
1
Biology 212: Anatomy and Physiology II
Lab #2: BLOOD/HEMATOLOGY
References: Saladin, KS: Anatomy and Physiology, The Unity of Form and Function 7
th
(2015). Be sure
you have read and understand Chapter 18 before beginning this lab.
Blood is one of the most important components of the human body. It transports materials (i.e., oxygen,
carbon dioxide, hormones, waste products, nutrients, etc.) from one area of the body to another and
allows tissues in distant areas to communicate with one another. In addition, blood protects us from
harmful things like bacteria and viruses via the coordinated actions of a variety of different types of
leukocytes (also known as white blood cells). The average human body contains roughly 5 liters of blood
that is constantly being forced through our arteries and veins by the heart.
Many pathologies of the human body involve blood. For example, anemia can result from excess blood
loss or the inability to form red blood cells which deliver oxygen to the body or parts of the body. An
increased risk of heart disease is associated with elevated levels of LDL (bad) cholesterol, low levels of
HDL (good) cholesterol, and high levels of triglycerides in the blood. Abnormal blood clotting, or
hemostasis, is associated with such disorders as stroke, pulmonary embolism, or hemophilia.
LEARNING OBJECTIVES:
Upon completion of this lab exercise students will be able to:
Describe the composition of blood plasma
Identify the five types of leukocytes typically seen in human blood and perform a differential
white blood cell count
Safely obtain a sample of blood by finger-stick to measure hematocrit and determine ABO and
Rh blood types
Describe the roles of hematocrit, mean corpuscular volume, and mean corpuscular
hemoglobin in maintaining normal oxygen delivery
Describe how erythrocyte production is regulated
Understand the relationship between blood group antigens and plasma antibodies in immunity
Blood is classified as a type of connective tissue which consists
of two fractions:
Formed elements – the cells and cell fragments found in blood
a. Erythrocytes (red blood cells)
b. Leukocytes (white blood cells)
c. Platelets
Plasma – the “liquid/matrix” portion of blood. Blood plasma
contains a great deal of water, ions, proteins, antibodies, and
clotting factors.
The analysis of blood and its components is very important
clinically since the body often changes the composition of blood
in response to changes in physiology or disease.

2
In this lab exercise, we will draw a small blood sample from a finger (not the arm). We will examine the
different components of blood as well as look at some of the basic diagnostic tests commonly used in
hematology.
Working safely with blood
In this lab exercise, we will be working with human blood (your own or that of your lab partners). If you
are not comfortable with drawing blood, if you know you are sick, if you have history of fainting, if you
consider yourself at risk for transmitting a blood born disease, etc., then please do not use your own
blood. Work to safely support your peers in your laboratory group.
While it is unlikely that someone in this class carries an infectious agent in their blood (bacteria, viruses),
it is a universal practice in all laboratories to assume that every blood, tissue, or fluid sample is tainted
with something harmful. As a result, we will follow the following safety protocols:
a) Always wear disposable gloves whenever you are handling blood or any materials that
have come into contact with blood (even if it is your own).
b) Any object which has (or may have) come into contact with blood must be disposed of in
appropriate receptacles. These are never discarded in the trash.
c) Any surface which has (or may have) been contaminated with blood or another body fluid
must be disinfected.
d) Even though you have been wearing gloves, wash your hands before leaving the lab.
Disinfecting solutions supplied by the Biology department are available in the lab for your use.
Microscope slides, gloves, lancets, paper towels, etc. must be placed in designated “biohazard”
receptacles. Your laboratory instructor will discuss these precautions with you.
A. BLOOD PLASMA:
It is important to understand some of plasma’s properties, even though it is not the major focus of this
lab. Plasma makes up approximately 55-60% of our blood volume and is nearly 95% water. The
remaining 5% of plasma consists of ions (also called electrolytes), many different proteins, antibodies,
hormones, nutrients, waste products, and clotting factors. When fresh blood is allowed to settle, the
formed elements sink to the bottom and a yellow-tan (straw colored) fluid rises to the top. This yellow
fluid is the blood plasma.
Since plasma is 95% water, it is a major reservoir for water in our bodies and it is considered one of the
major “fluid compartments” in the human body. When we become dehydrated our tissues pull water
from our plasma and our overall blood volume drops. If we are over-hydrated, the extra fluid volume is
added to the plasma where it can eventually be removed by the kidneys and excreted in the urine. In
addition to acting as a reservoir for water, plasma also plays an important role in maintaining the pH, or
acid/base, balance of the body. Plasma contains buffer molecules which allow the blood and most other
tissues of the body to maintain a relatively constant pH of approximately 7.4. Plasma also plays an
important role in maintaining body temperature near 98.6
o
F since water has a great capacity to absorb
and release heat. As a result, on a hot day plasma supplies the water in sweat that helps cool our bodies.
On a cold day, delivery of warm plasma from our body’s core to our extremities helps keep them warm
when we are outside enjoying the Minnesota winter! We will discuss more about the plasma when we
study our hematocrits later on in lab

3
B. FORMED ELEMENTS OF THE BLOOD:
Keep in mind that the formed elements of blood consist of erythrocytes, leukocytes, and platelets.
Examine Figure 18.1 and Table 18.6 of your Saladin text and note their appearances.
Exercise 1: Examination of Formed Elements
In this exercise, we will be studying the formed elements of
blood using the blood smear slides found in your slide boxes
(Slide #6). Since these are prepared slides and have been
sterilized, you won’t be needing gloves for this exercise.
Our focus will be on the morphology of erythrocytes as well as
the various different types of leukocytes found in human blood.
The identification of the different types of leukocytes is most
easily accomplished by looking at the relative size of the
leukocyte and also at the structure of the nucleus. The vast
majority of the cells that you see on a blood smear will be
erythrocytes, which do not have nuclei, so when identifying the
different leukocytes, just look for cells that have a dark-stained
nucleus.
That being said, you won’t be able to identify EVERY cell that has a nucleus since some cells will have
been damaged during the processing of the slide. As you proceed, make sure you look at the images in
your text book to familiarize yourself with what a “typical” leukocyte looks like and search your slide for
that rather than simply picking a random cell and trying to determine its identity. Make sure everyone in
your group can identify the various white cells. Figure 18.1, Figure 18.18 and Table 18.6 show what
these are supposed to look like, or you can use one of the Histology textbooks in the lab.
Part 1: Erythrocytes: By far, erythrocytes are the most numerous of the cells you will see on a blood
smear. From your Bio 211 experience, you will remember that erythrocytes are small (7.5 microns in
diameter), round, and have an indented center. Basically, they look like little doughnuts that lack a
nucleus. These are red in color because they contain large amounts of the protein hemoglobin to which
oxygen and carbon dioxide can bind as they are carried in the blood.
Part 2: Platelets: Platelets will often have an irregular shape and will be much smaller than erythrocytes
(1-2 microns in diameter). Platelets also lack nuclei since they are actually fragments of a much larger
cell which remains in the bone marrow. They tend to stain dark in color. Platelets play a vital role in
hemostasis, or blood clotting, when blood vessels are injured.
4
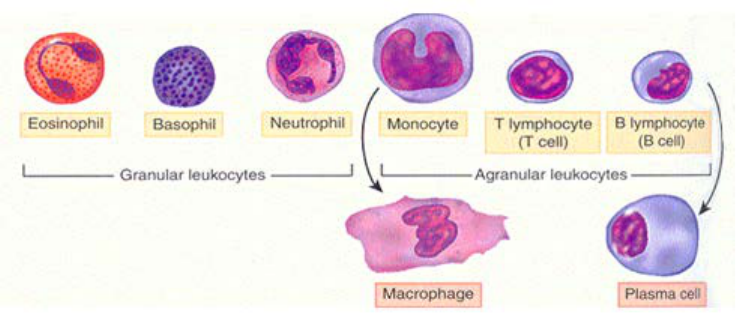
Part 3: Leukocytes: There are two main categories of leukocytes in human blood, granulocytes and
agranulocytes. Examples of each of these are shown in Figure 18.1 and Table 18.6 of your Saladin text.
Granulocytes will possess visibly stained granules within the cytoplasm which look like speckles within
the cell, while agranulocytes will not. Additionally, granulocytes tend to possess nuclei which are more
lobed in appearance and may even make them look like they are multinucleated, while agranulocytes
tend to possess more rounded nuclei that we commonly expect to see in most cells. All of the
leukocytes are involved in protecting the body from infections or other foreign materials.
Granulocytes:
1. Neutrophils are the most common granulocyte, and in fact they are about half of all the
leukocytes in the blood. These cells should be pretty easy to identify based on their sheer
numbers. A neutrophils typically possesses a blue nucleus consisting of three or more “lobes”
that often can be seen connected by thinner strands. However, some cells may simply appear to
have more than one nucleus, even though in reality there is only one. Their cytoplasm contains
many small granules, some of which stain red or pink and others of which stain purple or blue
Neutrophils are phagocytic cells which play an important role in protecting the body against
infections by destroying bacteria, fungi, viruses, and even abnormal or cancerous cells. Their
numbers will increase dramatically when an individual is sick with a viral or bacterial infection
anywhere in the body, and they are able to leave the blood to easily reach other parts of the
body.
2. Eosinophils are much less common than neutrophils, and you may need to spend a few
minutes to identify one. They typically have a blue nucleus which has divided into two lobes, and
they have large granules in their cytoplasm which stain red or orange because they bind onto a
dye called eosin.
Eosinophils are also phagocytic cells like the neutrophils, and they can also leave the blood to get
into other tissues of the body. They secrete chemicals which damage multicellular pathogens
such as parasites, and they destroy allergens and the antigen/antibody complexes which are
formed when the body is fighting an infection.
5
3. Basophils are even less common than neutrophils and eosinophils, so you will probably have
to search for quite a while and be quite lucky to find one. You will probably need to look at
different slides. The nucleus of a basophil is blue and is usually curved into a “U” or “S” shape,
but it will be very difficult to see because the large granules of this type of cell also stain a dark
blue or purple. You will not need to identify a basophil with the light microscope on the lab
exam, but even if you are unable to identify any of these you should be familiar with their
appearance from the photos in your textbook and you should know their function.
These granules contain histamine and heparin which are released in response to inflammation
and tissue injury, and like all of the leukocytes the basophils are able to leave the blood to reach
other tissues. Unlike the eosinophils and neutrophils, however, they are not phagocytic. They
increase the blood flow into injured tissues and they secrete chemicals which attract other
leukocytes to these tissues.
Agranulocytes:
4. Lymphocytes are fairly common in the blood. Since they are agranulocytes, you will see very
few if any granules in the cytoplasm of the cells. Lymphocytes in the blood usually appear to be
relatively small but they will be larger if the individual has an active infection anywhere in the
body. They have large rounded nuclei that may have slight indentations. The nucleus actually is
so large that you often will only be able to see a very small, thin ring of cytoplasm surrounding
the nucleus. This is in contrast to most other human cells we’ve seen that have a smaller nucleus
and a more expansive cytoplasm.
There are at least two functionally different types of lymphocytes known as “B”-lymphocytes
(or “B” cells) and “T”-lymphocytes (“T” cells), but they will have the same appearance under
the light microscope. A major function of “B” cells is to produce and secrete antibodies
needed by the immune system to fight infections. “T” cells play a slightly different role by
secreting factors which recruit phagocytes and macrophages to an infection site, while some
specialized “T” cells are also able to directly attack damaged or infected cells. You may learn
more about these cell types when we discuss the immune system later in this course.
5. Monocytes are relatively large agranulocytes and are usually the largest leukocytes you will
see in the blood. They are much less abundant than lymphocytes, but you should still be able to
identify them on your slides. The nuclei of monocytes typically stain a slightly lighter blue than
the nuclei of other leukocytes and usually have large indentation or a kidney bean appearance.
Like all of the leukocytes, monocytes leave the blood and enter other tissues where they will
mature into macrophages that phagocytose bacteria, viruses, and damaged cell debris.

6
Exercise #2: Differential White Blood Cell Count
In this exercise, we will be performing what is known as a differential white blood cell count. The goal
of this clinical test is to assess the relative numbers of different leukocytes in a given blood sample, each
of which will be expressed as a percentage of the total number of leukocytes. This is an important
diagnostic test since the numbers of certain leukocytes will rapidly change in response to an infection or
inflammation of a tissue.
Differential counts are important for the diagnosis of many diseases. For example, a high differential
count for lymphocytes may be suggestive of lymphocytic leukemia. A low differential count for
neutrophils is often suggestive of radiation exposure or chemotherapy. A high differential count for
eosinophils often results from intestinal parasitic infection. Allergic reactions often are associated with
high differential count for basophils. A chronic infection such as tuberculosis often results in a high
differential count for monocytes.
Again using your blood smear slide (slide #6), you will start at one
edge of the slide and systematically keep track of the numbers of
different leukocytes you see as you move the slide in a specific
pattern as shown in this diagram. Be sure you are not re-counting
the same cells. You can ignore all of the erythrocytes and platelets
you see since we are only interested in the leukocytes. Keep
moving to new adjacent regions of the slide until you have counted
and identified 100 leukocytes. Keep track of the numbers in the
table below. (You want a total of 100 when you are done.)
Cell Type
Number Observed
Neutrophil
Eosinophil
Basophil
Lymphocyte
Monocyte
Total Number of Cells Counted: _____________
(this should be 100)
Based on your reading of Chapter 18 of your Saladin text prior to
this lab, are these normal percentages of leukocytes in human blood?
If not: the percentages of which leukocytes are too high?
the percentages of which leukocytes are too low?

7
B. PHYSIOLOGY OF THE BLOOD:
Erythrocytes contain the protein hemoglobin. Examine Figure 18.5 in your Saladin text and note that
there are four parts to a hemoglobin molecule. Each part has a heme group with an iron ion (Fe
2+
) at its
center, and this is surrounded by a molecule of the protein globin which comes in two forms called
alpha or beta. Within the capillaries of the lungs, molecules of oxygen bind onto the iron of each heme
group and are carried from the lungs to all tissues of the body. In those tissues, the oxygen is released
and diffuses out of the erythrocyte, and carbon dioxide takes its place to be carried back to the lungs.
In this exercise, we will obtain samples of blood from a finger stick to measure your hematocrit, and we
will discuss average red cell size (MCV=Mean Corpuscular Volume), and the hemoglobin concentration
per red cell (MCH=Mean Corpuscular Hemoglobin).
Your hematocrit is simply the percentage of your blood which consists of erythrocytes. MCV, and MCH
are collectively called Red Blood Cell Indices and are values that describe the size and hemoglobin
content in red cells. Obviously, all of these are important in ensuring that your blood can supply the
other tissues of your body with the oxygen they need:
- you must have enough total erythrocytes in your blood (hematocrit)
- those erythrocytes must be the right size and shape
- each erythrocyte must have enough hemoglobin to carry enough oxygen
- that hemoglobin must be able to bind oxygen in the lungs, carry it to other cells
of the body, then release it for them to use for aerobic metabolism.
This is a prime example of homeostasis: If any one of these is too low or too high, your erythrocytes will
not be able to function normally.
Exercise #3: Erythrocytes, Oxygen Carrying Capacity, and Erythropoiesis
Based on your reading of Chapter 18 of your Saladin text prior to this lab, explain each of the following
to other members of your lab group:
a) The meanings of anemia, hypoxia, and polycythemia.
Discuss the causes of each of these, and the effects they have on the body.
b) Where erythrocytes are produced and released into the blood.
How old and damaged erythrocytes are removed from the blood.
c) How erythrocyte production is regulated by the hormone erythropoietin,
including where this hormone is produced.
d) How erythropoietin and erythrocyte production are affected by hypoxia or hypoxemia
e) In terms of intermittent hypoxia experienced during intense exercise, why athletes often
have higher than normal hematocrits.
f) Why cigarette smokers who are exposed to carbon monoxide in the smoke and experience hypoxia
often have higher than normal hematocrits?

8
Exercise #4: Measuring Hematocrit
In order to obtain your own blood to determine your hematocrit, you will be performing a “finger stick”
using a lancet with a very small needle. Because you will also be determining your blood type as
described in Exercise 7 below, you will also need two slides, three or four clean toothpicks, and antibody
solutions (called “antisera”) for specific blood antigens. This will allow you to get blood for both Exercise
4 (hematocrit) and Exercise 6 (blood type) without having to stick yourself a second time.
Before you begin, bring to your lab table an alcohol swab, capillary tube with a colored band on one end,
a lancet, and a paper towel. For blood typing, also bring to your lab table two clean slides, a wax pencil,
and three antisera: Anti-A, Anti-B, and Anti-D. Mark those slides and add antisera to them as described
in Exercise 6.
You are now ready to obtain a blood sample:
1. Wash your hands in warm water and dry vigorously with a paper towel. Hold the hand that you
plan to obtain blood from below your waist for a minute or so to allow more blood to flow to the
tips of your fingers.
2. Use an alcohol swab to clean the side of the fleshy tip of your ring or middle finger.
3. With your hand still below your waist, prepare the lancet (instructor will demonstrate) and press
it firmly against the side of your finger about halfway down your distal phalange (basically off to
the side of your fingernail).
4. Lance your finger and wipe away the first small drop of blood that appears with a paper towel.
5. Have one of your team members place the capillary tubes on the edge of the table and have that
person hold the tubes in place with their finger. As the second drop appears, move your finger
with the drop of blood on it up to one end of the capillary tube – it will automatically flow into
the tube by capillary action. You want the tube to be about 1/2 to 2/3rds of the way full, and you
may have to squeeze your finger a bit to keep the blood flowing (not too hard though).
6. Place your finger over the other end of the capillary tube and push it into the clay to seal off the
end of the capillary tube and place it flat on the paper towel.
7. Gently squeeze your finger to produce another drop of blood and add this to the drop of Anti-A
antiserum you placed on one of the slides. Wipe your finger with a paper towel, gently squeeze
your finger to produce another drop of blood, and add this to the drop of Anti-B antiserum you
placed on one of the slides. Wipe your finger with a paper towel, gently squeeze your finger to
produce another drop of blood, and add this to the drop of Anti-D antiserum you placed on one
of the slides.
8. Clean up any waste materials and disinfect contaminated objects. Do not forget to spray
disinfectant on the area where you were working! Be Smart - Be Safe.
In order to determine the hematocrit, which is the proportion of formed elements versus plasma in your
blood, we will spin the capillary tubes in a special centrifuge (your instructor will do this). After 3-5
minutes of centrifugation the heavier formed elements will accumulate at the bottom of the capillary
tube and the tan/yellow plasma will be seen at the top. The vast majority of the formed elements seen
at the bottom of the tube will be erythrocytes, but you will also notice a thin layer of leukocytes and
platelets in between the erythrocytes and plasma.
9
You can easily determine the percentage of formed elements versus plasma in your blood by using a g a
millimeter ruler or a fancier hematocrit reader (your instructor will demonstrate).
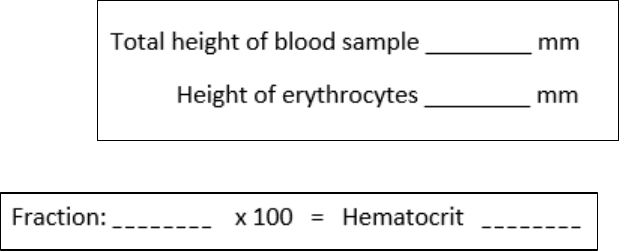
Use a millimeter ruler to measure two things and
record your values in the chart on the right:
a) The total height of the blood sample, from the
clay to the top of the plasma
b) The height of the erythrocytes, from the clay
to the top of the red blood cells
Divide the height of the erythrocytes by
the total height of the blood sample.
This should be a fraction less than “1”.
Multiply that fraction by 100 to get your hematocrit.
Subtract your hematocrit from “100”.
This is the percentage of your blood which is plasma ________%
“Normal” ranges of a hematocrit are given in you textbook and on many websites. Small deviations are
common especially in young women. But all values may be a little low if you had to squeeze your finger
to obtain a blood sample. An abnormally high hematocrit reading indicates an excessive number of
erythrocytes and is known as polycythemia. A low hematocrit is indicative of anemia.
Is your hematocrit within the normal range?
C. DETERMINATION OF BLOOD TYPE (ABO AND RH-FACTOR)
In this exercise, we will be determining your blood type. This is determined genetically, so your blood
type does not change during your life. Like almost all cells in our bodies, blood cells possess
characteristic groups of glycolipids and glycoproteins on the cell membrane that specify “self” versus
“non-self”. This allows our immune systems to recognize and attempt to destroy any cells which it views
as being foreign. While this is vital to protecting us from things that can harm us, it does present
problems in a clinical setting when tissue such as blood is transplanted from one individual to another.
These glycolipids and glycoproteins on the cell surface which may be attacked by our immune systems
are known as antigens. Every person in this room has a slightly different set of antigens on their cells,
making each of us unique. Erythrocytes also contain many antigens on their surfaces, but luckily for us
there are only a couple of different antigens that are clinically important. These are the “ABO” and “Rh”
antigens which produce the blood groups with those names.

10
The ABO blood group describes one set of antigens found on erythrocytes in human blood. There are
four possibilities:
a) A person with Type A blood will have erythrocytes with the “A” antigen but not the “B” antigen;
b) A person with Type B blood will have erythrocytes with the “B” antigen but not the “A” antigen;
c) A person with Type AB blood will have erythrocytes with both the “A” antigen and the “B” antigen;
d) A person with Type O blood will have erythrocytes with neither the “A” antigen nor the “B” antigen.
In order for our bodies to keep track of “self” versus “non-self” cells, the plasma of our blood will
contain antibodies which will detect and attack any erythrocytes which have “non-self” antigens.
a) plasma of a person with Type A blood will contain antibodies
that will detect the presence of cells possessing the “B” antigen.
b) plasma from a person with type B blood will contain antibodies
which will detect the presence of cells possessing the “A” antigen
c) plasma from a person with type O blood will contain antibodies
which will detect the presence of cells possessing either the
“A” antigen or the “B” antigen
d) plasma from a person with type AB blood will not contain either of
those antibodies
This is summarized in the table to the right.
The Rh blood group describes a different antigen found on erythrocytes in human blood, but in this case
there are only two possibilities: your erythrocytes either have the Rh antigen (Rh-positive) or they don’t
have the Rh-antigen (Rh-negative). Unlike the ABO blood groups, however, anti-Rh (also called Anti-D)
antibodies are not normally present in the blood of Rh-negative individuals. They are formed in the
plasma of Rh-negative individuals only after exposure to Rh-positive blood cells. This means the first
exposure of an Rh-negative individual to Rh-positive blood will initiate an immune response that
generates antibodies, but serious problems will not occur because it takes a few days or weeks for the
body to build these new -Rh antibodies. Thus, it is the second exposure of an Rh-negative individual to
Rh-positive erythrocytes when a life-threatening situation can occur. This is extremely important, for
example, during pregnancy when an Rh-negative mother is carrying an Rh-positive fetus for the second
time. She will form anti-Rh antibodies when she is exposed to the blood of her first Rh-positive child,
and during her second pregnancy with an Rh-positive child these antibodies will cross the placenta to
attack the fetus’s erythrocytes. This is called hemolytic disease of the newborn or erythroblastosis
fetalis and often results in death of the fetus or newborn. Fortunately, this situation can be prevented
by the administration of a drug called Rhogam to an Rh-negative woman to suppress her production of
those anti-Rh antibodies.
These antigens and antibodies of either the ABO blood groups or the Rh blood groups are why
transfusion of the wrong blood type to a person often has devastating consequences. For example if a
person with Type A blood receives Type B blood, the anti-B antibodies in their plasms will stick to the
transfused Type B blood cells and cause them to clump together. If a person with type “O” blood
receives either Type A or Type B blood, the anti-A and anti-B antibodies in their plasma will cause the
transfused cells to clump together. If an Rh-negative person receives Rh-positive blood, the anti-Rh
antibodies in their plasma will cause the transfused cells to clump together. This is called agglutination.
Large clumps of the transfused cells will create blood clots that quickly occlude blood vessels, often
leading to death.
11
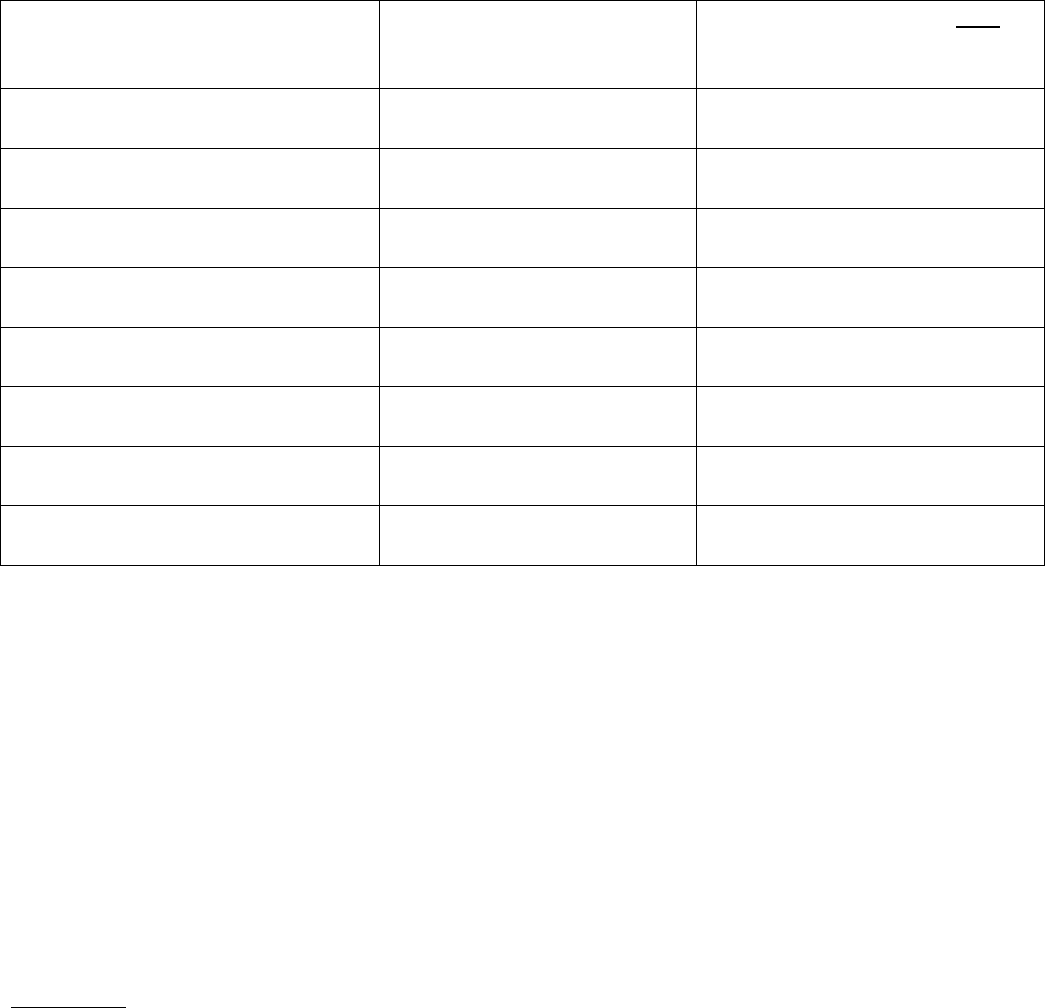
Exercise #5: Blood Transfusion
Discuss with your lab group which types of blood – including both the ABO and Rh groups – can and can
not be safely transfused into an individual with each of the following types of blood, and complete this
chart.
Recipient Blood Type
What types of blood can
safely be transfused into that
recipient?
What types of blood can NOT be
safely transfused into that
recipient?
A-positive blood
(that means Type A and Rh-positive)
B-positive blood
AB-positive blood
O-positive blood
A-negative blood
B-negative blood
AB-negative blood
O-negative blood
Based on that information, explain to other members of your lab group why a person with Type
O-negative blood is considered a “universal donor”, and why a person with Type AB-positive blood is
considered a “universal recipient”.
Exercise #6: Determining ABO and Rh Blood Types:
In this exercise we will be using commercial antibodies against either the “A” antigen or “B” antigen to
determine your ABO blood type, and a commercial antibody against the Rh antigen to determine if you
are Rh-positive or Rh-negative.
Remember: Type A blood will agglutinate (clump together) in the presence of antibodies against the “A”
antigen (these antibodies come from plasma of a person with Type B blood), Type B blood will
agglutinate in the presence of “anti-B” antibodies, Type AB blood will agglutinate in the presence of
either antibody, and Type O blood will not agglutinate at all in the presence of either anti-A or anti-B
antibodies. Regardless of the ABO blood type, Rh-positive blood will agglutinate in the presence of Anti-
Rh antibodies.
12
Procedure:
1. Remember to wear your gloves when dealing with blood.
2. Using a wax pencil label one side of a clean microscope slide “A” and the other half “B”
3. Use a wax pencil to label another clean slide “Rh”
4. Place one drop of Anti-A antiserum on the side of the slide you labelled A
5. Place one drop of Anti-B antiserum on the side of the slide you labelled B
6. Place one drop of Anti-Rh (also called “Anti-D”) antiserum on the slide you labelled Rh
You can now lance your finger as described for determining your hematocrit
7. Place one drop of blood on the microscope slides next to each of those drops of antiserum and
use clean toothpicks to mix each drop of blood with its antiserum.
8. Be careful not to let any of those drops dry out.
9. After one or two minutes, examine the slide to see if the blood exposed to either antibody has
clumped. If after 5 minutes you cannot detect any clumping in the presence of either Anti-A or
Anti-B antibody, it can be safe to assume that you have type O blood, and if you can not detect
clumping in the presence of Anti-Rh antibody you can assume you have Rh-negative blood
10. Remember to clean up your work area and place your used microscope slides in the appropriate
biohazard container OR in a container of bleach/water.
Draw your results in the circles below.
Anti-A Anti-B Anti-D
What is your blood type, both ABO and Rh? __________________
How common is your blood type
(that is, what percentage of people have it?) ____________________
What types of blood could you
safely receive in a blood transfusion? __________________________
