Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 1
DEVELOPMENTAL
DISABILITIES ADMINISTRATION
Person-Centered Plan Development and Authorization Guidance
Revised Date: March 29, 2022
Effective Date: October 15, 2020
*All text in red indicates added/revised language since the prior release date
Audience ..................................................................................................................................................... 1
Purpose ....................................................................................................................................................... 1
Definition ..................................................................................................................................................... 2
Overview ..................................................................................................................................................... 4
Applicability ............................................................................................................................................... 5
Person-Centered Plan - Pre-Planning ................................................................................................... 6
Person-Centered Plan - Development ................................................................................................. 10
Person-Centered Plan - Approval ........................................................................................................ 28
Person-Centered Plan - Authorization ................................................................................................ .32
● Coordinators of Community Services
● Fiscal Management Providers
● Support Brokers
● Developmental Disabilities Administration providers
● Developmental Disabilities Administration Regional Office (RO) Program and Fiscal Staff
This guidance outlines the Developmental Disabilities Administration (DDA) Person-Centered
Plan (PCP) development and funding authorization processes. Historic processes have been
updated to:
● Streamline and ensure the PCP is a living document reflecting the person entirely
throughout the year;
● Support team collaboration, planning, and flexibility for the plan year;
● Decrease the need for Revised PCPs throughout the year;
● Increase efficiencies in submitting, reviewing, and approving a PCP; and
● Ensure services are properly authorized within the Provider Consumer Information
System (PCIS2) until service billing transitions to Maryland’s Long-Term Services and
Supports (LTSSMaryland).

Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 2
A. “Annual Plan” means the person-centered plan completed within 365 days of the agreed
upon Annual PCP date. This date is chosen by the person when they first enter services,
and the initial PCP is developed.
B. “Coordinator of Community Services” means an individual who provides Coordination of
Community Services either as an employee or contractor of a provider organization.
C. “DDA Medicaid Waiver program” means each Medicaid Home- & Community-Based
Waiver program submitted by the Maryland Department of Health and approved by
the Centers for Medicare & Medicaid Services pursuant to § 1915(c) of the federal
Social Security Act, which is overseen and administered by DDA: Community
Pathways, Community Supports and Family Supports.
D. “Dedicated Hours” mean 1:1 and 2:1 staff-to-participant supports hours based on the
participant’s assessed needs.
E. “Designated representative” means an individual who acts on behalf of the participant
in managing the participant’s services under the self-directed services delivery model
in accordance with applicable requirements.
F. “Detailed Service Authorization” means the LTSSMaryland PCP section that lists the
DDA funded services including the specific service name, service provider, units per
month, annual service cost, and provider status.
G. “Direct Support Staff” or “Direct Support Professional” (DSP) means an individual
who is paid to provide direct care services to a participant.
H. “Family as Staff Form” means the form used by participants self-directing their services
to indicate their choice to hire a relative as staff.
I. “Fiscal Management Services provider” or “FMS provider” means a DDA provider
selected by and contracted with the DDA to provide fiscal management services to
support each participant enrolled in the Self-Directed Services delivery model.
J. “Good Life” means a person’s vision for what they want in their life, including what is
important to and for them.
K. “Initial PCP” means the first person-centered plan developed for a participant once they
are approved to apply for waiver services or is the new PCP for a different DDA
program type. It is the first step in applying for another waiver program when the
participant is already currently enrolled in another.
L. “LTSSMaryland” means an electronic information system, developed, and supported
by the Maryland Department of Health, used by DDA, the CCS, and DDA Providers
to create, review, and maintain records regarding an individual’s eligibility status for
DDA-funded services, the individual’s person- centered plan, and services and
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 3
funding authorized by the DDA.
M. “Milestone” means a DDA service unit that is paid based on the completion of a
particular deliverable such as an Assistive Technology Assessment, Behavioral Plan,
Employment - Discovery.
N. “Overnight Supervision” means residential overnight support services where staff may
be awake or asleep, depending on the participants’ needs and provider business model.
Supports are available within Supported Living, Community Living - Group Home, and
Community Living- Enhanced Services services.
O. “Participant” means an individual enrolled in, and receiving, DDA-funded services.
P. “Participant Agreement” means the form used by participants self-directing their
services to documents the participant’s choice to either (1) be the primary person
responsible for managing employer and budget authority responsibilities; (2) to
appoint a designated representative to be responsible for all tasks; or (3) to appoint
team members to assist with specific tasks related to roles and responsibilities under
self-direction.
Q. “Person-centered plan” means a written plan that is developed by a planning process
driven by the individual with a developmental disability in order to:
1. Identify the goals and preferences of the individual with a developmental
disability;
2. Identify services to support the individual in pursuing the individual’s personally
defined outcomes in the most integrated community setting;
3. Direct the delivery of services that reflect the individual’s personal preferences
and choice; and
4. Identify the individual’s specific needs that must be addressed to ensure the
individual’s health and welfare.
R. “Person-centered thinking” means thinking focused on the language, values, and actions
toward respecting the views of the participant and their loved ones. It emphasizes quality
of life, well-being, and informed choice.
S. “Rights and Responsibilities Form” means the form used to notify participants of their
rights and responsibilities as a participant in a DDA program.
T. “Relative” means a natural or adoptive parent, stepparent or sibling.
U. “Revised PCP” means a plan developed when an active Initial or Annual PCP requires
changes to services, outcomes, or other elements of the plan that reflect a change in the
person’s needs and wants. Reasons for a revision may include but are not limited to
discontinuation, initiation or increase in a service; newly identified outcomes, etc.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 4
As noted by the federal Administration for Community Living (ACL), a Person-Centered Plan
(PCP) “helps the person construct and articulate a vision for the future, consider various paths,
engage in decision-making and problem solving, monitor progress, and make needed
adjustments in a timely manner. It highlights individual responsibility, including taking
appropriate risks (for example, whether arranging for back-up staff is needed). Emergency
planning is often part of the process.” (Reference: ACL Person Centered Planning) The PCP
builds and describes the person’s vision for their future.
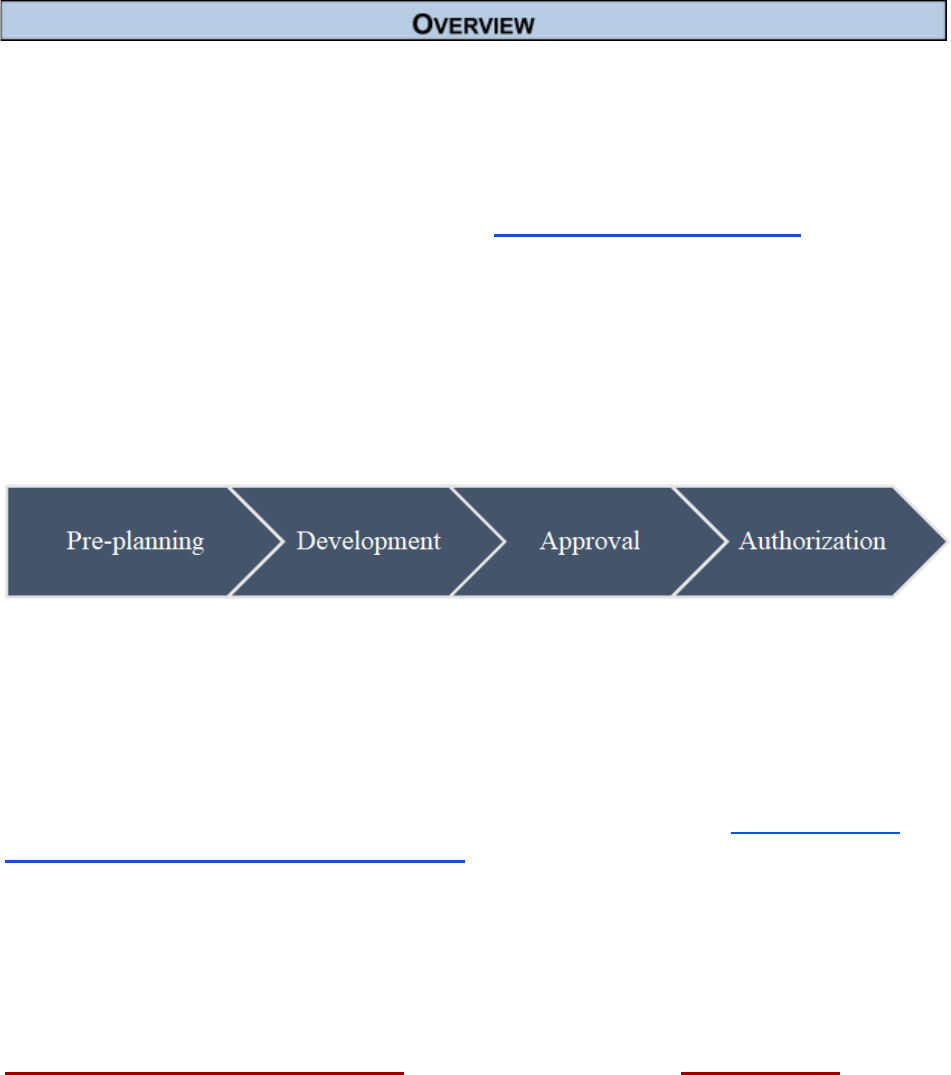
The PCP process always begins with and is about the person. The PCP format, approval, and
authorization are documented within the LTSSMaryland information system. The DDA’s PCP
processes include: (1) pre-planning, (2) plan development, (3) plan approval, and (4) plan
funding authorization. PCP services are authorized for a one-year period and must be
updated annually.
Until the DDA system has fully moved (transitioned) into the LTSSMaryland - DDA Module, the
DDA will be operating in two systems: LTSSMaryland - DDA Module and the current Provider
Consumer Information System (PCIS2). PCPs will be completed and approved in the
LTSSMaryland- DDA Module, and services will be authorized and billed through PCIS2 until the
service provider transitions to the LTSSMaryland- DDA Module fee for service billing.
As part of the DDA’s final transition to LTSSMaryland, the DDA issued the “ GUIDANCE FOR
OPERATING IN PCIS2 AND LTSSMARYLAND”, which includes information and process
changes for transitioning from the legacy services authorized in PCIS2 to the LTSSMaryland-
DDA Module PCP detailed service authorization request. The DDA has also shared guidance
related to the different service names, units, scope, and billing instructions to operate between
the two systems.
All participants will follow the same process for requesting services in their PCP. Under the
traditional services delivery model, DDA-licensed and DDA-certified providers will complete the
Detail Service Authorization Tool (DSAT) and submit to the CCS. The Cost Detail Tool is also
required under the traditional service delivery model for all providers listed in the PCP unless
the services have transitioned to the LTSSMaryland fee for service billing. The DSAT will help
teams identify the appropriate services and units for the LTSSMaryland - DDA Module PCP
detailed service authorization section. The Cost Detail Tool will be used to assist the Regional
Offices with service authorization in PCIS2. The LTSSMaryland - DDA Module PCP detailed
service authorization section and determines the self-directed budget allocation.

Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 5
Once the PCP has been completed, the CCS will submit it to the DDA via LTSSMaryland for
review as per current guidance and policy. Once approved, the DDA will ensure services are
documented and authorized in PCIS2 as applicable. It is important to note that some
LTSSMaryland services and units do not directly correlate to legacy services authorized in
PCIS2. This is due in part to the different rate structures and historical practices of distributing
authorized hours among several people residing in the same home. Therefore, teams and
DDA staff will need to carefully assess the authorized PCP services to the authorized PCIS2
services to determine if new or additional services or hours are needed or edits are needed to
the existing authorization in PCIS2.
Beginning on July 1, 2020, and until the DDA provider’s service transitions into LTSSMaryland fee for
service billing:
● Services under the traditional service delivery model will be authorized and billed
through PCIS2 with the exception of Personal Support, Supported living, and
participants and transition providers to the new fee-for-service payment
methodology.
Self-directed budgets and services will be authorized through PCIS2 and billed through the
FMS until the award and implementation of the new FMS providers.
This guidance focus includes: (1) pre-planning, (2) plan development, (3) plan approval, and (4)
plan funding authorization.
This guidance applies to all Initial, Revised, and Annual PCPs for both the self-directed and
traditional service delivery models.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 6
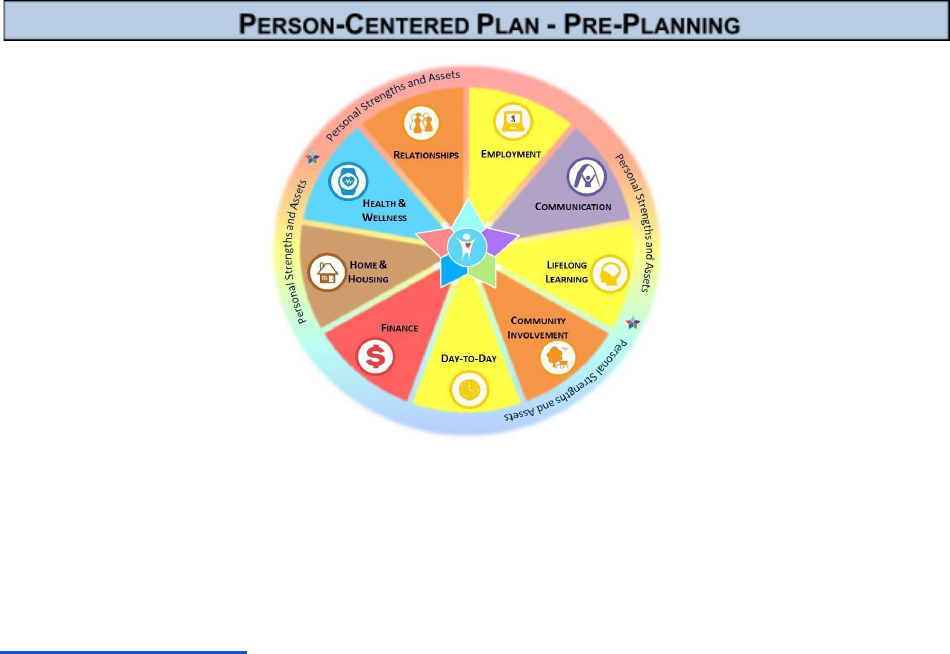
Everyone has the right to live, love, work, play, and pursue their aspirations in their community.
Since 2015, the Maryland Developmental Disabilities Administration (DDA) has been wholly
transforming our programs, policies, and funding processes to put people with developmental
disabilities at the center of our efforts.
People are the center of planning a vision for their personally-defined good life. This is done through
Person-Centered Planning. Our guide for Coordinators of Community Services provides more
information on how individuals can choose in “My Life, My Plan, My Choice.”
Comprehensive pre-planning is essential for Initial and Annual Person-Centered Plans (PCPs)
to support the participant’s life aspirations and address any unmet needs (i.e., immediate and
for the upcoming year) and also reduce the need for a Revised PCP. Pre-planning occurs in
collaboration with the participant’s PCP team which includes people chosen by the participant
but often includes their family members, friends, and provider agencies.
For Initial, Revised, and Annual PCP’s
1. Personally-Defined Good Life
a. The first and most important part of planning is getting to know the person. Who
are they? What do they want for their life, what don't they want? What is their
vision for their "Good Life?"
b. Before even discussing services and supports, teams need to know and
understand what aspirations and goals the participant has in order to assist them
with planning and helping the participant to achieve their self-defined good life.
c. Knowing the person; their strengths and assets, needs, goals and challenges
allows the team to discuss, plan and identify different resources, supports
and services, including DDA funded services to positively support their
trajectory toward their good life.
d. Before discussing DDA-funded and other services, it is important to understand
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 7
the participant’s trajectory so that planning can then begin on the steps to lead a
self-defined good life captured in the Focus Area Exploration (FAE).
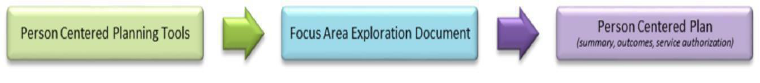
2. Person-centered Planning Tools and Strategies
a. There are several person-centered planning tools and strategies that may be
used in helping each participant to consider their personal strengths, assets,
gifts, and wishes across the Life Domains and over the lifespan.
b. The process involves finding out how each participant prefers to engage and
communicate. It can be done through a one-to-one conversation with the
individual or a meeting with family, friends, and/or others important to the
participant who knows them well. Formal planning processes such as Charting
the LifeCourse and the Integrated Support Star, Essential Lifestyle Planning or
PATH, etc. or a combination can be utilized.
c. Focus Area Exploration (FAE)
(1) Person-centered planning is a continual process of listening and learning
(e.g., exploration and discovery) to create a meaningful and relevant plan
that may be adjusted according to life circumstances.
(2) Discuss focus areas as identified by the participant and included in the PCP
as well as outcomes the participant wants to accomplish initially and
throughout the PCP year.
(3) The Employment FAE must be completed annually. All other FAEs are
driven by the participant and can be discussed at any time throughout the
year, however it is best practice that the team review and complete all
FAE’s particularly when there are revisions being made to authorized
services. The FAE’s provide a good overview of need and documentation of
need for authorized services.
3. Health Risk Screening Tool (HRST)
a. The HRST is used to identify health care needs, risks, and destabilization early.
The HRST assigns scores to 22 health and behaviorally related rating items. The
total points result in a Health Care Level with an associated degree of health risk.
Health Care Levels (HCL) can range from 1 through 6; Level 1 being the lowest risk
for health concerns and Level 6 being the highest risk of health concerns. It is
important to understand that the HRST measures health risk not disability.
b. The HRST can help inform teams of health risks that should be considered
during planning and also provides recommended staff training.
c. The HRST should accurately reflect current health needs.
(1) Teams should review the HRST to determine and document risks and
mitigation efforts to support those risks in the PCP.
(2) The HRST must be reviewed, updated, and approved within 90 days of
the PCP expiration date.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 8
(3) The HRST should be completed early on in the PCP pre-planning process
to ensure timely submission with the PCP to the regional office.
(4) The HRST must also be updated when there are major health status
changes.
4. Support Intensity Scale (SIS)
a. The SIS measures the participant’s support needs in personal, work-related, and
social activities in order to identify and describe the types and intensity of the
supports a participant may require. It can help provide information and
considerations during the person-centered planning processes by the participant
and their team.
b. The SIS is to be completed for all new participants and should be used
for development of the Initial PCP.
c. The DDA has been coordinating with the SIS contractor to conduct a SIS for all
other DDA participants. Since the DDA supports over 17,000 individuals, SIS are
being completed in phases.
d. Once completed, the SIS shall be reassessed every five years. The
LTSSMaryland system will automatically send a referral to the contractor to
complete the SIS and the CCS will also be alerted to the referral.
e. The CCS shall request completion or ensure a SIS is available for PCP team
review and utilization during the pre-planning process.
5. Assessed Need(s) and Risks
a. After the participant’s vision has been identified, the PCP team should utilize the
HRST and other tools/discussions to assess support need(s), including any that
have changed or have not been met and identify health care needs, risks, and
mitigation strategies.
b. To support an integrated “community life” versus a “service life”, the PCP team
should continuously explore generic, natural, community, local, and other
resources to meet need(s) and address risk.
■ The Charting the LifeCourse Integrated Star is a useful tool for people,
families, and teams to consider an array of integrated supports to achieve
the envisioned good life, including those that are publicly or privately funded
and based on eligibility, community supports that are available to anyone,
relationship-based supports technology, and also take into account the
assets and strengths of the individual and family. This tool is helpful to get a
more comprehensive look at all the services and supports that may exist in
a participant’s life; not just eligibility specific supports.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 9
c. After exploration of generic, natural, community, local, and other resources, the
PCP team should determine if any remaining unmet support needed can only be
met with a Waiver or Medicaid service.
(1) Natural Supports refer to the support and assistance that naturally flows
from the associations and relationships typically developed in natural
environments such as the family, school, work, and community.
(2) Generic service/support means support and services available to any
member of the population and is not specific to meeting specialized
needs of individuals with intellectual disabilities or developmental
disabilities. Essentially, it's the same as a community resource,
support, or service.
d. If an individual has Conditions of Release or Probation from a court, the court
documents need to be uploaded into LTSS. All Conditions of Release or
Probation need to be listed in the restriction section of the PCP and BP to
address those restrictions.
6. Annual Plan (in addition to the requirements noted above):
a. Preplanning should be initiated within 90 days of the PCP Annual Plan date.
b. HRST Reviewers should coordinate or complete the HRST as part of the pre- planning
process. HRST must be completed within 90 days of the Annual Plan date.
c. Behavioral Plan (as applicable) must be current, (i.e., completed and approved within the
last 12 months), reviewed, and updated.
Resources:
LifeCourse Integrated Star link
Maryland Long-Term Services and Supports Person-Centered Plan Overview
PCP CCS Guide
PCP Summary and Outcomes
PCP Focus Area Exploration
DDA PCP Planning web page
DDA HRST web page
DDA SIS web page
Person Centered Planning and Strategies Webinar
Person Centered Plan Authorization Webinar
Supporting Families Community of Practice
Charting the LifeCourse - PCP Foundational Tool
Employment Conversations

Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 10
Based on information and input gathered through the PCP Pre-Planning process, the next step
is the PCP Development process.
1. The CCS will develop, in collaboration with the participant and their PCP team, a
PCP that reflects the:
a. Participant's Vision;
b. Participant’s outcomes;
c. Identified risks, right restrictions, and needs; and
d. Requested services necessary to ensure the participant is:
■ Healthy
■ Safe
■ Achieving the “good life.”
2. PCP - Outcome Section
a. Personal outcomes are goals people set for themself and are defined from the
participant’s perspective. They are items that each participant identifies as
Important To them and standards by which we measure progress and quality of
service.
b. Teams should not only provide needed support, but also help the participant
develop natural supports in the community that will assist them in reaching goals.
c. Outcomes should be associated with each authorized service in the PCP.
d. Outcomes
(1) As per COMAR Chapter 10.22.01 B. (42) outcomes are tangible results
of goals that reflect the desired quality of life as defined by the participant.
(2) Outcomes are specifically linked to the participant’s vision,
values, and fundamental rights.
(3) Outcomes can be supported by or in combination of generic, natural,
community, local, and other resources in addition to Waiver services.
(4) The outcome description is a statement to further define what the person
wants to happen as a result of the support, to include person-specific
benefit or value. The outcome description(s) related to issues of
Importance To the participant should be based on their vision and
preferences related to daily life, employment, relationships, spirituality,
community engagement and membership, health, safety and
self-advocacy etc.
(5) Those outcomes which addressed solely issues of Importance FOR the
person addressed either functional/clinical needs, or compliance with a
service.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 11
e. To support an integrated “community life” and prevent a “service life”, PCP teams
should identify and note:
(1) How community resources and/or natural support are being used or
developed; and
(2) How non-DDA funded and other contributing resources are being used
to support the outcome.
3. PCP - Service Authorization Section
a. Requested DDA funded services are noted in the PCP’s detailed service
authorization section.
b. Requested services should be in accordance with the DDA’s Waiver service
descriptions taking into consideration:
(1) Other available resources;
(2) Assessed unmet need;
(3) Potential duplication of services; and
(4) Service scope and limitations.
c. The person-centered planning process in LTSSMaryland requires month-by-
month service planning. The CCS leads a conversation with the participant and
their PCP team to determine which services the participant needs, the amount,
and in which months services will be utilized.
d. Detail Service Authorization Tool (DSAT)
(1) The DSAT was created to improve and expedite the planning and
development process for requested services in the monthly detailed
service authorization section.
(2) The CCS will request the DSAT from Providers, selected by the
participant as a guide to help identify the proposed services to meet the
participant’s needs.
(3) Providers complete the DSAT, proposing the service, amount, and
duration, and to support the participant to achieve their goals and meet
the assessed needs and preferences.
(4) The provider agency submits the completed DSAT to the participant’s
CCS, who will review the DSAT with the participant and his or her support
team. As always, the participant may accept the proposed services or
choose to seek different services that best fit their needs.
(5) Once the DSAT is submitted to the CCS, the DSAT will be uploaded
into LTSSMaryland as an attachment to the PCP.
(a) The form should be saved and uploaded in this standardized
format:
1) PROVIDERNAME.DSAT.Participant’s
FIRSTLASTName.DATE (e.g.,
ABCAgency.DSAT.JonSmith.7-1-2020)
2) The DSAT shall be uploaded in the LTSSMaryland PCP
documentation section.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 12
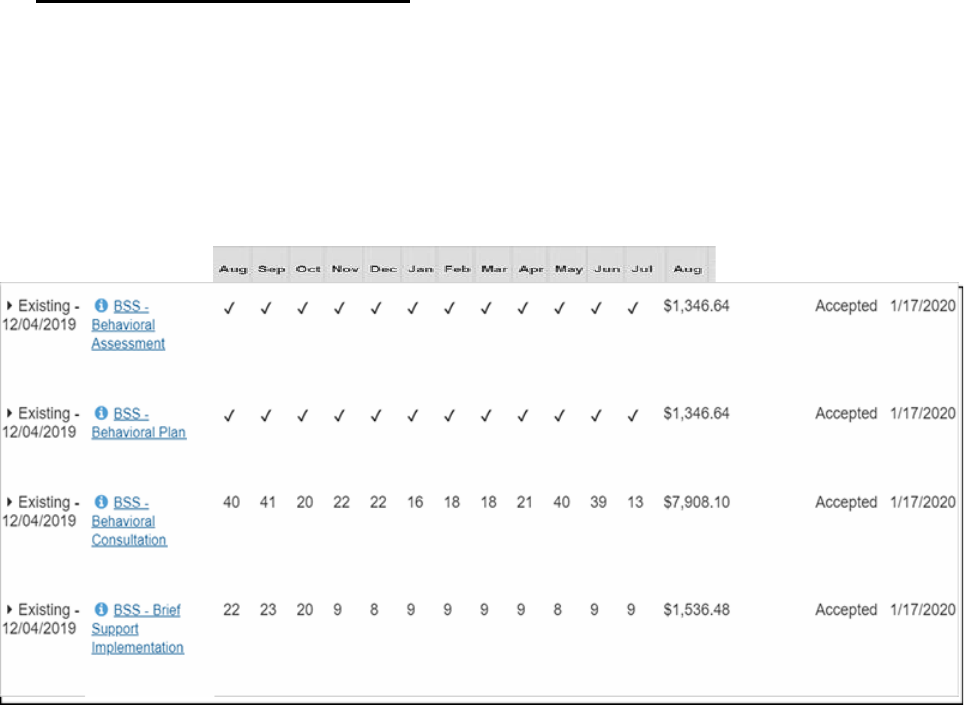
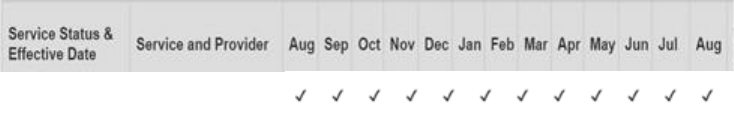
Detail Service Authorization Example: In the example on the next page, Behavior
Support Services (BSS) are being requested. The BSS-Behavioral Assessment and
BSS-Behavioral Plan milestone services are checked each month to support the
flexibility in service delivery and the provider’s ability to bill in the actual month that the
service was provided. Also, 15-minute unit BSS-Brief Support Implementation and BSS-
Behavioral Consultation services have units of service across the entire plan year to
support the participant’s needs and service flexibility.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 13
e. PCP - Service Referral (Traditional Service Delivery Model Only)
(1) After a DDA-funded service is identified to meet an unmet need and
assist the participant in meeting their goal(s), the CCS works with
the participant to select a provider for each service.
(2) Upon receipt of the DSAT and Cost Detail Tool as required from applicable
providers, the CCS will indicate the specific provider and site locations (if
applicable) in the PCP detailed service authorization section.
(3) LTSSMaryland will send a service referral to the provider:
(a) The provider reviews service referrals in the Provider Portal and
makes a decision to accept or reject the request.
(b) The provider must take action to accept or reject the referral
within five (5) days.
(c) If no action is taken the referral expires and will need to be resent
based on the participant’s choice.
(d) The CCS should also follow up with the provider to determine if
there are technical issues preventing acceptance or if the provider
is no longer interested in providing the service.
(e) If the provider is not responding, the CCS may contact the CCS
Lead at Regional Office for further assistance.
(f) If the provider is choosing not to accept the referral, the PCP team
should work with the participant, and as applicable, designated
representative to explore new providers or services to meet
assessed needs.
Note: The DSAT will assist with coordination and communication on the
service, frequency, and units prior to service referral and can prevent
delays in the PCP process.
(4) If either the provider or site that the participant prefers is not available
because the provider has not completed enrollment in ePrep or due to
a system issue, the CCS shall email the appropriate Regional Office as
noted below, who will follow-up with the provider:
● CMRO - Jessica Xander (Jessica.Xander@Maryland.gov)
● SMRO - KIANNA BLAKENEY (Kianna.Blaeney@Maryland.gov)
● ESRO - Andrea Jones (Andrea.Jones@Maryland.gov)
● WMRO - Timothy Jenkins ([email protected])
4. Cost Detail Tool (CDT)
a. The Cost Detail Tool is used to calculate the cost of services and map
LTSSMaryland PCP requested services to DDA’s historical services for
authorization into PCIS2 for services that have not transitioned to the
LTSSMaryland fee for service billing.
(1) It is important to understand that the cost detail tool is needed for all PCP’s (i.e.,
Initial, Revised, and Annual PCPs) that have not transitioned to LTSSMaryland fee
for services billing to ensure continued PCIS2 service authorization for applicable
services
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 14
(2) This tool is particularly important when there are changes made to
authorized services billed in PCIS2.
b. The justification tab
i. The justification tab is required to be completed for any PCP revisions
that occur during the annual planning meeting or during the PCP year.
ii. Briefly describe the need or risk resulting in the need for a PCP revision
or an Appendix K request. When describing needs, steer away from
talking about tangible items, rather, what is happening or not happening
that a waiver service is essential to ensure health, safety, or community
integration. Consider how the need is currently being met, what has
changed?
iii. Describe the resources (natural, community, school, DORS, CFC,
medical insurance, Medicaid State Plan) the team has exhausted? Why
were these resources unable to meet the need?
iv. Describe how these supports will reduce risk; How these services ensure
health/safety; and How these services increase community participation.
c. The use of the Cost Detail Tool, in collaboration with an initial, changes made at
the Annual, and Revised PCP and the DSAT tool replaces and eliminates the
legacy Service Funding Plan and Modified Service Funding Plan Request
(MSFPR) processes and forms.
d. For participants with selected providers, the provider completes the Cost Detail
Tool and submits it to the CCS.
e. The DDA has developed several resources to assist with service mapping
between the two systems including:
■ At a Glance - Meaningful Day Services
■ At a Glance - Support Services
■ At a Glance - Residential Services
■ At a Glance - Personal Supports Services
f. For participants that are (a) currently receiving employment related services from
a Meaningful Day provider; AND (b) seeking Employment Services, the
Meaningful Day service noted on the approved Cost Detail Tool will be
authorized in PCIS2 including Add-ons. Please refer to the DDA Meaningful Day
Services Relationship Between LTSSMaryland and PCIS2 Services At A Glance
for service mapping options.
g. After the CCS reviews and confirms with the participant that the Cost Detail Tool
meets their needs and preferences, they upload it in the PCP documentation
section so that it is included with the PCP for submission to the Regional Office.
(1) The form should be saved and uploaded in this standardized format:
(a) For Cost Detail Tool with no provider associated save as:
CostDetailTool.Participant’sFIRSTLASTNAME.DATE. (e.g.,
CostDetailTool.JonSmith.7-1-2020)
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 15
(b) For Cost Detail Tool with the provider indicated save as:
PROVIDERNAME.CostTool.Participant’sFIRST
LASTNAME.DATE (e.g., ABCAgency.CostTool.JonSmith.7-1-
2020)
(2) The Cost Detail Tool shall be uploaded in the LTSSMaryland PCP
documentation section.
5. Self-Directed Service Delivery Model Budget Determination and Approval
a. Participant’s using the self-directed delivery model, annual budget allocations are
based on the approved PCP detailed service authorization.
b. The PCP detailed service authorization includes the current DDA rate for
services, including any cost-of-living increase which are built into each
service rate.
c. The approved PCP establishes the self-directed budget allocation which is based
on the approved services and detailed services authorization total cost.
d. DDA Regional Offices Self-Direction Lead staff or designee review and authorize
all PCP and Self-Directed Budget Sheets for participant’s using the self-directed
service delivery model.
e. Self-Directed Budget Submission
(1) The Self-Directed Budget Sheet must be submitted with the PCP.
(2) The participant, with support of their CCS, creates the Self-Directed
Budget Sheet based on their PCP detail service authorization request
and anticipated budget allocation from the service cost total.
(3) The Self-Directed Budget Sheet must mirror the services and units
included in the PCP detail service authorization request and total cost
shall not exceed the anticipated budget.
(4) Participants set wages in the Self-Directed Budget Sheet based on the
reasonable and customary standards.
(5) The CCS uploads the Self-Directed Budget Sheet into the PCP
Documentation section of the plan when submitting the PCP.
(6) Upon receipt of PCP, the Regional Office will review the Self-Directed
Budget Sheet after completing the detail service authorization review
process.
(7) Any changes in service requests based on service and unit clarifications
may require adjustments to the Self-Directed Budget Sheet.
(8) Questions regarding the Self-Directed Budget Sheet shall be sent using
the PCP clarification function.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 16
f. Self-Directed Budget Submission for New or Increased Services:
(1) A request for new or increased services should be submitted via a
Revised PCP with all of the necessary elements of the PCP completed,
a description of the current needs, and documentation to substantiate
the request.
(a) The CCS shall include information in the Revised PCP text
box related to the purpose of the revision.
(b) To help facilitate the review, CCS shall include details to justify
new assessed needs such as:
1) What is the need/risk?
2) How will the service being requested meet the need or
mitigate the risk?
(c) Additional documentation to justify need shall be included in the
PCP such as a participant schedule, risk, and mitigation
strategies, HRST, Nursing Care Plan, Behavior Plan, and details
in the Focus Areas such as What’ working/What’s not working, as
applicable.
(2) The effective date noted in the PCP should allow the Regional Offices 20
business days for review and approval.
(3) All existing, new, or increased services should be captured in the Detailed
Service Authorization section of the PCP along with their frequency,
duration, and scope based on the effective date noted in the Revised
PCP. For example, if the effective date in the PCP is 03/01/2021, all
services in the DSA should reflect service units starting from 03/01/2021
to the annual plan date.
(4) The CCS will utilize the established overall budget that was produced in
the Detailed Service Authorization (DSA) Section of the PCP to develop a
revised Self-Directed Services budget sheet that aligns with the services
noted in the DSA and adheres to the DDA’s reasonable and customary
standards.
(5) The SDS Budget Sheet should contain the same effective date as noted
in the PCP.
(6) After inputting all the needed services in the SDS Budget Sheet, the
total annual budget amount in the SDS budget sheet should not exceed
the total cost generated in the DSA section of the PCP. However, it can
be less than what is noted in the DSA based on the chosen pay rates for
employees and vendors.
(7) The annual and actual columns of the SDS budget sheet will have similar
total budget amounts and does not require any further proration.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 17
g. Self-Directed Service Delivery Model Budget Approval Criteria and Process:
(1) The self-directed budget sheet must include the DDA services
authorized in the PCP based on the assessed need.
(2) Participants can determine staffing and pay rates based on the
reasonable and customary rate standards.
(3) The self-directed budget sheet for all PCP plan types (i.e., Initial, Revised,
and Annual) can contain allocation of funding for Individual and Family
Directed Goods and Services (based on cost savings) and for Staff
Recruitment and Advertising.
(4) The self-directed budget sheet must be uploaded into the PCP and
submitted to the Regional Office for review and approval.
(5) Regional Office staff will confirm that the service included in the
self-directed budget matches the assessed services needed in the
approved PCP.
(6) Once approved by the RO, they will send to the Fiscal Management
Services agency with the PCP and approved budget.
h. Self-Directed services start date is based on: (1) the DDA program enrollment date; (2)
PCP effective; (3) staff meeting required qualifications (e.g., background check, CPR,
First Aid Training, etc.); and (4) completion of required Fiscal Management Services
paperwork / requirements such as establishing the participant’s Employer Identification
Number.
6. PCP - Documentation Section
a. The PCP includes a section for PCP related documents that can be
uploaded into the system.
b. Based on the service delivery model chosen by the participant (i.e., self-directed,
traditional services delivery model), the documents uploaded may vary.
c. For participants using the self-directed service delivery model, documentation
includes self-direction related forms such as the Self-Directed Budget Sheet,
Participant Agreement Form, Family as Staff Form, and the Rights and
Responsibility Forms, and other documents as applicable.
d. For all participants using the traditional service delivery model, the
documentation section includes DSATs, Cost Detail Tools, and the Rights
and Responsibility Forms, and other documents as applicable.
7. Service Considerations and Flexibility
a. For participants still in school, it is important to consider services needed during
times school is not in session, such as winter, spring, and summer breaks.
b. For participants seeking Employment Services including Discovery, Follow
Along, Job Development, On-going Job Supports or Self-Employment
Development Supports:
(1) The effective LTSSMaryland service billing date can be no earlier than
July 1, 2021, unless the participant’s service transitions fully in
LTSSMaryland.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 18
(2) Activities that fall under each of these Employment Services (Discovery,
Job Development, On-going Job Supports, Follow Along Job Supports
and Self Employment Development Supports) can be supported under
the appropriate Meaningful Day service based on a participant's individual
outcomes and schedule. For instance, it may be common for a participant
not yet employed to take part in discovery or job development activities in
Community Development Services or Day Habilitation because most of
their activities in a given day are non-work related. While a participant
receiving supports to maintain their employment would fall under
Supported Employment. Please refer to the DDA Meaningful Day
Services Relationship Between LTSSMaryland and PCIS2 Services At A
Glance for service mapping options.
c. For participants seeking Co-Worker Supports, the effective LTSSMaryland
service billing date can be no earlier than July 1, 2021 unless the participant’s
service transitions fully in LTSSMaryland.
d. To support week-to-week flexibility under the traditional service delivery in the
participant’s employment, schedule, and services needs for Meaningful Day
Services, Meaningful Day services can be requested, and authorized by the
DDA, up to the weekly limit set forth in the DDA Medicaid Waiver program
application, subject to the following limitations.
(1) Although DDA may authorize up to the weekly limit for each Meaningful
Day Service requested,
(a) Teams should review and discuss service needs including taking
into consideration the hours a participant is working (i.e., daytime,
nighttime, and weekend hours) and not request the maximum
service units for each Meaningful Day service;
(b) Participants cannot receive and the provider will not be paid for
more than the limit for Meaningful Day services set forth in the
DDA Medicaid Waiver program application - a total of 40 hours per
week for all authorized Meaningful Day services combined.
(2) Neither a service provider nor a participant through a Fiscal
Management Services provider may submit a claim for payment to DDA
for Meaningful Day Services provided in excess of the weekly limit. Such
a claim for payment will be denied.
(3) For example, a participant may be authorized to receive Community
Development Services, Employment Services, and other Meaningful Day
Services. For maximum flexibility, the DDA can approve up to 40 hours
per week of combination of each of these services. However, in
combination, the participant may not use, and the provider may not bill
for, more than a total of 40 hours of Meaningful Day services within a
week.
(a) Week One: The participant may receive 10 hours of Community
Development Services and 30 hours of Employment Services.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 19
(b) Week Two: The participant may receive 20 hours of Community
Development Services and 20 hours of Employment Services.
(c) The participant may not receive 40 hours of Community
Development Services and 40 hours of Employment Services in
a single week.
(4) This flexibility is provided under the traditional services delivery model
only.
(5) Participants using the self-directed service delivery model have the
flexibility to make adjustments within their budget. Over authorization
of services will inflate the budget.
e. For Behavioral Consultation services, it is important to consider potential monthly
consultation units needed in addition to scheduled reviews, in the case of an
emergency or off-cycle review.
f. For participants seeking Community-Living - Enhanced Supports is available
when the participant’s service transitions fully in LTSSMaryland. Until the
transition, participants in need of residential services should request Community
Living - Group Home services which will be authorized as Residential in PCIS2.
g. Milestone units are indicated with a check mark in the detail service authorization
section. To support flexibility in the receipt of these services, each month can be
checked as shown below.
h. Residential Shared Hours
(1) The DDA recognizes that people who live together spend many hours together
and still have separate interests and activities, the LTSSMaryland – DDA
Module residential rates (including Community Living-Group Home,
Community Living - Enhanced Supports, and Supported Living) have been
developed using assumptions for shared staffing hours per home size with the
goal of ensuring adequate shared staffing hours to promote full lives in the
community and support individualized schedules.
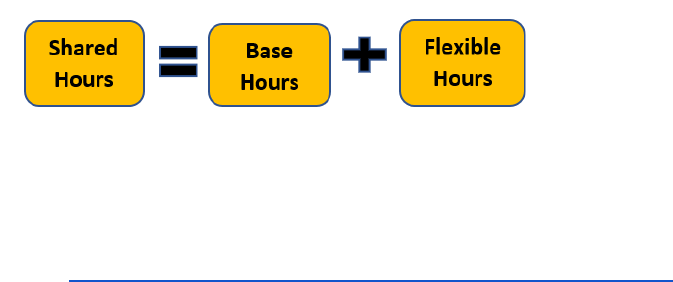
(2) Beginning April 1, 2022, residential shared staffing hours include an allocation
for base staffing hours plus an allocation of flexible hours per home to support
and promote individualized supports. These allocations together make up the
total shared hours and build the residential rates to support the home as a
whole through flexible staffing. It is expected that providers develop staffing
patterns reflective of the needs, interests and schedules of their residents and
maximize the base hours available ahead of requesting dedicated supports.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 20
(3) In addition to the use of shared hours, teams can request dedicated supports
per person due to support:
(a) Behavioral, medical, or community integration goals that require 1:1
or 2:1 staffing.
(b) Residential Dedicated Supports During Meaningful Day Hours up to
30 hours per week, Monday through Friday based on the
participant’s assessed need as per current policy.
(4) A person may receive a combination of base and dedicated hours based on
their assessed needs. For example, a person may require 1:1 dedicated
support during eating and base support hours during other times.
i. Residential Services: Dedicated Hours - For participants in need of dedicated
support hours for residential services, the following should be considered before
requesting.
(1) The PCP includes Community Living-Group Home, Community Living -
Enhanced Supports, and Supported Living and Dedicated Hours as
residential service options.
(a) Dedicated Hours are hours that provide 1:1 or 2:1 participant to
staff ratio based on the assessed need for habilitation and
community integration. They are reflected in LTSSMaryland as
follows:
1) Dedicated Hours for Community Living - Group Home (1:1)
2) Dedicated Hours for Community Living - Group Home (2:1)
3) Dedicated Hours for Community Living - Enhanced
Supports (1:1)
4) Dedicated Hours for Community Living - Enhanced
Supports (2:1)
5) Dedicated Hours for Supported Living (1:1)
6) Dedicated Hours for Supported Living (2:1)
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 21
(b) If the participant’s needs cannot be met through residential
shared hours or overnight supervision (as applicable
based on the provider’s business model), then a request
for dedicated staff hours may be requested.
1) The person-centered planning process should include a
discussion of:
a) The participant’s support needs including any
dedicated hours needed to maintain health and safety,
if applicable;
b) Existing dedicated support hours;
c) Number of shared hours available in the home; and
d) Availability of overnight supervision.
2) Provider’s assessed need for dedicated hours will be based on:
a) Participant’s assessed need (i.e., medical, behavioral,
community);
b) Number of people in the home supported by base
hours;
c) Provider’s business model (i.e., overnight supervision
staff vs no overnight supervision staff) and
d) Provider staffing model (e.g., use overnight
supervision staff vs hiring dedicated staff)
3) Based on these considerations, a request for dedicated
supports for any additional hours that the participant will
need can be made.
(c) Participants with an assessed need for additional supports can
request Dedicated Hours in addition to the main residential service
(i.e., Community Living-Group Home, Community Living -
Enhanced Supports, and Supported Living). If approved, the
participant will have both the main service and the dedicated
service listed in the PCP detail service authorization section.
(d) Dedicated 1:1 hours cannot be authorized when the house
reaches 1:1 support for each participant living in the home.
(e) Dedicated hours are not limited to services provided inside
the home and can support the participant with community
engagement.
(f) Dedicated hours to support community integration (for
participants without an assessed need for 1:1 or 2:1 due
to a medical or behavioral assessed need) beyond the
shared hours will need to be supported by a schedule
demonstrating how shared hours are utilized and the
additional hours needed.
(g) Dedicated hours for CL-GH and SL and residential add-on hours
are different
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 22
1) Dedicated hours are used in LTSSMaryland when a
person needs more staffing support than what is included
in the shared service hours and is based on the assessed
need for habilitation and community integration.
a) Rates for Community Living-Group Home,
Community Living - Enhanced Supports, and
Supported Living services include shared hours
based on the size of the home.
b) The option for shared overnight hours is captured in
the residential configuration and included in the
LTSSMaryland rates as shown in the chart below.
Service
Service
Supported Living: 1 w/ Overnight Supervision
Community Living/Group Home: 1 w/ Overnight Supervision
Supported Living: 2 w/ Overnight Supervision
Community Living/Group Home: 2 w/ Overnight Supervision
Supported Living: 3 w/ Overnight Supervision
Community Living/Group Home: 3 w/ Overnight Supervision
Supported Living: 4 w/ Overnight Supervision
Community Living/Group Home: 4 w/ Overnight Supervision
Supported Living: 1 w/o Overnight Supervision
Community Living/Group Home: 1 w/o Overnight Supervision
Supported Living: 2 w/o Overnight Supervision
Community Living/Group Home: 2 w/o Overnight Supervision
Supported Living: 3 w/o Overnight Supervision
Community Living/Group Home: 3 w/o Overnight Supervision
Supported Living: 4 w/o Overnight Supervision
Community Living/Group Home: 4 w/o Overnight Supervision
c) The residential configuration for Supported Living
(SL) is completed by the Regional Office
Provider Services (PS) team based on
information provided to PS by the provider (home
address, capacity, overnight support on or off).
d) To ensure that the correct Supported Living, Day,
and Community Living - Group Home address is
selected in the detailed service authorization by the
CCS, the “Notes” section of the DSAT should
indicate the SL address and configuration
information.
2) Displayed Rates for Community Living and Supported
Living Residential Services
a) As CCS create or revise PCPs in LTSSMaryland
for a person who needs residential services, the
LTSSMaryland PCP detailed service acceptance
section will calculate, and display rates based on
the number of people authorized for services in
the home
b) For example - For a home for three people, the
first person authorized will show at the one-
person rate. The second person authorized will
show at the two-person rate. If more authorized
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 23
people move into the home, then the service
acceptance process will display the proper rate.
The configuration applies to Community Living -
Group Home, Community Living - Enhanced
Supports, and Supported Living.
c) Overnight Supports function as either “On” or
“Off” for any given home in the system. Please
contact your regional office if Overnight Supports
need to be adjusted for the home based on your
agency’s business model.
d) Starting July 1, and the first of every month
thereafter, LTSSMaryland will recalculate all
residential rates, taking into account the number
of people who have been accepted by the
provider and authorized by the DDA and for that
home. Current residential rates based on the
number of people in the home can be viewed at
DDA Service Authorization and Provider Billing
Documentation Guidelines
3) Residential add-ons can be authorized in PCIS2 when a
person needs more staffing support than what is included
in the rate for the person’s matrix score.
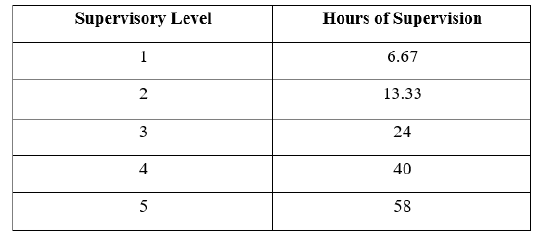
4) Rates for Residential services and Supported Living in
PCIS2 include supervision levels based upon the person’s
matrix score.
a) The number of supervision hours that are built into
the matrix score must be taken into account when
determining the number of residential add-on
supports that are needed.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 24
b) The Cost Detail Tool is used to calculate the cost of
services and map LTSSMaryland PCP requested
services (with the exception of Personal Supports
and Supported Living) to DDA’s legacy services for
authorization into the legacy PCIS2.
c) If PCIS2 rates apply, then any service
authorization by the provider or the DDA in
LTSSMaryland will not have any final legal
effect, unless the provider and participant are
participating in the fee-for-service payment
methodology.
5) For services that are being billed in PCIS2, the DDA will
review dedicated hours in LTSSMaryland and ensure that
the appropriate level is authorized in PCIS2.
6) Approved Appendix K COVID hours for Supported Living
should be reflected on the DSAT and captured in the DSA
as dedicated hours.
j. Meaningful Day Services: 1:1 and 2:1 Staffing
(1) If the participant’s needs cannot be met by the Day Habilitation Small or
Large Group services or Community Development Services (1- 4
participant groups) then a request can be made for Community
Development Services 1:1 / 2:1 staffing ratio or Day Habilitation 1:1 / 2:1
staffing ratio.
(a) The person-centered planning process should include a
discussion of the participant’s support needs, level of supports,
and hours needed.
(b) Based on these considerations, a request for 1:1 / 2:1 staffing
ratio hours that the participant will need can be made.
(c) The detail service authorization can reflect both (1) the
group services (i.e., Day Habilitation Small, Large Group, or
Community Development Services (1- 4 participant groups); and
(2) Community Development Services 1:1 / 2:1 or Day
Habilitation 1:1/ 2:1 staffing ratios.
(d) LTSSMaryland functionality was enhanced to support billing of
various Day Habilitation and Community Development Services
support models (e.g., small group, 1:2, etc.) during the same day.
(e) Career Exploration 1:1 / 2:1 Staffing Ratio funding is not available.
(2) Some Meaningful Day 1:1 and 2:1 staffing hours service authorization
can be directly mapped between LTSSMaryland 1:1 and 2:1 staffing ratio
to PCIS2 1:1 and 2:1 add-on hours. However, there are a few differences
for some services and how the rates are constructed.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 25
(a) Services authorized in LTSSMaryland detail service authorization
section include rates for:
1) Community Development Services 1:1 Staffing Ratio;
2) Community Development Services 2:1 Staffing Ratio;
3) Day Habilitation 1:1 Staffing Ratio; and
4) Day Habilitation 2:1 Staffing Ratio.
(b) Services authorized in PCIS2 include:
1) 1:1 and 2:1 add-ons hours can be included in the FY21
Cost Detail Tool and authorized in PCIS2 for Meaningful
Day Services when a participant needs more staffing
support than what is included in the rate for the
participant's matrix;
2) Add-ons can be associated with Supported Employment,
Employment Discovery & Customization, Career
Exploration, Community Development Services, and
Day Habilitation;
3) Rates based upon the participant’s matrix scores;
4) In PCIS2, 1:1 and 2:1 add-on hours are incorporated
into Meaningful Day Service main service and billed as
one rate.
k. Meaningful Day Services: Transportation Add On
(1) Providers in need of the Meaningful Day Transportation Add On shall
include it in their Cost Detail Tool. It does not need to be noted in the
LTSSMaryland PCP detailed service authorization.
(2) Once the Cost Detail Tool is approved, the Transportation Add On will be
authorized in PCIS2.
(3) Once the Meaningful Day Service is transitioned to LTSSMaryland, the
Meaningful Day Transportation Add On will be ended as the rate includes
a transportation cost component within it.
l. Respite (Traditional Service Delivery Model only)
(1) To support respite care services flexibility, hourly (15-minute units) and daily
total hours combined can be requested and authorized by the DDA, above the
720 hours limit within each PCP.
(a) This flexibility is provided under the traditional services delivery model
only.
(b) Participants using the self-directed service delivery model have the
flexibility to make adjustments within their budget. Over authorization
of services will inflate the budget.
(2) However, similar to the meaningful day service flexibility, participants cannot
receive, and providers will not be paid for more than the limit for respite daily
and hourly services combined.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 26
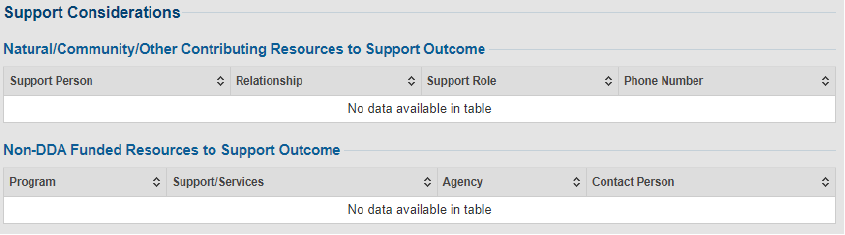
m. DDA Medical Day Care waiver services
(1) DDA Waiver Medical Day Care services will be added to the PCP service
authorization section in a future enhancement.
(2) Until this functionality is implemented the following process should be used for
authorized services
(a) Medical Day Care services shall be noted in the outcome under Support
Consideration > Non DDA Funded Resources to Support Outcome (see
below)
(b) ‘Program’ - should reflect Medical Day Care services
(c) ‘Support/Service’ - should specify the number of days per week the
participant is authorized to receive the service
(d) ‘Agency’ - should note the MDC provider authorized
n. Personal Supports - Awake Overnight Supports
(1) When awake overnight personal supports are necessary to meet the participant's
assessed behavioral or medical risk, which is documented in the participant's PCP
and approved Nursing Care Plan and/or Behavioral Plan, services may be authorized.
(2) The following information must be documented in the participant’s PCP:
(a) Overnight support must be documented in the PCP Risks section as one of
the mitigation efforts in addressing applicable behavior or medical risk.
(b) The PCP detail service authorization section should reflect the units for
Personal Supports (meaning overnight).
(c) Justification for overnight staffing and associated information must be
documented within the participant's PCP and either the Nursing Care Plan or
Behavior Plan, as applicable. Please refer to the updated Personal Supports
Policy for additional requirements.
(3) Participants enrolled in a DDA operated Waiver Program with DDA State Funded
overnight personal supports PCPs should be revised to move the services from Other
(State Only Funded) to Personal Supports.
o. DDA State Funded Services
(1) If a participant was authorized DDA State Funded services, the specific
services shall be noted in the DSA as follows:
(a) Services that directly align with a waiver service should be indicated in
the DSA with the Service Title that corresponds to the matching waiver
service.
(b) Service Title “Camp - Non-Respite (State Only Funded)” shall be used

Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 27
when the camp is not on the approved list or an out-of -state camp due to
unique circumstances and authorized by the DDA.
(c) Service Title “Nursing - Skilled Nursing Services (State Only Funded)” shall
be used when “skilled” nursing services were authorized. Note: This service
is only available to participants that were previously authorized by the DDA.
(d) Service Title “Rent - Individual Support (State Only Funded)” shall be
used when State-funded rent support were authorized by the DDA.
(e) Service Title “Other (State Only Funded)” shall be used for all other
items DDA authorized State funded services. Note: This service is only
available to participants that were previously authorized by the DDA.
(2) Additionally, the specific service must be noted in the Outcome Summary -
Support For field and a short summary of the service should be noted in the
Scope field.
(3) This process should be followed for all participants:
(a) That are Supports Only (i.e., not DD-eligible) State Funded
(b) Who receive waiver services and authorized State-funded services
(4) As per DDA’s policy on Use of State-Only Funds for DDA Services, the DDA
shall continue to maximize funds for services by using State funds solely for
Medicaid Waiver Services for which there is a federal fund match.
p. DDA Bundled Services
(1) In the past, some participants received State-funded services through
programs such as Family and Individual Support Services (F/ISS), in which
one or more services are “bundled” and provided to the participant by a
provider.
(2) The bundled services may include services that align directly with waiver
services as well as those that do not.
(3) Services that align directly with waiver services shall be unbundled during the
next Revised or Annual PCP process (whichever occurs first).
(4) Services that directly align with a waiver service should be indicated in the
DSA with the Service Title that corresponds to the matching waiver service.
(5) Service Title “Camp - Non-Respite (State Only Funded)” shall be used when
the camp is not on the approved list or an out of state camp due to unique
circumstances and authorized by the DDA.
(6) Service Title “Nursing - Skilled Nursing Services (State Only Funded)” shall be
used when “skilled” nursing services were authorized.
(7) Service Title “Rent - Individual Support (State Only Funded)” shall be used
when State-funded rent support were authorized
(8) Service Title “Other (State Only Funded)” shall be used for all other items
DDA authorized State funded services.
(9) Additionally, the specific service must be noted in the Outcome Summary -
Support For field and a short summary of the service should be noted in the
Scope field.
(10) For Providers services that are unbundled, the provider shall coordinate with
the DDA RO to update their FISS contract.
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 28
Resources
DDA Person-Centered Planning web page
DDA Waivers web page
DDA Waiver Programs Webinar
DDA Person-Centered Plan Development and Authorization Guidelines
DDA CCS PCP Checklist
DDA Provider PCP Checklist
Operating in PCIS2 and LTSS Guidance
Guidelines for Detailed Service Authorizations and Provider Billing Documentation
Link to Cost Detail Tool
Link to the SDS Budget sheet
Link to Support Broker Structured Interview Checklist
Participant Agreement
Family as Staff Form
DDA Participant Rights and Responsibilities
MDHDDA_Flyer_KnowYourRights
DDA Know Your Rights Final
At a Glance - Detailed Service Authorization Tool (DSAT)
The PCP Approval process includes: (1) the service referral acceptance from the provider;
(2) the participants or their legally authorized representatives’ approval; (3) the CCS
approval; and
(4) the final approval by the DDA.
Provider Approval - Service Referral Acceptance
1. The Provider's acceptance of the PCP service referral is their approval.
2. The Authorized Representative PCP signature page is requested when a
person has a legal guardian of the person. Note: The signature of the
authorized representative for the PCP does not mean the person is also
classified as a Designated Representative under the self-directed service
delivery model. The Designated Representative is noted on the SDS
Participant Agreement (see Option #2 that list the person by name).
3. When the provider accepts the service referral, the system will generate and
save the “Provider Signature Page” in the PCP “Signature” Section.
Participants or their Legally Authorized Representatives Approval
1. The CCS will review the draft PCP, providers' proposed service(s), scope, and
frequency with the participant and their legally authorized representatives (if
applicable) to see if the PCP clearly outlines their vision, goals, and supports
(including natural, community, and State funded supports).
2. If approved by the participant, the CCS facilitates the participant's agreement
on the “Participant Signature Page” and uploads in the PCP “Signature”
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 29
Section.
3. If approved by the legally authorized representative, agreement on the
“Authorized Representative Signature Page” and uploads in the PCP “Signature”
Section.
4. If not approved, the CCS facilitates further discussions with the team until agreement
or changes to the plan are made, including selecting different services or providers.
Coordinators of Community Services Approval
1. The CCS indicates their agreement to the PCP by completing the “Coordinators
of Community Services (CCS) Signature Page” and uploading it in the PCP
“Signature” Section.
2. Prior to approving the PCP, the CCS should complete a final review of the PCP to
ensure it meets all DDA requirements. The PCP Review Checklist is a good tool
that can be used for review of the PCP. Once finalized, they submit, via
LTSSMaryland, to the Regional Office.
a. Annual plans must be submitted no later than 20 business days prior to the
PCP annual plan date.
b. Initial and revised plans should be submitted within ten business days or
less after the participants or their legally authorized representatives’
approval.
Regional Office Program Team
The DDA Regional Office approval of the PCP is noted in the PCP “Service Plan Workflow
History” Section.
1. Regional Offices receive, review, request consults, request clarifications, and
approve Initial, Annual, or Revised PCP through LTSSMaryland.
2. Regional Office Program Team staff will:
a. Review PCPs within 20 business days of receipt.
b. Review PCP using the PCP Review Checklist.
c. Assess needs based on DDA Service Authorization guidelines.
d. Authorized services are based on an assessed need and the DDA
Medicaid Waiver program’s service requirements as noted in the
approved Medicaid Waiver program applications.
e. Verify that, for plans submitted after September 21, 2020, the DSAT has
been completed and uploaded unless otherwise directed. Plans for which
the DSAT has not been uploaded will be returned to the CCS for
resubmission after the DSAT is attached.
f. Review the correlation between the LTSSMaryland detailed service
authorization request to applicable PCIS2 authorizations until the service is
transitioned to LTSSMaryland fee-for-service billing
(1) Dedicated hours vs Add-On hours
(a) For participants currently in Residential (Community Living -
Group Home) and Supported Living services, the Regional
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 30
Office program staff will assess the PCP approved services
and Cost Detail Tool with the current authorization in PCIS2.
1) If there is no change in needs, the add-on hours
should remain the same.
2) If there is an increase/decrease in needs, the add-on
hours should be increased/decreased.
(2) For participants with a change in either services or needs, staff will
assess if there is a documented assessed need that indicates a
variance in current staffing supports from what is already included
through the Matrix score or PCIS2 authorization.
(3) For participants new to service, the following should be considered:
(a) Does the participant require overnight staffing? If so, are PCIS2
shared hours sufficient to meet the participant’s needs?
1) If the house does not already have PCIS2 shared hours,
or they are insufficient, or the participant needs one-to-
one supports should be reassessed.
2) If home PCIS2 share hours are sufficient, then
additional hours should not be authorized.
(b) Are there already PCIS2 shared hours in the home, or do
these need to be added?
1) If yes, then add or increase to add on hours.
2) If no, then make no changes to the current PCIS2
authorization.
(c) In addition to overnight supervision, is there a documented
assessed need that indicates a variance in staffing supports from
what is already included through the Matrix score or authorized in
PCIS2?
1) If yes, then add or increase to add on hours.
2) If no, then make no changes to the current PCIS2 authorization.
g. Review Cost Detail Tool to ensure:
(1) Correlation between requested services and correct PCIS2 rates;
(2) Matrix score and award number are accurate;
(3) No duplication of services;
(4) The agency chosen is licensed and certified to provide authorized
services; and
(5) An accurate start date of services is reflected;
h. If applicable, review the Self-Directed Service Budget sheet to ensure:
(1) Aligns with services authorized in the LTSSMaryland detailed service
authorization; and
(2) Utilizes rates in accordance with the reasonable and customary rate
standards.
i. Confirm an outcome is associated for every DDA funded service requested.
j. If a request is for a site change:
(1) Check PCIS2 to ensure capacity will not be exceeded; and
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 31
(2) Collaborate with Provider Service/Quality Enhancement staff for
Residential Site Configuration changes as applicable.
k. If clarification is needed, the PCP will be sent back to CCS via LTSSMaryland
clarification request functionality.
l. If internal consultation is needed for behavior support services, nursing, or
program related questions, send “CONSULT to applicable staff via
LTSSMaryland functionality.
m. If clarification is not necessary and PCP meets criteria for APPROVAL, RO
Program Staff will then finalize approval in LTSSMaryland and if there was a
change to authorized services (new or revised) specific to those in PCIS2 send
the Cost Detail Tool to the RO fiscal staff) for entry into PCIS2 and processing.
n. For all Annual and Revised PCPs (either at annual PCP meeting or through
mid- year PCP revision) that meet the DDA Regional Director PCP Revision
Review Criteria, the Program Staff will send a “CONSULT to Regional
Director/Deputy via LTSSMaryland functionality.
o. If an assessed need is not demonstrated or clarification returned still does
not document a substantiated need:
(1) For Initial and Annual PCPs, deny the plan;
(2) For Revised PCP, deny only if it is a mid-plan year revised
PCP, otherwise consult with program team supervisor for next
steps;
(3) Create a LTSSMaryland denial letter which include appeal rights; and
(4) Forward to the regional admin team for processing.
p. If PCP does not meet DDA Regional Director PCP Review Criteria and all
PCP criteria is met, the RO Program staff will then finalize approval in
LTSSMaryland and if there was a change to authorized services (new or
revised) specific to those in PCIS2 send the Cost Detail Tool to the RO fiscal
staff for entry into PCIS2 for processing.
DDA Regional Director PCP Review
1. As applicable, Program Staff will send a PCP CONSULT to the Deputy/Regional
Director for review if the PCP meets the DDA Regional Director PCP Review Criteria
as follows:
a. Total Plan Cost:
(1) Residential services plan cost of $350,000 or more;
(2) Personal Supports plan cost of $150,000 or more;
b. Authorization Threshold:
(1) Assistive Technology cost over $1,000;
(2) Employment Discovery request more than one time during a 24-
month period;
(3) Job Development service request from another provider;
(4) Overnight support and 2:1 service request;
(5) More than one Behavioral Assessment or Behavior Plan in a 12-
month period;

Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 32
(6) Environmental Modification over $2,000; and
(7) All service requests that exceed the Waiver service cost limits; and
c. Random 10% sample pull of submitted changes made to an Annual or a
Revised PCPs each month.
2. Upon receipt of the LTSSMaryland CONSULT from RO Program Staff based on
revision review criteria outlined above, the Deputy/Regional Director will authorize
continuation of the PCP review and determination process by RO program staff based
on service authorization guidelines.
Resources
PCP Review Checklist
Guidelines for Service Authorization and Provider Billing Documentation
A. LTSSMaryland Providers
The planned transition to DDA’s fee-for-service payment methodology, supported by
the new software system known as LTSSMaryland, has been delayed due to COVID-
19, as reflected in the approved Appendix K. MDH’s processing of claims and
payments for services funded by this Waiver program on a fee-for-service basis,
including updated rates, units, and service requirements, began with a small
transition group in December 2019.
1. If the provider and participant transitioned to the fee-for-service payment
methodology, the PCP Approval is the funding authorization, and no further
action is needed.
2. These providers and participants will follow applicable guidance for the fee-
for- service billing and supporting documentation.
B. Early Adopters/Transitioned Providers
To continue to ensure fiscal payment strategies used within LTSSMaryland are
functional, transitions will be implemented using small groups of providers who
volunteer to transition. This transition plan will continue to support the live testing of
the new detailed service authorization and fee-for service billing functionality in
LTSSMaryland and the Medicaid Management Information System (MMIS) prior to
full implementing these changes. This testing is being done to reduce the risk of
payment
issues for all participants and providers.
Initial providers who volunteered to transition all their services to test the system are
referred to as “early- adopters”. Beginning April 2022 additional providers will be
transitioning to test fee-for -service billing. These providers' services and sites will be
activated in LTSSMaryland to support billing functionality.

Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 33
1. The provider’s LTSSMaryland services billing date will be set for the first of
the agreed implementation month.
2. DDA Headquarter staff will end services in PCIS2 15-days after the
transition date to provide a buffer.
3. The LTSSMaryland PCP Approval is the funding authorization, and
no authorization is needed in PCIS2.
4. These providers and participants will follow applicable guidance for the fee-
for- service pilot program.
C. All Other Providers
1. For providers and participants not participating in the fee-for-service pilot
program, final authorization of services (and their approved scope,
frequency, duration, and rates) by both the provider and the DDA will occur
only in PCIS2.
Important Note:
For providers and participants not participating in the fee-for-service pilot
program, final authorization of services (and their approved scope, frequency,
duration, and rates) by both the provider and the DDA will occur only in
PCIS2. To crosswalk between LTSSMaryland and PCIS2, the provider (or
CCS for participants enrolled in self-directed services) must review the
requested services in the PCP in LTSSMaryland and then complete a Cost
Detail Tool to apply the rates from PCIS2. If PCIS2 rates apply, then any
services authorization by the provider or the DDA in LTSSMaryland will not
have any final legal effect, unless the provider and participant are participating
in the fee-for-service pilot program.
2. RO Review and Authorization Processes
a. Fiscal Staff
(1) Review Cost Detail Tool if there was a new or revised service authorized
in the PCP that is billed in PCIS2.
(a) Enter authorized services into PCIS2, OR
(b) Forward back to the program team supervisor if there are errors
that prevent entry into PCIS2.
(2) Once entered into PCIS2, fiscal staff will create a PDF that includes:
(a) Cost Detail Tool or SDS budget sheet; and
(b) Copy of the PCP Revision approval letter from LTSSMaryland.
(3) Send completed PDF to RO Fiscal Director /Designee designated email for
signatures.
b. RO Fiscal Director/Designee
(1) Receive and review fiscal PDF for accuracy and quality.
(2) As applicable, forward fiscal PDF to Deputy/Regional Director for final
signature if the revision meets the DDA Regional Director PCP Review
Developmental Disabilities Administration Find Out More: 844-253-8694 | dda.health.maryland.gov Revised: 03.29.2022 Page 34
Criteria.
(3) If fiscal PDF does not require Regional Director approval, sign off on PDF
and send to admin staff for processing.
(4) If errors are identified, they send the fiscal PDF back to applicable fiscal
staff for review, correction, and resubmission.
c. Regional Director or Designee
For PCPs that meet the DDA Regional Director PCP Review Criteria:
(1) Reviews fiscal PDF to ensure accuracy and quality.
(2) If approved, sign off on fiscal PDF and send via email to admin staff.
(3) If not approved, send back to fiscal and/or program directors for review,
correction, and resubmission.
d. DDA RO Admin Staff
(1) Receive approved fiscal PDF from Regional Director or designee.
(2) Log completion of fiscal PDF on RO tracker/ spreadsheet and save per
regional saving conventions.
(3) Send approval/denial letters with appeal rights (for denials) to individual.
(4) Scan or upload signed fiscal packet to regionally designated location.
(5) Email packet to applicable provider, CCS, and individual; and
(6) As applicable, for participant’s self-directing services, send the PCP,
approved self-directed budget sheet, signed Participant Agreement,
Family as Staff form, and other applicable documents to the Fiscal
Management Services provider.
