NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
Carol Rees Parrish, MS, RDN, Series Editor
32 PRACTICAL GASTROENTEROLOGY • AUGUST 2022
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
The Overlap Between Eating Disorders
and Gastrointestinal Disorders
Theresa Hedrick, MS, RDN, LD
Registered Dietitian Nutritionist, Oregon
Nutrition Counseling, LLC, Corvallis, OR
Eating Disorders (EDs) have a direct physiological effect on the gastrointestinal (GI) tract and
microbiota, which can lead to GI dysfunction. Additionally, there is a higher prevalence of EDs among
individuals with disorders affecting the GI tract compared to those without GI disorders. Several
simple screening tools exist to help clinicians identify EDs and should be utilized before prescribing a
restrictive diet. If an ED is detected, connections to an ED-specialized registered dietitian nutritionist
and mental health provider should be facilitated. This article reviews the connection between eating
disorders and GI disorders as well as provides ways to identify and manage EDs in the GI population.
Theresa Hedrick
INTRODUCTION
I
deally, eating is a exible behavior that balances
internal needs (e.g., hunger and satiety cues,
food preferences, nourishment needs, etc.)
with external constraints (e.g., food availability,
personal schedule, acceptable social behavior, etc.).
It is generally a neutral to positive experience to the
person eating. Thoughts about desired foods and
meal planning are a part of daily life, but do not take
up a disproportionate amount of time relative to
other tasks. Disordered eating involves food-related
behaviors that have a negative physiological and/or
psychological impact, yet do not meet the criteria
for an eating disorder diagnosis. Examples include
rigid self-imposed rules around food, feelings of
anxiety, guilt or shame associated with eating,
frequent dieting, a preoccupation with food, a loss
of control around food, and restricting intake to
compensate for eating “bad” foods. The severity of
these behaviors exists along a continuum, and some
of these behaviors are socially acceptable despite
not being supportive of health. An eating disorder
(ED) is a specic severity of disordered eating
that meets the criteria outlined in the American
Psychiatric Association’s (APA) Diagnostic and

NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
The Overlap Between Eating Disorders and Gastrointestinal Disorders
PRACTICAL GASTROENTEROLOGY • AUGUST 2022 33
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
There is some evidence that gut microbiota
could have a role in the initiation and progression
of anorexia nervosa (AN) by acting on the gut-
brain axis to distort hunger and satiety cues,
alter brain function, and disrupt gut barrier
function.
18
Restricted food intake in AN may
contribute to dysbiosis by lowering microbial
diversity, decreasing butyrate-producing bacteria,
and increasing mucin-degrading bacteria.
12,18,20
Additional research is needed to further elucidate
the bidirectional relationship between AN and the
microbiota, examine the role of and effects on the
microbiota in other EDs, and investigate potential
microbiota-targeted interventions.
EDs can cause GI dysfunction as a direct
physiologic result of restricting food intake,
purging, or weight loss.
3,5,21
As the body is denied
essential nutrients, GI motility is slowed, and GI
hormone release is altered.
3,19
Esophageal motility
is usually unaffected in AN, but patients can have
dysphagia, heartburn, and regurgitation.
2,3,19,21
Delayed gastric emptying is common in AN and
bulimia nervosa (BN), as are complaints of early
satiety, postprandial fullness, epigastric discomfort,
bloating, and nausea.
2,3,19,21
There have been reports
of gastric bezoars and need for gastric dilation in
AN.
2,21
Gallstones have been reported in those with
signicant weight loss.
3
Lack of food intake can
cause a reduction in the absorptive surface area of the
small intestine,
3,21
altered nutrient and ion transport,
and increased permeability to macromolecules.
18
Delayed gut transit time is common in AN and
BN.
2,19,21
Superior mesenteric artery (SMA)
syndrome in AN has also been reported due to loss
of the mesenteric fat pad between the abdominal
aorta and the SMA.
2,3,19,21
Constipation is common
in AN and BN for a variety of reasons including
smooth muscle atrophy, electrolyte abnormalities,
delayed intestinal transit, sick euthyroid syndrome,
and pelvic oor dysfunction.
2,3,19,21
Hepatic injury
and noninammatory brotic injury to the pancreas
are possible due to malnutrition from AN.
2,21
All of
these symptoms will improve with refeeding.
2,3,5
Specic to BN where purging is done by
vomiting, it is common for individuals to experience
heartburn, spontaneous vomiting, regurgitation,
chest pain, dysphagia, and nocturnal aspiration
when lying supine due to weakening of the lower
esophageal sphincter.
2,3,19,21
Mallory-Weiss tears
Statistical Manual of Mental Disorders, Fifth
Edition (DSM-5).
1
The consequences of EDs can affect any body
system, with impacts on the gastrointestinal (GI)
tract being particularly prevalent.
2,3
Postprandial
fullness and abdominal distention are the most
common GI complaints among individuals with
EDs, followed by bloating, early satiety, abdominal
pain, nausea, constipation, heartburn, and gastritis.
3
EDs can occur before, during or after the onset of
GI symptoms.
4
Individuals with GI disorders are more likely
to display disordered eating than healthy controls;
5
those with irritable bowel syndrome (IBS) in
particular are more likely to engage in disordered
eating behaviors (missed meals, irregular mealtimes,
not eating when hungry, vomiting after eating)
than healthy controls.
7-9
Dietary restriction to
manage GI symptoms may be an expected adaptive
response in some patients given that up to 90% of
individuals with IBS attribute their GI symptoms
to certain foods.
10
It may also be a maladaptive
coping mechanism in others as the severity and
duration of IBS have been positively correlated
with the number of ED symptoms/characteristics
self-reported on a standardized questionnaire.
11
EDs have one of the highest mortality rates
of any psychiatric illness.
3,12
There are numerous
adverse physiological consequences of EDs;
psychological comorbidities such as self-harm and
suicide are common. Therefore, it is important to
consider EDs when managing GI patients. This
article reviews reasons GI conditions and EDs
overlap, as well as how to identify EDs in the GI
patient and intervene for those individuals.
Why Eating Disorders and GI Disorders Overlap
EDs may exacerbate pre-existing GI disorders.
There is evidence of an increased prevalence
of EDs compared to the general population in
individuals with conditions such as celiac disease,
Ehlers-Danlos syndrome, and postural orthostatic
tachycardia syndrome.
13-15
Associations have also
been seen between EDs and both food allergies
and inammatory bowel disease.
16,17
Once an ED
has developed, it can be difcult to discern which
symptoms are due to the concurrent disease state
versus the ED.
34 PRACTICAL GASTROENTEROLOGY • AUGUST 2022
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
The Overlap Between Eating Disorders and Gastrointestinal Disorders
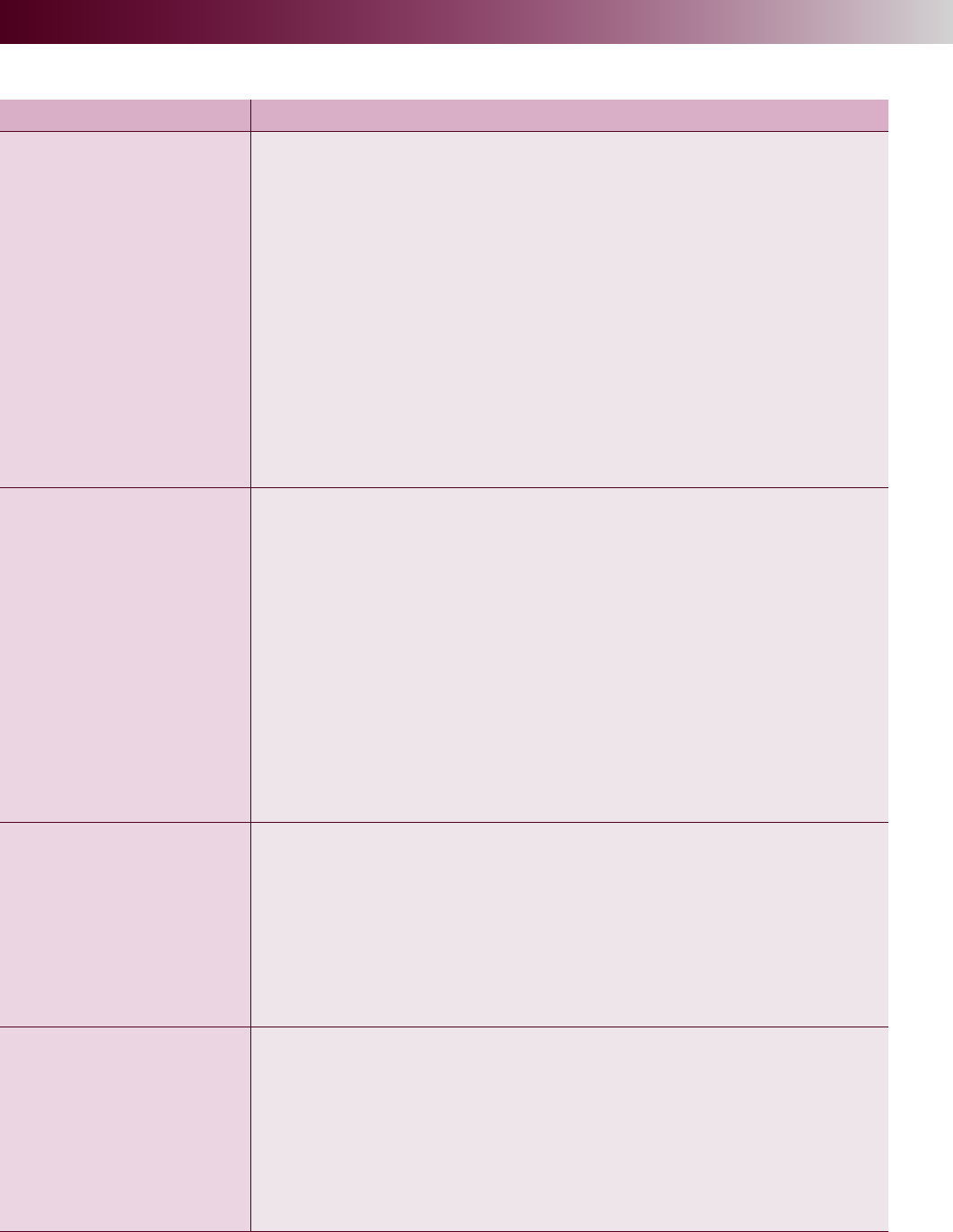
Table 1. GI Symptoms Associated with Eating Disorders
2,3,5,19,21,22
Eating Disorder Possible GI Symptoms
Anorexia Nervosa (AN)
·Dysphagia
·Heartburn
·Regurgitation
·Delayed gastric emptying
·Early satiety
·Postprandial fullness
·Epigastric discomfort
·Bloating
·Nausea
·Gastric bezoars
·Gallstones
·Delayed gut transit time
·Superior mesenteric artery syndrome
·Constipation
·Hepatic injury
·Pancreatic noninflammatory fibrotic injury
Bulimia Nervosa (BN)
·Delayed gastric emptying
·Early satiety
·Postprandial fullness
·Epigastric discomfort
·Bloating
·Nausea
·Heartburn
·Spontaneous vomiting
·Regurgitation
·Dysphagia
·Nocturnal choking when supine
·Mallory-Weiss tears
·Delayed gut transit time
·Constipation
·Rebound constipation & fluid retention with cessation of laxative abuse
Binge Eating Disorder
(BED)
·Heartburn
·Regurgitation
·Dysphagia
·Bloating
·Diarrhea
·Fecal urgency
·Fecal incontinence
·Non-alcoholic fatty liver disease
·Altered perception of satiety
Avoidant Restrictive Food
Intake Disorder (ARFID)
·Loss of appetite
·Dysphagia
·Esophagitis
·GERD
·Gastroparesis
·Gastritis
·Abdominal pain
·Nausea
·Constipation
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
PRACTICAL GASTROENTEROLOGY • AUGUST 2022 35
The Overlap Between Eating Disorders and Gastrointestinal Disorders
may occur
21
and individuals with BN may be at
risk for Barrett’s esophagus from frequent exposure
of esophageal mucosa to acidic emesis.
3,5
When laxatives are used to purge in BN, it
is common to see electrolyte abnormalities,
dizziness, and dehydration.
3,19,21
Individuals can
also experience rebound constipation and uid
retention (cathartic colon syndrome) if laxatives
are stopped.
3,19,21
In binge eating disorder (BED), binge
behavior can lower esophageal sphincter pressure,
exacerbating heartburn and regurgitation, while
the acid reux can potentially lead to dysphagia.
19
Other possible impacts of BED on the GI system
include bloating, diarrhea, fecal urgency, fecal
incontinence, non-alcoholic fatty liver disease,
and altered perception of satiety.
2,5,19,21
The most common GI complaints in those
with ARFID are nausea, constipation, loss of
appetite, and abdominal pain.
22
Dysphagia,
esophagitis, gastroesophageal reux disease
(GERD), gastroparesis, and gastritis have also been
reported.
22
See Table 1 for a list of GI symptoms
associated with each type of ED.
Recovery from an ED can also trigger GI
issues. When an individual increases their
energy intake after restricting food intake, it can
take weeks to months for their slowed motility
to return to normal depending on how quickly
the individual’s nutritional status and weight
are restored.
3,5
Because they are trying to eat an
increased amount with a slowed transit time,
they can experience early satiety, postprandial
fullness, abdominal pain/discomfort, bloating, and
distention. These symptoms are disconcerting to
the individual experiencing them. However, if they
continue to consume enough to meet their energy
needs despite the increase in GI symptoms, motility
will normalize, and symptoms will resolve. This
generally happens within a month of eating enough
to fully meet energy needs.
3
If the individual is
eating more than they used to, but is still in a
relative energy decit, this phase can be drawn out.
Screening for Eating Disorders
There are two validated screening tools to help
identify EDs for use in the primary and specialist
care settings: the Eating Disorder Screen for Primary
Care (ESP) and the Sick, Control, One, Fat, Food
(SCOFF) (Table 2).
23
These are not diagnostic;
rather, they indicate whether further investigation
is warranted. In general, 0-1 abnormal answers rule
out an ED. Two or more abnormal answers should
prompt a more complex assessment. In addition to
the screening tool questions, asking a patient to,
“Tell me about your relationship with food,” may
be helpful. If further information is needed, asking
hypothetical questions to the effect of, “Would
you be willing to eat more food if it resolved
(continued on page 43)
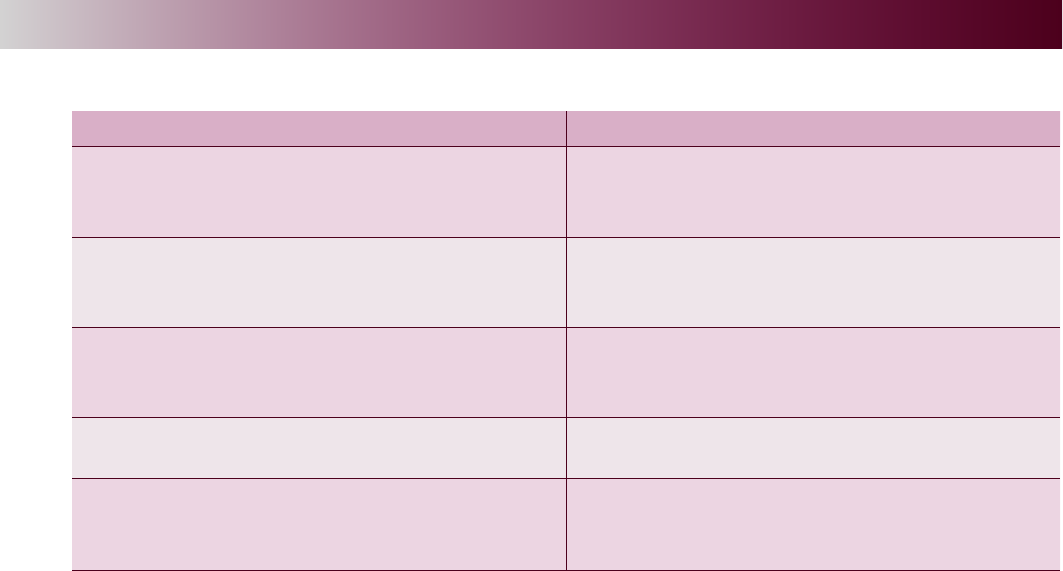
Table 2. Eating Disorder Screening Questions
23
ESP (Eating Disorder Screen for Primary Care) SCOFF (Sick, Control, One, Fat, Food)
• Are you satisfied with your eating
patterns? (A “no” to this question is
considered an abnormal response).
• Do you make yourself Sick because you
feel uncomfortably full?
• Do you ever eat in secret?
(A “yes” to this and all other questions
is considered an abnormal response).
• Do you worry you have lost Control over
how much you eat?
• Does your weight affect the way you
feel about yourself?
• Have you recently lost more than One
stone (14 lb or 7.7 kg) in a three-month
period?
• Have any members of your family suffered
with an eating disorder?
• Do you believe yourself to be Fat when
others say you are thin?
• Do you currently suffer with, or have you
ever suffered in the past with an eating
disorder?
• Would you say that Food dominates your
life?
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
The Overlap Between Eating Disorders and Gastrointestinal Disorders
PRACTICAL GASTROENTEROLOGY • AUGUST 2022 43
your GI symptoms?” or “Would you be willing
to gain weight if it resolved your GI symptoms?”
might also provide insight. Responses that express
rigidity, anxiety, shame, fear of judgement around
food, or an intense fear of weight gain may indicate
an ED. When determining if ED behaviors like
vomiting or laxative abuse are present, ask direct,
specic questions. Examples of these include,
“How often do you make yourself vomit?” and
“How often do you use laxatives when you are
not constipated?” Individuals with EDs may not
volunteer information about these behaviors.
Food-related fear and avoidance in individuals
with food intolerance are not always pathological.
However, if a patient is not distressed by multiple
dietary restrictions that would seem burdensome to
others, it may be a red ag. For example, restricting
dairy, wheat, and corn would eliminate many of the
foods Americans eat regularly and make it difcult
to consume an adequate balanced diet without a
tremendous amount of preplanning. If a patient
presented restricting those items, but did not feel
bothered by the inconvenience or limited choices,
it would be a red ag for an ED.
If a patient following a restrictive diet is
reluctant to reintroduce foods to their diet, it may
represent anxiety about the consequences of food
reintroduction or it may be a red ag for an eating
disorder. To elucidate, inquire about how restricting
is serving them. For a patient afraid of how the food
reintroduction may impact their quality of life or
activities of daily living, there may be a way to
work together and/or with a registered dietitian
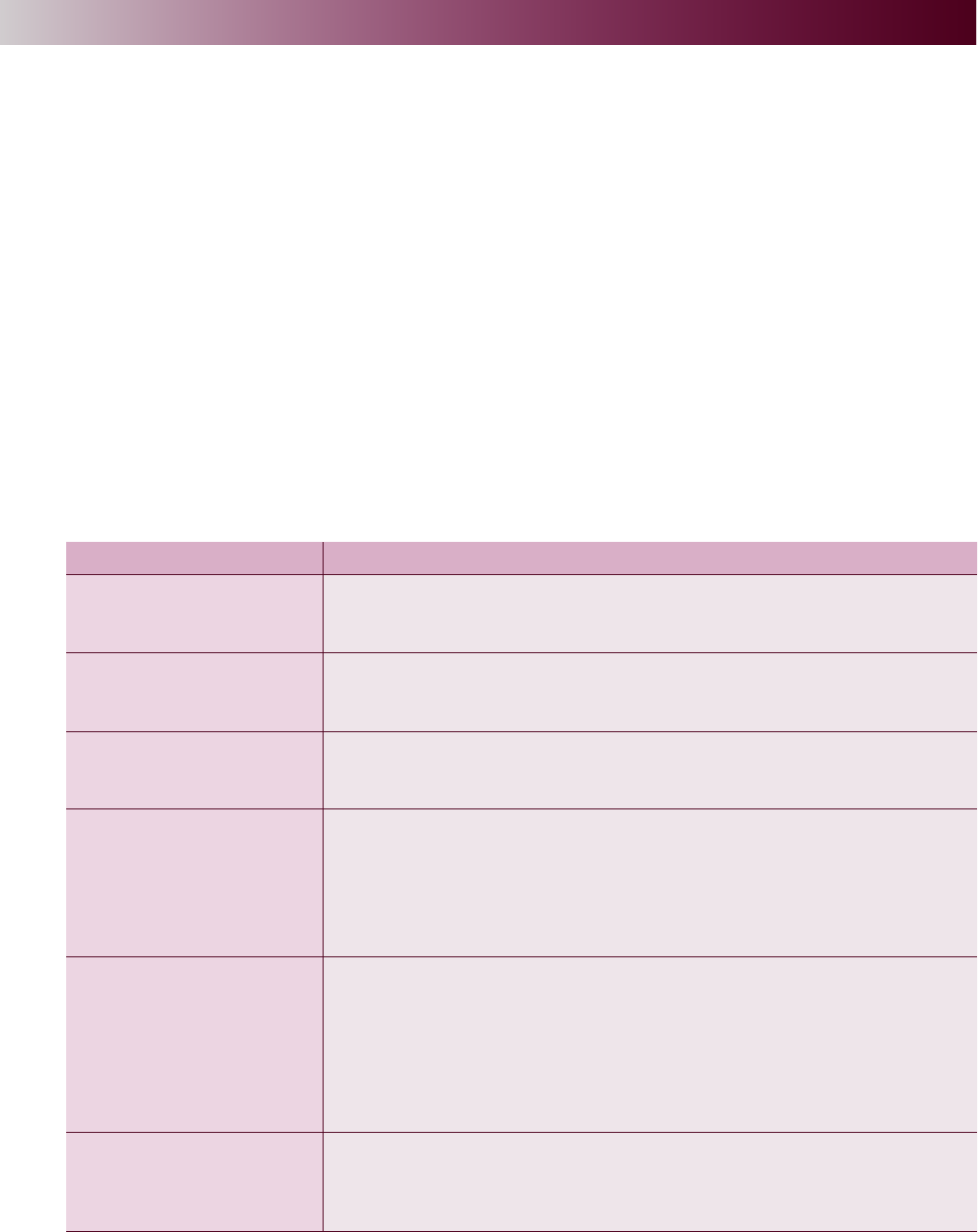
Table 3. Summary of Diagnostic Criteria for Eating Disorders
1,30
Eating Disorder Diagnostic Criteria
Anorexia Nervosa (AN)
·Restricted energy intake
·Intense fear of gaining weight
·Disturbance in the way weight/shape experienced
Bulimia Nervosa (BN)
·Episodes of binge eating
·Compensatory behavior to offset food intake
·Disturbance in the way weight/shape experienced
Binge Eating Disorder
(BED)
·Episodes of binge eating
·Marked distress about binge
·No compensatory behaviors
Avoidant Restrictive Food
Intake Disorder (ARFID)
Eating/feeding disturbance associated with ≥1 of the following:
·Significant weight loss (or failure to gain height or weight as expected in
children)
·Significant nutritional deficiency
·Dependence on enteral feeding or oral supplements
·Marked interference with psychosocial functioning
Other Specified Feeding or
Eating Disorders (OSFED)
(Previously Eating
Disorder Not Otherwise
Specified)
Behaviors do not meet the strict diagnostic criteria for one of
the other eating disorders, but are still significant including:
·Atypical Anorexia Nervosa
·Bulimia Nervosa of low frequency and/or limited duration
·Binge Eating Disorder of low frequency and/or limited duration
·Purging Disorder
·Night Eating Syndrome
Orthorexia*
·Pathological preoccupation with healthy eating
·Emotional consequences from non-adherence to self-imposed nutrition
rules
·Psychosocial impairment
*Not a separate diagnosis per the DSM-5. Considered an OSFED diagnosis.
(continued from page 35)

44 PRACTICAL GASTROENTEROLOGY • AUGUST 2022
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
The Overlap Between Eating Disorders and Gastrointestinal Disorders
the Diagnostic and Statistical Manual of Mental
Disorders (DSM–5).
1
EDs do not always fall neatly into categories.
For example, purging by vomiting does not
necessarily indicate bulimia nervosa; a diagnosis
of anorexia nervosa – binge/purge subtype might
be more tting. Being in a larger body does not
indicate binge eating disorder (BED); one could
have atypical AN. BN and BED are characterized
by objective binges, but individuals with AN may
report subjective binges.
What Clinicians Should Know
About Eating Disorders
The initiation of a weight loss diet can lead to the
development of an ED.
27
There is a lack of research
as to whether restrictive diets could precipitate a
similar progression, but a greater adherence to a
low-FODMAP diet has been associated with ED
behavior.
26
EDs do not have “a look.” Many individuals
with EDs fall within a normal BMI range.
5
Any ED
behaviors disclosed to a healthcare provider should
be taken seriously. Having ED behaviors dismissed
by a healthcare provider because the patient does
not appear thin enough may reinforce the ED and
delay treatment.
Individuals do not choose to have EDs.
28
There
is a strong genetic component to EDs inuenced
by hormonal, developmental, and environmental
pressures to initiate the illness.
28,29
Individuals
can choose to recover, but it is often not an easy
decision to come to or pursue for a multitude of
reasons such as resources, life circumstances,
ineffectiveness of prior treatment, and a lack of
availability of appropriate programs.
The duration of EDs is protracted, relapses are
common, and many individuals with EDs never
achieve recovery. If ED behaviors are lessened
but not fully resolved, the remaining ED behaviors
can continue to cause GI symptoms for the reasons
discussed earlier.
Individuals with EDs may knowingly or
unknowingly be looking for a physiological cause
of their symptoms. Both dismissing and repeatedly
evaluating GI complaints can have adverse effects
on ED recovery.
3
Ambivalence towards treatment is common in
EDs. The individual may recognize that their eating
nutritionist to empower them to partially or fully
liberalize their diet while mitigating the risks. For
example, if a patient is worried that reintroducing
a food could cause diarrhea while at work, the food
reintroduction trial could be done on the weekends
and/or the concerns could be offset with the use of
a medication or supplement. Or, if abdominal pain
is a primary complaint, implementing a medication
that lowers visceral hypersensitivity prior to
reintroducing foods might be helpful. Feeling
strongly about the need to keep the diet limited
without being able to give clear concrete reasons
as to why, or having an excessive fear of mild GI
consequences, may be suggestive of an ED.
Alternatively, reluctance to add foods back to
the diet may indicate an ED that is capitalizing on
a medically or socially acceptable reason to restrict
food. Making statements about being “healthy”
and adopting vegetarian or vegan diets are some
ways that people with EDs begin restricting in
socially acceptable ways.
24,25
A registered dietitian
nutritionist can conduct an in-depth assessment of
nutrition status and food-related behaviors when
a physician’s practice setting does not allow time
for detailed determination.
It is important to screen for ED risk before
further restricting an individual’s diet. It is generally
not recommended to initiate an elimination diet in a
patient with an ED or a history of an ED. However,
there may be instances where it is appropriate to
guide a patient through a modied version of a
necessary diet, while emphasizing the non-food
interventions like psychoeducation, medications or
supplements (motility agents, prebiotics, probiotics,
herbal supplements, etc.), toilet positioning and
routine, hypnotherapy, psychotherapy, etc. This
is best done under the supervision of a registered
dietitian experienced in eating disorders. Continued
screening for EDs is prudent given the association
between restrictive diets and ED behaviors.
26
Prevention of EDs is more effective than treatment.
Diagnosing Eating Disorders
Table 3 shows a synopsis of the diagnostic criteria
for anorexia nervosa (AN), bulimia nervosa
(BN), binge eating disorder (BED), avoidant
restrictive food intake disorder (ARFID), other
specied feeding or eating disorders (OSFED), and
orthorexia. Full diagnostic criteria can be found in
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
PRACTICAL GASTROENTEROLOGY • AUGUST 2022 45
The Overlap Between Eating Disorders and Gastrointestinal Disorders
patterns are causing issues, but the ED-related
thoughts will minimize the size, scope, and impact
of those issues. For these reasons, the clinician may
need to provide psychoeducation on the connection
between food intake and the function of the GI tract
more than once. Due to minimization, individuals
with EDs may have difculty following through on
scheduling recommended appointments with ED-
specialized providers. Assisting them in making
the appointments can be helpful.
The best chances of ED recovery are when
intervention is early and aggressive. The optimal
treatment of an ED involves the individual
concurrently seeing a registered dietitian
nutritionist, mental health provider, and physician,
all who specialize in treating EDs.
CONCLUSION
In summary, EDs have direct physiological effect
on the GI tract and microbiota. Several screening
tools exist to help clinicians detect EDs and should
be used prior to prescribing a restrictive diet. If an
ED is suspected, refer the patient to a registered
dietitian nutritionist and a mental health provider
who specialize in EDs and coordinate care. Several
ED professional groups have provider directories
to assist in locating nearby ED specialists (see
Table 4).
References
1. American Psychiatric Association. Feeding and Eating
Disorders. In: Diagnostic and statistical manual
of mental disorders, 5th ed. American Psychiatric
Association Publishing, Arlington, Virginia. 2013.
2. Hetterich L, Mack I, Giel KE, et al. An update on
gastrointestinal disturbances in eating disorders. Mol
Cell Endocrinol. 2019;497:110318.
3. Mehler PS. Gastrointestinal Complications. In: Mehler
PS, Andersen AE ed. Eating Disorders, 3rd Edition.
Johns Hopkins University Press, Baltimore, Maryland.
2017;126-142.
4. Salvioli B, Pellicciari A, Iero L, et al. Audit of digestive
complaints and psychopathological traits in patients
with eating disorders: A prospective study. Dig Liver
Dis. 2013;45(8):639-644.
5. McGowan A, Harer KN. Irritable Bowel Syndrome
and Eating Disorders: A Burgeoning Concern
in Gastrointestinal Clinics. Gastroenterol Clin North
Am. 2021;50(3):595-610.
6. Satherley R, Howard R, Higgs S. Disordered eating
practices in gastrointestinal disorders. Appetite.
2015;84:240-250.
practicalgastro.com
Visit our Website:
PRACTICALPRACTICAL
GASTROENTEROLOGYGASTROENTEROLOGY
Table 4. Resources for Clinicians
Websites
National Eating Disorder Association (NEDA): nationaleatingdisorders.org
The Academy for Eating Disorders (AED): aedweb.org
International Association of Eating Disorder Professionals (IAEDP): iaedp.com
Books
Eating Disorders: A Comprehensive Guide to Medical Care and Complications
4th Edition 2022; edited by Mehler and Andersen
Winning the War Within: Nutrition Therapy for Clients with Eating Disorders
3rd Edition 2020 by Myers ES, Caperton-Kilburn C. Helm Publishing, Inc.
Nutrition Counseling in the Treatment of Eating Disorders
2nd Edition 2013 by Herrin and Larkin
46 PRACTICAL GASTROENTEROLOGY • AUGUST 2022
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
The Overlap Between Eating Disorders and Gastrointestinal Disorders
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #224
7. Bavani NG, Hajhashemy Z, Saneei P, et al. The
relationship between meal regularity with Irritable
Bowel Syndrome (IBS) in adults. Eur J Clin Nutr. 2022.
8. Okami Y, Kato T, Nin G, et al. Lifestyle and
psychological factors related to irritable bowel
syndrome in nursing and medical school students. J
Gastroenterol. 2011;46(12):1403-10.
9. Reed-Knight B, Squires M, Chitkara DK, et al.
Adolescents with irritable bowel syndrome report
increased eating-associated symptoms, changes in
dietary composition, and altered eating behaviors:
a pilot comparison study to healthy adolescents.
Neurogastroenterol Motil. 2016;28(12):1915-1920.
10. Hayes P, Corish C, O’Mahony E, et al. A dietary survey
of patients with irritable bowel syndrome. J Hum Nutr
Diet. 2014;27(Suppl 2):36-47.
11. Kayar Y, Agin M, Dertli R, et al. Eating disorders in
patients with irritable bowel syndrome. Gastroenterol
Hepatol. 2020;43(10):607-613.
12. Voderholzer U, Haas V, Correll CU, et al. Medical
management of eating disorders: an update. Curr Opin
Psychiatry. 2020;33(6):542-553.
13. Nikniaz Z, Beheshti S, Farhangi MA, et al. A systematic
review and meta-analysis of the prevalence and odds of
eating disorders in patients with celiac disease and
vice-versa. Int J Eat Disord. 2021;54(9):1563-1574.
14. Baeza-Velasco C, Lorente S, Tasa-Vinyals E, et
al. Gastrointestinal and eating problems in women
with Ehlers–Danlos syndromes. Eat Weight Disord.
2021;26:2645–2656.
15. Benjamin J, Sim L, Owens MT, et al. Postural
Orthostatic Tachycardia Syndrome and Disordered
Eating: Clarifying the Overlap. J Dev Behav Pediatr.
2021;42(4):291-298.
16. Jafri S, Frykas TL, Bingemann T, et al. Food Allergy,
Eating Disorders and Body Image. J Affect Disord.
2021;6.
17. Ilzarbe L, Fabrega M, Quintero R, et al. Inammatory
Bowel Disease and Eating Disorders: A systematized
review of comorbidity. J Psychosom Res. 2017;102:47-
53.
18. Lam YY, Maguire S, Palacios T, et al. Are the Gut
Bacteria Telling Us to Eat or Not to Eat? Reviewing
the Role of Gut Microbiota in the Etiology,
Disease Progression and Treatment of Eating
Disorders. Nutrients. 2017;9(6):602.
19. Santonicola A, Gagliardi M, Pier Luca Guarino M,
et al. Eating Disorders and Gastrointestinal Diseases.
Nutrients. 2019;11(12):3038.
20. Di Lodovico L, Mondot S, Doré J, et al. Anorexia
nervosa and gut microbiota: A systematic review
and quantitative synthesis of pooled microbiological
data. ProgNeuro-Psychopharmacol Biol Psychiatry.
2021;106.
21. Bern EM, Woods ER, Rodriguez L. Gastrointestinal
Manifestations of Eating Disorders. J Pediatr
Gastroenterol Nutr. 2016;63(5):e77-e85.
22. Cooper M, Collison AO, Collica SC, et al.
Gastrointestinal symptomatology, diagnosis, and
treatment history in patients with underweight
avoidant/restrictive food intake disorder and anorexia
nervosa: Impact on weight restoration in a meal-
based behavioral treatment program. Int J Eat Disord.
2021;54(6):1055–1062.
23. Cotton MA, Ball C, Robinson P: Four Simple Questions
Can Help Screen for Eating Disorders. J Gen Intern
Med. 2003;18(1):53–56.
24. Sergentanis TN, Chelmi M-E, Liampas A, et al.
Vegetarian Diets and Eating Disorders in Adolescents
and Young Adults: A Systematic Review. Children.
2021;8(1):12.
25. Zickgraf HF, Hazzard VM, O’Connor SM, et
al. Examining vegetarianism, weight motivations,
and eating disorder psychopathology among college
students. Int J Eat Disord. 2020;53:1506-1514.
26. Mari, A, Hosadurg D, Martin L, et al. Adherence with
a low-FODMAP diet in irritable bowel syndrome: are
eating disorders the missing link? Eur J Gastroenterol
Hepatol. 2019;31(2):178-182.
27. Memon AN, Gowda AS, Rallabhandi B, et al. Have
Our Attempts to Curb Obesity Done More Harm Than
Good?. Cureus. 2020;12(9):e10275.
28. Steiger H, Booij L. Eating Disorders, Heredity and
Environmental Activation: Getting Epigenetic Concepts
into Practice. J Clin Med. 2020;9(5):1332.
29. Frank GKW, Shott ME, DeGuzman MC. The
Neurobiology of Eating Disorders. Child Adolesc
Psychiatr Clin N Am. 2019;28(4):629-640.
30. Bartel SJ, Sherry SB, Farthing GR, et al. Classication
of Orthorexia Nervosa: Further evidence for placement
within the eating disorders spectrum. Eat Beha. 2020;38.
EP IGENETIC SIT
P
N M X C V P H
INUL IN
MOTILITY
T
SET N N S C M
HEED
CELIAC AGE
E
U CUE U
LURE PRE GROWTH
I
E D O I A E
AUTO IMMUNE
DR
IP
L C U A D B E A
CHART BEAUMONT
F N TAX F P I
SCHLAFEN
AFFE
CT
I E LEA P E N I
PINT
D FIBRO
SIS
12345 67
8
91011
12 13
14 15 16 17 18
19
20 21 22 23 24
25 26
27 28 29
30
31 32
33
34 35 36 37
38 39
40 41
Answers to this month’s crossword puzzle:
