
APPENDIX A
https://www.congress.gov/115/plaws/publ182/PLAW-115publ182.pdf
APPENDIX B
1
MISSION Act Section 507: Medical Scribe Pilot Program
Training Manual
Revised June 2020
Medical Scribe Points of Contact:
- Katherine Williams, MPH, Health Systems Specialist
Katherine.Williams[email protected]
- Michael Davies, MD, Senior Medical Advisor
- Amanda Lyn, MPH, Contractor, Office of Veterans Access to Care
- Cathy Potts, MT (ASCP), Health Systems Specialists, Clinical Application Coordinator
- Donna Richardson (HOU), National Transformational Coach Captain
Donna.Richardson2@va.gov
- Donna Richardson (HAMPTON), National Transformational Coach Captain
Donna.Richardson5@va.gov

2
Table of Contents
Medical Scribe Points of Contact:.................................................................................................................................. 1
I. Purpose ....................................................................................................................................................................... 4
II. Background ................................................................................................................................................................ 4
A. Medical Scribes ..................................................................................................................................................... 5
III. Definitions ................................................................................................................................................................ 6
IV. Scribe Pilot Process ................................................................................................................................................ 10
A. Scribe Pilot Process ............................................................................................................................................. 10
B. Example Ramp Up Schedule for MISSION 507 Medical Scribes: ......................................................................... 13
C. Pilot Site Program Implementation Checklist ..................................................................................................... 13
D. Medical Scribe Onboarding Checklist ................................................................................................................. 14
V. Scribe Trainings and Orientation ............................................................................................................................. 14
VI. Policies and Procedures ......................................................................................................................................... 15
A. Policies and Procedures ............................................................................................................................. 15
B. Progress Notes ........................................................................................................................................... 16
C. Orders ........................................................................................................................................................ 17
Definition ................................................................................................................................................... 18
D. Orthopedics Orders Recommended ................................................................................................................... 18
E. Emergency Department Orders Recommended ................................................................................................ 19
F. Cardiology Orders Recommended ..................................................................................................................... 20
VII. Documentation ..................................................................................................................................................... 20
A. Tips and Guidelines for Excellent Clinic Notes .................................................................................................... 20
B. Copy and Paste Guidelines .................................................................................................................................. 21
C. Progress Note Critical Components .................................................................................................................... 22
1. Chief Complaint(s) ................................................................................................................................. 22
2. History ................................................................................................................................................... 23
3. Physical Examination (PE) and Test Results ........................................................................................... 23
4. Assessment for each problem evaluated/treated ................................................................................. 23
5. Treatment Plan ...................................................................................................................................... 23
VIII. Consultation Guidelines ....................................................................................................................................... 24
IX. Data Capture Tips ................................................................................................................................................... 25
X. Reference Materials ................................................................................................................................................ 26
3
A. Evaluation and Management (E/M) ................................................................................................................... 26
B. Examples of E/M Services Documentation Requirements ................................................................................. 27
XI. Service Connected and Treatment Factors ............................................................................................................ 29
A. Service Connected (SC) Determinations ............................................................................................................. 30
B. Combat Veteran .................................................................................................................................................. 31
C. Agent Orange ...................................................................................................................................................... 32
D. Ionizing Radiation ............................................................................................................................................... 34
E. Southwest Asia Conditions .................................................................................................................................. 35
F. Shipboard Hazard and Defense (SHAD)/Project 112 ........................................................................................... 37
G. Military Sexual Trauma (MST) ............................................................................................................................ 38
H. Head and Neck Cancer ........................................................................................................................................ 38

4
MISSION 507: Medical Scribe Pilot
I. Purpose
The purpose of the MISSION Act Section 507: Medical Scribe Pilot Program Training Manual is
to provide a comprehensive reference document for both Medical Scribes and their respective
facility’s teams in order to facilitate a smooth implementation of the medical scribe pilot at
their facility.
II. Background
Medical scribes are intended to take the burden of interacting with the computer off the
shoulders of the physician or Licensed Independent Practitioner (LIP) so these clinicians can
focus on diagnosis and treatment during the visit. Scribes are popular with some non-VA
practices in part because they allow clinicians to see more patients during their day. Congress
is asking VA to pilot scribes in VA to study the potential benefits and costs. The results of this
pilot will inform future VA policy.
The main role of scribes is to provide documentation assistance to a physician or LIP. The scribe
listens and records relevant information from the discussion between the clinician and patient
per the direction of the clinician. This information, while documented by the scribe, is the
clinician record for all medical purposes. The clinician is ultimately responsible and must
review, edit, and ultimately verify the record.
The Medical Scribe Pilot is authorized by law as documented in Section 507 of the VA
Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act.
Section 507 states “The Secretary of Veterans Affairs shall carry out a 2-year pilot program
under which the Secretary shall increase the use of medical scribes at Department of Veterans
Affairs (VA) medical centers”. The scribe program will be implemented at 12 medical centers of
the Department with the following criteria:
1. At least four such medical centers located in rural areas
2. At least four such medical centers located in urban areas
3. Two such medical centers located in areas with need for increased access or
increased efficiency, as determined by the Secretary
5
The following sites have been chosen to participate in the MISSION 507 Medical Scribe Pilot:
1. Oklahoma City Healthcare System (Oklahoma City, OK)
2. VA New Jersey Healthcare System (East Orange, NJ)
3. Fargo VA Hospital (Fargo, ND)
4. Clarksburg VA Medical Center (Clarksburg, WV)
5. Southern Arizona VA Healthcare System (Tucson, AZ)
6. Louisville VA Medical Center (Louisville, KY)
7. Hampton VA Medical Center (Hampton, VA)
8. South Texas Veterans Healthcare System (San Antonio, TX)
9. Togus VA Medical Center (Augusta, ME)
10. Montana VA Healthcare System (Fort Harrison, MT)
11. Department of Veterans Affairs Manchester Medical Center (Manchester, NH)
12. Olin E. Teague Veterans Medical Center (Temple, TX)
A. Medical Scribes
As part of the pilot program, four scribes will be assigned to each of the 12 pilot sites. Two of
the medical scribes will be hired as Department of Veterans Affairs term employees and the
remaining two will be provided by a VA Contract. Thus, each site will have two VA employee
scribes and two contract scribes. Two medical scribes will be assigned to one physician, and/or
LIP at each facility. According to the MISSION Act Section 507, thirty percent of the medical
scribes shall be employed in the provision of emergency care and seventy percent of medical
scribes shall be employed in the provision of specialty care in specialties with the longest
patient wait times or lowest efficiency ratings, as determined by the Secretary. For this pilot,
sites will have their scribes assigned to either the Emergency Department (ED), or Cardiology
and/or Orthopedic clinic
Medical Scribes (both VA employee and contract) will work directly with their assigned
physician and/or LIP to assist in medical documentation and any of the below duties:
1. Transcribing information into the electronic health record, as directed by physician
and/or LIP, during the patient visit
2. Record diagnostic results such as radiology interpretations and lab values, enter
medication orders, physical therapy orders, home exercises, educational handouts,
work restrictions and other orders per LIP instruction
6
3. Assisting the physician and/or LIP in navigating the health record and gathering
necessary information when directed
4. Researching additional information, as directed by the physician and/or LIP, for use
in coordinating referrals
5. Preparing reports, responding to messages, and other clerical tasks as directed by
the physician and/or LIP
6. Ensuring records are accurate, complete and reviewed for spelling, grammar, and
sequential order before review by the Treatment Team
7. Ensuring up-to-date record movement control and accountability through record
tracking in the health record
8. Ensuring forms are accurate and signed by appropriate individuals for request and
release. Requesting records from VA and non-VA facilities as directed by the
Treatment Team
9. Ensuring medical documentation complies with Joint Commission and other
accreditation body requirements
10. Using knowledge of qualitative and quantitative data collection methods to improve
the health records system by ensuring proper workload credit and statistical
information is maintained
III. Definitions
Scribes must know the meaning of a variety of medical terms in order to perform their
duties. Some of these terms include:
Adjunct Condition: although not service connected, is medically determined to be
associated with or is aggravating a disease or condition, which is service connected.
Agent Orange: is an herbicide that was used in Vietnam between 1962 and 1971 to remove
unwanted plant life that provided cover for enemy forces.
Chief Complaint: is a concise statement describing the symptom, problem, condition,
diagnosis, or other factor that is the reason for the encounter, usually stated in the patient’s
words.
Combat Veterans: served on active duty in a theater of combat operations during a period of
war after the Persian Gulf War or in combat against a hostile force during a period of hostilities
after November 11, 1998.

7
Consultation: is a type of service provided by a physician and/or LIP whose opinion or advice
regarding evaluation and/or management of a specific problem is requested by another
physician or other appropriate source.
Diagnosis: is the identity of a medical condition, cause or disease.
Encounter: is a professional contact between a patient and a clinician vested with primary
responsibility for diagnosing, evaluating, and/or treating the patient’s condition.
Encounter documents contain information needed for workload reporting (workload
ultimately funds the facility) and patient or insurance billing.
Family History: Record of health information about a person and his or her close relatives. A
complete record includes information from three generations of relatives, including children,
brothers and sisters, parents, aunts and uncles, nieces and nephews, grandparents, and
cousins.
1
A review of medical events in the patient’s family, including diseases that may be
hereditary or place the patient at risk.
History of Present Illness (HPI): is a chronological description of the development of the
patient’s present illness from the first signs and/or symptom or from the previous
encounter to the present. It includes the following elements:
• Location
• Quality
• Severity
• Timing
• Duration
• Context
• Modifying Factors
• Associated Signs and Symptoms
Medical Decision Making: Evaluation and Management (E/M) service levels are
documented on the encounter form and include four types of medical decision-making
services: straight-forward, low complexity, moderate complexity and high complexity.
Medical decision is one component involved in picking and E/M code which considers the
1
“Why Is It Important to Know My Family Medical History? - Genetics Home Reference - NIH.” U.S. National Library
of Medicine, National Institutes of Health, ghr.nlm.nih.gov/primer/inheritance/familyhistory.

8
complexity of establishing a diagnosis and/or selecting a management option as measured
by:
• The number of possible diagnoses and/or the number of management options
that must be considered.
• The amount and/or complexity of health records, diagnostic tests, and/or other
information that must be obtained, reviewed and analyzed; and
• The risk of significant complications, morbidity and/or mortality, as well as
comorbidities, associated with the patient’s presenting problem(s), the diagnostic
procedure(s) and/or the possible management options.
Medical Necessity: is defined as tests and services that are determined to be reasonable
and necessary. Documentation supporting diagnosis codes assigned for procedures
performed must be maintained in the record and be legible. Physicians must provide the
specific symptom, sign or diagnosis at the time the service is ordered.
Military Sexual Trauma (MST): Sexual trauma experienced while on active duty in the
military or while in active duty for training status. Sexual trauma is defined as sexual
harassment, sexual assault, rape and/or other acts of violence. Sexual harassment is further
defined as repeated unsolicited, verbal or physical contact of a sexual nature, which is
threatening in nature.
Operation Enduring Freedom (OEF)/Operation Iraqi Freedom (OIF): The Global War on
Terror (GWOT) includes Operation Enduring Freedom (OEF) and Operation Iraqi Freedom
(OIF); these have been ongoing conflicts since October 2001.
Outpatient Visit: Any visit made to a hospital outpatient department, or hospital unit
providing health and medical services to individuals who receive services but do not require
hospitalization overnight. (Note: definition adapted from reference 2 below)
2
Past, Family and/or Social History (PFSH): consists of a review of three areas:
• Past History
• Family History
• Social History
2
Healthcare Research. Medical Expenditure Panel Survey Topics,
meps.ahrq.gov/mepsweb/data_stats/MEPS_topics.jsp?topicid=38Z-1.
9
Past History: The patient’s past major illnesses, injuries, operations, hospitalizations,
current medications, allergies, age appropriate immunizations status, and age appropriate
dietary status.
Provider: is a person or organization that furnishes health care to a consumer and bills or is
paid for the health care in the normal course of business. This includes a professionally
licensed practitioner who is authorized to operate in a health care delivery facility.
Review of Systems (ROS): is an inventory of body systems obtained through a series of
questions seeking to identify signs and/or symptoms which the patient may be experiencing or
has experienced. For purposes of ROS, the following systems are recognized:
• Constitutional (fever, weight loss)
• Eyes
• Ears, Nose, Mouth, Throat
• Cardiovascular
• Respiratory
• Gastrointestinal
• Genitourinary
• Musculoskeletal
• Integumentary (skin, breast)
• Neurological
• Psychiatric
• Endocrine
• Hematologic/Lymphatic
• Allergic/Immunologic
Shipboard Hazard and Defense (SHAD)/Project 112: Program for both shipboard and
land-based biological and chemical testing that was conducted by the United States (U.S.)
military between 1962 and 1973.
Service Connected: VBA determination (rating) that a Veteran’s illness or injury was incurred in
or aggravated by military service.

10
Social History: An age appropriate review of past and current activities (such as marriage or
living arrangements, employment history, use of drugs, alcohol and tobacco, education,
sexual history and other related relevant social factors).
VA Video Connect (VVC): VA Video Connect allows Veterans and their caregivers to quickly and
easily meet with VA health care providers through live video on any computer, tablet, or mobile
device with an internet connection.
IV. Scribe Pilot Process
A. Scribe Pilot Process
For MISSION 507, each facility will employ in total, four scribes with two physicians and/or LIPs
participating in the pilot. Each physician and/or LIP will be assigned two scribes, one VA
employee scribe and one Contractor scribe. Effective incorporation of scribes into clinic
processes requires a clear understanding of the roles, processes, and tasks. The best resulting
system has the clinician (the most expensive resource) as the “constraint” or rate-limiting step
for clinic flow. This means the clinician must be maximally used in performing patient care
working at the top of their licensure and competency for as much of the day as possible. Below
is a potential clinic process flow for one physician and/or LIP, one VA or contractor scribe.
Two Rooms:
1. It is ideal for each practice (defined as 1 physician and/or LIP, 1 VA employee scribe,
and 1 Contractor scribe) to use two exam rooms for maximal efficiency. In this
model, one scribe is assigned to each exam room.
2. The physician and/or LIP will alternate between the two exam rooms seeing
patients.
While the physician and/or LIP is with VA employee scribe and patient in exam room
1, Contractor scribe will finish notes in exam room 2 from previous patient. As
physician and/or LIP is with Contractor scribe and patient in exam room 2, VA
employee scribe will finish notes in exam room 1 from previous patient.
Exam Room 1:
VA employee
scribe
Exam Room 2:
Contractor
scribe
Physician and/or LIP
moves between rooms
11
3. At the next break, physician and/or LIP reviews the scribes’ notes with the scribes.
Physician and/or LIP approves and signs.
One Room
If the practice (1 physician and/or LIP, 1 VA employee scribe, 1 Contractor scribe) only has
one room in which to work, it is possible that the room (not the clinician) could become the
constraint, or rate-limiting step in the clinic. Teams will have to be creative in designing the
clinic flow in this case and use the exam room for “only” things that need an exam room
and move as much of the other workflow outside the room. This scribe model will still
improve efficiency.
Below describes the process for one group (1 physician and/or LIP, 1 VA employee scribe,
and 1 Contractor scribe) using one room. Essentially, scribes (VA scribe and Contractor
scribe) will alternate between patients as the physician and/or LIP sees patients in one
exam room.
1. Physician and/or LIP and VA scribe will be with a patient in the exam room.
Meanwhile, the Contractor scribe will be outside of exam room finishing notes from
the previous patient.
2. When the physician and/or LIP is completed with the appointment, the VA employee
scribe, physician and/or LIP and patient will leave the room.
3. Follow regular procedures for prepping room and bringing in a new patient for their
appointment.
4. When exam room is ready and new patient is in the room, physician and/or LIP and
Contractor scribe enter room and complete appointment. Meanwhile, VA employee
Exam Room 1:
Physician and/or
LIP, VA Scribe,
and patient
Contactor Scribe
(outside of exam room)
Exam Room 1:
Physician and/or
LIP, Contactor
Scribe, and
patient
VA Scribe
(outside of exam room)
12
scribe will finish notes from previous patient outside of exam room.
5. Continue steps 1-4 (scribes alternating between patients) until physician has break
in clinic schedule.
6. At the next break, physician and/or LIP reviews the encounter notes with the
scribes. Physician and/or LIP approves and signs the note.
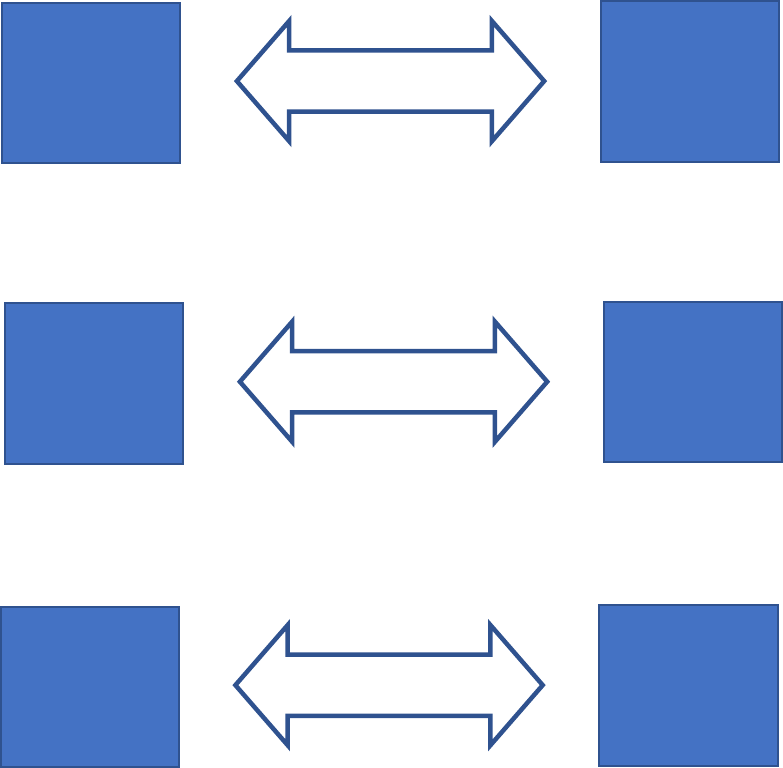
Virtual Scribe
There are several instances where the utilization of a virtual scribe could be accomplished.
Facilities with space constraints, provider/practice location and remote Veteran care are all
ideal situations where virtual scribing can be utilized.
Scenario 1: Provider and scribe together in the exam room at VA location and Patient is at a
remote location connecting via VVC on a computer or IOS app capable device.
Scenario 2: Patient and scribe are in an exam room at VA location and provider is at another VA
location.
Scenario 3: Provider and patient are in an exam room at a VA location and scribe is at a remote
location.
Provider and
scribe are at
the VA
Patient is at a
remote
location
All parties receive VVC
appointment invite
Scribe and
Patient at one
VA location
Provider at a
different VA
location
All parties receive VVC
appointment invite
Provider and
Patient at the
VA
Scribe is at a
remote
location
All parties receive VVC
appointment invite
13
Scenario 4: Provider, patient, and scribe are in different locations.
Emergency Room
Each facility will have some scribes available in the Emergency Room (ER). Consistent with the
principles above, ER teams must use the scribes to maximize the physician or LIP’s time.
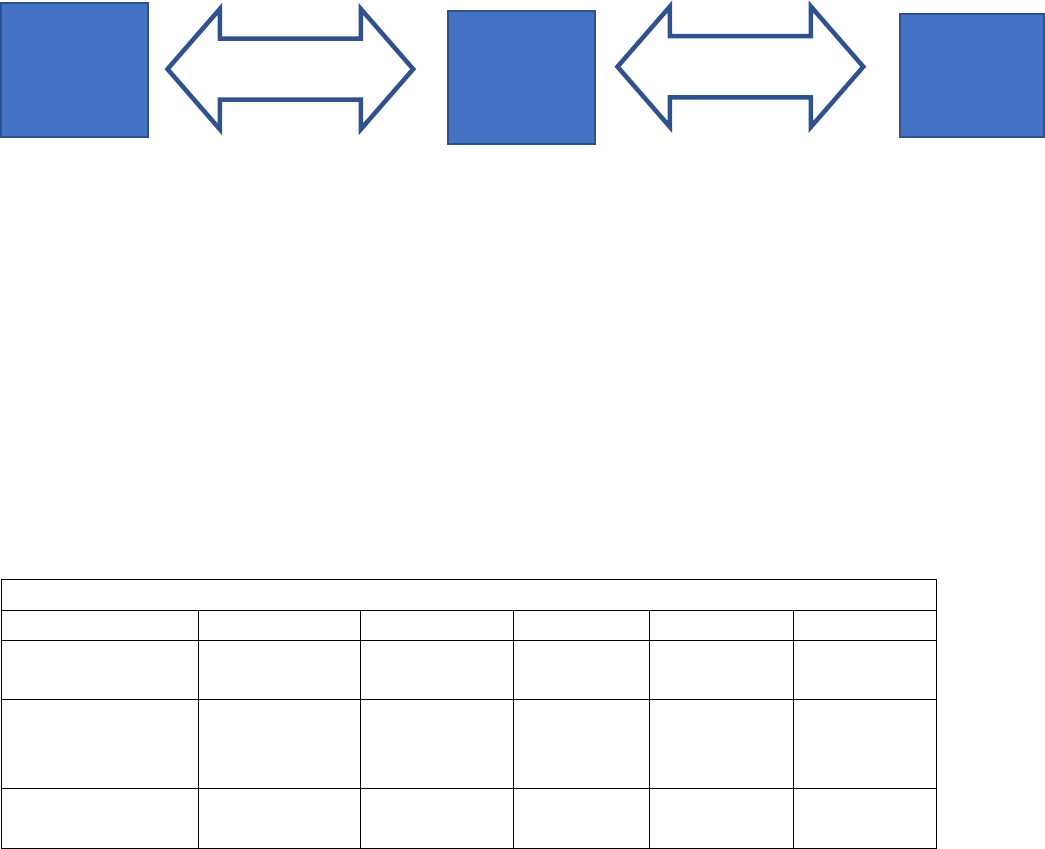
B. Example Ramp Up Schedule for MISSION 507 Medical Scribes:
Medical Scribes will need some time to gain confidence in their new position so it is expected
there will be ramp up period for them in terms of the number of patients seen per day. Please
do what works best for your facility, scribes and providers but below offers an example of a
schedule for a beginner medical scribe.
MISSION 507 Medical Scribe Beginner Schedule (Week 1)
Monday
Tuesday
Wednesday
Thursday
Friday
1 Provider
Patient #
14
14
14
14
14
VA Employee
Scribe
# of Patients/day
3
4
5
6
7
Contract Scribe
# of Patients/day
3
4
5
6
7
*** Please remember, this is just an example. Please adapt to whatever is best for your facility and provider
schedules
C. Pilot Site Program Implementation Checklist
The below checklist can be used by scribe pilot site administrators to ensure they have
completed all the necessary tasks prior to the arrival of their medical scribes for a successful
implementation of the medical scribe pilot:
Ensure all administrators and physicians/LIPs completed review and understand all
topics in Medical Scribe Training Manual
Provider is
at one
location
Scribe is a
different
location
All parties receive VVC
appointment invite
All parties receive VVC
appointment invite
Patient is
at another
location
14
Connected with local Systems Redesign Coordinator to develop current state and future
state process maps for facilitation of scribe into clinic flow
Ensure local facility CACs and local facility CPRS trainers completed quick order trainings
and are prepared to train scribes on how to enter notes and orders in CPRS
D. Medical Scribe Onboarding Checklist
The below checklist can be used by all medical scribes throughout their first weeks in the
position to ensure they have completed all onboarding tasks:
Completed VA New Hire Orientation (for VA medical scribes only)
Completed and understood concepts in Medical Scribe Training Manual
Completed CPRS training at the facility as a new employee
Met with facility CAC or CPRS trainer to learn how to enter notes and orders on CPRS
Obtained facility CAC or CPRS trainer contact information in case have further questions
on CPRS
Met with assigned Physician and/or LIP to discuss progress note template and other
general preferences
Received orientation of workspace and available equipment by scribe administrator or
Physician and/or LIP
Ensure understand ramp up schedule and number of patients seeing each day
V. Scribe Trainings and Orientation
Trainings to be offered by VA Central Office:
Trainings will be available on the MISSION 507 SharePoint:
Training Manual
The training manual developed by the OVAC MISSION 507 Medical Scribe Pilot team will cover
information on the overall pilot as well as documentation guidelines and tips for the medical
scribes.
Clinic Flow
Local Systems Redesign Coordinators will provide training on clinic flow and assist pilot sites
with developing current and future state flow maps to facilitate implementation of scribes into
clinic flow.
CPRS Order and Progress Note Trainings (Cardiology, Orthopedics and Emergency Department)
Training/Guide will be provided for Clinical Application Coordinators (CACs) to set up the
process in VistA/CPRS
15
Pilot sites’ Computerized Patient Record System (CPRS) trainers, CACs/Health Information
Management Service (HIMS), or other appropriate personnel will need to meet with the scribes
to train on entering the orders, notes, etc.
Trainings that should be conducted at Pilot Sites:
New Employee Orientation
All scribes will attend the mandatory New Employee Orientation conducted at their facility and
Training with facility CACs/CPRS trainers
Facility CACs/CPRS trainers are expected to meet with all scribes at pilot sites to discuss CPRS
and order entry and will act as a POC for scribes in the event they have further questions about
the Electronic Health Record (EHR).
Training with facility Systems Redesign or Improvement staff
Facilities should arrange time with the Systems Redesign staff to review the current state of
clinic flow and make adjustments to the new state, if possible.
Training with assigned Physicians and/or LIPs
Physicians and/or LIPs should review training manual and attend training manual presentation
to understand scribe pilot processes. It is also critical to remember that medical scribes (VA or
contract) cannot release orders. Providers and/or LIPs should work with their assigned scribes
through the clinic and documentation flow during their 1:1 training. Also, Physicians and/or LIPs
need to ensure there is time throughout their day to meet with the scribes, especially during
their first few weeks together, to review notes and help to build the scribe/provider
relationship. Physicians and/or LIPs should work together with their scribes during patient visits
such that the physician and/or LIP should organize the visit by following an agreed upon
documentation template so that the scribe knows where to input information.
Medical Record Documentation Guide for Scribing
VI. Policies and Procedures
A. Policies and Procedures
Each facility should have a policy/procedure regarding processes associated with scribes. Per
guidance from The Joint Commission, (reference: Perspectives Newsletter, August 2018,
Volume 38, Issue 8 – The Official Newsletter of The Joint Commission.)
The documentation should include:
16
• Support the use of scribes and performance of scribing actions
• Scribes enter information in the electronic health record (EHR) or chart, as
directed by a physician or Licensed Independent Practitioner (LIP).
• All documentation must be reviewed, edited, and submitted by the LIPs who will
be responsible for the content of the progress notes, orders, and other
documentation.
• Progress notes will not be viewable in CPRS prior to review, verification, editing,
and signature by the provider.
• All orders entered by personnel who are not authorized to submit orders should
be entered in CPRS entering the ordering provider’s name and held for signature
by the provider. The provider will review and submit the orders only after
verification.
• Transcribing orders in CPRS is NOT considered a verbal order.
• Scribes must use proper log-in procedures – such as prohibition of
documentation assistants from using the physician or LIP’s log-in
• An example policy is located on the MISSION Act Pilot SharePoint:
https://vaww.vha.vaco.portal.va.gov/sites/DUSHOM/10NA/ACAO/MISSION507/
Hiring%20Resources/Policy
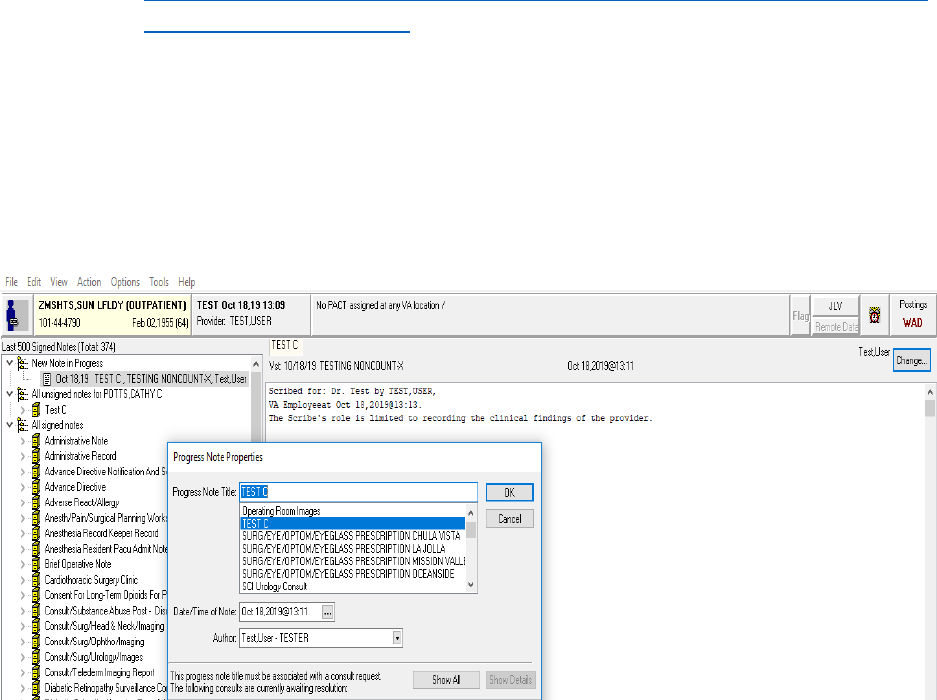
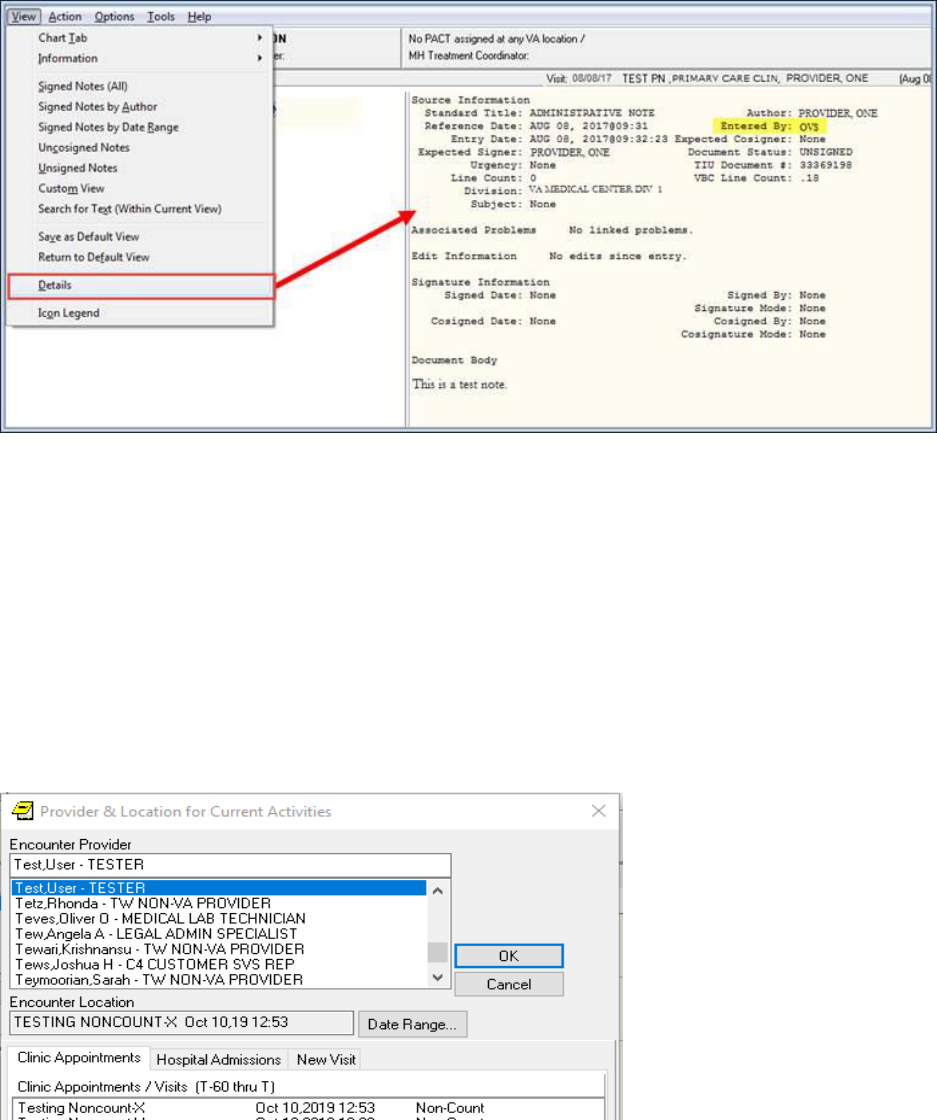
B. Progress Notes
When writing a progress note, once the scribe has entered all information in the note, the
scribe is to change the author’s name from the scribe’s own name to the physician or LIP for
this patient visit. This is performed on the CPRS notes Tab, as shown in Figure 1 below. The LIP
will then be displayed as the Author of the note.
Figure 1:
17
To serve as an audit trail, the scribe’s initials will appear in the “Entered by” field of the
document when displaying the details of the document as shown below in Figure 2.
Figure 2:
It is crucial that the scribe utilizes a templated progress note provided by the provider so that
the communications during the patient visit will be easier to document in the note. The note
may also contain data objects that automatically pull in laboratory or radiology results,
medications, etc. that will simplify the documentation.
C. Orders
Orders for non-clinical scribes should be set up to automatically accept orders to avoid clinical
decisions. The scribe should enter the order by entering the provider’s name in the Encounter
Provider. When the scribe clicks on the Orders Tab, and selects an order on a menu, the
provider name will need to be selected on the Provider & Location for Current Activities and
then click OK.
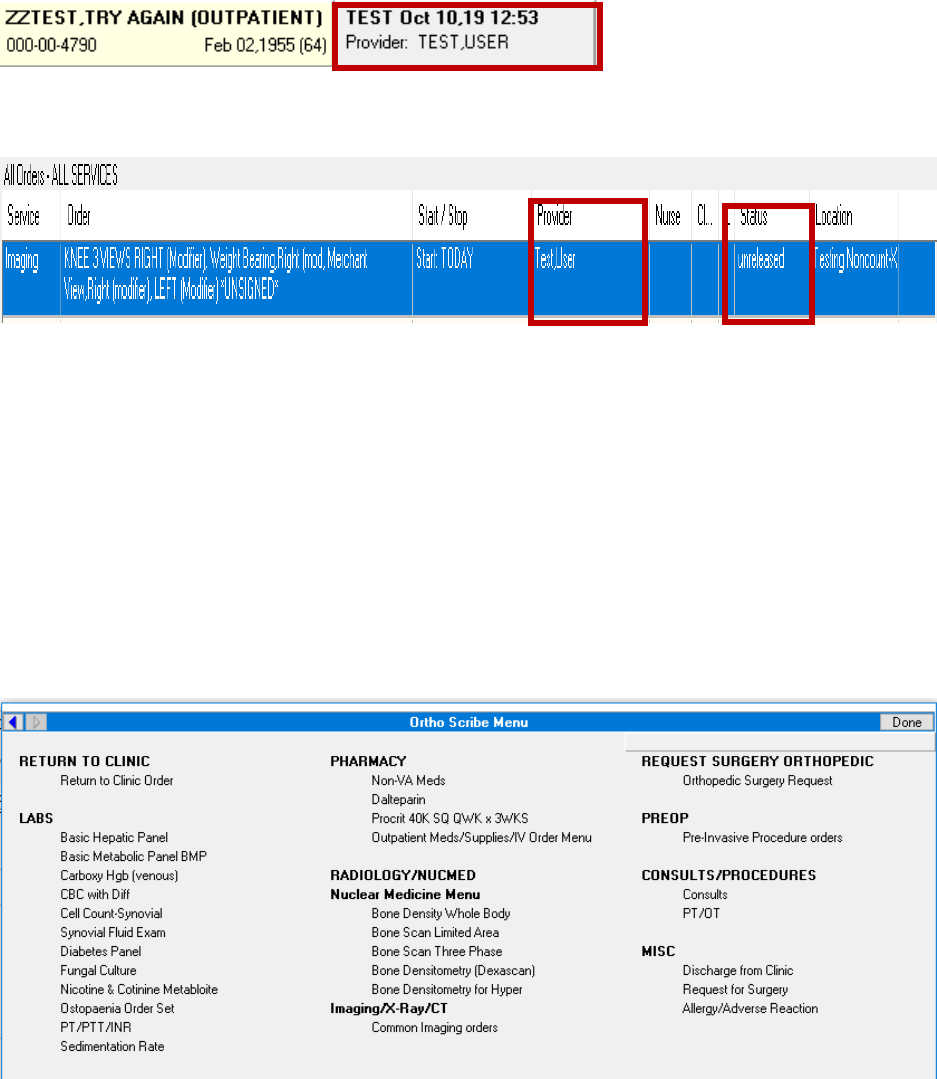
18
As a result, the Provider’s name will appear in the box next to the patient’s name at the top of
the screen.
The Imaging order below shows that the status of the order is Unreleased and the Provider’s
name Test,User is listed, not the Scribe’s name. Scribes cannot release any orders.
It is a best practice for the scribe to use the same or a similar menu as their provider so that
they are consistent. The scribe orders should be “auto accept” orders.
Please see recommended orders for each of the 3 scribe pilot specialties below. Each site can
review the suggested orders and set up orders for scribes if needed, based on the facility’s
needs.
Definition
Quick orders consist of a standard template of common orders scribes can choose from to limit
scribes from making clinical decisions.
D. Orthopedics Orders Recommended
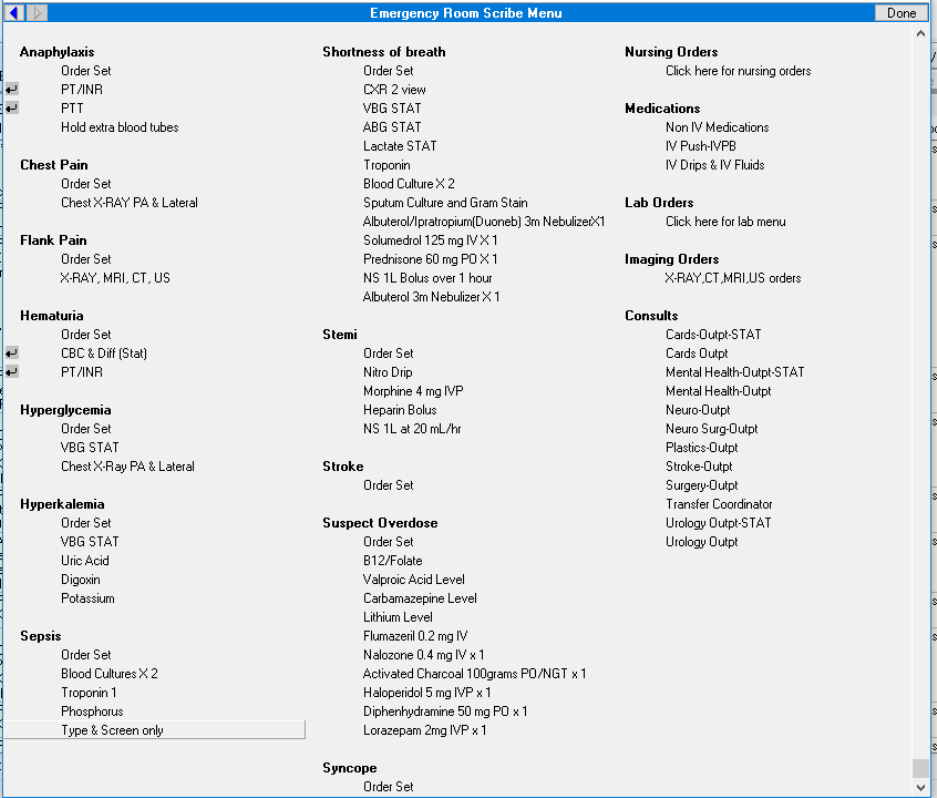
19
E. Emergency Department Orders Recommended
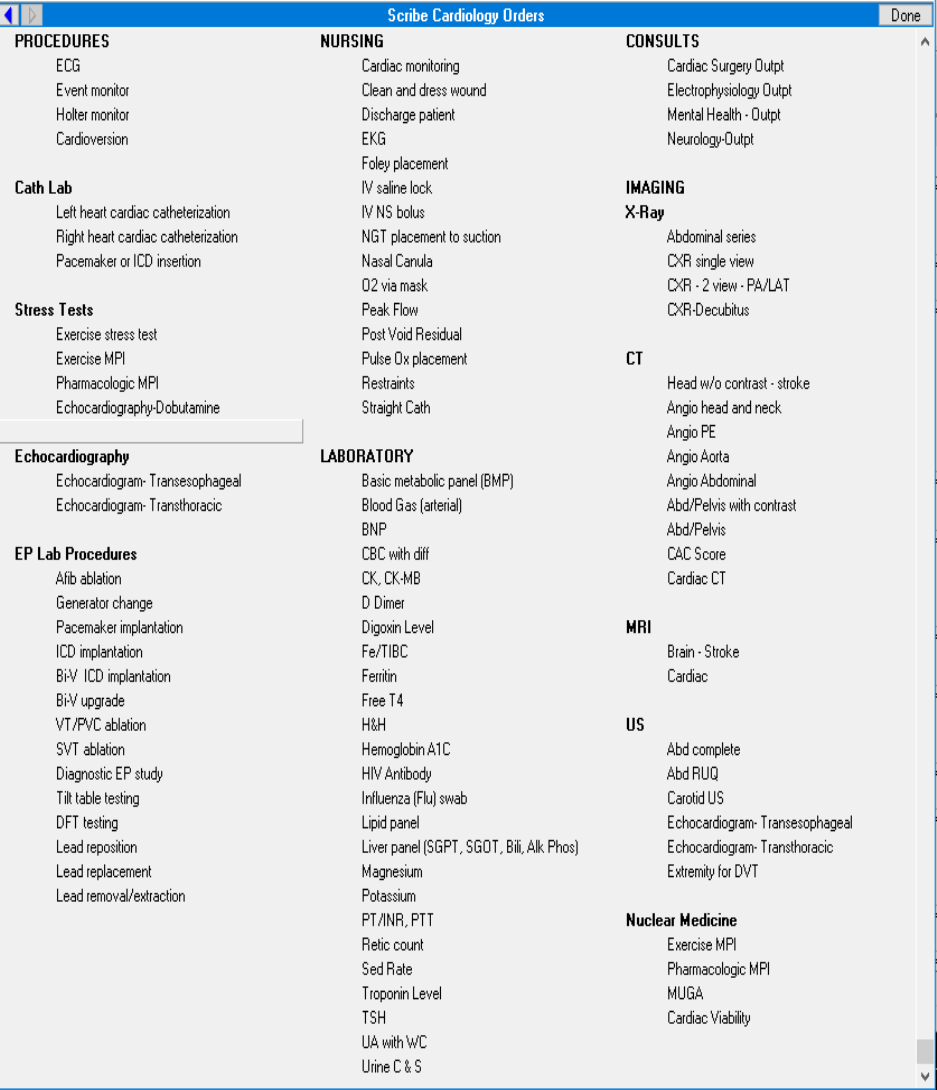
20
F. Cardiology Orders Recommended
VII. Documentation
A. Tips and Guidelines for Excellent Clinic Notes
1. The health record is complete and legible.

21
2. Documentation includes the reason for the visit and is timely, accurate and
authenticated.
3. Use key terms that have unambiguous meaning.
4. The final diagnosis is reflective of care documented.
5. If not specifically documented, the rationale for ordering diagnostic and other ancillary
services should be easily inferred by an independent reviewer. An example is
documenting in a progress note that a blood glucose level was ordered for a diabetic
patient.
6. Past and present diagnoses documented are accessible to the treating and/or
consulting physician.
7. Appropriate health risk factors are identified.
8. CPT, HCPCS and ICD-9-CM codes reported on the encounter form are supported by
the documentation in the health record.
9. Visit (Evaluation and Management) codes are based on:
a. History
b. Exam
c. Complexity of Medical Decision-making
10. Time can be used as an indicator if:
a. Counseling or coordination of care took >50% of the total visit time
b. Documentation includes what patient was counseled about
c. Documentation includes total time of visit
d. Documentation includes total time counseling
11. Medication reconciliation across the continuum of care is accurate and complete.
http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals/
12. Use appropriate note titles and templates.
13. All clinical treatments and procedures require the prior, voluntary informed consent
of the patient, or if the patient lacks decision-making capacity, the patient’s
authorized surrogate using iMedConsent™.
14. Ensure all documentation is professional and defensible.
B. Copy and Paste Guidelines
1. There is limited use of copy and paste in the electronic health record.
22
2. Documentation should only include information or data specific and pertinent
to the care provided for the particular date of service.
3. Copying unnecessary information from other documents in CPRS is redundant
and makes it difficult to read the progress note and quickly elicit pertinent facts.
4. Do not copy entire laboratory findings, radiology reports, entire problem lists,
and other information verbatim into a note. Refer to this information without
copying verbatim.
5. Documentation should not be a mirror image of previous notes.
6. Appropriate use of templates can reduce time spent documenting while
providing pertinent information. If templates are used, the wording is changed
from visit to visit to reflect the care provided for that episode of care. Note:
templates should not include pre-populated history or exam findings.
7. It is acceptable to refer to current documentation in CPRS that was reviewed
rather than repeating or inserting the information into the note. This can be
accomplished by a statement that the documentation was reviewed, e.g., nurse’s
note from 12/1/09 reviewed.
8. Do not copy the signature block into another note.
9. Providers are responsible for the content of their authenticated notes,
including copied items and information pulled into templates via object codes.
Plagiarized (copied) data, without attribution, in the patient record is
prohibited.
10. Additional information may be added in an addendum once a note has been signed.
C. Progress Note Critical Components
1. Chief Complaint(s)
Concise statements describing the main reason for the visit. This includes symptoms,
problems, conditions, diagnoses, or other factors that are the reasons for the
encounter. At least a portion of the statement should include the patient’s own
words.
Examples of a typical Chief Complaint include:
• “Tightness in my chest” for the past 4 days
• “I can’t pass my water” for the last day.
• “I just haven’t been feeling good all summer”
23
Things to avoid in writing a chief complaint statement are “Routine Visit”, “Here for
meds” or “Here because I had an appointment”. Remember to record the main
reason for the visit in this statement.
2. History
History of Present Illness (HPI) and interval history for chronic problems being followed.
The HPI should include as much as possible the time of onset of the complaint, the
duration, character and course, precipitating, alleviating and aggravating factors
associated symptoms, medications and pertinent negative questions from the
surrounding organ systems.
• ROS Entry
• Other History as Pertinent:
o Past History
o Social History
o Family History
o Military History
An example of the HPI might be this: Mr. Green is a 78-year-old man who comes in
complaining of chest pain for 4 days. This started Saturday evening after chopping a
chord of wood. He says the pain is in the chest and left shoulder. It is worse with
“putting on my shirt” and better when he rests. He has not taking any meds for it. Mr.
Green denies nausea, vomiting, shortness of breath, sweats, or palpitations. He has
never had heart problems and he believes it is tendonitis.
3. Physical Examination (PE) and Test Results
• Vital Signs
• Exam (Problem Related)
• Pertinent Test Results
4. Assessment for each problem evaluated/treated
An assessment of each problem being addressed during the visit. For example:
o Diabetes mellitus – Excellent glycemic control. No evidence of end organ disease.
5. Treatment Plan
Diagnostic
● Labs: with reasons for ordering
● Imaging
● Consults treatment
24
Treatment
● Medications
● Rx Changes
● Other treatments (operations, therapy, exercises, diet, over the counter
medications, etc.)
● Follow up:
○ Follow-up treatment
○ Patient Instructions
VIII. Consultation Guidelines
CPT defines a consultation as ‘‘a type of service provided by a physician whose opinion or
advice regarding evaluation and/or management of a specific problem is requested by
another physician or other appropriate source.’’
Key factors that define a consultation:
• A physician and/or LIP requests the opinion and/or advice of another
physician and/or LIP regarding the evaluation and/or management of a
specific problem.
• A consultant may initiate diagnostic and/or therapeutic services and the
initial service will still be considered a consultative visit.
• A “consultation” initiated by the patient and/or family, and not by another
physician or other appropriate source, is not reported using the consultation
codes but may be reported using the office visit, home visit, or domiciliary/
community living center care codes.
• A referral to take over the care for a condition is not reported using the
consultation codes but office visit codes, i.e., new patient code when seeing
the patient for the first time or established patient code when the specialty or
clinic has seen the patient within three years.
• The request and need for a consultation from the requesting clinician is
documented in the health record.
• The consultant’s opinion and any services that were ordered or
performed must also be documented in the health record. After the
consulting provider completes the initial consultation, if that provider
25
assumes responsibility for managing all or a portion of a patient’s
condition(s), the follow-up visits will be classified as Established Patient
visits.
• If an additional request for an opinion or advice regarding the same or a
new problem is received from the attending provider and documented in
the record, the provider consultant may report the office consultation
codes again.
IX. Data Capture Tips
• The most important skill to cultivate is to be prepared when the clinician walks into the
room, listen carefully and record accurately.
• Seek feedback from the clinician on your notes so you can continually work to record
the information in the way the clinician requests.
• Remember you are recording information in an interaction between the patient and
their provider. Don’t be afraid to ask questions, however, also don’t interfere with the
visit. Some questions may be best left for time with the clinician outside the exam
room.
• Always be professional, appropriate, and pleasant in your attitude.
• Time spent training and re-training on how CPRS works is invaluable and can help you
navigate the record and make the work easier.
• In addition to progress notes, you will likely interact with encounter forms. Remember
that an encounter is defined as a professional contact between a patient and a
practitioner vested with primary responsibility for diagnosing, evaluating and/or
treating the patient’s condition.
• An encounter can include face-to-face interactions or those accomplished via
telemedicine.
• Telephone contact is only considered an encounter if the contact is documented and
includes appropriate elements of a face-to-face encounter, namely history and medical
decision making. Telephone encounters are associated with a telephone clinic.
• Telemedicine encounter uses communication equipment to link health care
practitioners and patients in different locations.
• When there is a need to document an important note in the patient’s record without
patient contact, such as reviewing a record, leaving a message, documenting a no show,
or calling to cancel an appointment, enter a “historical” progress note. Historical notes
do not require encounter data, i.e., diagnosis or CPT code, as these notes do not
generate workload.

26
• Only one provider can be designated as PRIMARY for each encounter. If both the
Attending and Resident see the patient, then the Attending is selected as the primary
provider. If the provider you selected is the primary provider for the encounter, click on
the Primary button. If you are not listed as a provider and should be, you should enter
your name and add your name to the list of providers.
• When selecting a diagnosis, you may utilize the PROBLEM LIST. However, do not utilize
diagnoses associated with code 799.9 as this is an inaccurate code.
• The first diagnosis you select will always be listed as the primary diagnosis. When
another diagnosis is selected that should really be primary, highlight the correct
diagnosis, then click on the PRIMARY button located to the right. Diagnoses can also be
added to the problem list when highlighted and selected.
• Any incorrect information can be deleted before the note is signed by clicking the
encounter button and everything that was selected will appear. Click on the incorrect
item and then click on the remove button to delete the incorrect information.
• Nurse services without care by a physician or LIP, use CPT code 99211 or appropriate
procedure code for services ordered by a physician.
X. Reference Materials
A. Evaluation and Management (E/M)
Medical progress notes document the care provided to patients. Both new and established
patient notes are graded using an Evaluation and Management (E/M) scale, with visits
coded at level 1 being the least complex and those at level 5 the most complex. This system
is used for determining charges to insurance companies and for vesting patients in the VA
system.
History, exam and medical decision-making are considered the 3 KEY components that
must be performed when selecting a visit code.
The complexity of medical decision-making is dependent upon:
• The number of diagnoses or management options
• The amount and/or complexity or data to be reviewed, and
• The risk of complications and/or morbidity or mortality
Time becomes a key factor in selecting a level of service only when counseling or
coordinating care accounts for over 50% of the time spent with the patient.

27
B. Examples of E/M Services Documentation Requirements
Level 1
• Chief Complaint – history of present illness
• One body system/area examined, 1-5 elements (New Patient)
• One minor problem identified (e.g., common cold, insect bites, influenza) or
being seen for previously diagnosed problem that is stable or improving
• Minimal treatment required (i.e. injection, bed rest, and chest x-ray/lab tests)
Many Veterans have multiple chronic conditions, which may increase the level of care to:
Level 2
• Chief Complaint – history of present illness; minimum 1 element for either New
or Established Patient. One ROS taken from patient (New Patient)
• At least six bullets (New Patient)
Or
One to five bullets (Established Patient)
• One minor problem identified (i.e. cold, insect bites, influenza, etc.) or being
seen for a previously diagnosed problem that is stable or improving
• Minimal treatment required (i.e. injection, bed rest, and chest x-ray/lab tests)
Level 3
• Chief Complaint – history of present illness (must include 4 of 8 elements at a
minimum or 3 chronic conditions for a New Patient or 1 for an Established
Patient)
o ROS (verbal) (i.e. any problems such as weight loss, dizziness, etc.)
o Past medical history (patients)
o Family history
o Social history, 1-2 PFSH New Patient, None Established Patient
• At least 2 bullets from 6 areas or 12 bullets in 2+ areas (New Patient)
Or
At least 6 bullets (Established Patient)
• Conditions found – self-limiting or minor conditions (at a minimum) such as a
chronic condition – patient stable, and/or new problem to the physician or LIP
with no additional work-up planned

28
• Treatment recommendation usually an over the counter drug, minor surgery
with no identified risk factors, OR invasive diagnostic test
Level 4
• Chief Complaint – history of present illness (must include 4 of 8 elements at a
minimum or 3 chronic conditions)
o ROS (verbal) (10 ROS New Patient, minimum 2 ROS Established Patient)
o Past medical history
o Social or family history, all 3 PFSH New Patient, 1 PFSH Established Patient
• At least 2 bullets from 9 systems (New Patient)
Or
At least 2 bullets from 6 areas or 12 bullets in 2+ areas (Established Patient)
• New problem to the physician or LIP – additional workup planned; one or
more chronic problems with mild exacerbation; two or more stable chronic
illnesses; acute complicated injury. Normally three or more diagnoses are
documented.
• Order/review tests; prescription drug therapy; elective major surgery;
invasive diagnostic tests (i.e. scopes)
Level 5
• Chief Complaint – history of present illness (must include 4 of 8 elements at a
minimum or 3 chronic conditions).
o ROS (verbal) (10 or more systems reviewed with patient)
o Past medical history
o Social history
o Family history, all 3 PFSH New Patient, minimum 2 PFSH Established Patient
• At least 2 bullets from 9 systems
• New problem to the physician or LIP with additional work-up planned; two or
more chronic illnesses with severe exacerbation; acute injuries, illnesses that
pose a threat to life or bodily function; abrupt change in neurologic status
(i.e. seizure, TIA, sensory loss, etc.)
• Emergency or elective major surgery: drug therapy requiring intensive
monitoring for toxicity
29
XI. Service Connected and Treatment Factors
Veterans are eligible for cost-free (not charged co-pays nor have their billable health
insurance plan billed) medical care for conditions that have been adjudicated as a service
connected (SC) condition or for special treatment authorities related to exposures or
experiences. The special treatment authorities as of 2011 include:
• Combat Veterans. Care of conditions potentially related to combat service for
enrolled Veterans who were discharged from active duty on or after January 28,
2003 for 5 years post discharge
• Agent Orange (AO) exposure for Veterans who served in the Republic of
Vietnam from January 9, 1962 through May 7, 1975
• Ionizing Radiation (IR) Exposure for Veterans exposed during atmospheric
testing or during the occupation of Hiroshima and Nagasaki
• Southwest Asia conditions for Gulf War Veterans who served in Southwest Asia
from August 2, 1990 through November 11, 1998
• Shipboard Hazard and Defense (SHAD)/Project 112
• Military Sexual Trauma (MST)
• Head and/or Neck Cancer (HNC) related to nose or throat radium treatments
The provider must make a clinical decision to determine if an encounter is for a SC
condition or one of the special treatment authorities. If the Veteran is being treated
during the encounter for a condition that the provider believes is for a SC or a special
treatment authority, the provider will check “Yes” next to the appropriate category on
the encounter form. Neither the Veteran, nor the Veteran’s health plan will be billed for
the encounter if “yes” is checked. Clinical documentation must support the provider
marking the “Yes” box for SC or special treatment authority conditions.
Medication(s) related to a SC condition or special treatment authority condition must be
indicated during the outpatient medication ordering process. The Veteran will not be
charged a co-payment nor have his/her billable health insurance plan billed, for a
medication that is for SC condition or a special treatment authority.

30
A. Service Connected (SC) Determinations
Adjudicated service connection means that the facts, shown by evidence, establish that a
particular injury or disease resulting in disability was incurred coincident with service in the
Armed Forces, or if preexisting such service, was aggravated therein. The assignment of SC
percentage and disability code is based on the degree of disability as determined by the rating
board decision following the submission of a claim that a Veteran’s illness or injury was
incurred in or aggravated by military service. The very nature of some disabilities is to increase
in severity as time passes, regardless of the activities of the individual concerned. These later
manifestations of injury/disease in themselves that were not included in an original adjudicated
rating are not routinely service connected. Over a period of many years, a Veteran’s disability
claim may require evaluation for re-rating in accordance with changes in laws, medical
knowledge and his or her physical or mental condition to include such proportionate addition
and/or increase in percentage.
An adjunct condition, although not service connected, is medically determined to be associated
with or is aggravating a disease or condition, which is service connected. A Veteran is eligible to
receive treatment for an adjunct condition; however, because the adjunct is not a condition
that is specifically rated, VA can bill the insurance carrier as well as those Veterans responsible
for co-payments for treatment provided for the adjunct condition. Veterans should be
encouraged to file a compensation claim.
A secondary condition is defined as a condition that has been caused or is the result of a
service-connected condition. A Veteran is eligible to receive treatment for a secondary
condition. However, because the secondary issue is not a condition that is specifically rated, VA
can bill the insurance carrier, as well as those Veterans responsible for co-payments for
treatment provided for the secondary condition. Veterans should be encouraged to file a
compensation claim.
It is important that the provider be aware of the patient’s service-connected conditions. This
information is available by clicking the patient’s name in the square in the upper left corner in
31
CPRS. It is also found on the encounter form. If a patient is being treated for a service-
connected condition during a visit, the provider should check “yes” in the service-connected
box on the encounter form.
NOTE: Mentioning the service-connected condition does not constitute active treatment of a
SC condition. In order for the encounter to be marked as SC the provider must actually provide
treatment to include, but not limited to changing medications, ordering diagnostic services, etc.
Example of SC encounter: The provider ordered HCTZ for the Veterans SC
hypertensive condition. This will constitute active treatment and the visit
must be marked as SC.
Example of Non-Service-Connected (NSC) encounter: Provider documents that
the Hypertension is stable. Mentioning the SC condition in the note does not
constitute active treatment.
Utilization Review (UR) nurses have the responsibility to validate SC determinations made by
providers. If a determination is made without proper documentation, etc. the UR nurse will
contact the provider by various means to ensure the proper designation of the encounter.
Ultimately, it is the provider’s responsibility to make appropriate service connected and special
authority determination. Documentation must support the determination of the encounter.
Compensable Service-connected Veterans are not charged an outpatient co-payment. They
may be charged a medication co-payment if the medication is for a non-service-connected
condition and the Veteran is not rated greater than 50% service connected, not a former
Prisoner of War, in Priority Group 4 or exempt by virtue of low income. If the Veteran has
health insurance, a claim will be submitted to the insurance carrier for the treatment of non-
service-connected conditions.
B. Combat Veteran
A Veteran who served on active duty in combat operations during a period of war after the Gulf
War, or in combat against a hostile force during a period of hostilities after November 11, 1998,
is eligible for hospital care, medical services, and nursing home care for any illness, even if
there is insufficient medical evidence to conclude that such condition is attributable to such
service. Treatment provided under this authority is not subject to copayment requirements.
The law provides:
• Combat Veterans who were discharged or released from active service on
or after January 28, 2003, are to receive care and services at no cost for any
illness or condition possibly related to their combat service for five years
beginning from the date of their discharge.

32
Veterans Health Administration (VHA) providers have wide latitude in determining if a
Veteran’s condition may be possibly related to the Veteran’s combat service. This clinical
determination does not require the same rigor or standards used for adjudication of a service-
connected claim. It is a determination solely within the medical judgment of the treating
clinician. In general, VHA providers need to conclude that illnesses and conditions requiring
treatment or monitoring during the combat Veteran’s enhanced enrollment period (i.e., 5 year-
period post-discharge or release) are possibly related to combat service. Physical or mental
health evaluations needed to rule out combat-related health concerns are to be provided at no
cost to the enrolled combat Veterans.
However, the Under Secretary for Health has determined that certain conditions will invariably
be deemed to be due to causes other than combat service. These include, but are not limited
to:
• Congenital or developmental conditions, (e.g., scoliosis)
• Conditions which are known to have existed before military service unless there
is an indication that the condition has been aggravated or exacerbated by
combat service
• Conditions having a specific and well-established etiology that began after military
combat service, (e.g., bone fractures occurring after separation from military
service, a common cold)
Contrary to the other special treatment authorities, the “Combat Vet” (CV) status on the
encounter form is defaulted to Yes. This means that the provider must make a clinical decision
to determine if a visit or medication is not related to CV. If the Veteran is being treated for
conditions during this episode of care that the provider believes is NOT related to CV, the visit
should be un-checked and the “NO” box must be marked on the encounter form and the
medication should be designated as not related to CV.
On-line information on the intranet:
http://www.va.gov/healtheligibility/eligibility/CombatVets.asp
C. Agent Orange
Agent Orange (AO) is an herbicide that was used in Vietnam between 1962 and 1971 to
remove unwanted plant life that provided cover for enemy forces. VA has recognized the
following conditions as associated with but not necessarily caused by exposure to Agent
Orange. These are called “presumptive diseases”:
a. Diabetes (type 2)
33
b. Chloracne or other acneform disease consistent with chloracne (must occur
within one year of exposure to AO)
c. Porphyria cutanea tarda (must occur within one year of exposure to AO). Acute
and subacute peripheral neuropathy developed within one year of exposure
d. Parkinson’s disease (effective October 31, 2010)
e. Ischemic heart disease (effective October 31, 2010)
f. Chronic B-cell leukemias (effective October 31, 2010)
g. Numerous cancers:
i. Prostate cancer
ii. Hodgkin’s disease
iii. Multiple myeloma
iv. Non-Hodgkin’s lymphoma
v. Respiratory cancers (cancer of the lung, bronchus, larynx, or trachea)
(Must occur within 30 years of exposure to Agent Orange)
vi. Soft-tissue sarcoma (other than osteosarcoma, chondrosarcoma, Kaposi’s
sarcoma, or mesothelioma)
vii. Chronic lymphocytic leukemia
The conditions above represent the presumptive service-connected approved list by the
Veterans Benefits Administration (VBA). For VHA and medical care purposes, this list is used as
guidance for the provider, but is not an all-inclusive list for the Veteran to receive care under
the Agent Orange program. The provider may determine that a visit is potentially related to AO
without the condition being located on the VBA list. Again, documentation must support the
claim.
The VBA presumptive SC conditions are for SC adjudication purposes only. The presumptive
conditions allow a more rapid adjudication process without the need for the Veteran to prove
actual exposure to Agent Orange.
Note: Agent Orange was also used in Korea in 1968 and 1969 in an area from the Civilian
Control Line to the southern boundary of the Demilitarized Zone (DMZ). U.S. service members
in the area near spraying operations may have been exposed to Agent Orange during this
34
period. While Veterans who were exposed to AO in DMZ have no special eligibility for medical
care, they are eligible for Agent Orange registry examinations.
Check the following website for on-line training and updated information:
http://www.publichealth.va.gov/exposures/index.asp
D. Ionizing Radiation
Atomic veterans may have been exposed to ionizing radiation in a variety of ways at various
locations. Veterans exposed at a nuclear device testing site (the Pacific Islands, e.g., Bikini, NM,
NV, etc.) or in Hiroshima and/or Nagasaki, Japan, may be included. Atomic Veterans with
exposure to Ionizing Radiation (IR) are eligible to receive treatment for conditions related to
this exposure. VA has recognized the following conditions by statute or regulation as being
associated with radiation exposure; these are called “presumptive diseases.”
Conditions Associated with Ionizing Radiation
Leukemia, Lymphoid (except chronic lymphatic
leukemia)
Multiple myeloma
Leukemia, Myeloid
Posterior subcapsular cataracts
Leukemia, Monocytic
Non-malignant Thyroid Nodular Disease
Leukemia, Hairy Cell
Ovarian Cancer
Leukemia, other Leukemia, unspecified cell type
Parathyroid Adenoma
Thyroid Cancer
Malignant tumors of the brain and central
nervous system
Breast Cancer
Lymphomas other than Hodgkin’s Disease
Lung Cancer (malignant neoplasm of trachea,
bronchus, and lung)
Cancer of the rectum
Bone Cancer
Cancer of the small intestine
Primary Liver Cancer
Cancer of the pharynx
Skin Cancer
Cancer of the bile duct
Esophageal Cancer
Cancer of the gall bladder
Stomach Cancer
Cancer of the renal pelvis, ureters, and
urethra
Colon Cancer
Cancer of the prostate
Pancreatic Cancer
Broncho-alveolar carcinoma (a rare lung
disease)
Kidney Cancer
Benign neoplasms of the brain and central
nervous system
Urinary Bladder Cancer
Other malignancy/malignancies not listed in
the preceding diagnoses
Salivary Gland Cancer (malignant neoplasm of
major salivary gland)

35
The conditions above represent the presumptive service-connected approved list by the VBA.
For VHA and medical care purposes, this list is used as guidance for the provider but is not an
all- inclusive list for the Veteran to receive care under the Ionizing Radiation special authority.
The provider may determine that a visit is potentially related to IR without the condition being
located on the VBA list.
The VBA presumptive SC conditions are for SC adjudication purposes only. The presumptive
conditions allow a more rapid adjudication process without the need for the Veteran to prove
actual exposure to IR.
Note: Atomic Veterans do not have to receive an IR Registry Exam to qualify for this special
treatment authority. This is also true of Agent Orange.
The visit should be checked as related on the encounter form and the medication should be
designated as related to IR Exposure. This will mean that the Veteran does not have to pay a
co-payment for the visit or the medication nor will the Veteran’s health insurance be billed.
On-line training and updated information on website:
http://www.publichealth.va.gov/exposures/index.asp
E. Southwest Asia Conditions
Veterans who served in Southwest Asia between August 2, 1990 and November 11, 1998 were also
exposed to a wide variety of environmental hazards and potentially harmful substances during their
service in Southwest Asia. These include depleted uranium, pesticides, the anti-nerve gas pill
pyridostigmine bromide, infectious diseases, chemical and biological warfare agents, and vaccinations
(including anthrax and botulinum toxoid), and oil well free smoke and petroleum products. VA
recognizes that there are other health risk factors encountered by these Gulf War Veterans.
Treatment provided during the encounter that is for any disability that may possibly be associated
with service in the Southwest Asia Theater of operations during the Gulf War should be indicated on
the encounter form or medication order. This will mean that the Veteran does not have to pay a co-
payment for the visit or the medication, nor will the Veteran’s health insurance be billed. The
encounter must be marked as related to Southwest Asia Conditions.
VA recognizes the following presumptive diseases:
a. Brucellosis
b. Campylobacter jejuni
c. Coxiella Burnetii (Q fever)
36
d. Malaria
e. Mycobacterium tuberculosis
f. Nontyphoid Salmonella
g. Shigella
h. Visceral leishmaniasis
i. West Nile virus
j. Amyotrophic Lateral Sclerosis
Illnesses include medically unexplained clusters of symptoms that have existed for six
months or more, such as:
• Chronic fatigue syndrome
• Fibromyalgia
• Irritable bowel syndrome
• Any diagnosed or undiagnosed illness that VA’s Secretary determines should
be presumed to be associated with Gulf War Service
Signs and symptoms of an undiagnosed illness may include:
• Abnormal weight loss
• Cardiovascular signs and symptoms
• Fatigue
• Gastrointestinal signs or symptoms
• Headache
• Joint Pain
• Menstrual disorder
• Muscle pain
• Neurological signs or symptoms
• Signs or symptoms involving the skin
• Signs or symptoms involving the upper and lower respiratory system
• Sleep disturbances
The conditions above represent the presumptive service-connected approved list by the VBA.
For VHA and medical care purposes, this list is used as guidance for the provider, but is not an
all- inclusive list for the Veteran to receive care under the Southwest Asia special authority. The
provider may determine that a visit is potentially related to SW Asia without the condition
being located on the VBA list.
The VBA presumptive SC conditions are for SC adjudication purposes only. The presumptive
conditions allow a more rapid adjudication process without the need for the Veteran to prove
actual SW Asia conditions.

37
NOTE: The VA provider must determine and document if the conditions are related to the
Veteran’s Gulf War service. If treatment is related to Gulf War Service, the Veteran will be
exempt from first party copay and third-party billing for that date of service.
On-line training and updated information on website:
http://www.publichealth.va.gov/exposures/index.asp/
F. Shipboard Hazard and Defense (SHAD)/Project 112
Project Shipboard Hazard and Defense (SHAD) was part of a larger effort called Project 112
which was the overall program for both shipboard and land-based biological and chemical
testing that was conducted by the United States military between 1962 and 1973. Project
SHAD was the shipboard portion of these tests, which were conducted to determine:
a. The effectiveness of shipboard detection of chemical and biological warfare
agents
b. The effectiveness of protective measures against these agents, and;
c. The potential risk to American forces posed by the weapons
SHAD Veterans are to receive hospital care, medical services, and nursing home care at no
cost for any illness possibly related to their participation in these tests. However, these
Veterans may be charged a co-payment for care of conditions found to have resulted from a
cause(s) other than their participation in Project 112 tests.
Conditions Associated with Project SHAD/112:
a. Congenital or developmental conditions, e.g., scoliosis
b. Conditions which are known to have existed before military service
c. Conditions having a specific and well-established etiology and that began
after military service ceased (e.g., bone fractures occurring after
separation from military service, common cold)
Although the preceding types of conditions are not ordinarily considered to be due to military
service, if the staff physician finds that a Veteran requires care under this provision for one or
more of those conditions, the physician is to seek guidance from the facility Chief of Staff (COS)
and the Registry Physician (RP) regarding the authorization for such treatment. The decision
and its basis must be clearly documented in the medical record and charted by the RP.
VA facilities are responsible for ensuring that Project 112/SHAD Veterans who request either an
examination or enrollment in the VA health care system, whether or not they have previously
received health care from VA, are offered a complete “Primary Care New Patient History and
38
Physical Examination,” using the standardized template for this examination, and that the
results of the examination are documented in the patient’s health record.
The provider must make a clinical decision to determine if a visit or medication is related to
SHAD. If the Veteran is being treated for any condition during this episode of care that the
provider believes is related to SHAD, the visit should be checked as related on the encounter
form and the medication should be designated as related to SHAD. Clinical documentation
must support determination. This will mean that the Veteran does not have to pay a co-
payment for the visit or the medication nor will the Veteran’s health insurance be billed.
On-line information on the intranet:
http://www.publichealth.va.gov/exposures/shad/index.asp
G. Military Sexual Trauma (MST)
VA is authorized by law to provide counseling services to women and men Veterans who
experienced incidents of sexual trauma while they served on active duty in the military. Note:
This authority was extended to those whose service was only active duty for training. The Law
defines a sexual trauma as sexual harassment, sexual assault, rape and other acts of violence. It
further defines sexual harassment as repeated unsolicited, verbal or physical contact of a
sexual nature, which is threatening in nature.
The provider must make a clinical decision to determine if a visit or medication is related to
MST. If the Veteran is being treated for any condition during this episode of care that the
provider believes is related to MST; the visit should be checked as related on the encounter
form and the medication should be designated as related to MST. Clinical documentation must
support the determination. This will mean that the Veteran does not have to pay a co-payment
for the visit or the medication nor will the Veteran’s health insurance be billed.
On-line information on the intranet: http://vaww.mst.va.gov
Sexual Trauma Counseling Information website:
http://www.publichealth.va.gov/womenshealth/trauma.asp
H. Head and Neck Cancer
Veterans with cancer of the head and neck and a history of receipt of Nasopharyngeal (NP)
radium therapy are eligible for treatment. There are very specific dates and locations where
this activity occurred. Eligibility for this special class needs to be verified by the local Business

39
Office (not all Veterans receiving head and neck cancer treatment fall into this treatment
category).
During the 1920s, nasopharyngeal (NP) radium therapy was developed to treat hearing loss
caused by repeated ear infections. Radium-tipped rods were inserted into the nostrils and left
in place for several minutes. Military physicians used NP radium to treat aerotitis media
(barotrauma) in submariners, aviators, and divers. It is estimated that between 8,000 and
20,000 military personnel received NP radium treatments during World War II and into the
1960s. Veterans also included are those with documentation of NP radium treatment in active
military, naval or air service; those who served as an aviator in the active military, naval or air
service before the end of the Korean conflict; or underwent submarine training in active naval
service before January 1, 1965. Veterans with exposure to NP radium treatments are entitled
to receive treatment for conditions related to this exposure, including head and neck cancer.
If the Veteran is being treated for any condition during this episode of care that is related to
Head and Neck Cancer; the visit should be checked as related on the encounter form and the
medication should be designated as related to Head and Neck Cancer. Clinical documentation
must support the determination. This will mean that the Veteran does not have to pay a
copayment for the visit or the medication nor will the Veteran’s health insurance be billed.
On-line training and updated information on website:
http://www.publichealth.va.gov/exposures/index.asp
40
Appendix A: Scribe Weekly Deliverable Report
Medical Scribes should utilize the below form to track the name and type of
providers worked with throughout the week, the number of appointments
attended, their mode (in-person, telehealth, telephone, or other) and whether
any patients refused having a scribe in the exam room. Scribes will be asked to
submit this information on a weekly basis on the MISSION 507 SharePoint.
VISN:
Facility:
Report for Week of:
1. Scribe Type: VA or Contract
2. Name and Type (Physician or LIP) of Provider(s) worked with this week:
a. Name: and Type:
b. Name: and Type:
c. Name: and Type:
d. Name: and Type:
3. How many appointments did you attend each day and their mode
(telehealth, in-person, telephone, and other)?
a. Monday Total Appointments:
i. Number of Telehealth Appointments:
ii. Number of Telephone Appointments:
iii. Number of In-person Appointments:
iv. Number of Other Appointments:
b. Tuesday Total Appointments:
i. Number of Telehealth Appointments:
ii. Number of Telephone Appointments:
iii. Number of In-person Appointments:
iv. Number of Other Appointments:
c. Wednesday Total Appointments:
i. Number of Telehealth Appointments:
ii. Number of Telephone Appointments:
iii. Number of In-person Appointments:
41
iv. Number of Other Appointments:
d. Thursday Total Appointments:
i. Number of Telehealth Appointments:
ii. Number of Telephone Appointments:
iii. Number of In-person Appointments:
iv. Number of Other Appointments:
e. Friday Appointments:
i. Number of Telehealth Appointments:
ii. Number of Telephone Appointments:
iii. Number of In-person Appointments:
iv. Number of Other Appointments:
4. Did any patients refuse the use of scribes in their appointments?
a. If yes, how many refused?
b. What was their reason for refusal?
APPENDIX C
VACO, OFFICE OF VETERANS ACCESS TO CARE (10NG) SOP
MISSION 507: MEDICAL SCRIBE PILOT February 2020
DOCUMENTATION ASSISTANCE PROVIDED BY SCRIBES
1. PURPOSE
The Purpose of this Standard Operating Procedure (SOP) is to establish
documentation assistance procedures for Medical Scribe Progress Note and Order
Entry Policy for the MISSION 507 Medical Scribe Pilot at the following sites:
Manchester, NH; Togus, ME; East Orange, NJ; Clarksburg, WV; Hampton, VA;
Louisville, KY; San Antonio, TX; Temple TX; Helena, MT; Oklahoma City, OK;
Tucson, AZ; and Fargo, ND.
2. BACKGROUND
a.
The Medical scribes in this pilot will be placed in the Emergency
Department and/or Specialty Care Clinics (Orthopedics and Cardiology).
b.
Scribe Role versus Documentation Assistance by Licensed Staff
1.
A scribe enters information into the Electronic Health Record (EHR), or
chart as directed by a physician or Licensed Independent Practitioner
(LIP). The scribe may not act independently and is not permitted to
interject any documentation or opinion that is not specifically dictated
by the physician or LIP performing the physician examination.
2.
The Joint Commission recently relaxed restrictions on order entry,
allowing (non-licensed) Scribes to enter orders, which should benefit
sites participating in the MISSION 507 Medical Scribe Pilot.
3.
The Joint Commission has previously defined scribes as unlicensed
personnel and prohibited them from entering orders. However, due to
the widespread emergence of scribe models (including both licensed
and unlicensed personnel of varying levels of skill and clinical
knowledge performing scribe duties), that previous definition has
changed. There are individuals with the official title of “scribe” for
whom documentation assistance is their only role, and there are
individuals who perform dual roles that include clinical responsibilities
as well as documentation assistance. To clarify, the scribes in this pilot
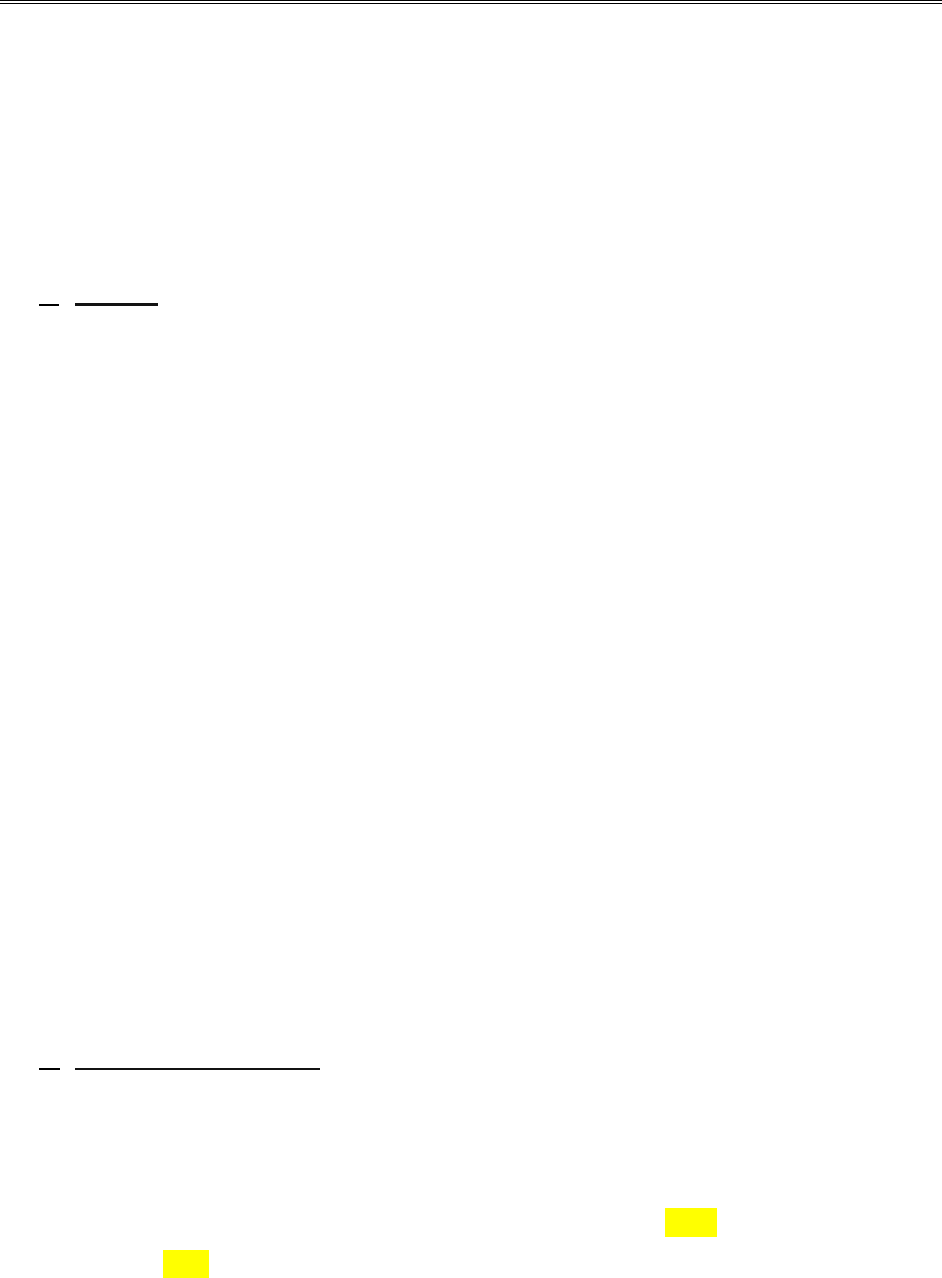
VACO, OFFICE OF VETERANS ACCESS TO CARE (10NG) SOP
MISSION 507: MEDICAL SCRIBE PILOT February 2020
Page 2 of 4
will not have any clinical responsibilities and documentation assistance
is their main role.
4.
The provider and or LIPs are ultimately responsible for the review,
approval, and signing of the scribe entries.
3. PROCEDURES/DOCUMENTATION
a.
Orders
1. The Acting Assistant Deputy Under Secretary for Health for Access for the
Office of Veterans Access to Care (OVAC) has made the decision that
Medical Scribes at the MISSION 507 Medical Scribe Pilot Sites can enter
orders, including medication orders. Pilot Sites have the option to not allow
nonclinical scribes to enter orders, if they prefer.
2.
All types of personnel functioning as a medical scribe at sites in this pilot may,
at the direction of a physician or another LIP, enter orders into the
electronic health record. The use of “read-back, repeat-back” of the order
by the scribe is encouraged, especially for new medication orders.
Scribes who are not authorized to submit orders must leave the entered
order in a pending status until a certified or licensed personnel activates or
submits the orders after verification.
3.
The process of a scribe’s entry of orders into the electronic health record
is not considered a verbal order. Verbal orders are orders received from a LIP and
are acted upon immediately by individuals practicing within the scope of
their licensure, certification, or practice in accordance with law and
regulation as well as with organizational policy.
b.
Order Entry Process
1. Scribes, as with all employees, will have their own log in information and are
prohibited from using any other log in credentials including the physician or
LIP’s log in information.
2. All non-clinical scribes should be provided with OREMAS key only, never the
ORELSE key.
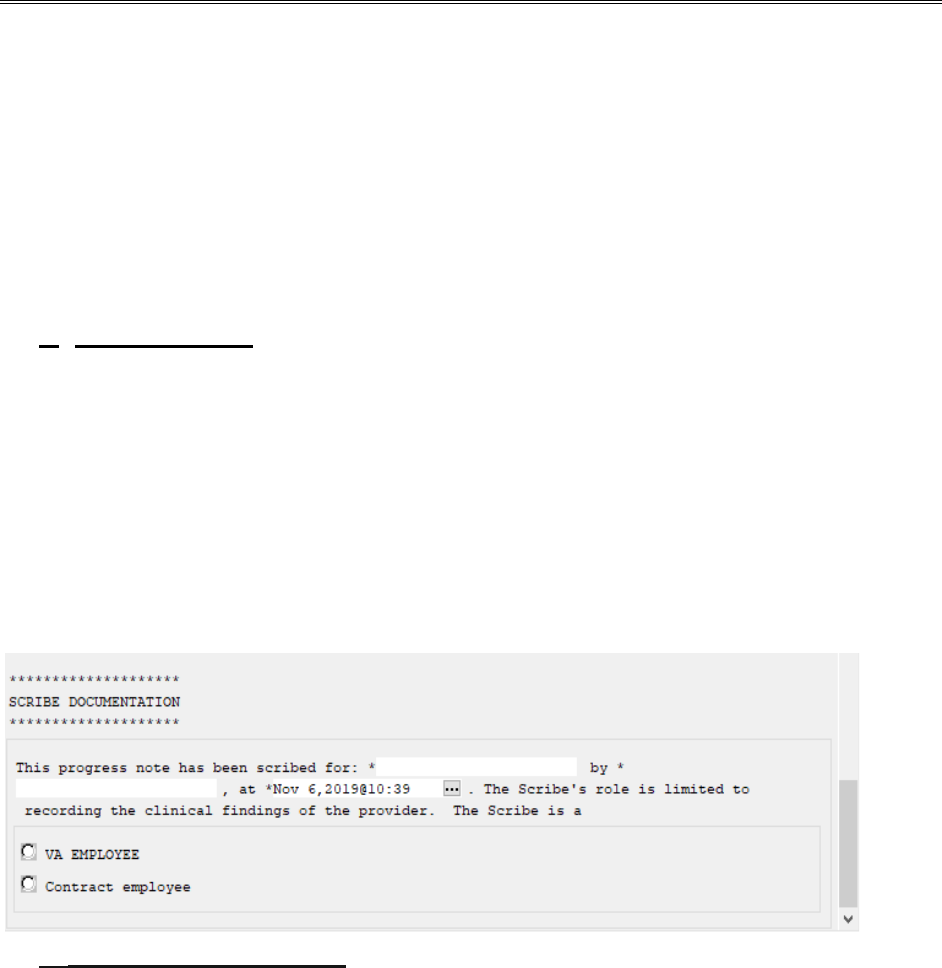
VACO, OFFICE OF VETERANS ACCESS TO CARE (10NG) SOP
MISSION 507: MEDICAL SCRIBE PILOT February 2020
Page 3 of 4
3.
Upon the direction of the provider, the scribe will enter medication orders
under the providers name.
The use of “read-back, repeat-back” of the
order by the scribe is encouraged, especially for new medication orders.
4.
After verification, the scribe will hold the order for signature.
5.
The provider or LIP is responsible for verifying all documentation,
including orders, entered by a scribe prior to signing and releasing the
order.
c. Progress Notes
1. Each progress note must use the below reminder dialog and health factors
in order to capture workload for the scribe. The reminder dialog consists of
scribe documentation in the progress note indicating “the progress note has
been scribed for Dr. X by Y at time and date. The Scribe’s role is limited to
recording the clinical findings of the provider. The scribe is a VA Employee
or Contract Employee.” A screenshot of the reminder dialog can be found
below:
d. Progress Note Process
1. Scribes, as with all employees, will have their own log in information and are
prohibited from using any other log in credentials including the physician or
LIP’s log in information.
2.
Scribe will document only what is dictated by the physician or LIP
performing the examination in the progress note.
3.
Once the scribe is finished writing the note, they will change the author to
the provider.
4.
Providers will review, edit, update, and sign the note.
VACO, OFFICE OF VETERANS ACCESS TO CARE (10NG) SOP
MISSION 507: MEDICAL SCRIBE PILOT February 2020
Page 4 of 4
5.
The note will not be viewable to others prior to the provider’s signature
and CPRS/VistA progress note business rules must ensure that this is
followed.
6.
Providers are responsible for the note content.
4. RESPONSIBILITY:
a. The Chief of Staff is responsible for the implementation of this policy with
all clinical staff and ensuring their compliance with this and all related
facility policies.
b. The Service Chiefs of those staff whose roles and responsibilities are
defined within this policy are responsible for ensuring their compliance
with the process and parameters outlined
c. Providers are responsible for:
(1) Functioning within the parameters outlined within their individual approved
clinical privileges/scope of practice.
(2) Assuring the appropriateness and completeness of all documentation
including orders entered into the patient’s medical record.
(3) Providing clarification to those staff responsible for the implementation
of these orders as needed or requested.
5. Dr. Michael Davies, Senior Medical Advisor in the Office of Veterans Access to
Care (OVAC), is the executive lead of the MISSION 507 Medical Scribe Pilot.
Katherine Williams is the project lead of the MISSION 507 Medical Scribe Pilot and
is the primary contact for all discussions regarding this agreement or conditions of
this SOP. She can be reached via email at [email protected].
APPENDIX D
DEPARTMENT OF Memorandum
VETERANS AFFAIRS
Date:
From:
Subj:
To:
October 4, 2018; revised October 10, 2019
Austin Frakt, PhD, Director, Partnered Evidence-Based Policy Resource Center (PEPReC)
National Access and Clinic Administration Evaluation
Susan Kirsh, MD, MPH, Acting Deputy ADUSH for Access to Care, Office of Veterans Access to Care
1. The purpose of this letter is to confirm that the VA Quality Enhancement Research Initiative
(QUERI) project entitled “National Access and Clinic Administration Evaluation” meets the criteria
for classification as non-research. This project is being conducted at the VA Boston Healthcare
System and is led by Steven Pizer. The project is designed to inform quality improvement efforts,
as part of the agreed-upon protocol established with QUERI and OVAC.
2. The purpose of this project is to support internal implementation and evaluation efforts to develop
and validate access metrics, such as return-to-clinic dates in primary and mental health care.
PEPReC is working with OVAC to measure the impact of a pilot program using new scheduling
software that has the potential to have profound effects on access and productivity in VA clinics
nationwide. Additionally, PEPReC is tasked with completing a quantitative analysis of MISSION Act
Section 507, a national two-year pilot of the use of medical scribes in emergency and specialty
care. These projects use secondary data collected using assessments that are part of routine care
and/or clinical management. The project will be collecting information that is designed for quality
improvement initiatives, as described in VHA Handbook 1058.05, for the purposes of program
implementation/evaluation.
3. These activities are designed and implemented for internal VA purposes and findings are
intended to be used to better inform care in the VA. This project is not designed to inform activities
beyond VA, produce information that expands the knowledge base of a scientific discipline or other
scholarly field, and does not involve collecting additional data or performing analyses that are not
needed for the purposes of this internal implementation.
Signature______________________________________________________
Susan Kirsh, MD, MPH, Acting Deputy ADUSH for Access to Care, Office of Veterans Access to Care
Partnered Evidence-Based Policy Resource Center Protocol #2019-001
APPENDIX E
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 1 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Find Studies
About Studies
Submit Studies
Resources
About Site
The safety and scientific validity of this study is the responsibility of the study
sponsor and investigators. Listing a study does not mean it has been evaluated
by the U.S. Federal Government. Know the risks and potential benefits of clinical
studies and talk to your health care provider before participating. Read our
disclaimer for details.
ClinicalTrials.gov Identifier: NCT04154462
Recruitment Status ! : Recruiting
First Posted ! : November 6, 2019
Last Update Posted ! : March 17, 2020
See Contacts and Locations
COVID-19 is an emerging, rapidly evolving situation.
Get the latest public health information from CDC: https://www.coronavirus.gov.
Get the latest research information from NIH: https://www.nih.gov/coronavirus.
Evaluation of the Use of Medical Scribes in VAMC Emergency Departments and
Specialty Care Clinics
Sponsor:
VA Boston Healthcare System
Collaborator:
US Department of Veterans Affairs
Information provided by (Responsible Party):
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 2 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Study Details Tabular View No Results Posted
Disclaimer
How to Read a Study Record
Melissa Garrido, VA Boston Healthcare System
Study Description
Brief Summary:
Background and study aims: Medical scribes are trained paraprofessionals that assist providers with
documenting patient encounters. Prior evidence suggests that scribes may be effective in
increasing provider productivity and satisfaction, and decreasing provider time spent on
documentation without negatively affecting patient satisfaction. Section 507 of the MISSION Act of
2018 mandated a two-year pilot of medical scribes, which will begin in March 2020 in specialty
clinics and emergency departments (EDs) of twelve VA Medical Centers (VAMCs) across the country.
The aims of this study are to understand how the introduction of scribes and scribe training affect
provider efficiency, patient and provider satisfaction, wait times, and daily patient volume in the VA
context.
Who can participate? Urban and rural VAMCs willing to be assigned medical scribes for use in EDs
or selected high wait time specialty clinics (cardiology, orthopedics).
What does the study involve? Four medical scribes will be assigned to each of the 12 VAMC sites
randomized into treatment with the VA hiring half as new employees and contracting out for the
remaining half. 30% of the scribes will be assigned to emergency departments and the other 70%
will be assigned to specialty care. Remaining sites that expressed interest in the pilot but were not
randomized treatment will be used as comparators. Provider productivity, patient volume, wait
times, and patient satisfaction from the treated sites will be compared to baseline (pre-scribe) data
as well as data from comparison sites.
What are the possible benefits and risks of participating? VAMCs where medical scribes are
introduced may see gains in provider efficiency, reduced wait times, and increased patient
satisfaction due to the shifting of administrative burdens associated with documenting patient
encounters in electronic health records from providers to these trained professionals. The
introduction of medical scribes could complicate patient encounters by making some patients
and/or providers uncomfortable.
Go to
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 3 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Where is the study run from? This study is being coordinated by the Partnered Evidence-based
Policy Resource Center (PEPReC) at the VA Boston Healthcare System in collaboration with the VA
Office of Veterans Access to Care (OVAC).
When is the study starting and how long is it expected to run for? March 2020 to February 2022
Who is funding the study? U.S. Veterans Health Administration
Condition or disease ! Intervention/treatment ! Phase !
Medical Scribes Other: Scribes Not Applicable
Study Design
Study Type ! : Interventional (Clinical Trial)
Estimated Enrollment ! : 12 participants
Allocation: Randomized
Intervention Model: Parallel Assignment
Intervention Model Description: A two-arm randomized field experiment is being used to
assess the effect of medical scribes on productivity, wait
times, and patient satisfaction. OVAC will work with
participating VAMCs to identify providers to participate in the
pilot. A varied provider pool will limit selection bias but must
be balanced with recruitment and retention of providers. The
goal is to keep the provider-scribe pairs consistent throughout
the pilot.
Each VAMC site randomized to treatment will have two VA
employee scribes and two contract scribes. Two medical
scribes, ideally one employee and one contract, will be
assigned to one physician, with two physicians and/or
Licensed Independent Practitioners (LIP) participating at each
facility. Scribes will work with others if the provider partner is
not available during a scheduled shift. Power analyses have
been conducted to determine the minimum effect size for each
outcome with 80% power, which will be useful for putting the
final results into context.
Go to
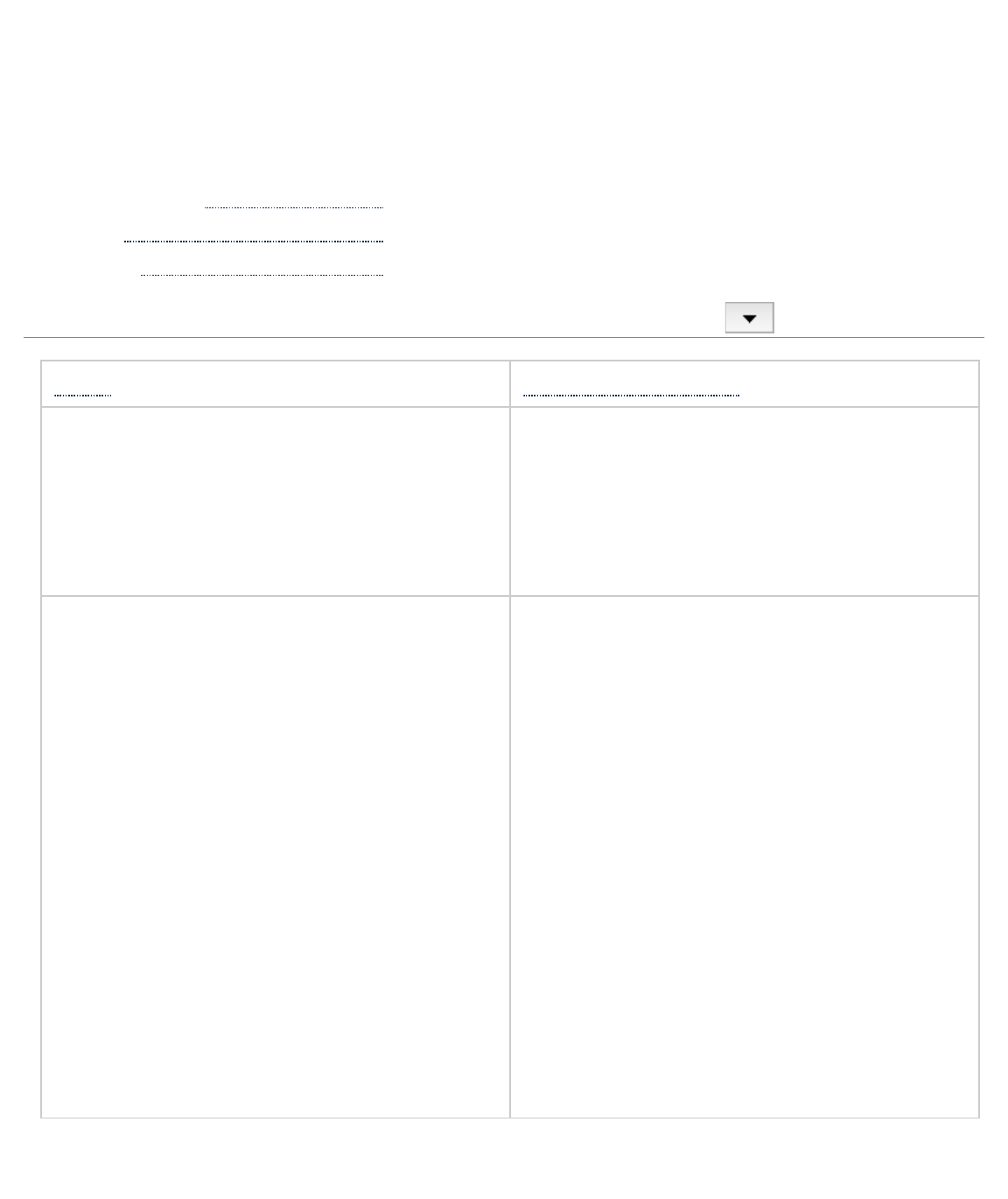
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 4 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Masking: None (Open Label)
Primary Purpose: Other
Official Title: Evaluation of the Use of Medical Scribes on Provider
Efficiency, Patient Satisfaction, and Wait Times in VAMC
Emergency Departments and Specialty Care Clinics
Actual Study Start Date ! : March 1, 2019
Estimated Primary Completion Date ! : February 28, 2022
Estimated Study Completion Date ! : May 31, 2022
Arms and Interventions
Arm ! Intervention/treatment !
No Intervention: No intervention
The VAMC sites randomized to the
comparison arm will not have medical
scribes introduced into emergency
departments or specialty clinics.
Experimental: Treatment
The VAMC sites randomized to the
treatment arm are each expected to have
four medical scribes, with two being VA
employees and two being contractors,
introduced into emergency departments or
specialty clinics to assist providers during
patient encounters.
Other: Scribes
Section 507 of the MISSION Act of 2018
mandates a two-year pilot of medical
scribes in VA specialty clinics and
emergency departments. Medical scribes
assist health care providers by helping to
administratively expedite an episode of care
through the recording of patient information
and updating patient records. Scribes are
trained but non-licensed professionals, often
deployed in emergency departments and
outpatient clinic settings, that observe and
document patient encounters but do not
participate in clinical care.
Go to

6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 5 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Outcome Measures
Primary Outcome Measures ! :
1. Pay period work relative value-based provider efficiency [ Time Frame: Approximately 42
months ]
Pay period work relative value-based provider efficiency is measured using administrative
data collected by the VA Corporate Data Warehouse in pay period increments
2. Pay period visit-based provider efficiency [ Time Frame: Approximately 42 months ]
Pay period visit-based provider efficiency is measured using administrative data collected by
the VA Corporate Data Warehouse in pay period increments
3. Daily visit-based provider efficiency [ Time Frame: Approximately 42 months ]
Daily visit-based provider efficiency is measured using monthly-based provider efficiency,
scaled by full-time-equivalent days; this is based on administrative data collected by the VA
Corporate Data Warehouse in pay period increments
4. Days to completed consult [ Time Frame: Approximately 42 months ]
Days to completed consult is measured using administrative data collected by the VA
Corporate Data Warehouse in pay period increments
5. Days to scheduled consult [ Time Frame: Approximately 42 months ]
Days to scheduled consult is measured using administrative data collected by the VA
Corporate Data Warehouse in pay period increments
6. Unique patient volume [ Time Frame: Approximately 42 months ]
Unique patient volume is measured using administrative data collected by the VA Corporate
Data Warehouse in pay period increments
7. Patient satisfaction [ Time Frame: Approximately 42 months ]
Patient satisfaction is measured using V-Signals survey data collected by the VA Office of
Go to

6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 6 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Veterans Experience in pay period increments
Eligibility Criteria
Information from the National Library of Medicine
Choosing to participate in a study is an important personal decision. Talk with
your doctor and family members or friends about deciding to join a study. To
learn more about this study, you or your doctor may contact the study research
staff using the contacts provided below. For general information, Learn About
Clinical Studies.
Ages Eligible for Study: Child, Adult, Older Adult
Sexes Eligible for Study: All
Accepts Healthy Volunteers: Yes
Criteria
Inclusion Criteria:
• Expression of interest by VAMC
Exclusion Criteria:
• Lack of appropriate site capabilities
The VA Office of Veterans Access to Care developed a list of 32 interested VAMCs based on email
surveying, which were categorized based on location (urban, rural), desired scribe deployment (ED,
specialty care), and underserved (based on high new patient specialty care wait times). 12 VAMCs
were then randomly selected for the treatment, accounting for the requirements of the law, OVAC
preferences, and site capabilities, with the remainder used as comparison sites.
Contacts and Locations
Go to
Go to
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 7 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
Information from the National Library of Medicine
To learn more about this study, you or your doctor may contact the study
research staff using the contact information provided by the sponsor.
Please refer to this study by its ClinicalTrials.gov identifier (NCT number):
NCT04154462
Contacts
Contact: Steven Pizer, PhD (857) 364-6061
Locations
United States, Arizona
Southern Arizona VA Health Care System
Recruiting
Tucson, Arizona, United States, 85723
United States, Kentucky
Robley Rex VA Medical Center
Recruiting
Louisville, Kentucky, United States, 40206
United States, Maine
Togus VA Medical Center
Recruiting
Augusta, Maine, United States, 04330
United States, Montana
Fort Harrison VA Medical Center
Recruiting
Helena, Montana, United States, 59636
United States, New Hampshire
Manchester VA Medical Center
Recruiting
Manchester, New Hampshire, United States, 03104
United States, New Jersey
Recruiting
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 8 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
East Orange VA Medical Center
East Orange, New Jersey, United States, 07018
United States, North Dakota
Fargo VA Medical Center
Recruiting
Fargo, North Dakota, United States, 58102
United States, Oklahoma
Oklahoma City VA Medical Center
Recruiting
Oklahoma City, Oklahoma, United States, 73104
United States, Texas
Audie L. Murphy VA Hospital
Recruiting
San Antonio, Texas, United States, 78229
Olin E. Teague Veterans' Medical Center
Recruiting
Temple, Texas, United States, 76504
United States, Virginia
Hampton VA Medical Center
Recruiting
Hampton, Virginia, United States, 23667
United States, West Virginia
Louis A. Johnson VA Medical Center
Recruiting
Clarksburg, West Virginia, United States, 26301
Sponsors and Collaborators
VA Boston Healthcare System
US Department of Veterans Affairs
Investigators
Principal Investigator: Steven Pizer, PhD Boston VA Healthcare System
More Information
Additional Information:
Go to
6/23/20, 11:34 AMEvaluation of the Use of Medical Scribes in VAMC Emergency Departments and Specialty Care Clinics - Full Text View - ClinicalTrials.gov
Page 9 of 9https://clinicaltrials.gov/ct2/show/NCT04154462
S.2372 - VA MISSION Act of 2018
Publications:
Pearson, E., Frakt, A., & Pizer, S. (2018, December). Medical Scribes, Productivity, and Satisfaction.
Partnered Evidence-based Policy Resource Center Policy Brief, 3(2).
Responsible Party: Melissa Garrido, Associate Director, VA Boston Healthcare System
ClinicalTrials.gov Identifier: NCT04154462 History of Changes
Other Study ID Numbers: PEPReC Protocol #2019-001
VA QUERI PEC #16-001 ( Other Grant/Funding Number: VA QUERI )
First Posted: November 6, 2019 Key Record Dates
Last Update Posted: March 17, 2020
Last Verified: March 2020
Individual Participant Data (IPD) Sharing Statement:
Plan to Share IPD: No
Studies a U.S. FDA-regulated Drug Product: No
Studies a U.S. FDA-regulated Device Product: No
Keywords provided by Melissa Garrido, VA Boston Healthcare System:
workforce
medical records
documentation
efficiency
patient satisfaction
Additional relevant MeSH terms:
Emergencies
Disease Attributes
Pathologic Processes

APPENDIX F
Measures
We will evaluate the impact of medical scribes on outcomes in several domains, including
provider efficiency, wait times, patient volume, and patient satisfaction (Table 3). Data will be
organized by facility-pay period for all outcomes to allow us to compare facilities with and without
scribes for one year before and during the intervention period. We will also assess the provider
efficiency outcomes at the provider-pay period level to allow us to describe differences between
providers within treatment facilities based on their pairing with scribes. Detailed descriptions of
each measure are contained in the appendix.
Productivity
Our primary productivity measure will be based on work relative value units (wRVUs) per
facility-pay period and provider-pay period using the following formula.
wRVU-based productivity = total wRVUs ÷ adjusted physician clinical FTE
wRVUs are a way to measure the amount of work associated with a clinical activity or procedure,
assigned by the Centers for Medicare and Medicaid Services (CMS). We will calculate wRVUs
using the CPT (Current Procedural Terminology) codes of all medical procedures performed by
specific providers during their encounters captured in the CDW. We will calculate the total
wRVUs by multiplying the volume of each CPT code performed with the respective wRVUs
assigned by CMS and then summing over all codes. We will divide by adjusted physician clinical
FTE for each facility-pay period to make the measure comparable across facilities and time. As a
sensitivity analysis, we will also use a productivity measure based on facility-pay period visit
volume using the following formula. The MISSION Act also requires reporting on visits per day
so we will also compute a version scaled by FTE days.

Visit-based productivity = total visits ÷ adjusted physician clinical FTE
Wait times
Consult wait times are a validated wait time measure for specialty care, and lower wait
times are associated with improved patient satisfaction.
7
We will use appointment and visit data in
CDW to create two average wait time variables, one capturing time to completion of consults
during the pay period and another capturing how long into the future patients are waiting for
consults recently ordered. The first is a retrospective measure of days to a completed consult and
is defined as shown below. Consults that are canceled or where the patient was a no show are not
included in this measure.
Days to completed consult = completed consult date – consult creation date
The second is a prospective measure of days to a scheduled consult and is defined as follows.
Days to scheduled consult = scheduled consult date – consult creation date
We will calculate the pay period average wait times for each physician in cardiology and
orthopedics as well as clinic-specific facility-pay period average wait times that include all
physicians within each specialty.
Patient volume
We will use the patient visits data from CDW to count the patients seen with the following
formula to calculate the patient volume:
Patient volume = unique patients per day ÷ adjusted physician clinical FTE
Patient satisfaction
We plan to use two V-Signals surveys to measure patient satisfaction: 1) Outpatient –
Scheduling an Appointment and 2) Outpatient – Health Care Visit. Each survey includes several
statements about the Veteran’s experience and the Veteran assigns a number from 1 to 5 on a

Likert Scale to indicate whether they agree or disagree with the statements (1 is strongly
disagree, 5 is strongly agree). We will use responses to seven questions in the V-Signals survey
shown in Table 3 to measure their satisfaction, with only the final three questions used for
emergency department patients. We will recode the Likert scales into binary variables to provide
a percentage change interpretation in patient satisfaction (where strongly disagree, disagree, and
neutral are set equal to zero; and agree and strongly agree are set equal to 1). We will calculate
the average percentage change in patient satisfaction for each facility-specialty combination.
APPENDIX G
Power Analysis
We conservatively assumed 24 pay periods (1 year) worth of data given that hiring and
training delays could result in less than two full years of implementation, with 24 providers (two
scribes per provider) at 12 treatment sites and 48 providers in comparison sites. We used the
observed standard deviation for each outcome in the baseline period, averaged across specialties,
as our assumption in the power analysis. For provider efficiency and patient volume, the number
of provider-pay periods corresponds to a sample size of 576 in the treatment group and 1,152 in
the comparison group. As wait times are only measured for specialty care, the number of provider-
pay periods corresponds to a sample size of 384 in the treatment group and 768 in the comparison
group. For patient satisfaction, we had to make additional assumptions about patient volume and
response rate to project the number of responses per provider-pay period. Based on baseline patient
volume and a 15% response rate (historically 20%), we project 12 completed patient satisfaction
surveys per provider-pay period, which yields sample sizes of 6,912 in the treatment group and
13,824 in the comparison group.
Under these assumptions, we would have 80% power to detect a 25.85 increase in wRVUs
per physician FTE and a 13.63 increase in visits per physician FTE related to the introduction of
scribes. Another study found a 95 wRVU increase on average per physician hour in a community
ED, much larger than our minimum detectable effect sizes if re-scaled appropriately.
6
We would
be powered to detect a 5.82 day decrease in wait times for specialty care and a 0.55 increase in
unique patients seen per day per physician FTE. For context, a prior analysis of 2012 VHA data
found a 28.8 days to completion average for specialty care consults.
13
A prior study examining
scribes in primary care found an increase of 0.16 patients per hour.
5
If we assume an 8 hour
workday and that these magnitudes are comparable for specialty and ED care, we would have
power to detect an effect size considerably smaller. Our minimum detectable effect size for patient
satisfaction, using “I am satisfied with the service I received from the VA clinic”, is an increase of
approximately 0.82 percent, small enough to detect any meaningful difference in patient
satisfaction. Assessment of differences in the effectiveness of VA-hired versus contract-hired
scribes is Congressionally mandated, but not powered for analysis. We will rely on descriptive and
qualitative analysis to explore whether there are any noteworthy differences by mode of hiring that
might inform how such an intervention would be scaled nationally.
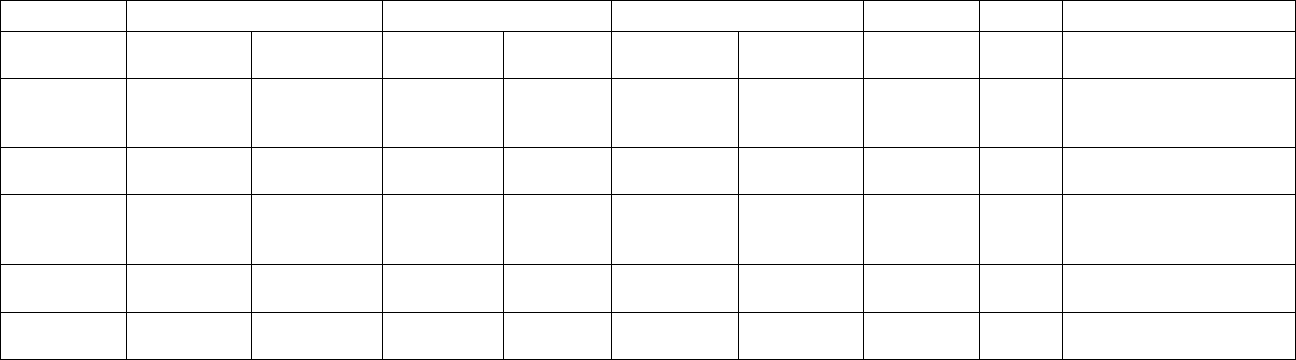
33
Table G.1. Minimum detectable effect sizes at 80% power
ICC – intra-class correlation
Size of clusters represents the number of pay periods for wRVU-based productivity, visit-based productivity, wait times, and patient volume, and number of
respondents per pay period for patient satisfaction. For patient satisfaction, the item “I am satisfied with the service I received from the VA clinic” was used in
our power analysis.
a
Applies to specialty care only
Number of providers
Size of clusters
Sample size
Outcome
Comparison
Treatment
Comparison
Treatment
Comparison
Treatment
Standard
deviation
ICC
Minimum detectable
effect size
wRVU-
based
productivity
48
24
24
24
1,152
576
163
0.01
+25.85
Visit-based
productivity
48
24
24
24
1,152
576
86
0.01
+13.63
Days to
completed
consult
a
32
16
24
24
768
384
30
0.01
-5.82
Patient
volume
48
24
24
24
1,152
576
3.5
0.01
+0.55
Patient
satisfaction
48
24
288
288
13,824
6,912
10
0.01
+0.82
