CONTRACTOR
NOTICE OF CONTRACT
NOTICE OF CONTRACT NO. MA XX
between
THE STATE OF MICHIGAN
and
CONTRACT SUMMARY
DESCRIPTION: Prepaid Inpatient Health Plan (PIHP)
INITIAL EFFECTIVE
DATE
INITIAL EXPIRATION
DATE
INITIAL AVAILABLE
OPTIONS
EXPIRATION DATE BEFORE
CHANGE(S) NOTED BELOW
October 1, 2023 September 30, 2024 N/A N/A
PAYMENT TERMS
DELIVERY TIMEFRAME
Net 45 As Needed
ALTERNATE PAYMENT OPTIONS
EXTENDED PURCHASING
☐
P-card ☐ Payment Request (PRC)
☐
Other
☐
Yes ☒ No
MINIMUM DELIVERY REQUIREMENTS
N/A
MISCELLANEOUS INFORMATION
N/A
ESTIMATED CONTRACT VALUE AT TIME OF EXECUTION
STATE OF MICHIGAN PROCUREMENT
Department of Health and Human Services
235 South Grand Avenue, Suite 1201, Lansing, MI 48933
Grand Tower Building, Suite 1201, PO Box 30037, Lansing, MI 48909
CONTRACTOR
Business Name
Street Address
City, State & Zip
First & Last Name
Phone Number
Email Address
V Cust#
STATE
Program
Manager
Kristen Jordan MDHHS
517-388-7421
Contract
Administrator
Danielle Walsh MDHHS
517-241-2110
Page 2 of 148
CONTRACT NO. MA XX
FOR CONTRACTOR:
Company Name
Authorized Agent Signature
Authorized Agent (Print or Type)
Date
FOR THE STATE:
Signature
Christine H. Sanches, Director,
Bureau of Grants and Purchasing
Name & Title
Michigan Department of Health and Human
Services
Agency
Date

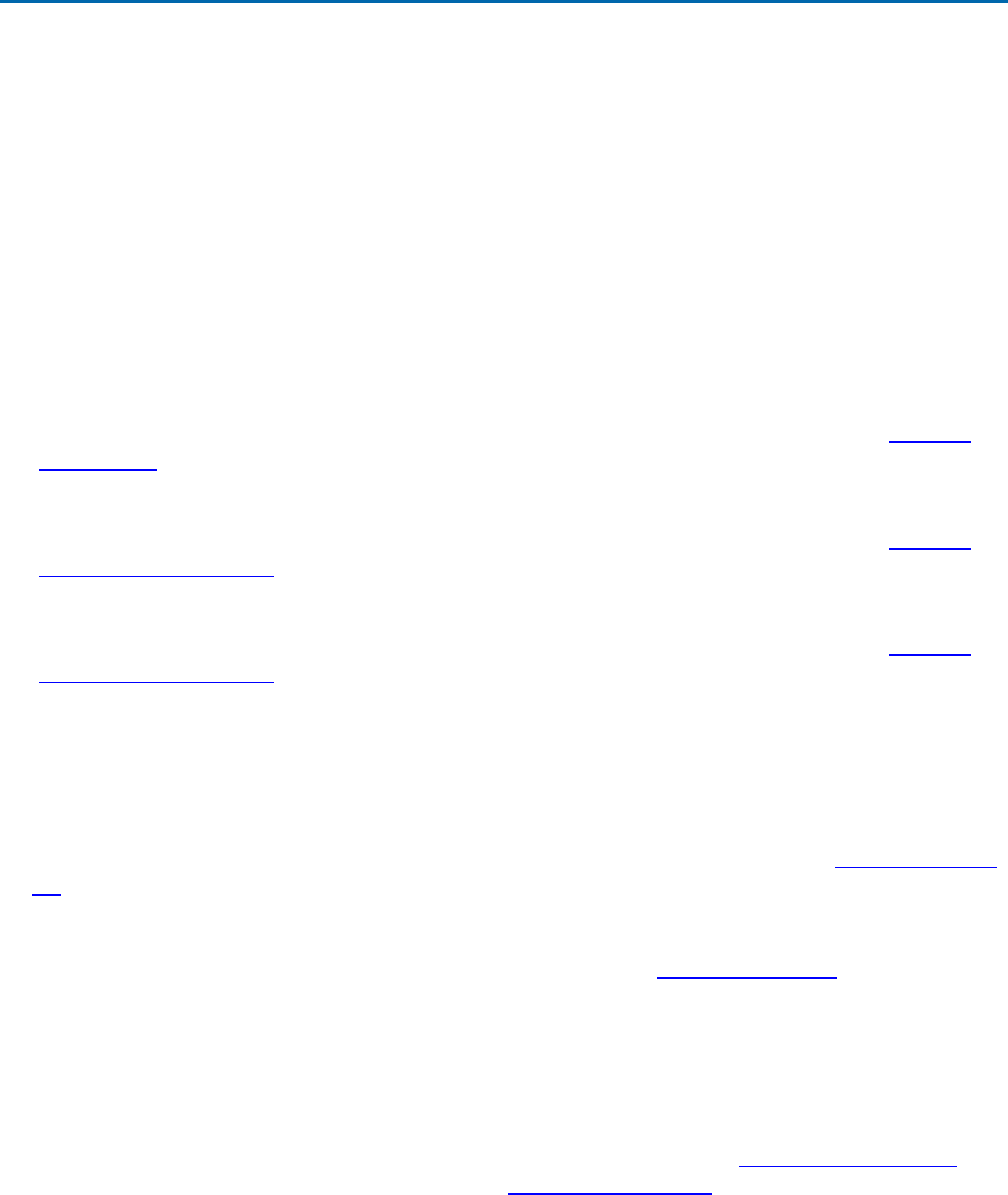
TABLE OF CONTENTS
Standard Contract Terms ........................................................................................................................... 4
Federal Provisions Addendum ................................................................................................................. 21
EXHIBIT 1 Byrd Anti-Lobbying Certification ............................................................................................. 27
Schedule A- Statement of Work Contract Activities .................................................................................. 29
BACKGROUND ....................................................................................................................................... 29
SCOPE .................................................................................................................................................... 29
A.
Service Area ............................................................................................................................... 30
B.
Customer Services Standards ..................................................................................................... 31
C.
Payment Reform ......................................................................................................................... 33
D.
Contract Remedies and Sanctions .............................................................................................. 35
E.
Access and Availability ................................................................................................................ 36
F.
Covered Services ........................................................................................................................ 44
G.
Contractor Governance and Board Requirements ....................................................................... 48
H.
Behavioral/Physical Health Integration ........................................................................................ 49
I.
Eligibility ...................................................................................................................................... 50
J.
Parity and Benefits ...................................................................................................................... 51
K.
Quality Improvement and Program Development ........................................................................ 52
L.
Grievance and Appeals Process for Beneficiaries ....................................................................... 53
M.
Beneficiary Services .................................................................................................................... 60
N.
Provider Services ........................................................................................................................ 63
O.
Health Information Systems ........................................................................................................ 69
P.
Legal Expenses .......................................................................................................................... 70
Q.
Observance of State and Federal Laws and Regulations ............................................................ 71
R.
Program Integrity......................................................................................................................... 78
S.
Fiscal Audits and Compliance Examinations ............................................................................... 91
1.1 Transition .................................................................................................................................... 94
2.
Staffing, Organizational Structure, Governing Body, and Subcontractors .................................... 96
3. P
roject Management ................................................................................................................. 101
4. Internal Service Fund (ISF) ....................................................................................................... 109
5. Authorizing Document ............................................................................................................... 110
6. Contractor Risk Management Strategy ...................................................................................... 110
7. Risk Corridor ............................................................................................................................. 111
8. Payment Terms ......................................................................................................................... 112
Schedule B- HIPAA Business Associate Agreement .............................................................................. 121
Schedule C- Definitions / Explanation of Terms ..................................................................................... 129
Schedule D- reserved ............................................................................................................................ 135
Schedule E- Contractor Financial Reporting Requirements ................................................................... 136
Schedule E- Contractor Non-Financial Reporting Requirements ............................................................ 138
Schedule F- Medicaid Mental Health Substance Use Disorder Authorization and Payment Responsibility
Grid .................................................................................................................................................... 142
Schedule G- Local Funding Obligation Schedule ................................................................................... 147
Schedule H- Behavioral Health Capitation Rate Certification ................................................................. 148

Page 4 of 148
STANDARD CONTRACT TERMS
This STANDARD CONTRACT (“Contract”) is agreed to between the State of Michigan
(the “State”) and [Insert Company Name] (“Contractor”), a Prepaid Inpatient Health
Plan (PIHP). This Contract is effective on October 1, 2023 (“Effective Date”), and
unless terminated, will expire on September 30, 2024 (the “Term”).
The parties agree as follows:
1. Duties of Contractor. Contractor must perform the services and provide the
deliverables (the “Contract Activities”) described in a Statement of Work, the initial
Statement of Work is attached as Schedule A Statement of Work. An obligation to
provide delivery of any commodity is considered a service and is a Contract Activity.
Contractor must furnish all labor, equipment, materials, and supplies necessary for
the performance of the Contract Activities unless otherwise specified in a Statement
of Work.
Contractor must: (a) perform the Contract Activities in a timely, professional, safe,
and workmanlike manner consistent with standards in the trade, profession, or
industry; (b) meet or exceed the performance and operational standards, and
specifications of the Contract; (c) provide all Contract Activities in good quality, with
no material defects; (d) not interfere with the State’s operations; (e) obtain and
maintain all necessary licenses, permits or other authorizations necessary for the
performance of the Contract; (f) cooperate with the State, including the State’s quality
assurance personnel, and any third party to achieve the objectives of the Contract;
(g) return to the State any State-furnished equipment or other resources in the same
condition as when provided when no longer required for the Contract; (h) assign to
the State any claims resulting from state or federal antitrust violations to the extent
that those violations concern materials or services supplied by third parties toward
fulfillment of the Contract; (i) comply with all State physical and IT security policies
and standards which will be made available upon request; and (j) provide the State
priority in performance of the Contract except as mandated by federal disaster
response requirements. Any breach under this paragraph is considered a material
breach.
Contractor must also be clearly identifiable while on State property by wearing
identification issued by the State, and clearly identify themselves whenever making
contact with the State.
2. Notices. All notices and other communications required or permitted under this
Contract must be in writing and will be considered given and received: (a) when
verified by written receipt if sent by courier; (b) when actually received if sent by mail
without verification of receipt; or (c) when verified by automated receipt or electronic
logs if sent by facsimile or email.
If to State:
If to Contractor:
Danielle Walsh
235 S. Grand Avenue, Suite 1201
Lansing, MI 48933
Walshd4@michigan.gov
[Name]
[Street Address]
[City, State, Zip]
[Email]
Page 5 of 148
If to State:
If to Contractor:
517-241-2110
[Phone]
3. Contract Administrator. The Contract Administrator, or the individual duly
authorized for each party, is the only person authorized to modify any terms of this
Contract, and approve and execute any change under this Contract (each a
“Contract Administrator”):
State:
Contractor:
Danielle Walsh
235 S. Grand Avenue, Suite 1201
Lansing, MI 48933
Walshd4@michigan.gov
517-241-2110
[Name]
[Street Address]
[City, State, Zip]
[Email]
[Phone]
4. Program Manager. The Program Manager for each party will monitor and coordinate
the day-to-day activities of the Contract (each a “Program Manager”):
State:
Contractor:
Kristen Jordan
400 South Pine Street
Lansing, MI 48913
jordank4@michigan.gov
517-388-7421
[Name]
[Street Address]
[City, State, Zip]
[Email]
[Phone]
5. Performance Guarantee. Contractor must at all times have sufficient financial
resources as objectively determined by the State, to ensure performance of the
Contract and must provide proof upon request.
6. Insurance Requirements. Contractor, at its sole expense, must maintain the
insurance coverage identified below. With respect to Privacy and Security Liability,
Contractor may, at the discretion of the DHHS Contract Administrator, defer
coverage up to no more than 30 days prior to beginning any work or deliverables
under this Contract. All required insurance must: (a) protect the State from claims
that may arise out of, are alleged to arise out of, or otherwise result from Contractor's
performance.
Required Limits
Additional Requirements
Commercial General Liability Insurance
Minimum Limits:
$1,000,000 Each Occurrence
$1,000,000 Personal & Advertising Injury
$2,000,000 Products/Completed Operations
$2,000,000 General Aggregate
Automobile Liability Insurance
If a motor vehicle is used in relation to Contractor's performance, Contractor must have
vehicle liability insurance on the motor vehicle for bodily injury and property damage as
Page 6 of 148
Required Limits
Additional Requirements
required by law.
Workers' Compensation Insurance
Minimum Limits:
Coverage according to applicable laws
governing work activities.
Waiver of subrogation, except where waiver is
prohibited by law.
Employers Liability Insurance
Minimum Limits:
$500,000 Each Accident
$500,000 Each Employee by Disease
$500,000 Aggregate Disease
Privacy and Security Liability (Cyber Liability) Insurance
Minimum Limits:
$1,000,000 Each Occurrence
$1,000,000 Annual Aggregate
Contractor must have their policy cover
information security and privacy liability,
privacy notification costs, regulatory defense
and penalties, and website media content
liability.
Professional Liability (Errors and Omissions) Insurance
Minimum Limits:
$3,000,000 Each Occurrence
$3,000,000 Annual Aggregate
If any of the required policies provide claims-made coverage, Contractor must: (a)
provide coverage with a retroactive date before the Effective Date of the Contract or
the beginning of Contract Activities; (b) maintain coverage and provide evidence of
coverage for at least three (3) years after completion of the Contract Activities; and
(c) if coverage is cancelled or not renewed, and not replaced with another claims-
made policy form with a retroactive date prior to the Contract Effective Date,
Contractor must purchase extended reporting coverage for a minimum of three (3)
years after completion of work.
Contractor must: (a) provide insurance certificates to the Contract Administrator,
containing the agreement or delivery order number, at Contract formation and within
twenty (20) calendar days of the expiration date of the applicable policies; (b) require
that subcontractors maintain the required insurance contained in this Section; (c)
notify the Contract Administrator within five (5) business days if any insurance is
cancelled; and (d) waive all rights against the State for damages covered by
insurance. Failure to maintain the required insurance does not limit this waiver.
This Section is not intended to and is not to be construed in any manner as waiving,
restricting or limiting the liability of either party for any obligations under this Contract
(including any provisions hereof requiring Contractor to indemnify, defend and hold
harmless the State).
7. Reserved.
Page 7 of 148
8. Reserved.
9. Relationship of the Parties. The relationship between the parties is that of
independent contractors, Contractor, its employees, and agents will not be
considered employees of the State. No partnership or joint venture relationship is
created by virtue of this Contract. Contractor, and not the State, is responsible for the
payment of wages, benefits and taxes of Contractor’s employees and any
subcontractors. Prior performance does not modify Contractor’s status as an
independent contractor. Neither party has authority to contract for nor bind the other
party in any manner whatsoever.
10. Intellectual Property Rights. If a Statement of Work requires Contractor to create
any intellectual property, Contractor hereby acknowledges that the State is and will
be the sole and exclusive owner of all right, title, and interest in the Contract Activities
and all associated intellectual property rights, if any. Such Contract Activities are
works made for hire as defined in Section 101 of the Copyright Act of 1976. To the
extent any Contract Activities and related intellectual property do not qualify as works
made for hire under the Copyright Act, Contractor will, and hereby does, immediately
on its creation, assign, transfer and otherwise convey to the State, irrevocably and in
perpetuity, throughout the universe, all right, title and interest in and to the Contract
Activities, including all intellectual property rights therein.
11. Subcontracting. Contractor may only delegate managed care functions to a
Community Mental Health Service Program with written and express approval from
the State. The State will provide an approval or denial of the delegation request
within 60 days. Contractor must submit existing delegation arrangements in the form
or format determined by the State within 30 days of execution of this Contract.
Thereafter, Contractor must submit to the State new or revised delegation
agreements at least 90 calendar days before the proposed delegation is to take
effect. Contractor will provide any additional information requests from the State to
assist in reviewing the delegation for approval. If a delegation request is approved,
Contractor must: (a) be the sole point of contact regarding all contractual matters,
including payment and charges for all Contract Activities; (b) make all payments to
the subcontractor; and (c) incorporate the terms and conditions contained in this
Contract in any subcontract with a subcontractor; (d) require the subcontractor to
comply with all of Contractor’s reporting requirements including but not limited the
reporting of administrative costs pursuant to the Medical Loss Ratio and the Standard
Cost Allocation methodology Contractor remains responsible for the completion of
the Contract Activities and the compliance with the terms of this Contract. The State,
in its sole discretion, may require Contractor to revoke the delegation agreement in
whole or part and require Contractor to resume delegated managed care functions
for deficiencies in the subcontractor’s performance of delegated duties or if the State
determines the delegation is not in the best interest for the proper administration of
the Contract.
12. Staffing. The State’s Contract Administrator may require Contractor to remove or
reassign personnel if the State provides a notice to Contractor. The State will provide
justification for the removal or reassignment and why it is in the best interest of the
Medicaid program.
Page 8 of 148
13. Background Checks. Contractor must perform background checks on all
employees and subcontractors and its employees prior to their assignment. The
scope is at the discretion of the State and documentation must be provided as
requested. Contractor is responsible for all costs associated with the requested
background checks. The State, in its sole discretion, may also perform background
checks.
14. Assignment. Contractor may not assign this Contract to any other party without the
prior approval of the State. Upon notice to Contractor, the State, in its sole discretion,
may assign in whole or in part, its rights or responsibilities under this Contract to any
other party. If the State determines that a novation of the Contract to a third party is
necessary, Contractor will agree to the novation and provide all necessary
documentation and signatures.
15. Change of Control. Contractor will notify the State, within 30 days of any public
announcement or otherwise once legally permitted to do so, of a change in
Contractor’s organizational structure or ownership. For purposes of this Contract, a
change in control means any of the following: (a) a sale of more than 50% of
Contractor’s stock; (b) a sale of substantially all of Contractor’s assets; (c) a change
in a majority of Contractor’s board members; (d) consummation of a merger or
consolidation of Contractor with any other entity; (e) a change in ownership through a
transaction or series of transactions; (f) or the board (or the stockholders) approves a
plan of complete liquidation. A change of control does not include any consolidation
or merger effected exclusively to change the domicile of Contractor, or any
transaction or series of transactions principally for bona fide equity financing
purposes.
In the event of a change of control, Contractor must require the successor to assume
this Contract and all of its obligations under this Contract.
16. Reserved.
17. Reserved.
18. Reserved.
19. Reserved.
20. Reserved.
21. Terms of Payment. The State is exempt from State sales tax for direct purchases
and may be exempt from federal excise tax, if Services purchased under this
Agreement are for the State’s exclusive use. Notwithstanding the foregoing, all prices
are inclusive of taxes, and Contractor is responsible for all sales, use and excise
taxes, and any other similar taxes, duties and charges of any kind imposed by any
federal, state, or local governmental entity on any amounts payable by the State
under this Contract.
The State has the right to withhold payment of any disputed amounts until the parties
agree as to the validity of the disputed amount. The State will notify Contractor of any
dispute within a reasonable time. Payment by the State will not constitute a waiver of
any rights as to Contractor’s continuing obligations, including claims for deficiencies
or substandard Contract Activities. Contractor’s acceptance of final payment by the

Page 9 of 148
State constitutes a waiver of all claims by Contractor against the State for payment
under this Contract, other than those claims previously filed in writing on a timely
basis and still disputed.
The State will only disburse payments under this Contract through Electronic Funds
Transfer (EFT). Contractor must register with the State at
http://www.michigan.gov/SIGMAVSS to receive electronic fund transfer payments. If
Contractor does not register, the State is not liable for failure to provide payment.
Without prejudice to any other right or remedy it may have, the State reserves the
right to set off at any time any amount then due and owing to it by Contractor against
any amount payable by the State to Contractor under this Contract.
22. Liquidated Damages. Liquidated damages, if applicable, will be assessed as
described in a Statement of Work. The parties understand and agree that
any liquidated damages (which includes but is not limited to applicable credits) set
forth in this Contract are reasonable estimates of the State’s financial loss and
damage in accordance with applicable law. The parties acknowledge and agree that
Contractor could incur liquidated damages for more than 1 event. The assessment of
liquidated damages will not constitute a waiver or release of any other remedy the
State may have under this Contract for Contractor’s breach of this Contract, including
without limitation, the State’s right to terminate this Contract for cause under Section
24 and the State will be entitled in its discretion to recover actual damages caused by
Contractor’s failure to perform its obligations under this Contract. However, the State
will reduce such actual damages by the amounts of liquidated damages received for
the same events causing the actual damages. Amounts due the State as liquidated
damages may be set off against any fees payable to Contractor under this Contract,
or the State may bill Contractor as a separate item and Contractor will promptly make
payments on such bills.
23. Stop Work Order. The State may suspend any or all activities under the Contract at
any time. The State will provide Contractor a written stop work order detailing the
suspension. Contractor must comply with the stop work order upon receipt. Within 90
calendar days, or any longer period agreed to by Contractor, the State will either: (a)
issue a notice authorizing Contractor to resume work, or (b) terminate the Contract or
delivery order. The State will not pay for Contract Activities, Contractor’s lost profits,
or any additional compensation during a stop work period.
24. Termination for Cause. (a) The State may terminate this Contract for cause, in
whole or in part, if Contractor, as determined by the State: (i) endangers the value,
integrity, or security of any facility, data, or personnel; (ii) becomes insolvent,
petitions for bankruptcy court proceedings, or has an involuntary bankruptcy
proceeding filed against it by any creditor; (iii) engages in any conduct that may
expose the State to liability; (iv) breaches any of its material duties or obligations
under this Contract; or (v) fails to cure a breach within the time stated by the State in
a notice of breach. Any reference to specific breaches being material breaches within
this Contract will not be construed to mean that other breaches are not material.
(b) If the State terminates this Contract under this Section, the State will issue a
termination notice specifying whether Contractor must: (i) cease performance
immediately or (ii) continue to perform for a specified period. If it is later determined
that Contractor was not in breach of the Contract, the termination will be deemed to
Page 10 of 148
have been a Termination for Convenience, effective as of the same date, and the
rights and obligations of the parties will be limited to those provided in Section 25,
Termination for Convenience.
The State will only pay for amounts due to Contractor for Contract Activities accepted
by the State on or before the date of termination, subject to the State’s right to set off
any amounts owed by Contractor for the State’s reasonable costs in terminating this
Contract for cause, including administrative costs, attorneys’ fees, court costs,
transition costs. Contractor must promptly reimburse to the State any fees prepaid by
the State prorated to the date of such termination, including any prepaid
fees. Contractor must pay all reasonable costs incurred by the State in terminating
this Contract for cause, including administrative costs, attorney’s fees, court costs,
transition costs, and any costs the State incurs to procure the Contract Activities from
other sources.
25. Termination for Convenience. The State may immediately terminate this Contract
in whole or in part without penalty and for any reason or no reason, including but not
limited to, appropriation or budget shortfalls. The termination notice will specify
whether Contractor must: (a) cease performance of the Contract Activities
immediately or (b) continue to perform the Contract Activities in accordance with
Section 26, Transition Responsibilities. If the State terminates this Contract for
convenience, the State will pay all reasonable costs, as determined by the State, for
State approved Transition Responsibilities to the extent the funds are available.
26. Transition Responsibilities. Upon termination or expiration of this Contract for any
reason, Contractor must, for a period of time specified by the State (not to exceed 2
years) provide all reasonable transition assistance requested by the State, to allow
for the expired or terminated portion of the Contract Activities to continue without
interruption or adverse effect, and to facilitate the orderly transfer of such Contract
Activities to the State or its designees. Such transition assistance may include, but is
not limited to: (a) continuing to perform the Contract Activities at the established
Contract rates and local match requirements; (b) taking all reasonable and necessary
measures to transition performance of the work, including all applicable Contract
Activities, training, equipment, software, leases, reports and other documentation, to
the State or the State’s designee; (c) transferring title in and delivering to the State,
at the State’s discretion, all completed or partially completed deliverables prepared
under this Contract as of the Contract termination date; and (d) preparing an
accurate accounting from which the State and Contractor may reconcile all
outstanding accounts (collectively, “Transition Responsibilities ”). This Contract will
automatically be extended through the end of the transition period.
27. Return of State Property. Upon termination or expiration of this Contract for any
reason, Contractor must take all necessary and appropriate steps, or such other
action as the State may direct, to preserve, maintain, protect, or return to the State all
materials, data, property, and confidential information provided directly or indirectly to
Contractor by any entity, agent, vendor, or employee of the State.
28. Indemnification. To the extent permitted by law, Contractor must defend, indemnify
and hold the State, its departments, divisions, agencies, offices, commissions,
officers, and employees harmless, without limitation, from and against any and all
actions, claims, losses, liabilities, damages, costs, attorney fees, and expenses
Page 11 of 148
(including those required to establish the right to indemnification), arising out of or
relating to: (a) any breach by Contractor (or any of Contractor’s employees, agents,
subcontractors, or by anyone else for whose acts any of them may be liable) of any
of the promises, agreements, representations, warranties, or insurance requirements
contained in this Contract; (b) any infringement, misappropriation, or other violation
of any intellectual property right or other right of any third party; (c) any bodily injury,
death, or damage to real or tangible personal property occurring wholly or in part due
to action or inaction by Contractor (or any of Contractor’s employees, agents,
subcontractors, or by anyone else for whose acts any of them may be liable); and (d)
any acts or omissions of Contractor (or any of Contractor’s employees, agents,
subcontractors, or by anyone else for whose acts any of them may be liable)
The State will notify Contractor in writing if indemnification is sought; however, failure
to do so will not relieve Contractor, except to the extent that Contractor is materially
prejudiced. Contractor must, to the satisfaction of the State, demonstrate its financial
ability to carry out these obligations.
The State is entitled to: (i) regular updates on proceeding status; (ii) participate in the
defense of the proceeding; (iii) employ its own counsel; and to (iv) retain control of
the defense, at its own cost and expense, if the State deems necessary. Contractor
will not, without the State’s prior written consent (not to be unreasonably withheld),
settle, compromise, or consent to the entry of any judgment in or otherwise seek to
terminate any claim, action, or proceeding. To the extent that any State employee,
official, or law may be involved or challenged, the State may, at its own expense,
control the defense of that portion of the claim.
Any litigation activity on behalf of the State, or any of its subdivisions under this
Section, must be coordinated with the Department of Attorney General. An attorney
designated to represent the State may not do so until approved by the Michigan
Attorney General and appointed as a Special Assistant Attorney General.
The State is constitutionally prohibited from indemnifying Contractor or any third
parties. Notwithstanding the foregoing, nothing in this section shall be construed as a
waiver of any governmental immunity for Contractor, its directors or employees as
provided by statute or modified by court decisions.
29. Infringement Remedies. If, in either party’s opinion, any piece of equipment,
software, commodity, or service supplied by Contractor or its subcontractors, or its
operation, use or reproduction, is likely to become the subject of a copyright, patent,
trademark, or trade secret infringement claim, Contractor must, at its expense: (a)
procure for the State the right to continue using the equipment, software, commodity,
or service, or if this option is not reasonably available to Contractor, (b) replace or
modify the same so that it becomes non-infringing; or (c) accept its return by the
State with appropriate credits to the State against Contractor’s charges and
reimburse the State for any losses or costs incurred as a consequence of the State
ceasing its use and returning it.
30. Limitation of Liability and Disclaimer of Damages. IN NO EVENT WILL THE
STATE’S AGGREGATE LIABILITY TO CONTRACTOR UNDER THIS CONTRACT,
REGARDLESS OF THE FORM OF ACTION, WHETHER IN CONTRACT, TORT,
NEGLIGENCE, STRICT LIABILITY OR BY STATUTE OR OTHERWISE, FOR ANY
CLAIM RELATED TO OR ARISING UNDER THIS CONTRACT, EXCEED THE
Page 12 of 148
MAXIMUM AMOUNT OF FEES PAYABLE UNDER THIS CONTRACT. The State is
not liable for consequential, incidental, indirect, or special damages, regardless of the
nature of the action.
31. Disclosure of Litigation, or Other Proceeding. Contractor must notify the State
within 14 calendar days of receiving notice of any litigation, investigation, arbitration,
or other proceeding (collectively, “Proceeding”) involving Contractor, a
subcontractor, or an officer or director of Contractor or subcontractor, that arises
during the term of the Contract, including: (a) a criminal Proceeding; (b) a parole or
probation Proceeding; (c) a Proceeding under the Sarbanes-Oxley Act; (d) a civil
Proceeding involving: (1) a claim that might reasonably be expected to adversely
affect Contractor’s viability or financial stability; or (2) a governmental or public
entity’s claim or written allegation of fraud; or 3) any complaint related to the services
provided in this Contract filed in a legal or administrative proceeding alleging
Contractor or its subcontractors discriminated against its employees, subcontractors,
vendors, or suppliers during the performance of Contract activities and during the
term of this Contract; or (e) a Proceeding involving any license that Contractor is
required to possess in order to perform under this Contract.
32. Reserved.
33. State Data.
a. Ownership. The State’s data (“State Data,” which will be treated by Contractor
as Confidential Information) includes: (a) the State’s data, user data, and any
other data collected, used, processed, stored, or generated as the result of the
Contract Activities; (b) personally identifiable information (“PII“) collected, used,
processed, stored, or generated as the result of the Contract Activities, including,
without limitation, any information that identifies an individual, such as an
individual’s social security number or other government-issued identification
number, date of birth, address, telephone number, biometric data, mother’s
maiden name, email address, credit card information, or an individual’s name in
combination with any other of the elements here listed; and, (c) protected health
information (“PHI”) collected, used, processed, stored, or generated as the result
of the Contract Activities, which is defined under the Health Insurance Portability
and Accountability Act (HIPAA) and its related rules and regulations. State Data is
and will remain the sole and exclusive property of the State and all right, title, and
interest in the same is reserved by the State. This section survives the
termination of this contract.
b. Contractor Use of State Data. Contractor is provided a limited license to State
Data for the sole and exclusive purpose of providing the Contract Activities,
including a license to collect, process, store, generate, and display State Data
only to the extent necessary in the provision of the Contract Activities. Contractor
must: (a) keep and maintain State Data in strict confidence, using such degree of
care as is appropriate and consistent with its obligations as further described in
this Contract and applicable law to avoid unauthorized access, use, disclosure, or
loss; (b) use and disclose State Data solely and exclusively for the purpose of
providing the Contract Activities, such use and disclosure being in accordance
with this Contract, any applicable Statement of Work, and applicable law; (c) keep
and maintain State Data in the continental United States and (d) not use, sell,
Page 13 of 148
rent, transfer, distribute, commercially exploit, or otherwise disclose or make
available State Data for Contractor’s own purposes or for the benefit of anyone
other than the State without the State’s prior written consent. This section
survives the termination of this contract.
c. Extraction of State Data. Contractor must, within 5 business days of the State’s
request, provide the State, without charge and without any conditions or
contingencies whatsoever (including but not limited to the payment of any fees
due to Contractor), an extract of the State Data in the format specified by the
State.
d. Backup and Recovery of State Data. Unless otherwise specified in a Statement
of Work, Contractor is responsible for maintaining a backup of State Data and for
an orderly and timely recovery of such data. Unless otherwise described in a
Statement of Work, Contractor must maintain a contemporaneous backup of
State Data that can be recovered within 24 hours. If backup of State Data cannot
be made within 24 hours, Contractor must request approval from the State for
additional time.
e. Loss or Compromise of Data. In the event of any act, error or omission,
negligence, misconduct, or breach on the part of Contractor that compromises or
is suspected to compromise the security, confidentiality, or integrity of State Data
or the physical, technical, administrative, or organizational safeguards put in
place by Contractor that relate to the protection of the security, confidentiality, or
integrity of State Data, Contractor must, as applicable: (a) notify the State as soon
as practicable but no later than 24 hours of becoming aware of such occurrence;
(b) cooperate with the State in investigating the occurrence, including making
available all relevant records, logs, files, data reporting, and other materials
required to comply with applicable law or as otherwise required by the State; (c)
in the case of PII or PHI, at the State’s sole election, (i) with approval and
assistance from the State, notify the affected individuals who comprise the PII or
PHI as soon as practicable but no later than is required to comply with applicable
law, or, in the absence of any legally required notification period, within 5
calendar days of the occurrence; or (ii) reimburse the State for any costs in
notifying the affected individuals; (d) in the case of PII, provide third-party credit
and identity monitoring services to each of the affected individuals who comprise
the PII for the period required to comply with applicable law, or, in the absence of
any legally required monitoring services, for no less than 24 months following the
date of notification to such individuals; (e) perform or take any other actions
required to comply with applicable law as a result of the occurrence; (f) pay for
any costs associated with the occurrence, including but not limited to any costs
incurred by the State in investigating and resolving the occurrence, including
reasonable attorney’s fees associated with such investigation and resolution; (g)
without limiting Contractor’s obligations of indemnification as further described in
this Contract, indemnify, defend, and hold harmless the State for any and all
claims, including reasonable attorneys’ fees, costs, and incidental expenses,
which may be suffered by, accrued against, charged to, or recoverable from the
State in connection with the occurrence; (h) be responsible for recreating lost
State Data in the manner and on the schedule set by the State without charge to
the State; and (i) provide to the State a detailed plan within 10 calendar days of
Page 14 of 148
the occurrence describing the measures Contractor will undertake to prevent a
future occurrence. Notification to affected individuals, as described above, must
comply with applicable law, be written in plain language, not be tangentially used
for any solicitation purposes, and contain, at a minimum: name and contact
information of Contractor’s representative; a description of the nature of the loss;
a list of the types of data involved; the known or approximate date of the loss;
how such loss may affect the affected individual; what steps Contractor has taken
to protect the affected individual; what steps the affected individual can take to
protect himself or herself; contact information for major credit card reporting
agencies; and, information regarding the credit and identity monitoring services to
be provided by Contractor. The State will have the option to review and approve
any notification sent to affected individuals prior to its delivery. Notification to any
other party, including but not limited to public media outlets, must be reviewed
and approved by the State in writing prior to its dissemination. The parties agree
that any damages relating to a breach of this Section 33 are to be considered
direct damages and not consequential damages.
f. State’s Governance, Risk and Compliance (GRC) platform. Contractor is
required to assist the State with its security accreditation process through the
development, completion and ongoing updating of a system security plan using
the State’s automated GRC platform and implement any required safeguards or
remediate any security vulnerabilities as identified by the results of the security
accreditation process.
34. Non-Disclosure of Confidential Information. The parties acknowledge that each
party may be exposed to or acquire communication or data of the other party that is
confidential, privileged communication not intended to be disclosed to third parties.
a. Meaning of Confidential Information. For the purposes of this Contract, the
term “Confidential Information” means all information and documentation of a
party that: (a) has been marked “confidential” or with words of similar meaning, at
the time of disclosure by such party; (b) if disclosed orally or not marked
“confidential” or with words of similar meaning, was subsequently summarized in
writing by the disclosing party and marked “confidential” or with words of similar
meaning; or, (c) should reasonably be recognized as confidential information of
the disclosing party. The term “Confidential Information” does not include any
information or documentation that was or is: (a) subject to disclosure under the
Michigan Freedom of Information Act (FOIA); (b) already in the possession of the
receiving party without an obligation of confidentiality; (c) developed
independently by the receiving party, as demonstrated by the receiving party,
without violating the disclosing party’s proprietary rights; (d) obtained from a
source other than the disclosing party without an obligation of confidentiality; or,
(e) publicly available when received, or thereafter became publicly available
(other than through any unauthorized disclosure by, through, or on behalf of, the
receiving party). For purposes of this Contract, in all cases and for all matters,
State Data is deemed to be Confidential Information.
b. Obligation of Confidentiality. The parties agree to hold all Confidential
Information in strict confidence and not to copy, reproduce, sell, transfer, or
otherwise dispose of, give or disclose such Confidential Information to third
parties other than employees, agents, or subcontractors of a party who have a

Page 15 of 148
need to know in connection with this Contract or to use such Confidential
Information for any purposes whatsoever other than the performance of this
Contract. The parties agree to advise and require their respective employees,
agents, and subcontractors of their obligations to keep all Confidential Information
confidential. Disclosure to a subcontractor is permissible where: (a) use of a
subcontractor is authorized under this Contract; (b) the disclosure is necessary or
otherwise naturally occurs in connection with work that is within the
subcontractor's responsibilities; and (c) Contractor obligates the subcontractor in
a written contract to maintain the State's Confidential Information in confidence.
At the State's request, any employee of Contractor or any subcontractor may be
required to execute a separate agreement to be bound by the provisions of this
Section.
c. Cooperation to Prevent Disclosure of Confidential Information. Each party
must use its best efforts to assist the other party in identifying and preventing any
unauthorized use or disclosure of any Confidential Information. Without limiting
the foregoing, each party must advise the other party immediately in the event
either party learns or has reason to believe that any person who has had access
to Confidential Information has violated or intends to violate the terms of this
Contract and each party will cooperate with the other party in seeking injunctive
or other equitable relief against any such person.
d. Remedies for Breach of Obligation of Confidentiality. Each party
acknowledges that breach of its obligation of confidentiality may give rise to
irreparable injury to the other party, which damage may be inadequately
compensable in the form of monetary damages. Accordingly, a party may seek
and obtain injunctive relief against the breach or threatened breach of the
foregoing undertakings, in addition to any other legal remedies which may be
available, to include, in the case of the State, at the sole election of the State, the
immediate termination, without liability to the State, of this Contract or any
Statement of Work corresponding to the breach or threatened breach.
e. Surrender of Confidential Information upon Termination. Upon termination of
this Contract or a Statement of Work, in whole or in part, each party must, within
5 calendar days from the date of termination, return to the other party any and all
Confidential Information received from the other party, or created or received by a
party on behalf of the other party, which are in such party’s possession, custody,
or control; provided, however, that Contractor must return State Data to the State
following the timeframe and procedure described further in this Contract. Should
Contractor or the State determine that the return of any Confidential Information is
not feasible, such party must destroy the Confidential Information and must certify
the same in writing within 5 calendar days from the date of termination to the
other party. However, each Party’s legal ability to destroy the other Party’s data
may be restricted by its retention and disposal schedule, in which case
Confidential Information will be destroyed after the retention period expires.
35. Data Privacy and Information Security.
a. Undertaking by Contractor. Without limiting Contractor’s obligation of
confidentiality as further described, Contractor is responsible for establishing and
maintaining a data privacy and information security program, including physical,

Page 16 of 148
technical, administrative, and organizational safeguards, that is designed to: (a)
ensure the security and confidentiality of the State Data; (b) protect against any
anticipated threats or hazards to the security or integrity of the State Data; (c)
protect against unauthorized disclosure, access to, or use of the State Data; (d)
ensure the proper disposal of State Data; and (e) ensure that all employees,
agents, and subcontractors of Contractor, if any, comply with all of the foregoing.
In no case will the safeguards of Contractor’s data privacy and information
security program be less stringent than the safeguards used by the State, and
Contractor must at all times comply with all applicable State IT policies and
standards, which are available to Contractor upon request.
b. Audit by Contractor. No less than annually, Contractor must conduct a
comprehensive independent third-party audit of its data privacy and information
security program and provide such audit findings to the State.
c. Right of Audit by the State. Without limiting any other audit rights of the State,
the State has the right to review Contractor’s data privacy and information
security program prior to the commencement of Contract Activities and from time
to time during the term of this Contract. During the providing of the Contract
Activities, on an ongoing basis from time to time and without notice, the State, at
its own expense, is entitled to perform, or to have performed, an on-site audit of
Contractor’s data privacy and information security program. In lieu of an on-site
audit, upon request by the State, Contractor agrees to complete, within 45
calendar days of receipt, an audit questionnaire provided by the State regarding
Contractor’s data privacy and information security program.
d. Audit Findings. Contractor must implement any required safeguards as
identified by the State or by any audit of Contractor’s data privacy and information
security program.
e. State’s Right to Termination for Deficiencies. The State reserves the right, at
its sole election, to immediately terminate this Contract or a Statement of Work
without limitation and without liability if the State determines that Contractor fails
or has failed to meet its obligations under this Section.
36. Reserved.
37. Reserved.
38. Records Maintenance, Inspection, Examination, and Audit. Pursuant to MCL
18.1470, the State or its designee may audit Contractor to verify compliance with this
Contract. Contractor must retain and provide to the State or its designee and the
auditor general upon request, all records related to the Contract through the term of
the Contract and for 10 years after the latter of termination, expiration, or final
payment under this Contract or any extension (“Audit Period”). If an audit, litigation,
or other action involving the records is initiated before the end of the Audit Period,
Contractor must retain the records until all issues are resolved.
The State, CMS, the Office of the Inspector General, the Comptroller General, and
their designees may, at any time, inspect and audit any records or documents of
Contractor, or its subcontractors, and may, at any time, inspect the premises,

Page 17 of 148
physical facilities, and equipment where Medicaid-related activities or work is
conducted. The right to audit under this section exists for 10 years from the final date
of the contract period or from the date of completion of any audit, whichever is later.
Within 10 calendar days of providing notice, the State and its authorized
representatives or designees have the right to enter and inspect Contractor's
premises or any other places where Contract Activities are being performed, and
examine, copy, and audit all records related to this Contract. Contractor must
cooperate and provide reasonable assistance. If financial errors are revealed, the
amount in error must be reflected as a credit or debit on subsequent invoices until
the amount is paid or refunded. Any remaining balance at the end of the Contract
must be paid or refunded within 45 calendar days.
This Section applies to Contractor, any parent, affiliate, or subsidiary organization of
Contractor, and any subcontractor that performs Contract Activities in connection
with this Contract.
39. Representations and Warranties. Contractor represents and warrants: (a)
Contractor is the owner or licensee of any Contract Activities that it licenses, sells, or
develops and Contractor has the rights necessary to convey title, ownership rights, or
licensed use; (b) all Contract Activities are delivered free from any security interest,
lien, or encumbrance and will continue in that respect; (c) the Contract Activities will
not infringe the patent, trademark, copyright, trade secret, or other proprietary rights
of any third party; (d) Contractor must assign or otherwise transfer to the State or its
designee any manufacturer's warranty for the Contract Activities; (e) the Contract
Activities are merchantable and fit for the specific purposes identified in the Contract;
(f) the Contract signatory has the authority to enter into this Contract; (g) all
information furnished by Contractor in connection with the Contract fairly and
accurately represents Contractor's business, properties, finances, and operations as
of the dates covered by the information, and Contractor will inform the State of any
material adverse changes;(h) all information furnished and representations made in
connection with the award of this Contract is true, accurate, and complete, and
contains no false statements or omits any fact that would make the information
misleading; and that (i) Contractor is neither currently engaged in nor will engage in
the boycott of a person based in or doing business with a strategic partner as
described in 22 USC 8601 to 8606. A breach of this Section is considered a material
breach of this Contract, which entitles the State to terminate this Contract under
Section 24, Termination for Cause.
40. Conflicts and Ethics. Contractor will uphold high ethical standards and is prohibited
from: (a) holding or acquiring an interest that would conflict with this Contract; (b)
doing anything that creates an appearance of impropriety with respect to the award
or performance of the Contract; (c) attempting to influence or appearing to influence
any State employee by the direct or indirect offer of anything of value; or (d) paying
or agreeing to pay any person, other than employees and consultants working for
Contractor, any consideration contingent upon the award of the Contract. Contractor
must immediately notify the State of any violation or potential violation of these
standards. This Section applies to Contractor, any parent, affiliate, or subsidiary
organization of Contractor, and any subcontractor that performs Contract Activities in
connection with this Contract.
Page 18 of 148
41. Compliance with Laws. Contractor must comply with all federal, state and local
laws, rules and regulations.
42. Reserved.
43. Reserved.
44. Nondiscrimination. Under the Elliott-Larsen Civil Rights Act, 1976 PA 453, MCL
37.2101, et seq., the Persons with Disabilities Civil Rights Act, 1976 PA 220, MCL
37.1101, et seq., and Executive Directive 2019-09. Contractor and its subcontractors
agree not to discriminate against an employee or applicant for employment with
respect to hire, tenure, terms, conditions, or privileges of employment, or a matter
directly or indirectly related to employment, because of race, color, religion, national
origin, age, sex (as defined in Executive Directive 2019-09), height, weight, marital
status, partisan considerations, any mental or physical disability, or genetic
information that is unrelated to the person’s ability to perform the duties of a
particular job or position. Breach of this covenant is a material breach of this
Contract.
45. Unfair Labor Practice. Under MCL 423.324, the State may void any Contract with a
Contractor or subcontractor who appears on the Unfair Labor Practice register
compiled under MCL 423.322.
46. Governing Law. This Contract is governed, construed, and enforced in accordance
with Michigan law, excluding choice-of-law principles, and all claims relating to or
arising out of this Contract are governed by Michigan law, excluding choice-of-law
principles. Any dispute arising from this Contract must be resolved in the Michigan
Court of Claims. Complaints against the State must be initiated in Ingham County,
Michigan. Contractor waives any objections, such as lack of personal jurisdiction or
forum non conveniens. Contractor must appoint an agent in Michigan to receive
service of process.
47. Non-Exclusivity. Nothing contained in this Contract is intended nor is to be
construed as creating any requirements contract with Contractor, nor does it provide
Contractor with a right of first refusal for any future work. This Contract does not
restrict the State or its agencies from acquiring similar, equal, or like Contract
Activities from other sources.
48. Force Majeure. Neither party will be in breach of this Contract because of any failure
arising from any disaster or acts of god that are beyond their control and without their
fault or negligence. Each party will use commercially reasonable efforts to resume
performance. Contractor will not be relieved of a breach or delay caused by its
subcontractors. If immediate performance is necessary to ensure public health and
safety, the State may immediately contract with a third party.
49. Dispute Resolution. The parties will endeavor to resolve any Contract dispute in
accordance with this provision. The dispute will be referred to the parties' respective
Contract Administrators or Program Managers. Such referral must include a
description of the issues and all supporting documentation. The parties must submit
the dispute to a senior executive if unable to resolve the dispute within 15 business
days. The parties will continue performing while a dispute is being resolved, unless
the dispute precludes performance. A dispute involving payment does not preclude
performance.
Page 19 of 148
Litigation to resolve the dispute will not be instituted until after the dispute has been
elevated to the parties’ senior executive and either concludes that resolution is
unlikely or fails to respond within 15 business days. The parties are not prohibited
from instituting formal proceedings: (a) to avoid the expiration of statute of limitations
period; (b) to preserve a superior position with respect to creditors; or (c) where a
party makes a determination that a temporary restraining order or other injunctive
relief is the only adequate remedy. This Section does not limit the State’s right to
terminate the Contract.
50. Media Releases. Any news releases (including promotional literature and
commercial advertisements) which contain specific reference to MDHHS and pertain
to the Contract or project to which it relates must not be made without the prior
written approval of the State, and then only in accordance with the explicit written
instructions of the State.
51. Schedules. All Schedules and Exhibits that are referenced herein and attached
hereto are hereby incorporated by reference. The following Schedules are attached
hereto and incorporated herein:
Document Title Document Description
Schedule A Statement of Work
Schedule B HIPAA Business Associate Agreement
Schedule C Definitions/Explanation of Terms
Schedule D Reserved
Schedule E Reporting Requirements
Schedule F
Medicaid Mental Health Substance Use Disorder
Authorization Payment Responsibility Grid
Schedule G Local Funding Obligation Schedule
Schedule H Behavioral Health Capitation Rate Certification
52. Entire Agreement and Order of Precedence. This Contract, which includes
Statement of Work, and schedules and exhibits, is the entire agreement of the
parties related to the Contract Activities. This Contract supersedes and replaces all
previous understandings and agreements between the parties for the Contract
Activities. If there is a conflict between documents, the order of precedence is: (a)
first, this Contract, excluding its schedules, exhibits, and Statement of Work; (b)
second, Statement of Work as of the Effective Date; and (c) third, schedules
expressly incorporated into this Contract as of the Effective Date. NO TERMS ON
CONTRACTOR’S INVOICES, ORDERING DOCUMENTS, WEBSITE, BROWSE-
WRAP, SHRINK-WRAP, CLICK-WRAP, CLICK-THROUGH OR OTHER NON-
NEGOTIATED TERMS AND CONDITIONS PROVIDED WITH ANY OF THE
CONTRACT ACTIVITIES, OR DOCUMENTATION HEREUNDER, EVEN IF
ATTACHED TO THE STATE’S DELIVERY OR PURCHASE ORDER, WILL
CONSTITUTE A PART OR AMENDMENT OF THIS CONTRACT OR IS BINDING
Page 20 of 148
ON THE STATE OR ANY AUTHORIZED USER FOR ANY PURPOSE. ALL SUCH
OTHER TERMS AND CONDITIONS HAVE NO FORCE AND EFFECT AND ARE
DEEMED REJECTED BY THE STATE AND THE AUTHORIZED USER, EVEN IF
ACCESS TO OR USE OF THE CONTRACT ACTIVITIES REQUIRES
AFFIRMATIVE ACCEPTANCE OF SUCH TERMS AND CONDITIONS.
53. Severability. If any part of this Contract is held invalid or unenforceable, by any court
of competent jurisdiction, that part will be deemed deleted from this Contract and the
severed part will be replaced by agreed upon language that achieves the same or
similar objectives. The remaining Contract will continue in full force and effect.
54. Waiver. Failure to enforce any provision of this Contract will not constitute a waiver.
55. Survival. Any right, obligation or condition that, by its express terms or nature and
context is intended to survive, will survive the termination or expiration of this
Contract; such rights, obligations, or conditions include, but are not limited to, those
related to transition responsibilities; indemnification; disclaimer of damages and
limitations of liability; State Data; non-disclosure of Confidential Information;
representations and warranties; insurance and bankruptcy.
56. Contract Modification. This Contract may not be amended except by signed
agreement between the parties (a “Contract Change Notice”). Notwithstanding the
foregoing, no subsequent Statement of Work or Contract Change Notice executed
after the Effective Date will be construed to amend this Contract unless it specifically
states its intent to do so and cites the section or sections amended.
Page 21 of 148
FEDERAL PROVISIONS ADDENDUM
This addendum applies to purchases that will be paid for in whole or in part with funds
obtained from the federal government. If any provision below is not required by federal law for
this Contract, then it does not apply and must be disregarded. If any provision below is
required to be included in this Contract by federal law, then the applicable provision applies,
and the language is not negotiable. If any provision below conflicts with the State’s terms and
conditions, including any attachments, schedules, or exhibits to this Contract, the provisions
below take priority to the extent a provision is required by federal law; otherwise, the order of
precedence set forth in the Contract applies. Further, Contractor agrees to, through a Contract
Change Notice, append or modify specific federal provisions to this Contract, if reasonably
necessary to keep the State and Contractor in compliance with federal funding requirements,
and comply with the terms set forth therein. Hyperlinks are provided for convenience only;
broken hyperlinks will not relieve Contractor from compliance with the law.
A. Equal Employment Opportunity
This Contract is not a “federally assisted construction contract” as defined in 41 CFR
Part 60-1.3.
B. Davis-Bacon Act (Prevailing Wage)
This Contract is not a “federally assisted construction contract” as defined in 41 CFR
Part 60-1.3, nor is it a prime construction contract in excess of $2,000.
C. Copeland “Anti-Kickback” Act
This Contract is not a “federally assisted construction contract” as defined in 41 CFR
Part 60-1.3, nor is it a prime construction contract in excess of $2,000 where the Davis-
Bacon Act applies.
D. Contract Work Hours and Safety Standards Act
The Contract does not involve the employment of mechanics or laborers.
E. Rights to Inventions Made Under a Contract or Agreement
If this Contract is funded by a federal “funding agreement” as defined under 37 CFR §401.2
(a) and the recipient or subrecipient wishes to enter into a contract with a small business
firm or nonprofit organization regarding the substitution of parties, assignment or
performance of experimental, developmental, or research work under that “funding
agreement,” the recipient or subrecipient must comply with 37 CFR Part 401, “Rights to
Inventions Made by Nonprofit Organizations and Small Business Firms Under Government
Grants, Contracts and Cooperative Agreements,” and any implementing regulations issued
by the awarding agency.
F. Clean Air Act and the Federal Water Pollution Control Act
If this Contract is in excess of $150,000, Contractor must comply with all applicable
standards, orders, and regulations issued under the Clean Air Act (42 USC 7401-7671q)
and the Federal Water Pollution Control Act (33 USC 1251-1387), and during performance
of this Contract Contractor agrees as follows:
(1) Clean Air Act
Page 22 of 148
(i) Contractor agrees to comply with all applicable standards, orders or regulations
issued pursuant to the Clean Air Act, as amended, 42 U.S.C. § 7401 et seq.
(ii) Contractor agrees to report each violation to the State and understands and
agrees that the State will, in turn, report each violation as required to assure
notification to the Federal Emergency Management Agency or the applicable
federal awarding agency, and the appropriate Environmental Protection
Agency Regional Office.
(iii) Contractor agrees to include these requirements in each subcontract
exceeding $150,000 financed in whole or in part with Federal assistance
provided by FEMA or the applicable federal awarding agency.
(2) Federal Water Pollution Control Act
(i) Contractor agrees to comply with all applicable standards, orders, or
regulations issued pursuant to the Federal Water Pollution Control Act, as
amended, 33 U.S.C. 1251 et seq.
(ii) Contractor agrees to report each violation to the State and understands and
agrees that the State will, in turn, report each violation as required to assure
notification to the Federal Emergency Management Agency or the applicable
federal awarding agency, and the appropriate Environmental Protection
Agency Regional Office.
(iii) Contractor agrees to include these requirements in each subcontract
exceeding $150,000 financed in whole or in part with Federal assistance
provided by FEMA or the applicable federal awarding agency.
G. Debarment and Suspension
A “contract award” (see 2 CFR 180.220) must not be made to parties listed on the
government-wide exclusions in the System for Award Management (SAM), in accordance
with the OMB guidelines at 2 CFR 180 that implement Executive Orders 12549 (51 FR
6370; February 21, 1986) and 12689 (54 FR 34131; August 18, 1989), “Debarment and
Suspension.” SAM Exclusions contains the names of parties debarred, suspended, or
otherwise excluded by agencies, as well as parties declared ineligible under statutory or
regulatory authority other than Executive Order 12549.
(1) This Contract is a covered transaction for purposes of 2 CFR. Part 180 and 2 CFR. Part
3000. As such, Contractor is required to verify that none of Contractor’s principals
(defined at 2 CFR. § 180.995) or its affiliates (defined at 2 CFR. § 180.905) are excluded
(defined at 2 CFR. § 180.940) or disqualified (defined at 2 CFR. § 180.935).
(2) Contractor must comply with 2 CFR. Part 180, subpart C and 2 CFR. Part 3000, subpart
C, and must include a requirement to comply with these regulations in any lower tier
covered transaction it enters into.
(3) This certification is a material representation of fact relied upon by the State. If it is later
determined that Contractor did not comply with 2 CFR. Part. 180, subpart C and 2 CFR.
Part. 3000, subpart C, in addition to remedies available to the State, the Federal
Government may pursue available remedies, including but not limited to suspension
and/or debarment.
Page 23 of 148
(4) The bidder or proposer agrees to comply with the requirements of 2 CFR. Part 180,
subpart C and 2 CFR. Part 3000, subpart C while this offer is valid and throughout the
period of any contract that may arise from this offer. The bidder or proposer further
agrees to include a provision requiring such compliance in its lower tier covered
transactions.
H. Byrd Anti-Lobbying Amendment, 31 U.S.C. § 1352 (as amended)
Contractor has applied or bid for an award of $100,000 or more and shall file the required
certification in Exhibit 1 – Byrd Anti-Lobbying Certification attached to the end of this
Addendum. Each tier certifies to the tier above that it will not and has not used federally
appropriated funds to pay any person or organization for influencing or attempting to
influence an officer or employee of any agency, a Member of Congress, officer or employee
of Congress, or an employee of a Member of Congress in connection with obtaining any
federal contract, grant, or any other award covered by 31 U.S.C. § 1352. Each tier shall also
disclose any lobbying with non-federal funds that takes place in connection with obtaining
any federal award. Such disclosures are forwarded from tier to tier up to the recipient who in
turn will forward the certification(s) to the federal awarding agency.
I. Procurement of Recovered Materials
If this Contract is a procurement to purchase products or items designated by the EPA
under 40 CFR. part 247 during the course of a fiscal year, then under 2 CFR 200.323,
Contractors must comply with section 6002 of the Solid Waste Disposal Act, as amended by
the Resource Conservation and Recovery Act.
(1) In the performance of this contract, Contractor shall make maximum use of products
containing recovered materials that are EPA-designated items unless the product cannot
be acquired:
(i) Competitively within a timeframe providing for compliance with the contract
performance schedule;
(ii) Meeting contract performance requirements; or
(iii) At a reasonable price.
(2) Information about this requirement, along with the list of EPA- designated items, is
available at EPA’s Comprehensive Procurement Guidelines web site,
https://www.epa.gov/smm/comprehensive- procurement-guideline-cpg-program.
(3) Contractor also agrees to comply with all other applicable requirements of Section 6002
of the Solid Waste Disposal Act.
J. Prohibition on Contracting for Covered Telecommunications Equipment or Services
Contractor acknowledges and agrees that Section 889(b) of the John S. McCain National
Defense Authorization Act for Fiscal Year 2019, Pub. L. No. 115-232 (the “McCain Act”),
and 2 CFR. §200.216, prohibit the obligation or expending of federal award funds on certain
telecommunication products or with certain entities for national security reasons on or after
August 13, 2020.
During performance of this Contract, Contractor agrees as follows:
Page 24 of 148
(a) Definitions. As used in this Section J. Prohibition on Contracting for Covered
Telecommunications Equipment or Services (“Section J”):
(1) the terms “backhaul,” “critical technology,” “interconnection arrangements,”
“reasonable inquiry,” “roaming,” and “substantial or essential component” have
the meanings defined in 48 CFR § 4.2101;
(2) the term “covered foreign country” has the meanings defined in § 889(f)(2) of the
McCain Act; and
(3) the term “covered telecommunications equipment or services” has the meaning
defined in § 889(f)(3) of the McCain Act.
(b) Prohibitions.
(1) Unless an exception in paragraph (c) of this Section J applies, neither Contractor
nor any of its subcontractors may use funds received under this Contract to:
(i) Procure or obtain any equipment, system, or service that uses covered
telecommunications equipment or services as a substantial or essential
component of any system, or as critical technology of any system;
(ii) Enter into, extend, or renew a contract to procure or obtain any
equipment, system, or service that uses covered telecommunications
equipment or services as a substantial or essential component of any
system, or as critical technology of any system;
(iii) Enter into, extend, or renew a contract with an entity that uses any
covered telecommunications equipment or services as a substantial or
essential component of any system, or as critical technology as part of
any system; or
(iv) Provide, as part of its performance of this contract, subcontract, or other
contractual instrument, any equipment, system, or service that uses
covered telecommunications equipment or services as a substantial or
essential component of any system, or as critical technology as part of
any system.
(c) Exceptions.
(1) This Section J does not prohibit Contractor from providing—
(i) A service that connects to the facilities of a third-party, such as
backhaul, roaming, or interconnection arrangements; or
(ii) Telecommunications equipment that cannot route or redirect user data
traffic or permit visibility into any user data or packets that such
equipment transmits or otherwise handles.
(d) Reporting requirement.
(1) In the event Contractor identifies covered telecommunications equipment or
services used as a substantial or essential component of any system, or as
critical technology as part of any system, during contract performance, or
Contractor is notified of such by a subcontractor at any tier or by any other
source, Contractor shall report the information in paragraph (d)(2) of this Section
J to the recipient or subrecipient, unless elsewhere in this contract are
established procedures for reporting the information. In the event of this
occurrence, reports should be submitted to the contract administrator.
Page 25 of 148
(2) Contractor shall report the following information pursuant to paragraph (d)(1) of
this Section J:
(i) Within one business day from the date of such identification or
notification: The contract number; the order number(s), if applicable;
supplier name; supplier unique entity identifier (if known); supplier
Commercial and Government Entity (CAGE) code (if known); brand;
model number (original equipment manufacturer number, manufacturer
part number, or wholesaler number); item description; and any readily
available information about mitigation actions undertaken or
recommended.
(ii) Within 10 business days of submitting the information in paragraph
(d)(2)(i) of this Section J: Any further available information about
mitigation actions undertaken or recommended. In addition, Contractor
shall describe the efforts it undertook to prevent use or submission of
covered telecommunications equipment or services, and any additional
efforts that will be incorporated to prevent future use or submission of
covered telecommunications equipment or services.
(e) Subcontracts. Contractor shall insert the substance of this Section J, including this
paragraph (e), in all subcontracts and other contractual instruments.
K. Domestic Preferences for Procurements
As appropriate, and to the extent consistent with law, Contractor should, to the greatest
extent practicable, provide a preference for the purchase, acquisition, or use of goods,
products, or materials produced in the United States. This includes, but is not limited to
iron, aluminum, steel, cement, and other manufactured products.
For purposes of this Section K – Domestic Preferences for Procurements:
“Produced in the United States” means, for iron and steel products, that all manufacturing
processes, from the initial melting stage through the application of coatings, occurred in the
United States.
“Manufactured products” mean items and construction materials composed in whole or in
part of non-ferrous metals such as aluminum; plastics and polymer-based products such as
polyvinyl chloride pipe; aggregates such as concrete; glass, including optical fiber; and
lumber.
L. Affirmative Socioeconomic Steps
For all contracts utilizing federal funding sources subject to Title 2 of the Code of Federal
Regulations (CFR) Part 200 issued on or after November 12, 2020, if subcontracts are to
be let, the prime contractor is required to take all necessary steps identified in 2 CFR. §
200.321(b)(1)-(5) to ensure that small and minority businesses, women’s business
enterprises, and labor surplus area firms are used when possible.
M. Copyright and Data Rights
Pursuant to 2 CFR
§ 200.315(b), the State may copyright any work which is subject to
copyright and was developed, or for which ownership was acquired, under a Federal
award. T
he Federal awarding agency reserves a royalty-free, nonexclusive and
Page 26 of 148
irrevocable right to reproduce, publish, or otherwise use the work for Federal purposes,
and to authorize others to do so.
N. Additional FEMA Contract Provisions
This Contract does not involve purchases that will be paid for in whole or in part with funds
obtained from the Federal Emergency Management Agency (FEMA).
O. Other Federal Contract Provisions
The following provisions also apply to purchases that will be paid for in whole or in part with
funds obtained from the federal government: Contractor must comply with federal
requirements in Title XIX of the Social Security Act, 42 CFR Part 438 and other applicable
laws, including requirements incorporated into the Medicaid and Children’s Health
Insurance Program Managed Care Final Rule published November 13, 2020 and effective
on December 14, 2020, and requirements in effect prior to the release of the 2020 Final
Rule (i.e., in effect in 42 CFR Part 438 contained in 42 CFR Parts 430 to 481, edition
revised as of May 6, 2016) and did not materially change within the 2020 Final Rule.

Page 27 of 148
EXHIBIT 1 BYRD ANTI-LOBBYING
CERTIFICATION
Contractor must complete this certification if the purchase will be paid for in whole or in part
with funds obtained from the federal government and the purchase is greater than $100,000.
APPENDIX A, 44 CFR. PART 18 – CERTIFICATION REGARDING LOBBYING
Certification for Contracts, Grants, Loans, and Cooperative Agreements
The undersigned certifies, to the best of his or her knowledge and belief, that:
1. No Federal appropriated funds have been paid or will be paid, by or on behalf of the
undersigned, to any person for influencing or attempting to influence an officer or employee
of an agency, a Member of Congress, an officer or employee of Congress, or an employee
of a Member of Congress in connection with the awarding of any Federal contract, the
making of any Federal grant, the making of any Federal loan, the entering into of any
cooperative agreement, and the extension, continuation, renewal, amendment, or
modification of any Federal contract, grant, loan, or cooperative agreement.
2. If any funds other than Federal appropriated funds have been paid or will be paid to any
person for influencing or attempting to influence an officer or employee of any agency, a
Member of Congress, an officer or employee of Congress, or an employee of a Member of
Congress in connection with this Federal contract, grant, loan, or cooperative agreement,
the undersigned shall complete and submit Standard Form-LLL, “Disclosure Form to Report
Lobbying,” in accordance with its instructions.
3. The undersigned shall require that the language of this certification be included in the award
documents for all subawards at all tiers (including subcontracts, subgrants, and contracts
under grants, loans, and cooperative agreements) and that all subrecipients shall certify and
disclose accordingly.
This certification is a material representation of fact upon which reliance was placed when
this transaction was made or entered into. Submission of this certification is a prerequisite
for making or entering into this transaction imposed by section 1352, Title 31, U.S.C. Any
person who fails to file the required certification shall be subject to a civil penalty of not less
than $10,000 and not more than $100,000 for each such failure.
Page 28 of 148
Contractor, enter contractor name here, certifies or affirms the truthfulness and accuracy of
each statement of its certification and disclosure, if any. In addition, Contractor understands
and agrees that the provisions of 31 U.S.C. Chap. 38, Administrative Remedies for False
Claims and Statements, apply to this certification and disclosure, if any.
Signature of Contractor’s Authorized Official
Name and Title of Contractor’s Authorized Official
Date
Page 29 of 148
SCHEDULE A- STATEMENT OF WORK CONTRACT
ACTIVITIES
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
The State hereby enters into a Contract with the specialty Prepaid Inpatient Health Plan (PIHP)
Contractor identified on the signature page of this Contract.
BACKGROUND
Under approval granted by the Centers for Medicare and Medicaid Services (CMS), the Michigan
Department of Health and Human Services (MDHHS) operates a 1115 Behavioral Health
Demonstration Waiver. Under this waiver, selected Medicaid State plan specialty services related
to mental health and developmental disability services, as well as certain covered substance use
disorder services, have been “carved out” (removed) from Medicaid primary physical health care
plans and arrangements.
CMS has also approved a 1115 Demonstration Waiver titled the Healthy Michigan Plan (HMP)
which provides health care coverage for adults who become eligible for Medicaid under Section
1902(2)(10)(A)(i)(VIII) of the Social Security Act. In Michigan, the 1115 Behavioral Health
Demonstration Waiver and the Healthy Michigan Plan are managed on a shared risk basis by
specialty PIHP contractors, selected through the Application for Participation (AFP) process which
can be found on the MDHHS website:
https://www.michigan.gov/-
/media/Project/Websites/mdhhs/Folder2/Folder64/Folder1/Folder164/2_6_2013_AFP.pdf?rev=d68
64822812b4c5fb1ace235562cbc71.
Services provided under the behavioral health managed care program include treatment for people
with Serious Mental Illness (SMI), Serious Emotional Disturbance (SED), Substance Use Disorder
(SUD) and Intellectual and Developmental Disabilities (I/DD). Behavioral Health Services include
State plan and Early Periodic Screening, Diagnosis and Treatment (EPSDT) services, 1915(i)
Waiver services and 1915(c) Waiver services:
•
Children’s Waiver Program (CWP)
•
Habilitation Supports Waiver (HSW)
•
Serious Emotional Disturbance (SED) Waiver
All the substance use disorder services are covered under the State plan (or alternative benefit
plan (ABP)) for the HMP population.
SCOPE
The purpose of this Contract is to obtain the services of Contractor to manage the 1115 Behavioral
Health Demonstration Waiver Program, the Healthy Michigan Plan and relevant approved Waivers
in a designated service area and to provide a comprehensive array of specialty mental health and
substance use disorder services and supports as indicated in this Contract. Contractor must
manage its responsibilities in a manner that promotes maximum value, efficiency, and
effectiveness consistent with State and federal statute and applicable waiver standards. This
includes limiting managed care administrative duplication thereby reducing avoidable costs while
maximizing the Medical Loss Ratio (MLR). Contractor must actively manage behavioral health
services for its geographical service area using standardized methods and measures for
determination of need and appropriate delivery of service. Contractor must ensure that cost

Page 30 of 148
variances in services are supported by quantifiable measures of need to ensure accountability,
value and efficiency. Contractor must minimize duplication of contracts and reviews for providers
contracting with multiple Community Mental Health Services Programs (CMHSPs) in the service
area.
RESPONSIBILITIES OF THE STATE
The State will administer this Contract with Contractor, monitor Contract performance, and perform
the following activities:
1.
Notify Contractor of the name, address, and telephone number, if available, of all Medicaid,
MI Child and Healthy Michigan eligibles in the service area. Contractor will be notified of
changes, as they are known to the State.
2.
The State has the authority to take whatever action is necessary to address repeated health
and welfare issues or emergencies or Contractor’s failure to provide medically necessary
services timely.
REQUIREMENTS
Contractor must provide Deliverables/Services and staff, and otherwise do all things necessary or
incidental to the performance requirements and performance of work, pursuant to the requirements
set forth in this Contract. Contractor must comply with all provisions of Medicaid policy applicable to
Contractors unless provisions of this Contract stipulate otherwise. All policies, procedures,
operational plans and clinical guidelines followed by Contractor must be in writing and available to
the State and CMS upon request. All medical records, report formats, information systems, liability
policies, provider network information and other details specific to performing the Contracted
Services must be available to the State and CMS upon request.
Contractor must have sufficient administrative staff and organizational components to comply with
the responsibilities reflected in this Contract. Contractor must ensure that all personnel has training,
education, experience, licensing, or certification appropriate to their position and responsibilities.
1. General Requirements
The following sections provide an explanation of the specifications and expectations that
Contractor must meet and the services that must be provided under the Contract. Contractor and
its provider network are not, however, constrained from supplementing this with additional services
or elements deemed necessary to fulfill the intent of the Medicaid Managed Specialty Services and
Supports Program (MMSSSP) and the Flint 1115 Waiver.
A.
Service Area
1.
Targeted Geographical Area for Implementation
a.
Contractor must manage the 1115 Behavioral Health Demonstration Waiver Program
and the Healthy Michigan Plan under the terms of this Contract for its geographic
service area. Counties included in each service area can be found at the following
website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/cmhsp.
2.
Target Population
a.
Contractor must serve Medicaid beneficiaries in the service area described in
Section 1.A.1.a. above who require the Medicaid services included under the 1115
Behavioral Health Demonstration Waiver; who are eligible for the Healthy Michigan
Plan, the 1915(i) State Plan Benefit the Flint 1115 Waiver; who are enrolled in the
1915(c) waivers (HSW, CWP, SED); who are enrolled in the MIChild program; who

Page 31 of 148
are enrolled in the Maternity Outpatient Medical Services (MOMS) program, or for
whom Contractor has assumed or been assigned County of Financial Responsibility
(COFR) status under Chapter 3 of the Mental Health Code.
3.
Home and Community Character
a.
Contractor must assure that the residential (adult foster care, specialized residential,
provider owned/controlled) and non-residential services (skill building, supported
employment, community living supports, pre-vocational, out of home non-vocational)
where individuals are supported by funds from the Medicaid 1915(c) waiver
programs (Habilitation Supports Waiver, Children’s Waiver, and Children’s SED
Waiver) maintain a home and community character setting as required by federal
regulation and the resultant, Michigan-specific, Home and Community Based
Services State Transition Plan.
B.
Customer Services Standards
1.
Introduction
Contractor must establish a Customer Services Unit. Contactor must convey an
atmosphere that is welcoming, helpful and informative. As per 42 CFR 438.66, these
standards apply to Contractor and to any entity to which Contractor has delegated the
customer service function in accordance with 42 CFR 438.230.
2.
Functions
a.
Welcome and orient individuals to services and benefits available, and the provider
network.
b.
Provide information about how to access behavioral health, primary health, and other
community services.
c.
Provide information about how to access the various rights processes.
d.
Provide the “Your Rights When Receiving Mental Health Services in Michigan”
booklet. Reference the following website for more information:
https://cmham.org/services/bookstore/
.
e.
Help individuals with problems and inquiries regarding benefits.
f.
Assist people with and oversee local complaint and grievance processes.
g.
Track and report patterns of problem areas for the organization.
3.
Requirements
Contractor must:
a.
Establish a Customer Services Unit with a minimum of one full-time equivalent
(FTE).
b.
Establish a toll-free customer service telephone line with access to alternative
telephonic communication methods (such as teletypewriter (TTY)).
c.
Publish customer service numbers in agency brochures and public information
material.
d.
Ensure initial calls are answered by a live voice during normal business hours, a
minimum of eight hours daily, Monday through Friday, excluding observed holidays.
e.
Publish how to access Customer Services information outside of normal business
hours in the Customer Services Handbook and on Contractor website.
f.
Provide each beneficiary a Customer Services Handbook within a reasonable time.
g.
Post the customer handbook on Contractor website.
h.
Provide the Customer Services Handbook to the beneficiary by one of the following
methods:
i.
Mailing a printed copy to the beneficiary’s mailing address.
ii.
Emailing an electronic version after obtaining the beneficiary’s written approval.
iii.
Notifying the beneficiary by providing a written statement that identifies where the
handbook can be found on the website.
iv.
Other alternate distribution method based on the request of the beneficiary.

Page 32 of 148
i.
Provide, upon request, each affiliate CMHSP’s current organizational chart, list of
Board members, board meeting schedule and minutes and annual report.
j.
Upon request, assist beneficiaries with filing grievances and appeals, accessing local
dispute resolution processes, and coordinating with Fair Hearing Officers and the
local Office of Recipient Rights (ORR). See Section L. Grievance and Appeals
Process for Beneficiaries.
k.
Ensure staff are trained and possess current, working knowledge in the following
areas:
i.
The populations served (serious mental illness, serious emotional disturbance,
developmental disability and substance use disorder) and eligibility criteria for
various benefits plans (e.g., Medicaid, Healthy Michigan Plan, MIChild).
ii.
Service array, medical necessity requirements and eligibility for and referral to
specialty services.
iii.
Person-centered planning.
iv.
Self-determination.
v.
Recovery and Resiliency.
vi.
Peer Specialists.
vii.
Grievance and appeals, Fair Hearings, local dispute resolution processes, and
Recipient Rights. Contractor must ensure that newly hired staff be trained in
Recipient Rights within 30 days of hire.
viii.
Limited English Proficiency (LEP) and cultural competency.
ix.
Information on covered items and services and benefits not covered under this
Contract.
x.
The Public Behavioral Health System.
xi.
Customer services functions and beneficiary rights and protections in accordance
with federal regulations.
xii.
Community resources (e.g., advocacy organizations, housing options, schools,
public health agencies).
xiii.
Public Health Code, Mental Health Code and Medicaid Provider Manual.
4.
Customer Services Handbook Requirements
Contractor must comply with 42 CFR 438.10, including the following:
a.
Include the date of publication/revision and version number in each Customer
Services Handbook.
b.
Provide a current version of the Customer Services Handbook to the beneficiary
upon first request of service and annually thereafter, or sooner if substantial revisions
have been made.
c.
To the extent possible, provide each beneficiary with at least 30 days’ notice before
the intended effective date of any change that the State defines as significant in the
information specified in 42 CFR 438.10(g)(2). Significant is defined as any change
that affects a beneficiary’s Medicaid benefits, including but not limited to: Contractor
contract information, authorization for services, covered benefits and copays.
d.
The topics with asterisks (*) below must use the standard language templates (which
can be found on
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/customer-services.)
e.
Ensure all information contained in the Customer Services Handbook is easily
understood.
f.
The information must be available in the prevalent non-English language(s) spoken
in Contractor’s service area.
g.
Obtain State approval, in writing, prior to publishing original and revised editions of
the Customer Services Handbook.
h.
Produce supplemental materials to the Customer Services Handbook, as needed, to

Page 33 of 148
ensure compliance with Contractual Requirements (e.g., inserts/stickers).
i.
Use the State’s description for each Medicaid covered service.
j.
Include the following contact information for Medicaid Health Plans (MHP) or
Medicaid fee-for-service programs:
i.
Plan/program name
ii.
Locations
iii.
Telephone numbers
k.
Include the following topics in the Customer Services Handbook:
i.
Topics Requiring use of MDHHS Template Language, which can be found on the
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/customer-services, include:
1) *Template #1: Confidentiality and Family Access to Information
2) *Template #2: Coordination of Care
3) *Template #3: Emergency and After-Hours Access to Services
4) *Template #4: Glossary or Definition of Terms
5) *Template #5: Grievance and Appeals Processes
6) *Template #6: Language Assistance and Accommodations
7) *Template #7: Payment for Services
8) *Template #8: Person-Centered Planning
9) *Template #9: Recipient Rights
10) *Template #10: Recovery and Resiliency
11) *Template #11: Service Array
12) *Template #12: Service Authorization
13) *Template #13: Tag Lines
14) *Template #14: Fraud, Waste and Abuse
ii.
Other Required Topics (not necessarily in this order), include:
1) Benefits Provided by Contractor.
2) How and where to access any benefits provided.
3) Access to out-of-network services.
4) Affiliate the names, addresses and phone numbers of the following
personnel:
a) Executive director.
b) Medical director.
c) Recipient rights officer.
d) Customer services.
e) Emergency (911) and after-hours contact numbers.
5) Transition of Care Policy
6) Community resource list (and advocacy organizations) .
7) Index.
8) Right to information about Contractor operations (e.g., organizational chart,
annual report).
9) S
ervices not covered under contract.
10) Welcome to the PIHP.
11) What are customer services and what it can do for the beneficiary
12) Hours of operation and process for obtaining customer assistance after hours
iii.
Other Suggested Topics
1) Customer services phone number in the footer of each page
2) Safety information
3) Web Address
C.
Payment Reform
1.
Behavioral Health Integration
Page 34 of 148
a.
Contractor recognizes the importance of integrating both physical health and
behavioral health services in order to effectively address beneficiary needs and
improve health status.
b.
Contractor agrees to work with the State to develop initiatives to better integrate
services covered by Contractor and the MHP(s) serving Contractor’s beneficiaries
and to provide incentives to support behavioral health integration.
c.
Contractor agrees to collaborate with MHPs and the State to develop shared metrics
to measure the quality of care provided to beneficiaries jointly served by Contractor
and MHPs.
2.
Data Reporting
a.
In order to continually improve the performance of its contracted providers,
Contractor must collect and report data in a consistent and coordinated manner in
collaboration with the State.
b.
Contractor agrees to work collaboratively with the State and with other Contractors to
develop standard measure specifications, data collection processes, baseline data,
and reports that will be provided to contracted providers and the State.
3.
Responsibility for Payment of Authorized Services
a.
Contractor will be responsible for payment for services that Contractor authorizes,
including Medicaid substance use disorder services. This provision presumes
Contractor, and its network providers/subcontractors are fulfilling their responsibility
to individuals according to terms specified in the Contract.
b.
Services must not be delayed or denied as a result of a dispute of payment
responsibility between two or more network providers/subcontractors. In the event
there is an unresolved dispute between Contractor and network
providers/subcontractor(s), either one may request the State’s involvement to resolve
the dispute and make a determination. Likewise, services must not be delayed or
denied as a result of a dispute of payment responsibility between Contractor and the
network provider/subcontractor.
c.
Contractor, or their designee, must be contacted for authorization for post-
stabilization care. Contractor is financially responsible for post-stabilization specialty
care services obtained which are pre-approved by Contractor, or their designee, if
authorization is delegated to it by Contractor in accordance with 42 CFR 438.230.
d.
Contractor is also responsible for post-stabilization care services when they are
administered to maintain, improve or resolve the beneficiary’s stabilized condition
when:
i.
Contractor does not respond to a request for pre-approval within one hour.
ii.
Contractor cannot be contacted.
iii.
Contractor’s representative and the treating physician cannot reach an
agreement concerning the beneficiary's care and a Contractor physician is not
available for consultation. In this situation, Contractor must give the treating
physician the opportunity to consult with a Contractor physician and the treating
physician may continue with care of the patient until a Contractor physician is
reached or one of the criteria of 42 CFR 422.133(c)(3) is met.
e.
Financial responsibility for enrollees who are children is the county where the child
and parents have primary residence. For temporary and permanent wards of the
State or court (including tribal), financial responsibility is the county where the child
current resides in the community (i.e., licensed foster care home, relative placement,
or independent living) as long as the foster care case remains open. Residential
treatment facilities licensed as a Child Caring Institution (CCI) including shelter
placements contracted by MDHHS child welfare are not considered “residing in the
community.” If a temporary or permanent court ward is residing in the community

Page 35 of 148
with a foster family, the county where the child is residing is responsible for
authorizing inpatient psychiatric hospitalization when medically necessary. If the child
is not residing in the community and placed by child welfare in a residential treatment
facility or a DHHS emergency shelter licensed as a CCI, the county of court record
would be responsible for assessing and authorizing the inpatient psychiatric
hospitalization and providing transition services (assessment for community-based
services, wraparound, case management or supports coordination) for up to 180
days prior to discharge.
f.
In accordance with 42 CFR 438.114(c)(1)(ii)(B), Contractor is prohibited from
denying payment for treatment obtained by a beneficiary when a representative of
Contractor instructs the beneficiary to seek emergency services. The attending
emergency physician, or the provider actually treating the beneficiary, is responsible
for determining when the beneficiary is sufficiently stabilized for transfer or discharge
in accordance with 42 CFR 438.114(d)(3).
g.
In accordance with 42 CFR 438.114(d)(2), Contractor may not hold an enrollee who
has an emergency medical condition liable for payment of subsequent screening and
treatment needed to diagnose the specific condition or stabilize the patient.
4.
Medicaid Services Verification
a.
Contractor must perform annual verification of Medicaid claims in accordance with
Medicaid Services Verification:
https://www.michigan.gov/mdhhs/keep-
mihealthy/mentalhealth/mentalhealth/practiceguidelines and must be finalized no
later than December 31.
5.
Liability for Payment
a.
Contractor must provide that its Medicaid beneficiaries are not held liable for Covered
services provided to the beneficiary, for which the State does not pay Contractor, or
Contractor does not pay the individual or health care provider that furnished the
services under a contractual, referral, or other arrangement.
D.
Contract Remedies and Sanctions
1.
The State will utilize a variety of means to assure compliance with Contract
requirements and with the provisions of Section 330.1232b of Michigan's Mental Health
Code. The State will pursue remedial actions and possibly sanctions as needed to
resolve outstanding contract violations and performance concerns. The application of
remedies and sanctions shall be a matter of public record. If action is taken under the
provisions of Section 330.1232b of the Mental Health Code, an opportunity for a hearing
will be afforded Contractor, consistent with the provisions of Section 330.1232b.(6)
and/or the Administrative Procedures Act 306 of 1969.
2.
The pursuance of any of remedial actions does not require a Contract amendment. The
Contract Compliance notice to Contractor is sufficient authority. The use of remedies
and sanctions will typically follow a progressive approach, but the State reserves the
right to deviate from the progression as needed to seek correction of serious, or
repeated patterns of substantial non-compliance or performance problems. Contractor
can utilize the dispute resolution provision of the Contract to dispute a Contract
compliance notice issued by the State or pursue other available legal remedies.
3.
Before imposing a sanction on a Contractor, the State will provide Contractor with timely
written Contract compliance notice that explains both of the following:
a.
The compliance issue along with its statutory/regulatory/contractual basis and the
objective evidence upon which the finding of fault is based.
b.
The opportunity for a hearing to contest or dispute the State's findings and intended
sanction, prior to the imposition of the sanction. A hearing under this Section is
subject to the provisions governing a contested case under the Administrative
Procedures Act of 1969, 1969 Public Act (PA) 306, MCL 24.201 to 24.328, unless

Page 36 of 148
otherwise agreed to in the specialty PIHP contract.
4.
The State may do any of the following:
a.
Require a plan of correction and specified status reports that becomes a Contract
performance objective.
b.
Retain a portion of the .002% contract withhold to be earned through timely and
accurate completion and resolution of corrective action plans associated with the
MDHHS conducted 1915(c) Waivers (CWP, HSW, and SEDW) site reviews of PIHP
operations as specified in the CAP Incentive Scoring Metric, which is located on the
MDHHS Reporting Requirements website at
https://www.michigan.gov/mdhhs/keep-
mi-healthy/mentalhealth/reporting
c.
Impose a direct dollar penalty and make it a non-matchable Contractor administrative
expense and reduce earned savings from that fiscal year by the same dollar amount.
d.
Delay up to 25% of scheduled payment amount to Contractor until compliance is
achieved.
i.
The State may apply this sanction in a subsequent payment cycle and will give
prior written notice to Contractor.
e.
Initiate Contract termination.
E.
Access and Availability
1.
Provider Network Services
Contractor is responsible for maintaining and continually evaluating an effective provider
network adequate to fulfill the obligations of this contract. Contractor remains the
accountable party for the Medicaid beneficiaries in its service area, regardless of the
functions it has delegated to its provider networks as specified in 42 CFR 438.230. In
this regard and in compliance with 42 CFR Parts 438.414; 438.10(g)(2)(xi)(C)(D)(E) and
457.1260, Contractor must:
a.
Maintain a regular means of communicating and providing information on changes in
policies and procedures to its providers. This may include guidelines for answering
written correspondence to providers, offering provider- dedicated phone lines, and a
regular provider newsletter.
b.
Have clearly written mechanisms to address provider grievances and complaints,
and an appeal system to resolve disputes.
c.
Provide a copy of Contractor's prior authorization policies to the provider when the
provider joins Contractor's provider network. Contractor must notify providers of any
changes to prior authorization policies.
d.
Provide a copy of Contractor's grievance, appeal and fair hearing procedures and
timeframes to the provider when the provider joins Contractor's provider network.
Contractor must notify providers of any changes to those procedures or timeframes.
e.
Provide to the State, in the format specified by the State, provider agency information
profiles that contain a complete listing and description of the provider network
available to recipients in the service area.
f.
Assure that services are accessible, taking into account travel time, availability of
public transportation, and other factors that may determine accessibility.
g.
Assure that network providers do not segregate beneficiaries in any way from other
individuals receiving their services.
2.
Network Requirements
a.
Contractor must maintain a network of qualified providers in sufficient numbers, mix,
and geographic locations throughout their respective service area for the provision of
all covered services. Contractor may also utilize qualified providers from outside
Contractor’s service area for the provision of covered services.
b.
Contractor must consider anticipated enrollment and expected utilization of services.
c.
Contractor must provide documentation on which the State bases its certification that
Page 37 of 148
Contractor complied with the State’s requirements for availability and accessibility of
services, including the adequacy of the provider network as referenced in 42 CFR
Parts 438.604(a)(5); 438.606; 438.207(b) and 438.206. Submission of
documentation will take place as specified by the State but no less frequently than
the following:
i.
At the time Contractor enters into a contract with the State.
ii.
On an annual basis.
iii.
Anytime there has been significant change (as defined by the State) in Contractor
operations that would affect adequacy of capacity and services, including changes in
services, benefits, geographic service area, composition of or payments to its
provider networks, or at the enrollment of a new population.
d.
Contractor must submit any other data, documentation, or information relating to the
performance of the entity’s obligations as required by the State as referenced in 42
CFR Parts 438.604(b) and 438.606.
e.
In accordance with 42 CFR 438.14, Contractor must demonstrate that there are
sufficient Indian Health Care Providers (IHCP) participating in the provider network to
ensure timely access to services available under the Contract from such providers
for Indian beneficiaries who are eligible to receive services.
i.
If timely access to covered services cannot be ensured due to few or no IHCPs,
Contractor must:
1) Allow Indian beneficiaries to access out-of-State IHCPs; or
2) Show good cause for disenrollment from both Contractor and the State's
managed care program in accordance with 42 CFR § 438.56(c).
ii.
Contractor must permit Indian beneficiaries to obtain services covered under the
Contract from out-of- network IHCPs from whom the beneficiary is otherwise
eligible to receive such services.
iii.
Contractor must permit an out-of-network IHCP to refer an Indian beneficiary to a
network provider.
3.
Changes in Provider Network
a.
Contractor must notify the State within seven days of any changes to the
composition of the provider network organizations that negatively affect access to
care. Contractor must have procedures to address changes in its network that
negatively affect access to care. Changes in provider network composition that
MDHHS determines to negatively affect recipient access to covered services may be
grounds for sanctions.
b.
The State may apply sanctions to Contractor if a network change that negatively
affects beneficiaries’ access to care is not reported timely, or Contractor is not willing
or able to correct the issue.
4.
Out of Network Providers
a.
Contractor must provide adequate and timely access to and authorize and reimburse
Out-of-Network providers and cover Medically Necessary services for beneficiaries if
such services could not reasonably be obtained by a Network Provider on a timely
basis inside or outside the State of Michigan. Contractor must cover such out-of-
Network services for as long as Contractor’s Provider Network is unable to provide
adequate access to covered Medically Necessary services for the identified
beneficiary(ies) as referenced in 42 CFR 438.206(b)(4).
b.
If Contractor cannot reasonably provide access to non-emergent Covered Services
by a Network Provider within access requirements of this Contract, Contractor must
include in its service authorization decision, the provision of Covered Services Out-
of-Network.
c.
Contractor must coordinate with Out-of-Network providers with respect to payment

Page 38 of 148
and follow all applicable MDHHS policies to ensure the beneficiary is not liable for
costs greater than would be expected for in network services including a prohibition
on balance billing in compliance with 42 CFR 438.106, 42 CFR 438.116, 42 CFR
438.206(b)(5) and the Medicaid Provider Manual.
d.
Contractor must comply with all related Medicaid Policies regarding authorization and
reimbursement for Out-of- Network providers.
i.
Contractor must pay Out-of-Network Medicaid providers’ claims at established
Medicaid fees in effect on the date of service.
ii.
If Michigan Medicaid has not established a specific rate for the Covered
Service, Contractor must follow Medicaid Policy to determine the correct
payment amount.
5.
1115 Behavioral Health Demonstration Waiver and Healthy Michigan Programs
a.
Services may be provided at or through Contractor service sites or contractual
provider locations. Unless otherwise noted in the Michigan Medicaid Provider
Manual, mental health and intellectual/developmental disabilities services may also
be provided in other locations in the community, including the beneficiary's home,
according to individual need and clinical appropriateness.
6.
Provider Procurement
a.
Contractor is responsible for the development of the service delivery system and the
establishment of sufficient administrative capabilities to carry out the requirements
and obligations of this Contract. Where Contractor and its provider network fulfill
these responsibilities through subcontracts, they must adhere to applicable
provisions of federal procurement requirements as specified in 2 CFR 200. In
complying with these requirements and in accordance with 42 CFR 438.12,
Contractor:
i.
May not discriminate for the participation, reimbursement, or indemnification of
any provider who is acting within the scope of his or her license or certification
under applicable State law, solely on the basis of that license or certification.
ii.
Must give those providers not selected for inclusion in the network written
notice of the reason for its decision.
iii.
Is not required to contract with providers beyond the number necessary to
meet the needs of its beneficiaries and is not precluded from using different
practitioners in the same specialty. Nor is Contractor prohibited from
establishing measures that are designed to maintain quality of services and
control costs and are consistent with its responsibilities to its beneficiaries. In
addition, Contractor's selection policies and procedures cannot discriminate
against particular providers that serve high-risk populations or specialize in
conditions that require costly treatments. Also, Contractor must ensure that it
does not employ or contract with providers excluded from participation in
federal health care programs under either Section 1128 or Section 1128A of
the Social Security Act.
7.
Access Standards
a.
Contractor must ensure timely access to supports and services in the preferred
language of the person served based on their language skills and in accordance with
the Access Standards
(https://www.michigan.gov/documents/mdhhs/Access_Standards_702741_7.pdf)
which can be found on the MDHHS website: https://www.michigan.gov/mdhhs/keep-
mi-healthy/mentalhealth/mentalhealth/practiceguidelines and the following timeliness
standards and report its performance on the standards in accordance with Schedule
E of this Contract.

Page 39 of 148
b.
Have written policies guaranteeing each beneficiary’s right to request and receive a
copy of their medical records, and to request that they be amended or corrected.
8.
Person Centered Planning
a.
The Michigan Mental Health Code, MCL 330.1712, establishes the right for all
individuals to have an Individual Plan of Service (IPOS) developed through a person-
centered planning process. Contractor must implement person-centered planning in
accordance with the MDHHS Person-Centered Planning Policy which can be found
on the MDHHS website: https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines. In accordance with 42 CFR
438.208(b)(2)(i), the person-centered planning process must include coordination of
services between settings of care which includes appropriate discharge planning for
short and long-term hospitalizations. This provision is not a requirement of
Substance Use Disorder Services.
b.
Contractor must ensure that its provider network uses a specially-constituted
committee, such as a behavior treatment plan review committee, to review and
approve or disapprove any plans that propose to use restrictive or intrusive
interventions with individuals served by the public mental health system who exhibit
seriously aggressive, self-injurious or other behaviors that place the individual or
others at risk of physical harm. The Committee must substantially incorporate the
standards in the Standards for Behavior Treatment Plan Review Committees,
https://www.michigan.gov/mdhhs/-
/media/Project/Websites/mdhhs/Folder4/Folder13/Folder3/Folder113/Folder2/Folder
213/Folder1/Folder313/Technical_Requirement_for_Behavior_Treatment_Plans.pdf?
rev=92e7d3739bf64c97991657af19362634&hash=E6D047EBF35C585C715665FF2
ACD9BCD which can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines
9.
Cultural Competence
a.
The supports and services provided by Contractor (both directly and through
contracted providers) must demonstrate an ongoing commitment to linguistic and
cultural competence that ensures access and meaningful participation for all people
in the service area. Such commitment includes acceptance and respect for the
cultural values, beliefs and practices of the community, as well as the ability to apply
an understanding of the relationships of language and culture to the delivery of
supports and services.
b.
To effectively demonstrate such commitment, it is expected that Contractor has five
components in place: (1) a method of community assessment; (2) sufficient policy
and procedure to reflect Contractor's value and practice expectations; (3) a method
of service assessment and monitoring; (4) ongoing training to assure that staff are
aware of, and able to effectively implement, policy; and (5) the provision of supports
and services within the cultural context of the recipient.
c.
Contractor must participate in the State’s efforts to promote the delivery of services
in a culturally competent manner to all beneficiaries, including those with limited
English proficiency and diverse cultural and ethnic backgrounds, and those who are
Deaf, Hard of Hearing, and Deaf and Blind. Treatment will be modified to effectively
serve individuals who are deaf, hard of hearing, and deaf and blind as determined by
their language skills and preferences.
10.
Self-Direction
a.
It is the expectation that Contractor will assure compliance among their network of
service providers all elements of Participant-Directed Services outlined in the
1915(i)(1)(G)(iii), 1915(c) Appendix E HCBS waiver authorities and the Self-Directing
Page 40 of 148
Services Policy which can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines. This provision is not a
requirement of Substance Use Disorder Services.
11.
Choice
a.
In accordance with 42 CFR 438.3(l), Contractor must assure that the beneficiary is allowed to
choose his or her health care professional, i.e., physician, therapist, etc. to the extent
possible and appropriate.
12.
Second Opinion
a.
If the beneficiary requests, Contractor must provide for a second opinion from a
qualified health care professional within the network or arrange for the ability of the
beneficiary to obtain one outside the network, at no cost to the beneficiary.
13.
Denials by a Qualified Professional
a.
Contractor must assure that any decision to deny a service authorization request or
to authorize a service in an amount, duration, or scope that is less than requested,
must be made by a health care professional who has appropriate clinical expertise in
treating the beneficiary's condition.
14.
Recovery Policy
a.
All Supports and Services provided to individuals with mental illness, including those
with co-occurring conditions, must be based in the principles and practices of
recovery outlined in the Michigan Recovery Council document, Recovery Policy and
Practice Advisory which can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/drugcontrol/reportstats/reportcontent/policies-and-advisories
15.
Nursing Home Placements
a.
Contractor agrees to provide medically necessary Medicaid specialty services to
facilitate placement from, or divert admissions to, a nursing home for eligible
beneficiaries determined by the Omnibus Budget Reconciliation Act (OBRA)
screening assessment to have a mental illness and/or developmental disability and in
need of placement and/or services.
16.
Nursing Home Mental Health Services
a.
Residents of nursing homes with mental health needs must be given the same
opportunity for access to Contractor services as other individuals covered by this
Contract.
17.
Payments to Federally Qualified Health Centers (FQHCs) and Rural Health Clinics
(RHCs)
a.
When Contractor pays FQHCs and RHCs for specialty services included in the
specialty services waivers, Contractor must ensure that payments are no less than
amounts paid to non-FQHC and non-RHCs for similar services.
18.
Indian Health Service/Tribally Operated Facility or program/Urban Indian Clinic (I/T/U)
a.
Contractor is required to pay any Indian Health Service, Tribal Operated Facility
Organization/Program/Urban Indian Clinic (I/T/U), or I/T/U contractor, whether
participating in Contractor provider network or not, for Contractor authorized medically
necessary covered Medicaid managed care services provided to Medicaid
beneficiary/Indian beneficiaries who are eligible to receive services from the I/T/U
provider either (1) at a rate negotiated between Contractor and the I/T/U provider, or (2)
if there is no negotiated rate, at a rate not less than the level and amount of payment that
would be made if the provider were not an I/T/U provider.
b.
In accordance with 42 CFR 438.14, when an Indian Health Care Provider is not enrolled
in Medicaid as a FQHC, regardless of whether it participates in the network of
Contractor, it has the right to receive its applicable encounter rate published annually
Page 41 of 148
in the Federal Register by the Indian Health Service, or in the absence of a published
encounter rate, the amount it would receive if the services were provided under the
state plan’s FFS payment methodology.
19.
Persons Associated with the Corrections System
a.
Under an arrangement between the Michigan Department of Corrections (MDOC) and
the Michigan Department of Health and Human Services (MDHHS), the PIHP must be
responsible for medically necessary community-based substance use disorder treatment
services for individuals under the supervision of the Michigan Department of Corrections
once those individuals are no longer incarcerated. These individuals are typically under
parole or probation orders. Individuals referred by court and services through local
community corrections (PA 511) systems must not be excluded from these
Medicaid/Healthy Michigan program funded medically necessary community-based
substance use disorder treatment services.
b.
Referrals, Screening and Assessment
i.
Individuals under MDOC supervision are considered a priority population for
assessment and admission for substance use disorder treatment services due
to the public safety needs related to their MDOC involvement. Contractor must
ensure timely access to supports and services in accordance with this
Contract. The Code of Federal Regulations and the Michigan Public Health
Code define the first four (4) priority population enrollees. The fifth population
is established by MDHHS due to its high-risk nature. The priority populations
are identified as follows and in the order of importance:
1) Pregnant injecting drug user.
2) Pregnant.
3) Injecting drug user
4) Parent at risk of losing their child(ren) due to substance use.
5) Individual under supervision of MDOC AND referred by MDOC OR individual
being released directly from an MDOC facility without supervision AND
referred by MDOC. Excludes individuals referred by court and services
through local community corrections (PA 511 funded) systems.
6) All others.
ii.
Contractor must designate a point of contact within each Contractor catchment
area for referral, screening and assessment problem identification and
resolution. The position title and contact information will be provided to the
State, which will provide the information to the MDOC Central Office Personnel.
Contractor must provide this contact information to MDOC Supervising Agents
in their regions.
iii.
The MDOC Supervising Agent will refer individuals in need of substance use
disorder treatment through the established referral process at Contractor. The
Supervising Agent will make best efforts to obtain from the individual a signed
Michigan Behavioral Health Standard Consent Form, MDHHS-5515, and
provide it to Contractor and/or designated access point along with any
pertinent background information and the most recent MDOC Risk Assessment
summary.
iv.
The Supervising Agent will assist the individual in calling Contractor or
designated access point for a substance use disorder telephonic screening for
services. Individuals that are subsequently referred for substance use disorder
treatment as a result of a positive screening must receive an in-person
assessment. If the individual referred is incarcerated, the Supervising Agent
will make best efforts to facilitate service initiation and appropriate contact with
Contractor/Designated Access Point. Provided that it is possible to do so,

Page 42 of 148
Contractor must make best efforts to ensure the individual receives a
telephonic, video or in-person screening for services at the designated location
as arranged by MDOC Supervising Agent. Contractor/designated access point
may not deny an individual an in-person assessment via phone screening.
v.
Assessments must be conducted in accordance with MDHHS-approved
assessment instruments (if any) and admissions decisions based on MDHHS-
approved medical necessity criteria included in this Contract. In the case of
MDOC supervised individuals, these assessments should include
consideration of the individual’s presenting symptoms and substance
use/abuse history prior to and during incarceration and consideration of their
SUD treatment history while incarcerated. To the extent consistent with HIPAA,
the Michigan Mental Health Code and 42 CFR Part 2, and with the written
consent of the individual, Contractor/designated provider will provide notice of
an admission decision to the Supervising Agent within one business day, and
if accepted, the name and contact information of the individual’s treatment
provider. If the individual is not referred for treatment services,
Contractor/designated access point will provide information regarding
community resources such as AA/NA or other support groups to the individual.
vi.
Contractor must not honor Supervising Agent requests or proscriptions for
level or duration of care, services or supports and must base admission and
treatment decisions only on medical necessity criteria and professional
assessment factors.
c.
Plan of Service
i.
The individualized master treatment plan must be developed in a manner
consistent with the principles of person-centered planning as applicable to
individuals receiving treatment for substance use disorders as defined in this
Contract and applicable portions of Person-Centered Planning Policy (which
can be found at:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines .
ii.
Contractor/designated provider agrees to inform the Supervising Agent when
Medication Assisted Treatment (MAT) is being used, including medication type.
If the medication type changes, Contractor/designated provider must inform
the Supervising Agent. Contractor/designated provider must obtain a release
of information from the beneficiary.
d.
Residential Services
i.
If an individual referred for residential treatment does not appear for, or is
determined not to meet, medical necessity criteria for that level of care, the
Supervising Agent must be notified with one business day. If an individual is
participating in residential treatment, the individual may not be given
unsupervised day passes, furloughs, etc. without consultation with the
Supervising Agent. Leaves for any non-emergent medical procedure should be
reviewed/coordinated with the Supervising Agent. If an individual is absent
from an off-site supervised therapeutic activity without proper authorization,
Contractor/designated provider must notify the Supervising Agent by the end
of the day on which the absence occurred.
ii.
Contractor/designated provider may require individuals participating in
residential treatment to submit to drug testing when returning from off property
activities and any other time there is a suspicion of use. Positive drug test
results and drug test refusals must be reported to the Supervising Agent.
Contractor/designated provider must obtain a release of information from the
beneficiary.
Page 43 of 148
iii.
Additional reporting notifications for individuals receiving residential care
include:
1) Death of an individual under supervision.
2) Relocation of an individual’s placement for more than 24 hours.
3) Contractor/designated provider must immediately, and no more than one
hour from awareness of the occurrence, notify the MDOC Supervising Agent
any serious sentinel event by or upon an individual under MDOC supervision
while on the treatment premises or while on authorized leaves.
4) Contractor/designated provider must notify the MDOC Supervising Agent of
any criminal activity involving an MDOC supervised individual within one hour
of learning of the activity.
e.
Service Participation
i.
Contractor must ensure the designated provider completes a monthly progress
report on each individual on a template supplied by the MDOC and must
ensure it is sent via encrypted email to the Supervising Agent by the fifth day of
the following month.
ii.
Contractor/designated provider must not terminate any referred individual from
treatment for violation of the program rules and regulations without prior
notification to the individual’s Supervising Agent, except in extreme
circumstances. Contractor/designated provider must collaborate with the
MDOC for any non-emergency removal of the referred individual and allow the
MDOC time to develop a transportation plan and a supervision plan prior to
removal.
iii.
Contractor must ensure a recovery plan is completed and sent to the
Supervising Agent within five business days of discharge. Recovery planning
must include an offender’s acknowledgment of the plan and Contractor’s
referral of the offender to the prescribed aftercare services.
f.
Testimony
With a properly executed release inclusive of the court with jurisdiction, Contractor
and/or its designated provider, must provide testimony to the extent consistent with
applicable law, including HIPAA and 42 CFR Part 2.
g.
Training
i.
In support of the needs of programs providing services to individuals under
MDOC supervision, the MDHHS will make available training on criminogenic
risk factors and special therapy concerns regarding the needs of this
population.
ii.
Contractor must ensure its provider network delivers services to individuals
served consistent with professional standards of practice, licensing standards,
and professional ethics.
h.
Compliance Monitoring
Contractor is not accountable to the MDOC under this Contract. Contractor must
permit the MDHHS, or its designee, to visit Contractor to monitor Contractor provider
network oversight activities for the individuals served under this Section.
i.
Provider Network Oversight
Contractor is solely responsible for the composition, compensation and performance
of its contracted provider network. To the extent necessary, Contractor must include
performance requirements/standards based on existing regulatory or contractual
requirements applicable to the MDOC-supervised population. Provider network
oversight must be in compliance with applicable sections of this Contract.
20.
Network Adequacy Standards.
Information regarding Network Adequacy Standards can be found at the following

Page 44 of 148
MDDHS website:
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
a.
Pursuant to 42 CFR Parts 438.68 and 457.1218, MDHHS created a Network
Adequacy Standard policy (MSA 18-49) and corresponding procedural document to
effectuate network adequacy standards for Michigan’s specialty behavioral health
delivery system. Contractor must comply with the network adequacy standards set
forth in the policy and procedure documents.
b.
Contractor must comply with the standards set forth in this Contract requirement.
The State will provide 90 days’ advance written notice to Contractor prior to the
effective date of any changes to the network adequacy procedure.
c.
Contractor must submit a plan on how the standards will be effectuated. Contractor
must consider at least the following parameters for their plans:
i.
Maximum time and distance
ii.
Timely appointments
iii.
Language, Cultural competence, and Physical accessibility
21.
Intensive Crisis Stabilization Services (ICSS)
Contractor must report its performance on the standards specific to ICSS for children on
behalf of the enrolled programs in their geographic service area in accordance with
Schedule E of this Contract.
22.
Transition of Care
Contractor must develop and implement a transition of care policy consistent with 42
CFR 438.62 and the MDHHS Transition of Care Technical Requirement to ensure
continuity of care for its enrollees. The Contractor transition of care policy must be
included in the enrollee handbook.
a.
Contractor’s transition of care policy must ensure continued access to services
during a transition from FFS to a managed care entity, or transition from one
managed care entity to another when a beneficiary, in the absence of continued
services, would suffer serious detriment to their health or be at risk of hospitalization
or institutionalism.
b.
The transition of care policy must include at a minimum:
i.
Transitioning Beneficiaries have access to services consistent with the access
they previously had.
ii.
Transitioning Beneficiaries must be permitted to retain their current provider for
the time period required in MDHHS’ transition of care technical requirement if
that provider is not in Contractor’s network.
iii.
Transitioning Beneficiaries are referred to appropriate providers within
Contractor’s network.
iv.
Contractor, if previously serving a beneficiary must fully and timely comply with
requests for historical utilization, data from the beneficiary’s new contractor or
MDHHS.
c.
Contractor must include instructions to beneficiaries and potential beneficiaries on
how to access continued services upon transition.
F.
Covered Services
1.
General
a.
Contractor must conform to professionally accepted standards of care and may not
arbitrarily deny or reduce the amount, duration, or scope of a required service solely
because of the diagnosis, type of illness, or condition of a beneficiary.
b.
Contractor must operate consistent with all applicable Medicaid policies and
publications for coverages and limitations. If new Medicaid services are added,
expanded, eliminated, or otherwise changed, Contractor must implement the
changes consistent with State direction and the terms of this Contract.

Page 45 of 148
c.
Contractor will be responsible for the operation of the 1115 Behavioral Health
Demonstration Waiver, the Healthy Michigan Plan, the 1915(i) State Plan Benefit,
those who are enrolled in one of the three 1915(c) waivers (Habilitation Supports
Waiver, Children’s Waiver Program, or the Waiver for Children with Serious
Emotional Disturbances) and other public funding within its designated service area.
Operation of the 1115 Behavioral Health Demonstration Waiver Program must
conform to regulations applicable to the concurrent program and to each (i.e., 1115
Behavioral Health Demonstration Waiver and 1915 (c)) Waiver. Contractor will also
be responsible for development of the service delivery system and the establishment
of sufficient administrative capabilities to carry out the requirements and obligations
of this Contract. If Contractor elects to subcontract, Contractor must comply with
applicable provisions of federal procurement requirements as specified in 2 CFR
200, except as waived for CMHSPs in the 1115 Behavioral Health Demonstration
Waiver.
d.
Contractor will be responsible for the Reciprocity Standards policy which can be
found on the MDHHS Policies & Practice Guidelines website,
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines
2.
1115 Demonstration Waiver
a.
State Plan Services: Under the 1115 Demonstration Waiver, Contractor is
responsible for providing the covered services as described in the Michigan Medicaid
Provider Manual.
3.
1915(c) Services
a.
Contractor is responsible for provision of certain enhanced community support
services for those beneficiaries in the service area who are enrolled in one of the
three Michigan’s 1915(c) Home and Community Based Services Waivers. Covered
services are described in the Behavioral Health and Intellectual and Developmental
Disability Supports and Services Chapter of the Michigan Medicaid Provider Manual.
4.
Healthy Michigan Plan
a.
Contractor is responsible for providing the covered services described in the
Behavioral Health and Intellectual and Developmental Disability Supports and
Services Mental Health/Substance Use Disorder Chapter of the Michigan Medicaid
Provider Manual as well as the additional Substance Use Disorder services and
supports described in the Medicaid Provider Manual for individuals who are eligible
for the Healthy Michigan Plan.
5.
MIChild
a.
Contractor must provide medically necessary defined mental health benefits to
children enrolled in the MIChild program.
6.
Flint 1115 Waiver
a.
The demonstration waiver expands coverage to children up to age 21 years and to
pregnant women with incomes up to and including 400 percent of the federal poverty
level (FPL) who were served by the Flint water system from April 2014 through a
State-specified date. This demonstration is approved in accordance with Section
1115(a) of the Social Security Act, and is effective as of March 3, 2016, the date of
the signed approval through September 30, 2026.
b.
Medicaid-eligible children and pregnant women who were served by the Flint water
system during the specified period will be eligible for all services covered under the
State plan. All such persons will have access to Targeted Case Management
services under a fee for service contract between the State and Genesee Health
Systems (GHS). The fee for service contract will provide the targeted case
management services in accordance with the requirements outlined in the Special

Page 46 of 148
Terms and Conditions for the Flint Section 1115 Demonstration, the Michigan
Medicaid State Plan and Medicaid Policy.
7.
Institution for Mental Disease (IMD) Services
a.
As per 42 CFR 438.3(e)(2)(iii), the covered services in an IMD will be offered to enrollees
at the option of the Contractor and with agreement from the enrollee up to 15 days per
month per individual if the following conditions are met:
i.
The IMD stay is a medically appropriate substitute for the covered setting
under the State plan.
ii.
The IMD stay is a cost-effective substitute for the setting under the State plan.
iii.
The beneficiary is not required to use the alternative setting.
8.
Early Periodic Screening, Diagnosis and Treatment (EPSDT)
a.
Under Michigan's 1115 Behavioral Health Demonstration Waiver, Contractor is
responsible for the provision of specialty services Medicaid benefits and must make
these benefits available to beneficiaries referred by a primary EPSDT screener, to
correct or ameliorate a qualifying condition discovered through the screening
process.
b.
While transportation to EPSDT corrective or ameliorative specialty services is not a
covered service under this waiver, Contractor must assist beneficiaries in obtaining
necessary transportation either through the State or through the beneficiary’s
Medicaid health plan.
9.
Special Health Care Needs
a.
Beneficiaries with special health care needs must have direct access to a specialist,
as appropriate for the individual’s health care condition, as specified in 42 CFR
438.208(c) (4).
10.
Opioid Health Home (OHH) (Optional Benefit to be provided by approved Contactors)
a.
The OHH will provide comprehensive care management and coordination services to
Medicaid beneficiaries with opioid use disorder who also have or are at risk of
developing another chronic condition. For enrolled beneficiaries, the OHH will
function as the central point of contact for directing patient-centered care across the
broader health care system. Beneficiaries will work with an interdisciplinary team of
providers to develop an individualized recovery care plan to best manage their care.
The model will also elevate the role and importance of peer recovery coaches and
community health workers to foster direct empathy and connection to improve overall
health and wellness. In doing so, this will attend to a beneficiary's complete health
and social needs. Participation is voluntary, and enrolled beneficiaries may opt out at
any time.
b.
OHH receives reimbursement for providing the following federally mandated core
services:
i.
Comprehensive care management
ii.
Care coordination and health promotion
iii.
Comprehensive transitional care
iv.
Patient and family support
v.
Referral to community and support services
c.
Contractor, serving as the Lead Entity (LE), must meet all requirements indicated in
the Opioid Health Home State Plan Amendment, Medical Services Administration
(MSA) Policy 18-27, Opioid Health Home Handbook, and all other Medicaid laws,
regulations, policies, and procedures (reference the following MDHHS website:
www.michigan.gov/ohh
)Contractor must utilize State Plan qualified Opioid
Treatment Programs (OTPs) and Office Based Opioid Treatment providers (OBOTs)
to execute the OHH via a “Hub and Spoke” system of care. Participation is voluntary
and enrolled beneficiaries may opt-out at any time. The OHH will provide

Page 47 of 148
comprehensive care management and coordination services to Medicaid
beneficiaries with an opioid use disorder diagnosis.
d.
Contractor, serving as the LE, will be responsible for the administrative oversight,
coordination, and provision of OHH services.
e.
Contractor is responsible for the selection and paneling of designated Opioid Health
Home Partners (OHHPs), coordination of enrollment through the Waiver Support
Application, payment, health information technology, coordination of services, and
other requirements cited in the approved State Plan, Policy, and the OHH Handbook.
f.
OHH providers will be required to enroll in Contractor’s provider panel.
g.
Contractor must execute a contract with OHHPs to ensure an adequate network of
providers to meet the state plan defined requirements.
h.
Contractor must provide technical assistance and training to current and prospective
OHHPs to successfully operationalize the OHH program.
i.
Provider Types
i.
Eligible provider types for the OHH include OTPs and OBOT providers.
11.
Behavioral Health Home (BHH) (Optional Benefit to be provided by approved
Contactors)
a.
BHH will provide comprehensive care management and coordination services to
Medicaid beneficiaries with a serious mental illness or serious emotional disturbance.
For enrolled beneficiaries, the BHH will function as the central point of contact for
directing patient-centered care across the broader health care system. Beneficiaries
will work with an interdisciplinary team of providers to develop a person-centered
health action plan to best manage their care. The model will also elevate the role and
importance of Peer Support Specialists and Community Health Workers to foster
direct empathy and raise overall health and wellness. In doing so, this will attend to a
beneficiary’s complete health and social needs. Participation is voluntary and
enrolled beneficiaries may opt-out at any time.
b.
BHH receives reimbursement for providing the following federally mandated core
services:
i.
Comprehensive care management
ii.
Care coordination and health promotion
iii.
Comprehensive transitional care
iv.
Patient and family support
v.
Referral to community and support services
c.
Contractor, serving as the LE, will be responsible for the administrative oversight,
coordination, and provision of BHH services.
d.
Contractor must meet all requirements indicated in the BHH Handbook, and all other
Medicaid laws, regulations, policies, and procedures (reference the following MDHHS
website: www.michigan.gov/bhh
)
e.
Contractor is responsible for the selection and paneling of designated Behavioral
Health Home Partners (BHHPs), coordination of enrollment through the Waiver
Support Application, payment, health information technology, coordination of
services, and other requirements cited in the approved State Plan, Policy, and the
BHH Handbook.
f.
Contractor must execute a contract with BHHPs to ensure an adequate network of
providers to meet the state plan defined requirements.
g.
Contractor must provide technical assistance and training to current and prospective
BHHPs to successfully operationalize the BHH program.
12.
Long-Term Support Services
a.
Long Term Services and Supports (LTSS) provided under this Contract must be
provided in a setting which complies with the 42 CFR 441.301(c)(4) requirements for
Page 48 of 148
home and community-based settings. Contractor must establish and maintain a
member advisory committee. The member advisory committee must include a
reasonably representative sample of the LTSS population, or other individuals
representing those beneficiaries, covered under this Contract.
13.
Maternity Outpatient Medical Services (MOMS)
a.
Contractor must provide medically necessary defined mental health benefits to
women enrolled in the MOMS program.
14.
CMS Certified Community Behavioral Health Clinic (CCBHC) Demonstration
Contractors with certified CCBHC Demonstration Sites in their regions will execute the
PIHP duties and responsibilities as cited and required by the MDHHS CCBHC Policy
and the MDHHS MI CCBHC Demonstration Handbook to implement the CMH CCBHC
Demonstration in accordance with Section 223 of the Protecting Access to Medicare Act
of 2014.
a.
Per the CCBHC Policy and MI CCBHC Demonstration Handbook, key PIHP
responsibilities and duties include, but are not limited to, the following:
i.
CCBHC Oversight and Support
ii.
CCBHC Enrollment and Assignment
iii.
CCBHC Coordination and Outreach
iv.
CCBHC Payment
v.
CCBHC Reporting
vi.
CCBHC Grievance Monitoring
b.
PIHPs must comply with the CCBHC Demonstration Policy and the most current
version of the corresponding MI CCBHC Demonstration Handbook, as authorized by
the policy. MDHHS may modify the MI CCBHC Demonstration Handbook as needed
in accordance with the following parameters:
i.
For minor changes (e.g., formatting, style, organization, grammar, etc.) or
technical modifications that do not substantively alter CCBHC operations,
MDHHS will draft and send an updated draft version of the MI CCBHC
Demonstration Handbook with proposed changes to the PIHPs for notice and
review. Upon receiving the proposed changes, the PIHPs will have up to 15
days to provide feedback. PIHPs will, as part of its review, notify and seek
feedback from its contracted CCBHCs on the proposed Handbook updates. A
majority of the PIHPs may waive the 15-day feedback period to allow the new
version of the MI CCBHC Demonstration Handbook to take effect sooner.
ii.
For all other changes, MDHHS will draft and send an updated draft version of
the MI CCBHC Demonstration Handbook with proposed changes to the PIHPs
for notice and review. Upon receiving the proposed changes, the PIHPs will
have up to 30 days to provide feedback. PIHPs will, as part of its review, notify
and seek feedback from its contracted CCBHCs on the proposed Handbook
updates. A two-thirds majority of the PIHPs may waive the 30-day feedback
period to allow the new version of the MI CCBHC Demonstration Handbook to
take effect sooner.
G.
Contractor Governance and Board Requirements
1.
For the purposes of this Contract, the designation as a Contractor applies to single
county Community Mental Health Service Program or regional entities (organized under
Section 1204b of the Mental Health Code or Urban Cooperation Act) serving Contractor’s
service areas as defined by the State. Contractor must either be a single county
CMHSP, or a regional entity jointly and representatively governed by all CMHSPs in the
service area pursuant to Section 204 or 205 of PA 258 of 1974, as amended in the
Mental Health Code.
2.
Contractor must establish a SUD Oversight Policy Board pursuant to Section 287 of PA

Page 49 of 148
258 of 1974, as amended in the Mental Health Code.
3.
Contractor must Provide timely notification to the Department, in writing, of any action by
its governing board or any other funding source that would require or result in significant
modification in the provision of services, funding or compliance with operational
procedures.
H.
Behavioral/Physical Health Integration
1.
Medicaid Health Plan (MHP) Agreements
a.
Many Medicaid beneficiaries receiving services from Contractor will be enrolled in an
MHP for their health care services. The MHP is responsible for non-specialty level
mental health services. It is therefore essential that Contractor have a written,
functioning Coordinating Agreement with each MHP serving any part of Contractor's
service area. The written Coordinating Agreement must describe the coordination
arrangements, inclusive of but not limited to, the exchange of information, referral
procedures, care coordination and dispute resolution. At a minimum, these
arrangements must address the integration of physical and mental health services
provided by the MHP and Contractor for the shared consumer base plans. A model
Coordination Agreement is provided on the MDHHS Policies and Practice Guidelines
website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines. Contractors must, in
collaboration with coordinating MHPs, update the Coordination Agreement to
incorporate any necessary remedies to improve continuity of care, care
management, and the provision of health care services, at least annually.
2.
Integrated Physical and Mental Health Care
a.
Contractor must initiate affirmative efforts to ensure the integration of primary and
specialty behavioral health services for Medicaid beneficiaries. These efforts must
focus on persons that have a chronic condition such as a serious mental health
illness, co-occurring substance use disorder, children with serious emotional
disorders or a developmental disability and have been determined by Contractor to
be eligible for Medicaid Specialty Mental Health Services and Supports.
i.
Contractor must implement practices to encourage all consumers eligible for
specialty mental health services to receive a physical health assessment
including identification of the primary health care home/provider, medication
history, identification of current and past physical health care and referrals for
appropriate services. The physical health assessment will be coordinated
through the consumer's MHP as defined in H.1.
ii.
As authorized by the consumer, Contractor must include the results of any
physical health care findings that relate to the delivery of specialty mental
health services and supports in the PCP process.
iii.
Contractor must make its best effort to conduct an initial screening of each
enrollee's needs, within 90 days of the effective date of enrollment for all new
enrollees. Contractor must make subsequent attempts to conduct an initial
screening of each enrollee's needs if the initial attempt to contact the enrollee
is unsuccessful. Since Contractor is not an enrollment model, screening once
an individual presents for services would meet this agreement.
3.
Primary Care Coordination
a.
In accordance with 42 CFR Part 2 Contractor must take all appropriate steps to
assure that substance use disorder treatment services are coordinated with primary
health care. Care Coordinating Agreements or joint referral agreements, by
themselves, are not sufficient to show that Contractor has taken all appropriate steps
related to coordination of care. Client treatment case file documentation is also
necessary. Client treatment case files must include, at minimum, the primary care
Page 50 of 148
physician’s name and address, a signed release of information for purposes of
coordination, or a statement that the client has refused to sign a release.
b.
Contractor must coordinate the services furnished to the beneficiary with the services
the beneficiary receives with Fee For Service (FFS) Medicaid.
I.
Eligibility
1.
Medicaid Eligibility
a.
The MDHHS MSA administers the Medicaid program in Michigan. Eligibility is
determined by the State with the sole authority to determine whether individuals or
families meet eligibility requirements.
2.
1915(c) Habilitation Supports Waiver
a.
Contractor must identify Medicaid Beneficiaries who are eligible for and meet criteria for
the HSW per the approved 1915(c) HSW application and submit eligible enrollees to the
State for review and approval.
b.
The 1915(c) HSW and 1915(i) uses an “attrition management” model that allows PIHPs
to “fill in behind” attrition with new beneficiaries up to the limits established in the
CMS- approved waiver. MDHHS has allocated slots to each of the PIHPs. The
process for filling a slot involves the following steps: 1) the PIHPs submit applications
for Medicaid beneficiaries for enrollment based on vacant slots within the PIHP and
includes required documentation that supports the eligibility for HSW; 2) MDHHS
personnel reviews the PIHP enrollment applications; and 3) MDHHS personnel
approves (within the constraint of the total yearly number of available waiver
certificates and priority populations described in the CMS-approved waiver) those
beneficiaries who meet the requirements described above.
c.
The State may reallocate an existing HSW slot from one Contractor to another if:
i.
Contractor has presented no suitable candidate for enrollment in the HSW
within 60 days of the certificate being vacated and
ii.
there is a high priority candidate (person exiting the ICF/ IID or at highest risk
of needing ICF/ IID placement, or young adult aging off CWP) in another
service area where no certificate is available.
d.
The State will review all disenrollments from the HSW.
e.
Contractor is responsible for the administration of the HSW and therefore must
adhere to the requirements outlined in CMS approved 1915 (c) HSW application.
3.
1915(c) Children’s Waiver Program
a.
Contractor must identify children who meet the eligibility criteria for the Children’s
Waiver Program Benefit Plan and submit to, the State, prescreens for those children.
For children determined ineligible for the CWP, Contractor, on behalf of the State,
informs the family of its right to request a Medicaid fair hearing by providing written
adequate notice of denial of the CWP to the family.
b.
Contractor must carry out administrative and operational functions delegated by
State to Contractor as specified in the CMS approved (c) waiver application. These
delegated functions include level of care determination; review of participant service
plans; prior authorization of waiver services; utilization management; qualified
provider enrollment; quality assurance and quality improvement activities.
c.
Contractor must determine the appropriate Category of Care/Intensity of Care and
the amount of publicly funded hourly care for each Children’s Waiver Program
recipient per the Medicaid Provider Manual.
d.
Contractor must assure that services are provided in amount, scope, and duration as
specified in the approved plan.
e.
Contractor must comply with policy covering credentialing, temporary/provisional
credentialing and re- credentialing processes for those individuals and organizational
providers directly or contractually employed by Contractor, as it pertains to the
Page 51 of 148
rendering of services within the Children’s Waiver Program.
f.
Contractor is responsible for ensuring that each provider, directly or contractually
employed, credentialed or non-credentialed, meets all applicable licensing, scope of
practice, contractual and Medicaid Provider Manual qualifications, and requirements.
4.
1915(c) Serious Emotional Disability Waiver (SEDW)
a.
The intent of this program is to provide Home and Community Based Waiver
Services, as approved by Centers for Medicare and Medicaid Services (CMS) for
children with Serious Emotional Disturbances Benefit Plan, along with state plan
services in accordance with the Medicaid Provider Manual.
i.
Contractor must assess eligibility for the SEDW and submit applications to the
State for those children Contractor determines are eligible. For children
determined ineligible for the SEDW, Contractor, on behalf of the State, informs
the family of its right to request a Medicaid fair hearing by providing written
adequate notice of denial of the SEDW to the family.
ii.
Contractor must carry out administrative and operational functions delegated
by the State to Contractor as specified in the CMS approved (c) waiver
application. These delegated functions include level of care determination;
review of participant service plans; prior authorization of waiver services;
utilization management; qualified provider enrollment; quality assurance and
quality improvement activities.
iii.
Contractor must assure that services are provided in amount, scope and
duration as specified in the approved plan of service. Wraparound is a
required service for all participants in the SEDW and Contractor must assure
sufficient service capacity to meet the needs of SEDW recipients.
iv.
Contractor must comply with credentialing, temporary/provisional credentialing
and re- credentialing processes for those individuals and organizational
providers directly or contractually employed by Contractor, as it pertains to the
rendering of services within the SEDW. Contractor is responsible for ensuring
that each provider, directly or contractually employed, credentialed or non-
credentialed, meets all applicable licensing, scope of practice, contractual and
Medicaid Provider Manual qualifications and requirements.
b.
SEDW Child Welfare Project Procedural Requirements
Contractor must:
i.
Develop local agreements with County local MDHHS offices outlining roles
and responsibilities regarding the MDHHS SEDW Child Welfare Project.
ii.
Identify a specific referral process for children identified as potentially eligible
for the SEDW, with the assistance of local MDHHS workers, Contractor SEDW
Coordinator, CMHSP SEDW Leads and Wraparound Supervisors.
iii.
Participate in required SEDW Child Welfare Project State/Local technical
assistance meetings and trainings.
iv.
Collect and report, to the State, all data as requested by the State.
J.
Parity and Benefits
1.
Contractor must ensure compliance with 42 CFR part 438, subpart K, Parity in Mental
Health and Substance Use Disorder Benefits. Contractor must comply with all applicable
federal regulations, including the information requirements in the parity regulations,
specifically 42 CFR 438.915 Availability of Information. The State will work with the
Contractor to ensure the necessary changes to achieve full compliance are successfully
implemented. The State will analyze parity compliance as part of routine monitoring of
Contractor.
2.
Contractor must use processes, strategies, evidentiary standards, or other factors in
determining access to out-of-network providers for mental health or substance use
Page 52 of 148
disorder benefits that are comparable to, and applied no more stringently than, the
processes, strategies, evidentiary standards, or other factors in determining access to
out-of-network providers for medical/surgical benefits as identified by the State, in the
same classification.
3.
Contractor must not apply any financial requirement or treatment limitation to mental
health or substance use disorder benefits in any classification that is more restrictive
than the predominant financial requirement or treatment limitation of that type applied to
substantially all medical/surgical benefits as identified by the State, in the same
classification furnished to beneficiaries (whether or not the benefits are furnished by the
same Managed Care Plan (MCP).
4.
Contractor may not apply any cumulative financial requirements for mental health or
substance use disorder benefits in a classification (inpatient, outpatient, emergency
care, prescription drugs) that accumulates separately from any established for
medical/surgical benefits as identified by the State, in the same classification.
5.
Contractor may not impose Non-Quantitative Treatment Limitation (NQTLs) for mental
health or substance use disorder benefits in any classification unless, under the policies
and procedures of Contractor as written and in operation, any processes, strategies,
evidentiary standards, or other factors used in applying the NQTL to mental health or
substance use disorder benefits in the classification are comparable to, and are applied
no more stringently than, the processes, strategies, evidentiary standards, or other
factors used in applying the limitation for medical/surgical as identified by MDHHS,
benefits in the classification.
K.
Quality Improvement and Program Development
1.
Utilization Management Incentives
a.
Contractor must assure that compensation to individuals or entities that conduct
utilization management activities is not structured to provide incentives for the
individual or entity to deny, limit, or discontinue medically necessary services to any
beneficiary.
2.
Quality Assessment/Performance Improvement Program (QAPIP) and Standards
a.
Contractor must have a fully operational QAPIP in place that meets the conditions
specified in the Quality Assessment and Performance Improvement Program
Technical Requirement (
https://www.michigan.gov/mdhhs/-
/media/Project/Websites/mdhhs/Folder4/Folder13/Folder3/Folder113/Folder2/Folder
213/Folder1/Folder313/QA_and_PIP__for_Specialty_Prepaid_Inpatient_Health_Plan
s.pdf?rev=d4dc2f2bff104f199c2c38c5d460185c&hash=7D31840A589904614DDE39
B83B790A8C.) which can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines
b.
External Quality Review
i.
The State will arrange for an annual, external independent review of the quality
and outcomes, timeliness of, and access to covered services provided by
Contractor. Contractor must address the findings of the external review
through its QAPIP. Contractor must develop and implement performance
improvement goals, objectives and activities in response to the external review
findings as part of Contractor's QAPIP. A description of the performance
improvement goals, objectives and activities developed and implemented in
response to the external review findings will be included in Contractor's QAPIP
and provided to the State, annually, by February 28. The State may also
require separate submission of an improvement plan specific to the findings of
the external review.
ii.
If Contractor has received accreditation by a private independent accrediting

Page 53 of 148
entity, it must authorize the private independent accrediting entity to provide
the State a copy of its most recent accreditation review, including the following:
1) Accreditation status, survey type, and level (as applicable).
2) Recommended actions or improvements, corrective action plans, and
summaries of findings.
3) Expiration date of the accreditation.
c.
LTSS Assessment
The comprehensive QAPIP program must include mechanisms to assess the quality
and appropriateness of care furnished to beneficiaries using LTSS, including an
assessment of care between care settings and a comparison of services and
supports received with those set forth in the beneficiary’s treatment/service plan.
Contractor is required to implement mechanisms to comprehensively assess each
Medicaid beneficiary identified as needing LTSS to identify any ongoing special
conditions of the beneficiary that require a course of treatment or regular care
monitoring. The assessment mechanisms must use appropriate providers or
individuals meeting LTSS service coordination requirements of the State or
Contractor as appropriate.
3.
Annual Effectiveness Review
a.
Contractor must annually conduct an effectiveness review of its QAPIP. The
effectiveness review must include analysis of whether there have been
improvements in the quality of health care and services for beneficiary as a result of
quality assessment and improvement activities and interventions carried out by
Contractor. The analysis should take into consideration trends in service delivery and
health outcomes over time and include monitoring of progress on performance goals
and objectives. Information on the effectiveness of Contractor's QAPIP must be
provided annually to network providers and to recipients upon request. Information
on the effectiveness of Contractor's QAPIP must be provided to the State annually,
no later than February 28.
4.
Service and Utilization Management
a.
Contractor must perform utilization management functions sufficient to control costs
and minimize risk while assuring quality care.
5.
Other Quality Requirements
a.
Contractor must disseminate all practice guidelines it uses to all affected providers
and, upon request, to beneficiaries. Contractor must ensure decisions for utilization
management, beneficiary education, coverage of services, and other areas to which
the guidelines apply are consistent with the guidelines. Contractor must assure
services are planned and delivered in a manner that reflects the values and
expectations contained in the following guidelines (which can be found on the
MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines) :
i.
Inclusion Practice Guideline
ii.
Housing Practice Guideline
iii.
Consumerism Practice Guideline
iv.
Personal Care in Non-Specialized Residential Settings
v.
Family-Driven and Youth-Guided Policy and Practice Guideline
vi.
Employment Works! Policy
L.
Grievance and Appeals Process for Beneficiaries.
1.
Grievance and Appeals Policies and Procedures
a.
Contractor must establish and maintain an internal process for the resolution of
Grievances and Appeals from beneficiaries. The Appeal and Grievance Resolution
Processes Technical Requirement
Page 54 of 148
(https://www.michigan.gov/documents/mdhhs/Appeal-and-Grievance-Resolution-
Processes-Technical-Requirement_704451_7.pdf ) which can be found on the
MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines
b.
Contractor must comply with 42 CFR 438.100, Enrollee Rights.
c.
Contractor must establish and maintain an internal process for the resolution of
Grievances and Appeals from beneficiaries.
d.
Contractor must have written policies and procedures governing the resolution of
Grievances and Appeals; A beneficiary, or a third party acting on behalf of a
beneficiary, may file a Grievance or Appeal, orally or in writing, on any aspect of
Covered services as specified in the definitions of Grievance and Appeal.
e.
Contractor must seek the State’s approval of Contractor’s Grievance and Appeal
policies prior to implementation. These written policies and procedures must meet
the following requirements:
i.
Except as specifically exempted in this Section, Contractor must administer an
internal Grievance and Appeal procedure according to the requirements of
MCL 500.2213 and 42 CFR 438.400 – 438.424 (Subpart F).
ii.
Contractor must cooperate with the Michigan Department of Insurance and
Financial Services (DIFS) in the implementation of MCL 550.1901-1929,
“Patient’s Rights to Independent Review Act”.
iii.
Contractor must have only one level of Appeal for beneficiaries. A beneficiary
may file a Grievance and request an Appeal with Contractor.
iv.
Contractor must make a determination on non-expedited Appeals not later than
30 Days after an Appeal is submitted in writing by the beneficiary. The 30-Day
period may be tolled; however, for any period of time the beneficiary is
permitted to take under the Medicaid Appeals procedure and for a period of
time that must not exceed 14 Days if (1) the beneficiary requests the extension
or (2) Contractor shows that there is need for additional information and how
the delay is in the beneficiary’s interest. Contractor may not toll (suspend) the
time frame for Appeal decisions other than as described in this Section.
v.
Contractor must make a determination on Grievances within 90 Days of the
submission of a Grievance.
vi.
If Contractor extends the timeframes not at the request of the beneficiary, it
must:
1) Make reasonable efforts to give the beneficiary prompt oral notice of the
delay.
2) Within two (2) calendar days, provide the beneficiary written notice of the
reason for the decision to extend the timeframe and inform the beneficiary of
the right to file a Grievance if he or she disagrees with that decision.
3) Issue and carry out its determination as expeditiously as the
beneficiaries’ health condition requires and no later than the date the
extension expires. (Per 42 CFR 438.404(c)(4); 42 CFR 438.408(c)(2);
438.410(c)(2))
vii.
If an Appeal is submitted by a third party but does not include a signed
document authorizing the third party to act as an authorized representative for
the Beneficiary, the 30-Day time frame begins on the date an authorized
representative document is received by Contractor. Contractor must notify the
Beneficiary that an authorized representative form or document is required. For
purposes of this Section, “third party” includes, but is not limited to, health care
Providers.
Page 55 of 148
viii.
Contractor must provide written notice of resolution in a format and language
that, at a minimum, meets the standard described in accordance with 42 CFR
438.10.
ix.
Contractor may extend the timeframe for processing a grievance by up to 14
calendar days if:
1) The beneficiary requests the extension.
2) Contractor shows there is need for additional information and that the
delay is in the beneficiary’s interest (upon the State’s request).
2.
Grievance and Appeal Procedure Requirements
Contractor’s internal Grievance and Appeal procedure must include the following
components:
a.
Contractor must give beneficiaries timely and adequate notice of an Adverse Benefit
determination in writing consistent with the requirements in 42 CFR 438.02, 438.10,
438.404 and this Contract. The notice must explain the following:
i.
The Adverse Benefit determination Contractor has made or intends to make.
ii.
The reasons for the Adverse Benefit Determination, including the right of the
beneficiary to be provided, upon request and free of charge, reasonable access
to and copies of all documents, records, and other information relevant to the
beneficiary’s Adverse Benefit Determination. Such information includes Medical
Necessity criteria, and any processes, strategies, or evidentiary standards used
in setting coverage limits.
iii.
The beneficiary’s right to request an Appeal of the Adverse Benefit
Determination, including information on exhausting Contractor’s one level of
Appeal and the right to request a State Fair Hearing.
iv.
The procedures for exercising their Appeal rights, the circumstances under
which an Appeal process can be expedited and how to request it.
v.
The beneficiary’s right to have benefits continue pending resolution of the
Appeal, how to request that benefits be continued, and, if allowed under State
policy, the circumstances under which the beneficiary may be required to pay the
costs of these services.
b.
Contractor must mail the Adverse Benefit Determination notice within the timeframes
specified in 42 CFR 438.404(c).
c.
Contractor must allow beneficiaries 60 Days from the date of the Adverse Benefit
notice in which to file an Appeal.
d.
Contractor must provide beneficiaries reasonable assistance in completing forms
and taking other procedural steps. This includes but is not limited to interpreter
services and toll-free numbers that have adequate TTY/TDD and interpreter
capability.
e.
Contractor must acknowledge receipt of each Grievance and Appeal
f.
Contractor must ensure that the individuals who make decisions on Grievances and
Appeals are individuals who:
i.
Are not involved in any previous level of review or decision-making, nor a
subordinate of any such individual; and
ii.
Are health care professionals who have the appropriate clinical expertise in
treating the beneficiary’s condition when the Grievance or Appeal involves a
clinical issue.
iii.
Must take into account all comments, documents, records and other information
submitted by the beneficiary or their representative without regard to whether
such information was submitted or considered in the initial Adverse Benefit
determination.
g.
Contractor must provide that oral inquires seeking to Appeal an Adverse Benefit
Page 56 of 148
determination are treated as Appeals to establish the earliest possible filing date for
the Appeal and must be confirmed in writing, unless the beneficiary or the Provider
requests expedited resolution.
h.
Contractor must provide the beneficiary a reasonable opportunity, in person and in
writing, to present evidence and testimony and make legal and factual arguments.
Contractor must inform the beneficiary of the limited time available for this sufficiency
in advance of the resolution timeframe for Appeals in the case of Expedited Appeal
resolution.
i.
Contractor must provide the beneficiary and his or her representative the
beneficiary’s case file, including medical records, other documents and records, and
any new or additional evidence considered, relied upon, or generated by Contractor
in connection with the Appeal of the Adverse Benefit Determination. This information
must be provided free of charge and sufficiently in advance of the resolution
timeframe for Appeals.
j.
Contractor must consider the beneficiary, his or her representative, or estate
representative of a deceased beneficiary as parties to the Appeal.
k.
Contractor must notify the beneficiary, in writing, of Contractor’s decision on the
Grievance or Appeal.
3.
Notice to Beneficiaries of Grievance Procedure
a.
Contractor must inform beneficiaries about Contractor's internal Grievance
procedures at the time of Initial Enrollment and any other time a beneficiary
expresses dissatisfaction by filing a Grievance with Contractor.
b.
The internal Grievance procedures information must be included in the member
handbook and must explain:
i.
How to file a Grievance with Contractor
ii.
The internal Grievance resolution process
4.
Notice to beneficiaries of Appeal Procedure
a.
Contractor must inform beneficiaries of Contractor’s Appeal procedure at the time of
Initial Enrollment, each time a service is denied, reduced, or terminated, and any
other time a Contractor makes a decision that is subject to Appeal under the
definition of Appeal in this Contract.
b.
The Appeal procedure information must be included in the member handbook and
must explain:
i.
How to file an Appeal with Contractor.
ii.
The internal Appeal process.
iii.
The member’s right to a Fair Hearing with the State after Contractor’s one level
Appeal process has been exhausted.
5.
Contractor Decisions Subject to Appeal
a.
When Contractor makes a decision subject to Appeal, as defined in this Contract,
Contractor must provide a written Adverse Benefit determination notice to the
beneficiary and the requesting Provider, if applicable. Contractor must mail the notice
within the following timeframes:
b.
For termination, suspension, or reduction of previously authorized Medicaid
Services, within the timeframes specified in 42 CFR 431.211,431.213, and 431.214.
c.
For denial of payment, at the time of any action affecting the claim.
d.
For standard service authorization decisions that deny or limit services, within the
timeframe specified in 42 CFR438.210(d)(1).
e.
If Contractor meets the criteria set forth for extending the timeframe for standard
service authorization decisions consistent with 42 CFR438.210(d)(1)(ii), Contractor
must:
i.
Give the beneficiary written notice of the reason for the decision to extend the
Page 57 of 148
timeframe and inform the beneficiary of the right to file a Grievance if he or she
disagrees with that decision; and
ii.
Issue and carry out its determination as expeditiously as the beneficiary’s
health condition requires and no later than the date the extension expires.
f.
For service authorization decisions not reached within the timeframes specified in 42
CFR 438.210(d) (which constitutes a denial and is thus an adverse benefit
determination), on the date that the timeframes expire.
g.
For expedited service authorization decisions, within the timeframes specified in 42
CFR 438.210(d)(2).
h.
Contractor must continue the beneficiary’s benefits if all the following conditions
apply:
i.
The beneficiary files the request for an Appeal timely in accordance with 42
CFR 438.402(c)(1)(ii) and (c)(2)(ii).
ii.
The Appeal involves the termination, suspension, or reduction of a previously
authorized services.
iii.
The services were ordered by an authorized Provider.
iv.
The period covered by the original authorization has not expired; and the
beneficiary timely files for continuation of benefits, meaning on or before the
later of the following:
1) Within 10 days of Contractor’s mailing the Adverse Benefit
determination notice.
2) The intended effective date of Contractor’s proposed Adverse
Benefit determination notice.
i.
If Contractor continues or reinstates the beneficiary’s benefits while the Appeal or
State Fair Hearing is pending, the benefits must be continued until one of the
following occurs:
i.
The beneficiary withdraws the Appeal or request for State Fair Hearing.
ii.
The beneficiary fails to request a State Fair Hearing and continuation of
benefits withing 10 days after Contractor mails an adverse resolution to the
beneficiary’s Appeal.
iii.
A State Fair Hearing decision adverse to the beneficiary is made.
iv.
The authorization expires or authorization service limits are met.
j.
If Contractor or State Fair Hearing Officer reverses a decision to deny, limit or delay
services, that were not furnished while the Appeal was pending, Contractor must
authorize or provide the disputed services promptly, and as expeditiously as the
beneficiary’s health condition requires but no later than 72 hours from the date it
receives notice reversing the determination.
k.
If Contractor or State Fair Hearing Officer reverses a decision to deny authorization
of services, and the beneficiary received the disputed services while the Appeal was
pending, Contractor must pay for those services.
6.
Adverse Benefit Determination Notice
a.
Adverse Benefit determination notices involving Service Authorization Request
decisions that deny or limit services must be made within the time frames described
in this Contract. Adverse Benefit Determination Notices pursuant to claim denials
must be sent on the date of claim denial for termination, suspension, or reduction of
previously authorized Medicaid-Covered Services. Contractor must mail Adverse
Benefit Determination Notices within the following timeframes:
i.
At least 10 Days before the date of action, except as permitted under 42 CFR
431.213 and 431.214.
ii.
Contractor may send an Adverse Benefit Determination Notice not later than
the date of action if (less than 10 Days before as required above):
Page 58 of 148
1) Contractor has factual information confirming the death of a beneficiary.
2) The beneficiary submits a signed written statement that:
a) He/she no longer requests the services or;
b) The beneficiary gives information that requires termination or
reduction of services and indicates that he/she understands that
service termination or reduction will result.
3) The beneficiary has been admitted into an institution where he/she is
ineligible under the plan for further services.
4) The beneficiary’s whereabouts are unknown, and the post office returns
Contractor’s mail directed to the beneficiary indicating no forwarding
address.
5) Contractor verified, with MDHHS, that the beneficiary has been accepted
for Medicaid services by another local jurisdiction, state, territory or
commonwealth.
6) A Change in the level of health care is prescribed by the beneficiary’s
Provider.
7) The notice involves an Adverse Benefit Determination with regard to
preadmission requirements.
iii.
Contractor may shorten the period of advance notice to five Days before the date
of action if:
1) Contractor has facts indicating that action should be taken because of
probable Fraud by the beneficiary; and
2) The facts have been verified, if possible, through secondary sources.
b.
The notice must include the following components:
i.
The Adverse Benefit Determination Contractor has taken or intends to take and
the reasons for that action.
ii.
The reasons for the Adverse Benefit Determination, including the right of the
beneficiary to be provided, upon request and free of charge, reasonable access
to and copies of all documents, records and other information relevant to the
beneficiary’s Adverse Benefit Determination. Such information included
medical criteria, behavioral health and any processes, strategies or evidentiary
standards used in setting coverage limits. The beneficiary’s right to request an
Appeal, including information on exhausting Contractor’s one level of Appeal
and the right to request a State Fair Hearing.
iii.
An explanation of Contractor’s Appeal process.
iv.
The beneficiary’s right to request a Fair Hearing.
v.
The circumstances under which expedited resolution is available and how to
request it.
vi.
The beneficiary’s right to have benefits continue pending resolution of the
Appeal and how to request that benefits be continued.
vii.
Must be mailed in a timely manner in accordance with 42 CFR 438.404(c).
c.
Written adverse action notices must also meet the following criteria:
i.
Be translated for the individuals who speak prevalent non-English languages
as defined by the Contract.
ii.
Include language clarifying that oral interpretation is available for all languages
and how the beneficiary can access oral interpretation services.
iii.
Use easily understood language written below the 6.9 reading level.
iv.
Use an easily understood format.
v.
Be available in Alternative Formats, and in an appropriate manner that takes
into consideration those with special needs.
d.
In accordance with 42 CFR 438.420(d), if the final resolution of the appeal or State Fair
Page 59 of 148
Hearing is adverse to the beneficiary, that is, upholds Contractor's adverse benefit
determination, Contractor may, consistent with the State's usual policy on recoveries
under 42 CFR 431.230(b), and as specified in this Contract recover the cost of services
furnished to the beneficiary while the appeal and State Fair Hearing was pending, to the
extent that they were furnished solely because of the requirements of this Grievance and
Appeals Section.
7.
State Medicaid Appeal Process
a.
The State must maintain a Fair Hearing process to ensure beneficiaries have the
opportunity to Appeal decisions directly to the State. Any beneficiary dissatisfied with
a State agency determination denying a beneficiary’s request to transfer
Contractors/disenroll has access to a State Fair Hearing.
b.
Contractor must include the Fair Hearing process as part of the written internal
process for resolution of Appeals and must describe the Fair Hearing process in the
member handbook. The parties to the State Fair Hearing may include Contractor as
well as the beneficiary and her or his representative or the representative of a
deceased beneficiary's estate.
c.
A beneficiary may request a State Fair Hearing only after receiving notice that
Contractor has upheld its Adverse Benefit Determination.
i.
If Contractor fails to adhere to the required Appeals notice and timing
requirements in 42 CFR 438.408, the beneficiary is deemed to have exhausted
Contractor’s Appeals process.
d.
Contractor must allow the beneficiary 120 Days from date of Contractor’s Appeal
resolution notice to request a State Fair Hearing.
8.
Expedited Appeal Process
a.
Contractor must establish and maintain an expeditated review process for appeals
when Contractor or provider, acting on behalf of the beneficiary, indicates that taking
the time for a standard resolution could seriously jeopardize the beneficiary’s life,
physical or mental health, or ability to attain, maintain, or regain maximum function.
42 CFR 438.410(a)
b.
Contractor’s written policies and procedures governing the resolution of Appeals must
include provisions for the resolution of Expedited Appeals as defined in the Contract.
These provisions must include, at a minimum, the following requirements:
i.
The beneficiary or Provider may file an Expedited Appeal either orally or in
writing.
ii.
The beneficiary or Provider must file an Expedited Appeal within 60 calendar
days of the Adverse Benefit Determination.
iii.
Contractor must make a decision on the Expedited Appeal within 72 hours of
receipt of the Expedited Appeal.
iv.
Contractor must provide written notice of resolution in a format and language
that, at a minimum, meets the standard described in accordance with 42 CFR
438.10.
1) For notice of an expedited resolution, Contractor must also make
reasonable efforts to provide oral notice.
v.
If Contractor denies the request for an Expedited Appeal, Contractor must
transfer the Appeal to the standard Appeal resolution timeframe and give the
beneficiary written notice of the denial within two Days of the Expedited Appeal
request.
vi.
Contractor must not take any punitive actions toward a Provider who requests
or supports an Expedited Appeal on behalf of a beneficiary.
9.
Grievance and Appeals Records
Contractor and its network providers/subcontractors as applicable, must maintain record
Page 60 of 148
of all Grievance and Appeals
a.
The record of each Grievance and Appeal must contain, at a minimum all the
following:
i.
A general description of the reason for the Appeal or Grievance.
ii.
The date received.
iii.
The date of each review or, if applicable, review meeting.
iv.
Resolution at each level of the Appeal and/or Grievance.
v.
Date of resolution for each Appeal and/or Grievance.
vi.
Name of covered person for whom the Appeal or Grievance was filed.
b.
The record must be accurately maintained in a manner accessible to the State and
available upon request to CMS.
c.
Grievance and appeal records must be retained for 10 years from the final date of
the contract period or from the date of completion of any audit, whichever is later.
M.
Beneficiary Services
1.
Provider Directory
a.
Contractor must maintain and publish a complete provider directory, including
pharmacies, medical suppliers, ancillary health providers, independent facilitators
and fiscal intermediaries, in hard copy and web-based formats.
b.
Information included in a paper provider directory must be updated at least monthly
and electronic provider directories must be updated no later than 30 calendar days
after Contractor receives updated provider information.
c.
Directory must be made available in a prominent, readily accessible location in a
machine-readable format, which can be electronically retained and printed.
d.
Paper form requests must be fulfilled within five business days, without charge to the
beneficiary.
e.
Contractor provider directory must be organized by county.
f.
Contractor’s provider directory must contain, at a minimum, the following information:
i.
provider name
ii.
address
iii.
telephone number
iv.
website URL
v.
services provided
vi.
whether the provider is accepting new patients
vii.
languages spoken, including American Sign Language (ASL)
viii.
cultural and linguistic capabilities
ix.
whether the providers’ office/facility has accommodations for people with
physical disabilities
2.
Written Materials
a.
All Informative materials, including the provider directory, intended to be distributed
through written or other media (e.g., Electronic) to beneficiaries or the broader
community that describe the availability of covered services and supports and how to
access those supports and services, including but not limited to provider directories,
beneficiary handbooks, appeal and grievance notices, and denial and termination
notices, must meet the following standards:
i.
All such materials must be written at or below the 6.9 grade reading level when
possible (i.e., in some situations it is necessary to include medications,
diagnosis and conditions that do not meet the 6.9 grade level criteria).
ii.
All materials must be in an easily understood language and format and use a
font size no smaller than 12 point.
iii.
All informative materials, including the provider directory, must be made
available in paper form upon request and in an electronic form that can be
Page 61 of 148
electronically retained and printed. It must also be made available in a
prominent and readily accessible location on Contractor’s website, in a
machine-readable file and format. Information included in a paper provider
directory must be updated at least monthly and electronic provider directories
must be updated no later than 30 calendar days after Contractor receives
updated provider information.
iv.
All materials shall be available in the languages appropriate to the people
served within Contractor's area for specific Non-English Language that is
spoken as the primary language by more than 5% of the population in
Contractor’s Region. Such materials must be available in any language
alternative to English as required by the Limited English Proficiency Policy
Guidance (Executive Order 13166 of August 11, 2000, Federal Register Vol.
65, August 16, 2000). All such materials must be available in alternative
formats in accordance with the Americans with Disabilities Act (ADA), at no
cost to the beneficiary. Beneficiaries must be informed of how to access the
alternative formats.
v.
If Contractor provides information electronically, it must inform the customer
that the information is available in paper form without charge and upon request
and provides it upon request within five business days.
vi.
Material must not contain false, confusing, and/or misleading information.
vii.
For consistency in the information provided to beneficiaries, Contractor must
use State developed definitions for managed care terminology, including:
appeal, durable medical equipment, emergency medical condition, emergency
medical transportation, emergency room care, emergency services, excluded
services, grievance, habilitation services and devices, health insurance, home
health care, hospice services, hospitalization, hospital outpatient care,
physician services, prescription drug coverage, prescription drugs, primary care
provider, rehabilitation services and devices, skilled nursing care, specialist, co-
payment excluded services, health insurance, medically necessary, network,
non-participating, plan preauthorization, participating provider, premium,
provider and urgent care, as defined in the this Contract and/or Medicaid
provider manual.
b.
Additional Information Requirements
i.
To take into consideration the special needs of beneficiaries with disabilities or
LEP, Contractor must ensure that beneficiaries are notified that oral
interpretation is available for any language, written information is available in
prevalent languages, and auxiliary aids, such as and Teletypewriter/Text
Telephone (TTY/TDY) and American Sign Language (ASL), and services are
available upon request at no cost, and how to access those services as
referenced in 42 CFR Parts 438.10(d)(3) and 438.10(d)(4). Contractor must
also ensure that beneficiaries are notified how to access alternative formats as
defined in 42 CFR 438.10(d)(6)(iv). In mental health settings, Video Remote
Interpreting (VRI) is to be used only in emergency situations, extenuating
circumstances, or during a state or national emergency as a temporary solution
until they can secure a qualified interpreter and in accordance with R 393.5055
VRI standards, usage, limitations, educational, legal, medical, mental health
standards.
ii.
All written materials for potential beneficiaries must include taglines in the
prevalent non-English languages in Contractor’s region, as well as large print,
explaining the availability of written translations or oral interpretation to
understand the information provided and the toll-free telephone number of the
Page 62 of 148
entity providing choice counseling services as required by 42 CFR 438.71(a)
and as defined in 42 CFR Parts 438.10 (d)(3) and 431.10(d)(4). In accordance
with 42 CFR Parts 438.10(d)(3) 438.10(d)(6) and 438.10(d)(6)(iv), Large print
means printed in a font size no smaller than 18 point.
1) Contractor must provide the following information to all beneficiaries
who receive specialty supports and services:
a) A listing of contracted providers that identifies provider name as
well as any group affiliation, locations, telephone numbers, web
site URL (as appropriate), specialty (as appropriate), the
provider’s cultural capability, any non-English languages
spoken, if the provider’s office/facility has accommodations for
people with physical disabilities, and whether they are accepting
new beneficiaries. This includes any restrictions on the
beneficiary's freedom of choice among network providers. The
listing would be available in the format that is preferable to the
beneficiary: written paper copy or on-line. The listing must be
kept current and offered to each beneficiary annually.
b) Their rights and protections, as specified in Section L. Grievance
and Appeals Process for Beneficiaries.
c) The amount, duration, and scope of benefits available under the
Contract in sufficient detail to ensure that beneficiaries understand
the benefits to which they are entitled.
d) Procedures for obtaining benefits, including authorization
requirements.
e) The extent to which, and how, beneficiaries may obtain benefits
and the extent to which, and how, after-hours crisis services are
provided.
f) Annually (e.g., at the time of person-centered planning) provide to
the beneficiary the estimated annual cost to Contractor of each
covered support and service he/she is receiving. Cost of Services
provides principles and guidance for transmission of this
information, this can be found at:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines.
g) Contractor is required to provide Explanation of Benefits (EOBs)
to 5% of the consumers receiving services. The EOB distribution
must comply with all State and Federal regulations regarding
release of information as directed by MDHHS. MDHHS will
monitor EOB distribution annually. A model Explanation of
Benefits which can found at:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines.
Contractor may, but is not required to, utilize the model
template.
2) Contractor must give each beneficiary written notice of a significant
change in its applicable provider network including the addition of new
providers and planned termination of existing providers.
3) Contractor must make a good faith effort to give written notice of termination
of a contracted provider to each enrollee who received his or her primary care
from, or was seen on a regular basis by, the terminated provider as defined in
42 CFR 438.10(f)(1). Notice to the enrollee must be provided by the later of 30

Page 63 of 148
calendar days prior to the effective date of the termination, or 15 calendar
days after receipt or issuance of the termination notice.
4) Contractor must provide information to beneficiaries about managed
care and care coordination responsibilities of Contractor, including:
a) Information on the structure and operation of the Managed Care
Organization (MCO) or Contractor.
b) Upon request, physician incentive plans in use by Contractor or
network providers as set forth in 42 CFR 438.3(i).
c) Contractor must provide information on how to contact their
designated person or entity for coordination of services as
referenced in 42 CFR 438.208(b)(1).
N.
Provider Services
1.
Provider Credentialing
a.
Contractor must have written credentialing policies and procedures for ensuring that
all providers rendering services to individuals are appropriately credentialed within
the State and are qualified to perform their services. Credentialing must take place
every two years. Contractor must ensure that network providers residing and
providing services in bordering states meet all applicable licensing and certification
requirements within their state. Contractor also must have written policies and
procedures for monitoring its providers and for sanctioning providers who are out of
compliance with Contractor's standards. Reference the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines.
2.
Health Care Practitioner Discretions
a.
Contractor may not prohibit, or otherwise restrict a health care professional acting
within their lawful scope of practice from advising or advocating in the following areas
on behalf of a beneficiary who is receiving services under this Contract:
i.
Beneficiary's health status, medical care, or treatment options, including any
alternative treatment that may be self-administered.
ii.
Any information the beneficiary needs in order to decide among all relevant
treatment options.
iii.
Risks, benefits, and consequences of treatment or non-treatment
iv.
Beneficiary's right to participate in decisions regarding his or her health care,
including the right to refuse treatment, and to express preferences about future
treatment decisions.
3.
Reserved
4.
Level of Care Utilization System (LOCUS) Contractor must:
a.
Ensure that the LOCUS is incorporated into the initial assessment process for all
individuals 18 and older seeking supports and services for a severe mental illness
using MDHHS approved methods for scoring the tool listed below:
i.
Use of the online scoring system through State approved vendor with costs
covered by the State.
ii.
Use of software purchased through State approved vendor with costs covered
the State.
b.
Ensure that each individual 18 years and older with a severe mental illness has a
LOCUS completed as part of any assessment and re-assessment process if they are
not receiving Early Periodic Screening Diagnosis and Treatment Services (EPSDT).
If the child / youth aged 18-21 years is receiving EPSDT in the CMHSP system, the
CAFAS needs to be completed at intake, quarterly, and exit up to age 21.
c.
Collaborate with the State for ongoing fidelity monitoring on the use of the tool.
d.
Provide to the State the composite score for each LOCUS that is completed in
Page 64 of 148
accordance with the established reporting guidelines.
5.
National Core Indicator (NCI) Surveys
a.
Contractor must provide, to the State, the mailing addresses, pre-survey and
background information, and demographics needed for the State or its designee to
schedule and conduct the face-to-face surveys for the identified survey participants
in their service area.
b.
Contractor must coordinate appointments and, if required, obtain consent from
beneficiaries.
c.
Contractor must disseminate the survey results to the stakeholders in their service
area(s) and utilize the results in their quality improvement activities.
d.
Contractor must identify a specific individual to be the primary point of contact
between Contractor, its designees, and the State.
6.
Standardized SUD Assessment Process
a.
The State requires the use of SUD assessment tools that utilize the American
Society of Addiction Medicine (ASAM) criteria. The selected assessment tool must:
i.
collect all necessary information to provide a Diagnostic and Statistical Manual
based diagnosis.
ii.
recommend ASAM placement needs.
iii.
be appropriate for the age of the individual.
iv.
comply with State-specified reporting requirements at the data element level
identified within the 1115 Behavioral Health Waiver’s standard terms and
conditions (STCs).
b.
Contractor is responsible for ensuring the State approved assessment tool is
implemented and fidelity is maintained.
c.
Contractor must honor network reciprocity requirements including valid SUD
assessment tool results performed by a qualified provider under agreement with an
alternate PIHP.
i.
Contractor must ensure appropriate release of information authorizations are
executed.
d.
Contractor must work with the State and its independent evaluators for data
collection and reporting as detailed in the approved 1115 Behavioral Health
Demonstration Waiver evaluation plan.
i.
Contractor must monitor the use of the approved assessment tool by sampling
case files on review.
ii.
An auditing tool will be provided by the State. This tool can be used to validate
the level of care determination and to monitor compliance with the STCs.
Cases where deviations from the assessment recommended level of care must
be justified by the clinician with clinical notes attached to the assessment.
7.
Claims Management System
a.
A valid claim is a claim for supports and services that Contractor is responsible for
under this Contract. It includes services authorized by Contractor, and those like
Medicare co-pays and deductibles that Contractor may be responsible for regardless
of their authorization.
b.
Contractor must assure the timely payments to all providers for clean claims. This
includes payment at 90% or higher of all clean claims from network providers within
30 days of receipt, and at least 99% of all clean claims within 90 days of receipt,
except services rendered under a subcontract in which other timeliness standards
have been specified and agreed to by both parties.
c.
Contractor must have an effective provider appeal process to promptly and fairly
resolve provider-billing disputes.
d.
Post-Payment Review
Page 65 of 148
Contractor may utilize a post-payment review methodology to assure claims have
been paid appropriately. Regardless of method, Contractor must have a process in
place to verify that services were provided.
e.
Total Payment
Contractor or its network providers/subcontractors must not require any co-
payments, recipient pay amounts, or other cost sharing arrangements unless
specifically authorized by the State. Network providers/subcontractors must not seek,
nor accept, additional supplemental payment for services authorized by Contractor.
f.
Electronic Billing Capacity
Contractor must be capable of accepting HIPAA compliant electronic billing for
services billed to Contractor, or Contractor claims management agent, as stipulated
in the Michigan Medicaid Provider Manual. Contractor may require its providers to
meet the same standard as a condition for payment.
g.
Vouchers
i.
Vouchers issued to individuals for the purchase of services provided by
professionals may be utilized in non- contract agencies that have a written
referral network agreement with Contractor that specifies credentialing and
utilization review requirements. Voucher rates for such services must be
predetermined by Contractor using the actual cost history for each service
category and average local provider rates for like services. These rates
represent total payment for services rendered. Those accepting vouchers may
not require any additional payment from the individual. Voucher arrangements
for purchase of individual-directed supports delivered by non-professional
practitioners may be through a fee-for-service arrangement. The use of
vouchers is not subject to the provisions of Section E.6 (Provider Procurement)
and Section 2.7 (Use of Subcontractors) of this Contract.
h.
Programs with Community Inpatient Hospitals
i.
Upon request from the State, Contractor must develop programs for improving
access, quality, and performance with providers. Such programs must include
the State in the design methodology, data collection, and evaluation. The State
and Contractor will develop revised methods for the programs with community
inpatient hospitals to ensure they comply with 42 CFR 438.6(c).
1)
Hospital Eligibility
Hospital eligibility is determined by the State. Community hospitals,
including Institutes for Mental Disease, are eligible for Hospital Rate
Adjustor (HRA) directed payments based on Contractor inpatient
encounters. Out of State hospitals are not eligible. The hospital
billing provider NPI on the original invoice must be enrolled in the
state Medicaid management information system (CHAMPS).
2)
Determination of the Hospital Payment Amount
Contractor reported community inpatient psychiatric encounters will
be used by the State as the basis for determining an annual add-on
rate. Directed payment allocations are based on room and board
encounters, identified by billing provider NPI. Encounters accepted
in CHAMPS during the prior quarter will be included in the directed
payment for that quarter. Medicaid and Healthy Michigan Plan
encounters will be included in allocation pool.
3)
State Payment Process
Contractor will receive a quarterly gross adjustment from the State.
The amount of a quarterly payment to Contractor will be equal to the
total amount shown on the HRA directed payment instructions for
Page 66 of 148
the prior quarter.
4)
Directed Payment Instructions
The State will provide directed payment instructions indicating the
payment amount per hospital, at the PIHP level. Instructions will be
provided to Contractor prior to the end of the 1st month in each
quarter.
5)
Contractor Payment Obligations and Payment Process
Payment is made by Contractor to each hospital identified in the
HRA directed payment instructions at the amount specified.
Payments are quarterly with no minimum payment threshold.
Payments are due to hospitals every three months within 10 State
business days of Contractor receiving the quarterly HRA gross
adjustment from the State. The State acknowledges that payments
can be made without a current contractual arrangement between
Contractor/affiliate CMHSPs and the hospital receiving an HRA
payment. Contractor delegation to affiliate CMHSPs is not
recommended.
6)
Contractor Reporting Requirements
Financial status reports will continue to include HRA payment
revenue and payment information requirements.
8.
MDHHS Standard Consent Form
Michigan PA 129 of 2014 was enacted to promote the use and acceptance of a standard
consent form. Contractor must implement a written policy that requires the provider
network to use, accept, and honor the standard consent form created as a result of the
Public Act (Form MDHHS-5515). Per PA 559 of 2016, the policy must recognize written
consent is not always required.
9.
Trauma Policy
Contractor must develop a trauma-informed system in accordance with the
MDHHS/BPHASA Trauma Policy, which can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines
10.
Substance Use Disorder (SUD) Services
a.
Contractor must comply with the SUD Services Policy and Advisory Manual, which
can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/drugcontrol/reportstats/reportcontent/policies-and-advisories.
b.
Contractor must:
i.
Develop comprehensive plans for substance use disorder treatment and
rehabilitation services consistent with guidelines established by the State.
ii.
Review and comment to the Department of Licensing and Regulatory Affairs
(LARA) on applications for licenses submitted by local treatment, rehabilitation,
and prevention organizations (SUD Rules can be found at the following website:
https://ars.apps.lara.state.mi.us/AdminCode/DeptBureauAdminCode?Departme
nt=Licensing%20and%20Regulatory%20Affairs&Bureau=Bureau%20of%20Com
munity%20and%20Health%20Systems (under the Substance Use Disorder
Programs titled document)).
iii.
Provide technical assistance for local substance use disorder service programs.
iv.
On request from MDHHS or LARA, subject to applicable regulations, collect and
transfer data and financial information from local programs to the LARA.
v.
Annually evaluate and assess substance use disorder services in the State-
designated community mental health entity in accordance with guidelines
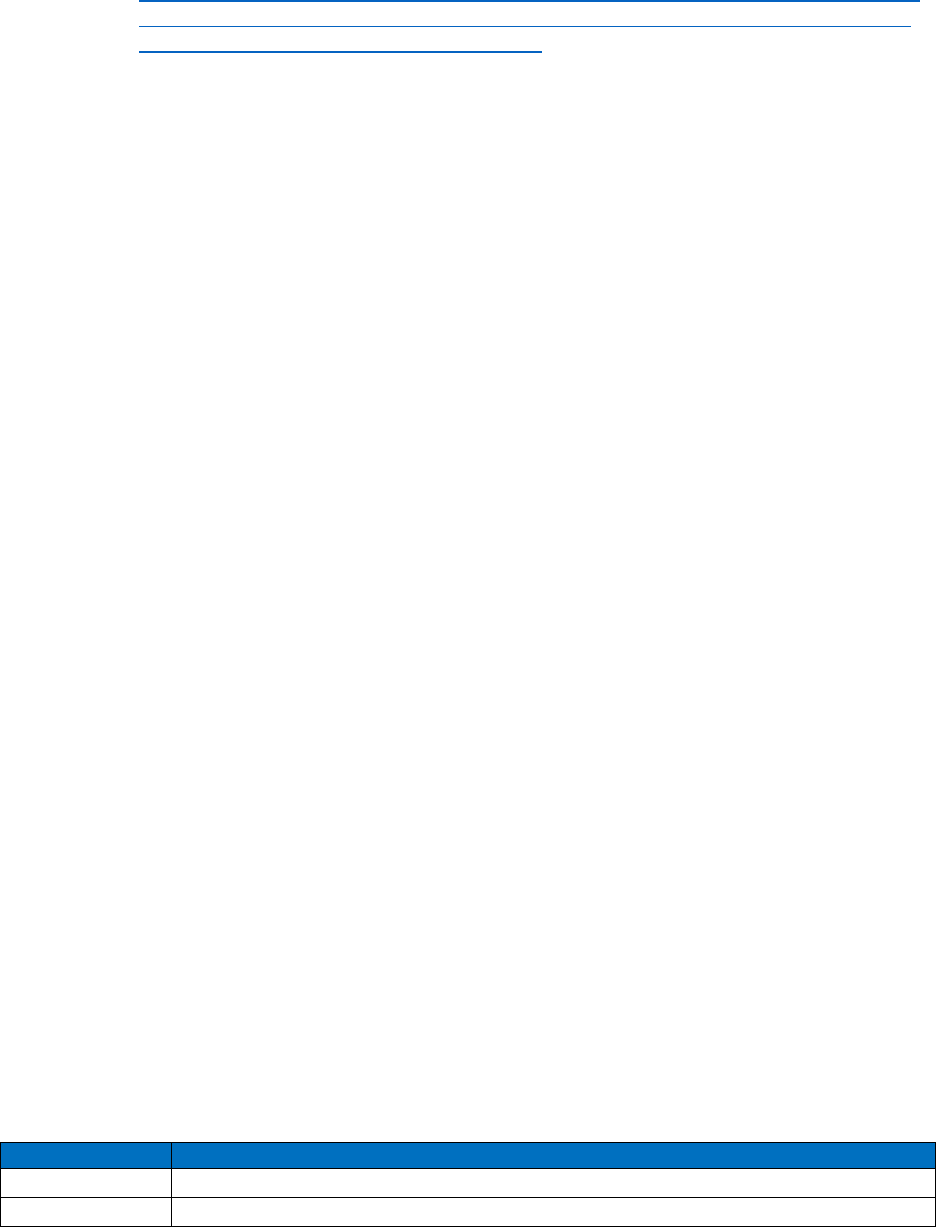
Page 67 of 148
established by the State. (SUD Rules can be found at the following website:
https://ars.apps.lara.state.mi.us/AdminCode/DeptBureauAdminCode?Departme
nt=Licensing%20and%20Regulatory%20Affairs&Bureau=Bureau%20of%20Co
mmunity%20and%20Health%20Systems (under the Substance Use Disorder
Programs titled document))
vi.
Follow financial requirements as described in this Contract and Schedule E.
vii.
Follow progress reporting requirements as described in Schedule E.
viii.
Enter into subcontracts with providers for SUD services.
ix.
Ensure network providers are appropriately licensed for the service(s) provided
in accordance with Michigan Public Health Code, PA 368 of 1978.
c.
Provider Network Oversight Management
i.
The provision of SUD treatment services must be based on the ASAM Level of
Care (LOC) criteria.
1)
If Contractor plans to purchase case management services or peer
recovery and recovery support services, and only these services, from
an agency that is not accredited per this Contract, Contractor may
request a waiver of the accreditation requirement.
ii.
To ensure compliance with contractual and administrative rule requirements,
fidelity to assessment process and ASAM LOC Criteria:
1)
Conducting an annual review of each network provider’s program,
policies, practices and clinical records.
2)
Documenting compliance with the purported LOC for each provider.
a) Include any corrective action that may have been taken and
documentation that indicates all LOCs are available in the service
area.
3)
Ensuring review documentation is available for the State during biennial
Contractor site visits for comparison with State provider reviews.
d.
Reimbursement for Services to Persons with Co-Occurring Disorders
i.
SUD funds may be used to reimburse providers for integrated mental health and
substance use disorder treatment services to persons with co-occurring
substance use and mental health disorders.
ii.
Contractor may reimburse a Community Mental Health Services Program
(CMHSP) or network provider for substance use disorders treatment services for
such persons who are receiving mental health treatment services through the
CMHSP or network provider.
iii.
Contractor may also reimburse a provider, other than a CMHSP or network
provider for substance use disorders treatment provided to persons with co-
occurring substance use and mental health disorders.
e.
American Society of Addiction Medicine (ASAM) Level of Care (LOC) for Network
Providers
i.
Contractor must enter into network provider agreements for SUD treatment with
organizations that provide services based on the ASAM LOC only.
ii.
The State Approved ASAM SUD treatment providers can be found in the
Customer Relationship Management (CRM) system. Contractor must ensure
that to the extent licensing allows all the following LOCs are available for adult
and adolescent populations:
Level of Care
ASAM Title
0.5
Early Intervention
1
Outpatient Services
Page 68 of 148
2.1
Intensive Outpatient Services
2.5
Partial Hospitalization Services
3.1
Clinically Managed Low Intensity Residential Services
3.3*
Clinically Managed Population Specific High Intensity Residential Services
3.5
Clinically Managed High Intensity Residential Services
3.7
Medically Monitored Intensive Inpatient Services
OTP Level 1**
Opioid Treatment Program
1-WM
Ambulatory Withdrawal Management without Extended On-Site Monitoring
2-WM
Ambulatory Withdrawal Management with Extended On-Site Monitoring
3.2-WM
Clinically Managed Residential Withdrawal Management
3.7-WM
Medically Monitored Inpatient Withdrawal Management
* Not designated for adolescent populations **Adolescent treatment per federal guidelines
iii.
It is further required that all SUD treatment providers complete the MDHHS LOC
Designation Questionnaire every two years and receive a formal designation for
the LOC that is being offered.
11.
Electronic Visit Verification (EVV)
a.
Contractor must ensure its network providers, and subcontractors comply with 42 USC
1396b (or sec. 1903(I) of the Social Security Act and the State’s implementation
timeline.
i.
Contractor must provide evidence of compliance upon request. Compliance
must be in the form of either:
1) An existing EVV system that meets State requirements as confirmed by
Contractor’s on- site review.
2) Participation in the State sponsored Statewide EVV system.
ii.
Personal Care Services (PCS) includes community living support and respite
services in a person’s home, in a non-licensed setting.
iii.
Contractor must ensure its subcontracts, or those of their CMHSP participants,
stipulates the EVV system supports self-directed arrangements and is minimally
burdensome or disruptive to care.
12.
Critical Incidents
a.
Contractor must require all its residential treatment providers to prepare and file critical
incident reports that include the following components:
i.
Provider determination whether critical incidents are sentinel events.
ii.
Following identification as a sentinel event, the provider must ensure that a root
cause analysis or investigation takes place.
iii.
Based on the outcome of the analysis or investigation, the provider must ensure
that a plan of action is developed and implemented to prevent further
occurrence of the sentinel event. The plan must identify who is responsible for
implementing the plan, and how implementation will be monitored. Alternatively,
the provider may prepare a rationale for not pursuing a preventive plan.
b.
Contractor must report the following incidents for beneficiaries enrolled in the CWP,
SEDW, HSW and the 1115/1915(i) State Plan: Suicide; Non-suicide death; Arrest of
Consumer; Emergency Medical Treatment due to injury or Medication Error: Type of
injury will include a subcategory for reporting injuries that resulted from the use of
physical management; Hospitalization due to Injury or Medication Error:
Hospitalization due to injury related to the use of physical management. Type of injury
will include a subcategory for reporting injuries that resulted from the use of physical
management.

Page 69 of 148
c.
Contractor must comply with the reporting requirements and guidelines identified in
the Critical Incident Reporting and Event Notification Requirements which can be
found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines
O.
Health Information Systems
1.
A Contractor organized as a regional entity must ensure that health plan information
technology functions are clearly defined and separately contracted from any other
function provided by a subcontractor CMHSP. A Contractor organized as a regional
entity may have a single subcontractor CMHSP perform Contractor health plan
information technology functions on behalf of the regional entity if each of the following
requirements are met:
a.
The contract between Contractor and the CMHSP clearly describes the CMHSP’s
contractual responsibility to Contractor for the health plan information technology
related functions.
b.
The contract between Contractor and the CMHSP for Contractor health plan
information technology functions must be separate from other EHR functions
performed as a CMHSP.
2.
Contractor must ensure that all Health Information Systems used by Contractor and/or
its subcontractors have the capacity to fulfill the obligations of this Contract. Contractor
must maintain a health information system that collects, analyzes, integrates, and
reports data and can achieve the objectives of this part. The system must provide
information on areas including, but not limited to, utilization, claims, grievance and
appeals, and disenrollment for other than loss of Medicaid eligibility. Contractor must
develop, implement and maintain policies and procedures that describe how Contractor
will comply with the requirements of this Section.
a.
Contractor must comply with the following:
i.
Section 6504(a) of the Affordable Care Act, which requires that State claims
processing and retrieval systems are able to collect data elements necessary to
enable the mechanized claims processing and information retrieval systems in
operation by the State to meet the requirements of Section 1903(r)(1)(F) of the
Act and as defined in 42 CFR 438.242(b)(1).
ii.
Collect data on beneficiary and provider characteristics as specified by the
State, and on all services furnished to beneficiaries through an encounter data
system or other methods as may be specified by the State.
iii.
Ensure that data received from providers is accurate and complete by:
1) Verifying the accuracy and timeliness of reported data, including data
from network providers is compensating on the basis of capitation
payments.
2) Screening the data for completeness, logic, and consistency.
3) Collecting data from providers in standardized formats to the extent
feasible and appropriate, including secure information exchanges and
technologies utilized for State Medicaid quality improvement and care
coordination efforts.
iv.
Make all collected data available to the State and, upon request, to CMS.
b.
Contractor must ensure all encounter data is complete and accurate for the purposes
of rate calculations and quality and utilization management and must provide for:
i.
Collection and maintenance of sufficient beneficiary encounter data to identify
the provider who delivers any item(s) or service(s) to beneficiaries.
ii.
Submission of beneficiary encounter data to the State at a frequency and level
of detail to be specified by CMS and the State, based on program

Page 70 of 148
administration, oversight, and program integrity needs.
iii.
Submission of all beneficiary encounter data that the State is required to report
to CMS under 42 CFR 438.818. Specifications for submitting encounter data to
the State in standardized ASC X12N 837 and NCPDP formats.
3.
Capabilities
a.
Health Information Systems capabilities are required for the following:
i.
Monthly downloads of Medicaid eligible information.
ii.
Individual registration and demographic information.
iii.
Provider enrollment.
iv.
Third party liability activity.
v.
Claims payment system and tracking.
vi.
Grievance and complaint tracking.
vii.
Tracking and analyzing services and costs by population group, and special
needs categories as specified by the State.
viii.
Encounter and demographic data reporting.
ix.
Quality indicator reporting.
x.
HIPAA compliance.
xi.
Uniform Business Practices (UBP) compliance.
xii.
Individual access and satisfaction.
xiii.
Utilization of Benefit Enrollment and Maintenance (834) and Payment Order
Remittance Advice (820) reconciliation files as the primary source for eligibility
determination for Contractor functions. Eligibility Inquiry and Response file
(270/271) is intended as the primary tool for the CMHSP and provider system
to determine eligibility.
4.
Beneficiary Service Records
Contractor must ensure that providers establish and maintain a comprehensive
individual service record system consistent with the provisions of MSA Policy Bulletins,
and appropriate State and federal statutes. Contractor must ensure that providers
maintain in a legible manner, via hard copy or electronic storage/imaging, recipient
service records necessary to fully disclose and document the quantity, quality,
appropriateness, and timeliness of services provided. The records must be retained
according to the retention schedules in place by the Department of Technology,
Management and Budget (DTMB) General Schedule #20 at:
https://www.michigan.gov/dtmb/services/recordsmanagement/schedules/GSLocal
.This
requirement must be extended to all of Contractor's provider agencies.
5.
Contractor must analyze claims and encounter data to create utilization reports. The
utilization data must be detailed for each CMHSP and consolidated for the entire
geographic service area. Contractor must utilize this information to develop and update
their risk management strategies and other health plan functions.
6.
Contractor must actively participate with the State to develop metrics the State will use
to provide reports to Contractor (i.e., benchmarking Contractor’s data against Statewide
data).
7.
Contractor must participate with the State and CMHSPs in activities to standardize and
consistently submit encounter data when the CMHSP identified as the County of
Financial Responsibility (COFR) is not part of Contractor’s geographic service area.
P.
Legal Expenses
1.
Sufficient documentation must be maintained to support the allowability of legal
expenses. Invoices must contain sufficient detail to evidence allowability. The following
legal expenses are allowed:
a.
Legal expenses required in the administration of the program on behalf of the State of

Page 71 of 148
Michigan or Federal Government.
b.
Legal expenses relating to employer activities, labor negotiation, or in response to
employment related issues or allegations, per 2 CFR 200.
c.
Legal expenses incurred in the course of providing consumer care.
d.
Legal expenses in response to enforcement action or audit findings issued by the
State or CMS under the following circumstances:
i.
Contractor prevails and the action is reversed, or any contested adjustment is
reduced by 50 percent or more; or
ii.
Contractor enters into a settlement agreement with the State or CMS prior to
any Hearing. The following legal expenses are not allowed:
e.
Legal expenses of responding to an action against Contractor by MDHHS or CMS
from initiating an enforcement action or issuing an audit finding, except those legal
costs described above as allowable.
f.
Legal expenses for the prosecution of claims against the State of Michigan or the
Federal Government.
g.
Legal expenses contingent upon recovery of costs from the State of Michigan or the
Federal Government.
Q.
Observance of State and Federal Laws and Regulations
1.
General
a.
Contractor must comply with all State and federal laws, statutes, regulations, and
administrative procedures and implement any necessary changes in policies and
procedures as required by the State.
b.
Federal regulations governing contracts with risk-based managed care plans are
specified in Section 1903(m) of the Social Security Act and 42 CFR Part 434 and will
govern this Contract.
2.
Compliance with False Claims Acts
If the Contactor makes or receives annual payments under this Contract of at least
$5,000,000, it must make provisions for written policies for all employees of the entity,
and of any network provider/subcontractor or agent, that provides detailed information
about the False Claims Act and other Federal and State laws described in Section
1902(a)(68) of the Act, including information about rights of employees to be protected
as whistleblowers.
3.
Third Party Liability Requirements
Third Party Liability (TPL) refers to health insurers, self-insured plans, group health
plans, service benefit plans, managed care organizations, pharmacy benefit managers,
or other parties that are, by statute, contract, or agreement, legally responsible for
payment of a claim for a health care item or service to pay for care and services
available under the approved Medicaid state plan. Contractors are payers of last resort
and will be required to identify and seek recovery from all other liable third parties in
order to be made whole, including recoveries from any related court judgment or
settlement if Contractor has been notified of the legal action. Contractor must follow the
“Guidelines Used to Determine Cost Effectiveness and Time/Dollar Thresholds for
Billing” as described in the Michigan State Medicaid Plan (which can be found at the
following link:
https://www.michigan.gov/mdhhs/assistance-
programs/medicaid/michigan-medicaid-state-plan ). Contractor may pursue cases below
the thresholds at their discretion.
i.
Contractor must seek to identify and recover all sources of third-party funds
based on industry standards and those outlined by MDHHS TPL Division.
ii.
Contractor may retain all such collections as provided for in Section 226a of the
Michigan Mental Health Code as applicable. If third party resources are
Page 72 of 148
available and liability has been established, Contractor is required to follow
Medicaid policy, guidance, and all applicable State and federal statutes, the
Medicaid Provider Manual, the State Plan, and the TPL Guidelines and Best
Practices Guidance for cost avoiding Medicaid covered services.
iii.
Contractor must follow Medicaid Policy, guidance and all applicable State and
federal statutes regarding TPL. MDHHS TPL policy information can be found in
federal regulations, Michigan Compiled Law, MDHHS Medicaid Provider
Manual, Medicaid State Plan, and TPL Guidelines, and are available upon
request. Contractor use of best practices is strongly encouraged by the State
and are available in the TPL Guidelines and Best Practices Guidance.
Contractor must develop and implement written policies describing its
procedures for TPL recovery. The State will review Contractor’s policies and
procedures for compliance with this Contract and for consistency with TPL
recovery requirements in 42 USC 1396(a) (25), 42 CFR 433 Subpart D.
iv.
Contractor must submit a Risk Mitigation Plan in a format required by the State,
to address any risk identified in the MDHHS TPL Dashboard within 30 days of
a State request. This requirement does not become effective until Contractor
has received two quarterly MDHHS TPL dashboards.
v.
Contractor must report third party collections through encounter data
submissions, and in aggregate, as required by the State.
vi.
Contractor must provide third party recovery data to MDHHS in the electronic
format prescribed by the State.
vii.
Contractor must collect any payments available from other health insurers
including Medicare and private health insurance for services provided to its
members in accordance with Section 1902(a)(25) of the Social Security Act
and 42 CFR 433 Subpart D and the Michigan Mental Health Code and Public
Health Code as applicable.
viii.
The State will provide Contractor with all known third party resources for its
beneficiaries. This information is available real-time within CHAMPS or through
Eligibility Inquiry and Response file 270 requests. The State will provide the
most recent data to Contractor on the daily Enrollment/Eligibility 834 HIPAA
file. The State will provide Contractor with a full history of known third party
resources for beneficiaries through a secure file transfer process.
ix.
If Contractor denies a claim due to third party resources (other insurance),
Contractor must provide the other insurance carrier ID, if known, to the billing
provider.
x.
When a beneficiary is also enrolled in Medicare, Medicare will be the primary
payer. Contractor must make the beneficiary whole by paying or otherwise
covering all Medicare cost-sharing amounts incurred by the beneficiary such as
coinsurance, co-pays and deductible whether Contractor authorized the service
or not.
xi.
If the State enters into a Coordination of Benefits Agreement (CBA) with
Medicare for FFS, and if Contractor is responsible for coordination of benefits
for individuals dually eligible for Medicaid and Medicare, the State requires
Contractor to enter into a CBA with Medicare and participate in the automated
claims crossover process.
xii.
Contractor must respond within 30 days of subrogation notification pursuant to
MCL 400.106(10).
xiii.
Contractor must cooperate with TPL subrogation best practices including, but
not limited to:
Page 73 of 148
1) Providing the State with most recent contact information of Contractor’s
assigned TPL staff including staff name(s), fax and telephone numbers.
2) Informing the State, in writing, within 14 Days of vacancy or staffing
change of assigned TPL staff.
3) Reporting TPL quarterly subrogation activities to the State on a template
developed by the State.
xiv.
Contractor is prohibited from recovering loss directly from the beneficiary.
4.
Confidentiality
a.
Contractor must maintain the confidentiality, security and integrity of beneficiary
information that is used in connection with the performance of this Contract to the
extent and under the conditions specified in HIPAA, the Michigan Mental Health Code
(PA 258 of 1974, as amended), the Michigan Public Health Code (PA 368 of 1978 as
amended), and 42 CFR Part 2.
b.
All beneficiary information, medical records, data and data elements collected,
maintained, or used in the administration of this Contract must be protected by
Contractor from unauthorized disclosure.
c.
Contractor must provide safeguards that restrict the use or disclosure of information
concerning beneficiaries to purposes directly connected with its administration of the
Contract.
d.
Contractor must have written policies and procedures for maintaining the
confidentiality of data, including medical records, client information, and appointment
records.
5.
Advance Directives Compliance
In accordance with 42 CFR 422.128 and 42 CFR 438.3(j), Contractor must maintain
written policies and procedures for advance directives. Contractor must provide adult
beneficiaries with written information on advance directive policies and a description of
applicable State law and their rights under applicable laws. This information must be
continuously updated to reflect any changes in State law as soon as possible but no
later than 90 days after it becomes effective. Contractor must inform individuals that
grievances concerning noncompliance with the advance directive requirements may be
filed with Customer Service. This must include prohibiting Contractor from conditioning
the provision of care based on whether or not the individual has executed an advance
directive.
6.
Pro-Children Act
Contractor must comply with Public Law 103-227, also known as the Pro-Children Act of
1994, 20 USC 6081 et seq, which requires that smoking not be permitted in any portion
of any indoor facility owned or leased or contracted by and used routinely or regularly for
the provision of health, day care, early childhood development services, education or
library services to children under the age of 18, if the services are funded by federal
programs either directly or through State or local governments, by federal grant,
contract, loan or loan guarantee. The law also applies to children's services that are
provided in indoor facilities that are constructed, operated, or maintained with such
federal funds. The law does not apply to children's services provided in private
residences; portions of facilities used for inpatient drug or alcohol treatment; service
providers whose sole source of applicable federal funds is Medicare or Medicaid; or
facilities where Women, Infants, and Children (WIC) coupons are redeemed. Failure to
comply with the provisions of the law may result in the imposition of a civil monetary
penalty of up to $1,000 for each violation and/or the imposition of an administrative
compliance order on the responsible entity. Contractor must assure that this language
will be included in any sub-awards that contain provisions for children's services.
Contractor must assure, in addition to compliance with Public Law 103-227, any service
Page 74 of 148
or activity funded in whole or in part through this Contract will be delivered in a smoke-
free facility or environment. Smoking will not be permitted anywhere in the facility, or
those parts of the facility under the control of Contractor. If activities or services are
delivered in residential facilities or in facilities or areas that are not under the control of
Contractor (e.g., a mall, residential facilities or private residence, restaurant or private
work site), the activities or services must be smoke free.
7.
Hatch Political Activity Act and Intergovernmental Personnel Act
Contractor must comply with the Hatch Political Activity Act, 5 USC 1501-1509, and
7324-7328, and the Intergovernmental Personnel Act of 1970, as amended by Title VI of
the Civil Service Reform Act, Public Law 95-454, 42 USC 4728 - 4763. Federal funds
cannot be used for partisan political purposes of any kind by any person or organization
involved in the administration of federally assisted programs.
8.
Limited English Proficiency
a.
Contractor must comply with the Office of Civil Rights Policy Guidance on the Title VI
Prohibition Against Discrimination as it affects persons with Limited English
Proficiency, 45 CFR 92.201 and Section 1557 of the Patient Protection and Affordable
Care Act. Contractor is expected to take reasonable steps to provide meaningful
access to each individual beneficiary with limited English Proficiency, such as
language assistance services, including but not limited to, services oral and written
translation. This includes interpretation services for deaf, hard of hearing and
deaf/blind populations in accordance with The MICHIGAN DEPARTMENT OF CIVIL
RIGHTS DIVISION ON DEAF, DEAF BLIND AND HARD OF HEARING QUALIFIED
INTERPRETER – GENERAL RULES (By authority conferred on the division on deaf
and hard of hearing by Section 8a of the deaf persons’ interpreters act, 1982 PA 204,
MCL 393.508a, Section 9 of the division on deafness act, 1937 PA 72, MCL 408.209,
and ERO 1996-2, MCL 445.2001, ERO 2003-1, MCL 445.2011, and ERO 2008-4,
MCL 445.2025.)
b.
Contractor must comply with all applicable federal requirements in Title VI of the Civil
Rights Act of 1964; Title IX of the Education Amendments of 1972 (regarding
education programs and activities, as amended); the Age Discrimination Act of 1975;
the Rehabilitation Act of 1973, as amended; the Americans with Disabilities Act of
1990, as amended; and Section 1557 of the Patient Protection and Affordable Care
Act.
9.
Health Insurance Portability and Accountability Act (HIPAA) and 42 CFR PART 2
To the extent that State and Contractor are HIPAA Covered Entities and/or Programs
under 42 CFR Part 2, each agrees that it will comply with HIPAA’s Privacy Rule,
Security Rule, Transaction and Code Set Rule and Breach Notification Rule and 42 CFR
Part 2 (as now existing and as may be later amended) with respect to all Protected
Health Information and substance use disorder treatment information that it generates,
receives, maintains, uses, discloses or transmits in the performance of its functions
pursuant to this Agreement. To the extent that Contractor determines that it is a HIPAA
Business Associate of the State and/or a Qualified Service Organization of the State,
then the State and Contractor will enter into a HIPAA Business Associate Agreement
and a Qualified Service Organization Agreement that complies with applicable laws and
is in a form acceptable to both the State and Contractor.
a.
Contractor must not share any protected health data and information provided
by the State that falls within HIPAA requirements except as permitted or
required by applicable law or to a network provider/subcontractor as
appropriate under this agreement.
b.
Contractor must ensure that any network provider/subcontractor will have the
same obligations as Contractor not to share any protected health data and
Page 75 of 148
information from the State that falls under HIPAA requirements in the terms
and conditions of the subcontract.
c.
Contractor must only use the protected health data and information for the
purposes of this Contract.
d.
Contractor must have written policies and procedures addressing the use of
protected health data and information that falls under the HIPAA requirements.
The policies and procedures must meet all applicable federal and State
requirements including the HIPAA regulations. These policies and procedures
must include restricting access to the protected health data and information by
Contractor’s employees.
e.
Contractor must have a policy and procedure to immediately report to the State
any suspected or confirmed unauthorized use or disclosure of protected health
data and information that falls under the HIPAA requirements of which
Contractor becomes aware. Contractor must work with the State to mitigate the
breach and will provide assurances to the State of corrective actions to prevent
further unauthorized uses or disclosures.
f.
Failure to comply with any of these Contractual requirements may result in the
termination of this Contract in accordance with Section 24 Termination for
Cause in the Standard Contract Terms. In accordance with HIPAA
requirements, Contractor is liable for any claim, loss or damage relating to
unauthorized use or disclosure of protected health data and information by
Contractor received from the State or any other source.
g.
Contractor must enter into a business associate agreement .
h.
All recipient information, medical records, data and data elements collected,
maintained, or used in the administration of this Contract must be protected by
Contractor from unauthorized disclosure as required by State and federal
regulations. Contractor must provide safeguards that restrict the use or
disclosure of information concerning recipients to purposes directly connected
with its administration of the contract.
i.
Contractor must have written policies and procedures for maintaining the
confidentiality of all protected information.
10.
Ethical Conduct
State administration of this Contract is subject to the State of Michigan State Ethics Act:
Act 196 of 1973, “Standards of Conduct for Public Officers and Employees. Act 196 of
1973 prescribes standards of conduct for public officers and employees.” The State
administration of this Contract is subject to the State of Michigan Governor’s Executive
Order No: 2001-03, “Procurement of Goods and Services from Vendors.”
11.
Conflict of Interest
Contractor and the State are subject to the federal and State conflict of interest statutes
and regulations that apply to Contractor under this Contract, including Section
1902(a)(4)(C) and (D) of the Social Security Act: 41 U.S.C. Chapter 21 (formerly Section
27 of the Office of Federal Procurement Policy Act (41 U.S.C. 423): 18 U.S.C. 207)): 18
U.S.C. 208: 42 CFR 438.58: 45 CFR Part 92: 45 CFR Part 74: 1978 PA 566: and MCL
330.1222.
12.
Human Subject Research
Contractor must comply with Protection of Human Subjects Act, 45 CFR, Part 46,
subpart A, Sections 46.101-124 and HIPAA. Contractor must, prior to the initiation of the
research, submit Institutional Review Board (IRB) application material for all research
involving human subjects, which is conducted in programs sponsored by the State or in
programs which receive funding from or through the State of Michigan, to the State’s
IRB for review and approval, or the IRB application and approval materials for
Page 76 of 148
acceptance of the review of another IRB. All such research must be approved by a
federally assured IRB, but the State’s IRB can only accept the review and approval of
another institution’s IRB under a formally approved interdepartmental agreement. The
manner of the review will be agreed upon between the State’s IRB Chairperson and
Contractor’s IRB Chairperson or Executive Officer(s).
13.
Fiscal Soundness of the Risk-Based Contractor
Federal regulations require that the risk-based Contractor maintain a fiscally solvent
operation and the State has the right to evaluate the ability of Contractor to bear the risk
of potential financial losses, or to perform services based on determinations of payable
amounts under the Contract.
14.
Medicaid Policy
Contractor must comply with provisions of Medicaid policy developed under the formal
policy consultation process, as established by the Medical Assistance Program.
15.
Service Requirements
a.
Contractor must limit Medicaid and MIChild services to those that are medically
necessary and appropriate, and that conform to accepted standards of care.
b.
Contractor must operate the provision of their Medicaid services consistent with the
applicable sections of the Social Security Act, the Code of Federal Regulations (CFR),
the CMS/HCFA State Medicaid & State Operations Manuals, Michigan’s Medicaid
State Plan, and the Michigan Medicaid Provider Manual: Mental Health-Substance
Use Disorder Section.
c.
Contractor must provide covered State plan or 1915(c) services (for beneficiaries
enrolled in the Michigan Medicaid Managed Specialty Services and Supports
Program) in sufficient amount, duration and scope to reasonably achieve the purpose
of the service.
d.
Consistent with 42 CFR 440.210 and 42 CFR 440.220, services to recipients must not
be reduced arbitrarily.
e.
Criteria for medical necessity and utilization control procedures that are consistent
with the medical necessity criteria/service selection guidelines specified by the State
and based on practice standards may be used to place appropriate limits on a service
(42 CFR 440.230).
16.
Home and Community Based Setting (HCBS) Transition Implementation
a.
In order to ensure compliance with the HCBS rule Contractor must complete the
following: administer the assessment process for new and existing providers, review
and analyze data collected from the assessment, notify providers of a need for
corrective action (if required), develop a corrective action plan, ensure corrective
action is implemented and monitor ongoing compliance. Contractor will develop a
process to ensure settings are surveyed with a frequency identified by the State.
Contractor will provide the State with its proposal to address those settings that do not
comply with the required HCBS assessment process, including timelines. Contractor
will provide updated reports to the State specifying assessment activities taken and
required remediation or validation activities as identified by the State.
b.
Contractor must ensure that all new providers of HCBS services complete the HCBS
Comprehensive Assessment. Contractor may provide provisional approval to the new
provider as long as the setting does not qualify for heightened scrutiny. When a
setting qualifies for heightened scrutiny, Contractor must communicate this to the
HCBS Transition team, who will determine the required next steps, that must include
an individualized consultation.
i.
Contractor must ensure that provisionally approved providers and beneficiaries
receive the comprehensive HCBS assessment within 90 days of the
beneficiaries’ IPOS. Contractors must ensure providers complete this

Page 77 of 148
assessment and subsequent remediation/validation processes in order to be
eligible for HCBS funding.
c.
Contractor must ensure that all HCBS final rule requirements are met, as described in
the Michigan Medicaid Provider Manual.
d.
Contractor must not enter into new contracts with new providers of services covered
by the Federal HCBS Rule (42 CFR Parts 430,431, 435, 436, 440, 441 and 447)
unless the provider has obtained provisional approval status through completion of
the HCBS New Provider Application, demonstrating that the provider does not require
heightened scrutiny. Provisional approval allows a new provider or an existing
provider with a new setting, service, or licensee to provide services to HCBS
participants pending the full assessment process. Providers and participants will
receive the comprehensive HCBS assessment during the first assessment cycle
occurring 90 days post provisional approval. Providers will complete the HCBS
assessment and cooperate with Contractor to demonstrate 100% compliance with the
Federal HCBS rule and State requirements as promulgated by the MDHHS and
documented in the Michigan Statewide Transition Plan. Failure to complete the
provisional approval process and the ongoing compliance assessments will result in
the exclusion from participating in Medicaid or Healthy Michigan Plan funded HCBS
services. Contractor must monitor their provider panel annually for ongoing
compliance with the HCBS rule and implement a system to remove providers from the
regions network due to failure to meet requirements of the rule. Contractor must
maintain documentation of this annual review and/or removal from its provider
network. Contractor must make all HCBS provider network status collected data
available to the State and, upon request, to CMS.
e.
Contractor shall conduct a physical assessment of the setting annually and the
comprehensive assessments at least once every two years to ensure that the setting
remains home and community based.
f.
Please reference the HCBS Technical Advisory which is located on the MDHHS
Policy and Practice Guidelines website,
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines for further detail on these
requirements.
17.
Electronic Visit Verification (EVV)
In accordance with Section 12006(a) of the 21st Century Cures Act, Contractor must
implement EVV for all Medicaid Personal Care Services (PCS) that requires an in home
visit by a provider. This applies to PCS provided under Sections 1905(a)(24), 1915(c),
1915(i), 1915(j), 1915(k), and Section 1115; and HHCS provided under 1905(a)(7) of the
Social Security Act or a waiver.
18.
Application Programming Interface (API)
In accordance with 42 CFR 438.242(b)(5), Contractor must implement an Application
Programming Interface (API) as specified in 42 CFR 431.60 (beneficiary access to and
exchange of data) as if such requirements applied directly to the Contractor.
19.
Methadone
Pursuant to 2023 PA 119 Section 965 and any properly promulgated successor
guidance issued, Contractor shall maintain a bundled rate at not less than $19.00 per
unit for the administration and services of methadone (procedure code H0020).
20.
Programs or Activities No Longer Authorized by Law
Should any part of the scope of work under this Contract relate to a State program that
is no longer authorized by law (e.g., which has been vacated by a court of law, or for
which CMS has withdrawn federal authority, or which is the subject of a legislative
repeal), Contractor must do no work on that part after the effective date of the loss of
program authority. The State will adjust capitation rates to remove costs that are specific
Page 78 of 148
to any program or activity that is no longer authorized by law. If Contractor works on a
program or activity no longer authorized by law after the date the legal authority for the
work ends, Contractor will not be paid for that work. If the state paid Contractor in
advance to work on a no-longer-authorized program or activity and under the terms of
this Contract the work was to be performed after the date the legal authority ended, the
payment for that work should be returned to the State. However, if Contractor worked on
a program or activity prior to the date legal authority ended for that program or activity,
and the State included the cost of performing that work in its payments to Contractor,
Contractor may keep the payment for that work even if the payment was made after the
date the program or activity lost legal authority.
R.
Program Integrity
The State, MDHHS-Office of Inspector General (OIG) is responsible for overseeing the
program integrity activities of Contractor and all subcontracted entities/network providers
consistent with this Contract and the requirements under 42 CFR 438.608.
1.
General:
a.
To the extent consistent with applicable Federal and State law, including, but not
limited to 42 CFR Part 2, HIPAA, and the Michigan Mental Health Code, Contractor
must disclose protected health information to MDHHS-OIG or the Department of
Attorney General upon their written request, without first obtaining authorization from
the beneficiary to disclose such information.
b.
Contractor must have administrative and management arrangements or procedures for
compliance with 42 CFR 438.608. Such arrangements or procedures must identify program
integrity compliance activities that will be delegated per 42 CFR 438.230 and how
Contractor will monitor those activities.
c.
Contractor that makes or receives annual payments under this Contract of at least
$5,000,000 to a provider, must make provision for written policies for all employees of
the entity, and of any contractor or agent of the entity, that provide detailed
information about the False Claims Act and other Federal and State laws described in
Section 1902(a)(68) of the Act, including information about rights of employees to be
protected as whistleblowers.
d.
Contractor must require all contracted providers that make or receive annual
payments under this Contract of at least $5,000,000 to agree to comply with Section
6032 of the Deficit Reduction Act (DRA) of 2005.
e.
Contractor must have written documentation of internal controls and policies and
procedures in place that are designed to prevent, detect, and report known or
suspected Fraud, Waste, and Abuse activities. The arrangements or procedures must
include the following:
i. Contractor must have a program integrity compliance program as defined in 42
CFR 438.608. The program integrity compliance program and plan must include, at
a minimum, all of the following elements:
1) Written policies, procedures, and standards of conduct that articulate
Contractor’s commitment to comply with all applicable Fraud, Waste,
and Abuse requirements and standards under this Contract, and all
applicable Federal and State requirements.
a) Standards of Conduct – Contractor must have written standards
of conduct that clearly state the Contractor’s commitment to
comply with all applicable statutory, regulatory and Medicaid
program requirements. The standards of conduct must be written
in an easy-to-read format and distributed to all employees. All
employees must be required to certify that they have read,
Page 79 of 148
understand, and agree to comply with the standards.
b) Written Compliance Policies and Procedures – Contractor must have
comprehensive written compliance policies and procedures, developed
under the direction of the compliance officer and Compliance
Committee, which direct the operation of the compliance program. The
written compliance policies and procedures must include, at a
minimum, the following elements:
i) Duties and responsibilities of the compliance officer and
Compliance Committees.
ii) How and when employees will be trained.
iii) Procedures for how employee reports of noncompliance will be
handled.
iv) Guidelines on how the compliance department/officer will
interact with other individuals and departments (e.g., human
resources, legal counsel, etc.).
v) Duties and responsibilities of management in promoting
compliance among employees and responding to reports of
non-compliance.
vi) Ensuring that prospective employees receive appropriate
background screening and agree to abide by the Contractor’s
code of conduct.
vii) Conducting periodic reviews, at least annually, of the code of
conduct and the compliance policies and procedures.
viii) Procedures for the monitoring of compliance in Contractor and
subcontractor/network provider systems and processes.
ix) Procedures for the monitoring of potential Fraud, Waste, and
Abuse in provider billings and beneficiary utilization.
x) Procedures for performing an investigation of targets selected
for audit, including triage and review processes.
xi) Reporting confidentiality and non-retaliation policy.
xii) Information about the False Claims Act and other Federal and
State laws described in section 1902(a)(68) of the Act, including
information about rights of employees to be protected as
whistleblowers.
xiii) Written policies and procedures pertaining to cooperation in
investigations or prosecutions.
2) The designation of a compliance officer who is responsible for developing
and implementing policies, procedures, and practices designed to ensure
compliance with the requirements of the contract and who reports directly to
the chief executive officer and the Board of Directors.
a) Contractor must designate a compliance officer whose primary
responsibility is to oversee the implementation and maintenance of the
compliance program.
b) The compliance officer must have adequate authority and
independence within the Contractor’s organizational structure in order
to make reports directly to the board of directors and/or to senior
management concerning actual or potential cases of non-compliance.
c) The compliance officer must also report directly to corporate
governance on the effectiveness and other operational aspects of the
compliance program.
d) The compliance officer’s responsibilities must encompass a broad
Page 80 of 148
range of duties including, but not limited to, the investigation of alleged
misconduct, the development of policies and rules, training officers,
directors, and staff, maintaining the compliance reporting mechanism
and closely coordinating with the internal audit function of the
Contractor.
3) Maintenance of a Regulatory Compliance Committee comprised of the Board
of Directors and senior management charged with overseeing the
Contractor’s compliance program and its compliance with requirements
under the Contract.
a) Contractor must establish a Regulatory Compliance Committee that
will advise the compliance officer and assists in the maintenance of the
compliance program.
b) The Regulatory Compliance Committee must not have the authority to
block or interfere with any actions taken or proposed to be taken by the
compliance officer.
c) The compliance officer will remain duty-bound to report on and correct
alleged fraud and other misconduct.
d) The compliance officer must chair the Regulatory Compliance
Committee.
e) The Regulatory Compliance Committee must meet no less than
quarterly.
4) A system for annual training and education for the compliance officer,
Contractor’s senior management, and Contractor’s employees regarding
fraud, waste and abuse, and the federal and State standards and
requirements under this Contract. While the compliance officer may provide
training to Contractor’s employees, “effective” training for the compliance
officer means it cannot be conducted by the compliance officer to
himself/herself.
a) Formal Training Programs – Contractor must provide general
compliance training to all employees, officers, managers, supervisors,
board members and long-term temporary employees that effectively
communicates the requirements of the compliance program, including
the company’s code of conduct and applicable Medicaid statutory,
regulatory, and contractual requirements.
i) Contractor must also determine under what circumstances it
may be appropriate to train nonemployee agents and
contractors.
ii) Employees, officers, managers, supervisors, and Board
members must be required to attend compliance training
sessions and to sign certifications that they have completed the
appropriate sessions.
iii) The initial compliance training for new employees must occur
within 90 days of the date of hire.
iv) Contractor must provide annual refresher compliance training
that highlights compliance program changes or other new
developments. The refresher training should re-emphasize
Medicaid statutory, regulatory, and contractual requirements
and the Contractor’s code of conduct.
b) Informal On-going Compliance Training – Contractor must employ
additional, less formal means for communicating its compliance
message such as posters, newsletters, and Intranet communications.
Page 81 of 148
The compliance officer must be responsible for the content of the
compliance messages and materials distributed to employees and
managers.
5) Effective lines of communication between the compliance officer and the
Contractor’s employees.
a) Hotline or Other System for Reporting Suspected Noncompliance –
Contractor must have mechanisms in place for employees and others
to report suspected or actual acts of non-compliance.
i) In order to encourage communications, confidentiality and non-
retaliation policies must be developed and distributed to all
employees.
ii) Contractor must use e-mails, newsletters, suggestion boxes,
and other forms of information exchange to maintain open lines
of communication.
iii) A separate mechanism, such as a toll-free hotline, must be
employed to permit anonymous reporting of non-compliance.
iv) Matters reported through the hotline or other communication
sources that suggest substantial violations of compliance
policies or health care program statutes and regulations must be
documented and investigated promptly to determine their
veracity.
v) Contractor must create an environment in which employees feel
free to report concerns or incidents of wrongdoing without fear
of retaliation or retribution, when making a good faith report of
non-compliance.
b) Routine Communication and Access to the compliance officer –
Contractor must have a general “open door” policy for employee
access to the compliance officer and the Compliance Department staff.
Staff must be advised that the compliance officer’s duties include
answering routine questions regarding compliance or ethics issues.
i) The compliance officer must establish, implement, and maintain
processes to inform the Contractor’s employees of procedure
changes, regulatory changes, and contractual changes.
6) Enforcement of standards though well-publicized disciplinary guidelines.
a) Consistent Enforcement of Disciplinary Policies – Contractor must
maintain written policies that apply appropriate disciplinary sanctions
on those officers, managers, supervisors, and employees who fail to
comply with the applicable statutory and Medicaid program
requirements, and with the Contractor’s written standards of conduct.
These policies must include not only sanctions for actual
noncompliance, but also for failure to detect non-compliance when
routine observation or due diligence should have provided adequate
clues or put one on notice. In addition, sanctions should be imposed
for failure to report actual or suspected non-compliance.
i) The policies must specify that certain violations, such as
intentional misconduct or retaliating against an employee who
reports a violation, carry more stringent disciplinary sanctions.
ii) In all cases, disciplinary action must be applied on a case-by-
case basis and in a consistent manner.
iii) Contractor may identify a list of factors that will be considered
before disciplinary action will be imposed. Such factors may
Page 82 of 148
include degree of intent, amount of financial harm to the
company or the government or whether the wrongdoing was a
single incident or lasted over a long period of time.
b) Employment of, and Contracting with, Ineligible Persons – Contractor
must have written policies and procedures requiring a reasonable and
prudent background investigation to determine whether prospective
employees and prospective non- employee subcontractors/network
providers or agents were ever criminally convicted, suspended,
debarred, or excluded from participation in a federal program.
i) Contractor must also conduct periodic reviews of current
employees and/or subcontractors/network providers and agents
to determine whether any have been suspended or debarred or
are under criminal investigation or indictment. If an employee or
non-employee agent or subcontractor/network provider is found
to be ineligible, Contractor must have a written policy requiring
the removal of the employee from direct responsibility for, or
involvement with, the Medicaid program, or for the termination
of the subcontract/network providers, as appropriate.
7) Establishment and implementation, and ongoing maintenance of procedures
and a system with dedicated staff for routine internal monitoring and auditing
of compliance risks, prompt response to compliance issues as they are
raised, investigation of potential compliance problems as identified in the
course of self-evaluation and audits, correction of such problems promptly
and thoroughly (or coordination of suspected criminal acts with law
enforcement agencies) to reduce the potential for recurrence, and ongoing
compliance with requirements under the Contract.
a) Auditing – Contractor must have a comprehensive internal audit
system to ensure that the Contractor is in compliance with the range of
contractual and other MDHHS requirements in critical operations
areas. The internal auditors must be independent from the
section/department under audit. The auditors must be competent to
identify potential issues within the critical review areas and must have
access to existing audit resources, relevant personnel, and all relevant
operational areas. Written reports must be provided to the compliance
officer, the Compliance Committee and appropriate senior
management. The reports must contain findings, recommendations
and proposed corrective actions that are discussed with the
compliance officer and senior management.
i) Contactor must ensure that regular, periodic evaluations of its
compliance program occur to determine the program’s overall
effectiveness. This periodic evaluation of program effectiveness
may be performed internally, either by the compliance officer or
other internal source - or by an external organization. These
periodic evaluations must be performed at least annually, or
more frequently, as appropriate.
b) Monitoring – Contactor must maintain a system to actively monitor
compliance in all operational areas. Contractor must have a means of
following up on recommendations and corrective action plans resulting
from either an internal compliance audit or MDHHS review to ensure
timely implementation and evaluation.
i) Contractor must have a Questionnaire that includes questions
Page 83 of 148
regarding whether any exiting employee observed any violations
of the compliance program, including the code of conduct, as
well as any violations of applicable statutes, regulations, and
Medicaid program requirements during the employee’s tenure
with the Contractor. The Compliance Department must review
any positive responses to questions regarding compliance
violations.
ii. Provision for prompt notification to MDHHS when it receives information about changes
in an Enrollee’s circumstances that may affect the Enrollee’s eligibility, including but not
limited to:
1) Changes in the Enrollee’s residence.
2) The death of an Enrollee.
iii. Provision for notification to MDHHS-OIG when it receives information about a change in
a network provider’s circumstances that may affect the network provider’s eligibility to
participate in the managed care program, including the termination for cause of the
provider agreement with the Contractor.
iv. Provision for a method to verify, by sampling or other methods, whether services that
have been represented to have been delivered by network providers were received by
Enrollees and the application of such verification processes on a regular basis.
1) Contractor must have methods for identification, investigation, and referral of
suspected Fraud cases (42 CFR § 455.13, 455.14, 455.21).
a) Contractor must respond to all MDHHS-OIG audit referrals with
Contractor’s initial findings report within the timeframe designated in
the MDHHS-OIG referral. Initial findings means prior to the provider
receiving a final notice with appeal rights.
2) Contractor may request a one-time extension in writing (email) to MDHHS-
OIG no less than two (2) business days prior to the due date, if the
Contractor is unable to provide the requested information within the
designated timeframe. The request must include a status update and
estimated date of completion.
3) Contractor must have adequate staffing and resources to investigate unusual
incidents and develop and implement corrective action plans to assist the
Contractor in preventing and detecting potential Fraud, Waste, and Abuse
activities.
a) Special Investigations Unit – The Contractor must operate a distinct
Fraud, Waste, and Abuse Unit, Special Investigations Unit (SIU).
i) The investigators in the unit must detect and investigate Fraud,
Waste, and Abuse by its Michigan Medicaid Enrollees and
providers. It must be separate from the Contractor’s utilization
review and quality of care functions. The unit can either be a
part of the Contractor’s corporate structure or operate under
contract with the Contractor.
ii) On a yearly basis, the Contractor’s SIU must conduct program
integrity training to improve information sharing between
departments within the Contractor, such as Provider
Credentialing, Payment Integrity, Customer Service, Human
Resources, and the General Counsel, and to enhance referrals
to the SIU regarding Fraud, Waste, and Abuse within the
Contractor’s Medicaid program.
1. The yearly training must include a component specific to
Michigan Medicaid and the Contractor’s approach to
Page 84 of 148
address current Fraud, Waste and Abuse within the
program.
iii) Data Mining Activities – Contractor must have surveillance and
utilization control programs and procedures (42 CFR § 456.3,
456.4, 456.23) to safeguard the Medicaid funds against
unnecessary or inappropriate use of Medicaid services and
against improper payments. Data Mining must be performed at
least annually. Contractor must utilize statistical models,
complex algorithms, and pattern recognition programs to detect
possible fraudulent or abusive practices. The Contractor must
report all data mining activities performed (including all program
integrity cases opened as a result) within the previous quarter to
MDHHS-OIG. See Quarterly Submissions section of this
Contract for the method and timing of such reporting.
iv) Preliminary Investigations – Contractor must promptly perform a
preliminary investigation of all incidents of suspected Fraud,
Waste, and Abuse. The Contractor must report all program
integrity cases opened within the reporting period to MDHHS-
OIG (see Quarterly Submissions section of this Contract for the
method and timing of such reporting). All confirmed or
suspected provider Fraud must immediately be reported to
MDHHS-OIG (see Reporting Fraud, Waste, or Abuse section of
this Contract).
v) Audit Requirements – Contractor must conduct risk-based
auditing and monitoring activities of provider transactions,
including, but not limited to, claim payments, vendor contracts,
credentialing activities and Quality of Care/Quality of Service
concerns that indicate potential Fraud, Waste, or Abuse. These
audits should include a retrospective medical and coding review
on the relevant claims.
vi) Prepayment Review – If the Contractor subjects a provider to
prepayment review or any review requiring the provider to
submit documentation to support a claim prior to the Contractor
considering it for payment, as a result of suspected Fraud,
Waste and/or Abuse, the Contractor must notify MDHHS-OIG in
accordance with the Quarterly Reporting requirements of this
Contract for the method and timing of such reporting.
v. Provision for written policies for all employees of the Contactor, and of any contractor or
agent, that provide detailed information about the False Claims Act and other Federal
and State laws described in section 1902(a)(68) of the Act, including information about
rights of employees to be protected as whistleblowers.
1) Contractor must include in any employee handbook a description of the laws
and the rights of employees to be protected as whistleblowers.
vi. Provisions for internal monitoring and auditing of compliance risks. Audits must include
post payment reviews of paid claims to verify that services were billed appropriately
(e.g., correct procedure codes, modifiers, quantities). Acceptable audit methodology
examples include:
1) Record review, including statistically valid random sampling and
extrapolation to identify and recover overpayments made to providers.
2) Beneficiary interviews to confirm services rendered.
3) Provider self-audit protocols.
Page 85 of 148
4) The frequency and quantity of audits performed should be dependent on the
number of fraud, waste, and abuse complaints received, as well as high risk
activities identified through data mining and analysis of paid claims.
vii. Provisions for Contractor’s prompt response to detected offenses and for the
development of corrective action plans. “Prompt Response” is defined in this Contract
as action taken within 15 business days of receipt and identification by Contractor of the
information regarding a potential compliance problem.
viii. Dissemination of the contact information (addresses and toll-free telephone numbers)
for reporting fraud, waste, or abuse by network provider/subcontractors of Contractor to
both Contractor and the MDHHS-OIG. Dissemination of this information must be made
to all Contractors network providers/subcontractors and members annually. Contractor
must indicate that reporting of fraud, waste or abuse may be made anonymously.
2.
Once all applicable appeal periods have been exhausted, Contractor must adjust all associated
encounter claims identified as part of their Program Integrity activities within 45 days. Failure to
comply may result in a gross adjustment for the determined overpayment amount to be taken
from Contractor.
a.
Contractor must resolve outstanding encounter corrections in the timeframe designated in
any authorization granted by MDHHS-OIG.
3.
Biannual meetings will be held between MDHHS-OIG and all Contractor Compliance Officers to
train and discuss fraud, waste, and abuse.
4.
Subcontracted Entities and Network Providers
a.
Contractor must include program integrity compliance provisions and guidelines in all
contracts with subcontracted entities and network providers.
b.
If program integrity compliance activities are delegated to subcontractors as outlined in 42
CFR 438.230, the subcontract must contain the following:
i.
Designation of a compliance officer.
ii.
Submission to Contractor of quarterly reports detailing program integrity compliance
activities.
iii.
Assistance and guidance by Contractor with audits and investigations, upon request
of the subcontracted entity.
iv.
Provisions for routine internal monitoring of program integrity compliance activities.
v.
Prompt response to potential offenses and implementation of corrective action plans.
vi.
Prompt reporting of fraud, waste, and abuse to Contractor.
vii.
Implementation of training procedures regarding fraud, waste, and abuse for the
subcontracted entities’ employees at all levels.
c.
Annually, Contractor must submit a list of their subcontracted entities and network
providers using the template created by MDHHS-OIG.
i.
Contractor must maintain a list that contains all facility locations where services are
provided, or business is conducted. This list must contain Billing Provider NPI
numbers assigned to the entity, what services the entity is contracted to provide, and
provider email address(es).
5.
Investigations
a.
Contractor must investigate program integrity compliance complaints to determine
whether a potential credible allegation of fraud exists. If a potential credible allegation of
fraud exists, Contractor must refer the matter to MDHHS-OIG (see Reporting of Fraud,
Waste, or Abuse) and pause any recoupment/recovery in connection with the potential
credible allegation of fraud until receiving further instruction from MDHHS-OIG.
b.
To the extent consistent with applicable law, including but not limited to 42 CFR Part 2,
HIPAA, and the Michigan Mental Health Code, Contractor must cooperate fully in any
investigation or prosecution by any duly authorized government agency, including but not
limited to: MDHHS-OIG or the Department of Attorney General, whether administrative,
Page 86 of 148
civil, or criminal. Such cooperation shall include providing, upon request, information,
access to records, and access to schedule interviews with designated Contractor
employees and consultants, including but not limited to those with expertise in the
administration of the program and/or in medical or pharmaceutical questions or in any
matter related to the investigation or prosecution. Contractor must follow the procedures
and examples contained within processes and associated guidance provided by MDHHS-
OIG.
i.
Contractor must maintain written policies and procedures pertaining to cooperation
in investigations or prosecutions.
6.
Reporting Fraud, Waste, or Abuse
a.
Upon receipt of allegations involving fraud, waste, or abuse regardless of entity (i.e.,
Contractor, employee, subcontracted entity and/or network providers, provider, or
member), Contractor must perform a preliminary investigation.
b.
Questions regarding whether suspicions should be classified as fraud, waste, or abuse
should be presented to MDHHS-OIG for clarification prior to making the referral.
c.
Upon completion of the preliminary investigation, if Contractor determines a potential
credible allegation of fraud exists, and an overpayment of $5,000 or greater is identified
(cases under this amount shall not be referred to OIG), Contractor must:
i.
Promptly refer the matter to MDHHS-OIG and Attorney General-Health Care Fraud
Division (AG-HCFD). These referrals must be made using the MDHHS-OIG Fraud
Referral Form. The form must be completed in its entirety, as well as follow the
procedures and examples contained within the MDHHS-OIG guidance document.
ii.
Share referral via secure File Transfer Process (sFTP) using Contractor’s applicable
MDHHS-OIG/AG-HCFD sFTP areas.
iii.
Cooperate in presenting the fraud referral to the OIG and AG-HCFD at an agreed
upon time and location.
iv.
Defend their potential credible allegation of fraud in any appeal should the referral
result in a suspension issued by MDHHS-OIG. After reporting a potential credible
allegation of fraud, Contractor shall not take any of the following actions unless
otherwise instructed by OIG:
1) Contact the subject of the referral about any matters related to the referral.
2) Enter into or attempt to negotiate any settlement or agreement regarding the
referral with the subject of the referral; or
3) Accept any monetary or other thing of valuable consideration offered by the
subject of the referral in connection with the findings/overpayment.
d.
Upon making a referral, the Contractor must immediately cease all efforts to take adverse
action against or collect overpayments from the referred provider until authorized by
MDHHS-OIG.
e.
If a draft/potential referral is declined prior to Contractor sending a final potential credible
allegation of Fraud, Contractor must follow MDHHS-OIG reporting procedures.
f.
If the State successfully prosecutes and makes a recovery based on a Contractor referral
where the Contractor has sustained a documented loss, the State shall not be obligated to
repay any monies recovered to the Contractor. Unless otherwise directed by the State, the
correction of associated encounter claims is not required.
g.
Contractor must refer all potential Enrollee Fraud, Waste or Abuse that the Contractor
identifies to MDHHS via the local MDHHS office or through (File a Complaint - Medicaid
Complaint Form). In addition, the Contractor must report all of Fraud, Waste and Abuse
referrals made to MDHHS on their quarterly submission described in the Quarterly
Submissions of this Contract.
h.
Contractor must report all suspicion of waste or abuse on the Quarterly Submission
described in the Quarterly Submissions section of this Contract.
Page 87 of 148
i.
Documents containing protected health information or protected personal information must
be submitted in a manner that is compliant with applicable Federal and State privacy rules
and regulations, including but not limited to HIPAA.
7.
Overpayments
Contractor must report identified and/or recovered overpayments due to fraud, waste, or
abuse to MDHHS-OIG.
a.
If Contractor identifies an overpayment involving potential fraud prior to identification by
MDHHS-OIG, Contractor refers the findings to MDHHS-OIG and waits for further
instruction from MDHHS-OIG prior to recovering the overpayment.
b.
If Contractor identifies an overpayment involving waste or abuse prior to identification by
MDHHS-OIG, Contractor must void or correct applicable encounters, should recover the
overpayment, and must report the overpayment on its quarterly submission (see Quarterly
Submissions section of this Contract).
c.
If a subcontractor/network provider identifies an overpayment, they must agree to:
i.
Notify Contractor, in writing, of the reason for the overpayment and the date the
overpayment was identified.
ii.
Return the overpayment to Contractor within 60 calendar days of the date the
overpayment was identified.
d.
Contractor shall include a provision in all contracts with subcontractors and/or network
providers giving Contractor the right to recover overpayments directly from providers for
the post payment evaluations initiated and performed by the Contractor. These
overpayment provisions do not apply to any amount of a recovery to be retained under
False Claims Act cases or through other investigations.
8.
Contractor must send all program integrity notifications and reports to the MDHHS-OIG sFTP.
The Contractor must follow the procedures and examples contained within the MDHHS-OIG
submission forms and accompanying guidance documents. See Schedule E for the listing of
notification forms and reports and their respective due dates.
9.
Quarterly Submissions
a.
Contractor must provide information on program integrity compliance activities performed
quarterly using the template provided by the MDHHS-OIG. Data mining activities must be
performed at least annually; monthly or quarterly application is considered the best
practice standard. Program integrity compliance activities must be included.
b.
All program integrity activities performed each quarter must be reported to MDHHS-OIG
according to Schedule E, Reporting Requirements.
c.
Contractor must provide MDHHS-OIG with documentation to support that these program
integrity compliance activities were performed by its subcontractors in its quarterly
submission to the MDHHS-OIG.
d.
Contractor must include any improper payments identified and amounts adjusted in
encounter data and/or overpayments recovered by Contractor during the course of its
program integrity activities. It is understood that identified overpayment recoveries may
span multiple reporting periods. This report also includes a list of the individual encounters
corrected. To ensure accuracy of reported adjustments, Contractor must:
i.
Purchase at minimum one (1) license for MDHHS-OIG’s case management
software. This license will be utilized to upload report submissions to the case
management system and to check the completeness and accuracy of report
submissions.
ii.
For medical equipment, supplies, or prescription provided, adjust any encounter for
an enrollee to zero dollars paid. If the encounter with a dollar amount cannot be
adjusted to zero dollars paid, then the encounters with dollars paid must be voided
and resubmitted with zero dollars paid.
iii.
Specify if overpayment amounts were determined via sample and extrapolation or
Page 88 of 148
claim-based review. In instances where extrapolation occurs, Contractor may elect
to correct claims, and thus encounters, as they see fit.
iv.
Specify encounters unavailable for adjustment in CHAMPS due to the encounter
aging out or any other issue.
1) These encounters must be identified by Contractor and reported to MDHHS-
OIG. MDHHS-OIG will record a gross adjustment to be taken out of
Contractor’s next capitation payment.
v.
Report only corrected encounters associated with post payment evaluations that
resulted in a determined overpayment amount.
10.
Pursuant to 42 CFR § 438.608(d)(3), on an annual basis, Contractor must submit to MDHHS-
OIG, in a format determined by MDHHS-OIG, an annual Program Integrity Report containing
details of the improper payments identified, overpayments recovered, and costs avoided for the
program integrity activities conducted by the Contractor for the preceding year. The report also
must address the Contractor’s plan of activities for the current and upcoming fiscal year. The
report must include all provider and service-specific program integrity activities.
a.
Pursuant to 42 CFR § 438.606, the annual Program Integrity Report must be certified by
either the Contractor’s chief executive officer; chief financial officer; or an individual who
reports directly to the chief executive officer or chief financial officer with delegated
authority to sign for the chief executive officer or chief financial officer so that the chief
executive officer or chief financial officer is ultimately responsible for the certification. The
certification must attest that, based on best information, knowledge and belief, the
information specified is accurate, complete, and truthful.
11.
Any excluded individuals and entities discovered in the screening described in the Contractor
Ownership and Control Interest section of this Contract, including the provider applications and
credentialing processes, must be reported to the federal HHS-OIG and MDHHS-OIG, in a format
determined by MDHHS-OIG, within 20 Business Days of discovery.
12.
Contractor must submit to MDHHS-OIG, in a format determined by MDHHS-OIG, a Quarterly
Provider Prepayment Review Placement Log for providers placed on prepayment review as a
result of a program integrity activity.
13.
Provider Manual and Bulletins – Contractor must issue Provider Manual and Bulletins or other
means of provider communication to the providers of medical, behavioral, dental and any other
services covered under this Contract. The manual and bulletins must serve as a source of
information to providers regarding Medicaid covered services, policies and procedures, statutes,
regulations, and special requirements to ensure all Contract requirements are being met. The
Contractor may distribute the provider manual electronically (e.g., via its website) as long as
providers are notified about how to obtain the electronic copy and how to request a hard copy at
no charge to the provider. Should these items be captured within the subcontract/agreements,
that would also meet contractual requirements.
a.
Contractor’s Provider Manual must provide all of its providers with, at a minimum, the
following information:
i.
Description of the Michigan Medicaid managed care program and covered
populations.
ii.
Scope of Benefits.
iii.
Covered Services.
iv.
Emergency services responsibilities.
v.
Grievance/appeal procedures for both Enrollee and provider.
vi.
Medical necessity standards and clinical practice guidelines.
vii.
Contractor’s policies and procedures including, at a minimum, the following
information:
1) Policies regarding provider enrollment and participation.
2) Policies detailing coverage and limits for all covered services.
Page 89 of 148
3) Policies and instructions for billing and reimbursement for all covered
services.
4) Policies regarding record retention.
5) Policies regarding Fraud, Waste and Abuse.
6) Policies and instructions regarding how to verify beneficiary eligibility.
viii.
Primary care physician responsibilities.
ix.
Requirements regarding background checks.
x.
Other subcontractors’/network providers’ responsibilities.
xi.
Prior authorization and referral procedures.
xii.
Claims submission protocols and standards, including instructions and all
information necessary for a clean claim.
xiii.
Medical records standards.
xiv.
Payment policies.
xv.
Enrollee rights and responsibilities.
xvi.
Self-reporting mechanisms and polices.
b.
Contractor must review its Provider Manual, Bulletins and all provider policies and
procedures at least annually to ensure that Contractor’s current practices and Contract
requirements are reflected in the written policies and procedures.
c.
Contractor must submit Provider Manual, Bulletin and or other means of provider
communications to MDHHS-OIG upon request.
14.
Subcontractor and/or Network Provider Agreements – Contractor must submit its subcontractor
and/or network provider agreements to MDHHS-OIG upon request.
15.
MDHHS-OIG Sanctions
a.
When MDHHS-OIG sanctions (suspends and/or terminates from the Medicaid Program)
providers, including for a credible allegation of fraud under 42 CFR 455.23, Contractor
must, at minimum, apply the same sanction to the provider upon receipt of written
notification of the sanction from MDHHS-OIG. Contractor may pursue additional
measures/remedies independent of the State. If MDHHS OIG lifts a sanction, Contractor
may elect to do the same.
16.
MDHHS-OIG Onsite Reviews
a.
MDHHS-OIG may conduct onsite reviews of Contractor and/or its subcontracted
entities/network providers.
b.
To the extent consistent with applicable law, including, but not limited to 42 CFR Part 2,
HIPAA, and the Michigan Mental Health Code, Contractor is required to comply with
MDHHS-OIG’s requests for documentation and information related to program integrity
and compliance.
17.
Contractor Ownership and Control Interest
a.
According to 42 CFR 438.610 Prohibited affiliations, Contractor may not knowingly have a
relationship of the type described in paragraph (c) of this Section with the following:
i.
An individual or entity that is debarred, suspended, or otherwise excluded from
participating in procurement activities under the Federal Acquisition Regulation or
from participating in non-procurement activities under regulations issued under
Executive Order No. 12549 or under guidelines implementing Executive Order No.
12549.
ii.
An individual or entity who is an affiliate, as defined in the Federal Acquisition
Regulation at 48 CFR 2.101, of a person described in paragraph (a)(i) of this
Section.
b.
Contractor may not knowingly have a relationship with an individual or entity that is
excluded from participation in any Federal health care program under section 1128 or
1128A of the act.
c.
The relationships described in paragraph (a) of this Section, are as follows:
Page 90 of 148
i.
A director, officer, or partner of Contractor.
ii.
A subcontractor and/or network provider of Contractor, as governed by 42 CFR
438.230.
iii.
A person with beneficial ownership of five percent (5%) or more of Contractor's
equity.
iv.
A subcontractor and/or network provider or person with an employment, consulting,
or other arrangement with Contractor for the provision of items and/or services that
are significant and material to Contractor's obligations under its Contract with the
State.
d.
Contractor must agree and certify it does not employ or contract, directly or indirectly, with:
i.
Any individual or entity excluded from Medicaid or other federal health care program
participation under Sections 1128 (42 U.S.C. § 1320a-7) or 1128A (42 U.S.C. §
1320a) of the Social Security Act for the provision of health care, utilization review,
medical social work or administrative services or who could be excluded under
Section 1128(b)(8) of the Social Security Act as being controlled by a sanctioned
individual.
ii.
Any individual or entity discharged or suspended from doing business with Michigan
Medicaid; or
iii.
Any entity that has a contractual relationship (direct or indirect) with an individual
convicted of certain crimes as described in Section 1128(b)(8) of the Social Security
Act.
e.
MDHHS may refuse to enter into or renew a contract with the Contractor if any person
who has an ownership or control interest in the Contractor, or who is an Agent or
managing employee of the Contractor, has been convicted of a criminal offense related to
that person’s involvement in any program established under Medicare, Medicaid, or the
Title XX Services Program. Additionally, MDHHS may refuse to enter into or may
terminate the Contract if it determines that the Contractor did not fully and accurately
make any disclosure required under this section of the contract.
f.
Contractor must comply with the Federal regulations to obtain, maintain, disclose, and
furnish required information about ownership and control interests, business transactions,
and criminal convictions as specified in 42 CFR 455.104-106. In addition, Contractor must
ensure that any and all contracts, agreements, purchase orders, or leases to obtain
space, supplies, equipment, or services provided under the Medicaid agreement require
compliance with 42 CFR §455.104-106.
g.
Pursuant to 42 CFR 455.104: the State will review ownership and control disclosures
submitted by Contractor and any of Contractor’s subcontractors and/or network providers.
Contractor is required to identify and report whether an individual or entity with an
ownership or control interest in the disclosing entity is related to another individual with an
ownership or control interest in the disclosing entity as a spouse, parent, child, or sibling
and/or whether the individual or entity with an ownership or control interest in any
subcontractor in which the disclosing entity has a five percent (5%) or more interest is
related to another individual with ownership or control interest as a spouse, parent, child,
or sibling. Contractor is also required to identify the name of any other disclosing entity in
which an owner of the disclosing entity has an ownership or control interest.
18.
Network Provider Medicaid Enrollment – Pursuant to 42 CFR § 438.602(b)(1), all network
providers of the Contractor must enroll with the Michigan Medicaid Program.
a.
The State will screen and enroll, and periodically revalidate all enrolled Medicaid
providers.
b.
Contractor must require all applicable network providers are enrolled in the Michigan
Medicaid Program via the State’s Medicaid Management Information System.
i.
Contractor may execute network provider agreements, pending the outcome of
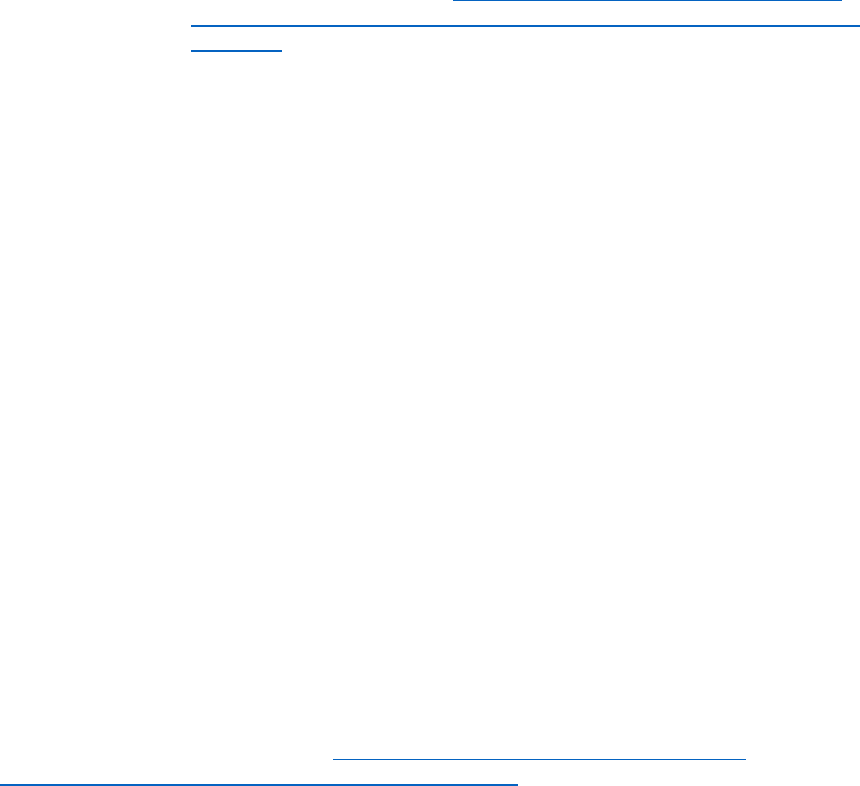
Page 91 of 148
screening, enrollment, and revalidation, of up to 120 days but must terminate a
network provider immediately upon notification from the State that the network
provider cannot be enrolled or the expiration of one 120-day period without
enrollment of the provider, and notify affected enrollees.
c.
Contractor must verify and monitor its network providers’ Medicaid enrollment.
d.
Exclusions Monitoring:
i.
At the time of provider enrollment or re-enrollment in Contractor’s provider network,
and whenever there is a change in ownership or control of the provider entity,
Contractor must search the following databases to ensure that the provider entity,
and any individuals with ownership or control interests in the provider entity (direct or
indirect ownership of five percent (5%) or more or a managing employee), have not
been excluded from participating in federal health care programs.
1) Office of Inspector General’s (OIG) exclusions database, which can be found
at /. This list includes parties excluded from federal programs and may also
be referenced as the “excluded parties lists” (EPLS).
2) The State of Michigan Sanctioned Provider list, which can be found at the
following internet address:
https://www.michigan.gov/mdhhs/doing-
business/providers/providers/billingreimbursement/list-of-sanctioned-
providers .
3) System for Award Management (SAM) information can be found in this
contract under the Federal Provisions Addendum.
ii.
Contractor must search the OIG exclusions database and the State of Michigan
Sanctioned Provider list monthly to capture exclusions and reinstatements that have
occurred since the last search, or at any time providers submit new disclosure
information.
iii.
Contractor must notify the MDHHS OIG immediately using the approved OIG
reporting form and process if search results indicate that any of their network’s
provider entities, or individuals or entities with ownership or control interests in a
provider entity are on the OIG exclusions database. Contractor must also provide
notification to MDHHS OIG if it has taken any administrative action that limits a
provider’s participation in the Medicaid program.
S.
Fiscal Audits and Compliance Examinations
1. Required Audit and Compliance Examination`
Contractor must submit to the State, a Financial Statement Audit and a Compliance
Examination as described below. Contractor must also submit a Corrective Action Plan for
any audit or examination findings that impact State-funded programs, and the management
letter (if issued) with a response.
2. Financial Statement Audit
Contractor must submit to the State a Financial Statement Audit prepared in accordance
with generally accepted auditing standards (GAAS).
3. Compliance Examination
Contractor must submit a contract end date (September 30) Compliance Examination
conducted in accordance with the American Institute of CPA’s (AICPA’s) Statements on
Standards for Attestation Engagements (SSAE) 18 Attestation Standards – Clarification and
Recodification AT-C Section 205, and the Compliance Examination Guidelines which can
be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines.
4. Due Date and Where to Send
The required Financial Statement Audit, Compliance Examination, and any other required
submissions (i.e. Corrective Action Plan and management letter with a response) must be

Page 92 of 148
submitted to the State within 30 days after receipt of the practitioner’s reports, but no later
than June 30 following the Contract year end by e-mail to
MDHHS-
[email protected]. The required materials must be assembled as one document
in a PDF file compatible with Adobe Acrobat (read only). The subject line must state
Contractor name and fiscal year end. The State reserves the right to request a hard copy of
the materials if for any reason the electronic submission process is not successful.
5. Penalty
If Contractor does not submit the required Financial Statement Audit, Compliance
Examination, and applicable Corrective Action Plans by the due date and an extension has
not been approved by the State, the State may withhold from the current funding an amount
equal to 5% of the audit year’s grant funding (not to exceed $200,000) until the required
filing is received by the State. The State may retain the amount withheld if Contractor is
more than 120 days delinquent in meeting the filing requirements and an extension has not
been approved by the State. This is a contract enforcement mechanism and not a sanction
per Sec 232b of the Mental Health Code.
6. Management Decisions
The State will issue a management decision on findings, comments, and questioned costs
contained in Contractor Financial Statement Audit and Compliance Examination Report.
The management decision relating to the Financial Statement Audit will be issued within six
months after the receipt of a complete and final reporting package. The management
decision relating to the Compliance Examination will be issued within eight months after the
receipt of a complete and final reporting package. The management decision will include
whether or not the finding or comment is sustained; the reasons for the decision, and the
expected Contractor action to repay disallowed costs, make financial adjustments, or take
other action. Prior to issuing the management decision, the State may request additional
information or documentation from Contractor, including a request for practitioner
verification or documentation, as a way of mitigating disallowed costs. The appeal process
available to Contractor relating to the State management decisions on Compliance
Examination findings, comments, and disallowed costs can be found on the MDHHS
website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines.
7. Other Audits
The State or federal agencies may also conduct or arrange for additional audits to meet
their needs.
8. Reviews and Audits
a.
The State and federal agencies may conduct reviews and audits of Contractor
regarding performance under this Contract. The State will make good faith efforts to
coordinate reviews and audits to minimize duplication of effort by Contractor and
independent auditors conducting audits and compliance examinations.
b.
These reviews and audits will focus on Contractor compliance with State and federal
laws, rules, regulations, policies, and waiver provisions, in addition to Contract
provisions and Contractor policy and procedure.
c.
The State reviews and audits will be conducted according to the following protocols,
except when conditions appear to be severe and warrant deviation or when State or
federal laws supersede these protocols.
i.
State Reviews
1) As used in this Section, a review is an examination or inspection by the
State or its agent, of policies and practices, in an effort to verify compliance
with requirements of this Contract.
2) The State will schedule onsite reviews at mutually acceptable start dates to
the extent possible, with the exception of those reviews for which advance
Page 93 of 148
announcement is prohibited by rule or federal regulation, or when the
deputy director for the Health Care Administration determines that there is
demonstrated threat to consumer health and welfare or substantial threats
to access to care.
3) Except as precluded in Standard Contract Terms 31. Disclosure of
Litigation, or Other Proceeding above, the protocol and/or instrument to be
used to review Contractor, or a detailed agenda if no protocol exists, will be
provided to Contractor at least 30 days prior to the review.
4) At the conclusion of the review, the State will conduct an exit conference
with Contractor. The purpose of the exit conference is to allow the State to
present the preliminary findings and recommendations.
5) Following the exit conference, the State will generate a report within 45
days identifying the findings and recommendations that require a response
by Contractor.
a) Contractor will have 30 days to provide a Correction Action Plan (CAP)
for achieving compliance. Contractor may also present new information
to the State that demonstrates it was in compliance with the questioned
provisions at the time of the review. (New information can be provided
anytime between the exit conference and the CAP). When access or
care to individuals is a serious issue, Contractor may be given a much
shorter period to initiate corrective actions, and this condition may be
established, in writing, as part of the exit conference identified in (d)
above. If, during a State on-site visit, the site review team member
identified an issue that places a participant in imminent risk to health or
welfare, the site review team would invoke an immediate review and
response by Contractor, which must be completed in seven calendar
days.
b) The State will review the CAP, seek clarifying or additional information
from Contractor as needed, and issue an approval of the CAP within 30
days of having required information from Contractor. The State will take
steps to monitor Contractor's implementation of the CAP as part of
performance monitoring.
c) The State will protect the confidentiality of the records, data and
knowledge collected for or by individuals or committees assigned a peer
review function in planning the process of review and in preparing the
review or audit report for public release.
6) State follow-up will be conducted to ensure that remediation of out-of-
compliance issues occur within 90 days after the CAP is approved by the
State.
ii.
State Audits
1) The State and/or federal agencies may inspect and audit any financial
records of the entity or its network provider/subcontractors. As used in this
Section, an audit is an examination of Contractor's and its contract service
providers' financial records, policies, contracts, and financial management
practices, conducted by the MDHHS Bureau of Audit, or its agent, or by a
federal agency or its agent, to verify Contractor's compliance with legal and
contractual requirements.
2) The State will schedule State audits at mutually acceptable start dates to the
extent possible. The State will provide Contractor with a list of documents to
be audited at least 30 days prior to the date of the audit. An entrance
meeting will be conducted with Contractor to review the nature and scope of

Page 94 of 148
the audit.
3) State audits of Contractor will generally supplement the independent
auditor’s Compliance Examination and may include one or more of the
following objectives (the State may, however, modify its audit objectives as
deemed necessary):
a) to assess Contractor’s effectiveness and efficiency in complying with the
Contract and establishing and implementing specific policies and
procedures as required by the Contract; and
b) to assess Contractor’s effectiveness and efficiency in reporting their
financial activity to the State in accordance with Contractual
requirements: applicable federal, State, and local statutory requirements;
Medicaid regulations; and applicable accounting standards; and
c) to determine the State’s share of costs in accordance with applicable
State requirements and agreements, and any balance due to/from
Contractor.
4) To accomplish the above listed audit objectives, State auditors will review
Contractor’s documentation, interview Contractor staff members, and
perform other audit procedures as deemed necessary. The audit report and
appeal process can be found on the MDHHS website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines.
9. Financial Management System
a.
Contractor must maintain all pertinent financial and accounting records and evidence
pertaining to this Contract based on financial and statistical records that can be
verified by qualified auditors. Contractor must comply with generally accepted
accounting principles (GAAP) for government units when preparing financial
statements. Contractor and their network providers/subcontractors must use the
principles and standards of 2 CFR 200 Subpart E for determining all costs related to
the management and provision of MMSSSP services reported on the financial status
report. The accounting and financial systems established by Contractor must be a
double entry system having the capability to identify application of funds to specific
funding streams participating in service costs for individuals.
b.
The accounting system must be capable of reporting the use of these specific fund
sources by major population groups. In addition, cost accounting methodology used
by Contractor must ensure consistent treatment of costs across different funding
sources and assure proper allocation to costs to the appropriate source. Contractor
must comply with the Standard Cost Allocation (SCA) methodology established by
MDHHS when assigning the fund source and ensure subcontractors comply with SCA
methodology.
c.
Contractor must maintain adequate internal control systems. An annual independent
audit must evaluate and report on the adequacy of the accounting system and internal
control systems.
1.1 Transition
A.
See Section 26 Transition Responsibilities of the Standard Contract Terms.
B.
If this Contract is canceled or expires and is not renewed, the following will take effect:
1. Within 45 days following the end date of this Contract, Contractor must provide interim
financial, performance, and other reports as required.
2. Within two years following the end date of this Contract, Contractor must provide final
financial, performance, and other reports as required.
3. Payment for any and all valid claims for services rendered to covered beneficiaries
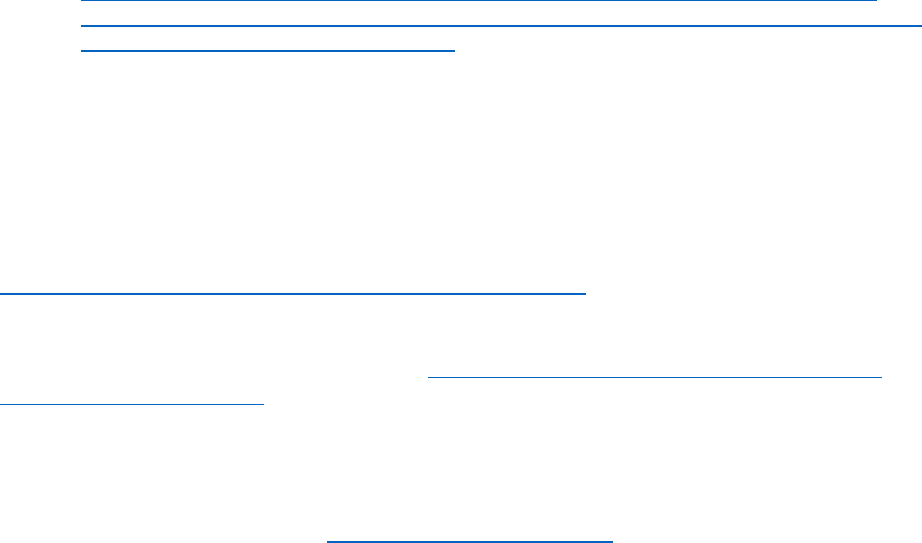
Page 95 of 148
prior to the effective end date are the responsibility of Contractor.
4. The portion of all Medicaid Internal Service Fund (ISF), Medicaid Savings, and any
other reserves, and related interest, held by Contractor that were funded with the
State’s funds are owed to the State within 90 days, less amounts needed to cover
outstanding claims or liabilities, unless otherwise directed in writing by the State.
5. Reconciliation of equipment with a value exceeding $5,000, purchased by Contractor
or its provider network with funds provided under this Contract, since January 1, 2015,
will occur as part of settlement of this Contract. Contractor must submit, to the State,
an inventory of equipment meeting the above specifications within 45 days of the end
date. The inventory listing must identify the current value and proportion of Medicaid
funds used to purchase each item, and whether or not the equipment is required by
Contractor as part of continued service provision to the continuing service population.
The State will provide written notice within 90 days or less of any needed settlements
concerning the portion of funds ending. If Contractor disposes of the equipment, the
appropriate portion of the value must be returned to the State (or used to offset costs
in the final financial report).
6. All financial, administrative, and clinical records under Contractor's responsibility must
be retained according to the retention schedules in place by the Department of
Technology, Management and Budget’s (DTMB) General Schedule #20 at:
https://www.michigan.gov/dtmb/-/media/Project/Websites/dtmb/Services/Records-
Management/RMS_GS20.pdf?rev=9df833feb31e40c9a7438d5c4ef711f1&hash=DC32
AC21A9F07F49855DB2B2550D7E10 unless these records are transferred to a
successor organization or Contractor is directed otherwise in writing by the State.
1.2 Specific Standards
A.
IT Policies, Standards and Procedures (PSP)
All services and products provided as a result of this contract must comply with all applicable State
IT policies and standards. Contractor is required to review all applicable links provided below and
ensure compliance.
Public IT Policies, Standards and Procedures (PSP):
DTMB - IT Policies, Standards & Procedures (michigan.gov)
B.
Acceptable Use Policy
To the extent that Contractor has access to the State’s computer system, Contractor must comply
with the State’s Acceptable Use Policy, see 1340.00.130.02 Acceptable Use of Information
Technology (michigan.gov). All Contractor Personnel will be required, in writing, to agree to the
State’s Acceptable Use Policy before accessing the State’s system. The State reserves the right to
terminate Contractor’s access to the State’s system if a violation occurs.
C.
SOM Digital Standards
All software items provided by Contractor must adhere to the State of Michigan Application/Site
Standards which can be found at www.michigan.gov/standards.
D.
ADA Compliance
The State is required to comply with the Americans with Disabilities Act of 1990 (ADA) and has
adopted standards and procedures regarding accessibility requirements for websites and software
applications. All websites, applications, software, and associated content and documentation
provided by Contractor as part of the Solution must comply with Level AA of the World Wide Web
Consortium (W3C) Web Content Accessibility Guidelines (WCAG) 2.0.
1.3 Hosting
Contractor must maintain and operate a backup and disaster recovery plan to achieve a Recovery Point
Page 96 of 148
Objective (RPO) (maximum amount of potential data loss in the event of a disaster) of 24 hours, and a
Recovery Time Objective (RTO) (maximum period of time to fully restore the Hosted Services in the
case of a disaster) of 24 hours.
2.
Staffing, Organizational Structure, Governing Body, and Subcontractors
2.1.
Contractor Representative
Contractor must appoint individuals, specifically assigned to State of Michigan accounts, that will
respond to State inquiries regarding the Contract Activities, answering questions related to ordering
and delivery, etc. (the “Contractor Representative”).
2.2.
Customer Service Toll-Free Number
Contractor must specify its toll-free number for the State to make contact with Contractor
Representative. Contractor Representative must be available for calls during the hours of 8:00 a.m.
to 5:00 p.m. EST.
2.3.
Work Hours
Contractor must provide Contract Activities during the State’s normal working hours Monday –
Friday, 8:00 a.m. to 5:00 p.m. EST, and possible night and weekend hours depending on the
requirements of the project.
2.4.
Key Personnel
A.
Contractor must appoint individuals who will be directly responsible for the day-to-day
operations of the Contract (“Key Personnel”). Key Personnel must be specifically assigned
to the State account, be knowledgeable on the contractual requirements, and respond to
State inquires within 48 hours.
B.
Administrative Personnel Requirements
1. Contractor must employ or contract with sufficient administrative staff to comply with all
program standards and applicable Mental Health Code requirements. At a minimum,
Contractor must specifically staff positions listed below:
a. Executive director/chief executive officer.
b. Medical director.
c. Quality improvement director.
d. Chief financial officer.
e. Chief information officer.
f. Compliance officer.
g. Grievance and appeals coordinator.
h. Special Investigations unit (SIU) manager/liaison
2. Contractor must ensure all staff have appropriate training, education, experience,
appropriate licensure and liability insurance coverage to fulfill the requirements of the
position.
a. Contractor must assure that all Contract employees receive annual training in
recipient rights protection. Contractor must forward any recipient rights complaints
filed against a Contract employee to MDHHS-ORR for review and possible
investigation.
3. Resumes for all staff listed above must be provided to the State upon request. Resumes
must include detailed, chronological work experience.
C.
Executive Personnel
1. Contractor must inform the State, in writing, within seven days of vacancies or staffing
changes for the staff listed above.
2. Contractor must fill vacancies for the staff listed above with qualified persons within six
months of the vacancy unless an extension is granted by the State.
2.5.
Criminal Background Checks
Page 97 of 148
A.
Contractor (or network provider/subcontractor), in accordance with the general purposes
and objectives of this Contract, must ensure that each direct-hire or contractually employed
individual health care staff and/or practitioner meets all background checks, applicable
licensing, scope of practice, contractual, and Medicaid Provider Manual (MPM)
requirements.
B.
Contractor must:
1. Conduct a search that reveals information substantially similar to information found on
an Internet Criminal History Access Tool (ICHAT) check and a national and state sex
offender registry check for each new employee, subcontractor, subcontractor
employee, or volunteer (including students and interns) who works under this Contract.
a. ICHAT: https://apps.michigan.gov/
b. Michigan Public Sex Offender Registry: https://mspsor.com/
c. National Sex Offender Registry: https://www.nsopw.gov/
2. Conduct a Central Registry (CR) check for each new employee, subcontractor,
subcontractor employee, or volunteer (including students and interns) who under this
Contract works directly with children.
a. Central Registry:
https://www.michigan.gov/mdhhs/0,5885,7-339-
73971_7119_50648_48330-180331--,00.html
3. Require each new employee, subcontractor, subcontractor employee, or volunteer
(including students and interns) who works under this Contract, works directly with
enrollees, or who has access to enrollee information to notify Contractor in writing of
criminal convictions (felony or misdemeanor), pending felony charges, or placement on
the CR as a perpetrator, at hire or within ten (10) days of the event after hiring.
4. Use information from the Medicaid Provider Manual (General Information for
Providers; Section 6 – Denial of Enrollment, Termination and Suspension; Item 6.1 –
Termination or Denial of Enrollment) and the Social Security Act (Subsection
1128(a)(b)), to determine whether to prohibit any employee, subcontractor,
subcontractor employee, or volunteer (including students and interns) from performing
work directly with enrollees or accessing enrollee information related to enrollees
under this Contract, based on the results of a positive ICHAT response, reported
criminal felony conviction, or perpetrator identification.
5. Use information from the Medicaid Provider Manual (General Information for
Providers; Section 6 – Denial of Enrollment, Termination and Suspension; Item 6.1 –
Termination or Denial of Enrollment) and the Social Security Act (Subsection
1128(a)(b)), to determine whether to prohibit any employee, subcontractor,
subcontractor employee or volunteer (including students and interns)from performing
work directly with children under this Contract, based on the results of a positive CR
response or reported perpetrator identification.
2.6.
Organizational Chart/Contractor Organizational Structure
Contractor must provide annually a current organizational chart that lists staff members and
subcontractors, by name and title. (see Schedule E for submission information). Contractor must
maintain an administrative and organizational structure that supports a high quality, comprehensive
managed care program inclusive of all behavioral health specialty services. Contractor's
management approach and organizational structure must ensure effective linkages between
administrative areas including provider network service, customer service, service area network
development, quality improvement and utilization review, grievance/complaint review, financial
management and health information systems. Effective linkages are determined by outcomes that
reflect coordinated management.
2.7.
Use of Subcontractors

Page 98 of 148
A.
Contractor must be able to demonstrate compliance with all contract activities set forth in
this Contract either directly or through formal delegation of a specified contract activity to a
subcontractor through a written subcontract agreement as specified in 42 CFR 438.230.
B.
In accordance with 42 CFR 434.6 and 42 CFR 438.230 the term “subcontract(s)” includes
contractual agreements between Contractor and any other entity, including a provider, that
performs any function or service for Contractor related to securing or fulfilling Contractor’s
required contract activities and obligations under the terms of the Contract. The term does
not include network provider agreements that are limited in scope to the provision of
covered services to enrollees (i.e., the actual delivery of clinical care). Examples of
subcontractor classifications include but are not limited to:
1. Engaging in provider network development
2. Health Benefit Managers (HBMs) – entities that arrange for the provision of health
services covered under this Contract.
3. Administrative Subcontractors – entities that perform administrative functions required
by this Contract such as claims payment, delegated credentialing, and utilization
management.
C.
All subcontracts must be in writing and incorporate the terms and conditions contained in
this Contract. Contractor must comply with all subcontract requirements specified in 42
CFR 438.230 and comply with federal and state laws, Medicaid regulations, and sub
regulatory guidance.
D.
All subcontracts, if using Medicaid funds, must fulfill the requirements of 42 CFR 434.6. All
subcontracts are subject to review by the State at its discretion.
E.
Contractor shall be held fully liable and retain full responsibility for the performance and
completion of all Contract requirements regardless of whether Contractor performs the work
or subcontracts for services. Contractor (and subcontractors, as applicable) must monitor
the performance of all subcontractors on an ongoing basis. This includes conducting formal
reviews consistent with industry standards. Both Contractor and subcontractor must take
corrective action on any identified deficiencies or areas of improvement.
F.
Contractor must obtain the approval of MDHHS before subcontracting any portion of the
Contract requirements and must submit the subcontractor agreement and delegation grid to
MDHHS annually, any time there is a material change, or upon request.
G.
Contractor must fulfill the requirements of 42 CFR 438.230 by ensuring there is a written
agreement that specifies the activities and report responsibilities delegated to
Subcontractors and provides for revoking delegation or imposing other sanctions if the
Subcontractor’s performance is inadequate, see the MDHHS Policies and Practice
Guidelines
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelinesfor a model agreement. All
agreements are subject to review by the State at its discretion.
1. If Contractor determines revocation of a delegation to a subcontractor is appropriate,
Contractor must provide notice of such action to MDHHS ten (10) business days in
advance of issuing such notice to the subcontractor.
2. If Contractor identifies deficiencies or areas for improvement, Contractor and the
Subcontractor must take corrective action, including when appropriate, revoking
delegation or imposing other sanctions if the Subcontractor’s performance is
inadequate. Contractor must provide:
a. Quarterly report to MDHHS of all subcontractor noncompliance and/or areas of
subcontractor performance that were below standards or expectations of this
Contract. This notice must include name of subcontractor and delegated functions;
a brief description of specific non-compliance or performance deficiency; what
action Contractor took to resolve the concerns; including specific monitoring is
being completed by Contractor; whether the concern has been resolved; and if not

Page 99 of 148
fully resolved what actions are occurring or planned to resolve the issue.
b. Any information or documentation related to subcontractor deficiency, inadequacy,
or non-compliance to MDHHS upon request. Responsive information to such
request by MDHHS must be produced to MDHHS within ten (10) business days.
H.
Contractor must develop, maintain, and submit policies and procedures addressing auditing
and monitoring subcontractors’ performance, data, and data submission, including
evaluation of prospective subcontractors’ abilities prior to contracting with the subcontractor
to perform services, collection of performance and financial data to monitor performance on
an ongoing basis and conducting formal, periodic, and random reviews. Contractor must
incorporate all subcontractors’ data into Contractor’s performance and financial data for a
comprehensive evaluation and identify subcontractor improvement areas.
I.
Fiscal Viability of Subcontractors.
Contractor must maintain a system to evaluate and monitor the financial viability of all
subcontractors and risk bearing provider groups, including but not limited to CMHSPs. At
least annually, Contractor must make documentation of its review available to MDHHS
upon request. MDHHS reserves the right to review these documents during Contactor site
visits.
J.
Delegation of Network Development.
When Contractor delegates network development responsibilities to a subcontractor
including a CMHSP, the subcontracts must address the following, in accordance with 42
CFR 438.230:
1. Duty to treat and accept referrals
2. Prior authorization requirements
3. Access standards and treatment timelines
4. Relationship with other providers
5. Reporting requirements and time frames
6. Quality Assurance/Quality Improvement (QA/QI) Systems
7. Payment arrangements (including coordination of benefits) and solvency requirements.
8. Financing conditions consistent with this Contract
9. Compliance with Office of Civil Rights Policy Guidance on Title VI “Language
Assistance to Persons with Limited English Proficiency"
10. Early and Periodic Screening, Diagnostic and Treatment (EPSDT) requirements
11. Requirement to comply with the “Quality Assessment and Performance Improvement
Programs for Specialty Prepaid Health Plans”, which can be found on the MDHHS
website:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/mentalhealth/practiceguidelines and require the subcontractor to
cooperate with Contractor's quality improvement and utilization review activities
12. Provisions for the immediate transfer of recipients to a different provider if their health
or safety is in jeopardy.
13. Network Providers right to discuss treatment options with a recipient that may not
reflect Contractor's position or may not be covered by Contractor.
14. Network Providers right to advocate on behalf of the recipient in any grievance or
utilization review process, or individual authorization process to obtain necessary
health care services.
15. Requirement to meet accessibility standards, both as established in Medicaid policy,
and this Contract.
K.
In accordance with 42 CFR 422.216, Contractor must establish payment rates for plan
covered items and services that apply to deemed providers. Contractor may vary payment
rates for providers in accordance with 42 CFR422.4(a)(3).
1. Providers must be reimbursed on a fee-for-service basis.
2. Contractor must make information on its payment rates available to providers that
Page 100 of 148
furnish services that may be covered under Contractor’s private fee-for-service plan.
3. Contractor must pay for services of noncontract providers in accordance with 42 CFR
422.100(b)(2).
L.
In accordance with 42 CFR 422.208, any physician incentive plan operated by a Contractor,
or its subcontractor, must meet the following requirements:
1. Contractor makes no specific payment, directly or indirectly, to a physician or physician
group as an inducement to reduce or limit medically necessary services furnished to
any particular enrollee. Indirect payments may include offerings of monetary value
(such as stock options or waivers of debt) measured in the present or future.
2. If the physician incentive plan places a physician or physician group at substantial
financial risk (as determined in this Section) for services that the physician or physician
group does not furnish itself, Contractor must assure that all physicians and physician
groups at substantial financial risk have either aggregate or per-patient stop-loss
protection in accordance with this Section.
a. For all physician incentive plans, Contractor must provide to CMS, and to any
Medicaid beneficiary, the information specified in 42 CFR 422.210.
b. Contractor must provide a copy of specific contract language used for incentive,
bonus, withhold or sanction provisions (including sub-capitations) to the State at
least 30 days prior to the subcontract effective date. The State reserves the right
to require an amendment of the subcontract if the provisions appear to jeopardize
individuals’ access to services. The State will provide notice of approval or
disapproval of proposed contract language within 25 days of receipt.
M.
In accordance with 42 CFR 447.325, Contractor may pay the customary charges of the
provider but must not pay more than the prevailing charges in the locality for comparable
services under comparable circumstances.
N.
Contractor, and its subcontractors, as applicable, must retain, as applicable, beneficiary
grievance and appeal records in accordance with 42 CFR 438.416, base data in 42 CFR
438.5(c), MLR reports in 42 CFR 438.8(k), and the data, information, and documentation
specified in 42 CFR 438.604, 438.606, 438.608, and 438.610 for a period of no less than 10
years.
O.
In accordance with 42 CFR 438.230(c), all subcontracts must allow the State, CMS, the
HHS Inspector General, the Comptroller General, or their designees to have the right to
audit, evaluate, and inspect any books, records, contracts, computer, or other electronic
systems of the subcontractor, or of the subcontractor's contractor, that pertain to any aspect
of services and activities performed, or determination of amounts payable under this
Contract with the State. The subcontractor must make available, for purposes of an audit,
evaluation, or inspection under this Contract, its premises, physical facilities, equipment,
books, records, contracts, computer or other electronic systems relating to its Medicaid
beneficiaries. The right to audit under this Contract will exist through 10 years from the final
date of the Contract period or from the date of completion of any audit, whichever is later.
P.
Accreditation of Network Providers
Contractor (and its subcontractors, as applicable) may enter into network provider
agreements for treatment services provided through outpatient, Methadone, sub-acute
detoxification and residential providers only with providers accredited by one of the
following accrediting bodies: The Joint Commission (TJC formerly JCAHO); Commission on
Accreditation of Rehabilitation Facilities (CARF); the American Osteopathic Association
(AOA); Council on Accreditation of Services for Families and Children (COA); National
Committee on Quality Assurance (NCQA), or Accreditation Association for Ambulatory
Health Care (AAAHC). Contractor, or its subcontractor, must determine compliance through
review of original correspondence from accreditation bodies to providers. Accreditation is
not needed in order to provide access management system (AMS) services, whether these
Page 101 of 148
services are operated by a Contractor or through an agreement with Contractor or for the
provision of broker/generalist case management services. Accreditation is required for AMS
providers that also provide treatment services and for case management providers that
either also provide treatment services or provide therapeutic case management.
Accreditation is not required for peer recovery and recovery support services when these
are provided through a prevention license.
3. Project Management
3.1. Reporting
A.
Release of Report Data
1. Written Approval
Contractor must obtain the State's written approval prior to publishing or making formal
public presentations of statistical or analytical material based on its beneficiaries other
than as required by this Contract, statute or regulations. The State is the owner of all
data made available by the State to Contractor or its agents, network
providers/subcontractors or representatives under the Contract.
2. Acceptable Use of State Data
Contractor must not use the State’s data for any purpose other than providing the
Services to beneficiaries covered by Contractor under any Contract or Program, nor
will any part of the State’s data be disclosed, sold, assigned, leased or otherwise
disposed of to the general public or to specific third parties or commercially exploited
by or on behalf of Contractor. No employees of Contractor, other than those on a
strictly need- to-know basis, have access to the State’s data, except as provided by
law.
3. Acceptable Use of Personally Identifiable Data
a. Contractor must not possess or assert any lien or other right against the State’s
data. Without limiting the generality of this Section, Contractor must only use
personally identifiable information as strictly necessary to provide the Services to
beneficiaries covered by Contractor under any Contract or Program and must
disclose the information only to its employees on a strict need-to-know basis.
b. Contractor must always comply with all laws and regulations applicable to the
personally identifiable information.
4. Acceptable Use of Contractor Data
The State is the owner of all State-specific data under the Contract. The State may use
the data provided by Contractor for any purpose. The State will not possess or assert
any lien or other right against Contractor’s data. Without limiting the generality of this
Section, the State may use personally identifiable information only as strictly
necessary to utilize the Services and must disclose the information only to its
employees on a strict need-to-know basis, except as provided by law. Other material
developed and provided to the State remains the State’s sole and exclusive property.
B.
Uniform Data and Reporting
1. To measure Contractor's accomplishments in the areas of access to care, utilization,
service outcomes, recipient satisfaction, and to provide sufficient information to track
expenditures and calculate future capitation rates, Contractor must provide the State
with uniform data and information as specified by the State as previously agreed, and
such additional or different reporting requirements (with the exemption of those
changes required by federal or state law and/or regulations) as the parties may agree
upon from time to time. Any changes in the reporting requirements, required by state
and federal law, will be communicated to Contractor at least 90 days before they are
effective unless state or federal law requires otherwise. Both parties must agree to

Page 102 of 148
other changes, beyond routine modifications, to the data reporting requirements.
2. Contractor's timeliness in submitting required reports and their accuracy will be
monitored by the State and will be considered by the State in measuring the
performance of Contractor. Regulations promulgated pursuant to the Balance Budget
Act of 1997 (BBA) require that the CEO or designee certify the accuracy of the data.
3. Contractor must cooperate with the State in carrying out validation of data provided by
Contractor by making available recipient records and a sample of its data and data
collection protocols. Contractor must certify that the data they submit are accurate,
complete and truthful. An annual certification from, and signed by, the chief executive
officer or the chief financial officer, or a designee who reports directly to either must be
submitted annually. The certification must attest to the accuracy, completeness, and
truthfulness of the information in each of the sets of data in this Section.
4. The State and Contractor agree to use the Encounter Data Integrity Group (EDIT) for
the development of instructions with costing related to procedure codes, and the
assignment of Medicaid and non-Medicaid costs. The recommendations from the EDIT
group have been incorporated into Schedule E (see Mental Health and Substance Use
Disorder Reporting Requirements website at:
https://www.michigan.gov/mdhhs/keep-
mi-healthy/mentalhealth/reporting .
5. Encounter Data Reporting
In order to assess quality of care, determine utilization patterns and access to care for
various health care services, affirm capitation rate calculations and estimates,
Contractor must submit encounter data containing detail for each recipient encounter
reflecting all services provided by Contractor. Encounter records must be submitted
monthly via electronic media in the HIPAA-compliant format specified by the State.
Encounter level records must have a common identifier that will allow linkage between
the State’s and Contractor’s health information systems.
6. Encounter Data Reporting Requirements
a. Due dates: Encounter data are due within 30 days following adjudication of the
claim for the service provided, or in the case of a Contractor whose business
practices do not include claims payment, within 30 days following the end of the
month in which services were delivered. It is expected that encounter data
reported will reflect services for which providers were paid (paid claims), third
party reimbursed, and/or any services provided directly by Contractor. Submit the
encounter data for an individual on any claims adjudicated, regardless of whether
there are still other claims outstanding for the individual for the month in which
service was provided. In order that the State can use the encounter data for its
federal and State reporting, it must have the count of units of service provided to
each consumer during the fiscal year. Therefore, the encounter data for the fiscal
year must be reconciled within 90 days of the end of the fiscal year. Claims for the
fiscal year that are not yet adjudicated by the end of that period, should be
reported as encounters with a monetary amount of "0." Once claims have been
adjudicated, a replacement encounter must be submitted.
b. Who to Report: Contractor must report the encounter data for all mental health
and developmental disabilities (MH/DD) Medicaid beneficiaries in its entire service
area for all services provided under the State’s benefit plans. Contractor must
report the encounter data for all substance use disorder Medicaid beneficiaries in
its service area. Encounter data is collected and reported for every beneficiary for
which a claim was adjudicated, or service rendered during the month by
Contractor (directly or via contract) regardless of payment source or funding
stream. Contractor’s and CMHSPs that contract with another Contractor or
CMHSP to provide mental health services should include that consumer in the
Page 103 of 148
encounter data set. In those cases, Contractor or CMHSP that provides the
service via a contract should not report the consumer in this data set. Likewise,
Contractor or CMHSPs that contract directly with a Medicaid Health Plan, or
subcontract via another entity that contracts with a Medicaid Health Plan to
provide the Medicaid mental health outpatient benefit, should not report the
consumer in this data set.
c. The Health Insurance Portability and Accountability Act (HIPAA) mandates that all
consumer level data reported after October 16, 2002, must be compliant with the
transaction standards.
i.
A summary of the relevant requirements is:
1.
Encounter data (service use) is to be submitted electronically on a Health
Care Claim form 837, version 5010.
2.
The encounter requires a small set of specific demographic data: gender,
diagnosis, Medicaid number, race, and social security number, and name
of the consumer.
3.
Information about the encounter such as provider name and identification
number, place of service, and amount paid for the service is required.
4.
The 837 includes a “header” and “trailer” that allows it to be uploaded to
the CHAMPS system.
5.
Every behavioral health encounter record must have a corresponding
Behavioral Health Registry record reported prior to the submission of the
Encounter. Failure to report a registry record prior to submitting an
encounter for a consumer receiving services will result in the encounter
being rejected by the CHAMPS system.
d. The information on HIPAA contained in this Contract relates only to the data that
the State is requiring for its own monitoring and/or reporting purposes and does
not address all aspects of the HIPAA transaction standards with which Contractor
must comply for other business partners (e.g., providers submitting claims, or third-
party payers). Further information is available at:
https://www.michigan.gov/mdhhs/doing-business/providers/hipaa
.
e. Data that is uploaded to CHAMPS must follow the HIPAA-prescribed formats for
encounter data. The 837/5010 includes header and trailer information that
identifies the sender and receiver and the type of information being submitted. If
data does not follow the formats, entire files could be rejected by the electronic
system.
f. HIPAA also requires that procedure codes, revenue codes and modifiers
approved by the CMS be used for reporting encounters. Those codes are found in
the most recent edition of the Current Procedural Terminology (CPT) Manual,
published by the American Medical Association, the Health Care Financing
Administration Common Procedure Coding System (HCPCS), the National Drug
Codes (NDC), the Code on Dental Procedures and Nomenclature (CDPN), the
International Classification of Diseases, Tenth Revision, Clinical Modification
(IICD-10-CM), ICD-10and the Michigan Uniform Billing Manual. The procedure
codes in these coding systems require standard units that must be used in
reporting on the 837/5010.
g. The State has produced a code list of covered Medicaid specialty and HSW, CWP
and SEDW supports and services names (as found in the Medicaid Provider
Manual) and the CPT or HCPCS codes/service definition/units as soon as the
majority of mental health services have been assigned CPT or HCPCS codes. This
code list is available on the MDHHS web site:
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
Page 104 of 148
h. Stored encounter data will be subject to regular and ongoing quality checks as
developed by the State. The State will give Contractor a minimum of 60 days’
notice prior to the implementation of new quality data edits; however, the State
may implement informational edits without 60 days’ notice. When encounter
corrections are needed, the encounters are to be voided and replaced. The
original encounter record number (Claim Number) is to be included when
encounter records are voided and resubmitted.
i. The following elements reported on the 837/5010 encounter format will be used by
the State for Federal and State reporting, Contract Management, and Actuarial
Services. The items with an ** are required by HIPAA, and when they are absent
will result in rejection of a file. Items with an ** must have 100% of values recorded
within the acceptable range of values. Failure to meet accuracy standards on
these items may result in Contract action. Refer to HIPAA 837 transaction
implementation guides for exact location of the elements. Contractor must consult
the HIPAA implementation guides, and clarification documents (on MDHHS’s web
site) for additional elements required of all 837/5010 encounter formats. The
Supplemental Instructions contain field formats and specific instructions on how to
submit encounter level data.
ii.
**1.a. PIHP Plan Identification Number (PIHPID or PIHP CA Function ID)
The State-assigned 7-digit payer identification number must be used to identify
Contractor with all data transactions.
iii.
1.b. CMHSP Plan Identification Number (CMHID)
The State-assigned 7-digit payer identification number must be used to identify
the CMHSP with all mental health and/or developmental disabilities
transactions.
iv.
**2. Identification Code/Subscriber Primary Identifier (see the details in the
submitter’s manual)
Ten-digit Medicaid number must be entered for a Medicaid or MIChild
beneficiary. If the consumer is not a beneficiary, enter the nine-digit Social
Security number. If consumer has neither a Medicaid number nor a Social
Security number, enter the unique identification number assigned by the
CMHSP or CONID.
v.
**3. Identification Code/Other Subscriber Primary Identifier (please see the
details in the submitter’s manual)
Enter the consumer’s unique identification number (CONID) assigned by the
CMHSP regardless of whether it has been used above.
vi.
**4. Date of birth
Enter the date of birth of the beneficiary/consumer.
vii.
**5. Diagnosis
Enter the ICD-10 primary diagnosis of the consumer.
viii.
**6. EPSDT
Enter the specified code indicating the child was referred for specialty services
by the EPSDT screening.
ix.
**7. Encounter Data Identifier
Enter specified code indicating this file is an encounter file.
x.
**8. Line Counter Assigned Number
A number that uniquely identifies each of up to 50 service lines per claim.
xi.
**9. Procedure Code
Enter procedure code from code list for service/support provided. The code list
is located on the MDHHS web site. Do not use procedure codes that are not on
the code list.
Page 105 of 148
xii.
*10. Procedure Modifier Code
Enter modifier as required for Habilitation Supports Waiver services provided
to beneficiaries; for Autism Benefit services under EPSDT; for Community
Living Supports and Personal Care levels of need; for Nursing Home
Monitoring; and for evidence-based practices. See Costing per Code List.
xiii.
*11. Monetary Amount :
Enter the charge amount, paid amount, adjustment amount (if applicable), and
adjustment code in claim information and service lines. (See
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
).
Click on Instructions for Reporting Financial Information – 837 Encounters;
then click Instructions for Reporting Financial Information)
xiv.
**12. Quantity of Service
Enter the number of units of service provided according to the unit code
type. Only whole numbers should be reported.
xxiv.
Place of Service Code
Enter the specified code for where the service was provided, such as an office,
inpatient hospital, etc. (See PIHP/CMHSP Encounter Reporting Costing Per
Code and Code Chart at
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting.)
xxv.
Diagnosis Code Pointer
Points to the diagnosis code at the claim level that is relevant to the service.
xxvi.
**15. Date Time Period
Enter date of service provided (how this is reported depends on whether
the Professional, or the Institutional format is used).
xxvii.
**16. Billing Provider Name
Enter the name of the Billing Provider for all encounters. (See Instructions for
Reporting Financial Information – 837 Encounters; Instructions for Reporting
Financial Information at
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting.)If the Billing Provider is a specialized licensed
residential facility, also report the LARA license facility number (See
Instructions for Reporting Specialized Residential Facility Details at
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting Click
on Instructions for Reporting Financial Information – 837 Encounters; LARA
License Reporting).
xxviii.
**17. Rendering Provider Name
Enter the name of the Rendering Provider when different from the Billing
Provider (See Instructions for Reporting Financial Information – 837
Encounters; Instructions for Reporting Financial Information at
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
.)
xxix.
18. Facility Location of the Specialized Residential Facility
In instances in which the specialized licensed residential facility is not the
Billing Provider, report the name, address, NPI (if applicable) and LARA license
of the facility in the Facility Location (2310C loop). (See Instructions for
Reporting Financial Information – 837 Encounters; LARA Licensing Reporting
at
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
.)
xxx.
**19. Provider National Provider Identifier (NPI), Employer Identification
Number (EIN) or Social Security Number (SSN) Enter the appropriate
identification number for the Billing Provider, and as applicable, the Rendering
Provider. (See Instructions for Reporting Financial Information – 837
Encounters; Instructions for Reporting Financial Information at
Page 106 of 148
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting.)
7. Reporting Requirements for Behavioral Health Treatment Episode Data Set (BH-
TEDS)
a. Technical specifications, including file formats, error descriptions, edit/error
criteria, and explanatory materials on record submission are located on MDHHS’s
website at:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting.)
b. Reporting covered by these specifications includes the following:
i.
BH-TEDS Start Records (due monthly)
ii.
BH-TEDS Discharge/Update/End Records (due monthly)
iii.
BH-TEDS Crisis Event Q record (due monthly)
c. Basis of Data Reporting
The basis for data reporting policies for Michigan behavioral health includes:
i.
Federal funding awarded to Michigan through the Combined SABG/MHBG
Behavioral Health federal block grant.
ii.
SAMHSA’s Behavioral Health Services Information Systems (BHSIS) award
agreement administered through Eagle Technologies, Inc that awards the
State a contracted amount of funding if the data meet minimum timeliness,
completeness and accuracy standards.
iii.
Legislative boilerplate annual reporting and semi-annual updates
d. Policies and Requirements Regarding Data
BH TEDS Data reporting will encompass Behavioral Health services provided to
persons supported in whole or in part with MDHHS-administered funds.
i.
Policy:
Reporting is required for all persons whose services are paid in whole or in
part with State administered funds regardless of the type of co-pay or shared
funding arrangement made for the services.
ii.
For purposes of State reporting, an admission, or start, is defined as the formal
acceptance of a client into behavioral health services. An admission or start
has occurred if and only if the person begins receiving behavioral health
services.
1) Data definitions, coding and instructions issued by the State apply as
written. Where a conflict or difference exists between the State definitions
and information developed by Contractor or locally contracted data
system consultants, the State definitions are to be used.
2) All SUD data collected and recorded on BH-TEDS must be reported
using the proper Michigan Department of Licensing and Regulatory
Affairs (LARA) substance use disorder services site license number.
LARA license numbers are the primary basis for recording and reporting
data to the State at the program level.
3) Ther
e must be a unique person identifier number assigned to each
individual. It must be 11 characters in length, and alphanumeric. This
same number must be used to report data for BH- TEDS and encounters
for the individual within Contractor’s service region. It is recommended
that a method be established by Contractor and funded programs to
ensure that each individual is assigned the same identification number
regardless of how many times he/she enters services in any program in
the service area, and that the client number be assigned to only one
individual.
4) Any changes or corrections made on Contractor on forms or records
submitted by the program must be made on the corresponding forms and
Page 107 of 148
appropriate records maintained by the program. Each Contractor and its
programs must establish a process for making necessary edits and
corrections to ensure identical records. Contractor is responsible for
making sure records at the State level are also corrected via submission
of change records in data uploads.
5) Contractor must make corrections to all records that are submitted but
fail to pass the error checking routine. All records that receive an error
code are placed in an error master file and are not included in the
analytical database. Unless acted upon, they remain in the error file and
are not removed by the State.
6) Contractor is responsible for generating each month's data upload to the
State consistent with established protocols and procedures. Monthly data
uploads must be received by the State via the DEG no later than the last
day of the following month.
7) Contractor must communicate data collection, recording and reporting
requirements to local providers as part of the contractual documentation.
Contractor may not add to or modify any of the above to conflict with or
substantively affect State policy and expectations as contained herein.
8) Statements of the State’s policy, clarifications, modifications, or additional
requirements may be necessary and warranted. Documentation will be
forwarded accordingly.
e. Method for submission
BH-TEDS data are to be submitted in a fixed length format, per the file
specifications.
f. Due dates
BH TEDS data are due monthly. Contractor is responsible for generating each
month's data upload to the State consistent with established protocols and
procedures. Monthly data uploads must be received by the State via the DEG no
later than the last day of the following month.
g. Who to report
Contractor must report BH-TEDS data for all individuals with mental health,
intellectual/developmental disabilities, and substance use disorders who receive
services funded in whole or in part with the State’s administered funding. If
Contractor is participating in the Medicare/Medicaid integration project, Contractor
must not report BH-TEDS records for beneficiaries for whom Contractor’s financial
responsibility is to a non-contracted provider during the 180-day continuity of care.
8. Coordination of Benefits information is required based on current CMS managed care
rules and MDHHS encounter reporting specifications.
C.
Ad Hoc Reporting
Notwithstanding the provisions of 3.1.B.1., the State may request from Contractor, on an ad
hoc basis, reporting to ascertain compliance with provisions of this agreement. These
requests will allow a minimum of 30 days for preparation and submission unless a different
time frame is agreed to by all parties.
D.
Reports and Annual Appropriation Boilerplate Requirements
Contractor must submit timely reports on annual appropriation boilerplate requirements.
E.
Medical Loss Ratio (MLR) Reporting Requirements
The MLR is a measure of the percentage of premium dollars that each Contractor spends
on clinical services and quality improvement activities. For each reporting year, MDHHS will
require each Contractor to submit an MLR report that includes at least the total incurred
claims, expenditures on quality improving activities, expenditures on fraud prevention
activities, non-claims costs, premium revenue, taxes and fees, and expenditure allocation

Page 108 of 148
methodologies. MDHHS will ensure Contractors are properly identifying and classifying
costs across these categories.
1. Contractor must submit a consolidated MLR report to the State for each reporting year
as directed by MDHHS and in accordance with 42 CFR 438.8, medical loss ratio
standards, and all other regulatory guidance as issued by CMS.
2. Contractor must use the reporting tool provided by MDHHS for MLR reporting
requirements and follow the state’s reporting instructions for completing the requested
information.
a. Technical specifications, including file formats, and explanatory materials are
located on the MDHHS website at:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting
3. The MLR reporting replaces Contractor obligation to complete an administrative cost
report. The MLR report must provide sufficient administrative cost reporting to meet
the actuarial needs. In addition to information required above this will include non-
benefit costs in the following categories:
a. Administrative costs.
b. Taxes, licensing and regulatory fees, and other assessments and fees.
c. Contribution to reserves, risk margin, and cost of capital.
d. Other material non-benefit costs.
4. In accordance with 42 CFR 438.8, each PIHP expense must be included under only
one type of expense, unless a portion of the expense fits under the definition of, or
criteria for, one type of expense and the remainder fits into a different type of expense,
in which case the expense must be pro-rated between types of expenses.
Expenditures that benefit multiple contracts or populations, or contracts other than
those being reported, must be reported on pro rata basis. Expense allocation must be
based on a generally accepted accounting method that is expected to yield the most
accurate results. Shared expenses, including expenses under the terms of a
management contract, must be apportioned pro rata to the contract incurring the
expense. Expenses that relate solely to the operation of a reporting entity, such as
personnel costs associated with the adjusting and paying of claims, must be borne
solely by the reporting entity and are not to be apportioned to the other entities.
5. The credibility adjustment is added to the reported MLR calculation before calculating
any remittances. Contractor may not add a credibility adjustment to a calculated MLR if
the MLR reporting year experience is fully credible. If Contractor experience is non-
credible, it is presumed to meet or exceed the MLR calculation standards.
6. Contractor must aggregate data for all Medicaid eligibility groups covered under the
Contract with the State unless the State requires separate reporting and a separate
MLR calculation for specific populations.
7. MLR must be equal to or higher than 85 percent and the MLR must be calculated and
reported for each MLR reporting year by Contractor.
8. Contractor is not required to make a remittance if it does not meet the minimum MLR
standard of 85 percent or higher.
9. Contractor must require any subcontractor providing claims adjudication activities to
provide all underlying data associated with MLR reporting to Contractor within 180
days of the end of the MLR reporting year or within 30 days of being requested by
Contractor, whichever comes sooner, regardless of current contractual limitations, to
calculate and validate the accuracy of MLR reporting.
10. In any instance where the State makes a retroactive change to the capitation
payments for a MLR reporting year where the MLR report has already been submitted
to the State, Contractor must re-calculate the MLR for all MLR reporting years affected
by the change. In any instance where the State makes a retroactive change to the

Page 109 of 148
capitation payments for a MLR reporting year where the MLR report has already been
submitted to the State, Contractor must submit a new MLR report meeting the
applicable requirements.
11. Contractor must attest to the accuracy of the calculation of the MLR in accordance with
the MLR standards when submitting required MLR reports.
F.
Finance Planning, Reporting and Settlement
1. The final expenditure report must reflect incurred, but not paid claims. Contractor must
provide financial reports on forms and formats specified by the State. Forms and
instructions are posted to the State website at:
https://www.michigan.gov/mdhhs/keep-
mi-healthy/mentalhealth/reporting (See Financial Planning, Reporting and Settlement
Section of Schedule E).
2. Contractor must comply with:
a. Governmental Accounting Standards Board (GASB) standards for Generally
Accepted Accounting Principles
b. Audit and Accounting Guide: State and Local Governments, current edition, by
AICPA
c. 2 CFR 200 Subpart E
G.
Public Health Reporting
PA 368 of 1978 requires that health professionals comply with specified reporting
requirements for communicable disease and other health indicators. Contractor must ensure
compliance with all such reporting requirements through its provider contracts.
H.
Annual Provider Survey Reporting
In compliance with MDHHS policy bulletin MSA 21-39 (and any properly promulgated
successor guidance issued) establishing annual cost reporting requirements for behavioral
health service providers contracted with Contractor and/or CMHSPs, Contractor must
support the data collection process by providing to MDHHS the contact information for all of
their network providers (regardless of whether such network providers contract directly with
Contractor or directly with a subcontractor, including a CMSHP). This information is due to
MDHHS annually upon request. Contractor must ensure all network providers comply with
the MDHHS cost reporting survey process and MDHHS cost reporting policy.
4. Internal Service Fund (ISF)
The establishment of an ISF is one method for securing funds as part of the overall strategy for
covering risk exposure. The ISF fund balance should be kept at a minimum to assure that the
overall level of Contractor funds is directed toward consumer services. Requirements for an ISF
are below:
A.
Contractor must establish an ISF.
B.
The purpose of the ISF is to ensure that Contractor has a reserve of funds to pay any
liabilities that Contractor may incur in a future year that are in excess of 100% of the risk
corridor-related operating budget for which Contractor is financial responsible, as described
in Section 7, Risk Corridor. For example, as specified in Subsection 7(C), a Contractor is
financially responsible for liabilities incurred between 100% and 105% of the risk corridor-
related operating budget, and Contractor may use funds in the ISF to pay those liabilities in
future years. Contractor may use funds in the ISF only for this defined purpose of paying for
liabilities in excess of the 100% of the risk corridor-related operating budget. Contractor
may not use funds in the ISF to pay liabilities incurred in previous years.
C.
Contractor may transfer Medicaid Capitation funds up to 7.5% of the Medicaid/Healthy
Michigan Plan pre-payment authorization to the ISF in any given year. Contractor may not
transfer any funds in excess of that percentage to the ISF in any year.
D.
The ISF must only be used for the defined purpose and not be used to finance any activities
or costs other than ISF eligible expenses.
E.
All programs exposed to the risk corridor must be charged their proper share of the ISF
Page 110 of 148
charges to the extent that those programs are covered for the risk of financial loss. Such
charges must be allocated to the various programs/cost categories based on the relative
proportion of the total contractual obligation, actual historical cost experience, or reasonable
historical cost assumptions. If actual historical cost experiences or reasonable historical
cost assumptions are used, they must cover, at a minimum, the most recent two years in
which the books are closed.
F.
A set of self-balancing accounts must be maintained for the ISF in compliance with
generally accepted accounting principles (GAAP).
G.
The amount of funds paid to the ISF will be determined in compliance with reserve
requirements as defined by GAAP and applicable federal and State financing provisions
contained in the State/Contractor Contract.
H.
To establish an adequate funding level to cover risk corridor requirements (e.g., to pay
liabilities incurred between 100% and 105% of the risk corridor-related operating budget in
a future year), Contractor may make payments up to the lesser of: (1) the total potential
liability relative to the risk corridor and the overall risk management strategy of Contractor’s
operating budget; or (2) the risk reserve requirements and the applicable financing
provisions contained in the State/Contractor Contract.
I.
Contractor must establish a policy and procedure for increasing payments to the ISF in the
event that it becomes inadequate to cover future losses and related expenses.
J.
Payments to the ISF must be based on either actuarial principles, actual historical cost
experiences, or reasonable historical cost assumptions, pursuant to the provisions of 2 CFR
200 sub part E. If actual historical cost experiences or reasonable historical cost
assumptions are utilized, they must cover, at a minimum, the most recent two years in
which the books have been closed.
K.
If the ISF becomes over-funded, it must be reduced within one fiscal year through the
abatement of current charges or, if such abatements are inadequate to reduce the ISF to
the appropriate level, it must be reduced through refunds in accordance with 2 CFR 200
Subpart E Cost Principles.
L.
Upon Contract cancelation or expiration, any funds remaining in the ISF and all of the
related claims and liabilities must be transferred to the new contractor that encompasses
the existing Contractor’s service area. When existing Contractor’s geographic service area
overlaps more than one new contractor service area, the State will provide the percentage
allocation to each new contractor.
5. Authorizing Document
The appropriate authorizing document for services will be this Contract.
6. Contractor Risk Management Strategy
A.
Risk Management Strategy
Each Contractor must define the components of its risk management strategy that is
consistent with general accounting principles as well as federal and State regulations.
B.
Contractor Assurance of Financial Risk Protection
1. Contractor must provide, to the State, upon request, documentation that demonstrates
financial risk protections sufficient to cover Contractor’s determination of risk.
Contractor must update this documentation any time there is a change in the
information.
2. Contractor may use one or a combination of measures to assure financial risk
protection, including pledged assets, reinsurance, and creation of an ISF. The use of
an ISF must be consistent with the requirements of Section 4 of the State/Contractor
Contract with the State.
Page 111 of 148
3. Contractor must submit a specific written Risk Management Strategy to the
Department (see Schedule E). The Risk Management strategy will identify the amount
of reserves, insurance and other revenues to be used by Contractor to assure that its
risk commitment is met. Whenever General Funds are included as one of the listed
revenue sources, the State may disapprove the list of revenue sources, in whole or in
part, after review of the information provided and a meeting with Contractor. Such a
meeting will be convened within 45 days after submission of the risk management
strategy. If disapproval is not provided within 60 days following this meeting, the use of
General Funds will be considered to be allowed. Such disapproval will be provided in
writing to Contractor within 60 days of the first meeting between the State and
Contractor. Should circumstances change, Contractor may submit a revision to its Risk
Management Strategy at any time. The State will provide a response to this revision,
when it changes Contractor’s intent to utilize General Funds to meet its risk
commitment, within 30 days of submission.
7. Risk Corridor
The shared risk arrangements must cover all MMSSSP Programs. The risk corridor is administered
across all services, with no separation for mental health and substance use disorder funding.
A.
Contractor must retain unexpended risk-corridor-related funds between 95% and 100% of
said funds. Contractor must retain 50% of unexpended risk-corridor related funds between
90% and 95% of said funds. Contractor must return unexpended risk-corridor-related funds
to the MDHHS between 0% and 90% of said funds and 50% of the amount between 90%
and 95%.
B.
Contractor may retain funds as noted above, except as specified in Section 1.1.D.
Transition.
C.
Contractor must be financially responsible for liabilities incurred above the risk corridor-
related operating budget between 100% and 105% of said funds contracted.
D.
Contractor will be responsible for 50% of the financial liabilities above the risk corridor-
related operating budget between 105% and 110% of said funds contracted.
E.
Contractor will not be financially responsible for liabilities incurred above the risk corridor-
related operating budget over 110% of said funds contracted.
F.
The risk corridor is calculated on an annual basis. The only expenditures counted in
calculating the risk corridor are those incurred for services delivered in, or other allowable
activities performed attributable to, the applicable year for which the risk corridor is being
calculated. The only revenue counted in calculating the risk corridor is revenue paid to
Contractor for the applicable year for which the risk corridor is being calculated.
G.
Contractor’s transfer of funds to the ISF shall be treated as an expenditure by Contractor for
purposes of calculating unexpended risk-corridor-related funds.
H.
The assumption of a shared-risk arrangement between Contractor and the State will not
permit Contractor to overspend its total operating budget for any fiscal year.
I.
Contractor must not pass on, charge, or in any manner shift financial liabilities to Medicaid
beneficiaries resulting from Contractor financial debt, loss and/or insolvency.
J.
Contractor’s financial responsibility for liabilities for costs between 100% and 110% must
first be paid from Contractor’s Internal Service Fund (ISF) for risk funding or insurance for
cost over-runs. The ISF balance must be tracked by Medicaid and Healthy Michigan funds
contributed. Each portion of the ISF must retain its character as Medicaid and Healthy
Michigan Funds but may be used for risk financing across the Medicaid and Healthy
Michigan programs. Medicaid ISF amounts may be used for Medicaid or Healthy Michigan
cost over runs into the risk corridor and Healthy Michigan ISF amounts may be used for
Medicaid or Healthy Michigan cost over runs into the risk corridor.
K.
If Contractor’s liability exceeds the amount available from ISF and insurance, then other
funding available to Contractor may be utilized in accordance with the terms of Contractor’s
Page 112 of 148
Risk Management Strategy.
L.
General Restrictions
Use of funds held in the ISF must be restricted to the following:
1. Contractor must restrict the use of the ISF to the defined purpose specified in Section
4, Internal Service Fund. No expenses from this fund will be match able-only the
payments to the ISF will be match able. No other expenses may be paid from the ISF.
2. Contractor may invest ISF funds in accordance with statutes regarding investments
(e.g., Mental Health Code 330.1205, Sec. 205(g)), provided that Contractor does not
use ISF funds in a manner inconsistent with the purpose of the ISF set out in Section 4
of the State/Contractor Contract with the State.)The earnings from the investment of
ISF funds must be used to fund the risk reserve requirements of the ISF in accordance
with Section 4 of the contract.
3. The ISF may not loan or advance funds to any departments, agencies, governmental
funds, or other entities in accordance with 2 CFR 200 Subpart E.
4. Funds paid to the ISF must not be used to meet federal cost sharing or used to match
federal or State funds pursuant to 2 CFR 200 Subpart E.
5. State funds paid to the ISF must retain its character as State funds in accordance with
the Mental Health Code and must not be used as local funds.
M.
General Accounting Standards
The ISF must be established and accounted for in compliance with the following standards:
1. Generally accepted accounting principles (GAAP).
2. GASB Statement No. 10, Accounting and Financial Reporting for Risk Financing and
Related Insurance Issues, or other current standards.
3. 2 CFR 200 Subpart E, Cost Principles, or other current standards.
4. Other financing provisions contained in the State/Contractor Contract.
5. The financial requirements set forth in the 1115 and 1915 (i) Waiver.
N.
Financing
The State will immediately notify Contractor of modifications in funding commitments in this
Contract under the following conditions:
1. Action by the Michigan State Legislature or by the Center for Medicare and Medicaid
Services that removes any State funding for, or authority to provide for, specified
services.
2. Action by the Governor pursuant to the Constitution 1963, Article 5, Section 20 that
removes the State's funding for specified services or that reduces the State's funding
level below that required to maintain services on a statewide basis.
3. A formal directive by the Governor, or the Michigan Department of Technology,
Management and Budget (DTMB) on behalf of the Governor, requiring a reduction in
expenditures.
8. Payment Terms
A.
Contract Financing
1. Contractor must accept transfers of all reserve accounts and related liabilities
accumulated by Contractor that formerly operated within the current Contractor’s
geographic service area. Contractor must accept transfer of all liabilities accumulated
by Contractor that formerly operated within Contractor’s geographic service area that
were incurred and paid on behalf of the new Contractor as start-up costs.
2. Local Obligation
a.
Contractor must provide to the State, for deposit into a separate contingency account,
local funds as authorized in the State Appropriations Act. These funds must not
include either State funds received by a CMHSP for services provided to non-
Medicaid recipients or the State matching portion of the Medicaid capitation payments
made to a CMHSP or an affiliation of CMHSPs. The amount of local funds and
Page 113 of 148
payment schedule is included in Schedule G. In the event Contractor is unable to
provide the required local obligation, Contractor must notify the State’s Program
Manager immediately.
b.
Local financial obligations exclude grants or gifts received by the county, Contractor,
or subcontractors, from an individual or agency contracting to provide services to
Contractor.
i. An exception may be made, where Contractor can demonstrate that such
funds constitute a transfer of grants or gifts made for the purposes of
financing mental health services and are not made possible by Contractor
payments to the network provider/subcontractor that are claimed as
matchable expenses for the purpose of state financing.
c.
The following are potential revenue sources for the local obligation:
i. Appropriations of general county funds to Contractor by the County Board
of Commissioners.
ii. Appropriations of funds to Contractor or its network provider/subcontractor
by cities or townships.
iii. Funds raised by fee-for-service subcontractors and/or network providers
as part of the network provider’s/subcontractor’s contractual obligation,
the intent of which is to satisfy and meet the local match obligation of
Contractor, as reflected in this Contract.
iv. Grants, bequests, donations, gifts from local non-governmental sources,
charitable institutions or individuals.
1) gifts that specify the use of the funds for any particular
individual identified by name or relationship may not be used
as local match funds.
v. Funds of participating CMHSPs from the Community Mental Health
Special Fund Account, consistent with Section 226a of the Michigan
Mental Health Code.
1) Federal Supplemental Security Income (SSI) does not qualify
for use under Section 226a of the Michigan Mental Health
Code.
vi. Interest earned on funds deposited or invested by or on behalf of
Contractor, except as otherwise restricted by 2 CFR 200 Subpart E.
1) Interest earned on the State’s funds by subcontractors and/or
network providers as specified in its contracts with Contractor
may not be used as local obligation.
vii. Other Revenues for Mental Health Services - As long as the source of
revenue is not federal or State funds, revenues from other county
departments/funds (such as childcare funds) or revenues from public or
private school districts for Contractor mental health services.
3. As per 42 CFR 438.608(c)(3) the Contractor and any subcontractor must report to the
State within 60 calendar days when it has identified the capitation payments or other
payments in excess of amounts specified in the contract.
B.
State Funding
The State’s funding includes MMSSSP and the Flint 1115 Waiver. The financing in this
Contract is always contingent on the annual Appropriation Act. CMHSPs within a PIHP
may, but are not required to, use General Funds to provide services not covered under
MMSSSP or underwrite a portion of the cost of covered services to these beneficiaries. The
State reserves the right to disallow such use of General Funds if it believes that the CMHSP
was not appropriately assigning costs in order to maximize the savings allowed within the
Page 114 of 148
risk corridors. Specific financial detail regarding the State funding is provided in Schedules
G and H. As per 42 CFR 438.608(c)(3), the Contractor and any subcontractors must report
to the state within 60 calendar days when it has identified capitation payments or other
payments in excess of amounts specified in the Contract.
1. Medicaid Payments
The State will provide to Contractor both the State and federal share of Medicaid funds
as a capitated payment based upon a per eligible per month (PEPM) methodology.
The State will provide access to an electronic copy of the names of the Medicaid
eligible people for whom a capitation payment is made. A PEPM payment is
determined for each of the populations covered by this Contract, which includes
services for people with a developmental disability, a mental illness or emotional
disturbance, and people with a substance use disorder as reflected in this Contract.
PEPM payment is made to Contractor for all beneficiaries in its service area, not just
those with the above-named diagnoses. The actual number of Medicaid beneficiaries
will be determined monthly, and Contractor will be notified of the beneficiaries in their
service area when the payment is made.
a. Medicaid Rate Calculation
The Medicaid Rate Calculation is based on the actuarial documentation letter from
the State's contracted Medicaid Actuarial Services Vendor. The State's contracted
Medicaid Actuarial Services Vendor letter documents the calculation rate
methodology and provides the required certification regarding actuarial soundness
as required by the Balanced Budget Act Rules effective August 13, 2002. The
chart of rates and factors contained in the actuarial documentation is included in
Schedule H.
b. Medicaid Payments
The State will provide Contractor with managed care payments each month for the
Medicaid covered specialty services listed under the Benefit Plan (BP). When
applicable, additional payments may be scheduled (e.g., retro-rate implementation
and up to six months retro eligibility). HIPAA compliant 834 and 820 transactions
will provide eligibility and remittance information. Monthly payment will include:
i.
Base Rates for each Benefit Plan (BHMA, BHMA-MHP, BHHMP, BHHMP-
MHP, HSW-MC**, SED-MC, CWP-MC)
**For HSW beneficiaries of a PIHP that includes the county of financial
responsibility (COFR), referred to as the “responsible PIHP”, but whose
county of residence is in another PIHP, referred to as the “residential
PIHP”, the HSW capitation payment will be paid to the COFR within the
“responsible PIHP” based on the multiplicative factor for the “residential
PIHP”.
ii.
Recovery of payments previously made for beneficiaries prior to MDHHS
notification of death.
iii.
Recovery of payments previously made for beneficiaries, who upon
retrospective review, did not meet all the Benefit Plan enrollment
requirements.
Contractor must be able to receive and transmit HIPAA compliant files, such as:
i.
834 – Eligibility
ii.
820 – Payment/Remittance Advice
iii.
837 – Encounter
c. Medicaid State Plan Payments
The capitation payment excludes individuals enrolled in a Program for All Inclusive
Care (PACE) organization, individuals incarcerated, and individuals with a
Page 115 of 148
Medicaid deductible.
d. Savings and Reinvestment
Provisions regarding the Medicaid, Healthy Michigan Plan, and the Flint 1115
Waiver savings and Contractor reinvestment strategy are included in the following
Section e. It should be noted that only a PIHP may earn and retain
Medicaid/Healthy Michigan Plan savings. CMHSPs may not earn or retain
Medicaid/Healthy Michigan Plan savings. Note that these provisions may be
limited or canceled per Schedule A, Statement of Work, Section 1.1 Transition and
may be modified by actions stemming from Schedule A, General Requirements,
Section 1.D Contract Remedies and Sanctions.
e. Medicaid Savings
Consistent with Section 7(“Risk Corridor”) of the contract, Contractor may retain
unexpended Medicaid Capitation funds up to 7.5% of the Medicaid/Healthy
Michigan Plan pre-payment authorization. The Contractor may not retain any
unexpended Medicaid Capitation funds in excess of that 7.5%. The unexpended
and retained funds described in this paragraph are hereafter referred to as
“Medicaid Savings funds.” These Medicaid saving funds may only be used on
Medicaid service expenditures made within one (1) year of the end of the Contract
year in which the Medicaid savings fund were realized. Any Medicaid savings
funds not spent consistent with the previous sentence must be returned to the
state within 60 days of the end of the contract year settlement process.
2. Habilitation Supports Waiver (HSW) Payments
a. The 1915(c) HSW capitation payment will be made to Contractor based on HSW
beneficiaries who have enrolled through the State enrollment process and have
met the following requirements:
i.
Has a developmental disability as defined by Michigan law.
ii.
Is Medicaid eligible as defined in the CMS approved waiver.
iii.
Is residing in a community setting.
iv.
Otherwise eligible for Intermediate Care Facilities for individuals with
Intellectual Disability (ICF/IID) level of care services.
b. Beneficiaries enrolled in the HSW Program may not be enrolled simultaneously in
any other 1915(c) waiver programs, such as the Children’s Waiver Program
(CWP) and Serious Emotional Disturbance Waiver (SEDW). The capitation
payment excludes individuals who reside, for an entire month, in any of the
following: ICF/IID, Nursing Home, Child Caring Institution (CCI), or who are
incarcerated. HSW capitation payments exclude individuals who are enrolled in a
PACE organization. The HSW capitation payment will be scheduled and/or
adjusted to occur monthly. When applicable, additional payments may be
scheduled.
c. Encounters for provision of services authorized in the CMS approved waiver must
contain the appropriate modifier to be recognized as valid HSW encounters.
Encounters must be processed and submitted on time, as defined in Section N.
Provider Services, 7. Claims Management System and the Reporting
Requirements (see Schedule E), in order to assure timely HSW service
verification.
3. The Children’s Waiver Program (CWP) Payments
a. The 1915(c) CWP capitation payment will be made to Contractor based on CWP
beneficiaries who have enrolled through the State’s enrollment process and have
met the following requirements:
i.
Has a developmental disability as defined by Michigan law.
Page 116 of 148
ii.
Is Medicaid eligible as defined in the CMS approved waiver.
iii.
Is residing in a community setting.
iv.
eligible for Intermediate Care Facilities for individuals with Intellectual
Disability (ICF/IID) level of care services
b. Beneficiaries enrolled in the CWP may not be enrolled simultaneously in any other
1915(c) waiver programs, such as the Habilitation Supports Waiver (HSW) and
Serious Emotional Disturbance Waiver (SEDW). The capitation payment excludes
individuals who reside, for an entire month, in any of the following: ICF/IID,
Nursing Home, Child Caring Institution (CCI), or who are incarcerated. CWP
capitation payments exclude individuals who are enrolled in a PACE organization.
The CWP capitation payment will be scheduled and/or adjusted to occur monthly.
When applicable, additional payments may be scheduled.
c. Encounters must be processed and submitted on time, as defined in Section N.
Provider Services, 7. Claims Management System and the Reporting
Requirements in order to assure timely CWP service verification.
4. Serious Emotional Disturbance Waiver Payments
a. The SEDW capitation payment will be made to Contractor based on SEDW
beneficiaries who have enrolled through the MDHHS enrollment process.
Beneficiaries enrolled in the SEDW may not be enrolled simultaneously in any
other 1915(c) waiver programs, such as the Children’s Waiver Program (CWP)
and HSW. The capitation payment excludes individuals who reside, for an entire
month, in any of the following: ICF/IID, Nursing Home, Child Caring Institution
(CCI), or who are incarcerated. The SEDW capitation payment will be scheduled
and/or adjusted to occur monthly. When applicable, additional payments may be
scheduled.
b. Encounters must be processed and submitted on time, as defined in Section N.
Provider Services, 7. Claims Management System and the Reporting
Requirements in order to assure timely SEDW service verification.
5. Expenditures for MMSSSP and the Flint 1115 Waiver.
a. Contractor may expend any funds received for MMSSSP. All funds must be spent
on Medicaid beneficiaries for Medicaid services. Surplus funding in either
Medicaid or Healthy Michigan may be utilized to cover a funding deficit in either
program. If a deficit still exists, the Medicaid or Healthy Michigan Plan risk reserve
may be utilized. Medicaid or HMP risk reserve can fund a deficit in either program.
The surplus funds must be used before the ISF can be utilized.
b. While there is flexibility in month-to-month expenditures and service utilization
related to the different funding sources in MMSSSP, Contractor must submit
encounter data on service utilization - with transaction code modifiers that identify
the service for each specific MMSSSP program. The encounter data (including
cost information) will serve as the basis for future MMSSSP capitated rate
development.
6. Capitated Payments and Other Pooled Funding Arrangements
Medicaid funds may be utilized for the implementation of, or continuing participation in,
locally established multi- agency pooled funding arrangements developed to address
the needs of beneficiaries served through multiple public systems. Medicaid funds
supplied or expensed to such pooled funding arrangements must reflect the expected
cost of covered Medicaid services for Medicaid beneficiaries participating in or referred
to the multi-agency arrangement or project. Medicaid funds cannot be used to supplant
or replace the service or funding obligation of other public programs.
7. OHH Payments
The State will provide a monthly case rate to Contractor based on the number of OHH

Page 117 of 148
beneficiaries with at least one OHH service during a calendar month. Contractor will
reimburse the OHHP for delivering health home services. Depending on the current
services provided by the OHH Contractor can negotiate a rate with the OHHP while
following the guidelines below, requirements in the approved SPA, MDHHS OHH
Bulletin MSA 20-31
and the OHH Handbook.
8. BHH Payments
The State will provide a monthly case rate to Contractor based on the number of BHH
beneficiaries with at least one BHH service during a calendar month. Contractor will
reimburse the HHP for delivering health home services. Depending on the current
services provided by the HHP, Contractor can negotiate a rate with the HHP for value-
based payment (VBP) while following the requirements in the approved SPA, policy,
and the BHH Handbook.
9. Premium Pay Hourly Wage Increase for Direct Care Workers (DCW)
a. Based on current year appropriations, MDHHS has implemented a wage increase
for direct care workers, to be included on an ongoing basis. This applies to
MDHHS programs and service codes as identified in MSA L Letters. The L Letters
can be found on the MDHHS website :
https://www.michigan.gov/mdhhs/doing-
business/providers/providers/medicaid/communicationtraining/173142 Contractor
must implement the hourly wage increase, with MDHHS providing increased
capitation rates to cover the actual cost of these mandatory pay increases.
Contractor must disperse these funds to eligible contracted providers employing
individuals that qualify for the increase.
b. As this is a base wage increase, Contractor must ensure that the full amount of
funds appropriated for a direct care worker wage increase is provided to direct
care workers through sustained increased wages. Agencies will be provided with a
per-hour amount to cover additional costs related to implementing the increase.
c. DCW wage increase funding will be a component of monthly capitation payments
made to Contractor. Contractor is responsible for maintaining a record of DCW
wage increase payments and is subject to the risk corridor cost settlement
procedures outlined in Schedule A Subsection 7 Risk Corridor of this contract.
d. All wage increase payments are subject to audit and potential recoupment.
Providers must retain documentation that demonstrates the distribution of
payments to eligible staff.
10. MDHHS Incentive Payment
a. The MDHHS Incentive Payment (DHIP) has been established to support program
initiatives as specified in the MDHHS Medicaid Quality Strategy, including
ensuring high quality and high levels of access to care. For the PIHPs to be
eligible for an incentive payment, the child must meet the following requirements:
i.
To receive the MDHHS Incentive Payment, the child must meet the
following eligibility criteria:
1) Have a Serious Emotional Disturbance as defined by Michigan Law.
2) Eligible for Medicaid.
3) Between the ages of 0 to 18.
4) Be served in the MDHHS Foster Care System or Child Protective
Services (Risk Categories I and II)
5) Meet one of the following criteria:
a) Service Criteria 1: At least one of the following services was
provided in the eligible month:
1. H2021 – Wraparound Services
2. H0036 – Home Based Services
3. H2033 - Multi-Systemic Therapy (MST) for juveniles
Page 118 of 148
b) Service Criteria 2: Two or more state plan behavioral health
services covered under the 1115 Demonstration Waiver,
excluding one-time assessments, were provided in the
eligible month.
ii.
Incentive Payments: The incentive payment will occur quarterly. Each
incentive payment will be determined by comparing the PIHP’s identified
eligible children with the encounter data submitted. Valid encounters must
be submitted within 90 days of the provision of the service regardless of the
claim adjudication status in order to assure timely incentive payment
verification. Once the incentive payment has taken place there will not be
any opportunities for submission of eligible children for a quarterly payment
already completed.
iii.
Quarterly incentive payments will occur as follows:
1) April: Based on eligible children and the supporting encounter data
submitted for October 1 – December 31.
2) July: Based on eligible children and the supporting encounter data
submitted for January 1 – March 31.
3) October: Based on eligible children and the supporting encounter
data submitted for April 1 – June 30.
4) January: Based on eligible children and the supporting encounter
data submitted for July 1 –September 30.
iv.
The State will provide access to an electronic copy of the names of those
individuals eligible for incentive payments, which incentive payment amount
they are to receive, and the COFR.
v.
PIHPS are expected to provide a one-page annual narrative report by each
CMHSP in their Region summarizing how the MDHHS incentive payment is
directly supporting mental health services for children involved in child
welfare. This report will be due at the same time as the CAFAS/PECFAS
annual reporting for the MDHHS Incentive. The PIHP shall also include the
total amount of annual MDHHS DHIP incentive funding they received and
total amount and percentage that they passed down to CMHSPs. If the
amount was less than 85% of the total amount received, please provide an
explanation.
11. CCBHC Payments
Per the requirements of the CMS CCBHC Demonstration, Contractor will receive from
the State the equivalent of the CMS-approved PPS-1 rate for each Medicaid CCBHC-
eligible service day. A portion of this PPS rate is included in the overall capitation rate,
and the remainder provided in a supplemental payment. The CCBHC supplemental
payment will be made to Contractor based on CCBHC beneficiaries who have been
enrolled through the MDHHS WSA/CHAMPS enrollment process. One component of
this supplemental payment reflects that estimated difference between the PPS rate
and the amount included in the capitation rates based on anticipated utilization of
CCBHC services for Medicaid beneficiaries. The State will also incorporate an amount
for CCBHC administration in this supplemental payment based on projected total
CCBHC demonstration costs. The State and Contractor will reconcile to the number of
daily visits delivered by the CCBHC to ensure the full PPS payment can be provided to
the CCBHC. Contingent on the availability of State General Funds or other grant
funding, the State will provide Contractor with an annual payment and/or prospective
payments based on anticipated utilization to offset the costs of non-Medicaid CCBHC
services. Contractor’s liability to the CCBHC’s non-Medicaid individuals served is
limited to the State General Funds and/or other grant funds earmarked for services to
Page 119 of 148
a CCBHC eligible population. To the extent that modifications to the CCBHC
Handbook conflict with this contract, the contract language shall govern.
C.
MIChild
The State will provide the federal and matching share of MIChild funds as a capitated
payment based upon actuarially sound Per Enrolled Child Per Month (PECPM)
methodology for MIChild-covered mental health services. The MIChild capitation payment
will be scheduled and/or adjusted to occur monthly. When applicable, additional payments
may be scheduled.
D.
Contractor Performance Bonus
Contract withholds and the Performance Bonus Incentive Program have been established
to support program initiatives as specified in the MDHHS Medicaid Quality Strategy.
Awards will be made to Contractors according to criteria established by the State. Criteria
for Performance Bonus awards will include, but is not limited to, assessment of
performance in quality of care, access to care and administrative functions. Each year, the
State will establish and communicate to Contractor the criteria and standards to be used for
the performance bonus awards.
1. Withhold Arrangements
a. The State will withhold 0.2% of BHMA, BHMA-MHP, capitation payments to
Contractor. The withheld funds will be issued to Contractor in the following
amounts within 60 days of when the required report is received by the State:
i.
0.03% for timely submission of the Projection Financial Status Report –
Medicaid
ii.
0.03% for timely submission of the Interim Financial Status Report –
Medicaid
iii.
0.04% for timely submission of the Final Medicaid Contract Reconciliation
and Cash Settlement
iv.
0.04% for timely submission of the Encounter Quality Initiative
v.
0.03% for timely submission of encounters (defined in Schedule E)
vi.
0.03% for timely resolution of corrective action plans. Scoring metric will be
available on the MDHHS reporting requirements website located at
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
.
b. Performance Bonus Incentive Pool (PBIP)
i.
Withhold and Metrics
The State will withhold 0.75% of BHMA, BHMA-MHP, BHHMP, BHHMP-
MHP, HSW-MC, CWP-MC, and SEDW-MC payments for the purpose of
establishing a PBIP. Distribution of funds from the PBIP is contingent on
Contractor’s results from the joint metrics, the narrative report, and
Contractor-only metrics available on the MDHHS reporting requirements
website located at
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting.
ii.
Assessment and Distribution
PBIP funding awarded to Contractor will be treated as restricted local
funding. Restricted local funding must be utilized for the benefit of the public
behavioral health system. The 0.75% PBIP withhold will be distributed as
follows:
1) Contractor-only Pay for Performance Measure(s): 45%
2) Contractor Narrative Reports: 25%
3) MHP/Contractor Joint Metrics: 30%
4) The State will distribute earned funds by April 30 of each year.
c. Opioid Health Home (OHH) Benefit
Page 120 of 148
The State will withhold 5% of monthly case rate payments to Contractor for
potential pay for performance (P4P) award payments for OHHPs meeting or
exceeding performance benchmarks. This withhold is outside of the actuarial
equivalent monthly case rate. The methodology for determining P4P payment,
including the metrics, specifications, and distribution is cited in the OHH
Handbook, which can be found at the following website:
https://www.michigan.gov/mdhhs/assistance-programs/medicaid/opioid-health-
home. If awarded, the State will distribute P4P payments to Contractor within one
(1) year of the end of the performance year. Contractor must distribute P4P
monies to OHHPs that meet the quality improvement benchmarks in accordance
with the distribution methodology cited in the OHH Handbook. OHH P4P funding
awarded to Contractor will be treated as restricted local funding. Restricted local
funding must be utilized for the benefit of the public behavioral health system.
d. Behavioral Health Home (BHH) Benefit
The State will withhold 5% of monthly case rate payments to Contractor for
potential pay for performance (P4P) award payments for BHHPs meeting or
exceeding performance benchmarks. This withhold is outside of the actuarial
equivalent monthly case rate. The methodology for determining P4P payment,
including the metrics, specifications, and distribution is cited in the BHH
Handbook, which can be found at the following website:
https://www.michigan.gov/mdhhs/assistance-programs/medicaid/behavioral-
health-home. If awarded, the State will distribute P4P payments to Contractor
within one (1) year of the end of the performance year. Contractor must distribute
pay for performance monies to BHHPs that meet the quality improvement
benchmarks in accordance with the distribution methodology cited in the BHH
Handbook. BHH P4P funding awarded to Contractor will be treated as restricted
local funding. Restricted local funding must be utilized for the benefit of the public
behavioral health system.
e. Certified Community Behavioral Health Center (CCBHC) Demonstration Quality
Bonus Payment (QBP)
The State will withhold 5% of the CCBHC benefit plan capitation payments for
potential CCBHC QBP award payments for CCBHCs that meet or exceed
federally defined QBP measures and benchmarks. This withhold is outside of the
actuarial equivalent PPS-1 rate payment. The methodology for determining QBP
payment, including the metrics, specifications, and distribution is cited in the
CCBHC Handbook, which can be found at the following website:
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/ccbhc
. QBP
funding awarded to Contractor will be treated as restricted local funding.
Restricted local funding must be utilized for the benefit of the public behavioral
health system.
Page 121 of 148
SCHEDULE B- HIPAA BUSINESS ASSOCIATE
AGREEMENT
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
HIPAA BUSINESS ASSOCIATE AGREEMENT
The parties to this Business Associate Agreement (“Agreement”) are the Michigan Department
of Health and Human Services and __________________________.
RECITALS
A. Under this Agreement, the Business Associate will collect or receive certain information on the
Covered Entity’s behalf, some of which may constitute Protected Health Information (“PHI”). In
consideration of the receipt of PHI, the Business Associate agrees to protect the privacy and
security of the information as set forth in this Agreement.
B. Covered Entity and the Business Associate intend to protect the privacy and provide for the
security of PHI collected or received by the Business Associate under the Agreement in
compliance with the Health Insurance Portability and Accountability Act of 1996, Public Law
104-191 (“HIPAA”) and the HIPAA Rules, as amended.
C. The HIPAA Rules require the Covered Entity to enter into an agreement containing specific
requirements with the Business Associate before the Business Associate’s receipt of PHI.
AGREEMENT
1. Definitions.
a. The following terms used in this Agreement have the same meaning as those terms in
the HIPAA Rules: Breach; Data Aggregation; Designated Record Set; Disclosure; Health Care
Obligations; Individual; Minimum Necessary; Notice of Privacy Practices; Protected Health
Information; Required by Law; Secretary; Security Incident; Security Measures, Subcontractor;
Unsecured Protected Health Information, and Use.
b. “Business Associate” has the same meaning as the term “business associate” at 45
CFR 160.103 and regarding this Agreement means __________________________.
c. “Covered Entity” has the same meaning as the term “covered entity” at 45 CFR 160.103

Page 122 of 148
and regarding this Agreement means the Michigan Department of Health and Human Services.
d. “HIPAA Rules” means the Privacy, Security, Breach Notification, and Enforcement
Rules at 45 CFR Part 160 and Part 164.
2. Obligations of Business Associate.
Business Associate agrees to:
a. use and disclose PHI only as permitted or required by this Agreement or as required by
law.
b. implement and use appropriate safeguards, and comply with Subpart C of 45 CFR 164
regarding electronic protected health information, to prevent use or disclosure of PHI other than as
provided in this Agreement. Business Associate must maintain, and provide a copy to the Covered
Entity within 10 days of a request from the Covered Entity, a comprehensive written information
privacy and security program that includes security measures that reasonably and appropriately
protect the confidentiality, integrity, and availability of PHI relative to the size and complexity of the
Business Associate’s operations and the nature and the scope of its activities.
c. report to the Covered Entity within 24 hours of any use or disclosure of PHI not
provided for by the Agreement of which it becomes aware, including breaches of Unsecured
Protected Health Information as required by 45 CFR 164.410, and any Security Incident of which it
becomes aware. If the Business Associate is responsible for any unauthorized use or disclosure of
PHI, it must promptly act as required by applicable federal and State laws and regulations. Covered
Entity and the Business Associate will cooperate in investigating whether a breach has occurred, to
decide how to provide breach notifications to individuals, the federal Health and Human Services’
Office for Civil Rights, and potentially the media.
d. ensure, according to 45 CFR 164.502(e)(1)(ii) and 164.308(b)(2), if applicable, that any
subcontractors that create, receive, maintain, or transmit PHI on behalf of the Business Associate
agree to the same restrictions, conditions, and requirements that apply to the Business Associate
regarding such information. Each subcontractor must sign an agreement with the Business Associate
containing substantially the same provisions as this Agreement and further identifying the Covered
Entity as a third party beneficiary of the agreement with the subcontractor. Business Associate must
implement and maintain sanctions against subcontractors that violate such restrictions and conditions
and must mitigate the effects of any such violation.
e. make available PHI in a Designated Record Set to the Covered Entity within 10 days
of a request from the Covered Entity to satisfy the Covered Entity’s obligations under 45 CFR
164.524.
f. within ten days of a request from the Covered Entity, amend PHI in a Designated
Record Set under, 45 § 164.526. If any individual requests an amendment of PHI directly from the
Business Associate or its agents or subcontractors, the Business Associate must notify the Covered
Entity in writing within ten days of the request and amend the information within twenty days of the
request. Any denial of amendment of PHI maintained by the Business Associate or its agents or
subcontractors is the responsibility of the Business Associate. § 164.526.
Page 123 of 148
g. maintain, and within ten days of a request from the Covered Entity make available, the
information required to provide an accounting of disclosures to enable the Covered Entity to fulfill its
obligations under 45 CFR § 164.528. Business Associate is not required to provide an accounting to
the Covered Entity of disclosures: (i) to carry out treatment, payment or health care operations, as set
forth in 45 CFR § 164.506; (ii) to individuals of PHI about them as set forth in 45 CFR § 164.502; (iii)
under an authorization as provided in 45 CFR § 164.508; (iv) to persons involved in the individual’s
care or other notification purposes as set forth in 45 CFR § 164.510; (v) for national security or
intelligence purposes as set forth in 45 CFR § 164.512(k)(2); (vi) to correctional institutions or law
enforcement officials as set forth in 45 CFR § 164.512(k)(5); (vii) as part of a limited data set
according to 45 CFR 164.514(e); or (viii) that occurred before the compliance date for the Covered
Entity. Business Associate agrees to implement a process that allows for an accounting to be
collected and maintained by the Business Associate and its agents or subcontractors for at least six
years before the request, but not before the compliance date of the Privacy Rule. At a minimum, such
information must include: (i) the date of disclosure; (ii) the name of the entity or person who received
PHI and, if known, the address of the entity or person; (iii) a brief description of PHI disclosed; and
(iv) a brief statement of purpose of the disclosure that reasonably informs the individual of the basis
for the disclosure or a copy of the written request for disclosure. If the request for an accounting is
delivered directly to the Business Associate or its agents or subcontractors, the Business Associate
must, within ten days of the receipt of the request, forward it to the Covered Entity in writing.
h. to the extent the Business Associate is to carry out one or more of the Covered Entity’s
obligations under Subpart E of 45 CFR Part 164, comply with the requirements of Subpart E that
apply to the Covered Entity when performing those obligations.
i. make its internal practices, books, and records relating to the Business Associate’s use
and disclosure of PHI available to the Secretary for purposes of determining compliance with the
HIPAA Rules. Business Associate must concurrently provide to the Covered Entity a copy of any PHI
that the Business Associate provides to the Secretary.
j. retain all PHI throughout the term of the Agreement and for a period of six years from
the date of creation or the date when it last was in effect, whichever is later, or as required by law.
This obligation survives the termination of the Agreement.
k. implement policies and procedures for the final disposition of PHI and the hardware and
equipment on which it is stored, including but not limited to, removal of PHI before re-use.
l. within ten days of a written request by the Covered Entity, the Business Associate and
its agents or subcontractors must allow the Covered Entity to conduct a reasonable inspection of the
facilities, systems, books, records, agreements, policies and procedures relating to the use or
disclosure of PHI under this Agreement. Business Associate and the Covered Entity will mutually
agree in advance upon the scope, timing and location of such an inspection. Covered Entity must
protect the confidentiality of all confidential and proprietary information of the Business Associate to
which the Covered Entity has access during the course of such inspection. Covered Entity and the
Business Associate will execute a nondisclosure agreement, if requested by the other party. The fact
that the Covered Entity inspects, or fails to inspect, or has the right to inspect, the Business
Associate’s facilities, systems, books, records, agreements, policies and procedures does not relieve
the Business Associate of its responsibility to comply with this Agreement. Covered Entity’s (i) failure

Page 124 of 148
to detect or (ii) detection, but failure to notify Associate or require Associate’s remediation of any
unsatisfactory practices, does not constitute acceptance of such practice or a waiver of the Covered
Entity’s enforcement rights under this Agreement.
3. Permitted Uses and Disclosures by the Business Associate.
a. Business Associate may use or disclose PHI:
(1) for the proper management and administration of the Business Associate or to carry
out the legal responsibilities of the Business Associate; provided, however, either (A) the disclosures
are required by law, or (B) the Business Associate obtains reasonable assurances from the person to
whom the information is disclosed that the information will remain confidential and used or further
disclosed only as required by law or for the purposes for which it was disclosed to the person, and the
person notifies the Business Associate of any instances of which it is aware in which the
confidentiality of the information has been breached;
(2) as required by law.
(3) for Data Aggregation services relating to the health care operations of the Covered
Entity;
(4) to de-identify, consistent with 45 CFR 164.514(a) – (c), PHI it receives from the
Covered Entity. If the Business Associates de-identifies the PHI it receives from the Covered Entity,
the Business Associate may use the de-identified information for any purpose not prohibited by the
HIPAA Rules; and
b. Business Associate agrees to make uses and disclosures and requests for PHI
consistent with the Covered Entity’s minimum necessary policies and procedures.
c. Business Associate may not use or disclose PHI in a manner that would violate
Subpart E of 45 CFR Part 164 if done by the Covered Entity except for the specific uses and
disclosures described above in 3(a)(i) and (iii).
4. Covered Entity’s Obligations
Covered entity agrees to:
a. use its Security Measures to reasonably and appropriately maintain and ensure the
confidentiality, integrity, and availability of PHI transmitted to the Business Associate under
this Agreement until the PHI is received by the Business Associate.
b. provide the Business Associate with a copy of its Notice of Privacy Practices and must
notify the Business Associate of any limitations in the Notice of Privacy Practices of the
Covered Entity under 45 CFR 164.520 to the extent that such limitation may affect the
Business Associate’s use or disclosure of PHI.
c. notify the Business Associate of any changes in, or revocation of, the permission by an
individual to use or disclose the individual’s PHI to the extent that such changes may affect
the Business Associate’s use or disclosure of PHI.
d. notify the Business Associate of any restriction on the use or disclosure of PHI that the
Covered Entity has agreed to or is required to abide by under 45 CFR 164.522 to the
extent that such restriction may affect the Business Associate’s use or disclosure of PHI.
Page 125 of 148
5. Term. This Agreement continues in effect until terminated or is replaced with a new agreement
between the parties containing provisions meeting the requirements of the HIPAA Rules, whichever
first occurs.
6. Termination.
a. Material Breach. In addition to any other provisions in the Agreement regarding breach,
a breach by the Business Associate of any provision of this Agreement, as determined by the
Covered Entity, constitutes a material breach of the Agreement and provides grounds for the Covered
Entity to terminate this Agreement for cause. Termination for cause is subject to 6.b.:
(1) Default. If the Business Associate refuses or fails to timely perform any of the
provisions of this Agreement, the Covered Entity may notify the Business Associate in writing of the
non-performance, and if not corrected within thirty days, the Covered Entity may immediately
terminate the Agreement. The Business Associate must continue performance of the Agreement to
the extent it is not terminated.
(2) Business Associate’s Duties. Notwithstanding termination of the Agreement, and
subject to any directions from the Covered Entity, the Business Associate must protect and preserve
property in the possession of the Business Associate in which the Covered Entity has an interest.
(3) Erroneous Termination for Default. If the Covered Entity terminates this
Agreement under Section 6(a) and after such termination it is determined, for any reason, that the
Business Associate was not in default, then such termination will be treated as a termination for
convenience, and the rights and obligations of the parties will be the same as if the Agreement had
been terminated for convenience.
b. Reasonable Steps to Cure Breach. If the Covered Entity knows of a pattern of activity or
practice of the Business Associate that constitutes a material breach or violation of the Business
Associate’s obligations under the provisions of this Agreement or another arrangement and does not
terminate this Agreement under Section 6(a), then the Covered Entity must notify the Business
Associate of the pattern of activity or practice. The Business Associate must then take reasonable
steps to cure such breach or end such violation, as applicable. If the Business Associate’s efforts to
cure such breach or end such violation are unsuccessful, the Covered Entity may either (i) terminate
this Agreement, if feasible or (ii) report the Business Associate’s breach or violation to the Secretary.
c. Effect of Termination. After termination of this Agreement for any reason, the Business
Associate, with respect to PHI it received from the Covered Entity, or created, maintained, or received
by the Business Associate on behalf of the Covered Entity, must:
(1) retain only that PHI which is necessary for the Business Associate to continue its
proper management and administration or to carry out its legal responsibilities;
(2) return to the Covered Entity (or, if agreed to by the Covered Entity in writing,
destroy) the remaining PHI that the Business Associate still maintains in any form;
(3) continue to use appropriate safeguards and comply with Subpart C of 45 CFR
Part 164 with respect to electronic protected health information to prevent use or disclosure of the
Page 126 of 148
PHI, other than as provided for in this Section, for as long as the Business Associate retains the PHI;
(4) not use or disclose the PHI retained by the Business Associate other than for the
purposes for which such PHI was retained and subject to the same conditions set out at Section
3(a)(1) which applied before termination; and
(5) return to the Covered Entity (or, if agreed to by the Covered Entity in writing,
destroy) the PHI retained by the Business Associate when it is no longer needed by the Business
Associate for its proper management and administration or to carry out its legal responsibilities.
7. No Waiver of Immunity. The parties do not intend to waive any of the immunities, rights,
benefits, protection, or other provisions of the Michigan Governmental Immunity Act, MCL 691.1401,
et seq., the Federal Tort Claims Act, 28 U.S.C. 2671 et seq., or the common law.
8. Data Ownership. The Business Associate has no ownership rights in the PHI. The covered
entity retains all ownership rights of the PHI.
9. Disclaimer. The Covered Entity makes no warranty or representation that compliance by the
Business Associate with this Agreement, HIPAA, or the HIPAA Rules will be adequate or satisfactory
for the Business Associate’s own purposes. The Business Associate is solely responsible for all
decisions made by the Business Associate regarding the safeguarding of PHI.
10. Certification. If the Covered Entity determines an examination is necessary to comply with the
Covered Entity’s legal obligations under HIPAA relating to certification of its security practices, the
Covered Entity or its authorized agents or contractors, may, at the Covered Entity’s expense,
examine the Business Associate’s facilities, systems, procedures and records as may be necessary
for such agents or contractors to certify to the Covered Entity the extent to which the Business
Associate’s security safeguards comply with HIPAA, the HIPAA Rules or this Agreement.
11. Amendment. The parties acknowledge that state and federal laws relating to data security and
privacy are rapidly evolving and that amendment of this Agreement may be required to provide for
procedures to ensure compliance with such developments. The parties specifically agree to take such
action as is necessary to implement the standards and requirements of HIPAA and the HIPAA Rules.
Upon the request of either party, the other party agrees to promptly enter into negotiations concerning
the terms of an amendment to this Agreement embodying written assurances consistent with the
standards and requirements of HIPAA and the HIPAA Rules. Either party may terminate the
Agreement upon thirty days written notice if (i) one party does not promptly enter into negotiations to
amend this Agreement when requested by the other party or (ii) the Business Associate does not
enter into an amendment to this Agreement providing assurances regarding the safeguarding of PHI
that the Covered Entity, in its sole discretion, deems sufficient to satisfy the standards and
requirements of HIPAA or the HIPAA Rules.
12. Assistance in Litigation or Administrative Proceedings. Business Associate must make itself,
and any subcontractors, employees or agents assisting the Business Associate in the performance of
its obligations under this Agreement, available to the Covered Entity, at no cost to the Covered Entity,
to testify as witnesses, or otherwise, if litigation or administrative proceedings are commenced
against the Covered Entity, its directors, officers or employees, departments, agencies, or divisions
based upon a claimed violation of HIPAA or the HIPAA Rules or other laws relating to the Business
Associate’s or its subcontractors use or disclosure of PHI under this Agreement, except where the
Page 127 of 148
Business Associate or its subcontractor, employee or agent is a named adverse party.
13. No Third Party Beneficiaries. Nothing express or implied in this Agreement is intended to
confer upon any person other than the Covered Entity, the Business Associate and their respective
successors or assigns, any rights, remedies, obligations or liabilities whatsoever.
14. Interpretation and Order of Precedence. Any ambiguity in this Agreement must be interpreted
to permit compliance with the HIPAA Rules. Where the provisions of this Agreement differ from those
mandated by the HIPAA Rules, but are nonetheless permitted by the HIPAA Rules, the provisions of
this Agreement control.
15. Effective Date. This Agreement is effective upon receipt of the last approval necessary and the
affixing of the last signature required.
16. Survival of Certain Agreement Terms. Notwithstanding any contrary provision in this
Agreement, the Business Associate’s obligations under Section 6(d) and record retention laws
(“Effect of Termination”) and Section 12 (“No Third Party Beneficiaries”) survive termination of this
Agreement and are enforceable by the Covered Entity.
17. Representatives and Notice.
a. Representatives. The individuals listed below are designated as the parties’ respective
representatives for purposes of this Agreement. Either party may from time to time designate in
writing new or substitute representatives.
b. Notices. All required notices must be in writing and must be hand delivered or given by
certified or registered mail to the representatives at the addresses set forth below or sent via email to
the Privacy Security Mailbox at MDHHSPrivacySecurity@michigan.gov.
Covered Entity Representative:
James Bowen
Privacy and Security Manager
MDHHS Compliance Office
333 South Grand Ave, 4
th
Floor
Lansing, MI 48933
(517) 284-1018
Business Associate Representative:
Name:
Title:
Department:
Address:
Phone:
Email:
Page 128 of 148
Name:
Title:
Department:
Address:
Phone:
Email:
Any notice given to a party under this Agreement shall be deemed effective, if addressed to such party,
upon: (i) delivery, if hand delivered; or (ii) the third Business Day after being sent by certified or
registered mail.
Business Associate
Covered Entity
[INSERT NAME]
By:____________________________
Date:__________________________
[INSERT NAME]
By:_______________________________
Date: _____________________________
Print Name: ____________________
Print Name: Kristen Jordan____________
Title:___________________________
Title: Director, Bureau of Specialty______
Behavioral Health Services____________
Covered Entity
[INSERT NAME]
By:_______________________________
Date: _____________________________
Print Name: Tony Weber
Title: Chief Compliance Officer

Page 129 of 148
SCHEDULE C- DEFINITIONS / EXPLANATION OF
TERMS
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
The terms used in this Contract will be construed and interpreted as defined below unless the Contract
otherwise expressly requires a different construction and interpretation.
Abuse: As defined in 42 CFR 455.2, provider practices that are inconsistent with sound fiscal,
business, or medical practices and result in an unnecessary cost to the Medicaid program, or in
reimbursement for services that are not medically necessary or that fail to meet the professionally
recognized standards for health care.
Actuarial Soundness: As defined in 42 CFR, (a) Actuarially sound capitation rates are projected to
provide for all reasonable, appropriate, and attainable costs that are required under the terms of the
contract and for the operation of the MCO, PIHP, or PAHP for the time period and the population
covered under the terms of the contract, and such capitation rates are developed in accordance with
the requirements in paragraph (b) of this Section.
(b) CMS review and approval of actuarially sound capitation rates. Capitation rates for MCOs, PIHPs,
and PAHPs must be reviewed and approved by CMS as actuarially sound. To be approved by CMS,
capitation rates must:
(1) Have been developed in accordance with standards specified in 42 CFR 438.5 and generally
accepted actuarial principles and practices. Any proposed differences among capitation rates
according to covered populations must be based on valid rate development standards and not based
on the rate of Federal financial participation associated with the covered populations.
(2) Be appropriate for the populations to be covered and the services to be furnished under the
contract.
(3) Be adequate to meet the requirements on MCOs, PIHPs, and PAHPs in 42 CFR 438.206,
438.207, and 438.208.
(4) Be specific to payments for each rate cell under the contract.
(5) Payments from any rate cell must not cross-subsidize or be cross-subsidized by payments for
any other rate cell.
(6) Be certified by an actuary as meeting the applicable requirements of this part, including that the
rates have been developed in accordance with the requirements specified in 42 CFR438.3(c)(1)(ii)
and (e).
(7) Meet any applicable special contract provisions as specified in 42 CFR 438.6.
(8) Be provided to CMS in a format and within a timeframe that meets requirements in 42 CFR 438.7.
(9) Be developed in such a way that the MCO, PIHP, or PAHP would reasonably achieve a medical
loss ratio standard, as calculated under 42 CFR438.8, of at least 85 percent for the rate year. The
capitation rates may be developed in such a way that the MCO, PIHP, or PAHP would reasonably
achieve a medical loss ratio standard greater than 85 percent, as calculated under 42 CFR 438.8,
as long as the capitation rates are adequate for reasonable, appropriate, and attainable non-benefit
costs.
Appropriations Act: An act to make appropriations, to the State, for each fiscal year, and to provide
for the expenditure of the appropriation.
Behavioral Health – Healthy Michigan Plan (HMP), Medicaid Health Plan (MHP) Unenrolled
(BHHMP): This plan covers Medicaid mental health and substance use disorder services managed by
Contractor for Healthy Michigan (HMP) recipients who have a specialty level of need and are not
Page 130 of 148
enrolled in a Medicaid Health Plan (Fee For Service- FFS).
Behavioral Health – Healthy Michigan Plan, MHP Enrolled (BHHMP-MHP): This plan covers
Medicaid mental health and substance use disorder services managed by Contractor for Healthy
Michigan (HMP) recipients who have a specialty level of need and are enrolled in a Medicaid Health
Plan for Managed Care (MC).
Behavioral Health – Medicaid, MHP Unenrolled (BHMA): This plan covers Medicaid mental health
and substance use disorder services managed by Contractor for MA recipients who have a specialty
level of need and are not enrolled in a Medicaid Health Plan (Fee For Service - FFS).
Behavioral Health – Medicaid, MHP Enrolled (BHMA-MHP): This plan covers Medicaid mental health
and substance use disorder services managed by Contractor for MA recipients who have a specialty
level of need and are enrolled in a Medicaid Health Plan for Managed Care (MC).
Capitated Payments: Is a fixed amount of money per beneficiary per month paid in advance to
Contractor for the delivery of behavioral health care services.
Capitation Rate: The fixed per person monthly rate payable to Contractor by the State for each
Medicaid eligible person covered by the 1115 Demonstration Waiver Program, regardless of whether or
not the individual who is eligible for Medicaid receives covered specialty services and supports during
the month. There is a separate, fixed per person monthly rate payable for each eligible person covered
by the Healthy Michigan Program.
Clean Claim: As defined in 42 CFR 447.45 Timely Claims Payment, b, a clean claim is one that can be
processed without obtaining additional information from the provider of the service or a third party. It
does not include a claim from a provider who is under investigation for fraud or abuse, or a claim under
review for medical necessity.
Community Mental Health Services Program (CMHSP): A CMHSP is a program that contracts with
the State to provide comprehensive behavioral health services in specific geographic service areas,
regardless of an individual’s ability to pay. (Michigan Mental Health Code 330.1100a, 330.1206). A
CMHSP is considered a “Network Provider” under this Contract when directly engaged in the delivery,
ordering, or referring of covered services to a beneficiary, and is considered a “Subcontractor” under
this Agreement when providing a function or service on behalf of Contractor related, directly or
indirectly, to the performance of Contractor’s obligations to the State under this Contract.
CMHSP Contractual Staff: CMHSP contractual staff are not W-2 employees of the CMHSP, but they
also do not have a network provider agreement. The following provides guidance regarding whether
these contractual staff can be considered “employees” for purposes of reporting, or whether the
CMHSP is required to have a network provider agreement with the contractual staff. To determine if a
provider without a network provider agreement can be considered an employee of the CMHSP for
purposes of the standard cost allocation methodology, EQI reporting, and MLR reporting, the provider
must:
1. Use the CMHSP NPI number for billing/encounter submission, and
2. Perform work under the control and direction of the CMHSP, i.e., what will be done and how it
will be done.
Relationships where the provider does not use the CMHSP NPI number, or the CMHSP has the right to
control and direct only the result of the provider’s work (i.e., not what will be done and how it will be
done) would be indicative of a network provider relationship.
CMHSP Employee: A CMSHP employee is a person employed by the CMHSP receiving a salary or
Page 131 of 148
wage and a W-2 for tax purposes, and where the work performed by the person is under the control of
the CMHSP (i.e., how, and where the work is done).
Critical Incident: Critical Incidents are defined as the following events: Suicide; Non-suicide death;
Arrest of Consumer; Emergency Medical Treatment due to injury or Medication Error: Type of injury will
include a subcategory for reporting injuries that resulted from the use of physical management;
Hospitalization due to Injury or Medication Error: Hospitalization due to injury related to the use of
physical management.
Delegation: an agreement between Contractor and an individual, provider, CMHSP or other
organization to perform certain functions that otherwise would be the responsibility of Contractor to
perform. Contractor oversees and is accountable for any functions or responsibilities that are delegated
to other entities whether the functions are provided by Contractor or other entities.
Early and Periodic Screening, Diagnosis, and Treatment Program (EPSDT): As defined in 42 CFR
440.40(b).
Excluded: Individuals or entities that have been excluded from participating in the Medicare, Medicaid,
or any other Federal health care programs. Bases for exclusion include convictions for program related
fraud, patient abuse, licensing board actions, and/or default on Health Education Assistance loans.
Fraud: As defined in 42 CFR 455.2, the intentional deception or misinterpretation made by a person
with the knowledge that the deception could result in some unauthorized benefit to himself or another
person. It includes any act that constitutes fraud under any applicable federal or State Law.
Flint 1115 Demonstration Waiver: The benefit describes Targeted Case Management (TCM) services
provided to pregnant women and children up to age 21 with household income up to and including
400% of the federal poverty level (FPL) who were served by the Flint water system on or between April
1, 2014, and the date the water is deemed safe by the appropriate authorities. Pregnant women will
remain eligible throughout their pregnancy and will receive two months of post-partum coverage. Once
eligibility has been established for a child, including those children born to pregnant women, the child
will remain eligible until age 21 as long as other eligibility requirements are met. TCM services assist
individuals in gaining access to appropriate medical, educational, social, and/or other services. TCM
services include assessments, planning, linkage, advocacy, coordination, referral, monitoring, and
follow-up activities.
Health Care Professional: Includes any of the following: physician, podiatrist, optometrist,
chiropractor, psychologist, dentist, physician assistant, physical or occupational therapist, therapist
assistant, speech-language pathologist, audiologist, registered or practical nurse (including nurse
practitioner, clinical nurse specialist, certified registered nurse anesthetist, and certified nurse midwife),
registered/certified social worker, registered respiratory therapist, and certified respiratory therapy
technician (this list is not all inclusive).
Health Insurance Portability and Accountability Act of 1996 (HIPAA): Public Law 104-191 of 1996
to improve the Medicare program under Title XVIII of the Social Security Act, the Medicaid program
under Title XIX of the Social Security Act, and the efficiency and effectiveness of the health care
system, by encouraging the development of a health information system through the establishment of
standards and requirements for the electronic transmission of certain health information.
Healthy Michigan Plan (HMP): Is a category of eligibility authorized under the Patient Protection and
Affordable Care Act and Michigan PA 107 of 2013.
Page 132 of 148
Healthy Michigan Plan Beneficiary: An individual who has met the eligibility requirements for
enrollment in HMP and has been issued a Medicaid card.
Intellectual/Developmental Disability: As defined in MCL 330.1100a(25) of the Michigan Mental
Health Code.
Institution for Mental Disease (IMD) Services: Means a hospital, nursing facility, or other institution
of more than 16 beds, that is primarily engaged in providing diagnosis, treatment, or care of persons
with mental diseases, including medical attention, nursing care, and related services.” (SSA
§1905(i).).
Intensive Crisis Stabilization Services (ICSS): Structured treatment and support activities provided
by a mobile intensive crisis stabilization team that are designed to promptly address a crisis situation in
order to avert a psychiatric admission or other out of home placement or to maintain a child or youth in
their home or present living arrangement who has recently returned from a psychiatric hospitalization or
other out of home placement. These services must be available to children or youth with serious
emotional disturbance (SED) and/or intellectual/developmental disabilities (I/DD), including autism, or
co-occurring SED and substance use disorder (SUD).
Limited English Proficiency (LEP): Means being limited in ability or unable to speak, read and/or
write the English language well enough to understand and be understood without the aid of an
interpreter.
Managed Care Administration: An administrative cost category to which non-encounterable costs of
Contractor or subcontractor must be assigned. Managed care administration are administrative costs to
fulfill the obligations of the Contract to organize, arrange, and coordinate clinical service delivery. Non-
exhaustive examples include eligibility and coverage verification, utilization management, network
development, contracted network provider training, claims processing, activities to improve health care
quality, and fraud prevention activities. Costs defined as shared managed care administration must be
excluded from the unit cost and the independent rate model.
Maternity Outpatient Medical Services (MOMS): A health coverage program operated by the State.
Medical Loss Ratio (MLR): Is the proportion of premium revenues spent on clinical services and
quality improvements. The Affordable Care Act establishes minimum MLR standards and requires
issuers to provide rebates when the MLRs are lower than the applicable MLR standard. Contractor
must maintain an MLR of 85% or higher or provide rebates.
Medicaid Managed Specialty Services and Supports Program (MMSSSP): This includes the
following: 1115 Behavioral Health Demonstration Waiver and the 1915(c) Habilitation Supports Waiver,
Children’s Waiver Program (CWP), Serious Emotional Disturbance (SED), the MIChild program, MOMS
program, and the 1115 Healthy Michigan Plan.
MIChild: A health care program for low-income, uninsured children under age 19 administered by
MDHHS. Beneficiaries receive a comprehensive package of health care benefits including vision,
dental, and mental health services.
Network Provider Agreement: An agreement between Contractor and a provider or between
Contractor’s subcontractor and a provider that describes the conditions under which the provider
agrees to furnish covered services to Contractor’s enrolled beneficiaries. Agreements with providers
that include additional functions or services beyond the provision of covered services to beneficiaries
are not network provider agreements and shall be considered subcontracts for the purposes of this
Page 133 of 148
Contract.
Network Provider: Any provider, group of providers, or entity that has a provider agreement with
Contractor or Contractor’s subcontractor, including a CMHSP, and receives Medicaid funding directly or
indirectly to order, refer or render covered services as a result. A network provider is not a
subcontractor by virtue of the network provider agreement, unless the network provider is responsible
for services other than those that could be covered in a network provider agreement related to the
delivery, ordering, or referring of covered services to a beneficiary.
Per Eligible Per Month (PEPM): A fixed monthly rate per Medicaid eligible person payable to
Contractor by the State for provision of Medicaid services defined within this Contract.
Post-stabilization Care Services: As defined in 42 CFR 438.114(a), covered services related to an
emergency medical condition that are provided after a beneficiary is stabilized in order to maintain the
stabilized condition, or, under the circumstances described in 42 CFR 438.114(e) to improve or resolve
the beneficiary's condition.
Prepaid Inpatient Health Plan (PIHP): A PIHP is an organization as defined in 42 CFR Part 438 and
meets the requirements of MCL 330.1204b.
Provider: An individual or entity engaged in the delivery, ordering, or referring of services.
Regional Entity: An entity established by a combination of community mental health services
programs under Section 204b of the Michigan Mental Health Code, A 258 of 1974 as amended.
Risk Mitigation Plan: For the purposes of Third-Party Liability, a Risk Mitigation Plan is a document
that will be provided by the Medicaid Health Plan outlining the actions the Medicaid Health Plan will
take to address risks identified by the State. Risks are issues that will affect a Medicaid Health Plan’s
ability to meet the minimum TPL requirements required by this Contract, federal, or state law in order to
reduce the likelihood of an adverse state or federal TPL audit finding.
Sentinel Event: Is an “unexpected occurrence” involving death (not due to the natural course of a
health condition) or serious physical or psychological injury, or risk thereof. Serious injury specifically
includes permanent loss of limb or function. The phrase “or risk thereof” includes any process variation
for which recurrence would carry a significant chance of a serious adverse outcome (JCAHO, 1998).
Any injury or death that occurs from the use of any behavior intervention is considered a sentinel event.
Serious Emotional Disturbance (SED): As defined in Section 330.1100c of the Michigan Mental
Health Code
Serious Mental Illness (SMI): As defined in MCL 330.1100d(3) of the Michigan Mental Health Code.
Subcontract: An agreement entered into by Contractor with any other individual, provider, CMHSP, or
other organization who agrees to perform any function or service on behalf of Contractor related to
securing or fulfilling Contractor’s required contract activities and obligations under the terms of this
Contract when the intent of such an agreement is to delegate the responsibility for any major service or
group of services required by this Contract. Examples of delegated activities include but are not limited
to overseeing quality management and assessing performance measurement and improvement,
developing or maintaining a compliance program, managing staff qualifications and training, overseeing
a utilization management program, assuring compliance with access standards, maintaining information
technology systems, overseeing finance system and procedures, providing customer service, upholding
enrollee rights and protections, managing the enrollee or provider grievance process, engaging in
Page 134 of 148
provider network selection and management, performing credentialing functions, managing the appeals
process, making ownership and control disclosures, and other general management functions
undertaken on behalf of Contractor related to fulfilling the Contract requirements. Agreements limited in
scope to the provision of covered services to enrollees are not subcontracts and shall be considered
network provider agreements for purposes of this Contract.
Subcontractor: An individual, provider, CMHSP, or other organization that provides any function or
service on behalf of Contractor related to securing or fulfilling Contractor’s obligations under this
Contract. Subcontractor does not include a network provider, unless the network provider is responsible
for services other than those that could be covered in a network provider agreement related only to the
provision of covered services to beneficiaries.
Substance Use Disorder (SUD): As defined in MCL 330.1100d(11) of the Michigan Mental Health
Code.

Page 135 of 148
SCHEDULE D- RESERVED
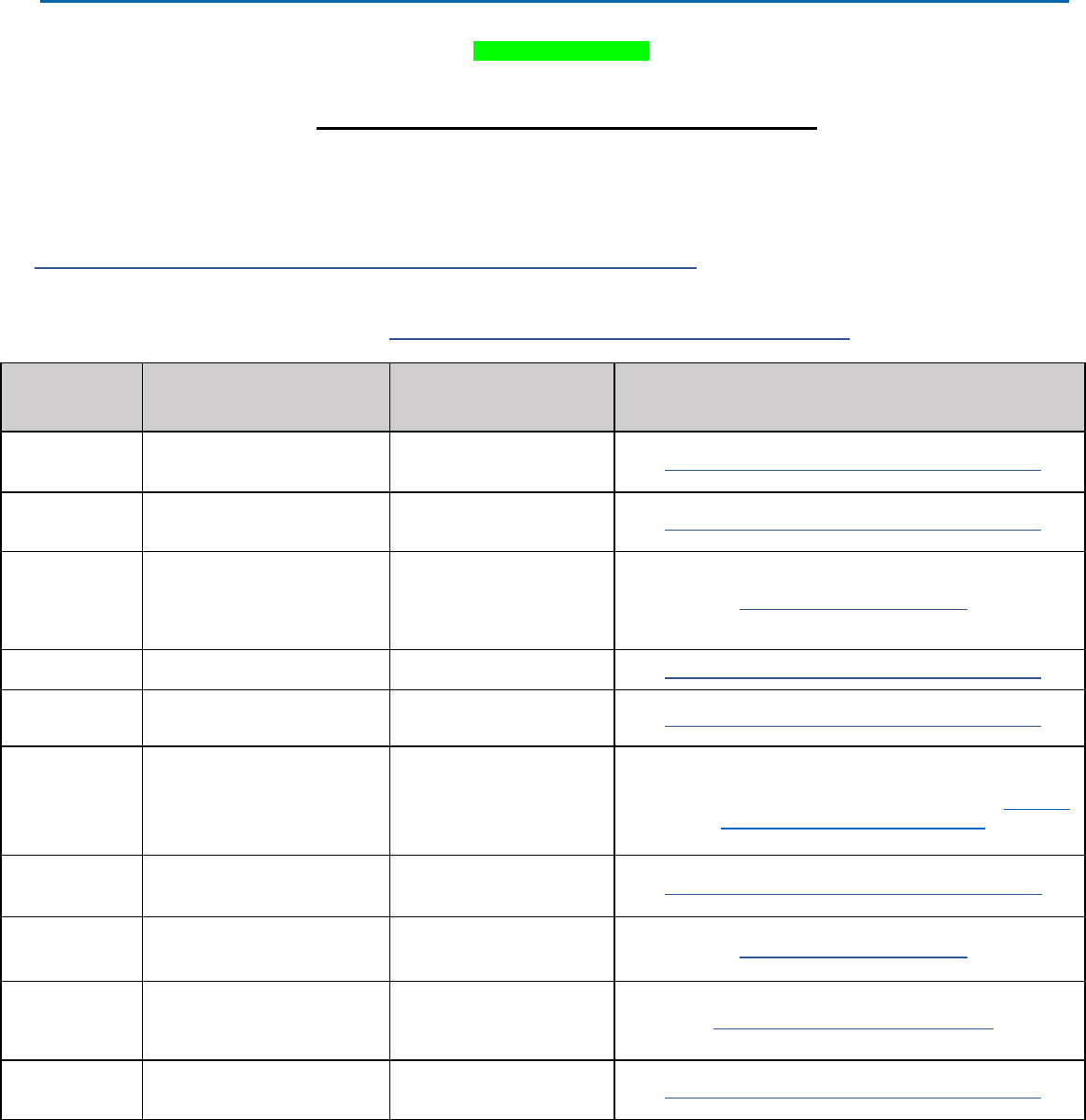
Page 136 of 148
SCHEDULE E- CONTRACTOR FINANCIAL
REPORTING REQUIREMENTS
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
FINANCIAL PLANNING, REPORTING AND SETTLEMENT
Contractor must provide the following financial reports to the State as listed below.
Mental Health and Substance Use Disorder (Non-Medicaid) Reporting Requirements, which includes forms,
instructions, and other essential resources, are located on the MDHHS website at:
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/reporting
Unless otherwise noted in the Reporting Mailbox column below, submit completed reports electronically
(Microsoft Excel or Microsoft Word) to: MDHHS-BHDDA-Contracts-MGMT@michigan.gov
Due Date Report Title Report Period Reporting Mailbox
February 28
SUD – Legislative
Report/Section 904
Annually
October 1 to September 30
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
February 28
PIHP Medicaid FSR Bundle -
MA, HMP
Final (Use tab in
FSR Bundle)
October 1 to September 30
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
February 28
Encounter Quality Initiative
Report (EQI) including
Attestation to accuracy,
completeness, and truthfulness
of claims and payment data
Annually
October 1 to September 30
QMPMeasures@michigan.gov
February 28
PIHP Executive Compensation
Reporting for Section 904(2)
Annually
October 1 to September 30
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
February 28 Medical Loss Ratio
Annually
October 1 to September 30
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
April 30
DHHS Incentive Payment DHIP
Report and Narrative
Annually
October 1 to September 30
Electronic version of the DHIP CAFAS report (and if
applicable PECAFAS report) for each CMHSP to
MDHHS-
BCCHPS-Reporting@michigan.gov
May 31 Mid-Year Status Report
Mid-Year
October 1 to March 31
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
May 31
Encounter Quality Initiative
Report (EQI)
Four months
October to January
QMPMeasures@michigan.gov
June 30 SUD – Audit Report
Annually
October 1 to September 30
(Due 9 months after close of
fiscal year)
MDHHS-AuditReports@michigan.gov
August 15
PIHP Medicaid FSR Bundle
MA, HMP
Projection (Use
tab in FSR Bundle)
October 1 to September 30
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
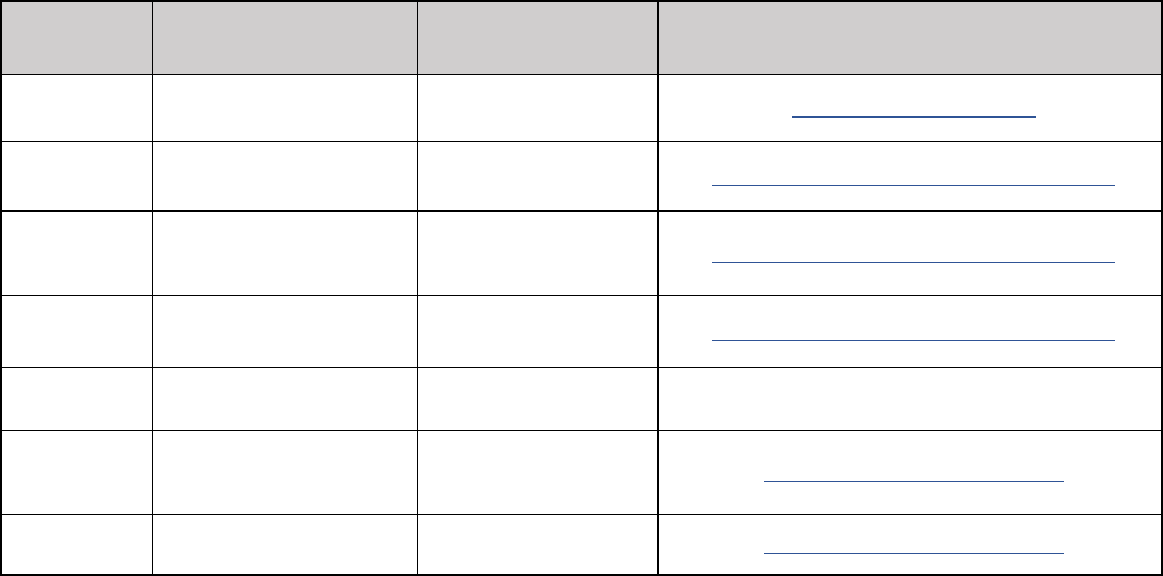
Page 137 of 148
Due Date Report Title Report Period Reporting Mailbox
September 30
Encounter Quality Initiative
Report (EQI)
Eight Months
October to May
QMPMeasures@michigan.gov
October 1 Medicaid YEC Accrual
Final
October 1 to September 30
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
November 1
PIHP Medicaid FSR Bundle
MA, HMP
Interim (Use tab in FSR
Bundle)
October 1 to September 30 -
Interim
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
December 3 Risk Management Strategy
Annually
To cover the current fiscal
year
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
December 31
Medicaid Services Verification
Report
Annually
October 1 to September 30
Contractor’s MDHHS-
OIG sFTP Area and/or Case
Management System
30 Days after
receipt
Annual Audit Report,
Management Letter, and
CMHSP Response to the
Management Letter.
Annually
October 1 to September 30
MDHHS-AuditReports@michigan.gov
30 Days after
receipt
Compliance exam and plan of
correction
Annually
October 1 to September 30
MDHHS-AuditReports@michigan.gov
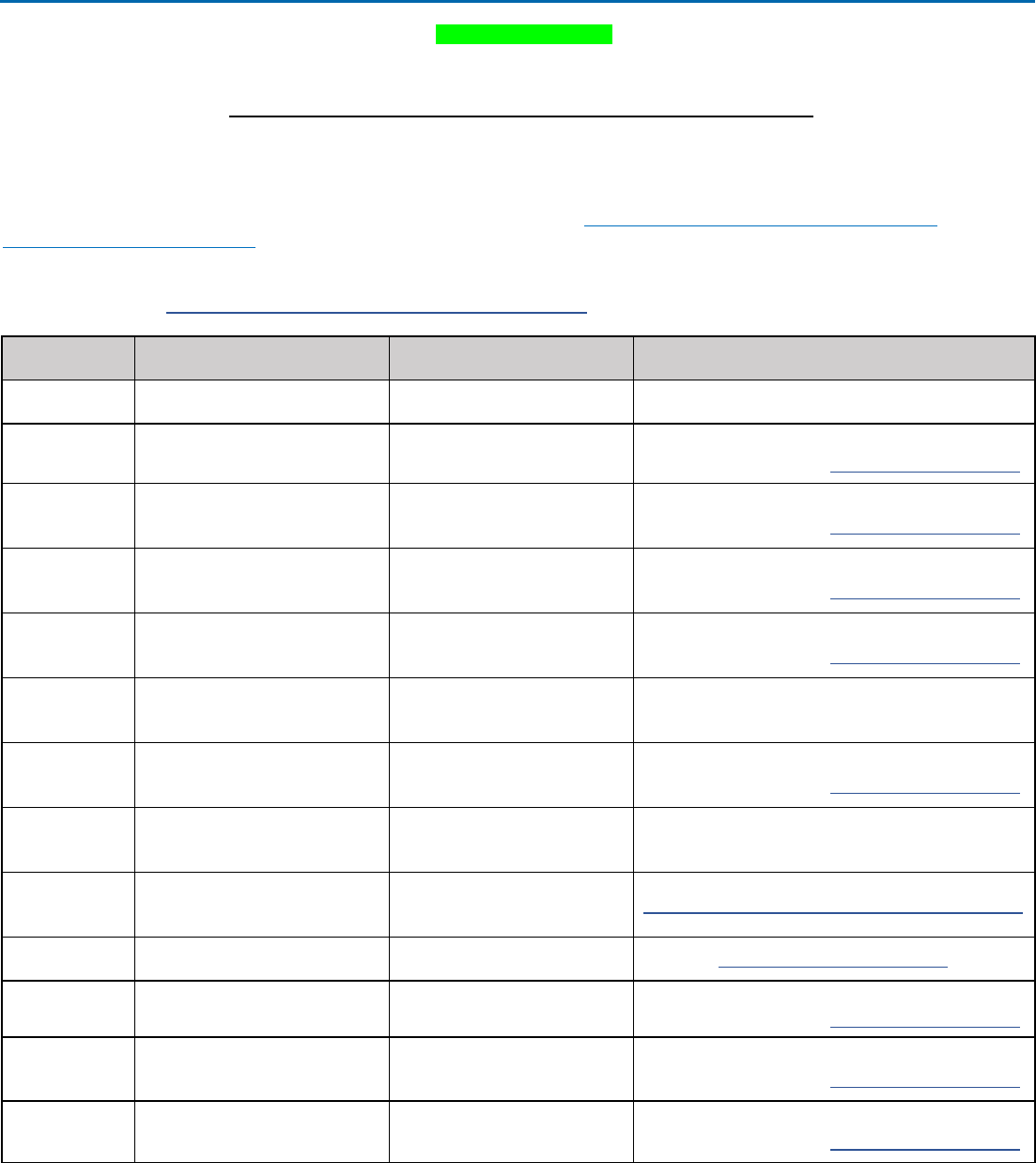
Page 138 of 148
SCHEDULE E- CONTRACTOR NON-FINANCIAL
REPORTING REQUIREMENTS
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
NON-FINANCIAL REPORTING REQUIREMENTS SCHEDULE
Contractor must provide the following reports to the State as listed below.
Mental Health and Substance Use Disorder (Non-Medicaid) Reporting Requirements, which includes forms, instructions,
and other essential resources, are located on the MDHHS website at:
https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting
Unless otherwise noted in the Reporting Mailbox column below, submit completed reports electronically (Microsoft Excel or
Microsoft Word) to: MDHHS-BHDDA-Contracts-MGMT@michigan.gov
Due Date Report Title Report Period Reporting Mailbox
January 15
Annual Program Integrity Report
October 1 through September
30 of the previous fiscal year
Contractor’s MDHHS-OIG sFTP Area and/or Case
Management System
January 27
Managed Care Program Annual
Report (MCPAR)
October 1 through September
30
prior fiscal year
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
February 15 Member Grievances Feb 15 for 1Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
February 15 Service Authorization Denials Feb 15 for 1Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
February 15 Member Appeals Feb 15 for 1Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
February 15 Program Integrity Activities October 1 to December 31
Contractor’s MDHHS-OIG sFTP Area and/or Case
Management System
February 28
Quality Assessment Performance
Improvement Program (QAPIP)
October 1 to September 30
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
March 15
Annual Compliance Program
Report
October 1 of prior fiscal year to
current
Contractor’s MDHHS-OIG sFTP Area and/or Case
Management System
April 30 Network Adequacy Report
October 1 to September 30 of
previous fiscal year
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
March 31 Performance Indicators October 1 to December 31 QMPMeasures@michigan.gov
May 15 Provider Credentialing May 15 for 1Q and 2Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
May 15 Member Grievances May 15 for 1Q and 2Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
May 15 Member Appeals May 15 for 1Q and 2Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
Page 139 of 148
Due Date Report Title Report Period Reporting Mailbox
May 15 Service Authorization Denials May 15 for 1Q and 2Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
May 15 Program Integrity Activities January 1 to March 31
Contractor’s MDHHS-OIG sFTP Area and/or Case
Management System
June 30 Performance Indicators January 1 to March 31 QMPMeasures@michigan.gov
August 15 Member Grievances Aug 15 for 1Q, 2Q & 3Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
August 15 Member Appeals Aug 15 for 1Q, 2Q & 3Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
August 15 Service Authorization Denials Aug 15 for 1Q, 2Q & 3Q data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
August 15 Program Integrity Activities April 1 to June 30
Contractor’s MDHHS-OIG sFTP Area and/or Case
Management System
September 1
Conflict of Interest
Attestation/Provider Screening
Information Collection Tool
(PSICT)
Upcoming New Fiscal Year
Submit through DCH File Transfer to: MDHHS-
Managed Care System Support and Operations
Notify Kim Heinicke at HeinickeK@michigan.gov
September 30 Performance Indicators April 1 to June 30 QMPMeasures@michigan.gov
October 30
Intensive Crisis Stabilization
Services (ICSS) for Children
Annual Data Report
October 1 to September 30 MDHHS-BCCHPS-Reporting@michigan.gov
November 15 Provider Credentialing
Nov 15 for 1Q, 2Q, 3Q & 4Q
data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
November 15
Performance Bonus Incentive
Narrative on “Increased
participation in patient-centered
medical homes characteristics.”
October 1 to September 30 MDHHS-BHDDA-Contracts-MGMT@michigan.gov
November 15 Member Grievances
Nov 15 for 1Q, 2Q, 3Q & 4Q
data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
November 15 Member Appeals
Nov 15 for 1Q, 2Q, 3Q & 4Q
data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
November 15 Service Authorization Denials
Nov 15 for 1Q, 2Q, 3Q & 4Q
data
Submit through: DCH-File Transfer
Notify Audra Parsons at ParsonsA@michigan.gov
November 15 Program Integrity Activities July 1 to September 30
Contractor’s MDHHS-OIG sFTP Area and/or Case
Management System
November 15
Subcontracted Entities and
Network Providers List
Annually
Current Fiscal Year
Contractor’s MDHHS OIG sFTP Area
November 15
PIHP Current Organizational
Chart
Annually
Current Fiscal Year
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
Page 140 of 148
Due Date Report Title Report Period Reporting Mailbox
December 31 Performance Indicators July 1 to September 30 QMPMeasures@michigan.gov
Within 120
calendar days
IET Data Files
PIHPs will be provided the IET
data files by January 31 and
within 120 calendar days return
their data validation
Submit via DEG at:
https://milogintp.michigan.gov
Monthly
All Behavioral Health Treatment
Episode Data Set (BH- TEDS)
October 1 to September 30 Due
last day of each month.
See resources at:
https://www.michigan.gov/mdhh
s/keep-mi-
healthy/mentalhealth/reporting
Submit via DEG at:
https://milogintp.michigan.gov
Monthly
(minimum 12
submissions per
year)
All Encounter Reporting via
HIPAA 837 Standard
Transactions
October 1 to September 30
See resources at:
https://www.michigan.gov/mdhh
s/keep-mi-
healthy/mentalhealth/reporting
Submit via DEG at:
https://milogintp.michigan.gov
Monthly*
Consumer-Level Data
1. Quality Improvement
October 1 to September 30.
See resources at:
https://www.michigan.gov/mdhh
s/keep-mi-
healthy/mentalhealth/reporting
MDHHS-BHDDA-Contracts-MGMT@michigan.gov
Monthly Critical Incidents
As identified in the Critical
Incident Reporting and Event
Notification Requirements
https://www.michigan.gov/mdhh
s/keep-mi-
healthy/mentalhealth/mentalhea
lth/practiceguidelines
Submit through the Customer Relationship
Management (CRM) System
Monthly
Crisis and Access Service
Information updated in the BH
CRM for MH and SUD per MCL
330.1206
Current and Ongoing
Update through the Customer Relationship
Management (CRM) System
For Technical Difficulties:
mdhhs-bh-crm@michigan.gov
On Request
Provider Network Stability Plan
Report
October 1 to September 30 MDHHS-BHDDA-Contracts-MGMT@michigan.gov
*Reports required if Contractor is participating in pilot and/or optional programs.
NOTE: To submit via Data Exchange Gateway (DEG) to the State/MIS Operations Client Admission and
Discharge client records must be sent electronically to:
Michigan Department of Health and Human Services
Michigan Department of Technology, Management & Budget
Data Exchange Gateway (DEG)
For admissions: use c:/4823 4823@dchbull
For discharges: use c:/4824 4824@dchbull
Behavioral Health-Treatment Episode Data Set (BH-TEDS) collection/recording and reporting requirements
including technical specifications, file formats, error descriptions, edit/error criteria, and explanatory materials on

Page 141 of 148
record submission are located on MDHHS’s website at: https://www.michigan.gov/mdhhs/keep-mi-
healthy/mentalhealth/reporting
The PIHP Policies and Practice Guidelines are located on the MDHHS website at
https://www.michigan.gov/mdhhs/keep-mi-healthy/mentalhealth/mentalhealth/practiceguidelines

Page 142 of 148
SCHEDULE F- MEDICAID MENTAL HEALTH SUBSTANCE USE
DISORDER AUTHORIZATION AND PAYMENT RESPONSIBILITY GRID
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
The attached grid is designed to be utilized as a general guideline to assist Medicaid Health Plans, Prepaid Inpatient Health Plans, Community Mental Health Service Programs,
and providers in determining the responsible entity for authorization and payment. These are general guidelines and all entities should follow Medicaid policy as described in the
Medicaid Provider Manual and in the agency’s contract with the State.
Acronyms:
– BHM - Behavioral Health Manager
– CMHSP - Community Mental Health Services Program
– DRG – Diagnosis Related Group
– ED – Emergency Department
– FFS – Fee for Service
– I/DD – Intellectual/Developmental Disability
– MHA – Mental Health Assessment
– MHP - Medicaid Health Plan
– MAT – Medication Assisted Treatment
– NF – Nursing Facility
– OBAT – Office Based Alcohol Treatment
– OBOT – Office Based Opioid Treatment
– OTP – Opioid Treatment Provider
– PAR – Pre-Admission Review
– PIHP - Prepaid Inpatient Health Plan
– SBIRT – Screening, Brief Intervention, and Referral to Treatment
Services
– SED – Serious Emotional Disturbance
– SMI - Serious Mental Illness
– SUD - Substance Use Disorder
Notes:
Diagnosis may be one of the factors considered in determining responsible payor but is not the only factor.
Unless otherwise indicated by the most current ICD-10-CM coding guidelines, list first the ICD-10 code for the diagnosis, condition, problem, or other reason
for the encounter/visit that is shown in the medical record to be chiefly responsible for the services provided followed by additional ICD-10 codes that describe
any coexisting conditions.
Specialty supports and services provided to individuals with an I/DD outlined in the Medicaid Provider Manual are the responsibility of the PIHP; mental
health, physical health and substance use disorder services for these individuals are handled by the appropriate agency as designated below.
When the grid below indicates that authorization and payment is the responsibility of the PIHP, refer to the contracted entity for specialty behavioral
health services (CMHSP or other).
When the grid below indicates that payment is the responsibility of the MHP, provider network requirements apply.
Post-psychiatric hospitalization crisis intervention is the responsibility of the PIHP.
Refer to the Medicaid Provider Manual for additional coverage and reimbursement information including information for those beneficiaries enrolled with
an Integrated Care Organization.
Page 143 of 148
Setting in Which Service is Provided
Outpatient Office
(FQHCs/RHCs/THCs,
Physician Office,
Psychiatrist,
Psychologist, Social
Worker)
Medical Emergency
Department
Mental Health Crisis
Center - Access and
Screening Center
Outpatient
Behavioral Health
(Crisis) Residential
Services
Outpatient
Substance Abuse
Office, Residential
Substance Abuse
Center or Sub-Acute
Detox Center
Including OTPs.
Inpatient Acute Care
Hospital (Medically
Managed)
Inpatient
Psychiatric
Hospital
(Excluding State
Psychiatric
Hospital
Services)
Nursing Facility
Mental Health Services to Individuals Who Have "Mild to Moderate" Mental Illness or whose severity has not yet been diagnosed.
NOTE: The authorization and payment responsibilities delineated hold true regardless if the individual has concurrent I/DD or SUD.
The MHP is
responsible for
outpatient mental
health services
including screening;
this service may or
may not require
authorization from
MHP. MHP must
coordinate care as
appropriate.
Payer responsible:
MHP or FFS based
upon beneficiary
enrollment.
After medical
screening and
stabilization, if a
medical health
professional believes
that pre-screening for
inpatient psychiatric
hospital services is
indicated, or if the
need for specialty
supports is identified,
the ED should contact
the PIHP for a PAR.
Authorization and
payment for PAR are
the responsibility of
the PIHP. The PAR
may be conducted
telephonically or face-
to- face in the ED by
the PIHP.
The MHP/FFS is
responsible for mild to
moderate mental
illness treatment
services, as
determined by the
discharge diagnosis,
provided by
practitioners in the ED
who are not
associated to a PIHP.
Payer Responsible:
mixed
Crisis intervention is
the responsibility of
the PIHP even if
individual is currently
categorized as "mild
to moderate" mental
illness.
Payer responsible:
PIHP
Mental health and
SUD services should
be coordinated with
the MHP—this is
especially true if the
individual has co-
occurring disorders
(mental health and
SUD).
Payer responsible:
PIHP
The PIHP is
responsible for
payment for services
provided by PIHP
contracted providers.
Payer responsible:
FFS or PIHP
depending upon
contract
arrangements.
Mental health
assessment while the
individual is in an
inpatient medical
acute care hospital is
the responsibility of
the MHP (or FFS if
applicable); the MHP
may require prior
authorization for the
assessment.
If the mental health
assessment finds that
admission for
inpatient psychiatric
hospital services is
indicated, the PIHP
must be contacted for
PAR. Authorization
and payment of the
PAR is the
responsibility of the
PIHP.
Payer responsible:
mixed - Inpatient
medical acute care
MHP/FFS, payment
for inpatient
psychiatric admission
PIHP
The PIHP’s
designated
screening unit
determines the
need for inpatient
mental health
services.
The PIHP
provides the
authorization for
mental health
inpatient
admission and is
responsible for
mental health
inpatient
admission costs
including
psychiatrists’ fees.
Payer
responsible:
PIHP
Nursing facilities complete the
Pre- admission Screening and
Annual Resident Review
(PASARR)
Mental health services provided
by the nursing facility staff, as
specified in the resident’s plan of
care, are included in the facility’s
per diem rate. Nursing facilities
must provide mental health,
intellectual/developmental disability
or related condition services that
are of lesser intensity than
specialized services to all
residents who need such services.
Payer responsible: MHP or FFS
based upon beneficiary
enrollment.
Page 144 of 148
Setting in Which Service is Provided
Outpatient Office
(FQHCs/RHCs/THCs,
Physician Office,
Psychiatrist,
Psychologist, Social
Worker)
Medical Emergency
Department
Mental Health Crisis
Center - Access and
Screening Center
Outpatient
Behavioral Health
(Crisis) Residential
Services
Outpatient
Substance Abuse
Office, Residential
Substance Abuse
Center or Sub-Acute
Detox Center
Including OTPs.
Inpatient Acute Care
Hospital (Medically
Managed)
Inpatient
Psychiatric
Hospital
(Excluding State
Psychiatric
Hospital
Services)
Nursing Facility
Mental Health Services to Individuals Who Have "Serious" Mental Illness.
NOTE: The authorization and payment responsibilities delineated in this row hold true regardless if the individual has concurrent I/DD or SUD.
The PIHP is
responsible for
services provided by
qualified providers
contracted with the
PIHP.
The MHP must
provide information to
the Enrollee regarding
the availability of
specialty behavioral
health services and
coordinate care as
appropriate.
Payer responsible:
PIHP
After medical
screening and
stabilization, if a
medical health
professional believes
that pre-screening for
inpatient psychiatric
hospital services is
indicated, or if the
need for specialty
supports is identified,
the ED should contact
the PIHP for a PAR.
Authorization and
payment for PAR are
the responsibility of
the PIHP. The PAR
may be conducted
telephonically or face-
to- face in the ED by
the PIHP.
The MHP/FFS is
responsible for
medical stabilization
treatment services for
individuals with
serious mental illness,
as determined by the
discharge diagnosis,
provided by
practitioners who are
not associated to a
PIHP.
Payer responsible:
mixed.
The PIHP is
responsible for
treating the individual
until the individual is
stabilized and no
longer meets the
criteria for serious
mental illness
treatment as outlined
in Medicaid policy.
Payer responsible:
PIHP
The PIHP is
responsible for
clinically managed
low-intensity
outpatient and
residential services
including but not
limited to clinically
managed high
intensity residential
services and
medically monitored
high intensity inpatient
services.
Mental health and
SUD services should
be coordinated with
the MHP—this is
especially true if the
individual has co-
occurring disorders
(mental health and
SUD).
Payer responsible:
PIHP
The PIHP is
responsible for
payment for services
provided by PIHP
contracted providers.
Payer responsible:
FFS or PIHP
depending upon
contract
arrangements.
Mental health
assessment while the
individual is in an
inpatient medical
acute care hospital is
the responsibility of
the MHP (or FFS if
applicable); the MHP
may require prior
authorization for the
assessment.
If the mental health
assessment finds that
admission for
inpatient psychiatric
hospital services is
indicated, the PIHP
must be contacted for
PAR. Authorization
and payment of the
PAR is the
responsibility of the
PIHP.
Payer responsible:
mixed - Inpatient
medical acute care
MHP/FFS, payment
for inpatient
psychiatric admission
PIHP
The PIHP
determines the
need for inpatient
mental health
services. The
PIHP provides the
authorization for
mental health
inpatient
admission and is
responsible for
mental health
inpatient
admission costs
including
psychiatrists’ fees.
Payer
responsible: PIHP
Specialized services are those
identified by the PASARR Level II
and are provided or arranged by
the PIHP. These services must be
available to nursing facility
individuals regardless of whether
they are identified and required by
the PASARR process, or whether
the individual is determined to
require additional services to be
provided or arranged for by the
State as specialized services.
Individuals with a primary
diagnosis of dementia are also
covered by this requirement, even
though the PASARR process
exempts individuals with a primary
diagnosis of dementia.
Specialized services are defined
as those mental health services for
residents who have a mental
illness, I/DD or related condition
which are 1) of greater intensity
than those normally required from
a NF, 2) provided in conjunction
with usual NF services, 3)
determined through the PASARR
process, 4) provided or arranged
for by the local CMHSP, OR
5) Result in the continuous and
aggressive
implementation of an individualized
plan of care.
Payer responsible: MHP or FFS
based upon
beneficiary enrollment.
Page 145 of 148
Setting in Which Service is Provided
Outpatient Office
(FQHCs/RHCs/THCs,
Physician Office,
Psychiatrist,
Psychologist, Social
Worker)
Medical Emergency
Department
Mental Health Crisis
Center - Access and
Screening Center
Outpatient
Behavioral Health
(Crisis) Residential
Services
Outpatient
Substance Abuse
Office, Residential
Substance Abuse
Center or Sub-Acute
Detox Center
Including OTPs.
Inpatient Acute Care
Hospital (Medically
Managed)
Inpatient Psychiatric
Hospital (Excluding
State Psychiatric
Hospital Services)
Nursing Facility
Substance Use Disorder Treatment Services
MAT services
provided by
practitioners enrolled
with or associated to a
PIHP are reimbursed
by the PIHP.
OBOT and OBAT
services provided by
practitioners not
enrolled with or
associated to a PIHP
are reimbursed FFS.
SUD services
provided in the office
setting (e.g., SBIRT)
by a practitioner not
enrolled with or
associated to a PIHP
are reimbursed by the
MHP or FFS based
upon beneficiary
enrollment.
FFS/MHP is
responsible for
ambulatory withdrawal
management.
If the patient is
admitted for acute
medical detoxification,
the ED costs are
rolled into the
inpatient DRG.
MAT services
provided by
practitioners enrolled
with or associated to a
PIHP are reimbursed
by the PIHP. MAT
services provided by
practitioners not
enrolled with or
associated to a PIHP
are reimbursed by
FFS.
Payer responsible:
PIHP
Payer responsible:
PIHP
The PIHP is
responsible for
clinically managed
and medically
monitored withdrawal
management in the
residential or licensed
outpatient program.
FFS/MHP is
responsible for
medically managed
intensive inpatient
acute detox and
associated potentially
life-threatening
substance-induced
toxic conditions
requiring acute
medical monitoring or
intervention and
detoxification services
in the acute care
setting. Services
include primary
medical and nursing
care services
including intensive
care services.
Payer Responsible:
MHP or FFS based
upon beneficiary
enrollment.
Payer responsible:
PIHP
Services rendered for the
treatment of alcohol and drug
abuse are an ancillary service
and are not included in the
facility’s per diem rate.
Payer Responsible: MHP or
FFS based upon beneficiary
enrollment.
Setting in Which Service is Provided
Outpatient Office
(FQHCs/RHCs/THCs,
Physician Office,
Psychiatrist,
Psychologist, Social
Worker)
Medical Emergency
Department
Mental Health Crisis
Center - Access and
Screening Center
Outpatient
Behavioral Health
(Crisis) Residential
Services
Outpatient
Substance Abuse
Office, Residential
Substance Abuse
Center or Sub-Acute
Detox Center
Including OTPs.
Inpatient Acute Care
Hospital (Medically
Managed)
Inpatient Psychiatric
Hospital (Excluding
State Psychiatric
Hospital Services)
Nursing Facility
Medical Services – Professional and Facility Services Including Diagnostic Tests
(e.g., Radiology and Laboratory Services Including Toxicology Screening)
Payer Responsible:
MHP or FFS based
upon beneficiary
enrollment and current
OBOT/OBAT policy
(MHP may require
authorization for non-
emergent care).
Payer Responsible:
MHP or FFS based
upon beneficiary
enrollment and
current OBOT/OBAT
policy (MHP may
require authorization
for post-stabilization
treatment).
Payer responsible:
PIHP
Payer responsible:
PIHP
Payer responsible:
PIHP
Payer Responsible:
MHP or FFS based
upon beneficiary
enrollment (MHP may
require authorization
for non-emergent
care).
PIHPs are
responsible for
costs related to
providing a
psychiatric
admission, history
and physical.
MHPs or FFS are
responsible for
medical services.
Ancillary services (defined
in the Nursing Facility
Chapter of the Medicaid
Provider Manual) should be
billed to the MHP or FFS
based upon beneficiary
enrollment.

Page 147 of 148
SCHEDULE G- LOCAL FUNDING OBLIGATION
SCHEDULE
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
Attachments to Schedule G: Local Funding Obligation Schedule include:
a. FY 2024 Local Funding Obligation Schedule.

Page 148 of 148
SCHEDULE H- BEHAVIORAL HEALTH CAPITATION
RATE CERTIFICATION
Contract No. MA
Prepaid Inpatient Health Plan (PIHP)
The Medicaid PEPM rates effective October 1 is included as follows. The actual number of Medicaid
beneficiaries will be determined monthly, and Contractor will be notified of the beneficiaries in their
service area via the pre-payment process.
Attachments to Schedule H: Behavioral Health Capitation Rate Certification include:
a.
State Fiscal Year 2024 Behavioral Health Capitation Rate Certification
b.
SFY 2024 Behavioral Health Entity Specific Factor Development
c.
SFY 2024 Behavioral Health Capitation Rate Certification Amendment
d.
April to September 2024 BH Capitation Rate Methodology
