
COMPASS
Winter 2023
2 0 23 WINTER
NEW SLETTE R
THE QUARTERLY
Winter 2024 Newsletter
2
President’s Message
Happy New Year to all! As I reflect on the
start to the new year and my short time
at the Health Alliance, I think about the
Saint Alphonsus promise, We Listen, We
Partner, We Make it Easy. This promise not
only applies to how we care for patients,
but believe it is no less important in how
we partner with clinicians. Given the strong
history of the Health Alliance clinically
integrated network(CIN) I think the new
year is a great time to reflect on HOW we
do this.
We Listen……we want to hear from you. How can we
at the Alliance help support you to ensure success
in caring for patients and being good resource
stewards? In addition to the Health Alliance sta,
our board and committees consist of both Saint
Alphonsus and independent clinicians who best
represent our network participants and ensure their
interests are prioritized. These individuals are listed
on our website or if you have questions or concerns
you wish to discuss, please reach to me directly.
We Partner…..our sta are often physically out
working in clinics to be an additional resource and
extra set of hands to help get the work done. We
share best practices, gather quality data and how
to create eciencies. Our team helps to ensure
providers are getting credit for the great care they
deliver and maximize performance under advanced
payment models/value-based contracts.
Warm Regards,
We Make it Easy….most things in healthcare are
not easy, but we at the Health Alliance strive to
eliminate barriers, smooth processes and bring the
caring, human-element to this work in support of
our network participants. Our role is to bring forth
resources that do make things easier to care for
patients, conduct the business of health care and be
reasonably compensated for the eort.
We look forward to the new year ahead and working
closely with you and your care teams to serve
patients in the Treasure Valley and surrounding
areas.
Stacy Meyr, DC
President
Saint Alphonsus Health Alliance

3
Annual Wellness and Preventative Care Visits
As we enter a new year, it is crucial for healthcare
providers to prioritize the scheduling of Annual
Wellness Visits (AWVs) to ensure comprehensive
care of their patients. Utilizing your patient roster(s)
at the beginning of the year to perform outreach can
significantly improve the success rate in scheduling
these important visits. Paying attention to the “new”
column on your roster is essential to ensure that
patients who are new to your practice, new to the
plan, and especially new to Medicare, are scheduled
for their AWVs or Preventative Care Visits (PCVs).
This approach allows for the capture of all active
conditions including those diagnosed prior to
Medicare enrollment.
In line with best practices and to reduce the need for
outreach, it is recommended to proactively schedule
each patient for next year’s AWV at the time of
checkout. AWVs may be our only face to face
opportunity to address all active chronic conditions
within the calendar year and should represent the
patient’s overall state of health at the time of service.
The Saint Alphonsus Health Alliance All in One
Report and Pre-Visit Planning Sheets are helpful
resources in performing some of the cognitive work
of the provider by identifying past reported chronic
conditions. By implementing these strategies and
staying diligent in scheduling AWVs, providers
can enhance patient care, improve recapture and
documentation of active conditions, contributing
to a more comprehensive and coordinated approach
to healthcare delivery.
A more accurate Risk Adjustment Factor (RAF) may
be measured by implementing The Saint Alphonsus
Health Alliance provided Clinic Rosters, All in One
Report, and Pre-Visit Planning Sheets to increase
both the number of AWVs scheduled and chronic
condition recapture rate in your daily practice.
4
Medicaid | Well & Sick Visits
Combining Well Visit with Sick Visits
Q: Can you bill Medicaid for a sick and well visit on the same patient encounter?
A: YES! Medicaid will accept and pay claims for a sick and well visit that occur during the same patient
appointment.
Report the additional CPT code with Modifier-25
Based on the guidelines from the AMA:
https://www.ama-assn.org/practice-management/cpt/can-physicians-bill-both-preventive-
and-em-services-same-visit
If provider has time to do so – conducting well visit services during sick visit appointment means:
• Patients receive additional, appropriate care.
• Practice receives increased reimbursement.
• VCO Program quality measures have better chance of being met.

5
Statin use with Diabetics (DM)
and Cardiovascular Disease (CVD)
CMS continues to grade how many of our patients with DM or CVD are prescribed and taking statins. But
what if the patient is intolerant to statins?
Patients will be removed from the list if there is documentation of an intolerance of statin, but one of
the following exclusion codes must be submitted at least annually within a visit:
• G72.0 Drug-induced myopathy
• G72.9 Myopathy, unspecified
• M60.80 Other myositis, unspecified
• M60.9 Myositis, unspecified
• M62.82 Rhabdomyolysis
Please remember to add to the problem list to ensure the code is submitted annually during the annual
wellness visit.

6
Hypertension in Patients 81-85
Did you know we are graded on blood pressure control in adults aged 18-85? For those who are on the
older age of that spectrum we can exclude those who are medically frail.
Patients will be excluded from the list if they are aged 81-85 and there is documentation of a frailty code.
One of the following must be submitted at least annually within a visit:
R53.1 Weakness
R53.83 Other fatigue
W01.0XXA-W01.198S, W06.XXXAW10.9XXS, W18.00XA-W19.XXXS Fall
Z73.6 Limitation of activities due to disability
Z74.09 Other reduced mobility
Z74.1 Need for assistance with personal care
Z91.81 History of falling
Please remember to add to the problem list to ensure the code is submitted annually during the annual
wellness visit.
7
Post-Acute Care and Treasure Valley
Skilled Nursing Facilities
We care about the care our patients receive in a
skilled nursing facility (SNFs) and if the facility
our patients choose, provides quality, optimized,
safe care. Our Post-Acute Care Management Team
monitors CMS quality metrics, Trinity Health quality
metrics and individual skilled facility data monthly.
We have recently updated our Quality of Care
Profiles (QoCP) which are patient materials provided
to patients and families when helping them choose a
facility for next site of care. We ask our SNF partners
listed as ‘quality’ to share in our quality measures
and hold them accountable for performance related
to readmissions, optimized length of stay, and
Star Ratings. We also monitor and track health
inspections, stang, and SNF quality measures to
ensure they provide safe and just care for all. When
necessary, we also meet with our SNF partners to
discuss concerning readmissions or patient care
issues that we have been notified of.
Quality of Care Metrics
To earn and maintain their listing on the QoCP,
SNFs must achieve and maintain an average length
of stay of less than 22 days, and have 30 and
60 day readmissions of less than 18%. The SNF
must also allow our RNs to participate in patient
care meetings, fax medication lists, discharge
appointments, and home health agency information
to our Health Information Management fax for
immediate uploading after discharge.
Our mission and expectations of the QoCP
is to provide safe and just care for all. Saint
Alphonsus understands there may be unique
circumstances where it is not possible to meet
all metric expectations. With regular and robust
communication, we can improve the quality of care
for our shared patients and safely transition them
back to the Primary Care Provider.
https://mytrinityhealth.sharepoint.com/sites/SAHS-PostAccuteCareMgmt/Shared%20Documents/Forms/
AllItems.aspx

8
Patient Care Liaisons
Saint Alphonsus Health Alliance has dedicated
clinical Patient Care Liaisons for your patients to
assist with navigation throughout our healthcare
system.
• Assist with coordination of referrals or scheduling,
including inpatient, outpatient, post-acute and
practice-based care settings
• Help your patients find in-network providers to
avoid/minimize patient out-of-pocket costs
• Assist with proactive gap authorization when out-
of-network services are truly required
• Assist with payer authorizations if you are running
into roadblocks in certain cases
• Assist with all pediatric referral questions
Please be aware that Saint Alphonsus Health Alliance network has providers who can handle certain
pediatric specialty services, the challenge is that many of these services have age-determined restrictions.
Referrals to non-network providers will likely cause a much higher out of pocket expense for your patients.
Call our patient care liason department:
Monday - Friday (8am-5pm MST)
Aetna/Trinity - Saint Alphonsus Colleague Plan
(208) 367-SAHS
Blue Cross of Idaho - Connected Care
Alpha Prefix: XMO, XMU, ISN
(208) 367-INFO
Saint Alphonsus Health Plan - formerly MediGold
(208) 367-INFO
Mountain Health Co-op - Access Care
(208) 367-INFO
Regence Blue Shield of Idaho - Individual & Family Network (IAFN)/Accord
(208) 367-INFO
MODA - Select Individual & Group Plans
(208) 367-INFO
Select Health - SAHA Individual & Group Plans
(208) 367-INFO

1
GLP-1
Prescriber Guide
A PRIMARY CARE RESOURCE FROM EXPERTS
Michael Twomey, MD | Julie Foote, MD | Christopher Reising, MD
Amber Kirtley-Perez, PA-C | Sara Heiner, PharmD

GLP-1 Prescriber Guide
A PRIMARY CARE RESOURCE FROM EXPERTS

As providers grapple with the right way to manage chronic diseases, medical
costs seem to be skyrocketing while quality of care appears just out of reach.
GLP-1 agonists are one class of medication at the crossroads of improved quality and pharmaceutical
profit. How can we use these drugs eectively? Can we be a steward of value in a landscape that
highlights financial and health inequities?
Our panel attempted to take a crack at these dicult questions and give primary care providers a guide
for how to interpret the myriad of studies. We strive to provide you with the knowledge of the current
prescription landscape, the true cost of GLP-1 medications, and philosophies of use in the chronic diseases
of diabetes and obesity.
1
GLP-1 Prescriber Guide
For too long, non-insulin diabetic treatments comprised of medications which exacerbated or worsened
cardiac disease. Treatment was necessary but came with a medical burden. With the advent of the
SGLT2i and GLP-1 classes came a paradigm shift. We now had treatments beyond Metformin with proven
reduction in the risk of heart attack, stroke, and death. Patients and providers flocked to these new classes
for good reason.
DATA
Speaking to the GLP-1 class alone, Ozempic
(semaglutide) showed a Number Needed to Treat
(NNT) to prevent one cardiovascular (CV) event
of 45 in the SUSTAIN
1
trial of diabetics while
Victoza (liraglutide) showed an NNT of 66 in the
LEADER trial.
2
For perspective, the NNT for statins
is 28 for our highest risk patients
3
and is 70 or
greater in the moderate to low-risk spectrum.
4
This class represents powerful A1c reduction for
your patients. A1c improvement ranges from 0.4
to 1.5 for non-insulin medications. GLP-1s routinely
score at the top of that spectrum representing
one of our best tools we have to optimize control.
The dierence between a controlled A1c and an
uncontrolled A1c could be over 3.5 years to your
patient’s life!
5
But enough about living longer—lets talk about
weight! For many, the most visible benefit of these
medications is the weight loss potential. Average
starting weight in these trials was 220 pounds
with a total weight loss of up to 12 – 46 pounds
depending on medication.
Brand Generic
Weight Loss
on Max Dose
Time Frame Trial
Mounjaro Tirzepatide 20.9% 26 weeks SURMOUNT
6
Victoza Liraglutide 5.8% 56 weeks SCALE
7
Ozempic Semaglutide 17.4% 68 weeks STEP
7
2

Of course, there is more to the story...
DATA
Here are some nuances to help us understand
how to apply these medications in our practices.
Ozempic’s SUSTAIN Trial was of course comprised
of diabetics, but 83% had established CV disease
or seen as high risk. In a low-risk patient, the NNT
for prevention of any CV event could be much
higher. In a population of high-risk obese patients
without diabetes, Wegovy (high dose semaglutide)
showed an NNT of 63. That number alone looks
intriguing, however the cost of prevention for each
event is $1.1 million.
8
As providers, we know quality of life is invaluable
and prevention of any event is important. However,
with many possible interventions regarding heart
disease, it is valuable to first prioritize those most
cost eective. Make sure that we do not lose sight
of the value of generic treatments such as ACEi,
statins, beta blockers and aspirin where appropriate.
Meanwhile, all weight loss studies used motivated,
engaged patients, with the addition of lifestyle
changes. The dierences between placebo and
medication were incredible, but it is dicult to
recreate the important support structure in a busy
primary care center. In the real world, only 50%
of patients are adherent to therapy at 12 months
9
and many suer from significant nausea or other
side eects.
ACCESS
As the popularity of these drugs has risen, it has
become increasingly more dicult to prescribe.
Insurances have initiated prior authorizations and
step-throughs to combat rising claim costs and
access is very dicult to ensure. Too often a patient
is calling multiple pharmacies searching for any
available prescription of a GLP-1. Some of the supply
issues will improve in time, but expect increasing
restrictions from insurance companies over the
next few years.
3
4
GLP-1 Prescriber Guide
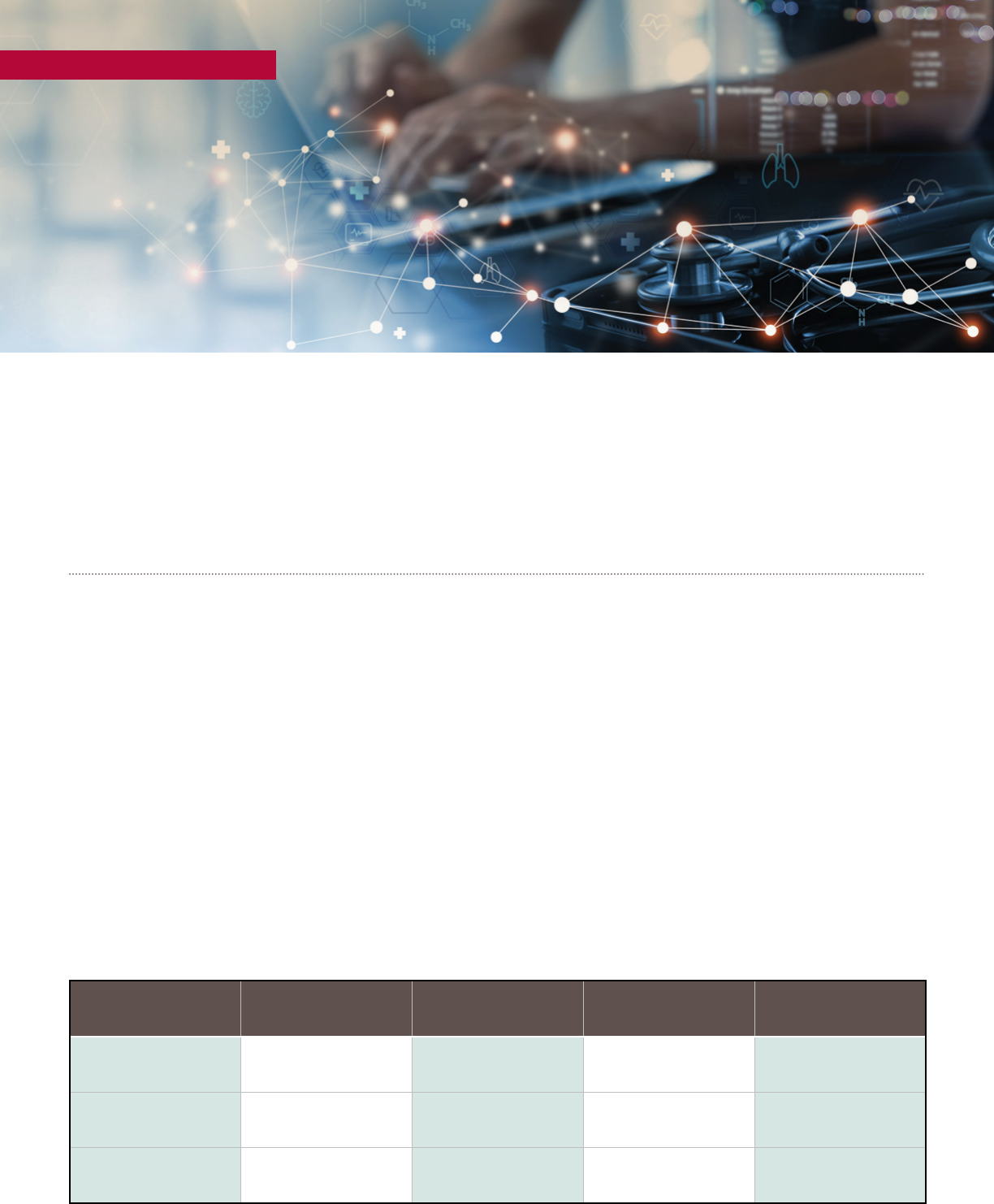
COST
Even compared to other branded diabetic medications, these drugs pack a heavy punch. SGLT2i are
$4,000-$7,000 per year prior to rebates. Unfortunately, GLP-1s are double the cost ranging from $10,800
for Byetta all the way to $19,200 for Wegovy. For comparison, an average hospitalization (4.5 days) cost
$12,974 in 2021! No matter what the patient’s copay, this represents a large medical cost to the system.
Overall, pharmacy spending accounts for 25% of total costs. Diabetic medication represents about a
quarter of the pharmacy claims. As costs increase, we continue see them often passed on to the patient
through higher deductibles, copays, and premiums.
In Medicare plans, the donut hole
represents an additional burden. Let’s
follow a patient example on a GLP-1:
As you can see, the donut hole
creates an expensive situation
where patients may be surprised
by the cost changes. With just a
GLP-1 medication, the patient will
be stuck in the donut hole for the
rest of the year but experience big
fluctuations to their out-of-pocket
cost. Non-compliance is common
during this period and some
patients end up discontinuing all
of their prescriptions due to cost.
JANUARY
At the beginning of the year, a patient’s
first fill will hit the deductible. This could
be up to $505 and depends on the plan.
FEBRUARY - MAY
The next few fills will be around $50 and will
represent just the plan’s branded co-payment.
JUNE - DECEMBER
After about five months of
therapy,
the patient will
fall into the donut hole
and suddenly be charged ~$275
per month (25% of the total
cost of the medication).
This will continue for the rest
of the year or until the patient
pays over $8,000 out of
pocket in drug costs!

Julie Foote, MD Christopher Reising, MD Michael Twomey, MD Amber Kirtley-Perez PA-C Sara Heiner, PharmD
So, what should you do?
To help guide us through the weight of these
complex medical decisions we empaneled Dr.
Foote, MD in Endocrinology, Dr. Reising, MD in
Bariatric Surgery, Amber Kirtley-Perez, PA-C in
Wellness, and Sara Heiner, Pharm-D to help.
TYPE 2 DIABETES
Diabetic care is inherently individual, and the right
class of medication will depend on many factors.
We still recommend starting with metformin. In
order to maximize the tolerance of this drug,
consider extended-release forms to reduce GI
upset and have them take it with their largest
meal. The most improvement in A1c occurs from
0 – 1000mg so any amount the patient can take
helps! Always consider ways you can restart or
increase metformin use. In patients on insulin, but
without current metformin, restarting therapy can
reduce insulin use by 7-20U per day! This could be
a cost savings of $1,200 per year while reducing
weight gain and insulin resistance.
Be careful of duplicate therapy! We still see patients
on both a DPP-4i and a GLP-1. These are easy to
identify in your practice by simply focusing on
reduced use of the DPP-4i class entirely. Most
would benefit more from a cardioprotective
standpoint by shifting to an SGLT2i for a similar
cost & A1c reduction.
Avoid adding on any diabetic medication if the
patient has a well-controlled A1c < 7. The risk of
side eects and polypharmacy is real, and the
benefit is less clear in these scenarios. The major
exception to this rule is patients with both diabetes
and established heart disease. Data is clear that
adding on an SGLT2i will reduce the risk of
cardiovascular hospitalization and they are
separately indicated in cardiovascular disease.
Afterwards, it really is a patient and physician
discussion. Consider co-morbid diseases and identify
if the patient will benefit greater from an SGLT2i vs
GLP1. From a quality standpoint, both classes are
superior in comparison to the older sulfonylureas
or thiazolidinediones. However, it is unrealistic to
expect all patients to be able to tolerate or aord
these medications and there is still room for use
of older medications classes. Most of the time,
your patients would benefit from both SGLT2i and
GLP1’s prior to adding insulin. If cost becomes a
concern, there are income programs provided by
the drug manufacturer that may help. Reach out
to a CHW or pharmacist through an EPIC referral
to help. Remember, you may be burdened by
multiple prescription rejections after dealing with
prior authorizations, drug shortages, and sticker
shock. In the end, the best medication is the one
your patient can take. Being honest about the total
cost of care will ensure both you and the patient
are realistic about medication adherence.
5

GLP-1 Prescriber Guide
OBESITY
No weight loss program works without providing
a multimodal and multidisciplinary treatment
approach. The right patient is motivated and
engaged to achieve a long-term outcome. The
bariatric philosophy is to provide this partnership
for at least six months prior to any surgical
intervention to gage this readiness. Those resources
are not always available in a busy clinical practice
and GLP-1s are not a panacea to a poor lifestyle
structure. Although they help with weight loss
in the first year, once discontinued, two-thirds
of the weight is gained back in one year and the
patient is usually back to initial weight just two
years later. In the end, the weight loss medications
are tempting, but there isn’t a BMI level where we
should be pushing them on patients. Instead,
a focus on managing macro-nutrients through
education and dietary services with medication
as an adjunct is the correct perspective. Here are
some helpful hints for your practice.
Best management for patients asking for GLP-1s
for weight loss is to create a strategic plan prior
to initiation. Start with a face-to-face appointment
with an initial weight and discuss the pros and
cons of therapy. Remind patients they will not
be successful in the long run without lifestyle
changes. Meet with them monthly with weight
loss, macronutrient, and activity (not necessarily
exercise) goals. Providers can benefit from
requiring a visit with a dietician during the initial
stages of management. Unfortunately, Medicare
does not cover dietician services and exceptions
may need to be made for those patients. If they
are not meeting goals (intolerance, lack of weight
loss, no-shows), the medication should be
discontinued, and alternative therapy should be
considered. Set clear expectations for when to
stop the medication and support the patients after
stopping to avoid rebound weight gain. Discourage
the use of compounded medications and non-FDA
approved forms of drugs as their safety is unclear.
Finally, refer to bariatrics for more extensive
support. Consider wellness and health coaches.
Utilize embedded community programs that
encourage socialization, accountability with
other like-minded members, and share education.
6

WELLNESS
As you know, we cannot manage these chronic
disease states with medication alone. Our aspirations
as providers must be greater to achieve true quality
in our practice. It is through community that
patients can help hold themselves accountable
outside of your oce visit—where all the magic
happens! Fortunately, help is on the horizon. The
exciting space of wellness medicine is focused on
building those small groups of patients—allowing
them to share and educate each other. Currently
working on heart health, our wellness team is
looking to touch every cardiac rehab patient to
improve outcomes. As we move forward, health
coaches, chronic case management from nurses,
and community health resources will be vital to
the management of both diabetes and obesity.
For now, use your existing resources. Get patients
engaged with nursing for education and management,
give a number to a local support group of patients
with the same disease, use diabetic education
regularly, refer to CHW’s for social determinants of
health, and refer to wellness medicine if appropriate.
Diabetic Education
Currently oered at Saint Alphonsus Glycemic
Boise, 12th Avenue in Nampa, West Chery Lane
in Meridian, and SW 9th Street in Ontario. As a
reminder there are four great times to refer for
Diabetic Education:
1. At diagnosis (10h)
2. Annually or when not meeting treatment
targets (2h)
3. When complicating factors develop (2h)
4. When a transition in life or care happens (2h)
Bariatric Support Group
Monthly free bariatric support group open to all
patients on at any stage. Currently meets on the
third Thursday of every month at 6:00 PM virtually.
To sign up for group email notifications patients
may fill out a form on the SAHS web:
SaintAlphonsus.org/specialty/bariatric-surgery/
education-and-support/support-groups
or call the Saint Alphonsus General Surgery
and Bariatric Clinic at (208) 302-2300
7
8
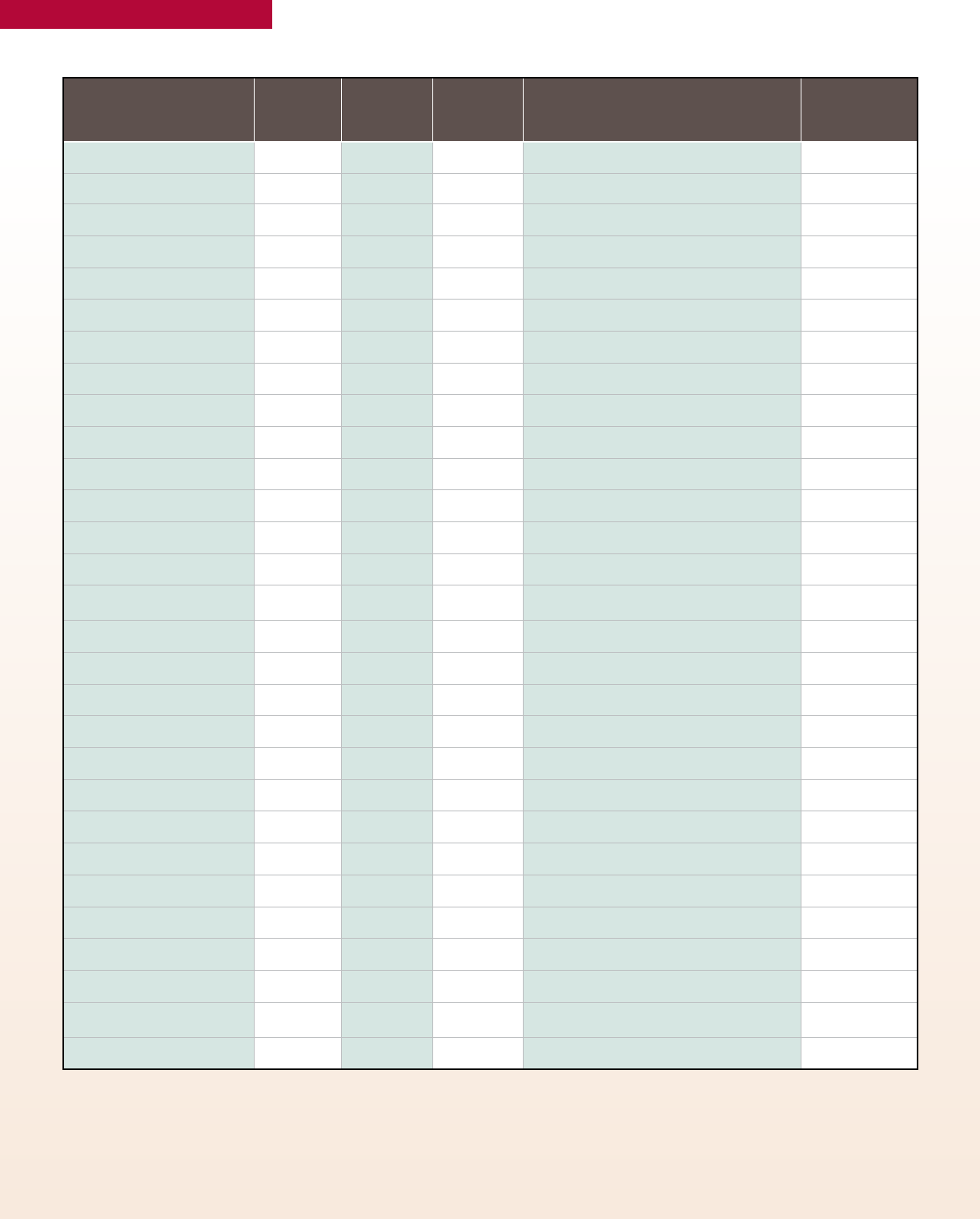
GLP-1 Prescriber Guide
REGISTERED DIETICIANS
LANGUAGE
SPOKEN
ACCEPTING
MEDICARE
ACCEPTING
MEDICAID
CLINIC NAME CITY
Erin Rae, RD No No Apex Chiropractic & Wellness Boise
Kelly Wood, RD No No Be Well Nutrition, LLC Boise
Jennifer Anthony, RD Yes Yes Full Circle Health – Raymond Boise
Kelsey Ruszel, RD Yes Yes Full Circle Health – Raymond Boise
Spring Bean, RD ASL Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Medina Blanchet, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Brenda Bourn, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Jennifer Buker, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Margaret Capron, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Maryanne Cunningham, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Deena La Joie, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Rachael Tatko, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Sariah Wilson, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Kelly Wood, RD Yes No Idaho Nutrition Associates, LLC – Wainwright Boise
Laura Nielsen, RD Yes Yes
Saint Alphonsus General Surgery & Bariatrics
– Mulvaney
Boise
Sandra Dammarell, RD Yes Yes Saint Alphonsus Glycemic Boise Boise
Sandra Horrocks, RD Yes Yes Saint Alphonsus Glycemic Boise Boise
Danielle Rich, RD Yes Yes Saint Alphonsus Glycemic Boise Boise
Alyson Bores, RD Yes Yes Saint Alphonsus Regional Medical Center Boise
Lynn Bailey, RD Yes No Whole Body Nutrition & Fitness Boise
Cindy Nebeker, RD No No Nutrition By Design Meridian
Marjorie Rich, RD Yes Yes Saint Alphonsus Glycemic – W. Cherry Ln. Meridian
Lynn Kipp, RD No No Nourish Your Life Nampa
Danielle Kipp, RD No No Nourish Your Life Nampa
Lynn Dammarell, RD Yes Yes Saint Alphonsus Glycemic – Caldwell 430 Caldwell
Laura Moulton, RD No Yes Mountain Home Nutrition Services Mountain Home
Valerie Lawrence, RD Yes Yes Valerie Lynn Lawrence Emmett
Sanjuanita Aguilar, RD Spanish Yes Yes Valley Family Health Care – Mobile Access Unit Payette
Andrea Aguilar, RD Spanish Ye s Yes Valley Family Health Care – Payette Payette

9
FOUR CRITICAL TIMES FOR DIABETES SELF-MANAGEMENT
EDUCATION AND SUPPORT SERVICES
At Diagnosis
When Complicating
Factors Develop
When Transitions in
Life and Care Occur
Annually and/or When Not
Meeting Treatment Targets
P
R
O
B
L
E
M
S
O
L
V
I
N
G
R
E
D
U
C
I
N
G
R
I
S
K
M
O
N
I
T
O
R
I
N
G
H
E
A
L
T
H
Y
C
O
P
I
N
G
T
A
K
I
N
G
E
D
U
C
A
T
I
O
N
H
E
A
L
T
H
Y
E
A
T
I
N
G
B
E
I
N
G
A
C
T
I
V
E
10
GLP-1 Prescriber Guide
Endnotes
1
Semaglutide and Cardiovascular Outcomes in Patients with
Type 2 Diabetes.
Steven P. Marso, Stephen C. Bain, Agostino Consoli, et al. The New
England Journal of Medicine. Nov 10, 2016.
2
Kalra S. Follow the LEADER-Liraglutide Eect and Action in Diabetes:
Evaluation of Cardiovascular Outcome Results Trial. Diabetes Ther. 2016
Dec;7(4):601-609. doi: 10.1007/s13300-016-0197-4. Epub 2016 Sep 9.
PMID: 27613064; PMCID: PMC5118235.
3
Mortensen MB, Nordestgaard BG. Statin Use in Primary Prevention of
Atherosclerotic Cardiovascular Disease According to 5 Major Guidelines
for Sensitivity, Specificity, and Number Needed to Treat. JAMA Cardiol.
2019;4(11):1131–1138. doi:10.1001/jamacardio.2019.3665.
4
Byrne P, Cullinan J, Gillespie P, Perera R, Smith SM. Statins for
primary prevention of cardiovascular disease: modelling guidelines
and patient preferences based on an Irish cohort. Br J Gen Pract. 2019
Jun;69(683):e373-e380. doi: 10.3399/bjgp19X702701. Epub 2019 Apr 23.
PMID: 31015226; PMCID: PMC6532821.
5
Kianmehr H, Zhang P, Luo J, et al. Potential Gains in Life Expectancy
Associated With Achieving Treatment Goals in US Adults With Type 2
Diabetes. JAMA Netw Open. 2022;5(4):e227705. doi:10.1001/
jamanetworkopen.2022.7705.
6
Jastrebo AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B,
Kiyosue A, Zhang S, Liu B, Bunck MC, Stefanski A; SURMOUNT-1
Investigators. Tirzepatide Once Weekly for the Treatment of Obesity.
N Engl J Med. 2022 Jul 21;387(3):205-216. doi: 10.1056/NEJMoa2206038.
Epub 2022 Jun 4. PMID: 35658024.
7
Jensterle M, Rizzo M, Haluzík M, Janež A. Ecacy of GLP-1 RA
Approvedfor Weight Management in Patients With or Without
Diabetes: A Narrative Review. Adv Ther. 2022 Jun;39(6):2452-2467. doi:
10.1007/s12325-022-02153-x. Epub 2022 May 3. PMID: 35503498; PMCID:
PMC9063254.
8
airfinity.com/articles/wegovy-costs-usd1-1m-to-prevent-one-heart-
attack-stroke-or-cardiovascular. Accessed 10/31/2023.
9
Weiss T, Carr RD, Pal S, Yang L, Sawhney B, Boggs R, Rajpathak S,
Iglay K. Real-World Adherence and Discontinuation of Glucagon-Like
Peptide-1 Receptor Agonists Therapy in Type 2 Diabetes Mellitus
Patients in the United States. Patient Prefer Adherence. 2020 Nov
27;14:2337-2345. doi: 10.2147/PPA.S277676. PMID: 33273810; PMCID:
PMC7708309.
10
GoodRx October 2023 prices.
