
Dental and Skeletal Maturity
The Journal of Clinical Pediatric Dentistry Volume 36, Number 3/2012 309
A
ccurate evaluation of patient’s growth is important
in many fields of dentistry. The practitioner placing
implants needs to know that skeletal growth is com-
plete.
1,2
The orthodontist benefits from assessing the amount
of skeletal growth already completed in planning orthopedic
treatment.
3
Surgeons likewise assess growth before planning
surgeries involving growing structures.
4
Hand-wrist radi-
ographs are accepted as the standard for skeletal growth
evaluation, but require additional time and exposure of the
patient to additional radiation.
5
For this reason, investigators
have searched for additional ways to assess growth with
commonly taken radiographs, such as periapical, panoramic
and cephalometric radiographs.
3
Dental formation has long been employed as a method to
assess chronological age and skeletal development.
6
Erup-
tion of the dentition was investigated but it is influenced by
systemic and local factors whereas root development is not.
7
Children and adolescents have multiple teeth to evaluate
development, as most of the teeth are still forming. About
the age of 14, most of the teeth cease development at the
apex except third molars.
8
The third molars are the last to
begin development and finish development, and are thus of
interest in evaluating the growth of mid to late teens.
9
This
paper reviews articles using dental development to assess
skeletal growth from routine dental radiographs.
PubMed was searched for the following keywords: skele-
tal maturity, skeletal growth, cervical vertebra maturity,
hand-wrist radiographs, dental maturity, tooth development,
dental staging, dental radiographic stage assessment, dental
mineralization, third molar development, and orthopan-
togram. In addition, hand searches from the references of
relevant studies were performed. All studies were gathered
and reviewed for similarities and differences.
&.)"*+)"' )(!*
There are three main radiographic means to determine
skeletal development: hand-wrist radiographs; cephalomet-
ric radiographs; and panoramic or periapical radiographs.
Skeletal evaluation of the hand can be evaluated by observ-
ing changes in the epiphysis in different joints of the hand,
fusion of plates, and the presence of the sesamoid bone.
Generally, the proximal, middle and distal phalanx of the
third finger, middle phalanx of the fifth finger, sesamoid
bone and the radius are analyzed. Skeletal maturity indices
(SMI) from 1–11 have been described by Fishman (Table
I).
10-12
These stages are useful in determining remaining
growth potential. These 11 stages are divided into four cate-
gories including ephiphyseal widening (SMI 1-3), ossifica-
tion of the sesamoid of the thumb (SMI 4), capping of the
third and fifth finger epiphyses over their diaphyses (SMI
5–7), and finally fusion the third finger epiphyses and
'))$+"'&'&+$+,)"+/."+!#$+$+,)"+/)'%
"' )(!"****%&+-".
John M. Morris * / Jae Hyun Park **
There have been many attempts to correlate dental development with skeletal growth. The relationship is
generally considered to be moderate at best. However, there is evidence that hand-wrist radiographic inter-
pretation of remaining growth can be augmented by taking into account the developing dentition. In addi-
tion, the practicality of evaluating routine dental radiographs and avoiding additional radiation is advan-
tageous. To this point, no system has been described to match apical development by Demirjian’s stages
and compare it to skeletal development and remaining growth. This study reviewed articles pertinent to the
relationship between developing teeth and skeletal maturity and remaining growth, and a system is proposed
to give practitioners an additional assessment for growth and development.
Keywords: dental maturity, skeletal maturity, cervical vertebrae maturity, mandibular third molar
J Clin Pediatr Dent 36(3): 309–314, 2012
* John M. Morris, DDS, DHSc, Private practice, Gilbert, AZ, Former
Postgradaute Orthodontic Resident, Arizona School of Dentistry & Oral
Health, A.T. Still University, Mesa, AZ.
** Jae Hyun Park, DDS, MSD, MS, PhD, Associate Professor and Chair,
Postgraduate Orthodontic Program, Arizona School of Dentistry & Oral
Health, A.T. still University, Mesa, AZ and International Scholar, the
Graduate School of Dentistry, Kyung Hee University, Seoul, Korea.
Send all correspondence to Dr. Jae Hyun Park, Postgraduate Orthodontic
Program, Arizona School of Dentistry & Oral Health, A.T. Still University,
5835 East Still Circle, Mesa, AZ 85206.
Tel: 480.248.8165,
Fax: 480.248.8180
E-mail: [email protected]
Downloaded from http://meridian.allenpress.com/jcpd/article-pdf/36/3/309/2192962/jcpd_36_3_l403471880013622.pdf by Bharati Vidyapeeth Dental College & Hospital user on 25 June 2022
Dental and Skeletal Maturity
tion of hand-wrist films.
23
In contrast, Sidlauskas et al
24
reported a close correlation between hand-wrist films and
m
andibular and maxillary growth. Growth may be difficult
to determine from hand-wrist radiographs during final
stages, such as determining whether an orthognathic patient
is ready for surgery.
25
Thus, additional information that can
be easily acquired should be considered in evaluating
r
emaining growth.
26
+)$(!$'%+)")"' )(!*
)-"$-)+)$%+,)+"'&
Lateral cephalograms show the cervical vertebrae, and
their morphologic changes in size and shape as an individual
grows. These changes are divided into 6 major stages
(Figure 1 and Table I). The vertebrae increase vertically and
horizontally during the stages, and the concavities become
more pronounced as growth occurs.
27
The cervical vertebral
maturation (CVM) stage 1 is correlated with initial of
growth (85-100% remaining); stage 2 with acceleration of
growth (65-85% remaining); stage 3 with transition of
growth (25-65%); stage 4 with deceleration of growth
(10–25%); stage 5 with maturation of growth (5-10%); and
stage 6 with completion of growth (0%).
13
Some have ques-
tioned the reproducibility of staging cervical vertebra, and
intra- and inter-observer consistency is questioned.
28
This
technique has been modified by Bacetti et al
2
9
to include 5
stages on the basis that it is difficult to differentiate between
cervical stage (CS) 1 and 2.
29
Reproducibility of this modi-
fied CVM technique is reportedly as high as 98.6%. With the
use of thyroid collars, CVM1 was revised to include only the
310 The Journal of Clinical Pediatric Dentistry Volume 36, Number 3/2012
diaphysis and radius (SMI 8–11). The clinician can quickly
gauge the remaining growth by first viewing whether the
a
dductor sesamoid bone of the thumb is present. If it is not,
then the epiphyses of the third and fifth finger can be viewed
for widening at select points, and the appropriate stage deter-
mined. If the sesamoid bone is present the third and fifth fin-
ger can be viewed for capping. If there is no capping, then
t
he individual is in the ossification stage. The capping stages
can be determined from the select points of the third and
fifth finger. If the sesamoid is present and capping is com-
pleted, the third finger and radius can be viewed for
fusion.
1
1,12
The peak growth spurt of an individual is between
stages 5–6.
13,14
Accuracy of hand-wrist predictions is greater right
around the peak growth spurt and when different time points
are viewed, which may require repeated radiographic expo-
sure.
15
In addition, single ossification events are not as accu-
rate as bone staging.
16
Hand-wrist radiographs are not difficult to assess or
acquire. However, to decrease radiographic exposure to
patients and when other indications may be utilized for
rough estimates, hand-wrist films may not be practical.
17
Many orthodontists can get adequate estimations of growth
from patient questionnaires, observed growth changes in
patients, and cervical vertebral changes on lateral cephalo-
grams.
Hand-wrist films and the developmental patterns from
the bones are regarded as the standard for evaluating growth.
In original publications, hand-wrist coordinated growth to
statural height, and this has been validated by other stud-
ies.
1
8,19
It is reported, though, that the correlation between
hand-wrist and remaining statural growth is around r = 0.7,
and predicting growth of the face is even lower r = 0.52.
17
Another study measured mandibular growth in three groups
of individuals during acceleration, peak and decelerating
phases of puberty (determined from hand-wrist radiographs)
and found that there were no statistical differences between
the groups.
20
There was, however, an acceleration of
mandibular growth during the peak growth spurt. The
mandibular growth has also been shown to be different in
early or late maturers, and in molar classifications (Class I,
II and III).
21,22
In addition, ethnic variations can introduce
variability in growth patterns, complicating the interpreta-
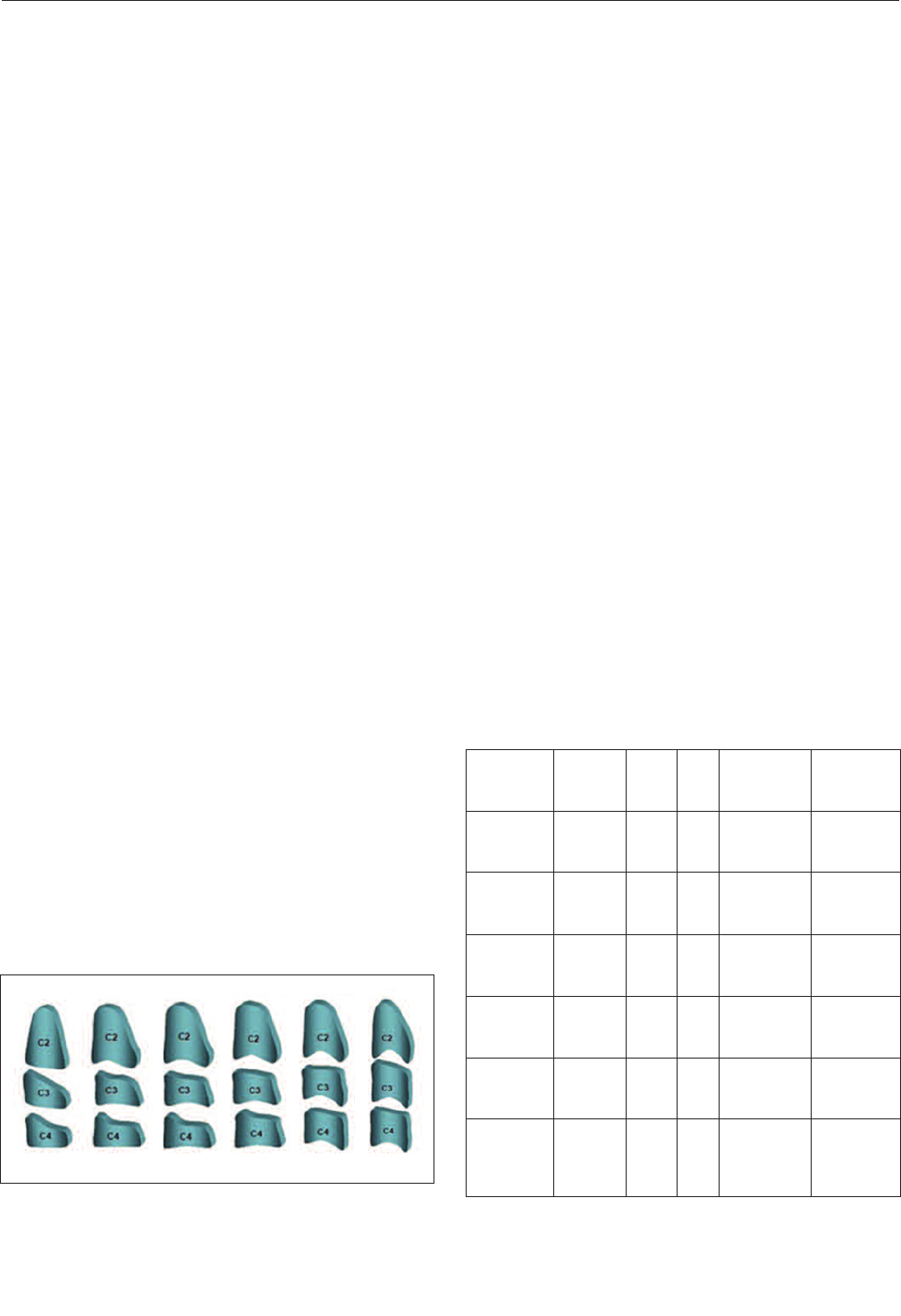
Figure 1. Cervical Maturation Stages. Remaining growth can be
assessed from the morphology of the vertebrae 2-4. As growth
occurs, the vertebrae bodies grow more vertically than horizontally,
and deeper concavities are observed on the lower borders.
CS1 CS2 CS3 CS4 CS5 CS6
Remaining
Pubertal
Growth
Velocity
of
Growth
SMI CS
Dental
Stage
G-H
Mandibular
Third Molar
85%-100% Slow 1-2 1 1st molars
and central
incisors
No bud, or
radiolucent
bud
65%-85% Moderate 3-4 2 1st molars
and central
incisors
Radiolucent
bud
25%-65% Peak 5-6 3 Mandibular
canines
Crown
formation
beginning
10%-25% Moderate 7-8 4 2nd
premolars
Crown
calcification
complete
5%-10% Slow 9-10 5 2nd molars Root
formation
beginning
0% Slow 11 6 All teeth
complete
except third
molars
Root
formation
1/3 to 2/3
SMI, skeletal maturity index according to Fishman;
10
CS, cervical
stage according to Hassel and Farman;
13
Demirjian dental stages
modified by Krailissari et al.
53
Table I. Relationships between skeletal and dental maturity and
their association with growth
Downloaded from http://meridian.allenpress.com/jcpd/article-pdf/36/3/309/2192962/jcpd_36_3_l403471880013622.pdf by Bharati Vidyapeeth Dental College & Hospital user on 25 June 2022
Dental and Skeletal Maturity
The Journal of Clinical Pediatric Dentistry Volume 36, Number 3/2012 311
2–4th vertebrae, as the 5-6th were no longer imaged.
13
Despite criticisms, CVM stages are consistently correlated
w
ith skeletal maturity indicators in the hand.
30-32
Gu and McNamara
3
3
measured mandibular growth
and cervical maturation. They determined that peak
mandibular growth occurs between CS2 and CS3. Average
intervals between stages were 16-17 months, except CS5-
C
S6, which was 12 months. Bacetti et al
29
a
lso investigated
CVM and determined peak mandibular growth and found
peak growth between cervical vertebral maturation stage
(CVMS) II and CVMS III (CS3-CS4). Postpubertal cranio-
facial growth prediction from CVM is modestly effective.
3
4
The cervical vertebrae as maturational indicators offer
several advantages and disadvantages. There is reduced radi-
ation exposure, and cephalograms are routinely taken in an
orthodontic office. Proper interpretation of the stages of
CVM can be problematic, as illustrated in a study where
clinicians trained in CVM interpretation only agreed with
themselves 62% of the time on repeated analysis.
28
The same
study showed an improvement when there are two longitu-
dinal radiographs to review. However, the clinician should
be aware of any and all indicators of growth when treatment
planning, as each individual has their own pattern of growth.
&')%"')()"("$)"' )(!*
&+$-$'(%&+
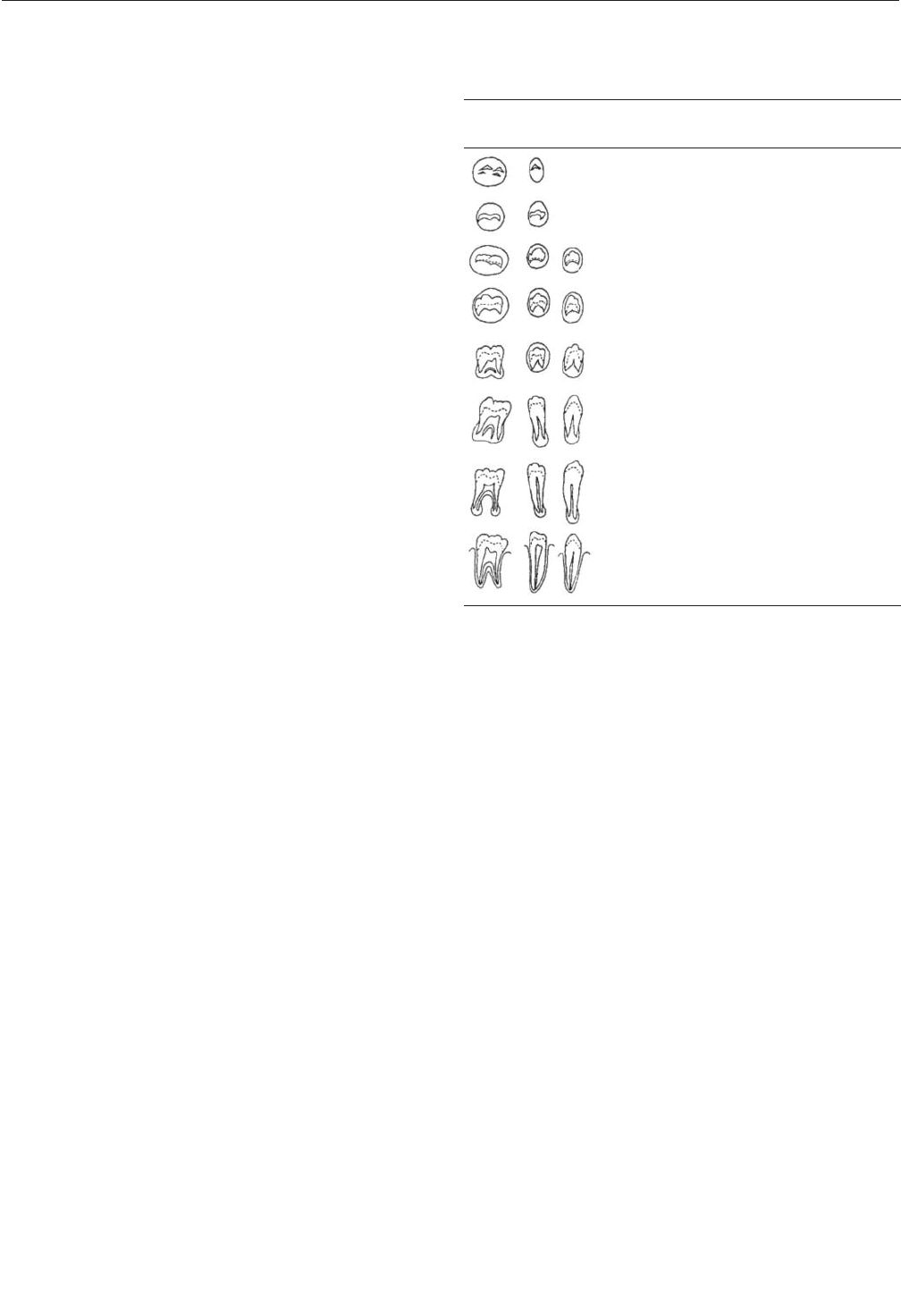
As the teeth develop, the roots undergo similar morpho-
logical stages. These stages have been described by several
authors, and compared to other growth indicators, such as
hand-wrist radiographs and cervical vertebrae. Some com-
mon morphological categories were reviewed.
3
5-39
Among
these, Olze et al
40
reported that Demirjian et al
36
offers the
most reproducible assessment of mandibular third molar
development and is thus employed frequently in staging the
third molar development. Furthermore, Dhanjal et al
41
reported intra-observer agreement was highest using Demir-
jian’s method. The development stages described by Demir-
jian are described in Table II.
Teeth vary in development.
42
This can be due to ethnicity,
sexual differences and on an individual basis. Some develop
early dentally and late skeletally, or vice versa.
43
Dental
maturity is generally accepted in the literature to be variable
and the relationship to skeletal development is reported as
moderate.
15,44-46
While some authors have reported high
correlations between skeletal growth and dental develop-
ment,
7,47-49
others findings have demonstrated low correla-
tions.
50
There is no denying that observing the developing denti-
tion is the quickest and most accessible test for maturity that
is available without additional exposure. For this reason,
several studies have suggested using routine radiographs for
a first estimate or adjunct, and if more detailed information
is needed about growth, additional sources can be
utilized.
3,5,15,51
The mandibular canine is of interest because just before
its apex calcifies it is correlated to other events of
puberty.
43–45,48
This can be useful for an indicator of an
impending growth spurt. The first molar and central incisor
is finishing development at the root apex during cervical
vertebral stage (CVS) 1 and 2, just before or at the beginning
of pubertal growth.
7
By the end of growth, all teeth except
third molars are likely to be finished or near finished in api-
cal development.
52
The mandibular second premolar has shown a high cor-
relation with skeletal markers of the hand, substantiated by
several investigators.
51-53
Basaran et al
7
demonstrated that the
second premolar was nearing completion of apex formation
at the CS4.
Mandibular third molars are useful especially in deter-
mining the remaining growth of a patient over the age of 14,
and offer a unique perspective because their development
lasts an extended period of time.
52,54
Also, in determining
remaining skeletal growth of an orthodontic patient, the
third molar is the only remaining tooth to undergo develop-
ment during final growth.
54
The correlation between mandibular third molar develop-
ment and skeletal development was investigated in several
studies, and some showed a strong relationship between
third molar development and skeletal maturity.
47-49,54,55
In con-
trast, some studies have reported poor relationships.
50,55
Third
molars vary in development by ethnicity and sex, and this
should be considered when evaluating their develop-
ment.
5,7,53,56
Relationships between skeletal, cervical, and
dental maturity associated with growth are summarized in
Table I.
Molar Premolar
Canine
Stage Morphologic Characteristics
A
Calcification of single occlusal
points without fusion
B Fusion of mineralization points
C
Enamel formation completed at the
occlusal surface, dentin formation
started
D
Crown formation complete to the
CEJ, root formation commenced
E
Root length less than crown height,
bifurcation commenced calcification
F
Root length equal or greater than
crown height, roots have distinct
form
G
The walls of the root canal are paral-
lel, apical end open
H
The root apex is completely closed,
periodontal ligaments are uniform
throughout
Table II. Stages of tooth development by Demirjian et al
3
6
modi-
fied by Krailassiri et al
53
(Used with permission from The
Angle Orthodontist)
Downloaded from http://meridian.allenpress.com/jcpd/article-pdf/36/3/309/2192962/jcpd_36_3_l403471880013622.pdf by Bharati Vidyapeeth Dental College & Hospital user on 25 June 2022

Dental and Skeletal Maturity
Dental development is variable. Similar to height measure-
m
ents, the current number or category may not be as impor-
tant as the change. Thus, evaluating the dentition over a
period of time may indicate an individual pattern. If an indi-
vidual is clearly an early dental developer, the teeth finish-
ing apical development may differ from those listed in the
c
hart. This is one of the difficulties of assessing growth – it
may be different for each patient, and skeletal growth can be
different than growth of the dentition or face. All helpful
information should be considered when evaluating growth.
25
Developing tooth apices have been correlated with
stature and menarche.
57
Stature is correlated with skeletal
development.
58
In fact, serial height measurements are a
good way to estimate growth patterns, with a reported high
correlation to height change and skeletal development.
59
In
females, menarche does not always happen before peak
height velocity, though it is a fairly good indicator of accel-
erating growth.
60
It does not appear to be strongly correlated
with dental development. In males, prepubertal to male
voice change can be used with other factors as an indicator
for pubertal growth spurt.
61
Insulin-like growth factor 1
(IGF-1) has also shown promise for use in assessing
growth.
62
Planning orthopedic treatment for orthodontics is impor-
tant. McNamara et al
6
3
reported that in patients treated with
the Frankel appliance, greater increase of mandibular length
was observed during ages closer to puberty. Pancherz and
Hagg
64,65
reported greater effects of Herbst appliance therapy
during peak growth periods. Malmgren et al
66
reported sim-
ilar findings with an activator and high pull headgear. Treat-
ing just before and during the time of peak growth allows for
more skeletal than dental change.
53
It is generally accepted that orthognathic surgery must be
planned to occur after growth has been completed according
to a survey of orthodontists.
67
Often cleft palate patients
undergo surgical intervention during growth, and decreased
postsurgical development of the maxilla has been docu-
mented.
68
This decreased growth and the potential for
changes deviant from the final surgical position can be
avoided by assessing growth and timing treatment when it is
complete.
69
It may be difficult to determine final stages of
growth from hand-wrist. For this reason, it is recommended
that other indicators of growth such as serial cephalometric
radiographs and vertical height changes be viewed, espe-
cially for Class III patients with condylar hyperplasia.
25
Likewise, implant placement requires careful timing. The
ideal treatment for missing teeth may involve either substi-
tution or single tooth implant placement.
70
Timing and treat-
ment is best determined by an interdisciplinary team and
outcomes are improved through a team approach.
71,72
In the
case of a growing patient, space must be managed carefully
for the final implant, which should only be placed when a
patient’s growth is completed. It is recommended that
implants be placed after vertical growth is complete, which
is in the second decade of life.
73
Nevertheless, mature adults
m
ay exhibit vertical growth similar to adolescents and verti-
cal steps due to growth have been observed.
7
4
In some cases,
such as ectodermal dysplasia, implant placement in a grow-
ing patient may be appropriate.
75
Thus, growth determination
is vital to various interdisciplinary treatment planning.
Environmental factors may influence the development of
teeth, but generally root formation is not affected by malnu-
trition, or other processes that interfere with growth.
7
6
Care
should be taken when the patient has any endocrine disor-
ders, or conditions that may cause delayed development of
the dentition. In categorizing dental formation, multiple
stages of development used for dental maturity assessment
and the method of evaluating skeletal maturity introduce
variability.
41
Although Demirjian et al
36
offers good intra-
observer agreement, developing crowns of molars may be
angled so that differing crown stages is not very practical. In
addition, in classification systems the more stages the
greater chance for error.
56
In an effort to increase accuracy,
more stages have been added, but this may make classifying
the stages more difficult.
41,77
Different radiographic techniques may introduce vari-
ables. Accurate radiographs are important in assessing both
the skeletal and dental development structures. It is interest-
ing to note that a study using periapical radiographs of the
third molars had a higher correlation than other studies using
panoramic radiographs.
76
Some advantages are seen with
improved imaging techniques like digital panoramic radi-
ographs.
78
Cone-beam computed tomography (CBCT) imag-
ing systems may further assist assessment of morphological
changes of developing teeth.
Each person has their own individual growth pattern, and
they do not necessarily follow the averages. Skeletal growth
of the long bones of the body does not always correlate
strongly to facial skeletal growth, which should be consid-
ered when treatment planning.
Hand-wrist examination is the gold standard for evaluating
remaining growth, yet it clearly can be augmented with addi-
tional information such as dental development. Cervical ver-
tebrae morphology can also be evaluated for remaining
growth as it correlates strongly with skeletal maturity indi-
cators. The relationship between dental maturity and skele-
tal maturity is reported to be strong, yet should not be the
only evaluation done in assessing growth when more
detailed information is required. There is some promise for
using the dentition as a rough estimator and an adjunct in
evaluating patients for skeletal growth and development. In
addition, in some situations it may obviate the need for addi-
tional exposure for hand-wrist radiographs.
312 The Journal of Clinical Pediatric Dentistry Volume 36, Number 3/2012
Downloaded from http://meridian.allenpress.com/jcpd/article-pdf/36/3/309/2192962/jcpd_36_3_l403471880013622.pdf by Bharati Vidyapeeth Dental College & Hospital user on 25 June 2022

Dental and Skeletal Maturity
The Journal of Clinical Pediatric Dentistry Volume 36, Number 3/2012 313
1. Sharma AB, Vargervik K. Using implants for the growing child. J Calif
Dent Assoc, 34: 719–724, 2006.
2. Carmichael RP, Sándor GKB. Dental implants, growth of the jaws, and
determination of skeletal maturity. Atlas Oral Maxillofac Surg Clin
North Am, 16: 1–9, 2008.
3. Sahin Sağlam AM, Gazilerli U. The relationship between dental and
skeletal maturity. J Orofac Orthop, 63: 454–462, 2002.
4. McIntyre GT. Treatment planning in Class III malocclusion. Dent
Update, 31: 13–20, 2004.
5. Uysal T, Sari Z, Ramoglu SI, Basciftci FA. Relationships between den-
tal and skeletal maturity in Turkish subjects. Angle Orthod, 74:
657–664, 2004.
6. Demisch A, Wartmann P. Calcification of the mandibular third molar
and its relation to skeletal and chronological age in children. Child Dev,
27: 459–473, 1956.
7. Başaran G, Ozer T, Hamamci N. Cervical vertebral and dental maturity
in Turkish subjects. Am J Orthod Dentofacial Orthop, 131: 447.e13–20,
2007.
8. Prieto JL, Barbería E, Ortega R, Magaña C. Evaluation of chronologi-
cal age based on third molar development in the Spanish population. Int
J Legal Med, 119: 349–354, 2005.
9. Lewis JM, Senn DR. Dental age estimation utilizing third molar devel-
opment: A review of principles, methods, and population studies used
in the United States. Forensic Sci Int, 201: 79–83, 2010.
10. Fishman LS. Radiographic evaluation of skeletal maturation. A clini-
cally oriented method based on hand-wrist films. Angle Orthod, 52:
88–112, 1982.
11. Fishman LS. Chronological versus skeletal age, an evaluation of cran-
iofacial growth. Angle Orthod, 49: 181–189, 1979.
12. Fishman LS. Maturational patterns and prediction during adolescence.
Angle Orthod, 57: 178–193, 1987.
13. Hassel B, Farman AG. Skeletal maturation evaluation using cervical
vertebrae. Am J Orthod Dentofacial Orthop, 107: 58–66, 1995.
14. Kamal M, Goyal S. Comparative evaluation of hand wrist radiographs
with cervical vertebrae for skeletal maturation in 10-12 years old chil-
dren. J Indian Soc Pedod Prev Dent, 24: 127–135, 2006.
15. Flores-Mir C, Nebbe B, Major PW. Use of skeletal maturation based on
hand-wrist radiographic analysis as a predictor of facial growth: a sys-
tematic review. Angle Orthod, 74: 118–124, 2004.
16. Hunter CJ. The correlation of facial growth with body height and skele-
tal maturation at adolescence. Angle Orthod, 36: 44–54, 1966.
17. Verma D, Peltomäki T, Jäger A. Reliability of growth prediction with
hand-wrist radiographs. Eur J Orthod, 31: 438–442, 2009.
18. van Rijn RR, Lequin MH, Robben SG, Hop WC, van Kuijk C. Is the
Greulich and Pyle atlas still valid for Dutch Caucasian children today?
Pediatr Radiol, 31: 748–752, 2001.
19. Thodberg HH, Neuhof J, Ranke MB, Jenni OG, Martin DD. Validation
of bone age methods by their ability to predict adult height. Horm Res
Paediatr, 74: 15–22, 2010.
20. Gomes AS, Lima EM. Mandibular growth during adolescence. Angle
Orthod, 76: 786–790, 2006.
21. Silveira AM, Fishman LS, Subtelny JD, Kassebaum DK. Facial growth
during adolescence in early, average and late maturers. Angle Orthod,
62: 185–190, 1992.
22. Alexander AEZ, McNamara JA, Franchi L, Baccetti T. Semilongitudi-
nal cephalometric study of craniofacial growth in untreated Class III
malocclusion. Am J Orthod Dentofacial Orthop, 135: 700–701, 2009.
23. Mora S, Boechat MI, Pietka E, Huang HK, Gilsanz V. Skeletal age
determinations in children of European and African descent: applica-
bility of the Greulich and Pyle standards. Pediatr Res, 50: 624–628,
2001.
24. Sidlauskas A, Zilinskaite L, Svalkauskiene V. Mandibular pubertal
growth spurt prediction. Part one: Method based on the hand-wrist radi-
ographs. Stomatologija, 7: 16–20, 2005.
25. Wolford LM, Karras SC, Mehra P. Considerations for orthognathic
surgery during growth, part 2: maxillary deformities. Am J Orthod
Dentofacial Orthop, 119: 102–105, 2001.
26. Sato K, Mito T, Mitani H. An accurate method of predicting mandibu-
lar growth potential based on bone maturity. Am J Orthod Dentofacial
Orthop, 120: 286–293, 2001.
27. Mourelle R, Barbería E, Gallardo N, Lucavechi T. Correlation between
dental maturation and bone growth markers in paediatric patients. Eur
J Paediatr Dent, 9: 23–29, 2008.
28. Gabriel DB, Southard KA, Qian F, et al. Cervical vertebrae maturation
method: poor reproducibility. Am J Orthod Dentofacial Orthop, 136:
478–480, 2009.
29. Baccetti T, Franchi L, McNamara JA. An improved version of the cer-
vical vertebral maturation (CVM) method for the assessment of
mandibular growth. Angle Orthod, 72: 316–323, 2002.
30. Gandini P, Mancini M, Andreani F. A comparison of hand-wrist bone
and cervical vertebral analyses in measuring skeletal maturation. Angle
Orthod, 76: 984–989, 2006.
31. San Román P, Palma JC, Oteo MD, Nevado E. Skeletal maturation
determined by cervical vertebrae development. Eur J Orthod, 24:
303–311, 2002.
32. Lai EH, Liu J, Chang JZ, et al. Radiographic assessment of skeletal
maturation stages for orthodontic patients: hand-wrist bones or cervical
vertebrae? J Formos Med Assoc, 107: 316–325, 2008.
33. Gu Y, McNamara JA. Mandibular growth changes and cervical verte-
bral maturation. a cephalometric implant study. Angle Orthod, 77:
947–953, 2007.
34. Fudalej P, Bollen A. Effectiveness of the cervical vertebral maturation
method to predict postpeak circumpubertal growth of craniofacial
structures. Am J Orthod Dentofacial Orthop, 137: 59–65, 2010.
35. Gleiser I, Hunt EE. The permanent mandibular first molar: its calcifi-
cation, eruption and decay. Am J Phys Anthropol, 13: 253–283, 1955.
36. Demirjian A, Goldstein H, Tanner JM. A new system of dental age
assessment. Hum Biol, 45: 211–227, 1973.
37. Gustafson G, Koch G. Age estimation up to 16 years of age based on
dental development. Odontol Revy, 25: 297–306, 1974.
38. Harris MJ, Nortjé CJ. The mesial root of the third mandibular molar. A
possible indicator of age. J Forensic Odontostomatol, 2: 39–43, 1984.
39. Kullman L, Johanson G, Akesson L. Root development of the lower
third molar and its relation to chronological age. Swed Dent J, 16:
161–167, 1992.
40. Olze A, Bilang D, Schmidt S, et al. Validation of common classifica-
tion systems for assessing the mineralization of third molars. Int J
Legal Med, 119: 22–26, 2005.
41. Dhanjal KS, Bhardwaj MK, Liversidge HM. Reproducibility of radi-
ographic stage assessment of third molars. Forensic Sci Int, 159 Suppl
1: S74–77, 2006.
42. Lewis AB. Comparisons between dental and skeletal ages. Angle
Orthod, 61: 87–92, 1991.
43. Nadler GL. Earlier dental maturation: fact or fiction? Angle Orthod, 68:
535–538, 1998.
44. Chertkow S. Tooth mineralization as an indicator of the pubertal
growth spurt. Am J Orthod, 77: 79–91, 1980.
45. Coutinho S, Buschang PH, Miranda F. Relationships between
mandibular canine calcification stages and skeletal maturity. Am J
Orthod Dentofacial Orthop, 104: 262–268, 1993.
46. So LL. Skeletal maturation of the hand and wrist and its correlation
with dental development. Aust Orthod J, 15: 1–9, 1997.
47. Engström C, Engström H, Sagne S. Lower third molar development in
relation to skeletal maturity and chronological age. Angle Orthod, 53:
97–106, 1983.
48. Sierra AM. Assessment of dental and skeletal maturity. A new
approach. Angle Orthod, 57: 194–208, 1987.
49. Lauterstein AM. A cross-sectional study in dental development and
skeletal age. J Am Dent Assoc, 62: 161–167, 1961.
Downloaded from http://meridian.allenpress.com/jcpd/article-pdf/36/3/309/2192962/jcpd_36_3_l403471880013622.pdf by Bharati Vidyapeeth Dental College & Hospital user on 25 June 2022

Dental and Skeletal Maturity
50. Demirjian A, Buschang PH, Tanguay R, Patterson DK. Interrelation-
ships among measures of somatic, skeletal, dental, and sexual maturity.
Am J Orthod, 88: 433–438, 1985.
51. Rózylo-Kalinowska I, Kolasa-Raczka A, Kalinowski P. Relationship
between dental age according to Demirjian and cervical vertebrae
maturity in Polish children. www.ncbi.nlm.nih.gov/pubmed/20558591
accessed August 15th, 2010.
52. Sisman Y, Uysal T, Yagmur F, Ramoglu SI. Third-molar development
in relation to chronologic age in Turkish children and young adults.
Angle Orthod, 77: 1040–1045, 2007.
53. Krailassiri S, Anuwongnukroh N, Dechkunakorn S. Relationships
between dental calcification stages and skeletal maturity indicators in
Thai individuals. Angle Orthod, 72: 155–166, 2002.
54. Cho S, Hwang C. Skeletal maturation evaluation using mandibular
third molar development in adolescents. Korean J Orthod, 39: 120,
2009.
55. Steel GH. The relation between dental maturation and physiological
maturity. Dent Pract Dent Rec, 16: 23–34, 1965.
56. Bai Y, Mao J, Zhu S, Wei W. Third-molar development in relation to
chronologic age in young adults of central China. J Huazhong Univ Sci
Technol Med Sci, 28: 487–490, 2008.
57. So LL. Correlation of sexual maturation with stature and body weight
& dental maturation in southern Chinese girls. Aust Orthod J,
14:18–20, 1995.
58. Moore RN. Principles of dentofacial orthopedics. Semin Orthod, 3:
212–221, 1997.
59. Moore RN, Moyer BA, DuBois LM. Skeletal maturation and craniofa-
cial growth. Am J Orthod Dentofacial Orthop, 98: 33–40, 1990.
60. Hägg U, Taranger J. Maturation indicators and the pubertal growth
spurt. Am J Orthod, 82: 299–309, 1982.
61. Kucukkeles N, Acar A, Biren S, Arun T. Comparisons between cervi-
cal vertebrae and hand-wrist maturation for the assessment of skeletal
maturity. J Clin Pediatr Dent, 24: 47–52, 1999.
62. Masoud MI, Masoud I, Kent RL, et al. Relationship between blood-
spot insulin-like growth factor 1 levels and hand-wrist assessment of
skeletal maturity. Am J Orthod Dentofacial Orthop, 136: 59–64, 2009.
63. McNamara JA, Bookstein FL, Shaughnessy TG. Skeletal and dental
changes following functional regulator therapy on Class II patients. Am
J Orthod, 88: 91–110, 1985.
64. Hägg U, Pancherz H. Dentofacial orthopaedics in relation to chrono-
logical age, growth period and skeletal development. An analysis of 72
male patients with Class II division 1 malocclusion treated with the
Herbst appliance. Eur J Orthod, 10: 169–176, 1988.
65. Pancherz H, Hägg U. Dentofacial orthopedics in relation to somatic
maturation. An analysis of 70 consecutive cases treated with the Herbst
appliance. Am J Orthod, 88: 273–287, 1985.
66. Malmgren O, Omblus J, Hägg U, Pancherz H. Treatment with an ortho-
pedic appliance system in relation to treatment intensity and growth
periods. A study of initial effects. Am J Orthod Dentofacial Orthop, 91:
143–151, 1987.
67. Weaver N, Glover K, Major P, Varnhagen C, Grace M. Age limitation
on provision of orthopedic therapy and orthognathic surgery. Am J
Orthod Dentofacial Orthop, 113: 156–164, 1998.
68. Wolford LM, Cassano DS, Cottrell DA, et al. Orthognathic surgery in
the young cleft patient: preliminary study on subsequent facial growth.
J Oral Maxillofac Surg, 66: 2524–2536, 2008.
69. Bailey LJ, White RP, Proffit WR, Turvey TA. Segmental LeFort I
osteotomy for management of transverse maxillary deficiency. J Oral
Maxillofac Surg, 55: 728–731, 1997.
70. Kokich VG, Spear FM. Guidelines for managing the orthodontic-
restorative patient. Semin Orthod, 3: 3–20, 1997.
71. Richardson G, Russell KA. Congenitally missing maxillary lateral
incisors and orthodontic treatment considerations for the single-tooth
implant. J Can Dent Assoc, 67: 25–28, 2001.
72. Lewis BRK, Gahan MJ, Hodge TM, Moore D. The orthodontic-restora-
tive interface: 2. Compensating for variations in tooth number and
shape. Dent Update, 37: 138–140, 142–144, 146–148, 2010.
73. Fudalej P, Kokich VG, Leroux B. Determining the cessation of vertical
growth of the craniofacial structures to facilitate placement of single-
tooth implants. Am J Orthod Dentofacial Orthop, 131(4 Suppl):
S59–67, 2007.
74. Bernard JP, Schatz JP, Christou P, Belser U, Kiliaridis S. Long-term
vertical changes of the anterior maxillary teeth adjacent to single
implants in young and mature adults. A retrospective study. J Clin Peri-
odontol, 31: 1024–1028, 2004.
75. Sharma AB, Vargervik K. Using implants for the growing child. J Calif
Dent Assoc, 34: 719–724, 2006.
76. Bhat VJ, Kamath GP. Age estimation from root development of
mandibular third molars in comparison with skeletal age of wrist joint.
Am J Forensic Med Pathol, 28: 238–241, 2007.
77. Moorrees CF, Fanning EA, Hunt EE. Age variation of formation stages
for ten permanent teeth. J Dent Res, 42: 1490–1502, 1963.
78. Introna F, Santoro V, De Donno A, Belviso M. Morphologic analysis of
third-molar maturity by digital orthopantomographic assessment. Am J
Forensic Med Pathol, 29: 55–61, 2008.
314 The Journal of Clinical Pediatric Dentistry Volume 36, Number 3/2012
Downloaded from http://meridian.allenpress.com/jcpd/article-pdf/36/3/309/2192962/jcpd_36_3_l403471880013622.pdf by Bharati Vidyapeeth Dental College & Hospital user on 25 June 2022
