©robertprzybysz/i Stock/Thinkstock
MARCH 2015
The
ORTHODONTIC
workforce
CONTENTS
www.nature.com/BDJTeam BDJ Team 02
©iStockphoto/Thinkstock
Highlights
04 The twenty-first century
orthodontic workforce
Highlights the changes that have
taken place over the past decade and
proles an orthodontic nurse and an
orthodontic therapist.
11 ‘There is a family atmosphere in
our lab’
BDJ Team meets Willette Jean Lati,
a dental technician who works in an
orthodontic laboratory in London.
22 Are you addicted to sugar?
Certied health coach and blogger
Laura omas explains how to control
your sugar cravings - and shares a low
sugar apjack recipe.
Regulars
03 News
28 New products
30 BDJ Team verifiable CPD
In this issue
13 Needlestick safety for the whole
dental team
An update on risk management and
the use of sharps.
16 The denture box
How the denture box facilitates
denture hygiene, reduces the chance of
accidental damage, and more.
20 Rules for shared parental leave
Parents of babies due on or aer
5 April 2015 will be able to share
statutory leave.
25 How to dispose of
hazardous waste
Waste segregation and management
in dentistry - with one hour of CPD.
From the Vital archive.
March
2015
04
25
CORE
CPD:
ONE HOUR
www.nature.com/bdjteam
22

NEWS
NEW APP FOR BRITISH DENTAL
CONFERENCE 2015
Delegates at this year’s British Dental
Conference and Exhibition will nd
everything they need at the tip of their ngers
thanks to a new app specially designed for the
event. A rst for 2015, the app is suitable for
both Apple and Android devices and makes
managing your time at the event and getting
around even easier than before. e app is
available to download now via the Apple App
Store or Google Play.
Key features of the new app include:
■
A personal agenda feature allowing
delegates to browse full programme
information and add sessions they would
like to attend to their own personalised
event diary
■
Full speaker bios
■
Venue and exhibition maps
■
Instant event notications
■
Access to special show oers
■
Visitor information from cash machine
locations to car parking
■
Direct access to Twitter and Facebook
allowing users to interact and share views
with other delegates and organisers
■
Notes section that allows you to save and
email notes to yourself.
Linda Stranks, Director of Marketing and
Membership at the British Dental Association
(BDA), said: ‘We have designed this app to
make the event experience as simple and
smooth as possible. Many of our delegates
now carry smartphones so it makes sense
to interact with them and provide show
information directly into their hands. We
want to make the event even more interesting
for visitors and more interactive for
exhibitors.’
is year’s event will take place from 7-9
May at the Manchester Central Convention
Complex with many of the sessions of interest
to the whole team. However, in addition,
there are also a number of sessions which
have been designed with particular team
members in mind.
Dental nurses
One session that’s not to be missed is the
Career Pathways presentation in the Training
Essentials theatre (Friday, 12 noon). In this
special session for dental nurses, BADN
President Fiona Ellwood will look at the
opportunities that are out there for dental
nurses. She will help dental nurses reect
on developing as a specialist practitioner
and consider what a new dental contract
might mean for dental nurses’ future career
pathways.
Dental hygienists and therapists
On Friday morning the BSDHT is hosting a
must-attend Conference Pass session at which
Paul Brocklehurst, Senior Clinical Lecturer/
Honorary Consultant, Dental Public Health
and NIHR Clinician Scientist, University
of Manchester will be looking at
the evidence supporting the
use of dental hygienists and
therapists in primary care.
Another highlight for
dental therapists is the
Paediatric Prevention
presentation in the
Training Essentials
theatre (Saturday,
11 am) in which
Amanda Gallie, Dental
Hygienist and erapist,
and DCP Advisor,
Health Education England
(East Midlands) will look
at systems for developing
a child friendly hygiene and
therapy practice. In total the Training
Essentials theatre oers 19 x 30-minute
sessions based on the BDA’s Training
Essentials portfolio. Topics include dealing
with emergencies, radiation doses in dental
radiography, child and adult safeguarding,
infection control and team working.
Practice managers
and administrators
One highlight that’s not to be missed is the
ADAM team leadership presentation in the
Training Essentials theatre (ursday, 4 pm).
In this special session Association Honorary
Vice President Tracy Stuart will walk through
the steps of building a team rather than a
group of people that turn up to the same
place of work each day. She will help you
understand the many hats you need to wear as
a business owner or manager. She will share
the changes in marketing, what is working
and what isn’t and how you can convert
calls into patients and treatment plans into
solutions the patients wants to pay for without
becoming an aggressive sales person.
Further event highlights include a large
exhibition featuring the live Demonstration
theatre, Speakers’ corner and Innovation
zone, free advice sessions with BDA advisors
and an evening social programme including
networking drinks, a Cuban party night. Up
to 15 hours’ CPD will be on oer with all core
CPD subjects covered.
Conference Passes for dental care
professionals oer great value with a one day
Conference Pass priced at £95 and a full three
day Conference Pass just £155. is gives you
access to all the lectures as well as the shorter
sessions in the Exhibition Hall.
Alternatively, you could attend the event
free of charge by registering for your FREE
Exhibition Pass which gives you access to the
shorter Training Essentials theatre sessions
outlined above as well as the other Exhibition
Hall sessions. Don’t miss out!
Further programme information and
booking details for both Conference
and Exhibition Passes is available at
www.bda.org/conference
Delegates can register online at www.bda.
org/conference or by calling 0870 166 6625.
Please note!
e UK general election will take place on
ursday 7 May 2015. If you are planning to
attend the event on this day and wish to vote
in the election you will need to apply for a
postal vote if you cannot attend your local
polling stations.
Do you have a news story that you would
like included in BDJ Team? Send your press
release or a summary of your story to
the Editor at bdjt[email protected].
©fu rtaev/iStockphoto/Th inkstock
03 BDJ Team www.nature.com/BDJTeam
bdjteam201530

©filiz76/iStockphoto/Thinkstock
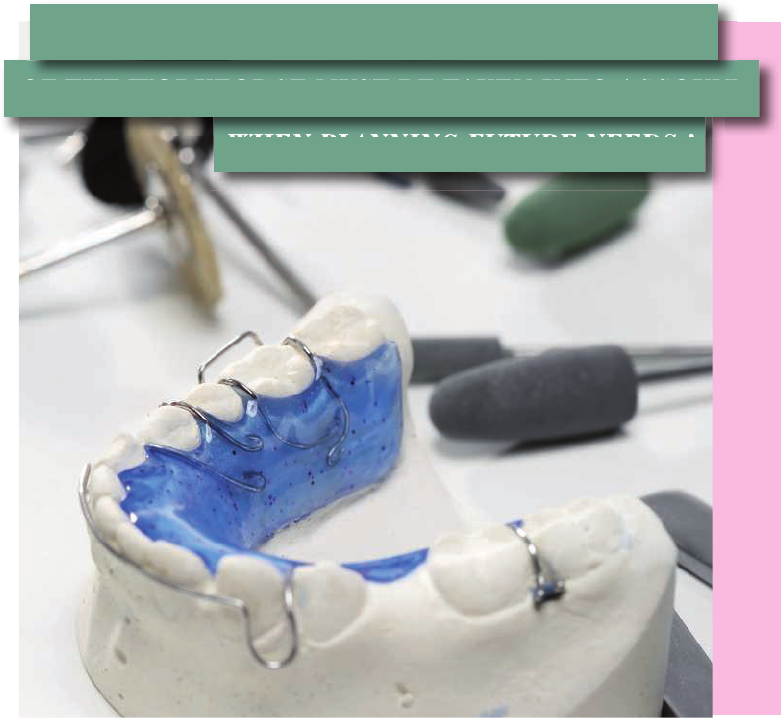
FEATURE
www.nature.com/BDJTeam BDJ Team 04
The twenty-first century
ORTHODONTIC
workforce
Orthodontic workforce planning
Historically, orthodontic workforce planning
has proved dicult. In 1985 Stephens et al.
1
predicted an oversupply of orthodontists
and yet only 13 years later the Task Group
for Orthodontics identied a shortfall and
recommended a target of 480 general dental
service specialist practitioners for the UK.
is wide ranging and perspicacious report
took into account training mechanisms,
European directives and wider drivers from
the Chief Medical and Dental Ocers. At
that time they were mindful of two other
unknowns in planning the workforce, the
inuence of ‘grandfathering’ onto specialist
lists and the potential impact of ‘orthodontic
auxiliaries’ as they were then known.
2
e rst complete survey of the
orthodontic workforce in the UK was carried
out during 2003 and 2004.
3
is survey was
commissioned by the Department of Health
and carried out by the University of Sheeld.
e aim was to assess the existing orthodontic
workforce in relation to current and future
population needs. It was questionnaire-based
and investigated the location of workforce
and the ratio of 12-year-olds per whole time
equivalent orthodontic provider in each
Strategic Health Authority. Type of provider,
case mix and productivity (assessed as
number of cases treated per year) were also
investigated. An orthodontic provider was
considered to be a specialist or non-specialist
who treated more than 30 cases per year.
Of the 1,660 UK orthodontic providers
identied, 919 were General Dental Council
(GDC) registered specialist providers. In the
hospital setting, 243 NHS consultants and
68 university teachers were identied. Fiy-
ve worked in a community setting and 221
were in training. e specialist practitioner
group was the largest group (548) and the
practitioner group (non-specialist providers)
represented 26% of the workforce (432).
At this time, orthodontic therapists did
not exist and attempts were not made to
measure their potential impact on workforce
need. Several scenarios were presented with
the problem of addressing the shortfall in
orthodontists and it was emphasised that the
demand for increased numbers of providers
could be lessened if those patients falling
T. Hodge
1
and N. Parkin
2
highlight the
changes that have taken place
in the orthodontic workforce over
the past decade and review the
roles of various members of the
orthodontic team.
1
Consultant Orthodontist, Leeds
Dental Institute;
2.
Consultant
Orthodontist, Charles Clifford
Dental Hospital, Sheffield
©robertprzybysz/i Stock/Thinkstock
FEATURE
05 BDJ Team www.nature.com/BDJTeam
into low index of treatment need categories
of treatment were not o ered orthodontic
correction. Following this survey, and
the introduction of contracting, for those
patients with a dental health component
(DHC) score of three and below orthodontic
treatment is no longer available on the
NHS. An exception to this rule is those who
fall in the DHC category three where the
aesthetic component scores six or higher. It
was also highlighted in the report that there
was considerable variation in geographic
distribution of providers, similar in fact to the
variation shown in the study by O’Brien and
colleagues.
4
In recent years, probably the most
signi cant change to the orthodontic
workforce has been the introduction of
orthodontic therapists. ere is anecdotal
evidence that this has already impacted on the
employment of some dentists and specialist
orthodontists in the workforce and continues
to impact on the employment of newly
quali ed specialists and clinical assistant
dentists. Future workforce issues will need
to be reassessed by the Centre for Workforce
Intelligence, with input from the British
Orthodontic Society (BOS). Consideration
should be given as to whether potentially
smaller numbers of specialists will be needed
to be trained in the future or whether there
needs to be a reduction in the number of
orthodontic therapist training providers.
In many ways this latter problem should
have been circumvented. e original pilot
study to establish training of orthodontic
therapists, and conducted in Bristol, made
it very clear that a very small number of
centres should be involved. It was recognised
that it was important to fully evaluate the
appropriateness of the training and skills
acquired from the initial courses over time
before further proliferation of programmes
around the UK. At the end of the Bristol pilot
it was suggested that there should initially
be an establishment of one or two auxiliary
training courses in the UK to ensure the
development of a national standard, and
that further courses would then be seeded
from these
THE CURRENT WORKFORCE
Orthodontic nurses
In 2000, a survey was undertaken to
investigate the delegation of orthodontic tasks
and the training of chairside support sta in
Europe.
6
At this stage in the UK the role of the
orthodontic therapist had not been developed.
From the nine tasks investigated, the only
one which was permitted to be undertaken
by a dental nurse in the UK was the taking
of radiographs. is survey highlighted that
UK dental nurses were allowed to work
without quali cations or formal training.
However, currently all dental nurses have to
be registered with the GDC. ose employed,
but not yet quali ed, need to be enrolled
within two years of commencing employment
or waiting to start on a recognised training
programme leading to GDC registration.
In addition, the clinical duties dental
and orthodontic nurses are permitted to
undertake have increased. Many nurses not
only take radiographs but routinely give oral
hygiene instruction, take impressions and
clinical photographs. ese roles, as with all
dental registrants in the team, are laid out in
the GDC Scope of practice documentation.
7
Finally, as well as the Certi cate in Dental
Nursing, the National Examining Board for
Dental Nurses (NEBDN) also run additional
post-quali cation courses leading to
certi cation that many orthodontic nurses
undertake in assisting them perform their
additional clinical roles competently
including the:
■
Certi cate in Orthodontic Nursing
8
■
Certi cate in Oral Health Education
9
■
Certi cate in Dental Radiography.
10
Orthodontic therapists
Orthodontic therapists are a grade of dental
care professional (DCP) introduced in 2007.
e recommendations for the training and
deployment of orthodontic auxiliaries in
the UK were based on the experiences of
the Bristol pilot study,
5
which provided a
foundation for the current training models
being used in Bristol and Leeds. ese were
the rst two training centres to qualify
orthodontic therapists.
11
It was also the
basis for those institutions that subsequently
established programmes (Swansea,
Edinburgh, King’s, Manchester, Preston
and Warwick).
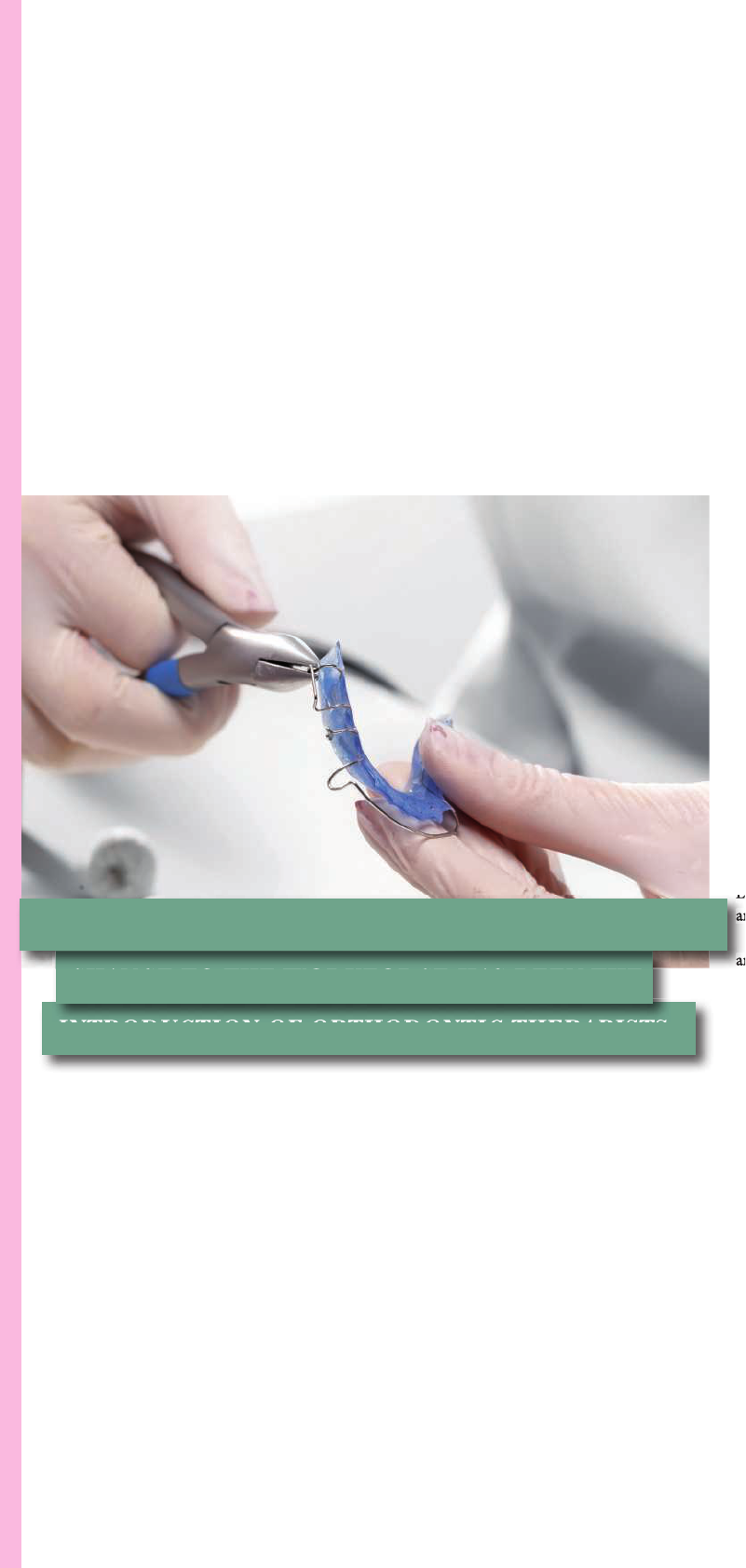
Working under appropriate supervision
12
and following a prescription, orthodontic
therapists are permitted to undertake
numerous reversible orthodontic procedures.
In reality this includes most orthodontic
procedures, such as bonding brackets,
changing archwires, tting functional
appliances and retainers and debonding
appliances.
e exact details of the scope of practice
for orthodontic therapists as laid out by the
GDC
7
are shown in Table 1 and the speci c
capabilities of orthodontic therapists can
be found in the GDC Preparing for practice:
Dental team learning outcomes for registration
document.
13
Since the rst orthodontic therapists
quali ed in 2008, 364 of these personnel are
now registered with the GDC (as of May
2014). is has signi cantly increased the
orthodontic workforce and in many areas
has led to an increase in access to a specialist
led orthodontic service. It is expected that
therapists will have had a bene cial e ect in
reducing geographical inequality of specialist
©robertprzybysz/i Stock/Thinkstock
INTRODUCTION OF ORTHODONTIC THERAPISTS.’
INTRODUCTION OF ORTHODONTIC THERAPISTS.’
CHANGE TO THE WORKFORCE HAS BEEN THE
Edinburgh, King’s, Manchester, Preston
and Warwick).
and following a prescription, orthodontic
CHANGE TO THE WORKFORCE HAS BEEN THE
‘IN RECENT YEARS, PROBABLY THE MOST SIGNIFICANT
FEATURE
www.nature.com/BDJTeam BDJ Team 06
care, although this has still to be conrmed
in the latest BOS survey expected to be
published in the near future.
ere have been possible concerns raised
about the quality of supervision of this
grade of dental registrant.
14
At the outset
many, including a number of educational
providers, were keen that while DCPs could
work independently from a dentist once they
had a treatment plan, due to the nature of
orthodontics where progress and mechanics
were constantly being re-evaluated, an
appropriate reassessment schedule would be
required every visit. erefore an orthodontic
therapist should never be le unsupervised.
15
Others felt this view was over prescriptive
and perhaps such guidelines would be a
disincentive to employing therapists.
16
As a
result, a working party from all the groups
of the BOS convened leading to a set of
guidelines being published on the supervision
of qualied orthodontic therapists by both
the BOS and the Orthodontic National
Group (ONG).
12
Orthodontic technicians
Orthodontic technicians are registered dental
professionals who construct custom-made
orthodontic appliances to a prescription from
a dentist or orthodontist. If they are trained,
competent and indemnied they can:
■
Review cases that come in to the
laboratory to decide how they
should progress
■
Work with the dentist/orthodontist on
treatment planning and appliance design
■
Modify orthodontic appliances according
to a prescription
7
■
Give appropriate patient advice and
carry out shade taking. is may be
especially useful mid-treatment when
constructing temporary pontics to replace
missing units.
17
With additional training, working alongside
an orthodontist, technicians may also
assist in the treatment of patients by taking
impressions, recording facebows and occlusal
registrations, tracing cephalograms and taking
photographs. e skill of an orthodontic
technician in the orthodontic workforce
is probably nowhere more central than in
delivering an orthognathic service where
accuracy, skill and good communication are
crucial for success in treatment outcomes.
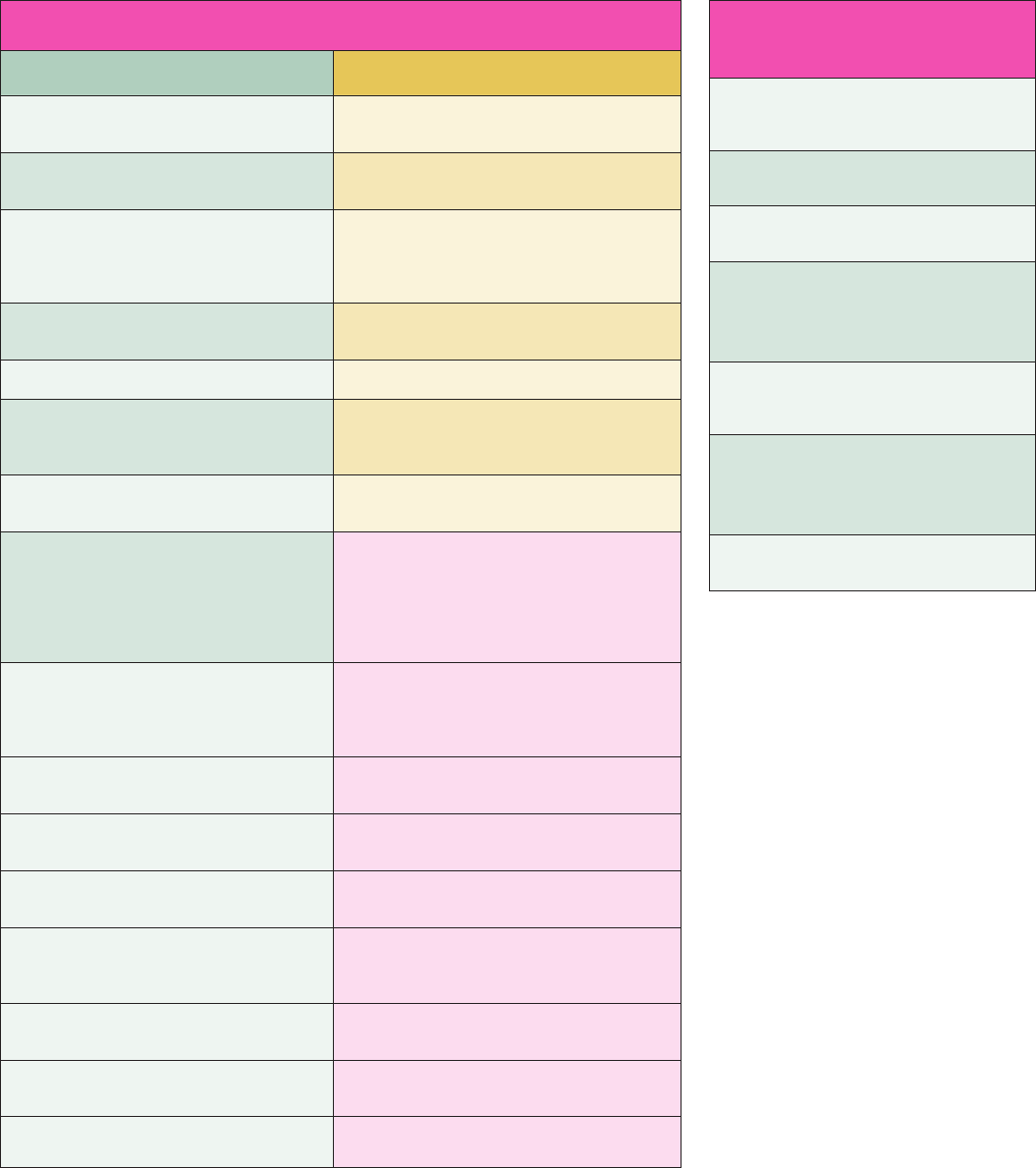
Table 1 Scope of practice of the orthodontic therapist
Orthodontic therapists can: Orthodontic therapists cannot:
Clean and prepare tooth surfaces ready for
orthodontic treatment
Remove sub-gingival deposits
Identify, select, use and maintain appropriate
instruments
Give local analgesia
Insert passive removable orthodontic
Appliances
Insert removable appliances activated or
adjusted by a dentist
Re-cement crowns
Remove fixed appliances, orthodontic adhe-
sives and cement
Place temporary dressings
Identify, select, prepare and place auxiliaries
Place active medications
Take impressions
Pour, cast and trim study models
They do not carry out laboratory work other
than previously listed as that is reserved to dental
technicians and clinical technicians
Make a patients’s orthodontic appliance safe
in the absence of a dentist
Diagnose disease, treatment plan or activate
orthodontic wires - only dentists can do this
Fit orthodontic headgear
Fit orthodontic facebows which have been
adjusted by a dentist
Take occlusal records including orthognathic
facebow readings
Take intra and extra-oral photographs
Additional skills which orthodontic therapists
could develop during their career include:
Place brackets and bands prepare, insert,
adjust and remove arch wire previously
prescribed or, where necessary, activated by a
dentist
Applying fluoride varnish to the prescription of a
dentist
Give advice on appliance care and oral health
instruction
Repairing the acrylic component part of
orthodontic appliances
Fit tooth separators Measuring and recording plaque indices and
gingival indices
Fit bonded retainers Removing sutures after the wound has been
checked by a dentist
Carry out Index of Orthodontic Treatment Need
(IOTN) screening either under the direction of a
dentist or direct to patients
Make appropriate referrals to other healthcare
professionals
Keep full, accurate and contemporaneous
patient records
Give appropriate patient advice
Table 2 GDC learning outcomes
for dentists–management of the
developing and developed dentition
1.13.1 Identify normal and abnormal
facial growth, physical, mental and dental
development and explain their significance
1.13.2 Undertake orthodontic assessment,
including an indication of treatment need
1.13.3 Identify and explain development or
acquired occlusal abnormalities
1.13.4 Identify and explain the principles
of interceptive treatment, including timely
interception and interceptiv orthodontics, and
refer when and where appropriate
1.13.5 Identify and explain when and how
to refer patients for specialist treatment and
apply practice
1.13.6 Recognise and explain to patients the
range of contemporary orthodontic treatment
options, their impact, outcomes, limitations
and risks
1.13.7 Undertake limited orthodontic
appliance emergency procedures

FEATURE
07 BDJ Team www.nature.com/BDJTeam
General dental practitioners and
dentists with enhanced skills
General dental practitioners (GDPs) perform
a key role in the orthodontic workforce acting
as diagnostic gatekeepers. e GDC Preparing
for practice documentation
13
it lists the
learning outcomes for dentists to be registered
with the GDC (Table 2).
Although orthodontics is a very specic
area of expertise, and only those registered
on the specialist list with the GDC can call
themselves a specialist orthodontist, any
registered dentist can carry out orthodontics
as long as they are competent to do so.
Historically, a signicant proportion of
orthodontic treatment has been carried out
by GDPs in the UK. e 2005 report revealed
that 17% of orthodontic providers had no
orthodontic qualication. e report also
highlighted that in some regions, Shropshire,
Staordshire, Trent, North and East Yorkshire
and Lincolnshire, the majority of orthodontic
provision was carried out by non-specialists.
Since 2006 the speciality has seen the end of
fee-for-item payments and the introduction
of the new individualised contracts. While the
majority of these contracts have been made
with specialist orthodontic practitioners,
contracting has occurred among a group of
existing NHS primary care general dentists.
Initially known as dentists with a special
interest in orthodontics,
18
these clinicians are
now known as dentists with enhanced skills
(DES). While not being eligible for specialist
list registration with the GDC these providers
will have gained additional experience
and training in orthodontics and can be
formally recognised by the commissioners
of orthodontic care (known as area teams
since April 2013). A DES is expected to treat
patients within their competence and refer
complex cases to a specialist orthodontist
or local hospital service as part of a local
clinical network. If this clinical network works
eciently and eectively, the likelihood of
population need being met and high quality
of care being maintained will be increased.
Training of DES oen used to take place on
two-year orthodontic clinical assistantship
schemes but now few, if any, of these remain.
Instead, there has been a recent increase in
longitudinal general professional training
(GPT) schemes for foundation dentists with
placements in orthodontic specialist practice
or in hospital departments.
Recently, GDPs have increased their
presence in the orthodontic workforce by
oering short-term orthodontics to adult
patients wanting an improvement in their
anterior smile aesthetics. While this has
caused debate
19
a move away from anterior
alignment using a handpiece to reshape
teeth together with ceramic restorations has
to be welcomed.
20
It should, however, be
appreciated by those practitioners oering
short-term orthodontics that it provides
a relatively limited range of outcomes and
frequently a specialist referral for correction
of a patient’s wider malocclusion may be
indicated.
Specialist practitioners
Specialist practitioners work in primary care
and are registered as specialists with the
GDC. At the time of the introduction of the
specialist lists in the late nineties a number
of people gained entry to this group via
‘grandfathering’. However, entry should now
only be on receipt of orthodontic training
in other EU member states or in the UK by
securing an orthodontic speciality training
registrar post. Entry to these salaried posts
by UK/EU applicants is competitive with
essential criteria for application including the
possession of a dental degree, registration
with the GDC and completion of a period
of dental foundation/vocational training
or GPT demonstrating experience in a
range of dental specialties. Interestingly, the
GDC are currently completing research,
including patient and public, stakeholders’
and registrants’ views on regulation of
the specialties and are asking these three
questions to gather evidence on the way
forward:
21
■
Does regulation of the specialties bring any
benets (potential and/or actual) in terms
of patient and public protection?
■
Is regulation of the specialties
proportionate to the risks to patients in
relation to more complex treatments?
■
Are the specialist lists the appropriate
mechanism for helping patients to make
more informed choices about care not seen
as falling within the remit of the general
dental practitioner?
Many consider that the reason specialist
lists are useful is because specialist training
and dened standards of practice help to
deliver better treatment and improve clinical
outcomes for patients who receive specialist
dental care. In orthodontics the likelihood
that a treatment will benet a patient is
increased if appliance therapy is planned and
carried out by an experienced orthodontist.
22
Orthodontists also spend less time on
treatment and achieve better quality outcomes
than cases treated by general dentists who
have not undergone a specialisation course in
orthodontics.
23
e training programme leading to
specialisation in orthodontics in the UK
is three years full-time (or part-time pro
rata)
24
and involves undertaking a university
postgraduate degree at the Masters
(MSc, MClinDent, MPhil) or Doctorate
(DClinDent, DDS) level and upon successful
completion of the programme, eligibility
to sit the Membership in Orthodontics
examination of the Royal College of Surgeons.
e training programmes are currently
monitored by the Postgraduate Deaneries
and the Specialist Advisory Committee but
with national developments through Health
Education England these arrangements are
likely to change. e workload undertaken by
specialist orthodontic practitioners reects
the comprehensive learning outcomes of
the specialist training programmes which
include being able to diagnose anomalies of
the developing dentition and facial growth,
carrying out a wide range of simple and
complex treatments both interceptive and
comprehensive in nature including multi-
disciplinary management of a variety of
treatments and understanding psychological
aspects relevant to orthodontics.
Community orthodontists
e community orthodontic service is a
long-established part of NHS provision.
In a changing climate of dental provision
over recent years, providing orthodontic
support for Trust-based ‘Personal Dental
Services’ schemes, under the umbrella of the
salaried primary dental care services, has
become increasingly important. Community
orthodontists are specialist-trained providers
who undertake orthodontic treatment for
a range of special care patients who have
limited access to other, appropriate specialist
treatment.
e majority of such patients who are
able to receive orthodontic treatment oen
require close liaison with other health care
professionals for a holistic approach to
management and not infrequently this service
provides a ‘safety net’ in those areas of the
country not well served by specialist practice
or hospital orthodontic providers.
Orthodontic consultants
Consultant orthodontists are those specialists
that have undergone an additional two years
of full-time training (or part-time pro rata),
in many cases sub-specialising for example,
cle lip and palate work, who collectively
can provide any orthodontic service which
the commissioners might require. In
addition eligibility for application to these
posts is subject to satisfactory completion
of the Intercollegiate Speciality Fellowship
FEATURE
www.nature.com/BDJTeam BDJ Team 08
Examination Exam in Orthodontics, FDS
(Orth), although foundation trusts are in a
position to write their own requirements for
appointment to a consultant post. While this
role can be varied, clinical activity is focused
upon the following:
■
Working in conjunction with consultant
oral and maxillofacial surgeons, plastic
surgeons or paediatric surgeons to correct
severe skeletal problems by means of
combined orthodontic and surgical
treatment approaches
■
Liaise with other key specialties to
provide coordinated care for patients
with cle lip and palate, and other
congenital dentofacial anomalies. ere
is also increasing collaboration with ENT
consultants and respiratory medicine to
manage patients with obstructive sleep
apnoea
■
Provide clinical training for undergraduate
dental students, career junior sta , future
specialists and trainee academics and
participate in continuing professional
programmes for all trained providers of
orthodontic care
■
Undertake personal research, innovation
and service evaluation including audit
■
Working with colleagues in primary
care and dental public health as part
of a professional network to manage
orthodontic services locally.
In summary, the role of the consultant
orthodontist is varied but centres on clinical
consultation, the treatment of severe and
multidisciplinary cases, service coordination,
training and research.
DISCUSSION
is article highlights the many varied
personnel involved in the delivery of
orthodontic treatment in the UK and
illustrates how the workforce has evolved in
recent years. From the extension of the role
of the orthodontic nurse, the introduction of
the orthodontic therapist into the team, the
mandatory registration of all DCPs and the
increase in uptake of short-term orthodontic
treatments being o ered in general dental
practice, much has changed over the past
decade.
While we may be clearer now as to who
does what in the orthodontic workforce,
perhaps the next workforce issue that will
arise as a result of these changes is how many
of these varied personnel will be needed to
deliver care and their appropriate training.
e Centre for Workforce Intelligence
published a strategic review in 2013 analysing
the future ‘supply and demand’ of the dental
workforce in England between 2012 and
2040
25
which revealed that there is likely to
be a surplus supply of dentists by as many
as 4,000 by 2040. e mechanisms for the
derivation of these gures is far from clear
and likely to be as hopeless as the information
which led to expansion of undergraduate
numbers in 2006. It is hoped that the report of
the current Workforce Survey Task and Finish
Group of the BOS will form the backbone of
negotiations with the Centre for Workforce
Intelligence, Health Education England
and the Department of Health and will be
instrumental in shaping the future training
of the workforce and delivery of orthodontic
services in England and Wales.
CONCLUSION
ere has been considerable change in the
composition of the orthodontic workforce
over the last decade. It is hoped that the
extension of roles performed by the various
members of the orthodontic team will lead to
increased accessibility of specialist care.
e impact of the change in composition
of the orthodontic workforce, in particular
the addition of orthodontic therapists, must
be taken into account when planning future
manpower needs.
1. Stephens C D, Orton H S, Usiskin L A. Future
manpower requirements for orthodontics
undertaken in the General Dental Service. Br J
Orthod 1985; 12: 168–175.
2. Lumsden K W, Brown D V, Edler R J et al. Task
group for orthodontics. Report. Br J Orthod 1998;
23: 222–240.
3. Robinson P G, Willmot D R, Parkin N A, Hall A C.
Report of the orthodontic workforce survey of the
United Kingdom. She eld: University of She eld,
2005. Online information available at: http://www.
bos.org.uk/Resources/British%20Orthodontic%20
Society/Migrated%20Resources/Documents/
Workforce_survey.pdf (accessed December 2014).
4. O’Brien K, Corkill C. Regional Variations in the
provision of orthodontic treatment by the hospital
services in England and Wales. Br J Orthod 1990;
17: 187–195.
5. Stephens C D, Keith O, Witt P et al. Orthodontic
auxiliaries – a pilot project. Br Dent J 1998; 185:
181–187.
6. Seeholzer H, Adamidis J P, Eaton K A, McDonald
J P, Sieminska-Piekarczyk B. A survey of the
delegation of orthodontic tasks and the training of
chairside support sta in 22 European countries. J
Orthod 2000; 27: 279–282.
7. General Dental Council. Scope of practice. 2013.
Online information available at: http://www.
gdc-uk.org/Newsandpublications/Publications/
©robertprzybysz/i Stock/Thinkstock
WHEN PLANNING FUTURE NEEDS.’
WHEN PLANNING FUTURE NEEDS.’
OF THE WORKFORCE MUST BE TAKEN INTO ACCOUNT
OF THE WORKFORCE MUST BE TAKEN INTO ACCOUNT
‘THE IMPACT OF THE CHANGE IN COMPOSITION
FEATURE
09 BDJ Team www.nature.com/BDJTeam
Publications/Scope%20of%20Practice%20
September%202013.pdf (accessed December 2014).
8. National Examining Board for Dental
Nurses. National certi cate examination.
2008. http://www.nebdn.org/documents/
NationalCerti cateProspectus_000.pdf (accessed
December 2014).
9. National Examining Board for Dental Nurses.
Certi cate in oral health education. 2011. http://
www.nebdn.org/documents/OHEProspectus_000.
pdf (accessed December 2014).
10. National Examining Board for Dental Nurses.
Certi cate in dental radiography. 2011. http://www.
nebdn.org/documents/DRPProspectus_001.pdf
(accessed December 2014).
11. Bain S, Lee W, Day C J, Ireland A J, Sandy J R.
Orthodontic therapists – the rst Bristol cohort. Br
Dent J 2009; 207: 227–230.
12. British Orthodontic Society and Orthodontic
National Group. Guidelines on supervision of
quali ed orthodontic therapists. 2012. Online
information available at: http://www.bos.org.
uk/Resources/British%20Orthodontic%20
Society/Author%20Content/Documents/
PDF/Supervision%20of%20orthodontic%20
therapistsBoard%201212.pdf (accessed December
2014).
13. General Dental Council. Preparing for practice.
2011. Online information available at http://www.
gdc-uk.org/newsandpublications/publications/
publications/gdc%20learning%20outcomes.pdf
(accessed December 2014).
14. Hodge T. Orthodontic therapists: a challenge for
the 21st Century. J Orthod 2010; 37: 297–301.
15. Littlewood S, Hodge T, Knox J et al. Supervision of
orthodontic therapists in the UK. J Orthod 2010;
37: 317–318.
16. Day C, Hodge T. Supervision of orthodontic
therapists:
what is all of the confusion about?
Fac Dent J 2011; 2: 192–195.
17. Hodge T M. Clinical pearl:
in-treatment replacement of
missing incisors. J Orthod 2005;
32: 182–184.
18. Department of Health/Faculty of
General Dental Practice (UK).
Guidance for the appointment of dentists with
special interests (DwSIs) in orthodontics. 2006.
Online information available at: http://www.bos.
org.uk/Resources/BOS/Documents/Careers%20
and%20GDP%20documents/dh_4133859.pdf
(accessed December 2014).
19. Maini A, Chate R A C. Short-term orthodontics. Br
Dent J 2014; 216: 386–389.
20. Kelleher M. Porcelain pornography. Faculty Dent J
2011; 2: 134–141.
21. General Dental Council. Reviewing regulation of
the specialties. 2014. Online information available
at http://www.gdc-uk.org/Aboutus/ ecouncil/
Council%20Meeting%20Documents%20
2014/5%20Reviewing%20Regulation%20of%20
the%20Specialties.pdf (accessed December 2014).
22. O’Brien K D, Shaw W C, Roberts C T. e use
of occlusal indices in assessing the provision of
orthodontic treatment by the hospital orthodontic
service of England and Wales. Br J Orthod 1993;
20: 25–35.
23. Marques L S, Freitas Junior Nd, Pereira L J, Ramos-
Jorge M L. Quality of orthodontic treatment
performed by orthodontist and general dentists.
Angle Orthod 2012; 82: 102–106.
24. Joint Committee for Postgraduate Training in
Dentistry Specialty Advisory Committee in
Orthodontics. Guidelines for the UK threeyear
training programmes in orthodontics for specialty
registrars. 2012. Online information available
at: http://www.rcseng.ac.uk/fds/jcptd/
higher-specialist-training/documents/
guidelinesfor-the-uk-three-year-training-
programmes-inorthodontics-for-
specialty-registrars-july-2012 (accessed
December 2014).
25. Centre for Workforce Intelligence.
A strategic review of the future dentistry
workforce: informing dental student
intakes. 2013. Online information
available at: http://www.cfwi.org.
uk/publications/a-strategicreview-
of-the-future-dentistry-workforce-
informingdental-student-intakes
(accessed December 2014).
is article was originally
published in the British
Dental Journal as
‘Who does what’ in the
orthodontic workforce
on 16 February 2015 (218:
191-195).
PROFILE - ORTHODONTIC
NURSE
Ruth Mackenzie, 34, is a dental
nurse at Giff nock Orthodontic
Centre in Glasgow. Ruth worked
at a specialist orthodontic
practice from 2002-2006, at
a private general dental practice from
2006-2010, and has been at her current
workplace since 2010. As well as her dental
nurse qualifi cation, Ruth has a certifi cate
in dental radiography, and enjoys
snowboarding, running and travelling.
What first attracted you
to dentistry?
I have always been interested in how
braces can make people’s teeth move. I
had upper and lower xed appliances
myself in the past. I was attracted to
working in orthodontics a er noticing
how much more people would smile
a er having braces tted. My interest
in orthodontics began when I read a
magazine article about clear braces.
I rst started working in an
orthodontic dental practice in 2002.
e general practice that I worked in
later on was far quieter. e sta at the
orthodontic practice were more involved
in the treatment of patients, which I
found very appealing.
We treat a broad mixture of child and
adult patients. It is very satisfying when
patients complete their orthodontic
treatment and are happy with the
outcome - especially with the patients
that were very self-conscious with their
smile before treatment.
Have you undertaken a Certificate
in Orthodontic Nursing?
No but it is something I am interested
in doing and feel I would bene t
from greatly.
Would you recommend working in
an orthodontic practice to other
dental nurses?
Yes, there are many opportunities within
orthodontics and it is very satisfying
to see patients happy with their smile
a er treatment.
Do you have any career plans you
would like to share with us?
I would like to volunteer in a work
placement in a third world country.
©macroart/iStock/Thinkstock
PROFILE - ORTHODONTIC
NURSE
Ruth Mackenzie
nurse at Giff nock Orthodontic
Centre in Glasgow. Ruth worked
at a specialist orthodontic
practice from 2002-2006, at
FEATURE
www.nature.com/BDJTeam BDJ Team 10
PROFILE - ORTHODONTIC THERAPIST
Fiona Carter, 53, is an orthodontic
therapist at Colchester Orthodontic Centre.
Fiona qualifi ed as a dental nurse in
1981 and completed a Certifi cate in Oral
Health Education in 1993, a Certifi cate in
Orthodontic Nursing in 2008, a Diploma in
Orthodontic erapy in 2009, and was PAR
calibrated in 2014 (Peer Assessment Rating
index). Ruth is a member of the Orthodontic
National Group (ONG) and enjoys running,
cycling, yoga and vintage shopping!
What first attracted you to dentistry?
Nursing was my chosen career but when
I le school I was too young to begin the
SRN (state registered nurse) training. I
saw an advertisement for an orthodontic
dental nurse so applied, not realising what it
entailed, and was successful. at was way
back in 1978 and by chance I had found a
profession I really enjoyed.
In 1978 there was no recognised
quali cation for orthodontic nursing so my
orthodontist enrolled me on a local NEBDN
course. I gained experience in general dental
nursing by spending half a day a week
working in various local general dental
practices to successfully gain the National
Certi cate. is con rmed that orthodontics
was the branch of dentistry that I wanted to
continue in.
Fixed appliances were still being made
with stainless steel tape so welding and
soldering attachments was part of the
orthodontic nurse role as was acrylic and
wire repairs to removable appliances,
preforming arch wires and making EOT face
bows which involved learning how to bend
wires, a great skill to have as an orthodontic
therapist (OT). is was together with all
the other duties of running a busy specialist
orthodontic practice.
Following a short break a er the birth
of my two sons I returned to work on a
part time basis in a multi-disciplinary
dental practice working for an orthodontic
specialist. Gaining my Certi cate in Oral
Health Education in 1993 was a great
advantage having a varied patient base and
the help and guidance of GDPs.
As my children got older and more
independent I had the opportunity to work
with the orthodontist I began my career
with in 1978 within the local Primary
Care Trust, treating a variety of complex
orthodontic cases and also dental nursing
in a special care dental department. ere
was a speci c managerial element to
this position as it involved setting up an
orthodontic practice within the community
dental department, sta recruitment,
department management and carrying out
audit, producing the department COSHH
manual, Dental Nurse Policy and Protocol,
following Trust guidelines and liaising with
multidisciplinary departments.
When did you decide to become an
orthodontic therapist?
OTs were being discussed as early as
1978 when I started my career. When the
orthodontic therapy course was introduced
in 2007 I knew that this was what I wanted
to do and that this may be my opportunity!
I applied for an orthodontic nurse position
and I was lucky in nding an orthodontic
specialist who had the con dence in me to
support my application and training and
was prepared to be my training provider.
I studied for the RCS Eng Diploma in
Orthodontic erapy at South Wales
Orthodontic erapy course, based at
Cardi Dental School. It was hard work
but also very exciting with excellent
course tutors.
Was it difficult to get a place?
I considered myself fortunate to be selected
for interview and I was so pleased to
be successful at my rst interview. My
employer/orthodontist also had to be
interviewed as a ‘training provider’.
Was it straightforward finding
employment as an orthodontic
therapist?
Yes because you are trained by the
orthodontic specialist that you work with.
S/he is your ‘trainer’ and a er such a big
investment in time, energy and emotion (not
forgetting nancial investment), successful
OTs tend to stay with their trainers/training
providers.
e transition
from orthodontic
nurse to orthodontic
therapist was very
exciting; however,
it was a change for
the whole practice.
Having a very supportive team made
it easier. Patients had to adjust too but
they were all very understanding and
encouraging. I am con dent working within
my clinical capabilities and I am aware of
my limitations. CPD is an essential and
important part of keeping up to date.
I treat a mixture of both adults and
children but a higher percentage of children.
I work within the limits of the OT GDC
scope of practice and following BOS
guidelines.
At Colchester Orthodontic Centre we
are a small but very happy team of ten:
Gareth Davies, the orthodontic specialist
practitioner; two orthodontic therapists;
four orthodontic nurses; a practice manager;
and two administrative sta .
e most satisfying part of my job is
seeing how delighted the patients are
when treatment is completed and the self-
con dence that this gives them. Not only
because they have a fantastic smile but
because they realise that have they achieved
this through their own hard work. Adult
patients may have missed the opportunity to
undertake orthodontic treatment as a child
and it is rewarding to see the con dence
they gain.
What is the future for OTs?
I think OTs are an asset to an orthodontic
practice and coming from a dental nursing
background OTs are empathetic to the
patient and parents. I think it is an excellent
career path for an orthodontic dental nurse
considering career progression.
bdjteam201531
WHEN TREATMENT IS COMPLETED.’
SEEING HOW DELIGHTED PATIENTS ARE
‘THE MOST SATISFYING PART OF MY JOB IS

Willette Jean Lati is a 26-year-old dental technician
and Clear Aligner Department Assistant Manager
at NimroDental Orthodontic Solutions in London.
FEATURE
Dental destiny
When I was at school, like most people, I was
quite indecisive about what I wanted to do
when I grew up. From a young age till about
secondary school it ranged from wanting to
be a palaeontologist, doctor, vet, chef, scientist
to artist.
I was born in the Philippines but because of
my mum’s work we were relocated to Sydney,
Australia when I was about two-years-old. Aer
ve years, we moved back to the Philippines to
further my education for about six years. We
moved to London in 2002 where I started at
Year 10.
Not doing particularly well during my
A-levels (chemistry, biology, maths and
psychology), I had to look for an alternative
course that catered to my interest in both art
and science. A google search turned me to the
direction of dental technology. So I guess it was
like destiny.
Work experience
To secure a place on a dental technology course
is not very dicult providing you have ve
GCSEs at A*-C (especially in maths, science
and English) and don’t mind getting your hands
dirty. It may be dicult, however, to nd a
dental laboratory to take you on as an apprentice
if you don’t have any prior experience. Work
experience before you start studying is also
recommended as it will give you a better idea of
what sort of business you’re getting yourself into.
I started work experience at NimroDental
in 2007 whilst I was studying my BTEC course
in Dental Technology and have been there
ever since.
I completed a Foundation degree in Dental
Technology in 2009. Both my BTEC and
Foundation Degree courses tried to condense
the principles and practical techniques of all
departments of dental technology (prosthetics,
orthodontics and prosthodontics) in a span of
three years. But I would say that courses focus
more on denture or crown and bridge work.
My class was attended by a majority of girls of
a wide range of dierent ages and backgrounds;
there with only two boys among us. But I
found that other groups or batches were quite
male dominated.
I enjoyed the practical aspect of my
foundation course more than the academic as
I am more of a hands-on sort of learner. It was
interesting to learn and make dierent sorts of
appliances used in dentistry that many would
take for granted. I enjoy being able to build,
recreate, add detail and nish things with my
hands using dierent mediums.
e academic side of my course was a bit
challenging, and also learning to make new
appliances - but practice and persistence does
help to improve and perfect new skills.
In the lab
At NimroDental I make a fair range of
appliances in the lab such as retainers, clear
aligners, removable appliances and Inman
aligners. I have worked my way up from plaster
room technician to assistant manager.
I am currently based on the famous Harley
Street although I wasn’t initially aware of its
reputation until I started working in the lab.
Previously we were located just o Paddington
Street; I used to personally do collections and
drop-os of impressions and appliances in the
Harley Street area and got to meet or see some of
London’s well known dentists and orthodontists.
It was fascinating to learn that a small area has
such a huge reputation of quality of care and
services both from the medical and dental eld.
It was also nice to bump into the odd celebrity
every now and then.
I am currently Assistant Manager of our
Clear Aligner Department headed by Agnieszka
Horton, specialising in the new digital clear
aligner movement system and 3D printed
models. I also attend dental tradeshows to
raise our company’s prole in the dental and
orthodontic industry.
I support my colleague Sophie Cook
11 BDJ Team www.nature.com/BDJTeam
‘ There is a family
atmosphere in our lab’

FEATURE
www.nature.com/BDJTeam BDJ Team 12
(@Nimrodental_SC on Twitter), who is Head
of Marketing, with our social media accounts.
I would like to make special mention of our
mentor Jowita Penkala of Uniqabrand for
teaching us the power of social media marketing
through Twitter and Facebook since November
2014. I have never used Twitter for personal use
but found that it is an amazing tool to connect
to all types of people in the dental industry.
As a lab it is rare for us to be involved with or
to interact with the general public, but we do
try to maintain good relationships with our
clients such as dentists, cosmetic dentists and
orthodontists across the UK and in Europe.
A family atmosphere
Having been at NimroDental for more than
seven years, there is an almost family-like
atmosphere. We are a continuously growing lab
with currently over 30 individuals including the
o ce team.
As a company we enjoy each other’s company
even a er work hours. We organise monthly
work drinks at nearby local pubs or bars.
A few of us have even been travelling around
Europe together.
Regarding my future career ambitions, this
may sound cheesy but they are to be the best at
what I do and to continue to improve and learn
every day, whether it is dental-related or not.
I subscribe to a yearly magazine to regularly
update my CPD hours and try to attend lectures
or nd free CPD websites online to keep my
skills up to date.
I usually nish work around 5 pm but stay
a little longer on busier days. To relax or let o
steam a er work I sometimes go to the gym to
swim or train, do a bit of hot yoga or even just
spend a couple of minutes in the sauna.
To be honest, I haven’t got a clue what I
would have done if I hadn’t become a dental
technician! Wherever the wind had taken me I
suppose. I don’t have a set path and just take any
opportunities that come my way.
If you are good with your hands and have
an interest in science, then I would de nitely
recommend a career in dental technology
to others.
TECHNOLOGY. SO I GUESS IT WAS LIKE DESTINY.’
TECHNOLOGY. SO I GUESS IT WAS LIKE DESTINY.’
TURNED ME TO THE DIRECTION OF DENTAL
TURNED ME TO THE DIRECTION OF DENTAL
ART AND SCIENCE. A GOOGLE SEARCH
ART AND SCIENCE. A GOOGLE SEARCH
THAT CATERED TO MY INTEREST IN BOTH
THAT CATERED TO MY INTEREST IN BOTH
‘...I HAD TO LOOK FOR AN ALTERNATIVE COURSE
What three things can Willette not
live without?
1. My iPhone to connect with people
2. The Internet to connect with
the world
3. Sour candies/sweets because
I have a bit of a sweet (sour) tooth
which is a naughty thing in
my profession!
bdjteam201532
FEATURE
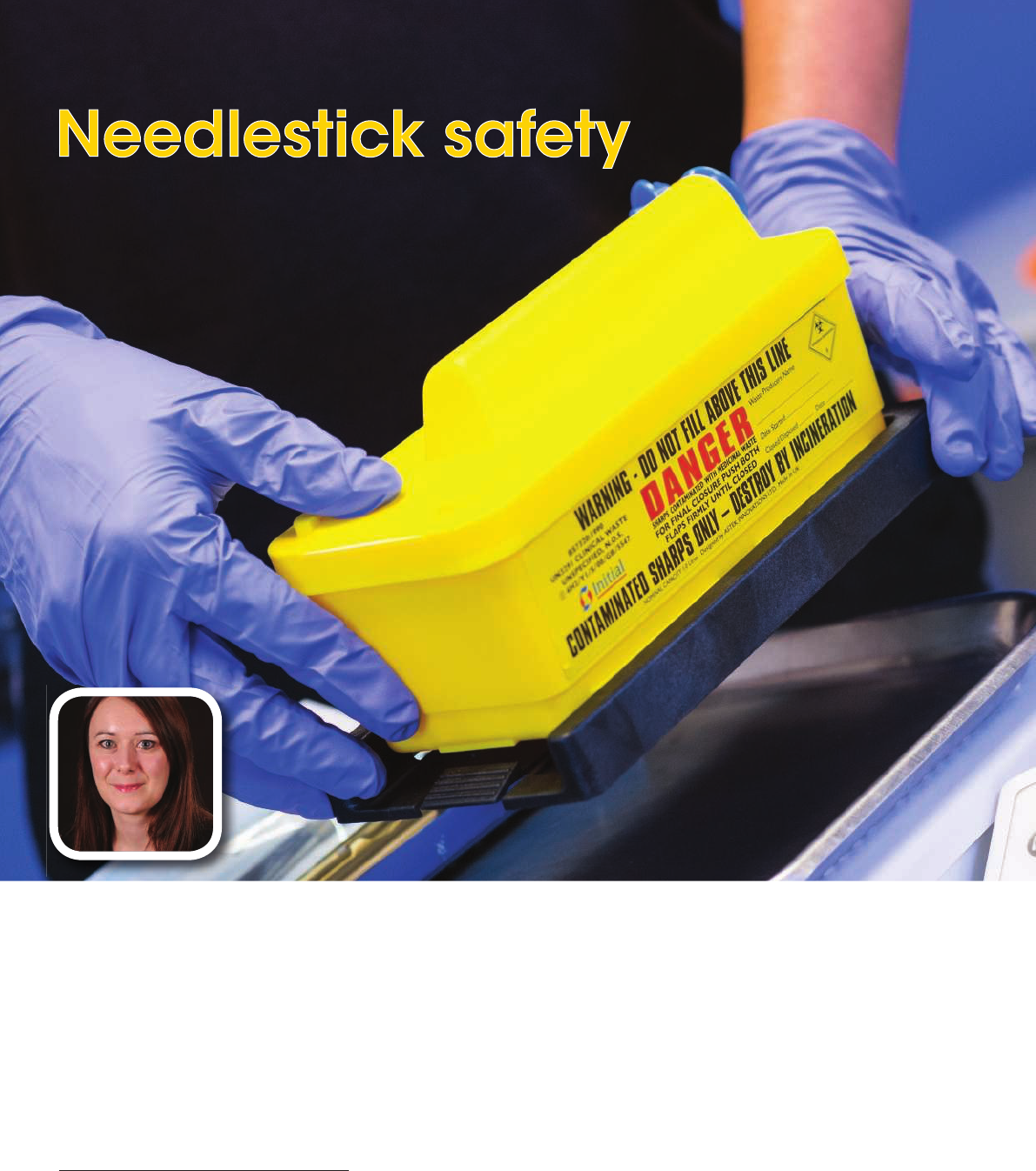
Consider the risk
As part of the dental team, needlestick safety
is something you should be acutely aware of in
your day-to-day role. A survey of 1,216 dental
nurses from the UK and Ireland conducted
in conjunction with the British Association
of Dental Nurses (BADN) in 2014 found that
51.2% of respondents had received a needlestick
injury at some point throughout their career,
with 60% of those saying they’d received more
than one. When you then consider the risk
of infection following a needlestick injury is
estimated to be one in three for Hepatitis B virus
(HBV), one in 30 for Hepatitis C virus (HCV)
and one in 300 for HIV (for healthcare workers
worldwide), it is vital that safety procedures are
put in place in all dental surgeries.
The use of sharps
Following the introduction of e Health &
Safety (Sharps Instruments in Healthcare)
Regulations 2013, all healthcare facilities must
ensure that:
(a) e use of medical sharps at work is avoided
so far as is reasonably practicable
(b) When medical sharps are used at work,
safer sharps are used so far as is reasonably
practicable
(c) Needles that are medical sharps are not
capped a er use at work unless:
i. that act is required to control a risk
identi ed by an assessment undertaken
pursuant to regulation 3 of the
Management of Health and Safety at
Work Regulations 1999 (a)
ii. the risk of injury to employees is
e ectively controlled by the use of
a suitable appliance, tool or other
equipment
(d) In relation to the safe disposal of medical
sharps that are not designed for re-use:
i. there should be written instructions for
employees
ii. clearly marked and secure containers
should be located close to areas where
medical sharps are used at work.
Health and safety law has always placed
general responsibilities on the employer to
provide their sta with a healthy working
environment. However, this legislation now puts
further emphasis on prevention. In reality it
would be di cult, if not impossible, to remove
all sharps from a dental practice, so the next best
thing is to assess the risk correctly, use devices
By Rebecca Allen
1
©Creatas/Thinkstock
1
Rebecca is Category Manager at Initial
Medical (http://www.initial.co.uk/
healthcare-waste/). She has worked
in the healthcare sector for the past
13 years and was a Research Chemist
with Bayer Cropscience prior to joining
Rentokil Initial in 2003. She keeps up to
date on all developments within the
clinical waste management industry
and is an active member of the CIWM,
SMDSA and BDIA.
for the whole
dental team
13 BDJ Team www.nature.com/BDJTeam
FEATURE
www.nature.com/BDJTeam BDJ Team 14
which limit the risk of injury and dispose of all
sharps in a safe manner.
Top tips for needlestick safety are shown in
Table 1.
Cradle-to-grave rule
It’s important to remember that when it comes
to hazardous and infectious waste such as
syringes and other sharps at a dental practice,
the cradle-to-grave rule applies. e producer
of waste will always be held responsible for the
safe and legal disposal of it, even a er it has been
passed onto the waste carrier collecting it. is is
why it’s important to work with comprehensively
trained sharps waste disposal experts who will
advise on the correct products that comply with
both the UK and EU legislation and safely and
securely dispose of sharps. Health and safety
law is criminal law and healthcare organisations
can be subject to enforcement action if they fail
to comply with the legal requirements. ere
is also always a threat of civil law action if an
employee is injured due to insu cient practices
and technologies being in place.
Staff wellbeing
Everyone has a role to play in the prevention
of sharps injuries, from trainee sta who are
learning the ropes, to practice owners who will
hold legal overall responsibility for the wellbeing
of their sta .
Another quick and simple way to reduce the
risk of needlestick injuries is to use innovative
solutions such as InSafe syringes – a safety
system providing comprehensive protection
for clinical sta from the beginning of the
procedure through to the disposal of the needle.
InSafe’s syringe and sharps box ensure that the
contaminated needle is never exposed except
during the actual injection. It feels and aspirates
just like a traditional syringe so there will be
no interruptions to the dental practice when
introducing the protective system. When the
injection has been administered, the protective
sleeve locks securely into place over the needle,
protecting clinical sta and patients when not
in use. e needle can then be safely disposed
of using a sharps container. Specially developed
sharps disposal bins are designed for such waste
and comply with all EU and UK regulations
and directives, and there are companies
available that provide a dependable and safe
collection service.
BDJ Team promotion
Initial Medical Waste Experts
Initial Medical is an expert in
healthcare waste management,
providing a complete collection,
disposal and recycling service for
hazardous and non-hazardous waste,
such as offensive waste produced
by businesses and organisations
within the UK. The safe management
of healthcare waste is vital to ensure
your activities are not a risk to human
health. Initial Medical’s healthcare
waste services ensure that all of
your waste is stringently handled in
compliance with legislation and in
accordance with Safe Management
of Healthcare Waste best practice
guidelines, providing you with the
peace of mind that you are adhering
to current legislation.
For further information visit
www.initialmedical.co.uk or call
0800 731 0802.
bdjteam201533
Always dispose of used sharps
directly into an approved sharps
container
It is essential that your sharps
are segregated and disposed of
correctly based on their medical
contamination. The lid colour and
label on the container relates to how
the waste should be treated and
disposed of.
Where possible, place the sharps
container at the point of use
This avoids the need to walk anywhere
with a needle, which creates higher
risk of an injury occurring.
Do not re-sheath needles
When the Health & Safety (Sharps
Instruments in Healthcare) Regulations
2013 came into place, the recapping
of needles was banned, so it is
now against regulations to do so.
The purpose of this is to prevent
needlestick injuries from occurring
when removing the needle. You should
use a safer sharps device to remove
needles from your syringe.
Do not leave sharps lying around
Although this may seem obvious,
sharps injuries are still known to occur
as a result of sharps being left lying
around, when other people are not
aware that they are there, so it is
extremely important that they are
disposed of immediately after use.
Report all sharps
injuries immediately
If a sharps injury does occur, you need
to ensure you follow the below steps:
■
Encourage bleeding from
the wound
■
Dry the wound and cover it with a
waterproof dressing
■
Seek urgent medical advice
■
Report the injury and ensure
all details are reported in your
practice’s accident reporting book.
Table 1 Top tips for needlestick safety
WELLBEING OF THEIR STAFF.’
WELLBEING OF THEIR STAFF.’
LEGAL OVERALL RESPONSIBILITY FOR THE
LEGAL OVERALL RESPONSIBILITY FOR THE
ROPES, TO PRACTICE OWNERS WHO WILL HOLD
TRAINEE STAFF WHO ARE LEARNING THE
PREVENTION OF SHARPS INJURIES, FROM
PREVENTION OF SHARPS INJURIES, FROM
‘EVERYONE HAS A ROLE TO PLAY IN THE
BE PART OF THE LARGEST EVER
CONFERENCE AND EXHIBITION
IN UK DENTISTRY
www.bda.org/conference or call 0870 166 6625
REGISTER TODAY
GAIN UP TO 15 HOURS
OF VERFIABLE CPD
• Widest variety of clinical sessions
• All CORE CPD covered
• Vibrant and FREE to attend Exhibition
GREAT PRICES FOR DCPS
1 day Conference Pass from £95
3 day Conference Pass from £155
M. J. Faigenblum
1
explains how the denture box facilitates denture
hygiene, reduces the chance of accidental damage and acts as a
means of identification.
1
UCL Eastman Dental Institute
Patients or their carers need
to maintain as low a level of
denture biofilm as possible. This
article notes that the handling
of dentures is unpleasant to
carers and suggests a method
of reducing this contact to a
minimum yet allowing efficient
cleaning by means of brushing.
It also highlights the potential
damage that can occur due
to mishandling or accident.
The denture box acts as a safe
storage unit and its ‘footprint’
allows accurate recovery in an
institution where dentures can
be inadvertently mingled.
www.nature.com/BDJTeam BDJ Team 16
The
denture
box
Edentulous patients
e programme for the 2013 British Dental
Association’s conference contained some
60 lectures, none of which dealt with the
treatment of edentulous patients. is
reects the subject’s relative absence from the
literature and reinforces the perception that
the need for complete dentures is waning.
Nonetheless, as recently as 2009, 6% of the
combined population of England, Wales and
Northern Ireland were edentate and in need
of prostheses.
1
Most of them are ‘elderly’, that
is 75+, and in consequence a proportion are
likely to be in care homes or incapacitated to a
greater or lesser degree.
e York consensus
2
declared that for the
edentulous mandible the minimal standard
of care is the provision of an overdenture
supported by two implants. However, in the
recent update on guidelines for the provision
of such treatment under the NHS,
3
the
authors note ‘…funding for implants on the
NHS is likely to be a precious resource.’ ey
suggest, ‘the decision to provide implants
needs to be balanced against alternative
modes of restoration, their ease of provision,
longevity and outcome rates’.
An alternative mode of restoration is the
provision of optimal dentures, if necessary,
at the hands of an experienced dentist.
is might preclude the need for surgical
intervention and is especially relevant for
patients who are not amenable to surgery.
4
An
added benet is that if correctly designed, the
denture(s) can act as a stent for implants if
they are subsequently required.
A well-made but retentively compromised
complete upper denture can be stabilised
with the judicious use of a dental xative
5
and severe bone resorption of either jaw too
is not necessarily a barrier to a successful
outcome. e eect of a resorbed, mobile
maxillary ridge can be ameliorated by a
careful impression technique.
6
Similarly, in
©Small_World/iStockphoto/Thinkstock
FEATURE
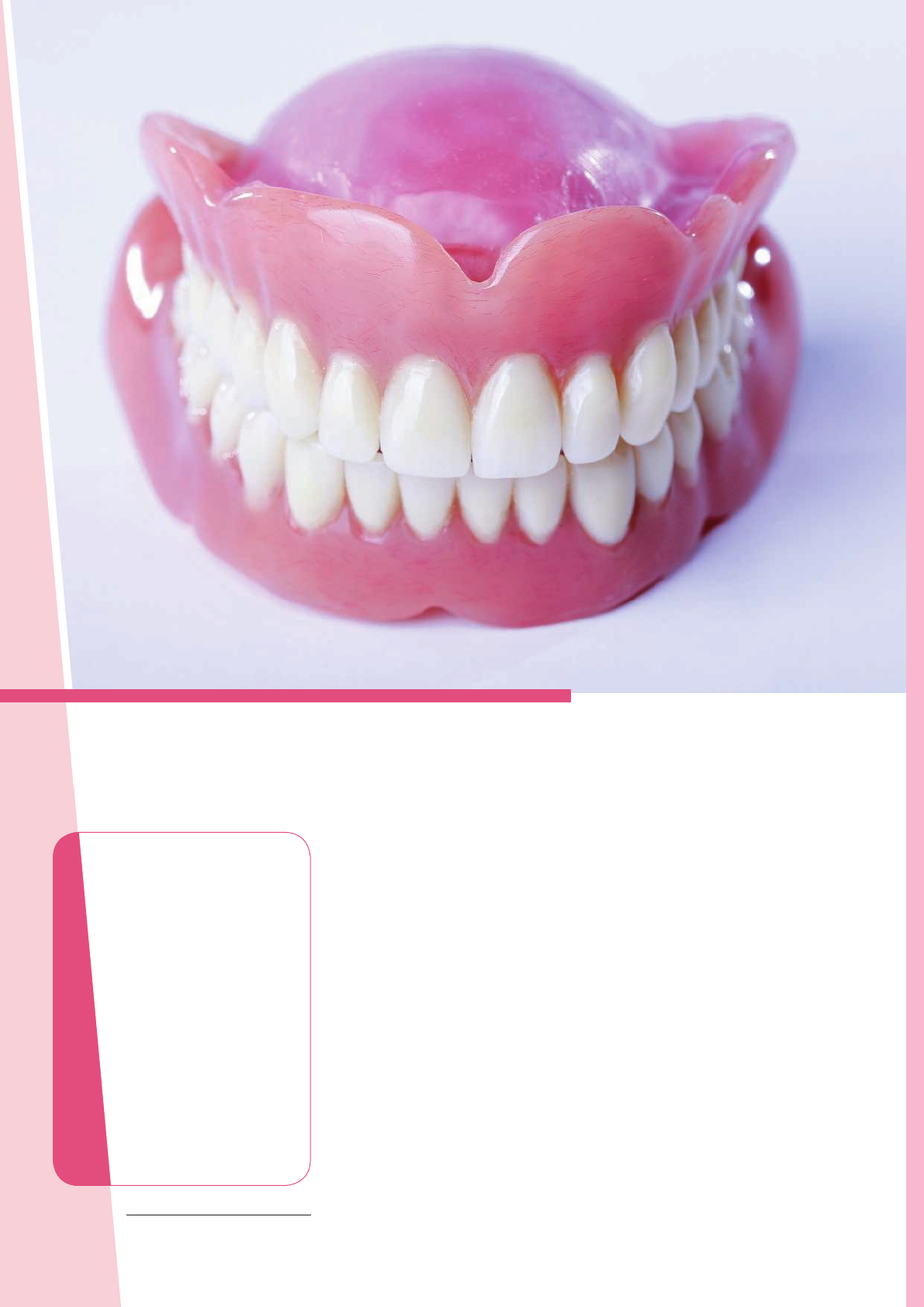
Fig. 2 Angular cheilitis associated with the
stomatitis in Figure 1
Fig. 1 Denture induced stomatitis under an
acrylic partial denture
Fig. 3 Using a plaque disclosing liquid and the result of simple cleaning with a brush and
detergent
Fig. 4 Probable cause for a carer’s
reluctance to handle a denture
FEATURE
17 BDJ Team www.nature.com/BDJTeam
the mandible a skilful technique can provide
a stable denture that can be so -lined if
discomfort cannot be eliminated. e updated
report
3
makes provision under the NHS for
patients who are intolerant to such treatment
and where the implant retained or supported
overdenture
2
would then be treatment of
choice.
e edentate state is most o en the result of
a lack of awareness of the importance of oral
hygiene. It is therefore unlikely that attention
to this will be radically altered when the teeth
are replaced by dentures. Even if this is not
always the case, patients may not be aware of
the potential harm of the denture bio lm.
Denture biofilm
Denture plaque (DP) di ers in its constituents
from the normal dental bio lm.
7
In the
physically healthy individual it can be
aesthetically objectionable with a build-up
of materials found in the mouth that can
produce an unpleasant odour.
8
ey can also
induce mucosal in ammation that is, denture
stomatitis, and a potentially dis guring
angular cheilitis (AC).
9,10
Denture stomatitis (DS) can appear in
di erent forms. Found typically under a
maxillary denture it produces a bright red
imprint of the outline of the denture on
the underlying mucosa (Fig. 1). Due to a
lack of symptoms, its presence is frequently
unnoticed by the patient and by the dental
professional.
Not infrequently, DS is associated with AC
described as a usually bilateral erythematous
ssuring of the corners of the mouth (Fig.
2). e poor appearance that this produces
is exacerbated by deep labial folds that
encourage maceration of the corners of the
mouth with saliva. ese folds are o en
present when the vertical dimension is
signi cantly reduced but is not a cause of the
cheilitis.
11
AC can sometimes be a result of
vitamin and iron de ciency anaemias.
12
Removal of denture plaque is therefore
important. e lm may not be visible but its
presence can be demonstrated to the patient
by the use of a plaque disclosing agent (Fig.
3). e two main denture cleaning methods
of brushing with a non-abrasive paste or
soaking in chemicals have been reviewed.
13
e authors found that there was a lack of
evidence to suggest that one method was
superior to the other. In the author’s opinion
the demonstration of the removal of disclosed
plaque by brushing is preferred to simply
advising chemical soaking. However, without
assistance brushing becomes a problem when
the patient is unable to use one hand, for
example due to injury or a stroke. A possible
solution is suggested below.
e healthy individual can be expected to
respond to oral hygiene advice but this may
not be the case with patients who are seriously
in rm and/or residents in care establishments,
and this can pose a serious problem. It is
now recognised that dental and denture
plaque allow the colonisation of respiratory
pathogens.
14
‘Dentures should be considered
an important reservoir of organisms
which could colonise the pharynx, and the
importance of controlling denture plaque
for the prevention of aspiration pneumonia
cannot be overemphasised.’
15
Where rigorous
oral hygiene procedures have been instituted
a reduction in the rate of pneumonia and
deaths has resulted.
16
Oral care assistance
A Swedish study
17
compared the di erences
in attitude to the maintenance of oral health
PNEUMONIA CANNOT BE OVEREMPHASISED.’
PLAQUE FOR THE PREVENTION OF ASPIRATION
‘THE IMPORTANCE OF CONTROLLING DENTURE

Fig. 6 Denture lightly impressed into the
laboratory putty
Fig. 5 A denture box
Fig. 7 Impression left by the denture
Fig. 9 Resin bonded bridge with
cingulum rests
Fig. 8 The patient is able to steady the box
with his left hand
Fig. 10 Kennedy Class 1 denture with a
cingulum bar major connector
Fig. 11 Kennedy Class 1 denture replaced
into the silicone impression to avoid
accidental damage when cleaning
FEATURE
www.nature.com/BDJTeam BDJ Team 18
in dependant elderly and severely disabled
patients in a group of 398 health workers.
ey were asked regarding a) personal oral
healthcare habits b) experience and attitudes
in assisting oral care and c) willingness to
assist patients/residents with their daily oral
hygiene. is study revealed that oral care
assistance is viewed as more disagreeable than
other nursing activities.
Another study
18
found that nursing sta
considered oral care the most distasteful
aspect of their work (Fig. 4). ey said they
would ‘rather clean up aer bowel movements
or attend to urinary incontinence accidents
than brush a resident’s teeth’.
e denture biolm attached to removable
partial dentures (Fig. 12) will place teeth
at risk, in particular the abutment teeth.
19
Acrylic resin partial dentures, as with
complete dentures, are prone to fracture if
dropped onto a hard surface whereas metal-
based dentures are more resistant to this
danger, but nonetheless can distort aer being
dropped or by mishandling during cleaning.
is is most likely to occur with a mandibular
denture
20
with a lingual or cingulum bar
major connector.
21
As with complete dentures,
cleaning partial dentures may be le to a carer
with the possibility of neglect or damage.
As has been stated, for most individuals the
simplest way to remove the denture biolm
is by mechanical cleaning with a toothbrush
and a non-abrasive paste, at least once a day.
As an adjunct to this, the denture can be
soaked twice a week in 0.1% hypochlorite
solution or chlorhexidine solution for 15-30
minutes.
22
Long-term nocturnal use should be
discouraged.
23
According to Manfredi et al.
22
leaving dentures to soak overnight is counter
to ‘hygienic logic’ because organisms that
inhabit the biolm do not survive prolonged
drying out. ere is no evidence to support
the view that leaving them to dry overnight
will cause warpage of the acrylic.
22
To summarise, both complete and partial
dentures require careful removal of the
denture biolm. However, this may not be
carried out because:
■
e patient is unaware of the need to
do this
■
e patient is unable to physically carry
out the cleaning
■
e carer nds the process unpleasant and
may do this perfunctorily or even avoid it
■
In the process of cleaning, the denture
may be prone to fracture or distortion
if mishandled.
The denture box
is is a simple device to hold the denture in
place during cleaning (Fig. 5). It reduces the
risk of fracture and distortion of a prosthesis.
It will also allow a carer minimal handling of
the denture and allow its storage with reduced
risk of ‘getting lost’. In an institution its
‘footprint’ will make positive discovery of the
owner certain.
One half of an orthodontic retainer or
denture box (or a soap box) is lled with
activated laboratory putty (Fig. 6). e
occlusal surface of the denture is pressed
into the putty suciently deeply to produce
rm retention. e denture can be replaced
in the negative impression and the surface
rigorously cleaned with a brush. Where the
patient has the loss of the use of a hand, the
box can be steadied while brushing or it can
be secured on its base with a suction pad or a
fabric fastener.
e occlusal surface of the denture can be
similarly displayed, following an imprint of
the intaglio surface in the lid of the box if it
has sucient depth (Fig. 7).
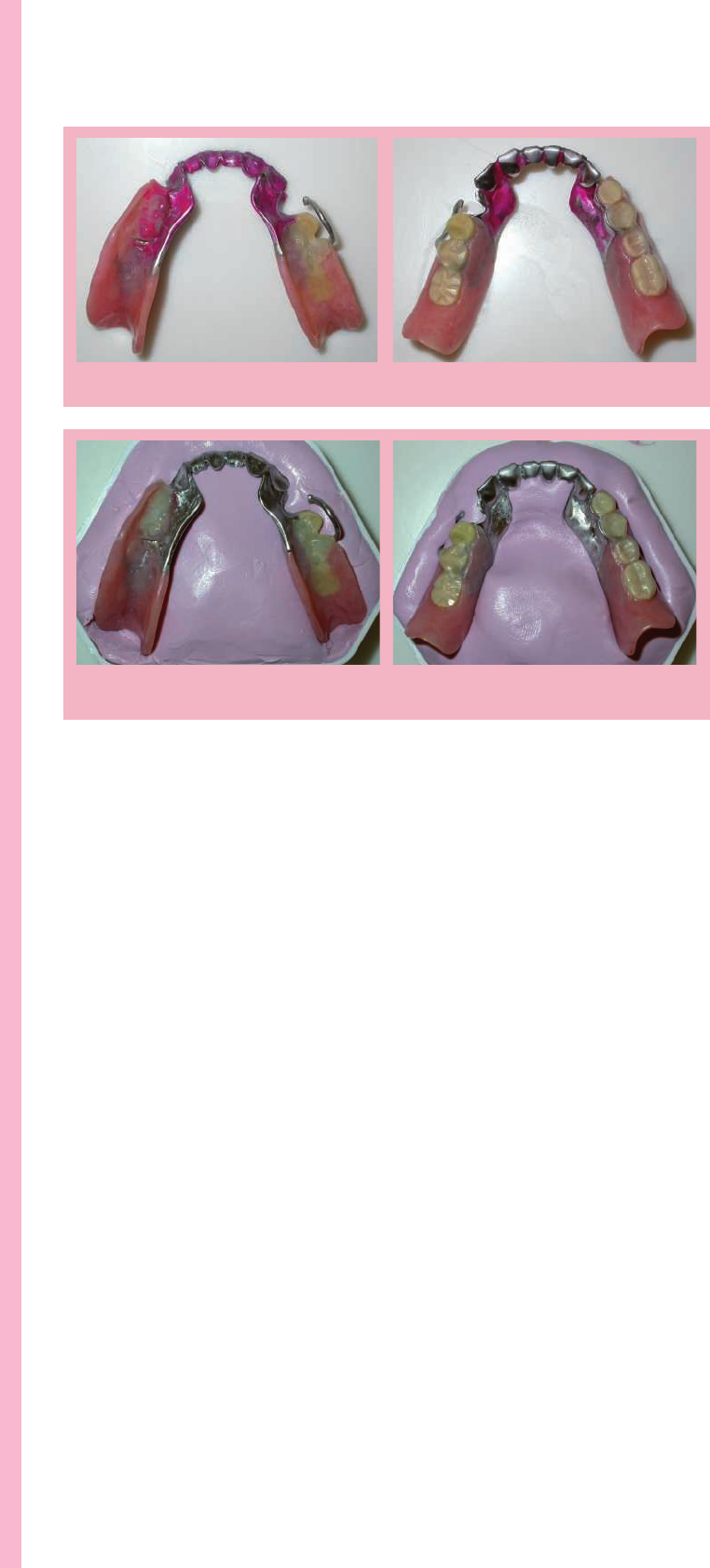
Fig. 12 The disposition of plaque on the denture is shown with a disclosing solution
Fig. 13 The occlusal surface of the denture is placed in the base of the denture box. The fitting
surface is impressed in the lid
FEATURE
19 BDJ Team www.nature.com/BDJTeam
Case history 1
An 80+ male patient in indierent health had
suered a recent stroke that prevented the
normal use of his le hand. He was provided
with an acrylic partial overlay denture,
primarily to replace his upper front teeth. e
denture was embedded in the silicone putty
and he was able to steady the box with the le
hand allowing the right hand to brush (Fig. 8).
Case history 2
e patient has been provided with a resin-
bonded bridge to replace the lower incisor
teeth with wings on the canines (Fig. 9).
Cingulum rests have been added to the canine
wings to receive the cingulum bar major
connector of the Kennedy Class 1 denture
(Figs 10 and 11).
Case history 3
e cingulum bar connector does not impinge
on the gingival margins but the abutment
teeth, in the presence of plaque, are still prone
to damage (Figs 12 and 13).
Storage
e denture box provides a secure method
of storage particularly in an institutional
environment where it is not unusual for
dentures to be wrapped in tissue and
inadvertently discarded. In addition, where
the denture is not marked for identication,
it is possible for the ownership of a denture to
be confused with others. e imprint of the
denture being unique to the individual can
be used to reclaim it to its owner. e imprint
can be kept clean by washing under a tap and,
if required, a small amount of chlorhexidine
gluconate can be le in situ when stored.
1. NHS Information Centre. Adult dental health
survey – rst release. 2009, amended 2010. Online
information available at http://www.hscic.gov.uk/
pubs/dentalsurveyrstrelease09 (accessed November
2014).
2. omason J M J, Feine J, Exley C et al. Mandibular
two implant-supported overdentures as the rst
choice standard of care for edentulous patients – the
York Consensus Statement. Br Dent J 2009; 207:
185–186.
3. Alani A, Bishop K, Renton T, Djemal S. Update
on guidelines for selecting appropriate patients to
receive treatment with dental implants: priorities
for the NHS – the position aer 15 years. Br Dent J
2014; 217: 189–190.
4. Ellis J S, Levine A, Bedos C, Mojon P, Rosberger
Z, omason J M. Refusal of implant supported
mandibular overdentures by elderly patient.
Gerodontology 2011; 28: 62–68.
5. Felton D, Cooper L, Duqum I et al. Evidence-based
guidelines for the care and maintenance of complete
dentures: a publication of the American College of
Prosthodontists. J Prosthodont 2011; 20 (Suppl 1):
S1–S12 .
6. Watt D M, MacGregor A R. Designing complete
dentures. 2nd ed. Bristol: Wright, 1986.
7. Coulthwaite L, Verran J. Potential pathogenic aspects
of denture plaque. Br J Biomed Sci 2007; 64: 180–
189.
8. Verran J. Malodour in denture wearers: an ill-dened
problem. Oral Dis 2005; 11 (Suppl 1): 24–28.
9. Scully C, EI-Kabir M, Samaranayake LP. Candida
and oral candidosis: a review. Crit Rev Oral Biol Med
1994; 5: 125–157.
10. Gendreau L, Loewy Z G Epidemiology and etiology
of denture stomatitis. J Prosthodont 2011; 20: 251–
260.
11. Chernosky M E. Collagen implant in management
of perléche (angular cheilosis). J Am Acad Dermatol
1985; 12: 493–496.
12. Basker R M, Davenport J C. Prosthetic treatment of
the edentulous patient. 4th ed. Oxford: Munksgaard,
2002.
13. de Souza R F, de Freitas O, Paranhos H, Lovato da
Silva C H, Abu-Naba’a L, Gurgan C A. Interventions
for cleaning dentures in adults. Cochrane Database
Syst Rev 2009; 4: CD007395.
14. Azarpazhooh A, Leake J L. Systematic review of the
association between respiratory diseases and oral
health. J Periodontol 2006; 77: 1465–1482.
15. Sumi Y, Kagami H, Ohtsuka Y, Kakinoki Y,
Haruguchi Y, Miyamoto H. High correlation
between the bacterial species in denture plaque and
pharyngeal microora. Gerodontology 2003; 20:
84–87.
16. El-Solh A A. Association between pneumonia and
oral care in nursing home residents. Lung 2011; 189:
173–180.
17. Wårdh I, Andersson L, Sörensen S. Sta attitudes to
oral health care. A comparative study of registered
nurses, nursing assistants and home care aides
Gerodontology 1997; 14: 28–32.
18. Dharamsi S, Jivani K, Dean C, Wyatt C. Oral care
for frail elders: knowledge attitudes, and practices of
long term care sta. J Dent Educ 2009; 73: 581–588.
19. do Amaral B A, Barreto A O, Gomes Seabra E,
Roncalli AG, da Fonte Porto Carreiro A, de Almeida
E O. A clinical follow-up study of the periodontal
conditions of RPD abutment and non-abutment
teeth. J Oral Rehabil 2010; 37: 545–552.
20. Pienkos T E, Morris W J, Gronet P M, Cameron
S M, Looney S W. e strength of multiple major
connector designs under simulated functional
loading. J Prosthet Dent 2007; 97: 299–304.
21. Meeuwissen R, Keltjens H M, Battistuzzi P G.
Cingulum bar as a major connector for mandibular
removable partial dentures. J Prosthet Dent 1991; 66:
221–223.
22. Manfredi M, Polonelli L, Aguirre-Urizar J M,
Carrozzo M, McCullough M J. Urban legends series:
oral candidosis. Oral Dis 2013; 19: 245–261.
23. Compagnoni M A, Souza R F, Marra J, Pero A C,
Barbosa D B. Relationship between Candida and
nocturnal denture wear: quantitative study. J Oral
Rehabil 2007; 34: 600–660.
bdjteam201534

FEATURE
www.nature.com/BDJTeam BDJ Team 20
Rules
for shared parental leave
By Alan Pitcaithley, practice management consultant
P
arents will soon be legally
entitled to share statutory
leave following the birth
or adoption of a child. is
‘shared parental leave’ will
apply to eligible parents of
babies due, or children placed for adoption,
on or aer 5 April 2015. It allows employees
to break their absence from work into
separate blocks and to share some of the
leave with their spouse or partner. Potentially,
eligible parents, in the rst year of a child’s
birth or adoption, will be able to dip in and
out of their job, taking time o to provide care
for the child.
Greater flexibility
e idea is to allow greater exibility for new
parents in setting their work-life balances in
their child’s rst year. is will have an impact
on employers and there are, therefore, precise
procedures to be followed.
e mother would normally be able to
take up to 52 weeks’ maternity leave. Shared
parental leave allows a mother to turn her
maternity leave into shared parental leave.
e actual amount of shared parental leave
available depends on how much maternity
leave is taken.
Since a mother must take at least two
weeks’ compulsory maternity leave following
the birth of their child, there could be up to
50 weeks of shared parental leave available.
Any week or weeks of maternity leave taken
by the mother before the birth of the child or
aer the two weeks of compulsory maternity
leave reduces the shared parental leave
available by a corresponding amount. e
remaining amount of shared parental
leave can be used by either the mother
or her spouse or partner to take time
o work to look aer the child.
It is the mother’s initial
choice whether
or not to opt
for shared
parental
leave, but
once that
choice
has been
made the
couple must
agree when
they should
take leave.
ey may
choose
to take
time o at
the same time,
consecutively or
alternately. Whatever their
decision, shared parental leave must be
taken by the child’s rst birthday – any
unused leave at that date would be lost.
Written notice
To use these rights, eligible parents (Table
1) must give their employer proper written
notice; in fact, three dierent notices.
First, the mother must give notice to end
her maternity leave and change over to shared
parental leave. Second, both parents must give
their employers a notice of entitlement letter
that sets out their basic eligibility (Table 2).
Finally, each must provide a notice of leave
letter that species the actual dates that the
employee wishes to take as shared parental
leave. It should include the start date, end
date and overall amount of leave to be taken,
which must be in full weeks. Each notication
fulls a specic purpose but the employee
could combine them all into one letter.
Time limits are important. Eight weeks’
notice must be given, both by the
mother to switch over from
maternity leave and by either
parent before the start of a period
of shared parental leave.
A mother must:
■
Be an employee entitled to
maternity leave or self-employed
and entitled to maternity allowance
■
Have given notice to end her
maternity leave and take shared
parental leave.
A partner must:
■
Be the mother’s spouse, civil
partner or partner (who is a person
in a long-term relationship with the
mother and living with the mother
and child), or the child’s biological
father (even if they are not in a
stable relationship with the mother)
■
Share the primary parental
responsibility for the child with the
mother at the time of the birth
■
Be an employee, who is entitled to
paternity leave.
Table 1 Who can share the leave?
©AnaBGD/iStockphoto/Thinkstock

FEATURE
21 BDJ Team www.nature.com/BDJTeam
Continuity
A major change introduced by shared parental
leave is the facility to divide leave into
separate blocks, where a parent can return to
work between blocks and go back on leave
later on. Each block must, however, be made
up of full weeks. is could cause diffi culties
for an employer, so how a practice responds
to a notice of leave letter will depend on if the
employee is asking for a continuous period of
leave or a series of separate blocks.
If a continuous period of shared parental
leave is requested, this request must be agreed.
But if the employee asks for two or more
separate blocks of leave – which would be
interspersed by periods back in work – this is
subject to the approval of the employer.
If you have an objective business or
operational reason to refuse a request for
leave to be taken in blocks you can. But you
must respond in writing, setting out your
reason within two weeks. In this situation, the
employee’s overall amount of requested leave
defaults to a single period of leave to begin
on the original start date for their intended
rst block of leave. You should ensure that
your employee understands these default
provisions because they can change the start
date by amending their notice of leave or
could withdraw their request altogether.
Being able to refuse a request for shared
parental leave to be taken in separate blocks
would seem to negate the employee’s new
right but an employee can submit three
separate notice of leave letters within the year.
If each one asks for a continuous block of
leave then, as currently understood, each of
these three blocks of leave would have to be
agreed. But this provision has given rise to the
misconception that shared parental leave can
only be taken in three distinct blocks. While
this is the default situation where an employee
gives you three separate notice of leave letters,
they could in any of these requests ask for
their leave to be split into many more parts.
It is therefore theoretically possible that an
employee could take 25 blocks of shared
parental leave, working one week on and one
week o up to the child’s rst birthday. is
pattern of shared parental leave would require
an employer’s agreement but in some job roles
could occur under the new arrangements.
Shared parental pay
Most mothers taking maternity leave will be
entitled to Statutory Maternity Pay (SMP),
which is available for up to 39 weeks. If an
employee opts into shared parental leave
then the Statutory Maternity Pay remaining
becomes available as Shared Parental Pay
(ShPP). is can be claimed by either partner
while on shared parental leave. e eligibility
for each partner is based on the same earnings
criteria for Statutory Maternity Pay and
Statutory Paternity Pay.
If both parents qualify for ShPP, they must
decide who will receive it or how it will be
divided. Each must inform their respective
employers of how much ShPP each parent
intends to take and when they expect to take
ShPP. ey must also include a declaration
from the employee’s partner con rming their
agreement to the employee claiming their
amount of ShPP. It is expected that this notice
would be given at the same time as a notice of
leave letter.
Another way to SPLIT it
e concept of Keeping-in-Touch (KIT)
days that apply to maternity leave has been
extended to shared parental leave. is allows
an employee to attend work during a period
of leave for training purposes or just to stay
up to date with what is happening in their
workplace.
Under shared parental leave these are
known as Shared-Parental-Leave-In-Touch
(SPLIT) days; up to 20 SPLIT days are
available overall to be shared by the parents.
e employees should contact their employers
to discuss the date or dates of SPLIT days
that they wish to work, though there is
no obligation on either party to agree to a
speci c date.
Sharing adoption leave
e right to opt into shared parental leave also
applies to employees who are on adoption
leave. From the end of a compulsory period
of adoption leave, that is two weeks a er the
placement of the child, the adopter can opt
into shared parental leave and share some
of this with their partner or co-adopter. e
same rules and procedures apply to giving
notice, taking leave and claiming ShPP.
More details
Shared parental leave is a new system and
exactly how it will work for businesses,
employers and employees remains to be seen.
If your principal is a BDA member, the BDA
Advice Employees maternity and parental leave
and pay (see www.bda.org/advice) provides
further information.
bdjteam201535
A notice of entitlement letter must
include the following:
■
The date that the child is expected
or their actual date of birth
■
The spouse’s or partner’s name
■
The spouse’s or partner’s address
and National Insurance number
■
Confirmation that the spouse
or partner shares childcare
responsibility
■
The amount of shared parental
leave available overall for both
parents
■
The dates of any maternity leave
that will be, or has been, taken
■
The amount of shared parental
leave that the employee intends to
take
■
The amount of shared parental
leave their spouse or partner
intends to take
■
A personal declaration that the
employee meets the eligibility
criteria for shared parental leave
and that all the information
provided is accurate
■
A signed declaration from the
employee’s spouse or partner that
they meet the eligibility criteria for
shared parental leave.
Table 2 Notice of entitlement letter
HAVE AN IMPACT ON EMPLOYERS AND THERE ARE,
employee’s spouse or partner that
they meet the eligibility criteria for
shared parental leave.
THEREFORE, PRECISE PROCEDURES TO BE FOLLOWED.’
criteria for shared parental leave
and that all the information
provided is accurate
■
A signed declaration from the
HAVE AN IMPACT ON EMPLOYERS AND THERE ARE,
LIFE BALANCES IN THEIR CHILD’S FIRST YEAR. THIS WILL
NEW PARENTS IN SETTING THEIR WORK-
NEW PARENTS IN SETTING THEIR WORK-
‘THE IDEA IS TO ALLOW GREATER FLEXIBILITY FOR
FEATURE
www.nature.com/BDJTeam BDJ Team 22
As a dental professional you often advise patients to cut down
their sugar intake, but are your own sugar cravings under
control? asks Laura Thomas
1
Practising what you preach
You know that your patients’ sugar habits end
up costing them greatly in terms of dental
treatment and you’re regularly dealing out low
sugar lifestyle advice to help them. However,
sometimes you nd yourself craving sugar
and succumbing to a few more chocolates
than you’d like. Keen to live by your messages,
what can you do to get more control over your
own sugar cravings and protect your own
health from the white stuff ?
Other impacts of sugar
In addition to attacking teeth and enamel,
an excess of sugar has all sorts of other
detrimental impacts on your body.
Re ned sugar, whether in its raw form or
in a processed food like a tomato sauce, is
made up of 50% glucose and 50% fructose.
You need to know that fructose is metabolised
very diff erently to glucose - it’s processed
exclusively by the liver. Consuming an excess
of fructose (sugar) puts serious strain on
this vital organ which can lead to a number
of ailments including non-alcoholic fatty
liver disease and elevated levels of uric
acid (contributing to gout). It’s also worth
noting that excess fructose consumption
over a sustained and long period of time
can increase the risk of the serious chronic
diseases (eg diabetes) that are plaguing the
Western world today.
Sugar also plays havoc on your blood sugar
management, impacting on your sleep quality,
concentration and energy levels. It weakens
your immune system and speeds up the
ageing process.
Finally, sugar is addictive. Over time, a
gradual increase in consumption can start
to negatively aff ect your behaviour. is can
result in you needing more sweet food to
satisfy your sweet tooth.
Reminding yourself of these reasons can
help motivate you to take consistent actions to
reduce the sugar in your diet.
So what can you do to shi your taste buds
away from sweet?
Stop drinking sugar
It’s likely that because you know about the
detrimental impacts of sugary so drinks
on teeth and
enamel, you
aren’t chucking back half a dozen zzy drinks
during the day. However, it’s worth being
aware of the more covert sources which may
be exposing your palate frequently to the
sweet taste that drives cravings.
e sweetener in your tea, the smoothie
drink on the go or that tonic water in your
gin tipple are all still sweet drink sources that
you may not realise have become somewhat
habitual in your routine or lifestyle. Seek to
identify those last few places where you are
drinking sugar and work to eliminate sugar
in all liquid forms. Adapt to unsweetened tea
or coff ee; use fresh lemon or lime to avour
water [editor’s note - but use a straw to protect
your tooth enamel!] and opt for the whole
bre rich fruit instead of a sugar condensed
smoothie.
Lower sugar substitutes of your
favourite foods
Quite o en there can be a big diff erence in
sugar content between brands of the same
food. Spending a little time researching and
nding the ones that don’t have as much
added sugar shaves off a few grams that
can make a diff erence if you’re eating these
products daily. Muesli, sauces and dressings
are all good items to do this with. By doing
this you’re also becoming aware of the great
lower sugar products that you can easily
recommend to your patients.
1
Laura Thomas is a certified health coach
and the founder of Happy Sugar Habits,
an organisation working to educate
and support individuals to reduce their
sugar consumption, and feel a sense of
control over their sweet cravings. Laura
runs a successful Mentor Me Off Sugar
detox programme and speaks nationally
about sugar, emotional eating and the
practicalities of a low sugar lifestyle.
Laura was the former the presenter of
The Sugar Diaries radio show for
UK Health Radio, has written for The
Telegraph and the Daily Mail and has
recently been featured in Elle and Grazia
magazines. Find out more at www.
happysugarhabits.com.
Are you addicted to
sugar?
©yelet/iStockphoto/Thinkstock
FEATURE
23 BDJ Team www.nature.com/BDJTeam
Being
mindful of
total sugar
(especially fructose)
As mentioned earlier,
fructose is the more
dangerous part of sugar.
Although fruits and natural sources of sugar
have nutritional benet and are healthy in
many respects, they are still sweet and you’re
likely to still experience powerful cravings if
you’re consuming them excessively.
To keep cravings at bay, be mindful of
the total amount of sweet food in your
diet (including fruit), the quantities you’re
consuming and how oen you’re eating it. Be
particularly wary of dried fruit products and
fruit purees that tend to be very concentrated
sources of sugar. If something says ‘rened
sugar free’ always check that it’s not just been
jam packed full of ‘natural’ dried fruit sugar.
Avoid hidden sugar
It goes without saying: avoid sugar that you
don’t know you’re eating. Double check
sauces, dressings, cereals, soups etc. Look to
make your own where you can and cut back
on processed foods as much as possible.
Consider your use of sugar
It’s very common for people to use sugar as
a stress coping mechanism. It’s accessible,
cheap, quick and easy. Take note if you’re
consuming sugar in response to emotional
hunger. Seek to build in other coping
mechanisms that don’t involve sweet food eg
some yoga or a run, something relaxing like a
walk or a simple breathing exercise.
Embrace the savoury foods you love
To avoid the doom and gloom feeling of
eating less sugar, embrace your favourite
savoury foods in all their forms. Try new
combinations of them, be more experimental
with foods and try to enjoy the process of
nding savoury alternatives that you really
get excited about.
Work through social challenges
Oen it’s the social side of sugar that can be
particularly challenging:
the birthdays, weddings
and numerous annual
occasions that are
closely associated
with excessively
sugary food. Seek to
understand if you’re
eating sugar because
bdjteam201536
Have you had a go at this recipe? Let
us know how your flapjacks turned
out and send a photo of the results to
bdjteam@nature.com or upload it on
the BDJ Team Facebook page www.
facebook.com/bdjteam.
These have all the satisfaction of a flapjack but with a savoury twist and no sugar
in sight. Great as a quick breakfast bar or as a substantial snack. The pumpkin and
chia seed topping is optional to simply boost the nutritional count and make them
look pretty!
RECIPE: Savoury olive & almond flapjacks
Makes 8 large bars or 16 smaller bites
Ingredients
200g rolled oats (2 cups)
300ml milk (1½ cups)
75g almonds (½ cup)
20g parmesan cheese (⅓ cup, grated)
60g black pitted olives (½ cup)
½ tsp salt
2 tbsp dried oregano
2 tbsp ground flaxseed
1 tsp cumin seeds
1 tsp chilli flakes
1 tbsp chia seeds (optional)
1 tbsp pumpkin seeds (optional)
Method
■
Preheat the oven to 180C and line
an 8-inch square tin with parchment
paper
■
In a medium bowl, mix the oats, salt,
herbs and spices together with the
ground flaxseed
■
Add the milk and leave it to soak for
10 minutes whilst you prepare the rest
■
Roughly chop the olives, almonds and
grate the parmesan cheese
■
Add these ingredients to the mixture,
stir well
■
Pour the mixture into the tin and
spread evenly
■
Sprinkle over the chia seeds and
pumpkin seeds
■
Bake for 45 minutes, remove and
let cool
■
Slice into bars or squares
■
Keep refrigerated in an airtight
container for up to 3 days
everyone else is, or if it’s closely tied to the
joy you feel at these events and celebrations.
Building awareness of your sugar habits
in social situations is the rst best step to
adjusting them.
For more tips, recipes and a free low
sugar snack guide to get control over sugar
cravings visit and sign up for updates at www.
happysugarhabits.com.
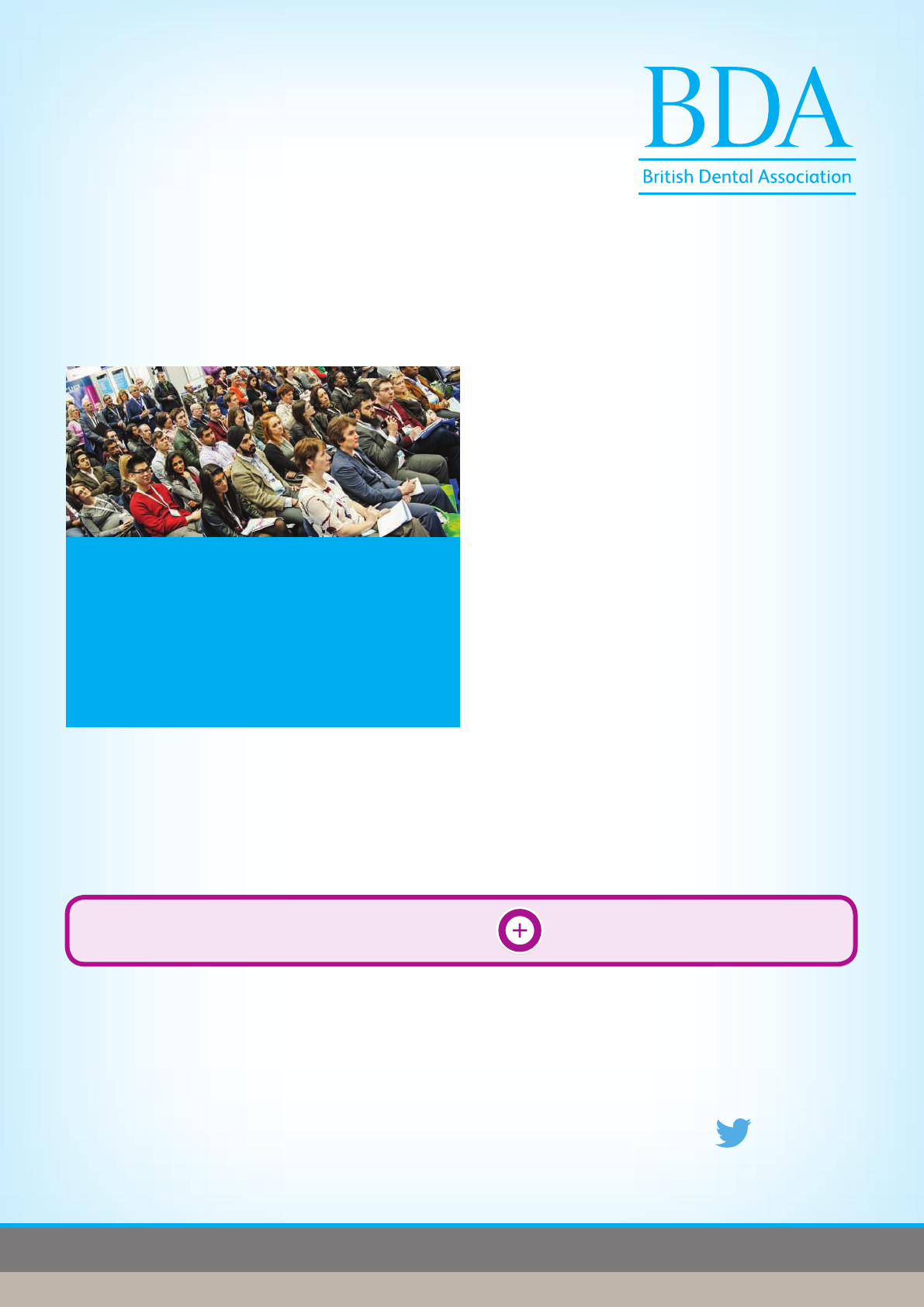
Training
Essentials
BDA special events oer
*This oer cannot be booked online and cannot be applied to events already booked or two day courses. For full terms and conditions please visit our website.
DCPs book one course for £135 Get one course FREE
Check the website www.bda.org/training for event details.
To book call:
020 7563 4590
@BDAEvents
Courses available cover CORE CPD,
GDC recommended, and business and
personal development topics:
Setting yourself up in practice
Management of medical emergencies
Safeguarding children and vulnerable adults
Growing your practice
Leading the dental team
Performance appraisals
An IRMER course in dental radiography
and radiation protection
Oral cancer
Online marketing and social networking
Handling complaints
Infection control
Getting better results with business planning
Book any Training Essentials
course* and get one Training
Essentials course FREE to
help top up your CPD hours
in 2015.
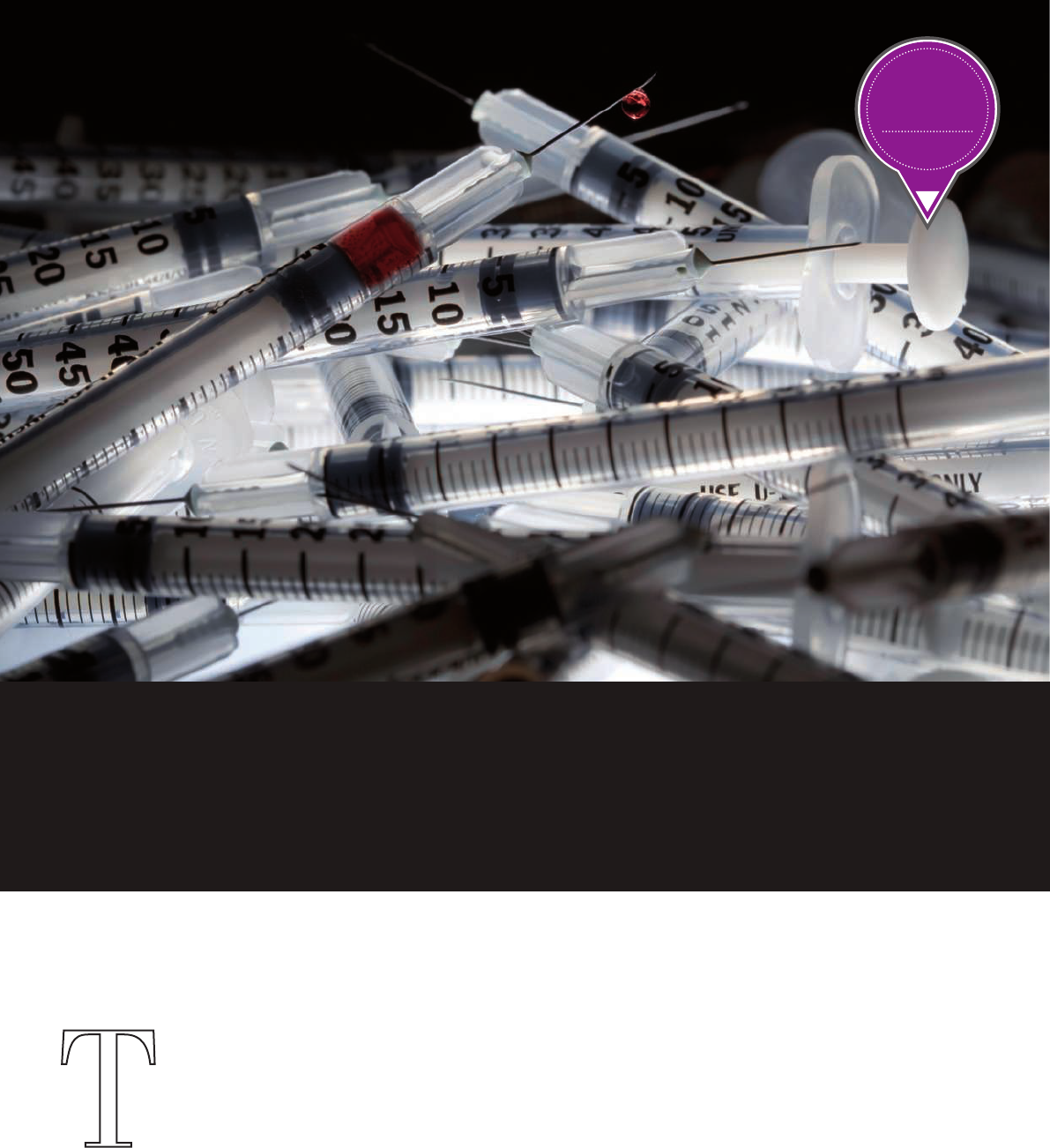
25 BDJ Team www.nature.com/BDJTeam
T
he aim of this article is to
give a practical approach
to the subject of waste
management and segregation
in general practice. It is my
intention that this could
be used as a tool in practice to develop the
waste management and segregation protocol
and policy. It can equally be used for an
individual’s development as veriable CPD in
the core subject of infection control.
Waste produced as a result of any
healthcare activity, like dentistry, is
classied as clinical waste. Health Technical
Memorandum 01-05 (HTM 01-05) states that:
‘e Registered Manager is solely
responsible for ensuring that waste is:
■
Correctly segregated
■
Stored safely and securely away from areas
of public access within the premises
■
Packaged appropriately for transport
■
Described accurately and fully on the
accompanying documentation when removed
■
Transferred to an Authorised Person for
transport to an authorised waste site
■
Appropriately registered, with necessary
records and returns at premises.
e Registered Manager should also
ensure that all sta are trained and aware
of the waste procedures.’
Most of the requirements can be found
in HTM 07-01 (Safe management of healthcare
waste) which is followed for England, Wales
and Scotland but not Northern Ireland.
Clinical waste
Clinical waste is any waste which consists
wholly or partly of human or animal tissue,
blood or other bodily uids, excretions,
drugs or other pharmaceutical products,
swabs or dressings, syringes, needles
or other sharp instruments, being waste
which unless rendered safe may prove
hazardous to any person coming into contact
with it.
Also, any other waste arising from medical,
nursing, dental, veterinary, pharmaceutical
or similar practice, investigation, treatment,
care, teaching or research, or the collection of
blood for transfusion, being waste which may
cause infection to any person coming into
contact with it.
It is vital that ONLY sta members
FEATURE
WASTE
How to dispose of hazardous
CORE
CPD:
ONE HOUR
Do you know what constitutes hazardous waste and how to dispose of it
correctly? Mhari Coxon RDH discusses waste segregation and management
in dentistry.
©iStockphoto
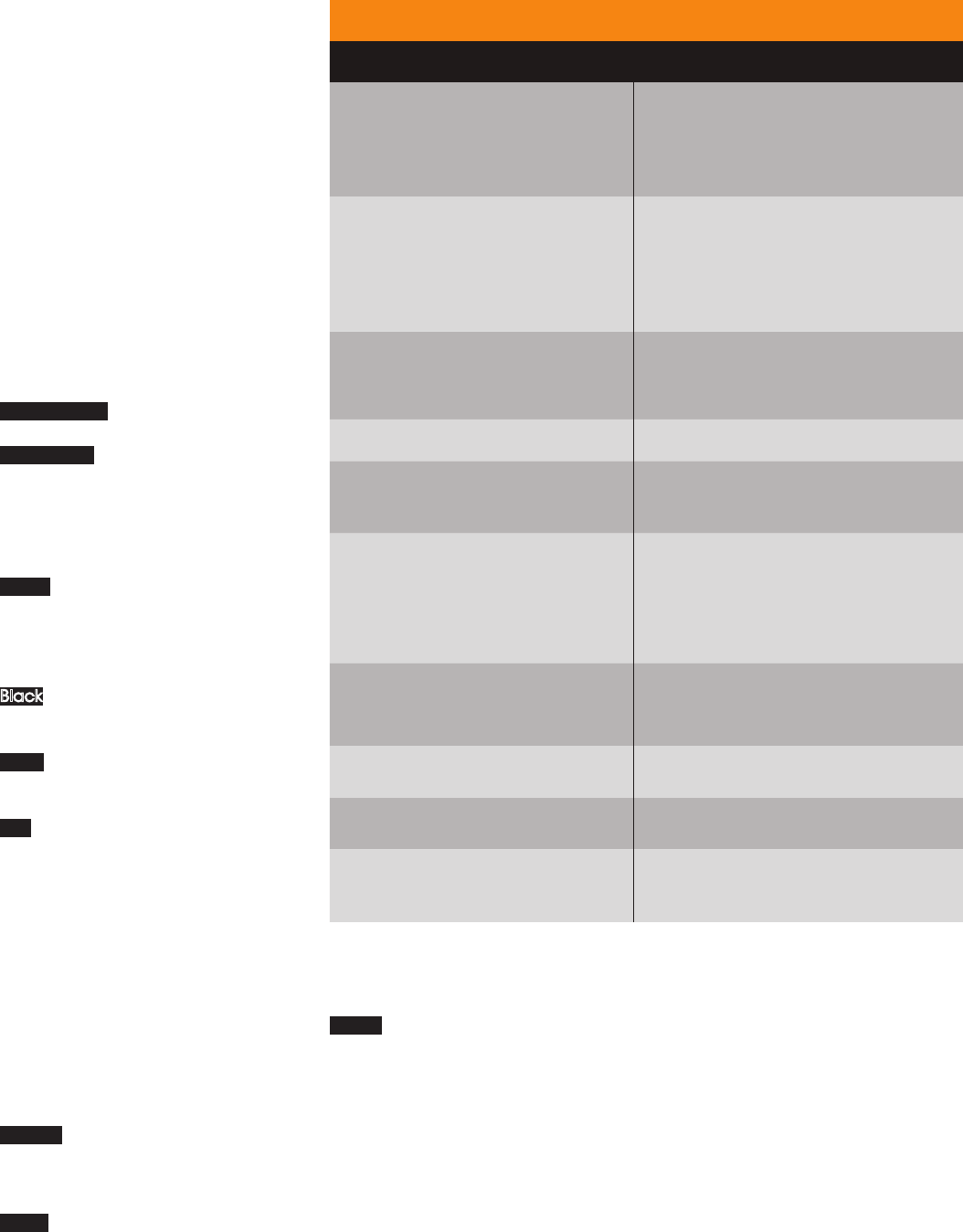
FEATURE
www.nature.com/BDJTeam BDJ Team 26
who have a certied Hep B immunisation
should be handling clinical waste. Cleaners
should NOT touch it unless they have been
immunised and are aware of the protocols and
polices and have had adequate training.
Correct segregation
Is the waste a healthcare waste? Table 1 shows
us how we can dene and categorise our waste
in practice.
Hazardous waste must be disposed of
without endangering human health or the
environment and be capable of being traced
from the point of production to the point of
disposal (Table 2).
Colour description for bagging day
to day waste
Orange bags – infectious or anatomical
waste which requires incineration.
Yellow bags with black stripes – continence
pads and other waste produced from human
hygiene (urine, faeces, sputum, tears, nasal
secretions, vomit). Disposed equipment that
does not pose a risk of infection (inhalers,
gowns, gloves, and plaster casts).
Purple cytotoxic and cytostatic waste (waste
which requires treatment to be ‘rendered safe’.
Unlikely to nd this in a dental environment
but you should recognise the danger of these
waste bags or buckets).
Black Domestic waste for landll – also most
authorities have recycling bags you can buy as
a business which vary in colour.
White Amalgam waste for recovery (includes
extracted teeth with amalgam present and
cages from suction if amalgam was removed).
Red Healthcare waste for special recovery eg
X-ray processing chemicals.
Lead foil
Lead foil is now classied as non-hazardous
waste and there is no longer any need for it to
be collected by licensed contractors.
Sharps waste
Sharps are items that could cause cuts or
puncture wounds – including needles,
syringes with needles attached, broken
glass ampoules, scalpels and other blades or
infusion sets.
Orange lidded sharps bins are for hazardous
sharps not contaminated by prescribed
medicines. is bin would include extracted
teeth with no amalgam in them and scalpels.
Yellow lidded bins are suitable for local
anaesthetic cartridges and botox ampules
as they are for sharps, including infectious
sharps, for incineration only. Marked with
‘Medicinal Sharps’. For use with sharps
waste including those contaminated with
medicines other than those which are
cytotoxic/cytostatic.
Again, not likely to be in general practice,
purple lids are for those medicines and
sharps which are cytotoxic/cytostatic.
Waste handling
NEVER:
■
row bags
■
Carry close to body
■
Empty one bin into another
■
Attempt to retrieve items from waste
■
Leave waste areas unsecured
■
Overll bags or containers
■
Allow waste to build up – contact
Environmental Manager if additional
collection is required.
ALWAYS:
■
Apply Standard Infection
Control Precautions
■
Wear Personal Protective Equipment (PPE)
■
Carry out hand hygiene
■
Provide patients with a
waste receptacle
■
Dispose of waste immediately at point
of use
■
Label and secure correctly
■
Give information to patients/carers on
appropriate waste disposal.
Storage of waste
Within the clinical area:
■
Solid sided, foot operated bin
■
Bags not more than three-quarters full
■
Segregation of waste streams
Table 1 Defining and categorising waste in the practice
Hazardous waste Non-hazardous waste
Infectious waste (eg sharps, anatomical
waste, implanted medical devices). Any
waste which poses a known or potential
risk of infection.
Offensive/hygiene waste (eg human
incontinence and other human hygiene,
sanitary waste, nappies, stoma bags).
Waste which may cause offence to those
coming into contact with it.
Cytotoxic and cytostatic medicines
Non-cytotoxic and cytostatic medicines
(expired, unused, spilt and contaminated
pharmaceuticals, bottles and boxes with
residue, masks, connecting tubing, syringes,
drug vials, vaccines, medicinal patches
and sera).
Health care chemicals and hazardous
properties
Domestic waste (uncontaminated
paper towels, flowers, materials which are
unsuitable for recycling).
Batteries (single-cell or Ni-cad batteries) Packaging waste
X-ray photo chemicals
Recyclable materials (cardboard, non-
confidential paper, drinks cans, bottles,
plastic, toner/ink cartridges, cooking oil).
Mercury (from dental amalgam,
spillage from thermometer/
sphygmomanometer, from electrical
switch/battery or fluorescent discharge
lamps).
Confidential paper waste
Other chemicals eg paint, solvents,
some cleaning materials, laboratory
chemicals
Grounds waste
Radioactive waste Food waste
Contaminated furniture or equipment
Uncontaminated, unwanted or broken
furniture or equipment
Asbestos and some construction/
demolition waste
Construction/demolition waste following
risk assessment

FEATURE
27 BDJ Team www.nature.com/BDJTeam
Table 2 Instructions for disposal of waste
Type of waste Instructions for disposal
Anatomical waste
Must be placed in appropriate UN approved container, labelled
and sealed for incineration. Container must not be placed inside
a bag.
Equipment and
furniture
If contaminated, contact waste contractor. If decontaminated
must have a certificate before disposal.
Radioactive waste
Contact Radiation Protection Supervisor or Environmental
Manager for advice.
Dental waste
Teeth are non-anatomical infectious waste – orange stream
Teeth with amalgam must be segregated into white rigid
container with mercury suppressant
Dental practices must have an amalgam separator
Mercury
Areas where mercury is in use must have a spillage kit. Staff
within the area must know how to use the kit. Instructions should
be looked at at intervals as a team.
Medicinal waste
Expired prescription drugs should be handed in to a local
pharmacy for disposal
Chemical waste
Any chemicals in use within healthcare must have a COSHH risk
assessment.
Staff in areas where chemicals are used/disposed must know
how to handle and dispose of them appropriately.
Surgical
instruments
Must be transported in designated, correctly labelled rigid,
locked container to/from decontamination area.
■
Not le in corridors or public spaces
■
Disposed of as soon as possible
■
Tied securely
■
Bins kept clean inside and out.
Aer removal from clinical area:
■
Securely away from public access
■
Safe from pests and animals
■
In locked wheeled bins (available from
your contractor)
■
Away from other items
■
In an area where hand hygiene facilities
are close by (could be wall mounted
hand disinfectant).
Sealing and tagging
Bags must be:
■
No more than three-quarters full
■
Release air to avoid bursting bag
■
Secure the bag using tags or double
tie method
■
Label with department/surgery in which
the waste was generated (for audit
purposes) and with correct European
Waste Code.
European Waste Catalogue (EWC) codes
are mandatory for all waste documentation
– ie it is necessary for the documentation
which accompanies the consignment of
waste containers to state what the waste
is, including its classication per the EWC
(Table 3). Contaminated sharps could t into
any one of approximately ten EWC codes
dependent on particular circumstances. If
the container label includes the EWC code,
then there is a likelihood either that the code
will be wrong or that a substantially greater
number of containers will be required. is is
why it must be written on by the clinician and
initialled again for audit purposes.
Personal Protective Equipment
ALL sta handling waste must have access to
appropriate PPE. In most instances disposable
gloves and an apron will suce. Heavy duty
gloves must be available for use if required.
If uniform/clothing becomes contaminated
they must be changed immediately.
Training
It is essential that every team member
handling clinical waste be aware of how to
segregate, label and dispose of waste safely.
Training should be reviewed annually and
audited at intervals. e sta members should
accept responsibility for how to manage
themselves in this regard once adequate
training has taken place.
Paper trail of safe disposal
It is essential that all documentation to
and from your registered waste collection
company is kept on le. Your waste collection
company will also be able to give you a copy
of their licence and policies for your le.
is article was originally published in Vital
in 2011 as e whys and wherefores of waste.
To take part in the veriable CPD questions
associated with this BDJ Team article,
visit www.nature.com/bdjteamcpd
(free subscription required).
bdjteam201537
Table 3 EWC codes
18 01 01
Sharps (except 18 01 03)
LA cartridges for example
18 01 02
Body parts and organs
including blood bags and
blood preserves (except
18 01 03)
18 01 03 Infectious waste
18 01 04 Offensive waste
18 01 08
Cytotoxic and
cytostatic medicines
18 01 09
Medicines other than those
mentioned in 18 01 08
18 01 10 Dental amalgam waste
‘ All staff
handling
waste must
have access
to appropriate
PPE.’
PRODUCTS
Products
& services
HELPING YOU IDENTIFY ACID WEAR
Product news is provided as a service to readers using text and images from
the manufacturer, supplier or distributor and does not imply endorsement
by BDJ Team. Normal and prudent research should be exercised before
purchase or use of any product mentioned.
CELEBRATING
THREE DECADES
OF TALKING POINTS
GSK, manufacturers of
Aquafresh, Corsodyl,
Poligrip, Pronamel
and Sensodyne,
is inviting dental
professionals
to join them to
celebrate 30 years of
Talking Points in Dentistry.
The postgraduate lecture series first
launched in 1985 and is open to all
members of the dental team.
This year in celebration of the 30-year
heritage of the programme we ask:
‘Who will be the patient in 2045 and
what will they want?’ The lectures will
reflect on the changes that have
occurred in the dental industry over
the last 30 years and how delivery of
dental care will continue to evolve in
the future.
Over the last 30 years more than
60 industry experts and professionals
have delivered lectures to thousands
of delegates. Many things have
evolved during that time, but the core
focus has remained to provide topical
and thought provoking content.
The lecture series will visit five venues
across the UK during May:
■
12 May 2015 – Titanic Belfast
■
14 May 2015 – Dynamic Earth,
Edinburgh
■
18 May 2015 – National Motorcycle
Museum, Solihull
■
20 May 2015 – National Museum,
Cardiff
■
27 May 2015 – Royal Institute,
London.
To book your place at your nearest
venue simply visit www.gsk-dentalpro-
fessionals.co.uk. Tickets are allocated
on a first come, first served basis and
limited to a total of six per practice, so
book now!
TAKE ACTION AGAINST PERIODONTITIS
New from oral healthcare specialist Curaprox is the perfect pocket minimiser for the
treatment of chronic and aggressive periodontitis.
Adjusan combines the active ingredient doxycycline with a novel design for easy
subgingival application, high tolerability and optimum efficiency. The effective and
uncomplicated single administration is easily applied via the practical cylinder
cartridge. The local antibiotic has the ability to kill key
microorganisms whilst remaining safe for the patient.
Adjusan’s most impressive characteristic is its
innovative gel-like consistency. The initial flowable form
allows you to reach the deep areas of the periodontal
pocket, remaining in place as its viscosity increases
in the aqueous environment. The active ingredient is
released continuously over at least 12 days, enabling
pocket depth to be reduced and attachment
level enhanced.
For more information call 01480 862084 or visit www.
curaprox.co.uk
The results of ESCARCEL, the first and
largest pan-European Epidemiology
study to assess the prevalence and risk
factors for acid wear, offers unparalleled
insights into the condition.
The study revealed just how
widespread acid wear is in young
adults across Europe, with one in three
exhibiting clinical signs. Of particular
concern is the evidence that this figure
is significantly higher in the UK.
1
ESCARCEL found that those aged
26-35 years were most affected by acid
wear, and exposed to what extent
conditions such as frequent heartburn
or acid reflux contribute.
1
Acid wear is an irreversible condition.
The best way to manage it is prevention.
As identification of the early clinical
signs is the first step in helping to
protect patients from further damage,
the BEWE (basic erosive wear
examination) tool can help support
your understanding. Developed
with Professor David Bartlett, Head of
Prosthodontics from King’s College
London Dental Institute, the tool is split
into three simple steps which can help
you to assess patients’ level of risk and
ultimately aid your treatment decision.
GSK has launched the Pronamel
BEWE and acid wear mobile app to help
support you in detecting acid wear. Use
the simple app on-the-go as an easy
reference guide for the background to
the condition, the BEWE tool and tips for
patient management. Download the
app from the iTunes App Store now, just
search ‘bewe’.
1. Bartlett D W,
Lussi A, West N X,
Bouchard P, Sanz
M, Bourgeois D.
Prevalence of
tooth wear on
buccal and
lingual surfaces
and possible risk
factors in young
European adults.
J Dent 2013; 41:
1007–1013.
If you would like to promote your
products or services direct to the
dental industry in BDJ Team, call
Andy May on 020 7843 4785 or
email a.may@nature.com.
www.nature.com/BDJTeam BDJ Team 28
Let us help your career
The most successful course available. Learn this crucial skill in your
own practice with support from our tutors at BDA Education and
gain the BDA qualication in dental radiography.
Dental Radiography
“ Very easy to follow and I would recommend
the course to anyone.”
For more information
visit www.bda.org/radcourse or call 020 7563 6888
Online course for DCPs
Over 600 dental nurses have used BDA Education’s Oral Health Education
course to boost their career. Why not join them and gain the BDA
qualication in oral health education.
Oral Health Education
“My OHE qualication has opened up so many
opportunities for me.”
For more information
visit www.bda.org/ohecourse or call 020 7563 4551
Online course for DCPs

www.nature.com/BDJTeam BDJ Team 30
CPD
CPD questions – March 2015
BDJ Team continuing
professional development
CPD ARTICLE: How to dispose of hazardous waste
1. Which of the following is categorised
as hazardous waste?
A. grounds waste
B. ink cartridges
C. nappies
D. sphygmomanometer spillage
2. According to HTM 01-05, who is
responsible for ensuring that waste
is described accurately and fully on
the accompanying documentation
when removed?
A. the cleaner
B. the Registered Manager
C. the bin men
D. whoever is last to leave the practice
3. Which of the following is incorrect?
A. red bags are for healthcare waste for
special recovery
B. yellow bags with black stripes are for
infectious or anatomical waste which
requires incineration
C. extracted teeth with no amalgam in
them should be placed in orange
lidded sharps bins
D. after removal from the
clinical area waste bags
should be kept in locked
wheeled bins
4. What is the correct
European Waste
Catalogue code for a
body part or organ?
A. 18 01 08
B. 18 01 10
C. 18 01 02
D. 18 01 01
CORE
CPD:
ONE HOUR
How do I take part
in BDJ Team CPD?
BDJ Team is offering all readers TEN hours
of free CPD in 2015 through our website.
The ten free hours of free CPD that we
offered in 2014 are also still available until
the end of 2015.
Just go to www.nature.com/bdjteam/
cpd to take part!
Missed core CPD?
You can complete BDJ Team CPD
through our website, any time
in 2014 and 2015.
Just go to www.nature.com/
bdjteam/cpd to find out how!
Topics covered so far
April 2014: Disposing of clinical and
dental waste
May 2014: Emergency oxygen
therapy in the dental practice
July 2014: Needlestick and
occupational exposure to infections
August 2014: Medical emergencies:
the drug box, equipment and
basic principles
October 2014: Radiation protection
in dental X-ray surgeries
CORE
CPD:
ONE HOUR
31 BDJ Team www.nature.com/BDJTeam
CPD
1. Please PRINT your details below:
First name: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ Last name: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Title: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Address: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ Postcode: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Job title: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
GDC registration no.: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
2. Payment details – SUBMISSIONS SENT IN WITHOUT PAYMENT WILL NOT BE PROCESSED
I enclose a cheque for £6 made payable to Nature Publishing Group for ONE hour of CPD
¨
I would like to pay for more than one person and enclose a cheque for £______ made payable to Nature Publishing Group
(£6 per person for an hour of verifiable CPD).
Or
Please debit the sum of £6 or £______ from the following credit/debit card (tick box):
Visa
¨
Mastercard
¨
Switch/Maestro
¨
Visa Debit
¨
Card number: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Expiry date: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Issue no. (Switch/Maestro): _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Name of cardholder: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Address of cardholder (if different to above): _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
3. I am answering the CPD questions in the __________________ issue (PLEASE ENTER MONTH):
A B C D
Q1
¨
¨
¨
¨
Q2
¨
¨
¨
¨
Q3
¨
¨
¨
¨
Q4
¨
¨
¨
¨
4. Please add any comments or feedback that you might have below or email bdjteam@nature.com.
BDJ TEAM POSTAL CPD FORM
Can I take part in BDJ Team CPD through the post?
YES! Just print off this page, complete the form and send it with your payment of £6, to cover administrative
costs. Send to: BDJ Team CPD, Nature Publishing Group, 4-6 Crinan Street, London, N1 9XW. We will check
your answers to the CPD questions, process your payment and send you a certificate through the post.
You can now participate in this BDJ Team CPD through the post until the end of December 2015.
BDJ Team CPD – through the post
