
Probiotics
BENJAMIN KLIGLER, MD, MPH, Albert Einstein College of Medicine of Yeshiva University, New York, New York
ANDREAS COHRSSEN, MD,
Beth Israel Residency Program in Urban Family Practice, New York, New York
P
robiotics are live microorganisms
that benefit the health of the host
when administered in adequate
amounts.
1
A large number of
organisms are being used in clinical practice
for a variety of purposes. The most widely
used and thoroughly researched organisms
are Lactobacillus sp. (e.g., L. acidophilus, L.
rhamnosus, L. bulgaricus, L. reuteri, L. casei),
Bifidobacterium sp., and Saccharomyces bou-
lardii, a nonpathogenic yeast.
Pharmacology
Several mechanisms have been proposed to
explain the actions of probiotics. In most
cases, it is likely that more than one mecha-
nism is at work simultaneously. In the pre-
vention and treatment of gastrointestinal
infection, it is likely a combination of direct
competition between pathogenic bacteria
in the gut, and immune modulation and
enhancement. In children with atopic der-
matitis, the mechanism is probably related
to the effect of probiotics on the early devel-
opment of immune tolerance during the
first year of life. Probiotics may help down-
grade the excessive immune responses to
foreign antigens that lead to atopy in some
children.
2
They may also contribute to sys-
temic down-regulation of inflammatory
processes by balancing the generation of
pro- and anti-inflammatory cytokines, in
addition to reducing the dietary antigen
load by degrading and modifying macro-
molecules in the gut.
3
Probiotics have been
shown to reverse the increased intestinal
permeability characteristic of children with
food allergy, as well as enhance specific
serum immunoglobulin A (IgA) responses
that are often defective in these children.
4
To be most effective, a probiotic species
must be resistant to acid and bile to survive
transit through the upper gastrointestinal
(GI) tract. Most probiotics do not colonize
the lower GI tract in a durable fashion. Even
the most resilient strains generally can be
cultured in stool for only one to two weeks
after ingestion.
3
To maintain colonization,
probiotics must be taken regularly.
Uses and Effectiveness
Most of the identified benefits of probiot-
ics relate to GI conditions, including anti-
biotic-associated diarrhea, acute infectious
diarrhea, and irritable bowel syndrome
(IBS) (Table 1). Some studies indicate a ben-
efit in treating atopic dermatitis in children.
Probiotics are also commonly used for con-
ditions in which firm evidence is lacking,
including vaginal candidiasis, Helicobacter
pylori infection of the stomach, inflamma-
tory bowel disease, and upper respiratory
infections. These uses are not addressed in
this review.
Probiotics are microorganisms with potential health benefits. They
may be used to prevent and treat antibiotic-associated diarrhea and
acute infectious diarrhea. They may also be effective in relieving
symptoms of irritable bowel syndrome, and in treating atopic der-
matitis in children. Species commonly used include Lactobacillus sp.,
Bifidobacterium sp., Streptococcus thermophilus, and Saccharomyces
boulardii. Typical dosages vary based on the product, but common
dosages range from 5 to 10 billion colony-forming units per day for
children, and from 10 to 20 billion colony-forming units per day for
adults. Significant adverse effects are rare, and there are no known
interactions with medications. (Am Fam Physician. 2008;78(9):1073-
1078. Copyright © 2008 American Academy of Family Physicians.)
COMPLEMENTARY AND
ALTERNATIVE MEDICINE
▲
See related editorial
on page 1026.
Downloaded from the American Family Physician Web site at www.aafp.org/afp. Copyright © 2008 American Academy of Family Physicians. For the private, noncommercial
use of one individual user of the Web site. All other rights reserved. Contact [email protected] for copyright questions and/or permission requests.
1074 American Family Physician www.aafp.org/afp Volume 78, Number 9
◆
November 1, 2008
ANTIBIOTIC-ASSOCIATED DIARRHEA
A meta-analysis of 19 recent studies showed
that probiotics reduced the risk of devel-
oping antibiotic-associated diarrhea by
52 percent (95% confidence interval [CI],
0.35 to 0.65; P < .001).
5
The benefit was great-
est when the probiotics were started within
72 hours of the onset of antibiotic treatment.
The species that were evaluated included
strains of L. rhamnosus, L. acidophilus, and
S. boulardii. The authors found that the
magnitude of the effect did not differ signifi-
cantly among the strains, although a limited
number of strains were represented.
5
In a second meta-analysis of 25 random-
ized controlled trials (RCTs; n = 2,810),
various probiotics were given to prevent or
treat antibiotic-associated diarrhea.
6
The
relative risk (RR) of developing antibiotic-
associated diarrhea with probiotics was 0.43
(95% CI, 0.31 to 0.58; P < .0001), which
was a significant benefit when compared
with placebo.
6
This analysis also found that
L. rhamnosus, S. boulardii, and mixtures of
two or more probiotic species were equally
effective in preventing antibiotic-associated
diarrhea. The mean daily dosage of the bac-
terial species in these studies was 3 billion
colony-forming units (CFUs), but studies
using more than 10 billion CFUs per day
showed that these dosages were significantly
more effective. The dosages of S. boulardii
were 250 mg or 500 mg per day.
6
The same meta-analysis examined the
prevention and treatment of Clostridium dif-
ficile disease.
6
Six RCTs were analyzed and
revealed a prevention benefit for participants
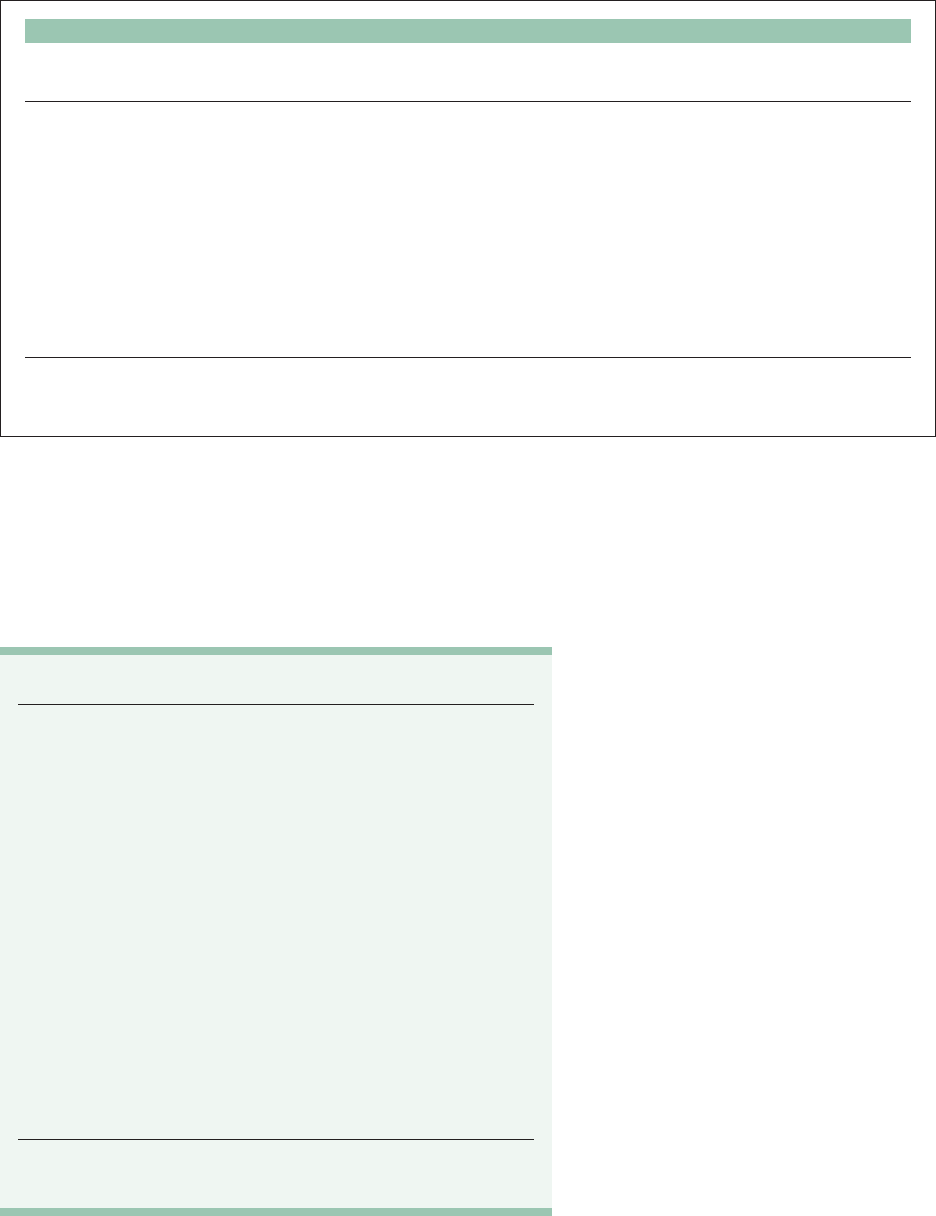
Table 1. Key Points About Probiotics
Effectiveness* Probably effective for antibiotic-associated diarrhea
and infectious diarrhea; possibly effective for
irritable bowel syndrome symptom reduction and
atopic dermatitis for at-risk infants
Adverse effects Common: flatulence, mild abdominal discomfort
Severe/rare: septicemia
Interactions None known
Contraindications Short-gut syndrome (use with caution); severe
immunocompromised condition
Dosage Dosage should match that used in clinical studies
documenting effectiveness: 5 to 10 billion CFUs per
day for children; 10 to 20 billion CFUs per day for
adults
Cost $8 to $22 for a one-month supply
Bottom line Safe and effective for preventing and treating
antibiotic-associated diarrhea and infectious
diarrhea; physicians should consult http://www.
comsumerlab.com or another objective resource for
information about the quality of various brands
CFU = colony-forming unit.
*—Effectiveness depends on probiotic strain and dosage.
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Clinical recommendation
Evidence
rating References Comments
Probiotics may reduce the incidence
of antibiotic-related diarrhea.
A 5-7, 9 Most validated products are Saccharomyces
boulardii and Lactobacillus rhamnosus GG
Probiotics may reduce the duration and severity
of all-cause infectious diarrhea.
A 5, 10-12 A large meta-analysis of all-cause infectious
diarrhea included studies with viral
diarrhea and traveler’s diarrhea
Probiotics may reduce the severity of pain
and bloating in patients with irritable bowel
syndrome.
B 17-19 Small trials to date
Probiotics may reduce the incidence of atopic
dermatitis in at-risk infants. There is preliminary
support for treatment of symptoms.
B 20-23, 25-28 —
A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-
oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to http://www.aafp.
org/afpsort.xml.
Probiotics

Probiotics
November 1, 2008
◆
Volume 78, Number 9 www.aafp.org/afp American Family Physician 1075
taking probiotics. The RR of developing
C. difficile disease was 0.59 (95% CI, 0.41 to
0.85; P = .005). Only S. boulardii showed a
reduction in recurrence with treatment.
A meta-analysis of six RCTs (n = 766) that
focused on preventing antibiotic-associated
diarrhea in children found a reduction in
risk from 28.5 to 11.9 percent (RR = 0.44; 95%
CI, 0.25 to 0.77) in those using probiotics.
7
This analysis showed no difference among L.
rhamnosus GG, S. boulardii, and a combina-
tion of Bifidobacterium lactis and Streptococ-
cus thermophilus. However, a recent Cochrane
review found that although a per-protocol
analysis of 10 trials showed a benefit in pre-
vention of antibiotic-associated diarrhea
in children, a more sensitive intention-to-
treat analysis failed to show a benefit.
8
The
authors did find greater effectiveness in the
studies that used dosages of more than 5 bil-
lion CFUs per day than those that used lower
dosages, regardless of the type of probiotic.
Preliminary evidence suggests that pro-
biotics delivered via fermented milk con-
taining L. casei DN-114 001 and the yogurt
starter cultures L. bulgaricus and S. ther-
mophilus may be useful dietary components
that can reduce the risk of antibiotic-
associated diarrhea and C. difficile toxin for-
mation in hospitalized patients.
9
ACUTE INFECTIOUS DIARRHEA
A Cochrane review examined 23 studies
(n = 1,917) that used different types of pro-
biotics to treat acute infectious diarrhea.
10
Definitions of diarrhea and specific out-
comes varied. The reviewers concluded that
probiotics significantly reduced the risk of
diarrhea at three days (RR = 0.66; 95% CI,
0.55 to 0.77; P = .02). The mean duration of
diarrhea was also reduced by 30.48 hours
(95% CI, 18.51 to 42.46 hours; P < .00001).
This analysis included all causes of infectious
diarrhea (e.g., viral diarrhea, traveler’s diar-
rhea). The authors concluded that probiotics
appear to be a useful adjunct to rehydration
therapy in treating acute infectious diarrhea
in adults and children.
A meta-analysis examining S. boulardii
for treatment of acute diarrhea in children
combined data from four RCTs (n = 619).
11
The authors found that S. boulardii sig-
nificantly reduced the duration of diarrhea
when compared with the control group, for
a mean difference of −1.1 days (95% CI,
−1.3 to −0.8). However, a large trial (n =
571) comparing several probiotic prepara-
tions to oral rehydration solution concluded
that L. rhamnosus GG or a combination of
Lactobacillus delbrueckii subsp. bulgaricus, S.
thermophilus, L. acidophilus, and Bifidobac-
terium bifidum was more effective than S.
boulardii or oral rehydration therapy alone
in reducing the duration and severity of
acute diarrhea in children.
12
Another trial examined the prophylac-
tic benefits of probiotics in preventing GI
infections in children.
13
In a double-blind,
placebo-controlled RCT at 14 child care
centers, infants four to 10 months of age
(n = 201) were fed formula supplemented
with L. reuteri SD2112, B. lactis Bb-12, or
no probiotic for 12 weeks. Both probiotic
groups had fewer and shorter episodes of
diarrheal illness, with no change in respira-
tory illness. Effects were more prominent
in the L. reuteri group, which had fewer
absences, clinic visits, and antibiotic pre-
scriptions during the study.
Therapeutic yogurts have also been stud-
ied in the prevention and treatment of
community-acquired diarrhea in chil-
dren.
14,15
Although a benefit is suggested,
more confirmatory studies are indicated.
A meta-analysis of 12 studies (n = 4,709)
found a modest decrease in the risk of trav-
eler’s diarrhea, with an RR of 0.85 (95% CI,
0.79 to 0.91; P < .0001) in patients taking
probiotics.
16
No difference was found among
organisms, including S. boulardii or mixtures
of Lactobacillus sp. and Bifidobacterium sp.
IRRITABLE BOWEL SYNDROME
Although definitive evidence is still lacking,
several studies have found probiotics to be
effective in relieving symptoms of IBS, par-
ticularly abdominal pain and bloating.
17-19
One study found a 20 percent reduction in
symptoms of IBS with Bifidobacterium infan-
tis 35624 at a dose of 1 × 10
8
CFUs compared
with placebo in 362 patients.
17
In another
study, 50 children fulfilling the Rome II

Probiotics
1076 American Family Physician www.aafp.org/afp Volume 78, Number 9
◆
November 1, 2008
criteria for IBS were given L. rhamnosus GG or
placebo for six weeks.
18
L. rhamnosus GG was
not superior to placebo in relieving abdomi-
nal pain, but there was a lower incidence of
perceived abdominal distention (P = .02).
IBS symptoms may also be managed by
adding components to patients’ diets. One
yogurt (Activia), which contains Bifidobacte-
rium animalis DN-173 010, improved health-
related quality of life scores and decreased
bloating symptoms in patients with IBS.
19
ATOPIC DERMATITIS
There may be a role for probiotics as prophy-
laxis in the development of atopic dermati-
tis in high-risk infants. One double-blind,
placebo-controlled RCT (n = 132) of chil-
dren with a strong family history of atopic
disease administered L. rhamnosus GG
(1 × 10
10
CFUs) or placebo to mothers for two
to four weeks prenatally and then to infants
postnatally for six months.
20
The incidence
of diagnosis of eczema by two years of age
was reduced by one half (23 percent in the
probiotic group versus 46 percent in the
placebo group [RR = 0.51; 95% CI, 0.32 to
0.84]).
Follow-up visits at four and seven
years of age showed no reduction in asthma,
food allergy, or allergic rhinitis, suggesting
that this intervention will not prevent other
manifestations of atopy.
21,22
A larger study (n = 925) using L. rhamno-
sus GG combined with L. rhamnosus LC705,
Bifidobacterium breve Bb99, Propionibac-
terium freudenreichii subsp. shermanii JS,
and 0.8 g of galacto-oligosaccharides (new-
borns only) showed similar effectiveness for
atopic dermatitis at two years of age.
23
A pla-
cebo-controlled study using L. acidophilus
LAVRI-A1 administered to 231 newborns at
high risk of atopic dermatitis failed to repli-
cate this finding, possibly because of a dif-
ferent strain or dosage.
24
Several small RCTs have shown some
benefit in children with established atopic
dermatitis treated with probiotics.
25-27
In
another study, 56 children six to 18 months
of age with moderate or severe atopic der-
matitis were recruited into a randomized,
double-blind, placebo-controlled trial.
28
The children were given a probiotic (1 × 10
9
Lactobacillus fermentum VRI-033) or an
equivalent volume of placebo twice daily for
eight weeks. A final assessment at 16 weeks
showed a significant reduction in the Sever-
ity Scoring of Atopic Dermatitis (SCORAD)
index over time in the probiotic group
(P = .03) but not in the placebo group. Sig-
nificantly more children receiving probiotics
(92 percent) had a SCORAD index that was
better than baseline at week 16, compared
with the placebo group (63 percent; P = .01).
However, other interventions to improve
allergic symptoms have not been successful.
Contraindications, Adverse Effects,
and Interactions
There are no absolute contraindications to
probiotics comprised of Lactobacillus sp.,
Bifidobacterium sp., S. thermophilus, or
S. boulardii. There are typically few or no
adverse effects; flatulence or mild abdominal
discomfort, usually self-limited, are reported
occasionally. There have been reports of
pathologic infection, including bactere-
mia with probiotic species following oral
administration. These are rare, occurring in
severely ill or immunocompromised hosts,
or in children with short-gut syndrome. It is
prudent to avoid probiotics in these patients,
or to be aware of the risk of sepsis. A recent
systematic review examined the safety of L.
rhamnosus GG and Bifidobacterium sp. and
concluded that the risk of sepsis is low, with
no cases reported in any prospective clinical
trial.
29
There are no reports of sepsis or other
pathologic colonization in healthy patients.
There are also no known interactions with
medications or other supplements.
Dosages
A wide range of dosages for Lactobacillus sp.
and other probiotics have been studied in
clinical trials, ranging from 100 million to
1.8 trillion CFUs per day, with larger dos-
ages used to reduce the risk of pouchitis
relapse. Most studies examined dosages in
the range of 1 to 20 billion CFUs per day,
although exact dosages for specific indica-
tions varied within this range. Generally,
higher dosages of probiotics (i.e., more than
5 billion CFUs per day in children and more
Probiotics
November 1, 2008
◆
Volume 78, Number 9 www.aafp.org/afp American Family Physician 1077
than 10 billion CFUs per day in adults) were
associated with a more significant study
outcome. There is no evidence that higher
dosages are unsafe; however, they may be
more expensive and unnecessary. The dos-
ages of S. boulardii in most studies range
between 250 mg and 500 mg per day.
Probiotics are generally sold as capsules,
powder, tablets, liquid, or are incorporated
into food. The specific number of CFUs
contained in a given dose or serving of food
can vary between brands. Patients should be
advised to read product labels carefully to
make sure they are getting the proper dose.
A recent study analyzed a range of
brands of probiotics and found that of the
19 brands examined, five did not contain
the number of live microorganisms stated
on the label.
30
Because some labels are
unreliable, physicians should recommend
specific brands known to be of reasonable
quality or encourage patients to research
brands before purchasing a specific product
(Table 2). Guidance on probiotics can be
found at http://www.usprobiotics.org and
at the National Center for Complementary
and Alternative Medicine’s Web site, http://
nccam.nih.gov/health/probiotics/.
For patients who dislike taking pills
or powder, therapeutic yogurt prepara-
tions may be preferred option. Traditional
yogurts likely do not contain sufficient
concentrations of probiotics to deliver the
type of CFU doses studied in the clinical
trials. Therapeutic fermented dairy prod-
ucts such as Danactive, which contains
10 billion CFUs of L. casei DN-114 001 per
serving, and Activia, which contains about
5 to 10 billion CFUs of B. animalis DN-173 010
per 4-oz. container, are currently available.
Yo-Plus and Stonyfield yogurts contain
well-studied probiotic strains B. lactis Bb-12
and L. reuteri ATCC 55730, respectively, but
at undisclosed levels. Danimals, a drink-
able yogurt marketed for children, contains
1 billion live L. rhamnosus GG. More studies
are warranted on many food sources of pro-
biotics to provide confidence in effective-
ness and dose recommendations.
The Authors
BENJAMIN KLIGLER, MD, MPH, is associate professor of
family medicine at the Albert Einstein College of Medicine
of Yeshiva University in New York, NY. He received his
medical degree from Boston (Mass.) University School of
Medicine and completed a residency in family medicine at
Montefiore Medical Center in New York, NY.
ANDREAS COHRSSEN, MD, is program director of the Beth
Israel Residency Program in Urban Family Practice in New
York, NY. He received his medical degree from the Johann
Wolfgang Goethe—Universität Frankfurt (Germany), and
completed a residency in family medicine at Lutheran
Medical Center in New York, NY.
Address correspondence to Benjamin Kligler, MD,
MPH, Continuum Center for Health and Healing, 245
Fifth Ave., 2nd Floor, New York, NY 10016 (e-mail:
bkligler@chpnet.org). Reprints are not available from
the authors.
Author disclosure: Nothing to disclose.
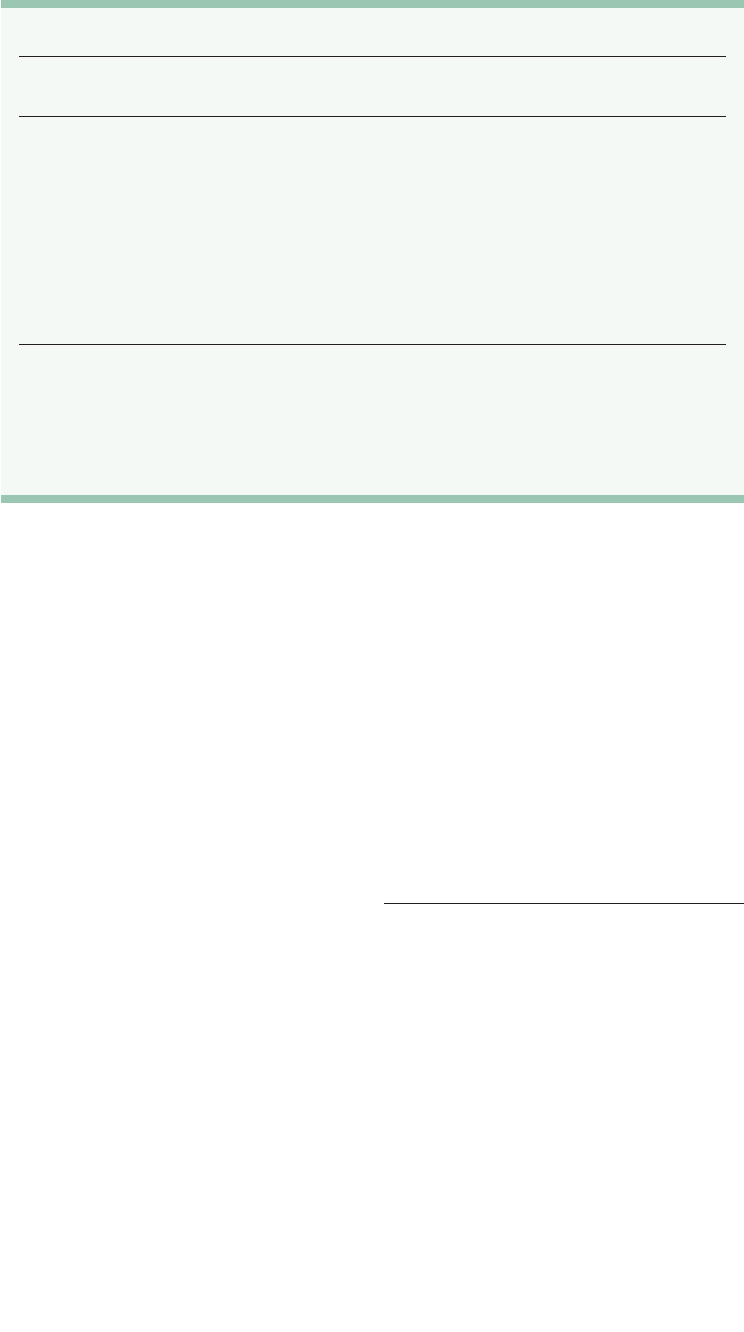
Table 2. Probiotic Strains and Preparations
Probiotic strain
Recommended
daily dosage Preparations*
Lactobacillus
rhamnosus GG
10 billion CFUs Capsules (Culturelle)
Therapeutic yogurts and fermented milks
Lactobacillus sp./
Bifidobacterium sp.†
100 million to
35 billion CFUs,
depending on
preparation
Capsules (Align, Primadophilus)
Powder (Primal Defense)
Capsules or powder (Fem-Dophilus, Jarro-Dophilus)
Therapeutic yogurts and fermented milks (Activia,
Danactive, Yo-Plus)
Saccharomyces
boulardii
250 mg to 500 mg Capsules (Florastor)
CFU = colony-forming unit.
*— This is not a complete list of commercially available preparations.
†—Most commercial brands contain a mixture of strains that may include Lactobacillus acidophilus, L. rhamnosus,
Lactobacillus bulgaricus, Bifidobacterium bifidum, Bifidobacterium longum, and others. Exact combinations of strains
vary among brands.
Information from references 30 and 31.

Probiotics
1078 American Family Physician www.aafp.org/afp Volume 78, Number 9
◆
November 1, 2008
REFERENCES
1. Food and Agriculture Organization of the United Nations
and the World Health Organization. Health and nutri-
tional properties of probiotics in food including powder
milk with live lactic acid bacteria. Cordoba, Argentina;
2001. http://www.who.int/foodsafety/publications/fs_
management/en/probiotics.pdf. Accessed July 2, 2008.
2. Prescott SL, Dunstan JA, Hale J, et al. Clinical effects
of probiotics are associated with increased interferon-
gamma responses in very young children with atopic
dermatitis. Clin Exp Allergy. 2005;35(12):1557-1564.
3. Doron S, Snydman DR, Gorbach SL. Lactobacillus GG:
bacteriology and clinical applications. Gastroenterol
Clin North Am. 2005;34(3):483-498.
4. Rosenfeldt V, Benfeldt E, Valerius NH, Paerregaard A,
Michaelsen KF. Effect of probiotics on gastrointestinal
symptoms and small intestinal permeability in children
with atopic dermatitis. J Pediatr. 2004;145(5):612-616.
5. Sazawal S, Hiremath G, Dhingra U, Malik P, Deb S, Black
RE. Efficacy of probiotics in prevention of acute diar-
rhoea: a meta-analysis of masked, randomised, placebo-
controlled trials. Lancet Infect Dis. 2006;6(6):374-382.
6. McFarland LV. Meta-analysis of probiotics for the
prevention of antibiotic associated diarrhea and the
treatment of Clostridium difficile disease. Am J Gastro-
enterol. 2006;101(4):812-822.
7. Szajewska H, Ruszczy ´nski M, Radzikowski A. Probiot-
ics in the prevention of antibiotic-associated diarrhea in
children: a meta-analysis of randomized controlled tri-
als. J Pediatr. 2006;149(3):367-372.
8. Johnston BC, Supina AL, Ospina M, Vohra S. Probiot-
ics for the prevention of pediatric antibiotic-associated
diarrhea. Cochrane Database Syst Rev. 2007;(2):
CD004827.
9. Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic
Lactobacillus preparation to prevent diarrhoea associ-
ated with antibiotics: randomised double blind placebo
controlled trial. BMJ. 2007;335(7610):80.
10. Allen SJ, Okoko B, Martinez E, Gregorio G, Dans LF.
Probiotics for treating infectious diarrhoea. Cochrane
Database of Syst Rev. 2004;(2)CD003048.
11. Szajewska H, Skórka A, Dylag M. Meta-analysis: Sac-
charomyces boulardii for treating acute diarrhoea in
children. Aliment Pharmacol Ther. 2007;25(3):257-264.
12. Canani RB, Cirillo P, Terrin G, et al. Probiotics for
treatment of acute diarrhoea in children: randomised
clinical trial of five different preparations. BMJ.
2007;335(7615):340.
13. Weizman Z, Asli G, Alsheikh A. Effect of a probiotic for-
mula on infections in child care centers: comparison of
two probiotic agents. Pediatrics. 2005;115(1):5-9.
14. Pedone CA, Arnaud CC, Postaire ER, Bouley CF, Reinert P.
Multicentric study of the effect of milk fermented by
Lactobacillus casei on the incidence of diarrhoea. Int J
Clin Pract. 2000;54(9):568-571.
15. Pedone CA, Bernabeu AO, Postaire ER, Bouley CF,
Reinert P. The effect of supplementation with milk fer-
mented by Lactobacillus casei (strain DN-114 001) on
acute diarrhoea in children attending day care centres.
Int J Clin Pract. 1999;53(3):179-184.
16. McFarland LV. Meta-analysis of probiotics for the
prevention of traveler’s diarrhea. Travel Med Infect Dis.
2007;5(2):97-105.
17. Whorwell PJ, Altringer L, Morel J, et al. Efficacy of an
encapsulated probiotic Bifidobacterium infantis 35624
in women with irritable bowel syndrome. Am J Gastro-
enterol. 2006;101(7):1581-1590.
18. Bausserman M, Michail S. The use of
Lactobacillus GG in
irritable bowel syndrome in children: a double-blind ran-
domized control trial. J Pediatr. 2005;147(2):197-201.
19. Guyonnet D. Chassany O, Ducrotte P, et al. Effect of a
fermented milk containing Bifidobacterium animalis DN-
173 010 on the health-related quality of life and symp-
toms in irritable bowel syndrome in adults in primary
care: a multicentre, randomized, double-blind, controlled
trial. Aliment Pharmacol Ther. 2007;26(3):475-486.
20. Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koski
-
nen P, Isolauri E. Probiotics in primary prevention of
atopic disease: a randomised placebo-controlled trial.
Lancet. 2001;357(9262):1076-1079.
21. Kalliomäki M, Salminen S, Poussa T, Arvilommi H, Iso
-
lauri E. Probiotics and prevention of atopic disease:
4-year follow-up of a randomised placebo-controlled
trial. Lancet. 2003;361(9372):1869-1871.
22. Kalliomäki M, Salminen S, Poussa T, Isolauri E. Probiotics
during the first 7 years of life: a cumulative risk reduc-
tion of eczema in a randomized, placebo-controlled
trial. J Allergy Clin Immunol. 2007;119(4):1019-1021.
23. Kukkonen K, Savilahti E, Haahtela T, et al. Probiotics
and prebiotic galacto-oligosaccharides in the preven-
tion of allergic diseases: a randomized, double-blind,
placebo-controlled trial. J Allergy Clin Immunol. 2007;
119(1):192-198.
24. Taylor AL, Dunstan JA, Prescott SL. Probiotic supplemen
-
tation for the first 6 months of life fails to reduce the risk
of atopic dermatitis and increases the risk of allergen sen-
sitization in high-risk children: a randomized controlled
trial. J Allergy Clin Immunol. 2007;119(1):184-191.
25. Viljanen M, Savilahti E, Haahtela T, et al. Probiotics in
the treatment of atopic eczema/dermatitis syndrome in
infants: a double-blind placebo-controlled trial. Allergy.
2005;60(4):494-500.
26. Sistek D, Kelly R, Wickens K, Stanley T, Fitzharris P,
Crane J. Is the effect of probiotics on atopic dermatitis
confined to food sensitized children? Clin Exp Allergy.
2006;36(5):629-633.
27. Passeron T, Lacour JP, Fontas E, Ortonne JP. Prebiot
-
ics and synbiotics: two promising approaches for the
treatment of atopic dermatitis in children above 2 years.
Allergy. 2006;61(4):431-437.
28. Weston S, Halbert A, Richmond P, Prescott SL. Effects
of probiotics on atopic dermatitis: a randomised con-
trolled trial. Arch Dis Child. 2005;90(9):892-897.
29. Hammerman C, Bin-Nun A. Safety of probiot
-
ics: comparison of two popular strains. BMJ.
2006;333(7576):1006-1008.
30. ConsumerLab.com product review: probiotic supple
-
ments (including Lactobacillus acidophilus, Bifido-
bacterium, and others. http://www.consumerlab.
com/results/probiotics.asp. Accessed July 2, 2008.
31. Usprobiotics.org. http://www.usprobiotics.org. Accessed
October 8, 2008.
