCXR
shouldbetakenandserial(over3days)earlymorningurinesamplestaken.
• Serum and urine protein electrophoresis (with immunofixation) are essential
testsinthe‘work-up’formyeloma.Ureaandcreatininearealsoimportantas
hypercalcaemia, and acute renal impairment have prognostic significance in
thiscondition.
• Routinebloodtestsmaypointtoanunderlyingmetabolicbonedisordersuch
asPaget’sdiseaseorosteomalacia.Thesetestsarenormalinpostmenopausal
osteoporosis.

• Ifosteoporosisisdiagnosed(see Chapter16)ascreenforsecondarycauses
shouldincludeESR(andifraised,serum,andurineproteinelectrophoresis),
calcium, phosphate, sex hormones, but also serum 25-hydroxyvitamin D,
parathyroidhormone(PTH),thyroidfunctiontests(TFTs),andliverfunction
tests(LFTs).
Treatmentoflowbackpain:adults
(Seealso Chapter21forgreaterdetail)
• Animportanttherapeuticinterventioninthecaseofacutepainistotakethe
patientseriously,takeapositiveview,andintheabsenceofsinistersigns,e.g.
nerverootpain,urgeearlymobility.
• Analgesics and muscle relaxants can be used in the short term, initially
regularly,thenasrequired.
• Physicaltherapywithgraded-activityprogrammesmaybeofvalue,certainly
earlyindiscdiseaseorspondylosis.
• Cordcompressionduetobonecollapsefromatumourisanacuteemergency
and should be discussed immediately with an oncologist or radiation
oncologist,andaspinalorthopaedicorneurosurgeon.
• Caseswithdiscprolapsefailingtorespond toconservativetherapy,orcases
wherethereisongoingorrapidlyprogressiveneurologicaldeficit,shouldbe
referredforsurgery.
• Available surgical techniques for acute or persistent disc disease include
decompression (e.g. nerve root decompression and partial facetectomy),
prostheticintervertebraldiscreplacement,intradiscalthermocoagulation, and
intradiscal steroid injections, although evidence for long-term efficacy is
lackingforalltheseprocedures.
• Surgeryforspinalstenosisisusefulforrelievinglegneurogenicfeatures,but
notindicatedifthereisnosignificantneurologicalcompromise.Surgeryisnot
usuallydoneiftheonlyeffectofspinalstenosisisbackpain.
• In chronic back pain, aerobic exercises combined with behavioural methods
maybemoreeffectivethanexercisealoneandcanhelpmotivatethepatient.
Methods may also incorporate psychological and social assessment and
management.
• Thecommontreatmentsavailableforchronicbackpaininclude:
• analgesicsandmusclerelaxants.
• antiepileptics/antidepressantsforneuropathicpain.
• localanaesthetic/steroidinjections.
• acupuncture.
• transcutaneouselectricalnervestimulation(TENS).
• physicaltherapy.See p.609
• ergonomicadvice.
• multidisciplinary programmes—counselling, cognitive therapy, education,
relaxation,corsetsandbelts.
• Timelysurgeryforstructuralscoliosiscanlessenspinalcurvature.
Lowbackpaininchildrenandadolescents
Synopsis
Childrenandyoungpeoplepresentwithacombinationofbackpain,deformity,
limp, systemic or neurological features. Many of the features of adolescents
overlapwithyoungadultsandthereaderisreferredtotheassessmentofadults
onpp.140–152.Seealso Chapter21,pp.618–621.
• Backpaininchildren andadolescentsiscommon(lifetime prevalenceupto
80%by20y)and,asinadults,mostcasesarenon-specific,self-limitingand
donotpresenttothemedicalprofession.
• Backpainismorecommonattimesofrapidgrowthingirlsandwithhighand
lowlevelsofactivity.Itisespeciallycommoninyoungathletes.
• Times of rapid growth are also associated with: progression of idiopathic
scoliosis; other spinal deformities; and (if excessive) volume expansion of
vertebraewhichconfersthepotentialforadiscrepancybetweenbonesizeand
bonemass(areasonforcorrectingDXAscan-derivedBMDmeasures).
• Thelikelihoodoffindingunderlyingpathology(see Table21.6,p.618)is
low,butmorelikelyatyoungerages(especially<4yold).
• Low back pain in adolescence is a significant risk factor for back pain in
adulthood.
Takingahistoryoflowbackpaininchildren
• Itisimportanttoconsiderbackpaininrelationtoageanddevelopment.Loss
of developmental milestones, refusal to walk, or irritability in a non-verbal
child,especiallyif<4y,warrantsimmediateinvestigation.
• Systemicfeatures,intractableornightpaininchildren<6yrequireassessment
forinfectiousorneoplasticcausesincludingTBinrelevantpopulations.
• Backpainismorecommonattimesofrapidgrowthingirlsandwithhighand
lowlevelsofactivity.Itisespeciallycommoninyoungathletes.(seealso
Box21.1).
• Trauma,especiallysuddenorrepetitivetwistinginadolescentsmayaggravate
orcauseaparsdefectleadingtospondylolisthesis.
• Disability(includingschoolabsence)disproportionatetoexaminationfindings

may indicate pain amplification. Social history including stresses and sleep
patternshouldbeelicited.
• Incongruence of history and examination raises suspicion of non-accidental
injury.
• Asinadults,differentiationbetweenbiomechanicalandinflammatoryclinical
featuresshouldbeelicited.
Examinationofbackpaininadolescents
• Be opportunistic with a young child, observe play and review findings in
contextofdevelopmentalstage.
• Focalbonytendernessidentifiedbypalpationorpercussionshouldbeassessed
furtherthroughradiologicalinvestigation.
• Examinegait(see pp.37–39)andposture,forlossorexaggeratedlordosis,
pelvictilt(fromleglengthdiscrepancy),neckjut,andkyphosis.
• Scoliosisisrarelypainful.
• Reduced hamstring flexibility (determined by popliteal angle) and tight hip
flexors(Thomas’stest)arecommonlyassociatedwithbackpain.
• New,unilateralorpersistenttoe-walkingsuggestsspasticity,tetheredcord,or
muscleweakness.
• Survey the skin for possible bruising, mid-line hairy patches, café-au-lait,
axillary freckling (neurofibromatosis). Soft tissue swelling may denote
extensionofaspinaltumour.
• Neurologicalexaminationin20%ofchildrenwithboneorspinalcordtumours
willshowmotorweakness.
Investigations
• Investigationsarethesameasforadultssee pp.148–151.
• AgeneralanaestheticiscommonlyrequiredforanMRIinyoungchildren.
Pelvic,groin,andthighpaininadults
Anatomy
Anatomyofthepelvisandhipregion
• The bony pelvis consists of two innominate bones (ilium above the
acetabulumandischiumbelowit)thatarticulatewitheachotherattheanterior
symphysispubisandposteriorlywiththesacrumattheSIjoints(SIJs).
• SIJs are initially synovial but become fibrous with age. A few degrees of
rotationcanbedemonstratedinchildrenandyoungadults.
• Strongligamentsstabilizetheposteriorpelvisthroughsacroinominate,lumbo
(L5)–sacral,andlumbo(L5)–iliacattachments.
• Thesymphysispubisisacartilaginousjointandnormallydoesnotmove.
• When standing, weight is transferred through the head of the femur. The
femoral head is stabilized in the acetabulum by the acetabular labrum and
strongpericapsularligaments.
• The ligamentum teres crosses the hip joint and carries blood vessels to the
headofthe femur inchildrenand young adults.Inold age, bloodsupply is
largelyviavesselsthatenterthefemoralneck.
• Twobursaearefoundattheinsertionofthegluteusmaximus:oneseparatesit
fromthegreatertrochanter,theotherseparatesitfromthevastuslateralis.
• The ischial bursa separates gluteus maximusfromtheischial tuberosity and
canbecomeinflamedfromoveruse.
Anatomyofpelvicmusculature
• Threegroupsofmusclesmovethehipjoint:thegluteals,theflexormuscles,
andtheadductorgroup.
• Themajorglutealgroupmusclesare:
• gluteusmaximus(L5,S1/2):arisesmainlyfromiliumandsacrum,projects
down posteriolaterally and inserts into the posterior femur and the lateral
tensorfasciaelatae.Itextendsandexternallyrotatesthehip(thehamstrings
alsoextendthehip).
• gluteus medius (L4/5, S1): lies deeper and more lateral. It inserts into the
lateralgreatertrochanterandabductsandinternallyrotatesthehip.
• piriformis,obturatorinternus,andquadratusfemorisarisedeepinthepelvis
andinsertintotheposteriorgreatertrochanter.Allexternallyrotatethehip.
• Themajorhipflexor,psoasmajor(L2/3),isamassivemusclethatarisesfrom
thelateralpartofthevertebraeandintervertebraldiscs(T12–L5)andlateral
processesofthelumbarvertebrae.Itrunsanteriorlyovertheiliacrim,across
thepelvis,undertheinguinalligament,andinsertsintothelessertrochanter.
Theiliacus(L2–L4)arisesfromthe‘inside’oftheiliacblade,passesunderthe
inguinal ligament medially to the lesser trochanter. Both flex, but the psoas
alsointernallyrotatesthehip.
• Thepsoasisenvelopedinafascialsheath.Retroperitonealorspinalinfections
thattrackalongsofttissueplanessometimesinvolvesthepsoassheathandcan
causeinflammationinthepsoasbursa,which separatesthemusclefromthe
hipjoint.
• Alladductormusclesarisefromthepubisorischiopubicrami.Theadductor
longus and gracilis are the most superficial; they arise from the pubis and
insertintothefemoralshaftandpesanserinus(‘goose’sfoot’)belowtheknee,

respectively. The adductor magnus (L4/5) is the largest of the deeper
adductors;itinsertsintothemedialfemoralshaft.
• Adductors stabilize movement around the hip towards the end of the stance
phaseofthegait.Bodyweightistransferredontoonelegduringthisaction
and,therefore,adductorsneedtobestrong,especiallyforrunning.
Functionalanatomyofthehip
• Withaflexedknee,thelimitofhipflexionisabout135°.
• Hipextension(at30°),internalrotation(at30–35°),andexternalrotation(at
45–55°)islimitedbystrong,pericapsularligaments.
• Abductionislimitedto45–50°bycontactbetweenthegreatertrochanterand
acetabularlabrumrim.Adductionislimitedto20–30°withafixedpelvis(see
Plate15).Theseareadultranges.
• Greater femoral neck anteversion (angle of the neck compared to the distal
femur) allows greater internal rotation of the hip (and reduced external
rotation).Tibialtorsioncancompensatebutthisandhipanteversionresultsin
atoe-ingait.Femoralneckretroversion(iftheangleisposteriortothefemoral
intercondylar plane) allows greater external rotation of the hip, usually
resultinginatoe-outgait.
• Normallyinfantshavemoreanteversionthanolderchildrenoradults(30–40°
atage2yearscomparedwith8–15°atage>18years).
Neuroanatomy
• The femoral nerve is formed from L2–L4 nerve roots and supplies mainly
musclesofthequadricepsgroupandsomedeeperhipadductors.
• WithcontributionsfromL4–S3roots,nervesfromtheplexusconvergeatthe
inferiorborderofthepiriformistoformthesciaticnerve.Thisisataforamen
formed by the ilium (above and lateral), sacrum (medial), sacrospinous
ligament(below),andsacrotuberousligament(posteromedial).
• Inabout10%ofpeoplethesciaticnervedividesbeforeexitingthepelvis.In
some a branch exits above the piriformis muscle. Nerve entrapment and
traumaatthissitemaygiverisetopiriformissyndrome,andmaybenefitfrom
physicaltherapy.
Takingahistory
Age
Ageisariskfactorforsomeconditions:
• Unless there has been previous hip disease (e.g. osteonecrosis, synovitis),
trauma, or a long-standing biomechanical abnormality (e.g. epiphyseal
dysplasia)hiposteoarthritis(OA)isuncommoninadults<55yearsold.
• Paget’s disease of bone is rare in adults <50 years old except in familial
disease.
Distributionandtypeofboneandsofttissuepain
• Allmechanicallesionsofthelumbarspinecanresultinreferredpainaround
the pelvis and thighs. It is often bilateral, localizes poorly, and is aching in
nature.
• Lateral pelvic pain is often referred from the lumbosacral spine. If pain
localizes (i.e. the patient points) to the greater trochanter, it may be due to
trochanteric bursitis, enthesitis, or meralgia paraesthetica (lateral femoral
cutaneousnervesyndrome,seeTable3.18).
• Hip joint pain is felt in the groin, but it can be located deep in the buttock
whenischialbursitisandsacroiliacpainshouldalsobeconsidered.Itmaybe
referreddistallytotheanteromedialthighandknee.
• Groin pain on weight-bearing suggests hip pathology such as synovitis,
osteonecrosisorOA,butitisnotspecific.Tendonitisoftheadductorlongus,
osteitispubis,afemoralneckstressfracture,osteoidosteoma,orpsoasbursitis
cangivesimilarsymptoms.
• Bonepathologytypicallygivesunremittingpain.Sleepisoftendisturbed.
• PainfromdeepMSKpelvicstructuresistypicallypoorlylocalized,although
can be severe. If the pain appears to be ‘catastrophic’ consider pelvic bone
disease (tumours, infection, Paget’s disease, osteomalacia, osteoporotic
fracture)(see Chapter16)oranunstablepelvis(chronicosteitispubiswith
diastasis/laxityofthesymphysispubisandsacroiliacjoints).
• EnthesitisoftheanteriorpelvisandosteitispubisassociatedwithSpAs(see
Chapter8)areprobablyunder-recognized.
• Achinginthebackofthelegsafterstandingisfoundwithspondylolisthesis
(i.e.anteriordisplacementofavertebra).
• Sacroiliacpainandstiffnessradiatestothebuttocksandposteriorthighs.
Table3.18Patternsofpainaroundtheproximallegandtheirmajorcausesinadults
Patternof
pain
Causes
Painin
buttockand
posterior
thighs
Referredpainfrom:lumbarspine,e.g.facet,OA,
spondylolisthesis;SIjointinflammation;lowerlumbarnerve
rootirritation;sciaticnerveentrapment(piriformissyndrome)
Localizedpain:ischialbursitis/enthesitisorfracture;
coccidynia
Diffusemuscularpain/stiffness:myositisorPMR
Paget’sorotherbonelesionofsacrum
Lateral
pelvicpain
Referredfromlumbosacralspine
Trochantericbursitis/enthesitis
Gluteusmediustear
Lateralhipjointpain,e.g.osteophyte
Groinpain Hipdisease,e.g.OA,osteonecrosis,synovitis,
femoroacetabularimpingement
Psoasbursitis
Adductortendonitis,osteitispubis,pubisfracture
Pelvicenthesitis
Paget’sdisease(pelvisorfemur)
Femoralneckorpubicramusfracture
Hernia
Anterior
thigh
Referredfrom:lumbarspine,e.g.facetOA,spondylolisthesis;
upperlumbarnerveroot;hipjoint,femoralneck
Myositis,PMR
Meralgiaparaesthetica(anterolateral)
Adductortendonitis,osteitispubis
Ischaemia(claudication)
Lymphnodes
Paininamusculardistribution
• DiffusepaininthebuttocksandthighsoccursinPMR.Itisoftensuddenor
subacuteinonset,associatedwithstiffness,andmaygivesimilarsymptomsto
thosecausedbysacroiliitisbutinvariablyoccursforthefirsttimeinamuch
olderagegroup.

• Pain is not invariably present for all types of autoimmune myositis (see
Chapter 14). When it does occur, it is unlikely to be confined to pelvic
musculature or to be unilateral, but should be considered where acute or
subacuteonsetdiffusepelvicgirdle/thighpainaccompaniesweakness.
• Multipleentheseallesions—particularlyofstructuresatthegreatertrochanter
—canpresentwithquitediffusepain—interpretedbypatientsas‘muscular’.
Qualityanddistributionofnervepain
• Nerverootpainisoftenclearlydefinedandsharp.Itmaybeburninginquality
and is often accompanied by numbness or paraesthesias. L5 or S1 lesions
generallycausepainbelowtheknee,butcanalsocauseposteriorthighpain.
L1–L3rootlesionscancausepainintheanteromedialthigh.
• Pain with paraesthesia on the anterolateral part of the thigh may be due to
entrapmentofthelateralcutaneousnerveofthethighunderthelateralpartof
theinguinalligament(i.e.meralgiaparaesthetica).Symptomsmaybereferred
to this area with L2 or L3 nerve root lesions, since this is where the nerve
originates.
• Diabetics with uncontrolled hyperglycaemia are at risk of diabetic
amyotrophy. Acute unilateral or bilateral thigh pain with muscle wasting
occurs.ItshouldnotbemisdiagnosedasPMR(inwhichweaknessorwasting
donotoccur)orinflammatorymyopathy.
• Footballersareatriskofadductortendonitis(often anadductor apophysitis)
and osteitis pubis owing to substantial mechanical forces placed on pelvic
structuresduringrunningandkicking.
• Althoughhipfracturesareusuallyobvious,theycanalsopresentsubacutelyin
a patient who continues to walk; this is particularly common among the
elderly,whomaydevelopstressfracturesofthehip.
Previoustrauma,lowback,andMSKproblems
• Previoustraumaordiseasecausingpermanentdeformityofanylumbosacral
orhipjointstructurecanbeconsideredariskfactorforasymmetry,poorcore
stabilityandMSKpains(Table3.19).
• Multiparity is a risk factor for osteitis pubis, sacroiliac, and pelvic pain,
particularlywherethereishypermobility.
• Trochanteric pain syndrome owing to enthesitis, bursitis or insertional
tendonitis/tendontearmaycoexistwithreferredbackpain.
• Enthesitis of the gluteus medius can occur at its greater trochanterinsertion
andgivesimilarsymptomstothosecausedbybursitis.
• Historically, tailors were at risk of ischial bursitis because of sitting on the
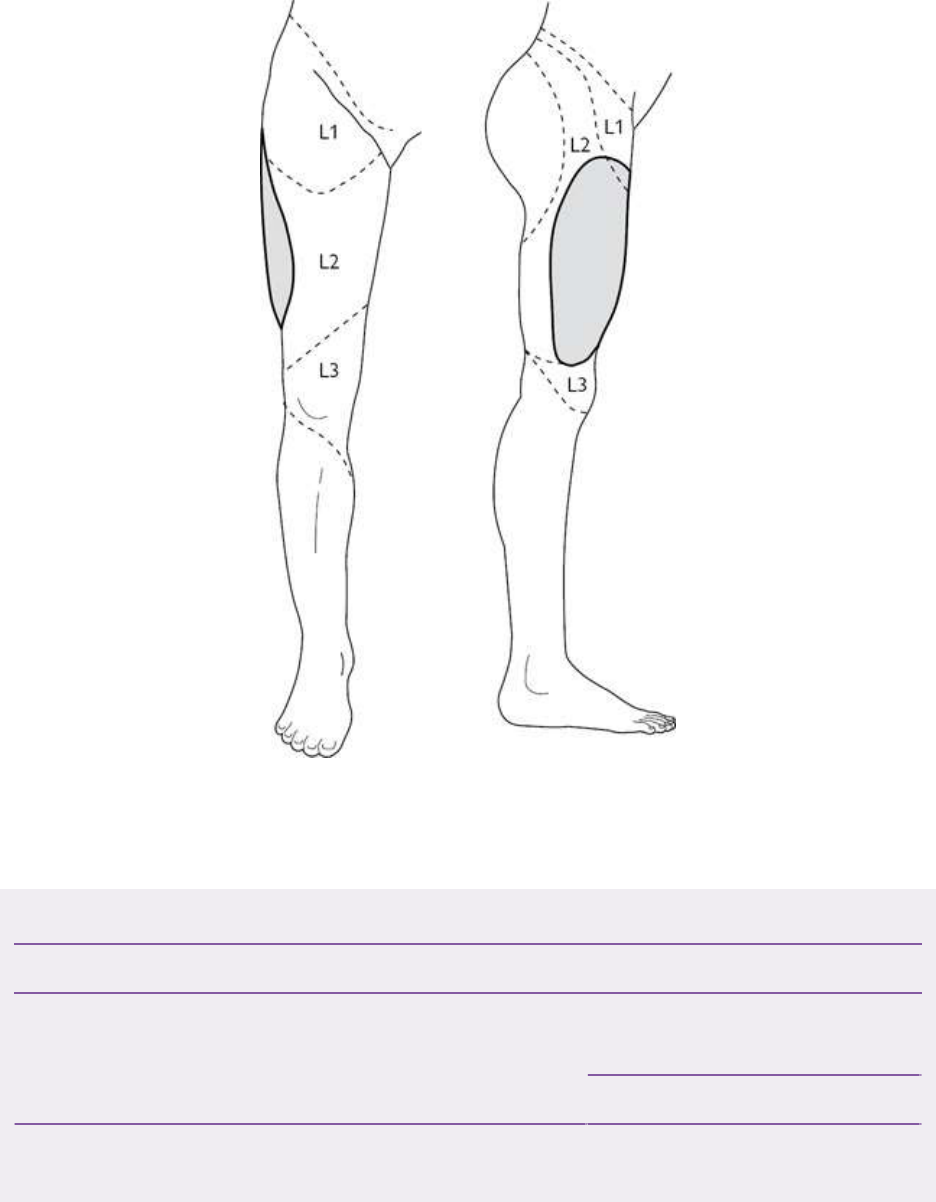
floorcontinuallycrossinganduncrossingtheirlegs,causingfrictionirritation
ofsofttissuesoverlyingtheischialtuberosity.
Fig.3.12Theapproximateareaswithinwhichsensorychangesmaybefoundinlesionsofthelateral
cutaneousnerveofthethigh(hatchedarea)andhighlumbarradiculopathy(brokenline).Shadedarea—
sensorysymptomsdistributionfrommeralgiaparaesthetica.
Table3.19Riskfactorsforpainfulpelvicorhiplesions
Riskfactor Pelvic/hippathology
Lowbacklesions(e.g.lumbarfacetdiseaseor
intervertebraldegenerativediscdisease)
Referrednon-dermatomal
pain
Sciaticpain
Hipjointstructurallesion(e.g.Perthes’disease,
slippedepiphysis,epiphysealdysplasia)
Hipdysplasia,avascular
necrosisorOA
Glucocorticoiduse Osteoporoticfracture
Osteonecrosisofthe
femoralhead(see Plate
17)
Autoimmuneandautoinflammatoryrheumatic
jointdisease(e.g.RA,JIA,axSpA,AS)
Synovitiship
SecondaryOAofthehip
Pyogenicarthritisofthe
hip
Periarticularenthesitis
CKD3b–5 CPPD/pseudogoutofthe
hipjoint
Multiplepregnancies Osteitispubis(±pelvic
instability)
Sports Adductor
tendonitis/apophysitis
Osteitispubis
Examinationofadultswithhipandpelvicpain
Thereaderisreferredtothesequenceofexaminationforthelowback,including
thesacroiliacandlowerlimbneurologicexaminationelsewhereinthischapter
(see ‘Examination of an adult with low back pain’, pp. 144–147). Always
consider lower spinal, muscle, or neurological pathology when assessing
weaknessandpainaroundthepelvis.
Observationandpalpation
Forobservationandpalpation,thepatientshouldbesupineonacouch:
• Look for leg length discrepancy (hip disease, scoliosis) and a leg resting in
externalrotation(hipfracture).
• Psoriasismaybeassociatedwithpelvicenthesitis/sacroiliitis.
• Swellinginthegroinmaybeahernia(reducible,moveswithcough),lipoma
(soft/non-tender/diffuse), a saphenous varix, or lymphadenopathy
(hard/rubberyandinvariablymobile).Ahipjointeffusioncannotbefelt.
• Tendernessoverthehipjointinthegroinisnotspecificforjointpathology:
thejointisdeep—musclesandpsoasbursaoverlieit.

• Ifthegroinisverytenderwithslighttouch,considerhipfractureorinfection.
Hyperpathia(andallodynia)isconsistentwithCRPS(see Chapter22).
• Numbness over the anterolateral thigh suggests meralgia paraesthetica (Fig.
3.12).
• The adductor longus tendon can be palpated at its insertion at the pubic
tubercleanddistallyalongtheuppermedialthigh.Thepubictubercleisfound
bypalpating slowlyand lightlydownwards fromumbilicusoverthebladder
untilboneisreached.
• Pain from osteitis pubis or adductor apophysitis is often significant, with
abdominal rectus contraction (ask the patient to slowly lift their head and
shouldersoffthecouchkeepingyourfingeronthepubictubercle).
Hipexamination
The patient is supine. Tests generally help to discriminate articular and extra-
articulardisease,butnotthecausesofarticulardisease:
• Measure and determine actual or apparent leg length discrepancy: measure
fromtheanteriorsuperioriliacspinetothemedialtibialmalleolus;byflexing
hipsandknees,thesiteofshorteningshouldbecomeapparent.
• A fixedloss of extensionisa signofintra-articular hipdisease.The patient
flexesthehipandkneeononesideuntilnormallumbarlordosisflattensout
(confirmedbyfeelingpressureonyourhandplacedundertheirlumbarspine
duringthemanoeuvre).Iftheotherhipflexessimultaneously,itsuggestship
extensionlossonthatside(Thomas’test).
• Usingthepatellaortibialtubercleaspointers,testtherotationalhiprangein
extensionbyrotatingthestraightenedlegsbyholdingtheheels.
• Rotationalmovementsarealsotestedbyliftingtheleg,flexed90°attheknee,
and swinging the foot out (internal rotation) or in (external rotation). Hip
flexioncanbe tested inthis position too(see Plate15a). Patients without
intra-articularpathologyshouldhaveapain-freerangeofmovement.
• Rotational ranges in hip flexion and extension may differ between left and
rightinanindividual.Also,variationsinfemoralneckanteversioncontribute
tovariationsinrotationrange.
• Totesthipabduction/adduction,fixthepelvistoavoidpelvictiltbyplacing
onehandfirmlyovertheiliaccrest(see Plate15b).Occasionally,painatthe
end of abduction or internal rotation occurs with a bony block (solid ‘end-
feel’).Inanolderpatientthismightsuggestimpingementofamarginaljoint
osteophyte.
• Barlow’s manoeuvre checks for congenitaldislocationof the hips in babies.
Flexandadductthehipsexertinganaxialforceintotheposterior‘acetabulum’
todemonstrateposteriordislocation.
• Greaterretroversion(allowingexcessivehipexternalrotation)usuallyoccurs
in cases of slippedfemoralepiphysis.External rotation is accentuated when
the hip is flexed. The slip (usually inferoposterior) is thought to occur in
associationwithaperiodofrapidgrowth.
Muscleactivationtests
Specific muscle activation against resistance can be used to elicit pain, but
resultsneedtobeinterpretedcautiouslyinthecontextofknownhipdisease:
• Hip adductionagainstresistance(slidingtheir leginwards towardsthe other
against your hand) reproducing pain is a sensitive test for adductor longus
tendonitis, but may be positive in osteitis pubis, hip joint lesions, and other
softtissuelesionsintheadductormuscles.
• Testpsoasbyresistedhipflexioninslightinternalrotation.Psoasbursitisor
infection tracking along the psoas sheath is likely to give intense pain with
minimalresistance.
• Hipabduction(slidingthelegoutwardsagainstyourhand)maybeparticularly
painful in cases of gluteus medius tears, but also in trochanteric bursitis or
intra-articularpathology.
Palpateposterolateralstructures
Askthepatienttolieontheirsideandpalpatetheposterolateralstructures(Fig.
3.13):
• Tenderness over the greater trochanter is usually well-localized, although it
maybeanteriororposterolateraltothetrochanterandrefersasmallwaydown
theleg.
• Theischialtuberosityanditsoverlyingbursalieattheapexofthebuttock.
• Thesofttissuesoverlyingthepointwherethesciaticnerveexitsthepelvisis
foundmidwaybetweentheischialspineandthegreatertrochanter.Theremay
betendernessasaresultofsofttissuelesionsortraumacausingsciaticnerve
entrapment(piriformissyndrome),whichcanleadtofootdrop.
• Atendercoccyx(coccidynia)canbepalpatedinthisposition.Itcanalsobe
palpated(andthesacrococcygealjointmoved)fromabi-digitalexamination,
thoughthisrequirestheindexfingertobeplacedinsidetherectum,thethumb
outside,thetwodigitsthenholdingthejoint.
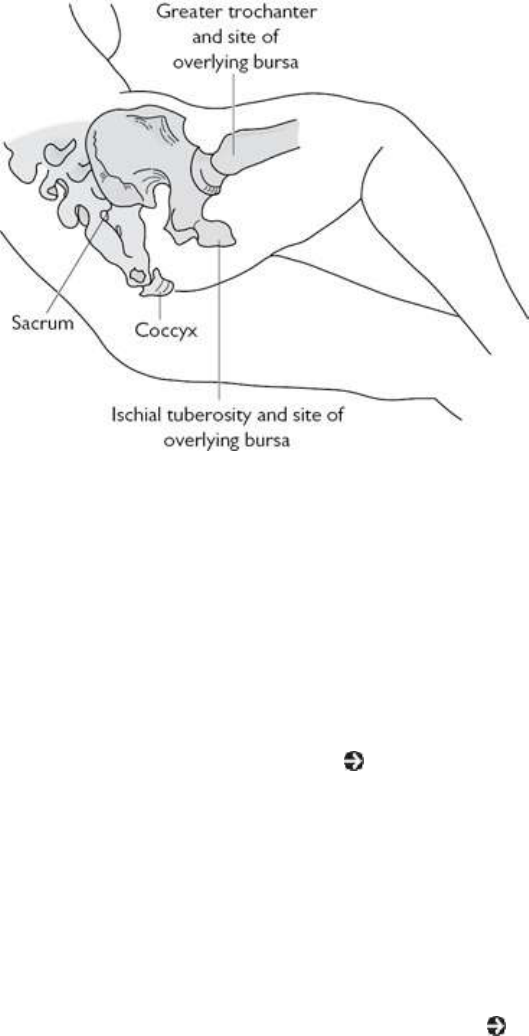
Fig.3.13Bonyanatomyoftheposteriorhipandpelvis,showingthepositioninwhichlesionsaroundthe
greatertrochanterandischialbursacanbepalpated.
Investigationofanadultwithhipandpelvispain
Radiographs
AnAPradiographofthepelvisisagoodinitialscreeningtestinpatientswith
pelvic,hip,orthighpain.APandlaterallumbarspinefilmsmaybewarranted:
• The pelvis is a common site of involvement in myeloma, metastatic
malignancy,andPaget’sdiseaseofbone(see Chapter16).
• Established, but often not early, sacroiliitis can be ruled out. The main
differentialdiagnosesofthecausesofsacroiliitisareAS,psoriaticorreactive
arthritis, enteric arthropathy, brucellosis and other infections,
hyperparathyroidismandosteitiscondensansilii (sclerosisofthe SIjoint on
theloweriliacside.)
• Wideningofthesymphysisinchildrenmaybeasignofcongenitaldisorders
of development (e.g. epispadias, achondrogenesis, chondrodysplasias,
hypophosphatasia),traumaandhyperparathyroidism(see Chapter16).
• Wideningofthesymphysispubis,osteitispubis(boneresorptionandsclerosis)
and osteitis condensans ilii are signs associated with chronic pelvic pain in
multiparouswomen.
• General osteopenia is a risk factor for general low bone mass measured by
densitometry; however, it is not a sensitive or specific indicator of
osteoporosis(i.e.maybeosteomalaciaorrickets).
• Regional osteoporosis confined to the femur is non-specific: hip synovitis,

infection,ortransientosteoporosisofthehiparepossible.
• Earlysynovitisandinfectionmaybedemonstratedthroughsubtleradiological
signssuchasjointspacewideningandchangeinsofttissuefatplanes.
• A‘frogleg’(lateral)viewofthehipshowstheanteriorandposteriorfemoral
head more clearly than an AP view (useful in early osteonecrosis/Perthes’
disease,slippedepiphysis).
• Theacetabulaearebestvisualizedon45°obliqueviews(acetabularfractures
canbemissedonaconventionalAPview).
• ‘Stork’ views of the symphysis pubis (standing on one leg) are useful for
confirmingdiastasisofthejoint.
Diagnosticultrasound
USisasensitiveandsimplewayofconfirmingahipjointeffusion.UsingUS,
fluid can be aspirated for culture and an assessment of the extent of synovial
thickeningcanbemade.
• TendondamageinthegroinareashouldbeidentifiablewithUSalone(guided
steroidinjectioncanthenbedoneifnecessary)butMRImaybeneededeither
tocharacterizepathologyfurtherorruleoutjointpathology.
Bonescintigraphy
Characteristic, though non-specific, patterns of bone scan abnormality are
recognizedinthehip/pelvicarea.
• The following conditions can be recognized: sacroiliitis, bone malignancy,
myeloma, Paget’s disease, hip fracture, femoral head osteonecrosis (see
Plate17),osteoidosteoma,OA,bursitis/enthesitisatthegreatertrochanterand
synovitisofthehip.
• Visualizing osteitis pubis/adductor apophysitis requires special seated ‘ring’
view.
CTandMRI
• MRIofthehighlumbarregionshouldbeconsideredtoconfirmanerveroot
lesioncausinggroinorthighpain.
• SpecificpatternsofX-rayattenuationorsignalchangearoundtheSIJsoccur
insacroiliitiswithCT/MRI,althoughactiveandpreviousinflammationcannot
easilybedistinguishedunlessbothmodalitiesofimagingarearranged.
• A suspicion of bony malignancy from radiographs of the pelvis requires
furthercharacterization.CTisthetechniqueofchoiceforcharacterizingbone
lesionsaroundthehip,suchasfemoralneckstressfracture,osteoidosteoma,
orotherbonetumours.CTmaygivemoreinformationaboutthelesion(andis
valuablefor‘guidedbiopsy’),butMRIisusefulincheckingforpelvicvisceral

lesions.
• MRIisthetechniqueofchoiceifhipinfectionorosteonecrosisissuspected.In
adults,patternsofsignalchangehavebeencorrelatedwithprognosis.
• During a single examination, the pattern of hip synovitis (vascularity and
thickness),cartilageloss,andsubchondralboneerosioncanbedocumented.
Laboratoryinvestigations
• ESRandCRPmaybenormalininflammatorySIJs,lumbarvertebraldisc,and
pelvicenthesisdisorders.
• PMRisinvariablyassociatedwithanacute-phaseresponse.
• MyelomaisunlikelyiftheESRisnormal.
• A high alkaline phosphatase is typically associated with an acute-phase
response,althoughintheelderly,itmightsuggestPaget’sdisease.
• ANAandRFareunlikelytohelpdiagnostically.
• Majormetabolicbonedisease,suchasosteomalaciaandhyperparathyroidism
isusuallyexcludedbyanormalserumcalciumandphosphate.
Treatmentofpelvicconditionsinadults
Treatmentofspinalandneuropathicpainiscoveredintheearliersectionon
‘Lowbackpaininadults’,pp.140–152andin Chapter21.
• NSAIDs may be required for a number of the conditions described earlier,
particularlyOA,hipsynovitis,andtendoninflammation.
• Physicaltherapyandrehabilitationplayavitalandearlypartinmanagement,
maintaining mobility, preventing tissue contracture, and re-
strengthening/stabilizingthelowerback,pelvis,andhip.
• Eitherphysicaltherapistsorpodiatristsmayhelpinaccuratelyevaluatingback
and lower limb biomechanics. Asymmetry and muscular imbalance may be
modifiablerelativelysimplywithfootorthotics,forexample.
• Steroidinjectionsmaybeimportantinthefollowingconditions:
• meralgiaparaesthetica.
• osteitispubis.
• trochantericbursitis/enthesitis.
• ischialbursitis/enthesitis.
• adductortendonitis.
• coccidynia.
• hipsynovitis(underimagingguidance).
• sacroiliitis—inintractablepainandunderX-rayorUSguidance.
• Injectiontechniquesarecoveredin Chapter24.
Surgery
• When the hip has been damaged by an inflammatory arthritis or OA the
principal surgical intervention is joint replacement. Osteotomy has been
mainlysupersededbymorereliablereplacement.
• Surgicalsynovectomyofthehipisadifficultprocedureandopeningthehip
carriesariskofavascularnecrosis.Thisprocedureisveryrarelydone.
• Excision arthroplasty is only really necessary where infection or poor bone
stockmakereconstructionunwise.Powerisoftengreatlyreducedandeventhe
previouslyfityoungpatientwillnotbeabletoambulatewithoutcrutches.
Pelvic,groin,andthighpaininchildrenand
adolescents
Generalconsiderations
Hipandpelvicproblemsinyoungchildrenusuallypresentwithalimpnoticed
bya parent.In anolderchildoradolescentpainmay bereported initially—in
groin,aroundbuttocksorgreatertrochanterareas.
• Thecommonestcausesof pelvic,hipandupperthighconditionsin children
are either due to developmental disorders, inflammatory lesions or
trauma/overuse(seeTable3.20).
• If stress fracture of the femoral neck is suspected in a teenage girl then
consider:amenorrhea,eatingdisorderandathleticover-training(‘femaletriad
syndrome’).
Table3.20Commoncausesofhipjointandpelvisareapainsinchildrenandadolescents
Typeofcondition Diagnosis Incidence(per10,000)
Developmental Perthes’disease 0.6
Slippedupperfemoral
epiphysis(SUFE)
0.1–1
Inflammatoryor
infection
Septicjoint,osteomyelitis
orpyomyositis
1(notknownfor
pyomyositis)
JIA 0.3
Irritablehip(transient
tenosynovitis)
8
Idiopathicchondrolysisof <0.1
thehip
Biomechanicaland
overuseinjury
Snappinghip ≈1
Tendinopathy/muscle
strain
Common
Enthesitis(apophysitis) Uncommon(numberdue
toSpAunknown)
Stressfracture(“female
triadsyndrome”)
Uncommon
Tumours Osteoidosteoma 0.1
Ewingsarcoma(femur) <0.1
Leukaemia/neuroblastoma <0.1
Other Intra-abdominalpathology
Examination
Examinationbeginswithgaitevaluation.Accountforthedevelopmentalstage.
Examinesquatting,single-leghopping,lunging,zig-zagrunningandabdominal
curls/sit-ups(todiscloseanysymphysealpain).
• Hip rangeof movementinchildrenissimilartoadults exceptthe degreeof
femoralanteversionisgreaterintoddlers(30–40°at2years)reducingto8–
15°by18yearsofage.
• Reduced range of movement and irritability at end of range is typical of
intraarticularpathology.Jointpainradiatesintothegroin.
• Palpate for tenderness over ASISs, iliac crests, iliac tubercles, greater
trochanters,SIJregionandpubictubercleswiththepatientstandingandlying
onthesidewithhipflexed(whenincludeposteriorsuperioriliacspinestoo).
• Includejointsaboveandbelow(lumbarspine,SIJ,knee)andtrytoreproduce
thehippainthroughpalpationandmanipulation.
• Also,examinegroinnodesandmassesandabdomen.
Leglengthdiscrepancy
Slightdifferencesarenormalandnotassociatedwithhiporkneerestriction.
• Broadly,leglengthdiscrepancycanbeascertainedbyassessmentofpelvictilt
andkneecreasesymmetrywhenstanding.
• Evaluationisthendonewiththepatientlyingpronemeasuringfromanterior
superior iliac spine to the medial malleolus and umbilicus to the medial
malleolus.Thelattermayneedtoaccountforpelvictilt,musclecontractureor
spasm.
• Unless leg length discrepancy is idiopathic, the shorter leg is usually the
abnormaloneandusuallyduetoeithershorteningofsofttissues,growthplate
trauma, Perthes disease, SUFE, tumours, or infection and secondary
degenerativechanges.
• Radiographicevaluationassesses skeletal,jointandepiphysealcausesofleg
lengthdiscrepancy.
Specificexaminationtests
Some tests in children and adolescents are similar to those in adults though
should beconsidereda guide to further tests/investigationsas none are highly
specificforpathology(Table3.21).
Table3.21Specialtests:pelvis/hipsinchildrenandadolescents
Test Manoeuvre Interpretation
Trendelenburg
(patient
standing)
Standingononelegortheother. Thenon-weight-
bearingsideofthe
pelvisdropswith
adjacenthipabductor
orpelvicstabilizer
deficiency(duetopain
inhibitionortrue
weakness)
Thomastest
(patient
supine)
Liftandflexonelegatthehip Aspelvistiltsthe
contralateralhipflexes:
fromatightpsoas,loss
ofhipjointextensionor
hipjointflexion
contracture
Obertest
(patient lying
onside)
Withtheaffectedleguppermost,
thelegisabductedandkneeflexed
to90°.Holdingthehipjointin
neutralwithslightextensionand
externalrotation,thelegis
released
Failureofthekneeto
adduct(fall)isa
positivetestindicating
contractionortightness
oftheiliotibialband
Faber/Patrick
test
(patientsupine)
Atthehipbringonelegpassively
intoflexion,abductionandexternal
rotationwiththefootrestingon
oppositeknee.Pressdowngently
butfirmlyontheflexedkneeand
thecontralateralanteriorsuperior
iliaccrest
Groinpainontheflexed
hipsidemayindicate
intraarticularhip
pathologybutalso
contralateralbuttock
painmayindicateanSI
lesiononthatside.
Kneepaininadults
Anatomyoftheknee
• Thekneeextends,flexes,androtates.
• The main extensor quadriceps consists of four muscle segments—rectus
femoris,vastuslateralis,medialis,andintermedius,whichconvergetoforma
tendon containing the patella that then inserts into the tibia. Rectus femoris
arisesfromthepelvisandvastusmusclesfromtheupperfemur.
• Thehamstringmuscles(bicepsfemoris,semitendinosus,semi-membranosus)
all arise from the ischial tuberosity and flex the knee. The biceps femoris
insertsaroundthefibularhead.Theothertwomusclesinsertintothetibiaon
themedialsideandcanexternallyrotatethefemur.
• Intheknee,thefemoralcondylesarticulatewithinsemicircularfibrocartilage
meniscionthetibialcondyles(Fig.3.14).Onlytheperipheral10–30%ofthe
menisciisvascularandinnervatedandcanpotentiallyrepairitself.
• Asthekneeapproachesfullextension,thefemurinternallyrotatesonthetibia
(bicepsfemorisaction)tighteningeachpairofligamentsrelativetoeachother.
Thisconfigurationconfersmaximumstability.
• Asflexionisinitiated,asmallamountoffemoralexternalrotationonthetibia
occurs.This‘unlocking’isdonebythepopliteus—amusclethatarisesfrom
theposteriorsurfaceofthetibiabelow.Itpassesupobliquelyacrosstheback
ofthekneeandinserts,viaacord-liketendon,intothelateralfemoralcondyle.
Thetendonpartlylieswithinthekneejointcapsule.
• Groovesonthefemoralcondylearticularsurfacesallowtightcongruitywith
theanteriorhornsofthemenisciwhenthekneeisextended.Iffullextension—
and this optimal articulation configuration—is lost, then articular cartilage
degenerationinvariablyfollows.Thisisparticularlyimportantininflammatory
arthritis.
• Thecruciateligamentsaretheprincipaljointstabilizers.Theanteriorcruciate
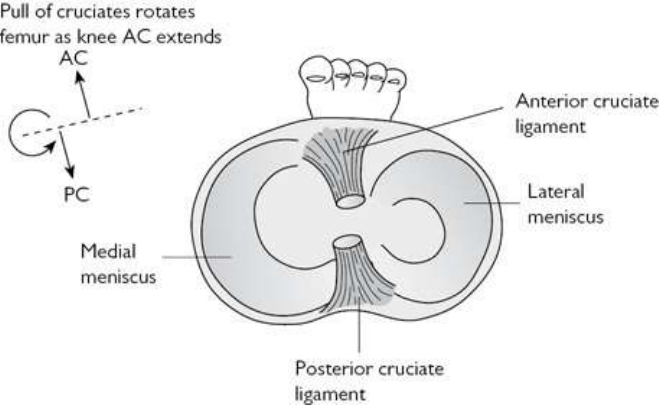
attachesabovetothe inside ofthelateral femoral condyle andbelowto the
tibiainfrontofthetibialspinesthoughaslipattachestotheanteriorhornof
thelateralmeniscus.Itsmainroleistocontrolandcontaintheamountofknee
rotationwhenthejointisflexed.
• The posterior cruciate attaches above to the inside of the medial femoral
condyle. At the other end, it attaches in a (posterior) groove between tibial
condyles. Its main role is to stabilize the joint by preventing forward
displacementofthefemurrelativetothetibiawhenthekneeisflexed.
• The cruciates are extra-articular and are covered by a layer of vascular
synovium.Bleedingusuallyaccompaniesdisruption.
• Thetibialormedialcollateralligament(MCL)hassuperficialanddeeplayers
(Fig.3.15).Itstabilizesthekneeagainstvalgusstresses,mostlyduringflexion.
• The superficial MCL overlies, and moves relative to, the deep part and is
separatedfromitbyabursa.ThelowerpartofthesuperficialMCLiscovered
bythelongadductors,gracilis,semitendinosus,andsartoriusmuscles,asthey
mergeintothepesanserinusbeforeinsertingintothetibia.
• TheMCLandpesanserinusareseparatedbytheanserinebursa.DeeperMCL
fibresattachto,andstabilize,themedialmeniscus.
Fig.3.14Axialsectionoftherightkneejoint(lookingdownonthetibialplateau,wherethefootisfixedon
thefloor).Thefemoralcondylesarticulatewithinthemenisci.Asthekneeextendsthecruciateligaments
tightenandpullthefemoralcondylesactingtointernallyrotatethefemurthroughthelastfewdegreesof
extension.Thekneetherefore‘locks’andisstablewhenthelegisstraight.
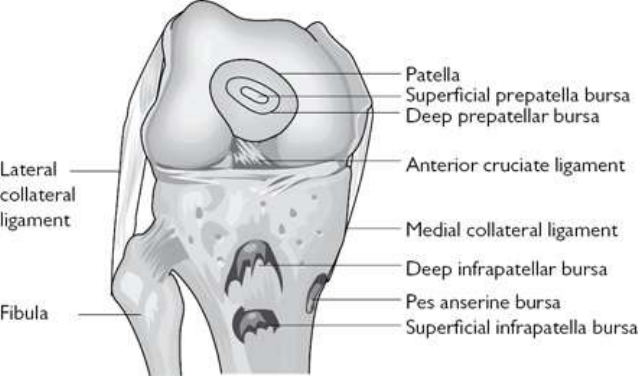
Fig.3.15Anteriorkneestructures.
• The fibular or lateral collateral ligament (LCL) joins the lateral femoral
condyletothefibularheadandisseparatedfromitbyabursa.Itstabilizesthe
kneeonitslateralside.Ithasnomeniscalattachment.Asmallbursaseparates
itfromtheoverlappingtendoninsertionofbicepsfemoris.
• Thepatellaisa seamedbonethatarticulatesinthe femoralcondylargroove
and makes quadriceps action more efficient. Patella articular facet
configuration can vary; congenital bi/tripartite patellae are associated with
anteriorkneepain.
• The strongest force on the patella is from vastus lateralis (Fig. 3.16).
Mechanical factors that increase the ratio of lateral to medial forces during
patellatrackingsuchasawidepelvis,amorelateraloriginofvastuslateralis,
femoralneckanteversion,externaltibialtorsion,andaweakvastusmedialis
areriskfactorsforpatellatrackingproblemsandanteriorkneepain.
• Therearebursaebetweenthequadricepstendonandthefemur(suprapatellar),
the patellartendon and tibial tubercle(deep infrapatellar), andoverlyingthe
patella (prepatellar) and patellar tendon insertion (superficial infrapatellar).
The suprapatellar bursa communicates with the knee joint and large joint
effusionsinvariablyfillit.
• Posteriorly, bursaeseparateeach ofthe headsofgastrocnemius (whicharise
fromfemoralcondyles)fromthejointcapsule.Thebursaecommunicatewith
thekneejointandcanfillfromjointeffusions.
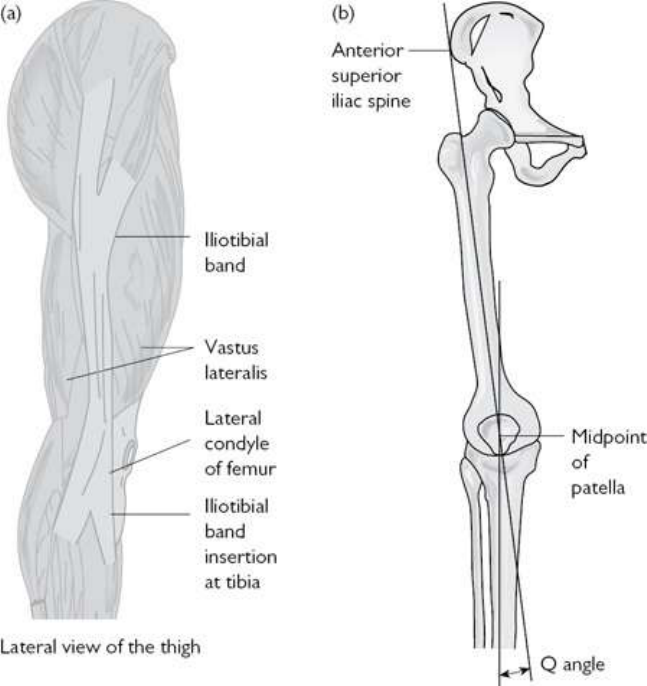
Fig.3.16(a)Theiliotibialband.(b)ThepatellaQangle(normalvalues—men10°,women15°).
Takingahistoryofkneepain:adults
Askaboutthesiteofpain
Try to establish whether pain is from articular, soft tissue, or anterior knee
structures.Isitreferredpain?
• Bursa,tendon,andmostligamentlesionscausewell-localizedpain.
• Localizedtibiofemoraljointlinepainsuggestsmeniscalpathology.
• Localized medial knee pain has a number of possible causes: MCL tear or
chronic inflammation (calcification of MCL origin termed the Pellegrini–
Stiedaphenomenon),medialmeniscustear,meniscalcyst,anserinetendonitis,
bursitis,orenthesitis(semimembranosusinsertion).
• Enthesitis of structures at their insertion to the patella margins can result in
considerablepain.
• Overuseinrunnersandcyclistscancauselocalizedinflammationandpainof
the iliotibial band (ITB) or its underlying bursa over the lateral femoral
condyle(asthebandmovesacrosstheboneasthekneeflexes).
• Anterior pain in adults invariably suggests an underlying mechanical
abnormality. In older adults, the most common cause is patellofemoral OA
(Table3.22).
• AnteriorkneepainmaybereferredfromthehiporL3nerveroot.Hippainis
anachingpain;nerverootpainissharpoftenwithparaesthesia.
• Posterior kneepainassociated with‘alump’isoften due tosynovitis in the
posteriorkneecompartmentwithpoplitealcystformation(Baker’scyst).
Table3.22Causesofanteriorkneepaininadults
Common(non-
inflammatory)
PatellofemoralOA(lookformechanicalfactorsand
generalizedOA)
Referredhippain,e.g.hipOA
Referredpainfromlumbarspine,lateralpelvis,ITB,
orgreatertrochanterlesions
Tear/cystofanteriormeniscalhorn
Patellarligamentfat-padsyndrome
Common
(inflammatory)
Patellaligamententhesitis(enteropathicSpA,PsA,or
axSpA)
Crystal-inducedMSKinflammation
Synovitisofanteriorjointcompartment(e.g.RA,
PsA)
Uncommon(non-
inflammatory)
Osteochondritisatpatellarlowerpole—overuseinjury
injumpingsports
*
Patellarfracture
Enthesopathyatpatellarmargins(maybepartof
DISH)
Uncommon
(inflammatory)
Bursitis(prepatellar,superficial/deepinfrapatellar)
Sepsisofjointoranteriorjointstructures
*
Sinding–Larsen–Johanssondisease.
Askaboutinjury
Kneeinjuriesarecommon;themostsignificantisanteriorcruciateinjury.Ask
aboutinjuryandifthekneefeelsunstableor‘givesway’:
• Anteriorcruciateinjuriesareinvariablyassociatedwithahaemarthrosis,thusa
painful effusion will have occurred immediately. Meniscus tears can cause
immediatepain,butsynovitisandswellingaredelayedforabout6hours.
• Patients mayvolunteerthat the knee‘keepsgiving out onme’.This feeling
may be the pivot shift phenomenon caused by reduced anterior cruciate
stabilityagainstavalgusstressasthekneeisflexing.
• AnteriorcruciateandMCLinjuriesoftencoexist(sincetheyareattached).Ask
aboutmedialkneepainoriginallyandsubsequently.
Askaboutkneelocking
Knee locking is a mechanical effect of disruption of normal articulation by
‘loosebodies’:
• Suspectmeniscusdamageinthemiddleagedorifthepatientplayssports.A
meniscustearisthemostcommoncauseofthekneelocking.Inadolescents,
locking may be due to a tear in a discoid meniscus (>98% lateral).
Morphologicallyabnormaldiscsarepronetodegeneration.
• Synovialchondromatosisisararecause.
• Somepatientswithanteriorkneepaindescribethekneelockingorgivingway.
Thisisduetoreflexquadricepsinhibitionratherthantrueinstability.
Askabouttheinitialonsetofpain
• Acutepainisusualwithinjuriesofcruciatesandverticalmeniscaltears.
• Acuteonsetpainwithouttrauma(butalwayswithswelling)suggestsinfection,
crystalarthritis,orspontaneoushaemarthrosis.
• Intheveryelderly,traumaticlesionsmaybemissed,sincethepresentationis
notalwaysstriking,e.g.intra-articularfracturewithhaemarthrosis.
• An insidious onset of pain is usual in cleavage tears of menisci (horizontal
tears), which occur typically in adults where the disc is degenerate, in
adolescentswithdiscoidmenisci,andinearlyosteochondritisdissecans.
Askaboutthepatternandtypeofpain
• Painfromsynovitisisoftenassociatedwithstiffnessandisoftenworseaftera
periodofimmobility.Almostwithoutexceptionkneesynovitiscanoccurinall
formsofarthritis.
• Painfromsubchondraldamage(e.g.OA)isalmostalwaysworseonweight-
bearing,butthisassociationisnotspecific.
• Painonkneeling/squattingischaracteristicofanteriorkneepain.
• Burningpainmaybeneurogenic,e.g.L3nerverootorosteodystrophypainor

iffocalmaybeenthesitic.
Pastmedical,family,occupational,andleisurehistory
• Knee synovitis and patellar enthesitis occur in all forms of SpA. Ask about
previous uveitis, low back pain, urethral discharge, sexually transmitted
disease,IBD-typesymptoms,andpsoriasis.
• Gout(see Chapter7)isnotuncommonaroundtheknee.Askaboutgoutrisk
factorsandwhetherthepatienthaseverhadacutefirstMTPJpain.
• There may be a family history of OA, an hereditary disease of connective
tissue,orhypermobilityinyoungadultswithOA.
• Prepatellar bursitis classically occurred in housemaids, hence the nickname
‘housemaid’sknee’.Frictioncausedbyrepeatedkneelingcancauseit.
• Sportsinjuriesarecommon.Anteriorcruciateinjuryoccurscharacteristically
inskiing.Meniscalinjuriesarecommoninsoccer.Jumpingevents(e.g.high
jump,basketball)canleadtopatellartendonapophysitis.Cyclingisassociated
withanteriorkneepain.MCLandmeniscalinjuriesarecommoninskiingand
weight-bearingactivitieswhererotationandchangeofdirectionarefrequent.
CyclingandrunningareassociatedwithITB/bursapainandinflammation.
Examinationofanadultwithkneepain
Fromfrontandbehind,observethepatientstanding
• Lookformechanicalabnormalitiesthatmightbeassociatedwithkneelesions:
patellaasymmetry,prominenttibialtuberclesfrompreviousOsgood–Schlatter
disease(anteriorkneepain),flat feet,andhypermobility(patelladislocation,
hyperextensionof>10°).
• Checkformechanicalabnormalitieswhichmightsuggestspecificpathology:
genu varum (bowed leg, typical appearance with primarily medial
compartment OA), obvious suprapatellarkneeswelling(synovitis), psoriasis
(associatedsynovitisorenthesitis),andgenuvalgum(knock-kneed).
Examinationofthesittingpatient
Ask the patienttositon the examination table with legs hanging, kneesbent.
Patellar tracking and pain from medial meniscus damage can be assessed. An
alternative approach is with the patient supine. Observe any muscle wasting.
Palpateanterior,medial,andlateralstructures:
• Inpatientswithanteriorkneepain,lookforsymmetricpatellaralignment.
• Observe active knee extension. Patellar movement should be smooth, pain
free,andsymmetric.
• Passivelyexternallyrotateeachlowerlegtoitsextreme.Thisisareasonably
sensitive test for conditions of the medial knee compartment (e.g. meniscus
tear)andmedialkneestructures.Discomfortwillbefelt.IftheMCListotally
deficient,anabnormallyincreasedrangeofexternalrotationmayoccur.
• Quadricepswasting(accentuateddepressioninmusclejustabovethepatella)
occurswithdisuseafterinjuriesandchronicarthritis.
• Sitesofbursae,patellartendon,andligamentinsertionsshouldbepalpatedin
patientswithlocalizedpain(Fig.3.17).
• Tibiofemoral joint line tenderness is likely to be due to either meniscus
pathologyormarginalosteophytes.Osteophytesgivebonyswelling.
• Anterior pain from patellofemoral joint disorders may be elicited by gentle
pressure down on the patella. Mobilizing the patella sideways will give an
impressionoftissuelaxity(possibleunderlyinghypermobility).
• Factors that predispose to patellofemoral pain syndrome include: high or
lateral patella, weak vastus medialis, excessive pronation, weak ankle
dorsiflexors,tighthamstrings,reducedmovementattheankle,andawideQ-
angle.TheQ-angleisformedbetweenalinefrom theanteriorsuperioriliac
spinetothecentreofthepatella,andalineextendedupwardsfromthetibial
tuberclethroughthecentreofthepatella.Thelargertheanglethegreaterthe
lateraltensilepullonthepatella(Fig.3.17).
• Localized tenderness of the femoral condyle is often the only sign of
osteochondritis dissecans in adolescents. The most common site is on the
insideofthemedialfemoralcondyle(75%).
Examineforjointsynovitis(synovialinflammationgivingsynovialthickening
and/ortenderness)andaneffusion
• The joint may be warm. Chronic synovitis doesn’t always result in a warm
joint,butinfection,acutecrystalarthritis,andhaemarthrosisusuallydo.
• Gross synovitis can produce obvious effusions and/or synovial thickening
mosteasilyfeltaroundthepatellaredges.
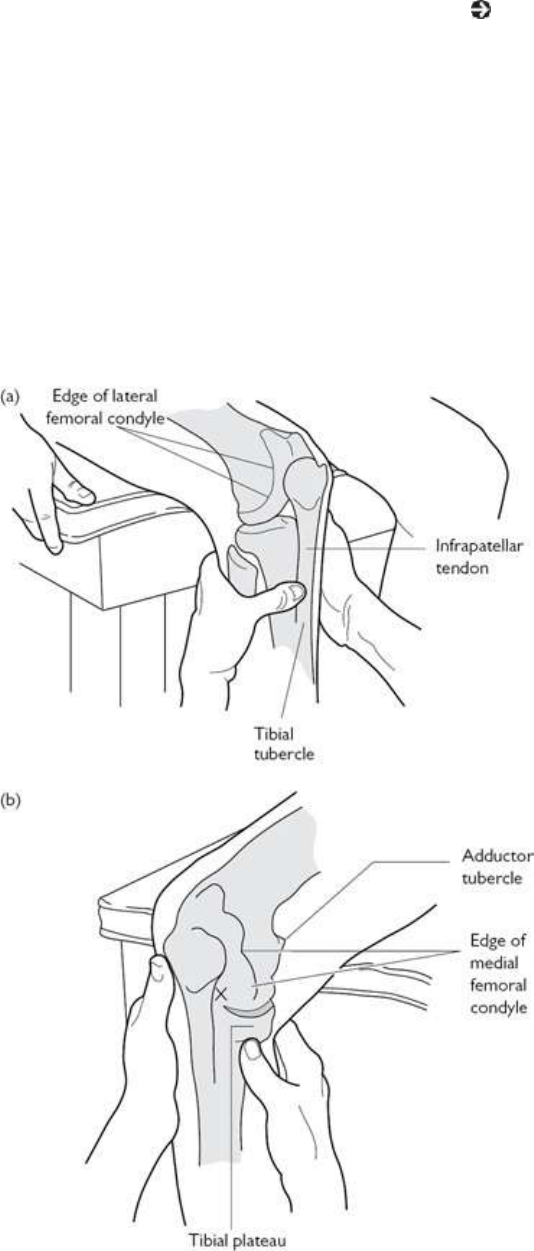
• Effusionsmaybeconfirmedbythepatellartaptest(see Plate18).
• Small effusions can be detected by eliciting the ‘bulge sign’. Fluid in the
medialcompartmentissweptfirmlyupwardandlaterallyintothesuprapatellar
pouch.Firmpressureonthelateralsideofthejointmaythenpushfluidback
intothemedialcompartment,producingabulge.
• Thickenedsynoviumcanbedetectedbyexperiencedexaminersintheabsence
ofadetectableeffusion.Itisnotalwaystender.
• Posteriorcompartmentsynovialthickeningandpoplitealcystscanbefeltby
wrappingthefingersaroundunderthekneewhenitisslightlyflexed.
• Incontrasttoadults,poplitealcystsinchildrenarenotusuallyassociatedwith
intra-articularpathology.Investigationisnotalwaysnecessary.
Fig.3.17Positionofthekneeforpalpationofmostofitsstructures.Palpatingforenthesitisatthepatellar
tendoninsertion.(a)Palpationovertheinsertionofsemimembranosusandpesanserinusunderthetibial
plateau(b)Thesiteofthemajorityofosteochondritislesionsinthekneeisshownbythe‘X’.
Testthekneeforstability
Therearemanytestsforinstability:instabilitymaybestraightorrotationaland
canbegradedaccordingtoconsensuscriteria(consultorthopaedicstexts).
• TheLachmanntest(Fig.3.18)isarguablythemostsensitivetestforeliciting
anterior cruciate disruption: hold the knee flexed between 20–30°, grasped
aboveandbelowthejoint.Attempttomovethetibiaforwardsandbackwards
onthefemur.Askaboutpainandfeelforlaxityora‘clunk’.
• Theanteriordrawtestisnot assensitive astheLachmanntestfordetecting
partial anterior cruciate tears, but is easier to do. The patient lies flat, hip
flexed,thekneeflexedat90°,withthefootflatonthetable.Fixthefootby
gentlysittingonitandpullthetopofthelowerlegforwardsinthelineofthe
thigh.Askaboutpainandfeelforlaxity.
• Theposteriordrawtestidentifiesposteriorcruciatedisruption:withtheknee
flexedto90°,pressthetopofthelowerlegbackwardsinthelineofthethigh,
askaboutpainandfeelforlaxity.
• Test medial stability at 0° and 30° of flexion (MCL stabilizes maximally at
30°) by holding the upper leg still and applying a valgus force to the tibia.
Laxity associated with widening of the tibiofemoral joint (with or without
pain)isapositivetestandsuggestsMCLdeficiency.
• Lateral(LCLandITB)stabilityissimilarlytested,thoughusingavarusforce
onthelowerleg.
• MCL tears can accompany anterior cruciate injuries and deep lesions are
associated with simultaneous tears of the medial meniscus. Such complex
pathologycanmakespecificexaminationmanoeuversdifficulttointerpret.
Testformeniscusdamage
• McMurraytest(Fig.3.19).Flextheknee,internallyrotatethelowerleg,then
extend the joint. Repeat with the lower leg externally rotated. The fingers
(overthejointline)mayfeela‘clunk’asafemoralcondylepassesoveratorn
meniscus. It isoftenpositive(21–65% of cases)whensurgery subsequently
revealsnotear.
• Askthepatienttoturnover.Whenprone,lookandpalpateforswellinginthe
poplitealfossaandproximalcalfthatmayindicatealowlyingpoplitealcyst.
• Inflammation ofthe bursaunderlying theITB mayresultintendernessover
thelateralfemoralcondyle.TheITBmaybetight.Thisisdemonstratedusing
theObertest.Withthepatientlyingontheirsideandaffectedleguppermost,
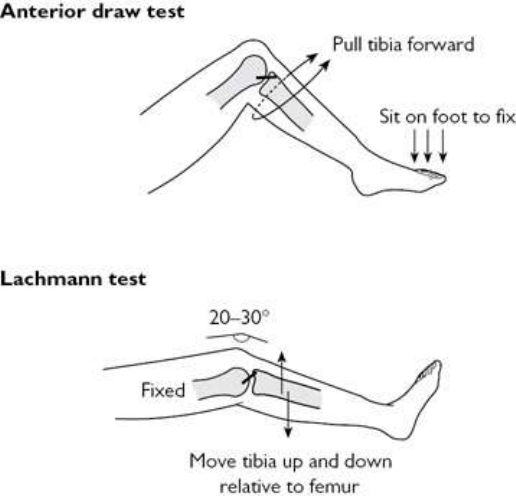
the leg is abducted and knee flexed to 90°. Holding the hip joint in neutral
withslightextensionandexternalrotation,thelegisreleased.Failureofthe
knee to adduct/fall is a positive test—leg length inequality and foot over-
pronationmaybecausativefactors.
• Detectingspecificstructuresintheposteriorfossaisoftendifficultbecauseof
the lack of bony landmarks and overlapping soft tissue structures. Synovial
cysts may form under pressure and are often hard and tender. Diffuse
thickeningsuggestsjointsynovitis.
RelevantproximalMSKexamination
As always examine the immediate proximal structures at the end of the
examinationsequence—hereexaminethehipandgait.
• Gaitexamination—considerthelowerlimbasfunctionallyinter-relatedfrom
lowerspinetotoes.
• Hip examination can help determine ante/retroversion at the hip—and the
configurationofsuchcanhaveabearingonlowerlegpronation,in-toeingand
painsatbothkneeandinfeet(seeFig.3.20).
Fig.3.18Dynamictestsofanteriorcruciatefunction.Patientsshouldberelaxedlyingsupineonacouch.
Excessivelaxityisthemostimportantsign.
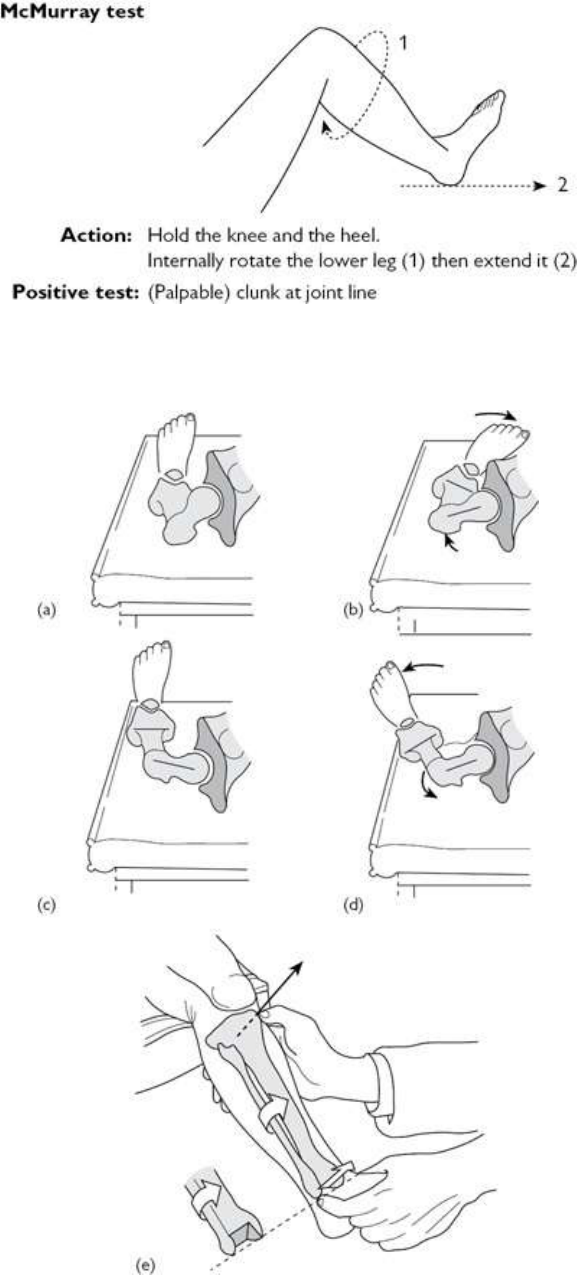
Fig.3.19Dynamictestdesignedtoelicitsignsofmeniscusdamage.‘Clunks’,intra-articularpain,and
coarsecrepitusmayindicatedamage.Thetestisnotspecificandisopentomisinterpretation.
Fig.3.20Femoralanteversion,retroversion,andtibialtorsion.(a)Wherethefemoralneckangulates
excessivelyforwardrelativetoanimaginaryaxisthroughthefemoralcondyles,thehipisanteverted.(b)
Femoralneckanteversioncanleadtoagreaterthanusualrangeofhipinternalrotationandatoe-ingait.(c)
and(d)Retroversion,wherethefemoralneckangulatesposteriorlyrelativetoafemoralcondyleaxis,can
causeatoe-outgait.(e)In-toeingcanalsobecausedbyexcessivemedialtibialtorsion.Normallytheankle
mortisefaces15°externallyrelativetoasagittalplaneaxisthroughthetibialtubercle(arrow)butinmedial
torsionitfacesforwardorinternally.
Investigationsofadultswithkneepain
Radiographs
AP and lateral weight-bearing radiographs are suitable screening views if the
diagnosisisunclearafterclinicalassessment:
• Early synovitis may only be evident from the presence of an effusion,
periarticular osteopenia, or soft tissue swelling. Patterns of bone damage in
chronicarthropathiesmayberecognized.
• Signsofjointinfection,whichmaynotnecessarilypresentacutely,arepatchy
boneosteolysisandirregularlossofbonecortex.
• Osteonecrosisisuncommoninthekneealthoughitisseeninfemoralcondylar
bone,oftenwithoutsymptoms,insicklecellanaemia.
• Loss of joint space, angulation deformity, osteophytes, subchondral bone
sclerosis,andbonecystsarehallmarkfeaturesofOA.
• Linear or vague intra-articular calcification suggests chondrocalcinosis
(associatedwithcalciumpyrophosphatedihydrate(CPPD)arthritis).
• Gross‘thumbprint’calcificationistypicalofsynovialchondromatosis.
Specializedradiographicviews:tomographicviews;‘skyline’(axialwithknee
bent)view;orlateralviewtakenwithatleast30°offlexion
• Tomographyisusefulforclarifyingnon-peripheralosteochondraldefects.
• Skyline views demonstrate anomalous patellar facet configuration and can
reveal patellofemoral incongruity though multiple views may be needed.
Subchondralpatellarpathologyisseenmoreclearlythanonlateralviews.
• Patellaaltaismostreliablyseenonalateralviewwith30°flexion.
Furtherimaging
Further imaging depends on differential diagnosis and a discussion with your
radiologist:
• PeriarticularsofttissuelesionscanbecharacterizedwithMRI,althoughwith
superficiallesionsadequateinformationneededforfurthermanagementmay
beobtainablewithUSalone.
• Patterns of meniscus damage are recognized on MRI, give an indication of
prognosis,andaidthesurgeon’sdecisiontoproceedtoarthroscopy.

• MRIisessentialifthereislikelytobeacombinationoflesions,e.g.anterior
cruciate,MCL,andmedialmeniscuslesions.
• Inanteriorkneecompartmentsymptomsalone,USisareasonablefirstoption
forimagingbecauseinflammatorylesionscanbeinjectedwithglucocorticoid
ifneededusingimagingguidance.
• MRIismoresensitivethanradiographsorUSatidentifyingjointerosionsin
RA(‘pre-erosions’).
• The place of CT or MRI in investigating radiographically detected bone
tumoursdependsonthenatureofthelesion.
Aspirationofjointandperiarticularfluidcollections
• Earlyaspirationisessentialifinfectionissuspected(see Plate19).
• Thekneeisacommonsiteofmonoarthritisformsofsystemicdiseases(e.g.
PsA,CPPDdisease).
• Sendjointfluidforcellcount,polarizedlightmicroscopy,andculture.
• Inadults,theusualdifferentialdiagnosisofsepsisofkneestructuresisgout,
sofluidshouldbeexaminedbypolarizedlightmicroscopyforuratecrystals.
• Blood-stainedfluideithersuggestsatraumatictaporchondrocalcinosis.Frank
blood suggests haemarthrosis, the major causes of which are cruciate tear,
bleedingdiathesis,intra-articularfracture,andPVNS.
• Bursa fluid may be more successfully detected and aspirated using US
guidance.
Laboratoryinvestigations
Theseshouldbedirectedtowardssuspectedunderlyingdisease:
• FBC,acute-phasemeasures(ESR,CRP).
• Bloodurea,electrolytes,creatinine,andurate.
• Bloodcalcium,phosphate,albumin,alkalinephosphatase,25-OHvitaminD,
andPTHtoscreenformetabolicbonedisease.
• Autoantibodies: rheumatoid factor (RF), ACPA, antinuclear (ANA), and
extractablenuclearantibodies(ENAs)tocharacterizeanautoimmuneprocess
wheresynovitisischronic.
• Serumangiotensinconvertingenzyme(ACE)forsarcoidosis.
• IgM Borrelia burgdorferi serology for acute arthropathy in Lyme disease,
streptococcal antibodies for reactive streptococcal arthritis and parvovirus
serology.
Treatmentofadultswithkneepainconditions
• Ingeneral,mostsofttissuelesionswillsettlewithrestandNSAIDs.
• Anterior knee pain may respond well to isometric exercises, adjustments to

foot alignment, e.g. with sensible shoes, orthotics (support insoles), and
hamstringstretchingexercises.
• The acute swollen knee requires aspiration, rest for 24 hours and gentle
mobilization.
• If infection is considered, broad-spectrum antibiotics against staphylococcal
andstreptococcalagentsshouldbestartedimmediatelywhileawaitingculture
data. In infection, intra-articular antibiotics and steroids should be avoided.
Thepatientshouldnotbearweightonanacutelyinfectedjoint(see Chapter
17).
• Acute and chronic inflammation can leadtojointdestruction and instability
thisisrelevantforRA—earlytreatmentmaypreventlong-termmorbidity.
• Physicaltherapyandsplintingplayanimportantroleinmaintainingfunction
andpreventingcontractures,etc.
Addressbiomechanicalfactors
Input from aphysicaltherapistmay be helpful in cases of anterior kneepain.
SuccessfromMcConnell(patellar)tapingismorelikelyinnon-patellofemoral
OA-relatedanteriorkneepain.
• Quadriceps strengthening exercises can be reviewed and reinforced by
physicaltherapistsincasesofkneeOA.
• Kneepain,particularlyanteriorpain,maybelinkedtofootabnormalities(e.g.
over-pronation),andhipalignment(Q-angle,above).
• Specificmusclestrengtheningexercises,footorthotics,andkneebracesshould
beconsidered.
Localsteroidinjection
Chapter24hasmoredetailonlocalsteroidinjections.
Localsteroidinjectionscanbehelpfulinthefollowingsituations:
• Acuteflareofnon-infectiveinflammatorydisease:
• OA(especiallywhenininflammatoryphase)—mildOAmayalsorespondto
hyaluronaninjections.
• autoimmunearthritis,e.g.RA.
• intra-articulargoutorCPPD/pseudogout.
• SpAormorelikelyPsAeffusion/monoarthritis.
• Bursitis(maybegout):
• pre-andinfrapatella(superficialanddeep)bursa(thelattermayrequireUS
guidance).
• anserine.
• Baker’s cyst (note: the knee joint is injected at the site of the pathology
assumingthereisintra-articularcommunicationbetweenjointandcyst.Direct
poplitealcystinjectionshouldbeunderUSguidanceonlytoavoiddamageto
vascularandnervetissues).
• Enthesitis,e.g.semimembranosusinsertion.
• Trauma,e.g.painoverMCLinsertion.
• Othersofttissue:ITBsyndrome.
• In patients with large joint effusions, merely aspirating the effusion may
provide some level of symptomatic relief—this procedure may need to be
done alone initially without steroid injection pending results from fluid
microscopyandculture.
• Knee OA may respond transiently to an injectable steroid, such as
methylprednisolone. Saline irrigation and injections with hyaluronan
preparationsarealsoused,butresponseisvariable.
• Note: all intra-articular injection therapies are more effectivewhenpatient’s
kneeisimmobilizedfor24hoursfollowingtheprocedure.
Drugs
• NSAIDs will invariably be helpful in cases of inflammatory and septic
arthritis.
• Colchicine 0.5 mg two to three times daily for 5 days is often useful in
relievingpainfromcrystalarthritisinpatientsintolerantofNSAIDs.
• Paracetamol/acetaminophenmaybeaseffectiveasNSAIDsforsomepatients.
• TheeffectofglucosamineandchondroitinforOAisdebated.Althoughsome
studiesdemonstrateimprovedpaincontrolandfunction,otherstudiesindicate
thatthesearenobetterthanplacebo.
Surgery
• Arthroscopy is often used as a diagnostic tool in cases of undiagnosed
monoarthritisandtoconfirmandtrimcartilagetears.Synoviumandsynovial
lesions (e.g. PVNS, synovial chondromatosis) can be biopsied or excised
(synovectomy)andthejointcanbeirrigated.
• Inappropriatecases,jointreplacementcanberemarkablysuccessfulandisan
importantoptiontoconsiderinOAandinflammatoryarthritis,wherepainis
severeandpresentatrest,andwhenmobilityissubstantiallyrestricted.
• Unicondylar osteotomycanaidrealignment of thetibiofemoral joint, e.g.in
metabolicbonedisease,suchasPaget’sdisease.
Other
• InOA,capsaicincreamappliedthreeorfourtimesdailytopainfulsuperficial
structures,e.g.patellarmarginsormarginal tibiofemoraljointpain,canease
symptoms.Responseiscumulativeandmaynotoccurfor6–8weeks.
• Yttrium-90radiationsynovectomyhasalonghistoryofuseforisolatedknee
synovitisoccurringasaresultofanumberofconditions.Y-90injectioncanbe
arrangedtofollowarthroscopicsynovectomyaimingtomaximizetheeffectof
bothprocedures.
• Topicallidocainepatchesmayalsobeusefulforcontrolofpainlimitedtoone
joint.
Kneepainandlowerlimbdevelopmentin
childrenandadolescents
Generalconsiderations
Inyoungerchildren,especially,knee,foot,andankleproblemsneedassessment
in light of developmental stage and with reference to any developmental
abnormalities.
History
• Growingpainsarecommonandoccurtypicallyinchildren<6years.Thereis
a nighttime predominance, hence the term ‘benign nocturnal pain of
childhood’.Kneeisoftenidentifiedasakeysitebutalsothigh,shins,andfeet.
• Osteochondrosesofkneestructuresarecommoninthegrowingskeleton(see
Table16.11).
• Osteochondritis can affect the articular cartilage (e.g. medial/proximal tibia
(Blount’s))oranenthesisoranepiphysealplate.
• The osteochondritis lesion becomes more severe if the cartilage becomes
separatedasafragment(‘dissecans’lesion).
• Cause of osteochondritis at an enthesis is assumed to be traction-trauma in
aetiologythoughthenumberofchildrenwiththeselesions,whomighthave
ERA,PsA,orJSpAisnotknown.
• Anteriorkneepainatallagesisrelativelycommon(theterm‘chondromalacia
patella’isasurgicalfindingwhichmayormaynotbeassociatedwithpain).
• The commonest cause of anterior knee pain in adolescents—termed
patellofemoral syndrome (PFS)—is attributable to abnormal loading of the
patellofemoral joint and patella mal-tracking. There is often underlying
biomechanical imbalance including muscle tightness and vastus medialis
obliqus(VMO)weakness.
• Anterior kneepain can besecondary topatellainstability. Thisis avariable
lesion which ranges from mild dynamic imbalance with lateral patellar

compressiontorecurrentpatelladislocationandchronicdislocation.
• Othercausesofanteriorkneepaininactivechildrenincludespatellaligament
originorinsertionalenthesitis(inERA,JSpAorJPsA),localbursitisorfatpad
syndrome.
• Impingement of the infrapatellar fat pad—which is richly innervated—
between patella and femoral condyle is amplified by mal-tracking of the
patella,kneeextension,prolongedstandingandkneeling.
• Thekneeisacommonpresentingsiteforinflammatorydiseaseparticularlyin
IBD-relatedarthritisandJPsA.
• A swollen knee can be a presenting sign of JIA, PVNS, tuberculous/septic
arthritis,andhaemarthrosis(trauma).
• Painisthemainpresentingfeaturesoftumours,whichcanoccuraroundthe
knee (e.g. osteoid osteoma, chondroblastoma, Ewing sarcoma, leukaemia,
neuroblastoma).
• Mechanical symptoms on movement (catching, knee giving way, painful
clunks, etc.) may occur with patellofemoral instability or with an internal
structurallesion—suchascruciateligamentdeficiencyorsynovialplica.
• Synovial plicae are embryonic remnants, with a septated structure, which
becometenderandinflamedwhentrappedbetweenpatellaandmedialfemoral
condyle. Snapping and catching during flexion differentiate it from other
biomechanicallesions.
• Finallyaskabouthip/groinpainsgivenreferredpainfromthehipjointmaybe
presentandcandenotePerthesdiseaseorSUFE.
Examination
A general overview of relative MSK stiffness, hypermobility, functional
movementability,andmuscletoneishelpfulbeforearegionalexaminationtakes
place.
• Functionalbiomechanicsareassessedbyevaluationofgait,andmanoeuvres
such asjumping,hopping, and squatting. This isfollowedby assessment of
musclegroupstrengthandstretch.
• Assessforthe‘J’signofpatellartracking.Thisismedialshiftofthepatellain
earlyflexion asit entersthe trochlea,suggestive ofVMO weaknessor tight
lateralpatellaretinaculum.
• Fixed loss of extension or loss of full flexion is indicative of intraarticular
pathology.
• Ajointeffusionisshownbysweep(orbulge)sign(seeearlier).
• Othertestsincludepatellarcompression(Clarketest),Lachmantest;anterior
and posterior draw tests; McMurray and Trendelenburg tests—see ‘Knee
paininadults’,pp.170–183.
Lowerlimbdevelopmentalfactorsandvariations
Developmentalfactors
• Developmentalcharacteristicsoftenimplythatdifferentagegroupsareprone
toadifferentspectrumofconditions.
• Duetoligamentouslaxity,whenbabiesbegintowalk,themidfootisflattothe
floor.Alongitudinalarchusuallydevelopsby5years.
• During growth, tendon insertions (apophyses) are often weaker than the
tendons themselves. Traction strain on tendons can lead to apophysitis
(osteochondritis).Thisisacommonpatternofinjuryinthefootinactiveolder
children.
Femoralanteversion
• Thiscausesinternalfemoraltorsionleadingtoamediallyrotatedpatellaand
in-toeing.
• SeeFig.3.20.
• Femoral anteversion is present at birth in 40% but decreases with age and
disappearsby10yearsofage.
• Mildpersistencewithin-toeingdoesnotusuallyresultinfunctionaldisability.
• Itmaypersistwithpatternsofsittingsuchasthe‘W’position.Sittingcrossed
leggedmayencourageexternalrotationatthehipsinstead.
Internaltibialtorsion
• Thisresultsinin-toeingandisnormalintoddlers,resolvingat2–4years.
• SeeFig.3.20.
• Thigh-foot axis angle of more than about −10° confirms the diagnosis,
althoughtreatmentisonlyconsideredwhengreaterthan−45°.
• Bycontrast,externaltibialtorsionisacommoncauseofanout-toegaitand
mayleadtoPFS.
• Osteotomy may be recommended for a thigh-foot axis angle of more than
+40°.
Genuvarum(bowlegs)
• Bow legs are normal in toddlers and normal beyond 4 years if mild and
symmetrical.
• Bowlegsappearmorepronouncedinanoverweightchildandassociatedin-
toeingmaygiveappearanceofaclumsygait,butdoesnotrequireintervention.
• Asymmetricorexaggeratedbowing andreportsofpainrequiresafull MSK
assessmentincludingmetrology(ofintercondylardistanceandlateralthrustat
theknee)andgaitassessment.
• Radiographs may disclose Blount’s disease (osteochondritis of the medial
aspectoftheproximaltibialphysis).
• Bowingcanoccurinrickets(checkvitaminDlevels).
• A full leg AP radiograph assesses hip, knee, and ankle contribution and
measuresjoint-to-diaphysisanglestoidentifywhichphysisiscontributingto
thedeformity.
• MRI,CT,andDXAarerarelyuseful.
Genuvalgum(knockknees)
• Knock knees is physiological between 2 and 6 years of age and does not
progressafter7years.Interventionwithbracesororthosesisunwarrantedand
meddlesome.
• Adolescentidiopathicgenuvalgummaybeassociatedwithcircumductedgait,
anterior knee pain and patellofemoral instability. Often hereditary, it may
progressintoadulthoodtoprematureOAofthepatellofemoraljointandlateral
compartmentoftheknee.
• Anangleof12°ofvalgusorintermalleolardistanceof>8cmshouldprompt
orthopaedicassessmentforadolescentgenuvalgum.
• Othercausesofgenuvalgumincludelocalpathologyfromtraumaorinfection
(usually unilateral), skeletal dysplasias, neurofibromatosis and vitamin D-
resistantrickets.
• Genuvalgumisbestassessedusingafull-lengthstandingAPradiograph.The
mechanical axis or centre of gravity (drawn from the centre of the femoral
head to the centre of the ankle) should bisect the knee and lie within the
intercondylarcentralareaoftheknee.
Lowerlegandfootdisordersinadults
Anatomy
Anatomyofbonesandjoints
• The leg absorbs six times the body weight during weight-bearing. Strong
ligaments secure the ankle (formed by tibia above/medially and fibular
malleolus laterally) and talocalcaneal (subtalar) joints and bones of the
midfoot(Fig.3.21).
• Anomalousossiclesinthefootarecommon.Someareassociatedwithspecific
pathology. There are many potential sites, though the sesamoids in flexor
hallucisbrevis(FHB)areinvariable.
• The foot is an optimal mechanical device to support body weight when
walking or running over flat, inclined and uneven types of terrain. The
configuration of bones at synovial articulations allows dorsal flexion (foot
pulledup),plantarflexion(towalkontoes),inversion(foottipsin),eversion
(foot tips out) and small degrees of adduction and abduction. Midfoot
movementsallowpronationandsupination.
• Thenormalanklejointrangeisabout25°ofdorsalflexionand50°ofplantar
flexionfromneutral(foot90°toleg).Therangeofsubtalarinversion–eversion
isnormally10–15°.
Anatomyofthelongmusclesandtendons
• In the lower leg, a strong fascia connects the tibia and fibula. Lower leg
muscles primarily move the foot. They are separated into compartments by
fasciaandarepronetopressureeffects.
• The foot dorsal flexors—tibialis anterior, extensor digitorum longus (EDL),
extensor hallucis longus (EHL), and peroneus tertius—lie adjacent to the
anteromedial side of the tibia. Their tendons pass in front of the ankle in
synovial sheaths held down by strong retinaculae (Fig. 3.22). The tibialis
anterior, the bulkiest flexor, inserts into the medial midfoot (medial
cuneiform).
• Intheposteriorlowerleg,thegastrocnemius(andplantaris),whicharisefrom
thefemur,plantarflexesthefootbypullingthebackofthecalcaneum.The
soleus,whicharisesinthelowerleg,mergeswiththemintheAchillestendon.
Thistendonhasadeepandsuperficialbursaatitsinsertionsite.
• Plantarflexionisassistedweaklybylongmuscles,whichariseinthelower
leg, pass behind the medial malleolus in synovial sheaths (Fig. 3.22), and
insertintothesole.Theymostlyinvertthefoot.Tibialisposterior,thebulkiest
plantarflexor,insertsintotheplantarsurfaceofthenavicular.
• Theperoneuslongusandbrevisarisefromthefibularsideofthelegandpass
around the lateral malleolus in a common synovial sheath held by a
retinaculum.Longuspassesintothesoleandinsertsintothemedialcuneiform.
Brevisinsertsintothefifthmetatarsalbase.Bothevertthefoot.
• Thetibialnerveandarteryfollowthecourseofthemedialtendonsunderthe
flexorretinaculum(Fig.3.22).
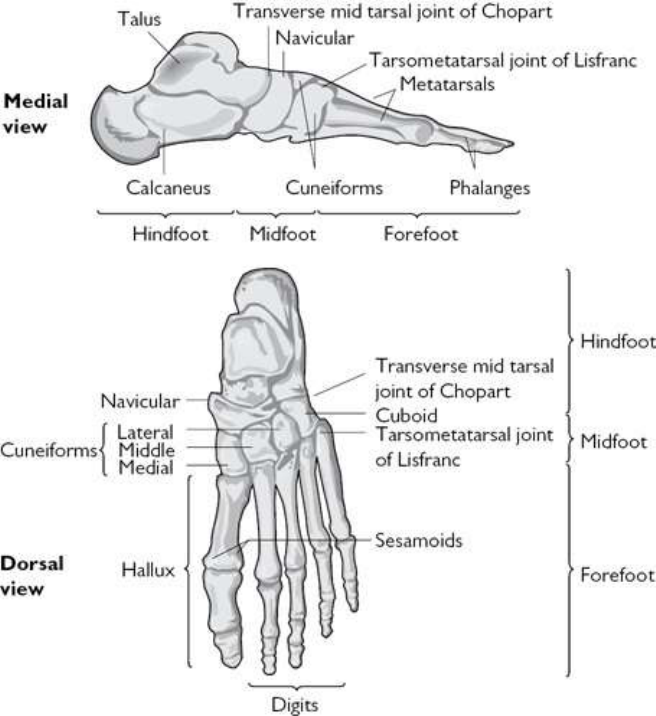
Fig.3.21Thebonesofthefoot.
Anatomyofintrinsicfootstructure
• Intrinsic foot structures have been greatly modified during evolution to
combine provision of a flexible platform for support and a rigid lever for
thrustingbodyweightforwardwhenwalking.
• Inthesoleofthefoot,musclesarealignedlongitudinallyinfourlayers.The
deepestlayersincludephalangealinterosseiintheforefeet, tibialisposterior,
peroneus longus, adductor hallucis, and FHB, which has two insertions into
theproximalgreattoephalanx,eachcontainingasesamoid.
• The superficial layers include flexor digitorum longus (FDL), which inserts
into the lateral four distal phalanges, the phalangeal lumbricals, flexor
digitorumbrevis,andabductorhallucis.Thelattertwomusclesarisefromthe
plantarsurfaceofthecalcaneumdeeptotheplantarfascia.
• Flexor tendons merge with the deeper part of the plantar fascia, a swath of
tissuethatextendsfromoscalcistothemetatarsalarea.
• Longitudinal muscles, ligaments, and fascia contribute to stabilize the foot
with a longitudinal arch—its apex at the talus, but also with some effect
laterally.Thefootarchestransversely—itsapexatmedialcuneiformlevel.
Neuroanatomy
• The sciatic nerve splits into tibial and common peroneal nerves above the
knee. The common peroneal is prone to pressure neuropathy as it runs
superficiallyaroundthefibularhead.Thenervethendivides.Adeepbranch
runsdistallywithEDLundertheextensorretinaculumtothefoot.Itsupplies
tibialis anterior, EHL and EDL. A superficial branch supplies the peroneal
musclesandmostoftheskinoverthedorsumofthefoot.
• The tibial nerve runs in the posterior lower leg compartment supplying
gastrocnemiusandsoleus.Itthenpassesunderthemedialflexorretinaculum
dividing into medial and lateral plantar nerves, which supply the intrinsic
plantarmusclesofthefootandskinofthesole.
Functionalanatomy
• Inanormalgaitpattern,thefootisdorsiflexedandinvertors/evertorsstabilize
thehindfootforheelstrike.Asweightistransferredforward,thefootplantar
flexes and pronates, the great toe extends (optimally between 65° and 75°),
andpushoffoccursthroughthemedialsideoftheforefoot.
• Allmetatarsalsbearweightandcansufferweight-bearinginjury.
• Ligamentousattachmentsaroundthehindfootarestrong.Afallonapronated
invertedfootwithoutdirecttraumacanresultinafractureofthedistalfibula.
This is probably a consequence of the relative strength of the talofibular
ligamentscomparedwithbone.
Conditionsofthelowerleg
• Patientswithlowerlegconditionspresentwithpainordeformity.
• Painsinthecalfmaybeduetolocalsofttissueormuscleconditions,andare
commonlyduetoreferredlumbosacralpain.Thesepainsareoftendescribed
by patients as ‘cramps’—suggesting a muscle problem at first. A detailed
historymaysuggestnerverootpathology.
• Imbalanceofmusclesinthefootcanleadtoincreasedtensionattendonand
fascialinsertionsinthecalfandshin,resultingin‘shinsplints’.Shinsplints
usuallypresentafteractivityandarerelievedbyrest.Conditionstoconsider
include:
• stressfracturesofthetibiaorfibula.
• tibialisposteriorfasciitis—oftenwithaflat,pronatedfoot.
• compartmentsyndrome(softtissueandvascularswelling).
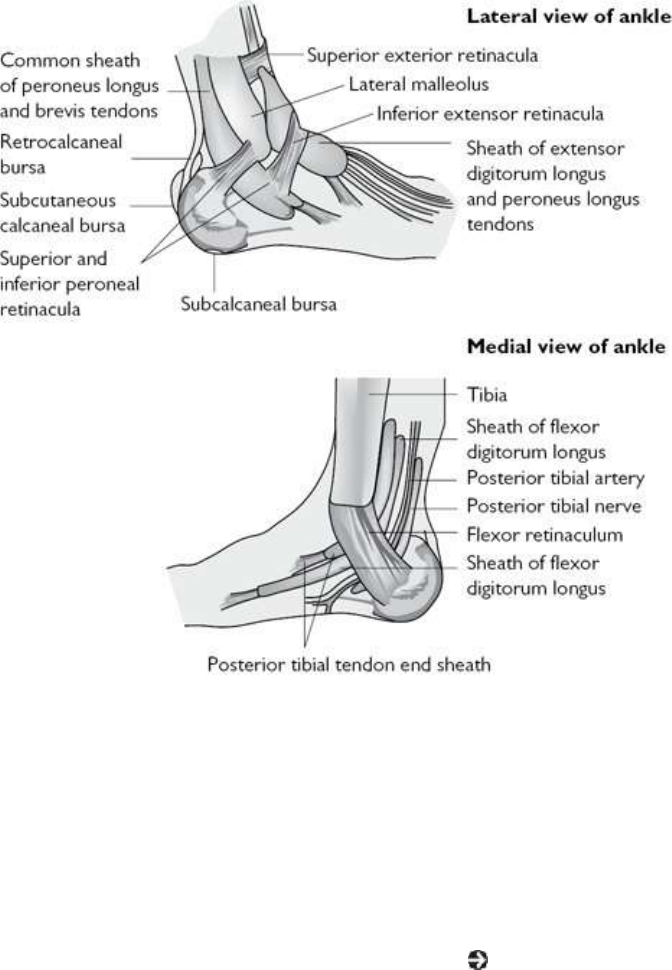
• poplitealarterystenosis.
• referrednervepain(spinalclaudication).
• peripheralvasculardisease(intermittentclaudication).
Fig.3.22Tendons,retinaculae,andbursaeofthehindfoot.
Takingahistoryfromanadultwithlowerlegorfootpain
Askaboutsiteandqualityofpaininthelowerleg
• Localizedanteriorpainoccursinbonylesionsoftheanteriortibia,e.g.stress
fractures,periostitis.
• Burning pain suggests a neurogenic cause. Diffuse burning pain may be
caused by peripheral neuropathy, CRPS (see Chapter 22), or (rarely)
erythromelalgia.
• Mostcommonlyoccurringintheelderly,bilaterallegpainwith‘heaviness’or
‘stiffness’limitingwalkingdistanceistypicalofspinalstenosis.Analternative
would be vascular claudication where often pain is more overt, and critical
ischaemiacangivenightpaineasedbyhangingthelegsoverthesideofthe

bed(gravityeffects).
• Simultaneouskneeproblemsmayberelevant.Escapeofsynovialfluidfrom
the knee into the soft tissues of the calf can present with acute pain and
swelling and be misdiagnosed as a deep vein thrombosis
(pseudothrombophlebitis).Often ahistory ofprecedingjointeffusioncanbe
elicited.
• Low-lyingsynovialcystsconnectingwiththekneecancausecalfpain(withor
withoutswelling).Thisinvariablyoccursonlywithchronicsynovitis.
Establishpossiblecausesofhindfootpain
(SeeTable3.23.)
• Establishing the cause of hindfoot pain from the history alone is difficult.
Thereareimportantclues,mainlyfrompatternsofinjuryoroveruse.
• Posterior heelpain has afew causes.Oftenclinically indistinguishablefrom
Achilles tendonitis or retrocalcaneal bursitis, enthesitis is usually associated
with axSpA (see Chapter 8). An os trigonum may become damaged
especiallyinsoccerplayersandballerinas(seelaterinsection).
• Theoriginofplantarheelpainisvaried.Mechanicalplantarfasciitisisthought
tooccurmorefrequentlyinpeoplewhoareontheirfeetforlongperiodsof
time, those who are obese, have thin heel fat pads, or poor footwear.
Symptomsofarthritisandenthesopathyelsewhere,lowbackpain(sacroiliitis),
eye inflammation (iritis), psoriasis, or previous gut or ‘urethral’ infection,
mightsuggestSpA.
• Lesscommoncausesofplantarheelpainincludefracturethroughacalcaneal
spur and lateral plantar nerve entrapment between the fascia of abductor
hallucis and quadratus plantae muscles (causing pain/paraesthesias on the
lateralsideofthesole).
• In the elderly and postmenopausal women, calcaneal stress fractures are a
recognizedfeatureofosteoporosisandcanpresentwithheelpain.
• Ankle and talocalcaneal synovitis, OA, ankle osteochondritis dissecans, and
tendonitisaroundthehindfootmaybedifficulttodistinguishfromthehistory
alone.SynovitisoraneffusionoftenaccompaniesOAofthesejoints.
EstablishpossiblecausesofmidfootandfirstMTPJpain
• Gout (see Chapter 6), OA (see Chapter 6), enthesitis, and referred L5
nerverootpainarethemostlikelydiagnosesofmidfootandfirstMTPJpain.
• Gout should alwaysbe considered a possiblecause of painfullesionsin the
footinpeopleatrisk.Goutisnotalwaysintra-articular,intra-bursalorintra-
tendon. Local or diffuse soft tissue inflammation is common and often
misdiagnosedascellulitis.
• The first toe and midfoot are common sites for PsA; check radiograph for
typicalPsAperiostealnewboneformation.
• L5painisreferredtothedorsumandS1paintothesole,ofthefoot.
• InolderadultsOAofmidfootjointsiscommon.Mildsynovitiscanoccurwith
itandmaybecausedbyCPPDdisease(see Chapter7).
Table3.23Conditionscausinglocalizedfootpaininadults
Siteofpain Commonlesions
Ankle
region
Ankleortalocalcanealjoint:synovitis(e.g.gout),OA.L4/L5
rootpain
Posterior
heel
Achillestendonitis.Retrocalcanealbursitis.Achillesenthesitis.
Osteonecrosisofostrigonum
Medialside
ofheel
Asforankleregion.Calcanealfracture.Tibialisposterior
tendonitis.Plantarfasciitis
Lateralside
ofheel
Asforankleregion.Calcanealfracture.Peronealtendonitis.
Fifthmetatarsalbasefracture
*
Underneath
heel
Plantarfasciitis.Calcanealfracture.Infra-calcanealbursitis.
Lateralplantarnerveentrapment
Topoffoot Midfootjointsynovitis(e.g.gout),OA.Navicular
osteochondritis.Enthesitis.L5rootpain
Soleoffoot S1rootpain.Plantarfasciitis.Metatarsalstressfracture.
Tibial/plantarnerveentrapment
Toes MTPsynovitis(e.g.RA,gout).MTPOA.Morton’s
metatarsalgia.Bursitis.Enthesitis/dactylitis
*
Robert–Jonesfracturefromaninversion–pronationinjury.
Establishpossiblecausesofforefootpain
• In those with forefoot pain, typically referred to as metatarsalgia, establish
whethertheconditionisfocalorduetoarthropathy.
• Painundertheballofthefootwhilewalkingisnon-specificbutmightsuggest
any MTPJ abnormality, distal metatarsal stress fracture, Freiberg’s disease,
plantarnerveneuroma,orbursitis.

• Patients with RA often describe pain under the MTPJs and a feeling of
‘walkingonpebbles’(duetojointswellingand/orsubluxation).Synovitisof
theMTPjointsisacommonfeatureofearlyRA.
• Acutepainundertheforefootspreadingintooneormore(adjacent)toesand
worseonwalkingsuggestsaplantarnerveneuroma(Morton’smetatarsalgia)
orintermetatarsalbursitis.
• Pain associated with paraesthesias or numbnessundertheforefootmight be
due to S1 root irritation (common) or entrapment of the tibial nerve in the
hindfoot(rare).Askaboutbackpainandotherhindfootproblems.
• Non-traumatic toe painassociatedwith swelling of theentiretoe suggests a
dactylitis (associated with axSpA). Although many toes may be affected,
dactylitismaybeunilateralandaffectjustonetoe.
• The development of hallux valgus is associated with tight footwear. The
deformityisassociatedwithalteredweight-bearingandasecondtoe(hammer)
deformity.
• Big toe pain might be due to hallux rigidus. It is usually due to OA and
importanttorecognizeasitmaypreventtoedorsiflexionsufficientlytoleadto
acompromisedgaitpattern.
• Painspecificallyunderthehalluxmaybeduetodamagetothesesamoidsin
theflexorhallucisbrevistendonandbemisdiagnosedasajointproblem.
Askforadescriptionofthepain
• Asinthehand,neurogenicpainiscommonandtypical.
• Severe or unremitting pain when at rest suggests intrinsic bone pathology.
Considerosteonecrosis,infection,fracture,andtumours,e.g.osteoidosteoma.
• Neurogenicpainmaybesharpandwelldefined(e.g.inacuteL5orS1root
pain),deep,achy,andlesswelldefined(e.g.chronicnerverootsymptomsas
in spinal or foramenal stenosis), or burning in quality. Paraesthesias and
numbnessmayaccompanyboth.
• If swelling accompanies neurogenic pain, consider a complex regional pain
syndrome.Therearenumeroustriggers,e.g.traumaandsurgery.Patientsmay
beunwillingtowalkandapparentdisabilitymayappearprofound.
Weakness
Iftrueweaknessisthemajorproblemratherthanpain,thediagnosisisusually
between a myopathic process, but more likely is a spinal or peripheral nerve
lesion(see ‘Examination’,p.194).
Examinationofanadultwithlowerlegorfootpain
Observation
Observe the lower legs and feet from front and back, while the patient is
standing.Noteanyswelling,deformities,orrashes:
• Lowerlegdeformitiestonote:tibiavarum(orbowlegs)inanolderadultmay
be due to Paget’s disease of the tibia. Muscle wasting might suggest disuse
atrophy, old polio, or spinal stenosis (bilateral and subtle usually in older
adults).
• Oedema or soft tissue swelling may be relevant to an underlying condition
causing ankle synovitis. Although it may cause discomfort, oedema from
cardiacfailure,venouscongestion,hypoproteinaemia,orlymphoedemaisnot
painfulunlessthereareulcersorthrombophlebitis.
• Gout can cause swelling anywhere; gouty tenosynovitis can mimic the
appearanceofacellulitisintheregionofajoint.
• Calfswellingmaybeduetoveinthrombosisorrupturedpoplitealcyst.
Commonpatternsoffootdeformityare:flatfeet(pesplanus),high-archedfeet
(pescavus)withhighmedialarch,halluxvalgusandrigidus,over-ridingtoes,
hammertoes,orclawtoes.
• Skinconditionsfromvenousabnormalitiesarecommonintheelderly.Other
skin lesions which may be relevant include purpura, panniculitis—which is
oftensubtleandovertheshins—andpyodermagangrenosum.
Askthepatienttowalkinbarefeet
Gaitpatternsshouldbenoted:
• Anantalgic(‘limp/wince’)gaitisanon-specificindicatorofpain.
• A wide-based gait (>10 cm wider than normal) suggests instability: joint
instability,muscleweakness,orneurologicallesionsmaybethecause.
• A foot that slaps down or a high stepping gait suggests tibialis anterior
weakness(L4nerverootorcommonperonealnervelesion).
• Significant weakness of gluteus medius and gluteus maximus in L5 and S1
rootlesions,respectively,canresultinlurchingduringgait.Intheformer,as
weight is taken on the affected side, gluteus medius may be weak in
controlling the small 2–3 cm lateral displacement in the weight-bearing hip
thatnormallyoccurs.Thiscanbecompensatedforifthebodycentreofgravity
isbroughtoverthehipbylurchingtheupperbodyovertheaffectedside.With
gluteus maximus lesions (S1) extension of the hip, which helps mediate
motionthroughthestancephasepriortotoeing-off,maybeweak.Thrusting
thethorax forwardwithanarchedback (forwardlurch)compensatesforthe
weaknessandhelpstomaintainhipextension.
• A flat-footed gait withlittleor weak toe-offmaysuggestanS1 root lesion;
however,‘flat-foot’(lossofthemedialarch)withassociatedhindfooteversion
andheelpain(plantarfasciitis)isextremelycommon.Oftenthearchweakness
correctswhenthepatientisaskedtowalk.
Examinethelowerleg
Withthepatientsupineonthecouch,examinethelowerleg:
• Afterarupturedpopliteal(Baker’s)cyst,calftissuesareoftendiffuselytender
and swollen. Calf circumferencescanbecompared(e.g.10cmbelowtibial
tubercle). There may also be mild skin erythema. Findings are not specific.
Goutandinfectionarethemainalternativesifthereismarkedtenderness.
• Checkforbruising,swelling,andtendernessaroundthefibulaheadinpatients
withfootdrop(possibleperonealnervepalsy).Neurologicalexaminationmay
bedoneatthispoint.
• Localized anterior tibial tenderness is often found in patients with stress
fracturesorwithpseudo-fractures.
• Tibialdeformityinadultsmaybeassociatedwithdiffusebonytendernessand
heat(arteriovenousshunting)inPaget’sdisease.
Examinetheankleandhindfoot
At the ankle and hindfoot, examine for joint and tendon synovitis, palpate
specificstructuresandtestpassivehindfootjointmobility:
• Synovitis of hindfoot joints is not always easily detected. With ankle joint
synovitis, thickened tissue may be felt anteriorly in the ankle crease (where
theremaybea‘springyfullness’)orlaterallyaroundthemalleoli.
• Posteriortibialandperonealtendonitisareassociatedwithsofttissueswelling
of the medial and lateral hindfoot, respectively. Synovial thickening from
ankleandtalocalcanealjointsmayalsobefelthereandsynovitisofstructures
maycoexistinRAorSpA.Painfromresistedmovementoftendonsmaynot
bespecific.
• Pathology of medial hindfoot structures may be associated with tibial nerve
entrapmentresultinginsensorysymptomsonthesoleofthefoot.Theremay
beapositiveTinel’ssign.
• Posterior heel pain may be due to Achilles tendonitis, enthesitis and
mechanicaldamagetothetendon,andretrocalcanealbursitis.Deeptenderness
maysuggestanostrigonumlesion.
• Thelossofpassivehindfootmovementsisnotspecificandcanbeassociated
withanycauseofankleorsubtalararthritis(20–30°ofdorsiflexionand45–
55°ofplantarflexionisaveragefortheankleanda10–20°inversion–eversion
range is average for the subtalar joint). Subtalar joint movement can be

difficulttotestaccurately.
• Thepainofplantarfasciitismay beelicitedbyfirmpalpationofthe medial
underside of the calcaneum. A negative test does not rule out pathology, as
oftenthehistoryismoresensitive.FullMSKexaminationisrequiredtocheck
forfeaturesofSpA,suchasarthritis/enthesitiselsewhereandsacroiliitis.
Examineformidfootlesions
Identifying specific midfoot lesions is difficult, though bony landmarks and
discretetenderareascanbenoted:
• Twisting the midfoot may elicit pain but locating the source in the midfoot
may be difficult. Common lesions include PsA, OA, gout, and enthesitis or
synovitisfromSpAorRArespectively.
• Bonytendernessalonewithoutsofttissueswellingdoesnotruleoutsynovitis
ofanadjacentjoint.
• Themidfootisatypicalsiteforneuroarthropathyindiabetes.
• Bonyexostosesthatmayhaveformedatsitesofpressurearecommoninthe
foot(e.g.medialordorsalaspectofthefirstMTPJ,baseorheadofthefifth
metatarsal,distaltalus,oroverthemidfoot).
• Bothgoutandinfectionresultinswelling,skinerythemaandlocaltenderness.
Gout of the first MTPJ occurs at any one time in 70% of patients with the
condition.Itcanoccuranywhereinthefoot.
Examinetheforefoot
Checkforbonyorotherswelling,digitseparation,andexaminethesoleofthe
foot.SqueezingthewholeforefootatthelineoftheMTPJsisanon-specific,but
usefulscreeningtestforpainfulforefootlesions:
• Tenderswellingofthewholetoe(dactylitis)occursinSpA,sarcoidosis(see
Chapter8),andHIVinfection.Swellingissoftnotbony.Tenderbonyswelling
suggestsabunionandiscommononthedorsalaspectofthetoesandthefirst
andfifthMTPJs.
• Forefoot splaying and interdigital separation suggests MTP synovitis or
interdigital bursitis. MTPJs may be individually tender (simultaneously
palpatedwiththumbbelowandfingerabove).
• Tenderness between metatarsal heads is typical in Morton’s metatarsalgia.
There may be a sensory deficit in the interdigital cleft. The differential
diagnosis (in adolescents) may be osteochondritis of the second and third
metatarsalhead.
• Check for hallux rigidus. Passive hallux dorsiflexion should be >50°.
Extendingthehalluxcanrevealanabilitytoformamediallongitudinalarchin

patientswithflatfeet(Jack’stest).
• Discretebonytendernesswithoutswellingoccurswithstressfractures.
• Uneven callus distribution under the forefoot may suggest an abnormally
focusedareaofweight-bearingandanunderlyingmechanicalabnormality.
• Rashes on the sole of the foot are uncommon but important to consider are
pompholyx, pustular psoriasis, and keratoderma blennorrhagica (‘reactive
arthritis’,see Chapter8).
• Loss of sensation under the forefoot may be due to an S1 root lesion,
peripheral neuropathy (e.g. diabetes), mononeuritis (e.g. vasculitis; see
Chapter15),Sjögren’ssyndrome(see Chapter12),otherAICTDsor,rarely,
tibialnerveentrapment(examinehindfoot).
Neurologicalexamination
Neurological examination of the feet is essential in cases where pain is
neurogenicandlikelytobereferredornerverootinoriginorthereisweakness,
numbness,orparaesthesias(Table3.24).
RelevantproximalMSKexamination
Asalwaysexamineproximally—here,theknee.
• Gaitexaminationisimportant—considerthelowerlimbasfunctionallyinter-
relatedfromlowerspinetotoes.
• Hip examination can help determine ante/retroversion at the hip—and the
configurationofsuchcanhaveabearingonlowerlegpronation,in-toeingand
painsatbothkneeandinfeet(seeFig.3.20).
Investigationsofanadultwithlowerlegorfootpain
Imagingofthelowerleg
• Suspectedtibialabnormalitiessuchasstressfracturesandpseudofracturesin
osteomalaciaandPaget’sdiseasehavecharacteristicradiologicalappearances.
• Periosteal changes occur intrauma,psoriatic arthritis (above ankle), HPOA,
andpachydermalperiostitis.
• Inathleteswithexercise-relatedpain,three-phasebonescintigraphyispartof
thework-upforanteriorshinpain.
• Insuspected(butradiograph-negative)casesofbonydisease,suchascortical
stressfracture,periostitis,orcorticalhyperostosis,bonescintigraphymaybe
usefultoidentifysubtlepathology.
• MRIisneededin suspectedcasesofmyopathy thoughimagingmaybdone
moreusefullyoftheupperleg.
Table3.24Patternsofcommonabnormalexaminationfindings(primarilyinthefeet)inlowerlumbar
nerverootlesions
Nerve
root
Abnormalfinding
L4 Weaknessofankledorsiflexion(tibialisanterior)
Patientfindswalkingontheirheelsdifficult(strongankle
dorsiflexonneeded)
*
Reducedkneereflex(L3andL4)
L5 Weaknessofbigtoedorsiflexion(extensorhallucislongus)
Weaknessoffooteversion(peronealmuscles,alsoS1)
Sensorydeficitoverdorsumoffoot
Reducedanklereflex(L5andS1)
S1 Weaknessofankleplantarflexion(gastrocnemiusandsoleus)
Patientfindswalkingon,orrepeatedlyrisingonto,tiptoedifficult
*
Sensorydeficitoversoleoffoot
Reducedanklereflex
*
Manoeuvresmaybeaffectedbypain,makinginterpretationdifficult.
Imagingofthefoot
Informationavailableonradiographsofthehindfootincludes:
• Increased soft tissue attenuation around the tendon insertion in cases of
Achillestendonitisorretrocalcanealbursitis.
• ErosionsorperiostitisattheAchillestendoninsertioninenthesitisassociated
withSpA.
• ErosionsingoutandRA-associatedretrocalcanealbursitis.
• Axial radiographs of the hindfoot are useful in showing talocalcaneal joint
abnormalities,e.g.inRA.
• If radiographs arenormal in patientswithposterior heel pain,UScan show
patternsoftendonandbursalinflammation.MRIcanfurthercharacterizeany
discretepatternoftendoninjury.
• Osteonecrosisofanostrigonumorposteriortalarprocessortarsalnavicular
maybeidentifiedbyradiographs.Itisinvariablylocatedbybonescintigraphy
andcanbecharacterizedfurther,usuallywithsofttissueswelling,byMRI.
• Aplantarspurmaydenoterecurrentplantarfasciitis.
• Plantarheelpainmaybeduetoafractureinaspur.Erosionsjustabovethe
spurmaybeseen.ThethicknessofheelfatpadcanbegaugedfromitsX-ray
attenuation(thin=riskforplantarfasciitis).Afatpad>23mmthickinmen
and>21.5mmthickinwomenisassociatedwithacromegaly.
• Calcaneal fractures or an osteoid osteoma can be seen in some cases with
radiographsalone.Bonescintigraphy/CTaremoresensitive.
• Patternsofjoint,enthesis,andtendoninflammationcanbedocumentedusing
MRIorbonescintigraphy.Thisisusefulinformationwhencharacterizingan
arthropathy.
• Bony abnormalities in the mid and forefoot are generally revealed by
radiographsalone,thoughmetatarsalstressfracturesmaybemissed.MRIcan
discriminateaplantarneuromafrominterdigitalbursitisandMTPJsynovitis.
TheformerareprobablybestinitiallydemonstratedbyUS.
Otherinvestigations
• Neurophysiology (NCS) is a useful adjunct to clinical examination in
diagnosis of lower limb neuropathies, and can help discriminate between
peripheral(commonperonealorsciatic)ornerverootcausesoffootdrop,and
alsoS1rootortibialnerveentrapmentcausesofparaesthesiasofthesoleof
thefoot.
• Joint/bursa fluid aspiration is mandatory in suspected cases of sepsis and
shouldbesentforculture(remembertoconsidergonococcusinyoungadults
andTBinpatientsfromendemicorinner-cityareas).Fluidshouldbesentfor
polarizedmicroscopyifacrystal-induceddiseaseissuspected.
• Laboratory tests requested should reflect suspicion of specific infective,
inflammatory,metabolic,ormalignantpathology.
Treatmentoflowerlegandfootconditions:adults
Lowerlegdisorders
• Anterior shin pain should be treated according to cause. If there is also a
problemoffootalignment,thenorthosesthatsupportboththehindfootand
midarchmaybeveryuseful.Patientsmayvolunteerthatgoodwalkingshoes
or‘trainers’(‘sneakers’)help(asisthecasewithplantarfasciitis).
• Exercise-induced lower leg pain has a number of causes and includes shin
splints and compartment syndrome. The latter may require further
investigationwithpressurereadingsorexercisescintigraphy(
99m
Tc-MIBI).In

cases resistant to rest, analgesia, and modification of triggering factors,
decompressivesurgerymayberequired.
• Patients with Paget’s disease of the tibia may require treatment with IV
zoledronateandwillneedabiomechanicalassessment.
Ankleandhindfootdisorders
• Tendonitis around the ankle should respond to treatment of its underlying
cause. Chronic posterior tibial tendonitis left untreated will eventually
acceleratethedevelopmentofhindfootvalgus.Considerheelandarchsupport
orthoticsearly.
• Steroid injection of inflamed ankle, subtalar and (both posterior tibial and
peroneal) tendons can be done easily (though with subtalar injection, image
guidanceisadvisable).See Chapter24.
• Plantarfasciitismayrespondtoanumberofmeasures:
• Hindandmidfootorthoticsand/orsupportiveshoes.
• NSAIDs.
• Modificationofweight-bearingactivity.
• Achillestendonstretching.
• Hindfootstrapping.
• Restingnightsplint(preventingankleplantarflexion).
• Steroidinjectionaroundthemedialcalcanealtubercle.
• surgery.
• Disease modifying anti-rheumatic drugs/immunosuppressants (e.g.
sulfasalazineormethotrexate)ifpartofPsAorSpA.
• Externalbeamradiotherapy.
Forefootdisorders
• Localizedforefootpain(e.g.metatarsalgia)mayrespondtosupportpadsanda
change to a wider, more supportive, low-heel shoe. A podiatry/chiropody
opinionshouldbesoughtasrequired.
• Forefoot stress fractures and metatarsal head osteochondritis require rest,
supportivefootwearandtimetoheal.
• Patientswithchronicforefootpainmaybenefitfromapodiatricassessment.
‘Stress offloading’ foot orthoses for metatarsalgia and other biomechanical
abnormalities (e.g. hallux rigidus) can be individually moulded using
thermoplasticmaterials.
Steroidinjections
Steroidinjectionsmaybeofvalueinthefollowing:
• Anklejointinflammation(e.g.RA,PSA, OA,acuteCPPDandgout)(see

Plate20a).
• Subtalarjointinflammation(imagingguidanceneeded).
• Tarsaltunnelsyndrome.
• Achilles peritendinitis (steroid injections for Achilles nodules should be
avoided as the risk of rupture is high. The same concern, though probably
lesserrisk,appliestoAchillesperitendinitis).
• Calcanealapophysitis(Sever’sdisease—Achillestendoninsertion).
• Retrocalcanealbursitis.
• Plantarfasciitis.
• Gout/OA/enthesitisatfirstMTPJ.
• InitialtreatmentofaMorton’sneuroma.
Surgery
• Minor surgical techniques can be curative in tarsal tunnel syndrome and in
excisinganinterdigital(Morton’s)neuroma.
• Consider excision of painful exostoses and troublesome rheumatoid nodules
andamputationofdeformedorover-ridingtoes.
• Majorsurgicalprocedureswithgoodoutcomesinappropriatepatientsinclude
fusion of hindfoot joints and forefoot arthroplasty in chronic inflammatory
arthritides.
• Osteotomyrealignmentofahalluxvalgusdeformitycanbesuccessfulinthe
longterm.
Lowerlegandfootdisordersinchildrenand
adolescents
Generalconsiderations
Footandankleproblemsarecommoninchildrenandadolescentsandmostare
attributabletominortraumaorrepetitivestress.Concernscanarisefromover-
interpretationofcommondevelopmentalvariationorcongenitalanomalies(see
Table2.1)andfailureofconditioningorrehabilitationafteracuteinjury.
Takingahistoryinchildrenandadolescents
• Overuse and acute trauma is common: tendinopathy, stress fractures,
osteochondritis and apophysitis. Taking an accurate history of trauma is
important.
• If stress fracture is suspected (e.g. second, third, or fifth metatarsals or
navicularorcalcaneal)inateenagegirlthenamenorrhea,eatingdisorderand
overtraining(inanathlete)needstobeconsidered(‘femaletriadsyndrome’).

• A history of initial trauma then chronic symptomology is recognized with
some lesions—particularly lateral tibiofibular ligament injury, ‘turf-toe’ and
tarso-metatarsaljointinjury.
• Pescavusorplanus,tarsalcoalitions(stiffnessandsometimespaininthehind-
midfoot),andmetatarsusadductuspresentinginyoungchildrenareprimarily
developmental/congenital in origin. Symptoms may have been present since
thechildstartedwalkingthoughnotalwaysandahistoryofdiscomfortmay
haveevolvedoveralongperiodoftime.
• Painundertheheelorareluctancetoheelstrikecandiscloseplantarfasciitis
(e.g.tractionapophysitis).
• Tendonitis may not be an isolated lesion. For example, posterior tibial
tendonitiscanoftenaccompanyanaccessorynavicularandperonealtendonitis
isassociatedwithexcessivepronation.
• Osteochondritisofdifferentstructurespresent acrosssomewhatdifferingbut
broad age ranges: fifth metatarsal base enthesis (9–15 years), Achilles
insertionalapophysitis(6–17years),naviculararticularchondritis(3–7years
old).
• A dissecans osteochondritis lesion of the dome of the talus presents with
hindfootpain±catching/lockingofthehindfoot.Severelesionscandevelop
osteonecrosis.
• JIAandpainamplificationsyndromescanpresentwithfootsymptomsthough
it is wise to rule out all trauma and developmental lesions initially. Dual
pathologyofcoursemayexist.
Examination
Examinationshouldbeginwithfunctionalassessmentofgait,jumping,hopping,
toewalking,walkingonheelsandininversion,andfigure-of-8running.Major
problemswillbecomeapparent.
• Observewhenstandingandlookforpelvictilt,hindfootvalgus,subtalarand
forefootposition,mediallongitudinalfootarch,clawtoesandaMorton’sfoot
(firstrayshorterthansecond).
• Palpateandmovethefoottoreproducepainandassessrangeofmovement.
• Beawarethatifthesubtalarisonlyexaminedoffloaded,abnormalitiesofthe
jointmaynotbeapparent.
• Testheelrisetoassessrigidorflexiblepesplanus.
• Check thigh–foot angle to screen for tibial torsion (see ‘Internal tibial
torsion’,p.180).
• Other examination: is there correctable forefoot adduction? Is there pain on
hindfoot external rotation suggesting a deficiency to the anterior talofibular

ligament?.
• Checkstrength(activemovementagainstresistance)ofankledorsiflexionand
plantar flexion, subtalar inversion (tibialis posterior), subtalar eversion
(peronealtendons),firstMTPJdorsiflexion(EHL)andplantarflexion(FHL).
• Finallyexaminetheknee(see p.185).
Commonfootconditionsinchildrenandadolescents
Metatarsusadductus(MTA)
This is a common exaggerated turning in of the forefoot typically identified
whenthechildstartstowalk.
• MTAmaybedetectedatbirth,whenattributedtoaninuterofootposition.
• Most MTA configurations are flexible and asymptomatic and require no
intervention.
• Stretching may help the foot move into a straighter position and may be
supportedbytheuseofaboot,althoughevidenceforthisislimited.Casting
andsurgeryarerarelyrequired—onlyinseverecases.
Calcaneovalgus
This excess dorsiflexion and valgus of the hindfoot, detected in neonates, is
typicallyidentifiedwhenthechildstartstowalk.
• Thepositionofthefootisusuallycorrectablebytheexaminer.
• Thereisnodislocationorbonydeformity.
• Muscleimbalanceduetoneurologicaldisturbancemayresultinweaknessof
theplantarflexorsandunopposedactionoftibialisanteriorandfootextensors.
• Radiographs typically show posteromedial bowing of the tibia and the first
metatarsalliningupwithaverticallyheldtalus.
• The condition differs from rocker bottom feet which are not correctable—
whenthetalusisplantartothefirstmetatarsal.
• Prognosis is good with spontaneous resolution. Passive stretching exercises
mayexpediteresolution.
Pesplanus
Pesplanus(flatfeet)isanormalvariantinyoungchildrenunlessthefootisrigid
fromaneurologicaldeficit(diplegia)orbonychanges.
• Associationsofpesplanusincludehindfootvalgus,tighteningoftheAchilles
tendon,andinwardrotationoftheforefoottobalancetheheelposition(orthe
footmaybegintoslantoutwardsfromthemiddleofthefoot).
• Hypermobilepesplanuscorrectsifthechildrisesontip-toe.
Radiographs need only be done for rigid flat feet or if pain suggests a tarsal
coalition,congenitalverticaltalus,oraccessorynavicular.
• Usuallynotreatmentisneededandthepatientshouldbeencouragedtowalk
barefootasmuchaspossible.
• Thevalueofarchsupportsisdebatedas thisdoes notimprovethedynamic
support of the foot and may make things worse, although can provide pain
relief.
Pescavus
A high medial longitudinal arch that does not flatten when weight-bearing is
termedpescavus.Itispresentin10%ofthepopulation.
• Afullneurologicalhistory(includingofmotormilestones)andexaminationis
wise.
• Pes cavus may rarely indicate neuromuscular disease (hereditary motor
sensoryneuropathy,Friedrich’sataxia,musculardystrophy,orcerebralpalsy).
• Ifpescavusisunilateralorrapidlyprogressive,thenconsidertheremaybea
spinaltumour.
• Associated clawing of the toes, contracture of the plantar fascia, and
dorsiflexedgreattoemaycausemidfootpain.
• Mayalsoaffectfootwear.
• Physiotherapy, foot orthoses, and foot wear modifications for pain or
instabilityshouldbeconsidered.
• Surgical treatment is reserved for cases where conservative measures have
failed.Surgeryincludestendontransfers,softtissuemanipulation,osteotomy
andarthrodesis
Talipesequinovarus(clubfoot)
• The flexible variant is a common congenital deformity and requires
physiotherapyguidancealone.
• Therigidform,whichisofgeneticaetiology,typicallyrespondstothePonseti
methodofmanipulationwithoutinvasivesurgery.
Tarsalcoalition
A tarsal coalitionis a congenitalanomalywhere there isanabnormal fibrous,
cartilaginousorosseousconnectionbetweenhindfootbones.
• Coalitionsareusuallyasymptomatic.
• Painoccurswhenthereisdecompensationofsupportingmusculature,arigid
flatfoot,hindfootvalgus,orperonealspasticity.
• The commonest coalitions are calcaneonavicular (presenting at 8–12 years
old)andtalocalcaneal(presentingin12–15-year-olds).
• RadiographsconfirmthelesionsbutMRIishelpfulincharacterizingfibrous
variantsandassessmentofbonestress(boneoedema).
• Managementincludes‘determined’physiotherapyworkingongaitandmuscle
supportofthefoot,which,ifsuccessfulavoidssurgery.
• Overallsurgeryisrarelyrequiredandnotdesired.
In-toeing
Clumsinessorregulartrippingafter2yearsofage iscommon.Mildin-toeing
maybeanormalvariant.However,assessmentrequiresathoroughexamination
ofpotentialcontributingfactorswhichmightbemodifiablewithphysiotherapy
and/orfootorthoses(e.g.femoralanteversion,MTA,oranyconditionresulting
inmuscleweakness).
Toeanomalies
• Congenitalcurlytoesresultfromshorteningofflexortendonsaschildstartsto
walk. Surgical tendon release can be considered in cases where there are
painfulblistersorrubbing.
• A hammer toe is a tendon contracture with progressive PIPJ flexion and
compensatoryextensionattheMTPJsandDIPJs.Management,includingfor
pain,isusuallyconservative.
• AmallettoeisacontractureoftheDIPJs.
• A claw toe is formedfromdorsaltoe subluxation at the MTPJs and flexion
deformitiesatthePIPJsandDIPJs.
• Toeinstability(dorsalsubluxationoftheproximalphalanxoverthemetatarsal
head)israreinyoungpeople.Oftenthereisahistoryofrepeattearing(pain)
andswellingoftheplantarplatewithlocaltendernessandswelling.
• Polydactyly occurs 1 in 500 live births with radial, ulnar, or central extra
digits.Thereisahighlikelihoodofsyndromicgeneticanomalyandchanceof
multiplegeneticdefects.Areferraltoageneticistisrecommended.
• Syndactylyisanembryonicfailureofapoptosisofthedigitwebbingatabout
16weeks’gestation.Mostlesionsareisolateddefectsbuttheremayalsobean
associationwithgeneticdefects.

Chapter4
Thespectrumofdisordersassociatedwithadult
rheumaticandmusculoskeletaldiseases
Skindisordersandrheumaticdisease
Skinvasculitisinadults
Cardiacconditions
Pulmonaryconditions
Renalconditions
Endocrineconditions
Gutandhepatobiliaryconditions
Malignancy
Neurologicalconditions
Ophthalmicconditions
Skindisordersandrheumaticdisease
Theimportanceofexaminingtheskin
• Theskinisthemostaccessibleorgantoexamine.
• Pattern recognition of skin symptoms and lesions is valuable in aiding
diagnosis(e.g.acuteorchronicsarcoid)andprognosisofrheumaticdiseases
(e.g.nodulesandvasculitisinRA).
• MSK abnormalities may be mirrored by skin abnormalities (e.g. joint
hypermobilityandskinlaxitywithbruising,scarring,andstriae).
• Someantirheumaticdrugsproducespecificandpotentiallyseriouscutaneous
reactionsthatrequirepromptmanagement.
• SomerareautoinflammatoryconditionsassociatedwithMSKsymptomscan
manifestprimarilywithskinpathology(see Chapter18).
Regionalabnormalities
Thescalp
Scalpsymptomsandlesionsmaybesubtle.
• ScalptendernessisasignofGCA.
• C2root/occipitalneuropathy(e.g.inC1–C3facetjointOAorcrowned dens
syndrome/CPPDdisease)orshinglesmaybeassociatedwithdysaesthesiaover
thescalpandoccipitalneuralgia.
• Alopeciamaybelocalized(areata)ordiffuse(e.g.inSLEorirondeficiency).
Scarringalopeciaistypicalofdiscoidlupus.
• Scalppsoriasismaybepatchyanddiscrete,andoftenaffectsthehairline.
Faceandears
Face and ears are in sun-exposed areas. Consider ultraviolet (UV) skin
sensitivity.
• AvarietyofpatternsofSLE-associated,UV-sensitiverashesmayoccur.The
rashisoftendiffuse.Shadedareas(e.g.nasolabialfolds)maynotbeaffected
(see Chapter13).
• AsinSLE,rosaceacanpresentwithanerythematousfacialrash.Distinctionis
sometimesdifficultwithoutbiopsy.
• Periorbitaloedemaoccursindermatomyositis,angio-oedema(whichmaybea
presentingfeatureofSLE),andinnephroticsyndrome.
• Heliotrope rash refers to violaceous oedema/erythema of the eyelids in
dermatomyositis(see Chapter14).
• Thecutaneousinfiltrationofchronicsarcoid(lupuspernio)(see Chapter18)
acrossthenoseandcheeksmaybeovert(papular)butalsomaybequitesubtle
(see Plate21).
• Saddle nose deformity/nasal cartilage destruction has a number of causes:
PR3-positiveANCA-associatedvasculitis(AAV;see Chapter15),relapsing
polychondritis ( Chapter 18), hereditary connective tissue disease (e.g.
Stickler’ssyndrome;see Chapter19),andlethalmidlinegranuloma.Nasal
septalperforationcanoccurfromcocaineuse.
• Oralaphthousulcersarecommon.Oralulcerationmayfollowdiseaseactivity
(e.g.inSLE).Ulcersinreactivearthritisaretypicallypainless.Oralaphthous
ulcersarefrequentlyidiopathic,andnotassociatedwithsystemicdisease.
• Large punched-out and numerous tongue and buccal ulcers that scar are a
hallmarkofBehçet’sdisease(see Chapter18).Theymayremainforseveral
weeks.
• Strawberryerythemaofthetongueandlipsshouldnotbemissedinchildren.It
may denote self-limiting streptococcal infections but may also herald the
desquamatingpalmar(andsole)rashofKawasakidisease(KD;see Chapter
15).

• Lacywhitestreaksonthebuccalmucosasuggestlichenplanus.
• The pinna is a common site for gouty tophi and discoid lupus. Relapsing
polychondritis typically causes softening and distortion of cartilage (but is
lobe-sparing).
• Lipidskindepositsaroundtheeyeoccurinhyperlipidaemiaandmulticentric
reticulohistiocytosis.
Handsandnails
Handsandnailsshouldbeexaminedclosely.
• Aphotosensitiveeruptionsparesthefingerwebsandpalms.
• Erythema on the back of the fingers may help distinguish dermatomyositis
fromSLE.
• InpatientswithRaynaud’sdisease(RD),fingerulceration,fingerpulpatrophy
(withsmoothtaperingofthefingertips),induration,andtetheringoftheskin
indicatescleroderma(see Chapter13).
• Unlikenormalskin,theskinofsclerodermadoesnotformfinewrinkleswhen
pinched.
• Onycholysis, nail-pitting, salmon patches, and subungual hyperkeratosis are
typicalofpsoriasis(see Chapter8).
• Subungual splinter haemorrhages may be associated with trauma, infective
endocarditis,vasculitis,orthromboangiitisobliterans.
• Nailfold capillariescan beexaminedwith anophthalmoscope at40dioptres
after applying a drop of oil (or surgical lubricant) to the cuticle. Enlarged
(dilated) capillary loops and capillary ‘dropout’ suggests an underlying
autoimmune connective tissue disease (AICTD), particularly systemic
sclerosis(SScl).
• Nailfold vasculopathy is non-specific, and can occur with vasculitis,
dermatomyositisandinfectiveendocarditis.
Typesoferuption
Macularrashes
Macularrashesareflat(non-palpable)areasofalteredskincolour.Papulesare
lumps<1cmindiameter.
• Maculopapularrashesaretypicalofviralinfections.
• Ashort-lived,pinkish,maculopapulareruptionoccursonthetrunkandlimbs
insystemic-onsetJIA(soJIA;see Chapter9)andadult-onsetStill’sdisease
(see Chapter18).Itisoftenprominentinthelateafternoon,andcoincides
with temperature spikes. If scratched, the rash may blanch (Koebner
phenomenon).

• Erythema that enlarges to form erythematous patches with pale centres
suggestsrheumaticfever(‘erythemamarginatum’).
• A ‘bulls-eye’ erythematous lesion around a tick bite may be the erythema
migransofLymedisease.
• Maculopapular eruptions can occur from NSAIDs, gold, sulfasalazine,
azathioprinehypersensitivity,andleflunomide(see Chapter23).
Pustulesandblisters
Blistersmaybevesicles(<0.5cm)orbullae(>0.5cm).
• Themostcommonpustularrashisduetofolliculitis.
• PustulesconfinedtothehandsandfeetsuggestreactivearthritisorSAPHO,
althoughlocalformsofpsoriasismaybeindistinguishable.Psoriasiscanalso
occuras‘raindrop’erythematouslesions,alsoknownasguttatelesions.
• Generalized pustular rashes can occur in vasculitis, the neutrophilic
dermatoses, intestinal bypass syndromes, Behçet’s disease, and gonococcal
bacteraemia.
• Bullous eruptions may be due to SLE and drug reactions, pemphigus, and
pemphigoid.
Plaques
Plaquesareslightlyraised,circumscribedareas—oftendiscshaped.
• Plaquesarethehallmarkofpsoriasis.Skinmaybescalyandflakeoffeasily.
Lesionsareoftenred.
• Psoriaticplaquescanoccuranywhereontheskin,buttypicalsitesareoverthe
extensorsurfacesofthejoints,intheinterglutealcleft,atsitesofskinfriction
(e.g.underwaistbandsoftrousersorunderwear)andtheumbilicus.
• Scaling may be a feature of discoid lupus; scaling tends to occur at the
peripheryofthelesion.
Vascularlesions
Bleedingintotheskinthatdoesnotblanchiscalledpurpura.Itmaysometimes
be palpable. Telangiectases are dilated small vascular lesions that blanch on
pressure.
• Non-palpablepurpuramaybeduetothrombocytopenia,plateletdysfunction,
trauma (± capillary/skin fragility, e.g. chronic steroid use), haemophilia,
anticoagulation, and hereditary connective tissue diseases (e.g. EDS; see
Chapter19).
• Palpable purpura suggests vasculitis, including drug-induced disease (see
Chapter15).
• Widespread telangiectasia occurs in limited cutaneous scleroderma (lcSScl;
see Chapter 13), hereditary haemorrhagic telangiectasia, and
dermatomyositis.
• Livedoid rashes can be subtle, occur mainly over the legs, can occur in
smokers but are also associated with SLE and antiphospholipid syndrome
(APS).
• Lumpy erythema on thelowerlegsespecially, which can be tender, may be
panniculitis (e.g. erythema nodosum), and related to systemic disease (e.g.
sarcoid,Crohn’s)
Ulcersandulceratingrashes
Ulcers are defined as a loss or defect of dermis and epidermis produced by
sloughingofnecrotictissue.
• Cutaneousulcerationmayhavemorethanonecauseinautoimmunediseases.
Forexample,vasculitis,venousstasisinanimmobilepatient,andulceration
overnodulesorpressurepointsmayallcontributetothesamesetoflesions.
Trauma may be an important cause of cutaneous ulcers in a patient who is
alreadypredisposedtowardsformingtheselesions.
• Anindurated,expanding,plum-colouredplaqueoracneiformpustulethatthen
ulcerates suggests pyoderma gangrenosum. The ulcer has irregular, bluish
margins.
• Neurotropiculcersareclassicsequelaeofdiabetes,buttheycanalsooccurin
associationwithmononeuritismultiplex(fromvasculitis)andotherrheumatic
diseases.
• Vasculitic ulcers in the context of livedo reticularis and antibodies to
phospholipids(e.g.cardiolipin)maydenoteAPS(see Chapter11).
Texturalabnormalities
Abnormalitiesofthetextureoftheskinmaybedifficulttodiscern.Atrophyand
thinning,laxity,thickening,andindurationmayallbeassociatedwithdisease.
• Generalizedskinatrophyandthinningisanage-relatedprocess,butthiscan
beacceleratedbychronicsteroiduse;hereditarydiseasesofconnectivetissue
shouldalsobeconsidered.
• Skinlaxitycanbestbedemonstratedoverelbowandkneeextensorsurfaces.
Generalized laxity of connective tissue may result in varicose veins and
internalorganprolapse.
• True acral and digital puffiness in a patient with Raynaud’s disease is
suggestiveofSScl.Skinthickeninghasa varietyof causes(seelaterinthis
topicand Chapter13).
• Sclerodermaandscleroderma-likeskinmaybelocalized,limited,ordiffuse—
thisdistinctionisimportant(Table4.1).
Diagnosticissuesinpatientswithskinthickening
• Raynaud’s disease (RD) invariably precedes the onset of SScl, but is not a
characteristicofmorpheaorlinearscleroderma.
• In patients with RD, abnormal nailfold capillaries on capillaroscopy may
indicateSScl(see Plate9).
• The specificities of autoantibodies are often predictive of SScl subtype. In
patientswithRD,ANAhaspredictivevalueforidentifyingpatientswhomay
progresstoSScl; anticentromereantibodycan predictprogressionto limited
cutaneous SScl; anti-topoisomerase I (SCL-70) and anti-RNA polymerase
antibodiesarelinkedwithprogressiontodiffusecutaneousSScl(dcSScl).
• PatientswithdcSSclhaveapreponderanceofvisceral organ involvementin
the first 5 years of disease; screening investigations are usually useful, and
shouldincludecardiovascularscreeningtests(referto Chapter13).
• Eosinophilic fasciitis (see Chapter 18) may occur as a paraneoplastic
syndrome,andisassociatedwithhaematologicalmalignancies.
• Linearsclerodermainchildrencanproducelifelongdeformitiesbecauselimbs
failtodevelopcorrectlengthandbulk.
Table4.1Patternrecognitioninpatientswithskinthickening
Classification Skinfeatures
Morphea
maybe
localized
(guttate)or
generalized
Earlysmallskinareasaffected(itchy).Progressionto
hideboundskin,typicallyontrunk(areolaspared)andlegs.
Lesionsbecomewaxyandhypo/hyper-pigmentedguttate
(small<10mm)papulesusuallyonneckandanteriorchest
Linear
scleroderma
Linearband-likepatternoftenindermatomaldistribution.
Atrophyofmusclesiscommon.Fixedjointdeformitiesand
growthabnormalitiescanoccur
‘Coupde
sabre’
Linearsclerodermaontheface/scalpcanbedepressed;ivory
inappearance.Hemi-atrophycanoccur
SScl(early) Earlymorning‘puffiness’inhandsandfeet,facial‘tightness’.
Non-pittingoedemaofintactdermalandepidermal
appendages.Highdegreeofsuspicionneeded
SScl(classic) Firm,taut,hideboundskinproximaltoMCPjoints.Skinmay
becoarse,pigmented,anddry.Epidermalthinning,lossof
hair,andsweatingcanoccur.Telangiectasiaandskin
calcinosisbecomeobvious.Skincreasesdisappear.Such
changeproximaltoelbowsorkneesinthelimbsorbelowthe
clavicles(inthosewithfaceandneckinvolvement)classifies
diseaseasdiffuseasopposedtolimitedsystemicsclerosis
SScl(late) 2–15yearsafteronsetofclassicalphase,skinsoftens,but
pigmentationchangesremain.Skinbecomesatrophicandcan
ulcerate
Eosinophilic
fasciitis
Phases:early—pittingoedema;progressive—peaud’orange;
late—induration(‘woodyfeel’)withvenousgutteringwhen
limbelevated.Armsandlegsmostcommonlyaffected,but
fingersmainlyspared.Synovitisandlow-grademyositismay
occur.Eosinophiliaisusuallystriking,butnotalwayspresent
Lipodermato-
sclerosis
Hyperpigmentationandindurationoflowerlegsassociated
withvenousstasis(‘champagne-bottlelegs’)
Diabetes Waxythickeningofextremities.Insidiousprogression.Joints
ofthehandsbecomestiff,thetendonscanthicken.Skin
changesproximaltowristandonthefaceveryunlikely,but
stiffeningofelbowandshoulderjointsnotuncommon
Dependent
lymphoedema
Feet/ankles/lowerlegs.Oftenpitting.Chronicpresencemay
givehyperkeratosis.Maincauses:R-orL-sidedheartfailure,
renalfailure,nephroticsyndrome,andlow-proteinstates
Skinvasculitisinadults
Background
Thereareavarietyofwaysinwhichsystemicvasculitismaypresent,including
fever of unknown origin, organ infarction, gastrointestinal (GI) bleeding, and
highacutephaseinagenerallyunwellpatient.Avasculiticskinrashisoneof
themostcommonpresentingfeaturesofsystemicvasculitis,andisanimportant
diagnosticclue(see Chapter15).
Whentoconsideradiagnosisofvasculitis
• Primarysystemicvasculitisisrare.
• Cutaneous vasculitis, however, is not rare; it can follow viral or bacterial
illness,canbetriggeredbydrugs,andisassociatedwithmalignancy.Biopsy
generally demonstrates degranulation of neutrophils (‘leucocytoclasis’) and
evidenceofvesseldestruction.
• Thelistofcausesislong(Table4.2);however,inabout50%ofcasesnocause
maybefound.
• Cutaneousvasculitismayalsooccurinassociationwithanotherautoimmune
disease not normally characterized by vasculitis, such as SLE, RA, and
Sjögren’ssyndrome.
Importantconsiderations
The following important points of clinical assessment should be followed in
patientswithpossiblevasculiticrashes.
• Determinewhetherthepatienthasbeentakinganewdrug.Manyantibiotics,
including penicillins, sulfonamides, and cephalosporins, cause cutaneous
vasculitis.Biologicsmaytoo,notablyanti-TNFα.
• Evaluatethepatientforevidenceofchronicinfection:hepatitisB,hepatitisC,
andHIVareworthconsidering.Endocarditisshouldalsobeconsidered(e.g.
theelderly,orpatientswhouseIVdrugs).
• Lookforevidenceofaprimaryautoimmunedisorderthatmaybeassociated
with cutaneous vasculitis. IBD, for example, can occasionally cause a
leucocytoclastic vasculitis in addition to oral ulcerations and pyoderma
gangrenosum.BecauseSLEiscommon,checkANAandserumcomplement
C3/C4.
• Lookforevidenceofcryoglobulinaemicvasculitis.Serumcryoglobulinstests
areoftenmishandled,leadingtofalse-negativeresults,primarilybecausethe
sampleneedstobekeptwarm(usuallybysimplyholdingintheclosedpalm
ofthehand)andshouldbetakenstraighttothelaboratory.
• RFisdetectedin80%ofpatientswithmixedessentialcryoglobulinaemia,and
maybeabetterscreeningtestthanthelatter.
• Age-appropriate screening for malignancy should be done. Serum and urine
electrophoresiswithimmunofixationmaybeofvalue.
• Urinalysis may demonstrate ‘active sediment’; evidence of haematuria,
proteinuria,or redbloodcell castsmay bethe firstcluethat apatient hasa
systemicvasculitis.
Systemicvasculitis
• Untreated primary systemic vasculitis is generally characterized by general
inflammation; many patients will complain of B-type symptoms, including
fevers,weightloss,andnightsweats.Patientswithcutaneousvasculitisalone,
ontheotherhand,oftenfeelquitewell.
• The extracutaneous signs and symptoms may provide clues to the correct
diagnosis:
• Henoch–Schönleinpurpura(HSP):colickyabdominalpain.
• Eosinophilic granulomatosis with polyangiitis: adult-onset asthma,
eosinophilia.
• PR3-positiveAAV:chronicsinusitis,pneumonitis.
• Microscopicpolyangiitis:haemoptysis,redbloodcellcasts.
• Mononeuritis multiplex, which presents as a ‘wrist drop’ or ‘foot drop’, is
suggestiveofsystemicvasculitisinanon-diabeticpatient.
Table4.2Precipitantsandassociationsofleucocytoclasticsmallvesselvasculitis
Drugs Sulphonamides,forexample(therearemany).Some
drugsmaycausealymphocyticvasculitiswithout
leucocytoclasis
Infections HepatitisB,hepatitisC,HIV
β-haemolyticStreptococcus
Foreignprotein E.g.serumsickness
Autoimmune
disease
Rheumatoidarthritis
Sjögren’ssyndrome(anti-Ropositive)
SLE(thoughlivedoidvasculitismayoccurinassociation
withsecondaryAPS,andthismaybelymphocytic
withoutleucocytoclasis)
Inflammatory
diseases
Sarcoid
Crohn’sdisease,ulcerativecolitis,chronicactive
hepatitis
Malignancy Myelo-andlymphoproliferativedisorders
Solidtumours
Cryoglobulinaemia
Investigations
Skinbiopsy
• Discussthecasewithahistopathologist.
• Punchbiopsyissimple,andmaybesufficienttoyieldadiagnosis.Elliptical
biopsyprovidesmoretissue,andmayincreaseyield.
• Useaneedletolifttheskinsample.Avoidforceps-induceddamage.
• Biopsy should extend to the subcutaneous fat, which generally includes the
arterioles and venules affected by primary systemic vasculitis. Idiopathic
leucocytoclastic vasculitis affects the capillaries but generally spares the
arteriolesandvenules.
• Biopsy should be sent for routine histology and for direct
immunofluorescence, which may yield important clues regarding the
underlyingcause:
• IgA:HSP.
• IgM,C3:cryoglobulinaemicvasculitis.
• IgG,IgM,IgA,C3:SLE.
• Lowimmunoreactantstaining:AAV.
• SamplesforimmunofluorescenceshouldbesnapfrozeninliquidN
2
ordryice
ortransported immediatelytothelaboratory.Immunofluorescence cannotbe
doneonsamplestreatedwithformalin.
• SeeTable4.3foralistoflaboratoryinvestigationstobecarriedoutinpatients
withsuspectedvasculitis.
Table4.3Laboratorytestsinpatientswithsuspectedvasculitis
Haematology FBC,ESR,lupusanticoagulant
Biochemistry Electrolytes,urea,creatinine,LFTs,ACE,CRP,serumand
urineproteinelectrophoresis
Microbiology Urinemicroscopyforredcellcasts,bloodculture,HepBand
Cserology,considerHIV,streptococcalantibodies.Also,save
10mLofclottedbloodforviralserologyandrepeatin2–3
weeksforpairedtitreanalysis
Immunology Immunoglobulins(includeIgGsubsetsifIgG4diseasebeing
considered),cryoglobulins,ANA,ENAs,RF,anti-cardiolipin
antibodies,ANCA,Complement(C3,C4,CH50/CH100,anti-
C1qantibodiesifconsideringurticarialvasculitis))
Cardiacconditions
SubclinicalcardiacinvolvementisfoundinmanyrheumaticMSKdiseases,and
itisnotuncommonforacardiacabnormalitytobediscoveredincidentally.As
our ability to treat the underlying rheumatic diseases improves, our ability to
identify and to treat the cardiac complications of these diseases becomes
increasinglyimportant.
Pericardium
• Pericardial effusion has been reportedinassociation with a large number of
rheumaticdiseases,includingSScl,Sjögren’ssyndrome,polymyositis,mixed
connectivetissuedisease(MCTD),RA,SpAs,andsystemicvasculitides.
• Inthemajorityofcases,effusionsarediscoveredincidentally,areoftensmall,
clinicallyasymptomatic,andrequirenospecifictherapy.
• Pericardial effusions can also occur in the setting of non-rheumatic illness.
Whenapatientwithaknownrheumaticdiseasepresentswithasymptomatic
effusion, it is important to consider other possible explanations, such as
infection(e.g.TB,viral),malignancy,andotherunrelatedconditions(uraemia,
hypothyroidism).
• Pericardial effusions are common in SLE and are due to immune complex
depositionintothe pericardium.Effusions canbe serous, serosanguinous,or
haemorrhagic. Analysis of the pericardial fluid generally demonstrates
evidenceofcomplement,immunecomplexes,andleucocytes,consistentwith
anactiveinflammatorystate.
• Although pericardial effusions are common with SLE, they are generally
trivial. Cardiac tamponade is found in <1% of patients with SLE.Sincethe
effusion tends to reflect the overall disease, generally treatment of the
underlying disease is adequate to resolve the effusion. Rarely, therapeutic
pericardiocentesismayberequired.
• Pericardial effusions are found in up to 30% of patients with RA, although
onlyasmallnumberofthesepatientswillpresentwithpericarditisorevidence
oftamponade.
• PericardialeffusionsaremorecommoninRF-positivepatientswithahistory
ofrheumatoidnodules.Chronicpericardialeffusionscanbecomeinfected,and
inrarecasesleadtoconstrictivepericarditis.
• Forbothgroupsofpatients,thepresenceofasymptomaticpericardialeffusion
isassociatedwithincreasedmortality.InonestudyofpatientswithSLEwho
presentedwithcardiactamponade,the5-yearsurvivalwasonly46%.
Myocardium
• Myocarditis isan uncommonfeature ofrheumatic diseases.Myocarditis can
befoundamongpatientswithactiveSLEandRA,althoughitgenerallydoes
notleadtoclinicallysignificantdysfunction.
• CardiomyopathyamongpatientswithRAandSLEismorelikelytobedueto
prematurecoronaryarterydisease,followedbythedevelopmentofischaemic
heartdisease.
• Although uncommon, the possibility of hydroxychloroquine-induced
cardiomyopathy should be considered in patients who develop congestive
heartfailureintheabsenceofcoronaryarterydisease. Thediagnosiscanbe
confirmed with myocardial biopsy, and the condition responds to drug
cessation.
• Eosinophilicgranulomatosiswithpolyangiitis(EGPA;formerlyChurg–Strauss
vasculitis) can lead to an acute eosinophilic myocarditis that can be life-
threateningifnottreatedpromptly.
• One-third of patients with AAV may have cardiac dysfunction as a
consequenceoftheunderlyingvasculitis.Themajorityofthesepatientswill
have wall motion abnormalities on echocardiography, but valvulitis and
ventricular aneurysm havealsobeenreported.The majority of these lesions
will be asymptomatic, but the 5-year survival rate for patients with cardiac
lesionsattributabletoAAVis57%.
Valvulardisease
• Aortic regurgitation is an important potential consequence of aortitis, which
can occur with any of the large-vessel vasculitides (including Takayasu
arteritis,GCA,andBehçet’sdisease).Theaortitisleadstoaneurysms,which
createvalvularincompetence.
• Aortic regurgitation can also occur as a consequence of AS. Unlike the
vasculitides, in AS there is inflammation at the aortic root leading to dense
scarringoftheaorticvalves.Althoughthemechanismisuniquetothisdisease,
itshouldbemonitoredandtreatedlikeanyformofaorticinsufficiency.
• Mitralregurgitationandmitralvalveprolapsearecommonmanifestationsof
SLE.
• MitralvalveprolapsemayalsobeafeatureofEhlers–Danlossyndrome.
• A more serious valvulitiscanoccurin association with SLE or APS. In the
processofhealing,thevalvesbecomescarredandcalcified,aprocessthatcan
eventuallyleadtoclinicallysignificantvalvulardisease.
• Libman–SacksendocarditisisaclassicmanifestationofSLE.Inthisdisease,
vegetations form from immune complexes, mononuclear cells, and fibrin,
which attach to the valves. Although not infectious, these vegetations can
embolize.
• Haemodynamically insignificant valve lesions have also been reported in
associationwithRA,MCTD,SScl,andSjögren’ssyndrome.
Coronaryarterydisease
• Surprisingly, the primary vasculitides rarely lead to coronary artery
inflammation, although coronary artery vasculitis has been reported in
associationwithPANandAAVs.
• APS is associatedwitha substantial increasedriskof myocardial infarction,
evenintheabsenceoftruecoronaryarterydisease.
• BothRAandSLEarestronglyassociatedwithcoronaryarterydisease.This
may be the result of systemic inflammation or a response to chronic
immunosuppression.Regardless,patientswiththesediagnosesshouldundergo
earlycardiacevaluationtoaddressmodifiableriskfactorsforcoronaryartery
disease.
• Accelerated atherosclerosis may be an important consequence of
glucocorticoidexposure. Evenchroniclow-doseprednisonemay placesome
patientsatincreasedriskofcardiovasculardisease.
Conductionabnormalities
• Clinically insignificant dysrhythmias and conduction defects are common
among patients with inflammatory myopathies (dermatomyositis,
polymyositis)andscleroderma.
• Clinically significant abnormalities (including heart block) can be seen in
patients with SpAs as a result of the same scaring process that leads to the
valvularabnormalitiesnotedearlier.
Pulmonaryconditions
Pleura
• An exudative pleural effusion is found in up to 50% of patients with SLE.
These effusions can be unilateral or bilateral, and frequently are found in
associationwithapericardialeffusion.
• Pleural disease is a common manifestation of RA, which is associated with
pleural effusions and pleural thickening. Effusions are generally
asymptomatic,andarefoundinthesettingofactivedisease.
• Asymptomaticpleuraleffusionscanalsobefoundin10–30%ofpatientswith
AAV.
• Pleural effusions are classified as transudates, typically arising as a
consequence of left ventricular, renal and hepatic failure, and SLE; or
exudates,usuallyduetoinfection,malignancyorpulmonaryembolism.
• Bythe‘Light’criteria(witha75–80%sensitivity)atransudateis:
• clear.
• specificgravity<1.012.
• fluidprotein<2g/dL.
• fluid:serumproteinratio<0.5.
• fluid:serumLDHratio<2/3.
• cholesterol<45g/dL.
• Inthesamecriteria,anexudateisdefinedas:
• cloudy.
• specificgravity>1.020.
• fluidprotein>2.9g/dL.
• fluid:serumproteinratio>0.5.
• fluid:serumLDHratio>2/3.
• cholesterol>45g/dL.
• Ifanexudateisidentifiedfluidshouldbeexaminedfor:
• amylase:inoesophagealrupture,pancreatitis.
• glucose:decreasedininfection,malignancyandRA.
• pH:lowinempyema.
• Gramstain.
• polymerasechainreaction(PCR)fortuberculosis.
Pulmonarynodules/masses
• BothPR3-positiveAAVandsarcoidosisareoftendiagnosedincidentally,after
the discovery of lung masses. Sarcoidosis is associated with hilar
lymphadenopathy, while PR3-positiveAAV generally presents with multiple
peripheralpulmonarynodulesthatcanbemistakenforlungcancer.
• Inapatientwithaknownrheumaticdiseasewhopresentswithalungmass,it
isalwaysimportanttoconsiderthepossibilityofmalignancy.Lungcancerrisk
isincreasedamongpatientswithRAandSScl,andmanyrheumaticdiseases
areassociatedwithanincreasedriskoflymphoma.
• PR3-positive AAV (and less commonly, AS and RA) can lead to cavitating
apicallesionsthatcanbemistakenforTB.
Interstitiallungdisease(ILD)
• ILD and pulmonary fibrosis (with a predilection for the lung bases and
periphery) is a common feature of both dcSScl and the inflammatory
myopathies.
• Pulmonary fibrosis is found in 20–65% of patients with SScl.
Radiographically, the lesions take on the appearance of ground glass ILD
infiltratesthatgraduallyleadtohoneycombingandfibrosis.
• ILD may be the initial manifestation of an inflammatory myopathy, and
pulmonarysymptomsmayprecedeclinicalevidenceofmuscleinvolvement.
• RAisalsoassociatedwithILD.
• Apicalfibrosiscanbefoundin1%ofpatientswithAS.Apicalfibrosisisalso
anuncommonfeatureofrheumatoidlung.
• Pulmonary fibrosis can also occur as the long-term sequelae of pulmonary
capillaritis,whichmayoccurinpatientswithAAV.
• ILDinprimarySjögren’ssyndromecanbesubtleandevolveinsidiously.The
usualpatternisnon-specific(NSIP).
• Bronchiolitis obliterans organizing pneumonia (BOOP) has been associated
withautoimmunerheumaticandconnectivetissuediseasesbuttheassociation
isnotfrequent.
Vasculature
• Haemoptysiscanbetheresultofpulmonarycapillaritis,whichcanbefoundin
association with the so-called pulmonary renal syndromes: SLE, AAV
(predominantly microscopic polyangiitis), and anti-glomerular basement
membrane syndrome. Acute or severe pulmonary vasculitis may require
promptplasmapheresis.
• Cryoglobulinaemicvasculitiscanalsocausepulmonarycapillaritis,although
thisisnotoneofitsmorecommonmanifestations.
• Pulmonary artery hypertension (PAH) is most commonly associated with
lcSScl. Isolated PAH can also be seen with dcSScl, although it generally
appearsasaconsequenceofpulmonaryfibrosis.
• SScl causes PAH by narrowing of the small arteries and arterioles that
graduallyleadstoobliterationofthepulmonaryvascularbed.
• RA,SLE,inflammatorymyopathy,MCTD,andSjögren’ssyndromecanalso
be associated with PAH, but it is considered an uncommon feature of these
diseases.
Airways
• RAcanleadtolaryngealobstructionwhenitaffectsthecricoarytenoidjoints.
Itusuallypresentswithhoarsenessorodynophagia.
• SubglotticstenosisisacommonfeatureofPR3-positiveAAV,whichcanlead
tosignificantstridor.
• Uncontrolled relapsing polychondritis can cause tracheomalacia, which is a
significantcauseofmorbidityforthisdisease.
• Any part of the airway can become symptomatic in primary Sjögren’s
syndrome:xerotrachea,xerostomia,sinussymptoms.
Renalconditions
Evaluationofrenalfailure:overview
Thekidneysareanessentialcomponentintheevaluationandmanagementofthe
rheumaticMSKdiseases.
• Intermsoftimecourse,renalfailuremaybesecondarytoacutekidneyinjury
(AKI)orchronickidneydisease(CKD).AKIcanoccurinpatientswithstable
CKD.
• AKI(grade1)isdefinedwhenoneofthefollowingcriteriaismet:
• Serumcreatininerisesby≥26µmol/Lwithin48hours.
• Serumcreatininerises≥1.5×fromthereferencevalue,which isknownor
presumedtohaveoccurredwithin1week.
• Urineoutputis<0.5mL/kg/hourfor>6consecutivehours.
• Theabove-listedindicesaretheminimumrequiredfordefinition(grade2and
3 AKI have definitions: http://www.renal.org/guidelines/modules/acute-
kidney-injury).
• UrgenturinalysisandrenalultrasoundshouldbeobtainedinallAKIpatients.
• Glomerularfiltrationratevalue(mL/min/1.73m
2
)classifiesrenal functionas
WHOstage:normal(grade1;>90),mild(grade2;60–89),moderate(grade3;
30–59),severe(grade4;15–29),severefailure(grade5;<15).
• The presenceofred bloodcells andprotein,or redbloodcell casts(i.e. ‘an
activesediment’)impliesglomerulonephritis,whichcanoccurwithvasculitis
andSLE.
Pre-renalazotaemia
• Hypovolaemia is an important cause of pre-renal AKI. Dehydration and
anaemiacanbothleadtopre-renalazotaemia(e.g.theelderlyRApatient).
• Renal hypoperfusion can also be caused by diminished blood flow to the
kidneys.Diseases involvingtherenalartery(such asrenalarterystenosisor
thrombosisorPANaffectingtherenalartery)maycausepre-renalazotaemia.
ThismaybeacuteleadingtoAKIorslowlyevolvingcausingCKD.
• Conditions associated with low cardiac output (including shock, congestive
heart failure, myocarditis, tamponade, and pulmonary arterial hypertension)
mayallpredisposethepatienttopre-renalAKI.
• Hyperviscosity,whichisseenwithtypeI(monoclonal)cryoglobulinaemia,is
averyrarecauseofpre-renalazotaemia.
• All of these conditions may be exacerbated by drugs that decrease renal
perfusion,includingNSAIDsandACEinhibitors.
• Withpre-renalazotaemia,thefractionalexcretionofsodium[FENa=(UNa×
PCr)/(PNa × UCr)] is <1.0; this test is not reliable in patients treated with
diuretics.
Post-renalazotaemia
• Nephrolithiasisisnotacommoncauseofpost-renalazotaemia,butshouldbe
consideredinapatientwithgout:5–10%ofrenalcalculiintheUnitedStates
arecausedbyuricacid;thisisparticularlycommonamongpatientswithgout
whohavebeentreatedwithuricosuricagents(e.g.probenecid).
• Sarcoidosis can cause hypercalcaemia and hypercalciuria, which in turn can
lead to nephrolithiasis and nephrocalcinosis, both of which can rarely cause
post-renalazotaemia.
• Methotrexate and trimethoprim/sulfamethoxazole can cause crystalluria and
renalobstruction.
• Ultrasoundisausefulmodalitytoevaluatebothforthepresenceofobstruction
leadingtohydronephrosisandrenalcalculi.
Intrinsicrenalfailure:‘activesediment’
• Intrinsicrenaldiseasefromarheumatologicalconditionscanpresentacutely
(AKI)orinsidiouslyasevolvingCKD.
• The nephritic syndromes are an important cause of moderate/severe AKI
amongpatientswithrheumaticdiseases,particularlyvasculitisandSLE.
• The presence of haematuria, proteinuria, and red blood cell casts strongly
suggeststhepresenceofglomerulonephritis.
• A renal biopsy is crucial to determining the underlying diagnosis and the
severity/chronicityofthedisease.
• Nephritic syndromes can be divided into ‘focal proliferative’ and ‘diffuse
proliferative’basedonhistology.
• CausesoffocalproliferativeglomerulonephritisincludeSLE,HSP,andother
formsofsmallvesselvasculitis.
• Diffuseproliferativeglomerulonephritisiscausedbycryoglobulinaemia,SLE,
anti-glomerular basement membrane disease (Goodpasture’s syndrome), and
small-vesselvasculitis(includingAAVandrenal-limitedvasculitis).
• Direct immunofluorescence can also provide valuable information regarding
the correct diagnosis: SLE biopsy demonstrates multiple immunoreactants
(‘fullhouse’stainingpattern);IgAdepositionimpliesHSP;cryoglobulinaemic
vasculitisleadstoIgG andC3deposition; sparseorabsentimmunoreactants

onbiopsyissometimescalled‘pauci-immune’,andimpliesanAAV.
Intrinsicrenalfailure:‘blandsediment’
• Ablandsedimentreferstoaurinesamplethatisacellular;transparenthyaline
castsmaybeseen.
• Ablandsedimentisalsoseeninpre-renalandpost-renalazotaemia.
• Acutetubularnecrosis(ATN)reflectsacute,intrinsicrenalfailureassociated
withaurinesedimentthathasmuddybrowncastsandtubularepithelialcells.
• NephrotoxictubularinjuryfromdrugsisacommoncauseofATNinpatients
withrheumaticdisease.
• Prolonged pre-renal azotaemia can lead to permanent kidney damage;
therefore,diseasesoftherenalartery(includingpolyarteritisnodosaandrenal
arterythrombosisfromAPS)shouldbeconsidered.
• Interstitial nephritis is most commonly seen as a drug reaction (e.g. gold,
penicillamine).
• Interstitialnephritiscanalsobeseenasamanifestationofseveralrheumatic
diseases,includingSjögren’s,SLE,sarcoidosis,andEGPA.
• NSAIDscauserenalvasoconstrictionandinterstitialnephritis,bothofwhich
caneventuallyleadtoachronicanalgesicnephropathy.
• UnliketheotherformsofAAV,themechanismofrenalfailureamongpatients
withtheEGPAisaninterstitialnephritis;glomerulonephritisisrelativelyrare
withthisdiagnosis.
• The most common causes of secondary renal amyloidosis are AS, RA and
FMF. Glomerular deposits of amyloid lead to proteinuria (which can be
nephroticrange)andprogressiverenalfailure.
SSclrenalcrisis
• SScl renal crisis is a rheumatologic emergency characterized by AKI and
malignanthypertension(see Chapter25,p.720).
• PatientswithdcSSclareatgreatestrisk.
• SSclrenalcrisisgenerallyoccurswithinthefirst4yearsafterdiagnosis,butit
canoccuratanytime.Patientswhoaretreatedwithhigh-doseglucocorticoids
andareanti-RNPpositiveareathighestrisk.
• Urinalysis generally demonstrates a bland sediment. Kidney biopsy
demonstrates evidence of a thrombotic microangiopathy that histologically
cannot be distinguished from malignant hypertensive nephrosclerosis,
haemolytic–uraemicsyndrome,SLE,orAPS.
• ThecornerstoneoftherapyisescalatingdosesofACEinhibitors,followedby
angiotensin II receptor blockers (ARBs) and calcium channel blockers if

adequatebloodpressurecontrolisnotachieved.
Renaltubularacidosis
• Renaltubularacidosis(RTA)isanon-aniongapmetabolicacidosiscausedby
afailureoftherenaltubulestomaintainacid–basestatus.
• Type I RTA, caused by an inability to excrete acid, is found with Sjögren’s
syndromeandSLE.
• Type IV RTA is most commonly caused by hyporeninaemic
hypoaldosteronism, can occur as a result of treatment with NSAIDs, ACE-
inhibitors,andARBs.Thisiscommonlyassociatedwithhyperkalaemia.
Endocrineconditions
Well-characterized MSK conditions occur in many endocrine disorders. Some
arespecificforcertaindisorders;othersarenon-specific,butoccurwithgreater
frequencyamongpatientswithendocrinedisease.MSKfeaturesoccureitheras
a result of metabolic disturbances or are influenced by a common link in
autoimmunepathophysiology.
Diabetes
• Dupuytren’s contracture, trigger finger, carpal tunnel syndrome, diffuse
idiopathicskeletalhyperostosis(DISH),andadhesivecapsulitisalloccurwith
greaterfrequencyamongpatientswithdiabetes.
• Someformoftissueorjointhypomobility/stiffnessiscommonamongpatients
with diabetes (Table 4.4); in some cases, this can appear similar to
scleroderma.Thesescleroderma-likeskinchangesaremoreprevalentamong
patientswithtypeIdiabetes.
• Handweaknessmaybeduetodiabeticneuropathyandmaybemistakenfor
carpal tunnel syndrome. Neurophysiology tests help discriminate between
thesetwodiagnoses.
• Calcificationofsofttissuesaroundtheshoulderoccursinapproximately20%
ofdiabetics,andisassociatedwithvariablesymptomsanddisability.
• Diabetic amyotrophyisuncommon. Itpresentsacutely with pain,weakness,
and wasting of the proximal lower limb muscles. It may be unilateral.
Differential diagnosis includes myositis (see Chapter 14) and PMR. It is
associatedwithuncontrolledhyperglycaemia.Theaetiologyisunknown,butit
isprobablyaneuromyopathy.
• Though rare (1:500 diabetics), neuropathic arthritis can occur in advanced
disease.Mostpatientsareaged40–60yearsandhavepoorglycaemiccontrol.
Tarsal and metatarsal joints are most frequently affected (60%). The usual
presentationisofswellingofthefootwithnoorlittlepain.Traumamayhave
occurred.EarlyradiographicchangescanresembleOA.
• Asymptomatic osteolysis can occur at the distal metatarsals and proximal
phalangeswithrelativejointsparing:aetiologyunknown.
• Osteomyelitisisnotuncommonandneedstobediscriminatedfromcellulitis
andneuropathicarthritis(Charcot’sjoint).Atriple-phasebonescanshouldbe
helpful. Osteomyelitis is usually disclosed by prominent blood flow in the
dynamic(first)phaseandincreaseduptakeoftracerbysofttissueandbonein
laterstages.Cellulitisisassociatedwithminimaluptakeoftracerin bonein
the delayed (third) phase. Neuropathic joints display minimal first-phase
abnormalitiesbutprominenttraceruptakeinthethirdphase.
• Diabeticmuscleinfarctioncanpresentasapainfulmusclemassandisaresult
of arterial narrowing. Often mistaken for thrombophlebitis, myositis or
vasculitis, this is a late complication of diabetes. Biopsy may be needed to
confirmthisdiagnosis.
• Diabetes may be associated with a ‘metabolic syndrome’ (diabetes +
hypertension,hyperuricaemia,obesity).
Table 4.4 Patterns of joint and tissue hypomobility/stiffness in diabetes by reported series. Tissue
changes are thought to occur from changes in hydration properties/kinetics of glycosaminoglycans
(consequenceofanexcesslocalproductionofsugaralcohols)
Patientseries Majorabnormalities Associations
Diabetics
overall
Inabout30–40%mainlyinlong-
standingdisease:slowdecreaseinhand
mobility;waxyskinthickening
(‘scleroderma-like’)
Occasionallung
fibrosis.
Microvascular
diabetic
complications
Adults 55–76%prevalenceofjoint
hypomobilityintype1/type2diabetes,
respectively
Notassociated
withdiabetic
complications
Mature-onset
diabetes(mean
61years)
Stiffeningofconnectivetissue(assessed
inhands)
Diabetic
nephropathy
Childrenwith
type1diabetes
31%havelimitedjointmobility Nonewith
glycaemic
control,
retinopathy,or
proteinuria
Juvenileand
youngadult
onset(age1–24
years)diabetes
34%hadskinthickening.Changesrarely
proximaltoMCPsandneverproximalto
wrists.Jointcontracturesin>50%,often
thirdorfourthfingers
Noflexortendon
rubs(asseenin
scleroderma)
Hypothyroidism
• Over 25% of patients with hypothyroidism have an arthropathy—cross-
sectional data. The likeliest explanation is coincidental arthritis disease:
generalized OA, CPPD-related (see next bullet point) or an autoimmune
arthritis (e.g. RA). Whether a specific arthritis occurs directly as a result of
thyroidabnormality,isdebatable.
• Radiographically-defined chondrocalcinosis is only marginally increased
comparedwithcontrols(17%vs10%).About1/10patientswithacuteCPPD
arehypothyroid.
• ThyroiddiseasemayalsobeautoimmuneandtheserumANApositive,again
oftenmistakenforassumingthepresenceofaprimaryrheumaticcondition.
• Carpaltunnelsyndromeiscommon(7%).Upto10%ofpatientswithcarpal
tunnelsyndromemayhavehypothyroidism.
• Hyperuricaemiaiscommon,butgoutattacksarerare.However,screeningfor
hypothyroidism in patients with gout is recommended. Treated
hypothyroidism then requires review of the need for uric acid-lowering
therapy.
• Myopathy isrelativelycommon. About1in 20 casesof acquired myopathy
are due to hypothyroidism. The presentation can mimic polymyositis with
elevation of muscle enzymes, but muscle biopsy typically shows no
inflammatory cell infiltrate. Improvement with thyroxine replacement is
sometimescomplicatedbymusclecramps,buttheseshouldresolveinafew
weeks.
• Thecombinationof weakness,muscularstiffness,andan increaseinmuscle
mass in an adult with myxoedema is termed Hoffman’s syndrome. Muscle
massincreaseissometimesstrikingandcantakemanymonthstoresolveon
treatment.
• Lymphocytic thyroiditis (Hashimoto’s) is an autoimmune condition
characterized by hypothyroidism and autoantibodies to thyroglobulin and

thyroid microsomes. These antibodies are found in 40% of patients with
primary Sjögren’s syndrome, but only about 10% are or have been overtly
hypothyroid.
Thyrotoxicosis
• Hyperthyroidismcancauseaproximalmyopathy(70%),shoulderperiarthritis
(7%),acropachy(thickeningofextremities),andosteoporosis.
• Graves’diseaseisfrequentlyassociatedwithfatigueandmuscularweakness.
Itisassociatedwithautoimmunerheumaticandconnectivetissuediseases.
Thyroidacropachy
This is rare (<2% of patients with thyrotoxicosis) and most often occurs in
treatedpatientswhoarehypo/euthyroid.
• Thereisclubbing,andpainfulsofttissueswellingofhandsandfeet.
• Periosteal new bone occurs on the radial aspect of the second and third
metacarpals.
• Acropachyoccursmostfrequentlyinpatientswhohavetheophthalmopathyor
dermopathyassociatedwithautoimmunethyroiddisease.
Hyperparathyroidism
See Chapter16.
Thefollowingpointsrefertobothprimaryandsecondarydisease:
• MSK symptoms are the initial manifestation in up to 16% of patients with
primaryhyperparathyroidism.
• Hyperparathyroidism,chondrocalcinosis,andCPPDfrequentlycoexist.Acute
CPPDcanbetriggeredbyparathyroidectomy.
• ChronicCPPDarthropathycanmimicRA.UnlikeRA,synovialproliferation
isabsent.Radiographically,erosionshaveapredilectionforthecarpus,mid-
feetandsecond/thirdMCPJs.Pericapsularcalcificationisoftenpresent.
• An erosive polyarthritis favouring the large joints can occur with renal
osteodystrophyinpatientswithchronicrenalfailureondialysis.Itmayrelate
to a number of different, or combination of, crystal induced inflammatory-
basedmechanisms(hydroxyapatite,basiccalciumphosphate,pyrophosphate,
urate).
• Hyperparathyroidism is associated with a specific shoulder arthropathy
characterizedbyintra/periarticularerosionsofthehumeralhead.Thismaybe
sub-clinical.
• Subjective muscle weakness and fatigability are common complaints.
Typically,muscleenzymesarenormalandbiopsyshowstypeIIfibreatrophy;
thefeaturesofaninflammatorymyopathyaregenerallyabsent.

• The hallmark of radiographic changes is bone resorption: sub-periosteal
(typically on the radial side of second and third phalanges), intracortical,
subchondral, trabecular, sub-ligamentous, and localized (Brown’s tumours)
resorptionpatternsareseen.Bonesclerosis,periostitis,andchondrocalcinosis
alsooccur.
• Fragility fracture is common and often precedes a diagnosis of primary
hyperparathyroidism. Although significant and fast accretion of bone occurs
aftersurgery,bonemassoftenremainslowlongterm.
Acromegaly
• Over-stimulation of bone and connective tissue cells from excessive growth
hormone can result in several features: bursal and cartilage hyperplasia,
synovial and bony proliferation, an OA-like picture, backache, and
hypermobility.
• Joint complaints usually manifest about 10 years after the onset of clinical
acromegaly.Kneesarefrequentlyaffected.
• Jointsymptomsarenottypicalofaninflammatoryarthritis.Morningstiffness
isnotprominentandjointswellingispresentin<50%.
• Carpaltunnelsyndromeaffects>50%andisfrequentlybilateral.
• Backandneckpainandradicularsymptomsfromnerverootcompressionor
spinalstenosisarenotuncommonandarerelatedtoaxialbonyproliferation.
• Apainlessproximalmyopathyoccursinfrequently.
• Radiographs characteristically show widened joint spaces (e.g. >2.5 mm in
adult MCPJs) and a thickened heel pad (>23 mm in men and >21.5 mm in
women).
• Diagnosis relies on demonstration of a failure of growth hormone to be
suppressedbyaglucosetolerancetest,butalateralskullradiographisagood
screeningtestas90%haveenlargementofthepituitaryfossa.
Gutandhepatobiliaryconditions
MSK features frequently occur in patients with gut or hepatobiliary disease
(Table4.5).
• Dataonthefrequencyofrheumatologicalfeaturesarelargelybasedonstudies
ofhospitalpatientswithclinicallyovertgutorbiliarydisease—leadingtoan
underestimateofthefrequencyofassociation.
• Well-establishedassociationsinclude:
• toxiceffectsofmedications(e.g.NSAIDs;see Chapter3).
• irritablebowelsyndromeandfibromyalgia.

• functionalGImotilitydisorders(e.g.SScl,EDS).
• sacroiliitis,arthritis,andenthesitisinpatientswithSpAandIBD.
• degenerativearthritisinhaemochromatosisandWilson’sdisease.
• The frequency of enthesitis in patients with IBD may be underestimated.
Enthesitismaybedetectedatthemedial/lateralhumeralepicondyles,Achilles’
tendon insertion, calcaneal plantar fascia origin and insertion, greater
trochanters, and the patellar tendon origin and its insertion at the tibial
tubercle.
• Radiology studies in patients with IBD suggest that sacroiliitis is under-
recognizedbyclinicians.
Severityofrheumatologicmanifestations
• Optimal surveillancestrategiesfor the MSKmanifestationsof gut or biliary
diseasearenotknowninmanyinstances.
• Faecalcalprotectinisasensitivemeasure forIBDscreeninginpatientswith
SpA,butmodestelevationscanoccurinanumberofscenarios.
• Life-threateningvasculitismayoccurfromchronicviralinfection.HepatitisB
is associated with polyarteritis nodosa, and hepatitis C may lead to
cryoglobulinaemicvasculitis.
• In mostpatients whodevelopjoint inflammationor enthesitisafterbacterial
dysentery,theconditionisself-limiting.Chronicityandseveritymaybelinked
toHLA-B27.Progressivespondylitisisrare.
Gutandhepatobiliaryconditionsinpatientswithrheumaticdiseases
(Tables4.6and4.7;alsosee Chapter15,‘Vasculitis’)
• Themostcommon problemamongpatientswithRAisdyspepsiaassociated
withgastroduodenalerosionsorulcersduetoNSAIDs.Pepticlesionsmaybe
clinicallysilentandmaypresentwithdroppinghaemoglobinlevelsoranacute
bleed.
• RAmaybethemostcommoncauseofAAamyloidosis.Biopsiesoftheupper
GI tract will demonstrate amyloid deposits in 13% of patients. There are
numerous GI manifestations of amyloidosis, including GI haemorrhage,
malabsorption,obstruction,andhepatosplenomegaly.
• InSLE,seriousgutandhepatobiliarymanifestationsarerelativelyuncommon
(5%),butnausea,anorexia,vomiting,anddiarrhoeaarequitefrequent.
• SSclhasnumerousGImanifestationsincludingrefractorygastro-oesophageal
reflux disease, gastric antral vascular ectasia (‘watermelon stomach’),
oesophagealdysmotility,bacterialover-growth,andfaecalincontinence.
• TherefluxassociatedwithSScloftenrequirestreatmentwithhigh-doseproton
pumpinhibitors.
• ‘Watermelonstomach’canleadtosignificantacuteandchronichaemorrhage.
• In SScl, bloating and abdominal distension caused by bacterial overgrowth
mayrespondtocycliccoursesofantibiotics.
• Mesentericvasculitisisclassicallycausedbypolyarteritisnodosa,butcanbe
seenwithavarietyofrheumaticillnesses,includingTakayasuarteritis,AAV,
and (rarely) with SLE. Although mesenteric angina is the symptom most
strongly associated with mesenteric vasculitis, the earliest sign of intestinal
ischaemiaisdiarrhoea.
• HSP is an IgA-mediated small vessel vasculitis that presents with colicky
abdominal pain and purpura (adults and children). Although generally mild
and self-limited in children, it can occasionally cause intussusception and
bowelnecrosis.
Table4.5Associationsbetweengastrointestinal(GI)andrheumaticdisorders
GIdisorder> Rheumatic
disorder
Association
Entericinfection Reactivearthritis:
self-limitinginmost
Arthritisin2%whogetShigella,
Salmonella,Yersinia,
Campylobacter,Clostridium
difficileoverallbutin20%of
infectedwhoareHLA-B27+
Crohn’sdisease Arthritis20%.AS
10%.Sacroiliitisin
26%
60%ofspondyloarthritispatients
havehistologicalevidenceof
bowelinflammation.Seealso
belowintable
Ulcerativecolitis Arthritis20%.AS
7%.Sacroiliitis
15%
Seealsoaboveintable.Severity
ofgutandjointinflammation
variesinitsassociationbutSI
joint/pineinflammationdoesnot
Whipple’sdisease Migratoryarthritis
in>60%
Tropherymawhippleiidentifiedin
smallbowel.Diarrhoeaoccursin
>75%ultimately
Intestinalbypass
surgery(blindloop
Polyarticular
symptoms50%in
Intestinalbacterialovergrowthin
smallbowel?Associatedwith
syndrome) scleroderma jointsymptoms
Coeliacdisease Arthritisisrare ?Increasedintestinalpermeability
Viralenteritis Rare(<0.5%) Mostcommon:Coxsackieorecho
HepatitisA Arthralgia15%.
Vasculitisrare
Causalassociation
HepatitisB Arthralgia10–25%.
PAN
Aetiological
HepatitisC Sialadenitisin
>50%.Vasculitis
(cryoglobulinaemic)
?AetiologicalinSjögren’s
syndrome.HepatitisCidentified
in27–96%ofpatientswith
cryoglobulinaemia
Primarybiliary
cirrhosis
Polyarthritis19%.
Scleroderma18%.
Sjögren’s50%
Autoimmune‘overlap’.Features
maybesubclinical
Chronicactive
hepatitis
Polyarthralgiaor
arthritisin25–50%
Autoimmunity
Haemochromatosis OA50% Ironstoragedisease
Wilson’sdisease OAin50%adults.
Chondrocalcinosis
Copperstoragedisease
Table4.6GutandhepatobiliarymanifestationsofrheumatologicaldiseasesI:general
Disease Abnormalities Presentationwith
Rheumatoidarthritis(see
Chapter5)
TMJarthritis.
Oesophageal
dysmotility
Impaired
mastication
Dysphagia,reflux
GIvasculitis(0.1%) Ulcers,pain,
infarction
Portalhypertension Splenomegaly
(Felty’s)
Liverinvolvement
(Felty’s)
Enzyme
abnormalities
Hepatosplenomegaly Palpableviscera
Systemiclupus(see Chapter
10)
Oesophageal
dysmotility
Dysphagia,reflux
GIvasculitis Ulcers,pain,
perforation
Protein-losing
enteropathy
Hypoalbuminaemia
Peritonitis Ascites(10%),
serositis
Hepatosplenomegaly
(30%)
Palpableviscera
Scleroderma(see Chapter13) Oesophageal
dysmotility
Heartburn/dysphagia
Delayedgastric
emptying
Aggravatedreflux
Intestinal
dysmotilityand
fibrosis(80%)
Malabsorption,
pseudo-obstruction
(<1%)
Pseudo-andwide-
mouthdiverticula
Haemorrhage,stasis,
bacterialovergrowth
Polymyositisand
dermatomyositis(see Chapter
14)
Muscleweakness Aspiration,
dysphagia
Disorderedmotility Dysphagia,
constipation
Vasculitis(rare) Ulcers,perforation
MCTD Hypomobility Dysphagia,reflux,
pseudo-obstruction
Sjögren’ssyndrome(see
Chapter12)
Membrane
desiccation
Xerostomia,
dysphagia
Oesophagealwebs
(10%)
Dysphagia(>60%)
Gastric
infiltrates/atrophy
Masses,dyspepsia
Pancreatitis Pain,amylasaemia
Hepaticdysfunction Hepatomegaly
(~25%)
Hepaticcirrhosis Primarybiliary
cirrhosis
Spondyloarthritis(see
Chapter8)
Ileocolonic
inflammation
Maybe
asymptomatic
Adult-onsetStill’sdisease Hepatitis,peritonitis,
hepatosplenomegaly
Painorabnormal
enzymes(~75%)
SystemicJIA
(see Chapter9)
Serositis Abdominalpain
Hepatomegaly Abnormalenzymes
Marfansyndrome,joint
hypermobilitysyndrome,
Ehlers–Danlossyndrome(see
Chapter19)
Defectivecollagen Hypomotility,
malabsorption,
visceral
rupture/laxity
Functional GI
disorders
Table4.7GutandhepatobiliarymanifestationsofrheumaticdiseasesII:vasculitis.Seealso Chapter
15
Disease FrequencyofGIvasculitisandfeatures
Polyarteritis
nodosa
80%(mesenteric).Buccalulcers,cholecystitis(15%),
bowelinfarction,perforation,appendicitis,pancreatitis,
strictures,chronicwastingsyndrome
Henoch–
Schönleinpurpura
44–68%.Abdominalpain,melena,haematemesis,
ulcers,intussusception,cholecystitis,infarction,
perforation,appendicitis
EGPA ~40%.Haemorrhage,ulceration,infarction,perforation
Behçet’sdisease Buccalandintestinalulcers,haemorrhage,perforation,
pyloricstenosis,rectalulcers
Systemiclupus
erythematosus
2%.Buccalulcers,ileocolitis,gastritis,ulceration,
perforation,intussusception,volvulus(1%),pneumatosis
Kawasakidisease Abdominalpain,intestinalobstruction,non-infective
diarrhoea
AAV <5%.Cholecystitis,appendicitis,ileocolitis,infarction
Juvenile
dermatomyositis
Wellrecognized.Perforation,pneumatosis
MCTD Rare.Ulceration,perforation,pancreatitis
RAandJIA 0.1%.Buccalulcers,abdominalpain,pepticulcers,
acalculus-cholecystitis,gutinfarction,andperforation
Polymyositisand
dermatomyositis
Veryrare.Mucosalulcers,perforation,andpneumatosis
Cryoglobulinaemia Rare.Ischaemiaandinfarction
Gutandhepatobiliarysideeffectsfromdrugsusedintreatingrheumatic
andbonediseases
(Seealso Chapter23.)
Themainrheumatologydrugscausingsideeffectsare:
• NSAIDs—whichareacommoncauseofGIdistress.COX-2inhibitorswere
developed to decrease the risk of peptic ulcer disease; most have been
withdrawn from the market due to concerns regarding increased risk of
cardiovascular events and those remaining may be no more effective than
takingaconventionalNSAIDwithaprotonpumpinhibitor.
• Glucocorticoidsmaycausegastritis,pepticulcerdisease,andGIhaemorrhage.
Althoughtheabsoluteincreaseineventsissmall,thecombinationofsteroids
andNSAIDsresultsinasynergisticincreaseintheriskofGIsequelae.
• Methotrexate (MTX) may cause stomatitis, which may respond to
supplemental folate. Nausea, emesis, and dysgeusia may respond to dose
reduction. MTX can cause a transaminitis; it is therefore recommended that
patientsminimizealcoholintake.
• Sulfasalazinegutandhepatobiliarysideeffectsarecommonandmayoccurin
up to 20% of patients. The most frequent are mild: indigestion, nausea,
vomiting,anorexia,andabdominalpain.Gutulceration,bloodydiarrhoeaand
seriousliverproblems arerare;in 65%ofpatients, sideeffects occurin the
first3monthsoftreatment.
• Azathioprine(AZA)cancausenausea(15%),vomiting(10%),andabdominal
pain(8%).Diarrhoeaisrare(5%).Liverenzymeabnormalitiesareoftenmild
andmayremitonloweringthedose.TheGIsideeffectscanoccurinpatients
withnormallevelsofthiopurinemethyltransferase.
• Penicillaminecausesalteredtaste(25%withinthefirst3–6months),nauseaor
vomiting (18%), and stomatitis/mouth ulcers (5%). Hepatotoxicity and
haemorrhagiccolitisarerare.
• Chloroquine and hydroxychloroquine, can cause non-specific GI intolerance
(10%).Theonsetisofteninsidious.
• Ciclosporin causes gingival hyperplasia, nausea, diarrhoea, and elevation in
hepaticenzymes.
• Effects of cyclophosphamide on the gut are frequent: nausea, vomiting,
diarrhoea,andstomatitis.Serioushepatotoxicityisrare.
• Leflunomidecancausenausea(8–13%),diarrhoea(upto25%),andabnormal
liverenzymes.Instudies,mostrisesintransaminaseshavebeenmild(<2-fold)
andarereversibleondrugwithdrawal.
• Oralbisphosphonates(suchasalendronicacidandrisedronate)andstrontium
ranelate cancausenausea, dyspepsia, and diarrhoea.Oesophagealulceration
has occasionally been noted with alendronate, although it is thought this
occurs only in people who do not follow the instructions for taking them.
Myalgiasandarthralgiascanalsooccurwithbisphosphonates.
• Calcitonin either given as subcutaneous injection or as nasal spray cangive
abdominalpainsanddiarrhoea.
Malignancy
Rheumatic MSK features may be clues to the existence of cancer. Symptoms
may arise directly from neoplastic tissue invasion or indirectly as a
paraneoplasticphenomenon.
Primaryandsecondaryneoplasticdiseasesofboneandjoints
• Synovialtumoursarerare.Sarcoma(synovioma)ismorecommoninmenthan
womenandunusualinthose>60years.Itusuallyoccursinthelegs(70%)and
can occur around tendon sheaths and bursa. At diagnosis, pulmonary
metastasesarecommon.
• Para-articular involvement by bone tumours may give a monoarticular
effusion.Invasionofsynoviummayoccurandmalignantcellscanbedetected
injointfluid.Breast,bronchogeniccarcinoma,GItumours,andmelanomacan
allmetastasizetojoints.
• Lymphomas and leukaemias may simulate various conditions especially in
childrenandcausesynovitisinasingleorinmultiplejoints.
• Arthritiscomplicatingthepresentation ofmyeloma oran acuteleukaemiais
mostlikelytobepolyarticularandasymmetric.
• Inadults,arthritiscomplicatingleukaemiaisrare(5%ofcases).
• Leukaemia is the most common cause of neoplastic skeletal symptoms in
childhoodandadolescence(15%ofleukaemiacases).
• Neuroblastomasarethemostfrequentcauseofasolidtumourmetastasizingto
theskeletoninchildren.
CluesthatmayleadtoasuspicionofmalignancydirectlycausingMSK
symptoms
• Constitutionalsymptomswithoutevidenceforvasculitis.
• Thecoexistenceofbonepainfrommetastases(see Plate16).Also,consider
metabolicbonediseases,sarcoid,SAPHOsyndrome,andtheSpAconditions.
• Haemorrhagic joint fluid (also consider trauma, PVNS,
chondrocalcinosis/pseudogout).
• Radiographsthatshowadjacentbonedestruction,perhapswithlossofcortex
(alsoconsiderinfection).
• Radiographiccalcificationinsofttissuemass(considersynovioma).
Paraneoplasticidiopathicinflammatorymyopathy(IIM)
• IIMsmaybeduetocarcinomatousneuromyopathy.
• Polymyositis, dermatomyositis, Eaton–Lambert myasthenic syndrome
(ELMS), and hypophosphataemic (oncogenic) osteomalacia are all found in
associationwithmalignancy(Table4.8).
• Carcinomatous neuromyopathy is characterized by symmetric muscle
weaknessandwastingandcanpre-datethemalignancy.
Table4.8Myopathyandlinkswithmalignancy
Condition Typical
patternof
weakness
Commoncancer
associations
Otherfeatures
Carcinomatous
neuromyopathy
Pelvicgirdle
—symmetric
Lung:15%men,
12%women.
Ovary:16%.
Stomach:7%men,
Wasting,EMG
abnormality,and
increaseinmuscle
enzymesarenot
13%women invariable
Dermatomyositis
(+?PM)
Proximal
limb.Truncal
Reflectsunderlying
cancerfrequencyin
localpopulation
Responsetosteroids
isusual
Myasthenia
gravis(MG)
Frequently
ocularand
bulbar
muscles
involved
Thymus.Any Musclestrength
fluctuates
(fatiguability).
Respondstoanti-
cholinesterases
Eaton–Lambert
myasthenic
syndrome
(ELMS)
Pelvicgirdle
muscles.
Alteredgait.
Ocular
musclesnot
affected
Smallcelllung.Can
occurupto2–3
yearsafterELMS
Autonomic
disturbances.EMG
+poorresponseto
anticholinesterase
distinguishfrom
MG
Oncogenic
osteomalacia
Generalized.
Develops
insidiously
Small,discrete
mesenchymal
tumoursinbone,soft
tissues,andsinuses.
Neurofibromatosis
Bonepainand
osteomalacia.High
FGF23,
hypophosphataemia
andlow1,25(OH)
2
-
vit-D
Non-myopathyparaneoplasticsyndromes
• Thenon-myopathicparaneoplasticsyndromesarerare.
• Hypertrophic pulmonary osteoarthropathy consists of clubbing, periostitis of
diaphysisoflongbones,andanarthropathy(variesfromarthralgiastodiffuse
polyarthritis). Suspicion of HPOA should be investigated with bone
scintigraphy,whichtypicallyshowsincreasedradionuclideuptakeinaffected
bones.Radiographsoftenshowperiostealelevation.
• HPOA complicates 20% of primary lung tumours, but it is associated with
othermalignancies.
• Polyarthritis may be the presenting feature of cancer. Most cases occur >60
years old. The arthritis associated with malignancy tends to be asymmetric,
anddoesnotcauseerosions.
• Eosinophilic fasciitis, severe bilateral palmar fasciitis (often mistaken for
scleroderma), and fasciitis associated with panniculitis have been associated

withmalignancy.
• Casesof‘shoulder–hand’syndrome(aformofosteodystrophy;see Chapter
22)havebeenreportedinassociationwithmalignancy.
Rheumatologicaldiseasesassociatedwithanincreasedincidenceof
malignancy
AnumberofrheumaticMSKdiseasesareassociatedwithanincreasedincidence
ofmalignancycomparedwithhealthypopulations.
• Non-Hodgkin’slymphomaismoststronglyassociatedwithRA.Myelomaand
paraproteinaemiaarealsofoundinRApatients.
• TherelativeriskofcoloncanceramongRApatientsis0.77;thismaybedueto
theuseofchronicNSAIDsinthispatientpopulation,whichmaybeprotective.
• Non-Hodgkin’s lymphoma develops in a subset of patients with Sjögren’s
syndrome(4%).Itsonsetmaybeindicatedbyrapidenlargementofsalivary
glands, the appearance of a paraprotein, or decrease in circulating
immunoglobulinsorRFtitre.
• SSclhasbeenassociatedwithanincreasedriskofbothlungcancerandnon-
Hodgkin’slymphoma.
• Dermatomyositisisprobablyassociatedwithmalignancyinadults,thoughas
convincing evidence for an association of polymyositis with malignancy is
lacking.Gonadaltumoursarerelativelycommonamongsuchpatients.
• Eosinophilicfasciitismaybeassociatedwithmalignancy.
Rheumatologicaldrugsandmalignancy
(Seealso Chapter23.)
• Chronicazathioprineuseisassociatedwithanincreasedriskofskincancerso
patients taking azathioprine long term should be counselled regarding sun
protectionandmonitoringforskincancer.
• Use of cyclophosphamide is associated withanincreasedriskof lymphoma
andbladdercancer.
• Anti-TNFαdrugtherapyistheoreticallyassociatedwithariskofmalignancy.
However,patientdiseaseregistrieshavenotidentifiedanexcessincidencein
patientstreatedlong-termwiththetherapy.
• If malignancy develops while a patient is taking anti-TNFα then usually its
correcttostopthetherapy.
• Thereisincompletedataonwhetherstartinganti-TNFαincreasestheriskof
relapse of malignancy in patients previously treated successfully for their
cancer.
• Though very high dose per weight teriparatide is associated with sarcoma

developmentinrats,thereisnoevidence,atdosesusedinhumans,thatthere
isanincreasedrisk.
• Thefollowinghavenotbeenassociatedwithanincreasedriskofmalignancy
(as of 2016): sulfasalazine, leflunomide, rituximab, abatacept, apremilast,
ustekinumab,secukinumab,belimumab,anddenosumab.
Neurologicalconditions
Entrapment neuropathies and radicular lesions are discussed in Chapter 3.
Also,radiculopathyisincludedin Chapter21.
Inflammatoryperipheralneuropathy
• Inflammatory neuropathies can occur as part of any AICTD, though are
probably most likely to occur in association with SLE and Sjögren’s
syndrome.
• Vasculitis(andprobablyAPS)cancausesmallvesselvascularlesionswhich
compromiseperipheralnervefunctionandcausesensory,andifsevere,motor
featuresofnervedamage.
• Nerveconductionstudiesmayformpartoftheinvestigationsattheoutsetof
characterizingsystemicvasculitisandsevereAICTDs.
• Mononeuritis occurring as part of RA is possible but nowadays is very
unlikelyunlesssevereRAdiseaseisleftuntreated.
Entrapmentneuropathies
• Entrapmentneuropathiesarecommoninrheumatologicalpractice.Symptoms
arising from these lesions include paraesthesiae, a feeling of swelling,
numbnessandaburningqualitytopaininthedistributionofthetrappednerve.
• Median nerve irritation/entrapment may be secondary to carpal OA or
inflammationsecondarytoinflammatoryarthritis.
• Ulnar nerve irritation (fourth and fifth finger territory symptoms) is most
commonlyassociatedwithmedialelbowlesions.
Spinalcordlesions
Spinal cord lesions usually arise due to intrinsic spinal canal or extrinsic
compressionorinflammation.
• Tumours andischaemicspinal cord lesionsoftenpresent acutely withupper
motor neuron features distal to the affected level and issues of bladder and
bowelsphinctercontrol.
• Sometumoursandsyrinxes(thoracic,neck)cancausesubacuteevolutionof
pyramidalfeaturesinthelegs(oftennotpainbutstiffnessandmotorfunction
problems).
• Extrinsic cord compression can occur secondary to tumours, osteoporotic
vertebral and a combination of (usually degenerative) lesions. In the latter,
spinalcordcompressionisrarelyacuteandbecauseitevolvesveryslowlyis
oftenoverlookedintheelderly.
• Transverse myelitis causes acute focal back pain and distal spinal cord
symptoms and features including acute lower limb motor symptoms. It is a
featureofSLEandAPS.
Cerebrovascularlesions
• Acute cerebellar or stroke-like symptoms can be a presenting feature of
ischaemiclesionssecondarytoAPS.Ifoccurringinthenon-elderly<60years
thenscreeningforAPSandSLEismandatory.
• Cerebrallupuscanbepresentwithprofoundsymptomsofconfusionandbrain
functiondecompensationormaybesubtlerpresentingwithmildcognitiveor
frontalcortexdysfunction.
• Conventional stroke disease is a complication of many inflammatory
rheumatic diseases, probably most associated with APS and ongoing poorly
controlledinflammatorydiseaseandinthecontextofotherriskfactors(e.g.
smoking, metabolic syndrome in PsA, glucocorticoid-associated
hyperlipidaemia).
Headache
• Among the causes of headache in rheumatological practice, neurological
causesareprobablyrare.
• The hemicranialheadache (withscalp sensitivity)of GCA anddrug-induced
headachearethemostlikelycausesofheadacheencounteredinrheumatology
patients.
• Other causes of headache occasionally encountered are the global headache
fromcranialsinusthrombosisinBehçet’sdisease,andmeningeallesions(e.g.
inneurosarcoid).
Neuromyopathy
• Neuromyopathies may present to rheumatologists with focal pain or
generalizedpainandweakness.
• Focal neuromyopathies can occur after nerve trauma or infection. Marked
acutewastingwithpain,often withraisedCKand amyositis-typesignalon
MRI,canbeseen.
• Fluctuatingneuromyopathiceffectscanoccurinmyastheniagravis.Theremay
beavariationofeffectsoveradaywithmusclefatigueinfluencingthetiming,
characteristics, and severity of weakness. Symptoms can be focal—as in
orbital muscle myasthenia, which can present initially with diplopia—or
generalinvolvinglargermusclegroups.
Ophthalmicconditions
Blepharitis, conjunctivitis, uveitis, and ischaemic lesions can all occur with
rheumaticMSKdiseases.
Dryeye(xerophthalmia)
• Xerophthalmiaoftenpresentswithsoreorgrittyeyesandsensitivityincertain
atmospheric environments (e.g. air-conditioning). Oddly patients can get
epiphoraeiftearfilmisnotdrainedbecauseofinferiororbitalductblockage
throughtothesinuses.
• Blepharitisisoftenaconsequenceofdryeye—lidscanget‘sticky’.
• XerophthalmiaismostsevereinprimarySjögren’ssyndromebutcanoccurin
SOX syndrome and all autoimmune joint and connective tissue diseases
(secondarySjögren’ssyndrome).
Uveitis
• Anterior uveitiscanbe acuteorchronic. Symptomsincludeocular painand
photophobia.Theeyebecomesvisiblyerythematous.
• The most common associations of anterior uveitis include SpAs, sarcoid,
Behçet’sdisease,andJIA.
• All children and adolescents diagnosed with any form of JIA, regardless of
ANAstatus,shouldhaveaneyeexaminationtoruleoutuveitis.
Ischaemicophthalmiclesions
• Retinalexaminationisthemostdirectandaccessiblewaytovisualizeblood
vesselsinvivo.
• Ophthalmicexaminationisvaluableintheassessmentofsystemicvasculitis.
• The input of an experienced medical ophthalmologist is essential in
departmentsthatofferaservicetomanagevasculitispatients.
• The ischaemic lesions of GCA can present variably but most typically with
amaurosissymptoms(visualfieldcurtaining).
Scleralandcornealdisease
• Lesions ofthe scleraand corneaare rarein rheumatologypatientsexceptin
severe(usuallyhigh-titreseropositive)RApatients.
• ScleralorcornealdiseaseinanRApatientshouldpromptconsiderationofthe
presenceofsystemicRAvasculitis.
Other
• ProptosisisarecognizedfeatureofAAVandisusuallyduetogranulomatous
inflammationintheretro-orbitalspace.
• Conjunctivitis can accompany many diseases but is an acute lesion insome
casesof(SpA-associated)reactivearthritis.
• Ophthalmoplegiaisarecognizedpresentingfeatureofmononeuritisassociated
with systemic vasculitis. Cerebrovascular disease (thus APS and GCA also)
shouldbeconsideredaspossibleinrelevantpatientsalso.

Chapter5
Rheumatoidarthritis
Introduction
Clinicalfeatures
Investigations
Management
Introduction
Epidemiology
Rheumatoidarthritis(RA)isthemostcommoninflammatoryarthritis,withan
incidence in the general UK population of 1.5 and 3.6 per 10,000 people per
year,formaleandfemalesrespectively.
• RAaffectspeopleworldwideandaffectsfemalesmorefrequentlythanmales,
withaF:Mratioof~3:1.
• RAmostcommonlyoccursatage45–65yearsalthoughitcanoccuratanyage
—occurringasadistinctdiseaseinchildhood.
Classification
The updated ACR/EULAR 2010 classification criteria (Table 5.1) have been
designedtoidentifyearlyRA.However,theyshouldnotbeusedtoexcludethe
diagnosisifallcriteriaarenotmet;clinicaljudgementshouldbeused.
Pathogenesis
RA is an autoimmune inflammatory disease, manifest primarily in synovial
tissues, mediated by interaction between T lymphocytes, B lymphocytes, and
synovialfibroblasts,leadingtodysregulationoftheinflammatorycascade.
• SmokingincreasestheriskofdevelopingRA.
• FamilialRAdoesexistbuttheoddsratioofdevelopingRAifthereisafirst-
degreerelativewiththediseaseisonly1.1.
Immunopathology
Overproductionofinflammatorycytokines,inparticulartumournecrosisfactor-
α(TNFα)andinterleukin-6(IL-6),iscentraltothepathologyofRA.
• Persistentinflammationleadstoincreasedvascularityandinflammationofthe
synovialliningofjoints(synovitis),andsecondarycartilagedegradation(joint
spacenarrowing)andboneerosion.
• Autoantibodies are seen in 50–80% of RA cases, in particular rheumatoid
factor(RF)andanticitrullinatedpeptideantibodies(ACPA).
• ThesensitivityandspecificityofACPAforidentifyingRAisgreaterthanthat
ofRF(67%and95%forACPAvs69%and85%forRF,respectively).
1
• PositivityforbothRFandACPAhasanear100%positivepredictivevaluefor
subsequentdevelopmentofRA.
• Genetics also contribute to the risk of developing RA. HLA-DRB1 is most
commonlyassociatedwithRA,andisoftenreferredtoasthe‘sharedepitope’.
Table5.1ACR/EULAR2010classificationcriteriaforrheumatoidarthritis
Target population is patients who have ≥1 joint with definite clinical
synovitis(swelling)*withthesynovitisnotbetterexplainedbyanother
disease.
Classification criteria for RA. Add score of categories A–D; a score of
≥6/10isneededforclassificationofapatientashavingdefiniteRA.
‡
Score
A.Jointinvolvement
§
1largejoint
¶
2−10largejoints
1−3smalljoints(±involvementoflargejoints)**
4−10smalljoints(withorwithoutinvolvementoflargejoints)
>10joints(>1smalljoint)
0
1
2
3
5
B.Serology(atleast1testresultisneededforclassification)
‡‡
NegativeRFandnegativeACPA
Low-positiveRForlow-positiveACPA
High-positiveRForhigh-positiveACPA
0
2
3
C.Acute-phasereactants(atleast1testresultisneeded)
§§
NormalCRPandnormalESR
AbnormalCRPorabnormalESR
0
1
D.Durationofsymptoms
<6weeks
≥6weeks
0
1
*Criteriaareaimedatclassificationofnewlypresentingpatients.Patientswitherosivediseasetypical
ofRAplushistorycompatiblewithfulfilmentofthe2010criteriaandpatientswithlong-standing
disease,shouldbeclassifiedashavingRA.
‡
Althoughscores<6/10arenotclassifiedashavingRA,criteriamaybereassessedandfulfilled
cumulativelyovertime.
§
Jointinvolvementreferstoanyswollenortenderjoint,whichmaybeconfirmedbyimagingevidence
ofsynovitis.DIPJs,1stCMCand1stMTPjointsareexcluded.
¶
‘Largejoints’areshoulders,elbows,hips,knees,andankles.
**‘Smalljoints’areMCPJs,PIPJs,2ndto5thMTPJs,thumbIPJsandwrists.
‡‡
‘Negative’referstointernationalunit(IU)valuesthatare≤totheupperlimitofnormal(ULN)forthe
laboratoryassay;low+vereferstoIUvaluesthatarehigherthantheULNbutlessthan3×theULNfor
thelaboratoryandassay;high+vereferstoIUvaluesthataremorethan3×theULNforthelaboratory
andassay.Ifonly+veor−veRFinformationisavailable,a+veresult=low-positiveforRF.
§§
Normal/abnormaldeterminedbylocallaboratorystandards.
ACPA,anti-citrullinatedproteinantibody;CRP,C-reactiveprotein;ESR,erythrocytesedimentationrate
GuidelinesreproducedfromAletahaDetal.2010‘RheumatoidArthritisClassificationCriteria’(2010)
Arthritis&Rheumatism62:92569–2581withpermissionfromJohnWileyandSons.
Synovialpathology
Theexactreasonwhysynoviumistargetedisunknown.Synoviuminjointsand
tendons becomes inflamed and local tissue damage of cartilage, bone, and
surroundingtissuesensues.
• Thereisincreasedsynovialvascularity,influxofmonocytesandplasmacells,
andactivationoftissuemacrophagesandfibroblasts.
• Synovialplasmacellsarenumerousandproduceantibodieswhichwillhavea
proinflammatorylocaleffect.
• Cellular activation of cytokines locally results in bone resorption activating
osteoclastscausingboneerosion.
• Inseverecases,cellularaggregationcanleadtolymphoidfolliclesformingin
thesynovialtissue.
• Extra-synovial inflammation includes rheumatoid nodule formation and
inflammationoflungandcardiactissue.
Reference
1. NishimuraK,SugiyamaD,KogataY,etal.Meta-analysis:diagnosticaccuracyofACPAandRFfor
RA.AnnInternMed2007;146:797–808.
Clinicalfeatures
RAischaracterizedbyswelling,pain,andstiffnessofsynovialjoints,systemic
features,andinvolvementofextra-articularorgansandtissue.
Jointsandtendons
RA typically affects the small joints of the hands and feet, but can affect any
joint (bursa or tendon) where there is synovial tissue (e.g. elbows, shoulders,
ankles,knees,hips,andTMJs).
• Symptomscharacteristicallyincludestiffnessworseinthemorning,andlasts
for>30min.
• Joint symptoms develop over weeks, but can also do so over a few days.
Occasionally symptoms can have a migratory onset over months, with
temporaryperiodsofresolution/improvement.
• Movementoftheaffectedjointsoftenalleviatesstiffnessanddiscomfortinthe
earlystagesofthedisease.
• Active movement ofaninflamed joint can cause‘gelling’ wherethepatient
describesanabruptmomentary‘paralysis’ofmovement.
• The functional impact of joint symptoms should be assessed. The Health
Assessment Questionnaire (HAQ) is helpful to provide a standardized
assessmentofdisability.
• Examinationshouldfocusonanyaffectedjoints,assessingforthedegreeof
swelling,warmth,andrangeofmovement.
• Joint or tendon synovitis may not be detectable clinically in the early/mild
stages of disease. Boggy swelling over the joint line is indicative of joint
synovitis.Ballotablejointeffusionscanbepresentiflargerjointsareinvolved.
• In the early stages of the disease, deformities are not seen; however, in
aggressive,longstanding,oruntreateddisease,deformitycanoccurandleadto
significantdisability.
• DeformitiesseeninRAinclude:
• ulnardeviationatthewrist,oftenaccompaniedbyadepressibleprominent
ulnastyloid(piano-keysign).
• swan-neckandboutonnieredeformitiesmay beidentifiedinthefingersin
advanceddisease.
• fixedlossofextensiondeformities.
• limited shoulder movement, due to joint erosion, effusion, or ligament
rupture.
• lateraldeviationofthetoes.
• subluxation of the metatarsal heads leads to discomfort when walking.
Callosities, skin degradation, soft tissue infection, and osteomyelitis may
ensue.
• Attheatlanto-axialjoint,erosionoftheodontoidcanleadtoanunstableC1–
C2 articulation, with potentially life-threatening consequences from cord or
brainstemcompression.
• Symptoms of atlanto-axial joint involvement can include occipital pain,
syncope,andheadaches.
• Theconsequencesofsmallcervicalfacetjointinvolvementcanbeupperlimb
radicular symptoms and hand weakness, and if the spinal cord is affected,
stiffness(includingoflegs).
• The differentialoflower cervicalradiculopathyiscarpal tunnelsyndrome—
alsoasecondarylesioninRAfromwristjointdisease.
Extra-articularfeatures
• Rheumatoid nodules are associated with seropositivity (RF and ACPA) and
canoccuranywhereinthebody,butaremostcommonlyfoundonthehands,
feet,andelbows.Whenasmallmass/noduleisidentifiedinanyinternalorgan
in a RA patient, cancer must be excluded before attributing the lesion to a
rheumatoidnodule.
• RA is associated with pulmonary fibrosis, exudative pleural effusions, and
pleurisy.
• Splenomegaly is common, and may be part of Felty’s syndrome (RA,
neutropenia,andsplenomegaly).
• LymphadenopathycanbeduetoRAbutpatientsalsohaveagreaterlikelihood
ofdevelopinglymphomacomparedtothegeneralpopulation,soinvestigation
of‘Bsymptoms’isveryimportant.
• Neurological examination may reveal nerve impingement due to synovitis,
tenosynovitis (e.g. carpal tunnel syndrome), joint damage, or bony
impingement(e.g.spinalnerverootimpingement).
• Rheumatoidvasculitiscanpresentasamononeuritismultiplex.
• Leucocytoclasticrashesarerarebutmaycauseskinulceration.
• Themostcommonophthalmicmanifestationisdryeyes(sicca).
• Painful scleritis, leading to scleromalacia, is a serious sight-threatening
condition. Scleral thinning may manifest as a darkening of the sclera, and
requiresurgentophthalmicinput.
Systemicfeaturesandassessment
• Fatigueisoftenaprominentsymptomandischallengingtomanage.
• Disease activity should be assessed using a standardized clinical outcome
measure at each clinical review. The most commonly used measure is the
DiseaseActivityScoreof28joints(DAS28).
• Other disease activity measures include the Clinical Disease Activity Index
(CDAI),andtheSimplifiedDiseaseActivityIndex(SDAI).
Associatedclinicalmanifestations
• PatientswithRAhaveanincreasedriskofdevelopingsepticarthritisdueto
pre-existingjointdamageanduseofimmunosuppressants.
• Active RA commonly is associated with muscle atrophy, primarily due to
reduceduse,butalsoduetosystemicinflammation.
• Osteoporosis is more common in RA than the general population, due to
systemicinflammation,reducedmobility,andsteroids.
• Osteoporosisriskshouldbeassessedinpatients>40yearsusingFRAX
®
(
http://www.shef.ac.uk/FRAX) and in postmenopausal women and men >50
yearsusingFRAX
®
andDXAscanning.
• Patients with RA have an increased cardio- and cerebrovascular risk profile
due to chronic inflammation promoting atherosclerosis. Active risk
managementisimportant.
• Secondaryamyloidosisisincreasinglyuncommon,butshouldbeconsideredin
patientswithlong-standingactivedisease.
Investigations
RA is primarily a clinical diagnosis. However, a set of baseline investigations
can assist in making the diagnosis, and provide a point of reference for
monitoringdiseaseprogression,drugresponse,andtoxicity.
• Laboratory tests should be done to aid diagnosis, as a baseline before and
when monitoring disease-modifying antirheumatic drugs (DMARDs; Table
5.2).
• Imagingcanconfirmaclinicaldiagnosisandcharacterize synovitisin joints
andtendons,evaluatejointandbonedamagefromjointinflammation,andcan
helpexcludealternativediagnoses(Table5.3).
• Key to diagnosis is detection of ACPA and RF. ACPA are as sensitive for
diagnosisofRAasRFbutaremorespecific.
Table5.2SuggestedbaselinelaboratoryinvestigationsforRA
Investigation Interpretation
Fullblood Hb↓/↔ Duetochronicinflammation/bonemarrow
count suppression.OftenlowMCVandMCHowing
topoorutilizationofironintoerythrocyte
precursors
Platelets↑/
↔
Duetoinflammatoryresponse
WCC↑/↔
Neuts↑/↔
Lymph↓
Eos↑/↔
Total WCC/neut count often ↑ from
inflammatoryresponse,with infection andin
haematologicalmalignancies.
GCscause↑neuts(↓vascularmargination).
Mild ↑ in eosinophils. If persistent ↑ then
investigate alternative causes (e.g. EGPA,
parasiticorhelminthinfection).
Renaltests Creat↑/↔
GFR↓/↔
Urea↑/↔
K ↔; Na
↔
NSAIDs can cause renal impairment. Many
DMARDsarerenal-excreted∴baselinerenal
functionimportant.
If unexplained renal dysfunction, consider
amyloidosisordrugcause.
Liverfunction
tests
ALT↔
ALP↔
Albumin
↔
INR↔
MostDMARDsaremetabolizedinliver.If↑
considerdrugeffect
Inflammatory
markers
CRP↑
ESR↑
TypicallyelevatedinactiveRA,although
normalinflammatorymarkersdonotexcludea
diagnosisofRA
Autoantibodies RF
ACPA
ANA
One/both/neither may be present but if both
negative be rigorous about making a correct
diagnosis (differential inflammatory OA,
CPPD polyarthritis, PsA). The autoantibody
titresarenotrelatedtodiseaseactivity.
ANApositivitycanoccurwithoverlap(SLEor
primarySjögren’s)
ALP,alkalinephosphatase;ALT,alanineaminotransferase;AST,aspartateaminotransferase;CPPD,
calciumpyrophosphatedihydratediseaseCr,creatinine;CRP,C-reactiveprotein;EGPA,eosinophilic
granulomatouswithpolyangiitis;ESR,erythrocytesedimentationrate;GFR,glomerularfiltrationrate;
Hb,haemoglobin;K,potassium;Na,sodium;WCC,whitecellcount.
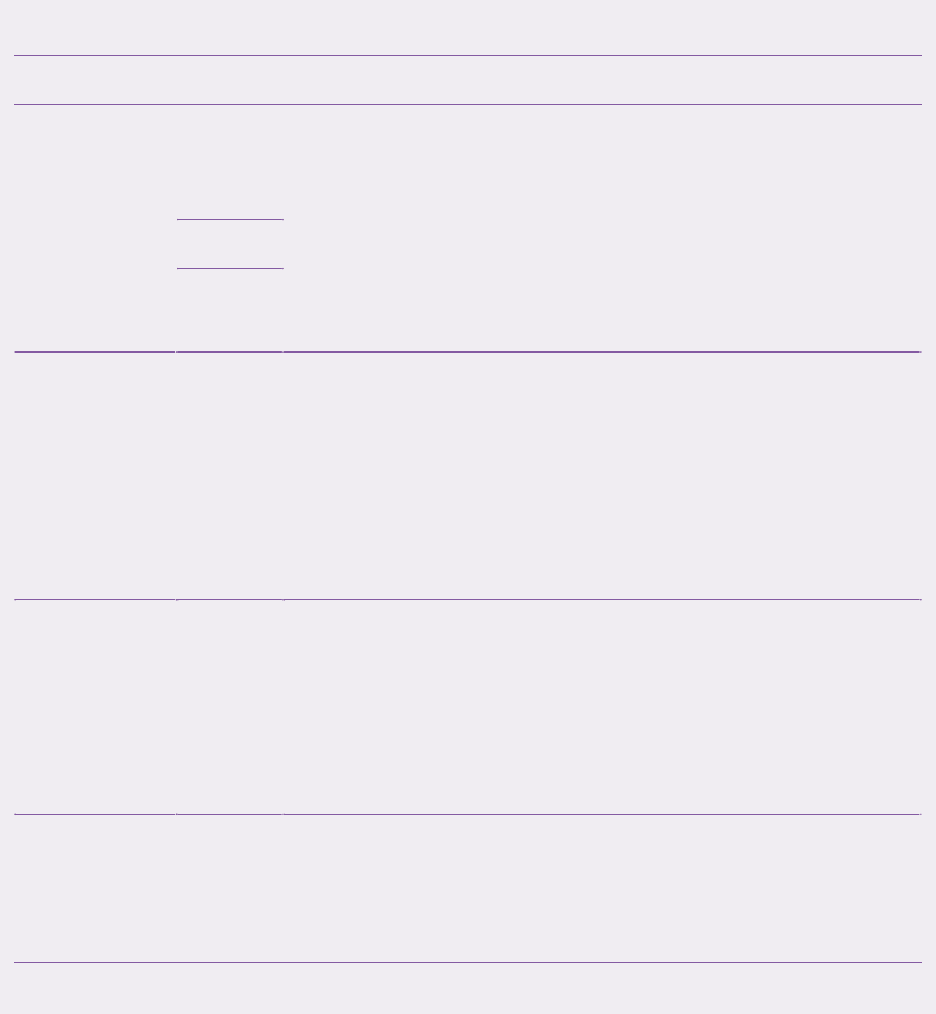
Table5.3BaselineimaginginvestigationsusefulinRA
Investigation Interpretation
Radiographs Hands
and
feet
Hands (including wrists) and feet to assess for
erosions, periarticular osteopenia and soft tissue
swelling
CXRtoassessforpulmonaryfibrosispriortostarting
DMARDs
Flexion/extensionsagittalC-spinefilmstoassessfor
C1/C2instability
CXR
Other
Ultrasound Hands
and
wrists,
feet
and
other
joints
Helpfulforassessingforsynovitis,hypervascularity,
effusion,andearlyerosions.Canaiddiagnosisiflittle
clinicalsynovitispresent,orifitisunclearifjoint
painisduetoinflammationorstructuraldamage.
Effectiveatprovidingdynamicjointimaging(e.g.
shoulder,ankle,wrist)
MRI C-
spine,
specific
joints
EssentialtoassessforcervicalmyelopathyifC1/C2
instabilitysuspected
Joint MRI helpful to confirm joint and tendon
synovitis, identify pre-erosions and erosions, and
rule out other MSK lesions at (symptoms/sign-
affected)sites
DXA RAisariskfactorforosteoporosis.DXA(hipandspine)
shouldbedoneatanyageifthepatientisonsteroidsorhashad
afragilityfracture,andinallpostmenopausalwomenandmen
>50yrsold
CXR,chestX-ray,MRI,magneticresonanceimaging.
Management
Generalconsiderations
Intensive target-driven treatment of RA, aiming for disease remission, is
recommended.
2,
3
AllpatientswithRAshouldhaveaccesstoregularmeetings
with a rheumatologist. Patient involvement and shared decision-making is
essentialintreatmentplanning.Forexample,foraguidetoRAmanagementby

auditablestandards,seeNICEClinicalGuideline79.
2
• Remissionisdefineddependingonthediseaseactivityscoreused(e.g.<2.6
usingDAS28).
• Early institution of DMARD therapy, usually with conventional synthetic
DMARDs(csDMARDs)initiallybeforetheonsetofjointdamage,isessential
(see Chapter23forDMARDnomenclature).
• A‘treat-to-targetapproach’hasbeenshowntoimproveoutcomesinRAand
involvessettingarealistictreatmenttarget(e.g.remission)withthepatientand
escalatingtreatmentuntilthegoalisreached.Thisapproachcanbeintensive
andrequiresfrequentpatientmeetingsorcontactstoassesstreatmentresponse
untilthetargetisachieved.
• Whileremissionisanappropriatetargetinearlydisease,patientswithlong-
standing disease may require a more pragmatic target, such as low disease
activity.
• AmultidisciplinaryapproachisessentialwhenmanagingRA:
• Earlyandregularspecialistpractitionerconsultscanhelpbothdiseaseand
medicinesmanagement,aswellasself-managementthrougheducationand
adeeperunderstandingofthepatientoftheirRA.
• Earlyreferraltophysiotherapyandoccupationaltherapyisrecommendedto
advise patients on appropriate exercises to maximize joint movement,
function,andstrength.
• Livingaids,pacing,copingskills,andself-managementofdiseaseactivity
flares/fatiguecanalsobelearnedthroughtherapyandpractitionerinput.
• Early institution of strategies to help patients to continue to participate in
workandsocialactivitiesisessentialtomaintainingagoodqualityoflife
forindividualswithRA.
• Podiatric orfoot orthoticsinput canbe helpfultoalleviatefootsymptoms
anddeformity.
• RA can lead to problems with low mood and depression so screening for
psychologicaldysfunctionandreferralforspecialistinputisveryimportant.
• Patients with RA have a higher risk of developing cardiovascular and
cerebrovasculardisease.Anannualreviewandmanagementofriskfactorsis
thereforemandatory.
Figure5.1SummaryofUKNationalInstituteforHealthandCareExcellence(NICE)guidanceforthe
managementofRA*ThissummarizesUK(NHScare)NICEguidelines.Local/regionalguidelinesmay
vary.GuidelinesadaptedfromNICEhttps://www.nice.org.uk/guidance/cg79.
Generalpain-relievingmeasuresandanalgesia
Analgesia can help manage symptoms while csDMARD and/or biologic
DMARDtherapy(bDMARD)takeseffect,andtotreatflaresofdiseaseactivity.
• Paracetamoland/orweakopiates(orincombination)willreducepainandcan
bewelltolerated.
• ConcomitantNSAIDs(preferentiallyselectiveCOX-2inhibitorsareinvariably
effectivethoughtheyaretoleratedvariably.
• NSAIDsshouldbeprescribedatthelowesteffectivedoseandfortheshortest
timepossible.
• Aprotonpumpinhibitortoreducetheriskofgastrointestinal(GI)ulcersand
toreduceGORDsymptomsshouldbeconsidered, especiallyinpatientaged
>65years,orwithahistoryofGIdisease.
• WhenchoosingaNSAID/COX-2inhibitor,considerapatient’sindividualrisk
factors,andchooseadrugwhichleastincreasestheserisks.Patientsshouldbe
counselledaboutthepossiblecardiorenal,GI,andliversideeffects.
• Transcutaneouselectricalnervestimulation(TENS)canbeahelpfulmeasure
to manage local/regional pain, and poses few side effects. Broken skin and
areaswithreducedsensation(i.e.diabeticneuropathy)shouldbeavoided.
SyntheticDMARDmedications(sDMARDs)
Foramoredetaileddiscussion,see Chapter23.
RA immunotherapeutics need planning with each patient. Objectives and a
time-frameforachievingobjectiveshouldbesetbyagreement.Thereneedsto
be a baseline safety assessment (Box 5.1) and careful monitoring of disease
activity,anydisability,comorbidity,anddrugeffects(Box5.2).
• Methotrexate (MTX) is the first-line conventional sDMARD of choice.
sDMARDdosesshouldbeescalatedrapidlyiftolerated.
• All sDMARDs and bDMARDs have a variable time to onset of efficacy,
between3and6months.
• Combinationtherapy(>1sDMARD),ideallyincludingMTX,isrecommended
iftolerated.
• Thereisgoodqualityevidencethatusinglow-doseGCtherapyduringthefirst
6months(e.g.‘COBRA-lite’30mgprednisolonedailyinitially),inorderto
achieveearlydiseasecontrol,reduceslong-termstructuraljointdamage.
• Once disease control is achieved, GCs should be tapered and stopped as
quicklyaspossible.
• Intra-articular (IA) GC injections can be efficacious for particularly swollen
joints.IMandIVGCscan behelpful tomanage flaresofjointpain/disease
activity.
• IfcombinationsDMARDtherapyisineffective,earlyescalationtobiological
therapyshouldbeconsidered.
• MTX should be co-prescribed with biologic therapy (particularly with anti-
TNFα)wherepossible,asitimprovesanti-TNFαresponseandpersistence.
• If first-line biologic therapy is inefficacious, switching to another biological
agentisrecommended.
Box5.1Investigationsandassessmentstoconsiderbeforestarting
sDMARDsforRA
Height,weight,bloodpressure
SomesDMARDscause↑bloodpressure,soabaselinemeasureisrequired.
Heightandweightarerequiredfordrugsprescribedby(‘ideal’)bodyweight.
Laboratorytestsandimaging
SeeTable5.2andTable5.3,respectively.
Comorbidities
Reviewcomorbidities,especiallyanyrespiratory,hepatic,orrenalconditions
thatmayaffectsDMARDchoice.Considerscreeningforoccultviralinfection
(suchashepatitis/HIV).
Pregnancy,fertilityandbreastfeeding
Discuss current and future plans for pregnancy and breastfeeding and tailor
treatmentaccordingly.
Vaccinations
VaccinationsagainstpneumococcusandinfluenzabeforestartingsDMARDs
or biologicsarerecommended.Live vaccines are not recommended(except
withhydroxychloroquineorSSZ).Theshinglesvaccineisalivevaccineand
evidence is limited on the use in immunocompromised individuals. Local
recommendations and clinician discretion should guide decisions. Prior to
commencinganti-TNFα, hepatitis Bvaccinationshould be considered inat-
riskindividuals.
DatafromLedinghamJetal.BSRandBHPRguidelinefortheprescriptionandmonitoringofnon-
biologicdisease-modifyinganti-rheumaticdrugs.Rheumatology2017;56(6):865–8.
Methotrexate(MTX)
• Once-weeklyoralpreparation,orsubcutaneous(SC)injection.Folicacidco-
prescription,oftenthedayafterMTXadministration.
• Therapeuticrangeisapproximately10–25mgweeklyandtimetotherapeutic
effect:8–12weeks.
• Toxicity(stomatitis,GIdisturbance,dysphoria-lassitudeeffects,andalopecia)
maybeaddressedbytheadditionoffolicaciddaily(apartfromdayofMTX
dosing).
• SCadministrationisausefuloptioniforaltreatmentisnottolerated.Thereis
some evidence of improved efficacy with SC compared with oral
administration,duetothehigherbioavailability.
• Milddrug-inducedhepatitisisrelativelycommonandisoftencorrectedbythe
additionoffolicacid.Routineliverbiopsyisnotnecessary,butcanbehelpful
in patients with other liver disease or persistent low-grade liver function
abnormalities.
• Liverfunctionabnormalitiesfluctuateandmayrequirethedrugtobestopped
forashortperiodiftransaminaselevelsriseabove2–3timestheupperlimitof
normal, with re-introduction after a period of time when levels have
normalized,withclosemonitoring.
• Myelosuppressionisrarelysevere.Antifolatedrugssuchastrimethoprimand
folatedeficiencyincreasetheriskoftoxicity.
• RenalimpairmentreducesMTXclearanceandmayleadtotoxicity.
• Concomitant NSAID use is not contraindicated, but monitoring for
hepatotoxicityisrecommended.
Sulfasalazine(SSZ)
• Dailyoralpreparation.Therapeuticrange1.5–3gdailyintwice-dailydoses.
• Timetotherapeuticeffect:12weeks.
• Toxicity:maycauseleucopenia,pancytopenia,haemolysis,aplasticanaemia,
andhepatictransaminitis.Bonemarrowtoxicityunusual.
• SSZ can rarely cause a hypersensitivity reaction characterized by LFT
abnormalities,lymphadenopathy,andrash.
• Spermatogenesis and libido can be affectedbySSZ,butitisreversible.No
apparentadverseeffectonfemalefertility.
Hydroxychloroquine(HCQ)
• Dailyoralpreparationwithusualtherapeuticdose200mgtwicedaily.
• Timetotherapeuticeffect:about12weeks.
• Retinal toxicityandmaculopathy are rare. Therisk increases with abnormal
liver or kidney function; after a cumulative dose >1000 g; and treatment
duration>5–7years.
Leflunomide(LFN)
• Dailyoralpreparation.Therapeuticdose20mgdaily.
• Timetotherapeuticeffect:12weeks
• LFNisaninhibitoroftheenzymedihydro-orotatedehydrogenaseandshows
antiproliferativeactivity,inhibitingpyrimidinesynthesis.Ithasalonghalf-life
of2weeks.
• Initially,itwasadministeredwithaloadingdoseof100mgdailyfor3days
followedbymaintenancetherapywith10–20mgdaily.Theloadingdosewas
associated with diarrhoea in many patients, and clinicians now use
maintenancetherapydosefromthestart.
• Side effects include myelosuppression, elevation of liver transaminases,
diarrhoea,andhypertension.Severehepatitisisuncommonandusuallyoccurs
inthefirst6monthsoftreatment.
• The long half-life has implications for drug withdrawal. If rapid washout is
required,cholestyramineforbetween14daysto6weeksshouldbeprescribed,
followedbytwobloodteststoensuredruglevelsarebelow0.02mg/L.
Azathioprine(AZA)
• Daily oral preparation dose range 2–2.5 mg/kg/day in twice-daily or three
timesadaydoses.
• Timetotherapeuticeffect:12weeks.
• InfrequentlyusedforRAastherapeuticeffectrelativelyweak.
• Toxicity: may cause leucopenia, pancytopenia, haemolysis, and aplastic
anaemia; especially in individuals with low/absent thiopurine
methyltransferase(TPMT)activity.AZAshouldnotbeprescribedforpatients
with‘low-activity’-associatedTPMTalleles.
Gold(myocrisin)
• IMpreparationwithloadingdosesthenusually50mgmonthly.
• Timetotherapeuticeffect:variable.
• Infrequently used for RA nowadays (and auranofin, the oral gold salt
preparation,isevenlessseldomused).
• Toxicity: hypersensitivity to injections, permanent blue/grey skin
discoloration,renalandliverdysfunctioncanoccuruncommonly.
Glucocorticoids(GCs)
• Oral,IM,IV,orIAuse.
• Timetotherapeuticeffect:dependsonthemodeofadministration;hours/days.
• IM and oral GCs can be very effectiveto manage flares and as a bridge to
sDMARDstakingeffect.
• IAinjectionsareofvalueinsymptomcontrol,inbothearlydiseaseandflares.
However,theireffectistransient,withlittleimpactontheoverallprocessof
RA,andshouldnotberepeatedanymorethan3-monthly.
• Caution should be exercised if considering IA injection in anticoagulated
patientsastheriskofhaemarthrosisisincreased.
• Thereisnoevidencetosuggestanincreasedriskofjointinfection,aslongas
anaseptictechniqueisused.
• Long-term systemic GCs can have sequelae, including cataracts, premature
coronary artery disease, osteoporosis, muscle atrophy, insulin
resistance/diabetes,andosteonecrosis.Appropriatefracturepreventiontherapy
should be given to patients expected to be on glucocorticoid therapy for >6
weeksatadose≥7.5mg.
Box5.2ManagingandmonitoringsDMARDs:BritishSocietyfor
RheumatologyUKrecommendations
Methotrexate(MTX)
Co-prescribedwithweeklyfolicacid(e.g.5mg/dayafterMTX).
Teratogenic. Notsafe inbreastfeeding. Adviselow alcoholintake.Rarely
causes pneumonitis (caution with pre-existing lung disease/poor respiratory
reserve).Rarelycausesmyelosuppression.
Monitoring: FBC, Cr/GFR, ALT, albumin all 2-weekly until dose/results
stablethenmonthlyfor3monthsthen3-monthlythereafter.
Sulfasalazine(SSZ)
GIsideeffectsearlyintreatmentcoursegenerallymildanddooftensubside.
Very rarely causes leucopenia, pancytopenia, haemolysis, and aplastic
anaemiainearlytreatment.Reducedpotencyinmen.
Monitoring:FBC,Cr,ALT,albuminall2-weeklyuntildose/resultsstable,
then monthly for 3 months, then 3-monthly until 12 months and no routine
monitoringrequiredthereafter.
Hydroxychloroquine(HCQ)
Cumulativedoseshouldnotexceed6.5mg/kgofbodyweight.
Monitoring: no routine lab monitoring required. Eye screening within 1
yearofstartingandthenannuallyifondrugfor>5years.
Leflunomide(LEF)
Diarrhoearelativelycommonsideeffect.Cancausehypertensionsoavoidif
BPuncontrolled.Notrecommendedinpregnancyorbreastfeeding.Longhalf-
lifedrugand requiresactive washoutifthere isseveretoxicity(e.g.10-day
cholestyramine).Rarelycausespneumonitis.
Monitoring:FBC,Cr,ALT,albumin:all2-weeklyuntildose/resultsstable
thenmonthlyfor3monthsthen3-monthlythereafter.BPmonthly.
Azathioprine(AZA)
Assess thiopurine methyltransferase (TPMT) genotype before treatment. If
likelyabsentTPMTactivitydonotprescribeAZA.Avoidco-prescriptionwith
allopurinol(blocksexcretionofAZA).GIdisturbancerelativelycommonbut
oftenmild.Relativelysafeinpregnancy.
Monitoring: FBC, Cr, ALT, albumin: 2-weekly until dose/results stable,
thenmonthlyfor3monthsthen3-monthlythereafter.
IMgold
Can cause bone marrow and liver disturbance. Contraindicated in
pregnancy/breastfeeding. Rarely: hypersensitivity reactions from injections.
Long-termtreatmentcancausechrysiasis(grey/blueskinpigmentation).
Monitoring:FBC,Cr,ALT,albumin:all2-weeklyuntildose/resultsstable
thenmonthlyfor3monthsthen3-monthlythereafter.Urinalysisforbloodand
proteinpriortoeachdose.
DatafromLedinghamJetal.BSRandBHPRguidelinefortheprescriptionandmonitoringofnon-
biologicdisease-modifyinganti-rheumaticdrugs.Rheumatology2017;56(6):865–8.
Anti-tumournecrosisfactorαtherapy(anti-TNFα)
Baselineassessmentisadvisable(Box5.1andBox5.3).
• GivenSC(e.g.etanercept,adalimumab)orIV(e.g.infliximab).
• Timetoeffect:2–24weeks.
• TNFαisapotentpro-inflammatorycytokinewhoselevelsareelevatedinRA.
• Anti-TNFα therapiesare availableasoriginator orbiosimilar drugs—mainly
either monoclonal antibodies or receptor fusion proteins (infliximab,
etanercept,adalimumab,certolizumab,golimumab).
• Common adverse effects include infection, headache, nausea, and injection-
sitereactions,andincreasedriskofinfection.
• Rarely can trigger a (ANA-positive) lupus-like syndrome responsive to
therapywithdrawal.
• Veryrarelycancausedemyelination.
• Withdrawifcardiacfailureworsens.
• Considerwithdrawalifinterstitiallungdiseasedevelopsorworsens.
• CancausepsoriasiswhenusedtotreatRAandevenworsenspsoriasisinPsA
patients(‘paradoxicalpsoriasis’).Thisisaclasseffectandwillre-occurifan
alternativeanti-TNFαistried.
• Antibodies can develop versus the therapeutic antibody/fusion protein. Such
antibodies can be detected by specific immunoassays. MTX therapy may
reduceanti-anti-TNFαdrugantibodyformation.
B-celldepletion(anti-CD20):rituximab(RTX)
Baselineassessmentisadvisable(Box5.1andBox5.3).
• GivenIV.Adoseconsistsof1ggiventwicebyinfusionsgiven2weeksapart.
Mostrheumatologistsadvocateaminimumof6monthsbetweensubsequent
doses, but often required less frequently. Usually co-administered with IV
GCs.
• Timetotherapeuticeffect:12–24weeks.
• BcellsplayanimportantroleinthepathogenesisofRAandadministrationof
rituximab leads to rapid CD20 positive B-cell depletion in the peripheral
blood.NormalB-cellrepopulationoccurswithinthenext3months.
• The best responses are seen in RF-seropositive patients, and when co-
prescribedwithMTX.IfpatientsareunabletotakeMTXthenconsiderLFN
orRTXmonotherapy.
• RTXiscontraindicatedifthereishypogammaglobulinaemia.
• Veryrarelycausesprogressivemultifocalleucoencephalopathy.
CTLA4-Ig:abatacept(ABA)
Baselineassessmentisadvisable(Box5.1andBox5.3).
• GivenSC(125mgweekly)orIV(maintenancedoseevery4weeksaccording
toweight).
• Timetoeffect:12–24weeks.
• Abatacept disrupts the CD80/86 co-stimulatory signal required for T-cell
activationbycompetingwithCD28forbinding.
• Co-prescriptionwithMTXisadvisable.
Box5.3Investigationsandconsiderationsbeforestartingbiologictherapy
TBinfection
Allpatientsshouldbescreened(history,CXR,T-spot/IgRAtest)forpresence
of active or latent mycobacterial infections and treated according to current
guidelinesbeforestartingbiologictherapy.
Hepatitis
ScreenallpatientsstartingabiologicforhepatitisBandC.Increasedriskof
infusionreactionsinpatientswithhepatitisCtreatedwithRTX.
HIV
Athoroughhistoryisrequiredandifanyriskfactorsarepresent,HIVtesting
shouldbeundertaken.
Malignancy
See ‘RA-associatedcancerrisk’,p.260.
ANAtesting
Anti-TNFα therapy has been associated with development of lupus-like
syndromeinrarecases.ObtainabaselinetestofANA.
Demyelination(includingopticneuritis)
Anti-TNFαtherapyhasbeenassociatedwithdemyelination,anditshouldnot
beprescribedtopatientswithahistoryofdemyelination.
Cardiacfailure
Anti-TNFαisnotrecommendedwithNYHAgrade3/4cardiacfailure.
Interstitiallungdisease(ILD)
There is mixed evidence on the association of anti-TNFα therapy and ILD.
Monitoringlungfunctionshouldbeconsidered.
Uveitis
Anti-TNFα should be used cautiously in patients with pre-existing uveitis.
Somestudieshaveidentifiedanincreasedriskofuveitis.
Fastinglipids
Patients starting on tocilizumab (TCZ) should have a baseline fasting lipid
profile. A repeat profile is recommended after 3 months of treatment. If
worsening lipid level, consider reviewing treatment. Ongoing monitoring
shouldbeinlinewithlocalguidelinesandindividualriskfactors.
Immunoglobulins
Immunoglobulins should be checked in patients starting RTX, 4–6 months
after an infusion, and before each treatment. There’s an increased risk of
infectionwithIgG<6g/L.
ANA,antinuclearantibodies;NYHA,NewYorkHeartAssociation;RTX,rituximab.
InformationsummarizedfromDingT,etal.BSRandBHPRrheumatoidarthritisguidelinesonsafetyof
anti-TNFtherapies.Rheumatology2010;49:2217–9.
Anti-interleukin-6receptorblocker:tocilizumab(TCZ)
Baselineassessmentisadvisable(Box5.1andBox5.3).
• GivenSC(162mgweekly)orIV(8mg/kgevery4weeks).
• Timetoeffect:12–24weeks.
• IL-6 is a potent pro-inflammatory cytokine. High levels have beenfoundin
serum and synovial fluid of RA patients, and levels correlate with disease
activity.
• Tocilizumabbindsspecificallytobothsoluble(sIL-6R)andmembrane-bound
IL-6receptors(mIL-6R).
• Best results are when it is co-prescribed with MTX, but is licensed as
monotherapy.
• Use with caution inpatientswitha history of diverticulitis duetoincreased
riskofgutperforation.RiskiselevatedifpatienttakingGCsand/orNSAIDs.
Patientsneedcounsellingabouttherisk.
Box5.4TheBritishSocietyforRheumatologyconsensusguidelinesfor
biologictherapiesforRA
Anti-TNFα*
Local guidelinesvaryon blood monitoring requirementfor anti-TNFα. It is
prudent to check FBC with WCC regularly to screen for neutropenia and
malignancysuchaslymphoma.
4
Anti-IL-6receptor(TCZ)
Check WCC and neutrophil count monthly for 6 months. If no neutropenia
occursinthefirst6months,monitoringcanbereducedto2-3monthly.For
TCZmonotherapy,checkLFTsmonthlyforthefirst6-months,thenevery2-3
monthsifresultsarestable.ForTCZco-prescribedwithsDMARDs,monthly
LFTmonitoringisrecommended.
5
Abatacept(ABA)
Noneavailable.Forsafetyandmonitoring,seeinformationonitsSPCat
http://www.medicines.org.uk
Anti-CD20(RTX)
Check immunoglobulins 4–6 months after each infusion. If there is active
infection, IgG levels <6g/L or very low CD4/CD8 counts, withhold
treatment.
6
SeealsoitsSPCat http://www.medicines.org.uk
FBC,fullbloodcount;LFTs,liverfunctiontests;RTX,rituximab;WCC,whitecellcount.
*2010BSRGuidelinestobeupdatedin2017.PleaseseeBSRwebsite:
https://www.rheumatology.org.uk/
BiologicDMARDbiosimilars
TheEuropeanMedicinesAgencydefinesbiosimilarsas‘abiologicalmedicine
thatissimilartoanotherbiologicalmedicinethathasalreadybeenauthorisedfor
use’.Thisusuallyoccursafterapatentexpiresonanoriginatordrug.SeeBox
5.4.
• Sincebiologictherapiesarederivedfromyeastorbacterium,biosimilarsare
notidenticaltotheoriginatordrugandassuch,cannotbeclassedasageneric
drug.
• For this reason, caution should be exercisedifswitchingbetween originator
andbiosimilarcompounds.
• At the time of writing, three anti-TNFα biosimilar therapies were available.
Experienceinthewidespreaduseofbiosimilarsislacking.
• Therearecurrentlynolong-termdataontheuseofbiosimilars.Ifstartingor
switchingapatientintoabiosimilardrug,considerenrollingthepatientontoa
patient(national)registry.
• Guidanceregardingusage(includingswitching)ofbiosimilarsvarieswidely,
soitisadvisedtofollowlocalpolicies.
Novelmedicationsonthehorizon
• Inadditiontocurrentlylicenseddrugs,numerousdrugsareindevelopmentfor
useinRA.Mostnotableofthesearesmallmoleculesthattargetintracellular
processesinvolvedinRA.
• Smallmoleculedrugscanbeadministeredorally.
• Januskinase(JAK)inhibitorshavebeenextensivelyinvestigatedandoneJAK
inhibitor (tofacitinib) is currently available in the USA for the treatment of
RA.
• Further biologic therapies continue to be developed and trialled in RA,
includingIL-17inhibitorsandvariationsonIL-6blockade.
Managinginfectionswhileonimmunosuppression
Themainriskofimmunosuppressionisinfection.‘Seriousinfection’isgenerally
definedasan infection thatrequires hospitalizationorparenteral antimicrobial
treatment.
• Seereferences4and7attheendofthechapterforfulldetails.
• Generally, all sDMARDs (with the exception of HCQ) should be stopped
duringanyseriousinfection,anduntilrecoveryiscomplete.
• BiologicDMARDsshouldbediscontinuedduringseriousinfection.
• Anti-TNFα therapy increases the risk of getting a serious infection, and
infectioncanpresentatypically,sovigilanceisrequired.
• A careful review of the risks and benefits of anti-TNFα therapy should be
undertaken,especiallyinpatientswith:
• chronicinfectedlegulcers.
• septicarthritisofanativejointwithinthelast12months.
• sepsis of a prosthetic joint within the last 12 months (if removed) or
indefinitely(ifjointremainsinsitu).
• persistent/recurrentchestinfections.
• indwellingurinarycatheter.
• bronchiectasis.
• hypogammaglobulinaemia.
Tuberculosis(TB)
• IfapatientdevelopssymptomssuggestedofTBinfectionwhileonanti-TNFα,
anti-mycobacterialtreatmentshouldbeinitiated.
• If the patient remains systemically well, anti-TNFα therapy may continue
whiletheTBinfectionistreated.
• Patientsonanti-TNFαtherapyaremorelikelytodevelopextra-pulmonaryTB.
• Non-TBmycoplasmainfectionsarerareandrequireexpertadvice.
• Evidencefor theoccurrenceofTBwithotherbiologicagentsislimited,but
appearstobelessthanforanti-TNFα.
Opportunisticinfectionriskissues
• Whilerare,monitorforopportunisticbacterial(e.g.Listeria,Salmonella)and
fungal (e.g. histoplasmosis, candidiasis, aspergillosis, Coccidioides,
Pneumocystisjirovecii)infectionsinpatientstreatedwithanti-TNFα.
• Consider treatment with varicella zoster immunoglobulin in all
immunocompromised RA patients who have had significant contact with an
individualwithvaricellazoster.
• Treatshinglesandherpeszosteraccordingtostandardguidance.
RA-associatedcancerrisk
ThereisanincreasedriskofmalignancywithRA,withastandardizedincidence
ratio(SIR)of1.1.TheriskisgreatestforHodgkin’s(SIR3.21)andlungcancer
(SIR1.64).
8
• ArecentstudyfromtheBSRBiologicsRegisterforRAreportednoincreased
riskofsolidtumourswithanti-TNFαtherapywhencomparedtoRApatients
treatedwithsDMARDs.
9
• Thereissomeevidencethatskincancers(bothnon-melanomaandmelanoma)
maybemorelikely.
• There is a theoretical increased risk of cancer in patients treated with anti-
TNFα therapy who have previously had a cancer, or have risk factors for
cancer(e.g.smoking).Treatmentdecisionsshouldbemadeonacase-by-case
basis. However, because patients with previous cancer have been excluded
frommostRCTs,littleisknownabouttheriskinthiscontext.
• Data on cancer risk are scarce for other biologics; primarily due to smaller
numbersofpatientstakingthesedrugsandshorterexposuretimessincedrug
licensing.
PregnancyandbreastfeedingwithRA
Thetopichasbeenextensivelyreviewedquiterecently.
10
• RAoftenimprovesinpregnancy,particularlyinthethirdtrimester.
• Preconceptioncounsellingisessential,asmanysDMARDsarecontraindicated
inpregnancyandbreastfeeding,andsomesDMARDscanaffectfertility.
• Ideally, conception should be planned and medications optimized prior to
conception.
• ThemanagementofRAinpregnancyshouldbediscussedwithallwomenof
childbearingage,andmenconsideringhavingchildren.
• Itisimportanttoreviewhowthepregnancyandbirtharelikelytoproceed.If
possible,earlyreferraltoaspecialistobstetricclinicwithexpertisemanaging
pregnantwomenwithRAisrecommended.
• If RA affects the hip, pelvis, or spine, an obstetric review is necessary to
discussbirthplansandanalgesia.
• RAmaymakecertaintasksmoredifficultforthenewmotherorfatherwith
RA(e.g.changingnappies,bathingthebaby).Planningandaddressingthese
problemsprospectivelyisrecommended.
• Patients should have a method of contacting the rheumatology team (e.g.
telephoneadviceline)shoulddifficultiesarise.Amanagementstrategyshould
beagreedwiththepatientandobstetricandprimarycareteamshouldtheRA
flareintheperinatalperiod.Arrangementforanearlyrheumatologyreviewin
thepostnatalperiod,toensureoptimaldiseasemanagement,isrecommended.
• Drug use in pregnancy needs careful planning. Guidelines updating practice
havebeenrecentlypublished(Box5.5).
• Paracetamolissafeinpregnancyandbreastfeeding.Intermittentusemightbe
reasonable given restrictions on NSAID use (see Box 5.5). Avoid regular
paracetamoluse duringweeks8–14 ofpregnancy asthere isasmallriskof
cryptorchidism. There are no data on paternal exposure, but paracetamol is
likelytobesafe.
• Biologictherapyexperienceisemergingforanumberofthetherapiesbutfor
abatacepttherearestillveryfewdataonitssafety.
Box5.5TheBritishSocietyforRheumatology2016guidelinesfor
prescribingNSAIDs,GCs,sDMARDs,andbDMARDsinpregnancyand
breastfeeding
NSAIDs(includingCOX-2selectiveNSAIDs)
Limited evidence. Possible ↑ risk of miscarriage and fetal malformation ∴
caution in first trimester. Stop NSAID by 32 weeks’ gestation to avoid
premature closure of ductus arteriosus. NSAIDs are excreted in breast milk
butnoevidenceofharm.Compatiblewithpaternalexposure.
Glucocorticoids(GCs)
Compatiblewithpregnancyandbreastfeeding.
Hydroxychloroquine(HQC)
Compatiblewithpregnancyandbreastfeeding.
Methotrexate(MTX)
Contraindicatedinpregnancyandbreastfeeding.StopMTX>3monthsbefore
conception. In accidental pregnancy, stop MTX and start folic acid (5
mg/day).Low-doseMTXpaternalexposureprobablynotrisky.
Sulfasalazine(SSZ)
Compatiblewithpregnancy(usefolicacid5mg/day)andbreastfeeding.
May↓fertilityinmen,however,don’tstopSSZtoimprovefertilityunless
conceptionisdelayed>12months.
Leflunomide(LEF)
Notrecommendedin pregnancyor whenbreastfeeding.Women considering
pregnancy should undergo cholestyramine washout prior to conception. If
accidental conception occurs, cholestyramine washout should be instituted
untilLEFplasmalevelsareundetectable.
Azathioprine(AZA)
Compatiblewithpregnancyatdoses≤2mg/kg/dayandinbreastfeedingand
withpaternalexposure.
Anti-TNFα
Infliximab:stopafter16weeks’gestation.Compatiblewithpaternalexposure.
Etanercept: stop by third trimester. Compatible with paternal exposure.
Adalimumab: stop by third trimester. Compatible with paternal exposure.
Certolizumabpegol:compatiblewithalltrimestersofpregnancy.Compatible
with paternal exposure. Breastfeeding probably safe on any anti-TNFα
therapy,althoughevidenceislimited.
Rituximab(RTX)
Stop6monthsbeforepregnancy.NoevidenceonRTXduringbreastfeeding.
Second/third trimester exposure associated with neonatal B-cell depletion.
Limitedevidenceonpaternalexposure—likelynotharmful.
Tocilizumab
Stop3months<conception.Nodataonbreastfeeding.
DatafromFlintJetal.BSRandBHPRguidelineonprescribingforrheumatologicalconditionsin
pregnancyandbreastfeeding.Part1andII.
https://www.rheumatology.org.uk/Knowledge/Excellence/Guidelines

SurgeryinRApatients
Athoroughperioperativeplanshouldbemadeforallpatients.
• Inform the surgical and anaesthetic team of the diagnosis of RA and any
relevantcomplications/comorbidities.
• Spinal involvement should be highlighted to the anaesthetist, to inform
intubation,positioning,andspinalanaesthesia.
• Respiratory involvement may make artificial ventilation challenging, and
increasetheriskofpostoperativeinfection.
• Postoperative occupational and physiotherapy will need to be tailored to
accommodatethepatient’sRA.
• For elective procedures, advance assessment and preparation of the home
environmentshouldbeundertakentofacilitaterehabilitation.
• Generally, sDMARDs should be continued throughout the perioperative
period,tominimizetheneedforGCs(asthelatterincreaseriskofsurgicalsite
infectionandnon-healing).
• For high-risk (‘dirty’/lengthy) procedures and when patients have
comorbidities,sDMARDsmayneedtobestopped.
• Closemonitoringofrenalfunctionisessentialintheperioperativeperiod,to
monitorforsDMARD-relatedtoxicity.
• Anti-TNFα therapy should be stopped before surgery. ‘Washout’ times for
biologicsvarydependingonhalf-lifeofthedrug.
• Biologics can be restarted after surgery once good wound healing has
progressed and there is no evidence of infection. Please refer to local
guidelines,but atypical currentpractice isto stopbiologic therapy2 weeks
priortosurgery,andrestart2weeksaftersurgery.
ComplementarytherapiesforRA
• Some patients will want treatment from complementary therapists, either in
advanceorduringtheirlong-termmanagementofRA.
• Some commonly used complementary therapies include acupuncture,
chiropractic,homeopathy,aromatherapy,andfaithhealing.
• Patientsoftenfindtreatmentsbeneficial,andprovidedtheydonoharm,there
isgenerallynoreasontoadvisepatientstostoptreatment.
• Itisimportanttohighlighttheabsenceofrobustevidenceforthesetreatments,
andtheyarenotasubstitutionforstandardmanagement.
• Spinal/neck manipulation is generallynotrecommended, especially if RA is
knowntoaffectthespine.
• Inquire about any supplements, herbal, or other medication use that might
interferewiththemetabolismofanalgesicsandsDMARDs.
• Please refer to Chapter 9 for information on juvenile RF-positive
polyarthritis.
References
2. NICE.RheumatoidArthritisinAdults:Management(Lastupdated:December2015).London:NICE.
http://www.nice.org.uk/guidance/cg79
3. SmolenJS,LandewéR,BijlsmaJ,etal.EULARrecommendationsfor the managementofRAwith
synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis
2017;76:960–77. http://ard.bmj.com/content/early/2017/03/06/annrheumdis-2016-210715
4. Ding T, Ledingham J, Luqmani R, et al. BSR and BHPR RA guidelines on safety of anti-TNF
therapies.Rheumatology2010;49:2217–9.
5. Malaviya AP, Ledingham J, Bloxham J, et al. The 2013 BSR and BHPR guideline for the use of
intravenous tocilizumab in the treatment of adult patients with rheumatoid arthritis. Rheumatology
2014;53:1344–6.
6. Bukhari M, Abernethy R,Deighton C, et al. BSR and BHPR guidelines on theuse of rituximab in
rheumatoidarthritis.Rheumatology2011;50:2311–3.
7. LedinghamJ,GullickN,IrvingK,etal.BSRandBHPRguidelinefortheprescriptionandmonitoring
ofnon-biologicDMARDs.Rheumatology2017;56:865–8.
8. SimonTA,ThompsonA,GandhiKK,etal.Incidenceofmalignancyinadultpatientswithrheumatoid
arthritis:ameta-analysis.ArthritisResTher2015;17:212.
9. MercerLK,LuntM,LowAL,etal.Riskofsolidcancerinpatientsexposedtoanti-tumournecrosis
factortherapy:resultsfromtheBritishSocietyforRheumatologyBiologicsRegisterforRheumatoid
Arthritis.AnnRheumDis2015;74:1087–93.
10. Flint J, Panchal S, Hurrell A, et al. BSR and BHPR guideline on prescribing for rheumatological
conditions in pregnancy and breastfeeding. Part 1 and II.
https://www.rheumatology.org.uk/Knowledge/Excellence/Guidelines

Chapter6
Osteoarthritis
Introduction
Epidemiology
Pathology
Aetiology
Clinicalfeatures
Investigation
Management
Prognosis
Introduction
Osteoarthritis (OA) is a chronic disorder characterized by cartilage loss, bone
remodelling,jointdeformity,andsynovialinflammation.Itisthemostcommon
jointdiseaseinhumans.
Epidemiology
• Itisestimatedthat8.5millionpeopleintheUKhavejointpainattributableto
OA, and that 15% of the UK population aged >55 years have symptomatic
kneeOA.
• TheprevalenceofradiographichandOAintheUKisestimatedat4.4million
people,significantradiographickneeOAat0.5millionpeople,andsignificant
radiographichipOAat0.2million.
1
• By 2020, OA is expected to be the fourth leading cause of disability in the
world.
• OA poses a significant economic burden on the UK economy, using 1% of
grossdomesticproduct,andcausing36millionworkingdaystobelosteach
year.
2
References
1. Arthritis and Musculoskeletal Alliance. Standards of Care for People with Osteoarthritis. London:
ARMA,2004.
2. NICE. Osteoarthritis: Care and Management of Osteoarthritis in Adults. Clinical Guideline 59.
London:NICE,2008.
Pathology
• Although there are recognized associations between OA, age, and trauma,
advances in knowledge of cartilage biochemistry and the recognition of
crystal-associateddiseasehaverenewedinterestinOAasadynamiccondition
ofcartilageloss(chondropathy)withperiarticularbonereaction.
• Atpresent,OAisassessedandmanagedclinicallyasastructural,ratherthan
physiologicalcondition,withanemphasisonestablisheddiseaseanddisease
prevention.
• Chondrocyte dysfunction leads to changes in the extracellular matrix, and
metalloproteinaseenzymerelease.
• Proteoglycandegradationleadstooedemaandmicro-fissuresinthecartilage.
Micro-fissuresprogresstosubchondralcystsanderosions.
• Cartilage degradation products stimulate synovial inflammation and the
productionofpro-inflammatorycytokines(e.g.IL1andTNFα).
• MacroscopicchangesinOAincludecysticbonedegeneration,cartilageloss,
andgrowthofboneatjointmargins(osteophytes).
• Microscopicchangesincludeflakingandfibrillationofarticularcartilagewith
variations in vascularity and mineralization of subchondral bone, leading to
sclerosisandnewboneformation.
• MostsurveysofOArelyonradiographicfeaturesfordefinitionandseverity—
this is problematic because of poor correlation of radiographic change with
clinicalstatus,symptoms,orfunction.
• Radiographic staging is best done at the hip and knee, but is poorest in the
handandspine.Thecorrelationbetweenpathologyandradiologyisshownin
Table6.1.
Table6.1Radiographic–pathologycorrelatesinOA
Pathologicalchange Radiographicabnormality
Cartilagefibrillation,erosion Localizedjoint-spacenarrowing
Subchondralnewbone Sclerosis
Myxoiddegeneration Subchondralcysts
Trabecularcompression Bonecollapse/attrition
Fragmentationofosteochondralsurface Osseous(‘loose’)bodies
Aetiology
• FemalesareathigherriskofOA(relativerisk(RR)2.6)andtendtodevelop
structuraldamagemorequickly,andaremorelikelytoproceedtoatotalhip
arthroplasty.
• Hip OA is more common in Europeans than in Asians or in African
Americans.
• TheFraminghamstudyfoundthat27%ofpeopleaged63–70years,and44%
ofpeopleaged>80yearshadradiographickneeOA.
• AUKstudyshowedthat50%ofadultsaged>50yearswithradiographicknee
OAhadsymptoms.SimilarfiguresareseeninhipOA.
• Notably only 3–7% of people with radiographic features of hands OA, are
symptomatic.
• RiskfactorsassociatedwithOAincludethefollowing:
• Familyhistory;particularlywithgeneralizednodalOA.
• Genetics:increasedconcordanceforOAinmonozygoticvsdizygotictwins,
andparticularlyfornodalOA.
• Genome-wide association studies have identified genetic loci associated
withOA:handOAwithchromosomes1,7,9,13,and19;kneeOAwiththe
LRCH1 gene on chromosome 13; hipOA with chromosome 11 (RR 1.4–
1.6).
• Geneticsofboneorarticularcartilagestructure(COL2A1gene).
• Highbonedensity.
• Calciumcrystaldepositiondiseaseandacromegaly.
• Obesity(closeassociationwithonsetandprogressionofkneeandhandOA,
butnothipOA).
• Femoraldysplasia(hipOA).
• Trauma(repeatedorsingleevent).
• LowvitaminCandDlevels(progressionofkneeOA).
• Factorswithless,orno,evidencefortherebeingariskforOA:
• For hip OA: previous hip disease (e.g. Perthes disease), acetabular
dysplasia, avascular necrosis of the femoral head, severe trauma,
generalizedOA,andoccupation(e.g.farming).
• ThereislittleevidencetolinkOAwithrepetitiveinjuryfromoccupationor
sports, such as running in those with normal joints, except perhaps knee-
bendinginmen.
Clinicalfeatures
Thesymptoms,andtoadegree,mostfeaturesofOA(Table6.2),oftendonot
correlatewithfunctionaloranatomicalchangejudgedradiographically.
Table6.2Clinicalfeaturesofosteoarthritis
Parameters Features
Symptoms Painoftenworseafteruse,betterwithrest
‘Gelling’afterinactivity
Withoutsignificantinflammatoryfeatures
Minimalstiffness,evenings>mornings
Signs Bonyenlargement
Crepitus
Reducerangeofmovement
Tendernessonpalpation
Malalignmentorinstability
Site 1stcarpometacarpaljoint(CMCJ)
Proximal(PIPJ)anddistalinterphalangealjoints(DIPJ)
1stmetatarsophalangealjoint(MTPJ)
Largejoints:hip,knee
1stmetatarsaljoint
Cervicalorlumbarspine
• Severalpotentialmechanismsmayberesponsibleforthepainassociatedwith
OA.
• Since cartilage is aneural, pain may arise from a number of other sites:

inflammatory mediators causing intra-articular hypertension, capsular
distension, and/or stimulation of synovial and subchondral bone nerve
fibres.
• Concomitantenthesopathyorbursitismayleadtopain.
• Morningstiffnessof<30miniscommoninOA.
• Muscleweaknessandatrophyduetoalteredjointuseiscommon.
• SeveralsubsetsofOAexist,withmigrationbetweenpatterns:
• PrimaryOA.
• GeneralizednodalOA(GNOA).
• Inflammatory/erosiveOA(iOA).
• LargejointOA(kneeandhip).
• SpinalOA.
• SecondaryOA(Table6.3).
GeneralizednodalOA(GNOA)
• This common condition (see Plate 7d), more common in women than in
men,ischaracterizedbypolyarticularinvolvement.
• ItischaracterizedbyHeberden’snodes(DIPJ)andBouchard’snodes(PIPJ).
• GNOApredisposestoOAofknee,hip,andspine.
• Theisoftenastrongfamilyhistory.
• ThereisoftenMCPJinvolvement,particularlythesecondandthird.Ifthereis
MCPJinvolvement,furtherinvestigationtoexcludecausesofsecondaryOA
arerecommended.
Inflammatory/erosiveOA(iOA)
• Sometimes called erosive OA, iOA is characterized by interphalangeal joint
involvement,flaresofinflammatorysymptomswithrapidprogression,anda
tendencytojointankylosis.
• Centraljointsubchondralerosionsandassociatedbonyremodelling.
• Thepeakonsetisaroundthemenopause.
• FunctionalimpairmentismorelikelythanwithnodalOA.
• The key differential diagnosis is psoriatic arthritis. Unfortunately, the two
conditions can be indistinguishable on plain radiographs in the early stages
and on ultrasound unless there are other psoriatic disease features such as
skin/nailpsoriasisortenosynovitis.
LargejointOA
• The knee is commonly affected; most often the patellofemoral and medial
tibiofemoralcompartments.
• Severeboneandcartilagelossleadstoinstabilityandvarus(bow)deformity.
• Instability and ‘giving way’ of a knee may be exacerbated by quadriceps
weakness.
• Hip OA tends to present as groin, buttock, or anterior thigh pain on weight
bearing,ratherthanlateralhipdiscomfort.
• Differential diagnosis for hip and groin pain include iliopsoas dysfunction,
ischialbonelesions,symphysis,andtrochantericpainsyndrome.
• SubdivisionofhipOAisusuallymadeonthebasisofacetabularcartilageloss
patterns:
• Superiorpole:commonpattern,oftenunilateral,morecommoninmen,and
likelytoprogress.
• Central(medial):lesscommon,usuallybilateral,morecommoninwomen,
andlesslikelytoprogress.
• Indeterminateacetabular-concentricpatternsarealsodescribed.
SecondaryOA
SecondaryOAisassociatedwithawidevarietyofdisordersaslistedinTable
6.3.
Table6.3SecondaryOA
Trauma Inflammatoryarthritis
Metabolic/endocrine:
Haemochromatosis
Acromegaly
Hyperparathyroidism
Ochronosis(alkaptonuria)
Crystaldepositiondisease:
Calciumpyrophosphate
Uricacid
Hydroxyapatite
Neuropathicdisorders:
Diabetesmellitus
Anatomicalabnormalities:
Bonedysplasia
Investigation
• ThediagnosisofOAisbasedonclinicalandradiologicalfindings.Thereare
nospecificlaboratorytests.
• As the disease progresses, other findings may appear and aid diagnosis,
includingosteophytes,subchondralbonesclerosis,andsubchondralcysts.
• Radiographscorrelatepoorlywithsymptomsandclinicalfunction.Manyolder
patients will have radiographic changes consistent with OA, but will be
asymptomatic.
• MRI is better at identifying early articular cartilage loss, subchondral bone
oedema,andlow-gradesynovitis,butitisrarelyused.
• Laboratorytests(includingsynovialfluidanalysis)maybeusefultoexclude
other causes of joint pain, such as RA, though abnormalities and pattern of
acute phase may be similar for PsA and calcium pyrophosphate deposition
disease.
• There are biomarkers of tissue destruction and inflammation that may
eventuallytranslatefromresearchsettingstoclinicaluse,including:
• cartilageoligomericmatrixprotein(COMP).
• pyridinolineandbonesialoprotein.
• metalloproteinases.
• hyaluronan.
• C-terminalcross-linktelopeptideoftypeIIcollagen(CTX-II).
• Opticalcoherencetomography(OCT)imaging:usesinfraredlight(inasimilar
waytosonography)toproducehigh-resolutiondynamicimages.Thisresearch
toolmaytranslatetoclinicalpractice.
Management
Management is based on symptoms and the impact of symptoms and joint
structuralchangesincluding the effect on qualityoflife, function, occupation,
leisure,andsleep.
• Functional requirements are addressed by therapists following therapy
assessment(occupationalandphysiotherapy).
• Occupational therapy can provide splints, aids, safe environment, and joint
protectiontechniques.
• Exerciseisakeytreatmentinmanycasesasitimprovesmusclestrength,joint
proprioception,andaerobicfitness.
• Patient expectations influence the use of analgesia and referral for surgical
procedures.
• Weight isassociatedwith anumber of typesof OA inweight-bearingjoints
and islinkedto poor prognosis. Weightlossistherefore important asakey
intervention.
• Psychosocial factors (mood and relationships) may influence symptoms and
impactofOAandrequiretherapeuticinputoccasionally.
• A multi-disciplinary approach is sensible. In the UK, NICE has produced
guidelinesformanagementofOAinadultsthatemphasizeaholisticapproach
tailoredtothepatient’sspecificneeds.
3
• NICE identifies core treatments that should be offered to all patients, in
addition to the use of pharmacological and adjunctive treatments based on
patientneeds(Box6.1).
Pharmacotherapies
• NSAIDsandCOX-2inhibitorsmaycanbeeffectiveforuseinshortperiods
duringinflammatorydiseaseflares.
• UK NICE guidance emphasizesNSAIDusefor the shortest time and atthe
lowestdosepossibleandwithcautioninolderpatients.
• Cardiovascular adverse events appear equal between conventional NSAIDs
andCOX-2inhibitors.
• The addition of local anaesthetic to intra-articular GC injection does not
improveefficacy,butmayreducepainfromtheinjections.
• Asymptomaticeffusionsdonotrequireintra-articularinjection.
• Most jointinjection dataarefor kneeOA.Infection israre (<1:10,000),but
care should be taken to clean overlying skin and avoid injecting through
infectedskinorpsoriaticlesions.Patientsshouldbewarnedoftheriskofskin
depigmentationandfatatrophy.Itisadvisedthatpatientsreceivenomorethan
3–4injectionsperyear,each≥3monthsapart
• Intra-articularinjectionofhyaluronicacidderivatives(viscosupplementation)
isnotsupportedbyrobustdataandisnotsupportedbyUKNICEguidance.
• Oralglucosamineandchondroitinsulphatesupplementshavebeenshownin
RCTs and meta-analyses to be no better than placebo, and are not
recommendedbyNICEintheUK.
• Evidence that avocado/soybean unsaponifiable supplementation, evening
primroseoil, rosehipextract,blue-lipmusselextract,and omega-3fish oils
improvepainislimited.
Box6.1OA:Diseasemanagementprinciples
Coretreatments
• Holistic,patient-centredcareplan.
• Provisionofwrittenandverbalinformation.
• Adviceonfootwear.
• Exercise.
• Weightloss.
Adjunctivetreatments
• TENSmachine.
• Braces,walkingaids,andinsoles.
• Thermotherapy:cold/warmmeasurestoreducesymptoms.
Pharmacologicaltreatments
Initial
• Regularparacetamol1g3–4timesdaily.
• Topicalanti-inflammatorygels(NSAIDs).
• Topicalcapsaicincream.
Subsequent
• OralNSAIDs/COX-2inhibitors±protonpumpinhibitor.
• Intra-articular glucocorticoids (useful during flares; duration of benefit
variable).
Rarely
• Codeine–paracetamolcombinationanalgesics.
• Buprenorphine.
• Gabapentinorpregabalin.
Surgical
• Arthroscopiclavage/debridementifmechanicallocking.
• Jointreplacementforactivity-limitingsymptomaticOA—mayreducepain
ratherthanincreasefunction.
Futuretherapeuticstrategies
CurrentOAresearchisfocusingondisease-modifying anti-osteoarthritisdrugs
(DMOADs),withtheaimofpreventingjointdamage.Approachesinclude:
• Inhibition of RANK ligand-mediated subchondral bone resorption using
monoclonalantibodies.
• Bisphosphonates reducing bone loss—putatively anti-(subchondral bone)
resorption.
• InhibitionofcathepsinK,apotentproteaseinvolvedindegradationoftypeI
collageninbonematrix.
• Vitamin D supplementation, which will optimize calcium absorption and
reducePTH,slowingboneresorption.Studiesareyettobedone.
• Diacerein,anIL1blocker,hasbeenshowntoreducejointspacelossinhipOA
over3yearsinoneRCT.Furtherstudiesneedtobeperformed.
• Mesenchymal stem cell therapy—precursor cells capable of differentiating
intoosteogenic,chondrogenic, or adipogeniccells. Several clinicaltrials are
ongoinginearlyphases.
Reference
3. NICE. Osteoarthritis: Care and Management. Clinical Guideline 177. London: NICE, 2014.
https://www.nice.org.uk/guidance/cg177
Prognosis
KneeOA
• Progressioninthekneemaytakemanyyears.Cohortstudieshavefoundthat
radiographicdeteriorationoccursinone-thirdofcases.
• BMIpredictsprogressionofpatellofemoralOA.
• For tibiofemoral compartment OA, patients with contralateral knee OA, a
baselineindexkneeOAgradeof1,higherbodymassindex(BMI)andhigher
baseline Western Ontario and McMaster Universities arthritis index total
scoresaremorelikelytodevelopKellgren&Lawrencegradeof3or4within
5years.
HipOA
• Progressionofhipdiseaseisvariable.ADanishstudyfoundthat66%ofhips
worsened radiologically over 10 years, although symptomatic improvement
wascommon.
• Heterogeneity of prediction factors is found across studies and within study
populations.
• Clinicalcharacteristics(highercomorbiditycountandpresenceofkneeOA),
healthbehaviourfactors(nosupervisedexerciseandphysicalinactivity),and
sociodemographics(lowereducation)havebeenfoundtopredictdeterioration
ofpain(weakevidence).
• Ahighernumberofcomorbiditieshavebeenfoundtopredictdeteriorationof
physicalfunctioning(strongevidence).

Chapter7
Crystal-inducedmusculoskeletaldisease
Goutandhyperuricaemia
Calciumpyrophosphatedepositiondisease
Basiccalciumphosphatecrystal-associateddisease
Calciumoxalatearthritis
Goutandhyperuricaemia
Goutisacommon,painful,andpotentiallydestructiverheumatologicdisorder,
related to hyperuricaemia. The clinical consequences of uric acid or urate
(monosodium urate (MSU)) crystal deposition include acute and chronic
arthritis,tophusformation,nephrolithiasis,andgoutynephropathy.
Epidemiology
• Several epidemiologic studies from different countries suggest that the
incidence and prevalence of gout is increasing, perhaps related to better
recognition,andchangesinlifestyleanddiet.
• In the UK, gout affects 25 per 1000 of the population, and accounts for
250,000 GP consultations per year. Prevalence data from the USA on self-
reportedgoutestimatethat13.6per1000adultmalesand6.4per1000adult
femalesareaffected.
• Goutismorecommoninmiddle-agedandelderlypeople.
• Theriskfactorsforgoutarethesameasthoseforhyperuricaemia(Table7.1).
Classificationcriteria
• ThecurrentACR/EULARguidelinesstipulate,for theclassificationof gout,
the occurrence of ≥1 episode (‘attack’) of joint or bursal swelling, pain or
tenderness.
• MSUcrystalsin(symptomatic)synovialfluidorfromatophusissufficientfor
diagnosisofgout.

• Thedomainsofthecriteriainclude:
• clinical (pattern of joint involvement, characteristics, and time course of
symptomaticepisodes).
• laboratory(serumuricacid(SUA)levels).
• synovialfluid(aspirateanalysisforcrystals).
• imaging (radiographic gout-related erosion, double-contour sign on
ultrasound,orMSUcrystalsondual-energyCT).
Clinicalfeatures
• Thefirststageoftheconditionisusuallyasymptomatichyperuricaemia(SUA
>680mg/L)oftenstartingyearsbeforesymptomsdevelop.
• Thisconcentrationmarksthephysiologicalpointabovewhichuratesaltsare
no longer soluble in the serum at physiologic pH and temperature. Not
everyonewithhyperuricaemiadevelopsgout,however.
• Inflammation to MSU crystals is typically sudden and severe and is often
referredtoasan‘attack’ofgout.
• Theinitialattackcommonlyoccursinthefourthtosixthdecadeoflifeinmen,
andinpostmenopausalwomen.
• The initial attack is usually monoarticular, affecting the first
metatarsophalangealjoint(podagra)inupto60%ofpatients.
• Otherfrequentlyinvolvedjointsincludetheankle,midfoot,knee,wrist,elbow
(olecranonbursa),andthesmalljointsofthehands.
• Axialandlargejointsandspinalstructuresarerarelyinvolved.
• With an attack, pain reaches its maximum intensity in 4–12 hours, with
marked limitation of physical function. Symptoms usually resolve in 3–14
days.
• 70–80%ofindividualswillhaveanotherattack(s)within2years.
• Theinitialattacksareusuallyseparatedbyasymptomaticinter-criticalperiod,
lastingmonthstoyears.
• Asthediseaseprogresses,acuteattacksmaybecomemorepolyarticular,with
associated joint damage and deformity. Intervals between attacks tend to
shorten. Disability, chronic pain, and tophi formation can be observed if
treatmentissuboptimal(see Plate7).
• TophiaredepositsofMSUembeddedinamatrixcomposedoflipids,proteins,
andcalcificdebris:
• Tophi are usually subcutaneous, but have been reported to occur in bone,
eyes,andotherorgans.
• Classicsitesfortophiformationincludeearpinna,elbowandkneebursae,
Achillestendon,anddorsalsurfaceoftheMCPJs.
• Tophi are usually painless, although the overlying skin may ulcerate and
becomeinfected.
• Those most at risk of tophi are patients with prolonged severe
hyperuricaemia,polyarticulargout,andtheelderlywithprimarynodalOA
ondiuretics.
• Someclinicianswilltreatasymptomatichyperuricaemiatopreventtheonset
of‘uratenephropathy’;butthisiscontroversial.
• Hyperuricaemia and gout are associated with the metabolic syndrome
(dyslipidaemia,hypertension,obesity,andinsulinresistance).
Investigation
• Synovialfluidanalysisisthemostimportantinvestigation.
• Negativelybirefringent,needle-shapedcrystalsonpolarizedlightmicroscopy
confirmsthediagnosis.
• Crystalsmaybeextra-orintracellular.However,theabsenceofcrystalsdoes
notruleoutthediagnosis.
• MSU crystals are identifiable in the synovial fluid from previously affected
joints and about 70% of those receiving SUA-lowering therapy during the
asymptomaticinter-criticalperiod.
• SUA concentrations may be normal during an acute attack in up to 30% of
cases, and may not reflect pre-flare levels. Therefore, SUA concentration
cannotbeusedtoexcludethediagnosisduringanacuteflare.
• SUAconcentrationsareofvalueinassessingthepatientonlyoncetheacute
flare has subsided; either to confirm hyperuricaemia or to monitor the
effectivenessoftherapy.
Table7.1Thecausesofhyperuricaemiaandriskfactorsforgout
Primarygout Malegender
Increasingage(inwomen)
Ethnicity
Beingoverweight
Diet(purinerichdiet)—particularlyredmeat,oily-fish,
shellfish,sugarydrinks,andfructose-richfoods
Alcoholuse(beerappearingtoposethehighestrisk)
Renalinsufficiency
Hypertension
Inherited
metabolic
syndromes
X-linkedHPRTdeficiency(Lesch–Nyhan),X-linked
raisedPRPPsynthetaseactivity.AutosomalrecessiveG6P
deficiency(vonGierke’sdisease)
Uricacid
overproduction
Cell lysis: tumour lysis syndrome, myeloproliferative
disease,haemolyticanaemia,psoriasis,trauma.
Drugs:alcohol,cytotoxicdrugs,warfarin
Uricacid
underexcretion
Renalfailure
Drugs:alcohol,salicylates,diuretics,laxatives,ciclosporin,
levodopa,ethambutol,pyrazinamide
Leadtoxicity Renalimpairmentandalteredpurineturnover
G6P,glucose-6-phosphatase.G6Pdeficiencyleadstoincreasedactivityofaminophosphoribosyl
transferaseandpurineformation;HPRT,hypoxanthineguaninephosphoribosyltransferase—asalvage
enzymeconvertinghypoxanthinebacktoprecursorsandthereforecompetingwithitsconversionto
xanthineandthenuricacid;PRPP,phosphoribosylpyrophosphatesynthetase—acomponentenzymein
purineringsynthesis.
Imaging
• Imagingfindingsvaryatdifferentstagesofgout.
• Plainradiographsareoftennormalduringtheearlyphaseofthedisease,but
softtissueswellingcanbeapparent.
• Radiographs are useful to assess for other conditions such as trauma or
infection (Box 7.1). Subcortical bone cysts may be suggestive of tophi or
erosions. Para-articular erosions with ‘overhanging edges’ of bone are
characteristicofgout.
• Later in the disease, radiographs may demonstrate tophi near joints, tissue
swelling, para-articular erosions, periosteal new bone formation, and joint
deformity.ManyfeaturesmimicRA.
• US can be useful to detect early disease and monitor treatment. Diagnostic
featuresincludea lineardensity paralleltothe jointsurface (double-contour
sign), or tophaceous deposits which appear as oval stippled signal
(hyperechoiccloudyarea).
• Dual-energyCTspecificallyidentifies MSUdepositsanddistinguishesthem
fromcalciumdeposition.
Box7.1Clinicalconditionsthatcanmimicgout
• CPPDdisease(pseudogout)
• Basiccalciumphosphate(BCP)arthritis
• Cellulitis
• Infectious(septic)arthritis
• Trauma(cancoexistwithgout)
• Rheumatoidarthritis(polyarticular)
• Psoriaticarthritis(monoarthritis/dactylitis)
• Erythemanodosum
• Reactivearthritis(monoarthritis/dactylitis).
Management
Themanagementofgoutshouldbeapproachedintwophases:thetreatmentof
theacuteattackandthetreatmentofchronicortophaceousgout(Fig.7.1).
Theacuteattackofgout
• Rest,elevation,andicepackscanpartlyeasesymptoms.
• The principal therapies are NSAIDs, colchicine, and oral and intra-articular
(IA)glucocorticoids(GCs).
• SUA-loweringdrugsareineffectivein acutegout. Patientsalready onSUA-
loweringdrugs,shouldcontinuewithoutinterruption.
• NSAIDsdecreasepain,swelling,anddurationofgoutattacks.
• All NSAIDs, including COX-2 selective NSAIDs, have potentially similar
efficacyforgout.
• NSAIDsaremosteffectivewheninitiatedwithin48hoursofsymptomonset.
Thedosemaybereducedafterareductioninsymptoms,anddiscontinued1–2
daysaftercompleteresolutionofsigns.
• The typical duration of NSAIDs required for an acute attack is 5–7 days.
NSAIDsarecontraindicatedinrenalinsufficiency(e.g.CKD3b–5).NSAIDs
shouldbeusedwithcautionintheelderlyandpatientswithGIriskfactors.
• Colchicine can be very effective in acute gout, and have a rapid onset of
action. Oral colchicine 0.5 mg, two to four times daily, for 5 days can be
effectivebutmaycausediarrhoeaathigherdoses.
• ColchicineisoftengiveninadditiontoNSAIDs,althoughthereisnoevidence
to support this. IV colchicine is no longer used due to high risk of bone
marrowsuppressionanddeath.
• Oralprednisone10–30mgdailyiseffectiveforimmediatereliefofgout,with
dosethentaperedover7–10days.
• ParenteralGCsmaybeusedinindividualsunabletotakeoralformandwith
polyarticulargout.A study comparingintramuscular triamcinolonewith oral
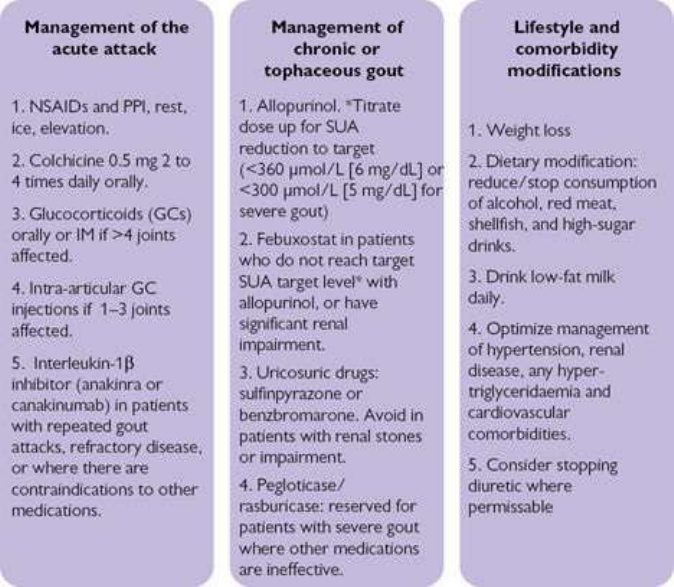
indometacinfoundnosignificantdifferenceintimetorecovery.
• IAGCsareusefulif≤4jointsareaffected.Asystematicreviewonthesafety
andefficacyofIAGCsforacutegoutcouldnotidentifyanyRCTsoftheiruse.
• IAGCsshouldbeavoidedifsepticarthritisispossible.
• IL-1 inhibitors are under study for acute gout. IL-1β is the predominant
mediatorofacuteinflammation.
• Anakinra 100 mg SC daily has been used until symptoms improve with
goodeffect.
• Canakinumab150mgSCislicensedforacutegoutinEurope.
• In one study comparing SC canakinumab with IM triamcinolone,
canakinumabachievedbetteroutcomesintermsofpainrelief,jointswelling
reduction,andpatient-assessedglobalresponse.
• Canakinumab is effective in patients either with multiple gout ‘flares’ or
whosedisease isrefractory toother treatmentorhavecontraindicationsto
othermedications.
• However, canakinumab is associated with increased infections, and at the
timeofwritingis5000×thecostoftriamcinolone.
Fig7.1Themanagementofgout.GC,glucocorticoid;IM,intramuscular;NSAID,non-steroidalanti-
inflammatorydrug;PPI,protonpumpinhibitor;SUA,serumuricacid.
Treatmentofchronicortophaceousgout
• Addressing adverse lifestyle factors and comorbidities should be a priority,
includingto:
• attainanormalBMI(20–25)/reducecentripetalobesity.
• reduce, orpreferentiallystop, consumptionofalcohol, red meat,shellfish,
andsugarydrinks.
• managehypertensionandassociatedhypertriglyceridemia.
• encouragetodrinklow-fatmilkdaily(anaturaluricosuric).
• remainwellhydrated.
• consider how best to minimize treatments which can aggravate
hyperuricaemia (e.g. thiazide, furosemide, indapamide, ciclosporin,
levodopa,theophylline).
• The target SUA with all drug therapy is <360 µmol/L (6 mg/dL) or <300
µmol/L(5mg/dL)wherethereisseveregout.Goutattacksareveryunlikely
whereSUAisbelowtarget.
• DrugsthatdecreaseSUAlevelsareindicatedinindividualswithfrequentor
disabling attacks of gout, clinical or radiological evidence of chronic gouty
arthropathy, tophaceous disease, with secondary renal impairment, or
urolithiasis.
• SUA-loweringdrugsareinitiated2–4weeksafteranacuteflaresubsides,as
theymayprolongorworsentheacuteflare.
• Allopurinol(axanthineoxidaseinhibitor)isthefirst-linetreatment:
• Allopurinolisinitiatedat100mgdailywithincrementaldosetitrationevery
month,aimingtolowerSUAto≤300mg/L.
• Thedoserangeofallopurinolis100–900mgdaily.
• Mostpatientsrespondto400mgdailyofallopurinol.
• Dosingshouldbeadjustedforrenalimpairment.
• Allopurinoltakes4daysto2weekstotakeeffect.
• Approximately 5–10% of patients develop significant drug intolerance:
nausea,diarrhoea,elevatedtransaminaselevels(3–5%).
• Severe hepatic disease including granulomatous hepatitis, cholestatic
jaundice,andhepaticnecrosisarerare.
• About2%ofpatientsdevelopapruritic,maculopapularrash.Pruritisalone
canheraldtheonsetofrash.
• Bonemarrowsuppressionoccursrarely—athighdoses.
• HLA-B*5801 status increases the risk of developing allopurinol drug
reactioneosinophiliaandsystemicsymptoms(DRESS).
• Inmildtomoderateintolerance,allopurinolcanbereintroducedatverylow
levels(e.g.10mgdaily)andtitratedupslowly.
• Allopurinolcaninterferewiththemetabolismofazathioprineandwarfarin,
increasingtheriskofsideeffects.
• Concomitant colchicine (0.5 mg twice daily orally) is recommended as
prophylaxis against acute flares for the first 3–6 months of allopurinol
treatment.
• Febuxostatisanon-purinexanthineoxidaseinhibitor:
• FebuxostatismoreeffectiveatloweringSUAthanallopurinol,andmaybe
usedinpatientsallergictoallopurinol,patientsnotattainingtargetSUAat
maximalallopurinoldose,andinpatientswithmoderaterenalinsufficiency.
• Dosesrangefrom40to120mg/day.
• Dosereductionisrequiredinpatientswithrenaldysfunction.
• Sideeffectsincludenausea,liverdysfunction,arthralgia,andrash.
• Somestudieshaveshownahigherincidenceofcardiovascularsideeffects
withfebuxostatcomparedwithallopurinol.
• Febuxostatissubstantiallymoreexpensivethanallopurinol.
• Some patients may respond to allopurinol and a uricosuric agent (e.g.
probenecid)wheneitheralonehasbeenineffective.
• Uricosuric drugs should be avoided in patients with renal insufficiency or a
historyofnephrolithiasis.
• Fenofibrate decreases SUA by increasing renal uric acid clearance. It may
haveanunlicensedroleinpatientsresistantorintoleranttoothertreatments.It
should be avoided in hepatic and biliary disease, hypothyroidism and
pregnancy.Sideeffectsincludemyoarthralgias.
• Sulfinpyrazoneisauricosuricdrugwhichiseffectiveandwelltolerated,butis
contraindicated in patients with renal stones and is ineffective in those with
renalinsufficiency.
• Benzbromarone is a uricosuric agent available in Europe. It is effective in
patientswithrenalinsufficiency.Liverfunctionmustbemonitoredfordrug-
inducedhepatitis(fulminantliverfailurereported).
• Pegloticase is a porcine uricase reserved for patients with severe gout, in
whomothergouttreatmentshavebeenineffective.Administrationis8mgIV
every 2 weeks.Concomitantcolchicine prophylaxis is recommended forthe
first6monthsofuse.Anti-pegloticaseantibodieshavebeenreported.
• Rasburicase is a non-pegylated recombinant uricase. It may be more
immunogenicthanpegloticase.
• Patients with uric acid stones are best managed with adequate hydration,
urinary alkalization, and allopurinol. This regimen is also effective in
preventingcalciumoxalatestones.
• Goutytophimaybeamenabletosurgicalremoval.
Calciumpyrophosphatedepositiondisease
• SeeBox7.2foranoverviewofEULARdefinitionsandclinicalpresentations.
• Precipitationofcalciumpyrophosphate(CPP)crystalsintissuesisextremely
common and arguably the most common reason why previously ill
hospitalizedpatientsdevelopMSKproblemswhenunwellinhospital.
• The spectrum of CPP crystal deposition disease includes acute and chronic
arthropathy, inflammation and symptoms at entheses or within/involving
tendons, soft tissue and bursal inflammation, asymptomatic cartilage
calcification,andsymptomsfromspinalcanalandintervertebraldisccrystals.
Box7.2EULARdefinitionsofcalciumpyrophosphate(CPP)deposition
(1–3)andclinicalpresentationsofCPPdeposition(CPPD)disease
1.CPPcrystals
Simplifiedtermforcalciumpyrophosphatecrystals.
2.CPPD
TheumbrellatermfordepositionofCPPcrystals.
3.CC
Cartilage calcification, identified by imaging or histology—but not always
duetoCPPD.
AsymptomaticCPPD
Maybeofnoclinicalconsequence;butthedegreetowhichcartilageorother
soft tissue CPP crystals increase the risk of significant MSK lesions (e.g.
osteoarthritis, intervertebral disc degeneration, chronic enthesopathy, spinal
stenosis)islargelyunknown.
AcuteCPPDarthritis
Acuteself-limitingsynovitis.
CPPDdiseasewithosteoarthritis(OA)
CPPcrystalsinajointwhichisosteoarthritic.
ChronicCPPDarthritis
Typicallyaffectswrists,2nd/3rdMCPJs,hips,knees(mimicsRAbutisACPA
negative).
SpinalCPPDdiseasetypes
Inflammation proven or suspected around the odontoid (‘crowned dens
syndrome’),causingorcomplicatingintervertebraldiscdiseaseorassociated
with ligament flavum thickening contributing to spinal and/or lateral recess
stenosis.
OtherCPPD(possiblyallCC)-relatedlesions
Tendoninsertion/enthesis-basedinflammationassociatedwithCPPD;boxing-
glove-likehand/wristswellingfeaturesofacutedisease.
• TheriskofCPPD-relateddiseaseincreaseswithage.Presentationinayoung
adult<50yearsoldshouldpromptasearchforanassociatedmetaboliccause.
• Definite associations with CPPD disease and chondrocalcinosis (i.e.
calcificationof fibrocartilageandhyaline cartilagetypically oftheknee and
wrist)include:
• Hypomagnesaemia (check Mg, PTH, vitamin D, bone profile and renal
function).
• Hypophosphatasia (low ALP, raised serum pyridoxal-5 phosphate and
increasedurinaryphophoethanolamine).
• Haemochromatosis (positive family history, abnormal LFTs, raised
haemoglobin, ferritin and transferrin saturation, and disease-associated HFE
genotype).
• Wilson’s disease (neurological disease, abnormal LFTs, eye disease, and
abnormallylowserumcaeruloplasmin).
• Hyperparathyroidism (primary, secondary, and tertiary in renal disease). So
checkPTH,boneprofile,renalfunction/estimatedGFR,andvitaminD).
• Vitamin D deficiency—chronic (through causing secondary
hyperparathyroidism).Checkasforhyperparathyroidism.
• Possible CPPD disease associations include gout, ochronosis, hypocalciuric
hypercalcaemia,diabetes,DISH,andXLHR.
• ThemainprecipitantsofanacuteCPPDdiseaseepisode(ifinajointhistorical
termwas‘pseudogout’)arelistedinBox7.3.
Box7.3FactorsthatmaytriggeracuteCPPD-inducedinflammation
• Acuteillness(e.g.chestorurinaryinfection).
• Directtrauma(e.g.jointcartilagedamageortendontear/strain).
• Post-surgical.
• Especiallypost-parathyroidectomy.
• BloodtransfusionorIVfluids.
• Commencementofthyroxinereplacement.
• Jointlavage.
Investigation
• CPPDdiseaseisdefinedbythepresenceofpositivelybirefringent,rhomboid-
shaped crystals under polarized light microscopy of synovial fluid. Crystals
maybeintra-orextracellular.
• Radiographs of the affected joints may not be helpful in establishing the
diagnosis.However,thepresenceofchondrocalcinosisincreasesthelikelihood
of CPPD disease. Radiographic clues that may help to distinguish CPPD
diseasefromOAinclude:
• axialinvolvement.
• sacroiliacerosions.
• corticalerosionsofthefemur.
• osteonecrosisofthemedialfemoralcondyle.
• associated hyperparathyroid disease signs: endocortical erosions of long
bonesinthehandsandfeet,corticaltunnelling,andosteopeniainphalanges.
• US features indicative of CPPD include a thin hyperechoic band along the
cartilage, running in parallel to the bony cortex (‘tram-lines’). Sites can
include the MCPJs, wrists, knees, and tendons. Nodular deposits in bursae,
entheses,andhyperechoiclinesparalleltotendonscanalsobeobserved.
• BothCTandMRImaybeneededtodisclosediseaseinspinalstructures:MRI
to show inflammatory changes and CT to disclose the distribution of
calcification(see Plate22).
Management
AcuteCPPD-relatedarthritis
• ThemanagementofacuteCPPDdiseaseissummarizedinFig.7.2.
• Rest,ice,andsplintingintheacutephasewillhelpsymptoms.
• NSAIDsintheacutephase.
• Oralcolchicine(0.5mg,twotofour timesaday)canbe usedinpatients in
whomNSAIDsarecontraindicatedintheacutesettingorasprophylacticuse
topreventrecurrentflares(seeFig.7.2).
• JointaspirationandIAGCinjectionforacutejointinflammation,oncejoint
infectionhasbeenexcluded(see Chapters24).
• Oral GCs will undoubtedly help in the acute setting but the dose should be
reviewedandminimizedtoavoidlong-termuseandsteroiddependency.
• AnakinrahasbeenusedinpolyarticularacuteCPPDdisease,unresponsiveto
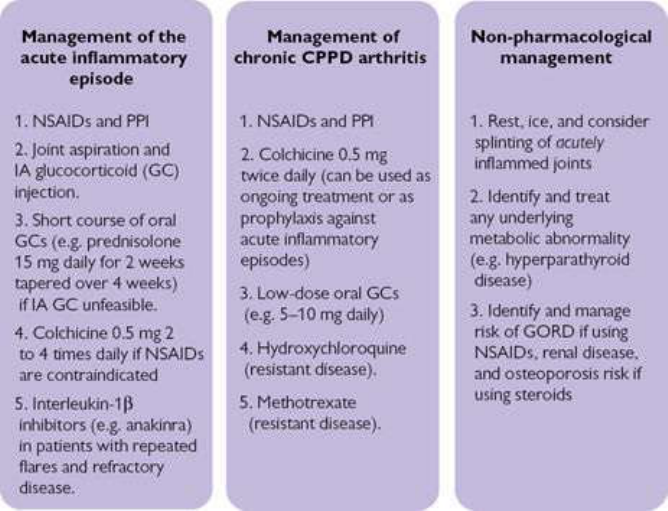
othermedications.
• AsinallCPPDcases,identifyandmanageassociatedmetabolicabnormalities.
ChronicCPPDarthritis/disease
• DiseasemaymimicRAifpolyarticularandcancausepersistentinflammatory-
typespinalsymptoms.
• Ongoing metabolicinfluencesof CPPDdiseasemay need addressing.Renal
disease, hyperparathyroidism (primary, secondary, or tertiary (but for
secondaryalsoconsidervitaminDdeficiency)),andchronicdehydrationmay
allplayarole.
• Hydroxychloroquine(200–400mgdailyintwice-dailydosesfortrialperiodof
4monthsforexample)ormethotrexate(e.g.15mgweeklyfortrialperiodof6
monthsinitially)maybetriedinpatientswithresistantdisease.
• Arguably there is more evidence to support the use of methotrexate than
hydroxychloroquine.
1
Fig.7.2Managementofcalciumpyrophosphatedeposition(CPPD)disease.GC,glucocorticoid;GORD,
gastro-oesophagealrefluxdisease;IA,intra-articular;NSAID,non-steroidalanti-inflammatorydrug;PPI,
protonpumpinhibitor.
Reference
1. Zhang W, Doherty M, Pascual E, et al. EULAR recommendations for calcium pyrophosphate
deposition.PartII:management.AnnRheumDis2011;70:571–5.
Basiccalciumphosphatecrystal-associated
disease
• Basiccalciumphosphate(BCP)crystalsincludehydroxyapatite,octacalcium
phosphate,andtricalciumphosphate.
• BCP and associated crystals are associated with several rheumatological
diseases(Table7.2).
• ThetreatmentoftheseconditionsisasperCPPDdisease,withNSAIDsand
colchicine(see Chapter23,forfurtherdetails).
Table7.2BCPcrystal-associatedconditions
Articular
disease
Milwaukeeshouldersyndrome(severedegenerative
arthropathy,morecommononthedominantsideandinelderly
women)
Osteoarthritis(synovialfluidcrystalsfoundin60%ofOA
patients)
Erosivearthritis
Mixedcrystaldeposition
Periarticular
disease
Pseudopodagra,calcifictendonitis,andbursitis
Calciumoxalatearthritis
• Crystals are positively birefringent and bipyramidal under polarized light
microscopyofsynovialfluid.
• Radiographsandlaboratorytestsarenotdiagnostic.
• Mostlabswillnothavetheexpertisetospecificallyidentifythesecrystalson
synovialsamples.
• TreatmentisasforCPPDdisease.
• Severalconditionsareassociatedwithcalciumoxalatearthritis(Box7.4).
Box7.4Conditionsassociatedwithcalciumoxalatearthritis
• End-stagerenaldiseaseondialysis.
• Shortbowelsyndrome.
• Dietrichinrhubarb,spinach,andascorbicacid.
• Thiaminedeficiency.
• Pyridoxinedeficiency.
• Primaryoxalosis:recessivetrait,earlyrenalfailure(inthethirddecadeof
life),arthritis,tendonitis.

Chapter8
Thespondyloarthritidesincludingpsoriatic
arthritis
Introduction
Spondyloarthritis(SpA):aparadigmshift
AxialSpAincludingankylosingspondylitis
Psoriaticarthritis
SpA-associatedreactivearthritis
Inflammatoryboweldisease-relatedSpA
Juvenilespondyloarthritis
Introduction
Allspondyloarthropathies(SpAs)arecommonlycharacterizedbyinflammatory
backandaxialskeletalpains,enthesitis,andanassociationwithHLA-B27.
• TheSpAsare:
• Axialspondyloarthritis(axSpA).
• Ankylosingspondylitis(AS;encompassedbyaxSpAdefinition).
• Psoriaticarthritis(PsA).
• Reactivearthritis(ReA).
• Inflammatoryboweldisease-relatedSpA.
• JuvenileSpA/enthesitis-relatedarthritis(ERA;see Chapter9).
• Considered together the SpAs are the most common form of chronic
inflammatoryarthritis;morecommonthanRA.
• AllSpAsarepotentiallymanifestby:
• enthesitis.
• inflammatorybackpain.
• asymmetricperipheralarthritis.
• inflammatorybowellesions.
• psoriasis.

• dactylitis.
• osteitis.
• sterileurethritis.
• uveitis(typicallyacuteanterioruveitis).
• aorta/aorticvalvelesions(rare).
• abnormalantigenpresentationassociatedwithHLA-B27.
• Similarities exist between SpAs and the SAPHO (synovitis, acne,
palmoplantar pustulosis, hyperostosis, aseptic osteomyelitis) syndrome;
SAPHOisnotconsideredtobeaSpA;see Chapter16.
• Pathologicalchangesaremainlyatenthesesbutalsointissuesofthegut,uveal
tract,urethra,aorta,bone,synovium,andskin.
• Acommoninflammatory‘target’orprecisecommonreasonwhysuchtissues
mightbeaffectedispostulatedthoughnotyetproven.
• Linesofimmunopathologyresearchcurrentlyfocusongeneralandlocaltissue
resident Th17 cell activation by Il-23 and subsequent activating effects
specifictothelocaltissueenvironment.
Spondyloarthritis(SpA):aparadigmshift
KeytoclassifyingallSpAsisthepresenceofinflammatorybackpain(Box8.1)
and,forday-to-dayclinicalrecognition—thepresenceofenthesitis(Box8.2).
• Sadly,thereisstilla7–10-yeardelayinasizablenumberofpatientsbetween
symptomonsetanddiagnosisofankylosingspondylitis(AS)—similardatato
data derived>30years ago. One reason isthatit takes many years insome
patientstoconfirmASasitisbasedpartlyonradiographiccriteria(ofSIJs)
whichcantakeyearstoevolve(Box8.3).
• The classification of axial spondyloarthritis (axSpA; see the Assessment of
Spondyloarthritis International Society (ASAS) working group criteria:
http://www.asas-group.org)includesclassicalASaswellasearlierstagesand
abortive courses of the disease, in which structural alterations have not yet
occurred.
• ASAS has facilitated classification of SpA in terms of axial or peripheral
predominantdisease.
• The new ASAS criteria (for axSpA; Box 8.4) potentially allow all patients,
who will ultimately develop AS, to be identified earlier in their disease
comparedwiththemodifiedNewYork(mNY)criteria.
• However, it is likely that not all ASAS axSpA classifiable patients will
progresstoanASphenotypeclassifiablebythemNYcriteria.
• Previously, early SpA disease was recognizable formally only through a
definition (ESSG) of ‘undifferentiated SpA’ (USpA). Many such patients
would now be classifiable by the newer ASAS working group criteria for
(peripheral)SpA(Box8.5).
• Recently,classificationcriteriaforPsAhavealsobeendeveloped(CASPAR;
see ‘Psoriaticarthritis’,pp.308–313).
Box8.1Inflammatorybackpain(IBP)
AhistoryofIBPiskeytoconsideringaxialsymptomsassecondarytoSpA—
forpeopleinwhomitstartsat<40yearsofage.Applicableforbackand/or
posterior pelvic symptoms.A number of descriptionsexist(e.g.after Calin,
Rudwaleit,orASAS).Typically,IBP:
• comesongraduallyovertime(insidiousonset).
• isimprovedwithexercise.
• doesnotimprovewithrest.
• causespainatnightwithimprovementongettingup.
• isreportedbypatientsasoccurringwith“stiffness”.
• improveswitha(‘once-daily’)modified-releaseNSAIDtakenatbedtime.
Box8.2Enthesitis
Anenthesisisthenamegiventospecializedtissuewhichattachesaligament
ortendontoabone.ExamplesincludetheattachmentsoftheAchillestendon
to os calcis, the origin of the finger extensor tendons at lateral humeral
epicondyle, the gluteus tendon insertion at the greater trochanter, or the
attachmentsofthepatellaligament.
AxialSpAincludingankylosingspondylitis
The diagnosis of axial spondyloarthritis (axSpA) includes classicalankylosing
spondylitis(AS)aswellasearlierstagesandabortivecoursesofthedisease,in
which(radiologicalevident)structuralalterationshavenotyetoccurred.Cases
ofthelattermightbealsoclassifiedasnon-radiographicaxSpA(nr-axSpA).
For a comparison of the ASAS criteria for classification for axSpA and
peripheralSpA,seeBox8.4andBox8.5.
EpidemiologyofAS(onmodifiedNewYorkcriteriaorearlierdefinitions)
• There isanextensive wealthofdata ontheepidemiology ofASdefined on
mNYandearliercriteria.
• Patientsaretypically<40yearsofagewithaM:Fratioof3:1.
• TheconditionoccursmostfrequentlyinCaucasians.
• In Pima American Indians, where HLA-B27 prevalence is high, AS is
particularly frequent, whereas the condition is less common in African
Americans, and rarer still in sub-Saharan Africans, reflecting the low
prevalenceofHLA-B27inthesegroups.
• Prevalenceestimateis0.5–0.8/100,000inCaucasianadults.
• Epidemiology data necessarily depend on patients satisfying criteria for
diagnosisthatnecessarilymeanstheyhavehadtheirdiseasearelativelylong
time(tohaveradiographicchangesatSIJs).
EpidemiologyofaxSpA
• OneimplicationofthisparadigmshiftisthatadefinitionofaxSpAresultsina
definedpatientprevalencemuchhigherthanhasbeenacceptedforAS(based
onmNYcriteria,forexample).
• There is an evolving understanding of the prevalence of axSpA based on
ASAScriteria.
• Studies of modelling disease prevalence suggest that axSpA is considerably
morecommonthanAS.
• ItislikelythatthefrequencyofaxSpApatientsinanygivencohortofIBPor
chronic back pain patients, is higher than previously defined for an AS
definition (e.g. 29% of patients with IBP met the criteria for nr-axSpA and
39%ofpatientswithchroniclowbackpainhadIBP).
1
Box8.3ModifiedNewYork(mNY)criteriaforclassifyingAS
Clinicalcriteria
• Lowbackpainandstiffnessfor>6months,improvingwithexercise,butnot
relievedbyrest.
• Limitationoflumbarspinemovementsinsagittalandfrontalplanes.
• Limitationofchestexpansionrelativetonormalvaluesforageandsex.
Radiologicalcriteria
• Greaterthanorequaltograde2bilateralsacroiliitis.
• Grade3or4unilateralsacroiliitis
Combineddiagnosticcriteria
• DefiniteASifradiologicalandclinicalcriterion.
• ProbableASifthreeclinicalcriteriaoraradiologicalcriterionwithoutsigns
orsymptomssatisfyingtheclinicalcriteria.
Adapted from Van der Linden et al. ‘Evaluation of diagnostic criteria for
ankylosingspondylitis.’ArthRheum,1984;27:361–368withpermissionfrom
Wiley.
Box8.4ASAScriteriaforclassificationofaxialSpA
Inpatientswith≥3months’backpainandageatonset<45years:
either
Sacroiliitisonimagingplus≥1SpAfeature
or
HLA-B27plus≥2otherSpAfeatures.
SpA features: IBP, arthritis, enthesitis (heel), uveitis, dactylitis, psoriasis,
Crohn’s/colitis,NSAIDresponse,familyhistoryofSpA,HLA-B27,CRP+
Sacroiliitis on imaging: either active (acute) inflammation on MRI highly
suggestive of sacroiliitis associated with SpA, or definite radiographic
sacroiliitisaccordingtothemNYcriteria
InformationfromRudwaleitMetal.ThedevelopmentofAssessmentofSpondyloArthritisinternational
Societyclassificationcriterialforaxialspondyloarthritis(partII):validationandfinalselection.Ann
RheumDis2009;68:777–783.
Box8.5ASAScriteriaforperipheralSpA
Arthritisorenthesitisordactylitis
(clinicallyassessed)
plus
≥1SpAfeature
(uveitis,psoriasis,Crohn’s/colitis,precedinginfection,
HLA-B27,sacroiliitisonimaging)
or
≥2otherSpAfeatures
(arthritis,enthesitis,dactylitis,IBP(ever),
familyhistoryforSpA)
InformationfromRudwaleitMetal.ThedevelopmentofAssessmentofSpondyloArthritisinternational
Societyclassificationcriteriaforperipheralspondyloarthritisandforspondyloarthritisingeneral.Ann
RheumDis2009;70:25–31.
Pathogenesis
HLA-B27andgenetics
• HLA-B27 is associated with the SpAs in 50–95% of patients. In most
populations,HLA-B27isprevalentinabout10%.
• HLA-B27isinheritedasautosomalco-dominant:50%offirst-degreerelatives
ofprobandswithHLA-B27possesstheantigen.
• 5–10%ofHLA-B27-positivepeopledevelopASovertime.
• 20% of people with HLA-B27 develop a reactive arthritis after bacterial
infectionwithChlamydiaorSalmonella.
• About 50% of patients with psoriatic or inflammatory bowel disease-related
spondylitisareHLA-B27positive.
• 50%ofnon-CaucasianswithASareHLA-B27positive(<theprevalenceof
HLA-B27inCaucasianswithAS;95%).
• Concordanceinmonozygotictwinsis70%vs13%indizygotictwins.
• HLA-B27 isfound inupto 40%of casesof uveitis,evenin theabsence of
underlyingrheumaticdisease.
• ThereisanexcessofHLA-B27prevalenceinpatientspresentingwithisolated
aorticrootorvalveinsufficiency.
• HLA-B27 has been found in 90% of males with a combination of aortic
regurgitationandconductionsystemabnormalities.
• GenotypingstudieshaveshowntwoASsusceptibilitylociinadditiontoHLA-
B27:ERAP1andthegeneencodingtheIL-23receptor.Theformercodesfor
anaminopeptidaseoftheERinvolvedintrimmingpeptidestoanoptimalsize
forbindingtoMHCclassImolecules.
• HLA-B27 is probably relevant to pathogenesis by (possibly non-exclusive)
mechanismscurrentlysummarizedaseither:
• allowingabnormallyrestrictedT-cellimmuneresponsestoself-antigensor
arthritogenicpeptides.
• itself misfolding during assembly and leading to endoplasmic reticulum
stressandautophagyresponses.
• itself triggering innate T-cell, NK cell pro-inflammatory responses by
presentingonthecellsurfaceashomodimersandbeingrecognizedbythese
cells.
Immunopathology
• Thereisdebateoverwhetheroneoranumberofmicroorganismscontributeto
pathophysiology.
• IncreasedfaecalcarriageofKlebsiellaaerogeneshasbeenreportedinpatients
with established AS and may relate to exacerbation of both joint and eye
disease.
• ThereisincreasingevidencethataxSpAandASareduetoanabnormalhost

response to the intestinal microbiota with involvement of Th17 cells, which
playakeyroleinmaintainingmucosalimmunity.
• ThisleadstoproductionofvariousinflammatorycytokinesincludingIl-12,Il-
23,Il-17,andTNFαwhichplaykeyrolesinthepathogenesisofenthesitisand
otherinflammatorylesions.
• Th17cellsmayberesidentintissuesandactivatedtherecausinglocaltissue
inflammationandtriggeringlocaltissuechanges.
ClinicalfeaturesofaxSpAandAS
• HallmarkfeaturesofaxSpAareIBP,fatigue,andenthesitis.
• MostaxSpAlesionsoccuratentheses,subenthesialbone(osteitis),intendons
andsynovium(see Plate24).
• Typical entheses affected include plantar fascia origin at os calcis medial
calcanealtubercle,Achillesinsertionsatoscalcis,extensordigittendonorigin
at lateral humeral epicondyle, and gluteus medius insertion at greater
trochanter(seealsoTable8.4).
• Synovitiscanoccur,typicallyinthelargerperipheraljoints(hipsandkneesin
particular).Though20–40%ofpatientshaveperipheraljointdiseaseatsome
stage,studieshavenotpreviouslyshownwhetherthefeaturesaresynovitisor
enthesitisorboth.
• About50%ofpatientswithadultASwilldevelophiparthritis.
• The standardized mortality ratio for AS is 1.5, due to cardiac valve and
respiratorydisease,amyloidosis,andfractures.
• ASpatientsarehighriskforhavingtoalterorgiveupwork.
• Although recognizedastypical ofAS,few patientsprogressto the classical
late‘bamboospine’.
• When spine segments do fuse in AS (syndesmophytes bridging the gap
betweenvertebralbodies),microfracturescanoccurleadingtoacuteepisodes
ofseverepain.
• Spondylodiscitisisanuncommonthoughseverelesion:acuteasepticdiscand
end-plateinflammation.
• Theburdenofspinaldiseaseistypicallyvariablechroniclow-gradeIBPand
stiffnesswithevidenceofreductioninspinalmobility.
Non-musculoskeletalclinicalfeatures
• Constitutionalfeaturesof fatigue,weight loss,low-grade fever,andanaemia
are common. Fatigue is often the most troublesome symptom for many
patients.
• IBD lesionsarepresent inabout50% ofASpatients thoughlesionsare not
symptomaticinallpatients.
• Uveitis occurs in up to 40% of cases, but has little correlation with disease
activityinthespine.
• Therearenoknowntriggersforuveitisandalthoughself-limiting,topical,or
systemic steroids may be required in severe cases. The uveitis is
predominantlyanteriorandmostlyunilateral.
• Upperlobe,bilateralpulmonaryfibrosisisarecognizedbutrarefeatureofAS.
Occasionally, the fibrotic area is invaded by Aspergillus with changes
mimickingtuberculosis.
• InlateAS,fusionofthethoracicwallleadstorigidityandreductioninchest
expansion. Ventilation is maintained by the diaphragm; however, there is a
threefoldincreasedriskofdeathfromarespiratorycausecomparedwiththe
normalpopulation.
• Cardiac involvement includes aortic incompetence, cardiomegaly, and
conductiondefects.Ofthe20%ofASpatientswithaorticvalvedisease,the
majorityareclinicallyundetectable.
• NeurologicallesionsarearareconsequenceofspinalMSKdisease:nerveroot
entrapmentandcaudaequinasyndrome.
• Sterileurethritisisanunder-recognizedSpAlesion.
• RenalinvolvementisrarebutcanbeduetoNSAIDuse(interstitialnephritis)
orrenalamyloidosis.
• Osteoporosisisanunder-recognizedfinding:
• ASpatientsareathighriskofvertebralfracture.
• Micro-fractures may occur with trauma and fractures can occur through
syndesmophytes.
• Systemic osteoporosis occurs and is identifiable through hip and forearm
BMDmeasurement.
• Estimates of osteoporosisprevalencerange from 20–60%, increasingwith
ageanddiseaseduration.
• DXAevaluationoflumbarspineBMDwillbeinaccurateinadvancedAS
duetothepresenceofsyndesmophytes.
• Studies suggest that bone loss occurs early and during the acute
inflammatorystageofthedisease.
InvestigationsinaxSpA
• Systemicmeasuresofacute-phaseresponseareoftendetectedthoughtypically
alsocanbenormaldespitesymptoms.
• Plain AP, or ‘coned’ view radiographs of the posterior pelvis are
conventionallyusedtodetectestablishedsacroiliitis.

• RadiographicSIJchangesmayinitiallybeasymmetric.Latechangesinclude
subchondralsclerosis,erosions,andfinallyankylosis.
• Conventional axial skeletal signs on spine and pelvis radiographs include
squaringofvertebrae,syndesmophytes,spinalligamentossification,Romanus
lesions,pelvicenthesophytes,andosteitispubis.
• Radiograph detection of syndesmophytes requires a distinction to be made
between DISH and AS syndesmophytes. Generally, DISH patients present
later than AS patients, have paramarginal syndesmophytes, frequently
asymmetric in thoracic spine and have OA (DISH may be associated with
chondrocalcinosisandCPPDdisease).
•
99m
Tc-MDPbonescintigraphyissensitiveforSIJinflammation,andscanscan
identify significant peripheral skeletal lesions from a single study through
obtaining‘spot’peripheralviews.
• CTprovidesexcellentimagesoftheSIJsandsensitivelydetectspreviousSIJ
lesionsbutcannotdatethelesionsandisnotaninvestigationtousetodetect
currentinflammation.
• MRI of SIJs show active inflammatory lesions but subtle previous SIJ
pathologycanbemissed.
• MRIdiscriminatesspinalDISHfromASindoubtfulcases.
• Bothfat-suppressedMRIandUScandetectinflammationatenthesesthough
theabsenceofinflammatory‘signal’onMRIorDopplersignalonUS,does
notruleoutenthesisdiseaseaspartofSpA.
DiseasestatusandprognosticindicatorsinaxSpA/AS
TherearevalidatedinstrumentsmeasuringdiseasestatusinASincludingBath
indices,ASASresponsecriteria,andqualityoflifeindicators.
• Historically,forstagingandmonitoringAS,theBathindiceshavebeenused
(devisedinBath,UKbyAndreiCalin’sgroup):
• BathAnkylosingSpondylitisFunctionalIndex(BASFI).
• BathASDiseaseActivityIndex(BASDAI;Box8.6).
• BathASMetrologyIndex(BASMI).
• BathASRadiologyIndex(BASRI)(seeTable8.1).
• The AS disease activity score (ASDAS) combines simplified self-reported
clinicalindiceswithameasureofESRorCRP.TheperformanceofASDASto
discriminatelowandhighdiseaseactivityandcut-offvaluesarequitesimilar
in patients with AS and axSpA ( http://www.asas-
group.org/clinicalinstruments/asdas_calculator/asdas.html).
• ASAS have defined response criteria for therapies used in AS.
2
These
measures (ASAS 20, ASAS 40, ASAS 5/6; see Box 8.7) incorporate some
Bathmeasures,areincreasingusedandmorewidelyvalidated(inanaxSpA
definition of disease), and may update the BASDAI (alone) as favoured
disease(treatment)responsemeasures.
• Anumberofqualityoflifemeasurescanbeused(e.g.ASQoL
3
).
• A number of enthesitis indices have been developed (Table 8.1). In clinical
practice,eitherMASESorSPARCCaremostuseful:
• Themostfrequentlyusedradiographicindexofskeletalspinechangesisthe
Modified Stoke AS Spinal Score. It is based on the degree of vertebral
erosion, sclerosis, and squaring and the presence of syndesmophytes and
theirdegreeofvertebralbridging.
• MRIspinalosteitisscoringforresearchpurposes:SPARCCindex.
• ThemainpredictivefactorsofpooroutcomeinASaretobe:
• hipinvolvement,earlylossoflumbarspinemobility.
• oligoarticulardisease;lowsocial–educationalbackground.
• sporadicdiseaseratherthanfamilial;onset<16years;ESR>30.
• poorinitialresponsetoNSAIDs;presenceofdactylitis.
Box8.6MeasuringdiseaseactivityinASandaxSpA:BathASDisease
ActivityIndex(BASDAI)andASdiseaseactivityscore(ASDAS)
BASDAIdescription
The assessment comprises six questions. Patients score each as 0–10 on a
linearscale.Scoresareweightedandacompositescoreisgenerated.
ASDASdescription
Ona0–10scale,thepatientscoresbackpain,durationofmorningstiffness,
their assessment of global disease, a score of peripheral pain and stiffness,
thenacontributionofeitherCRPorESRisaddedandacompositescoreis
generated.
Availability
ABASDAIcalculatorisavailableonlineat http://basdai.com/
ASDAS is available online at http://www.asas-group.org/clinical-
instruments/asdas_calculator/asdas.html
Performanceofindices
• In AS, BASDAI has long since been shown to have validity in
discriminatinghighandlowdiseaseactivityindifferentpopulationsandis
responsive to change over a practical duration of disease. BASDAI has
historicallybeenadoptedwidelyasausefulindexofASdiseaseactivity.
• ASDAS-CRP and ASDAS-ESR have similar performance to BASDAI in
discrimination of high and low disease activity, and change in disease
activitygenerallyandwithanti-TNFαtherapy,bothinASandinaxSpA.
Table8.1Enthesitisindices(EIs)forASassessment
Enthesitisindex
(reference)
Comments
MANDER(Ann
RheumDis
1987;46:197–
202)
TheoriginalEI.Scorestendernessat66entheses.
Impracticalandusedlittleinresearch
MASES(Heuft-
Dorenbosch.
AnnRheumDis
2003;62:127–
32)
Relativelywellvalidated.Scores13enthesesaseither
‘tenderornon-tender’.IncludesASIS,PSIS,iliaccrest,
Achillesinsertion,sternalattachment1stand6th/7thrib
andoveruppersacrum
SPARCC
(Maksymowych.
AnnRheumDis
2009;68:948–
53)
Scores18enthesesaseither‘tender’or‘non-tender’
(superiomedialgreatertrochanter,quadricepsinsertionat
patella,inferiorpatellapole,tibialtuberosity,Achilles
insertion,plantarfasciaorigin,medialandlateral
epicondylesandsupraspinatusinsertion)
BERLINEI
(Braun.Lancet
2002;359:1187–
93).
Notextensivelyvalidated.Scores12entheses.
UCSFEI
(Gorman.NEngl
JMed
2002;346:1349–
56).
Scores17entheses.Performswellinassessmentofanti-
TNFαinAS
Box8.7ASASresponsecriteria
ASAS improvement criteria (ASAS-IC). Four domains, based on the
discriminationbetweentreatment(originallyNSAID)andplacebo:
• Physicalfunction,measuredbytheBASFI.
• Spinalpain,measuredona0–100mmvisualanaloguescale(VAS).
• Patientglobalassessmentinthelastweek,ona0–100mmVAS.
• Inflammation,measuredasthemeanofthelasttwoBASDAIquestions
ASAS20%responsecriteria(ASAS20).Treatmentresponsedefinedas:
• ≥20% and ≥10 mm VAS on a 0–100 scale in at least 3 of 4 ASAS-IC
domains,andnoworseningof≥20%and≥10mmVASona0–100scalein
4thdomain.
ASAS40%responsecriteria.Treatmentresponseisdefinedas:
• ≥40%and
• ≥20mmVASona0–100scaleinatleast3of4ASAS-ICdomains,andno
worseningof≥40%and≥20mmVASona0–100scalein4thdomain.
ASAS5outof6responsecriteria(ASAS5/6).Developedforuseintrialsof
anti-TNFα therapy. Treatment response defined as improvement in 5 of 6
domainswithoutdeteriorationinthe6thdomain,usingpredefinedpercentage
improvements:
• Pain
• Patientglobalassessment
• Function
• Inflammation
• Spinalmobility
• C-reactiveprotein(acute-phasereactant).
ThetreatmentofaxSpAincludingAS
Generaltreatment
• UKNICEguidelineformanagementofaxSpA2017.
4
• Treatmentprinciplesareindicatedandincludethefollowing:
• Patienteducation.
• Exercises(see http://www.nass.co.uk).
• Otherphysicaltherapyandhydrotherapy.
• Avoidsmokinggivenitspro-inflammatoryeffects.
• NSAIDsforIBPandenthesitis.
• Oralglucocorticoid(GC)orIMmethylprednisolone.
• With exercise the emphasis is placed on the need to maintain posture and
physical activity. Spinal extension exercises are important as the natural
historyofthediseaseotherwiseleadstospinal‘stoop’,lackofbackextension,
andlossofheight.
• Physiotherapy provides benefit in the short term. Spa treatment improves
functionforupto9monthsandreduceshealthresourceuse.
• Fatigue isnot easilytreatedthough someeffort toimprovesleep healthand
maintainsomeaerobicexercisemayplayapositiverole.
NSAIDsandsyntheticDMARDs(sDMARDs)
• Forthemajorityofpatients,NSAIDsremainthetreatmentofchoice.Regular
full-doseNSAIDuseisoftenrequired.
• Continuous, rather than intermittent NSAID (including COX-2 selective
NSAIDs)mayslowradiographicprogressionofaxialskeletalchangesbutthe
researchevidenceoverallisweak.
• Sulfasalazine(SSZ)hasbeenshowninameta-analysistobeefficaciouswhen
compared with placebo for peripheral joint disease only. However,
improvementinsymptomsandqualityoflifeisnotdramatic.
• Mixedresultshavebeenfoundwithmethotrexate.ACochranemeta-analysis
concludedthatthereisinsufficientevidencetosupportitsuseinAS.Benefit
maybelimitedtopatientswithperipheraldisease.
• Joint inflammation can be managed in acute, severe cases with IA GC
injections.
• CareshouldbetakeninjectingGCaroundtendons,asrupturecanoccurifthe
injectionisplacedintothetendonitself.
• Steroid injection around the Achilles tendon can help/is safe if there is
paratenoninflammationalone(precedingimagingadvisable).
• TopicalGCeyedropsshouldbeusedtotreatuveitis.Ifthesymptomspersist
for>3daysanophthalmologicalopinionshouldbesought.
• IV bisphosphonates can help spinal osteitis symptoms. Pamidronate 90 mg
monthlycanbeused.Zoledronicacidcanresolveosteitislesionsfor3months
inamajorityofpatients.
BiologicDMARDs(bDMARDs)
• Anti-TNFα bDMARDs are effective in AS in reducing symptoms and
inflammation though there is debate on whether they can reduce the
progressionofstructuralskeletalchanges(infliximab,etanercept,adalimumab,
certolizumab,andgolimumab).
• IntheUK,NHSanti-TNFαisrecommendedfortreating‘severeactive’ASin
adultswhosedisease hasresponded inadequatelyto,or whocannottolerate,
NSAIDs.Infliximabisrecommendedonlyiftreatmentisstartedwiththeleast
expensiveinfliximabproduct.
• Infliximab is licensed to treat AS at a dose of 5 mg/kg (compared with 3
mg/kg used in RA), though published data suggest AS can be frequently

treatedtoremissionwith3mg/kgdosing.
• Remission of disease following anti-TNFα treatment is more common the
earlier in the disease course anti-TNFα is used. These consistent findings
highlight the need for early identification of AS and prompt treatment plan
implementation.
• Evidence overall now supports the efficacy and safety of anti-TNFα in nr-
axSpA. Secukinumab is the first drug targeting the Il-17 pathway in
radiographic-axSpA(AS)thathasshownefficacy.
• Anti-TNFα therapy recommendations in UK (NICE TA383)
5
are now
availablebasedontheASASdefinitionofnr-axSpA.
• Secukinumab (monoclonal anti-IgG1
k
) is the first drug targeting the Il-17
pathway(ittargetsIl-17A)andislicensedtotreatASandPsA.Atadoseof
150 mg(monthly SCafter 4initial weeklydisease) ithas shownefficacyin
twophaseIIIRCTs(NNTtoachieveASAS40response:3–4).
• Ustekinumab(monoclonalantibodytargetingthecommonsubunitofbothIl-
12 and Il-23) and tofacitinib (JAK inhibitor) have shown positive results in
phaseII/proof-of-concepttrials.
References
1. Burgos-Vargas R, Wei JCC, Rahman MU, et al. The prevalence and clinical characteristics of
nonradiographicaxialspondyloarthritisamongpatientswithinflammatorybackpaininrheumatology
practices:amultinational,multicenterstudy.ArthritisResTher2016;18:132.
2. Zochling J, Braun J. Assessment of ankylosing spondylitis. Clin Exp Rheumatol 2005;23(Suppl
39):S133–41.
3. DowardL,SpoorenbergA,SCookS,etal.DevelopmentoftheASQoL:aqualityoflifeinstrument
specifictoankylosingspondylitis.AnnRheumDis2003;62:20–6.
4. NICE.SpondyloarthritisinOver16s:DiagnosisandManagement.[NG65]London:NICE,2017.
https://www.nice.org.uk/guidance/ng65
5. NICE. TNF-alpha Inhibitors for Ankylosing Spondylitis and Non-Radiographic Axial
Spondyloarthritis.[TA383]London:NICE,2016. https://www.nice.org.uk/guidance/ta383
Psoriaticarthritis
Epidemiology
Psoriasis(Ps)affectsupto3%ofthepopulation.Theheterogeneityofclinical
featuresofpsoriaticarthritis(PsA),thenumerousclassificationcriteriaexisting
forithistorically,anduntilrecentlypoorunderstandingofitslesionsandtheir
detection,haveimpliedgreatuncertaintyinknowingthetrueprevalenceofPsA
(seeBox8.8).
• HistoricestimatesoftheprevalenceofPsAsuggestitispresentinupto40%
ofpatientswithPs.MoreconservativeestimatessuggestPsAoccursinabout

10–20%ofthePspopulation(i.e.0.5–1%ofthewholepopulation).
• However, estimates have not adequately considered the overall likely
prevalenceofPsAinallitsforms,andgivenobviousdifficultiesinidentifying
PsA sine Ps and defining disease without peripheral joint synovitis (e.g.
enthesopathic forms and forms characterized by tendonitis and/or enthesitis
and/orspinaldiseasealone).
• Theconditionaffectswomen andmen equallywithusualonsetbetween the
agesof20and40years.
Box8.8CASPARclassificationcriteriaforPsA
CASPAR updates previous criteria: Moll and Wright 1973; Vasey and
Espinoza1984;Gladman1987,McGonagle1999,Fournie1999.
Inflammatoryarticulardisease(joint,spineorenthesis)
with≥3pointsfromthefollowing:
(1pointeachunlessstated)
• CurrentPs(scores2points)
• HistoryofPsin1st-or2nd-degreerelative
• Psoriaticnaildystrophy
• IgMRFnegative*
• Currentdactylitis
• Historyofdactylitis
• Juxta-articularnewbone.**
*Byanymethodexceptlatex.
**Ill-definedossificationnearjointmargins(excludingosteophytes)onradiographsofhandsorfeet.
Pathophysiology
Genetics
• Ps is familial. There are about 40–50 genes which are associated with an
increasedoddsratioofdevelopingpsoriasis.
• Genetic factors also have an important role in PsA and family studies have
suggestedthattheheritabilitymayexceed80%.
• VariantsintheHLA-BandHLA-Cgenesarethestrongestgeneticriskfactors
butothervariantsexist.
Immunopathogenesis
• Many variants overlap with those implicated in Ps where there may be >40
susceptibility loci, and lie within or close to genes in the IL-12, IL-23, and

NFκBsignallingpathways.
• Itisthoughtthatanenvironmentaltrigger,probablyamicroorganism,triggers
thediseaseingeneticallysusceptiblepeople,leadingtoactivationofdendritic
andTcells.
• CD8+Tcells,whichrecognizeantigenpresentedinthecontextofHLAclass
I,aremoreabundantthanCD4+Tcellswithinthejointwhichisinkeeping
withthegeneticassociationbetweenPsAandHLA-Cand-Bvariants.
• Il-23/Il-17pathwayplaysapivotalroleinPsA.
• A triggering stimulus maycauseover-production of Il-23bydendriticcells,
which then promotes differentiation and activation of Th17 cells which
produceIl-17A.
• Il-17Aand Th1cytokinessuchasIFNγ andTNFα,act onmacrophages and
tissue-resident stromal cells at entheses, in bone, and within the joint to
produce additional proinflammatory cytokines and other mediators which
contributetoinflammationandtissuedamage.
Clinicalfeatures
• Ps-relatedMSKsymptomscanpresentwith,before,oraftertheonsetofPs.
The situation for nail disease is the same. In some cases, gaps between
presentationsofthedifferentaspectsofPsdiseasecanbemanyyears.Some
patientscangothroughlifewiththeirPsAandnevergetPs.
• MSK imaging research has shown lesions exist at entheses of tendon and
ligaments,inthenailbed,inbone,andonbonesurfaces(adjacenttoentheses,
probablyperiostea).Synovitismaywellbeasecondarylesionduetoadjacent
enthesitisandbynomeansanessentiallesionofPsA.
• Naillesionsarenotalwayspresentbutdistinctive.Naillesionsoccurin40%
ofpatientswithPsalone.See Plate8.
• FatigueisaconsistentandoftenseveresymptomofPs-relateddisease.
• Dactylitis,swellingofthewholefinger,occursinoverone-thirdofclassically
definedPsApatients.
• In about 20% of PsA cases there is a chronic, progressive, and deforming
arthropathy with an often-asymmetrical pattern including DIPJ involvement,
orarthritismutilans,and/orpolydactylitisand/orlargejointdeterioration.
• Some clinical patterns of PsA that have been written about historically are
listedasfollows.However,itisprobablethatpatternsdonotalwayspersistin
anyindividualandasyetnodistinctgenotypeorimmunopathologicalfeatures
segregateinassociationwiththesedescriptivepatternsofdisease:
• DIPJpredominantdisease.
• Asymmetricoligoarthritis.

• Symmetricalpolyarthritis.
• Spinepredominantdisease(estimates2–40%).
• Enthesopathicpredominantdisease.
• Arthritis mutilans is a classic but uncommon manifestation of PsA. Bone
resorption leads to collapse of the soft tissue in the digits, creating
‘telescopingfingers’.
• It is not clear, however, if the patterns of disease have any prognostic
significanceinthemselves.
• Adverse prognostic factors in the 1995 Toronto cohort were polyarthritis,
greaterHAQ,andincreaseinuseofsDMARDs.
• Persistentdactylitisisamarkerofassociateddigitsmalljointdeterioration.
• TheradiologicalfeaturesassociatedwithPsAthathelptodifferentiateitfrom
RAandinflammatorygeneralizedOAinclude:
• absenceofjuxta-articularosteoporosis.
• absenceofsubchondralplatechangesinearlydisease.
• DIPJ disease (with marginal changes initially and an absence of early
subchondralplatechanges).
• ‘whittling’(lysis)ofterminalphalanges.
• asymmetryofjointinvolvement.
• ‘pencil-in-cup’deformities.
• ankylosis.
• periostitis (often ‘fluffy’ juxta-articular periosteal new bone—see Plate
23).
• spondylitis (asymmetric ‘floating’ syndesmophytes, spondylodiscitis, facet
joint(FJ)changes—thoughFJappearancesinPsAarenotatallwell-defined
givenapresumedcommonfindingofOAaffectingFJsandpoordefinition
todateofjuxta-articularnewboneinPsAFJs).
ClinicalassessmentinPsA
• The variationin clinicalfeaturesbetween patients,the potentialformultiple
MSK lesions, and involvement of spine structures has historically led to a
difficulty in establishing agreed and universal classification criteria for PsA
andconsequentlyindesigningapplicabletreatmentoutcomeassessmenttools
forPsA.
• Typically,assessmentshavebeenadoptedfromtheiruseinRA.Somesalient
pointsare:
• DAS68shouldbeusedratherthanDAS28forassessingjointtendernessand
swelling.
• Though all have been developed for AS, different enthesitis indices (see

Table8.4)canbeappliedtoPsA.
• Thoughrepresentingsomemethodologicalchallenges,thePASIremainsthe
bestassessmentofPsskinresponsetotreatment.
• Comprehensive PsA assessment requires an index (indices) to allow
measurementofthe responseofjoint, tendon, enthesis,nail, spine, andskin
diseasetotreatment,butalsotomeasuregeneralhealthandfunctionchanges
capturingtheeffectsoffatigueandmood.
• Composite indices have been proposed. DAPSA: Disease Activity for
Psoriatic Arthritis; PsAJAI: Psoriatic Arthritis Joint Activity Index; CPDAI:
CompositePsoriaticDiseaseActivityIndex.Indiceshavebeensummarized.
6
• TheonlyenthesitisindexwhichhasbeendevelopedspecificallyforPsAisthe
LeedsEnthesitisIndex(LEI).Itscoressixenthesesscoringtenderness(1)or
no tenderness (0) at lateral humeral epicondyles, over medial femoral
condyles,andatAchillesinsertions.
• An index of minimaldiseaseactivity(MDA) has been proposed.
7
A patient
withPsAisdefinedashavingMDAwhen5of7ofthefollowingarepresent:
• Tenderjointcount≤1.
• Swollenjointcount≤1.
• PASI≤1orBSA≤3.
• PatientpainVAS≤15/100.
• PatientglobalactivityVAS≤20/100.
• HAQ≤0.5.
• Tenderentheses≤1.
Theextendedpsoriasis-relateddiseasecomorbidities
• Comorbidities, which require screening for in Ps patients, include arterial
hypertension, dyslipidaemia, obesity, diabetes mellitus, metabolic syndrome,
non-alcoholic steatohepatitis (NAFLD), depression, nicotine abuse, alcohol
abuse,chronicinflammatoryboweldisease,andlymphoma.
• In the UK, screening Ps patients for PsA using PEST is currently
recommended( http://www.bad.org.uk/library/).
• TheassociationofmetabolicsyndromewithPsAinpatientswithorwithoutPs
isunknown.
• Hyperuricaemia is associated with Ps and PsA. An association of PsA with
gouthasbeenrecognizedforalongtime.
TreatmentofPsA
Generaltreatment
• Patient education about the various lesions of PsA, their relapsing and

remitting nature, and about the risk of long-term comorbidity risk is of
increasingimportance.
• Encouraging patient group participation may be helpful (e.g. in the UK:
PAPAA( http;//www.papaa.org).
• Localizedlesionsmayrespondtorest,ice,andphysiotherapy.
• Comorbidities need to be addressed: obesity, cardiovascular risk,
hyperuricaemia,depression(e.g.screenwithHADS).
• PhysiotherapyassessmentparticularlyifthereisIBP.
NSAIDsandsyntheticDMARDs(sDMARDs)
• TreatmentistailoredtothesiteandnumberofMSKlesions.
• NSAIDswouldbeexpectedtohelp.
• sDMARDs have conventionally been reserved for patients who have
inflammatory disease threatening joint integrity; however, with multiple site
and/or severe symptoms, fatigue, Ps, and a potential impact from multiple
symptoms on function and contributing to comorbidities, many specialists
regardsDMARDtherapyintroductionwhollyreasonablewhenbasedonsuch
symptom-basedand‘holistic-view’criteria.
• Evidence for unequivocal sDMARD efficacy is not strong though some
evidenceexistsformethotrexate(MTX),leflunomide(LEF),andciclosporin.
Evidence is weaker still for SSZ, hydroxychloroquine (HCQ), gold,
penicillamine,andazathioprine(AZA).
• The first-line sDMARD choice of many rheumatologists for PsA remains
MTX.ThisisreflectedintheEULARguidelineformanagingPsA.
8
• Essentially,theEULARguideadvocates:
• Phase1:NSAIDsandGCinjections.
• Judgephase1responseagainsttreatmenttarget.
• Iftargetnotreached:phase2—startMTX.
• IfcontraindicationstoMTX:startLEF.
• Iftargetnotreached:phase3—startanti-TNFα.
• Ifaxialdiseasealone,onfailureofphase1:startanti-TNFα.
• Many clinicians would advocate relevant efficacy only occurs at the higher
weeklydosesofMTX(20–25mg/week).
• HCQcanaggravatepsoriasis(seeSummaryofProductCharacteristicsforthe
drug).
• Oral and IM GCs might be generally avoided in patients with Ps because
althoughtheskindiseaseresponds,afterthesteroidsthere canbearebound
worseningofskindisease.
• GoodefficacyonjointdiseaseinPsAisestablishedwithallanti-TNFαdrugs;
however, criteria for study recruitment and judging outcome with all anti-
TNFαdrugshasbeensetfairlyconventionallyandhasfocusedonjoints,and
therefore to a significant degree, on synovial disease (i.e. using ACR 20/50
outcome criteria or DAS28—both adopted from their development in
assessingRA,notPsA).
• In the UK, etanercept, infliximab, adalimumab and golimumab (see NICE
TechnologyappraisalguidanceTA199andTA220)
9,
10
areapprovedbyNICE
for the treatment of PSA. All have positive effects on skin, as well as joint
disease.
• For UK NHS funded anti-TNFα treatment, PsA patients need to have
peripheral arthritis with ≥3 tender and ≥3 swollen joints and have not
respondedto,orfailedtotolerate,atleasttwostandardsDMARDsaloneorin
combination.
• EssentiallymergingUKNICErequirementsandEULARguidancesuggests
UKcliniciansneedtochooseMTXfirstthenLEFsecond,pre-anti-TNFα.
• IntheUK,NICErequiresanti-TNFαtreatedPsApatientsareassessedat12
weeks using validated outcome measures such as Psoriatic Arthritis
ResponseCriteria(PSARC)measurements.
• NICE rules do not require PsA patients to be simultaneously treated with
MTXwhilereceivinganti-TNFα.
• Forpatientswithsignificantnaildiseaseforwhomtopical(GC±calcipotriol)
therapy has failed, treatment with adalimumab, etanercept, intralesional
steroid,ustekinumab,MTXandacitretinarerecommended.
• Certolizumab pegol has shown efficacy in PsA also with specific effect
demonstrated on different MSK lesions and nail disease; however, it is not
authorizedfortreatmentinUKbyNICE.Someconcernhasbeenraised
11
that
this anti-TNFα drug is associated with greater risk for adverse effects
comparedwithotheranti-TNFαdrugs.
• Ustekinumab, a monoclonal antibody which binds to, and neutralizes IL-23
(specifically binds the p40 subunit common to Il-12 and Il-23 preventing
receptorbinding)hasbeenlicensedtotreatPsforsomeyears.
• Efficacy of ustekinumab in PsA importantly shows significant responses in
joint,dactylitis,andenthesitisextendingtoayearaftertreatmentinphaseIII
trials.
• IntheUK,NICEhasauthorizeduseofustekinumabforPsApatientswhohave
failedanti-TNFα.
• ThefindingthatIl-23stimulatedTh17cellactivation(includinggeneratingIl-
17) in SpAs and psoriasis has heralded a new approach to developing

bDMARDs targeting this immune activation pathway (e.g. the anti-Il-17A
monoclonalsecukinumabinphaseIIIdevelopment).
• Apremilast,anorallyavailablesmallmoleculeinhibitorofphosphodiesterase
4(PDE4),waslicensedbytheFDAintheUSAin2014andintheEuropean
UnionfortreatingPsA.
• In the UK, NICE has not authorized the use of apremilast (in the USA
marketedasOtezla
®
forPsandPsA)forbothPsandPsA.
• Apremilast compares favourably to placebo in patients failing previous
sDMARDtherapyinPsAbuthasnotdirectlybeencomparedwithhigh-dose
MTXtherapyalone.Apremilastisassociatedwithfrequentmildtomoderate
adverse effects but also weight loss, worsening depression, and suicidal
ideation.
References
6. WongPC,LeungYY, Li EK,etal.Measuringdiseaseactivityinpsoriaticarthritis.IntJ Rheumatol
2012;2012:839425.
7. CoatesL,FransenJ,HelliwellPS.Definingminimaldiseaseactivityinpsoriaticarthritis:aproposed
objectivetargetfortreatment.AnnRheumDis2010;62:48–53.
8. GossecL,SmolenJS,Gaujoux-VialaC,etal.EuropeanLeagueAgainstRheumatismrecommendations
forthemanagementofpsoriaticarthritiswithpharmacologicaltherapies.Ann RheumDis2012;71:4–
12.
9. NICE. Etanercept, Infliximab and Adalimumab for the Treatment of Psoriatic Arthritis. [TA199]
London:NICE,2010. https://www.nice.org.uk/guidance/ta199
10. NICE. Golimumab for the Treatment of Psoriatic Arthritis. [TA220] London: NICE, 2011.
https://www.nice.org.uk/guidance/ta220
11. SinghJA,WellsGA,ChristensenR,etal.Adverseeffectsofbiologics:anetworkmeta-analysisand
Cochraneoverview.CochraneDatabaseSystRev2011;2:CD008794.
SpA-associatedreactivearthritis
Backgroundandclinicalfeatures
• SpA-associated reactive arthritis (ReA) is a (‘lesion-aseptic’, i.e. lesions not
directly infected) inflammatory condition affecting spine and axial skeletal
structures, joints, tendons, and entheses triggered by infection with certain
bacteriaincludingChlamydia,Campylobacter,Salmonella,Shigella,Yersinia,
andpossiblyalsoClostridia,Ureaplasma,andMycoplasma.
• The risk of developing ReA after having one of these infections is ~1–4%
generallybut20–25%inpeoplewhoareHLA-B27positive.
• Non-SpA-associatedReAcanoccurafterviruses(particularlyparvovirus)and
Streptococcus (β-haemolytic), gonococcus, HIV, Borrelia (Lyme disease),
Mycobacterium (Poncet’s disease) and possibly other pathogens but the
characteristicsofReAfollowingtheseinfectionsarenotSpA-likeinclinical
featuresnorimmunopathologyandhavenoassociationwithHLA-B27.
• SpA-associatedReAisbasicallyanacuteformofSpA.Indeed,itispossible
that ReA is the triggering event in developing long-term SpA—a semantic
issue perhaps when considering the alternative—‘chronic ReA’, which
historicallyisregardedtooccurinasmallminorityofpatientswithacuteReA.
• A high index of suspicion of sexually acquired ReA (SARA) is required
particularlyinwomenwheregenitalChlamydiainfectioncanbeasymptomatic
inupto50%.
• The onset of reactive arthritis is usually acute with systemic symptoms and
inflammatoryMSKsymptoms.
• Differentialdiagnosisincludessepticarthritis,gout,andotherSpAs.
• Non-MSK symptoms worth noting are mucocutaneous features including
painless circinate balanitis of the glans penis, conjunctivitis, and pustular
psoriasisofthepalmsorfeet(keratodermablennorrhagica).
• InGIinfection-triggeredReA,theacuteGIsymptomsmayprecedetheMSK
symptomsby1–4weeks:
• InitialGIsymptomsmaybesomildastobeignoredbythepatientandoften
the provoking bacterium has cleared from the gut before the MSK
symptomsarise.
• Persistent bowel symptoms, particularly pain and diarrhoea should raise
suspicionofinflammatoryboweldisease.
• Recurrent or repeated infections do not always lead to a recurrence of ReA
MSKlesionsand,inthecaseofSARA,mayoccurintheabsenceoffurther
sexualintercourse.
InvestigationofSpA-associatedReA
• Acute-phaseresponsemeasuresareinvariablyhigh.
• IfSARAissuspectedfromsymptomaticurethritis,prostatitis,orcervicitis,or
if suspicion of SARA is high based on MSK and non-genitourinary (GU)
symptomsalone,referralforrigorousGUinvestigationisrecommended.
• Withtriggeringbowelinfections,oftenbythetimeReAisapparent,thenstool
culturewilllikelybenegative.
• Serological evidence of recent Yersinia or Campylobacter can be sought
(IgM+) but often delays from initial infection to ReA issues with assay
specificityimpedeuse.Forexample,recentparvovirusB19infectionleadsto
false-positiveELISAsforanumberofthesepathogens.
• SerologyforChlamydiainfection—C.pneumoniaeorC.trachomatis—isnot
recommended.
• Radiographs are of limited use. The distribution of inflammatory lesions at
SIJs,joints,andenthesescanbeconfirmedwithbonescintigraphy.
• Lumbar spinous processes and posterior pelvis MRI may show typical SpA
inflammatorylesions(osteitis,sacroiliitis,enthesitis).
• Regional MSK US may be useful in selected cases (e.g. of ‘hindfoot’ may
showenthesitisatAchillesinsertion,plantarfasciaorigin,anysynovitis,and
its site and fluid can be aspirated under US guidance for Gram stain and
cultureandforpolarizedlightmicroscopyexamination,toruleoutgout).
ManagementofSpA-relatedReA
• NSAIDs and local joint or enthesis GC injections are the mainstay of
therapeuticintervention.
• If symptoms persist >6 months and there is clinical evidence of ongoing
synovitisandjointdestruction,thenasyntheticDMARD(sDMARD)suchas
SSZormethotrexatemaybeconsidered.
• PhysiotherapyshouldbeconsideredifthereispersistentIBP.
• The majority of patients are in complete remission at the end of 2 years of
sDMARDtherapy,mostwithin6months.
• Balanitis and keratoderma may persist—predictors of poor prognosis. Other
factors that may be predictive of poor outcome include arthritis of the hip,
persistentlyraisedESR,B27positivity,poorresponsetoNSAIDs,dactylitis,
andlumbosacralspineinvolvement.
• Asepticurethritisandearlyconjunctivitisresolvequicklyandspontaneously.
• Antibiotictherapywillclearunderlyinginfections,butthismaynothaveany
effectonthedurationofReAdisease.
• Uveitis should be treated in the usual way with topical steroid drops and a
referraltoanophthalmologistiftherehasbeennoresponsewithin3days.
• Patienteducation,particularlyinthecontextoffoodhygieneandpreventionof
exposuretosexuallyacquiredinfection,isimportant.Contacttracingisvitalin
casesofsexuallytransmittedinfection.
• Anti-TNFαisreservedforcasesofsDMARDfailure.IntheUK,thereareno
specificNICEguidelinesfortreatingSpA-relatedReA.
Inflammatoryboweldisease-relatedSpA
Clinicalpresentation
• The clinical characteristics of inflammatory MSK symptoms presenting in
patientswithactiveCrohn’sdiseaseand(ulcerative)colitisareoftentypicalof
SpAlesionsandoccur,broadlyspeakingconsideringallstudies,inasizeable
minorityofIBDpatients.
• Epidemiologydatadependonwhetherpatientgroupsaredefinedfirstbytheir
IBDorbytheirSpA.
• InoneseriesofIBDpatients,sacroiliitiswaspresentin17%detectedbyMRI;
thoughofnote,non-inflamed,non-currentSIJdiseasemaybemissedbyMRI.
• Bycontrast,whenASoraxSpApatientsareinvestigatedforIBDrigorously,
bowellesionsareseeninabout50%ofpatients.
• WhetherIBD-relatedSpAisdistinctfromaxSpA(newASASdefinition)will
needtobeestablished;however,pre-ASASaxSpAdefinition,many,ifnotall
IBD-relatedSpApatientsmightbeclassifiedusingtheESSGcriteriaforSpA.
• In summary, there is still some uncertainty as to whether all cases of IBD-
relatedarthritisaretrueSpAs.
• The association of the inflammatory arthritis with IBD is arguably stronger
with Crohn’s disease than with UC. The association might be more visible
giventhelikelihoodthatthecorrelationbetweenactivityofIBDandseverity
ofMSKsymptomsisgreaterforCrohn’sthanitisforUC.
• In Crohn’s-associated inflammatoryarthritis/SpA, thearthritis tendstoremit
after surgical removal of diseased bowel tissue or tight control of enteric
inflammation.
• It is observed that MSK symptoms associated with IBD are greater if the
integrity of the ileocecal valve is lost. Speculatively, then, it may be that
bacterialcolonizationofpreviouslybacteria-freesmallbowelisakeytrigger
inpathogenesisoftheSpA.
• Lesionscanbediscordantbysomeyears.IBDcanevolve(sometimesyears)
followingtheonsetofSpA(e.g.seereference12).
• Non-MSKextra-intestinalfeaturesofIBDinclude:
• aphthousstomatitis.
• fatigue.
• anaemia.
• uveitis(inabout10%).
• erythemanodosum.
• pyodermagangrenosum.
ManagementofIBD-relatedSpA
• NSAIDsareusuallycontraindicatedifthereisknownIBD.
• IA or IM GCs are used relatively early in the disease course given the
avoidanceofNSAIDs.
• Mesalazine and AZA, used to treat IBD, is not recognized for its effect on
MSK symptoms but SSZ and MTX do have effect. Their use may require
liaison with the gastroenterologist as mesalazine/AZA needs to be

discontinuedinmostcases.
• Anti-TNFαchoicesneedtobemadecarefullygivenbothSpAandIBDlesions
inrelevantpatients.EtanercepthasnoefficacyinIBD.
• The use of anti-TNFα in UK NHS patients with IBD-related SpA requires
qualificationforfundingfortreatmentbasedoneitherAS,PsA,orIBDcriteria
alone.
Reference
12. Vavricka SR, Rogler G, Gantenbein C, et al. Chronological order of appearance of extraintestinal
manifestationsrelativetothetimeofIBDdiagnosisintheSwissInflammatoryBowelDiseaseCohort.
InflammBowelDis2015;21:1794–800.
Juvenilespondyloarthritis
Epidemiologyandclassification
• JuvenileSpA(JSpA)isan‘umbrella’termencompassingagroupofdiseases
withsharedgeneticpredispositionthataffectchildren<16yearsofage.
• The classification of JSpA (International League of Associations for
Rheumatology(ILAR);Table8.7)acceptedbymostis:
• enthesitis-relatedarthritis(ERA).
• juvenile psoriatic arthritis (JPsA), which can be sub classified into SpA
similartoPsAinadultsorperipheralarthritissimilartoANA-positiveJIA.
• undifferentiatedSpA(ifERAandJPsAfeaturesarepresent).
• JuvenilePsAandERAareclassifiableusingtheILARclassificationendorsed
byWHOin1999(see Table8.2,p.318).
• OtherJSpAsnotspecificallyaccountedforintheILARclassificationinclude
juvenile AS (JAS) who fulfil the mNY criteria before they are 16 years,
reactivearthritis,andIBD-relatedSpA.
• Estimates of JSpA prevalence are based on data for JIA and do not include
JAS.
• ERAandJPsAtogetheraccountfor10–20%ofJIA,whichgivesanestimated
2–60casesper100,000children.
• OfadultswithAS,8–15%haveonsetinchildhood.
• JSpA mostly occurs in late childhood or adolescence with peak onset at 12
years;60%aremale.
• Approximately50%ofJSpApatientsareHLA-B27positiveand20%havea
familyhistoryofHLA-B27-associateddisease.
• RheumatoidfactorandANAcharacteristicallyarenegative.
Clinicalpresentation
• Arthritis is usually oligoarticular, asymmetric, and primarily of the lower
extremity.
• Hip and midfoot arthritis are suggestive of JSpA and dactylitis is typical of
JPsA.
• Enthesitisispresentin66–82%ofJSpApatients,affectingmainlytheinferior
pole of the patella, Achilles tendon insertion, plantar fascia origin and
insertions at metatarsal heads, and gluteus medius insertion into the greater
trochanter.
• Axialinvolvementatonsetoccursin10–24%ofchildrenfrequentlypresenting
assacroiliacpainandstiffness.
• Two-thirdsofMRI-positivesacroiliitismaybeasymptomatic.
• Byage10years,two-thirdsofJSpApatientshaveaxialdisease.
• Othermanifestationsincludeacuteanterioruveitis(unilateralpainfulredeye
with photophobia in 25% of children over time), bowel inflammation,
psoriasis,nailpitting,and,rarely,cardiacdisease.
Table8.2ILARclassificationofJIA—SpArelevantcriteria
Inclusioncriteria Exclusioncriteria
JPsA Arthritispluspsoriasis(Ps)
or
arthritisplus≥2of:
• dactylitis;
• nailpitting/onycholysis;
• psoriasis in a 1st degree
relative.
• Arthritis in a HLAB27 positive
male>6y.
• AS, ERA, or IBD with sacroiliitis,
reactive arthritis or acute anterior
uveitis or history of one of these
disordersina1stdegreerelative.
• • Presence of IgM RF on ≥2
occasions>3monthsapart.
• Systemic-onsetJIA.
ERA Arthritisplusenthesitis
or
arthritisorenthesitisplus≥2
of:
• Presence or history of SIJ
tendernessand/orIBP;
• HLAB27positive;
• onsetofarthritisinboy>6y;
• acute symptomatic anterior
uveitis;
• Psoriasisorahistoryofpsoriasisin
thepatientora1stdegreerelative.
• PresenceofIgMRF≥2occasionsat
least3monthsapart.
• SystemicJIA.
• history of: AS or ERA or
sacroiliitis with IBD or
reactive arthritis or anterior
uveitis - in a 1st degree
relative.
Approachtodiagnosis
• Thereisnostandardizedenthesitisindexforpaediatricpatients.
• Recent evidence suggests a role for whole-body MRI as enthesitis can be
overestimatedinchildrenbyphysicalexamination.
• TypicalclinicalfindingsinJSpAinclude:
• insidious onset of low back pain with morning stiffness of >30 min that
improveswithexercise.
• tendernessondirectcompressionovertheSIJ.
• decreasedlumbarflexion.
• positive FABER (Patrick) test ( http://www.physio-
pedia.com/FABER_Test).
• MRIutilityinasymptomaticandsymptomaticdiseaseisunclear.Correlation
of positive MRI findings with symptomatic improvement on bDMARD
therapyhasyettobeshown.GadoliniumenhancementofMRIispreferredby
somepaediatriccentres.
• WhereJSpAfulfilstheNewYorkcriteriaforAS,adiagnosisofjuvenileASis
made.
ManagementofJSpA
• JSpAconditions,likeallformsofJIA,canbeseverelydebilitatingandplaces
aheavyphysicalandpsychologicalburdenonchildrenandfamiliesaffected
bythedisease.Multidisciplinaryteam(MDT)supportisessential.
• The principles of treatment include patient and parental education, physical
therapy,splints,orthotics,NSAIDs,andIAGCforperipheralarthritis.
• With joint involvement, there is a high risk of permanent joint contractures
withpersistentdisease.IntensivephysiotherapyandjudicioususeofIAsteroid
isimportant.
• Treatment guidelines for JIA, including JSpA, have been published by the
AmericanCollegeofRheumatology.
• MTX, SSZ, and LEF are used for peripheral arthritis, but efficacy for
enthesitisandaxialdiseasehasnotbeenfullyassessedinERA.
• Responsetoanti-TNFαtherapyappearstobesimilartothatofASandaxSpA
in adults. It is not clear whether treatment halts progression of structural
damage.
• DrugsthattargetIl-12/23andIl-17mayhavearoleinJSpAtreatmentbutare
notyetapprovedinJSpAorJIA.
OutcomeofJSpA
• JSpA may have a poorer overall prognosis than JIA and <20% of patients
experiencediseaseremissionwithin5years.
• Persistent disease activity is associated with midfoot arthritis/disease, hip
arthritiswith6monthsofdiseaseonset,familyhistoryofAS,HLA-B27,and
HLA-DRB1*08.
Furtherreading
Colbert RA. Classification of juvenile spondyloarthritis: enthesitis-related arthritis and beyond. Nat Rev
Rheumatol2010;6:477–85.
GmucaS,WeissPF.Juvenilespondyloarthritis.CurrOpinRheumatol2015;27:364–72.
Hugle B, Burgos-Vargas R, Inman RD, et al. Long-term outcome of antitumor necrosis factor alpha
blockadeinthetreatmentofjuvenilespondyloarthritis.ClinExpRheumatol2014;32:424–32.
Rachlis AC, Babyn PS, Lobo-Meuller E, et al. Whole body magnetic resonance imaging in juvenile
spondyloarthritis:willitprovidevitalinformationcomparedtoclinicalexamalone?ArthritisRheum
2011;63:S292.
Chapter9
Juvenileidiopathicarthritis
Introduction
ManagementofJIA
Transitionservices
JIAsubtypesandtheirspecificfeatures
Macrophageactivationsyndrome
Uveitis
Introduction
Inflammatory arthritis, resulting in stiffness, swelling, joint restriction and
damage,wascharacterizedinchildrenin1896byGFStillandisnowrecognized
asoneofthe commonestcausesofdisabilityinchildhood.Juvenile idiopathic
arthritis(JIA)isthe ‘umbrella’term,acceptedbytheinternationalcommunity,
for several forms of arthritis (summarized into subtypes for practical terms in
Table 9.1; for JSpA conditions there are many similarities with adult
presentations,see Chapter8).
Epidemiology
• JIAaffects1in1000childrenandyoungpeopleupto16yearsofage,from
bestavailableUKestimatesandhassimilarprevalencetodiabetes(1in700).
Morerecentinternationalstudiesindicateahigherprevalenceof167–400per
100,000person-years.
• TheannualincidenceofJIAis~1in10,000children/youngpeople.
• A majority of patients with JIA have a phenotype distinct from adult
inflammatoryarthritiswhichincludesanassociationwithuveitis.
• The diagnosis of JIA requires the presence of arthritis for 6 weeks to
distinguish it from reactive arthritis etc.; however, the treatment of JIA and
referraltoophthalmologyshouldnotwait6weeks.
• In most forms of JIA, there is inflammation of the joint lining (synovium).
Circulating activated lymphocytes migrate into joints and the resulting
generationofpro-inflammatorycytokinesleadstoactivationofmacrophages
and joint stromal cells (e.g. fibroblasts) similar to that seen in adult RA. In
affectedjoints,thereisexcesscytokineproduction,ofTNFα,IL-6,andIL-17.
Classification
The classification of JIA was radically changed in 2001. For years, there was
confusion between North America and European conventions for naming the
differentformsofjuvenilearthritis.
• Classificationhasbeensubsequentlycomplicatedinpracticebytheevolving
understanding of the breadth of effects in the spondyloarthritis (SpA)
conditions.
• WeincludejuvenileSpAalsoin Chapter8.
Table9.1TheclassificationofJIAsubtypes
Diagnosis Peakage-
range(s)
Extra-articular
features
Oligo-
JIA
≤4joints 2–4yrs Uveitis
Poly-JIA
(RF or
ACPA
+ve)
>4joints >9yrs Nodules,malaise,
weightloss
Poly-JIA
(RF and
ACPA
−ve)
>4joints 2–4yrs
7–12yrs
Uveitis,poorgrowth
SoJIA Fever,rash,hepatomegaly
splenomegaly
4–7yrs Serositis,carditis,
coronaryectasia,MAS
ERA Enthesitis,asymmetricallarge
jointarthritisandSIJs
>6yrs Acuteuveitis
JPsA Psoriasis±in1st-degree
relative,nailpitting,dactylitis
9–11yrs Psoriasis,bone
oedema,panuveitis
InformationfromPettyREetal.InternationalLeagueofAssociationsforRheumatologyclassification
ofjuvenileidiopathicarthritis:secondrevision,Edmonton,2001.JRheumatol2004;31:390–2.

ManagementofJIA
Nationalguidelinestoaidmanagement
The following key documents promote best practice in JIA and paediatric
rheumatology:
• National service specification for paediatric rheumatology (E03/S/b):
http://www.england.nhs.uk/commissioning/spec-services/npc-crg/group-e/e03/
• NHS Commissioning Quality Dashboard:
http://www.england.nhs.uk/commissioning/spec-services/npc-crg/spec-
dashboards/
• British Society of Paediatric and Adolescent Rheumatology (BSPAR)
guidelines: http://www.bspar.org.uk/clinical-guidelines
• ArthritisandMusculoskeletalAlliance(ARMA)StandardsofCareforJIA:
http://www.arma.uk.net/resources/standards-of-care
• BSPARwebsitewww.bspar.org.uk
• InterimClinicalCommissioningPolicyStatement:BiologicTherapiesforthe
treatment of Juvenile Idiopathic Arthritis (JIA):
http://www.engage.england.nhs.uk/consultation/specialised-services-
policies/user_uploads/biolgcs-juvenl-idiop-arthrs-pol.pdf
• NICE—abatacept,adalimumab,etanercept,andtocilizumabfortreatingJIA:
http://www.nice.org.uk/guidance/TA373
Diagnosingarthritisinchildren
TherearenodiagnostictestsforJIA.Diagnosisrequiresathoroughhistoryand
examinationtodistinguishJIAfromothercausesofjointpainorswelling(Table
9.2).
• Inflammatory arthritis in children is characterized by prolonged morning
stiffness(typically>20min),swelling,restriction,andlossofjointfunction.
• JIAshouldbeconsideredwhen:
• joint swelling from presumed trauma (including knee and ankle) persists
beyond2weeks.
• thereisinvolvementofseveraljoints.
• aspiratedjointfluidisshowntobeaseptic.
• thereismorningstiffness.
• thereisjointrestrictionintheabsenceofamechanicallesion.
• Carefulexaminationaimstoconfirmswelling,whichmaybesubtle,identify
jointrestriction(typicalofactivelyinflamedjointsinchildren)andestablish
thedistributionofaffectedjoints.
• Quick and methodical assessment of other joints is achieved using pGALS
(see Chapter1,‘ThepaediatricGALSscreen’).
• The examination technique of specific joints uses a systematic approach
identifiedinpREMS( http://www.pmmonline.org).
• Abnormal signswhichmightrevealJIA summarizedfrom atypicaldetailed
regionalexaminationareshowninTable9.3.
• Involvement of multiple joints increases the likelihood that arthritis is JIA,
especiallyintheabsenceofsystemicsymptoms.
• Juxta-articularchangesinJIAincludemuscleatrophy,leglengthdiscrepancy
due to limb overgrowth from knee involvement, reduced limb length from
early closure of growth plates adjacent to inflammation during adolescence,
andsynovialcysts.
• SoJIApresentswithsystemicfeaturesandthedifferentialdiagnosisiswideso
abroadapproachtoassessmentandinvestigationsisessential(Table9.4).
Table9.2ThedifferentialdiagnosisofJIAconditions
Condition Examples Investigations
Monoarticular
disease
Septicarthritis,TB,PVNS,foreign-
bodysynovitis,sicklecelldisease,
haemophilia,leukaemia,non-bacterial
osteomyelitis
Bloodandsynovial
fluidculture,
Mantoux,IGRA,
US,MRI,synovial
biopsy,bloodfilm,
genetics,
coagulationfactor
assays
Arthritis
following
infection
Lymedisease,viralarthritis,post-
streptococcalarthritis,HSP,Kawasaki
disease
AIserology,ASOT,
anti-DNAseB,
throatswab,
transthoracicecho
Inflammatory
backpains
conditions
HLA-B27-associatedreactivearthritis,
ERA,IBD-associatedSpA,enthesitis
Biomechanical
and
orthopaedic
conditions
Trauma,haemarthrosis,NAI,
patellofemoralpain,osteochondroses,
osteochondritisdissecans,
osteonecrosis,osteoidosteoma,tarsal
coalition,biomecanicalimbalance
Radiographs,MRI
fromdeconditioning,muscletightness
andhypremobilityconditions
Painconditions Complexregionalpainsyndrome
(CRPS),chronicwidespreadpain
Differencesfromadultarthritis
• Arthritis in children directly affects limb growth and may have an overall
effectonheightandweightattainment.
• Joint restriction is often a more sensitive sign of inflammatoryjointdisease
activityinchildrenthanitisinadults.
• Witheffectivediseasecontrolandbeforepubertythereisalikelihoodofrepair
ofjointdamage.
• Medicationhastoaccountforbodysizeanddifferentpharmacodynamicsand
pharmacokinetics.
• Bloodmonitoringofmedicationsuseisfrequentlydifferent.
Table 9.3 Key signs compatible with a diagnosis of JIA, summarized from a (necessarily) detailed
regionalMSKexamination
Joint AbnormalsignstoidentifyinJIAconditions
Wrist Volardisplacement,reducedgripstrength,poorordifficultyin
handwriting
Fingers Dactylitis,nailpitting,nodules,handwriting(asforwrist)
Elbow Flexiondeformity,inabilitytotouchshoulder
Shoulder Lossofabduction,difficultydressing
Neck Lossofnormalcervicothoracicspinelordosis,reducedrotation
Spine Lossoflumbarspinelordosis,positiveSchöbertest,midlineor
sacralbonytenderness,reducedorasymmetriclowerlimbmuscle
length
Hips Apparentleglengthdiscrepancy,Trendelenburggait,lossofhip
swingongait,painatendofrangeof(passive)rotation,positive
FABERtest,positiveThomastest
Knees Lossofextension(especiallyifasymmetrical),synovial(including
popliteal)cysts,vastusmedialiswasting
Ankle
andfoot
Abnormal/antalgicgait:no/abnormalheelstrike,foot
pronation/inversion,calfmusclelengthasymmetry,midfoot
rigidity
TMJ Restrictedorasymmetricjawopening,TMJcrepitus
Investigations
Atpresentation,investigationshelpdistinguishdifferentialdiagnosessincethere
arenodiagnostictestsforJIA.
• ESRandCRPdonotcorrelatewellwiththeextentorseverityofinflammation
andmaybenormal.
• A particularly high ESR may indicate the presence of inflammatory bowel
disease(IBD)or(veryrarely)leukaemia.
• Alowhaemoglobinmayindicateanaemiaofchronicdiseaseratherthaniron
deficiency.
• ANApositivityoccursin 40–75%ofJIApatientsandindicatesanincreased
riskofeyedisease.Itisnotadiagnostictestorpredictiveofoutcome.
• Rheumatoid factor (RF) positivity is rare in JIA and difficult to interpret in
oligoarticularJIA.HightitreANAandRFmayindicateSLE.
• US is the radiological investigation of choice to corroborate arthritis and
evaluate tenosynovitis and joint damage. Its false-negative rate is higher in
footandanklediseasethanforotherjoints.
• Radiographs may show soft tissue swelling, periarticular osteopenia. and
erosionsinlong-standingarthritis.
• ArthroscopyshouldbeavoidedunlessabiopsyisrequiredasinPVNS.
• Synovial fluid aspiration, but not arthroscopy, is essential when considering
sepsisandTB.
• Tomonitordiseaseactivity,drugtherapyandtissuedamage:
• ESR and CRP frequently do not reflect the extent or severity of
inflammation.
• A falling ESR and haemoglobin with climbing ALT/AST may indicate
macrophageactivationsyndrome(see Chapter25)asmayaferritinlevel
>10,000ng/mL.
• USisusedtomonitorchangesinsynovialinflammationandjointdamage
butcontrast-enhancedMRImayprovidemoreusefulimagesincludingthe
presenceofboneoedema.
• MonitoringofdrugsideeffectsincludesthemeasurementofFBCandLFTs.
Table9.4ConditionsandinvestigationstoconsiderwhensuspectingSoJIA
Conditions Investigations
Acute
lymphoblastic
leukaemia
Bloodfilm,bonemarrowaspirate,whole-bodyMRI
(includingfat-suppressedsequence)
Neuroblastoma Urineorbloodadrenaline/noradrenaline
Lymphoma CXR,abdominalUS,whole-bodyMRIorCT
Sepsis,TB Bloodcultures,serology,PCR,Mantoux,IFNγrelease
assay,jointaspiration,MRI
SLE,APS Coagulation,complementC3andC4,autoantibodies,
urinalysis
JuvenileDM QuadricepsMRI,CK,LDH
Reactivearthritis,
rheumaticfever
Lyme,BartonellaandBrucellaserology,ASOT/anti-
DNAaseBandthroatswab,transthoracic
echocardiogram(TTE)
Vasculitides TTE,ECG,urinalysis,ANCA,detailedhistory,
angiography,biopsy
Viruses Serology(EBV,CMV,Parvovirus,Rubella)
Travel-associated
diseases
Testsaccordingtosuspicion
Periodicfever
conditionsand
porphyrias
Genotyping(see Chapter18),IgD,urinarymevalonic
acid,urinaryporphyrins
Inflammatory
boweldisease
Faecalcalprotectin,endoscopy,bariumswallow
Treatment
The overall approach to treatment in JIA is to gain early rapid control of
inflammation,minimizetheadverseeffectsoftreatment,andsupportthegeneral
physicalandmentalhealthofthepatient.Thispatient-centredholisticapproach
requires the participation of a full multidisciplinary team—each member with

dedicatedexperienceofJIA.
Treatmentoftheacuteswollenjoint
Themanagementoftheacuteswollenjointshouldprimarilyfocusonrulingout
sepsis(see Chapter25,pp.708–709).
• Ibuprofen,naproxen,diclofenac,orotherNSAIDS,shouldbeused,especially
whenwaitingforapaediatricrheumatologyreview.
• For an effective NSAID response (managing inflammation as opposed to
simplypain),therecommendeddosingfrequencyshouldbecontinuedfor>2
weeks+/–gastroprotection.
• IAglucocorticoids(GCs)canbeconsideredfor:
• limp,disability,jointrestriction,othercomplicationsofarthritis.
• persistentlymarkedjointswelling.
• a bridging strategy whilst awaiting long-term medication to become
effective.
• OralorIVGCsshouldbeusedtosupplement,orasanalternative,toIAGC,if
therearemanyjointsinvolvedor jointinjectionstherapyisnotimmediately
feasibleortheeffectofIAGCshasbeentriedandwaslimited.
Long-termmanagementofJIA
• Long-termmanagementofJIArequiresclosecollaborationbetweenmembers
oftheMDTwitheffectivecommunicationbothwithintheserviceandacross
theregionalnetwork.
• Members of the MDT include a clinical nurse specialist, physiotherapist,
occupational therapist, orthotist or podiatrist, ophthalmology colleagues,
musculoskeletalradiologist,psychologist,socialwork,anddieteticsupport.
• Medicationformsonlyapartofthelong-termmanagementofJIA.
• Fundamentalisthepromotionofphysicalactivitywhichencouragesareturn
of the strength and stamina lost from active arthritis, and correction of
muscularimbalancesthatresultinpain,injury,andlossofjointprotection.
• Provisionofinformationandeducationforparentsandpatientsisaconstant
requirement.Thisiscriticalfortheirparticipationinjointdecision-makingand
adherencetoagreedtreatmentplansandhelpsdissipatelingeringanxiety.
• Pain management frequently involves strategies other than the use of
medication.
• Vaccination advice is usually given at the outset and changes in national
guidelines (August 2017) indicate that it is safe to give live vaccines to
patients before treatment or whilst on low to moderate doses of GCs and
csDMARDs (
http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/655225/Greenbook_chapter_6.pdf
• Inindividualcases,givinglivevaccinesevenifimmunosuppressionisbeing
taken far outweighs the risks. All routine non-live vaccines may be given
withoutcomplication.
• Effective liaison is required with schools, primary care, and community
services.
• Effectivetransition,whichincludesage-appropriateservicesforyoungpeople
frompubertyonwards,isalsoanessentialrequirementtooptimizethewell-
being and self-efficacy of this age group. This should continue well after
transfertoadultservices.
• Ahealthydietavoidssomeoftheproblemsofgrowthrestrictionordelayand
excessweightgainfromlowphysicalactivityorGCuse.
• Although close collaboration with orthopaedics ensures timely referral of
patientsandgoodmedicalmanagementoforthopaedicconditions,therateof
surgicalinterventioninJIAhasgreatlydiminished.
• Surgicalsynovectomy,softtissuerelease(tenotomiesandcapsulotomies)and
jointreplacementarenowrare.
Long-termmedicationinJIA
Theaimofmedicationinthelongtermistoreducethefrequencyandimpactof
flaresofarthritisanduveitis.
• Long-term medications in the form of (synthetic) disease-modifying
antirheumaticdrugs(sDMARDs)areusedfor:
• Persistentarthritisoruveitisrefractoryto,orincompletelycontrolledby,IA
orperiocularGCs.
• Presenceofchroniccomplicationsortissuedamage.
• Extensiontootherjointsoreye.
• Joint-specificeffectsonthewristandhandfunction,thehipandmobility,or
jaw.
• sDMARDtreatmentstypicallytakeafewweekstobecomeeffectiveandmay
requireabridgingcourseofGCseitherIA,orally,orIV.
• Given the extensive support and experience required, sDMARDs are best
institutedbyaspecialistserviceordelegatedresponsibilitytosecondarycare
withinaclinicalnetwork.
• There is now extensive experience of the valuable role of primary care in
monitoringtreatmentwiththeback-upofanaccessiblesecondaryortertiary
service.
• ThestandardsDMARDusedinJIAanduveitisismethotrexate(MTX).
• MTXinSCform,ratherthantabletsorliquidpreparations,istypicallyusedin

theyoungchildandwherethereisextensiveorsevereinflammation.
• AlternativesDMARDS forarthritisincludeleflunomide(LEF),sulfasalazine
(SSZ),andhydroxychloroquine(HCQ).
• Azathioprine (AZA) and ciclosporin may have a role in both arthritis and
uveitis, whereas mycophenolate and tacrolimus are considered to have a
specificroleinuveitis.
• ThevalueofsDMARDcombinationsisnotwellstudiedinJIAbutareused
withgoodeffectinsomepatientsandhavenotbeenshowntohaveincreased
levelsofadverseeffects.
• BiologicDMARD(bDMARD)therapiesincludinganti-TNFαtherapieshave
been shown in high-quality studies to be effective in JIA and are now a
standard treatment in the presence of refractory disease to or intolerance of
MTXorothersDMARDs:
• IntheUK,thereisNHS(NICE)approvalfortheuseofabatacept(afusion
protein of the extracellular domain of human cytotoxic T-lymphocyte-
associatedantigen4(CTLA-4)linkedtoamodifiedFcportionofIgG1),the
anti-TNFαtherapiesadalimumabandetanercept,andtocilizumab(ananti-
IL-6 receptor monoclonal bDMARD) in JIA. In England there is also an
agreement with NHSE to use anakinra, infliximab and rituximab under
certainconditions.
• bDMARD use in England is directed by NICE and NHSE (
http://www.england.nhs.uk/commissioning/wp-
content/uploads/sites/12/2015/10/e03pd-bio-therapies-jia-oct15.pdf).
• Supplementarymedicationsincludethoseforpain,gastritis,andnauseaandto
optimizebonedensityandstrengthinthepresenceofGCsorreducedphysical
activity.
Outcomeandprognosis
GiventheprogressinmanagementstrategiesandadventofbDMARDtherapies,
old published outcome data will no longer be applicable. Current paediatric
rheumatologist consensus is that there has been a marked improvement in
outcomeandmanypatients.
• Theincidenceofjointreplacementhasreducedconsiderablyfromreportsin
theearly2000swhen80%ofpatientswithRF-positiveJIAfollowedupovera
periodof20yearsrequiredarthroplasty.
• Thereisstrikinglylittlehigh-qualitydata measuringlong-termremission off
medication.
• About 50–75% of patients with persistent oligo-JIA will achieve long-term
remission by their early teens but may still experience flares at any time in
adulthood.
• About20–30%ofpatientswith(RFandACPA)seronegativepolyarticular-JIA
achievedrug-freelong-termremissionintoadulthood.
• The concept of minimal disease activity has only recentlybeenvalidatedin
JIA and may be a better outcome variable for those patients who do not
achievecompleteremission.
• Despitechangesintreatmentstrategiesandoutcome,suboptimaloutcomesdo
occurandareassociatedwith:
• delayeddiagnosis.
• delayedreferraltoaspecialistMDT.
• suboptimalcontrolofactivedisease.
• inadequateengagementandcollaborationwiththepatient,parent,orother
carers(seepsychologysupportlaterinthislist).
• presentationwithuveitisandoculardamage.
• ongoingdiseaseactivityinsystemic-onsetJIA(SoJIA)at6months.
• SoJIAinmales.
• youngageofonsetinoligoarticularandpolyarticulardisease.
• psoriaticarthritis.
• hipinvolvement.
• rapidearlyonsetofJIAinsmalljointsofhandsandfeet.
• inassociationwithearlyradiographicchanges.
• Psychologysupportimprovesoutcomeby:
• reducingtheimpactofMTX-associatednausea.
• reducingtheimpactoffearandanxietyarounddiagnosisandtreatment.
• identifying,managing,andreferringanymentalhealthconcerns.
• alleviatingfactorsthatadverselyimpactonqualityoflifeandengagement
withschool.
• addressingadversebodyimageconcerns.
• managing thefrustration ordisappointment ofpersistent orflaring disease
activityandsideeffectsfrommedication.
Transitionservices
‘Transition’ means, and hopes to achieve, the seamless and appropriate care
transfer from paediatric/adolescent services to a young-adult or adult service.
Thedevelopmentofage-appropriateclinicsisawell-regardedstrategytoreduce
thebarrierstoeffectivetreatment.
• Atransitionserviceisachievedthroughoptimizingengagementofadolescents
oryoungadults,promotionofself-efficacy,andenhancementofself-advocacy
andadherencetoagreedmanagementplans.
• Manycentresnowofferadolescentclinicsforpatientsagedfrom10–13years
to17–18yearsandyoungadultclinicsforthoseaged17–25years.
• Theimplementationandoptimizationofadolescentandyoungpersons’clinics
requires:
• closecollaborationbetweenpaediatricandadultclinicians.
• age-specificnursingexpertise.
• age-appropriateenvironmentandinformationresources.
• thatthepatientbeseen(first)withoutparentspresent.
• thepromotionofanunderstandingofconfidentialityandconsent(orassent).
• the promotion of effective health-related behaviours including joint
decision-making,self-advocacy,andself-efficacy.
• support for the attendance and performance at school, college, and
universityandwhenseekingemployment.
• theearlyidentificationofmentalhealthproblemsthatmaybe abarrierto
care.
• respectfordevelopingbodyawareness.
• assistancewithfamilyplanningandsexualhealth.
• earlyanticipationofanysurgicalneeds.
• GuidelinestosupportthedevelopmentofyoungpersonclinicsincludeYou’re
Welcome Quality Criteria (Department of Health) and Transition to Adult
Care:ReadySteadyGo(UniversityofSouthampton).
JIAsubtypesandtheirspecificfeatures
OligoarticularJIA(oligo-JIA)
• Oligo-JIA is the commonest subtype, accounting for 30–40% of JIA and is
characterizedbytheriskofuveitis.SeeTable9.1
• Itpredominantlyaffectsfemaleswithpeakagesofonsetbetween2to4years
and7to13years.
• About50%ofcasesaremonoarticularinpresentation.
• If>4jointsbecomeinvolvedafter6monthsofdiseaseactivitytheconditionis
reclassifiedasextendedoligo-JIA.
• Extension to polyarticular JIA is more likely in those with uveitis and rare
beyond5yearsfromdiagnosis.
• Thecommonestjointsinvolvedareelbow,knee,andankle.
• Jointoralimbdeformityisofgreatconcerninthegrowingpatient.
• Leglengthdiscrepancyismorecommonwhenarthritisofthekneebegins<3
yearsofage.Toaccommodatefortheexcesslength,thechildstandswiththe
kneeflexedresultinginaflexioncontracture.
• HipmonoarthritisorprimarycoxitiscanoccurespeciallyinperipubertalAsian
girls,butasearchtoruleoutothercausesisessential.Thefollowingshouldbe
considered: septic arthritis, leukaemia (e.g. in an at-risk population such as
Down’s syndrome), psoriatic arthritis, IBD-associated arthritis, and juvenile
SpA.
• Studies have shown that over 80% of patients have little or no disability or
jointdamageafter15yearsoffollow-up.
• TheHLAassociationswitholigo-JIAincludeHLA-DRB1*08withadditional
susceptibilityhaplotypesHLA-DRB*1103/1104.
• HLA-DRB1*0401,foundinRA,isprotectiveforselectedsubtypesofJIA.
PolyarticularJIA(poly-JIA)
• Poly-JIAisdiagnosedwhen>4jointsareinvolvedwithinthefirst6monthsof
disease activity (excluding psoriatic arthritis, IBD-associated arthritis, and
enthesitisrelatedarthritis).
• Pragmatically, decision-making for extended oligo-JIA is similar to that for
poly-JIAandlong-termdataindicatesasimilaroutcome.
• A polyarticular course occurs in 20–30% of JIA and is subdivided by the
presence or absence of RF, which should be checked (on latex) on two
occasionsatleast3monthsapart.
• RFpositiveJIAoccursin<5%ofJIA,ismostcommoninfemalesandhasa
phenotypeverysimilartoRAinadults.
Rheumatoidfactor-negativepolyarticularJIA
• InRF-negativepoly-JIAthereisoftenincompletecontrolofarthritisdespite
majoradvancesintreatment.
• RF-negativepoly-JIAisassociatedwithhigherlevelsofdisabilityespecially
duringflaresofthearthritis.
• Joint restriction often indicates disease activity and is commonly associated
withmuscleatrophy,disability,andjointdamage.
• Thereisapoly-JIAphenotypewithboggysynovitisthatisnotassociatedwith
muchpainordisabilityandjointsarecommonlywellpreserved.Tenosynovitis
cancoexistwithjointsynovitisandcanremainundisclosedunlesssuspected.
• Another poly-JIA subtype is characterized by predominantly foot and ankle
involvement, the consequences of which can be a reduction in generalized
mobility,tarsalfusion,tenosynovitis,andbursitis.
• TMJ involvement is often insidious in onset. It is unlikely to be missed if
pGALS (see Chapter 1) is undertaken at each clinic visit. If left
undertreated, TMJ arthritis may result in micrognathia and dental
malocclusion.
• Neckinvolvementcancausemarkedirritabilityandbeparticularlydisabling
intheclassroom.Occupationaltherapyassessmentisadvisable.
Juvenilepsoriaticarthritis(JPsA)
• JPsA is considered as one of the juvenile spondyloarthritides (JSpA; see
Chapter8;andforILARdiagnosticcriteriasee Chapter8,p.318).
• FeaturesofJPsAaresimilartoadultPsA(see Chapter8,p.318).
• JPsAshouldbeconsideredevenifthereisnopsoriasisbutthereisahistoryof
psoriasisinafirst-degreerelative.
• Nail pitting, dactylitis, previous or concurrent acute panuveitis, and
inflammatorybackpainhistorymaybepresent.
• JPsAcanbeoligo-orpolyarticular.
• JPsAisfrequentlyresistanttoconventionaltreatmentstrategiesincludingGC
resistance.
Juvenilespondyloarthritis(JSpA)andenthesitis-relatedarthritis(ERA)
• See Chapter8foradditionaldetail.
• JSpA should only be considered in patients older than 6 years, especially
males,andwhenthereisasymmetriclargejointinvolvement.
• Enthesitis is the inflammation at the sites of bony insertion of tendons and
ligaments. In ERA, enthesitis can be very painful and disproportionate to
examinationfindings.
• HLA-B27 is found in 30–50% of ERA patients and is associated with an
increasedriskofdevelopingjuvenileankylosingspondylitis.
• ERA is generally associated with a low-grade grumbling disease persisting
intoadulthoodbutassociatedwithlittleerosivejointdisease.
• In a minority of patients with ERA there may be high levels of disability
responsivetoanti-TNFαtherapy.
Systemic-onsetJIA(SoJIA)
ThisformofJIA,presentingwithfeverandrash,affectsjust5–8%oftheJIA
population. A broad approach to diagnosis is essential—many conditions can
presentwithMSKpains,rash,andsystemicsymptoms.
• SoJIA is best considered as an umbrella term that covers several
autoinflammatory disorders (see Chapter 18 and Table 18.1, p. 544) and
poly-JIAtriggeredbyorpresentingwithaviralinfection.
• Previouslyknownas‘Still’sdisease’,thistermisnowdiscouragedduetothe
confusionitmaycause.
• Incidence:M=F.SoJIAoccursatanyageincludinginfantswithpeakonset
between2and3yearsold.
• Typically:highlevelsofIL-1andIL-6inserumandsynovialfluid.
DiagnosisofSoJIA
• Nospecificdiagnostictestsexist.
• Thereisabroaddifferentialdiagnosisthatrequiresassessmentbyapaediatric
rheumatologist.
• Many of the characteristic features including fever, rash, polyarthritis,
lymphadenopathy,andhepatosplenomegalyoverlapwithotherconditions(see
Table9.4).
• Similarly, acute lymphoblastic leukaemia can present with fever, rash, and
joint/limbpains(attributabletomarrowinvasion).
• Neuroblastomashouldbeconsideredinpatients<5yearsold.
• Ahistoryoftravelandcontactwithanimalsorticsshouldbetaken.
• Truepersistentjointinflammationmaynotbefoundatdiagnosisorformany
months(upto9yearsold)afterdiagnosis.
• Thefever,ofupto39°C,istypicallyquotidian—occurringonceortwiceper
day in a diurnal distribution with return to a normal baseline between fever
spikes.
• TypicalbloodresultsincludehighESRandCRP,neutrophilia(oftheorderof
20×10
9
/L),thrombocytopenia(often>600×10
9
/L),andanaemiaofchronic
inflammation(often<80g/L).
TreatmentofSoJIA
The initial treatment of SoJIA focuses on the need to allow time for
investigationstoexcludeothercausesoffeverandmanagepainanddisability.
• AtrialofNSAIDsfor2weeksisusedinitially,thoughNSAIDsmayhaveno
effectonserositis,orfloridpolyarthropathy.
• SoJIAisaGC-responsivecondition,butthere’slittleevidencethatGCsalter
thelong-termoutcome.
• GCsmaybeusedonceotherconditionshavebeenruledout.Ashortorlimited
courseofGCsmaybeusedtotemporizepain,fatigue,anddisabilitytoseeif
inflammationofapost-infectiousoriginsettlesonitsown.
• GCs provide effective symptomatic relief while waiting for a sDMARD
(typicallyMTX)response.
• BiologicDMARDs(bDMARDs)areusedwhen:
• unabletoweanoffGCsdespiteuseofMTX.
• MASispersistent.
• when a flare of joint pains/disease occurs despite MTX being taken at a
therapeuticdosefor>3months.
• If SoJIA isunresponsive toanakinra (ananti-IL-1 bDMARD)after 4weeks
treatment,thentreatmentshouldbeswitchedtotocilizumab.
• TocilizumabisrecommendedintheUKbyNICE.
• Anti-TNFα therapy can be used for children with a polyarticular course of
SoJIAoncesystemicfeatureshavesettled.
• Other less routine treatments for SoJIA include ciclosporin, canakinumab,
IVIg,andstemcelltransplantationinseveredisease.
Macrophageactivationsyndrome
Macrophageactivationsyndrome(MAS)israrebutislife-threatening(mortality
is8–22%).MAScancomplicateotherdiseases.MASisalsotermedsecondary
haemophagocytic lymphohistiocytosis (HLH). For a summary see
http://www.the-rheumatologist.org/article/macrophage-activation-
syndrome/6/)ThereaderisreferredtoChapter25
Uveitis
This important association of JIA occurs in 10–20% of patients and within 7
yearsofarthritisonset.
• Visuallossoccursin~25%ofJIA-associateduveitisandirreversibleblindness
occurswithoutsymptomsorchangesineyeappearance.
• Irreversiblecomplicationsmayoccurafteronlyafewweeksofuncontrolled
uvealinflammation.
• However, abouthalfof children with anteriororintermediate uveitis do not
experiencevisuallossdespiteprolongedinflammation.
• Therearenumerouscausesofuveitis(Table9.5).
Table9.5Thedifferentialdiagnosisofcausesofpaediatricuveitis
Infectious Non-infectious
Toxoplasma
Varicella
Herpessimplex
CMV
Trauma (sympathetic
ophthalmia)
Inflammatoryboweldisease
Sarcoid
TB
Borrelia(Lymedisease)
Bartonella
Other: toxocariasis, Ascaris, fungal,
histoplasmosis,Syphilis
Tubulointerstitialnephritis
Blausyndrome
Behçet’sdisease
Periodicfevers
Multiplesclerosis
Vogt–Koyanagi–Harada
Vasculitis (including
Kawasakidisease)
Uveitissurveillance(screening)programmes
Allpaediatricrheumatologyunits/physiciansshouldhaveanagreedmechanism
of systematically screening for, managing, and having emergency access to, a
suitably resourced ophthalmology team skilled in examining very young
children.
• UveitissurveillanceinJIAisessentialbecauseuveitis:
• issight-threatening.
• is rarely apparent from routine history and examination, especially in
children<8yearsofage.
• isnotpredictableandisunrelatedtotheseverityofarthritis.
• ispresentin40%casesatthetimeofthefirsteyescreen.
• complications,especiallycataract,occurinupto40%.
• ismostlikelytorespondwithaggressivetreatment.
• Other major ophthalmological concerns include glaucoma, macular oedema,
retinaldetachment,bandkeratopathy,andhypotony.
• There should be immediate access to advice and assessment should eye
symptomsdevelop.
• A uveitis screening interval schedule should be adopted (e.g. Table 9.6) to
avoidirreversibleeyedamage.
• Uveitissurveillanceschedulesshouldbeadaptedtotheriskofuveitis,andin
thecontextoftreatmentuse(e.g.whenstoppingMTX).
• Eyescreeningcontinuesuntil12yearsofagewhenapatientcanreliablyself-
reportfeaturesofinflammationsuchasfloatersandpain.
• Cessationofeyescreeningat12yearsolddoesnotindicatethatuveitismay
notoccur,buttheriskbeyondthisageissufficientlylowtomakeself-report
morereliable.
Table9.6Uveitissurveillance:recommendedfrequencyofslitlampexamination(summarisedfromthe
UKRoyalCollegeofOphthalmologyGuidelines)
Condition Frequency
SoJIA Yearly
Onsetof
JIA<7
yrsold
ANA+ve:every2monthsfor6months,thenevery3monthsfor
3.5 yrs, then 6 monthly for 3 yrs or until aged 12 yrs, then
yearly(ifpreviousuveitishasoccurred)
ANA−ve:every6monthsfor7yearsoruntilaged12yrs,then
yearly(ifpreviousuveitishasoccurred)
Onsetof
JIA≥7yrs
old
6monthlyfor4yrsthenyearly(ifpreviousuveitishasoccurred)
Managementofuveitis
Uveitismanagementaimstobalancelong-termriskofvisuallosswithshort-and
long-termrisksoftreatment.
• First-linetreatmentofanterioruveitis:topicalGCs(e.g.Maxidex
®
orPredsol
®
eyedrops)givenuptohourlydependingontheseverity.TopicalGCsareless
effectiveinintermediateorposterioruveitis.
• There is a dose-dependent increase in risk of cataract formation from using
steroideyedrops.Theriskfromonedropperdayis0.1%peryearandrises
withmorefrequentandprolongeduse.
• Othertopicalagentsincludemydriaticstoreducetheriskoftheirisstickingto
thelens(posteriorsynaechiae)andglaucomaagents.
• SystemicorperiocularGCsareusedinthepresenceofpanuveitisandfeatures
inadequatelyresponsivetoeyedrops.
• Aggressive or long-term treatment should be confined to those with a
significantriskofpermanentvisualloss.
• sDMARDsorbDMARDsareusedwhenrecurrentcoursesorprolongeduseof
steroideyedropsisrequiredtomaintaininflammationtolessthe0.5+activity
usingtheSUNcriteria.
3
• Poor outcome from uveitis is associated with presence of ocular damage at
presentation,whenuveitisprecedesarthritis,whenthereisdelayintreatment
initiation,andwithfailuretoachieveearlyremission.
Reference
3. ScottishUveitisNetwork(SUN).Guidelines. http://www.sun.scot.nhs.uk/guidelines.html

Chapter10
Systemiclupuserythematosus
Introduction
Pathophysiology
Clinicalfeaturesofsystemiclupuserythematosus(SLE)
AntiphospholipidsyndromeandSLE
PregnancyandSLE
Assessmentofdiseaseactivity
Drug-inducedSLE
ManagementofSLE
Prognosisandsurvival
JuvenileSLE
Neonatallupussyndrome
Introduction
Systemic lupus erythematosus (SLE/‘lupus’) is a multisystem autoimmune
disorderwithabroadspectrumofclinicalfeaturesinvolvingalmostallorgans
andtissues.
• SLEisachronicdiseasewhichremitsandrelapses.Apreclinicalphaseexists
characterized by autoantibodies common to other autoimmune diseases,
followedbyadisease-specificautoimmunephase.
• Variations exist in the incidence of clinical features between ethnic groups
necessitating a keen sense of awareness of a variety of multisystem
pathologiesandappreciationthatSLEhastakenonthemantleofsyphilisas
thegreatmimicofotherconditions.
Epidemiology
• Prevalencevariesworldwide,butintheUKitis97per100,000.
• SLEis10–20×morecommoninwomenthanmen,andmostlikelytodevelop
betweentheagesof15and40years.
• It is more common and often more severe in certain ethnic groups such as
thoseofAfrican-Caribbean,India,Hispanic,andChineseoriginlivinginthe
USAandEuropethaninwhiteCaucasians.
Classification
• TheAmericanCollegeofRheumatology(ACR)publisheditsrevisedcriteria
fortheclassificationofSLEin1997(Table10.1).
• Criteria are for the classification of SLE for epidemiological and research
purposes and not for diagnostic purposes. In practice, however, criteria
naturallytendtoformthecornerstoneforclinicaldiagnosis.Thecriteriawere
developedandvalidatedinpatientswithestablished,long-standingdiseaseand
thereforemayexcludepatientswithearlyorlimiteddisease.
• TheSystemicLupusInternationalCollaboratingClinic(SLICC)classification
criteria for SLE are similar to the ACR classification criteria. The main
differencesarethat,fortheSLICCclassification:
• Haematologicalabnormalitiesneedbepresentononlyoneoccasion.
• ThereisinclusionoflowC3,C4,andCH50levelsandapositiveCoombs
testintheabsenceofhaemolyticanaemia.
• The criteria also include non-scarring alopecia and a broader range of
cutaneousandneurologicalmanifestations.
Table 10.1 1997 update of the 1982 American College of Rheumatology revised criteria for the
classificationofSLE
1 Malarrash Fixederythemaflatorraisedovermalareminencestending
tosparethenasolabialfolds
2 Discoid
rash
Erythematousraisedpatcheswithadherentkeratoticscaling
andfollicularplugging;atrophicscarringmayoccurin
olderlesions
3 Photo-
sensitivity
Skinrashasaresultofanunusualreactiontosunlightby
patienthistoryorphysicianobservation
4 Oralulcers Oralornasopharyngealulceration,usuallypainless
observedbyphysician
5 Non-
erosivearthritis
Involving2ormoreperipheraljointscharacterizedby
tenderness,swelling,oreffusion
6 Serositis Pleuritis(historyofpleuriticpainorrubheardbyphysician
orevidenceofpleuraleffusion)orpericarditis(documented
byECGorruborpericardialeffusion)
7 Renal
disorder
Persistentproteinuria>0.5g/24hrsor>3+ifquantitation
notdoneorcellularcasts(redbloodcell,Hb,granular,
tubularormixed)
8
Neurological
disorder
Seizuresorpsychosisintheabsenceofoffendingdrugsor
knownmetabolicderangements,e.g.uraemia,ketoacidosis,
orelectrolyteimbalance
9
Haematological
disorder
Haemolyticanaemiawithreticulocytosisorleucopenia
<4.0×10
9
/Lon≥2occasionsorlymphopenia<1.5×109/L
on≥2occasionsorthrombocytopenia<100,000/mm
3
inthe
absenceofoffendingdrugs
10
Immunological
disorder
Anti-dsDNAantibodytonativeDNAinabnormaltitreor
anti-Smantibodyorantiphospholipid(APL)antibodies
(abnormallevelofIgMorIgGcardiolipinantibodiesor
positivelupusanticoagulantor‘false-positive’testresultfor
>6monthsconfirmedbyT.pallidumimmobilizationor
fluorescenttreponemalantibodyabsorptiontest)
11 Positive
ANA
AbnormalANAtitrebyimmunofluorescenceorequivalent
assay(anypointintimeandintheabsenceofdrugs)
SLEmaybediagnosedif4ormoreofthe11criteriaarepresenteitherseriallyorsimultaneously
ReproducedfromHochberg‘UpdatingtheAmericancollegeofrheumatologyrevisedcriteriaforthe
classificationofsystemiclupuserythematosus’(1997)Arthritis&Rheumatology40(9):1725with
permissionfromWiley.
Pathophysiology
ThecauseofSLEisincompletelyunderstoodbutgenetic,immunological,and
environmentalfactorsallplayanimportantrole.
Genetics
• There is a higher concordance in monozygotic twins and the disease is
stronglyassociatedwithpolymorphicvariantsattheHLAlocus.
• In a few cases, SLE is associated with inherited mutations in complement
componentsC1q,C2,andC4,andintheimmunoglobulinreceptorFcγRIIIbor
intheDNAexonucleaseTREX1.
• Genome-wide association studies have identified common polymorphisms
nearseveralothergenesthatpredisposetoSLE,mostofwhichareinvolvedin
regulatingimmunecellfunction.
Serologyandimmunecomplexes
ThecharacteristicfeatureofSLEisautoantibodyproduction.
• Autoantibodies have specificity for a wide range of targets, but many are
directedagainstantigensinthecellorwithinthenucleus.
• SLEmayoccurbecauseofdefectsinapoptosisorintheclearanceofapoptotic
cells,whichcausesinappropriateexposureofintracellularantigensonthecell
surface, leading to polyclonal B- and T-cell activation and autoantibody
production.
• Followingautoantibodyproduction,immunecomplexformationisthoughtto
beanimportantmechanismoftissuedamageinSLE,leadingtovasculitisand
organdamage.
Environmentalfactors
• Environmentalfactorscauseflaresoflupus.
• UVlightandinfectionsincreaseoxidativestressandcausecelldamage.
• StresscanaggravateSLE.
Clinicalfeaturesofsystemiclupuserythematosus
(SLE)
ThereisanextensivenumberofclinicalfeatureswhichcanoccurinSLE.Ofthe
severalnon-specificfeaturesthatarecommontomanychronicdiseases,lethargy
andfatigueareoftenthemostdisabling.
Mucocutaneous
Approximately half of patients diagnosed with SLE will have the classic UV-
sensitive‘butterfly’rashoverthenasalbridgeandmalarbones.Thecutaneous
manifestations of SLE include a combination of acute, subacute, chronic, and
otherrashes,listedinTable10.2.
Musculoskeletalfeatures
• Musculoskeletal immobility-related stiffness and polyarticular, symmetrical
arthralgiaorarthritisoccurin90%ofcases.
• In most cases, symptoms outweigh objective clinical signs, and overt joint
damagefromsynovitisisconfinedto<10%ofpatients.
• Reversiblesubluxationofjointswithouterosivedisease(Jaccoudarthropathy)
canalsooccur.
• Osteonecrosis occurs in 5–10% of patients; most cases are associated with
previous glucocorticoid (GC/‘steroid’) use or secondary to antiphospholipid
syndrome(APS).
• Raynaud’s disease, vasculitis, fat emboli, GCs, and APS can result in bone
ischaemia.
• Myalgiaiscommon,buttruemyositisisseenin<5%.
• Myopathymaybeaconsequenceofsteroidtreatment.
Cardiovasculardisease
• Pericardialdiseaseisthemostcommonmanifestation.
• Most cases of pericardial disease are asymptomatic. A mild pericarditis is
more common than a clinically significant pericardial effusion. On
echocardiography, pericardial thickening is seen more frequently than
pericardialeffusions.
• AlthoughSLEcanleadtolife-threateningpericardialeffusionsorconstrictive
pericarditis,thesemanifestationsarequiterare.
• Myocarditis,presentin8–25%ofpatients,isoftenasymptomatic.
• Clinicalmyocarditis(definedbycombinationsoftachycardia,dysrhythmias,a
prolongedPRintervalonECG,cardiomegaly,orcongestivecardiacfailure)is
considerablylesscommon.Bloodtestingoftenrevealsaraisedtroponinlevel
andN-terminalpro-BNP.DiagnosisisconfirmedbycardiacMRI.
• Valvular heart disease iscommon.Themost frequent abnormality is diffuse
thickening of the mitral and aortic valves followed by vegetations, valvular
regurgitation,andstenosis.Anyvalvevegetationsidentifiedinapatientwhois
febrile should raise the possibility of bacterial endocarditis. Libman-Sacks
endocarditis is characterised by immune-complex dominant vegetations
classically on the mitral or the aortic valves in patients with SLE. The
vegetations are associated with lupus duration, disease activity and
anticardiolipinantibodies,amongothers.
• SLE patients have increased morbidity and mortality from cardiovascular
disease. Patients are 5–10× more likely to have clinically evident coronary
arterydiseasethanthegeneralpopulation.
• Subclinical cardiovasculardiseaseis alsoseen,with increasedprevalenceof
carotidplaqueandfasterprogressionofplaqueformation.Thepathogenesisof
earlycardiovasculardiseaseismultifactorialincludingtraditionalriskfactors
(smoking, obesity, hypertension, diabetes mellitus, hyperlipidaemia, and
positivefamilyhistory),SLE-relatedriskfactors(diseaseactivityanddamage,
GC use, disease duration), and factors related to the inflammatory process
(raised C-reactive protein and pro-inflammatory cytokine levels, elevated
homocysteinelevels).
• Reducing cardiovascular morbidity and mortality requires management of
traditional risk factors, using antihypertensive agents and statins as
appropriate, as well as minimizing GC and NSAID use and achieving early
andprolongedcontrolofdiseaseactivity.
• GCs, althoughindicated forinflammatorycardiac disease,are anaddedrisk
factor for atherosclerosis given its propensity to induce hypertension,
hypercholesterolaemia,andobesity.
Table10.2MucocutaneousmanifestationsofSLE
Frequency Feature
Common(20–50%) Malarrash
Photosensitiverash
Chronicdiscoidlesions
Non-scarringalopecia
Lesscommon(5–20%) Mucosalulcers
Occasional(5%) Periorbitaloedema
Bullouslupus
Severescarringalopecia
Subacutecutaneouslupus
Legulcers
Panniculitis
Cutaneousvasculitis
Pulmonarydisease
• Because of the tendency for disease to be subclinical, CXR and pulmonary
function tests invariably indicate a greater degree of involvement than is
evidentclinically.
• Patients may present quitelatein the disease process following ahistoryof
slow-onsetnon-productivecoughandincreaseddyspnoea.
• Pulmonaryfunctionteststypicallyshowreducedtotallungcapacityandpeak

flowrates.
• Shrinking lung is associated with unexplained dyspnoea, initially exertional,
butthenatrestandonlyingflat,smalllungvolumesonCXR,diaphragmatic
elevation, and restrictive pulmonary function tests in the absence of
parenchymallungdisease.
• Pleuritic pain/pleuritis is present in up to 60% of cases, with a clinically
apparentpleuraleffusioninupto50%.
• Pleural effusions are a feature in one-third of patients, but they are usually
smallandclinicallyinsignificant.
• Interstitialfibrosis,pulmonaryvasculitis,andpneumonitisarefoundinupto
20%ofpatients.
• Pulmonaryhaemorrhageisrarebutpotentiallyacatastrophiccomplicationof
SLE.
• Pulmonary hypertension is found in ~10% of patients with SLE, and is
associatedwithRaynaud’sdisease,vasculitis,andAPLantibodies.
• Patientspresentingwithpleuriticpainand/orpulmonaryhypertensionshould
beinvestigatedforthepresenceofpulmonaryemboliandAPS(see Chapter
11).
Renaldisease
Assessment of blood pressure for hypertension, urine for protein, blood, and
casts,andtheserumcreatinine,urea,andalbuminisanessentialpartofregular
proactivemonitoring.
• Symptoms suggesting renal failure rarely become obvious until substantial
damagehasoccurred.
• If early disease is suspected, a spot urine protein:creatinine ratio(uPCR),is
moreaccuratethanurinedipstickandmoreconvenientthantheconventional
24-hoururinecollectionforproteinandcreatinine.
• Even low levels of proteinuria (<100 mg/mmol) may indicate renal
involvement.
• Theglomerularfiltrationrate(GFR)andrenalfunctionmayalsobeassessed
bynuclearmedicinetechniques.
• A uPCR of >50 mg/mmol should be investigated in a patient with SLE. A
uPCRof>300mg/mmolissuggestiveofnephroticrangeproteinuria.
• Renal biopsy should be considered if there is any evidence of new-onset
proteinuria,increasingproteinuria,haematuria,casts,oracutekidneyinjury.
• Biopsyshouldbedoneincentreswithahighdegreeofexperience.
• In2003,theInternationalSocietyofNephrology(ISN)andRenalPathology
Society (RPS) released a new classification of SLE (‘lupus’) nephritis
designedtostandardizedefinitions.The2003ISN/RPSclassificationoflupus
nephritis replaced the 1982 modified World Health Organization (WHO)
classification:
• ClassI:minimalmesangiallupusnephritis.
• ClassII:mesangialproliferativelupusnephritis.
• ClassIII:focallupusnephritis(<50%ofglomeruli).
• ClassIII(A):activelesions.
• ClassIII(A/C):activeandchroniclesions.
• ClassIII(C):chronicinactivelesions.
• Class IV: diffuse lupus nephritis (50% glomeruli), divided into diffuse
segmental(IV-S)orglobal(IV-G)lupusnephritis.
• ClassIV-(A):activelesions.
• ClassIV-(A/C):activeandchroniclesions.
• ClassIV-(C):chronicinactivelesions.
• ClassV:membranouslupusnephritis.
• Class VI: advanced sclerosing lupus nephritis (90% globally sclerosed
glomeruliwithoutevidenceofactivity).
• Chronicinactivelesions(glomerulosclerosis)areapoorprognosticfeature.
• Arepeatrenalbiopsymaybeconsideredwhenthereisincreasingproteinuria
orprogressiverenalfailureintheabsenceofanalternativecause(i.e.poorly
controlled blood pressure, intercurrent infection, or non-compliance with
medication).
• Active lupus nephritis may be present in otherwise clinically quiescent
disease.
• Patientswithlupusnephritisshouldhavegoodbloodpressurecontrolwitha
targetof≤130/80mmHg.
Haematologicalfeatures
• A microcytic anaemia may be due to anaemia of chronic disease, NSAID-
relatedpepticulcerdisease,dietarydeficiencyofiron, gastrointestinalblood
loss,haemoglobinopathy,ormenorrhagia.
• A normocytic anaemia can be due to myelosuppression from
immunosuppressants, chronic kidney disease due to nephritis, macrophage
activationsyndrome(MAS),orrarelyacutebleedinginalveolarhaemorrhage
orinthecontextofautoimmunethrombocytopenia.
• Macrocytosiscanbecausedbyimmunosuppression(e.g.azathioprine(AZA)
or methotrexate (MTX)) or as a consequence of hypothyroidism, alcohol
excess,vitaminB12,orfolatedeficiencyoroccasionallywithareticulocytosis
afterhaemolysis.

• Autoimmune haemolytic anaemia causes fragments on blood film, an
increased reticulocyte count, low haptoglobin, raised lactate dehydrogenase
(LDH)andbilirubin,andapositiveCoombstest(directantiglobulintest).
• Leucopeniaandlymphopeniaarecommonabnormalities,in50%and80%of
patients,respectively.
• Aleucocytosisisrare,suggestinginfectionorGCtherapy.
• Thereareseveralformsofclinicalthrombocytopenia.Chronic,indolent,and
uncomplicated thrombocytopenia (<100 × 10
9
/L) is present in up to 20% of
patients,particularly amongpatientswith APL antibodies.A rareracute and
life-threatening severe thrombocytopenia is also recognized, as well as
thromboticthrombocytopenicpurpura(TTP).
• Some patients may also present with immune thrombocytopenia, later
followedbyothermanifestationsofSLE.
• ThrombocytopeniaalsooccursinthecontextofMAS.This‘cytokinestorm’
requiresurgenttreatmentwithhigh-doseGCs(see Chapter9and 25).
Neurologicaldisease
Featuresofneurologicaldiseaserangefromcognitiveimpairment(inupto50%
ofpatients)topsychosesandseizures(in5–10%ofpatientsoverthecourseof
theirdisease).
• About 10% of patients develop a sensory (or, less often, sensorimotor)
peripheralneuropathy.
• Cranialnerveinvolvementisnotcommon.
• Upto70%prevalenceofpsychiatricillnesshasbeenquotedintheliterature
(includesanxietyanddepression).
• WhileitisacceptedthatGCscaninducepsychiatricsymptoms,ingeneralitis
felt the drugs given in SLE are not responsible for most of the psychiatric
manifestationsobserved.
• ExaminationofCSFinneuropsychiatricdiseaseshouldbedoneaspartofthe
initialevaluation—itmayrevealaraisedproteinand/orwhitecellcount,and
glucosemaybelow.CSFcanalsobenormal,makingdiagnosischallenging.
• Electroencephalographyisoftennon-specific.
• MRI with contrast is more sensitive than CT in detecting small vessel
vasculopathyassociatedwithSLE.
• Brain biopsy can be used to exclude opportunistic infection or neoplastic
diseasebutisoftennotrequired.Thepathologicalfindingsinlupuscerebritis
areofasmallvesselvasculopathy.
Otherclinicalfeaturesandimportantcomorbidities
OtherclinicalfeaturesarelistedinTable10.3.
VitaminDdeficiency
Thismaybeassociatedwithlossofimmunetolerance.MostpatientswithSLE
haveinsufficientlevelsofvitaminD,andtheeffectofreplacementondisease
activityremainsuncertain.
Osteoporosisandosteopenia
There is a high prevalence of fractures in young patients with SLE, due to a
reductioninbonedensity.
• Factors that contribute to osteopenia and osteoporosis include GCs, renal
osteodystrophy, low vitamin D levels due to sun avoidance, premature
menopause,orcyclophosphamide(CYC)treatment.
Malignancy
There is a 7× increased risk of non-Hodgkin lymphoma with SLE. There is
increasedincidenceofcervicalcancerduetohumanpapillomavirusinSLE.
Table10.3OtherclinicalfeaturesofSLE
Vascular Raynaud’sdisease
Cutaneousvasculitis
Digitalulcersandgangrene
Gastrointestinal
Hepatomegaly(25%)
Abdominalserositis(10–20%)
Splenomegaly(10%)
Mesentericvasculitis(rare)
Pancreatitis(rare)
Immunological Hypergammaglobulinaemia(60%)
Ocular Keratoconjunctivitissicca
Episcleritis
Scleritis
Anterioruveitis
Retinalvasculitis
Retinalvesselocclusion
Investigations
• ImportantinitialinvestigationsareshowninBox10.1.
• There are a variety of circulating autoantibodies to a range of nuclear,
cytoplasmic,andplasmamembraneantigens(Table10.4).
• Most patients (≥98%) will have antinuclear antibodies (ANAs). ~60% have
double-strandedDNA(dsDNA)antibodies (detectedbyimmunofluorescence
oncrithidialucillaeorbyELISAorradioimmunoassay).
• Somepatientshavevaryingcombinationsofantibodiesthatmaychangeover
thecourseofthedisease.
• SLE is associated with deficiencies of the early classical pathway of
complement(e.g.C1q,C1r,C1s,andC2).
• ReducedlevelsofcomplementC3andC4arecommoninSLE,particularlyat
thetimeofadiseaseflare.
• A subset of patients will be ‘serologically active but clinically quiescent’,
meaning they will have low complement levels and raised dsDNA antibody
titre,butnosignsofactivedisease.
• Patientsshouldalwaysbetreatedonthebasisofsymptomsratherthanblood
tests alone, but should be closely monitored for a flare in the context of a
risinganti-dsDNAantibodylevelandfallingC3.
• Some individuals may have high levels of RF and features of RA (thus an
‘overlap’syndrometermed‘rhupus’).
Box10.1Initialinvestigationsinpatientswhohave,oraresuspectedof
having,SLE
• Fullbloodcount
• Ureaandelectrolytes
• ESRandCRP
• Liverfunctiontests
• Urinalysis
• Urinemicroscopy
• Bloodpressure
• Urinaryprotein:creatinineratio
• ANAandextractablenuclearantigens(ENAs)
• ComplementC3andC4
• Anti-dsDNAantibodytitre(ELISA)
• Directantiglobulintest(Coombstest)
• Anticardiolipinantibodies
• Lupusanticoagulant(diluteRussellvipervenomtest)
• Rheumatoidfactor
Table10.4AutoantibodiesinSLE
Autoantibodyspecificity Prevalencein
SLEpatients
Associations
Intracellular: dsDNA 40–90% Renaldisease
Histone 30–80% Drug-inducedSLE
Sm 30% (Afro-
Caribbeans)
10%
(Caucasians)
Renalorneurologicaldisease
U1RNP 20–30% Mixedconnectivetissuedisease
Ro/SS-A 25–40% Sjögren’ssyndrome,cutaneous
SLE,congenitalheartblock
La/SS-B 10–15% AsforRo/SS-A(seeabovein
table)
Cell
membrane
Cardiolipin 20–40% Pregnancyloss,thrombosis
Redcell <10% Haemolyticanaemia
Platelet <10% Immunethrombocytopenia
Extracellular RF 25%
C1q 50%
AntiphospholipidsyndromeandSLE
(See also Chapter 11.) Abnormal procoagulant factors occurring in SLE
patientsincludeapositivelupusanticoagulanttest,anticardiolipinandanti-β
2
glycoprotein-1(GP1)antibodies.
• Antiphospholipid(APL)antibodiesoccurinupto33%ofSLEpatients.
• Although the presence of APL antibodies alone is not sufficient to make a
diagnosis of APS, 50% of SLE patients with positive APL antibodies will

develophypercoagulopathy.
• The manifestations of SLE-associated APS include venous and arterial
thrombosis, thrombocytopenia, cerebral disease, recurrent fetal loss,
pulmonaryhypertension,andlivedoreticularis.
• Some patients with APL antibodies develop renal impairment (e.g.
hypertensionorproteinuria)duetomultiplesmallthrombi.
PregnancyandSLE
• Thereisdebateaboutwhetherpregnancyisassociatedwithanincreasedrisk
of SLE flare. However, pregnancy does not appear to worsen the long-term
outcomeofSLE.
• A USA study
1
has shown that SLE patients suffer more from gestational
diabetes mellitus, hypertension, pulmonary hypertension, renal failure, and
thromboticepisodesinpregnancy.
• Incidenceofintrauterinegrowthretardation,pre-termdelivery,andincidence
ofcaesareansectionsarealsoincreased.
• Activediseaseincreasestheriskofmiscarriageandpretermbirth.
• A major complication is pre-eclampsia—it occurs in 22.5% of women with
SLE.Pre-existingrenaldiseaseisanimportantriskfactor.
• SLEisassociatedwithanincreasedrateoffetaldeathlateinpregnancy.~10%
ofSLEpregnanciesresultinfetalloss.
• APS-associatedcomplicationsarediscussedin Chapter11.
• Anti-Roassociateswithfetalheartblockandneonatallupus.
• Women who wish to conceive should receive appropriate counselling to
discussdiscontinuationofteratogenicdrugs.
• Features of a high-risk pregnancy include increasing age, significant organ
impairment/damage, lupus nephritis, active disease, high-dose GCs, and
presenceofAPL/Ro/Laantibodies.
• Womenathighriskshouldbemanagedinacombinedmedical-obstetricclinic,
and care should continue into the postpartum period, when flares and
thromboemboliceventscanoccur.
Reference
1. ClowseMEB,JamisonM,MyersE,etal.Anationalstudyofthecomplicationsoflupusinpregnancy.
AmJObstetGynecol2008;199:127.e1–127.
Assessmentofdiseaseactivity
Assessmentof changesinSLEactivityis anessentialpartofdecision-making
anddrugtreatment.
• Severalglobalactivityindiceshavebeenproducedthatcorrelatewellandare
reliable.
• Global scoring systems such as the Systemic Lupus Erythematosus Disease
Activity Index (SLEDAI) and the British Isles Lupus Assessment Group
(BILAG)activityindexareofsomevalue,bothinthecontextofclinicaltrials
andlong-termfollow-upofpatients.
• Equally constructive is the concept of an index of damage as distinct from
diseaseactivity.Forexample,apatientwithdyspnoeamayhaveanactivebut
reversiblepneumonitisorirreversiblefibrosis.
• The distinction between disease activity and damage is important since
treatments/managementforeachsituationaredifferent.
• The SLICC damage index has been developed as a method of recording
damageinpatientswithSLE.
2,3
References
2. Gladman DD, Goldsmith CH, Urowitz MB, et al. Sensitivity to change of 3 Systemic Lupus
ErythematosusDiseaseActivityIndices:internationalvalidation.JRheumatol1994;21:1468–71.
3. GladmanDD,GinzlerE,GoldsmithC,etal.ThedevelopmentandinitialvalidationoftheSystemic
Lupus International Collaborating Clinics/American College of Rheumatology damage index for
systemiclupuserythematosus.ArthritisRheum1996;39:363–9.
Drug-inducedSLE
Drug-inducedlupuserythematosus(DILE)shouldbesuspectedinpatientswith
nohistoryofSLE,whodevelopapositiveANAandatleastoneclinicalfeature
ofSLEafteranappropriatedurationofdrugexposure.
• DrugsmostcommonlyassociatedwithDILEare:
• minocycline.
• hydralazine.
• procainamide.
• isoniazid.
• quinidine.
• methyldopa.
• chlorpromazine.
• sulfasalazine(SSZ).
• anti-TNFαdrugs.
• Hydralazine-associated DILE is considered to be dose dependent, and
procainamide,timedependent.
• Upto90%ofpatientstakingprocainamidedevelopapositiveANAand30%
ofthesedevelopDILE.
• Renal, central nervous system, and skin features of SLE are rare in DILE.
OtherfeaturesofSLEsuchasmusculoskeletal,pulmonary,andserosaldisease
arecommon.
• Inthemajorityofcases,theconditionsubsidesonwithdrawingthedrug.
ManagementofSLE
Generalmeasures
• ItisimportanttoavoidoverexposuretoUV/sunlight.
• Sunblock should be SPF30orgreater, and shouldprotectagainst both UVA
andUVB.
• Advice should include supplement intake of vitamin D and in some cases
calcium to maintain adequate vitamin D levels (>50 nmol/L 25-
hydroxyvitaminD(25OHD)).
• Postmenopausalwomenandmen>50yearsoldonlong-termGCsshouldbe
offered a bisphosphonate as prevention against GC-induced osteoporosis
(GIO).
• In premenopausal women and men <50 years old, a DXA scan should be
obtained, and FRAX assessment done, and fracture risk—and need for
bisphosphonates—assessedaccordingly.
• Livevaccines(e.g.yellowfever,polio)arecontraindicatedinpatientstaking
immunosuppressants. Other vaccinations are not contraindicated though the
degreeofresponsetoavaccinemaydifferfromthehealthyindividual.
• Oestrogen-containing contraceptives should beavoidedideally. Progesterone
only contraceptives or other methods of contraception are advised in
preference.
• AlloralcontraceptivesshouldbeavoidedbywomenwithSLEwhohaveAPL
antibodies(orpositivelupusanticoagulant).
• Manypatientstoleratehormonereplacementtherapy(HRT)butuseofHRTin
themenopauseiscontroversial.Thereis,forexample,a20%increaseinSLE
flaresamongwomentakingHRT.
Reductionofcardiovasculardiseaseriskfactors
Thereisanexcessincidenceofcardiovascular disease(CVD) inSLE patients
comparedwithnon-SLEgeneralpopulation.
• ManagementofbasicCVDrisksisessential(smoking,hypertension,diabetes,
obesity).
• Considerstatinsforhypercholesterolaemia.
• AspirinorformalanticoagulationinthepresenceofAPSorifAPLantibodies
arepresent(butseealso Chapter11).
• TightcontrolofSLEdiseasemayreducerisk(seeTable10.5)
Table10.5RecommendationsfordruguseinSLE
Symptom Drug Regimen
Arthralgia/fever NSAIDs(caution
withrenaldisease)
Nospecial
recommendation
Arthralgia/myalgia/lethargy Hydroxychloroquine 200–400mgdaily
Malar/discoidrash Prednisolone,
hydroxychloroquine,
sunscreen,topical
steroid,or
tacrolimus
Arthritis/serositis/myositis Prednisolone,MTX,
AZA
20–40mgof
prednisolonedailyfor2–
4weeks,thenreducing
dosein5mgstepseach
week.Requiresbone
prophylaxisagainst
osteoporosisifdose
treatmentlastsfor>3
months
Autoimmuneanaemiaor
thrombocytopenia(ITP)
Prednisolone,IVIg,
AZA,rituximab
(RTX)
IVmethylprednisolone
followedby60–80mg
prednisolonedailyfor2
weeks,reducingin10
mgstepsperweek,
dependingonresponse.
ITPoftenrequires
immunoglobulin.
Refractorycasesmaybe
treatedwithRTX,AZA,
orsplenectomy
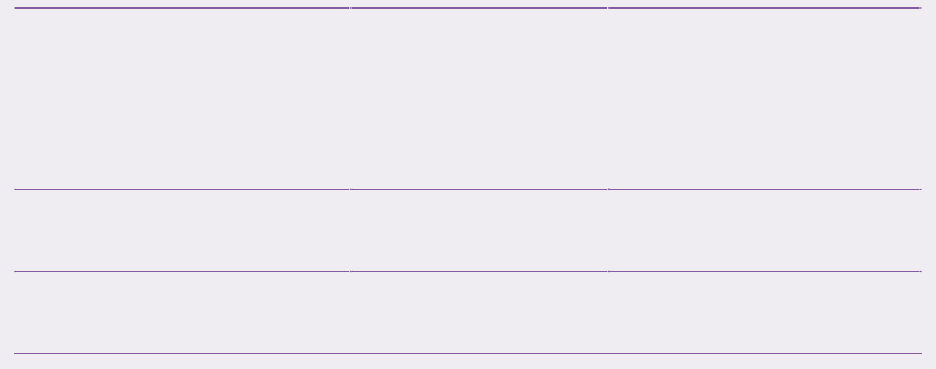
Renal Prednisolone,AZA,
CYC,
mycophenolate
mofetil(MMF),
RTX,tacrolimus
Control BP with ACE
inhibitororangiotensin
receptorblocker:
BP target <130/80
mmHg
Centralnervoussystem Prednisolone,AZA,
MMF,CYC,RTX
Raynaud’sdisease Calciumchannel
blockers,losartan
Immunosuppression
(SeeFig.10.1.)
Glucocorticoids(GCs)
• Prednisolone is frequently used with immunosuppressive drugs to rapidly
reduceSLEdiseaseactivity.
• DosingofGCsvarieswidelydependingontheseverityofdiseaseactivity,and
isgraduallytapered.
• Intravenous‘pulsed’methylprednisolone0.25–1guseddailyfor3consecutive
daysispreferredinseriousorganorlife-threateningdisease.
Antimalarialdrugs
• Hydroxychloroquine (HCQ) 200–400 mg/day is an initial treatment for
patientswithmildSLEsymptoms.
• HCQreducesthefrequencyofflaressoisnormallycontinuedinallpatients,
evenwhentheyrequireadditionalimmunosuppression.
• Patientsshouldbeadvisedabouttheneedforannualeyetesting,andafter5
yearsofusetheyshouldbereferredtoanophthalmologisttoassessforretinal
toxicity.
• Eyeexaminationshouldincludeexaminationofcentralvisualfield,visualand
readingacuity,slitlampofthecornea,andstereoscopicslitlampoftheretina.
• For patients intolerant of HCQ, chloroquine phosphate 250 mg daily is a
usefulalternative.
• MepacrineisanantimalarialeffectiveintreatingSLEskinrashes,butdoesnot
treatothermanifestationsofthedisease.
Azathioprine,mycophenolatemofetil(MMF),andmethotrexate
• Azathioprine (AZA) 2–3 mg/kg/day or mycophenolate mofetil (MMF) 0.5–
3g/dayareusedinmoderatetoseveredisease.
• MMF is often preferred to AZA for lupus nephritis after the ALMS trial
4
demonstrated superiority as a maintenance treatment with significantly less
timetotreatmentfailure(andequivalenceofMMFtoIVCYCasaninduction
agent
5
).
• TrialdatashowMMFisusefulintreatingnon-renalmanifestations.
• MTX isusedwhen arthritisisthe mainclinicalmanifestation ofSLE,or in
overlapsyndromeswithRA.
• A recent systematicreviewfound MTX is alsoassociatedwith a significant
reductioninSLEDAI.
Rituximab
RTXdepletescirculatingBcellsthroughtargetinganti-CD20.Itisamonoclonal
antibody that was first used effectively in 2002 in patients with active SLE
whichhadfailed,oronlyhadpartiallyrespondedto,conventionaltreatments.
• Open-label studies using pulse IV infusions of RTX confirmed the efficacy,
withbenefitsextendingto6months.
• However, a major RCT failed to demonstrate that RTX was beneficial to
patientswithmoderate-to-severeSLE.
• In NHS England healthcare,RTX is allowed forusein SLE, as long asthe
patient has one BILAG A and/or 2B scores or SLEDAI-2K score >6, in
additiontohavingfailedatleasttwoimmunosuppressivedrugs(atleastoneof
thesemustbeMMForCYC).
• B-celldepletioncanbetestedbymonitoringtheCD19count.
• Significantsideeffectsincludeinfusion-relatedreactionsandinfection.Rarely,
progressive multifocal leucoencephalopathy (PML) has been reported in
associationwithRTX,butPMLisalsoseeninSLEpatientswhohavenever
receivedRTX.
• Low IgG levels can occur with successive cycles, with very low levels
occasionally preventing further treatment, or necessitating the use of
maintenanceimmunoglobulin.
Cyclophosphamide(CYC)
• IV‘pulsed’CYCiscommonlyusedformanyoftheseveremanifestationsof
SLE, and has been demonstrated to be particularly effective for renal and
neurologicaldisease.
• The ‘Euro-Lupus’ regimen (low-dose IV CYC) is often used with clinical
outcomessimilartothehigher-doseregimens.
• As an alkylating agent with a broad effect on different cells, CYC depletes
bothBandTcells.
• Major side effects include infection, hair fall, premature menopause, and
bladdertoxicity(nowrareduetoco-treatmentwithmesna).
• ThereissomeevidencethatusingGnRHagonistsgivenpriortoeachdoseof
CYC may prevent premature menopause and preserve fertility following
treatment.
Belimumab
• Belimumabisa fully-humanizedantibodythatneutralizesthe activityofthe
soluble B-lymphocyte stimulator (BLyS)/B-cell activating factor (BAFF).
BLyS/BAFF is also known as TALL-1, and THANK, and is a TNF
superfamilymember(TNFSF13B)bestknownforitsroleinthesurvivaland
maturationofBcells.
• It is the first drugtobelicensed for SLE in approximately50years, and is
currentlyapprovedbyNICEintheUK.
• GivenIV,belimumabhasprincipallydemonstratedapositiveeffectinMSK
andmucocutaneousdisease,aswellasreductionindiseaseactivityandflares.
• ItsefficacyinneurologicalandrenalSLEremainsuncertain.
Plasmaexchange(PE)
• PE is a treatment option for severe manifestations of SLE such as alveolar
haemorrhage,refractorynephritis,orassociatedcatastrophicAPS,thoughthe
limitedtrialdataforitsuseareconflicting.
Stemcelltransplantation
• Haemopoieticstemcelltransplantation(HSCT)isusedtotreathaematological
disease,buthasalsobeenusedinpatientswithsevererefractorySLE.
• HSCTiseffectiveininducingremissionbutiscurativeonlyin<50%.
• Mortalityishighandlong-termeffectsareunknown.
• NewautoimmuneconditionshavebeenreportedafterHSCT.
• Itiscurrentlyusedonlyinthosewithlife-threateningSLE.
• Mesenchymalstemcelltransplantationhasrecentlyemergedasanalternative
treatment.It significantlyreducesSLEactivityandmayinduce remissionin
upto50%ofpatients.
Otheragents
• Tocilizumab hasbeenshown to improve diseaseactivity scores and dsDNA
antibodytitresinopen-labelstudies.
• Epratuzumab,ananti-CD22monoclonalantibody,reducesdiseaseactivityand
seemstodepleteamore‘lupus-specific’setofB-cellsthanRTX.Itiscurrently
undergoingphaseIIItrials.
• Ofatumumabisafullyhumanizedanti-CD20monoclonalantibodythatmay
be usefulinSLE as an alternative toRTX when there hasbeenan infusion
reaction.
• Eculizumab,afullyhumanizedmonoclonalantibodyagainstcomplementC5
haspassedphaseItrialsinSLE.Therearecasereportsofitsbenefit.
• Atacicept is a recombinant fusion protein that acts on B cells inhibiting
BAFF/BlySandaproliferation-inducingligand(APRIL).Inrecentstudies,it
significantlyreducedtheSLEflarerate.PhaseIIbtrialsareongoing.
• Tacrolimus,acalcineurininhibitor,may beusedinlupusnephritis.A recent
RCT suggests it may be non-inferior to MMF when used as an induction
agent.
• Pooled immunoglobulin (IVIg) may be of use in severely ill patients not
respondingtoothertherapies,andespeciallyinsituationswheresepsisisthe
triggerandlife-threatening.
• IVIg may have a role in drug-resistant membranous and
membranoproliferative nephritis, and has been used in severe immune
thrombocytopeniaandhaemolyticanaemiawithgoodeffect.
For additional detail on all drug therapies used for rheumatic disease,
includingimmunosuppressants,seeChapter23.
Fig.10.1Managementoflupusnephritis.DatafromBertsiasGK,TektonidouM,AmouraZ,etal.Joint
EuropeanLeagueAgainstRheumatismandEuropeanRenalAssociation–EuropeanDialysisandTransplant
Association(EULAR/ERA-EDTA)recommendationsforthemanagementofadultandpaediatriclupus
nephritis.AnnRheumDis2012;71:1771–82.
References
4. Dooley MA, Jayne D, Ginzler EM, et al. Mycophenolate versus AZA as a maintenance therapy for
lupusnephritis.NEnglJMed2011;365:1886–95.
5. Appel GB, Contreras G, Dooley MA, et al. Mycophenolate mofetil versus cyclophosphamide for
inductiontreatmentoflupusnephritis.JAmSocNephrol2009;20:1103–12.
Prognosisandsurvival
Many studies of the duration of disease and survival rates are confounded by
inadequateattentionpaidtotheethnicgroup,ageofonset,andsocioeconomic
status of individual patients. The number of patients lost to follow-up is also
high.
• In relevant studies, with the division of patients into those with or without
overtnephritis,thereisa5-yearsurvivalinSLEof90%.
• At 15 years, only 60% of those with nephritis will be alive compared with
85%ofthosepatientswithoutrenaldisease.
• Abi-modal mortalitycurveis consideredtoexist.Patients whodiewithin5
years usually have very active disease, requiring high doses of
immunosuppressivedrugs.
• Patientsdyingafter5yearstendtodoso fromcardiovasculardisease,renal
disease,andpossiblyinfection.
• Thecombinedeffectofthediseaseanditstreatmentistoincreasetheriskof
infectionmarkedly.Thepossibilityofinfectionmustalwaysbeconsideredand
treatedaggressivelyasoutcomesfromsepsiscanbeverypoor.
• SLEincreasestheriskofallmalignanciescomparedtothegeneralpopulation,
particularlynon-Hodgkin’slymphoma.
• CervicaldysplasiaisincreasedinSLEpatientsandregularmonitoringshould
beemphasized.
• The exact contribution of disease activity, duration, and immunosuppressive
drugexposuretotheriskofdevelopingamalignancyrequiresfurtherresearch.
Cliniciansshouldbeawareofthisincreasedriskandbealerttoinvestigating
worryingsymptomspromptly.
JuvenileSLE
Epidemiology
Approximately 20% of patients with SLE present before 18 years of age,
commonlybetween12and14years.
• Increasedincidenceofrenal,haematological,andneuropsychiatricdiseaseis
seeninjuvenileSLE(JSLE).
• TheoverallincidenceofJSLEis0.4–0.6per100,000,butismuchhigherin
Afro-CaribbeanandAsianpopulations.
• F:Mratioislesspronouncedthaninadultsandis3:1prepubertybutincreases
to9:1postpuberty.
Clinicalfeatures
TheclinicalfeaturesofJSLEareextremelyvariable,rangingfromamildillness
with rash, fatigue, and joint involvement to severe life-threatening organ
involvement.
• JSLE tends to be a more severe phenotype than adult disease, accruing a
greaterburdenoforgandamage.
• JSLE has a similar presentation to adult disease and follows a
relapsing/remittingcourse.
• Otherdifferencesfromadultdiseaseinclude:
• Raynaud’sdiseaseislesscommon(10–20%ofpatients).
• AvascularnecrosisofthehipismorecommoninJSLE.
• InJSLE,thediseaseitselfanditstreatmentshavesignificantconsequences
ongrowthandphysicaldevelopment.
• Malarrashoccursin30%ofcasesatdiagnosis.
• Prevalenceofrenaldiseaseishighatdiagnosis,upto60%ofcases.
• Neuropsychiatricdiseaseispresentinupto40%ofcases.
Diagnosisandinvestigations
• Similar to adult SLE, diagnosis is based on both clinical and laboratory
features.
• The ACR revised classification criteria for SLE have alsobeenvalidatedin
JSLE.
• Of the ACR criteria features, the commonest found in JSLE include ANA
positivity, arthritis, haematological disorders, malar rash, renal and
neuropsychiatricinvolvement.
• Assessment of JSLE includes history, examination, and disease activity
assessmentusingtoolsusedinadultSLE,includingBILAGandSLEDAI.
Initialassessmentinvestigations
• ANA(+vein>95%),dsDNA(+vein60%),ENAs—mostcommonlyinclude
anti-RoandLa,anti-Smantibodies.
• Lupusanticoagulant(LA),ACLIgGandIgM,β
2
GP1antibodies.
• Clottingscreen—prolongedinAPLSandMAS.
• Fibrinogen—increasedininflammation,lowinMAS.
• Coombstest/DAT—positiveinautoimmunehaemolyticanaemia.
• ImmunitystatustomeaslesandvaricellaIgG.
Ateachreview
• FBC (Hb low in anaemia of chronic disease or autoimmune anaemia,
leucocytecountincreasedininfectionandserositis,lowplateletsoften).
• IfpancytopeniaonFBCinunwellpatient—considerMAS.
• ESRtypicallyincreasedinflares,lowinMAS.
• CRP—ifincreasedconsiderinfection,serositis,polyarthritis.

• Complement:lowC3andC4levelscancorrelatewithdiseaseactivitybutwith
lowsensitivity.
• Urinalysis for blood and protein to check for renal involvement. If protein
present,quantificationisneededwithuPCR.
ManagementofJSLE
Early and aggressive therapy is key to improve outcome and prevent organ
damage.Thisincludesinductionandmaintenancetherapies.
• Management is similar to adult SLE (see ‘Management of SLE’, pp.
360–365).
• ThecurrenttreatmentparadigmistotreatallchildrenwithHCQtominimize
flares,skindisease,andlimitatherogenicandthromboticrisksassociatedwith
JSLE.
• ProvideadviceregardingsunandUVavoidanceanduseofsunblock(SPF50)
toreduceflaresandphotosensitiverashes.
• Induction therapy typically includes use of IV GCs (e.g. IV
methylprednisolone on 3 consecutive days), followed by a dose reduction
regimenoforalprednisolone(from1–2mg/kg/day)togetherwithasDMARD.
• TheroleofIVCYCininductionislessclearandMMFistypicallypreferred
inJSLEnephritis.
• CYC isstill usedinneurological disease,systemic vasculitis,andrefractory
JSLEnephritis.
• MildtomoderatediseaseatpresentationistreatedwithGCs,MMF,orAZA.
MTX is used when arthritis or cutaneous manifestations (including discoid
lupus)predominate.
• MaintenancetreatmentiswithAZA,MMF,orMTX—similartoadultdisease.
• RTX is effective in JSLE and can be used in disease refractory to first-line
induction therapy or in patients experiencing unwanted adverse effects of
alternativetreatments.
• Anticoagulants(heparinand/orwarfarin)shouldbeconsideredinAPLS,and
low-dose aspirin in cases of positive LA or ACL antibodies. Optimum
anticoagulationregimens,arenotknown,however.
• Hypertension and proteinuria should be aggressively managed with ACE
inhibitorsandcalciumchannelblockerstopreventorgandamage.
• Closesurveillanceofpatientsatintervalsof1–3monthsisnecessarytoensure
therearenounexpectedcomplicationsofJSLEoritstreatment.
Prognosisandsurvival
• TheprognosisofJSLEisoftendeterminedbytheseverity,management,and
outcomeofrenaldisease.
• Risk factors for poor outcome include severe JSLE flares, infection,
neuropsychiatricmanifestations,andsomefeatures,seennotablyinblackand
Hispanic populations, such as persistent anaemia, high creatinine,
hypertensionandpersistentlylowC3.
• JSLE continues to have a 2× higher mortality than adult SLE, although
outcomehasimprovedinrecentyears.
• 5-yearsurvivalofJSLEnowexceeds90%.
Furtherreading
BrunnerHI,HugginsJ,Klein-GitelmanMS.PaediatricSLE–towardsacomprehensivemanagementplan.
NatRevRheumatol2011;7:225–33.
MidgleyA,WatsonL,BeresfordMW. New insightsintothepathogenesisandmanagementoflupusin
children.ArchDisChild2014;99:563–7.
Thorbinson C, Oni L, Smith E, Pharmacological management of childhood-onset systemic lupus
erythematosus.PediatrDrugs2016;18:181–95.
Neonatallupussyndrome
Neonatallupuserythematosus(NLE)isanautoimmuneconditionattributableto
transfer of maternal autoantibodies across the placenta, such as anti-SSA/Ro
and/oranti-SSB/Laantibodies.
• Theconditioncanpresentinuteroorpostnatally.
• ~50% of mothers of babies with NLE are healthy at childbirth with no
recognizedsymptomsofAICTD.
• Only1–2%ofautoantibody-positivemotherswillhaveaninfantwhodevelops
NLE,althoughsubsequentriskincreasesto10–25%forfuturepregnancies.
• NLE is transient in cases other than those with heart block. Skin and
haematologicalmanifestationsresolveasmaternalantibodiesdisappearat3–6
monthspostbirth.
• Severe hepatitiscanbe life-threateningandmortality incardiacNLE is20–
30%.
Clinicalfeatures
There should be suspicion of the presence of NLE where there is a persistent
bradycardia or a combination of non-scarring rash, transaminitis, and
cytopeniainababy0–6monthsold.
Skin
• Rashesoccurin70%ofNLEbabies—typicallypresentatbirth.
• Typical lesions are transient and similar to subacute cutaneous LE with
annularpinkscalyplaques.
• Lesionsmaybecrustedandmayaffectheadandneckaselsewhere.
• Telangiectasiaandpetechiaearealsocommonandmayoccuralone.
Cardiacmanifestations
• Cardiaclesionsoccurin65%ofNLEbabies.
• Athirdofaffectedbabieshavecongenitalcompleteheartblock,whichusually
developsbetween18and20weeksofgestation.
• Other problems include bradycardia, prolonged QT interval, ventricular
tachycardias,valvedisease,cardiomyopathy,andheartfailure.
Othermanifestations
• Haematological effects usually appear during the second week of life and
includethrombocytopenia,haemolyticanaemia,andneutropenia.
• Liver involvement includes transaminitis in half of patients and conjugated
jaundice.
• OthereffectsofNLEcanincludetransientneurologicalandlunginvolvement.
Theformermaybemanifestbyasymptomaticneuroimagingabnormalities.
Investigations
• AllwomenofchildbearingagewithanAICTDshouldbetestedforanti-Ro
andanti-Laantibodiesearlyintheirpregnancy.
• Women testing positive for anti-Ro and/or anti-La antibodies should be
referred to a specialist obstetric unit for weekly fetal US-echocardiography
from16weeks’gestationonwards.
• ThefrequencyofUS-echomaybereducedinabsenceofcompleteheartblock
afterweek26.
• Diagnosis is made on the basis of clinical features and in the presence of
positiveautoantibodiesinneonatalormaternalserum.
ManagementofNLE
• Incompleteheartblock,64%oflivebirthsrequireapacemaker,almostallin
thefirstyearoflife.About60%ofcasesrequireapacemakerduringthefirst
10daysafterbirth.
• GCs, HCQ, and IVIg may reduce the risk of NLE-related cardiac lesions
overall.
• Skin lesions can be managed with UV avoidance, sun block, and topical
steroids(±HCQ).
Prognosis
• Affectedbabiesmaybeatincreasedriskoffutureautoimmuneconditionsbut
developmentofJSLEisrare.
• Otherinflammatoryconditionsininfantsthatmaysubsequentlyoccurinclude
autoinflammatoryconditionssuchasCINCA/NOMID,Kawasakidisease,and
systemic-onsetJIA.
Furtherreading
Brito-ZerónP,IzmirlyPM,Ramos-CasalsM,etal.Theclinicalspectrumofautoimmunecongenitalheart
block.NatRevRheumatol2015;11:301–12.
JohnsonB.Overviewofneonatallupus.JPaediatHealthCare2014;28:331–41
Saxena A, Izmirly PM, Mendez B, et al. Prevention and treatment in utero of autoimmune associate
congenitalheartblock.CardiolRev2014;22:263–7.
Chapter11
Antiphospholipidsyndrome
Antiphospholipidsyndrome
Catastrophicantiphospholipidsyndrome
Antiphospholipidsyndrome
Classification
Antiphospholipid syndrome (APS) is a systemic autoimmune disease
characterizedbyrecurrentarterialorvenousthrombosis.APScanbeprimaryor
secondary to an underlying autoimmune disease—commonly SLE (see
Chapter10).
• Patients may be classified in terms of the antibody present. Anticardiolipin
(ACL) and anti-β
2
glycoprotein 1 (β
2
GP1) are detected by quantitative
enzyme-linkedimmunosorbentassays(ELISA).SeeTable11.1.
• Lupus anticoagulant (LA) is a functional test that quantifies coagulation in
vitro.
Table11.1Classificationcriteriaforantiphospholipidsyndrome
Clinicalcriteria
Vascular
thrombosis
Oneormoreclinicalepisodesofarterial,venous,orsmall
vesselthrombosisinanytissueororgan,confirmedby
objectivecriteria.Histopathologyshouldshowthrombosis
withoutsignificantinflammationinthevesselwall
Pregnancy
morbidity
Oneormoreunexplaineddeathofamorphologicallynormal
fetusatorbeyond10weeks’gestation
or
Oneormoreprematurebirthofamorphologicallynormal
neonateatorbefore34weeks’gestationduetopre-eclampsia,
eclampsia,orplacentalinsufficiency
or
Threeormoreunexplained,consecutive,spontaneous
abortionsbefore10weeks’gestation,excludingmaternal
anatomicalorhormonalabnormalities,andexcludingmaternal
andpaternalchromosomalcauses
Laboratorycriteria
ACL
antibodies
Medium/hightitreofIgGand/orIgMisotypeanticardiolipin
antibodyinbloodon2ormoreoccasionsatleast12weeks
apartusingstandardassays
Anti-β
2
glycoprotein
1antibodies
Anti-β
2
glycoprotein1IgGorIgMinbloodon2ormore
occasionsatleast12weeksapartusingstandardassays
Lupus
anticoagulant
(LA)
LApresentinplasmaon≥2occasions>12weeksapart
AdiagnosisofAPSrequiresthepresenceofonepositiveclinicalcriterionmanifestedbythrombosisor
pregnancyloss,plusonepositivelaboratorycriterion(anyoneofthethreeantibodies)ontwodifferent
occasionsseparatedby12weeks.
AdaptedfromMiyakisSetal.Internationalconsensusstatementonanupdateoftheclassification
criteriafordefiniteantiphospholipidsyndrome(APS).JThrombHaemostasis2006;4:295–306with
permissionfromWiley.
Epidemiology
• Case–controlstudiesestimatetheprevalenceofACLantibodiesinthenormal
populationtobe1–4%.
• Prevalence of ACL antibodies in people >65 years increases to 12–50%
dependingonthestudy.
• Age-dependentreferencerangesdonotexistbuthavebeensuggestedbysome
authors.
• PrevalenceofACLantibodiesandLAinSLEpatientsisestimatedat20–40%
and10–20%,respectively.Thesedifferencesariseduetotreatmenthistoryand
thelackofuniformityofassaymethods.
Pathophysiology
• APL antibodies are directed against phosphorus-fat components of cell
membranescalledphospholipids.
• Certain blood proteins will bind with phospholipids to form complexes to
whichantibodiesmayoccur.
• ACL antibodies are a family of the immunoglobulins IgG, IgM, IgA, or a
combinationoftheseisotopes.TheIgGsubtypeshaveastrongerassociation
withclinicalcomplicationscomparedwithIgM.
• HighlevelsoftheIgMisotypecanbeassociatedwithautoimmunehaemolytic
anaemia.
• TheclinicalconsequencesofIgAACLantibodiesareunclear.
• β
2
GPIisaplasmaglycoproteinco-factortowhichACLbinds.Anti-β
2
GPIis
morespecificthanACLantibodyinpredictingthrombosis,andcanoccurin
~10%ofAPSpatientsastheonlypositivetest.
• LA is a functional measurement of the capacity of heterogeneous APL
antibodies that interferes with phospholipid-dependent stages of blood
coagulationinvitro,inhibitingboththeintrinsicandextrinsicpathways.
• Hence, in vitro, LA exhibits anticoagulant properties, whereas in vivo it
functions as a procoagulant. APL antibodies are therefore paradoxically
associatedwiththrombosis,ratherthanhaemorrhage.
• Apart from clinical suspicion, a clue to the presence of APS is prolonged
clottingtimeinassaysforthe‘internalpathway’clottingcascade.Around50%
of patients with positive LA antibodies have a prolonged activated partial
thromboplastintime(APTT).
Differentialdiagnosis
The most characteristic feature of APS is thrombosis in the presence of
thrombocytopenia.
• The main differential diagnosis to consider is thrombotic thrombocytopenic
purpura(TTP).
• TTPisamicrovasculardisorder,oftenassociatedwithneurologicalfeaturesof
confusion,seizures,andalteredconsciousness.
• Thedifferentialdiagnosisofunexplainedthrombosisincludesgeneticcauses
(e.g.proteinCandS,andantithrombinIIIdeficiencies)anddrugs(including
oestrogen,thalidomide,IVIg).Thereforeafullthrombophiliascreenshouldbe
carriedoutinpatientswithrecurrentvenousthrombosis.
Clinicalfeatures
(SeealsoTable11.2.)
Thrombosis
• Vesselsofallsizes,venousorarterial,maybeaffectedwithoutevidenceofan
inflammatoryinfiltrate,hencetherangeofclinicalfeaturesiswide.
• Unlike in most clotting disorders, arterial thrombosis is a major feature of
APS.
• Thrombosis can be present with or without a history of relevant pathology
associatedwithpregnancy.
• Occlusion of the intracranial arteries is the most common arterial
manifestation,withthemajorityofpatientspresentingwithstroke.
• APL antibodies should be sought in the younger stroke patient, where they
mayaccountforupto20%ofcases.
Catastrophicantiphospholipidsyndrome
• Widespread thrombosis is the feature of life-threatening ‘catastrophic
antiphospholipidsyndrome’(cAPS).
• cAPSmaypresentwithacutecollapse,severethrombocytopenia,multiorgan
failure (notably cerebral and renal), and adult respiratory distress syndrome
(ARDS).
Fetalloss
• Recurrent spontaneous pregnancy loss is a common manifestation of APS,
whichoccursaseitherrecurrentearlymiscarriageorintrauterinefetaldemise.
• ScreeningforAPLantibodiesinthecontextofpreviouspregnancyhistoryis
ofimportanceindeterminingthesignificanceofpositiveAPLantibodies.
• InAPLantibody-positivepregnanciesthatdonotendinmiscarriage,thereisa
high incidence of early onset pre-eclampsia, intrauterine growth restriction,
placentalabruption,andprematuredelivery.
Skinlesions
• Themostfrequentmanifestationsarelivedoreticularisandskinulcers.
• Livedo reticularis is characterized by a mottled purple reticular pattern.
Appearances look similar to a fishnet pattern and in APS is usually
disseminated.Livedoisamarkerofpoorprognosisanddiseaseseverity.
• Skinulcerscanbefoundintheextremities,andextensivecutaneousnecrosis
hasbeenreported.Digitalgangrenehasalsobeendescribed.
• Subungual splinter haemorrhages are seen in ~5%, and may suggest the
occurrenceofotherthromboticevents.
• Other cutaneous lesions also described include purpura, tender nodules,
papules,palmar–plantarerythema,andanetoderma.
Liverandgastrointestinaltract
• LiverabnormalitiesarecommoninAPS,possiblyduetovascularsludgingor
smallvesselthrombosis.
• Budd–ChiarisyndromewasafeatureoftheoriginaldescriptionofAPS.Itis
causedbythrombosisofthehepaticveins,presentingasatriadofabdominal
pain, ascites, and liver enlargement. It may be fulminant, acute, chronic, or
asymptomatic.
• Intestinal ischaemia and perforation due to thrombosis and coeliac artery
stenosishavealsobeendescribed.
Musculoskeletal
• OsteonecrosisisacomplicationofAPS.Itismostcommonlyofthefemoral
headbutcanaffectotherbonessuchasthenavicular.
• Non-specificarthralgiamayoccur.Jointpainsandstiffnessaremorecommon
inAPSassociatedwithSLEandotherautoimmunerheumaticandconnective
tissuediseases.
• Metatarsal fractures and other spontaneous vertebral and rib fractures have
alsobeenreported.
Endocrine
• Adrenalinsufficiencyisthemostcommonendocrinologicalmanifestation,and
canbethepresentingfeatureofAPS.
• Afewcasesofhypopituitarismandovarian/testicularinvolvementhavebeen
reported.
Kidney
• ThekidneyisamajortargetorganinAPS.
• Renalarteryocclusionandrenal arterystenosishavebeendescribed inAPS
patientswithhypertension,andmayresultinrenalinfarction.
• Thrombosis of the renal veins and thrombotic microangiography has been
described.
• DistinguishingbetweenSLEnephritis(immunecomplexmediated)andAPS
nephritis(thromboticdisease)canonlybeestablishedbyrenalbiopsy.
Lungs
• Pulmonaryembolismandinfarctionisthemostcommonlungmanifestationof
APS.
• Pulmonaryhypertensionisfoundinaround2%ofAPSpatients.
• ARDSisrarewithhighmortalityof~50%,usuallyseenincAPS.
Centralnervoussystem
• Cerebral ischaemia associated with APL antibodies is the most common
arterialthromboticmanifestation.Lesscommonlyassociatedissagittalvenous
sinusthrombosis.
• Migraineisacommoncomplaint,andcognitivedeficitscanoccur.
• APSpatientsmayexhibitfeaturesseenwithmultiplesclerosis,andMRIsmay
failtodifferentiate.
• Seizures can occur, thought to be secondary to the interaction of APL
antibodiesandneuronaltissue.
• Transverse myelopathy, though rare, has a strong association with APL
antibodies.
• Other lessfrequentmanifestations include chorea,Guillain–Barré syndrome,
sensorineuralhearingloss,andretinalischaemia.
Cardiacfeatures
• APSmaybeassociatedwithmultiplecardiovascularcomplicationsincluding
acceleratedatherosclerosis,valvularheartdisease,andintracardiacthrombi.
• CardiacmanifestationsofAPSresultinsignificantmorbidityinaround5%of
patients.
• InaEuropeancohort,myocardialinfarctionwasapresentingfeatureofAPS
in3%ofpatients,andwasseenduringfollow-upin5.5%.
• The prevalence of APL antibodies in patients with myocardial infarction is
estimatedat5–15%,butscreeningisnotindicated,exceptinyoungerpatients,
patients with other symptoms and signs of APS, and those with a family
historyofautoimmunedisease.
• Mitral and aortic valve thickening and dysfunction is commonly seen on
echocardiography,butsignificantmorbidityisuncommon.
• IntracardiacthrombusisararemanifestationofAPS.
Laboratoryfeatures
Thrombocytopenia
• Thrombocytopenia is common, seen in ~25%. It is rarely severe enough to
causebleeding.
• ACLantibodieshavebeenfoundinupto30%ofpresumedcasesofimmune
thrombocytopenicpurpura.
• Haemolyticanaemiawithapositivedirectantiglobulintestmayco-existwith
thrombocytopenia(Evanssyndrome).
Generalaspects
• Given an association with all AICTDs, extensive autoantibody screening
shouldbeconsidered:ANA,RF,anti-CCPantibodies.
• C3, C4, Coombs test/DAT, bilirubin, LFTs, FBC, ESR, CRP, and organ
functiontestsshouldbechecked.
Table11.2Clinicalfeaturesofantiphospholipidsyndrome
Feature Subgroup Frequency(%)
Thrombosis Deepveinthrombosis 39
Pulmonaryembolism 14
Arterialthrombosis,legs 4
Arterialthrombosis,arms 3
Stroke 20
Transientischaemicattack 11
Valvethickening/dysfunction 12
Livedoreticularis 24
Pregnancy
manifestations
Earlyloss(<10weeks) 35
Lateloss(≥10weeks) 17
Livebirth 48
Prematurebirth 11
Thrombocytopenia 30
Associated
features
Skinulcers,livedoreticularis,thrombophlebitis
Heartvalvelesionsandmyocardialinfarction
BuddChiari,transverse myelitis,chorea, cognitivedeficits,
pulmonaryhypertension
Lesscommon
features
Splinterhaemorrhages,digitalgangrene,amaurosisfugax,
retinalarteryandveinocclusion,renalartery
stenosis/thrombosis,osteonecrosis,Addison’sdisease,ARDS
ReproducedfromCerveraRetal.Antiphospholipidsyndrome:clinicalandimmunologicmanifestations
andpatternsofdiseaseexpressioninacohortof1000patients.ArthritisRheum2002;46:1019–27with
permissionfromWiley.
TreatmentofAPS
There is no evidence for the role of warfarin in primary prevention (‘primary
prevention’definedbypreventionbeforediagnosedthrombosis).Modifiablerisk
factors for thrombosis and cardiovascular lesions should be addressed (e.g.
smoking, high cholesterol, increased blood pressure, systemic inflammation,
oestrogenuse).
• Hydroxychloroquine has antiplatelet, anti-inflammatory, and anticoagulant
properties,andisrecommendedinSLEpatientswithpositiveAPLantibodies
(Table11.3andTable11.4).IthasalsobeenshowntoreduceAPLantibody
titres.
• HMG CoA reductase inhibitors lower cholesterol levels and have anti-
inflammatory,immunoregulatory,andantithromboticeffects.
• Studieshaveshown thatfluvastatinmaypreventthrombosisinpatientswith
APSbyinhibitingtissuefactorandothermonocytemarkersthatcontributeto
activation of the coagulation pathway, in addition to reducing thrombus
formationbiomarkers.
1
• Rituximab (RTX), an anti-CD20 monoclonal antibody that depletes CD20-
positiveB-cellpopulations,hasbeenusedinAPS-relatedthrombocytopenia,
haemolytic anaemia, venous and arterial thrombosis, ischaemic cardiac and
bowel events, cutaneous lesions, diffuse alveolar haemorrhage, nephropathy,
andcAPS.
• RTXmaybeusedinrefractorycasesofAPSafterfailureofanticoagulation.
• Glucocorticoids (GCs), immunosuppressive drugs, IVIg, or plasmapheresis
have been used in the treatment of APS with thrombosis, but the latter are
morejustifiedincAPS.
• Over the last 4 years, successful treatment with eculizumab (a complement
inhibitor) has been reported in a few cases, showing benefit in preventing
recurrenceofAPSamongtransplantrecipients,andinrefractorycAPS.
Anticoagulationinprimarythromboprophylaxis(APLantibodypositive
withoutpreviousthromboticevent)
• RecommendationsforprimarythromboprophylaxisinAPSsupporttheuseof
low-doseaspirin(75–100mg/day).
Anticoagulationinsecondarythromboprophylaxis(APS—afterfirstvenousor
arterialevent)
• After the first thrombotic event (either arterial or venous), recurrence of
thrombosisiscommon,butcanbepreventedbytreatmentwithwarfarin.
• Patients <50 years of age with cerebrovascular events and positive APL
antibodies,havea5×increasedriskoffurtherischaemicstroke.
• Invenousthrombosiswithtransientorreversibleriskfactorsorlow-riskAPL
antibody profile, 3–6 months of treatment may be adequate, aiming for an
internationalnormalizedratio(INR)of2–3.
• High-intensity anticoagulation (an INR of 3–4) is associated with increased
bleedingriskcomparedtostandardintensitytreatment(INRof2–3)withno
clearreductioninthromboticeventsaccordingtostudies.
• Hence, high-intensity anticoagulation is not recommended, but could be
considered in complicated cases where thrombosis occurs despite
warfarinizingwithanINRof2–3.
• Forpatientswithrefractorythrombosis,fluctuatingINRlevels,orhighriskof
major bleeding, alternative therapeutic options to warfarin should be
considered, such as long-term low-molecular-weight heparin (LMWH),
hydroxychloroquine,orstatins.
• Table 11.4 summarizes APS treatments in patients refractory to
anticoagulationorwhoareunabletotakewarfarin.
• Mild thrombocytopenia need not be treated but severe cases (<50 × 10
9
/L)
should be treated with oral GCs in the first instance. In those failing to
respond,IVIg,danazol,andsplenectomyhavebeenusedwithvaryingsuccess.
AnticoagulationinobstetricAPS
SeeTable11.5.
Noveloralanticoagulants(NOACs)
• Anticoagulation with warfarin is limited by drug and food interactions,
teratogenicity, high variability in response and necessity of frequent blood
monitoring.
• NOACsdirectlyinhibitasingleenzymeofthecoagulationcascade,andseem
tobepromisinginthepreventionofthrombosisinAPS(butnoAPStrials).
• Minimaldrugandfoodinteractionsandfixeddrugdosingwithouttheneedfor
laboratory monitoring contribute to the advantage of NOACs compared to
warfarin. However, the lack of antidotes remains a limitation. Some studies
reportariskofmajorbleedingofupto10%ofcasesperyear.
• NOACsincludedirectthrombininhibitorssuchasdabigatran,anddirectanti-
Xainhibitorssuchasrivaroxaban,apixaban,andedoxaban.TheRivaroxaban
forAntiphospholipidAntibodySyndrome(RAPS)studyiscurrentlyunderway
comparing the effects of warfarin versus rivaroxaban in thrombotic APS
patients.
Table11.3ThetreatmentofAPSandclinicalscenariosinvolvingAPLantibodies/positiveLA:summary

Clinicalsituation Treatment
Non-SLE
patientswith
high-riskAPS
profile
Noprevious
thrombosis
Low-doseaspirin75–150mg/day
(LDA)
SLEpatients
withLA/APL
antibodiesat
hightitres
Noprevious
thrombosis
Hydroxychloroquine200–400
mg/day±LDA
DefiniteAPS
withthrombosis
After1stvenous
event
Lifelongwarfarin(INR2–3)or3–
6monthswarfarin(INR2–3)if
low-riskAPLprofileorother
transient/reversibleriskfactorsat
timeofthrombosis
After1starterial
thrombosis
* Lifelong warfarin (INR 3–4) or
combined warfarin (INR 2–3)
withantiaggregantanticoagulant
therapy
*Assessbleedingrisk
After1stnon-cardio-
emboliccerebral
arterialeventwith
lowAPLprofile±
reversiblefactors
Considerantiplateletagents
CatastrophicAPS IVheparin
IVmethylprednisoloneplus
plasmapheresisorIVIg
DefiniteAPS
withpregnancy
Recurrent
miscarriage(<10
weeks’gestation)or
latecomplications
(>10weeks’
gestation)
Low-dose aspirin plus
unfractionated LMWH at
thrombo-prophylacticdoses
ConsiderLDAalonefor
selectedcaseswithin
1sttrimester
Pregnancyand
previousthrombosis
LDAplusLMWHattherapeutic
doses

Repeatfetalloss
despiteheparinand
aspirin
Unknown
DefiniteAPS
with
thrombocytopenia
Mild
(100–150×10
9
/L)
Observe
Moderate(50–100×
10
9
/L)
Observe
Severe(<50×10
9
/L) GCs(asITP),IVIg,
immunosuppression(e.g.RTX)
Table 11.4 Summary of the recommendations for refractory/difficult APL cases from the 14th
InternationalCongressonAPStreatmenttaskforce
2
Noveloral
anticoagulant
(NOAC)
Considerinafirstorrecurrentvenous
thromboembolismifwarfarinallergy/intoleranceor
pooranticoagulantcontrol
Oldernon-
heparin/warfarin
anticoagulants
Danaparoid,fondaparinux,andargatrobancanbeused
inheparin-inducedthrombocytopenia
Hydroxychloroquine RecommendedinSLEpatientswithAPLantibodies.
Considerinrefractorycases(adjuvanttreatment).No
evidenceforuseinprimaryAPS
Statins Maybeofbenefitinpatientswithrecurrenthistoryof
thromboembolismdespiteadequateanticoagulation
B-cellinhibition RecommendedforrefractorycasesofAPSpossiblyin
patientswithhaematologicalandmicro-angiopathic
manifestations
Complement
inhibition
monoclonalantibody
therapy
Notrecommendedyet.Dataonlyfromanimalstudies.
Mayhavearoleasadjuvantormaintherapyfor
patientsrefractorytoanticoagulation
Table11.5SummaryoftreatmentofobstetricAPLsyndrome
Recurrentearly
miscarriage(<10weeks’
gestation)
Latecomplications
(>10weeks’gestation)
Pregnantpatients
withprevious
thrombosis
Low-doseaspirin0.75–150
mg/day(LDA)plus
unfractionated/LMWH
combinationat
thromboprophylacticdoses
LDAplus
unfractionated/LMWH
combinationat
thromboprophylactic
doses
LDAplus
unfractionated/LMWH
combinationat
therapeuticdoses,then
warfarin(INR2–3)
postpartum
LDAaloneinselectedcases
Catastrophicantiphospholipidsyndrome
Introduction
ThisrarevariantofAPS(<1%cases)affectssmallvesselsandvisceralorgans
andwasfirstdescribedin1992.
• Catastrophic antiphospholipid syndrome (cAPS) is an important and serious
conditionthatcanpresentinpreviouslyasymptomaticpatients.
• Thetriggerisaninfectionin20%ofcases.Otherprecipitatingfactorsinclude
trauma/surgery, malignancy, warfarin withdrawal in a patient with APS,
pregnancy,andoralcontraceptives.However,itisestimatedthat45%ofcAPS
caseshavenoknowntrigger.
• cAPS is associated with other autoimmune conditions such as SLE (see
Chapter10),RA(see Chapter5),andSScl(see Chapter13).
• Mortalityishighat50%,andmostpatientsrequirecareinanintensivecare
unit.
Clinicalfeatures
• Diffuseperipheralandcentralthrombosisoccursleadingto:
• limbarterialandvenousocclusion.
• intra-abdominalorganinfarctionincludingrenalfailure.
• pulmonaryemboliandARDS.
• smallvesselcerebrovasculardisease.
• aorticandmitralvalvedefects,andmyocardialinfarction.
• other thrombotic complications, such as ovarian, testicular, and retinal
vesselocclusion.
• Livedoreticularis, gangrene,andpurpura arevisiblemarkersofthedisorder
ontheskin.
• Bonemarrowinfarctionhasalsobeenreported.
• Followingtheproductionofclassificationcriteria,datafrom300patientsina
cAPS registry have shown the majority are female (72%), almost half had
primaryAPS(46%),andaprecipitatingfactorwasfoundin53%.
2
• Data from the cAPS registry also show the most common sites are renal
(71%),pulmonary(64%),cerebral(62%),andcardiac(51%).
• The presence of systemic immune response syndrome, in which pro-
inflammatorycytokines arereleasedfromaffectedtissues,isalsothought to
contributetomorbidityandmortality.
Laboratoryfeatures
• Moderate-to-severethrombocytopenia.
• Haemolysiswithschistocytes.
• Disseminatedintravascularcoagulation.
• HighlevelsofIgGACLantibodiesorpresenceofaLA.
Differentialdiagnosis
• Theclinicianshouldconsiderthefollowingconditions:
• Thromboticthrombocytopenicpurpura(redcellfragmentsmorenumerous
thanincAPS).
• HELLPsyndrome(haemolysis,elevatedliverenzymesandlowplatelets).
• Haemolytic–uraemicsyndrome.
• Cryoglobulinaemia.
• Vasculitis.
Treatmentandprognosis
• Apartfromtechniquesandtherapiesusedintheintensivesupportofmultiple
organfailure,IVheparin,GCs,plasmaexchange,andIVIg(for4–5daysata
doseof0.4g/kg/day)canbeused.
• Case reports exist in single patients describing the use of epoprostenol,
defibrotide(notlicensedintheUK),andfibrinolytics.
• RTXcanbeusedinrefractorycasesorinthepresenceofmicro-angiopathic
haemolyticanaemia.
• CYChasbeenshowntobebeneficialincAPSwiththepresenceofsecondary
autoimmunediseasesuchasSLE.
• ARCTonbelimumab(aB-cellactivatingfactorinhibitor)inSLEpatientshas
shownadecreaseinACLIgA.
• Mortality remains >50% and 25% of survivors will develop further APS-
relatedevents.
• RecurrenceofcAPSisveryrare.
References
1. Merashli M, NoureldineMH,UthmanI,et al. Antiphophopholipid syndrome: anupdate.Eur J Clin
Invest2015;45:653–62.
2. CereveraR.Catastrophicantiphospholipidsyndrome(cAPS):updatefromthe‘cAPSRegistry’.Lupus
2010;19:412–18.
Chapter12
Sjögren’ssyndrome
Epidemiologyandpathophysiology
Clinicalmanifestationsandclassificationcriteria
Investigations
Treatment
Prognosis
Epidemiologyandpathophysiology
Sjögren’ssyndrome(SS)isachronicautoimmunediseaseofunknownaetiology,
characterizedbylymphocyteinfiltrationofexocrineglandsresultingindryness
ofmucosalsurfacesincludingmouth(xerostomia),eyes(xerophthalmia),nose,
pharynx,larynx,andvagina.
• SSmaybeprimary,associatedwithspecificextraglandular(systemic)disease,
or secondary, in association with a number of other autoimmune diseases
including RA (see Chapter 5), SLE (see Chapter 10), thyroid disease,
coeliacdisease,andprimarybiliarycirrhosis(PBC).
• SSis(rarely)associatedwithprogressiontolymphoidmalignancy.
• SShasaF:Mratioof14–24:1inthelargestreportedseries,andiscommon
between40and60yearsofage.
• Populationprevalenceisestimatedat1%,similartothatofRA.
• EBVandretroviruseshavebeenimplicatedinpathogenesis.
• AntibodiestonuclearproteinsRo/SSAandLa/SSBmaybeformedwhenRo
andLaareexposedonthesurfaceofapoptoticcells.
• Rheumatoid factor (RF) and a positive ANA are also common and patients
maybeerroneouslydiagnosedwithRA.
• HLA-DR3isstronglyassociatedwithSS.
Table 12.1 Classification criteria for primary Sjögren’s syndrome for use in the context of sicca
symptoms
Criteria Comment Score
PositiveSchirmertest <5mm/5min 1
Lowunstimulatedsalivaryflow <0.1mL/min 1
Anti-Roantibodypositive 3
Abnormallipbiopsy ≥1foci/4mm
2
3
Abnormalocularstainingscore ≥5 1
Individualswithsignsand/orsymptomssuggestiveofSSwhohaveatotalscoreof≥4fortheabove-
listeditemsmeetthecriteriaforprimarySS.
DataadaptedfromShiboskiCH,ShiboskiSC,SerorR,etal.2016AmericanCollegeof
Rheumatology/EuropeanLeagueAgainstRheumatismclassificationcriteriaforprimarySjögren’s
syndrome:aconsensusanddata-drivenmethodologyinvolvingthreeinternationalpatientcohorts.Ann
RheumDis2017;76:9–16.
Clinicalmanifestationsandclassificationcriteria
The classification criteria for primary SS are listed in Table 12.1. These
representanupdateofthe1993EuropeanCommunityCriteriaforclassifyingSS
and have been adopted by the scientific community worldwide. They have a
sensitivityandspecificityofaround94%.
• Exclusionsincludeheadandneckirradiation,hepatitisC,AIDS,pre-existing
lymphoma,sarcoidosis,graftvshostdiseaseandanticholinergicdruguse.
• Extraglandular diseaseis seenin one-thirdof patientswithprimarySS.The
main symptoms are fatigue, low-grade fever, myalgia, and arthralgia (Table
12.2).
Glandulardisease
• The initial manifestations can be non-specific and 8–10 years can elapse
beforethediagnosisisestablished.
• Typicalinitialfeaturesof‘sicca’syndromeincludedryeyes(xerophthalmia)in
>50% at presentation, dry mouth (xerostomia) in 40%, and parotid/salivary
gland enlargement in 25%. The prevalence of these manifestations increase
withthedurationofdisease.
• Concurrentcornealandconjunctivaldamage(keratoconjunctivitissicca),and
dentalcariesfrompoortearandsalivaryflowrespectively,canoccur.
• Lackofsecretionsmayalsoaffecttherespiratorytract(nasaldryness,cough,
orhoarsevoice),oesophagusandpharynx(dysphagia)orvagina(dyspareunia
andpruritus).
• Anumberofconditionscancausexerostomiaandother‘dryness’symptoms
andalsoparotid/salivaryglandswelling(seeTable12.3).
Joints
Joint disease needs careful assessment. Associated (‘overlap’) RA can occur
(ACPA positive and typical RA erosions on radiographs) and generalized
inflammatory osteoarthritis (OA) is common in the same age/gender
demography as primary SS. Whether a true SS-associated arthritis or (or)
whether(thereis)thereisasignificantassociationbetweengeneralizedOAand
PSS,isdebatedbutessentiallyisnotknown.
• Non-erosivearthritisismorefrequentinpatientswithRaynaud’sphenomenon,
andthelattercanpre-dateSSbymanyyears.
• AmilderformofSShasbeenlinkedtogeneralizedOAandhasbeentermed
‘SOXsyndrome’(sialadenitis,osteoarthritis,xerostomia).
Table12.2ThefrequencyofextraglandularmanifestationsofprimarySjögren’ssyndrome
Condition Frequency(%)
Arthralgia/arthritis 37
Raynaud’sdisease 16
Cutaneousvasculitis 12
Pulmonarydisease 9
Lymphadenopathy 7
Peripheralneuropathy 7
Renaldisease 6
Autoimmunehepatitis 2
Lymphoproliferativedisease 2
Myositis 1
Table12.3ThedifferentialdiagnosisoftheglandularfeaturesofSjögren’ssyndrome
Feature Differentialdiagnosis
Parotidandothersalivary
glandenlargement
Neoplasia
Infections(e.g.EBV,mumps,HIV,CMV)
Granulomatousdiseases(sarcoid,TB)
Endocrinecauses(diabetes,hypothyroidism,
acromegaly)
Chronicrecurrentidiopathicparotitis
Calculi
Amyloidosis
IgG4-relateddisease
Xerostomiaandxerophthalmia
(‘dryness’)
Age/elderly
Drugs(diuretics,antihypertensive,
parasympathetic,psychotropic)
Dehydration
Psychogenic
Irradiationdamage
SOXsyndrome
Congenital
Graftvshostdisease
HepatitisC
IgG4-relateddisease
Skin
• Itchy annular erythema, alopecia, and hyper/hypopigmentation can occur. A
hypersensitivityvasculitismayalsodevelop.
• Vascular involvement in SS affects small- and medium-sized vessels. The
most common manifestations are cutaneous purpura, urticaria, and skin
ulceration.
• SkinvasculitisinSSisbenignandtreatmentwithglucocorticoids(GCs)not
alwaysneeded.
• Cryoglobulins are present in 10–20% of patients with skin vasculitis in SS

(andmaybeassociatedwithhepatitisCpositivity).
• IncontrasttoSScl(see Chapter13),Raynaud’sdiseaseinSSisnottypically
associatedwithdigitalulcerationandinfarcts.
Pulmonarydisease
Pulmonarydiseaseiscommon.
• Pulmonaryfunctionabnormalitiesareseenin25%ofpatients,althoughthey
arenotusuallyclinicallysignificant.
• Rarely a lymphocytic interstitial pneumonitis (LIP) may occur, causing
pyrexia,cough,anddyspnoea.
• In LIP, lymphocytic infiltration occurs around bronchioles, leading to
cryptogenicorganizingpneumonia.ThisrespondswelltoGCs.
Renaldisease
Overtrenaldiseaseisfoundin10%ofpatientswithprimarySS.
• A renal tubular acidosis (RTA) may occur, causing a normal anion gap
metabolicacidosis,aurinepHof>5.5,andhypokalaemia.
• RTAistypicallytype1distaltubulepredominantinSS.
• Long-termRTAcanresultinnephrocalcinosisornephrolithiasis.
• GlomerulonephritisisrareandseenmainlyinthosewithSS/SLEoverlap.In
many cases, a consistent finding is cryoglobulinaemia and
hypocomplementaemia.
Gastrointestinalandhepatobiliarydisease
• Dysphagiaduetodrynessofthepharynxandoesophagusiscommon.Chronic
atrophicgastritismayoccurduetolymphocyticinfiltrationsimilartothatseen
inthesalivaryglands.
• Subclinicalhyperamylasaemiaisacommonfindinginupto25%ofcasesand
there may be a close link between the ‘autoimmune cholangitis’ of SS and
PBC.Siccasyndromeisfoundin50%ofPBCcases.
• Transaminitis may be due to hepatitis C, which can cause a Sjögren’s-like
diseaseofteninassociationwitha‘mixed’cryoglobulinaemia.
Neuromusculardisease
• Peripheralsensoryneuropathyisthemostcommonneuromuscularfeatureof
SS.Thismaybeasensoryataxicneuropathy(dorsalrootganglionopathy)ora
painfulsmallfibreneuropathy.
• Autonomicneuropathyisrarelyseen.
• Mononeuritismultiplexasaconsequenceofvasculitisiswellrecognizedasis
theisolatedinvolvementofcranialnerves,particularlythetrigeminalandoptic

nerve.
• Involvement of the central nervous system remains a controversy.
Demyelinating,multiplesclerosis-likesyndromesmaybeseen.
• Myalgia is common but myositis is rare. The pattern of myositis is like
polymyositisandistreatedassuchaccordingly(see Chapter14).
Lymphoproliferativedisease
• Patients with SS have an ~16% increased risk of developing a lymphoma,
comparedtoage-,gender-,andrace-matchednormalcontrols.
• The lymphomas are primarily B cell in origin, usually expressing the
monoclonalIgMκ, andof twomajortypes,eitherhighlyundifferentiated,or
well-differentiatedimmunocytomas.
• Theclinicalpictureisdiverse.Theapproachtotherapyshouldbedetermined
bythestageandhistologicalgradeofthedisease.
• Thesalivaryglandsarethemainsiteoflymphomatouschange.Thepresence
of lymphadenopathy, organomegaly, or persistent, painful, and continuously
enlarged salivary glands, in the absence of infection, should raise suspicion
andwarrantsbiopsy.
• Other organsand systems may beaffected includinglungs,kidneys,and GI
tract.
• Risk factors include monoclonal gammopathy, cryoglobulins,
hypocomplementaemia,andganglionopathy.
Cardiovascularsystem
• Anti-Ro andLaantibodies crosstheplacenta andcancause fetal congenital
heartblock.Mothers with theseantibodieshave a 1in 20 riskofhaving an
affectedpregnancy(see Chapter10).
• Fetalheartratemonitoringinspecialistcentresisneeded.
• Oraldexamethasonegiventomothersearlyfollowingdetectionofheartblock
mayreversethecondition.
• Neonatallupuserythematosus(NLE)isalsoseen(see Chapter10).
Fatigue
• FatigueisoftentheworstsymptomformanypatientswithSS.
• Patientsoftenlearntocopewithfatiguewiththemostsuccessfuladoptinga
frame of mind that ‘accepts’ the fatigue; having close relatives and family
realize that fatigue is part of the disease; pacing their activities; and
undertakingsomeregularaerobicexercise.
• Failuretocopewithfatiguemayleadtochronicpain.
OtherpathologyinSS
• Over 50% of patients have antithyroid antibodies and altered thyroid
biochemistrywithoutnecessarilyovertclinicalsymptoms.
• Non-bacterialinterstitialcystitisduetoanintenseinflammationofthemucosa
cancausefrequency,nocturia,andperinealpain.
• Mild normochromic,normocytic anaemiais common.Leucopenia isseen in
15–20%ofpatientswithSS.TheESRisoftenraised(requiringaparaprotein
tobeexcluded),buttheCRPisusuallynormal.
Otherautoimmunediseases
Inarecentretrospectivecasereviewof114patientswithprimarySS,33%had
an additional autoimmune disease, 6% two diseases, and 2% three diseases.
Hypothyroidismwas themost commonconditionseen.Coeliacdiseaseisalso
commonlyassociated.
Investigations
CommonlaboratoryfindingsinprimarySSaredetailedinTable12.4.
Assessmentofsiccasymptoms
• Salivaryflowrates(sialometry)canbemeasuredforwholesalivaorseparate
secretionsfromdifferentsalivaryglands,withorwithoutstimulation.
• Patients with overt SS have decreased unstimulated salivary flow rates.
Measuringsalivaryflowrateissimplebutcanbeconfoundedbyconcomitant
useofdrugswithanticholinergicproperties.
• However, a simple screening test is to have a patient spit all saliva into a
graded measuring sample pot for 10 min. More than 2 mL (>0.2 mL/min)
makesprimarySSunlikely.
• Anatomical changes in the ductal system can be assessed by radiocontrast
sialography.Thiscan,however,bepainfulandthereissomecontroversyasto
itssensitivityandspecificity.
• Scintigraphy,withuptakeof
99
Tc,mayprovideafunctionalevaluationofall
thesalivaryglandsbyobservingtherateanddensityofuptakeandthetimefor
it to appear in the mouth after IV administration. Scanning has a high
sensitivity albeit low specificity, but has a greater sensitivity and specificity
thanunstimulatedsialometry.
• TheSchirmertestisusedfortheevaluationoftearsecretion.Stripsof filter
paper30mminlengthareslippedovertheinferioreyelidbyafoldatoneend
ofthestrip. After 5minthe lengthofpaper that hasbeenmade wetbythe
tearsismeasured;wettingof<5mmisastrongindicationofdiminishedtear
secretion.
• SalivaryglandUSisemergingasausefulnon-invasivetoolinthediagnosisof
SS.Ithasahighspecificityandhasbeenshowntocorrelatewellwithlabial
glandbiopsyfindings.Itisusedinsomecentrestoestablishwhetheralabial
glandbiopsyisrequired.
Biopsy
AlabialglandbiopsyisoftenessentialtotheestablishmentofadiagnosisofSS,
particularlywhenthepatientlacksanti-Rooranti-Laantibodies.
• Becausethereisariskofsensorynervedamage,thebiopsyshouldbedoneby
asurgeonwithexperienceinthetechnique.
• At least 4–6 glands must be biopsied, since the pathologic process is
invariablyfocal.
• Biopsies shouldnot betaken ifthereismucosalinflammationoverlyingthe
biopsysiteorthereisapasthistoryoftherapeuticheadandneckirradiation.
• Thebiopsymustbescoredforthenumberoflymphocyticfoci(i.e.aggregates
of 50 or more lymphocytes) that surround ducts or blood vessels, and are
adjacenttohistologicallynormalacini.
• Ascoreof1ormorefociper4mm
2
iscompatiblewithSS.However,focal
lymphocytic sialadenitis can also be seen in hepatitis C, HIV, graft vs host
disease, and patients with autoimmune disease in the absence of sicca
symptoms.
Table12.4CommonlaboratoryfindingsinprimarySS.
Finding Frequency(%)
General Anaemia 20
Thrombocytopenia 13
Leucopenia 16
RaisedESR 22
Monoclonalgammopathy 22
Hypergammaglobulinaemia 22
Cryoglobulinaemia 9
Autoimmuneserology ANA 74
Rheumatoidfactor 38
Ro/SS-A 40
La/SS-B 26
ANCA 6
Antimitochondrial 5
ReproducedfromGarcia-CarrascoM,etal.PrimarySjögrensyndrome:Clinicalandimmunologic
diseasepatternsinacohortof400patients.Medicine2002;81:270–80withpermissionfromWolters
Kluwer.
Treatment
Table12.5summarizesthegeneralandorgan-directedtreatmentoptionsforSS.
Formoreextensivedetailthereaderisdirectedtothe2017BSRGuidelinefor
themanagementofadultswithprimarySjögren’ssyndrome.
• Dentalinputandclosecollaborationisessential.
• Patientsshouldbeencouragednottosmoke,toavoidsugar-ladenfoods,andto
attenddentalhygienistsessionsregularly.
• Periodically, swabbing palate, tongue, and pharynx for oral Candida
overgrowthisprudent,especiallyifdysgeusiadevelops.
• Thereismeritinpatientstriallingtopicalpreparationsforxerophthalmiaand
xerostomiaastheremaybepersonalpreferencetoonepreparationoranother.
• Manypatientsfavourthecombinationuseofarunnyeyedropforfrequentuse
duringthedayandamoreviscouspreparationatnightorinsituationswhere
frequentdropinsertionisimpracticable.
SyntheticDMARDs(sDMARDs)
• Hydroxychloroquine (HCQ) is the most commonly used sDMARD though
evidenceforitseffectivityinSSisweak.
• Significant improvements have been described in a retrospective study in
termsofthesiccafeatures,parotidglandenlargement,oralinfection,myalgia,
arthralgia,fatigue,andjointswellingfollowing12monthsoftreatmentwith
HCQ.
• In a 2014 study reported in JAMA, HCQ was no better than placebo in
improvingpain,fatigue,ordryness.
• There is no evidence that other sDMARDS or anti-TNFα therapies are
effectiveinprimarySS.
BiologicDMARDs(bDMARDs)
• Rituximab(RTX;anti-CD20/anti-B-cellmonoclonalantibody)hasonlyshown
short-lasting benefit in clinical trials, but may be useful for SS-related
cryoglobulinaemia or neuropathy, as well as for other coexisting immune-
drivenconditions,e.g.coeliacdisease.
• Belimumab (anti-BAFF monoclonal antibody (B-cell activating factor, also
known as BLyS, TALL-1, and THANK), is a TNF superfamily member
(TNFSF13B)bestknownforitsroleinthesurvivalandmaturationofBcells)
hasdemonstratedefficacyinopenlabelphaseIItrials,butsalivaryflowand
theSchirmertestdidnotimprove.
• Tocilizumab(anti-IL-6receptormonoclonalantibody)iscurrentlyundergoing
phaseII/IIItrials.
• Epratuzumab,(humanizedanti-CD22monoclonalantibody)hasdemonstrated
responseinanopenlabelphaseI/IIstudy.
For greater detail on all drug therapies including immunosuppressants,
seeChapter23
Prognosis
TherearefewstudiesontheprognosisofprimarySS.
• Some studies suggest the presence of vasculitis, cryoglobulins, or low
complementmaybeadverseprognosticmarkers.
• OutcomesinsecondarySSarelikelytocorrelatewiththeassociatedcondition.
Table12.5ThetreatmentofSjögren’ssyndrome
Condition Treatment
Xerophthalmia Artificialtears(preferablypreservativefree)
Topicalciclosporindrops
Punctalocclusion(plugs)
Treatmentofmeibomianglanddysfunction(withwarm
compresses).Inpersistentinflammationandblepharitis,
doxycycline50mgoncedailyforatleast3monthsmaybe
considered
Xerostomia Frequentsipsofwater,goodoralhygiene(e.g.chlorhexidine
mouthwash),high-concentrationfluoridetoothpastes)
Sugar-freegumandlozenges(e.g.Salivix
®
orSST
®
pastilles)
Artificialsalivaormouthlubricatingsprays
Siccafeatures Mayimprovewithpilocarpine5mgupto4timesdaily
(side-effectsincludeflushing/sweating),orcevimeline,
whichiscurrentlynotlicensedintheUK(fewerside-
effects)
Vaginal
dryness
Patientsmayrespondtopropionicacidgels.Rigorous
treatmentofinfection.Adviceonlubricants,useof
pessaries,andforintercourse,thepresenceofdyspareunia
Salivarygland Infection—tetracycline(500mg,4timesaday)and
NSAIDs.Persistentpainandswelling—biopsy
Arthralgia Hydroxychloroquine200–400mg/dayifRAandgeneralized
inflammatoryOAhavebeenruledout(though
hydroxychloroquinemaybeeffectiveforjointsymptoms
associatedwiththesediagnoses)
Systemic
vasculitis
Necrotizingvasculitisandglomerulonephritis—prednisone
and/orcyclophosphamide.Leucocytoclasticvasculitis—no
specifictherapybutMMForazathioprinemayhavearole.
Liverdisease Cholestasismayrespondtoursodeoxycholicacid10–15
mg/kg/day
Chronic
erythematosus
candidiasis
Topicalnystatin,miconazole,orketoconazole
Interstitiallung
disease(LIP)
Prednisolone,cyclophosphamide
Chapter13
Systemicsclerosisandrelateddisorders
Introductionanddefinitions
Epidemiologyandpathophysiologyofsystemicsclerosis(SScl)
ClassificationofSScl
ApproachtodiagnosisofSScl
ClinicalfeaturesofSScl
TreatmentandprognosisofSScL
Morphoea,localizedscleroderma,andscleroderma-likefibrosingdisorders
Introductionanddefinitions
Systemicsclerosis(SScl)isageneralizedautoimmuneconnectivetissuedisease.
Scleroderma—thecutaneouslesionwhichisprominentandkeytoadiagnosisof
SScl—is epidermal-dermal tethering associated with microangiopathy and
excessive collagen production and fibrosis. Morphoea essentially describes
localizedsclerodermaanditcanexistinanumberofformsthoughallformsare
notassociatedwithsystemicdisease/internalorganlesions(unlikeinSScl).
• TheclassificationofSSclisshowninTable13.1.
• Raynaud’s disease (RD) describes (usually cold-induced) peripheral digital
vasospasmandishighlyassociatedwithSScl(See Plate25).
• Thespectrumofmorphoeaconditionsincludes:
• Generalized morphoea which is characterized by widespread indurated
plaquesandpigmentarychanges.
• Linear scleroderma is localized scleroderma, which is characterized by a
lineofthickenedskinwhichcanaffectthebonesandmusclesunderneathit.
Itmostoftenoccursinthearms,legs,orforehead.Itisalsomostlikelytobe
onjustone sideofthebody.Linearsclerodermagenerallyfirstappearsin
youngchildren.
• Other: morphoea profunda, morphoea-lichen sclerosis et atrophicus,
frontolinearscleroderma(morphoeaencoupdesabre).(See ‘Morphoea,
localized scleroderma, and scleroderma-like fibrosing disorders’, pp.
422–423)
Table13.1ACR/EULARclassificationcriteriaforSScl
Feature Details Weight/score
Skinthickeningofthefingersof
bothhandsextendingproximalto
MCPJs(sufficientcriterion)
9
Skinthickeningofthefingers(only
countthehigherscore)
Puffyfingers 2
Sclerodactylyofthe
fingers(distaltoMCPJs,
proximaltoPIPJs)
4
Telangiectasia 2
Abnormalnailfoldcapillaries 2
Pulmonaryarterialhypertension
and/orinterstitiallungdisease
2
Raynaud’sdisease 3
SSc-relatedautoantibodies
(anticentromere,anti-topoisomerase
I,anti-RNApolymeraseIII)
3
Addtomaximumweightineachcategorytocalculatethetotalscore
Patientshavingatotalscoreof≥9areclassifiedashavingSScl
ReproducedfromvandenHoogenFetal.2013Classificationcriteriaforsystemicsclerosis:an
Americancollegeofrheumatology/Europeanleagueagainstrheumatismcollaborativeinitiative.Annals
oftheRheumaticDiseases2013;72:1747–1755withpermissionfromtheBMJ.
Epidemiologyandpathophysiologyofsystemic
sclerosis(SScl)
Epidemiology
• TheincidenceandprevalenceofSSclvariesindifferentpopulations.
• SSclappearstobelessprevalentinEurope(80–150casespermillionadults)
comparedwiththeUSA(276casespermillionadults).
• There isaracial difference in theprevalence of SScl—greaterin Europeans
thaninAsians.
• Mild disease often remains undiagnosed. Therefore, the true prevalence of
SSclisprobablyunderestimated.
• Annualincidenceisreportedat1–20casespermillion.Malesandfemalesare
bothaffected.
Pathophysiology
SScl is characterized by three main pathogenetic features: microvasculopathy,
immune activation with inflammation, and increase of extracellular matrix
depositionintheskinandinternalorgansresultinginfibrosis.
General
(For a recent review, see reference 1). Currently, the mechanisms involved in
SSclpathogenesisremainunknownandarelikelytobeverycomplex.Evidence
suggests a close connection between environmental factors and SScl
pathogenesis.
Immunecellactivationandcytokines
• The activation of T cells is considered to play an important role in the
developmentofthevasculopathyandfibrosisinSScl.
• ActivatedoligoclonalCD8Tcellsmaybedetectedinthebloodandlungsof
SScl patients and effector memory CD8 T cells may be involved in the
pathogenesisoforganinvolvementinSScl.
Genetics/epigenetics
• ThegeneticheritabilityforSSclis<0.01;however,thereisahigherincidence
inpatientswithafamilyhistorythaninthegeneralpopulationandapositive
familyhistorysignificantlyincreasestherelativerisk(RR)ofSSclby15–19-
foldinsiblings—indicatingageneticinfluenceonpathogenesis.
• EpigeneticeffectssuchasDNAmethylation,histonemodification,non-coding
RNAeffects(microRNA) areallthought toplayakeyrole inpathogenesis.
Forexample,hypomethylationofthegeneencodingintegrin-α9,amembrane
glycoproteinthatmediatescell–cellandcell–matrixadhesion,canproducean
overexpression of integrins causing myofibroblast differentiation and
increasedTGFβproductionpromotingfibrogenesis.
Environmentalfactors
Several chemical agents have been implicated in the development of
scleroderma, although exposures account for only a small fraction of patients
whodevelopsclerodermaorsimilarconditions.
• Possible chemical triggers of scleroderma include silica, organic chemicals,
aliphatic hydrocarbons (e.g. vinylchloride,naphtha),aromatic hydrocarbons
(e.g. benzene, toluene), drugs (e.g. hydroxytryptophan, carbidopa,
fenfluramine,bleomycin).
Vasculopathy
Vascular injury may be the primary pathophysiological event either by
vasomotor instability or microvascular intimal proliferation and vessel
obliteration. Intravascular pathology in the form of increased platelet activity,
redcellrigidity,andthrombosismayalsobeafactor.
Inflammation
Occurs early in SScl, and may no longer be present at the time of diagnosis.
Causesoedematous(notindurated)skin.
Fibrosis
Consequence of inflammation, widespread and non-organ-specific in SScl.
Excessextracellularmatrixproteinintheskinandinternalorgans.
• TGFβ plays a crucial role particularly through the activation of collagen
productionthatleadstofibrosis.
Reference
1. Barsotti S, Stagnaro C, d'Ascanio A, et al. One year in review 2016: systemic sclerosis. Clin Exp
Rheumatol2016;(34Suppl100):S3–S13.
ClassificationofSScl
Classificationanddiseasepatterns
Patients with SScl have a potentially wide range of features of pathology
affecting different organ systems, and can present in varied ways. The
ACR/EULAR2013classificationcriteriaforSScl(Table13.1)haveasensitivity
of91%andspecificityof92%.
• Clinicalfeaturesarewiderangingandtheirclassification,inassociationwith
typicalserologicalfindings,withindiseasepatternsisshowninTable13.2.
• Table13.2highlightsthetwomainclinicalformsofSScl:limitedcutaneous
(lcSScl)anddiffusecutaneous(dcSScl).Over60%ofcasesareinthe‘limited’
subset,wherevisceralinvolvementislate,andsome10–30yearsafteronsetof
Raynaud’sdisease(RD).
• The definition of ‘limited cutaneous’ subsumes the definition of CREST
(Calcinosis, Raynaud’s disease, (o)Esophageal dysmotility, Sclerodactyly,
Telangiectasia) syndrome,althoughthis acronymis ausefulreminder ofthe
commoncharacteristicsoflcSScl.
• SScl can develop insidiously and in early disease non-SScl scleroderma-
associateddisordersneedtobeconsidered(see Table13.3,p.409).
Table13.2Patternsofclinicalandserologicalfeaturesinthedifferentformsofsystemicsclerosis(SScl)
EarlySScl Raynaud’sphenomenon,nailfoldcapillarychanges
Disease-specificantinuclearantibodies(ANAs):
• Antitopoisomerase-1(Scl-70)
• Anticentromere(ACA)
• Anti-RNApolymeraseIII
• Nucleolar
Diffuse
cutaneous
SScl
Skinchangeswithin1yearofRaynaud’s.Truncalandacral
(face,arms,hands,feet)skininvolvement
Tendonfrictionrubs
Early,significantorgandisease:
• Interstitiallungdisease
• Sclerodermarenalcrisis
• Myocardialdisease
• GIdisease
Nailfoldcapillarydilatationand/or‘dropout’
Scl-70antibodiesinupto60%ofpatients
Limited
cutaneous
SScl
Raynaud’sphenomenonformanyyears
Acralskininvolvement
Lateincidenceofpulmonaryhypertensionwithorwithout
interstitiallungdisease
Skincalcificationandtelangiectasia
Nailfoldcapillarydilatationand/or‘dropout’
ACAantibodiesin70–80%ofpatients
SSclsine Raynaud’s
scleroderma
Noskininvolvement
Presentationwithlungfibrosis,renalcrisis,cardiac,orGI
disease
ANA
ApproachtodiagnosisofSScl
Differentialdiagnosis
Theprinciplesthatunderliediagnosisincludeconsideringfirstwhetherthereisa
form of systemic sclerosis (dcSScl or lcSScl; Table 13.2) or a disease that
mimicsSScl(Table13.3)orascleroderma-associatedfibrosingdisease(seelater
in this chapter, ‘Morphoea, localized scleroderma, and Scleroderma-like
fibrosing disorders’, p. 422. Then, if SScl is likely, establish the extent of
disease.
• The input of a dermatologist may be very helpful if a scleroderma-like
fibrosingdisorderispossible.
• Nephrologyinputshouldbeconsideredearly.
• Askinbiopsyshouldnotbetakenunlessdiscussedwithadermatologistand
pathologistfirstandprobablyshouldonlybedoneoncethepatienthasseen
thedermatologist.
• The extent of involvement of SScl requires a methodological approach to
evaluatingorgansandbodilysystems(seelaterinthistopic).
• Assessmentmaybeaidedbyanappreciationofhowearlyorlatethediseaseis
likelytobe(Table13.4).
Essentialinitialinvestigations
The extent of organ involvement disease should be assessed by baseline
investigationsasfollows:
• Bloodpressuremeasurementandurinalysis.
• Bariumswallow/GIendoscopydependingonsymptoms.
• Chestradiographandlungfunctiontests.
• High-resolutionCTlungscanifauscultationofthelungsrevealscracklesorif
lungfunctionabnormal.
• Laboratorytests:renalandliverfunction,paraprotein,FBC,ESR,CRP,TSH,
randomglucose,ANA/ENAs;RF,complementC3,immunoglobulins.
• ECGandtransthoracicechocardiography (withestimateofpulmonaryartery
pressure).
• Nailfold capillaroscopy and distal upper limb thermography with cold
stimulationchallenge(inspecialistcentres)canhighlightabnormalpatternsof
diseaseandcanpointtosystemicdiseaseincaseswithlimitedearlyfeatures.
Table13.3ThedifferentialdiagnosisofSScl
Metabolicand
inherited
conditions
Carcinoid
syndrome
Scleroderma-likelesionscanbefoundwith
malignantcarcinoid
Acromegaly Associatedwithskinpuffinessand
increaseinsebumandsweat
Phenylketonuria Phenylalanine-restricteddietmayimprove
skinchanges
Amyloidosis Plaquesfromdirectdermalinfiltrationcan
mimicSScl;morecommonarealopecia,
ecchymoses,andnaildystrophy
Immunological
and
inflammatory
conditions
Chronicgraftvs
hostdisease
Skinchangesfavourthetrunk,hips,and
thighs,butcanaffecttheentirebody.
Associatedwithpruritusand
hypopigmentation
Eosinophilic
fasciitis
Associatedwithpainfulindurationofthe
skin,hypereosinophilia,and
hypergammaglobulinaemia.Earlyskin
changesdescribedas‘peaud’orange’
Scleroedema Occurswithdiabetes,monoclonal
gammopathies,andafterinfections(e.g.
post-streptococcalthroatinfection).
UnlikeSScl,canoccurwithoutRaynaud’s
phenomenon
Sclero-
myxoedema
Waxyindurationoftheskinalongthe
forehead,neck,andbehindtheears.Not
associatedwithRaynaud’sphenomenon
Nephrogenic
fibrosing
dermopathy
Rapidindurationoftheskinandother
organsassociatedwithexposureto
gadolinium-basedcontrastusedforMRI
POEMS Polyneuropathy,organomegaly,
endocrinopathy,M-protein,andskin
changes.Hyperpigmentationismost
common,butacrocyanosis/skin
thickeningareseen
Acquired Lipodermato-
sclerosis
Hyperpigmentationandindurationof
lowerlegsassociatedwithchronicvenous
insufficiency/stasis(‘champagnebottle
legs’)
Eosinophilic
myalgia
syndrome
AcutesyndromecausedbyexposuretoL-
tryptophan
Bleomycin
exposure
Usedasamodeltostudyscleroderma
Table13.4Characteristicfindingsinearly-andlate-onsetSScl
Earlyonset(<3yrs
fromdiseaseonset)
Lateonset
(>3yrsfromdiseaseonset)
dcSScl
Constitutional Fatigue,weightloss Minimal
Vascular Raynaud’s(often
mild)
SevereRaynaud’s.
Telangiectasia
Cutaneous Rapidprogression
involvingarms,face,
andtrunk
Stableorsomeregression
Musculoskeletal Arthralgia,myalgia,
stiffness
Flexioncontractures
Gastrointestinal Dysphagiaand‘heart
burn’
Moreseveredysphagia.Midgut
andanorectaldisease
Cardiopulmonary Myocarditis,
pericarditis,lung
fibrosis
Progressionofestablished
disease/pulmonaryhypertension
Renal Maximumriskof Crisisuncommonafter4years
sclerodermarenal
crisis
lcSScl
Constitutional None Worsenedbyvasculopathy,GI
symptoms.
Vascular SevereRaynaud’s.
Telangiectasia
Digitalulcerationorgangrene
Cutaneous Mildsclerosison
face
Stable,calcinosis
Musculoskeletal Occasionaljoint
stiffness
FlexioncontracturesMoresevere
symptomscommon.
Gastrointestinal Dysphagiaand‘heart
burn’
Midgutandanorectaldisease
Cardiopulmonary Rarelyinvolved Slowprogressivelungfibrosis.
PulmonaryhypertensionRight-
sidedheartfailure
Renal Nodirect
involvement
Rarelyinvolved
ClinicalfeaturesofSScl
Raynaud’sdisease(RD)
The overall prevalence of RD is 3–10% worldwide, variation depending on
climate,skincolour,andracialbackground.
• InSScl,RDispresentin95%ofcases.
• History:classictriphasicresponsetocoldstartingwithepisodicpallorofthe
digits (due to ischaemia, see Plate 25), followed by cyanosis (due to
deoxygenation),andthenrednessandsuffusion.Thelaststageofrednessisa
reactive hyperaemia following the return of blood and is the most painful
phase,alsoassociatedwithtingling/numbness.
• Continuous blueness/cyanosis with pain is not characteristic of RD and the
maindifferentialdiagnosisthenischilblainsorvasculitis.
• SymptomsthatmightsuggestsecondaryRDincludeanonsetinmen,patients
>45years,symptomsallyearround,digitalulceration,andasymmetry.
• ANAshouldbe testedand nail-foldcapillaroscopy obtained(see Plate 9).
Pathological changes seen on capillaroscopy include nailfold capillary
dilatation,haemorrhage,anddrop-out.Bothhaveahighpredictivepowerfor
detectingthosepatientslikelytodevelopSScl.
• Conservativemeasuresshouldbedirectedatkeepingthecorebody(i.e.base
ofneckanduppertrunk)temperaturewarm.
• Smokingcessationisessential.
• SevereRDcancausedigitalulceration(DU).Ulcerscanbecomeinfectedand
mayleadtoosteomyelitis.Treatmentisusuallyconservativewithantibiotics.
• Earlyfingerpulptissuethreat/pathology(hardening,cracks,callusandsmall
erythematouslesions)—canbepainful.Skininfectioncanensue—theprocess
worsened by subcutaneous calcification. Regular application of fusidic acid
andhydrocortisonecreamcanhelpsoftentheskinandlessenpain.
• Digitalgangrenemayoccurfollowingprolongedischaemia,leadingtoauto-
amputationofdigits.Surgeryisusuallyavoidedduetopoorwoundhealing.
• RDcanoccurinfingers,toes,earlobes,andevengenitaliainSScl.
Table13.5ThetreatmentofRaynaud’sdisease
Treatment Examples Comments
Simple Handwarmers.Protective
clothing
Universallyhelpful
Eveningprimroseoil Effectiveinclinicaltrials
Fish-oilcapsules
Parenteral
vasodilator
Nifedipineoramlodipine
(calciumchannel
blockers)
Effective,butmaycauseoedema,
hypotension,headache,resultingin
poortolerabilityetc.
Losartan(angiotensinII
receptorblocker)
25–50mgoncedaily
Fluoxetine 20–40mgoncedaily
Sildenafil
(phosphodiesterase
inhibitor)
25–50mgthreetimesdaily
Topicalglyceryltrinitrate Highrateofdiscontinuationdueto
sideeffects
Epoprostenol Forsevereattackswithprolonged
ischaemia,digitalulceration
gangrene,andpriortohandsurgery.
Sideeffectsincludeheadache,
nauseaandhypotension
Bosentan(endothelin
receptorantagonist)
Endothelinreceptorantagonist.In
England—forusewhendigital
ulcersarepresentdespitetreatment
withsildenafilandepoprostenol
Surgery Chemicaloroperative
lumbarordigital
sympathectomywithor
withoutbotulinumtoxin.
Debridement.Amputation
Cautionpriortoanysurgeryas
woundhealingispoor.
Skin—scleroderma
SclerodermaindcSSclandlcSSclusuallyproceedsthroughthreephases:early,
classic,late.Intheearlystagetheremaybenon-pittingoedemaofthehandsand
feet,markedin the morningsandassociated with RD.Theskin then becomes
taut, the epidermis thins, hair growth ceases, and skin creases disappear—the
‘classic’ changes of scleroderma become pronounced. The classic changes
remainstaticformanyyears.
• Thelatephasemayevolveatanytime.Truncalandlimbskinsoftenssuchthat
itcanbedifficulttoknowthatapersoneverhadsclerosis.However,thehand
changes rarely resolve and continue to show the ravages of fibrosis and
contractures.
• During the late phase, digital pitting scars, loss of finger pad tissue, ulcers,
telangiectasia,andcalcinosiscanoccur.
• AllpatientswithSSclwillhavesomeinvolvementofthefaceandthedigits
(although this involvement may be mild). Skin thickening limited to the
fingers,butsparingtheproximalupperextremitiesiscalledsclerodactyly.
• lcSScl is associated with skin involvement limited to the face and distal
extremities(belowtheelbowsandknees).
• dcSScl is associated with taut hypo- or hyperpigmented skin involvement
proximaltotheelbow,knee,orclavicle.
Gastrointestinal
The GI tract is probably the most commonly involved system in SScl (Table
13.6).
• Over 90% of all patients with lcSScl and dcSScl develop oesophageal
hypomotility,with>50%ofpatientswithlcSSclhavingseriousdisease.
• ThecauseofGIdysfunctioninSSclisnotentirelyclear.Possiblecontributing
factorsincludeneuraldysfunction,tissuefibrosis,andmuscleatrophy.Inthe
earlieststagesofneuraldysfunctionmostpatientsareasymptomatic.
• Prokinetic drugs such as metoclopramide may help some patients with
oesophagealhypomotility.
• Manypatientsdeveloprefluxoesophagitis.Simpleadvicesuchasraisingthe
headofthebed,takingfrequentsmallmeals,andavoidinglatenightsnacks,
mayhelp.Patientsoftenrequirehigh-doseproton-pumpinhibitors.
• Small bowel disease with hypomotility can lead to weight loss and
malabsorption; bacterial overgrowth may exacerbate the situation requiring
rotationalcoursesofantibioticsandtheuseofprokineticdrugs.Ultimately,the
smallbowelmayfail,necessitatingtotalparenteralnutrition.
• Atony and hypomotility of the rectum and sigmoid colon may cause
constipation and incontinence, best managed with bulking agents, although
severe cases may need limited surgery or the use of implantable sacral
stimulators.
• AnaemiaduetovascularlesionsintheGImucosaisnowwidelyrecognized.
The classic appearance in the stomach is now called gastric antrum venous
ectasia(watermelonstomach),andtheselesionsmaybetreatedbyargonlaser
therapyifbloodlossissignificant,althoughthisisnotcurative.
Pulmonaryandcardiacdisease
PulmonarydiseaserankssecondtooesophagealdiseaseinSSclinfrequencyof
internalorganeffects(Table13.7).
• PulmonarydiseaseisnowthemajorcauseofdeathinSScl.
• The major lesions are parenchymal lung disease (interstitial lung disease,
organizing pneumonia, and traction bronchiectasis) and pulmonary vascular
disease(isolatedpulmonaryhypertension,pulmonaryhypertensionassociated
withinterstitiallungdisease,andpulmonaryoedema).
• Far less common lung conditions include pleurisy, aspiration pneumonia,
drug-inducedpneumonitis,andspontaneouspneumothorax.
• Interstitiallungdisease oftendevelopsinsidiouslyand establishedfibrosisis
currently untreatable. Early diagnosis is therefore vital. Most centres would
now treat active disease with oral GCs and either oral or IV
cyclophosphamide.
• TheCXRisnotasensitivetestforearlyfibrosis.Lungfunctiontestscanbe
discriminatory.Thesingle-breathdiffusiontest(diffusioncapacityforcarbon
monoxide(DLCO))isabnormalin>70%ofearlycasesandlungvolumesare
oftendecreased.
• LowDLCOwithnormallungvolumesmaysignifypulmonaryhypertension.
• High-resolution lung CT will confirm and stage lung disease and serial
imagingcanbecomparedwithchangesinDLCOandfunctionalindices(e.g.
6-mintimedwalkingtest).
• Fibrosis tends to occur mainly in dcSScl and is associated with anti-
topoisomerase I antibodies; and pulmonary artery hypertension (PAH)
associateswithlcSSclandanti-centromereantibody.
• Heartblockhasbeenreported,butisrare.
• Severe left ventricle impairment from myocarditis is treated with
cyclophosphamideandanimplantablecardioverterdefibrillator(ICD)maybe
indicatedtotreatventriculararrhythmias.
• RecentstudiessuggestaprevalenceofPAHof12–15%inSScl.
• Right heart catheterization is the gold standard method of diagnosis, but
screening using this method is not practical. Annual transthoracic
echocardiographydonebyexperiencedpractitioners,lungfunctiontests,and
clinicalassessmentareessentialtohelpdetectsubclinicaldisease.
• DETECT( http://detect-pah.com/home)is acompositedata calculatorthat
canbeusedtoscreenforpatientswithSSclwhomayhavePAH,toidentify
patientswhoshouldproceedtorightheartcatheter.DETECThasasensitivity
of96%andspecificityof48%andcomprises:
• FVC%predicted/DLCO%predicted.
• current/pasttelangiectasia.
• anticentromereantibody.
• serumNTpro-BNP.
• serumurate.
• right-axisdeviationonECG.
• echofindingsofrightatrialareaandTRvelocity.
Table13.6GastrointestinalpathologyassociatedwithSScl
Site Disorder Investigation Treatment
Mouth Caries,sicca
syndrome
Dental
radiographs
Oralhygiene.Artificial
saliva
Oesophagus Hypomotility Bariumswallow Metoclopramide(dopamine
receptorantagonist)
Strictures Endoscopy Dilatation
Stomach Gastroparesis Endoscopy Metoclopramide
Gastro-
oesophageal
refluxdisease
Bariumswallow
Endoscopy
Proton-pumpinhibitor.
Dopaminereceptor
antagonist
Small
bowel
Hypomotility Bariumfollow-
through
Metoclopramide
Malabsorption Hydrogenbreath
test
Pancreaticsupplements.
Low-doseoctreotide.
Nutritionalsupport
includingparentalfeedingif
refractory,antibiotics
Jejunal
aspiration/biopsy
Ifserologicevidenceof
coeliacdiseaseispresent
Stoolcultures
Large
bowel
Hypomotility Bariumenema Stoolbulkingagents
Anus Incontinence Rectal
manometry
Surgery.Neurostimulator
Table13.7CardiopulmonarypathologyinSScl
Disease Frequency Investigation Treatment
Pulmonarydisease
Pulmonary
fibrosis
Most
commonin
dcSScl(Scl-
70+)
Chest
radiograph,lung
functiontests,
high-resolution
CTscan
LowdoseGCs,
mycophenolateor
cyclophosphamide
(alkylatingagent)
dependingonextentof
disease.Rituximabisused
inrefractorydiseasewhere
thereisextensivelung
involvement
Pleurisy Uncommon Chest
radiograph
NSAIDs.Low-doseoral
prednisolone
Bronchiectasis Rare ChestCTscan Antibiotics.Physiotherapy
Pneumothorax Rare Chest
radiograph
Chesttube,pleurodesis
Pulmonary
artery
hypertension
(PAH)
10–15%
overall
Doppler
echocardiogram.
Catheterstudies
Endothelial 1 receptor
antagonists (bosentan),
epoprostenol, sildenafil,
ambrisentan/tadalfil
combination, macitentan
orriociguat.
Anticoagulation.Long-term
oxygentherapy
Cardiacdisease
Dysrhythmias
and
conduction
defects
Common,
butrarely
symptomatic
ECG.24h
ambulatory
cardiacmonitor
Dependentonrhythm—
drugs,pacemaker,ICDif
indicated
Pericarditis 10–15%
overall
Echocardiogram Asforpleurisy(seeabove
intable)
Myocarditis Rare Prednisolone,
cyclophosphamide.
Diuretics.ICDifindicated,
betablockersmaybeused
butmaycauseworsening
RDand/ordigitalischaemia
Myocardial
fibrosis
30–50%of
dcSScl
Controversial;consider
diuretics,ACEinhibitors
TreatmentofPAHassociatedwithSScl
• Thetreatmentoptionsandoutcomehavedevelopedrapidlyoverthelast5–10
years.
• Historically continuous parenteral epoprostenol was used for moderate and

severe PAH. However, the treatment improves symptoms and pulmonary
arterypressures,butnotmortality.
• Bosentan,anoralendothelinreceptorantagonist,improvesfunction.
• Sildenafilinhibitsphosphodiesterasetype 5(PDE5),enhancingrelaxationof
vascularsmoothmuscleandalsoinhibitsendothelialcellgrowth.
• Arecentdouble-blindplacebo-controlledstudyofpatientswithidiopathicor
autoimmune connective tissue disease-associated PAH found that sildenafil
significantly improves the 6-min walk times and mean pulmonary artery
pressures.
• Combination treatment with ambrisentan (another endothelin receptor
antagonist) and tadalafil (a PDE5 inhibitor) have improved functional status
andhaemodynamicsinarecentopenlabeltrial.
• Macitentan is a dual endothelin receptor antagonist with a better side effect
profileandlongerdurationofaction,withsimilaroutcomesintherapystudies
ofPAH.
• Riociguat is a soluble guanylate cyclase stimulator that has demonstrated
efficacyinPAH.
Renaldisease
Renaldiseasehasbeensupersededbylungdiseaseasthemaincauseofdeathin
SSclduetotheimpactofACEinhibitorsinthetreatmentofSSclhypertensive
renalcrisis(seealso Chapter25).
• Both epithelial and endothelial damage typically occurs before becoming
clinicallydetectable.
• A renal crisis characteristically occurs in dcSScl within the first 5 years of
diseaseonset.Riskfactorsincludeexposuretoprednisoloneatdoses>20mg,
rapidlyprogressiveskindisease,diffusecutaneousdisease,andthepresenceof
antibodies to Scl-70 or RNA polymerase III. In high-risk patients, the
incidencemaybeashighas20%.
• A renal crisis presents acutely with features of hypertension, acute kidney
injury (mild haemoproteinuria and sometimes casts), micro-angiopathic
haemolytic anaemia often with thrombocytopenia and fragments on blood
film, pulmonary oedema, hypertensive retinopathy, encephalopathy, and
convulsions.Mortalitymayreach10%.
• Essentialbasicinvestigationstoestablishanypresenceofrenalinvolvementin
all patients are blood pressure measurement, urea and electrolytes, NT pro-
BNP, troponin, serum urate, creatinine clearance, and urinalysis for
proteinuria.
• In some patients, a renal crisis can begin indolently, initially with just
hypertension.
• Hypertensionshouldbetreatedrapidly,eveninthepresenceofacutekidney
injury,withACEinhibitorsandtitratedtoaimforatargetbloodpressureof
<150/85mmHg.
• Continuousepoprostenolisoftenalsogivenduringarenalcrisis.Dialysismay
becomenecessary.Itisimportanttoknowthatconsiderablerecoveryofrenal
functioncanbemadeafteranacutecrisisandthatdecisionsinvolvingrenal
transplantationshouldbewithheldforupto2years.
• APL antibodies or lupus anticoagulant can contribute to renal SScl disease
(includingacrisis).
Otherorganinvolvement
Table13.8summarizestheinvolvementofotherorgansinSScl.
Table13.8.OtherorganpathologyassociatedwithSScl
Organ Effect Frequency
Thyroid Hypothyroidismiscommon 20–40%
Liver Primarybiliarycirrhosis 3%oflcSScl
*
Nervoussystem Trigeminalneuralgia 5%
Carpaltunnelsyndrome 3%
Sensorimotorneuropathy
Autonomicneuropathy
Genital Cavernosalarteryfibrosiscausingimpotence Upto50%
*Antimitochondrialantibodiesfoundinupto25%ofpatientswithSSclandanticentromereantibodies
foundin10–20%ofpatientswithprimarybiliarycirrhosis.
TreatmentandprognosisofSScL
Generaldiseasetreatments
Currently no treatment can induce complete remission of the disease. Some
therapiescanofferpartialreliefandcontrolofend-organdamage,andmanyof
theseareadvised bythe2016 BSR andBHPR guidelinesforthe treatmentof
SScl.
• The evaluation of treatments is extremely difficult given the complexity,
heterogeneity,andepisodicnatureofSScl,aswellasthepaucityofpatients
forrecruitment.
• Active phase skin disease is treated with methotrexate (MTX) or
mycophenolate mofetil (MMF) 1g twice daily, sometimes with low-dose
prednisolone(≤10mgdaily).
• MMFcanbeusedforlungfibrosiswhenthediseasenotextensive.
• TocilizumabimprovesskinscoresinphaseIItrialsandcouldbeanimportant
newtherapyforSScl.
• Cyclophosphamidemayofferbenefitincardiacorlungdisease.
• Rituximabisusedinrefractorycasesofseverepulmonaryfibrosis,withtrial
evidence demonstrating prevention of progression of lung disease and
improvementinskinscore.
• IVIg is useful in SScl overlap syndromes with myositis and may have a
beneficial effect on severe GI manifestations. There are ongoing trials
assessingIVIgeffectivenessintreatingskindisease.
• Autologous stem cell transplantation has been undertaken in severe SScl
disease,buthasahighmortalityrate.
For additional detail on all drug therapies including
immunosuppressants,seeChapter23
Prognosis
SScl has the highest case-specific mortality of any autoimmune rheumatic or
connectivetissuedisease.However,majoradvancesinthemanagementofSScl
havetakenplaceoverthepastdecade,confirmingtheeffectivenessoftreatment.
• Estimatesof 5-yearmortalityinSSclrangefrom34%to73%.Standardized
mortalityratioshavebeenestimatedat3–4×expected.
• Logistic regression modelling suggests three factors (proteinuria, elevated
ESR,andlowDLCO)are>80%accurateatpredictingmortality>5years.
• Patients with renal crisis had a mortality of 50%, although the use of ACE
inhibitors and renal replacement therapies may have reduced this figure in
recentyears.
• Anti-topoisomerase I and anti-RNA polymerase antibodies have also been
associatedwithahigherincidenceofSScl-relatedmortality.
• AdvancesintheunderstandingofmechanismsleadingtoPAHhasledtonew
therapies that, with time, may show significant impact in slowing disease
progression.
Morphoea,localizedscleroderma,and

scleroderma-likefibrosingdisorders
Morphoea
Morphoeamaybe‘circumscribed’withjustoneortwolesionsor‘generalized’.
Thegeneralizedformmaybeverysymptomaticanddistressingasitprogresses.
• The rash is often itchy, violaceous or erythematous, and progresses to firm
‘hide-bound’skinwithhypo-orhyperpigmentationandsubsequentatrophy.
• The‘circumscribed’lesiontendstoresolvewithin3–5yearsandtreatmentis
oftenunnecessary.
• The‘generalized’morphoeaformcanbedisfiguring,leadingtocontractures,
ulceration,andoccasionallymalignancy.
• GeneralizedmorphoeamayrespondtoPUVA,systemic/topicalorintralesional
GC,topicaltacrolimus,MTX,ciclosporin,orMMF.
• Guttatemorphoeaisavariantwithsmall1cmdiameterpapulesandminimal
sclerosis,resemblinglichensclerosusetatrophicus.Thelesionsusuallyoccur
ontheneck,shoulders,andanteriorchestwall.
Linearscleroderma
This describes a band-like pattern of sclerosis, often in a dermatomal
distribution.Thescleroticareasoftencrossoverjoints,andareassociatedwith
softtissueandboneatrophy,andgrowthdefects.
• Treatment is similar to that previously described for generalized morphoea.
Physiotherapyandappropriateexercisesmayhelptominimizegrowthdefects
inthechildhoodform.
• Encoup-de-sabreislinearsclerosisinvolvingthefaceorscalp,andassociated
with hemi-atrophy of the face on the same side. The lesion assumes a
depressedappearancelikeascarfromasabre.
Eosinophilicfasciitis
(Seealso Chapter18.)
• Characterized by the rapid spread of skin changes (‘peau d’orange’) over
extremities.Skinbecomesindurated.
• UnlikeSScl,theepidermis isspared(i.e.superficialwrinkling isintact)and
nail-foldcapillaroscopyisnormal.
• TheconditionmayresolvespontaneouslyorrespondtoGCs.
• The condition may be a paraneoplastic phenomenon in some patients
(haematologicalmalignancy).
• MTXandMMFcanbeusedaswellasGCs(noRCTs).
Nephrogenicsystemicfibrosis
Nephrogenic systemic fibrosis (NSF)—also known as nephrogenic fibrosing
dermopathy—isasystemicdisease,whichcanleadtofibrosisinskeletalmuscle,
myocardium,lungs,kidneys,andtestes.
• NSFischaracterizedbythepresenceofskininduration,nodularplaques,and
flexioncontracturesintheabsenceofRD.
• Lesionsdevelopoverdaystoweeks,andinitiallyfavourthelowerextremities.
• The majority of patients will have end-stage renal disease and a history of
exposuretogadolinium-basedcontrast.
• Histologically,NSFlesionsarecharacterizedbycollagenbundlessurrounded
byfibroblast-likeepithelioidorstellatecells,andmucindeposition,whichcan
extendintothefasciaandmuscles.
• Responsetoimmunosuppressiveagentsisdisappointing.
• Early institution of physical therapy to prevent contractures and muscle
wastingisimportant.Painmanagementmaybeespeciallychallenging.
Scleromyxoedema
Ischaracterizedbywaxyindurationoftheskinalongtheforehead(glabella),the
neck,andbehindtheears.
• Scleromyxoedemamayalsoaffectthemiddleoftheback,whichisgenerally
sparedinSScl.
• Scleromyxoedema can be associated with oesophageal dysmotility and
myopathy.
• Case reports have shown an association with severe neurological sequelae,
includingencephalopathy,seizures,coma,andpsychosis.
• ScleromyxoedemamayrespondtoIVIg.
Scleroedema
Scleroedema is a fibromucinous connective tissue disease, a scleroderma-like
disorder associated with doughy induration of the skin along the back, neck,
face,andchest.
• UnlikeinSScl,theextremitiesaretypicallyspared.
• It is seen in association with poorly controlled diabetes, monoclonal
gammopathyorfollowinginfections(e.g.Streptococcus).
• Prognosisdependsontheunderlyingaetiology.Scleroedemathatoccursafter
infection may resolve spontaneously. Scleroedema associated with diabetes
mayimprovewithbetterglucosecontrol.
• For some patients, ultraviolet light therapy (such as UVA-1, PUVA, and
photopheresis)maybebeneficial.

Chapter14
Idiopathicinflammatorymyopathiesincluding
polymyositisanddermatomyositis
Idiopathicinflammatorymyositis
Polymyositisanddermatomyositis
Investigations
Treatment
Inclusion-bodymyositis
Other(adult)inflammatorymyopathies
Juvenileidiopathicinflammatorymyopathy
Idiopathicinflammatorymyositis
Generalconsiderationsandclassification
The idiopathic inflammatory myopathies (IIMs) are a heterogeneous group of
conditions characterized by varied patterns of inflammation within striated
muscleandevidenceofautoimmune-mediatedmusclebreakdown.TheIIMsare
believedtobeautoimmuneinnature.Theyhavedistinctpathologicalfeatures,
buttheaetiopathogenesisofeachsubtyperemainslargelyunknown.
• The strongest genetic association of IIMs is with HLA class II alleles. In
Caucasians, HLA-DRB1*0301 and -DQA1*0501 are strongly associated,
compared to HLA-B7 in Asian populations. HLA-DQA1*01 seems to be a
protectivefactor.
• Proximal,symmetrical,andpainlessweaknessof musclesis thehallmark of
IIMs.
• Polymyositis(PM)anddermatomyositis(DM)arethemostcommonformsof
IIM,thelatterdistinguishedbythepresenceofacharacteristicrash.
• Overlapwithotherautoimmunediseasesoccurin15–20%ofcases.
• TheclassificationofIIMconditionsisshowninBox14.1.
• Secondarycausesofmyopathiesarediscussedlaterinthischapter.
• IIMhasanestimatedincidenceof2–8permillion.
• PM and DM are more common in women than in men (2:1), and peak
incidenceisat50–60yearsold.
• The F:M ratio is lower in myositis associated with malignancy, and higher
duringchildbearingyears(5:1).
• There is a latitude gradient of prevalence of PM and DM. DM is more
common closer to the equator correlating directly with UV-light irradiation,
andPMismorecommoninnortherncountries.
• ThecriteriaforPMandDMdiagnosisareshowninBox14.2.
• TheprincipalfeaturesofPMandDMarelistedinTable14.1.
Box14.1ModifiedBohanandPeter’sclassificationofPMandDM
1. Primaryidiopathicpolymyositis.
2. Primaryidiopathicdermatomyositis.
3. 1or2aboveinlist,withmalignancy.
4. Juvenilepoly(dermato)myositis.
5. Overlapsyndromeswithotherautoimmunerheumaticdiseases.
6. Inclusion-bodymyositis.
7. Raremyositis:granulomatous,eosinophilic,focal,orbital.
8. Drug-induced.
InformationfromBohanA,PeterJ.Polymyositisanddematomyositis.NEnglJMed1975;292:344–7.
Polymyositisanddermatomyositis
ApplicationofthecriteriafordiagnosisofPMorDMassumesinfective,toxic,
metabolic,dystrophy,andendocrinemyopathiesareexcluded.
Pathogenesis
• DM has been conceptualized traditionally as a complement-mediated
microangiopathy,butthisparadigmhaslimitations.
• PMarisesfromacytotoxicT-cellimmune-mediatedinflammationonmuscle.
• TypeIinterferonsignatureisupregulatedinDMandPM,butnotinIBM.
• Aberrant expression of major histocompatibility complex (MHC) proteins
contributes to muscle damage bothdirectlyandindirectlyin all subtypes of
IIM.
• A characteristic pattern of autoantibody production often occurs, in PM and
DMandinoverlapmyositisdisorders.
• ThereisevidenceofinflammasomecomplexactivityintheIIMs.
• Toll-like receptors (TLRs) are upregulated in IIMs and may link innate and
adaptiveimmuneprocesses.
• Autophagy is upregulated in IIM tissue, particularly within regenerating
myofibres,andthismayoccurviaactivationofTLR3andTLR4.
• Immatureandregeneratingmusclecellsmayperpetuatetheimmune-mediated
attackinIIMs.
Clinicalfeatures
Myositis
• Muscleweaknessisthemainclinicalfeatureinbothconditionsandisalmost
universal,tending todevelopinsidiouslyovermonths,butoccasionallywith
greatspeed.
• Weaknessisusuallysymmetricalanddiffuse,involvingtheproximalmuscles
oftheneck,shoulders,trunk,hips,andthighs.Thelowerlimbmusclestendto
beclinicallysymptomaticfirst.
• Weaknessofthedistalmusclesisrare,butcanoccurlateinthedisease.The
faceandocularmusclesmayalsobeinvolved.
• Myalgiaoccursinabout50%ofcases:itcanbemildandsometimesdifficult
todistinguishfrompolymyalgiarheumatica.
• Theremaybemuscleatrophyinchronicdisease,moresoinPMthanDM,and
contracturesmayoccurindiseaseoflongduration.
• Oftenthedistinctionbetweenautoimmunerheumaticdiseaseoverlappingwith
PM or DM and an autoimmune rheumatic disease with myositis as a
manifestationcanbeverydifficult.
Box14.2DiagnosticcriteriaforthediagnosisofPMandDM
1. Symmetrical proximal muscle weakness developing over weeks or
months.
2. Elevated serum muscle enzymes: creatine kinase (CK), aldolase, AST,
ALT,andlactatedehydrogenase.
3. Typicalelectromyographicfindings:myopathicpotentials(lowamplitude,
short duration, polyphasic) fibrillation, positive sharp waves, increased
insertionalactivity,complexrepetitivedischarges.
4. Typicalmusclebiopsyfindings.
5. DermatologicalfeaturesofDM:
• Gottron’spapules,involvingfingers,elbows,knees,andmedialmalleoli.
• Heliotropesignaroundtheeyes.
• Erythematousand/orpoikilodermatousrash.
DefinitePM:allofcriteria1–4;probablePM:3ofcriteria1–4;possiblePM:2ofcriteria1–4.
DefiniteDM:3ofcriteria1–4pluscriterion5;probableDM:2ofcriteria1–4pluscriterion5;possible:
1ofcriteria1–4pluscriterion5.
AfterBohanA,PeterJ.Polymyositisanddematomyositis.NEnglJMed1975;292:344–7.
Table14.1KeyfeaturesofPMandDM
PM DM
Typicalpatient Anyage
Unusual in
children
Female and
African
American
predominance
Anyage
Juvenileformcommon
Female and African American
predominance
Musclegroups
affected
Proximal >
distal
Symmetrical
Proximal>distal
Symmetrical
CKelevation 40–50×normal
notunusual
40–50×normalnotunusual
Weaknesssometimesoutofproportionto
CKlevel
Myositis
specific
antibodies
(MSAs)
Anti-aminoacyl
t-RNA
synthetase
antibodies;anti-
SRP
Anti-aminoacylt-RNAsynthetase
antibodies;anti-Mi-2
Histopathology Endomysial
inflammation
CD8+ cells
invading non-
necrotic
musclefibres
Perivascular
Interfascicularinflammation
CD4+ predominance; complement
membrane attack complex present;
capillary obliteration; endothelial
damage;perifascicularatrophy
Malignancy
association
Yes Yes
Otherfeatures Interstitial lung Skin
disease(ILD)
Cardiac
Malignancy
ILD
Cardiac
Intramuscularcalcification
Vasculitis
Malignancy
Skinandcutaneousdisease
• TherashofDMcommonlyprecedestheweaknessbyweekstomonths.The
rash may parallel the weakness or remain independent, persisting after the
myositisresolves.
• Erythematousorviolaceouspapulesorplaques(Gottron’spapules)ormacular
patches (Gottron’s sign) may occur over the metacarpophalangeal and
proximal(occasionallydistal)interphalangealjoints.Therashispresentinup
to80%ofcases.
• Occasionally, these lesions may be found on the extensor surfaces of the
knees,wrists,elbows,ormedialmalleoli.
• PeriungualabnormalitiesaffectingthecapillarynailbedsinDMandPMwith
erythemaandinsomecasestendernesscanbeseen.
• Vascular changes observed at the nailbed resemble those found in other
connective tissue diseases, e.g. systemic sclerosis and SLE. Abnormal
capillaryloopsmayalternatewithareasofvasculardilatationanddropout.
• Amaculareruptionmayinvolvetheupperchest,neck,shoulders,extremities,
face, and scalp. This may develop into poikiloderma, hyper- or
hypopigmentationwithatrophyandtelangiectasia.Typicalfeaturesincludethe
‘V’signatthebaseoftheneckanteriorly,andthe‘shawl’signatthebackof
theneckandacrosstheshoulders.
• The heliotrope rash, found in 30–60% of cases, is a purple/lilac coloured
suffusion around the eyes, often associated with periorbital oedema. It is
characteristic,butnotpathognomonic.
• SomepatientshavetypicalcutaneousDM,butdonotdevelopovertmyositis.
The term ‘amyopathic DM’ is applied. The same risk of malignancy and
systemiccomplicationsremains.
• Calcinosis,cutaneousvasculitis,andulcerationaremorecommoninjuvenile
DM.
Joints
Coexistent polyarthralgia is quite common. It is usually non-erosive and
glucocorticoid(GC)responsive.
Cardiacdisease
• ClinicalfeaturesofheartinvolvementarerareinPMandDM.
• Asymptomaticsubclinicalmanifestationsareoftenreported,andcanoccurin
up to 70% of patients. These are mainly conduction abnormalities and
arrhythmiasdetectedbyECG.
• Cardiovasculardiseaseisamajorriskfactorfordeathinmyositis,andshould
therefore not be overlooked. The most frequently overt manifestations are
congestiveheartfailure,conductionabnormalities,andcoronaryheartdisease.
• The underlying pathophysiological mechanisms responsible include
myocarditis,coronaryarterydisease,andinvolvementofthesmallvesselsof
themyocardium.
Pulmonary
• Shortness of breath may be a consequence of diaphragmatic and intercostal
muscle weakness (as well as other causes that will be discussed later), and
shouldbeassessed.
• ILDiscommon,withavariableresponsetoimmunosuppression.
Gastrointestinal
• Dysphagiaoccursinupto30%.
• Cricopharyngealmyotomyisoccasionallyneeded.
Malignancy
• Studiessuggestamodestincreaseinmalignancieswithin1–2yearsofonsetin
DM.Inthemajorityofcases,cancerandmyositishaveanindependentcourse.
• Thelargestpopulationstudiessuggestmalignancyoccursin15%ofcasesof
DM(relativeriskinmen2.4/inwomen3.4)and9%ofcasesofPM(relative
riskinmen1.8/inwomen1.7).
• CancerdeathsinstudiessuggestanincreaseinDM,butnotPM,supportinga
trueassociationwithDM,ratherthanastudybiasduetointensivesearching.
• The highest cancer riskappearsto be in men >45yearswith DM who lack
myositisautoantibodiesoroverlapautoimmuneconnectivetissuedisease.
• Tumours thatarefrequent in thegeneralpopulation are frequentin PM and
DM. However, there appears to be an increase in ovarian, breast, lung,
stomach,colon,andbladdercancersoutofproportiontothatofothertumours.
• The extent of investigations required is debated. Thorough physical
assessment should always include rectal, pelvic, and breast examination.
Specificinvestigationsshouldincludeachestradiograph,urinalysis,prostate-
specific antigen in men, faecal occult blood testing, mammography, and
cervicalsmear,andprobablypelvicultrasoundandCA125levelsinwomen.
• Furtherbowelinvestigationsareopentodebateanddeterminedbyindividual
patient symptoms. An elevated ALT may be from muscle and need not
indicateliverpathology.
• Malignancycanmanifestasparaneoplasticmyopathy(see Chapter4).
Clinicalassessments
FeaturessuggestinganalternativediagnosistoIIM
It is important to consider whether there are features of non-inflammatory
myopathy,which maypointtowardsstorage diseases,geneticmyopathies, and
neuropathy.
• Drug history: anumberof medications areassociatedwith causing myositis
(Table14.2).
• Weakness/cramp worsened by exercise or dietary changes (e.g. fasting,
carbohydrate intake), which might suggest a metabolic or mitochondrial
myopathy.
• Muscle atrophy without pain or hypertrophy can suggest a muscular
dystrophy.
• Fasciculationormyotoniaandotherneurologicalsignsmaysuggestaprimary
neurologicaldisease(e.g.motorneurondisease).
• Facial and shoulder girdle muscle involvement may suggest
facioscapulohumeraldystrophy.
• Afamilyhistoryofmyopathymaysuggestageneticmyopathy.
Table14.2Drug-inducedmyopathy
Clinicalpicture Examples
Myopathywithweakness,myalgia,
andhighCK
Penicillamine
Anti-TNFα
Cimetidine
L-tryptophan
Zidovudine
Colchicine
Hydroxychloroquine
Lipid-loweringagents
Ciclosporin
Vincristine
Carbimazole,propylthiouracil
Alcohol
NSAIDs—rarewithaspirin
Rhabdomyolysispicture Alcohol
Recreationaldrugs—cocaine,heroin,
ecstasy
Amphetamines
Barbiturates
Statins(particularlyhighdose)
Anaesthetics—malignant
hyperthermia
Psychotropics—neuroleptic-
malignantsyndrome
Assessmentofdiseaseimpact
SeeTable14.3.
Changes in muscle strength and function may change slowly with indolent
disease, or with treatment, and measures of long-term muscle and general
function are important to take regularly. General (Likert scale) patient and
physicianglobaldiseaseactivityscoresareeasytotakeandreproduce:
• HAQorSF36maybeused.
• Musclemetrologyfromanexperiencedphysiotherapist.
• Themanualmuscletest(MMT)isthemostoftenusedtestofmusclestrength,
althoughonlypartlyvalidatedinadultmyositis.
• Quantitativemuscleatrophy(e.g.byMRI).
• Several scalesof compositemeasures areavailable e.g.MYOACT(activity)
andMYODAM(damage)andMDI(diseaseindex).Thelatterhaverecently
beendemonstrated tohavegoodconstructand validityin adultand juvenile
IIM.
1,2
Table14.3SystemicmanifestationsofPMandDM
Organ/system Features
General Fatigue,malaise,weightloss
Fevers—in40%overall
Raynaud’sphenomenon
Pulmonary Duetomuscleweakness:aspirationpneumonia,respiratory
failure(lowTLC,VC,highRV)
Duetolocaldisease:interstitialfibrosis,pulmonary
vasculitis,pulmonaryhypertension(common)
Duetotreatment:hypersensitivitypneumonitis,
opportunisticinfection
Gastrointestinal Oesophagealdysphagia—in30%
Striatedmuscledysfunction
Cricopharyngealdysfunction
Lowoesophagealdysfunction
Stomachandboweldysmotility*
Cardiovascular Cardiomyopathy—<5%
Pericardialeffusion—upto20%
Hypertensionandischaemicheartdisease(common)
3
Heartblock—rare
Dysrhythmias—uncommon
Skeletal Arthropathy
Deformity,milderosivearthritis
Renal Veryrare.Possiblemyoglobinuria
*Intestinalvasculitis,perforation,andpneumatosiscystoidesintestinalis,featuresofjuvenileDM,are
veryrareintheadult.
RV,residualvolume;TLC,totallungcapacity;VC,vitalcapacity.
References
1.IsenbergDA,AllenE,FarewellV,etal.Internationalconsensusoutcomemeasuresfor patients with
idiopathic inflammatory myopathies. Development and initial validation of myositis activity and
damageindicesinpatientswithadultonsetdisease.Rheumatology2004;43:49–54.
2. Rider LG, Lachenbruch PA, Monroe JB, et al. Damage extent and predictors in adult and juvenile
dermatomyositis and polymyositis as determined with the myositis damage index. Arthritis Rheum
2009;60:3425–35.
3.BohanA,PeterJB.Polymyositisanddermatomyositis.NEnglJMed1975;292:344–7.
Investigations
TheinvestigationofpotentialmalignancyinDM/PMhasbeendiscussedearlier
inthischapter.
Muscleenzymes
• Serum levels of enzymes released from damaged muscle are helpful in the
diagnosisandmonitoringofthedisease.Creatinekinase(CK)ismostwidely
used.Aldolasemaybemoresensitiveinsomecases.
• ThereareanumberofothercausesforraisedCKlevels(Table14.4).Muscle
bulkinfluencestheCKlevels.Butitisalsopossible,despiteactivemyositis,
for the CK levels not be elevated (i.e. relative chronic muscle atrophy). In
these cases, imaging such as MRI may be a useful indicator of
damage/severity.
• The isoenzyme CK-MB can be elevated in myositis and less often in
myocarditis. It is released from regenerating skeletal muscle fibres and also
damagedmyocardiocytes.
• As a guide, patients with myositis without cardiac involvement may have a
CK-MB/totalCKratioof>3%.
• A more specific marker for myocardial damage in myositis is the cardiac
isoformtroponinI.
• Other cardiac troponin isoforms such as troponin C (cTnC) and troponin T
(cTnT)arelessspecificandexpressedinskeletalmuscle,hencelevelscanbe
raisedinvariousmuscledisorders.
Musclebiopsy
• All patients should have a muscle biopsy to confirm the diagnosis and to
excludeconditionsthatmayresembleIIM.
• There is an argument for not obtaining a biopsy in patients with proximal
weakness,elevatedenzymes,typicalEMGchanges,arashofDM,confirmed
myositis-specificautoantibodies,oranoverlapautoimmunerheumaticdisease
andmyositis-associatedautoantibodies.
• Formostpatientshowever,itisimportanttorememberthatthemimicsofIIM
aremorecommonthantheIIMsthemselves.Therefore,patientswithaclinical
diagnosisofPM/DMwhodonotrespondtoimmunosuppressivetreatmentas
expectedshouldhaveabiopsyinordertoconfirmanalternativediagnosis.
• Anegativebiopsydoesnotexcludemyositis,asinflammatorychangescanbe
focal.Therefore thesiteofbiopsyshould bepreferablyfromasymptomatic
musclewhichisnotatrophic.
• Musclebiopsysamplesarestainedwithhaematoxylinandeosin.
• Further immunohistochemical staining for MHC class antigens provide
additionalusefulinformation.ThepresenceofMHCclassIandIIantigensin
musclefibresisafeatureofinflamedmusclestissue.
• There are important histological descriptions that associate with specific
diagnoses:
• Fibrehypertrophysuggestsdystrophy.
• InclusionbodiesareseeninIBM.
• Widespread necrosis with profuse regeneration is the typical finding in
rhabdomyolysis.
• Inflammation affects striated muscle and occasionally heart muscle, but not
smoothmuscle.
• Histologically, the cellular infiltrates of skeletal muscle involve mainly T
lymphocytesandmacrophages.Dendriticcells,Bcells,andplasmacellscan
alsobefound.
• IIMsoftenhavespecificbiopsyfeatures:
• In DM, there are mainly perivascular and perimysial inflammatory
infiltrateswithapredominanceofCD4+Tcells.
• InPM,thereis endomysial(intramuscular)inflammatoryinfiltrateswitha
predominance of CD8+ T cells causing destruction of muscle fibres and
fattyreplacement.
• In IBM, the early disease may be indistinguishable from the histological
appearances of PM. Characteristic findings are intracellular amyloid
deposits or basophilic intracellular vacuoles (‘inclusion bodies’) seen on
electronmicroscopy.
• Optimal processing, evaluation, and minimizing of artefacts require
coordination with the pathologist prior to biopsy, to ensure appropriate
handlingofsamplesandmaximumdiagnosticinformation.
Table14.4Causesofaraisedcreatinekinase
Cause Examples
Strenuous
prolonged
exercise
Delayed-onsetmuscularstrain(DOMS)
Muscletrauma
Diseasesaffecting
muscle
Myositis
Metabolic(e.g.glycogenstorage)
Musculardystrophy
Myocardialinfarction
Rhabdomyolysis
Drugs(alsosee
Table14.7)
Necrotizingmyopathy(statins,ciclosporin,labetalol,
alcohol,anti-TNFα)
Inductionofmyositis(L-tryptophan,L-dopa,phenytoin,
lamotrigine,hydroxycarbamide)
Amphiphillic((hydroxy)chloroquine,amiodarone)
Microtubule(colchicine,vincristine)
InhibitionofCKexcretion(morphine,diazepam)
Metabolic
abnormalities
Hypothyroidism
Hypokalaemiaincludingdruginduced(diuretics,
laxatives,GCs)
Ketoacidosis
Renalfailure
Normalvariants Ethnicgroup(oftenhighernormalvaluesintheblack
population)
Increasedmusclemass
Technicalartefact
Autoantibodies
• Autoantibodies are present in ~60–70% of patients with PM and DM. The
mainantibodyisantinuclearantibody(ANA).
• Myositis-specificautoantibodies(MSAs)areassociatedwithspecificclinical
phenotypes,andfavourPM/DMoverothermyopathies.
• ThemostprevalentMSAisanantibodydirectedagainsthistidyltransferRNA
synthetase(anti-Jo1)presentinaround11–33%ofpatientswithPM/DM.
• Histidyl isoneof anumberof amino-acyl transferRNA synthetaserelevant
targetsforantibodyformation.
• Thevariousclinicalassociationsofthemainmyositis-associated(MAAs)and
MSAsareshowninTable14.5.
• Anti-signal recognition peptide (SRP) antibodies occur in ~5% of myositis
patientsandheraldanacute-onsetaggressivedisease.Itisnotlinkedtoskin
manifestations.Musclebiopsytendstoshowanecrotizingmyopathywithfew
inflammatorycells.Treatmentresponseisoftenpoor.
• Anti-Mi2andanti-CADM-140arefoundin10–20%ofDMcases.
• Statin-induced myopathy is associated with anti-HMG-CoA antibodies. The
presenceoftheseantibodiesisnotlinkedtostatinexposureineverycase.
• Anti-p155/p140(anti-MJ)isfoundinupto25%ofcasesofjuvenileDMand
isassociatedwithcalcinosis.
• DetaileddescriptionofallMAAs/MSAsisbeyondthistext.Newantibodies
aredescribedregularly.Itisworthnotingup-to-datepublicationsinthisarea
given that antibody immunological tests through specialist labs can help in
difficultcaseswheremalignancyanddrugsarebeingconsideredascauses.
Electromyography
• Electromyography (EMG) cannot establish the diagnosis of PM/DM with
certainty, but can demonstrate a myopathic process, and help to exclude
neuropathiesanddistinguishsomemyopathies.
• 90%ofpatientswillhaveabnormalEMGstudies.
• Early findings include low-amplitude, short-duration, polyphasic potentials,
with early recruitment and full interference patterns (i.e. more fibres are
required to achieve a given force). The latter features are in contrast to
neuropathieswherethereisdecreasedrecruitmentandinterference.
• Withtime,re-innervationofdenervatedfibresleadstohigh-amplitude,long-
duration,polyphasicpotentials.
• Otherfeaturesincludespontaneousactivityinupto75%ofcases,fibrillations,
and repetitive discharges akin to myotonia, but of constant amplitude and
startingandstoppingabruptly.
Imaging
• Magnetic resonanceimaging (MRI),ultrasound (US),computed tomography
(CT),
99m
Tc,andthalliumhavebeenusedtoassessthedistributionofdisease.
• MRI with T2-weighted images and fat suppression or short tau inversion
recovery(STIR)isbestatidentifyingareasofmuscleinflammation,atrophy,
orfattyinfiltration.
• OnMRI,activemyositisresultsintheappearanceoffluidsignalchangesin
muscle—interpretedasoedema.
• When evaluating a patient for weakness, MRI may be particularly useful in
distinguishing weakness due to active inflammation from weakness due to
previous damage or GC myopathy (which would not be expected to show
muscleoedema).
• Becausemuscleinvolvementmaybepatchy,MRIcanhelpidentifyanoptimal
siteformusclebiopsy.
Table14.5AntibodiesinPMandDM
Antibodyclass Antibody
subclass
Percentageof
PM/DM
Myositissubgroup
Myositis-
specific:
Intotal30–40
Anticytoplasmic Anti-Jo-1 20 Antisynthetase
syndrome
Anti-PL-7/PL-
12/OJ/EJ
<5each
Anti-SRP 4 PM
Antinuclear Anti-Mi-2 8 DM
Anti-56kDa 90 All
Myositis-
associated
Anti-PM-Scl 8 PM/DM–SScloverlap
Anti-U1-RNP 12 PM/DMoverlap
syndromes
Anti-U2/U5-
RNP
<2 PM
Anti-Roand
Anti-La
5–10 SLE.PrimarySjögren’s
syndrome

Othertests
• The ESR is elevated in 50% of cases, but correlates poorly with disease
activityandresponsetotherapy.
• CRPisnotspecific;highlevelssuggestaconcurrentinfection.
• ComplementlevelsinPM/DMareusuallynormal.
• Proteinuriamaybetheresultofmyoglobinuria.
• Serialspirometryforrespiratorymuscleweaknessmayberequired.
Treatment
Treatment should be started promptly pending completion of investigations,
particularly in acute-onset weakness, dysphagia, respiratory insufficiency, and
systemiccomplications.
• GCs have never been tested adequately in randomized, placebo-controlled
trials,butarethecornerstoneoftherapy.
• 90% of patients will have at least a partial response to GC therapy. Most
requiretreatmentwithaGC-sparingagenttomaintaindiseaseremissionand
tominimizeGCexposure.
• Anexerciseprogrammehelpsimprovefatigueandmusclestrength.Exercise
shouldbeusedwithcautionduringperiodsofdiseaseactivity,butthereisno
evidence that it causes prolonged worsening in muscle enzyme levels or
inflammation.
Glucocorticoids.
Seealso p.660
• Most clinicians use a starting oral prednisolone dose of 1–2 mg/kg until a
declineinCKand/orasubstantialimprovementinmusclestrengthisseen.
• LowerGCdosesof0.5mg/kgmaybesufficient.Severecases(orextraskeletal
involvement) may be treated with IV methylprednisolone 0.5–1 g/day for 3
daysbeforestartingoralprednisolone.
• As high doses are required for several months, early vitamin D/calcium
supplementation and bisphosphonates should be considered to prevent GC-
inducedosteoporosis.
• IIM patients are at increased risk of developing osteoporosis also due to
decreasedskeletalloadingandimmobility.
• Acase–controlstudyhasalsoshownthatmostIIMpatientshavelowserum
levels of vitamin D. This may confer a risk factor for developing adult
myositis,suggestingvitaminDreplacementtherapyisimportant.
• Mostpatientswillrespondtotreatment,butthiscanbeslowandpartial.CK

levelsoftenimprovequickerthananyapparentimprovementinstrength.
• Failure to respond despite 4–6 months of treatment may be due to one of
severalreasons(especiallyiftheANAisnegative):
• Incorrectdiagnosis.
• Hereditarymyopathyor‘inclusion-body’myositis.
• GCmyopathy.
• Permanentlossofstrength.
• NoresponsetoGCtherapy.
Syntheticdisease-modifyingantirheumaticdrugs(sDMARDs).Seealso
pp.662–80
• Methotrexate (MTX) and azathioprine (AZA) have demonstrable efficacy;
AZAmaybeabetteroptionforpatientswithILDorhepatitis,butmaytake
longertoshoweffectiveness.
• StudieshaveshownasynergisticeffectofMTXandAZAwhereasingledrug
hasfailed.
• Cyclophosphamide (CYC) has had variable results and is used in resistant
casesorinthosecaseswherethereissevereextraskeletalinvolvementsuchas
vasculitisorlungdisease.
• Tacrolimus has been used in refractory patients with PM/DM-ILD, with
improvementinmusclestrength,lungfunction,andcutaneousmanifestations.
• Ciclosporin can be a useful therapy in patients where MTX and AZA have
beenineffective/nottolerated.IthasbeenusedincombinationwithMTXor
IVIg.
• Mycophenolate mofetil (MMF) and chlorambucil have been reported to
achievediseaseremissioninsomerefractorycases.
Intravenousimmunoglobulin(IVIg)
• EfficacyofIVIghasbeendemonstratedinsmalldouble-blindcontrolledtrials
andoneopen-labeltrial,showingsignificantclinicalimprovementinmuscle
strength and reduction in CK levels after 3 months of treatment, compared
withplacebo.
• CasereportshavesuggestedefficacyofIVIginthetreatmentofPM/DM-ILD,
andithasbeenusedinonecaseofrefractoryamyopathicDM-ILDwithgood
response.
• High-doseregimensintheformof2g/kg/dayfor2–5dayseverymonthfor3–
6 months have been advocated, and can be used concomitantly with other
sDMARDs.
• Durationofefficacyofeachtreatmentmaybelimitedtoafewmonths,butthe
dose or interval can be changed based on severity of disease and treatment
responsiveness.
• A major advantage of IVIg is that it is safe to use in the context of active
infections,butitshighcostmayrestrictlong-termuse.Thereisalsoariskof
tachyphylaxis.
Biologictherapies
There is growing interest in evaluating biologics that target various pathways
involvedinthepathogenesisofIIM.
• Anti-TNFαtherapyhasbeenstudiedinsmallpatientseries.Therehavebeen
suggestionsthatitmaytriggerIIM,thereforetheyshouldbeusedwithcaution.
• Inopenlabelstudies,rituximab(RTX)hasbeenusedinrefractoryDMwith
reportsofclinicalimprovement.
• The first placebo-phase trial to assess the efficacy of RTX in refractory
myositis did not show a significant difference between the two treatment
groups.
• ArecentsummaryofpublishedevidenceforRTX effectinIIMsuggesteda
majority of patients derived benefit though markers of response varied and
therewasofcoursemarkedheterogeneityofdiseaseattheoutset.
• Further research is required to assess the role of biologic therapies though
manytreatmentshavebeentried(Table14.6).
Treatmentofextramusculardisease
• The rash of DM may respond to the treatment of the myositis. If lesions
persist,hydroxychloroquine(HCQ)at200–400 mg/dayortopicaltacrolimus
maybeofbenefit.Photosensitivitycanrespondtosunscreens.TopicalGCsare
oftennotsuccessful.
• ThetreatmentofamyopathicDMiscontroversial.SunscreensandHCQcan
beusedandinsome severecases, GCsor immunosuppressivesarejustified
for the cutaneous disease. If treatment is withheld due to an absence of
myositis,thepatientshouldbefollowedclosely,especiallyinthefirst2years
afteronsettoavoiddelayintreatmentshouldmyositisdevelop.
• Calcinosis, principallya problemin juveniledisease, isdifficultto treatand
does not respond to immunosuppression. Surgical resection may help for
accessibledeposits.
• Activeexerciseisdiscouragedduringacuteinflammation,butpassiverangeof
motion exercises should be commenced early to avoid joint contractures.
Isometric exercise should be introduced once inflammation subsides. This
mustbesupervisedbyaphysiotherapisttoavoidmuscleoveruse.
• ILDismanagedasinotherautoimmuneconnectivetissuediseaseswithoral
GCsandoralorIVCYC.
• Distal oesophageal dysmotility does not generally respond to
immunosuppression,butmeasuressimilartotreatmentofrefluxmayhelp.
PrognosisinPMandDM
• PM and DM are diseases with a high mortality and morbidity. One
retrospective study estimated a mortality rate of 22%, mostly due to
malignancyandpulmonarydisease.
• Inmostcases,thecourseofdiseaseiseithermonophasic,remitting/relapsing,
orchronicprogressive.
• Asmallnumber(5–10%)makeafullrecoveryfollowingtreatment.
• The use of prolonged immunosuppressive therapy increases the risk of
infection,especiallywithunusualorganisms.
• Casereportshavedescribedatypicalmycobacterialinfectionsinpatientswith
long-standingPM/DM.
• A worse prognosis is associated with increasing age, bulbar muscle, and
cardiopulmonaryinvolvement.
Table14.6BiologictherapiesusedfortreatingIIMs
Biologic Levelofevidence
Adalimumab Onecasereportofa‘hard-to-treat’patientshowingincreased
musclestrengthandreducedCKlevels
Etanercept Pilottrialof16treatmentnaïvepatientsshowednobenefits,
apartfromGCsparing
4
Infliximab Retrospectivestudies.UtilityinIIMslimitedduetopotential
forinducingPMandDM.Notrecommended
Rituximab Double-blindtrialshowingprimaryoutcomesnotmet,but
mostachievedtheIMACS*definitionofimprovement
Tocilizumab 3casereportsofrefractoryIIM.Someclinicalbenefitsseen
withreducedenzymelevelsineachcase
Anakinra 12-monthopenlabeltrial.Improvementin7/15patientswith
refractorymyositis.Inflammatoryinfiltratesinrepeat
biopsiesdidnotresolveandIL-1expressionwasnot
correlatedtoclinicalresponse
5
Alemtuzumab 1casereport(PM/ILD)showingrapidimprovement.Post
infusion-relatedreaction/respiratorycompromise.Concerns
aboutimmunosuppressivepropertiesandinfectionrisk
Abatacept Ongoingclinicaltrial(ARTEMIS).Favourableoutcomesin
JDMwithcalcinosisandrefractoryanti-SRPmyositis
Sifalimumab Phase1btrial.Suppressionofgenesinducedbytype1IFNγ
(bloodandmuscle)withimprovedmusclestrength
*InternationalMyositisAssessmentandClinicalStudiesGroup(IMACS)
AdaptedfromMoghadam-KiaSetal.ModernTherapiesforIdiopathicInflammatoryMyopathies
(IIMs):RoleofBiologics.ClinRevAllergyImmunol.2017Feb;52(1):81–87withpermissionfrom
Springer.
References
4. Muscle Study Group. A randomized, pilot trial of etanercept in dermatomyositis. Ann Neurol
2011;70;427–36.
5.ZongM,DorphC,DastmalchiM, et al. Anakinratreatmentinpatientswithrefractoryinflammatory
myopathiesandpossiblepredictiveresponsebiomarkers:amechanisticstudywith12monthsfollow-
up.AnnRheumDis2014;75;913.
Inclusion-bodymyositis
• Inclusion-bodymyositis(IBM)isadistinctdisorderthatcomprises20–30%of
idiopathicmyositiscases.IBMusuallybeginsaftertheageof50yearsandis
3×morecommoninmen.ThedifficultyindistinguishingitfromPMandits
insidiousonsetcanleadtoconsiderabledelayindiagnosisby3–5years.
• Distalweaknessandwastingcanbeascommonasproximal,ofteninvolving
thelowerlimbsbeforetheupper,andsparingtheface.
• Unlike PM or DM, IBM can present with diminished hand-grip strength, in
additiontoproximalmuscleweakness.
• Dysphagiaisafeaturein40%ofcases,andmyalgiasin20%.
• Anopenbiopsy(asopposedtoneedlebiopsy)isessentialtodiagnoseIBM.
• A needlebiopsy maynotbe sufficient toallow therecognitionof important
cluesthatpointawayfromotherformsofmyositis.
• Thereisasignificantinflammatorycomponentearlyinthediseasecourse,that
may partially respond to GCs, though generally patients are usually non-
responsivetoGCs.
• Theremaybeaperiodofstabilizationforafewmonthsbutthismayreflect
thenaturalhistoryofdisease.
• ProlongedadministrationofGCsmayresult inworsening ofdisease despite

improvementsinCKlevels.
• Treatmentusuallybeginswithhigh-doseGCsfor3months,addinginMTXor
AZA if clinical improvement or in patients with another autoimmune
connectivetissuedisease.Ifthereiscontinueddeclineinstrengthorfunction,
immunosuppressionshouldbediscontinued.
• Anti-T-lymphocyte globulin, interferon-β, MMF, and anabolic GCs such as
oxandrolone,mayhavebeneficialeffectsasinsomereports.
• Weakness willprogress inmost patientsbut thisis oftenvery slow. Patients
may need assistance with daily activities within 10 years and some may be
wheelchairboundwithin15yearsfromonsetofsymptoms.
Other(adult)inflammatorymyopathies
Drug-inducedmyopathies
• The range of myositis severity caused by different drugs varies, from
asymptomatic increases in CK to necrotizing severe myopathies resulting in
rhabdomyolysis.
• HMG-CoAreductaseinhibitors(statins)cancausemyalgiaandcrampsalong
withanelevatedCKlevelandmaybeexacerbatedbytheuseofotherdrugs
(ciclosporinandfibrates)orotherdiseases(hypothyroidism).
• Patientsonanydrugssuspectedofcausingmyositis,presentingwithmyalgia,
shouldhavetheirrenalfunctionandCKcheckedandthedrugstopped.
• See Table14.2,p.431foranoverview.
PM/DMwithinterstitiallungdisease
Polymyositisordermatomyositisoccurringtogetherwithinterstitiallungdisease
(PM/DM-ILD)maybeadistinctcondition.
• Characteristicfeaturesincludemyositis,ILD,Raynaud’sdisease,‘mechanic’s
hands’(i.e.dry,crackedskinacrossthedigits),andsmalljointpolyarthritis.
• Associatedwitharangeofautoantibodiesdirectedagainstaminoacyltransfer
RNA synthetases includinghistidyl-tRNA synthetase (HRS; termedtheanti-
Jo1autoantibody).
• Anti-Jo-1ispresentin~20%ofPM/DMpatientsandtitreofantibodycanbe
associatedwithdiseaseactivity.
• Canbeassociatedwithfeversatonsetorduringflares.
• SomepatientspresentingwithILDorarthritismaygoontodevelopmyositis
later,sopresentationofcomponentsofthediseasemaynotbeconcordant.
• Patientsneedtobemanagedwithachestphysicianmonitoringlungfunction
testsandinflammatorydiseaseactivity.

• CYC, MMF, and RTX give alternative choices for therapies in addition to
GCs.
Juvenileidiopathicinflammatorymyopathy
Introduction
• ThejuvenileIIMsareheterogeneousinflammatoryconditionsinyoungpeople
<17yearsofagecharacterizedbyproximalmyopathy,rashes,andotherorgan
involvement.
• Juvenile IIMs are classified into groups that share similar clinical and
laboratoryfeatures,treatmentresponses,andprognosis.
• ThejuvenileIIMsare:
• juveniledermatomyositis(JDM):80%.
• juvenilepolymyositis(JPM):5%.
• overlapmyositis:10%.
• rare forms: macrophagic myofasciitis, focal myositis, granulomatous, and
graft-vs-hostmyositis.
• inclusion body myositis and cancer associated myositis are exceptionally
rareinchildren.
• Aformofinclusionbodymyositisalsooccursincriticalillnessmyopathyseen
inintensivecareunits.
• Benign acute childhood myositis is self-limiting and typically presents with
calfpain,walkingdifficulty,andveryhighCKlevels.
• Benign acute myositis can be misdiagnosed as something more severe or
complexresultinginunnecessarytests,admission,andfollow-up.
• Although the 1975 ‘Bohan and Peter’ criteria
6
remain in principle the
diagnosticcriteria(see Box14.2,p.427),theinvasivenatureofEMGand
biopsymeanstheyarerarelyusedandMRIandUSareoftensubstitutedfor
confirmationofmuscleinvolvement.
Differentialdiagnosisofmuscleweaknessinchildhood
Muscleweaknessmaybeasignofmusclediseaseoramanifestationofamuscle
function-relatedpathologyorevengeneralpathology.
• Viralmyositisorbenignacutechildhoodmyositis.
• Drug-inducedmyopathy.
• Criticalillnessmyopathy(e.g.patientsinintensivecareunits).
• Musculardystrophyandcongenitalmyopathy.
• Juvenilefibromyalgia.
• Othermultisysteminflammatorydiseases(MCTD,SLE,vasculitis).
• Skeletaldysplasias.
• Electrolyteimbalances(potassiumandcalcium).
Juveniledermatomyositis(JDM)
• JDM is by far the commonest inflammatory myopathy in children and
adolescents and in typical circumstances does not require a search for
neoplasia.
• Theincidenceis2–4permillion(USAandUK)withamedianageofonsetof
7yearsold(25%are<4yearsoldatdiagnosis).
• Presentation is typically with a classical rash and insidious onset of muscle
weakness.
• A facial rash is common with a photosensitive malar distribution and
nasolabial-sparingcharacteristicofSLE.
• DistinguishingJDMfromSLEisimportant.WithJDMthereareshinyraised
redmarksontheknuckles,elbows,knees,andankles(Gottron’spapules)and
aduskypurple-redhuetotheuppereyelids(heliotroperash).
• Weaknessmanifestsasdifficultygettingupstairsoroutofbed,difficultywith
puttingonajumperorT-shirt,ortiringmorequicklythanusualduringsport.
• Other features include low-grade fever, weight loss, arthralgia, abdominal
pain,melaena,changeincharacterofvoice,anddifficultyswallowing.
• ILDanddilatedcardiomyopathymayoccurinchronicdisease.
• TheclinicalcourseofJDMfallsintodifferentpatterns:
• Monocyclic(lastingupto3years)in25–40%.
• Polycyclic (periods of remission and relapse relapse) or chronic, both of
whichcanbelifelong,in50–60%.
• Ulcerativein10–20%.
Myositis-specificautoantibodies(MSAs)
• MSAshavebeenidentifiedin~70%ofJDMpatients.
• AllautoantibodiesareseeninJDM.MorecommonMSAsinclude:
• anti-TIF1-gamma associated with classical JDM (18%), extensive skin
involvement(andlipodystrophy),andchroniccourse.
• anti-MJ, anti-NPX2(15%): bothassociated witha monocycliccourse, but
moreseverecalcinosis,dysphonia,andjointcontractures.
• MDA5 (6%):patientsare lesslikelyto be weak,but cutaneous ulceration
andarthritisarecommon.AssociatedILDisuncommon.
Treatment
• Managing JDM requires a multidisciplinary approach to optimize muscle
strength,function,andqualityoflifewhilecontrollinginflammationofskin,
muscle,gut,andotherorgans,andaimingtoavoidcalcinosisevolving.
• Calcinosiscutis(occurringinupto35%ofJDMcases)canbeamajorcause
ofmorbidityduetopain,cosmeticproblems,tetheringofskin,muscles,and
nerves,andasanidusforinfection.
• GCs are the mainstay of treatment and universally supplemented with
syntheticDMARDs(MTX,HCQ,ciclosporin,andIVIg).
• Earlyaggressivetreatmenttorapidlyandcompletelycontrolinflammationis
essentialtofullyrestoremusclefunctionandavoiddamageandcalcinosis.
• Consensus guidelines (CARRA 2012, USA) recommend escalating
immunosuppressionforthefirst2monthsdependingondiseaseseverity.
• ThetreatmentregimensutilizeSCMTX,andaGCtaperingschedulebasedon
weightandseverityofdisease(e.g.seeTable3inreference7).
• IV methylprednisolone is added for rapid induction especially for severe
diseaseandtoreplaceoralprednisolonewhenthereisgutinvolvement.
• If there is initialclinical improvement, then prednisolonedoseis reduced at
weekly intervals initially and then monthly at lower doses with the aim of
beingoffGCsby10–12months.
• CYCistypicallyusedforulcerativecases,severemuscledisease,andILD.
• IVIg is used for refractory and skin-predominant disease, or when there is
severeweakness.
• More recently MMF, RTX, and anti-TNFα agents have been used for
refractorydisease.
AmyopathicJDM
• Hasthecharacteristicrashbutnoobviousmuscledisease,althoughtypically
muscleinflammationandweaknessissubclinicalandinsidiousinonset.
• AmyopathicJDMisnotgenerallyassociatedwithcalcinosisorILD.
Overlapmyositis
• Occurswithscleroderma,SLE,JIA,Sjögren’sdisease,andtype1diabetesand
moreofteninnon-Caucasianpopulations.
• ItisoftenassociatedwithRaynaud’sandILDresultinginahighermortality.
Juvenilepolymyositis
• Isveryrareandresultsinmoreclinicallyapparentproximalanddistalmuscle
weaknesswithlittleskininvolvement.
• Itisusuallysevereatonsetwithvery highCK levels,affectsolderchildren
(adolescents),andfrequentlyhascardiacinvolvement.
• A muscle biopsy is required to differentiate from muscular dystrophy and
showsendomysialinfiltrates.
References
6.BohanA,PeterJB.Polymyositisanddermatomyositis.NEnglJMed1975;292:344–7.
7. Huber AM, Robinson AB, Reed AM, et al. Consensus treatments for moderate juvenile
dermatomyositis: beyond the first two months. Results of the second Childhood Arthritis and
RheumatologyResearchAllianceconsensusconference.ArthritisCareRes2012;64:546–53.
Chapter15
Primaryvasculitides
Introduction
Largevesselvasculitis
Takayasuarteritis
Polymyalgiarheumaticaandgiantcellarteritis
Polyarteritisnodosa
ANCA-associatedvasculitides
Smallvesselvasculitis
Childhood-onsetvasculitides
Introduction
• Thevasculitidesareaheterogeneousgroupofrelativelyuncommondiseases
that can arise as primary conditions or secondary to an established disease
such as rheumatoid arthritis (RA) (see Chapter 5) or systemic lupus
erythematosus(SLE)(see Chapter13).
• The vasculitidesarelinkedbythepresenceofvascularinflammation, which
canleadtooneoftwocommonoutcomes:
• Vesselwalldestruction:leadingtoaneurysmorrupture.
• Stenosis:leadingtotissueischaemiaandnecrosis.
• In 1990, the American College of Rheumatology (ACR) developed a
classification system based on vessel size, with the inclusion of a division
betweenprimaryandsecondaryvasculitis(Table15.1).
• Thisclassificationsystemisnotperfect.Patientswith‘largevesselvasculitis’
and‘smallvesselvasculitis’canhavediseasethataffectssomemedium-sized
vessels.Moreover,notallpatients with‘antineutrophilcytoplasmicantibody
(ANCA)-associated vasculitis (AAV)’ have detectable levels of ANCA.
However, thisis ausefulframeworkfortheclinician,sincecategorizingthe
patient into one of these groups can narrow the differential diagnosis
considerably.
• The Chapel Hill Consensus Conference (CHCC)in1994haddeveloped the
mostwidelyusednomenclaturesystemformostformsofvasculitis.Thiswas
revisedinthe2012CHCCtoincludenewinsightsgainedoverthepasttwo
decades, add new forms of vasculitis, and address issues surrounding
eponyms.(Box15.1).
• Thenotablechangesofthe2012CHCCare:
• theadoptionofnewnamesforseveralconditions,consistentwiththetrend
ofreplacingeponymswithdiseasenamesthatreflectpathology.
• formallyadoptingthetermANCA-associatedvasculitis(AAV)forthemajor
systemicsmallvesselvasculitissubtypes.
• adoption of additional categories to include variable vessel vasculitis and
secondaryformsofvasculitis.
• Thisnomenclaturedoesnotsubstitutetheclassificationcriteria.
• TheAAVshaveapredilectionfortherespiratorytractandkidneys.
The AAVs are granulomatosis and polyangiitis (GPA; formerly Wegener’s
granulomatosis), microscopic polyangiitis (MPA), and eosinophilic
granulomatosiswithpolyangiitis(EGPA;formerlyChurg–Strausssyndrome).
Antineutrophilcytoplasmicantibody
• ANCA exists in two main forms based on neutrophil autoantibody
immunofluorescencepatterns:
• Cytoplasmic(C-ANCA;antibodiesagainstproteinase-3(PR3)).
• Perinuclear(P-ANCA;antibodiesagainstmyeloperoxidase(MPO)).
• Other ANCA-staining patterns (i.e. non-cytoplasmic, non-perinuclear) can
occur.
• P-ANCA pattern may be caused by antibodies against antigens other than
myeloperoxidase.Thesearesometimesreferredtoas‘atypicalANCA’,anddo
not predict the presence of vasculitis, although they can be found in
inflammatory bowel disease, immune-mediated neutropenia, and other
autoimmunediseases.
• C-ANCAisfoundinpatientswithGPA.
• PatientswithMPAandEGPAtendtobeP-ANCApositive.
• Counterintuitively,patientswithAAVcanbeANCAnegativeinupto50%of
cases.
• AAV patients with active or untreated disease are more likely to be ANCA
positive.

• The role that ANCAs play in the pathogenesis of vasculitis remains
controversial.
Table15.1Aclassificationofsystemicvasculitis
Dominantvessel Disorders
Largearteries Giantcellarteritis.Takayasu
arteritis.Isolatedcentral
nervoussystemangiitis
AortitisinAS.Infection,
e.g.syphilis
Mediumarteries Classicalpolyarteritisnodosa,
Kawasakidisease
Infection,e.g.hepatitisB.
Hairycellleukaemia
Medium
arteries/small
vessel
AAVs(e.g.GPA,
EGPA/Churg–Strauss,
microscopicpolyangiitis)
Vasculitis secondary to
autoimmune disease.
Malignancy.Drugs.
Infection,e.g.HIV
Smallvessel
(leucocytoclastic)
Henoch–Schönleinpurpura.
Essential mixed
cryoglobulinaemia.
Cutaneousleucocytoclastic
angiitis
Drugs.Malignancy.
Infection,e.g.hepatitis
B/C
Box15.1The2012CHCCnomenclatureofvasculitis
Largevesselvasculitis
• Takayasuarteritis(TA)
• Giantcellarteritis(GCA).
Mediumvesselvasculitis
• Polyarteritisnodosa(PAN)
• Kawasakidisease(KD).
Smallvesselvasculitis
AAVs
• Microscopicpolyangiitis(MPA)
• Granulomatosiswithpolyangiitis(GPA)
• Eosinophilicgranulomatosiswithpolyangiitis(EGPA).
Immune-complexsmallvesselvasculitis
• Anti-glomerularbasementmembrane(anti-GBM)disease
• Cryoglobulinaemicvasculitis
• IgAvasculitis(Henoch–Schönleinpurpura)(IgAV)
• Hypocomplementaemicurticarialvasculitis(HUV)(anti-C1qvasculitis).
Variable-sizedvesselvasculitis
• Behçet’sdisease(BD)
• Cogan’ssyndrome(CS).
Single-organvasculitis
• Cutaneousleucocytoclasticangiitis
• Cutaneousarteritis
• Primarycentralnervoussystemvasculitis
• Isolatedaortitis
• Others.
Vasculitisassociatedwithsystemicdiseases
• Lupusvasculitis
• Rheumatoidvasculitis
• Sarcoidvasculitis
• Others.
Vasculitisassociatedwithprobableaetiology
• HepatitisCvirus-associatedcryoglobulinaemicvasculitis
• HepatitisBvirus-associatedvasculitis
• Syphilis-associatedaortitis
• Drug-associatedimmunecomplexvasculitis
• Drug-associatedAAV
• Cancer-associatedvasculitis
• Others.
Modified from Jennette et al. ‘2012 Revised International Chapel Hill Consensus Conference
NomenclatureofVasculitides’Arthritis&Rheumatism,65:1–11withpermissionfromWiley.
Generalprinciplesofvasculitismanagement
• Tobecomplete,anyevaluationofachronicdisease(suchasprimarysystemic
vasculitis)mustincludebothanassessmentofdiseaseactivityandofdisease
damage. The concept of damage denotes the aspects of disease that are
unlikely to reverse with immunosuppression (such as pulmonary fibrosis or
renalinsufficiency).
• ClinicaltrialsofvasculitiscommonlyusetheBirminghamVasculitisActivity
Score (BVAS) and Vasculitis Damage Index (VDI) to assess activity and
damage,respectively.
• Other clinicalindicesexist. The French Vasculitis Study Group(FVSG)has
developedaprognosticFive-FactorScore(FFS).Thisindexprovidesanother
useful method of classifying patients with vasculitis. Patients with PAN or
AAVwhohaveaFFS>0havesubstantiallyhighermortalitythanpatientswith
aFFS=0.
• TheFFSwasrevisedin2008,andnowincludesthefollowing:age>65,renal
insufficiency, cardiac involvement, and gastrointestinal (GI) manifestations.
The presence of ear, nose, and throat signs was found to correlate with an
improvedoutcomeamongpatientswithGPA.
Largevesselvasculitis
• The‘largevessels’includetheaortaanditsmainbranches(i.e.thesubclavian,
carotid, andbrachiocephalicarteries). Primary and secondary forms oflarge
vesselvasculitisareshowninTable15.2.
• TheclassicformsofprimarylargevesselvasculitisareTA(see ‘Takayasu
arteritis’,pp.454–455)andgiantcellarteritis(GCA).GCAisassociatedwith
PMR.
• Recent studies demonstrate that many patients with polymyalgia rheumatica
(PMR) have subclinical aortic inflammation, which seems to validate this
classificationscheme.
• Theclinicalmanifestationsof largevesselvasculitiscanbepredictedbythe
patternofvesselinvolvement.Archaortitisleadstoaneurysmaldilatationand
aortic regurgitation. Subclavian involvement causes arm claudication and
diminished pulses on examination. Carotid involvement may lead to visual
loss,jawclaudication,andstroke.Involvementofanymajorbloodvesselmay
causebruitsofphysicalexamination.
Table15.2Causesoflargevesselvasculitis
Primary Takayasuarteritis
Giantcellarteritis
*
Secondary
†
Infection:bacterial,fungal,mycobacterial,spirochaete
Rheumatoidarthritis
Seronegativespondyloarthritis
Systemiclupuserythematosus
Sarcoidosis
Relapsingpolychondritis
Juvenilearthritis
*
Giantcellarteritisisdiscussedinthischapterinthesectiononpolymyalgiarheumatica.
†
Thesecondarycausesoflargevesselvasculitisarediscussedintheirrespectivesections.
Takayasuarteritis
Takayasuarteritis(TA)isachronicgranulomatousarteritisthataffectstheaorta
andthegreatvessels.Thepulmonaryarteriescanalsobeinvolved,althoughthis
isrelativelyuncommon.
Epidemiology
• ItismostcommoninJapan,SoutheastAsia,India,andMexico.Itisrareinthe
UKandintheUSA,itsannualincidenceisestimatedat2.6permillion,where
itisnotlimitedtopatientsofAsiandescent—themajorityofpatientsinthe
USAareCaucasian.
• TAtendstoaffectwomen(90%ofcases)withadolescentsandyoungadults
20–40yearsoldatgreatestrisk.
• The hallmark of the disease is arteritic inflammatory infiltrates that cause
luminal narrowing or occlusion presenting with bruits, claudication, and
diminished(orasymmetric)pulses.
Presentation
• Systemicsymptomsarecommonintheearlyphaseofthedisease,including
fever,malaise,weightloss,andfatigue.
• As the disease progresses, consequences of vascular inflammation and
insufficiencycanbecomeapparent.
• Arthralgiasandmyalgiasarecommon.
• Clinicallyevidentsynovitisisrare.
• Lightheadedness, visual disturbance,andstrokes can occur. Subclavian steal
canbeanimportantcauseofneurologicalsymptoms.
• Hypertensionmaydevelopasaconsequenceofrenalarterystenosis.
• Myoarthralgiasarenotuncommon.
• Cardiovascularcomplicationsareanimportantcauseofmorbidity,andinclude
aorticinsufficiency,congestiveheartfailure,systemichypertension,andostial
involvementofthecoronaryarteries.
Investigation
• Traditionally, the diagnosis of TA has depended on angiography to
demonstrate the characteristic changes of arterial dilatation, thrombosis, and
aneurysmformation.
• Conventional angiography has the added benefit of allowing a comparison
betweencentralandperipheralbloodpressures—importantbecausesubclavian
stenosis is a common consequence of this disease and a standard arm cuff
blood pressure reading may underestimate hypertension. Angiography may
also allow for therapeutic intervention, e.g. angioplasty or stenting of the
stenoticvessels.
• Magnetic resonance imaging/angiography (MRI/MRA) have excellent
resolutionatthelevelofthelargevessels.MRIcanalsodemonstrateevidence
ofvesselwallinflammation,whichcouldsupportadiagnosisofTA.
• High-resolutionUSissensitivefordetectingcarotidlesions.
•
18
F-FDG PET-CT scanning is useful for identifying the presence of large
vesselvasculitis,butitisnotclearwhetheritcanbeusedtomonitorresponse
totherapy.
Treatment
• Initial medicaltreatment is withglucocorticoids (GCs) suchasprednisolone
40–60mgperdayinanaverage-sizedadult.
• Tapering GC dose is attempted when symptoms and laboratory tests of
inflammation subside. About one-half of all patients have steroid-resistant
disease. In this group, methotrexate (MTX), azathioprine (AZA),
mycophenolatemofetil(MMF),orleflunomide(LEF)maybetried.
• In severe forms of the disease, or if there is continuing evidence of disease
activity,cyclophosphamide(CYC)maybegiven.
• Experiencewithbiologicsislimited.Anti-TNFαagentsortocilizumab(anti-
IL6r)maybetriedinsevereorresistantcases.
• Hypertension can be difficult to manage, and may require angioplasty or
surgerytoaddressrenalarterystenosis.
• Surgicalmanagementrangesfromangioplastytobypassprocedures.Theseare
bestperformedduringtheinactivephaseofdisease.
• Angioplastyisoftenatemporizingmeasure,andlesionstendtorestenoseover
time.Restenosisislesslikelyfollowingbypassgrafting.Operativemortalityis
4%—mostlywithaneurysmrupture.
• The prognosis depends mainly on the presence of hypertension and aortic
incompetence.Themajorityofpatients(75%)willhavesomeimpairmentof
dailyliving,and50%arepermanentlydisabled.
• Mortalityislow,with5-yearand10-yearsurvivalratesreportedas80%and
90%,respectively.
• TAisnotacontraindicationtopregnancy.Cytotoxicagentsshouldbestopped
andGCskepttoaslowadoseaspossible.
• Obstetric decisions can be made on their own merits and not because of
coexistenceofTA.Themaincomplicationsareexacerbationofhypertension
andcongestivecardiacfailure.Theanaesthetistshouldbemadeawareofthe
diagnosis, as the patient may require invasive blood pressure monitoring
duringdelivery.
Polymyalgiarheumaticaandgiantcellarteritis
Polymyalgiarheumatica
Polymyalgiarheumatica(PMR)ischaracterizedbypainandstiffnessaffecting
structuresoftheshoulderandpelvicgirdleareas.Neckpainandstiffnessisalso
afeature.
Epidemiology
• PMRisrareinpatients<50yearsold.Themeanageofonsetis70years.
• Prevalence among patients older than 50 years is 1 in 133, and women are
affectedmorethanmen(ratio2:1).
• Thereisahigherfrequencyofdiagnosisinnorthernlatitudes.
Pathology
• Parainfluenza, parvovirus B19, Mycoplasma pneumonia, and Chlamydia
pneumoniae infections have been shown to have a temporal relation to
incidencepeaksofPMR,althoughotherstudieshavefoundnorelationship.
• HLA-DRB1
*
04and-DRB
*
01predictdiseasesusceptibility.
• PMR and GCA have a close clinical relationship. One-half of patients with
GCA have symptoms of PMR and up to 20% of patients with PMR have
histologicalorclinicalevidenceofGCA.
• Thepathogenesisofbothconditionsisnotknown.
Presentation
• ThediagnosisofPMRisbasedonclinicalfeatures.ThecriteriaofJonesand
Hazleman1981
1
aresuccinctandpractical(Box15.2).
• The European League Against Rheumatology (EULAR) and the ACR have
proposedclassificationcriteriatobeusedasaresearchtooltoidentifypatients
withPMR.
2
• EULAR/ACRcriteriainclude3requiredcriteriaand4pointsfromadditional
criteria:
• Required criteria include age ≥50 years, bilateral shoulder aching, and an
abnormalESRorCRP.
• Ascoringalgorithmwasdevelopedfortheadditionalcriteria,whichinclude
morningstiffness≥45minutes(2points);painorlimitedrangeofmotionat
hip(1point);absenceofRForanti-CCP(2points);absenceofperipheral
jointpain(1point).
• Theremaybeapparentmuscleweaknessontesting,whichisduetopainrather
thanintrinsicmuscledisease.
• Symptomsmaystartasymmetrically,butsoonbecomebilateral.
• Systemicfeaturesofmalaise,weightloss,low-gradefever,anddepressionare
common.
• Arthralgia and synovitis may occur. Up to 5% of patients with RA (see
Chapter5)haveaninitialPMR-likepresentation.
Investigation
• The lack of specific clinical features, a specific laboratory test, and the
presence of several conditions that can present with PMR-like symptoms,
makesPMRadiagnosisofexclusion(seeBox15.3).
Box15.2CriteriaforthediagnosisofPMR
Allthefollowingneedtobevalid/relevant:
1. Shoulder and pelvic girdle pain which is primarily muscular in the
absenceoftruemuscleweakness.
2. Morningstiffness.
3. Durationofatleast2months(unlesstreated).
4. ESR>30mm/hourorCRP>6mg/dL.
5. Absenceofinflammatoryarthritisormalignancy.
6. Absenceofmuscledisease.
7. Promptanddramaticresponsetoglucocorticoids.
CriteriafromJonesJG,HazlemanBL.TheprognosisandmanagementofPMR.AnnRheumDis
1981;40:1–5.
Box15.3ConditionsthatcanpresentwithPMR-typesymptoms
1. Rheumatoidarthritis
2. Inflammatorymyopathy
3. Hypo/hyperthyroidism
4. Myelomaorothermalignancy
5. Chronicsepsis
6. Bilateralshouldercapsulitis
7. Calciumpyrophosphatedepositiondisease
8. Spondyloarthritis/PsA
9. Inflammatoryphaseosteoarthritis
10. Parkinsonism.
Giantcellarteritis(GCA)
GCA is a granulomatous arteritis of the aorta and larger vessels, including
extracranialbranchesofthecarotidartery.Fordiagnosticcriteria,seeTable15.3.
Epidemiology
• GCA is the most common form of primary systemic vasculitis. In North
Americatheannualincidenceisestimatedat18per100,000.
• LikePMR,thefemaletomaleratiois2:1.
Pathology
• InfectiousandgeneticassociationsarealsosimilartoPMRwithevidenceof
disease‘clustering’.
• Increasing ageandethnicity arethemajor riskfactorsfor developingGCA.
GCAisrareamongAfricanAmericans.
Presentation
• Severeheadacheandscalptendernesslocalizedtotheocciputortemporalarea
arecommoninitial symptoms, andarepresent in 70%ofcases. The critical
featureoftheheadacheisthatitisnew.
• Headache is often localizedtothetemples, but may be frontal,occipital,or
generalized.
• Thetemporalarterycanbeswollen,tender,andpulseless.
• Jawclaudicationispresentinabouthalfofthepatients.Somepatientsreport
tongue claudication. Jaw claudication is strongly associated with a positive
biopsy.
• Scalpnecrosishasalsobeenreported.
• Large arteries are affected in 15% of cases, leading to claudication, bruits,
absentneckandarmpulses,andthoracicaortaaneurysmanddissection.
• Visualdisturbanceisusuallyanearlyfinding.Patientsmaydescribesymptoms
ofamaurosisfugaxbytemporary ‘curtaining’ofthevisualfield.Visual loss
dueto retinalischaemiamay beirreversiblewithin hours.Ahistory ofprior
transientvisuallossisthestrongestpredictorforsubsequentpermanentvisual
loss.
• Diplopiaandptosismayalsooccur.
• Fundoscopy may show optic disc pallor, haemorrhages, and exudates. Optic
atrophyisalatefinding.
• Arteriticanteriorischaemicopticneuropathyisthemostcommonfinding,and
mustbedifferentiatedfromnon-arteriticanteriorischaemicopticneuropathy,a
causeofvisuallossthatdoesnotrespondtosteroids.
• Malaise,fatigue,weightloss,fever,andanaemiaarecommon.
Investigation
• TheESRandCRParecharacteristicallyelevated,butcanbenormalinupto
3%ofcases.
• PatientssuspectedofhavingGCAshouldbeevaluatedwithbilateraltemporal
arterybiopsies,takingsegmentsof1.5cmeach.
• Treatment should not be delayed. Biopsies may be helpful to confirm the
diagnosisupto2weeksaftersteroidsarestarted.
• Unlike mostformsof vasculitis,GCA does notcausefibrinoid necrosisand
thepresenceoffibrinoidnecrosisonatemporalarterybiopsyshouldprompta
search for another form of vasculitis, such as GPA or cryoglobulinaemic
vasculitis.
• Temporal artery biopsies may be negative in 12% of patients. A negative
temporalarterybiopsydoesnotexcludeadiagnosisofGCA.
• DataregardingtheusefulnessofDopplerultrasoundforthediagnosisofGCA
aremixed.Variousabnormalitiesdescribedincludestenosis,occlusionandthe
presenceofahypoechoic‘halo’(halosign)aroundthetemporalarteries.
• ThesensitivityandspecificityofthehalosignforthediagnosisofGCAare
69%and82%,respectively.
• MRA is useful to diagnose GCA, identify regions of temporal artery
involvement,helpgaugediseaseactivity,andassessresponsetotreatment.
•
18
F-FDG-PET-CT may be useful in showing abnormal metabolic activity in
theaortaofmanypatientswithGCA(see Plate26).Directevaluationofthe
temporalarteriesisnotpossibleusing
18
F-FDG-PET-CT.
Table15.3DiagnosticcriteriaforGCA
Jonesand
Hazleman
Allthefollowing:
• Positivetemporalarterybiopsyorcranialarterytenderness.
(1981)
• One or more of: visual disturbance, headache, jaw pain,
cerebrovascular insufficiency; ESR >30 mm/hour or CRP >6
mg/L;responsetoglucocorticoids
ACR
criteria
Threeormoreof:
• Ageatonset>50years.
• Newheadache.
• Temporalarterytendernessordecreasedpulsation.
• ESR>50mm/hour.
• Abnormal artery biopsies showing necrotizing arteritis with
mononuclearinfiltrateorgranulomatousinflammationusually
withmultinucleatedgiantcells
InformationfromJonesJG,HazlemanBL.TheprognosisandmanagementofPMR.AnnRheumDis
1981;40:1–5andHunderGetal.TheAmericanCollegeofRheumatology1990criteriaforthe
classificationofthegiantcellarteritis.ArthritisRheum1990;33:1122–8.
TreatmentofPMRandGCA
• Both conditionsrequire GCtreatment;however, the amountand durationof
treatmentrequiredarequitedifferent.
3,4
• PMRrespondsdramaticallytolow–moderatedosesofGC(i.e.prednisone15–
20mgdaily)within24hours.
• Somepatientsrespondimmediatelytoprednisolone,andthevastmajorityof
patientshaveasubstantialimprovementwithindaysofstartingtreatment.
• ACR/EULAR suggest use of the minimum effective dose of prednisolone,
rangingfrom12.5–25mgprednisolone(orequivalent)perday.
• Lowerdosesof7.5–10mgprednisolonemaybesufficientinthosewithmild
symptoms.
• Persistent symptoms despitetreatmentmandate consideration ofanalternate
diagnosis.
• Aftertreatmentfor2–4weeks,theprednisonedosemaybedecreasedby2.5
mgevery2weeksuntilthepatientreachesamaintenancedoseof10mg/day.
Prednisonemaysubsequentlybetaperedin1mgpermonthincrements.
• GCArequirestreatmentwithhigh-doseGCs(i.e.prednisone40–60mgdaily)
andthepatientmaytakeaweekorlongertoexperiencesubstantialrelief.
• Treatment with GCs should be instituted once a diagnosis of GCA is
suspected,evenbeforeitisconfirmed.
• Aftertreatmentfor1month,prednisonemaybegraduallytaperedover9–12
months.
• In patients who have GC-resistant or GC-dependent disease, or develop
significant adverse effectswithtreatment,MTX may be added as a steroid-
sparingdrug.
• Ameta-analysis (of161 patients)showedthattheuseofMTXresultedin a
cumulativereductioninthesteroiddoseover48weeks.
• TocilizumabcanbeeffectiveasGC-sparing,asdemonstratedinasmalltrialof
30patientswithnewlydiagnosedorrelapsingGCA.
• SmalluncontrolledstudieshavesuggestedthatCYCmayalsobeconsidered
forthisindication.
• Patients with visual symptoms associated with GCA should be treated with
intravenouspulse methylprednisolonetherapy(1gdaily for3days)priorto
initiatingtherapywithprednisone.
• Daily low-dose (e.g. 75 mg) aspirin may prevent cranial ischaemic events,
such as stroke and blindness, and should be considered if there is no
contraindication.
• OsteoporoticfractureprotectionagainstGC-inducedosteoporosisisessential.
All patients with either GCA or PMR should be commenced at the time of
starting GCs,oneither a weekly oralbisphosphonateor IVzoledronicacid,
alongsidedailycalciumandvitaminDsupplements.
References
1. JonesJG,HazlemanBL.Theprognosisandmanagementofpolymyalgiarheumatica.AnnRheumDis
1981;40:1–5.
2. Dasgupta B. 2012provisional classificationcriteria for polymyalgia rheumatica: a European League
Against Rheumatism/American College of Rheumatology collaborative initiative. Arthritis Rheum
2012;64:943–54.
3. DasguptaB,BorgFA,HassanN,etal.BSRandBHPRguidelinesforthemanagementofpolymyalgia
rheumatica.Rheumatol(Oxf)2010;49:186–90.
4. DasguptaB,BorgFA,HassanN,etal.BSRandBHPRGuidelinesforthemanagementofgiantcell
arteritis.Rheumatol(Oxf)2010;49(8):1594–s7.
Polyarteritisnodosa
Polyarteritisnodosa(PAN)wasthefirstformofsystemicvasculitisdescribedin
the literature. It is characterized by a necrotizing vasculitis of medium-sized
arteries,whichcanleadtocutaneousulcers,kidneyinfarction,GIhaemorrhage,
andmononeuritismultiplex.
The CHCC created a distinction between ‘classic’ PAN (i.e. an ANCA-
negative, medium vessel vasculitis associated with renal infarcts) and
microscopic PAN (i.e. an ANCA-positive, medium vessel and small vessel
vasculitis characterized by glomerulonephritis). This re-classification (and the
hepatitisBvaccine)hasmadePANincreasinglyuncommon.
Aetiology
• SomecasesofPANhavebeenlinkedtoinfectionwithhepatitisB.
• PatientswithPANshouldbescreenedforviralhepatitis,asantiviraltherapy
maybeneededinadditiontoimmunosuppression.
Presentationandclinicalfeatures
• TheclinicalfeaturesareshowninTable15.4.
• Patientsoftenpresentwithnon-specificfeaturesofsystemicdiseaseincluding
myalgias,arthralgias,weightloss,andfever.
• About 50% of cases develop a vasculitic rash, which includes purpura,
nodules, livedo reticularis, bullous and vesicular lesions, ulcers, often with
‘punchedout’borderinthelowerextremities.
• GIinvolvementoccursin upto 50%ofcases.Non-specificabdominal pain,
gut/gallbladderinfarction,andpancreatitisareallfeatures.
• Renalinvolvementoccursinupto50%ofcasesintheformofrenalinfarct
andhypertension.Renalimpairmentisoftenmildandpresentinaround20%
ofcases.
• Mononeuritismultiplexoccursinupto70%ofpatients.
• Isolated organ involvement is rare, but disease affecting the skin, testes,
epididymis,breasts,uterus,appendix,andgallbladderhasbeenreported.
Treatment
• Treatmentandprognosisinallthesmallvesselandmediumvesselvasculitides
AREdiscussedattheendofthissection.
Table15.4Clinicalfeaturesatpresentation(as%ofcases)
Clinicalfeature PAN MPA EGPA
Renalimpairment 25% 90% 50%
Pulmonarydisease 40% 50% General50%,asthma100%
Fever 60% 40%
Skinvasculitis 40% 50% 50%
Gastrointestinaldisease 45% 20% 60%
Cardiovascular 15% 20% 45%
Peripheralneuropathy 10% 10% 60%
Ear,nose,andthroat 10% 20%

Oculardisease 10% 20%
ANCA-associatedvasculitides
Granulomatosiswithpolyangiitis(formerlyWegener’sgranulomatosis)
• Granulomatosis with polyangiitis (GPA) is the most prevalent of the AAVs.
Renal-limitedvasculitisanddrug-inducedAAVareless-commonmembersof
thisgroup.
• The CHCC has defined GPA as: ‘necrotizing granulomatous inflammation
usually involving the upper and lower respiratory tract, and necrotizing
vasculitis affecting predominantly small to medium vessels (e.g. capillaries,
venules, arterioles, arteries and veins). Necrotizing glomerulonephritis is
common.’
Epidemiology
• GPAisaworldwidediseasewithanincidenceof4–9permillion.
• Itisslightlymorecommoninmenthanwomen.
• Itmostoftenappearsinthefourthandfifthdecades.
Presentationandclinicalfeatures
• GPAisoftenaclinicaltriadwithmanifestationsaffectingtheupperrespiratory
tract,lowerrespiratorytract,andkidneys.
• Patientscanpresentwithawiderangeofclinicalmanifestations.
• Somepatientshaveanindolentpresentationcharacterizedbyrespiratorytract
involvement,suchassinusitisandpulmonarynodules.
• However,rapidlyprogressiveglomerulonephritisandpulmonaryhaemorrhage
canoccur(Box15.4).
Musculoskeletalsymptoms
• Rheumaticsymptomsareseenin60%ofcases.
• Symptomscanrangefrommildmyalgias(in50%ofthecases)andarthralgias
to overt arthritis. 20–30% of rheumatic symptoms may be related to a non-
erosiveandnon-deformingpolyarthropathy.
• MigratoryarthralgiasareaclassicpresentationforGPA.
Box15.4AmericanCollegeofRheumatology1990classificationcriteria
ofGPA*
Diagnosisrequirestwoormoreofthefollowing:
1. Nasal or oral inflammation: development of painful or painless oral
ulcersorpurulentorbloodynasaldischarge.
2. Abnormal chest radiograph: the chest radiograph may show nodules,
cavities,orinfiltrate.
3. Urinarysediment:microscopichaematuriaorredcellcasts.
4. Histologicalchangesofgranulomatousinflammationonbiopsy.
5. PR3-ANCA(C-ANCA)positivity.
*Thenknownas‘Wegener’sgranulomatosis’.
ReproducedfromLeavittetal.(1990),TheAmericanCollegeofRheumatology1990criteriaforthe
classificationofwegener’sgranulomatosis.Arthritis&Rheumatism,33:1101–1107withpermission
fromWiley.
Ear,nose,andthroatsymptoms
• Upto90%ofpatientshaveear,nose,andthroatinvolvement.
• ChronicsinusitisisacommoninitialpresentationforGPAandtypicallymany
patientswill havebeentreatedwithseveralcoursesof antibioticsbefore the
correctdiagnosisisreached.
• Othermanifestationsincludenasalseptalperforation,bloodynasaldischarge
(‘crusts’), and nasal bridge collapse due to erosion of underlying cartilage
(‘saddlenose’).
• Patientsmayalsocomplainofdiminishedhearing,eitherduetosensorineural
hearinglossorEustachiantubedysfunction.
• Subglottic stenosis is a classic feature of GPA and may present with
hoarsenessandstridor.Subglotticstenosismayworsenevenwhenapatientis
otherwiseinremission,andrespondsbettertosteroidinjectionsthansystemic
therapy.
• Intheoralcavityandoropharynx,inflammationcanleadtomucosalulcersor
gingivitis(‘strawberrygums’).
• It is thought that Staphylococcus aureus has a role in disease pathogenesis.
NasalcarriageinGPApatientsis3×thatofthehealthypopulation.Theexact
mechanismsleadingtodiseaseareunclear,buttrimethoprim/sulfamethoxazole
maybenefitpatientswithGPAbyeliminatingS.aureuscolonization.
Pulmonarydisease
• 80%ofcaseshavepulmonarydisease.
• The tracheobronchial tree may be locally involved before any signs of
generalizeddisease.
• Subglottic pseudo-tumours and/orstenosiscause stridor or dyspnoea.Lower
bronchialstenosismaycauseatelectasisandobstructivepneumonia.Multiple
nodules with or without cavitation are found in the lungs of asymptomatic
patients.
• Severepulmonarydiseaseisassociatedwithalveolarcapillaritis,haemorrhage
and haemoptysis, with infiltrates on CXR (typically an alveolar or mixed
alveolar–interstitial pattern; the distribution is often like that of pulmonary
oedemaandfocalinfection).
Renaldisease
• Upto90%ofpatientswith‘severe’GPAhaverenalinvolvement.
• Renal involvement can range from milder focal and segmental
glomerulonephritistofulminantdiffusenecrotizing(rapidlyprogressive) and
crescentic glomerulonephritis, which can rapidly lead to end-stage renal
disease.
• The milder form of the condition is most common, manifesting in the
asymptomaticpatientasanephriticpictureofmicroscopichaematuria,active
sediment,andmildrenalimpairment.
Skindisease
• 40%ofcaseshaveskindisease.
• Featuresincludepalpablepurpuraduetoaleucocytoclasticvasculitis,necrotic
papules (‘Churg–Strauss nodules’), livedo reticularis, and pyoderma
gangrenosum.
Nervoussystem
• About 30% of patients with GPA have involvement with mononeuritis
multiplexanddistalsensorimotor polyneuropathy themainlesions. Seizures
andcerebritisaremuchlessfrequentevents.
• Disseminated granulomatous lesions (‘pachymeningitis’) can involve the
retropharyngealareaandskullbaseaffectingcranialnervesI,II,III,VI,VII,
andVIII.Pachymeningitiscanalsobeassociatedwithdiabetesinsipidusand
meningitis.
Eyedisease
• Granulomatous lesionsmayobstruct thenasolacrimalduct and causeorbital
pseudotumour, with optic nervecompressionfrommasses developing in the
retrobulbarspace.
• Rarely a purulentsinusitismay spread andcausesecondary bacterial orbital
infection.
• ManifestationsinthegeneralizedstageofGPAincludeepiscleritis(redeye),
vasculitisoftheopticnerve,andocclusionofretinalarteries,inadditiontothe

granulomatouslesionsdescribedearlier.
Investigation
(See Table4.3,p.214forlaboratoryteststoconsider.)
• A biopsy should be done in patients with suspected AAV to confirm the
diagnosis. In some patients, biopsy is not feasible and so a presumptive
diagnosisismadeontheclinicalfeaturesandANCA.
• Laboratory investigation should include FBC with differential, routine
chemistry,ESR,CRP,andurinalysistolookforactivesediment.
• ApositiveANCAstronglysuggeststhediagnosisofvasculitis;however,false-
positiveandfalse-negativeresultsareseen.
• About 82% of patients with GPA have a positive ANCA. This is usually
specificforproteinase-3.
• 10%ofGPAcasesareANCAnegative.AnegativeANCAdoesnotexclude
thediagnosis.
• CXR and HRCT chest should be considered in all cases as the chance of
pulmonarylesionsishighdespitesometimesfewsymptoms.
Treatment
• TreatmentandprognosisofGPAisdiscussedlaterinthissectionwiththeother
AAVs.
ANCA-associatedvasculitides:microscopicpolyangiitis
• MPAisclassifiedasapulmonary-renal(haemorrhage)syndrome,agroupthat
also includes Goodpasture’s disease and SLE. GPA may also occasionally
presentasapulmonary-renalsyndrome.
• MPA lacks the granulomatous manifestations characteristic of GPA, such as
sinusdiseaseandpulmonarynodules.
• Unlike GPA, MPA is characterized by MPO-ANCA antibodies, which are
associated with a P-ANCA immunofluorescence pattern. Up to 80% of
patientswithMPAwillbeANCApositive.
• LikePAN,themaletofemaleratiois2:1,withthemajorityofpatientsbeing
Caucasian.Themeanageofpresentationis50years.
• MostpatientswithMPAwillpresentwithrenalinvolvementintheformofa
necrotizingglomerulonephritis,similartowhatcanbeseenwithGPA.Unlike
mostformsofvasculitis,glomerulonephritisfromAAVis‘pauci-immune’(i.e.
there is only minimal immunoglobulin deposition on immunofluorescence
stains).
• Pulmonary haemorrhage presents as haemoptysis, and can be surprisingly
subtle in some patients. Bronchoscopy with bronchoalveolar lavage will
demonstratehaemosiderin-ladenmacrophages.Chronicpulmonarycapillaritis
mayeventuallyleadtopulmonaryfibrosis.
• OtherclinicalfeaturesofthediseaseareshowninTable15.4.
ANCA-associatedvasculitides:eosinophilicgranulomatosiswith
polyangiitis(EGPA/formerlyChurg–Strausssyndrome)
• EGPAisoftendescribedasaclinicaltriadofadult-onsetasthma,eosinophilia,
andvasculitis.
• Typically,theasthmagraduallyworsensinintensityuntilthepatientrequires
dailyoralsteroidsforsymptomcontrol.Manyofthesepatientswillhavebeen
treated with a leukotriene inhibitor (although leukotriene inhibitors do not
causethedisease).
• Peripheral blood hyper-eosinophilia is typically mild and resolves quickly
upontreatmentwithoralsteroids.
• Other manifestations of hyper-eosinophilia include ‘fleeting’ pulmonary
infiltrates, myocarditis, and interstitial nephritis; frank glomerulonephritis is
muchlesscommoninthisdiagnosis.
• Nerve involvement is a common manifestation of vasculitis among patients
with EGPA, and patients should be examined for evidence of a sensory
neuropathyormononeuritismultiplex.
• Cutaneous granulomata that form along the elbows and fingers are called
‘Churg–Strauss nodules’. Ironically, they appear more commonly in
associationwithGPA.
• Cardiac involvement is one of the more serious manifestations of EGPA,
accountingforapproximatelyhalfofalldeathsinpatientswithEGPA.Clinical
manifestationsincludearrhythmias,pericarditis,andheartfailure.
• Treatmentandprognosisinallthesmallvesselandmediumvesselvasculitides
arediscussedattheendofthissection.
ThetreatmentofANCA-associatedvasculitides
• Assessment of disease activity in GPA or MPA is usually done using the
BVAS.
• BVASrangesfrom0to68;withascoreof0indicatingremission.
• AAVaremanagedwithtreatmentaimingtoprovideremissioninductionand
thenremissionmaintenance.
• Currenttreatmentchoicesarebasedonclassifyingpatientsashaving‘severe
generalized disease or poor prognosis’ versus ‘localized, early systemic
diseaseorgoodprognosis’.
• InitialimmunosuppressivetherapyconsistsofGCsincombinationwitheither
CYCorrituximab(RTX).MTXwithGCscanbeusedinpatientswithmild
extrarenaldisease.
• Inaselectgroup,thosewhopresentwithseveredisease,plasmaexchangemay
betried.
SeveregeneralizedGPAandMPA
• TheNationalInstitutesofHealthregimenconsistedof1yearoforalCYC(2
mg/kg daily) with prednisolone (1 mg/kg daily tapered over 6–12 months).
ThishasbeenmodifiedinthelastdecadetominimizeexposuretoCYCand
GCs.
• Theinductionphaseconsistsof3–6monthsofCYC,followedbyeitherAZA
(CYCAZAREMtrial)
5
orMTX(WEGENTtrial)
6
tomaintainremission.
• MMF was found to be inferior compared to AZA in a randomized trial
(IMPROVEtrial).
7
• IVIgleflunomideandcalcineurininhibitorshavebeenusedinasmallnumber
ofpatients,butdatatoaccesstheirefficacyisinsufficient.
• Etanerceptwasfoundtobeineffectiveinmaintainingremissioninaplacebo-
controlledtrial(WGETtrial).
8
• Theoptimallengthofmaintenancetherapyisunclearbutcontinuationfor12–
18monthsafterremissionisreasonableasthemajorityofpatientsflareafter
therapyisdiscontinued.
• The CYCLOPS trial compared daily oral to IV pulse CYC.
9
Bothregimens
resultedinsimilarratesofremission.Extendedfollow-upforadurationof4.3
yearsshowedcomparablesurvivalratesofabout80%,andsimilarsideeffect
profile.However,relapsesweremorecommonwithpulsetherapy.
• RTXhasdemonstratedefficacyandshort-termsafetycomparabletoCYCand
AZA.
• In the RAVE trial, 64% of patients who received RTX for 6 months
discontinuedprednisolonecomparedto53%whohadCYC.
10
RTXwasmore
efficacious compared with CYC in those who had relapsing disease at
baseline.
• At 12 months, 42% of patients in the RTX arm remained in remission
comparedwith38%intheCYCarm.
• IntheRITUXIVAStrial,about90%ofpatientsattainedremissioninboththe
RTXandCYCarms,and90%and85%respectivelyremainedrelapsefreeat
12months.
11
• RTX may be preferable to CYC for induction of remission in patients with
concernsaboutfertilityorthosewithahighriskofmalignancy.
LocalizedandearlygeneralizedGPAandMPA
• Disease may respond to a combination of MTX and prednisolone. In the
NORAMtrial,
12
whichcomparedMTXwithCYC,remissionat6monthswas
achievedinabout90%ofpatientsinbothtreatmentarms.Butrelapsesafter
drugdiscontinuationweresignificantlyhigherinthosegivenMTX.
• Trimethoprim-sulfamethoxazole may decrease the risk of relapse in patients
withlocalizeddisease.
Othertreatments
• Plasma exchangehasbeen used with someeffectinthose with severerenal
disease,althoughthebenefitistransient.
• IVIg has a short-lived benefit, but may be used in patients at high risk of
systemicinfection.
• Treatmentofavasculitis associatedwith aninfectiousdisease(e.g.hepatitis
B-associatedPAN,hepatitisC-associatedcryoglobulinaemicvasculitis)should
includetreatmentofthepathogen.
• There is evidence that respiratory tract infections may trigger a relapse of
GPA. Trimethoprim-sulfamethoxazole in patients with stable disease on
maintenancetherapymaydecreaserespiratoryinfection,andisalsousefulfor
preventionofpneumocystisamongpatientstreatedwithCYC.
EGPA
• Patientswithoutpoorprognosticfactors(FFS=0)achieveremissionwithGCs
alone in >90% of cases. Although about a third may relapse, the long-term
prognosisisexcellent.
• Inpatientswithpoorprognosticfactors(FFS≥1)IVCYCpulsesareeffective.
Flares are frequent on CYC discontinuation. Extrapolating results from
GPA/MPAtrials,AZAmaybeusedformaintainingremission.
• Successful treatment with RTX has been described in case series and case
reports.
• Mepolizumab, an anti-IL5 monoclonal antibody, has demonstrated
encouragingresultsinpilottrials.
PrognosisofANCA-associatedvasculitides
• Prior to the introduction of CYC and GCs, mortality associated with AAV
approached 100%. Modern immunosuppressive regimens have transformed
thesediseasesintochronicconditions,characterizedbycyclesofrelapseand
remission.
• For many patients, the consequences of treatment (such as GC-associated

complications) may lead to greater morbidity than the underlying disease
itself.
• Mortality due to infection continues to be an important consideration for
patients treated for AAV; indeed, patients with ‘treatment-resistant’ AAV
shouldbe carefullyevaluatedforthepresenceofNocardia,Aspergillus, and
otherinfectionsthatcanmimicsomeofthemanifestationsoftheAAV.
References
5. JayneD,Rasmussen N, AndrassyK, etal. A randomized trialof maintenancetherapy for vasculitis
associatedwithantineutrophilcytoplasmicautoantibodies.NEnglJMed2003;349:36–44.
6. Pagnoux C, Mahr A, Hamidou MA, et al. Azathioprine or methotrexate maintenance for ANCA-
associatedvasculitis.NEnglJMed2008;359:2790–803.
7. Hiemstra TF, Walsh M, Mahr A, et al. Mycophenolate mofetil vs azathioprine for remission
maintenanceinantineutrophilcytoplasmicantibody-associatedvasculitis:arandomizedcontrolledtrial.
JAMA2010;304:2381–8.
8. Wegener'sGranulomatosisEtanerceptTrial(WGET)ResearchGroup.Etanerceptplusstandardtherapy
forWegener'sgranulomatosis.NEnglJMed2005;352:351–61.
9. de Groot K, Harper L, Jayne DR, et al. Pulse versus daily oral cyclophosphamide for induction of
remissioninantineutrophilcytoplasmicantibody-associatedvasculitis:arandomizedtrial.AnnIntern
Med2009;150:670–80.
10. Stone JH, Merkel PA, Spiera R, et al. Rituximab versus cyclophosphamide for ANCA-associated
vasculitis.NEnglJMed2010;363:221–32.
11. JonesRB,TervaertJW,HauserT,etal.RituximabversuscyclophosphamideinANCA-associatedrenal
vasculitis.NEnglJMed2010;363:211–20.
12. De Groot K, Rasmussen N, Bacon PA, et al. Randomized trial of cyclophosphamide versus
methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-
associatedvasculitis.Rheum2005;52:2461–9.
Smallvesselvasculitis
The definition of small vessel vasculitis is open to different interpretations.
Small vessel disease can be one feature of GPA, MPA, and EGPA. However,
therearearangeofclinicalandpathologicalfeaturesthatdefineaspecificgroup
ofsmallvesselvasculitidesoutlinedinTable15.5.Seealso Table4.3,p.214
foradviceonlaboratoryinvestigation.
Leucocytoclasticvasculitis
• Histologically,leucocytoclasticvasculitisappearsasaneutrophilinfiltrationin
and around small vessels, with fragmentation of the neutrophils
(leucocytoclasis), fibrin deposition, and endothelial cell necrosis. Immune
complexdepositionappearstobeimportantinpathogenesis.
• Small vessel vasculitis usually presents in the skin, although the
microvasculatureofanytissuemaybeaffected.
• Some forms ofcutaneousvasculitis are predominantly lymphocytic,without
evidence of neutrophils or leucocytoclasis. However, the division into
leucocytoclastic and non-leucocytoclastic (lymphocytic) vasculitis is not
absolute.Likewise,theclinicalpresentationofcutaneousvasculitiscanvary
considerably.
• The finding of leucocytoclasis should prompt a thorough review of drug
treatment (e.g. sulfonamides, penicillin, thiazides), a search for infection
(hepatitis B, HIV, β-haemolytic streptococcus), a screen for autoimmune
rheumaticdisease, malignancy(in particularmyelo- andlymphoproliferative
diseases), inflammatory bowel disease, chronic active hepatitis, and
cryoglobulinaemia(seelater).
Allergic(hypersensitivity)vasculitis
(Seealso Table4.2,p.212.)
• Allergicvasculitisisthemostcommonpatternofpresentationinadults,both
sexesbeingaffectedequally.
• Non-blanching haemorrhagic papules (palpable purpura), purpuric macules,
plaques, pustules, bullae, and ulcers may occur, classically distributed
maximallyoverthelowerleg.
• A low-grade fever, arthralgias, and microscopic haematuria may accompany
suchpresentation.
• Oftentheconditionisself-limitingandidentifiablecausesshouldbemanaged
as appropriate. Analgesia may be needed and systemic steroids may be
requiredforacuteorgandisease,especiallyprogressiverenalimpairment.
• AZAmaybeappropriateforrefractorydiseasebutremovaloftheoffending
drugorexposureisthemosteffectivetreatmentstrategy.
Table15.5Conditionsassociatedwithsmallvesselvasculitis
Leucocytoclastic
vasculitis
Allergicvasculitis(hypersensitivityangiitis):drugs,
infection,inflammation,autoimmunedisease,malignancy,
Henoch–Schönleinpurpura
Urticarialvasculitis(hypocomplementaemicvasculitis)
Cryoglobulinaemia
Hypergammaglobulinaemia
Erythemaelevatumdiutinumandgranuloma
faciale
Non-
Drugs(penicillins,thiazides)
leucocytoclastic
vasculitis
(lymphocytic
vasculitis)
Nodularvasculitis(see ‘Panniculitis’,p.560)
Livedoidvasculitis
Pityriasislichenoides
Henöch–Schönleinpurpura(HSP;IgAvasculitis)
• HSPoccursmostofteninchildren(see ‘Childhood-onsetvasculitides’,pp.
474–481),butcanaffectadultsofanyage.IgAisusuallydetectedinskin,gut,
orrenalbiopsies.
• The classic presentation is with purpura, and in adults: arthritis (50%),
haemorrhagicGIdisease(40%),andglomerulonephritis(50%).
• GCs given early may relieve joint and GI symptoms, but there is little
evidence that they prevent progression of renal disease or influence overall
outcome.
• If renal function is rapidly deteriorating, pulsed methylprednisolone and/or
plasmapheresismaybeofbenefit.
• Patientswhopresentwithanephriticornephroticsyndromehaveanincreased
lifetimeprevalenceofrenalcomplications,includinghypertension.
• Although most cases are self-limited, HSP can (rarely) become a chronic,
relapsing disease. Such patients should be evaluated for the presence of a
monoclonalIgAantibody,whichmayheraldapre-malignantlesion.
Urticarialvasculitis
• Urticarial lesions with arthralgias are the most common features of this
condition,withmenoutnumberingwomenby2:1.Thetypicalageofonsetis
40–50years.
• Morphologically, theskinlesions resembleordinary urticariaandsometimes
maybemistakenforerythemamultiforme.
• Unlikeordinaryurticaria,urticarialvasculitistendstolastfordays(nothours)
andtendtobeburningandpainful(notpruritic).
• Patientswithhypocomplementaemicurticarialvasculitistendtodevelopmore
systemic features such as renal, GI, and pulmonary disease. Less common
manifestations include lymphadenopathy, uveitis, and benign intracranial
hypertension.
• Systemic antihistamines are widely used, but their effects tend to be
disappointing.
• Thereareanecdotalreportsofsuccesswithindometacin,hydroxychloroquine
(HCQ), colchicine, ciclosporin, and dapsone. AZA may be particularly

effective.
• For the majority of patients, the condition is chronic and benign. For those
withend-organdamage,chronicimmunosuppressionmaybenecessary.
Cryoglobulinaemicvasculitis
• Cryoglobulins are immunoglobulins that precipitate when cold. They are
dividedintothreetypes:typeI(monoclonal),typeII(mixedmonoclonaland
polyclonal),andtypeIII(polyclonal).
• Mixed cryoglobulins are associated with autoimmune rheumatic diseases,
infection,andlymphoproliferativedisorders.HepatitisBandCviralinfection
shouldalwaysbeexcluded;thelatterinparticularisstronglyassociatedwith
mixedessentialcryoglobulinaemia.
• Mixed essential cryoglobulinaemia presents with purpuric skin lesions
showing a leucocytoclastic vasculitis on biopsy; polyarthralgias (70%),
weakness, progressive renal disease (55%), and transaminitis (70%) are
common.
• Womenareaffectedtwiceasfrequentlyasmen.
• Lesscommonproblemsincludeoedema,hypertension,legulcers,Raynaud’s
disease, abdominal pain, neuropathy, and susceptibility to bacterial
pneumonia.
• Theprognosisisworsewithrenaldisease.
• The main causes of death among patients with cryoglobulinaemia include
renalfailureandinfection.
• Treatmentrequiresmanagementoftheunderlyingcause;immunosuppression
byitselfisfrequentlyunsatisfactory.
• Choice of immunosuppression should be dictated by the disease
manifestations;themostsevereformsmayrequiretreatmentwithCYC,pulse
steroids,andplasmapheresis.
Hypergammaglobulinaemicpurpura
• This is a rare, benign IgM condition presenting as long-standing
leucocytoclastic purpura similar to the cutaneous features of Sjögren’s
syndrome(see Chapter12).
• It should not be confused with Waldenström’s macroglobulinaemia, a
monoclonalIgMparaproteinaemiaassociatedwithlymphoma.
Erythemaelevatumdiutinumandgranulomafaciale
• These are rare distinctive forms of chronic localized leucocytoclastic
vasculitis.Therearenosystemiceffectsandtheaetiologyisunknown.
• Erythema elevatum diutinum (EED) is characterized by slowly enlarging

oedematous purplish-brown plaques or blisters over the backs of the hands,
elbows, or knees. They heal very slowly (months to years) with fibrosis. It
mayrespondtodapsone.
• Granuloma faciale (GF) presents as single or multiple pink-brown, well-
defined,smoothpapulesandplaquesontheface.Theypersistforyears.Itis
distinguished histologically from EED by the presence of eosinophils and a
normal collagen beneath the epidermis. It may respond to intralesional
steroids.
Non-leucocytoclastic(lymphocytic)vasculitides
• Thedifferentialdiagnosisofnodularformsofcutaneousvasculitisembracesa
wide range of disorders, including the panniculitides (see Chapter 18 and
Chapter4,p.206).
• Nodular vasculitis is regarded as a distinct group characterized by recurrent
subcutaneous nodules. Patients are otherwise healthy though it may be
associatedwithstreptococcalinfection.
• Bazin’s disease is sometimes used to describe the nodular vasculitis that
occurs in tuberculosis. The condition resolves spontaneously, but may take
manyyears.Intralesionaltriamcinolonemayhelp.
• Livedoid vasculitis is characterized histologically by endothelial cell
proliferationandintraluminalthrombosisleadingtoischaemia.
• Livedoid vasculitis has been attributed to defects in the tissue plasminogen
activator (tPA) gene, although similar lesions can be seen in the
antiphospholipid syndrome. The lesions heal with white atrophic scar
(‘atrophieblanche’).
• Pityriasislichenoidesisanuncommondisorderofpinkpapules,whichenlarge
rapidly and may become haemorrhagic before becoming necrotic and heal
with scarring. It is usually self-limiting and may respond to ultraviolet B
irradiation.
Childhood-onsetvasculitides
• The primary vasculitides in children are rare but life-threatening conditions.
ThecommonestareKawasakidisease(KD)andtheacuteusuallyself-limiting
Henoch–Schönleinpurpura(HSP).
• Suspicion of the chronic vasculitides (Table 15.6) arises in the presence of
fever(oftenlowgrade),weightloss,rash,andmultisystemclinicalfeatures.
• Asinadults,perivascularinflammationoccursandthesiteandsizeofaffected
vesselsinfluencesthespectrumofpresentation.
• Ahistoryshouldbetakenofinfection,immunizations,familyhistoryanddrug
exposure.
• The first paediatric specific classification of vasculitis by EULAR and the
PediatricRheumatologyEuropeanSociety(PRES)wasdevelopedin2005and
validatedin2010.
Table15.6Childhood-onsetvasculitides
Predominantlylargevessel Takayasuarteritis
Predominantlymedium-sizedvessel Kawasakidisease
SystemicPAN
Cutaneouspolyarteritis
Predominantlysmallvessel Non-granulomatous:
HSP,leucocytoclastic,MPA,
urticarialvasculitis
Granulomatous:
GPA/Wegener’s;EGPA/Churg–
Strauss
Variablesizedvesselinvolvement Behçet’sdisease
Childhoodprimaryangiitisof
theCNS
Cogan’ssyndrome
Associatedwithsystemicdiseasesor
clearaetiologicfactors
Relapsingpolychondritis
Cryoglobulinaemia(/hepatitisC)
Malignancies
Autoimmuneconnectivetissue
diseasesDrugs
Epidemiologyofchildhoodvasculitis
Theincidenceandprevalenceofchildhood-onsetvasculitidesarenotaccurately
describedandvarydependingonthepopulationstudied.
• TheprevalenceofHSPis3–20per100,000ofthegeneralpopulation,andof
KDis9–32per100,000ofthepopulationintheUSAand134per100,000of
thepopulationinJapan.
• The other childhood-onset vasculitides occur in 1–10 per million of the
population.
Kawasakidisease
• KD is the leading cause of childhood acquired heart disease in developed
countries and includes coronary artery aneurysms (in 15–25% of untreated
cases)whichoftenappearlate.
• Pericarditis,myocarditis,andmyocardialinfarctionmayoccur.
• WithrapiddetectionandIVIgtreatment,aneurysmsoccurinlessthan5–10%
ofpatientsandmortalityisreducedfrom3–4%to<1%.
• The burden of adult cardiovascular disease and premature atherosclerosis is
thesubjectofongoingresearch.
Epidemiologyandpathogenesis
• TheannualUKincidenceofKDis5–8per100,000ofthepopulation,witha
peakincidenceinchildrenaged1–2years (0–5years typically),differingto
Japanwithapeakat6–12monthsofage.
• 5–10%ofKDcasesoccurinchildrenaged5–10years.
• Theaetiologyisunknown.Pronouncedseasonalityandclusteringsuggestsan
infectiousorenvironmentaltriggeringeneticallysusceptibleindividuals.
• Recentepidemicshavebeenlinkedtolarge-scaletroposphericwindcurrents
originatingincentralAsia.
Presentation
• Diagnosticcriteriarequireahighspikingfever(usually≥40°C)for≥5days;
plus≥4ofthefollowing(allcriteriaarenotrequiredatonetime):
• Widespreadpolymorphicerythematousrash.
• Bilateralconjunctivalinjectionorcongestion.
• Reddening of the palms and soles, indurative oedema, and subsequent
desquamation(Beaulinesareseeninretrospect).
• Reddening/cracking of lips, strawberry tongue, oral and pharyngeal
injection.
• Acute,usuallysingle(>1.5cm),non-purulentcervicallymphadenopathy.
• Fevermayoccurabruptlybutthereisaprodromeincludingcoryza,abdominal
pain,diarrhoea,vomiting,andarthralgia.
• Irritabilityisconsidereduniversal.
• KDisalsodiagnosedwhenthereare<5featureswithcoronaryaneurysmor
dilatationorinaninfantwithpronouncedirritability.
• Incomplete KD is diagnosed in patients with a fever and fewer than 4
additionalfeaturessothattheyreceiveIVIgbefore10daysfromfeveronset.
Thisismostcommonininfants.
• Atypical KD is diagnosed in children older than 9 years, younger than 6
months,andwhenthereareadditionalinflammatoryfeatures.
• Other features include induration or redness at the BCG inoculation site;
arthritis, uveitis, aseptic meningitis, pneumonitis, intestinal obstruction,
hydrops of the gallbladder and jaundice, encephalopathy, macrophage
activationsyndrome,andSIADH.
• Persisting additional features should raise the possibility of alternative
diagnoses.Coronaryectasiacanoccurinotherconditionsincludingsystemic
onsetJIA,TA,andPAN.
Investigations
• Echocardiographyshouldbedoneatdiagnosis,2weeks,and6–8weeksafter
disease onset to detect myocardial inflammation and coronary aneurysmal
formation.
• ECGwillshowconductiondefects.
• There are no diagnostic blood tests but marked thrombocytosis may alert
clinicianstoKD.
• Viral serology (IgG and IgM) for mycoplasma pneumonia, enterovirus,
adenovirus,measles,parvovirus,Epstein–Barrvirus,andcytomegaloviruscan
bepositive.
Treatment
Thereductioninriskoflong-termcardiacdiseaseisbestachievedwithIVIgand
aspirinstartedwithin10daysofonsetoffever.
• IVIgreducestheriskofcoronaryarteryaneurysmformationfromabout20%
to6%.
• IVIg(2g/kg)isadministeredover10–12hours,exceptininfantswithcardiac
failurewhenthedoseissplitover2–4days.
• If the fever recurs or persists 36 hours after initial IVIg, a second dose is
given.
• Although the evidence supports early use of IVIg, it may be given after 10
daysofillness.
• Aspirinisinitiallygivenatadoseof80–100mg/kg/day,andreducedto2–5
mg/kg/daywhenthefeverhassettled(lowdose).
• Low-dose aspirin can be continued for a minimum of 6 weeks. It is then
stopped if echocardiography is normal or when aneurysms have returned to
normal.
• However,thereisdebateovertheuseofaspirinasRCTdataarenotavailable,
andthepositiveconsiderationsofitsusemustbebalancedagainsttheriskof
Reyesyndrome.
• Clopidogrel or dipyridamole may be temporarily substituted for aspirin in
patients who develop influenza or varicella. Warfarin is substituted in the
presenceofgiantaneurysms(>8mm).
• FeverthatrecursaftertwodosesofIVIgistermedIVIgresistanceandoccurs
in10–20%ofcases.Itisassociatedwithanincreasedriskofaneurysm.
• IVIg resistance is often treated with IV methylprednisolone 30 mg/kg
(maximum1g)for1–3daysfollowedbyoralprednisolone(1–2mg/kgdaily)
thenwithgradualdosereduction.
• Alternatively,infliximab(5mg/kg)isassociatedwithfewerdaysoffeverand
hospitalization compared to a second dose of IVIg, but a reduced rate
aneurysmformationhasnotyetbeendefined.
Henoch–Schönleinpurpura
• HSPisthemostcommonsystemicvasculitisinchildhood.
• HSP is a small vessel, non-granulomatous IgA leucocytoclastic vasculitis of
unknownaetiology.
• HSP is generally a benign, self-limiting disease with most patients
experiencingafullresolutionwithin8weeks(<5%ofpatientsdevelopchronic
symptoms).
• One-thirdofchildrenhavesymptomsforuptoafortnight,andanotherthird
foruptoa1month.
• Recurrentdiseaseoccursin50%within6weeks.
• HSPnephritisaccountsforupto3%ofallchildhoodcasesofend-stagerenal
failure(ESRF)intheUK.
Epidemiology
• UK incidence is 20 per 100,000 of the general population per year
(0.8/100,000inadults).
• 75%occursattheageof2–11years,andisrareininfancy.
• HSP is most prevalent during the winter and spring, and associations have
been considered with infectious disease such as group A streptococci,
hepatitis,CMV,HSV,humanparvovirusB19,coxsackievirus,adenovirus,and
somevaccinations.
Presentationandclinicalfeatures
• HSPhasacharacteristicpurpuricrash(in95%atpresentation)affectingbacks
ofthelegs,buttocks,andarms,andinchildrenneedstobedistinguishedfrom
meningococcalsepticaemia, acutehaemorrhagic oedemaof infancy, immune
thrombocytopenic purpura, acute post-streptococcal glomerulonephritis,
haemolytic-uraemicsyndrome.
• Purpurararelyinvolvestrunkorface.Urticaria,angio-oedema,deepbruising,
ornecroticappearancesmayalsooccur.
• Abdominalpainmayprecedetherashby2weeksandmaybeassociatedwith
vomiting,haematemesis,andmelena.
• GI complications are rare but include intussusception, appendicitis,
cholecystitis,pancreatitis,ulceration,infarction,andperforation.
• Arthralgiaorarthritis(47%ofcases),typicallyofthekneesandankles,tends
tobeself-limiting.
• Nephritisaffects25–60%ofpatients.
• However,<5%ofcasesprogresstoCKD,andonly1–2%toESRF(20%of
childrenwithrenaldiseaseandover10–25years).
• Renalprognosisisbestinchildren<7years.
• Renaldiseaseoccursin97%ofchildrenwithin3monthsofdiseaseonsetbut
generally <10% of patients require renal biopsy (usually for persisting
haematuriaandnephropathy).
• Rare manifestations include orchitis, pulmonary haemorrhage, and cerebral
vasculitis.
Treatmentandmonitoring
• NotreatmenthasbeenshowntoshortenthedurationofHSPorsignificantly
improvelong-termrenaloutcome.
• Treatmentisprimarilysymptomatic(rest,analgesia,andhydration).
• Admission can be helpful where there is severe abdominal pain, GI
haemorrhageandrenalfailureandoccasionallyforarthritis.
• Glucocorticoids (GCs) are used for symptomatic improvement and severe
facialorscrotaloedema.Prednisolonedoseisadjustedaccordingtoresponse
and typically started at 1 mg/kg/day orally for 5 days. If higher doses or
methylprednisoloneareused,tertiarycentreinputisrecommended.
• GCs are also used for persisting renal disease and where there are >50%
crescenticglomerularinvolvementonrenalbiopsy.
• Severe renal involvement may require GC-sparing immunosuppression,
antiproteinuric,andantihypertensiveagents.
• Monitoring of the condition should be weekly for the first month, alternate
weeks for 1 month and then monthly—the frequency increasing with renal
involvement.
• Monthlyurinalysisscreeningisrecommendedupto6months.
Leucocytoclasticvasculitis
Leucocytoclasticvasculitisisacommonsmallvesselvasculitisinchildrenand

presents as palpable purpura often with urticaria, vesicles, bullae, or pustules,
butnotitch,pain,orburning.
Presentationandclinicalfeatures
• Internalinvolvementmayincludejoints,GIsystem,andrenalsystem.
• About 50% of cases may be idiopathic, 10–15% secondary to autoimmune
disease (e.g. RA, SLE, IBD),about5%areassociatedwithmalignancy and
other cases attributed to medications or herbal remedies, food additives, or
primarilyunderlyinginfection.
• ~10%ofpatientshavechronicorrecurrentdisease.
• Erythemaelevatumdiutinumandgranulomafacialeareraredistinctiveforms
ofdisease(withpink/purple-brownwell-definedlesions).
Investigations
(Seealso Table4.2,p.212andTable4.3,p.214.)
• Investigations are for underlying infections (group A streptococci, viral
hepatitis,andHIV),autoimmunityormalignancy.
• Measure total haemolytic complement (CH50 or CH100), C3, C4, anti-C1q
antibodiesifurticarialvasculitisisbeingconsideredandcryoglobulinsifthere
isasuggestionofprevioushepatitisC.
• Consider askinbiopsy ifthere ismultisysteminvolvementandappearances
arenottypicalofHSP.
Treatment
• Treatunderlyingconditionsandwithdrawsuspiciousmedications
• TreatmentofprimarydiseaseincludesGCs,colchicine,HCQ,dapsone,AZA,
orMTX.
• RTXhasbeenshowntobemoreeffectivethanCYCforthosewithsystemic
involvement.
Cutaneouspolyarteritisnodosa
CutaneousPANisapaediatricconditionthatrunsabenigncourse,overmonths
toyears,distinctfromsystemicpolyarteritisnodosa.
Presentationandclinicalfeatures
• Arthralgias, myalgias, and neuralgia may occur, but there is invariably no
internalorgandamage.
• Distinct from a leucocytoclastic vasculitis, cutaneous PAN results in larger
inflammatoryplaques,tenderlumpsanderythemanodosum(orotherformsof
panniculitis),ulceration.

• Infarcts attributable to medium vessel and pan-arteritis involvement. Post-
inflammatorypigmentationmayoccur.
• TriggersincludeStreptococcusA,hepatitisBandC,HIV,andparvovirusB19.
Investigations
• Skinbiopsyshouldconfirmthediagnosis.Seealso Table4.3,pp.213–214.
Treatment
• Prednisolone is considered the mainstay of treatment, although there are no
RCTsforglucocorticoids,colchicine,IVIg,orMTX.
• PenicillinisgivenforStrepAinfection.
• Symptomatictreatmentisoftenrequiredforpainandulcers.
(Systemic)Polyarteritisnodosa
• PANisthethirdmostcommonvasculitisinchildrenandadolescents.
• Childhood PAN is now more common than PAN in adults since the
introductionofhepatitisBvaccine.
• PANhasanincidenceof3–7per100,000peryear.
• PAN characterized by a necrotizing vasculitis of medium-sized arteries,
aneurysmal formation, thrombi, ischaemia, and infarction. It spares the
smallestvesselsandvenules.
Presentationandclinicalfeatures
• PANshouldbeconsideredinpatientswithmalaise,fever,weightloss(>5%),
myalgia,arthropathy,and:
• vasculiticrash(especiallyonthelegs,palms,orsoles).
• mono/polyneuropathy(puresensoryormotorormixed).
• testiculartendernessorpain.
• muscletendernessorfocalweakness.
• PANisusuallyidiopathic,butmaybesecondarytoviralhepatitis.
• Permanent morbidity is relatively rare but relapses occur in 35–50% over a
meanof6years.
• Mortalityis4%over5yearsimprovedfrom87%withouttreatment.
• Complicationscaninclude:
• ulcerationsandgangrene.
• stroke,encephalopathy,myelopathy,andneuropathy.
• pericarditis,coronaryaneurysms,MI,andheartfailure.
• GIbleedingandinfarction.
• renalfailure.
• However,lungsarerarelyaffected.

Investigations
• Routine haematology, ESR, CRP, liver and renal biochemistry, CK, and
hepatitisserologyshouldbechecked.Seealso Table4.3,p.214.
• Conventional renal and mesenteric angiography shows aneurysms and
stenoses(notgenerallyshownbyCTorMRIangiography).
• ConsiderEMG,suralnerve,andmuscle(e.g.vastuslateralis)biopsy.
• Biopsy ofnodules anddeepdermalulcermarginsmaybehelpful; however,
renalbiopsyisunhelpfulandoftenassociatedwithpostoperativebleedingand
fistulae.
• Other features include hypertension, retinal vasculitis, unexplained
tachycardia, psychiatric symptoms, polymyositis, livedo reticularis, and
Raynaud’sdisease.
Treatmentandprognosis
• Active or latent hepatitis B may require concurrent antiviral therapy (e.g.
lamivudine)inadditiontoimmunosuppression.
• GCtherapyshouldbecombinedwitheitherMMF,MTX,orAZA.
• CYCisusedforseriousorganinvolvementorsteroid-refractorydisease.
• Theroleofplasmapheresisremainstobedetermined.
• Prognosticscoring,usingtheFFSmaybeuseful(FFS=1hasamortalityof
25%;FFS =2 hasamortalityof45%;etc.).The fivefactors—each scoring
one—are.
• Renalfailure.
• Proteinuria(>1g/dL).
• GIbleedorperforationorinfarctionorpancreatitis.
• Cardiomyopathy.
• CNSinvolvement(<10%).
Primaryangiitisofcentralnervoussysteminchildren(cPACNS)
• CNSvasculitisisincreasinglyrecognizedinchildrenbutpresentsadiagnostic
challenge.Alackofconsensusondiseaseclassificationhasmadeitdifficultto
establishthetrueincidenceofthedisease.
• Brainworks ( http//www.sickkids.ca/research/brainworks/) is helping to
better clarify this condition and provides support when there is diagnostic
uncertainty.
• Secondary CNS vasculitis occurs in a broad set of systemic conditions,
includingneurosarcoidosis,whichisadifferentialdiagnosis.
Presentationandclinicalfeatures
• Clinical presentation is typically with non-focal symptoms including
headachesandalteredmentalstate(in50%ofcases).
• Alternatively, children present with localizing symptoms include lateralized
weakness(30%),aphasia,ataxia,visualsymptoms,andseizures(each~15%).
• Thespinalcordisinvolvedin5–15%ofcases.
• Systemicfeaturesarerare.
• MimicsofCNSvasculitisshouldbeconsidered,andinclude:
• Moyamoyadisease.
• Thrombophilicconditions(e.g.antiphospholipidsyndrome).
• Neurologicalconditions(e.g.multiplesclerosis,Devic’sdisease).
• Metabolicconditions.
• Sarcoidosis.
• Malignancy.
Investigations
• Diagnosticcriteria
13
require:
• Anacquiredneurologicaldeficit.
• Angiographicand/orhistopathologicalfeaturesofCNSangiitis.
• Absenceofasystemiccondition.
• Catheterarteriographyisthegoldstandarddiagnostictestduetoanabilityto
detect distal lesions affecting smaller vessels and identify lesions in the
posteriorpartofthebrain.
• MRI of brain and/or spine and MRA may demonstrate acute ischaemia of
varying patterns dependent on size of vessel involve and use of diffusion-
weightedimaging(forlargevesseldisease).
• Meningeal enhancement may be seen with MRA which can reveal beading,
tortuosity,stenosis,andocclusionofthevessels.
• Brain biopsy should be considered for difficult cases when arteriography is
negativeorincaseswithapoorresponsetotherapy.
Treatmentandprognosis
• Current therapeutic recommendations are similar to those for systemic
vasculitis:
• InductionwithIVCYC,GCsandlow-doseaspirin.
• 1–2-yearmaintenancetherapywithMMForAZA,simultaneouslyreducing
thedoseofprednisolonebutcontinuingaspirin.
• Fullanticoagulationmayneedtobeconsidered.
• A poor prognosis is suggested by presentation with neurocognitive
dysfunction, seizures, multifocal parenchymal lesions on MRI, or distal
stenosisonarteriography.
ANCA-associatedvasculitides(AAVs)
• Using internationally recognized diagnostic criteria and algorithms, 80% of
paediatricAAVpatientsareGPA,15%areMPA,and5%areEGPA.Casesof
renal-limitedvasculitis(crescenticglomerulonephritis)arealsoincluded.
• The Paediatric Vasculitis Activity Score, PVAS (modified from BVAS), has
beenvalidatedforobjectiveassessmentofchildhoodvasculitis.
• Of all AAV childhood cases, 55% are cANCA positive (almost consistently
PR3 positive), 30% are pANCA positive (90% MPO positive), and 3% are
mixedcytoplasmicandperinuclear.
• Medianageatdiagnosisis14yearswitharelativelyhighburdenofdisease
(medianPVASof19).
• Timefromsymptomonsettodiagnosis isnowquick,averaging2.5 months,
butratesoforgandamageatthistimearestillhigh.
• 80%ofpatientshavepulmonaryorrenaldisease;60%haveboth.
• Pulmonary presentations include alveolar haemorrhage and massive
haemoptysis.
• 10–20%ofcasespresentinrenalfailurewhichrequiresdialysisand5%have
end-stagerenaldisease.
• ENTinvolvementoccursin60%andMSKin50%.
• CYCandGCshavebeenusedmostcommonlytoinducediseaseremissionbut
inkeepingwithpracticewithadultcases,RTXisincreasinglyused.
• The choice of maintenance therapy after induction of remission includes
MTX,AZA,andMMF.
• Plasmapheresis is usually for pulmonary-renal syndrome and alveolar
haemorrhage.
• Low-doseaspirinisusedtodecreasethrombosisrisk.
• Co-trimoxazoleusefornasalStaphylococcuscarriageiscontroversial.
• Highlevelsoforgandamagestilloccur.InonelargestudyofGPAinchildren,
40%hadchronicrenalimpairmentat3yearsofdiseaseduration.
Reference
13. CalabreseLH,FurlanAJ,GraggLA,etal.Primaryangiitisofthecentralnervoussystem:diagnostic
criteriaandclinicalapproach.CleveClinJMed1992;59:293–306.
Chapter16
Metabolicbonediseases
Osteoporosis
VitaminDdeficiency,osteomalacia,andrickets
Hypercalcaemia,parathyroiddisease,andrelateddisorders
Paget’sdiseaseofbone
Childhoodautoinflammatorybonediseases
SAPHOsyndrome
Theosteochondroses
Osteonecrosis
Fibrousdysplasia
Sclerosingbonedisorders
Bonetumours
Osteogenesisimperfectaisincludedin Chapter19
Osteoporosis
Osteoporosiscanbedefinedasadecreaseinbonemassandstrengthresultingin
anincreasedriskoffracturewithminimalornotrauma(‘fragilityfracture’).
• OsteoporosiscanbedefinedusingdualX-rayabsorptiometry(DXA)toderive
anestimateofbonemineraldensity(BMD).
• The clinical consequence of osteoporosis is fragility fracture and its
consequences, which include pain, skeletal deformity, functional loss
(includinglossofmobilityandindependenceintheelderly),andreducedlife
expectancy(e.g.hipfractureintheelderly).
• Theriskofosteoporoticfractureisgreaterinwomenthaninmenandvaries
withsite(Table16.1).
Table16.1Riskofosteoporoticfracturewithsite
Fracturesite Overalllifetimeriskoffracture(%)
Men Women
Hip 6 18
Vertebral 5 16
Distalforearm 2–3 16
Anyofabove 13 40
Pathogenesisandclassification
• Duringchildhoodandadolescence,growthandskeletalmodellingleadtoan
increaseinthesize,shape,strength,andcompositionofbone.Growthceases
with the closure of the growth plates (epiphyseal cartilage). However,
remodelling and mineral homeostasis continue throughout life with bone
resorptionanddepositioncoupledbytheinteractionbetweenosteoclastsand
osteoblasts,respectively.
• Peakbonemass/BMDormaximalbonedensityisusuallyachievedinthethird
decade. Peak bone mass is determined by both genetic and environmental
factors.
• Afterabouttheageof35years,theamountofboneproducedislessthanthat
resorbed during each remodelling cycle. The net effect is an age-related
decreaseinbonemass.TrabecularandcorticalBMDdeclineby~6%and3%
respectivelyperdecade.
• Acceleratedbonelossoccursatthetimeofmenopausewithdecliningovarian
functionandcirculatingoestrogen.Upto15%ofbonemasscanbelostover
the 5-year period immediately after menopause. The andropause (decreased
circulatingbioavailabletestosterone,sodecreasedaromatizationtooestrogen)
occursformanymenovermanyyearsthroughlate-middleandadvancedage.
ThereisamoderatecorrelationbetweenserumtestosteroneandBMD.
• Themechanismofage-relatedbonelossismultifactorialandisaconsequence
ofgenetic,environmental,andcomorbidinfluences:
• decreasedintestinalcalciumabsorption.
• decreasedsynthesisofvitaminD.
• hyperparathyroidism(causedbytheabove).
• factorsincreasingosteoclastfunction(e.g.oestrogenlack).
• reduced osteoblast development (e.g. ageing-related stem cell fate—away
fromosteoblastinfavourofadipocyte).
• increasing immobility reducing the physical stress on bone leading to
activationofboneresorption.
• Riskfactorsforosteoporosis(seealsoTable16.2)include:
• race(CaucasianorAsian>AfroCaribbean).
• increasingageandfemalegender.
• positivefamilyhistory(especiallyparentalhipfracture).
• previous‘fragility’fracture.
• drugs(e.g.glucocorticoid(GC)therapy).
• chronicinflammatorydiseases(e.g.RA,Crohn’sdisease,AS)
• malabsorption(e.g.coeliacdisease)
• endocrinopathies(e.g.hyperparathyroidism,Cushing’ssyndrome)
• lowbodymassindex(BMI<18).
• shortfertileperiod(latemenarche,earlymenopause).
• diseasesofbonemarrow(e.g.mastocytosis,Gaucherdisease)
• immobility,sedentarylifestyle.
• lowintakeofcalcium(<240mgdaily).
• excessivealcoholintake.
• smoking.
• The World Health Organization has developed a Fracture Assessment Tool
(FRAX; htpp://www.shef.ac.uk/FRAX) to identify patients at risk of
fragility fracture. BMD measurement is incorporated into FRAX. Assessing
BMD alone to predict fragility fracture may lead to an incomplete fragility
fracture risk profile. FRAX takes account of many of the major BMD-
independentfragilityfractureriskfactors(withtheexceptionoffallsrisk)and
allowsacalculationofa10-yearriskoffragilityfracture:
• age,lowBMI,andgender.
• priorfragilityfracture.
• GCuse.
• parentalhistoryofhipfracture.
• rheumatoidarthritis.
• secondaryosteoporosis(selectedcauses).
• currentsmokeranddailyalcohol>3units.
Table16.2Diseasesthatcause,orareassociatedwith,osteoporosis(incomplete)
Malignancies Multiplemyeloma
Leukaemia
Lymphoma
Endocrine Hyperparathyroidism
Hypopituitarism
Thyrotoxicosis
Hypogonadism
Cushing’ssyndrome
Diabetes(T1DM/T2DM)
Turner’ssyndrome
Chronicinflammatorydiseases Rheumatoidarthritis
Ankylosingspondylitis
Crohn’sdisease
Cysticfibrosis
Metabolicdiseases Gaucherdisease
Chronickidneydiseases
3b–5
Alcoholism
Skeletaldiseases Osteogenesisimperfecta
Mastocytosis
Diseasesandconditionsassociatedwith
immobilization
Multiplesclerosis
Paraplegia
Spaceflight
Drugs Glucocorticoids(GCs)
Anticonvulsants
Calcineurininhibitors
Levothyroxine(inexcess)
Heparin
Idiopathicjuvenileosteoporosis
• Idiopathic juvenile osteoporosis (IJO) is uncommon. It occurs before or at
onsetofpuberty.Itaffectsthesexesequally.Thecauseisunknownandthere
arenoconsistentbiochemicalabnormalities.
• IJOshouldbediscriminatedfromosteogenesisimperfecta(OI;see Chapter
19)andosteoporosisfromsecondarycauses(e.g.seeTable16.2).
• The child presents with pain, non-traumatic fractures around the weight-
bearingjoints,andcollapsedvertebrae.Nospecifictreatmentisavailableand
for most, bone mass increases to normal values as puberty progresses;
however,insomecasesfracturesmayleadtodeformity.Supportivephysical

therapyshouldbemadeavailable.
• ChildrenwithIJOandallformsofosteoporosishavelowBMDfortheirage
andskeletaldevelopment.ItisessentialthatDXAscan-derivedBMDdataare
adjusted for skeletal growth if growth deviates from average velocity
significantly (see ISCD position statements online:
https://www.iscd.org/official-positions/) using skeletal growth adjustment
algorithms(forUKdata,usingbonemineralapparentdensity(BMAD)).
Glucocorticoid-inducedosteoporosis(GIO)
• GIO is a common and (as published audits continually suggest) a poorly
managedcondition.
• Numerous guidelines for managing GIO risk exist (e.g. ACR, EULAR,
American Society of Bone Mineral Research (USA), National Osteoporosis
Foundation(USA),NationalOsteoporosisSociety(UK))
• The effects of GIO are greatest in the older patient given the additional
osteoporosisriskfactorsandcomorbiditieslikely.
• TheeffectofGCsontheskeletonismostprofoundwithearlyGCtreatment,
sopreventiveosteoporosisstrategiesneedconsideringatthebeginningofGC
use,particularlyintheelderly.
• Any vitamin D deficiency and secondary hyperparathyroidism requires
correctingattheoutsetofanyGCtreatment.
• GP patient databases suggest patients on long-term inhaled GCs may be at
increased of osteoporosis defined by DXA, but there is no overall evidence
that there is an increased risk of fracture compared to control patients with
underlyinglungdiseases.
• ThepathogenesisofGIOiscomplex.TherearedirecteffectsofGCsonbone
cells and indirect effects through an influence of metabolic and endocrine
factorsthoughconvincingdatainhumansforalltheseeffectsbeingsystematic
arelacking(Table16.3).
• A bisphosphonateshould berecommended,to patients≥65 yearsand50–65
years old with multiple risk factors for osteoporosis, who will take GCs ≥3
monthsandshouldbestartedsimultaneouslywiththeGCs.
• For younger patients FRAX ( http://www.shef.ac.uk/FRAX) is useful to
predictmajorfragilityfractureriskorverylowriskinpatientsbeforestarting
GCs. FRAX can be used without DXA scan data and can be adjusted
dependingonGCdose.
Table16.3Pathogenesisofglucocorticoid-inducedosteoporosis(GIO)
Mechanism Effect
Directeffectsonbone
cells
Reducedrecruitmentofosteoblastsfrombone
marrowprecursors
Induceapoptosisofosteocytes
Possiblecontributing
indirecteffects
Reduceproductionofsexhormones
IncreasedPTHproductionandPTHsensitivity
ReducedGIcalciumabsorption
Decreasedcalciumreabsorptionfromkidney
DecreasedefficiencyofvitaminDactivation
Sarcopeniceffectofsteroids(fallsrisketc.)
Clinicalfeatures
• Osteoporosisfrequentlypresentswithlow-traumafracture.
• Otherpresentationsincludebackpain(vertebralfractureduetoosteoporosis),
lossofheightevidentinthespineby‘xmas-tree’foldsofskinofthebackor
the lower rib cage margin approximating to the iliac crests, thoracic spine
kyphosis (multiple vertebral fractures can cause this though this is not the
commonestcauseforkyphosis).
• Features of the cause of osteoporosis may be obvious or not. For example,
immobilityduetospinalcordinjuryandparaplegia(potentcauseofboneloss)
buthypogonadisminmen,thoughdetectabletoanexperiencedclinician,may
besubtleandrelatively‘invisible’.
• Obviousand/orimportant clinicalfeaturesthatmightbe detectedtoindicate
conditions highly associated with osteoporosis include stigmata for chronic
alcoholexcess,hypogonadismfeaturesinmen,Cushing’sdiseaseappearance,
etc.
• Highfallsriskisanimportantclinicalfeature.Thoughhighfallsriskdoesnot
define osteoporosis, it is arguably the main risk factor for fracture in the
elderly,anditcanbedetectedsystematicallyusingguidelines(seeUKadvice
inNICEClinicalGuideline161).
1
Investigations
• Peopleaged>50yearsoldwhohaveafragilityfractureshouldbeinvestigated
to exclude secondary causes of osteoporosis (e.g. hyperparathyroidism,
CKD3b–5,myeloma,etc.).
• Anyfractureinaperson>75yearssuggestssomedegreeofskeletalfragility,
regardless of DXA scan-derived BMD; tests for underlying disease is
advisable.
• Plainradiographsareaninsensitivemethodofassessingbonemassbutlateral
spinalimagesare useful for stagingpreviousvertebral fractures, whichmay
haveoccurredwithminimalsymptomology.
• ThestandardtechniqueformeasuringBMDisDXA.Itisquick,accurate,low
inradiationdose,andisfairlyprecise.Sitesmeasurableincludelumbarspine,
femoralneck,forearm,andwholebody.
• DXAistypicallyinterpretedintermsofthe T-scoreorZ-score.TheT-score
(usedonlybyconventionforpostmenopausalwomenandmen>50yearsof
age) is the SD multiple difference between the individual’s BMD compared
withthemeanpeakBMDachievedinthethirddecadematchedforgenderand
ethnicity. The Z score (used by convention in premenopausal women and
childrenandallmen<50yearsofage)isthestandarddeviation(SD)multiple
difference between the individual’s BMD and the age/gender/ethnicity-
matched average. T- and Z-scores can be minus values. In postmenopausal
women,foreverySDdecreaseinBMDthereisatwofoldincreaseintherisk
offracture.
• Quantitative CT allows volume measurements and can distinguish between
corticaland trabecularbone invertebrae. Itis, however,costlyandentailsa
highradiationexposure.
• Boneultrasound(US)oftheoscalcishasbeenusedtopredictfracture.Both
theattenuationandspeedofUSinbonemayrelatetomaterialpropertiesof
bonerelevanttofragilityandfracture.
• Bone biopsy (undecalcified transiliac) may be useful in cases of multiple
comorbiditytodiscriminatehighandlowturnoverdiseaseandwhetherthere
isdemineralizationbutisnotroutinelyintheassessmentofosteoporosis.
• Routine biochemical and haematological tests are usually normal in
osteoporosis. High bone turnover disease may be indicated by high bone
turnovermarkers(e.g.collagencrosslinks(CTX)).
• ReductionofCTXhasbeenlinkedwithbisphosphonateresponseandmaybe
anindicatorofdrugadherence.
Preventionofosteoporosisandfragilityfractures
• The prevention of a first fragility (osteoporotic) fracture is termed ‘primary
prevention’ and prevention of second and subsequent fragility fractures
—‘secondaryprevention’(/treatmentofosteoporosis).

• All people who have a fragility fracture after the age of 50 years (or for
women, if post-menopausal) should be assessed for their risk of further
fragilityfractureand osteoporosis.Typically, thiswillbedoneby aFracture
LiaisonService (FLS)linked totheOrthopaedicUnit(secondaryprevention
assessment).
• Underlyingdiseases(knownorunknown)andmodifiableclinicalorlifestyle
issuesrelevanttoskeletalhealthwillbeidentifiedinmanypatientsbysuchan
assessment. FLSs will triage patients for specialist assessment or secondary
fracture prevention management including DXA scanning and considering
osteoporosismedications.
• Primarypreventionisbestundertakenbycase-findingbasedonthepresence
of osteoporosis risk factors, utilizing the FRAX risk factor tool (
http://www.shef.ac.uk/FRAX) then obtaining DXA in people with multiple
riskfactorsorhighscoresonFRAX.Osteoporosistreatmentcanbeconsidered
basedonBMDandfracturerisk.
Calcium
• Calcium intake, either increased by dietary intake or supplements, has not
beenshowntopreventosteoporoticfractures.
• However,chroniccalciumlackleadstosecondaryhyperparathyroidismwhich
cancauseaccelerated bonelossand this maycontribute to osteoporosisand
bonefragility.
• Providingcalciumsupplementsiswiseifthereisalow-calciumdiet(e.g.poor
indairyproducts)and/orsecondaryhyperparathyroidism.
• Calcium supplementation in pre-pubertal children enhances the rate of
increaseinBMDwithagebutwhetherthistranslatesintohigherpeakBMDis
unknown.
• Atpresenttheuseofcalciumsupplementsisrecommendedfor:
• calcium deficiency indicated by secondary hyperparathyroidismifvitamin
Dlevelsarereplete(butreasonablethentoruleoutcoeliacdisease/poorGI
absorption).
• poorcalciumdietparticularlyinchildren(<400mg/day).
• tooptimizetheeffectofbisphosphonatetherapy.
• Therehasbeenconsiderabledebateastowhethercalciumsupplementationis
associatedwithanincreasedriskofcardio/cerebrovasculardisease.
Exercise
• Thereissomeevidencetosuggestthatweight-bearingactivitydecreasesthe
rateofbonelossaroundthemenopause,althoughthelevelandtypeofactivity
remainsunclear.
• Thereislittleimpactof exerciseinimprovingbonemassonceosteoporotic,
althoughitmayaidinpreventingfurtherloss.
• ProfoundlossesofhipBMDintheelderlymaybehighlyandpredominantly
influencedbyreductionofmobility/weight-bearing.
Hormonereplacement
• Oestrogen replacement therapy is an effective way of preventing post-
menopausal bone loss. The addition of a progestogen allows endometrial
sheddingandminimizesriskofneoplasia.
• The minimum oral dose of estradiol required is 1 mg/day, and conjugated
oestrogen 0.3 mg/day. Estradiol gels and transdermal treatments should be
startedat1mg/dayor25micrograms/day,respectively.
• EvidencesuggeststhattheuseofHRTincreasesriskofDVT,coronaryartery
disease,breastcancer,andstroke.HRTshouldthereforebeusedwithcaution,
shouldbetimelimited,andusedwhentherisksofthesediseasesotherwiseis
lowest.
Bisphosphonates
• Weeklyoralbisphosphonates(risedronateoralendronicacid)reducefragility
fracturesby35–50%atthespineandbylessatthehipinwomenwhohave
hadafragilityfractureorosteoporosis-rangeBMD.
• Monthly ibandronic acid 150 mg is also licensed for postmenopausal
osteoporosis.Cyclicaletidronateisnowadaysseldomused.
• Fracturepreventiondatawithoralbisphosphonatesisnotasextensiveformen
as for women but treatment is considered effective for men with fragility
fractureandwithDXA-definedosteoporosis.
• IV zoledronic acid 5 mg given yearly (×3 years original RCT data), is
available if oral therapies fail, are not tolerated or contraindicated. Fracture
preventionisasmuchas70%forvertebralfracturesin3years.
• Ibandronic acid 3 mg IV (‘push’ injection taking just a few seconds) once
every 3 months is licensed also for postmenopausal women and some bone
physicians considered it relatively safe in mild renal impairment, where
zoledronicacidisnotused(i.e.estimatedGFR25–35mL/min/1.73m
2
)and
denosumabiscontraindicated.
• Currently most physicians will review the balance of risks and benefits of
long-term bisphosphonate therapy after 5-year oral, and 3-year parenteral,
bisphosphonate use. For those patients still at high fracture risk though,
treatmentcanbecontinuedforafurther3–5yearsaccordingly.
• The emerging concern about the incidence of atypical femoral fractures
(AFFs)inlong-termbisphosphonateusershaspromptedchangesinstrategic
long-term planning of medications for osteoporosis. AFFs can present with
proximalfemoralbonepainformanymonthsbefore(somewhatcatastrophic)
subtrochantericfracture,andcanbebilateral.Causeisunknownbutthoughtto
beacombinationoflowboneturnover/bonereplacementatasiteofcritical
weight-bearingstressonthefemoralbone.
• Ingeneral,bisphosphatesarewelltolerated,butshouldbeusedwithcautionin
renal impairment (estimated GFR <30 mL/min/1.73 m
2
), history of
oesophagealreflux/hiatushernia,orpoordentitionrequiringdentalwork(risk
ofmandibularosteonecrosis).
• Oralmedicationsshouldbetakenfasting.Absorptionmaybeoptimumiffood
intake is avoided for 60 minutes following taking the tablet. Symptoms of
nauseaandrefluxcanbe lessenedby takingwithplentyofwater andavoid
lyingdownaftertakingthetablet.
• AdherencewithoraltherapyisvariablewithreportsfromtheUSAof<30%,
butreportsintheUKof>80%at2–4years’therapy.Adherenceisbestwhen
treatment is started by a FLS following fragility fracture in comparison to
startingaspartofprimaryfragilityfracturepreventiontreatmentplan.
• TheeffectsofbisphosphonatesareoptimizedifvitaminDremainsrepleteand
there is sufficient calcium intake to prevent deficiency (e.g. no secondary
hyperparathyroidism).
• The therapeutic effect of bisphosphonates can be predicted to a degree by
demonstration of a reduction in bone resorption biomarkers (e.g. CTX)
measuredonserumorplasmabeforeand2monthsaftertreatmentisstarted.
Strontiumranelate
• Strontiumranelate2gdailywasshowntodecreasefractureriskover3years
in men and postmenopausal women (by about 40%), but its use has been
considerably restricted in recent years because it increases vascular disease
risk (e.g. CVD, IHD, and thrombosis). Strontium has now been withdrawn
fromuse.
• Strontium is similar to calcium chemically but much ‘heavier’. It is
incorporatedintothehydroxyapatitebonematrixandnaturallyleadstolarge
increases in BMD, though the relationship of change in BMD to change in
fractureriskisneitherlinearnorproportionaltoBMDchangesassociatedwith
fractureriskreductionseeninothertherapies,forexample.
• The association with markedly increased BMD is important to note when
reviewingserialDXAscandataonpatientspreviouslytreatedwithstrontium.
Teriparatide
• TeriparatideisaparathyroidhormoneanaloguegivenasaSCinjectiondaily
for2years.
• Licensed for use in postmenopausal osteoporosis, though not in men, it
reducedvertebralfractureriskbyabout70%.
• Teriparatideinitiallytriggersosteoblast-mediatedbonematrixproductionthen
an increase in bone turnover. It may achieve therefore a gain in bone
(‘anabolic’)unlikeanti-resorptiontherapies.
• IntheUK,teriparatideisheavilyrestrictedforuseforNHSpostmenopausal
osteoporosis by NICE and cannot be used without specialist application for
individualfundingformenwithosteoporosis.
Denosumab
• Denosumab is a fully human monoclonal antibody that inhibits the RANK
ligand,andisapotentinhibitorofboneresorption.
• DenosumabislicensedinEuropeforarangeofbonelossconditionsincluding
post-menopausal osteoporosis and bone loss in patients being treated with
hormoneablationforprostateandbreastcancer.
• Denosumab 60 mg SC injection once every 6 months reduces vertebral
fractureratebyabout70%inpostmenopausalwomenwithosteoporosisover3
years(FREEDOMtrial).
• TheFREEDOMtrialextensionnowshowsfractureprevention,BMDaccrual,
andnomajorsafetyissuesforupto8years’continuoususe.
Odanacatib
• OdanacatibwasdevelopedacathepsinKinhibitortoinhibitosteoclasticbone
resorption,thenslowingboneloss.
• Phase II data indicate that 50 mg once weekly inhibits bone resorption and
increasesBMD,withonlyatransientdecreaseinboneformation.
• InaphaseIIIRCT,fracturereductionwas shownbutsubsequentlythedrug
waswithdrawnduetoanunacceptablyhighnumberofcerebrovascularevents
inpatientsinthetreatmentarm.
Romosozumab
• Themonoclonalantibodyromosozumabbindstosclerostinthusinhibitingthe
effect of sclerostin, which is an osteocyte-derived inhibitor of osteoblast
activity,thusincreasingboneformation.
• In the phase III FRAME (FRActure study in postmenopausal woMen with
ostEoporosis) study, which enrolled 7180 women, SC 210 mg dose of

romosozumab resulted in a statistically significant 73% reduction in the
relative risk of a new vertebral fracture at 12 months compared to those
receivingplacebo(fractureincidence0.5%vs1.8%,respectively(p<0.001).
• Attimeofgoingtopressthelicensingforromosozumabisonholdpending
furtherinvestigationintocardiovascularadverseeventsinclinicaltrials.
Abaloparatide
• AbaloparatideisanovelsyntheticanalogueofhumanPTHrP(1–34).
• Itcanstimulateboneformationwithlessaccompanyingboneresorptionand
hypercalcaemiceffectsthatcanoccurwithPTH(1–34).
• In postmenopausal osteoporosis, weekly SC abaloparatide, compared with
placebo,reducedtheriskofnewvertebralandnon-vertebralfracturesover18
months(ACTIVEstudy).
• Treatment with a bisphosphonate after an 18-month course of abaloparatide
mayconsolidateBMDandfractureriskreductiongains.
Othertherapies
• Vertebroplasty is the percutaneous injection of bone cement into painful
fractured vertebrae. It can be used to treat osseous haemangiomas and
fracturescausedbymalignancy.
• Initiallyvertebroplastywasreportedtoreducethepainofvertebralfractures
thoughRCTsthenshowedconflictingresults.CurrentlyalargeRCT(vssham
procedure)isinprocess(VERTOSIV).
• Kyphoplasty(ballooninflationinthevertebralbodythenballooninjectedwith
bonecementasforvertebroplasty)isunprovenbyrobuststudyastowhether
there is cost-effectivity of the procedure vs conservative fracture pain
managementorvsvertebroplasty.
Guidelinesformanagingosteoporosis
• In the UK, Europe and North America, numerous societies have generated
guidelinesformanagingosteoporosis.
• IntheUK,NICEguidelinesoperatetocontrolfundingtreatmentsintheNHS.
Guidelinesarebasedoneconomicmodelsofdiseaseandtreatmenteffects,not
on clinical factors alone. The reader is advised to consult the NICE
Technology Appraisal Guidance (TA204 and TA464) and ClinicalGuideline
146.
2
• In the UK the National Osteoporosis Guideline Group regularly posts
consensusguidelines(e.g.see: https://www.shef.ac.uk/NOGG/).
References

1. NICE. Falls in Older People: Assessing Risk and Prevention (CG161). London: NICE, 2017.
https://www.nice.org.uk/guidance/cg161
2. NICECG146. https://www.nice.org.uk/guidance/cg146
VitaminDdeficiency,osteomalacia,andrickets
• Osteomalacia (adults) and rickets (children) are characterized by defective
mineralization of bone and cartilage and the accumulation of unmineralized
bonematrix(osteoid).
• Ricketsisthetermusedforthisdefectingrowingchildrenbeforetheclosure
oftheepiphyses.
• There is considerable debate over the level of 25-hydroxyvitamin D
(25(OH)D)thatconstitutes‘repletion’and‘deficiency’.Forthemajorityofthe
UK population a reasonable ‘repletion’ level is >50 nmol/L and deficiency
level<30nmol/L.Intheelderly,levelsof‘insufficiency’(30–50nmol/L)may
bepathologicallyrelevantandabetter‘repletion’leveltakenas>75nmol/L.
• Therearemanycausesofosteomalacia,butessentiallytheyalloccurdueto
either a deficiency (low sunlight exposure, dietary lack, or suboptimal
metabolism)orresistancetovitaminD,oranon-PTHrelateddefectinrenal
handlingofphosphate(Table16.4).
• Inbothosteomalaciaandrickets,PTHisinvariablyraisedduetovitaminD-
associatedcalciumlack.HighPTHcanincreaseboneturnover/bonelossand
amplifybonelossinosteoporosis.
• BothvitaminD
2
(ergocalciferol)fromvegetablesinthediet,andvitaminD
3
(cholecalciferol) from animal tissues and de novo synthesis in skin, are
metabolizedinthe liverto 25(OH)D(25(OH)D
2
/25(OH)D
3
) and then in the
kidney to 1,25-dihydroxyvitamin D
2
/D
3
respectively: the active forms of
vitaminD.
• 1,25-dihydroxyvitaminD
3
is considered more biologically potent than 1,25-
dihydroxyvitamin D
2
and negatively affects both 1α-hydroxylase (its own
activating enzyme), and transcription of the PTH gene, but increases the
capacityofGIcalciumabsorptionbyenhancingthetranscriptionandtherefore
effectofcalciumsensingreceptors(CaSRs).
• 1,25-dihydroxyvitamin D
3
stimulates bone formation through stimulating
osteoblast differentiation and activity thereby increasing coupled bone
turnover.
• 25(OH)D
3
canbealsobeconvertedinto24,25-dihydroxyvitaminD
3,
whichis
biologicallyinactiveanddestinedforexcretion.

Clinicalandlaboratoryfindings
• Classical symptoms of osteomalacia are bone pain and tenderness, bone
deformity (depending on age of onset), and proximal muscle weakness
(waddlinggait);muscleenzymesandbiopsyarenormal.
• Thehypocalcaemiaofosteomalaciausuallydoesnotcausesymptomsbutcan
cause paraesthesia and tetany. Rarely, it is severe enough to cause cardiac
dysrhythmia,convulsions,orpsychosis.
• Childrenwithricketsmaybehypotonicandapatheticwithgrowthretardation
anddelayedwalking.Onweight-bearing,bonesbecomebowed,andthereis
irregularity of the metaphyseal–epiphyseal junction, usually at the wrist and
costochondraljunctions.The lattergives risetothe feature‘rachitic rosary’.
An indentationmay also arisealongthe attachment ofthediaphragm to the
softenedribs(Harrison’sgroove).Rapidgrowthofthesoftenedskullleadsto
craniotabes,parietalboneflattening,andfrontalbossing.Dentitionisdelayed
andpoor.
• In rickets, many bony deformities persist despite treatment (unless due to
simpledietarydeficiencyandtreatedearly)andmayrequiresurgery,e.g.tibial
osteotomytocorrectlowerlimbalignment.
• The classical radiographic change of osteomalacia is the pseudo-fracture
(Looser’szone).Theseareincompleteradiolucentfracturelinesperpendicular
to the cortex, with poor callus formation and found most often at ribs,
clavicles,pubicrami,femoralneck,metatarsals,andouterborderofscapulae.
• Laboratory investigationsshow low25(OH)D,a loworlow referencerange
serumcalciumand phosphate, elevatedALP, lowurinarycalcium excretion,
andsecondaryhyperparathyroidism.
• Osteomalaciamayexistwithreferencerangelevelsofcalcium,phosphate,and
ALP;thusonlyraisedPTH,reduced25(OH)D,andlowurinarycalcium(24
hour),testedsimultaneously,disclosethediagnosis.
• Levels of 1,25-dihydroxyvitamin D may be in the reference range and are
thereforenotroutinelytested.
• Vitamin D deficiency throughpoordietintake is rare unlesscombinedwith
exposuretosunlight.Itisaphenomenonseenmostofteninthehousebound
elderly,andinimmigrantAsianpopulations.
• Intestinal disorders that lead to fat malabsorption can cause vitamin D
deficiency,asvitaminDisfatsoluble.
Table16.4Asimpleclassificationofosteomalacia
Low Reducedavailability Poordiet,UVskinexposureor
25(OH)D malabsorption
Metabolic Chronicrenalfailure
Anticonvulsantdrugs
Hepatobiliarydisease
Normal
25(OH)D
1α-hydroxylase
mutations
VitaminD-dependentricketstypeI
VitaminDreceptor
mutations
VitaminD-dependentricketstypeII
Phosphate
loss
FGF23excess X-linkedhypophosphataemia
Oncogenic—hypophosphataemia
Tubulardysfunction Fanconisyndrome
Skeletal
toxicity
Defective
mineralization
Aluminium,fluoride
ManagementofhypovitaminosisD,rickets,andosteomalacia
• Thestrategyshouldbetoreplace25(OH)Dtotargetrepletionlevel,provide
enough calcium to mineralize bone normalizing any secondary
hyperparathyroidism, control skeletal pain, pursue a physio-led muscle
rehabilitation regimen if there is any myopathy, and finally prevent the
conditionfromrecurring.
• Quite commonly there may be two lesions in the elderly: osteomalacia and
osteoporosis. It is unknown to what degree bisphosphonate therapy for
osteoporosiswillimpairmineralization/osteomalaciarecoveryiftreatmentfor
bothconditions isgivensimultaneously.Delayingosteoporosistreatment for
4–6weeks isunlikelyto harmandmaygivevaluabletimeforosteomalacia
healingbasedonnecessaryhigherboneturnover(canbeindicatedbyan‘ALP
flare’).
• Bone pain and muscle weakness respond quickly to successful replacement
therapythoughlaboratoryandradiologicalfeaturesmaytakelongertoreturn
tonormal.
• In adults, various regimens for cholecalciferol replacement might be
recommended (e.g. 20,000 IU cholecalciferol weekly for 5 weeks), though
cautionisadvisedinregardof‘over-replacementregimens’,whichhavebeen
associatedwithanincreasedfallsandfracturerisk.
• An alternative (and potentially well-adhered-to regimen) is 3200 IU
colecalciferoldailyintwice-dailydosesforacalendarmonth.Repletionstatus
should then be tested with repeat 25(OH)D check and repeat course of
treatmentgivenifrequired.
• Vitamin-D (and calcium) lack may be habitual as it depends on UV-skin
exposure and dietary preferences. Identification of repeat deficiency then in
futureisfacilitatedbyperiodic25(OH)Dtesting.
• Co-treatment with calcium supplements isn’t necessary in all cases but is
usually safe at daily supplement doses of 500–1000 mg without causing
hypercalcaemia.
VitaminD-dependentrickets
• Type I vitamin D-dependent rickets is a rare autosomal recessive disease
caused by inactivatingmutations in the 1α-hydroxylase gene. Low levels of
1,25-dihydroxyvitamin D result. Children are often affected with rickets
beforetheageof2 years,andfailtorespond tonormallevels ofvitaminD
replacement. Treatment is most effective with physiological doses of 1,25-
dihydroxyvitaminD(e.g.calcitriol).
• TypeIIvitaminD-dependentricketsisanautosomalrecessivedisordercaused
bylossoffunctionmutationsinthevitaminDreceptor(VDR).About70%of
patientswillhavealopecia—animportantprognosticfeaturewhendiscussing
likely outcome of treatment. In patients with normal hair, remission can be
achieved with high levels of 1,25-dihydroxyvitamin D. Only about 50% of
patientswithalopeciawillrespondtoasimilartherapeuticapproach.
Osteomalaciafromalteredphosphatehomeostasis
• Osteomalacia from phosphate depletion is histologically the same in the
skeleton as 25(OH)D deficiency, although serum calcium and 25(OH)D
are/canbenormal.
• X-linked(AD)hypophosphataemicrickets(XLHR)isadisorderofvitaminD
resistance. It is important to diagnose early in young children as treatment
preventsbonedeformity.
• XLHR manifests as delayed growth, short stature, lower limb skeletal
deformity,andrickets.
• InXLHR,dentaldevelopmentcanbedelayedbutdentitionisusuallynormal.
Proximal myopathy is not a feature. Laboratory tests show a low serum
phosphate, normal serum calcium and PTH, and low/normal 1,25-
dihydroxyvitamin D with high FGF23. The renal tubular maximum
reabsorption of phosphate for GFR is low for the degree of

hypophosphataemia(TMP-GFR).
• The treatment of XLHR is a combination of calcitriol (0.125–1.5
micrograms/day)andphosphate(25mg/kg/dayininfants,and1–3gelemental
phosphorusinadults).
• Complications of long-term treatment include hypercalcaemia,
hypercalciuria/renallesions,andhyperparathyroidism.
• TherequirementsforcalcitriolandphosphorustherapyinadultswithXLHRis
generallyreducedandmanagementoftheconditionrefocusesontheneedto
address tertiary hyperparathyroidism, address osteoarthritis, and MSK
symptomscausedbyorassociatedwiththeenthesopathywhichevolvesover
time.
• Renaltubularacidosis(RTA)andFanconisyndromemaybeassociatedwith
osteomalaciaandrickets.
• In RTA, there is a disorder of bicarbonate handling leading to low plasma
bicarbonate,metabolicacidosis,andaninappropriateurinepH.TypeIdistal
tubularRTAoccursasaresultoffailuretosecretehydrogenions.
• Type II proximal RTA is a consequence of bicarbonatewastingandis often
associatedwithFanconisyndrome.Thedevelopmentofricketsinbothforms
of RTA is due to hypophosphataemia. The acidosis should be treated and
vitaminDsupplementsgiven.
• Fanconi syndrome is associated with a number of acquired or inherited
disordersincludingmultiplemyeloma,amyloidosis,heavymetaltoxicity,and
disordersofcarbohydratemetabolism.
• Theneteffectofproximalrenaltubulardefectsisglycosuria,aminoaciduria,
phosphaturia, and hypophosphataemia. Treatment is with phosphate and
calcitriolsupplements.
Oncogenichypophosphataemicosteomalacia
Alsoknownastumour-inducedosteomalacia,thisiscausedby(usuallysmall)
benignmesenchymaltumours,whichsecreteFGF23.See Plate16.
• The condition is cured after removal of the tumour though detection of the
tumourcanbedifficult.
• Tumours can be anywhere including in bone. Many anecdotal reports of
tumoursexistinginoddpositionsexist(e.g.sinuses,in skin,deepfattissue,
labia,etc.).
• Functional imaging with somatostatin receptor or PET scintigraphy (e.g.
gallium-67gadopentetate)isoftenusedasfirst-lineimagingwithCTorMRI
thenusedtopreciselylocatethelesions.
• A milder form of the condition occurs in fibrous dysplasia and
neurofibromatosis.
• Intheabsenceofcurativesurgery,treatmentinvolveslong-termphosphateand
calcitriol supplements and careful monitoring for phosphate-induced
hyperparathyroiddiseaseandeffectsofhypercalciuria.
Hypercalcaemia,parathyroiddisease,andrelated
disorders
Hypercalcaemia
• Theclinicalpictureofhypercalcaemiacanrangefromtheasymptomatictoan
acutemedicalemergency.
• Serumcalciumisnormallybalancedbetweenhomeostaticmechanismsinthe
gut,skeleton,kidneys,andextracellularfluids.
• Hypercalcaemia arises most often from excessive mobilization of calcium
frombonebyosteoclasticresorption,butmayalsooccurduetoexcessivegut
absorption(Table16.5).
• The excessive bone loss, a failure of the kidneys to handle high loads of
calcium,andafailureofbonetoreclaimmineralsquicklyenough,leadstothe
imbalance.
• Accelerated osteoclast activity may be driven by several causes including
excess parathyroid hormone (PTH) or PTH-related protein (PTHrp) and
cytokines(e.g.IL-6,IL-1,TNFα,andTGF-β).
• Clinicalpresentationofmoderatetoseverehypercalcaemiaincludes:
• joint,bone,musclepain.
• muscleweakness.
• dehydrationandpolyuria.
• lethargy.
• fatigue.
• acuteconfusionalstate—unconsciousness.
• abdominalpainsandvomiting.
• renalcolicpains.
• ECGfindings—shortQTinterval,etc.
• Primary hyperparathyroidism(PHPT) andmalignancyare themost common
causes of hypercalcaemia (90% of cases). Other causes include sarcoid,
lymphoma,andgranulomatousinflammatoryconditions.
• ActivevitaminD
3
(calcitriol/1,25-dihydroxyvitaminD
3
)canbe producedby
tissue macrophages which generate 1α-hydroxylase.
Macrophage/inflammatory cell calcitriol production (e.g. in sarcoid) is not

regulated as occurs in renal vitamin D
3
activation as there is no feedback
inhibitionof1α-hydroxylasenordiversionofitssubstrate(25-hydroxyvitamin
D
3
)toaninactiveform(24,25-dihydroxyvitaminD
3
)byincreasingamountsof
calcitriol,whichhappensinnormalrenalcalcitriolproduction.
• Treatment of hypercalcaemia (Table 16.7) depends on the level of serum
calcium, the presence of symptoms, renal impairment, and the underlying
cause. For example, borderline high serum calcium in an asymptomatic
individualwithamildlyelevatedPTHmaysimplywarrantobservationinthe
absenceof renalimpairment orvitamin Ddeficiency. Onthe otherhand, an
individualwithseverehypercalcaemia,dehydration,andrenalimpairmentdue
toatreatablemalignancywouldrequireurgentaggressivemanagement.
• Withacutehypercalcaemia,dehydrationisverycommon.Earlyrehydrationis
very important and often given for 24–48 hours prior to review of serum
calciumlevelsandtheinstigationoffurthertherapiessuchasbisphosphonates
andloopdiuretics(Table16.6).
Table16.5Somecausesofhypercalcaemia
Common Primaryhyperparathyroidism
Malignancy Lyticmetastasesto
bone
EctopicPTH
(PTHrp)
Tumour-derived
1,25
dihydroxyvitaminD
Uncommon/rare
Drugs Thiazidediuretics
Lithium
Aminophylline
Granulomatousdisease(tissue
macrophageproductionof1α-
hydroxylase)
Sarcoidosis
Tuberculosis
Histoplasmosis
Endocrine/metabolic Thyrotoxicosis
Phaeochromocytoma
ExcessvitaminAor
D
Renalfailure
Paget’sdiseaseof
bone
Other Immobility±
calcium
supplementation
Table16.6Treatmentofhypercalcaemia
General
principles
Rehydratewithnormalsaline4Lin24hrsifneeded
Correcthypokalaemiaandhypomagnesaemia
Mildmetabolicacidosisneednotbetreated
Specific
treatment
Loopdiureticswhenhydrated
Bisphosphonates
Calcitonin
Glucocorticoids(haematologicalmalignanciesand
granulomatousdiseases)
Hypercalcaemiaininfancyandchildhood
• Chronic hypercalcaemia of infancy may not be associated with the more
commonclinicalfeaturesmentionedpreviously.Moreoftenthereisafailure
tothrive,abdominalpain,andirritability.Acutehypercalcaemiaisveryrarein
children.
• ConditionstoconsiderarelistedinTable16.7.
Table16.7Conditionsthatmayberesponsibleforhypercalcaemiaininfancyandchildhood
Williams’syndrome Aspectrumofaorticvalvestenosisandfacial
dysmorphism(‘elfin’facies)
Idiopathicinfantile
hypercalcaemia
SimilarmilderappearancetoWilliams’syndromecan
beseen.Therearealsofeaturesofinguinalhernias,
hypertension,strabismus,andkyphosis
Familial
hypocalciuric
hypercalcaemia
Seelaterinthissection
Neonatalprimary
hyperparathyroidism
Other Fatnecrosis,sarcoidosis,Jansensyndrome
(metaphysealdysplasia),overdosingofmilk/vitaminD
Parathyroiddisorders
Primaryhyperparathyroidism
• Primary hyperparathyroidism (PHPT) is a relatively common condition;
incidence1in1000.Itoccursatallages,althoughismuchmorecommonafter
theageof60withafemaletomaleratioof3:1.Itisunusualinchildhood—
when it should raise the possibility of familial multiple endocrine neoplasia
(MEN)typeIortypeII.
• Asinglebenignadenomaaccountsfor80%ofcasesofPHPT.
• Generalizedfour-glandhyperplasiaaccountsfor15–20%ofcases.
• Parathyroidcarcinomaisveryrare.
• PHPT is associated with bone, renal, GI, and neuromuscular complications.
BonyproblemscanbeseenonplainradiographsandrangefromlowBMDon
DXA scanning and mild sub-periosteal bone resorption to osteitis fibrosa
cystica, bone resorption of the distal phalanges and clavicles, patchy
osteosclerosis(classic‘ruggerjersey’spine),andmultiplelyticlesionsofthe
skull.
• Generalsymptomsincludefatigueandmyalgias(myopathyisrare).
• CPPD disease is a relatively under-recognized association (look for joint
chondrocalcinosis,crowneddenssyndromeSee Plate22,typicalfeaturesin
OA joints (‘OA-plus’)). Kidney stones are uncommon. GI manifestations
includepepticulcerationandpancreatitis.
• PHPT is easily diagnosed with raised PTH in the context of replete level
25(OH)D,andhigh(orhighreferencerange)serumcalciumandlow(orlow-
reference range) phosphate. Often 24-hour urinary calcium levels are
uninformative.
• Medical management includes adequate rehydration and avoidance of high
calcium intake and calcium supplements, gentle correction of 25(OH)D
deficiencyandabisphosphonatetolimitboneloss.
• Successful parathyroidectomy from minimally invasive targeted surgery is
feasible in the majority of cases for single adenomas identified by imaging
(e.g.
99m
Tc-MIBI scintigraphy and US though (contrast-enhanced, delayed
phase)CTisalsousedinequivocalcases).
• Neckexplorationsurgeryisrequiredifimagingfailstoidentifyanadenoma.
Surgeryshouldonlybedonebyexperiencedsurgeons.
• Conservativemanagementisacceptableifpatientsareasymptomatic,anddo
nothaveosteoporosisthoughalsomaybenecessaryifsurgeryisnotfeasible.
BisphosphonatesdostabilizeBMDlossasindicatedbyDXAandcanbeused
long-term.
• Clinical trials with calcimimetic agents (stimulates the PTH gland Calcium
sensing receptors with consequent inhibition of PTH secretion) such as
cinacalcet,canbeusedincaseswhereparathyroidectomyisnotfeasible/failed
andtherearehypercalcaemicsymptoms.
Secondaryandtertiaryhyperparathyroidism
• SecondaryHPT(SHPT) occursasaconsequenceoflowserum calciumand
PTHglandCaSR‘sensing’ofcalciumlevels.
• CalciumlackandthusSHPTareoftenduetovitaminDdeficiency.
• SHPTfrom calciumlackalone (where thereis replete 25(OH)D)is unusual
thoughmaypointtoasevereGIabsorptionproblem.
• With time, persistent SHPT can lead to autonomous PTH release (tertiary
HPT). This is most often seen in severe or prolonged renal bone disease or
fromlong-termcalcitrioluse(e.g.XLHR).
• CalcimimeticsmayhaveanimportantroletoplayincontrollingtertiaryHPT
butatpresentparathyroidectomyisthebestoption.
Familialhypocalciurichypercalcaemia(FHH)
• FHH is extremely rare. It is inherited as autosomal dominant with high
penetrance. Radiographs, PTH, and renal function are normal in
uncomplicated cases. Although parathyroid gland hyperplasia occurs,
parathyroidectomy is invariably unsuccessful at lowering serum calcium
levels.
• Thetwoindications forparathyroidectomyinFHHareneonatalsevereHPT
andadultrelapsingpancreatitis.
• Useofdiuretics,oestrogens,orphosphatetoregulateserumcalciumhasbeen
unsuccessful. Patients should therefore be followed without intervention
unlesscomplicationsarise.
• FHHneedstobeconsideredwhendiagnosingPHPT(wherehypercalcaemia
andelevatedPTHlevelsaremodest).Firstdiscriminationismadebyrepleting
25(OH)D to 100 nmol/L then retesting all biochemistry. PTH usually
normalizesinFHH,unlessthereistertiaryHPT,butwon’tinPHPT.Alsoif
thecalcium:creatinineclearanceratiois<0.02thenFHHis98%likely(CCCR
=uCa/(uCr×sCr)).
• Inpregnancythethreesituationstobeawareofare:
• asymptomatichypercalcaemiainanaffectedbabyofacarrier.
• neonatal hypercalcaemia in an affected baby of an unaffected mother
(intrauterineSHPT,whichresolvesspontaneously).
• hypocalcaemia in an unaffected baby of an affected mother (fetal
parathyroidsuppression).
Familialprimaryhyperparathyroidsyndromes
• Up to 10% of cases of PHPT may have a hereditary syndrome. The most
commonoftheseisMEN.
• MEN1isautosomaldominant(M=F),isassociatedwithpancreatic,thymic,
gastric,andpituitaryadenomas,andadrenalhyperplasia.
• Pancreatic, thymic, and bronchial neuroendocrine tumours are the leading
causeofdeathinpatientswithMEN-1andshouldberegularlymonitoredfor
(e.g.biannualcomputedtomographyimaging).
• The MEN1gene consistsoftenexons,spanning 10kb, andencodesa 610-
aminoacidprotein(‘menin’—itsfunctionasyetnotfullyknownbutmayplay
aroleintumoursuppression).
• MEN2A (Sipple syndrome) is autosomal dominant and is characterized by
phaeochromocytomas and medullary thyroid carcinoma and is highly
associatedwiththeRETproto-oncogene.
Parathyroidhormoneresistantsyndromes
• Pseudohypoparathyroidism(PHP)isatermappliedtoaheterogeneousgroup
ofdisorderswhosecommonfeatureisend-organresistancetoPTH.PHPtype
1A(PHP1A)ischaracterizedbyresistancetootherhormones,includingTSH
andgonadotropins.
• PHP1A isassociated withclinical featuresreferredto asAlbright hereditary
osteodystrophy (AHO; includes short stature, obesity, round facies,
subcutaneousossifications,brachydactyly,otherskeletalanomalies,andsome
patientshavementalretardation).
• In PHP1A, there is decreased cellular cAMP response to PTH infusion,
decreased erythrocyte Gs activity, and a GNAS1 mutation in the maternally
derivedallele.
• In PHP1B,thereis renalPTHresistance, decreasedcAMP responseto PTH
infusion,normalerythrocyteGsactivity,andimprinting/methylationdefectsat
theGNASlocusresultinginlackofexpressionofthematernalalleleinrenal
tissue.Classically,patientsdonothavefeaturesofAHO.
• PHP1B is not associated with generalized hormone resistance, although
resistancetothyroid-stimulatinghormonehasbeenreported.
• Individuals with AHO without endocrine abnormalities, a normal cellular
cAMP response to PTH infusion, decreased erythrocyte Gs activity and a
GNAS1 mutation in the paternally-inherited allele have
pseudopseudohypoparathyroidism(PPHP).
CKD-mineralandbonedisorders(CKD-MBD)incorporatingrenal
osteodystrophy(ROD)
• Thekidneysarekey inregulatingcalcium andphosphate,areatargetorgan
for PTH and FGF23, and are the primary source for 1α-hydroxylation
mediatedactivationof25(OH)D.
• CKD-MBD (the term was first proposed by Kidney Disease: Improving
Global Outcomes (KDIGO) in 2005) describes a broad clinical syndrome
whichincludesskeletal,softtissue,andvascularabnormalitiesthatdevelopas
aresultofCKD.Renalskeletaldiseasealoneistermed‘renalosteodystrophy
(ROD;Table16.8).
• RODcanbeaspectrumofbonediseasefrom‘highturnover’(duetoprimary
or tertiary hyperparathyroidism) to ‘low turnover’ (termed adynamic) bone
disease where PTH levels are generally low (reference range or modest
elevation).
• Phosphate retention (secondary), FGF23 elevation, hypovitaminosis D,
hypocalcaemia,impairedcalcitriolproduction,andskeletalresistancetoPTH
all contribute to secondary HPT in CKD with relevant effects beginning in
CKD3(estimatedGFR30–60mL/min/1.73m
2
).
• Historically low turnover, adynamic ROD has been related to excess
aluminium deposition in bone in dialysis patients—thus more prevalent in
peritonealdialysispatientscomparedwithhaemodialysis.
• Bone fragility and increased fracture risk is a consequence of all types of
ROD.ClinicalmanifestationsofRODareinTable16.8.
Table16.8Theclinicalmanifestationsofrenalosteodystrophy
Clinical
feature
Comment
Bonepain Common
Skeletal
deformity
Common.Affectsappendicularandaxialskeleton
Children:onset<3yrs,rachitic;onset<10yrs,bowingoflong
bones,widenedmetaphyses,pseudoclubbing,slipped
epiphyses
Adults:lumbarscoliosis,kyphosis,distortedthorax
Growth
retardation
Proximal
muscle
weakness
Ectopic
calcification
Soft-tissues.Visceral.Vascular—ifsevere,individualsmay
developischaemicnecrosis
GeneralmanagementofROD
• Earlydietaryrestrictionofphosphatecanmaintainnormalcalciumlevels,but
low-phosphate diets are often unacceptable and normal phosphate levels are
bestachievedwithbindingagents(somecontaincalcium).
• Small doses of calcitriol (vitamin D) may help to lower serum PTH levels.
Someindividualsmaybesensitivetocalcitriolandserumcalciumlevelsmay
increase.Mostpatientsrequiredosesof0.25–0.5microgramsdaily;children
mayrequirehigherdoses.
• Parathyroidectomy is indicated in persistent symptomatic hypercalcaemia,
ectopiccalcification,andseverebonepain.
Ectopiccalcificationandossification
• Ectopic calcification can arise from any one of a number of causes of
hypercalcaemia or hyperphosphataemia. These include renal failure,
hyperparathyroidism, familial hyperphosphataemia tumoural calcinosis
(OMIM211900)andsarcoidosis.Dystrophiccalcificationisalsoafeatureof
systemic sclerosis (see Chapter 13), dermatomyositis (see Chapter 14),
andprimarycalcinosis.
• Ectopicossificationcanbeseenposttraumaandfollowingmyositis.Itisalso
a feature of several rare conditions including PHP and myositis ossificans
progressiva. Early signs of muscle ossification are best detected with MRI
scanning.Laterossificationiseasilyvisibleonplainradiographs.Treatmentis
difficult, but includes physiotherapy to maintain suppleness and possibly
heparinsorbisphosphonatestohaltboneformation.
Paget’sdiseaseofbone
• Paget’s disease of bone (PDB) is a localized disorder of bone remodelling
resultinginexpansionanddeformityofbone.
• PDB is common (about 5% of the population >55 years) in the UK, North
America,Australia,andNewZealand,withamaletofemaleratioof3:2.It’s
uncommoninAsia,Africa,Scandinavia,andSouthAmerica.
• The ‘lesion’ in PDB is substantially increased (coupled) bone remodelling,
driven by an excess number of multinucleated, highly active osteoclasts,
producing excessive woven bone (immature bone characterized by erratic
collagenorientation).
• TheoriesofPDBbeingcausedbyviruseshavelargelybeendisproved.
• PDBhasageneticbasis;15–30%PDBpatientshaveapositivefamilyhistory;
there isa7× risk of developing PDBifyour first-degree relative has itand
30%offamilialcaseshavegenemutationsat5q35(thegeneencodesforan
ubiquitin-bindingproteinsequestasome-1(SQSTM1/p62)).
• SQSTM1mutationsindicateseverityofPDB,theproteinplayinganimportant
roleinNFKβsignalling.
• PDBpatientswithSQSTM1mutationscanhaveavariableclinicalphenotype
however,indicatingmodifyinggeneorenvironmentaleffectsalsoarerelevant.
• TheclinicalfeaturesofPDBareshowninTable16.9.
Table16.9ClinicalfeaturesofPaget’sdiseaseofbone
Clinicalfeature Details
Pain Deepunremittingpain,possiblycorrelatedtoblood
flow(e.g.headachefromskullinvolvement)
Boneinvolvement Pelvis75%,skull35%,femur35%,sacrum35%,tibia
30%,radius15%,handsorfeet10%ofcases
Fractures Vertebralfractures,‘fissure’fracturesatsiteof
convexityoflongbone
Neurological
sequelae
Spinalcordcompression,radiculopathy,deafness,
High-output
cardiacfailure
Rarebutcanoccurif>40%oftheskeletonisinvolved
Osteosarcoma 0.1%ofcases
Hypercalcaemia
andhypercalciuria
Unusual.Linkedtopolyostoticdiseaseandimmobility.
Can,ifsevere,leadtokidneystonedisease
Osteoarthritis PDBinboneadjacenttojoint,canacceleratejoint
degeneration
Retinalangioid
streaks
Causeunknown
Investigationandtreatment
• Serum alkaline phosphatase (ALP), a measure of osteoblast-derived bone
formation, is the most useful marker of high bone remodelling and may be
elevatedasmuchas30×abovenormal.
• ReferencerangeALPcanmeanboneturnoverislow(‘inactivePDB’)butis
not specific. The degree of abnormality of ALP often associates with the
number of bones affected, polyostotic disease being associated with higher
ALPvalues.
• The differentialdiagnosis of increased (bone) ALP includes metastatic bone
disease, osteomalacia, hyperparathyroidism, and osteomyelitis or
inflammation.
• Because of the increased bone turnover, other biomarkers will beabnormal:
e.g.increasedurinehydroxyproline,serum/plasmaCTX,P1NP.
• Thereisawidevariationinradiographicappearanceoftheconditionbutthe
main features are localized sclerosis, coarse and irregular trabecular
patterning,andboneexpansion.
•
99m
TC methylene diphosphonate (MDP) bone scintigraphy is a sensitive
investigationfordefiningtheextentoflesions.See Plate22.
• ThereareseveralindicationsfortreatmentofPaget’sdisease:
• Painarisingfromaffectedsites.
• Deformingdisease.
• Fissurefractures.
• Skulldisease.
• Reductionofvascularityinbonenexttoajointplannedforsurgery.
• Complications—progressiveneurology,hypercalcaemia,high-outputcardiac
failure.
• PDBandrelatedosteoarthriticpainmaybereducedbysimpleanalgesics,but
purepageticbonepainrespondspoorlytothis.
• Full biomechanical assessment, particularly looking for correctable
deformitieswithjudiciousorthosisuse,isinvariablyhelpful.
• First-linetreatmentofPDBisasingledoseofzoledronicacid5mgIV.
• Analternativeisrisedronate30mgdailyfor2months.Therelapseratewith
risedronateissignificantlyhigherthanwithzoledronicacid.
• Historically,etidronate(e.g.6monthsatadoseof5mg/kg/day),pamidronate
(e.g. 90 mg IV ×2 doses fortnight apart) and calcitonin (50–100 IU SC
injectiondaily,reducingto50IU2or3timesperweekonceasymptomatic
responseisachieved(usuallyafter4–8weeks)haveshownbenefitinreducing
PDBpainandALP.However,relapseriskismoderatelyhighcomparedwith
zoledronicacid.Calcitoninoftencausesnausea,flushing,anddiarrhoea.
• Many PDB patients achieve long-term biochemical remission with just a
singletreatmentofzoledronicacid5mg.
• Typicalsideeffectsofzoledronicacid,aswithpamidronate,includestransient
‘flu-like’symptomsoffever,myalgia,andarthralgia.
• Zoledronicacid5mgIVusedforALPrisealonedoesnotappeartobenefit
PDBpatientscomparedwithpatientstreatedonthebasisofPDBsymptoms
alone (PRISM-EZ); indeed, it may be associated with a greater risk of
fractures(innon-pagetoidbone).
• ZoledronicacidiscurrentlybeingstudiedforitsroleinPDBdevelopmentin
high-risk(SQSTM-1mutation-positive)patients.
• Typicalsurgicalinterventionsincludearthroplasty—whereacceleratedOAhas
evolved in joints adjacent to pagetoid bone, fixation of fractures, and
realignment osteotomies where there is significant deformity amenable to
surgicalcorrection.
• VitaminDdeficiencyisincreasedinfrequencyinPDBpatientscomparedto
expected,thusitshouldbesoughtandcorrected.
• Denosumab ispredicted tobe effective atreducing boneturnover, pain,and
ALP in PDB but treatment will be relatively expensive, relapse of PDB is
likely to occur on treatment cessation, and the rebound increase in bone
turnoveratthattime,islikelytoprecludeitsadoptionasaroutinetreatment
forPDB.
Childhoodautoinflammatorybonediseases
Introduction
Autoinflammatorybonediseasesaredisordersprimarilydrivenbyabnormalities
oftheinnateimmunesystem.
3
• The most common disorders include chronic non-bacterial osteomyelitis
(CNO); synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO)
syndrome;Majeedsyndrome; deficiency ofinterleukin-1 receptor antagonist
(DIRA);cherubism;andjuvenilemandibularchronicosteomyelitis(JMCO).
• Bone inflammation is typically characterized by a subacute or chronic
inflammation that is bacterial culture negative and with no demonstrable
organismonhistopathology.
• NSAIDs are typically used as first-line therapies in CNO. Bisphosphonates
and anti-TNFα drugs have been used for second-line therapies to prevent
pathologicfractures,pain,anddiseaserelapse.
• CNOandSAPHOarediscussedingreaterdetaillaterinthissectionandfor
therarerautoinflammatorybonediseasesseeTable16.10.
Table16.10Featuresoftherarestautoinflammatoryboneconditions
Features DIRA Cherubism Majeedsyndrome
Fever Uncommon No Highfevers
Common
CNOsites
Longbones
especiallyproximal
femur,vertebral
bodies,ribs,
clavicles
Maxillaand
mandible
Femur,tibia,pelvis,
calcaneus,ankle,
vertebrae,and
clavicle
Areaoflong
bones
affected
Metaphyses
predominantly
Longbones
rarelyaffected
Metaphyses
predominantly
Extraosseous
features
Skinpustulosis,
systemicorgan
involvement
Cervical
lymphadenopathy
Congenital
dyserythropoietic
anaemia,
dermatitis,growth
failure,
hepatomegaly,joint
contractures
Inflammatory
markers
Elevated Normaltomildly
elevated
Elevated
Inheritance AR AD AR
Genedefect IL-1RN SH3BP2 LPIN2
Ethnic
distribution
PuertoRican,
European,Lebanese
Worldwide Arabic,Turkish
CNO
The terminology for CNO has changed over the last 40 years. The most
commonly used term is chronic recurrent multifocal osteomyelitis (CRMO);
however,notallpatientshavemultifocalbonelesionsornumerousrecurrences,
hence the term chronic non-bacterial osteomyelitis (CNO) encompasses all
possiblediseasepresentations.
• CNO is a systemic disease that predominantly occurs in childhood. It has
manysimilaritiestoSAPHOsyndrome,adisorderprimarilyseeninadults.
• TheincidenceandprevalenceofCNOisunknown,butthemajorityofreports
are from Scandinavia, Europe, Australia and North America. Female
predominance/meanageofonsetabout10yearsofage.
• CNOisadiagnosisofexclusionestablishedbyclinicalpresentation,imaging
studies,andaculture-negativebonebiopsy.
• Painoccurswithorwithoutswellingatthesiteofabonylesion.Inflammatory
markersarenormalormoderatelyraised.
• Bonelesionstendtoclusteraroundmetaphysis,butcanoccuratsitessuchas
theclavicle(commonlythemedialthird).
• The most common CNO sites include the femur, pelvis, calcaneus, ankle,
vertebrae, and clavicle. Multifocal lesions tend to have a symmetrical
distribution.Unifocaldiseaseoccursin10–20%.
• CNOpatientsfrequentlyhaveothercoexistingchronicinflammatorydiseases
such as psoriasis, arthritis, inflammatory bowel disease, vasculitis,
myositis/fasciitis,andparotitis.
• Imaging to clarify diagnosis: radiographs and MRI. CT can be used, but
exposeschildrentohighradiation,soisnotrecommended.
• Whole-body MRI can assess for asymptomatic (polyostotic) lesions, and
shouldbeconsideredforindeterminateCNOcases.
• Typical radiographic findings include a lytic lesion at or around the
metaphysis,whichmayprogresstosclerosisorhyperostosis.

• Bonebiopsyisoftenrequiredtoconfirmthediagnosis—importantinisolated
bonelesions,asmalignancycanmimicCNO.
Treatment
• NSAIDsarethegoldstandardinitialtherapy.
• CasereportssuggestGCs,methotrexate(MTX),andsulfasalazine(SZP)may
bebeneficial,butresultsareinconclusive.
• Reports on use of anti-TNFα are inconclusive: some responses are
unsustained.
• IV bisphosphonate (e.g. pamidronate) has been used due to its effect on
reducingosteoclast-drivenosteitispathophysiology.
• Several studies have demonstrated high efficacy rates and good clinical
response occurring in the first 3 days, and inducing remission for 12–18
months.
• However,thereareconcernsregardingtheuseofbisphosphonatesinchildren
giventhelackoflong-termsafetydata.
• Themostcommonadverseeventofpamidronateisminorflu-likesymptoms.
Osteonecrosis of the jaw is a rare but serious complication and to date
unreportedinpaediatricuse.
• CNOcanbeadifficultconditiontotreat,withhighratesofnon-responders.If
untreated,thereisincreasedriskofpathologicalfractures,inadditiontoother
possible morbidities such as generalized growth failure, scoliosis, and
hyperostosis.
Reference
3. SternSM,FergusonPJ.Autoinflammatorybonediseases.RheumDisClinNorthAm2013;39:735–49.
SAPHOsyndrome
SAPHO syndrome was originally an acronym from the French term: le
Syndrome Acne, Pustulose, Hyperostose et Osteite but later changed and
terminology anglicized in terminology to Syndrome of Synovitis, Acne,
Pustulosis, Hyperostosis and Osteitis. However, the original description is
notable for the absence of synovitis, which probably is quite an uncommon
lesionofthecondition.
• SAPHO syndrome has similarity to CNO but can also be classified as an
osteoscleroticbonedisease.Furthermore,theremaybeoverlapwiththeSpA
diseases—some features exist in both SAPHO and some forms of psoriatic
arthritisthoughSAPHOisnotB27related.
4
Patternsandspectrumofdisease
• Typicalpresentationage30–50yearsoldthoughchildhoodformsexist.
• Pathogenesismayderivefromanamplifiedabnormalinnateimmuneresponse
to pathogens, with the most likely triggering pathogen being
Propionibacteriumacnes.
• Apatient’sdiseasephenotypecanbeindistinguishablealsofromaxialskeletal
sarcoid.
• Therearesimilaritiestoandoverlapwithformsofpsoriaticarthritis.
• CRMOhasbeendescribedasthepaediatricpresentationofSAPHO.However,
thelocalizationofinflammationisdifferentbetweenthetwoconditionswith
the extremities more often affected in CRMO than SAPHO whereas for the
latter,axialskeletonwithcosto-sternoclavicularregionisthefocus.
• Both enthesitis and spondylodiscitis are likely to be associated SAPHO
lesions.
Clinicalfeatures
• Painfulosteitislesions,enthesitis,andspondylodiscitisarelikelytoalloccur
inSAPHOlesions.
• Palmoplantar pustulosis (PPP) and severe acne (acne conglobata, acne
fulminans, hidradenitis suppurativa) are among the typical lesions seen in
SAPHO.
• PPPismoreoftenseeninwomenandsevereacneinmen.
• Other skin lesions described in SAPHO include various types of psoriasis;
pyodermagangrenosum;Sweet’ssyndrome;Sneddon–Wilkinsondisease.
• Systemicsymptomsoffeverandfatiguefrequentlyoccur.
Differentialdiagnosis
• Psoriatic arthritis. This can pose diagnostic dilemma since psoriatic arthritis
manifest by spondylodiscitis, osteitis, entheseal/juxta-articular hyperostosis
andpustularpsoriasiscanmimicSAPHO.
• Infection (osteomyelitis) and neoplasia should be considered though MRI is
usuallydiscriminatory.
• Inchildren,thefollowingshouldalsobeconsidered:Ewingsarcoma,Majeed
syndrome,histiocytosis,andDIRA.
Investigations
•
99m
TC MDP (bone) scintigraphy is characteristic in most cases showing
markedtracer accumulationat sternoclaviculararea lesions(e.g.Bull’s head
sign).
• Onradiographslesionsareoftenprimarilyexpandedandsclerotic.

• MRIdiscriminatesosteitisfrominfectionandmalignancy.
• Laboratory tests are not specific and features of inflammationmaybeseen:
raised CRP, ESR, platelets, C3, ACE. Immunoglobulins are usually normal
andautoantibodiesnotdetected.
• BoneshouldbeculturedforTB,Propionibacterium,andgeneralpathogens.
• Histology ofboneoften showsdense disorganized sclerosiswithfeatures of
increasedboneturnover.
• Histology of skin lesions can show neutrophilic infiltration and pseudo-
abscesses(differentialdiagnosis—Sweet’ssyndrome).
Treatment
• NSAIDsareusedforpain.
• Appropriateantibioticsforculture-positivebonebiopsy.
• Colchicine, GCs, oral and IV bisphosphonates, and sDMARDs (e.g. MTX)
haveallbeenusedwithvariableeffects.
• Anti-TNFα and anti-IL-1 receptor antagonist (anakinra) have shown good
effectpersistentdisease.
• Forskinmanifestations,topicalsteroids,PUVA,andretinoidshavebeenused.
Reference
4. RukavinaI.SAPHOsyndrome:areview.JChildOrthop2015;9:19–27.
Theosteochondroses
Osteochondrosis is a trauma-induced focal disturbance of cartilage in a joint
(articular), at a periarticular epiphyseal plate or tendon or ligament insertion
(apophysis/enthesis).
• Lesionstypicallyoccurinactivechildrenandadolescents.
• Osteochondritis may be associated with a delay in growth-associated
endochondral ossification, with a potential consequence of joint or other
biomechanicaldeformity(see Table16.11).
• Wherethelesionisassociatedwithcleftformationthrougharticularcartilage,
thenthelesionistermed‘dissecans’.
Scheuermann’sdisease
Although not consistently defined, Scheuermann’s disease is a vertebral
epiphysealosteochondritisthatoccursinadolescence.Seealso p.620
• Althoughanincidentalradiographicfinding,Scheuermann’sisalsoassociated
with diffuse spinal pain which is more likely to be present if the
osteochondritisisthoracolumbar(25%),ratherthanthoracic(75%)andifthe
childisanathleteorveryactive.
• It can present with painless dorsal kyphosis with compensatory lumbar
lordosisandlateralspineradiographsshowirregularityofvertebralend-plates,
anterior vertebral wedging, and kyphosis—the latter can develop in late
adolescenceorgraduallyoveryears.
• Inadultswhopresentlate,thevertebraldeformitiesmaybemistakenforgrade
1vertebralfractures.
• Management is with physiotherapy—working on extensor spinal muscular
strength,andjudicioususeofanalgesics.
Legg–Calvé–Perthesdisease
Perthesdiseaseisanosteonecrosisofthefemoralepiphysisandoccursintheage
range3–8years,mostfrequentlyinboys(ratio4:1).
• Perthesdiseaseisbilateralin10–20%ofcases.
• Symptomsincludeaninsidiousonsetoflimpandpaininthegroinorreferred
totheknee/thighthatisrelievedbyrest.
• Theremaybelimitationofhipinternalrotationandabduction(duetoadductor
spasm).
• Leg length inequality suggests femoral head collapse. There may be
spontaneousresolution,especiallyinyoungerpatients,inwhomconservative
managementisindicated.
Osgood–Schlatterdisease
Thisosteochondrosisisprobablyduetorepetitivetraumaatthesiteofpatellar
tendoninsertionintothetibialtubercle.
• Ittypicallyoccursinathleticadolescents,especiallyyoungmalesaged14–16
years.
• Painisusuallyonexerciseandeaseswithrest.
• Thediagnosisismadeclinicallyandondemonstratinganenlargedfragmented
tibialtubercleonalateralviewradiograph.
• Bilateralkneeviewshelptodistinguishnormalfromabnormal.
• DifferentialdiagnosisincludesSpA-relatedenthesitis.
Sinding–Larsen–Johanssondisease
Thisosteochondrosisoccursasaconsequenceofoverloadingofthepatellaatits
secondary centre of ossificationproducingatraction apophysitis at the patella
lowerpole.
• Although not exclusive to the group, it is a typical sports-related injury in
adolescentathleteswhojump,e.g.high-jump,basketball.
• TreatmentiswithsimpleanalgesiaorNSAIDs,andrest.
Köhlerdisease
Thisosteochondrosisisessentiallyanosteonecrosislesionofthetarsalnavicular.
Changesmayrepresentadevelopmentalvariationinossificationanditpresents
witha painfullimp. Weight-bearingis morecomfortable onthe outsideof the
footandthenavicularistender.
Freibergdisease
Anosteonecrosisofthemetatarsal(usuallythesecond)headfollowingtrauma,
ismostcommoninadolescentfemales.Painislocalizedandworseonweight-
bearingwithswellingsometimesdetectable.
Anosteochondritis‘dissecans’lesion
An articular osteochondritis lesion can become a ‘dissecans’ lesion when a
fragment ofarticularcartilage and subchondral bone becomes demarcatedand
mayformanintra-articularloosebody.
• Symptomsofadissecanslesionaremainlyacute-onsetpain,aneffusion,and
limitedmovementofthejoint.
• Plainradiographswillshowawell-circumscribed,scleroticlesion.
• Inyoungpatientsbeforeskeletalmaturitythereisagoodchanceofdissecans
healing.
• Aftertheepiphysishasclosed,however,thereismoreriskofaloosebodyand
secondaryosteoarthritisifadissecanslesionpersists.
• Arthroscopycanassistinassessingthedegreeofdamageandremovingloose
bodies.
• Surgeryrangesfromdrillingthelesioninsituto encouragehealing, tobone
osteochondralallografts.
Table16.11Osteochondritisconditions
Type Site Details
Articular Metatarsalhead
(Freiberg’s)
Typically,2ndmetatarsalhead;bilateralin
10%
Hip(Legg–
Calvé–Perthes)
Slippedcapitalfemoralepiphysis;4–10years
ofage;morecomplicationsif>8yearsofage;
isbilateralin10%
Navicular
(Kohler’s)
3–7yearsofage;maletofemaleratio5:1;
occasionallybilateral
Talus Laterallesionsmostlikelytobeassociated
withsingletraumatrigger
Lunate
(Kienbock’s)
Rare<15yrsold;commonlymales;maybe
associatedwithshortulnarelativetoradius
Non-
articular-
atan
enthesis
Vertebralend-
plate
(Scheuermann’s)
13–17yrs;male:femaleratioequal;usually
lowerthoracic>thanupperlumbar;often
severalvertebraeaffected(3–5)
Tibialtubercle
(Osgood–
Schlatter)
Enthesitisofinsertionofpatellarligament;
typically10–15yrsofage;moreoftenmales
thanfemales;bilateralin25%
Inferiorpatella
pole
‘Jumper’sknee’;typicallymaleadolescents
involvedinsportsandexercise;
5thmetatarsal
base(Iselin’s)
9–15yrsold;typicallysports-relatedtrauma
Calcaneus
(Sever’s)
‘TractionenthesitisatAchilles’tendon
insertion;incidence4/1000children6–17yrs
Epiphyseal
plate
Ulnamedial
epiphysealat
elbow
(Panner’s)
AvulsionenthesitisfrompitchinginLittle
Leaguebaseballtermed‘LittleLeague
elbow’;males<16yrsold;associatedwith
increasedheightvelocity;extensively
reportedinthesportsmedicineliterature
Medial/proximal
tibia(Blount’s)
‘Tibiavara’;infantile<3yrsoldorlateonset
Slippedupper
(capital)femoral
epiphysis
(SUFE)
Commonestadolescenthipdisorder;20%
bilateral;risks:obesity,coxaprofunda,
femoraloracetabularretroversion,
hypothyroidism,ROD,hypopituitarism;25%
riskofprogressiontoosteonecrosis;almostall
casesneedsurgery
Osteonecrosis
Osteonecrosis is regional ischaemic skeletal injury, which can be caused by
trauma,drugs(e.g.GCs),orsystemicconditions—metabolic,haematological,or
endocrine(e.g.sicklecelldisease,antiphospholipidsyndrome).

• Ifsevereand/orprolonged,ischaemiacancauseskeletalcelldeathleadingto
necroticbone,whichcancompromiseregionalskeletalintegrityandstrength
andleadtofracture,damagetoadjacentcartilage,anddeformity.
• Osteonecrosiscanbesymptomaticallysilentandpersist,withnoorminimal
symptoms,foryearsinsomecases.
• Ischaemia occurs after mechanical interruption of blood delivery, non-
traumaticintravascularocclusion,thrombosis,cholesterol,expandingnitrogen
bubblesorothermechanismsthatleadtocriticalischaemia;thendepositionof
vascularizedconnectivetissuecanaccumulateattheinterfaceofnecroticand
normal bone. Calcification can follow and necrotic tissue remains as an
‘island’ofinviablebone.
• Localskeletalfeaturesincludepainordiscomfort.Painevolutionmaydenote
the onset of subchondral bone collapse. If secondary adjacent joint damage
evolvesandprogressesthenfeaturesofmechanicaljointdiseasewillevolve—
painanddiscomfortonmovement,stiffness,swelling,andafunctionalimpact
accordingly.
• There may be tenderness on palpating over osteonecrotic bone and signs of
jointeffusionifthelesionhasaffectedtheadjacentjointcausingcartilageloss
ormicrofracture.
• MRIsignsarecharacteristicandcancontributetograding(e.g.femoralhead
afterFicat).Seealso bonescintigraphyPlate17.
• Practical radiographic-based osteonecrosis grading can be done using
Steinberg(2001)orevenARCO(1992)gradingsystems.
• Laboratorytestingshouldfocusonsystemiccauses(Table16.12).
• Initialmanagement:paincontrol,addressingremediableunderlyingsystemic
causes/associated disease,agreeingand planning what amount of weight-or
load-bearingoftheaffectedboneispermissible.
• In the absence of data from controlled studies of treatment, management is
basedonstageofthelesionanddegreeofeffectontheadjacentjoint,thusfor
early disease with reversible cause, or repair or revascularization possible
before any collapse of the subchondral bone, conservative measures are
appropriate.Butinlatediseasewithsubchondralbonecollapse,arthroplastyis
considered.
• Forosteonecrosisofthefemoralhead(ONFH)consideran8-weekperiodof
non-weight-bearing.
• Evidenceforbisphosphonateuseanditseffectisanecdotalonly.
• Core decompressionforONFH involves removingbone from themedullary
cavityormultiplesmallerholesthroughthebonesurface.Thecavitymaybe
then filled with a vascularized fibular graft or by non-vascularized cortical
bone.
• Osteotomy attempts to shift the weight from the necrotic segment but
subsequent joint replacement is technically more difficult. Hemi-resurfacing
preserves the bone for later arthroplasty and is an option for femoral head
collapseinyoungerpatients.
• Skeletalstemcellscombinedwithimpactionbonegraftingisanoveltreatment
translatedtothetreatmentofONFH.
Table16.12Conditionscausing,orassociatedwith,osteonecrosis
Condition Notes
Trauma Fracturesandfracture-dislocations,Legg–Calvé–Perthes
disease,orthopaedicprocedures
Glucocorticoids
(GCs)or
Cushing’s
disease
Associatedwithacuterepeatedhigh-doseGCsorhigh
cumulativeGCdoses.GCscausehypertrophyand
hyperplasiaofmarrowfatcells.GCsdivertmesenchymal
cellstowardanadipocytelineageasopposedtoosteoblast-
osteocyteone
Alcohol Riskincreases>3-foldinthoseconsuming40 unitsper
weekormore.
Drugs Cocaine;bisphosphonatesanddenosumab(monoclonal
antibodytoRANKL)bothcausingONJ;oral
contraceptives(rare);proteaseinhibitors;thalidomide
Gaucher
disease
Inthetotalpopulationof5894ICGGGaucherDisease
Registrypatients,544experiencedatleastoneepisodeof
osteonecrosis;associatedwithanaemia
SLE Osteonecrosisreportedinupto27%ofpatientstaking
GCs,oftenmultifocal;riskhigherifthereis
hypertriglyceridemia
Transplantation Likelymultifactorialrisks.MainlyassociatedwithGCs
Sicklecell
disease
Prevalenceveryhigh.Mostcommonlyhumeralhead(28–
48%prevalence);ONFHmostprevalentinpatientswith
SCD-SSα-thalassemia
Prothrombotic
risks
Upto50%ofcasesofmultifocalosteonecrosisassociate
withpro-thromboticconditions(e.g.antiphospholipid
syndrome)
Dysbaria Predominantlyaffectsfemoralheadandproximalhumerus
indivers,caissonandtunnelworkers.
HIV Proteaseinhibitor-inducedhyperlipidaemiaandHIV-
associatedantiphospholipidsyndrome
Malignancy All;notablychildhoodleukaemia
Otherprobable
associations
Pancreatitis,hyperlipidaemia,diabetes,pregnancy,
hyperuricaemia/gout
Fibrousdysplasia
Fibrous dysplasia (FD) manifests as either an isolated (monostotic) or
polyostoticconditionasfibrousbonecysts.
• FD presents most often in the second to third decade of life as monostotic
disease,orusually<10yearsofageinpolyostoticdisease.
• FDismanifestbycysticexpansionofbones.Lesionscancausepainandlocal
mechanical effects due to their site and proximity to critical structures (e.g.
nerveforamenintheskeleton).
• FDisduetoactivatingorgain-of-functionGNAS1mutations.
• McCune–Albrightsyndrome isatriadof polyostoticfibrousdysplasia,hyper
pigmented ‘café-au-lait’ patches, and endocrine abnormalities (Cushing’s,
thyroid,precociouspuberty).
• Thereisgenetic mosaicismgiventhemutationinFDandMcCune–Albright
syndromeissomaticinorigin.Thedegreeofextentofpathologyandseverity
therefore depends on the stage of development at which the postzygotic
somaticmutationoccurred.
• When the mutation occurs at an early post-zygotic development stage, the
conditionismoresevere(agermlineGNAS1mutationwouldbelethal).
• FD bone lesions grow under the influence of growth hormone (/IGF-1) and
maystopgrowingatskeletalmaturity,butneedmonitoring.
• AnyFDbonelesioncanproduceFGF23andmildhypophosphataemiaisnot
uncommonandadditionalosteomalaciacanresult.
• Bonepainiscommonanddifficulttotreat.
• Bonepainissometimessevereanditscauseunexplained.
• PaincanbetreatedwithserialIVpamidronateinfusions.Doseregimensvary
andoptionshavenotbeensystematicallystudied.

• SomeFDlesionsdonotcausesymptomsthoughcancausecomplicationssuch
asfracture,neuralcompromise(expansionofboneadjacenttoanervecanal),
orbonecollapsedependingontheirsite.Fracturehealingdoesnotappearto
becompromisedhowever.
• Patient information is available at: http://www.gosh.nhs.uk/fibrous-
dysplasia and support at: http://www.fibrousdysplasia.org and also at:
http://www.fdssuk.org.uk
Sclerosingbonedisorders
Sclerosingbonedisorderscomprisethoseaffectingcorticalbone(hyperostotic)
andthoseaffectingtrabecularbone(osteosclerotic).
• Therearemanysclerosingbonedisorders.
5
Themostcommonaredealtwith
herebutseealsoTable16.13.
Osteopetrosis
Isatermthatdefinesarangeofosteoscleroses(‘theosteopetroses’).
• The osteopetroses are caused by one of a number of genetic abnormalities
which result in functional deficit (mostly regulation of acidification) in
osteoclastic bone resorption (e.g. CLCN7, GL, CA II (causes carbonic
anhydraseIIdeficiency)).
• AD andARforms exist—theformer lethalinchildhood unlesstreated—the
latteroftenbenignandpresentslaterinlife.(See http://www.omim.orgfora
comprehensivereviewofgenetics.)
• Diagnosisismadeonradiographswheretheeffectsofosteoclastfailureduring
endochondralboneformationresultin‘islands’or‘bars’ofcalcifiedcartilage
withintrabecularbone.
• HLA identical bone marrow transplant has been very effective for some
infantileformsofosteopetrosis.
Camurati–Engelmanndisease(CED)andRibbingdisease(RD)
• CED and RD are manifest by slowly evolving long bone hyperostosis in
childrenandadolescents(CED)andinadolescentsandyoungadults(RD).
• Bone sclerosis may be drivenbyrelease of active TGF-β from bone matrix
whichdrivesthedevelopmentandactivityofosteoblasts.
• CEDislikelyaconsequenceofoneoranumberofgermlinemutationinthe
TGF-βgeneorpeptideswhichregulateTGF-βactivation.
• It is unclear whether RD is similar but with variable penetrance or whether
thereareacquiredsystemicfactorsthatcan,similartothefunctionaleffectin
CED,‘switchon’TGF-βactivity.
Primaryhypertrophicosteoarthropathy(HOA)
• HOA is a familial disorder characterized by digital clubbing, hyperhidrosis,
facialskinthickening,andlongbonehyperostosis.
• Therearevariablefeaturesofpachydermia,delayedclosureofthefontanelles,
andcongenitalheartdisease.
• The AD form (pachydermoperiostosis) is very rare and the genetic cause
unknown. AR primary hypertrophic osteoathropathy-1 (PHOAR1) is caused
byahomozygousmutationintheHPGDgeneonchromosome4q34.1.
Pulmonary(secondary)hypertrophicosteoarthropathy(HPOA)
• HPOAdiffersfromHOAandischaracterizedbydigitalclubbingsecondaryto
acquireddiseases,mostcommonlyintrathoracicneoplasm.
Endostealhyperostosis
Theprocessofsclerosischaracterizestwoconditions:VanBuchemdiseaseand
sclerosteosis.
• Both diseases are autosomal recessive and are caused by mutations in the
SOSTgene,whichencodesforsclerostin.
• A loss of function in sclerostin results in de-suppression of osteoblast
differentiation and function thus causing generalized bone sclerosis and
hyperostosis.
• The diseases have informed the development of a therapeutic inhibitor of
sclerostintotreatosteoporosis.
Osteopoikilosis
Is a benign condition often disclosed incidentally on radiographs (‘spotted
bones’).
• Occasionally the condition is associated with the occurrence of connective
tissue nevi and dermatofibrosis (Buschke–Ollendorf syndrome) and
melorheostosis.
HepatitisCosteosclerosis
HepatitisC canbeassociatedwithseveregeneralizedosteosclerosis(cranium-
sparing).
• Remodellingofgoodqualityexcessiveboneseemsacceleratedduringactive
disease, though it will respond to anti-resorption treatment and gradual
spontaneousremissioncanoccur.
• TheconditionmaybecausedbyeffectsofIGFasthereareincreasesinIGF
bindingprotein(‘bigIGF2’).
Table16.13Thespectrumofsclerosingbonedisorders
Type Conditions
Dysplasias
and
dysostoses
Autosomaldominantosteosclerosis;centralosteosclerosiswith
ectodermaldysplasia;craniodiaphysealdysplasia,
craniometaphysealdysplasia;dysosteosclerosis;endosteal
hyperostosis(VanBuchemdiseaseandsclerosteosis);
frontometaphysealdysplasia;infantilecorticalhyperostosis
(Caffeydisease);juvenilePDB;melorheostosis;metaphyseal
dysplasia(Pyle’sdisease);mixedsclerosingbonedystrophy;
oculodentoosseousdysplasia;osteopathiastriata;osteopetrosis;
osteopoikilosis;progressivediaphysealdysplasia;Ribbing
disease;pycnodysostosis;tubularstenosis(Kenny–Caffey
syndrome)
Metabolic CarbonicanhydraseIIdeficiency;fluorosis;heavymetal
poisoning;hepatitisCassociated;hypervitaminosisD/A;
primaryhyperparathyroidism;hypoparathyroidism,
pseudohypoparathyroidism;LRP5gain-of-function(highbone
mass);milk-alkalisyndrome;renalosteodystrophy;X-linked
hypophosphataemicrickets
Other Axialosteomalacia;DISH;Erdheim–Chesterdisease;
fibrogenesisimperfectaossium;pachydermoperiostosis;
hypertrophicosteoarthropathy;ionizingradiation;leukaemias,
lymphoma;mastocytosis;multiplemyeloma;myelofibrosis;
osteomyelitis;osteonecrosis;Paget’s;sarcoidosis;sicklecell
disease;sclerotictumourmetastases(e.g.prostate);tuberous
sclerosis
Reference
5. WhyteMP.Sclerosingbonedisorders.In:RosenCJ(ed)PrimerontheMetabolicBoneDiseasesand
DisordersofMineralMetabolism(8thedn),pp.767–85.NewYork:Wiley-Blackwell,2013.
Bonetumours
Primarytumoursofbonesandjointsarerare,haveapeakincidenceinchildhood
andadolescence,andcanbebenignormalignant.Paget’sdiseaseaccountsfor
mostcasesofosteosarcomaoccurring>40yearsofage.
Osteoidosteoma
An osteoid osteoma (OO) is a benign osteoid-forming tumour that can be an
elusivecauseofintensefocalbonepaininchildrenoradults.
• OOsareuncommonandaccountsfor10%ofbenignboneneoplasia.
• OOsare2–3×morecommoninmenthanwomenandtheincidenceishighest
in the second and third decades of life; >66% occur in long bones and
especiallythefemurandtibia.
• OOlesionsareidentifiedonradiographs(ormorecommonlyCT)asawell-
definedareaof sclerosiswith radiolucentnidusoften containingspeckles of
calcium.
•
99m
TcMDPscintigraphyisasensitivemethodofisolatingalesionandCTis
valuableforlocalizingthenidusbeforesurgicalresection.
• Pain will respond, in part, to aspirin or NSAIDs. Provided the nidus is
completelyresected,surgeryiscurative.
Osteosarcoma
Thisisararetumourwithanincidenceof0.6–0.9per100,000population.Itis
thecommonestprimarybonetumour.
• Mostpatientspresentat<30yearsofage.
• Thepresentationiswithlocalpainandswelling.
• Radiographsshowexpansionofthebonewithasurroundingsofttissuemass,
oftencontainingislandsofcalcification.
• MRIorCTshouldbearrangedtodeterminetheextentoftumour.
• Patientssuspectedtohaveosteosarcomashouldbereferredtoaspecialistteam
forbiopsy.
• Treatmentdependsonhistologybutgenerallyinvolvessurgicalremovalofthe
tumour (and often radical field surgery including amputation), followed by
chemotherapyandradiotherapy.
• The prognosis is generally good in cases that present in childhood and
adolescence,butpoorinelderlypatientswithosteosarcomarelatedtoPaget’s
diseaseofbone.
Chondrosarcoma
• Thisisthesecondmostcommonprimarybonetumour.Presentationissimilar
to osteosarcoma. Treatment choice is between surgical resection and
radiotherapy. Chondrosarcomasare relatively resistantto chemotherapy. The
prognosisisgoodforlow-gradetumoursbutpoorforanaplastictumours.
Chapter17
Infectionandrheumaticdisease
Introduction
Septicarthritis
Mycobacteriumtuberculosis
Osteomyelitis
Lymedisease
Rheumaticfever
Introduction
Microorganisms have been linked directly and indirectly (through organism-
specific and autoimmune responses) to a number of acute and chronic
inflammatoryrheumaticdiseases.Thischapterwillintroducesomeexamplesof
theinflammatorymechanisms(summarizedinTable17.1)andmicroorganisms
(summarizedinTable17.2)linkedtorheumaticdisease,andthendiscussseptic
arthritis, Mycobacterium tuberculosis, osteomyelitis, Lyme disease, and
rheumaticfever.
Table17.1Pathogenesisofrheumaticdiseaseassociatedwithinfection
Inflammatory
process
Basicprocess Example Susceptibility
Local
infectionat
MSKsites
Infection.Tissue
inflammationanddirect
tissuedamage
Pyogenic
septic
arthritis
Diabetes,
complementand
immunoglobulin
deficiencies
Pathogenand
pathogen-
specific
Infectionandorganism-
specificresponse.Immune
responsetointactorganism
Syndromes
associated
withviral
Notgenerally
established
immune
response
orfragments,probable
immunecomplex-mediated
tissueinjury
hepatitis,e.g.
Sjögren’s
syndrome
Pathogens,
immune
responseand
autoimmunity
i.Cross-reactiveimmune
response.ii.Infection
inferred,butnotestablished,
autoreactivity
Rheumatic
fever,RA,JIA
SLE
HLAclassIand
IIgenes,T-cell
receptorgenes
Table17.2.Examplesofmicroorganismsassociatedwitharthritis
Class Examples Disorder
Bacteria Staphylococcusand
Streptococcus
Septicarthritis,osteomyelitis
Neisseriaspp. Gonococcalarthritis
Brucella Septicmonoarthritis
Klebsiella Spondyloarthritis
Chlamydia Reactivearthritis
Mycobacteria Mycobacterium
tuberculosis
Osteomyelitis,oligoarthritis
Atypical
mycobacteria
M.aviumcomplexM.
malmoense
Septicarthritisin
immunosuppressedpatients
Spirochaete Borreliaburgdorferi Lymedisease
Viruses ParvovirusB19 Fifthdisease
Rubella Polyarthropathy
HepatitisB Polyarteritisnodosa
HepatitisC Cryoglobulinaemia,Sjögren’s
syndrome
HIV Polyarthralgia,myopathy,
vasculitis,Siccasyndrome
Protozoa Toxoplasma Polyarthritis
Giardia Oligoarthritis
Trypanosoma Myopathy
Helminths Toxocara Allcausemyositisandarthritis
Schistosoma
Fungi Histoplasma Monoarthropathy
Cryptococcus
Septicarthritis
Septic arthritis caused by a bacterium is a medical emergency. See also
Chapter25,p.708formanagementinadultsandchildren.
Epidemiology
Incidenceinthegeneralpopulationis2–10per100,000andrisingto30–70per
100,000 in those with autoimmune rheumatic disease or prosthetic joint
replacements.
Pathology
• Most cases are due to haematogenous seeding during transient bacteraemia,
butsepticarthritiscanalsobecausedbydirectpenetrationthroughtheskin,or
bylocalspreadfromacontiguousinfectedsite.
• Jointsdamagedbychronicarthritis(e.g.RAandOA)andprostheticjointsare
atincreasedriskofinfection.
• Riskfactorsincludeadvancingage(>80years),recentjointsurgery,IVdrug
use, alcoholism, previous intra-articular steroid injection, immunodeficiency
states,CKD3b-5,anddiabetes.
• ThemostcommonpathogensareStaphylococcusaureus (including MRSA),
Streptococcusspp.,andNeisseriagonorrhoeaeinadults.
• The clinical features and natural history of gonococcal and non-gonococcal
arthritisaresufficientlydistincttodiscussthemseparately(Table17.3).
• Gram-negativebacillimaybeinvolvedinpatientswithacurrenthistoryofIV
drugabuse,orthosewhoareimmunosuppressed.
• Salmonella isa commoncause ofsepticarthritisamongpatientswithsickle
cell disease, although Staph. aureus remains the most common organism in
thisgroup.
Presentation

• Themostcommonlyaffectedjointistheknee(>50%).
• Wrists,ankles,andhipsarealsocommonlyinvolved.
• Intravenous drugusers(IVDUs) are predisposedtoseptic arthritisinvolving
theaxialjoints,e.g.sternoclavicularjoint.
• Transientsynovitis,particularlyofthehip,isnotuncommoninchildren,and
generallyoccursinthesettingafterupperrespiratorytractinfection.
• Patients with septic arthritis usually present with joint pain, swelling, and
restrictedrangeofmovementoftheaffectedjoint(s).Mostpatientsarefebrile;
however,theelderlydonotalwaysshowasystemicresponse.
Investigation
Every attempt should be made to undertake joint aspiration prior to starting
antibiotics.
• The aspirate should be sent for Gram stain, cell count and differential,
microscopy,culture,andsensitivity,andbloodcultures.
• A fluid sample should be analysed with polarized light microscopy for
crystals.
• Dependingonlikelysourceofinfection,skin,oral,andgenitalswabsshould
beconsidered.
• For a septic joint, the leucocyte count (predominantly neutrophils) in the
aspirateisusually>50,000cells/mm
3
.
• Routinebloodtestsshouldbedone:FBC,ESR,CRP,renalfunction,andliver
functiontests.
• Plain radiographs are a useful baseline investigation for assessing for
osteomyelitis or alternative pathology. In untreated septic arthritis, patchy
lucencies in periarticular bone and evidence of articular cartilage loss (joint
spacenarrowing)canbeseen.
• UScanconfirmajointeffusionandaiddiagnosticaspirationofsmalljoints.
• Ifosteomyelitisissuspected,MRIistheinvestigationofchoice.
Management
Seealso Chapter25.
Three principles determine outcome: (i) prompt diagnosis; (ii) immediate
institutionofappropriateantibiotics;and(iii)adequatejointdrainage.
• Thejointshouldbeaspiratedtodryness.
• Surgicaldrainage/washout,ordailyarthrocentesismayberequired.
• An affected joint should be rested and non-weight-bearing until the
inflammation and pain have subsided enough to allow passive mobilization.
Mobilizationshouldbeencouragedassoonaspossible.
• Empiric therapy should be started while awaiting culture results. See local
guidelines, but common regimensincludeflucloxacillin2 g IV four times a
day±gentamicinIV,oranoralthird-generationcephalosporin.
• In casesofsuspectedMRSAinfection, discussionwith amicrobiologistand
considerationofvancomycinisadvised.
• Pseudomonasspp.shouldbesuspectedinIVDUs.
• IVantibioticsareusuallycontinuedfor2weeksfollowedby4weeksoforal
antibiotics. Prolonged courses of up to 6 weeks of IV antibiotics may be
required in severe cases until swelling subsides, inflammatory markers
normalize,andculturesbecomenegative.
• Therearenostudiescomparinglongandshortcoursesofantibiotics.
• Infection of a prosthetic joint is a challenging surgical problem, and the
management should only be undertaken by specialist arthroplasty surgeons,
ideallyaspartofaprostheticjointinfectionMDT.
• Infectionofaprosthesissoonaftersurgeryorwithinashortperiodfollowinga
bacteraemicepisodecansometimesbemanagedwithprosthesisretention,but
oftenrevisionoftheprosthesisisrequired.
• Prosthesisrevisioniseitherasingleoperationordoneinastagedmanner,with
an interval period during which an antibiotic impregnated cement spacer
replacestheprosthesis.
• A joint should not be injected with glucocorticoid (GC) if intra-articular
infectionissuspected,orifthereissuperficialinfectionovertheskincovering
ajoint(e.g.cellulitisorpsoriasis).
• There is no benefit from intra-articular antibiotics. Indeed, antibiotics can
causeachemicalsynovitis.
Septicbursitis
Thetwomostcommonsitesaretheolecranonandprepatellarbursae.
• Septic bursitis should be managed with serial fluid aspiration and oral
antibiotics.
• Non-responders will need IV antibiotics, and will probably need surgical
incisionanddrainage.
• Chronicallyinfectedbursitiscanleadtoosteomyelitis.
Gonococcalarthritis
GonococcalarthritisiscausedbyNeisseriagonorrhoea.
• May present as an acute monoarthritis but is more commonly a migratory
polyarthritiswithtenosynovitisanddermatitis.
• Thepolyarthritisisusuallyasymmetric.
• Patientsareusuallyafebrile.
• Investigations should include synovial fluid analysis, blood cultures,
skin/urethral/rectal/pharyngealcultures.
• If patients are found to have gonococcal infection they should be tested for
othersexuallytransmittedinfections.
• There is increasing resistance, including multidrug resistance, of N.
gonorrhoeatoawiderangeofantibiotics.
• Treatment should be guided by local policies but a common regimen is
ceftriaxone1gIMorIVevery24hours,withasingledoseofazithromycin1
gorallyforpotentialChlamydiatrachomatisco-infection.Anoralswitchcan
beconsideredafter24–48hourswhenclinicalimprovementisseen.Treatment
shouldcontinuefor7days.
Table17.3Comparisonofclinicalfeaturesofgonococcalandnon-gonococcalsepticarthritis
Gonococcalarthritis Non-gonococcalsepticarthritis
Causativeagent:
Neisseriagonorrhoeae
Causativeagents:
Staph.aureus(50%ofcases)
Staph.epidermis(15%ofcases)
Strep. pyogenes/pneumonia (20% of
cases)
Gram-negative bacteria (10% of
cases)
Anaerobes(5%ofcases)
Mostofteninyoungadults Mostcommonintheelderly,or
underlyingjointormedicalcondition
Women>men Men>women
Hipdiseaseuncommon Hipdiseasecommon(20%ofcases)
Migratorypolyarthritiscommon Polyarthritisuncommon
Monoarthritisverycommon
Rash,skinblisters/pustules,
tenosynovitiscommon
Extra-articularmanifestations
uncommon
Synovialfluidanalysis:
Gram stain-positive in 25%, culture
positivein50%,lactatenormal
Synovialfluidanalysis:
Gram stain-positive in 60%, culture
positivein90%,lactateraised
Rapidresponsetotherapy Oftenslowresponsetotherapy.May
requiresurgery
Fullrecoveryinmostcases 10%mortality;one-thirdhaveresidual
jointdamage
Mycobacteriumtuberculosis
Epidemiology
• Until 1985, the number of tuberculosis (TB) cases in the USA and Europe
declined. More recently, the recurrence of TB has become an important
complicationofnewbiologicDMARDs.
• Itisthoughtthat30%oftheworld’spopulationisinfectedwithTB.
• Inindustrializedcountries,<5%ofcasesofTBdevelopinfectionofboneor
joints.
Pathology
• TBcanaffectanyMSKstructure.
• Predisposing factors for MSK TB infection include pre-existing arthritis,
alcoholism,useofGCs,andimmunosuppression.
Presentation
• TBofboneisusuallyalow-gradeandslowlyprogressiveinfectionassociated
withavariabledegreeoflocalandsystemicsymptoms,suchasfatigue,weight
loss,ornightsweats.
• Onsetisinsidiousandusuallymono-articularormonostotic.
• The spine is the commonest site, whether within a vertebral body (Pott’s
disease),disc,oraparavertebralabscess.
• Spinal cord compression due to vertebral destruction and/or soft tissue
swelling due to an abscess is a serious complication and must be treated
urgently.
• Spinal stabilization procedures carry a good prognosis in preventing
neurologicalsequelae.
• Monoarticulardiseaseisseenmostofteninweight-bearingjoints(hip,knee,
ankle,sacroiliacjoint—inorder).Thewristandshoulderarelesscommonly
affected.
• Osteomyelitismayaffectanylongboneandisassociatedwitheithersolitary
ormultifocalcysts.
• InTBarthritis,typicalfeaturesofsepticarthritis(e.g.warmthanderythema)
areoftenabsent.
Investigation
• ThediagnosisofTBismadebyidentifyingacid-fastbacillifromalesionor
byhistopathologicalchangesinexcisedtissue.
• Synovialfluidanalysisisnotusuallydiagnosticandasynovialtissuebiopsy
mayberequired.
• Ahighlevelofclinicalsuspicion,intheabsenceofotheridentifiedpathology,
mightleadthecliniciantotreatempirically.
Management
• Standardanti-TBregimensshouldbeusedforprophylaxisortreatment,and
surveillancefor1yearaftertreatmentisrecommended.
• Treatment is usually continued for 6–9 months, or 9–12 months for more
advanceddisease.
• Surgical intervention may be necessary—tissue biopsy, debridement of
necrotictissue,orstabilizationofajointorlongbone.
• Owing to an association between biologics therapy (particularly anti-TNFα)
anddisseminatedTB,theidentificationoflatentTBhasbecomeincreasingly
importantinpatientsbeingtreatedforchronicarthritis.
• Insuchpatients,atuberculinskintest(PPD)isuseful.Indurationof>5mm
shouldbeconsideredpositiveinpatientswhoareimmunosuppressed.
• Quantiferon-TBgold,whichisablood-basedIFNγreleaseassay,isalsouseful
forthediagnosisoflatentTB.
Atypicalmycobacterialinfections
• Patients with autoimmune rheumatic or connective tissue diseases who are
taking immunosuppressant medications are at risk of developing atypical
infections.
• Theseinfectionsareusuallychronicinnatureandcanmimicaninflammatory
flareofrheumaticdisease,thusmakingadiagnosiscanbedifficult.
• Atypicalinfectionsshouldbeconsideredinpatientswithautoimmunediseases
who present with MSK symptoms that do not respond to conservative
treatment.
• Mycobacterium malmoense has been described causing tenosynovitis and
septicarthritisoftheknee.
• M.aviumcomplexand M.chelonae osteoarticular infections have also been
described.
Osteomyelitis
Osteomyelitisreferstoanyinfectioninvolvingboneorbonemarrow.
Pathology
• Staphylococcus aureus is the most common cause of osteomyelitis. Other
importantpathogenstoconsider,particularlyintheimmunosuppressedpatient,
areTB,Pseudomonas,andSalmonella.
• Thelongbonesaremostcommonlyaffectedinchildren,andthevertebraein
adults.
Investigations
• Nosinglelaboratoryinvestigationisreliableenoughtobeusedroutinelyfor
thediagnosisofosteomyelitis.AnelevatedwhitecellcountandESRmaynot
beseen.
• Imagingisimportantinestablishingthediagnosis.Whichimagingtechnique
is successful at identifying osteomyelitis depends partly on the stage of the
infectiveprocess.
• Once the pathogen has reached bone, a suppurative reaction and marrow
oedemaoccurs.ThiscanbeseenusingMRI.
• The next stage—vascular congestion, ischaemia, thrombosis, and soft tissue
swelling—isreadilydetectedbyCT.After2–3weeks,bonereactionincluding
newperiostealboneformationanddecalcificationcanbeseenonradiographs.
• Radiographs should be requested as routine as they provide a point of
reference,andassessforotherdisease.
• Vertebral osteomyelitis is often seen early on radiographs. There may be
erosionofthevertebralbodyordisc,andparavertebralabscessesandvertebral
collapsearecommoncomplications.
• Bone scintigraphy can help localize an area of abnormality.
99m
Tc-
bisphosphonate scans, however, are not specific and the negative predictive
valueisoftengreaterthanthepositivepredictivevalue.
•
111
In-labelledleucocytescintigraphyisanalternative.
• Bonebiopsyisthegoldstandardinvestigationtoconfirmlocationofinfection,
identifyspecificorganisms,toinformtreatmentchoices.
Management
Several general, local, and systemic factors need to be considered in the
managementofosteomyelitis(Table17.4).
• Initialtreatmentintheacutephaseisthesameasthatforsepticmonoarthritis.
Ingeneral,antibioticsareneededfor6weeks,althoughchronicinfectionmay
requirelong-term(>3months)low-dosetreatment.
• Antibiotic choice should be guided by tissuemicroscopyandculture results
andlocalantibiotictherapypolicy.
• Surgery may be required early in the acute phase especially if there is an
abscessorspinalinvolvementwithneurologicalcompromise.
• Chronic osteomyelitis implies that dead bone is present, and will require
surgicaldebridement.
• Hyperbaric oxygen has also been used successfully in the treatment of air
embolism,osteonecrosis,myonecrosis,andburnspatientswithinfection.
Table17.4Factorsrelevanttothemanagementofosteomyelitis
Factors Examples
General Age:neonatestendtoharbourS.aureus,Enterobacteriaceae,and
β-haemolyticstreptococci.Inchildren>4yrs,H.influenzaeis
common,andinadultsS.aureus.
Bone:longbones(especiallylowerlimb)aremoresusceptible
thanshortbonestoinfection.Pelvicandcranialbonesare
infrequentlyinvolved
Local Chroniclymphoedema
Venousstasis
Arterialdiseasewithpoorflow
Scars
Sensoryneuropathy
Prostheticmaterial
Systemic Malnutrition
Renalandliverfailure
Immunodeficiency
Diabetes
Malignancy
Extremesofage
Chronichypoxia
Parenteraldruguse
Lymedisease
Lyme disease is a tick-borne infection caused by the spirochaetes Borrelia
burgdorferi,B.afzeli,andB.garinii.
Epidemiology
• AllthreespirochaetesarefoundinEuropebutBorreliaburgdorferiistheonly
speciesidentifiedincasesofLymediseaseintheUSA.
• Cases of Lyme disease have been reported from most statesintheUSA, as
wellasthroughoutEurope,China,andJapan.
• Highestincidenceisinchildren<15yearsandmiddle-agedadults.
• Seasonalvariation:commoninthesummermonthsofJuneandJuly.
• ThetickvectorIxodesisfoundonrodents,boarordeer—animalsinhabiting
wooded,brush,orgrassyareas.
• Ahistoryofpotentialexposureinanendemiccountrywithinthelast30days
isanimportantfacttoestablishinconsideringthediagnosis.
Presentation
• The diagnosis is made on epidemiological history and presenting features
(Table17.5),andisconfirmedwithlaboratorytests.
• Aclearhistoryofatickbiteisnotnecessarytomakethediagnosis.
Investigations
• Diagnosisismadeby eitherisolationof thespirochaetefromtissue orbody
fluidordetectionofdiagnosticlevelsofIgMorIgGantibodiesintheserumor
cerebrospinalfluid(CSF)andchangesinantibodylevelsbetweenacute-phase
andconvalescentpairedsera.
• False-positiveresultsoccurinotherinfections(e.g.syphilis),RA,andSLE.
• Western blotting is available as a confirmatory test, distinguishing between
trueseroreactivityandfalse-positiveserology.
• If the serological status is negative, then the diagnosis is unlikely and an
alternativediagnosisshouldbesought.
Management
The management of Lyme disease is primarily with antibiotics with choice of
therapyvaryingdependingonorganaffected.
• Erythemamigransistreatedwithdoxycycline100mgtwicedailyfor3weeks,
orwithcefuroxime500mgtwicedailyfor3weeks.
• Septic arthritis is treated similarly but antibiotic treatment may need to be
continuedfor30days.
• The choice of antibiotics for neurological or cardiac disease includes IV
penicillin,cefotaxime,orceftriaxone/imipenem.
• Lyme disease can cause a post-infective inflammatory (‘reactive’) arthritis
which is typical migratory (differential: sarcoid, post-streptococcal,
palindromicRA).
Table17.5ThepresentationofLymediseases
Organ
affected
Symptoms
Skin Erythemamigrans(EM):beginsasaredmacule/papule
expanding,overdaysorweeks,tobecomealargeround
lesionoftenwithpartialcentralclearing.Thelesionusually
measures5cmormore.Theremaybesmallersecondary
lesions
*
Anexpandinglesionisoftenaccompaniedbygeneral
symptoms:fever,fatigue,arthralgia,myalgia,headache
Monthslaterachroniclesion,acrodermatitischronicum
atrophicans(AChA),canappear.Itisaviolaceous
infiltrativerashformingplaquesornodules)
MSK Recurrent, brief attacks of joint swelling in one or a few
joints (may become chronic in 60% of untreated cases
weekstoyearsafterinfection).
A post-Lyme syndrome of fatigue, arthralgia, and myalgia
hasbeenreported.Ongoinginfectionhasbeendifficultto
prove.Itmaybefibromyalgiasyndrome
Neurological
(mayoccur
weeksto
monthsafter
tickbite)
Lymphocyticmeningitis
Cranialneuritis(especiallyfacialnervepalsy)
Radiculoneuropathy(differentialGuillain–Barrésyndrome)
Encephalomyelitis
Cardiovascular Acutesecond-orthird-degreeatrioventricularconduction
(mayoccur
weeksto
monthsafter
tickbite)
defectsoftenassociatedwithmyocarditis.Resolvesindays
toweeks.
Carditis—rareandremitsspontaneously
*Asimilarlesionoccurringwithinhoursofatickbiteisusuallyahypersensitivityreactionanddoesnot
qualifyasEM.
Rheumaticfever
Rheumatic fever is a delayed, non-suppurative sequelae to a pharyngeal
infectionwithLancefieldgroupAβ-haemolyticStreptococcus.
Epidemiology
• Although there has been a dramatic decline in incidence in Europe and the
USA, rheumatic fever still occurs, and remains common in developing
countries.
• There are an estimated 10–20 million cases per year worldwide, with an
annualincidenceof100–200per100,000ofthepopulation.
Pathology
• AssociationshavebeendescribedwithHLA-DR2,-DR3,and-DR4.
Presentation
• Thereisalatentperiodof2–3weeksaftertransmissionbeforetheappearance
oftheillness.
• Asymptomaticpharyngitisisseenin60%ofcases.
• Patients can present with migratory arthritis (typically of the large joints),
myocarditis,orvalvulitis,thoughwithchoreaisunlikely.
• Diagnosisfollowstherevised‘Jones’criteria(Table17.6)
• Patients who have had previous acute rheumatic fever are at risk of repeat
episodes following reinfection with group A β-haemolytic streptococci. In
repeat episodes, 2 major, or 1 major and 2 minor or 3 minor criteria are
sufficientfordiagnosis.
Arthritis
Joint involvement is more common and often more severe in teenagers and
youngadults.
• Arthritis tends to start in the large weight-bearing joints and tends to occur
early.Thepaincanbesevere.Oftenthereisanabsenceofobjectivesignsof
inflammation.Itlasts2–3weeksandisself-limiting.
• NSAIDsaretherecommendedfirst-linetreatment.
• Discriminating post-streptococcal reactive arthritis (seen in the absence of
carditis) from rheumatic fever can be difficult. Most patients will fulfil the
Jonescriteriaand,therefore,shouldbeconsideredashavingrheumaticfever.
Cardiacdisease
• Rheumaticheartdiseaseisthemostsevereoutcomeofacuterheumaticfever.
Itremainsthemajorcauseofacquiredvalvularheartdiseaseintheworld.
• Rheumaticheartdiseaseusuallyoccurs10–20yearsaftertheinitialinfection.
Themitralvalve(stenosis)ismostfrequentlyinvolved.
• When left untreated, cardiomegalyandcardiac failure secondary to valvular
diseasemayensue.
• Carditismayalsooccurandisassociatedwithcardiomyopathyandconduction
defectsincludingsecond-orthird-degreeheartblock.
Table17.6TherevisedJonescriteriaforthediagnosisofacuterheumaticfever
Thediagnosisrequires2major;or1majorand2minorcriteria
Majorcriteria Carditis
Arthritis
Chorea
Erythemamarginatum
Subcutaneousnodules
Minorcriteria
Fever(≥38.5°C)
Arthralgia
Previousrheumaticfeverorrheumaticheartdisease
RaisedESRorCRP
ProlongedPRintervalonECG
Supportingevidence RaisedASOtitre*
PositivethroatculturesforgroupAstreptococci
Recentscarletfever
Normochromicnormocyticanaemia
*
ASO,anti-streptolysinOantibodies.Titrespeakatabout4weeks,whichisabout2weeksintothe
clinicalillnessthentitresfallrapidlyoverthefollowing2–3months.
Chorea
• Sydenham’s chorea (St Vitus’ dance) consists of abrupt, purposeless
movements,muscleweakness,andemotionaldisturbance.
• The hands and face are usually the most obviously affected parts. The
movementsarenotpresentduringsleep,butdooccuratrestandmaybemore
markedononesideofthebody.
• Choreamaybethesolefeaturesuggestingrheumaticfever(beyondobserving
new cardiac murmurs) and may occur weeks to months after onset of an
arthropathy.
Skin
• Subcutaneous nodules of rheumatic fever are firm and painless. They range
fromafewmmto2cminsize.Theyarelocatedoverbonysurfacesornear
tendons.Lesionsare presentfor 2–4weeksonly, andmoreoften inpatients
withcarditis.
• Erythema marginatum is an evanescent, non-purpuric rash, usually affecting
thetrunkandproximalpartofthelimbs,butsparingtheface.Becausetherash
oftenappearstomakearing,itisalsocalled‘erythemaannulare’.Thelesions
comeandgoinamatterofhours,heatcanmakethemappearworse,andthey
aremorecommoninassociationwithcarditis.Theyresolvespontaneously.
• Erythemanodosumisrare.
Investigation
• Thereisnodiagnostictest.
• DiagnosisisbasedondetectionofgroupAstreptococcalinfectionfollowedby
thetypicalclinicalmanifestations.
• Raisedinflammatorymarkersandmildanaemiaareoftenseen.
• Serial rises in ASO antibody (or anti-DNAaseB) titres may be seen if
measuredevery14days.
• CXRandECGtolookforconductiondefects/cardiomegaly.
Management
• The three goals of management include symptomatic relief, eradication of
group A β-haemolytic streptococci, and prophylaxis against future infection
withgroupAβ-haemolyticstreptococci.
• NSAIDsshouldbegivenuntilallsymptomshaveresolved.
• Heartfailureshouldbetreatedwithconventionalmedications.
• Penicillinisgivenfor10days,evenintheabsenceofpharyngitis.
• Chorea is treated with haloperidol 1–2 mg/kg/day. GCs are sometimes also
given,thoughthereislittleevidenceofaddedbenefit.
• Recurrencecanoccurwithinthe first2years.However, recurrenceratesare
low,andtheriskofrecurrencedeclineswithageoffirstattack.Recurrenceis
associatedwithincreasedriskofcardiacdisease.
• Prophylaxisshouldbestartedassoonasantibiotictreatmenthasfinishedwith
oralphenoxymethylpenicillinorbenzylpenicillin1.2millionunitsIMevery3–
4 weeks. Duration of prophylaxis depends on severity of disease.
Erythromycin250mgdailycanbeusedinpatientsallergictopenicillin.

Chapter18
Rareautoinflammatoryandmiscellaneous
diseases
Rareautoinflammatorydiseases
Behçet’sdisease
Sarcoidosis
Miscellaneousskinconditionsassociatedwitharthritis
Relapsingpolychondritis
Amyloidosis
Adult-onsetStill’sdisease
Eosinophilicfasciitis
ImmunoglobulinG4-relateddisease
Raredisordersofsynovium
Rareautoinflammatorydiseases
Introduction
Rare autoinflammatory diseases (RAIDs) are mostly rare monogenic
immunological disorders that typically present in childhood with recurrent
fevers,highinflammatorymarkers,andsystemicfeatures.
• The typical presentation is with bouts of fever, and associated symptoms
betweenwhichthepatientiswell(‘periodic’fever).
• The term ‘autoinflammatory’ arose from the understanding that gene
mutationsresultinswitchingonofinnateimmunitythathasasecondaryeffect
on adaptive immunity. This differs from autoimmunity where failure of
recognition between self and non-self is caused by self-reactive T cells,
involvesMHCclassIIandleadstocirculatingantibodies.
• Since the discovery of the gene for familial Mediterranean fever (FMF),
MEFV (pyrin innate immunity regulator), the genes of many other RAIDs
have been identified and collectively have proven extremely valuable in
understandinginflammatorypathways.
• AlthoughRAIDsarenotgenerallylife-threatening,earlydiagnosismayavoid
repeated hospital visits, unnecessary investigations and treatment, reduced
qualityoflife,andmorbidityfromAAamyloid.
Pathogenesis
• RAIDsaredisordersoftheinnateimmunesystem.Innateimmunityisthefirst
line of defence against pathogenic microbes and mediates host responses
against cellular stress (e.g. against lipopolysaccharide or peptidoglycan
constituents).
• Highly conserved molecular processes, known as pathogen-associated
molecularpatterns(PAMPs),aredetectedbyintracellularpattern-recognition
receptors (PRRs) such as Toll-like (TLRs) and nucleotide-binding
oligomerizationdomain(NOD)-likereceptors(NLRs),whichareexpressedby
macrophages,monocytes,neutrophils,andlymphocytes.
• PRR signalling drives (the ‘inflammasome’) cytokine production such as
interleukin-1β(IL-1β).
• Genotype-influencedinflammasomefunctioncancauseRAIDsandcontribute
to other diseases (e.g. NOD2 mutations can causes Blau syndrome and
contributetoIBDphenotypealso).
Epidemiology
• FMF, the commonest RAID, has a carrier frequency in Middle Eastern
populationsof30–50%.
• Fewerthan200familieshavebeenreportedwithtumournecrosisfactor(TNF)
receptor-associated periodic syndrome (TRAPS) and there are 100 reported
casesoffamilialcoldautoinflammatorysyndrome(FCAS)andMuckle–Wells
syndrome(MWS).
• AsanexampleofotherRAIDs,therearefewerthan10familiesreportedto
haveMajeedsyndrome,mostlyarisingfromJordan.
Table18.1Thespectrumofrareautoinflammatorydiseases
Mainfeatures Diagnosis;moleculardefect Inheritance;gene;
genelocation
Periodicfever,
macularorpapular
rash,abdominal
pain
MKD(MVAandhyperIgD
syndrome(HIDS));MVK
deficiency
AR;MVK;
12q24.11
FMF;pyrindeficiency AR;MEFV(pyrin
innateimmunity
regulator);16p33.3
TRAPS;TNFreceptorsignalling AD;TNFRSF1A;
12p13.31
Feverandurticarial
rash
CINCA,MWS,andFCAS;
aberrantcryopyrinproduction
andinflammasomeresponses
AD;NLRP3;1q44
Granulomatous
diseasewithlow-
gradefever
Blausyndrome AD;CARD15;
16q12.1
Early-onsetIBD AR;IL-10R
Pyogenicrash PAPA AD;PSTPIP1;
15q24.3
Majeedsyndrome AR;LPIN2;18p11
CAMPS;abnormalactivationof
NFκB
AD;CARD14;
17q25
DIRA;uncheckedIL-1α
activation
AR;IL-1RN;
2q14.1
DITRA;asforDIRA AR;IL-36RN;
2q14.1
CANDLE;defectinIFN
signalling
AR;PSMB8;
6p21.3
Skeletaldisorders Majeedsyndrome/DIRA Seeabove
CNO Notknown
Caffey’sdisease AD;COL1A1;
17q21.33
Cherubism AD;SH3BP2;
4p16.3
MultisystemRAID Behçet’sdisease Notknown
Systemic-onsetJIA Variousgenes
AD,autosomaldominant;AR,autosomalrecessive;CANDLE,Chronicatypicalneutrophilicdermatosis
withlipodystrophyandelevatedtemperatureCAMPS,CARD14-mediatedpsoriasis;CINCA,chronic
infantileneurologicalcutaneousandarticularsyndrome;CNO,chronicnonbacterialosteomyelitis;
DIRA,deficiencyofIL-1receptorantagonist;DITRA,deficiencyofinterleukin36receptorantagonist;
FCAS,familialcoldautoinflammatorysyndrome;FMF,FamilialMediterraneanfever;IBD,
inflammatoryboweldisease;MKD,mevalonatekinasedeficiency;MVA,mevalonicaciduria;MVK,
melavonatekinase;MWS,Muckle–Wellssyndrome;PAPA,pyogenicarthritis,pyodermagangrenosum
andacne;SAPHO,synovitis,acne,pustulosis,hyperostosis,osteitis;TRAPS,tumournecrosisfactor-
associatedperiodicsyndrome;TNFRSF,tumournecrosisfactorreceptorsuperfamily.
Approachtodiagnosis
Diagnosisisbasedonclinicalsuspicion,mostlyinchildren,attimesofrecurrent
feversormultisysteminflammationofunknownaetiology.
• Treatable causes of fever such as infection, neoplasia, and autoimmune
diseasesshouldbeexcluded.
• Familyhistory,ethnicity,ageofonsetoffever,especiallywithinfirstyearof
life, characterizationofthefever, and rash and manifestations are important
cluestodiagnosiswithRAIDs.
• Characterization of the fever includes its duration and periodicity. This also
helpstounderstandtheburdenofdiseaseonqualityoflife.
• High inflammatory markers and a neutrophilia are typical during febrile
episodesandnormalizeduringdisease-freeintervals.
• Associatedfeaturesalsoincludeabdominalorlimbpainand:
• Diarrhoea—presentin75%ofcaseswithMVKdeficiency.
• Uveitis.
• Sensorineuralhearingloss.
• Inflammatoryepisodesprovokedbyvaccination.
• Arthritis.
• ConfirmationofaRAIDcanbesoughtwithgenetictesting;however,>50%of
RAIDpatientshavenegativegeneticresults.
• IntheUK,genetictestingisundertakenbytheNationalAmyloidosiscentreat
UniversityCollegeHospital,London( http://www.ucl.ac.uk/amyloidosis).
• InformationaboutthelatestgeneticabnormalitiesisavailableontheIn-Fever
websiteat http://http://fmf.igh.cnrs.fr/ISSAID/infevers/.
• Urinalysis should be requested to screen for proteinuria which raises the
possibilityofsecondaryAAamyloidosis.
CutaneousmanifestationsofRAIDs
• Urticarialeruptions—typicalofpatientswiththecryopyrinopathies—areoften
indistinguishablefromthemorecommonmastcell-mediatedchronicurticaria.
The latter is usually asymmetric with itchy recurrent wheal and flare and
angio-oedema.

• Urticarial vasculitis, which is fixedinshapefor >24 hours and also seen in
cryopyrinopathies.
• Multiple sterile abscesses—seen in pyoderma gangrenosum, acne and
pyogenic arthritis (PAPA) syndrome, SAPHO syndrome, Majeed syndrome,
DIRA,early-onsetIBD,andseveralotherRAIDs.
• Psoriaform rashes: seen in congenital forms of psoriasis (e.g. CAMPS) and
pustularskinlesionsasinSAPHOsyndrome.
• Ichthyosiform rash:tan-colouredand scalyisseen in~90%of patients with
Blausyndrome.
RAIDpresentations
RAIDs might be considered in a differential diagnosis on the basis of age of
presentation,familial inheritance(seeTable18.1), and typical clinical features
commontocertaingroupingsofRAIDs.
Neonatalandinfantileperiodicfevers
• ARAIDisconsideredininfancywhenafeverisunresponsivetoantibioticsor
recurrent, when an associated rash is persistent or unusual, and there are
atypicalfeatures,suchasboneoedema.
• Alternative diagnoses for consideration include neonatal lupus (NLE; see
Chapter10),Kawasakidisease,Behçet’sdisease,andsystemic-onsetJIA.
• ARAIDinthefirstyearoflifeincludes:
• chronicinfantileneurologicalcutaneousandarticularsyndrome(CINCA),a
cryopyrinopathy also known in the USA as NOMID (neonatal-onset
multisysteminflammatorydisease).
• FCAS.
• Majeedsyndrome.
• deficiencyofIL-1receptorantagonist(DIRA).
• Blausyndrome.
• chronic atypical neutrophilic dermatosis with lipodystrophy and elevated
temperature(CANDLE).
Childhoodperiodicfevers(cryopyrin-associatedperiodicsyndromes)
CAPS are a group of autosomal dominant RAIDs that share the same gene
mutation(NLRP3)butpresentatdifferentageswithvariationsofphenotypethat
includesanurticarialrash.
• NLRP3geneencodestheproteincryopyrin.Cryopyrinisakeycomponentof
the inflammasome (an intracellular multi-protein complex), which regulates
theprocessingofIL-1β.
• CAPS result in excess IL-1β and respond to anti-IL-1 therapy (anakinra,
canakinumab,andrilonacept).
• AAamyloidosisoccursin~25%generallyinallCAPS.
• InCINCA,feversareusuallyshortlived,lowgrade,orabsent.
• Typical features in CINCA are frontal bossing, saddle nose, midface
hypoplasia;arthritisandbonyovergrowthofknees,handsandfeet,clubbing,
CNSandophthalmicinvolvement.
• Radiographs in CINCA may show irregular ossification of metaphyses and
epiphyses.
• FCASisalsoknownasfamilialcoldurticariaandassociatedwithlow-grade
feverandarthralgia.Itpresentswithinthefirst6monthsoflife.
• TypicallyinFCAS,coldprecipitatessymptomswithin1–2hoursandattacks
last<24hours.
• MWS typically presents in an older child with high fever, typically in the
afternoon.
• InMWS,feverattackslast1–2daysalthoughtherashcanbepersistentand
sensorineural deafness is common usually appearing in childhood or even
earlyadulthood.
FamilialMediterraneanfever(FMF)
FMFismostcommoninnon-AshkenaziJews,Arabs,Turks,andArmeniansasa
result of a mutation in the gene which encodes pyrin. Pyrin is expressed in
myeloidcellsandregulatestheinflammasome.
• Diagnosisisbasedonthepresenceof:
• short,intense,self-limitingepisodesoffever(1–3days)withaleucocytosis
andhighESR.
• serositis(peritonitisandlesscommonlypericarditisorpleuritis).
• comprehensive response to oral colchicine, which achieves remission in
65% of patients and 20–30% experience a reduction in the severity and
numberoffeverattacks.
• Less common features include large joint lower limb arthritis, meningitis
headache,orchitis,vasculiticrash,andmyalgia.
• Geneticanalysisisnotalwayshelpful.
• Therecommendeddoseofcolchicineis0.5mg/dayforchildren<5yearsof
age,1mg/dayforchildren5–10years,and1.5mg/dayforchildren>10years.
Dosesaretitratedupwardsforlackofefficacyanddownwardsforabdominal
pain/diarrhoea in 0.25 mg steps (max. 2 mg/day). Colchicine virtually
eliminatestheriskofAAamyloid.
• Anti-IL-1 (e.g. anakinra) may be effective in colchicine-resistant FMF
patients.
TNFreceptor-associatedperiodicsyndromes(TRAPS)
Previously known as Hibernian fever, TRAPS affects 1 per million in Europe
andiscausedbymutationsinthep55TNFreceptor1(TNFR1).50%haveno
familyhistory.
• Presentation is often by 4 years with prolonged, although milder, periodic
fevers,lasting1–3weeks.In30%,symptomsarealmostcontinuous.Feveris
alwaysassociatedwithhighESR.
• Common features are myoarthralgia, tender macular rash on the extremes
and/or torso, and abdominal pain, headache, pleuritic pain, conjunctivitis,
periorbitaloedema,andlymphadenopathy.
• Genotypingishelpfulbuttwopolymorphismsarepresentin4%ofthenormal
population(andmaybeassociatedwithmildsymptoms).
• Acuteflaresaretreatedwithglucocorticoids(GCs)andflaresbestprevented
withanakinraorcanakinumab.Etanercept(notinfliximab)maybeeffective.
• Withouteffectivelong-termtreatment25%developAAamyloid.
Mevalonatekinasedeficiency(MKD;mevalonicaciduria(MVA)/hyper-IgD
syndrome(HIDS))
• Thecondition(s)wasfirstidentifiedin1984insixpatientsofDutchancestry
withalonghistoryofrecurrentattacksoffeverandhighserumIgDlevels.
• AnARcondition,mutationsinthemevalonatekinase(MVK)generesultina
deficiency of mevalonate kinase, essential in cholesterol biosynthesis.
Complete absence of MVK activity results in mevalonic aciduria (MVA)
associated with developmental delay, progressive ataxia, visual loss, and
failuretothrive.
• MKDstartsinearlychildhoodandpresentswithfeverslasting3–7days.
• Characteristicallytheconditionisprecipitatedbyvaccination.
• Other features include abdominal pain, diarrhoea, lymphadenopathy,
arthralgia,aphthousulcers,andpolymorphicrash.
• DiagnosisissupportedbyanIgDconcentration>100IU/mLduring/between
attacksandincreasedurinemevalonicacidduringfever.
• MVKgenemolecularanalysisisusedtoconfirmthediagnosis.
• Treatmentissymptomaticduringaflarewhichmayalsorespondfavourablyto
GCs.TheremaybearoleintreatmentforinhibitorsofIL-1orTNFα.
• SymptomsimprovewithageandAAamyloidosisisrare.
Periodicfever,aphthousstomatitis,pharyngitis,adenitis(PFAPA)syndrome
PFAPAsyndromeisincludedhereasitisthecommonestsyndromeassociated
withrecurrentfever,althoughitisnotaRAID.
• Itisdefinedbydebilitatingepisodesofabruptonsetoffeverlasting3–6days
withrecurrenceevery2–6weeks.
• Otherfeaturesincludesorethroat,smallmouthorlipulcers,tenderswellingof
thecervicallymphnodes.
• The syndrome usuallypresentsbeforethe age of 5yearsandspontaneously
resolvesduringtheseconddecadeoflife.
• CRP/ESR and neutrophils are elevatedduringattacksand normal (or settle)
betweenthem.
• 1–2daysofprednisolone(1–2mg/kg)maybegivenatthestartofanattack,
whichmaybepreventedbycolchicine,anti-IL-1therapy,orevencimetidine
insomecases.
Late-onsetFMF
ThisformofFMFisamildervariantoftheconditioninchildren.
• Itoccurstypicallyinmenandwithabdominalattacks.
• Chronicmanifestations(e.g.amyloid)rarelyoccur.
Late-onsetTRAPS
OfallpatientswithTRAPS,9%presentinadulthoodwithmeanageofonsetof
35yearsandasimilarphenotypetopaediatriconset.
Schnitzler’ssyndrome
Veryrareandusuallyfrom50yearsofagewithurticarialrashandfatigue.
Whendiagnosisisunclear
Thereisconsiderableoverlapinfeaturesoftheinheritedperiodicfeversmaking
diagnosischallenging.
• Insomecasesgeneticanalysisisinconclusive.Thismaybebecauseofasingle
mutation in an AR disorder or identification of variants of unknown
significance (e.g. low-penetrance mutations, functional polymorphisms, and
novelvariantsofunknownfunctionalimpact).
• As a guide to diagnosis in general, the Eurofever Project has produced a
validatedevidence-basedtool(Table18.2).
Table18.2TheEurofevertoolforindicationformolecularanalysisorclinicalclassification*ofpatients
withsuspectedRAIDsaftercarefulexclusionofothercauses.
FMF MKS CAPS TRAPS
Presence Score Presence Score Presence Score Presence
Durationof 9 Ageofonset<2 10 Urticarialrash 25 Periorbital

episodes<2
days
years oedema
Chestpain 13 Aphthous
stomatitis
11 Neurosensorial
hearingloss
25 Duration
of
episodes
>6days
Abdominal
pain
9 Generalized
enlargementof
lymphnodesor
splenomegaly
8 Conjunctivitis 10 Migratory
rash
†
Eastern
Mediterranean
‡
ethnicity
22 Painfullymph
nodes
13 Myalgia
North
Mediterranean
‡
ethnicity
7 Diarrhoea
(sometimes/often)
20 Relatives
affected
7
Diarrhoea
(always)
37
Absence Absence Absence
Absence
Aphthous
stomatitis
9 Chestpain 11 Exudative
pharyngitis
25 Vomiting
Urticarialrash 15 Abdominal
pain
15 Aphthous
stomatitis
Enlarged
cervicallymph
nodes
10
Durationof
episodes>6
days
13
Cut-off ≥60
Cut-off ≥42 Cut-off ≥52 Cut-off
*Theclinicalfeaturesshouldberelatedtothetypicalfeverepisodes(i.e.exclusionofintercurrent
infectionorothercomorbidities).
†Centrifugalmigratory,erythematouspatchesmosttypicallyoverlyingalocalareaofmyalgia,usually
onthelimbsortrunk.
‡EasternMediterranean:Turkish,Armenian,non-AshkenaziJewish,Arab.NorthMediterranean:
Italian,Spanish,Greek.
CAPS,cryopyrin-associatedperiodicsyndromes;FMF,familialMediterraneanfever;MKD,mevalonate
kinasedeficiency;TRAPS,receptor-associatedperiodicfeversyndrome.
ReproducedfromFederici,Silviaetal,Evidence-basedprovisionalclinicalclassificationcriteriafor
autoinflammatoryperiodicfevers,AnnRheumDis2015;74:799–805,withpermissionfromtheBMJ.
RAIDswithprominentskinmanifestations
Pyodermagangrenosum,acne,andpyogenicarthritis(PAPA)syndrome
PAPAsyndromeischaracterizedbymultiplesterileabscessesorpyodermawith
severecysticacneandpainfulhotarthritis.
• PAPAisattributabletomutationsofthePTSTPIP1genethatencodesaprotein
whichinteractswithpyrin.
• PAPAmayberesponsivetoanti-TNFαorIL-1blockade.
DeficiencyofIL-1receptorantagonist(DIRA)
DIRApresentsintheneonatalperiodwithapustularrash,arthritis,periostitis,
and osteolytic lesions of ribs and long bones. An excellent response to IL-1
inhibition(e.g.anakinra)isseen.
Chronicatypicalneutrophilicdermatosiswithlipodystrophyandelevated
temperature(CANDLE)syndrome
CANDLE syndrome is AR with increased IFN-γ expression. It appears to be
responsive to drugs inhibiting Janus kinases (JAKs), which mediate IFN-γ
signalling.
Blausyndrome
Blausyndrome isan ADRAID characterizedbyatan-colouredichthyosiform
rash (90%) and non-caseating granulomas. Blau syndrome is indistinguishable
fromsarcoid,similarlyaffectingthejoints,skin,anduvealtract.
CARD14-mediatedpsoriasis(CAMPS)
InCAMPs,severegeneralizedpustularpsoriasispresentsbefore3yearsofage.
Feversareuncommonhowever.
Furtherreading
GattornoM,FedericiS,PelagattiMA,etal.Diagnosisandmanagementofautoinflammatorydiseasesin
childhood.JClinImmunol2008;28:S73–S83.
Koné-PautI,PiramM.Targetinginterleukin-1βinCAPSsyndromes.Whatdidwelearn?AutoimmunRev
2012;11:77–80.
Lachmann HJ, Kone-Paut I, Kuemmerle-Deschner JB, et al. Use of canakinumab in the cryopyrin-

associatedperiodicsyndrome.NEnglJMed2009;360:2416–25.
Behçet’sdisease
Epidemiologyandpathophysiology
Behçet’s disease (BD) is a systemic inflammatory disorder of unknown
aetiology.ItismostcommonintheMediterraneanbasin,theMiddleEast,and
Asia.
• Prevalenceisestimatedat80–370cases/100,000inTurkey.
• Theusualonsetofthedisorderisinthethirdtofourthdecades.Onsetisrare
beforepubertyorafterthesixthdecade.
• TheM:Fratioisequal,butthediseasetendstorunamoreseverecoursein
menandtheyoung.
• PatientsfromEasternAsia,MiddleEast,andMediterraneancountriesshowa
higherprevalenceofHLA-B51;InIsraelisthereisanassociationwithHLA-
B52,andintheUKHLA-B57.
• BD is considered to have a strong angiopathic basis and considerable
morbidityoveralliscausedbythrombosisinadditiontoinflammation.
• Mildanaemiaofchronicdiseaseandneutrophiliaisseenin15%ofpatients.
ESR and CRP are often only moderately raised with episodes of arthritis,
erythemanodosum(EN)andthrombophlebitis.
• Autoantibodiesarecharacteristicallyabsent(i.e.ANCAnegative).
Clinicalfeaturesandtheirmanagement
Full-blownBDmightbeeasytoidentify,butthereareconditionsthatmimicthe
incomplete picture, including reactive arthritis, antiphospholipid syndrome
(APS), multiple sclerosis, IBD, erythema multiforme, and neutrophilic
dermatoses.TheInternationalStudyGroup(ISG)criteriapublishedin1990are
the most widely accepted diagnostic and classification criteria (see Table
18.3).Forclinicalmanifestationfrequencies,see Table18.4.
Skinandmucosalinvolvement
• Skinlesionsmaybenodular(likeEN),acneiform,orvasculitic.
• The pathergy reaction, a hyper-reactivity of the skin to a needle prick, is a
nonspecificphenomenon, butmaybehelpfulin diagnosisof BD(note: also
positiveinIBDandSweet’sSyndrome).Afterskinpuncturewithaneedle,a
papuleorpustuleformsin24–72hours.Thereactionisthoughttobeunusual
inpatientsfromNorthernEuropeortheUnitedStates,butispositivebetween
60–70%ofpatientsfromJapanandTurkey.

• Painful oral aphthous ulcers may precede other features by several years.
Idiopathicoralaphthousulcersarecommon,andalonedonotimplyBD.The
ulcers may resemble ordinary aphthae, but tend to be more frequent and
multiple,andmayhealwithscarring.
• Genital ulceration in men is most prominent over the scrotum (90%).
Urethritisis notseen unlessthereisameatalulcer. Inwomen, thelabia are
commonlyaffected.
Table18.3InternationalStudyGroupcriteriaforthediagnosisofBehçet’sdisease
Clinical
feature
required
for
diagnosis
Definedas:
Recurrent
oral
ulceration
Minoraphthous,majoraphthousorherpetiformulcers,observed
byaphysicianorreportedreliablybythepatient,recurrentat
least3timesinone12-monthperiod
Plus,any2ofthefollowing:
Recurrent
genital
ulceration
Recurrentgenitalaphthousulcerationorscarring,observedbya
physicianorreportedreliablybythepatient
Eye
lesions
Anterioruveitis,posterioruveitis,orcellsinvitreousonslitlamp
examination;orretinalvasculitisobservedbyan
ophthalmologist
Skin
lesions
Erythemanodosum-likelesions,observedbyaphysicianor
reportedreliablybythepatient,pseudofolliculitisor
papulopustularlesions;oracneiformnodulesobservedbya
physicianinpost-adolescentpatientsnotreceivingGCs
Positive
pathergy
test
Testinterpretedaspositivebyaphysicianat24–48hrs,done
withanobliqueinsertionofa20-gaugeorsmallerneedleunder
sterileconditions
Skinandmucosalinvolvementtreatment
• MildoralandgenitalulcerationmayrespondtotopicalGCpreparationsorGC

inhalers.
• Colchicine 1.5 mg/day (0.5mg tds) can be used to treat frequent attacks of
aphthousulceration.
• More resistant cases may respond to azathioprine (AZA) 2.5 mg/kg/day,
mycophenolate mofetil (MMF) and/or brief courses of prednisolone 20
mg/day.
• Anti-TNFα(etanerceptandinfliximab)havebeenshowntobebeneficialfor
mucocutaneousdisease.
• Ciclosporin and interferon alfa have been shown to be effective in RCTs.
NSAIDsarefrequentlyusedforpaincontrol.
• Thalidomidehas modestbenefitsinmucocutaneousBD,butitisdifficultto
obtain and carries a significant risk of peripheral neuropathy and
teratogenicity. Itisgenerally reservedforhighly resistantdisease inpatients
whowillfollowstrictcontraception.
Eyedisease
• Eyediseaseisaseriouscomplicationandapoorprognosticfactor.
• Itismorecommoninmen,inthe<25yearsagegroup,isusuallyseenduring
thefirst2yearsofhavingBD,andisbilateralin70–80%.
• The most frequent eye involvement is chronic relapsing panuveitis. The
presence of a hypopyon occurs in ~20% of patients and is almost always
associated with severe posterior retinal vasculitis. Recurrent bouts of
inflammationresultinstructuralchange,andtotallossofvisionoccursin20%
ofcasesdespitetreatment.
Eyeinvolvementtreatment
Topical GC and mydriatics with close supervision may be sufficient in mild
disease, but severe disease requires AZA 2.5 mg/kg/day, ciclosporin, up to 5
mg/kg/day, anti-TNFα therapy (especially infliximab), and cyclophosphamide
(CYC)forrefractorycases.
Musculoskeletalinvolvement
Arthritisorarthralgiaisseeninabout50%ofpatients.
• MSKsymptomsmayprecedetheotherfindingsbymonthsoryears.
• Arthritis might commonly involve knees, ankles, hands, and wrists, or
occasionallysymmetrical.Itisusuallyaself-limitingsynovitis,andtendstobe
non-erosiveandnon-deforming.
• Back painis rare.However,asubgroupofpatientshave areactive arthritis-
like features, presenting with acne, arthritis and enthesopathy (see main
differential:SAPHOsyndrome, Chapter16).
Musculoskeletalinvolvementtreatment
PainmayrespondtoNSAIDsandcolchicine(e.g.0.5mgthreetimesaday).
• Inflammatorydiseaseoften requirestheintroductionof AZA2.5mg/kg/day.
OthertherapiesincludeSSZ2–3g/dayorMTX10–20mgweekly.Infliximab
couldalsobeconsidered.
Table18.4FrequencyofclinicalmanifestationsinBehçet’sdisease
Lesion Prevalence(%)
Aphthousulcers 97–100
Genitalulcers ~85
Skinlesions
Papulopustularlesions
Erythemanodosum
Pathergyreaction
~80
85
50
~60%(Mediterraneancountries,Japan)
Eyelesions/uveitis 50
Arthritis 30–50
Subcutaneousthrombophlebitis 25
Arterialocclusion/aneurysm ~4
Gastrointestinallesions 1–30(moreprevalentinJapan)
Epididymitis ~5
Deepveinthrombosis 5–20
Neurologicaldisease ~5
Secondaryamyloidosis 0.04–3
Cardiovascularandpulmonaryinvolvement
• BD can affect both arteries and veins. In spite of the thrombotic episodes,
thereisarelativeabsenceofembolicphenomena.
• The heart is rarely involved in BD, but may manifest as endocarditis,
myocarditis, pericarditis, coronary vasculitis, and ventricular aneurysms.
Right-sided endomyocardial fibrosis with intracardiac thrombi is an unusual
manifestationthathasbeenobservedinyoungmaleswithwidespreadvascular
disease.
• Thrombophlebitisoccursin25%ofpatients.Lowerlimbvenousthrombosisof
the deep veins is often seen. Occlusion of suprahepatic veins (Budd–Chiari
syndrome)isararecomplicationofBDthatcarriesahighdeathrate.
• Artery involvement (1.5–7.5%) carries significant associated mortality.
Lesions are typically aneurysmal with a risk of rupture, or uncommonly,
occlusive. The abdominal aorta is the most frequently affected resulting in
abdominalpain.Peripheralarterialinvolvementmayresultinreduced/absent
pulseswithintermittentclaudication,coldextremities,orevengangrene.
• The pulmonarypathologyofBDisrelatedtoarterialvasculitis. Aneurysms,
thromboses,andinfarctsarefound.Pulmonaryembolismisraredespitehigh
ratesofthrombophlebitis.
Cardiovascularandpulmonaryinvolvementtreatment
• AspirinandNSAIDscanbeusedforphlebitis.
• Aneurysms and arterial occlusion can be treated with endovascular surgery
including intra-arterialembolization if combination immunosuppressantsfail
orareconsideredinappropriate.
• Thereremainsdebateastowhethertouseheparinororalanticoagulantsfor
BD thrombophlebitis. Most physicians will choose to treat with
anticoagulation in addition to immunosuppression. If patients have BD-
associatedaneurysms,anticoagulationincreasestherisksofhaemorrhage.
Neurologicalinvolvement
Neurologicalinvolvementisseenin5%ofpatientswithBD.Itusuallyoccurs
after the first 5yearsofthedisease,and is almost never a presenting feature.
Patternsofinvolvementareeithervascularorparenchymal.
• Parenchymal disease is usually manifested by bilateral pyramidal signs,
unilateralhemiparesis,behaviouralchanges,andheadaches.
• Themostcommonlyaffectedsiteisthebrainstemandbasalganglia.Cerebral
corticesseemtobespared.Meningealirritationanddementiamayalsooccur.
As is the case with eye disease, central nervous involvement is often more
severeinmen.
• Cerebrospinal fluid (CSF) changes such as pleocytosis and increased
cellularityoccurin60%ofpatientswithparenchymalinvolvement.
• MRI is more sensitive than CT for imaging. Signal changes, with contrast
enhancement in the brainstem and basal ganglia regions, occur but are not
specific(considerMS,sarcoid,APS).
• Dural sinus thrombosis is a feature characterized by headache, sixth nerve
palsy, papilloedema, and raised CSF pressure.Ithasabetterprognosisthan
parenchymalinvolvement.Anassociationbetweenduralsinusthrombosisand
deepveinthrombosisexists.
• Incontrasttoothervasculitides,peripheralneuropathyisunusual.
Neurologicalinvolvementtreatment
• Thrombosisoftheduralsinusesandincreasedintracranialpressureshouldbe
treatedwithIVmethylprednisolone1gfor3–5days.
• ParenchymalinvolvementisusuallytreatedwithCYCorAZAcombinedwith
GCs.
• AsmalltrialhasfoundMTXmaystoptheprogressionofchronicneurological
involvement,butlargerstudiesareneeded.
• A few case reports suggest infliximab may be beneficial in refractory
parenchymaldisease.
Gastrointestinalinvolvementanditstreatment
• Whileseeninuptoone-thirdofpatientsinJapan,gastrointestinal(GI)disease
israreinpatientsfromtheMediterraneanbasin.
• Thepathologyismucosalulceration,mostlyinileumandcaecum.
• The course is one of relapse and remission, and a tendency for bowel
perforation.ItcanbedifficulttodistinguishthefindingsofGIBDfromthose
ofCrohn’sdisease.
• IntreatingGIBD,ulcerationmayrespondtoprednisolone0.5–1mg/kg/day,
SSZ2–3g/day,orinfliximab.AZAisanalternative.
• Surgicalevaluationmaybenecessarytomanageseveresequelae.
• Largeulcers,highCRPandperforationarepredictorsofrecurrence.
Renalinvolvementanditstreatment
Renaldiseaseisseenmuchlessthanmightbeexpectedwithsystemicvasculitis.
• There are occasional reports of glomerulonephritis, ranging from IgA
nephropathytorapidlyprogressiveglomerulonephritis.
• Secondary amyloidosis AA usually presents with nephrotic disease, and has
beenreportedinabout1%ofpatients.
• Epididymitisisseeninupto20%ofmales.Otherurologicalproblemsinclude
cystitisanderectiledysfunction.
• Treatmentfocusesonsymptomcontrol.PatientswithAAamyloidosisrequire
therapyforBD.
• ColchicinecanbeusedtotreatbothBDandamyloidosis.
Sarcoidosis
Sarcoidosisisamultisystemdiseaseofunknownaetiology,characterizedbythe
presenceofmultiple,non-caseatinggranulomas.
Epidemiologyandpathophysiology
• Sarcoidosis is found worldwide but the prevalence, clinical features, and
outcomevariesconsiderably.
• Itmaypresentatanyage,butprevalencepeaksinthe20–40yearsagegroup
withasecondpeakinwomen>50yearsold.
• Itisseenmoreoftenindevelopedvsunderdeveloped,WesternvsEastern,and
inNorthernvsSouthernEuropeancountries.
• SwedenandDenmarkhaveprevalenceratesof60per100,000,TheUK20per
100,000. In the USA, sarcoidosis is 10–15× more prevalent in African
American people than in Caucasians, and in this ethnicity, disease is often
severe. Studies have suggested a link between HLA-B8, HLA-DR3, acute
sarcoidosis,andarthritis.
• Granulomata and associated tissue inflammation can occur in virtually any
tissueinthebodyandcanmanifestlocalsymptomsalone.Systemiceffectsare
notalwayspresent.
Generalpatternsofdisease
Acutesarcoidosis(Lofgren’ssyndrome)
• Thispresentswithrapid-onsetfever,acutearthritis/arthralgias,EN,andhilar
lymphadenopathy.
• LÖfgren’ssyndromehasahighrateofremissionandagoodprognosis.
• TreatmentusuallyrequiresNSAIDsonly.
• Ithasbeenreportedtooccurinseasonalclusters,especiallywinterandearly
spring,suggestingenvironmental/infectioustriggers.
• Thechestradiographclearswithin1yearin60%ofcases.
• Around15%ofpatientswithLÖfgren’ssyndromehave araisedangiotensin
convertingenzyme(ACE)levelatpresentation.
Chronicsarcoidosis
• Chronic sarcoid is less common than LÖfgren’s syndrome and has an often
subtle, insidious, progressive, and highly variable clinical course. Clinical
manifestationscanbeextensive(Table18.5).
• Granulomata can occur in virtually any tissue in the body and can manifest
localsymptoms.Systemiceffectsarenotalwayspresent.
Early-onset(childhood)sarcoidosis
EOS refers to disease onset in the first 5 years of life and has a clinical
phenotypedistinctfromadult-onsetdiseaseandverysimilartoBlausyndrome
(seeearlierinthischapter).
• A typical presentation is with rash, polyarthritis (typically a ‘boggy’
tenosynovitis),anduveitis(littlepulmonaryinvolvement).
• The rash occurs in 77%andisoften unusual including a soft yellow-brown
papillomatouslesion,hypopigmentation,andulceration.
• Eye disease is often asymptomatic and uveitis requires screening withaslit
lamp.Lacrimalhypertrophyandconjunctivalgranulomamaybefound.
• Other organ involvement is rare but may include parotids glands, testes,
vasculitis,lungs,andrenalinvolvementfromhypercalciuria.
• Treatmentisasdescribedlaterinthissection.Thereisaguardedprognosisfor
EOSasnearlyalldeveloplong-termmorbiditydespiteintervention.
• Olderchildrenhaveaclinicalphenotypesimilartoadult-onsetdisease.
Musculoskeletalmanifestationsofsarcoid
Joints
• Distinctive patterns of arthropathy are seen in both acute and chronic
sarcoidosis. In acute disease, migratory arthralgias may precede other
symptoms.
• Acutesarcoidarthritisismainlyoligoarticular,occasionallypolyarticular,but
rarely monoarticular. It commonly involves the lower limb joints, often
resultinginsymmetricaleffusionsaffectingthekneesandanklejoints.After
recovery,recurrenceratesarelow.
• Chronic polyarthritis is uncommon. It is more frequent in women and in
associationwithpulmonarydisease.
• Different forms of chronic arthritis can occur: non-deforming with
granulomatous synovitis, non-erosive deformity (Jaccoud’s), dactylitis, and
tenosynovitis.Kneesandanklesareofteninvolved.
• Rheumatoidfactorispositivein10–47%ofchronicarthritis.
Bone
• Bone involvement is estimated to occur in up to 15% of all patients with
sarcoidosis,andisusuallyaccompaniedbyskindisease.
• Approximately50%ofaffectedpatientsareasymptomatic.
• Different types of bone involvement are seen: cystic (most common), lytic,
scleroticfocallesions,andosteopenia/osteoporosis.
• Bonecystsareoftenfoundincidentallyonplainfilms,andseenmostoftenin
phalangesbutmayalsooccurintheskull,facialbones,ribs,spine,pelvisand
longbones.
• Bonecystsarefrequentlyseenwithpersistentdiseaseand/orlupuspernio(i.e.
erythematousindurationoftheskinacrosstheface).
• Dactylitisappearsas‘sausage-like’swollendigits.
• Otherradiologicalfeaturesincludethickeningofcorticalbone,acrosclerosis,
andjointdestruction.
• Lyticlesionswhichappearinvertebralbodiescanleadtobackpain,andbea
causeofvertebralfractures.
Table18.5Clinicalmanifestationsinchronicsarcoidosis
Organ/system Clinicalfeatures
Lung Parenchymaldiseasein>90%ofcases
Skin Lupuspernio,plaques,nodules,vascularpurpura
Ocular Uveitis,conjunctivitis,xerophthalmia
Lymphatics Lymphadenopathy,splenomegaly
Bonemarrow Infiltration
Hepatic Failure,granulomas,portalhypertension
Renal Nephrocalcinosis,granuloma,glomerulardisease
Gastrointestinal Granulomas(alsoinsalivary,lacrimalglands,nose,
tonsilsandlarynx),xerostomia
Cardiac Arteritis,cardiomyopathy,conductionabnormalities
Nervoussystem Centralandperipheralneuropathy.Intracerebral
lesions.Meningealinflammation.Seizures
Endocrine/reproductive
organs
Granulomas
Muscles
• Skeletalmuscleinvolvementoccursin~50–80%ofpatientswithsarcoidosis,
but is often asymptomatic. Itmaypresentasproximalpain, tenderness, and
weakness.
• Myopathymaybefocalwithpainfulnodulargranulomatousmasses,insidious
withasymmetricaldiffusepattern,oracutewithelevatedmuscleenzymes.
• Muscleweaknessisoftenmorepronouncedthaneitherthesymptomsofpain
orthelevelofraisedCK.
• Acutesarcoidmyopathymayinvolvetherespiratorymuscles.
• Electromyographyisabnormalasforpolymyositis.
Diagnosisandinvestigations
Diagnosis relies on the combination of clinical and radiographic findings,
histologicalproofofnon-caseatinggranulomas,andexclusionofotherdiseases
withsimilarpresentation.
• All patients with suspected sarcoidosis should undergo the following
investigations: electrocardiogram (ECG), pulmonary function tests, PA chest
radiograph, slit-lamp examination, tuberculin skin test, urinalysis, 24-hour
urinarycalciumandbloodtests(urea,electrolytes,creatinine,FBC,ESR,bone
profile, vitamin D, PTH, LFTs, CRP, ACE, CK) in addition to a thorough
physicalexaminationandsymptom-drivenevaluation.
• ACTchestwillalso benecessaryto assessthedegree ofparenchymallung
involvement.
• Leucopenia can be seen in around 30% of cases, and eosinophilia in 25%.
Thrombocytopeniaisalsorelativelycommon.
• TheESRmaybeelevatedintheacutephase,particularlyifENispresent(see
laterinchapterforEN/panniculitis).
• Hypercalciuria and/or hypercalcaemia is seen in 10–20%, secondary to
increased 1α-hydroxylation of 25-hydroxyvitamin D to active 1,25-
dihydroxyvitamin D (1,25(OH)
2
D) by inflammatory cell-derived 1α-
hydroxylase. Hypercalciuria can exist without there being (supra-reference
range)hypercalcaemia(butPTHwillbesuppressed).
• Liverfunctiontestsmaybederangedandathirdofpatientshavesignificant
proteinuria.
• GranulomaepithelialcellsproduceACE.SerialmeasurementsofACEmaybe
usefulinmonitoringthecourseofthedisease.
• The distribution of inflammatory tissue in sarcoid and guidance to site of
potentialbiopsycanbeidentifiedusingeitherGa-67orsomatostatinreceptor
scintigraphy.
• Other causes of granulomatous disease include tuberculosis and other viral,
parasitic, bacterial, or fungal infections, lymphomas, Crohn’s disease,
granulomatosiswithpolyangiitis,anddrugreactions.
• Sincesarcoidosiscanresembleotherdiseases,thediagnosisshouldideallybe
confirmedbyhistology.
• Bronchoalveolarlavage(BAL)maydemonstratelymphocytosisandisuseful
in excluding other diagnoses. Transbronchial lung biopsy or mediastinal
lymphnodebiopsymayalsoberequired.
Treatment(seealsopp.662–80)
• Acute, transient disease may resolve spontaneously, and require only
supportive care. NSAIDs alone may be effective, and should be used in
conjunctionwithprotonpumpinhibitors.
• More severe disease may require treatment with GCs, either alone or in
combinationwithMTX.
• Addition of HCQ may also help the skin and joint manifestations. Several
reports also describe its use in pulmonary and neurological disease, and in
hypercalcaemia.
• AZA is most often used as second-line drug therapy in patients with
progressivediseasedespiteGCs.
• CYChasbeenusedinneuro-andcardiacsarcoidosis.
• Infliximab may be effective for refractory forms of this disease, including
lupus pernio; however, relapse of sarcoidosis has been observed upon
discontinuation.
• Colchicinehasbeenusedinpatientswithsarcoidarthritisatdosessimilarto
thoseusedingout.
• No therapy is required for asymptomatic osseous or cystic bone disease, or
asymptomaticmuscledisease.TheplaceforGCsinchronicsarcoidmyopathy
remainsuncertain.
• Mortality is <5% and mainly results from respiratory failure secondary to
pulmonaryfibrosisandrefractoryneurologicalorcardiacdisease.
Miscellaneousskinconditionsassociatedwith
arthritis
Panniculitis
Panniculitisisinflammationinfattissue.Itisaninflammatoryprocessinvolving
neutrophils,leucocytes,andhistiocytesthatcausesfibrosisandgranulomas.
• The categories of panniculitis, based on histopathology are septal, lobular,
mixedtypeseptalandlobular,panniculitiswithvasculitis.
Septalpanniculitis
• This includes erythema nodosum (EN) and Vilanova’s disease (subacute
nodular migratory panniculitis). EN is a common, acute, and self-limiting
condition (typically in lower legs). It usually heals in 4–6 weeks without
scarring.Arareformcancauseulcerationandamigratoryformcanoccurfor
severalyears(women40–50yearsold).
• AssociationsofENarenumerous(seeTable18.6).
Lobularpanniculitis
Numeroussyndromeshavebeendefined:
• Weber–Christian disease: a relapsing, febrile, nodular non-suppurative
disorder. Multiple recurrent nodules and fever, arthralgia, myalgia, and
abdominal pain. Any area of the body containing fat can be involved, e.g.
mesentery, heart, lung, liver, kidney. There is a 10–15% mortality.
Investigationsmayshowtypicalhistologicalfeaturesonbiopsy,elevatedESR,
anaemia,leucopenia,orleucocytosis.
• Lipogranulomatosis: this group of conditions tends to occur in children.
Multiplelesions,oftenontheextremities,resolvewithsubcutaneousatrophy.
• Post-GC use: the pathogenesis of this rare condition is not understood. It
seemstobelimitedtochildren.ItoccursonwithdrawalofGCs,andmayclear
uponGCre-administration.
• α1-antitrypsin deficiency: may predispose to panniculitis in many types—
worth checking genetic status if severe, recurrent, or family history of
panniculitis.
• Calcifyingpanniculitis:afeatureofchronicrenalfailure.Itisnotthesameas
metastatic calcification. The prognosis is poor even with good calcium–
phosphatebalance.Parathyroidectomymayhelp.
• Lipodermatosclerosis: may be a result of venous insufficiency and
thrombophlebitis. It should be treated with compression stockings.
IntralesionalGCsorlow-doseaspirinmayalsohelp.
• LupusprofundusisararemanifestationofchroniccutaneousSLE,occurring
in<3%ofcases.Thelesionsareusuallytenderandmayulcerateandcalcify,
commonlyoccurontheface,upperarms,andbuttocks,andmayunderliean
area of discoid lupus. The lesions do not seem to follow the course of the
systemicdisease.ItmayrespondtoGCs.
• Associatedwithacutepancreatitisandacutevasculitis.
Table18.6Causes/associationsoferythemanodosum
Cause Examples
Infections Streptococcal,TB/leprosy,Yersinia,Salmonella,histoplasmosis,
blastomycosis,psittacosis
Drugs Penicillin,sulfonamides
Pregnancy
Diseases Sarcoidosis,IBD,SLE,SScl,dermatomyositis,malignancy,
Sweet’ssyndrome
Neutrophilicdermatoses
• The neutrophilic dermatoses are a group of non-infectious disorders
characterized by the presence of an angiocentric, primary neutrophilic
inflammatorycellinfiltrate(Table18.7).
• The disorders can be divided into those that cause vessel wall destruction
(vasculitis)andthosethatdonot.
Sweet’ssyndrome
• Thisconditionisrareandoccursmoreinwomenthanmen(4:1),between30
and70years.Ithasoccasionallybeenreportedinchildren.
• It is otherwise known as acute febrile neutrophilic dermatosis and was
originally described following respiratory infection, but is more commonly
seen in patients with malignancy. It is also caused by drugs, especially
granulocyte-colonystimulatingfactor.
• The characteristic features are fever, neutrophilia, and tender erythematous
cutaneouslesions(plaques,nodules,andpapules).
• Lesionscanresemblevasculitis,especiallyinafebrileillpatient.
• Skin biopsy shows intense infiltrate of mature neutrophils, typically in the
upperdermis.
• Untreated,thelesionsresolveover6–8weeks,butnewlesionswillcontinueto
appear.
• The condition is usually an acute, GC-responsive self-limiting disorder. If
longer-termtreatmentisrequired,GCdosagemaybereducedbytheaddition
ofanNSAID,dapsone,colchicine,orpossiblyMTX.
• Asecondarycausefortheconditionshouldbesought(Table18.8).
Table18.7Non-infectiousneutrophilicdermatoses
Group Examples
Non-
angiocentric
Psoriasis,reactivearthritis,acnefulminans
Angiocentric
andvessel
destruction
Leucocytoclasticvasculitis,polyarteritisnodosa
Angiocentric,
novessel
destruction
Sweet’ssyndrome,pyodermagangrenosum,bowel-associated
dermatosis–arthritis,Behçet’sdisease,rheumatoidarthritis,
ulcerativecolitis,familialMediterraneanfever
Table18.8AssociationsofSweet’ssyndrome
Associations Examples
Haematological
malignancy
Leukaemia,lymphoma,myelodysplasticdisorders
Solidtumours Breast,gastric,bladder,colon
Infectiousdiseases HIV,hepatitisB/C,TB,salmonella
Inflammatorybowel
disease
Ulcerativecolitis,Crohn’sdisease
Autoimmunediseases Rheumatoidarthritis,SLE,Sjögren’ssyndrome,
Behçet’sdisease
Pyodermagangrenosum
• This is an uncommon, ulcerative, cutaneous lesion associated with AAVs,
SLE,severeRA,andIBDsandrarelyspondyloarthritis.
• Thelesionischaracterizedbyanerythematous,violaceousborderoverhanging
acentralareaofulcerationandnecrosis.
• The lesions start as discrete pustules, most often on the legs, and are often
extremelypainful,healingwithscars.
• There is no specific treatment. An underlying disease should be excluded.
Treatmentsincludetopicalsodiumcromoglicateor5-aminosalicylicacid,oral
sulfonamides,dapsone,andGCs.
Multicentricreticulohistiocytosis
• Thisisararesystemicdisease,occurringinadultsintheir50s.Itsrecognized
clinicallybythecombinationofpapularandnodularskinlesionsandasevere
destructivepolyarthritis.
• Itisassociatedwithmalignancy(25%).

• ThearthritismimicsRAbutnotablyinvolvesDIPJs.Thedestructionmaygive
apicturesimilartoarthritismutilans.See Plate7c.
• Theskinlesionsoccurin~90%ofcases.Histologically,theinfiltrateconsists
of multicentric giant cells and histiocytes from the monocyte-macrophage
lineage. The lesions are often numerous, non-pruritic, skin coloured (or
yellow/brown),sizemm–cmindiameter,andoccurmostonthedorsumofthe
hands and face (nose, corner of the mouth, and ears). Extensive facial
involvementmayleadtoa‘leonine’facies.
• About25%ofcaseshavexanthelasma.
• The differential diagnosis includes RA, PsA, sarcoid dactylitis, xanthoma,
histiocytosis X, histiocytoma or tendon sheath giant-cell tumour—usually
solitary.
• Theconditionwaxesandwanes.Spontaneousremissionscanoccur.
• Forpatientswithmilddisease,MTXmaybesufficient,buttheconditioncan
beaggressivesomanypatientsrequiretreatmentwithCYCorchlorambucilto
preventprogressivedamage.
Relapsingpolychondritis
Relapsing polychondritis (RP) is a rare multisystem disorder of unknown
aetiology,characterizedbyepisodicandsometimesprogressiveinflammationof
cartilageleadingtodestructionandfibrosis.
• Commonsitesofinvolvementincludetheear,nose,larynx,joints,heart,and
eyes.Characteristically,thecartilaginouspartofthepinnaisinvolved,sparing
thenon-cartilaginouslobe.
• Arthralgiainvolveslargeandsmalljoints.
• SimilarpatternsofdiseasemaybeseeninPR3-positiveAAV.Somepatients
withrelapsingpolychondritisareANCApositive.
• ThediseasepredominantlyaffectsCaucasians,withpeakincidenceinthefifth
decade(M=F).
• 50paediatriccaseshavebeenreportedworldwideandthereappearstobean
associationwith(monogenetic)autoinflammation.
• ThereisalsoanassociationwithHLA-DR4.
• Approximately 30% of cases are associated with other inflammatory or
autoimmune diseases, such as systemic vasculitis, RA, SLE, Sjögren’s
syndrome,thyroiditis,andIBD.
• Therearenospecificlaboratorytests.Diagnosisismadeonclinicalgrounds.
Thecourseofthediseaseisgenerallynotlife-threateningunlessitinvolvesthe
laryngotrachealcartilageormajorarteryroots.
• MAGICsyndrome(MouthAndGenitalulcerswithInflamedCartilage)might
represent a distinct condition but is exceptionally similar to BD with
secondaryRP.
Treatment
• Treatmentisbasedonanecdoteandconsensus.TherearenoRCTs.
• Ifinvolvementislimitedtoexternalearandnasalcartilagewithnoapparent
destructionorarthritis,symptomsmaybecontrolledwithNSAIDsalone.
• Dapsone(50–200mg/day)mayalsobeofvalueandsomeprefersmalldoses
ofGCs(10–20mg/day)formilddiseasealso.
• For destructive disease in the cartilage or laryngotracheal, vestibuloneural,
lung,eye,heart,kidneyinvolvement,orsystemicvasculitis—highdoseGCs
areused(prednisolone~60mg/day).
• CYC at 1–2 mg/kg/day has been considered in severe life-threatening lung,
heart,orrenaldisease.
• PersistentorseverecasesmayalsobetreatedwithAZA,MTX,orciclosporin
(withdueattentiontorenalfunction).
• Patientsshouldbeassessedfortrachealinvolvement(e.g.stridor).Somecases
may require temporary or permanent tracheostomy and stents if laryngeal
involvementissevere.Othermeasuresmayincludecontinuouspositiveairway
pressureatnight.
• There have been a few case reports regarding the use of biologic therapies
includinganti-TNFα,andbothIL-6andIL-1inhibitors,butclinicaloutcomes
havebeenvariable.
Table18.9Featuresofrelapsingpolychondritis
Organ Clinicalfeatures Prevalence
(%)
Externalear 95
Arthritis Non-deformingandnon-erosive 85
Nose Cartilagedestruction,saddle-nose 48
Eye Episcleritis,uveitis,retinalvasculitis 57
Respiratory
tract
Dysphonia,dyspnoea,stridor 67
Innerear 53
Skin Erythemanodosum,vasculitis,Behçet’s-like
ulceration
38
Kidney Glomerulonephritis(poorprognosis) 8
Heart Pericarditis,aorticvalveincompetence,heart
block
8
Bloodvessels Aneurysms(aorticrootandabdominalaorta). 12
ReproducedfromTrenthamDE,LeCH.RelapsingPolychondritis.AnnInternMed1998;129:114–22
withpermissionfromWoltersKluwer.
Amyloidosis
Amyloid—a proteinaceous, fibrillar material—is associated with many
conditions. The low solubility of amyloid and its relative resistance to
proteolyticenzymescontributestotheirreversibleandoftenprogressivecourse
ofamyloidosis.
• Despite morphological similarities (including the formation of a β-pleated
sheet),amyloidisaheterogeneousgroupofproteins(atleast20).Alltypesof
amyloidfibrilshaveacarbohydratemoietyintheformofglycosaminoglycans
and proteoglycans. Most forms of amyloid also contain the extrafibrillar
protein,amyloid-P.
• Twoformsareimportantasmanifestationsofaresponsetochronicsystemic
inflammation:amyloid-L(AL)andamyloid-A(AA).
• AL consists of monoclonal immunoglobulin light chains and is seen in
idiopathicandmyeloma-associatedamyloidosis.Itisthecommonestsystemic
amyloidosisinWesterncountries.
• AAisderivedfromserumamyloidA(SAA),anacutephaseapolipoprotein,
andissecondary‘reactive’amyloidosis.
• It is unclear whynotall chronic inflammatory disordersareassociated with
amyloidosis and how various precursor proteins are converted to insoluble
amyloidfibrils.
• Inthecontextofrheumaticdisorders,AAamyloidosisismainlyseeninadult
RAandAS.
• SeveralconditionsarerarelyassociatedwithAAamyloidosisduetorelatively
lowlevelsofacute-phaseSAAprotein.TheseincludeSLESScl,andSjögren’s
syndrome(SS).
• Other conditions associated with AA include chronic infections, periodic
fevers,IBD,andlessfrequentlymalignancies.
Investigations
Thediagnosisofamyloidosisismadebytissuebiopsy.
• Althoughspecimenscanbeobtainedfromtheliver,heartorkidneys,increased
bloodvesselfragilityassociatedwithamyloiddepositioncarriesanincreased
bleedingrisk.Thereforereadilyaccessibleabdominalsubcutaneousfatisthe
standardaspiration (ASFA),withasensitivity of57–88%, andspecificity of
100%.
• If the ASFA is negative, or contraindicated, biopsy of the salivary gland or
rectalmucosamaybeuseful.Peripheralnervebiopsiesvaryintheirdiagnostic
valueandcancauseresidualdysaesthesia.
• AlkalineCongoredstainshowsamyloiddepositsasapplegreen/yellowunder
thepolarizingmicroscope.
• Immunofixation of serum and urine, as well as an Ig free light chain assay
should be done to confirm AL amyloidosis. If the diagnosis is uncertain, a
bonemarrowbiopsycouldbeconsidered.
• If ALandAA amyloidosesare excludedon immunofixation,furthergenetic
testingmayhelpidentifyotherweaklyamyloidogenicproteinsknowntomake
upthehereditaryamyloidoses.
• Inpatientswithchronicinflammatorydiseaseandproteinuriaand/orchronic
renalfailure,increasedSAAconfirmsAAamyloidosis.
• Echocardiogramisthegoldstandardfordiagnosingcardiacamyloid.Cardiac
MRIisalsohighlysensitiveforheartinvolvement.
• Theserumamyloidproteincontributestostabilityofamyloiddepositsinvivo.
This property is used diagnostically in radiolabelled serum amyloid protein
scintigraphy to detect amyloid in the body and is of value in assessing
responsetotreatment.
Treatment
• Theconditionisprogressiveandthereisnocure.Markedheterogeneityofthe
hereditaryamyloidosesmakescounsellingdifficult.
• The processes by which the disorder may be controlled include liver
transplantationforlysosomalamyloidosisandbonemarrowtransplantation.
• In the rheumatic diseases, the main goal is to control underlying disease to
suppressSAAproduction.VariousimmunosuppressiveagentsincludingMTX,
chlorambucil,LEF,andCYC(oftenincombinationwithGCs)haveimproved
theprognosisinRAandJIApatients.
Table18.10TheclinicalfeaturesofALandAAamyloidosis
Organ/condition Comment
AL Heart Deathoccursin50%ofcasesfromrestrictive
cardiomyopathy,congestiveheartfailure,
conductiondisturbances
Lungs 90%developcoughanddyspnoea
Skin 40%ofcases:papules,nodules,tumours
Neuropathy 10%ofcasesdevelopcarpaltunnelsyndrome
Macroglossia
Vasculopathy
Amyloid
arthropathy
Autonomic
disturbance
AL
and
AA
Weakness
Fatigue
Weightloss
Renal Nephroticsyndrome/renalfailure—majorcauseof
deathinAA*,causeofdeathinone-thirdofAL
patients
Gastrointestinal
tract
Malabsorption,obstruction,diarrhoea,
hepatosplenomegaly
*InAAamyloidthespleen,liver,andkidneysareofteninvolvedfirst.
Adult-onsetStill’sdisease
Epidemiologyandpathogenesis
• Adult-onsetStill’sdisease(AOSD)isararesystemicinflammatorydisorderof
unknownaetiology,characterizedbydailyspikingofhighfeversaccompanied
byafleetingrash,arthritis,andsystemicmanifestations.
• Menandwomenareequallyaffectedwithbimodalpeaksatages15–25and
36–46yearsthoughcaseserieshavesuggestedanassociationwithpregnancy
andinthepost-partumperiod.
• Theremaybeageneticpredisposition.ACanadianstudyfoundapossiblelink
with HLA-B17, -B18, -B35, and -DR2, but this has not been confirmed in
otherstudies.GeneticpolymorphismsoftheIL-18genemayalsobelinkedto
AOSDsusceptibilityand/orseverity.
• Variousinfectioustriggershavebeenpostulated,suggestingAOSDmaybea
reactive syndrome. These include EBV, echovirus, CMV, parvovirus 19,
coxsackievirus, influenza, and bacteria including Mycoplasma pneumoniae,
Chlamydiapneumonia,Brucellaabortus,andBorreliaburgdorferi.
• Thelper1(Th1)cytokinespresentinbloodandtissuesarethoughttoplaya
roleinthepathogenesisofAOSDinadditiontoIL-1,IL-6,IL-18,TNFα,and
IFN-γ.
Clinicalfeatures
Severalsetsofclassificationcriteriahavebeenproposedandarewelldeveloped
fromretrospectivedata.TheYamaguchicriteria(Box18.1)providethehighest
sensitivity(93.5%).
• Fever:acuteonsetofdailyspikinghighfeverexceeding40°Cisoftenthefirst
symptom. Typically peaks once daily in late afternoon or early evening
(quotidian), lasting <4 hours, and normalizing in 80% without antipyretics.
Theremaybeadoublequotidianpattern,withhighestspikesoccurringinlate
afternoon.
• Rash: evanescent salmon-pink, macular or macular papular eruption,
predominantlyinvolving proximallimbs andtrunk.Theoverallincidenceof
therashinAOSDis~70%.Therashusuallyappearsinconjunctionwithfever,
and may exhibit Koebner phenomenon. There may be pruritus and
appearancesconfusedwithdrugallergy.
• Musculocutaneousdisease:arthritismay initiallybemild,oligoarticular,and
transient, and may evolve gradually into a more severe, destructive, and
symmetrical polyarthropathy—affecting mainly knees, wrists, and ankles.
Elbows,shoulders,hipsinterphalangealjoints,andtemporomandibularjoints
mayalsobeinvolved.Generalizedmyalgiaswithfeverspikesareseeninthe
majorityofpatients,butinflammatorymyopathyisrare.
• Pharyngitis:estimatedtooccurin~70%ofAOSDcases.
• Liver: hepatomegaly occurs in 50–70%, partly influenced by NSAID use.
Casesoffulminantliverfailurehavebeendescribed.
• Tender cervical lymphadenopathy and splenomegaly occur in 50%. Lymph
node biopsy may resemble lymphoma on light microscopy, but
immunohistochemistrydemonstratesbenignpolyclonalB-cellhyperplasia.

• Cardiopulmonarydisease:serositisoccursin30–40%(pleuritis,pericarditis),
transientpulmonaryinfiltrates.ILDprogressingtoARDS,cardiactamponade,
andmyocarditishavebeendescribed.
• Haematological disease: is rare, but pancytopenia secondary to macrophage
activationsyndrome(MAS)mayoccur(~40%ofpatients),whichcanbelife-
threatening (see Chapter 25). There have been reports of pure red cell
aplasia,thromboticthrombocytopenicpurpura(TTP),andhaemolyticuraemic
syndrome(HUS).
Laboratoryandradiographicfindings
• ThereisnospecificdiagnostictestinAOSD,andnoassociationwithRFor
positiveANA.
• ESRisraisedinvirtuallyallcases,andCRPmaybeelevated.
• Marked elevations in serum ferritin occurin~70%,correlating with disease
activity. A threshold of greater than fivefold the upper limit of normal as a
diagnostic tool for AOSD is thought to have a sensitivity of 80%, but a
specificity of 45%. Levels of 3000–30,000 ng/mL are not uncommon,
normalizingwithdiseaseremission.
• Aferritinlevelof>1000ng/mLwithaglycosylatedfractionof20%orless,
hasdiagnosticspecificityof>90%.
• There is leucocytosis (>10 × 10
9
/L), with a granulocyte predominance.
Normocyticnormochromicanaemiaandreactivethrombocytosisiscommon,
especiallyduringactivedisease.
• ThereisincreasedriskofelevatedintravascularcoagulationinAOSD,andthis
maybeassociatedwithhaemophagocytosis(macrophageactivationsyndrome)
resultinginpancytopenia,requiringpromptimmunosuppression.
• Elevated liver transaminases, lactate dehydrogenase, and bilirubin levels are
seenin75%ofcases,rangingfrommildtofulminant.Liverbiopsychanges
arenon-specific.
• VeryhighlevelsofIL-18havebeendemonstratedinanumberofstudiesof
AOSD.
• Pregnancyandthepost-partumperiodmaybefacilitativeonthedevelopment
ofAOSD(highIL-18responsescanoccurinassociationwithpregnancy).
• Secondary haemophagocyticsyndrome(HS) can occur:diffuse intravascular
coagulation (DIC), hepatosplenomegaly, pancytopenia, a decrease in ESR,
hypofibrinogenaemia,markedhyperferritinaemia,andraisedtriglyceridesand
liverenzymes.
• EarlysuspicionofHSiscrucialasthereishighmorbidityandmortality.The
goldstandarddiagnostictestisbonemarrowaspiratetoidentifythepresence
of haemophagocytosis, but appearances may be visible on a blood film, in
additiontofeaturesofhaemolysis.
• Therearenospecificradiographicfindings.Classically,thereisbilateralnon-
erosiveintercarpalandcarpometacarpaljointspacenarrowingonradiographs,
whichmayprogresstoankylosisoverseveralmonths.Rapiddestructionofthe
hipandkneejointscanoccurinsomecases,requiringtotaljointarthroplasty.
Box18.1TheYamaguchicriteriaforAOSD
Diagnosis requires the presence of ≥5 criteria, including at least 2 major
criteria,withoutthepresenceofanyexclusioncriteria.
Majorcriteria
• Feverof>39°C,intermittent,≥1week.
• Arthralgiasorarthritis,≥2weeks.
• Typicalrash.
• Leucocytosis(>10×10
9
/L)with≥80%granulocytes.
Minorcriteria
• Sorethroat.
• Recentsignificantlymphadenopathy.
• Hepatomegalyorsplenomegaly.
• AbnormalLFTs(includinglactatedehydrogenase).
• NegativetestsforANAandRF.
Exclusioncriteria
• Infections.
• Malignancies.
• Otherrheumaticdisease,i.e.vasculitis.
InformationfromYamaguchiMetal.PreliminarycriteriaforclassificationofadultStill’sdisease.J
Rheumatol1992;19:424–30.
Treatment
Treatment strategies are based on organ involvement and disease severity,
aimingtocontrolfever,arthritis,andsystemicdisease.
• NSAIDs can beused first line,andoften a highdoseof aspirin isrequired.
AlthougheffectiveforMSKsymptomsandfever,efficacyratesarelow,~20%
inAOSDpatients
• GCsremainfirst-linetreatment,regardlessofpresentation.Theusualdoseis
0.5–1 mg/kg/day of prednisolone. Pulsed methylprednisolone is helpful in
severediseaserefractorytooralGCs.GCscontroldiseaseactivityin~60%,
butefficacyseemshigherforsystemicratherthanarticularsymptoms.
• ForrefractoryAOSD,MTXisacommonlyusedGC-sparingagent,inducing
remissionin~70%.
• There is also reported efficacy of AZA, HCQ, D-penicillamine, ciclosporin,
andtacrolimus.
• Intravenousimmunoglobulin(IVIg)seemstohaveasuspensiveeffect,butis
welltolerated andsafetouseifconcomitantinfection. Usualdose is2g/kg
over2–5days.Tworandomizedopenlabeltrialshavedemonstratedefficacy
ofIVIgifusedearlyinthecourseofAOSD.Itshouldalsobeconsideredin
the context of macrophage activation syndrome, life-threatening
complications,andinthecaseofAOSDflareduringpregnancy.
• BiologicDMARDsusedincludeanakinra(IL-1antagonist),tocilizumab(IL-6
inhibitor)withbeneficialeffectsonsystemicandarticularfeatures,andanti-
TNFαespeciallyinchronicpolyarticulardisease.
• Adalimumab and etanercept may have led to macrophage activation in two
reportedcasesof AOSD,and have beenassociated withparadoxicaldisease
flares.Furtherprospectiveevidenceisrequiredontheiruse.
Courseofdiseaseandprognosis
Therearethreemainpatternsofdisease,with~1/3ofpatientsfallingintoeach
category.
• Self-limitingormonophasicpatterncharacterizedbyasinglediseaseepisode.
Mostachievecompleteremissionwithin1year.
• Intermittentorpolycyclicsystemicpatternconsistingofrecurrentattacks,with
remissionbetweenflares. Subsequent diseaseflaresare often less severe,of
shorterdurationandmaybeyearsapart.
• Chronicarticularpatternassociatedwithpoorprognosis.Diseaseispersistent
with predominantarticular symptoms resulting inseveredestructive arthritis
andarthroplastyfrequentwithin2years.
• Predictors of a chronic disease course include rash, polyarthritis, and
involvement of shoulders and hips. Patients with systemic disease generally
haveafavourablediagnosis.Seriouscomplicationsfromdiseaseortreatment
arerare,butamyloidosisisthoughttobeacommoncauseofdeath.
Furtherreading
JamillouxY,Gerfaud-ValentinM,HenryT,etal.Treatmentofadult-onsetStill’sdisease:areview.Ther
ClinRiskManag2015;11:33–43.

Eosinophilicfasciitis
Eosinophilicfasciitisisanuncommonidiopathicconditionthatischaracterized
bytherapidspreadofskinchangesovertheextremities.
• Skin—usuallyinthelimbs—initiallytakesona‘peaud’orange’ appearance,
whichisreplacedbyinduration.
• LikeSScl(see Chapter13),flexioncontracturesandRaynaud’sdiseasemay
bepresent.UnlikeSScl,theepidermisisspared(i.e.superficialwrinklingis
intact)andnailfoldcapillaroscopyisnormal.
• Other localized scleroderma conditions (see Chapter 13) will be in the
differentialdiagnosisinearlydisease.
• Theconditionmayresolvespontaneously.Otherwise,70%ofcasesrespondto
GCs.
• Theconditionmaybeaparaneoplasticphenomenon.
• Itisover-representedinwomenandinthehaematologicalmalignanciesinthis
respect. The paraneoplastic condition often fails to respond to GCs and
resolvesonsuccessfultreatmentoftheunderlyingmalignancy.
• MTX and MMF may be effective and are used as GC-sparing
immunosuppressants.
ImmunoglobulinG4-relateddisease
Epidemiologyandpathophysiology
Immunoglobulin G4-related disease (IgG4-RD) is a rare systemic fibro-
inflammatorydisorderofunknownaetiology.
• ThepathophysiologyandroleoftheimmunesysteminIgG4-RDisnotwell
understood.ThereisTh2cellinvolvementwithnumerousTh2cytokines(IL-
4,IL-5,andIL-13)presentalongsideT-regs(IL-10andTGF-β).Circulating
plasmablastlevelscorrelatewithdiseaseactivity,suggestingtheimportanceof
Bcellsinpathogenesis.
• Characteristichistopathologicalfindingsarealymphoplasmacyticinfiltration
withIgG4-positiveplasmacells,storiformfibrosis(irregularlywhorledpattern
offibrosis),andobliterativephlebitis.
• Itcanaffectmultipleorgansites(seelaterinsection)andmaybelocalizedor
systemic,butmostcommonlyaffectstheextra-pancreaticbileducts,lacrimal
orsalivaryglands,orpancreas.
• IgG4-RD often presents with a tissue mass and so may mimic a solid
malignancyorlymphoma.
• It is more common in males and appears to predominantly affect patients
betweentheageof50–70years.
Clinicalmanifestations
• Multiple organs can be affected: extra-pancreatic bile ducts, lacrimal or
salivaryglands,orpancreas(Table18.11).
• Disease is often incidentally identified on imaging or histopathology
examinationofatissuespecimen.
Investigations
• Tissuebiopsyisdiagnostic.
• SerumIgG4levelsmayberaised,althoughthesecanbenormal.
• ESRandCRPmaybeelevated.
• Hypergammaglobulinaemiaisoftenseen.
• Lowserumcomplementlevelsoccurinaroundone-thirdofpatientswithrenal
involvement.
Treatmentandprognosis
• There areno RCTstoguidetreatment.GCsareeffective,particularlyin the
inflammatoryphasebutlesssointhefibroticphase.
• Though frequently used, there is a lack of consensus as to whether a GC-
sparingagentshouldbeused.
• RTXhasbeenshowntobeeffectiveinacaseseriesandarecentprospective
open-labeltrial.
• MMF, MTX,and AZA aresuggested astreatment options,butthereislittle
evidencebasefortheiruse.
• The natural history and prognosis are poorly described. Significant organ
dysfunction may result from uncontrolled and progressive inflammationand
fibrosis in involved tissues. Relapses are common on weaning GCs,
particularlyinsystemicdisease.
Table18.11OrganinvolvementinIgG4-relateddisease
Organ/system Pathologies
Hepatobiliary Pancreatitis,sclerosingcholangitis,andcholecystitis
Salivaryand
lacrimalglands
Sialadenitis,submandibularglanddisease,
dacryoadenitis,parotitis
Endocrineglands Thyroid(Riedel’sthyroiditis)
Ophthalmic Orbitalmyositis,pan-orbitalinflammation,orbital
pseudo-tumour
Vascularand
cardiac
Aortitisandperiaortitis(retroperitonealfibrosis),
pericarditis
Pulmonary Pleuritis,lungmass/nodules,mediastinitis
Lymphaticsystem Lymphadenopathy
Neurological Pachymeningitis,hypophysitis
Renaland
genitourinary
Membranousglomerulonephritis,tubulointerstitial
nephritis,renalpyelitis,prostatitis
Skinand
cutaneous
Papulo-nodules,plaques,maculopapularrash,purpura,
urticarial,psoriatic-likelesions
Raredisordersofsynovium
Pigmentedvillonodularsynovitis(PVNS)
• PVNS is a rarenon-malignantcondition (2 per million)characterized by an
uncontrolledproliferationofsynoviocytes.
• Itisassociatedwithironandfatdeposition.
• Repeatedsmallhaemorrhagesandlipiddepositsstainthesynoviumred-brown
andyellow,respectively.
• Thecauseoftheconditionisunknown,althoughsomestudieshaveproposeda
linkwithchronicrepetitivetraumaorhaemarthroses.
• Anyagemaybeaffected(mainlythirdtofourthdecade;bothsexes).
• Theclassicpresentationiswithmonoarthritis.
• The knee is the most commonly affectedjointand‘diffuse’ disease is more
aggressiveandmorelikelytorecur.
• PVNScausesaninsidiousonsetofpainandswelling,blood-stainedsynovial
fluidaspirate,withcharacteristicsynovialbiopsyfindings.
• Differential diagnosis: malignant synovioma, TB arthritis, synovial
haemangioma,synovialchondromatosis,amyloidosis,haemophilia.
• Radiographs are often normal. Calcification is not a feature of PVNS and
might suggest another cause (e.g. malignant lesion, chondromatosis, gout,
CPPD,trauma,etc.).
• Erosions and subchondral cysts (also on non-articular surfaces) can occur.
Lossofjointspaceoccurslate.MRIisdiagnostic.
Treatment
• Monoarticular PVNS is treated by excision of the lesion with or without
precedingYttrium-90(Y-90)radiationsynovectomy(RS).
• Y-90RSisessentiallyonlysuitablefortheknee.
• Y-90RScanbecoadministeredwithintra-articularsteroid.
• Re-186HEDPRScanbegivenformid-sizejoints(e.g.elbow,ankle).
• DiffuseformsofPVNStendtobeprogressiveandrecurrent.
• There are no robust treatment trials of PVNS. Treatment is based on
radiologicalstagingandtechnicalfeasibility.
Synovialchondromatosis
• Synovial chondromatosis is a chondrometaplasia of the sub-synovial
connectivetissue.Thejointcontainsthickened,white-bluenodularsynovium.
• The cause is unknown, the disorder uncommon, and the process non-
malignant. It tends to occur more often in middle-aged men and has never
beenreportedinprepubertalchildhood.
• Clinically thecondition resemblesPVNSbut tendsto beslowlyprogressive
andsometimescanbeself-limiting.
• Radiographsmayshowpunctatecalcificationatthejointmargin.
• The diagnosis should be confirmed on synovial biopsy. In rare cases, there
maybetransformationtoachondrosarcoma.
• Treatmentissurgicalandusuallymanagedwitharthroscopy,removingloose
bodiesand/orthesynovialmembrane.

Chapter19
Hereditarydisordersofconnectivetissue
Background:molecularabnormalitiesofcollagenandfibrillin
Osteogenesisimperfecta
Distalarthrogryposes
Marfansyndromeandrelateddisorders
Ehlers–Danlossyndrome
Hypermobilityspectrumdisorderinadults
Hypermobilityinchildrenandadolescents
Sticklersyndrome
Background:molecularabnormalitiesofcollagen
andfibrillin
Collagen and fibrillin are major connective tissue proteins with important
mechanicalfunctionsparticularlyintissuesrelevanttoMSKintegrity,strength,
and flexibilityintendons,ligaments, and bone. In thischapter, we outline the
conditions manifest by abnormalities in collagen and fibrillin: osteogenesis
imperfecta(OI),Marfansyndrome(MFS),Ehlers–Danlossyndrome(EDS),and
hypermobilityspectrumdisorder(HSD)—themostcommonhereditarydisorders
ofconnectivetissue(HDCT).
Osteogenesisimperfecta
Osteogenicimperfecta(OI)isacollectionofgeneticdisorderscausedbyalack,
or deficiency, of type I collagen historically known as brittle bone disease.
Variedgenotypescanresultinrelatedbonephenotypes.
Epidemiology
• OIisuncommon—about1:20,000livebirths.
Genetics
• OI occurs, in >90% of cases, because of mutations in the COL1A1 or
COL1A2gene.
• In most cases of OI type I there is a ‘functional null’ allele of COL1A1 on
chromosome17orCOL1A2onchromosome7leadingtoreducedamountsof
normalcollagenI.
• Historicallyfourmaintypeshavebeendefinedonclinicalcriteria(Table19.1)
thoughatleast17distinctgenotypesarenowrecognized.
• OI may exhibit considerable interfamilial and intrafamilial variability in the
numberoffracturesanddegreeofdisability.
Pathophysiology
• PathologyarisesasaresultofdefectsinstructureorquantityoftypeIcollagen
foundinbone,ligaments,teeth,sclerae,andskin.
Clinicalfeatures
Fractures, bone deformity, ligament laxity, joint hypermobility, easy bruising,
poordentition,andhearingdeficitarecommonfeatures.
• Generalized osteopenia and fractures early in childhood are common.
Fractures are rare in the neonatalperiod;fracturetendencyis constant from
childhood to puberty, decreases thereafter, and often increases following
menopauseinwomenand>60yearsinmen.
• OIcanpresentinyoungadultswithlowBMDorfragilityfracturesincluding
recurrentinsufficiencyfractures.
• FracturesinOIare treatedwithstandard orthopaedicproceduresappropriate
forthe typeoffractureandthe age,andhealrapidlywith evidenceofgood
callusformation(sometimeswithhypertrophiccallusformation)andwithout
deformity.
• Using clinical, radiographic, and genetic criteria, Sillence developed the
classificationcurrentlyinuseintoOItypesItoIV:adominantformwithblue
sclerae, type I; a dominant form with normal sclerae, type IV; a perinatally
lethalOIsyndrome,typeII;andaprogressivelydeformingformwithnormal
sclerae,typeIII.
• Hearing loss of conductive or mixed type occurs in about 50% of families,
beginning in the late teens and leading, gradually, to profound deafness,
tinnitus,andvertigobytheendofthefourthtofifthdecade.
• Individuals with OI type I have blue sclerae which remain intensely blue
throughoutlife,incontrasttothescleraeinOItypeIIIandOItypeIVwhich
mayalsobeblueatbirthandduringinfancy.
• Theintensityofbluescleraefadeswithtimesuchthattheseindividualsmay
havescleraeofnormalhuebyadolescenceandadultlife.
• Adifferentialdiagnosistoconsiderinyoungchildrenisnon-accidentalinjury
(NAI) and depending on the time of presentation, idiopathic juvenile
osteoporosis,Cushing’s,andhomocystinuria.
Table 19.1 The clinical and collagen abnormalities in the (historically clinically defined) four main
osteogenesisimperfecta(OI)phenotypes(Sillenceclassification)
Type Clinicalfeatures Inheritance Defect
I Normalbonegrowth.Normaldentition.
Hearinglossin50%.Bluesclera
AD Decreased
productionof
typeI
procollagen
(nullallele)
II Lethal.Stillbirths AD
AR(rare)
Rearrangement
ofcollagen
IA/2Agenes
III Oftendeformedgrowthatbirthand
worsens.Poordentitioncommon.
Hearinglosscommon.Mayhaveblue
sclera
ADorAR Mutationsin
α1andα2
collagen
chains
IV Oftenbonedeformityandshortstature.
Poordentitioncommon.Hearingloss
uncommon.
AD Mutationsin
theα2chains
AD,autosomaldominant;AR,autosomalrecessive.
Management
• Fractures heal rapidly with evidence of a good callus formation, and, with
goodorthopaediccare,withoutdeformity.
• Short-term use of bisphosphonates in children and adults with type I OI is
associatedwithBMDgainsandfractureriskreduction.
• In children, IV bisphosphonate is favoured over oral treatment—mostly
pamidronatehistoricallybutnowzoledronicacidisbeingincreasinglyused.
• Treatmentwithbisphosphonatescanreducebonepainandfractures,increases
BMD,resultsinmorenormalskeletalgrowth,andiswelltolerated.Greatest

gainsareprobablyinthefirst2–4yearsoftreatment.
• Inchildren,pamidronateisgivenat1mg/kgbodyweightover4hourson3
successivedays;infusioncyclesarerepeatedevery4months.
• Some evidence for a positive effect on BMD, bone pain, and fracture
prevention from teriparatide exists anecdotally. Intuitively teriparatide may
offer a better ‘treatment fit’ for OI compared with bisphosphonate in low
collagenproductionOI.
• Thelong-termskeletaleffectsofanti-resorptiontherapyinadultswithOIare
unknown.
• ThereareanecdotalreportsoftheuseofteriparatideinadultswithOIwhere
gainsinBMDaredocumented.
• RCTsofteriparatideandabaloparatideareinplanning.
• Regular hearing evaluations after adolescence and early stapedectomy or
stapedotomyarerecommended.
• Patient information is available at: http://www.brittlebone.org and
http://www.oif.org.
Distalarthrogryposes
Case reports of congenital contractural arachnodactyly (CCA; Beal’s
syndrome/distalarthrogryposistypeIX)highlightthewidevariationinclinical
features representing variable genetic expressivity in the distal arthrogryposes
(DAs).
• In the DAs, the MSK features of joint contractures, arachnodactyly,
camptodactyly,andkyphoscoliosispredominateinCCA.
• The DAs types 1–10 are a groupofdisordersthatmainly involve the distal
partsofthelimbsmanifestbycongenitalcontracturesoftwoormoredifferent
body areas without primary neurologic or muscle disease. The prototypic
distalarthrogryposisistype1(DA1)—characterizedlargelybycamptodactyly,
clubfoot,andheterozygousmutationintheTPM2geneonchromosome9p13
(thegeneencodingbeta-tropomyosin).
Marfansyndromeandrelateddisorders
Marfan syndrome (MFS) is due to heterozygous mutations (numerous) in the
fibrillin1gene(FBN1)onchromosome15q21.1.
• MFS is an autosomal dominant condition with complete penetrance and
prevalenceof1in25,000;criteriafordiagnosisareshowninTable19.2.
• MFS is characterized by long extremities (span/height ratio >1.05), long
fingers and feet (arachnodactyly) with a hand/height ratio >11% and
foot/heightratio>15%, tallstature(with uppersegment/lowersegment ratio
<0.89), pectus deformity of the chest wall, high-arched palate, mandibular
hypoplasia,lensdislocationsandmyopia,andjointlaxity.
• Othercommonorpeculiarmanifestationsincludestriaedistensae,pulmonary
blebs(whichpredisposetospontaneouspneumothorax),andspinalarachnoid
cystsordiverticula.
• AllfeaturesarelistedinTable19.2.
• Mitral valve prolapse, mitral regurgitation, dilatation of the aortic root, and
aortic regurgitation are cardiovascular features. Aneurysm of the aorta and
aorticdissectionarelife-threatening.
• About35%ofaffectedpersonshaveMVprolapse,aorticrootenlargementor
both on echocardiography, despite normal auscultatory findings on cardiac
examination, thus all MFS patients should have an echocardiogram and
thoracicCT/MRtoassesstheaorticvalveandarch.
• Betablockadehasbeenusedonthepremiseitwilldecreasetherateofaortic
dilatationandimprovesurvival.
• IncomparingMFSwithnon-MFSchildren,heightisadiscriminantcriterion
when>3.3standarddeviationsabovethemeanforage.
Beal’ssyndrome
• MFSshowspleiotropismandclinicalvariability.Itsharesoverlappingfeatures
withcongenitalcontracturalarachnodactyly(alsotermedBeal’ssyndromeand
distal arthrogryposis type IX), which is caused by a mutation in the FBN2
gene(chromosome5q23–q31).
Loeys–Dietzsyndrome(LDS)
LDShassimilaritiestoMFS.
• LDScharacteristicsincludecraniofacialdysmorphism(craniosynostosis,cleft
palate, hypertelorism), arachnodactyly, camptodactyly, scoliosis, joint laxity,
talipes equinovarus, translucent and hyperelastic skin, umbilical hernia, and
vascularlesions,e.g.dilatationoftheascendingaorta.
• LDS1iscausedbyamutationintheTGF-βR1gene.
• LDS2iscausedbyabymutationintheTGF-βR2gene.
• LDS3, which is associated with early-onset osteoarthritis, is caused by a
mutationintheSMAD3gene.
• LDS4iscausedbyamutationintheTGF-β2gene.
• LDS5iscausedbyamutationintheTGF-β3gene.
Table19.2TheGhent1996criteriaforMarfansyndrome(MFS)
Majorcriteria
1.Skeletal—
fourormore
of:
Pectuscarinatum
Pectusexcavatum(requiringsurgery)
Marfanoidhabitus
Arachnodactyly
Scoliosis>20°
Reducedextensionattheelbow(to<170°)
Pesplanus
Protrusioacetabulae
2.Cardiovascular:dilationoftheascendingaortainvolvingatleastthe
sinusesofValsalvaordissectionoftheascendingaorta
3.Ocular Ectopialentis
4.Dura LumbosacralduralectasiaonCTorMRI
5.Genetic Parent,child,orsiblingmeetingthecriteriaorpresenceofa
mutationinfibrillingeneknowntocauseMFS
Minorcriteria
1.Skeletal Mild–moderatepectusexcavatum
Jointhypermobility
High-archedpalate
Facies:dolichocephaly,malarhypoplasia,enophthalmos,
retrognathia
2.
Cardiovascular
Mitralvalveprolapse
Dilatationofpulmonaryarterybelowage40years
Dilatationordissectionofthedescendingthoracicor
abdominalaortabelowage50years
Calcificationofthemitralannulusbelowage40years
3.Ocular Flatcornea,myopia
4.Skin Striae;recurrentincisionalhernia
5.Pulmonary Spontaneouspneumothorax;apicalblebs
Intheabsenceofgeneticconfirmation,2majorcriteriaand1othersysteminvolvementarerequiredfor
thediagnosis.Inacasewheregeneticmutationsareknowninthefamily,1othermajorcriterionis
requiredwithinvolvementofoneotherorgansystem.
Ehlers–Danlossyndrome
Ehlers–Danlos syndrome (EDS) is a clinically heterogeneous condition
characterized by skin fragility, ligament laxity, short stature, spinal deformity,
vascularfragility,and(rarely)retinaldetachment.
Classification
TheVillefranchenosologyforEDShas beenupdated.Villefrancherecognized
nine subtypes based on the severity of the clinical features, the underlying
biochemicalandgeneticdefect,andthepatternofinheritance.The2017updated
classification (Table 19.3) lists 13 subtypes and is available online at:
https://ehlers-danlos.com/wp-content/uploads/2017-EDS-
Classification_March_2017.pdf
Table19.3The2017classificationofEDS
NameofEDSsubtype Inheritance Geneticbasis
Classical(cEDS) AR COL5A1,COL5A2
Classical-likeEDS(clEDS) AR TNXB
Cardiac-valvularEDS(cvEDS) AR COL1A2
VascularEDS(vEDS) AD COL3A1(rarelyCOL1A1)
HypermobilityEDS(hEDS) ?? Unknown
ArthrochalasiaEDS(aEDS) AD COL1A1,COL1A2
DermatosparaxisEDS AR ADAMTS2
KyphoscolioticEDS AR PLOD1,FKBP14
Brittlecorneasyndrome(BCS) AR ZNF469,PRDM6
SpondylodysplasticEDS
(spEDS)
AR B4GALT7,B3GALT6,
SLC39A13
MusculocontractualEDS
(mcEDS)
AR CHST14,DSE
MyopathicEDS(mEDS) ADorAR COL12A1
PeriodontalEDS(pEDS) AD C1R
AD,autosomaldominant;AR,autosomalrecessive.
Genotypingandclinicaldiagnosis
• Thereisconsiderableoverlapbetweensubtypes.
• Diagnosis is increasingly though genotyping—available on blood or saliva
DNAsequencinganalysis.
• ForthosewhomeettheminimalclinicalrequirementsforanEDSsubtype,but
whohavenoaccesstomolecularconfirmation;orwhosegenetictestingshows
one(ormore)genevariants ofuncertain significancein thegenes identified
foroneoftheEDSsubtypes;orinwhomnocausativevariantsareidentifiedin
anyoftheEDS-subtypespecificgenes,thena‘provisionalclinicaldiagnosis’
ofanEDSsubtypecanbemade.
• If no diagnosis is made by genotyping and if there is an extreme clinical
phenotype,thenexpandedmoleculartestingcanbeconsidered.
• Embryonic testing can be done either by pre-implantation genetic diagnosis
(PGD) and pre-natal testing in utero. PGD is only approved for use in the
vascularandclassicalEDStypes.
ClassicalEDS(cEDS)
• cEDS is often predominantly initially manifest by disability. It affects skin,
woundhealing,andjoints.Theeffectsoftenworsenovertimeashypermobile
joints can be unstable, causing painful dislocations, subluxations, arthritis,
bursitis,tendonitis,and(later-adult)painfulOA.
• Hyperextensibleskiniseasilytornanddoesn’trepairitselfwell,causingpain
anddisfiguringscarring.
• Difficulties may arise during pregnancy: joint pain from increased body
weight, early rupture of membranes and premature birth, cervical
incompetence and spontaneous abortion, excessive tissue trauma during
delivery, and MSK complications in the post-natal period due to lifting and
caringforthenewborn.
• Patientsareoftenpartlyresistanttolocalanaesthetic—causeunclear.
• PhysicaltherapyforEDSshouldfocusongradedexerciseandjointandskin
protection.Someindividualsrequirejointsplints.Spinaldeformitymayneed
bracingorsurgery,andretinaldiseaserequiresophthalmicexpertise.
HypermobileEDS(hEDS)
The1997criteriafordiagnosinghEDSwereupdatedin2017.Formerly,criteria
for diagnosis were met if there was either hyperextensibility (and/or smooth
velvety skin) and/or generalized joint hypermobility and the presence of ≥1
minorcriteria(recurringjointdislocations,chronicjoint/libpain,positivefamily
history.
• The2017criteriasupercedetheBrightoncriteria.SeeareTable19.4.
• hEDS evolves over time. Contortionism and propensity for sprains and
dislocationsoccursinhEDSbutisnotspecifictothediagnosis.
• Paininitiallyisoftenlimitedtolowerlimbs.
• Theremaybeeasyfatiguabilityandvoidingdysfunction.
• The‘pain’phase(whichstartsinthesecondtofourthdecadeoflife)includes
more widespread and progressively worsening MSK pain, pelvic pain in
women,andheadache.
• The ‘stiffness’ phase (observed in a few adults and elderly only) results in
general reduction of joint mobility, significant reduction in function due to
disabling pain and fatigue, and limitations from reduced muscle mass and
weakness,priorinjuriesandarthritis.
• Patients with all types of EDS, may be at risk of developing postural
orthostatictachycardiasyndrome(PoTS)—anabnormalincreaseinheartrate
thatoccursaftersittinguporstanding,causingdizziness,fainting,andother
symptoms.
• However, the EDS-PoTS association is disputed as PoTS can be a benign
conditionaffectingmostcommonlygirlsandwomenaged15–50years.
• PoTScanbetreatedwithsaltandfluidsupplementation.
VascularEDS(vEDS)
Uterine,arterial,orvisceralruptureandahistoryofspontaneousbleedingraises
thepossibilityofvascular(typeIV)EDS.
• Thereisanexpectedshortenedlifespan(median49yearsformenand53years
forwomen).Acrogeriaiscommon.
• Appearance is often characteristic: translucent skin, increased visibility of
veins,thin lips,small chin,thin nose,largeeyes, recedinggums. Alsooften
seen:recedinggums,easybruising,congenitalclubfoot.
• vEDS can cause massive bleeding (e.g. intracranial aneurysm, arterial
dissection,uterineandGIbleeding).
• In vEDS, operative therapy is reserved for compelling indications in which
benefitclearlywarrantsriskbecauseofbleedingrisk.
Table19.4The2017criteriafordiagnosinghypermobileEDS(hEDS)
Criteria1
Thereisgeneralizedjointhypermobilitybasedona‘positive’Beightonscore
(seeTable19.6)of:
• ≥6inprepubertalchildrenandadolescents.
• ≥5inmenandwomen,post-pubertyuptoageof50years.
• ≥4inmenandwomenolderthan50years.
Criteria2
Twoormoreofthefollowingfeaturesapply.Thereis/are:
A.Atleast5systemicmanifestationsofamoregeneralizedconnectivetissue
disorderarepresent(fromfollowinglist).
B.Apositivefamilyhistory(≥1first-degreerelativesindependentlymeeting
criteriaforhEDS).
C.Musculoskeletalcomplications(≥1fromfollowinglist)
A:anunusuallysoftorvelvetyskin,mildskinhyperextensibility,unexplained
striaewithoutahistoryofsignificantweightchange,bilateralpiezogenic
papules of the heel, recurrent or multiple abdominal hernias, atrophic
scarring involving at least 2 sites and without the formation of truly
papyraceousand/orhaemosidericscarsasseenincEDS,dentalcrowding
andhighornarrowpalate,pelvicfloor,rectaland/oruterineprolapsein
childrenmenornulliparouswomenwithoutahistoryofmorbidobesityor
other predisposing condition, arachnodactyly defined by bilateral
Steinberg and/or Walker signs, arm span to height ratio ≥1.05, mitral
valveprolapse,aorticrootdilatationwithZ-score>+2.
C: MSK pain in ≥2 limbs, recurring daily for at least 3 months, chronic
widespread pain for ≥3 months, recurrent joint dislocations or frank
instability, in the absence of trauma (requiring both ≥3 atraumatic
dislocations in same joint or more atraumatic dislocations in 2 different
joints occurring at different times and medical confirmation of joint
instabilityat≥2sites,unrelatedtotrauma.
Criteria3
Allthefollowingarerequired:
• Absence of skin fragility, which should prompt consideration of other
typesofEDS.
• Exclusion of other heritable and acquired connective tissue disorders
includingautoimmunerheumaticconditions.
• In patients with an acquired/autoimmune connective tissue disorder
additionaldiagnosis ofhEDSrequiresmeetingbothfeaturesAandB of
criterion2.FeatureCofcriterion2cannotbecountedtowardsadiagnosis
ofhEDS.
• Exclusionofotherdiagnosesthatmayalsoincludejointhypermobilityby
meansofhypotoniaand/orconnectivetissuelaxity.
AdiagnosisofhEDSismadewhenallthreecriteriaaremet.
Hypermobilityspectrumdisorderinadults
Hypermobilityisnowcharacterized through theterm‘hypermobility spectrum
disorder’(HSD).Generalizedandlocalizedforms arerecognized(Table19.5).
Notably, havinganHSDcan be an advantage ifitis not severe; for example,
flexibility/hypermobility may present greater opportunity for enhanced motor
competence and sporting prowess through increased agility, as with gymnasts
andsomedancers.
• Associated features of HSD include chronic widespread pain, fatigue,
cardiovascular autonomic dysfunction, bowel dysfunction, pelvic organ
prolapse.
• Inadults,thediagnosisofbothhEDSandanHSDrequiresknowledgeofthe
Beightonhypermobilityscale(Table19.6).Thescalehasbeenvalidatedacross
somebutnotallethnicgroupswheretherangeofconnectivetissuelaxitymay
vary.
• ThegeneticsoftheHSDsispoorlyunderstood.
• Althoughhypermobilitydiminisheswithage,thesymptomstendtocontinue
andmayworsen.
• Itisimportanttorememberthatolderpatientsmayhavebeenpreviouslymore
mobile and that the Beighton score may not be an appropriate measure. A
historyofjointlaxityshouldbesought.
Table19.5Thespectrumofjointhypermobility(JH)inadditiontohEDS
Type Beighton
score
MSK
involvement
Notes
Asymptomatic
generalizedJH
Positive Absent
Asymptomatic
peripheralJH
Usually
negative
Absent JHtypicallylimitedto
handsandfeet
Asymptomatic
localizedJH
Negative Absent JHlimitedtosinglejoints
orparts
Generalized-HSD Positive Present
Peripheral-HSD Usually
negative
Present JHtypicallylimitedto
handsandfeet
Localized-HSD Negative Present JHlimitedtosinglejoints
orparts
Historical-HSD Negative Present HistoricalpresenceofJH
Table19.6Beighton(‘Bye-ton’)adulthypermobilityscore
Subjecthastheabilityto: Right Left
1 Passivelydorsiflexthefifthmetacarpophalangealjointto90° 1 1
2 Opposethethumbtothevolaraspectoftheipsilateralforearm 1 1
3 Hyperextendtheelbow10° 1 1
4 Hyperextendtheknee10° 1 1
5 Placehandsflatonthefloorwithoutbendingtheknees 1
Possibletotalscore 9
Treatmentofjointhypermobilitysyndromeinadults
• It is importanttode-medicalize simple situations offlexiblejoints and mild
hypermobilitywherepossible.
• Patients should be reassured that unlike other forms of heritable connective
tissue disease, there are often no serious long-term complications of most
HSDs and the mainstay of treatment is a combination of conservative
measuressuchasphysiotherapyandpainrelief.
• Analgesicsareoftenunhelpfulforchronicpain,buthavetheirplaceinacute
symptoms.Painandfatiguecausesignificantmorbidity.
• Joint stabilizing exercises withparticularreference to core stability, posture,
and proprioception are beneficial, as may be advice on avoiding overuse
injuries and practical ways of managing day-to-day activities. A global
approach to joint stability and function, as opposed to just treating regional
symptoms,iseffective.
• ‘Pain management’ should be considered in chronic pain cases. This might
include for example, cognitive behavioural therapy and management plans
similartothoseusedinfibromyalgia.
• The role ofserotonergic/noradrenergic agents inthesepatients is unclear. In
parttheremaybeeffectivecontrolofdepression;however,theremayalsobe
directanalgesicpropertiestotheseagents.
• Neurolepticagentsforneuropathicpainhavenotbeenstudiedinthisgroupof
patients.However,gabapentinorpregabalinandothersimilaragentsmayhave
arole.
• Cardiovascular autonomic dysfunction requires specialist assessment and
advice.
• Pregnancyisoftenaconcern.UnliketherarerformsofEDS,hEDSandthe
HSDsarenotassociatedwithanymajorvascularhazardduringpregnancyand
labour. However, in hEDS, and generalized HSD there are a number of
considerations:
• Jointpain/dislocationmayincreaseduringpregnancy.
• Positioning during delivery should be carefultoavoidexcessivestrain on
joints.
• Labourmayberapid.
• Membranesmayruptureprematurely.
• Thereisanapparentresistancetotheeffectsoflocalanaesthetics.
• Healingmaybeimpairedandsurgicaltechniquemayneedtobemodified
accordingly.
• Thereisnoabsoluteindicationforcaesareansection.
• Severe pelvic floor problems (uterine prolapse, etc.) May occur than
otherwiseanticipated.
Hypermobilityinchildrenandadolescents
A robust definition of the HSDs in children and/or adolescents has not been
established,sodistinguishing‘themorehypermobileoftherangeofnormal’(i.e.
familialconnectivetissuelaxity)from‘pathological’ischallengingifbasedon
hypermobilityalone.
• Historically,useofthediagnosticterms‘benignjointhypermobilitysyndrome’
andEhlers–Danlossyndromehypermobilitytype(EDStype3)hadatendency
to draw attention to a heterogeneous population of children and adolescents
with widespread pain and other clinical features whose level of stress and
disabilitywaspoorlyserved.
• InconsideringmakingadiagnosisofhEDSoranHSDinachildoradolescent
itisimportanttoconsiderthat:
• Beightoncriteriahaveneverbeenvalidatedinchildren.

• in the past, diagnostic labels such as EDS type 3 have been over- and
misusedwithoutreferencetovalidatedcriteria.
• thatjointhypermobilityandconnectivetissuelaxityisamanifestationofa
numberofdisorders—see Box19.1,p.592.
Box19.1Childhoodconditionsassociatedwithjointhypermobility
• Osteogenesisimperfecta.
• Ehlers–Danlossyndrome(e.g.classical,vascular).
• Marfansyndrome.
• Loeys–Dietzsyndrome.
1
• Sticklersyndrome.
• Distalarthrogryposis/Beal’ssyndrome.
• Trichorhinophalangealsyndrome(TRPS).
• Meier–Gorlinsyndrome(OMIM613805).
Epidemiology(ofasymptomatichypermobility)
• Hypermobility is present at high levels in the normal paediatric population.
ThereareracialvariationsandaBeightonscoreof≥4isespeciallycommonin
preschoolchildren.
• Inteenagegirlsandboys(mean14years),alargeUKstudyfoundgeneralized
joint laxity in 27.5% and 10.6%, respectively, using a cut-off of four
hypermobilejoints.
• Hyperextensibilityatthelittlefingerhasbeenfoundin>40%girlsand>30%
scored positively for thumb apposition. One explanation of this is that
hypermobilitymaybenormalinateenagepopulation.
Therelationshipofhypermobilityandchronicpaininchildren
• A theoretical basis for problems with hypermobility is that individuals with
hypermobility require greater muscular control to avoid stress, and possible
damage,ofthejointcapsuleorassociatedligaments.Asaresult,ithasbeen
inferredthathypermobilitymaybeariskfactorforchronicMSKpain.
• However,althoughthereissome,ifinconsistentevidence,thathypermobility
inchildrenandadolescentsisassociatedwithanincreasedriskofMSKpain,
thetruevalueofadiagnosticlabelofHSDasthecauseofpainisunclearand
mayevenbeharmfulinassertingalife-longconditionwhenthisisunproven.
• Painassociatedwithhypermobilityshouldalsobeseeninthecontextofthe
generalprevalenceofMSKpain.SeveralstudieshaveshownMSKpaincan
occurinathirdofpeoplefromthegeneralpopulation.
• Itisprudenttoconsiderthatifthereislong-termpaininachildwhohassome
featuresofhypermobility,thepainandhypermobilitymaynotnecessarilybe
linkedthroughacausalmechanism:
• A prospective study of the relationship between hypermobility (Beighton
score≥6)andMSKpaininthesamepopulationfoundatwofoldincreased
riskofpaininshoulders,knees,feet,andankles,butnototherjoints.
• In the same study, the impact of pain on daily activities was found to be
unrelatedtohypermobility.
• The lack of association between chronic widespread pain, hypermobility,
andpainintensityisconsistentacrossstudies.
• Inastudyofjuvenilefibromyalgia,painscoresweresimilarinthosewith
andthosewithouthypermobility.
• Asaresultoftheabove-listedpoints,inachildwithchronicpainwherethere
issomeevidenceforhypermobility,rehabilitationandfunctionalrestorationis
bestachievedbya‘needs’ratherthan‘diagnostic’focus.
Reference
1.VanLaerL,DietzH,LoeysB.Loeys-Dietzsyndrome.AdvExpMedBiol2014;802:95–105.
Sticklersyndrome
Sticklersyndromeisaclinicallyvariableandgeneticallyheterogeneousdisorder
characterizedbyocular,auditory,skeletal,andorofacialabnormalities.
MostformsofSticklersyndromearecharacterizedbytheeyefindingsofhigh
myopia,vitreoretinaldegeneration,retinaldetachment,andcataracts.Additional
findingsmayincludemidlineclefting(cleftpalateorbifiduvula),PierreRobin
sequence, flat midface, sensorineural or conductive hearing loss, mild
spondyloepiphysealdysplasia,andearly-onsetosteoarthritis.
TherearefivegeneticsubtypesofStickersyndrome:
• Type I is caused by heterozygous mutation in the COL2A1 gene on
chromosome12q13.
• SticklersyndrometypeII(STL2),sometimescalledthebeadedvitreoustype,
iscausedbymutationintheCOL11A1geneonchromosome1p21.
• SticklersyndrometypeIII(STL3),sometimescalledthenon-ocularform,is
causedbymutationintheCOL11A2geneonchromosome6p21.STL1–3are
ADinherited.
• ARformsincludeSticklersyndrometypeIV(STL4),causedbymutationin
theCOL9A1geneonchromosome6q12–q14,andtypeV(STL5),causedby
mutationintheCOL9A2geneonchromosome1p33–p32.2.
Chapter20
Commonupperlimbmusculoskeletallesions
Subacromialimpingement
Adhesivecapsulitis
Lateralhumeralepicondylitis
For a detailed view on the differential diagnosis of the entire range of upper
limblesions,see Chapter3
Forsteroidinjectionofupperlimblesions,see Chapter24
Subacromialimpingement
Subacromialimpingement(SAI)isimpingementoftissuesbetweenthehumeral
head(oftenthegreatertuberosity)andanarchofoverlyingtissuesformedbythe
acromion, coracoacromial ligament, and coracoid. The tissue most frequently
affectedispartoftherotatorcufftendon,thesupraspinatustendon.
Clinicalfeatures
Impingementcausesshoulderpainwhenthepatientreachesuporbehindtheir
back,orrollsoverontheshoulderatnight.
• SAIisthemostcommontypeofpresentationofshoulderpaininadults.
• Painisoftenreferredtotheupperarm.
• Causesareacuterotatorcufftendonitis(whichmaybecalcific),subacromial
bursitis, rotator cuff tear with cuff instability and impingement, and
glenohumeral(GH)instabilityduetoanumberofdifferentlesions(e.g.labral
tear,synovitisduetocrystalarthritis).
• Inferior acromial osteophytes/acromioclavicular joint (ACJ) osteoarthritis
(OA)canaccompanyanysubacromiallesion,andoftenprecedethemandthus
areriskfactorsforrecurrentrotatorcuffdisease.
• Weaknessandlossofrangeofmotionoccurparticularlyifthetendontears.
• Long-termrotatorcuffdiseasecanleadto‘cuffarthropathy’,withOAofthe
GHjoint(GHJ)andsignificantchronicmorbidity.

• In children or young adults with SAI, consideration of an underlying GH
(instability)lesionismandatory.
Makingadiagnosis
• Exclude alternative causes of shoulder pain, including rotator cuff tear,
adhesive capsulitis, and referred pain from the neck or abdomen (e.g.
cholecystitiswithpainreferredtotheshoulder).
• Signs:painfularconactivearmelevation,painonactivereachbehindback,
positiveNeerorKennedy–Hawkinstest(see Fig.3.5p.91;Table20.1).
• An AP radiograph can show changes identifying GH or bony pathology,
calcifictendonitis,andchronicchangesatsupraspinatusinsertiononhumeral
head.
• ConsiderrequestinganAPviewwith30°externalrotationatthearm,anoutlet
Yview,andanaxillaryview.
• In manycases,USisthemainstayof furtherclarifyingthenatureofrotator
cuff pathology, detecting structural damage, and identifying alternative
explanationsforshoulderpain.
• MRIalsocharacterizessitesofcuffinflammationandismoresensitivethan
USinidentifyingcufftearsandcanprovidemoreinformationaboutthewhole
shouldercomplexincludingGHJlesions,deeperlyingenthesitis,theACJ,and
bonelesions.
• Thegoldstandardfordiagnosingcufftearsisdirectvisionatarthroscopy.
Management
• Avoidoverheadarmactivities.
• Trialafull-doseregularNSAIDfor2weeks.
• If the rotator cuff is convincingly not torn (feasible to tell only for
supraspinatusbytestingshoulderabductionagainstsubmaximalresistanceat
position of downward vertically held arm), consider steroid (e.g.
methylprednisolone40mg;see Plate5)withlocalanaestheticinjection(e.g.
5 mL 1% lidocaine). Approach laterally or posteriorly under acromion—see
also Chapter24.
• Follow-upinjectionwithcuffphysiotherapy2weekslater.Physiotherapycan
addressrotatorcuffmuscle(s)weaknessandimbalanceandabnormalposture.
• Patients should be given realistic expectations that physiotherapy may take
severalmonthstoproviderelief,andmuchself-motivationisneeded.
• Considerasecondinjectionnotbefore6weeksafterthefirst(Fig.20.1;see
also Chapter24forinjectionprocedure/technique).
• Refer for surgical opinion if symptoms persist, as some are amenable to
arthroscopicdebridementofimpingingacromialosteophytes.
• A full-thickness tear that is identified early and not fully retracted, can be
amenabletosurgicalrepair.
Table 20.1 The range of disorders presenting with subacromial impingement pain. Clinical testing,
thoughit canbe elaborate,has beenshown repeatedlyin studiesnot to be asspecific as the original
literatureappearedtosuggest
Condition Diagnosismadeby
Supraspinatus/cufftendonitis MRIorUSor
arthroscopy
Subacromialbursitis(e.g.trauma,gout,CPPD) US/MRI
Rotatorcufftear(partialorfull) MRI
Longheadofbicepstendonitis Clinical,US/MRI
OAACJ(impingementofosteophytesoncuff) Clinical,
radiographs,MRI
GHinstabilityduetolabraltrauma(e.g.SLAPlesion),
arthritisGHJ
MRI
Enthesitis(e.g.deltoidoriginatacromion)inSpAs
(see Chapter8)
Clinical,US,MRI
Lesionatsuprascapularnotch(e.g.cyst,tophus) MRI
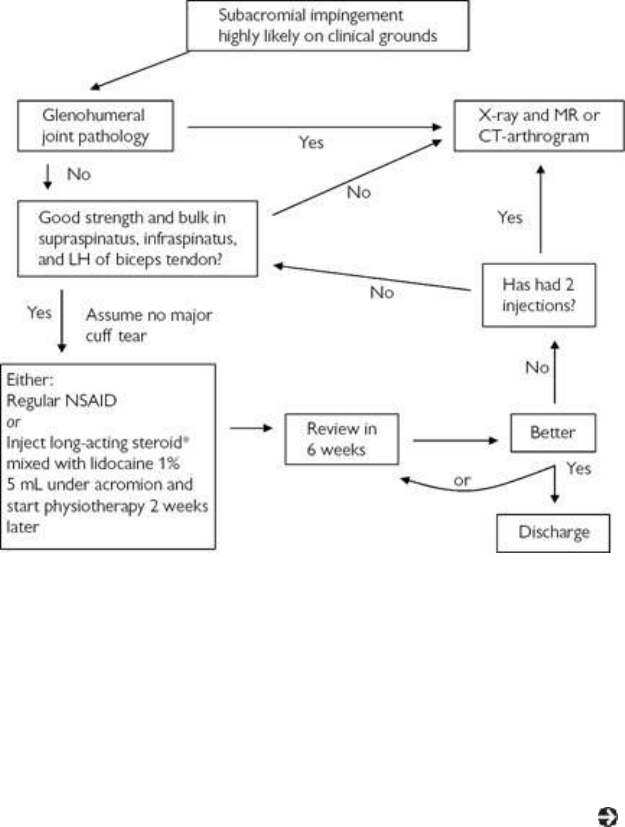
Fig.20.1Pragmaticalgorithmformanagingsubacromialimpingement.
*Use20–40mgtriamcinoloneacetonideormethylprednisoloneacetate.LH,longhead.
Adhesivecapsulitis
Adhesivecapsulitis(AC)—aetiologyunknown,thoughitinvolvescapsularand
coracohumeralligamentcontractures—issuggestedbyagradual,painfullossof
bothactiveandpassiverangeofmovementoftheGHJ(seealso Chapter3for
clinicalassessmentanddifferentialdiagnosisonpresentation).
Epidemiology
• ACismorecommoninfemalesthanmales,andisfourtimesmorecommonin
diabeticsthanthegeneralpopulation.
• Femalesaretypicallyaffectedbetweentheagesof40and60years.
• ACoccursbilaterallyin15%ofpatients.
• Recurrenceisunusual.
• Withoutintervention,thepainusuallyresolvesin<2years,butthepatientmay
beleftwithlong-termrestrictionofshouldermovement.
Presentationandinvestigations
• AC should not be confused with SAI, though the two lesions can co-exist.
With SAI, passively induced GHJ movements remain intact and are less

painfulthanactivemovements. WithAC,passiveandactivemovementsare
equallyimpaired.
• Cluestothediagnosisfromexaminationincludemarkedrestrictionofexternal
rotation, early scapular abduction (normally the scapula doesn’t move until
30°ofabductionhasbeencompleted).
• If the presentation is delayed (e.g. >6 months), a secondary SAI may have
evolvedandisexposedassomerangeofmotionbeginstoreturn.
Management
• Rule out associated conditions: diabetes, hypothyroidism, lung carcinoma,
myocardial infarction, stroke, and protease inhibitor use for human
immunodeficiencyvirus(HIV)infection.
• Control pain during the initial painful/stiff phase of the condition. Consider
NSAIDs,IAsteroidinjection(e.g.40mgmethylprednisolonewith5mL1%
lidocaine), suprascapular nerve block, or a short course of prednisone 30
mg/dayfor3weeks.
• Ifrotatorcuffintact(confirmwithUS),considerimage-guidedhydrodilatation
ormanipulationunderanaesthesia(MUA),early.
• Hydrodilatation improves pain and function to a greater degree than MUA
whencomparedinRCTs.
• Mobilizewithphysicaltherapyearly,butbeawarethismaybelimitedbypoor
paincontrol.
Lateralhumeralepicondylitis
Lateralhumeral epicondylitis(LHE)—oftencalled tenniselboworapophysitis
of the common extensor tendon origin—is essentially an enthesitis. It is
common,andaffects 1–3%oftheadultpopulation,typicallyage40–60years.
Thedominantarm ismostaffected.It is rarein elitetennisplayers, butupto
40%ofsocialplayersgetitatsometime.Enthesitisatthesiteiscommonandis
typically associated with the SpA conditions (see Chapter 8). For clinical
assessmentanddifferentialdiagnosis,see Chapter3.
Pathophysiology
LHE is thought to be due to either cumulative trauma overuse disorder from
mechanical overloading or typical SpA-related pathophysiology if an
inflammatorycause.
• Ifchronic,itcanleadtotendondegenerationandbonechanges.
• Trueinflammationoftheenthesiscanoccurbutpaincanexistwithoutthere
beinganyidentifiableinflammation.
• Poorprognosisisassociatedwithmanualwork,highlevelphysicalstrain at
work,andhighbaselinepainanddistress.
• Consider that the lesion may be part of SpA if bilateral, recurrent without
traumaorassociatedwithotherSpAfeatures.
Presentationanddiagnosis
(Seealso Chapter3.)
• Painiselicitedbyresistedforceinforearm/wristpronation(e.g.handshakes,
turningdoorknobs,carryingbags)orresistanceoffingerorwristextension.
• Pain often extends from the LHE down the extensor compartment to the
forearm.
• Enthesitis,tendontears,andjointlesionsmaybediagnosedbyanexperienced
MSKultrasonographer.
• MRImaymissmildLHE/enthesitisandappearancesarenotspecific.MRIis
moreusefulforrulingouttendontearsandjointlesions.
• IflesionsarebilateralthenspecificallyconsiderSpA.
• The main differential diagnoses are elbow joint lesions, referred neck pain,
andenthesitis(e.g.DISHorenthesitislinkedtoSpA,particularlyPsA;see
Chapter8).
Management
(Seealso Chapter24.)
• During the acute phase, LHE can be treated with activity restriction, pain
control,anelbowclasp,andimmobilization.
• NSAIDs and gabapentin/pregabalin may help in some cases. Employ a
treatmenttrialforalimitedperiodoftimeandreview.
• Injection around the epicondyle with methylprednisolone 20 mg should be
considered if conservative therapy fails—see Chapter 3 for details (see
Plate6).
• Isometricgripexercisesandstretchingforearmextensortissues(gradedwrist
flexionmobilisations)mayalsohelpwithrecovery.
• IfotherinflammatoryMSKlesionsareevidentthenexaminingforwidespread
enthesitislesionsandotherfeaturesofSpAisindicated.WithsubstantialSpA-
related enthesopathic disease then DMARDs may be considered (e.g.
sulfasalazineormethotrexate).
• Surgery is rarely indicated, and should be considered for patients with
persistentsymptomsdespiteothertherapies(Fig.20.2).
• Unproven therapies include autologous blood injection of tendon origin,
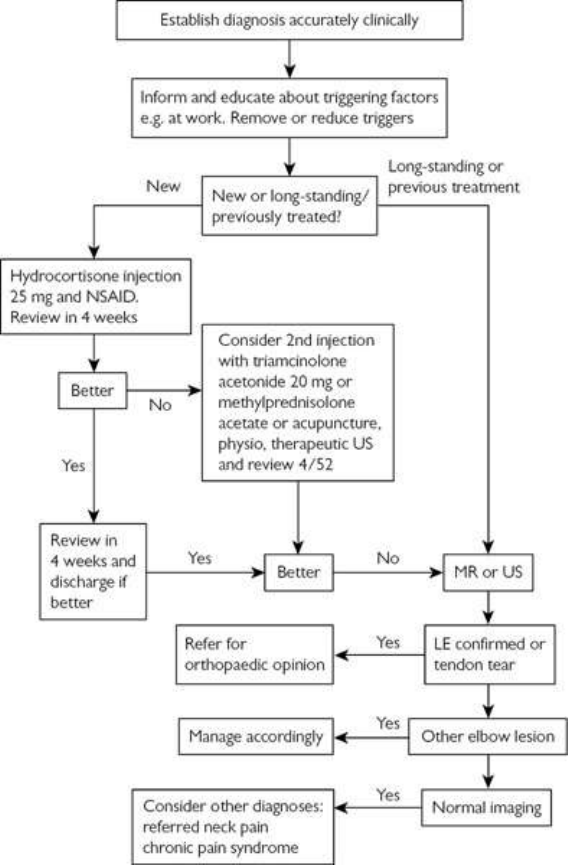
lithotripsy,andtherapeuticUS.
Fig.20.2Pragmaticalgorithmformanaginglateralepicondylitis(LHE).
Chapter21
Spinaldisordersandbackpain
Introduction
Acategorizationofbackpain
Acuteandsubacutebackpain(adults)
Chronicbackpain(adults)
Backpaininchildrenandadolescents
Introduction
Forareviewofspinalanatomyandfunctionalanatomy,see Chapter3under
relevantsectionsforthoracicorlumbarspineinadults.
• The differential diagnosis of symptoms located to the neck and back is
includedintherelevantpartof Chapter3.
• Relevant review of issues and tables on spinal conditions include the
following:
• Painful neurological and MSK conditions of the thoracic spine and chest
wall.See Table3.12,p.132.
• Commonand/orseriouscausesofneckpaininadults.See Table3.1,p.
75.
• Testingnerveroottensioninpatientswithlowbackpainandassociatedleg
pain.See ‘Testingnerveroottension’,p.146.
• Testingmusclestrengthinthelowerlimbs(inpatientswithneurogenicleg
painassociatedwithlowbackpain).See Table3.15,p.147.
• Principal combinations of signs used for identifying lumbar nerve root
lesions.See Table3.16,p.148.
• Commonly reported patterns of radiographic abnormality in adults with
spinal symptoms: the interpretation, and suggested reaction. See Table
3.17,p.149.
• Reviewofchoiceofimaging:radiographsandCTorMRI?See Chapter3,
p.150)
Acategorizationofbackpain
Non-spinalbackpain
Painmayradiatetothebackfromlesionsinotherstructures,e.g.renal,aortic
aneurysmal, pleuriticorpancreatic disorders, and periaortitis. Forsummaryof
conditionscausingspinalpainsee ‘Thoracicbackandchestpaininadults’,p.
132and‘Lowbackpain:adults’,p.140).
Acutenon-specificbackpain
• Thisaccountsfor80–85%ofallacutebackpain.
• Typically, 90% of cases will recover in <6 weeks (the threshold for
reassurance).
• Most causes will be ‘mechanical’ in origin but some causes will be
neuropathicandothersinflammatoryinnature.
Chronicbackpain
• Describespainthathasbeenpresentfor>12weeks.
• Some causes will be neuropathic, others inflammatory in nature, but the
majoritycanbecategorizedas‘mechanical’.
Neuropathicpain
• This typeof painaccounts forapproximatelyone-thirdofacuteandchronic
lowbackpain.
• ThepainDetect
®
questionnaireisausefulassessmenttool,aswellasanaide
memoire for the typical symptoms of neuropathic pain: burning, prickling,
hot/colddysaesthesia,sensitivitytotouchandpressure,numbness,andsudden
‘electricshock’-likesymptoms.
‘Redflags’and‘yellowflags’
Thisterminologyisusedtoidentifypotentiallyserioussecondaryphysical(red)
andpsychosocial(yellow)pathologies(Table21.1).
Table21.1Warningsignsforsinisterpathologycausingbackpain
‘Redflags’ ‘Yellowflags’
• Ageofonset<20years
• Ageofonset>55years
• Recenttrauma
• Beliefthatpainandactivityareharmful
• Abnormal ‘sickness behaviour’, e.g.
extendedrest
• Pain constant, progressive,
andnoreliefwithrest
• Intensenight-timepain
• Thoracicpain
• Pasthistoryofmalignancy
• Osteoporosisrisk
• Infection risk
(immunosuppressed)
• Systemically unwell—
weightloss/fever,etc.
• Progressive neurological
signs including bladder
dysfunction
• Structuraldeformity
• Low/negativemood
• Work environment (low
support/satisfaction conflicting evidence
forhighpace/demand)
• Seekingtreatmentsthatseemexcessiveor
inappropriate
• Inappropriateexpectations
• Lack of social support in private life
(moderateevidence)
• Compensationclaims
Acuteandsubacutebackpain(adults)
Acutemechanicalbackpain
• Mostcasesinaprimarycaresettingareduetolumbarmusclestrainorsprain
presenting with diffuse pain in the lower back to buttocks, which resolves
spontaneously.
• Ifpainisrelatedtopostureormovement,especiallyofthethoraciccage,and
local tenderness is felt at the lumbosacral junction then the pain is highly
likelytobeMSKinorigin.
• Withinthegravid population,two-thirds ofthepregnant womensufferfrom
lowbackpain,typicallyincreasingwithgestationalstage,impactingonsleep,
work,andday-to-dayfunction.
• ‘Red flags’ merit more thorough investigation. Although far less common
(<15%ofallcases),thefollowingshouldbeconsidered(%ofcasesinback
painpopulation):
• Fracture.
• Symptomaticherniateddisc(4%).
• Spinalstenosis(3%).
• Malignancy(0.7%).
• Axialspondyloarthritis(axSpA)/ankylosingspondylitis(0.3%).
• Caudaequinasyndrome(0.04%)causingsaddleanaesthesia,legweakness,
bilateralsciatica,andbladderdysfunction).
• Spinalinfectionorinflammatoryradiculopathy(0.01%).
• Herniateddiscsaccountfor4%oflowerbackpain.Discherniationpresents
withlegpainradiatingpasttheknee,andismostcommoninpatientsbetween
20and50yearsofage.
• Degenerative causes of backpain,includingdegenerative disc disease, facet
joint OA, and lumbar canal spinal stenosis, are more common in older
patients.
• The immediate management is a combination of adequate and regular
analgesia, titrating as per patient response, as well as encouraging gentle
mobilizationandnormalizationofactivities.
• Intheshortterm,asdiazepammaybeconsideredtodecreasemusclespasm
andaidsleep.
• The clinician should explore patient fears (‘yellow flags’) and, where
appropriate,reassurethatseriousillnessisunlikely,thattestsarenotusually
needed,andseverepainisoftenshort-lived.
• Radiographsarelikelytobeunhelpfulformanagementinmostcasesunless
redflagsignsarepresent.
• MRI of the lumbar spine, for example, frequently demonstrates abnormal
findingsinasymptomaticpatients;therelationshipbetweensuchfindingsand
clinicalsymptomsisnotalwaysclear.
• Arehabilitationapproachshouldbeconsidered(Table21.2).Theevidencefor
therapies is variable. Adherence may be augmented by providing patient
educationliterature.
Table21.2Therapiesusedinfacilitatingrehabilitationafteracutemechanicallowbackpain
Manipulation Eitherdonebyanosteopath,chiropractor,orphysiotherapist.
Cochranereview(2012)demonstratedlackofefficacy
comparedtoinerttreatmentorshammanipulation.Smaller
studiessince2015demonstrateaslightbenefit,however
McKenzie
exercises
Passive extension exercises designed to improve pain and
stiffness associatedwith discand anteriorspinal structure
pathology. May aggravate pain from posterior spine
structures,e.g.facetjoints,spinousprocesses.
A systematic review in 2011 has demonstrated a modest
benefit in patients undertaking directional preference
exercisewithintheMcKenzieframework
Hydrotherapy
or
Poorlystudied,butwarmthcaneasemovementandaugment
land-basedexercises.Mightbeconsideredafterinitial
balneotherapy
painfulphasetoregainnormalmovementsandmobility.May
onlysuitafewpatientsandresourcesmaybelimited
Graded
activity
programmes
Usefulforpatientswhorequireguidanceandwouldbe
unabletogainoptimallyfromhomeexerciseregimen.Aplan
forrehabilitationwithmilestonesisusefulforsomepatients
Behavioural
programmes
Focusesonpsychologicalaspectsofpain,involvesmoderate
supervisionandplannedwithdrawaloftreatment.Differs
fromsomeotherapproachesinthatthetherapisttakesover
the‘control’ofthebackpain.Limitedresourcesmayrestrict
provisionofthisapproach
Backpainandnerverootlesions
See also ‘Low back pain: adults’, pp. 144–147 for review of anatomy and
functionalanatomy.
• Nerve root compression occurs mostly because of acute or subacute disc
prolapseorforaminalstenosis.Thepeakincidence isage 30–50years. 70%
resolvewithin3monthsand90%within6months.
• Nerverootcompressionshouldbesuspectedifacuteorsubacutebackpainis
associatedwithsegmentalnerveorsciaticlegpain.
• Acute sciatic pain (‘sciatica’ affecting the outer and posterior leg) is often
sharporburninginnature,andmostfrequentlyarisesfromacutediscprolapse
ofeitherL4/5orL5/S1(>90%ofcases).
• Sciaticaischaracterizedbylegpainprojectingpasttheknee, whichmaybe
moreseverethantheassociatedbackpain.
• Apatientwithaherniateddiscmaypresentwithsciatica.
• Evidence of disc herniation may be elicited by straight leg raise or crossed
straightlegraise(i.e.elevationofunaffectedleg).Thesetestsarepositiveif
painisfeltinthebuttockorinthebackatalegangleof30–60°.Painelicited
atalegangle<10°isconsistentwithMSKbackpain.
• L5 nerve root lesions give decreased strength of the foot and great toe
dorsiflexion,standingonheel,anddecreasedanklereflexandsensationover
greattoe.
• S1 root lesions give decreased strength in plantar foot flexion, difficulty in
weight-bearingontoes,anddecreasedanklereflexandsensationonthesoleor
outerpartoffoot.
Principlesofmanagement

• Thenaturalhistory:30–60%ofpatientsrecoverin1week.
• Analgesia such as paracetamol (acetaminophen) and NSAIDs should be
consideredfirst.
• Useofdiazepammaybeofbenefitintheshorttermtolessenmusclespasm.
Some patients may need opiate therapy for pain control, e.g. codeine
phosphate, tramadol, buprenorphine, and short- or long-acting morphine
sulfate.
• Bedrestshouldbediscouraged:prolongedbedrestleadstoworseoutcomes.
Gentlemobilizationshouldbeencouraged.
• Anepiduralsteroidinjectioncanimprovepainintheshortterm,butdatafrom
RCTsdoesnotshowbetterlong-termoutcomeat3monthsorlongercompared
withcontrols.
• A meta-analysis showed that 1 in 7 patients having a steroid epidural
experienced >75% improvement in pain in the short term, and 1 in 13
experienced>50%symptomimprovementinthelongterm.
• Physicaltherapyandsupervisedrehabilitationusinglumbarextensorexercise
regimensmaybeofbenefit.
• MRI can characterize lesions, but 25% of asymptomatic people have frank
disc protrusions; so MRI gives poor specificity. MRI should be used to
confirmadiagnosis,nottoreachforone.
• Theabsoluteindicationsforsurgery(Table21.3)arecaudaequinasyndrome,
progressivemuscleweakness,andneuropathycausingfunctionaldisability.
Facetjointarthritis/syndrome
• Lumbar spine facet joint (FJ) osteoarthritis (OA) is common in middle
aged/elderlyadults,andcanbepartofgeneralizedOA.
• FJOA is associated with degenerativeandspondylolyticspondylolistheses—
forwardslippageofavertebraeonthevertebraebelowit.
• Psoriatic arthritis (see Chapter 8) and calcium pyrophosphate disease
(CPPD; see Chapter 7) can also affect FJs and are under-recognized as
causesoflowbackpain.
• Typicalsymptomsincludepainonextensionorrotationofthelowerback.The
painisoftenreferredtotheupperbuttocks,isworsewhilestandingstill,and
easedbyforwardlumbarflexion.
• Facethypertrophyitselfcannotbefelt,buttrueFJsyndromeisaccompanied
bymusclespasmandsuperficialsofttissuetenderness.
• ArthriticFJsmaybeseenonobliquespinalradiographs;however,imagingin
generalcannotreliablyidentifysymptomaticFJs.FJinjectionwithanaesthetic
mayconfirmthediagnosisifthisresultsinsignificantpainrelief.
Table21.3Surgicalapproachesforlumbardiscprolapse
Discectomy Essentialfordiscscausingcaudaequinasyndromeand
progressiveneurologicaldeficits.Excludingabove
indications,comparedwithconservativetherapy,ina
randomizedcontroltrial(RCT)66%vs33%patients
weresatisfiedfollowingsurgeryat1year,and66%vs
51%weresatisfiedat4years;thus,benefitofsurgeryin
thelongtermissmall.Adverseeventswithsurgery
includemortality(<0.2%),duraltears(4%),and
permanentnerverootinjuries(<1%).70%successratein
shortterm.Riskoffailurefromsurgeryrelatestohysteria
orhypochondriasisscoresonMMPI*andpresenceof
litigationclaims
Microdiscectomy Smallersurgicalfieldresultsinearliermobilizationand
lesspostoperativedisability.Outcomessimilartothose
ofconventionaldiscectomyfromCochranereview,2014
Percutaneous
discectomy
Suctioningofcentraldiscmaterialcausingdisc
decompressionandrelievingnerverootpressure.
Associatedwithlowcomplicationrateandrapid
rehabilitation.SmallRCTstudiessuggestsimilar
efficacytodiscectomyandmicrodiscectomy
Chemonucleolysis Injectionofproteolyticenzymeintodisc.RCTssuggest
standarddiscectomyissuperior.Rare,butdevastating
neurologicalcomplications;riskofanaphylaxis(0.3%)
Laserlumbar
discectomy
Vaporizingofpartofdiscbylaserthroughaneedle
probe.Efficacysimilartodiscectomy.NoRCTdata
Prosthetic
intervertebraldisc
replacement
Also,indicatedfordegenerativediscdisease,post-
laminectomysyndromeandnon-specificpersistentlow
backpain.Artificialdiscsconsistoftwoend-plates
separatedbypliableinnercore.RCTcomparativestudies
haveshownashort-termbenefitinamelioratingback
painandlong-termbenefitinreducinglegpain,
comparedwithdiscectomy.Complicationratemaybe
high(upto45%)andserious:discitis,re-herniation,
haematoma
*MMPI=MinnesotaMultiphasicPersonalityInventory.
ManagementofFJarthritis/syndrome
• Patients can be treated according to principles applied for all patients with
acutemechanicalbackpainexceptthatextensorexercisesarecontraindicated
astheywillaggravatesymptoms.
• Shortcoursesofanalgesicsand/orNSAIDsasforOA.
• Generally,adviseminimalbedrest.
• Steroid injection of FJs is frequently used, although studies have failed to
demonstratebenefitoverplaceboinjection.
• RadiofrequencydenervationofmedialbranchesofdorsalramisupplyingFJs
can help, but the procedure should only be considered if local anaesthetic
blockworksfirst.
Lumbarcanalspinalstenosis
• Thediagnosisisfrequentlymissedintheelderly.
• Itpresentsmainlywithachy,stiffpainsinthelegsincreasedonwalkingand
easing if the patient stops walking, sits, or leans forward (neurogenic or
pseudo-claudication).
• Pain, numbness/tingling, and weakness are the most common symptoms.
Neurologicallegsignscanbeaccentuatedafterexercise.
• ThediagnosisismadeusingMRIofthelumbarspine.
• Non-surgical management (including pain control and physical therapy) is
oftenadequate.
• Decompressive laminectomy is required for progressive neurological
symptoms,bladderdysfunction,orcaudaequinasyndrome.
Non-traumaticvertebralfracture
• A fragility (minimal or not) trauma vertebral fracture is usually due to
osteoporosis,collapseofanabnormalvertebra(e.g.vertebralhaemangioma),
orsecondarytomalignancyorinfection.
• Thehistoryshouldfocusonidentifyingriskfactorsfortheseconditions.Post-
menopause or hypogonadism, previous fracture history, steroid use, and
alcoholismmayallcontributetoosteoporosis.
• WeightlossorB-typesymptomsmayindicatethepresenceofmalignancyor
infection.
• Kyphosisandlossofheightcanoccuraftervertebralfracture.
• A full examination should be done to evaluate the possibility of cord
compressionormalignancy.

• Investigate with anteroposterior and lateral spinal radiographs, MRI, bone
biochemistry(boneprofile,PTH),morningluteinizinghormone(LH)andfree
testosterone,25-OHvitaminD,CRP,thyroidfunctiontests(TFTs),serumand
urineelectrophoresis.
• MRIisgoodatdiscriminating infectionandtumoursfromosteoporosis,and
candatefractures,butbiopsyforhistologyandcultureisessentialiftumouror
infectionhasnotbeenruledoutbyMRI.
Managementofnon-traumaticvertebralfracture
• The patient should be carefully monitored for evolving neurological deficits
withalowthresholdforMRIwholespine.
• Pain control often requires long-acting narcotics, with short-acting narcotics
forbreakthroughpainasparacetamol(acetaminophen)andNSAIDsaloneare
unlikelytobesufficient.
• Calcitonin 100–200 IU twice-dailySCor 200 IU/day by nasal spray hasan
analgesiceffectandreducesboneturnoverinosteoporosis.
• Osteoporosisshouldbetreatedaggressivelyinduecourse(see Chapter16)
but bisphosphonates should not be regarded to have/relied on to provide an
analgesiceffect.
• Discuss any pathological malignancy-related fracture with a clinical
oncologist.
• Considervertebroplastyorballoonkyphoplastywherepainisuncontrolledby
analgesia.
Post-surgicalbackpain
• Therearenumerouscausesandnosingleentity(Table21.4).
• Post-surgicalbackpainpresentsamanagementchallenge.Amulti-disciplinary
approach is often need in providing optimization of analgesia, physical
therapy, behavioural modification via psychotherapy, use of nerve blocks,
epidurals, and spinal cord stimulators, radio-frequency ablation as well as
consideringtheneedforre-operation.
• Somepreoperativefactorssuchasnerverootexitforaminalstenosis,smoking,
obesity,andpre-morbidpsychiatricconditionscanleadtohigherprevalenceof
post-surgicalbackpain.
• Imaging with gadolinium-enhanced MRI may be helpful to delineate
inflammatorytissuearoundthesurgicalsite.
• Persistentpainaftersurgerymaybeassociatedwithadversepsychologicaland
socialfactors,outstandinglitigation,orinsuranceclaims.
Non-septicdiscitis
• Inflammation of the intervertebral disc is often associated with annulus
enthesitisatthevertebralend-platesandvertebralosteitis.
• The causes include disc degeneration, CPPD disease, axSpA/ankylosing
spondylitis(‘romanus’lesions)andotherSpAs;also,SAPHO(see Chapter
16.
• The lesion should be identified with MRI and treatment should include
aggressiveanalgesiaadjustedastolerated.
• In RCTs, intradiscal steroid injections have been shown to be little help
overall.IVbisphosphonate(e.g.pamidronate60–90mg)hasanecdotallybeen
shown to help the symptoms of axSpA and SAPHO discitis
(‘spondylodiscitis’).
Table21.4Implicatedcausesofpost-surgicalbackpain
Recurrent
disease
Example:furtherdiscprotrusionandradicularfeatures.Ifre-
operationnotappropriateconsidernerverootblock,steroid
epidural,etc.
Operationfor
wronglesion
MRIcanshowlesions,whichmaynotberelevanttoclinical
features.Morethan1or2lesionscancoexist.Detailed
clinicalassessmentpriortoimagingisessential
Misdiagnosis
originally
Astructurallesiontreatedwhenaninflammatorydisease,
typicallySpA-relateddisease,waspresentandcausing
ongoingsymptoms
Altered
biomechanics
Increasedloadburdenovertheadjacentstructures,leadingto
accelerateddegenerativechangesinareasbothaboveand
belowthesurgery.Also,alteredbiomechanicsmay
potentiallyresultinincreasedtensionoverthepre-vertebral
andpost-vertebralmuscles,leadingtostiffness,spasm,and
pain
Adverse
rehabilitation
conditions
Resolutionofsymptomsandregainingfunctionalcapacityif
slowhasbeenassociatedwithsignificantpsychologicaland
socialfactors.Poorresultofsurgeryalsoassociatedwithan
outstandinginsuranceclaimorlitigation
Arachnoiditis Thoughttobeadirecteffectofsurgery.Duraltissuebecomes
inflamed.Innerveroot/discsurgeryoftenassociatedwith
sensoryrootsymptomsforsomemonthsafterwards.
Diagnosiswithcontrast-enhancedMRI.Whereassociated
withsensoryradicularsymptoms,mayrespondtosteroidroot
block,epidural.Ifradicularsymptomschronicanddisabling
considerspinalcord(implanted)stimulator
Chronicbackpain(adults)
TheGlobalBurdenofDiseaseStudy2010publishedinTheLancet delineated
howMSKdisordersarethesecondmaincauseofdisabilityworldwidemeasured
by years lived with disability (YLDs). Low back pain was the leading
contributortotheYLDsattributablefromMSKdisorders.
• Further analysis demonstrated how low back pain was the sixth out of 291
causesofglobalburdenofdiseasemeasuredbydisability-adjustedlifeyears
(DALYs).InWesternEurope,itisthefirstcause.
• In 2010, the global age-standardized prevalence of chronic back pain was
9.4%,withahigherrateinmen(10.1%)thaninwomen(8.7%).
• In WesternEurope,theprevalenceof lowback painwas 15.5%inmen and
14.5%inwomen.
• Managingchronicbackpainrequiresanemphasisonpsychologicalandsocial
management.
• Patients with chronic back pain are likely to have set beliefs about their
problem,theabilityofhealthcaresystemstohelpthem,andaremorelikelyto
have developed coping strategies than patients with acute or subacute back
pain.
• People with chronic back pain who continually seek further and different
healthcareoptionsarelikelytohavelesssuccessfulcopingstrategies.
Initialapproachtomanagingchroniclowbackpain
(SeeTable21.5.)
• Be confidentthatthere isnoundiagnosed conditionaffecting backpain and
thatnonewneurologicallesionshaveevolved.Ifexaminationraisesconcern,
useMRItoruleoutlesions.
• Establishempathyandtrust,takingtimetogetinformationaboutpatients’:
• socialsituation.
• healthandillnessbeliefs.
• intra-familydynamics.
• workandhomerole.
• perceptionoftheirroleatwork.
• viewonconventionalandcomplementarytherapies.
• viewonwhatdoesanddoesn’twork.
• specificviewofexercisetherapy.
• Plan the managementapproachwith the patient andestablishshort-to mid-
termgoals,includingwhether,andwhattypeof,supervisionisrequired(e.g.
gradedprogrammeofexercise)andhowoftenareviewisneeded.
• Consider‘domains’oftherapyunderthefollowingheadings:
• Physicaltherapy.
• Work/lifecommitments.
• Psychologicalandsocialsupport.
• Painkillersandmedications.
• Education(insightandcopingstrategies).
• Plantoreviewprogressatregularintervals.
• Evaluate patients carefully at baseline if considering long-term opiate use.
There may be an increased risk of dependency if the patient currently or
previously abused drugs, there is a high level of psychological distress, if
short-actingopiatesareused,ordrugsareprescribed‘asneeded’.
• Although many strategies, especially those that combine techniques, can be
costly, these costs to healthcare are likely to be offset by the saving in lost
wages.
Table21.5Managementoptionsforchroniclowbackpain:adults
Exercises RCTevidencesupportsuse.Greaterevidenceofeffect
whencombinedwithbehaviouralmethods.Aerobic
exercisesaugmenteffectof‘backschool’.Shouldbe
essentialpartofoutpatientphysicalretrainingprogramme.
Nodifferenceinefficacybetweenindividualorgroup
programmes
Manipulation Trialsshowefficacyonpaininthelongterm
Transcutaneous
electricnerve
stimulation
(TENS)
DisappointingresultsfromRCTsinchronicbackpain,
althoughefficacyforotherspecificdiagnosesareunknown
Posturetraining Maybemoreappropriatethancorsetuseandeasyto
combinetrainingwithsupervisedexercisetherapy
Pilates Low-levelevidenceforshort-termbenefit
Medications Paracetamol,especiallyusedinconjunctionwithopiatesto
obtainasynergisticeffect.
NSAIDsbestforacute-on-chronicpainflares,for
regulatingpainintensity,asshownbycurrentRCTs.
COX2-selectiveNSAIDsmayhavebetterGIsideeffect
profile.
Systemicreviewandmeta-analysishasdemonstrated
efficacyofopiatesintermsofpainreductionintheshort
term.Themedicationscanbedeliveredinavarietyof
ways:oral,trans-dermal,andbuccal.Chronicopiateusefor
chroniclowbackpainhasnotbeenextensivelystudied.A
mentalhealthevaluationbeforelong-termprescribingis
essentialtoavoidtriggeringdependency(seetext);short
courses,initiallyforatrialperiod,aresensible.Best
supervisedbyaspecialistwithexperienceinpain
management.
Low-dosetricyclics(e.g.amitriptyline,nortriptyline)are
usefulparticularlyifchronicneuropathicpainispresent.
Otherneuropathicagentssuchasgabapentin,pregabalin,
andduloxetinecanbeused.
Musclerelaxants:diazepamhasbeenshowntohaveshort-
termbenefitsinacute-on-chronicexacerbationsofback
pain.Evidenceforeperisoneiscurrentlylimited.
Topicallidocainecanbeusedasadjunctivetreatmentfor
neuropathicpain,thoughasyetnoclearevidencebase.
Systemicanti-nervegrowthfactoragents:limitedevidence,
experimentalphase
Backschool Regularprogrammecarryinganeducationalcomponent.
Programmesvaryfromonetomanysessions.Maybemore
effectiveinoccupationalsetting.Non-complianceand
relapseareproblems.Recentmeta-analysesshow
inconsistentresultswithregardtoefficacy
Psychology-
orientated
rehabilitation
programmes
Intensivecoursesoftenrunbypsychologistsand‘hands-
off’physicaltherapistscanhelp(highly)selectedpatients.
Focusisonlearningtocopewithpainandincreased
controlofeffectsofpainonfunctioningandpsyche.Not
suitableformanypatients.Coursesfewandfarbetween.
Cost-effectivenessofcoursesnotproved.Goodefficacy
comparedtostandardcare,especiallywithworkoutcomes
Complementary
therapies
Increasinglyused.Byconsensus,chiropractichasbeen
showntobehelpfulforchroniclowbackpain.
Acupuncturehasyettobeprovedsuccessfulinrobust
studies.Poorevidencebaseotherwise
Epiduralsteroid
injections
Goodlevelofevidenceforshort-andmedium-term
efficacyinreducingbackandradicularlegpain.
Greaterbenefitestablishedwithregimenconsistingoflocal
anaestheticandsteroid
Epidural
etanercept
therapy
Doesnotseemtohaveadverseeventscomparedtoplacebo
butfurtherstudiesneededtoestablishrobustefficacy
Intrathecal
opiates
Conflictingresultsfrom(only)non-controlledstudies.
Generally,resultsshowoverallshort-termimprovements
regardingpainperception,butnotfunction.Bestreserved
forpatientswhereallelsehasfailed
Spinalcord
stimulator
(SCS)
AnumberofgoodstudiesshowthataSCSiseffectivefor
neuropathicincludingradicularpain.Techniqueis
relativelysafe.Carefulpatientselectionisimportant.
Studiesshow50%reductioninpaininthelongterm
Percutaneous
adhesiolysis
RobustevidencefromRCTsdemonstratingshort-andlong-
termefficacyindiminishingchronicbackpainand
improvingfunctionalimpairment
Additionalsourcesofreferencesonthevalueofinterventions
ChouR,HuffmanLH;AmericanPainSociety,etal.Nonpharmacologictherapiesforacuteandchronic
lowbackpain:areviewoftheevidenceforanAmericanPainSociety/AmericanCollegeofPhysicians
clinicalpracticeguideline.AnnInternMed.2007;147:492–504.
Van Tulder MW, Becker A, Bekkering T, et al. Chapter 3 European guidelines for the management of
acutenonspecificlowbackpaininprimarycare.EurSpineJ2006;3(Suppl2):161–191.
RelevantCochranedatabaseevaluations
2003:MultidisciplinaryBio-psychosocial,Rehabilitation,Musclerelaxants.
2004:Backschools.
2005:Bedrest,Exercisetherapy,Behaviouraltherapy,Acupuncture.
2007:Herbalmedicine,Traction,Insoles,Opioids,Injectiontherapy,ProlotherapyandLasertherapy.

Backpaininchildrenandadolescents
Children with spinal problems present with deformity, back pain, limping,
systemicorneurologicalfeatures,oracombinationofeffects.
• Backpaininadolescentsiscommon—by20yofage,occursinupto80%,but
is rare in children<8years.Painina child <4y and pain requiring hospital
admissiontypicallypredictunderlyingpathology.
• Age determines the likelihood of cause, with infection and tumours being
morecommoninyoungchildrencomparedwithadolescents(Table21.6).
• Theprinciplesofhistorytakingandexaminationinchildrenarediscussedin
Chapter3,Seepp.154–155.
Non-specificlowbackpain
• Theannualincidenceis13–24%inschoolchildren.
• Adolescent back pain is linked with familial clustering, physical inactivity,
sportsinjuries,andpsychosocialfactors.
• Particular risk factors from a recent birth cohort studies includefemalesex,
muscle deconditioning previous sports injuries, sleeping problems, and
persistentfatigue.
• Mostchildrenandadolescentshaveself-limitingsymptoms.
• Management should focus on an explanation of the short natural history,
reassurance, addressing predisposing factors that remain a trigger for
recurrenceandincreasingexercisetoimprovemusclestrength.
• Back pain associatedwithhyperlordosis and pain on lumbarextensionof is
commonlyassociatedwithtighthamstringsorhipflexors,weakcoreandtense
paraspinalmuscleswithreducedforwardflexion.
• A thorough assessment of gait, posture, core stability, limb strength and
muscletightnesswillhelpdirectphysiotherapy-ledhomeexerciseplan.
Idiopathicscoliosis
Themajorformofidiopathicscoliosisisvertebralmalalignmentinthecoronal
planeassociatedwithspinalrotationaccentuatedonspinalflexion.
• Overall prevalence is reported to range from 0.5% to 5%, with the highest
prevalencewithinthe12–14yearsagegroups.
• About70%areasymptomatic.Theincidenceofbackpainisprobablyhigher
thaninthebackgroundpopulation.Progressionismorelikelyinthepresence
of pain or thoracic curve convex to the left—conditions that should be
investigatedforseriousunderlyingspinalpathology.
• Potential interventions include scoliosis specific exercises, bracing, and
surgery. There is poorqualityevidence for scoliosis-specificexercises as an
adjunctivetreatmentalongsideotherinterventions.
• Progressivescoliosis(Fig.21.1)requiresbracingorsurgery.Usuallycurvesof
25–45° are braced; rigid bracing seems to be superior compared to elastic
bracing.
• A child with a curve >40° would be considered for surgical intervention.
Similaroutcomes areachievedatshorttermfollowup forboth traditionally
opensurgeryversusminimallyinvasiveprocedures.
• An MRI to look for tumour, syrinx, neural tethering or infection should be
doneifthereisacurveconcavetotheleftandpain.
• It’simportanttodifferentiatethecauseofscoliosis(e.g.biomechanical,post-
traumatic,neuromuscular,metabolic,congenital,idiopathic).
Congenitalandneuromuscularscoliosis
Congenitalscoliosis(CS)isassociatedwithgenitourinarymalformations(20%)
and,rarely,congenitalheartdisease.Itisararecondition,occurringinabout1in
10,000 newborns. Neuromuscular scoliosis (NMS) is associated with cerebral
palsy,musculardystrophy,spinomuscularatrophy,andmyelodysplasia.
• CSisassociatedwithspinaldysraphism(20%),myelodysplasia,andKlippel–
Fielsyndrome.
• Toavoidrapidprogressionandincreasedlong-termmorbidityanddisability,
referforpromptcorrectionofprogressivecurves.
Table21.6Causesofbackpaininchildren
Developmental Painfulscoliosis,
Spondylolysisandspondylolisthesis,
Scheuermann’sdisease
Infection Discitis,
Vertebralosteomyelitis,
Spinalepiduralabscess
Inflammation Juvenilearthritis,
Osteoporosis
Mechanical Herniateddisc,
Musclestrain,
Fractures
Neoplasms Benign(osteoidosteomas,osteoblastoma,
aneurysmalbonecyst),
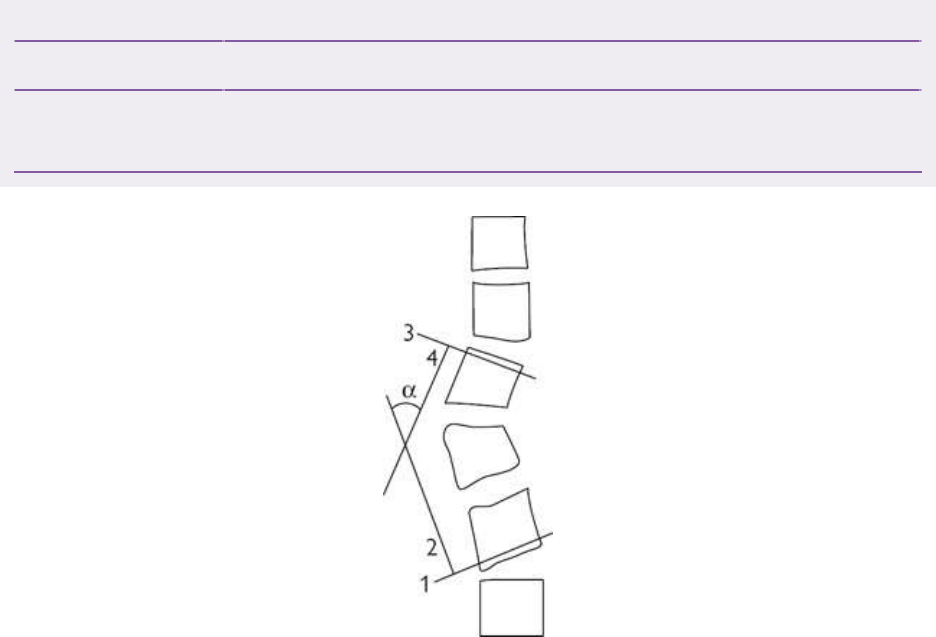
Malignant(leukaemia,lymphoma,sarcoma)
Visceral Pyelonephritis,appendicitis,retroperitonealabscess
Non-accidental Fractures—ribs,spinousprocesses,
Softtissueinjuries,burns
Fig.21.1MeasurementofthedegreeofscoliosisbytheCobbmethod:1,thelowestvertebrawhosebottom
tiltstotheconcavityofcurve;2,theerectperpendiculartoline1;3,thehighestvertebrawhosetoptiltsto
theconcavityofcurve;4,thedropperpendiculartoline3;α,theintersectingangle.Curveslessthan20°are
consideredtobemild,20–40°aremoderate,andabove40°aresevere.
Scheuermann’sosteochondritis
• This is perhapsthemost commoncauseof spinal deformityinchildren and
adolescents(1–8%ofalladolescentsusually13–17years).
• Theaetiologyisunknown.
• Most casesareasymptomaticandpresent withconcernsabout thekyphosis.
Pain occurs over the apex of the deformity often related to activity or
prolonged sitting. Lumbar pain occurs with a compensatory hyperlordosis.
Tightnessoccursinanteriorshouldermuscles,hipflexorsandhamstrings.
• Thetypicalradiographicpatternisofmildwedgevertebraldeformities(<10°)
ofthoracicvertebraeandirregularend-plates.
• Delayedpresentationoccursinadultseitherwith(degenerative)backpainsor
disclosedonaspinalradiographas‘vertebralfractures’(erroneously—asthe
wedgeshapedoesnotdenotefracture).
Management
• Minorkyphosisistreatedwithanexercise programtoincreaseflexibilityof
trunk, hamstring and pectoral muscles, and is monitored with radiographs,
obtainedperiodicallyuntilskeletalmaturity.
• Bracingisindicatedforakyphosis>55°orathoracolumbarscoliosis>40°and
shouldcontinueuntiloneyearafterfusionoftheiliacapophyses.Surgeryis
typically reserved for a thoracic kyphosis >70° or thoracolumbar scoliosis
>60°.
Spondylolysisandspondylolisthesis
Spondylolysisisadefectintheparsinter-articularis,mostcommonlyatL4or
L5.Aloneasalesionitiscommon(4%preschoolchildrenand6%<18years).It
occursinupto15%ofeliteadolescentathletes.
• Spondylolysis is a risk factor for asymptomatic and symptomatic
spondylolisthesis(forwardslip ofavertebra on theone below facilitatedby
thebilateralspondylolysis.(Fig.21.2)).
• Progressiveslippagemayoccurduringtheadolescentgrowthspurt.
Management
• If the slip is >25% (grade II, III, or IV), then effective physical therapy is
important, to stabilise the spine (which is at risk of lumbar hyperextension)
beforeareturntosports.
• Advice should be given on regular abdominal muscle exercises, avoiding
gainingabdominalobesity,andconsiderregularbracing.
• SurgeryisconsideredforprogressivevertebralslippageorgradeIII/IVslip.
Herniateddisc
Herniateddiscsareinfrequentinchildren<11y,butdiscprotrusionaffectsupto
20%by18yofage.
• How much pain can be attributed to the disc protrusion is often unclear.
Buttockorhippainexacerbatedbyforwardbend,coughorsneeze,orpositive
legraise,suggestspainisduetothediscprotrusion.
Management
• Withoutnerverootimpingement,managementisconservativeandincludesa
shortperiodofbedrest,adequateanalgesics,andNSAIDswithearlyexercise-
basedrehabilitationregimen.
• Over 50% improve with conservative treatment, but reported results from
surgeryforsignificantnerverootlesions,areverygood.
Spinaltumours
• Althoughrareinchildren,spinaltumourspresentwithnightpainincreasingin
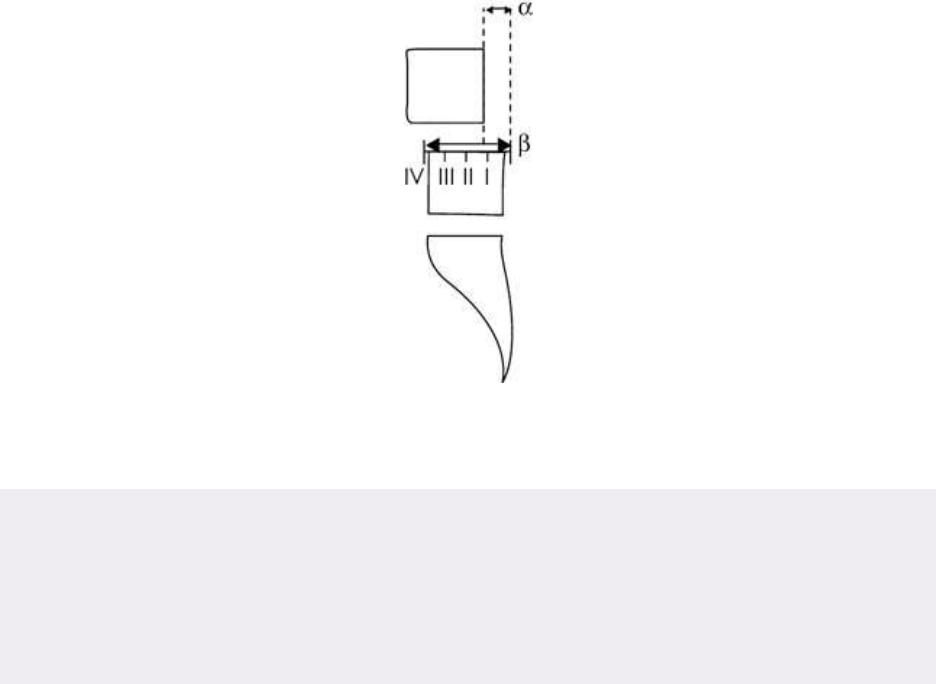
intensity over time and associated with weight loss, radicular features, and
focaltenderness.
• Other typical (though not specific) features include painful scoliosis and
effectivenessofNSAIDs.
Management
• Radiographs (may be negative in early disease) and MRI are essential with
bonescintigraphy(+SPECT)orCTtoidentifyposteriorelementtumours(e.g.
osteoidosteoma).
• Adequateanalgesiaisrequired.NSAIDs:ibuprofeninrecommendedbutdoses
for weight may not be sufficient. Consider naproxen 15 mg/kg/day for
adolescents.
• Bed rest is not essential, although wise if scans suggest risk of vertebral
collapseorcordcompression.Ifthelatter,discussurgentlywithapaediatric
spinalsurgeonandradiotherapist-oncologist.
• Initiateasearchforothertumoursknowntometastasizetospine(Box21.1).
• Investigation within an adolescent unit is advisable given the specific
multidisciplinaryinputoftenneeded.
Fig.21.2Spondylolisthesismeasuredasa%slipofL4onL5(α/β).GradeI<25%,gradeII25–50%,grade
III50–75%,andgradeIV>75%.
Box21.1Primaryspinaltumoursinchildrenandadolescents
Osteoidosteoma
Benign.Notuncommon.Mainlyadolescents.Posteriorvertebralboneusually.
Paincanbesevere.Discriminatefromosteoblastomasbysize(osteomasare
<1.5cm,osteoblastomas>1.5cm)ashistologyisoftenidentical.Lesionsare
associatedwithscoliosis(63%).Surgicalexcisionistreatmentofchoice.
Aneurysmalbonecyst
Benign. Symptoms often triggered by vertebral collapse. Take care when
consideringbiopsy todiscriminate frommalignant lesions.Discuss indetail
withMSKradiologist.
Eosinophilicgranuloma
Benign—oftenoccursaround10yearsofage.Rare.Lytic.Mayoccasionally
be multiple/disseminated—staging important. Symptoms often triggered by
vertebralcollapse.Cordandradicularcompressioncanoccur.Biopsyessential
to discriminate from malignant lesions. Surgical excision or internal spine
fixation not usually needed. Consider radiotherapy if cord compression
threatened. Consider external brace fixation in all and monitor for
spontaneous resolution. Disseminated lesions can be treated with
chemotherapy.
Ewingsarcoma
Overall rarely affects spine (~10% cases). Can affect any part of spine
including sacrum (latter cases often delayed diagnosis). Suspicion of it
requiresbiopsy.Treatwithcombinationchemotherapyandlocalradiotherapy.
5-year survival ~50%. Outcome better for tumour sizes <8 cm or localized
disease.
Leukaemia
Considerinallcasesofspinalosteopeniaorsingle/multiplevertebralcollapse.
Maybereferredpainfromhipandorpelviclesions.
Notoriousassociationwithdelayeddiagnosis.Associatedsystemicsymptoms
may not necessarily be present, but normal FBC at presentation unlikely
(~10% cases only). Also look for eosinophilia and hypercalcaemia, and
considerbonemarrowaspirate.
Lymphoma
Rarelypresentswithbackpain;however,knowncauseofpersistentbackpain.
MRI is imaging of choice: can show vertebral collapse and soft tissue
paraspinal mass. Biopsy is diagnostic. Case reports of plasmacytomas
presentingsimilarly.
Secondarymalignanttumour
Neuroblastoma, rhabdomyosarcoma, Wilms tumour, retinoblastoma, and
teratoblastomaareknown to present withback pain. Positive biopsyshould
triggerasearchfortheunderlyingprimaryneoplasm.

Chapter22
Chronicpainsyndromes
Pain
Generalizedpainsyndromes
Localizedpainsyndromes
Chronicpaininchildrenandadolescents
Complexregionalpainsyndromeinchildrenandadolescents
Pain
Introduction
Acutepainisadangersignal.Painsignalsa‘threat’andstimulatesabehavioural
response and memory toenableavoidingfuture ‘threat’. By nuanced contrast,
chronicpainistypicallyamaladaptiveprocessofreportingsucha‘threat’.
• Painisdefinedby theInternationalAssociationfortheStudyof Painas‘an
unpleasant sensory and emotional experience associated with actual or
potentialtissuedamageordescribedintermsofsuchdamage’.
• Thepainneuropathwaycanbemodified—eitherbyamplificationordamped
at various levels including peripherally—at the spinal cord and centrally.
Modificationsmayoccurinresponsetoavastarrayofinterpretivesensessuch
asbeliefs,earlierlifeexperiences,emotions,andemotionalresponses.
• The physiology and pathophysiology of pain is thus complex and it is best
viewedinthe contextof aneuromatrixrather thana pain nerveor asimple
gatetheory.
• Chronicpainisconsideredamaladaptivesensationthatbothover-reportsthe
peripheralthreatsignalssotypicalofacutepain,anddirectlycontributesto,or
maybetheprincipalexplanationfor,thepatient’sdistress.
• Viewed another way, tissue damage or inflammation cannot explain the
presence or level of distress and effective pain management requires an
understandingofallfactorsthatinfluencepainperception.
• Itisnowwidelyrecognizedthateffectiveexplanationofpainprocessingthat
integratesthepatient’sownexperiencesisinitselftherapeuticandallowsthe
patienttobuildonthepainmanagementstrategiesrecommended.
• Chronicpainmanagementstrategiesrecognizethebiopsychosocialmodelof
pain interpretation and are most effective when they integrate a
multidisciplinaryapproachtargetingspecificneeds.
Foreaseofexplanation,chronicpainsyndromeshavebeensub-dividedinto
chronic widespread (or diffuse) pain (CWP) and regional (or focal) pain
syndromes. Pragmatically this helps with considerations of differential
diagnoses and targeting investigations effectively. Management strategies
oftenoverlap.
Painneurophysiology:peripheries
Noxiouspainfulstimuliaredetectedintheperipherybynociceptorsonprimary
afferentneuronsandtransmittedtothedorsalhornofthespinalcord.
• Nociceptive primary afferents are specialized sensory neurons: either small
myelinatedAδfibresorunmyelinatedCfibres.
• ThesesynapsemainlyinlaminaIandIIofthespinaldorsalhornwithspinal
second-order interneurons. This is also one of the principal sites of pain
amplification.
• Itispossiblethatduringinflammation,nociceptorsmaybecomeactivatedat
lowerthresholdsthanusual,thusgivingadegreeofperipheralsensitization.
Painneurophysiology:central
Thebrainandspinalcordareresponsibleforcentralpainprocessingofnoxious
stimulitransmittedfromtheperiphery.Numerousareas(upwardsof700centres)
withinthebraininfluencepainperception.
• Nociceptiveimpulsesascendbytwomainspinalpathways.
• Information from Aδ fibres encodes ‘fast pain’ through the anterolateral
neospinothalamic tract (ALNT), which transmits pain and temperature and
discriminativequalitiesofpain:location,quality,andintensityofpain.
• This ALNT projects to the lateral thalamus with further connections to the
sensorycortexallowingpainlocalization.
• InformationfromC fibresencodes‘slow pain’transmittedthroughthe more
primitive-origin spino-reticulo-diencephalic tract in the posterolateral cord.
This projects to the reticular system of the brainstem, thalamus, and
hypothalamus and onwards to the limbic system. These connections are

responsiblefortheaffective,emotionalaspectsofpain.
• Connectionstothesympatheticnervoussystemmediatearousal.
Theoriesofpainpathophysiology
Over the years, various theories have been proposed to try and explain the
complexnatureofpainsensationandhowthisismodulated.
• René Descartes first postulated the existence of pain nerves which directly
transmitperipheralpainfulstimulitothebrain.
• ThegatecontroltheoryofpainwasputforwardbyMelzackandWall.This
statesthatthereisagateinthespinalcordthatinfluencespaintransmission.
Non-noxious stimulation inhibits upward transmission of pain (closes the
gate),henceotherstimuliaffectingthesameperipheralnervedistribution(e.g.
rubbing)reducesacutepain.
• Dissociation between peripheral stimuli and activation of the pain
neuromatrix,aprocess knownas centralsensitization,is thoughtto underlie
chronicpainthatpersistsintheabsenceoftissuedamage.
Furtherreading
Wedirectthoseseriousintheirintentiontohelppatientswithchronicpaintoothertextsandto‘Explain
Pain’ delivered by the Neuro-orthopaedic Institute ( http://www.noigroup.com/en/Category/EP)or
similarcourses.
Generalizedpainsyndromes
Chronicwidespreadpain
Chronicwidespreadpain(CWP)isacommonfindingpresentin5–10%ofthe
general population. In the absence of diffuse degenerative or
inflammatory/autoimmune rheumatic MSK, fibromyalgia (FM) is the
commonestmanifestation.
• CWPaffectswomenmorethanmenwitharatioof1.5:1andisdefinedaspain
for>6monthsintwoormoresitesbothaboveandbelowthepelvis.
• CWPmaypresentalone,maybemisinterpretedasanothercondition,ormay
beassociatedorcomplicateanothercondition.
• Conditions that can be associated with CWP or give rise to CWP as a
secondaryeffectareshowninBox22.1.
• CWPisoftenassociatedwithdisturbedandunrefreshedsleep.
• PeoplewithCWPoftenhavefatigueandmanymayultimatelybediagnosed
withchronicfatiguesyndrome.
• Peripheral threat (/pain) signals will often be amplified by other threats
including anxiety, depression, and any other persistent or unresolved
psychological conflict. Assessment of these should be considered a normal
partofthe historyand should beconsidered sympatheticallyas contributory
butnotthesolecause.
Box22.1Some(ofthemostcommon)conditionsinadultsthatcaneither
causeCWPormaybeassociatedwithit
• SLE.
• PrimarySjögren’ssyndrome.
• SOXsyndromeandearlygeneralizedOA.
• UndifferentiatedAICTD.
• Chronicsarcoidosis.
• Antiphospholipidsyndrome.
• Psoriatic-relatedMSKdisease.
• SAPHOsyndrome.
• AxialorperipheralSpA.
• Thyroiddisease.
• Primaryhyperparathyroiddisease.
• Osteomalacia.
• Largevesselarteritis.
Fibromyalgiaand‘syndromic’fibromyalgia
Fibromyalgia (FM) is the term given to patients who have CWP that satisfies
classificationcriteria:eitherACR1990criteriaforFMorACR2010criteriafor
FMwhichexpandstheearliercriteriatoincludeawiderspectrumofsymptoms
andtheirseverity(‘syndromic’FMorFMsyndrome).
Historyofuseofthetermfibromyalgia
FM is a type of CWP that has the cardinal feature of sleep disturbance.
Historicallythiswaspreviouslylabelledasmuscularrheumatismorfibrositisto
describeaconditionwithpain,fatigue,andpsychologicalinvolvement.
• BothFMandCWPareoftenassociatedwithothersomaticsymptoms,suchas
chronicfatigue,IBS,multiplechemicalsensitivities,andheadachesyndromes.
Other causes of fatigue should always be excluded, e.g. hypothyroidism,
hypoadrenalism,primarySjögren’ssyndromeandanaemia(Box22.1).
• Both CWP and FM are associated with alterations in peripheral and central
pain processing. Painful stimuli are detected at lower levels in affected
patients. Allodynia (pain in response to non-painful stimuli) found in these
conditionsisthoughttobeduetocentralsensitizationandan‘amplification’
phenomenon.
DiagnosisofFM
TherearetwoclassificationcriteriaforFM(ACR1990andACR2010criteria).
The 1990 criteria require diffuse tenderness at discrete anatomical sites. The
2010criteriaarebasedonmood,pain,andsleepdisturbance.The2010criteria
are designed to provide an alternative method of classification to allow long-
termfollow-upofFMpatientsandamethodofevaluatingthesymptomseverity
ofFM.
• ManyFMtenderpoints(Box22.2)areoverentheseswhicharescoredforpain
in enthesitis indices when assessing SpA conditions. It is of exceptional
importancethatSpAisdistinguishedfromFM.Ofcourse,bothmaycoexist.
An enthesitis predominant form of psoriatic arthritis is not uncommon (see
CASPARcriteriafordiagnosisofPsAin Chapter8).
• FMisalsofoundinupto25%ofpatientswithRA(see Chapter5),andSLE
(see Chapter 10). It is also commonly found in association with
hypermobilityspectrumdisordersandhypermobility-EDS( Chapter19).
• Care must be taken to avoid misdiagnosing CWP/FM as the only cause for
painwhenthereisanAICTD,axSpA,orPsApresent.
• FM cases tend to aggregate within families but no genetic contribution has
beendefinedasyet.Itisimplausiblethatgeneticinfluenceswillnoteventually
bedefined;thuscommonenvironmentaltriggersshouldbeconsidered.
• The2010criteriaforclassificationofFMareshowninBox22.3.
Box22.2ACR1990criteriafordiagnosisoffibromyalgia
1.Historyofwidespreadchronicpain
Painisconsideredwidespreadandchronicwhenallofthefollowingare
present:
• Painintheleftandrightsideofthebody
• Painaboveandbelowthewaist
• Axialskeletalpain
• Painpresentfor3months
and
2.Paininatleast11/18tenderpointsitesondigitalpalpationwith4kg
pressure*.Onepointisgivenforeachsideofthebodyatthefollowing
9sites:
1. Occiput:atthesuboccipitalmuscleinsertions
2. Lowcervical:attheanterioraspectsoftheinter-transversespacesat
C5–C7
3. Trapezius:atthemidpointoftheupperborder
4. Supraspinatus:atoriginsabovescapulaspinenearmedialborder
5. 2ndrib:at2ndcostochondraljunction
6. Lateralhumeralepicondyles:2cmdistalfromepicondyles
7. Gluteal:inupperouterquadrants
8. Greatertrochanter:posteriortotrochanter
9. Knees:atmedialfatpadproximaltojointline
*Positivetenderpointwhensubjectsayspalpationwaspainful,(‘tender’isnotconsideredpainful).
FMissaidtobepresentwhenbothcriteria(CWPandtenderpointcount)aresatisfied.FMisnot
excludedbythepresenceofanotherdisorder.
CriteriatakenfromWolfeFetal.TheAmericanCollegeofRheumatology1990Criteriaforthe
ClassificationofFibromyalgia.ArthritisandRheumatism1990;33(2):160–72.
Box22.3ACR(revised)2010fibromyalgiacriteria
ApatientsatisfiescriteriaforFMifthefollowingthreecriteriaaremet:
1.Widespreadpainindex(WPI)≥7andasymptomseverity(SS)scalescore
of≥5orWPI3–6andSSscalescore≥9.
2.Symptomshavebeenpresentatasimilarlevelfor≥3months.
3. The patient does not have a disorder that would otherwise explain the
symptoms.
WPI=thenumberofareasinthelastweekwheretherehasbeenpain(score
0–19): left and right—shoulder girdle, upper arm, lower arm, ‘hip’
(buttock/trochanter),upperleg,lowerleg,jaw.Also:upperback,lowerback,
chest,abdomen,neck.
SSscalescore(0–12)iscalculatedby:
Scoringeachofthese3symptoms:wakingunrefreshed,fatigue,andcognitive
symptoms,onascaleof0–3where:
0=noproblem
1=slightormildproblems,generallymildorintermittent
2=moderate,considerableproblems,oftenpresentand/oratamoderatelevel
3=severe:pervasive,continuous,life-disturbingproblems.
Andadding
ascorefortheextent(severity)ofsomaticsymptoms*where:
0=nosymptoms
1=fewsymptoms
2=amoderatenumberofsymptoms
3=agreatdealofsymptoms.
*Somaticsymptomsthatmightbeconsidered:musclepain,IBS,fatigue/tiredness,thinkingor
rememberingproblem,muscleweakness,headache,pain/crampsintheabdomen,numbness/tingling,
dizziness,insomnia,depression,constipation,painintheupperabdomen,nauseanervousness,chest
pain,blurredvision,fever,diarrhoea,drymouth,itching,wheezing,Raynaud’s,hives,welts,ringingin
ears,vomiting,heartburn,oralulcers,lossof/changeintaste,seizures,dryeyes,shortofbreath,lossof
appetite,rash,sunsensitivity,hearingdifficulties,easybruising,hairloss,frequenturination,painful
urination,bladderspasms.
NewcriteriasummarizedfromWolfeFetal.TheAmericanCollegeofRheumatologyPreliminary
DiagnosticCriteriaforFibromyalgiaandMeasurementofSymptomSeverity.ArthritisCare&Research
2010;62:600–10.
ManagementofCWPandfibromyalgia
Theultimategoalofpainrehabilitationistoimprovequalityoflifeandsenseof
well-being rather than focus on pain reduction. With improvement in factors
such as sleep or anxiety and improvements in physical activity and general
participation,distraction frompain isimprovedandtheoverall senseof threat
reduced.Thiswillinturnreducethevolumeofpainsignal.
1
Managementissue1:explanationandreassurance
It is of paramount importance to consider carefully the way in which an
explanationisgivenastothenatureofthecondition.Thismaytakesometime
and may be best approached in the context of a multidisciplinary team
(psychologists,physiotherapists,OTs,doctors).
• It is important to assess the effect of symptoms on the patient’s life, and
developagoodrapportsopsychosocialissuescanbediscussed.
• Theemphasisintheexplanationshouldbereassurancethatthereisnoserious
underlyinginflammatoryorsystemiccondition,thatnothinghasbeenmissed,
andthereisnodamagetothejointsandmuscles.Thisfearblocksengagement
withexplanationsandunderminesrehabilitationstrategies.
• Effectiveexplanationusesappropriatelanguageandstoriestohelpthepatient
understand:
• moreaboutthecomplexityofpainprocessingandwhyitgoeswrong.
• whythereisn’taquickswitchtoturnitoff.
• why a return to activities and routines including normalization of sleep
helps.
• whythereneedstobeachangeincopingstrategies.
• Explanations also challenge the value of ongoing litigation and it may be
necessarytowaitforthistoberesolvedbeforebeginningapainmanagement
programme
• Educationoffamilyandpartnersisinvariablyhelpfulandoftenessential.
• BothCWP/FMareconditionswithrelapsesandremissions.Mostpatientswill
have ongoing symptoms. Patients with appropriate coping strategies,
improvementsinpsychosocialstressors,andgoodsocialsupportnetworksare
morelikelytohaveabetteroutcome.
Managementissue2:symptommanagement
OftenpeoplewithCWPlimitactivityduetoafearofprovokingmorepain.In
addition to addressing physical symptoms such as pain and fatigue,
psychologicalinput(e.g.cognitivebehaviouraltherapy)ishelpfulinproviding
toolstomanagepainandactivitylevels.
• Althoughexercisemaycauseashort-termincreaseinpain,agradedexercise
programmehasbeenshowntobebeneficial.
• Low-impactexercise,suchasPilatesmaybehelpful.Pilatesishelpfulbecause
it:
• requirescontrolavoidingjarringandunpredictablemovements.
• worksallindividualmusclegroupsincludingthosethathavebecomeweak
frompreviousunhelpfulpatternsofmuscleuse.
• istiringandreleasesendorphins.
• encourageseffectivestretching.
• buildsconfidenceandresilience.
• A physiotherapist should help support and guide engagement with Pilates,
yoga, and gym classes and may indicate what specific activity might be
avoidedinthefirstinstance.
• Pacing ofactivities isimportant, avoiding‘boom andbust’ patternsofover-
activitywhenfeelingwell,followedbyperiodsofinactivityduetosubsequent
painandfatigue.
• Cognitive behavioural therapies (CBTs) provide a small incremental benefit
overcontrolinterventionsinreducingpain,negativemoodanddisabilityatthe
endoftreatmentandatlong-termfollow-upinFM.
2
• Lack of adequate forms of sleep reduces resilience and promotes pain
amplification.Poorsleepisoneofthemajorbarrierstoimprovementandis

tackledattheoutsetofmostpainprogrammes.
• Sleepdisturbanceneedstobeaddressedthroughsleephygienemeasures(e.g.
haveaquietbedroom,reducelightandnoisewherepossible,avoideatinglate,
reducingcaffeineintakeintheevening).
• Sleep health information is available at:
https://www.sleepassociation.org/patients-general-public/insomnia/sleep-
hygiene-tips/
Managementissue3:pharmacologicaltherapy
The role of medication is to help establish and reinforce good sleep routines,
reduceanxietyandfearofpain,andwherepossibleallowimprovementsinpain
severitytoallowengagementwithpainprogrammerecommendations.Manyof
thetechniqueslearntinpsychological-basedtreatmentstrategieshelpwiththis,
reducingtherelianceonoftenunhelpfulpainmedications.
• NSAIDs and GCs are not effective and may cause morbidity due to side
effects.
• Narcoticsshouldbeavoided.
• Many patients will have tried analgesics with little effect. This in itself can
fuel anxiety as to the cause and severity of their underlying condition, and
frustrationandlackofconfidenceintheirdoctor.
• Tricyclic antidepressants such as amitriptyline (10–50 mg 2 hours before
bedtime) are often helpful in embedding changes to sleep routines and
improvingqualityofsleep,decreasingmorningstiffness,andalleviatingpain.
• Patientsshouldbewarnedofsideeffectsoftricyclicssuchasdrymouth,self-
limiting morning somnolence and weariness, and that they may take 3–4
weekstotakeeffect.
• Patientsareoftenalsowaryofbeinggivenan‘antidepressant’.Anexplanation
thatatricyclicisbeingusedasamodifieroftheimpactofpainisimportantto
improveadherence.Amitriptylineisoneofagroupofdrugsthatincrease5-
hydroxytryptamine.
• Amitriptylinecanbeusedwithtramadolandthiscombinationmaybehelpful
inthosewithsevereexacerbationsorwavesofpain.
• The efficacy of selective serotonin reuptake inhibitors (SSRIs) is debated
given variable evidence of efficacy. The use of fluoxetine, duloxetine
sertraline,or citalopramimprovesmoodandanxiety, butSSRIsmaybeless
effectivethantricyclicsintreatingpain,fatigue,andsleepdisturbance.
• Venlafaxine(aserotoninandnoradrenalinereuptakeinhibitor)inhighdosesis
effective in treating multiple symptoms in FM. Low-dose treatment is
ineffective.

• Pregabalinhasshownefficacyonpaininsomestudiesandcanbecombined
effectivelywithduloxetine.
3
• Sedative hypnotics have been reported to improve sleep in severe
circumstances.
• A recent meta-analysis of RCTs
4
showed that duloxetine 60 mg, pregabalin
300mg,milnacipran100mg,and200mgweremoreefficaciousthanplacebo.
However, there was no significant difference in the efficacy and tolerability
betweenthemedicationsattherecommendeddoses.
• Overall however, when treatments are judged against quite strict criteria for
improvementthereisnotstrongevidenceforefficacy.
4
• The conclusion from the meta-analysis report
4
was: ‘The available data
regardingefficacy...(treatingpain,sleep,physicalfunction,fatigue,anxiety,
depression,andcognition)...wereinsufficienttodrawdefiniteconclusions..
. (regarding response of FM patients to reported treatment modalities). . . .
Indirect evidence indicates that efficacy may be expected with the use of
serotonin noradrenaline reuptake inhibitors (SNRIs), noradrenaline reuptake
inhibitors(NRIs),andmultidisciplinarytreatment....’
• A number of meta-analyses of drug therapies are available in the Cochrane
Library( http://onlinelibrary.wiley.com/cochranelibrary).
References
1. Okifuji A, Gao J, Bokat C, et al. Management of fibromyalgia syndrome in 2016. Pain Manag
2016;6:383–400.
2. Bernardy K, Klose P, Busch AJ, et al. Cognitive behavioural therapies for fibromyalgia. Cochrane
DatabaseSystRev2013;9:CD009796.
3. Gilron I, Chaparro LE, Tu D, et al. Combination of pregabalin with duloxetine for fibromyalgia: a
randomizedcontrolledtrial.Pain2016;157:1532.
4. Papadopoulou D, Fassoulaki A, Tsoulas C, et al. A meta-analysis to determine the effect of
pharmacological and non-pharmacological treatments on fibromyalgia symptoms comprising
OMERACT-10responsecriteria.ClinRheumatol2016;35:573–86.
Localizedpainsyndromes
Localized pain syndromes are chronic pain conditions in a defined area. The
diagnosis of a localized pain syndrome is a diagnosis of exclusion given
conditions that can present with similar features. Often there is underlying
neuropathicpainandabnormalneuralactivity.
Chronicregionalpainsyndrome(CRPS)
Generalconsiderations
CRPSischaracterizedbyvariabledysfunctionoftheMSK,skin,neurological,
andvascularsystems.CRPSmayoccurinavarietyofsituationswithanumber
ofclinicalmanifestationsvaryingaroundcentralcorefeatures.
• Severaltermshaveevolved,describingaspectsofthesamecondition:reflex
sympathetic dystrophy, Sudeck’s atrophy, shoulder–hand syndrome, and
transientosteoporosis.
• ThesetermshavebeensupersededbythetermCRPS,whichisrecognizedby
theInternationalAssociationfortheStudyofPain.
• TherearetwosubtypesofCRPS:type1describessymptomsintheabsenceof
peripheralnerveinjury,andtype2(‘causalgia’)inthepresenceofinjurytoa
specificperipheralnerve.
Epidemiologyandaetiology
CRPSisacommondisorder.Itaffectsbothsexesequally,andoccursatanyage
in allracesand geographical regions. Althoughtheexact aetiology is unclear,
thereislikelytobeacombinationofperipheralandcentralneurologicalfactors
involved.
• Trauma(e.g.fracture,burn,surgery,etc.)isthemostcommontriggeringevent.
Theeventmaybetrivial.Oftennocauseisidentified.
• CRPSisreportedinuptoathirdofseriesofdistalforearmfracture.
• Several neurological conditions may act as triggers, including, for example,
hemiplegiaandmeningitis.Peripheralnerverootinjurymayalsoleadtothe
syndrome.
• Pregnancy, tumours,and prolongedimmobilization havealso beenlinked as
possibletriggeringfactors.However,25%ofcaseshavenocleartrigger.
• Itisimportanttotryandidentifypsychosocialstressesasthesemayhavean
effectonthepersistenceofsymptoms.
Clinicalfeatures
Typically,thesyndromeinvolvesthedistalpartofalimb,e.g.forearmorfoot.
Early clinical features of the condition include pain, soft tissue swelling (e.g.
maybesynovitisifoverajoint),reticular/livedorash,warmthoveraffectedpart.
Occasionallytheremaybelocalized,sweatingandpiloerection.
• The pain has several particular characteristics and is often described as
‘burning’.Thefeaturesinclude:
• allodynia—anotherwiseinnocuousstimulusproducespain.
• hyperalgesia—increasedpainperceptiontoagivenstimulus.
• hyperpathia—delayed over-reaction, often after repetitive cutaneous
stimulus.

• Theaffectedlimbisoftenguardedtoavoidanycontactasallodyniaisusually
extreme.
• NovelclinicalsignsdescribedinrecentyearssupportinvolvementoftheCNS
andMRIstudiesshowevidenceofcorticalreorganization.Theseclinicalsigns
include digit misperception, astereognosis, altered hand laterality, and
abnormalbodyschema.
• Patientsbecome‘depersonalized’fromtheiraffectedlimbwithafeelingthatit
nolongerbelongstothemandadesiretoremovethatlimb.
Investigation,staging,anddiagnosis
Clinical suspicion and knowledge, and a good history and examination will
makethediagnosisofCRPSinallcases,butitisimportanttorecognizechanges
thatmayoccurinsomeradiologicalandfunctionalimaging.Thesetestsmaybe
misinterpretedinothersettingsandmayhelpwithexplanationswithpatients.
• Laboratory tests need to be interpreted cautiously. ESR, CRP, and FBC
abnormalities may be present if there is underlying inflammatory rheumatic
MSKdisease.
• However, there may be evidence of bone demineralization (osteopenia on
radiographs, CT or low bone density estimated using regional DXA) if the
lesionissevere.
• High bone resorption can be indicated biochemically by hypercalciuria
(hypercalcaemia would be very unlikely), and raised plasma/serum collagen
crosslinks(e.g.CTX).
• Thermographycandemonstratechangesincutaneoustemperature.
• Perhaps of most value, and high specificity, is the triple-phase bone
scintigraphy(
99m
Tc-MDPscintigraphy).
• An experienced nuclear medicine physician can specify CRPS based on
characteristicpatternsofbonescintigraphyabnormalityinthe earlyregional
bloodflowdistribution,bloodpoolappearances,andlateskeletalradionuclide
uptake.
• CRPS stage I is essentially regional pain and swelling. In most cases, the
symptomsfluctuate,thengraduallyresolve.
• StageIICRPSisaperiodofdystrophicchange(see Plate10).Thistendsto
occurseveralmonthsafteronsetofthedisorder.Theaffectedregionbecomes
cool, pale, and often cyanosed in colour with abnormal sensation
(dysesthesia).
• StageIIICRPSismanifestbyadecreaseinhairandnailgrowth,osteopenia,
and eventually atrophy of skin and subcutaneous tissue. Stage III CRPS is
difficulttotreatandreverse.

• MostcasesofCRPStendnottoprogressbeyondstageI,oratmostearlystage
II.
• TheBudapestcriteriafordiagnosisofCRPSareshowninTable22.1.
Table22.1.TheBudapestcriteriafordiagnosisofCRPS.ForadiagnosisofCRPS,allfourcriteria(A–
D)mustbemet
Criteria A:continuingpaindisproportionatetotheincitingeventand
B:≥1symptomin≥3categories(below)
and
C:≥1signin≥2categories(below)
and
D:nootherdiagnosisbetterexplainsthesymptomsandsigns
Categories Sensory:allodynia(tolighttouchand/ortemperaturesensation
and/ordeepsomaticpressureand/orjointmovement)and/or
hyperalgesia(topinprick)
Vasomotor:temperatureasymmetry(>1°C)and/orskincolour
asymmetrybetweenlimbs
Sudomotor/oedema:oedemaand/orsweatingchangesand/or
sweatingasymmetry
Motor/trophic:decreasedrangeofmotionand/ormotor
dysfunction(weakness,tremor,dystonia)and/ortrophictissue
changes(hair,nail,skin)
ManagementofCRPS
Success treating CRPS relies on an early and accurate diagnosis and early
treatmentinordertopreventchronicity.
• OnceCRPSpersistsbeyond6–8months,itisdifficulttoreverse.
• Early and ongoing treatment should focus on the whole individual and not
simplytheregionalsymptoms.
• Treatment is based around the broad categories of physical therapies
(physiotherapy and desensitization therapy), psychological therapies
(cognitivebehaviouraltechniques),andpharmacotherapy.
• Attention to anxiety, psychosocial stressors, pain behaviour, and sleep
disturbanceisimportant.
• Patientsoftenrequirerepeatedreassuranceandcounselling.
• The aim should be to resume premorbid levels of activity so early physical
therapy(/hydrotherapy)inputshouldbeconsidered.
• Desensitization therapy of the affected region can help to normalize the
sensationsofhyperalgesiaandallodynia.
• Desensitizationisachievedbyapplyingdifferenttexturestotheaffectedarea,
concentrating particularly on the interface between normal and abnormal
sensations.
• Mirror therapyto reflectthe unaffected limbwhile performingsynchronized
movements can also help in regainingfunctionandrangeofmovement and
relievingpain.
• In early acute disease, IV pamidronate may be helpful in relieving pain,
especially if there are bony changes on imaging. Short courses of
glucocrticoids(GCs)mayalsobehelpfulintheacutestages.
• Tricyclic antidepressants canhelpcorrect sleep disturbance and increase the
painthreshold.
• Gabapentinorpregabalinmayalsobeofvalue.
• Transcutaneouselectricalnervestimulation(TENS)mayhelppaincontroland
allowentryintoaphysicalactivityprogramme.
• In some severe cases, regional sympathetic or ganglion blocks have been
reported to control pain sufficiently to facilitate engagement with pain
managementprogrammes.
• Patients may request limb amputation as a result of their depersonalization
fromthatlimb.However,thisshouldbediscouragedasitdoesnotguarantee
improvement in pain and such patients may suffer with intractable phantom
limbpain.
Otheradultregionalpainsyndromes
Post-herpeticneuralgia
Thisneuropathicpainconditiondevelopsinadermatomaldistributionfollowing
an episode of herpes zoster. It is defined as pain that continues for 3 months
following an attack of herpes zoster. Typically, the neuralgia begins as the
vesiclesstarttohealandcrustover.
• Paincanbevariableinseverityandisneuropathicinnature.
• Antivirals such as aciclovir are often used at the beginning of an attack of
herpes zoster to limit the duration of the attack and reduce the chances of
developing post-herpetic neuralgia. However, these are not useful in
establisheddisease.
• Treatmentincludesanticonvulsantssuchascarbamazepineandgabapentinas
wellastricyclicantidepressantssuchasamitriptyline.
• Ganglionregionalnerveblockscanbeconsideredforseverecases.
• Analgesicssuchasparacetamol,anti-inflammatories,andopioidsmayallbe
helpfulinmanagingpain.
• ShortcoursesofGCsareoftenusedtoreducethedurationofpain.
• ConservativemeasuresthatmaybehelpfulareTENS,acupuncture,relaxation
techniques,andheat/coldtherapy.
Trigeminalneuralgia
This is a type of neuropathic pain affecting the trigeminal nerve and causing
intense facial pain along the trigeminal nerve divisions. There are two main
types:typicalandatypicaltrigeminalneuralgia.
• Thetypicalformcausesattacksofseveresuddenpainononesideoftheface
whichcanlastforsecondstominuteswhiletheatypicalformcausesconstant
burningpain.
• Theexactaetiologyisunknownbutisthoughttobeduetolossofthemyelin
nervesheath.
• Treatmentis withanticonvulsantssuch ascarbamazepineandtricyclicssuch
asamitriptyline.Opioidsareusuallynoteffective.
• Surgerymaybeanoptionifconservativemeasuresfail.
Temporomandibularjoint(TMJ)dysfunction
ThemostimportantfeatureofTMJdysfunctionispainandrestrictedmandibular
opening.
• Thereisoftenclickingassociatedwithmovementofthejoint.
• About 20–30% of the general population have some degree of TMJ
dysfunction.
• Thereisalinktothehabitofteethgrindingsooftenprostheticmouthguards
arefashionedtowearparticularlyatnight.
• TheTMJcanbeaffectedinallinflammatoryarthritidessuchasRAandPsA
andsuchcausesshouldalwaysbeconsideredasanunderlyingcauseofTMJ
pain.
Chronicpaininchildrenandadolescents
Introduction
In childhood and adolescence, pain is a ubiquitous experience affecting over
80%ofindividualsinanygivenpreceding3–6-monthperiod.Asinadults,this
threat, or danger, sensation is associated with neuroendocrine, MSK, and
inflammatory responses, and provokes threat appraisal and behavioural
adaptationthatmaybeattentiveoravoidant.
• Prevalence rates of chronic (recurrent or persistent) pain in children and
adolescentsarehigh(11–38%)with5%experiencingsignificantpain-related
dysfunction.
• Chronicpainaffectsmostbodysiteswithaprevalencethatincreaseswithage
(seeTable22.2)
Table22.2Prevalenceofchronicpaininchildrenandadolescents
Paintype Prevalencerangefromvariousstudies(%)
Headache 8–83
Abdominalpain 4–53
Backpain 14–24
MSKpain 4–40
Multiplepains 4–49
Other/generalpains 5–88
• Over 10% of all GP contacts with adolescents are attributable to MSK pain
and of thoseseekingmedicalintervention the direct cost to the USA is $19
billion.
• Although the international criteria for chronicity is 3 months’ duration
(constantorintermittent),takenfromthedefinitioninadults,adiagnosiscan
oftenbemadesooner.
• On careful enquiry the site, character, and severity of pain, and any loss of
function, are often incongruous with the mechanism of any injury or
backgrounddiseasestate(JIA,sickle,IBD,etc.)andthisfrequentlyoverrides
therelevanceofduration.
Associationsofchronicpaininchildrenandadolescents
Most chronic MSK pain might reasonably be attributed to biomechanical
imbalancesandstressesthattypicallyresultfromtissuetightnessandchangesin
patternsofmuscleusewithnormalgrowthanddevelopment.
• Inappropriate patterns of muscle use may also derive from previous injury,
repetitive sport or dance activities, or commonly from deconditioning when
sedentarybehaviourpredominates.
• Othercommonassociationswithchronicpainandpainamplificationinclude

obesity, poor sleep health, lower socioeconomic status, parental
catastrophizing, risk aversion, thought and attention problems, anxiety, low
mood, rule breaking, aggressive behaviour and hypermobile joints, but the
extenttowhichthesefactorsarecontributoryinchildhoodvary.
• Pain in multiple sites, including chest, abdomen, and head, is strongly
associated with obesity in girls and a high number of psychosocial and
mechanicalfactors.
• MultipleMSKpainsinadolescencehaveahightendencytopersist(>2years)
with both psychosocial factors and lifestyle factors contributing to this
vulnerability.
Chronicwidespreadpaininchildrenandadolescents
Thediagnosistermchronicwidespreadpain(CWP)ispreferredtojuvenileFM
orjointhypermobilitysyndrome/hypermobilityspectrumdisorderorotherlabels
which intimate poorly established aetiologies, have overlapping diagnostic
criteria,markedheterogeneity,andmayunnecessarilyinculcate(ortrap)patients
intoanexpectationoflifelongdisability.
• Duetovariationindiagnosticlabelsandcriteria,theepidemiologyofCWPis
poorlyunderstood.
• The prevalenceof juvenilefibromyalgia(JFM), definedby ACRcriteriafor
adults(chronicMSKpain,multiplediscretetenderpoints,fatigue,andsleep
disturbance),isupto6%.
• JFM accountsfor8% ofdiagnoses madebypaediatric rheumatologists.The
prevalenceofjointhypermobilitysyndromeinchildrendiagnosedwithJFMis
probablythesameasinthegeneralpaediatricpopulation.
• Enigmaticsymptomsofdizziness,fatigue,blurringofvision,‘blackouts’,and
tachycardia occur in 50% of children and adolescents with CWP and might
reasonably be attributable to variations in ‘threat signalling’ and may be
exacerbatedbyanxiety.
• Labels of ‘postural orthostatic tachycardia syndrome’ PoTS, ‘autonomic
dysfunction,’or‘chronicLymedisease’areusuallyunhelpfulandmostofthe
clinical symptoms resolve with effective explanation and engagement in a
rehabilitativeprogramme.
• CWP maybetriggered by or coexistin5–20% of cases withanunderlying
disorder such as sickle cell disease, heart disease, or cancer. CWP in the
presenceofaSpAconditionrequirescarefuldisentanglingasenthesitislinked
toSpAmaybepresent(see Chapter8).
ManagementofCWP:generalprinciples
• Irrespective of the medical setting there is always a potential to positively
intervene,beginningwithrecognitionofaprimarypaindisorderandmaking
time for the patient to explain their history, the impact, and their
understanding.
• Thetherapeuticconsultacknowledgesthepainandexplainstheroleofpainas
athreatsignal.
• Further explanations about pain processing, in appropriate language, should
assist an understanding to promote engagement in the treatment strategies
describedinthenextsubsectionandreduceasenseofhelplessness.
• Effective explanations of pain are therapeutic and can be enormously
motivational.
• In particular, there should be an understanding of disruptions to the ‘4Ss’
(sleep,sports/physicalactivity,sociallife,andschool).
• A focus on returning to normal 4S routines should improve resilience and
improve quality of life, with consequent reductions in the psychological
impactofpainandenhancedbiofeedbacktocounteractpainsignals.
ProgrammesofcareforCWP
• Effectiveprogrammesofcaretargetanappropriateamountofresourcetothe
levelofneed.
• Integrationacrossanetworkofservicesisoftenrequiredwithcommunityand
secondarycareservicesworkingwithatertiaryhub.
• Thefocusofcareistoreturntonormalfunctionwithanincidentdecreasein
pain.
• Corefeaturesofaprogrammeofcareinclude:
• adequateexplanationaboutpainandrehabilitation.
• an interdisciplinary and goal-orientated approach with a specific focus on
self-management.
• medication used to enhance engagement with advice and other self-
managementstrategies.
• Pain workshops inform and educate in an engaging way, dispel myths, and
create a narrative that helps to increase participation and improvements in
qualityoflifedespiteminimalchangeslevelsofpain.Workshopsalsoprovide
thebenefitofpeersupport.
• Physical therapiessuch asphysiotherapyand occupationaltherapytreatment
strategiesaremosteffectivewhengoaloriented.
• Physiotherapistshelptoreducethefearofmovementandguidethepatient
through a programme of exercise and increase participation in general
physicalactivity.
• Physiotherapypromotesresilience,aswellasreducingmuscletightnessand
buildingstrength,stamina,balance,andnormalpatternsofmuscleuse.
• Occupationaltherapistssupportupperlimbphysicalactivity,agradedreturn
toschool,sleep advice,management ofbullyingand areturnto anactive
sociallife.
• Physiotherapists often support such re-engagement with regaining normal
4Sfunctiontoo.
PsychologicaltherapiesforCWP
• Psychologicalinterventionnowdrawsfromanarrayoftreatmentstrategiesin
additiontoCBT.
• Effectivepsychologyprogrammesincludeafocusonresilienceandpromotion
ofpatientstrengthsinadditiontoreducingbarrierstoengagementandcoping
modification.
• ACochranereviewin2014showedpsychologicaltreatmentsareeffectivein
reducing pain intensity and disability in various forms of CWP and the
benefitsappeartobemaintained.
• Evidencefortheeffectsofpsychologicaltherapiesonmoodislimitedasitis
foreffectsondisabilityinchildrenwithheadache.
Activemind–bodytechniques
• Techniquesareusefulinpromotingself-management.
• Techniquesincludebreathingstrategies(squarebreathing,diaphragmaticand
slow exhale breathing), mindfulness, yoga, Pilates, and progressive muscle
relaxation.Thisisnotanexclusivelistandthebenefitvariesbetweenpatients.
Parentcoaching
• A child or adolescent in pain exerts a considerable emotional, and often
financial,tollonfamilylife.
• Pain-relateddisabilityismoreconsistentlyrelatedtopoorfamilyfunctioning
thanpainintensity.
• Parenting behaviours can act to maintain or even enhance their child’s pain
experience; e.g. if the child has to interpret ambiguous emotional parental
expressions.
• Thereisariskofincreasedanxietyanddepressionforachildofaparentwith
CWP.Familialdysfunctioncanfollow.
• Normalizing parental protectiveness reduces guilt and defensiveness and
refocusesparents’attentiononhealthyandadaptivebehaviours.
• Parentsaretaughthowtocalmthemselvesanduseskillstodistractandavoid
emotionalescalation.Afocusshouldbemaintainedontheirchild’s function
andparticipation.
• Parents’painexperiencesshouldbeaddressedanddiscussedopenlywiththe
childpresent.Itshouldbeclearlypointedoutthatthechild’spainisdifferent
from the parent’s disability and pain, with an expectation that the child can
becomepainfree.
• Parents are taught how to optimize the independence of teenagers and
encourageself-managementskills.
PharmacotherapyinCWP
• Thereislittleevidencetosupportthesoleuseofmedicationbutitmayhavea
roleintheintegratedmanagementplandescribedhere.
• There are no RCTs which confirm the benefit of paracetamol in treating
paediatricCWPbutthereissomelimitedevidenceforibuprofenalthoughboth
are associated with potential long-term side effects including overuse
headaches.
• Opiates should be avoided inprimarypain disorders due to poor safetyand
sideeffectprofilesassociatedwithworseoutcomes.
• Care should be taken with opiate use when IBD or sickle cell disease is
associatedwithaprimarypaindisorder.
• CodeinehasbeenwithdrawnfromtheWHOpainladderforchildren.
• Adjuvant therapies including low-dose tricyclic antidepressants,
gabapentinoids,SSRIs,andmelatoninmaybehelpful.
• TherearenoRCTswhichsupporttheuseofgabapentinintreatingpaediatric
CWP,anditsusemayresultincognitiveimpairmentandreducedresilience.
• The anxiolytic effects of tricyclics and SSRIs may help to improve
engagementwithmanagementstrategiesandresiliencefromimprovingsleep.
• MedicationisassociatedwithastrongplaceboeffectinCWP.Forexample,in
variousRCTsformigrainetherapies,aplaceboresponse istypically seenin
50–60%ofstudyparticipantsandcandecreaseheadachefrequencyfromsixto
threeheadaches/month.
Complexregionalpainsyndromeinchildrenand
adolescents
CRPS is clinically distinct from adult CRPS in that the lower limb is more
commonly involved than the upper limb, there is a marked female
predominance, dystrophic changes and long-term disability are less common,
andmultiplelimbscantypicallybecomeinvolved.
• Thepeakincidenceisinearlyadolescence(median13years).

• MRIshowsincreasedbonesignal(‘oedema’)earlyinthecondition.
• Thermographyhighlightsabnormalregionalbloodflowchanges,whichcanbe
comparedtotheotherlimbs.
• Laterinthediseaseradiographsshowosteopenia.
• Ultimately,limbdeformityoccursinthemostseverecases.
ManagementofCRPS
• EffectivemanagementofCRPSrequiresacarefulexplanationofthecondition
to the child or adolescent and their family, a graded exercise programme
supervised by a therapist experienced in chronic pain management, and
frequentdesensitization.
• Workonrestoringnormal4Sfunctionimprovesresilienceandmostpatients
respondwithin4–6therapysessions.Patientscanexpecttobecomepainfree
andreturntoallactivities.
• 25–35% of children and adolescents with CRPS are resistant to routine
management techniques and will benefit from more intense programmes of
careasdescribedforCWP(see ,‘Chronicwidespreadpain’,pp.639–641).
Chapter23
Drugsusedinrheumatologypractice
Introduction
Painrelief
Glucocorticoids
Disease-modifyingantirheumaticdrugs
Othermedications
Introduction
A variety of pharmacological agents are used across the breadth of rheumatic
diseases. Therapeutic options are discussed in each of the disease-specific
chaptersinPartIIofthisbook.
Thischapterhighlightscommonthemespertinenttoprescribingforpainrelief
and control of autoimmune rheumatic disease. It is not the intention of this
chaptertodescribealloftheseindetail,althoughspecificissuesarediscussed.
Protocolsfortheuseofcertainagentssuchaspooled-immunoglobulinwillalso
bedescribed.
Foradetaileddescriptionofaspecificdrugitisrecommendedthereaderuse
a National Formulary and in the UK all medicine summary of product
characteristics(SPCs)areavailableat http://www.medicines.org.uk
Table23.1liststhecommonclassesofdrugusedinrheumatologyandisthe
frameworkforthecontentofthischapter.
Table23.1Pharmacotherapyofrheumatologicaldiseases
Drugtype Examples
Painrelief Paracetamolandcompound
analgesics
Opioidanalgesics
NSAIDs
Antidepressants
Gabapentinandpregabalin
Hypnoticsandmusclerelaxants
Topicalagents
Glucocorticoids(GCs) Prednisolone,triamcinolone,
methylprednisolone
Conventionalsyntheticdisease-
modifyingantirheumaticdrugs
(sDMARDs)
Azathioprine
Ciclosporin
Cyclophosphamide
Gold(Myocrisin
®
IMorauranofin
oral)
Hydroxychloroquine(HCQ)
Leflunomide
Methotrexate(MTX)
Mycophenolatemofetil(MMF)
Penicillamine
Sulfasalazine
TargetedsDMARDs Tofacitinib
Apremilast
BiologicalDMARDs Anti-TNFα:etanercept,infliximab,
adalimumab,certolizumab,
golimumab
AntiB-cell(CD20):rituximab(RTX)
AntiBLyS/BAFF:belimumab
IL-1receptorantagonists:anakinra
IL-6receptorantagonists:tocilizumab
IL-12/23antagonists:ustekinumab
IL-17Aantagonists:secukinumab
CTLA4-Ig:abatacept
Other Hyperuricaemia/gout:allopurinol,
febuxostat
Osteoporosis:bisphosphonates,
denosumab,strontium,teriparatide
Pulmonaryhypertensionand
Raynaud’sdisease:iloprost,
sildenafil,bosentan
Intravenousimmunoglobulin
Painrelief
Generalconsiderations
Thedescriptorsandassessmentoftheimpactofpainarediscussedin Chapters
1 and 22. Good pain management is associated with improvement in various
physiologicalandpsychologicaloutcomemeasures.
• In general, pain management may be broadly divided into pharmacological
and non-pharmacological methods. The individual description of each non-
pharmacologicalmethodisbeyondthescopeofthischapterbutmayinclude
thefollowing:
• Hot/cold/pressurecompress.
• Physicaltherapies—landbasedandhydrotherapy.
• Transcutaneouselectricalnervestimulation(TENS).
• Acupuncture.
• Hypnosis.
• Cognitiveandbehaviouraltherapy(CBT).
• Pulsedradiofrequencyandnerveablationtherapies.
• Low-levellasertherapy(LLLT).
• Massage,relaxationtherapy,andmeditation.
• Othercomplementarymedicinemethods.
• Effective pain management must begin with a thorough assessment of the
patient’spain,treatmentexpectations,andconcerns.
• Unrealistic expectations or misunderstanding of pain could mean that the
managementstrategymayfailfromthebeginning.
• In chronic painful conditions please refer to Chapter 22. Patients should be
aware that there might be a period of trial and error before the optimal
combination of pain relief is found although in many circumstances
medicationmaybeunhelpful.
• Inassessingefficacyofanoralanalgesic,itisimportanttoconsider:
• theanalgesiceffect.
• thefrequencyandmaximumdosetried.
• anyunwantedsideeffects.
• Iftherewastemporaryreliefthatthenworeoff,thismaybeduetoeitheran
insufficientdose,ortheintervalbetweendosesistoolong.
• Unpleasantsideeffectsmayalsoputpatientsoffsomemedications.
• Patientsmayusetheterm‘addiction’toexpressconcernsoverthelong-term
useofanalgesics,inparticular,opioid-basedpainrelief.Ifsuchconcernsare
notaddressed,patientsmaybereluctanttotakeopioidsregularlywhichinturn
leadstopoorpaincontrol.
• Rather than ‘substance abuse’, the patient is most likely reflecting on the
possibilityof‘tolerance,’whenciting‘addiction’,i.e.‘becomingusedto’the
analgesicsothatahigherdoseisrequiredtosustaintheeffectovertime.This
oftenneedsclarificationduringconsultation.
• Abuse of opioids—addiction or recreational use and deliberate self-harm by
overdosing—isalegitimatecauseforconcern.
• The safety and suitability of these agents are very much dependent on
assessmentoftheindividualpatient.
• Follow-up appointments are important to allow both the patient and the
cliniciantoevaluatetheefficacyofatreatmentregimenandtothenmakethe
necessaryadjustments.
• Thereisverylittlehigh-qualityevidencefortheuseofanalgaesiainpaediatric
pain.
Analgesicescalation:the‘analgesicladder’
TheWHOanalgesicladder(Fig.23.1)isausefulframeworktoconsiderwhen
commencing patients on pharmacological pain treatment. But see also more
specificguidesformanagingandprescribingstronganalgesicsinchronicpain
(e.g. SIGN-136: www.sign.ac.uk; and at CDC:
www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm).
• Escalationofpainreliefmodalityfollowsastepwiseapproachdependingon
theassessmentoftheseverityofpain.
• Movement up the analgesic ladder is a balancing act between increasing
analgesicpotencyversusincreasingriskofsideeffects.
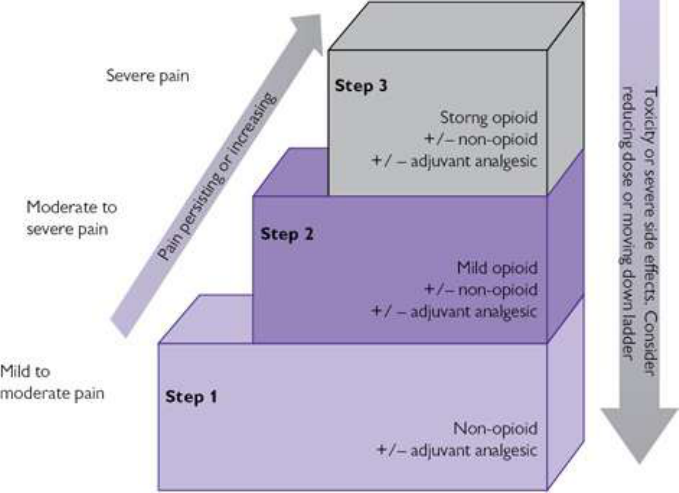
Fig.23.1WHOanalgesicladder.ReprintedfromWHO’scancerpainladderforadults,Copyright(2014)
http://www.who.int/cancer/palliative/painladder/en/.AccessedMay2017.
• Atthebottomoftheladder(Step1)arenon-opioidcompoundswithrelatively
good safetyprofilesuch as paracetamol andnon-steroidalanti-inflammatory
drugs(NSAIDs).Theseareeffectiveformildtomoderatepainseverity.
• Step2involvesaddinginweakopioidssuchastramadolorcodeinephosphate
for painof moderate severity, although codeineisno longer includedinthe
WHOladderforpainreliefinchildren.Thisisbecausechildrenarevariable
metabolisersofcodeine,leadingtoanunpredictableeffect.Codeineshouldnot
beusedinchronicpaininlongtermpaediatricconditions.
• Iflongtermopioiduseistobemaintainedconsiderconvertingtosustained-
release form as a basal analgesia. This is supplemented with instant-release
opioidforbreakthroughpain.Cautionshouldbetakenwhenusingopioidsin
longtermpaediatricconditionsandalternativestrategiestopainmanagement
shouldbesought.
• Opioids used for an extended period lead to tolerance, create physical
dependency,andshouldnotbewithdrawnabruptly.
• If an episode of acute pain is superimposed upon chronic pain requiring
regularstrongopioids,anyanalgesiaprescribedshould bein additionto the
regularopioidregimen.
• Someanalgesics,whentakentogether,haveasynergisticeffectthatisgreater
than the sum of its individual effects. It makes sense therefore to have a
compoundform(e.g.co-codamolwhichcontainscodeineandparacetamol).

• Acompoundagent maybe easierforthepatientto manageby reducingthe
numberofseparatepillstoingest.However,theabilitytoalterthedoseofone
of the componentagentswithoutaltering the other is lost. There is alsothe
additional risk of patients double dosing on a medication from failure to
recognize the active components of the drug (e.g. taking co-codamol and
paracetamoltogether).
• Clearadviceonthe optionsfor increasingdoseaccordingtotolerabilityand
efficacyshouldbegiven,includingtheprincipleofstartingatthelowestdose
wheneverpossible(particularlyintheelderly).Clearguidanceputsthepatient
incontroloftheirpainrelief.
Simpleandcompoundanalgesics
Paracetamol(acetaminophen)
Paracetamol is thought to reduce pain by inhibiting prostaglandin synthesis
withinthecentralnervoussystem. Ithasboth analgesicandantipyreticactivity
withoutanti-inflammatoryactivity.
• Itisavailableoverthecounterinmanycountriesandiseffectiveinmanaging
softtissueinjury,jointpain,dentalpain,andheadache.
• Itisusuallygivenorallyat4g/day(children30–60mg/kg/day;max4g)given
in4divideddoses.ItisalsoavailableinsuppositoryandIVformulations.
• Itisreasonabletotryparacetamolfirst.MostGPswillanditisimportantto
assurethepatientofitsefficacy.Thespecialistmayhearpatientssay‘myGP
justgavemeparacetamol’.
• CommonconcernsandinteractionsareshowninTable23.2.
Table23.2Cautionsandsideeffectswithparacetamol
Caution Comment
Hepatictoxicity Avoidinknownsignificantliverdiseaseandalcoholabuse
Renaltoxicity Notethattheeffervescentformulationscontainsodium—
avoidinmoderate–severerenalimpairment
Blooddyscrasia E.g.thrombocytopeniaandleucopeniacanbeinducedor
worsened
Pregnancyand
breastfeeding
Notknowntobeharmful
Commoninteractions
Coumarin
(warfarin)
Paracetamolmayenhancetheanticoagulanteffect
Absorptionand
metabolism
Metoclopramideincreasesabsorption;carbamazepine
acceleratesmetabolismofparacetamol
Paracetamolcompounds
• Paracetamol 500 mg is also available in compound analgesics, such as co-
codamol (paracetamol and codeine), co-dydramol (paracetamol and
dihydrocodeine),andparacetamolandtramadol.Thesearenotrecommended
inchronicpaediatricconditions.
• Careshouldalwaysbetaken,aswith‘over-the-counter’aspirinproductsand
otherNSAIDs,thatpatientsensuretheydonottakemorethanthemaximum
daily dose of paracetamol, irrespective of the combination of single and
compoundmedicationsusedtogether.
• Thecodeinecontentvariesintheseformulationsbetween10,15,and30mg
pertablettoamaximumtotaldailydoseof240mgdividedinto8tabletsand
takenas2tabletsfourtimesaday.
• Codeineisdiscussedlaterunderopioidanalgesics.
• Because of safety concerns (related to toxicity in overdose) co-proxamol
(paracetamolanddextropropoxyphene)isonlyavailableintheUKbyspecial
arrangementonanamed-patientbasis.
Opioidanalgesics
Opioiddrugsactasagonistsatopioidreceptorswhicharefoundmainlyinthe
brainandspinalcordandalsoperipherally.
• Forallopioiddrugs,therearenumerouscautions(See Table23.3)andcare
shouldbetakeninallchronicconditions,especiallyinchildren.
Table23.3Cautionsandsideeffectsofopioidanalgesics
Caution Comment
Hypotension Particularcarewhenalsotakingantihypertensives,
antipsychotics,orantidepressants
Sedationand
respiratory
suppression
Avoidinchronicobstructivepulmonarydisease,head
injury,anysituationofreducedlevelofconsciousness;
takeparticularcarewhenalsotakingantipsychotics,
antidepressants,orantihistamines.Counselcautionover
drivinganduseofmachinery
Hepatictoxicity Avoidinknownsignificantliverdisease,reducedosein
milddisease
Renaltoxicity Avoidinknownsignificantrenaldisease,reducedosein
milddisease
Blooddyscrasia E.g.thrombocytopenia;leucopeniacanbeinducedor
worsened
Porphyria Avoid
Pregnancy Avoid
Breastfeeding Preferablyavoid.Notecodeineisnotknowntobeharmful
asconcentrationareverysmall;however,individualsvary
inrateofmetabolismandcloseobservationshouldbe
madeforsignsofinfantmorphineoverdose
Gastrointestinal Opioidsinducenausea,vomiting,constipation,
pancreatitis,obstruction
Neuropsychiatric Opioidsinduceheadache,confusion,dys/euphoria,
hallucinations,moodchange,seizures
Genitourinary Sexualdysfunction,urinaryretention,avoidinsignificant
obstructiveprostatichypertrophy
Age Reducedosageintheelderly,avoidinchildhood
Commonlyusedweakopioids:codeineanddihydrocodeine
• Codeineanddihydrocodeine(alsoavailableasmodifiedrelease)canbeused
asasingleagenttomaximumdailyadultdosageof240mg(usually2×30mg
tabletsfourtimesaday).Itisavailablein15mgor30mgtablets.
• Itisalsoavailableincompoundagentswithparacetamolasdescribedearlier
andwithibuprofenoraspirin.
• Codeine is marketed in various salt compounds including phosphate and
sulfate (typical in the USA, Canada, and UK), hydrochloride (continental
Europe),hydro-iodide,andcitrate.
• Low-dosecodeineisavailable‘overthecounter’insomecountriesandisalso
foundincoughsuppressants.Inthemajorityofcountrieshowever,itremains
prescriptiononlyduetoconcernsoverdependencyandmisuse.Itsuseisstill
classedasillegalinafewplaces.Travellerswithlegitimateprescriptionsare
advisedtocarrydocumentationoftheirconditionfromtheirphysician.
• Cimetidine,actingasaP450enzymeinhibitor,increasesplasmaconcentration
ofcodeineanddihydrocodeine.
• Metoclopramide and domperidone are antagonized by codeine and
dihydrocodeine.
Tramadolandmeptazinol
Tramadolisaweakopioidagonist.Itinhibitsthereuptakeofbothserotoninand
norepinephrine(noradrenaline)atthedorsalhorn.
• Themaximumrecommendedadultdoseis400mg/dayindivideddoses.Itis
availableinmodified-release12-hourlypreparations(200mgtwicedaily)and
incombinationwithparacetamol.
• Meptazinolisapartialopioidreceptorantagonistandisgivenat800mg/day
individeddoses.Itsmixedeffectreducestheriskofdependenceandisless
likelytobeusedasasubstanceofabuse.
• Theseagentsareoftentriedafterorinsteadofcodeinecompoundsgiventhe
differenceinmechanismsofaction.
• They have a more favourable gastrointestinal (GI) side effect profile than
codeineandmaybeoneofthereasonsfortryingthembeforecodeineinthose
pronetoconstipation.However,thisisoffsetbyagreaterriskofintolerance
fromneuropsychiatriceffects.
Commonlyusedstrongopioids
Theseincludemorphinesulfateandoxycodonehydrochloride5–10mg,both4–
6-hourly(canbetitratedupto400mgperdayinseverecases);thelatteralsohas
a compound of oxycodone/naloxone, which may be beneficial in those with
severe constipation from opioids despite trials of different classes of laxative.
Thereafter,escalationmightmovetomorphinesalts,butbeforeanyoftheseare
utilizeditiscommontotrypatchformulations.
Opioidsdeliveredthroughtransdermalpatches
Theseareappliedtotheskinand,therefore,inadditiontotheabove-mentioned
cautions,beawareofallergicreactionwithlocalizedsensitivity.
• Buprenorphine (also available in the UK as Temgesic
®
200 micrograms
sublingual)isproducedasBuTrans
®
andTranstec
®
.Both haveformulations
that allow a wide variety of dosing, e.g. BuTrans 5 micrograms/hour 7-day
patch,graduallybuildingdose,perhapsevery2weeksdependingontolerance
andresponseofsymptoms.
Non-steroidalanti-inflammatorydrugs
NSAIDs are commonly used. Most have a licensed indication for OA (see
Chapter 6) and RA (see Chapter 5); some have a licence for ankylosing
spondylitis(see Chapter8).
• Inreality,mostNSAIDsareprescribedineffect‘offlicence’foranumberof
rheumatic conditions outside these diagnoses, but based on being effective
analgesics with the capacity to reduce inflammation such as occurs in soft
tissues,tendonitis,andsynovitis.
• NSAIDsareclassifiedbytheirinhibitoryactiononcyclooxygenase1(COX-
1), e.g. ibuprofen, naproxen, and diclofenac, or COX-2, e.g. celecoxib and
etoricoxib.Some agents(e.g.oxicams)demonstrateinhibitory actionagainst
bothenzymepathways.
• ItisreasonabletotryaNSAIDfromadifferentclasswhenanotherhasfailed.
• Ibuprofen and aspirin compounds are available over the counter in many
countries.Naproxen(250–500mgtwicedaily)anddiclofenac(150mgdaily
in divided doses) probably represent the two most commonly prescribed
NSAIDsworldwide.
• COX-2inhibitorsarediscussedlaterinthissection.
• Oral preparations are most often used. Some are available as slow-release
formulations,e.g.diclofenac.
• Althoughperrectumagentsarealsoavailableinsome,thesedonotappearto
reducesideeffect(specificallygastric)enoughtowarranttheirpreferenceover
oralagentsinthemajorityofcases.
• Topicalagentshavevariableefficacy,oftenwithlimitedevidenceofbenefit.
Thatsaid,theyarepopularwithpatientsaspartoftheirmanagement.
• Paediatricdosingincludes:Ibuprofen10mg/kg4-6timesdaily;naproxen10–
20mg/kg/dayin 2–3divideddoses;diclofenac3–5mg/kg/dayin2–3 divided
doses.
AdverseeffectsofNSAIDs
Anumberofadversereactionsarerecognized.CautionappliestoallNSAIDs,
particularlyavoidingtheiruseinhepaticandrenalimpairment,pregnancy,and
GIulceration(Table23.4).
• Using the lowest possible dose for the shortest period of time lessens the
adverseeffectsriskofNSAIDs.Itisinevitable,however,thatthosewithlong-
termconditionsforwhichremissionislessthanoptimalwillrequirelong-term
therapy.
• Whilecardiovascularcomplicationsoccur,manypatientswithcardiovascular
diseaseandriskfactorsuseNSAIDs,particularlyifthebenefitisconsideredto
outweigh the risk (e.g. improved function/exercise tolerance encourages a
healthierlifestyle).
• Itisimperativethatbloodpressureandrenalfunctionaremonitoredregularly
(preferablyevery3months).
• The highest risk of cardiovascular complications is with diclofenac, COX-2
NSAIDs, and high-dose ibuprofen (2.4 g daily). The lowest risk is with
naproxen(1gdaily)andibuprofen(1.2gorlessdaily).
• It is not uncommon for individuals to also be on aspirin for its platelet
inhibitoryfunction.
• AllNSAIDsarecontraindicatedinsevereheartfailure.
• GIrisksaredocumentedinTable23.4.
• ThehighestGIriskisseenwithpiroxicamandketoprofen; intermediaterisk
withdiclofenac,etodolac,indometacin,naproxen,andoxicams;andthelowest
riskwithibuprofen.
• Inrenaldisease,NSAIDsshouldbeusedwithcautionandavoidedifpossible.
• NSAIDs can induce acute kidney injury, as well as exacerbate chronic
impairment.The‘ruleofthumb’oflowestpossibledoseforshortestpossible
periodoftimeapplies.
• NSAIDs can exacerbate asthma; however, it should not be an absolute
contraindicationtoprescribing.
• Manypatientsmaywellhaveinadvertentlytriedaspirinandibuprofenover-
the-counter compounds without complication. The clinician may therefore
gain some sense of tolerability. The decision to prescribe should always be
based on the severity and responsiveness/stability of asthma in each
individual.
NSAIDcautions:sDMARDco-prescribing
• Concern is often expressed over the co-administration of sDMARDs and
NSAIDs.Toxicitymonitoringisafundamentalresponsibilitywhenmanaging
sDMARDs.
• sDMARDmonitoringappliesirrespectiveofNSAIDuse.
• Inprinciple,asdiseasecomesundercontrolonsDMARDsitisappropriateto
reducethefrequencyofNSAIDuseifpossible.
NSAIDcautions:pregnancyandbreastfeeding
ItisgenerallyadvisedthatNSAIDsshouldbeavoidedinpregnancyunlessthe
benefitstowell-beingsignificantlyoutweightherisk.
• NSAIDscanbeusedwithcautioninthefirstandsecondtrimesterbutshould
beavoidedinthethirdtrimesterduetotheaddedriskincludingclosureofthe
fetalductusarteriosusinutero,delayinonset,andanincreaseintheduration
oflabour.Inaddition,pulmonaryhypertensionmayaffectthenewborninfant.
• Insomecases,studiesshowconcentrationsofcertainNSAIDstobetoolowin
breast milk to warrant concern. In general, manufacturers advise avoiding
NSAIDsforthedurationofbreastfeeding.
• Low-dose aspirin may be continued throughout pregnancy but high-dose
aspirinshouldbeavoided.
• There are limited data for COX-2 inhibitors, which have been shown to be
teratogenicinanimalstudiesandhencetheseshouldbeavoidedinpregnancy
andbreastfeeding.
Table23.4AdverseeffectsofNSAIDs
Organ/complication Occurrence Comments
GItract Common Gastritis,bleeding,and
perforation.Highriskinthe
elderlyandthosewithahistoryof
ulcers
Renal Common Fluidretention,papillarynecrosis
Hypertension Common Interferencewithdrugssuchas
thiazidediuretics
Cardiac/myocardial
infarction
Increasedriskin
thosewith
cardiovascularrisk
factors
COX-1andCOX-2drugs
Lung Notuncommon Exacerbationofasthma,
pneumonitis(naproxen)
Skin Notuncommon Hypersensitivity,erythema
multiforme
Centralnervous
system(CNS)
Notuncommon Tinnitus,fatigue,cognitive
disturbance
Rare Asepticmeningitis
Liver Uncommon Drug-inducedhepatitis
Haematological Rare Bonemarrowdyscrasias

Aspirin
• As the prototype NSAID, aspirin is available in single and compound
formulationsoverthecounter.WhileitisrarelyprescribedasanNSAID,itis
importanttoacknowledgeitsavailability,aswellasitscommonuseinlower
dosage(75–150mgdaily)asacardio-protectiveagent,whenprescribingother
NSAIDs,andadvisingonsideeffectsanddruginteractions.
• For analgesic effect, aspirin is dosed at 300–900 mg four times a day
(maximum adult dose 4 g/day). It is available in oral and suppository
formulations.
• Low-dose aspirin may be continued throughout pregnancy but high-dose
aspirinshouldbeavoided.
• Aspirin isavoidedin childrenunderthe ageof16 years (exceptfor cardiac
conditionssuchasKawasakiDisease)duetotheriskofReyesyndrome.
Oxicams
• ThisgroupofNSAIDswasdevelopedfortheirlongerhalf-life.
• Meloxicam(7.5–15mgdaily)andpiroxicam(20mgdaily)arethetwomost
commonlyusedagents.
• Piroxicamhasarelativelyhighrelativetoxicity:efficacyratioforGIadverse
effectscomparedwithotherNSAIDs.
Coxibs/COX-2inhibitors
• TheseagentswereintroducedbecauseoftheirefficacyandselectiveCOX-2
inhibition, recognizing the value of preserving COX-1 ‘protective’ enzyme
activity,particularlyinrelationtoGItolerability.
• However, large-scale phase III control trials, an integral part of modern
pharmacological practice and essential in seeking approval for a licence,
demonstrated an appreciable cardiovascular risk. As a consequence, several
COX-2drugs(e.g.rofecoxib)havebeenwithdrawn.
• Celecoxib(100–200mgtwicedaily)andetoricoxib (30–120mgonce daily)
areavailableinEurope.CelecoxibisavailableintheUSA.In2007,theFood
andDrugAdministration(FDA)votednottoapproveetoricoxib.
• Regularbloodpressuremonitoringisrequired.
Antidepressants
Severalantidepressantsareusedinthemanagementofpain,usuallyasasingle
agent given at bedtime, sometimes in combination with other drugs using
differentmechanismsofaction,andoftenatlowerdosesthantypicallyusedfor

controllingdepression.Thereisnocompellingevidencefortheiruseinchronic
paediatricpain.
• Thereisoftenaneedtoexplaintopatientsthatthesedrugsarebeingusedfor
pain control and not for depression, even if there is a degree of reactive-
depressionpresentasaconsequenceofchronicpain.
• Educatingthepatientandexplainingthemechanismsofaction(blockingpain
messages from travelling up the spinal cord and modifying the response to
pain in the midbrain), one can gain greater compliance and enhance the
clinician–patientrelationship.
• Adetailedexplorationofthemechanismsisbeyondthescopeofthisbook,but
mostagentsarethoughttohaveadualeffectbymodifyingresponsivenessof
spinalopioidreceptors,andchangingmoodandperceptioncentrally.
• Theseagentsareperhapsmostlogicallyusedwhenpaindisturbssleep.Amild
sedativeandrelaxanteffectmayalsobebeneficial.
Serotoninandnorepinephrinereuptakeinhibitors
Tricyclics
Tricyclics are predominantly serotonin and/or norepinephrine re-uptake
inhibitors.The‘typical’agentsinthisgroupincludeamitriptyline,clomipramine,
imipramine,anddosulepin.
• Amitriptyline is the agent most frequently used (although sometimes
nortriptylineisbettertolerated).Givenatdosesupto75mg/daytakenbefore
bedtime, it is often titrated from a baseline of 10–25 mg in 10 mg steps
gradually until a balance between maximum efficacy and tolerability is
reached.
• CommonsideeffectsandinteractionsareshowninTable23.5.
Selectiveserotoninreuptakeinhibitors(SSRIs)
• Thisgroupincludesfluoxetine(20–40mgoncedaily),sertraline(50mgonce
daily),andparoxetine(20mgoncedaily).
• Randomized control trials in fibromyalgia (FM; see Chapter 22)
demonstrate SSRI efficacy similar to 25 mg amitriptyline; however, the
averageimpactonpainreductionandqualityoflifeisonlyabout15–20%and,
assuch,theseagentsareprobablynotsuitablecandidatesasanalgesicswhen
usedinisolation.ThesideeffectprofileinTable23.5applies.
Mixedserotonin-norepinephrinereuptakeinhibitors(SNRIs)
• Increasinginterestinthecomplexitiesofcentralpainpathwaysandtheaction
ofSNRIshasledtoseveralstudiesdemonstratingSNRIefficacyinFM(see
Chapter22).
Table23.5Cautionsandsideeffectsofserotonin/norepinephrinereuptakeinhibitors
Caution Comment
Sedative Careneededwhenusedwithotherpotentiallysedating
agent.Note:CNStoxiceffectsoftramadolcanbe
enhanced(serotoninsyndrome).Alsonotecautionwith
drivingorusingmachinery
Antimuscarinic
action
Cautioninthosewithocular(closed-angleglaucoma),
genitourinary(retention,prostatichypertrophy),dry
eyes/mouth,constipation
Cardiovascular Riskofdysrhythmiasespeciallyventricular(e.g.increased
withconcomitantuseofsotalolandamiodarone)
Hypotension Increasedriskinpatientsondiuretics
Thyroiddisease Amitriptylineenhanceseffectsofthyroiddrugs
Epilepsy Amitriptylineantagonizesantiepilepticsreducingthe
thresholdforseizures
Sexual
dysfunction
Sexualdysfunctionmayoccur.
Hyponatraemia Usuallyintheelderlyandpossiblyduetoinappropriate
secretionofantidiuretichormones.
Hepatic
impairment
Trytoavoidinsevereliverdisease—riskofsedation
Pregnancyand
breastfeeding
Avoidunlessbeingusedforpsychiatricreasonsandinthe
bestinterestsofwell-being
Neuropsychiatric Inductionofhallucinations,delusions,(hypo)mania,
neurolepticmalignantsyndrome,andsuicidalbehaviour
Motorfunction Tremor/extrapyramidalsigns
Endocrine Breastenlargement,galactorrhoea
• The FDA (USA) approved duloxetine (2008) and milnacipran (2009) for

treatmentofFMinadults.Neitherisapprovedforuseinchildren.
• Duloxetine is given as 60–120 mg daily and milnacipran at 100 mg twice
daily.Sideeffectsincludenausea,headache,insomnia,dizziness,constipation,
hepaticdysfunction,hyponatraemia,andorthostatichypotension(duloxetine)
andhypertension(milnacipran).
• Likeallantidepressantsduloxetinecarriesawarninghighlightinganincreased
riskofsuicide,especiallyinchildrenandyoungadults.
• Tramadol should not be co-administered with duloxetine; there is a risk of
developing serotonin syndrome. Through cytochrome P450 enzyme system
interactions,duloxetinemayprolongopioideffects.
Otheradjuvantanalgesics
Gabapentin and its analogue pregabalin (both structural analogues of γ-
aminobutyric acid (GABA)), has been shown to have efficacy, particularly in
studiesofFM (see Chapter22), although the NNT is 9 and there is a high
incidence of side effects. There is no compelling evidence for their use in
chronicpaininchildrenandadolescents.
Gabapentin
• Dose:oral,titratedfrom300mgdailytomaximum3600mgdailyindivided
doses,e.g.300mgoncedailyonday1,then300mgtwicedailyonday2,then
300 mg 3 times daily on day 3, then increased according to response and
tolerabilityinincrementof300mgdailyevery2–3daystomaximumdoseof
3600mgdaily.
• DoseneedstobereducedinrenalimpairmentaccordingtoGFR.
• Side effects: dizziness/light-headedness, oedema, weight gain, and
sedation/mental impairment. Other concerns include leucopenia, ataxia,
Stevens–Johnsonsyndrome,hepatitis,andpancreatitis.
• Avoidduringpregnancyandbreastfeeding.
• Discontinuationhastobedonegraduallyoverminimumof1week.
Pregabalin
• Dose:oral,titratedafter3–7daysfrom150mgtomaximum600mgdailyin
2–3divideddoses.
• DoseneedstobereducedinrenalimpairmentaccordingtoGFR.
• Side effects: dizziness/light-headedness, oedema, weight gain, and
sedation/mental impairment. Other concerns include visual disturbance,
neutropenia,ataxia,arrhythmia,Stevens–Johnsonsyndrome,andpancreatitis.
• Avoidduringpregnancyandbreastfeeding.
• Discontinuationhastobedonegraduallyoverminimumof1week.
Musclerelaxants
Themostlikelyagenttoconsiderisdiazepam,abenzodiazepine.
• Givenatdosesof2–5mgthreetimesadayforupto14daysdiazepamcanbe
helpful in alleviating acute severe pain associated with spasm, particularly
acrosstheneckandshouldergirdle,andthelumbarspine.
• Diazepamshouldbeavoidedinhepaticandrenalimpairment,pregnancy,and
breastfeeding.
• As with opioids, care should be taken to counsel the patient over perceived
riskofdependencyofbenzodiazepines,andprescriptionshouldbeavoidedif
thereareanyconcernsoverpotentialabuse.
• Drugssuchasbaclofen,dantrolene,methocarbamol,andtizanidineusuallysit
withintherealmoftheneurologistandmaybevaluableincontrollingmuscle
spasm and pain in conditions such as stroke and multiple sclerosis. Where
indicated,therheumatologistshouldseekadvicefromaneurologistifspasm
painisconsideredtobetheconsequenceofaneurologicalcondition.
• Quinine sulfate is often used in doses of 200–300 mg to control cramps. It
shouldbeprescribedwithcautioninpatientswitharrhythmiaandavoidedor
dosehalvedinhepaticandrenalimpairment.
• Quinine sulfate is contraindicated in haemoglobinuria, myasthenia gravis,
optic neuritis, and tinnitus; and it may be teratogenic (certainly in higher
dosage)inthefirsttrimesterofpregnancy,butsafeduringbreastfeeding.
Topicalagents
• The most common classes to be used (excluding opioid transcutaneous
delivery by patch) include a variety of ‘over-the-counter’ preparations
(rubefacients),NSAIDs,andcapsaicin.
• Capsaicinisanactivecomponentofchilipeppers.Itislicensedtotreatpost-
herpeticneuralgiaanddiabeticneuropathy.Itcanbeconsideredanadjunctto
treatingOA.Oneriskisasevereburningandirritationifcontactismadewith
mucous membranes, including the lips and conjunctiva. Hand-washing after
useshouldbemeticulous.
• Capsaicinisprescribedasa45gtubeof0.025%or0.075%concentration,to
be applied twice daily in the smallest of volume; literally a tiny amount
squeezed ontothetip of thelittlefinger and thenrubbedin over thesiteof
pain.
Glucocorticoids
Glucocorticoids(GCs;‘steroids’)arepowerfulanti-inflammatoriesandrangein

usefrom shortdurationoflowand highdosagetogaincontrol ofacondition
(including intra-articular; see Chapter 24), through to prolonged and even
lifelongtherapy.
Commonly used GCs are prednisolone, methylprednisolone, and
triamcinolone. Disease-specific indications and dosing regimens are stated in
eachrelevantchapterofthisbook.
Table 23.6 highlights the major and common cautions and concerns that
shouldbemonitoredanddiscussedwiththepatient.Patientson long-termGC
treatmentshouldbeencouragedtoholdasteroidtreatmentcardorsomeformof
alertbracelet,etc.
Table23.6Cautionsandcomplicationsofglucocorticoiduse
Caution Comment
Adrenal
insufficiency
Long-termusecanleadtoadrenalatrophy
Abruptwithdrawalshouldbeavoided
Replacement(evenhigherdosing)shouldbegivenduring
surgery, inter-current illness (especially associated
vomiting)
Diabetes Inductionandexacerbationofhyperglycaemia
Hypokalaemia Cancausehypokalaemia
Infection GCs are immunosuppressive—there is an increased
susceptibility to infections and severity of infections
especiallyafterprolongeduse
Liveviralimmunizationshouldbeavoided
Exposure to chickenpox or measles leading to concern
over significant infection should be managed with
passiveimmunoglobulin
MayexposelatentTB
Neuropsychiatric Caninducemania,confusion,delirium,andsuicidal
thoughts—canoccurearlyafterstartingcorticosteroid(3–
5daysonaverage)andtakeseveralweekstoresolve
havingdiscontinuedtherapy
Weightgain Thismaybeeitherasaconsequenceofperipheraloedema
orincreasedappetite—patientsshouldbewarnedtobe
carefulofthisandtousetrickslikedrinksofwaterto
reducesenseofhunger
Skin Long-termuseleadstoatrophyandbruising
Eyes Increasedriskofcataractsandglaucoma
Cardiovascular Inductionandexacerbationofhypertensionand
congestivecardiacfailure
Pepticulceration
Boneandmuscle Inductionandexacerbationofosteoporosis
Growthretardation
Myopathy
Osteonecrosis
Pregnancy GCscanbeusedorcontinuedifindicated—preferably
lowestdosepossible.Noevidenceofteratogeniceffects;
occasionalneonataladrenalsuppressionwhichusually
resolvesspontaneously
Breastfeeding Dosesofprednisoloneupto40mgdailyareunlikelyto
resultinsystemiceffectininfants
Glucocorticoidinteractions
• Because of the tendency for GCs to increase blood pressure, the effect of
antihypertensivesmaybeblunted.Monitoringiskey.
• BarbituratesandantiepilepticsincreasethemetabolismofGCs.
• DiureticsmaybeantagonizedbyGCs.
• ErythromycinandazolesmayinhibitthemetabolismofGCsthusincreasing
theireffect.
• GCsmayamplifytheseverityofNSAIDspepticulcerationrisk.
• GCs may increase the risk of bone marrow suppression with methotrexate
(MTX).
• GCsincombinationwiththeophyllineincreaseshypokalaemiarisk.
• GCsmayincreaseordecreasetheanticoagulanteffectofwarfarin.
Disease-modifyingantirheumaticdrugs
Disease-modifying antirheumatic drugs (DMARDS) are the cornerstone of
disease management aimed at the slowing or arrest and remission of chronic
inflammatoryrheumaticdisease.Foradditionaldetailseealso Chapter5(RA)

and Chapter8(SpAs).Terminologycanbeconfusingsincetheintroductionof
‘biologics’, which are also ‘disease-modifying’. A new nomenclature of
DMARDterminologyhasbeenproposedbySmolenetal.
1
:
• Firstly: ‘synthetic DMARDs’, which are subdivided into conventional
synthetic DMARDs (csDMARDs), i.e. traditional DMARDs, and targeted
syntheticDMARDs(tsDMARDs),whichareoralsyntheticdrugsdesignedto
targetaparticularmolecularstructure.
• Secondly: ‘biologic DMARDs’ (bDMARDs), which are subdivided into
biologic original DMARDs (boDMARDs) and biosimilar DMARDs
(bsDMARDs).
• Atthetimeofwritingitisunknownwhetherthisproposednomenclaturewill
be generally accepted. In this book we have mainly used the terminology
sDMARDs and bDMARDs, and have avoided introducing the other terms
extensively, with the exception being this chapter with the distinction being
madeclearinthefollowingsubsections.
ConventionalsyntheticDMARDs
Generalconsiderations
ConventionalsyntheticDMARDs(csDMARDs)areslow-actingdrugsthattake
8–12weekstobegintodemonstratebenefit,andeventhen,possiblylongerto
achievemaximumbenefitasthedoseisescalated(typically>6months).Patients
should always be informed of this, clarifying expectations and improving
compliance.
• It is not uncommon for combinations of csDMARDs to be used either by
sequential ‘step up’ (adding one after the other over time) or ‘step down’
(startingwithtwoorthree,andreducingtooneovertime).
• IntheUK,itisunlikelythatmorethanthreecsDMARDswouldbeusedsince
theintroductionofbDMARDs:UKguidanceallowsuseofbDMARDsafter
failureofatleasttwocsDMARDs(seelater).
• The most common drugs used are: hydroxychloroquine (HCQ), leflunomide
(LEF),MTX,andsulfasalazine(SSZ).
• Ofthesedrugs,MTXisprobablythedrugoffirstchoiceformostconditions
(e.g.RA,PsA,JIA)atdosesof7.5–30mgweekly.
• csDMARDsarenotwithouttheirtoxicityandtheproteancomplicationsand
monitoringrequirementscanseemdaunting.
• Tables23.7–23.10describeprinciplesapplicabletoallcsDMARDs.
• Advice on immunization and risk assessment of viral infection is shown in
Box23.1.
• GeneralmonitoringofcsDMARDs—seeTable23.7(pleaserefertoBox23.2
forcommon sideeffectstoassessfor, atevery bloodtestcheckandclinical
review).
• CommoncsDMARDsideeffectsandadviceoninitialactiontobetaken—see
Box23.2.
• Useinpregnancyandbreastfeeding—seeTable23.10.
• AllcsDMARDsshouldbeusedwithcautioninhepaticandrenalimpairment,
blood dyscrasias (including suspected or known G6PD deficiency and
porphyria),recurrentinfection,andintheelderly.
Box23.1Immunizationandassessmentofinfectionriskbefore
commencingcsDMARDs
Disclaimer: all readers should refer to their own local practice guidelines.
Informationhereisincompleteandbriefandaskeletonguideonly.
• In some circumstances it may be appropriate to give live vaccines to
patients on DMARDs. Refer to local guidelines. (e.g. oral polio, BCG,
MMR,yellowfever).
• Patientsshouldreceivethepneumococcalvaccine.
• Annualfluvaccinationisrecommended.
• Patientsexposedtochickenpox(whohavenoclearhistoryofchickenpox
in the past) or to shingles, should receive passive immunization using
varicellazosterimmunoglobulin.
• Patients should be screened for hepatitis B and C risk by history, and, if
required,serumantibodies.
• PatientsshouldbeassessedforriskofHIVandtestedifapplicable.
• Patientsshouldbeassessedforriskofactive/latentTB.
csDMARDmanagementforsurgeryandduringinfectiveillness
• csDMARDs do not need to be discontinued before surgery though some
surgeons/surgicalspecialtiesrequestcsDMARDsarediscontinued.Thereisa
lackoverallofrobustdataasfewrandomizedtrialshavebeenundertaken.
• IfthesurgeonwishescsDMARDstobestoppedthen,asa‘ruleofthumb’,itis
reasonabletodiscontinuefor2weeksbeforeandupto2weeksaftersurgery.
• It is not possible to predict the risk of a flare of inflammation during this
period,althoughmanypatientsreportaleveloftoleranceforupto4weeks.
• csDMARDsarediscontinuedduringsevereinfectiveillnessifthereisconcern
theirimmunosuppressanteffectoutweighstheriskofadiseaseflare.
Table23.7PrinciplesofmonitoringofcsDMARDs.
Disclaimer: all readers should refer to their own local practice guidelines. Information here is
incompleteandbriefandaskeletonguideonly.
Timeline Action
Pre-
treatment
assessment
FBC,creatinine,U&E,LFTs,CRPandESR,urinalysis
(protein),CXR(pre-MTX),bloodpressure,excludecurrent
infection,excludeunexplainedrash/skinlesion,complete
applicablediseaseactivityassessmenttools,requestvisual
acuitymeasurementbeforestartingHCQ
Monitoring
forthefirst
6–8weeks
FBCandLFTevery2weeks(4weeklyinchildrenforMTX
andAzaand2weeklyMMFandLFD)for6–8weeks(except
forAZAandMMF(weekly),HCQ(notrequired),gold(FBC
andurinalysisbeforeeverydose),SSZ(every4weeks)).Also,
creatinine,U&Eforciclosporin
6–8-week
clinical
assessment
FBC,creatinine,U&E,LFTs,CRP,ESR,urinalysis,blood
pressure,excludeinfectionandskinlesions,complete
applicablediseaseactivityassessmenttools
Monitoring
between2
and6
monthsif
drugdose
stable
FBCandLFTevery4weeks(exceptforHCQ(notrequired),
gold(beforeeverydose),SSZ(3-monthlyifstableinfirst3
months)).Somedrugsrequireclosemonitoringofcreatinine
andurinalysis—seeciclosporin
6-month
clinical
assessment
FBC,creatinine,U&E,LFTs,CRPand/orESR(aspartof
assessmentcriteria),urinalysis(proteinandblood),blood
pressure,excludecurrentinfectionandrash/skinlesions,
completeapplicablediseaseactivityassessmenttools
Monitoring
after6
monthsif
stabledrug
dose
FBCandLFTevery8–12weeks.Somedrugsrequireclose
monitoringofcreatinine,U&E,andurinalysis—seeciclosporin
Yearly
clinical
assessment
FBC,creatinine,U&E,LFTs,CRP,andESR
Assessment
every6
monthsif
dosestable
Urinalysis(protein),bloodpressure,excludecurrentinfection,
excludeunexplainedrash/skinlesion,completeapplicable
diseaseactivityassessmenttools
Generalprinciples
Returntotheearlymonitoringprotocolwheneverincreasingdrugdoseaftera
periodofstabledosage,orwhenintroducinganothercsDMARDoran
NSAIDorotherpotentiallytoxicdrug(byinteraction)forthefirsttime.
Seepublishedguidelines,e.g.atBritishSocietyofRheumatology:
http://www.rheumatology.org.uk/resources/guidelines/default.aspx
Familyplanning,pregnancyandbreastfeeding,whiletakingcsDMARDs
• Some csDMARDs can be taken reasonably safely while pregnant and
breastfeeding;seeguidelines(e.g.BSRguidelineonprescribingforpregnancy
and breastfeeding can be found at:
http://www.rheumatology.org.uk/resources/guidelines/default.aspx).
• Table 23.8 shows specific regimens advised before trying to conceive, and
whichdrugstoavoidduringpregnancyandbreastfeeding.
• LEFshouldbestopped2yearsbeforetryingtoconceive,or‘washed’outas
describedlaterinthissection(see ‘Leflunomide’,p.670).
• AdviceonuseofanalgesicsandGCsinpregnancyandbreastfeedingisgiven
intheprevioussections.
MalignancyriskwithcsDMARDs
• EstablishingtheriskofmalignancyfromcsDMARDsischallengingowingto
theexcessincidenceofmalignancyinsomeoftheconditionsbeingtreatedand
alackof‘real-world’dataofcsDMARDuse.
• MMF,CYC,andAZAareassociatedwithincreasedincidenceofmalignancy
butSSZ,HCQ,MTX,andLEFareprobablynot.
SharedcareinformationoncsDMARDsandtheiruse
• ItisessentialthatthepatientreceivesinformationandadviceoncsDMARDs
and their primary care physician has access to correspondence from the
prescribingclinicianandresultsofmonitoring.
• It is essential that there is clarity over the roles and responsibilities of the
prescribingandprimary/communitycliniciansandthepatient.
• Various guidelines on csDMARD monitoring exist (e.g. see UK BSR
guidelines 2017 at:
http://www.rheumatology.org.uk/resources/guidelines/default.aspx).
• Box23.2broadlyoutlinesmanagementofcsDMARDsideeffects.
Box23.2csDMARDmonitoringandsideeffectsmanagement
Disclaimer: all readers should refer to their own local practice guidelines.
Informationhereisincompleteandbriefandaskeletonguideonly.
• AbnormalASTorALT.StopcsDMARDifenzymelevel>twiceupperlimit
of normal. As with all blood indices listed below, repeat weekly until
normalized.
• Abnormalleucocytecount.StopcsDMARDifneutrophils<1.5×10
9
/L,or
ifsteepdownwardtrendincount,andassessforinfection.Witheosinophilia
>0.5×10
9
/L,increasedvigilancerequiredbutmaybeunassociatedatopy.
• Low platelets. Stop csDMARD if platelet count <100 × 10
9
/L or serial
resultsshowsignificanttrenddownwards.
• Abnormal bruising. Check clotting screen and platelets urgently. If
abnormal withhold csDMARD immediately. Bruises are common in
children.
• AbnormalMCV.IfMCV>110fL,checkfolate,vitaminB12,TSH,andfor
excess alcohol intake. MCV+ may be an effect of AZA, MTX, SSZ, or
allopurinol
• Proteinuria. Send urine for microscopy/culture + treat infection. Quantify
proteinuria,checkcreatinine,U&E,excludehaematuria+urinarycastsand
obtaining‘KUB’ultrasound.ConsiderwithdrawingcsDMARD.
• Note: proteinuria may indicate worsening disease so stopping the
csDMARDmaybeinappropriate.
• Rash.Ifmildinadults,dropcsDMARDdose.Ifmoderate/severe,thenstop
csDMARD.Rashesarecommoninchildrenbutadvicemaybesought.
• Mucosalulceration.Considercauseofulcerationandaddfolate(forMTX)
andadjustdoseifpersistent.IfsevereconsidertrialoffcsDMARD.
• Hairloss.Considercauseofalopeciaandadjustdoseifpersistent.Atrial
off treatment may be appropriatebuthairgrowth may not recover for ≥1
haircycle,i.e.severalmonths.
• Hypertension.Ifmildrise,mayrespondtosmalldropincsDMARDdoseor
leavealoneandmonitor.Ifmoderatetosevere,treathypertensionfirst(see
adviceforciclosporinondosereduction).
• Weightloss.Considerthecauseofweightlossandreducethedoseorstop
foratrialperioddependingontheseverity.
• Dyspnoea. Chest exam + CXR. Treat infection and cardiac failure. If
pulmonary fibrosis suspected stop csDMARD and arrange further
investigation.
• Advisable actions if stopping a csDMARD. Repeat bloodtestafter1or 2
weeks. Assess foranyrecent change in medication, alcoholconsumption,
illness, csDMARD dosing error. Treat disease ‘flare’ with GCs. If trend
downwards in laboratory indices, then csDMARD should be reviewed
irrespectiveoflaboratoryvalue.Onceabnormalitiesreturntonormal,start
csDMARD at a lower dose, or switch to a new csDMARD, and in both
casesreturntotheearlymonitoringphase.
Azathioprine
Azathioprine (AZA) is prescribed for a number of autoinflammatory and
autoimmune conditions. AZA inhibits purine synthesis by generating
thioguaninenucleotidesfromitsmetabolite:6-mercaptopurine(6-MP).
• The typical dose of AZA is 0.5–1 mg/kg/day orally in twice-daily divided
doses, increasing after 4–6 weeks to 2–3 mg/kg/day with an anticipated
responsewithin6–12weeks.
• Thiopurinemethyltransferase (TPMT)activitystatus canbecheckedbefore
AZAisstarted:
• 99%ofpeoplewillhavehighorintermediateTPMTlevelsandbe atlow
riskofAZAtoxicity(fromslowAZAclearance).
• In a TPMT deficiency homozygous state (0.3% of population (1:300)) it
maybefatal—toxicityoccurringinthefirst6weeks.
• Intheheterozygousstate(10%ofpopulation),theremaybedelayed(upto6
months),butusuallyreversible,bonemarrowtoxicity.
• Although measurement of TPMT is advised in guidelines, it may be
impracticalsocloseFBCmonitoringinthefirst6–12weeksoftreatmentis
imperative.
• AZAcancauseaphotosensitivityreaction—patientsshouldbeadvisedtowear
sunscreensandprotectivecovering.
• AZAhassomespecificdruginteractions:
• Allopurinol:AZAdoseshouldbereducedto0.25–0.5mg/kg/day.
• Angiotensin-converting enzyme (ACE) inhibitors: co-prescription may
exacerbateanaemia.
• Anticonvulsants:AZAmayreduceabsorption.
• Aminosalicylates: (mesalazine (ME)/SSZ): increase risk of bone marrow
toxicity.
• Ciclosporin:AZAcandecreaseciclosporinlevels.
• Co-trimoxazole/trimethoprim:bonemarrowtoxicity.
• Warfarin:AZAinhibitsanticoagulanteffects.
Ciclosporin
Ciclosporin is considered in PsA, RA, AICTDs, uveitis, and MAS. It is a
calcineurininhibitorandhasafairlyselectiveactiononlymphocytes:blocking
mitosisandinhibitinglymphokinerelease.
• Ciclosporindoseistypically2.5mg/kg/dayorallyintwice-dailydosesfor6
weeks,thenmaybeincreasedat4-weeklyintervalsin25mgincrementsupto
amaximumof4mg/kg/day.Responsein<12weeks.
• Pre-monitoring(Table23.8)shouldincludefastinglipids,repeated6-monthly
andthedrugdiscontinuedifanuncontrollablesignificantriseinlipidsoccurs.
• Monitoring includes checking creatinine clearance/GFR. A rise in creatinine
>30% above baseline on two consecutive readings 7 days apart warrants
stoppingthedrugandreassessing.
• It is essential that blood pressure monitoring be commenced at baseline. If
uncontrollablehypertensionoccurs,thedrugshouldbestopped.
• Electrolyte balance should be checked every 2 weeks until stable dose
achievedandthenevery3monthswithotherroutinemonitoring(Table23.8).
If the potassium rises above the laboratory threshold the drug should be
stoppedandre-assessed(havingensureditisnotaresultofothermedication
changes).
• Grapefruit (including juice) increases the bioavailability of ciclosporin.
Grapefruitshouldbeavoidedforanhourbeforeandaftertakingthedrug.
• Ciclosporinhassomespecificdruginteractions.Ciclosporinisaninhibitorof
CYP3A4,whichmetabolizessomedrugs:
• Calciumchannelblockers:reducedoseofciclosporinto50%.
• Statins:useinlowdoseasciclosporincanelevateconcentrationofallthese
drugs.
• Colchicine:shouldbeavoided.
• Diclofenac:reducethemaximumdoseofdiclofenacto75mgdaily.
• Digoxin: measure levels and reduce dose accordingly as ciclosporin can
increaseserumlevels.
• Diuretics:cautionwithelectrolyteimbalance.
• Hydroxychloroquine (HCQ): may increase plasma concentrations of
ciclosporin.
• PUVA: avoid ciclosporin given significant increase risk of invasive
squamouscellcarcinoma.
• Concomitantuse of potentially nephrotoxicdrugs requiresspecialconcern
andmonitoring.
• Simvastatin:avoiddosingabove10mg/day.
• St.John’swort:decreasesciclosporinactivity.
Table23.8Disease-modifyingantirheumaticdrugsinpregnancyandbreastfeeding
Drug Effects
Azathioprine Pregnancy:compatiblethroughoutpregnancywithdose≤2
mg/kg/day
Breastfeeding:compatiblewithbreastfeeding
Ciclosporin Pregnancy: compatible throughout pregnancy with lowest
possible dose. Suggested monitoring of blood pressure,
renalfunction,bloodglucoseanddruglevels
Breastfeeding:compatible—thoughfromlimiteddata
HCQ Pregnancy:compatiblethroughoutpregnancy
Breastfeeding:compatiblewithbreastfeeding
Leflunomide
(LEF)
Pregnancy:potentialteratogenic—avoid
Note:LEFhasalonghalf-life.Rapidremovaloftheactive
metabolite can be achieved using washout with
colestyramine8gthreetimesadayoractivatedcharcoal
50gfourtimesadayfor11days.Bloodconcentrations
should be checked twice, 14 days apart prior to
conceiving(levelsshouldbe<0.02mg/L)
Breastfeeding:avoidLEF
Methotrexate
(MTX)
Pregnancy: teratogenic and abortifacient. Termination not
mandatory.StopMTX3monthsbeforestartingtotryto
conceive
Breastfeeding:avoiddrug
Mycophenolate
mofetil(MMF)
Pregnancy:teratogenicandabortifacientavoidMMF.Stop
MMF >6 weeks before starting to try to conceive.
Recommenduseoftwoformsofcontraceptionotherwise.
Breastfeeding:avoidMMF
Sulfasalazine Pregnancy: compatible throughout pregnancy with folate
supplementof5mg/day
Breastfeeding:compatiblewithfull-term,healthyinfants
CYC,gold,
penicillamine
Avoidinpregnancyandbreastfeeding
Cyclophosphamide
Themainuse ofthe cytotoxicdrugcyclophosphamide (CYC)is for organ- or
life-threatening manifestations of autoimmune connective tissue diseases
(AICTDs)andforremissioninductionofvasculitis.
• CYC can be administered either orally at a dose of 1.5–2 mg/kg/day or IV
givenasapulsedregimen.
• IVCYCdoseistypicallycalculatedbasedonweightorbodysurfaceareaand
adjustedforrenalfunctionandage;givenonceevery2–4weeksforupto3–6
months.
• For ANCA-associatedvasculitis(AAV), the CYCLOPSregimen is used:IV
CYCatdoseof15mg/kg(reducedforageandrenalfunction)each2weeks
for6weekstheneach3weeksfor3months.
• Pulsed IV CYC regimens are associated with lower total lifetime doses and
reducedtoxicity.
• CYC-inducedsuppressionofgametogenesisisoftenirreversible.Priortothe
decision to use CYC, patients should be counselled about infertility and
offered the use of GNRH analogue and/or harvesting and storage of
sperm/ova.
• Urothelial toxicity from the active CYC metabolite acrolein can cause
haemorrhagiccystitis.PatientsshouldbewellhydratedbeforereceivingCYC
andfor24–48hoursafterIVadministration.
• MesnaisgiventoreduceriskofCYC-inducedurothelialtoxicity. Theusual
doseis2gbeforeandrepeated2and6hoursafterIVtherapy.
• Commonsideeffectsincludenausea,vomiting,diarrhoea,arthralgia,fatigue,
headache,tachycardia,andhypotension.
• Prophylactic antiemesis treatment should be offered to patients who are
receivingIVCYC.
• Co-trimoxazole 960 mg three times a week should be prescribed for
prophylaxisagainstPneumocystisduringtreatmentwithCYC.
• Leucopenia/neutropeniaisasignificantriskandCYCdoseshouldbereduced
ifthishappens.FBCmaybecheckedondays0,7,10,and14afterthefirst
infusion and with any subsequent infusions where the dose is changed. An
FBC is often checked on day 12 (the usual nadir in neutrophil count) in
anticipationofthenextinfusion.

• Afterinductionofdiseaseremission,theusualpracticeistoswitchfromCYC
to alternative maintenance therapy such as AZA or MTX) to maintain
remission.
• ThereareafewCYCdruginteractions:
• Avoidclozapine:increasedriskofagranulocytosis.
• Digoxin:CYCreducesabsorption.
• Phenytoin:CYCreducesabsorption.
Gold(auranofinandsodiumaurothiomalate)
Gold was used extensively in the management of RA and JIA but its use has
becomeinfrequentsincethewidespreadadoptionofrelativelyhigh-doseMTX
andtheavailabilityofbDMARDs.
• The precise mode of action of gold is unknown though numerous in vitro
actionswhichmayberelevanthavebeenobserved.
• Gold is given as 3 mg 2–3 times daily (oral; auranofin) or as a 50 mg IM
injection(sodiumaurothiomalate),usuallymonthly.
• Atestdoseof10mgIMsodiumaurothiomalateshouldbegivenonthefirst
treatment;thereafter 50mg isgivenweeklyuntildiseaseresponseachieved.
Thereafter,theinjectionisgivenevery4weeks.
• Inchildren,IMgoldisgivenat1mg/kguptoamaximumof50mg.
• Ifnoresponseisseenafteracumulativedoseof1g(about20weeklydoses)
ofsodiumaurothiomalate,itshouldbediscontinued.
• Both formulations of gold are contraindicated in severe renal or hepatic
disease,ulcerativecolitis,historyofmarrowdysplasia,porphyria,exfoliative
dermatitis,SLE,pulmonaryfibrosis,andbronchiolitis.
Hydroxychloroquine(HCQ)andchloroquinephosphate
HCQandchloroquinephosphateare(old)antimalarials.Theiruseiscommonin
themanagementofRA,andinalltheAICTDs.HCQisespeciallypopularforits
useasmaintenancetreatmentinSLE(see Chapter10).
• Antimalarial drugs have a number of anti-inflammatory and
immunomodulatoryactions.
• HCQ is produced as a sulphate. Some side effects to HCQ may be a
consequence of the sulphate component of the drug (e.g. rash) thus a
phosphateformofHCQcanbeusedinstead.
• The therapeutic dose of HCQ is 200 mg once or twice daily. The dose of
chloroquinephosphateis250mgoncedaily.
• The dailydoseof chloroquineshouldnot exceed 6.5mg/kg. Alternate daily
regimesmaybeusedinsmallchildren.
• Enquire about visual impairment and measure acuity. Near-vision testing
should demonstrate the capacity to read small print N8 or N6 on an acuity
chart.
• Athoroughbaselinevisualassessment,includingaviewoftheretina,maybe
requestedofanoptometrist,opticianorophthalmologistpriortodrugonset.
• Once on an antimalarial, patients should report any changes in visual
acuity/blurring; this would trigger re-assessment at any time and immediate
withdrawal of the drug until the nature of the problem is found. Otherwise,
accuratevisualacuityassessmentshouldtakeplaceannually.
• Antimalarialscanexacerbatepsoriasis.
• Antimalarials can cause skin rash, nausea, diarrhoea and can in rare cases
causecardiacconductionabnormalities.
• Thereareafewdruginteractions:
• Antimalarialscanincreasetheplasmaconcentrationofdigoxin,MTX,and
ciclosporin.
• Avoid antimalarial use with amiodarone, quinine, mefloquine, and
quinolonesforriskofhypersensitivityreaction.
Leflunomide
LEFisusedin RA,PsA,andJIAandcanbeusedincsDMARDcombination
regimens. LEF is an ‘antiproliferative’ drug inhibiting the enzyme dihydro-
orodatedehydrogenase.
• Aloadingdoseof100mgdailyfor3daysissuggested(seeSPC)butoften
thiscausesGI upset andmostrheumatologists avoid it,startingat the long-
termmaintenancedoseof20mgdaily.
• Adoseof10mgdailymaybesufficientiftherearesideeffectson20mg.
• Thedoseinchildrenover3yearsofageis5mgdailyif<10kg;10mgdailyis
10-40kg;20mgdailyif>40kg.
• LEF has a long half-life and requires a washout when severe toxicity is
suspected.Awashoutisachievedusingcolestyramine8gthreetimesadayor
activated charcoal 50 g four times a day for 11 days. Blood concentrations
shouldbecheckedtwice,14daysapartpriortoconceiving(levelsshouldbe
<0.02mg/L).
• CautionisrecommendedwhenusingLEFwithMTX,sincethiscombination
hasbeenassociatedwithliverdysfunctionandfailure.Cytopeniahasalsobeen
observed.
• BloodpressureismonitoredwithbloodmonitoringsinceLEFmaycausean
increaseinBPanddestabilizecontrolledhypertension.
• Rarely,LEFcancausepneumonitis,acuteallergicreactionandneuropathies.
• WomenplanningafamilyshouldhavestoppedLEFfor2years(teratogenic)
(andmen3months)beforetryingtoconceive.
• ThereareafewdruginteractionswithLEF:
• LEFcanincreasetheanticoagulanteffectofwarfarin.
• LEFenhancesthehypoglycaemiceffectsoftolbutamide.
• LEFmayleadtoincreasedconcentrationsofanticonvulsants.
Methotrexate
MTX is the most commonly used csDMARD. It is used as a first-line
csDMARD in RA, JIA and PsA, and in managing some AICTDs and
vasculitides.
• TheactionofMTXasanimmunomodulatorisnotclear,althoughitisknown
tobeaninhibitorofdihydrofolatereductaseinhighdoses.Thisisassociated
with aninhibitionofDNA, RNA, and protein synthesis andmayeffect cell
division.
• ThetypicalmaintenancedoseofMTXis15–25mgonceaweek.
• TheuseofMTXvariesacrosscentres,buttypicallybeginsat10–15mgper
weekandincreaseby2.5–5mgevery2weeksforaperiodof6–8weeks.
• In children and adolescents the subcutaneous route is commonly used at
initiationatadoseof10–15mg/m
2
.Higherdosesofupto20–25mg/m
2
maybe
usedbutareassociatedwithmoresideeffectsandalowerrateofadditional
benefit.
• A lowerdoseand slower escalationisrecommended in theelderly and frail
andwherethereisreducedrenalclearance.
• ThesubcutaneousrouteisassociatedwithreducedriskofGIsideeffectsand
higherbioavailability,comparedtooral.
• MTXtabletsshouldbetakenwhole,notcrushedorchewed.
• MTXtabletscomein2.5mgand10mgformulations.Itisrecommendedthat
only2.5mgtabletsareprescribedanddispensedtoavoidconfusionandrisk
ofoverdose.
• Folic acid (5mg once per week) is often given to reduce the risk of side
effects.Itmaybeincreasedupto6daysoftheweekavoidingthesamedayas
MTX.
• Folic acid may be increased when there is: raised MCV, mildly deranged
LFTs,anaemia,mucositissymptoms,nausea,mucosalulceration;hairloss.
• Emergencyfolinicacid‘rescue’(15–25mgfourtimesadayIVororal)should
be given if any concern over severe toxicity (primarily pneumonitis and
marrowsuppression)andinoverdoseusuallyaboveacumulativeof100mg
MTX.IfserumMTXlevelscanbemeasureditisadvisabletocontinuerescue
until MTX levels fall below <0.1 µmol/L. In most cases, the response is
judgedbythedailyimprovementinhaematologicalindices.
• Theroleofliverbiopsyandserumpro-collagenIII(PIIINP)testingremains
unclear.Somecentresconsiderobtainingaliverbiopsywhentherehasbeen
threeconsecutiveelevationsinPIIINPovera12monthperiod.Thedecisionto
stoptherapywouldbebasedonarisk/benefitassessmentineachindividual.
• History should be taken at each monitoring visit for new dyspnoea as a
screening assessment for pneumonitis or pulmonary fibrosis. Further
investigationmayrequirehigh-resolutionCTandlungfunctiontestsdetailing
lungvolumeandgastransfercoefficients.
• The antifolate effect of some drugs, particularly co-trimoxazole and
trimethoprim,mayincreasethetoxicityofMTX.
• MTXconcentrationcanbeincreasedslightlybyregularNSAIDs.
Mycophenolatemofetil
MMFhasbeenroutinelyusedinorgantransplantation.MMFhasalsobeenused
in the control of lupus nephritis, myositis, and vasculitis, often in ‘remission
maintaining’orin‘steroid-sparing’roles.
• MMFisthe2-morpholinoethylesterofmycophenolicacid(MPA).MPAisa
potent, selective, uncompetitive and reversible inhibitor of inosine
monophosphatedehydrogenase,andthereforeinhibitsthedenovopathwayof
guanosinenucleotidesynthesiswithoutincorporationintoDNA.
• BecauseTandBlymphocytesarecriticallydependentfortheirproliferation
onde novo synthesis of purines whereas other celltypescanutilize salvage
pathways, MPA has more potent cytostatic effects on lymphocytes than on
othercells.
• MMFdoseis1–3g/day(300–600mg/m
2
inchildrenandadolescents)orallyin
divideddoses,startingat500mgdailyforthe7days,then500mgtwicedaily
for7days,buildingsequentiallybyanadditional500mgdailyevery7days
overtheensuingweekstoanoptimal/tolerabledose.
• MMF is monitored using FBC, LFTs, and urinalysis (screening for
nephrotoxicity).
• MaindruginteractionsofMMF:
• Decreased absorption of MMF can occur with antacids (magnesium and
aluminiumhydroxide)andcolestyramine.
• Increasedconcentrationmayarisewiththeuseofaciclovir.
• ConcomitantNSAIDsmayaddtonephrotoxicrisk.
Sulfasalazine
Sulfasalazine (SSZ) is a useful csDMARD in treating peripheral and
enteropathicSpA andRA. Thereis weakto moderateevidenceforefficacyin
PsA.
• A SSZ is an active substance although most is converted by bacteria in the
colon into the active metabolites colon where bacteria split the drug into
sulfapyridine(SP)andmesalazine(ME).MostSPisabsorbed,hydroxylated,
orglucuronidatedandamixofunchangedandmetabolizedSPappearsinthe
urine. Some ME is taken up and acetylated in the colon wall. SSZ is also
excretedunchangedinthebileandurine.
• OverallSSZanditsmetabolitesexertimmunomodulatoryeffects,antibacterial
effects, effects on the arachidonic acid cascade, and alteration of activity of
certainenzymes.
• SSZtherapeuticdoserangeisfrom1.5gto3gdailyindivideddoses.The
dose in children and adolescents is 30-50mg/kg/day (maximum 3g daily) in
twodivideddoses.
• A dose increment regimen is typically advised starting at 500 mg/day
(approximately 10mg/kg in children) for 7 days and increasing by an
additional500mgdailyevery7daysovertheensuingweekstotheplanned
therapeuticdose.
• Patientsshouldbewarnedthatbodilyfluidsmayturnadarkeryellow/orange
andnottobealarmed.
• SSZmayleadtostainingofcontactlenses.
• Theenteric-coatedformulationiswelltolerated.SSZalsocanbeprescribedin
liquidform.
• SlowacetylatorsofSSZmaydevelopadrug-inducedlupus-likesyndrome.It
isnotnecessarytocheckacetylatorphenotypesincethedrugwillhavebeen
stoppedwhensuspicionoccurs.
• The majority of patients who develop SSZ side effects do so in the first 3
monthsoftakingthedrug.Correspondingly,laboratorytestmonitoringcanbe
relaxedandinmostguidelines,inlong-termuse,isonlyadvisedonceevery3–
6months.
• Ahistoryofhypersensitivitytosulfonamides/co-trimoxazoleshoulddeteruse
ofthedrug.
• SSZcontainsinpartsalicylicacidthusitcanproduceaspirinandNSAID-like
sideeffects(e.g.pepticlesions,interstitialnephritis,tinnitus).
• SSZcanreducespermcountandviabilitydirectlyandcanaffectfertilityby
reducinggonadotrophinproduction.
• SSZincombinationwithAZAmaypotentiatetheriskofbonemarrowtoxicity
fromeitherdrug.
TargetedsyntheticDMARDs(tsDMARDs)
Tofacitinib
Tofacitinib is a JAK (Janus kinase) inhibitor that impairs the JAK-STAT
signallingpathwayandaffectsimmunecellfunction.
• Tofacitinib has been shown to be effective in RA as monotherapy or co-
therapywithMTX.Trialshavealsotakenplaceinpsoriasisandcolitis.
• IthasbeenapprovedintheUSAfortreatmentofRAanditisbeingreviewed
byNICEintheUK.
• Itisgivenorally5mgtwicedailyfortheimmediate-releasetabletor11mg
oncedailyfortheextended-releasetablet.
• Thedoseneedstobeadjustedinmoderaterenalandhepaticimpairmentto5
mgoncedailyandavoidedinsevereimpairment.
• It is not recommended to co-prescribe tofacitinib with strong CYP3A4
inducerssuchasrifampicinandthedoseshouldbereducedwithconcomitant
useofCYP3A4inhibitors.
• TestandtreatmentforlatentTBisrecommendedpriortocommencementof
tofacitinib.
• Lymphomaandothermalignanciesincludingskincancershavebeenreported.
• EBV-associated post-transplant lymphoproliferative disorders have been
reported in renal transplant patients treated with tofacitinib and concomitant
immunosuppressants.
• Bone marrow suppression, lipid abnormalities, and hepatotoxicity can occur
and hence monitoring should include FBC, lipid profile, and liver function
tests.
• GI perforation has been reported in clinical trials so use with caution in
patientsatincreasedrisksuchasdiverticulitis.
Apremilast
Apremilastisaphosphodiesterase4(PDE4)inhibitor,whichresultsinincreased
intracellularcAMP levelsand consequentlyaffectsthe regulationof numerous
inflammatorymediatorsincludingdecreasingtheexpressionofTNFα:
• ApremilastislicensedfortheuseofPsA.
• ItisapprovedintheUSAandEuropebutitisyettobeapprovedbyNICEas
‘cost-effective’intheUK.
• Apremilastisgivenorallyinitiallyat10mginthemorningonday1,titrate
upwardbyadditional10mgperdayondays2to5andmaintenancedoseof
30mgtwicedailyfromday6.
• Doseneedstobeadjustedwhencreatinineclearanceis<30mL/min.
• Apremilast maycauseweight lossanddiscontinuation should beconsidered
withsignificantweightloss.
• Neuropsychiatric effects such as depression and mood changes have been
reported.
BiologicalDMARDs
Anti-TNFαtherapy
TNFα is a potent pro-inflammatory cytokine and the levels are elevated in
autoinflammatory/autoimmuneinflammatoryconditions.
• Atpresent,therearefivemainanti-TNFαbDMARDsavailable:adalimumab,
etanercept,certolizumabpegol,infliximab,andgolimumab.
• Infliximab is a chimeric human–murine anti-TNFα monoclonal antibody,
etanerceptarecombinanthumanTNFαreceptorfusionprotein,certolizumab
pegol a pegylated Fab fragment of a fully humanized anti-TNF monoclonal
antibody, adalimumab and golimumab are both fully humanized anti-TNFα
monoclonalantibodies.
• InfliximabisadministeredbyslowIVinfusionat0,2,4,andevery4–8weeks,
thereafterdependingonresponse.
• Etanercept is administered by SC injection and can be given once (50 mg)
insteadoftwice(25mg)weekly.
• CertolizumabpegolisgivenbySCinjectionatadoseof400mginweeks0,
2,and4,followedbyadoseof200mgevery2weeks.
• Adalimumab is given by SC injection: 40 mg (20mg if the child weighs
<30kg)every2weeks.
• Golimumabis givenbySCinjectionatadoseof50mgevery4weeks.An
increaseindoseto100mgevery4weekscanbegiveninpatientswhoweigh
>100kg.
• Withallanti-TNFαagents,co-administrationwithMTXisrecommendedfor
treatingRAandJIAwhenMTXistoleratedasthishasbeenshowntoincrease
efficacy. Inaddition,MTX usewithinfliximabandadalimumab reducesthe
riskofantibodiestotheanti-TNFagent.
• ForefficacyalonethereappearstobenoadditionaleffectofaddingMTXto
anti-TNFαtherapyforPsAorAS/axSpA.
• For RA patients who cannot take MTX, adalimumab, etanercept and
certolizumabpegolcanbeusedasmonotherapy.
• Notably,andparticularlyinPsAandaxSpA/AS,thereisevidencethatpatients
mayrespondtoasecondanti-TNFαifthereisaninadequateresponsetoafirst
therapy.
• In the UK, anti-TNFα is restricted by criteria for use (NICE has published
guidelinesforNHSusebasedoncost-effectivenessassessments;Table23.9).
• Infliximab has been used to treat conditions (‘off-licence’) such as Behçet’s
disease(see Chapter18).
Table 23.9 Summary ofUK (NICE) guidelinesfor the useof the anti-TNFα therapyin RA in NHS
practice
1 PatientswithclinicaldiagnosisofRA:‘recentonset’(diseaseduration
ofupto2yearsandestablished(>2years)
2 ADiseaseActivityScore(DAS28)of>5.1
3 Adequatetrialofatleast2conventionalDMARDs,oneofwhichshould
bemethotrexate.Anadequatetrialisdefinedas:
Treatmentforatleast6months,withatleast2monthsatstandardtarget
dose(unlesstoxicity)
Treatment for <6 months where treatment was withdrawn due to
intoleranceortoxicity, normally after atleast 2 months oftherapeutic
doses
4 Exclusioncriteria:activeinfectionorhighriskofinfection.Malignantor
pre-malignantstates
5 Criteriaforwithdrawaloftherapy:adverseeventsorinefficacy
6 Analternativeanti-TNFαtherapymaybeconsideredforpatientsinwhom
treatmentiswithdrawnduetoanadverseeventbeforetheinitial6-month
assessmentofefficacy
Informationtakenfrom https://www.nice.org.uk/guidance/TA375and
https://www.nice.org.uk/guidance/CG79.
Anti-TNFα:cautionsandmonitoring
AlltheassessmentandmonitoringprinciplessetoutinTable23.7,Table23.8,
and Box 23.2 apply to bDMARDs as much as they do to csDMARDs,
particularlytheassessmentofinfectionandmalignancyrisk.
• Active bacterial or severe viral infection and current/recent malignancy are
exclusion criteria for treatment with anti-TNFα. Paediatric judgment is
requiredinchildren.
• Anti-TNFαshouldnotbegiventopatientswithahistoryofmultiplesclerosis
orsevereheartfailure(NYHAgrade3or4).
• Guidelines for using anti-TNFα therapy in pregnancy have recently been

published(Table23.10).
• Commonreactionsincludeheadache,nausea,andinjection-sitereactions.
• Serious bacterial infections have been reported, and patients with active
infectionshouldhavetheirtreatmentstopped.
• For patients at risk of recurrent infection (e.g. in-dwelling urinary catheter,
immunodeficiency states) it is usually recommended to avoid anti-TNFa
therapy.
• Otherreportedsideeffectsincludedemyelination,worseningofheartfailure,
lupus-likesyndromes,andblooddyscrasias.
• ReactivationofTBhasbeenreportedmainlywithinfliximabandadalimumab
use (3–4× increased risk compared with etanercept) and most commonly
within3monthsofbeginningoftreatment.PatientsshouldbeassessedforTB
risk.
• ThereareguidelinesforassessingriskandmanagingTBinfectioninpatients
duetostartanti-TNFαtherapy(e.g.BritishThoracicSocietyavailableat:
http://www.brit-thoracic.org.uk). Use of anti-TNFα therapy is not
contraindicatedbutpatientsmayrequireupto3–6months’treatmentforlatent
TB.
• Thelong-termsafetyofanti-TNFαespeciallywithregardtomalignancyisnot
known. It is well known that RA patients have a 2× risk of developing
lymphoma compared with the general population. Debate continues as to
whetherreports oflymphomainRA patientson anti-TNFαtherapyreflect a
realdrugeffectortheknownincreasedincidenceoflymphomainRApatients.
• There is no increased risk of developing solid tumours. However, there
appearstobeanincreasedriskofsomeskincancersespeciallymelanomaand
hencepatientshouldbeadvisedonpreventiveskincareandclosemonitoring
ofskin.
B-celldepletiontherapy
BcellsplayanimportantroleinthepathogenesisofRAandotherautoimmune
conditions generating antibodies and, through their surface receptors, in
processingandpresentingantigentoTcells.
Rituximab
RTXisachimericmonoclonalantibodyagainsthumanCD20thatispresenton
developingBcellspriortotheplasmacellstage.AdministrationofRTXleadsto
rapid CD20 positive B-cell depletion in the peripheral blood. Normal B-cell
repopulation (measured by monitoring the CD19 count) occurs variably but
typicallyoverthenext6–9months.
• RT.RCTshaveshownthatinRF-positiveRApatientswhohavefailedseveral
csDMARDs, a course of RTX (two infusions, 1 g 2 weeks apart with
methylprednisolone infusions) achieves a significant improvement in RA
diseaseactivityat6monthscomparedtoMTXalone.
• InRA,thetimetonextinfusionregimencanrangefrom6to18months,but
hasameanof9months.
• There is concern about persistent hypogammaglobulinaemia after repeated
courses of RTX. The possibility of increased risk of infection with
hypogammaglobulinaemia should be discussed with patients before re-
treatment.
• IntheUK,NICEallowsRTXtobeusedwithMTXinthetreatmentofsevere
RA forNHSpatients, wherethere hasbeenan inadequateresponseto other
DMARDsandoneormoreotheranti-TNFαtherapy.
• Open-labelstudiesin SLEinitiallysuggestedefficacyofRTX,withbenefits
extending to 6 months; however, a RCT failed to show that RTX was
beneficialtopatientswithmoderate-to-severeSLE.
• Repeated RTX infusions in SLE appear to increase BAFF/BLyS (see later),
whichisassociatedwith increasingseverityofpost-treatmentflaresinsome
patients.
• Rituximab is as effective as CYC in the treatment of AAV as induction or
maintenancetherapyandisusedifavoidanceofCYCispreferableorthereis
aninadequateresponsetoCYC.
• There is a growingliterature suggesting benefit ofRTX in other conditions,
e.g.polymyositisanddermatomyositis.
• Theseriousconditionprogressivemultifocalleucoencephalopathy(PML)has
been reported with RTX in a small number of patients. Patients should be
counselledappropriatelybeforetreatment.
• The assessment and monitoring recommended for RTX is similar to that
recommendedforanti-TNFαtherapy.
• A lymphocyte CD19 count can be checked before and 6 weeks after
administeringRTX.Theobservationofitfallingwithtreatmentandthenrising
asthe disease‘flares’ isevidenceinfavourofdrugefficacyandameansof
predictingneedforretreatment.
Belimumab
• Belimumab is monoclonal antibody that depletes B cell by blocking the
bindingofsolubleBAFF/BLyStoreceptorsonBlymphocytes,reducingthe
activity of B-cell-mediated immunity. BAFF/BLyS is a TNF superfamily
member(TNFSF13B)bestknownforitsroleinthesurvivalandmaturationof

Bcells.
• BelimumabmaybeusedinSLEresistanttootheragents.
• Belimumabisgivenasaninfusioninitiallyat10mg/kgevery2weeksfor3
dosesandmaintenanceof10mg/kgevery4weeks.
Interleukin-1receptorantagonists
Interleukin-1(IL-1)isapro-inflammatorycytokine.AnakinraisanIL-1receptor
antagonistthatcompeteswithIl-1forbinding.
• Anakinraisgivenby100mg(inchildren1–4mg/kg)SCinjectiondaily.
• RCTs have shown that anakinra is more effective than placebo in RA but
smallerdiseaseresponsesareevidentcomparedtoanti-TNFα.
• AnakinraisusedintreatingMAS,systemiconsetJIAandautoinflammatory
conditions, e.g. TNF receptor-1 associated periodic syndrome (TRAPS),
SAPHOsyndrome,andadult-onsetStill’sdisease(see Chapter18).
• Sideeffectsincludeinjection-sitereactions,blooddyscrasias,andinfection.
• Anakinrashouldnotbeusedtogetherwithanti-TNFαtherapies.
• Clearanceisreducedinrenalimpairment.
Interleukin-6inhibition
Interleukin-6(IL-6)isapotentpro-inflammatorycytokineandmediatorofthe
acute-phaseresponse.HighlevelsofIl-6havebeenfoundinserumandsynovial
fluidofRApatients.
• Recent work has shown that both upstream and downstream signalling
pathwaysforIL-6differbetweenmyocytesandmacrophages.
• ItappearsthatunlikeIL-6signallinginmacrophages,whichisdependenton
activation oftheNFκB signalling pathway, intramuscular IL-6expressionis
regulatedbyanetworkofsignallingcascades,includingtheCa
2+
/NFAT and
glycogen/p38MAPKpathways.
• IL-6 signalling in monocytes or macrophages, creates a pro-inflammatory
response, whereas IL-6 signalling in muscle (independent of a preceding
TNFαresponseorNFκBactivation)isanti-inflammatory.
Tocilizumab
TocilizumabisahumanizedmonoclonalantibodyspecificfortheIl-6receptor.It
islicensedforuseintreatingRA,systemicJIA,andCastleman’sdisease.
• TocilizumabisgivenbymonthlyIVinfusionatadoseof8mg/kg.Itisalso
availableasSCinjectionat162mgeveryotherweekifweightis<100kgor
162mgeveryweekifweight>100kg.Inchildren>2ywithsystemicJIAthe
doseis:weight<30kg–12mg/kgeverytwoweeksbyinfusion;weight>30kg–
8mg/kg every two weeks. In children with polyarticular JIA the dose is 8–

10mg/kgevery4weeksbyinfusion.
• Tocilizumab is effective in controlling disease and limiting radiographic
progressioninRApatientsinwhomMTXandanti-TNFαtherapyhavebeen
ineffectiveornottolerated.
• Tocilizumab can be used as monotherapy if MTX is not tolerated or
contraindicated.
• Tocilizumab is currently under trial for use in large vessel vasculitis and
uveitis.
• Lipids should be monitored 6-monthly given the association with drug-
inducedhyperlipidaemia.
• Bone marrow side effects are more frequent in the first few months of
treatment.FBCandliverfunctiontestsshouldbemonitoredmonthly.
BiologicDMARDstargetingTh17cellactivation
Commontoanumberofconditions,Th17cellactivationisdrivenbyIl-12and
Il-23, which triggers the activated T-cell to produce Il-17 and elaborate other
cytokines, whichhavedownstream pro-inflammatory effects in varioustissues
then having tissue-specific effects. Diseases where Th17 cell activation is
pertinentincludepsoriasisandtheSpAs(see Chapter8).
Ustekinumab
Ustekinumab is a human monoclonal antibody directed against the pro-
inflammatory cytokines IL-12 and IL-23. Ustekinumab binds to the (common
sequence) p40 subunit of both cytokines so that they cannot activate their
receptorsonTh17cells.
• In PsA, ustekinumab has shown superior efficacy in treating synovitis,
dactylitis and enthesitis compared to MTX alone. Responses are positive in
bothanti-TNFαnaïveandanti-TNFαtreatedpatients.
• UstekinumabisgivenbySCinjection:dose45mg(weight<100kg)or90mg
(weight>100kg)atweek0,4,and12-weeklythereafter.
• IntheUK,NICEhasapproveduseforNHSpatientswithPsAwhendiseaseis
stillactivedespitetreatmentwithDMARDsandifanti-TNFαhasfailedoris
contraindicated.
• Commonsideeffectsincludeinfection,fatigue,andheadache.
• Uncommon side effects include exfoliative dermatitis, encephalopathy, and
facialpalsy.
Secukinumab
SecukinumabisarecombinantfullyhumanmonoclonalIgG1kantibodywhich
binds Il-17A inhibiting its receptor binding. It is licensed for use in treating
plaquepsoriasisandhasshownefficacyintreatingAS.
2
• For AS, the recommended dose is 150 mg once weekly subcutaneously at
weeks0,1,2,and3;followedbyamaintenancedosemonthlyfromweek4.
• Secukinumab may be effective in some adults with PsA whose response to
csDMARDshasbeeninadequate.Casereportssuggesteffectivityinpatients
definedashavingaxSpA.
• ItshouldbeusedwithcautioninpatientswithCrohn’sdiseaseasitcancause
exacerbationofinflammatorydisease.
OtherbiologicDMARDs
Abatacept(CTLA4-Ig)
Abatacept disrupts the CD80/86 co-stimulatory signal required for T-cell
activationbycompetingwithCD28forbinding.
• AbataceptiseffectiveinpatientswithRAwhosediseaseisnotcontrolledwith
oneormorecsDMARDsincludingMTXoranti-TNFα.
• AbataceptisadministeredIVatadoseaccordingtobodyweight;500mg(<60
kg),750mg(60–100kg),and 1000mg(>100kg)atweeks0, 2,and4and
thenmonthlythereafter.Inchildren<75kgthedoseis10mg/kgbyinfusionin
thesamefrequencyasadults.
• Abatacept can also been given SC at a dose of 125 mg once weekly. In
children25–50kgthedoseis87.5mgandif>50kganadultequivalentdoseis
used.
• Arecentsystematicreviewhasshownthattheincidenceofseriousinfections
waslow,andcomparedwithplacebowasequal.
TheuseofbDMARDsinpregnancyandbreastfeeding
There is a paucity of data on the effect of bDMARDs in pregnancy and in
women breastfeeding but consensus opinion is summarized in a number of
guidelines (e.g. UK BSR guidelines available at:
http://www.rheumatology.org.uk/resources/guidelines/default.aspx).
Table23.10Biologicsinpregnancyandbreastfeeding
Disclaimer: all readers should refer to their own local practice guidelines. Information here is
incompleteandbriefandaskeletonguideonly.
Drugs Effects
Infliximab Pregnancy: compatible peri-conception and with first
trimester,stopat16weeks
Breastfeeding:compatible
Etanercept
Adalimumab
Pregnancy: compatible peri-conception and with first and
secondtrimester,stopatthirdtrimester
Breastfeeding:compatible
Certolizumab Pregnancy: compatible peri-conception and throughout
pregnancy
Breastfeeding:compatible
Golimumab Pregnancy:nodatatorecommend
Breastfeeding:nodatatorecommend
Rituximab Pregnancy:stop6monthsbeforeconception
Breastfeeding:nodatatorecommend
Tocilizumab Pregnancy:stop3monthsbeforeconception
Breastfeeding:nodatatorecommend
Anakinra
Abatacept
Belimumab
Pregnancy:nodatatorecommend
Breastfeeding:nodatatorecommend
References
1.SmolenJS,vanderHeijdeD,MacholdKP,etal.Proposalforanewnomenclatureofdisease-modifying
antirheumaticdrugs.AnnRheumDis2014;73:3–5.
2.BaetenD,SieperJ,BraunJ,etal.Secukinumab,aninterleukin-17Ainhibitor,inankylosingspondylitis.
NEnglJMed2015;373:2534–48.
Othermedications
Drugsusedintreatingosteoporosis
The treatment of osteoporosis is described in Chapter 6. A summary of
currentlylicensedosteoporosisdrugsisshowninTable23.11.
Table23.11Drugsusedinthetreatmentofosteoporosis
Drugs Dose Comments
Alendronic
acid
70mgorally
onceweekly
Fracture reduction broadly 20–40% for oral
bisphosphonates over 3–5 yrs and 70% for
vertebralfracturereductionforzoledronateat
3yrs.Initialtreatmentcourseis3–5yrs
Optimum response occurs if not calcium and
Risedronate 35mgorally
onceweekly
Ibandronic
acid
150mgoral
monthlyor3
mgIVevery3
months
vitaminDdeficient
Avoidallbisphosphonatesinrenalimpairment
(estimatedGFR<30mL/min)
Oral bisphosphonates can cause dyspepsia,
oesophagitis,andoesophagealulcers
Oral bisphosphonates must be taken with
water,fastingandatleast1hrbeforefoodor
liquid(otherthanwater)
Regularreviewforadherenceisadvisable
Atypicalfemoralfractures have been reported
—but rarely and chiefly with long-term
treatment
Osteonecrosisofthejawisveryrare
Zoledronic
acid
5mgIVonce
yearly
Denosumab 60mgSC
injectiononce
every6
months
Fracture reduction risk about 70% over 3 yrs
forvertebralfractures
Side effects include cellulitis, urinary tract
infection, and upper respiratory tract
infection
Hypocalcaemia can occur and the risk is
increased if estimated GFR <30 mL/min—
givecalciumsupplementsandmonitorserum
calcium
Atypicalfemoralfracturesandosteonecrosisof
jaw(advisedentalcheck-up)arerarebutcan
occur
Strontium
ranelate
2goraldaily;
avoidfoodfor
2hrsbefore
and2hrsafter
RCTsshowedfracturepreventionafter3yrsof
continuous use. Continued use to 8 yrs
suggestedmaintainedfractureprevention
Sideeffects:GI;nowusedsparinglybecauseof
increased risk of cardiovascular disease and
venous thrombosis. Use banned in some
countries
Teriparatide 20micrograms
SCinjection
dailyfor2
years
Side effects include GI disorders, palpitation,
hypercalcaemia,myalgia
Contraindicated in hypercalcaemia, skeletal
malignanciesorbonemetastases,Paget’s,and
previousradiationtotheskeleton
Avoidinsevererenalimpairment
DrugsusedinthetreatmentofRaynaud’sdiseaseandpulmonaryartery
hypertension
The treatment of Raynaud’s disease (RD) and pulmonary artery hypertension
(PAH)associatedwithSSclisdescribedin Chapter13.Table23.12providesa
summaryofthedrugsused.
Table23.12DrugsusedinthetreatmentofRaynaud’sdisease(RD)andpulmonaryarteryhypertension
(PAH)
Drugs Adverseeffects
Nifedipine:5–20mgthreetimesadayfor
RD.Startdoselowwithdoseadjustments
followingresponse
Amlodipine5–10mgdailyforRD
Oedema,hypotension,
headache,nausea
Losartan:25–50mgoraldailyforRD Hypotension,
hyperkalaemia
Fluoxetine:20–40mgoraldailyforRD SeeSNRIcautions, p.658
andTable23.5,p.657
TopicalGTN:availablein5mg/24hrs.For
RD.Applytoaffectedareaforuptill12hrs
Hypotension,headache,
applicationsitereactions
Sildenafil:25–50mgorallythreetimesaday
forRD,or
Tadalafil:40mgorallydaily.
Reducedosesinrenalandhepatic
impairment
Hypotension,priapism,
headache,flushing,diarrhoea,
visualdefects
Iloprost(prostacyclinanalogue)
NebulizedformforPAH.Firstinhaleddose
shouldbe2.5microgramsincreasedto5.0
microgramsiftoleratedandgiven3–4-
hourly.Typically,6–9doses/daybutnomore
than45micrograms/dayadvisable.
IVinfusionforPAHinitially0.5ng/kg/min
for30minsthenincreasedatintervalsof30
Hypotension,headache,jaw
orlimbpain.Monitorpulse,
bloodpressure,andoxygen
saturation.Ifeffectssevere
considerreducingdoseor
stoppinginfusiontemporarily
andrestartingatlowerdose
minsinstepsof0.5ng/kg/minupto2
ng/kg/min.Exactinfusionrateshouldbe
calculatedonbodyweighttoeffectinfusion
raterangeof0.5–2ng/kg/min.Finaldose
givenover6hrsdaily(e.g.over5days).
Bosentan:forPAH.Initially62.5mgtwice
dailyorallyincreasedafter4weeksto125
mgtwicedaily.
Macitentan:forPAHonly:10mgoraldaily.
Ambrisentan:forPAHonly:5mgoraldaily,
increasedifnecessaryto10mgdaily
Lowhaemoglobin(Hb)so
monitorHbbeforeandduring
treatment.AlsocheckLFTsat
startandatmonthlyintervals
ontreatment
Riociguat:forPAHonly;initially1mgthree
timesadaydailyfor2weeks,increasedby
0.5mgeachdoseevery2weeksupto
maximum2.5mgthreetimesaday
Hypotension—reducedoseif
systolicBPfalls<95mmHg
Drugsusedintreatinggoutandhyperuricaemia
The management of gout is described in Chapter 7. The treatment of acute
goutiswithNSAIDs,colchicine,andGCs.Urateloweringdrugsareusedifgout
issevere(e.g.chronic/tophaceous)and/orrecurrent.SeealsoCochranereview
CD010069( http://www.cochranelibrary.com).
Colchicine
• Colchicineisanti-inflammatoryandusedingoutandCPPDdiseaseforboth
acuteattacksandchronicdisease.
• ColchicinecanalsobeusedlongterminthetreatmentofBehçet’sdiseaseand
familialMediterraneanfever.
• Itisgiveninitiallyatadoseof0.5mgtwicedailyinacutegoutandCPPD.
Thedoseinchildrenis0.3–2.4mginonetotwodivideddosesincreasingin
0.3mg/dayincrementsastolerated.
• Dose should be adjusted with renal impairment and avoided completely in
severerenalimpairment(estimatedGFR<10mL/min).
• Dose is increased to three or four times daily but is limited by dose-related
diarrhoea.
• Colchicine frequently causes nausea, vomiting, and abdominal pain. Larger
doses may cause profuse diarrhoea, GI haemorrhage, skin rashes, and renal
andhepaticdamage.
• Theraresideeffectsaremyopathy,rhabdomyolysis,alopecia,withprolonged
treatment,bonemarrowsuppressioncanoccur.
Allopurinol
• Allopurinolisaxanthineoxidaseinhibitorwhichisusuallythefirst-lineurate-
loweringdrug.
• Initiate at 100 mg orally daily then adjust according to plasma uric acid
concentrationeachmonthby100mgtomaximum900mgdaily.
• The dose should be adjusted down in renal impairment, and in severe renal
impairment,reducedailydosebelow100mg.
• Thedoseshouldbechangedinversely (e.g.each4–6weeks)titrated against
urateleveltoatarget<360nmol/Lorinseveredisease<300.
• About 2% of patients develop a rash which is typically pruritic and
maculopapular.Ifmild,withdrawtherapyandre-challengecanbeundertaken
withcautionbutdiscontinuepromptlyifrecurrence.
• LifethreateninghypersensitivityreactionssuchasStevens–Johnsonsyndrome,
toxic epidermal necrolysis, or drug rash with eosinophilia and systemic
symptoms (DRESS) can occur rarely and re-challenge should not be
undertaken.
• GI disorders, e.g. nausea and diarrhoea, are uncommon and bone marrow
suppressionisrareeveninhighdoses.
• AllopurinolcaninterferewiththemetabolismofAZAand6-MP,potentiating
sideeffects.ThedoseofAZAor6-MPshouldbe~25%oftheusualdoseif
theyaregivenconcurrentlywithallopurinol.
• Otherinteractionsincludewarfarin(monitorINR),theophylline(monitordrug
level),andACEinhibitors(haematologicalreactions).
Febuxostat
Febuxostat is a non-purine xanthine oxidase inhibitor used to treat
hyperuricaemia.Itisappropriateforpatientswhoareallergictoallopurinol,do
not reach the target uric acid level with maximal allopurinol doses, or have
severerenalinsufficiency.
• Febuxostatisinitiatedat80mgorallydailythenincreaseto120mgdailyafter
2–4weeksifserumuricacid>6mg/dL.
• Themostcommonsideeffectsarediarrhoea,nausea,headache,liverfunction
testabnormalities,andrash.
• Severe hypersensitivity reactions such as Stevens–Johnson syndrome, toxic
epidermalnecrolysis,orDRESSoccurbutarerare.
• Mild liver function abnormalities were observed in 5% in clinical studies,
hence checking LFTs is recommended before starting febuxostat and
periodicallythereafter.Inknownmildhepaticimpairment,thedoseisreduced
to40–80mgdaily.
• Febuxostat is not advised for people with ischaemic heart disease or heart
failurebecauseinitialtrialsshowedahigherincidenceofcardiovascularside
effects fromfebuxostatcomparedwithallopurinol; however,theobservation
hasnotbeensubstantiatedinfurthertrials.
• Febuxostat can interfere with metabolism of AZA and 6-MP and hence
concomitantuseisnotrecommended.
Probenecid
Probenecidisauricosuricagent,whichiseffectivebyalteringrenalhandlingof
urate and increasing urine excretion. It has been used to increase the
concentrationofsomeantibiotics.
• The recommended dose is 250 mg oral twice dailyfor1weekand500mg
twicedailythereafter.
• Probenecidshouldnotbestarteduntilafteranacuteattackofgout.
• In some countries, including the UK, probenecid is only available from
‘special-order’manufacturersordistributors.
• Itisimportanttoensureadequatefluidintake.
• Probenecid is contraindicated in patients with a history of blood disorders,
renalstones,andrenalimpairmentwhereestimatedGFRis<30mL/min.
Sulfinpyrazone(sulphinpyrazone)
Sulfinpyrazoneisauricosuricagent.Itshouldnotbestartedduringanacutegout
attack.
• Sulfinpyrazone is initiated at 100–200 mg orally daily with food increasing
over2–3weeksto600mgdailyuntiltargetserumuricacidconcentrationis
reachedandthenreducedtomaintenancedosewhichmaybeaslowas200mg
daily.
• Dose shouldbe reducedin renalimpairment.Itshouldbeavoidedinsevere
renalimpairmentandisineffectiveifGFRis<30mL/min.
• Itiscontraindicatedinpatientswithhistoryofblooddisorders.
• RegularFBC/CBCmonitoringisadvisableassulfinpyrazonecancauseblood
disorders.
• Caution is advised in prescribing wherethereiscardiac,cerebrovascular, or
hypertensiondiseaseasthedrugmaycausesaltandwaterretention.
• Other side effects include GI disturbances and ulceration, allergic skin
reactions,acutekidneyinjury,andhepatitis.

• Seealso: http://www.medicines.org.uk/emc/medicine/26935.
Benzbromarone
Benzbromaroneisauricosuricagentandnon-competitiveinhibitorofxanthine
oxidase,availableinEurope.BenzbromaronealsoinhibitscytochromeCYP2C9,
whichisresponsibleformetabolizinganumberofdrugsincludingdrugswitha
narrowtherapeuticindexsuchaswarfarinandphenytoinandotherdrugssuchas
tolbutamide,losartan,andsomeNSAIDs.
• Benzbromarone offers advantages over some uricosuric drugs as it may be
saferandbettertoleratedinpatientswithrenalinsufficiency.
• Liverfunctionmustbemonitoredfordrug-inducedhepatitis;fulminantliver
failurehasbeendescribed.
• Given itseffectsonCYP2C9cautionwith co-prescribing,any medicationis
mandatory.
Rasburicase
Rasburicase is a recombinant uricase/urate-oxidase enzyme produced by
genetically modified Saccharomyces cerevisiae strain. Urate oxidase exists in
manymammalsbutdoesnotoccurinhumans.
• Rasburicase catalyses enzymatic oxidation of uric acid into a metabolite,
allantoin,whichis5–10×moresolublethanuricacid,withCO
2
andhydrogen
peroxideasby-productsinthechemicalreaction.
• Rasburicase is licensed in the USA and Europe for treatment of acute
hyperuricaemia associated with tumour lysis syndrome in patients receiving
lymphomaorleukaemiachemotherapy.
• Therecommendeddoseis0.2mg/kg/daygivenasaonce-daily30-minuteIV
infusionin50mLof0.9%saline.
• Thedurationoftreatmentmaybeupto7days,theexactdurationshouldbe
based upon adequate monitoring of uric acid levels in plasma and clinical
judgement.
• Long-termuseforhyperuricaemiaassociatedwith goutat dosesof 0.15–0.2
mg/kgisbeinginvestigated.
Pegloticase
Pegloticase is a recombinant porcine-like uricase and like rasburicase it
metabolizesuricacidtoallantoin.
• Pegloticaseispegylatedtoincreaseitseliminationhalf-lifefromabout8hours
to 10–12 days and to decrease the immunogenicity of the foreign uricase
protein.Sopegloticaseisgivenevery2–4weeks.
• Pegloticasemightbeconsidered*forpatientswithseveregoutinwhomother

urate-loweringagentshavebeenineffective.
• Pegloticaseproducesrapidreductioninsignsandsymptomsofgout.
• PegloticaseisgivenasanIVinfusion,8mgevery2weeks,infusedover>2
hours with premedication to decrease infusion reactions including oral
paracetamol,hydrocortisone,andantihistamine.
• Allpatientsshouldbegivenprophylaxisforpreventionofacutegoutduring
thefirst6monthsoftreatment.
• Trials haveshown thattheurate-lowering effect canbe attenuatedorlost in
somepatientsduetohightitreanti-pegloticaseantibodies.
• IntheUK,pegloticasehasnotbeensanctionedforuseingoutbyNICEfor
NHS-treated patients, citing poor cost-effectivity but also noting reported
severeanaphylaxisreactionshaveoccurredwithit.
• * In 2016, the European Commission withdrew the marketing authorization
forpegloticaseintheEU.
Pooledintravenousimmunoglobulin(IVIg)
Pooled IVIg is primarily used as replacement therapy in primary
immunodeficiencyconditions. However,IVIgcan havean immunosuppressive
effect though the mechanism of effect is not precisely known. A number of
theoriesexist.
• Apartfromimmunodeficiency,themainindicationsforIVIgareinGuillain–
Barrésyndrome,myastheniagravis,immunethrombocytopenicpurpura,SLE
(see Chapter 10), dermatomyositis (see Chapter 14), and Kawasaki
disease(see Chapter15).
• The typical dosing regimen is 400 mg/kg/day as a single infusion over 2–4
hoursastoleratedandfor5days;or1g/kg/dayfor2days.Thisisrepeated
every4–8weeksforupto6monthsinthefirstinstanceaccordingtoefficacy.
• Side effectsoccur in <5% ofpatientsand most often within 24hoursofan
infusion.
• However, the FDA (USA) requires IVIg products to carry a black box
warning, cautioning that IVIg has been associated with renal dysfunction,
acutekidneyinjury,osmoticnephrosis,anddeath,especiallyintheelderlyor
withsimultaneoususeofothernephrotoxicdrugsorotherpre-existingissues
thataffectthekidneys.
• Sideeffectsatthetimeofinfusionincludeheadache,flushing,chills,myalgia,
wheezing, tachycardia, lower back pain, nausea, and hypotension. If these
occur,theinfusionshould beslowedorstopped.Mostcaseswillrespond to
antihistaminesandIVhydrocortisoneifsymptomspersist.
• Other significant, but rare complications include acute kidney injury,

arteriovenous thrombosis, disseminated intravascular coagulation, transient
serum sickness, transient neutropenia, aseptic meningitis, post-infusion
hyperproteinaemia with pseudohyponatraemia, eczematous dermatitis, and
alopecia.
Resources
AllUK-licenseddrugSPCsareavailableatEMC: http://www.medicines.org.uk
Patientdruginformationavailableat: http://www.arthritisresearchuk.org
Selectivetherapymeta-analysesat: http://www.cochranelibrary.com

Chapter24
Glucocorticoidinjectiontherapy
Introduction
Principlesofinjectiontechniques
Theshoulder
Theelbow
Thewristandhand
Thehipandperiarticularlesions
Thekneeandperiarticularlesions
Theankleandfoot
Relevant anatomical drawings for each region of the body are found in
Chapter3
Introduction
Local anaesthetic and glucocorticoid (GC; ‘steroid’) injection into joints,
tendons,bursae,andsofttissuesisaveryeffectivetreatmentforlocalizedpain
andinflammation.
• Injection offers a local maximal anti-inflammatory effect with minimal
systemicabsorption.
• Asageneralrule,itisrecommendedthatanyonejointshouldnotbeinjected
more than four times in 12 months and there are at least 6 weeks between
injections.
• Theindicationsforlocalsteroidinjectioninclude:
• reductionofinflammation.
• reliefofpainfrominflammatorylesions.
• reliefofinflammationatsitesofnervecompression.
• reducethesizeofnodulesandganglia.
• Thecontraindicationsare:

• absolute: septic arthritis/sepsis, a febrile patient with cause unknown,
seriousallergytopreviousinjection,sicklecelldisease.
• relative: unknown cause of lesion, neutropenia, thrombocytopenia,
anticoagulation,orbleedingdisorder.
• Commonsteroidpreparationsusedinclude:
• hydrocortisone acetate—a short-acting, weak steroid useful for superficial
lesionssuchastendonsandbursae:25mgistypical.
• methylprednisoloneacetate40mg/mL.
• prednisoloneacetate25mg/mL.
• triamcinoloneacetonide10and40mg/mL.
• Thelatterthreeagentsarelong-actingsyntheticglucocorticoids.
• Choiceofstrengthofsteroidremainsempiric.
• Volumeofsteroid/anaesthetic‘accepted’byjointsvaries:
• Smalljointsacceptonlyasmallvolume;thus,forIPJs,MCPJs,MTPJs,and
temporomandibularjoints,0.5mLonlyisappropriate.
• Allotherjointsshouldacceptatleast1mL.
• There may be merit in diluting the steroid in sterile saline, to increase
volumeforbetterdistributioninlargerjoints.
• alternatively,largervolumelevobupivacaine(10mL)isofvalue.
• Potential,thoughuncommon,sideeffects(seealso Chapter23)are:
• exacerbationofpainfor24–48hours.
• septicarthritisandreactivationofTB.
• tissueatrophy(lesslikelywithhydrocortisonethanothers).
• depigmentationofskin.
• anaphylaxis.
• nervedamage.
• tendonrupture.
• osteonecrosis.
• cartilagedamage.
• softtissuecalcification.
• temporaryexacerbationofhyperglycaemiaindiabetes.
Principlesofinjectiontechniques
Theprocedureneednotnecessarilybedoneinasterileenvironment.However,
thereisaneedtomaintainanaseptictechnique.Efficacymaybegreaterusing
US-guided injection but will be more accurate. US should only be done by
appropriatelyqualifiedclinicians.
• Marktheexactspotofneedleinsertion.
• Washhands.Usesterileglovesfortheprocedure.
• Cleantheskinwithpovidone-iodineandallowittodry.
• Anaesthetize the skin (either with local anaesthetic or refrigerant alcohol
spray).Childrenandsomeadolescentsmayrequirealightgeneralanaesthetic
giventheprocedurecanbetraumatic.Analternativeistouselocalanaesthetic
gelpads(e.g.EMLA
®
patch).
• Insertacleanneedlewithemptysyringeandaspirateback.
• Leavetheneedleinplace,detachthesyringe,andplacethesyringecontaining
steroid/localanaestheticontotheendofanewneedle.
• Insertneedleintositetobeinjected.
• Pull back the syringe plunger again before injecting to confirm placement,
ensuringtheneedleisnotinabloodvessel.
• Introductionofsteroidshouldbeeffortless.Resistanceimpliestheendofthe
needleisinthewrongspace.Stopifitcausesmorepain.
• On completion of the procedure, remove the syringe and needle and throw
awaythe‘sharps’.
• Covertheinjectionsitewithcleangauzeorabandage.
• Restthejointfor24hours(considerupto48hoursforaweight-bearingjoint),
includingusinganon-rigidsplint(e.g.Velcro
®
attachedsemi-rigidsplintfor
wrist,ormodifiedRobert-Jonesbandagingfortheknee).
• Advisethaticingthearea/jointmayreducepost-injectiondiscomfort,andre-
emphasizepossiblesideeffectsandbenefits.
Theshoulder
Theglenohumeraljoint(forglenohumeraljointsynovitisoradhesive
capsulitis)
US-guidedinjectiontechnique
Itisdifficulttobeconfidentaneedleisplacedintheglenohumeraljointspace
withoutconfirmationimagingwithUS.Thedefaulttechniqueforinjectingthe
glenohumeraljointshouldbewithUS.
• US-guided injection is the gold standard for comparing therapy options in
researchstudies(e.g.steroidinjectionvshydrodilationforadhesivecapsulitis).
• USisprobablynotrequired,however,whenaninjectionisdoneasthesecond
partofalinkedprocedurewhenthefirstpartisaspiratingalargeeffusion(e.g.
inCPPD-pseudogout).
Non-US-guidedinjectiontechnique

SometimesitisnotpossibletoobtainUSanda‘blind’injectionmayneedtobe
done.Itisessentialthatanyoneundertakingtheinjectionshasbeenappropriately
trained or is supervised and is knowledgeable about anatomy and functional
anatomy.
• Theapproachmaybeanteriororposterior.
• The anterior approach is favoured for adhesive capsulitis given the
predominant pathology involves the anterior part of the joint complex
includingcoracoacromialligamentandsubscapularisbursa.
• Theanteriorrouteisundertakenthus:
• Palpatethecoracoidprocessanteriorlyandacromionposteriorly.
• The injectionismade just lateraltothe coracoid withtheneedle pointing
towardstheacromion(see Plate4).
• Theposteriorrouteisdonethus:
• Theclinicianpalpatesthespineofthescapulawiththethumbtoitslateral
endwhereitbendsforwardastheacromion.
• Withtheforefinger,palpatethecoracoidanteriorly.Thelinebetweenfinger
andthumbthenmarksthepositionofthejointline.
• Theneedleisadvancedfrombehind,1cmbelowtheacromion,andtowards
thecoracoid.Thereshouldbenoresistance.
• By either approach, the joint can be injected with relatively large volumes
such as 1 mL (40 mg) methylprednisolone acetate mixed with 5 mL 1%
lidocaine.
• Alongneedleisneeded.
• Withdrawingtheneedleslightlyandredirecting30°upwardwillallowoneto
reachtherotatorcuffwiththesameprocedure.
Subacromialspace(forsubacromialimpingementdisorders)
US-guidedinjectiontechnique
Itisdifficulttobeconfidentaneedleisplacedinthesubacromialspacewithout
confirmationwithUS.Thedefaulttechniqueforinjectingthesubacromialspace
shouldbewithUS.
• USmaybeuseddiagnosticallyand,withappropriatesonographerexperience
andskill,calcificsupraspinatuslesionsandtearscanbeidentified.
• Radiologicalexpertisevariesfromdepartmenttodepartmentandlocaladvice
onchoosingMRIorUSforspecificlesionidentificationwouldbeappropriate.
Non-US-guidedinjectiontechnique
SometimesitisnotpossibletoobtainUSanda‘blind’injectionmayneedtobe
done. It is essential that anyone undertaking such an injection has been

appropriatelytrainedorissupervisedandisknowledgeableaboutanatomyand
functionalanatomy.
• Thesubacromialspaceisinjectedmosteffectivelyfromthelateralaspectof
theshoulder.
• The arm is placed in a neutral position, hanging to the side, and the gap
betweentheacromionandthehumeralheadispalpated.
• A long, narrow-gauge (e.g. 23) needle is directed medially and slightly
posterior(butonahorizontalplane)forabout2–3cm(see Plate5).
• Usuallyavolumeof3–4mLcanbeaccepted(e.g.40mgmethylprednisolone
acetatein1mLwithupto5mL1%lidocaine).
• Advise avoidance of overarm activity or heavy lifting for a few days and
considerarrangingphysiotherapytostart2weeksaftertheinjectiontowork
onrestoringrotatorcufffunction.
Acromioclavicularjoint(ACJ)
TheACJissometimesvery difficulttolocate soUS tohelpmarkthejoint is
desirable. US is somewhat limited in its utility however, given the amount of
bonepresent—usuallyanACJwhichneedsinjectingissomewhatarthriticwith
osteophytesandperiarticularsclerosis—thusinterferingwithUSimagingdata.
• TheACJislocatedbyfollowingtheclaviclelaterallytoaridgeinthebone.
Thejointisoftentendertopalpate.
• Markingthebonyedge/landmarkswithapenwillbehelpful.
• Withthepatient eithersitting orlyingsupine, asmall-gauge needlewith20
mgmethylprednisolone(orequivalent)in0.5mLmixedwith0.5mLof1%
lidocaineisdirectedintothejoint.
Theelbow
Lateralepicondylitis/‘tenniselbow’/commonextensortendonorigin
enthesitis
Pleasesee Chapter3foradviceonclinicalassessmentandmakingadiagnosis.
ThislesionmaybesecondarytotraumaorassociatedwithaSpAconditionor
PsA.
• US imaging is not required. The injection is best placed at the point of
maximumtenderness.Thetargetisusuallyverysuperficial.
• The lateral humeral epicondyle and surrounding tissue is injected with the
elbowrestingonapillow—orsimilar—ontheexaminationtableandflexedat
90°.
• Use hydrocortisone initially 25 mg because other steroid preparations may

causelocalfatatrophyanddepigmentation(asthisisnecessarilyoftenavery
superficialinjectionjustundertheskin).
• Use0.5–1mL1%lidocainemixedwiththehydrocortisone.
• Theinjectionisaimedat45°totheendofthetendonorigin.
• A fair amount of pressure is required for this injection. Efficacy of the
injectionmayrelypartly on disruption oftheperiosteum of the epicondylar
bone.Itisoftenpainful(see Plate6).
• Adviserestandicingpostprocedure.
• Autologousbloodinjectionhasbeenreportedanecdotallyaseffective,though
thetechniqueiscontroversial,convincingdataonefficacyislackingandinthe
UKNHS,thetechniqueisnotrecommended.Guidanceonthisproceduremay
befoundat: https://www.nice.org.uk/guidance/ipg438/.
Medialepicondylitis/‘golfer’selbow’/commonflexortendonoriginenthesitis
Pleasesee Chapter3foradviceonclinicalassessmentandmakingadiagnosis.
ThislesionmaybesecondarytotraumaorassociatedwithaSpAconditionor
PsA.
• US imaging is not required. The injection is best placed at the point of
maximumtenderness.Thetargetisusuallyverysuperficial.
• The medial humeral epicondyle and surrounding tissue is injected with the
elbow extended and resting on a pillow—or similar—on the examination
table.
• Use hydrocortisone initially 25 mg because other steroid preparations may
causelocalfatatrophyanddepigmentation(asthisisnecessarilyoftenavery
superficialinjectionjustundertheskin).
• Use0.5–1mL1%lidocainemixedwiththehydrocortisone.
• Theinjectionisaimedat45°totheendofthetendonorigin.
• The needle is directed to the flexor tendon origin. However, care should be
takentoavoidthegroovejustbehindthemedialepicondyle—thesiteofthe
ulnarnerve.
• Adviserestandicepostprocedure.
Olecranonbursitis
AnolecranonbursacanbeaspiratedandinjectedwithoutUSguidance.Needle
positionisconfirmedbytheaspirationoffluid.
• Theusualcausesofbursitisaregout,infection,andRA.
• Fluid aspirated may reasonably be sent initially for microscopy and culture
andinfectionruledoutbeforesteroidisinjected.
• Alwayssendfluidforpolarizedlightmicroscopy.

• Usetriamcinoloneacetonideormethylprednisoloneatadoseof20–40mgand
adviseicingandrestfor48hours.
• Arrange appropriate follow-up as the olecranon bursa is prone to develop
infectionandmayneedpromptreassessment—advisethepatientaccordingly.
Elbowjoint(e.g.RAsynovitis)
USguidancemayhelpthoughoften,whenthereisaneffusion,needleplacement
isrelativelystraightforwardandcanbeconfirmedbyfluidaspiration.
• Theelbowjointismosteasilyreachedbyaposteriorapproach.
• Use40mgmethylprednisoloneorequivalent,with2–3mL1%lidocaine.
• Injection into a swollen elbow joint after fluid aspiration, when there is a
distendedcapsuleis relativelystraightforward;however, aneffusionmaybe
present and not readily clinically identified—so landmark identification is
necessary.
• Placethethumbonthelateralepicondyleandthethirdfingerontheolecranon.
Thegroovebetweenthetwofingersidentifiesthejointline.
• Injectat90°totheskin,justaboveandlateraltotheolecranon.
• Alternatively,theradialheadcanbepalpated(byfeelingforitduringforearm
pronation/supination)andtheneedlesitedtangentiallyjustunderthecapsule
(ananterolateralapproach).
• Advise rest and icing postprocedureand advise to avoid lifting orgripping
withthearmforafewdays.
• Considerarrangingphysiotherapytoencourage/exercisetheelbowbacktofull
range. There is a high chance, with persistent inflammatory disease in the
elbow,ofprogressiontopermanentlossofelbowextension.
Thewristandhand
Lesionsofthewrist
Radiocarpaljoint
(Pleaseseealso Chapter3.)
• Theradiocarpaljointisbestidentifiedforinjectionwiththepatient’sforearm
supportedandtheirhand—alsosupported—palmdownwiththewristthenin
slightflexion.Atriangulargapisfeltbetweentheradiusscaphoidandlunate.
• Theneedle(smallgauge)ispointeddirectlydownintothespace.
• For most causes of wrist joint inflammation and synovitis, 40 mg
methylprednisoloneacetatewith2mL1%lidocaineisappropriate.
• Image-guidedinjectiontechniqueisnotusuallyneededforthisinjectionasthe

wristspaceiseasilygained.
Carpaltunnelsyndrome
For anatomy and clinical assessment see ‘Upper limb peripheral nerve
lesions’,pp.124–127.
• The carpal tunnel is injected on the palmar surface of the wrist in the first
crease,midline. Positionthepatient’ssupportedarm,volar sideup andwith
gentleextensionatthewrist;handsupportedalso.
• USguidanceforthisinjectionisnotneeded.
• Sitoppositethepatientsotheir armand handispointingtowardsyourown
position.
• Advancetheneedleat30–45°totheskintowardsthehandforabout2cm(i.e.
towardsyou).
• Improvementofneurogenicsymptomscanbegainedwithhydrocortisone25
mg but most rheumatologists will use triamcinolone 20 mg or
methylprednisoloneacetate20mg.
• Donotuselidocaine.
• Ifthepalmaristendonispresent,theinjectionshouldbesitedjustmedial(i.e.
closertothe‘littlefinger’)tothemidline,byabout1cm.
• Thereshouldbenoresistanceoninjectionornervepain(see Plate12).
Extensorpollicisbrevis/abductorpollicislongus
De Quervain’s tenosynovitis should be injected at the point of maximal
tenderness, advancing the needle through the tendon sheath at a very shallow
angletotheskin,alongthelineofthetendonratherthanat90°tothetendon.
• For functional anatomyandclinical assessment please, see ‘Wrist pain in
adults’,pp.106–110.
• Inject25mghydrocortisoneinitially.Ifasecondinjectionisrequired,consider
eitherusingmethylprednisoloneoraskingforaUS-guidedinjection.
• AUScanalsoruleoutotherlesionsofthewristandtendonarea(e.g.ganglia,
carpal bone disruption, lateral wrist compartment synovitis, 1st CMCJ
synovialcyst,etc.).
Thesmallhandjoints
Thesmalljointsofthehandarefrequentlyaffectedbysynovitisinpatientswith
chronic inflammatory arthritis. Excess joint fluid and capsule extension and
thickeningcanbeconfirmedbyUS.Effusionsareusuallyunderhighpressure,
thoughcannoteasilybeaspiratedwithoutalarge-gaugeneedle.Useofthelatter,
however,issomewhatbrutalandisbestnotattemptedexceptunderanaesthetic.
• US to confirm joint synovitis is often very useful and there are specific
diagnostic signs potentially available with it (e.g. double contour sign in
detectingMSUcrystalsingoutandcalciumpyrophosphatedepositsinCPPD
arthritis).
• TheMCPJsandPIPJswillnormally‘accept’0.5–1mLofinjectedfluid(e.g.
0.5 mL triamcinolone acetonide or methylprednisolone(20mg)and0.5 mL
1%lidocaine).
• ForMCPJinjection,ensurethepatient’sforearmandhandaresupported.Sit
oppositethepatient.
• Useasmall23-or25-gaugeneedleand‘run’theneedleundertheskinparallel
tothefingerjusttothesideofthemetacarpalhead(Fig.24.1),awayfromyou
butaimingveryslightlytowardsthemetacarpalhead—envisageenteringthe
needleunderthedistendedjointcapsuleandinthisway,avoidcontactingthe
bone(whichwillbepainful).Lookforasubcutaneousblebappearing(asign
ofnotgettingtheinjectionintothejoint).
• Usingthesameneedleaccesspointbutanglingtheneedleappropriately,two
MCPJscanbeaccessedintheoneprocedure(butplanthisandfillthesyringe
withappropriateamountofsteroid/lidocaine).
• TheapproachtoaPIPJisprobablybestundertakenfromtheulnarsideofthe
digitbutthetechniqueissimilartoMCPJinjection.
• The small joint injections can cause discomfort and so advise icing and
NSAIDuseinthepost-injectionperiodfor2–3days.
• Asalwayswithjointinjections,adviseagainstmobilizingthejointtoomuch
inthefirstfewdaysafterinjection.
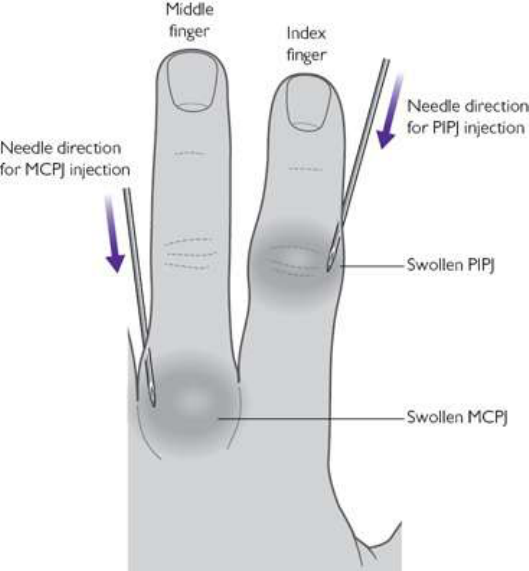
Fig.24.1Directionofneedleaccesstoaswollenmetacarpophalangealjoint(MCPJ)orproximal
interphalangealjoint(PIPJ).Synovitisswellsthejointcapsulewhichcanbeaccessedbyrunningtheneedle
virtuallyparallelwiththedigitbutslightlyangled.
Thehipandperiarticularlesions
Hipjoint
Hipinjectionis notaroutineoutpatientprocedure.Aspirationandinjectionof
thejointeitherunderUSorfluororadiographicguidanceisrecommended.
Greatertrochanterpainsyndrome
Pain at and around the greater trochanter may be due to referred lumbosacral
pain,gluteusmedius(orothertendon)tearorinsertionaltendonitis/enthesitis,or
alocalbursitis.Lesionscancoexist.
• Imagingtoconfirmthelesionandtoruleoutatendontear—whenaninjection
wouldbecontraindicated—isadvisable.
• Trochantericbursitisorenthesitisatthissite,however,oftenrespondswellto
localsteroidinjection.
• US-guided injection is preferable as the inflamed tissue is deep and ‘blind’
injectionplacementmaybequiteinaccurate.
• However,occasionally‘blind’injectionisappropriate.

• Thepatientshouldlieontheirsidewithkneesdrawnupandthemosttender
arealocatedwithmarkers—e.g.withpenontheskin.
• The usual point of maximum tenderness in gluteus medius enthesitis is just
posteriorandhightothegreatertrochanterapex.
• Thesiteofinjectionisatthepointofmaximaltenderness.
• Theinjectiontargetisdeepandthereforeapragmaticapproachusingalarge
volumeissensible(e.g.5–10mL).
• Use20–40mgtriamcinoloneormethylprednisolone(thus1–2mL)andthen
dilutedwithsterilesalineor1%lidocaine.
• InjectionfailureshouldraisethepossibilityofpoorneedlepositionthusUS-
guidanceonasecondinjectionattemptisadvisable.
Otherlesionsaroundthepelvisandhip
• Meralgia paraesthetica occurs as a consequence of lateral cutaneous nerve
entrapment(see Chapter3)asittraversesthefascia10cmbelowandmedial
to the anterior superior iliac spine. If this spot can be clearly demarcated
because of localized tenderness, steroid injection has a greater chance of
success.
• Theischialtuberositiesarelocateddeepinthemedialsideofthebuttocks.The
hamstringenthesesoroverlyingbursaecanbecomeinflamed,causingpainon
sitting. These tender points can be injected. The differential diagnosis is
coccidynia.
• Thecoccyxcanbepalpatedwiththepatientproneorlyingontheirside)andis
amenabletolocalanaestheticandsteroidinjection.
• Adductorenthesitis/insertionaltendonitisisamenabletosteroidinjectionbut
is technicallydifficult. Imaging initially isessentialas there is adifferential
diagnosis—which includes symphysitis, osteitis pubis, ischiopubis fracture,
inguinalhernia,andmedialhipjointlesions.Aninflamedsymphysispubisis
bestinjectedunderUSguidance.
Thekneeandperiarticularlesions
Thekneejoint
Knee joints are, with appropriate training and experience, straightforward to
accesswithaneedlewithoutimagingguidance.
• Accesstothejointisperhapssimplestbythelateralapproachsotheprocedure
doesnothavetotakeplace‘over’thepatient’sotherleg/knee,andtheperson
undertaking the procedure can sit comfortably without having to reach over
thepatient.

• The patient should be supine and comfortable with support under the knee
(whichmaynot,whenthereisaneffusion,beabletoextendfullyandreston
thecouch).
• Markapointaboutathirdofthewaydownthepatellabutmidwaybetween
the upperandlower parts of theleg—thisshould be whereaneffusion will
‘balloon’ out because of pressure distribution within the joint, and thus be
mosteasilyaccessed.
• Awide-gaugeneedleismostappropriategivenaspirationofsynovialfluidis
oftenalsorequiredforsymptomreliefanddiagnostics.
• If theprocedure maybelongbecauseof anticipationthat alargevolume of
fluid will need to be aspirated, then consider anesthetizing the skin and
subcutaneoustissuesfirst.
• Theneedleisadvancedat90°totheskinsurface(see Plate19).
• Ajointeffusionshouldbereached,inallbutthemostobesepatients,within2
cm.Acommonmistakethatinexperiencedoperatorscanmakeistoinsertthe
needle too far and cause pain by hitting the femur or patella bone with the
needle.
• Ifsepsisorcrystalarthritisissuspected,sendasampleoffluidformicroscopy
andculture,andpolarizedlightmicroscopy,respectively.
• If a sample is needed to assess for infection, take great care to harvest the
sampleinasterileway—withtheaidofanassistanttohelpcollectthesample
inasterilepot.
• Aspiratethe jointtodrynessor untilaspirationbecomesdifficult.Trynotto
repositiontheneedletoomanytimesasthiswillcausetraumaandbleeding—
effusionswithPsAandinfectioncanbelarge(e.g.author’spersonalrecordis
300mLfromaTBeffusion!).
• Access to the joint space may be improved, and greater fluid removal
facilitated, by pressing on the medial side of the knee and pressing on, and
tilting,thepatellawithyourotherhand.
• Disengage the needle from the syringe and re-attach the syringe containing
steroid: 40 mg triamcinolone or methylprednisolone is appropriate for most
sizejointsandconditions—butaddperhaps5mLofeithersterilesalineor1%
lidocainebecausethejointspaceispotentiallyquitelarge.
• Theefficacyofasteroidinjectionmayrelatetotheamountofrestfollowing
the procedure—avoidance of weight-bearing on a flexed knee for example.
Advise48hoursrestideally.
• Icing and NSAIDuse for 24 hoursafterthe procedure mayeasediscomfort
associatedwiththeprocedure.
• Consider follow-up physiotherapy if there is poor extension range and/or

quadricepswastingassociatedwithchronicityofthekneesynovitis.
Kneeperiarticularinjections
• Prepatellar bursitis, patellar ligament enthesitis, pes anserinus enthesitis or
bursitis,andtriggerpointsaroundthekneemayallrespondtolocalsteroidand
anaesthetic.
• US scanning to confirm diagnosis may reasonably be combined with a US-
guidedprocedurebutthedetailsofthisneedtobeagreedwithanappropriate
radiologistinadvance.
• Popliteal cysts can be directly aspirated and injected but due to the risk of
damaging superficial neurovascular structures, should be done under US
guidance.
Theankleandfoot
Ankleandsubtalarjointsandtarsaltunnel
The ankle joint can sometimes be accessed without US guidance though the
techniqueisdifficultwhenaffectedbythecommonoccurrenceofsubcutaneous
oedema.
• Theanklejointislocatedmosteasilywiththepatientsupineonacouchand
wholelegrestedandsupported.
• Thejointlinecanbepalpatedjustlateraltotheextensordigitorumtendonasit
crossestheanklecrease.
• The needle is initially advanced downwards over the dome of the talus and
paralleltothesoleofthefootforabout1–2cminmostcases—whenthereis
aneffusion,theswellingwillballoonout/forwardtowardsthispoint.
• Itisquitefrequenttohitbonewiththeneedlesocautioninneedleplacement
isadvised(see Plate20a).
• It is unusual to be able to aspirate fluid from an ankle joint though a small
volumeisaccessiblewithalarger-gaugeneedle.Theankleisacommonjoint
tobeaffectedbygoutandCPPDarthritissosendinganysampleforPLMis
appropriate.
• For an inflammatory ankle arthritis, 40 mg of triamcinolone or
methylprednisoloneacetatewith2–3mLof1%lidocaineistypical.
• Adviseelevation,rest,andicingpostprocedureandavoidingallbutnecessary
weight-bearingfor48hours.
• Subtalarjointcanbeaffectedbysynovitisandinfectionbutaccessingthejoint
withoutUSguidanceisverydifficult.
• The tarsal tunnel (see Plate 20b) is injected under the flexor retinaculum

betweenthecalcaneumandthemedialmalleolus.
Plantarfasciitis
Theoriginoftheplantarfasciaatthemedialcalcanealtubercleoftheoscalcisis
frequently affected by recurrent trauma and inflammation. The latter occurs
commonlyinaxSpA,PsA,reactive(SpA-associated)arthritis,and IBD-related
arthritis.
• The plantar fascia origin is injected from the medial side after carefully
localizingthepositionofmaximalpain(see Plate20c).
• Neverinjectthroughthesoleofthefoot(i.e.at90°totheskin)butapointof
needle entry at the medial edge of the foot, angled towards the point of
maximaltendernessmaybeoptimal.
• Some clinicians will numb the area with local anaesthetic injection of the
posteriortibialnerve,inthetarsaltunnel(see Plate20b).
• Use40mgtriamcinoloneacetonideormethylprednisolonemixedwith1–2mL
of1%lidocaine.
• Advisepost-procedurefootelevation,restrictingofweight-bearing,andicing
iftheheelissore.
• Manyrheumatologistswillconsideritappropriatetoofferasecondinjectionif
thefirstisonlypartlyhelpful.Allow4–6weekstotellifthefirstinjectionhas
beensatisfactorilyeffectiveornot.
Smalljointsofthefeet
• The MTPJs are injected most easily via the dorsal approach (20 mg
triamcinoloneormethylprednisolone)throughthetoeweb.
• Theneedleisdirectedtowardstheappropriatemetatarsalhead.
• Thesametechniqueisusedtoinjectaroundaninterdigitalneuroma(Morton’s
neuroma).
• Careshouldbetakenwithsterilizingtheskinpriortotheprocedureasthereis
aparticularriskofinfectionaftertheprocedure.

Chapter25
Rheumatologicalemergencies
Septicarthritis
Infectionsinpatientsonbiologics
Acutesystemiclupuserythematosus
Systemicvasculitis
Systemicsclerosis‘crises’
Methotrexate-inducedpneumonitis
Macrophageactivationsyndrome
Paediatricosteomyelitis
Malignanciespresentingwithmusculoskeletalsymptomsinchildren
Septicarthritis
Infectionina joint can progressrapidly, causingtissuedestruction, permanent
deformity, and disability. When septic arthritis is suspected, investigation and
antibiotic initiation should be prompt, and where feasible, infected tissue
resected.Theepidemiologyandaetiopathogenesisofsepticarthritisisreported
in Chapter17.
Septicarthritis:inadults
• Patients may not appear systemically unwell, so a high index of clinical
suspicionisrequired.
• Septic arthritis is more common in patients with established joint disease,
prostheticjoints,andwheretherearecomorbiditiessuchasdiabetes,chronic
renaldisease,immunosuppression,andIVdrugabuse.
• Staphylococcus and Streptococcus are the most common pathogens. Septic
arthritis from Haemophilus influenzae type b is becoming rare due to
vaccinationprogrammes.
• Crystalarthropathyandcellulitisaredifferentialdiagnoses.
• Considerprimaryorsecondaryinfectiveendocarditisinhigh-riskcases,(e.g.
IVdrugusersandprosthetic/diseasedcardiacvalves).
• Gonococcalarthritisisthemostcommoncauseofmonoarthritisinayoung,
sexually active adult; women during menstruation may be at particular risk.
Disseminatedgonococcalinfectionmaypresentasaclinicaltriadofpustular
skin lesions, tenosynovitis, or migratory arthralgias. The cutaneous
manifestationsarefleetingandarenotrequiredtomakethisdiagnosis.
Septicarthritis:inchildren
• Diagnosisisconsideredifthereishighorspikingfever,lossofweightbearing
or limp, or joint swelling. There may be focal bony tenderness if there is
associatedosteomyelitis(especiallyininfants).
• Mostcasesoccurinyoungchildren(50%ofcasesaged<2years).
• Thelowerlimbisinvolvedin75%ofcases(knee>hip>ankle).Theshoulder
isacommonlyaffectedsite.
• Presentationdependson organismand hostimmunity.Infants mayhavefew
signsandnotappearunwellorpyrexial.
• Although >2 joints may be affected, this is rare, and alterative diagnoses
shouldbeconsidered,e.g.JIA.
• Theyieldfromjoint/boneaspirateandbiopsyispoor.
• Staphylococcusaureusisthemostcommoncauseinchildren,butcommunity-
acquired methicillin-resistant Staphylococcus aureus (MRSA-CA) is
increasinglycommon.Considerotherpathogensbyage:
• Neonates:EscherichiacoliandgroupBstreptococci.
• 2monthsto5ygroupAStrep,andStrep.pneumoniae.
• Adolescents:Neisseriagonorrhoeae.
• Mycobacteriumtuberculosisisanincreasinglyrecognized,albeitrarecauseof
chronicpyogenicarthritis.MantouxandanIFNγreleaseassay(IGRA)should
bedoneinhigh-riskcases.
• ConsiderHaemophilusinfluenzaetypeBinnon-vaccinatedchildren.
• Viral-induced transient synovitis of the hip is an important differential
diagnosis.Itisabenigncondition,farmorecommonthansepticarthritisofthe
hip, presenting with hip pain, impaired mobility, apyrexia, and without
systemicupset.
Immediatemanagementofsepticarthritisinadults
• Jointimmobilization,analgesia,andfluidresuscitationifseptic.
• Laboratory testing (FBC, U&E, creatinine, LFT, ESR, and CRP) and blood
cultures.
• CompletejointdrainagesynovialfluidanalysiswithGramstain,culture,and
polarizedlightmicroscopy.
• Joint fluid with a white blood cell count >50,000/mm
3
(mainly neutrophils)
andaglucose<400mg/Lishighlysuggestiveofinfection(see Chapter17).
• Ifcrystalsareevident,andculturesarenegativeafter48hours,adiagnosisofa
crystalarthropathyshouldbeconsidered(see Chapter7).
• Antibiotic therapy initiation immediately after joint samples have been
obtained.Cultureandsensitivityresultsmaychangeantibiotictherapyasthey
becomeavailable,butbroad-spectrumIVtherapyshouldbegiveninitially.
• Joints with implants or prostheses should not be aspirated without prior
discussion with an orthopaedic specialist, and should only be aspirated in
steriletheatreenvironments;ideallypriortoantibioticadministration.
• Foranon-gonococcalsepticarthritis,seekorthopaedicinputforjointwashout,
and microbiology input to arrange a Gram stain of joint fluid and set up
cultures/special tests for atypical organisms (especially for a septic arthritis
resistanttoempiricantibiotics).
• EmpiricantibiotictreatmentintheabsenceofapositiveGramstaininadults
inastraightforwardclinicalscenarioshouldbeguidedbylocalpolicies;some
examplesregimensaredetailedasfollows:
• Common regimens include flucloxacillin 2 g IV four times a day ±
gentamicinIVorathird-generationcephalosporin.
• In cases of suspected MRSA infection, discussion with microbiology and
considerationofvancomycinisadvised.
• Pseudomonas spp. should be suspected in IV drug users (Table25.1) and
treatedwithcephalosporinIVwithanaminoglycoside(e.g.gentamicin3–5
mg/kgIV).
• Forfurtherinformationsee Chapter17.
Managementofsepticarthritisinchildren
Followsasimilarlinetoadultsandincludesahipultrasoundinchildrenifthe
cause of the limp is not obvious. IV antibiotics and analgesia will depend on
localpolicies,butasaguideaccordingtoage(seeTable25.1andTable25.2)the
followingarerecommended
Table25.1Post-immediatemanagementofsepticarthritisinchildren
Diagnosticstatus Management
Diagnosisnotconfirmed
Clinicallyimproved
SplintandcontinueIVantibiotic1–2weeks
Then switch to oral co-amoxiclav for a total
treatmentof4–6weeksaccordingtoclinical
condition
Confirmeddiagnosis
(pus ± 50,000 leucocytes ±
pathogenisolatedinblood
orsynovialfluid)
Splint and continue IV antibiotic 1–2 weeks
andadjustbasedonculture/susceptibility
Then switch to oral co-amoxiclav for a total
treatmentof4–6weeksaccordingtoclinical
conditionandpathogen
Weeklyclinicalandlaboratoryfollow-up
Diagnosisnotconfirmed
Clinicallynotimproved
Reviewantibiotics
Obtain paediatric infectious disease specialist
advice
Further evaluation to consider other types of
non-infectiousarthritis
Table25.2Summaryofantibioticsbyagegroup
Neonate(<3
months)
Benzylpenicillinandgentamicin
Orcefotaxime
Addamoxicilliniflisteriasuspected
Oralswitchtoco-amoxiclav
3months–5
years
Cefuroxime
Oralswitchtocefalexinorco-amoxiclav
>5years Flucloxacillinorclindamycin
Considerceftazidimeorciprofloxacinifpseudomonas
suspected
Oralswitchtoco-amoxiclavsuspensionorflucloxacillinor
clindamycintablets
ReproducedfromWattsetal.(2013)OxfordTextbookofRheumatologywithpermissionfromOxford
UniversityPress.
• <3monthsold:IVcefotaximeandamoxicillin.
• 3months:5yearsold:IVcefuroxime.
• >5yearsold:IVflucloxacillin
Post-immediatemanagementofsepticarthritisinadults
• Regularanalgesiareview.
• Assessformultiplefociofinfection.

• Discontinueanyimmunosuppressants,butconsiderstress-doseglucocorticoids
(GCs)ifthepatientissystemicallyunwellandhasbeenonlong-termGCs.
• Adjustantibioticsaccordingtoculturesensitivitiesandindiscussionwithan
infectiousdiseasespecialist.
• For affected weight-bearing joints, keep non-weight-bearing until there is
obviousimprovementinpainandswelling,andyouareconfidentthepatientis
onappropriateantimicrobials.
• Physical therapists should be involved early to help passive mobilization of
jointbeforepatientweight-bears.
• The evidence for routine duration of antibiotic course is not strong and the
regimen should be tailored to the individual. A common protocol is IV
antibioticsfor1–2weeks,followedbyoralantibioticsfor2–4weeks.
• Reasonsforlimited/noresponsetotreatmentcaninclude:
• Alternative diagnosis. Consider crystal-induced MSK disease (see
Chapter7),RA(see Chapter5),andspondyloarthritis(see Chapter8).
• Concomitantcrystal-inducedMSKdisease,reactivearthritis,foreignbody,
orflareofunderlyingarthritis,e.g.RA.
• Inappropriate antimicrobial choice for an atypical organism (e.g.
Mycobacteriummarinum,Borrelia,fungus)ormultipleinfectingorganisms
(see Chapter17).
• Secondary osteomyelitis—especially if treatment had been delayed (see
Chapter17).
• Surgical lavage may need to be repeated, and surgical synovectomy
considered. Recalcitrant cases may require joint excision ± subsequent
arthroplasty.
Gonococcalsepticarthritis
• Synovial fluid and blood cultures can be negative. If gonococcal infection
suspected,re-culturebloodbutalsourethra,cervix(80–90%positive),rectum,
pharynx,anyskinpustules,andjointfluid.
• UrinecanbetestedforgonococcalnucleicacidbyPCR.
• Treatment should be guided by local policies but a common regimen is
ceftriaxone1g IM orIV every24hours. An oralswitch can beconsidered
after 24–48 hours when clinical improvement is seen. Treatment should
continuefor7days.
• Duetoincreasingorganismmicrobialresistance,treatmentwithciprofloxacin
isnolongeradvisable.
• ConsiderempirictherapyforChlamydiawithdoxycycline100mgfor7days
oronedoseofazithromycin1g,andconcurrenttestingforHIVandsyphilis.

• All sexual partners should receive one dose of ceftriaxone 125 mg IM and
empirictreatmentforChlamydia.
Infectionsinpatientsonbiologics
• Overthelast10years,immunosuppressantsthatspecificallyinhibittheactions
ofTNFα, Il-6,and Tcells,anddeplete Bcells havebecomewidelyusedto
treatmultiplerheumaticdiseases(see Chapter23).
• Theriskofinfectionsisincreasedwithuseofthese‘biologic’drugs,although
isprobablygreaterwithanti-TNFαagentsthanotherclasses.Patientswitha
history of serious infections should be treated with this class of drug with
extremecautionandvigilance.
• Theriskandseverityofinfectionsmaybeincreasedinthosealsotakingother
immunosuppressants,typicallyMTXorGCs.
Commonpathogens
• Patientsareatparticularriskfortuberculosis(TB).
• Disseminatedfungalandviralinfectionscanoccur(Table25.3).
• Reactivationoflatentinfectionsmaybeaparticularproblem.
• Latenthistoplasmosisshouldbeconsideredinpatientsfromendemicregions
orwithahistoryofpotentialexposure(e.g.caving/potholing,construction).
• Listeriosis should be considered in the context of unpasteurized dairy
consumption.
Tuberculosisanditsrisk
ReportsofTBoccurringwithbiologicsadvocatetakingprecautions:
• ScreenforlatentTBpriortoinitiationoftherapy.
• Screenpeoplewhotraveltoendemicareasandhealthcareworkers.
• Screenusingintradermalinjection ofPPDandCXRgiven thepossibilityof
anergy.
• With PPD injection, induration of ≥5 mm should be considered a positive
responseformostpatientswithrheumaticdisease.
• If active TB is found, patientsshouldbetreated as per the British Thoracic
SocietyGuidelineandtreatmentshouldbepostponeduntil≥2monthsofanti-
TBtherapyhasbeenreceived.
• Reactivation of TB should be considered in biologic-treated febrile patients
andthosenotscreenedforTBbeforebiologictreatment.
• Patientsmayneedalongerthannormalcourseofantibioticsandneedcareful
reassessmentbeforerestartingtherapy.
Varicellainfections
• Ifapatientonabiologic,orahouseholdcontact,developsprimaryvaricella
(chickenpox),thenvaricellaimmunityshouldbechecked.
• People not immune and at significant risk of infection should be given
varicellazosterimmunoglobulinwithin72hours.Thiswillprovidetemporary
immunity.
• If a patient develops shingles, standard treatment should be given and the
biologicwithheld.
Table25.3Organismsandinfectionsreportedwithbiologics
Organisms Natureofinfection
Bacteria Mycobacteriumtuberculosis Disseminated
Pulmonary
Atypicalmycobacteria
Listeria Septicaemia
Septicarthritis
Meningitis
Staphylococcus Septicaemia
Cavitatingpneumonia
Salmonella Septicaemia
Septicarthritis
Moraxella Septicarthritis
Actinobacillus Septicarthritis
Nocardia Respiratorytract
Viruses Varicella
Herpessimplex
HepatitisB/C
CMV
Disseminated
Severe
Reactivation
Disseminated
Fungi/yeasts Candida
Cryptococcus
Aspergillus
Sporothrix
Pneumocystis
Septicaemia
Pneumonia
Disseminated
Skin
Pneumonia
Histoplasmosis Disseminated
Parasites Leishmania Visceral
Acutesystemiclupuserythematosus
Acute systemic lupus erythematosus (SLE) will manifest either as a flare in
patientswithanestablisheddiagnosisorasthefirstpresentationofthedisease.
Declining C3 and increasing dsDNA titres may predict acute disease flares in
somepatients.Thereaderisreferredto Chapter13forSLEandto Chapter
11forantiphospholipidsyndrome(APS)andcatastrophicAPS.
DiagnosingSLEinanacutemedicalcontext
• Consider SLE as a diagnosis in all young and middle-aged women who
presentwithahistoryofjointpain,photosensitiverash,orpleuriticchestpain.
• Raynaud’sdisease(RD)andrecurrentmouthulcersarenon-specific,butmay
alsoappearinassociationwithSLE.
• ANA serology and complement levels may not be available at initial
assessment.
• InflammatorymarkerssuchastheESRorCRParenotreliableindicatorsof
SLEactivity.
• Although pericardial effusions are common with SLE, they are generally
trivial. Cardiac tamponade is found in <1% of patients. Since the effusion
tendstoreflecttheoveralldiseasestate,generallytreatmentoftheunderlying
disease is adequate to resolve the effusion. Rarely, therapeutic
pericardiocentesisisrequired.
AcuterenalSLE(adults)
• ChecktheBP,sendbloodforcreatinine,U&E,sendurineforculture,aspot
urine protein/creatinine ratio (as an estimate of proteinuria) and organize a
renaltractUStoruleoutpost-renalobstruction.
• Quantification of urinary protein and creatinine grades severity of the renal
lesionandguidesmanagementapproach(Fig.25.1).
• Control BP aggressively. Use an ACE inhibitor or ARB for those with
proteinuria.
• Biopsy can inform treatment decisions. Induction treatment is usually given
withGCsandoralmycophenolatemofetil(titrateto1–1.5gtwicedaily)orIV
cyclophosphamide.
• GC-inducedosteoporosisandcardiovascularriskshouldbemanagedfromthe
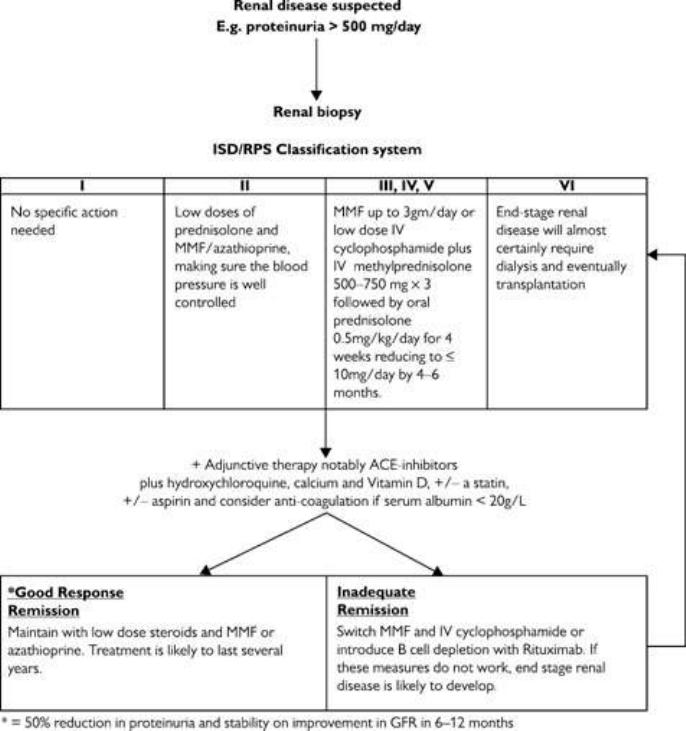
outset.Considergettingthefollowingdoneearly:DXAscan,ECG,andfasting
lipidpanel.
• Daily calcium (1000–1500 mg) and vitamin D (800 IU) should be
administeredtoallpatientsreceivingGCs.
• Withcyclophosphamide,thereisaneedtocounselpatientsabouttherisksof
infertility, malignancy, and haemorrhagic cystitis, the dosing schedules (e.g.
using mesna), monitoring (FBC at day 10 after and prior to IV pulse), and
Pneumocystisprophylaxischemotherapy(e.g.trimethoprim-sulfamethoxazole;
Fig.25.1).
Fig25.1Flowdiagramofthemanagementofrenalsystemiclupuserythematosusbasedonourown
practice.ReproducedfromWattsetal.(2013)OxfordTextbookofRheumatologywithpermissionfrom
OxfordUniversityPress.
AcutecardiorespiratorySLE(adults)
• CardiacandisolatedpulmonarymanifestationsofSLEarerare andinmany
patientswithSLE,acutecardiacandpulmonaryfeaturesmaybeduetoother
commonconditions(Table25.4).
• CRP elevation may reflect infection or significant pleuropericardial SLE.
Lupus pericarditis alone without evidence of cardiac compromise can be
treated with NSAIDs and prednisone 20–40 mg daily for 2–4 weeks with
subsequentGCdosetaper.
• Ifnotduetocardiacfailure,acutedyspnoeainSLEmaybeduetointercurrent
infection, pneumonitis, pulmonary vasculitis, pulmonary embolism,
pulmonaryhypertension,ordyspnoeafromthepainofpleuralserositis.
• Cyclophosphamide should be considered for severe or life-threatening
manifestationsofSLE.
AcutehaematologicalSLE(adults)
• ManypatientswithSLEareCoombs(directantiglobulin)testpositivewithout
havinghaemolysis(anddonotneedtreatingassuch).
• Features of haemolysis include fever, shivers, pyrexia, anaemia, elevated
bilirubininserumandurine,lowserumhaptoglobins,andreticulocytosis.
• Acutethrombocytopeniaisarelativelyfrequentpresentation.
• If severe, both haemolytic anaemia (Hb <70 mg/L) and thrombocytopenia
(platelets<25,000)require high-doseprednisone60–80 mg/day andAZA or
CYC(pulsedIVororal).
AcuterenalSLE(paediatrics)
• ThemostcommonlesionisClassIVdiffuseproliferativeglomerulonephritis
(30–45%ofcases),andcarriestheworstprognosis.
• One-third of children with acute renal SLE have hypertension which often
needsaggressivemanagement.
• All have microscopic haematuria and proteinuria >3 mg/kg/day. Most have
>25mg/kg/dayproteinuria.Upto33%haveserumalbumin>35g/L.About
50%maintainGFR>100mL/min/1.73m
2
.
• PrognosisandtherapyofnephritisisguidedbythehistopathologyactiveISN-
grade pathological lesion and chronicity index, thus obtaining a biopsy is
important.
• Management shouldbe ina specialistunit,andincludeshigh-doseGCsand
MMF600mg/m
2
BD.InsomecasesIVCYCuitilisingthelow-orhigh-dose
Eurolupusprotocolisusedforinductionorflareoflupusnephritis.
• The value of plasma exchange and IVIg in crescenteric or fulminant renal
disease is unclear but its often considered, and dialysis may ultimately be
necessary.
Table25.4Importantaspectsinmanagementofacutecardio-respiratorySLE(adults)
Initialclinical
cardiacassessment
ECG,bloodforCK,troponinT,echo
Initiallung
assessments
ABGs,CXR,spirometry,HRCTchest,VQscan
Consider
pulmonaryembolus
Considerempiricalanticoagulationearlyandcheckfor
lupusanticoagulant,APLantibodies,andcomplete
thrombophiliascreen
Pulmonary
vasculitis(very
rare)
Features:severedyspnoea,CXRabnormal.Requires
ICUandrespiratoryphysiciansupportandconsider
plasmaexchange
Interstitiallung
disease
Requireshigh-dosesteroidsandeither
cyclophosphamide,azathioprine,ormycophenolate
mofetil
Antiphospholipid
syndrome
PE-associatedwithAPLsyndromeinSLErequires
lifelonganticoagulation
Specifictherapies
Glucocorticoids Assumingnon-viralinfectionsexcludedortreated
mostcardiopulmonarySLEfeaturesrespondtooral
prednisone0.5–1mg/kg/day.Consider
methylprednisolone1gIV×3daysifclinicalsituation
extreme
Mycophenolate Mycophenolatemofetil(0.5mgtwicedailyinitially
increasingafter1–2weeksto1–1.5gtwicedaily)can
beconsideredifAZAorcyclophosphamide
contraindicatedorpatientintolerant.Itisincreasingly
beingusedinsteadofcyclophosphamideforinducing
remissioninlupusnephritis
Anti-CD20 Thoughevidenceminimal,rituximab(anti-CD20)1g
infusionrepeatedafter2weeksmaybeconsideredif
otherimmunosuppressantsarecontraindicatedorcause
sideeffects
Fragility AllpatientstreatedwithGCsrequiredailycalcium(1
fracture/osteoporosis
prevention
g)andvitaminD(800IU).Forall>50yrsa
bisphosphonateshouldbeofferedinitially(and
withdrawnifDXAscanandoverallfracturerisk
assessment(e.g.FRAX)suggestsfractureriskislow.
Localguidelinesmayexist
AcutehaematologicalSLE(paediatrics)
• Overthaemolysisoccursin<10%,thrombocytopeniain15–45%.
• Bleedingisuncommon.
• AutoimmunehaemolyticanaemiaistreatedwithoralGCs,but,whenthereis
rapidlyprogressinganaemia,IVmethylprednisoloneandIVIgmaybeneeded.
• Most patientswiththrombocytopenia respondtooral GCs.Ifthere is active
haemorrhage or no response to oral GCs, then IV methylprednisolone and
IVIgmaybeneeded.
• Splenectomyshouldbeavoided.
• A high index of suspicion is needed to diagnose catastrophic APS. It is
characterizedbymultipleorganthrombosesandmicroangiopathy.
• Leucopeniausuallyresolvesasdiseaseactivityimproves.
• If there is neutropenia with infection, granulocyte colony stimulating factor
can be used to increase the neutrophil count. If neutropenia is due to drug
toxicity and infection is absent, this usually improves with stopping or
decreasingthedoseoftheoffendingmedication.
• Close working with haematologists will assist interpretation of coagulation
studiesandadviseonanticoagulantuseincludingfactor10ainhibitors.
Systemicvasculitis
A vasculitis flare should be treated aggressively because permanent damage
from tissue ischaemia may occur rapidly. Patients diagnosed with pulmonary
capillaritisorglomerulonephritiswilltypicallybenefitfromtreatmentwithpulse
GCs. The specific management of each type of vasculitis is outlined in
Chapter 15. See Table 4.2 p. 212 for precipitants and associations of
leucocytoclasticsmallvesselvasculitisand Table4.3p.214fortherangeof
laboratorytestsneededinpatientswithsuspectedvasculitis.
Giantcell(temporal)arteritis
• Sincegiantcellarteritis(GCA)canleadtocranialischaemiceventsincluding
blindnessandstroke,treatempiricallyifsuspected.

• TheprevalenceofGCAincreaseswithage.Visualchanges,jawclaudication,
and diplopia in the setting of B-type symptoms all support the diagnosis of
GCA.
• Empirictherapyiswithprednisone40–60mgdailyfor1monthbutifthereare
visualsymptoms,urgentophthalmologyexaminationisessential.
• IschaemicGCA-relatedocularpathologyistreatedwithmethylprednisolone1
gIVfor3days.
• Daily low-dose aspirin decreases the risk of cranial ischaemic events, and
should be used as part of standard therapy unless there is a clear
contraindication.
• Treatmentshouldnotbedelayed.Biopsyisdiagnosticallyusefulupforsome
weeksafterGCtherapyisinitiated.
• To optimize yield, temporal artery biopsy should be bilateral, with samples
>1.5cminlength.
‘Severe’vasculitis
• Patientswithactivevasculitiscanquicklydevelopmanifestationsthatthreaten
lifeorthefunctionofavitalorgan.
• Patients with a potential flare of vasculitis, already on immunosuppression,
needthoroughassessmenttoruleoutinfectioninitially—see Tables4.2and
4.3(p.212andp.214).
• Severe manifestations of the small vessel vasculitides include pulmonary
haemorrhage(orcapillaritis)andglomerulonephritis.Severemanifestationsof
mediumvesselvasculitisincludemononeuritismultiplex(e.g.footdrop/wrist
drop)andmesentericangina/ischaemia.
• When glomerulonephritis is suspected, renal biopsy should always be
considered.
• Severevasculitisisgenerallytreatedwithpulsemethylprednisolone1gIVfor
3days,followedbyprednisone1mg/kg/day.
• Most patients with severe vasculitis will also be treated with
cyclophosphamide 1.5–2.0 mg/kg/day. Lower doses should be used in the
elderlyorinpatientswithrenalinsufficiency.
• Plasmapheresis can belife-savingfor AAV-related pulmonary vasculitis;not
allcentreshaveafacilitytogiveplasmapheresisthough.
• Cyclophosphamide places patients at risk for Pneumocystis infection, and
appropriatechemoprophylaxisshouldbeinstituted.
• Inpatientswhodeclineonclinicalgrounds,despiteimmunosuppression,then
infectionsmimickingvasculitisshouldbeconsidered.

Systemicsclerosis‘crises’
Renalcrisis
• Thismaymanifestasanacuteorsubacutehypertensivecrisis,usuallywithin
thefirst4yearsafterdiagnosisofdiffusesystemicsclerosis(dcSScl).Itcanbe
thepresentingfeatureofSScl(see Chapter13).Itrarelyoccursinlimited
cutaneousSScl(lcSScl).
• AnabruptincreaseinBP>150/85andnewrenalinsufficiencyareconsistent
with this diagnosis. Very occasionally patients are normotensive, and
paradoxicallysubjecttoapoorerprognosis.
• Other manifestations include those of a hypertensive emergency:
microangiopathic haemolytic anaemia, encephalopathy, and hypertensive
retinopathy.
• Urinalysisisusuallynormal.
Management
• ACEinhibitorsarethecornerstoneofrenalcrisismanagement.
• The patient should be treated with escalating doses of captopril until BP is
broughtundercontrol.Calciumchannelblockerscanbeaddedsequentiallyif
captoprilisinadequate.
• FastdropsinBPshouldbeavoided,aslowperfusionpressuresinabnormal
renalvesselsmayworsenrenalfailure.
• Early consulting with a nephrologist about the potential need for
haemodialysisisprudent.
• Promptinitialtreatmentcanleadtoreturnofgoodrenalfunction.
Pulmonaryhypertensioncrisis
(Seealso Chapter13.)
• Primary pulmonary arterial hypertension (PAH) occurs as a complication of
lcSScl, although it can also occur in dcSScl (both as a primary feature and
secondarytopulmonaryfibrosis).
• Echocardiography can be used to screen for PAH. A RVSP estimate of >40
mmHg is suggestive, but the diagnosis must be confirmed by right heart
catheterization.
• Decompensated PAH presents with dyspnoea, syncope, raised JVP, loud P2
heartsound,andankleoedema.
Management
• Intensivecoronarycareunitmonitoringisessential.
• Patients withrapidly decompensatingheart failuresecondary toPAHshould
betreatedwithsupplementaloxygen,diuresis.
• ContinuousIVepoprostenolcanbeconsideredbutdecreasingcardiacpreload
toomuchcanreduceoverallpulmonaryperfusionifthePAisnotresponsive.
• Diuretics decrease right ventricular preload, and can lead to significant
symptomaticrelief.
• AlargepulmonaryembolismcanalsoresultinrapidlyworseningofPAH,and
should be considered contributory if the PAH was known to be high
previously,ifthereisAPSandintheappropriatesetting.
Methotrexate-inducedpneumonitis
Thisisrarebutcanoccurinanypatienttakingmethotrexate(MTX).
Epidemiologyandriskfactors
• Incidence5–70 per1000patientsperyeartakingMTX.Itis probablymuch
rarerinchildren/adolescentscomparedwithadults.
• Life-threatening pneumonitis requiring hospital admission occurs in <1%
patientstakingMTX.
• Mildpneumonitislikelyresolvesondrugwithdrawalalone.
• Mostpatientssufferingfrompneumonitisdosowithinthefirstfewmonthsof
startingMTXorafterasignificantdosechange.
• In patients on stable-dose MTX, blood levels may change in the setting of
progressiverenalinsufficiencyorlowlevelsoffolate.
• ConsiderthediagnosisinallpatientsonMTXwithacuteonsetofdrycough,
dyspnoea,headache,andfever.
• The differential diagnosis lies between chest infection, acute pulmonary
oedema, or acute interstitial lung disease associated with the underlying
condition.
Managementofseveretoxicity
• StopMTX.
• Intensiverespiratorycareisnotoftenneededbutshouldbeconsidered.Severe
casesneedsupplementaloxygenandbloodtransfusion.
• Assessforinfection.Considerbronchoalveolarlavagefor samplesandhigh-
resolutionlungCT.Itmaybenecessarytotreatempiricallyforthemostlikely
pathogens,whileawaitingresults.
• Optimal therapy for MTX-induced pneumonitis has not been well defined.
Folinicacid(15–25mgorallyfourtimesaday)mayreverseMTXtoxicity.
• Anecdotally, GCs accelerate recovery. In cases of severe respiratory

decompensation,treatwithmethylprednisolone1gIVfor3days,followedby
prednisone1mg/kg/day.Prednisonecanbetaperedoverthesubsequent1–6
months,dependingondiseaseseverity.
• Most patients with MTX-induced lung injury will recover, but may have
chroniclungdamageasaresult.
Macrophageactivationsyndrome
Macrophageactivationsyndrome(MAS)israrebutislife-threatening(mortality
is8–22%).MAScancomplicateotherdiseases.MASisalsotermedsecondary
haemophagocytic lymphohistiocytosis (HLH). For a summary, see
http://www.the-rheumatologist.org/article/macrophage-activation-syndrome/6/
Pathology
• Activatedmacrophagesengulfotherhaematopoieticcellsinthebonemarrow,
liver,andspleen.
• PolyclonalT-andNK-cellactivationisassociatedwithacytokine‘storm’with
consequentextensiveimmunologicalabnormalities.
Presentationandclinicalfeatures
• A high level of suspicion remains key to MAS diagnosis as it may present
insidiouslyinanalreadyunwellchild.
• Unremitting fever and high levels of persistent inflammation despite broad-
spectrumantibioticsoranunexpectedfallinESRassociatedwithnew-onset
cytopeniaandhyperferritinaemiashouldraisesuspicionofMAS.
• MAScanbetheinitialpresentationoracomplicationofoncologic,infectious,
and rheumatic disorders, including systemic-onset JIA, SLE, and Kawasaki
diseaseandlesscommonlyjuvenileDM,PAN,polyarticularJIA,MCTD,and
otherautoimmuneandautoinflammatoryconditions.
• Sepsisshouldbeconsideredasacause.
• Infective triggers of MAS include EBV, VZV, CMV, coxsackievirus,
parvovirusB19,hepatitisA,Salmonella,andenterococcus.
• If MAS is the initial presentation of an inflammatory illness, assessment
shouldbemadeformalignancy.
• BycontrasttoMAS/secondaryHLH,primaryHLHisusuallyseeninchildren
<2yearsold,withconsanguineousparents.Theremaybeahistoryofdeathof
youngfamilymemberwithunexplainedfever,andaprimarycentralnervous
systempresentation.
Diagnosis
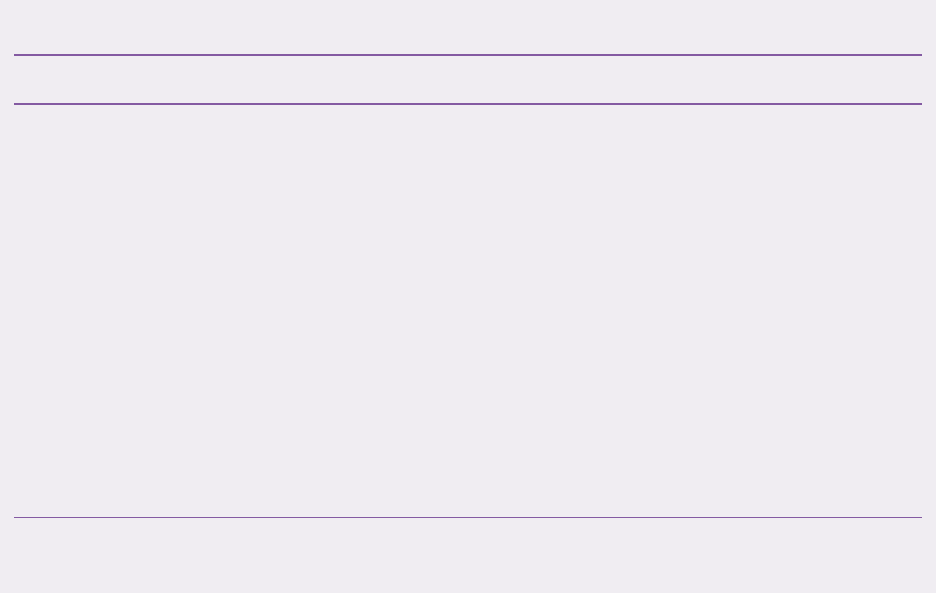
Clinicalfeaturesarenotspecificfordiagnosis.Combinationsoftypicalfeatures
are often present and high suspicion for the diagnosis remains important; see
Table25.5.
• NewdiagnosticcriteriaforMASinthecontextofactiveSoJIA
1
include:
• Ferritin>684ng/mL.
• Plus ≥2 of the following: platelet count <181 × 10
9
/L, AST >48 U/L,
triglycerides>156mg/dL,fibrinogen<360mg/dL.
• The valueoftesting forCD25 andCD163positive circulatinglymphocytes,
low NK-cell activity, haemophagocytosis in bone marrow, liver, spleen, or
lymphnodes,highD-dimer,andabnormalperforinexpression,isdebatable.
Table25.5Clinicalandlaboratoryfeaturesofmacrophageactivationsyndrome
Clinicalsigns Laboratoryfindings
• High, persistent, unremitting
fever or change in pattern of
fever
• New-onsethepatosplenomegaly
• Neurological manifestations
includingirritability
• Lymphadenopathy
• New-onsetheart,lung,orkidney
failure
• Petechiaeorhaemorrhages
• Low/falling ESR in context of active
inflammatorydiseaseorhighCRP
• Low/rapidlyfallingwhitebloodcells,
Hb,orplateletcount
• Low/falling or unexpectedly normal
plateletcount
• Low/falling or unexpected normal
fibrinogen
• Rising AST, ALT, GGT, bilirubin,
triglyceridesandLDH
• Ferritinhigherthanwouldbeexpected
forpatient’sdiagnosis
Haemophagocytosisinthebonemarrowaspirateispresentin60%ofMAScases,andtendstobea
relativelylatesign.AbsenceofhaemophagocytosisdoesnotruleoutMAS.
Treatment
• Treatmentshouldbestartedpromptlyasdelayedtreatmentisassociatedwith
poorprognosis.
• Broad-spectrumantibiotictreatmentisusuallystartedincasesotherthanthose
withactiveautoimmuneconditions.
• First-line treatment of IV then oral GCs is effective in >50% of cases. For
example:methylprednisolone30mg/kg/day(maximum1g)for3consecutive
days,followedbyoralprednisolone1mg/kg/dayandthendosetapering.
• Ifthereisapoorresponsetosteroids,IVIg1–2g/kgisrecommended.

• IL-1 inhibition (e.g. anakinra) is dramatically effective in MAS associated
with SoJIA (and increases survival rate vs placebo in adult sepsis + MAS
features).AnakinraisgivenSCorIV2–8mg/Kg/day(max100mg/dose)in1–
4divideddoses.
• In refractory disease other options include anti-IL-6r (tocilizumab), anti-
TNFα, etoposide, rituximab (anti-CD20+ B-cell therapy) for EBV-driven
MAS,andcyclophosphamideinSLE-associatedMAS.
Reference
1. RavelliA,MinoiaF,DavìS,etal.2016ClassificationCriteriaforMacrophageActivationSyndrome
Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against
Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials
OrganisationCollaborativeInitiative.AnnRheumDis2016;75:481–9.
Paediatricosteomyelitis
Inchildren,osteomyelitisismostcommonininfants;50%ofcasesoccurbefore
5yearsofage.
• Thereisusuallyahistoryoftrauma,typicallyinvolvingthemetaphysisoflong
bones.
• Osteomyelitis can arise from haematogenous spread of pathogens from a
primarysite(e.g.lung,skinear,nose,orthroat)orbydirectinoculationfrom
openfracturesorpenetratingwounds.
• Thereareacute,subacute(2–3weeks’delay),chronic(rareinchildren),and
non-bacterial (e.g. CRMO or SAPHO) forms of osteomyelitis (see also
Chapter17).
Malignanciespresentingwithmusculoskeletal
symptomsinchildren
Causes
The annual incidence of primary malignant tumours of bone, synovium, or
muscle is 6 per 1 million children. The main causes are osteosarcoma (about
50%ofcases)andEwingsarcoma(40–45%ofcases).
• Widespread MSK symptoms may of course be from bone metastases from
osteosarcomaorEwingsarcoma.
• Bone marrow infiltration by different lymphoproliferative disorders can
presentwithMSKsymptoms.
Presentationandclinicalfeatures
• Malignancy should be suspected, particularly in an adolescent if there is
persistentpainoflongbonesorvertebraeof>2weekswithassociated:
• pointtenderness.
• nightawakening.
• painoutofproportionforclinicalfindings.
• Otherfeaturescanincludebonyswellingorenlargement,weightloss,malaise,
pathologicalfracture(5–10%),andrarely,lunginvolvement.
• A mass increasing in size, extending deep into soft tissues, or a presumed
exostosis>5cm,shouldraisethepossibilityofmalignancy.
• The associated arthritisusually involves large joints, ismild,migratory, and
oftenwithoutmorningjointstiffness.
Investigationandmanagement
• Earlyreferraltoapaediatriconcologistisessential.
• Making a diagnosis prior to metastasis greatly enhances the prognosis.
Mortalityratefollowingmetastasisis40%.
• BloodtestsmayshowincreasedinflammatorymarkersandLDH.FBCisoften
normal initially, but there may be a reduction trend in platelet count and
haemoglobin.Alowleucocytecountisalatesign.
• Abloodfilmshowingblastcellsispathognomonicforleukaemia.
• Abonemarrowaspirateortissuebiopsyprovidesahistologicaldiagnosisand
canfacilitatetumourgrading.
• Tumour staging is dependent on the diagnosis, histological grade, and both
sizeandlocationofthetumour.
Imaging
• Plainradiographscharacterizetheprimarybonetumour.
• US is important to screen for hepatosplenomegaly, lymphadenopathy, and
furtherdefinesofttissuemassessuchaslipomaorvascularmalformation.
• MRIprovidesspecificinformationregardingthetumournatureandsizeand
thesurroundingsofttissueinvolvement.
• MRIimagesfacilitatetheplanningofabiopsy.
• CT helps define tumour anatomy prior to surgery and to evaluate for
metastases locally, though bone scintigraphy or whole-body MRI are useful
investigationstogetanoverviewofanyskeletalmetastases.
Treatment
• Therapy measures are beyond the scope of the text here. However, for
overviews see references 2 and 3 for osteosarcoma and Ewing sarcoma
managementrespectively.
Othermalignancies
ManychildhoodmalignancieshaveMSKfeaturesatpresentation,inparticular
acutelymphoblasticleukaemia(ALL),lymphoma,andneuroblastoma.
• Isolated hip or back involvement in a young child raises the suspicion of
leukaemia in the absence of sepsis. Risk factors for leukaemia include
conditionssuchasDown’ssyndrome.
• Backpaincanbeapresentingfeatureofneuroblastomainyoungchildrenand
toddlers and is attributable to metastases which occur in 75% of patients at
diagnosis.
• Limb pain in leukaemia and lymphoma is due to marrow invasion. Pain is
usually intense and continuous and associated with night awakening. Local
signs,suchasarthritisorerythema,maybeabsent.
• All malignancies can be associated with systemic features such as pallor,
petechiae,bruising,weightloss,andfever.
• In lymphoma, there may be hypertrophic osteoarthropathy associated with
painfulperiostitisandlymphadenopathy.
• Investigations should include checking FBC, LDH, LFTs, a blood film,
measuringurinarycatecholamines/metadrenalines,CXR,andabdominalUS.
• Bone marrow aspirate and whole-body MRI are then more definitive
investigations.
References
2. LindseyBA,MarkelJE,KleinermanES.Osteosarcomaoverview.RheumatolTher2017;4:25–43.
3. KridisWB, Toumi N, Chaari H, et al. A review of Ewing sarcoma treatment: is it stilla subject of
debate?RevRecentClinTrials2017;12:19–23.
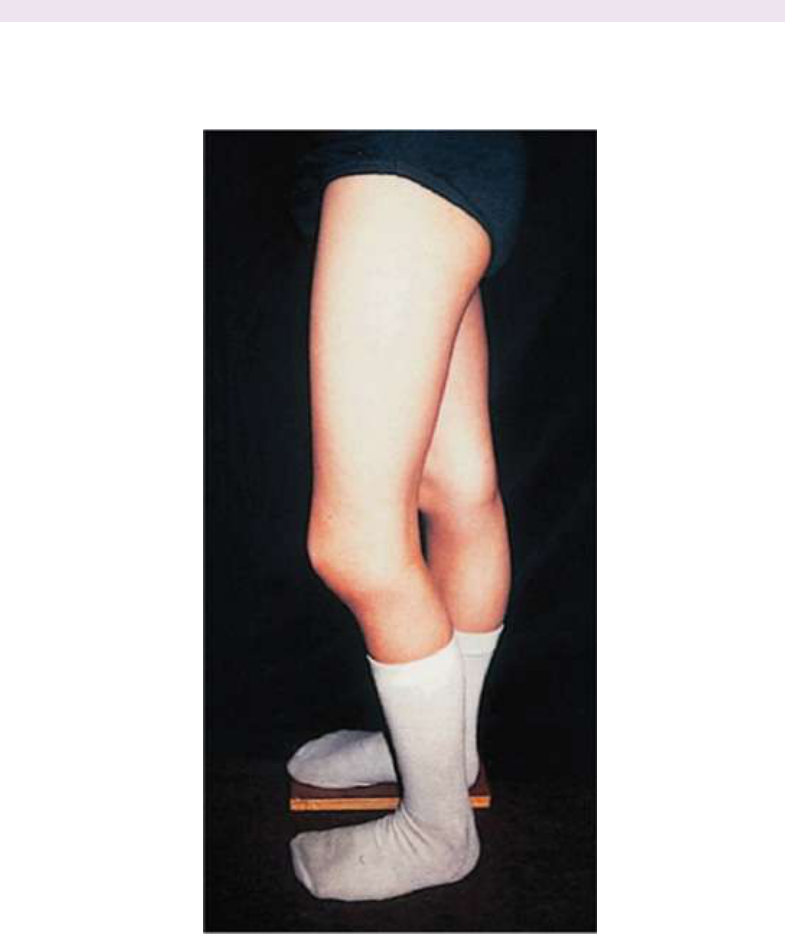
Plates
Plate1Increasedgrowthoftheleftlowerlimbduetochronickneeinflammationin(rheumatoidfactor-
negative)juvenileidiopathicarthritis.
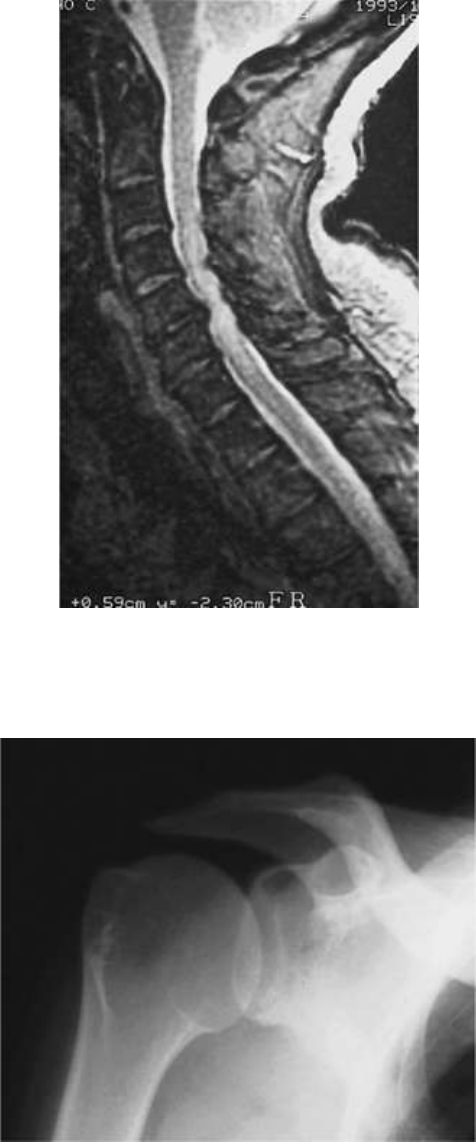
Plate2Magneticresonancescanoftheneckshowinglossofheightandsignalaffectingseveraldiscswith
multisegmentalspondyloticbars,compressionofthecordfromprotrusionoftheC5/6disc,and
myelopathicchanges(highsignal)inthecord.
Plate3Patternsofradiographicabnormalityinchronicsubacromialimpingement:sclerosisandcystic
changesinthegreatertuberosity.
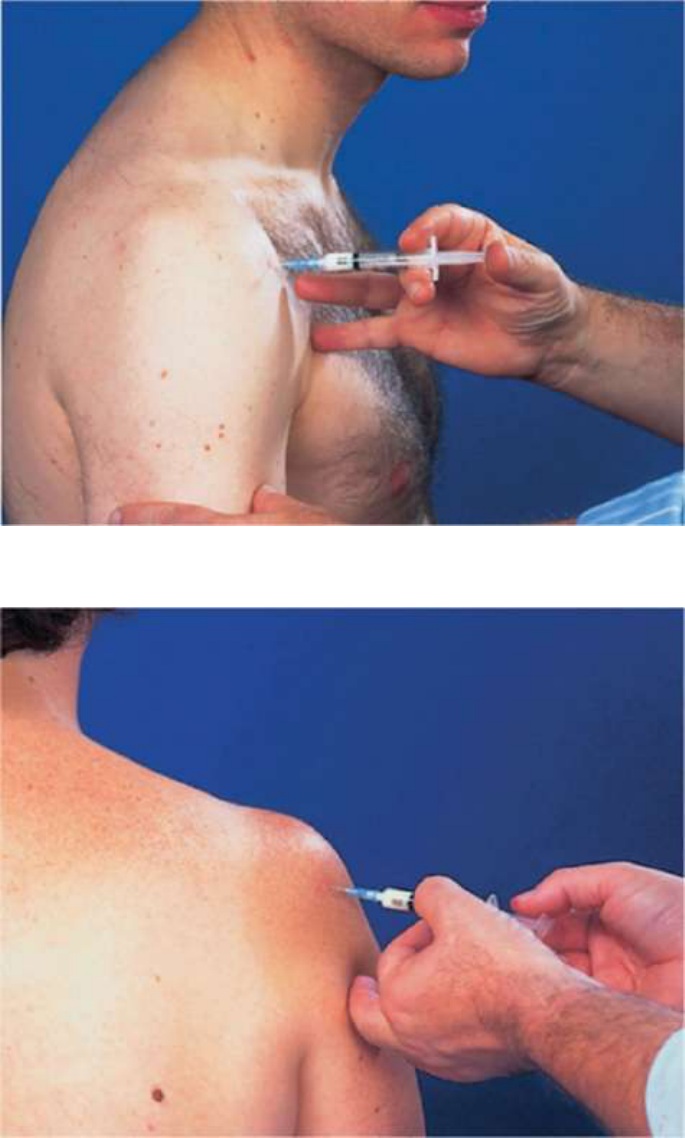
Plate4Injectionoftheglenohumeraljointviatheanteriorroute.
Plate5Injectionofthesubacromialspace.
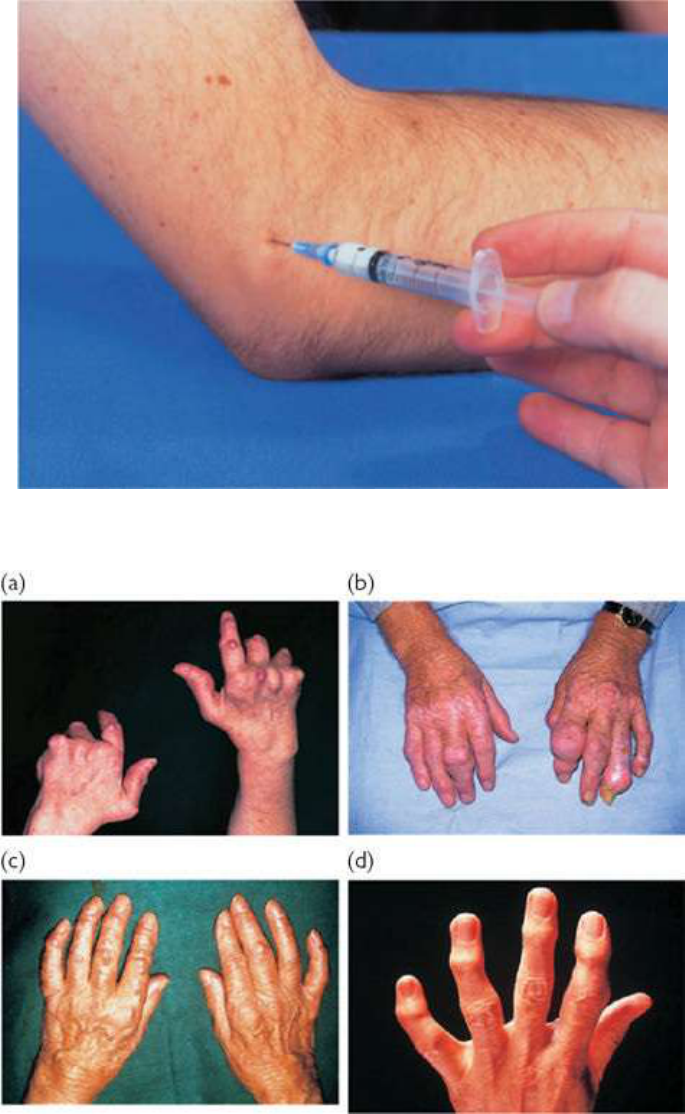
Plate6Injectionoftenniselbow(lateralhumeralepicondylitis/enthesitis).
Plate7Nodulesassociatedwithjointdiseases.(a)RA:typicallyoverextensorsurfacesandpressureareas.
(b)Chronictophaceousgout:tophicanbeindistinguishableclinicallyfromRAnodulesthoughmayappear
aseccentricswellingsaroundjoints(imageprovidedcourtesyofDrR.A.Watts).(c)Multicentric
reticulohistiocytosis:nodulesareintheskin,aresmall,yellowish-brown,andareoftenaroundnails.(d)
NodalOA:swellingisbony,typicallyatPIPJsandDIPJs.

Plate8Dactylitis,nailchanges,andDIPJarthritisinpsoriaticarthritis.
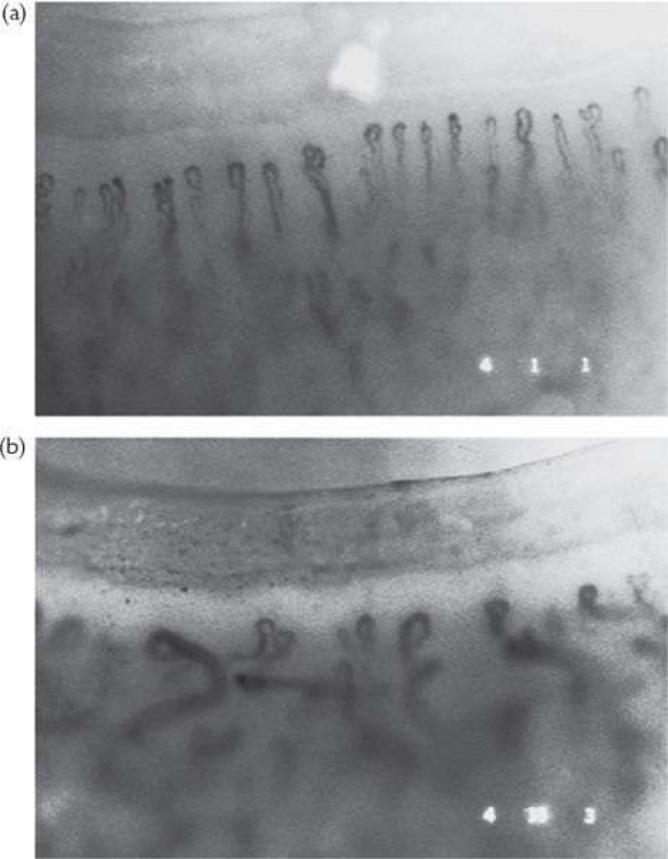
Plate9(a)Normalnailfoldcapillaries.(b)Nailfoldcapillariesinsclerodermashowingavascularareasand
dilatedcapillariesinanirregularorientation(originalmagnification×65).

Plate10Diffusearmandhandswellinginchronicregionalpainsyndrome(osteodystrophy)ina13–year–
oldgirl.
Plate11Slightflexionoffourthandfifthfingersasaresultofanulnarnervelesionattheelbow.Thearea
ofsensorylossisindicatedbythedashedline.
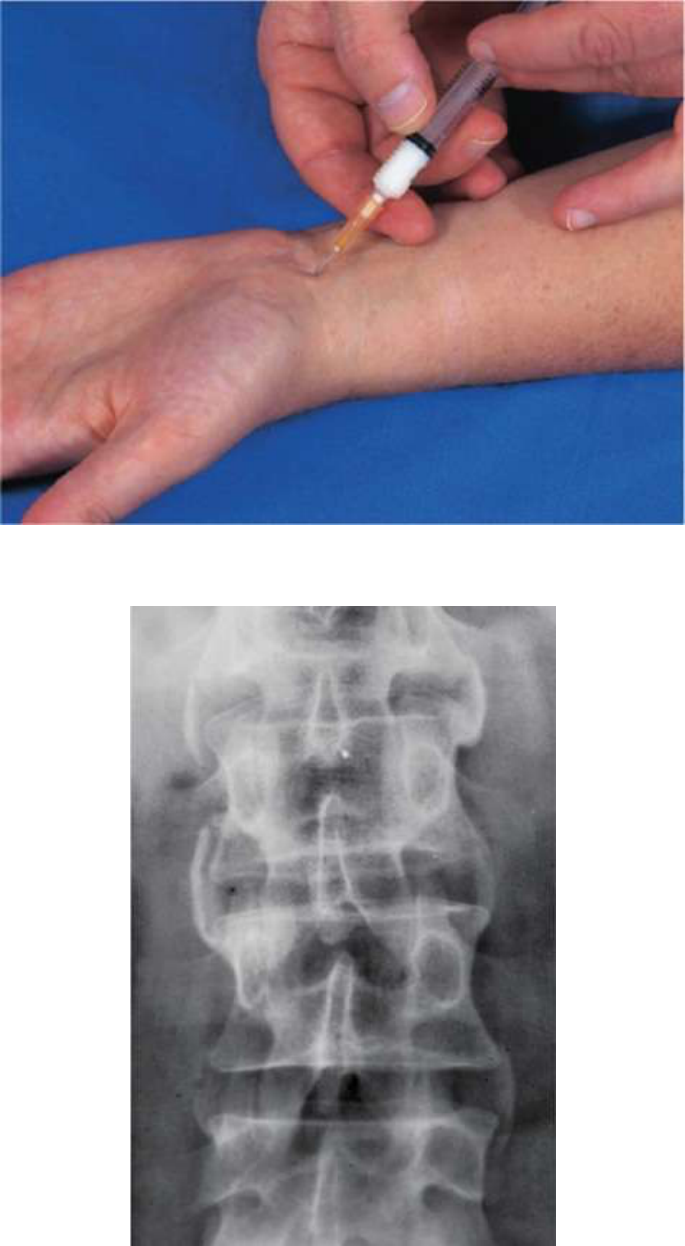
Plate12Injectionofthecarpaltunneltotheulnarsideofpalmarislongustendon.

Plate13Psoriaticspondylitis:non-marginaland‘floating‘(non-attached)syndesmophytes.
Plate14Spondylolysis.Thedefectintheparsinterarticularis(blackarrows)mayonlybenotedonan
obliqueview.Thepatienthashadaspinalfusion(openarrows).
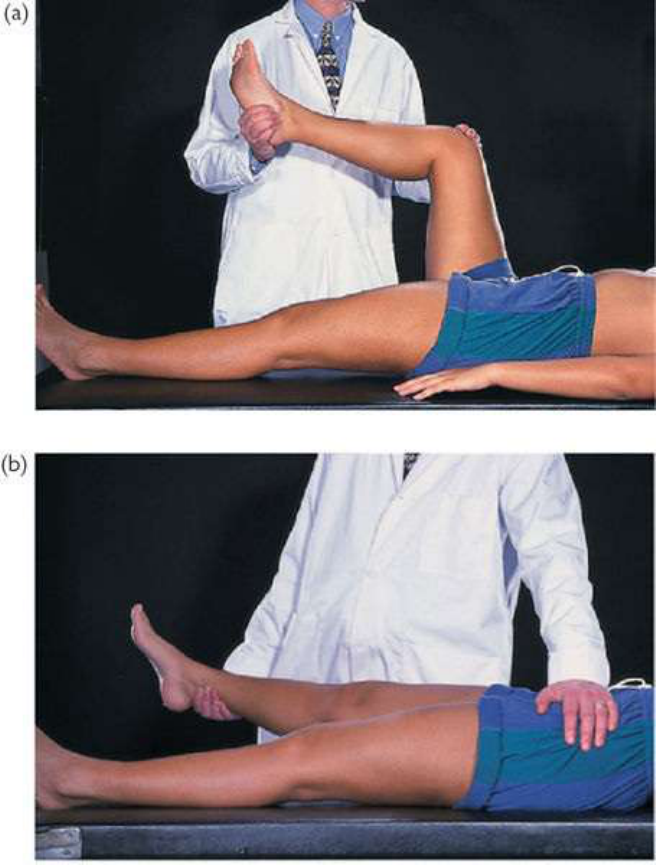
Plate15Testingpassivehipflexionandrotationalmovements(a)andhipabduction.(b)Thepelvisshould
befixedwhentestingabductionandadduction.
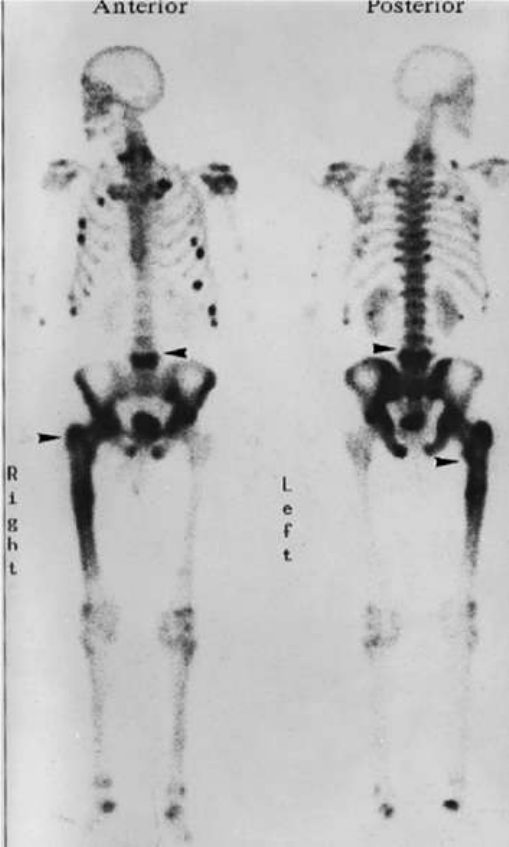
Plate16Bonescintigraphy(
99m
Tc-MDP)ofa65-year-oldmanwithwidespreadbonepainandweakness
suspectedtohavemetastaticmalignancy.Anteriorview(left);posteriorview(right).Undecalcified
transiliacbonebiopsyconfirmedsevereosteomalacia.TherewascoincidentalrightfemoralPaget’sdisease
(arrowedlesions).
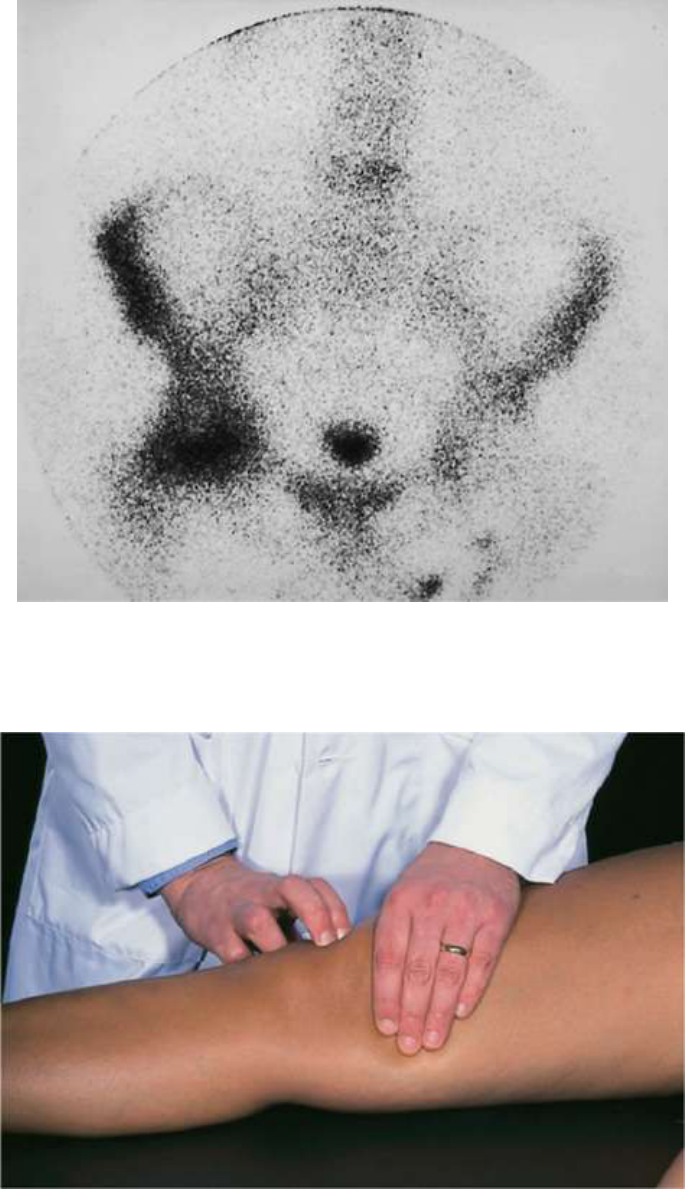
Plate17Bonescintigraphyshowingosteonecrosisoftheleftfemoralhead(ontheright-handsideasthisis
ananteriorview).Hightracerlocalisationindicatesincreasedboneturnoverthoughinsomeinstancesthere
maybephotopenia(anearlysign)whichcorrespondstoischaemia.
Plate18The‘patellartap’test.Anyfluidinthesuprapatellarpouchissqueezeddistallybythelefthand.
Thepatellaisdepressedbytherighthand.Itwillnormallytaptheunderlyingfemurimmediately.Any
delayinelicitingthetaporafeelingofdampingasthepatellaisdepressedsuggestsajointeffusion.
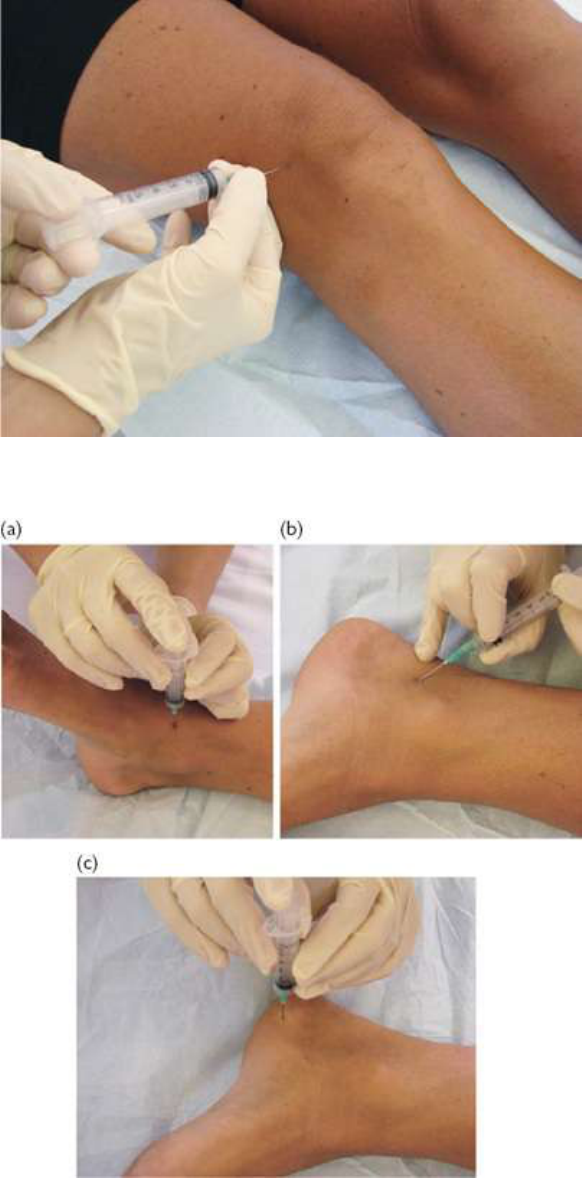
Plate19Injectionoftheknee.CourtesyofMrsCareyTierney.
Plate20(a)Injectiontoanklejoint,(b)tarsaltunnel,and(c)plantarfascia.ImagescourtesyofMrsCarey
Tierney.
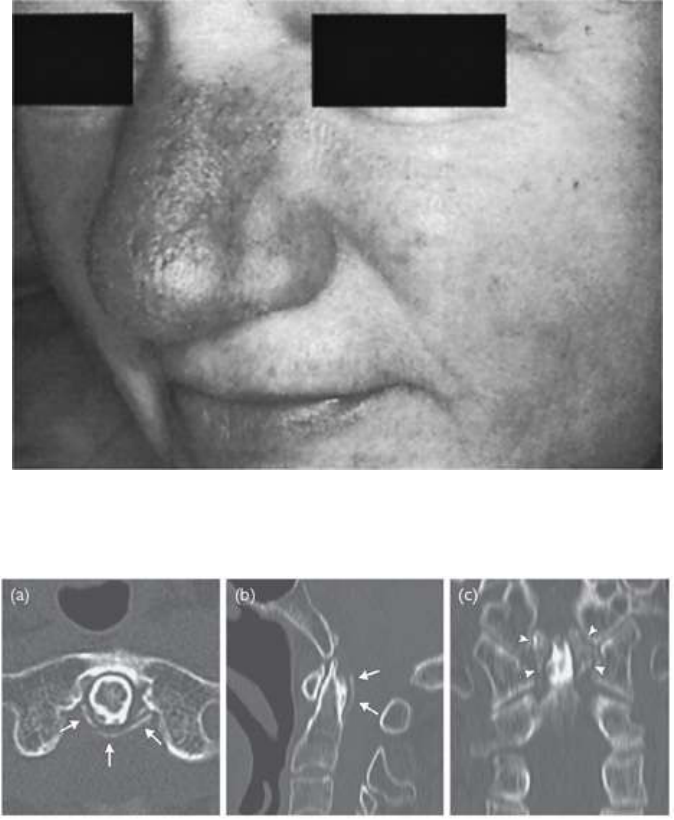
Plate21Lupusperniopresentingasabluish–redorviolaceousswellingofthenoseextendingontothe
cheek.
Plate22Calciumpyrophosphatedepositiondisease(CPPD).ThisisatypicalaxialskeletalCPPDlesion:
calcificationofperiodontoidligamentsandsoft-tissue(termed‘crowned-denssyndrome’)shownonCT
scan:(a)axialview;(b)sagittalview;(c)coronalview.
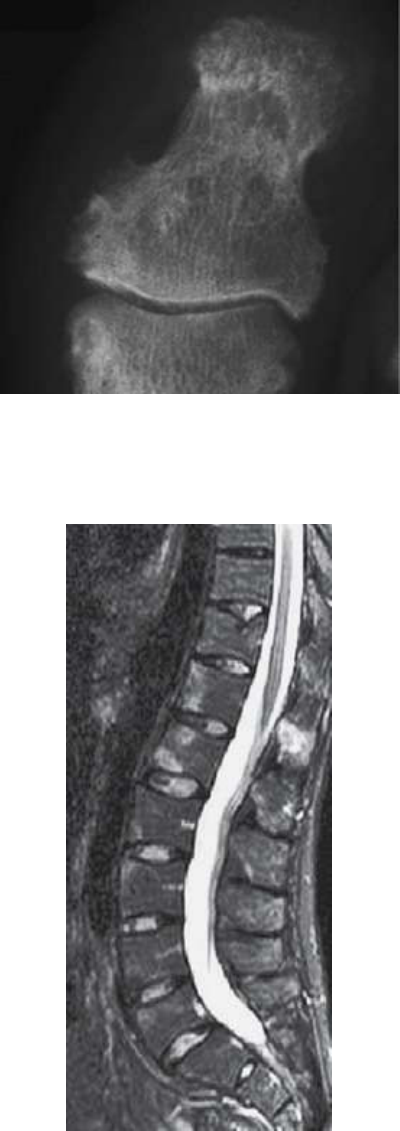
Plate23Psoriaticarthritis(PsA).Lesionsat/aroundadistalgreattoeinterphalangealjoint.Inearlydisease
thearticularsurfacesoftenappearnormalandthereis‘fluffy’juxta-articularnewbone.SeeCASPAR
criteriafordiagnosisand‘Investigations’forPsAinEChapter8.
Plate24Osteitisinaxialspondyloarthritis(axSpA).Vertebral(corner)osteitisisseenashighsignalonthis
fat-suppressedsagittalspinalmagneticresonanceimage,indicatingcurrentinflammationonfour
contiguousvertebrae(T12–L3)andfaintlyinL5.Intervertebraldiscsappearnormal(highsignalindicating
wellhydrated)sonotdegenerate—suggestingagainstthevertebralhighsignalbeing‘Modiclesions’
(associatedwithdegeneratediscdisease).
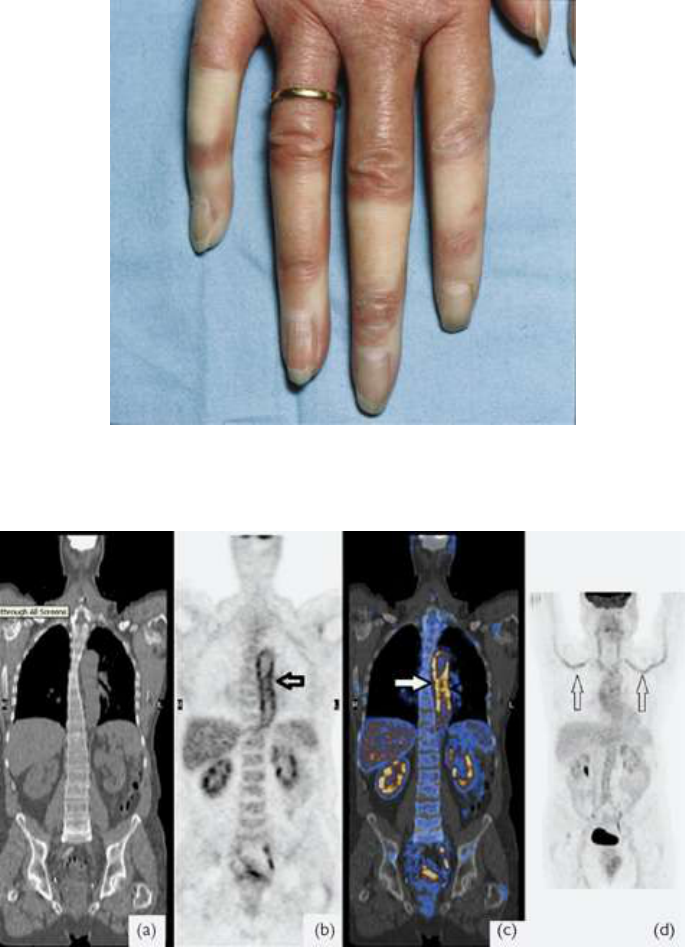
Plate25Raynaud’sdisease(RD)insystemicsclerosis(SScl).Noteclearmarginstoischaemic(white)
areas.
Plate26ContiguousCT(a)and
18
F-FDG-PET(b)imagesshowingaortitis(arrowedin(b)andinCT-PET
registeredimage(c))andvasculitisofsubclavianarteries(arrowedin(d)innon-contiguous
18
F-FDG-PET
scanimage)invasculitis(ina75-year-old,treatedasgiantcellarteritis).

Index
Note:Tables,figures,andboxesareindicatedbyanitalict,f,andbfollowing
thepagenumber.
A
abaloparatide492,581
abatacept680
rheumatoidarthritis258,259b
juvenileidiopathicarthritis329
polymyositisanddermatomyositis440t
pregnancyandbreastfeeding676t
abdominalpain63
abductordigitiminimi115t
abductorpollicislongus696
acetaminophenseeparacetamol
Achillesperitendonitis199
aciclovir637
acitretin312
acromegaly227,409t
acromioclavicularjoint90,597t
acropachy,thyroid226
activemind–bodytechniques641
acuteorsubacutebackpain,conditionscausing608–613
facetjointarthritis/syndrome610–611
lumbarcanalspinalstenosis611–612
lumbardiscprolapse611t
mechanical608–609,609t
nerverootlesions609–610
non-septicdiscitis613
non-traumaticvertebralfracture612
post-surgical612–613,613t
therapies609t
adalimumab674–675,676
axialspondyloarthritisandankylosingspondylitis305–306
juvenileidiopathicarthritis329
polymyositisanddermatomyositis440t
pregnancyandbreastfeeding676t
psoriaticarthritis312
rheumatoidarthritis262b
Still’sdisease571
adductorapophysitis162
adhesivecapsulitis(frozenshoulder)88,224–225,600
adolescents
assessment32–45
backpain618–621
chronicpain44–45,638–641
conditionsnottobemissed28b
elbowpain104
endocrinemanifestations224t
fatigue23
fever23
handpain122
hypermobility592–593
inflammatoryarthritis33–37
jointpainswithsystemicfeatures40
kneepainandlowerlimbdevelopment184–186
limpandgaitconcerns22
lowbackpain154–155
lowerlegandfooddisorders200–203
musclepainandweakness39–40
neckpain82
non-inflammatorymusculoskeletalconditions40–44
normalmusculoskeletalvariants32–33
painassessment20
pelvic,groin,andthighpain168–169
pyrexia23
referralforfurtherassessment,triggeringfeatures28–30
regionalmusculoskeletalpain4
shoulderpain96
thoracicbackandchestpain136–138
unexplainedacute-phaseresponse23
wristpain122
airways219
Albrighthereditaryosteodystrophy504
alemtuzumab440t
alendronicacid682t
allergic(hypersensitivity)vasculitis471
allopurinol667,684
ambrisentan417,683t
aminosalicylates667
amiodarone669–670
amitriptyline615t,631–632,637,657
amlodipine683t
amyloid55
amyloidosis50,222,247,409t,566–567,567t
amyopathicjuveniledermatomyositis446
anakinra678
macrophageactivationsyndrome723
polymyositisanddermatomyositis440t
pregnancyandbreastfeeding676t
SAPHOsyndrome513
Still’sdisease571
systemic-onsetjuvenileidiopathicarthritis336
analgesia
analgesicescalation649–650
opioidanalgesics651–653,652t
rheumatoidarthritis252
aneurysm217
aneurysmalbonecyst622b
angina131t
angiotensin-convertingenzyme(ACE)inhibitors667,684
ankle18t,147t,195,198–199
glucocorticoidinjectiontherapy704–705
ankylosingspondylitis298–306
BathAnkylosingSpondylitisDiseaseActivityIndex(BASDAI)302–304,303b
classifying297b
clinicalfeatures300–301
diagnosticcriteria296
diseaseactivityscore302–304,303b
diseasestatusandprognosticindicators302–304,303b,304b
enthesitisindices303t
epidemiology298
treatment304–306
anserinetendonitis173–174
antalgicgait38–39
anteriorcruciatefunctiontests178f
anteriordrawtest177,178f
antibioticsforsepticarthritis710t
anticonvulsants667
antidepressants656
antiepileptics660
antihypertensives660
anti-interleukininhibitors258,259b,678–679
antimalarialdrugs361,669–670
antineutrophilcytoplasmicantibody(ANCA)450
-associatedvasculitides464–469,481
antinuclearantibodies67t
antiphospholipidsyndrome356
anticoagulation383–384
cardiacfeatures380
catastrophic378,386–387
centralnervoussystem380
classification376–377
clinicalfeatures378–380
differentialdiagnosis377
endocrinefeatures379
epidemiology377
fetalloss379
kidney380
laboratoryfeatures380–381
liverandgastrointestinaltract379
musculoskeletalfeatures379
pathophysiology377
pregnancy378t,384t
pulmonaryfeatures380
skinlesions379
thrombocytopenia378t,380
thrombosis378
treatment381–384
antirheumaticdrugs206
seealsodisease-modifyingantirheumaticdrugs
anti-TNFαtherapy674–675
axialspondyloarthritisandankylosingspondylitis305–306
cautionsandmonitoring675–677
chronicnon-bacterialosteomyelitis511
inflammatoryboweldisease-relatedspondyloarthritis317
juvenileidiopathicarthritis329
juvenilespondyloarthritis320
macrophageactivationsyndrome722
NICEguidelines675t
polymyositisanddermatomyositis439
psoriaticarthritis312
rheumatoidarthritis256,257b,259b,260,262b
SAPHOsyndrome513
spondyloarthritis-associatedreactivearthritis315
Still’sdisease571
systemic-onsetjuvenileidiopathicarthritis336
Takayasuarteritis455
α1-antitrypsindeficiency560–561
aorticdissection131t
aorticregurgitation217
apixaban384
apremilast313,674
arachnoiditis613t
argatroban382t
arthralgias392t
arthritis
calciumoxalate291
calciumpyrophosphatedeposition48t
crystal174
facetjoint610–611
gonococcal48t,529t,530–531
followinginfection324t
andjuvenileidiopathicarthritis,differencesbetween326
Lyme49,50
microorganisms527t
monoarthritis,acute46–47
non-gonococcal529t
oligoarticularjuvenileidiopathic334
post-streptococcal34
reactive33–34,51,206–207
andrelapsingpolychondritis565t
rheumaticfever539
andSjögren’ssyndrome392t
spondyloarthritis48t,230t
seealsoinflammatoryarthritis;juvenileidiopathicarthritis;osteoarthritis;psoriaticarthritis;rheumatoid
arthritis;septicarthritis;skinconditionsassociatedwitharthritis
arthropathy
sarcoid54–55
seealsocrystalarthropathies;entericinfection;spondyloarthropathies
articulardisorders108t,290t
articularlesions87t
aspirin653–656
antiphospholipidsyndrome381t,383,384t
giantcellarteritis460
Still’sdisease570–571
atacicept364–365
ataxicgait39
auranofin255,669
autoantibodiesinsystemiclupuserythematosus355t
autoimmunediseases
ascausesofmyopathiesandmyalgia59t
andskinvasculitis212t
autoimmunehepatitis392t
autoimmunerheumaticdisease67t,160t
autoinflammatorybonediseases,childhood510–511
axialspondyloarthritis296,298–306
classification298b
clinicalfeatures300–301
diseasestatusandprognosticindicators302–304,303b,304b
epidemiology299
HLA-B27andgenetics299–300
immunopathology300
investigations301–302
pathogenesis299–300
treatment304–306
azathioprine673,685
ANCA-associatedvasculitides468,469
immunoglobulinG4-relateddisease574
inflammatoryboweldisease-relatedspondyloarthritis317
juvenileidiopathicarthritis329
lupusnephritis362f
polymyositisanddermatomyositis438–439
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
relapsingpolychondritis564
rheumatoidarthritis254b,255,262b,667
Still’sdisease570–571
systemiclupuserythematosus361t,363
Takayasuarteritis455
azithromycin530–531
azoles660
azotaemia220–221
B
Bcelldepletors677–678
Bcelltherapyseerituximab
backpain605–621
acutenon-specific607
adults614–617
categorization607
causesinchildren618t
childrenandadolescents618–621
chronic607,614–617,615t
congenitalandneuromuscularscoliosis620
herniateddisc621
idiopathicscoliosis619
neuropathic607
non-specificlowbackpain618
non-spinal607
‘red’and‘yellow’flags607
Scheuermann’sosteochondritis620
spinaltumours621,622b
spondylolysisandspondylolisthesis620,621f
seealsoacuteorsubacutebackpain,conditionscausing;lowbackpain;thoracicbackandchestpain
backschool615t
baclofen659
bacteria527t,712t
Baker’scyst173–174
balanitis51
balneotherapy(backpain)609t
barbiturates660
Barlow’smanoeuvre162
basiccalciumphosphatecrystal-associateddisease290
Bazin’sdisease473
Beal’ssyndrome584
behaviouralprogrammes(backpain)609t
Behçet’sdisease51,550–554
clinicalfeaturesandmanagement550–554,551t
diagnosticcriteria551t
epidemiologyandpathophysiology550
gutandhepatobiliarymanifestations231t
skindisorders206–207
belimumab364,387,398,676t,678
benignmyositisofchildhood39–40
benignnocturnallimbpainofchildhood45,32t,184–185
Bennett’sfractures106–108
benzbromarone686
benzylpenicillin540
biliarycirrhosis,primary228t
biologicaltherapies647t,674–677
abatacept(CTLA4-Ig)680
anti-TNFαtherapy674–675,675t
axialspondyloarthritisandankylosingspondylitis305–306
Bcelldepletors677–678
belimumab678
infectionsinpatientson712–714
juvenileidiopathicarthritis329
polymyositisanddermatomyositis439,440t
pregnancyandbreastfeeding676t,680
relapsingpolychondritis564
rheumatoidarthritis257b,258,259b
rituximab677
secukinumab679
Sjögren’ssyndrome398
Still’sdisease571
systemic-onsetjuvenileidiopathicarthritis336
Takayasuarteritis455
targetingTh17cellactivation679
ustekinumab679
biomechanicalconditions
ofback132t
ofchestwall132t
differentialdiagnosis324t
kneepain182
biomechanicalpaininchildrenandadolescents41
bisphosphonates
chronicnon-bacterialosteomyelitis511
non-septicdiscitis613
osteogenesisimperfecta581
osteoporosis490–491
SAPHOsyndrome513
Blausyndrome542,549
bleomycinexposure409t
blindloopsyndrome228t
blisters208
bloodvesselsandrelapsingpolychondritis565t
Blountdisease515t
bonedisorders/manifestations
backpain141t
hand/wrist120t
sarcoidosis558
shoulderpain87t
seealsometabolicbonediseases
bonelesions75t
bonemarrowmanifestationsandsarcoidosis557t
bonepathology60–61,108t
bonetumours524
chondrosarcoma524
osteoidosteoma524
osteosarcoma524
bosentan417,683t
brachialplexuslesions75t
breastfeeding
biologicaltherapies676t,680
DMARDs663,665t
NSAIDs655
rheumatoidarthritis261,262b
bronchiectasis416t
Brown’stumours227
Buerger’sdisease116
buprenorphine610,653
bursitis173–174
children184–185
Busche–Ollendorfsyndrome523
buttockpain158t
C
calcanealfractures198
calcaneovalgus201
calcificsupraspinatustendonitis,acute89–90
calcitonin507–508,612
calcium489
calciumchannelblockers668
calciumoxalatearthritis291
calciumpyrophosphatedepositionarthritis47,48t,50
calciumpyrophosphatedihydratedisease286–289
definitions286b
inflammation,triggeringfactorsof287b
investigations288
management288–289,289f
pseudogout,triggeringfactorsof287b
calf14t
Camurati–Engelmanndisease522
canakinumab336
CANDLEsyndrome549
capsaicin659
carbamazepine637
carcinoidsyndrome409t
carcinomatousneuromyopathy235t
cardiactamponade216,714
cardiopulmonarydisorders/manifestations,systemiclupuserythematosus715,716t
cardiovasculardisorders/manifestations216–217
antiphospholipidsyndrome380
Behçet’sdisease553
conductionabnormalities217
coronaryarterydisease217
immunoglobulinG4-relateddisease575t
Lymedisease537t
myocardium216–217
non-steroidalanti-inflammatorydrugs654–655
pericardium216
polymyositisanddermatomyositis429,432t
relapsingpolychondritis565t
rheumaticfever539
andsarcoidosis557t
Sjögren’ssyndrome395
systemiclupuserythematosus349,360
systemicsclerosis415–417
valvulardisease217
carditis537t
carpaltunnelsyndrome116,127,224–225,225–226
glucocorticoidinjectiontherapy696
caudaequinasyndrome142–143
cavitatingapicallesions218
cefotaxime536
ceftriaxone530–531,536
Lymedisease536
celecoxib653–656
centralnervoussystem
antiphospholipidsyndrome380
non-steroidalanti-inflammatorydrugs654t
cerebrovascularlesions238–239
certolizumab305–306,676t
certolizumabpegol262b,312,674–675
cervicaldystonia(torticollis)77
cervicalnerves74f
cervicalradiculopathy87
cervicitis51
chemonucleolysis611t
cherubism510–511,511t
chestpain62
seealsothoracicbackandchestpain
children
assessment32–45
autoinflammatorybonediseases510–511
backpain154–155,618–621
chronicpain44–45,638–641
conditionsnottobemissed28b
elbowpain104
endocrinemanifestations224t
fatigue23
fever23
gait,arms,legs,spine(GALS)screen14–19,24
gaitassessment37–39
gaitconcerns22
handpain122
hypercalcaemia501–502,502t
hypermobility592–593
idiopathicinflammatorymyopathy444–446
idiopathicosteoporosis485–486
inflammatoryarthritis33–37
jointpainswithsystemicfeatures40
juvenilespondyloarthritis318–320
kneepainandlowerlimbdevelopment184–186
limp22,37–39
lowbackpain154–155
lowerlegandfootdisorders200–203
malignanciespresentingwithmusculoskeletalsymptoms726–727
musclepainandweakness39–40
neckpain82
non-inflammatorymusculoskeletalconditions40–44
normalmusculoskeletalvariants32–33
osteogenesisimperfecta581
osteomyelitis724
painassessment20–21
pelvic,groin,andthighpain168–169
primaryvasculitides474–481
pyrexia23
rareautoinflammatorydiseases545
referralforfurtherassessment,triggeringfeatures28–30
regionalmusculoskeletalpain4
sarcoidosis556–557
septicarthritis708–710
shoulderpain96
systemiclupuserythematosus368–370,717
thoracicbackandchestpain136–138
unexplainedacute-phaseresponse23
wristpain122
seealsojuvenileidiopathicarthritis
chlorambucil439,567
chloroquinephosphate669–670
chondrocalcinosis225–227
chondromalaciapatella184–185
chondrosarcoma524
choreaandrheumaticfever539
chronicatypicalneutrophilicdermatosiswithlipodystrophyandelevatedtemperature(CANDLE)
syndrome549
chronicgraftvshostdisease409t
chronickidneydisease-mineralandbonedisorders504–505
chronicnon-bacterialosteomyelitis510–511
chronicpainsyndromes623–642
childrenandadolescents44–45,638–642
chronicwidespreadpain626,628–632,639–641
complexregionalpainsyndromeinchildrenandadolescents642
fibromyalgiaand‘syndromic’fibromyalgia626–632,628b,629b
generalized626–632
localizedpainsyndromes634–637
withoutidentifiablemusculoskeletalabnormalities44–45
seealsochronicregionalpainsyndrome;chronicwidespreadpain
chronicrecurrentmultifocalosteomyelitis510–511
chronicregionalpainsyndrome634–637
Budapestdiagnosticcriteria636t
clinicalfeatures634–635
epidemiologyandaetiology634
investigation,staging,anddiagnosis635
management635–637
chronicwidespreadpain626
activemind–bodytechniques641
careprogrammes640
causative/associatedconditions626b
childrenandadolescents639–641
management628–632,639–640
parentcoaching641
pharmacotherapy641
psychologicaltherapies640
Churg–Strausssyndromeseeeosinophilicgranulomatosiswithpolyangiitis
ciclosporin667–668,669–670
juvenileidiopathicarthritis329
macrophageactivationsyndrome722
polymyositisanddermatomyositis439
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
relapsingpolychondritis564
Still’sdisease570–571
systemic-onsetjuvenileidiopathicarthritis336
citalopram631–632
clawtoe203
clicks12
clomipramine657
clozapine669
clumsygait39
clunks12
coccidynia163–164
coccyx700
codeine651
codeinephosphate610
coeliacdisease228t
cognitivebehaviouraltherapies630
colchicine513,668,684
colitis232,316–317
collagenandfibrillin,molecularabnormalitiesof578
seealsohereditarydisordersofconnectivetissue
Colles’fracture106–108
commonextensortendonoriginenthesitis694
compartmentsyndrome198
complementaryandalternativemedicine263,616t
complexregionalpainsyndrome28,44–45
childrenandadolescents642
management642
conductionabnormalities217
congenitalscoliosis620
conjunctivitis240
connectivetissueseealsohereditarydisordersofconnectivetissue
constitutionalsymptoms12–13
cornealdisease240
coronaryarterydisease217
cortex,lossof149t
corticosteroidsseeglucocorticoidinjectiontherapy;glucocorticoids
costochondritis133
co-trimoxazole672,673,667
cough62
coupdesabre210t,422
coxibs/COX-2inhibitors656
creatinekinase,raised434t
Crohn’sdisease228t,316–317
cruciateligamentdeficiency185
cryoglobulinaemia213,231t,472
cryopyrin-associatedperiodicsyndromes545
crystalarthritis174
crystalarthropathies277–291
basiccalciumphosphatecrystal-associateddisease290
calciumoxalatearthritis291
calciumpyrophosphatedihydratedisease286–289
seealsogoutandhyperuricaemia
CTLA4-Igseeabatacept
curlytoes,congenital203
cutaneousdisease428–429
cutaneousmanifestations
immunoglobulinG4-relateddisease575t
rareautoinflammatorydiseases543
cutaneouspolyarteritisnodosa478–479
cutaneousvasculitis392t
cyclophosphamide664,668–669
amyloidosis567
ANCA-associatedvasculitides467–469
catastrophicantiphospholipidsyndrome387
giantcellarteritis460
lupusnephritis362f
polymyositisanddermatomyositis439
pregnancyandbreastfeeding665t
relapsingpolychondritis564
systemiclupuserythematosus361t,363
systemicsclerosis420
Takayasuarteritis455
cytokines404
D
dabigatran384
dactylitis(sausagetoe)51,117
danaparoid382t
danazol383
dantrolene659
dapsone564
DeQuervain’stenosynovitis99,109,110,115
defibrotide387
deficiencyofinterleukin-1receptorantagonist510–511,549
features511t
degenerativecausesofbackpain141t
degenerativeconditionsofspineandchestwall132t
degenerativedisease78
degenerativelesions75t
deltoid92t
denosumab492,508,682t
dermatomes
cervicalandupperthoracicnerves74f
upperlimb128f
dermatomyositisseepolymyositisanddermatomyositis
developmentalcausesofbackpaininchildren618t
diabetes210t,224–225
jointandtissuehypomobility/stiffness224t
diabeticamyotrophy225
diabeticneuropathy225
diarrhoea63,231
diazepam610,615t,659
diclofenac327,653–656,668
diffuseconditionsandshoulderpain87t
diffuseidiopathicskeletalhyperostosis(DISH)134
digoxin668,669–670
dihydrocodeine651
discspace,narrowed149t
discectomy611t
discitis143,613
disease-modifyingantirheumaticdrugs647t,662–680
abatacept680
anti-interleukin6inhibitors678–679
anti-TNFαtherapy674–675,675t
apremilast674
axialspondyloarthritisandankylosingspondylitis305–306
azathioprine667
Bcelldepletors677–678
belimumab678
biological674–680
ciclosporin667–668
co-administerednon-steroidalanti-inflammatorydrugs655
conventionalsynthetic662–673
cyclophosphamide668–669
familyplanning,pregnancy,andbreastfeeding663,665t
gold(auranofinandsodiumaurothiomalate)669
hydroxychloroquineandchloroquinephosphate669–670
immunizationandassessmentofinfectionriskbeforecommencement663b
interleukin-1receptorantagonists678
juvenileidiopathicarthritis328–329
leflunomide670
malignancy664
methotrexate671–672
monitoring664t,666b
mycophenolatemofetil672
polymyositisanddermatomyositis438–439
pregnancyandbreastfeeding680
psoriaticarthritis311–313
rheumatoidarthritis248,250–258,253b,254b,259b
rituximab677
SAPHOsyndrome513
secukinumab679
sharedcareinformation665–667
sideeffects666b
Sjögren’ssyndrome398
spondyloarthritis-associatedreactivearthritis315
sulfasalazine672–673
surgeryandinfectiveillness663
systemic-onsetjuvenileidiopathicarthritis336
targetedsynthetic673–674
tocilizumab678–679
tofacitinib673–674
ustekinumab679
uveitis341
distalarthrogryposes582
diuretics660,668
dorsalinterossei114f
dosulepin657
doxycycline536
D-penicillamine570–571
drug-inducedlupuserythematosus(DILE)359
drugsascauseofmyopathiesandmyalgia59t
drugsusedinrheumatology645–687
antidepressants656
biologicaltherapies647t
glucocorticoids660
goutandhyperuricaemia684–687
non-steroidalanti-inflammatorydrugs653–656
opioidanalgesics651–653,652t
osteoporosis682–683
pharmacotherapy647t
pooledintravenousimmunoglobulin687
pulmonaryarteryhypertension683–684
Raynaud’sdisease683–684
seealsobiologicaltherapies;disease-modifyingantirheumaticdrugs;painrelief
dryeye240
duloxetine615t,631–632,658
Dupuytren’scontracture115,119,224–225
dysphagia63
dyspnoea62
dysrhythmias217
systemicsclerosis416t
E
ears
andgranulomatosiswithpolyangiitis465
andrelapsingpolychondritis565t
andskindisorders206–207
Eaton–Lambertmyasthenicsyndrome234–235,235t
ectopiccalcificationandossification505
eculizumab364–365,383
edoxaban384
Ehlers–Danlossyndrome230t,586–589
classical587
classification586
genotypingandclinicaldiagnosis586–589
hypermobile587,588t,592–593
vascular589
elbow
glucocorticoidinjectiontherapy694–695
joint695
lateralepicondylitis/tenniselbow694
medialepicondylitis/golfer’selbow694
olecranonbursitis695
physicalexamination14t,17t
seealsoelbowpain;lateralepicondylitis(tenniselbow);medialepicondylitis(golfer’selbow)
elbowpain98–104
activeflexionandsupination/pronation100
acuteorchronic(overuse)trauma,historyof98–99
adults98–102
bonyconfigurationatelbow98f
causesinchildrenandadolescents104t
childrenandadolescents104
distalarmsymptoms101
distalradiation99
electrophysiology102
examination100–101
exclusivepaininelboworreferredfromelsewhere98
flexingandextension,passive101
functionalanatomy98
historytaking98–99
lateralepicondyleofhumerus,palpationof100
locking99
medialhumeralepicondylepalpation100
needlearthrocentesis/olecranonbursocentesis102
peripheralnervefunctiontesting101
prominentstiffness99
radiographsandotherimaging101
supinationandpronationofforearm101
symptomsinotherjoints99
treatment102
unremittingandsevere99
visualinspection100
emergencies,rheumatological707–727
infectionsinpatientsonbiologicaltherapy712–714
macrophageactivationsyndrome722–723,723t
malignanciespresentingwithmusculoskeletalsymptomsinchildren726–727
methotrexate-inducedpneumonitis721
paediatricosteomyelitis724
septicarthritis708–711
systemiclupuserythematosus,acute714–717
systemicsclerosiscrises720
systemicvasculitis718–719
emptycantest91f
‘end-feel’101
endocrinedisorders/manifestations224–227
acromegaly227
antiphospholipidsyndrome379
diabetes224–225
hyperparathyroidism226–227
hypothyroidism225–226
myopathiesandmyalgia59t
thyroidacropachy226
thyrotoxicosis226
endocrineglands575t
endostealhyperostosis522–523
entericinfection228t
enthesitis134,173–174,597t
children184–185
indices303t
oligoarticular47
spondyloarthritis297b
trochanteric158–159
enthesitis-relatedarthritis318–319
juvenile335
enthesophytes101
entrapmentneuropathies238
eosinophilicfasciitis209,210t,235,409t,422,572
eosinophilicgranuloma622b
eosinophilicgranulomatosiswithpolyangiitis213,217,231t,467
treatment469
eosinophilicmyalgiasyndrome409t
eperisone615t
epiduraletanercepttherapy616t
epiduralsteroidinjections616t
epiphysealdysplasia157,160t
epratuzumab364–365,398
erythemaelevatumdiutinum472
erythemamarginatumseerheumaticfever
erythemanodosum52,560
erythromycin540,660
etanercept674–675,676
ANCA-associatedvasculitides468
axialspondyloarthritisandankylosingspondylitis305–306
backpain616t
juvenileidiopathicarthritis329
polymyositisanddermatomyositis440t
pregnancyandbreastfeeding676t
psoriaticarthritis312
rheumatoidarthritis262b
Still’sdisease571
etidronate507–508
etodolac655
etoricoxib656
Eurofevertool548t
Ewingsarcoma622b
inchildren726
exercise490,615t
chronicpainsyndromes630
extension145
extensorhallucislongus147t
extensorpollicisbrevis696
externaltibialtorsion186
extraglandulardisease392t
extramusculardisease,treatmentof440–441
eyedisorders/manifestations240
Behçet’sdisease552
dryeye(xerophthalmia)240
granulomatosiswithpolyangiitis466
immunoglobulinG4-relateddisease575t
ischaemicophthalmiclesions240
relapsingpolychondritis565t
sarcoidosis557t
scleralandcornealdisease240
systemiclupuserythematosus352t
uveitis240
F
Faber/Patricktesttest169t
face206–207
FacesPainScale20–21
facetjointarthritis/syndrome610–611
familialcoldautoinflammatorysyndrome542–543
familialMediterraneanfever546
late-onset547
familyplanninganddisease-modifyingantirheumaticdrugs663
Fanconisyndrome497
fatpadsyndrome184–185
fatigue226
childrenandadolescents23
Sjögren’ssyndrome395
febuxostat685
Felty’ssyndrome247
femaletriadsyndrome200–201
femoralanteversion32t,185
Fenbid
®
653–656
fetalloss379
fever23
fibrillinseecollagenandfibrillin,molecularabnormalitiesof
fibromyalgia626–628
ACR(revised)2010criteria629b
diagnosis627–628,628b
historyofuseofterm627
juvenile44–45,639–641
management628–632
sitesoftendernessin65f
‘syndromic’626–627
fibrosis
nephrogenicsystemic422–423
systemicsclerosis405
fibrousdysplasia520
fingers17t,112f,117
Finkelstein’stest110
flatfeet(pesplanus)32t,201–202
flexordigitiminimiBrevis115t
flexortendinopathy119
fluoxetine631–632,657,683t
fluvastatin383
folicacid671–672
folinicacid671–672
fondaparinux382t
foot18t
forefoot193,196,199
glucocorticoidinjectiontherapy704–705
hindfoot14t,189f,191–192,195,198–199
midfoot14t,192–193,195–196
smalljoints705
seealsolowerlegandfootdisorders
forefoot193,196,199
foreignprotein212t
fractures
Bennett’s106–108
calcaneal198
Colles’106
hip161–162
non-traumaticvertebral612
andosteoporosis489–493
stress191
Freibergdisease515t,516
Froment’ssign125–126
frozenshoulder(adhesivecapsulitis)88,224–225,600
fungi527t,712t
G
gabapentin615t,636,637,641,658
gait,arms,legs,spine(GALS)screen14–19,15–16f,17t,19f
paediatric14–19,24
gaitconcerns,childrenandadolescents22
gaitpatterns144–145
children37–39
gametogenesis668–669
ganglia116,118
gastritis232
gastrocnemiusandsoleus(ankleplantarflexion)147t
gastrointestinaldisorders/manifestations228t
antiphospholipidsyndrome379
Behçet’sdisease554
non-steroidalanti-inflammatorydrugs654t
polymyositisanddermatomyositis429,432t
sarcoidosis557t
Sjögren’ssyndrome394
systemiclupuserythematosus352t
systemicsclerosisandrelateddisorders414–415
gastrointestinalhaemorrhage229–231,232
genitalia418t
genitourinarymanifestations,immunoglobulinG4-relateddisease575t
genuvalgum(knockknees)32t,175
childrenandadolescents186
genuvarum(bowlegs)32t,175
childrenandadolescents186
giantcellarteritis457–460,458t,718
gingivalhyperplasia232
glandulardisease392,393t
glenohumeralinstabilityduetolabraltrauma597t
glenohumeraljoint90,692
glomerulonephritis220
glucocorticoidinjectiontherapy689–705
acromioclavicularjoint693
ankleandfoot704–705
carpaltunnelsyndrome696
elbow694–695
extensorpollicisbrevis/abductorpollicislongus696
glenohumeraljoint692
greatertrochanterpainsyndrome700
hipandperiarticularlesions700
kneeandperiarticularlesions702–703
lateralepicondylitis/tenniselbow694
medialepicondylitis/golfer’selbow694
olecranonbursitis695
plantarfaciitis704
principlesofinjectiontechniques691
radiocarpaljoint696
shoulder692–693
subacromialspace693
subtalarjoints704
tarsaltunnel704
wristandhand696–698
glucocorticoids256,262b,647t,660
ANCA-associatedvasculitides467–469
cautionsandcomplications661t
chronicnon-bacterialosteomyelitis511
chronicpainsyndromes631–632
chronicregionalpainsyndrome636
interactions660
juvenileidiopathicarthritis327
lobularpanniculitis560–561
macrophageactivationsyndrome722
osteoporosis487–488
pelvicorhiplesions160t
polymyositisanddermatomyositis438
post-herpeticneuralgia637
rheumaticfever540
SAPHOsyndrome513
Still’sdisease570–571
systemiclupuserythematosus360
systemic-onsetjuvenileidiopathicarthritis336
Takayasuarteritis455
seealsoglucocorticoidinjectiontherapy
glutealgroupmuscles14t,156–157
glyceryltrinitrate683t
gold(auranofinandsodiumaurothiomalate)669
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
rheumatoidarthritis254b,255
golfer’selbowseemedialepicondylitis
golimumab305–306,312,674–675,676t
gonococcalarthritis48t,529t,530–531
Goodpasture’ssyndrome221
goutandhyperuricaemia48t,225–226,278–284
acuteattackofgout281–282
causesandriskfactors278t
chronicgout282–284
classificationcriteria279
clinicalconditionsmimickinggout280b
clinicalfeatures279–280
drugs684–687
epidemiology278
imaging280–281
investigation280
management281–284
tophaceousgout282–284
gradedactivityprogrammes(backpain)609t
granulomafaciale472
granulomatosiswithpolyangiitis
classificationcriteria464b
ear,nose,andthroatsymptoms465
eosinophilicseeeosinophilicgranulomatosiswithpolyangiitis
epidemiology464
eyedisease466
investigation466
musculoskeletalsymptoms464–465
nervoussystem466
presentationandclinicalfeatures464
pulmonarydisease465
renaldisease465
skindisease465
treatment466,468
grapefruit668
Graves’disease226
greatertrochanterpainsyndrome700
Guillain–Barrésyndrome39–40
gutandhepatobiliarydisorders/manifestations228–232
immunoglobulinG4-relateddisease575t
rheumaticdiseases229–231
sideeffectsfromdrugsusedintreatment231–232
Sjögren’ssyndrome394
H
haemarthrosis46–47,48t,174
haematologicaldisorders/manifestations
non-steroidalanti-inflammatorydrugs654t
systemiclupuserythematosus351,716–717
haematuria213
haemochromatosis54,228t,229
haemophagocyticlymphohistiocytosis,secondaryseemacrophageactivationsyndrome
haemoptysis62,219
haloperidol540
hammertoe203
hamstrings(kneeflexion)147t
hand112–122
adults112–121
bonescintigraphy119
childrenandadolescents122
conditions/featuresdiagnosedonradiograph120t
deformityofdigits118
diffuseswelling118
dorsalinterossei114f
dorsum118
Dupuytren’scontractureandflexortendinopathy119
examination117–119
extensorexpansionoffinger112f
functionalanatomy112–115
glucocorticoidinjectiontherapy696–698
grip113–115
historytaking115–117
hypermobile32t
hypothenareminencemuscles114f,115t
immobilityandstiffness,painassociatedwith115
intrinsicmuscles113
ischaemicpain116
jointsandnodules,palpationof118
laboratorytests120–121
longtendons112–113
lumbricalmuscles114f
magneticresonanceimaging119
musclewasting118
nailsandfingers,examinationof117
neurologicalqualitiestopainorcommonnervelesions115
painarisingfrombone116
painfulconditions108t
palm118
palmtendons,palpationof119
physicalexamination17t
radiographs119,120t
skindisorders207
smalljoints697–698
stiffness,localordiffuse115
‘swelling’116
thenareminencemuscles113t,114f
tingling/pinsandneedles/numbness116
treatmentofdisorders121
triggerfinger117,224–225
ultrasound119
‘weakness’117
Hashimoto’sthyroiditis226
headache239
helminths527t
Henoch–Schönleinpurpura213,231t,471,476–478
heparin381t,383,384t,387
hepaticmanifestationsandsarcoidosis557t
hepatitis58t,228t,229,392t
hepatitisCosteosclerosis523
hepatobiliarydisordersseegutandhepatobiliarydisorders/manifestations
hepatosplenomegaly229–231
hereditarydisordersofconnectivetissue577–594
Beal’ssyndrome584
distalarthrogryposes582
Ehlers–Danlossyndrome586–589
hypermobilityspectrumdisorderinadults590–591
hypermobilityspectrumdisorderinchildrenandadolescents592–593
Loeys–Dietzsyndrome584
Marfansyndrome584
molecularabnormalitiesofcollagenandfibrillin578
osteogenesisimperfecta580–581
Sticklersyndrome594
herniateddisc621
herpeszoster132t
Hibernianfeverseetumournecrosisfactor(TNF)receptor-associatedperiodicsyndrome
highsteppinggait39
hilarlymphadenopathy218
hindfoot14t,191–192,195,198–199
tendons,retinaculae,andbursae189f
hip
flexion/internalrotation147t
functionalanatomy157
glucocorticoidinjectiontherapy700
osteoarthritis276
andperiarticularlesions700
physicalexamination18t,162
Hoffman’ssyndrome226
hormonereplacement490
housemaid’sknee175
hydrotherapy(backpain)609t
hydroxychloroquine668,662–663,664,669–670
antiphospholipidsyndrome381–384,382t
dermatomyositis440–441
juvenileidiopathicarthritis329
lupusnephritis362f
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
rheumaticarthritis254b,255,262b
Sjögren’ssyndrome398
Still’sdisease570–571
systemiclupuserythematosus361t
hypercalcaemia500–501
causes501t
childhood501–502,502t
familialbenign503
familialhypocalciuric502t
idiopathicinfantile502t
treatment501t
hypergammaglobulinaemicpurpura472
hyper-IgDsyndrome546–547
hypermobilityseejointhypermobilitysyndrome
hyperparathyroidism54,226–227
familial503–504
neonatalprimary502t
primary502–503
secondaryandtertiary503
hypertension654t
seealsopulmonaryarteryhypertension
hypertrophicosteoarthropathy
primary522
pulmonary(secondary)235,522
hyperuricaemiaseegoutandhyperuricaemia
hyperviscosity220
hypophosphataemicosteomalacia234–235
hypothenareminencemuscles114f,115t
hypothyroidism225–226
hypovitaminosisD496
I
ibandronicacid682t
ibuprofen327,641,653–656
idiopathicarthritisseejuvenileidiopathicarthritis
idiopathiccausesofmyopathiesandmyalgia59t
idiopathicinflammatorymyopathiesseepolymyositisanddermatomyositis
idiopathicscoliosis619
iliopsoas(hipflexion/internalrotation)147t
iliotibialband172f
iloprost683t
imipenem536
imipramine657
immunecellactivation404
immunoglobulin,intravenous687
ANCA-associatedvasculitides468–469
polymyositisanddermatomyositis439
Still’sdisease570–571
immunoglobulinG4-relateddisease574,575t
immunologicalfeatures,systemiclupuserythematosus352t
immunosuppressivetherapies259–260
impingement89–90
indomethacin655
infection
acutepolyarthritis58t
arthritisfollowing324t
backpain141t,151,618t
enteric228t
kneepain174
managementwhileonimmunosuppression259–260
non-osseous75t
skinvasculitis213
seealsoinfectionandrheumaticdisease
infectionandrheumaticdisease541–576
autoimmune67t,160t
Lymedisease536,537t
Mycobacteriumtuberculosis532–533
osteomyelitis534–535,535t
pathogenesis526t
rheumaticfever538–540
septicarthritis528–531
inflammatoryarthritis
characteristicrashes36
childrenandadolescents33–37
examination35
familyhistory34
imaginginvestigations36
infectiousfeatures33–34
jointaspirationandsynovialbiopsy37
jointinvolvement,typicalpatternsof33t
laboratorytests36–37
regionalmusculoskeletalexamination35
responsetomedication35
systemsenquiryandpastmedicalhistory34
trauma,historyof34
travelhistoryandinfectiouscontacts35
inflammatorybackpain
differentialdiagnosis324t
spondyloarthritis296b
inflammatoryboweldisease-relatedspondyloarthritis316–317
clinicalpresentation316
management317
inflammatorydisorders/manifestations75t
backpain141t,618t
skinvasculitis212t
systemicsclerosis405
inflammatoryperipheralneuropathy238
infliximab674–675,676
axialspondyloarthritisandankylosingspondylitis305–306
polymyositisanddermatomyositis440t
pregnancyandbreastfeeding676t
psoriaticarthritis312
rheumatoidarthritis262b
infraspinatus92t
interleukin-1receptorantagonistsseeanakinra
internaltibialtorsion186
interstitiallungdisease219
interstitialnephritis222
intestinalbypasssurgery228t
in-toeing32t,203
ischaemicophthalmiclesions240
ischialtuberosities700
Iselindisease515t
seealsoosteochondritis
J
Jack’stest196
januskinaseinhibitors259
jointhypermobilitysyndrome29,64t,99,206,230t
adults46,590–591
Beightonhypermobilityscale590–591,592
childrenandadolescents41,592–593,639–641
hands32t
knees32t
jointinjectiontherapies182–183
seealsoglucocorticoidinjectiontherapy
joints
painswithsystemicfeatures40
polymyositisanddermatomyositis429
sarcoidosis557–558
Sjögren’ssyndrome393
synovitis177
juveniledermatomyositis231t,444–445
amyopathic446
juvenileenthesitis-relatedarthritis335
juvenileidiopathicarthritis321–341
andadultarthritis,differencesbetween326
classification323
diagnosis324–326
differentialdiagnosis324t
epidemiology322–323
gutandhepatobiliarydisease231t
investigations326–327
keysigns325t
macrophageactivationsyndrome338,722
management324–330
nationalguidelinestoaidmanagement324
oligoarticular334
outcomeandprognosis329–330
polyarticular334
rheumatoidfactor-negativepolyarticular334–335
subtypes322t,334–336
systemic-onset40,326t,335–336
transitionservices332
treatment327–329
uveitis340–341
juvenileidiopathicinflammatorymyopathy444–446
juvenileidiopathicosteoporosis485–486
juvenilemandibularchronicosteomyelitis510–511
juvenilepolymyositis446
juvenilepsoriaticarthritis335
juvenilespondyloarthritis318–320,335
clinicalpresentation319
diagnosticapproach319
epidemiologyandclassification318–319
management319–320
outcome320
juvenilesystemiclupuserythematosus368–370
K
Kawasakidisease207,231t,475–476
childrenandadolescents40
Kennedy–Hawkinstest91f
keratodermablennorrhagica52
ketoprofen655
kidneysseerenaldisorders/manifestations
Kienbockdisease515t
knee
extension147t
flexion147t
glucocorticoidinjectiontherapy702–703
hypermobile32t
osteoarthritis276
periarticularlesions703
physicalexamination18t,14t
seealsokneepain
kneepain170–186
adults170–183
anatomy170–173
anteriorcruciatefunctiontests178f
anteriorpain,causesof173t
anteriorstructures171f
axialsection171f
biomechanicalfactors182
capsaicincream183
childrenandadolescents184–186
computedtomography181
drugs183
examination175–179,185
examinationandobservationofpatientstanding175
examinationforjointsynovitisandeffusion177
examinationofsittingpatient175–177
femoralanteversion,retroversion,andtibialtorsion180f
historytaking173–175,184–185
iliotibialband172f
initialonset174
injury174
jointaspirationandperiarticularfluidcollections181
jointinjectiontherapies182–183
laboratoryinvestigations181
lidocainepatches183
locking174
magneticresonanceimaging181
meniscusdamagetesting178
pastmedical,family,occupationalandleisurehistory174–175
patellaQangle172f,177
patternandtypeof174
positioningofkneeforpalpation176f
proximalmusculoskeletalexamination179
radiographs179
siteofpain173–174
stabilitytesting177
steroidinjection,local182–183
surgery183
treatment181–183
ultrasound181
yttrium-90radiationsynovectomy183
Köhlerdisease515t,516
kyphoplasty493
L
Lachmanntest177,178f
lacrimalglands575t
lactationseebreastfeeding
largevesselvasculitis452
causes452t
laryngealobstruction219
Laseague’stest146
laserlumbardiscectomy611t
lateralepicondylitis(tenniselbow)100,602–603,603f
glucocorticoidinjectiontherapy694
leflunomide662–663,664
amyloidosis567
ANCA-associatedvasculitides468
juvenileidiopathicarthritis329
juvenilespondyloarthritis320
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
rheumatoidarthritis254b,255,262b,670
Takayasuarteritis455
legdisorders
developmentalfactors185
femoralanteversion185
genuvalgum(knockknees)186
genuvarum(bowlegs)186
internaltibialtorsion186
seealsolowerlegandfootdisorders
leglengthdiscrepancy169
Legg–Calvé–Perthesdisease514,515t
leisureactivities/history77,109,174–175
leucocytoclasticvasculitis470,478
associatedconditions470t
precipitantsandassociations212t
leukaemia622b,727
Libman–Sacksendocarditis217
lichenplanus207
lidocaine615t
limp
assessment38–39
causes38t
childrenandadolescents22,38–39
linearscleroderma402,422
lipodermatosclerosis561,210t,409t
lipogranulomatosis560–561
livedoreticularis209
livedoidvasculitis473
liver418t
antiphospholipidsyndrome379
non-steroidalanti-inflammatorydrugs654t
localizedpainsyndromes634–637
chronicregionalpainsyndrome634–637,636t
post-herpeticneuralgia637
temporomandibularjointdysfunction637
trigeminalneuralgia637
Loeys–Dietzsyndrome584
Lofgren’ssyndrome556
longheadofbicepstendonitis597t
losartan361t,683t
lowbackpain140–155
adults140–152
assessment140–141
bonescintigraphy150
childrenandadolescents154–155
commonand/orseriouscauses141t
computedtomography150
descriptionofpain143
epidemiology140
examination144–147,148–151
extensionandlumbarrotation145
familyhistory143
gaitpattern144–145
historytaking141–143
lumbarandsacralspineanatomy140
lumbarnerverootlesions148t
magneticresonanceimaging150
musclestrengthtestinginlowerlimbs147t
nerveroottensiontest146
neurologicalexamination146
observationofactivemovementswhilepatientstanding144
occupationalhistory143
previousbackpainandtrauma143
pronepatient146
radiationofpainandsymptomsinlegs142–143
radiographs148–150,149t
sacroiliacjointsandhips145
screeningforinfection,malignancy,ormetabolicbonedisease151
slumptest145f
straightleg(Laseague’stest)146
treatment151–152
visualinspection144
lowerlegandfootdisorders188–203
adults188–199
anatomyofbonesandjoints188–189
anatomyofintrinsicfootstructure190
anatomyoflongmusclesandtendons189–190
ankleandhindfootexamination195
childrenandadolescents200–203
conditions191,201–203
conditionscausinglocalizedfootpain192t
descriptionofpain193
examination194–196,200
footbones188f
footimaging197
forefootexamination196
forefootpain,causesof193
functionalanatomy190–191
gaitpatterns194
hindfootpain,causesof191–192
historytaking191–194,200
investigations197–198
joint/bursafluidaspiration198
laboratorytests198
lowerlegimaging197
lowerlumbarnerverootlesions197t
midfootandfirstMTPpain,causesof192–193
midfootlesionsexamination195–196
neuroanatomy190
neurologicalexamination196
neurophysiology198
observation194
relevantproximalmusculoskeletalexamination196
siteandqualityofpain191
steroidinjections199
surgery199
tendons,retinaculae,andbursaeofhindfoot189f
trauma,historyof200–201
treatment198–199
treatmentforankleandhindfootdisorders198–199
treatmentforforefootdisorders199
treatmentforlowerlegdisorders198
weakness194
lucentlesions,localized149t
lumbarcanalspinalstenosis611–612
lumbardiscprolapse611t
lumbarflexionmeasurement15–16f
lumbarnerverootlesions148t,197t
lumbarpedicles,short149t
lumbarrotation145
lumbarspine17t,140
lumbosacralanomalies149t
lumbricalmuscles114f
lunateosteochondritis(Kienbock’sdisease)515t
lungsseecardiopulmonarydisorders/manifestations;pulmonarydisorders/manifestations
lupusnephritis362f,364–365
lupuspernio206–207
lupusprofundus561
Lymearthritis49,50
Lymedisease58t,536,537t
lymphadenopathy392t
hilar218
lymphaticdisorders/manifestations
immunoglobulinG4-relateddisease575t
sarcoidosis557t
lymphoblasticleukaemia,acute727
lymphocyticthyroiditis226
lymphocyticvasculitis(non-leucocytoclastic)470t,473
lymphoedema,dependent210t
lymphoma622b,727
lymphoproliferativediseaseandSjögren’ssyndrome392t,395
M
McCune–Albrightsyndrome520
McGillpainscale7t
McGregor’sline78–79
macitentan417,683t
McKenzieexercises609t
McMurraytest178,179f
macrophageactivationsyndrome338,722–723
clinicalfeatures722,723t
diagnosis722
laboratoryfeatures723t
pathology722
treatment723
macularrashes207
Majeedsyndrome510–511,542–543
features511t
malignancy75t,234–236
causingmusculoskeletalsymptoms234
disease-modifyingantirheumaticdrugs664
lowbackpain151
myopathy235t
neoplasticdiseases,primaryandsecondaryofbonesandjoints234
non-myopathyparaneoplasticsyndromes235
paraneoplasticmyopathies234–235
polymyositisanddermatomyositis430
presentingwithmusculoskeletalsymptomsinchildren726–727
rheumaticdiseasesassociatedwithincreasedincidenceof236
rheumatoidarthritis-associatedrisk260
rheumatologicaldrugs236
secondary622b
skinvasculitis212t
systemiclupuserythematosus352
andwidespreadpain69–70
seealsotumours
malletfinger118
mallettoe203
manifestationsandsarcoidosis557t
manipulation(backpain)609t,615t
Marfansyndrome230t,584
Ghent1996criteria585t
mechanicaldisorders/manifestations
backpain141t,160,618t
hip157
seealsobiomechanicalconditions
metabolicbonediseases483–524
bonetumours524
childhoodautoinflammatorybonediseases510–511
fibrousdysplasia520
lowbackpain151
osteochondroses514–516
osteonecrosis518–519
Paget’sdisease506–508
SAPHOsyndrme512–513
sclerosingbonedisorders522–523
seealsoosteomalaciaandrickets;osteoporosis;parathyroiddiseaseandrelateddisorders
metaboliccausesofmyopathiesandmyalgia59t
metabolicsyndromes225
metatarsalheadosteochondritis(Freiberg’sdisease)515t
metatarsalphalangealjoint192–193
metatarsusadductus201
methocarbamol659
methotrexate660,662–663,664,669–670,671,674–675,677
amyloidosis567
ANCA-associatedvasculitides467–469
axialspondyloarthritisandankylosingspondylitis305
chronicnon-bacterialosteomyelitis511
eosinophilicfasciitis572
giantcellarteritis460
immunoglobulinG4-relateddisease574
-inducedpneumonitis721
inflammatoryboweldisease-relatedspondyloarthritis317
juvenileidiopathicarthritis329
juvenilespondyloarthritis320
polymyositisanddermatomyositis438–439
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
relapsingpolychondritis564
rheumatoidarthritis253,254b,262b
SAPHOsyndrome513
spondyloarthritis-associatedreactivearthritis315
Still’sdisease570–571
systemiclupuserythematosus361t,363
systemic-onsetjuvenileidiopathicarthritis336
systemicsclerosis420
Takayasuarteritis455
methylprednisolone660,677
antiphospholipidsyndrome381t
giantcellarteritis460
lupusnephritis362f
macrophageactivationsyndrome722
polymyositisanddermatomyositis438
Still’sdisease570–571
systemiclupuserythematosus360
mevalonatekinasedeficiency546–547
microdiscectomy611t
microscopicpolyangiitis213,466–467,468
midfoot14t,192–193,195–196
milnacipran631–632,658
Milwaukeeshoulder/kneesyndrome50,89
miscellaneousconditionsseerareautoinflammatoryandmiscellaneousdiseases;skinconditionsassociated
witharthritis
mitralvalveprolapse217
mixedconnectivetissuedisease230t,231t
mixedserotonin-norepinephrinereuptakeinhibitors658
monoarthritis,acute46–47
monoarticulardisease324t
monoarticularpain46–47
mononeuritismultiplex213
morphinesulfate610,653
morphoea210t
circumscribed422
generalized402,422
guttate422
Morton’smetatarsalgia192t,196
Muckle–Wellssyndrome542–543
mucocutaneousmanifestations,systemiclupuserythematosus348
mucosalinvolvementandBehçet’sdisease550–552
multicentricreticulohistiocytosis562
muscleactivationtests162–163
musclebiopsyandpolymyositisanddermatomyositis435–436
muscleenzymelevelsandpolymyositisanddermatomyositis434–435
musclerelaxants659
musclesandsarcoidosis558
musculardystrophies59t
musculoskeletalassessmentandpatternsofdisease25–70
adults46–70
childrenandadolescents32–45
featuresnottobemissed26
normalvariants32–33,46
musculoskeletaldisorders/manifestations
antiphospholipidsyndrome379
Behçet’sdisease552
granulomatosiswithpolyangiitis464–465
Lymedisease537t
sarcoidosis557–558
systemiclupuserythematosus348
musculoskeletallesionsseeupperlimbmusculoskeletallesions
musculoskeletalsymptoms,evaluationof3–24
clunks,snaps,andclicks12
constitutionalsymptoms12–13
elicitedpainonexamination10
fatigueinchildrenandadolescents23
feverinchildrenandadolescents23
gait,arms,legs,spine(GALS)screen14–19,15–16f,17t,19f
inflammatorymusculoskeletalpain8
limpandgaitconcernsinchildrenandadolescents22
McGillpainscale7t
mechanicalpain8
painassessmentinchildrenandadolescents20–21
paininadults6–13
painlocalization6–7
physicalexamination14t,15–16f,17t,19f
pyrexiainchildrenandadolescents23
qualityofpain7
rashes13
stiffness12
swelling12
unexplainedacute-phaseresponseinchildrenandadolescents23
myalgias59t,60,65–67
myastheniagravis235t
mycobacteria527t
Mycobacteriumtuberculosis532–533
mycophenolatemofetil672
ANCA-associatedvasculitides468
eosinophilicfasciitis572
immunoglobulinG4-relateddisease574
juvenileidiopathicarthritis329
lupusnephritis362f
polymyositisanddermatomyositis439
pregnancyandbreastfeeding665t
systemiclupuserythematosus361t,363
systemicsclerosis420
Takayasuarteritis455
myeloma236
myocardialfibrosis416t
myocardialinfarction131t
myocarditis216–217,416t
myocardium216–217
myocrisin(gold)254b,255
myofascialpain87
myopathy59t
drug-induced431t,443
idiopathicinflammatory426,430–431,440t,444–446
andmalignancy235t
paraneoplastic234–235
proximal226
screeningexamination66f
myositis392t,428
autoantibodiesin436–437
benignmyositisofchildhood39–40
chronic39–40
inclusion-body438,442
infectious59t
overlap446
-specificautoantibodies445
N
nails63,117,207
naproxen327,653–656
navicularosteochondritis(Köhler’sdisease)515t
neck,physicalexaminationof14t,17t
neckpain
acutewithtrauma76
adults74–79
backgroundepidemiology74
bonescintigraphy79
causesinadults75t
causesinchildren83t
childrenandadolescents82
computedtomography79
dermatomaldistributionofcervicalandupperthoracicnerves74f
examination77–78,82
functionalanatomy74–76
historytaking76–77
magneticresonanceimaging79,80f
newand/orassociatedsymptoms76–77
occupationalandleisureactivities77
radiographs78–79
site,radiation,anddescriptionof76
trauma,previous77
treatment79,80f
Neertest91f
neonatallupuserythematosus372–373
neoplasmsascausesofbackpain141t,618t
neoplasticdiseases,primaryandsecondaryofbonesandjoints234
nephriticsyndromes221
nephritis,interstitial222
nephrogenicfibrosingdermopathy409t
nephrogenicsystemicfibrosis422–423
nerveentrapment124
nerveirritation132t
nervelesionsseeupperlimbperipheralnervelesions
nerverootlesions609–610
nervoussystemdisorders/manifestations
granulomatosiswithpolyangiitis466
sarcoidosis557t
systemiclupuserythematosus351–352
systemicsclerosis418t
seealsoneurologicaldisorders/manifestations
neuroblastoma727
neurologicalconditions238–239
cerebrovascularlesions238–239
entrapmentneuropathies238
headache239
inflammatoryperipheralneuropathy238
neuromyopathy239
spinalcordlesions238
neurologicaldeficit,rapidlyprogressive151–152
neurologicaldisorders/manifestations
Behçet’sdisease553–554
immunoglobulinG4-relateddisease575t
Lymedisease537t
shoulderpain87t
wristandhand108t
neurologicalexaminationandlowbackpaindisorders146
neuromusculardiseaseandSjögren’ssyndrome394
neuromuscularscoliosis620
neuromyopathy239
neuropathy
entrapment238
inflammatoryperipheral238
neutrophilicdermatoses208,561–562
non-infectious561t
Sweet’ssyndrome561–562,562t
nifedipine683t
nodularvasculitis473
non-accidentalcausesofbackpaininchildren618t
non-bacterialosteomyelitis,chronic510–511
non-gonococcalarthritis529t
non-gonococcalsepticarthritis47
non-Hodgkin’slymphoma236
non-inflammatorymusculoskeletalconditions
childrenandadolescents40–44
contributoryfactorsandtheirimpact42
diagnosis,principlesof40–41
examination43
history42–43
laboratorytests44
magneticresonanceimaging44
radiographs44
typicaldisordersinchildrenandadolescents41b
ultrasound44
non-myopathyparaneoplasticsyndromes235
non-osseousinfections75t
non-septicdiscitis613
non-steroidalanti-inflammatorydrugs653–656,660,672
adverseeffects654–655
axialspondyloarthritisandankylosingspondylitis305
backpain610,615t
cautions655
chronicnon-bacterialosteomyelitis511
chronicpainsyndromes631–632
andco-administereddisease-modifyingantirheumaticdrugs655
inflammatoryboweldisease-relatedspondyloarthritis317
juvenileidiopathicarthritis327
non-traumaticvertebralfracture612
psoriaticarthritis311–313
rheumaticfever540
rheumatoidarthritis252,262b
SAPHOsyndrome513
spondyloarthritis-associatedreactivearthritis315
Still’sdisease570–571
systemiclupuserythematosus361t
systemic-onsetjuvenileidiopathicarthritis336
non-traumaticvertebralfracture612
norepinephrinereuptakeinhibitors657–658
nortriptyline615t,657
nose
andgranulomatosiswithpolyangiitis465
andrelapsingpolychondritis565t
O
Obertest169t,178
occupationalactivities/history77,109,174–175
oculardisordersseeeyedisorders/manifestations
odanacatib492
oesophagealdysmotility229–231
oesophagealreflux131t
olecranonbursitis695
oligoarticularjuvenileidiopathicarthritis334
oligoarticularpain
adults47–55
affectedjoints50,51
associatedfeatures51
commoncausesandtypicalpatternsofpresentation48t
examination49,51–52
familyandsocialhistory50–51
generalexamination51
history48–49,50
inflamedjoint,assessmentof47
investigations52
jointaspiration52–53
jointfluidcharacteristics53t
laboratoryinvestigations54
magneticresonanceimaging54
musculoskeletalstructures,examinationof51
precedingfactors50
radiographs53–54
skinrashesandinflammation52
synovialbiopsy54–55
ultrasound54
oncogenicosteomalacia235t
hypophosphataemic498
onycholysis207
ophthalmicsymptomsseeeyedisorders/manifestations
ophthalmoplegia240
opiates,intrathecal615t
opioidanalgesics651–653
cautionsandsideeffects652t
opponensdigitiminimi115t
orthopaedicconditions,differentialdiagnosis324t
Osgood–Schlatterdisease514,515t
osteitispubis159,162
osteoarthritis48t,265–276
aetiology268
clinicalfeatures270–271
epidemiology266
facetjoint149t
futuretherapeuticstrategies275
generalizednodal270–271
hip276
inflammatory/erosive271
investigation272
knee276
largejoint271
management274–275,275b
pathology267
pharmacotherapies274
prognosis276
radiographic-pathologycorrelates267t
secondary271
osteochondritis514–516
childrenandadolescents42–43,184–185
dissecans42–43,174,514–516
Scheuermann’s132t,134,620
osteochondroses514–516
childrenandadolescents42–43,184–185
conditions515t
Freiberg’sdisease516
Köhlerdisease516
Legg–Calvé–Perthesdisease514
Scheuermann’sdisease514
Sinding–Larsen–Johanssondisease516
osteogenesisimperfecta580–581
Sillenceclassification580t
osteoidosteoma524,622b
osteolysis225
osteomalaciaandrickets494–498
fromalteredphosphatehomeostasis497
classification494t
clinicalandlaboratoryfindings495–496
hypophosphataemic234–235
management496
oncogenichypophosphataemic(tumour-induced)498
oncogenicosteomalacia235t
ricketyrosary132t
thoracicbackandchestpain132t
vitaminD-dependentrickets496
X-linkedhypophosphataemicrickets497
osteomyelitis225,534–535,535t
chronicnon-bacterial510–511
osteonecrosis106–108,518–519
causative/associatedconditions519t
osteopenia352
generalized149t
osteopetrosis522
osteopoikilosis523
osteoporosis484–493
abaloparatide492
bisphosphonates490–491
calcium489
causative/associateddiseases486t
clinicalfeatures488
denosumab492
drugs682–683
endocrinemanifestations226
exercise490
fractureprevention489–493
glucocorticoid-induced487–488
guidelinesformanaging493
hormonereplacement490
idiopathic485–486
investigations488–489
juvenileidiopathic485–486
kyphoplasty493
odanacatib492
pathogenesisandclassification484–488
rheumatoidarthritis247
riskoffracturewithsite484t
romosozumab492
strontiumranelate491
systemiclupuserythematosus352
teriparatide491
thoracicbackandchestpain133
vertebroplasty492–493
osteosarcoma524
inchildren726
out-toeing32t
overlapmyositis446
oxicams653–656
oxycodonehydrochloride653
P
pachydermoperiostosis522
paediatricgait,arms,legs,spine(pGALS)screen14–19,24
paediatricsystemiclupuserythematosus,acute717
Paget’sdisease132t,157,198,506–508
clinicalfeatures506t
investigationandtreatment507–508
pain624–625
acute624–625
inadults6–13
elicitedpainonexamination10
gatecontroltheory625
hypermobilityandchronicpaininchildren593
inflammatorymusculoskeletalpain8
localization6–7
McGillpainscale7t
mechanical8
monoarticular46–47
neurophysiology624
pathophysiology625
qualityof7
referred75t,87t
siteof88
seealsochronicpainsyndromes;chronicregionalpainsyndrome;painrelief
painconditions,differentialdiagnosis324t
painrelief647t,648–659
analgesicescalation649–650
antidepressants656
gabapentin658
musclerelaxants659
non-steroidalanti-inflammatorydrugs653–656
opioidanalgesics651–653
pregabalin658
rheumatoidarthritis252
serotoninandnorepinephrinereuptakeinhibitors657–658
simpleandcompoundanalgesics650,651t
topicalagents659
painfularctest91f
palpitations62
pamidronate305,511,581,613,636
Pannerdisease515t
panniculitis560–561
calcifying561
lobular560–561
septal560
withvasculitis561
paracetamol(acetaminophen)650
backpain610,615t
cautionsandsideeffects651t
chronicwidespreadpaininchildrenandadolescents641
compounds650
non-traumaticvertebralfracture612
post-herpeticneuralgia637
paraesthesias124
paraneoplasticmyopathies234–235
paraneoplasticsyndromes,non-myopathy235
paraproteinaemia236
parasites712t
parathyroiddiseaseandrelateddisorders483–524
chronickidneydisease-mineralandbonedisorders504–505
ectopiccalcificationandossification505
familialhyperparathyroidsyndromes503–504
familialhypocalciurichypercalcaemia503
hypercalcaemia500–502,502t
hyperparathyroidism,primary502–503
hyperparathyroidism,secondaryandtertiary503
parathyroidhormoneresistantsyndromes504
renalosteodystrophy504–505,505t
parathyroidhormoneresistantsyndromes504
parentcoaching641
paroxetine657
parsinterarticularis/defect/fracture149t
parvovirusB1958t
patellaQangle172f,177
patellofemoralsyndrome42,184–185
patternsofdiseasepresentationseeoligoarticularpain;widespreadpain
peg-leggait38–39
pegloticase686–687
Pellegrini–Stiedaphenomenon173–174
pelvic,groin,andthighpain156–169
adults156–166
ageofpatient157
areaswithinwhichsensorychangesmaybefound161f
boneandsofttissuepain,distributionandtypeof158–159
bonescintigraphy165
bonyanatomyofposteriorhipandpelvis163f
causesinchildrenandadolescents168t
childrenandadolescents168–169
computedtomography165
diagnosticultrasound164
examination160–164,168–169,169t
hip,functionalanatomyof157
hipexamination162
historytaking157–160
laboratoryinvestigations165
leglengthdiscrepancy169
magneticresonanceimaging165
muscleactivationtests162–163
musculardistribution,painin159
nervepain,qualityanddistributionof159–160
neuroanatomy157
observationandpalpation161–162
painpatternsandcausesaroundproximalleg158t
pelvicandhipregion,anatomyof156
pelvicmusculature,anatomyof156–157
pelvicorhiplesions,riskfactorsfor160t
pelvicphysicalexamination14t
posterolateralstructures,palpationof163–164
previoustrauma,lowback,andmusculoskeletalproblems160
radiographs164
surgery166
thigh,posterior,painin158t
treatment165–166
pemphigoid208
pemphigus208
penicillamine311–313,665t
penicillin536,540
pepticulcerdisease131t,231–232
percutaneousadhesiolysis616t
percutaneousdiscectomy611t
periarticulardisorders108t,290t
periarticularinjections
hip700
knee703
periarticularlesions87t,700–703
pericarditis416t
pericardium216
effusions216
inflammation131t
periodicfever,aphthousstomatitis,pharyngitis,adenitis(PFAPA)syndrome547
periostitis227,191
peripheralneuropathy392t
peripheralspondyloarthritis299b
peritendonitiscrepitans99
Perthesdisease160t
children42–43
pescavus32t,202
pesplanus(flatfeet)32t,201–202
Phalen’smanoeuvre127
phantomlimbpain637
phenoxymethylpenicillin540
phenylketonuria409t
phenytoin669
photosensitivityreaction667
physicalexamination14–19,15–16f,17t,19f
physiotherapy640
pigmentedvillonodularsynovitis576
Pilates615t,630
piriformissyndrome157,163–164
piroxicam655,656
pityriasislichenoides473
plantarfasciitis51,195,200–201
glucocorticoidinjectiontherapy704
plantarspur198
plaques208
plasmaexchange
ANCA-associatedvasculitides467–469
systemiclupuserythematosus364
pleura/pleuraleffusion218
pleurisy416t
pleuriticinflammation131t
pneumonitis,methotrexate-induced721
pneumothorax416t
POEMS409t
polarizedlightmicroscopy53
polyangiitis,microscopic213,466–467,468
polyarteritisnodosa231t,462
aetiology462
clinicalfeatures463t
cutaneous478–479
presentation462
systemic479–480
treatment462
polyarthropathy68
polyarticularabnormalityinwrist/hand120t
polyarticularjuvenileidiopathicarthritis334
rheumatoidfactor-negative334–335
polychondritis,relapsing52,206–207,564,565t
polydactyly203
polymyalgiarheumatica159,456–457,457b,459–460
polymyositisanddermatomyositis206–207,226,234–235,235t,425–446
antibodies436t
assessmentofdiseaseimpact431–432
autoantibodies436–437
biologictherapies439,440t
BohanandPeter’sclassification426b
cardiovascularfeatures429,432t
children444–446
clinicalassessments430–432
clinicalfeatures428–430
creatinekinase,raised434t
diagnosticcriteria427b
electromyography437
extramusculardisease,treatmentof440–441
gastrointestinalfeatures429,432t
glucocorticoids438
gutandhepatobiliarymanifestations230t,231t
idiopathicinflammatorymyopathy430–431
imaging437
inclusion-bodymyositis438,442
withinterstitiallungdisease443
intravenousimmunoglobulin439
investigations434–437
joints429
juveniledermatomyositis231t
keyfeatures427t
malignancy235t,430
musclebiopsy435–436
muscleenzymelevels434–435
myopathy,drug-induced431t,443
myositis428
pathogenesis428
prognosis441
pulmonaryfeatures429,432t
skinandcutaneousdisease428–429
systemicmanifestations432t
treatment438–441,445–446
pooledimmunoglobulin365,687
posteriordrawtest177
post-herpeticneuralgia637
post-renalazotaemia221
post-streptococcalarthritis34
posturetraining615t
prednisolone660
ANCA-associatedvasculitides468
lupusnephritis362f
macrophageactivationsyndrome722
polymyalgiarheumatica459–460
polymyositisanddermatomyositis438
relapsingpolychondritis564
Still’sdisease570–571
systemiclupuserythematosus360,361t
systemicsclerosis420
Takayasuarteritis455
prednisone459–460
pregabalin615t,631–632,636,658
pregnancy
antiphospholipidsyndrome378t,384t
biologicaltherapies676t,680
disease-modifyingantirheumaticdrugs663,665t
multiple,andpelvicorhiplesions160t
non-steroidalanti-inflammatorydrugs655
rheumatoidarthritis261,262b
systemiclupuserythematosus357
Takayasuarteritis455
prepatellarbursitis(housemaid’sknee)175
pre-renalazotaemia220
presentationofrheumaticdisease205–240
cardiacconditions216–217
endocrineconditions224–227
gutandhepatobiliaryconditions228–232
malignancy234–236
neurologicalconditions238–239
ophthalmicconditions240
pulmonaryconditions218–219
renalconditions220–222
skindisorders206–209
skinvasculitis212–214
primaryangiitisofcentralnervoussysteminchildren480–481
primaryvasculitides447–481
ANCA450
ANCA-associatedvasculitides464–469,481
childhood-onset474–481
cutaneouspolyarteritisnodosa478–479
eosinophilicgranulomatosiswithpolyangiitis467
giantcellarteritis457–460,458t
granulomatosiswithpolyangiitis464–466
Kawasakidisease475–476
largevesselvasculitis452
leucocytoclasticvasculitis470,478
microscopicpolyangiitis466–467
polyarteritisnodosa462
polymyalgiarheumatica456–457,457b,459–460
primaryangiitisofCNSinchildren480–481
smallvesselvasculitis470–473
systemicpolyarteritisnodosa479–480
systemicvasculitis,classificationof448t
Takayasuarteritis454–455
vasculitis,CHCCnomenclatureof449b
vasculitismanagement,generalprinciplesof450
seealsosmallvesselvasculitis
probenecid685
proptosis240
prostacyclin418,387
prostheticintervertebraldiscreplacement611t
proteinuria213
protozoa527t
proximalmyopathy226
pseudogout47,50
triggeringfactorsof287b
pseudohypoparathyroidism504
psoriasis206
psoriaticarthritis50,308–313
CASPARclassificationcriteria308b
clinicalassessment310–311
clinicalfeatures309–310
comorbidities311
epidemiology308
genetics308
immunopathogenesis309
juvenile318–319,335
NSAIDsandsyntheticDMARDs311–313
pathophysiology308–309
treatment311–313
psychologicaltherapies640
psychology-orientatedrehabilitationprogrammes616t
pulmonaryarteryhypertension
drugs683–684
systemicsclerosis416t,417
pulmonarydisorders/manifestations218–219
airways219
antiphospholipidsyndrome380
arterialhypertension219,720
Behçet’sdisease553
fibrosis219,416t
granulomatosiswithpolyangiitis465
immunoglobulinG4-relateddisease575t
interstitiallungdisease219
nodules/masses218
non-steroidalanti-inflammatorydrugs654t
pleura218
polymyositisanddermatomyositis429,432t
sarcoidosis557t
Sjögren’ssyndrome392t,394
systemiclupuserythematosus349–350
systemicsclerosisandrelateddisorders415–417
vasculature219
pulmonaryhypertrophicosteoarthropathy522
pustules208
PUVA668
pyodermagangrenosum209,562
pyodermagangrenosum,acne,andpyogenicarthritis(PAPA)syndrome547–549
pyrexiaofunknownorigin(PUO)23
Q
quadricepsfemoris(hipflexion/kneeextension)147t
quadricepsphysicalexamination14t
quinine669–670
quininesulphate659
quinolones669–670
R
radialnerve101,126
radiculopathy78–79
radiocarpaljoint696
rareautoinflammatoryandmiscellaneousdiseases541–576
amyloidosis566–567,567t
approachtodiagnosis543
Behçet’sdisease550–554
Blausyndrome549
CANDLEsyndrome549
CARD14-mediatedpsoriasis549
childhoodperiodicfevers545
cutaneousmanifestation543
deficiencyofIL-1receptorantagonist549
eosinophilicfasciitis572
epidemiology542–543
Eurofevertool548t
familialMediterraneanfever546,547
immunoglobulinG4-relateddisease574
mevalonatekinasedeficiency546–547
neonatalandinfantileperiodicfevers545
pathogenesis542
PFAPAsyndrome547
pigmentedvillonodularsynovitis576
polychondritis,relapsing564,565t
presentations543–547
prominentskinmanifestations547–549
pyodermagangrenosum,acne,andpyogenicarthritissyndrome547–549
sarcoidosis556–559
Schnitzler’ssyndrome547
skinconditionsassociatedwitharthritis560–562
spectrum544t
Still’sdisease568–571
synovialchondromatosis576
TNFreceptor-associatedperiodicsyndromes546,547
reactivearthritis33–34,51,206–207,314–315
clinicalfeatures314
investigation314–315
management315
‘redflags’(backpain)607
referralforfurtherassessment
adults31
childrenandadolescents28–30
referredpain75t,87t
regionalmusculoskeletalconditions71–203
elbowpain98–104
hand112–122
kneepain170–186
lowbackpainanddisordersinadults140–155
lowerlegandfootdisorders188–203
neckpain74–82
pelvic,groin,andthighpain156–169
shoulderpain84–96
thoracicbackandchestpain130–138
upperlimbperipheralnervelesions124–127
wristpain106–110
regionalpainsyndrome106–108
relapsingpolychondritis52,206–207,564,565t
renaldisorders/manifestations220–222
antiphospholipidsyndrome380
Behçet’sdisease554
granulomatosiswithpolyangiitis465
immunoglobulinG4-relateddisease575t
intrinsicrenalfailure–‘activesediment’221
intrinsicrenalfailure–‘blandsediment’221–222
non-steroidalanti-inflammatorydrugs654t
polymyositisanddermatomyositis432t
post-renalazotaemia221
pre-renalazotaemia220
relapsingpolychondritis565t
renalfailureevaluation220
renaltubularacidosis222
sarcoidosis557t
sclerodermarenalcrisis222
Sjögren’ssyndrome392t,394
systemiclupuserythematosus350–351,714–715,717
systemicsclerosisandrelateddisorders417–418
renalosteodystrophy504–505,505t
renaltubularacidosis222,497
repetitivestraininjury72,109
respiratorydisorders/manifestations
non-steroidalanti-inflammatorydrugs654t
relapsingpolychondritis565t
reticulohistiocytosis207,562
rheumaticdiseaseseeinfectionandrheumaticdisease
rheumaticfever52,54,58t,538–540
acute34
rheumatoidarthritis48t,243–263
abatacept258,259b
anti-interleukin-6receptorblocker–tocilizumab258,259b,262b
anti-TNFαtherapy256,259b,260,262b
associatedclinicalmanifestations247
azathioprine254b,255,262b
baselineimaginginvestigations249t
baselinelaboratoryinvestigations248t
B-celldepletion–rituximab256–258,259b,262b
cancerrisk260
classification244,245t
clinicalfeatures246–247
complementarytherapies263
epidemiology244
extra-articularfeatures247
glucocorticoids256,262b
gold254b,255
gutandhepatobiliarymanifestations230t,231t
hydroxychloroquine254b,255,262b
immunopathology244
infectionmanagementwhileonimmunosuppression259–260
investigations248
januskinaseinhibitors–tofacitinib259
jointsandtendons246
leflunomide254b,255,262b
management250–263
methotrexate253,254b,262b
NICEguidance251f
novelmedications259
NSAIDs252,262b
painreliefandanalgesia252
pathogenesis244
pregnancyandbreastfeeding261,262b
sulfasalazine254b,255,262b
surgery261–263
synovialpathology244–245
systemicfeaturesandassessment247
rheumatoidfactor-negativepolyarticularjuvenileidiopathicarthritis334–335
rheumatoidnodules118
rhupus354
Ribbingdisease522
ricketsseeosteomalaciaandrickets
rifampicin673–674
riociguat417,683t
risedronate507–508,682t
rituximab
ANCA-associatedvasculitides467–469
antiphospholipidsyndrome383,387
immunoglobulinG4-relateddisease574
polymyositisanddermatomyositis439,440t
pregnancyandbreastfeeding676t
rheumatoidarthritis256–258,259b,262b,677
Sjögren’ssyndrome398
systemiclupuserythematosus361t,363
systemicsclerosis420
rivaroxaban384
romosozumab492
rosacea206–207
rotatorcufflesions85–87
rotatorcufftear597t
rubefacients659
rubella58t
S
sacralspineanatomy140
sacroiliacjoints145
sacroiliitis51,143,164,229
sailsign101
St.John’swort668
salivaryglands575t
sarcoid
arthropathy54–55
conditions206–207
sarcoidosis556–559
acute(Lofgren’ssyndrome)556
chronic556,557t
clinicalmanifestations557t
diagnosisandinvestigations558–559
early-onset(childhood)556–557
epidemiologyandpathophysiology556
musculoskeletalmanifestations557–558
patternsofdisease556–557
treatment559
scalp206
Scheuermann’sdisease46,143,514,515t
Scheuermann’sosteochondritis132t,134,620
Schnitzler’ssyndrome547
Schöbertest15–16f,144
sciaticnerveentrapment163–164
scleraldisease240
sclerodactyly413
scleroderma230t,412–413
diffusecutaneous209
-likefibrosingdisorders422–423
limitedcutaneous208
linear210t,402,422
renalcrisis222
scleroedema409t,423
scleromyxoedema409t,423
sclerosingbonedisorders522–523
Camurati–Engelmanndisease522
endostealhyperostosis522–523
hepatitisCosteosclerosis523
osteopetrosis522
osteopoikilosis523
primaryhypertrophicosteoarthropathy522
pulmonary(secondary)hypertrophicosteoarthropathy522
Ribbingdisease522
spectrum523t
sclerosis149t,227
crises720
lipodermato-210t,409t,561
sclerosteosis522–523
scleroticlesions,localized149t
scoliosis133
congenital620
idiopathic619
measurement619f
neuromuscular620
secukinumab306,313,679
selectiveserotoninreuptakeinhibitors631–632,657
septicarthritis247,528–531,708–711
adults708
antibiotics710t
children708–709
epidemiology528
gonococcal711
immediatemanagementinadults709
investigation528–529
andLymedisease536
management529–530
managementinchildren709–710,710t
non-gonococcal47
pathology528
post-immediatemanagementinadults710–711
post-immediatemanagementinchildren710t
presentation528
septicbursitis530
serotoninandnorepinephrinereuptakeinhibitors657–658
serotoninreuptakeinhibitors657t
serratusanterior92t
sertraline631–632,657
Severdisease515t
shinsplints191
shoulder
acromioclavicularjoint693
glenohumeraljoint692
glucocorticoidinjectiontherapy692–693
physicalexamination14t,17t
subacromialspace693
seealsoshoulderpain
shoulderpain84–96
acromioclavicularjoint90
adults84–95
anatomyofshoulder84
arthrography93–94
bilateralshouldermovements89–90
bloodtests94
bonescan94
causesinadults87t
causesinchildrenandadolescents96t
childrenandadolescents96
electrophysiologicaltests94
examination89–93
glenohumeraljointmovement90
historytaking85–88
isolatedmuscletestingofshouldergirdlemuscles91–92,92t
jointaspiration94
localanaestheticinjection94
magneticresonanceimaging93–94
majorshoulderstructuresandjointcapsule85f
musclesoftheshoulder86f
onsetofpain85–87
painandshoulderlesions84–85
radiographs93
spinalsymptoms88
subacromialimpingement90,91f
supineshoulderexamination92–93
tenderness89
treatment94–95
ultrasound93–94
variationinpain88
visualinspection89
sifalimumab440t
sildenafil417,683t
simvastatin668
Sinding–Larsen–Johanssondisease516
Sipplesyndrome504
Sjögren’ssyndrome389–400
autoimmunediseases,co-existing395
biopsy397
cardiovascularsystem395
classificationcriteria390t,392–395
clinicalmanifestations392–395
endocrinemanifestations226
epidemiologyandpathophysiology390
extraglandulardisease392t
fatigue395
gastrointestinalandhepatobiliarydisease394
glandulardisease392,393t
gutandhepatobiliarymanifestations230t
investigations396–397
joints393
laboratoryfindings396t
lymphoproliferativedisease395
neuromusculardisease394
prognosis400
pulmonarydisease394
renaldisease394
siccasymptoms,assessmentof396–397
skin212,393–394
treatment398,399t
skeletaldysplasias43
skeletalmanifestationsandpolymyositisanddermatomyositis432t
skier’sthumb115
skinconditionsassociatedwitharthritis560–562
multicentricreticulohistiocytosis562
neutrophilicdermatoses561–562
panniculitis560–561
pyodermagangrenosum562
skindisorders/manifestations206–209
antiphospholipidsyndrome379
Behçet’sdisease550–552
diagnosticissuesinskinthickening209
eruption,typesof207–209
examination,importanceof206
faceandears206–207
granulomatosiswithpolyangiitis465
handsandnails207
immunoglobulinG4-relateddisease575t
Lymedisease537t
macularrashes207
non-steroidalanti-inflammatorydrugs654t
patternrecognitioninskinthickening210t
plaques208
polymyositisanddermatomyositis428–429
pustulesandblisters208
rareautoinflammatorydiseases547–549
regionalabnormalities206–207
relapsingpolychondritis565t
rheumaticfever539
sarcoidosis557t
scalp206
Sjögren’ssyndrome212,393–394
systemiclupuserythematosus206–207,212,348
texturalabnormalities209
ulcersandulceratingrashes208–209
vascularlesions208
widespreadpain63
seealsoskinconditionsassociatedwitharthritis;skinvasculitis
skinvasculitis212–214
diagnosis212
importantconsiderations213
investigations213–214
laboratoryinvestigations214t
precipitantsandassociationsofleucocytoclasticsmallvesselvasculitis212t
skinbiopsy213–214
systemic213
sleep630
slippedepiphysis160t
slippedupperfemoralepiphysis515t
adolescents42–43
slumptest145f
smallvesselvasculitis470–473
allergic(hypersensitivity)471
cryoglobulinaemic472
erythemaelevatumdiutinum472
granulomafaciale472
Henoch–Schönleinpurpura471,476–478
hypergammaglobulinaemicpurpura472
leucocytoclastic470,478
non-leucocytoclastic(lymphocytic)470t,473
urticarial471–472
snaps12
sodiumaurothiomalate669
softtissuelesions75t
soleus147t
spinalcordcompression78,151–152
spinalcordlesions238
spinalcordstimulator616t
spinaldisordersseebackpain
spinalstenosis142–143,151–152,611–612
spinaltumours621,622b
spinealignment,physicalexaminationof14t
spirochaete527t
splinterhaemorrhages207
spondylitis78–79
spondyloarthritis48t,230t
-associatedreactivearthritis314–315
inflammatoryboweldisease-related316–317
juvenile318–320,335
paradigmshift296
spondyloarthropathies132t,134,293–320
axialspondyloarthritisandankylosingspondylitis298–306
classifying296,298–299
inflammatoryboweldisease-relatedspondyloarthritis316–317
juvenilespondyloarthritis318–320
psoriaticarthritis308–313
seealsoankylosing-spondylitis;spondyloarthritis
spondylodiscitis613
spondylolisthesis144,620,621f
spondylolysis620
statins668
stemcelltransplantation364
stenosingtenosynovitis(triggerfinger)117,224–225
steroidinjections182–183,199
Sticklersyndrome206–207,594
stiff-leggedgait38–39
stiffness12
Still’sdisease207,230t,568–571
clinicalfeatures568–569
courseofdiseaseandprognosis571
epidemiologyandpathogenesis568
laboratoryandradiographicfindings569–570
treatment570–571
Yamaguchicriteria569b
stomatitis232
stoopedgait39
straightlegraise(Laseague’stest)146
stressfractures191
stridor219
strontiumranelate491,682t
subacromialbursitis597t
subacromialimpingement84–85,87t,596–597,597t,598f
subacromialspace693
subluxation78–79
subtalarjoints704
sulfasalazine662–663,664,672–673
axialspondyloarthritisandandankylosingspondylitis305
chronicnon-bacterialosteomyelitis511
inflammatoryboweldisease-relatedspondyloarthritis317
juvenileidiopathicarthritis329
juvenilespondyloarthritis320
pregnancyandbreastfeeding665t
psoriaticarthritis311–313
rheumatoidarthritis254b,255,262b
spondyloarthritis-associatedreactivearthritis315
sulfinpyrazone685–686
suprascapularnerve124–125
suprascapularnotchlesion597t
supraspinatus92t
supraspinatus/cufftendonitis597t
Sweet’ssyndrome561–562,562t
swelling12
symphysitis700
syndactyly203
syndesmophytes134
synovialchondromatosis53–54,576
synovialplica185
synovitis108
acne,palmoplantarpustolosis,hyperostosis,asepticosteomyelitis(SAPHO)syndrome52,510–511,
512–513
joint177
oligoarticular47
pigmentedvillonodular576
synoviumdisorders576
systemicconditionsandshoulderpain87t
systemiclupuserythematosus67t,343–373
acuteseesystemiclupuserythematosus,acute
antimalarialdrugs361
andantiphospholipidsyndrome356
assessmentofdiseaseactivity358
atacicept364–365
autoantibodies355t
azathioprine363
belimumab364
cardiovasculardisease349,360
classification344,345t
clinicalfeatures348–352,352t
cyclophosphamide363
drug-inducedlupuserythematosus(DILE)359
eculizumab364–365
environmentalfactors346
epidemiology344
epratuzumab364–365
gastrointestinalclinicalfeatures352t
genetics346
glucocorticoids360
gutandhepatobiliarymanifestations230t,231t
haematologicalfeatures351
immunologicalclinicalfeatures352t
immunosuppression360–365,362f
investigations354
juvenile368–370
malignancy352
management360–365
methotrexate363
mucocutaneousmanifestations348
musculoskeletalclinicalfeatures348
mycophenolatemofetil(MMF)363
neonatallupussyndrome372–373
neurologicaldisease351–352
ocularclinicalfeatures352t
osteoporosisandosteopenia352
pathophysiology346
plasmaexchange364
pooledimmunoglobulin(IVIG)365
andpregnancy357
prognosisandsurvival366
pulmonarydisease349–350
recommendationsfordruguse361t
renaldisease350–351
rituximab363
serologyandimmunecomplexes346
skin206–207,212,348
stemcelltransplantation364
tacrolimus364–365
tocilizumab364–365
vascularclinicalfeatures352t
vitaminDdeficiency352
systemiclupuserythematosus,acute714–717
cardiorespiratory715,716t
diagnosis714
haematologicalmanifestations716–717
paediatric–haematologicalmanifestations717
paediatric–renalmanifestations717
renal714–715,715f
systemic-onsetjuvenileidiopathicarthritis326t,335–336
conditionsandinvestigationstoconsider326t
diagnosis336
treatment336
systemicpolyarteritisnodosa479–480
systemicsclerosisandrelateddisorders210t,401–423
ACR/EULARclassificationcriteria402t
cardiacdisease415–417,416t
characteristicfindings410t
classificationanddiseasepatterns406
clinicalfeatures412–418
diagnosis408
differentialdiagnosis408,409t
diffusecutaneous406,407t,410t
earlysystemicsclerosis407t
environmentalfactors405
eosinophilicfasciitis422
epidemiology404
essentialinitialinvestigations408
fibrosis405
gastrointestinaltract414–415
genetics/epigenetics404
genitalia418t
immunecellactivationandcytokines404
inflammation405
limitedcutaneous406,407t,410t
linearscleroderma422
liver418t
morphoea422
nephrogenicsystemicfibrosis422–423
nervoussystem418t
pathophysiology404–405
prognosis420
pulmonaryarteryhypertension417
pulmonarydisease415–417,416t
Raynaud’sdisease412,413t
renaldisease417–418
scleroderma-likefibrosingdisorders422–423
scleroedema423
scleromyxoedema423
sinescleroderma407t
skin412–413
thyroidgland418t
treatment420
vasculopathy405
systemicsclerosiscrises720
pulmonaryhypertension720
renalcrisis720
systemicvasculitis448t,718–719
T
tacrolimus
dermatomyositis440–441
juvenileidiopathicarthritis329
polymyositisanddermatomyositis439
Still’sdisease570–571
systemiclupuserythematosus361t,364–365
tadalafil417,683t
Takayasuarteritis454–455
epidemiology454
investigation454
presentation454
treatment455
talipesequinovarus(clubfoot)202
talusosteochondritis515t
tarsalcoalitions202
tarsaltunnel704
tearsofmenisci174
telangiectasia208
temporomandibularjointdysfunction637
tendonitis
acutecalcificsupraspinatus89–90
anserine173–174
supraspinatus/cuff597t
tendonsandrheumatoidarthritis246
tenniselbowseelateralepicondylitis
tenosynovitis47,117,119
teriparatide491,581,682t
thenareminencemuscles113t,114f
theophylline660,684
thighpainseepelvic,groin,andthighpain
thiopurinemethyltransferase(TPMT)deficiency667
Thomastest162,169t
thoracicbackandchestpain130–138
adults130–135
bonescintigraphy135
cardiachistoryandexamination137
causesinchildrenandadolescents136t
characteristicsfromnon-neurologicalandnon-musculoskeletalpathology131t
childrenandadolescents136–138
examination133–134,136–138
historytaking130–133,136–138
magneticresonanceimaging135
musculoskeletalfeatures137
painfulneurologicalandmusculoskeletalconditions132t
palpation133
pulmonarydiseasefeatures137
qualityofpain132
radiographs134
symptoms,other,andriskfactors132–133
thoracicspinalinvolvement134
visualinspection133
thoracicconditions87t
thoracicnerves74f,124
thoracicspine,physicalexaminationof17t
thoracicvertebraldisease132t
throatandgranulomatosiswithpolyangiitis465
thrombocytopenia378t,380
thrombosis378
thyroidacropachy226
thyroiddisease54
thyroidgland418t
thyroiditis,lymphocytic226
thyrotoxicosis226
tibialtorsion186
tibialisanterior(ankledorsiflexion)147t
tibialisposterior(ankleinversionanddorsiflexion)147t
Tinel’ssign127,195
tizanidine659
tocilizumab
giantcellarteritis460
juvenileidiopathicarthritis329
polymyositisanddermatomyositis440t
pregnancyandbreastfeeding676t
rheumatoidarthritis258,259b,262b,678–679
Sjögren’ssyndrome398
Still’sdisease571
systemiclupuserythematosus364–365
systemic-onsetjuvenileidiopathicarthritis336
systemicsclerosis420
Takayasuarteritis455
toeanomalies203
toewalking32t,39
tofacitinib259,306,673–674
tolbutamide670
topicalagents659
torticollis77
Toxoplasmagondii58t
tramadol610,631–632,652,658
transaminitis232
transcutaneouselectricnervestimulation252,615t,636
Trendelenburglimp/gait38–39
Trendelenburgtest169t
triamcinolone660
trichorhinophalangealsyndrome46
tricyclicantidepressants631–632,636,641,657
trigeminalneuralgia637
triggerfinger117,224–225
trimethoprim667,672
trimethoprim-sulfamethoxazole468,469
trochantericbursitis/enthesitis158–159,700
T-score488–489
tuberculosis260,713
tubularnecrosis,acute221–222
tumour-inducedosteomalacia498
tumournecrosisfactor(TNF)receptor-associatedperiodicsyndrome(TRAPS)546
late-onset547
tumours
bone524
Brown’s227
spinal621,622b
U
ulcerativecolitis228t
spondyloarthritis316–317
ulcersandulceratingrashes208–209
ulnarnerve125,125–126,128f
unexplainedacute-phaseresponse23
upperlimbmusculoskeletallesions595–603
adhesivecapsulitis600
lateralhumeralepicondylitis(tenniselbow)602–603,603f
subacromialimpingement345t,596–597,598f
upperlimbperipheralnervelesions124–127
carpaltunnelsyndrome127
dermatomesofanteriorandposterioraspects128f
mediannerve126–127
radialnerve126
suprascapularnerve124–125
thoracicnerve,long124
ulnarnerve125–126
urethritis51
urgentrheumatologicalassessment30
urothelialtoxicity668–669
urticarialvasculitis471–472
ustekinumab306,312–313,679
uveitis51,240
differentialdiagnosisofcauses340t
juvenileidiopathicarthritis340–341
management341
surveillance(screening)programmes340–341,341t
V
valvulardisease217
VanBuchemdisease522–523
vancomycin530
varicellainfections713
vasculardisorders/manifestations
immunoglobulinG4-relateddisease575t
systemiclupuserythematosus352t
vascularlesions208
vasculature219
vasculitis117
allergic(hypersensitivity)471
CHCCnomenclatureof449b
cutaneous392t
large-vessel452
leucocytoclastic470,478
livedoid473
management450
nodular473
non-leucocytoclastic(lymphocytic)470t,473
withpanniculitis561
‘severe’718–719
skindisorders208
systemic448t,718–719
urticarial471–472
seealsoskinvasculitis;smallvesselvasculitis
vasculopathy405
venlafaxine631–632
vertebralend-plateosteophytes,marginal149t
vertebroplasty492–493
Vilanova’sdisease560
viralenteritis228t
viruses527t,712t
visceralcausesofbackpaininchildren618t
vitaminDdeficiency494–498
clinicalandlaboratoryfindings495–496
management496
systemiclupuserythematosus352
vitaminD-dependentrickets496
W
waddlinggait38–39
warfarin660,667,670,684
antiphospholipidsyndrome381–384,382t
Weber–Christiandisease560–561
Wegener’sgranulomatosisseegranulomatosiswithpolyangiitis
Whipple’sdisease228t
widespreadpain55–63
abnormality,patternsof64–65
affectedjoints57
age,gender,andracialbackground56
antinuclearantibodies67t
bonepathology60–61
categoriesofconditions55t
chestpain,dyspnoea,palpitations,cough,andhaemoptysis62
commoninfectionswithacutepolyarthritisandraisedacutephaseresponse58t
drughistory62
dysphagia,abdominalpain,anddiarrhoea63
electrophysiologyandimaging69
examination63–70
familyhistory62
fibromyalgia,sitesoftendernessin65f
historyofpainatdifferentsites56
historytaking56
initialimpressions55
investigations67
ischaemicpains60
jointexamination63
jointhypermobilitysyndrome64t
jointpainatrest,afterrest,orwithjointuse57
laboratorytests68–69
malignancy,investigationsfor69–70
musclebiopsy69
musclepain58,69
myalgiasandweakness59t,60,65–67
myopathies59t,66f
pastmedicalhistory61
patternofjointsymptomsovertime57–58
patternofmusclepainsovertime60
polyarthropathy,basictestsin68
previousdiagnoses56
psychosocialandsexualhistory61
skinandnailsexamination63
travel61
Williams’syndrome502t
Wilson’sdisease228t,229
work-relateddisorder(WRD)72
wrist
glucocorticoidinjectiontherapy696–698
physicalexaminationof17t
seealsowristpain
wristpain106–110
adults106–110
bonescintigraphy119
childrenandadolescents122
dorsumexamination110
examination109–110
flexion/extensionrangetests109
flexorandextensortendonsheaths107f
functionalanatomy106
historytaking106–109
job/leisureactivities109
locationofpain106
magneticresonanceimaging119
painfulconditionsanddiagnoses108t
qualityof108
radiographs119,120t
synovitis108
tendonintegritytesting110
traumahistory106–108
treatment110,121
ultrasound119
visualinspection109



