
1
P4 - ADVANCED PHARMACY PRACTICE EXPERIENCE
(APPE)
PRECEPTOR MANUAL
2017-2018
2
Contents
INTRODUCTION ........................................................................................................................................ 4
NEOMED Experiential Program Contact Information ................................................................................. 5
ADVANCED PHARMACY PRACTICE EXPERIENCE (APPE) ............................................................. 6
APPE General Descriptions .......................................................................................................................... 7
Goals, Objectives and Activities ................................................................................................................... 9
PRECEPTOR STANDARDS ....................................................................................................................... 9
STUDENT STANDARDS ......................................................................................................................... 10
PRECEPTOR GUIDELINES ..................................................................................................................... 11
E*Value .................................................................................................................................................. 11
Preceptor Checklist: Before the Student Arrives ................................................................................... 11
Orientation .............................................................................................................................................. 12
Scheduling and Workload ....................................................................................................................... 12
P4 - APPE Academic Schedule .............................................................................................................. 14
Policy Regarding Time Off During P4 (APPE) Rotations...................................................................... 15
Evaluations and Grading ......................................................................................................................... 17
Feedback ................................................................................................................................................. 18
Student Performance during the Rotation ............................................................................................... 19
Student Evaluation of Preceptor ............................................................................................................. 19
APPENDIX ................................................................................................................................................. 20
ADVANCED PHARMACY PRACTICE EXPERIENCE OBJECTIVES ............................................ 21
Advanced Community Pharmacy & Leadership ................................................................................. 21
Advanced Hospital/Health System & Leadership ............................................................................... 27
Adult Acute Care/Internal Medicine ................................................................................................... 31
Ambulatory Care ................................................................................................................................. 34
Underserved ........................................................................................................................................ 37
Geriatrics ............................................................................................................................................. 40
Pediatrics ............................................................................................................................................. 44
Clinical Patient Care Selective ............................................................................................................ 47
E*VALUE INSTRUCTION GUIDE FOR COLLEGE OF PHARMACY PRECEPTORS .................. 50
P4 STUDENT APPE EVALUATION ................................................................................................... 58
ABSENCE REQUEST FORM ............................................................................................................... 63
TEMPLATE JOURNAL ARTICLE PRESENTATION FORM ............................................................ 64
TEMPLATE JOURNAL ARTICLE CRITIQUE ................................................................................... 66
3
EVALUATION OF JOURNAL CLUB .................................................................................................. 70
CASE PRESENTATION EVALUATION ............................................................................................. 72
STUDENT PHARMACIST OBSERVATION FORM .......................................................................... 73
EVALUATION OF ORAL CLINICAL QUESTION CONSULT ......................................................... 74
EVALUATION OF WRITTEN CLINICAL QUESTION CONSULT .................................................. 75
VERBAL Patient Counseling Rubric ..................................................................................................... 76
APPE PRECEPTOR /SITE EVALUATION FORM ............................................................................. 77
4
INTRODUCTION
Welcome and thank you for your service as a preceptor for the Northeast Ohio Medical
University (NEOMED) College of Pharmacy. As preceptor, your role is one of teacher, mentor,
and advocate for our students’ professional development. You are guiding our students through
their final year of pharmacy school as they acquire the skills and knowledge necessary to become
a practicing professional pharmacist.
APPEs are designed to enhance the knowledge base and skills students need in order to
fulfill the competencies required for the professional pharmacy degree. Students should further
develop their skills in patient care, critical thinking, decision making, ethical judgment and
professionalism.
This preceptor manual is a guide for preceptors to utilize in one’s development and
throughout a student’s APPE. We have included information on APPE policies, procedures,
objectives, and assessments. You are making an enormous contribution to individual students,
NEOMED and the profession of pharmacy. Please do not hesitate to contact the college if you
have any questions; we are more than willing to assist you.
Best wishes for a rewarding experience!
Charles Cather R.Ph., MBA, FASCP
Director of Experiential Education
Updated 02/27/2017
5
NEOMED Experiential Program Contact Information
Mailing Address:
Northeast Ohio Medical University
College of Pharmacy
Office of Experiential Programs
4409 St Rt 44
PO Box 95
Rootstown, Ohio 44272
NEOMED Preceptor Website:
http://www.neomed.edu/pharmacy/academics/preceptor/
E-Value:
https://www.e-value.net
Contacts:
Charles Cather, R.Ph., M.B.A., FASCP
Director of Experiential Education
Phone: 330-325-6228
Email: [email protected]
Debbie Frank
Senior Curriculum Coordinator
Phone: 330-325-6339
Email: [email protected]
Patti Pfeifer
Administrative Assistant
Phone: 330-325-6390
Email: ppfeifer@neomed.edu
6
ADVANCED PHARMACY PRACTICE EXPERIENCE (APPE)
COURSE DESCRIPTION
The Advanced Pharmacy Practice Experiences or APPEs consist of seven professional
experiences that provide students the opportunity to develop their skills and knowledge base in
pharmacy practice. This series of experiences follows the first three years of the Pharm.D. didactic
curriculum as well as a series of Introductory Pharmacy Practice Experiences (IPPEs) students
have completed. APPE rotations take place over 10 months, from June following through April of
P4 year. There are no rotations scheduled for the months of December and May.
The rotations include:
• Inpatient/Acute Care Internal Medicine (2-month rotation)
• Underserved (1 month)
• Ambulatory Care (2-month rotation)
• Advanced Community Pharmacy Practice* (1 month)
• Advanced Hospital Pharmacy Practice* (1 month)
• Selective Leadership (1 month added to either of the above*)
• Clinical Patient Care Selective (1 month)
• Elective (1 month)
APPE rotations reinforce the ability to apply skills and knowledge students received during
the previous three years in the curriculum. APPEs provide students the opportunity to serve
various patient populations in a variety of settings and to collaborate with other healthcare
professionals. These experiences offer exposure to disease states that pharmacists are likely to
encounter in practice. Students complete these experiences under the general supervision of a
licensed pharmacist or other college appointed preceptor.
7
APPE GENERAL DESCRIPTIONS
Clinical - (Acute Care Internal Medicine, Ambulatory Care, Clinical Selective)
These experiences take place primarily in hospital and ambulatory care practice settings.
Clinical Selective experiences focus on a particular patient population (e.g. pediatrics, geriatrics)
or specific clinical specialty (e.g. Infectious disease, Psychiatry, Cardiology, Oncology,
Palliative care). Students are exposed to diverse patient populations with a broad range of acute
and chronic medical problems. Students will learn and demonstrate the ability to assess patients,
identify medical- and drug-related problems, develop therapeutic care plans, make
recommendations to health care practitioners, monitoring drug therapy, and counsel patients.
Advanced Community Pharmacy Practice
These experiences occur in retail settings such as chain store pharmacies, independent pharmacies
or managed care pharmacies. In addition to medication dispensing, these experiences focus on the
identification, resolution and prevention of drug related problems dealing with general medicine
issues. Students may participate in patient care services such as administration of immunizations,
medication therapy management (MTM), disease state management, counseling, blood pressure
checks, and adherence monitoring.
Advanced Hospital/Health System Pharmacy Practice
These experiences take place in hospitals or other systems of integrated pharmaceutical
services. These experiences focus on patient-specific care and medication use systems. Emphasis
is placed on the drug-use decision-making process, monitoring of individual patient drug therapy,
formulary management and the communication of information and analysis to other health
professionals and patients. These experiences may include medication order processing,
dispensing, sterile product preparation, clinical services, inventory management, and
administration.
8
Underserved
These experiences take place primarily in ambulatory settings (e.g. Federally Qualified
Health Centers, charitable pharmacies, hospital-based ambulatory clinics) which provide
pharmaceutical care services to those who face barriers to timely access to health services. These
experiences focus on identification, resolution and prevention of drug related problems in the
underserved patient. Students may participate in activities such as dispensing, patient counseling,
medication therapy management, disease state management, adherence monitoring, development
of care plans, monitoring drug therapy, and making recommendations to health care practitioners.
Leadership
These experiences take place in a community or institutional setting in which the student
focuses on the administrative and management aspects of the setting. These experiences occur as
an additional one-month extension of a student’s Advanced Community or Hospital Practice
experience. Activities a student may perform on these experiences include spending time with a
manager or director of pharmacy services, attend administrative related meetings, and develop
policies and procedures, and human resource/financial/inventory/operational management.
Electives
Elective APPEs may be either patient-care or non-patient care experiences. These rotations
provide students with an adequate breadth of knowledge in areas of interest and should
complement the required APPEs to develop the student pharmacist into a competent and mature
professional. Elective experiences give students the opportunity to gain insight in areas such as
academia, research, drug information, compounding, and professional association management
among others. Students may also take additional clinical selective rotations, community, or
hospital rotations as elective experiences.
9
Goals, Objectives and Activities
The goals and objectives for each experience align with the ability statements needed to
fulfill the requirements for the Doctor of Pharmacy degree. Students must demonstrate a minimum
level of proficiency for all the abilities by the end of the experiential education. The goals and
objectives for the APPEs are listed in the Appendix. Preceptors may include their own site-specific
goals and objectives for their rotations. Students should also work with preceptors to incorporate
his or her interests or areas of needed skill improvement into the goals and objectives of the
rotation.
PRECEPTOR STANDARDS
The Preceptor shall:
1. Recognize that the relationship with the student is one of preceptor-student rather than
employer-employee.
2. Recognize that learning requires mutual respect, courtesy and communication between him
or herself and the student.
3. Take responsibility for the professional and legal supervision of the student during the
experience.
4. Demonstrate the principles of professional ethics.
5. Plan and prepare for the student’s rotation experience. This includes review of the rotation
goals and objectives, review of assessment forms, develop a schedule of activities for the
student, and notify staff of their responsibilities when working with a student.
6. Give the student a thorough orientation to the site and experience early in the rotation to
facilitate a smooth transition and an optimal use of available resources.
7. Clearly outline expectations of the student regarding professional dress, conduct,
scheduling of hours/activities, assignments, and performance.
8. Afford the student sufficient time, preparation and patience for the learning experience.
9. Do not assume the student’s level of competence but determine this by discussing previous
experiences the student had and observing performance of his/her basic skills.
10. Expose and involve the student in all aspects of practice consistent with the student’s
ability, needs and interest as determined by the goals and objectives as set forth by the
College.
10
11. Establish a schedule of student’s activities for the rotation in consultation with the student.
If the schedule includes experiences with other practitioners, the preceptors should clearly
communicate with these individuals and the student.
12. Provide the student with feedback and constructive criticism on a continuous basis and
convey this information in a private manner.
13. Familiarize site personnel with the experiential program objectives to avoid
misunderstanding about the student’s role during the rotation.
14. Review with the student their performance at the midpoint and end of the rotation in a
timely, accurate and objective manner.
STUDENT STANDARDS
The following are standards, which all students must meet before participating in APPE site
visits:
• Be in good academic standing at NEOMED including successful completion of all didactic
course work
• Up to date with all required immunizations including annual TB skin test and influenza
vaccination
• Pass a criminal background check and urine toxicology screen
• Be a licensed pharmacy intern in Ohio (Note: for rotations occurring outside Ohio students
will obtain an intern license in accordance with that state or site’s requirements)
• Have successfully completed Basic Life Support and Immunization Provider certification
• Not have a family member, employer or previous employer as a preceptor or site
• Will not receive monetary compensation for site visits
Students on practice experiences represent the College of Pharmacy. Students are expected to
conduct themselves in a professional manner in all interactions while on rotations.
During experiential rotations, the student shall:
1. Be professional in both appearance (dress) and conduct.
2. Work to master assigned activities quickly so more time can be devoted to gaining the widest
experience possible.
3. Recognize that learning requires mutual respect and courtesy and an open line of
communication between preceptor and student.
11
4. Not divulge any patient or business related information of a confidential nature.
5. Not make professional decisions without preceptor supervision and approval.
6. Adhere to a specified schedule predetermined with the preceptor.
7. Be punctual and be required to notify preceptor of lateness or absence.
8. Comply with all applicable pharmacy laws and regulations.
9. Comply with all policies and procedures of the College and training sites.
10. Complete all assignments from the preceptor in a timely manner
11. Complete a constructive evaluation of the preceptor.
PRECEPTOR GUIDELINES
E*Value
E*Value is a management software system used by NEOMED to track all experiential training
rotations and associated information. Every student and preceptor will be able to use the system,
via Internet, to check for rotations updates, maintain personal addresses, complete student
evaluation forms and communicate with student. Detailed instructions for using this system can
be found in the Appendix.
Preceptor Checklist: Before the Student Arrives
The following are several items which you may want to check off before the rotation begins.
You may also wish to provide some of this information to your student when he or she contacts
you prior to the start of the rotation.
1. Review goals and objectives for the APPE experiential site visits. (see Appendix)
2. Prepare a list of student tasks/activities/assignments in accordance with goals and objectives.
3. Inquire about additional orientation sessions and/or procedures student must attend and/or
follow for your facility such as orientation sessions, additional ID badges, etc.
4. Have information available regarding parking location, permits, fees, etc.
5. Remind staff of arrival of student, what the student’s roles and responsibilities will be and
the role staff members will have in regard to the rotation.
6. Prepare a list of your facility’s contact names and numbers for student use in case of
emergency, absence, etc.

12
Orientation
Preceptors should provide students with a comprehensive orientation to the site and the
experience within the first few days of the rotation. The orientation should clearly outline
expectations of the student and what the student may expect from the experience. Students should
be informed of their role and responsibilities at the site as well as the role of the preceptor. The
orientation should include general information such as introductions to professional and office
staff, a tour of the facility, location of drugs, materials and equipment, ID badges, parking and
other relevant information. The orientation would also serve as an opportunity for preceptors to
discuss the following with students:
1. The site’s policies and procedures, as they apply to students including:
• confidentiality
• lines of authority
• absence and tardiness procedures
• safety and emergency procedures
2. Scheduling of student’s hours.
3. The goals and objectives for the experience as set forth by the College and the preceptor.
Preceptors should ask the student if he or she has any goals of their own or specific areas
of interest which might be incorporated into the experience.
4. How the experience will be structured and how the preceptor plans to work with students.
Preceptors should discuss when they plan to meet with the student and how that time would
be spent, e.g. discussing patient cases, reviewing student activities or performance.
5. Activities the student can expect to do at the site, as well as written assignments and/or
formal presentations, which he or she will be required to complete.
6. Expectations for the student to receive and request on-going informal feedback.
7. Grading and evaluation – What areas will be evaluated and what level of performance
will garner favorable evaluation marks.
Scheduling and Workload
The following policies apply to student scheduling and workload. Preceptors are encouraged to
work with students when determining a work schedule.
1. Rotations are scheduled to start on the first working day of the month and end on the last
working date. The preceptor can modify start and stop dates (must be within the month)
at their discretion. For example, if the first working date is a Friday, the preceptor may
have the student start on Monday. Preceptors are not required or expected to accommodate
any student requests to change start and stop dates.
2. A minimum of 160 hours per month of participation is required between the start date of
the APPE and the ending date. These do not have to be contact hours and may include
research and writing time away from the site.
13
3. Rotations are to be scheduled during the day Monday through Friday unless the learning
needs of the student at the site are such that weekend or evening activities is necessary.
Students should be informed in advance of the rotation if weekends or evening activities
will be part of the experience. This allows time for the students to make appropriate
arrangements with employment, childcare needs, or other personal issues.
4. Student outside employment should not interfere with APPE activities. The last
professional year is not designed for additional student employment and preceptors should
not expect to schedule around outside employment work hours.
5. Workload will not be considered excessive unless it exceeds 10 hours per day of contact
time and an additional 4 hours of study/research time daily.
6. Students are not allowed to receive compensation under any circumstances for hours
worked during APPEs.
14
P4 - APPE Academic Schedule
2017-2018
Class of 2018
June 1 – June 30
July 3 – July 31 (Holiday – Independence Day – July 4)
August 1 – August 31
September 1 – September 29 (Holiday – Labor Day – September 4)
October 2 – October 31 (Career Day Interviews October 6 optional)
November 1 – November 30 (Holiday – Thanksgiving – November 23 & 24)
December 1 – December 31 (no rotations scheduled)
January 2 – January 31 (Holiday – New Year’s Day – January 1)
February 1 – February 28
March 1 – March 30
April 2 – April 30
May 1 - 11 CAPSTONE (On-campus) Mandatory
May 19 Graduation!
15
Policy Regarding Time Off During P4 (APPE) Rotations
Due to the intensity of each rotation and the need to achieve the required objectives, it is advised
that students avoid taking time away from their rotations. Students completing APPE rotations
do not follow the P1 – P3 academic calendar for NEOMED. Students are not allowed to take
vacation time during their rotation schedule. However, it is recognized that students may need
time off for off from rotations for professional or personal reasons. The following are the
approved guidelines regarding absence from rotations:
1. Approvable absences from rotations are those which the preceptor deems important to the
professional development of the student (i.e. residency/job interviews, attendance to a
professional meeting) or for a personal illness or a family related emergency. Absences
related to on campus activities such college committees are approvable at the discretion of
the preceptor. Time off for personal vacations, weddings, honeymoons, family reunions,
etc. are not considered valid reasons for taking time off from the rotation.
2. Students will be allowed no more than TEN (10) days of approved absences including
personal illness or emergencies from their assigned rotations over the entire APPE program
(10 months). The ten days are not meant to be an entitlement and cannot be used or saved
for an extended break from rotations including personal or family vacations. Each student
is responsible for assuring that the maximum number of days away from the ten-month
program is not exceeded. Exceeding the maximum number days can result in a student not
successfully completing the requirements of the APPE program necessary for graduation.
3. Students will be allowed no more than TWO (2) days of approved absences during any
one month. Exceptions to this requirement as in the case of residency interviews can be
granted only if approved by the preceptor prior to scheduling an interview. If additional
absences are allowed the preceptor may require the student to work extra time at the site or
complete additional activities (e.g. projects, written assignments, presentations) to insure
achievement of rotation objectives. Additional absences maybe denied if the preceptor
believes the student will be unable to achieve the objectives of the rotation.
4. Students with approved absences are expected to complete all rotation objectives
responsibilities as assessed by the preceptor. The preceptor may require the student to
make-up any absence time from the rotation.
5. Time off is to be taken only with the PRIOR approval of the preceptor. The student is
required to complete the “Request for Approval of Absence from APPE Activities
Form” for your approval and signature FIVE (5) business days before a planned absence.

16
Students should not make any travel arrangements until they have received approval from
their preceptor to be absent. The signed absence form should be forwarded to the Director
of Experiential Education for review.
6. Students are authorized specific holidays off from rotation (refer to the P4 APPE Academic
Schedule for a list of approved student holidays). Preceptors should allow students to be
off for these approved holidays.
7. In the case of personal illness or emergency, the student is required to notify the preceptor
or his /her designee as soon as possible prior to the scheduled arrival time to the site. The
method of notification (i.e. email, phone call) shall be predetermined by the preceptor and
communicated to the student at the start of the rotation. If the student is absent for more
than TWO (2) days from the rotation due to illness or emergency, both the preceptor and
the student must notify the Director of Experiential Education. The “Request for Approval
of Absence from APPE Activities Form” must be completed upon the student’s return to
the rotation.
8. Time off for religious reasons is allowed in accordance with NEOMED policy. Students
requesting time for this reason are required to receive prior approval from the Director of
Experiential Education TWO (2) months prior to the start of the time off. The student is
required to inform the preceptor of these approved absences upon initial notification of the
preceptor. Students may be required to make up any missed time resulting from these
types of absences at the discretion of the preceptor.
9. Unexcused absences include any failure to be present on a scheduled rotation day(s), failure
to notify the preceptor of an illness or emergency in a reasonable period of time, or any
absence that was not approved by the preceptor. Unexcused absences will not be tolerated
and jeopardize the student’s successful completion of the program. Any unexcused
absence may result in failure of the rotation in which it occurred. Preceptors should
immediately notify the Director of Experiential Education if such absences occur.
10. Time off requests for travel to or from a distant rotation is to be arranged only within that
rotation at the discretion of the preceptor. Generally, no more than ONE (1) business day
should be taken for travel.
11. Preceptors should consult with the Director of Experiential Education regarding any
concerns surrounding a student’s absence from a rotation.
17
Evaluations and Grading
APPEs are required courses within the College of Pharmacy and students must treat them
as they would any other course. Preceptors monitor student performance, identify strengths and
weaknesses and provide necessary feedback to ensure student development in established
competency areas. Preceptors must complete a student evaluation in E*Value for each student
they precept (see Appendix). The evaluation consists of six sections:
Section 1: Professionalism
Section 2: Communication
Section 3: Drug Disease Knowledge
Section 4: Application
Section 5: Interprofessional Collaboration
Section 6: Medication Distribution/Dispensing
Section 7: Administrative Skills
• Midpoint Evaluation: The preceptor is strongly encouraged, by the university and ACPE,
to complete a student evaluation at the midpoint of the rotation. The midpoint evaluation
is required if the student is not meeting rotation expectations or performing at an
unsatisfactory level. The evaluation should be discussed with the student and submitted to
the college via E*Value. If a student is not meeting performance expectations at the
midpoint, the preceptor should contact the Director of Experiential Education to discuss
the issues and discuss a plan for improvement.
• Final Evaluation: The preceptor is required to complete a final student evaluation during
the last week of the rotation. The final evaluation will be used to determine the student’s
grade for the rotation. Narrative comments are required to support “Unsatisfactory
Performance”, “Needs Improvement”, and “Exceeds Expectations” ratings.
• The final evaluation should include a summary of any presentations and/or projects the
student completed. This information allows future preceptors to recognize what was
accomplished during past rotations and build in activities during subsequent rotations to
fulfill all the expectations of a student’s APPE rotations.
• Preceptors are encouraged to comment on student needs to improve for subsequent
rotations. (Note: Preceptors are able to view Overall Comments and Areas for
Improvement sections of earlier APPE evaluations of the students they are precepting.
Information on how to view these evaluations is in the E*Value instruction guide)
• The final evaluation should be reviewed and discussed directly with the student at the
end of the rotation. It is important to complete the evaluation in a timely manner so the
student’s grade can be posted for the rotation.
18
Grading Scale
Final grades for rotations will be based on an average score of all the components of the
evaluation using the following scale:
Less than 2.5 overall or less than 2.0 in an individual section = FAIL
2.5 to 3.5 overall = PASS
Greater than 3.5 overall = PASS with HONORS
Feedback
In addition to the guidelines above, preceptors should be aware that feedback is an integral
part of the evaluative process and more importantly, integral to the development of the
student. Effective feedback provides positive reinforcement for what the student is doing
correctly and steps the student can take to improve those areas, which need improvement.
Without appropriate feedback, students may miss crucial skills development and/or
knowledge base enrichment. The following are some guidelines for preceptors reading
feedback:
1. Students want to receive feedback on their performance - Students desire and expect
preceptors to provide them feedback on their performance whether it is positive or
negative. One can only improve or change if they are provided honest, specific, and
timely feedback. It is suggested to tell the student “I want to give you some feedback,
…” before giving feedback.
2. Feedback should be specific and based on direct observation – Feedback should refer to
actions that are specific and which the preceptor has observed first-hand.
3. Feedback should include positive aspects and areas for improvement – Ideally
feedback should not just be all positive or all negative. Include both when you are
discussing individual performance with a student. Some find it effective to “sandwich”
negative feedback between positive feedback given at the beginning and the end.
4. Provide feedback in a consistent and timely manner – If possible, preceptors should
provide feedback immediately after a task, patient-counseling session or other activity. As
this is not always possible, a time should be determined for providing feedback to the
student, once a week for example “Feedback Friday”. Preceptors should take notes as
soon as possible after observing students and not rely on memory to ensure accurate and
helpful feedback. Preceptors might find the Journal Club Evaluation, Case Presentation
Evaluation Form, Drug Information Evaluation Form and Pharmacist Observation Form
(see Appendix) helpful for recording observations.
5. Feedback should focus on remediable behavior and should offer suggestions for
improvement – Feedback should focus on behaviors that can be corrected. Feedback
should not deal with assumed intentions or preceptor interpretations. Preceptors should
provide suggestions to correct or improve the behavior; judgment statements should be
avoided. Discussing the potential negative outcome of a certain behavior can help to
explain to the student why a change is needed
6. A record of feedback should be saved – Preceptors should keep copies of all written
feedback and forms completed. The College of Pharmacy may request copies of this
documentation on as needed basis.
19
Student Performance during the Rotation
Students are expected to maintain a high level of professionalism and demonstrate and an
acceptable level of competence in the practice and clinical skills necessary to becoming a
licensed pharmacist. Successful completion of the rotations goals and objectives is a
reliable measure of one’s performance during a rotation. Since a student’s level of
competence in any specific skill may vary from their peers it is important that preceptors
identify and work with their student on those skills needing improvement. Identifying
those areas for improvement and discussing with the student as early as possible into the
rotation will allow opportunity for the student to show improvement. The preceptor and
student developing a plan with specific, measurable, attainable, relevant, and timely
(S.M.A.R.T) goals is an ideal approach to help one meet the expectations of the rotation.
This may require the student spending additional time mastering a particular activity or
task (e.g. counseling patients, dispensing, reviewing patients drug therapy, answering drug
information questions, etc.) rather than activities one is comfortable doing. Providing
effective feedback (see above) throughout this time is vital. Ideally the student should be
allowed the time to demonstrate a progressive improvement in one’s performance needed
to successfully pass the rotation. The preceptor should consider the student’s effort and
degree of progression in mastering a skill when completing the midpoint or final
evaluation.
Preceptors who are having difficulty with a student’s performance, developing a plan for
improvement, or believe improvement is not being achieved should contact the Director of
Experiential Education for assistance as soon as possible.
In instances of unacceptable professional behavior or performance, the preceptor should
contact the Director of Experiential Education to report the situation and determine the
appropriate actions to be taken. Actions may include immediate dismissal from the rotation
and the student being referred to the NEOMED Council on Academic Performance &
Professionalism.
For students who are performing at or above the rotation expectations the preceptor is
encouraged to allow the student to participate in higher-level activities. This may include
but not limited to a greater amount of independence, mentoring/training other learners, and
completion of special projects or research. In these situations, a preceptor should not feel
limited by the established list of rotation objectives when working with high performing
students. Providing feedback to the high-performers is also essential during this time.
Student Evaluation of Preceptor
• Following the completion of an APPE, the student is required to complete an assessment
of their preceptor, the rotation, and the site (see appendix). The student will also provide
a self-assessment following each rotation.
• Preceptors have access to the student assessment in the E*Value system. The information
should be utilized as a tool to make potential enhancements to their program.
• Preceptors who have a concerns or questions about the evaluations submitted by their
student can contact the college.
20
APPENDIX
ADVANCED PHARMACY PRACTICE EXPERIENCE OBJECTIVES ............................................ 21
Advanced Community Pharmacy & Leadership ................................................................................. 21
Advanced Hospital/Health System & Leadership ............................................................................... 27
Adult Acute Care/Internal Medicine ................................................................................................... 31
Ambulatory Care ................................................................................................................................. 34
Underserved ........................................................................................................................................ 37
Geriatrics ............................................................................................................................................. 40
Pediatrics ............................................................................................................................................. 44
Clinical Patient Care Selective ............................................................................................................ 47
E*VALUE INSTRUCTION GUIDE FOR COLLEGE OF PHARMACY PRECEPTORS .................. 50
P4 STUDENT APPE EVALUATION ................................................................................................... 58
ABSENCE REQUEST FORM ............................................................................................................... 63
TEMPLATE JOURNAL ARTICLE PRESENTATION FORM ............................................................ 64
TEMPLATE JOURNAL ARTICLE CRITIQUE ................................................................................... 66
EVALUATION OF JOURNAL CLUB .................................................................................................. 70
CASE PRESENTATION EVALUATION ............................................................................................. 72
STUDENT PHARMACIST OBSERVATION FORM .......................................................................... 73
EVALUATION OF ORAL CLINICAL QUESTION CONSULT ......................................................... 74
EVALUATION OF WRITTEN CLINICAL QUESTION CONSULT .................................................. 75
VERBAL Patient Counseling Rubric ..................................................................................................... 76
APPE PRECEPTOR /SITE EVALUATION FORM ............................................................................. 77

21
ADVANCED PHARMACY PRACTICE EXPERIENCE OBJECTIVES
Advanced Community Pharmacy & Leadership
The goal of the Advanced Community Pharmacy Experience is to provide the opportunity for the student
to build upon information acquired in his/her didactic and early experiential education and apply the
knowledge and skills in direct patient care activities in a community pharmacy setting. The student will
complete all activities in a professional manner under the facilitation of a preceptor.
Upon completion of the experience, the student will be able to:
I. Demonstrate the ability to appropriately process new and refill prescriptions.
• Utilize the patient profile to assess the prescription for allergies, drug interactions,
therapeutic duplication, contraindications of use, dosage, and potential for adverse
effects
• For each prescription assess appropriate:
• Indication
• Legality
• Completeness
• Dose
• Dosage form
• Route of administration
• Directions of use
• Duration of therapy
• Demonstrate the ability to communicate with prescribers and office staff when
necessary regarding the processing of a prescription including the receipt and review
(with preceptor) of a new prescription
• Demonstrate the ability to transfer a prescription to and from another pharmacy
• Demonstrate the ability to perform any necessary pharmaceutical calculations
• Demonstrate the ability to resolve issues regarding third party billing, prior
authorizations, managed care formulary guidelines
• Develop a systematic approach to verifying the accuracy of one’s own entry before final
completion of the prescription
II. Demonstrate the ability to properly prepare a product for dispensing to a patient.
• Accurately select the appropriate medication to include strength, dosage form, and
amount
• Using the concepts of pharmaceutics, appropriately compound non-sterile products for
patient use
• Gain an understanding of pharmacy automation and central fill procedures when
applicable
• Develop a systematic approach to ensure the five principles of drug delivery: Right drug,
Right patient, Right dose, Right time, Right route
III. Communicate health information (drug, disease, other) to the patient, which shall include, but
not be limited to:
• Assessment of patient’s health beliefs
• Assessment of patient’s health literacy
22
• Effective verbal communication when advising, counseling, and educating patients
about their medications
Prescription medications – The student shall demonstrate the ability to:
Establish a dialogue with patients concerning medications to:
• Clarify proper medication dosing
• Clarify the directions of use
• Clarify length of therapy and refill information
• Review potential medication side effects and action(s) to be taken by the patient if/when they
occur
• Clarify storage instructions of the medication
▪ Verify the patient knows who to contact with questions or if specific medication-related
issues arise.
▪ Handle difficult patients and/or difficult situations (i.e. misfilled prescriptions)
Counsel patients on sensitive issues
Non-prescription medications including natural products- The student shall demonstrate the ability to:
▪ Respond to patient’s questions
▪ Determine if the patient is a self-care candidate using the QuEST/SCHOLAR process
▪ Recommend and counsel the patient on a self-care product if the patient is deemed to be a
good self-care candidate
▪ Verify the patient knows who to contact with questions or if specific medication-related issues
arise.
Non-pharmacologic:
▪ Develop and communicate an appropriate non-pharmacologic treatment plan (i.e. diet, exercise,
sleep hygiene, home monitoring, etc.) based on patient specific factors (i.e. age, diet, work
schedule, financial resources available, etc.)
IV. Participate when applicable in services provided by a pharmacist to include but not limited to:
• Medication Therapy Management Service (MTMS)
• Collaborative Practice Agreements
• Chronic Disease State Management
• Adherence Counseling
• Immunization services
• Disease Screening/Health and Wellness programs
• Community health fairs
• Patient home visits
• MD office visits
• Screening and Brown Bag programs
• Other community outreach programs such as presentations to nursing homes
• Marketing presentations to employer and payor groups
V. Demonstrate the ability to appropriately assess patients, which shall include, but not be
limited to, obtaining or discussing the following information:
• Signs and symptoms of patient complaint or disease
• Demographics
• Allergies (to include description of the reaction)
23
• Medication history (including previous treatments and nonprescription products)
• Available past medical, family, social, and surgical history
• Immunization history
• Adherence to a medication regimen
• Physical assessment
• Measure basic physical assessment data (i.e. blood pressure, lipid panel,
glucose, weight, height, etc.) where available and when appropriate
• Obtain physical assessment and lab data from patient health record when
record is available
• Insurance/healthcare coverage
VI. Demonstrate the ability to analyze the appropriateness of treatment (both prescription and
non-prescription) for each disease, incorporating:
• Pathophysiology
• Etiology (especially drug-related causes)
• Treatment guidelines and primary literature
• Cost
• Benefits versus risks
• Lifestyle factors unique to the patient
VII. Identify and prioritize a patient’s problems including the following drug related problems:
• Indication
• Unnecessary drug therapy (i.e. duplicate therapy, no indication)
• Additional drug therapy needed (i.e. untreated indication)
• Effectiveness
• Different product required (i.e. superior product available, therapy is not
achieving goals, medication not effective for the condition being treated)
• Dose too low [inadequate dosing frequency or duration, drug interaction
(i.e. induction of metabolism), incorrect administration]
• Safety
• Drug interaction (with another drug, natural product, disease, food, lab)
• Contraindication (allergy, organ dysfunction, pregnant or breastfeeding,
previous issue such as an adverse effect)
• Inadequate or Inappropriate monitoring (efficacy, toxicity)
• Dose to high [excessive dosing frequency or duration, drug interaction
(i.e. inhibition of metabolism)]
• Compliance
Inadequate patient knowledge (i.e. directions or need for medication not
understood)
• Unavailable product (i.e. not on the market, supply problems, etc.)
• Concern about adverse effects
• Cost
• Patient forgets to take
• Patient cannot tolerate dosage form
24
VIII. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Key patient education talking points
• Cost of therapy
IX. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
• State the desired and achievable pharmacotherapeutic goals for each identified problem
• Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
• Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
• Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
• Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
X. Demonstrate the ability to measure and document patient outcomes.
• Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
• Measure, record, and appropriately track the therapeutic response and toxicity
• Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
• Identify, assess, and report identified adverse drug reactions and medication errors
using the appropriate reporting system
XI. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques.
• Create an audience-appropriate response and communicate this in a timely manner.
• Document the question, response, and resources/references used on an appropriate
documentation form
XII. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals, others involved in the healthcare continuum (payors, employers) and
patients. Examples include but are not limited to:
• Medication and disease education
• Responses to drug information requests either verbally or in writing
• Documentation of interventions
• Communication to health care professionals regarding medication therapy plans and
drug related problems

25
• Communication to patients summarizing their prescription coverage if applicable
XIII. Prepare and present at least one patient case presentation and deliver this to the preceptor
and/or pharmacy staff.
XIV. Complete at least one of the following:
• Journal club
• A formal presentation to a community group
• Newsletter article
• Patient education document or flip chart
• Create a disease state management protocol or program
XV. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
• Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
• Mentoring pharmacy students currently on an early experiential site visit if applicable
• Arriving on time and prepared for all rotation activities
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning
For an Advanced Community with Leadership Experience the following objectives should be
included:
I. Review the mission statement, strategic plans, and management plans for the pharmacy
or corporation.
II. Identify the pharmacy or corporation organizational structure with respect to lines of
authority, function, and responsibilities.
III. Review the pharmacy or company administrative and professional policies and procedures
to include but not limited to:
• Detection, evaluation, and reporting of medication errors and adverse drug reactions
• Quality control
• Inventory control
• Budgeting and financial management
• Record keeping
• Theft reporting
IV. Review the process by which the pharmacy meets and maintains compliance with all
federal and state laws and regulations that pertain to the practice of pharmacy.
V. Review key components of human resource management, including but not limited to:
• Hiring and interview process
• Personnel evaluation process
• Formal disciplinary procedures
• Staff development and training
26
• Development of staff schedule
VI. Identify methods of implementing, maintaining, and evaluating pharmacy services in the
pharmacy or corporation.
VII. Discuss the methods for planning, implementation, and maintaining pharmacy related
technology and informatics within the pharmacy or corporation.
VIII. Discuss the future trends that will impact community pharmacy services.
IX. Complete a management related or quality assurance project, for example:
• Time study
• Financial analysis
• Review and analysis of medication errors or adverse drug reactions
• Assessment of the medication use process
• Patient satisfaction survey
• Assessment of a new or existing pharmacy service

27
Advanced Hospital/Health System & Leadership
The goal of the Advanced Hospital/Health System Pharmacy Experience is to provide the
opportunity for the student to build upon information acquired in his/her didactic and early
experiential education and apply the knowledge and skills in direct patient care activities in
Hospital Pharmacy. The student will complete all activities in a professional manner under the
facilitation of a preceptor. Upon completion of the experience, the student will be able to:
I. Demonstrate the ability to appropriately analyze and process medication orders.
• Utilize the patient profile to assess the order for allergies, drug interactions, therapeutic
duplication, and potential for adverse effects
• For each medication order assess appropriate:
• Indication
• Completeness
• Dose and pharmacokinetics
• Route of administration
• Dosage form, if injectable consider:
▪ IV compatibility
▪ Stability
▪ Administration rate
▪ Reconstitution
• Compliance with federal/state regulations, hospital policies and procedures,
including formulary restrictions
• Duration of therapy
• Medication safety issues (i.e. look-alike/sound alike, legibility, unapproved
abbreviations)
• Demonstrate the ability to prioritize medication orders considering work load and
clinical status of patients (i.e. STAT vs routine orders)
• Demonstrate the ability to perform any necessary pharmaceutical and pharmacokinetic
calculations
• Develop a systematic approach to verifying the accuracy of one’s own entry before final
completion of the order
• Know when to discontinue and or restart medications when situations warrant per
hospital policies and procedures
• Demonstrate the understanding and ability to properly use on-site technology utilized in
the medication dispensing process (i.e. Robotics, bar-coding, automated dispensing
cabinets)
II. Demonstrate the ability to properly prepare a product for dispensing to a patient.
• Accurately select the appropriate medication to include strength, dosage form, and
amount
• By following USP 797 guidelines and appropriate aseptic technique competently
compound sterile products
• Using the concepts of pharmaceutics, appropriately compound non-sterile products for
patient use
• Develop a systematic approach to ensure the five principles of drug delivery: Right drug,
Right patient, Right dose, Right time, Right route
28
III. Demonstrate the ability to appropriately assess patients which shall include, but not be
limited to, obtaining or discussing the following information:
• Signs and symptoms of the patient complaint or disease
• Medication history (including previous treatments)
• Available past medical, family, social, and surgical history
• Medication administration review
• Data from the patient chart/medical record and/or the patient, i.e. including but not
limited to vital signs, height/weight, and laboratory tests
IV. Demonstrate the ability to appropriately assess patient information to identify the following
drug related problems, and as a result be able to recommend medication therapy changes:
• A problem or disease state of a patient not being treated or is not optimally treated
• A medication that a patient is receiving that is not indicated or is contraindicated
• Therapeutic duplication and/or polypharmacy
• An adverse effect(s) that may be caused by a medication(s)
• Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
• A drug interaction or potential drug interaction including interactions with labs, food,
and disease states
• Inappropriate medication dose or duration of therapy (including consideration of
hepatic/renal impairment, and age of the patient)
• Inappropriate route or dosage form to include consideration of IV to oral therapy
• The patient has a medication regimen that can potentially lead to non-compliance
• A cost ineffective medication regimen
V. Demonstrate a firm understanding of drug therapy. For each drug encountered the student
should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Cost of therapy
VI. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques
• Create an audience-appropriate response and communicate this in a timely manner
• Where applicable document the question, response, and resources/references used
VII. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
• Patient disease and medication counseling
• Responses to drug information requests either verbally or in writing
• Documentation of interventions through the utilization of the standard SOAP note
format
• Communication to the health care professionals regarding medication therapy plans and
drug related problems

29
VIII. Prepare and present at least one formal presentation delivered to pharmacists or an
interdisciplinary committee from the following list:
• Monograph for formulary review
• Journal club
• Patient case presentation
• Patient safety initiative
• New formulary agent overview
IX. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibits self-control in all
interactions
• Maintaining confidentiality regarding patient information and displays honesty and
integrity in all activities
• Arriving on time and prepared for all rotations activities
• Mentoring pharmacy students currently on an early experiential site visit if applicable
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning
For an Advanced Hospital with Leadership Experience the following objectives should be
included:
I. Review the mission statement, strategic plans, and management plans of the pharmacy
department.
II. Identify the departmental organizational structure with respect to lines of authority,
function, and responsibilities.
III. Review the department’s administrative and professional policies and procedures to
include but not limited to:
• Detection, evaluation, and reporting of medication errors and adverse drug reactions
• Infection control
• Formulary system
• Emergency preparedness
• Sterile and non-sterile compounding
• Investigational drug handling
IV. Review the process by which the department meets and maintains compliance with Joint
Commission and USP 797 Standards.
V. Demonstrate a working knowledge of state and federal laws pertaining to hospital
pharmacy practice and how these are met by the department.
VI. Compare and contrast various fiscal budgeting, inventory control, purchasing,
reimbursement systems, and financial analyses used by the department.
VII. Discuss the function of the Pharmacy & Therapeutics committee and how institutional
formulary decisions are made.
30
VIII. Review key components of human resource management, including but not limited to:
• Hiring and interview process
• Personnel evaluation process
• Formal disciplinary procedures
• Staff development
IX. Identify methods of implementing, maintaining, and evaluating clinical pharmacy services
in an institution.
X. Discuss the methods for planning, implementation, and maintaining pharmacy related
technology and informatics within an institution.
XI. Attend any interdisciplinary committee meetings deemed appropriate by the preceptor.
XII. Participate in a management related or quality assurance project, for example:
• DUE or MUE
• Time study
• Financial analysis
• Review and analysis of medication errors or adverse drug reactions
• Assessment of a new or existing pharmacy service
• Patient safety initiative

31
Adult Acute Care/Internal Medicine
The goal of the Adult Acute Care/Internal Medicine Experience is to provide the student with
experience in the pharmacotherapeutic management of adult patients with common acute and
chronic medical illnesses. The activities of the experience are to build upon information
acquired in a student’s didactic education and develop skills related to assessment and drug
therapy management of hospitalized patient in an internal medicine environment. The student
will complete all activities in a professional manner under the facilitation of a preceptor. Upon
completion of the experience, the student will be able to:
I. Demonstrate knowledge of the pathophysiology and pharmacotherapy of the common
disease states seen in patients in an acute care/internal medicine setting. This includes but
not limited to disorders of the following:
• Cardiovascular
• Pulmonary
• Endocrine
• Renal
• Gastrointestinal
• Neurology/Psychiatry
• Immunity/Infectious Disease
II. Develop and implement a systematic approach to gathering, organizing and prioritizing
pertinent data of assigned patients by:
• Utilizing current and past health records, patient interviewing, and interaction with
other health care professionals to obtain any or all of the following information:
• Signs and symptoms of the patient complaint or disease
• Physical assessment
• Available past medical, family, social, and surgical history
• Laboratory values
• Tests and procedures
• Medication history both past and current
• Performing and relevant physical assessments not otherwise available
III. Identify and prioritize the health /medical problems including the following drug related
problems in the assigned patients:
• A problem or disease state of a patient not being treated or is not optimally treated
• A medication that a patient is receiving that is not indicated or is contraindicated
• Therapeutic duplication and/or polypharmacy
• An adverse effect(s) that may be caused by a medication(s)
• Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
• A drug interaction or potential drug interaction including interactions with labs, food,
and disease states
• Inappropriate medication dose or duration of therapy (including consideration of
hepatic/renal impairment, and age of the patient)
• Inappropriate route or dosage form
• Non-adherence to a prescribed medication(s)
32
IV. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
• State the desired and achievable pharmacotherapeutic goals for each identified problem
• Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
• Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
• Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
• Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
V. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Key patient education talking points
• Cost of therapy
VI. Demonstrate the ability to measure and document patient outcomes.
• Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
• Measure, record, and appropriately track the therapeutic response and toxicity
• Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
• Identify, assess, and report adverse drug reactions and medication errors using the
appropriate reporting system
VII. Educate patients, caregivers, and health care professionals regarding the appropriate use of
drugs in common acute and chronic medical illnesses in adults.
• Implement patient-specific education plans. These plans should include purpose,
directions for use/administration, storage, potential adverse effects and potential
interactions with other medications and food
• Assist in facilitating patient transition from one care setting to another by
communicating the pharmaceutical care plan to another pharmacist and or health care
provider(s)
• Educate professional colleagues, including pharmacists, physicians, and nurses regarding
drug therapy using formal or informal methods.
VIII. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques
33
• Create an audience-appropriate response and communicate this in a timely manner
• Where applicable document the question, response, and resources/references used
IX. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
• Patient disease and medication counseling
• Responses to drug information requests either verbally or in writing
• Documentation of interventions through the utilization of the standard SOAP note
format
• Communication to the health care professionals regarding medication therapy plans and
drug related problems
X. Prepare and present at least one patient case presentation delivered to pharmacists or the
health care team.
XI. Prepare and present at least one journal club article delivered to pharmacists or the health
care team.
XII. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
• Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
• Arriving on time and prepared for all rotation activities
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning

34
Ambulatory Care
The goal of the Ambulatory Care rotation is to provide the student with experience in the
pharmacotherapeutic management of adult patients with common chronic medical illnesses.
The activities of the experience are to build upon information acquired in a student’s didactic
education and develop skills related to assessment and drug therapy management of the
patient in an ambulatory care setting. The student will complete all activities in a professional
manner under the facilitation of a preceptor. Upon completion of the experience, the student
will be able to:
I. Demonstrate knowledge of the pathophysiology and pharmacotherapy of the common
disease states or medical conditions seen in patients in an ambulatory care setting. This
includes the following:
• Key conditions required for review:
• Hypertension, Diabetes, Dyslipidemia, Anticoagulation, COPD/Asthma
• Other conditions to review include but not limited to:
• Congestive heart failure
• PUD/GERD
• Depression
• Pain management
• Osteoporosis
• Hematologic disorders
• Rheumatoid arthritis
• Thyroid disorders
• Gout
• Seizures
II. Demonstrate knowledge and participate when applicable in services provided by a pharmacist
in an ambulatory care setting to include but not limited to:
• Medication counseling
• Medication reconciliation
• Medication therapy management service (MTMS)
• Collaborative practice agreements
• Chronic disease state management
• Adherence counseling
• Immunization services
• Disease prevention/health wellness
III. Develop and implement a systematic approach to gathering, organizing and prioritizing
pertinent data of assigned patients by:
• Utilizing current and past health records, patient interviewing, and interaction with
other health care professionals to obtain any or all of the following information:
• Signs and symptoms of the patient complaint or disease
• Physical assessment
• Available past medical, family, social, and surgical history
• Laboratory values
• Tests and procedures
35
• Medication history both past and current
• Performing relevant physical assessments not otherwise available
IV. Identify and prioritize the health /medical problems including the following drug related
problems in the assigned patients:
• A problem or disease state of a patient not being treated or is not optimally treated
• A medication that a patient is receiving that is not indicated or is contraindicated
• Therapeutic duplication and/or polypharmacy
• An adverse effect(s) that may be caused by a medication(s)
• Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
• A drug interaction or potential drug interaction including labs, food, and disease states
• Inappropriate medication dose or duration of therapy (with consideration of
hepatic/renal impairment, and age of the patient)
• Inappropriate route or dosage form
• Non-adherence to a prescribed medication(s)
V. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
• State the desired and achievable pharmacotherapeutic goals for each identified problem
• Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
• Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
• Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
• Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
VI. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Key patient education talking points
• Cost of therapy
VII. Demonstrate the ability to measure and document patient outcomes.
• Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
• Measure, record, and appropriately track therapeutic response and toxicity
• Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
36
• Identify, assess, and report adverse drug reactions and medication errors using the
appropriate reporting system
VIII. Educate patients, caregivers, and health care professionals regarding the appropriate use of
drugs in common acute and chronic medical illnesses in adults.
• Describe the role of the pharmacist as an educator in the ambulatory care setting
• Implement patient-specific education plans. These plans should include purpose,
directions for use/administration, storage, potential adverse effects and potential
interactions with other medications, natural products, and food
• Educate professional colleagues, including pharmacists, physicians, and nurses regarding
drug therapy using formal or informal methods.
IX. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques
• Create an audience-appropriate response and communicate this in a timely manner
• Where applicable document the question, response, and resources/references used
X. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
• Patient disease and medication counseling
• Responses to drug information requests either verbally or in writing
• Documentation of interventions through the utilization of the standard SOAP note
format
• Communication to the health care professionals regarding medication therapy plans and
drug related problems
XI. Prepare and present at least one patient case presentation delivered to pharmacists and/or
other health care professionals.
XII. Complete at least one of the following:
• Journal club
• Creation of guidelines of medication use within the practice
• A drug utilization review for the practice
• A formal presentation to a group of patients or health care professionals
• Newsletter article
• Peer reviewed article or patient case for potential publication
• Patient education document
XIII. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
• Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
• Arriving on time and prepared for all rotation activities
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning

37
Underserved
The goal of the Underserved Rotation is for the student to develop experience in the provision
of care to those who face barriers to timely access to health services which provide the best
health outcomes. The activities of the experience are to build upon information acquired in a
student’s didactic education and develop skills related to assessment and drug therapy
management of the patient in an underserved care setting. The student will complete all
activities in a professional manner under the facilitation of a preceptor.
Upon completion of the experience, the student will be able to:
I. Demonstrate knowledge of the challenges and opportunities of providing pharmaceutical care
to underserved patients.
• Demographic and economic characteristics of underserved patients in this setting
• Common acute and chronic medical disorders seen in underserved patients in this
setting
• Social, medical, prescription assistance service available to the underserved patient in
this setting
II. Demonstrate knowledge and participate when applicable in services provided by a pharmacist
in an underserved care setting to include but not limited to:
• Medication counseling
• Medication Therapy Management service
• Chronic Disease State Management
• Adherence counseling
• Immunization services
• Device teaching
• Disease Prevention/Health Wellness
• Medication dispensing
• Assisting a patient in identifying and applying for a specific prescription assistance
program
III. Develop and implement a systematic approach to gathering, organizing and prioritizing
pertinent data of underserved patients by:
• Utilizing current and past health records, patient interviewing, and interaction with
other health care professionals to obtain any or all of the following information:
• Signs and symptoms of the patient complaint or disease
• Physical assessment
• Available past medical, family, social, and surgical history
• Laboratory values
• Tests and procedures
• Medication history both past and current
• Performing and relevant physical assessments not otherwise available
IV. Identify and prioritize the health /medical problems including the following drug related
problems in the assigned patients:
• A problem or disease state of a patient not being treated or is not optimally treated
• A medication that a patient is receiving that is not indicated or is contraindicated
• Therapeutic duplication and/or polypharmacy
• An adverse effect(s) that may be caused by a medication(s)
38
• Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
• A drug interaction or potential drug interaction including interactions with labs, food,
and disease states
• Inappropriate medication dose or duration of therapy (including consideration of
hepatic/renal impairment, and age of the patient)
• Inappropriate route or dosage form
• Non-adherence to a prescribed medication(s)
V. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
• State the desired and achievable pharmacotherapeutic goals for each identified problem
• Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
• Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
• Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
• Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
VI. Assess patient medication adherence and develop strategies for improving adherence in
underserved patients.
VII. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Key patient education talking points
• Cost of therapy
VIII. Demonstrate the ability to measure and document patient outcomes.
• Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
• Measure, record, and appropriately track the therapeutic response and toxicity
• Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
• Identify, assess, and report identified adverse drug reactions and medication errors
using the appropriate reporting system
• Medication adherence
39
IX. Educate patients, caregivers, and health care professionals regarding the appropriate use of
drugs in common acute and chronic medical illnesses in underserved patients.
• Implement patient-specific education plans. These plans should include purpose,
directions for use/administration, storage, potential adverse effects and potential
interactions with other medications and food
• Educate professional colleagues, including pharmacists, physicians, and nurses regarding
drug therapy using formal or informal methods.
X. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques
• Create an audience-appropriate response and communicate this in a timely manner
• Where applicable document the question, response, and resources/references used
XI. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
• Patient disease and medication counseling
• Responses to drug information requests either verbally or in writing
• Documentation of interventions through the utilization of the standard SOAP note
format
• Communication to the health care professionals regarding medication therapy plans and
drug related problems
XII. Complete at least one of the following:
• Patient case presentation
• A formal presentation to a group of underserved patients
• Journal club presentation
XIII. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
• Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
• Arriving on time and prepared for all rotation activities
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning

40
Geriatrics
The goal of the Geriatrics Experience is to provide the student with experience in the
pharmacotherapeutic management of elderly patients with common acute and chronic medical
illnesses. The activities of the experience are to build upon information acquired in a student’s
didactic education and develop skills related to assessment and drug therapy management of
the patient in a geriatric setting. The student will complete all activities in a professional
manner under the facilitation of a preceptor.
Upon completion of the experience, the student will be able to:
I. Describe the general principles of aging to include the following:
• Demographic and economic characteristics of seniors (i.e. gender, ethnicity, geographic,
socioeconomic, and population)
• Biology and theories of aging
• Socioeconomics of aging including ethical issues, economic issues, elder abuse, and
cultural competencies
• Social and medical services available to seniors, including home health services and
geriatric institutions
II. Describe the physiologic changes associated with aging and how they impact medication
therapy to include:
• Pharmacokinetic alterations associated with aging including absorption, distribution,
metabolism, and excretion of drugs
• Pharmacologic alterations of aging in terms of altered receptor and organ sensitivities
and homeostasis
• Factors that predispose the geriatric patient to adverse drug reactions and identify
those drugs to which seniors are particularly sensitive
• Common drug interactions seen in the geriatric patient and factors which predispose
them to these interactions
• The medication adherence problems in the geriatric patient and modalities to promote
proper use of drugs by the patient
III. Demonstrate knowledge of the pathophysiology and pharmacotherapy of the common
disease states seen in the geriatric population. This includes but not limited to the following
disorders:
• Cardiovascular
• Pulmonary
• Endocrine
• Renal and Urologic
• Gastrointestinal
• Neurology/Psychiatry
• Immunity/Infectious Disease
• Musculoskeletal
• Nutritional/Hydration
• Ophthalmology
IV. Discuss the potential etiology, prevention and management of the common syndromes or
problems seen in the geriatric patient to include but not limited to the following:
• Mobility Deficiencies and Falls
41
• Pain
• Anxiety
• Insomnia
• Depression
• Cognitive decline
• Delirium
• Behavioral and psychological symptoms of dementia
• Altered Elimination
• Altered nutrition and weight disorders
• End of Life Issues
V. Develop and implement a systematic approach to gathering, organizing and prioritizing
pertinent data of assigned geriatric patients by:
• Utilizing current and past health records, patient/family interviewing, and interaction
with other health care professionals to obtain any or all of the following information:
o Signs and symptoms of the patient complaint or disease
o Physical assessment
o Available past medical, family, social, and surgical history
o Laboratory values
o Tests and procedures
o Medication history both past and current
• Performing and relevant physical assessments not otherwise available
VI. Identify and prioritize the health /medical problems including the following drug related
problems in the assigned patients:
• A problem or disease state of a patient not being treated or is not optimally treated
• A medication that a patient is receiving that is not indicated or is contraindicated
• Therapeutic duplication and/or polypharmacy
• An adverse effect(s) that may be caused by a medication(s)
• Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
• A drug interaction or potential drug interaction including interactions with labs, food,
and disease states
• Inappropriate medication dose or duration of therapy (including consideration of
hepatic/renal impairment, and age of the patient)
• Inappropriate route or dosage form
• Non-adherence to a prescribed medication(s)
VII. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
• State the desired and achievable pharmacotherapeutic goals for each identified problem
• Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
• Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
• Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
42
• Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
VIII. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Key patient education talking points
• Cost of therapy
IX. Demonstrate the ability to measure and document patient outcomes.
• Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
• Measure, record, and appropriately track the therapeutic response and toxicity
• Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
• Identify, assess, and report identified adverse drug reactions and medication errors
using the appropriate reporting system
X. Educate patients, caregivers, and health care professionals regarding the appropriate use of
drugs in common acute and chronic medical illnesses in geriatrics.
• Implement patient-specific education plans. These plans should include purpose,
directions for use/administration, storage, potential adverse effects and potential
interactions with other medications and food
• Assist in facilitating patient transition from one care setting to another by
communicating the pharmaceutical care plan to another pharmacist and or health care
provider(s)
• Educate professional colleagues, including pharmacists, physicians, and nurses regarding
drug therapy using formal or informal methods.
XI. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques
• Create an audience-appropriate response and communicate this in a timely manner
• Where applicable document the question, response, and resources/references used
XII. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
• Patient disease and medication counseling
• Responses to drug information requests either verbally or in writing
• Documentation of interventions through the utilization of the standard SOAP note
format
• Communication to the health care professionals regarding medication therapy plans and
drug related problems
43
XIII. Complete at least one of the following:
• Patient case presentation
• Journal club
• Medication or guideline review
XIV. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
• Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
• Arriving on time and prepared for all rotation activities
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning

44
Pediatrics
The goal of the Pediatrics Experience is to provide the student with experience in the
pharmacotherapeutic management of pediatric patients with common acute and chronic
medical illnesses. The activities of the experience are to build upon information acquired in a
student’s didactic education and develop skills related to assessment and drug therapy
management of the patient in a pediatric setting. The student will complete all activities in a
professional manner under the facilitation of a preceptor.
Upon completion of the experience, the student will be able to:
I. Describe the anatomical and physiological differences between the pediatric and adult patient
and how these impact medication therapy to include:
• Growth and development changes of the child at various ages (i.e. premature, neonate,
infant children, adolescents) and how this influences drug therapy
• Pharmacokinetic alterations associated with pediatrics including absorption,
distribution, metabolism, and excretion of drugs
• Factors that predispose the pediatric patient to adverse drug reactions and identify
those drugs to which pediatrics are particularly sensitive too.
• Common drug interactions seen in the pediatric patient and factors which predispose
them to these interactions
• The medication adherence problems in the pediatric patient and modalities to promote
proper use of drugs by the patient.
II. Demonstrate knowledge of pathophysiology and pharmacotherapy of the common disorders
seen in the pediatric population. This includes but not limited to disorders of the following:
• Cystic fibrosis
• Asthma
• Infectious diseases (otitis media, meningitis, sepsis, HIV)
• Seizures
• Fluid & Electrolyte disorders
• Hematological disorders
• Nutritional disorders
• Pain
• Toxicology /Poisonings
III. Describe the appropriate immunization schedules required in specific pediatric patient
populations.
IV. Develop and implement a systematic approach to gathering, organizing and prioritizing
pertinent data of assigned pediatric patients by:
• Utilizing current and past health records, patient/family interviewing, and interaction
with other health care professionals to obtain any or all of the following information:
• Signs and symptoms of the patient complaint or disease
• Physical assessment
• Available past medical, family, social, and surgical history
• Laboratory values
• Tests and procedures
• Medication history both past and current
• Performing and relevant physical assessments not otherwise available
45
V. Identify and prioritize the health /medical problems including the following drug related
problems in the assigned patients:
• A problem or disease state of a patient not being treated or is not optimally treated
• A medication that a patient is receiving that is not indicated or is contraindicated
• Therapeutic duplication and/or polypharmacy
• An adverse effect(s) that may be caused by a medication(s)
• Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
• A drug interaction or potential drug interaction including interactions with labs, food,
and disease states
• Inappropriate medication dose or duration of therapy
• Inappropriate route or dosage form
• Non-adherence to a prescribed medication(s)
VI. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
• State the desired and achievable pharmacotherapeutic goals for each identified problem
• Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
• Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
• Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
• Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
VII. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
• Pharmacology
• Pharmacokinetics
• Dose and routes of administration
• Contraindications and precautions
• Adverse reactions
• Interactions (drugs, dietary supplements, food, laboratory, disease)
• Monitoring parameters for efficacy and toxicity
• Key patient education talking points
• Cost of therapy
VIII. Demonstrate the ability to properly determine the correct dose of a medication for a pediatric
patient.
• Utilization of appropriate pediatric drug references to determine the dose of a particular
medication (including over the counter medications)
• Accurately calculate appropriate medication doses for pediatric patients to include
surface pharmacokinetic and body surface area calculations
• Determine appropriate route of administration for various medications used in pediatric
patients
• Recommend dosage forms or specials compounds for medications not available in a
form for pediatric us
46
IX. Demonstrate the ability to measure and document patient outcomes.
• Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
• Measure, record, and appropriately track the therapeutic response and toxicity
• Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
• Identify, assess, and report identified adverse drug reactions and medication errors
using the appropriate reporting system
X. Educate patients, caregivers, and health care professionals regarding the appropriate use of
drugs in common acute and chronic medical illnesses in pediatrics.
• Implement patient-specific education plans. These plans should include purpose,
directions for use/administration, storage, potential adverse effects and potential
interactions with other medications and food
• Assist in facilitating patient transition from one care setting to another by
communicating the pharmaceutical care plan to another pharmacist and or health care
provider(s)
• Educate professional colleagues, including pharmacists, physicians, and nurses regarding
drug therapy using formal or informal methods.
XI. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
• Identify the specific question using appropriate techniques
• Create an audience-appropriate response and communicate this in a timely manner
• Where applicable document the question, response, and resources/references used
XII. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
• Patient disease and medication counseling
• Responses to drug information requests either verbally or in writing
• Documentation of interventions through the utilization of the standard SOAP note
format
• Communication to the health care professionals regarding medication therapy plans and
drug related problems
XIII. Complete at least one of the following:
• Patient case presentation
• Journal club
• Medication or guideline review
XIV. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
• Maintaining a professional manner in both appearance and behavior at all times
• Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
• Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
• Arriving on time and prepared for all rotation activities
• Demonstrating the ability to complete assignments in an accurate and timely manner
• Developing the habits consistent with life-long learning.

47
Clinical Patient Care Selective
The goal of a clinical patient care selective is to provide the student with experience in the
pharmacotherapeutic management of patients in a specialized clinical setting/service (i.e.
infectious disease, critical care, psychiatry). The activities of the experience are to build upon
information acquired in a student’s didactic education and develop skills related to assessment
and drug therapy management of patients in these types of settings. The student will complete
all activities in a professional manner under the facilitation of a preceptor.
Including elective specific objectives determined by the preceptor, the student should upon
completion of the experience be able to:
a. Demonstrate knowledge of the pathophysiology and pharmacotherapy of the common
disease states or disorders seen in patients in the elective setting. These disorders are to be
determined by the preceptor.
b. Develop and implement a systematic approach to gathering, organizing and prioritizing
pertinent data of assigned patients by:
a. Utilizing current and past health records, patient interviewing, and interaction with
other health care professionals to obtain any or all of the following information:
• Signs and symptoms of the patient complaint or disease
• Physical assessment
• Available past medical, family, social, and surgical history
• Laboratory values
• Tests and procedures
• Medication history both past and current
b. Performing and relevant physical assessments not otherwise available
c. Identify and prioritize the health /medical problems including the following drug related
problems in the assigned patients:
a. A problem or disease state of a patient not being treated or is not optimally treated
b. A medication that a patient is receiving that is not indicated or is contraindicated
c. Therapeutic duplication and/or polypharmacy
d. An adverse effect(s) that may be caused by a medication(s)
e. Inappropriate or missing medication monitoring parameters (efficacy, toxicity,
pharmacokinetics)
f. A drug interaction or potential drug interaction including interactions with labs, food,
and disease states
g. Inappropriate medication dose or duration of therapy (including consideration of
hepatic/renal impairment, and age of the patient)
h. Inappropriate route or dosage form
i. Non-adherence to a prescribed medication(s)
d. Develop a pharmaceutical care plan to manage a patient’s identified health/medical problems
including drug related problems. The plan should:
a. State the desired and achievable pharmacotherapeutic goals for each identified problem
b. Provide appropriate pharmacologic and non-pharmacologic treatment
recommendations supported by primary literature and or in accordance with known
established clinical guidelines
c. Consider factors such as comparative efficacy, pharmacokinetics, toxicity, appropriate
dosage form, adherence, formulary, and cost of therapy
48
d. Include a drug therapy monitoring plan that states the parameters to be measured and
frequency of measurement, including measures of therapeutic response and toxicity
e. Be communicated to the patient and other members of the health care team in an
accurate, concise and timely manner, and where appropriate, written in an audience-
appropriate format
e. Exhibit a firm understanding of drug therapy. For each pharmacotherapeutic option the
student should be familiar with the following:
a. Pharmacology
b. Pharmacokinetics
c. Dose and routes of administration
d. Contraindications and precautions
e. Adverse reactions
f. Interactions (drugs, dietary supplements, food, laboratory, disease)
g. Monitoring parameters for efficacy and toxicity
h. Key patient education talking points
i. Cost of therapy
f. Demonstrate the ability to measure and document patient outcomes.
a. Implement the pharmaceutical care monitoring plan to determine the outcome(s) of
drug therapy
b. Measure, record, and appropriately track the therapeutic response and toxicity
c. Modify the pharmaceutical care plan appropriately based on data collected from patient
monitoring or when other data becomes available
d. Identify, assess, and report identified adverse drug reactions and medication errors
using the appropriate reporting system
g. Educate patients, caregivers, and health care professionals regarding the appropriate use of
drugs in common acute and chronic medical illnesses in adults.
a. Implement patient-specific education plans. These plans should include purpose,
directions for use/administration, storage, potential adverse effects and potential
interactions with other medications and food
b. Assist in facilitating patient transition from one care setting to another by
communicating the pharmaceutical care plan to another pharmacist and or health care
provider(s)
c. Educate professional colleagues, including pharmacists, physicians, and nurses regarding
drug therapy using formal or informal methods.
h. Demonstrate the ability to use the most appropriate resources to respond to drug information
questions from patients and health care professionals in an accurate and timely manner.
a. Identify the specific question using appropriate techniques
b. Create an audience-appropriate response and communicate this in a timely manner
c. Where applicable document the question, response, and resources/references used
i. Demonstrate the ability to effectively communicate, both in writing and verbally, with health
care professionals and patients. Examples include but are not limited to:
a. Patient disease and medication counseling
b. Responses to drug information requests either verbally or in writing
c. Documentation of interventions through the utilization of the standard SOAP note
format
49
d. Communication to the health care professionals regarding medication therapy plans and
drug related problems
j. Complete at least one of the following:
a. Patient case presentation
b. Journal club
c. Medication or guideline review
k. Conducts oneself in a professional and ethical manner when interacting with patients and
health care professionals by:
a. Maintaining a professional manner in both appearance and behavior at all times
b. Demonstrating courtesy and respect towards others and exhibiting self-control in all
interactions
c. Maintaining confidentiality regarding patient information and displaying honesty and
integrity in all activities
d. Arriving on time and prepared for all rotation activities
e. Demonstrating the ability to complete assignments in an accurate and timely manner
f. Developing the habits consistent with life-long learning
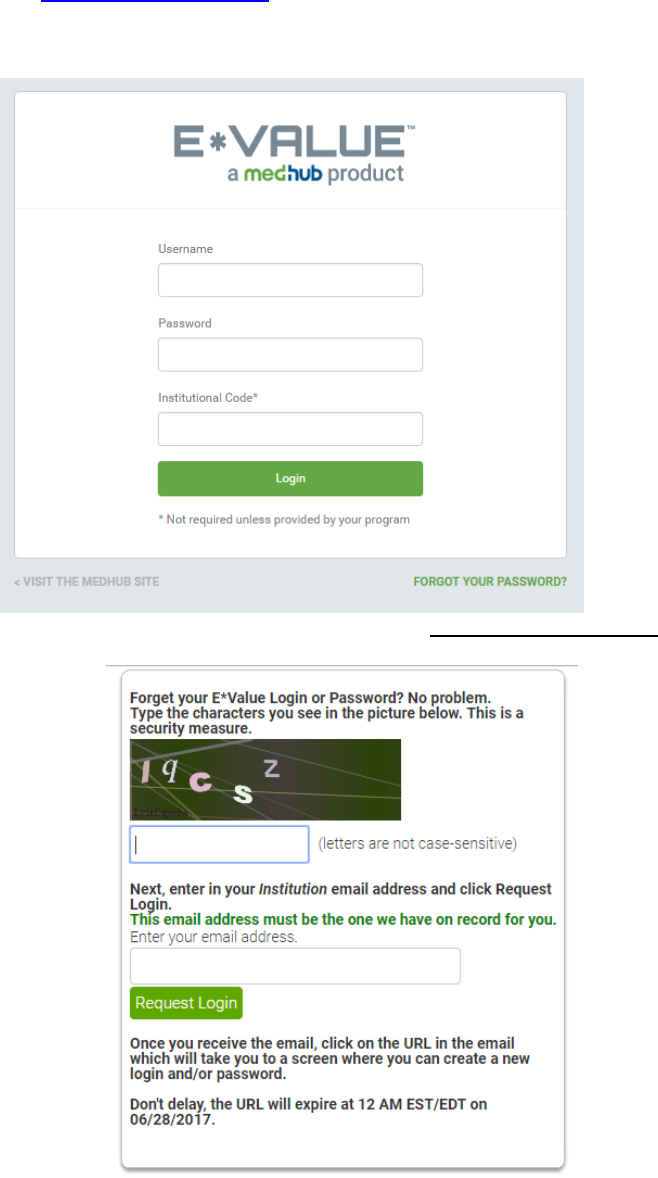
50
E*VALUE INSTRUCTION GUIDE FOR COLLEGE OF PHARMACY PRECEPTORS
➢ You will receive an e-mail with your login and password information. E*Value’s website
address is: https://www.e-value.net.
➢ Using the information in the e-mail, log into E*Value: (Ignore the institution code field).
➢ If you have forgotten your password, click on the ‘Forgot Your Password’ link and
follow the directions to have your password e-mailed to you.
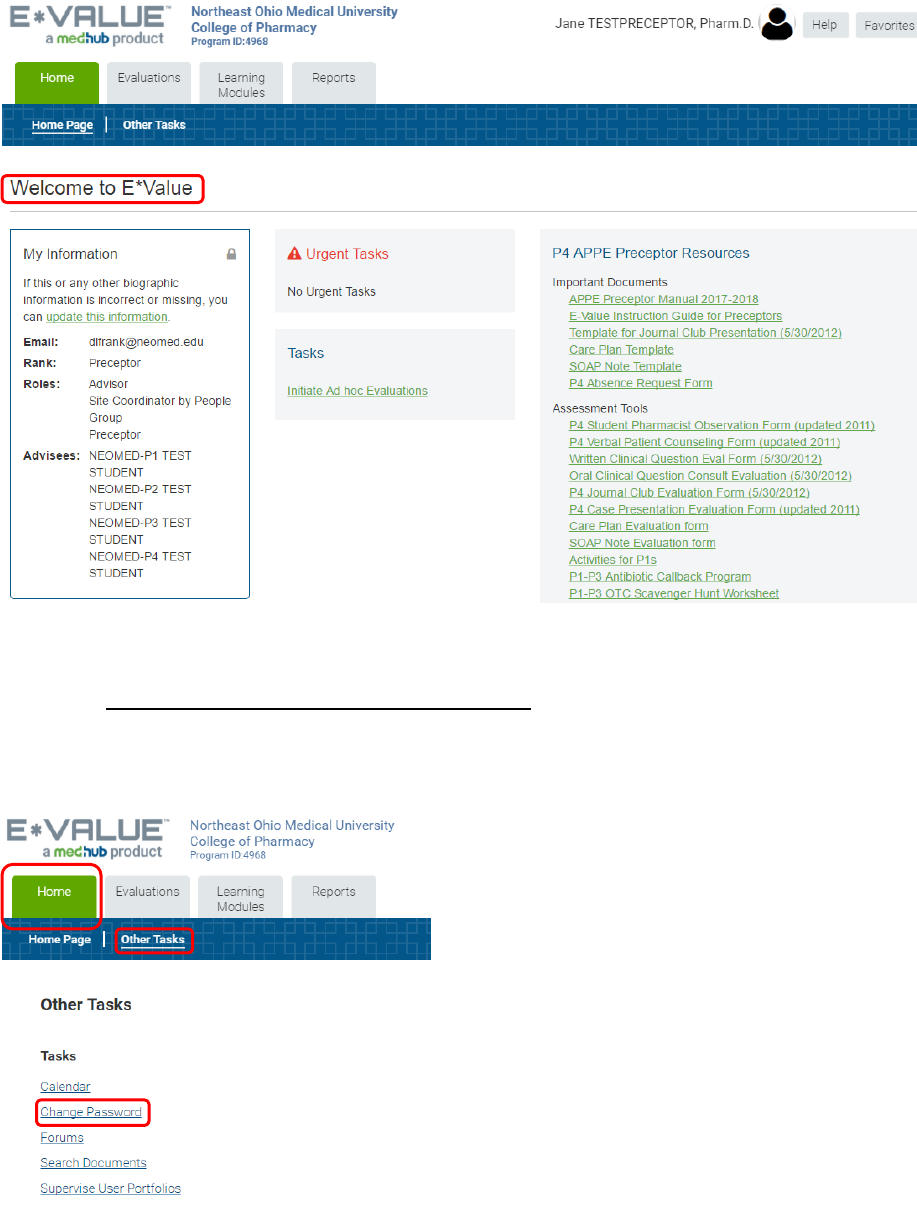
51
Once you are logged in, you will see the welcome page.
➢ To change your password and/or your login, click the ‘Home’ icon, then click ‘Other
Tasks.’ Click ‘Change Password.’ You do not have to change your login if you are
satisfied with it, but you may want to change it for consistency. To change it, type in a
New Login or New Password and re-type it. Then click ‘Update.’
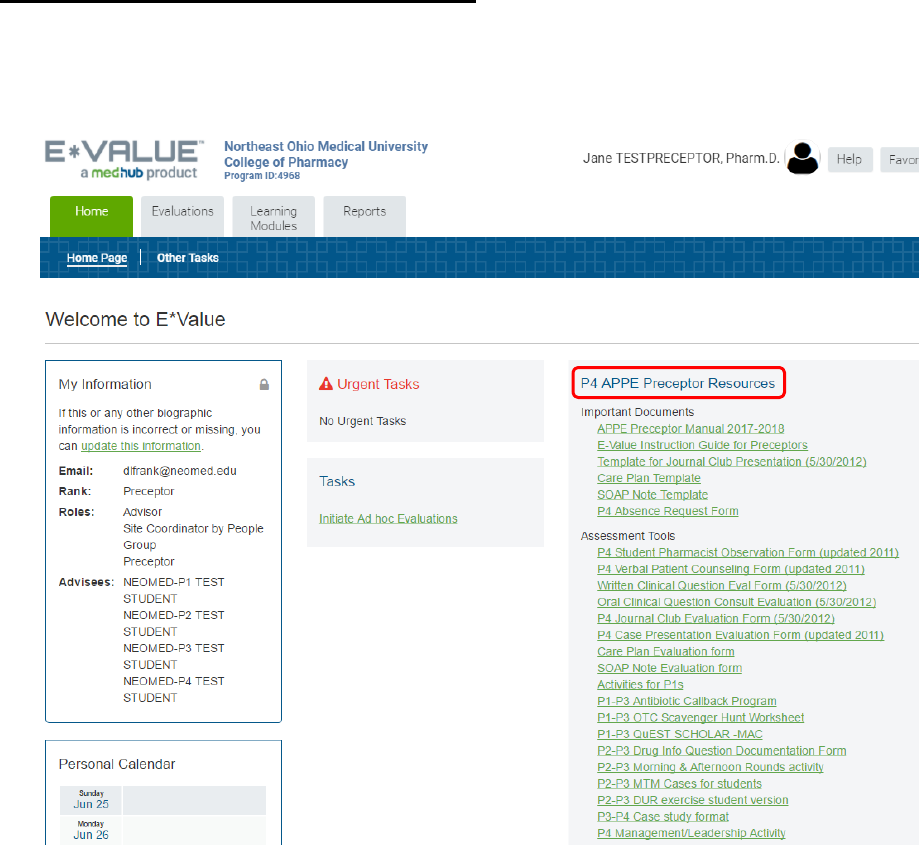
52
PRECEPTOR RESOURCES (Announcements)
➢ On the Welcome page, you will be able to access important documents and tools for
APPE and IPPE student rotations (i.e. Preceptor Manuals, Evaluation forms,
Assessment tools).
➢ Evaluations: These are here for your reference only! You will receive an email from E-
Value with a link to the actual evaluation form you will need to complete for your
students.
➢ Preceptor Manuals: These manuals provide helpful information on the experiential
programs including important policies and rotation objectives.
➢ Assessment Tools: These are to assist you in assessing a student while on rotation.
You are not required to return these to the college unless requested!
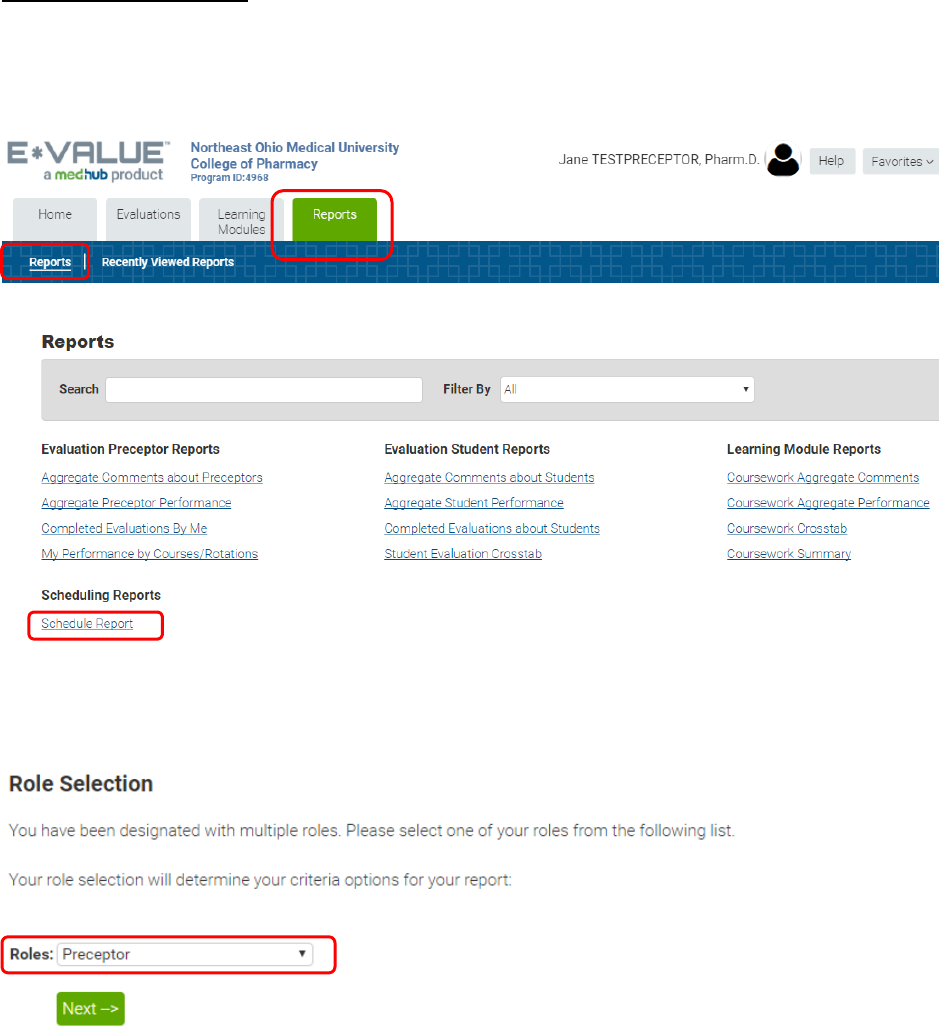
53
STUDENT SCHEDULES
➢ E*Value will have a schedule of students assigned to you which you will be able to see
by clicking the ‘Reports’ icon | Reports | Schedule Report.
➢ The Role Selection should be ‘Preceptor.’ Then click next.
➢ Note: If you have the role of “Site Coordinator” (for those who are responsible for
multiple preceptors) you will have to select “Site Coordinator” at Role Selection. At the
‘Schedule Report’ you can either click on Next or filter based on certain criteria.
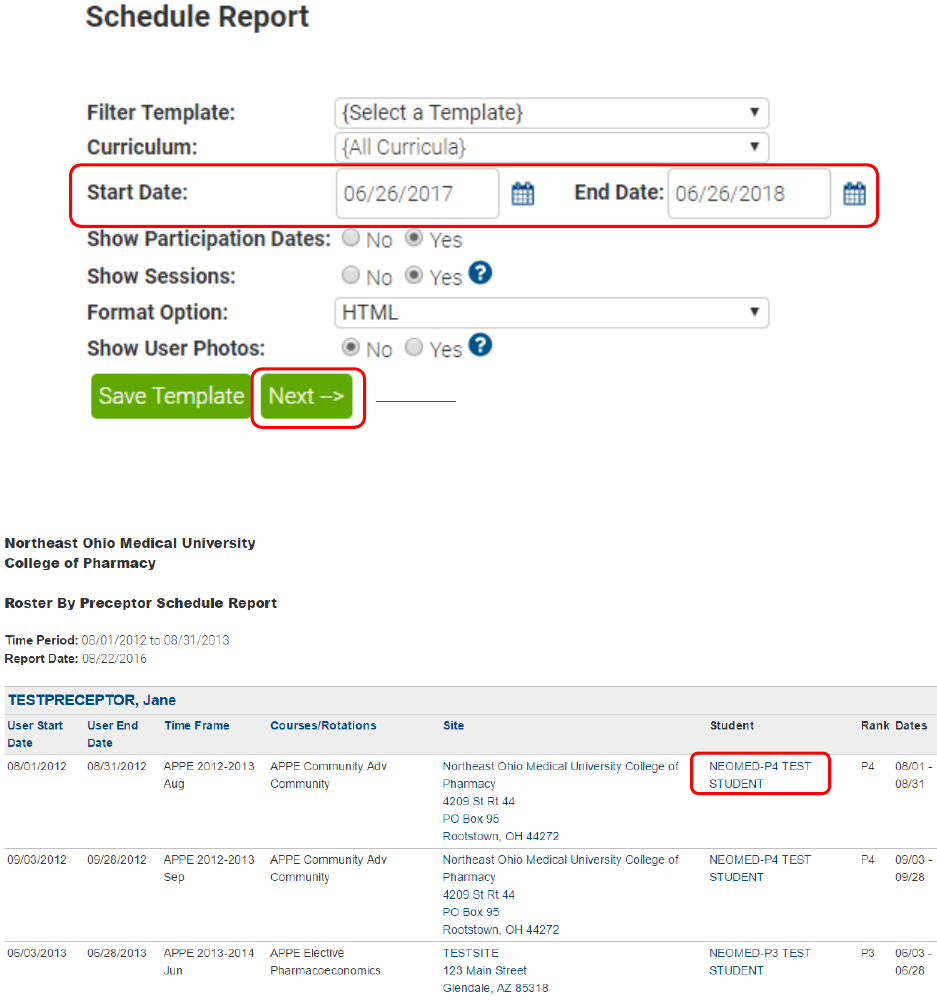
54
➢ By default, the date range will be the current date plus one year. You can modify it by
clicking on the calendar icon
➢ The student schedule will look something like this.
➢ Clicking on the student’s name will give you more information about the student
(picture, email, rotation schedule, portfolio) about the student
Click on ‘Next’ to view schedule
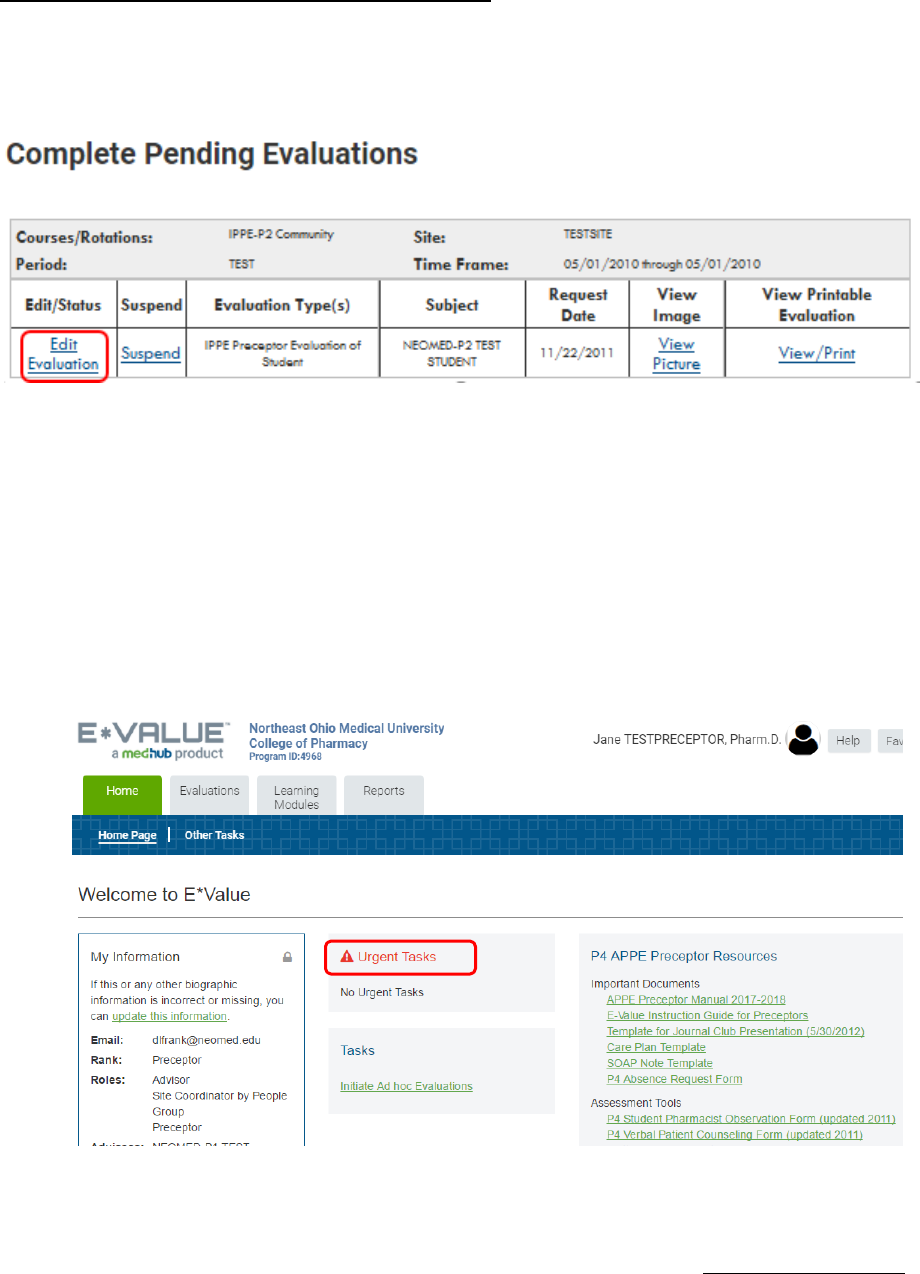
55
COMPLETING FINAL STUDENT EVALUATIONS
➢ When you are scheduled to complete the final Student Evaluation, an e-mail will be
sent to you (within 1 week prior to the end of the rotation) with a link. Clicking on the link
will automatically take you to your pending evaluations queue:
➢ To complete the evaluation, click ‘Edit Evaluation.’
➢ You should complete all applicable sections of the evaluation form to include providing
comments. Comments are required if the student receives “Unsatisfactory
Performance”, or “Needs Improvement” grades.
➢ E-Value will automatically calculate the final rotation grade.
➢ Once the evaluation is completed, you will need to click on Submit at the bottom of the
evaluation.
➢ NOTE: The final Student Evaluation is due on the last day of the rotation. A reminder
notice from E-Value will be sent if you have not completed the evaluation!
➢ Scheduled evaluations you need to complete will also appear in the middle of your
‘Welcome Page’ under Urgent Tasks.
➢ You can also navigate to the pending evaluations by clicking the ‘Evaluations’ icon |
Evaluation Management | Complete Pending Evaluation.
➢ For APPE Only - Please Note: On-the-Fly Evaluations are now called Ad Hoc
Evaluations. Preceptors can create an Ad Hoc Evaluation for a Mid-Point Evaluation or
when a scheduled student final evaluation has not yet been generated by the system.
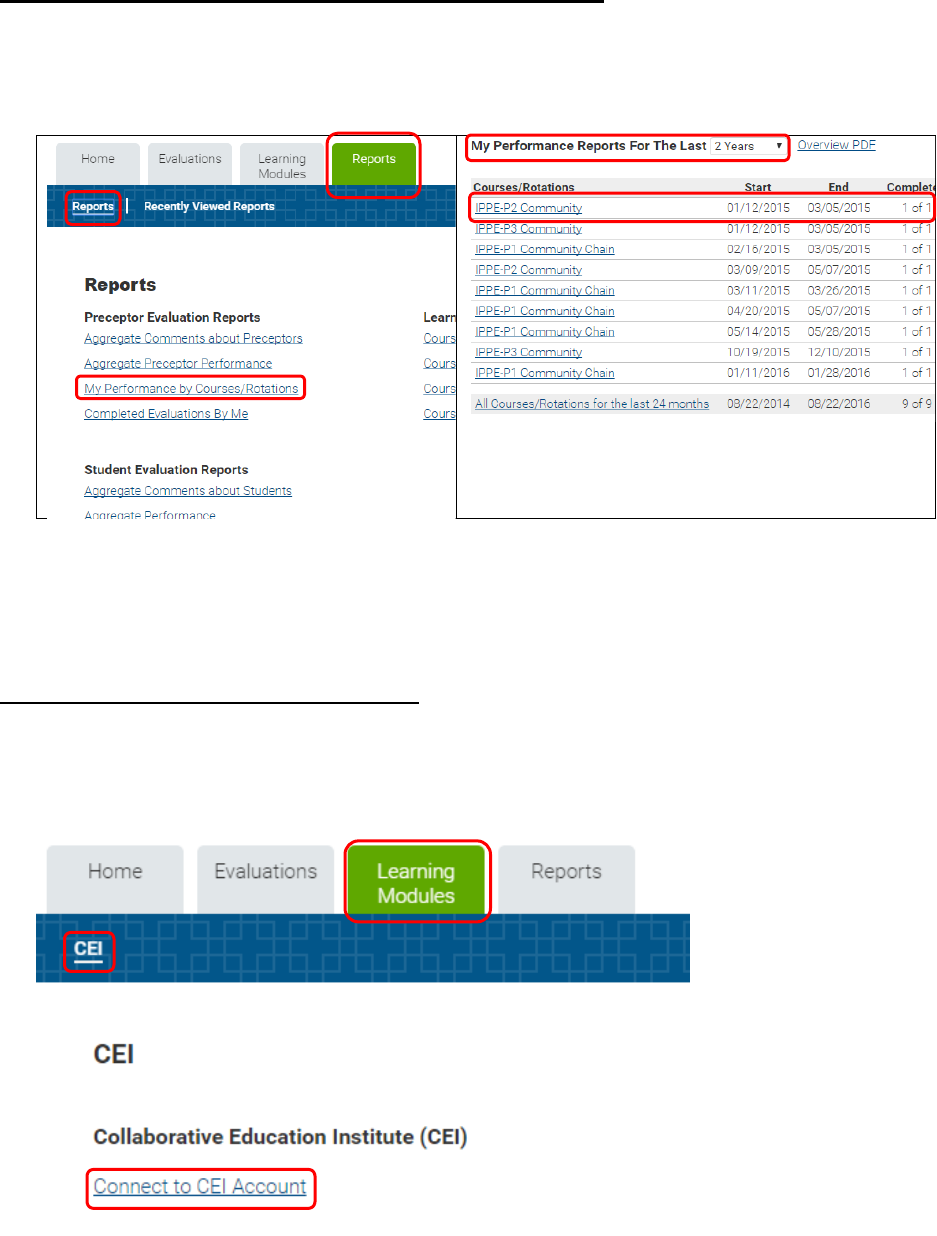
56
VIEW STUDENT EVALUATION OF PRECEPTOR AND SITE
➢ Students are required to complete an evaluation of the preceptor and site. To view an
anonymous evaluation summary, click the ‘Reports’ icon | Reports | My Performance by
Courses/Rotations. Select the time frame. Then click the appropriate rotation.
PRECEPTOR CONTINUING EDUCATION
➢ E*Value offers CEI (Collaborative Education Institute) continuing education. You can
access this on-line CE approved preceptor development program by clicking the
‘Learning Modules’ icon | CEI | Connect to CEI Account.
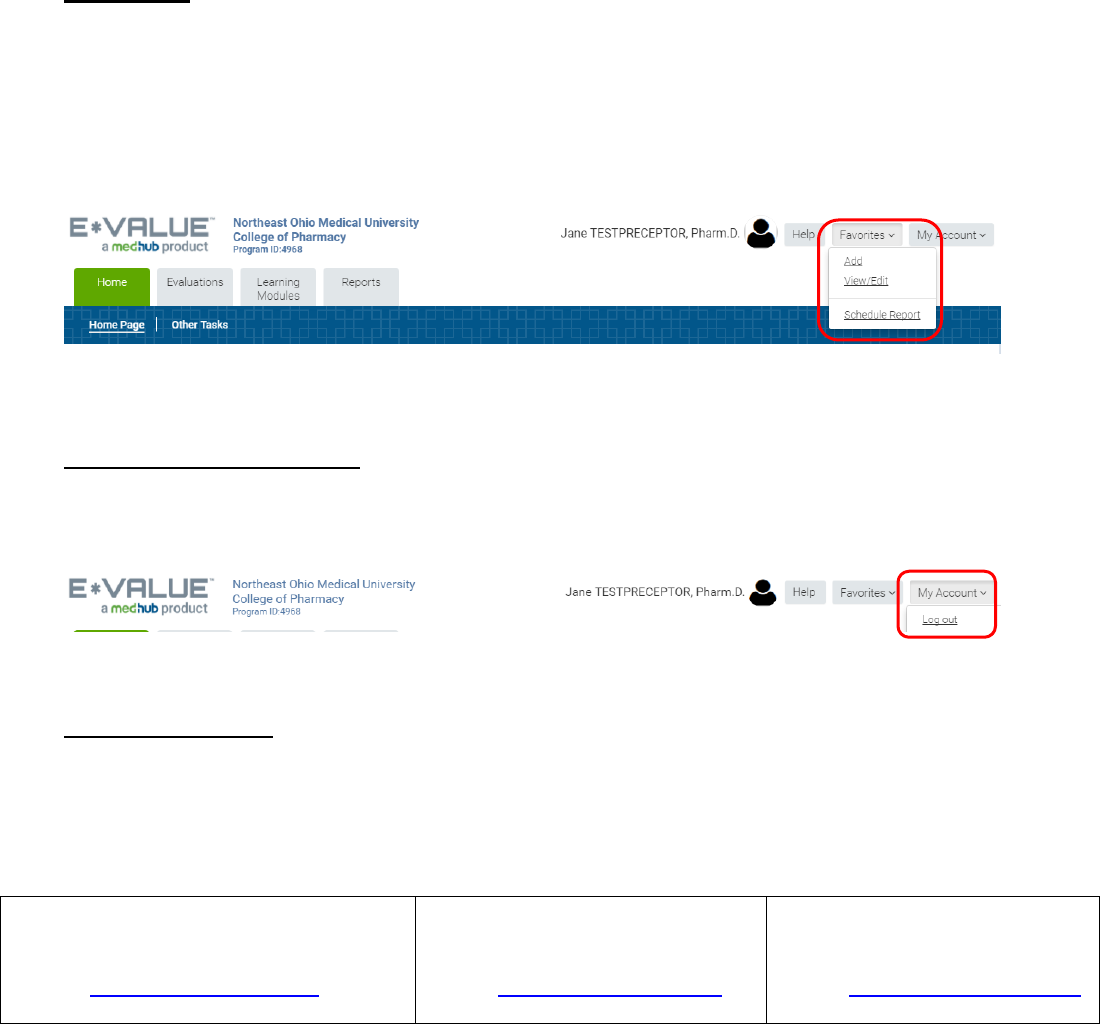
57
FAVORITES
➢ For convenience, you can customize your site by using the ‘Favorites’ feature at the top
right which allows you to create a list of your most frequently used pages within the site.
➢ Click to the page you want to add to the list. Click ‘Favorites’ and choose ‘Add’ from the
drop-down menu. This will add the page name under the ‘Favorites’ bar. You can
change the list order or name by choosing View/Edit | Edit.
LOGGING OUT OF E-VALUE
➢ To logout of E*Value, click on the ‘My Account’ button on the top right of the page. Then
click ‘Log Out.’ This will end your E*Value session.
NEED ASSISTANCE
➢ If you are experiencing any difficulties logging in, navigating, or completing the
evaluation forms, please contact:
Charles Cather, RPh., M.B.A., FASCP
Experiential Director
Phone: 330-325-6228
Email: ccather@neomed.edu
Debbie Frank
Senior Curriculum Coordinator
Phone: 330-325-6339
Email: dlfrank@neomed.edu
Patti Pfeifer
Administrative Assistant
Phone: 330-325-6390
Email: ppfeifer@neomed.edu
58
P4 STUDENT APPE EVALUATION
Please evaluate the student during the midpoint and final week of the rotation using the
following scale for evaluation. A midpoint evaluation is required for any student who is
currently performing at an unsatisfactory or needs improvement level. Preceptors are
required to provide narrative comments to support Unsatisfactory Performance, Needs
Improvement, and Exceeds Expectations scores.
1
Unsatisfactory
Performance
Student does not
meet requirements.
Student is unable to
complete
basic/routine tasks
despite guidance and
prompting.
2
Needs Improvement
Student meets some
minimum
requirements.
Student frequently
requires guidance
and/or prompting to
complete basic or
routine tasks.
3
Progressing
Satisfactorily
Student consistently
meets requirements.
Student completes
basic and some
complex tasks
independently with
minimal or no
guidance and/or
prompting.
4
Exceeds
Expectations
Student exceeds
requirements.
Student consistently
and independently
completes all basic
and complex tasks
going beyond what
is required.
The FINAL rotation grade will be based on student achieving an average of ≥ 2.0 in each
section and the average score for the all the sections based on following distribution:
Grading Distribution
Less than 2.5 = Fail
2.5 to 3.5 = Pass
Greater than 3.5 = Pass with Honors
59
SECTION I: PROFESSIONALISM
Midpoint
Final
Week
1. Participates in the process of self-assessment and displays
an interest in life-long learning and continuous professional
development
2. Maintains a professional manner in both appearance and
behavior at all times
3. Demonstrates courtesy and respect towards others and
exhibited self-control in all interactions
4. Maintains confidentiality
5. Displays cultural sensitivity and tolerance
6. Arrives on time and prepared for all rotation activities
7. Demonstrates appropriate time-management skills and the
ability to prioritize
8. Demonstrates initiative and responsibility for providing
patient care and completing assignments
Comments
Section Scores
SECTION II: COMMUNICATION
Midpoint
Final Week
1. Demonstrates active listening skills and empathy
2. Effectively communicates both verbally and in writing with
patients and other health care professionals
3. Demonstrates the ability to establish effective
relationships with other health care professionals and
patients
4. Appropriately demonstrates a willingness to form an
opinion, express observations and/or ask questions
5. Displays effective presentation skills
6. Demonstrates assertiveness and confidence when making
recommendations
7. Responds to questions in a clear and concise manner with
supporting evidence/rationale via written or verbal
communication as appropriate to the situation
Comments:
Section Scores
60
SECTION III: DRUG/DISEASE KNOWLEDGE
Midpoint
Final
Week
1. Demonstrates knowledge of disease states appropriate for
this clinical setting
2. Describes the expected mechanism of action, therapeutic
response, adverse effects, and monitoring parameters for a
given drug or combination of drugs
3. Applies physical assessment skills as appropriate to assist in
evaluating a patient and his/her medication therapy
4. Demonstrates knowledge of evidence based medicine and
clinical practice guidelines
Comments:
Section Scores
SECTION IV: APPLICATION
Midpoint
Final Week
Problem Assessment
1. Utilizes a systematic problem-solving approach to patient
care
2. Obtains and interprets information from the medical chart,
computer system or patient to assess therapy
3. Consistently and accurately identifies and prioritizes all
medication-related problems
Plan Development
1. Designs and evaluates regimens for optimal outcomes,
incorporating pharmacokinetic, formulation data, and
routes of administration into decision
2. Adjusts regimens based patient physiologic parameters
and response to therapy
Monitoring Parameters
1. Create and implement a monitoring plan to assess the
outcomes of drug therapy for a patient
2. Prospectively measure, record, and track a patient’s
therapeutic response and toxicity to drug therapy
3. Identify, assess, and appropriately report drug related
problems, adverse events, and toxicities
4. Assesses patient adherence to medications and risk factors
for non-adherence
Use & Interpretation of Drug Information
1. Identifies and thoroughly evaluates current literature and
effectively apply this information to patient care
2. Given a drug, health or operational information question,
formulates a timely efficient, thorough and effective
answer using appropriate sources of information
61
3. Provides and appropriately document references and
resources
Comments:
Section Score
SECTION V: INTERPROFESSIONAL ACTIVITIES
Midpoint
Final
Week
1. Demonstrates the ability to interact effectively with
prescribers/student prescribers to address and resolve
patient’s drug therapy problems
2. Demonstrates the ability to actively participate as a
healthcare team member in providing direct patient care
and engaging in shared decision-making
3. Demonstrates competence in the roles and responsibilities
of members of the interprofessional healthcare team
Comments:
Section Score
SECTION VI: MEDICATION DISTRIBUTION / DISPENSING
Midpoint
Final
Week
4. Demonstrates proficiency in processing new and refill
prescriptions/medication orders in accordance with
regulatory requirements
5. Accurately selects and prepares appropriate medication for
prescription or medication order
6. Develops a systematic approach for final verification to
ensure the five principles of drug delivery: right drug, right
patient, right dose, right time, right route
7. Using the concepts of pharmaceutics, and applying best
practice guidelines, appropriately compounds products for
patient use
Comments:
Section Score
62
SECTION VII: ADMINISTRATIVE SKILLS (To be completed for
leadership/management rotations only)
Midpoint
Final
Week
1. Discusses use of management principles (e.g. planning,
organizing, directing and controlling) for simple/individual
tasks and complex activities
2. Discusses and/or participates in resource management
related to Time, people, finances and
technology/informatics
3. Discusses and/or participates in quality assurance and/or
patient safety activities
4. Discusses marketing principles and how they are applied
5. Identifies methods to enhance pharmacy services
6. Reviews and applies all site related policies and procedures.
7. Demonstrates an understanding of leadership needs and
opportunities in pharmacy practice
Comments:
Section Score
PRESENTATIONS, JOURNAL CLUBS, ETC.
Provide description/title of presentation & comments on student performance:
PROJECTS, RESEARCH, PUBLICATIONS, ETC.
Provide description of project & comments on student performance:
OVERALL COMMENTS: It is important to provide an accurate overall written assessment of the
student’s performance on the rotation. Information in this section is available to the student’s
other preceptors.
LIST AREAS IN NEED OF IMPROVEMENT FOR SUBSEQUENT ROTATIONS: Information in this
section is available to the student’s other preceptors.
MIDPOINT ROTATION GRADE: ________________
FINAL OVERALL ROTATION GRADE: _____________
By submitting this evaluation, you confirm that the student has fulfilled all attendance
requirements
63
ABSENCE REQUEST FORM
Template Journal Article Presentation Form
Student : _____________________________________________________________________________________
Clerkship Site/Rotation: _________________________________________________________________________
Number of days’ absence included in this request: ____________________________________________________
Approval is requested for absence from rotation activities on ____/___/_____ for reason indicated below.
Approval is requested for absence from rotation activities from ___/___/_____ through ___/___/_____ for the reason indicated
below.
REASON FOR ABSENCE:
______ Illness
______ Death in Family
______ Job/Residency Interview
______ Attend Professional Meeting
______ Personal Reason
______ Other _________________________________________________________________________
FURTHER REASON FOR ABSENCE CAN BE GIVEN HERE IF EXPLANATION IS REQUIRED:
Approval requested _______________________________________________________ _____/_____/_____
(Student) (Date)
Approval ________________________________________________________________ _____/_____/______
(Preceptor) (Date)
Received ________________________________________________________________ _____/_____/______
(Director of Experiential Education) (Date)
This form should be faxed to: 330-325-5951 to the attention of: Pharmacy Practice, Director of Experiential Programs.
A copy should be kept on file with the Preceptor.

64
TEMPLATE JOURNAL ARTICLE PRESENTATION FORM
I. Background/overview:
A. Article title/citation
B. Study objective/hypothesis
C. Introduction/background
D. Funding sources/sponsorship/role
II. Methods:
A. Study design/demographics
1. Study design
2. Intervention
3. Institution setting
4. Study population
B. Methodology
1. Inclusion criteria
2. Exclusion criteria
3. Study methods
C. Outcome Measures
1. Primary endpoint
2. Secondary endpoint(s)
3. Statistical analysis
a. Sample size
b. Power
c. Statistical significance
d. Statistical methods/tests
65
III. Results:
A. Baseline characteristics
B. Outcomes
1. Primary results
2. Secondary results
3. Miscellaneous results
4. Adverse effects/side effects
IV. Author’s discussion/conclusions:
A. Brief summary of author’s main discussion points
B. Author’s acknowledged limitations
C. Author’s conclusions
V. Student’s discussion/conclusions:
A. Positive attributes
B. Negative attributes/bias
C. Student’s conclusions
D. Clinical applicability/impact on healthcare providers
VI. References:

66
TEMPLATE JOURNAL ARTICLE CRITIQUE
The following questions should be considered when critiquing a journal article. The student should
discuss the answers to any questions that apply to their journal article in their presentation.
I. Background/overview:
A. Article title/citation
What is the professional reputation of the journal? Are manuscripts peer-reviewed?
What is the professional background of the investigators? Do they have the appropriate
qualifications to conduct the study?
B. Study objective/hypothesis
Are the objectives clear, unbiased, specific, and obtainable?
C. Introduction/background
Does the study’s introduction provide adequate and current background information?
Have the investigators described the results of previous related research and do they explain
why the current study is necessary (why is it important)?
D. Funding sources/sponsorship/role
Who funded the investigation? Could this lead to bias?
What role (if any) did the drug manufacturer have in the study (such as authorship, investigator,
collection/analysis of study data)? Could this lead to bias?
Do the investigators have any relevant disclosures?
II. Methods:
A. Study design/demographics
1. Study design
What types of control groups (parallel, cross-over, historical) were used to compare the
effectiveness of the studied treatment?
Were patients randomized to treatment groups?
Was everyone (patients, physicians, study personnel, etc.) blinded to treatments? Does the
type of blinding, or lack thereof, introduce any potential bias?
2. Intervention
Is the study intervention (and control group) feasible and relevant in today’s practice? Were
appropriate doses and regimens used for the disease state under study?
67
3. Institution setting
Was the study conducted at a single institution or multicenter? If there were multiple
observers, how was variation among their observations minimized?
4. Study population
B. Methodology
1. Inclusion criteria
2. Exclusion criteria
Are the inclusion and exclusion criteria specific enough and is there a logical rationale for
these criteria? Are additional criteria needed?
Are sample subject’s representative of the target population (patients commonly treated)?
Does selection bias exist (consider the severity of illness, type of population, etc.)?
3. Study methods
Is enough detail provided so that a different investigator could repeat the study?
Were patient groups treated similarly during the study, except for the study treatment?
Are other interventions (such as medications on non-pharmacologic treatments) that were
used/allowed in the trial feasible and relevant in today’s practice? Were appropriate doses
and regimens used for the disease state under study?
Was patient adherence monitored and assured?
C. Outcome Measures
1. Primary endpoint
2. Secondary endpoint(s)
Is the primary outcome a DOE (Disease-Oriented Evidence) or POEM (Patient Oriented
Evidence that Matters)? Does this study look at outcomes my patients care about?
Was the test period large enough for the treatment effect to be measured adequately?
How were the measurements made (observer report, self-report, interview, lab tests)? Do
they appear to be appropriate, reliable/accurate, and standardized? Were they made at the
appropriate times and frequency? If a lab or diagnostic test is used to measure the
outcome(s), is it feasible and relevant in today’s practice?
3. Statistical analysis
a. Sample size
Did the authors explain how they determined the number of patients to study?
68
b. Power
Was the power stated?
Was the β (Type II error) stated?
c. Statistical significance
Was the α level to determine significance stated?
d. Statistical methods/tests
Were descriptive statistics used properly to describe the results?
Were inferential statistical tests used to examine the results? Were significance levels
set a priori? Are the statistical tests used appropriate for the data (consider whether
the data is nominal, ordinal, or continuous)?
Are potential confounding variables explained and statistical measures taken to adjust
for these variables?
Was data analyzed based on the groups the patients were initially randomized to
(intent-to-treat analysis) or was data analyzed based on the treatment the patients
received (per protocol analysis)?
III. Results:
A. Baseline characteristics
Were treatment and control patient groups similar at the beginning of the study?
B. Outcomes
1. Primary results
2. Secondary results
Are the results of the study statistically significant? How is statistical significance
determined/reported (p values, ratios and confidence intervals, etc.)?
How clinically important are the reported differences between the experimental and control
groups?
What is the ARR, RRR and NNT (or NNH) for the outcomes of the study?
What is the null hypothesis of the study? Was it accepted or rejected? Was there a chance
a type I or a type II error was made?
3. Miscellaneous results
Were all patients accounted for at the end of the study? If not, were the missing patients
addressed or adjusted for? Was the sample size of patients analyzed adequate to achieve
power for the primary outcome?
Were confounding variables present that could have affected the study results?
Were any post-hoc or subgroup analyses conducted (if so, were they determined prior to
starting the study)?
Adverse effects/side effects
69
Were adverse effects monitored prospectively?
Are adverse effects presented in sufficient detail along with the rates of occurrence?
IV. Author’s discussion/conclusions:
A. Brief summary of author’s main discussion points
Were the study results interpreted appropriately?
Were all deviations from the described methods reported and managed appropriately?
Author’s acknowledged limitations
Did the investigators explain study limitations?
Did the investigators compare their study results to the results of similar studies?
Author’s conclusions
Do the conclusions follow logically from the data?
V. Student’s discussion/conclusions:
A. Positive attributes
B. Negative attributes/bias
C. Student’s conclusions
D. Clinical applicability/impact on healthcare providers
To assess applicability of the results, compare your population (or patients commonly
treated) to the study population.
Do the benefits of the treatment outweigh the risks (and costs)?
Will the study affect recommendations that you will make as a pharmacist?
Should/can practice be changed based on these results? If so, how can practice be changed
based on these results?
What additional questions does the study raise?
VI. References:
70
EVALUATION OF JOURNAL CLUB
Student Name: ____________________ Evaluator: __________________________ Date: __________
Key: MC = Meets Competency; NI = Needs Improvement; O = Omitted
MC
NI
O
Criteria
COMMENTS:
Strengths and areas for
improvement
BACKGROUND
• States the title, journal of publication and author affiliations (if
relevant)
• Background information from the article was succinctly presented
• Other literature (e.g., previous articles, guidelines, etc.) was
discussed in context of the article being presented
• The study objective(s) was/were clearly stated
• The study’s sponsor and their role are identified (If applicable)
METHODS
• The study design (e.g. randomized controlled, cohort, case-control,
etc.) was clearly and concisely described
• The study intervention was clearly and concisely described
• The study population was characterized
• Relevant inclusion/exclusion criteria were presented
• The primary (and secondary where applicable) endpoints were
presented
• An accurate summary of the statistics was given
• Appropriateness (or lack thereof) of the statistical tests used was
vocalized by the presenter
RESULTS
• Baseline characteristics of the study population were discussed
• The primary (and secondary where applicable) results were
presented
• The statistical significance (or lack thereof) of the results was noted
• The clinical significance (or lack thereof) of the results was noted
CONCLUSIONS
• The author(s) conclusion(s) were presented
• Strengths and limitations as noted by the authors was presented
• Strengths and limitations identified by the student (aside from the
authors) were presented
• The student’s conclusion(s) were presented
• How the trial may or may not impact clinical practice was presented
71
MC
NI
Criteria
COMMENTS:
Strengths and areas for
improvement
ABILITY TO ANSWER QUESTIONS
• Answered questions logically and accurately. If unsure of answer, the
student clearly stated so.
• Responded to >50% of questions without assistance from instructor or
other participants.
OVERALL PRESENTATION / DELIVERY
• Presentation was generally presented in a logical sequence
• Presentation was within the allotted time
• Spoke audibly to the audience
• Used few (or no) distracters (e.g. “um”) OR distracting mannerisms (e.g.
clicking pen)
• Referred to notes occasionally, but did NOT read from notes
HANDOUT
• Handout was well organized, clear and succinct
• Appropriate references were cited in the proper format
•
PASS or FAIL (Circle One)
(Passing: ≥70% of MC’s for applicable items)
Professional Conduct (failure to achieve in this area will result in a meeting with the course director)
The student was:
dressed appropriately
wearing a clean white coat
displaying their name badge
respectful to other presenters
Additional Comments:
72
CASE PRESENTATION EVALUATION
STUDENT:
DATE:
PRECEPTOR:
Student has excelled in
performance. Student
has completed work
above and beyond the
requirements of the
assignment. Requires
no intervention.
5
Student performs with
minimal preceptor
assistance or
guidance. Rarely
requires intervention.
4
Student performs at an
acceptable level.
Assistance or guidance
from preceptor is
frequently necessary.
3
Student has attempted
but not performed at an
acceptable level in all
areas. Needs
significant
improvement.
2
Unacceptable. Below
expectations. Student
requires extensive
intervention.
1
I. PREPARATION
1. Patient Presentation
1. ID, CC, HPI, FH, SH, Med history, ROS, VS, physical exam and lab/test, problem list
5
4
3
2
1
2. Chronological course adequately detailed.
5
4
3
2
1
3. All relevant data presented for necessary assessment.
5
4
3
2
1
II. KNOWLEDGE
1. Discussion of diseases states/pathophysiology
1. Overview of disease epidemiology, etiology, pathophysiology and therapy.
5
4
3
2
1
2. Signs, symptoms and risk factors reviewed.
5
4
3
2
1
2. Drug Therapy
1. Understands and explain patient’s current drug therapy.
5
4
3
2
1
2. Identifies drug related problems.
5
4
3
2
1
3. Develops pharmacy care plan to resolve drug related problem(s).
5
4
3
2
1
4. Provides evidence-based rationale for recommendation(s). (Primary literature support preferred)
5
4
3
2
1
3. Monitoring
1. Used appropriate parameters to assess drug regimen efficacy and toxicity.
5
4
3
2
1
2. Defines endpoints of therapy, including patient follow up.
5
4
3
2
1
4. Patient Information/Counseling
1. Explains purpose(s) of drug therapy.
5
4
3
2
1
2. Important instructions for drug use.
5
4
3
2
1
3. Side effects/precautions that should be communicated to the patient.
5
4
3
2
1
4. Other (blood glucose testing, home BP monitoring, peak flow use, etc.)
5
4
3
2
1
III. STYLE OF PRESENTATION
1. Delivery
Diction, voice projection, personal appearance, eye contact with audience, reliance on notes
5
4
3
2
1
2. Organization
Well organized, pertinent information, slides/overheads.
5
4
3
2
1
3. Handout (also includes visual aids if applicable)
Includes at least two current primary references.
5
4
3
2
1
Professionally prepared, neat and free of typographical errors. All sources appropriately referenced.
5
4
3
2
1
4. Responses to Questions
Responses appropriate and straightforward.
5
4
3
2
1
Comments:
73
STUDENT PHARMACIST OBSERVATION FORM
Student Pharmacist Name: ________________________________________________
Preceptor name: __________________________________ Site: __________________
Today’s date: ____________________________________
Use the following scale to rate the student pharmacist’s daily activities:
1
2
3
4
Unsatisfactory
Needs Improvement
Progressing
Exceeds Expectations
Performance
Satisfactorily
Student does not meet
requirements. Student is
unable to complete
basic/routine tasks
despite guidance and
prompting
Student meets some
minimum requirements.
Student frequently
requires guidance
and/or prompting to
complete basic or
routine tasks.
Student consistently
meets requirements.
Student completes basic
and some complex tasks
independently with
minimal or no guidance
and/or prompting
Student exceeds
requirements. Students
consistently and
independently complete
all basic and complex
tasks going beyond what
is required.
What activities did you see the student pharmacist perform today? Score _____________
______________________________________________________________________________
______________________________________________________________________________
What did the student pharmacist do particularly well?
______________________________________________________________________________
______________________________________________________________________________
What improvements or suggestions should you provide the student pharmacist to increase his or
her proficiency/skill level?
______________________________________________________________________________
______________________________________________________________________________
The above assessment was discussed with the student on: ______________________________
Date
_________________________________________ _________________________________
Preceptor Signature Student Signature
74
EVALUATION OF ORAL CLINICAL QUESTION CONSULT
Student/Group Name: _____________________ Evaluator: __________________________ Date: __________
Key: MC = meets competency; NI = needs improvement
PASS or FAIL (Circle One)
(Passing: ≥ 70% of MC’s for applicable items)
Professional Conduct (failure to achieve in this area will result in a meeting with the course
director)
The student was:
dressed appropriately
wearing a clean white coat
displaying their name badge
respectful to other presenters
Additional Comments:
MC
NI
Criteria
COMMENTS:
Strengths and areas for
improvement
Presentation Style
□
□
1. Maintained eye contact most of the time
□
□
2. Did not rely solely on notes
□
□
3. Appeared generally relaxed
□
□
4. Movements and gestures enhanced delivery
□
□
5. Most sentences were complete and grammatically correct
□
□
6. Most words were precise and appropriate for the
audience
□
□
7. Voice was clear and audible
□
□
8. Pronunciation was correct for most words
□
□
9. Pace was appropriate
Organization and Timing
□
□
10. Sequence was logical
□
□
11. Transitions were clear
□
□
12. Within 1 minute of allotted time (e.g. within 7 to 11
minutes for an 8 to 10-minute presentation)
Depth of Knowledge
□
□
13. Most information was relevant to the question
□
□
14. Explanations of concepts and theories were mostly
accurate and complete
□
□
15. Literature presented generally supports claims
Ability to Answer Questions
□
□
16. Answered questions concisely
□
□
17. Appeared confident when answering questions
□
□
18. Answered >50% of questions without assistance
75
EVALUATION OF WRITTEN CLINICAL QUESTION CONSULT
Student Name: _____________________ Evaluator: __________________________ Date: __________
Key: MC = meets competency; NI = needs improvement; O= omitted
PASS or FAIL (Circle One)
(Passing ≥ 70% of MC’s for applicable items)
Additional Comments:
MC
NI
O
Criteria
COMMENTS:
Strengths and areas for
improvement
Question/Introduction
□
□
□
1. Identified and restated the drug information question
□
□
□
2. The introduction of the paper orients the reader to the
main themes
Literature Review
□
□
□
3. Identified all relevant literature resources
□
□
□
4. Evaluated the strengths and weaknesses of the literature
□
□
□
5. Properly analyzed and synthesized study data to answer
the drug information question
Discussion/Summary
□
□
□
6. The recommendation is logical and clinically sound
□
□
□
7. The recommendation is stated clearly with the
appropriate level of certainty (or uncertainty)
□
□
□
8. The recommendation takes into account relevant patient-
specific information
□
□
□
9. The consult is objective and does not impose bias upon
the reader
Quality of References / Citation
□
□
□
10. Appropriate information resources are used to answer
the question (Must use primary literature where
appropriate)
□
□
□
11. References are appropriately numbered (as superscripts
and in the order, they appear) throughout the consult.
□
□
□
12. Reference citation formats are appropriately formatted
(consistent with the Uniform Requirements)
Quality of Writing
□
□
□
13. The consult is clear and succinct.
□
□
□
14. Paragraphs are organized logically/appropriately.
□
□
□
15. Sentences and paragraphs transition smoothly.
□
□
□
16. Correct grammar and spelling are used throughout the
consult.
76
VERBAL Patient Counseling Rubric
Student name: Date:
1 = unsatisfactory, 3 = satisfactory, 5 = exceptional
PATIENT CARE DIMENSION
COMMENTS: Strengths and areas for
improvement.
INTRODUCTION: Greeted patient; introduced self,
verified patient name, used open invitation to talk,
smooth opening overall.
1 3 5
PRIME QUESTIONS: Asked all 3 questions during
encounter*
1 3 5
PURPOSE: Explained (or assured understanding of) the
purpose of the medication(s).
1 3 5
GOALS OF THERAPY: Properly communicates goals of
therapy for the medication. Describes what response
to expect, when to expect response.
1 3 5
GENERAL DRUG INFO: Told the patient the name,
strength, and frequency of administration for the
medication, or reinforced existing patient knowledge.
1 3 5
TIMING OF ADMINISTRATION: Explained how to take
medication relative to meals or other pertinent daily
activities (statins in the evening, bisphosphonates 1
st
thing in AM, etc.).
1 3 5
STORAGE: Explained the proper means of storing the
medication.
1 3 5
SIDE EFFECTS: Described the most common / clinically
significant side effects for each medication.
1 3 5
DURATION/FOLLOW UP: Told the patient how long to
take the medication, what to do if miss a dose, and
who to contact if symptoms continue, worsen, and/or
there are side effects.
1 3 5
EXIT: Communicated end of counseling session; gave
patient a chance to ask questions and responded
appropriately; ended effectively.
1 3 5
*Prime Questions: “What did your doctor tell you about this medication?”
“How did the doctor tell you to take it?”
“What response do you expect to receive from this medication?”
TOTAL SCORE ________________________
(maximum score=50)
ADDITIONAL COMMENTS:

77
APPE PRECEPTOR /SITE EVALUATION FORM
Using the following scale to indicate your agreement with the following statements:
4 = Strongly Agree
3 = Agree
2 = Disagree
1 = Strongly Disagree
NA = Not applicable to the Rotation or Site
MY PRECEPTOR:
1. Adequately oriented me to the APPE site.
2. Outlined and/or explained the goals and objectives of the rotation.
3. Clearly identified the performance expectations and approach to evaluation of my performance
at the beginning of the rotation.
4. Had an organized approach to precepting.
5. Regularly and in a timely manner provided feedback which identified both my strengths and
weaknesses.
6. Encouraged problem solving and professional decision making.
7. Spent sufficient time to guide me and address any questions or concerns I had.
8. Treated me with respect.
9. Served as a positive role model.
10. Provided and reviewed a final evaluation of my performance at the end of the rotation.
Additional Comments including preceptor strengths and suggestions for enhancement (required):
THE ROTATION ALLOWED ME TO:
1. Assess patients and recognize health and drug related problems.
2. Develop and recommend pharmaceutical care plans to manage a patients’ health and/or drug
related problems.
3. Define the therapeutic goals or outcomes of pharmaceutical care plans for a patient.
4. Monitor drug therapy for efficacy, adverse effects, and compliance.
5. Process and dispense prescription or medication orders.
6. Respond to drug information questions from patient and/or healthcare professionals.
7. Provide patient education/counseling.
8. Develop my written communication and documentation skills.
9. Develop my formal presentation skills.
10. Enhance my understanding of the leadership and administrative aspects of the practice setting.
11. Collaborate with other healthcare professional (other than pharmacists) interprofessionally in
providing quality health care to patients.
Additional Comments including rotation strengths and suggestions for enhancement:
THE SITE:
1. Provided a professional environment to enhance and expand student learning.
2. Provided access to reference materials, either hard copy or via electronic means.

78
3. Had staff that was receptive and willing to interact with students.
4. Afforded the necessary space to complete assignments and meet with the preceptor.
5. Provided adequate contact opportunities with patients and/or healthcare providers.
Additional Comments including site strengths and suggestions for enhancement:
INTERPROFESSIONAL ACTIVITIES:
1. Provided An opportunity to interact in a meaningful way with non-pharmacy healthcare
professionals (e.g. physician, physician assistants, nurses, social workers, dentists, etc.)
2. Provided an opportunity to interact in a meaningful way with other non-pharmacy healthcare
profession students (e.g. medical, nursing, social work, etc.)
Additional Comments including interprofessional activity strengths and suggestions for
enhancement:
Please add comments below. Your feedback is important for continued improvement of the
experiential program.
1. Describe the positive aspects of your learning experience.
2. What changes, if any, do you suggest that may have enabled you to learn more from this
rotation?
3. List the areas/skills that you believe you need to further develop/improve on future
rotations.
4. How did this experience contribute to your career planning?
5. Additional Comments\Suggestions:
